Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as award number NIHR127367. The contractual start date was in August 2019. The draft manuscript began editorial review in July 2023 and was accepted for publication in March 2024. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ manuscript and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Permissions
Copyright statement
Copyright © 2024 Rhys et al. This work was produced by Rhys et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Rhys et al.
Chapter 1 Introduction
This report presents the findings from a study funded by the UK National Institute for Health and Care Research Health and Social Care Delivery Research programme. Its purpose was to develop a qualitative understanding of the experience of making a complaint from the perspective of the NHS patient. The process of making a complaint within the healthcare system, including the final outcome, frequently fails to meet patient expectations. This has significant implications for the NHS, as dissatisfaction and the perception of an ineffective system can lead to legal action by patients. Litigation not only takes a toll on the health and well-being of both the complainants and the complained-about staff, but also imposes financial burdens both on the individuals and on the NHS budget.
The NHS as a public funded system of free healthcare has now existed for 75 years but is currently under huge threat from pressures on the services given tightened resources, increased demand, clinical complexity, and the fall-out from the COVID pandemic and its associated expense. In two recently published books marking the NHS’s 75th anniversary, Isabel Hardman1 and Andrew Seaton2 comment on its current existential crisis: ‘The NHS continues to operate at a pace and level of stress that it simply has not seen in its entire history’ and ‘patients are starting to lose faith with it in an unprecedented way’. 1 In our data, many of our complainants allude to the ‘crisis’ in the NHS, the sense that it is ‘on its knees’, in ‘utter chaos’, with wards ‘like a war zone’. It is therefore unsurprising that both the reasons to complain and the volume of complaints are increasing (e.g. written complaints to NHS England doubled to 208,626 between 2008 and 2018 and continue to grow, with 225,570 written complaints reported in 2021–23). Moreover, the complaints emerging from the current crisis are also more likely to lead to costly litigation for the NHS.
A significant body of research documents how dissatisfaction with complaint handling results from unmet expectations not only of the outcome of the complaint but also of the interpersonal conduct of NHS staff [both complaint handlers (CHs) and medical professionals]. 4 Moreover, the way in which a complaint is handled may be more consequential to a complainant’s decision to litigate than the gravity of the complained-about incident. For example, in an Australian incident, 11 patients received a contaminated solution during heart surgery, leading to 5 deaths. However, due to the Chief Executive’s genuine apology and his earnest commitment to investigate the issue, none of the affected families pursued legal action. 5 Similarly, a recent systematic review points to a recognised need for patient-centric ways of responding to complaints in order to improve complainant satisfaction. 6 One of the aims of this study therefore is to analyse whether and how good communication may contribute positively to the avoidance of a decision to pursue legal action.
While existing NHS guidance acknowledges the importance of communication in complaint handling, the current recommendations are broad and lack specific guidance on how to achieve effective communication. The current study was based on a pilot study conducted by Benwell, Rhys and McCreaddie7–12 on complaints calls to a Scottish NHS Health Board. The pilot highlighted contrasting patterns in the outcomes of the calls as an effect of the differing communication styles of the CH in the corpus. This pointed to the need for a more extensive observational study of the specific interactional practices influencing the outcomes of encounters between complainants and NHS staff. In addition, Friele et al. 13 demonstrated that complainants have nuanced expectations regarding the interpersonal conduct of CHs and clinical staff, with different expectations prioritised at different stages of the complaint process. These evolving expectations and shifting levels of satisfaction emphasise the need for a longitudinal approach to build knowledge of complainants’ lived experience of the complaints journey, understood as a series of communicative encounters (both spoken and written).
Our study thus investigated the following research question:
-
How can the power of language be harnessed to transform complainants’ experience of complaining in the NHS and reduce their recourse to litigation?
This was addressed through six research objectives:
-
to examine complainants’ lived experience of interacting with the ‘system’ through detailed micro-analysis of direct communications, both spoken and written, with NHS representatives
-
to audit patients’ perceptions of cultural bias in NHS contexts and show how this may create patterns of social relations that can help or hinder effective complaint resolution
-
to record self-reported expectations and experiences of the complaint's journey and its timeline, focusing on evolving perceptions of the complaints experience and the complained-about issue, and the impact of the process on complainant well-being and satisfaction
-
to identify and cross-reference moments of change and key drivers of change in complainants’ responses and intentions (including intentions to litigate) throughout their complaints journey
-
to develop an evidence-based ‘Real Complaints’ communication training resource to provide effective, evidence-based intervention that addresses the specific interactional and interpersonal challenges of NHS complaints handling
-
to disseminate good-practice recommendations to service users, NHS staff, local and national policy-makers and ombudsmen that will improve NHS complaint-handling processes and experiences.
The term ‘Real’ in the title of our training package (‘Real Complaints’) refers to the use of authentic recorded examples of complaints communication (written and spoken) to inform the identification of best practice and development of training, and foregrounds a significant contrast with the more common use of invented/role-played examples in existing training materials.
Structure of the report
Chapter 2 sets the context with key literature. Chapter 3 outlines our bespoke combination of observational and qualitative methods and our approach to developing the communication intervention as well as protocol changes made over the duration of the project. The subsequent analytic chapters detail the findings from our different data streams: the cultural audit (see Chapter 4), the longitudinal case studies (see Chapter 5), the written response letters (see Chapter 6) and finally the interactional findings (see Chapter 7). Chapter 8 discusses how our findings have been translated into Real Complaints Training and Guidance resources. Lastly, Chapter 9 presents our overall reflections and conclusions along with recommendations for further research.
Chapter 2 Literature review
Study context: complaining to the National Health Service
Patient satisfaction with the complaints-handling process in healthcare institutions, specifically the NHS, has been identified as an area of concern in the existing literature. Prior studies highlight that patient dissatisfaction is largely rooted in poor communication, leading to unmet service-user needs and, in extreme cases, litigation. 14,15 Although the actions of NHS staff managing complaints profoundly affect the outcomes, limited knowledge exists on this aspect. 4 Moreover, recent reports still highlight major failings with the current complaints system in the NHS. 16–18 This lack of insight underscores the need for comprehensive empirical research on the practices of responding to complaints.
The significance of effective communication in healthcare contexts is widely accepted, yet a troubling discrepancy persists between policy and practice. Even when strategies such as the ‘disclose and apologise’ policy were introduced, the expected reductions in litigation were not observed. 19,20 Mazor et al. 21 argued that this is due to a lack of understanding of how such disclosure should be executed. Similar gaps exist in the domain of complaints handling, where vague prescriptions for communication, such as adopting a non-judgemental, transparent and appropriate manner, provide insufficient guidance for actual implementation.
Healthwatch England has noted that previous improvements focused predominantly on systems rather than on understanding and enhancing the patient’s experience. 22 The preoccupation with system design and process optimisation has overshadowed the need for fostering trust and positive relationships between healthcare staff and complainants. The existing literature indicates a pressing requirement for adopting a relational, interpersonal view of the complaints process. 6,23,24
Certain principles, such as the ‘Power of Apology’ and ‘Duty of Candour’, have underpinned the complaints process in recent years. However, the assumptions that communicative events linked to these principles improve patient satisfaction require further empirical evidence. 25,26 While the ‘Power of Apology’ initiative outlines the components of a successful apology, understanding the precise timing and manner of apology delivery remains underexplored. 27–29 Furthermore, the complaints journey often involves a series of interactions, adding another layer of complexity. 30
According to Simmons and Brennan,31 the public expects the NHS to be responsive during their times of need. Both patients and complaint staff acknowledge the significance of communication quality in determining the outcome of the complaint journey. 8,23,27 Despite these insights, there is still a notable gap in the understanding of service users’ experience during the ‘complaints journey’ and the behaviour of staff managing patient complaints. 4
Complaint handling is a complex and sensitive social activity, significantly shaped by the social and institutional context. 32 The emotionally charged nature of the complaints topic, the potential defensive reactions of the clinical staff, and the varying needs and expectations of complainants all contribute to the intricacy of the complaints journey. 7,8,15,33 Hence, promoting empathy, reducing insensitivities, and avoiding alienation are essential for patient engagement and satisfaction, yet are often thwarted by institutional, procedural, and interpersonal factors. 31,34,35
Sociology and health services research on complaints
The expectations of complainants
A significant body of research indicates that complainants have diverse expectations and desired outcomes when initiating a complaint. Importantly, complainant expectations of responses to complaints or the accessibility/navigability of complaints systems have been shown to be important in terms of deciding whether or not actually to initiate a complaint in the first place. Complainants fear that they could potentially become victimised (with potential impacts on access to and quality of care) or that professionals will act defensively and ‘club together’ to undermine the complaint or complainant – thus may be reluctant to complain. 36 In this way, the types of expectations held by a potential complainant certainly feed into a very significant ‘moment’ in the complaints journey: where the decision is made about whether to make a complaint or not.
Where a complaint does proceed, complainants expect the complaints procedure to be fair and impartial. 26 More specifically, Bouwman et al. 37 argue that what complainants expect to achieve when complaining can be divided into three categorie: (1) complaints to improve healthcare quality, (2) complaints for personal benefit and (3) complaints to provoke consequences for care providers. This typology is particularly useful because it captures complainant expectations and hopes as reported in a range of other empirical research.
In the first dimension, which was found to be the most significant for complainants, complaints are made to improve healthcare quality in terms of intending institutions to learn from complaints, to prevent similar events happening to others,34 or to improve healthcare safety or stop poor practice. 38,39 In the second, types of personal benefit expected include solutions to a specific problem, prevention of occurrence or recurrence, financial reparations, justice, an apology, expressions of regret, explanations or accounts of what happened26,40–42 or simply cathartic benefit found in vocalising a grievance. 39 Interestingly, research additionally highlights how, perhaps surprisingly, negative expectations exist amongst complainants about receiving sympathy from professionals and the hope for the revival of relationships with professionals. 26 In this respect, it seems that complainants see initiating a complaint as damaging significantly or terminating existing relationships with professionals. Finally, complainants’ expectations include punishment (including loss of ability to practise), regulatory scrutiny, organisational or department closures, and financial consequences for organisations. However, it is important not to overstate the expectation of punitive action. Bismark et al. ,34 in the Australian context, show that fewer than one in five complainants expected or hoped that sanctions would be taken against specific staff or organisations, indicating that punitive action is a relatively uncommon factor in complaints. Where complainants call for punishment of professionals, this is linked most clearly to the occurrence of a death. 43 Complaining in this instance can be interpreted as forming part of period of mourning39 and motivated by a sense of ‘owing’ it to the deceased. 26 It is also important to note that financial considerations (which can be argued to fit within both of the latter dimensions) have been shown to be of only limited significance to participants34,39,44 and, where complainants have held financial expectations, they are primarily related to costs incurred. 40
Complainant experiences and the ‘expectation gap’
Research shows that complainants are often left dissatisfied with the outcome of their complaint. 13,14,26,45 Indeed, complainants’ expectations and the subsequent experience of making a complaint are often significantly different. 13,34,37,40 It has been argued26 that complainants will not be satisfied with a complaints procedure unless it meets their expectations. As noted above, complainants expect corrective measures and improvements to be made relating to healthcare quality following their complaint. However, most complainants report feeling that no significant institutional changes or improvements were made following their complaint. 13 Research by Bismark et al. 34 clearly highlights an ‘expectations gap’, a mismatch between complainants’ initial desires and expectations and what they ultimately felt was achieved. In this research, 57% of complainants sought communication in the form of information about what had happened, an expression of responsibility, or an apology; 46% sought corrective action to reduce the risk of harm to future patients. Seventeen per cent of complainants sought sanctions (in the form of disciplinary action or other punitive measures) against specific individuals or organisations. While some form of communication-related remedy was nearly always offered to patients, only 1 in 5 complainants who sought correction were given assurance that changes had been or would be made to reduce the risk of others experiencing a similar issue, and fewer than 1 in 10 who sought sanctions experienced processes to achieve this outcome. 14 If correspondence during and/or at the end of the complaint journey does not clearly communicate steps taken or changes made, then this is potentially significant in the creation of the expectations gap. Many complainants are also left disappointed by the reactions of professionals involved in the complaint,13 particularly when there is no admission of error.
Conversation analysis research on complaints
Conversation analytic research examines complaints as a social action, and as an interactional activity, which can offer a window into how institutions function and how morality is produced in interaction through people’s attention to something as good/bad or right/wrong. Conversation analysis (CA), like other forms of ethnomethodological research, empirically examines what people do, and not what people think they do. CA specifically is an approach to understanding the organisations of interaction, and how those organisations fit within an understanding of social relations. 46
Conversation analytic research has examined both informal complaints in conversational settings and formal complaints in institutional settings. Researchers have noted that complaining is a delicate and accountable activity47 with negative social connotations. 48,49 Strategies used to manage complaints and enhance their legitimacy include expressing moral indignation, displaying anger through prosody and pitch, engaging in painful self-disclosure,48 using extreme case formulations50 and idiomatic expressions,51 and employing identity categories like ‘reasonable complainer’ and ‘normal person’ to manage accountability and strengthen the grievance. 52,53 Another observation is that complaining expects agreement or affiliation54 from the recipient,7,8 but that the provision and extent of affiliation can be influenced by the institutionality of the complaint encounter, potentially conflicting with patients’ expectations. 33
Designing a complaint as actionable
Across various environments, research has shown how service users design their trouble as relevant for the institution that they are contacting. To make a legitimate request for assistance, or a relevant complaint to the institution, the talk needs to have a sense of actionability,55 whereby something can be done about the trouble. Callers work to establish themselves as having a legitimate reason to call; it will be seen below how they craft themselves as reasonable users of the service and thus worthy of attention. In institutional contexts, that means presenting the problem as one for which seeking assistance or making a complaint is a reasonable action. 46 However, what is ‘actionable’ can be unknown, so it requires work by both the caller and call handler to jointly construct the request/complaint as something which can be solved. 56
The interactional environment of complaints to the NHS is a particular context where callers are not ‘just complaining’, but are calling to resolve some problem that they have encountered while using the service. 52,57–60 Building a case for help can thus be accomplished in a number of ways sensitive to local interactional environments; however, complainants must also consider how they can build their case genuinely without facing accusations of being someone who is simply ‘moaning’.
Legitimate complainant identities
Registering a complaint as legitimate is achieved using a variety of discursive devices. These focus on the construction of the complaint itself; however, a common feature of complaints is how people produce themselves as reasonable people who have a legitimate complaint. It should not be argued that these are divorced projects; rather, offers of personal information are contextually bound performances of the individual as part of impression management. 61
Complaining is considered face-threatening;62 indeed, the delivery of complaints typically attends to cultural acceptability of an act where complainants tread a line where they are directly speaking to how one should act and how one should not act,63 so they need to be heard as rational speakers. 49 Cultural values are indexed in how people produced themselves in complaints – it is common (certainly in British culture) for stoicism to be valued and complaining to be treated as ‘moaning’, ‘whingeing’, etc. 49 In institutional settings, complaining does not usually attract such negative judgements, but complainants nonetheless work to be taken seriously.
A large body of work on producing oneself as a legitimate complainer comes from discursive psychology on characterological formulations64 where the ‘type’ of person someone is gets worked up in and through the interaction. Alexander and Stokoe focused on the formulation ‘[positive description] person’, for example, ‘I am an extremely tolerant person’. 64 They argue that these formulations implicate the conduct of the complained-about person by rendering them responsible for the caller’s actions (i.e. calling to complain). Consequently, characterological formulations are a resource for action and for identity work. 65 Investigating how complainants produce themselves (and the object of complaint) can provide insights into complainants’ stance, attitude and disposition towards the world, their social reality, and ultimately the complainable matters. 66
Institutional perspectives: relationships and constraints
Building rapport
An overriding concern for institutions when interacting with service users is to establish and maintain a good relationship; in social relation terms this is commonly referred to as rapport. 55,67 Institutions clearly have a stake in rapport-building, which ostensibly means better outcomes and thus increased client satisfaction. Rapport is demonstrably useful for service users; as described above, it goes some way to lend credence to their complaint if they can be seen as working with the institution to solve a problem, and not against the institution to create new problems. Rapport is actively sought and tied up with how institutions manage their relationship with their users. 68
Gatekeeping
Gatekeeping is an action accompanying the interactional role of call handling;69–71 call handlers decide whether and how the complaint/request etc. progresses. Whether calls result in a complaint or request does not necessarily result from the actions of individual call handlers, as the institution will have its own frameworks and workflows; they are merely responsible for navigating these procedures and ensuring that the service user fulfils the remit of the service. Though gatekeeping is characterised by decisions made by the institution, it comprises a negotiation wherein service users are tasked with convincing the service provider of the legitimacy of their trouble/request/complaint. Examining gatekeeping thus provides a window into the frameworks, processes and culture of an institution.
Navigating and signposting
Calling an institution often requires some navigation of that institution, whether it be form-filling, answering questions, telling one’s story, etc. Part of the call handler’s role is to support the caller to navigate that system to make their complaint, such as by eliciting details or being empathetic to the complainant’s experience. One method of navigating is signposting. Alexander72 offers a detailed review of signposting as an interactional activity where direction is provided to service users. Interlocutors attend to a preference for helping and providing a service even when the request/complaint cannot be fulfilled. 72,73
Signposting is organised with respect to the goal-orientedness of these approaches to the services. 67 The ‘goal’ is often bound up with how service users make requests to service providers to fulfil a course of action,74 for example, whether a current problem such as the removal of stitches is formulated as a request for help (to remove the stitches) or as a complaint (their non-removal thus far). These constructions have implications for the trajectory and ultimate outcome of the encounter.
Summary and opportunities for research
The central question explored in this literature review relates to complainant and professional expectations and experiences of complaining. Core findings include that complainants have three types of expectations when they make a complaint. They complain (1) to improve healthcare quality, (2) for personal benefit and (3) to provoke consequences for care providers. 37 However, very significantly, Bismark et al. 34 highlight an ‘expectations gap’ between expectations at the beginning of a complaint and what complainants ultimately felt was achieved – particularly relating to the expectation of corrective measures and improvements being undertaken.
Saliently, the sociological and health services research into complaints highlights the significance of poor communication and interpersonal problems as the cause of complaints. 75 Importantly for our purposes, however, only passing references are made about communication during the complaints journey, despite the evidence for the potential significance of poor communication for complainant (dis)satisfaction and the creation of the ‘expectations gap’ during the complaints process. It is clear that complainants expect certain communicative approaches and events, but, in the sociological and health services research literatures, little is said, for example, about what an effective apology or explanation would look like and how it might be received in an actual interaction. This provides scope for our project to attend to some of these gaps in the research field, specifically in engaging with longitudinal research. Such a longitudinal perspective offers the opportunity to identify whether certain forms or types of interaction with particular individuals or types of staff or, indeed, other specific moments during the complaints journey are especially important.
Chapter 3 Methodology
The aim of this project was to conduct primary research that would have implications for improving the patient experience of making a complaint. Our focus on communication stemmed from the existing research evidence indicating that the interpersonal conduct of NHS staff is a key factor in complainant dissatisfaction and that dissatisfaction with communication is the strongest predictor of litigation. 76,77 Our primary research therefore adopted a novel mixed-methods approach to provide a detailed, contextualised examination of the relationship between complainants’ observable, complaint-handling experiences and their personal, evolving perspective on both the complaint issue(s) and the complaints process.
Protocol history
In the course of this study, it became necessary to make certain changes to the protocol as originally designed. The original timeline called for data collection to begin early in 2020; however, the COVID-19 pandemic made it impossible to engage in face-to-face data collection until restrictions were relaxed, while the additional burdens placed on the NHS Trusts affected the ways in which they were able to participate. Some of the changes necessitated were on a relatively broad scale:
-
One Trust withdrew from the project completely, so the data sample consists of complaints journeys from two Trusts.
-
The remaining Trusts found that it was no longer feasible to involve clinical staff to document their role in the complaints process.
Other changes affected the nature of researchers’ interactions with complainants:
-
Face-to-face contacts with complainants were largely replaced with communication by telephone or online meeting.
-
Written communication by e-mail was offered as an alternative to post.
-
Complainants were not issued with recording devices to record their own telephone communication with the Trusts.
To compensate for some of the limitations imposed by these measures, other changes were made that increased the quantity of data available:
-
The number of longitudinal participants recruited was increased from 20 to 30.
-
Complainants were recruited even when their initial contact with the Trust regarding their complaint had occurred before the beginning of data collection, and as much information as possible on the earlier stages of their journey was obtained through interviews.
Despite these changes to the protocol, the data obtained are comparable in scope to what was envisaged in the original protocol design.
Patient and public involvement in project design
Three patient and public involvement (PPI) participants acted as consultants for the design of the data-collection tools. Of particular concern was the potential burden of longitudinal participation, particularly the diary method. All three participants were supportive of the use of diaries and recommended offering both ‘pen & paper’ and digital formats. The PPI members of the Project Management Group were consulted on the wording of the Participant Information Sheets and Consent forms.
Data sources
The project was conducted across three data-collection sites in Northern Ireland: two Health and Social Care Northern Ireland (HSCNI) Trust complaints services and one Patient Advocacy Service (PAS). Note that the health service in Northern Ireland is unique in the NHS in incorporating social care under the same organisational banner as healthcare. While clearly organisationally significant, this does not appear to be consequential for the communication phenomena in our analysis. The wider cultural context of these data-collection sites was examined via a quantitative cultural audit which explored the degree of congruence/dissonance between patient expectation and experience of the NHS in order to determine whether the patterns of social relations that matter most to patients are supported in the health service cultures they encounter.
The focus of the project was the observational microanalysis of language-in-use in both spoken and written communication between complainants and the NHS Trusts, complemented by a parallel analysis of participants’ subjective reflections on their complaint journey, both during and after the journey.
The observational data were structured in two key data sets: initial encounters (by telephone or e-mail) and longitudinal case studies following individual complainants through their entire complaint journey. The primary complaints data were either recorded phone calls, meetings or written correspondence (letters and e-mails). These observational data in the longitudinal case studies were complemented by a parallel qualitative data set of participant diaries and semistructured interviews with each of the longitudinal participants in order to cross-reference the findings of the observational analysis with participant appraisal of their complaints experience. Qualitative semistructured interviews with both complainants and complaint staff were conducted online with members of the research team and diaries were submitted online or by telephone with a researcher.
A total of 80 participants were recruited, of whom 23 ultimately became longitudinal participants. This yielded a final data set of 23 complaint journeys and a total of 86 phone calls (1155 minutes), 113 written communications and 6 recorded meetings as well as 36 participant diaries and 23 interviews. Both Trusts provided both spoken and written data, but there was a preponderance of written cases in Trust A and of spoken in Trust B. While our analysis was mindful of the differences between the Trusts, it was not the focus of the study. Both sites adhere to the same complaint-handling policy and our aim was to focus on commonalities in order to ensure the widest relevance of the training developed. The cultural audit yielded 115 cultural-audit responses.
Data on individual complaint journeys
A total of 30 longitudinal participants were recruited. Of these, 7 subsequently withdrew, leaving 23 longitudinal participants, 8 from Trust A and 15 from Trust B. Differences in practices in the two Trusts had a substantial effect on the nature of the longitudinal journey data available. All Trusts adhere to the standards for complaint handling set out by the Department of Health Social Services and Public Safety but operationalise those standards differently. Trust A has a telephone line for general enquiries but requires the complaint itself to be submitted in writing and issues written responses for all complaints. In Trust B, formal complaints may be logged by telephone and, in relatively simple cases, also resolved solely by telephone.
For Trust A, our data include all the written communication between the complainant and the Trust. Some complainants were also supported by the PAS and their journeys include recordings of telephone calls and face-to-face meetings between the complainant and a PAS representative.
For Trust B, we recorded all telephone calls between participating complainants and front-line CH made during the data-collection period. Two calls to complainants from complaints managers were also recorded. Where a complaint was closed by telephone, the Trust provided copies of the internal telephone resolution form (TRF). Where the final response to a complaint was in writing, these letters were also provided.
Complainants also provided diaries in the form of an online questionnaire (see Report Supplementary Material 1). Some participants preferred to update the research team by means of free-form e-mails or telephone calls from the researchers. In the latter case, the data that they provided have been treated as interview data.
A final interview was carried out with all complainants who consented and were available before the end of the data-collection period. These interviews were conducted using a semistructured format (see Report Supplementary Material 1); complainants were invited to reflect on their complaints journey as a whole, or, for those whose complaints were still ongoing at the end of the study, on their journey so far. These interview data are augmented by recordings of other contacts between complainants and researchers. It was found that many complainants wanted to discuss their complaints journey during the call to recruit them as longitudinal participants; as their comments were a potentially valuable source of data, some recordings of these calls were also made.
All data presented in this report and in related publications or presentations relating to the research have been anonymised in line with the project’s ethics protocol. Pseudonyms were used in place of real names (of people and places).
Complaint-handler interviews
Using a semistructured format (see Report Supplementary Material 1), three front-line CHs, two complaints managers (one from each Trust), and a PAS representative were interviewed, yielding 6.79 hours of data.
Cultural audit
The online cultural audit (see Chapter 4, Sample survey) was distributed through the mailing list of a PAS with a remit to engage the public in health research. Membership of this mailing list is open to the general public as service users of the NHS. One hundred and fifteen responses were obtained.
Modes of analysis
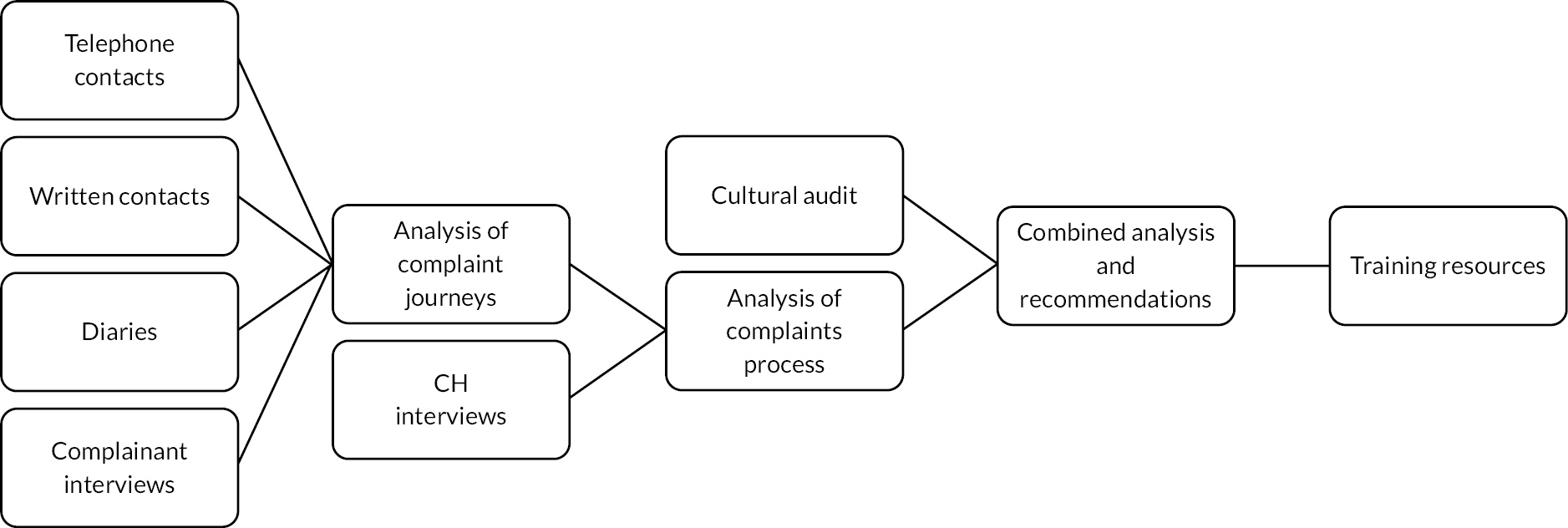
This study thus combines multiple modes of analysis to investigate the complaints process, as shown in Figure 1.
FIGURE 1.
Research pathways.
At the heart of this project is the application of CA to the spoken (mostly telephone) interactions between complainants and CHs. CA is a form of observational research that studies in fine-grained detail how conversation participants methodically display their understanding of each other’s turns-at-talk and how those understandings are negotiated in interaction. CA involves turn-by-turn analysis of communication practices in context to understand what matters to speakers moment-by-moment in the interaction and to reveal the impact of particular language choices on the ongoing conversation. In this way, the ‘next turn proof procedure’ of CA78 provides robust evidence of the effectiveness (or otherwise) of individual interactional practices by examining participants’ own situated sense-making practices. While formal quantitative measurements of frequency are therefore not relevant to the CA approach, ‘informal quantification’, described by Schegloff79 as ‘an experience or grasp of frequency’, nonetheless informs the selection of analytic foci and of trainables (see Chapters 7 and 8). In presenting our findings in Chapter 7, we focus on the interactional patterns that recurred both within and across encounters.
Similarly, discourse analysis (DA) is a linguistic approach to the analysis of written texts, which focuses on the meanings, intentions, ideologies and consequences of particular language choices by the writer, and views discourse as a form of social action or practice. 80 The written communication in our observational data set was analysed focusing on choices in grammar, word choice and pragmatic meaning (what is implied or presupposed), to provide an empirically grounded account of good and poor written communication.
The analysis of the observational data in our longitudinal case studies was triangulated by thematic analysis of participant diaries and interview data for a holistic account of the key factors within and between cases. An iterative process of open coding, informed by the microanalysis of the observational data, was applied across all data sources for each individual journey to uncover central themes and detect inconsistencies across sources. These themes were subsequently categorised into two primary axes, ‘process’ and ‘c-concepts’ (causes, consequences, correlations, constraints), for the analysis of longitudinal case studies. The cumulative effects of multiple encounters in an overall complaint journey were examined to provide a deeper understanding of the relationship encounter-by-encounter between the personal and the systemic.
Finally, the themes from the longitudinal case studies were cross-referenced with insights from the cultural audit into the sociopolitical context of the patient–healthcare provider relationship within which these complaint journeys were taking place. The cultural audit applied a validated measurement tool81,82 to assess the relative influence of cultural perspectives on four key aspects of service users’ relational expectations and experiences within the NHS: ‘courtesy and respect’; ‘how knowledge is valued’; ‘how fairness and equity issues are resolved’; and ‘how voice is expressed’. Responses were analysed using descriptive and paired-sample statistics in SPSS 25 (IBM Corp. Released 2017. IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY: IBM Corp.) to identify important gaps between expectations and experiences.
Communication skills training methodology
Communication skills training that draws on the outcomes of CA microanalysis of real recordings is well-established as delivering effective, evidence-based interventions. 76,83 The particular strengths of this approach are the authenticity and flexibility of the interactional skills identified using CA. 68,84 There are multiple benefits from the authenticity generated by inductive analysis of real recordings compared to, for example, role-play or simulation-based training approaches. To begin with, inductive analysis of real data reveals the tacit knowledge deployed in natural examples of good practice. This establishes an authentic evidence base for the targeted communication skills that clearly demonstrates their effectiveness in practice. This then also ensures the transferability of the communication behaviours from training to real-world experience. 85 In addition, the authenticity of using real examples has been shown to be particularly effective in encouraging reflection and learning about emotionally challenging communication. 86 The question of flexibility is tied to the evidence base for the training. At the heart of any CA is the recognition that turns at talk are context sensitive; each turn-at-talk both responds to the immediately prior talk and creates the context for the next turn-at-talk. 78 A key implication of this is that ‘trainables’, the communication practices targeted by a communication skills intervention, cannot be taught as standalone behaviours but as actions in a sequence of actions. Presenting trainables in their interactional context facilitates the development of reflective practice and enhanced awareness of how particular interactional strategies are not a priori effective but effective in particular interactional and sequential contexts. As our data analysis shows, this is particularly significant for some of the trainables in Real Complaints Training.
Presenting our findings
In the chapters to follow, the findings are presented from the macro to the micro. In Chapter 4, insights from the cultural audit provide the patient perspective on the sociopolitical/institutional backdrop against which individual complaints take place. Chapter 5 focuses on how the longitudinal case studies provide a nuanced understanding of patient complaints as a dynamic journey with evolving narratives and shifting expectations where each experience and encounter is shaped by preceding ones and, in turn, influences subsequent interactions and perceptions. Chapters 6 and 7 focus on the analysis of the language of first written and then spoken encounters, providing the microlevel analysis of the associations between communicative practices and outcomes that underpins the Real Complaints Training resources presented in Chapter 8.
Chapter 4 Cultural audit
Introduction
This chapter examines the influence of cultural–institutional factors in NHS/HSCNI which provide a context for the likely stance and expectations of patients/carers making a complaint. The ‘cultural audit’ tool developed by Simmons,81,82 based on Grid-Group Cultural Theory (CT), is used as part of a broader survey to structure the perceptions and opinions of service users of the NHS.
This analysis shows particular tensions between how patients think the service ‘should be’ and how they think the service ‘actually is’. Additional evidence from the survey is used to assess these findings: in particular, in the relationships between ‘good opportunities’ for patient/carer voice and the perceived quality of public service relationships and service performance.
This chapter thus addresses study objective 2.
Detailed background
The importance of relationships
The relationships between patients/carers and providers of NHS/HSCNI services are often an under-emphasised feature of public administration. Using CT as a way to structure the complexity of public service relationships, we examine whether the cultural–institutional arrangements in NHS/HSCNI services are congruent or dissonant with expectations of patients/carers.
Tensions persist in the realm of public service interactions. These arise from issues like bureaucratic paternalism, where agencies often disregard the perspectives of their users; target cultures, where relational aspects are seldom prioritised or quantified; and an emphasis on managerialism and public relations, leading to the technical handling or trivialising of relational concerns. This approach frequently results in users feeling impersonalised and powerless. 87,88 Consequently, there is a growing demand for a ‘relational state’ that emphasises meaningful service relationships over superficial transactions. 89,90
Patterns of social relations
This aspect of our study examines the extent to which the culture of NHS/HSCNI services is attuned to the patterns of social relations that matter most to patients/carers. Institutional theories offer insights into the behaviour of public service organisations and their responsiveness to user feedback. Yet, these theories fall short in clarifying the specific nature of what service users request or in identifying the initiatives that link these demands with their desired solutions. 91 The purpose of the ‘cultural audit’ is to establish the extent of compatibility between users’ perspectives about what patterns of social relations are present and what patterns are desired, as a way of setting the institutional context for the findings from this study’s microanalysis using CA.
Relational concerns, institutional work and cultural innovation
Relational concerns include aspects such as relational justice, relational satisfaction and relational morality. Notions of relational justice and relational fairness refer to the interpersonal treatment associated with decision-making. 92,93 As Waldron94 points out, people anticipate being heard, respected, taken seriously and having the chance to address any injustices in their relationships. Their sense of relational satisfaction partly stems from how well these unspoken agreements are adhered to. On the other hand, stories of relational betrayal are often told using vivid and resentful language, highlighting the strong emotions involved when expectations are not met.
Particular resonance for NHS/HSCNI services arises from further considerations of relational morality, whereby such factors as close proximity, forced interdependence and vulnerability to abuses of power may require users to develop with providers an unwritten code of relational ethics to supplement formal rules. 94 This requires institutional work,95 which may involve cultural innovation, or ‘a reprioritisation or rebalancing within organisational value systems that can help reframe the conceptual or emotional view of a situation, customize new strategies and promote new behaviours’. 96 Yet insufficient research has been directed toward the influence of broader cultural factors on how relational issues are constructed and negotiated within NHS/HSCNI services and organisations.
Understanding cultural diversity
Applying the Cultural Theory framework
Our initial discussion of cultural issues focuses on values such as relational justice, norms such as relational morality and practices that promote relational satisfaction. These are fundamental for understanding how institutional cultures preserve cultural values and norms, give them authority and provide a context for the practices of social interaction97,98 that are discussed in microanalytic detail in this study.
If we accept that patterns of social relations shape people’s preferences and justifications so that ‘everything human beings do or want is culturally biased’,99 CT, which distinguishes a limited number of cultural biases, provides a useful mechanism for simplifying system complexity in ways that are congruent with ‘real world’ processes. 100
The Cultural Theory framework and public services
Here we introduce the key elements of CT101–104 as a tool for understanding cultural diversity.
