Notes
Article history
The research reported here is the product of an HSDR Rapid Service Evaluation Team, contracted to undertake real time evaluations of innovations and development in health and care services, which will generate evidence of national relevance. Other evaluations by the HSDR Rapid Service Evaluation Teams are available in the HSDR journal.
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as project number NIHR131295. The contractual start date was in October 2018. The final report began editorial review in July 2020 and was accepted for publication in October 2020. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2022 Sidhu et al. This work was produced by Sidhu et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2022 Sidhu et al.
Chapter 1 Background, context and objectives
Parts of this report have been reproduced with permission from Sidhu et al. 1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Summary of key points
-
The evaluation reported here is of instances where organisations running NHS acute hospitals have taken on the responsibility of also running some general practices.
-
This change in practice has been happening in several locations in England and Wales, with the first instances commencing in 2016, but it is not yet widespread practice.
-
An acute hospital taking responsibility for running general practices is an example of ‘vertical integration’, that is, integration between organisations operating at different stages along the patient pathway.
-
Vertical integration can occur in any area of the economy and can be seen as a way of attempting to reduce transaction costs and to reduce risks for the integrating entities. Vertical integration can make decision-making, monitoring and information-sharing more efficient. In health care, this might translate as better mutual understanding between general practitioners (GPs) and hospital specialists, better communication and flows of patient information between GPs and hospital specialists, and reduction of risks through better demand management.
-
The NHS across England and Wales is working towards systems of care that offer better co-ordination across the primary and secondary care interface. One innovative approach to achieving stronger integration of care is via vertically integrating primary care organisations with secondary care organisations (i.e. co-ordination within a single management entity of staff, infrastructure, functions and activities that contribute to different levels of patient care).
-
There has also been growing interest in extending the range of health-care services that are delivered in primary care settings. However, at the same time, in the face of growing patient demand combined with GP workforce constraints, the long-term sustainability of primary care has become an increasing focus of concern.
Background
This report presents a rapid evaluation of arrangements whereby NHS organisations operating acute hospitals have additionally taken over the running of general practices at scale in a few locations in the NHS in England and Wales (i.e. a new form of vertical integration). There is little systematic information on the rationale for, or desired impact of, such vertical integration in a UK NHS setting, or on why it is developing in some places despite not being an explicit part of current NHS policy in England or Wales. There is, correspondingly, limited understanding about how to implement vertical integration in a UK NHS setting (e.g. contractual/governance and commissioning issues) and the enablers of and barriers to its implementation. The number of examples of vertical integration is, nevertheless, growing and so it is timely to evaluate their implications.
The initial impetus for the evaluation of vertical integration was a desire to understand the logic of this form of integration in the provision of health care across primary and secondary care settings. However, as the study progressed, it became clear that a major driver of vertical integration is a response to difficulties with sustaining general practices and, therefore, local access for patients to primary health care.
In this chapter, we first describe the institutional context. We then locate the form of vertical integration that is the focus of this evaluation within the landscape of types of health-care integration, before going on to describe the current and recent past policy context relevant to such vertical integration. We finish the chapter by stating the aims of the evaluation reported here and outlining the structure of the rest of the report.
Institutional context
Within the NHS, acute hospitals do not usually run primary care services. Indeed, at the founding of the NHS in 1948, although hospital services were nationalised, GPs remained as independent practitioners. GPs were, and usually still are, contracted by the NHS to provide primary care medical services to the patients who register with them. GPs also have the responsibility of acting as ‘gatekeepers’ to other NHS services, including acute hospitals; however, GPs are not employees of the NHS. 2 This separation between primary and secondary care has been maintained through numerous NHS reforms, including the major reorganisations in 1974 and 1990. 3 Indeed, the 1990 reforms arguably deepened the divide by casting GPs in the role of fundholders and, therefore, ‘purchasers’ from secondary care providers (i.e. NHS trusts). In the past 20 years, the role of GPs as purchasers or commissioners of care for their patients from other NHS organisations, as individual practices, has reduced. However, as members of Clinical Commissioning Groups (CCGs) and primary care networks (PCNs) in England, GPs’ involvement in purchasing hospital care remains strong. At the same time, the desirability of better integration of patient care across primary and secondary care settings has become firmly established as a policy objective, as described later in Policy-drivers for integration.
Acute hospitals are providers of hospital-based emergency and/or elective specialist health care. In England, acute hospitals are run by a publicly owned organisation known as an ‘NHS foundation trust’ or an ‘NHS trust’ (hereafter referred to collectively as trusts). There are 152 acute hospital trusts in England. 4 The institutional set-up of the NHS in Wales is different from that of the NHS in England. In Wales, NHS acute hospitals are run by seven territorially defined Local Health Boards (LHBs). The services of acute hospitals are contracted for by both national and local NHS ‘commissioners’ of care. In England, the commissioning organisations are NHS England (London, UK) (nationally) and CCGs (locally). In Wales, the commissioners are NHS Wales (Cardiff, UK) (nationally) and LHBs (locally).
Until the last few years, hospital trusts in England had no role in running general practices. Although it remains most often the case that hospital trusts do not run general practices, in recent years, a small number of departures from this have occurred (i.e. a few hospital trusts in England have started to run general practices). In Wales, the LHBs directly run hospitals and community health services. LHBs also contract with independent general practices, but LHBs do not usually operate general practices directly. However, in recent years, this has started to change in a few locations in Wales. It is these recent changes in England and Wales that provide the initial stimulus for the evaluation reported here. Our focus is on those cases where organisations running acute hospitals have taken on general practices at scale (i.e. more than just one or two practices). Such vertical integration at scale is a relatively new phenomenon in the NHS – occurring over the period since 2015 – and the number of examples is currently small and scattered geographically. Nevertheless, interest in vertical integration is growing and during the study we became aware of new examples starting up.
The arrangements for general practices are essentially the same in both England and Wales; they provide primary medical care to their registered populations, which are effectively the total national population in aggregate. General practices are staffed by GPs and, increasingly, other health-care professionals (e.g. nurses and pharmacists). In England, as of September 2019, there were around 7000 general practices with 34,586 GPs (headcount), of whom there were 26,958 full-time equivalent qualified permanent GPs (i.e. excluding locums and trainees). 5 In Wales, as of September 2018, there were 421 general practices6 with 1964 GPs (headcount). 7
There are, in both England and Wales, three types of contract by which the NHS buys the services of GPs: (1) General Medical Services (GMS), (2) Personal Medical Services (PMS) and (3) Alternative Provider Medical Services (APMS) (Box 1). GMS contracts are the most common and are between GP-owned practices and NHS England (in England) or their LHB (in Wales); PMS and APMS contracts, which resulted from primary care reforms in 1997,8 are less common. However, the traditional GMS contract, where GP partners own the practice, has been declining in popularity. The UK Government’s 2019 GP Partnership Review9 stated that ‘The numbers of GP partners are falling as a proportion of the general practice workforce’ (contains public sector information licensed under the Open Government Licence v3.0) (although the report did not provide any relevant data).
The GMS contract is agreed nationally. This type of contract provides the contracting general practice with an income stream to pay for the staff, premises and other costs of providing a menu of compulsory ‘essential’ services. Under the GMS contract, a practice may also voluntarily provide, and be paid for, ‘additional services’ and ‘enhanced services’. Around 55% of general practices have GMS contracts.
Personal Medical ServicesPMS contracts are negotiated locally (with the local CCG in England or LHB in Wales). The GPs are paid to provide a defined service as agreed locally. Around 40% of general practices have PMS contracts.
Alternative Provider Medical ServicesAPMS contracts can be let to private-sector – both commercial and voluntary – organisations, as well as to traditional general practices. This type of contract tends to be used in areas where it is difficult to recruit and retain GPs. Around 5% of GP services are provided via APMS contracts.
Source: Healthcare Financial Management Association 2016, pp. 40–1.
In both England and Wales, there are many areas where recruitment and retention of GPs is a challenge. The number of GPs per 100,000 population has fallen in England since 2009 (from 66 then to 58 in 2018) and in Wales since 2013 (from 64 then to 63 in 2018) in a context, in both countries, of increasing demand from the population for health care, including primary care. 10
The evaluation reported here is of those instances where acute hospitals have taken on the responsibility for fulfilling GP contracts. This change in practice has been happening in several locations in England and Wales, with the first instances commencing in 2016; however, it is not yet widespread practice and so it is now timely to evaluate such arrangements.
Vertical integration
An acute hospital taking responsibility for these GP contracts and, therefore, for running general practices, is an example of ‘vertical integration’, that is, integration between organisations operating at different stages along the patient pathway. This kind of integration is distinct from ‘horizontal integration’, whereby organisations at similar stages along the patient pathway merge, such as when one acute hospital trust merges with another, or when one general practice merges with another or joins a network of general practices. 11,12 Vertical integration between acute hospitals and general practices in the NHS often entails an element of horizontal integration. When hospitals merge with more than one general practice, those practices are effectively integrated horizontally with one another, as well as vertically with the hospital. Our focus is on the vertical aspect of the integration. There are many other types of horizontal integration between general practices (Smith J and Sidhu M, University of Birmingham, 2020; Parkinson S and Harshfield A, RAND Europe, 2020; personal communication), but horizontal integration is not the focus of the evaluation reported here.
The concept and term ‘vertical integration’ has a long history in the economics literature13 and is seen as having three main aspects: (1) market power, (2) risk management and (3) transactions costs. Some associated perspectives on vertical integration have emerged in the context of competitive product markets; these perspectives are likely to be of limited relevance in an NHS context. For example, no UK NHS acute hospital has ever set up new general practices, as they might, in principle, were they in a competitive market where they were keen to channel patients to themselves rather than to rival hospitals. Nonetheless, the economic perspective does offer the following additional insights of potential relevance to the case of acute hospitals running general practices.
Vertical integration can be seen as a way of attempting to reduce transaction costs, as it can make decision-making, monitoring and information-sharing more efficient. 14 In the context of our evaluation, this might translate as better mutual understanding between GPs and hospital specialists, and better communication and flows of patient information between GPs and hospital specialists. A vertically integrated organisation can use more informal and less time-consuming procedures to resolve conflicts internally than would independent agents from separate organisations. 13
Vertical integration could also be a strategy to reduce risk. If risk grows over time, then the attractiveness of this strategy may increase correspondingly. In a competitive market, this may involve securing a segment of potential customers who might otherwise purchase from a rival, but it is also relevant in an NHS context, where the risk to be reduced may be that of demand growing faster than the capacity of the hospital and its sources of NHS funds to meet that demand. A hospital integrating with general practices from which patients are referred to it may offer the prospect of greater demand management. Less positively, vertical integration may mean that patients find themselves less able to exercise choice between alternative providers of hospital care because their GP is inclined to default to referring them to the hospital that employs them.
Laugesen and France15 reviewed the applicability of economic theories of integration to the health-care sector, with specific reference to the UK and the USA. Laugesen and France15 were particularly interested in the scope for risk management and transactions cost reduction via vertical integration. The study15 does not mention a specific example from primary care but vertical integration in the UK is such an example. Here, risk management might mean not only the risks to a hospital of insufficient or excessive demand, but also the financial risks faced by the owners of individual general practices that are facing difficulties in recruiting and retaining new partner GPs. In the US context, Laugesen and France15 highlighted Kaiser Permanente (Oakland, CA, USA) as a well-developed vertically integrated health-care organisation. Kaiser Permanente and other international examples of vertical integration in health care are briefly described in Chapter 2.
In the health-care context, vertical integration has been defined by Ramsay et al. 16 as being of six types: organisational integration (organisations merge into one or bind themselves together contractually), functional integration (non-clinical activities for multiple organisations are combined), service integration (clinical services are integrated within the same organisation), clinical integration (where patient care becomes a single integrated process both within professions and across them, e.g. by using shared guidelines), normative integration (the sharing of values in collaborating to deliver health care) and systemic integration (making rules and policies coherent across all organisational levels).
Conrad and Dowling17 have argued that vertical integration requires (1) the clinical integration of the processes involved in delivering patient care and (2) administrative (functional) integration at both inter- and intraorganisational levels. Therefore, strong administrative integration (e.g. management support, governance and strategy formation) is required to support clinical integration whereby patient care is improved over time. Subsequently, to achieve near-complete vertical integration of care across primary, community and secondary sectors, health care for patients should cut across health promotion and disease prevention all the way through to treating short-term episodic acute illness. Shortell et al. 18 identified a number of limiting factors that need to be considered prior to commencing vertical integration. These factors include (but are not limited to) the need to establish trust among clinicians and institutions, well-integrated information systems and non-clinical support services (i.e. back office functions) and consensus on practice and care delivery guidelines. Robinson and Casalino19 go further, suggesting that vertical integration needs to go beyond a physician’s desire for professional autonomy and a hospital’s desire for organisational co-ordination to show how services in primary care can be delivered through greater horizontal integration, achieving ‘integrated delivery systems’ (known as PCNs and primary care clusters in England and Wales, respectively). Theoretically, vertical integration between acute hospitals and integrated delivery systems can lead to efficient use of services across the care pathway (particularly post-acute care) and avoid duplication of administrative tasks; but, more importantly, vertical integration should lead to a single hierarchy of authority with shared goals and strategies.
Policy-drivers for integration
Despite the historical institutional separation between general practices and hospitals, integration between the multiple levels and providers of health and social care has increasingly been seen, in both England and Wales, as important for the effectiveness and efficiency of the NHS in the long term and to improving the care provided to patients. The NHS across England and Wales is working towards systems of care that offer better co-ordination across the primary and secondary care interface. One innovative approach to achieving stronger integration of care is vertically integrating primary care organisations with secondary care organisations (i.e. providing co-ordination within a single management entity of staff, infrastructure, functions and activities that contribute to different levels of patient care). 12,16,17 Such organisational integration can range from virtual integration that entails the formation of relatively flexible alliance arrangements to a fully integrated organisational model in which a single body holds contracts to deliver both secondary and primary care services. 20 In this evaluation, we are interested in the fully integrated model of vertical integration, specifically NHS acute hospitals taking over the management of general practices.
In England, the NHS Five Year Forward View21 described, among other options for stronger integration between primary and secondary care, what it termed primary and acute care systems (PACS), which would combine general practice and hospital services ‘for the first time’21 (contains public sector information licensed under the Open Government Licence v3.0),21 although not yet within single vertically integrated organisations. There were nine PACS ‘vanguards’ at a variety of locations scattered across England. 22 In 2018, a report from The King’s Fund recommended that acute hospitals should play a greater role in primary care provision:
. . . acute hospitals will need to play a fundamentally different role within local health economies. This will involve: . . . working more closely with local partners, including primary care . . . developing integrated service models that span organisational boundaries . . .
Naylor et al. 23
Evaluations of the PACS ‘vanguards’ have found evidence of considerable change activity, but have not yet yielded clear conclusions on the outcomes achieved as a result. The National Audit Office (London, UK) has found early signs that PACS and other new models of care focused on integration are having a beneficial effect on emergency admissions to hospitals,22 and there have been ‘significant amounts of innovation in terms of both front-line services and wider structures supporting system-wide collaboration’. 20 However, data and findings are limited across the vanguard sites, with questions about the reliability of outcomes data and, consequently, uncertainty about the impact of PACS on key dimensions of health service delivery. 24,25
Five years on from the NHS Five Year Forward View,21 the 2019 NHS Long Term Plan26 announced the intention that all general practices in England should combine into PCNs covering populations of 30,000–50,000. 26 Since July 2019, all but a small number of practices have become horizontally integrated in that way with other practices, although remaining separate legal entities with separate contracts. Findings from a recent BRACE (Birmingham, RAND and Cambridge Evaluation Centre) rapid evaluation (Smith J, Parkinson S, Harshfield A, Sidhu M, personal communication) of PCNs show that there have been a number of facilitators of and challenges to horizontal integration achieving sustainable primary care, addressing growing workload issues and improving the availability and co-ordination of local primary care services. The evaluation (Smith J, Parkinson S, Harshfield A, Sidhu M, personal communication) revealed a tension between the desire for local autonomy and influence over PCNs, and the top-down nature of PCN policy (i.e. the need for effective leadership). Notably, rural case study sites from the evaluation felt that PCN policy had been developed with urban practices and collaborations in mind, and did not adequately account for the experience of primary care in rural areas. Vertical integration was not specifically mentioned in the NHS Long Term Plan,26 but is, nevertheless, happening in a few locations.
In 2015, the Welsh government published a plan for primary care services in Wales over the following 3 years. The plan set out a specific aim for the 64 ‘primary care clusters’ (i.e. collaborations between general practices) that had recently been set up in Wales, each covering a population of 30,000–50,000, to ‘play a significant role in planning the transfer of services and resources out of hospitals and into their local communities for the benefit of their local populations’ (© National Assembly for Wales Commission Copyright 2017. Inquiry into Primary Care: Clusters). 27 Reviewing progress with primary care clusters, the National Assembly for Wales Health, Social Care and Sport Committee reinforced the desirability of that form of integration. 27 The subsequent Strategic Programme for Primary Care in 2019 built further on these initiatives through an enhanced community-based model of primary care. 28 This model arose, in part, from the national Pacesetter Programme, in which LHBs received funding to support innovations within primary care. Research by University of Birmingham (Birmingham, UK) found that, although the Pacesetter Programme had enabled some positive developments, overall, it was hampered by a lack of clarity about its objectives, insufficient evaluation capacity and underdeveloped opportunities to share learning. 28 Similarly to the situation in England, vertical integration between acute hospitals and general practices is not currently being specifically advocated by NHS policy-makers in Wales, but it is happening spontaneously in a small number of places.
Alongside the push for better integrated care, there has been growing interest in extending the range of health-care services that are delivered in primary care settings. 21 However, at the same time, the long-term sustainability of primary care has become an increasing focus of concern in the face of growing patient demand combined with GP workforce constraints. 29,30
With this background of pressure to better integrate secondary and primary care services and to increase the range of services available in primary care settings, combined with concerns about the sustainability of general practices, there are a number of potential pragmatic reasons that might drive vertical integration between acute hospitals and general practices. Vertical integration brings the opportunity to redesign services; address problems with governance, funding, differing objectives and drivers; reduce transactions costs; enhance the ability to involve both primary care and secondary care clinicians in the design of effective and efficient clinical pathways; and, for patients, improve continuity of care and foster more seamless transitions between teams and services. Organisational vertical integration between hospitals and general practices might help to overcome co-ordination challenges that result from the discrete financial ‘silos’ in which primary care and secondary care otherwise find themselves (e.g. where investment in one sector yields cost savings in the other). Vertical integration, which entails practice staff becoming salaried employees of an acute hospital NHS trust (England) or LHB (Wales), may particularly suit younger GPs, many of whom are showing reluctance to buy into the traditional ‘partner model’ of general practice and are showing a preference to be sessional or salaried. 16,31
There are also potential downsides to the implementation of acute hospital and general practice vertical integration, including fears among some GPs of reduced GP autonomy and, therefore, damage to what they see as the entrepreneurialism and innovation of general practice;16,32 mistrust from local primary care stakeholders;33 and doubts over how much inappropriate health service utilisation can be reduced through vertical integration, especially compared with other models of integration. 34
Chapter 2 Scoping the evaluation
Summary of key points
-
The study team took a narrative-based descriptive thematic approach to synthesising findings drawn from a rapid scoping review guided by existing theory on vertical integration.
-
The reasons most commonly cited in the literature for integrating acute hospitals and primary care services (i.e. vertical integration) were concerned with expectations of providing better-quality, more effective health care, with better patient experiences of care being delivered at lower, or at least no higher, costs to the health-care system as a whole.
-
Vertical integration can be undertaken by recourse to different types of contractual and governance arrangements, but evidence as to which are more effective, and in which circumstances, is not yet available.
-
Core characteristics and enablers of vertical integration include establishing continuity of care; the management of finance, human resources (HR), information technology (IT) and planning being closely co-ordinated across the units being integrated; and building relationships with doctors who actively participate in management and are economically linked to their organisation.
-
Barriers to the successful implementation of vertical integration include professional silos, unlinked and differing information systems, difficulties sharing patient records between organisations and organisations’ different approaches to case management.
-
There is a lack of robust evidence on the impact and effectiveness of vertical integration in health care, particularly with respect to patient outcomes.
The first stage of the evaluation comprised a pragmatic rapid scoping review of the literature, supported by interviews with key informants, discussion with the members of the BRACE Steering Group (which includes experienced health services evaluators, commissioners and health-care practitioners) and a project design workshop with policy-makers and external researchers. This was a key stage in the evaluation to understand the existing evidence, develop research questions and identify potential case study sites. We obtained an overview of the evidence already reported on vertical integration of acute hospitals with general practices and identified knowledge gaps to be filled and propositions to be tested later through comparative case studies, following principles outlined by Munn et al. 35 In this chapter, we present our findings from the scoping of the literature and key learning from interviews with informants, and the research questions that subsequently emerged.
To scope the evaluation, we reviewed published literature, including grey literature (i.e. literature that is not formally published in sources such as books or journal articles such as NHS trust reports and/or working papers from policy groups or committees). We used a selective but systematic approach to searching and provided a descriptive summary of our findings.
The study team took a narrative-based descriptive thematic approach to synthesising findings drawn from the rapid scoping review, guided by existing theory on vertical integration. 17 We thematically categorised literature according to differing models of vertical integration to aid the identification of core characteristics that act as enablers of successful implementation. We then sought to draw connections between core characteristics and desired outcomes for vertical integration within a UK NHS context. A more detailed description of our literature review method is provided in Appendix 1, along with our search terms (see Appendix 1, Box 2) and a PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow chart with regard to screening results (see Appendix 1, Figure 8).
Discussions with key experts
In parallel with the scoping review, members of the study team completed telephone interviews (using a structured topic guide informed by the literature; see Report Supplementary Material 1) and face-to-face meetings with academics, policy analysts and NHS staff involved in the implementation of vertical integration across different sites in the UK (total n = 13). The study team sought (1) their initial insights and perspectives on why vertical integration was introduced and (2) their views on which research questions should be prioritised in a rapid evaluation. The team also sought to better understand the current climate of primary and acute care working more closely together and what the possible advantages and disadvantages of vertical integration would be for acute trusts and general practices. Telephone interviews with NHS staff helped the research team to identify potential case study sites across the UK that would be eligible to partake in a rapid evaluation.
Following the review of the literature and the scoping interviews, the research team held a stakeholder project design workshop to consider the scope of an evaluation of vertical integration between acute hospitals and general practices, and to refine the research questions. 36 The workshop took place in Birmingham in March 2019. In addition to research team members, participants included an independent researcher expert in the field of integration in the NHS and employees of the Department of Health and Social Care (England) and NHS England.
Findings from the literature
Several examples of vertical integration between organisations involved at various stages of the care pathway were identified in the UK, some of which are examples of an NHS acute hospital taking responsibility for the delivery of GP services.
South Somerset’s Symphony Project (2016 to present)
-
The South Somerset’s Symphony Project involved integration between Yeovil District Hospital NHS Foundation Trust (Yeovil, UK) and local primary care providers through stronger partnerships, supporting practices and improving joint work between GPs and hospital services. 37
Southwark and Lambeth Integrated Care (2012–16)
-
Southwark and Lambeth Integrated Care was a 4-year integrated care programme across two adjacent south London boroughs, which attempted to integrate care across primary, acute, community, mental health and social care. 33
The Royal Wolverhampton NHS Trust primary care vertical integration (2016 to present)
-
Primary care vertical integration at the Royal Wolverhampton NHS Trust (Wolverhampton, UK) involved nine practices in the West Midlands being run by the Royal Wolverhampton NHS Trust. 38
Closer to Home (2006–7)
-
The Closer to Home project involved the moving of selected specialist services for less complex conditions from hospital into a community setting in five different sites across six specialties in each. 39
Northumbria Primary Care (2015 to present)
-
Six practices in Northumbria were run by the Northumbria Healthcare NHS Foundation Trust (Newcastle-upon-Tyne, UK). 40
The Willow Group (April 2017 to present)
-
The Willow Group comprised four practices in Gosport (Hampshire, UK) being run by the Southern Health NHS Foundation Trust (Southampton, UK). 41
Some international examples of specific relevance were also identified:
The Alzira model (1999–2018)
-
The Alzira model involved a single health-care provider receiving a fixed annual sum per inhabitant to supply free universal access to a range of primary, acute and specialist hospital services in Valencia, Spain. 42,43 It is worth noting that, in 2018, the contract with the private provider was terminated after nearly 20 years by Valencia’s health authority and the services then reverted to public ownership. According to Comendeiro-Maaløe et al. ,44 the termination was for a combination of reasons relating to ‘Financial concerns, governance failures and politics’.
The Kaiser Permanente Community Health Initiative (2003 to present)
-
The Kaiser Permanente Community Health Initiative is an integrated health-care delivery system that provides care for more than 12 million members in the USA. 45
Odense University Hospital co-operation model between the hospital and general practitioners, including co-location of primary and secondary services (2013–16)
-
The Odense University Hospital co-operation model involved an on-call GP facility located alongside the accident and emergency (A&E) department at a hospital in Odense, Denmark. 46
The remainder of this section draws on information from the literature on acute hospital/general practice vertical integration. The following themes emerged from the scoping of the literature and are used to organise the scoping results that are presented in the remainder of the chapter:
-
the rationale behind vertical integration schemes
-
contractual and governance arrangements
-
the core characteristics and enablers of vertical integration
-
concerns about and barriers to such programmes
-
the outcomes identified.
Rationale
As noted in Chapter 1, it is possible to hypothesise several reasons for integration between acute hospitals and general practices. It might bring the opportunity to redesign services; address problems with governance, funding, differing objectives and drivers; reduce transactions costs; enhance the involvement of both primary care and secondary care clinicians in the design of effective and efficient clinical pathways; and, for patients, improve continuity of care and foster more seamless transitions between teams and services.
Primary and acute care systems were a new model of care that was introduced in the hope that they would deliver on the ‘triple aim’ of the new care models programme as a whole (i.e. better patient experience, better population health and more efficient use of resources). 20 It is hoped that these aims will be met through better decision-making and a more sustainable use of resources, with a stronger focus on prevention and integrated community-based care and less reliance on hospital care. 21
The rationale for/drivers of integration in some UK examples from the literature are outlined in Table 1. The first of these – Southwark and Lambeth Integrated Care – is an example of where vertical integration stops short of the acute trusts concerned taking ownership of general practices. The Royal Wolverhampton NHS Trust has taken over a number of the general practices in its local area. Northumbria Primary Care is a not-for-profit company wholly owned by Northumbria Healthcare NHS Foundation Trust and is an example of where an organisation running acute hospitals (i.e. the trust) has taken over responsibility for running some general practices.
| Case study example | Description | Rationale/drivers |
|---|---|---|
| Southwark and Lambeth Integrated Care | Socioeconomically relatively deprived areas, with multiethnic populations, high burden of disease and fragmented health and social care services |
|
| The Royal Wolverhampton NHS Trust | Socioeconomically relatively deprived areas, with multiethnic populations, high burden of disease and fragmented health and social care services |
|
| Northumbria Primary Care | Socioeconomically relatively deprived areas, with an elderly white British population, high burden of disease and fragmented health and social care services |
|
With respect to the international examples, the institutional contexts in the respective health-care systems differ from England and Wales. However, the examples are interesting indications that the option of acute hospitals operating primary care practices has attracted interest beyond the UK. The rationales highlighted in the literature vary across the different vertical integration examples, but, in all cases, are potentially highly relevant in a UK context. The Alzira model was introduced with the expectation of efficiency improvements, leading to cost savings and, at the same time, providing services of a higher quality. 42,43 The Kaiser Permanente Community Health Initiative integrated health care at all levels to tackle local public health issues, such as reducing obesity in low-income communities. 45 In Denmark, the Odense scheme focused on improving co-ordination between hospital A&E services and GP services. 46
Overall, the rationales we found to be most commonly cited for integrating acute hospitals and primary care services were concerned with expectations, or hopes, of providing better quality and more effective health care, with better patient experiences of care being delivered at lower, or at least no higher, costs to the health-care system as a whole.
Contractual and governance arrangements
Vertical integration can be undertaken by recourse to different types of contractual and governance arrangements, but evidence as to the advantages and disadvantages of different approaches is not available.
With respect to PACS, three contracting models are possible. 47
Virtual primary and acute care systems
Virtual PACS are when providers in different parts of the health-care system, including acute hospitals and general practices, are bound by an alliance agreement (i.e. where two or more independent entities agree to work together, without forming a jointly owned entity, to deliver care for the local population). PACS are not a new contractual model, but, instead, overlay an alliance agreement on top of the existing system of contracts by which acute hospital and primary care services are governed in the NHS (as described in Chapter 1). An alliance agreement could establish a shared vision and ways of working, and the role for each provider in the PACS.
Partially integrated primary and acute care systems
Partially integrated PACS go further than virtual PACS and require most providers, but excluding primary care practices, to have a single contract with the commissioner of health-care services, implying, in turn, that those other providers must have a contractual relationship with one another, but general practices are explicitly outside this. The single contract holder would be required to integrate directly with primary medical services delivered under GMS, PMS and APMS contracts (see Box 1).
Fully integrated primary and acute care systems
The PACS hold a single, whole-population budget for the full range of services in scope, including primary medical services. No fully integrated PACS yet exist.
Vertical integration between acute trusts and general practices would imply either partially integrated or fully integrated PACS. The Royal Wolverhampton NHS Trust and south Somerset’s Symphony Project have taken partially integrated PACS approaches. 37,38 Elsewhere, the evaluation of the Southwark and Lambeth Integrated Care programme, which adopted a ‘virtual’ approach rather than formal contracting, highlighted the importance of shared ownership and leadership among the stakeholders. 33
The health-care system in Spain is, like that in the UK, tax funded and largely provided by publicly owned organisations. With respect to the Alzira model, payment to the providers of the integrated services was made through a capitation system, whereby a budget is assigned according to population size and range of service provision. Furthermore, hospital doctors and many GPs were employed directly by the private organisation providing the integrated services. 43 Therefore, the Alzira model was equivalent to a fully integrated PACS approach.
Relatively little information was present about the governance of existing vertical integration programmes referred to in the literature. However, details were provided for the Southwark and Lambeth Integrated Care programme. The Southwark and Lambeth Integrated Care programme was set up as a partnership across local general practices, three NHS foundation hospital trusts, two CCGs, one mental health foundation trust and two local government authorities. 33 The Southwark and Lambeth Integrated Care programme was run by four main boards: (1) a sponsor board for strategic direction and high-level decision-making, (2) a provider group for turning strategy into action, which also acted as a programme board, (3) an operations board, which oversaw delivery, and (4) a citizens’ board, which gathered input from patients and local citizens. Importantly, citizens and primary care were also represented on the other three boards.
The Royal Wolverhampton NHS Trust employs a public health consultant and registrar to ensure that the general practices are up to date on ways to improve health in the area and reduce unnecessary demand for health-care services. Moreover, there is a ‘command centre’ that handles calls to all practices, which also employs social services staff. General practices run by the Royal Wolverhampton NHS Trust also have access to a live data set showing their patients’ contacts with acute, primary and community services, and the practices can book patients directly into hospital beds at the Royal Wolverhampton NHS Trust. 38
Core characteristics and enablers of vertical integration
The information found on core characteristics and enablers of vertical integration is drawn from the international literature, in particular relating to the USA, but many of the observations are relevant to a UK setting. Sheaff et al. 31 identified seven core characteristics of successful vertically integrated health-care organisations in the USA:
-
hierarchical governance or long-term relationships between organisations that vertically integrate
-
continuity of care and provision by teams, enabling less costly models of care
-
capitation payment, creating incentives for preventative care
-
competing with other providers on quality rather than price
-
good management and information systems, with ‘functional integration’ (i.e. support functions, such as the management of finance, HR, IT and planning, being closely co-ordinated across the units being integrated)
-
sufficiently large organisation and population served to ensure long-term stability of the organisation and enable the development of care pathways for common diseases
-
doctors who actively participate in management and are economically linked to their organisation.
Furthermore, Sheaff et al. 31 identified two strong enablers of vertical integration: (1) a ‘front-door’ triage of patients coming into hospital as emergencies and (2) an integrated electronic patient record system accessible by both hospital and primary care professionals. 31 Despite the major differences between the US health-care system and the systems in England and Wales, the characteristics and enablers of vertical integration identified by Sheaff et al. 31 are all relevant to the case of acute hospitals running general practices in the UK.
The Alzira model established a unified information system, becoming the first public hospital in Spain with a fully integrated computerised medical history system. 43 Moreover, the Alzira model introduced medical links between secondary and primary care, with a secondary care consultant physician associated with each primary care health centre and working with the same patients as the GP; integrated primary care centres with an increased scope of services provided (e.g. X-ray imaging); and integrated medical care pathways, from prevention through to palliative care, to enable the integration of primary and secondary care.
Concerns about, and barriers to, vertical integration
There is rather more evidence available on concerns about vertical integration and barriers to its success, particularly with respect to acute hospital integration with general practices. In their analysis, Sheaff et al. 31 found that obstacles to care co-ordination can remain within integrated organisations for reasons such as professional silos (with rivalries and self-imposed isolation of occupational groups from one another), discrepant IT systems for different divisions or care groups within one organisation, difficulties sharing patient records between organisations and organisations’ different approaches to case management. 31 All of these potential obstacles are familiar within the UK context too.
