Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as award number 17/99/85. The contractual start date was in April 2019. The draft manuscript began editorial review in July 2022 and was accepted for publication in June 2023. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ manuscript and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Permissions
Copyright statement
Copyright © 2024 Adams et al. This work was produced by Adams et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Adams et al.
Chapter 1 Introduction and background
Introduction
This three-phased, qualitative, realist study aimed to identify and investigate the critical factors that underpin improvements in the disclosure and discussion of avoidable harm with families in NHS maternity care. This chapter describes the policy and research background on disclosure in health care and in NHS maternity care and outlines the structure of the report.
Open disclosure: policy and research background
Since the mid-2000s, the term ‘open disclosure’ has been adopted internationally by policy-makers and researchers to capture the process of ongoing communication with patients and families after adverse events. 1,2 Open disclosure (OD) is defined by Manser (2011) as: ‘the open and timely communication about adverse events to keep patients and family members informed, to acknowledge their suffering and grief and help in reducing feelings of abandonment’. 3–5 OD communication involves providing accurate information about the critical incident, its immediate consequences and appropriate remedial action, as well as providing an expression of regret and information about what will be done to avoid harm reoccurrence. 5
Internationally, OD of adverse events to affected patients and families has been recognised as an important ethical and patient safety concern for several decades. 6–13 Additionally, evidence suggests that OD reduces long-term emotional distress and injury to families and healthcare staff. 5,14–22 As an added benefit, greater openness with families post incident might enhance their confidence in service transparency, thereby reducing their need for investigatory and legal processes and, when practised routinely and in the longer term, may enhance the public’s trust in services. 14,19,23–29
Yet, services consistently providing OD that meets the needs and expectations of patients, families and staff remains a challenge. Barriers to OD are deeply rooted and widely documented, and include factors like physician management fears over loss of reputation or litigation and second victim trauma,11,12,30–33 fear of reprisals in punitive workplaces,34 lack of clarity over accountability for injury,15,35,36 varying perspectives on when disclosure is appropriate12 and heavy-handed procedural systems that can constrain empathic communication. 12,23,37,38 Furthermore, since the inception of OD policy initiatives, researchers have noted a tension between what patients and families expect after injury and what healthcare providers (HCPs) think that they should provide. 8,39,40 For HCPs, post-incident communication with families encompasses a complex array of legislative, policy, professional, organisational, local workplace and interpersonal considerations. 12,17,37 In the English NHS, and particularly in NHS maternity care since 2013, the development and implementation of a raft of legislative, policy and safety improvement initiatives have given rise to complex and sometimes contradictory OD improvement contexts. The following sections outline the rationales, components and effects of the most significant of these.
Open disclosure initiatives in the English National Health Service
The ‘Being Open’ framework
The ‘Being Open: Communicating Patient Safety Incidents’ best practice framework was launched to improve communication and ongoing support for patients and families injured during NHS care. 41 The guidance describes Being Open as a flexible, ongoing process, rather than a one-off meeting with a family and is underpinned by 10 principles. Among these, providing acknowledgement of the incident, taking patient reports seriously and reporting them as soon as possible and ensuring truthfulness, timeliness and clear communication to families throughout the investigation process in face-to-face meetings. The guidance highlights the importance of corporate and clinical governance (CG) structures for the support of staff reporting patient safety incidents, for the integration of Being Open into management and system improvements and for assuring ongoing care and confidentiality for all involved.
While this document remains an important reference for all health providers in England, the initial reception of this guidance by health service providers indicated a widespread lack of interest in implementation, including in staff training. 12 Birks et al. found that there was an ‘in-principle’ agreement of senior clinicians on the value of OD. However, in practice, it was expected that workplace attitudes and fear of litigation inhibited incident reporting, while the moral dilemmas over when and how to be fully open with patients inhibited efforts to invest in the guidance. 12
The statutory Duty of Candour
In 2014, the statutory Duty of Candour (DoC), Regulation 20 of the Health and Social Care Act42 was introduced for acute health providers following recommendation 181 of the Francis public inquiry. 43 It was to complement the existing professional DoC that applies to healthcare professionals.
The DoC obliges organisations to disclose to patients or families if there has been a notifiable safety incident during their care. Organisations that fail to comply are liable to criminal prosecution. The DoC also established expected disclosure standards, in particular, the timing of disclosure, how disclosure should be made (to include an apology that is ‘an expression of sorrow or regret’ regarding the incident) and documentation. A ‘two-stage’ approach to the DoC was written into the NHS contract in 2015. This made services responsible for ‘feedback of the findings of the inspection report to an appropriate person’. 44
In 2020, joint statements by the professional councils and regulators reiterated the professional DoC, with application of the duty to all situations of actual or potential harm. 45 The imposed (rather than negotiated) application of this duty has been questioned. 46 In 2021, the Care Quality Commission (CQC) (the arm’s length body of the Department of Health and Social Care with expertise in dispute, claims and resolution) reissued the Regulation 20 guidance to providers to emphasise the need for completion of the regulation for all notifiable safety incidents, for clarification of how these incidents can be defined and to emphasise that an apology is not an admission of fault on the part of individual or the service. 47
The effectiveness of the DoC in promoting honesty for injured patients and families has been widely debated. In particular, the emphasis on compliance (or ‘box ticking’) over a sensitive approach to patient or family needs has been contested. 48 Additionally, the higher threshold of statutory DoC reporting requirements, compared to professional DoC requirements, was anticipated to result in a downgrading of assessments of harm by organisations or HCPs. 12 This could confuse whether incidents meet the threshold for reporting or lead providers to neglect to report some cases. Furthermore, the effects of the DoC on litigation rates have also been debated. While honesty about an incident, as stipulated by the DoC, might reduce the need for some patients and families to initiate litigation action to find the answers they seek, disclosure might also encourage litigation as cases of avoidable injury are illuminated. 36 Regardless, there is evidence of varying compliance with the DoC,49 along with initially inconsistent inspection of compliance. 50 Despite this, across the NHS provision, the prosecution of organisations for breach of this duty has been infrequent. 51 At the time of research, the DoC did not apply to other NHS or independent investigating bodies. 52,53
Open disclosure in NHS maternity services
The Morecombe Bay Investigation Report made a powerful case for the need for disclosure of serious incidents (SIs) to affected families and for their involvement in incident review and investigation. 54 Concurrently, increasing costs of obstetric litigation claims were noted, with overall costs of settlement equating to 40% of the £1.1 bn paid by the NHS in 2016 and escalating to 50% in 2017 and 62% of all secondary claims in 2021–2. 55,56
NHS and professional bodies began to attend more closely to post-incident communication with families as a sign of wider and significant shortcomings in maternity safety, including incident investigation, and thus introduced multiple incentivised improvement programmes. 57 Since 2018, the Clinical Negligence Scheme for Trusts (CNST) administered by National Health Service Resolution (NHSR) (the arm’s length body of the Department of Health and Social Care with expertise in dispute, claims and resolution) requires participating Trusts to contribute an additional 10% of CNST premium that is then refunded if they can demonstrate that they have met all 10-of-10 identified safety actions (that range from workforce and training to completion of safety improvement programmes). 58 Safety improvement and parent engagement initiatives in maternity services are focused on both reviews, where the avoidability of some adverse events is not known, and on investigations, where avoidability is anticipated and the factors contributing to the event are unknown.
The most significant initiatives were:
Parent involvement in the Perinatal Mortality Review Tool (now UK-wide)
In 2017, an online, multidisciplinary reporting tool was developed by clinicians with families with the aim of improving and standardising all reviews of perinatal deaths across the NHS. The tool has three questions on parent involvement: if they have been notified of a review; if they have been invited to ask questions or raise concerns; and what responses to these questions were given. Bespoke implementation materials for parent engagement in NHS services include evidence-based timeline and flowcharts, and guidance on writing an effective report for parents. 59,60
Tool completion was financially incentivised by NHSR’s CNST as 1 of 10 actions requiring board-level reporting. In 2019, the reporting standard for the inclusion of parents in 95% of all perinatal deaths (from 22+ weeks gestation; stillbirths and neonatal deaths up to 28 days) in each Trust. 61 Findings from the Perinatal Mortality Review Tool (PMRT) are also thematically reviewed, with recommendations for clinical, service management and patient engagement published annually. 62–64 Up to 2021, of 9174 completed PMRTs, there was an overall increase in the number of parents told of a review. However, a more targeted investigation of parent engagement indicated that many parents (one in three) felt only partially heard by investigating clinicians. 65 Reported progress on family involvement facilitated by the PMRT is presented in Report Supplementary Material 1. Annual reporting on implementation progress of the PMRT in Trusts highlights the ongoing challenges on in-service resourcing, variability in multidisciplinary time or investment in reviews and weaknesses in action planning following review findings. 62–64
The Healthcare Safety Investigation Branch maternity investigation programme (England)
Initiated amid growing concerns with variations in the quality, rigour and timeliness of investigations conducted internally by Trusts, this programme was established for independent investigation of some serious maternity incidents in 130 NHS Trusts and 11 ambulance services in April 2019. 66 It was an extension of the wider HSIB, an arm’s length body of the Department of Health and Social Care that investigates harm to NHS patients. For families, this promised that investigations would not be biased by the defensiveness of service providers. The HSIB was funded to develop a standardised investigation and post-incident learning approach that was heavily influenced by human factors methodology. The primary purpose of the programme was to identify common themes and influence systemic change in clinical practice. 66
With parent consent (for the sharing of their data from the Trust), incidents that met certain clinical criteria (e.g. incidents affecting term babies, caused during labour or during the postnatal period, as well as some maternal deaths) were referred for investigation by the Trust to the HSIB. 67 Since 2020–1, 100% Trust reporting of these incidents to the HSIB has been incentivised under the NHSR CNST scheme.
The programme has invested in a detailed family engagement model, with regular, one-to-one contact with investigators that included an interview about the family’s experience, discussion of the investigation terms of reference (ToR), updating of investigation progress, access and explanation of a draft copy of the report, receipt of the final report with the possibility of a three-way meeting led by the Trust and invitation to feedback on the HSIB investigation process. 68 The Trust carries responsibility for families after their incident has been investigated and reported on.
The NHSR Early Notification Scheme (England)
Established in 2017, and incentivised since 2018, the Early Notification Scheme (ENS) incentivises the prompt initial investigation of incidents of suspected severe brain injury associated with birth. The scheme offers some financial assistance to families if it is agreed by an ENS panel (comprising doctors and midwives, solicitors and expert witnesses working independently of the Trust) that there is sufficient evidence for them to legal claim against the Trust. From 2020, investigation criteria for suspected cases were tightened to align with Royal College of Obstetricians and Gynaecologists (RCOG) established risk indicators. 69 The additional objective of the scheme is the thematic analysis of incidents for rapid dissemination of learning from incidents at Trust, regional and national levels, for the benefit of families and staff. The notification of families that an ENS investigation is ongoing was identified as important (and was incentivised) from 2020 to 2021; however, families are unable to access ENS investigation documents about their own case. 70 Since 2020–1, family consent has been required for ENS cases (as these are also reported to the HSIB). 71 Until 2020, communication with families after incident investigation under the NHSR ENS happened outside maternity services and after investigation completion. Therefore, the study is not directly focused on this intervention.
Interim summary of Chapter 1
Our brief overview of ongoing OD initiatives in place in 2021–2 indicates the complex background for service managers, as well as for front-line clinicians (doctors and midwives), involved in improvement efforts to engage with families post incident, along with the potential for confusion among families themselves.
We note that while regular reports on the progress on OD initiatives indicate a gradual, if uneven, overall improvement in post-incident communication with families, these reports are usually by organisations responsible for intervention development. We note that many of the long observed and widely noted challenges to OD improvement are evident in recent OD initiatives in the English NHS and NHS maternity care. These include professional and service concerns over litigation and reputational risk; differing perspectives on when and how far the exercise of openness with families should extend, including the application of different clinical thresholds by different improvement programmes for the incentivisation of openness with families; uncertainties over who is responsible for communication with families throughout the OD process; and the sometimes-unclear relationship between the imperative for family involvement and wider patient safety agendas. These questions underpin the fluid and uncertain conditions within improvements in post-incident communication with families unfold.
We note that while general and uneven improvements in OD processes have been described previously, these findings are most often drawn from progress reports on the implementation of interventions. Particularly in NHS maternity care, where multiple interventions to improve OD are ongoing and sometimes overlapping, there is limited understanding of how, in what circumstances, and to what effect OD happens in practice. More specifically, there is a need to identify what critical factors are required for improvements in OD.
Study aims, research question and objectives
The study aims were to:
-
identify and explore the critical factors underpinning OD improvements
-
capture the perspectives of national stakeholders, local service leads and practitioners, families, doctors and midwives (henceforth clinicians), and local managers during various situations of avoidable harm and their viewpoints on OD.
The overarching research question was: ‘What are the critical factors that can improve the incidence and quality of Open Disclosure in NHS maternity services?’.
We addressed this question and sought to achieve these aims through five sequential study objectives:
-
OBJECTIVE 1: To establish initial hypotheses to focus the realist investigation of OD improvements in NHS maternity services.
-
OBJECTIVE 2: To establish the scope of OD in NHS maternity services in England.
-
OBJECTIVE 3: To refine the initial hypotheses and conduct a stakeholder analysis with national and regional stakeholders, establishing a suitable dissemination and impact plan.
-
OBJECTIVE 4: To conduct an in-depth study of OD improvement interventions.
-
OBJECTIVE 5: To verify data interpretation and study output development with stakeholders.
Report structure
The following section details the contents of each of the upcoming chapters:
-
Chapter 2: Restates the study aims and objectives and describes the study design and methods.
-
Chapter 3: Details our scoping review of the changing assumptions that underpin policy about the purpose of post-incident involvement of injured families in NHS maternity service provision (2015–22).
-
Chapter 4: Details our realist synthesis and identifies the five initial hypotheses on the factors that underpin OD from the perspectives of families, clinicians and services.
-
Chapters 5–9: Examine and develop each of these five initial hypotheses. Each chapter includes findings from each study phase (SP) and explores the initial propositions from different viewpoints and fields of experience. The perspectives of national stakeholders, managers, front-line staff and families are included. We use these findings towards a ‘Best Practice Guidance Document’ draft (see Appendix 9).
-
Chapter 10: Discusses the overall study findings to identify the critical factors that underpin disclosure improvements, reconsidering the preliminary theories that guided our research questions, focusing on what works, in what contexts and for whom for OD to be successful. Here, we also reflect on the possibilities and constraints of our approach to the study question. Additionally, we briefly situate our findings in the wider national context of the coronavirus disease 2019 (COVID-19) pandemic and reflect on the impacts of the pandemic on our research.
-
Chapter 11: In the final chapter, we identify recent policy changes that will impact on OD in the UK, and identify implications from the findings for service managers, professional bodies, families, policy-makers and researchers.
Chapter 2 Research design, methods and data sources
Introduction
This report is based on findings from a three-phased evaluation of factors strengthening the disclosure and discussion of harm with families in NHS maternity care. We used a realist evaluation approach to understand how, for whom and in what contexts interventions to improve post-incident communication with injured families are effective. The aim of the research was to identify the critical factors that can improve the incidence and quality of OD in NHS maternity services to enable the generation actionable evidence for maternity providers on how to strengthen OD.
Overview of study
Following realist evaluation principles,72 a 36-month qualitative study was conducted in three sequential SPs. Families who had experienced injury in NHS maternity care were recruited into each of the SPs and acted as study advisors.
Our qualitative methods enabled us to meet the five study objectives as represented in Table 1. The overall study design is detailed in the research protocol. 73
| Study objective | Method | |
|---|---|---|
| 1 | Establish initial hypothesis to focus realist investigation of disclosure improvements in NHS maternity services | Realist synthesis with stakeholder consultation |
| 2 | Establish the scope of disclosure in NHS maternity services in England | Telephone interviews with national and regional stakeholders |
| 3 | Refine initial hypotheses and conduct stakeholder analysis with national and regional stakeholders | Telephone interviews with national and regional stakeholders |
| 4 | Conduct in-depth study of disclosure improvement interventions | Comparative ethnographic case studies of three services (Trusts or hospitals) |
| 5 | Conduct data interpretation and study output development with stakeholders | Interpretive forums |
Realist methodology
A realist, theory-driven approach underpins the study design. 74 Realism, as used in health service research, examines the interaction between a complex social intervention or ‘programme’ (e.g. a policy implementation, a programme of work or an operational system), the context in which it is implemented in everyday practices and the intended or unintended outcomes that are produced for different participants. 75,76 These interactions are examined by the identification of contingent and generative mechanisms (or critical factors) that trigger effects in particular contexts. 72 Realist evaluations approach understanding these interventions by asking ‘what works, for whom, in what circumstances, in what respects and why?’72,77 This is often expressed as a context–mechanism–outcome (C–M–O) heuristic. A summary of the realist terms and principles used in this study are in Report Supplementary Material 2.
A key aspect of the realist approach is the identification and later refinement of one or more initial hypotheses (in realist terms, ‘initial programme theories’) of how interventions have effect. Initial hypotheses are identified by literature scoping and realist synthesis and in discussion with different topic experts. 78,79 A realist evaluation generates a series of interconnected hypotheses on the critical factors that drive and direct improvement work. 80 The study design reflected this theory-driven approach as described below.
Study phase 1: scoping
Study phase 1a: policy scoping review and realist literature synthesis
Our scoping review examined guidance related to family involvement issued in the time between two landmark reports, the Kirkup report and the Ockenden report, to map what, if any, changes have occurred in this area. The aims of the review were to synthesise and examine key reports and policy documents to evaluate the evolution of recommendations for and discussion of family involvement in reviews and investigations in maternity care in England. A scoping review was selected as the approach to address the aims of this study because in contrast to systematic reviews, which aim to answer discrete questions, scoping reviews enable the researcher to collate a broad overview of a topic to synthesise evidence. 81
The scoping review aimed to address the following primary question: How has family involvement been conceptualised and how have recommendations for family involvement shifted over time in policy documents, reports and recommendations for reviews and investigations in English NHS maternity care?
To answer this question, we used three further questions to guide our review:
-
What language and terminology have been used to describe family involvement and how have these evolved?
-
What is the impetus for family involvement and has this changed over time?
-
What actions are suggested to improve family involvement and have these changed over time?
The policy review involved four steps: searching for key policy documents; searching within key documents for sections on family involvement; data extraction; and inductive thematic analysis. This process is detailed in Appendix 1, Section A: Stages of the policy scoping literature review and the findings of the policy review are reported in Chapter 3.
Our realist synthesis of the international literature on disclosure improvements in maternity services addressed the overarching research question of: ‘what are the critical factors that can improve the incidence and quality of disclosure in NHS maternity services?’ Recognising that diverse forms of evidence contribute to realist synthesis and theory development,82 the researchers sought the views and experiences of two mixed groups of expert stakeholders [from the established Project Advisory Group (PAG) and Co-investigator Group (CIG)] to help focus on the synthesis and prioritise the findings. The synthesis was conducted in five steps: a two-stage literature search; realist document appraisal; retroductive theorisation with data extraction; and consolidation of extracted data into Explanatory Accounts (EAs). The process is detailed in Appendix 1, Section B: Stages of the realist literature review and Figure 3. The findings of the realist synthesis are reported in Chapter 4. A comprehensive account of the realist synthesis methods is available in Adams. 83
Study phase 1b: national and regional interview study
We developed our SP1b interview topic guides following the SP1a programme theory findings. Sampling, approach and recruitment of national and regional stakeholders were designed to prioritise national policy-makers, including senior representatives from NHS Resolution; NHS England; HSIB maternity programme; PMRT design and implementation; the Royal Colleges; and third-sector organisations actively participating in national OD or safety improvement work within local or national services. This initial sample included 12 families who were actively participating in national- and local-level safety improvement work. As interviews progressed, this sampling framework was revised to include participants with more localised or informal experiences of OD improvement work (e.g. clinical fellows on rotation through national organisations and families without formalised roles in service improvement).
Participants were identified by purposive and snowball sampling. Following university-approved ethical procedures to protect research participants from coercion and identification, initial participants were identified and approached by PAG members. Next, snowball sampling through organisational networks was utilised to identify additional participants. Informed written consent was obtained from all participants prior to interview and each participant was given a unique identifier code to protect their anonymity and confidentiality. Both study information and the interview topic guides were forwarded in advance of all interviews to facilitate reflection and discussion. Advice on sources of post-incident support and a follow-up call were offered by the research team due to the sensitivity of the research topic. The interview topic guides, study information sheet and interview consent forms approved by university ethics panels are available as project documents (www.fundingawards.nihr.ac.uk/award/17/99/85).
One-to-one, audio-recorded telephone interviews with national and regional stakeholders were conducted between September 2019 and November 2020 by author MA. These interviews were intended to capture perspectives and experiences of OD in different service settings and conditions with different interest groups. 84 Sixty-seven one-to-one interviews were conducted, lasting between 40 and 120 minutes each. One group interview, lasting 90 minutes, was conducted with four families. Fifty-eight of these interviews were with participants who had a national role in OD improvement and nine of the interviews were with families who had experience of any OD improvement (see Appendix 2, Table 4). The interview guides for families were adjusted reflexively for families depending on the family’s readiness to consider the perspectives of clinicians and services. 84
Study phase 2: ethnography
Identification of case-study services
Three case-study services were selected for positive deviance85 using purposive sampling for maternity services that had high or improving performance in disclosure improvements. To select the case-study services, first we examined most recent CQC ratings of Trust and maternity service performance (2014–20) and 2019 NHS Staff Survey Results (Trust-level benchmark reports) to identify metrics that were indicative of an environment supporting disclosure improvements (e.g. metrics on transparency, incident reporting and staff-reported organisational or service responsiveness of incident reporting). We also included the rating from the 2015 to 2016 ‘Learning from Mistakes League Table’ as comparative case data. These surveys established a picture of how well all 134 Trusts in England were engaging in disclosure improvement work. Next, we shortlisted Trusts and services that indicated better performance for leadership and learning from incidents to be approached through an open call for study participation. Due to the sensitivity of the research topic and anticipated challenges with research engagement, we followed Stake’s principles of case-study sampling that prioritise (1) maximum changes of ongoing research engagement, (2) diversity of cases across contexts and (3) cases that provide learning about complexity and context. 86 Due to COVID-19-related delays in research engagement, the study team was obliged to prioritise criteria (1). The sampling process for case-study site selection is documented in Appendix 3, Figure 4.
The three services selected for case study had the following attributes:
-
Trust-level CQC ratings and Board minutes that indicated a notable emphasis on DoC improvement work or transparency (e.g. long-established practices of SIs in maternity reporting in Board minutes).
-
Service-level variation in the consistency and seniority of leadership.
-
Service and Trust-level variation in ongoing practices of listening to families (most notably, provision of postnatal and post-incident support for families).
Further general and topical features of the selected case-study sites are presented in Appendix 4, Table 7.
Ethnographic case studies
Following a series of one-to-one and group meetings at each case-study service, where the study was introduced and concerns and questions addressed, key informants and initial case-study interviewees were approached. Initial interviewees were identified using purposive sampling with assistance from service gatekeepers and site-specific principal investigators (PIs). Subsequent case-study interviewees were identified using snowballing techniques. After the identification and approach of clinicians with a central role in disclosure (notably, clinical and service leads and CG teams), the sampling approach was to maximise the diversity of interviewees with experience of disclosure. For clinicians, this was to explore variations in the clinicians’ experiences based on clinical and corporate roles, place of work, seniority and clinical profession. MA and JH conducted 75 interviews with clinicians in a range of front-line to senior management positions and across the three case-study services. For families, we sought to identify families that reflected social and ethnic diversity, as well as differences in clinical events and histories. To protect anonymity and confidentiality, if an individual decided to participate, they were asked to contact the research team directly. The realist topic guides from SP1 were reflexively adapted for use in SP2 to explore the initial programme theories. Informed, written consent was obtained from all interviewees. We conducted interviews with four families recruited from one service. Other services were reluctant or unable to facilitate family approaches. All services had challenges recruiting families that were socially or ethnically diverse. Appendix 2, Table 5 summarises participation in the case-study interviews by case-study service. The case-study services also included observations of formal and informal meetings and collection of relevant organisational documents. Appendix 2, Table 6 documents the formal meetings observed by the researchers at the case-study sites.
A detailed account of research processes employed in the case-study data collection, iteration and analysis is presented in Appendix 2.
Study phase 3: interpretation and output development
Finally, we facilitated five interpretive forums: one at each organisational case-study site (two online and one in-person), one national forum with the PAG and one online family forum (FF) (online due to COVID-19 travel concerns). The interpretive forum research process is described in Appendix 2. Appendix 2, Table 3 details participation at the interpretive forums.
Data organisation and analytical approach
Pseudonymised interview and forum transcripts, fieldnotes of observations and all redacted site documents were stored on a dedicated, password-protected drive hosted on a secure university server. Transcripts, notes and documents were analysed using NVivo (QSR International, Warrington, UK) (March 2020 release). A realist, retroductive, thematic analysis of the data was completed. This analytical approach is directed to the ‘unearthing of causal mechanisms’. 87 The approach starts with the empirical and seeks to explain events and outcomes by theorisation of the underlying mechanisms and structures that are likely to produce them. 88 This interrogation of the data and consideration of underlying generative possibilities was conducted by the researchers in several stages. This involved ongoing discussion with the CIG, who were topic and policy experts, and sense-checking the findings and interpretations during the interpretive forums.
This staged, iterative analysis of data generated more findings than could be accounted for in the five programme theories. Three additional programme theories were developed in retrospect using a thematic analytical approach and are described in Chapter 10. Additional findings that extended beyond the study aims included: family strategies of help seeking, including families investigating their own incidents; the personal careers of family support champions; and practices of epistemic injustice across perinatal care.
Further development of findings and dissemination
-
The development of formative practice guidance for OD improvement was generated from the analysis of findings in collaboration with our CIG and some interpretive forum participants (see Appendix 9). This guidance is to be further developed in collaboration with two PIs from our case-study services and with wider clinical (service) and corporate (Trust) governance teams.
-
Study findings are being used to inform a 5-minute animation for families, front-line clinicians and service managers to illustrate what many families and clinicians experience during post-incident communication.
The study was assessed against RAMSES II reporting standards for realist evaluations (see Report Supplementary Material 3).
Summary
This chapter reports on the methods used in the study. The SPs conducted were:
-
SP1a. Realist synthesis of the literature and policy review of family involvement in OD.
-
SP1b. Interview study with national and regional stakeholders. This SP also included interviews with nine families recruited through support associations.
-
SP2. Ethnographic case studies in three maternity services in two English NHS Trusts that included clinician interviews, family interviews and ethnographic observations.
-
SP3. Interpretive forums conducted in the case-study services, with a national PAG, and with a family group.
Governance arrangements included steering committee meetings and reporting, as well as PAG meetings. During the research period (April 2019–March 2022), the research scope and timelines were adjusted, with a 9-month extension including a 3-month costed extension, so that all study objectives were met despite two waves of the COVID-19 pandemic.
Chapter 3 Scoping review of policies and interventions informing disclosure and discussions with injured families
Introduction
This chapter situates the study within recent policies designed to foster family involvement in maternity safety, focusing particularly on the inclusion of families after incidents affecting them. Our policy review traces two trajectories, the first related to the DoC and the second to maternity safety, to describe the various ways that the involvement of harmed families has been envisaged and prioritised post incident.
Family involvement in disclosure and maternity safety
Independent investigations54,89–91 have exposed several system failures that led to potentially avoidable harm in maternity care in NHS Trusts in the UK. Although these investigations span incidents occurring over two decades of maternity care, during which time many recommendations and improvements have been advised by various stakeholders, common themes persist. One area that is emphasised in investigation reports is that families’ voices were not heard, both during their care and in the aftermath of harm during incident reviews and investigations. 54,89–91 The importance of increasing support for families, personalised care and family involvement in decision-making, reviews and investigations is recurrently highlighted. Despite this, recent studies have shown that family involvement in reviews and investigations is not yet consistently taking place in practice. 59,60,92–94 The lack of translation of these recommendations into changes in practice could be due, in part, to the inconsistency of recommendations over time and the lack of actionable recommendations provided. Accordingly, the aim of this review was to synthesise and examine key reports and policy documents to evaluate the development of recommendations and discussion of family involvement in reviews and investigations in NHS maternity care in the time since the statutory DoC requirement came into effect.
Results
We identified two overlapping policy trajectories (see Report Supplementary Material 4): one related to the DoC (see Report Supplementary Material 5) and one related to maternity safety more generally (see Report Supplementary Material 6).
Ten total documents were included in the DoC trajectory. Of these, nine discussed family involvement in reviews and investigations42,49,95–101 and one document did not. 102 Forty-three documents were included in the Maternity Safety Trajectory. Of these, 31 discussed family involvement in reviews and investigations54,55,57,68,90,93,94,98,103–125 and 12 documents did not. 66,126–136 Within and across each of these trajectories, we identify shifts and continuities in how service user (SU) and family involvement are understood. The language, priorities and recommendations surrounding family involvement over time are discussed.
Building trust in organisations
In 2014, the impetus for involving SUs in reviews and investigations was to build individual and public trust in organisations. 95,101 A shift from ‘paternalism’ to ‘partnership’ and the ability to have candid conversations were emphasised for improving trust. 101 Recommendations related to SU involvement were focused on organisational obligation to provide patients and families their rightful access to their health information101 and to notify, acknowledge and apologise for what happened. 95,101 This was described not only as a professional obligation, but also as ‘the right thing to do’; a key priority was creating an organisational culture of openness. At the time, SUs were one-directional recipients of information about their case. Care Quality Commission Guidance recommended a single point of contact in case of SU questions or queries about what happened, but the emphasis was on organisational communication rather than SU involvement. 95 The CQC recommended the provision of emotional support and other relevant assistance for SUs, but details on how this should be facilitated were not provided. 95
Improving systems of care and ensuring accountability
The Kirkup report, published in early 2015 on the independent investigation into Morecambe Bay NHS Trust, uncovered numerous failures in safety, care and respect for injured families within the Trust. 54 Recommendations addressed organisational failings in admission of the ‘extent and nature’ of injuries caused to families. The Trust was instructed to review family involvement practices, particularly with respect to complaint procedures. It was noted, for the NHS more widely, that there was a ‘strong case’ for standardising the internal investigation process to include input and feedback from families, with families offered the opportunity contribute evidence to their investigation. Shortly after the Kirkup report, strategy documents began to highlight the importance of reducing stillbirths and neonatal deaths. 105,107 These documents did not include SU involvement recommendations for when harm occurred, but did suggest that post-mortem examinations were important in the event of stillbirth or neonatal death so that counselling could be provided for future pregnancies. 105,107
Around the same time, the rationale for conducting investigations into incidents of injury shifted from building and restoring public trust in the NHS to improving systems of care while encouraging public accountability. 96,98,106 Although documents did not make explicit recommendations for family involvement, they still warned that the relationship between patients and organisations was in danger of remaining merely ‘transactional and contractual’ without changes and improvements in leadership. 104 When involvement was included, it was envisaged as more two directional than in previous documents, with a language shift from ‘apologising, acknowledging, providing and telling’42,99 in earlier documents to ‘engaging’,96,98 ‘hearing’106 or ‘involving families’97,98 as ‘active participants’96 ‘at the centre’ of investigation processes98 from ‘start to finish’. 106 Policy documents continued to advise on the provision of a single point of contact for families during the investigation process,96–99 along with the opportunity for SUs to ask questions. 98,99 For the first time, the importance of establishing family expectations and preferences for communication96,98 was described as part of active engagement. Although little detail was provided on how to achieve active engagement or involvement,106 the unique perspective SUs offer on their adverse events was acknowledged and it was noted that these perspectives should be shared and listened to as part of the review process. 96,98 The specifics on how these contributions were to be garnered and used remained unclear.