Cultural Theory has its roots in Durkheim’s105,106 two dimensions of social organisation: social regulation (‘grid’) and social integration (‘group’) (Figure 2). ‘High grid’ cultures are heavily constrained by rules and ascribed behaviour; ‘low grid’ cultures much less so. In ‘high group’ cultures, group membership is strong; in ‘low group’ cultures, much weaker. CT thus helps frame institutional analysis of the NHS/HSCNI service environment.
FIGURE 2.
The dimensions and cultural biases of CT.

The four cultural biases of Cultural Theory
Hood107 uses CT to describe four cultural biases describing ideal-typical patterns of relations in public administration:
-
Hierarchy (strong social regulation, strong social integration) sums up a bureau-professional relationship in which experts define users’ needs, and services are delivered according to strict rules of eligibility.
-
Individualism (weak social regulation, weak social integration) constructs service users as rational, utility-maximising individuals, negotiating the role to support their private needs and wants.
-
Egalitarianism (weak social regulation, strong social integration) is represented by ‘mutualistic’ forms of relationship, in which a sense of membership/ownership confers rights (but also responsibilities) on users to co-produce services through more collective processes.
-
Fatalism (strong social regulation, weak social integration) sees social relations as imposed by external structures. Fatalists consider the expression of voice as pointless, and therefore tend to feel isolated from the public service system.
Understanding cultural tensions
Cultural Theory includes two further theoretical propositions. First, the ‘requisite variety condition’ states that the four cultural biases need each other to be viable and define themselves against. 104 Elements of all four cultural biases should be expected to be present but exist with one another in a state of permanent disequilibrium, tension and flux. 104,108
Second, the ‘compatibility condition’ states that these different and mutually irreconcilable biases nevertheless need to be accommodated to maintain the viability of the system. 108 Hence, viable patterns arise when social relations and cultural biases are mutually supportive of each other. 104
Research methodology and operationalisation of Cultural Theory
General research approach
The survey tool was developed by Simmons,81,82 based on research in public service contexts which elicited four key themes in the patterns of social relations that mattered most to service users:
-
‘how fairness and equity issues are resolved’
-
‘how knowledge is valued’
-
‘courtesy and respect’
-
‘how rules are set and policed’
After review with staff at the PAS, the fourth theme was replaced with ‘expression of voice’ as more relevant in NHS settings.
Sample survey
The PAS membership list was contacted by e-mail and via the PAS newsletter, with a link to the survey on Jisc Online Surveys. Of 260 members receiving the link, there were 115 responses, a response rate of 44%. Cross-tabulation showed no significant mediating effects between survey responses and other basic differentiating sample characteristics (see Appendix 1, Table 10).
Operationalising Cultural Theory
The above thematic work defined the key elements of social relations in NHS/HSCNI services that could be evaluated using CT. Accordingly, these themes were applied in each corner of the CT framework to produce 2 sets of 16 attitude statements: first, about how NHS/HSCNI services actually are, then, in parallel, how these services should be (see Appendix 1, Table 11). Respondents used a five-point Likert-type scale (strongly agree, agree, neither agree nor disagree, disagree, strongly disagree). To avoid response bias, statements were mixed up by both theme and cultural bias, and respondents were unable to refer to their previous answers.
Findings from the cultural attitude statements
Visualising cultural characteristics
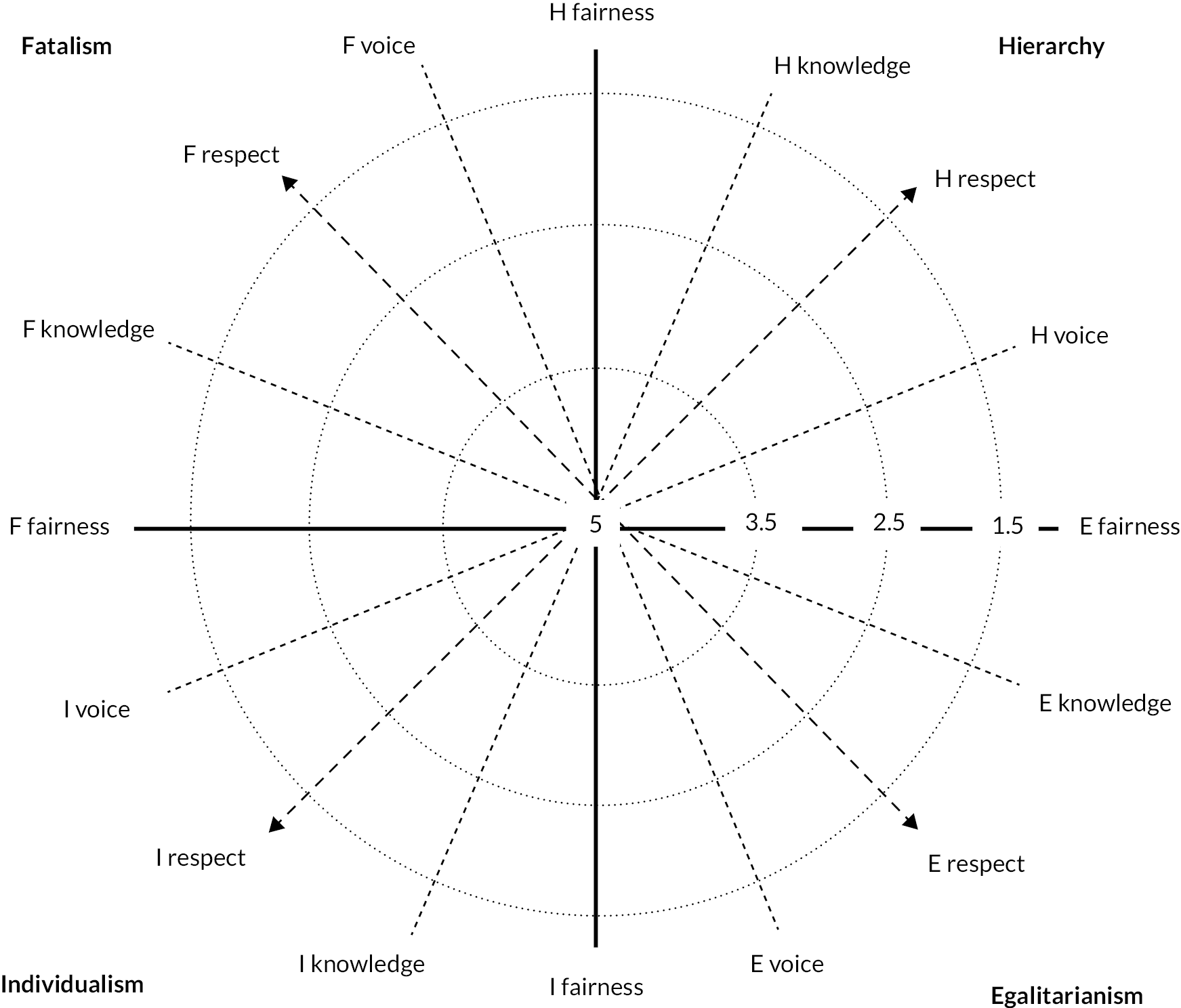
Patients’/carers’ scores against each of the attitude statements were combined to calculate a mean aggregate score for each statement. These scores were plotted on a concentric graph to represent the tension-bound nature of the cultural context in each case (Figure 3).
FIGURE 3.
Template for radial plot showing dimensions and values. Note: lower scores represent greater agreement.
Patterns in the way patients/carers felt the service relationship actually is are displayed in the visual ‘shape’ formed by these scores in Figure 4, which displays a greater degree of development or attenuation of particular ‘cultural biases’ (red line). The inconsistencies in these patterns stood in some contrast with the way patients/carers felt the service relationship should be (shaded area).
FIGURE 4.
Patient Advocacy Service members’ perceptions of how the service ‘is’ (red line) vs. how it ‘should be’ (shaded area). E, egalitarianism; F, fatalism; H, hierarchy; I, individualism.

Statistical comparison between ‘is’ and ‘should be’ statements
Such patterns indicate certain cultural ‘blind spots’; patients/carers tended to agree that their relationships with the service should be less hierarchical, much less fatalistic, more individualistic and much more egalitarian. Table 1 provides the results of a paired-samples t-test analysis comparing PAS members’ responses, showing the variations between patients’/carers’ perceptions of what ‘actually is’ and what ‘should be’ on each indicator. This analysis shows that work remains to close the gap on all four dimensions, with statistically significant differences between many of the ‘is’ and ‘should be’ statements.
| Ideal types and themes | t-test results | ||
|---|---|---|---|
| t | df | p | |
| Hierarchy | |||
| How fairness/equity issues are resolved | 3.760 | 114 | < 0.001*** |
| Whose knowledge is valued | 5.987 | 114 | < 0.001*** |
| Courtesy and respect | 1.106 | 114 | 0.136 |
| Expression of voice | 11.676 | 114 | < 0.001*** |
| Egalitarianism | |||
| How fairness/equity issues are resolved | 13.872 | 114 | < 0.001*** |
| Whose knowledge is valued | 12.625 | 114 | < 0.001*** |
| Courtesy and respect | 16.720 | 114 | < 0.001*** |
| Expression of voice | 2.496 | 114 | 0.014* |
| Individualism | |||
| How fairness/equity issues are resolved | 3.233 | 114 | 0.002** |
| Whose knowledge is valued | 7.819 | 114 | < 0.001*** |
| Courtesy and respect | 8.205 | 114 | < 0.001*** |
| Expression of voice | 2.271 | 114 | 0.013* |
| Fatalism | |||
| How fairness/equity issues are resolved | 14.528 | 114 | < 0.001*** |
| Whose knowledge is valued | 1.207 | 114 | 0.230 |
| Courtesy and respect | 10.673 | 114 | < 0.001*** |
| Expression of voice | 12.157 | 114 | < 0.001*** |
This is confirmed in Table 2, which uses a paired-samples t-test with the means of the ‘is’ and ‘should be’ scores for each cultural bias. This demonstrates both high levels of statistical significance and large effect sizes. These results appear to illuminate patients’/carers’ expectations and experiences on a range of factors, regarding patterns of social relations that would otherwise be hidden from view.
| t-test results | Effect size | ||||
|---|---|---|---|---|---|
| Cultural bias | t | df | p | Cohen’s d | Effect size |
| Hierarchy | 9.824 | 114 | < 0.001*** | 0.916 | Large |
| Individualism | 7.984 | 114 | < 0.001*** | 0.745 | Medium |
| Egalitarianism | 15.594 | 114 | < 0.001*** | 1.454 | Large |
| Fatalism | 14.621 | 114 | < 0.001*** | 1.363 | Large |
Value of the cultural audit tool
Achieving ‘relational justice’
These findings display a level of cultural dissonance. As predicted by the ‘requisite variety’ and compatibility’ conditions of CT, the value of the cultural audit lies in showing how action can be taken, to work in a number of complementary ways in the pursuit of greater congruence (or ‘dissonance reduction’).
For this complaints study, where the patient/carer voice is relevant to achieving relational justice, factors in the culture of public service organisations are important in assessing the ‘possibility spaces’ or ‘opportunity structures’ they open up or close off. 109 Survey respondents were therefore asked: ‘Are there are good opportunities available to express your views about the service?’. Yet only 22% said ‘Yes’ – 49% said ‘No’ and 27% said ‘Don’t know’.
Links with service relationships and service performance
The expression of voice could also be cross-tabulated with two further variables (service relationships and service performance), where patients/carers were asked: ‘On balance, how good a service do you think you get?’, and ‘On balance, how positive or negative is your relationship with the people who deliver this NHS service?’. Chi-squared analysis confirmed clear relationships between these variables. Hence, the more likely patients/carers were to say there were ‘good voice opportunities’, the more positive their perceptions of both relational quality and service performance (Table 3). This confirms the findings of previous research and provides an important consideration for NHS/HSCNI service managers and staff.
| ‘Are there good opportunities available to express your views about the service?’ | |||||
|---|---|---|---|---|---|
| Relationship | Yes (%) | No (%) | Performance | Yes (%) | No (%) |
| Very good | 56.0 | 7.1 | Very good | 56.0 | 8.9 |
| Quite good | 36.0 | 32.1 | Quite good | 36.0 | 23.2 |
| Neither good nor poor | 4.0 | 33.9 | Neither good nor poor | 8.0 | 12.5 |
| Quite poor | 0.0 | 19.6 | Quite poor | 0.0 | 35.7 |
| Very poor | 4.0 | 7.1 | Very poor | 0.0 | 19.6 |
| χ2 value | 41.575 | χ2 value | 49.658 | ||
| df | 12 | df | 12 | ||
| sig. (two-sided) | < 0.001*** | sig. (two-sided) | < 0.001*** | ||
Tackling fatalism
Finally, we found that the more patients/carers/complainants felt unable to engage effectively in public service relationships, the more likely they were to feel isolated and fatalistic. Those who said ‘no’ to the ‘good opportunities to express your views’ question were significantly more likely to exhibit more fatalistic perceptions (Table 4).
| ‘Are there good opportunities available to express your views about the service?’ | ||||||
|---|---|---|---|---|---|---|
| PAS members | ||||||
| Yes | N | No | N | Don’t know | N | |
| Fatalism mean score | 3.22 | 25 | 2.09 | 56 | 2.52 | 31 |
| χ2 value | 62.518 | |||||
| df | 32 | |||||
| sig. (two-sided) | < 0.001*** | |||||
As Hood107 observes, fatalist approaches arise in conditions where co-operation is rejected, distrust widespread, and apathy reigns. In promoting greater relational justice in public services, it is therefore important for greater efforts to be made to listen, engage and respond more carefully with patients/carers. 110
Conclusions
Four interconnected themes seem worthy of note in concluding this analysis.
The value of the cultural audit in understanding the cultural–institutional context
Cultural Theory analysis helps illuminate ways in which dissonance can be addressed and greater congruence promoted in NHS/HSCNI service cultures and service relationships. This added considerable value in triangulating, interpreting and assessing the microanalytical data at the analysis stage of this study.
Culture as context for complaining
Cultural dissonance between deontological (what should be) and ontological (what actually is) dimensions of service relationships constitutes a background against which a person makes a complaint. Participants’ answers portray the current relational condition in HSCNI as mostly fatalistic and hierarchical, meaning that these cultural predispositions create barriers and low expectations of the complaints process from the outset to the point of reluctance to complain. At the same time, the dissonance may encourage people to seek more congruent relationships with the service through systemic change, and the complaints procedure may be seen as an appropriate channel for such reform.
The extent to which National Health Service/Health and Social Care Northern Ireland services are attuned to relational aspects with patients/carers
This study suggests that less positive and productive contexts are created under conditions of relative dissonance. This supports calls for a more relational system that prioritises ‘deeper’, more person-centred service relationships,90 which links a need for a relational competence that goes beyond simple technical competence to the pursuit of more ‘person-centred’ approaches to public services,111,112 with concomitant prescriptions for changes in service systems, values and practices. 113,114
Whether cultural innovation can help manage emergent contradictions and incongruences within the service system
As stated above, cultural innovation involves a reprioritisation, recombination or rebalancing within organisational value systems to help reframe the conceptual or emotional view of a situation, customise new strategies and promote new behaviours. 96 In the context of this study, cultural innovation and the emergence of more congruent relational conditions may encourage patients/carers to contribute more often and more productively to the health of NHS/HSCNI services through their engagement with providers, harnessing the productive energy of emergent cultural conflict to build more harmonious relationships.
Chapter 5 The complaint as journey: longitudinal analysis
Introduction
Understanding the complaint as a journey
One of the main insights of our study is that the complaint should be understood as a journey. The concept ‘complaints journey’ captures the entire process of filing, handling, and resolving a complaint, including all the interactions and experiences that occur from the moment the complainant initiates the complaint until its resolution. This concept goes beyond just procedural elements and incorporates interpersonal elements such as the behaviour, expectations, thoughts and emotions of the complainants at each stage.
Studying complaints as journeys allows for a nuanced understanding of complainants’ expectations and satisfaction levels, which can vary at different stages of the process. Moreover, a journey-focused approach facilitates the discovery of interactional patterns and how one instance of interaction may lead to the next. This helps to understand how complainants build their future actions and understandings based on past interactions.
This chapter examines complainant evaluations of complaints journeys and thus addresses study objectives 1, 3, 4.
Data and methods
The analysis in this chapter relies on 21 full complaints journeys, 8 from Trust A and 13 from Trust B. RC18 and RC27 contributed to the recruitment quota for longitudinal participants, but their journeys provided too little data for inclusion in this chapter. (See the ‘List of abbreviations’ for the notation used to refer to participants and data sources.) Complaint journeys were varied in duration, ranging from 5 days to over 2 years (and ongoing). Figure 5 provides information on the communicative modalities used by the Trusts across the journeys.
FIGURE 5.
Communication methods across complaints journeys in two Trusts (excluding acknowledgement and holding letters).

Open coding was employed on all data sources associated with each individual journey to uncover themes and detect inconsistencies across sources (see Report Supplementary Material 2 for a coding template). The themes identified were subsequently categorised into two primary axes: ‘process’ and ‘c-concepts’ (causes, consequences, correlations, constraints). 115 This categorisation formed the foundation for the analysis that follows.
Survey data and qualitative appraisal data (diaries, interviews) capture complainants’ perceptions and expectations. Consequently, analysing these different data sources using multiple methods is expected to produce findings that reinforce and enrich one another. Meanwhile, the analysis of observational data (written correspondence, calls and meetings) offers an additional dimension. The insights from this type of data can either converge or diverge from the findings revealed by the survey and qualitative data.
Complaints journeys as processes
The complaints journey, as a temporal sequence, begins with certain negative events concerning medical care and treatment. Across our longitudinal data we see common themes uniting the patient experience in a number of cases. In addition, complainants’ broader reflections on the state of the NHS constitute a context to their complaint.
Entering the complaints process
Prior to the initiation of the complaints process, the complainant already carries a set of assumptions and expectations. In this section, we analyse how pre-existing beliefs and expectations influence the perception of the complaint journey.
Context of complaining
First, we explore how the cultural predispositions, identified in the cultural audit, are manifested in the qualitative data sources from the longitudinal journeys.
Cultural predispositions
The NHS is a revered public service to which the British public feel a strong sense of emotional attachment116 but this arguably coexists with the implicit expectation that the service should be delivered to a high standard. 7,109,117 A majority of longitudinal participants (15/21) make reference at some point in their complaint journey to a loss of confidence in the NHS as a system of healthcare. These reflections tend to emerge out of their individual experiences as they seek to understand the local failings leading to their complaint within a wider context of policy, management and funding decisions:
... there’s no such thing as the NHS anymore because they’re not providing the healthcare, they’re not providing it to the public. Because [daughter]’s not receiving any care.
RC21[Rc]
[S]omething went badly wrong with the nursing aftercare this time which made me feel afraid and lacking confidence in NHS.
RC28[D]
This perception of the NHS as a ‘failing’ institution, combined with a sense of regret at this development, is a strong theme threading through our participants’ descriptions of circumstances and motivations that lead people to complain. Sometimes the loss of faith is framed in terms of a more existential evaluation of the NHS as a whole institution:
I think the NHS is finished […]. I think the NHS is on its knees as it is.
RC28[I]
The system is just broken and the system is abused […]. The whole infrastructure, the whole environment doesn’t work.
RC30[I]
The relationships with healthcare are frequently characterised as hierarchical, and the NHS is framed as a faceless, bureaucratic and anonymous ‘system’ by our participants. In this context, individuals can feel ‘lost’, leading to negative experiences with healthcare that ultimately trigger complaints:
[S]he was just caught in the system and it was a vicious circle and nobody was, no one was there to help her.
RC02[I]
But somewhere in the great bureaucracy in the sky, this letter has gone missing, and I was left with not belonging to anyone.
RC24[I]
You’re in a system. You put up with it. You think, ‘Oh well, this is the way it is’.
RC26[I]
This perception primarily originates from the system’s perceived failure to effectively communicate and provide adequate healthcare and aftercare. The examples of RC20, RC22, RC24 and RC29 illustrate this theme vividly.
RC20, reliant on ‘extension kits’ for her nutrition, is stuck in an endless cycle of promises for the kits’ delivery, raising doubts about the truthfulness of what she is told. Similarly, RC22 recounts his father’s experience, who was negligently discharged from the Emergency Department (ED) without proper arrangements. He describes his father as being ‘pushed out of the door’ with ‘absolutely nothing’, characterising the situation as a ‘let-down’. RC24’s missing referral, despite significant numbness in her legs, left her feeling abandoned and ‘in limbo’, resulting in her complaint as a final resort. This sentiment is mirrored in RC29’s experience of continuous surgical delays for her daughter due to overlooked referrals and unreturned calls, leaving them feeling stranded and uncertain about their next steps: ‘You’re just left with that “what the heck do we do?”’
These four cases underscore the problematic anonymity of a system which is too large and under-resourced to properly care for its patients. It is clear from these examples that the system’s impersonal nature fails to address the individual needs and unique circumstances of patients. This perception of the inhuman bureaucracy of the NHS leads many complainants to feel cynical and fatalistic about the possibilities of complaints being dealt with adequately:
[D]ealing with the bureaucracy of the NHS even at the higher levels can be a waste of time.
RC09[D]
[T]he reality of how difficult it is to implement change in such a large organisation.
RC11[I]
With many of the participants expressing their disappointment in the healthcare system, we see two polar consequences. On the downside, this loss of confidence creates a pessimistic outlook on the system from the outset of the complaints journey. Complainants embark on this journey already frustrated, disillusioned and cynical about the outcomes. As a result, they may perceive the complaints process not as a channel for resolution but as a part of a system that is fundamentally flawed. On a positive side, the disillusionment with the system’s failings motivates complainants to seek changes. The drive to ‘fix’ the system becomes one of the main reasons to lodge complaints, signifying a hope to bring about meaningful reform.
These findings offer a more detailed understanding of individuals’ cultural predispositions at the beginning of their complaints journey, as identified through the cultural audit: the reverence for the NHS juxtaposed with an expectation of high-quality service leads to significant dissonance when these expectations are not met. This cultural dissonance is further exacerbated by a perceived hierarchical and bureaucratic healthcare system, resulting in a sense of alienation and fatalism. It is against this cultural backdrop of lost confidence and the desire for change that the complaints journey commences.
Drivers of complaints
Certain issues leading to the initiation of a complaint can be seen to be repeated across our corpus of longitudinal participants (Table 5).
| Complainable issue | Count |
|---|---|
| Failure to communicate/provide adequate healthcare/aftercare | 10 |
| Attitudes of and communication with staff (healthcare and receptionists) | 8 |
| Problems caused by being passed back and forth between different departments | 7 |
| Chaotic state of ward/admissions | 5 |
| Concerns regarding patient dignity | 4 |
| Clinical error/medical negligence | 4 |
| Operation waiting times | 4 |
| Seemingly minor conditions with more serious impact on patient’s life | 3 |
| COVID (and other safety) concerns | 2 |
The most frequent problems stem from communication shortcomings, reaffirming the significance of this study. Although the issues outlined probably reflect real problems with healthcare, some narrative elements are frequently emphasised or magnified. They bring to the table the work of identity construction performed by complainants, which is often used in the service of framing the initiation of a complaint as ‘reasonable’.
Reasonable complaint/complainant identity
Across our data we find frequent general references to ‘reasonable’, ‘thoughtful’, ‘normal’ person identities, often in descriptions of themselves as patients or carers, for example, ‘I can imagine a lot of people a lot of parents kicking off and like we didn’t kick off’ (RC21). RC23 defends her ‘reasonable patient’ identity in the way she describes her own behaviour (compared to the ‘rude’ doctor) as beyond reproach:
I wouldn’t even lower myself to be cheeky back to him to give him a reason to say anything about me like I don’t drink alcohol or take drugs or anything I’m genuinely sick.
RC23[T]
RC28 constructs herself as a ‘good patient’:118
I am a very independent person as my records the last time will show that at 12 week check up my recovery was brilliant as surgeon couldn’t get over work I had put in.
RC28[D]
Complainants also regularly appeal to membership of the implicit category ‘reasonable complainant’ by distancing from the activity of complaining and stressing that complaining is exceptional or not something the caller usually does (e.g. ‘we’re not really complaining people’; ‘I don’t usually complain’) or through the announcement of explicit membership of particular kinds of ‘reasonable’ identity categories (e.g. ‘I’m not an ignorant man’; ‘I’m sort of the type that doesn’t like to bother anyone’), or through attributes or activities tied to the category ‘reasonable person’ (e.g. ‘don’t want anybody getting into trouble’; ‘it’s not about punishing the system … it’s trying to make a change’).
The moral accountability of complaining sets a threshold of ‘tolerance’ before initiating or progressing complaints. RC23 (a long-term and frequent patient at the hospital) states that her perception of poor staff attitudes began at a much earlier stage but it is only now that she has decided to complain formally: ‘over the course of the twelve years … it’s just getting worse and worse and worse’. Similarly, RC29, calling on behalf of her daughter, emphasises the period of waiting prior to making the complaint; RC21 also implicitly refers to his reasonableness and patience in waiting before ‘taking a stand’:
I’ve let this go on for seven weeks now. And I feel, it’s got to the stage now where I feel like I’m letting my daughter down and I’m neglecting her because I’m her father and I’m letting her suffer. So that’s why I have now taken this stand. I’ve had enough.
RC21[Rc]
Complaining is portrayed as a ‘last resort’, only taken when extraordinary circumstances demand it. Thus, the potential social disapproval associated with the act of complaining might deter some individuals from lodging a complaint at an earlier stage. It also influences how complainants present their motives in the decision and justification to complain.
Motivation to effect change for others (‘altruistic’ reasons)
One of the most common motives voiced by our participants is the hope that the complaints process may lead to positive change for others in the future:
I don’t want anything else it’s not for financial benefit … it’s just about getting my child home and helping any other kids in the same position that we’re in.
RC21[I]
This notion of giving a ‘voice’ to or leaving a legacy for future patients through the act of complaining is a strong theme characterising patients’ motivations for complaining, a finding previously observed by other researchers. 24 RC30 expresses this perspective repeatedly in her interview, and RC02 (complaining on behalf of her sister, who is a vulnerable adult) expresses the explicit objective for her complaint to lead to the development of a protocol for dealing with hospital admissions of brain-injured adults:
If there is any learning to come out of this investigation, I would like this to benefit Brain Injured adults who require treatment.
RC02[CW]
[T]here are people like him [her father] there who couldn’t speak for themselves and had no relative with them, but I’m making this complaint. I’m making it for every single person.
RC30[I]
Similarly, RC11 sets out her motivation for complaining in the outset of her letter:
I am writing this letter in the hope that another patient does not have to endure these issues in the future.
RC11[CW]
The nature of complaining makes the will for systemic change a fundamental driving force.
Pursuing/gaining validation of complaint as legitimate
Much of the work around the construction of a reasonable complainant identity indirectly pursues a validation of the complaint as valid, legitimate and reasonable, which we observe in different strategies complainants use to justify their concerns.
Adding to the rhetorical devices reviewed above, another means of presenting a complaint as reasonable is to emphasise the exceptional status of the events leading to the complaint and the lifeworld impact of these medical circumstances. Complainants may focus on explaining the details that show that they have grounds for complaining, such as the impact of the complained-of events on their daily lives:
I was so annoyed because I was in so much pain.
RC16[T]
This exceptional poorness of care and communication is used to underpin the justification for the complaint being made:
I don’t normally complain but this individual’s behaviour was so bad and uncalled for I felt I had to highlight it.
RC09[CW]
A complainant may also mitigate the negative connotations of a complaint by bestowing praise on another aspect of their healthcare experience. They laud elements such as the excellence of staff, their exceptional workloads, or the high-quality care received in a different setting or occasion. These positive remarks serve to demonstrate their reasonableness, showing that their complaints are not blanket criticism but rather targeted at specific issues, separate from the overall competence of the healthcare system.
In the service of a reasonable complainant identity, participants also show an explicit awareness of the potential negative impact and inconvenience of their complaint, as well as an appreciation of the resource constraints on the NHS, while regretting the necessity of complaining. They appreciate the substantial demands on the healthcare system and acknowledge the pressures and challenges staff face. This self-awareness underpins their commitment to being reasonable, with complainants distancing their grievances from systemic issues like long waiting times, staff shortages or the under-resourcing of services.
Other ways to highlight their reasonable complainant identity observed in our data include: the appeal to what others said; displayed understanding that their concerns are ‘minor’; emphasis on professional experience (often working in healthcare settings) and epistemic authority.
The validation to be seen as reasonable is sometimes explicitly offered by CHs and commented on with gratitude by complainants. RC24’s case is one of the most positive endorsements of the initial call we have in our data collection:
[T]hank you so much you’ve made me feel that I’m not a – not (.) being silly about this.
RC24[T]
I think the main thing that was important was he said to me, and quite soon into the phone call, ‘You’re absolutely right to have phoned us’. It was a validation because that was my biggest concern.
RC24[I]
In this section, we have seen the kinds of rhetorical patterns around the presentation of complainant identity which largely strive to persuade the listener (CH, Trust, researcher) that the complaint is legitimate, substantive and reasonable, and that as both patients and complainants, they have behaved rationally, thoughtfully and with consideration for the significant challenges currently faced by the NHS. The work of identity construction emerges as a key moment in longitudinal journeys, supporting the analysis of the more fine-grained conversational bids for affiliation discussed in Chapter 7 (also predominantly underpinned by an orientation to ‘reasonableness’). This observation leads us to a pivotal connection between the ‘reasonable complainant identity’ and the motivations underlying the act of complaining which are tightly linked to complainants’ expectations and beliefs about the complaints process.
Preconceptions about the complaints process and motivation to complain
When an individual contacts a complaint line, they generally have an anticipated resolution in mind. Complainants often desire an acknowledgement of fault, an apology and the assurance that steps will be taken to prevent the recurrence of the issue. However, their expectations might also extend to ‘help’, which can be interpreted in a broader sense as any enhancement to their present circumstances or remedies to their issues (this is confirmed by the analysis of complainants’ reasonable motives, which demonstrated that many turn to the complaints process as a last resort). In our sample, 15 participants had ongoing concerns regarding treatment and care at the time of making a complaint. The expectation that their complaint might lead to improvements could have heightened their dissatisfaction when those changes did not occur.
We have a clear illustration of how misrepresentation of functions of the complaints department could lead to an escalation of frustration in the case of RC21. Conversations with the complainant revealed that he expected the complaints department to be independent and to advocate for him:
I put all my trust into the complaints […] I do believe that the complaints will help and they act independently and they will push my side as much as possible.
RC21[TD]
He also did not understand that the complaints team do not carry out the investigation, as is evident from the following quote where he comments on being unexpectedly drawn into a meeting about his complaint without prior notice during a ward visit:
Surely that goes against the whole complaint process because it’s then not allowing the complaint people to effectively investigate the complaint. (emphasis added)
RC21[I]
Unrealistic expectations regarding the role of the complaints department probably exacerbated this complainant’s frustration. Although he had been through the complaints process before with an equivalently complex complaint, that experience did not adequately prepare him for the current one. It indicates that there is a lack of clarity about the complaints department’s function.
Indeed, confusion exists regarding the various entities handling complaints and their responsibilities. For example, two participants believed the only complaint channel was the Ombudsman. RC30 stated, ‘I didn’t know how to complain or who I could complain to’ (RC30D), and turned to the Ombudsman with her previous complaint, but made no progress. RC26 saw the Ombudsman ‘advertised somewhere on the TV’ (RC26[T]), but was unaware of her right to complain, and only learnt about the complaint line after inquiring about her surgery waitlist status.
I think if the public were more aware that they could complain I think there would be a lot more complaints about the NHS.
RC26[I]
Understanding the right to complain does not equate to knowing how to complain, and in one of our cases the NHS staff were equally unaware of the process:
[T]hey told me they don’t know how to do that […] so I’ve actually just googled.
RC20[T]
Although instances of misunderstanding/non-awareness are infrequent in our study, their existence within our limited sample suggests that complainants have varied interpretations of the complaints process.
The tension between complaint and problem-solving becomes evident in those cases where the complaints process did resolve some problems for the complainant. RC17 was a woman who fractured her toe and found her subsequent medical care experience unsatisfactory. While she didn’t initially expect her complaint to lead to a resolution, she has the impression that her complaint contributed to her being seen by a helpful consultant:
[W]hen I phoned up to complain it was really just to complain, it wasn’t, I wasn’t thinking that they would intervene and get me an appointment, but for whatever reason they did.
RC17[I]
Nevertheless, she believes this kind of advocacy shouldn’t be necessary.
Her case also vividly demonstrates how problem-solving could be an underlying motive and expected outcome of the complaint. At the time of complaining its motivation was expressed as getting justice and effecting change for others, but it appears from the interview 7 months later that the complainant’s primary motive was to resolve the issues with her care (‘Well just to get the issue resolved really it was […] I was just hoping somebody would have sorted it out in some way and then they did’). The pressure to be seen as reasonable subsided over time and the complainant’s personal care became more prominent.
Similarly, RC30 and RC24 experienced positive shifts in care after lodging formal complaints. For RC30, it brought about an immediate enhancement in their father’s care, making him ‘treated like a king’. This positive outcome, however, sparked reflections on the privilege inherent in the ability to complain, not afforded to everyone. RC24, stuck in healthcare ‘limbo’ due to an unrecorded referral, reluctantly lodged a complaint. This led to a swift response from the service and an operation date, leading the patient to view the complaint as a direct tool for resolution. Nevertheless, RC24 expresses discomfort over the need to complain for prompt healthcare and concern for the potential system bias favouring assertive complainants. She mirrors RC30’s reflection on the privileged status of those able to voice concerns and effect change.
While RC17, RC24 and RC30 seemed satisfied with the resolution of their grievances, they were not necessarily satisfied with the resolution of the complaint. For example, RC17, in the interview, diaries and e-mail to the research team, expresses ongoing concern about whether the staff member in question who was rude to her was disciplined or addressed. It becomes evident that the complaints process, while often seen as a mechanism for justice and systemic change, frequently serves as a vehicle for problem-solving and individual care improvement. The cases reviewed above highlight this dual role. Yet, these case studies also underscore the complexity and multifaceted nature of satisfaction within the complaints process. Although the complainants saw positive changes in care, questions remained about broader systemic change and accountability.
This suggests that there are broadly two types of motivations to complain: ones directed at systemic issues (justice, change for others in the future) and ones aimed at personal care/treatment (problem-solving). The former is explicitly stated and serves to maintain the reasonable complainant identity while the latter usually stays in the background but nevertheless impacts complainants’ satisfaction.
In sum, misrepresentations and lack of clarity about the complaints process can have a significant impact on the satisfaction of complainants. This implies the necessity for clearer communication strategies and perhaps more widespread education about patients’ rights and avenues for complaint within the NHS.
Dynamics of an ongoing complaint
In this section, we study how the complaint transforms over time and how the modality of communication impacts this process.
The power of personal communication
The complaints process starts when the complainant calls a complaint line or submits their concerns in writing. When the complaint is lodged via telephone, the CH is the first point of contact in the journey. The primary contention for the importance of initial interaction lies in the fact that the first conversations with the complaints team significantly impact complainants, a fact supported by the substantial amount of positive feedback received about the complaints staff. Nine out of 13 participants who lodged their complaint via phone expressed appreciation for the call, either during the call itself, or in subsequent interviews.
Personal communication is generally appreciated by our participants, whose stories often report the lifeworld impact of their complaints which calls for the understanding of the background of a unique individual case:
I requested that [a meeting with the complaints team] when I first logged my complaint […]. You know I just thought that was standard because it is such a complex thing to do via email.
RC01[I]
… but somebody maybe just had a discussion about what my complaint is, and find out a bit about the person that they were talking about. I know it’s a big organisation but still, we’re all humans.
RC02[I]
In a system dominated by written correspondence, the complaints process can be perceived as a ‘cosmetic activity’, a ‘tick-box exercise’.
[H]ow can an in depth investigation take place without contact being made and an understanding of the person involved?
RC02[D]
It is just a process for them […], they are like ‘that’s great tick the box’.