The impact of cultural barriers to integration across organisations and professions can be significant. Differences in practices, cultures and values may exist between different general practices being combined within a vertical integration arrangement, or between primary care staff and hospital staff; if so, such differences are likely to influence the extent and quality of joint working. (See Mannion et al. 48 for an example and a helpful summary of the meaning and use of organisational culture in health care.)
In their review of the evidence base for vertical integration for health care, Ramsay et al. 16 identified three major concerns:
-
integration that focuses mainly on bringing organisations together is unlikely to create improvements in care for patients
-
integrating providers in certain geographical areas may create a monopoly and, therefore, may restrict patient choice
-
top-down attempts to integrate (e.g. that impose mergers of service providers) often have less happy outcomes than those that are motivated from the bottom up.
The issues appear to be directly relevant to acute trust and general practice vertical integration because of the geographical proximity of the organisations, the natural focus it has on bringing different organisations together and the risk that it might be driven by top-down integration (i.e. instigated by the acute trust and, therefore, seen by general practices as being done ‘to’ them rather than ‘with’ them).
International literature on vertical integration schemes also points to various concerns and barriers. When considering the Alzira model in the context of the UK NHS, concerns raised by the NHS Confederation were that:43
-
commissioners of health services would have less control over how health care is provided, as more of the care process would be internal to an organisation and that organisation would be more powerful than individual unintegrated organisations would be
-
commissioners might even be subject to ‘regulatory capture’, meaning that the vertically integrated provider might control the local health economy to such an extent that independent oversight by the commissioner would cease to be effective
-
the vertically integrated model could squeeze out all other providers, such as social enterprises, charitable providers and other niche services, creating a local monopoly.
To some extent, these concerns stem from the involvement of a private sector organisation running the vertically integrated services for the publicly funded health-care system in that region of Spain. However, these concerns might, in principle, also apply to any vertically integrated group of health-care providers. The concept of regulatory capture of, and loss of control by, commissioners of/payers for health care appears not to have been a subject of much research in the NHS and comparable publicly run health-care systems.
With respect to the Odense University Hospital vertical integration in Denmark, the different incentives in primary care and secondary care around professional approach, culture and reimbursement made integration there challenging. 46 Such differences between primary and secondary care exist in the UK too. These difficulties are not necessarily removed by employing both primary care and secondary care staff in the same organisation.
Outcomes
There is a lack of robust evidence on the outcomes and effectiveness of vertical integration in health care, particularly with respect to patient outcomes. In the scoping review, all the evidence we found on the outcomes achieved by acute hospital integration with general practices was anecdotal. Caution is needed when interpreting the transferability and robustness of the data we collected, because (1) very little high-quality published evidence was available on the outcomes and impact of vertical integration and (2) in the evidence that was available, many of the findings demonstrated inconclusive or mixed results.
Ramsay et al. 16 concluded the following when considering the impact of vertical integration between different organisations on a care pathway:
-
Some evidence of strengthened partnerships [between the integrating organisations] . . .
-
Some reports of improved capacity, for example personnel, and improved focus on governance and adherence to guidelines
-
Little evidence of impact on health outcomes
-
Limited evidence of impact on cost. 16
The Southwark and Lambeth Integrated Care programme did not achieve the radical reductions in hospital and nursing home utilisation that were initially expected. 33 Although a reduction in admissions to nursing homes was observed and there was no increase in the rate of emergency admissions to hospital, this fell some way short of targets set at initiation. 34 Despite this lack of impact on health-care utilisation, other benefits did emerge. Effective efforts at integration took place between partners across health and social care, there was greater citizen engagement and co-production, and there was a reported shift in investment away from acute care towards community and primary care. 34
Similarly, the Closer to Home project saw a general improvement in patient-reported waiting times, quality of care, overall satisfaction and improved access compared with existing services. However, in this case, care co-ordination did not improve and neither did interpersonal quality of care. 39
Information on the outcomes of acute hospital vertical integration with general practices is largely limited at present, being drawn from providers’ own websites and/or online articles. However, the Royal Wolverhampton NHS Trust has conducted its own evaluation of the impact of vertical integration on A&E attendances, emergency admissions and emergency readmissions. This evaluation was published just as the current report was about to be submitted for publication. Yu et al. report a statistically significant 11% reduction in emergency admissions and a 2% reduction in emergency readmissions for patients of vertically integrated general practices compared with patients of equivalent non-vertically integrated practices in the same area. 49
According to the Northumbria Primary Care website, its vertical integration programme has seen the following results for its general practices: all of its practices had achieved > 98% in the Quality and Outcomes Framework for 2016/17, patient satisfaction was high (with more than 88% of patients likely or extremely likely to recommend their service to friends and family) and the Care Quality Commission (CQC) had rated all of its practices as ‘good’. 40
The Willow Group website41 states that its acute trust and general practice vertical integration programme has yielded positive outcomes in terms of improved access to care and the range of care provided, and has improved the integrated organisations’ resilience to respond to capacity challenges; however, no supporting data are provided.
With respect to the international examples, Caballer-Tarazona et al. 50 found that the Alzira model performed better than average, compared with the rest of the national health service in Spain, in terms of costs and efficiencies between 2009 and 2010, but was outperformed by some public provision models. López-Casasnovas and Del Llano51 found no difference in clinical or economic indicators when comparing the Alzira model with other public provision models from 2012 to 2015. Moreover, Comendeiro-Maaløe et al. 42 found that, generally, the Alzira model did not outperform other (public provision) models in respect of 15 out of 26 performance indicators (e.g. low-value care, potentially avoidable hospitalisation, hospital case fatalities and technical efficiency and expenditure), although in some areas of care its developments were outstanding (e.g. lower mortality after percutaneous coronary intervention).
Summary of findings from the literature
The evidence on vertical integration of health services from the literature found by the scoping review is relatively sparse and highlights the need for many questions to be addressed empirically. The reasons offered for vertical integration between acute hospitals and general practices are wide-ranging, from the desire to share expertise and knowledge, to the expectation of improved health outcomes. However, evidence on the advantages and disadvantages of different contractual and governance arrangements for implementing vertical integration was not apparent. Concerns about some effects of vertical integration are evident, as well as expectations of beneficial outcomes. However, evidence to either support or refute the stated rationale for vertical integration is largely lacking. There are reports that vertical integration can lead to stronger partnerships and greater collaboration across a wider range of stakeholders, but robust evidence on the impact on quality of care and patient experience is so far absent. We concluded, therefore, that evaluation of vertical integration of hospital care with primary care was necessary to fill an identified evidence gap.
Findings from discussions with key experts
Policy experts and academics expressed their concerns about the rationale given for vertical integration, as it appeared to be driven more by structural/organisational integration than better co-ordination of care delivery. Policy experts and academics perceived a paucity of evidence for vertical integration between acute hospitals and general practices, noting that some of the impetus was from international examples, which may not be transferable to UK settings, and they were keen to hear more about primary care-related outcomes and patient views, as distinct from the hospital perspective. In addition, NHS staff were concerned about the impact that vertical integration might have on general practices working in the same area but outside the vertically integrated arrangement and, therefore, having to compete with acute hospital-managed practices, which would have a greater pool of resources (e.g. finance, clinical staff and administrative capacity) to rely on. All stakeholders raised a number of questions with regard to the impact of vertical integration on the wider health economy, specifically how the delivery of community care services might change as a direct result of integration.
During scoping interviews, NHS staff and policy experts recognised benefits of vertical integration, especially for younger GPs, as younger GPs could be given greater opportunities to acquire specialist training across the primary and secondary interface and would be more likely to have a set/defined workload and greater back office support (e.g. legal, indemnity, procurement), creating more time for clinical contribution. This relates strongly to the current shift in primary care working among GPs, where almost half of GPs in the NHS in England are employed on a salaried or sessional basis (as opposed to having equity ownership of the practice) and a majority are women (many of whom work part-time and/or wish to have portfolio careers, as do some of their male colleagues). 52 However, a number of academics were cautious that there would be a marked difference of leadership styles between salaried GPs and GPs as partners. The closer integration of primary and secondary care might also lead to increased data-sharing aligned with improved management in primary care of high-risk patients who are more likely to access emergency secondary care. Policy experts also expressed a desire to understand how the ‘success’ of vertical integration would be measured. Would success be measured by general practice sustainability, by understanding the ‘right’ professional mix of multidisciplinary teams (MDTs) in primary care or by improved financial and outcomes-based performance by the acute trust? As a result, one academic interviewee felt that it would be appropriate for the study team to develop individual programme theories for each vertically integrated organisation so as to better understand the rationale for, and consequences of, vertical integration in a variety of approaches.
The project design workshop was an opportunity to consider, as a whole, the material gathered from the scoping interviews and literature review, and to identify and prioritise, in discussion with policy and academic stakeholders in the area, which questions to pursue for evaluation of vertical integration between acute hospitals and general practices. These discussions led the team to identify the following six research questions for an initial evaluation:
-
What are the drivers of and rationale for acute hospitals taking over the management and governance of general practices? What does this type of vertical integration aim to achieve?
-
What models/arrangements exist for acute hospital organisations to manage general practices (including different contractual/legal/organisational arrangements across primary, secondary and community health services)?
-
What is the experience of implementing this model of vertical integration, including barriers to and enablers of vertical integration, as well as the lessons learnt?
-
In what ways, if any, has this model of vertical integration influenced the extent and type of health service provision delivered in primary care?
-
What are the views of the primary and secondary care workforces about working together in this way across the care interface?
-
In what ways, if any, has this model of vertical integration had impact so far? What are the expected longer-term impacts? How is progress being measured?
Addressing these questions informs the development of a theory of change for vertical integration between acute hospitals and general practices, describing its desired outcomes and the mechanisms by which these are expected to be achieved.
A conclusion of the discussion at the workshop was that a rapid evaluation could not address all of the main knowledge gaps and that it would be better to adopt a phased approach. This phased approach would comprise an initial evaluation (which is the subject of the present paper) followed by a second phase evaluation somewhat later. The second phase would start from the theory of change and then more fully assess the impact of vertical integration, in particular on patients and on the efficiency and effectiveness of the health-care system.
The method adopted for the initial rapid evaluation is described in the next chapter.
Chapter 3 Methods
Summary of key points
-
This rapid evaluation had two distinct aims.
-
Aim 1: to understand the early impact of vertical integration, including its objectives, how it is being implemented, if and how vertical integration can underpin and drive the redesigning of care pathways, if and how services offered in primary care settings change as a result, and the impact on the general practice and hospital workforces.
-
Aim 2: to develop a theory of change for vertical integration, including identifying what outcomes this model of vertical integration is expected to achieve in the short, medium and long terms, and under what circumstances.
-
-
We completed a qualitative cross-comparative case study evaluation that comprised three work packages (WPs).
-
WP1: rapid review of the literature, telephone scoping interviews and a stakeholder workshop.
-
WP2: comparative case studies of three vertical integration sites with interviews with key staff involved in the conceptual design, implementation and analysis of this model of vertical integration; analysis of key documentation (both internal and publicly shared and that related to patient experience); and non-participant observation of strategic meetings.
-
WP3: development of a theory of change for each case study site and an overall theory of change for vertical integration.
-
-
We undertook a purposive sampling to select three case study sites, based on identifying appropriate sites where vertical integration was happening at scale.
-
A content analysis approach to documentary reviews and observations was undertaken. Data analysis for interviews was informed by a framework method for the analysis of qualitative data in multidisciplinary health research. Our analysis was guided by theoretical literature on vertical integration between acute trusts and general practices.
General approach
This rapid evaluation had two distinct aims.
Aim 1
To understand the early impact of vertical integration, including its objectives, how it is being implemented, if and how vertical integration can underpin and drive the redesigning of care pathways, if and how services offered in primary care settings change as a result, and the impact on the general practice and hospital workforces.
Aim 2
To develop a theory of change for vertical integration, including identifying what outcomes this model of vertical integration is expected to achieve in the short, medium and long terms, and under what circumstances.
As a result of the scoping work, we identified six research questions by which to address these aims(see Chapter 2, Findings from discussions with key experts).
Our general approach to meeting the aims and answering the research questions was a cross-comparative case study qualitative evaluation, comprising three WPs: (1) a rapid review of the literature, telephone scoping interviews and a stakeholder workshop, (2) interviews with key stakeholders across three case study sites, alongside observations of strategic meetings and analysis of key documents, and (3) development of a theory of change for each case study site, as well as an overall theory of change for this model of vertical integration (Table 2). 5
| WP | Description |
|---|---|
| WP1: rapid review of the literature, telephone scoping interviews and a stakeholder workshop | An overview of the evidence already reported on vertical integration of secondary and primary care services to inform the development of propositions to be tested through comparative case studies |
| WP2: comparative case studies of three vertical integration sites | Interviews with those involved in the conceptual design, implementation and analysis of this model of vertical integration at their respective sites; analysis of key documentation (both internal and publicly shared and that related to patient experience); non-participant observation of strategic meetings; and interpretation of existing metrics and cost information being collected by, and any quantitative analyses undertaken at, the case study sites |
| WP3: development of theory of change | A workshop meeting of the full research team plus other senior qualitative researchers from University of Birmingham and RAND Europe to develop a theory of change for each case study site, as well as an overall theory of change for this model of vertical integration |
The original project design additionally included a stakeholder workshop at each case study site and a further workshop with stakeholders from the Department of Health and Social Care and NHS England plus peer policy analysts active in the field of care integration. The workshops were intended to refine the theories of change and to contribute to the dissemination of evaluation findings. However, as a result of the COVID-19 pandemic and associated research-related restrictions from March 2020, the study team followed National Institute for Health and Care Research guidance on suspending research activity with NHS staff and temporarily omitted the workshops prior to report submission so as not to delay reporting for an indefinite, and likely protracted, period. Workshops were subsequently completed in August and September 2020.
Protocol sign-off
The study topic was identified and prioritised for rapid evaluation through BRACE’s approach of identifying innovations through horizon scanning. An initial topic specification (first-stage protocol) was prepared (February 2019) and, once approved, was used as the basis for writing the full research protocol (May 2019), which drew on the findings of the initial scoping review and workshop (WP1).
Ethics approval
An application for ethics review to the University of Birmingham’s Research Ethics Committee was made by the project team and approval was gained in July 2019 (reference ERN_13-1085AP35). The project team received confirmation from the Health Research Authority (London, UK) that this study was to be categorised as a service evaluation and, therefore, approval by the Health Research Authority or an NHS Research Ethics Committee was not required. At each case study site, we approached relevant local research and development offices to register our service evaluation and received confirmation that all were content for the evaluation to proceed in their local area.
The method and findings from WP1 are presented in the preceding chapter (see Chapter 2). The second and third WPs are described in the following paragraphs.
Comparative case studies of three vertical integration sites
In January 2019, through grey literature searching (of Pulse, the Health Service Journal and GPonline), during the scoping of the evaluation, the research team identified five sites (Table 3) across England and Wales where vertical integration between an acute hospital and general practices was already being delivered at scale (i.e. four practices or more integrated with the local trust/LHB). Members of the study team sent e-mail correspondence to vertical integration organisational strategic and/or clinical leads (or their equivalent) on behalf of the principal investigator (JS).
| Case study site | Rationale | Location | Legal framework | Date of commencement | Number of general practices |
|---|---|---|---|---|---|
| 1 | Better management of secondary demand | England | Subcontracting GMS contract | June 2016 | 10 |
| 2 | Primary care stability and sustainability | Wales | Health board control over primary and secondary care | March 2016 | 22a |
| 3 | Primary care sustainability | England | Creation of a subsidiary limited company managed by local trust | April 2016 | 13 |
| 4 | Primary care stability | England | Subcontracting GMS contract | April 2017 | 4 |
| 5 | Primary care sustainability | England | Creation of non-profit limited company | April 2015 | 6 |
The selection of case study sites was purposive, with the aim of seeking variation across three sites in terms of (1) their rationale for implementing vertical integration and intentions for growth (i.e. management of more general practices operating under this model in future), (2) their geographical location and population served (i.e. a mix of rural and urban locations), (3) their legal and governance working frameworks and (4) the amount of time that has elapsed since vertical integration was introduced. One site declined to participate as it was already taking part in another research study, whereas another site was addressing pertinent local challenges to health-care delivery. Three sites were selected and approached to seek their agreement to participate in the study through face-to-face meetings at each respective site. All three sites agreed by sending formal confirmation of participation letters/e-mails.
Stakeholder interviews
The aim of completing interviews with stakeholders was to understand the rationale for, drivers of and challenges involved in the conceptualisation and implementation of vertical integration and interpret the experiences of primary and secondary care staff working together across the interface. The evaluation team planned to complete 15–20 interviews across each case study site or until data saturation (i.e. once data were triangulated, no new information was being discovered during data analysis, with the data confirming only existing themes and conclusions). The point of saturation was agreed by all members of the study team. Fieldwork was completed in parallel across all three case study sites (August–December 2019) by three members of the research team with experience of undertaking interviews and qualitative data analysis (led by MS). Manbinder Sidhu was responsible for all communication and data collection at two sites, and Jon Sussex and Jack Pollard were responsible for communication and data collection at the third site. A small number of interviews (n = 3) were conducted with both Jon Sussex and Jack Pollard present, at a single site, as the principal investigator wished to embed himself appropriately within the data collection process to better inform data analysis.
Participants for interview were purposively sampled and were approached through each case study site’s contact person/gatekeeper. 53 A gatekeeper was defined as a person based at our case study sites who could act as an intermediary between a researcher and potential participants, with the authority to deny or grant permission for access to potential research participants. 54 The gatekeeper facilitated the identification of key individuals (informants) involved in the design, implementation, governance and analysis of the model of vertical integration at the levels of strategic decision-making and delivering patient care. Informants included LHB and acute hospital chief executives, directors (clinical and non-clinical) and other NHS managerial-level staff (related to integration and strategy, delivery of health care services, as well as financial and governance-related management); staff and board members (from CCGs); GPs/general practice cluster leads and primary care staff who had, and some who had not, implemented the vertical integration model in each area; and members of patient participation groups.
The study team followed Johl and Renganathan’s55 phased framework for responsible engagement with organisations and gatekeepers to build their trust and support for the project, starting with formal e-mail requests for invitation, including a participant information sheet (see Project management information). Individuals participated in a semistructured interview with either one or two members of the study team, completed at their place of employment, at any other suitable location convenient to the interviewee or via telephone. Each participant was provided with the participant information sheet at least 48 hours in advance to enable them to make an informed decision regarding whether or not to participate. Interviewees had the opportunity to ask questions about the study and/or wider BRACE-related work. Participants signed a consent form (see Project management information) prior to participating in the interview. This included giving consent or not to the recording of the interview. Participants were informed that they were entitled to withdraw from the study at any time and were given information about how to find out more about the study and how to raise any concerns about its conduct. In total, the study team approached 67 potential participants to complete an interview across all three sites, with 52 participants agreeing to take part. Salient characteristics of stakeholders interviewed across our three case study sites are given in Table 4.
| Area of specialism | Generic description of role | Number of participants (participant identifiers) |
|---|---|---|
| Primary care | Clinical | 12 (A03, A12, A15, B12, B13, B17, C04, C07, C09, C15, C16, C17) |
| Organisational management | 9 (A17, A18, B01, B05, B08, B09, B10, B11, C08) | |
| Professional representation | 2 (B02, B04) | |
| Clinical and managerial | 1 (B03) | |
| Patient participation group | 2 (A08, B16) | |
| Primary and secondary care | Clinical | 1 (A07) |
| Clinical and managerial | 1 (B06) | |
| Organisational management | 3 (B14, C03, C11) | |
| Primary care commissioning | Organisational management | 1 (B15) |
| Secondary care | Clinical | 2 (A16, C10) |
| Organisational management | 15 (A01, A02, A06, A09, A10, A11, A13, A14, B07, C01, C02, C05, C06, C12, C14) | |
| Senior management | 3 (A04, A05, C13) | |
| Total | 52 |
A topic guide was developed and used by researchers as an aide-memoire during the interviews (see Report Supplementary Material 2). The main themes the topic guide covered were understanding the rationale behind the implementation of vertical integration, the clinical/legal/governance arrangements to facilitate this model, understanding the experiences of primary care and secondary care staff involved with the implementation of this model, and the outcomes the vertical integration model is expected to deliver in the short, medium and long term.
Interviews were audio-recorded (subject to consent being given), transcribed verbatim by a professional transcription service, anonymised and kept in compliance with the General Data Protection Regulation 201856 and the Data Protection Act 2018. 57
Non-participant observation of meetings
We observed meetings (at an executive and managerial level at the acute trust and at the general practice level among senior staff) between key stakeholders at case study sites to develop a better understanding of how decisions regarding implementation and delivery of vertical integration are made at local and executive board level. Non-participant observation provided the opportunity to gather data with regard to the ongoing challenges of sustaining the vertical integration model across a number of general practices, with input from stakeholders ranging from those who were more concerned with strategic decision-making to GPs and other practice staff who were familiar with the everyday effects of vertical integration on their work.
A participant information sheet and consent form (see Project management information) were circulated to all invited attendees 1 week in advance of the meeting that was to be observed. At the start of each meeting, prior to observations commencing, a member of the study team provided a verbal explanation of the project and its aims, and gave everyone present the opportunity to ask questions. Individuals who did not consent were omitted from recorded observation notes. During meetings, team members were seated appropriately to record observations but remain non-obtrusive to the discussion. Interactions were recorded on an observation template (see Report Supplementary Material 3) based on the agenda for the meeting, as well as by using sociograms (i.e. visual representations of relationships between individuals in a given setting) to map the nature of interactions. 58
Throughout the evaluation, arranging to attend meetings proved difficult across all three case study sites. Organisations at the case study sites were selective with regard to the nature of the meetings that study team members were permitted to attend. For example, it was difficult to gain access to meetings where individual practices were likely to divulge information that may have compromised their anonymity. This had a significant impact on the number of observations that were carried out.
Document review
Members of the study team gathered documents containing and describing data on the aims, drivers and challenges associated with the implementation of vertical integration across the case study sites. Documents were acquired either directly from gatekeepers across the case study sites or by searching the relevant NHS organisations’ websites for publicly available information. The types of data and documents the project team gathered included minutes from meetings where the implementation of vertical integration had been discussed and presentations describing the progression of vertical integration at each site. Information was extracted from source documents using a structured Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA) extraction template (see Report Supplementary Material 4).
Modes of analysis/interpretation
Development of a theory of change
What is a theory of change?
According to Weiss,59 a theory of change provides a framework that encourages stakeholders to develop comprehensive descriptions and illustrations of how and why a desired change is expected to happen in a particular context. The process is outcomes based and helps to clearly define long-term goals and then map backwards to identify the necessary preconditions that are required for success. It is worth noting the difference between logic models and theory of change: logic models connect programme activities and outputs to stakeholder outcomes, whereas theory of change attempts to identify how to create a range of conditions that helps programmes deliver on the desired outcomes. 60 For Weiss,59 conducting evaluations on programme theories serves four main purposes:
-
It concentrates evaluation attention and resources on key aspects of the programme.
-
It facilitates aggregation of evaluation results into a broader base of theoretical and programme knowledge.
-
It asks programme practitioners to make their assumptions explicit and to reach consensus with their colleagues about what they are trying to do and why.
-
Evaluations that address the theoretical assumptions embedded in programmes may have more influence on both policy and popular opinion.
The development of theory of change often incorporates a form of diagrammatic representation and accompanying narrative (i.e. causal chains, assumptions and the contextual conditions that influence how a programme works captured in a single diagram). However, vertical integration, and its implementation within the UK, can be difficult and challenging to evaluate. Vertical integration is a complex programme, comprising multiple services across a number of health sectors made up of multiple processes, causal chains and outcomes. 61 In addition, across our three case study sites, vertical integration has been in place for a number of years, and, therefore, it might be difficult for stakeholders to clearly remember the nature of steps taken to reach a desired outcome. All of these factors make it difficult for researchers to uncover all aspects of a programme that may have led to change. However, applying theory of change methodology can be valuable to understanding how each of our three case study sites interprets how vertical integration is making a difference to the local health economy.
For Vogel,60 developing a theory of change is not a one-off exercise, but rather an ongoing discussion between different stakeholders groups and researchers to detail the assumptions of how change has come about, which may affect whether or not the activities and outputs are appropriate for influencing the desired changes in a given context. Vogel60 suggests that the process of developing a theory of change involves (in order):
-
defining the context for the programme, including social, political and environmental conditions, detailing the dilemma the programme is seeking to influence and identifying stakeholders who are able to influence change
-
presenting the long-term outcomes that the programme seeks to support and for whose ultimate benefit
-
establishing the broad sequence of activities anticipated (or required) to lead to the desired long-term outcome
-
presenting assumptions about how these changes might happen, and about contextual drivers that may affect whether or not the activities and outputs are appropriate for influencing the desired changes in a given context
-
displaying a diagram and narrative summary that represents the sequence and captures the discussion.
As a result, the study team attempted to follow the above steps as closely as possible to develop theories of change and a narrative summary for each case study site. The process of how these steps were applied throughout the rapid evaluation is provided below.
Application of theory of change within this rapid evaluation
We have developed a working theory of change and accompanying narratives for vertical integration specific to each case study site, as well as a generic model for cross-case comparison. Throughout our findings, we have focused on mapping out or ‘filling in’ what has been described as the ‘missing middle’ between what a programme or change initiative does and how this leads to desired goals being achieved. 62 We recognise, given our qualitative data collection methods, that theories of change will be grounded in the assumptions of stakeholders with regard to how vertical integration is meant to work and may overestimate the nature of its impact with respect to local contexts. In addition, participants will be providing retrospective accounts of the implementation of vertical integration, which has evolved over the past 2–4 years. In addition, we recognise that stakeholders may vary in their accounts when distinguishing between the expected and aspirational outcomes that vertical integration is expected to achieve. Therefore, we have produced not final theories of change but, rather, theories of change and summaries that are in development, which can be tested and can then be refined in a follow-up impact evaluation (see Chapter 9, Conclusions, for more information about a phase 2 evaluation).
In February 2020, the project team held a workshop to develop and refine theories of change and accompanying narratives for each case study site, with input from those with expertise in theory of change and theory-based evaluation within the BRACE partner organisations. As part of the workshop, participants first identified from the case study material the long-term goals of the site as presented by stakeholders, and then worked backwards to identify all the conditions (outcomes) that must be in place (and how these related to one another causally) for the goals to occur. 62 In addition, we attempted to map longer-term goals that go beyond the identification of programme outputs. 62 Therefore, the theory of change workshop supported the identification of outcomes that vertical integration is expected to achieve. The team’s intention had been to validate emerging theories of change with each respective case study site; however, the team was able to deliver workshops and receive feedback from only two case study sites. These workshops were designed to ascertain whether or not the study team correctly understood the context within which vertical integration was being implemented, differentiate between the aspirational and expected long-term outcomes and how they were expected to be achieved, and comprehend any further changes, relevant to our research questions, since data collection. Note that the development of theories of change was not an iterative process with a number of feedback sessions with each site, but was delivered once data collection and analysis was complete.
Data analysis
Between November 2019 and April 2020, the insights gained through interviews, documents and non-participant observations were analysed for each case study site.
We took a content analysis approach to documentary reviews and observations and, therefore, an iterative process of reading appropriate vertical integration literature and engaging in interpretation. To aid the process of analysing and interpreting data, the team (MS, JP and JS) held weekly 1-hour telephone meetings for the duration of the project (June 2019 to June 2020) to discuss project progress and emerging findings. Furthermore, the team undertook three face-to-face half-day workshops from November 2019 to March 2020 (in addition to the theory of change workshop with methodological experts) to discuss data in the context of findings from the scoping review, identify any unexplored gaps in data that could be addressed in further interviews and develop theories of change. Manbinder Sidhu and Jon Sussex continued to have regular weekly video calls (March–June 2020) to discuss the write-up of findings (JP had left the project by April 2020). These meetings took place online, as the evaluation team was working from home as per government guidance for the COVID-19 pandemic.
Our interview analysis was informed by the Gale et al. 63 framework method for the analysis of qualitative data in multidisciplinary health research. This method of analysis is a systematic method of categorising and organising data, while continuing to make analytical and interpretive choices transparent and auditable. Specifically, the framework facilitated constant comparison across the three case studies. There are seven stages to the analysis:
-
transcription of interviews
-
familiarisation with the interview/observation/documentary material
-
coding
-
developing a working analytical framework
-
applying the analytical framework
-
charting data in a framework matrix
-
interpreting the data.
Stage 1: transcription
All interviews across three case study sites were transcribed verbatim by a professional outsourced transcribing company. A single organisation, specialising in transcribing health-related qualitative interviews, was used for all interviews. The quality of transcriptions was checked against recordings by one of member of the project team (MS) on two transcripts, which also supported early immersion and familiarity with the data.
Stage 2: familiarisation with the material
The members of the project team established familiarity with the data by each reading two transcripts from each case study site and holding an early data analysis meeting, while data collection was still ongoing (November 2019). During the meeting, team members were able to reflectively discuss and share preliminary thoughts and impressions of early findings. These thoughts and impressions were fed back into the conduct of how members of the team completed further interviews/observations.
Stages 3 and 4: coding and developing a working analytical framework
Stages 3 and 4 of the analysis took place in tandem. The study team applied a deductive approach, having developed predefined codes focusing on specific areas of interest identified from our scoping review. These codes were reviewed, refined and added to. Two interview transcripts were independently coded by all three project team members (MS, JP and JS) to ensure that no important aspects of the data were missed. NVivo 12 (QSR International, Warrington, UK) was used to undertake coding. After the completion of the data analysis meeting (November 2019), and the independent coding of two transcripts, an analytical coding framework was agreed with all project team members (see Appendix 2). The codes were categorised under the following broad themes: rationale/drivers for integration; description of the current model of integration; contracts, governance and legal arrangements; implementation of vertical integration; financial implications; outcomes of vertical integration; changes in health service provision; alignment of vertical integration with other existing models of primary care; impact on staff; uptake of vertical integration in other areas; and future steps. The analytical coding framework was reviewed at subsequent data analysis meetings of the research team in January and February 2020 (as and when more interviews/observations were completed and were simultaneously being coded).
Stage 5: applying the analytical framework
The working analytical framework was then applied by indexing by all three project team members across all interview transcripts [i.e. the systematic application of codes (n = 61) from the agreed analytical framework to the whole data set and subsequent transcripts using the existing categories and codes]. The same codes were applied to notes from non-participant observations and to extracting data from the documentary review.
Stage 6: charting codes
The project team took a novel, rapid approach to charting codes by developing a matrix based on summaries of each code (once the analytical framework had been applied to all transcripts). This process was led by a single researcher (MS) within the project team, with input from the other team members. The matrix was structured according to research questions and how best to develop integrative themes. As a result, summarised codes were merged to support the development of themes.
Stage 7: interpreting the data
The project team held a final data analysis workshop in March 2020 to finalise case-specific theories of change and the development of themes. Key to this meeting was to understand the characteristics of vertical integration across the three case study sites and differences across the data, interrogating theoretical concepts relational to our research questions and mapping connections across our themes. Once all members of the project team agreed on the final themes, writing up of the findings commenced. In June 2020 the project team circulated a summary of findings (a digital slide deck) to each case study site, providing an opportunity to give comments (i.e. member validation).
In summary, we followed a framework analysis model adapted for rapid evaluation, including repeated discussion across the whole project team and calling on additional evaluation experts, in the development of our findings. Our approach supported engagement with the data in a timely fashion, while retaining wider context discussed within interviews and other sources. The approach was flexible enough to be applied to interview, non-participant observation and documentary data, and to incorporate perspectives of multiple stakeholders. We include a COREQ (consolidated criteria for reporting qualitative research) checklist (see Report Supplementary Material 5) to add rigour to our reporting.
Chapter 4 Overview of case study sites
Summary of key points
-
This chapter provides a brief overview and context for each of the three case study sites, along with their core characteristics.
-
Urbanville comprises an acute hospital trust that is one of the largest acute and community providers of health services in a socioeconomically disadvantaged, ethnically diverse urban area of England. Integration with primary care practices was initiated in 2016, when three general practices approached the acute trust. As of March 2020, the acute trust had integrated 10 general practices, treating approximately one-third of the local primary care population.
-
The acute trust–general practice vertical integration model in the Greenvale case study serves a dispersed rural population, a relatively high proportion of whom are elderly compared with the national average in England. The vertical integration model takes the form of the acute hospital trust 100% owning a limited company, which by late 2019 was running GP services for a group of 13 practices covering a total registered population of approximately 80,000.
-
Seaview comprises a LHB in Wales that provides a full range of primary, community, mental health and acute hospital services for a population of around 700,000 people across a largely rural and coastal area. As of March 2020, the LHB had received resignations from 22 GMS contract-holding practices, which were, consequently, being directly managed by the LHB.