Notably, the serious incident framework (SI Framework), which involved some families in its production, was the first document to detail specific actions and resources to produce meaningful involvement (e.g. the provision of letter templates to facilitate the initial communication with families). 98 The SI Framework suggested the following actions: arranging meetings with families, ensuring that investigation teams have expertise in facilitating family involvement, keeping families informed of investigation progress, providing support and opportunity to express concerns and questions, enabling families to inform ToR and give evidence, sharing findings with families, giving media advice as appropriate and providing the opportunity for families to comment on findings and recommendations. 98 The SI Framework included expectations that investigation reports include a description of how families have been engaged in the investigation process and how they were supported following the incident. Finally, after the conclusion of the investigation, the framework recommended that families be offered opportunities for continued involvement should they wish. The rationales for family involvement were to ensure accountability and build service-user confidence that the investigation findings were ‘robust, meaningful and fairly presented’. 98
Improving the safety of maternity care and saying sorry
Most documents in 2016 were focused on improving the safety of maternity care, rather than improving the processes after harm has happened. 126–129 However, in the Better Births National Maternity Review, where recommendations for improving family involvement were made, the language used to describe this involvement matched the shift in late 2015. 108 Recommendations focused on improving communication with families, putting families at the centre of processes and enabling informed decision-making. In addition to informing families of what was involved in reviews and investigations, the importance of individualised, relational care in maternity care and in investigation practices was foregrounded. 108 The importance of a single point of contact, especially in the wake of trauma, was described as essential to communicating family involvement options. 108
Despite these recommendations, evidence from the CQC in 2016 suggested SU involvement in investigation processes was still inadequate. 49 SUs reported that they were not always told that an investigation was happening, what their rights were in this process, what an investigation involved or how to access support and advocacy. 49 Family involvement was perceived by families as ‘tokenistic’ rather than ‘meaningful’. 49 This suggests that, although the language had shifted towards promoting meaningful involvement after publication of the Kirkup report, there was a lag in translating these priorities into practice. To combat this, the CQC review recommended production of a complementary family engagement framework, developed in partnership with families, for learning from deaths.
Throughout this period, a central concern was how to manage NHS staff concerns with liability and organisational obligations to meet the DoC. In 2016, the NHSR ‘Saying Sorry’ poster was released for circulation through Trust services. Its purpose was to encourage more NHS staff to apologise to injured families. The poster sought to clarify the difference between an apology and an admission of liability. 100 It also alerted staff to their obligations, as employees and professionals, to ‘apologise’, ‘acknowledge’, ‘share information about what went wrong’, ‘provide truthful information’ and ‘inform’ families after an incident. 100 In addition to this reminder of obligations, NHS staff were encouraged to see that apologising had a wider moral basis, in that it is ‘the right thing to do’. The poster also touched on the challenges of standardising communication with injured families, suggesting the ‘tailoring the apology’ to individual patient’s needs. 100
Shifting to individualised, relational care
In 2017, the shift to individualised, relational care was even more pronounced. A new vocabulary was adopted: rather than ‘active participants’ as in previous publications, families were described as ‘equal partners’. 109,110 This was captured in the recommendations, which were extended to incorporate individual choice. In addition to communicating openly and honestly about what happened, services were advised to communicate investigation and complaint procedures with families55,109,110,112 and to involve families to whatever extent they wish in these processes. 55,109–112 This involvement was envisaged as providing the opportunity for families to ask questions and voice concerns during reviews,55,109,110 inviting families to contribute to evidence, inform ToR and comment on findings and recommendations,55,110 providing families a meaningful, plain English explanation of what happened and what could have prevented what happened,112 and finally, offering the option of involving families in service learning efforts after the conclusion of the review or investigation. 109,110 However, it was also noted that it should be made clear that SU feedback may not be included if was not considered ‘relevant or appropriate’. 110 Who determines what is ‘relevant or appropriate’ was not described in this guidance, which was produced for Trust Boards. However, this creates an interesting paradox: families cannot truly be considered equal partners if their contributions to reviews can be dismissed.
Additional new recommendations, such as providing a sympathetic environment for disclosure, also surfaced at this time. 109,110 Improved communication between healthcare professionals across services was also recommended, for instance, increasing communication with outside facilities during transfer and with the family’s general practitioner (GP), to improve continuity and handover. 109,110 Although these recommendations were more actionable than their predecessors, it was still suggested that more detailed guidance on family involvement was required. 109,111 In some cases, recommendations signposted to existing outside guidance, such as that by the stillbirth and neonatal death charity (Sands). 55,111,112 Concurrently, two consultation documents were produced to inform policy development in ways that aligned the interests of families and HCPs. 57,113 These stated that both parties value the opportunity for meaningful apology,57 increased family involvement in reviews and investigations,57 a single point of contact57 and continuity of carer. 113
Enhancing communication
Despite mounting recommendations in previous years for increasing family involvement, in 2018, a progress update on the Each Baby Counts (EBC) programme revealed that only 41% of parents were invited to be involved in reviews. This was an increase from 34% in the previous EBC report, but still startlingly far from involvement ambitions. 116 The EBC recommendations that followed these statistics were mainly focused on procedural compliance, but reiterated that families should be informed of any reviews and investigations taking place and be invited to contribute according to their wishes. 116 The Maternity Safety Training (MST) Fund, one of the other mechanisms set out for achieving the national maternity ambitions, also released an evaluation report in 2018 which listed the training opportunities provided to staff around maternity safety. Disappointingly, none of the offered trainings were related to family involvement or disclosure, other than training on the DoC. 130 The content of this training was not described, and it was not one of the ‘popular’ courses selected by the Trust. The course was also not featured in the MST catalogue, but rather was included as a course funded by the programme in the ‘other’ category.
Also in this year, National Health Service Improvement (NHSI) launched their scheme for ‘Maternity Safety Champions’ operating at the front-line, regional and national levels. 114 Maternity Safety Champions are representatives who act as ambassadors for improving safety in maternity care by learning and sharing best practice. Notably, this programme does not include a SU representative; however, the guidance recommends that champions ‘work with service users to address their needs, particularly in the redesign of new services’ (p. 10). Although no advice on how to achieve this work is given, it is the first time that a co-design approach to family involvement in maternity safety/service improvement is recommended.
The year 2018 did not yield many new recommendations for SU involvement; however, NHSI produced a document on promoting effective spoken communication between clinicians and patients. 115 This highlighted factors like providing the right environment for communication, ensuring information is accurate and understood, listening, conveying an attitude of respect and aligning expectations as facilitators to effective communication. 115 Although not specifically about disclosure, these principles can be applied to the practice. However, as Iedema et al. pointed out the following year in their report on the findings of this initiative, translating these principles from work-as-imagined to work-as-done presents a number of challenges. 137 Namely, there are differences between factually accurate communication and cultural, emotional and situationally sensitive communication, between imagined calm contexts for communication and the reality of the hospital setting, and between structured, evidence-based communication templates and individual, flexible, situated judgement. As such, it is unsurprising that these recommendations were not carried into future policy documents.
Conceptualising families as active partners rather than passive recipients
In mid-2019, the publication of the new NHS Patient Safety Strategy (PSS) marked a significant shift in the potential for patient and family involvement. 120 Transparency, providing opportunity for families to raise concerns and the use of the Patient Safety Incident Response Framework (PSIRF) and ENS were emphasised, and family involvement was embedded in a wider national strategy. The first ENS progress report, published in 2019, highlighted that the programme would enable families to receive answers, support and compensation more quickly. The ENS report did not reflect any of the developments in family involvement recommendations since 2015, instead integrating the original DoC steps of apology, openness, candour and providing support. 121 The biggest addition to existing recommendations in the PSS was the explicit recommendation to approach patients not as ‘passive recipients’ but ‘active partners’. In other publications published that year, the language matched that of 2017, employing phrases like ‘meaningful engagement’ and family as ‘equal partners’. 118 The PSS differentiated itself terminologically, opting for the word ‘active’ instead of ‘equal’. This new status was to be embodied by the ‘Patient Safety Partner’ who was to represent patient interests in their work with innovators on co-production, safety, strategy and policy developments. 120 Other publications signposted to existing recommendations for family involvement from the SI Framework, Sands or HSIB rather than producing new recommendations. 117,119 A report of qualitative findings on the implementation of the learning from deaths national guidance was published, reporting that good practice involved engaging families. 118 The report revealed that environments where there is a culture of openness and staff are supported/trained help with achieving engagement, but did not give specific recommendations beyond that. Several reports published between 2019 and 2020 on maternity safety topics by NHS England, NHSI, NHSR and HSIB did not include any sections on family involvement. 66,125,131–136
Enabling families to guide the process
As in previous years, 2020 policy recommendations by professional, NHS and inspection bodies focused on reminding services of the importance of informing families that a review or investigation was taking place,93,94,122 offering an opportunity for families to share their perspective on their care and raise any questions that they have,93,94,122 enabling families to contribute to evidence,68 personalising care123 and providing a point of contact. 124 Interventions that include family notification, such as the PMRT93,122 and ENS,122 were also signposted. The impact of the gradual recommendation changes and specification on steps for boosting involvement was evidenced in the EBC progress reports published in 2020, which revealed that invitations for family involvement in reviews had increased from 40% to 51% from 2016 to 201793 and to 70% by 2018. 94 These results were approximated in PMRT annual review reports (see Report Supplementary Material 1).
The language shifted slightly in some documents from ‘partnership’ and ‘active engagement’ to allowing patients and families to ‘guide’ their own engagement122,124 with flexibility, inclusivity and transparency during the review process. 93,94 The transition of SUs from recipients to equal partners, to active partners, and finally to guides, demonstrates the changes in perception of family involvement over time. HSIB stressed that families offer unique perspective as the only individuals with insight into what transpires at all stages of the healthcare journey and that families should have continuous involvement. 68 Fittingly, new recommendations at this time included encouraging and instructing patients, families and carers on how to record and share information about patient safety incidents,124 proactively seeking feedback about service openness and transparency,124 having a discussion with families about incidents124 and helping families to understand reports and recommendations. 68 Although national guidance remained the same, HSIB published a diagram illustrating the different steps for family involvement throughout HSIB-led reviews and investigations, illustrating their process for continuous engagement. 68 The process spans the initial contact with the family through investigation completion, with opportunities for family engagement at each stage. Each step has a section with additional information on questions to ask families, considerations to keep in mind and advice for where, when and how meetings with families should take place. 68 For the first time, this process involves giving the family access to a draft report for their input in addition to shaping ToR. 68
Healthcare Safety Investigation Branch reports on their progress for involving families in their investigations indicates the success of organisational investment in an adequately staffed, systematic and flexible family involvement strategy. It also indicates the neglected interests of many families in involvement. In 2019–20, 88% of families were involved in HSIB maternity investigations, whereas, in that same year, 34% of families were involved in Trust investigations. 103
In late 2020, the preliminary findings of the Ockenden report were published with immediate actions and recommendations. 89 Disappointingly, as in Kirkup,54 few of these recommendations were related to processes of family involvement. While Ockenden reports that families want their questions answered and want systems to learn, the only recommendation related to families made is that family voices must be heard and that families must have an advocate. 89 This advocate is to provide an oversight of meetings that happen with families in services. The final Ockenden report, published in 2022, builds on these recommendations to some degree, adding that families should be the primary concern during incident investigations, that families must be actively involved, that feedback must be shared with families openly and transparently by senior team members, that governance teams must work with the Maternity Voices Partnership (MVP) and that bereavement care and other support should be provided. 90 In 2021, an inquiry report published by the House of Commons Health and Social Care Committee recommended that families should be involved in a ‘compassionate manner’ and acknowledged that investigations have often failed to involve families in a ‘meaningful’ way. 103 It was again stressed that families need to be heard and that lessons need to be learnt; HSIB’s family engagement pathway68 was cited as a programme that had boosted family involvement. The report concludes that: ‘… it is important that [HSIB] continue to pursue improvements in this area to ensure that all investigations are informed by the experience of families’ (p. 22). 103 What improvements were needed, or how these might be achieved, were not noted.
Conclusions
This review of policy and report recommendations for family involvement in reviews and investigations in maternity care has several key findings. The first is that many recommendations have remained consistent over time but with limited guidance or resourcing for their implementation in NHS Trusts or maternity services. The importance of providing each family with a sincere apology, information about the review and open and honest communication throughout the investigation or review process, and of facilitating their access to the service with a single point of contact has been reiterated over time. Recommendations have also gradually extended to stress the need for continuous family engagement and for the provision of multiple opportunities for families to ask questions and raise concerns. The reimagining by policy-makers of injured families from those who passively receive information to those who can actively contribute evidence is notable. In policy terms, the recognition that families offer a unique and valuable perspective on patient safety has resituated them as subjects whose experiences of harm might become useful resources for learning and safety improvement. These additions evidence the fact that progress has been made in promoting the active and meaningfully involvement of families in documentation. Yet, there is still work to be done to meaningfully action these aspirations at the service level. Critically, this review also highlights that, in practice, families are not as involved as they would like to be, that different stakeholders in reviews and investigations (for instance, NHS England, NHSR, NHSI, HSIB, various charities and the NHS Trusts themselves) may have different perspectives on what family involvement entails and thus, the complete application of the principles for involving families is inconsistent.
Chapter 4 Realist literature synthesis of open disclosure in international maternity services
Introduction
This chapter reports the results of our realist synthesis and is the first step to meeting research objective one: to establish initial hypotheses to focus realist investigation of OD improvements in NHS maternity services. The research question guiding this synthesis was: ‘What key factors (resources and relationships) underpin successful disclosure in maternity care for different social groups, families, clinicians and managers of services in different circumstances?’
Identification of the literature
The documents included in the synthesis were identified using a two-stage literature search that included consultations with stakeholders. This process is detailed in Appendix 1.
In total, 39 documents were identified. After quality appraisal of the 39 documents for ‘fitness for purpose’ by relevance and rigour,75,138 38 documents were included in the realist synthesis (see Report Supplementary Material 7). A summary of our realist assessment criteria to establish ‘fitness for purpose’ is in Report Supplementary Material 8.
Realist data extraction and synthesis
Following RAMESES guidance,78 a data extraction tool was developed and piloted incorporating C–M–O configurations. For each paper, the rationales for interventions discussed or investigated were extracted as sets of ‘if …, then … ’ propositions using the tool.
This data extraction yielded 135 EAs from the 38 papers and were reported separately for families, staff and services. These EAs were organised by two researchers into a series of themes based on semi-predictable patterns in the accounts. 139 Following realist review principles,138 neither reported EAs nor reported intervention outcomes were necessarily the primary study focus of the papers. These EA statements were then mapped across two pathways: the ‘ideal-type’ temporal trajectory of OD (from event to resolution) and in relation to context/mechanism relationships that could be identified in relation to this trajectory. The outcomes of this data extraction for families, staff and services are available in Report Supplementary Materials 9, 10 and 11, respectively.
This data extraction from the perspectives of three distinct interest groups (families, staff and services) helped us to surface points of divergence and commonality in how OD was envisaged (its purpose, benefits and how it might be achieved). For example, OD as a service imperative to protect or enhance organisational reputation and to manage litigation may be antithetical to OD envisaged by families as greater transparency. These documents were discussed with our CIG and some members of our PAG. The PAG included national policy experts (n = 5), senior clinicians (n = 4) and family members with lived experience (n = 5). These stakeholder groups advised on the consolidation and prioritisation of the mapped EAs (or partial C–M–Os). They directed our attention towards key elements of OD experiences for families and staff, for example:
-
the initial responses of staff to a catastrophic incident and how this is felt by the parents or family
-
the significance of family involvement in reviews or investigations over time
-
the importance of understanding what happened and why for families
-
the complications of this work for staff during periods of rapid procedural change
-
the different ways in which some relief from the injury of harm happens for a family, including:
-
sincere recognition by clinicians of the effects of the incident on the family
-
knowing that changes have been made because of what happened to them
-
the value of clinicians’ OD skills.
-
-
the immediate and ongoing social and emotional effects of OD on healthcare staff as being fundamental to the ongoing quality and extent of disclosure with families
-
and finally, given the diversity of interventions identified, that an overview of intervention outcomes would deepen our understanding of the assumptions underpinning these programmes of work.
The outcome of these discussions was a honing of the synthesis into 68 consolidated EAs across the three interest groups: families (n = 20), staff (n = 28) and services (n = 20). These consolidated EAs were further synthesised into C–M–Os or elements of C–M–Os through independent analysis by two researchers (MA and JH) and in discussion with the CIG. CIG discussions refined the five ‘when/then’ mechanism sets. These were identified as C–M–Os expected to have a notable and identifiable effect on OD.
Results
Realist data extraction of the 38 documents identified 135 underlying assumptions or theories about what is required for effective OD events. The 38 identified documents include peer-reviewed publications (n = 22), policy research (n = 14) and evidence-based improvement updates with training resources (n = 2). They included findings from England (n = 18), the USA (n = 7), Australia (n = 4), ‘High-Income Countries’ (sic) (n = 3), Scotland (n = 2), Ireland (n = 1), France (n = 1), Europe (n = 1) and ‘International’ (sic) (n = 1). One paper was a systemic review, and two papers were evidence reviews. The complete list of included documents, organised by comparable interventions, publication details, realist quality appraisal ratings and key study characteristics, is presented in Report Supplementary Material 7.
Across all papers, there was limited primary research investigating families’ experiences of OD and what families consider necessary for OD in maternity services (with the exception of Iedema,37 Quinn140 and Stanford and Bogod141). Only two papers considered social diversity as a factor that might influence experiences of OD and felt outcomes. 37,142 Evidence of the direct use of family experience for practice or systems change was limited to one paper. 141 ‘Culture change’ towards either ‘no blame’ or ‘fair’ behavioural or organisational principles was often mentioned as an overarching cause49,55,92,121,140,143,144 or effect49,143 of OD improvements.
The empirical studies and reports documenting the effects of OD interventions (n = 21) were reviewed for descriptions of intervention design and intervention outcome. These fell into three broad categories of intervention and the nature of the evidence on outcomes varied between studies. First, three quantitative and mixed-methods studies examined the outcomes of simulated training sessions for individual trainees or professionals that were designed to enhance clinical communication skills. 145–147 These studies all suggested that there was an improvement in individual or team skills to conduct OD conversations after the interventions, with one identifying some of the benefits from the use of an evidence-based cognitive aid. 147 However, these clinical educational studies were small scale (n = between 15 and 60 participants), conducted in simulated environments and, most significantly, did not include patients or the public perspectives on the study design or assessments of outcomes.
The second group of studies (n = 5) included progress reports and one qualitative study. These documented the progress of parent or patient involvement in safety improvement interventions, including consideration of perinatal mortality reviews (PMRs) or audits62,63,148 and SI investigations. 49,118 These studies indicated the slow progress in improving parent involvement when doing so as one element of a wider safety improvement initiatives.
Third, a series of studies and reports (n = 8) documented the effects of multifaceted interventions to strengthen OD practices across a sector, service or hospital. 9,37,140,149–153 These interventions were often described as including the development and dissemination of faculty-tailored protocols and guidance, formation of CG revisions, introduction of general and more specialist clinician training and wider awareness-raising across staff teams. Overall, these studies acknowledged the long-term, uneven quality and extent of OD. A few individual, positive experiences of honest apologies in clinician–patient relationships were described. In many cases, the tension between clinicians’ support for OD in principle and their apprehension about reputational risk was captured. One study described a widespread increase in OD practices following a hospital-based quality assurance audit. 151 The increase was attributed to a long-term (at least 27-month) consequence of dedicated resourcing and focus by senior leadership, consistent messaging throughout the organisation, investment in enthusiastic and established champions working close direct care provision and insurer-approved protocols and specialist OD leads. However, with few exceptions,9,140 the views and experiences of patients, families and staff on the quality of OD events and their felt consequence were not a focus of these accounts of service-based OD improvements.
Initial programme theories hypothesised
The following sections describe the synthesised underlying factors for OD as a series of generalised hypotheses and explore how these are considered in the included papers. We summarise the realist data extraction findings in relation to the five identified programme theories in Appendix 5, Table 8.
The five identified programme theories are summarised as:
-
receiving a meaningful acknowledgement of the harm that has happened
-
being involved during the review/investigation process
-
making sense of what happened
-
receiving care from clinicians who are skilled and feel safe during post-incident communication
-
knowing that things have changed because of what has happened.
Receiving a meaningful acknowledgement of the harm that has happened
When a family feels that their experience of harm and its aftermath has been acknowledged in a meaningful way, their trust in clinicians and the service is more likely to be rebuilt, clinicians involved feel some relief and ongoing care and communication post incident is more likely.
Early and meaningful acknowledgement of harm, irrespective of questions of whether the harm was avoidable, was significant to families (24 papers) and staff (5 papers). Three studies stressed the importance of a family-centred perspective on the severity of harm and its aftermath. 49,141,154 Meaningful acknowledgement was emphasised as including recognition of the uniqueness of the experience on a family. This interpretation involved clinicians recognising and understanding the experience of the family and was additional to professional and regulatory duties. 49,121 The rationale for this acknowledgement differed from the organisationally and professionally prescribed OD tasks of giving honest information and explanation of what happened. This was also different from family involvement guidance, in which the clinician’s primary responsibility was to ensure that the family was invited to ask questions or raise concerns. 62,149 Only one paper considered the possibility that injured families could introduce clinicians to alternative perspectives on harm when involved. 153
As part of the meaningful acknowledgement of harm, the value of an honest and direct apology to a family during initial and subsequent OD conversations was noted in many studies. 37,118,141,149,155,156 Sometimes, a sincere expression of regret was found to enable some restoration of trust in a clinician or the service for the family. 37,141 Indeed, clinicians expressed surprise and relief that a family may offer understanding after an honest expression of regret. 9,149 Several studies indicated the disappointment of families when these apologies did not translate to their subsequent experiences of care. Many harmed families felt the injustice of poor ongoing care and expressed that they felt insensitivity from general maternity staff to their trauma and loss. Several papers suggested that the lack of ongoing recognition of harm may be because clinically defined incidents fall below procedural or regulatory thresholds of severity deemed to merit investigation;49,141,154 however, studies noted that clinicians also require information, time and determination to understand and discuss these ‘less severe incidents’. 141,157 Three studies explored the experiences of families after stillbirth, noting experiences of marginalisation, unrecognised distress and ignoring of their distinctive needs. 142,156–158
When evidence of harm was clinically uncertain and so interpretation of the extent or presence of harm gradually evolved, meaningful acknowledgement by a clinician was more complex and sometimes involved expert diagnosis and discussion with families and a wider clinical team. 156,158,159 Additionally, maternal harm or significant harm to babies could be identified weeks or months after the incident; in these circumstances, OD was initiated by clinicians or services far removed from the originating events and the clinicians involved. 121,141,154 These aspects of multiprofessional, multiservice OD work raise challenges around maintaining trust and communication with affected families. 141
Two papers from the same study found that the timing and conduct of OD meetings were often interpreted by those affected as indicators of how seriously the event was taken by the service. 37,153 Creating the space and time for exploration and discussion of events and their consequences communicated acknowledgement of the family’s situation. 153 Family preference for the presence of particular clinicians at their OD meeting also suggests the importance of personalising these events from the perspective of the family. While families more often wanted to meet with a senior clinician already known to them,159,160 some also wanted to meet those directly involved in the incident so that this family better understand events and their aftermath37,147 or can receive a more personal expression of regret. 37 A recognised barrier to meaningful acknowledgement during OD meetings was the inhibiting effects of clinicians’ worries about the risk of disciplinary action or litigation following OD. The distorting effects on conversations where legal or organisational representatives were present, or where legally protected ‘safe spaces’ were uncertain, limited the possibility for openness and honesty. 49,140
The meaningful acknowledgement of harm was secured by the conversational skills of empathic clinicians in cases where families might accept an honest expression of regret and explanation of what happened. 37,141 However, when a family needed material compensation or assistance, uncomplicated and timely settlements by the service were also important for diffusing anger and the chances of litigation, as well as preserving clinical relationships. 121,140,144 More immediate, short-term assistance with ‘out-of-pocket’ expenses, along with the provision of any further or specialist care, were valued as expressions of acknowledgement of harm. 37,68,140,148 Surprisingly, few included papers considered the divisive effects of tort legal principles on clinician–family relationships after harm in maternity care. In some cases, these principles could shape ongoing adversarial relationships between families, clinicians and services, especially when it was felt that a genuine acknowledgement of harm did not take place after an incident. 121,140,144
Being involved during the review/investigation process
When families are included in these processes if they decide, and have support for this involvement, then they are less likely to feel alienated and distrustful of services and are more likely to be heard in discussions about the event and their care.
Nine studies highlighted the value of a named, expert, family contact to act as the ‘link person’ through organisational processes, individualised care and information giving. 9,49,59,68,118,121,149,150,156,160 In addition to OD meetings offered by clinical leads, named contacts were expected to be more readily available and responsive to families, even offering an ‘open door policy’ for families to return with questions should they desire. 49,68 In this dedicated role, named contacts responded to changing situations and personalised needs of a family, representing family interests and perspectives during review and investigation meetings. The role prioritised keeping families present and visible within busy services,68 where unexpected delays and complications in bureaucratic processes might not otherwise be explained to them,160,161 and could cause further upset and suspicion. 49,144
Although this role was commonly suggested as an important element of OD, reviews and investigations, the composition of this role as an advisor, information giver or family advocate was not fully explored. The requirements of this role were only briefly noted as ‘training and support’150,161 and protected time. 68 The legal implications of family advocacy were not explored. The anticipated duration of family involvement with a service after an incident, along with the duration of a ‘named link’ relationship with a family, varied considerably in the literature. For example, some suggested closure at discharge from a service49,68 and others proposed that the relationship be sustained until inquest or retriggered on future re-admissions to a service. 49,59,68,160 Inherent tensions between different responsibilities were rarely discussed in the identified papers. For example, the work of the named contact might span from care co-ordination to family advocacy, with different implications for families depending on the context. Some review and service redesigns identified bereavement midwives160 or community midwives149,150 as the contacts for families because of their ability to champion and translate family concerns and questions to clinical teams more effectively than non-clinicians. 59,149 However, the expectations of the named contact’s employers, managers, peers and wider professional identities may be in direct conflict with their role as family advocates. The development of the role of a fully independent family advocate is not fully explored or evaluated in the identified literature, but it is noted as a possibility for families in better-resourced maternity units. 59
The wider significance of keeping affected families informed and updated on review and investigation processes was discussed in eight studies. 55,63,121,142,144,150,158,161 These studies focused less on issues of family entitlement to information and more on the challenges of producing and circulating accessible, written, standardised materials to families with differing needs and expectations. 55,59,63,92,158,160 The guidance circulated to families highlighted the shortcomings of some services that neglect to provide family-centred advice. 55,121 Information content and delivery, designed with staff and parent advisors, were expected to have greater relevance for families. 62,150,162 Yet, prescriptive, standard information for families about review and investigation processes was often considered inadequate. For example, guidance for families on recommended time frames for review/investigation completion could be reassuring to families but was also found to enhance disappointment and distrust when delays happened. 49,144 Furthermore, in some circumstances, families felt irritated or confused when information was duplicated or reinforced by services;121 however, in other cases, this was necessary as families in shock and crisis may not grasp information the first time it was shared. 62 These findings suggest the importance of personalised information sharing rather than standardisation.
Similarly, the adaptation of guidance literature in response to social diversity,92,152 including the provision of translation,68 was seen to ‘solve’ the task of recognising family differences. 49,68 However, others found that this approach may overlook more fundamental concerns about family expectations of OD in relation to socioreligious background. 142 Four studies made clear that for pre-designed information materials for families to have relevance and resonance, they had to be introduced and discussed during ongoing OD meetings, ideally by a clinician or advocate who already knows that family. 37,92,142,160 One paper identified the need for the development of a family-centred pathway for embedding pre-discharge routines of post-incident enquiry and care planning discussion in maternity services. 154
Making sense of what happened
When families feel that they can make sense of what happened, and that clinicians and the service have sought to help them do this, then they feel less dismissed and are more likely to begin some recovery.
Fifteen studies indicated that a crucial and ongoing aspect of OD was helping families make sense of ‘life-shaping’ events. 49,55,59,60,62,63,68,92,121,141,143,156,158–160 When an explanation was offered, this could reduce family distress and mistrust in a service, help families recover from grief156 and progress their ability to plan for the future. 142,156 However, not uncommonly, families felt that explanations given were incomplete, misleading or incompatible with their understanding of what happened. 9 Not all reviews or investigations can establish causality158 or have sufficient scope to address all questions raised by a family. 59,68 One study noted that the invitation to a family to raise questions about what happened, does not, in itself, ensure meaningful or empathic family involvement. 49 Systems-based explanations disappointed families who felt that issues of personal accountability were also important to them. 68 Additionally, a series of perspectives may be captured in reports. These diverse interpretations impact how the incident is managed by clinicians, families and managers. While one paper proposed clarification for all investigation routes and ‘hierarchies’ to reduce complexity to an orderly explanation,161 another argued the need for ‘expectation management’ (informing families of the limited and pre-defined scope of the investigation body for examining the incident),68 and a further paper advocated for the future production of a single, integrated report to reduce family experiences of discordant interpretations. 62
Receiving care from clinicians who are skilled and feel psychologically safe during post-incident communication
When clinicians are skilled and feel psychologically safe to conduct disclosure conversations with families, then these conversations are less likely to be avoided, questions of responsibility are more likely to be addressed and OD is more likely to become embedded in ongoing clinical practice.
Eight studies discussed the importance of active listening, language, posture and conversational tone as crucial interaction and improvisational skills in communicating meaningfully with families. 37,121,141,145–147,149,158 While one study described the effectiveness of ‘best practice’ staff guidelines for improving disclosure conversations with senior clinicians,147 another noted the necessity of ongoing, clinician, situated judgement for adjusting guidance and protocols. 153 This skill was considered crucial for OD to become more than an ‘in-principle’ agreement. 153 OD communication training for trainees,145 for all labour and delivery clinicians,151 and multidisciplinary OD leads147 was shown to increase self-reported confidence, competence and cross-disciplinary collaboration in conducting OD conversations121,145,146,149 and was also suggested as a means of potentially reducing the risk of workplace burn-out. 146 One study found that while training clinicians to use ‘appropriate words’ did not make the task of OD feel easier, it helped them to express their feelings in ways that encouraged a more honest conversation with families. 151 This could indicate that the performative skills and personal and moral aspects of OD conversations both require careful nurturing.
In addition to the implementation of awareness and skills training for dedicated OD leads, three studies identified the importance of promoting OD skills and awareness across clinical teams and as part of the wider service ethos. 143,151,163 The inclusion of more junior or non-specialist clinicians in incident review meetings was one approach to demystify OD without seeking blame. 161 Seven studies considered the expectations and needs of clinicians after incidents, such as including them in updates on progress and outcomes of reviews/investigations55,121,143,149,151,161 and updating them on resulting changes across teams or departments. 156 Clinicians’ knowledge that changes have been made was associated with a reduction in their post-incident trauma. 156 Four included studies proposed that the exclusion of affected front-line staff from OD and investigation processes may heighten post-event anxiety, fearfulness and felt isolation,156 while familiarity with reliable, no-blame processes may alleviate these worries and decrease uneasiness when reporting and disclosing future incidents. 143,151,163,164
Dedicated, confidential, post-incident support was considered a necessary investment for normalising OD practices and for sustaining the confidence of clinical teams. 55,121 However, the acceptability of existing, dedicated post-incident support systems to staff remained unclear. 121 It is possible that informal peer support, without fear of blame or loss of reputation, is more relevant to some healthcare professionals. 49,141,143,147,149,151 Given the vibrant social and organisational discourse on ‘open cultures’ and ‘fair cultures’ in health care, there was limited exploration and discussion of these values and practices concerning OD in the included studies. 121
Knowing that things have changed because of what has happened
When families and staff see that aspects of the service have changed after the incident that has affected them, they are more able to deal with loss and trauma in the longer term and are less likely to feel alienated from the service.