RC01[I]
In contrast, in our data the overall impression about the initial calls was that the complainants’ concerns were heard, understood and taken seriously, all actions that validate the complainant’s need to be seen as ‘reasonable’. Moreover, when triangulating different data sources, it becomes noticeable that complainants tend to exaggerate the degree to which the CH sympathises with their perspective. The case of RC26, who has been waiting for a preoperative consultation for over 4 and a half years, vividly illustrates this tendency:
The words that stick in my mind from that conversation were that the lady didn’t believe how long I had waited for an actual first appointment. She said it’s a ridiculous amount of time you’ve had to wait for a first consultation with somebody, from whenever my consultant had sent the letter in. Again, I think she thought it was the system at fault rather than the consultant or the doctor.
RC26[I]
However, the transcript of the call reveals that the CH demonstrated a neutral stance, quickly moving to information gathering and closing phases of the conversation, and that the caller regularly relaunched their narrative to resist the CH’s institutional agenda. Contrary to the complainant’s recollection, the CH’s response did not strongly validate the complainant’s frustration, the only explicit recognition of the long wait time occurring at the very end of the call: ‘that’s far far ahead to see’ (see Chapter 7, Extract 38). Therefore, the complainant’s perception of the initial call appeared to amplify the level of empathy demonstrated by the CH, compared to the more institutional and objective approach taken during the actual call.
A similar pattern is noted in other cases. For example, RC21 in the telephone diary recalls the CH saying that the lack of medical supplies in the hospital was ‘unacceptable’ though the CH did not actually evaluate this. RC17 generalises the sympathetic behaviour of CHs, despite her CH also refraining from making explicit judgements:
[T]hey just say things are unacceptable and, you know, I suppose that’s what you want to hear.
RC17[I]
In addition, conversations with CHs, while being important for the overall experience of complaining, often escape complainants’ deliberate reflection. They were rarely commented on in the diaries, while other encounters, such as calls from the service, holding or response letters, warranted commentary. Participants mentioned initial calls in the interviews only after prompts from the researcher, and some had trouble recalling them (as an extreme case, RC21 did not remember that the initial complaint was lodged with a different CH from subsequent contacts). The inconspicuousness of first encounters arises from the CH’s perceived role as mere intermediary, although our study shows that CHs are fully fledged mediators119 who can modify the content/course of the complaint rather than simply passing it on.
The spoken register thus adds personalisation to the complaints process and makes the complainants feel ‘part of the investigation’ (RC02) and listened to. In contrast, lack of personal communication can lead to a feeling of alienation:
[A]t no stage was I made to feel part of the complaints procedure, other than a letter.
RC02[I]
Chapter 7 presents CA findings on the spoken encounters which reveal the mechanisms behind such positive perceptions.
Comparison with Patient Advocacy Service
In our sample we have three cases where the complainants had recourse to the PAS (RC15 used their help from the outset; RC01 and RC21 during their complaints journeys).
The experiences of RC01 and RC15, despite representing individual cases, demonstrate shared themes of dissatisfaction with the complaints-handling process, contrasted with significant appreciation for the assistance provided by the PAS:
It feels like you have better support somewhere because with the hospital, we’ve had none. So it feels like he is supporting us as a family.
RC15[I]
RC01 considered the assistance from the PAS ‘brilliant’ and ‘invaluable’. RC15 repeatedly praised their PAS advisor for being ‘amazing’, ‘brilliant’ and someone they ‘couldn’t have done without’.
The experiences of RC01 and RC15 highlight the fundamental role that individualised support plays in facilitating complaints journeys. In contrast, RC21 only mentions PAS support in reference to complaining in writing in a follow-up call.
Similar to front-line CHs, PAS representatives can influence perceptions of complainants. Their role seems to be a double-edged sword. On one hand, the PAS representative serves as an ally, validating the complainant’s frustrations and experiences. On the other hand, their input can potentially reinforce negative perceptions, contributing to further distrust and cynicism towards the Trust. For example, the PAS representative’s comment, ‘they don’t want to hold their hands up and admit things’, underpins and validates RC01’s lack of confidence in the Trust investigation. Similarly, the expression of cynicism concerning the delays in the complaints process (‘are these delays convenient?’) feeds into the complainant’s suspicion that these delays are strategic and deliberate.
Thus, the roles of both CHs and PAS representatives significantly influence the complaints journey, albeit in different ways.
The importance of personal communications prompts an inquiry into whether such interactions alone suffice for complainant satisfaction. The following section delves into why this is not the case.
Balancing formality and humanity in the complaints process
The observations and cultural predispositions revealed through cultural audit and qualitative data mirror findings from a recent study on systems for responding to concerns and complaints in healthcare,117 informed by Habermas’s systems theory. 120 According to Habermas, there are two interconnected levels of society, the lifeworld and the system. The former represents culturally transmitted and linguistically organised shared values, understandings and norms that people use in everyday interactions. The latter, on the other hand, consists of the formal institutions that operate based on a logic of efficiency, money and power. They are autonomous and abstract systems of action that follow their own instrumental logic, separate from the lifeworld.
When a person makes a complaint, their concerns are made sense of in the lifeworld, whereas the drivers for their complaint and desired outcomes are usually systemic issues. Martin et al. 117 use this distinction to explain why their participants expressed frustration with systems and processes (part of the system) which are ill-equipped to deal with lifeworld concerns of people’s everyday lives.
Our study reveals that some people feel that they had already started to express their dissatisfaction with what was going on before they reached the complaints team. This finding highlights an important distinction between complaint and care. In their narratives complainants vacillate between healthcare events leading to the complaint and the complaint process itself. If this distinction is blurred, it may mean that the complaints process is ‘invisible’ for the complainant, and all actions and communications from the healthcare service are treated as inseparable from the complaints journey.
Many participants said that they saw the beginning of their complaint at a moment in time prior to lodging it. Their discontent with the provided services, which eventually compelled them to complain, primarily stemmed from either being shuffled between various departments (RC17, RC20, RC24) or the highlighted chaotic conditions in hospital (RC17, RC29, RC30). These two themes cover almost the whole sample in the Trust B (except RC19 and RC25); therefore we cannot say that they correlate with the blurred boundary between complaint and care. What can be said though is that these factors hindered the ability of the complainants to rectify the issues within the service.
RC20 recasts the distinction between complaint and care as formal and informal complaint:
[I]t was more like an informal sort of complaint to the service and then when I took it to the complaints office that was me sort of, like almost formalising the complaint, outside of the service, because I wasn’t getting anywhere directly with the service then.
RC20[I]
RC21 says almost the same things but feels that the complaint started when it was formalised through the complaints team. The differences between these two accounts stress that, while the formal complaint might become invisible for the complainant, the ‘informal complaint’ tends to be left unattended by the service. Formalisation is a way to make the complaint ‘heard’ by the institution and a tool to have changes implemented. In terms of Habermas’s systems theory, the lifeworld and the system should coexist as systemic change is only possible on the level of formal structures and instrumental action. 120 In the words of RC26, ‘what the public need is for the system to be fixed’.
This complex interrelation between the lifeworld and the system is reflected in our participants’ attitudes to written communication, which they largely find impersonal (as RC02 notes in her interview: ‘I don’t think their complaints system is people orientated, no’). However, they sometimes recognise that the written register is more advantageous when attempting to implement and monitor changes in formal protocols of conduct of service providers.
But you see, that as a case as a learning experience, that means nothing. Really. Unless that’s put in, into part of the protocol or you know it’s put in writing. Him saying that to me doesn’t mean anything.
RC02[I]
I would like all of the assurances provided in the letter to be acted upon and monitored closely until established practice.
RC11[D]
A written register makes words durable and thus accountable for, which is also reflected in re-evaluation of how the complaint is lodged and handled.
I believe my information being relayed to the complaints department was being mis-intro-trued [sic, probably ‘misconstrued’] and maybe noted down slightly differently than what I was saying and just, yes the communication there would have been better if I had of sat down and put it all in writing.
RC21[I]
Yes, well I’ve learned now that people deny things when you talk to them on the phone so that’s why I’ve started learning to send emails because then they can’t deny it, it’s in writing.
RC32[I]
The written register, while being formal and somewhat impersonal, serves a crucial role in the complaints process. It provides a concrete, unalterable record of the complaint, ensuring accuracy and accountability which may not always be guaranteed in oral communication. However, the challenge lies in balancing this formality with the need for a person-centred approach to address and resolve the grievances effectively.
If complaining does not help the complainant to achieve results, next-level options may be considered, such as the Ombudsman, litigation or publicity. The legal path is just a more formalised option to enforce accountability, compel corrective action and ultimately seek resolution to the issues raised in the initial complaint. This escalation is evident in RC23 case study where she initially expresses dissatisfaction with the ‘informal complaint’ to the service (‘I’m fed up trying to complain to them’). This sentiment eventually broadens to the entire complaints process: in the interview the complainant reveals her intent to involve the media and hire a solicitor, feeling she can no longer manage the situation by herself.
Additional case studies also reinforce the perception that legal action is regarded as the most potent strategy for exerting influence over the system, a measure which should be invoked ‘in the right circumstances’ (RC17):
… if something has happened that is sort of negligent, you do need to go down that road [of litigation], otherwise, you know, nothing would ever change.
RC17[I]
… probably that the only way of really changing something when there is obviously gonna be costs involved, dealing with something legally. They tend to sit up and listen when something goes legal.
RC01[I]
In sum, spoken interaction is associated with an informal and thus more ‘human’ register, whereas written discourse is considered formal and thus more impersonal. Ultimately, understanding and improving the complaints journey means effectively bridging the divide between people’s lifeworld concerns and procedural formalities of the system.
In the next section, we examine how the central points of a complaint can evolve and change throughout the course of the complaints process.
Shift over time in complaint focus
When the complaint is lodged, it takes on a life of its own. The complaints journey may comprise multiple instances of communication, both with the complaint-handling staff and with service providers. Each instance forms impressions about the complaints process and expectations of what happens next. A following encounter in a sequence may (in)validate the impressions and expectations created by the previous one. During its lifespan the focus of complaint could shift, due to both the experience of the complaints process and the evolving nature of the underlying issues, alongside the complainant’s changing perceptions and expectations.
Devastating effects of unsuccessful encounters are most evident in the patterns of complainant satisfaction self-reported in their diaries.
The ‘peaks’ indicate that a successful encounter was followed by a communicative failure. If communication fails at the end of the journey, the overall experience will be negative, no matter how many instances of successful communication preceded it. In the patterns observed in Figure 6, two out of three sharp peaks are related to the contrast between impressions and expectations created before and after final response letters were received (Table 6).
FIGURE 6.
Complainant satisfaction throughout complaints journeys, based on diary entries (excluding participants who made fewer than two entries).
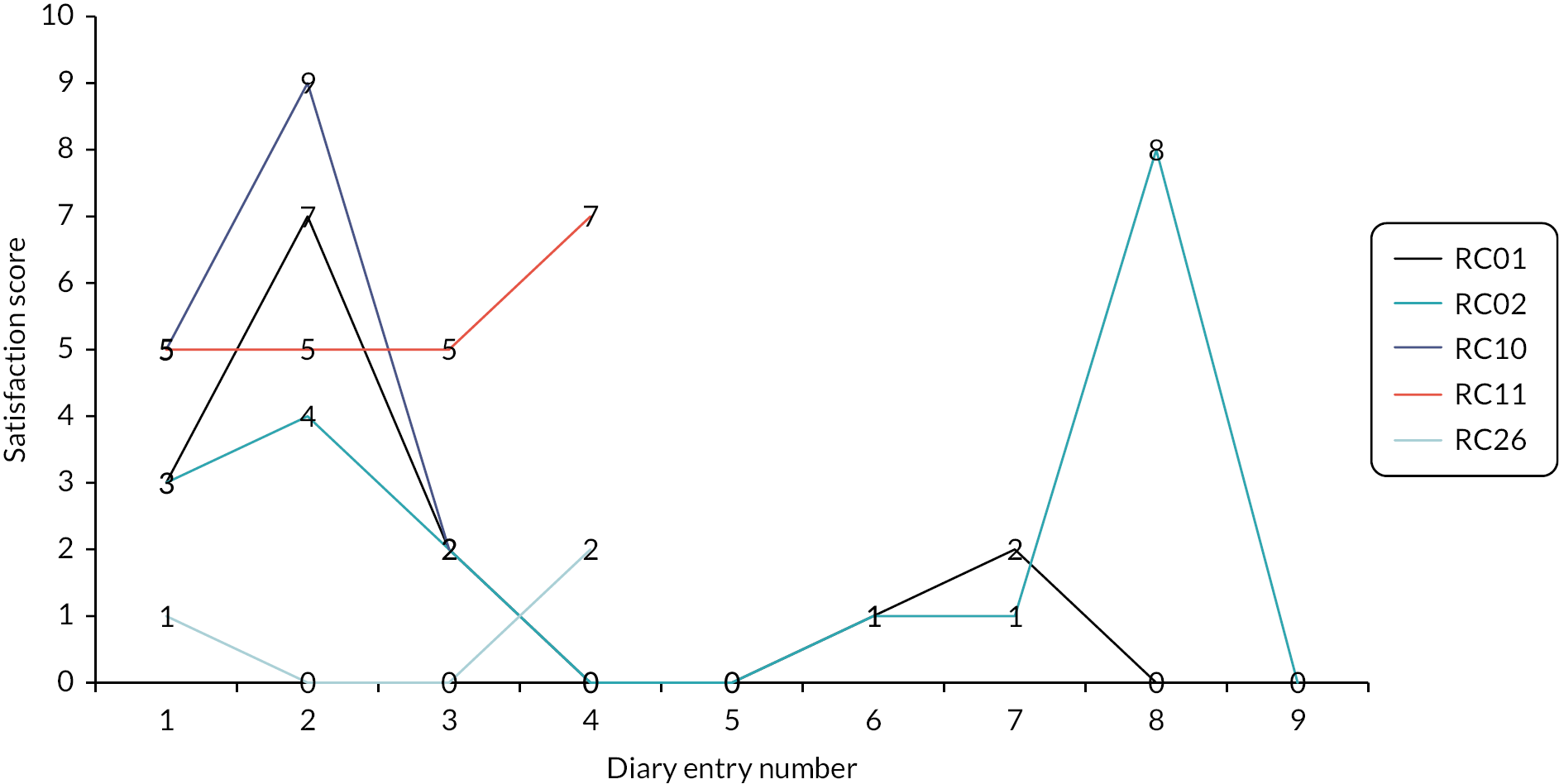
| Complainant | Peak | Trough |
|---|---|---|
| RC02 | I am happy that a full review and meeting (in person) has been offered. | They have disregarded the previous correspondence of a meeting and again addressed the complaint not taking into consideration my grievances and missing the objection of the complaint all together. […] I am very disappointed and deflated. |
| RC10 | Tone and content of phone conversation was positive and I felt listened to and validated afterward. | Despite speaking to the manager of cardiology department for 20+ minutes a couple of weeks ago about the crux of the complaint this was not addressed in the letter. […] I was very clear during my last conversation with the department manager and she obviously did not listen. |
Our analysis of participant reactions to the written Trust responses charts how well expectations of complaining map onto their experiences. In a number of case studies, we have encountered instances of contrasting anticipations and actual experiences.
By the end of her complaints journey RC02 was already disappointed with the results of her complaint and wrote a follow-up letter clarifying the main points of complaint, including the expectation of a face-to-face meeting. The offer of a meeting was a positive moment of change for her which was subsequently completely invalidated by the Trust’s reluctance to fulfil their offer (the evaluation of satisfaction rose from 1 to 8 then fell to 0). RC10’s experience is a similar reflection that the complaint journey is often derailed at the point at which the complainant receives their final written response to the complaint. Her second diary entry reveals a marked improvement in her perception of the complaint handling, following a telephone call with the service (scored 9), but this impression was reinterpreted in a negative way after she received a written response from the Trust (scored 2). In the interview RC10 points out that the expectation created in the telephone call with the service manager made the actual receipt of the unsatisfactory written response harder to take. She says ‘I would have been happy to end it at that phone call’, suggesting that the written response has harmed the complaint process. In both cases the dissatisfaction was caused by the fact that preceding communication instances were disregarded, that is, the complaints journeys lacked connectivity.
The dynamics of complainant satisfaction may be also influenced by the evolving nature of the complaint itself. The complaint may encompass a range of concerns, and what is pressing may change over time. The initial lodging of complaints may be affected by emotions which fade away as time passes. For example, RC10 is repeatedly at pains to explain that her initial complaint was made in annoyance and therefore did not make clear what the ‘crux’ of the complaint was. In effect, the complaint appears to evolve over time. The initial e-mail complains about several things: the missed appointment and time lost as well as the consultant’s erroneous claim that she had not picked up the phone when they called. Subsequent communication from the complainant clarifies that it was the fact of being ‘blamed’ for not answering a phone call that never came that made her angry and was the ‘real reason’ for the complaint.
Similarly, RC17 focuses mainly on the rudeness of a single staff member in the initial call. The service manager who resolved the complaint via phone noted that the complainant ‘was just annoyed at the way she was spoken to and would hate to think this person would talk to other patients in the same way’ (emphasis added). In her diaries though the scope of the complaint extends beyond the rudeness. RC17 highlights poor communication, lack of information and an overall lack of interest from the staff in treating minor injuries.
In complex ongoing cases, the focus of complaint tends to shift as circumstances may change and new issues may arise. This is particularly true in long-drawn-out situations like the one faced by RC01. Her case differs from the cases reviewed above as it is the cumulative negative experiences with the complaints process which led to a sharp drop in satisfaction (7 to 2).
RC01’s complaints journey spans a 2-year period and is not fully diarised. Her initial intent to lodge a complaint was primarily to improve her mother’s care and to facilitate her transfer closer to home. However, after a lengthy wait she gained access to additional medical records, following a subject access request. The information she found there fundamentally altered the trajectory of her journey. There were contradictions within the notes, primarily revealing that the hospital had knowledge of her mother’s spinal fracture much earlier than they had communicated.
I did not expect such a complex complaint when I put it in […] did not think two years down the line we’d be talking broken back.
RC01[I]
The peak we have in our data (see Figure 6) reflects the complainant’s call with the representative of the PAS she sought help from after her first unsatisfactory experience of complaining. She reports the PAS adviser as ‘helpful and supportive’ and making ‘the task feel easier’. In the next diary entry, written after receipt of her mother’s medical records, RC01 expresses weariness with the complaints process, indicating reluctance to file another formal complaint to address additional issues due to the anticipated burden of work and a concern that the issues raised may be again ‘brushed off with excuses’. She had expected more help from the complaints-handling team and ends up seeking help from her local MP to expedite the complaint process. Reflecting on her complaints journey more generally RC01 indicates a range of examples of conflicting experiences and expectations:
I didn’t expect to have to keep looking to other external departments for help. Like I rang so many legal departments to do with health … because I couldn’t get basic help from the Trust.
RC01[I]
In this case it was the poor quality of prior experiences combined with the arduousness of the process which led to frustration.
RC03 similarly indicates conflicting expectations and experiences:
Honestly, I think I expected them to hold their hands up and say ‘look we’re sorry and this is what we will change in the future’. And I probably expected too much in that sense erm because as I’ve said it was quite the opposite. They didn’t see any wrongdoing.
RC03[I]
Here the complainant identifies a disparity between the anticipated receipt of an apology and a promise of change in response to their complaint, versus the actual defensive stance and denial of accountability expressed in the response to the complaint.
RC21’s case study exemplifies how the focal point of a complaint can evolve over the course of an ongoing case. The initial grievance was about the complainant’s child being discharged despite being in significant pain. However, subsequent follow-up calls introduced new issues concerning his child’s ongoing care, such as a lack of necessary hospital equipment, exposure to infections and a lack of beds which led to the hospital’s repeated attempt to prematurely discharge the child. Additional issues were not addressed in the response letter, which probably exacerbated dissatisfaction with the complaints journey.
The pattern described, albeit relating to only a small number of observations, showcases that both poor quality of separate interactional encounters and their insufficient connectivity may affect the experience of the complaints journey. Although it is easiest to see from the scores in the diaries, changing levels of satisfaction can also be traced discursively. For example, RC09 reports being happy with the complaints procedure, yet expresses significant dissatisfaction with the final response letter, feeling that it dismisses his concerns and unjustly attributes all blame to him for allegedly violating hospital policy. In a follow-up letter to the research team, he reflects that ‘The Patient Complaints Procedure was actually very good for me – good communication, very quick – it was just the Response that I found unfortunate’.
Since the complaints journey unfolds in time, each next instance of communication has more bearing on the entire experience and may even ‘overwrite’ the effects of a previous encounter (as in RC10: ‘I felt listened to’ → ‘she obviously did not listen’). This insight is explicitly formulated by RC29 commenting on the resolution call from the service: ‘So that was really difficult to deal with and felt, I don’t think patronising is the word, but it just felt like it devalued the positive encounters that we had up to then’ (emphasis added). In the case of RC15, the family explain in their interview that face-to-face encounters with healthcare staff were invariably positive but stalled when the stage of written communication was reached: ‘They are different to your face than they are in how they’re overall dealing with it’.
In sum, the complaints journey is a multifaceted process marked by successive instances of interaction, each having a cumulative effect on the overall satisfaction of the complainant, with one impression potentially overhauled by a succeeding instance. The quality of these interactions, their sequential coherence, and the passage of time significantly impact the perception of the process and may shift the complaint focus.
Written responses, often marking the final stage of the complaints process, have the most significance for the evaluation of the journey as they either meet or not the expectations and match the impressions formed at earlier stages. Due to their paramount importance, we analyse potential challenges involved in providing written responses in Chapter 6.
Afterlife of the complaint
When the complaints process concludes, there can be a pronounced disparity between initial expectations and the outcome. If the resolution does not align with the complainant’s anticipated outcome, it may result in dissatisfaction and a sense of injustice. Such a mismatch can trigger the escalation of the complaint, pushing the complainant to seek further redress. In this section, we analyse when complainants feel that their complaints are resolved and explore the drivers behind complaints escalation.
Navigating the grey area: when is a complaint really resolved?
A complainant’s (dis)satisfaction with the process is not just confined to the formal resolution of the complaint. It extends to the actualisation of pragmatic solutions to their concerns and how their individual care experience improves as a result. This problem-solving aspect can greatly influence the complainant’s overall evaluation of the complaints journey. Thus, dissatisfaction may arise from a perceived lack of concrete action taken to address the issues identified in the complaint.
This is clearly the case of RC01. Her complaints journey, driven by the desire to improve her mother’s care, was marked by a pervasive sense of frustration. She struggled to navigate the system alone, grappling with a lack of proactive support and unfulfilled expectations, including an unresolved data-protection issue and an ignored request for a meeting. RC01 had anticipated more support throughout the complaint journey, but the reality was a challenging process, described by her as ‘really hard to negotiate’. Despite a formal response to her complaint, she did not consider the matter resolved and proceeded to send a second formal complaint letter to the Trust about the inadequacy of the first response:
So I thought that was very sly and inappropriate that they sent a letter saying we are now reopening your complaint … so I know what they did was try to make this look like it was resolved. It wasn’t. It strongly wasn’t resolved. They were, they should be very clear on that.
RC01[I]
RC01’s journey underscores the importance of recognising the difference between a formal resolution and the resolution experienced by complainants. In her case, dissatisfaction arose from a lack of anticipated support and the Trust’s failure to fulfil a problem-solving function. The opposite scenario is more prevalent in our data, where the complaint leads to a problem being resolved, yet the broader issues associated with the complaint, such as the pursuit of justice and systemic change, remain unaddressed. A complaint might feel resolved at the level of personal care but may continue to remain unaddressed in the context of complainables relating to systemic issues and formal procedures. This is fairly common in Trust B, where complaints are often resolved via a telephone resolution call.
As previously touched upon, a fundamental incentive for RC17 was to rectify her personal concerns regarding the care she was receiving. Nevertheless, her motive to get justice and effect change for others went nowhere when the practical problem was solved. Throughout different data sources, the complainant conveys a persistent worry about whether the staff member complained-about was reprimanded or dealt with. In essence, RC17 seems to be less satisfied with the resolution than suggested in the telephone resolution form (TRF):
I believe the last person I spoke to asked did I consider the matter resolved, which I didn’t, but I got the impression they regarded it as resolved! I’d be interested to hear how the member of staff involved was approached about the issue, if it was recorded in her personnel file and what changes would be made, going forward.
RC17[E]
In analysing the cases of RC22 and RC30, we also see a common theme of mismatched understandings between the complainant and the institution regarding complaints resolution.
For RC22, the core complaint originated from a disjointed discharge process for his father with a cast, which left the complainant in an exhausting chase between the ED, fracture clinic and the General Practitioner (GP). Despite the Trust’s view of the complaint as resolved, the complainant did not regard the call from the service as conclusive. The TRF centred merely on the appointment with the fracture clinic, framed the issue narrowly as a ‘poor experience’ in ED and a ‘delay’ in referral, which did not fully encompass the complainant’s frustrations with ‘going round in circles banging my head off the proverbial brick walls’ (initial call) and his father’s follow-up care including physiotherapy. A notable contradiction emerges between the Trust’s perception of a closed complaint and the complainant’s ‘surprise that there’s not been some contact’ (interview) from the CH.
RC30 similarly aimed to address her father’s current health status as well as provide feedback on the accident and emergency (A&E) department. While her complaint immediately led to significant improvement in her father’s care, the absence of a formal response or apology from the Trust left her with the impression that they believed the issue to be resolved once better care was initiated:
What I get a feeling is they’re palming me off, ‘Your father was taken care of so therefore it’s fine’.
RC30[I]
However, she maintains that a formal response is desirable.
The lack of a formal response can not only leave complainants with the impression that their complaint has been neglected (with only their immediate care being addressed), but also create ambiguity about whether their complaint has been officially closed and if they should expect further communication. While RC20 expressed satisfaction with the telephone resolution provided by the service, there was ambiguity as to whether the complaint was officially closed with the complaints team. This points towards a slight disconnection, suggesting the complaints loop was not fully closed.
The complaint and care distinction further illuminates the complex dynamics in our data, where a complaint might lead to a resolved care issue, while broader systemic and justice aspects remain unaddressed. The absence of formal apology or acknowledgement, along with the lack of clarity about the official closure of the complaint, indicates the presence of loose ends. Hence, healthcare institutions should strive to ensure not only the formal resolution of complaints but also the resolution experienced by complainants, addressing their concerns at both the care and systemic levels.
Escalation of the complaint
When the complaint is closed but the complainant is dissatisfied with its resolution, they may consider pursuing it further and escalate via an external third party. The different avenues for this escalation can include the Ombudsman, independent PAS, media, politicians or legal recourse. The choice of a particular path depends on different factors, which necessitates a separate investigation. However, our study identified potential risk factors associated with escalation, which may shed light on why certain external entities are chosen for pursuing unresolved complaints.
The initial factor pertains to the problem-solving aspect of complaining. The complaints process is often seen as a last resort for individuals seeking to resolve issues and improve their or their loved one’s care. However, if it does not yield results, complainants may escalate their concerns to other institutions. The legal path is seen in this regard as a way to enforce accountability and prompt corrective actions, seeking a resolution to the issues originally addressed in the complaint.
A significant role in the escalation is played by the failure to investigate the complaint quickly and effectively. The subject of long delays in the complaints process emerges in some of our case studies:
I was like, three years down the line we still have no answers.
RC15[I]
This particularly characterises RC01’s complaint and her feelings about the process. RC01’s very lengthy waits to receive both her mother’s medical records and a formal response to her complaint (she received nine holding letters during the investigation) cause immense frustration:
I am beyond fed up with the ridiculous delay in responding to my letter with 7 closed questions which can be answered from the medical notes.
RC01[D]
The frustration is arguably compounded by repeated written apologies for the delay which never seem to alter the response rate.
Similarly, RC21 reaches a point of frustration about what he sees as the lack of progress with his complaint:
I got to the stage of so frustration that I had to contact my MP and say, ‘Look, I need you now involved, because I’m not getting anywhere with this’. […] I lodged a complaint [last year] and I’ve only just received on Saturday the response.
RC21[I]
The extensive delays to receiving a formal response have consequences with both complainants considering escalation.
[the complaints service failed] to meet their own timeframe or to communicate with me as to why. I will wait for a bit longer for the trust to make contact. If there is none, ironically, I may decide to complain about the complaints procedure.
RC12[D]
RC01 in particular is minded to ‘email them with a not very polite email stating their incompetence’ and expresses the view that the experience has made her ‘more determined’ and that she has become ‘hell-bent on making them pay’ [RC01(I)]. She elsewhere states her intention to go to the Ombudsman ‘in time’ [RC01(D)] and to ‘go legal’ [RC01(I)].
In her interview, RC01 also expresses the perception that the Trust’s efforts were focused on ‘batting away complaint’ and ‘sweeping under carpet’ rather than diligently attending to the detail and focus of the complaint. She construes these delays as an avoidance strategy:
… feel they don’t care and are hoping I will just give up.
RC01[I]
This is a view shared by RC21 and RC12:
but the two letters were just biding time.
RC21[I]
I would like assurance that they are investigating and not just waiting for me to forget about it.
RC12[D]
RC01 and RC23 (who are also considering escalation) both comment on the contradiction between assurances offered in holding/response letters that the complaint is being treated seriously and lack of any response (hence a perception of insincere communication):
I don’t believe they are looking at the complaint, just kicking the can down the road.
RC01[D]
The attitude to their [previous complaint response] apology was disgusting. If the doctor didn’t do anything wrong, then why did he have to take six months to reflect on what happened?
RC23[I]
Another consequence of the delays and subsequent frustration is the profound cynicism that develops, with many references to ‘no faith’ or ‘zero confidence’ in the complaint process. 121 More work is arguably necessary to reassure complainants when there are repeated delays, but complainants are cynical about expressions of sincerity and commitment as they are perceived to simply ward off any potential inference that the delay may be due to a lack of concern.
Another driver of escalation is the lack of acknowledgement of lifeworld impact. It implies that the complaints process should encompass the wider context of the complainants’ lives instead of concentrating solely on specific points of complaint. This need is most pronounced in serious complaints. In the case of RC02, the failure of the Trust to adequately acknowledge the lifeworld impact in her sister’s care was a prominent factor leading to dissatisfaction. Her sister’s undetected fractured hip, which probably resulted in an inability to walk and rapid deterioration of health, were the focus of the complaint. Despite two formal responses from the Trust, RC02 expressed disappointment with the replies – because they did not acknowledge the sister’s brain damage and dementia (first letter) and her human dignity (second letter). Despite RC02’s dissatisfaction, in the interview she expresses the decision to not proceed with the Ombudsman. However, she plans to pursue a copy of the protocol for treating patients in her sister’s condition, in hope of reopening the complaint, indicating that the acknowledgement of the full context of her sister’s condition and its impact on her quality of life was a crucial missing element in the resolution process:
Nobody has acknowledged the life that they’ve taken away from her, the life they’ve given her now.
RC02[I]
The case of RC02 exemplifies an internal escalation when the complainant seeks to resolve their grievances within the complaints process. In contrast, RC15’s case is emblematic of a situation where the complaints process fails to adequately address the issue at hand, prompting the family to consider more drastic measures such as litigation. The complaint pertains to the hospital’s treatment of the complainant’s mother. The family alleges that the failure to initially consider her alcoholism, which led to a rapid increase in her sodium levels, caused her brain damage. Frustration over the Trust’s lack of acknowledgement of their distress and the current state of the complainant’s mother has deepened the family’s dissatisfaction with the complaints process and led them to consider legal recourse. The interview indicates the family’s feeling of being disregarded and a sentiment that drives the escalation to litigation:
They’re just not acknowledging what we’ve went through and how my mammy is.
RC15[I]
The next risk factor of escalation is the lack of comprehension of the essence of the complaint or acknowledgement of complainant’s reasoning. When the complaint is lodged via telephone, the CH takes on a role of the interpreter who can reformulate the complaint but also has a chance to clarify any ambiguities during the conversation. In contrast, when the complainant puts their issues, concerns or grievances in writing, they have more control over the narrative they present. This written record leaves less room for immediate misinterpretation as it is directly from the complainant’s perspective. However, without the interactive dialogue characteristic of a phone call, there is less opportunity for immediate clarification of misunderstood elements.
In our data, problems with comprehension were more common in written complaints, the reaction to which is exemplified in the following quotes:
not taking into consideration my grievances and missing the objection of the complaint all together.
RC02[D]
Letter outlined reason for the decision made, with no real resolution or new information. It did not address the root cause of my complaint.
RC12[D]
RC02 and RC12 pursued different forms of escalation: RC02 decided to stay within the complaints process, while RC12 arranged the meeting with the Head of Service (suggested in the response letter) and extended it to other service users.
Incomprehension may also be construed as an avoidance strategy to not engage properly with the substance of the complaint. This relates to a perceived contrast between a thorough and substantial investigation and a superficial ‘tick-box’ exercise:
Their response and the procedure to investigate the complaint was a cosmetic activity. The complaint was only superficially read which resulted in my concerns and worries to be disregarded.
RC20[D]
The comprehension of the complaint is closely linked with acknowledging complainants’ reasoning. Misunderstandings may challenge the latter, creating contradictions between complainant and Trust accounts. This conflict is never well received. It can explain the extremely negative reactions of RC03, RC09 and RC10 to the final response letters.
RC03 describes how the response to her complaint was used to dispute the grounds of the complaint and to argue that the complainant had misremembered or was distorting the situation in the hospital. The lack of acknowledgement of the traumatic experience endured by RC03 as well as a lack of accountability ultimately motivates her to seek complaint resolution through the Ombudsman. In RC09’s case, the complainant felt that his complaint about being treated rudely and unfairly by a hospital staff member was overlooked, with the Trust’s response letter placing all the fault with him for acting against hospital policy. Similarly, RC10’s complaint was primarily about the false claim that she had failed to answer the call leading to a missed appointment. The Trust, however, focused its resolution letter on the delay of her appointment, failing to address her chief issue. In all three instances, the complainants perceived that their reasoning was undermined, which created a significant disconnection between their experiences and the Trust’s responses.
Shaken reasoning can contribute to a pessimistic perspective towards the complaints process. In her interview, RC03 for instance says ‘I felt angry with outcome but also expected it’, concluding that the complaint has been a ‘waste of time’. RC02 in a diary entry expresses her ‘disappointment and anger’ that her ‘fears’ around making the complaint have come true. RC10 also reveals a retrospective expectation that the outcome would be disappointing:
[It was] frustrating and it was long and it was ultimately unsatisfactory so it was exactly what I – what I imagined it to be.
RC10[I]
Negative outcomes are often presented as a predisposition to be cynical in advance of the process but it is clear that the experience of the complaint journey itself generates this cynicism since there is an underlying hope for change and improvement:
See I was hoping, even that I would maybe meet somebody with vision and would look at my, look at my complaint and think, ‘God, you know, if we don’t have these, if we don’t have these protocols set in place, right, they have highlighted something to us. We will look at that’.
RC02[I]
As time’s gone on I have become more cynical […] I kind of think it wasn’t a waste of effort because I did feel strongly about it at the time.
RC11[I]
This tendency to present negative outcomes as predispositions sheds new light on the results of the cultural audit, which revealed cultural predispositions as a background for complaining (see Chapter 4). Understanding the complaints process as a journey adds a temporal dimension to it, showing that people navigate cultural landscapes in their evaluations of relational practices and may transition, for example, from egalitarianism to fatalism in their views on service relationships. This conceptualisation therefore allows us to show exactly how culture is constituted through interactions.
The retroactive trajectory of expectations works for supporting reasonable complainant identity: negative outcomes redefine positive expectations as naïve, and people renounce them to construct themselves as knowledgeable:
Realistically I knew what I wanted I wasn’t gonna get because I know how it works. (emphasis added)
RC10[I]
For some complainants, cynicism regarding the complaints process could lead to apathy:
Realistically I knew I was never gonna get that I don’t even know why I bothered it certainly wouldn’t lead me to complain again.
RC10[I]
I have become a little bit apathetic I suppose and cynical erm about further correspondence on the matter at all […] I have never made a complaint before about any medical treatment I’ve received and this experience – following this I shall never make another one.