In this chapter, a brief overview is given of the background and context to each of the three case study sites, along with their core characteristics. Particular attention has been paid to the context into which vertical integration has been introduced. The way in which these sites were selected for study is set out in Chapter 3. Taken together, the three case studies offer a mix of very urban and very rural geographies, and a variety of organisational arrangements to vertical integration. In that way, we are able to examine a range of vertical integration experience, providing relevant learning for much of the NHS in England and Wales and, indeed, in the rest of the UK and, to some extent, internationally.
The site-specific information on each location has been derived from local, public domain documentation, including published reports and minutes, plus supporting papers from trust board meetings. Interviewees corroborated much of the information during the conversations we had with them.
Urbanville
The Urbanville acute hospital trust is one of the largest acute and community providers of health services in a socioeconomically disadvantaged and ethnically diverse urban area of England. There is a significant gap between healthy life expectancy and life expectancy, which is reflected in a high demand on health and social care services in the area. This is coupled with a large ageing population living with a range of long-term health conditions, and often with multiple conditions. The trust delivers care across three acute sites and more than 20 community settings working with third-sector organisations and the local authority. The acute trust is the largest employer in the local area, with nearly 10,000 staff.
Integration with primary care practices was initiated in 2016, when three general practices approached the acute trust. Vertical integration offered the opportunity to redesign patient services and clinical pathways across primary and secondary care in a better co-ordinated way to improve (appropriate) access and positively impact on patient outcomes. As of March 2020, the acute trust had integrated 10 general practices, treating approximately one-third of the local primary care population.
As part of the integration, the acute trust has established a governance team, comprising both primary care clinicians and secondary care managerial staff, to oversee the merger. A diagram of Urbanville’s vertical integration organisational structure is provided in Figure 1.
FIGURE 1.
Urbanville vertical integration organogram.
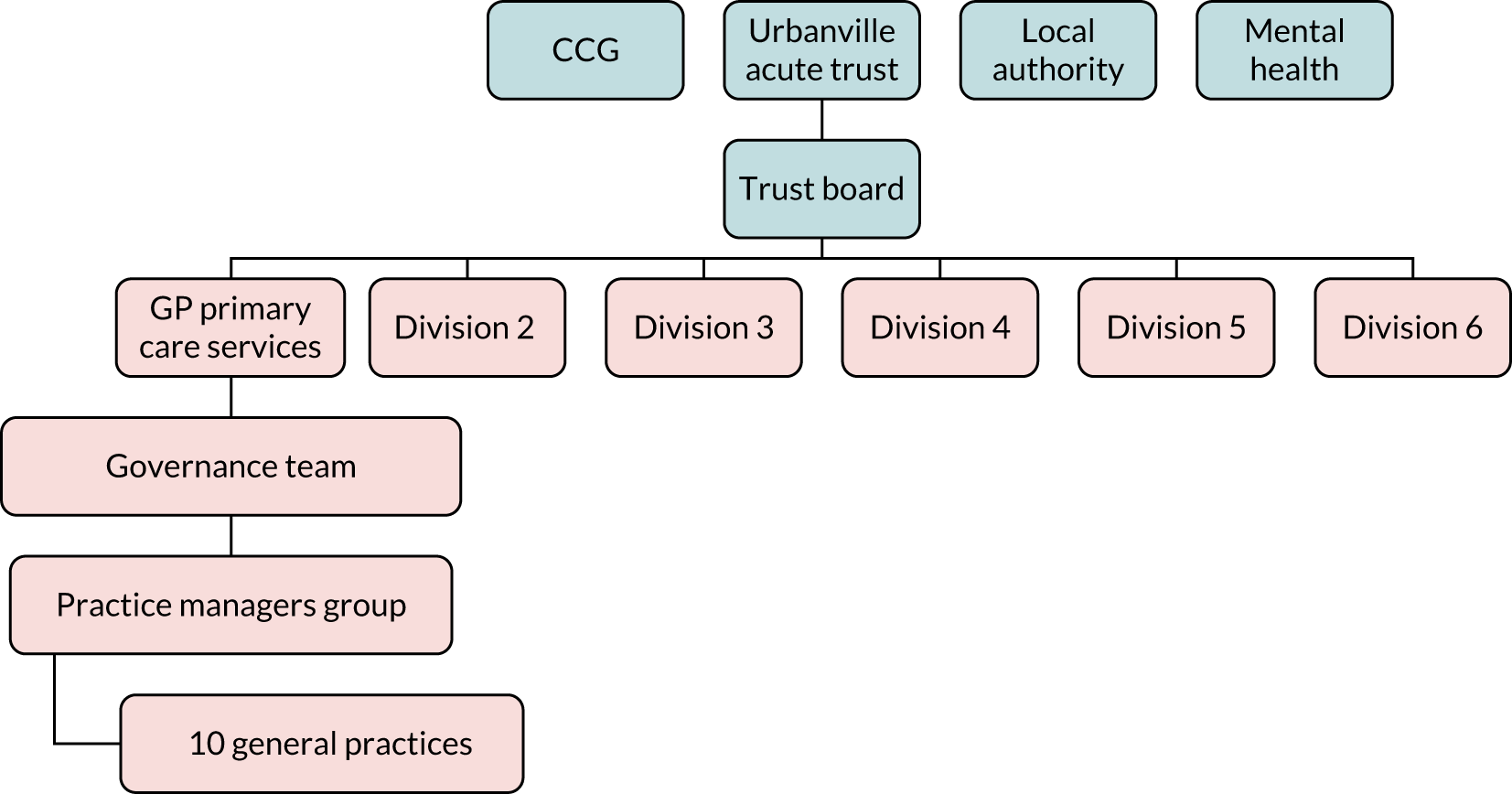
Greenvale
The acute trust–general practice vertical integration model in the Greenvale case study serves a dispersed rural population, a relatively high proportion of whom are elderly compared with the national average in England. There is a small acute hospital in a market town. There is also rural deprivation and a limited transport infrastructure, with substantial journey times between villages and the market town. Some general practices increasingly struggle to recruit and retain GPs and have to rely heavily on the use of locums.
In 2015, prior to the official formation of the acute trust–general practice vertical integration model, the local health economy became a vanguard for a PACS new model of integrated primary and secondary care. The main focus of the vanguard was on:
-
complex care teams focusing on patients with complex and multiple conditions who are heavy users of health-care resources (analysis showed that 50% of resources in the local health economy were being used for just 4% of patients)
-
enhanced primary care to offer greater local practice-based support for people with long-term conditions [enhancements included a wider range of health-care professionals (e.g. musculoskeletal practitioners, mental health workers, pharmacists), use of health coaches to support patients and free up GP time, and providing GPs with easier access to advice from secondary care specialists].
As a result of the vanguard programme, strong relationships were developed between primary care and secondary care in the area.
The vertical integration model began in 2016, after three general practices experiencing difficulties approached the acute trust. The vertical integration model takes the form of the acute hospital trust 100% owning a limited company, which by late 2019 was running GP services for a group of 13 practices (together holding nine GP contracts, following mergers between some practices), covering a total registered population of approximately 80,000. The NHS trust-owned primary care company reports directly to the hospital board. A diagram of Greenvale’s vertical integration organisational structure is provided in Figure 2.
FIGURE 2.
Greenvale vertical integration organogram.
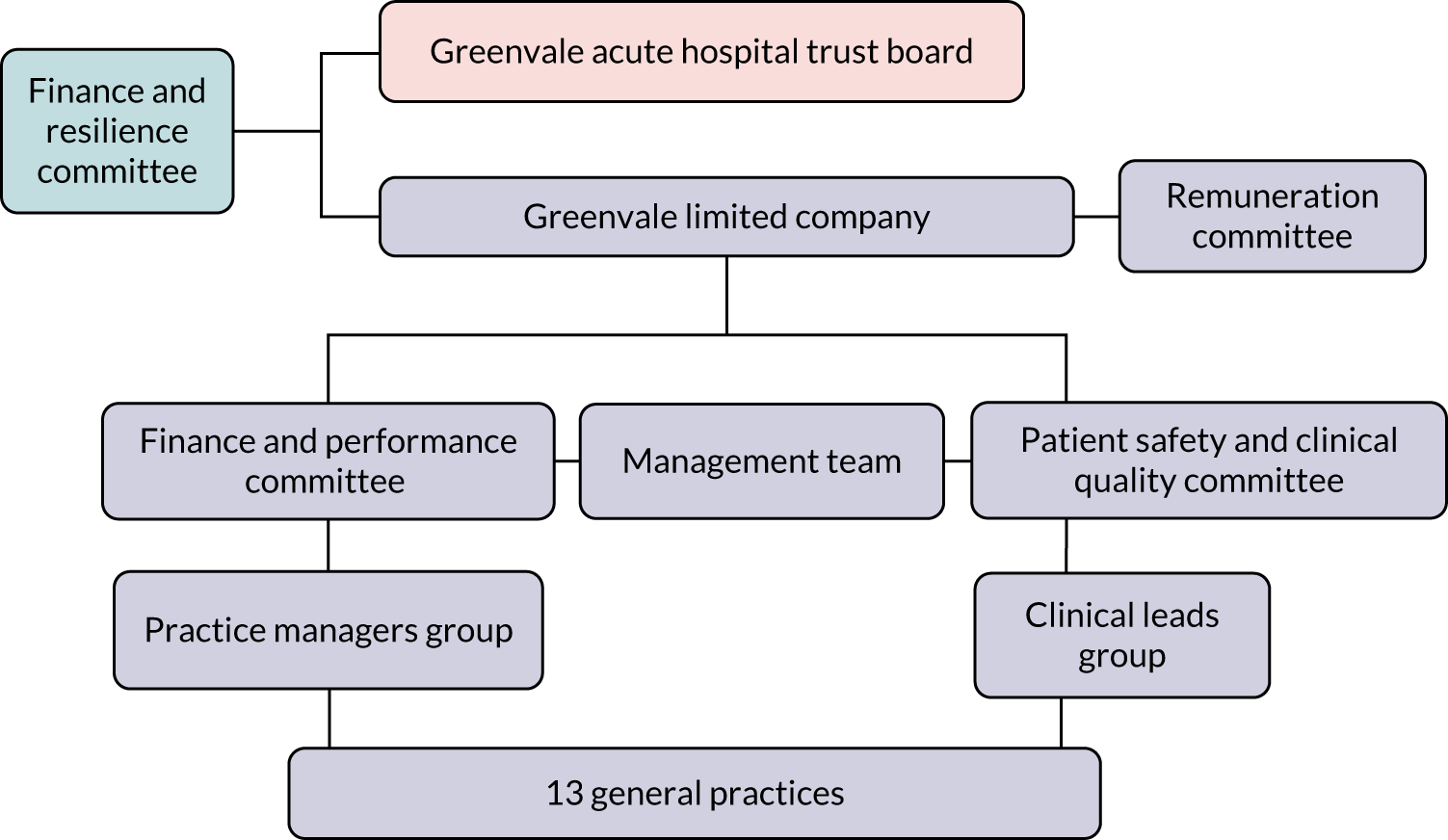
Seaview
Seaview comprises a LHB in Wales that provides a full range of primary, community, mental health and acute hospital services for a largely rural and coastal area. The area serves a large elderly population, many of whom live with long-term health conditions, as well as a transient population of holidaymakers during the summer months.
There are three main hospitals, along with a network of community hospitals, health centres, clinics, mental health units and community team bases. The LHB also co-ordinates the work of more than 100 general practices and NHS services provided by dentists, opticians and pharmacists. The LHB was, at the time of the study, in the second half of 2019, under ‘special measures’ by the CQC.
Since 2015, the LHB has been directly managing general practices as a result of GP resignations. There was no strategic intention for the LHB to directly manage general practices. As of March 2020, the LHB had received resignations from 22 GMS contract-holding practices, which were consequently being directly managed by the LHB. Some of these 22 practices have been merged or their patients have been dispersed to other LHB-managed practices.
The LHB has created a governance team of staff from the LHB and managed practices, and also GPs from non-managed practices in the area. In addition, regional teams have been developed (east, central and west) to oversee general practices. Managed practices continue to work with regional primary care clusters comprising both managed and non-managed practices. A diagram of Seaview’s vertical integration organisational structure is provided in Figure 3.
FIGURE 3.
Seaview vertical integration organogram.
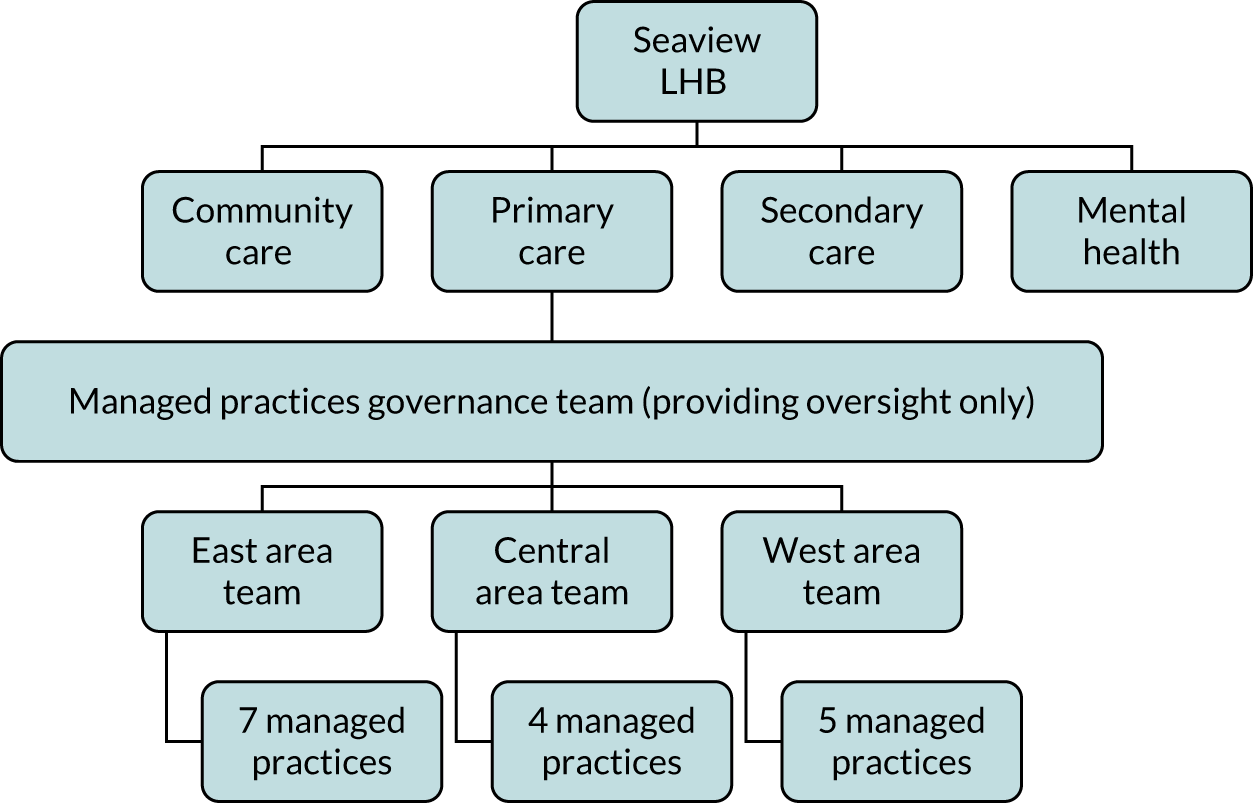
Chapter 5 Results: Urbanville
Summary of key findings
-
The rationale for vertical integration for Urbanville was to better manage demand in the local health economy through (1) improving patient access to primary care services, (2) increasing quality of care and (3) increasing opportunities for innovation.
-
GP contracts have been directly taken on by the acute hospital trust.
-
The vertical integration strategy was built on shared values between primary care and acute trust colleagues about how best to deliver care to patients and the ability to adapt pathways so that more patients could be treated in the community rather than in acute hospital settings.
-
Urbanville was able to develop a primary care-specific division within the acute trust to support the restructuring of back office functions to serve the vertical integration organisation. Despite this, many in primary care felt that back office tasks now took longer to complete than they did before integration.
-
Primary care leads have taken up prominent positions within the acute trust to oversee and govern the process of integration, alongside secondary care managerial colleagues.
-
Initial investment from the acute trust prioritised the recruitment of salaried GPs and locums, alongside upskilling the primary care workforce.
The study team carried out 18 interviews with stakeholders and a single observation of a strategic planning event hosted by the acute hospital with primary and secondary care practitioners in attendance. Further observations were scheduled in March 2020; however, because of the COVID-19 pandemic, the research team was advised not to attend meetings in clinical settings. The acute hospital shared documents that were discussed in the meetings.
Theme 1: understanding the need for and purpose of acute hospital integration with primary care
For a number of years, the traditional partner model of primary care was considered unsustainable in the face of such challenges as a limited primary care workforce, fewer GPs and the increasing number of patients living with complex multimorbidities. Furthermore, greater integration of primary care with secondary and community health provision was understood to be one remedy to alleviate pressures elsewhere in the health economy. For example, poor access to primary care often meant patients accessing A&E departments in secondary care. Therefore, it was imperative to break this cycle:
I mean, the rationale that was given to me, and I think it was the rationale that was out there just in the landscape, was . . . firstly, primary care isn’t sustainable as it is . . . we were already talking about an ICA [Integrated Care Alliance] anyway.
A14, secondary care, organisational management
. . . so, basically they wanted to integrate primary and secondary care and try to break that divide between purchaser/provider, that was their main thing.
A03, primary care, clinical
. . . and I came to the conclusion the only way I can manage demand in secondary care is from primary care.
A04, secondary care, senior management
A key premise for Urbanville was that vertical integration would allow practitioners in primary and secondary care to create a shared vision of how best to design health services and manage back office functions (e.g. payroll, HR, estates and legal planning) to improve population health and manage resources effectively. Therefore, a key driver of vertical integration was how to make the most of resources through collaborative working and the development of a formal legal arrangement between general practices and the local acute trust, which would reduce primary care workload:
. . . there was that shared vision of ‘How is this going to work? What is it going to look like?’ We got that shared vision that primary care was . . . sinking. We were doing our best, but we just could not get on top of the amount of work we were being asked to do.
A09, secondary care, organisational management
Many participants, both in primary care and in the acute trust, considered that, by moving GPs from being partners to salaried positions as employees of the trust, the maximisation of personal/practice income was no longer an incentive to improve delivery of services to the local population:
. . . so the whole idea that you merge with the hospital and you become salaried – so the money, you take the money out of the equation.
A09, secondary care, organisational management
The GPs like the idea of having a regular salary because they’re all employees of the trust, they liked the idea of having a regular salary.
A02, secondary care, organisational management
However, the nature and introduction of vertical integration did give rise to concerns as to whether or not a shared vision could be reached between general practices and the acute trust. It is not uncommon for there to be a cultural divide and mutual mistrust and lack of understanding between those working in primary care and those working in secondary care. For this reason, many GPs whom we interviewed felt that they had much to lose by entering into a legal arrangement that might lead to a loss of autonomy:
I think there’s always been a concern about the big monster, which is the trust, so it’s about being engulfed into an organisation and losing to some degree your autonomy. So the one advantage of being a partner and being a GP is it’s your business; you’re autonomous.
A15, primary care, clinical
It was a new project; we were three practices, and of course, secondary care don’t know anything about primary care. We find them an anomaly; they find us an anomaly.
A02, secondary care, organisational management
Although former GP partners shared their genuine concerns about the sustainability and future of primary care in the area, they also noted that vertical integration is one way of addressing this and that there were few, if any, alternative options to consider. In addition, GPs may have recognised that there was limited gain for the acute trust too:
If you can’t get any partners and your estates are falling apart and you can’t do anything about it and you’ve got no way of expanding, it might be the right thing for you. It really is down to individual practices.
A12, primary care, clinical
Other GPs in the patch, obviously, became very nervous. Where a big organisation starts to throw their weight around primary care, you know, it’s kind of worrying for their business model. But our counter view to that is, ‘Actually, we’re trying to provide better care. We know there’s no money in primary care, so we’re not doing it for the money’.
A05, secondary care, senior management
Theme 2: developing an integration model and implementation strategy
The implementation of the vertical integration model was instigated by three general practices collectively approaching the acute hospital to discuss how best to deliver primary care services and improve patient management in the local area. Although these practices were, relatively speaking, financially stable, they were encountering other challenges:
. . . the practices that had joined seemed to be those that have had difficulty recruiting staff and, therefore, were struggling generally; they’ve had problems with their estates maybe and felt that the hospital could help them with that, and that seems to have been the main driver for people moving. The practices that are quite stable, are happy running their own businesses, seem to be making money, having no staff problems, don’t seem to be that interested.
A12, primary care, clinical
Very early stages of the integration were characterised by due diligence meetings, whereby a team from the acute trust would visit an interested practice to understand more about its financial and legal viability:
It’s looking at their income and expenditure, it’s looking at salaries, anything to do with finance, so it would be looking at, you know, all of their bills, you know, things like leases and things like that, just to get an overall picture of financial viability and, actually, almost mapping that against, for example, another similar practice of similar size to see what that looks like and what the financial envelope would look like.
A14, secondary care, organisational management
The due diligence process enabled both parties to understand, and develop an offer of, how best to integrate, and establish whether or not becoming salaried employees would be financially viable for the general practice partners. According to senior managers at the acute trust, integration was not restricted to financially better-performing practices, but was extended to those that had the ethos and infrastructure in place to support redesigned primary care. The acute trust recognised (and accepted) that there would be significant financial impact when integrating practices. Furthermore, the process of integration often highlighted other concerns too:
. . . why has that person been off sick for that amount of time? Is there a problem here . . . are they ill, is there another thing going on? . . . I think there’s also something about understanding clinically their current way of working with the way of working that we aspire to, and how far away are they? What is the shift or change we need to make and what’s that going to mean for us in terms of resource, whether it’s time or bodies or money? Because that’s what we actually find. When they come to us, there’s a huge amount of work and could we have known that, could we have planned for that work better? Or, actually, some of it you just don’t find out until you’ve got them.
A11, secondary care, organisational management
Depending on the nature and complications associated with a practice, due diligence and integration took between 3 and 6 months.
The expansion and sustainability of vertical integration has faced challenges with respect to NHS England and NHS Improvement’s (NHSE&I’s) introduction of PCNs. All but one of the practices aligned with the acute trust to form a single PCN to discuss service delivery and quality improvement, whereby financial resources that would otherwise go directly to general practices instead go to the acute trust. The PCN model, more contextually, has strengthened the position of non-integrated practices in the local area that felt uneasy about the potential influence the acute hospital would have by having greater control in primary care through their managed practices model. Conversely, GPs working within the acute hospital felt that PCNs were supporting the work of the vertical integration model. For example, the PCN model may support the introduction of a single contract (rather than GPs individually subcontracting their contracts) that covers all practices, and it may offer better employment prospects for new types of staff joining general practice:
. . . they’re looking at the PCN holding the GMS [contract] for all of our practices, so they’re looking at one GMS contract for the PCN, which is all the vertical integration practices.
A17, primary care, organisational management
The recruitment of staff has been an interesting one . . . one new person working in a PCN in a new type of role is really vulnerable to getting them to stay. You’ve got to be a particular type of person who can work in a new role, change work and be on your own within a PCN, and I think that’s one of the failings of it. I think the – and this is what we argue – as [a] PCN, we can recruit six of those types . . . they have the care and support of each other.
A11, secondary care, organisational management
To support the implementation and integration of general practices, the acute trust restructured staff and resources to specifically manage back office functions (March 2018). This will be explored further in the next theme.
Theme 3: making the change – from General Medical Services to subcontracted providers of primary care
Throughout this theme, we provide further details of how practices transitioned from being GMS contract-holding providers of primary care to providers within a subcontracting model with the acute trust.
Changes to contract holding
The acute trust sought the advice of NHS England with appropriate legal counsel prior to integrating general practices. The acute trust was unable to directly hold GMS contracts and, therefore, a subcontracting arrangement was developed to pursue integration:
. . . we’ve got a subcontracting arrangement, essentially the practices have subcontracted the delivery of the contract to [the acute trust], but they are actually still accountable for the contract, which makes it slightly difficult sometimes when, you know, if we want to do certain things or we want to have certain conversations, it’s that we’re still almost having a provider/commissioner kind of conversation between us and the practices, whereas it should really just be us and the CCG at the moment.
A14, secondary care, organisational management
This contractual arrangement brought about an unusual set of circumstances of GPs being named contract holders, but not, ultimately, being responsible for delivering the contract:
. . . so there’s this slightly bizarre situation that we’re the contract holders, we’ve subcontracted the contract, and [the acute trust] have re-employed us to deliver that contract, and if we’re not delivering on that contract, who holds us to account? Because it isn’t the trust, it’s the CCG holding us to account.
A09, secondary care, organisational management
Contractual arrangements allow for practices, where former partners have taken up salaried positions, to return to GMS contract providers. To date (June 2020), only one practice has left the vertical integration arrangement, although reasons as to why the practice left were not divulged to the research team because of confidentiality restrictions.
Estates management
As part of the contract, the acute trust effectively becomes the new landlord of general practice premises (in cases where buildings were previously owned by the practice, not leased):
So from the estates perspective, as part of our subcontracting arrangement, we have a licence to occupy. So, basically, we become the landlord for the practice, and that’s the arrangement that we have, so [the acute trust] cannot claim notional rent, which is what the GP practices get. So what they have is because it’s their building, so to speak, because it’s a GP practice and they are supplying health care, they then get their rent reimbursed and they get things like council tax, water rates, things like that are reimbursed as well; so actually, they keep all of that.
A14, secondary care, organisational management
From the acute trust’s perspective, the growing concern with regard to the complexity of this arrangement was how best to individually manage the increased number of buildings. For instance, according to CQC guidelines for secondary care provision, some general practice premises were unfit to treat patients. This led to high costs falling on the trust to meet standards:
. . . things like the quality of the clinic facilities, infection prevention control, so some of the practices, for example, had carpeted areas and wouldn’t meet quality standards of the CQC.
A01, secondary care, organisational management
Where premises were in significant disrepair, the acute trust converted existing, available hospital spaces in and around the vicinity of practices. Therefore, the management of a growing number of buildings via vertical integration was increasing the work placed on the acute trust’s estates staff.
Reorganising back office functions
As part of the trust’s process of integrating general practices, a separate department was created to manage back office functions (e.g. HR and recruitment, finance, payroll, legal and indemnity, estates management and quality improvement). Many interviewees felt that structural integration of back office functions would free up more time for primary care clinical and non-clinical staff to focus on how best to deliver front-line services:
Clearly, we [general practice] don’t do any payroll or anything like that. Well, we don’t employ an accountant anymore, because don’t need to. We don’t have any HR; all the HR is dealt with through [the acute trust], so you’re not worried about staff causing a problem, you know, and suing you, and you end up being taken to an industrial tribunal – none of that’s an issue anymore.
A09, secondary care, organisational management
However, many of the staff working across primary care felt that, although additional back office support was provided, it was often slower and more bureaucratic in comparison with pre-integration, and it created considerably more reporting back to the acute trust with regard to quality improvement:
As part of a vertical integration practice, obviously, there’s a lot of reporting that we do, which feeds back.
A18, primary care, organisational management
Biggest frustration I think is probably the HR processes, without doubt. Everyone on the primary care side of things is hugely frustrated at how long they think it takes us to recruit anybody, and they are very vocal.
A11, secondary care, organisational management
You know, with GPs you’re quite slick and quick and everything happens quickly, you know. We’re running out of rubber gloves, that’s absolutely fine: ‘Can you order 50 boxes of rubber gloves?’ ‘They’ll be here tomorrow [and] we get 20% discount.’ Couldn’t do that with the trust, so they’ve got a procurement process. You want rubber gloves? You’ve got to have a procurement thing and they’ll be here a week on Thursday. But we’ve run out today. So we started having to borrow disposable scissors and stuff like that.
A09, secondary care, organisational management
The nature of implementation has resulted in a number of new roles and committees being created to oversee the management and the progression of vertical integration. Some GPs have moved into more managerial/clinical oversight roles based at the acute trust, whereas some GPs feel that time could be better spent elsewhere, possibly back in primary care:
So if you are employing people who were doing clinical before vertical integration, now coming to vertical integration doing just management, it’s a loss, you know.
A03, primary care, clinical
In addition, a number of committees and meetings were arranged between the trust and primary care providers to discuss accountability and governance, attended by senior GPs and senior colleagues of the acute trust. To prepare for these, general practice leads continued to meet once a month to ensure that they had opportunities to share their concerns from a GP perspective before reporting back to formal meetings with the acute trust.
Cross-cultural misunderstandings and tensions
A common thread during interviews with primary care stakeholders was misunderstanding by colleagues working in secondary care of how primary care is delivered. Many staff in primary care felt that the acute trust was, initially, poorly prepared to manage general practices and lacked understanding of how everyday decisions were made in a timely manner in an environment that was poorly resourced:
They didn’t really understand primary care . . . they’re jumping to something, but they didn’t really know how to run it.
A03, primary care, clinical
A fundamental challenge for the acute trust was establishing and building relationships with stakeholders across primary care, mainly GPs and practice managers. These stakeholders were accustomed to making their own decisions with regard to how to run and manage their general practice, with significant independence and autonomy. However, integration with the acute trust, with the implication of having standardised working practices across all general practices within the vertical integration organisation, brings tensions between primary care and acute trust colleagues:
. . . lots of personality clashes, but it’s about managing those personalities and, actually, how you use the strengths of all of the people, actually, within the group to make sure that you get the best out of them, so definitely culture, personality clashes and just a willingness to change and understanding that. You know, saying that you want to change and actually making that change are two different things.
A14, secondary care, organisational management
Collectively, there was a perception that the acute trust was trying to bridge a divide that has long existed within the English health-care system, and that being able to address tensions and mistrust while implementing a standardised approach to manage practices across a cultural chasm was proving difficult:
. . . the culture gaps between primary, community and acute are vast, you know, and the differences and the mindsets are completely different. So what I was hearing was we’re all on the same path and we’re all on the same journey, and there was a little bit of me that thought ‘Hmm, well that’s great, but that would be, you know, that’s almost unheard of’.
A11, secondary care, organisational management
Nevertheless, primary care colleagues, overall, understood the reasoning for a more standardised approach to managing practices across 10 surgeries that had integrated with the trust. Yet, it was still taking time for primary care colleagues to become accustomed to their now more limited capacity with regard to decision-making:
I think looking at it as an outsider, I think a lot of the changes that have been implemented are for the better, because [before] you would have surgeries just doing what they wanted. There was no standardisation, no structure. So in one respect, I think it’s a good thing, but also, some practice managers feel like they’ve lost a bit of control.
A18, primary care, organisational management
Theme 4: impact on patient management – changes to primary care and secondary care delivery
The nature of clinical integration between primary and secondary care at Urbanville was driven by the acute trust, with the aim of treating a larger number of patients in the community and reducing utilisation of secondary care services. However, it had taken considerable time to set up back office support functions, with the consequence that attention had only recently been directed to service redesign. This centred on primary care services. The following example highlights possible savings that could be made by moving community services into primary care:
So phlebotomy at the moment is delivered through the community contract, community services, which is actually very expensive. If you start to train up your primary care nurses and, actually, you’re delivering through extended access or extended hours or putting on specific specialised clinics, actually, you start to pool your resource. Those nurses then that are in community that were doing phlebotomy . . . you’re freeing them up then.
A14, secondary care, organisational management
In addition, the acute hospital being integrated with general practices allowed the development and application of innovative methods for managing highly complex patients who are likely to be frequent users of secondary emergency care. The vertically integrated organisation was able to develop its own database to identify and track high-risk patients across primary and secondary care, sharing real-time information with practitioners across the care interface:
It’s like a dashboard, so it tells us what patients have been admitted overnight, what procedures they’ve had done, and we get a copy of that each day and the GPs look at it and think, ‘Oh, Mrs so-and-so was in there last night; I might give her a call and see if she’s OK’. So it links the care up better.
A02, secondary care, organisational management
Although new roles were being introduced in primary care, the acute trust was still struggling to rectify GP shortages. Many of the GP partners in the practices that were integrated had either moved to being salaried or had left primary care prior to or shortly after integration. This led to locums being used as a short-term measure across managed practices until suitable salaried GPs could be recruited. For some in primary care, the use of locums was a source of tension:
. . . salaried partners, they worked as hard as us and contributed to the teamwork in exactly the same fashion, which is different than locums when you have to use them.
A07, primary and secondary care, clinical
Many of the non-clinical staff working across practices felt that both locums and salaried GPs had a different approach to managing and delivering general practice services compared with GP partners. In general, non-clinical staff felt that former partners of their practice (which was now part of the vertical integration organisation) had been much more involved in, and focused on, the everyday challenges of delivering primary care, whereas locum and salaried GPs focused only on delivering care to patients. This was seen as leading to a lack of cohesiveness among primary care teams:
I mean, none of the GPs here have been a partner before but they behave like partners, if you like. So, like, with holiday, we all say: ‘Unwritten rule: no one has time off at Christmas, because it’s not fair for one or the other’. They do what they like and they book time off, which upsets everybody else, which upsets the girls, because I’m saying, ‘You can’t have time off’. They’re, like, ‘Well, they’re salaried like I’m salaried, so why do they get it and not me?’.