Twenty-six studies described a relationship between OD and learning for improvements in safety after an incident. Many families anticipate that a review will address two imperatives: first, an explanation of what happened in their case, and second, the use of this knowledge to prevent the same thing from happening again in the future. 157 Assurance that similar incidents will be prevented in the future was found to help families to make sense of their loss. 49,92,140,161 However, family expectations of improvements from learning were often not met,49,68,161 because changes had not happened, were happening gradually or were not communicated to the family. 49,141 One study found that 83% of families felt that their incident investigation had made no positive difference to the service and 73% of families were unclear on what learning had happened. 49
Seven studies identified the need to embed OD processes in well-functioning, CG systems to ensure systems-level learning. 9,149–151,153,163,164 In some cases, it was implied that this learning might include the incorporation of family perspectives and experience. 62,63,121 Organisational changes to facilitate the shift from learning to service improvement systems included strengthening assurance systems in directorates with regular reviews, implementing unit reporting for external benchmarking for ‘candour training’ and increasing guideline compliance to promote learning and acting on lessons. 55,118,149 The need for clarification of service commissioners’ and Trust Board members’ responsibilities for meeting OD guidance or candour regulation, for enhancing family involvement in reviews and investigations and for completing assurance of recommended action plans from these incidents was noted in some studies. 49,55,121 However, some studies also suggest that the quality assurance frameworks supporting greater openness with families were often ineffective and could even undermine this,49,118,121,143,144,151,161 for example, by the stipulation of inflexible time frames for family involvement. 49
Comprehensive reviews of whole care pathways, requiring multidisciplinary and cross-service contribution, were noted as especially valuable for maximising possibilities for learning within62,152,158,162 and beyond maternity care. 141 Particularly in situations when harm was less immediately obvious, collaborative learning networks beyond maternity care (e.g. with GPs) enabled a reduction in misunderstanding and treatment delays for individual women and families. 141,154 Such networks relied on material and social investment in cross-sector relationships, which required the clarification of leadership responsibilities,62,143 reporting timelines,49,62 peer-review and ‘fresh-eyes’ contributions,55,62,162 agreement on investigation methodologies and administrative co-ordination. 49 Further service investment in review and investigation data with external quality improvement (QI) bodies and the dissemination of learning from these external bodies through services, units and teams was expected to enhance learning for safety revisions beyond single Trusts. 63,121 The more complex task of translating these lessons into ongoing practice and systems revisions was rarely addressed in the literature. Only one study described the pivotal role of a professional body in promoting members’ learning from one woman’s experience of unrecognised harm in maternity care. 141
With notable exceptions,9,118,141,152,161 the identified papers did not consider the possibilities for family participation in wider QI work in services where they had experienced incidents. Some studies noted that family representation on review/investigation and wider quality assurance committees sustained awareness of family perspectives for service managers and clinical leads, encouraged a wider sense of service-user involvement in informing appropriate improvement priorities118,165 and normalised wider consumer engagement in strategic healthcare management. 143 Some included studies cautioned that radical changes in the assumptions of clinical professionals and organisational managers would be required before the involvement of families in service improvement gains traction and becomes ‘taken-for-granted’. 62,149,165 Legacy work with families, along with sustained prioritisation of investments in the necessary skills and resources to manage this work, was expected to be unevenly distributed across maternity provision. 62,63,118,150,165 One paper described the effects of collaborative work between a harmed woman and a senior clinician, which led to promising changes in clinical practice and more egalitarian perspectives on knowledge and learning. 141
Discussion
This realist synthesis identified five underlying factors significant for OD in maternity settings that carry felt effects in different ways for different people. These factors are not unusual in studies of OD in general health care12,14,16,29,30,35,166–168 or more recent NHS England policy intervention. 120 However, our synthesis of these issues, incorporating the perspectives of families, staff and service managers, shows where tension and alignment in both expectations and experience occur. For example, the meaningful acknowledgement of harm to a family during an OD conversation with a clinician can later ring hollow when wider aspects of care or post-incident support or learning are felt to be lacking. 169 For families who anticipate that their experience will affect change, creating these legacies may be hindered when family insights are not translated into knowledge for clinical or service improvement. At the same time, sensitive invitations to families to discuss their experiences on their terms may disrupt the administrative pace and purpose of OD as an auditable output. 14 Further tensions emerge as families and clinicians rely on investigation findings to make sense of what happened. Different frameworks require families and staff to negotiate and reconcile multiple sources and perspectives. As different approaches to investigations of the same incident draw different conclusions, the confidence of families and affected staff in service or wider investigating bodies can be compromised.
Our focus on interventions intended to improve OD practice, rather than focusing on OD practice itself, highlights a series of underlying assumptions about how educators and policy-makers expect OD to happen, what underpins effective OD and how improvements are fostered. We identified a wide range of interventions designed to strengthen OD in maternity settings. Overall, evidence regarding the effectiveness of interventions is weak, with limited possibilities for comparison. However, with notable exceptions,141,151,153 the included reports and papers included limited suggestions for family involvement in understanding the incidents affecting them, despite over 16 years of international improvement efforts. The included papers more often documented evidence of what improvements people want, rather than what improvements have happened and to what end.
One series of OD interventions were inserted within wider improvement programmes or strategies intended to improve incident analysis or audits. OD events were reduced to single components of toolkits or items for audit, with the question of how OD is conducted and experienced largely overlooked. In these interventions, OD was considered a predictable and reportable task rather than an ongoing relationship that might address wider family needs. The extent to which these approaches meet families’ expectations of recognition and understanding of incidents of harm requires further exploration. Another series of OD improvement interventions focused more narrowly on clinician training and guidance for OD conversations. These interventions, conducted in educational rather than clinical settings, fail to consider the demands and unpredictability of unfolding OD conversations in pressurised, emotive and distracting care environments. 120 Without recognition of the organisational and local workplace conditions in which OD conversations take place, responsibilities for OD improvements are assumed to reside with trained individuals. In contrast to more singular interventions, other studies described system-wide interventions designed as forms of ‘culture change management’ for open OD improvement across local hospitals, units or services. These studies anticipate that OD improvements will be slow-paced, uneven and complex. Evaluation studies of this approach documented expected changes in staff attitudes towards openness and transparency, responsibility and risk and family involvement. In these approaches, OD improvements intersected with and informed a range of activities associated with CG, maternity safety strategies and improvements in families’ experience of maternity care. For example, in the Lexington Veterans Affairs Medical Centre directives,151,170 a ‘systems-based approach’ to OD improvement incorporated a range of technologies that included local policy development and implementation, training events, awareness raising and dedicated championship and leadership approaches. These multiple initiatives were expected to stimulate gradual shifts in formal and informal workplace practices that included local translation and adjustment of protocols and guidance in relation to work settings and circumstances. 171 In these evaluations, the implementation of OD policy found that service managers formulated their local approaches in relation to strategic principles underlain by a clear ethos and supported by co-ordinated guidance. 151,153
The recent introduction of the PSIRF in the English NHS120 also incorporates an organisational strategic approach to the involvement of patients or families in investigations and governance of these processes. 120 Some of our included studies9,151–153 considered a wider sociopolitical promise of OD as an ethical practice. As such, it encapsulates an ethos of care and communication with patients and families that includes consideration of both alternative forms of expertise and user entitlement. 9,168 This ethos is challenged in situations of poor outcome,152,172 when resources required to support harmed families and staff are eroded29 and when expectations of learning for future improvement evaporate.
Conclusions
This realist synthesis highlights the main contingencies, underlying factors and effects of OD interventions and OD practices in international maternity settings between 2000 and 2020. The focus of the most recently published documents in our synthesis has been on OD interventions in English NHS settings, where public inquiries have driven an accumulation of safety improvement initiatives and associated quality assurance measures. Our discussion unpacks some of the tensions that can arise during OD for families, staff and service managers. We question the expectation of policy-makers that disclosure, when effectively implemented, will satisfy a multitude of social and health policy interests ranging from patient justice to safety improvement and savings for services. Instead, our synthesis suggests that the anticipated effects and valuations of incident OD are more fluid, negotiable and differ in practice for different families, clinicians and service representatives. A more detailed understanding of the various organisational and wider social spaces where these negotiations occur is required to better understand how underlying relationships and resources of acknowledgement, safety, advocacy, sense-making of an event and learning are enacted in rapidly changing and challenged maternity service.
Strengths and limitations of the realist synthesis
The strength of this analysis is that the identified underlying factors for OD have been developed iteratively with input from discussions with stakeholders and recent policy interests in this field. The programme theories have been constructed based on their pragmatic relevance in guiding future ethnographic research within maternity services. 73 Following realist principles,173,174 a non-linear approach to data searching, along with the inclusion of heterogeneous evidence sources, allowed us to develop and refine our approach during the synthesis process. More traditional search strategies would have excluded many relevant sources that were not peer reviewed. At the same time, this approach included data that might not have the same rigor as data extracted in a traditional systematic review. While we have maintained a focus on international maternity settings, the most recent documents are from English health services, where there is a notable policy drive for maternity safety improvement. This may decrease the external validity of the results. These themes should be explored more widely in empirical research in both the English NHS and other health systems. In the following five chapters, which are drawn from the results of SP2 and SP3, we explore each programme theory from the perspectives of national and regional stakeholders and research participants from the three case-study services.
Chapter 5 Programme theory 1 – receiving a meaningful acknowledgement of the harm that has happened
Programme Theory 1:
When a family feels that their experience of harm and its aftermath has been acknowledged in a meaningful way, their trust in clinicians and the service is more likely to be rebuilt, clinicians involved feel some relief and ongoing care and communication post incident is more likely.
Introduction
This chapter focuses on three different aspects of post-incident communication with families: the initial communication, post-incident communication (including the organisationally mandated DoC) and the ongoing care of the family post incident. These aspects of post-incident communication are explored as crucial practices of acknowledgement of the injured family, which means that neither the incident nor the family’s experience of this is denied by clinicians or the service.
Perspectives and experiences of national stakeholders
General reflections
Most participants highlighted the importance of communication by clinicians as soon as possible after the incident for injured families to begin to feel acknowledged. Several also noted the importance of honesty. Two national leads described that OD stood as the ‘litmus test’ of an open organisation and committed safety culture. Few QI leads felt that there has been significant improvement in OD in NHS maternity care. There was an overall sense that the reported OD improvement did not capture the quality of communication required by families. A senior charity lead commented:
Parents say the same thing today that I would have said 19 years ago or someone else would have told me 10 years ago. Parents are not being told.
SG2
Few participants felt the organisational DoC had encouraged meaningful discussion with or involvement of families but rather had ‘just become another process you’ve got to do’ (Qi17). Participants rarely discussed the practice of acknowledgement beyond spoken apologies and later explanations of what happened. The provision of tailored postnatal care or compensation was rarely mentioned. Rather, participants focused on the practical and ethical challenges of honest conversations with families, particularly in relation to the demands of corporate assurance measures. As significant variations between thresholds of clinical harm determined the application of particular review and/or investigation procedures and guidelines for family involvement in these procedures.
The ‘human’ and the ‘technical’
Many participants noted a difference between the ‘human’ and ‘technical’ aspects of candour. This captured the tensions between what constituted honesty in clinical relationships, who had authority to determine how harm is defined and categorised and what this authority conveyed about organisational, professional and family interests.
For most clinicians, candour was envisaged as honesty embedded in a taken-for-granted relationship of care. Some objected to the notion of the organisation of a conversation of candour as a series of procedural steps in a mandated time frame. Referring indirectly to the DoC, they stressed the importance of a situated and responsive approach to honesty within an ongoing clinical relationship.
A senior obstetrician commented:
Candour is the start of your relationship with a patient [and is] built upon many things: integrity of what you are saying, how you are saying it and the relationships that you have developed with that person, be it long or short term. We tend to make up for that by having policies and procedures. The other day at our clinical governance meeting a senior member said: ‘did you do candour?’ and I put my hand up and said: ‘It’s not a thing!’
Qi13
Many clinicians felt that the demands of organisational compliance had diverted attention away from ‘the human story’ (FS9), thus narrowing the care of injured families. Some charity leads and defence solicitors also noted the effects of the ‘legal imprint’ on conversations with families, with clinicians fearful of ‘getting it wrong’ (PB1) and with conversations reduced to ‘legal transactions’ (ML2). Overall, many clinicians and some others considered that the organisational DoC had undermined the relational care of injured families.
Apologising
All participants agreed that an apology in person after any incident was important to all families, irrespective of the circumstances of an event. However, many commented on the difference between interpersonal expressions of regret offered by those caring for a family and routine apology initiated by organisational directives, which were less likely to be attuned to the family.
For senior clinicians, apologising was seen as the ‘human thing to do’. Many described the long-term impact of the difficulties with expressing regret to families injured in their care. These descriptions differed from the more consumer-orientated, instrumental apologising described by stakeholders from governance and commissioning backgrounds. A former commissioner commented:
And it doesn’t matter [about your Band], you say ‘I’m really, really sorry, I’ve done this.’ The family anger is when ‘they didn’t even say sorry.’ To just apologise reduces the level of anger and not admitting that you’ve done something wrong is going to cost the Trust money.
Qi15
In the discussion between clinicians and families, apologising had value as a strategy for reducing conflict between a family and a service, with legal action implied. However, for clinicians anxious about litigation, a misinterpreted claim of individual accountability made apologising feel risky. For some, the blurring of personal and organisationally directed apology was complicated by evolving understanding of the ‘avoidability’ of an incident. The risk of misconstrued apologies was also discussed by participants from Trust legal teams. Their concern was that an apology for ‘distress caused’ could be an admission of liability. Overall, the emphasis of legal teams on ‘right words’ and ‘right time’ was observed to make already difficult conversations more challenging.
In summary, in their reflections of the conditions and effects of personal apology, participants reiterated the felt tension between organisationally prescribed behaviours and personal responses to injured families. For those in corporate management, technical processes and procedures were essential to the management of risk to the organisation.
Degrees of candour
Duty and situated judgement
For many clinicians, in contrast to family representatives in charities or legal firms, a further aspect of candour in the clinical relationship was that it could be approached as a matter of judgement in relation to the family situation rather than an unquestionable ethical responsibility. For some, the questions of how and when to disclose news of an injury was a question of ‘human’ sensitivity and professional judgement.
The difference between mandated truth-telling and professional, situated judgement was especially complicated in circumstances when the severity of injury to a baby or a mother could only be established over time. For example, in situations of suspected hypoxic–ischaemic encephalopathy (HIE) which can lead to cerebral palsy, the severity might not be established for several years. In some situations, lack of certainty and clinicians’ concerns about causing families unnecessary distress became a rationale for Trust corporate teams to avoid OD. For family representatives, such avoidance was strongly opposed; for them, OD should include discussions of uncertainty because ‘families expect to be knowing what the Trust knows about the incident’ (SG6).
Reflections on the acceptability or necessity of OD in situations of uncertain harm highlight the more fundamental difficulties involved in discretionary OD practices. While sometimes exercised benevolently in the interests of a family, withholding knowledge to families could open the possibility for a strategic management of knowledge by organisations and for generalised judgements to be made about what would be best for families to know. At the same time, the support needs of families harmed by ongoing anxiety over uncertain prognoses also required a response from services.
Thresholds of inclusion
The categorisation of incident severity by governance teams defined the possibilities for families to receive the DoC. Two clinicians (FS1; FS7) identified the NHSE Revised SI Framework98 as one way that OD varied for different families with the same injury in different services. The tensions between learning opportunity and service capacity in decisions about incident classification were highlighted by several participants. The arbitrary criteria for the inclusion of families into different safety improvement initiatives could also determine a family’s access to an investigation and support. Some participants commented on the effects on families who fell outside of target populations because of cut-off criteria like gestational age.
In discussions about how (and for whom) criteria should be revised, participants touched on two distinct rationales that underpinned family inclusion in recent interventions. These were the anticipated outcomes to a family when their loss was acknowledged and the potential benefits to future families, where some individual cases contribute information for systems learning. These rationales are not mutually exclusive but did carry different implications for families at different times.
Summary of stakeholder perspectives on acknowledgement
Apart from family representatives, national stakeholders felt that the regulation of candour had disabled the situated judgement of clinicians to shape family-centred OD. At the same time, situated judgements opened the possibility for OD to be avoided or delayed for reasons besides the family’s best interests. Maternity safety improvement schemes also contributed to a managerial/procedural stance of individual family entitlement.
Perspectives and experiences of families
For family participants, acknowledgement of harm had a considerable impact on their overall journey after injury. While immediate priorities varied between families depending on the context, the way their harm was disclosed mattered. The ‘human’ aspects of this communication were fundamental to their experience. Clarity about what was known at the time of the event made a positive difference to families who were overwhelmed and confused. They understood that full explanations were not always possible soon after an event, but nevertheless valued the sharing of available information. Honesty was important even if the news was difficult to hear. Sometimes this news came as a shock, but open communication was appreciated, especially if the message was delivered in a kind and caring way. For some families, communication that harm might have been avoidable occurred as events were unfolding. For others, it came later, during or after the arrival of the incident investigation report. Whatever the situation, empathic and responsive communication was key.
Few families identified formal DoC processes, but instead referred to meetings with staff in which they learnt about the harm experienced. Families often appreciated immediate appointments followed by further scheduled meetings, which provided time for processing information and sent a message to them that questions and discussion were welcome. Participants whose injuries were not identified as avoidable, or who had no interest in raising questions about avoidability, were more likely to feel that staff had been open with them:
I think genuinely everything was done that could have been done, so therefore they could be completely honest with everything.
SU1-5,7
Honest conversations led to trust in practitioners that was lacking if there were concerns that information was being withheld. Some participants described tight guarding of information and defensive behaviour from clinical staff during initial and later conversations. This generated a climate of suspicion and a concern that staff were ‘closing ranks’ (SU7) to control information and prevent access to answers. Yet, in some situations, families revisited these initial impressions. For example, a family who experienced a neonatal death in 2015 later acknowledged that it was more likely that staff were overwhelmed with work. However, their suspicion that clinicians were guarding information affected confidence in immediate care post injury (SU7).
Irrespective of questions of avoidability, sincere expressions of regret for the injury were important to participants, even if these were sometimes delayed or prompted by a family’s insistence on further conversations (e.g. after a complaint about how they were treated). Impersonal, written apologies were more defensively phrased and less welcome. ‘Non-apologies’ (‘I’m sorry you feel that way’ SU20) were distressing for families, particularly when they conveyed the impression that the family was somehow responsible for the situation. Other unhelpful responses include being told ‘it is one of those things’, especially when, as with one family whose baby required cooling following his birth in 2008, families were discouraged from asking questions and suspected that information was being withheld (SU14).
The physical setting where OD happened was remembered as important. Although families appreciated invitations from the service after the event to discuss what took place, checking with them about how and where they would like these conversations to take place did not always occur. Women reported being ‘being crammed in a tiny room and really hot’ (SU17), which was particularly hard if the space was close to where the harm happened. One family, whose baby was stillborn in 2020, was obliged to return to the place where the event happened to receive post-mortem results:
And we got a letter through the post … asking us to attend an appointment at that hospital, where we would have to go and sit in the waiting room amongst all the other pregnant women whilst we wait for the second half of the post-mortem results.
SU16
The right words used at the right time matter, but the location also needs to be considered for the message(s) to be delivered with sensitivity. Honest, prompt and in-person OD conversations were important to families. It was appreciated that a complete picture of what happened would not be immediately available.
Perspectives and experiences of in the case-study services
The purpose of open disclosure
Clinicians with OD responsibilities from all case-study services noted that the overall purpose of OD was to recover a family’s trust in the service. Several clinical and service leads noted the negative effects of the wider public mistrust because of some untrustworthy maternity units and felt the need to mitigate these concerns for each injured family who ‘think we are not going to be honest’ (SCSi16).
Several senior clinicians felt that having to respond to families in the light of this public concern, rather than to a family’s experience of an incident itself, was the most challenging aspect of OD work. Four key elements were felt to be necessary for OD that helped families to recover trust. These were the speed at which the initial conversation with a family happens, the tone of initial OD meetings, the management of information at the meetings and the organisation of investigation procedures to minimise complications and confusion for families.
The first moments of the initial conversation were also considered to be crucial in opening a dialogue with that family otherwise ‘you’ve lost the trust of patients’ (SCSi16).
A family’s wider experience of care was also discussed by participants as important to the undermining or nurturing of trust:
The care has been like, what the outcome has been, the support they got after that, whether they felt supported during their labour or their admission, whether they felt that had a good MDT around them, I think there are many factors.
SCSi08
One of the three case-study families vividly remembered the care they received from one member of the staff involved in their immediate post-incident care. During a difficult labour and after care, they remembered her as the ‘one person there to support them’ (SAFi3). This family felt that, apart from later OD conversations, very few front-line staff were able to acknowledge the immediate effects of the injury on the family.
Completing the Duty of Candour
A narrative overview of OD processes and practices in the three participating maternity units is presented in Appendix 4, Box 6.
The first stages of OD comprised two distinct activities: an initial conversation and apology soon after the incident, ideally done by a senior clinician where incidents were expected to have serious outcomes, and a mandated organisational directive completed by a member of the CG team or Head of Midwifery (HoM). Depending on the time of the incident, different clinicians, risk midwives, risk leads, unit or shift leads or clinical ‘debriefing’ leads might lead initial conversations. In contrast to the national stakeholders interviewed, not all maternity staff considered the tension between ‘procedural’ and ‘human’ aspects of OD. For many clinicians, the completion of the DoC was not felt to be onerous or distracting from providing care. Some clinicians felt that this regulation had benefited families and staff because there was now greater local acceptance of this previously marginal practice. However, clinicians widely agreed that completion of the regulated duty (represented by a Datix tick box) failed to capture the nuanced and time-consuming work involved in this wider process. A clinical lead at Site A argued that the way any clinician manages good OD is ‘only out of kindness because it hasn’t been resourced properly’ (SASi36).
Staff involved in initial meetings
In Sites B and C, clinical or service leads usually led all daytime meetings with injured families. At Site A, the CG team, and usually risk midwives, completed the DoC, and sometimes, the initial discussion with a family. Clinical and service leads were more confident and better positioned to convey trustworthiness. They were also likely to be more distanced from the events immediately surrounding the incident. Their involvement was expected to ameliorate harm caused ‘on the shop floor’ (SASi12).
There were mixed views whether staff more directly involved in a family’s care should be present at initial or ongoing OD meetings. Depending on their personal experiences, some clinical leads felt that while some families would find comfort in these meetings, some families might also use any unguarded expressions of regret as later evidence at inquest or to bolster a future complaint against the service or clinician. These different views on inclusive OD as a potential source of healing or potential source of professional risk to a clinician or a service highlight the ongoing concerns by clinical leads over the unclear boundaries of ‘safe space’ within actual judicial processes.
The risk midwives at Site A were differently positioned in OD processes because ‘this is where their relationship starts’ (SASi12). This relationship with the family was envisaged as a first opportunity to acknowledge injury to the family and rebuild trust in the service, rather than with individual clinicians or teams. However, families did not necessarily envisage CG work in this way. For example, Fay’s parents described their shock at being first approached by a risk midwife and what this could mean:
So this risk midwife turned up and we were like, wow, right, this is really serious and we go the impression that there was some sort of litigation reason for her to be there which was really alarming then she said ‘You potentially have grounds to sue the NHS because of what happened’, that’s the message we got.
SAFi1
For these parents, already angry with the maternity care they had received, clinicians involved seemed to be avoiding them. They never encountered this clinical team again, and, several years later, felt that they ‘never truly acknowledged us and learned from their mistakes’ (SAFi1). However, they later came to appreciate the honesty of the risk midwife.
In all study services, bereavement midwives distanced themselves from conversations that might relate to avoidable harm. They emphasised their role in the support of all bereaved families, with the support of families affected by avoidable injuries often passing to risk midwives or senior clinicians in the CG team.
Contexts of early disclosure conversations
Clinicians also often noted that early conversations after an incident were poorly remembered by most families because of exhaustion or shock. However, our family interviews indicate that initial events and the tone of conversation are vividly remembered by families for attitudes conveyed, if not for the information given. Clinical scenarios where prognosis is uncertain presented greater difficulties to offering solace to a family:
Where it’s clear that there has been an absolutely devastating outcome, then it’s ‘I’m sorry for your loss’. It’s easier to offer with a hard outcome. Whereas for the babies that are having ongoing care you don’t want it to sound like you think that baby’s going to die because hopefully the cooling is going to help.
Clinical Lead SDSi06
Two of the four Site A families remembered the immediate shock of the first conversations where clinicians raised the possibility of avoidable harm. Hearing this news came as a ‘bomb shell’ (SAFi1) or ‘like being hit by a bus’ (SAFi04), regardless of if this news was given in person or by phone. However, as most clinicians noted, the initial moments or hours between the incident and the initial meeting are vividly remembered by families. This timing sets a tone of trust or suspicion for this conversation and the wider process. Three of the Site A families felt that these initial meetings were honest because they were prompt.
Overall, all disclosure leads agreed that conversations, more than written correspondence, were important for mitigating the distrust of a family that was often inevitable post incident. Ideally, initial, formal OD could be conducted in the hospital, where families could be met in person. Even then, detailed co-ordination of family care was needed across day and out-of-hour shifts, where clinical leads and risk teams were often concerned about misinformation or misunderstandings that could undermine fragile relationships. Out-of-area communication with families, more often required at Site B, where neonatal intensive care required hospital or service transfers, was especially difficult to organise. Many risk midwives found that completing the formal DoC conversation with a family discharged home without an initial meeting, especially difficult for everyone. The invisible and ongoing work of some risk midwives, HoMs and clinical leads to manage some consistency in OD processes for some families against the flux of staffing and the speed of family transfers is notable. However, for families themselves, careful written correspondence was an important and memorable way that clinicians acknowledged them. The enduring emotional value of carefully personalised DoC correspondence was highlighted during some interviews with families.
Participants often noted the differences in the responses of individual families to both injury and initial and subsequent disclosure meetings. One experienced CG lead described each meeting as ‘just so very unique’ (SCSi01). The need to understand each family’s response to an incident, in terms of what they want to know and how far they want to engage, was emphasised by most participants. Senior clinicians described a range of embodied and material techniques for adjusting a meeting to the family situation.
As indicated above, meeting preparation was described by experts as vital for minimising further distress to the family. All participants described the need for time and space to prepare for initial conversations with a ‘knowledge of the facts (by reading the notes)’ (SCSi14) and by checking with colleagues ‘to just get a barometer of how things are’ (SASi01). One risk midwife noted the importance of memorising all first names and the baby’s weight in advance of the meeting, not only to personalise the conversation but to ‘look like you’ve made some degree of effort’ (SASi01). Meeting preparations were, then, important resources for recognising the injured family by ‘ethical performance’. 175 Preparation and anticipation allowed for degrees of proximity, opacity and engagement to be adjusted in response to the family’s behaviour and apparent needs.
Ongoing care of injured families
Many clinicians, including CG teams, envisaged care and acknowledgment of some families as extending far beyond meetings, letters, direct expressions of regret and the support offered in multidisciplinary pregnancy aftercare pathways or specialist midwifery debriefings. One risk midwife spoke of ‘that special treatment’ (SASi16) that some families received. This was offered to a few families where individual clinicians built closer relationships and a strong moral investment in their situation over time. Sometimes, this support for a family’s interests continued against the advice or support of service managers or Clinical Directors. The interviews with most clinical and service leads in Sites A, B and C indicate that their extended care of families is not reducible to instrumental concerns with ‘complaints reduction’ or the management of litigation risk. Rather, this compensatory work, sometimes discussed as the most rewarding aspect of CG work, was about the alleviation of injustices faced by some families (e.g. a family being denied an investigation in into their incident because they fell below agreed investigation criteria).
The four Site A families expected that, given what had happened to them, the service would be interested in them after their discharge. In some cases, this happened. For example, a clinical debrief lead at Site A had stayed in touch with one woman over several years in an advisory capacity. This woman described how this ongoing attentiveness after her baby’s death was important to her in both practical and emotional terms. This family was the only one that felt that ‘things were changing’ and who described a change in their position from ‘a lot of mistrust’ to ‘having some confidence’ because of this clinician (SAFi4).
This ‘special treatment’ of some families relied on considerable discretionary effort. However, this ‘ethics on the ground’176 created procedural exceptions, with this care unavailable to those less well situated for building rapport and relationships with some staff. Also, as the experience of the Site A family illustrates, in some situations, this recovery of trust was in individual clinicians rather than wider teams or services and could undermine, as often support, the recovery of confidence in services or organisational processes.
Avoidance of disclosure
Given the social and emotional complexity of OD work, it is unsurprising that some clinicians avoided these conversations. Particularly in 2021, at the most highly pressured services, senior clinicians discussed the intensity of shift patterns, escalating workload and associated risk contributing to situations where staff ‘sometimes feeling that they were moving from one incident to the next’ (SASi36). Clinical leads in all services felt that a traumatised workforce without the ‘bandwidth or capacity to have those conversations’ (SDSi19) made avoidance inevitable. Notwithstanding these issues, clinicians who led OD processes at all services, felt that, irrespective of possible training opportunities through services, Royal Colleges or charities, several of their colleagues would continue to avoid any involvement in OD conversations because personal admissions of error or the sense that ‘we could have done something differently, this could have been different’ (SCSi05) challenged fundamental aspects of their professional identity.
More generally, it was felt that many clinicians continued to fear the implications of offering an apology to a family for an incident due to wider social assumptions about the admission of liability. Additionally, several senior clinicians recounted the personal stress and professional upheaval of coronial investigations ‘that can happen to anyone, whether you’re doing a great job or not and it’s a process that takes a heavy toll’ (SASi20). Particularly, for less senior clinicians, the most significant barrier to acknowledgement of injury and its effects on a family was the fear of investigation by professional regulators, a coroners’ court summons, or the risk of becoming drawn into a family’s legal claim against the Trust.
Some clinical staff in all sites drew a distinction between actual incidents of this kind and their ‘omnipresent threat’ (SASi01). This view contrasted with that of trust solicitors who felt that the challenge was to make clinicians more aware of litigation risk. A senior Trust and service lead observed this fundamental contradiction between ‘safe space and nervousness of the legal’ (SCSi14) and the differing objectives of CG and the legal team. They described:
I’ll get my legal team saying ‘No, we can’t share that information with a family because it’s just opening another claim’. It’s a conflict between being open transparent and doing that in a safe way, the systems don’t align, to be honest.
SCSi14
This contradiction placed CG teams in a difficult position with some families. More often, and particularly in situations where outcomes for a family were expected to be costly or unjust, they informally supported the families in taking legal action against their Trust.
The outcomes of disclosure for families
All clinical and service managers interviewed commented that they usually had little idea of the way that they managed disclosure process, and the ongoing care of some families was successful in re-establishing a family’s trust in them or confidence in the maternity service or NHS. Governance leads might estimate overall success from changing number of complaints when non-disclosure had occurred; however, these estimates relied on variable aggregations of data from complaints services. The organisation of complaints reporting within and between services made trends difficult to follow unless they were actively identified. At Site A, some service and corporate leads simply explained that ‘candour is something that we just don’t have a problem with’ (SASi31). Across the services, it was agreed that the impact of post-incident communication on any family’s decision to take legal action was complex and often unpredictable. More often, clinicians gauged the success of OD by incidental discovery that a family they knew had returned to that service for a subsequent pregnancy. However, this informal indicator of success overlooked variations in access to other services.
In all, it was often difficult for clinicians to gauge the success of their efforts to shape OD in ways that acknowledged different families’ responses and ongoing bereavement.
Interim findings and chapter summary
In contrast to many national stakeholders, most clinicians in the case-study services did not feel that the introduction of an NHS DoC had cramped or undermined OD conversations with families. This contrast may indicate some success in the case-study services in promoting practices of openness that were not overly constrained by regulatory demands. However, the escalating demands of safety assurance within the maternity service were perceived as taking time away from meeting the needs of injured families. From the perspectives of clinicians in the case-study services, the more immediate challenges of disclosure work were the variation in incident and OD situations as well as investigation process, as well as the unpredictability of family needs and situations. Without service recognition and resourcing of disclosure communication, and of the co-ordination work across and beyond services to sustain this communication, clinicians tended to provide exceptional care to a few families who became their ‘just cause’. The sometimes uncomfortable and largely unknown consequences of OD work also encouraged the discretionary care of injured families.
Nevertheless, the FF and the PAG forum encouraged us to revisit the tension between an impersonal ‘tick box’ procedures driven by service needs and a personalised and empathic approach that many families desired. At these forums, families commented on a system that automatically presumed that families were interested in blame and retribution and that interrupted the possibility of their need to find out what happened. Forum discussions began to explore what an empathic approach would look like, in terms of the adjustment of initial conversations, and highlighted the need for clinicians to be ‘empowered to embrace their own humanity’ (FF participant) in their relationships with family post incident.