RC11[I]
Others, despite disappointment and disillusionment, remain resilient and believe in the necessity of their actions. Thus, cynicism could not only fuel the willingness to escalate, but also contribute to the selection of escalation routes. In RC23 we see the complainant excluding the option to go to the Ombudsman just because the letter from the complaints department advises it:
Well, [the response letter] said about speaking to the Ombudsman but I’m going to the papers and I’m getting a solicitor because I can’t do it anymore.
RC23[I]
Like the proverbial King Midas, for RC23 the complaints process spoils everything that it touches.
Reasonable complainant identity can also influence the choice of escalation route. Because of the awareness of the extreme resource challenges faced by the NHS, it is common for complainants to state explicitly that complaining is not motivated by desire to gain financially. This often deters complainants from escalating to litigation:
No, no, my goodness, they’re under enough pressure, the health service.
RC16[I]
I don’t want money from them. I just want the help and support that I’m supposed to get.
RC23[I]
Money would never pay me for what they’ve taken away from me. And it was never about money.
RC02[I]
While negative experiences may dampen complainants’ optimism, they are also instrumental in shaping their decisions on the escalation route. A strong sense of reasonableness and awareness of the constraints faced by the healthcare system may steer complainants away from financially motivated escalation, such as litigation. Nevertheless, we cannot say if this conviction transfers beyond narratives into action.
In conclusion, our exploration into the reasons for escalated complaints underscores the fundamental importance of person-centredness in the complaints process. While external escalation pathways exist and can be pursued, the goal is to address complaints at their origin effectively and efficiently. Delays and the perceived avoidance of accountability can prompt complainants to escalate their concerns further. A greater focus on the lived experiences of complainants can also significantly improve the perceived legitimacy and efficacy of this process. Equally important is the need for a clear comprehension of the essence of the complaint and the complainant’s reasoning (which does not mean agreeing with the complainant’s perspective). Misinterpretations or a lack of comprehension can shake the complainant’s trust in the system, leading to a negative outlook and potential escalation of the complaint.
Complaints staff views on the complaint journey
Although our study focused on the complainants’ experiences, they represent only one side of the complaint process. To gain insights into the other side, semistructured interviews were conducted with complaint-handling staff at different levels: three front-line CHs, two complaints managers (one from each Trust) and a representative from the PAS. Conversations covered various aspects of the complaint journey: context, process, person-centredness, responses, learning.
In terms of Context a number of challenges were identified, in a recent increase in complaint volumes; key operational challenges resulting from day-to-day pressures (‘we would never bury our own services, because our services are working hard’); and the complexity of complaints as a key factor in handling complaints (‘the more people involved, the more complicated it becomes’). Culture was also identified as a key factor, with regard to the (lack of) fit of complaints with cultural norms, and a ‘need for cultural change in this organisation’. Examples included where ‘hierarchy causes delay’, and an ‘unspoken but widely accepted cultural norm to “protect our staff”’. Fatalistic attitudes amongst complainants were also evident: ‘you’ll have this “what’s the point” attitude’. These observations fit well with the findings of the cultural audit (see Chapter 4).
In terms of Process, complaints staff had a clear belief in its design, feeling supported by what one CH called ‘that luxury of a process’. However, this consistency was lacking in service areas, where follow-ups varied and updates were hard to enforce. Staff were often frustrated by the ‘sheer length of time it takes’ and ‘lack of effective communication’, which led to a sense from the PAS of ‘a lot of wasted time in the complaints process’. Complaints staff also had mixed feelings about imposed 20-day response times, viewing them as challenging and potentially hindering a meaningful process. Despite these frustrations, there was a shared understanding of the process’s purpose: to provide accountability (‘we try to be held to accountability as best we can’), and balance (e.g. as ‘a means of escalating for complainants, to get it sent to a service area’, or ‘de-escalating the complaint to avoid legal cases’), by gaining greater understanding of each case and providing ‘a bit of clarity’ as a ‘trusted middleman’.
In terms of person-centredness, respondents spoke about complainants’ expectations. One noted that complainants sometimes expected them to be ‘on their side’, but acknowledged that this was ‘not a fair representation – we have to be very impartial. But this is such a difficult balance to strike’. Others put it succinctly: ‘they want empathy and they want to be respected’; ‘they want reassurance that they have done the right thing’. These notions fit well with this study’s key findings regarding affiliation and reasonableness. The latter was widely recognised by staff: ‘most people are reasonable and will accept an explanation if you give it to them’. Respondents also spoke about their experience of interactions with complainants. Good interactions were considered to include ‘taking time to listen’, ‘keeping them informed’ and ‘providing reassurance’.
Empathy was also commonly raised as an important factor, ‘acknowledging they have been through a difficult time’, providing ‘openness and transparency’, and seeing them ‘as a person, not a number’ by understanding the wider context of their lives – although as one CH noted, ‘what becomes a difficulty is the wording you use’. In short, as one manager put it, good interactions mean: ‘Have they been heard? Have they been answered? Have we listened? Have we responded? Have we done that empathically?’ The PAS felt these elements were sometimes missing from interactions across the complaint journey, and that claims ‘to put the patient first’ were ‘insincere’, and yet that ‘sometimes stars align’ between a reasonable family member and a reasonable person from the Trust: ‘if everybody was more reasonable, there would be more resolution and it would be great’.
In terms of responses, respondents discussed how service areas communicate with complainants, highlighting their advisory role in supporting these areas in fulfilling their responsibilities. It was universally recognised that ‘it is the inadequacy of the response that often leads to escalation and litigation’. One complaints manager picked up on ‘something about the language and phraseology’ that was often problematic in written responses. Another identified that ‘face-to-face responses can work so much better’, whereby two-way communication ‘helps to clarify’, is ‘more meaningful’ and makes it ‘easier to get closure’. A significant concern among respondents was the variability in the response from service areas; some were proactive and prompt, while others had poor response times and issues with updates. For serious cases, the PAS noted that such delays without updates were a common cause of escalation, including moves to litigation that could otherwise have been avoided.
Finally, with regard to the value of complaints, respondents noted various processes in place to capture trends and learning, both from individual and aggregate complaints data. However, one complaint manager noted that ‘generally speaking, complaints do not prompt changes. This would be worth exploring further – we may benefit from questioning ourselves more about this’. The same manager also noted the benefits of research and training (‘I do think the work you are doing is important, and it’s part of the solution’) and expressed an interest in ‘encouraging further research in this area, if there was an opportunity to do that and to participate’. This included take-up of the training from this project, where it was recognised that ‘it’s very difficult getting training around communication like that’.
Notions of the ‘system’ are evident in the responses of complaint service staff around the broader cultural context, which often produces inadequate responses and is behaviourally resistant to learning and change that may add significant value. This acknowledgement of the potential inadequacy of responses leading to escalation and litigation reflects the dissatisfaction expressed by some complainants. The process attempts to bridge between system and lifeworld. CHs thus emphasise the importance of person-centredness, empathy and respect – principles that align with the expressed needs of complainants. Ultimately, the alignment of staff and complainant perspectives in many key areas, along with the staff’s expressed uncertainty about ‘good communications’ (and their interest in learning), validate the need for the fine-grained interactional training from this study (see Chapter 8). However, the ability to consistently deliver such communications in practice, through a process that is often insufficiently equipped from end-to-end of a complaint to deal with the real concerns that affect people’s everyday lives, remains a challenge. In particular, as a ‘trusted middleman’, there is an awareness of the tension between this and not ‘burying our own services, because our services are working hard’.
Conclusion
In Chapter 5, we have delved deeply into the complexities of the complaints process and portrayed complaints as dynamic, evolving narratives rather than static accounts. It is clear that a focus on improving individual instances and connectivity across the complaints journey is paramount. Each interaction point within the journey serves to mould the complainant’s perceptions and future expectations, thus having a cumulative effect on their overall satisfaction.
This chapter supports the insights from the cultural audit, where we explored the reverence for the NHS and the expectation of high-quality service. Our findings here highlight how these expectations, when unmet, lead to a significant dissonance and a sense of alienation within a perceived hierarchical and bureaucratic healthcare system.
Furthermore, this chapter has illuminated how these cultural predispositions, identified in Chapter 4, set the stage for the complaints process. By understanding the complaints process as a journey, we add a temporal dimension that allows us to see how individuals navigate through various cultural landscapes, potentially shifting their views on service relationships from egalitarian to fatalistic.
Understanding the complaint as a journey has opened up several avenues for detailed exploration. As we transition to Chapter 6, we will focus on the pivotal role of written responses in the complaints process. These responses, often marking the journey’s conclusion, are critical in meeting or failing to meet the complainants’ expectations and in shaping their overall perception of the process.
Our findings revealed the importance of a person-centred approach within the complaints process. It comprises the following priorities: acknowledging the ‘lifeworld impact’ of the complaint; appreciating the essence of the complaint and the complainant’s reasoning. Looking ahead to Chapter 7, we delve into the conversational bids for affiliation which orient to the same priorities. This analysis will provide a deeper understanding of the moment-by-moment dynamics of communication between complainants and CHs.
Finally, the alignment of perspectives between staff and complainants, coupled with the staff’s desire for improved communication skills, paves the way for the interactional training detailed in Chapter 8. This training is rooted in the fine-grained analysis of initial calls and personal encounters, demonstrating the practical application of our findings in improving the complaints-handling process.
Chapter 6 Written responses to complaints
As mentioned in the previous chapter, written responses to complaints are often the culmination of the complaint journey and can be pivotal in the sense of providing a conclusion to the investigation, while being the opportunity to provide some kind of resolution for the complainant. While our corpus of complaint responses is quite limited (Table 7), it provides plausible evidence, in line with other reports,18,121,122 that the point at which the written response is received is also the point at which complainants express the most dissatisfaction and disappointment with the whole complaint experience (see Chapter 5). While this is sometimes because the complaint is not upheld, it is more often than not because the reporting of the investigation and its conclusions is felt to not meet the complainant’s expectations. Often this disappointment revolves around lack of admission of responsibility by the relevant service, lack of recognition of the reasonableness of the complaint (and complainant), failure to acknowledge the lifeworld impact of the events leading to the complaint and failure to deliver a sincere apology.
| Trust | Number of responses |
|---|---|
| Trust A | 15 (including multiple responses to a single complaint) |
| Trust B | 3 |
As mentioned in Chapter 3, Data on individual complaint journeys, the Trusts from which we gathered written data adopt quite different approaches to responding to complaints. Trust A conducts most of its communication in written form, encouraging complainants to put their complaint in writing, with also a written response. Trust B relies more on spoken interaction; complaints are often resolved via a telephone call which is then summarised briefly in an internal TRF, which records whether the complainant is satisfied with the outcome. Where Trust B does issue written responses, these are informed by guidance and a template letter (see below).
While there were insufficient data to make significant generalisations about the effectiveness of written responses to complaints, or to compare the effectiveness of one Trust’s approach to written responses to the other, we noted in Chapter 5 some tentatively significant patterns suggesting that written responses are not only more poorly received than resolutions through conversations, but are actually points at which a complaint will often escalate, sometimes prompting the complainant to end the relationship with the Trust and move to contacting the Ombudsman (e.g. RC03) or even to litigation (RC01). In this chapter, we explore the language choices and communicative approaches made in complaint response letters in more detail as a means of attempting to understand how these negative impressions of complainants are formed. The analysis of these written responses is triangulated with the qualitative responses of the relevant participants reflecting on their impressions of this written correspondence in diary entries and post-journey interviews. Themes emerging from the analysis of the longitudinal journey are picked up again in this chapter, particularly relating to a clash between expectation for the complaint process and its actual outcome.
This chapter thus addresses the study objectives 1 and 4.
Reforms to complaint handling procedure at Trust B
An Independent Inquiry into a high-profile case involving multiple complaints against a specialist at Trust B noted a number of failings and proposals to reform the complaints system. As a result, reforms were introduced to complaints handling at Trust B, including a ‘clinical record review’ (currently limited to complaints involving doctors) where one or both of the following categories of complaint are assigned – ‘quality of treatment and care’ and ‘staff/attitude and behaviour’. These two broad concerns are reflected in the ‘drivers of complaint’ whose frequency is detailed in Table 6. Further recommendations arising from this report are discussed below.
Complaints procedure within Trusts
We were unable to gain information from Trust A about their formal procedures for drafting a written response to a complaint, despite repeated attempts. This was due to significant staffing challenges, leading to repeated changes to the point of contact and general inaccessibility of staff. However, it is clear from the response letters that a template is adopted. The following sequence can be observed across most of the first response letters:
-
Thanks for raising concerns.
-
Apology for delay in responding (usually due to need to investigate complaint thoroughly).
-
Information about who was consulted during process of investigation.
-
Detailed case history of patient’s care.
-
Relevant versions of events from clinical staff (including those that refute complainant’s narrative).
-
Apologies where relevant (sometimes phrased as e.g. ‘I wish to support Dr X in making this apology’).
-
Invitation to respond to complaints department if complainant feels complaint has not been adequately resolved.
-
Alternatively, invitation to contact Ombudsman if not satisfied with response (and details of how to contact them).
We were provided with an account of the production of written responses from Trust B. Written responses are usually developed as a team response led by the lead manager investigating the complaint but with input from all parties relevant to the complaint, including the Co-Director of the relevant service. This draft is then amended or approved and signed off by the Executive Director of the Trust on behalf of the Chief Executive and issued to the complainant. Trust B also provides a letter template which includes an apology for the complainant’s dissatisfaction with the services provided and an assurance that the matter has been properly investigated. It includes the advice to respond to each of the complainant’s concerns in turn, and in the order they were raised. The letter ends with the hope that the response has addressed all their issues satisfactorily but inviting them, if not, to contact the complaints department again to raise any outstanding issues or to contact the Ombudsman, providing contact details.
In addition to the letter template, Trust B provides guidance and tips (unpublished) for people writing responses to complaints. It invites writers to consider whether it is clear to them exactly what the complaint concerns are and to devise a plan for investigating whether these concerns are valid or not. Writers are also encouraged to take into account any sensitive issues (e.g. named staff in the complaint) and to properly record the steps and process of the investigation and how it was conducted. Investigators writing a response are required to state the outcome of their investigation, to be prepared to stand by this if interviewed by the Northern Ireland Public Services Ombudsman (NIPSO) or as a witness in a court. They are also invited to consider whether they have remained impartial and how this can be evidenced if required. In terms of the content, order and style of the letter itself, the guidance includes a checklist of relevant information to include (e.g. accurate personal and administrative details of complainant and complaint, any apology for any delay beyond the agreed 20-day deadline and information about who has conducted the investigation). The advice then moves to the substantive content of the letter, including a response
to the concerns raised, taking each of the complainant’s issues in turn and providing a clear reply to these. It is useful to actually use the issues provided by the complainant as headings in bold, followed by the Service reply in normal font.
See Chapter 5 on the disadvantages of not recording a complaint in writing.
The guidance then goes on to suggest that ‘the next paragraph should indicate any apology where appropriate, and our wish for the response to address the complainant’s concerns’. A final point of guidance relates to style and tone and the recommendation that the writer reads ‘with the view if it was your loved one receiving this reply about their concerns, would you be content with how it is worded and the style etc.?’ The recommendation to consider receiving the letter as if it had been addressed to ‘your [own] loved one’ points to the Trust’s recognition of the importance of empathy, and respect.
Data
Summary
There are a number of potential pitfalls accompanying the provision of written responses. Most prominently there is a common perception that the apology is ‘insincere’ or ascribes the problem to the complainant’s feelings or perceptions (‘politician’s apology’/‘fauxpology’). 121,122 Another complaint about written responses arising in follow-up interviews and diary entries is the way in which staff rudeness is presented as ‘exceptional’ or ‘excusable’ (e.g. stressful environment). More broadly there is a perception that complaint responses operate defensively and largely refute, avoid or mitigate responsibility for the complainable. 121 Written responses have a tendency to seek out all ‘sides’ of a story (judicial register) which implicitly undermines the ‘truth’, ‘reason’ or legitimacy of the complaint/complainant. A final very common complaint is that letters adopt a formula encouraging the lengthy rehearsing of clinical histories not necessarily relevant to the complaint, which can also entail a perception that the points of the complaint have not been directly addressed. This final tendency was one identified and strongly criticised in the recent Independent Inquiry.
Key themes
This section discusses a number of key themes emerging from our analysis of the written responses to complaints (and supported by complainants’ accounts). In line with our ethical approval, all names mentioned in the data are pseudonyms.
Defensiveness of Trust/lack of accountability as a barrier to successfully resolving a complaint
A recurring theme in our participants’ view of the Trust’s written response was that it ultimately evaded or at least mitigated responsibility for the poor experience or poor healthcare.
I think they’re trying to cover up everything that happened. That’s the feeling we get, that they want to cover it up. They don’t want to admit that they’ve done wrong.
RC15[I]
The source of this perception of defensiveness can be identified in the response letters, which adopt a number of strategies to avoid admission of direct responsibility for the complainable – for example, locating responsibility for the events with other actors (including the patients themselves), appealing to factors such as healthcare workers’ ‘experience’, ‘professionalism’ and ‘good intentions’ as well as referring to ‘exceptionality’ in order to avoid or mitigate blame. Sometimes the wording of a complaint response is designed to subtly evade accountability for errors. In the case of RC01, a fracture belatedly detected on an X-ray (following routine review of historic X-ray data) leads to the request for a renewed X-ray, but the mistake is vaguely framed without any overt agent as ‘after the report of L1 was available’, thus obfuscating responsibility for the error. A similar example of obfuscation can be seen in the second response to RC15, ‘the Clinical Biochemist has no record that he was informed of a significant alcohol consumption history’ – a vague and agentless formulation that is speculated about at length in conversations between the family and PAS advisor.
There are some (relatively rare) examples of transparent accountability in our corpus of written responses which admit responsibility for mistakes and explain what should have happened.
Dr Gow adds that if Dr Martin had correctly identified and recorded your son’s blood results this would have had an impact on his formulation of his management plan. He would have sought a second opinion as to the appropriateness of discharge and possible escalation of treatment.
IW01[W]
However, responses that evade or mitigate culpability are more common. For instance, RC10, complaining about a call that a consultant failed to make, focuses on the implication in the response letter that the blame is being shifted to herself.
My main reason for the complaint was the consultant, via his secretary, said he had tried to contact me and couldn’t get me suggesting that it was my fault the appointment did not happen.
RC10[D]
In her interview she reiterates the impression that ‘all these excuses’ have been offered in lieu of a proper apology and that this is ‘bordering on defensive’. Similarly, in the response letter sent to RC02, the trust shifts blame for the complainant’s sister’s fracture remaining undetected to the sister herself: ‘your sister denied having any limb or pelvic pain’, thus implicitly blaming her sister for misleading staff about her pain. This phrasing is explicitly picked up by RC02 in one of her diary entries:
The complaint response refers to my sister having DENIED having any limb or pelvic pain, I find this UNBELIEVABLE. This has little to do with her being reluctant but more to do with her state of mind and brain injury with dementia and old age combined.
RC02[D]
At a later point in this response letter the Trust states that ‘this team is very experienced in managing patients with mobility issues and would have intervened if they suspected any hip injury at this time’. By mentioning the medical delivery team’s ‘experience’ here, an appeal is made to their good intentions, but it also implicitly suggests the injury was not present at this time. The phrase ‘would have intervened’ is epistemically certain and thus casts doubt on the complainants’ view of events. However, the fact that the fracture was later detected and deemed to have most likely dated from this admission presumably means that this handling of the situation needed to be questioned, not just defended. When asked by the interviewer whether RC02 felt that the Trust ever ‘acknowledged or accepted responsibility for what went wrong’, she replies, ‘no no they didn’t. Not when I look at the letters, no’.
In RC01’s case, the mention of good intentions is designed to mitigate the error committed by the doctor.
Dr Crossland believes that the doctor who made the decision to transfer was doing it with the best of intentions but had unfortunately overlooked the statement made in the notes that your mother was unsuitable for surgery.
RC01[W]
Similarly, complaint responses often refer to lack of intentionality as a way of mitigating blame.
[S]taff did not mean to cause any further distress to you at an already distressing time […] It was not Sister Murphy’s intention to cause any upset or distress at the time of this interaction […] I do hope you will be reassured that it was certainly not the intention of any of the staff involved in your care to add to your distress.
RC03[W]
These formulations of lack of intentionality arguably add to an impression that the complainant’s version of events differs from reality and contribute to the sense that their lived experience is being undermined (see Presentation of ‘alternative’ or contradicting narratives of staff).
Blame mitigation is also achieved by appealing to standard practice and what is normally done in such circumstances. 121 In the case of RC01, whose mother had a lengthy stay in hospital during which it was discovered she had sustained a lumbar fracture, RC01 expressed concerns that her mother’s injury may have been made worse by being manoeuvred by staff without knowledge of this fracture and was told that ‘Dr Crossland advised that immobilisation is not standard practice in vertebral fractures’. Moreover, the admission by the Trust that the spinal fracture was missed on an X-ray is mitigated by the information that ‘an abdominal X-ray is not a standard view to look for lumbar spine fractures’. Similarly, the letter states that the decision to transfer the complainant’s mother to another hospital (against the family’s wishes) was due to the spinal surgeon’s wish to assess her and that ‘staff would normally defer to them’. Similarly, in RC21’s response letter the Trust appeals to ‘standard practice’ (‘seeking tertiary opinions from specialist teams in such circumstances would be standard practice’), thus subtly undermining RC21’s account that the doctor had admitted being unable to diagnose his daughter’s condition.
Sometimes fault is implicitly acknowledged but mitigated by reference to challenging circumstances.
Dr Jones recognises that patients who are re-attending because of advice received from the ED should be prioritised for reassessment. We do aim to do this wherever possible, but it can be difficult when the ED is under pressure.
IW03[W]
Here the formulation suggests an ideal procedure (‘should be’) from which the service is exempt when mitigating circumstances arise. Similarly, RC10’s missed phone consultation is explained with reference to ‘unforeseen circumstances’.
Blame evasion can be highly consequential to a complainant’s evaluation of how the complaint has been handled, especially in highly distressing or stressful complaints where it is seen to compromise the Trust’s empathy for the patient and their loved ones. In response to RC03’s complaint (detailing the responses and attitudes of allegedly unsympathetic and unhelpful staff while she was suffering a miscarriage in A&E), the Trust reports, ‘I am unable to identify who this may be and therefore unable further investigate or to comment’. By prioritising a formulation designed to avoid admissions of fault, this becomes a missed opportunity to express regret for the patient’s traumatic experience. RC03 comments on her perception of this stance in her interview, stating that there was ‘no admission of any fault’ and ‘if they’re not going to take responsibility for what happened, how is it going to change for anyone else?’; she goes on to comment cynically that ‘they stick together and look out for each other … remembering events in a way that suits them’. In one of our most complex and lengthy longitudinal cases, involving a very young baby, the response from the Trust contains only one apology: for the delay in responding. The response is otherwise a point-by-point refutation of each element of RC21’s complaint, and while it is possible that the Trust’s response is entirely factually accurate, the absence of any acknowledgement of the complainant’s feelings, perceptions, experiences or the ‘reasonableness’ of his complaint seems likely to exacerbate his sense of grievance and his fatalist view that complaining has been ‘pointless’.
Occasionally this perspective is aligned with the assumption that the relevant Trust is concerned more about legal ramifications than attempting to understand what lies behind the complaint, and this is clearly picked up on by our longitudinal participants. RC01 for instance describes the response letter as demonstrating ‘no accountability for what had gone wrong’. She expresses the view that the Trust should not spend so much time and energy defending their position/avoiding culpability; that she would prefer more admission of culpability and less defensive promotion of ‘here’s what we did right’. Interestingly this is a view shared by staff at the PAS who have been supporting RC01: ‘from my experience of dealing with trust in these complaints y-y- they’re they’re- y’know they don’t want to hold their hands up and admit things’. This perception is shared by other longitudinal participants. RC15, for instance, states, ‘I think they’re trying to cover up everything that happened’ and ‘we feel they just don’t want to admit that they’ve made a mistake’. RC11 similarly comments in her interview that ‘when it was investigated lots of excuses were made’ and when asked by the interviewer if she felt excuses were made says:
[I]sn’t that everybody’s response ((laugh)) to not taking responsibility … try to come up with excuses rather than putting their hands up and saying mea culpa my fault and I’ll have to do something, I have to do more work on this.
Sometimes complainants comment explicitly on their perception that this is linked to fear of legal redress.
[T]hey’re obviously very worried about litigation et cetera erm but – with regards to complaints sometimes the best thing to do in my opinion is just to own up and say ‘we’re wrong, we shouldn’t, we didn’t and we don’t but in the future we’re going to try to do that better’ and that’s all that’s needed as far as I was concerned erm was a genuine – like authentic response.
RC11[I]
RC15’s family comments that for them closure could be achieved if the Trust acknowledged responsibility for what happened to their mother: ‘we will feel better about the whole situation. We’d feel that they’ve took responsibility for what they’ve done’.
The need sometimes exhibited in Trust responses to defend their practices against possible charges of negligence, errors or incompetence arguably takes precedence over the need to make complainants feel ‘listened to’, empathised with, respected and that their complaints are ‘reasonable’ and worth making.
Lack of sincere apology
Apologies are an important component of complaint response letters, especially where blame, error or harm is being acknowledged. Guidance on apologies from the Scottish Public Services Ombudsman (SPSO) reinforces the legislative point that apologies are not an admission of liability and busts the myth that when an organisation issues an apology it is more likely to lead to litigation: ‘Research into the impact of apologies consistently shows that a well-made, timely apology diminishes people’s wish for compensation’. 3,123 Given the clear value of an apology in the context of responding to a complaint, why do we find that so many of our complainants remain dissatisfied following receipt of an apology?
A common theme in complainants’ responses to complaint resolution letters is the sense that the apology was not ‘proper’ or ‘sincere’ (‘an insincere story about the delay’; ‘she kinda brushed over sorry for the delay’; ‘if someone had come on the phone initially with a sincere apology explaining … I would not have complained in the first place’). Since an apology (at the very least for a delay in providing a final response) seems to be an obligatory element of complaint response letters, it is worth analysing why these apologies are seen to be inadequate.
The impression of ‘insincerity’ is likely to be connected to the way in which apologies are worded. In a previous analysis of written responses to complaints122 it was noted that apologies tended to be mitigated by treating complainants’ accounts as subjective and by providing explanations for substandard experiences of care that appealed to unintentionality or exceptionality (see also above). The analysis also noted the common appearance of what has sometimes been described as the ‘fauxpology’ or ‘politician’s apology’ (e.g. ‘I’m sorry you feel that …’) which ‘imputes the cause of distress to the subjective (and possibly misguided) impressions of the complainant’. 122 In this way the complaint responses avoid admission of accountability for the complainable action by ‘implying that the complainants’ feelings do not align with the facts’122 or seeming to ‘question whether the person has actually suffered’. 123 This phenomenon was repeatedly noted in our own data and was also explicitly picked up on by participants in interviews and diary entries. In a written response to RC01’s complaint, the letter states that ‘Sister Morgan would like to sincerely apologise that you felt your mother was treated in a “derogatory” manner’. Here the writer effectively apologises for the subjective and possibly incorrect impression experienced by the complainant (‘that you felt that’), thus rendering the apology insincere. The use of scare quotes for ‘derogatory’ implies distance from the evaluation, mitigating the authority of account and distancing itself from its veracity. Similarly, RC02’s letter states that ‘Dr Dryden is sorry that you and your family were upset about the lack of communication’. In this way, the lack of communication is mediated through the feelings of the family. The letter provides another mitigated apology for the complainant’s sister’s experience using low modality: ‘I wish to support Dr Dryden in making this apology to your sister for the distress she may have suffered as a result of these matters’ (emphasis added). An apology where there is no admission of responsibility, or even an attempt to investigate the cause/timing of the injury the complainant’s sister has sustained more thoroughly, is inadequate and possibly worse than no apology at all.
Interestingly, there is evidence that complaints managers compiling response letters are aware of the nuances of these linguistic choices. In a memo from the doctor asked to respond as part of the investigation into RC03’s complaint, he says: ‘In summary I would like to extend my apologies to Miss Whitehead regarding her experience in the Emergency Department […]. I recognise that this fell below your expectations and has caused distress’. Here the emphasis is on the subjective perception of the patient, ‘your expectations’, which could cast doubt on its objectivity. By contrast, the version that is actually sent to the patient has amended the wording: ‘Dr Carradale is sorry that your experience in the ED … fell below the standard of care that would be expected and for the distress this caused’. Though a subtle change, the amended version suggests that this is a more objective standard of care that would be expected by anyone.
Written responses do often contain direct, unmitigated and ‘model’ forms of apology.
Dr Martin deeply regrets that there appears to have been an error in this case and wishes to advise that he has learned from this and will reflect on this case in the future.
IW01[W]
On behalf of [the Trust] I wish to support Dr Crossland, Dr Richards and Mrs Morgan in making this apology to you for the distress you have suffered.
RC01[W]
The distress in the latter example is presented as a matter of fact rather than linked to the subjective view of the complainant. It is therefore interesting that the perspective of the longitudinal participant about this response remains negative overall and she still seems to feel that the response and apology is inadequate. One reason may be that the potentially ‘good work’ achieved by sincere apologies is often ‘cancelled out’ by what co-occurs with it. For instance, RC03’s response letter contains the following model apology and efforts at redress (invitation to a meeting) ‘he does acknowledge the distress you have suffered and would therefore like to offer you the opportunity to meet with him’. Unfortunately, this is preceded by ‘On review, whilst Dr Carradale … feels the issues raised in your original complaint have been adequately responded to’. Here the insistence that there is nothing to apologise for does nothing to make the offer of a meeting attractive. In RC09’s complaint (about an ‘aggressive and rude’ doorman) the offer of a ‘sincere apology to you for the experience you encountered’ is arguably undermined by the subsequent text explaining that the complainant was entirely in the wrong for failing to observe hospital health and safety measures around food and COVID. The complainant comments on this in his diary following the response: ‘He basically was more concerned that I was bringing outside food (Takeaway) than how rude and aggressive the Porter was to me’. Similarly, the response to RC11’s complaint ideally states ‘we can only sincerely apologise for the experience that you had’ but this is prefaced by the qualification that ‘all concerns raised appear to be environmental’, suggesting that they were not necessarily linked to staff actions. Such formulations arguably detract from the sense of the trust being accountable for failings or poor healthcare experiences and contribute to RC11’s sense of dissatisfaction with the response.
A detailed and full apology may also seem to be eclipsed or undermined by accompanying ‘excuses’. This can be seen in RC10’s complaint about a call by a consultant that never happened. The letter begins by saying ‘he would like to offer his sincere apologies for the inconvenience caused’ but then proceeds to offer a long and slightly convoluted list of events that led to this omission.
[M]aking excuses in a letter of apology doesn’t make a full apolo- it feels like you’re saying ‘sorry but’ so just say sorry without giving two paragraphs of ….
RC10[I]
A number of our other participants also raise the juxtaposition of apology with excuse: ‘Had hoped for an apology that wasn’t followed by “but”’; ‘it was at least one paragraph anyway of excuses it (tended) to detract from the apology if I’m honest’. Even where a written apology seems to be full and sincere, the appearance of lengthy ‘excuses’ seems to detract from its positive effects. This is an interesting finding that potentially contradicts other research pointing to the value of providing ‘reasons’ to accompany an apology. 123
The following apologies are offered in the response sent to RC03:
Dr Carradale wishes to reiterate his apologies to you for the distress caused to you at an already stressful time […] Ms Murphy [nurse] acknowledges the distress you were in during this time and would like to reiterate her apology that your experience was not made more comfortable with a visible amount of compassion and empathy.
RC03[W]
However, RC03 remains deeply unhappy with the response overall and signals her intention to take her complaint up with the Ombudsman. The letter contains a number of accounts of the events reported by the complainant which contradict her own account and thus cast doubt on her integrity (see also Presentation of ‘alternative’ or contradicting narratives of staff). One can only assume then that these sincere apologies are compromised/cancelled out by other elements of the letter that are defensive and fail to admit fault or accountability. This pattern is also referred to by RC23, describing a previous written response she received and which she remains deeply dissatisfied about:
It took them six months to get back to me and then the fact it says, ‘The doctor has had time to reflect, and he apologises blah blah blah’, and then in the next page it was like, ‘This was correctly done, and this was correctly done’. No, it wasn’t.
RC23[I]
She goes on to describe the response as ‘a half-assed apology. They apologise and then in the next breath they are saying, “This was in order and that was in order”’.
The problem with inadequate, insincere or incorrectly focused apologies was also an observation of the Independent Inquiry mentioned above. The findings point to an institutional preference for apology over a clear analysis of events and admission of accountability where relevant.
Medical jargon
The use of complex terms and a medical and specialised register in written communication is a theme that emerged in some of our case studies. Written responses tend to be constructed using medicalised language and descriptions of conditions which non-specialists may have difficulties understanding.
The urinalysis at this stage showed ketones ++, + blood, + protein, leucocytes ++ and this time nitrates were positive.
IW01[W]
[S]he had a water-soluble contrast enema […]. This revealed a normal recto-sigmoid ratio […] the subsequent results were normal which helped to exclude Hirschsprung’s disease.
RC21[W]
Longitudinal participants comment on the confusing effects of this use of language and the work it creates for them to understand the significance of the terms used.
[W]e found like anything we’ve asked has been avoided then answered in terms that we don’t understand […] all medical, like we don’t understand it at all. I know that we couldn’t understand anything that it meant, so we went back and asked for it in simpler terms.
RC15[I]
The same family reported having to do the work of research themselves to make sense of the communication in written responses.
Aye, it’s like us, as a family, are trying to work it out ourselves, you know, because they’re not explaining it to us properly. And we’re not medically trained. We don’t know what’s what, but you’re just doing a lot of research yourself.
RC15[I]
RC01 also reported finding the written response letter to her complaint about her mother’s care to be ‘longwinded … not really answering anything’. She also finds the volume of her mother’s requested medical records to be overwhelming and intimidating (‘I’m a bit overloaded with all the notes. Hard to understand them’) and expresses the wish that they would be ‘easily understandable, legible and detailed’. She contrasts her encounters with the Trust’s communications with those of the contact at the PAS (who helped her to work through the medical records): ‘He talks normally and makes the task feel easier’. In recorded calls and meetings with the PAS they discuss the use of ‘medical language’ and ‘shorthand terminology’ that excludes the non-expert, and express appreciation of the more ‘plain English’ communications they have received. There are also numerous self-identifying references by the PAS officer to himself as a ‘layman’, ‘not a medical person’, which presents a deliberate contrast to the obscure and medical register of the Trusts.
Another consequence of the use of a medicalised register is that it can detract from the empathy that is needed particularly in cases involving trauma and suffering. RC21’s description of his baby daughter’s pain (‘she was screaming in pain … her whole body was going into spasms … her body was fitting because she was in pain … uncontrollable fits where her knees were swinging about’) is in stark contrast to the more formal and medical register used by the Trust to respond to his complaint and which conveys a kind of downplaying or restraint around the description of the baby’s condition: ‘increased work of breathing … reduced feeding … very unsettled with a high-pitched cry … at times distressed and irritable … any discomfort’. The use of this kind of professional register therefore risks undermining the account provided by the complainant.
Responses which summarise medical care rather than addressing substance of complaint
A common formula adopted by complaint response letters is to methodically detail the stages of care given to the patient/complainant. Often this involves repeating or ‘confirming’ (in more formal, medicalised language) the series of events or treatment already set out by the complainant in their original written complaint and usually comprises the majority of the response. This seems to be a component of the formula prescribed by Trust A, as all their written responses involved a detailed case history of the patient’s care, but it is not part of Trust B’s letter template. This strategy is, however, perceived to be an irrelevance and distraction by complainants:
[…] it was just literally a summary of why she was in hospital and what infection she had. It was a summary of her medical care and I was just like, that’s not what we asked about, so I was very deflated with that […] I cannot believe it has taken 9 months for a 3 page letter to be issued which merely documents my mother’s stay and a high level overview of her care.