A17, primary care, organisational management
However, salaried GPs could focus more on patient care, which might be a good thing for both the GPs and the patients:
I think from a clinician’s perspective, especially the GP’s, they’re actually able to concentrate on their clinical work because all of that admin side of things, that has been taken away; so they’re actually able to be GPs and see patients and provide that clinical care.
A14, secondary care, organisational management
One fundamental and very significant opportunity that vertical integration created was for training and career development, for both clinical and non-clinical staff in primary care. Some staff from primary care had already moved into positions at the acute trust (e.g. to manage and provide quality assurance for the running of managed practices):
When you get to the top of the band, there might be an opportunity to change, you know, to a higher band. You know, it’s just a bit more organised, I guess, and fair. But, yeah, there’s loads of opportunities within the hospital.
A17, primary care, organisational management
Primary care itself, there’s no career prospects; basically, it’s a dead-end job. You start off as a receptionist, and if you want to be a practice manager, it’s dead man’s shoes. But within this [vertical integration], you’ve got the opportunity to move into the trust, perhaps on the same grading, and develop your career, and you’ve also got more education and training. A couple of the staff have been supported through NVQs [National Vocational Qualifications]. There’s two people in my team who have come from primary care; they’re doing their degrees, and the trust is financing that for them. Things they would never have been able to do before.
A02, secondary care, organisational management
Therefore, vertical integration opened a number of opportunities for those working in primary care, especially those currently in non-clinical positions. Notably, perhaps as a result of our sampling frame, there were very few references within the participants’ accounts of staff from secondary care finding opportunities to work with, or in, primary care. However, we heard, anecdotally, a view that some younger medical students at the acute trust were becoming more interested in working in primary care as a result of the vertical integration model. The following quotation is from a GP working as part of the vertical integration model, relating being approached by a medical student:
‘I came to your talk, I was there, but now I think I want to come and talk to you about what it’s like to be a GP and what other roles could I have’. So it’s almost putting those seed thoughts in place, isn’t it, about what this is going to look like for the future? So I think it’s playing to the strengths of being part of a much bigger organisation.
A09, secondary care, organisational management
Theme 5: measuring success and identifying any areas of unintended impact
Given the stage that the acute trust had reached with vertical integration at the time of our evaluation, much of the described impact focused on non-clinical outcomes. Financially, the acute trust was carrying a significant burden, which was a result of having to use locums to cover former GP partners who had left and difficulties in recruiting salaried GPs. In addition, the trust encountered high staff costs, with the majority of primary care staff being ‘TUPE-ed’ [i.e. Transfer of Undertakings Protection of Employment (TUPE)] over onto Agenda for Change (AfC) NHS contracts, resulting in increased salary levels for some and increased National Insurance contributions:
So employer’s National Insurance is more expensive than self-employed. That’s the first obstacle. Then you’re taking a lot of risk. So if a partner leaves or becomes ill or a salaried GP leaves or becomes ill, the risk is then on us to fill that with locums, agency, which can be very expensive. To recruit we may need to pay more than has been paid in the past because of the increasing shortage of GPs.
A13, secondary care, organisational management
Meanwhile, the stakeholders interviewed from the acute trust felt that it had taken time for the trust’s finance managers to understand how best to maximise primary care income and ensure primary care activity was recorded accurately owing to the rather different ways in which acute hospitals and GPs are funded:
I think there’s something around, actually, in terms of how primary care funding also works. It’s been a real learning curve for the finance department within [the acute trust], because from an acute perspective, this is how much you’re getting. That’s a block contract, so you’ve only got that much to spend. There’s a little bit of variation here or there but, actually, that’s the envelope that you have to work with, and that’s the constant money that you know that you’re going to get. Whereas in primary care, you’ve got your GMS contract money, which more or less stays the same but, actually, if you then don’t do any in-house services, direct enhanced services, public health initiatives . . .
A14, secondary care, organisational management
In an attempt to maximise income for its primary care activity, the acute trust established a back office function that was focused on ensuring complete, accurately coded recording of activity. Some of the vertical integration general practices had been continuing to record some of the details of their activity as ‘free text’ within patient records, rather than fully coding that activity. As a result, there was a significant amount of lost revenue, for example through failing to ensure that eligible patients were invited for consultations:
. . . patients with mental health or patients that were reaching the end of the age eligibility so that they could call them in and not miss that point of care. By inviting those patients in, [the practice] would get a set amount for an invitation. So our reporting structure highlights if a patient has actually had a health check but hasn’t had an invitation coded.
A16, secondary care, clinical
For the acute trust, the main outcome that vertical integration intended to achieve was a reduction in secondary care emergency admissions, while, at the same, reducing the number of ‘did not attends’ and increasing the number of appointments available in primary care. Comments on early data collected from the trust had indicated a reduction in referrals to A&E following vertical integration, as well as fewer patients being readmitted to hospital within 30 days of discharge. However, the trust was unwilling to share these data with the research team until their analysis was complete and ready for wider dissemination.
Nevertheless, there have been some notable successes with regard to other outcomes, specifically recruitment. As a larger organisation with greater availability of resources, the trust has been able to fill GP vacancies more quickly; however, this came at a significant financial cost:
So there was one practice that lost quite a lot just because they could never fill the vacancy, because there were three GPs required. They could never recruit anybody. Cost us a fortune. I think we may have recruited now.
A13, secondary care, organisational management
Notably, since the commencement of vertical integration, only one practice had left the collaboration (mutually agreed by both parties). There is engagement across practices. Back office functions have been established and contribute to a more cohesive and collective approach to improved service provision across the area, and this has led to lower staff turnover and to some staff reporting of higher levels of job satisfaction. For those in primary care, the greatest success of vertical integration is that the acute trust ultimately provides additional financial resources:
I think success otherwise for me is how engaged are the practices when we get them all together to talk about what does the future look like and things like that. You know that is big; we moved away from some basic level conversation to, actually, we’re now talking about doing something quite different, and we’ve gone up a level . . .
A11, secondary care, organisational management
So, personally, primary care has probably been underfunded. If we had to put in a certain amount of money into a practice, lose a bit of money on the practice, but it makes it a better practice that supports people that are frail, that diverts patients from A&E, all those good things, if we spend a bit of money on that, that’s great. So that probably is value for money.
A13, secondary care, organisational management
Theory of change
A theory of change illustration for this case study site is presented in Figure 4. The central rationale for integration between the acute trust and primary care practices was to better manage demand in the local health economy through (1) improving patient access to primary care services, (2) increasing quality of care and (3) increasing opportunities for innovation. Collectively, this would, it was hoped, lower the whole-system cost of treating patients. The acute trust was feeling the impact of poorly resourced general practices on secondary care, with many patients accessing emergency care at the trust because GPs were experiencing increasing workloads with fewer full-time clinical staff.
FIGURE 4.
Urbanville vertical integration theory of change. PPG, patient participation group; STP, Sustainability and Transformation Partnership.
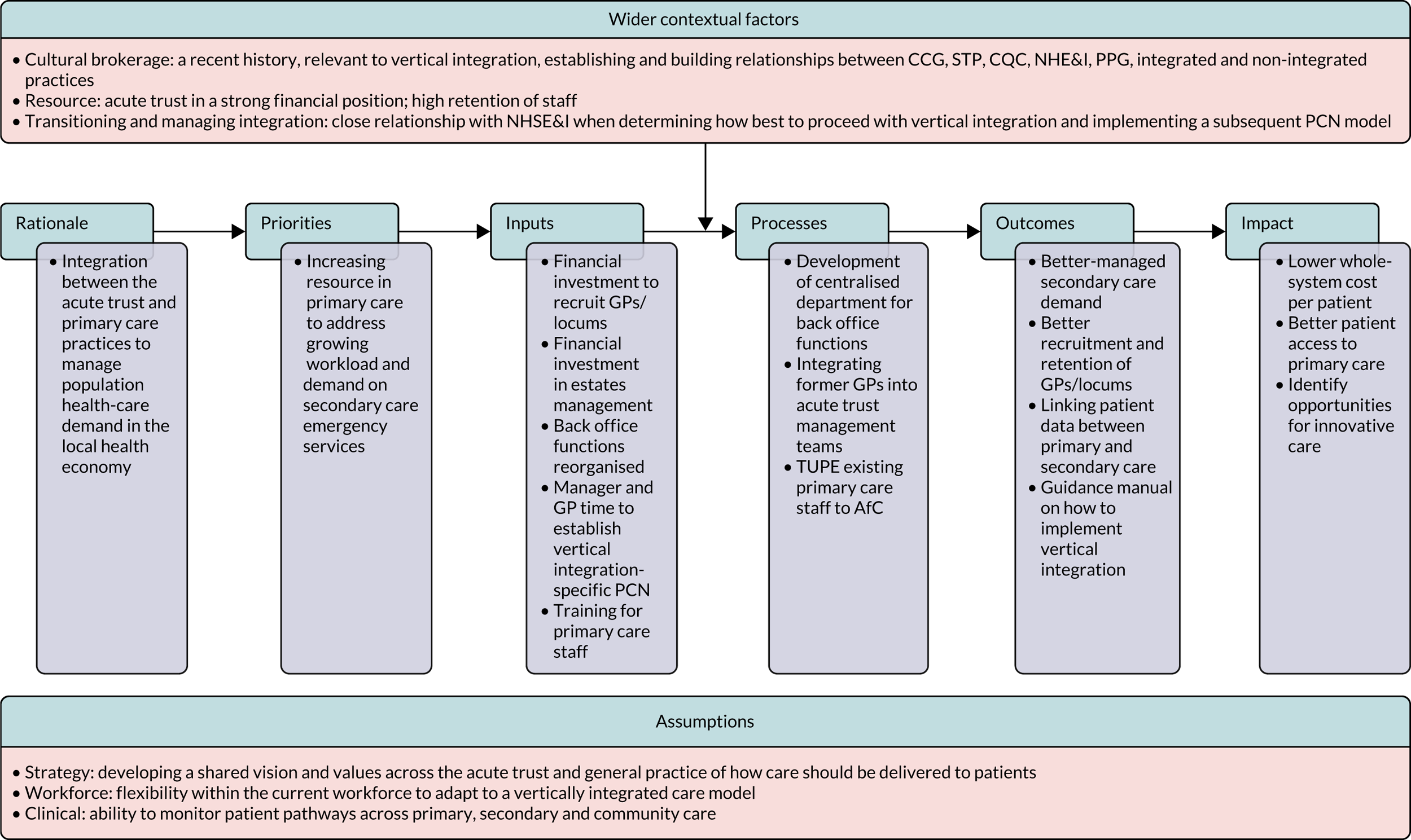
Integration required stakeholders from primary and secondary care to establish a strategy, built on shared values, on how best to deliver care to patients and have the ability to adapt pathways so that more patients could be treated in the community rather than in acute hospital settings. This was achieved, in part, by sharing real-time data from secondary care with primary care practitioners to manage high-risk patients (i.e. those most likely to require emergency secondary care). This strategy was further strengthened with ties built by the trust with the local CCG and Sustainability and Transformation Partnership, by establishing a vertical integration-specific PCN and by working with NHSE&I, which advised the trust on how this model of integration could legally occur. Therefore, significant time was spent establishing a clear line of communication between primary and secondary care.
Initial investment from the acute trust prioritised the recruitment of salaried GP and locums, as well as the introduction of non-GP clinical staff who would be better suited to address the needs of patients living with long-term complex health conditions. This coincided with skilling up the primary care workforce. Positively, integration created a number of opportunities for clinical and non-clinical staff to further their careers in a larger organisation that could afford to fund time away from their main roles. Such opportunities were welcomed by staff, alongside the transition to AfC contracts. In addition, there was substantial investment in managing estates-related costs where buildings were owned and not leased.
Urbanville prioritised, early in the implementation of its vertically integrated model, functional integration and developed a primary care-specific division within the acute trust to support the restructuring of back office functions, with a mixture of new and existing staff to support financial management, procurement and estates. This shared ethos was largely achieved by certain primary care leads taking up prominent positions within the acute trust to oversee and govern the process of integration alongside secondary care managerial colleagues. This was largely received as a positive step to having balanced representation and ensuring that the interests of primary care remained at the foreground of vertical integration decision-making, with effective communication with the acute trust board. However, despite large-scale restructuring, many in primary care felt that back office tasks now took longer to complete when compared with pre-integration. This was despite the acute trust appointing a number of senior primary care clinical staff to oversee the management and governance of integration.
As a result, the acute trust achieved a number of short-, medium- and long-term outcomes with regard to implementation (see Figure 4), but some areas still required further exploration to comprehend their effectiveness. The trust continues to bridge the cultural divide between primary and secondary care, establishing shared values among its managed practices to make the most out the resources available in the local health economy. Yet, in the long term, it remains to be seen whether or not the high cost of locums can be sustained and whether or not linking patient data across the interface leads to a reduction in secondary care demand.
Chapter 6 Results: Greenvale
Summary of key findings
-
The main rationale for vertical integration at Greenvale was to enable general practices to continue to operate in the face of recruitment and financial difficulties, and in the context of rising demand for care.
-
Vertical integration was implemented by setting up a limited company to run the GP services, with the company 100% owned by the acute hospital trust.
-
The financial backing of the acute hospital trust, centralised back office functions within the primary care company and the creation of a central management team for the primary care company have contributed to the viability of primary care at Greenvale.
-
Vertical integration benefited from active and supportive leadership, both at the acute trust and in the local primary care community. Relationships had developed and strengthened during a prior PACS vanguard in the area.
-
Recruitment and retention of GPs, now all salaried, has been supported by the vertical integration arrangement, and no practices have had to close.
-
Primary care practices have more MDTs than previously, share staff across practices and have access to some specialist services via outreach from the acute hospital.
The study team completed 17 interviews with stakeholders and two non-participant observations of meetings. The two meetings observed were of the management team of the primary care company owned by the acute trust and of the practice managers from the practices within the company.
Theme 1: understanding the need for and purpose of acute hospital integration with primary care
It was a clear theme across all of the interviews at Greenvale that the principal driver of vertical integration was the risk of general practices closing and the scope for vertical integration to prevent that happening. Therefore, the main purpose of vertical integration at Greenvale was to sustain primary care in the area; subsequently, it would be possible to continue to develop better integrated care, not least to carry on the changes commenced by the PACS vanguard, with its focus on better managing care for people with complex needs and multiple long-term conditions.
The acute trust-owned company that was to operate a number of general practices in its catchment area was set up in April 2016. According to our interviewees, it was clear by that time, and has become clearer in the years since, that the traditional model of general practice was unattractive to some GPs:
GPs going in just don’t want that responsibility any more. They don’t want to run a business and have a mortgage and manage people. They just don’t want it.
B08, primary care, organisational management
Not only do potential GP recruits not want to take on the responsibilities and personal financial risks of co-owning a small business (i.e. a general practice co-owned by partner GPs, which is the traditional model of general practices in England and Wales), but some existing GP partners would like to relinquish them. This was particularly the case for practices where, owing to a recent departure, only one GP partner remained or where the remaining partner(s) were approaching retirement age and becoming increasingly concerned about how they might sell on their practice. The consequence was that some practices in the area were on the verge of handing back their contract to the CCG:
. . . it was quite apparent there was several practices that would fold, because – well, as you’ve heard a million times before – so elderly GPs having to retire, no one to take over the practice, or no desire to move it forward. Expensive locums to fill people, long-term vacancies.
B14, primary and secondary care, organisational management
. . . certainly our local experience, it’s been largely a response to crisis, although there have been some very good practices where the partners have simply said, you know, ‘We trained to be doctors, we don’t want to be partners, we don’t want to own the business, we don’t want to employ all these staff, we’d just like someone to come and do that, and we’ll stay on and serve our patients’ and that’s fine, but I think the majority of practices that both [name of another vertical integration organisation] and [name of case study B organisation] have taken on have been, you know, in a bit of a pickle, really.
B15, primary care commissioning, organisational management
The formation of the acute trust–general practice vertical integration, in April 2016, and its subsequent enlargement were in direct response to this pressure. In 2015, the acute trust was approached by a group of three general practices with a proposal to integrate. Links between practices in the area and the acute hospital were already good, in part because of the work around the PACS vanguard model. In addition, the acute trust’s chief executive had been active in integrating health and social care in his previous post in another part of the country and was known to be supportive of integration:
So, basically, they applied for the vanguard, got all this research done about new models of care, and, at that point, as they started to work with primary care and were looking at the benefits of sustaining primary care, some practices came forward to the hospital . . .
B09, primary care, organisational management
. . . because of the vanguard work, the relationships between primary care and the acute trust were very strong, and I think that is a very, quite an important point.
B01, primary care, organisational management
[Name of individual] was very much around sustaining primary care when he was chief executive in the hospital. And he was approached by the [name of general practice] surgery, and then also [name of another general practice], who owned [names of two health centres], about formally taking that step further to support primary care within [area]. And that’s when they integrated as part of [acute hospital] . . .
B11, primary care, organisational management
Alongside the strong pre-existing relationships between primary care and secondary care in the area, one interviewee said that the vertical integration model was formed partly because of the appetite of the acute trust to take on the challenge:
The management at the time, and this continues today, have a probably higher appetite for risk-taking and transforming at pace than perhaps elsewhere . . . So there was an appetite amongst the leadership to take this on, which perhaps doesn’t exist everywhere.
B14, primary and secondary care, organisational management
By sustaining practices that were in particular difficulty, the vertical integration arrangement not only helped the practices that were integrated with the acute hospital, but also avoided the imposition of a burden on the general practices that remained (i.e. practices that would otherwise have had to take on patients from the failed practices):
Yeah, the whole premise was around sustaining primary care. And, obviously, not just about sustaining those practices, but, obviously, taking the pressure off the other practices in [name of county], because if you disperse lists, that then has pressure on the other practices because they’ve then got to take a cohort of patients . . .
B11, primary care, organisational management
Vertical integration of general practices with the acute hospital trust was, from the outset, clearly seen to be beneficial to the trust, as well as to the GPs concerned:
. . . there was a clear and sort of symbiotic relationship, I guess, between primary care and the acute trust. So if primary care starts to get into difficulty, then that has significant impacts across the health and care system. So if practices start to hand back contracts and start to dissolve, then that has a big impact on the hospital, because those patients end up going somewhere else. And for a lot of them on their, sort of, urgent, on-the-day demand, that would come here if there wasn’t access to primary care. So that was the first reason.
B07, secondary care, organisational management
They’d looked at lots of other options but were at the point of handing back their lists to the CCG, and if they did that, we know within the hospital the impact would have been most greatly felt within the hospital. And if those patients aren’t being cared for appropriately in primary care, where will they go? They’ll rock up to A&E.
B08, primary care, organisational management
Therefore, in addition to safeguarding the survival of some general practices that were in difficulties, another major purpose of vertical integration at Greenvale was to manage demand for acute care in the local health economy:
. . . where practices are understandably focusing on their cost base, actually, what they haven’t traditionally done is focused on their impact on the wider health and care system. And so . . . if you can start to standardise and you can start to make some resource decisions that are different, then you can start to affect the way that cost is attributed across the healthcare system in quite a dramatic way. That was kind of part of the logic.
B07, secondary care, organisational management
. . . the acute trust wanted strong primary care, and they wanted to make sure that the people that came into the hospital were the right people that came into hospital, and when they came in, that they were there for the minimum amount of time, and we got them home, living independently in the community, supported by their GPs and the community staff.
B01, primary care, organisational management
This joint rationale of sustaining primary care and thereby enabling better responding to, and management of, patient demand has remained unchanged so far.
Theme 2: developing a model of integration and an implementation strategy
Various models of integration were considered for the local health economy, particularly before and during the PACS vanguard, which commenced in 2015. When the acute trust was approached by three general practices in difficulty and wanting to integrate, various specific models for achieving that were considered, drawing on the research that was undertaken during the vanguard programme. The decision was made to establish an organisation to run the general practices that was at arm’s length from the acute trust to lessen the likelihood that it would be perceived as a secondary care takeover of primary care:
. . . it was very strongly felt by all those that primary care needed to be an arm’s-length body from the hospital, so that it had, it was still very clear that it was a primary care organisation.
B08, primary care, organisational management
So the advantage of having a limited company, which was arm’s length from the hospital, is it meant that the focus would be kept on primary care by a team of people that would be running that organisation at arm’s length, as opposed to the practices being swallowed up by the hospital and then the focus becomes all about secondary care, not primary care.
B09, primary care, organisational management
The arm’s-length relationship with the acute hospital was reported by some in primary care to have achieved that aim:
If you’re on the ground . . . you don’t even particularly think about [the acute trust] owning you.
B05, primary care, organisational management
We heard no reports from interviewees about the general public being concerned about who was running their local GP services, and it seems unlikely that clinicians at the hospital were concerned about whether or not any particular patient was a patient of a hospital-owned practice. Indeed, these seemed to be non-issues:
So I think as soon as you start discussing that relationship between the hospital, [the vertical integration company] and the practice – I’m not being uncharitable – I think it goes over people’s heads or, quite frankly, they’re not interested. It’s the ‘So what? Can I get an appointment tomorrow?’ that I’m interested in.
B16, primary care, patient participation group
I suspect a lot of the secondary care teams don’t know who are in [the vertical integration company] and who aren’t when it comes to the practices.
B13, primary care, clinical
The arm’s-length limited company that managed the general practices had its own board, which was chaired by a non-executive director from the acute trust’s board, but had more primary care than secondary care representatives. The company board reported directly to the acute trust board. Voting power on the company board was effectively split 50/50 between primary care and the acute trust. The organisation had a central management team and staff, as well as the staff in each of the constituent practices, all of whom focus on the running of primary care, while drawing on the resources of the acute trust where appropriate:
. . . if you have a subsidiary of the hospital which is at arm’s length, has its own management team, it can focus solely on the day-to-day running of the primary care, which has its different constraints, different contracts. But being under the same hood, it can borrow resources.
B14, primary and secondary care, organisational management
Another feature of the implementation of the vertical integration model at Greenvale was the concern to ensure that the GP contracts taken over by the primary care company owned by the acute trust could be reversed, that is, the GPs of the practice can take back the contract (i.e. leave the company) if they wish to at some future date, including, for example, if the vertical integration company decided it no longer wished to run the practice or wanted to sell it to a non-NHS-owned company:
As with any new initiative, there were concerns that it would not work out. Practices have retained their contracts to alleviate this concern, i.e. reversibility.
B04, primary care, professional representation
. . . what was put in was that if at any point [the vertical integration company] decided to stop doing what it does and potentially sell up to a private provider, within the contract, the partners that were there before have first opportunity to take it back.
B08, primary care, organisational management
However, concerns were raised when the acute trust–general practice vertical integration model was designed and established. Some primary care stakeholders in the region worried that secondary care was taking over primary care, leaving the traditional partnership model under threat:
I think there’s still a lot of negative sentiment and a belief that [the vertical integration company] was set up as a trojan horse to kind of take over general practice as part of the overall kind of conspiracy against the partnership model.
B15, primary care commissioning, organisational management
There was also a concern that if the acute hospital trust was looking to take over primary care in the area, then this would create a single monopoly provider of primary care to the local population:
I mean, obviously, patients still need to have choice where they go, so in terms of GP practices, you wouldn’t want [the acute trust] . . . to take all of the practices in [the area].
B11, primary care, organisational management
There were still concerns that, even if a single monopoly provider of primary care did not materialise, general practices in the area that were not part of the integrated organisation would suffer. As a result, the central management team of the trust-owned primary care company sought to reassure other general practices in the area that this would not be the case. Furthermore, of the three GP positions on the vertical integration company board, one position was specifically for a local GP who was not part of the vertical integration arrangement.
By taking over general practices in difficulty, the acute trust was thereby taking over the financial losses those practices were incurring. Nevertheless, senior trust managers considered this to be ultimately beneficial to the trust, and to the local health economy overall, because it ensured that the continuance of primary care would support better demand management and more efficiency in care provision to the local population. Analysis undertaken by the trust indicated that the cost to the wider system (i.e. through increased secondary care utilisation as a result of failing primary care) would be much greater without vertical integration:
. . . there’s a question whether you ever can get [the general practices] financially stable, but the cost to the system would be so much greater [without integration], and that’s where the argument, you know, goes back and forth.
B08, primary care, organisational management
With respect to the implementation of the vertical integration model at Greenvale, each practice was still responsible for running itself, while drawing on the support of the central team within the primary care company. This central team provided back office support functions, such as HR, payroll and accounts, to all integrated practices:
. . . practices still very much run themselves, with support from a central team; it is different to how it first started out, as the central management team is much smaller now.
B04, primary care, professional representation
. . . we are a central team, and we brought in, like, our [the acute trust’s] HR and our finance and corporate governance and, like, management policy procedures, which is now managed centrally.
B11, primary care, organisational management
Within each general practice, there was an operational manager who was responsible for running the practice on a day-to-day basis, supported by a clinical lead and, often, a nurse. The clinical leads of each general practice were supported by a MDT of other health-care professionals:
. . . we’ve got a mixture of not just GPs, but we’ve got advance nurse practitioners, nurse practitioners, practice nurses, highly skilled HCAs [health-care assistants] and apprentice HCAs. We’ve got MSK [musculoskeletal] practitioners, and we’re piloting mental health workers. And we have health coaches, which is, obviously, which came from the vanguard programme. So we really do work as a multidisciplinary team.
B11, primary care, organisational management
Practices within the vertical integration organisation also collaborated with one another, as they would in a horizontally integrated network. Staff worked across different sites where necessary (e.g. if there was a shortage of staff in one practice):
. . . one of the things that can happen is to phone another [vertical integration company] practice and say, ‘Have you got a bit of slack on the system today? Have you got a GP that’s got an admin[istration] morning that might sacrifice that to do a couple of hours for us?’ I mean, I use ‘GP’ as an example. It can be any of the clinical staff, where the pressure is on in one place. Now I think that it’s beginning to operate in an informal way, and without treating all the clinicians as a pool, because I don’t think that’s helpful, but to have a protocol or, if you like, contingency plans, where the sharing of resources at times of pressure becomes the norm rather than something that kicks in at the last minute.
B16, primary care, patient participation group
After the first three general practices approached the acute trust, which led to the formation of the vertical integration model, several others joined, so that by late 2019 the primary care company had 13 general practices (i.e. 13 sites), which were covered by nine contracts with NHS England. The acute trust and the primary care company it owns had not actively sought to recruit additional practices. All of the new additions had approached the trust/company. A due diligence process had been developed around the decision as to whether or not additional general practices were suitable for integration. There were three core perspectives considered in the current due diligence process: (1) quality regulation, (2) finances and (3) workforce.
Interviewees acknowledged that, initially, the due diligence process was not stringent enough, leading to unexpected issues arising after some practices had been integrated. However, the process had since been tightened up:
. . . one of the initial risks was around due diligence and our due diligence process – the risk being that our due diligence process wasn’t robust enough to pick up some of the issues. And so then you, kind of, you think you’re doing one thing and you’re actually, once you get in there, you find there’s a whole heap of other things that you should have found out about that before.
B07, secondary care, organisational management
Since the NHS Long Term Plan’s21 formalisation of PCNs and their near-100% coverage across England since July 2019, the vertical integration model has operated within a new landscape of horizontal networks of general practices. At Greenvale, approximately half of the vertical integration practices together formed a single PCN that was made up solely of those vertical integration practices. The other vertical integration practices were spread thinly across other PCNs that also incorporated non-integrated practices. These latter vertical integration practices had been allowed the freedom to support their PCN in whatever way necessary, with one interviewee even suggesting practices should look towards their PCN, rather than the vertical integration company, to provide some collaborative services:
. . . we’ve given our practices that aren’t in the main PCN, if you like, permission to just go and support their PCN to do whatever it needs to do and not worry about the fact that they’re a [vertical integration company] practice.
B03, primary care, clinical and managerial
It makes much more sense for our practices to be looking at their PCN as the way to then provide services collaboratively, rather than look at [the vertical integration company].
B03, primary care, clinical and managerial
However, the view was expressed that an arrangement such as the vertical integration company model would continue to be important because, unlike with PCNs, the acute trust that owns the vertical integration company is able, in effect, to underwrite general practices in financial difficulties:
. . . when you get to a point where you’re trying to support practices that get into big financial difficulties, the PCN isn’t the risk-holding entity. So the question then is: who holds the financial liability for that practice? So I think the PCN will change the nature of the relationship with [the vertical integration company], and it will almost put a step in place before you get to an entity like [the vertical integration company], that scale provider of local practices trying to support a practice that is in difficulty and kind of keep it stable. But there’s likely to still be a requirement for an at-scale provider like [the vertical integration company], who can then come in.
B07, secondary care, organisational management
Theme 3: making the change – from General Medical Services to subcontracted providers of primary care
Changes to contract holding
The specifics of the arrangements for holding GP contracts required lengthy prior discussions with NHS England and substantial legal fees. This process was particularly difficult for the acute trust, as it had no prior experience of GP contracts. Getting through all this represented a significant up-front learning, negotiation and legal advice cost to establishing the vertical integration model:
The way it [the new contractual arrangement] was actually created was a bit kind of Byzantine . . .
B15, primary care commissioning, organisational management
The arrangement that was agreed by the acute trust with NHS England and the local practices was that PMS contracts would now be held by the vertical integration company and GMS contracts (there were no APMS contracts in the area) would now each be held by two nominee GPs (the medical director of the vertical integration organisation and a nominated GP in each practice). These two individual GPs then subcontracted to the vertical integration company (of which they are employees) to provide the GP services and staff. The two GPs were, therefore, in theory, still responsible for the contract, but the liability and indemnity had been moved to sit with the acute trust so that the individual GPs were no longer liable:
. . . for the GMS have a nominee GP structure of which [name] is our main GP on all of our contracts as medical director, and, in theory, it then needs to be someone else that is from the practice – it doesn’t have to be a GP, but we tend to have got then a GP from the practice – to be the other name on the GMS contract . . .
B08, primary care, organisational management
The existing general practice staff had been allowed, after more than a year of negotiation with the Department of Health and Social Care, to be retained on the NHS pension scheme. More generally, staff in the practices that became part of the vertical integration company had the option to move, following TUPE, across to the company on their existing terms and conditions or to move to the company’s terms and conditions. Therefore, the staff were all no worse off as a result, and some were better off than when they had been when working in individual general practices:
We had access to the NHS pension scheme on a limited basis, but now we have direct access because, you know, it’s now deemed that we [the vertical integration company] are a provider of NHS services, which indeed we are.
B01, primary care, organisational management
Former GP partners who were now receiving a salary had a large amount of financial risk removed and no longer had the worry of finding new GP recruits to replace them when they wanted to move on or retire. The acute trust adds the financial deficits of the general practices within the company it owns to its own financial deficit; however, as already described, the trust board so far accepts the view that, overall, the trust’s deficit is smaller than it would have been had general practices been allowed to fail and, as a result, patient demand had not been so appropriately and effectively managed and met.
Estates management
The vertical integration organisation does not actively seek to take on ownership of property – not seeing itself as being in the business of property management – but it has done so as a short-term fix before selling property on to dedicated property managers. This contributes to further risk reduction for GPs, but without the vertical integration company having to become property managers:
We [the vertical integration company] take over the lease . . . that’s a big reason why GPs want to integrate as well, because of that responsibility of having a mortgage; so we do take that on. We do have one property that is fully owned by us, but otherwise we take on the lease. [The GPs in the practices that join the vertical integration company] will sell, if they’ve got the building, to another property provider and get the money from that, and we then, then we hold the lease after that so they have nothing to do with the property then.
B08, primary care, organisational management
You know, they can continue to own the property if they want to, but what we tend to find is that when they join, they want to get rid of all of their risks in one go and just move on.
B10, primary care, organisational management
Reorganising back office functions
At Greenvale, back office functions were provided to the constituent general practices centrally by the primary care company owned by the acute trust. This approach was taken, rather than utilising the acute hospital’s resources, because the acute trust’s staff were unfamiliar with the requirements of supporting general practices and to ensure that sufficient priority was accorded to those requirements. Therefore, the vertical integration company provided HR, finance, IT and data management, and publicity services to all of its general practices, as well as practice management:
So finance and HR, payroll, legal, to the extent that we need it, all of those are provided, and there’s a lot of data integration, analysis-type work as well, so that’s all done from here. We’ve got a team of, I think, it’s about 15 whole-time equivalent people in the central office that do all of that, plus the kind of management, the ongoing management of the practices.
B10, primary care, organisational management
I think a lot of the things like processes and protocol, decisions around immunisation, vaccination, a lot of clinical and non-clinical things are an issue for multiple practices at the same time, and where they can be decided centrally, they are decided centrally. It saves each practice having to reinvent the wheel.