Paradoxically, while all clinicians saw OD work as important for re-establishing relationships of trust with a family, OD was hedged by various measures, both personal and corporate, to regulate the flow of knowledge to families whose responses to this information might compromise reputations or threaten legal action.
Chapter 6 Programme theory 2 – being involved during the review/investigation process
Programme Theory 2:
When families are included in these processes if they decide, and have support for this involvement, they are less likely to feel alienated and distrustful of services and are more likely to be heard in discussions about the event and their care.
Introduction
This chapter examines the potential and the challenges of including the experiences and perspectives of injured families during NHS reviews and investigations. Representation is explored, examining factors such as the organisational structures that might facilitate the inclusion of family priorities in review and investigation processes, the framing of family insight and its associated credibility within organisational procedures and in clinical practice and the wider institutional contributors to these processes. The implementation of a series of national and local interventions to encourage family involvement is examined, primarily from the perspectives of clinicians and other staff leading on this work.
As in Chapter 5, these issues are explored from the perspectives of national and regional stakeholders, including families (who had experienced avoidable harm between 2007 and 2021), and from in-depth organisational case studies in three maternity services. Interpretations have been refined in discussions with staff, families and managers in interpretive forums.
Perspectives and experiences of national stakeholders
What is meant by family involvement
Across the case-study services, there were a range of definitions of family involvement. Clinicians understood involvement as the process of asking a family if they had any questions or concerns during a DoC conversation, offering a meeting to discuss family questions, requesting questions about the draft report and providing a final explanation when the report content was agreed by the Trust. By contrast, charity and HSIB leads envisaged a more open and reciprocal approach whereby family perspectives and concerns informed the scope of a review or investigation, the ToR, the emergent findings, draft reports and final action plans. Without this sort of involvement, these participants felt:
it’s not unusual for a Trust to do what they think is a good job investigating and to share it with the family at a very advanced stage when in fact it has already been signed off and can’t really be changed.
SG6
A widespread experience of national stakeholders was that there was a lack of family representation in internal SI investigations. Informal and less visible work on CG teams and clinical leads to represent family interests and perspectives in service-level reviews and Trust-level investigations was overlooked as involvement work.
In addition to holding individuals and services accountable, families needed to revisit the events, in their own terms, as they experienced them to make sense of what happened. One charity lead explained:
This gap between what clinicians know and what parents go away with, it is about the entire narrative of that day and the need to process a life-changing event for a family.
SG2
To meet this need, this participant noted, the incident must be approached in ways that were different to clinical or safety improvement frameworks and that had the inclusion of family personal experience as a starting point.
The Perinatal Mortality Review Tool
Nine participants considered the variable effects of the implementation of the financially incentivised (in England) PMRT, which includes prompts for disclosure and inviting questions from parents about their or their baby’s care. Several noted the importance of this tool to provide ‘a coherent answer to what happened’ (Qi6) because it was designed to include multidisciplinary and family perspectives. However, most participants agreed that PMRT implementation in Trusts was stymied by a widespread lack of service-level investment in skilled staff with time for ‘that type of conversation’ (FS5) to ‘understand how a family is feeling’ (ML2). Local service capacity for the review determined whether families were ‘invited into the investigation process or just … asked “can you send us some questions?”’ (FS5).
Some participants noted the increase in the percentage of parents reported to have been informed of a review. Some improvement leads also suggested that the online prompts for reporting family engagement that were built into the tool could act as an important ‘signalling exercise’ (Qi6). However, most also noted the practical and ethical difficulties of asking time-squeezed staff to initiate ‘people-related difficult conversations where you just don’t know what a family is going to need’ (Qi20). They worried that the simplification of this work from ‘actual engagement and the desire to change things for families to a tick-box’ (Qi11) was enhanced by the financial incentivisation of the tool through the Maternity Incentive Scheme. Participants cited examples of midwives responsible for tool completion limiting family engagement to e-mail correspondence or simply asking colleagues for any signs of family questions or concerns.
As with the discussions about the DoC, participants who were clinicians stressed their concerns that the implementation of national safety improvement programmes reduced the emotionally demanding, skilled, intricate and unpredictable conversations with families into an administrative procedure. Several participants noted that despite the provision of sensitive guidance on family engagement, the completion of the financially incentivised tool was directed by organisational rather than family needs.
Family representation in Healthcare Safety Investigation Branch investigations
Almost all participants who were also practising clinicians felt that family engagement in the HSIB maternity programme had been positively received by these families. They felt that this had encouraged a wider reconsideration of family engagement in Trust-based (or internal) investigations. Several factors contributing to the success of HSIB’s family engagement approach were identified. First, it was felt that more families would engage with HSIB because it was independent and perceived as trustworthy. A senior HSIB lead commented that before this programme, ‘families would have felt that nobody was even vaguely in their corner’ (Qi4). HSIB leads described family involvement as a ‘moral compass’ with guiding values of ‘openness, honesty and transparency throughout relationships with the family’ (Qi1). They felt that concerns about reputational and litigation risk for the Trust created a conflict of interest when applying these values. Second, the HSIB approach was underpinned by centralised strategic planning and funding. Senior HSIB operational and family engagement leads brought practical expertise from non-maternity healthcare settings, emphasising the need for interpersonal and organisational support systems for investigation teams and the ongoing development of family engagement support tools and facilities. Finally, responsiveness to family needs was central to the practice of the investigation teams. In some situations, senior leads modelled an approach to family engagement that included home visits, which created ongoing opportunities for families to ‘talk through their story’ (Qi8) and to develop family care directly from knowledge of their needs.
Some services, particularly senior midwives, worried that HSIB family engagement work undermined the relationship between families and the NHS. Some midwives also reflected on the impact of external investigations on the morale of service staff. Despite this, the contrast between the type of family representation promoted by some PMRT questions and the type of representation that occurred through a well-resourced national organisation with the capacity to develop strategic and operational plans for family engagement was stark.
The impact of national safety developments on staff and families
Many participants noted that the introduction of multiple review and investigation systems was a barrier to improving disclosure with families. This was a point of frustration for some clinicians. Participants felt that, particularly since 2018, both families and clinicians have been faced with an ever-expanding range of national safety improvement initiatives. Many identified a sense of disconnect between national ambitions of maternity safety improvement, the implementation approaches used (notably, incentivised schemes with regular assurance reporting), and actual, felt changes in services. This situation left clinical and service leads feeling ‘frustrated’ (FS11), ‘overburdened’ (Qi5) and ‘overwhelmed’ (SG2) with a ‘well-intentioned, brilliant, but complicated jigsaw’ (ML2). Misunderstandings over referral criteria or thresholds of severity led to situations where some injured families ‘slipped though the investigation net’ (SF5).
Attempts by national safety improvement leads to consolidate the reporting tasks of clinicians with the construction of single reporting portals were welcome. However, the need for clinicians to respond to multiple initiatives with different information requirements remained. The overall effect was that ‘people still feel there is just lots of different bits (of reporting activity) without specific purpose’ (Qi4). Participants also indicated that families required ongoing advice for understanding these schemes, yet this task often fell to families themselves. The ongoing efforts demanded of staff to stay abreast of complex and changing schemes could reduce the time spend with families and a sense that this time diverted attention away from systems designed to include them. The introduction and rapid development of multiple and sometimes overlapping programmes to improve maternity safety investigation and family involvement were complicated by a lack of capacity to keep up to date on changes, rendering clinicians ill-equipped to provide the expert reassurance that families required.
Perspectives and experiences of families
The maternity care reported by the participants of this stakeholder group spanned the years from 2007 to 2021 and the landscape of reviews and investigations varied considerably in that time. Despite this, few reported good experiences of inclusion in reviews and investigations. In common with our findings related to receiving a meaningful acknowledgement of the harm that has happened, those with good experiences appreciated being fully informed, even if they were not directly involved.
Most of the families received care before the HSIB maternity investigations programme began. Of the more recent cases, only six triggered a HSIB investigation. Positive experiences of these investigations were reported by two families who had more recently been involved. The independence of HSIB was reassuring for them during the investigation process. Being part of the process included contributing to the HSIB review ToR and being given periodic updates on timescales as well as a draft report to comment on. ‘Being kept in the loop’ (SU5) was helpful for families. However, HSIB involvement was not as positive an experience for the other four families. Some parents wanted closer involvement (e.g. to meet with reviewers or attend meetings themselves) and some families felt that providing statements about their experience and its impact on them was too demanding of them. This highlights the importance of a personalised approach to family inclusion.
Rather than being an integral part of Trust-level investigation processes, families often reported being excluded. Even if asked for information, their contribution felt separate from the rest of the investigation.
Some women whose cases were reviewed by HSIB were not asked for any input, which was particularly upsetting if perceived ‘crucial moments’, such as when SU17 reported reduced fetal movements in response to a question from a midwife on the antenatal ward, were missing from the report:
That moment haunts me and it angers me because when they did the investigation, that moment was not mentioned at all. It was not in there. And when I called and said, ‘Why is this not in here?’ they then went away, did some research and said, ‘Nobody remembers this happening’.
SU17
Even when reports were received, they did not always provide answers to women’s questions and finding out what was happening during investigations ‘felt like a battle’ (SU5). Most families hope that reviews and investigations will lead to lessons being learnt by the service but often families were looking for more information for their own learning too. Absent or incorrect information created limitations on the learning that could occur, both for the service and for parents who wanted to find out what happened.
Families in this stakeholder group were clear about the support they would have found helpful. Feeling on their own in the immediate aftermath of harm occurring was a common experience. Several families mentioned how much they would have appreciated clear information on the review and investigation processes and who they could contact for support. A helpline or procedure document and named contact/family advocate were suggested. Being able to trust their contact was important to families, which often meant having someone independent of the hospital. Families who have experienced harm, especially if they have felt excluded from investigations, find it hard to believe what they are told by the service and many are suspicious of the independence of reviews. Our data support the proposition that inclusion in reviews and investigations is important in helping families develop greater confidence in clinical teams and the reviews produced and helping them to feel less excluded. Where this does not happen, harm can be increased.
Perspectives and experiences in the case-study services
The organisation of post-incident family involvement
Data from the three case-study services were used to establish a diagrammatic representation of family involvement in reviews and investigations, focusing on Trust and service-level processes (see Appendix 6, Figure 5). All case-study services followed DoC procedures including identifying a named linked person for each family. Some clinicians also initiated responsive link arrangements with families already known to them, occasionally working across services and teams as an ongoing contact. Most clinical leads and CG teams felt that service resourcing, to develop more coherent structures for family representation post incident, was inadequate and were aware that ‘many families with questions [were] falling through the gaps’ (SDSi06). While some clinicians justified this as a difference in families’ interest in engagement, others highlighted a lack of time for family outreach and the poor commissioning of language services as contributory factors. Issues of service capacity were interconnected with distinctive patient-flow patterns in maternity services. The most prominent of these were the rapid throughput of families from hospital to community services and the transfer of babies requiring intensive care across hospital sites and services or between Trusts.
Communication with families was difficult and incomplete when conducted by e-mail or telephone. The situation was improved when families were visited in person at nearby neonatal units. For example, a senior neonatologist described that the ongoing updating of families on the emergent process and findings of reviews and investigations was more an aspect of day-to-day communication within the unit because, compared to maternity professionals, ‘it is more in our nature to be constantly explaining’ (SASi06).
Service capacity for encouraging family representation in review and investigations differed between the case-study services and in relation to the differing attitudes of the CG teams towards the risks and advantages of family involvement. In Site A, where there was greater reluctance to establish processes for involving injured families, CG teams were more likely to work within DoC procedures, where families were invited to contact a named link person if they had concerns or questions. At Sites B and C, a more proactive approach to involving these families had been introduced. One senior obstetrician explained:
Historically, we have situations where even when the woman had the letter, they didn’t know who to contact so they felt very alone so we’ve tried to build in gentle touch points to update them and say, ‘is there anything you want us to make sure we’ve covered?’ And some will send an e-mail and other families we’ll meet with them.
SDSi06
Nevertheless, even in services taking a more progressive and proactive approach to the involvement of injured families, initiating and sustaining this process required the staff to encourage first contact, respond to expressed needs and to incorporate family perspectives into panel presentations, discussions and reports. The value and undeveloped possibility of community midwives representing injured families during investigation processes was noted across all three services.
Determining facts with families
Across the case-study services, both CG and lead clinicians described several different rationales for ensuring that families were represented in review and investigation meetings and different ways that insights from families were elicited and included in investigation processes. Most often, family representation was understood to be about the exchange of factual details about the incident between CG teams and families. These exchanges happened in response to those families who had themselves contacted the CG team with a question about the incident. However, CG staff valued these family enquiries:
And when they come back to us with an e-mail full of questions, of this is what we want answered by the review panel. Which is great because it gives us a real steer and you feel like you are doing a good job for them [because] you can answer what is actually on their mind rather than what we think the priorities are.
Risk Midwife, SASi01c
Without ‘getting a steer’ on what a family might want to know, the CG teams felt less able to anticipate how a family might respond to report findings and might overlook what is important to a particular family.
In some situations, families were invited to draft their own factual accounts and chronologies of events for incorporation into the risk scenario, which was otherwise derived from clinical records. However, these contributions were most likely to be included where a family could produce ‘hard evidence’ (SASi1b), such as smartphone records or photographs where there can be ‘no debate’ (SASi1b). CG teams often noted the difficulties of dealing with unsubstantiated accounts from families, especially where these insights were missing from or contradicted the clinical notes. In these situations, it was almost always assumed that the family had forgotten or had misinterpreted events or conversations. CG teams agreed that the reason for building a factually detailed risk narrative of the event was to improve the depth of information available to panels and, from this, to improve the quality of a report sent to the service and parents. The inclusion of information from the family meant the CG team ‘don’t feel the need to revisit things after the report is published’ (SCSi04) and avoided a situation where ‘if there was some crucial bit of information that they had, and we didn’t know then the whole thing slightly unravels’ (SCSi06). There was an awareness amongst CG teams that without inclusion of a family perspective, reports produced by them could be dismissed by some families as ‘full of lies’ (SASi16). Additionally, CG teams felt that the inclusion of family perspective in the incident investigation was important for demonstrating that their service was not defensive or duplicitous.
Of the four case-study families (all from Site A), two had had their incidents investigated internally rather than through HSIB and all had contributed towards their investigations by adding factual knowledge of events that was absent from clinical records. One family had not been notified of the internal investigation of a serious near-miss medication error. They felt that ‘the service had shown itself as defensive’ (SAFi03) by not informing them of the planned investigation, and ‘unwilling to learn’ by not including their perspectives on the incident. A clinical risk and debrief lead met with them to re-examine the incident. Using this family’s factual account with time-stamped photographs, the clinical risk lead initiated changes to drug administration equipment in the department and across the Trust. However, this consultant described his meetings with this family as unusual. He felt that, unlike some families he met, this family was interested in system safety concerns as well as their isolated case (SASi20).
The significance of family experiences
In addition to determining the facts and timeline of the case, at least initially, most families wanted to determine their own frames of reference for their engagement with services. These were more often highly detailed, personalised narratives, related to feelings and memories surrounding the event. This immediate priority for families often eluded staff who were more engaged with evidence gathering for risk identification and learning. For example, a risk midwife commented that, when you start to ask a family what they want to know:
We ask ‘is there anything that you want us to raise on your behalf so it can be discussed?’ Nine times out of ten, we will get questions from the patient to say, ‘This is how I felt’ and you have to respond to that.
SASi01
Clinical governance teams and other clinicians, as this risk midwife indicates, engaged with injured families because the experience of these families demanded in-principal acknowledgement of their situation.
There were several ways that CG teams and risk midwives managed the tension between collecting facts from families and recognising other means of family representation. For example, in Site A, some risk midwives kept separate notebooks of family reflections on the impact of their injury. At least during the research period, the use of family reflection documents appeared to be for personal reference only. These documents were managed in addition to records of family descriptions of events for the risk record. Across all services, the stories of some families were remembered by CG teams and clinical leads as important and enduring reference points that informed their personal approaches to injured families. These also became integrated into in-service teaching sessions as it was hoped that they would enhance collective approaches to care.
As mentioned in the previous chapter, some clinicians developed close relationships with some injured families, that often extended beyond their core work responsibilities. For example, they sometimes called to check if a family was prepared for a meeting, accompanied them around the hospital and arranged or escalated various outpatient appointments. At Site A, risk midwives identified themselves as family representatives because of their wider interest in the experiences of families beyond the risk record. According to one risk midwife there:
So we say before at the end of the panel meeting, in summary, ‘if the parents were watching us now, are we agreed and assured that we have discussed everything you would want to know as a parent? that we’ve done everything that we possibly can’. Just to draw people’s attention back to the fact that this is a woman and baby that we’re talking about. That there’s a family hurt at the end of it.
SASi04
Our field-work observations were that the possibilities for improving panel meetings to better accommodate family perspectives were very limited at this site. For the most part, panel discussions focused on questions of informed choice about maternity care and on the reliability of a family’s memories about events. Despite CG team and some clinicians’ best intentions, most panel meetings observed pivoted on the construction and defence of risk and its management (see further discussion below).
Parent involvement in the Perinatal Mortality Review Tool
Five PMRT panels were observed in two services (Sites A and B) and 10 staff regularly involved in PMRT work were interviewed. One of the panels observed reviewed a case of serious harm that was also investigated internally. In all three case-study services, attitudes towards parent involvement in the PMRT were entangled with the wider implementation challenges of the PMRT.
There was a significant difference in the attitudes towards the PMRT at Site B (a PMRT pilot service), and the other services. At this former pilot site, a consultation obstetrician led on bereavement care and PMRT completion and, from their perspective, the PMRT carried significant value for learning across the service and the Trust:
We feed the findings up to the mortality surveillance group within the hospital [and] it’s increased the awareness of the importance of mortality review so now maternity had helped lead improvement of reviews of death in other specialities.
SDSi12
This PMRT lead also noted the ‘huge potential’ of the PMRT across her local network that was lost without ‘having the time and resource to be able to do everything as you would like it to be done’ (SDSi12). However, this PMRT lead noted, along with risk midwives and clinical leads at Sites A and B, that improvements to the design and content of the tool to avoid the need to complete many questions that appeared to her to be unnecessary would avoid some duplication.
It is quite laborious and quite repetitive, but I think you can get useful stuff out of it if you used it properly.
SDSi12
Without a clear understanding of the potential of the tool to generate learning for their own service or Trust, staff involved tended to feel that ‘the PMRT is a lot of work for not very much insight’ (Fieldnotes, PMRT meeting, Site C, 2 September 2021). This perspective was notable at Site A, where staff learning forums had been significantly diminished in recent years (see later discussion). Site A risk midwives and clinical leads were particularly frustrated with the prescriptive design of the tool and the poor functionality of the web pages.
Across the three case-study services, responsibility for tool completion was differentiated between maternity and neonatal cases. However, at Sites A and C there was an ongoing lack of clarity over who was responsible for family involvement and for completion of these sections of the tool. The senior risk midwife at Site A reflected:
There’s a tension between where responsibility for the PMRT sits, in clinical governance or in bereavement. It feels like the bereavement team feel like it’s their thing, but they don’t really want it. But they’re pissed off when the clinical governance team get involved.
SASi1c
At Site C, where a recently appointed obstetrics lead for maternity quality and safety was especially keen to engage staff, it had been possible for the lead bereavement midwife to negotiate the PMRT responsibilities that had originally fallen to her. They explained that until recently,
I would complete the PMRT summary of care and then complete all sections of PMRT [but] now we’ve got a wider team to grade the care as it’s always weighed heavily on me to ensure I’m grading someone’s care.
SCSi04
At the same time, and most notable in neonatal care settings, senior medical staff questioned the effects of the tool on undermining their own clinical expertise:
There is no space for judgement about what questions you should be asking. You can’t actually get to anything important.
SASi06
Besides the ongoing tensions evoked over clinical responsibilities and judgement, the implementation of the PMRT was particularly challenging during 2020. During this year of exceptional pressures on staffing and maternity care, staff worried about care quality and how to reach judgements of care. Additionally, time for discussion with colleagues was often surrendered to meeting reporting timelines into the Trust and so guarantee financial benefit.
Clinicians’ frustrations with the PMRT at this time impacted on staff attitudes towards the representation of parents during these reviews. Of the panel meetings observed, the time and space given to considering parents’ concerns and questions were limited because of scheduling and difficulties with accessing the website pages for uploading information. There were parent questions that were not mentioned at all because the panel agreed that a bereavement midwife had already answered them. There were also questions considered to be so unfocused that an answer during the time and space available was not possible:
Ginny (the obstetric risk lead) notes that one question asked by the parent. Jane (the risk midwife) says: ‘it’s a very vague question which is “what happened?”’ The panel quickly decide that they will explain to her about a Strep B infection as that is what they believe the case of death was.
Fieldnotes, PMR panel, 2 August 2021
Panels tended to reduce explanations to parents into single clinical causalities (e.g. ‘it was a failing of the placenta’ or ‘it was a severe infection’). Overall, an indifference of clinicians to the consideration of baby deaths during the PMRT process was noted by researchers as they were often considered to be the responsibility of the bereavement midwife:
At the close of two PMRT meetings, both completed in less than 30 minutes, the risk midwife chairing the panels exclaimed ‘that was record speed! We can fit a few more in next time!’
Fieldnotes, PMRT meetings, 5 July 2021
In all, the PMRT had most significance for staff as a means of including families when it was used alongside responsive family updates and in-person debriefings where ‘you have that meeting people and interacting on a face-to-face human basis’ (SDSi12). One approach for improving a more empathic approach to families during the PMRT was to include a family representative onto the panels.
Other approaches to the representation of families
Family involvement leads
Possibly in response to reported challenges of PMRT implementation, in 2019, Site C introduced arrangements for a long-established patient and public involvement (PPI) and MVP lead to represent the interests of families during PMRs. This arrangement at that time was triggered by a family request by an obstetric risk lead who ‘had felt for a long time that this is part of the national ambition’ (SCSi07).
Since then, several families have been offered this option for their PMR. This took considerable time to introduce to staff and essentially relied on a long-established working relationship between this lead and service and clinical managers. She was able to reassure clinical and management staff about their concerns about patient confidentiality (with parents consenting to sharing of their notes) and about risks to her own emotional well-being. Her contribution as a family representative at the review panels appeared to vary from case to case, but essentially involved her overseeing the panel. For example, in more complex cases where the impact of care on outcome was discussed, she sought to ensure that ‘parents; wishes were respected’. More generally, she saw her role as making sure that the panel was objective and held the service responsible if necessary.
The outcome of family representation in PMRs led to change in the tone of panel discussions, with greater awareness over the use of language in ‘an almost humanising way’ (SCSi07). She felt that the PMR was less of a ‘tick box exercise’ (SCSi07) with a parent representative present at the panel. The future of this intervention at Site C was uncertain as its success relied on the vision of an obstetric risk lead and her long-established relationship with several service managers and one PPI lead.
Families representing themselves on investigation panels
Some families at Site C were invited to attend their own investigation panels. This intervention was supported by a member of the Trust Board. She explained:
Parents at the meeting presents a very different meeting that’s not actually the clinical facts, and the perception of what’s really important. SI panels can be very mechanical with no one taking to the parents. When you put parents in the room, they can’t avoid it. And they don’t get a report they’ve never had sight of before.
SCSi14
Family presence at panels was seen as changing the tone of the meeting. Besides encouraging professionals to communicate more clearly and effectively with one another and to ‘stop using abbreviations’ (SCSi14), clinicians were less likely to approach the event as an ‘inhuman procedure’, and as more than ‘just looking at sets of notes and statements’ (SDSi07).
However, for a variety of reasons, many clinicians working at service level did not share in this aspiration for panel reform. For them, the issue was ‘getting the best out the panel for the best report for parents’ (SCSi01) and direct parent involvement was expected to confuse this objective. More immediately, some clinicians noted concerns that families may feel alienated, out of their depth or may be ‘needing translations of the jargon all the time’ (SASi01). CG and risk leads anticipated that the differing concerns of the panel and family would lead to a ‘clash in priorities with our focus on guidelines and procedures and families being bothered about other aspects of their care that was only to do with their case’ (SASi01). Some clinical leads proposed the organisation of two separate panels to deal with each of these different objectives.
A central concern for many staff was that the presence of families would inhibit their opportunities for honest conversation about clinical risk. Such conversations, they noted, could create misunderstandings and concerns among families who heard discussions about the potential for service improvement as observations about service failings. A consultant midwife described this honesty as ‘like where you are almost devil’s advocate to push the conversation to be sure that we have robustly considered all options’ (SDSiO7). A senior risk lead described:
For some families, the reason why you discuss things is because it is wrong. Whereas we want to interrogate a service to make it better. Then they hold us to that, asking ‘well, actually, why didn’t you do that? They might interpret us as giving substandard care.
SCSi03
These concerns were underpinned by professional and personal uncertainties; some felt families might be more likely to report staff to regulatory bodies or initiate legal action after attending their investigation panel. Despite the promotion of direct family involvement at service and Trust level, clinicians remained concerned that direct family involvement in panels would lead some to ‘pick up on things they don’t quite understand and twist it all a little bit’ (SCSi03) or ‘finger point’ (SASi20). On the other hand, some clinicians reflected that it may benefit families to witness professional or clinical uncertainty. A consultant lead for risk and family debriefings reflected:
I do think that we like to present ourselves as knowing everything and being very good at our jobs, which we are but behind that there is uncertainty, there is a seeking out of information. It may actually benefit those families to see that.
SASi20
This participant reflected on the more fundamental question of the relationship between medical authority and trustworthiness when disclosure to families might expose uncertainty or disagreement between risk as well as clinical experts.
The management of knowledge during investigation and reporting
Although the above efforts were proposed to increase involvement of families in the construction of risk or incident scenarios, clinicians struggled with whether it was best to share of incomplete understandings in the form of draft reports and emerging findings. Clinicians trod a difficult line between fostering relationships of trust with a family while meeting that family’s expectations for knowledge sharing when this knowledge was either uncertain or not officially sanctioned for sharing. Some clinicians managed this situation by reference to process: ‘I always tell them honestly where we are up to and that we are still looking into everything’ (SDSi02). Others found that this situation more difficult to manage with families. Particularly at Site A, CG teams were cautious when offering meetings with families while investigation panel meetings were being prepared or reported.
So, there was only one time where we offered to meet with a family to give them an update. I didn’t find it was a particularly fruitful meeting because they want answers and we haven’t got answers at that minute and it would be irresponsible to suggest what we were writing in the final report, before we had finalised it.
Risk Midwife, SASi01
For some staff, as this risk midwife illustrates, there was an ongoing reluctance to share uncertainty with families. Others felt that sharing emerging knowledge was essential to maintaining trust:
If a family wants an answer you don’t say ‘Sorry, I can’t. I know the answer to that, but I can’t tell you until I’ve had a meeting’. That says ‘what are you hiding?’ If they want to talk then we talk to be responsive to the family wants.
SASi06
From this senior clinician’s perspective, the confidence of families relied on her sharing of information not yet agreed or approved by investigation panels. While the guarding of knowledge on forthcoming report findings was often explained as an ethical practice, to avoid confusion or contradiction for families, it was also an approach determined by corporate imperatives. The need for corporate approval of internal and external investigation report documents overshadowed efforts of CG and clinical teams to foster trust in them or their service.
Interim findings
This chapter has taken a broad approach to family inclusion during reviews and investigations, considering how legitimacy is ascribed to families who want their views and experiences represented as well as the organisational structures that facilitate and shape their representation. The organisation of social spaces and relationships, the PMRT and HSIB maternity safety programme are examined, along with informal practices of family representation assumed by some clinicians during Trust-based reviews and investigations. We find that family representation within services was often discretionary with the recovery of some trust by a family focused on individual staff rather than the service. 177 Additionally, this representation can meet a variety of purposes ranging from the elicitation of factual questions and answers for event analysis to the accommodation of narratives of experience.
Chapter 7 Programme theory 3 – making sense of what happened
Programme Theory 3:
When families feel that they can make sense of what happened, and that clinicians and the service have sought to help them do this, they feel less dismissed and are more likely to begin some recovery.
Introduction
This chapter focuses on the ways families and services sought to understand an incident. This process is partially shaped by DoC requirements for the Trust to feedback the findings of the investigation to the appropriate person within 10 days of the investigation being conducted. 178 The chapter explores the implications, for some families, of the use of different ways used by services of explaining an incident. We also examine how the crafting and circulation of incident report documents, along with family debriefs and reflections/listening clinics, represent different approaches to the construction and legitimation of knowledge of an incident.
Perspectives and experiences of national stakeholders
Many national stakeholders agreed that OD processes were intended to help the family to understand what had happened to them and why. Most agreed that families expected an explanation from the service about the events that lead to the incident, along with a recognition of their experience of these events. One claims solicitor explained:
One of the main reasons for families coming to me is because they haven’t got any knowledge of what has gone on.
ML1
However, meeting these expectations was complicated because as investigations unfolded, families were often presented with several authoritative accounts of ‘what had gone on’.
Explanations
Several participants considered the importance of a family’s search for explanations. Participants from clinical backgrounds often commented that they were sometimes unable to offer completeness and certainty to a family, and this could generate suspicion of their motives in the light of wider public expectations of medical expertise:
To the outside world there is always a definitive answer that something did or didn’t happen. There is no grey area, and it is this idea of us being infallible or able to discover some deeper truths. You have got clinicians being as transparent as they can be, but that transparency comes across as fudging it.
Qi14
Many participants also reflected on how multiple programmes and perspectives contributed to a family’s attempts to ‘uncover what really happened’ (Qi11). They noted situations where families had received ‘two reports with conflicting information’ (Qi11) from services, leading families to struggle to determine ‘what bit of all of that do you believe?’ (Qi6). The need for families to receive ‘one coherent report’ (Qi6) from a service was emphasised. However, this approach did presume that one ‘coherent answer’ could be gleaned from reports based on different investigation methodologies or viewpoints where questions and answers were framed differently (e.g. to explain the action or decisions leading to an incident or the contexts in which these actions or decisions occurred).
Healthcare Safety Investigation Branch leads viewed the challenge of multiple perspectives differently. They felt that the solution was to remind families of the purpose of each report:
Reminding the family all the time that this is about shared learning for cases in the future and not particularly about them is hard to hear when the investigation is about you, your baby and your incident.
Qi5
Several charity leads felt that this approach failed individual families when the particularity of their incident and its outcomes were marginalised as a result:
From a family perspective, these reports are not focusing closely on what should have happened in an individual’s treatment.
SG3
Participants working outside the health system also noted the tension between explanations of events focused on systems-learning and explanations focused on the affected family. For example, a coroner commented:
We have SI reports looking at standards of care and learning lessons, so where is the test of a root cause? Where is the balance of probabilities? A family may have an expectation that we will reach the same conclusion at inquest, but there are so many types of investigation all with different approaches. It’s a bit of a minefield. And can you imagine a family trying to navigate all this?
Qi6
This coroner’s view summed up a wider feeling that multiple investigation and reports, while constructed for different purposes, frustrated families’ attempts to come to an acceptable understanding of what happened. The ‘evidence’ that families relied on differed between reports constructed as learning documents and investigations of a case initiated to determine legal causality.
In summary, participants identified incident reporting as a significant process that epitomises the tensions between family expectations of OD and service offerings. A central dilemma identified across the interviews was that many families lacked confidence in their report findings and Trusts and services may be defensive of these findings due to the perceived reputation and litigation risk posed by injured families. Family misinterpretation of the purpose of reports was expected to contribute to this risk, as families often desired a coherent, linear and sometimes reductionist account of what happened. Participants indicated that organisational learning frameworks clashed with adversarial assumptions and legislative frameworks. This tension was compounded by investigation approaches that sought to involve families as contributors of learning for the future. A perceived danger of the system approach to learning was the potential marginalisation of families’ needs for acknowledgement and understanding of their case.
Perspectives and experiences of families
In the aftermath of an incident, families valued opportunities to quickly piece together what had happened to them. This was sometimes facilitated through effective multidisciplinary team (MDT) effort and was found ‘absolutely crucial’ for processing information by SU3 who received care in 2008:
And so it was almost like I could put together this jigsaw puzzle of what happened. They came and sat with us and shared all their different parts of the story, whether it was the one who was running to get the blood and bring it back, the one who was pushing my son down the corridor; all these different things, and that has been so incredibly helpful.