RC01[I]
Participant RC03 also comments on this tendency to focus on irrelevant details of care. In the written response she received, the assessment, diagnosis and speed of referral was reiterated and deemed satisfactory (‘I therefore have no concerns regarding the clinical assessment and management made by the doctor at that time’) yet the focus of the complaint was about the attitudes of staff and neglect of her dignity while experiencing a miscarriage while waiting in A&E. In her written response to this, RC03 stresses that the focus is incorrect:
I’m not sure why Ward 21 were brought into this as I had no issues whatsoever once I was handed over to them. The team were fantastic and done everything they could for me. I also had no complaint about having to return to ED as the team were in theatre, that couldn’t be helped.
RC03[RP]
Similarly, in her interview she says, ‘it was a lot of information in the response that I received that was totally irrelevant to my complaint’.
This pattern of spending some time narrating the details of the patient’s care is observed across written responses from both Trusts; in part it seems motivated by desire to show proper healthcare procedures have been observed and could be seen to impart a slightly defensive tone. Significantly, this kind of practice was criticised in the Independent Inquiry report.
Presentation of ‘alternative’ or contradicting narratives of staff
A significant source of dissatisfaction with complaint response letters is the tendency to present alternative narratives to the complainants’ version of events, provided by responses from relevant staff gathered by the investigating officer. 124 Where these narratives contradict those of the complainant they are seen to undermine the complainant’s lived experience and the basis and legitimacy of their complaint and cast doubt on their integrity/truthfulness. While it is obviously sometimes necessary for a complaint response to refute factual inaccuracies in a complaint, this becomes more problematic where the experience is a subjective one involving perspectives on staff attitudes and behaviour for instance.
This is particularly apparent in the case of RC03. In her post-complaint interview she commented that she felt that the response suggested that the grounds for her complaint were dismissed due to the seeking out of accounts which contradicted her experience.
[T]hey said ‘that didn’t happen’. Implied I was lying or too emotionally distressed to realise what was happening. But that wasn’t the case.
RC03[I]
We can see how the letter may have contributed to this impression:
The staff member that has been mentioned does not recall sending you back to the waiting room, and has stated that, when she noticed you were requiring help, she spoke with a staff nurse to arrange a cubicle space, which she then brought you into.
RC03[W]
The letter also makes reference to the possibility of misinterpretation:
Mrs Murphy recognises that this communication may have been misinterpreted as the staff member has intended this to be communicated in a compassionate way and apologises to you sincerely for any hurt caused.
RC03[W]
Despite the inclusion of a ‘sincere’ apology here, the effects are arguably cancelled out by these references to an exonerating lack of intent and misinterpretation on the part of the complainant, and the complainant’s overwhelming impression is that her truthfulness is being brought into question:121
I wouldn’t have gone to the bother of complaining if it hadn’t all been true – wouldn’t just make things up.
RC03[I]
The patient’s reply to this written response (in which she expresses dissatisfaction with the outcome) is dominated by her sense of grievance that her account of what she experienced is being denied and contradicted and leads to a doubling down on her own version of events:
Dr is recalling that night incorrect […]. As for the auxiliary nurses recollection of events, again that is completely incorrect. She called me in for bloods and said quite loudly ‘do you know you’re covered in blood, you’d need to get someone to bring you a change of clothes’ […]. Not once was I offered a gown or anything for that matter to cover myself […]. If what the members of staff are saying were true then there would have been no complaint made or any issues. If given half the chance to preserve my dignity do you not think I would have taken it with both hands? I remember every detail of that night very clearly, it’s a night that will stay with me for the rest of my life.
RC03[DP]
She ends her letter with an expression of intent to escalate her complaint to the Ombudsman’s office: ‘The fact both members of staff are making out I’m lying is just an added insult. I will be forwarding the complaint to the ombudsman’. Finally, her sense of dismay and frustration around the questioning of the veracity of her account leads her to resort to including visual evidence of the events – a kind of counter-empirical evidence to the testimonies provided by the Trust: ‘I have attached pictures to this email of just how I was left in the waiting room’.
A similar pattern of response can be seen in the letter provided to RC21 after a long, complex and protracted complaint about his baby daughter’s care. The written response takes RC21’s issues in turn and refutes or corrects some of his assumptions:
As such, our teams would not be in agreement with your statement that the GI consultant was the first person to do further tests […]. It is generally accepted that Paracetamol and Ibuprofen are not classed as sedative agents.
RC21[W]
It also ‘recasts’ some of the complainant’s perspectives about the team being unable to diagnose his daughter’s condition:
to the best of his knowledge, Dr Li does not feel that he stated that he thought he had missed something.
RC21[W]
The response also points to contradictions between the complainant’s view that his daughter was too sick to be discharged, and his partner’s express wishes that she take the child home. There is some mitigation here with ‘regrets that your opinions had not been communicated to him’, though this could also imply the complainant was not clear. It also refutes the complainant’s perception about the results of a scan, though it does mitigate this with an apology for the possibility that this confusion arose from poor communication: ‘I apologise if this was the case or if there was any misunderstanding in what you were advised, as this is also incorrect’. While it is reasonable for the Trust response to refute points of fact that can be shown to be inaccurate, it seems unfortunate that there is no acknowledgement in the response that any of the complainant’s concerns (especially around his child’s suffering) had any substance to them. The only real apology (and agreement with the complainant) relates to the delay in providing a response.
There is also little acknowledgement of the family’s stressful experience and the pain experienced by the child – rather, the condition and experience is ‘normalised’; ‘in pain’ is recast as ‘distressed and irritable’ and the conclusion of the medical team is that there is nothing really wrong with his child: ‘am pleased to learn and hope that it was some reassurance to you, that GOSH explained that they did not find anything unusual with all the tests they carried out’. There is a stark contrast between this written response and the highly empathic response provided by the front-line call handler in our recording of the initial complaint call. The written complaint response overall is deemed to have addressed all the complainant’s concerns and considers the case ‘closed’. However, in his follow-up interview with the project team, RC21 expresses dissatisfaction with this response and notes its defensive approach. He goes on to comment on his negative view of the whole process as well as his consideration of escalating the complaint.
Well, as I say yes they’ve apologised on one or two points, but I feel like it’s just much covering their tracks and then saying there is nothing more we could have done, like we done everything in our power and so I think to me it was just very much excuses, in a point they actually said that it was my partner’s my fault that it was the mum’s fault […]. Nothing has been addressed. No. I don’t feel anything has come out of it, as I said, you know, the whole process has been a complete waste of time and it’s now in my hands whether, as you say, I want to pursue it and go on to the next level and get somebody else to reinvestigate it.
RC21[I]
This semi-judicial approach to investigation where staff (especially named in a complaint) have a ‘right to reply’ tends to produce responses which are defensive in tone, and are seen to undermine the veracity of the complaint and by extension question the reasonableness and integrity of the complainant. One obvious drawback with this approach (which is ostensibly about fairness and right to reply) is that the version provided by the Trust (through questioning relevant employees) ends up being the definitive one, impossible to question or cross examine as would be the case in the more dialogic context of an actual judicial review. This was also noted by van Dael et al. :
It … positions the provider and patient perspectives as antagonistic, with any inconsistency leading to the dismissal of one account, rather than seeking to understand and explore dissonance and realising its potential to reveal institutional blind spots or failures in communication. 124
Conclusion
Our analysis of longitudinal complaint journeys demonstrated that poorly received final responses are often turning points for complaint journeys which make the complainant more determined not to give up and sometimes propel them to take their complaint further – either to the Ombudsman or to legal recourse. Key issues identified by longitudinal participants (in follow-up interviews or diary entries) include the tendency for written responses to avoid acknowledging responsibility/accountability for the poor experience or error; the provision of the ‘false’ or insincere apology; the inclusion of medical ‘jargon’ which alienates complainants and makes them feel they are not being effectively addressed; the tendency to detail the history and sequence of the patient’s healthcare (even where this is not relevant to the complaint) and finally the compulsion to provide all ‘sides’ to a reported event, which frequently involves an undermining of the original complaint. The upholding of the ‘reasonableness’ of the complainant’s submission and the damage incurred by undermining it is an important theme across all our data sets and is picked up again in Chapter 7, exploring spoken complaint interactions. The perceived lack of empathy accompanying some of these tendencies is at odds with the explicit recommendation in Trust B’s guidelines that ‘[t]he first read through should be taken with the view if it was your loved one receiving this reply about their concerns, would you be content with how it is worded and the style etc.?’.
The complainant testimonies in this chapter and the longitudinal analysis of the complaint journey in Chapter 5 suggest that there is potential to reform the process of providing responses to complaints, both through the consideration of alternative modes of communication (e.g. face-to-face meetings) but also through greater attention to language choices in written responses. While apologies are an important component of response letters, they are ineffective without other components such as validation of the reasonableness of the complaint and some acknowledgement of responsibility. 123,125 This supports the conclusion of Lewicki et al. that ‘when an apology contains an Explanation for the offense, an Acknowledgment of Responsibility, and an Offer of Repair (EAO), the apology is perceived as significantly more effective than when it only contains an Expression of Regret, a Declaration of Repentance, and a Request for Forgiveness (RDF)’. 126 Sometimes practical steps to institute permanent changes to prevent the complainable occurring again (‘offer of repair’,127 ‘indication of future intention’,128 ‘remedy’123) are actually seen as far more valuable than an apology. 26 In Appendix 2, we present formal guidance for reforming the construction of written responses to complaints by Trusts.
Chapter 7 Interactional findings
The interactional analysis of our spoken data is focused on understanding complainants’ experience of the communication and identifying interactional patterns that contribute either positively or negatively to that experience. The value of the CA approach for this is the reliance on the moment-by-moment participant orientations that provide robust evidence for what matters to complainants in each encounter. This participant orientation evidence reveals the interactional/interpersonal priorities for complainants and the impact on the progress and outcomes of an encounter if those priorities are not met. The inductive analysis of the individual encounters provided candidate phenomena – structures, patterns and practices that were significant for the encounter and might be found in other encounters; our analysis then focused on those that were found to recur across encounters in the corpus. The insights emerging from the inductive examination of each encounter were also iteratively cross-referenced with complainant appraisals of that encounter where such were available (see Chapter 5).
Examining the practices that complainants deploy to bid for and pursue what matters to them also allows us to identify CH practices that work to meet the needs of the complainant (C). Our analysis shows that these practices enhance call-handling effectiveness and efficiency by facilitating effective identification of the key point(s) of complaint, as well as efficient progress through the call. Not only does this avoid escalation, but it can be deployed to negotiate challenging contexts such as individual criticism and blame during an encounter. A further value of our moment-by-moment analysis is that it clearly demonstrates that it is not just the practices but, as we will show, the timely, context-sensitive use of these practices that matters for a positive outcome for a call.
In the next chapter, we discuss how our findings are applied in the development of Real Complaints Training. In this chapter, we present our findings and the participant orientation evidence that supports them. This chapter thus addresses the study objectives 1 and 4 and provides the core evidence base for study objective 5.
Caller priorities
Our inductive analysis identified three key priorities that complainants are observably oriented to and that pervade the communication across all complaints encounters: the need to tell their story; the need to be heard; and the need to be acknowledged as ‘a reasonable complainant’. These priorities demonstrably influence how complainants approach complaining as an interactional project and, where these needs are not met, how complainants observably orient to pursuing these needs. Moreover, when implicit pursuit fails, complainants explicitly express these needs. (For illustrative purposes, some data from the pilot corpus7 are also presented.)
Extract 1
PI05
Extract 2
IC75
Extract 3
PI07
From an analytical perspective, pursuit of these needs provides turn-by-turn participant orientation evidence of the salience of those needs for participants. From an applied perspective, it is highly significant that pursuit of these needs also has an impact on the progress and outcomes of each encounter, so the overarching needs and the forms of pursuit of those needs have clear relevance for Real Complaints Training.
The need to tell their story
Callers typically orient to talking about their complaint as a form of storytelling, where what matters to them is to tell their story in its entirety. This is observable in how callers launch the explanation of their complaint with story prefaces129 such as ‘anyway it’s a wee bit of a story so I hope you’ll bear with me’, which make a bid for the interactional space to tell a story in ways that not only orient to their sense of the size and shape of their story, but also orient to the telling of the complete story as imposing an accountable burden on the call handler. For example, in Extract 4, the CH’s response (line 2) orients to the caller’s turn not only as a bid to tell a story but also as an implicit apology28 for the ‘longwindedness’:
Extract 4
PI12
Callers’ bids to tell their story are thus often combined with forms of accounting for the additional details involved in telling the story, for example accounting for the role of the details in the story, for example, as ‘background’. (In Northern Irish English, one very recognisable story preface is ‘I’ll tell you what it is’.)
Extract 5
RC30
Sometimes the overarching need to be seen as reasonable is also embedded in how the caller launches and accounts for their lengthy complaint narrative:
Extract 6
RC29
Callers also orient to concerns with the ‘(in)completeness’ of their story. This may involve invoking additional information or additional complainable issues:
Extract 7
IC55
Extract 8
RC21
More often, orientation to the ‘(in)completeness’ of the complainant’s story is evidenced by callers’ interactional moves to resist CHs’ attempts to progress through the institutional requirements of the call. 130 These moves implicitly orient to the complaint story as ‘not yet complete’ – as requiring further elaboration to satisfy the caller’s overarching needs. Benwell and Rhys130 show how callers orient to moments of transition through the structure of a call as opportunities to re-launch their story and how the practices used to re-launch their story are revealing of the various ways that the caller perceives their complaint story as incomplete. For example, callers may re-launch their story to address the ‘hearably factual, recordable’ details of their complaint or to pursue acknowledgement of their subjective experience of those details. This reflects the important finding that telling their story, for complainants, involves not just the facts of the complaint story but also their subjective experience of the events of the story and, importantly, its impact on their life beyond the experience of care itself, that is the lifeworld impact. For example, in Extract 9, the caller resists the CH’s moves to close the call with a return to his complaint narrative that explicitly focuses on ‘how I’ve felt’:
Extract 9
IC45
And in Extract 10, the caller resists the move to close with practices oriented to the completeness of their story with respect to both the factual details (their status as a vulnerable adult), and the associated lifeworld impact (‘it’s really affecting me’):
Extract 10
IC69
Thus, caller orientation to the completeness of their story is closely tied to the other overarching priorities/needs as the practices through which callers orient to their story as incomplete serve as vehicles to re-launch their complaint narrative in pursuit of caller-handler acknowledgement of those wider priorities.
The need to be listened to
Closely related to the need to tell their story is the complainant’s need to feel listened to. This is the interactional counterpart to the telling of the complaint story in that it is a product of the CH’s listening practices in response to the storytelling. 131–133 Just as callers often launch their complaint with an explicit bid to tell their complete story, so they also close their calls with explicit recognition where they have felt ‘listened to’:
Extract 11
RC22
Extract 12
RC22
These overt evaluations provide evidence to support the claim that the need to be listened to is an overarching priority for complainants that significantly impacts their experience of the communication in an encounter. They confirm that the caller’s need to be listened to has been met by the CH’s listening behaviours; however, they don’t evidence which listening behaviours contribute to meeting that need. The specific practices through which caller handlers accomplish this are discussed below. First, we turn to established CA insights relating to different listening practices and show how callers pursue responses134 that meet the need to feel listened to.
It is well-established that listening requires not just hearing the speaker but orienting to them as interlocutor by displaying attentiveness to, and understanding of, the ongoing talk and the speaker. In the context of an extended narrative, the speaker typically signals production of an extended ‘telling’, making relevant displays of listenership that show an understanding that the current speaker’s turn is continuing. Listeners draw on an array of minimal response tokens to display listenership, each of which conveys different perspectives on the prior turn. Gardner,135 for example, differentiates between continuers such as mm hmm that simply pass the turn back to the speaker and other forms of minimal response that display some kind of understanding of the prior turn, for example newsmarking tokens (‘oh’). On the other hand, the speaker may design their turn to make relevant a listening response that is sensitive to the particular action or stance embodied in the current speaker’s turn. 54 In the latter case, the listener is expected to provide more than a minimal response token in order to provide a responding next action or to display a responsive stance.
In the listening practices in our data, there is an observable tension for the CHs between, on the one hand, meeting the institutional requirements of information gathering and, on the other, meeting the interpersonal and subjective needs of complainants, who, as described above, are oriented to narrating not only the facts of their complaint but also their subjective experience and how it has impacted them. Call handling thus involves listening practices oriented to both types of caller need. This distinction is illustrated by the following contrast involving time references:
Extract 13
PI03
Extract 14
PI05
In Extract 13, the caller gives the exact date for her husband’s admittance. Giving a date involves being specific and precise and is oriented to being factual136 and we see here that the CH responds with an information-oriented response marking the event as a ‘fact’ on the recordable timeline of the complaint. Time references can, however, be used to convey an evaluative stance towards the passage of time. 8 We see this in Extract 14, where the caller uses the time reference to imply that they have faced an unreasonable delay and the CH’s response makes explicit the implied complainability of the delay.
Pursuit of the caller’s needs
Meeting the caller’s need to be listened to requires CHs to provide responses that recognise where and how callers’ turns convey more than the recordable ‘facts’. In the absence of this, complainants display their unmet needs by observably pursuing responses that meet their needs. For example, in Extract 15, similar to Extract 14, the caller’s temporal formulation conveys an implicit negative evaluation of the timeline but unlike in Extract 14, the CH’s minimal response provides no recognition of the caller’s stance towards the date. The caller responds by pursuing recognition of their evaluative stance through a form of repetition that makes the evaluative stance explicit. This response thus displays an orientation to the CH’s uptake as insufficient, that is, as ‘not listening’.
Extract 15
PI13
Our data show that repetition is a recurring practice that callers use to convey that their need to be listened to has not been met by the CH’s prior turn and to pursue a more relevant response from the CH. Callers use different forms of repetition, from verbatim repetition of the same form (e.g. Extract 16), to repetitions that make explicit unaddressed aspects of the caller’s previous turns (e.g. Extract 15).
Extract 16
IC32
As noted above, repetition may even involve re-launching the complaint narrative in the closing phase of the call to pursue unmet concerns. 130 For example, in the following extract we see that while the CH has already recorded the facts of the complaint (waiting times in A&E), the caller orients to having not been heard and re-launches her complaint story with ‘It’s just …’ and re-tells the story to explain why she took her daughter to A&E and why she was so frustrated by the length of the wait.
Extract 17
IC42
Callers may also escalate the evaluative stance expressed in their repetition. For example, in the following extract, the caller describes herself as ‘terrified’. In the absence of CH uptake, she upgrades her self-description to ‘absolutely petrified’. This escalated description again gets no CH uptake and the caller repeats ‘terrified’ but escalates the scope of their fear with the addition of ‘to go anywhere near them’.
Extract 18
RC23
Following the caller’s third repetition of her escalated state of fear, the CH produces a non-specific expression of regret, ‘I’m sorry to hear that’. This allows the CH to proceed to institutional fact gathering, but does not meet the caller’s need to feel listened to and she later produces a further escalated repetition of her self-description that repeats the frame ‘it’s got to the stage now’ but this time provides a heightened description of the impact of her fear: ‘I’ve started taking pseudo-seizures and everything’:
Extract 19
RC23
This time the CH explicitly acknowledges the caller’s original description of her emotional state, which appears to meet the caller’s need to be listened to as she does not return to this element of her complaint.
Extract 18 also illustrates a second key interactional resource that callers deploy to pursue a CH response, namely silence – the noticeable absence of further talk. CA research has long recognised the interactional significance of moments where talk is expected but absent and hence oriented to as noticeably absent. 137 Key to the significance of noticeably absent talk are the structural, turn-taking features of the environment in which the talk is absent, producing not just an absence of talk but an absence of a particular kind of talk and a particular speaker’s talk.
The structural environment influences the specific turn-taking rule applicable at each transitional relevance place, the moments where change of speakership becomes potentially relevant. In the complaint narrative phase of a complaint call, participants orient to an asymmetry in which callers primarily orient to ‘telling their story’ through extended turns of talk and CHs primarily orient to listenership, displayed through various listening practices. In this phase of the call, there are two positions in which silences are oriented to pursuit of CH uptake. The first is following a caller assertion that displays some kind of heightened evaluative or affective stance. There are two aspects of turn-taking management at stake in this position. On the one hand, it is a storytelling environment so there is a shared orientation to the caller producing multi-unit turns. On the other hand, the caller’s heightened stance makes relevant a response from the call hander that attends to the caller’s stance, so a silence in this position is hearable as an absence of acknowledgement from the CH. This type of silence was seen in Extract 18 above, lines 3–11.
The heightened affect in the caller’s turns make relevant acknowledgement by the CH, so the silences in lines 5, 7 and 10 are hearable as a noticeable absence of empathy and the marked duration can be heard as caller pursuit of affective uptake as the caller delays continuation of their complaint narrative, that is, they delay application of the ‘current speaker continues’ turn-taking rule that applies in the context of multi-unit storytelling turns of talk.
The second position in which silence is oriented to pursuit of CH uptake occurs immediately following CH response turns. As discussed above, minimal responses such as ‘mm hmm’ and ‘yeah’ display listenership while also passing the floor back to the teller. A regular pattern in our data shows lengthy silences following CH minimal responses. Through this noticeable absence of caller continuation, the caller orients to the CH’s minimal uptake as insufficient and pursues a more ‘fitted’ response. This is illustrated in Extract 20 where the caller repeats her complaint that her mental health support worker shouldn’t have contacted her following an agreement that she would be assigned a new support worker because her relationship with the current support worker had broken down:
Extract 20
IC68
The CH responds with a continuer ‘yeah’ (line 3), but the caller does not immediately continue with her complaint. Instead, there is a noticeable absence of talk for 1.7 seconds, following which the caller pursues a more substantive uptake with ‘you know’ (line 5). This gets the same minimal response, ‘yeah’ followed by a further noticeable silence of 1.4 seconds after which the CH moves to the ‘service delivery’ phase of the call. (Note that the caller’s needs remain unmet here and following the procedural talk from the CH, the caller returns to her criticism of the mental health support worker.)
These features of repetition, escalation and silence often, perhaps unsurprisingly, cluster together at moments where the caller’s need to be listened to is not being met. This is clearly illustrated in the following example from earlier in the same call as Extract 20. Here the caller is illustrating why her relationship with her mental health worker has broken down:
Extract 21
IC68
Here we see the caller pursue acknowledgement of what she sees as inappropriate ‘help’ from her support worker in response to the caller’s distress. The caller initially pursues acknowledgement through repetition of the inappropriate help – the advice to ‘join Weight Watchers’. This receives silence and then a minimal response, and the caller escalates her pursuit with an explicit bid for agreement (line 21): ‘Surely that’s not right’. When this receives only minimal uptake, we see escalation in the caller’s criticism of her support worker, imputing deliberately harmful intentions in lines 26 and 32. Alongside these repetitions and escalations, we also see repeated silences displaying noticeable absence of caller continuation following the CH’s minimal responses in lines 11, 19, 23 and 28. These silences are hearable as oriented to pursuit of uptake of the prior complainable, which the CH does not provide and which leads then to the escalation of the complainable.
Repetition, escalation and silence thus serve as observable interactional resources through which callers display that their needs are not being met and pursue alternative responses from the CHs. Close examination of pursuit of particular listening responses also shows that being listened to from the complainant’s perspective includes not just the facts of their complaint experience, but also their subjective, felt experience of the issues and the wider lifeworld impact of their complaint. Where CHs accurately record the point of a complaint but don’t acknowledge these more subjective aspects of a complaint story, callers will resist progress through the call in pursuit of this acknowledgement. These analytical observations translate into very effective training insights to support the development of reflective practice for CHs.
The need to be treated as a ‘reasonable complainant’
The third priority for complainants is the need to be seen as a reasonable complainant. 7 This relates to the CA observation that complaining is a stigmatised ‘accountable activity’49,51,59,138 oriented to as a breach in expectable behaviour through the practice of accounting. 139 Even in complaints-handling settings, we see evidence of a moral onus on complainants to justify complaining. This is particularly so in the NHS where resources are known to be catastrophically stretched and loyalty to the institution is paramount. Interactional displays of reasonableness thus index this ‘moral accountability’. 140
Our longitudinal analysis showed that the need to be seen as reasonable permeates the entire complaint journey, including complainants’ reported reflections in participant diaries and post-completion interviews (see Chapter 5). Here, we focus on how the need to be seen as reasonable is evidenced in the interactional data and how it impacts the progress and outcomes of individual encounters.
As with being listened to, the importance of the reasonable complainant identity is reflected in how callers sometimes overtly compliment CHs. (Note: it is striking that these formulations presuppose being treated as unreasonable as expected.)
Extract 22
RC16
Extract 23
RC24
Callers regularly draw on practices that orient to the act of complaining as stigmatised and therefore accountable to seek validation of their decision to complain. Most straightforwardly, callers often make an explicit bid for recognition as a reasonable complainant through references to seldom complaining:
Extract 24
PI16
Extract 25
PI14
Bids for recognition of a reasonable complainant identity are also made more implicitly through references to not liking to make a fuss or not having malicious intentions:
Extract 26
PI17
Extract 27
RC17
Callers also display reasonableness through reference to complaining as a last resort (Extract 28) or to the extreme circumstances driving them to complain (Extract 29):
Extract 28
RC20
Extract 29
PI12
Callers also orient to the accountability of complaining by using the ‘I know X but Y’ structure to preface their complaint with a concession that displays their reasonableness through recognition of difficult circumstances (Extract 30) and/or of good aspects of their care (Extract 31):
Extract 30
RC22
Extract 31
PI07
In addition, as recognised in previous qualitative studies of patient complaints,22,141 complainants often demonstrate a ‘reasonable complainant’ identity by claiming altruistic grounds for complaining:
Extract 32
IC68
The need to be seen as reasonable is also observable throughout callers’ narratives in the ways that callers include details designed to display reasonableness, often marked with the adverbial ‘obviously’ (e.g. Extract 33) and/or through an emphasis on explaining the complainability of the details, for example through repeated references to the severity of pain as a justification for complaining (e.g. Extract 34).
Extract 33
IC07
Extract 34
IC13
NB: in Northern Irish English, ‘whenever’ is used to refer to a single instance, i.e. where ‘when’ would be used in Standard English.
The breadth of practices through which complainants seek validation as reasonable speak to the importance of this particular priority for complainants. Moreover, where these bids to be seen as reasonable are not met, callers deploy the practices for pursuing unmet concerns discussed above, that is, repetition, escalation and silences. Particularly striking is the observation that callers resist attempts to close the call in contexts where the details of the complaint have been accurately recorded but the caller has not yet been validated as reasonable. For example, the following extract occurs in the closing phase of a call where the CH has already accurately summarised the caller’s complaint about the duration of her wait at A&E with her young child:
Extract 35
IC42
We see here that the CH has completed service provision and is in the final closing phase when the caller re-launches her complaint with ‘It’s just that …’. With this re-launch, the caller pursues recognition of her reasoning-oriented justifications for being annoyed about the duration of their wait. In other words, although her complaint has been accurately recorded, she orients to not having been treated as reasonable in making the complaint and here pursues validation of her decision to complain.
The data extracts discussed have shown how complainants orient to these three overarching priorities in explaining their complaint: the need to tell their story; the need to be heard; and the need to be acknowledged as ‘a reasonable complainant’. Although our discussion has examined each priority in turn, these priorities necessarily interact. For example, callers need to feel heard in order to feel that they have told their story; they observably repeat elements of their story or relaunch their story in pursuit of the need to feel heard, but these pursuits also provide evidence of the caller’s perspective on what it means to tell their story in its entirety. Callers also orient to the reasoning that underpins the complainability of their story as a fundamental component of the overall complaint story. The need to tell their story thus includes the need to convey the logic of their story and being listened to includes having that logic acknowledged. The need to be seen as reasonable is thus a fundamental component of the need to feel heard firstly because meeting this need involves recognition of the logic of the complainability of the story, and secondly, because complainants orient to the moral accountability of complaining and being listened to includes recognising orientations to moral accountability. These interactions together thus make the case that while all three priorities matter to complainants, the need to be seen as reasonable is the driving force in these complaint interactions. Moreover, our analysis of the need to be seen as reasonable makes the case that orientation to the moral accountability of complaining is a feature not just of the action or the activity but of the entire interactional project.
The interactional practices associated with callers’ priorities form a foundational element of Real Complaints Training as they provide a recognisable set of interactional behaviours that can support CHs to become aware of how their own language behaviours influence the trajectory of a complaints call.
Affiliation
Having examined the needs of the callers and their interactional practices in pursuit of those needs, the complementary observations we address next relate to the interactional behaviours that CHs can deploy to listen and respond effectively to complaints and ensure that they meet the needs of the callers as well as the institutional requirements of complaints handling. Our analysis points to practices associated with the technical concept of affiliation from CA (not to be confused with Fisher and Shapiro’s concept142 of affiliation as a core emotional concern) as key to effective communication for CHs. The concept of affiliation recognises that there is a layer of communication in the interactional to-and-fro of conversation that relates not to simple information exchange, nor even to the actions accomplished through talk (at least not straightforwardly), but instead relates to the affective or evaluative stance that a speaker conveys towards the events she/he is describing. Affiliation is widely defined as involving ‘taking a stance that matches the teller’s stance toward the event(s) being described’. 54 While stance is sometimes narrowly defined as referring to affect,54 it is also used to refer to a broader range of attitudinal positions. 143 As our analysis shows, this means that affiliation should not be conflated with empathy. In focusing on affiliation, we also maintain Stivers’s54 distinction between affiliation and alignment. Alignment is structural, operating at the level of the activity or project-in-progress and hence, in the context of complaints, is oriented to progressing the complaint-telling but not necessarily ratifying the complainability. Affiliation, on the other hand, ratifies complainability by attending to the negative stance conveyed by the complainant. Progressing the institutional requirements of the call thus requires both alignment and affiliation, but we argue that it is affiliation that meets the interpersonal needs of the complainant. Crucially, affiliating does not necessarily equate to agreeing with the blameworthiness of any particular third party, but rather shows ‘that the complaint recipient recognizes that the complaint teller’s (negative) feelings are justified, i.e., that her/his situation is complainable’144 (emphasis added). This clearly indicates why and how affiliation is important for addressing complainants’ need to be treated as reasonable.
Our analysis has shown that where CHs display affiliation at relevant moments, it helps to progress the call and de-escalate the complaint; conversely, where opportunities to affiliate are missed or mis-timed, affiliation is pursued, the CH’s agenda is delayed and the complaint may escalate. 145 Real Complaints Training has thus been developed around the core insights from our analysis of how affiliation applies in complaint-handling interaction. In the wider CA literature, different types of affiliation are linked to the type of stance involved (e.g. affective, evaluative, epistemic etc.). In addition, recent work by Pino146 has demonstrated the value of a more precise specification of the object of the affiliation. Our own analysis of affiliation in our complaints data has adopted a similarly fine-grained focus on the object of affiliation to reveal three key categories of affiliation that CHs deploy to negotiate the statements of ‘hurt and blame’ that are constitutive of the caller’s story as a complaint story,146 as well as expressions of distress, and claims to a ‘reasonable complainant’ identity.
Types of affiliation
The types of affiliation that emerge as significant in our data relate to (1) callers’ displays of emotion; (2) callers’ evaluative stance towards the complainability of the information presented; and (3) callers’ appeals to reason. These different aspects of the callers’ stance towards their complaint story each make relevant a different form of affiliation in response. The different types of affiliation relate to the three key priorities of complainants discussed above, but not in a simple one-to-one mapping. Just as the key priorities interact and overlap, so we find that these different aspects of affiliation interact and overlap, particularly as more than one type of caller stance may be at play at any one moment and similarly a single turn may orient to more than one type of affiliation. In the following sections, we discuss each type of affiliation in turn to examine what each offers to the progress and outcomes of an encounter, but we will also show how the different types of affiliation co-occur and interact.
Affiliation to affective stance and overt empathy
There is clearly an affective dimension to complaints communication: complainants are typically emotionally affected by the complaint issue and often also by the complaints process itself. Thus, while callers are telling their story, they usually also convey an affective stance towards their experiences. However, a striking feature of our data is the relative lack of overtly empathic uptake by CHs of complainants’ affectual displays. This observation has also been noted for other institutional settings where there is a tension between expressing empathy and dealing with the institutional task at hand; there is often an orientation on the part of the professionals to prioritising the institutional task and avoiding directly addressing the client’s affective concerns. 147
In our data, the CHs do not generally respond to callers’ displays of emotional stance with overt expressions of empathy/sympathy. This is not to suggest that empathy is not important in complaints communication. Professional guidance to CHs includes the recommendation that complainants should be treated with ‘professional empathy’. Complainants also clearly value empathy and comment, in interview, on whether they felt they were treated with empathy. Moreover, CHs in our corpus are often perceived as highly empathic despite never using overtly empathic expressions. Conversely, as Chapter 6 demonstrates very starkly, communication experiences that include overt expressions of empathy are not always perceived as empathic.
This apparent contradiction relates to the challenges in conceptualising empathy. Empathy is broadly seen as ‘a matter of understanding, of knowing the other person’s experience’. 148 In CA, empathy is conceptualised as an interactional accomplishment, an observable product of how we talk, and prior research in CA has been on examining ‘empathy displays’. However, what constitutes an empathy display and how the boundary is drawn between talk that displays empathy and talk that is perceived as empathic remain somewhat contested. For example, while Hepburn and Potter149 restrict empathic responses to those involving an explicit formulation of the other’s mental state, and a marker of the epistemic contingency of the mental state formulations, others include a broader set of formulations that claim understanding without necessarily constructing mental states. 150 Empathy displays may also be defined as including non-verbal behaviours and prosodic resources that mirror the affective stance of the prior speaker,151,152 although Ford and Hepburn153 argue that the latter, non-semantic, practices are sympathetic rather than empathetic.
For our purposes, we differentiate between CH responses that directly affiliate with the caller’s affective stance and forms of talk that achieve empathy as a perceived impact without overtly addressing the caller’s affective stance. Drawing the distinction in these terms supports the translation of our findings into useful training resources by focusing on the features of the callers’ stance that convey bids for different kinds of affiliation; as our analysis demonstrates, CHs who make effective use of other forms of affiliation are often perceived as highly empathic, but there are moments when affiliation with affective stance appears to be important. Here, we turn to the moments in our data where CHs recurringly affiliate with the affective stance displayed by the caller.
Complaints calls are typically focused on concerns that are recognisably upsetting for callers; there are moments in some calls where the caller moves from talking about distressing details to becoming hearably distressed. CHs need to negotiate this distress sensitively in order to be able to proceed with the institutional tasks of complaint recipiency. These are the moments where CHs respond with empathy and directly address the caller’s emotions. For example, in Extract 36, the caller is reflecting on the care she receives from her doctors in contrast to the mental health support worker who is the focus of her complaint. This triggers her distress, first hearable through her ‘wobbly voice’ which indexes incipient crying and then made more explicit by the hearably tearful ‘give me a wee second’:
Extract 36
IC68
The CH’s responses in this extract focus directly on the caller’s displayed distress with repeated uses of ‘take your time’149 and explicit recognition that the complaints process is difficult for the caller. The latter works as a form of explicit empathy in so far as it formulates the caller’s subjective experience as ‘difficult’ and claims hedged understanding of that experience: ‘I understand this may be difficult’.
As with the evidence from other institutional settings with tension between information gathering and expressions of distress, the CH’s primary orientation here is to the caller’s difficulty in proceeding. 147 Hepburn and Potter149 suggest that ‘take your time’ is deployed in helpline contexts to acknowledge that the caller’s distress is preventing further talk and to license that momentary break in talk. As such, they argue that it is not an overt expression of empathy but is highly affiliative and its absence in contexts of caller distress is perceived as unsympathetic. For our purposes, the consequential observation is that it involves a switch to directly attending to (and affiliating with) the caller’s emotional state rather than the substance of their complaint narrative. Interestingly, a related context in which CHs express similar affiliation with the caller’s affective stance is where the CH formulates the caller’s subjective experience of making the complaint as ‘difficult’ or ‘upsetting’, as a vehicle for accounting for prioritising non-empathic, institutional tasks such as recording personal details.