B17, primary care, clinical
The vertical integration company was, at the time of our interviews, also piloting with four of its general practices a ‘workflow hub’ to make paperwork more efficient:
So ‘workflow’, it will have an administrative team, have a protocol, and, basically, look at documents coming in, and they can be all sorts of things, like A&E reports, consultant letters, to incoming mail. They have a protocol for sorting out how urgent they are, whether a GP needs to see them. There’s a protocol for filing some that don’t need clinical oversight. The ones that do, they will be allocated to the appropriate surgery, but that is centralised. And they come in centrally and they’re dealt with promptly. So individual practice teams on site don’t have the first hit of dealing with that aspect of the workflows. So there’s a reduced workload . . .
B17, primary care, clinical
Four practices were piloting a ‘prescribing hub’, which, if successful, would be spread across all of the vertical integration practices:
Prescription requests go in centrally, so whether they’re electronic requests or telephone requests. And we have a team of prescription clerks supported by a pharmacist who would deal not just with issuing prescriptions, but also things like medication reviews for people who need to be reviewed, and prescription queries. They tackle clinical queries like medication as well. Again, if you imagine, because that’s centralised, that takes the pressure off not just doctors on four surgery sites, but also off the other members of the team.
B17, primary care, clinical
The vertical integration company not only had the size to achieve cost savings in provision of back office functions, it could also employ appropriately specialised staff, which would be difficult for an individual general practice to do. For example, the vertical integration organisation achieved economies of scale in responding to quality regulation and inspections by the CQC:
A good example was when we had CQC inspections, which came up roughly at the same time for all the practices, and we have one particularly experienced person who’s been a practice manager for a long, long time, many CQC inspections, who’s involved in supporting multiple practices in getting all the documentation together . . .
B17, primary care, clinical
. . . ultimately, I’ve got that support that is the organisation, so a good example of that, I think, is CQC, right? So I’ve been through a CQC inspection as a GP partner, I’ve been through several, actually, because of the length of time I was partner, and that is absolutely you’re there on your own sorting out a fire policy at 9 o’clock on a Sunday night. You know, it’s depressing! And [now, with the vertical integration company] my role in our CQC inspection was honestly clinical. It was ‘What’s your opinion on this? How are you running this?’ It was all about the clinical side patient safety.
B06, primary care, clinical and managerial
Cross-cultural misunderstandings and tensions
As already noted, the trust had sought to put in place measures to mitigate concerns that vertical integration was, in effect, a secondary care takeover of primary care. The vertical integration company owned by the trust was seen to be primary care led, that is, the contracts were reversible so that GPs who become dissatisfied were not forced to remain within the vertical integration company, and a non-vertical integration GP sat on the company board so as to provide a channel for the wider GP community voice to be represented. Perhaps as a consequence, we heard of few examples of cross-cultural misunderstandings either between primary care and secondary care (e.g. secondary care colleagues failing to recognise the urgency of recruitment needs in primary care) or across primary care. The corollary of this, however, is that the interviewees did not describe a picture where secondary care and primary care had become much more integrated with one another, although with some exceptions, as described in Theme 4: impact on patient management – changes to primary care and secondary care delivery. The research team’s observations of a meeting of practice managers within the vertical integration arrangement and of a separate meeting of managers from the vertical integration company were consistent with this. We found that the meeting agendas and discussions focused almost exclusively on primary care operational issues, with hardly any reference to interaction between primary care and the acute hospital.
Theme 4: impact on patient management – changes to primary care and secondary care delivery
In spring 2020, at the time of writing, the vertical integration company had been in operation for 4 years. We have described how the main purpose of the vertically integrated model at Greenvale had been to sustain primary care in the face of severe staffing and financial difficulties being experienced by some practices in the area. Changing the way that health care was provided to patients had evidently not been the number one preoccupation. Changes were happening, but it was unclear to what extent these were due to the vertical integration arrangement rather than a result of the PACS vanguard and county-wide initiatives that were also affecting non-vertical integration general practices in the area, or if these were purely in line with more general trends in the rest of the NHS in England and Wales.
For example, in primary care, the health-care teams at the vertical integration company’s general practices had become more multidisciplinary, but this was a widespread trend:
I think we’ve really focused on the multidisciplinary team, so how we probably differ from most traditional practices is we’ve got a much smaller ratio of doctors to patients . . . So we’ve got more of multi-disciplinary team members and less GPs . . .
B08, primary care, organisational management
. . . what we’ve done in [vertical integration company] is to, firstly, create a much flatter multidisciplinary team structure, where the GP effectively sits in the middle of it rather than the top of it and acts partly as a consultant to the other members of the team to support them, but also focuses on complex patients, with the idea that most of the other work that GPs historically provided is done by other members of the team.
B03, primary care, clinical and managerial
By contrast, two interviewees who were not part of the vertical integration organisation stated that, as far as they knew, there had been:
. . . no changes to health service provision due to [the vertical integration company].
B04, primary care, professional representation
No, I think . . . it feels like a – I won’t say a missed opportunity – it feels like an opportunity we haven’t yet grasped.
B15, primary care commissioning, organisational management
We heard from several interviewees about health coaches working at general practices and a complex care team focused on people with complex and/or multiple conditions. However, these coaches and teams had been introduced before vertical integration, as part of the PACS vanguard.
We also heard about initiatives to bring some specialist care out of the acute hospital and into general practices, which were being introduced with the vertical integration practices:
We have got some links with the hospital, so we have got a couple of the specialist nurses coming and helping us with doing chronic disease clinics, for example, in our practices and supporting our practice nurses who run these clinics to provide slightly more complex care for who are the most difficult patients to manage.
B03, primary care, clinical and managerial
. . . a good example of that is we’ve got a respiratory specialist nurse, OK? So she’s based at the hospital, she was doing her job completely at the hospital, right? So she now comes out into [vertical integration company] practices to see the complex patients . . .
B06, primary and secondary care, clinical and managerial
We also heard from one interviewee a view that primary care staff in the vertical integration model had been given more scope than before to develop special interests/skills for the benefit of patients:
I think there’s been more creativity and imagination about special provisions . . . when I say special provisions, let’s think in terms of diabetic clinics, provision for the elderly, special needs and so on. That a great deal of attention has been given to what needs need special, particular attention and can we provide clinics for that . . . And this may be . . . that some of the existing staff are given special responsibilities, are trained, which is attractive to them. If they have – I’ll give the example of diabetes – they’re particularly interested in diabetic care, one of those practitioners will be trained or focused on that.
B16, primary care, patient participation group
None of the interviewees we spoke to felt that the vertical integration model had, as yet, had any impact on service delivery in secondary care.
Theme 5: measuring success and identifying unintended impacts
We asked interviewees how the success of the vertical integration model, or the opposite, was being, or could be, measured. We also discussed unexpected or unintended impacts. Measures of success related to the maintenance of patient access to local general practices, the net financial impact on the local health economy and recruitment and retention of primary care staff. The last of these three categories (i.e. recruitment and retention of primary care staff) was where unintended and undesired consequences were noted.
The vertical integration model had, so far, been successful in sustaining primary care in the short term, apparently saving at-risk general practices from closing and recruiting new staff there. No practices taken on by the vertical integration company had closed, despite several of them having been in severe staffing and financial difficulty when they were taken on by the acute trust-owned primary care company. Keeping local practices open is essential to maintaining patient access to primary care in rural areas with poor transport links, that is, areas such as Greenvale:
. . . if [the vertical integration company] didn’t exist now and I looked at our practices, I think three of them definitely would not be in the NHS.
B03, primary care, clinical and managerial
I know that morale in our team is good. People feel listened to. We’ve had, the practice I’ve had, hasn’t been [vertical integration company] for a huge amount of time, but going from being a practice that was really struggling to getting very positive patient feedback now is very nice. And to have people happy where they’re working, feel that they can actually make a difference, can develop things themselves, I think that’s a sign of success.
B17, primary care, clinical
Taken together, the vertical integration general practices are not yet breaking even, with a total deficit (expenditure in excess of income) of nearly £1M expected for financial year 2019/20, despite savings on the cost of back office functions. This reflects, in part, continuing high costs of employing locum GPs.
Offsetting that, there appears to be preliminary evidence (from Greenvale summary reports identified from documentary analysis) that the vertical integration model is supporting a reduction in growth of attendance and admittance to secondary care among patients of integrated practices. The creation of the vertical integration model took place on the basis that, although expenditure on general practice is much less than on acute hospital care, how general practice works can have a large impact on the finances of acute hospitals:
If you just measure primary care on their contract value, which actually in comparison to how much it would cost to run an acute trust is miniscule, you know, is a fraction of the cost, but if you look at their impact and influence on spend in the system, i.e. how many referrals they make, how many they signpost, how many they recommend someone to go to residential nursing care, how many they refer, you know, into other services, to how much they try, you know, how much testing they do, their costs are something like seven times what their contract value is.
B01, primary care, organisational management
I know that things like admission rates and readmission rates and all the classic kind of markers of control had improved because of what [the vertical integration company] were doing.
B02, primary care, professional representation
Senior managers at the acute trust argued that the vertical integration model had saved them money as a result of lower secondary care utilisation, achieved by stopping patients inappropriately entering secondary care (often as emergencies), as a result of better primary care provision. This also saves the local health economy overall, as the primary care provided is less costly than the secondary care it obviates:
[The financial impact on the acute trust] has been positive in the sense that we’ve avoided all of those emergency costs.
B15, primary care commissioning, organisational management
I firmly believe that if [the vertical integration company] wasn’t here, the cost to the system and the cost to the commissioner would be far greater, because a number of these practices would have handed back contracts and they would have been subject to transition funding and dispersal costs and all the rest of it . . . The counterfactual case is that we think the [vertical integration company] has saved the system between £6M and £8M each year. So there’s a £1M hit sitting on the [acute trust’s] books because that’s kind of where it sits, but the counterfactual deficit to the system could have been up to £6–8M, so £5–7M more than that.
B07, secondary care, organisational management
There were indications that the vertical integration model was having a net positive effect on recruitment and retention of GPs to the area, as the vertical integration arrangement enables more attractive career options for GPs and other staff, which aids recruitment and retention:
We can offer that the career is working partly in the hospital, partly in primary care, which a lot of GPs seem to want. We can offer portfolio careers, where you’re not just working in one practice. You can be moving around the practices, which, again, some people that might appeal to . . .
B10, primary care, organisational management
Although recruitment of new GPs by the vertical integration company had proved quite successful, GPs remained the main staffing problem and it had proven impossible to recruit GPs to work full time:
GPs are the key issue, definitely. We are able to recruit. We do, unlike a lot of partnerships, the traditional practices, we have been able to recruit. We’ve recruited quite a lot of GPs over time . . .
B10, primary care, organisational management
We’ve recruited something approaching 40 GPs in the last two and a half years, but not one single one of them is full time.
B03, primary care, clinical and managerial
The recruitment of non-GP staff seems to have been little affected either positively or negatively by the vertical integration model:
In terms of other clinicians, so nurse practitioners, practice nurses, again, it really varies in our practices – overall there’s probably been a balanced exodus and recruitment – but we have some practices where at the moment we’re really struggling to provide chronic disease management, for example, because we don’t have enough practice nurses. But there are others that are completely fully staffed.
B03, primary care, clinical and managerial
So, yeah, I don’t think on the non-clinical, I don’t think that’s any different than any other practice. People do come and go; that’s the way of life.
B05, primary care, organisational management
One negative unintended effect of the vertical integration company taking over some practices, which was remarked on by several interviewees, was that the remaining GP(s) at practices joining the vertical integration company had, on occasion, taken the opportunity to then retire or move to become locums soon afterwards. Likewise, GPs had been more inclined to take sick leave (for which they get paid when they are salaried) once the practice ‘business’ had been taken off their hands. Consequently, it is possible that, in the short term, the need to recruit new GPs had been increased in a few practices:
When we took on that practice, we knew they were in trouble because they’d tried to recruit for 4 years and they hadn’t been able to. There were three partners there and a salaried GP, and, at the time, we had assurances from everyone, including the CCG, that those partners would stay if [the vertical integration company] took them on and helped stabilise the practice. Within . . . a week of taking them on, the salaried GP retired, and then one of the partners resigned, and then subsequently the other two partners both went off sick.
B09, primary care, organisational management
I think integration is a big shock, and we do seem to lose GPs sometimes at integration. I think they’re not used to not being their own boss maybe. And usually I think they have plans to leave that we don’t necessarily know about.
B05, primary care, organisational management
Theory of change
The research team’s analysis of the findings from Greenvale is summarised in a theory of change map, which is presented in Figure 5. The predominant rationale for vertical integration between the acute hospital and several general practices in its catchment area was to enable those practices to continue in the face of recruitment and financial difficulties, where the traditional partnership model was no longer sustainable as a result. The preceding PACS vanguard in the area, which was focused on improving care for people with multiple conditions or other complex health needs, had reinforced and strengthened relationships, thereby providing fertile ground for the vertical integration idea, which also benefited from active and supportive leadership, both at the acute trust and in the primary care community locally.
FIGURE 5.
Greenvale vertical integration theory of change. CEO, chief executive officer.
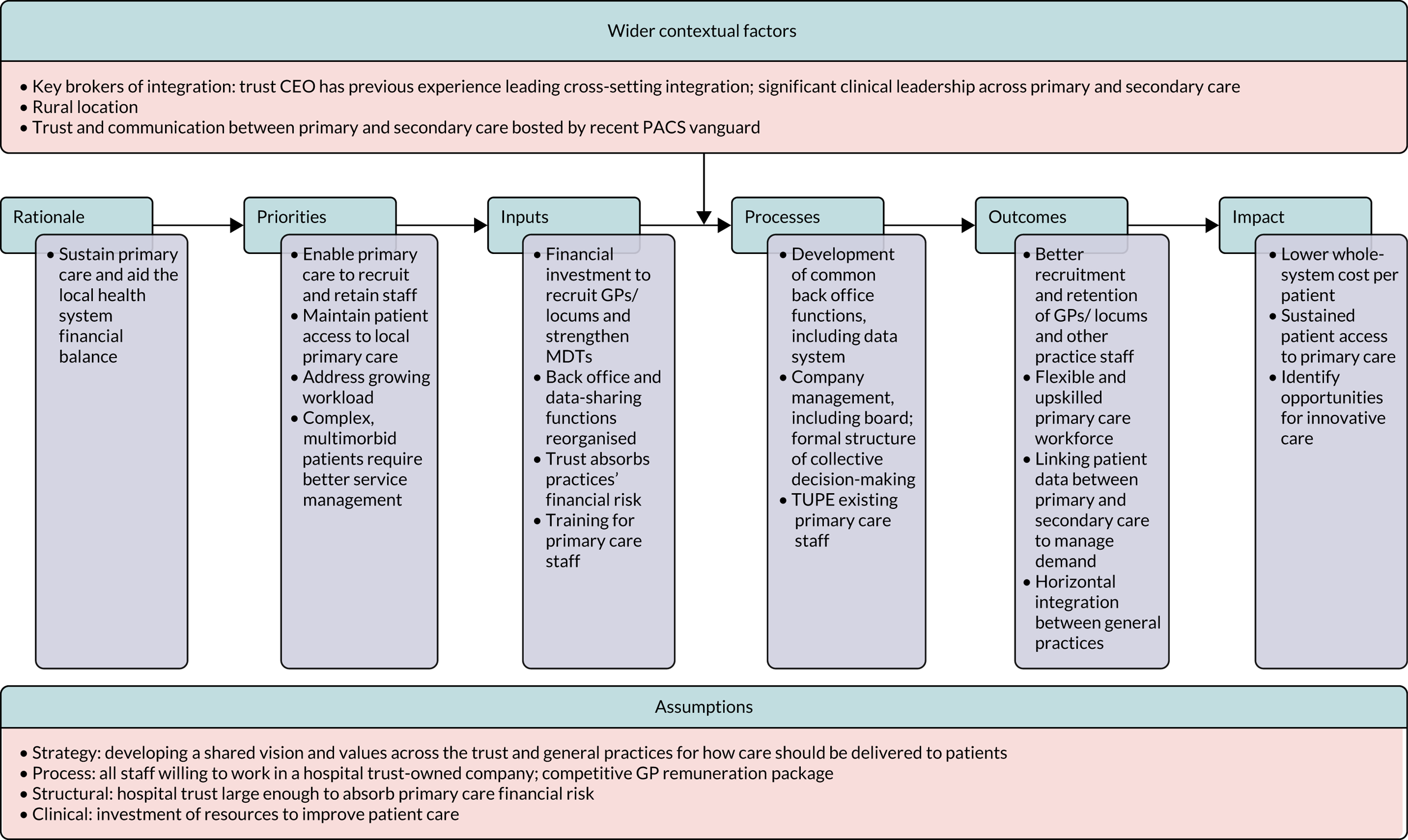
Implementing the local vertical integration solution – which entails a limited company running the GP services, with the company 100% owned by the acute hospital trust – required a substantial up-front investment of time and effort by senior management at the trust and leading GPs. The trust’s then chief executive and one of the leading GPs were singled out in several of the interviews as having provided strong and active leadership. Creating the novel legal and governance structure preferred at Greenvale required detailed discussions with NHSE&I and the Department of Health and Social Care, as well as expert legal and VAT-related advice. The provision of centralised back office functions, drawing on those of the acute trust, to achieve both functional and systemic integration, along with the creation of a central management team for the vertical integration company’s constituent general practices, appears to have been successful and may have contributed to the viability of primary care financially, but it is still operating at a loss.
Recruitment and retention of GPs, now all salaried, had been supported by the vertical integration arrangement and no practices had to close. This is important for the maintenance of patient access to primary care in this rural area with poor transport links. Recruitment and retention of non-medical staff at primary care practices had been maintained.
The success in sustaining primary care and stabilising recruitment had enabled the continuation of the PACS model’s innovations for people with multiple morbidities and the gradual introduction of other changes in patient care. Primary care practices had more MDTs than previously and they had access to some specialist services via specially trained practice staff and some limited outreach from the acute hospital.
Finally, the acute trust and its board were strongly of the view, based on their own analyses (not in the public domain), that, despite the financial deficit for both their own trust and the vertical integration primary care company (with the latter contributing to the former), the trust’s financial position was considerably stronger than it would have been without implementation of vertical integration. Comparing vertical integration practices with patient flows from non-vertical integration practices in the county, the acute trust sees apparent reductions in the volumes of both emergency and elective work they are called on to deliver to the vertically integrated practices, which imply net savings to the local health economy to the tune of a few millions of pounds per year relative to the position that would be expected without vertical integration.
Chapter 7 Results: Seaview
Summary of key findings
-
The rationale for implementing vertical integration at Seaview was to address the potential problem of a large number of general practices closing by integrating them within the LHB, as there were no other viable alternatives.
-
There was a shift in strategy from a desire to return practices to GMS contract-holding providers, to holding onto practices and applying a MDT model of working.
-
The LHB was able to set up a governance team specifically to address the management of integrated practices, comprising primary care and secondary care stakeholders in the region.
-
Attracting GPs to a rural/coastal area remains difficult, especially in remoter locations, and locums remain costly and scarce.
-
In the vertical integration arrangement, the LHB was able to create attractive portfolio-based career opportunities for salaried GPs, and practice managers were given opportunities for greater responsibility.
-
Little is known so far about the impact on demand for secondary care.
The study team carried out 17 interviews with stakeholders and a single observation of a governance meeting hosted by the LHB, which had primary and secondary care practitioners in attendance. Further observations had been scheduled in February and March 2020; however, because of the COVID-19 pandemic, the LHB advised the research team not to attend meetings in its clinical settings to prevent the unnecessary risk of spreading the virus.
Theme 1: understanding the need for and purpose of acute hospital integration with primary care
Integrating with, and managing, primary care practices was a predicament that was placed on the LHB, with a considerable number of general practices handing back their contracts over a sustained period of time. Initially, the LHB was unprepared to manage a large number of practices more centrally. As a result, there was no initial model for integrating the practices with the health board, rather the strategy developed as the number of managed practices grew. The key goal for the LHB was to return practices to independent contractors:
In the last four years, we’ve received – I can get the number for you – so we’ve got 16 managed practices, we’ve probably received around 20 – over 20 resignations from contract. So for some of them I’ve managed in the central area, two of them that didn’t become managed were very small, single-handed practices, that had been ticking over for years – the GP has just retired, and they’re so small you wouldn’t do anything else but disperse them [their patients].
C02, secondary care, organisational management
There were a number of reasons why the LHB was being asked to manage practices. The main reason was the inability of some independent providers to recruit and retain GPs. Often, these practices were led by GPs who were nearing retirement and who were unable to find suitable successors to take over their practice, whereas, for a significant number of other GPs, the pressures of running a practice, increasing workloads and tensions arising with their partners were all contributory factors:
. . . there’s sometimes things going on behind the scenes that we don’t know about, in terms of partnership fall-outs and things like that – but I think the main reason is burn-out. It’s: ‘Don’t want to be responsible for the whole business anymore, had enough, but I’m quite happy to continue as a GP, seeing my patients, but I don’t want to run a, you know, work 12-hour days and run a practice’. Can’t recruit GPs; the age profile of GPs in [Seaview] is going up. You know, they’re getting older and older. And we’re not – I don’t think we’re replacing as quickly as they’re retiring . . .
C02, secondary care, organisational management
However, according to accounts from LHB employees, GPs and primary care staff, not all the practices had been performing poorly:
. . . it was a very good practice and certainly not a practice you would have expected to have resigned.
C06, secondary care, organisational management
Notably, as the number of general practices being managed by the LHB increased, in parallel with being unable to find suitable independent primary care providers to take over practices, the LHB changed its rationale and its understanding of how to make best use of the opportunity of having direct involvement in the delivery of primary care services:
. . . there was always the feeling this is the way the health board wants to go, so there was an awful lot of discussion about that: ‘Is this now the health board strategy? How hard have they tried to find GMS providers?’ And I think certainly early on, it was ‘No this is about us; don’t want anymore, please, no more!’.
C03, primary and secondary care, organisational management
Yet, given this new opportunity, there were still a number of challenges that persisted, primarily how to achieve standardisation across managed practices over a very dispersed and varied geographical landscape, where local knowledge of service provision was required to treat a complex patient population. Therefore, the immediate challenge was to address the nature of horizontal integration, before attempting to make gains through vertical integration between the LHB and general practices:
. . . if we have them all in one area, in one geographical area, and it’s much easier to make that horizontal integration than it is separately, so it’s working out, I think, going forward, how we do that horizontal integration. The vertical integration, we’ve just scratched the surface of, and that would be my next bit, I suppose, primary, community, but we keep saying, ‘Actually, the vertical integration is where we’ve got the greatest gains potential, because of clinical pathways being changed’.
C03, primary and secondary care, organisational management
Theme 2: developing a model of integration and an implementation strategy
The strategy and processes of taking over a practice at Seaview became more refined over time. The first step for the LHB was to speak with a practice to understand more about the specific challenges that it was facing at the time and to try to encourage the partners not to return their contract to the LHB:
I mean, with any practice, when they first resign, if we didn’t know they were going to resign, in the situation we’re in at the moment with this latest one, the first thing we would do is meet with the GPs, first of all to try and see if there’s any way that possibly they might not wish to change their minds, to try and understand why they’ve done it, and for us to get a better feel of what the problems are and also to understand whether they themselves, as GPs, are interested in continuing in any shape or form.
C06, secondary care, organisational management
In most cases, when a practice returned its GMS contract to the LHB there was a three-pronged approach, among which integration was considered the third and final option. (However, in a small number of cases, a decision to directly manage a practice following conversations with primary care clusters was taken immediately.) First, the LHB would attempt to readvertise the practice to see whether or not there were GPs in the local cluster, the UK or internationally who would be interested in working in the area. Up to autumn 2019, this option had yielded only one former GP from the local area, who agreed to acquire and manage three practices in a staggered sequence. Second, if there were no interested parties, then the LHB would decide whether or not the practice patient list could be dispersed to neighbouring practices. Third, the LHB would decide whether to integrate the practice as it is or to merge the practice with another geographically local practice that had already integrated with the LHB:
. . . the process was fairly established, so for single-handers, you obviously only have 3 months to sort it out, for group practices 6 months. So the single-handers – it had to be moved quite quickly. So it went out to the cluster GPs to see what their feeling was about what should happen next, and the options on the table of course at any time you get a resignation are: dispersing, taking over, re-advertising or possibly combining two lists, so if there was a willing nearby practice.
C03, primary and secondary care, organisational management
A fundamental action soon after integration was to invest in the workforce to address the shortage of GPs. This led to the development of greater and more widespread use of models of MDTs working across the LHB area. As a result, in one area within the LHB, a model was developed to encourage interdisciplinary working, supporting patients living with complex multimorbid conditions and reducing medicine prescribing. The model was brought about following the quick resignation and return of GMS contracts of five general practices in a small geographical area covering a population of approximately 20,000 patients. Clinical teams were established within this model to treat groups of 5000–6000 patients, using a range of primary care staff:
So within one of the normal teams, there’s – depending on the hours that they work – sort of perhaps one and a half full-time equivalent GPs. We have nurse practitioners, possibly some ANPs’ [advanced nurse practitioners’] involvement, there’s an occupational therapist linked to that, a pharmacist and then we also have a team co-ordinator, who tries to manage the team’s work and direct it according to where’s best to be dealt with for the patient.
C09, primary care, clinical
There have been early attempts, using this model, to integrate into primary care settings some specialised services that are usually delivered in secondary care settings. However, there were certain caveats:
. . . secondary care diabetic care and doing it much more holistically in the community, it’s a piece of work, but it is not . . . it’s very difficult to realise the potential of doing that in other subjects without a lead who’s previously worked in secondary care, coming out to primary care and going ‘Woo!’ So the separate management structures, I think, between the hospital specialties and the centralisation of them limits it . . .
C03, primary and secondary care, organisational management
A number of primary and secondary care colleagues were critical of this MDT primary care model. First, many interviewees felt that the nature of the additional funding the first area received could not be replicated widely across the LHB. Second, recruitment of staff is difficult in rural and/or coastal areas farther away from the English border. Third, many interviewees questioned the effectiveness of the MDT model:
I mean, the idea when [subsite within Seaview] was set up was that it was going to offer a different type of service, there’s mixed messages about how that’s worked, you know, the idea, I know everybody talks about it, but there are some, sort of . . . sometimes you do get a bit of feedback that, actually, there are problems with it.
C06, secondary care, organisational management
Last, although practices have been integrated with the LHB, they continue to maintain a reasonably integral role in local primary care, working via local clusters. Managed practices’ involvement in cluster working has been a cause of tension with non-managed practices, which feel disadvantaged because managed practices continue to have access to cluster funding and also receive additional resources from the LHB:
This is going to sound crude, but because the GP clusters have – because they are still GP clusters – but they are going to have to change – and some of them are much more mature than others – but they have funds, and of course you’ll have the GMS practices who, some of them, tend to think, ‘Well, why are the managed practices getting cluster funds?’.
C06, secondary care, organisational management
Theme 3: making the change – from General Medical Services to subcontracted providers of primary care
Changes to contract holding
The nature of transitioning at Seaview differs from that at the other two case study sites. At Seaview, there is no subcontracting model with the LHB, as the LHB manages service provision in both primary care and secondary care.
Prior to addressing contracting and other practical issues, as well as completing the due diligence process, the LHB will communicate with a number of stakeholders to discuss the wider impact of taking over the management of a general practice:
So we’ll be agreeing a letter with the practice that can go out. We’ll be communicating with everybody else from [national] government to social services to local councillors, obviously the patients. And meeting with people. The other night, we met with the local councillors for the practice that’s just resigned.
C06, secondary care, organisational management
Unusually, there is no formal/legal contractual arrangement between the LHB and a general practice once it has been integrated into the LHB. There is an informal contractual arrangement, overseen by the national government, which states that the LHB will continue to deliver services in line with GMS contract guidance:
So we have no GMS contract. So, again, it’s very different to – so, obviously, we have GMS contracts, under [Seaview] regulation with the independent practices. There’s been no diktat from [national] government, because we’ve got other health boards with managed practices, in terms of you must have an internal contract, GMS contract arrangement. Having said that, it’s always been taken as read that we, in the main, you continue to deliver services under those specifications within GMS contracts.
C02, secondary care, organisational management
Many interviewees felt that having a relatively loose legal arrangement between general practices and the LHB led to some practices too easily giving up their GMS contract without seeking alternative arrangements to remain independent providers of care. Therefore, as part of the LHB’s due diligence, the health board continues to support practices to first identify alternatives to direct management.
Estates management
Senior staff across the LHB felt that there were significant challenges associated with managing GP premises. The LHB was reluctant to take over GPs’ leases for their premises. Given the larger number of practices that were becoming integrated with the LHB, they felt that they were coming to terms with primary care estates management and how best to minimise the nature of the risk this involves. Nevertheless, this process was time-consuming and resource-intensive:
We don’t make an assumption that we take the lease . . . It’s something we’re getting better at because we’re having to learn as we go along, really, and it’s very complicated sometimes, because all the leases are different; there’s nothing straightforward about any of these leases. I mean, what’s supposed to happen is the GPs, there’s a survey done for dilapidations and then we have a look at and negotiate with the GPs about what they should be paying for and what – before we take it over – and that can be a sticking point as well.
C06, secondary care, organisational management
There were a number of other challenges with taking greater responsibility for premises. Where premises were shared with non-managed practices, the LHB often found itself taking greater responsibility for the costs of managing the building. Where existing building leases were taken over, the LHB often found that buildings were in disrepair and/or did not meet the standards required to safely deliver health-care services. Finally, buildings may have limited space, which can affect the LHB’s aim of introducing MDT working across managed practices:
For example, health and safety, I know that provided a lot of challenges. A lot of the estate is not up to scratch. Now the health board’s taken liability for that and not the GMS partners.
C03, primary and secondary care, organisational management
Reorganising back office functions
In general, the management, setting up and alignment of back office functions within the LHB were being absorbed into staff’s current roles and responsibilities. Therefore, there was no development of specific departments. However, there were new roles created across the LHB to manage the responsibilities of managed practices. Back office staff were more accustomed to addressing issues with secondary care employment concerns and, therefore, there was a steep learning curve for them when it came to addressing challenges in primary care:
. . . there’s no recognition from the health board as a whole that managed practices are part of what we do now, you know. We’ve got 17 or something, so that’s what we do. So it’s never really been built into other departments, so procurement, payroll, estates, HR, there’s not been, say, it’s not part of their day work and it needs to be, because when we come along, say, to procurement, and say, ‘Oh, we’re trying to sort this out’, and they can be as helpful as they can, but half the time, they don’t understand it because they don’t understand primary care . . .
C06, secondary care, organisational management
Practice managers were playing a crucial role as providers of real-time information to ensure correct recording of service delivery and, especially, payroll. The following quotation highlights the pressures placed on practice managers, including pressures that were formerly within the remit of senior partners of the practice or pressures from increased bureaucracy within the vertically integrated organisation relative to when their practice was independent:
I think within the [LHB] managed practices, for me certainly, it’s the bureaucracy. And tick boxes constantly. I feel that we have a lot more to do. I certainly have a lot more to do as practice manager in terms of form filling.
C08, primary care, organisational management
Similar to our other case study sites, there were significant issues at Seaview with regard to recruitment of staff into existing and new roles. We heard that recruitment processes were taking significantly longer inside the vertically integrated organisation than with the previous situation. This was simultaneously coupled with existing staff being ‘TUPE-ed’ across to their new employment contracts with the LHB, which was creating additional work for LHB staff on top of maintaining other responsibilities:
. . . we interviewed and got a health-care assistant post – this was ages after the person had left in that post – so it was advertising a vacant post, somebody was appointed but then they [dropped out], so we had to go back all the way through the whole process again, so it just meant that you were without the HCA [health-care assistant] for months and months and months, which impacts, you know, when you’re already running quite bare bones, you know, we haven’t got a lot of people, there was a lot of people, but considering the workflow and the patient numbers . . . so that’s just really disheartening.
C09, primary care, clinical
. . . there’s so much restrictions on recruitment at the moment. But somebody could pop their notice in from there, then you have to do an establishment control, and from there it goes on to the advert, then you have to go out to our venue interview, your shortlist you interview, then the actual recruitment process. Where it could take you a month in GMS-land, it could take you now up to 6 months to recruit someone.
C05, secondary care, organisational management
To address some of the aforementioned challenges, the LHB established a new management structure across its three constituent regional areas, consisting of medical, area and assistant area director roles, with practice managers reporting to them to communicate day-to-day challenges. In addition, area and assistant area directors were responsible for engaging with practice managers. The LHB had established quarterly governance meetings with colleagues from the LHB, as well as GPs and practice managers from both managed and non-managed practices.
Cross-cultural misunderstandings and tensions
The most fundamental tension was between those working in primary care who felt that the LHB had struggled to get to grips with the challenges of managing general practices and those at the LHB who were trying to manage practices according to how they were running secondary care services:
So I think the health board have sort of got to look at how we run alongside the secondary care, because when you think of [the LHB], it is very secondary care orientated, isn’t it? Or you think of the general hospitals, you don’t actually think of managed practices or . . . But I don’t think there’s any benefits in being a managed practice.
C08, primary care, organisational management
I think the balance in secondary care – very management heavy. General practice – very clinical leadership heavy. And the realignment of that, I think, is a real challenge.