SU3
An opportunity to talk through events with the Consultant Obstetrician and go through medical records with the Bereavement Midwife meant that this family did not want to see the internal investigation report because she had the answers she needed. Few women experienced such a systematic approach, but rather used multiple sources to make sense of their experience.
Reports were important to families. For some, receiving written reports was helpful, especially if they had been warned of their arrival, because it gave them time to read them and identify questions they wanted to ask during future meetings. Some struggled with technical language, but still appreciated the opportunity to review the reports, especially if offered the option for a staff member to translate unfamiliar medical terms. Reports were less helpful when families did not recognise their own experiences in them.
This was also true for the medical records accessed by families. When families discovered information in records that they felt was incorrect, incomplete or redacted, it was unsettling and led to suspicion that ‘there was a cover-up going on’ (SU1–5, 7). In some cases, ‘key moments’ were not reflected in the clinical records and were subsequently missing from HSIB reports. Conclusions about what happened could not be reached because it was the family’s word against the clinician’s. In these cases, families felt their experiences had been marginalised.
Some families had to re-process what happened to them on receipt of official reports. It was difficult for them to learn of shortcomings in the care they had received when they had been told that everything possible had been done immediately after the event, especially if they learnt that the death of their baby could have been prevented if more appropriate care had been given. Recognition that incomplete information was available at the time of the event would have facilitated making sense of the event at that stage. Honest, open communication and the inclusion of families in reviews helped them to make sense of what happened. When disagreements continued, there was further distrust in the service.
Five of the 23 families interviewed had previously taken legal action. They indicated that they took this action to gather information on their events and would not have sought this had information been more forthcoming. One of the families, who received maternity care in 2011, had been told that registration of their baby as a stillbirth meant that a coronial inquest was not available to them. They felt litigation was the only way they could have an independent review of their care. Another woman needed more information on how the conclusions of the SI review into her daughter’s death had been reached.
However, there were mixed experiences for families who became involved in litigation. One family, whose case was settled out of court with the Trust issuing an apology and financial compensation, continued to contact the Trust and professional regulators with Freedom of Information and disclosure requests because they wanted reassurance that safety had improved in that service.
Perspectives and experiences in the case-study services
Review and investigation reports
Senior clinicians widely agreed that most families had three main questions to ask of an incident review or investigation: ‘what went wrong, was anybody at fault and how can we stop this happening again?’ (SASi04b). Those experienced in bereavement or trauma care also felt that these questions overlay a more fundamental need for many families for services and clinicians to fully recognise the impact of their injuries. CG and clinical leads were aware that a family’s receipt and discussion of their investigation or review report were critical times for them. Readings of the report, and discussions with debrief leads, were times when the integrity of the service from the perspective of the family were at stake. The final drafting and design of reports received by families often conveyed a sense that their own interests and experiences were marginal to service interests in limiting the sharing of knowledge with them.
Clinical governance teams rarely shared draft investigation reports with families, even though some families had raised complaints about this. The demands of additional administrative processes, along with the personal risks of sharing knowledge that was unapproved by corporate leads, conspired to prevent the sharing of this information with families:
Bits [of the draft report] go to the clinical director and Trust safety people and then they say ‘maybe don’t write that’ or ‘that isn’t right’ so do we send the report to families before or after this? We could end up getting into some legal hot water.
SASi01c
Instead, CG teams tended to focus attention on ensuring that families received a signed-off report that was a ‘good, finished product, the distilled thing that is the most useful thing’ (SASi01). A widespread sense of risk that some families might report staff or seek legal advice of knowledge acquired during the investigation process hindered family inclusion in the construction of this knowledge.
Service and family interests in the report
Additionally, the open question of who the report was for complicated the design of the report and the satisfaction of families with this document.
Clinical governance teams and clinical leads highlighted the purpose of a report as a response to the injured family’s search for answers and some also noted that the purpose of the report was to contribute to ‘learning that would benefit other women’ (SDSi02). Less often mentioned, but observed, was the use of incident reports as evidence in business case submissions for investment in infrastructural improvement. A CG midwife at Site B reflected on how they managed the different objectives of investigation and reporting:
So it’s not about the family, it’s more about Trust learning, but in all these cases I’ve always got the families in the back of my mind with thinking ‘I want to do this on your behalf’.
SDSi03
At Site A, the CG team emphasised that incident reviews and investigations were conducted in the interest of the injured family rather than for organisational learning:
'So, you are telling them that actually,' what you are struggling with here, we actually think is really quite serious. It is serious enough that we are going to galvanise this process, and I have come to talk to you about it because I don’t want this going on without you knowing about it, and you being at the absolute centre of it.
Risk Midwife, SASi1c
At Sites B and C, service and clinical leads were more likely to explain the benefits of an investigation for future events or other families:
I always say upfront ‘look, really sadly, we can’t change the outcome of what happened here but what we really need to do is to do all the learning we can to make services safer'. Most parents are really engaged in that.
SCSi14
Healthcare Safety Investigation Branch investigations, which required family consent for data sharing, were explained to families in more immediate, relational terms:
I always explain ‘If you have another baby, we want things to be safer moving forward. If your baby girl has a baby, we want her maternity care to be better, and we’ve got to look at that wider picture’. And I think most people are very receptive of that.
SDSi11
Service leads and risk midwives assumed the complicated interpretive tasks of making reports relevant to families. Sometimes, a ‘systems approach’ (SASi04) meant that clinicians felt family questions and concerns were ‘just personal to them’ (SASi04) or ‘actually don’t have a bearing on the outcome of the investigation at all but have to be heard at some point’ (SASi13). In other cases, particularly at Site A, where clinical teams had less confidence that interventions would lead to tangible improvements, CG teams and some clinical leads emphasised the importance of responding to individual family concerns.
Crafting reports and balancing interests
Irrespective of the ultimate purpose of the report, across all three services, clinicians felt that a report that give a clear explanation of what had happened, would help a family ‘be able to close that incident off a little better’ (SCSi08). A risk midwife commented:
Normally it’s quite a lengthy document and it all looks quite official, so generally families are quite pleased with what you have done even if they might not be pleased with what we’ve said as the outcome.
SASi1b
The production of the report was, in itself, an indication of care by the service. Teams described how reports should also generate action plans, thus contributing to organisational learning and in some cases committing the service to the completion of improvement requirements.
A difficult aspect of investigation report drafting described by CG midwives was the need to balance both family and service priorities. Where possible, reports were drafted to include any previously shared findings with ‘everything tied together so that they resemble one another’ (SCSi04) or ‘woven in’ (SASi08). This was to minimise variation in perspectives on the incident shared with families and to create consistency. Reports were also crafted for accessibility to families with understanding of their emotional situation:
[It’s important to make] sure that the language used is weighted correctly so that a family understand as best as we understand what the truth is behind the events. There’s a lot of guilt families carry about so when things aren’t black and white like when there’s uncertainty, we need to make sure that we say it in a measured way.
SDSi06b
However, from the perspective of families, their own information and experience were often marginalised, for example, added into the report as an addendum or excluded from this document:
If that’s something important [to a family] but not significant, then we verbalise that in the debrief meeting [and] put in a letter so that the parents are very clear that we’ve acknowledged whatever bit the report hasn’t addressed.
SDSi06
Exclusion of family information from the report also happened when there was a discrepancy between a family’s view of events and the risk scenario drawn from clinical records. For example, a clinical lead at Site A reflected on why a recent incident report was poorly received by a family whose understanding of events had been excluded from the report:
So, they raised things like ‘the doctor in the night’. I can’t know what the doctor in the night may have said, so this is a flaw in the process isn’t it? People often write in the notes their own interpretation of what the woman feels rather than what the woman felt.
SASi16
Site C developed a way for the experience of parents to be incorporated alongside the clinical notes; this process was informed by the inclusion of parents in investigation panels (as described in the previous chapter). The governance lead explained that even when some families had not submitted detailed accounts of the event from their perspective, there was a different tone to reports:
The report is better balanced and rather than saying ‘and then this is what happened to the woman and that is what happened to the woman’ we put ‘well actually the woman’s perspective was that she came in’. When you look at the clinical documentation and staff statements it doesn’t always reflect what the woman felt. So the way we’ve made our actions, it’s woman-centred because it’s about experience. So, yes, perhaps we have less questions and it’s less contentious and I think it’s more digestible when people give their own perspective and it’s fed into the report.
SCSi08
This participant describes an approach to report drafting that does not necessarily include greater depth or breadth of event information but offers a different way of framing the events described. She indicates the benefits of this approach to families, staff and services because the report produced is accessible and prioritises the narrative of family experience.
More generally across the case-study services, the management of knowledge reported extended more often extended beyond questions of accessibility and recognition of the family. Reports were more often about the management of different sets of interests with an awareness that the more the report identified, the more likely it was for a family to ‘give it to their lawyers’ (SCSi05).
For the four Site A families, receiving their incident report was a critical moment that determined their view of the service. For them, a key aspect of reporting was that their views, experiences and questions were included in the body of the report. These families interpreted omissions as a sign of the unwillingness of the service to learn from the event:
I made the point that [my baby] should have been brought out earlier and I don’t think there was a satisfactory answer for why it shouldn’t have happened so, for me, I was satisfied with the process and the apology but there can’t be a change in practice.
SAFi01
Family debriefs
In all case-study services, families were invited to meet with members of the CG team to discuss the findings of their incident investigation or report. These meetings were expected to alleviate underlying tensions that were likely to surface in the disclosure process. Debrief leads noted the importance of these discussions to bring ‘cohesiveness’ to a family’s understanding of events and to mitigate any growing suspicions that a service was not being entirely honest. Another purpose was for the service to attempt to acknowledge the situation of the injured family.
Meetings with families to discuss report findings was an onerous task for all but the most experienced CG and clinical leads. They explained that planning for timing, tone and content of debrief meetings was difficult:
And they are all so different. You can have some awful cases that are the nicest debriefs to do and you can have some that are awful. They are unique, there’s never a common theme to them all.
SCSi14
One experienced lead in family debriefs explained the principles he had developed himself, over time, to mitigate this:
So, I tell people that it’s their time and whatever is going to be most useful. We can go through the timeline, if they would like, or if they would like us to hear their story then we will listen to that and draw out the points as to whether we can learn something or whether there’s been a misconception of why something was done, if it’s helpful.
SASi20
The accommodation of family needs was sometimes difficult:
Before Lola’s family meeting, the HoM and clinical lead met to plan for ‘getting the meeting right for the family’. Timing was a consideration for both of them. They agreed on an hour to discuss the HSIB report on Lola’s HIE injuries, but ‘who knows they might have four questions or their might have 47 questions’. At the meeting, Lola’s mother said that she had ‘loads of questions with no answers yet’ and they said that a further meeting was possible to ‘cover everything’. Lola’s mum became very distressed, saying ‘we’ve already waited four-and-a-half months and things really need to be wrapped up now’.
Fieldnotes, Report Debriefing with Family, 6 July 2021
Power dynamics at meetings became more tangible when the clinical leads neglected to translate terminology used in the report:
Lola’s mother asks ‘and what’s macrosomia? I don’t even know what macrosomia is and I know for a fact that wasn’t mentioned to me before birth’. The clinical lead explains ‘macrosomia is just a word for a big baby. You were informed of the possibility of a big baby several times’. Lola’s mother snapped ‘big words shouldn’t be used because most people don’t know what they mean’.
Fieldnotes, Report Debriefing with Family, 6 July 21
Investigations conducted using interpretations of human factors methodology could generate further tension over the language used and the report priorities implied, exacerbating suspicion by families and defensiveness by clinicians:
The neonatologist sought to respond to Lola’s mother’s question of what happened to Lola just after she was born. She explained ‘it’s all done by human factors that are meant to help with the messiness of humans by asking like, how can we maintain safety alongside the humanness of interactions. Like making an incorrect call’. Lola’s mother asked, ‘so is human factors the panicking that staff were doing?’ She replied ‘yes, we work hard to standardise what happens in emergencies, but we can’t guarantee what will happen when people are under stress. So, those kinds of incidents don’t happen very often and we’re trying to train staff’. Lola’s mother looked confused and moved on to another question.
Fieldnotes 7 June 2021
This case study illustrates the difficulties for families of report debrief meetings where matters of timing, the use of specialist terminology or explanatory frameworks and the difficulties of challenging organisationally determined frames of reference.
For Lola’s mum, as for the four Site A families interviewed, debriefing conversations opened the opportunity for them to discuss issues with their care that fell beyond the interests of investigation panel and scope of the report. During debrief meetings observed and described, families often felt that investigators’ classification of events and experiences that families felt were connected to their incident as ‘incidental’ was symptomatic of a myopic or disingenuous attempt at addressing service shortcomings. In some meetings, where families discussed a completely different version of events to those in the report document, CG and risk leads sought to ‘unify and iron things out, just to maintain trust really’ (SASi16); however, it is not clear how far this approach satisfied families themselves. For example, Lola’s mother was expected to return several times more to continue her conversations with the clinical lead and other staff involved in her care.
Three of the four families interviewed from Site A had decided not to seek legal action because of the quality of post-incident communication. It was particularly their experience of the attention given to them and responsiveness to their needs in person-to-person debrief meetings, which led them to conclude that they would not seek legal action.
The background conditions and costs of successful family debriefs
Most generally, for clinicians, the success of the family debriefs rested on the acceptance of responsibility of the service for the incident. Some senior clinicians described the most difficult meetings to be those where no explanation of what caused the injury can be offered but ‘the apology is probably really valuable’ (SASi13).
There are things we don’t know, we don’t necessarily have an explanation for. And as one of the patients put it ‘don’t tell me it was just one of these things’. But sometimes it is one of these things, it is bad luck, you happen to be 1 : 10,000 and that is very, very difficult to accept.
SASi16
In these situations, families were more likely to become suspicious that a clinician or the service was hiding things. Both CG teams and families felt more satisfied when the service directly and immediately accepted responsibility:
The last debrief I was at they said ‘absolutely, 100% said this is our fault. Your baby is dead because of a fault in our administration processes. We are truly sorry. We will try to do everything we can, but this is nothing that you have done. We have failed you’. Now these are the kind of debriefs I can get behind.
SASAi1b
Several clinical leads agreed that if responsibility for the incident is clearly assumed by the service, families are less likely to hold individual staff accountable. For example, Fay’s family’s meeting with a clinical lead left the family unconvinced that the service had really addressed what mattered to them. For them, ‘real point of things, that she should have been brought out earlier was missed’ (SAFi1) and without this clarification they felt that the obstetric team who delayed the C-section were both ‘off the hook’ and ‘unlikely to change their practice’. All case-study families felt frustrated with family meetings and clinical debriefings that appeared to avoid a clear identification of who was accountable for what happened. However, questions of responsibility acceptance were more complicated in situations where parents’ own decisions were implicated in poor outcomes.
Senior clinicians who were expert in family debriefings were often resigned to withholding clinical judgements when family choices might have contributed to an incident. This was particularly so in services that actively promoted the value of women-centred care over risk management (i.e. at Sites B and C). 179,180 However, this position was more challenging for junior clinicians to sustain, particularly where they were themselves directly involved in incidents are perceived as connected to decisional autonomy that is unsupported by the obstetric or maternity team.
Listening services
All case-study services offered injured families some access to reflections or after-thoughts services. These services were described by a Professional Midwifery Advocate (PMA) as ‘about families feeling like we understand how they are feeling’ (SDSi08). Depending on the approach of individual clinicians as well as the family, these one-to-one sessions with clinicians were described as providing families with a clearer explanation of what happened to them, often by a careful reading of their notes with them, or as a ‘another opportunity for families to be able to voice how they felt, their perspectives, their concerns’ (SCSi06).
The PMA started the session by explaining to the woman that this was a chance for ‘me to listen to your story and to see if there are any areas where I can offer a perspective, either by filling in any gaps by looking at the medical notes or to explain things so you have a better understanding of why things happened the way they did’. The woman was silent and the PMA suggested ‘why don’t you explain to me your birth. Start at the beginning’.
Fieldnotes, Reflections Clinic, 24 September 2021
While some matters raised by families were seen as a more straightforward need for ‘filling in the gaps’ of what happened, often to more immediately relieve families of feelings of confusion or guilt, others were more complicated by families sharing experiences of poor care or questioning documented events. A Practice Development Midwife (PDM) explained:
People are unhappy and have been treated badly. I never want read the notes in too much detail because I want their story; you don’t really get that from the notes and I don’t want to go in with preconceived ideas of what happened.
SASi30b
The legitimisation of family’s experiences of injury in their own terms was central to the service, as was an approach to understanding events that were different to those offered by clinical or incident explanatory frameworks. Service managers noted the success of these services in reducing informal complaints; however, percentage changes were difficult for them to calculate due to data collection methods in that department.
The organisation of the service differed across the case-study services (see Appendix 2) At Site A, the service was always oversubscribed with families arriving by self-referral or matron referral following a complaint. At Sites B and C, referral into this multidisciplinary pathway for injured families was more responsive, with therapeutic approaches determined by family need. As noted in Chapter 6, service managers felt that care through this pathway was important for families who wanted to attend their own incident investigation meetings. Across the services, according to staff there was high demand for the service even though these services were not always publicised to families themselves.
Unplanned opportunities to make sense of events
In home birth settings, where relationships extended beyond incident management or a hospital stay, some families and staff found less-formal ways of making sense of incidents.
A few days after the emergency admission of a baby following a home delivery, the mother contacted the preceptor midwife present at the birth with baby photos and updates. She felt a ‘special connection’ with this midwife. The midwife replied to the mother’s invitation to meet in the hospital cafe. The midwife described: ‘she did ask me “was there anything wrong with my birth?”. I did say to her ‘No I was as surprised as you were until the baby came out it all looked perfect and that I didn’t have a lot of experience but from my perspective, everything sounded perfect’. Then her husband said, ‘yes, everything was perfect, but she blamed herself’.
SDSi17
Most service and clinical managers from hospital settings were wary of these informal meetings during which families might search for explanation and some resolution. However, several staff recalled the importance to them of meeting a family months or years after an incident as both found comfort in hearing one another’s perspectives. Where families remained feeling unacknowledged and unheard by the service, staff often found these accidental meetings ‘very terrifying because it was just me and my face was the face that they remembered’ (SCSi08).
Interim findings
This chapter explored how families seek to make sense of incidents, focusing on the influence of clinicians and impact of corporate teams on these dynamic processes. The impact of organisational defensiveness is clear, particularly with respect to the management of knowledge shared with families. In this context, debrief meetings with families to discuss the report were significant spaces where the relevance, coherence or legitimacy of investigation findings could be reconfigured to accommodate a family perspective. At the same time, families could be marginalised when discussion relied on the translation of specialist expertise or did not focus on their experience. A central question for injured families, which was also significant for some clinicians, was around the assumption of retrospective responsibility for certain incidents (or alleviation of a family’s concerns about their own responsibility). The possibility for affected families and clinicians to explore the circumstances and consequences of an incident together to find personal relief relied on Trusts and services being willing to support these meetings and most were unwilling to risk this.
Chapter 8 Programme theory 4 – receiving care from clinicians who are skilled and feel psychologically safe during post-incident communication
Programme Theory 4:
When clinicians are skilled and feel psychologically safe to conduct disclosure conversations with families, these conversations are less likely to be avoided, questions of responsibility are more likely to be addressed and OD is more likely to become embedded in ongoing clinical practice.
Introduction
This chapter examines the contexts and outcomes of post-incident communication with families from the perspective of clinicians’ support needs and their acquisition of skills. We draw on our national interview study, which included clinical fellows on national programme placements (n = 5), as well as interviews and fieldwork observations during case-study research that included front-line clinicians and junior midwives.
Senior stakeholder perspectives and experiences
Disclosure training
Few senior stakeholders who also worked clinically had any formal communication skills training, despite several leading on debriefing work with families in their service. They described how they, like others, had ‘just learned on the job’ (FS1) and ‘got wheeled out because [I’m] quite good at talking to families’ (Qi13). Five participants were actively involved in developing pilot training for legal firms, national charities or professional colleges.
Eight participants commented on the lack of central investment in training for OD. Bursary and sponsorship opportunities were available in some services (FS5). Although attending an investigation panel and a family debrief is part of the obstetrician training curriculum, clinicians more often prioritised updates of technical skills and funding for midwives or allied maternity care professionals was also very limited (FS5; ML5). Interest in training approaches to prepare for less defensive OD varied between maternity services and between individual professionals. Most staff had a brief induction session by a Trust legal representative on meeting the statutory DoC with advice on minimisation of professional and organisational litigation risk:
You get told how you can handle this in a way that best protects yourself from unwanted attention from the CQC, litigation or other unwanted outcomes.
SG3
The lack of NHS training investment in communication with families was contrasted to the HSIB maternity safety programme that was designed around ‘what investigators on a daily basis cope with’ (Qi8). Investigator training and support ranged from introductory workshops on ‘steps’ to involvement over the investigation time frame (first phone call, home visits and closing relationships after investigation reporting) to bespoke sessions on resilience, bereavement and trauma care. Routine regional team meetings, ongoing peer support and expert telephone advice on family engagement issues were described as ‘a must for our wellbeing’ (Qi5):
There is a lot we take on like sometimes families who aren’t coping and the dynamics of the families. Lots of tears and support and open talking within our teams.
Qi5
The connection between HSIB’s investment in training of their investigation teams and the better experience of families was noted by many participants. Overall, discussions about disclosure training noted the comparative underinvestment in disclosure training in services and by professional bodies. Participants also emphasised the value of acquired practical knowledge over training programmes. Training offered by national charities was welcome but had not yet been evaluated for immediate and longer-term outcomes.
The care of staff post incident
Surprisingly, few national stakeholders identified post-incident support for staff as important to families, services or staff themselves. Those who identified this need were more often former or practising clinicians who drew on their own personal experiences of post-incident trauma and approaches to recovery. Two other participants who considered this were from mediation rather than clinical or safety improvement backgrounds. They noted the psychosocial challenges of disclosure ‘when you take it as personal failure’ (Qi1) and ‘need to start acknowledging the impact of incidents or you get stuck’ (Qi19). Five safety improvement leads discussed the importance of ‘fair’ or ‘open’ workplace culture for supporting OD; these discussions were of general principles and their implications for practice. It is significant that the support needs of clinicians conducting OD were widely overlooked. It may be related to a wider ethos amongst some staff in NHS maternity units where discussion of post-incident support needs is unsupported by many colleagues in this speciality. 181,182
Clinician care and disclosure: workplace features and variations
However, the clinical fellows recruited from our national study highlighted the relationship between local unit practices of staff support as well as ongoing mentoring and the quality of their post-incident communication with families. Significantly, they did not identify connections between formal systems of post-incident staff support and their behaviours towards families.
Several of these participants reflected on the impact of the first moments after the incident on their subsequent conversation with the affected family. The immediate reactions of colleagues, particularly of senior colleagues or managers, were described as critical for providing non-judgemental support to trainees. This, in turn, influenced how comfortable the trainee was to share what had happened with the service. One trainee described this:
If I do a Cat 1 section at 02:00 in the morning and that baby looks like they’re going to have brain damage, if I know that at 8 a.m. when I discuss that it’s going to be ‘Are you okay? Do you want to talk about it? Have you spoken to the mum about it?’. Whereas if you think ‘I know so-and-so is on in the morning and they’re going to be … Oh no, you’ve sent a term baby to the Neonatal Intensive Care Unit (NICU)’ then you’ve got that kind of reticence. You’re not going to go into it as much. You’re going to keep things a bit to yourself because you’re scared of being judged. If you can’t have conversations like ‘I feel like I’ve done something wrong’ or ‘maybe I should have done that quicker’ with your team, then you’re not going to have them with the patient.
Qi7
This description highlights the impact of the attitudes and behaviours of immediate colleagues on the ways that incidents are discussed, and initial OD might unfold.
Opportunities to observe differences in the behaviours and skills of clinical shift leads as they communicated with a family post injury was also important. Learning on the job by informal mentoring, often by senior colleagues and bereavement midwives, was envisaged as a gradual building of the necessary expertise for meeting with families after traumatic events and situations. One senior trainee described:
You see things that you think are wonderful, that person has just told somebody the worst imaginable thing that you can hear and in an incredible way. I want to be like that or equally, I never want to be like that.
Qi10
These learning experiences were recognised by trainees and clinical leads as essential to developing the embodied skills of reflexivity and being attuned to a family’s situation. However, clinical fellows agreed that there were declining opportunities to observe post-incident conversations with families due to lack of time or a reluctance of senior colleagues to invite them.
Clinical fellows also identified leadership in CG as a significant factor affecting the possibility of their post-incident communication with families. Where CG was more risk adverse, these relationships were actively discouraged. One experienced trainee described the effects of a CG approach that ‘disempowers patient-facing clinicians’ who feel ‘too junior to say sorry’ because it has become ‘only something matron does …’ (FS2). She continued:
We work intimately, with lots of honesty and openness with families then when something goes wrong it’s like everyone is on the defensive and then it’s something for governance. That’s quite harmful from both sides when someone says, ‘No you can’t go and see her and her baby’ or ‘if they ask questions just tell them to talk to so-and-so.’ It entrenches the thing. Then the parents will say ‘nobody spoke to us’.
FS2
This trainee, and other clinicians, indicated their interest in seeking some early resolution with families and the reluctance of many services to facilitate these opportunities. However, clinical fellows recruited for our national interview study described that while these meetings might be organised at the request of a family, service or clinical leads lacked the protected time or mediation skills to steer these events. Two clinical fellows described ‘disastrous meetings’ with families. One became a ‘shouting match’ (FS2) with a family when all attendees were ill prepared for the meeting and the Chair had been called away. Both fellows were now determined to revise attitudes towards incidents and OD.
In summary, the post-incident support experiences of clinical fellows (both obstetricians and midwives) were highly varied across services, units and shifts. In the absence of any post-incident support from immediate colleagues and managers, these staff looked to partners and friends, particularly their former student peers, for care and advice.
The perspective and experiences of staff in the case-study services
‘Putting out the flames’
During the case-study research (April–November 2021), there was a growing public awareness of the importance of staff well-being in NHS services. This was reflected in interviews with senior and specialist clinicians in the case-study services where, despite some recent investment in staff well-being interventions, many participants highlighted the inadequacies of the post-incident care of front-line clinicians. A series of factors contributed to this. Most immediately, there was limited time available for post-incident support and recovery:
When everybody’s go, go, go, you feel like you’re just putting out flames.
Matron for Quality and Safety, SASi17b
We just make them a cup of tea, we do a hot debrief, we rub them off and send them back off out into the battlefield, let’s be truthful.
Director of Midwifery, SCSi16
I think as a Trust we are not very good at it. Not good at it at all.
Clinical Lead, SDSi19
Particularly at Site A, senior clinicians felt that service attrition and sickness rates were directly related to the lack of post-incident support of clinicians:
Staff used to think that when if anything happened, they would be 100% supported and it would be fine. Now I believe that staff don’t feel that and that’s why they think twice about coming to work unless they feel completely right.
PMA, SASi22
Reflections on the inadequacy of post-incident support for staff were also shaped by a sense of wider workforce neglect and demoralisation. Some clinicians at all case-study services described feeling ‘disempowered’ or ‘defensive’ in the face of corporate systems that managed the complaints of families who assume poor clinical outcomes or experiences of care centred on the behaviours of single individuals (SASi36; SDSi19). Some front-line clinicians felt ‘forgotten’ or ‘neglected’ by their immediate managers or by their service more widely.
Several clinical leads noted the need for individualised post-incident support for clinicians that would include the possibility of ongoing care by the service and the commissioning of specialist support. This approach relied on the provision of collectively agreed guidance on post-incident support. At the same time, some clinical leads were wary that such provision was a salve for more fundamental issues of staff welfare, while post-incident workplace response was the more pressing issue to be addressed.
Workforce trust, flux and diversity
In the case-study services, we examined the formal resources and interventions for post-incident staff support with service, clinical and business managers. Our detailed interview and observational findings on the organisation and reception of post-incident support for staff are presented in Appendix 7, Table 9.
We note that all case-study services invested in formal post-incident staff support structures (ranging from weekend coverage of PMAs, who provided personal and educational for midwives and sometimes doctors; PMA group and individual reflection sessions, Trust counselling services and, at Site A, a dedicated service psychologist). Despite this, front-line staff described a lack of both formal and informal support resources during our fieldwork and interviews. This may have been because of a lack of available time for staff to access formal resources as well as various structural and cultural factors undermining the embedding of the resources in the case-study services. For senior clinicians, in particular, informal arrangements of ‘one-off’ informal peer support, occurred between team members sharing the same office space. For example, a senior clinical lead at Site A described the common practice of ‘talking to office colleagues and then literally closing the book and hoping the next time is easier’ (SASi12) as her way of coping post incident.
The puzzle for post-incident support specialists was the tailoring of post-incident support so that staff could reach it at critical times (which were frequently out of office hours). This was complicated by patterns of part-time working, night work and long shifts, as well as by a significant workforce turnover in Sites A and C. Several PMAs and Consultant Midwives were also aware that as long-standing, senior employees, they may not be immediately trusted by junior staff. Specialist leads and advisors at all case-study services reflected on the ongoing difficulties of engaging with many midwives who ‘get anxious because they think they are going to be blamed for something’ (SDSi08). At the same time, trainees interviewed and observed at the case-study services had highly varied experiences of support from educational supervisors.
Some senior medical staff were not keen to encourage junior colleagues to seek MDT post-incident support and preferred to have issues discussed only in trainee meetings. While PMAs were available for them at some services, obstetric trainees rarely made use of this resource. Indeed, 8 months after Trust commissioning of a full-time staff psychologist at Site A, there was widespread reluctance of medical staff to make use of scheduled group sessions (e.g. breaking bad news and self-care after events) or individual appointments (SASi35). Some managers also noted the shortcomings of commissioned post-incident support for diverse staff groups that have different attitudes to counselling and psychological services.
In all, the fluidity and diversity of clinical teams, workforce churn and protectiveness over professional identities contributed to the difficulties of embedding support interventions in practice. Additionally, access and use of these resources and interventions often relied on workplace histories where individuals had the time and opportunity to develop an ongoing trusting and confidential relationship with a clinical specialist. Our interviews with junior clinicians at the case-study services (n = 6) highlighted important parallels between the post-incident needs of families and of junior front-line staff.
The immediate impact of an incident on clinicians directly involved
When incidents were out of hours, and the mother was conscious, junior clinicians were often the first staff to engage with the family immediately after the event. In these situations, senior trainees led the initial conversation with the woman and her family. Although two junior staff had completed various training courses on conducting the DoC and its implications for staff, both still felt poorly prepared and anxious about these encounters with families. One trainee described this first conversation as ‘an aspect of the fear of a serious incident’ (SASi19).
As with clinical fellows recruited in our national study, front-line post-incident staff support in the case-study services was described as highly varied, and changeable from shift to shift depending on floor or shift leads. As also indicated in our national study, better experiences of post-incident support were described as having significant more immediate effects for the family, and longer-term effects for the development of clinician confidence and skills.
For example, Roberta, a senior trainee, described the effects of immediate and unjudgemental collegial support at Site B. Immediately after an intrapartum stillbirth on the unit where Roberta was shift lead, her senior colleague from another area came over. This colleague ‘stood right next to me’ (SDSi18) during the very difficult and initial conversation with the distraught father. This colleague was with Roberta again, the following night, when the baby’s mother wanted to meet only with her:
Like I know it wasn’t down to me but when I arrived the following night I was physically shaking. I was still really upset myself. So, I got the mother’s permission to talk to her with my colleague. Then we spent about 40, 45 minutes talking with the family. She was present for support for me and to answer any questions I couldn’t. Then the next four nights I had more conversations [with the family] to answer any questions they thought of.
SASi18
These examples highlight the importance and impact of senior support for junior members of staff, both for their own well-being, the development of post-incident care of a family and for the informal acquisition of OD skills.