Comprehending complainability as affiliation
Given the relative lack of overt empathy in our data, along with the importance to participants of feeling that they have been treated with empathy, a priority in our analysis was to understand the CH practices that lead to this sense of having been treated empathically. Careful analysis of calls that were rated by the caller as highly empathic pointed to a set of affiliative practices that can be categorised as displaying comprehension turn-by-turn of the complainability of the details of the caller’s complaint narrative. In contrast to overt empathy (which was infrequent and deployed in specific contexts with an orientation to institutional progressivity), comprehending complainability as a set of practices was evident across our entire corpus; the noticeably empathic calls were differentiated by the high frequency of this type of affiliation within the single call, creating a cumulative empathic impact.
Extract 37 provides a good example of two different practices that achieve this type of affiliative uptake. The caller, at this stage, has provided a lengthy narrative about an X-ray the previous year which led to a diagnosis of a crumbling spine, her subsequent collapse with a broken femur a month later, and issues with her recovery. Here, she is describing a follow-up appointment several weeks later:
Extract 37
PI05
In this extract, the caller narrates the moment where she learns that she had had a hairline fracture in her femur the previous year. The CH’s responses in lines 6 and 8 deploy ‘appendor questions’154 to make explicit two significant, but implicit, elements of this story: firstly, that the hairline fracture had been visible in an X-ray that had been taken before she collapsed with a broken femur and, secondly, that she had not been informed. In The need to be listened to, we described different practices for displaying listenership. This listenership practice doesn’t just receipt the information from the caller but actively displays a ‘candidate understanding’ of the implications of the information – specifically how it contributes to the caller’s complaint. In other words, the responses affiliate with the complainability of the story by displaying on-record understanding of what makes it complainable, while the repair initiation format still orients to the epistemic authority of the complainant by seeking confirmation of that understanding by the caller. 155
The final lines of this extract illustrate a second practice used to affiliate with complainability: a ‘so’-prefaced formulation. These foreground information that has particular contextual salience;156 in complaints handling, they are thus often used to formulate the CH’s candidate understanding of the ‘point of complaint’. 130 In this extract, the caller has confirmed the CH’s candidate understanding of the elements foregrounded by the CH’s appendor questions, then narrates her reaction at the time using direct reported speech. The CH’s ‘so’-prefaced formulation then reformulates the implications of his previous appendor questions as a candidate understanding (‘I guess what you’re asking me today is’) of the point of complaint of the call (‘why wasn’t it picked up in August?’).
An interesting feature of this particular use of a ‘so’-prefaced formulation is that it occurs in response to the caller’s display of affective stance, animated through the use of direct reported speech and marked prosody. The caller’s turn makes relevant both affiliation with the caller’s affective stance but also validation of the complainability of the revelation. By summing up the point of complaint with a formulation, the CH neatly validates the complainability, thus displacing the opportunity to provide affective affiliation. In other words, as noted above, the CH prioritises the institutional focus on formally recording the complaint but does so in a highly affiliative manner.
In Extract 38, the CH demonstrates comprehension of complainability by producing a second assessment that makes explicit the implied negative assessment in the caller’s prior turn. In this extract, the caller is complaining about waiting times:
Extract 38
RC26
In line 5 the caller clarifies the waiting time she has been given. This conveys an implicit negative assessment of the duration of the wait and the CH affiliates with the implicit negative assessment by making it explicit, ‘that’s far far ahead’. By making explicit a caller’s implicit evaluation in this way, the caller affiliates with the complainability of the assessment. Expressions of time are frequently involved in this type of implicit assessment as waiting times are a significant feature of NHS complaints. But other types of complainable negative assessments are also affiliated with in this way. For example, in this next extract the caller is complaining that he was left on his own to get from reception to A&E with a knee injury (in a hospital where porters usually provide wheelchairs from A&E):
Extract 39
PI02
The CH first provides an appendor question that makes explicit the caller’s implied complaint about the lack of help to get to A&E. As in Extract 37, the caller confirms the CH’s candidate understanding with an Extreme Case Formulation that foregrounds the complainability of the concern8 before elaborating on the details of his struggle to get to A&E, including an implied evaluation of distance (‘eventually got within twenty yards or thirty yards’). The CH responds to the implied negative assessment by making it explicit (‘that’s a long walk up there’). This extract provides an interesting comparison with Extract 38 because although it uses the same practice and affiliates with the complainability of the assessment, overall, it is less affiliative in outcome; the issue of distance is not produced as the ‘point of complaint’ so much as an exacerbating factor, whereas in Extract 38 the duration was the point of complaint.
What we have shown is that CH practices demonstrating an understanding of the complainability of the details of the caller’s experience provide a vehicle for affiliative uptake that meets the caller’s need to feel listened to. These practices involve moment-by-moment negotiated sense-making, often offering candidate understandings of the caller’s perspective for the caller to accept or reject as well as making explicit aspects that were implicit in the complainant’s narrative. This perhaps accounts for why these calls are perceived as highly empathic despite the lack of overt empathy. While some authors argue that empathy involves explicit orientation to another’s emotional state,149,157 others158 refer more widely to displays of understanding of the other’s perspective. Affiliation that demonstrates comprehension of the caller’s stance towards the complainability of their story can thus be understood as achieving empathy by negotiating shared understanding of the complainant’s perspective on their complaint story. These practices for displayed understanding of the caller’s perspective have been incorporated into Real Complaints Training as a detailed approach to meeting the requirements for active listening to ensure that complainants feel listened to.
Affiliation to reason
The final type of affiliation revealed as important for complaint handling is affiliation to reason. This type of affiliation is obviously closely tied to the complainant’s need to be acknowledged as reasonable which, as our longitudinal case analysis has shown, permeates the entire complaint journey, influencing how complainants talk (and feel) about their complaint at every stage. Previously we discussed the practices callers use to pursue acknowledgement of their identity as a reasonable complainant. In this section, our focus turns to the practices CHs use to validate callers as reasonable without being heard as agreeing with the caller’s complaint. Some of these practices relate directly to callers’ practices for pursuing recognition as reasonable, while others relate to the reasoning explicitly or implicitly conveyed in the callers’ complaint narratives. One striking feature of CH turns oriented to affiliating with reason is that they usually involve combining multiple forms of affiliation.
One set of practices for affiliating with reason focuses on directly affiliating with the caller’s self-presentation as a ‘reasonable complainant’ by validating either their decision to complain or their motivations for complaining.
In Extract 40, the CH validates the caller’s decision to complain, with ‘you’re right to come to us’:
Extract 40
IC40
Note, the CH first demonstrates comprehension affiliation in a ‘light touch’ form with the anticipatory completion in line 8 of the caller’s turn in line 7. 159 The CH thus first displays understanding of the complainability of the caller’s concerns before validating the decision to make the complaint.
In Extract 26 above, the CH also validates the decision to complain but does so implicitly first through aligning and affiliating with the caller’s assessment that they are ‘not malicious or anything like that’ and then through a formulation that presents the caller’s motivation for complaining as reasonable (‘you just want yourself to get sorted’). The CH’s formulation directly affiliates with the caller’s reasoning motivating their complaint and emphasises the reasonableness with ‘just’ which frames the motivation as proportional and restrained. Again the CH deploys a form of anticipatory completion that is maximally affiliative in that it demonstrates anticipatory understanding of the motivation that the caller was formulating.
Callers often construct their reasonable complainant identity through accounts that frame their decision to complain as a last resort or driven by extreme circumstances. In Extract 41, the caller has been describing his ‘horrendous experience’ of having a heart attack and waiting in A&E in one hospital before being transferred to a different hospital where he had another heart attack. Although his complaint centres on the duration of his wait to be seen in the first hospital and the damage to his heart caused by that wait, his narrative leading up to this point focuses on his extreme pain and distress during the whole experience.
Extract 41
PI16
The caller formulates his complaint with an extreme case formulation, ‘an absolute disgrace’, before pursuing recognition of a reasonable complainant identity. The CH responds to this appeal with a reformulation of the caller’s ‘awful experience’ as a reasonable account for making the complaint. This affiliates both with the caller’s affective stance and with the caller’s appeal to reasonableness, while avoiding affiliation with the caller’s negative stance towards his wait in the first hospital. This pattern repeats throughout this call: the caller handler recurringly affiliates with the caller’s heightened affective stance (she is unusually empathic) and with his multiple bids to be acknowledged as reasonable, whereas her uptake of the core part of the complaint, which she summarises for him three times during the call, remains entirely oriented on a neutral recording of the complaint, for example, ‘so basically we’re focusing on why did it take so long to be seen in the out of hours (.) at Barlett, that’s kinda the (.) the crux of the (.) the problem’. Interestingly, the caller is highly complimentary at the end of the call, commenting that ‘it has been smashing talking to you, smashing manner’, providing strong support for the claim that these forms of affiliation matter to the caller experience of complaints interaction.
While the previous set of extracts involved affiliating directly with caller’s bids to be acknowledged as a reasonable complainant, Extracts 33 and 30 show how CHs can validate the caller as reasonable by validating the caller’s reasoning in their complaint narrative.
In Extract 33, the caller makes a clear appeal to reason by invoking common-sense reasoning and general knowledge160 The use of the adverbial obviously frames the turn as presenting common-sense reasoning and the switch to generic, non-specific somebody combined with the present tense (‘when somebody waits’) indexes a generalisation. Thus, although what she describes in this turn is her personal experience that has led to her complaint, these linguistic features frame it not as personal but as an obvious (and therefore reasonable) generalisation. The CH’s response, on the other hand, first claims understanding and then demonstrates understanding by switching back to invoking the caller’s first-hand experience to affiliate with the complainability before explicitly claiming affiliation with the caller’s reasoning with ‘I understand where you’re coming from’.
In Extract 30, lines 9–12, we see a concise example of affiliation to reason in response to the caller’s use of the concession structure ‘I know X (concession), but Y (complaint)’. What is interesting in this extract is the CH’s orientation to the recognisability of this reasoning structure as a practice for emphasising reasonableness, as revealed by the position of the CH’s affiliative response which comes in overlap with but and affiliates with reasonableness by denying the need for the concession. Note that again, this affiliation to reason is combined with comprehension affiliation that underscores the affiliation to reason by providing a formulation of the ‘main point’ of the caller’s complaint.
Caller priorities and affiliation
This analysis shows that complainants’ overarching priorities are observable in the interaction both in the callers’ turns and importantly in the responses that they observably pursue from CHs. Those responses typically involve context-sensitive use of the three kinds of affiliation discussed above. The boundaries between different types of affiliation are somewhat fuzzy but some key insights have emerged about the different kinds of affiliation. We have shown that comprehension-oriented affiliation meets caller’s need to be listened to and to tell their story. By meeting these needs, it is perceived as highly empathic, so is an important interactional resource for meeting the emotional needs of the complainant. This is significant because although complainants expect to be treated empathically, overt empathy and affiliation to affective stance do not appear to be prioritised in these complaints encounters. Our analysis also shows that treating the caller as reasonable overlaps with comprehension in that when CHs demonstrate understanding of the complainability of the caller’s experience they also imply that the caller is being reasonable in making the complaint by showing that the complainability is recognisable. A similar interaction arises between reason and affect: our analysis of hypothetical reported thought as an affiliative practice in complaints advocacy makes the case that interactional orientation to affect involves both emotive states and the reasons for them. Affiliation to reason thus can also serve to meet the wider affective needs of complainants. These interactions begin to account for our overarching claim that participant orientations to the caller’s need to be seen as reasonable are a driving force in the overall trajectory and outcomes of complaints encounters and therefore foundational for any complaint-handling communication training.
Affiliation in challenging contexts
Negotiating blame and criticism
Complaining involves not just an expression of ‘feelings of discontent about some state of affairs’ but also attribution of responsibility for the state of affairs causing the discontent. Pino’s analysis146 of third-party complaints in an institutional setting labels these two components of complaining as ‘hurt’ and ‘blame’ and argues that they are constituent components of the action formation of complaining. Blame, however, may be quite implicit and diffused or non-specific. For example, complaints are sometimes expressed with passive voice or with non-specific ‘they’:
Extract 42
RC22
Here the caller uses multiple linguistic devices to leave the agent of his father’s poor treatment, that is the blame, unspecified: passives (‘unbelievably let down’), non-specific they (‘they said he’s still showing as an in-patient’) and noun phrases that avoid specifying agency (‘nothing, no medication, no referral letter, no doctor’s letter’).
In the context of the NHS, blame is often left implicit161 or, as our longitudinal findings show, generalised to failings of the wider NHS ‘system’. Sometimes, however, blame is explicit, personalised and directed at a specific individual. This presents obvious challenges for CHs who need to accurately (and affiliatively) record the complaint without appearing to agree with or uphold the caller’s still-uninvestigated blaming of a particular individual. We investigated this particular interactional challenge to identify CH practices that either escalate or de-escalate individual blame and to understand how CHs avoid agreeing with explicit blaming without appearing to undermine, disbelieve or disagree with the caller’s account of their complaint.
Extract 43
IC68
The complainant is ringing to complain about the breakdown in her relationship with her mental health support worker and to make sure that she is allocated to a different support worker. At this point in the call, the caller makes an explicit criticism of her support worker: namely that she patronises her by addressing her as ‘pet’. The CH responds with a continuer and the caller pursues a more substantive response with a more specific and somewhat escalated illustration of this criticism. Further lack of uptake from the CH leads to more explicit stance-taking from the caller along with escalation of the blame to explicitly impute negative intentions to the support worker. This extract illustrates how receipting explicit blame as if it were neutral information leads to the patterns of pursuit previously discussed. This is unsurprising as complaining makes affiliation relevant, so each of the CH’s neutral responses represents a noticeable absence of affiliation leading to pursuit of affiliation.
Pino’s analysis146 of the negotiation of blame demonstrates very persuasively that complaint recipients can ‘decouple’ hurt and blame and affiliate just with the affective stance embodied in the hurt. Pino’s data, however, come from a therapeutic setting. In our complaints data, CHs also decouple hurt and blame but deploy particular forms of comprehension affiliation and of affiliation to reason as effective resources for the negotiation of blame. These forms of affiliation directly or indirectly validate the caller as a reasonable complainant without agreeing with the blame or the assessment of the complained-about person.
The first set of practices directly validates the caller either by affiliating with the caller’s decision to make a complaint or by acknowledging the seriousness of the complaint issues. For example, in Extract 44 the caller has made extended allegations of abuse by staff in a mental health ward. The CH validates the caller by labelling the accusations as serious and focusing on the procedural implications:
Extract 44
IC15
In this second extract, the CH validates the caller by focusing on their decision to complain:
Extract 45
IC30
Here we see that the CH responds to the caller’s accusation (repeated from earlier in the call) that ‘the guy’s actions were outrageous’ by validating the caller’s decision to make a complaint and making extended generalised assertions about welcoming feedback (though it should be noted that the downgrading of the call to ‘feedback’ rather than a complaint would not be seen as good practice). These response strategies that treat the caller as a ‘reasonable complainant’ help to move the focus of the call away from the individual blaming, and we see in both examples that the caller accepts the response and the call moves swiftly to call closure.
The shift to speaking in general terms noted in this last extract is another practice for providing affiliative uptake in contexts of blame. For example, in Extract 46 the caller has been criticising her social worker and the CH switches to ‘what usually happens’:
Extract 46
IC68
We see a slightly different application of this generalising type of response in the next extract from the call seen in Extract 44. Here, we see the caller make multiple allegations of different kinds of abuse and then list their belongings that have been taken, ending with their mobile phone:
Extract 47
IC15
The caller handler responds to this series of allegations by generalising about the process for ‘some patients’ in mental health wards. This frames the caller not having their mobile phone as a ‘normal’ part of being in hospital and provides a resource to raise the potential of face-to-face contact, which the caller accepts as a positive offer.
Each of these applications of the idea of generalisation is context-specific but, in each case, it serves to treat some aspect of the caller’s experience as ‘normal’ and ‘expectable’ and thus indirectly treats the caller as a ‘normal’ ‘reasonable’ person going through a ‘normal’ and ‘reasonable’ process. In each case, we see that the move to generalisation facilitates progressivity through the call, supporting the claim that it is perceived as affiliative by the caller.
The first set of practices for negotiating blame was, to varying degrees, oriented to affiliation to reason. Our data also show that caller handlers may negotiate blame with comprehension affiliation through reformulating what the caller has said in ways that help to mitigate or diffuse the blame. For example, in Extract 48 the caller is complaining about a rude receptionist. The caller had asked the receptionist whether they could take pain relief while waiting for triage and complains that the receptionist was very rude to them and accused them of trying to ‘jump the queue’. In the extract, we see the CH reformulate the issue as ‘a wee bit of a communication issue’:
Extract 48
RC16
Notice that while this practice of reformulating addresses the explicit criticism of the receptionist, it is combined with other forms of affiliation oriented to validation of the caller. The CH displays comprehension of the complainable, showing comprehension of the caller’s perspective of her own behaviour as reasonable, as well as affiliating with reason through the practice of validating the caller’s decision to complain by valuing the complaint as feedback to improve the service. This practice of combining reformulation with other forms of affiliation seems to work to mitigate the risk that it might otherwise be seen as distorting or undermining the version of events presented by the caller.
Our final set of practices for negotiating blame demonstrate taking the caller’s concerns seriously through the practices used for receipting and recording those concerns. This is sometimes done by paraphrasing, and sometimes by what we call ‘typing aloud’ –citing back the caller’s own words to them as a form of record-taking. We see both these practices in Extract 49, which is from a complaint about a social worker who blocked the caller’s contact visits with his children on the grounds that he ‘smelled of drink’ (the caller is adamant that he does not drink):
Extract 49
IC23
In line 1, we see the CH overtly preface typing aloud with a reference to his task of recording the complaint (‘I’m gonna say’). Prefacing it in this way provides an anticipatory account of the extra time it takes, which is often more explicitly referenced with phrases like ‘bear with me a wee second’. The typing aloud follows and is prosodically highly distinctive, marked with multiple silences and continuing intonation. Note the caller collaborates with this very overt display of getting the complaint ‘on record’. The CH’s turn of typing aloud in lines 10–12 also illustrates the practice of paraphrasing as he types aloud ‘her comments regarding his hygiene’ rather than the caller’s words (‘she called me scruffy and smelly’).
Sometimes the typing aloud, as an audible form of the act of writing the caller’s words, is further signalled through the use of the first-person pronoun as a way of marking the text as the caller’s own words. We see this in Extract 50, which is a continuation from Extract 47:
Extract 50
IC15
As with the previous example, we see here the typing aloud prefacing and the explicit reference to what has been recorded (‘I’ve taken a note …’). This last set of practices that focus on explicitly orienting to recording the caller’s own words might be seen as a strategy of last resort. It works very effectively in some calls, where CH and caller collaborate on the recording of the details, but we also see in many of our calls that callers orient to ‘mere’ recording of their complaint as insufficiently affiliative and pursue a more affiliative response from the CH through repetition and escalation.
Our analysis thus shows that affiliation provides effective resources for the negotiation of blame. It also reinforces our claim that orientations to the reasonable complainant identity are a key driver in these conversations. These particular forms of affiliation directly or indirectly validate the caller as a reasonable complainant without agreeing with the blame or the assessment of the complained-about person. We again saw that the various practices are often most effectively used in combination, particularly with more risky practices such as reformulation which otherwise might be heard as undermining the complaint. Our data also show that in some cases, individual blaming may be an effect of anger and frustration rather than the key point of the complaint. A significant task for CHs is thus to deploy comprehension affiliation effectively to determine where this is the case.
Affiliation, context sensitivity and timing
Our analysis thus shows the effectiveness of affiliation across a wide range of complaint contexts. Crucially, however, the effectiveness of affiliation relies on fine-tuning responses by attending to the cues in the immediately prior turn. An important implication of this is that when applying these findings to training, affiliation cannot be presented as a decontextualised set of response strategies.
This final section draws on the insights developed in the previous sections to demonstrate the importance of the context sensitivity of affiliation. We examine examples where there is a poor fit between the affiliative practice used by the CH and the immediately prior talk by the complainant to show that timing matters for a practice to achieve its affiliative potential.
In Extract 51, the caller has been left with a catheter following post-operative complications and is upset at the length of time he has to wait to get a test before they can consider removing the catheter. Here the caller complains that he hasn’t seen a doctor – he has been treated by nurses for his follow-up care. Note that the caller has already twice raised his concern at not seeing a doctor without any uptake of this concern from the CH [‘I mean ah- I have not seen a doctor (1.8)’ and ‘I- I (really) (1.0) I want to see a doctor (.) but (0.4) they want to do a test’].
Extract 51
PI04
The CH in line 11 deploys a version of the generalising practice: a practice which we have seen can work very effectively to frame the caller’s experience as ‘normal’ and ‘expectable’. However, in this instance, we see that the caller interrupts the CH’s attempt to explain the expertise of the Extended Nurse Practitioners (ENPs) to express escalated distress at not knowing ‘what is happening with my body’ and in subsequent turns his complaint escalates further. 145 The generalising practice here is thus not only not effective, it leads to further escalation of the complaint. This example illustrates the importance of turn-by-turn analysis, what is made relevant turn-by-turn in the sequence and the position of the practice in the sequence. From this perspective, we can see that an explanation of the care provided by specialist nurses was made relevant following the caller’s turns in line 3 and line 5 (as well as following the two earlier complaints about not seeing a doctor) but these turns are met with silence and a continuer, following which the caller’s complaint escalates to focus on his heightened emotional state. This is when the CH, following a 0.6-second silence, moves to explain the expertise of ENPs. In other words, this practice is located in a position where the caller’s affective stance has been made relevant and the caller subsequently pursues acknowledgement of his affective stance (line 16), orienting to the account of ENPs as irrelevant/insufficient. The point here is that an explanation of the expertise of the ENPs might have been reassuring if delivered at the first opportunity (i.e. when the caller first expresses concern at not seeing a doctor), but, following multiple missed opportunities, the effect of the position of the explanation here is to seem defensive and uncaring. This illustrates a key issue for the effectiveness of affiliative practices which is timing: an effective practice deployed too late at best is ineffective and at worst escalates the complaint.
A brief overview of a single call further illustrates how timing matters for the effective use of affiliation. For this we return to the call illustrated in Extracts 20 and 21. These extracts were taken from early in the call and showed how the early phases of the call were marked by a lack of affiliation by the CH and a significant amount of repetition and escalation by the caller. This is also the call where we saw explicit blaming emerge as part of that escalation (Extract 43). Looking at this call as an overall encounter, further observations emerge about the timing of the affiliation opportunities and the impact of the timing of the CH’s use of affiliation. This call is about the breakdown in the caller’s relationship with her mental health support worker. The first observation is that the caller initially frames the problem as ‘me and her have been bumping heads’:
Extract 52
IC68
This early framing is significant firstly because it is repeated but also because the framing is less critical and less accusatory, so the missed opportunities for affiliation are actually missed opportunities to maintain this less personal, less critical framing. We saw in Extract 21, lines 26–32, that the missed opportunities to affiliate led to escalation and the suggestion that the mental health support worker was trying to be deliberately harmful. In that extract, the CH finally produced an affiliative response, ‘it’s having an impact on you’ (line 30), following the caller’s escalation and pursuit of affiliation through noticeable silences. This response acknowledged the impact of the complaint on the caller but deployed at this late stage of the call, the reference for ‘it’ was the alleged harmful intent of the mental health worker rather than the relationship breakdown, the ‘bumping heads’ (Extract 52). In other words, the affiliation with lifeworld impact comes too late so feeds the escalation to increasingly personal criticism.
In the closing phase of the same call, we see that the caller’s unmet concerns persist, which delays progress of the call through to closing as the caller relaunches and escalates narration of those unmet concerns. The CH attempts to use the practice of validating the caller but the caller ignores the CH’s turn and relaunches her complaint with her key point that she won’t attend appointments with the mental health support worker:
Extract 53
IC68
The repeated noticeable absence of affiliative uptake leads to an extended retelling of her criticism of the mental health worker, labelling her as ‘condescending’ and her actions as ‘degrading’. After this extended retelling, which is marked with all the features of pursuit of affiliation, the CH deploys the practice of overtly referencing the recording of the details [‘Okay. Well, I have taken a note of that Edith uhmm (1.2) I will type all that out’] to transition into closing but again the caller resists the closing move and relaunches her complaint narrative, this time not retelling details already noted but escalating the complaint with a bid for validation as a reasonable complainant in relation to the blame that extends her criticism to include the support worker’s interactions with others:
Extract 54
IC68
Again, we see repeated pursuit of affiliation before the CH validates the caller but with a rather downgraded labelling of the caller’s stance: ‘You’re just concerned, yeah. No, I understand’. The caller accepts the move to close but only after a further 0.7 second noticeable silence. Examining the overall progression of this single call illustrates not only how multiple missed opportunities to affiliate result in an extended and escalated complaint but also how affiliative practices deployed later in the call are much more limited in their effectiveness.
Conclusion
The interactional analysis presented here has focused on the aspects of the analysis that underpin Real Complaints Training. Overall, our analysis has shown that affiliation is key for effective and efficient complaints handling. Within that overall insight, we have seen that being seen and treated as reasonable is, for complainants, the driving force for much of the pursuit of affiliation. This provides interactional/observational weight to the insights about complainant perspectives and priorities emerging from the appraisal data examined in Chapter 5. Callers consistently pursue recognition not just of the details of their complaint narrative but of the reasoning driving their complaint, which very often includes reference to the subjective experience and lifeworld impact of the complaint. As such, the affective stance-taking in the complaint narratives primarily functions as a vehicle to convey the seriousness of the concerns rather than primarily as bids for empathic uptake. In this way, we see that the affective aspects of a complaint narrative are closely tied to the reasoning and the need to be seen as reasonable in making the complaint. These interactions between different kinds of bid for affiliation shed light on the observation, also seen in Chapter 6, that overt expressions of empathy and/apology are insufficient, and potentially even counterproductive, without other forms of affiliation, particularly validation of the caller as reasonable.
Additionally, our detailed examination of the turn-by-turn progress of individual calls demonstrates powerfully that timing matters. Affiliative practices are highly effective in meeting callers’ needs when used context-sensitively as a timely response to particular bids for affiliation. However, where callers’ bids for affiliation don’t receive affiliative uptake, affiliation is pursued turn-by-turn in ways that not only extend the duration of the call but often lead to escalation of the scale, scope and emotional intensity of the complaint. Our analysis also showed that where affiliative practices are sequentially deferred, they are problematic in a number of different ways. For example, we saw that a generalising explanation left too late was perceived as defensive and that affiliative practices deployed following escalation can exacerbate the escalation.
Thus while the cultural audit in Chapter 4 and the longitudinal analysis in Chapter 5 reveal the importance of a person-centred approach to the complaints process, our microanalysis of real complaints communication shows empirically what person-centredness looks like in actual interactions, while also persuasively demonstrating that simple prescriptions to ‘apologise’ and ‘show empathy’ are clearly inadequate as guidelines for successful complaint handling.
In Chapter 8, we demonstrate how these findings have informed the development of Real Complaints Training.
Chapter 8 Real Complaints Training and guidance
Research objectives 5 and 6 of the project are focused on translating our research outcomes into bespoke communication training resources and good-practice recommendations for NHS complaint handling.
In this chapter, we focus on the process and outcomes of the development of Real Complaints Training and the emerging guidelines for good practice for written responses.
Development of Real Complaints Training
Real Complaints Training has been developed from our microlevel examination of the real-life progress of encounters between complainants and the NHS throughout the complaints journey (see Chapter 5). The value of this approach is discussed in Chapter 3. Here, we focus on how our analysis of complaints interactions has been translated into effective and accessible training resources for CHs. We will outline the design of the training package and how it relates to our underpinning research and then move to explaining how we engaged with stakeholders during both the design phase and subsequent evaluation to ensure accessibility and useability.
Real Complaints Training
The design of Real Complaints Training is focused on providing experiential, reflective learning to foster in participants enhanced awareness of how their interactional conduct affects the progress and outcomes of their conversations with complainants. Our analysis of real-time, actual complaints encounters provides us with evidence firstly of the specific interactional challenges involved in complaints encounters and secondly of the particular practices that CHs naturally deploy to address these challenges. In this way, we make visible the ‘tacit’ communication competencies employed by CHs and build training based on practices that demonstrably work in real-world conversations.
The specific interactional challenges of the healthcare complaints encounter relate to the tensions between competing institutional and interpersonal agendas – the institutional requirements for accurate objective information-gathering to support complaint investigation and the interpersonal significance of the subjective, typically highly emotive experience at the heart of the complaint. Our analysis showed that affiliation is key to the effective negotiation of these competing agendas, because affiliation operates at the interpersonal, relational level in interaction without displacing the informational. As our data analysis showed, timely use of context-sensitive affiliation facilitates efficient and effective complaint handling, while missed opportunities to affiliate lead to repetition and escalation in the complainant’s explanation of their complaint and consequently also to potentially significant delays in the CH’s institutional agenda.
Real Complaints has thus been designed to build CHs’ interactional awareness specifically of (1) how callers signal and pursue their interpersonal needs, (2) how they can meet caller’s needs while staying within the professional constraints of their institutional role as CH and (3) how their own language behaviours influence the trajectory of a complaints encounter. The training is designed around extracts from our corpus of recorded encounters (transcript and recordings) selected to illustrate specific communication practices and outcomes and to stimulate reflection on how those practices impact on the trajectory of the conversation as well as wider discussion of the needs and priorities of complainants.
The content, structure and design of the training have been through multiple phases of stakeholder evaluation to ensure maximal useability and accessibility as well as ensuring that the final set of resources meet the professional and practical needs of participants. This evaluation process has led to a modular structure to facilitate flexible use of the materials to meet training needs and accommodate practical constraints on delivery (Table 8). The materials include workbooks and presentations as well as ‘train the trainer’ documentation. The presentations include sound files (with accompanying transcript) for the data extracts. The workbooks include the data sets and exercises as well as supporting materials such as a guide to transcription practices, references for the underpinning research and, importantly, a ‘key take-aways checklist’ that participants can use to reflect on their own practice. The ‘train the trainer’ materials provide accessible explanations of the primary research and guidance on the use of the data sets to ensure retention of the integrity of the relationship between the training and the underpinning research.
| Module | Content |
|---|---|
| 1 | Focusing on listening |
| 1.1 | Listening as a moment-by-moment skill |
| 1.2 | Ways of listening |
| 2 | Listening to callers’ needs |
| 2.1 | Recognising cues to callers’ priorities |
| 2.2 | Recognising cues that callers’ needs aren’t being met |
| 3 | Using affiliation to meet callers’ needs |
| 3.1 | Dealing with emotion and distress |
| 3.2 | Using affiliation to listen effectively |
| 3.3 | Respecting the complainant as a reasonable person |
| 3.4 | Why timing matters |
| 4 | Affiliation in challenging contexts |
| 4.1 | How and why blaming occurs |
| 4.2 | Successfully negotiating blame with affiliation |
| 5 | Affiliation-focused reflective practice |
| 5.1 | Applying the affiliation framework to reflect in professional practice |
The training materials may be used to complement existing training either:
-
as separate training modules that complement and sit alongside existing training, or
-
by trainers integrating the data sets and their insights into existing training courses on empathy, active listening and professional neutrality.
Real Complaints module content
Module 1: focusing on listening
This section of the training establishes the Real Complaints CA framework for reflecting on communication in terms of the moment-by-moment experience of a conversation and the context-dependent nature meaning. The module provides training on listening skills that draws on core conversation analytic insights about the relationship between turn-taking and listening, as well as on our research on how particular call handler choices of listening response influence whether (or not) callers feel ‘heard’. This framework-setting module works as a standalone module to stimulate reflection on foundational communication skills but is primarily designed as introductory resources for the other modules in the training package.
Module 2: listening to callers’ needs
Our research revealed three key communication priorities for callers with implications for the listening practices of CHs, who need to listen for what matters to a caller both in the moment and overall in a call and to take that into account when replying. The module focuses on developing CHs’ awareness of the cues that callers display to convey that their interactional needs are not yet being met. Our findings indicate that this is a key training objective as not meeting callers’ needs causes delays and disruption to a call and may lead to escalation of the complaint. These cues provide an early indicator of potential problems as they emerge in a call. Sensitivity to these cues thus helps avoid escalation. This module encourages reflective practice for even the most experienced of call handlers because of the microlevel focus on callers’ cues which supports the development of CHs’ ‘conscious competence’.
Module 3: using affiliation to meet callers’ needs
This module stimulates reflections on best practice in responding to complaints, focusing on how the skill of affiliation supports active listening and professional empathy. The module applies our findings relating to how affiliation needs are interactionally signalled and met, as well as how different types of affiliation interact and intersect and the impact of not meeting affiliation needs. The module provides exercises relating to each of the relevant categories of affiliation in turn, as each is significant to complaint handling in a different way. A central objective is supporting trainees to recognise different patterns of interactional behaviours relating to the different categories of affiliation but also to develop a critical awareness of the inherent context sensitivity of the different forms of affiliative response and how they interact. This is fundamental to appreciating that affiliation cannot be understood simply as a decontextualised set of response options. The module also includes data sets that demonstrate how affiliation needs evolve over the trajectory of an encounter, building on our analysis of the significant impact of timing on the outcomes of the use of affiliation.
Module 4: affiliation in challenging contexts
This module focuses on the interactional challenges of negotiating explicit, personalised blaming. The module reflects on the contexts in which explicit blaming emerges and the affiliative strategies that are used to successfully negotiate blaming without either agreeing with the blame or undermining the complaint/complainant. The workbook tasks also extend the critical reflections on context sensitivity and timing that were introduced in module three.
Module 5: affiliation-focused reflective practice
This final module offers opportunities to practise applying the take-away checklists from the previous modules to case-study calls, either from participants’ own practice or from the Real Complaints corpus of calls.
Training design and evaluation: stakeholder engagement
The development of Real Complaints Training involved extensive stakeholder engagement throughout the design, development and evaluation process as follows.
Round-table event
The first event was a round-table discussion of the communication challenges in complaint handling and associated training needs. Seventeen people signed up to attend, including CHs and managers from across all six HCSNI Trusts as well as a representative from the PAS. It included a presentation from NIPSO’s Complaints Standards Manager on the recently approved Statement of Principles for complaints handling by public bodies. A key insight from this session related to the challenge of combining empathy with professional neutrality. This became an important theme in the development of our training.
Stakeholder training design workshops
During the training design phase, a co-design workshop was held to seek stakeholder perspectives on the training focus and data sets as well as guidance on preferred formats. The workshop was attended by five people, including complaints managers and PAS representatives, and led to invaluable feedback which was incorporated into the training.
Stakeholder training evaluation workshops
Lastly, we hosted three ‘taster’ sessions at which draft versions of the training resources were presented. These were delivered to the SPSO (11 attendees), the NIPSO (22 attendees), and the Parliamentary and Health Service Ombudsman (3 attendees), as ‘critical friends’ with expertise, experience and insight to feed into the training development. Attendees ranged from senior leadership to managers responsible for training design and CHs dealing directly with the public. They engaged with interactive exercises to experience working with real complaint data and reflect on their own interactions. Time was provided for discussion and comments; the feedback received was then reflected in the design of new versions of the resources. Feedback was overwhelmingly positive, with many participants expressing the view that such training, particularly the use of transcripts of real recorded data, was useful to their reflective practice and professional development.
Training design and evaluation: an iterative process
Each stakeholder event included time for reflection and discussion, and the feedback was applied to revise and refine the materials in preparation for the next event. Here we discuss how the events contributed to the iterative process of design – deliver – reflect – refine.
At the roundtable discussion, the challenge of responding empathically while maintaining professional neutrality was identified as a major training priority. While NIPSO guidance emphasised ‘active listening’ and ‘professional empathy’, Trust participants asked, ‘what do effective “active listening” and “professional empathy” look like in context?’ This question set the overarching goal for Real Complaints Training and ultimately led to the focus on affiliation. Additional training priorities raised by participants and incorporated into Real Complaints were: early warning signs that a call is going badly; closing calls empathically; responding empathically without agreeing; active listening while note-taking; coping with angry, emotional or abusive callers.