C03, primary and secondary care, organisational management
However, others felt differently. A number of stakeholders we interviewed across primary and secondary care were very understanding of the predicament that the LHB was initially in (i.e. being asked to take over the management of general practices). Many stakeholders felt that certain tensions had pertained well before the integration with the LHB, whereby primary care practitioners felt burdened because they believed that secondary care delivered via acute hospitals risked them being seen as doing an inadequate job of managing complex patients. Yet, going forward, newer challenges centred on the difficulty of managed practices to learn, adapt and accommodate more innovative ways of delivering services as salaried GPs:
We still have some GPs – going to choose my words carefully – who work in a very traditional model of practice, where it all comes to them. But most of them are now very on board and are referring to us regularly. And that was about making some allies, making some of those initial contacts, and then once other people started to see, actually see, that’s the OT [occupational therapist], something might change.
C04, primary care, clinical
Theme 4: impact on patient management – changes to primary and secondary care delivery
A significant challenge faced by the LHB was how to best treat an ageing population living with complex multimorbidities who were dispersed across a large geographically rural/coastal area, along with more transient tourists who access health services during seasonal peak times throughout the year. In response to this challenge, there was a strong focus on developing services that support patient self-management, with the hope that this would bring about a subsequent reduction in health service demand:
We work with people with chronic long-term conditions, so looking at self-management. So things like COPD [chronic obstructive pulmonary disease], pain – pain is a big one – and looking at trying to reduce the impact of those conditions on people’s lives. So, essentially, increase their function in the community and reduce demand on health services . . .
C04, primary care, clinical
The mechanism, as stated in Theme 2: developing a model of integration and an implementation strategy, was the introduction of distinct clinical and non-clinical allied health professionals, using a model of MDT working within managed practices. The majority of primary care staff welcomed the introduction of additional resource to manage patient demand. However, this introduction of new staff contradicted patients’ perceptions of how care should be delivered, with many patients still continually requesting to be seen by GPs:
I think surgeries are trying to get away from, in some parts, of always seeing the same patients, because you’re not, actually – at one time you used to be registered with a particular GP – and some patients still think you are, so they want to see that GP. So we’re obviously trying to move away from that and get patients to see other clinicians, so signpost them. They don’t always have to see a doctor, but some people have got it in their head they’ve got a problem, they need to see a doctor. So it’s educating, trying to educate the patients as well.
C08, primary care, organisational management
And so we have had, probably the biggest difference would be, having the occupational therapists that have particularly linked with the community and a lot of things like social prescribing have raised the profile of that, I think, within the practice.
C09, primary care clinical
However, although patients might be seen more readily, the new system does not necessarily preclude the patient being seen by their preferred choice of health professional:
So, I think, for me, availability of appointments is always what everyone talks about in practice, but actually getting the person to the right practitioner is something that perhaps patients didn’t appreciate right at the beginning, whereas now they probably do. So I think over time probably patient opinions have changed. And there’s a lot of noise initially; if you get a lot of noise in the system that ‘That’s a managed practice, so you won’t be able to get an appointment’, it ends up becoming the truth, even though, actually, you’re getting an appointment with the appropriate person.
C03, primary and secondary care, organisational management
Overall, there remained a dichotomous relationship between primary and secondary care, whereby there remained some lack of communication and a lack of data/IT integration across the interface. There were instances where secondary care specialists were becoming more involved in delivering primary care-based services; however, such instances remained rare:
Just small little pockets of, so, for example, one orthopaedic consultant is coming to work at one of the managed practices alongside. But, again, really difficult to get the processes, just things, like, because it’s a GP practice, you can’t get notes delivered to it and they work on clinical notes system, you know. The barriers sometimes between historically very different organisations are difficult.
C03, primary and secondary care, organisational management
I think we need more connection with the secondary care physicians as well. I think, you know – and I recognise it’s really difficult because there are vast differences and secondary care’s under a lot of pressure as well, so I do recognise that – but that would be helpful that we’re actually working together.
C09, primary care, clinical
With regard to staffing, the main concern for the LHB was how to attract health professionals to the area and get them to remain for a sustained period of time. The greatest challenge was the employment of locums, which was creating competition across the three regional areas. Therefore, the LHB tried to develop attractive packages to entice GPs, while, at the same time, co-ordinating across its whole area so that practices were not competing against one another within the LHB area for the limited pool of potential recruits:
One of the main things we sorted out early, one of the initial things we sorted out as a group, was terms of conditions of locums – because we’re all fishing in the same pond for the locums – and making sure they don’t play us off on each other, and we’re all paying the same rate and setting expectations . . .
C02, secondary care, organisational management
I described the training offer, support with training, special-interest development. Obviously, they get the terms and conditions that are better. We try and put support in, so they are there doing what they want to do, . . . the running of the practice isn’t their problem anymore, if that’s what they want. We offer, yeah, all sorts of different things, anything, really, just to incentivise them!
C02, secondary care, organisational management
Non-clinical staff faced challenges working with locum GPs compared with permanently employed GPs. Some staff commented on locums who were working to rule, placing greater pressure on the remaining staff:
So I feel bad for some of them because some of them, they get away with not – they’re like, ‘Oh, I’m a locum; I won’t do that kind of thing’. And then there’s other ones that are long-term locums and I forget that they’re long-term locums but they’re not a salaried GP, because they act almost like a salaried GP, and then they’re, like, ‘Oh, we’ll be around now for a few months’, and it’s, like, [sighs]
C07, primary care, clinical
And just the admin[istration], like looking at letters and things, relying on salaried GPs when you’ve only got, like, one salaried GP and they only work 2 or 3 days a week, it’s just . . . you just rely on the regular locums, and when they all go to go off in the holidays and stuff, sometimes it’s just not safe because you don’t have the consistency and . . . they can just be, like, ‘Yeah, I’m not coming in for the next few weeks; good luck’ kind of thing, and we don’t have anyone. And then you feel bad for the . . . because if there’s just one locum that’s on and they end up leaving because they’re, like, ‘Well, I’m a locum, like, this is more salaried GP job’ kind of thing.
C07, primary care, clinical
The greatest tension for existing staff was the transition to AfC contracts and the recruitment of new employees in primary care being paid more, as a consequence of that, than those who have been working for longer as part of independent practices:
Well, it’s a mess, basically. There’s an understandable want from the staff in the practices when they’re transferring to us [the LHB] that, obviously, they transfer on their own terms and conditions, and then the problem always comes in when we recruit new staff who are on Agenda for Change and then you’ve got one member of staff who’s been there 20 years on this much money and then you bring in a new kid of about 16 and they’re on more money and you think, ‘Well, I can understand why you don’t like that, but it’s because of AfC’.
C06, secondary care, organisational management
. . . we’ve got some existent staff whose morale is very low. For me, I would love them all on Agenda for Change, but it’s a higher decision than me, and we are working towards getting them all over there. So, for example, we have one of our practices has three members of staff. They’re the eldest, the longest-serving members of staff, on their own terms and conditions. And we have a junior who’s just started on an AfC getting better paid, better terms and conditions, and they’ve never known the role before; they’re new to the role.
C05, secondary care, organisational management
Theme 5: measuring success and identifying unintended impacts
The revenue generated from primary care practices was considered an important marker of success. However, of greatest importance was the amount the LHB was currently spending to bring practices into a sustainable model. Therefore, a fundamental marker for measuring success was to control the expenditure being made to manage and redesign health service delivery across managed general practices:
. . . we’ve got a, sort of, a set budget based on what we would generate as a GMS practice. They’re all overspent . . . But they’re overspent for a plethora of reasons. One of the obvious ones is reliance on locums, so – for [subsite within Seaview], we’re not too bad now, so that overspend has come right down. So their overspend has come down. Reliance on locums.
C02, secondary care, organisational management
. . . there’s always that because we have restrictions within the health board, so we can’t always spend the money as freely as GMS practices. For instance, if we wanted a new phone system, GMS can just go out and purchase whatever. We have to actually go through the procurement process . . . , so we have a lot more restrictions.
C05, secondary care, organisational management
Monitoring financial expenditure was important to show potential interested parties that the general practices that were being managed by the LHB were both financially stable and a viable business opportunity if someone was willing to take them over:
So you’d want to see the accounts, effectively, wouldn’t you, of a new business? So I think although, you know, I’ve heard people say, ‘Well, what’s the point in doing the enhanced services, because the health board are paying themselves?’ but I think it’s also important to have that service still running because then at least there is – and for the health board as well – to see how much that the practice are worth and that it is a viable option having a practice within the health board.
C08, primary care, organisational management
One of the opportunities the LHB envisaged when taking over general practices was the ability to train staff to undertake a larger number of responsibilities and also to identify candidates who were already skilled enough to progress their careers across the LHB:
I think in terms of development for staff, that’s clinical and administrative, I think there’s a lot more opportunities. I think within an independent practice you’re very restricted, because, for example, if you’re a practice nurse, unless the practice, depending on its size and, sort of, financially, whether they’d be able to encourage them to work towards an advanced nurse practitioner role, or if you were a nurse practitioner, where do you go after that?
C08, primary care, organisational management
There were some notable drawbacks. One drawback was a lack of leadership at practice level, seen as a result of the shift within the GP workforce from partnered GPs to part-time salaried GPs or locums. In addition, there was a perceived sense of competitiveness and tension across staff in certain areas within the LHB, who found themselves, unintentionally, competing with one another for the same small pool of resources:
And one of the huge differences is the onus on the GPs working within the practice to take on clinical leadership, such as they would do were they partners, and not just turn up and see the patients, as they would do under a salaried GP contract. So I think the big – for me, one of the huge – differences is that establishing clinical leadership within the practices. There are huge differences of course: as a partner, you’re running the business, so there’s no timesheets or whatever, so you expand the work – no, you expand your time to fit the work – whereas one of the big differences, I think, in directly managed practices is people are on salaried contracts, so they’ve got no responsibility to stay when the work is not done. And so the shift of leadership towards management, I think, is one of the biggest challenges that if you’d had more time you could have planned.
C03, primary and secondary care, organisational management
I think it’s a very ‘us and them’ kind of scenario . . . Central on one table, East on another table, West on another table.
C07, primary care, clinical
Yet there were some widespread successes from the integration. Although many of our stakeholders recognised that there was still plenty to do to improve the nature of functional integration with the LHB, many felt that noteworthy changes had been made to health service delivery and, having the opportunity to deliver beyond the GMS contract (known locally as ‘GMS plus’), better communication across the care interface had been established (mostly between primary and secondary care, rather than primary and community care), ratings with the CQC had improved and patient satisfaction had improved (i.e. fewer complaints had been received):
I think communication has improved. Referrals are quicker. The access to information is there. Unfortunately, IT systems aren’t as cohesive as they could be.
C01, secondary care, organisational management
And from a CQC perspective, we know that all of our practices have got higher ratings since they’ve been with us.
C01, secondary care, organisational management
. . . we also try to do a lot of engagement with patients about satisfaction and things, so we’ve got some of that information.
C02, secondary care, organisational management
More recently, the LHB has been committed to understanding more about the changes that the integration of practices with the LHB had achieved. This played a role in allowing access to the research team to speak with stakeholders:
. . . we know from [subsite within Seaview], although I haven’t looked at it for the last 12 months, is medicines, pharmacy spend has come right down, prescribing spend. And in terms of the cluster, they are within the lowest users of the ED [emergency department], that practice population.
C02, secondary care, organisational management
Theory of change
A theory of change map for this case study site is presented in Figure 6. The rationale for Seaview was to address the immediate crisis of a large number of general practices closing and, consequently, integrate them within the LHB because there were no other viable alternatives. The reasons for closure were an ageing profile of existing GPs, being unable to attract new GPs within a traditional partner model and increasing GP workload.
FIGURE 6.
Seaview vertical integration theory of change. BMA, British Medical Association; LMC, local medical committee.
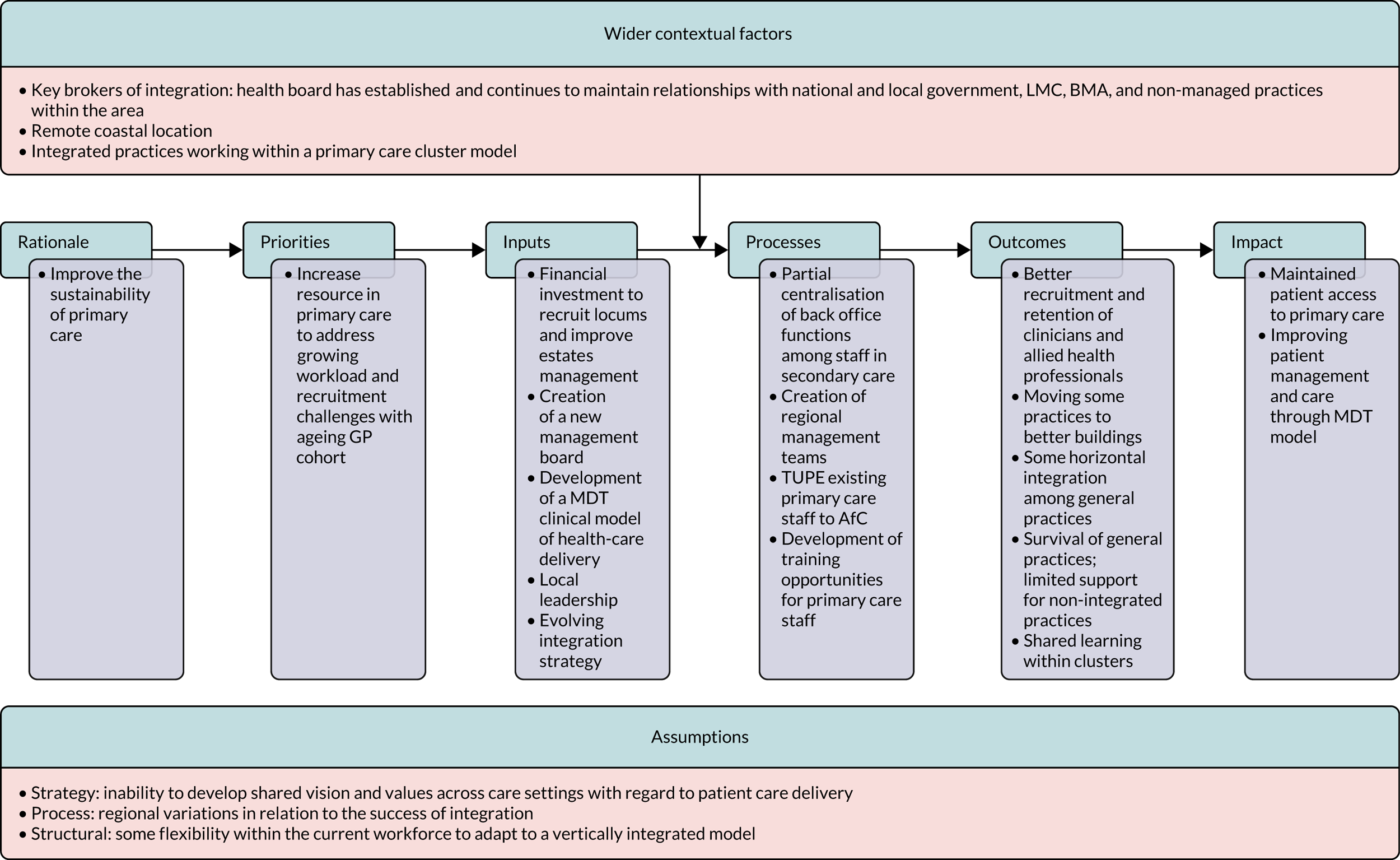
Different from our other case study sites, the desired impact of integrating and managing general practices at Seaview was to eventually be able to return general practices to GMS contract-holding providers. However, owing to the ever-increasing number of general practices returning their contracts to the LHB, the strategy for managed practices has now shifted. Therefore, although general practices remained integrated with the LHB, the rationale was to improve patient care through the regional application of a MDT model. There was little or no reference within interviews and observations of achieving clinical integration across primary and secondary care in the immediate term.
This came with a number of caveats. There remained significant variation in the management of integrated practices across the LHB’s area. A ‘one size fits all’ approach to MDT care was considered difficult by both primary and secondary care stakeholders. Nevertheless, many staff recognised that having integrated practices made it easier to make changes to clinical pathways for patients, especially between primary and community care (more so than between primary and hospital care because of geographical constraints faced by patients attending distant acute hospitals). In particular, stakeholders found it difficult to comprehend how a MDT model should be implemented if the rationale was based on ultimately returning practices to GMS contract-holding providers. Therefore, a clear long-term strategy for the sustainability of primary care was desired.
There was a substantial cost associated with integrating practices, especially for a LHB in special measures, as was the case at Seaview. Attracting GPs to a rural/coastal area remained difficult, especially in remote locations, and locums remained an expensive and scarce resource. There were also significant estates-related costs, with a number of managed practices being moved to new premises that were fit for purpose and could accommodate a MDT model.
Nevertheless, integration had a number of advantages. The LHB was able to create attractive portfolio-based career opportunities for salaried GPs and practice managers were given opportunities for greater responsibility. Nearly all staff would eventually receive improved contractual terms on AfC, which brought perceived greater employment security. In addition, the LHB was able to set up a governance team specifically to address the management of integrated practices, with primary and secondary stakeholders, both within and outside the model.
As a result, Seaview had achieved some sustainability with regard to the number of general practice closures, but little is known so far about the effect on secondary care demand or the financial cost of integration.
Chapter 8 Discussion
Summary of key themes
-
The main rationale for the introduction of a vertically integrated model, evident in all three case studies, was to sustain primary care by supporting local general practices that are in financial and recruitment difficulties and, at the same time, manage demand effectively and efficiently across primary, secondary and community care.
-
Our overall theory of change shows that the early implementation of vertical integration is focused more on achieving functional than clinical integration.
-
Closer integration was attributed to previous good relationships between primary and secondary care locally, and to historical planning and preparation for integrated working across the local health economy.
-
Our initial evaluation of three case studies, two in England and one in Wales, implies that vertical integration may, indeed, have a role to play as a route to better integration of patient care, at least in some geographical areas. Although there have been innovations in patient care, these do not appear to be specifically attributed to the vertically integrated model.
-
The inevitable corollary of salaried doctors replacing independent GP contractors is a degree of loss of autonomy for GPs.
-
Making the shift to vertical integration imposes a significant short-term challenge on acute trust/LHB staff (who are used to operating in large organisations focused on secondary care) to learn about and understand the practicalities and culture of running primary care.
-
Improving care pathways, and the efficiency of the local health economy, for patients who are high users of emergency secondary care and/or living with complex or multiple morbidities was a particular focus at two of our three case study sites. We will explore impact and effectiveness in greater depth in our phase 2 evaluation.
Chapters 5–7 demonstrate overlapping, but not completely congruent, findings from the three case study sites. Our study design deliberately selected three sites that, although similar in the core feature that general practices were effectively being run by local acute hospital services, had clear differences in the ways that they were set up. At Urbanville, in England, the acute trust ran the integrated general practices as a division of the trust, and employed the GPs and other primary care staff of those practices just as it employed the medical and other staff at its hospitals. At Greenvale, in England, the acute trust set up a wholly owned subsidiary company to run the integrated GP services and employ the primary care staff. At Seaview, in Wales, the LHB, which had previously been focused mainly on managing secondary care, took over the direct management of GP services in practices that otherwise would have handed back their contracts, alongside the management of hospital services.
A strong theme at all three sites was that the rationale for vertical integration was to enable the continued existence of general practices in difficulty and thereby support a local health-care system in which patient demand would be better managed and patient pathways more appropriate than if general practices were allowed to fail. At all three sites, the establishment of vertical integration created opportunities for better integration of patient care across secondary and primary care settings and for rationalisation of common functions, such as back office functions. However, the extent to which these opportunities were being exploited differed across sites.
In the following section, we present and discuss an overall theory of change for vertical integration between acute hospitals and general practices, before going on to consider similarities and differences across the case studies, referring to the same themes as in the individual case study chapters. The chapter concludes with reflections on the strengths and weaknesses of the evaluation, and highlights issues that are candidates to be the focus of a second evaluation of vertical integration.
An overall theory of change for vertical integration
Overview
With reference to Weiss’59 four main purposes when conducting evaluations on programme theories (as detailed in Chapter 3), we have spoken to a range of stakeholders across sites to make their assumptions of vertical integration explicit. In developing our overall theory of change and accompanying illustration, following Vogel’s60 criteria, we have provided a detailed description of the wider context of vertical integration in the light of wider primary care policy in both England and Wales, and provide the long-term outcomes that vertical integration aims to achieve, detailing as many assumptions of how these outcomes are perceived to be achieved. An overall theory of change map is presented in Figure 7, drawing out the common features of the individual theories of change for the three case study sites. Although no single theory of change can do full justice to the specific aspects of all cases of vertical integration, there are some core aspects, and this overall theory of change map provides a framework to understand how, at a high level, the implications of vertical integration between primary and acute care in the UK can vary considerably across sites with regard to local feasibility (e.g. setting, context and resources). In addition, our theory of change illustrations remain in development and reflect that different sites are at different stages (i.e. from conception to achieving clinical integration).
FIGURE 7.
Overall vertical integration theory of change.
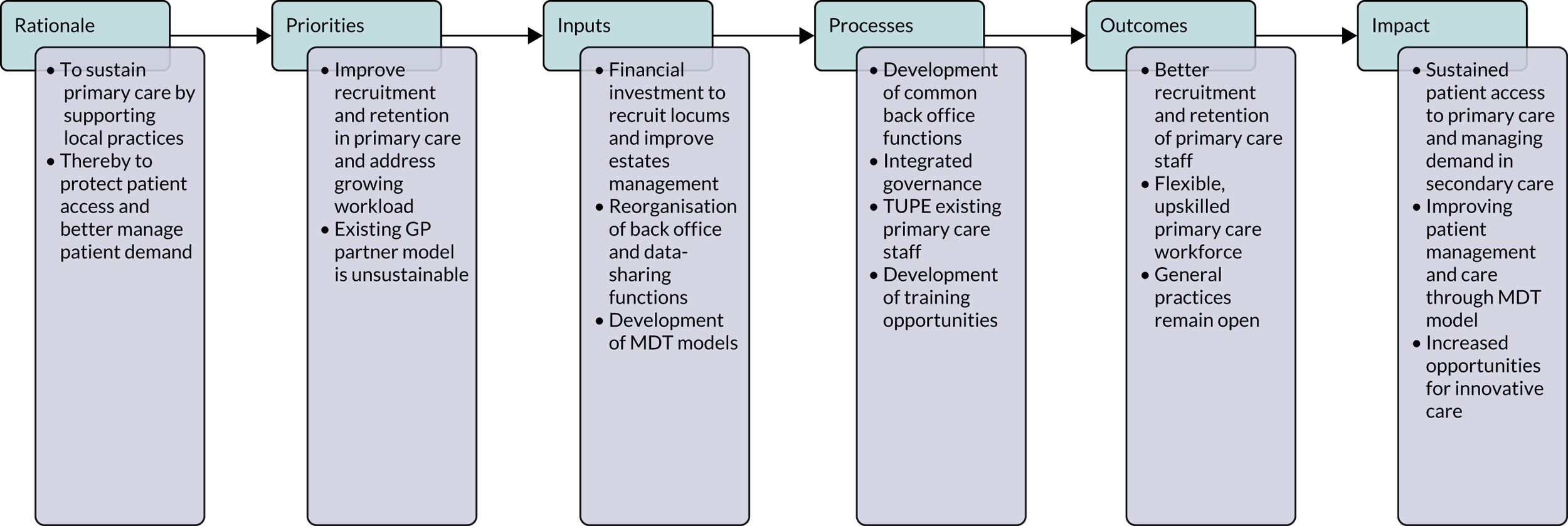
As the theory of change map illustrates (see Figure 7), the main rationale for the introduction of a vertically integrated model, a rationale that was evident across all three case study sites, was to sustain primary care by supporting local general practices that are in financial and recruitment difficulties and, at the same time, manage demand effectively and efficiently across primary, secondary and community care. This focus differs, to some extent, from international examples (e.g. Kaiser Permanente and the Alzira model)42,45,64 where rationale and implementation were focused principally on closer integration of primary and secondary care to improve quality of care and increase efficiency, with no explicit reference to sustaining primary care in the face of growing recruitment/retention and workload pressures.
In our case studies, the introduction of vertical integration across sites led to increased interdependencies among individual general practices and the acute trust or LHB with regard to controlling costs, responding to patient needs and developing legitimacy throughout the local health economy. Similar to their international predecessors, UK examples of vertical integration are challenged with initial costs and barriers, and with limited co-ordination of care across settings. However, despite these challenges of implementation, the desire to integrate both clinically and functionally across primary and secondary care has persisted.
The theory of change shows that the early implementation of vertical integration is primarily centred on achieving functional integration as opposed to clinical integration. 65 As Lasker et al. 66 further emphasise, key to achieving vertical integration is integration of information systems and financial arrangements. Therefore, functional integration can be synergistic with clinical integration. At all three case study sites, stakeholders sought to achieve greater ‘closeness of working’ to achieve functional integration,67 whereby organisational arrangements and designated staff to oversee the introduction of vertical integration led to more cohesive working, both among general practices and between them and the acute trust/LHB.
Description of overall theory of change map
Our explanation of the theory of change map for the implementation of vertical integration between acute hospitals/health boards and primary care general practices begins with intended impact. Although the rationale for implementation is centred on sustaining primary care, each site varied in terms of intended impact (i.e. eventually returning practices to GMS contract-holding providers was the aim at Seaview, whereas managing secondary care demand and achieving financial and clinical efficiencies across the health-care system were emphasised more at both Greenvale and Urbanville).
Across the three case study sites, we found that there were, in practice, four key inputs with regard to the investment required to achieve a vertically integrated model at any site. The inputs were economic in nature. There appeared to be much less emphasis on other inputs, such as steps to align values, cultures and ways of working, among the primary care practices in the vertical integration arrangements and between those practices and the acute hospitals.
Foremost among the inputs we heard about was the significant financial investment required to attract, recruit and retain salaried and locum GPs. The attraction of salaried posts for existing partners was in receiving an appropriate salary while no longer having to bear the financial risks of running the practice as a business they themselves owned. The attraction of salaried positions for new GPs was having posts that offered less financial risk, the opportunity for portfolio careers and career development paths across primary, community and secondary care. Nevertheless, although many vacancies were filled in two sites (Urbanville and Greenvale), questions remained about the ratio of salaried to locum GPs and about the higher cost due to continued reliance on locums.
At all three sites, the vertically integrated organisation also had to absorb significant estates costs related to managing additional buildings, carrying out repairs, dealing with landlords and, in some cases, moving practices to buildings owned by the acute trust or LHB.
In addition, there was major restructuring of back office functions, which were centralised in all three case studies, either at the acute trust/LHB or in a trust-owned primary care company.
The final input was to achieve a model of health-care delivery in primary care that relied much more than previously on MDTs. This can be seen as a response to the difficulties and costs of recruiting and retaining GPs, but also as a more strategic response to remodelling primary care on a sustainable basis while providing appropriate care locally.
A number of processes have taken place to achieve vertical integration. At a very practical and day-to-day working level, back office functions were centralised at all three sites. Therefore, rather than relying on within-practice resources for HR, payroll, accounts, dealing with CQC regulation, etc., the vertically integrated practices were served by a single central team. This appears to lead to economies of scale, although the magnitude of any savings is unknown. However, when back office functions are provided by hospital trust or LHB departments, it may also have led to some increased ‘bureaucracy’ with administrative processes and, consequently, lengthening of the timescales to make and implement decisions.
Significant to enabling and implementing functional and clinical integration was the setting up and creation of governance teams/meetings for the vertically integrated practices. All sites developed management teams comprising primary and secondary care staff. In addition, GPs from practices outside the vertically integrated arrangement were included in governance arrangements, in an attempt to ensure fair treatment of both ‘managed’ and ‘non-managed’ practices.
For staff, especially those in primary care, and particularly the non-clinical staff there, vertical integration brought new opportunities for further training, with the prospect of developing their careers within the acute trust or LHB. The process of moving the employment of existing primary care staff to the hospital trust or LHB, or to a new primary care company owned by the hospital trust, entailed significant up-front efforts to negotiate with national bodies and legal costs to establish arrangements, such as continued access to the NHS pension scheme. Some of the staff being transferred received slight pay increases or improved terms and conditions as a result, implying some increase in costs.
With regard to the outcomes of vertical integration, the main beneficial impact evident was that general practices remained open that otherwise would very likely have closed (i.e. ‘handed back their contracts’). Therefore, the consequence that was avoided was the patients of closed practices being dispersed to other practices’ lists, with increased pressure on the remaining practices (in the face of continuing recruitment difficulties) and leaving patients with greater distances to travel to access primary care. In this initial evaluation, we have not determined the magnitude of the impact of vertical integration on patient flows, including patient demand for secondary care, but evidence at Urbanville and Greenvale suggests that integration has supported smaller growth in patient flows to secondary care than from non-vertically integrated practices in the same areas.
Recruitment of salaried GPs and locums to the vertically integrated practices has evidently been possible. The spread of MDTs and opportunities for staff to upskill, and to see improved career prospects and security of employment, can be expected to have led to better staff recruitment and better staff retention. This may also lead to opportunities to improve clinical continuity of care across primary and secondary care. For one site in particular, Urbanville, substantial strides were made to improve continuity of care through data-sharing between general practices and secondary care (i.e. being able to monitor high-risk patients living with multimorbidities entering emergency secondary care and following them up in the community).
Synthesis of case study findings
As part of the analysis, we identified five major themes, as well as four subthemes, that provided a framework for evaluation of all three case studies. In the following section, we reflect on the cross-case study implications within each theme.
Understanding the need for, and purpose of, acute hospital integration with primary care, in a context of primary care networks and clusters
In spring 2019, at the outset of the study, the trend of health-care policy in the UK had, for many years, favoured greater integration of care. Such integration had, and has, many dimensions. Vertical integration of general practices with organisations running acute hospital services had been discussed, along with a small number of international examples, but had been accorded less policy attention than horizontal integration, including across primary care. In England, the NHS Long Term Plan,26 published in January 2019, emphasised the creation of (horizontal) PCNs of general practices covering registered populations of 30,000–50,000 patients, but made no mention of vertical integration. Nevertheless, we anticipated at the outset of the evaluation that we would hear about increased integration of patient care across secondary and primary care settings.
Our initial evaluation of three case studies, two in England and one in Wales, implies that vertical integration may, indeed, have a role as a route to better integration of patient care, at least in some areas. However, it was clear that the single most important driver of vertical integration was not integration of care, but rather maintenance of primary care local to where patients live. In all three areas we studied, vertical integration has been used to address the difficulty faced in maintaining the traditional model of GP partnership-based primary medical care. Vertical integration in these places has provided a more stable financial platform for primary care than the model based on individual practices run as separate businesses. At the case study sites, GPs no longer risk personal financial loss when the practice suffers from high costs (e.g. due to employing locums). At the same time, the acute trust- or LHB-backed general practices are able to offer staff training and career development opportunities, as well as job security, which increases their chances of recruiting and retaining primary care staff.
The inevitable corollary of salaried doctors replacing independent GP contractors is a loss of autonomy for GPs. A frequent eventuality that followed vertical integration was that GPs in the integrated practices not only sought that trade-off, but took it one step further once the integration was in place by leaving their practices, either to become locums or to cease practising as GPs.
The importance, from a system perspective, of sustaining primary care was not only to maintain local access for patients, but, at the same time, to manage demand effectively and efficiently across primary, secondary and community care. If primary care practices had closed, local acute hospitals feared a consequent increase in emergency demand on their services (demand that could have been appropriately managed locally in a primary care setting were that still an option).
Although the official endorsement in the NHS Long Term Plan26 of horizontal integration of general practices in PCNs, which together covered the whole of England from 1 July, at least in name, had not been in place long at the time of our study, many places had various forms of interpractice networking before then. Therefore, we were able to seek informed expectations from our case study interviewees at Urbanville and Greenvale about the likely future interaction of vertical integration with horizontally integrated PCNs (in England). We also asked about the interaction of vertical integration with primary care clusters at Seaview (in Wales). Expectations evidently differ. At Urbanville, all but one of the vertically integrated general practices together formed a single large PCN. The one other vertically integrated practice was part of a PCN with a majority of non-vertical integration practices. Therefore, with the exception of this last practice, the PCN was coterminous with the vertical integration organisation and could be run as one and the same organisation, without any consequent disturbance to existing arrangements. Hence, the nature of PCNs being coterminous with vertical integration relates closely to Robinson and Casalino’s19 concept of developing integrated delivery systems through increased horizontal integration among general practices. However, it was nationally mandated primary care policy driving the changes to clinical care provision and management structures in general practice, rather than being solely led by strategy developed by the acute trusts.
At Greenvale, the vertical integration practices were split across several PCNs. One PCN comprised vertical integration practices alone, but several other PCNs had one vertical integration practice plus a handful of non-vertical integration practices. In the latter case, the vertical integration practices have two potential ‘homes’ for sharing services, supporting each other with staffing, co-ordinating more specialised practice-based services, etc. The interviewees we spoke to at Greenvale who offered views on the future interaction of the vertical integration company with the local PCNs took the view that the two forms of integration could co-exist. The vertical integration company and its practices were able to co-operate with all of the PCNs with which they had links and there was no need, yet, for any practice to decide to plump for one organisation rather than another. It was also too early to tell whether or not PCNs would take advantage of, for example, the centralised back office functions offered by the vertical integration company.