However, in all case-study services, junior doctors considered that, because they lacked a formalised ‘risk or governance brief’, they struggled to negotiate time to adequately prepare, both emotionally and practically, for initial and subsequent family meetings. The importance of ‘being given at that very time the headspace for a considerate response to a family’ and ‘to start to “absorb”’ (SASi27) or ‘process’ (SASi19) the event was expected to be crucial for everyone concerned. This relied on, to some extent, an immediate staffing capacity during a shift but also on senior colleagues recognising this as important.
There were significant differences in post-incident leadership support between the case-study services. At Site A, it was often felt that ‘we don’t have that luxury’ (SASi01), whereas, at Sites B and C, senior service managers sometimes ‘ended up staying there and being with them or sending them home when they are safe to leave’ (SCSi16).
Sometimes, the fast-paced environment of the maternity unit was not conducive to discussing events with an injured family. In these instances, the regret for not meeting with that family lingered with junior clinicians, sometimes for years. For example, an experienced trainee senior described how 3 years after an event she still experienced enduring regret for being unable to return to speak to a woman whose delivery had led to severe harm to the baby and who was transferred, rapidly and unexpectedly, to another unit.
When junior clinicians were directly involved with a traumatic incident, they experienced initial and ongoing emotions of self-blame, regret, self-doubt and isolation. These initial feelings ‘weighed heavy’ (SASi28), irrespective of issues of avoidability. This was also the case where junior clinicians felt that families had opted for care that contradicted clinical advice. Being offered some time to begin some recovery was highly valued, often as a sign that their distress had been acknowledged by senior colleagues.
Ewa, a Band 7 midwife, was involved in a difficult neonatal resuscitation while covering a colleague’s lunch break. Two years later she remembered:
So, when I finished the notes then it hit me as a really big deal because it’s a baby’s life, like you know for a fact it’s going to be severely disabled. The second I walked out the room, the midwife-in-charge just said ‘Oh well, your other patient needs you’ so I just went back to my unit. It would have been nice for someone to say ‘just go and get a cup of tea and I’ll deal with your patient, just recognizing what had happened and that I might have needed five minutes to collect myself. It was that desensitized.
SASi28
From Ewa’s perspective, the failure of her immediate manager to acknowledge the impact of the incident on her came to summarise the attitude of the wider service. This experience, and the neglect of the service to update her on what happened to the baby, contributed to her decision to leave the Trust the following year.
Particularly for more junior clinicians, there was also an important interplay between the acquisition of disclosure skills and immediate post-incident support for junior clinicians by practising experts. For example, Roberta’s support by a senior colleague, described above, was also an opportunity to observe and then develop disclosure skills. Apprenticeship learning, involving graduations of shared practice, focuses on the needs of one particular family ‘as a locus for embodied work practice rather than a Site of contemplation’. 183 Several clinical leads described significant moments in their own careers where they had worked out, from memorable events of tangible success or disaster when interacting with a family, certain tacit points of convention or ‘rules of thumb’ for OD. For example, a clinical and debriefing lead at Site A described the impact of a SI and his acquisition of OD expertise:
Years ago, I had a hideous case where someone died, and I made an error. I went through a lot of emotions. The single most important thing I did was to immediately talk about it to the family so that I wasn’t going down to them the next day. It was a roller coaster. It might be why I approached risk job afterwards. I felt very strongly that it was the speed at which I told them the truth.
SASi20
This clinical lead occasionally shared this experiential learning with staff in his team. He implied that this might encourage better OD. Opportunities for this learning were under considerable strain during the period of fieldwork. Learning-in-practice and through story telling relied on the ‘in-the-moment’ availability and accessibility of expert clinicians. Also, senior clinicians and specialists who had not previously met a family were understandably cautious of exposing them to any unnecessary attention from additional, unknown staff. As often, however, expert clinicians tended to overlook OD conversations as clinical learning opportunities for a trainee or midwife already involved in that families’ care.
Notably, very few CG teams or lead clinicians from the case-study services had attended professional or in-service training on disclosure skills. As far as the research team could establish, in-service staff inductions into the DoC at the case-study services were conducted by representatives from the Trust legal team, rather than by clinicians who were expert in this practice.
Clinicians’ experiences of reviews and investigations of incidents involving them
Junior clinicians across all the case-study services often felt that their involvement in internal incident review and investigation processes was poorly considered or planned by CG teams. Many felt that after initial support from senior colleagues, they were treated with less sensitivity as time went on (e.g. being told of a HSIB investigation in front of colleagues, being texted for information about a family complaint on days off and having to complete time-consuming and emotional written reports in their own time). For some trainees, distress was compounded by requests for statements for inquests arriving years after an incident that had happened on a previous rotation. With variable support from senior staff in their previous service, they often completed these alone and without professional advice. While trainees worried about the consequences of investigations as well as potential legal action by a family because of emotional strain and impact on career, they also felt it a necessary recourse for families in need of financial support after injury. Not knowing how a review or investigation was progressing left them feeling confused and anxious. Lack of follow-up after an investigation has been reported, was also a problem, with one midwife at Site B describing how:
You just get an e-mail from management asking for a statement and nothing else comes of it.
Fieldnotes, shift observations, 21 September 2021
In situations where front-line staff felt ignored or misrepresented in internal investigation processes or report findings, they often felt frustration and resentment towards families whose perspective was (they assumed) better represented. A CG lead confirmed this sense of neglect of front-line clinicians post incident:
We go back to them as individuals ‘are you Ok, do you need anything?’ and then there’s the investigation and there’s learning and I don’t think we actually come back together with them.
SCSi06
Most interviewees had not received final reports of investigations involving them and those who did felt that an e-mailed report without opportunity for further discussion did not help their understanding of events or their personal recovery. The interplay between post-incident learning and the care of staff post incident was complex. It was approached differently across the case-study services.
Staff debriefs
Immediate and longer-term post-incident team debriefs were the most common way that services supported all staff directly involved in the incident to begin to make sense of events. However, as indicated in Appendix 7, Table 9, immediate (end-of-shift) debriefs were initiated at the discretion of shift leads and might be conducted for different purposes (e.g. reflecting on immediate feelings, composing a clinical picture and advising on investigation processes). No one mentioned immediate debriefs as an important aspect of their post-incident experience. However, some clinicians did discuss later post-event debriefs as important for their recovery of feelings of guilt and isolation. For example, a few weeks after the incident involving Ewa, a MDT meeting was organised by a risk midwife. Several senior clinicians involved in the neonatal resuscitation attended and the service psychologist facilitated the discussion. Ewa described the positive effects of this meeting on her self-esteem and personal recovery:
I realised I wasn’t the only one blown away by how unexpected it was. It reassured me that as a relatively junior member of such a team, I wasn’t the only one who didn’t know what to do. That you just do as much as you can do.
SASi28
Clinical leads in the case-study services (who were senior doctors) often remarked on the difficulties of organising these debriefs. Identifying and reassembling the team involved in the incident (including those who had witnessed events) was a ‘major headache’ (SASi13) when staff came from different service areas, had different work patterns and differing seniority. The impetus to organise these events could diminish as collective memory of the incident seemed to fade. However, several junior clinicians directly affected by incidents described these meetings as invaluable to their recovery post incident.
Meeting with families
As already discussed, in some circumstances, it was possible for injured families to contact clinicians involved in their incident. Some clinical leads identified the valuable potential of these encounters for clinicians and families. In hospital births, especially where families were quickly discharged or transferred, these meetings were rarely suggested or initiated. However, some service managers and midwives found ways of reconnecting with families, on the advice of colleagues, when families were re-admitted to the unit in later pregnancies. Pamela, a Band 6 midwife, described spotting the name of a woman on an admissions board ‘a name I’ll never forget’, as she felt responsible for this family’s intrauterine death (IUD) several years earlier:
We had an opportunity to chat then, and very interesting to see how she perceived the event. I certainly did feel a huge amount of guilt and sadness. She didn’t harbour any feelings of anger or sadness towards us. That was my closure, after all these years that was my closure.
SASi27
The possibility for facilitated meetings that might contribute towards resolution, for families as well as for staff, was considered by some service and governance managers. However, it was generally felt that the unpredictability of these meetings, with possibilities of further trauma for staff and for families, and risks for the service if legal action was progressed, meant that they were unlikely to be formally encouraged.
Personal and service investments in post-incident learning
The organisation and processes of post-incident learning in the case-study services are examined in detail in Chapter 9. However, from the perspective of more junior front-line trainees as well as midwives, this service work had limited reach to them. Interviewees had little knowledge of changes being implemented because of an investigation of an incident they had been involved in. However, most felt a personal responsibility to make changes to their own or others’ clinical practice, either by learning more about the clinical aspects of the adverse event (with three becoming recognised specialists and teachers in that area of practice) or by becoming involved in related QI programmes risk governance (three clinicians). A senior obstetric trainee described the aftermath of a disastrous delivery that resulted in the admission of a baby to NICU. A delayed investigation of the incident (that happened outside of the three case-study services), generated considerable personal concern about her own safety as a clinician.
It all makes you very apprehensive. It was such an awful thing and I wanted to leave medicine at that time. Then I did a lot of my own research. These skull fractures do happen with some vaginal deliveries and perhaps it’s a little bit like a lottery. But it’s very hard to change your practice when you don’t know what happened.
SASi29
The significance of post-incident learning for both future patient safety and ongoing personal recovery was highlighted by trainees. As one trainee expressed it: ‘when you look at it more clinically and less emotionally, you start to realise that you did your best’ (SASi19). This realisation was, for all participants, a necessary step towards the rebuilding of professional confidence.
The support needs of governance teams and clinical leads
The emotion work and support needs of clinicians less directly involved in incidents but communicating with injured families and distressed staff on a regular basis were rarely directly considered by participants.
Particularly for risk governance teams and HoMs, office spaces were the usual forum for listening, learning, encouragement and skills development between colleagues.
The researcher walked into the offices of the risk team just as there was a round of applause for the HoM by everyone present. They explained ‘she had just managed to talk a really upset family down from a formal complaint, it was so well done!’
Fieldnotes, office observations, 11 July 2021
Particularly at Sites B and C, mentoring support for challenging conversations extended beyond the HoM to senior managers, where the escalation of family concerns was identified as important for families as well as for service leads (senior midwives) themselves. A Director of Nursing explained:
These need to be dealt with at a senior level and when they go wrong, they usually haven’t been. I absolutely want sight on all of them. My Director of Midwifery just did a second debrief of a family that had already contacted me, and I said: ‘Look, I’m aware you’ve got a debrief meeting on Wednesday. Have that meeting and let’s catch up after to see how I can support,’ like follow-up.
SCSi14
These mentoring systems were reported to be highly valued by distressed families as well as by staff responsible for communicating with them.
Interim summary
Our findings identify how front-line staff expectations and experiences influence OD with families both directly and indirectly. The immediate, non-judgemental responses of colleagues and managers to an incident, and these initial moments of post-incident support, are particularly important for initial discussions with families and for clinicians’ sense of care by their service. The dread of an incident and felt personal responsibility for an adverse event, which can impact on both clinical care and staff attrition, might be alleviated where immediate line managers and clinical leads enable space for staff to process these feelings and prepare for family conversations and accompany them through this encounter.
Our findings concur with related research that shows that without clinicians acquiring an understanding of what happened to a case involving them, they feel less secure in their clinical work and more likely to practise defensively. 184 We found that the service-wide support interventions were often not designed appropriately for the demands of maternity units and that interventions that encourage ongoing discussions with colleagues, and regular MDT learning events that included junior staff (notably, doctors at senior registrar level), carried more promise for clinicians’ personal and professional post-incident recovery. 184–186 The chapter also identifies the informal ways that staff and family interests might align over time, providing possibilities for both parties to work together to develop understanding and resolution, and the ways that both front-line staff and families can become marginalised from organisational processes.
Chapter 9 Programme theory 5 – knowing that things have changed because of what has happened
Programme Theory 5:
When families and staff see that aspects of the service have changed after the incident that affected them, they are more able to deal with loss and trauma in the longer term and are less likely to feel alienated from the service.
Introduction
This chapter examines the relationship between OD and approaches to post-incident learning. We explore how different attempts to improve safety arising from action planning, as well as communication of this information, impact injured families as well as clinicians. As in previous chapters, our findings draw from our national interview study (n = 67 participants, including 23 families) and our observational and interview case-study findings, where 75 interviews were conducted, including four interviews with families, and 52 observed meetings.
Perspectives and experiences of national stakeholders
Anticipating the needs of families
Most stakeholders commented on the overlapping interests of families and services as both wanted to avoid the reoccurrence of similar incidents. One charity lead identified the importance for everyone involved in the incident for services to:
Act on those moments where you go ‘Oh, if only something different had happened there then things would have been different’.
SG4
However, some participants were cautious of assuming an automatic alignment of interests between services, staff and injured families. For instance, clinicians who were trauma and bereavement specialists commented on the need to prioritise and give families time to grieve before involving some in service improvement agendas. It was also recognised that families’ interests in sharing their experience for the benefits of a service was one of many approaches they might take to make sense of what had happened to them.
Furthermore, several participants from clinical backgrounds were cautious that families might be promised changes in action plans that either were difficult to achieve or had marginal effects on underlying systems:
I’ve heard it all the time. They want to make changes so that it doesn’t happen again to someone else. Having a report that says we’ve done things might appease them so that feel that. Whether that is truly making a difference? It’s a fine balance between how do you do an investigation so that people get their answers at the same time as having a wider, deeper level investigation that is going to make a difference? Can you do both or just one?
FS1
Discussions like this centred on concerns about how the focus and scope of both report recommendations and action plans were negotiated to meet the interests of both services and families.
The positioning of families in service improvement work
For the most part, participants’ reflections on organisational learning and safety improvement after incidents rarely involved an expectation of families actively participating in informing action plans or holding services to account for implementing them.
The national stakeholders who reflected on the question of how service changes were demonstrated to families and staff identified several key considerations. First, participants noted the potential for alignment of family and service priorities for organisational learning. They described the importance of identifying and acting on ‘pinch points’, or the critical loci where learning can be translated into significant service improvement to impact outcomes. Finally, some national stakeholders suggested the need for a rethinking of improvement approaches, recognising the potential to involve families as active participants to drive improvement, rather than as passive recipients of improvement efforts.
Perspectives and experiences of families
After the death or injury of babies, especially babies who were healthy and at term when labour began, suggestions that lessons would be learnt were not necessarily well received in the early stages of grief:
… she’s not a learning opportunity, it’s not a test case, it’s not just a tragic accident.
SU19
However, the perspective of families often changed over time, with a concern with ensuring that the same thing did not happen again to them or to other people:
… we’re always going to be unhappy with the result, yes, of course we are. Our daughter is dead, I can’t change that, but if we can make sure it doesn’t happen to us again and hopefully doesn’t happen to other babies, then that’s an added bonus for us.
SU19
Some families felt personal responsibility for ensuring that services took steps to avoid repeated mistakes. The importance of ensuring women feel safe during their maternity care was highlighted by women who had experienced traumatic births. They needed reassurance that the specific issues would be addressed with the staff concerned so that other women would not experience the same. However, for some, this did not go far enough. There was recognition of the breakdown of trust in a service that happens when harm has occurred and the need for senior manager involvement to support staff ‘to do the right thing’ (SU11). Two families who received care in 2010 and 2020, respectively, had experienced similar issues with spinal anaesthesia, both becoming active in ensuring that change happened. One woman was active in local service improvement, and another, Anthea, had engaged a senior professional lead who worked with her to promote her story and their proposals for improvement through professional networks and journals. She had received feedback that practitioners had changed their practice after listening to her.
Families appreciated being told about action plans agreed after incident investigations and what Trusts were doing to address recommendations. However, some discovered that although HSIB makes recommendations, Trusts do not have to implement them and felt that they ‘were being fobbed off’ (SU22). Several families indicated that knowing who at the Trust would read reports would have made a difference, as would evidence of changes that had been made because of their experiences. The SI investigation into the neonatal death of one family’s daughter in 2015 identified that staffing levels needed improvement; however, there was no reference to learning from the investigation on the Trust website:
So it’s just like she died for nothing, basically, and they’ve got away with it.
SU16
When babies have died, knowing that changes have happened ensured a legacy for them and families fought to secure this:
Because I can’t be her mum in any other way, I need to make some sort of change [tearful] because it can’t keep happening to other people because they’re not listening.
SU16
Not being heard was a frequent complaint from our participants that they hoped to address through being part of the study. Anthea recognised how powerful birth stories and their public and professional accessibility could be. Her view was that the discomfort professionals feel being confronted by such stories, and an understanding of their position, would lead to practice change.
If families could see that changes had been made because of learning from their harm, it helped them process their trauma. However, all too often, families were frustrated by the lack of evidence that any lessons had been learnt and were left with little trust in services going forward.
Perspectives and experiences in the case-study services
Implementing actions plans for safety improvement (April–November 2020)
The period of fieldwork was a time when staff were ‘just about getting by, from shift to shift’ (Site C clinical lead, Fieldnotes, 23 July 2022). Across all case-study services, there was a sense that organisational learning post incident and communication of this learning to harmed families were particularly inadequate. Also, clinical and service leads discussed two longer standing difficulties with this work. These were, first, how to balance the desire for ‘quick wins’ with longer-term change in a service. The pace of change was a concern for some injured families as well as front-line staff and, second, how to communicate ongoing changes to staff.
Site A’s CG lead was especially outspoken about the undermining effects of extensive reporting requirements of Trust and external QI programmes.
They, along with many senior clinicians, felt that required action for learning from incidents had become an exercise in the pragmatics of demonstrable success organised around service risk registers rather than a response to clinical realities. 187
At Site A, staff were frustrated that learning from incidents simply bypassed some service areas and front-line staff. A risk midwife commented:
There’s lot of learning that needs to be known more widely. Like for junior doctors and labour ward. It’s really important for them to see the same issues come up time and time again.
SASi01
Improvement leads at Sites B and C were also tired of assurance and audit that did not seem to contribute to any new learning or service change. Site C’s CG lead remarked:
I feel like learning could be better. I feel like it all gets fed upwards, and you go to meetings, and you explain what actions you’re going to take and why but actually it needs to trickle back down to staff.
SCSi08
However, reasons for disappointment at the pace and spread of service changes post incident were significantly different across the case-study services.
At Site A, where safety improvement was less embedded in regular service business, many staff interviewed felt demoralised by the lack of investment in learning opportunities and in ongoing safety improvements. At Sites B and C, where clinical leads were more actively engaged in Local Maternity and Neonatal System (LMNS) and service-level improvement projects and ongoing initiatives, staff were more often frustrated by the technical and political complexity of securing changes to systems [e.g. revisions in care pathways or information technology (IT) systems]. At Sites B and C, many clinical leads were invested in professional and service development work (e.g. site selection for national pilots; leadership in LMNS projects, specialist training initiatives and secondments into national schemes). These investments were evident in service-level expertise, commitment to and ownership of quality and safety improvement processes along with knowledge of organisational change.
‘Quicker wins’ and system changes
Across the case-study sites, post-incident action plans were constructed pragmatically, with an eye to service capacity and ambitions, as well as to the interests of injured families who might want to know whether changes highlighted from their own incident investigations had happened.
‘Quicker wins’ or local changes that did not require inclusion on the risk register or a business case could sometimes be identified as a way of demonstrating safety improvements to families and front-line staff as well as meeting requirement for local audit. However, there was understandable caution that action plans drafted for more rapid completion were not always the most beneficial for managing ongoing safety concerns. A clinical lead commented:
We change the guideline, share message of the day, put individual training in place, do an e-learning module, we do all these things to share learning. We will get 10 to 20 people to alter their behaviour but that won’t alter the system. And that, I think, is the challenge.
SDSi06a
Changes to the physical environment were often expected to be the most straightforward to implement. However, a relatively straightforward change to the workplace could be difficult and time-consuming to secure, as the changes required the support of business cases and external recommendations before they were taken seriously:
Getting a second printer for Maternity Admissions triage should have been simple stuff so that the midwife did not have to leave triage and walk 30 paces to another printer. When we got an actual anonymised external report, then all the things we’d been saying, when it was in the report, the changes happened overnight because some external came in an explained it.
Clinical Lead, SDSi06a
Indeed, action plans established from incident report recommendations often involved complex as well as protracted revisions across a service.
So, we met with the family whose baby died 18 months ago and that was an HSIB investigation with recommendations for us. We’ve got traction on quite a few of them, but not all are completely completed. Some things are big: antenatal storage of CTGs requires a business case, capital investment, finance committee investment, then you have to tender, then you have to buy the equipment …
Director of Midwifery, SCSi16
Changes to care pathways were particularly complex and time-consuming to develop and embed in practice. Site C’s Clinical Director explained what was involved in the 2-year project of revising the ‘Induction of labour pathway’ that involved changes in guidelines and working practices, staff attitudes and ongoing improvement cycles. Senior clinicians at Sites B and C sometimes reflected on how best to balance the ambitions of service improvement and the completion of action plans. The clinical director explained:
We need to close on actions. Making sure these actions are caught when some people were not aware an action had their name on. But they all have to be realistic and with a reasonable timescale to deliver it but seeing impact on the shop floor.
SCSi03
This clinical lead was commenting on previous situations where clinicians had been overly ambitious in drafting action plans, identifying service changes that were out of reach for improvement teams. She felt that this lack of change would be difficult to justify to a family. She noted that overambitious post-investigation action plans could also alienate staff and showed in failing audits. In this service, there has been some initial discussions to involve some families with insights into the demands of this work in the prioritisation of identified safety improvement work streams.
Communicating changes to front-line clinicians
Many senior clinicians involved in safety improvement highlighted a tension between the demands of ‘upward reporting’, auditing and assurance to service and Trust committees and the felt need to communicate ‘down to the shop floor’ (SASi17a; SDSi12) and to injured families. While CG teams and clinical leads recognised the importance of involving front-line staff in learning and service change, they also stressed the difficulties of engaging highly fluid teams in multiple units and across geographically dispersed parts of a service.
Appendix 8, Table 10 documents service communication approaches in the three services and how they were received by different clinicians working in the three case-study services.
In brief, we found that none of the services were able to implement a post-incident communication strategy to reach front-line clinicians. Most notably, the effectiveness of newsletters, bulletins and e-mail updates for sharing learning was questionable, with messages lost within other correspondence; e-mail overload and difficulties with accessing IT systems for staff e-mail updates during working hours. Special learning events, dedicated safety weeks and invitations to reviews panels often missed staff working shifts on busy units or out of hours. We found that more organic informal networks of learning188,189 were more accessible and enjoyable for staff. Multidisciplinary team learning meetings and informal outreach activities were reported as the most effective approaches to knowledge sharing. As discussed below, these approaches were effective for influencing the attitudes of junior clinicians towards families post incident as well as for sustaining the work of CG teams and clinical leads.
Particularly at Site A, the CG team was acutely aware of the tense division between their team and front-line clinicians affected by incidents. Risk midwives tried various approaches to improve awareness of their work and foster better relationships. For example, they networked to ‘tempt people to risk meetings’ and invited Band 6 midwives to the PMRT and SI review meetings to ‘take up any learning and spread an understanding by word of mouth of what we do far more effectively than we can’ (SASi01). They composed letters of reassurance to staff before HSIB interviews, ran ‘tea and cake trolleys’ to update staff on learning from investigations and worked some clinical shifts ‘so that people don’t say how can you judge my clinical care’ (SASi04b). Overall, the clinical risk team were aware that without service-learning forums, their engagement with clinical teams was limited:
When I work clinically, I get asked all the time ‘Whatever happened to that woman who had so-and-so?’ and I’m like ‘it’s this, and this,’ and everybody’s interested. I just feel that we have got this huge gap here. Because you experience these things, you see all these things, but the circle doesn’t close for you because you don’t know.
SASi01a
Another aspect of this informal outreach work of risk midwives, some nurse consultants and PMAs was post-incident support of some midwives and, occasionally, junior doctors (see also Chapter 8).
Most senior clinicians at Sites B and C described the services where they worked as places of learning for quality and safety improvement. Weekly MDT learning meetings were the tangible expression of this organisational focus and ethos. Significantly, detailed case studies of SIs that had happened in the service, which were narrated from precipitating events to learning and change outcomes, were included amongst other learning topics. The inclusion of these case studies normalised discussion of SIs as events of learning and collective reflection:
During a weekly zoom learning meeting 30 staff discussed a recent SI and its investigation. The clinical lead and some staff from the unit where the incident happened were at the meeting. Discussion initially focused on flaws in tools and systems until the Chair asked who admitted the woman. The clinical lead replied it was midwifery triage, adding ‘we try our best under immense pressure. We manage the best we can. Maternity Assessment Services in all units are under such high risk at the moment.’ The Chair quickly added ‘yes, yes, there is city-wide action on awareness of these problems at the moment. It’s just not manageable.’
Fieldnotes, Weekly Multi-Disciplinary Learning Forum, 4 August 2021
As this example shows, case-study discussions took account of wider service conditions beyond individual clinical scenarios. Particularly where staff involved were present, there were frank discussions about service pressures and limitations. These discussions also drew attention away from more immediate assumptions about individual clinical error. In addition, during these meetings clinicians pondered ethical questions, for example, on the role of families in their own safety.
During this learning meeting, some participants reflected on the role of women themselves in drawing staff attention to a change in signs of illness. Some meeting participants suggested that if a woman felt any changes, she should be listened to. A senior clinician commented on the difficulty of this:
'We’ve got to think about how much onus we leave for families if we wait for this.’ There was a pause and some agreement before the meeting moved on.
Fieldnotes, Weekly Multi-Disciplinary Learning Forum, 4 August 2021
Multidisciplinary team learning meetings were also an important space where service and clinical leads could promote ongoing reflection and shared discussion. The examples given above illustrate how complex questions of accountability were explored through case-study examples. As often, ‘one-off’ remarks at these meetings could express and reiterate a wider service ethos of shared responsibility for events of harm.
At the start of a SI case presentation, about a baby who required admission to NICU after a home delivery, the presenter mentioned that a Band 5 midwife had been called for this delivery. The maternity safety lead chairing the meeting blurted out ‘how could we put her [the midwife] in this position?’ (Fieldnotes, Weekly Multi-Disciplinary Learning Forum, 2 August 2021).
At Sites B and C, there were multiple examples of senior clinicians reflecting, individually and in small groups, on the best ways to approach teams and families post incident to communicate subsequent learning. ‘Learning how to learn’ was a noticeable dimension of approaches to SIs and action plans and their implementation. Reflecting on the difficulties of including all staff in learning meetings, a senior clinical lead commented:
So it’s quite hard to sort of spread the message wider. I just need to make sure that whatever allowed a Band 6 midwife or doctor to drift into that error, I need to fix that, and not them.
SCSi05
The situation was very different in Site A where there was less capacity for learning by MDT discussion and learning; there was widespread resistance to systems-based approaches to events, and consequently staff sometimes felt scapegoated for incidents. At Site A, a senior clinical lead complained of the loss of this clinical space in recent years leading to a ‘denudation of our culture’ (SASi12). A ‘lack of manpower’ to ‘look into things’ (SASi35) or to ‘work out who was involved’ (SASi01; SASi04b) was repeatedly noted by senior clinicians. During the fieldwork period, Site A had also disengaged from many LMNS activities and had no regular forum for multidisciplinary engagement and learning. Senior leads talked of ‘the luxury of learning’. At Site A, CG and clinical teams more often described their exhaustion and cynicism towards the narrative of safety improvement. At this site, there was a widespread sense that service or systems-wide learning and improvement post incident were either ‘just not done very well’ (SASi1c) or ‘not disseminated effectively’ (SASi14). One long-established clinical lead noted the ‘disintegration’ of opportunities for learning and QI in recent years due to the sheer increase of patient numbers and pressures on clinical time. The gradual erosion of maternity teams to protect time for learning also appeared to correspond with a hiatus in service leadership (see also Appendix 2 on general and topic-relevant features of the case-study sites).
This meant that QI practices were not routinely embedded through learning forums and ongoing safety improvement work. Without this, staff felt, there were limited opportunities to share knowledge and make changes, resulting in demoralisation.
It all does nothing. Absolutely nothing. I end up just feeling like a monkey. It does nothing. Don’t pat yourselves on the back that we’ve spread a learning message because we haven’t.
Risk Midwife, SASi1b
As described above, for injured families wanting to be involved in service improvement, this lack of capacity was interpreted as a lack of interest in collaborative working to make improvements.
In contrast, at the same time, clinical leads at all case-study services were keen to use the voices of injured families to strengthen the case for front-line staff to attend to various practice and service improvement work. This inclusion depended on the availability of time between more pressing clinical learning priorities. Family stories or experiences were considered a ‘soft side of safety learning’ that encouraged staff to be ‘better, more empathic listeners’ (SDSi04). Also, when these stories impacted directly on clinical leads during debriefs, they might have a more significant impact on approaches to clinical care:
The clinical director at Site C described: ‘an incident that really hit me. [The woman] said she didn’t want forceps and the doctor just ignored her and put the forceps in and pulled the baby out. The debrief will always stay in my mind. She felt, at the time, raped. That’s what she said. Violated, is the word she used. Violated. “A piece of meat”. This really stayed with me all the way. We use that in teaching when the junior doctors join us, we bring up listening and not making a woman feel violated’.
SCSi05
The possibilities for injured family experiences to contribute to formal teaching events were also important to clinicians who contributed these stories. However, in contrast to situations where families shared their stories more directly, there were relatively few opportunities for families themselves to shape these narratives for different audiences or to have a sense of the impact of the experiences they had shared.
Communicating changes to families
As previously described, all case-study services routinely invited families to at least one in-person or virtual meeting to discuss the findings from their finalised incident report. Some of this discussion was to reassure families that ‘learning had happened’ (SASi08b). For more expert debrief leads, this aspect of the meeting was carefully considered in relation to the interests and expectations of that family.
Several clinicians who were expert in developing relationships with injured families (before, during and after debriefs) were cautious of assuming that all families are interested in knowing about service and systems changes. Some families were still dealing with the ‘raw emotions’ (SASi01b) of family injury, and for them, such promises of changes made were irrelevant or insulting. A risk midwife described:
An angry woman said to me ‘I don’t want my baby to be your f***ing learning curve. I want my baby alive’. At the end of the day, you’re going home to an empty cot and I don’t suppose you give two shits then as to whether we are taking learning forward.
SASi01b
For some clinicians, another consideration of the debrief meeting was how to respond to a family’s expectations of the outcomes of safety improvement work. For example, a specialist midwife commented:
Always have to say to a family ‘I can’t promise you that this will never happen again’ but I can say we will make improvements.
SDSi08
She felt that promising too much to families risked the further erosion of trust in the service. Clinicians involved in the longer-term support of injured families (CG teams or specialist clinicians) were also aware that families had different expectations for the pace and the scope of changes. The completion of safety improvement measures that were rapid and more tangible was sometimes expected to offer some families greater reassurance that changes were happening:
By the time we’ve done the debrief following the SI closure, we’ve normally completed most of the actions so that’s why we can sit with them and say to them that is what we’ve done, so not many families come back for more closure.
Risk Midwife, SDSi03
However, some senior clinicians felt that a more honest approach to what was possible for services was important to many families:
So I say there’s certain things that I cannot fix but at the same time there are things that I can influence straightaway, so this shows learning and improving on things all the time.
CG Lead, SCSi01
Debrief leads were also aware that the pace of some changes in services change left families with the impression that nothing had been done.
Families want that meeting quite early and actually it takes us time to work out what’s happened and then institute changes. So, like changes to our CTG monitoring off the back of a couple of cases with some really awful outcomes, we told the families we were going to do that, actually now that’s three or four years ago and they wouldn’t know that we’ve actually done that and are doing that.
SASi13
This senior clinician highlights the difficulty of demonstrating long-term changes to families without a Trust or service strategy for keeping injured families updated on long-term improvements and without public access to risk registers.