Following the research-led decision to focus on affiliation as a solution to the challenges raised at the roundtable, the Training Design Workshops sought stakeholder feedback on the implementation. Participants confirmed the value of the focus on affiliation to resolve the dilemma between professional distance and empathy and to avoid/minimise escalation. A significant outcome was the decision not to develop training based on the ‘angry call’ data in our corpus as the data raised too many intersecting issues. Recommendations incorporated from these stakeholder workshops were: defining terms more simply to improve accessibility but retaining the technical term affiliation; focusing on practical applications; adopting a problem–solution structure to make training goals more explicit. Additional considerations around the structure and format of the training package were also discussed and led to development of a three-module structure: (1) why affiliation matters; (2) how to affiliate; (3) affiliation in challenging contexts.
The ‘taster event’ workshops presented an outline of the overall project before delivering a subset of the training materials for evaluation and feedback. Participants commented very favourably on the benefits of working with real data and detailed case studies, the value of reflective practice (particularly the microlevel attention to interactional cues and response options) and the relevance of the difficult-caller training. Team reflection on the participant feedback led to a restructuring into a five-module structure with clearly defined trainables as well as the following more specific revisions and refinements:
-
inclusion of ‘key take-aways for reflective practice’ and a single extended case study exercise for practice in applying the key takeaways
-
greater emphasis on examples of good practice and on presenting the training as a means of improving efficiency and balancing the agendas of callers and call handlers
-
more explanation and illustration of how affiliation relates to the concepts of active listening and empathy.
Building on the experience and feedback of the taster events, the full suite of Real Complaints Training modules was developed and two half-day workshops were delivered with the NIPSO complaints teams to evaluate the training for useability and accessibility. Approximately 20 people attended each session. Suggestions for improvements focused on the desire to see more data and have more opportunities to hear ‘whole calls’ rather than extracts. Individual feedback in a post-event survey was overwhelmingly positive (e.g. ‘a very enlightening and worthwhile training event’) and reinforced the value of each of the trainables delivered.
Each of these stakeholder events has thus significantly contributed to the iterative design process and provided indicative feedback on the potential value of the training. A full pilot to measure the effectiveness of the training, although outside the scope of the current project, is in development.
Development of best-practice guidelines for the writing of formal response letters
The Real Complaints Guidance on Best Practice for writing response letters deploys the research insights that emerged from our linguistic analysis of the language used in formal response letters informed by our analysis of our longitudinal participant reflections on the impact of the letters on their overall experience of making a complaint (see Chapters 5 and 6). It was also informed by informal engagement with Trust stakeholders to gather contextual information about practices and processes involved in writing formal final response letters and by discussions at the stakeholder events discussed above which focused primarily on complainant dissatisfaction with final response letters. In this section, we outline how our research insights have been distilled into practical guidance (see Appendix 2) on best practice for both the response writing process and the final response letter itself.
The value of the longitudinal case study approach was in providing an evidence-based understanding of formal response letters as one moment in a journey taking place in a wider organisational cultural context. This more contextualised, relational perspective on the formal response letter led to the inclusion of a section on the preparation for writing and one on the role of the written response in the overall complaint journey. The former draws on our research evidence around complainant dissatisfaction when there is a poor fit between the complaint as understood from the complainant’s perspective and as represented in the final response letter. The latter draws on the evidence from our longitudinal case studies on the dynamic relationship between encounters within a complaint journey, issues with connectivity between encounters and the potential for any one encounter (particularly the final response letter) to ‘overwrite’ positive experiences in previous encounters.
The remaining sections of our best practice guidance draw on the evidence from our analysis of the structure, content and language of our corpus of formal response letters to provide practical guidance on format and structure, what to include, what not to include and importantly how to make effective language choices. The guidance is thus structured around the main sections of a response letter (the opening, the main body of the response, the closing) and provides illustrations of good and poor practice from our data along with examples of complainants’ reflections on their response letters (Table 9).
| Section | Content |
|---|---|
| 1 | How to read/understand complaints |
| 2 | How to write responses |
| 2.1 | How to begin |
| 2.2 | Structure of response |
| 2.3 | Guiding principles |
| 2.4 | Apologies |
| 2.5 | How to conclude |
| 3 | Written responses and the complaint journey |
Our analysis of the language used to respond to specific points of complaint identified specific pitfalls that can lead to marked dissatisfaction. These insights led into five guiding principles for responding to a complaint: acknowledge responsibility; avoid ‘blame evasion’; acknowledge the lifeworld and emotional impact of the complained-about event on the complainant; avoid introducing ‘alternative’ narratives that undermine the complainant’s account of events; make a clear commitment to change/reform. The guidance discusses the challenges in meeting these guiding principles as well as providing plenty of examples to ensure that the principles are translated into concrete advice on language formulations and their effects. Lastly, given the importance of apologising and the persistence of complainant dissatisfaction with the apologies embedded in response letters, the guidance document provides a section on apologies that draws on the empirical evidence in our corpus to reflect on and reinforce existing good-practice guidance on how make an apology.
Patient guidelines
The PAS has already developed a comprehensive guide on how to make a complaint which comprises three simple questions future complainants need to ask themselves before initiating a complaint:
-
What am I unhappy about?
-
What do I want to achieve?
-
Who do I raise my concerns with?
Our findings validate this guidance by showing that they perform important functions: (1) clarifying the point(s) of complaint; (2) formulating a desired outcome; and (3) forestalling potential preconceptions about the complaints process.
Based on our findings, we can add to this list:
-
What can I expect from the complaints process?
and
-
What should I do if the focus of my complaint has changed?
The fourth question will help to form realistic expectations of the complaints procedure (e.g. that problem-solving is not its function), and the fifth, to add a temporal dimension to the complaints journey which is neglected in most guidance on complaining.
These will be developed in collaboration with the PAS to ensure acceptability and useability within the framework of the sixth project objective, which is ongoing.
Chapter 9 Discussion and conclusions
Review of evidence
This section briefly reviews how each of the research objectives listed in Chapter 1 was met and synthesises key findings from across our data sources.
Objective 1 – the complaints’ lived experience
The microanalysis of our observational data (spoken and written) provided robust evidence for examples of both good and poor practice and led to the identification of affiliation as a key communication skill for CHs and the ‘reasonable complainant’ identity as a key priority for complainants.
Objective 2 – patient perceptions of cultural bias in the National Health Service
Our cultural audit survey revealed the need for cultural innovation within the NHS to develop more congruent relational conditions as a precursor for effective complaint resolution.
Objective 3 – complainant appraisals of the complaints journey
Self-reported data and interview data provided important triangulation of the evidence from the observational data as well as demonstrating the significant cumulative effective of successive complaints encounters and the dynamic nature of complainant expectations and experiences at each stage of the complaint journey.
Objective 4 – key drivers of change
Each longitudinal case study was analysed across all data sources to identify, examine and cross-reference key moments. The findings were synthesised across all journeys to identify recurring themes and these insights were cross-referenced with the participant orientation evidence from the micro-analysis of the wider set of interactional data to draw conclusions about recurring patterns in the complainant experience and related communication practices.
Objective 5 – communication training
Real Complaints Training was developed through an iterative process of data analysis and stakeholder engagement to ensure that resources met the needs of complaint-handling teams.
Objective 6 – dissemination
Stakeholder engagement meetings have begun the dissemination of Real Complaints Training and good-practice recommendations. This objective is ongoing.
Main findings and conclusions
Reasonableness as a driving force in the complaints experience
A key finding from both our interactional and qualitative data streams is the pervasiveness of the discursive work by complainants to present themselves as both ‘reasonable patients’ (during the complainable events) and ‘reasonable complainants’ (in the decision to complain and manner by which they raise a complaint). Crucially we have shown the extent to which complainants pursue recognition of their reasonableness in their interactions with complaints staff and the impact this has on the progress and outcomes of a call, as well as the significant benefits of language choices that validate the complainant as reasonable. This finding is central to the unique contribution of Real Complaints Training for CHs.
The emergence of the reasonable complainant identity as significant demonstrates the value of discursive research in revealing and evidencing tacit priorities that nonetheless have a profound influence on experience. More conventional methodologies recognise complainants’ explicit priorities such as the desire for an apology162 and empathic treatment163 or values such as fairness, transparency and timeliness. 164 Our findings demonstrate the importance of understanding how the need to be seen as reasonable interacts and intersects with these more explicit priorities in ways that are consequential for the overall experience of the complaint journey.
This finding is highly significant for recommendations, guidance and training around communication (both spoken and written) as our data show that meeting the complainant’s need to be seen as reasonable is fundamental to achieving a more person-centred approach to complaint handling, but to date has not been discussed in previous research, guidance or policy documents.
The complaint experience as a dynamic journey
Our multiple data sources in our longitudinal case studies reveal the complaint experience as a dynamic journey with evolving narratives reflecting complainants’ shifting perceptions, expectations and experiences of the ‘system’, both moment by moment and encounter-by-encounter. Each interaction within the journey moulds these perceptions and future expectations; hence the paramount importance lies in improving individual instances and enhancing connectivity throughout the complaint journey as each next encounter can ‘overwrite’ the effects of the previous. Our study shows that written responses, which are typically the final stage of the journey, have the most significance for the overall evaluation of the experience. Written responses often miss the mark by not acknowledging accountability, providing insincere apologies, using obscure medical jargon, and detailing irrelevant patient histories. Such issues can propel complainants to escalate their complaint, emphasising the need for more nuanced written communication.
More broadly, our analysis illuminates the dual nature of complaints: as personal expressions of dissatisfaction with care and as systemic critiques, reflected in the motivations to complain. 117 Attitudes towards communication methods manifest themselves in a preference for more personal, ‘human’ spoken interactions to address individual concerns, contrasted with a reliance on formal, written responses to ensure accountability and effect systemic changes. Understanding this duality – complaint and care – is vital to improving the complaint-resolution process by ensuring both the validation of individual lived experiences and effective systemic response. This suggests that scrutinising communication within the service sector is as important as examining process in any investigation into complaints.
Finally, the cornerstone of a successful complaints process is a person-centred approach. It should include: understanding the complainant’s broader life context and recognising the ‘lifeworld impact’ of the complaint and respecting the complainant as reasonable in making the complaint. Inadequacies in addressing these factors, coupled with misunderstandings, misrepresentations and ambiguity, can jeopardise the complaints process, fostering dissatisfaction, mistrust and escalation. This finding mirrors the CA finding about the significance of affiliation in complaints interactions. Therefore, our study revealed complainants’ priorities which are fundamentally important on different levels of communication processes.
Transforming experience through affiliation, person-centredness and congruence
Collectively, our findings show that resolving the dissonance in complainants’ experience stemming from unmet expectations and concerns requires:
-
affiliative interactions with Trust staff in which complainants feel heard and respected as a reasonable complainant
-
person-centred complaints journeys in which both individual and systemic concerns are recognisably understood and addressed
-
congruence in the cultural context to support patterns of service relationships within which patients see themselves as having a legitimate voice.
Our research considers each of these aspects to be mutually supportive within healthcare settings. Indeed, weaknesses in one of these aspects can undermine good work in each of the other two. We therefore see this as a ‘chain’, in which each link needs to be made as strong as possible if overall complaint outcomes are to be strengthened (Figure 7).
FIGURE 7.
The relational complaint chain.
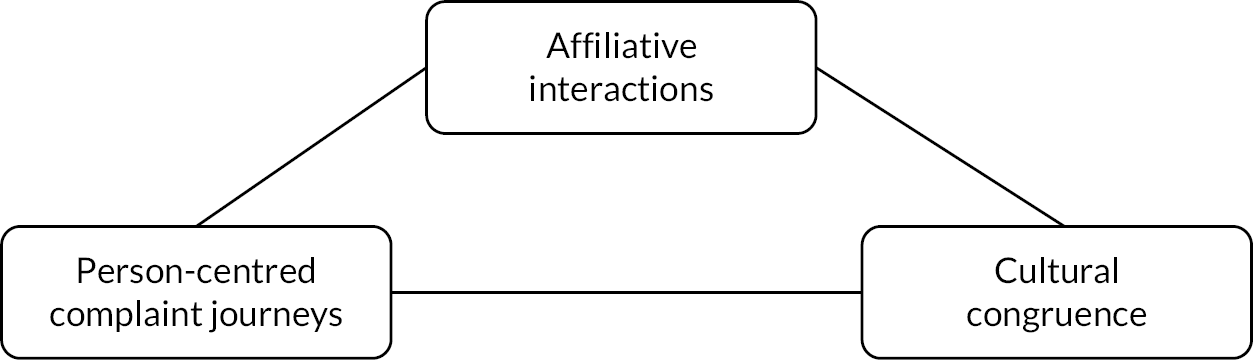
The chain metaphor emphasises the importance of the links being connected up effectively. For instance, it is insufficient to train people in affiliative skills, unless appropriately person-centred contexts and opportunities are going to be provided to use those skills. Similarly, it is insufficient to argue for a person-centred approach when the cultural context is insufficiently congruent with the values and norms of complainants or when complaint-handling staff lack the affiliative skills for person-centred interaction. The links in the chain need to be joined together, in a co-ordinated way, if complaints processes are to be strengthened.
In sum, different factors working at different levels of the ‘relational complaint chain’ have a role to play in whether or not complaints are resolved effectively. Our focus at the microlevel of affiliation was broadened to include other influencing factors. This approach reveals complaint handling as fragile, with numerous potential points of failure. Employing the relational complaint chain framework, we show that effective complaint management involves predictable, plannable and actionable strategies.
Implications for decision-makers
In strengthening the ‘affiliative interactions’ link in the ‘relational complaint chain’, our project points to a role for staff development and training, including encouragement of professional reflection, to build CH awareness, skills and confidence. The Real Complaints Training developed in this project provides ground-breaking new support for innovation at this level of microanalysis.
Strengthening the ‘person-centred journeys’ link depends on the more open, honest and empathic engagement of patients and carers across the duration of their complaint journey, provision of relevant, timely and appropriate communications and interactions that meet complainants’ reasonable expectations, and negotiating a path to sincere and shared agreements on the ‘closure’ of complaints. Our complainant and CH interviews demonstrate both the importance and the challenges involved in joining up these elements, especially in complex complaints.
Strengthening the ‘cultural congruence’ link in the chain involves institutional work to ensure that the complaints process works with the grain, rather than against it, in relation to these factors. This may be supported by more extensive use of the cultural audit tool within healthcare settings.
Robustness and limitations
Robustness
The robustness of the empirical evidence for our findings comes from the empirical and ethnomethodological rigour of the CA research practice at the heart of this project combined with innovative triangulation with the additional data sources all working together to provide a holistic perspective on the complaint journey from the patient perspective. CA also provides robust evidence for the development of Real Complaints Training. An important premise of CA communication training is that practitioners often develop effective communication practices, and training should thus be built around these naturally occurring communication practices that demonstrably work in context. Equally, post hoc reflection is rarely a reliable source of evidence for what exactly those communication practices are or what makes them effective, because ‘people’s “memories” of their communicative encounters are shaped by stereotypes and normative assumptions’. 68 By contrast, the ‘next turn proof procedure’ of CA provides objective empirical evidence for the effectiveness (or otherwise) of individual interactional practices.
Limitations
Delivering this project during the COVID pandemic inevitably placed restrictions on the implementation of the original research proposal, so while we are confident in the value of the data set finally collected, there are some limitations.
Firstly, the pressures of COVID and post-COVID recovery severely impacted the capacity of the Trusts and the PAS to participate and the volume and types of data they could collect. Only one PAS staff member participated; one Trust withdrew completely; one Trust engaged 19 months after the start date but staffing pressures severely limited their participation; one Trust only began data collection in project month 34 and data recording was restricted to staff within the complaints team. Hence, despite every effort and despite initial commitments, encounters between complainants and clinical staff/service managers were not recorded. This leaves a gap in the observational data for the longitudinal case studies. We could still follow the complainant experience of their complaint journey through the participant diaries and interviews, but while we could assess the impact of those encounters, we could not examine differences between communication with service managers/clinical staff and complaints staff.
A further limitation was that while most complainants consented to recording, complaints staff reported that many of the callers they would describe as ‘challenging’ refused to be recorded. Our data set does include examples of challenging calls, including with people who were expressing anger or emotional distress or where accounts were inconsistent or unreliable, but we had hoped to see more of these challenging calls. In addition, there were complainants whom we did not approach for the longitudinal study because their evident mental health vulnerabilities raised ethical issues for participation. While this was in line with our ethical approval, there is a very pressing need to understand how complainants with mental health vulnerabilities fare within the complaints procedures.
A third limitation comes from the recent introduction of ‘telephone resolution’ in Trust B. This had a twofold impact. Firstly, it reduced the proportion of longitudinal journeys that end with a final response letter because the telephone resolution replaces the formal letter. Secondly, because we could not record those calls, we have no observational data for how those journeys end. We do have interview and diary evidence for how those conversations were perceived by complainants, but without observational data, we cannot draw conclusions about the communication involved.
While we did not collect demographic information about participants, one noticeable limitation is the lack of ethnic diversity in the research participants (both complainants and CHs). Every complainant who approached the participating Trusts during the data-collection phase was invited to participate, so this may be an effect of the relative lack of ethnic diversity in the overall population in Northern Ireland, but it may also point to significant issues with access to complaints procedures.
Recommendations for future research
Following this study, we propose the following avenues for further study:
-
Research is needed to examine complaints communication with service managers and clinical staff. Our longitudinal data show that these conversations can be highly consequential for the overall complaints experience (both positively and negatively) and that they can interact with and impact the experience of care.
-
There is a need to understand more about issues with access to complaints procedures. Our data show that many people struggle to understand how to make a complaint and are often confused by the process. Moreover, the lack of diversity in our data suggests that some communities may struggle to access complaints procedures.
-
Wider rollout of the cultural audit would be an effective way to strengthen the ‘relational complaint chain’, given the importance of understanding cultural congruence/dissonance in healthcare settings at the level of values, systems and practices.
-
Recruiting participants at the start of their complaints journey yielded a large proportion of relatively short complaint journeys. Research is needed to understand the impact of very long complaint journeys. This could be achieved by recruiting participants who continue to pursue their complaint following the final response letter either with the Trust or with the ombudsman. This would also permit further stratification of complainants to explore different types of complaint.
-
Our stakeholder engagement has shown that complaints investigators in the ombudsman’s offices operate with different institutional constraints but still need to meet the interpersonal needs of complainants. Given the seriousness of the complaints that go to the ombudsman, and the level of frustration that those complainants have already experienced, research is needed to provide primary data to adapt Real Complaints Training for ombudsman complaint investigators.
-
Lastly, Real Complaints Training has been evaluated to assess useability and accessibility but a full pilot of the effectiveness of the intervention is required.
Patient and public involvement and stakeholder involvement
Patient and public involvement
Patient and public involvement in this project contributed to the research design, data interpretation and direction of the research. Initially, PPI participants contributed to decision-making about the design of the data-collection tools to ensure accessibility and feasibility. PPI representation on both the Study Steering Committee and the Project Management Group aimed to ensure PPI views were consistently reflected in the decision-making of the project. The PPI members of the Project Management Group were particularly active and contributed substantially to decision-making during the management of the project through the pandemic. A PPI training design workshop was convened following the development of the Real Complaints Training focus and potential data sets to gain PPI perspectives on the goals and implementation of the training.
Stakeholder involvement
As detailed in Chapter 8, the team hosted a number of events for stakeholder organisations to seek their perspectives, disseminate findings and introduce Real Complaints Training. Initially we held a round-table discussion with CHs and managers from all six HCSNI Trusts and the PAS. The aim was to elicit stakeholder perspectives on the communication challenges in complaint handling and associated training needs to inform our training development from the outset. During the training design phase, a co-design workshop was held with complaints managers from three Trusts and the PAS to seek their input on the training focus and data sets as well as guidance on preferred formats. Lastly, ‘taster’ sessions were delivered to the Scottish Public Services Ombudsman, the NIPSO, and the Parliamentary and Health Service Ombudsman, as ‘critical friends’ with expertise, experience and insight to feed into the training design evaluation. Attendees ranged from senior leadership to managers responsible for training design and CHs dealing directly with the public.
Impact and learning
These outreach activities led to additional impact work beyond the scope of the original grant. Following an invitation from NIPSO, the research team delivered specialised training to their staff using the Real Complaints Training resource. This training took the form of two half-day in-person sessions with separate teams. The participants also had the opportunity for discussion and feedback, providing valuable insights to the research team for further refinement of the training materials. This event was supported by Stirling University’s Faculty of Arts and Humanities Impact Funding Scheme.
Equality, diversity and inclusion
Participant inclusion
Given the focus on observational data, the restriction to ‘live’ complaint journeys was a necessary feature of participant recruitment. All complainants who made a complaint to one of the participating Trusts were invited to participate, and most complainants consented to be recorded. Among the measures taken to maximise the diversity of participants were the use of plain-English consent scripts (see Report Supplementary Material 3) and the provision of opportunities for potential participants to find out more about the study. The resulting corpus includes some groups who might be classed as ‘under-served’ (particularly older patients, mental health patients, illiterate patients and socially marginalised patients), but it undoubtedly lacks ethnic diversity. This is perhaps to some degree a reflection of the overall population in Northern Ireland but may also point to the inaccessibility of HSCNI complaints procedures to some communities. This is a concern that should be examined by future research.
Research team
The project involved a small research team (three permanent staff, two advisory consultants, two research associates). The fixed-term team members were supported (including with funding) to avail themselves of career development opportunities that arose during the project. PPI participants were invited through the PAS and were representative of the wider cohort of complainants in Northern Ireland. The recruitment process for researchers was conducted through Ulster University, in accordance with the University’s stringent equality, diversity and inclusion (EDI) policies.
Additional information
Acknowledgements
The authors would like to thank the PAS and the NHS Trusts and Boards that gave their support for this research, as well as all the complaint handlers and complainants who agreed to participate. The authors would also like to thank all the PPI participants who supported the project throughout its lifespan, the Study Steering Committee, the participants in the Real Complaints round-table event, and the staff of the Parliamentary and Health Service Ombudsman, the Scottish Public Services Ombudsman, and the Northern Ireland Public Services Ombudsman who provided feedback on the project’s training resources. We also thank University of Stirling and Ulster University for additional support through funding and sabbaticals granted to Benwell and Rhys. The authors wish to express their especial gratitude to project consultants Carolyn Hirst, for her feedback on the project’s training resources and her work as liaison for training and stakeholder events, and Professor Ruth Parry for her insights and input into the analysis of interactions and the development into training resources, and to Morgan Macleod, who went above and beyond in supporting the production of this final report and kept us within the editorial requirements.
CRediT contribution statement
Catrin S Rhys (https://orcid.org/0000-0002-8111-2543): Conceptualisation, Data curation (lead), Formal analysis, Funding acquisition (lead), Investigation, Methodology, Resources, Supervision, Visualisation, Writing – original draft, Writing – reviewing and editing.
Bethan Benwell (https://orcid.org/0000-0003-4638-6888): Conceptualisation, Data curation, Formal analysis, Funding acquisition (supporting), Investigation, Methodology, Resources, Visualisation, Writing – original draft, Writing – reviewing and editing.
Maria Erofeeva (https://orcid.org/0000-0002-0874-5272): Data curation (supporting), Formal analysis, Investigation, Resources, Visualisation, Writing – original draft, Writing – reviewing and editing.
Richard Simmons (https://orcid.org/0000-0002-3843-6542): Conceptualisation, Formal analysis, Funding acquisition (supporting), Investigation, Methodology, Visualisation, Writing – original draft, Writing – reviewing and editing.
Other contributions
Carolyn Hirst: Project consultant.
Morgan Macleod: Data curation (supporting), Project administration, Visualisation, Writing – original draft, Writing – reviewing and editing.
Carol Stitt: Data curation (supporting), Formal analysis, Investigation.
Ruth Parry: Formal analysis, Funding acquisition (supporting), Supervision.
Jack B Joyce: Formal analysis, Investigation, Writing – original draft.
Tom Douglass: Investigation, Writing – original draft.
Helen Baron: Project administration.
Disclosure of interests
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, are available in the toolkit on the NIHR Journals Library report publication page at https://doi.org/10.3310/NRGA3207.
Primary conflicts of interest: There is no interest declared for any of the research team.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Ethics statement
Ethics approval for this study was granted by the Office for Research Ethics Committees Northern Ireland (20/NI/0026) on 1 April 2020, amended 7 August 2020.
Information governance statement
Ulster University is committed to handling all personal information in line with the UK Data Protection Act (2018) and the General Data Protection Regulation (EU GDPR) 2016/679. Under the Data Protection legislation, Ulster University is the Data Controller, and you can find out more about how we handle personal data, including how to exercise your individual rights and the contact details for our Data Protection Officer here: www.ulster.ac.uk/about/governance/compliance/gdpr
Department of Health and Social Care disclaimer
This publication presents independent research commissioned by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by the interviewees in this publication are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, MRC, NIHR Coordinating Centre, the Health Services and Delivery Research programme or the Department of Health and Social Care.
This monograph was published based on current knowledge at the time and date of publication. NIHR is committed to being inclusive and will continually monitor best practice and guidance in relation to terminology and language to ensure that we remain relevant to our stakeholders.
Publications
Benwell B, Rhys CS. Phase structure and resistance to progressivity in complaints calls to the NHS. J Lang Soc Psychol 2023;42:523–43. https://doi.org/10.1177/0261927X231185751
Benwell B, Erofeeva M, Rhys CS. Why affiliation matters: a conversation analysis of complaints calls to the NHS. Patient Educ Couns 2024;119:108077. https://doi.org/10.1016/j.pec.2023.108077
Disclaimers
This article presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- Hardman I. Fighting for Life: The Twelve Battles that Made Our NHS, and the Struggle for its Future. London: Penguin; 2022.
- Seaton A. Our NHS: A History of Britain’s Best Loved Institution. New Haven, CT: Yale University Press; 2023.
- NHS Digital . Data on Written Complaints in the NHS n.d. https://digital.nhs.uk/data-and-information/publications/statistical/data-on-written-complaints-in-the-nhs (accessed 6 July 2023).
- Mirzoev T, Kane S. Key strategies to improve systems for managing patient complaints within health facilities – what can we learn from the existing literature?. Glob Health Action 2018;11. https://doi.org/10.1080/16549716.2018.1458938.
- Wheeler C. Apologies: overcoming public sector reluctance. AIAL Forum 2006;51:47-66.
- van Dael J, Reader TW, Gillespie A, Neves AL, Darzi A, Mayer EK. Learning from complaints in healthcare: a realist review of academic literature, policy evidence and front-line insights. BMJ Qual Saf 2020;29:684-95. https://doi.org/10.1136/bmjqs-2019-009704.
- Benwell B, McCreaddie M. Identity Struggles: Evidence from Workplaces Around the World. Amsterdam: Benjamins; 2017.
- Benwell B, Rhys CS. Negotiating relevance in pre-operative assessments. Soc Sci Med 2018;200:218-26. https://doi.org/10.1016/j.socscimed.2018.01.034.
- Benwell B, Rhys CS. The Role of Affiliation in Responses to Complaints to the NHS n.d.
- Rhys CS, Benwell B. Temporal Formulations in NHS Complaints n.d.
- Benwell B, Rhys CS. ‘The Most Horrendous Experience’: ECFS and Forms of Experience in NHS Complaints n.d.
- Rhys CS, Benwell B. Complaining and the Preference for Non-Recognitional Third-Party Formulations n.d.
- Friele RD, Sluijs EM, Legemaate J. Complaints handling in hospitals: an empirical study of discrepancies between patients’ expectations and their experiences. BMC Health Serv Res 2008;8. https://doi.org/10.1186/1472-6963-8-199.
- Cowan J, Anthony S. Problems with complaint handling: expectations and outcomes. Clin Gov 2008;13:164-8. https://doi.org/10.1108/14777270810867366.
- Adams M, Maben J, Robert G. ‘It’s sometimes hard to tell what patients are playing at’: how healthcare professionals make sense of why patients and families complain about care. Health 2018;22:603-23. https://doi.org/10.1177/1363459317724853.
- Healthwatch England . Shifting the Mindset: A Closer Look at Hospital Complaints n.d. www.healthwatch.co.uk/sites/healthwatch.co.uk/files/20191126%20-%20Shifting%20the%20mindset%20-%20NHS%20complaints%20.pdf (accessed 6 July 2023).
- Independent Medicines and Medical Devices Safety Review . First Do No Harm n.d. www.immdsreview.org.uk/downloads/IMMDSReview_Web.pdf (accessed 6 July 2023).
- Ockenden D. Findings, Conclusions and Essential Actions from the Independent Review of Maternity Services at the Shrewsbury and Telford Hospital NHS Trust. London: TSO; 2022.
- Pelt JL, Faldmo P. Physician error and disclosure. Clin Obstet Gynecol 2008;51:700-8. www.doi.org/10.1097/grf.0b013e3181899c6d.
- Giraldo P, Sato L, Castells X. The impact of incident disclosure behaviors on medical malpractice claims. J Patient Saf 2020;16:e225-9. https://doi.org/10.1097/PTS.0000000000000342.
- Mazor KM, Simon SR, Gurwitz JH. Communicating with patients about medical errors: a review of the literature. Arch Intern Med 2004;164:1690-7. https://doi.org/10.1001/archinte.164.15.1690.
- Healthwatch England . Suffering in Silence: Listening to Consumer Experiences of the Health and Social Care Complaints System 2014. www.healthwatch.co.uk/sites/healthwatch.co.uk/files/hwe-complaints-report.pdf (accessed 29 June 2023).
- NHS England . Annual Report and Accounts 2017.
- Simmons R, Brennan C. Grumbles, Gripes and Grievances: The Role of Complaints in Transforming Public Services. London: NESTA; 2013.
- Pettker CM, Thung SF, Lipkind HS, Illuzzi JL, Buhimschi CS, Raab CA, et al. A comprehensive obstetric patient safety program reduces liability claims and payments. Am J Obstet Gynecol 2014;211:319-25. https://doi.org/10.1016/j.ajog.2014.04.038.
- Friele RD, Sluijs EM. Patient expectations of fair complaint handling in hospitals: empirical data. BMC Health Serv Res 2006;6. https://doi.org/10.1186/1472-6963-6-106.
- Armstrong D. The power of apology: how saying sorry can leave both patients and nurses feeling better. Nurs Times 2009;105:16-9.
- Robinson JD. The sequential organization of ‘explicit’ apologies in naturally occurring English. Res Lang Soc Interac 2004;37:291-330. https://doi.org/10.1207/s15327973rlsi3703_2.
- Heritage J, Raymond CW. Are explicit apologies proportional to the offenses they address?. Discourse Process 2016;53:5-25. https://doi.org/10.1080/0163853X.2015.1056695.
- Birks Y, Harrison R, Bosanquet K, Hall J, Harden M, Entwistle V, et al. An exploration of the implementation of open disclosure of adverse events in the UK: a scoping review and qualitative exploration. Health Serv Deliv Res 2014;2:1-196. https://doi.org/10.3310/hsdr02200.
- Simmons R, Brennan C. User voice and complaints as drivers of innovation in public services. Public Manag Rev 2017;19:1085-104. https://doi.org/10.1080/14719037.2016.1257061.
- Heinemann T, Traverso V. Complaining in interaction. J Pragmat 2009;41:2381-4. https://doi.org/10.1016/j.pragma.2008.10.006.
- Weatherall A. Producing and Managing Restricted Activities: Avoidance and Withholding in Institutional Interaction. Amsterdam: Benjamins; 2017.
- Bismark MM, Spittal MJ, Gogos AJ, Gruen RL, Studdert DM. Remedies sought and obtained in healthcare complaints. BMJ Qual Saf 2011;20:806-10. www.doi.org/10.1136/bmjqs-2011-000109.
- Public Administration Select Committee . More Complaints Please! 2014.
- Allsop J, Mulcahy L. Dealing with clinical complaints. Qual Heath Care 1995;4:135-43. https://doi.org/10.1136/qshc.4.2.135.
- Bouwman R, Bomhoff M, Robben P, Friele R. Patients’ perspectives on the role of their complaints in the regulatory process. Health Expect 2015;19:483-96. https://doi.org/10.1111/hex.12373.
- Allsop J. Two sides to every story: complainants’ and doctors’ perspectives in disputes about medical care in a general practice setting. Law Policy 1994;16:149-83. https://doi.org/10.1111/j.1467-9930.1994.tb00121.x.
- Mulcahy L. Disputing Doctors: The Socio-legal Dynamics of Complaints About Medical Care. Maidenhead: Open University Press; 2003.
- Mazor KM, Greene SM, Roblin D, Lemay CA, Firneno CL, Calvi J, et al. More than words: patients’ views on apology and disclosure when things go wrong in cancer care. Patient Educ Couns 2013;90:341-6. https://doi.org/10.1016/j.pec.2011.07.010.
- Bark P, Vincent C, Jones A, Savory J. Clinical complaints: a means of improving quality of care. Qual Heath Care 1994;3:123-32. https://doi.org/10.1136/qshc.3.3.123.
- Vincent C, Young M, Phillips A. Why do people sue doctors?: a study of patients and relatives taking legal action. Lancet 1994;343:1609-13. https://doi.org/10.1016/S0140-6736(94)93062-7.
- Allsop J. A Form of Haunting n.d.
- Bismark M, Dauer E, Paterson R, Studdert D. Accountability sought by patients following adverse events from medical care: the New Zealand experience. Can Med Assoc J 2006;175:889-94. https://doi.org/10.1503/cmaj.060429.
- Daniel AE, Burn RJ, Horarlk S. Patients’ complaints about medical practice. Med J Aust 1999;170:598-602. https://doi.org/10.5694/j.1326-5377.1999.tb127910.x.
- Heritage J. The New Blackwell Companion to Social Theory. Oxford: Blackwell; 2008.
- Holt E. Reporting and reacting: concurrent responses to reported speech. Res Lang Soc Interact 2010;33:425-54. https://doi.org/10.1207/S15327973RLSI3304_04.
- Dewar J. Calling to Complain: An Ethnographic and Conversation Analytic Account of Complaints to an Industry Ombudsman 2011. http://hdl.handle.net/10063/2271 (accessed 3 July 2023).
- Edwards D. Moaning, whinging and laughing: the subjective side of complaints. Discourse Stud 2005;7:5-29. https://doi.org/10.1177/1461445605048765.
- Pomerantz A. Extreme case formulations: a way of legitimizing claims. Human Stud 1986;9:219-29. https://doi.org/10.1007/BF00148128.
- Drew P, Holt E. Complainable matters: the use of idiomatic expressions in making complaints. Soc Probl 1988;35:398-417. https://doi.org/10.2307/800594.
- Stokoe E, Hepburn A. ‘You can hear a lot through the walls’: noise formulations in neighbour complaints. Discourse Soc 2005;16:647-73. https://doi.org/10.1177/0957926505054940.
- Benwell B, Stokoe E. Discourse and Identity. Edinburgh: Edinburgh University Press; 2006.
- Stivers T. Stance, alignment and affiliation during storytelling: when nodding is a token of affiliation. Res Lang Soc Interact 2008;41:31-57. https://doi.org/10.1080/08351810701691123.
- Hofstetter E. Citizens Getting Help: Interactions at the Constituency Office 2016.
- Lee SH. Extended requesting: interaction and collaboration in the production and specification of requests. J Pragmat 2009;41:1248-71. https://doi.org/10.1016/j.pragma.2008.09.013.
- Alexander M, Stokoe E. Problems in the neighbourhood: formulating noise complaints across dispute resolution services. J Community Appl Soc Psychol 2019;29:355-70. https://doi.org/10.1002/casp.2405.
- Edwards D, Stokoe E. Self-help in calls for help with problem neighbors. Res Lang Soc Interact 2007;40:9-32. https://doi.org/10.1080/08351810701331208.
- Stokoe E. Doing actions with identity categories: complaints and denials in neighbor disputes. Text Talk 2009;29:75-97. https://doi.org/10.1515/TEXT.2009.004.
- Stokoe E, Edwards D. ‘Did you have permission to smash your neighbour’s door?’: silly questions and their answers in police-suspect interrogations. Discourse Stud 2008;10:89-111. https://doi.org/10.1177/1461445607085592.