In 2019, in Wales, there was no new initiative promoting horizontal integration between general practices, but, as in England, there had, for many years, been development of such ‘primary care clusters’. 27 The emphasis at Seaview on stabilising general practices to return them, if possible, to independent operation implies that vertical integration was seen as a temporary state of affairs. To the extent that horizontal clusters of general practices are expected to continue by default, they may be seen as the intended way forward in that location. However, the number of general practices within the vertical integration arrangement with the LHB were growing and practices had not yet returned to independent operation, and so there is the prospect of vertical integration becoming at least semi-permanent, despite original hopes to the contrary. Nevertheless, the motivation for primary care clusters seems not to depend on whether or not any members of a cluster are operated by the LHB or operating as independent contractors.
Progress with developing an integration model and implementation strategy
There were notable differences across the three case study sites in the changes visible so far, despite implementation of vertical integration occurring for a relatively similar duration of time. Seaview did not intend any one general practice to remain LHB-run indefinitely and so definite moves to perpetuate that arrangement should not be expected. The other two case study sites had achieved a greater scale of organisational and functional integration, as well as some clinical integration, between the acute hospital and the integrated general practices because of a longer-term rationale and (at Urbanville at least) more of a protocol-based implementation of how integration was to occur with primary care practices.
Achievement of closer organisational integration was helped by previously established good relationships between primary and secondary care locally, and by historical planning and preparation towards integrated working across the local health economy. Therefore, the basis for vertical integration at Greenvale was partly laid by the PACS vanguard model of care that had been operating since 2015, which was focused on better managing care across primary and secondary care settings for patients with complex and multiple morbidities. The vanguard had, arguably, been made possible by committed leadership and some strong pre-existing relationships between primary care and secondary care providers locally. However, the vanguard also reinforced those relationships. The result was a platform that enabled the subsequent vertical integration to seem a natural solution both to general practices facing difficulties and to the local acute hospital trust whom they approached to take over their GP contracts. Similar strong relationships had already existed at Urbanville, although without reinforcement from a PACS vanguard.
At all three sites, the historical division between primary and secondary care represents a non-negligible challenge to vertical integration. Vertical integration with an acute hospital is evidently not attractive to every GP. Many local practices had chosen to remain outside the vertical integration arrangement, even though they would be free to join it (subject to due diligence investigation by the acute trust or LHB). Clearly, vertical integration with an acute hospital is not sought by all GPs, even in areas where recruitment of GP colleagues and/or other practice staff may be difficult. The majority of interviewees in each case study were part of the vertical integration arrangement, and it was noticeable that the non-vertical integration interviewees were more equivocal in their descriptions of the vertical integration arrangement in place. We do not want to overinterpret what was a matter of stress and tone rather than opposing viewpoints, not least because, particularly at Seaview, but at the other sites too, the rationale and strategy for vertical integration was being developed as and when integration was occurring, and in all three sites vertical integration had only been in existence for 3 or 4 years. It could be difficult, therefore, to develop shared values and an ethos towards integration when the greatest priority was to simply prevent the closure of general practices that appeared about to fail.
Making the change: from General Medical Services to subcontracted providers of primary care
The scoping work for the evaluation had prepared us to expect to hear more mention of lost GP autonomy than was the case. This is no doubt, in part, owing to the majority of interviewees being part of the vertical integration arrangement at the case study site. GPs who wished to remain autonomous were still autonomous and at none of the three case study sites did the acute trust or LHB seek to take over general practices, rather they took on practices they were approached by.
An unintended consequence of the transition to vertical integration may have been that some GPs gave up practising sooner than they might otherwise have done (because vertical integration meant that they could do so without financial cost to themselves). The transition from GP partner to salaried GP was, therefore, characterised by many of the GP partners apparently viewing being a salaried employee at the practice they had formerly (co-)owned as only a temporary state. Some GP partners remained for only a short period of time post-vertical integration and then left general practice, despite one site (Greenvale) providing a financial incentive for GPs to stay on as salaried GPs for at least 2 years (note that this financial incentive has since been removed and replaced with a more balanced performance-related remuneration package).
However, learning from a BRACE evaluation (Smith J, Parkinson S, Harshfield A, Sidhu M, personal communication) suggests that PCNs in England can better support GPs with regard to workload, provide greater local autonomy over commissioning (with respect to the local CCG) and provide additional funding that is channelled directly to general practice, all of which may encourage GPs to remain in general practice for longer (Smith J, Parkinson S, Harshfield A, Sidhu M, personal communication). Yet, the GP role continues to change across England and Wales in a context of GP shortages in deprived and rural/coastal areas, whereby GPs are expected to deliver a larger number of services within the community, working as part of MDTs. In addition, NHSE&I has re-stated its commitment to the GP partnership model, with the introduction of a one-off £20,000 payment to GPs or other staff who enter into a practice partnership, and new GPs and nurses will be offered a new 2-year fellowship to support their first steps in a primary care career. 68 Experienced GPs will also be reimbursed for mentoring their newly qualified colleagues.
Perhaps unsurprisingly, the legal and administrative practicalities of moving staff from independent general practices to employment directly by an NHS trust or LHB entailed considerable efforts. The three case studies had rather different legal and governance arrangements. In Seaview, where the stated intention was for general practices to be returned to independent operation as soon as the practice staff were able and willing, the GP contracts had, in effect, simply been taken up by the LHB, which then employed the salaried staff and locums. In Urbanville, the practices had been absorbed into the management structure of the NHS trust, of which they formed a division. In Greenvale, the practices were run by a purpose-created limited company, which was, in turn, owned by the NHS trust. Acute trust managers and leading GPs at Greenvale and Urbanville, over time, built up working relationships with NHSE&I and with the Department of Health and Social Care. There was no already-cleared path to follow for transitioning general practices to vertical integration with trusts, either as a part of a trust (Urbanville) or as a wholly owned subsidiary company (Greenvale). Legal arrangements had to be found to transfer responsibility for GMS contracts. For example, in Seaview, the LHB continued to manage general practices according to GMS contract income and expenditure and attempted to pool resources and make efficiencies based on an overall available expenditure across all managed practices, therefore moving resources where they were most required. Hence, this contractual responsibility led to opportunities for economies of scale and, in some instances, following investment, made some practices more attractive to those willing to take them over as independent providers of care.
Yet, the transfer of responsibility for GMS contracts from GPs to the acute trust in England can also lead to difficulty in leaving the vertical integration model. As stated in the Urbanville findings, practices were able to leave the arrangement (where former partners remain as salaried GPs); however, this can be time-consuming and expensive because of legal due diligence. To date, only one practice had left vertical integration arrangements across our three sites. Nevertheless, despite LHB and acute trusts taking over GMS contracts, many GPs still decided to leave general practice altogether rather than remain as salaried GPs. Inevitably, the absence of former partners led to an absence of strong clinical leadership within managed practices, particularly in practices where the use of locums was common practice.
NHS pension scheme rules had to be adapted to avoid transferred staff losing future access to that highly valued scheme and its benefits. VAT arrangements had to be clarified. Practice staff generally had their terms and conditions of employment protected, and sometimes enhanced, with more job security and improved pay and conditions for some. However, the transition also meant greater scrutiny with regard to job specifications and whether or not individual members of staff fulfilled them.
Now that different sites have pioneered this transition, the precedents have been created for others to follow. At Urbanville, guidance to others interested in implementing vertical integration had been formalised in written form, and both Urbanville and Greenvale interviewees reported a steady trickle of approaches to them by organisations in other parts of the NHS contemplating the option of vertical integration.
Transitioning to vertical integration also evidently imposed a significant requirement on acute trust/LHB staff who are used to operating in large organisations focused on secondary care to learn about and understand the practicalities and the culture of running primary care. The distance between front-line staff and decision-makers about day-to-day management, equipment purchases, minor adjustments to practice, etc., is much shorter in a general practice than in a hospital. Consequently, we heard some frustrations from primary care staff about much slower and more bureaucratic decision-making. At the same time, however, the centralisation of back office functions was often welcomed as taking an unwanted and tedious burden off the backs of health-care professionals who would prefer to be seeing patients and not staying late to sort out the paperwork.
The primary and secondary care staff (i.e. clinicians and managers) we interviewed at the three case study sites did not venture many views about how vertical integration was affecting working relationships across the primary–secondary care interface. The impression given by staff was still largely of separate primary care and secondary care, albeit with some increase in outreach of specialist services (which is also evident in non-vertically integrated areas). There was an absence of normative integration across all three sites with respect to developing shared values and securing collaboration in delivering health care. We hope to return in a future further evaluation to focus more on questions around working across the primary/secondary care interface.
Changes to patient care
Although changing patient care was not stated as the prime motivation for vertical integration in any of the three case studies, the platform it created by stabilising primary care provided an opportunity to progress with some changes to patient care. It is hard to tell the extent to which the changes, such as specialist musculoskeletal or diabetic services being provided at general practices, might have occurred in the absence of vertical integration; however, without financially stable, fully staffed primary care practices, changes would have been much harder to introduce. The nature of innovation in care provision to address local needs varied across our case study sites. At Urbanville and Greenvale, opportunities for innovation centred on more MDT working in primary care based on local population needs. Increased use of MDTs was also apparent in Seaview. Other innovations included sharing information in real time across primary and secondary care (Urbanville) and targeting high-risk patients who are most likely to access emergency secondary care, but could be better managed in the community (Greenvale). Therefore, despite having strong administrative integration (e.g. management support, governance and strategy formation), at intraorganisational levels, as described by Conrad and Dowling,17 all our sites had limited clinical integration with secondary care health services. The maintenance of primary care practices was a necessary condition for there to be innovations of these kinds in delivering care to patients. However, similar innovations had been occurring in non-vertically integrated primary care. Therefore, vertical integration per se does not appear to have been the driver of innovations in care. We hope to return, in a second stage of evaluation, to investigate further the extent of any causal linkages between vertical integration and changes to patient care.
Impact of vertical integration
To the best of our knowledge, the net impact of vertical integration on the costs of patient care in the local health economies has not been comprehensively analysed. The acute trusts and the LHB at the three case study sites had to invest significant financial resources with regard to recruiting clinical staff to rectify GP shortages and operating primary care practices in difficult circumstances. Urbanville and Greenvale had undertaken local exercises to assess the impact of vertical integration on total health system costs. At Urbanville, a quantitative impact evaluation had been commissioned from independent researchers to assess if, and to what extent, vertical integration had resulted in changes in the demand for unplanned hospital care. At Greenvale, we were told about a similar analysis (which we have not been able to see) that was presented by management of the vertical integration company to the trust board, which showed net savings in annual operating costs in the local health economy of a few million pounds per year, mainly resulting from reduced emergency admissions to hospital as a result of patient care being better managed in primary care in the vertical integration practices.
All three sites had some success in recruiting salaried GPs to work within vertical integration practices. The financial de-risking consequent on the acute trust or LHB taking responsibility for the GP contracts is itself a benefit. Combined with increased training and special interest development opportunities, the opportunity to focus on clinical work and leave running the ‘business’ aspects to others makes vertical integration practices more attractive to some potential GP recruits. However, recruitment of GPs is not easy, even for vertical integration organisations, and all sites continued to encounter high costs associated with continued employment of locums. In addition, increased training opportunities for non-clinical staff in primary care to upskill and ‘move up’ within a larger organisation prompted many staff to stay and work within a vertically integrated model.
As a result either of due diligences processes prior to integrating practices or of experience post-integration, the acute trusts/LHB identified the need for a number of expenditures associated with either improving the standard of current primary care buildings and/or transitioning practices to buildings suited to safer and more comprehensive health service delivery (e.g. having enough consultation rooms to maximise delivery of direct enhanced services). The result may be better care for patients or, at least, a better experience of care than would otherwise have pertained.
From our initial evaluation, it remains unclear to what extent patients will have experienced changes as a result of vertical integration, whether for the better or the worse. Patients are likely to have been introduced to new GPs and to new, but still local, buildings/facilities, which may be better than previous buildings/facilities. Patients are also more likely to have encountered health-care professionals other than GPs in primary care settings, as part of the spread of MDTs that had taken place within the vertical integration sites.
Improving care pathways, and the efficiency of the local health economy, for patients who were high users of emergency secondary care and/or living with complex or multiple morbidities was a particular focus at Urbanville and Greenvale; however, in the latter case, this appears to have been a consequence of the PACS new model of care that was established the year before the commencement of vertical integration, which applied to the local non-vertical integration practices as well as to the vertical integration practices.
Perhaps the main benefit to patients, and the most important measure of success, is the continued existence of fully functioning primary care in their local practice, rather than its demise, where that can be expected to have been the counterfactual. Therefore, potentially the greatest benefit to patients is one that they may well not have perceived (i.e. the absence of a worsening in access to primary care near where they live).
Feedback workshops with case study sites
In July 2020, the study team approached all three case study sites to feed back results from the rapid evaluation and learn how the vertical integration arrangements fared during the COVID-19 pandemic. Workshops were delivered with two sites (Greenvale and Seaview) in August and September 2020, sharing and discussing overall and site-specific findings and theory of change illustrations. The study team made a number of attempts to arrange a workshop with Urbanville, but was unable to arrange and deliver a brief session with key stakeholders prior to submitting this report.
At Greenvale, the workshop was attended by six colleagues, including medical, HR, operations directors, business and finance managers and a GP, all of whom were from within the primary care company. Attendees, in general, agreed with the findings presented, but stressed the development of forthcoming changes to patient care and the collaborative innovation happening across the limited company and general practice. However, the attendees recognised that it was difficult to distinguish innovation as a direct result of vertical integration rather than stemming from working as part of PCN. In addition, attendees felt that the governance and managerial framework that had been established was vital to sharing services across primary care and would create opportunities to do more with secondary care in the future.
In relation to the COVID-19 pandemic, general practices within the vertical integration arrangement felt that the were able to have a ‘greater voice with commissioners’ than might otherwise have been the case and, therefore, were able to help shape the local response to the pandemic better as part of the vertical integration limited company. Furthermore, the GP in attendance felt that the centralised governance team was crucial with regard to working collaboratively with neighbouring PCNs (as opposed to working more closely with the local acute hospital). GPs employed by the limited company were happy to move across practices to provide greater clinical oversight and care during early stages of the pandemic. A novel finding from the workshop was that the limited company had experienced a significant surge in the number of GPs recruited on permanent contracts since 1 April 2020. In total, 18 GPs, the majority of whom were working as locums within managed practices, had been recruited on, predominantly, permanent but part-time contracts. Anecdotal evidence suggests that GPs may have been seeking greater job security as the pandemic continues.
At Seaview, the workshop was attended by three heads of managed services for east, west and central areas, and two assistant directors of primary care and community services. Between the time data collection was completed (February 2020) and the time of the workshop (September 2020), a number of new practices were being managed, whereas other practices had returned to independent providers of primary care. As a result, as of September 2020, five practices in the eastern area, four in the central area and five in the western area were being managed. In addition, there had been greater integration with community services, such as district nursing and medicines management, but less so with mental health services, for all general practices under the remit of the LHB, but still no integration with acute hospitals.
Attendees welcomed the presentation and were surprised to learn that their experiences of managed practices had such strong similarities with English sites. The attendees were generally in consensus with the study team with regard to ‘overall’ findings. One attendee expressed challenges with working on the basis of GMS contracts and the need to stay within global sum payments, which can vary widely between practices, even on a per registered patient basis, and, therefore, suggested a need to move away from working towards this contractual model. Another attendee felt that the LHB was still able to deliver services beyond the contract model, but that provision of additional services comes at a greater cost for the LHB. Notably, the two attendees felt that the process of managing practices was a challenging learning experience, whereby ‘rolling up your sleeves and running primary care is quite different from commissioning it’.
During the COVID-19 pandemic, the scale and spread of technology in primary care had been very rapid and encouraged by Welsh government, with far greater use of telephone triage. Although appointments using such technology can be much longer because of patient unfamiliarity with using technologically grounded services, in managed practices, the LHB was able to redeploy staff to areas of most need to create ‘upstream prevention’ to a greater extent than was possible in non-managed practices. However, there remains a patient backlog to work through across managed practices (e.g. annual reviews for those living with long-term conditions), which will be challenging with respect to treating COVID-19, as well as managing seasonal flu vaccinations and cases.
Reflections on the robustness of the results
The study team completed a qualitative mixed-method comparative evaluation, following established methodology and guided by previous evidence of implementation, 69–71 while iteratively engaging with published literature. The robustness of our findings has been shown in a number of ways throughout the evaluation. The use of triangulation (i.e. collecting data through interviews, non-participant observation and documentary analysis)72 enabled the team to develop a comprehensive understanding of the rationale and the process of implementation demonstrated by our theory of change maps. We completed a large number (n = 52) of interviews with a range of stakeholders across primary and acute care settings (however, we had fewer interviews with clinical staff working in acute settings and those working within the community). Given the extent of our data collection (despite recruitment of interviewees guided by local gatekeepers and fewer completed interviews of secondary care professionals at one site) and the scope of the evaluation, we are confident that data saturation was achieved. 73
Member validation occurred throughout data analysis among study team members,74 senior members of the BRACE executive team and external colleagues with expertise in theory development and in undertaking evaluations. In addition, theories of change were developed with significant input from evaluation experts (however, these have not been confirmed/checked by case study sites) and consolidated with numerous analysis workshops.
The team encountered a number of challenges that resulted in a longer than anticipated period to complete the evaluation (i.e. 18 months between the identification of sites to the submission of the report). Notably, the team encountered difficulties in obtaining documents for analysis due to data-sharing governance issues between an acute trust and the University of Birmingham, which led to the team relying on publicly available information. Therefore, the team was often subject to meeting the criteria for studies categorised as research when dealing with NHS trusts and university governance teams, with standards and processes for service evaluation remaining unclear. As a result, processes for ethics, data-sharing and appropriate governance remains difficult to complete for rapid evaluations within 12 months in NHS settings. With respect to project management, a small three-person team with a clear hierarchy, roles and responsibilities (i.e. principal investigator, project manager and researcher) consistent throughout the project was a significant positive, alongside weekly communication to facilitate rapid working.
Finally, there was significant cross-learning with another BRACE project75 that is specifically exploring the early implementation of PCN working across England. This cross-learning supported nuanced interpretation of how vertical integration was being implemented in tandem with wholesale primary care policy changes involving horizontal integration.
Limitations
There were a number of limitations when completing our rapid evaluation. The team found it challenging, when deciding the scope of this qualitative rapid evaluation and the nature of exploration, to determine what could (1) be completed in a relatively short timescale and (2) be responsive to NHS health care policy. Following the project design workshop, research questions were identified and, alongside discussions with senior members of the BRACE centre, it was deemed appropriate to split our research questions into two separate evaluations (i.e. implementation and impact). In comparison with the wider BRACE programme, this rapid evaluation has informed early learning on best practice with regard to engagement with stakeholders in relation to design, patient and public involvement (PPI) and data collection, as well as resources required. Across all three sites, fewer than intended non-participant observations were completed because of meetings being rescheduled/cancelled at short notice as a result of the onset of the COVID-19 pandemic. Access to such data would have further strengthened the robustness of our findings, as well as potentially giving the study team increased access to a wider number of stakeholders to approach for interview, rather than being reliant solely on our gatekeepers.
The success of our interviewing approach was largely dependent on the relationships members of the study team established with gatekeepers over a relatively short period of time. In addition, the success of our recruitment approach also depended on the strength of the relationship between the gatekeeper and the interviewee. This may explain why the study team had limited success in recruiting NHS colleagues working outside vertical integration, which would have counteracted potential bias in our sample of interviewees and further strengthened our critique. In addition, the study team recognises that the balance of interviewees from primary and secondary care varied between sites. Despite concerted efforts by researchers, poor recruitment of secondary care practitioners could be explained by their limited contribution to the vertical integration model thus far, as well as gatekeepers potentially highlighting participants who they implicitly felt were more involved with the implementation of vertical integration. This is despite the study team completing a stakeholder mapping exercise with gatekeepers to identify a range of stakeholders. Notwithstanding contacting a range of stakeholders at each site, a small number of stakeholders did not respond to initial e-mail invitations. On reflection, the team does not believe that this imbalance across primary and secondary participants influenced the overall data set, but rather focused our interpretation on the most pertinent purpose for vertical integration (i.e. creating stability and sustainability in primary care). However, exploration of the impact on secondary care will be a key area in any possible impact evaluation (phase 2) and we remain cautious over the conclusions drawn with regard to this. Yet, given the nature of the relationships established with gatekeepers and senior colleagues across all three sites, all three sites remain interested in taking part in a further evaluation on the effectiveness of vertical integration.
Another methodological limitation was the varied pace of data collection across case study sites. The study team experienced a ‘stop-start’ approach to early data collection, which made it difficult to share learning simultaneously; specifically, the study team experienced considerable delay in collecting data from one site. We encountered significant difficulty with regard to signing a data-sharing agreement between one case study site and the University of Birmingham (study sponsor) because of differing interpretations of how best to share relevant documentation that may contain sensitive and/or personally identifiable information. Last, owing to the onset of the COVID-19 pandemic during project write-up, the team was unable to undertake a site-specific and an overall face-to-face workshop with policy experts.
We recognise that there are a number of advantages and drawbacks of using theory of change methodology and developing accompanying diagrammatic illustrations as part of this evaluation. The approach provides a rigorous systematic method of determining how, why and if a programme works. Given that acute hospitals managing general practices is a recent phenomenon and with limited literature, there was a clear need to determine the rationale, inputs, processes and desired outcome as to what vertical integration is expected to achieve in a UK-wide setting. Furthermore, the study team has outlined all contextual factors drawn from documentary analysis and interviews, although there may be other political, social and economic factors at play and having an impact on vertical integration at each site. In addition, theory of change is able to bridge process (phase 1) and effectiveness (phase 2) evaluations.
We also recognise that our understanding of theories of change is based on post hoc rationalisation by stakeholders who we were able to interview at the time of data collection, and may not be wholly representative of vertical integration as it happened. However, we were able to obtain feedback from two sites with regard to our illustrations and narrative.
Reflections on the experience of conducting a rapid evaluation
We have summarised our experiences of conducting a National Institute for Health and Care Research-funded rapid evaluation, as defined by following three overarching principles (see also Chapter 2).
Responsiveness
The team completed a rapid scoping review as opposed to a formal systematic literature review, which saved considerable time and resources; however, there was limited evidence available on the topic of vertical integration in health-care systems relevant to the NHS. The onset of the COVID-19 pandemic has been detrimental to real-time feedback to case study sites, especially with those sites seeking to learn from our findings to inform their vertical integration implementation strategy. The evaluation has taken longer to complete than stated in the original protocol because of delay in gathering data through document-sharing and non-participant observation, exacerbated by recent changes to General Data Protection Regulation. 56 However, the study team anticipates potentially easier access to sensitive meetings in the future to complete ‘remote observations’ if appropriate [i.e. joining meetings via Zoom (Zoom Video Communications, San Jose, CA, USA), Skype™ (Microsoft Corporation, Redmond, WA, USA) or Microsoft Teams (Microsoft Corporation, Redmond, WA, USA)]. This consideration will be shared with colleagues across the BRACE centre with regard to future rapid evaluations.
Relevance
There has been continued and close collaboration with the BRACE Health and Care Panel (which includes members of the BRACE PPI group) to discuss the priority of our evaluation, comment on our participant-facing material (e.g. information sheets) and listen to our emerging findings. The involvement of key stakeholders and policy experts in the project design ensured that the team answered the most appropriate research questions with regard to current health policy changes. However, collaboration from stakeholders has been largely in the form of consultation rather than co-production.
Rigour
The team iteratively engaged with theoretical- and policy-relevant literature throughout the design, data collection and analysis/interpretation stages of the evaluation. A key learning from undertaking this rapid evaluation was the value of validation with appropriate methodological experts. For example, holding workshops with theory of change experts increased the rigour of findings and of presenting our findings appropriately within this report. Our theories of change remain a work in progress and we plan to develop them further in a future evaluation. Having validated theories of change would consolidate and improve understanding of how inputs and processes are intended to achieve desired outcomes. As a result, we have proceeded cautiously when synthesising our findings.
Chapter 9 Conclusions
Summary of key points
-
Vertical integration is enabling locally accessible primary care to continue to be provided for patients in areas in which general practices have faced particular difficulties.
-
Vertical integration appears to provide an opportunity to further develop and integrate care for general practice patients.
-
Vertical integration developed further where there were good pre-existing relationships between primary and secondary care, and where key individuals were active in providing leadership, energy and focus for the integration.
-
The vertical integration sites have acted as pioneers, and we have heard that they are being approached by others in the NHS who wish to learn about such models of care organisation.
-
The net impact of vertical integration on health system costs is argued by local stakeholders to be beneficial.
-
We propose a follow-up evaluation, quantitative as well as qualitative, returning to one or more of our original case study sites and potentially including other vertical integration sites in the UK to address the following questions.
-
Is vertical integration improving recruitment and retention of primary care staff, including, but not limited to, GPs?
-
To what extent has there been service redesign as a result of the vertical integration arrangement, as distinct from horizontal integration via PCNs?
-
What are the views of patients in relation to their experience of accessing primary care services?
-
Are these views different among patients with multiple morbidities?
-
What impact is vertical integration having on secondary care service utilisation (e.g. A&E admissions, readmissions, length of stay in bed-days) and patient access (e.g. GP and practice nurse appointments) to primary care?
-
Is this impact different for patients with multiple morbidities?
-
Are there economies of scale in provision of back office functions?
-
Aims
This rapid evaluation had two distinct aims:
-
To understand the early impact of vertical integration, namely its objectives, how it is being implemented, if and how vertical integration can underpin and drive the redesigning of care pathways, if and how services offered in primary care settings change as a result, and the impact on the general practice and hospital workforces.
-
To develop a theory of change for vertical integration, identifying what outcomes this model of vertical integration is expected to achieve in the short, medium and long terms, and under what circumstances.
In addressing these aims we have attempted to answer six research questions suggested to us by our initial scoping work. We return to these questions, and how far we have found answers to them, in the following paragraphs and, in addition, we identify where further research would be desirable.
Research question 1: what are the drivers of and rationale for acute hospitals taking over the management and governance of general practices? What does this type of vertical integration aim to achieve?
Our initial evaluation of vertical integration of general practices with organisations focused on running secondary care has identified that the main driver of and rationale for such vertical integration at all three case study sites was the need to sustain primary care provision locally by avoiding closure of general practices. Sustaining primary care would not only enable patients to continue to have local access to primary care, but would also serve the end of managing demands on secondary (especially emergency) care. The stable platform provided by vertical integration would then create the opportunity for patient care development in future.
Research question 2: what models/arrangements exist for acute hospital organisations to manage general practices (including different contractual/legal/organisational arrangements across primary, secondary and community health services)?
At Seaview, the contracts for GP services were run directly by the LHB. At Urbanville, the practices were part of the NHS trust organisation. At Greenvale, a separate company was created to run GP services, but it is wholly owned by the NHS trust. Therefore, the specific arrangements for implementing vertical integration differ across the three case study sites. The inevitable details of these new arrangements, in particular the legal aspects and resolving such matters as access to the NHS pension scheme and clarification of the application of VAT rules, took considerable time and effort to resolve, in discussion with NHSE&I and the Department of Health and Social Care in the case of the English sites, for example. The vertical integration sites have, therefore, acted as pioneers, and we have heard that they are being approached by others in the NHS who wish to learn about such models.
Research question 3: what is the experience of implementing this model of vertical integration, including barriers to and enablers of vertical integration, as well as the lessons learnt?
The opportunity created by vertical integration’s successful continuation of primary care (i.e. to develop patient services in primary care settings and integrate them better with secondary care) was exploited to differing degrees across the three sites. It was a substantial focus at Urbanville, rather more opportunistic at Greenvale and not much evident at Seaview (which was largely focusing on developing patient services in primary care and community settings). Vertical integration developed further where there were good pre-existing relationships between primary and secondary care, and where key individuals were active in providing leadership, energy and focus for the integration. Recruitment and retention of GPs and practice staff was difficult, but positive progress was made at all three case study sites. Reliance on locums had been reduced, but remains a considerable cost burden, especially in Seaview. The approach to increasing the number of general practices included in the vertically integrated arrangement is different across the three sites. In Seaview, new candidate practices continue to present themselves, although the LHB expresses no wish to manage them in the long term. In Greenvale, the door remains open to new practices, but it is not being actively courted. In Urbanville, no additional practices are expected to be taken on.
Research question 4: in what ways, if any, has this model of vertical integration influenced the extent and type of health service provision delivered in primary care?
It seems clear that, in all three case study locations, without vertical integration of general practices with organisations running acute hospitals, at least some general practices would have closed and their patients dispersed, which would have increased the pressure on remaining general practices and forced patients to travel further to receive care. However, it is less clear to what extent vertical integration has otherwise influenced the extent and type of primary care provision. The development and use of MDTs has certainly taken place and there has been some increase in providing specialist outreach from hospitals to primary care locations. Yet, similar changes can be seen among non-vertically integrated practices.
Research question 5: what are the views of the primary and secondary care workforces about working together in this way across the care interface?
The different operational practicalities and cultures of primary care and secondary care have required effort to bridge. We have found signs that clinical and non-clinical staff in primary care and secondary care have gained a greater understanding of each other’s work and perspectives as a result of vertical integration. The main impact we found on ways of working has been in primary care hitherto. We detected little change to patient care in secondary care settings as a result of vertical integration. This is a question we intend to return to in our proposed second-stage evaluation.
Research question 6: in what ways, if any, has this model of vertical integration had an impact so far? What are the expected longer-term impacts? How is progress being measured?
The net impact of vertical integration on health system costs appears either to be neutral or is argued by local stakeholders (in Greenvale and Urbanville) to be beneficial. The main benefit to efficiency is the scope for better management of emergency patient flows to acute hospitals. Centralisation of back office functions may also offer modest savings as a result of economies of scale. We plan to return to the question of costs and savings in a further phase 2 evaluation of vertical integration.
As in the pre-existing literature16–19 on vertical integration, we were not able to determine the impact of vertical integration on patient experiences or outcomes, or to quantify the effect on the ability to recruit and retain primary care staff. The relative novelty of vertical integration arrangements in the NHS suggests that the presence or absence of impacts and effects may be easier to detect in future. As described below, we intend to return to these issues in a second phase of evaluation of vertical integration.
Overall assessment and implications for decision-makers
In this rapid evaluation we have been able to develop a theory of change for each of the case study sites. In addition, there has proven to be sufficient commonality between sites for it to be possible to derive an initial overall theory of change for vertical integration (see Figure 7). We intend to test and develop these theories of change in a follow-on phase 2 study of vertical integration.
Although vertical integration is being implemented in a number of locations in England and Wales, some urban, some rural, it is not evident that it is a generally desired way forward for health-care provision. Even where it has been introduced, many general practices choose to remain outside the vertical integration arrangement. The spread of (horizontally integrated) PCNs and primary care clusters may, if successful, enable sustainable primary care without vertical integration as well.
The implication is that, based on the rapid evaluation reported here, vertical integration is a valuable option to consider when general practices look likely to fail. However, it is not an option that should be imposed from the top down. Many GPs evidently do not wish to join such arrangements, as they have not taken that option even when available to them locally. By contrast, there are clearly some GPs who prefer to give up the autonomy and responsibility of owning and running a business (as necessitated by the partnership model) to retire or take up other opportunities. Some GPs and other practice staff are clearly content to be salaried employees. Primary and secondary care workforces are divided by decades of separate working and bringing them together is easier to achieve when strong and positive relationships already exist or can be built up between primary and secondary care leaders. Even then, we have not seen much evidence of greater clinical integration in providing care to patients.
A variety of specific forms of legal and governance arrangements for vertical integration is evident. All three varieties we have studied are viable and all entailed a good deal of detailed work to design and agree the specifics of arrangements, including staff terms and conditions, to enable previously independent practices to be integrated with NHS trusts and LHBs.
It remains to be seen whether the major changes that have occurred in primary care practice as a result of the COVID-19 pandemic, with patients communicating with primary care professionals by telephone and online, rather than face to face, affect the case for or against vertical integration. If GP workloads and lifestyles were to become more manageable as a result, the pressure from failing practices would abate; however, the need and opportunities for better integration of primary care with secondary care would likely remain.
Whatever the future, vertical integration can claim some successes so far in having maintained patient access to primary care in some locations at a higher level than would have otherwise happened. Improvements to patient care, including better integration of that care, would not be possible in the absence of such foundations. Therefore, although vertical integration has not been highlighted in current NHS policy in England and Wales, it appears to have an important role to play in some locations in enabling the continuation and development of locally accessible patient care.