Indeed, all four families recruited from Site A highlighted that the lack of proactive communication from the service about changes made. This lack of public communication led families to conclude that the service, rather than all staff working there, was untrustworthy with respect to what they had committed to do for this family and others. For example, 3 years on, Fay’s mother remembered that the appointment of two specialist cardiotocography (CTG) midwives was identified as a priority action following Fay’s injuries. The family had not been informed that these appointments had happened. For Fay’s family, this situation reflected a wider disinterest of the service in their daughter and their avoidance of any responsibility for learning. She felt that the harm that had happened to her should be used as a case study for staff to demonstrate where things went wrong to promote learning (SAFi1). However, Fay’s mother remained unsure about the learning that had happened in clinical teams after her daughter’s avoidable injuries. She wanted assurance that the doctors who had dismissed the midwife’s concern about the CTG and who ‘didn’t even ask my name, just looked at the chart and walked off again’ knew of the outcome for her family (SAFi1).
These views illustrate the importance of ongoing service efforts to sustain relationships, provide acknowledgement and demonstrate learning to injured families. For some families, the attribution of events surrounding the incident as ‘incidental’ by investigation panels overlooked their lived impression of that time. They stressed the connection between their poor relational care on their incident and its immediate aftermath.
While CG leads and clinical leads tended to focus on providing reassurance of specific changes connected with the SI, many families were as concerned with improvements to the general care before and after their incident (e.g. the cleanliness of a room or how staff spoke to one another). These aspects of care quality indicated a wider interest in their experience and in making improvement. However, without Trust or service prioritisation of and support for updating injured families on service changes made, CG teams or clinical leads responded to family enquiries on a discretionary basis.
Involving families in ongoing learning
The involvement of some injured families in safety changes in more active ways was noticeable at Sites B and C, where experience-based learning and learning networks were already embedded in other aspects of maternity care provision.
At Site B, in-person invitations to injured families to become part of maternity quality and safety improvement work fostered a wider ethos of reconciliatory practice as well as in family engagement. Family engagement was envisaged as ‘the most powerful way of getting change’ (SDSi04). For example, small grant and service funding secured by clinical leads supported two women from injured families to join the ‘User Experts by Lived Experience’ panel that influenced the reorganisation and renaming of the maternal mental health service. Another woman, with perineal injuries was directly involved in the development of the ‘new pelvic floor programme’. Programme completion and promotion gave further social capital to improvement work with injured families.
Three (of four) families recruited from Site A expressed the desire to become directly involved in changes that would prevent the reoccurrence of similar injuries. For example, Hugh described that he had offered to contribute to teaching events for the service:
I offered, it think, on multiple occasions to speak to whoever wanted to speak to me about my experiences. I would have been happy to speak to a room full of midwives or obstetricians or anaesthetists or whatever. I would argue that would be a lot of use if you are going to change the system.
SAFi3
For these families, the apparent lack of interest of the service to learn from their own events, and to include them directly in their learning, led to disappointment and continued distrust. At the same time, some families were more ambitious than clinicians in driving service improvement. While some clinical teams were satisfied in framing successful change as that happening in their unit, hospital or LMNS, some families sought to address these issues on a national scale.
The development of working relationships with some injured families was described by several CG and clinical leads working in some services. For example, the CG lead described her relationship with one father where:
He actually stayed in contact and phoned me like every 3 or 4 months. He did chase me up on it. It actually made me realise [that] it’s good when [families] do that because it means you follow through on these actions, people get busy and actions slip off into the file on some computer somewhere.
SCSi01
This emphasis on giving time and personal attention to disappointed parents, understanding what exactly the family expected and voicing dissatisfaction to Trust leads encouraged some demonstration of trustworthiness to families despite the slow pace of service improvements during 2020–1 (due to the COVID-19 pandemic).
This service approach also opened the possibilities for a realignment between ‘work with injured families’ and ‘accounting upwards’ as families came to inform some of the priorities of senior committees or the Board. The Director of Midwifery (DoM) at Sites C and D took the view that families played a significant part in holding CG and clinical leads to account:
Families are quite searching, they’ll go through the Public Board minutes. Literally, I’ve had families go and look and try to identify their case. They’re anonymised but they’ll recognise them. If you haven’t presented things at Trust Board you wouldn’t get away with it.
SCSi16
This perspective was informed by the attitudes of Trust Board members towards taking family voice seriously and by an embedded ethos of family involvement in different aspects of the service. Where families were proactive and able to access systems for holding services to account for changes to be made in the longer term, families could effect changes in services that had a service ethos that welcomed their involvement and the associated development of new family involvement perspectives.
Chapter summary
This chapter has explored service efforts and challenges in implementing sustainable changes, communicating these changes to those involved and involving families in staff in long-term QI efforts. Analysis of case-study findings highlights the pragmatics of post-incident safety improvement, with action plans shaped to accommodate Trust and service level risk management and assurance systems, the temporal demands of different types of improvement work and the expected needs of some families to know that post-incident improvements identified from their investigation is not overlooked. Alongside the challenges of sustaining safety improvements, services also faced the difficulties of communicating this improvement work to front-line staff and to families. Without service support for collective learning events, many risk management and QI staff felt that their work was devalued, and families continued to distrust a service that seemed to still neglect them.
The possibility for some families to become more actively engaged in safety improvement work is explored in relation to a service ethos shaped by wider organisational leadership and practice examples of service leads. These collaborations are situated in ways that might dissolve the felt tensions between ‘upward reporting’ and actual maternity safety work. Concurrently, the need for an organisational strategy for communicating post-incident changes to all families is identified across the case-study services and the outcomes for families who are never informed of post-incident changes are examined. Techniques for sharing post-incident learning and for conveying attitudes towards incidents with front-line clinicians are explored and two approaches (the regular multidisciplinary learning meetings and risk team outreach) are examined to understand what is required for these techniques to be effective and for whom.
Chapter 10 Synthesis and discussion of findings
Introduction
This chapter addresses Research Objective 5: conduct data interpretation and study output development with stakeholders. The discussion of findings is organised in three main sections. First, we summarise the development of the realist analysis, from the initial programme theories to the evidence-informed C–M–O configurations that suggest ways to strengthen disclosure in NHS maternity services. This section integrates findings from national and regional stakeholder interviews, including those with families (study phase 1b), the service case studies (study phase 2) and the forum discussions (study phase 3). Second, we identify and explore three additional programme theories derived from the study findings that were examined thematically and developed in co-investigator discussion and with critical reflections of some SP3 forum participants. Finally, we reflect on inclusion in the study and the study’s strengths and weaknesses.
Recap of study aims and objectives
We aimed to understand how OD works, for whom and in what circumstances in NHS maternity care to identify the impacts on different stakeholders and to generate actionable evidence to inform maternity providers. Appendix 9 presents our Draft Best Practise Guidance, currently in development with stakeholders.
These aims were met through a staged realist analysis that included:
-
the establishment of initial hypotheses for a realist investigation of OD improvements in NHS maternity services
-
refinement of these hypotheses through an interview study of national stakeholders and in-depth ethnographic case studies of OD improvement interventions
-
further interpretation of data (initial and new hypotheses) with national and case-study stakeholders.
Realist theory development
Initial programme theories
Table 2 summarises the if/then hypotheses that structured our five initial programme theories and the a priori propositions identified from our realist literature synthesis (see Chapter 4). These working hypotheses were used to guide data collection and analysis of our national interview and service case-study findings. These differ from the stages of the ‘Being Open’ guidance41 as they are focused on outcomes, particularly from the perspective of families and front-line clinicians.
| Title | Proposition | |
|---|---|---|
| 1 | Receiving a meaningful acknowledgement of the harm that has happened | When a family feels that their experience of harm and its aftermath has been acknowledged in a meaningful way, their trust in clinicians and the service is more likely to be rebuilt, clinicians involved feel some relief and ongoing care and communication post incident is more likely |
| 2 | Being involved during the review/investigation process | When families are included in these processes if they decide, and have support for this involvement, they are less likely to feel alienated and distrustful of services and are more likely to be heard in discussions about the event and their care |
| 3 | Making sense of what happened | When families feel that they can make sense of what happened, and that clinicians and the service have sought to help them do this, they feel less dismissed and are more likely to begin some recovery |
| 4 | Receiving care from clinicians who are skilled and feel safe during post-incident communication | When clinicians are skilled and feel safe to conduct disclosure conversations with families, these conversations are less likely to be avoided, questions of responsibility more likely to be addressed and OD is more likely to become embedded in ongoing clinical practice |
| 5 | Knowing that things have changed because of what has happened | When families and staff see that aspects of the service have changed after the incident that affected them, they are more able to deal with loss and trauma in the longer term and are less likely to feel alienated from the service |
Revised evidence-informed development of the programme theories: what this study adds to knowledge of open disclosure policy and practice improvement
Evidence-based development of initial context–mechanism–outcome configurations
Receiving a meaningful acknowledgement of the harm that has happened
We identify the significance of the national medicolegal context that often interrupted the meaningful acknowledgement of families in the aftermath of harm. First, we noted the pervasiveness of professional and organisational defensiveness against OD in both nationally and within the services used as case-study services. This exists against a national policy tension between the management of public concerns and of transparency and respect for injured families and uncertainties over the consequences of candour to the number and costs of claims. 52,88,121 Second, our findings suggest ongoing clinician concerns related to the reputational and personal costs of incident investigation, both during inquest and in internal service contexts where accessible practical and emotional support is currently lacking. In this environment, organisational and professional judgement, adequate resourcing and support for OD are more likely to be compromised. These findings support recent evidence that many clinicians are reluctant to risk being open because they fear disciplinary or legal consequences and that these fears continue despite an NHS claims management system where the defendant is always the organisation and not the individual clinician. 52,103 Trust legal teams within the case-study services felt responsible for protecting employees from these risks as often as defending the interests of the organisation.
We also identify situations where OD is undermined by the inflexibility of post-incident communication procedures. For instance, timing, thresholds and interaction or written communication families can be tightly prescribed. 38,190 This was described as a tension between the ‘technical’ and ‘human’ aspects of OD. Furthermore, our findings across all SPs suggest a lack of agreement between clinicians over the details and timing of disclosure. Clinicians want to be truthful with families and are also concerned about avoiding further distressing families by providing incomplete information; this was especially the case when there were initial uncertainties about the nature and extent of injury. Ethical dilemmas regarding truth telling have been widely debated in the literature on clinician–patient relationships. 191,192 For instance, Birks et al. 12 examine this in relation to disclosure in the English NHS prior to the introduction of the DoC. They identify the ethical argument for a duty-based ethic of care, where truth-telling is not conditioned by the specific details of the situation; a rights-based approach to patients’ unconditional knowledge of their medical situation also supports this position. 193 This position is supported by the DoC. Others have argued that situated truth-telling, underpinned by therapeutic exception, where a clinician makes a judgement about the withholding or giving of information in relation to the patient’s situation or condition, is more ethical. 193 Indeed, we note this ongoing tension and that the DoC has not solved this dilemma. Rather, ongoing questions about thresholds of family entitlement to information and the timing and details of ongoing conversations remain unclear. Many clinicians remain uncertain about how, when and how much information should be shared with families, not because clinicians want to deceive families, but rather because they want to protect families from further distress when uncertainties remain. Our empirical research findings lend weight to recent ethical arguments about the necessity of an approach to candour as a multifocal and dynamic practice, which includes practices of personal, professional and organisational integrity and accountability. 46,194 In practice, as we show, OD processes operate less as a duty and more as an interactive space of tension and moral reflexivity.
However, our findings illustrate that there is a lack of opportunity for shared deliberation on these ethical questions for clinical teams, even in services that are more committed to the post-incident care of families. In addition, we find that notions of therapeutic exception have entered the discourse of Trust legal teams, potentially minimising possibilities for families to raise complaints or initiate legal action. In these cases, we note the significant impact of Trust-level clinical leads who can mitigate the defensive behaviours of corporate governance teams and strengthen the influence of service-level CG and clinical leads so that provisional information sharing practices with injured families are integrated into organisational culture and completed without reluctance.
Finally, from the perspective of families, we highlight the importance of clinicians’ communication skills and organisational capacity for meaningful acknowledgement by the service. Our findings provide empirical support for the long-standing argument111 for the need of junior clinicians can leverage senior colleagues for support and guidance during OD; the tone of these colleagues’ initial response to incidents involving them impacts the initial communication with families and learning for future events. These factors and corresponding C–M–O configurations (Box 1) will be used to develop OD improvement implication in Chapter 11.
-
In the context of the defensive environment of NHS maternity care, the influence of senior clinical leadership in promoting ethics of OD at both Trust and service levels is important for establishing and sustaining a situation where OD is a cultural practice in services.
-
In the context of ongoing uncertainties experienced by clinical and service leads, as well as out-of-hours leads, over when and how to initiate disclosure in particular family and/or clinical circumstances, meeting the expectations of families to be informed of the possibilities of injury as soon as possible after the event, must be paramount.
-
In the context of variability and fast-moving situations for completing prompt initial as well as ongoing disclosure with families, the inclusion of OD discussions as part of the transfer of injured families between units and services is important.
-
In the context of initial and statutory disclosure conversations initiated at pace, and under strain to all concerned, the psychological safety, reflexive clinical skills and expertise of the clinician leading these are important, along with the access to necessary service resources for this work (e.g. private or off-site rooms).
-
In the context of ongoing care of injured families, the confidence and expertise of all service staff to be able to respond to the wider care needs of injured families are important.
-
In the context of ongoing uncertainties of many senior clinicians over if and how disclosure meetings led by them are successful, the development and ring-fencing of regular opportunities for shared reflection and learning are important.
Being involved during the review/investigation process
We identified a variety of approaches and justifications for the inclusion of injured families in reviews and investigations. Some variation is explained by differences in the social and clinical contexts of injury. For instance, later discovery of an incident, especially after a family was discharged from the service, required different organisational processes and communication approaches to those after an obvious and catastrophic event. In some cases, variation was also related to the wider integration of family involvement across the organisation. Indeed, the prompt provision of support services for families affected by significant injury (e.g. Birth Reflections clinics, meetings with PMAs and counselling services) is a significant factor for family recovery, engagement in OD processes and withdrawal or withholding of costly formal complaints. Most families interviewed from the national and case-study research noted the lack of a personalised approach to inclusion as well as limited explanation of what to expect from review and investigation processes. Services sometimes lacked the capacity or interest in including families in the development of ToR for investigations or in the drafting of reports. A lack of protected resourcing and service-level planning for inclusion of injured families led to patterns of family involvement that relied on a responsive approach to complaints or discretionary involvement by clinical staff. The reported contrast between family involvement during HSIB investigation processes and PMRT reviews, as described by clinicians, highlights disparities in staff time and resourcing for prioritising family inclusion. For many staff, the Trust-level demands of incentivised completion of the PMRT combined with staff shortages undermined the ability to prioritise inclusive practices.
Our findings present new evidence on the introduction and impact of more innovative approaches to family involvement, such as the presence of a lay representative (MVP lead) or the presence of families themselves in Trust investigation meetings. Representation, the ‘humanisation’ of both clinical cases and clinical teams and oversight of investigation practices were all rationales for MVP or family presence. In these cases, staff continued to navigate the tension between fostering the trust of families by encouraging open practices and protecting the service and families from sharing incomplete knowledge that might be subject to misinterpretation and might lead to distress. We found that in services where there was leadership-supported, wider expertise and confidence in engaging families in safety and QI work (as in Trust B) proactive inclusion were possible. Therefore, we identify the ongoing influence of senior leads to champion and disseminate an ethos of family entitlement to information for the strengthening of OD. Strategies for communicating information that is incomplete or uncertain must be developed to avoid ethical dilemmas and reduce distress for families and clinicians (Box 2).
-
In the context of the varying needs and circumstances of families who might choose to be included in their incident review or investigation, the development and embedding of a flexible involvement guidance that includes a proactive approach to inclusion, initial (and return) discussions to clarify family expectations, explanations on review and investigation processes and the opportunity to inform the ToR of an investigation and review provisional report drafts need to be available to families and to clinicians. This, coupled with a proactive approach to initiating and continuing family inclusion, is important to avoid current inconsistencies in inclusion practices. The option of independent advocacy should be available to families, along with an option to attend reviews of their own case.
-
In the context of the differing approaches to family involvement (from fact finding to testimonies of injury), families and staff require opportunities to reflect on expectations of information sharing.
-
In the context of the emotional demands and potential distress that many injured families experience during reviews and investigations, provision of structured support by or commissioned by the investigating service (e.g. Birth Reflections or counselling) is necessary.
Making sense of what happened
Our findings on Trust-level investigations and reporting, as well as on the management of external (HSIB) reports within a service, further indicate the cramping effects of corporate governance and Trust legal teams on knowledge sharing with families. While this effect has often been explained as the effect of the prioritisation of service ‘compliance’ over sensitivity to family situation and need,46,48 our findings also provide strong empirical evidence of the impact of corporate risk aversion on the construction and sharing of investigation findings with families. The investigation report, in particular, captures the dynamic of mistrust that can emerge as organisations seek to manage sensitive information while families anticipate and experience information concealment. The drafting and redrafting of the wording of reports, along with adjustments to the reporting on panel conclusions arising from different investigation methodologies, might, in one respect, lend clarity to information generated by complex and sometimes inconsistent organisational processes. At the same time, however, the truthfulness of reports may be compromised by the interests of those guiding the search for knowledge. 195 This could result in a situation where certain facts were de-emphasised and families could be misled. 196 This conflict between a family’s need for information and the management of information by the service underpins the difficulties experienced by senior leads in services where families are present at their own investigation panels. Here, families observed constructive discussions of service improvement that were deemed to be not directly relevant to their case. It was sometimes anticipated that families might misconstrue this information as grounds for legal action. Similarly, all but a few exceptional clinical leads encouraged injured families and affected staff to meet informally to reflect on the effects of the incident. There were few opportunities created for junior staff involved in an incident to participate in or observe subsequent disclosure conversations with the family.
Different expectations around the main purpose of incident reviews and investigations – for understanding of what happened for a family or for systems learning – could further undermine family confidence in investigators and the service. This was particularly the case when families were unable to recognise their own experiences and questions in the report or when these were marginalised in favour of issues that were considered central to overall findings. The use of unfamiliar language or concepts in reports and family debriefs exacerbated this marginalisation. The service accepting responsibility for the incident reduced the likelihood of families seeking to blame the behaviours of front-line clinicians. However, sometimes this can lead to the same incidents being repeated by the same clinical teams if wrong-doing and systems learning are never fully addressed. 197 Given the overall context of defensive reporting, conversations with clinicians about the report, the incident and its impact were significant for families (Box 3). The development of formal care pathways that not only supported family inclusion in investigations, but also encouraged alternative ways of making sense of the event, was critical for some. Our research provides new findings on the sociopolitical processes and moral practice of report drafting, an aspect of OD that is critical to families but rarely examined empirically. While several researchers52,198 have surmised the cramping effects of the national medicolegal climate on post-incident communication with families, our empirical research documents how this cramping can happen at the interface between corporate concerns of the Trust (to manage litigation and reputational risk) and some service and individual professional concerns with OD improvement.
-
In the context of embedded organisational defensiveness over the sharing of provisional knowledge with families, clarification for corporate and clinical teams on the likely legal status of sharing provisional knowledge is required.
-
In the context of differing (and often fluid) expectations for families and clinicians over the primary and secondary purposes of reviews and investigations, ongoing clarification and discussion of how different needs can be met over time are required.
-
In the context of reports and later discussions, inclusion of the perspectives and questions raised by the injured family is required as a central part of the report.
-
In the context of formal reporting requirements, in-person discussion of the report during which a family’s version of events can be further explored and documented is required. This should later be integrated into the report as an important, credible and legitimate perspective to ensure the entire picture of what happened is visible.
-
In the context of a family’s search for a wider understanding of what happened and for some alleviation of their harm, the possibility for families to meet with staff more directly involved in their incident should be explored and offered where all parties agree and the presence of a skilled Chair and mediator is ensured.
Receiving care from clinicians who are skilled and feel safe during post-incident communication
The impact of involvement in adverse events on clinicians has been noted over decades,33 with shorter-term emotional reactions of distress, self-blame, guilt and shame,199,200 often intensified when there are poor patient outcomes and a strong sense of self-responsibility for the event. 5 These experiences can become life altering, leaving a ‘permanent imprint on the individual’ with those affected ‘dropping out, surviving or thriving’. 181 Slade et al.’s recent findings highlight the relationship between traumatic work-related events for obstetricians and gynaecologists, attitudes and behaviours of blame relating to incidents and the stigmatisation of discussion of work-related trauma. 181,201 These are consistent with our findings, which also highlight the importance of clinical skills, psychological safety and opportunities for OD. These relationships are less clearly understood. We also explore the experiences of clinicians with different roles and seniority related to OD work and consider the various support strategies required for this work at all levels.
The anticipation of OD is associated with anxiety for those directly involved in the incident, particularly where they are already feeling undermined and isolated by colleagues. 11 However, these conversations can sometimes bring emotional relief, help psychological coping, reduce guilt and shame and even open the possibility for relationship reparation with a family. 13,14,20,29,33 Manser (2011) identifies the need for investment in accessible and relevant staff support to alleviate the impact of critical incidents on all involved. 5 Discussions with medical staff during our interpretive forums noted the interest of junior doctors (Senior Registrars) in ‘closing the loop’ after they had been involved in an incident. Many shared experiences of not knowing what had happened to injured families after the event. One doctor commented:
It’s not so much about wanting to learn as much as wanting to know that the mother and baby are alright.
Forum 5
They also wanted to be present in immediate and later family debriefs, suggesting that they could offer a closer understanding of events during these discussions. The forum reflected on the harmful sense of separation of front-line clinicians and families in the immediate and longer-term aftermath of an incident (Box 4).
Our findings present a more comprehensive picture than previous studies of post-incident staff support initiatives and also explore and seek to explain the reception of these initiatives within a service across different clinical groups and levels of seniority.
-
In the context of ongoing attitudes and practices of blame and self-blame for incidents, an immediate, non-judgemental response of shift leads and the wider team, along with practical support, is critical for the emotional care of staff involved as well as for skills development and learning.
-
In the context of a dependence on legal teams to deliver ‘DoC’ guidance, there is a pressing need for investment in disclosure skills training for clinical and service leads as well as in wider OD awareness training (on the ongoing needs of injured families and affected colleagues) for all staff.
-
In the context of incidents happening in complex and fast-moving workplaces, service and Trust-level support for externally facilitated ‘cool’ debriefs that involve both senior and junior staff from the incident and where the events and effects of events are discussed is valuable.
-
In the context of events involving junior staff, opportunities for them to be present (if the family consents) in ongoing OD meetings offer possibilities for reconciliation and skills development.
-
In the context of increasing demands on CG leads and service leads to lead multiple OD processes, Trust and service-level support for opportunities to develop local and national support networks for the discussion of personal and professional OD demands, and of best practice examples of how to address them, is important.
Knowing that things have changed because of what has happened
Recent research by Martin et al. highlights the significance of organisational practices of reflection, learning and improvement for fostering cultural change towards greater openness. 38,190 This involved an approach that moved beyond ‘projectness’ towards an open-ended and continuous perspective on implementation and the ongoing identification of complementary impact across an organisation. 190,202 We found that one Trust was seeking to embed less-guarded discussions about incidents and injured families into ongoing learning events. This differed significantly from the ‘post-incident learning meeting’ that maintained a separation of discussions about incidents (that people would prefer to not have to deal with) and news of less uncomfortable or comprising service learning or change. Some families’ hopes for safety changes that would eliminate the possibility of their incident happening again, and for these changes to happen at speed, were challenging for a service to explain or address.
A central question raised from the desire of both families and clinicians to know that changes have happened because of the incident that affected them is the extent to which perspectives on relevance and severity are shared. Perceptions of what classifies an event as significant and what constitutes acceptable risk may vary between clinicians, families and services. 203 Furthermore, simultaneous pressures impinging on a healthcare organisation may necessitate complex risk trade-off decisions. 204 We identified a perspective of front-line staff that corporate and service leads were more likely to uphold the complaints of families over clinical failings and communication difficulties, rather than investigating and understanding the full picture of complexity. We also identified a competing perspective of many families that service managers would protect their own staff at all costs.
Our research findings document the often-unexplored challenges of both securing and sustaining significant safety improvement work within a service and of communicating this work to affected families and front-line clinicians. We provide new evidence of the challenges of this work, which are rooted in a lack of organisational staff communication strategies and limited investment and attention to the needs of injured families after discharge from secondary or tertiary maternity services (Box 5).
-
In all contexts where investigation and review reports recommend specific safety improvements, a service-level communication strategy for updating affected families of the progress of these changes is necessary.
-
In contexts where families anticipate both rapid and in-depth service changes resulting from their incident review or investigation, the involvement of family representatives or service leads to account for the pace and extent of service change would prevent further family distrust in a service.
-
In situations where injured families have interest and feel sufficiently recovered, service expertise and capacity to involve them in safety improvement roles in that service should be available.
-
In maternity services, where the communication of post-incident learning to all staff is important, a review of staff communication strategies to ensure that ongoing changes are known about is important.
-
In service and team contexts where defensive views and practices towards incidents and their impact continue, regular and non-judgemental discussion of these difficult events during ongoing multidisciplinary learning forums can inform attitude change.
Additional programme theories informing disclosure
In the above sections, we have presented our initial programme theories, discussed our deeper interpretation of the key elements of these programme theories as informed by our empirical research and have offered realist C–M–O configurations to illustrate what works, for who and in what contexts for successful OD. In addition to our five original programme theories, throughout our empirical research, we inductively identified three additional programme theories during thematic analysis and in discussion with our CIG and interpretive forums. We tentatively propose that these additional theories also encompass mechanisms that underpin effective disclosure in many circumstances for many families. These programmes theories are:
-
RECOGNITION: If attempts to understand the incident prioritise the family’s own experience and position, as well as their unfolding priorities for making sense of their incident, then some families might rebuild some sense of trust in those who recognise these priorities.
-
INCLUSION: If maternity services were proactive in the inclusion of injured families in ongoing safety and QI work, then family interests and experiences would be more effectively integrated into this work.
-
RECOVERING TRUST: If lead clinicians and services are both engaged in the recovery of a family’s trust (rather than the management of their complaint), then families are more likely to consider the service, rather than a few individuals working there, trustworthy.
Recognition of family experiences of event
We understand recognition as different from acknowledgement, which is the ‘non-denial’ of an injury and the effects of the injury on an individual, family or community. 205,206 Recognition is considering a family’s experiences of injury and its effects in their own terms. 207,208 Our national interview and service case-study findings identify and examine various situations where the priorities and perspectives of injured families are not aligned to the organisationally defined imperatives of safety improvement agendas. Misalignment is most immediately felt when a family’s incident of harm falls outside clinically recognised thresholds of significant injury as defined by the DoC or outside service-defined thresholds for maximum learning as defined by EBC and UK-MBRRACE criteria. 105,209,210 Second, we explore a range of situations where a family’s need to understand the details of what happened in their case becomes obscured by organisational priorities to generalise learning for ongoing and future-oriented systems improvement. Third, misalignment arises during incident investigation and reporting practices, for example, when a family’s sense-making of the event becomes categorised as ‘incidental’ or is excluded from recommendations and related action plans. In these situations, family concerns become irrelevant as they were filtered through limited definitions of safety with a short-sighted interpretation of the information seen as necessary for identifying risk. 211 Finally, in reviews and investigations, family testimonies of what happened, along with broad questions of ‘why?’, sat uncomfortably with a risk investigation focused on establishing ‘objective’ facts. 212
Families who offered experiential testimonies rather than objective evidence were disregarded because this knowledge did not fit neatly into review and investigation systems or wider safety improvement priorities. This marginalisation was sorely felt by families as further injustice. In these situations, families encountered what is described as a ‘double injury’: their experiences are silenced by both the difficulty of communicating aspects of their experience and by the assumed inaccessibility of understanding these personal experiences. 213 Birth Reflections clinics were positively experienced by many families for this reason; their experiences were legitimised.
In the absence of meaningful inclusion in reviews, investigations or responses to their concerns, some families initiate their own searches for explanation. Our 27 in-depth family interviews indicate that the injured families from Shrewsbury and Telford NHS Trust and from East Kent are not exceptional in this regard. Discussions during the SP3 FF and Project Advisory Forums (PAF) identified and considered a fundamental difference between the interests of families and the interests of services in disclosure improvements. Participants identified a ‘mismatch’ between family and service interests that underpinned our findings (PAG forum participant). This mismatch was identified in the tensions between the personalisation of acknowledgements of harm and the standardisation of these acknowledgements in ‘tick box’ procedures required for services. Sometimes, organisations’ ‘family involvement’ agendas differed from the at-that-time needs of families. For example, considering an example of a family feeling deluged by information and visits from different staff (a risk midwife, complaints team, clinical lead and HoM) soon after receiving the news that their baby was likely to have been seriously harmed after a traumatic labour and delivery, a forum participant reflected:
[Your data] suggests that the organisation is deploying resources to meet four or five different things it needs to be, but it’s not thinking about how you support the person who had suffered the problem. So I wonder if it’s not so much ‘is the family involved or not involved’ as ‘what is the mismatch between the needs of families and the things that drive the processes’.
PAG forum participant
This emphasis on the experience of families as the credible starting point for inclusive practices was elaborated in this same forum discussion:
[The best approach is not] ‘this is what it looks like, now ask questions’, but actually: ‘tell us how it was, what’s your part of this whole experience so that we can get all of the information together’.
PAG forum participant
Standardised review and investigation procedures, while important, have set in motion a practice where the stories, voices and concerns of families have been muted or shaped for standardisation to be achieved. 171 In improving future disclosure work, it is important not to lose sight of the importance of enabling practices that prioritise listening, discussing and integrating family voices during review and investigations. Previous research has highlighted that without an open conversation about what happened, many patients and families feel that their experience has been disrespected by providers. 13,214 Reflections Clinics and responsive post-investigation debrief meetings were some interventions that opened the possibility for families to rebuild confidence in a service, yet ensuring that families also contribute their experiences should still be a necessary care priority. Like Wu et al., we identified some conflict between patient safety theory and patient expectations. 11 However, we were unable to characterise these families as intent on focusing on individual clinician failings and involved in a ‘blame game’. Instead, we found the families wanted an assumption of responsibility from them by services and, more significant, time for a hearing of events in their own terms.
We are currently exploring the sociopolitical issues raised by our findings on family experiences of post-incident care through the paradigms of epistemic injustice215,216 and knowledge encounters. 217
Family inclusion in service change
In our PAG and FFs, proposals for co-production arising from the study findings were discussed by families as a means of achieving change and partnership. Family participants described a desire to help services lobby for resources and design better processes. Participants wanted to be apprised of any challenges with making service changes and be involved with overcoming any barriers to change. Also in these discussions, several families expressed an empathy with clinicians, who were identified as victims of ‘process’:
[If] you had just had something go really wrong and almost like you’re in a war zone, you’ve just got to go straight on to the next one. There is no time … for personalised care where you actually treat the people in front of you … There’s this feeling … [of] … process, process, process. And that sucks the humanity out of the staff.
FF participant
Families were cognisant of challenges faced by staff during OD and acknowledged the potential for incidents to deeply affect the healthcare team. They were keen to work with staff in improving OD and safety processes. 218–220
However, our findings show that the marginalisation of injured families in organisational systems and processes that promise to be inclusive is deeply rooted in health care. 219,221 The importance of a ‘whole systems’ and multilevelled approach to the development of more meaningful PPI and partnership working with patients within health care has been noted. This approach encourages cultural shifts that place patients at the centre of safety and address taken-for-granted paternalism. 218 Our case-study findings present new evidence on the wider value of ongoing organisational PPI and partnership working. It is the organisational foundation for listening to injured families. Also, we emphasise the need for this inclusion to extend beyond the imperatives of maternity safety improvement.
An issue not addressed in our forums were accountability structures to encourage ongoing family involvement in interventions to strengthen OD. In contrast to most of the NHS, the development of mechanisms for gathering maternity SU feedback and for promoting service-user involvement in the co-production of local services has been incentivised at Trust level. 58 However, the effects of this intervention on promoting empathic and meaningful engagement of injured families in OD work have yet to be explored.
During our data analysis, we surfaced the two critical factors for strengthening disclosure for a family’s perspective that underpinned others. These were, first, recognition of the incident in the family’s own terms and, second, the need for skilled clinicians who feel safe and have time to practice in ways that are responsive to family needs. Figure 1 shows how the programme theories map against the general steps of SI management within organisations.
FIGURE 1.
Programme theories mapped against the general steps of SI management within organisations.