- Antaki C, Barnes R, Leuder I. Self-disclosure as a situated interactional practice. Br J Soc Psychol 2005;44:181-99. https://doi.org/10.1348/014466604X15733.
- Brown P, Levinson S. Politeness: Some Universals in Language Use. Cambridge: Cambridge University Press; 1987.
- Billig M. Rhetoric and the unconscious. Argumentation 1998;12:199-216. https://doi.org/10.1023/A:1007795814561.
- Alexander M, Stokoe E. Characterological formulations of persons in neighbourhood complaint sequences. Qual Res Psychol 2020;17:413-29. https://doi.org/10.1080/14780887.2020.1725950.
- Robles JS, Parks ES. Complaints about technology as a resource for identity-work. Lang Soc 2019;48:209-31. https://doi.org/10.1017/S0047404518001379.
- Edwards D, Potter J. Some uses of subject-side assessments. Discourse Stud 2017;19:497-514. https://doi.org/10.1177/1461445617715171.
- Drew P, Heritage J. Talk at Work: Interaction in Institutional Settings. Cambridge: Cambridge University Press; 1992.
- Stokoe E, Sikveland R. Formulating solutions in mediation. J Pragmat 2016;105:101-13. https://doi.org/10.1016/j.pragma.2016.08.006.
- Heritage J, Clayman SE. Talk in Action: Interactions, Identities, and Institutions. Chichester: Wiley Blackwell; 2010.
- Whalen J, Zimmerman DH, Whalen MR. When words fail: a single case analysis. Soc Probl 1988;35:335-62. https://doi.org/10.2307/800591.
- Whalen MR, Zimmerman DH. Describing trouble: practical epistemology in citizen calls to the police. Lang Soc 1990;19:465-92. https://doi.org/10.1017/S0047404500014779.
- Alexander M. Formulating and Managing Neighbourhood Complaints: A Comparative Study of Service Provision 2018.
- Feo R, LeCouteur A. Dealing with third-party complaints on a men’s relationship-counselling helpline. Discourse Stud 2017;19:131-47. https://doi.org/10.1177/1461445617691701.
- Couper-Kuhlen E, Etelämäki M. Requesting in Social Interaction. Amsterdam: Benjamins; 2014.
- Jangland E, Gunningberg L, Carlsson M. Patients’ and relatives’ complaints about encounters and communication in health care: evidence for quality improvement. Patient Educ Couns 2009;75:199-204. https://doi.org/10.1016/j.pec.2008.10.007.
- Durand MA, Moulton B, Cockle E, Mann M, Elwyn G. Can shared decision-making reduce medical malpractice litigation?: a systematic review. BMC Health Serv Res 2015;15. https://doi.org/10.1186/s12913-015-0823-2.
- Tingle J. The chasm between theory and practice in NHS complaint handling. Br J Nurs 2022;31:510-2. https://doi.org/10.12968/bjon.2022.31.9.510.
- Heritage J. Garfinkel and Ethnomethodology. Cambridge: Polity Press; 1984.
- Schegloff EA. Reflections on quantification in the study of conversation. Res Lang Soc Interact 1993;26:99-128. https://doi.org/10.1207/s15327973rlsi2601_5.
- Gee JP. An Introduction to Discourse Analysis: Theory and Method. London: Routledge; 2014.
- Simmons R. Improvement and public service relationships: cultural theory and institutional work. Public Adm 2016;94:933-52. https://doi.org/10.1111/padm.12257.
- Simmons R. Using cultural theory to navigate the policy process. Policy Politics 2018;46:235-53. https://doi.org/10.1332/030557318X15230060606081.
- Parry R. Are interventions to enhance communication performance in allied health professionals effective, and how should they be delivered?: direct and indirect evidence. Patient Educ Couns 2008;73:186-95. https://doi.org/10.1016/j.pec.2008.05.029.
- Sikveland RO, Moser T, Solem MS, Skovholt K. The effectiveness of the Conversation Analytic Role-Play Method (CARM) on interactional awareness: a feasibility randomized controlled trial with student teachers. Teach Teach Educ 2023;129. https://doi.org/10.1016/j.tate.2023.104136.
- Stokoe E. The Conversation Analytic Role-play Method (CARM): a method for training communication skills as an alternative to simulated role-play. Res Lang Soc Interact 2014;47:255-65. https://doi.org/10.1080/08351813.2014.925663.
- Parry R, Pino M, Faull C, Feathers L. Acceptability and design of video-based research on healthcare communication: evidence and recommendations. Patient Educ Couns 2016;99:1271-84. https://doi.org/10.1016/j.pec.2016.03.013.
- Skelcher C. Involvement and empowerment in local public services. Public Money Manag 1993;13:13-20. https://doi.org/10.1080/09540969309387770.
- Power Inquiry . Power to the People 2006.
- Clark M, Denham-Vaughan S, Chidiac MA. A relational perspective on public sector leadership and management. Int J Leadership Public Serv 2014;10:4-16. https://doi.org/10.1108/IJLPS-03-2013-0006.
- Muir R, Parker I. How the Relational State Will Transform Public Services. London: IPPR; 2014.
- Lieberman RC. Ideas, institutions, and political order: explaining political change. Am Polit Sci Rev 2002;96:697-712. https://doi.org/10.1017/S0003055402000394.
- Greenberg J. Organizational justice: yesterday, today, and tomorrow. J Manag 1990;16:399-432. https://doi.org/10.1177/014920639001600208.
- Bies RJ, Shapiro DL. Voice and justification: their influence on procedural fairness judgments. Acad Manage J 1988;31:676-85. https://doi.org/10.5465/256465.
- Waldron VR. Emotion in Organizations. London: Sage; 2000.
- Lawrence T, Suddaby R. SAGE Handbook of Organization Studies. London: Sage; 2006.
- Van Ess Coeling H, Simms LM. Facilitating innovation at the nursing unit level through cultural assessment, part 1: how to keep management ideas from falling on deaf ears. J Nurs Adm 1993;23:46-53. https://doi.org/10.1097/00005110-199304000-00013.
- Brett JM. Culture and negotiation. Int J Psychol 2000;35:97-104. https://doi.org/10.1080/002075900399385.
- Douglas M. How Institutions Think. London: Routledge; 1987.
- Mamadouh V. Grid-group cultural theory: an introduction. GeoJournal 1999;47:395-409. https://doi.org/10.1023/A:1007024008646.
- Jessop B. Governance as Social and Political Communication. Manchester: Manchester University Press; 2003.
- Douglas M. Natural Symbols: Explorations in Cosmology. London: Barrie and Rockliff; 1970.
- Douglas M. In the Active Voice. London: Routledge; 1982.
- Douglas M. Risk and Blame: Essays in Cultural Theory. London: Routledge; 1992.
- Thompson M, Ellis R, Wildavsky A. Cultural Theory. Boulder, CO: Westview Press; 1990.
- Durkheim E. Suicide. London: Routledge; 1897.
- Durkheim E. Moral Education. New York: Free Press; 1925.
- Hood C. The Art of the State. Oxford: Oxford University Press; 1998.
- Perri 6 . Institutional viability: a neo-Durkheimian theory. Innovation 2003;16:395-41. https://doi.org/10.1080/1351161032000163593.
- Simmons R, Birchall J, Prout A. User involvement in public services: ‘choice about voice’. Public Policy Adm 2012;27:3-29. https://doi.org/10.1177/0952076710384903.
- Simmons R. Leadership and listening: the reception of user voice in today’s public services. Soc Policy Adm 2011;45:539-68. https://doi.org/10.1111/j.1467-9515.2011.00790.x.
- Entwistle VA, Watt IS. Treating patients as persons: a capabilities approach to support delivery of person-centered care. Am J Bioeth 2013;13:29-3. https://doi.org/10.1080/15265161.2013.802060.
- Murphy D, Duggan M, Joseph S. Relationship-based social work and its compatibility with the person-centred approach: principled versus instrumental perspectives. Br J Soc Work 2013;43:703-19. https://doi.org/10.1093/bjsw/bcs003.
- Francis R. Report of the Mid-Staffordshire NHS Trust Inquiry. London: TSO; 2013.
- Kings Fund . Patient-Centred Leadership 2013.
- Corbin J, Strauss A. Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory. London: Sage; 2015.
- Mulgan G, Tucker S, Ali R, Sanders B. Social Innovation: What It Is, Why It Matters and How It Can Be Accelerated. Oxford: Said Business School; 2007.
- Martin GP, Chew S, Dixon-Woods M. Why do systems for responding to concerns and complaints so often fail patients, families and healthcare staff?: a qualitative study. Soc Sci Med 2021;287. https://doi.org/10.1016/j.socscimed.2021.114375.
- McCreaddie M, Wiggins S. Reconciling the good patient persona with problematic and non-problematic humour: a grounded theory. Int J Nurs Stud 2009;46:1079-91. https://doi.org/10.1016/j.ijnurstu.2009.01.008.
- Latour B. Reassembling the Social: An Introduction to Actor-Network-Theory. Oxford: Oxford University Press; 2005.
- Habermas J. Lifeworld and System: A Critique of Functionalist Reason. Boston: Beacon Press; 1981.
- Robinson J. How to get sued: the step by step guide to increase litigation against your trust. Br J Midwifery 1997;5. https://doi.org/10.12968/bjom.1997.5.10.641.
- McCreaddie M, Benwell B, Gritti A. A qualitative study of National Health Service (NHS) complaint-responses. BMC Health Serv Res 2021;21. https://doi.org/10.1186/s12913-021-06733-5.
- Scottish Public Services Ombudsman . How to Make a Good Apology n.d. www.spso.org.uk/sites/spso/files/csa/ApologyGuide.pdf (accessed 3 July 2023).
- van Dael J, Reader TW, Gillespie AT, Freise L, Darzi A, Mayer EK. Do national policies for complaint handling in English hospitals support quality improvement?: lessons from a case study. J R Soc Med 2022;115:390-8. https://doi.org/10.1177/01410768221098247.
- Tomlinson EC, Dineen BR, Lewicki RJ. The road to reconciliation: antecedents of victim willingness to reconcile following a broken promise. J Manag 2004;30:165-87. https://doi.org/10.1016/j.jm.2003.01.003.
- Lewicki R, Polin B, Lount R. An exploration of the structure of effective apologies. Negot Confl Manag Res 2016;9:177-96. https://doi.org/10.34891/9awp-8644.
- Lewicki RJ, Polin B. Restoring Trust: Challenges and Prospects. New York: Oxford University Press; 2012.
- United Nations Ombudsman and Mediation Services . The Power of Apologies n.d. www.un.org/ombudsman/resources/tips/power-of-apologies (accessed 3 July 2023).
- Sacks H. Explorations in the Ethnography of Speaking. Cambridge: Cambridge University Press; 1974.
- Benwell B, Rhys C. Phase structure and resistance to progressivity in complaints calls to the NHS. J Lang Soc Psychol 2023;42:523-43. https://doi.org/10.1177/0261927X231185751.
- Schegloff EA. Georgetown University Roundtable on Languages and Linguistics. Washington DC: Georgetown University Press; 1982.
- Goodwin C. Structures of Social Action: Studies in Conversation Analysis. Cambridge: Cambridge University Press; 1984.
- Goodwin C. Audience diversity, participation and interpretation. Text 1986;6:283-316. https://doi.org/10.1515/text.1.1986.6.3.283.
- Pomerantz A. Structures of Social Action: Studies in Conversation Analysis. Cambridge: Cambridge University Press; 1984.
- Gardner R. When Listeners Talk: Response Tokens and Listener Stance. Amsterdam: Benjamins; 2001.
- Pomerantz A. Talk and Social Organisation. Clevedon: Multilingual Matters; 1987.
- Sacks H, Schegloff EA, Jefferson G. A simplest systematics for the organization of turn taking for conversation. Language 1974;50:696-735. https://doi.org/10.2307/412243.
- Benwell B, Stokoe E. The Routledge Handbook of Language and Identity. London: Routledge; 2016.
- Heritage J. Analysing Everyday Explanation: A Casebook of Methods. Thousand Oaks, CA: Sage; 1988.
- Jayyusi L. Ethnomethodology and the Human Sciences. Cambridge: Cambridge University Press; 1991.
- Parliamentary and Health Service Ombudsman . Breaking Down the Barriers: Older People and Complaints about Healthcare 2015. www.ombudsman.org.uk/sites/default/files/Breaking_down_the_barriers_report.pdf (accessed 5 July 2023).
- Fisher R, Shapiro D. Beyond Reason: Using Emotions as You Negotiate. New York: Viking; 2005.
- Muntigl P, Knight N, Horvath AO, Watkins A. Client attitudinal stance and therapist-client affiliation: a view from grammar and social interaction. Res Psychother Psych Process Outcome 2012;15:117-30. https://doi.org/10.4081/ripppo.2012.119.
- Traverso V. The dilemmas of third-party complaints in conversation between friends. J Pragmat 2009;41:2385-99. https://doi.org/10.1016/j.pragma.2008.09.047.
- Benwell B, Erofeeva M, Rhys CS. The Role of Affiliation in Managing Progressivity of Complaints Calls n.d.
- Pino M. Hurting and blaming: two components in the action formation of complaints about absent parties. Res Lang Soc Interact 2022;55:260-78. https://doi.org/10.1080/08351813.2022.2101298.
- Antaki C, Richardson E, Stokoe E, Willott S. Dealing with the distress of people with intellectual disabilities reporting sexual assault and rape. Discourse Stud 2015;17:415-32. https://doi.org/10.1177/1461445615578962.
- Ruusuvuori J. ‘Empathy’ and ‘sympathy’ in action: attending to patients’ troubles in Finnish homeopathic and general practice consultations. Soc Psychol Q 2005;68:204-22. https://doi.org/10.1177/019027250506800302.
- Hepburn A, Potter J. Crying receipts: time, empathy, and institutional practice. Res Lang Soc Interact 2007;40:89-116. https://doi.org/10.1080/08351810701331299.
- Pudlinksi C. Doing empathy and sympathy: caring responses to troubles tellings on a peer support line. Discourse Stud 2005;7:267-88. https://doi.org/10.1177/1461445605052177.
- Couper-Kuhlen E. Emotion in Interaction. Oxford: Oxford University Press; 2012.
- Weiste E, Peräkylä A. Prosody and empathic communication in psychotherapy interaction. Psychother Res 2014;24:687-701. https://doi.org/10.1080/10503307.2013.879619.
- Ford J, Hepburn A. How Emotions Are Made in Talk. Amsterdam: Benjamins; 2021.
- Schegloff EA. Practices and actions: boundary cases of other‐initiated repair. Discourse Process 1997;23:499-545. https://doi.org/10.1080/01638539709545001.
- Sidnell J. Turn-continuation by self and by other. Discourse Process 2012;49:314-37. https://doi.org/10.1080/0163853X.2012.654760.
- Hutchby I. ‘Active listening’: formulations and the elicitation of feelings-talk in child counselling. Res Lang Soc Interact 2005;38:303-29. https://doi.org/10.1207/s15327973rlsi3803_4.
- Hepburn A, Potter J. Emotion in Interaction. Oxford: Oxford University Press; 2012.
- Heritage J. The Morality of Knowledge in Conversation. Cambridge: Cambridge University Press; 2011.
- Lerner GH. Interaction and Grammar. Cambridge: Cambridge University Press; 1996.
- Koskela H. Invoking different types of knowledge in celebrity interviews. SKY J Linguistics 2005;18:93-118.
- Benwell B, Rhys CS, Stitt C. Third-Party Formulations in Complaints to the NHS n.d.
- Skär L, Söderberg S. Patients’ complaints regarding healthcare encounters and communication. Nurs Open 2018;5:224-32. https://doi.org/10.1002/nop2.132.
- Parliamentary and Health Service Ombudsman, Opinion Research Services . Complainant Feedback: Charter Commitment 10 n.d. www.ombudsman.org.uk/sites/default/files/ORS_Summary_Report_on_Impartiality_March_2020.pdf (accessed 6 July 2023).
- Biggar S, Lobigs LM, Fletcher M. How can we make health regulation more humane?: a quality improvement approach to understanding complainant and practitioner experiences. J Med Regul 2020;106:7-15. https://doi.org/10.30770/2572-1852-106.1.7.
Appendix 1 Additional cultural audit data
| Gender | Female: 82% | Male: 18% | |||
| Age | Under 60: 40% | Over 60: 40% | |||
| Qualifications | Non-university: 39% | University degree or higher: 61% | |||
| Length of PAS membership | < 3 years: 25% | 3–5 years: 37% | > 6 years: 38% | ||
| HSCNI trust | Trust A: 19% | Trust B: 21% | Trust C: 24% | Trust D: 12% | Trust E: 22% |
| Main services used | Hospital inpatient: 10% | Hospital outpatient: 16% | Community treatment: 12% | GP services: 55% | Care at home: 3% |
| Themes and cultural biases | How NHS services ‘actually are’ | How NHS services ‘should be’ |
|---|---|---|
| Theme 1: How fairness and equity issues are resolved | ||
| Cultural bias: Hierarchy | ‘NHS services are only provided for those who need them most’ | ‘NHS services should only be provided for those who need them most’ |
| Cultural bias: Individualism | ‘Individuals are not given enough choice about the services they get from the NHS’ | ‘Individuals should be given more choice about the services they get from the NHS’ |
| Cultural bias: Egalitarianism | ‘Everybody in my community has the same chance of accessing the service provided by the NHS’ | ‘Everybody in my community should have the same chance of accessing the service provided by the NHS’ |
| Cultural bias: Fatalism | ‘People rely on their luck to get NHS services’ | ‘People should rely on their luck to get NHS services’ |
| Theme 2: How knowledge is valued | ||
| Cultural bias: Hierarchy | ‘Patients/carers trust NHS services to decide what is best for them’ | ‘Patients/carers should trust NHS services to decide what is best for them’ |
| Cultural bias: Individualism | ‘NHS services give priority to what individuals say they want’ | ‘NHS services should give priority to what individuals say they want’ |
| Cultural bias: Egalitarianism | ‘NHS services are run in line with the views of patients/carers as a whole’ | ‘NHS services should be run in line with the views of patients/carers as a whole’ |
| Cultural bias: Fatalism | ‘I am wary of those who claim to know what is best for the NHS services’ | ‘Patients/carers should be wary of those who claim to know what is best for the NHS services’ |
| Theme 3: Courtesy and respect | ||
| Cultural bias: Hierarchy | ‘Patients/carers respect the decisions of professionals delivering NHS services’ | ‘Patients/carers should respect the decisions of professionals delivering NHS services’ |
| Cultural bias: Individualism | ‘NHS services accept that individuals know best what they need’ | ‘NHS services should accept that individuals know best what they need’ |
| Cultural bias: Egalitarianism | ‘NHS services take heed of what the patient/carer community has to say’ | ‘NHS services should take heed of what the patient/carer community has to say’ |
| Cultural bias: Fatalism | ‘In my experience, patients/carers do not have any power’ | ‘Patients/carers should not expect to have any power’ |
| Theme 4: Expression of voice | ||
| Cultural bias: Hierarchy | ‘Patients/carers are only consulted on what NHS professionals have already decided’ | ‘Patients/carers should only be consulted on what NHS professionals have already decided’ |
| Cultural bias: Individualism | ‘In practice, I would only speak out about things that affect me as an individual’ | ‘In principle, I feel I should only speak out about things that affect me as an individual’ |
| Cultural bias: Egalitarianism | ‘In practice, I would only speak out about things that affect patients/carers as a whole’ | ‘In principle, I feel I should only speak out about things that affect patients/carers as a whole’ |
| Cultural bias: Fatalism | ‘Patients/carers do not expect their views to make any difference to NHS services’ | ‘Patients/carers should not expect their views to make any difference to NHS services’ |
Appendix 2 Real Complaints guidance on best practice for writing response letters
This guidance emerges from the empirical findings of the ‘Real Complaint’ project (specifically analysis of written complaint response and longitudinal journeys) combined with engagement with and advice from Trust stakeholders. It comprises practical guidance about how to approach the writing of responses to complaints based on our findings from the analysis of written complaints: what to include, what not to include and how to make effective language choices. All examples/cases provided within this guidance are real and derived from the Real Complaints corpus. All names are pseudonyms and other identifying details anonymised.
How to read/understand complaints
The most important stage of responding to a complaint is the reading of or listening to the complaint itself. Where complaints are made by telephone, the call handler has a challenging task to record the details of the complaint in a way that prioritises the important information and focus of the complaint. Telephone complaints are often less ordered and structured than written complaints, so their focus can be harder to discern. The quality of the typed-up record of this complaint will be crucial for the investigating team’s handling of the complaint. The record of the complaint will then either be an original written complaint by the complainant or a typed-up record of the complaint made by telephone, at which point the focus of the complaint can be accurately identified.
Start by identifying the points of complaint – what is it about? Often there are several points that need to be addressed, and a careful reading/listening will identify what these are, what their relative importance is, and what the complainant is seeking in making their complaint. For instance, in one case the complainant wanted (1) the doctor to acknowledge that he did not call her and (2) a sincere apology for her wasted time. A careful reading of the letter reveals that the first objective is more important to the complainant than the second (as it links to her integrity as a patient and complainant).
TIPS
-
Identify the key focus of the complaint by paying attention to the way it is framed by the complainant. For instance, one participant complains about excessive waiting times for surgery but frames this in terms of it arising due to her consultant retiring and her not being reassigned to someone new. The response only acknowledges that COVID pressures have led to excessive waiting times (and thus seems to evade some element of blame for the error).
-
Consider the context and details a complainant gives when formulating a complaint. They are not random and point to what is important to the complainant. For example, one complainant foregrounds the fact that her sister was brain-injured and had dementia. Her ongoing dissatisfaction and frustration primarily relate to both response letters failing to acknowledge this (1) in relation to her inability to clearly communicate her symptoms to health professionals and (2) because the events led to her sister losing any remaining capacity and autonomy.
-
Look at repetitions – what information is repeated several times? Repeated information is likely to indicate what is important to the complainant. In the telephone complaint made by one participant, she repeats the information that the receptionist in the service area was ‘rude and abrupt’ multiple times. The sense that this element of the complaint remains unresolved (despite other elements being seen to be highly satisfactory) haunts the post-complaint interview: ‘I did get seen, but then it’s still the fact that you know, is that the way she’s phoning everybody and speaking to them and you would never find that out’.
How to write responses
How to begin
The importance of the initial careful reading of the original complaint is that it ensures that the response is properly focused on the actual concerns raised. Therefore, following thanks for bringing concerns to the Trust’s attention and any apology for delay in responding, it is ideal to begin the response with a summary of what the investigating officer understands to be the main points of the complaint: for example, ‘we understand your complaint to relate to …’. These may involve multiple strands, and it is important to ensure all are listed.
Opening of letter
-
Thanks for raising concerns and expression of commitment to resolving complaint.
-
Any apology for delay in responding.
-
Summary of complaint as the Trust understands it.
Structure of response
The complaint itself should be used to structure the main text of the response so that it is clear that each point of the complaint has been addressed to take each of the issues in turn, using them as headings, especially where there are multiple strands to a complaint. The summary of the complaint in the opening lines of the letter should help to provide this structure.
Attend carefully to the details in the original complaint and ensure that responses do not seem to overtly contradict or avoid addressing these details. For instance, in one response letter, there is an apology for ‘any confusion regarding the reason your mother was transferred’. The original complaint letter had explicitly stated a contradiction between what they were told about the transfer (that it was for assessment only and would only be 1 day) and what actually happened (she was admitted for spinal surgery and ended up there for a lengthy stay) and asked for this to be explained/accounted for, but this phrasing implies that the complainant was ‘confused’ about this. It is also crucial that where differences of opinion (between complainant and staff) are expressed, these differences are made explicit. Any kind of failure to address issues directly or to seem to obfuscate around the point of a complaint will be poorly received by complainants, as we can see from the following comment by one participant in her interview:
When I got my letter I was like oh my god, they’ve missed everything that I said. I felt that they hadn’t addressed the issues that I had highlighted.
The response should avoid the formula of recounting or summarising the care and treatment process unless this is directly relevant to the substance of the complaint. The inclusion of so much extraneous and often irrelevant detail about care and treatment may mean that points where the complaint is being addressed get lost and adds to the impression that the response is simply defending its processes and not actually addressing the point of the complaint.
Preserve the chronology of events where possible. Where more than one report obtained by relevant staff members is being incorporated into the response, ensure that they inform each stage of the events leading to the complaint rather than being simply summarised in turn. This will avoid confusing chronology and contradictory accounts by different staff members.
Guiding principles
Acknowledge responsibility
A study by Lewicki et al. 126 found that ‘Acknowledgement of Responsibility’ is seen as the most important component in an apology. Where the investigation concludes that an error has been found to be made or behaviour found to be wanting, it is most effective to admit this in clear and transparent terms. The following, from a Trust response, is an example of good practice since it clearly and honestly states that the outcome would have been different if the mistake had not been made:
Good practice
Dr Gow adds that if Dr Martin had correctly identified and recorded your son’s blood results this would have had an impact on his formulation of his management plan. He would have sought a second opinion as to the appropriateness of discharge and possible escalation of treatment.
Avoid explicit ‘blame evasion’
Obvious defensiveness or an unwillingness to acknowledge responsibility where it is due is one of the most salient expressions of dissatisfaction about complaint response letters made by longitudinal participants in follow up diaries and interviews.
We feel they just don’t want to admit that they’ve made a mistake, like that’s just how it feels.
Blame evasion can be very explicit or more subtle, perhaps pointing to blame mitigation, though it is striking that participants pick up negatively on even the most subtle forms of mitigation. Blame evasion can be realised through:
-
blaming others
-
using obfuscatory formulations that make the agency of the actions unclear (who does what)
-
excuses and mitigating circumstances (multiple excuses or excuses that seem designed to exonerate the complained-about subject from the need to apologise are most negatively received)
-
good intentions/no intentionality to cause harm.
Sometimes it is valid and effective for a response letter to offer explanations about what events occurred as they did, but it is important that these are not seen to undermine the accountability of the Trust or to obviate any need to apologise. An example of a good-practice response is as follows:
Good practice
While we have been committed to much clinical care during the Pandemic our duty to complete the investigation and communicate with you remains irrespective, so I do not offer it as an excuse, but as context from which I offer my apology to you.
One of our case studies illustrates how good writing is unnecessarily compromised by the inclusion of excuses. The participant has complained about the provision of clean linen and water, and safety measures around COVID. While the response contains appropriate apologies and assurances about measures that will be taken to ensure the problems do not reoccur in the future, the letter adopts a defensive tone about the usual exemplary processes in place in the ward and challenges the complainant’s point that she had difficulties obtaining a pillow.
Sister Langton is sorry if there was difficulty in obtaining a pillow for you whilst in the department but she is content that one was provided.
A more effective response should ideally acknowledge and validate the patient’s experience and might be formulated as follows:
Good practice
We apologize for this incident; it should not have happened. Normally there is a procedure …. We will ensure that the procedure is followed in the future [ideally with a concrete expression of how it will be done].
Acknowledge the lifeworld and emotional impact of the complained-about event on the complainant (‘Be Affiliative’)
In the SPSO’s guidance on apologies, they recommend that complaint responses include ‘an acknowledgement of the effect the problems have had for the other person’, for example, ‘you experienced significant delays and were left not knowing what was happening’.
The kinds of lessons about the importance of affiliation described in the interactional analysis section also apply to written complaints. Complainants have explicitly constructed their complaints in a way that stresses the evidentiality of the right and need to complain and also in ways that constructs their own identities as ‘reasonable complainants’. These constructions need to be recognised and affiliated with in the written responses. Sometimes this kind of affiliation can involve an expression of overt empathy: ‘I was sorry to hear about the difficulties you encountered and understand that this was an upsetting experience’. However, possibly of even more value is a complaint response that acknowledges the impact the complainable has had on the complainant (or their loved one). Where this kind of acknowledgement is lacking, we find this reflected in post-complaint evaluations by study participants:
-
Nobody has acknowledged the life that they’ve taken away from her, the life they’ve given her now.
-
There’s been no acknowledgement of how her life has changed or how it’s affected her and us as a family […].
-
[In the context of considering engaging a solicitor] They’re just not acknowledging what we’ve went through and how my mammy is.
In contrast, the quotation below from a Trust response is an example of good practice:
Good practice
The Trusts are very sorry that waiting times are very long presently and do not underestimate the impact that long waiting times have on individuals awaiting surgery.
Further examples of how a complaint response can be more affiliative include:
-
the repetition of words/formulations that complainants have employed themselves in formulating their complaint
-
using less formulaic language, avoiding the passive voice, and avoiding medical/bureaucratic register.
Avoid introducing ‘alternative’ narratives that undermine the complainant’s account of events
Complainants report feeling particularly aggrieved when a response includes alternative accounts of events which seem to directly contradict those presented by the complainant.
The staff member that has been mentioned does not recall sending you back to the waiting room.
These are felt to be particularly grievous when the experience being contradicted is an emotional, traumatic and necessarily subjective one. While the purpose of an investigation is to establish the ‘facts’ of the complaint, and to allow a ‘right of reply’ by individuals named in the complaint, the presentation of these conflicting perspectives as the substance of a response to the complaint risks framing the complaint response as a ‘defence’ by the Trust and is better avoided. Such responses are then construed as partial and ‘one-sided’ rather than being an even-handed investigation of all perspectives. This is an observation remarked on by family members in one case complaining about a serious adverse event experienced by their mother.
We were happy to leave the investigation with the Trust, as we believed it would be impartial and comprehensive. Unfortunately, we feel that the response so far has been one-sided, and we are very disappointed about this.
While it is important for a complainant to understand that concerns have been raised with relevant staff about their behaviour, a simple account that this conversation has taken place and an apology or expression of empathy would be more effective, as we see in the following good-practice formulation in the response to a participant’s complaint:
Good practice
Dr Hurst would like to extend his apologies to you regarding your experience in the ED. He recognises that this … has caused distress.
Make a clear commitment to change/reform
The most valuable outcome of a complaint for many complainants is the promise of future change and a guarantee that the complained-about event will not affect future patients. Evidence of practical steps to institute permanent changes (‘offer of repair’, ‘indication of future intention’, ‘remedy’) is a crucial key to the success and effectiveness of complaint handling.
Complaint responses should give concrete details of the changes that were made as a result of the complaint, as in the following good-practice example:
Good practice
Going forward from your complaint, more water jugs will be ordered for the department …. We have also increased the provision of bottled water for the department and this will be available for all patients.
Vague offers of or paying lip service to ‘learning points’ are insufficient (e.g. ‘we welcome your contribution to the service learning around clinic scheduling that we have taken on board as a result of your experience’; ‘He will incorporate this case into the teaching programme and ask the junior doctors to strongly consider …’). Complainants want evidence that permanent changes will be made as a result of their complaint, and they need to know these will be properly implemented and monitored (e.g. via the introduction of protocols). Vague appeals to good intentions and future learning are usually felt to be insufficient. Complainants express this view clearly in their statements that protocols need to be established and then monitored:
As time’s gone on I have become more cynical and felt if nobody’s monitoring the implementation of these changes then nothing going to- long term erm and (large systems) being as they are.
On the other hand, do not make false promises – do not promise what will not follow. It may be satisfactory at some point in the complaint journey but will enhance negative attitudes when it becomes clear that the promises weren’t kept. For example, in one of our cases, the complainant was promised a personal apology from the doctor which she didn’t ultimately receive, and her overall experience therefore worsened.
Apologies
Where a complaint investigation reveals the need for an apology, it is important that this is delivered effectively.
An apology should be personal, written for the specific occasion and be sensitive to the context in which the apology is being made.
SPSO guidance
The composition of an apology matters.
Lewicki et al. 2016126
In the SPSO’s guiding document, they point out that written apologies can be less effective than face-to-face apologies: ‘When we speak to another person directly we come over as fellow humans and not a faceless organisation’. For this reason, the composition of an apology in written communication is really important to get right.
Writers should avoid the ‘faux/politician’s apology’ (see also McCreaddie et al. ). 122 In other words, avoid framing the apology in terms of the patient’s feelings (and thus implicitly reducing the experience to something merely subjective): ‘I am sorry that/if you felt’. Acknowledge the reality of the experience for the patient. Also avoid expressions that suggest the patient’s experience may be in doubt, for example, ‘I wish to apologise for the distress she may have suffered’, ‘I apologise if this was the case’. Apologies that minimise the ‘hurt’ of the complaint (e.g. by suggesting ‘someone else is worse off than you’: ‘Mrs Khan acknowledges that at present you have been waiting 71 weeks and Mr Wright’s longest waiting knee replacement is currently waiting 247 weeks’) undermine the complaint and the complainant’s sense that they are being reasonable.
Where apologies are offered, avoid mitigating with appeals to exceptional circumstances, good intentions or standard practice. The following are good-practice examples that acknowledge and accept responsibility for the error without mitigation and apologise for it:
Good practice
It would appear that the ED doctor did not pick up this L1 fracture when she examined her x-ray picture and for this oversight, Dr Crossland sincerely apologises.
Dr Crossland wishes to apologise that the doctor did not communicate the plan and decision he had made based on discussions with the specialist tertiary team to your family. Further discussion could have changed the outcome. Dr Crossland acknowledges that the lack of communication has caused your family a lot of distress and for that he is sorry.
How to conclude
Our analysis demonstrated that complainants may be uncertain if the complaints process has concluded if they feel their concerns remain unmet. Therefore, it is important to communicate clearly that the complaints process has come to an end, so they can decide on their next actions if unsatisfied with the outcome (rather than waiting for some other actions from the Trust). An example of good practice is as follows:
Good practice
The Trust has now endeavoured to answer your questions and as such, this is our final response and concludes the internal complaints procedure.
Written responses and the complaint journey
As it is impossible to take into account every detail, it may be a good general practice to offer calls/appointments to complainants to make them feel heard, a part of the process, to express what are their actual concerns during the investigation (not after), at least for more serious cases.
It is important to take very brief notes of each point of communication with the complainant. In this way the trajectory of the complaint is uninterruptible. Complainants get very annoyed when they are told something, for example, via a phone call, and there are no traces this information was acknowledged in the response letter. Notes should be brief so they may be retrieved quite easily by the staff member who will be the next point of communication.
Finally, the overwhelming evidence of our analysis of longitudinal journeys points to the value of face-to-face conversations between complaint handlers and complainants. While written responses are an important record of the investigation and any reparations being offered, they are often deemed to fall short in terms of presenting complainants with a satisfactory outcome to their complaint. While the guidance above points to ways in which written responses can be improved, our recommendation would be that face-to-face meetings (especially in the more serious cases) are offered to discuss the outcome of a complaint alongside the written response.
References
Lewicki R, Polin B, Lount R. An exploration of the structure of effective apologies. Negot Confl Manag Res 2016;9:177–196. https://doi.org/10.34891/9awp-8644122
McCreaddie M, Benwell B, Gritti A. A qualitative study of National Health Service (NHS) complaint-responses. BMC Health Serv Res 2021;21:696. https://doi.org/10.1186/s12913-021-06733-5
Scottish Public Services Ombudsman. How to Make a Good Apology. www.spso.org.uk/sites/spso/files/csa/ApologyGuide.pdf (accessed 3 July 2023).
List of abbreviations
- A&E
- accident and emergency
- C
- complainant
- CA
- conversation analysis
- CH
- complaint handler
- CT
- Cultural Theory
- [CW]
- data from complaint in writing to Trust
- D
- data from diary
- DA
- discourse analysis
- [E]
- data from e-mail to study member
- ED
- Emergency Department
- ENP
- Extended Nurse Practitioner
- GP
- General Practitioner
- HSCNI
- Health and Social Care Northern Ireland
- [I]
- interview data
- NIPSO
- Northern Ireland Public Services Ombudsman
- PAS
- Patient Advocacy Service
- PInn
- pilot project participant nn
- PPI
- patient and public involvement
- [Rc]
- data from recruitment call
- RCnn
- Real Complaints longitudinal participant nn
- [RP]
- data from response by patient to Trust
- SPSO
- Scottish Public Services Ombudsman
- [T]
- data from telephone call to Trust
- [TD]
- data from telephone diary
- TRF
- telephone resolution form
- [W]
- written response from Trust
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/NRGA3207).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