Recommendations for future research
Our rapid qualitative evaluation based on three case studies has found much of interest, but important questions remain. Vertical integration shows promise, particularly in areas where GP retention and recruitment is particularly problematic. It may well remain a feature of the NHS in England and Wales, and may spread, given expectations that pressures on the GP workforce are set to increase over the coming years. It is unclear how vertical integration might develop in a primary care world where PCNs (England) and primary care clusters (Wales) are general, but our a priori expectation is that vertical integration will continue. After all, vertical integration has developed in an NHS where alliances, federations, networks, clusters, etc., of general practices have been very common, if not quite universal. Therefore, vertical integration has come about simultaneously with horizontal integration, rather than in advance of it.
There remain questions about vertical integration and its impacts and we intend to address some of them in a follow-up phase 2 quantitative and qualitative evaluation. This evaluation would investigate how far the current local instances of vertical integration are proving to be sustained and would test and develop the case-specific and overall theories of change created in the initial evaluation.
In a future mixed-methods follow-up evaluation, we intend to test and develop further the theories of change set out in this report. In particular, we intend to examine outcomes and impacts, including patient and carer experience, associated with hospitals managing GP services, and to explore the impact of vertical integration on local health-care systems in total. Within that, we will investigate how well vertical integration is adapted to the health-care needs of people with multiple long-term morbidities, for whom local access and well-integrated care are particularly important and in respect of whom the impact of vertical integration on the health-care system might be expected to be most prominent.
We propose to return, if possible, to one or more of the original case study sites and potentially to include other vertical integration sites in the UK to address some, or all, of the following evaluation questions:
-
Is vertical integration improving recruitment and retention of primary care staff, including, but not limited to, GPs?
-
To what extent has there been service redesign as a result of the vertical integration arrangement, as distinct from being a result of horizontal integration via PCNs?
-
What are the views of patients in relation to their experience of accessing primary care services?
-
Are these views different among patients with multiple morbidities?
-
What impact is vertical integration having on secondary care service utilisation (e.g. A&E attendances, emergency admissions and readmissions, length of stay in bed-days) and patient access (e.g. GP and practice nurse appointments) to primary care?
-
Is this impact different for patients with multiple morbidities?
-
Are there economies of scale in provision of back office functions?
Where possible, quantitative analysis based on administrative (primary care and secondary care) data will be included, alongside further qualitative research.
Any future evaluation of vertical integration would necessarily take place in the context of the great changes to primary care practice that have come about as a result of the COVID-19 pandemic. Therefore, a second evaluation could provide an early indication of whether or not those changes have affected the desirability or otherwise of vertical integration in different types of local health economy.
A longer-term assessment of the impact of vertical integration in a world where telephone and digital consultations in primary care have become more common than face-to-face consultations could represent an important body of work for the wider research community in future. Other knowledge gaps that could also be targeted in a future research agenda for the wider research community include the following:
-
the role of changing organisational culture, both as an enabler and a consequence of vertical integration
-
the impact of vertical integration on innovation in health services
-
the impacts of other types of vertical integration than that between acute hospitals and general practices.
Many interesting questions remain about the scope for integration across primary and community care, and between community and hospital care, whether for physical or mental health services, respectively.
The potential future research agenda around vertical integration is large, but we hope that the initial rapid evaluation presented in this report represents an informative first step.
Acknowledgements
We are very grateful to all of the participants in this study and to our contacts at each case study site who helped to co-ordinate our interactions with interviewees and provided documents. We thank our BRACE colleagues and members of the BRACE Health and Care Panel for their input and constructive comments throughout the duration of the study, and we thank our colleagues from the Department of Health and Social Care, NHS England and The King’s Fund for their contributions at the project design workshop. Specifically, we thank Richard Allen and Dr Nishma Manek for advising on our study protocol from a PPI and GP perspective, Cathy Dakin (BRACE Administrator, University of Birmingham) for reviewing our Plain English summary and Professor Russell Mannion, Professor Judith Smith, Dr Joanna Ellins (all University of Birmingham) and Professor Nicholas Mays (London School of Hygiene and Tropical Medicine) for undertaking a critical review of the draft report. Any errors in the report are the sole responsibility of the authors.
Patient and public involvement
The proposal for the evaluation was reviewed by a PPI member of the BRACE Health and Care Panel. The Plain English summary of the report has been reviewed by another PPI adviser. Project findings will be shared and discussed at a meeting of the full BRACE Health and Care Panel, which includes eight patient and public members, and we will seek the advice of those members concerning how best to communicate the evaluation’s findings to patient and public audiences.
The phase 2 vertical integration evaluation, which was planned to follow up on the initial evaluation that is the subject of this report, will include assessment of the impacts of vertical integration on patients’ experience of, and access to, secondary and primary health care. Therefore, we intend to involve PPI members from the BRACE Health and Care Panel in the design of the phase 2 project at the protocol stage and, later on, in the design of project materials as the evaluation progresses.
Contributions of authors
Manbinder Sidhu (https://orcid.org/0000-0001-5663-107X) (Research Fellow, University of Birmingham) was the project manager and a researcher for the study. He contributed to the conception and design of the study, the theoretical framework, data collection at two study sites, overall data analysis and interpretation, and he is the lead author of the final report. He contributed to integrating the findings of the study and to all chapters, and he made critical revisions to the report for important intellectual content and approved the final manuscript.
Jack Pollard (https://orcid.org/0000-0002-2403-2635) (Researcher in Health Economics, University of Oxford) was a research analyst (employed by RAND Europe) for the study. He contributed to the conception and design of the study, the theoretical framework, data collection at one study site, overall data analysis and interpretation, and he is a co-author of the final report. He contributed to integrating the findings of the study and to Chapters 2 and 6.
Jon Sussex (https://orcid.org/0000-0001-8970-4546) (Chief Economist at RAND Europe and Co-Director of the Cambridge Centre for Health Services Research, a collaboration between RAND Europe and University of Cambridge) was the principal investigator for the study and led the study. He contributed to the conception and design of the study, the theoretical framework, data collection at one study site, overall data analysis and interpretation, and he is corresponding author of the final report. He contributed to integrating the findings of the study and to all chapters, and he made critical revisions to the report for important intellectual content and approved the final manuscript.
Publications
Sidhu MS, Pollard J, Sussex J. Acute Hospitals Managing General Practice Services in the UK: Why, How and What are the Consequences for Primary Care Delivery? Oral presentation at the Health Services Research Virtual Conference, 1 July 2020.
Sidhu M, Pollard J, Sussex J. Vertical integration of primary care practices with acute hospitals in England and Wales: why, how and so what? Findings from a qualitative, rapid evaluation. BMJ Open 2022;12:e053222.
Data-sharing statement
Owing to the consent process for data collection at case study sites within this evaluation, there are no data that can be shared. Please contact the corresponding author with any queries.
Disclaimers
This report presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- Sidhu M, Pollard J, Sussex J. Vertical integration of primary care practices with acute hospitals in England and Wales: why, how and so what? Findings from a qualitative, rapid evaluation. BMJ Open 2022;12. https://doi.org/10.1136/bmjopen-2021-053222.
- Webster C. The National Health Service: A Political History. New York, NY: Oxford University Press; 2002.
- Webster C. National Health Service Reorganisation: Learning from History?. London: Office of Health Economics; 1998.
- NHS Confederation . NHS Statistics, Facts, and Figures 2019. www.nhsconfed.org/resources/key-statistics-on-the-nhs (accessed 11 June 2020).
- NHS Digital . General Practice Workforce 30 June 2019 n.d. https://digital.nhs.uk/data-and-information/publications/statistical/general-practice-workforce-archive/final-30-june-2019 (accessed 14 March 2022).
- Welsh Government . GP Access: 2018 n.d. https://gov.wales/gp-access-2018 (accessed 25 June 2020).
- Welsh Government . General Medical Practitioners: As at 30 September 2018 2018. https://gov.wales/general-medical-practitioners-30-september-2018 (accessed 4 May 2022).
- Great Britain . National Health Service (Primary Care) Act 1997 (Commencement No. 1) Order 1997 1997.
- Department of Health and Social Care . GP Partnership Review. Final Report 2019. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/770916/gp-partnership-review-final-report.pdf (accessed 26 June 2020).
- Palmer W. Is the Number of GPs Falling Across the UK? 2019. www.nuffieldtrust.org.uk/news-item/is-the-number-of-gps-falling-across-the-uk (accessed 21 August 2020).
- Bienkowska-Gibbs T, King S, Saunders C, Henham M-L. New Organisational Models of Primary Care to Meet the Future Needs of the NHS: A Brief Overview of Recent Reports 2015.
- Rumbold B, Shaw S. Horizontal and vertical integration in the UK: lessons from history. J Integrated Care 2010;18:45-52. https://doi.org/10.5042/jic.2010.0652.
- Joskow PL, Menard C, Shirley MM. Handbook of New Institutional Economics. Boston, MA: Springer; 2005.
- Williamson OE. The vertical integration of production: market failure considerations. Am Econ Rev 1971;61:112-23.
- Laugesen MJ, France G. Integration: the firm and the health care sector. Health Econ Policy Law 2014;9:295-312. https://doi.org/10.1017/S1744133114000139.
- Ramsay A, Fulop N, Edwards N. The evidence base for vertical integration in health care. J Integrated Care 2009;17:3-12. https://doi.org/10.1108/14769018200900009.
- Conrad DA, Dowling WL. Vertical integration in health services: theory and managerial implications. Health Care Manage Rev 1990;15:9-22. https://doi.org/10.1097/00004010-199001540-00003.
- Shortell SM, Gillies RR, Anderson DA, Erickson KM, Mitchell JB. Integrating health care delivery. Health Forum J 2000;43:35-9.
- Robinson JC, Casalino LP. Vertical integration and organizational networks in health care. Health Aff 1996;15:7-22. https://doi.org/10.1377/hlthaff.15.1.7.
- Naylor C, Charles A. Developing New Models of Care in the PACS Vanguards: A New National Approach to Large-Scale Change? 2018. www.kingsfund.org.uk/publications/developing-new-models-care-pacs-vanguards (accessed 11 June 2020).
- NHS England . Five Year Forward View n.d. www.england.nhs.uk/wp-content/uploads/2014/10/5yfv-web.pdf (accessed 11 June 2020).
- National Audit Office . Developing New Care Models Through NHS Vanguards 2018. www.nao.org.uk/report/developing-new-care-models-through-nhs-vanguards/ (accessed 26 June 2020).
- Naylor C, Alderwick H, Honeyman M. Acute Hospitals and Integrated Care. London: The King’s Fund; 2015.
- Tallack C. Lessons from the Vanguards for Rapid Evaluation 2019. www.nuffieldtrust.org.uk/media/lessons-from-the-vanguards-for-rapid-evaluation (accessed 11 June 2020).
- Wilson MP, Billings J, MacInnes J, Mikelyte R, Welch ME, Richey MR, et al. Investigating Locally Commissioned Evaluations of the NHS Vanguard Programme 2019. www.research.manchester.ac.uk/portal/files/118897237/Investigating_Locally_Commissioned_Evaluations_of_the_Vanguard_Programme_Final_Report.pdf (accessed 14 March 2022).
- NHS England . NHS Long Term Plan 2019. www.longtermplan.nhs.uk/ (accessed 25 June 2020).
- National Assembly for Wales . Inquiry into Primary Care: Clusters 2015. https://senedd.wales/laid%20documents/cr-ld11226/cr-ld11226-e.pdf (accessed 25 June 2020).
- Miller R, Weir C, Gulati S. Critical Appraisal of the Pacesetter Programme: Scientific Report 2018.
- Kumpunen S, Curry N, Farnworth M, Rosen R. Collaboration in General Practice: Surveys of GP Practice and Clinical Commissioning Groups 2017. www.nuffieldtrust.org.uk/research/collaboration-in-general-practice-surveys-of-gp-practice-and-clinical-commissioning-groups (accessed 11 June 2020).
- Smith J, Holder H, Edwards N, Maybin J, Parker H, Rosen R, et al. Securing the Future of General Practice: New Models of Primary Care 2017. www.nuffieldtrust.org.uk/research/securing-the-future-of-general-practice-new-models-of-primary-care (accessed 11 June 2020).
- Sheaff R, Halliday J, Øvretveit J, Byng R, Exworthy M, Peckham S, et al. Integration and continuity of primary care: polyclinics and alternatives, a patient-centred analysis of how organisation constrains care coordination. Health Serv Deliv Res 2015;3. https://doi.org/10.3310/hsdr03350.
- Roberts N. Could Hospitals Take Over Primary Care? 2014. www.gponline.com/hospitals-primary-care/article/1229322 (accessed 11 June 2020).
- Round T, Ashworth M, Crilly T, Ferlie E, Wolfe C. An integrated care programme in London: qualitative evaluation. J Integr Care 2018;26:296-308. https://doi.org/10.1108/JICA-02-2018-0020.
- Wolfe I, Sigfrid L, Chanchlani N, Lenton S. Child health systems in the United Kingdom (England). J Pediatr 2016;177S:S217-S242. https://doi.org/10.1016/j.jpeds.2016.04.058.
- Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Meth 2018;18. https://doi.org/10.1186/s12874-018-0611-x.
- Ørngreen R, Levinsen K. Workshops as a research methodology. Electron J E-Learning 2017;15:70-81.
- Collins N. New Care Models: Emerging Innovations in Governance and Organisational Form 2016. www.kingsfund.org.uk/publications/new-care-models (accessed 11 June 2020).
- The Royal Wolverhampton NHS Trust . Primary Care Network (RWT PCN) n.d. www.rwtprimarycare.nhs.uk (accessed 26 May 2022).
- Sibbald B, Pickard S, McLeod H, Reeves D, Mead N, Gemmell I, et al. Moving specialist care into the community: an initial evaluation. J Health Serv Res Policy 2008;13:233-9. https://doi.org/10.1258/jhsrp.2008.008049.
- Northumbria Primary Care . About Us n.d. https://northumbriaprimarycare.co.uk/about-us (accessed 11 June 2020).
- The Willow Group . About Us n.d. www.thewillowgroup.nhs.uk/about-us/ (accessed 11 June 2020).
- Comendeiro-Maaløe M, Ridao-López M, Gorgemans S, Bernal-Delgado E. A comparative performance analysis of a renowned public private partnership for health care provision in Spain between 2003 and 2015. Health Policy 2019;123:412-18. https://doi.org/10.1016/j.healthpol.2018.11.009.
- NHS Confederation . The Search for Low-Cost Integrated Healthcare: The Alzira Model – from the Region of Valencia 2012.
- Comendeiro-Maaløe M, Ridao-López M, Gorgemans S, Bernal-Delgado E. Public-private partnerships in the Spanish National Health System: the reversion of the Alzira model. Health Policy 2019;123:408-11. https://doi.org/10.1016/j.healthpol.2019.01.012.
- Schwartz PM, Kelly C, Cheadle A, Pulver A, Solomon L. The Kaiser Permanente community health initiative: a decade of implementing and evaluating community change. Am J Prev Med 2018;54:105-9. https://doi.org/10.1016/j.amepre.2018.02.004.
- Blom A, von Bulow LL. Vertical integration across hospital acute care and on-call general practitioners: an evaluation of a cross sectional cooperation model at Odense University Hospital, Southern Region of Denmark. Int J Integrated Care 2013;13. https://doi.org/10.5334/ijic.1481.
- NHS England . Integrated Primary and Acute Care Systems (PACS) – Describing the Care Model and the Business Model 2016. www.england.nhs.uk/publication/integrated-primary-and-acute-care-systems-pacs-describing-the-care-model-and-the-business-model (accessed 11 June 2020).
- Mannion R, Brown S, Beck M, Lunt N. Managing cultural diversity in healthcare partnerships: the case of LIFT. J Health Organ Manag 2011;25:645-57. https://doi.org/10.1108/14777261111178538.
- Yu V, Wyatt S, Woodall M, Mahmud S, Klaire V, Bailey K, et al. Hospital admissions after vertical integration of general practices with an acute hospital: a retrospective synthetic matched controlled database study. Br J Gen Pract 2020;70:e705-13. https://doi.org/10.3399/bjgp20X712613.
- Caballer-Tarazona M, Clemente-Collado A, Vivas-Consuelo D. A cost and performance comparison of public private partnership and public hospitals in Spain. Health Econ Rev 2016;6. https://doi.org/10.1186/s13561-016-0095-5.
- López-Casasnovas G, Del Llano J. Colaboración Público-Privada En Sanidad: El Modelo Alzira. Madrid: Fundación Gaspar Casal; 2017.
- Salisbury H. Helen Salisbury: oh, those lazy, part time GPs!. BMJ 2019;367. https://doi.org/10.1136/bmj.l6813.
- Ritchie J, Lewis J, Nicholls CM, Ormston R. Qualitative Research Practice: A Guide for Social Science Students and Researchers. London: SAGE Publications Ltd; 2013.
- Andoh-Arthur J, Atkinson P, Delamont S, Cernat A, Sakshaug JW, Williams RA. SAGE Research Methods Foundations. London: SAGE Publications Ltd; 2020.
- Johl S, Renganathan S. Strategies for gaining access in doing fieldwork: reflection of two researchers. Electron J Bus Res Methods 2010;8.
- Great Britain . General Data Protection Regulation 2018 2018.
- Great Britain . The Data Protection Act 2018 2018.
- Tubaro P, Ryan L, D’angelo A. The visual sociogram in qualitative and mixed-methods research. Sociol Res Online 2016;21:1-18. https://doi.org/10.5153/sro.3864.
- Weiss CH, Connell J, Kubisch A, Schorr L, Weiss C. New Approaches to Evaluating Community Initiatives: Concepts, Methods and Contexts. New York, NY: Aspen Institute; 1995.
- Vogel I. Review of the Use of ‘Theory of Change’ in International Development 2012. www.theoryofchange.org/pdf/DFID_ToC_Review_VogelV7.pdf (accessed 14 March 2022).
- Mackenzie M. The practice and the theory: lessons from the application of a theories of change approach. Evaluation 2005;11:151-68. https://doi.org/10.1177/1356389005055538.
- Taplin DH, Clark H. Theory of Change Basics: A Primer on Theory of Change. New York, NY: ActKnowledge; 2012.
- Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol 2013;13. https://doi.org/10.1186/1471-2288-13-117.
- Zanon E. The Alzira Model Gives Us a Great Deal to Think About 2014. www.nhsconfed.org/articles/alzira-model-gives-us-great-deal-think-about (accessed 11 June 2020).
- Conrad DA, Shortell SM. Integrated health systems: promise and performance. Front Health Serv Manage 1996;13:3-40.
- Lasker R, Weiss E, Miller R. Partnership synergy: a practical guide for studying and strengthening the collaborative advantage. Milbank 2001;79:179-205. https://doi.org/10.1111/1468-0009.00203.
- Øvretveit J. Five ways to describe a multidisciplinary team. J Interprofessional Care 1996;10:163-71. https://doi.org/10.3109/13561829609034099.
- Baird B, Beech J. The 2020 21 Update to the GP Contract Explained 2020. www.kingsfund.org.uk/publications/updated-gp-contract-explained#:~:text=The%20updated%20contract%20sets%20out,number%20of%20other%20roles%20including%3A&text=care%20co%2Dordinators (accessed 25 June 2020).
- Bardsley M, Steventon A, Smith J, Dixon J. Evaluating Integrated and Community-Based Care: How Do We Know What Works? 2017. www.nuffieldtrust.org.uk/research/evaluating-integrated-and-community-based-care-how-do-we-know-what-works (accessed 11 June 2020).
- Davidoff F, Dixon-Woods M, Leviton L, Michie S. Demystifying theory and its use in improvement. BMJ Qual Saf 2015;24:228-38. https://doi.org/10.1136/bmjqs-2014-003627.
- Lamont T, Barber N, de Pury J, Fulop N, Garfield-Birkbeck S, Lilford R, et al. New approaches to evaluating complex health and care systems. BMJ 2016;352. https://doi.org/10.1136/bmj.i154.
- Flick U. Triangulation in qualitative research. Companion Qual Res 2004;3:178-83. https://doi.org/10.1007/978-3-322-97512-6.
- Fusch P, Ness L. Are we there yet? Data saturation in qualitative research. Qual Rep 2015;20:1408-16. https://doi.org/10.46743/2160-3715/2015.2281.
- Pope C, Ziebland S, Mays N. Analysing qualitative data. BMJ 2000;320. https://doi.org/10.1136/bmj.320.7227.114.
- Parkinson S, Smith J, Sidhu M. Early development of primary care networks in the NHS in England: a qualitative mixed-methods evaluation. BMJ Open 2021;11. https://doi.org/10.1136/bmjopen-2021-055199.
Appendix 1 Literature review method
We completed a scoping review to undertake a preliminary assessment of the potential size and scope of available UK and international research literature on vertical integration and to identify the nature and extent of research evidence on this topic.
The scope of the initial review of literature, undertaken on 14 December 2018, was completed in two stages. First, the study team completed a search of published peer-reviewed literature (including reviews) restricted to key search terms in the title and abstract. Searches were undertaken in Ovid MEDLINE (Health Management Information Consortium), Web of Science, Scopus (restricted to the following subject areas: medicine, social sciences, nursing, multidisciplinary and health professions), Social Policy & Practice and Applied Social Sciences Index and Abstracts (ASSIA). Publications were eligible for inclusion if they were in the English language and were published between 2008 and 2018. This period was selected to achieve a broad sweep, but with a focus on recent evidence and thinking on vertical integration. Search terms were refined in collaboration with an experienced health services research librarian [Emma Green, Health Services Management Centre (HSMC) Knowledge and Evidence Service, University of Birmingham]. Our search terms and strategy are presented in Box 2.
“vertical” OR “structural”
AND
“integration” OR “integrate” OR “integrat*” OR “integrated care” OR “model of care” OR “models of care”
AND
“general practice” OR “gp” OR “primary care” OR “acute primary”
AND
“acute trust*” OR “NHS trust*” OR “NHS hospital trust*” OR “hospital trust*” OR “hospital” OR “secondary care” OR “admissions” OR “cost*”
Second, to allow for a possible paucity of peer-reviewed literature relevant to vertical integration of general practices with acute hospitals, an internet search was additionally undertaken to identify further relevant material. Specifically, the term ‘vertical integration general practice’ was searched in Google (Google Inc., Mountain View, CA, USA) (first three pages) and the results were sifted through. Snowballing from references found in the literature and from relevant websites was also undertaken to identify further sources. Records were managed within an EndNote library (version X6; Clarivate Analytics).
Titles and abstracts were screened by two study team members (MS and JP), independently and in duplicate, for relevance to the integration of general practices with acute hospitals. The full text of all ‘included’ papers was then obtained for further full-text screening and manual searching of references for further relevant literature.
We identified 12 peer-reviewed primary research studies and reviews, seven UK government policy reports, seven relevant websites detailing examples of acute hospitals integrating into general practice and a single online news article, bringing the total number of included publications in this scoping review to 27. We present these numbers using an adapted version of the PRISMA flow diagram (Figure 8).
FIGURE 8.
A PRISMA flow diagram of screening decisions (2008–18 inclusive). ASSIA, Applied Social Sciences Index and Abstracts.
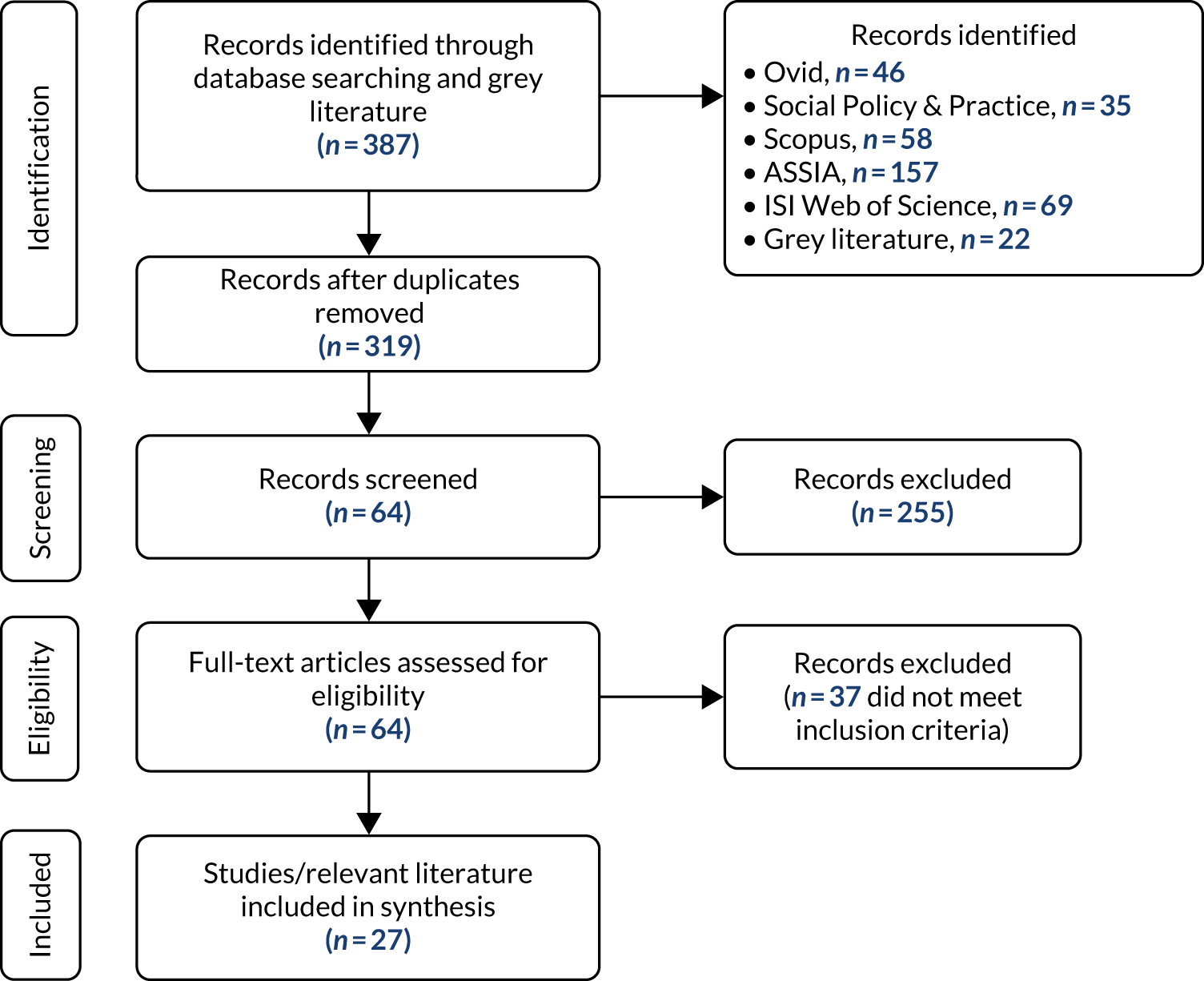
Appendix 2 Coding framework
| Integrative theme | Subcode | Description of subcode | Research question |
|---|---|---|---|
| Understanding the need and purpose of integration with primary care | Change in rationale | Has the rationale changed since the model was first implemented? | 1 |
| Concerns | What concerns were raised? By whom? | 1 | |
| Initiation | Who initiated this model of vertical integration? | 1 | |
| Other models | Were any other models considered? Which ones? | 1 | |
| Rationale | What was the rationale from the perspective of the acute trust/health board and/or general practices? | 1 | |
| Scale up | Do you think vertical integration is an attractive (or viable) model for the NHS in the UK, and does it have potential for ‘scale up’? | 1 | |
| Developing an integration model and implementation strategy for general practices | Alignment of vertical integration 1 | How does the introduction of vertical integration align with the delivery of primary and secondary care services within your area? (Integrated care systems, PCNs?) | 2 |
| PCN future | The future of the current vertical integration model in the context of developing PCN working/collaboration arrangements in England | 2 | |
| Contextual information | Background and wider contextual information with regard to landscape of where the vertical integration model has been implemented | 2 | |
| Current model and maturity | Please describe the current model of the acute trust/health board taking over and directly managing general practice services. When did it first take place? | 2 | |
| Current stakeholders | Who are the current stakeholders involved? Are these stakeholders different from those involved in the implementation? | 2 | |
| Number of practices | How many practices are involved? Has this increased/decreased since implementation? | 2 | |
| Selection process | How are practices selected to join the model? Against what criteria are they measured? | 2 | |
| Transitioning: from GMS to a subcontracted provider of primary care | Contracts | Who is holding the APMS/GMS contract? | 3 |
| GP property | Who now owns/leases general practice properties? | 3 | |
| Impact among GPs | How has the vertical integration model affected governance, contractual and legal arrangements among general practices? | 3 | |
| Impact between acute trust or health board and GPs | How has the vertical integration model affected governance, contractual and legal arrangements between acute trust/health board and the general practices? | 3 | |
| Indemnity | What changes have occurred (if any) with regard to indemnity? | 3 | |
| Limited company | Was there creation of a limited company? | 3 | |
| Regulation | New governance and management teams providing oversight to integration. The nature of governance and oversight provided of the vertical integration model (e.g. CQC) | 3 | |
| Risk management | What about risk management both on behalf of the acute trust/health board and general practices themselves? | 3 | |
| Culture | The lack of understanding of the working of primary care compared with secondary care | 3 | |
| Back office | Is there sharing of ‘back office’ functions? | 3 | |
| Implementing vertical integration | Could you please describe the process of implementing vertical integration in your area? How has the process evolved? | 3 | |
| New management board | Has there been an introduction of a new board overseeing management/performance of integration? Who is involved? Frequency of meetings? | 3 | |
| Tensions | Have there been issues of tension among stakeholders? | 3 | |
| Impact on patient management: changes to primary and secondary care delivery | Differential impact | Does the impact differ for patients from vertical integration practices from those registered with non-vertical integration practices? Are patients experiencing something new/different? | 4 and 5 |
| Health service provision | How has the delivery of services changed in given settings (e.g. primary and secondary care, and wider community services)? | 4 and 5 | |
| Pathways and processes | What changes have there been with regard to referral pathways/processes? (If not now, will it change in the future?) | 4 and 5 | |
| Patient access | What has been the impact on patients accessing services across the care interface? | 4 and 5 | |
| Patient management | Has integration led to changes to how certain groups of patients are managed? | 4 and 5 | |
| Career progression | Has the introduction of vertical integration had an impact on career progression (e.g. early career GPs)? | 4 and 5 | |
| Challenges | What have been some of the key changes that staff have noticed in their everyday working practices? | 4 and 5 | |
| Impact on recruitment and retention | What has been the impact of the recruitment and retention across both primary and secondary care? | 4 and 5 | |
| Job satisfaction | Has working within a vertical integration model had any impact on job satisfaction among staff? | 4 and 5 | |
| New personnel | Has there been an introduction of new personnel (e.g. new types of staff/roles, additional staff numbers)? | 4 and 5 | |
| Measuring success and identifying the unintended impact of integration | Leavers and joiners | Why have some practices decided to leave or join? | 6 |
| Drawbacks | Are there any financial drawbacks of this model? | 6 | |
| Financial implications | Financial implications of this model? | 6 | |
| General practices | What has been the financial performance of general practices? | 6 | |
| Incentives | What are the financial incentives? | 6 | |
| One-off costs | What have been the one-off cost implications for trusts/boards? | 6 | |
| Ongoing costs | What have been the ongoing cost implications for trusts/boards? | 6 | |
| Next steps | How are you planning to further develop the vertical integration model (what are the next steps)? | 6 | |
| Intended outcomes | What are the intended outcomes (clinical and non-clinical)? | 6 | |
| Short and long term | How is progress and impact being tracked (using what data) for the short and long term? | 6 | |
| Success | How is ‘success’ being determined and/or measured? What process measures are being considered? | 6 | |
| Unintended outcomes | Have any unintended outcomes occurred? What are they? | 6 | |
| Advice | What advice would you give such prospective areas if they were thinking about adopting this model of vertical integration? | 6 | |
| Expression of interest | Have any other trusts/health boards expressed interest in adopting a similar vertical integration model? | 6 | |
| Miscellaneous | Further comments | Is there anything else you wanted to tell us about that has not already been covered in the interview? | |
| Gold dust | Great quotation to use in the final report | ||
| Site, participant and date | Which site is the interview relevant to? Who is being interviewed? Date of interview? | ||
| Participant role and stakeholder type | What is your job title? Please describe your current role and key responsibilities? How long have you been in your role? Stakeholder category? |
List of abbreviations
- A&E
- accident and emergency
- AfC
- Agenda for Change
- APMS
- Alternative Provider Medical Services
- ASSIA
- Applied Social Sciences Index and Abstracts
- BRACE
- Birmingham, RAND and Cambridge Evaluation Centre
- CCG
- Clinical Commissioning Group
- CQC
- Care Quality Commission
- GMS
- General Medical Services
- GP
- general practitioner
- HR
- human resources
- IT
- information technology
- LHB
- Local Health Board
- MDT
- multidisciplinary team
- NHSE&I
- NHS England and NHS Improvement
- PACS
- primary and acute care systems
- PCN
- primary care network
- PMS
- Personal Medical Services
- PPI
- patient and public involvement
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- TUPE
- Transfer of Undertakings (Protection of Employment)
- VAT
- value-added tax
- WP
- work package
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/TLLA3317).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