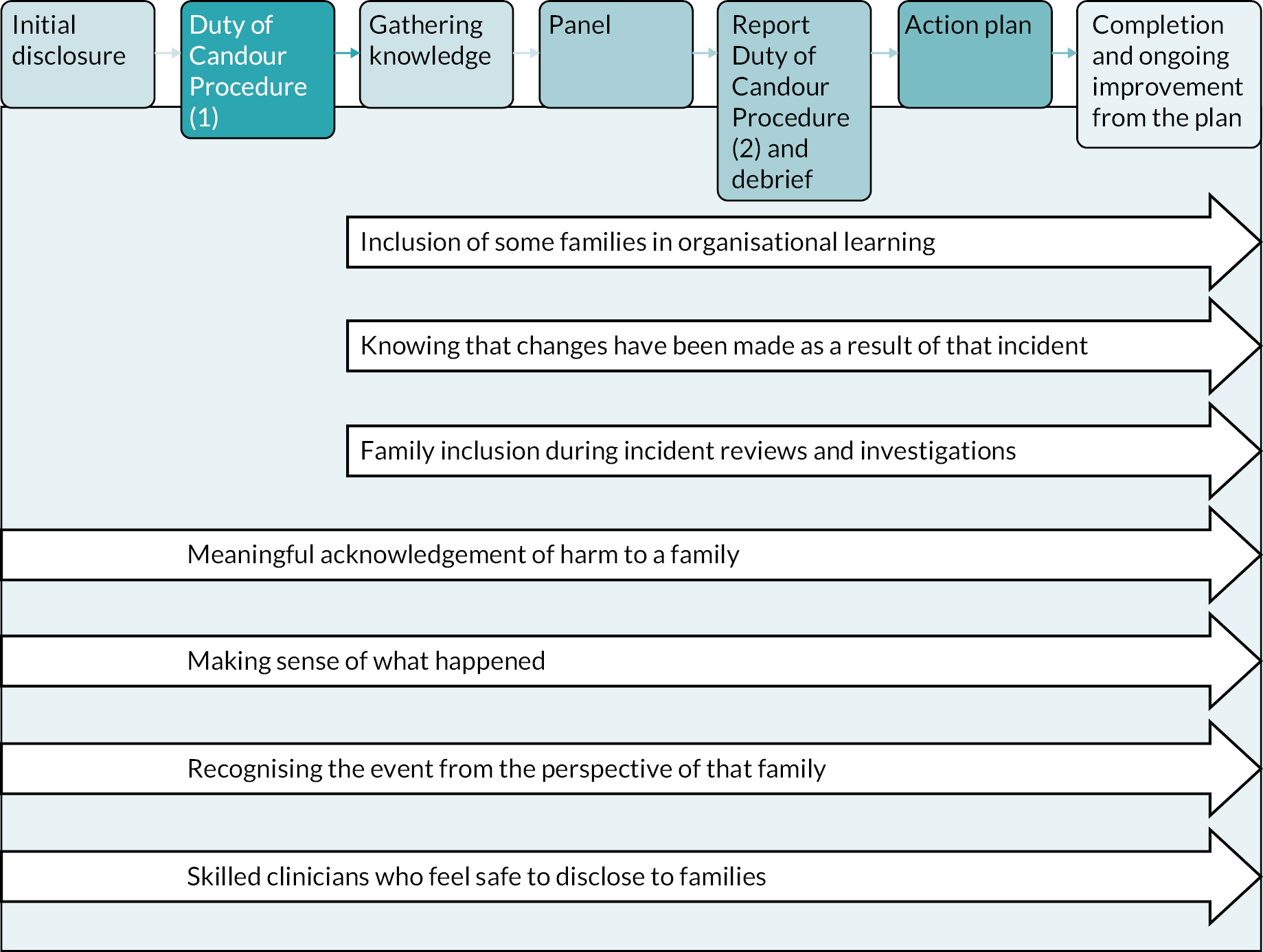
However, we found that underlying service or clinician efforts to strengthen OD was a medicolegal background that undermined this, compromising staff and families. Figure 2 illustrates how the programme theories interconnect to explain how disclosure can be improved.
FIGURE 2.
How the programme theories interconnect to explain how disclosure can be improved for some families.
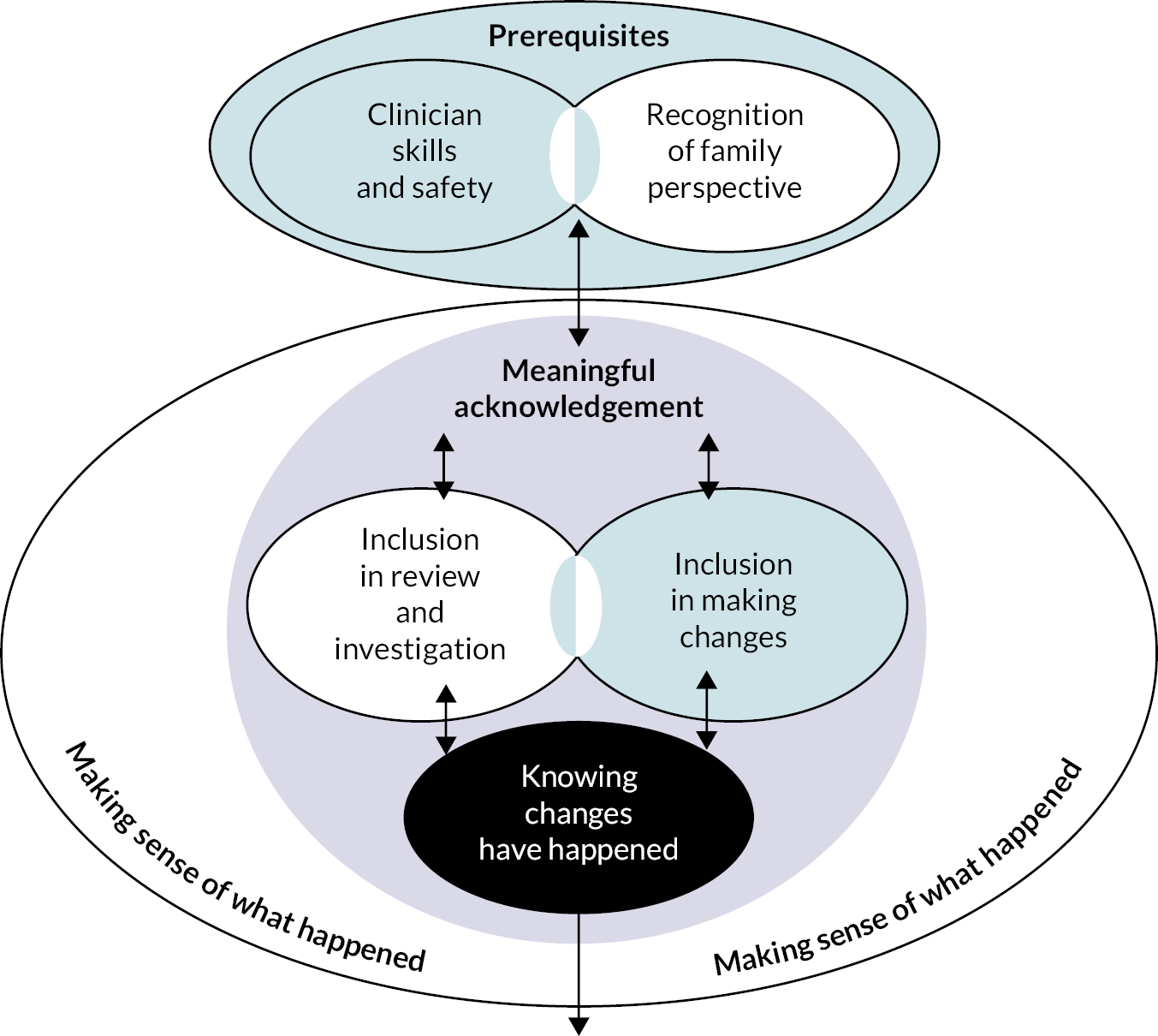
Summary of contexts of open disclosure
We identified several contextual layers that influenced the strengthening of OD. These were:
-
A national context that promotes openness with families by services and clinical professionals. This is most often known by how openness is cramped or negated in an adversarial medicolegal context that created anxiety about reputational and litigation and investigation risk.
-
A Trust context where senior clinical leadership, that included mentoring of service leads, played a significant part in clinicians’ attitudes towards family involvement, experience and reputational and professional risk taking.
-
A service context where services that supported OD were already developed and embedded in routine work (e.g. family involvement in service improvement; post-pregnancy support services for families disappointed with perinatal care); and where there was capacity and continuity of staffing for supportive working relationships to be developed between CG and clinical teams.
-
An individual professional context where post-incident communication with a family was honed from previous experience, with that person emerging as a local expert in this practice (with this expertise largely unrecognised across a service).
-
An individual family context shaped by the location of initial disclosure conversations; positioning in different review and investigation pathways based on revisable clinical or organisational learning criteria; and the candidacy of those actively seeking out post-incident support in situations where some individual clinicians championed their case.
However, we note the importance of empirically understanding how these various contexts interface in different policy and practice situations. Following some strands of realist theory79 and recent theoretical challenges to efforts to infer causality in realist research and qualitative comparative analysis more generally,222 we consider our programme theories partial and corrigible. The significant context and mechanisms important for OD improvement are multilayered and support for OD practice in different situations is likely to carry some unpredictability.
Reflections on involvement, diversity, study strengths and study weaknesses
Patient and public involvement
As described in Chapter 2 and Appendix 2, public and family involvement were embedded in all stages of the research cycle in four ways. First, one experienced PPI representative and parent was an active member of our Study Steering Group (SSG). Their concerns with the practical outcomes and impact of the study were an important public contribution to this academic group. Second, three PPI co-investigators were included in the study team from the outset of the project. The entire study team met 6-weekly for meetings and ongoing correspondence. This was essential to reaching an agreement on the refinement of study methods, adjustments in research design, identification and prioritisation of study findings, report design and drafting, and research dissemination and impact priorities. The three PPI co-investigators supported study progress in practical ways, for example, in networking the researchers into new campaign groups promoting diversity, so extending the scope of our PAG and promoting the study across their charity and association networks from where most members of the national family cohort were recruited. However, the most positive outcome of the PPI co-investigators was their ongoing involvement in the discussions about study progress and research findings. They became a trusted and critical ‘sounding board’ for the researchers to ensure the relevance of work to injured families and the wider public. Third, our PAG included six families, who became the direct voice of SUs during these meetings. The outcome of this direct involvement within the PAG was to ensure that disclosure improvement for families remained the focus of discussion. The inclusion of these families was a central focus of the second PAG meeting where two researchers worked with the families to prepare and present their own stories of disclosure and their expectations for service and practice change. Finally, a second family group (recruited from SP1 and SP2 family research participants) gathered to contribute towards the interpretation of study findings and research dissemination and impact plans. In all, the study engaged in four ways with a variety of PPI representatives. This inclusion of different voices was important so that differences were not muted and critical engagement with the research team and study findings were possible. 223 Nevertheless, the study team recognises that the families who expressed participated in the study represent a population who are more proactively involved in post-incident service change.
Reflecting on the overall outcomes of multifaceted PPI for the study, the study process and outcomes have been enriched by a multifaceted PPI approach (e.g. the study team have been able to identify key issues that would otherwise have been overlooked by those without this experience). At the same time, particularly for the CIG teamwork, the project has benefited from exceptionally experienced PPI contributors who had worked on previous studies together or were aware of one another’s work. We feel that this level of expertise and collaboration is critical for the success of multifaceted PPI. Our PPI included lively debates on the value of immediate recommendations over theorisation and generalisation from findings.
Diversity and inclusion
Although the research was designed for relevance to all families and clinicians involved in disclosure, during year 1 of the study, it became clear that black and ethnic minority families, families with non-heteronormative sexual orientations or gender identities and families with disabilities had been less actively included in the study (as co-applicants, project advisors and research participants). We addressed this to some degree by identifying and directly inviting representatives of two black parenthood groups on to our PAG. We also purposively identified and approached four families from ethnic minority backgrounds as study participants, with three consenting to interview. The challenge with accessing and recruiting these families echoes our findings about systemic inequalities for families who wish to engage with improvement work. It is important that we recognise whose experiences our work captures and ensure that we work to amplify marginalised voices, thus accurately representing the experiences, needs and wants of a diverse population in our improvement interventions. This is an important and salient reminder that engaging in research, accessing networks and advocating for one’s own care requires privilege and resources which may not be available to all families. Breaking down these systemic barriers is an essential priority for all interventions related to family involvement.
Study strengths and weaknesses
A key strength of the study is generation and integration of in-depth and extensive qualitive research findings to develop a nuanced understanding of the critical factors shaping disclosure practices and outcomes, from the multiple perspectives of three stakeholder groups. These groups have also been directly involved in research design, ongoing study management, data collection, analysis and decisions over dissemination and impact. The research was structured around a realist evaluation methodology. A realist synthesis of international disclosure work in maternity settings underpinned the development of initial theories to guide investigation of the complex causal processes of disclosure improvement. This methodological strategy also allowed for the iterative development of previously unidentified theoretical insights from the research findings. Interviews with injured families and ethnographic observations of disclosure practices including them have generated new perspectives on the relationships and disconnections between the expectations of injured families and the imperatives of services. Given the significant variation in disclosure nationally, the participation of families recruited from the case-study services where disclosure improvements were ongoing strengthens the reliability of findings.
A limitation to the in-depth case-study research is its limitation to three services in two NHS Trusts due to difficulties of accommodating non-COVID-related research during the pandemic. These services were selected for their positive deviance in OD improvement. Therefore, the generalisability of enablers to OD improvement beyond these case-study services has not been examined. Additionally, families were recruited from only one case-study service and so the impact of OD improvement in two case-study services has been explored without direct communication with families affected. However, the research team was able to identify and explain considerable variation within and across these three services, as well as to explore the generalisability of findings in interpretive forums with national stakeholder groups, including a family group. A significant limitation to the study findings has been a lack of access to HSIB investigators and HSIB investigation practices, where many SIs in NHS maternity care are now investigated. As a qualitative study, inevitably influenced by relational aspects of data collection, researchers’ personal perspectives may have influenced the interpretation of study findings.
The inclusion of a co-investigator engaged with families who had experienced marginalisation during maternity care, whether because of sexual orientation, gender identification, ethnicity or disability, would have generated findings that better reflected population diversity. Our well-networked third-sector co-investigators enabled some mitigation of this during the study. Finally, while the study has followed a realist evaluation methodological strategy, co-investigators have found the conceptualisation of findings in realist evaluation terms particularly challenging in terms of jargon and causal modelling. Clear differentiations between programme interventions and mechanisms could not always be established, particularity where programme improvement was explicitly directed to issues of attitude or cultural change in the workplace. Our analysis of findings in terms of programme theories highlights the cumulative and interlinked quality of factors underpinning disclosure improvements.
The impact of coronavirus disease 2019 on the study findings
Our ethnographic case studies were conducted between April and October 2021, immediately after some decline in service pressures associated with the second wave of the COVID-19 pandemic. However, service leads in consenting case-study services as well as our site PIs were aware of more enduring declines in staff morale and critical staff shortages within midwifery and obstetrics. The pandemic magnified longer-standing issues of short staffing, escalating organisational demands and increasing barriers to the provision of relational care,224 along with anticipated increases in preventable incidents associated with care modifications. 225–227 Our research, while conducted in unusual circumstances, documents magnified rather than exceptional situations in which post-incident care and communication with families and staff were conducted.
Chapter 11 Conclusions and implications
Introduction
This chapter briefly summarises the main findings of our research, considers their relevance in the context of recent policy developments in maternity safety and family involvement, identifies future research needs and outlines implications of study findings for policy and practice. Our main study findings are discussed in relation to our SPs and then in relation to our overarching research question.
Findings from study phase 1a (literature reviews)
Our scoping review of recent perspectives and recommendations on family involvement in reviews and investigations in English maternity services identified evolving terminology for conceptualising family involvement, but a consistency of message that families ought to be involved to a greater extent. In the last decade, there has been a shift from a paternalist view of injured families as passive recipients of care and reporting to active contributors to investigations, reports, and learning. A lack of specific, actionable guidance was noted.
From our realist literature synthesis and discussions with stakeholders, we established five initial hypotheses (programme theories) to focus our investigation of OD improvements in NHS maternity services. These were meaningful acknowledgement of harm; family inclusion in reviews and investigations; having the opportunity to make sense of what happened; care by skilled clinicians who feel psychologically safe to conduct OD; and knowing that the service is learning and changing because of the incident. We found weak evidence of the effectiveness of improvement interventions identified from the international literature. The difference between post-incident family involvement interventions that were embedded in safety improvement programmes and those designed to improve OD was described. We also identified a recent UK bias in documents with primary data on OD improvement.
Findings from study phase 1b (stakeholder interviews) and study phase 2 (ethnographic case studies of three services)
Building on the programme theories from phase 1a, phase 1b and phase 2 data were thematically analysed. Key findings are presented below, organised by programme theory and drawing from both the national stakeholder interviews and three case studies.
Receiving a meaningful acknowledgement of the harm that has happened
We identified ongoing tensions over the ethical need and learning benefits of OD, particularly in relation to concerns with litigation and reputational risk. Our evidence from families suggests that for over a decade, post-incident communication has been limited, closed and suspicious. Incentivisation of reviews and reporting, which included a family inclusion element, was felt to have taken time and energy from relational care. While these views were recognised in the case-study services, staff managed these tensions personally. A few staff were experts in in-person communication for the purpose of recovering the trust of the injured family. This work was poorly recognised or resourced by services. Inconsistency in OD processes was managed by informal staff networks and against the churn of shifts, hospital discharges and transfers.
Being involved during the review/investigation process
We found widespread agreement that this aspect of OD required improvement. The implementation of family involvement as an aspect of the PMRT highlighted the lack of resourcing for necessary post-incident relational care. By contrast, external reviews such as those conducted by HSIB were perceived as well-resourced, integrating more structured family involvement and ultimately more successful. Many families felt that they, their views and their experiences were excluded from NHS organisational processes. In the case-study services, some staff attempted more proactive approaches to family involvement, and sought to incorporate family perspectives into panel presentations, discussions and reports. Nevertheless, the interests of families (to understand their case) and wider service interest (to extract learning) sometimes clashed, and the unclear status of uncertain knowledge discussed in report drafts or panels could undermine the intentions of staff to foster trust. Involvement of harmed families in service improvement was unusual. In the one example of this that we were made aware of, a senior Trust lead had independently championed this work.
Making sense of what happened
We identified widespread challenges of establishing explanations for an incident when they are examined through multiple review and investigation approaches and when there is a reliance on often inconsistent or patchy clinical records. In the case-study services, enabling participation in report crafting, providing in-person support and ensuring ongoing report debriefs were identified as crucial practices for the regaining of family confidence in clinicians and services and making sense of what happened. We also explore informal opportunities for injured families and affected staff to explore the consequences of an incident. From our national and case-study injured families, we briefly note the capacity of some to gather information and garner professional networks and expertise independently of a service. We identified the value of post-pregnancy support and Birth Reflections services when injured families were referred into them.
Receiving care from clinicians who are skilled and feel psychologically safe during post-incident communication
We identified a national underinvestment in OD training for clinicians, as well as a lack of awareness raising of the needs of injured families across services. We found that immediate workplace responses to an incident were crucial for the quality of OD, both in terms of the quality of the communication with the family and in terms of the experience of the clinicians, many of whom felt unsupported in conducting OD. While the case-study services were investing in post-incident staff support, we found that this was often inappropriate and underutilised. The value of facilitated, ‘cool’ post-incident staff debriefings, informal staff support systems and informal meetings with some families, as well as being informed of system changes and learning, were important for post-incident staff recovery.
Knowing that things have changed because of what has happened
We found that knowing that learning and service improvement had happened was a crucial aspect of OD for most families. Evidence of post-incident learning and ongoing communication, even after the review or investigation had concluded, was often critical for families to begin regaining trust in a service. However, services did not proactively communicate news of the progress of changes with families, and improvement leads often sought to demonstrate ‘quick wins’ rather than longer-term and more significant improvement investments, both of which were disappointing to families and created additional feelings of mistrust. Correspondingly, we found there was a lack of effective, post-incident, learning communication strategies across services. The non-judgemental discussion of an incident and its implications, in either ongoing MDT meetings or during outreach work by risk midwives, were found to be important in shaping staff attitudes towards incidents and injured families.
Findings from study phase 3 (interpretive forums with families, clinicians and service leads)
We found family insights from forum discussion especially helpful in clarifying our findings. The marginalisation and underinvestment in the support of injured families were highlighted. Families identified the importance of ‘recognition’, describing the need for staff, services and reports to demonstrate understanding of the incident from the family’s own perspective and position. The forums also illuminated the pertinence of staff being supported in developing the skills to do so and feeling psychologically safe to do so as a central aspect of high-quality OD. Forum discussions with front-line junior clinicians involved in incidents identified their desire not to be removed from contact with families post incident and the need for their inclusion in OD processes, rather than solely relying on specialists or senior colleagues to take part to OD meetings. We identified the potential disjuncture between service imperatives of safety improvement; families’ imperatives to learn what happens and make sure it does not happen again; and clinicians’ imperatives to learn what happened, recover trust and clarify personal responsibilities. The complex and contradictory medicolegal field in which OD happens, the underfunding of service-led OD improvements and the discretionary and risky nature of this work by a few experts were described.
Overall findings – summary
This study contributes original and in-depth empirical research, detailing the complex and multilayered quality of OD. The study demonstrates how the medicolegal and ethical complexity of disclosure work can lead to OD quickly becoming reduced to a fixed, ‘tick box’ procedure. This is especially true in the context of the imposition of strict incentives by external bodies and in the pressurised healthcare environment, which is notoriously and increasingly understaffed, under-resourced and undersupported. In the absence of adequate time, training, expertise and organisational support for OD, and when openness is interpreted as a reputational or litigation risk, the quality of OD is decreased. This has detrimental consequences for the family, clinicians and service alike, inhibiting the quality and completeness of reports, the possibility for recovery, the formation or rebuilding of trust, as well as systems learning and improvement. We note the greater success of post-incident communication with families in organisations where family engagement strategies and practices are better developed and highlight opportunities for increasing scalable, actionable guidance for OD nationally.
Recent policy developments
The research was undertaken during a time of exceptional stress in maternity care delivery and of significant revisions in maternity safety and patient safety policy. The relevance of the study’s findings in this new landscape of post-incident communication and care is discussed below.
Findings from the Ockenden Independent Review of Maternity Services at The Shrewsbury and Telford Hospital NHS Trust surface a series of issues that we have examined as ‘programme theories’ for strengthening OD in maternity care. 89,90 The development of the new Independent Senior Advocate (ISA) role is an important initiative for supporting the needs of injured families. However, the findings suggest that if the role is to extend beyond the oversight of due process during meetings, time and support are required for advocates to develop communication and support plans that are appropriate and bespoke to each individual family. Without time and proactive post-incident communication, the needs of many families will be overlooked. The potential for MVPs to identify and overview service progress in post-incident communication with families is unclear. We note the influential work of some risk midwives in developing relationships of trust with families post incident, along with their role in promoting a non-judgemental attitude towards incidents and their aftermath by outreach to peers into wards and units. Their family-facing and staff-facing work requires some protection in the light of enhanced CG accountability processes. Moreover, given the time required for safety improvement to secure significant change within a services (e.g. making a business case, securing funding), a promise of ‘service change from maternity incidents to be introduced into clinical practice within six months of the incident occurring’ could disappoint families and staff. 90
Our research was initiated when the new PSIRF (NHS England) was in preparation for phased implementation across England. 124 None of our case-study services were early adopter sites; however, clinical directors at Site B were involved in preparation for later adoption. This strategy includes a shift in Trust-led incident investigations decided on the basis of hard-to-define clinical thresholds to a proactive and strategic determination of what to investigate based on an approach to maximise organisational learning for patient safety improvement. 228 Women and families will be actively involved in these investigations concerning them. While national training investments in candour and Being Open guidance are available, it is not clear how services will be further encouraged to meet the support and communication needs of families whose incidents are not identified for patient safety investigation. The strategy offers positive examples in training materials of resolution approach (e.g. for staff directly involved in an incident meeting with injured patients). 124 However, it is unclear how these more open approaches will be received in maternity services where ongoing anxiety over the organisational and professional risks of openness is notable.
Finally, the Health and Care Act that establishes the Health Services Safety Investigations Body (HSSIB) as an independent statutory body also surfaces long-standing issues related to openness with injured families. 229 Agreement to not allow ‘safe space’ for Trust-level investigations, and all maternity investigations, highlights a policy emphasis on the DoC in maternity care. At the same time, however, policy support for candour with families is sustained within an adversarial litigation system. A shift from a litigation system that relied on proof of clinical negligence rather than agreement on avoidability, as supported by the Health and Social Care Select Committee, is more likely to foster the engagement and support of injured families, as well as encourage learning by clinical teams. 103,230
Recommendations for future research
This study has identified the need for research in the following areas:
-
Examination of the experience of post-incident communication and care for under-represented or marginalised families for the purpose of the development of responsive OD with them, for instance minority ethnic groups, people of different sexual orientations or identities and people who are socially marginalised in other ways.
-
Examination of the relationship between the programme theories identified and the progress of OD improvement in higher, medium and lower performing services, including examination of the impact of the relationship between DoC training and practice expectations and the current English medicolegal framework that pertains to avoidable SIs.
-
Development of fit-for-purpose outcome assessments of OD practice improvement within maternity services (e.g. timeliness and quality of communication, reflexive practice and peer support, responsiveness to needs, provision of appropriate staff training and staff and family support).
-
Given recent investments in perinatal mental health services, evaluation of their adequacy and reach for addressing the needs of harmed families.
-
Evaluation of the role and impact of the ISA from the perspective of families, clinical leads and services.
-
Examination of the scope, requirements and outcomes of the direct representation of families in their own reviews or investigations.
-
Examination of the reception and impact in maternity services of restorative practice approaches (e.g. as promoted by the NHSE PSIRF Framework, by third-sector organisations like the ‘Harmed Patients Alliance’, and independent mediators).
-
Development and implementation, with clinicians, of simulation training that supports non-judgemental discussions of incidents within clinical teams.
Implications for policy and practice
The study identifies some key components that support the strengthening of OD within services. These include prompt initial disclosure with a clinician skilled in this work, face-to-face meetings where possible, an approach to OD as a relationship (not a one-off event), opportunities for referral of families affected by incidents into post-pregnancy support services (e.g. Birth Reflections), initial and ongoing discussions to clarify family needs and expectations (including information to them on how to escalate OD concerns within the service, proactive updating of harmed families, including after report debrief meetings), space and time for a family to develop and share their own views on the incident and to have these views fully recognised in incident investigations and investigation reports.
These components and others are expanded on in our more detailed recommendations for policy and practices in our draft guidance for staff and service managers for strengthening OD (see Appendix 9).
Higher-level implications for policy and practice indicated from this study are as follows:
-
Our findings indicate the importance of the newly developed ISA position to be a main point of contact and support for families outside of the service where the incident happened.
-
Our findings point towards the marginalisation of harmed families when their needs do not correspond to service imperatives of learning for safety improvement. Organisational support for the development of a ring-fenced, service-level role for leading the planning and implementing of OD processes for family benefit and in collaboration with family advocates across and beyond a hospital or service is suggested:
-
This service or regional planning would include the development and regular updating of an assessable, visual aid to be used as a guide for injured families through organisational processes and in conjunction with face-to-face communication.
-
-
Our findings suggest the need for the re-design of review processes and adjustment of incident reporting processes to place families at the centre of this work. The progress of PSIRF in supporting this is anticipated.
-
Our findings also highlight the importance of consensus-based development of post-incident care pathway, processes and communications that includes families in this co-production.
-
Our data also identify the value of OD that extends beyond the closure of investigation debriefs and includes as proactive and personalised update on the progress of anticipated post-incident improvements. This is important for recovering family trust in a service. Services (rather than individual staff) should be responsible for this.
-
Our findings revealed a widespread lack of investment in post-incident family communication training and wider OD processes for clinicians at both junior and senior levels. Professional bodies and training schools should consider the development of a coherent and consistent approach to OD expertise. This should include opportunities for reflection on wider ethical and practical issues, as well as opportunities for simulation training, extending beyond present obstetric trainee and midwifery curriculums. Services must consider training investments so that OD is not only presented as a regulation during routine staff induction by Trust legal teams.
-
Our research indicates that investment in staff awareness raising of the care needs of injured families is important across maternity services.
-
We identified limited explicit acknowledgement within services of the emotional and practical work involved in developing and maintaining contact with injured families. This needs to be adequately resourced and supported (e.g. by protected opportunities for reflective discussion between colleagues). We identified that HSIB family engagement processes work well for their staff because of well-resourced support structures.
-
We identified a significant relationship between immediate and non-judgemental post-incident support for staff from colleagues and managers who were expert in OD improve OD and promote ongoing learning. Immediately post incident, families and staff would benefit from the 24-hour availability of a clinical lead who is expert in OD. This person should be an expert by experience but should also receive formal training.
-
Our research suggests that despite investment in post-incident staff support by some organisations, utilisation is poor. Organisations need to include staff groups in commissioning decisions and ensure that services are considered appropriate to promote uptake.
-
Organisational support for multiple, facilitated staff debriefs during the weeks following an incident should be implemented to support staff recovery and learning.
-
Our research identified the importance of updating staff by the incident, as well as wider teams, on investigation findings and on ongoing improvement work. There are challenges to this communication work; however, we identified the value of regular informal outreach by risk midwives and of periodic discussions of incidents and post-incident learning in already embedded MDT learning forums. These approaches were significant spaces where a service ethic was clarified.
-
Likewise, communicating with and updating families on ongoing improvement work (and involving them in this if they wish) supports recovery, the reformation of trust and the quality and sustainability of improvements.
-
For some injured families and affected clinicians, we identified a mutual need to meet and reflect together on the effects of an incident. Clinical and service leads should consider the creation of supported opportunities for these currently informal processes.
-
Given the ongoing defensiveness with respect to OD within maternity services, a series of wider dialogues is required between families, medicolegal experts and NHS representatives to clarify practices for sharing uncertain knowledge with families. These ethical dialogues, with external guidance, are required within Trusts, between clinical leads, Trust legal teams and clinical negligence lawyers.
Additional information
Acknowledgements
We want to thank the participants in this study, who generously gave their time during an exceptionally difficult time in maternity services. We thank the staff and families who trusted us with their information. We particularly want to thank the families who shared their experiences of loss and bereavement with us. The loss of their children continues to be felt.
We are grateful for the advice, support and enthusiasm of our Study Steering Group, James Duffy (Chair), Alessandro Alagna (Patient and Public Advisory Expert), Billie Hunter, Graham Martin, Rebecca Randell and Justin Waring.
We are grateful for the insights and guidance of our Project Advisory Group, chaired by Graham Martin, and in particular, to Natasha Adams, Joanna Bigsby, Natasha East, Karen Fourneaux, Lisa Hirst, Elisha Nunhofer and Harriet Williams, who provided us with careful and invaluable expertise by experience. We want to thank Daghni Rajasingam and Louise Page for their contribution and expertise in supporting the conduct of the study.
We thank colleagues at the National Institute for Health Research, particularly Martin Simpson-Scott and our project funders.
The study was funded by the Department of Health and Social Care, HS&DR Programme (17/99/85) and sponsored by King’s College London. The views expressed in this report are those of the authors and not necessarily those of the NHS, the National Institute for Health Research or the Department of Health and Social Care.
Contributions of authors
Mary Ann Adams (https://orcid.org/0000-0003-1276-617X) (Senior Research Fellow, Social Science and Health and Maternity Service Research) co-led research concept and protocol development, co-led the research study, led and drafted the realist review and co-led the policy review, led and conducted the primary research, led data analysis and led and co-drafted study write-up.
Charlotte Bevan (https://orcid.org/0000-0002-6361-4398) (Senior Research and Prevention Advisor, The Stillbirth and Neonatal Death Charity) contributed to research concept and protocol development, contributed to analysis of findings and contributed to study write-up.
Maria Booker (https://orcid.org/0000-0002-2748-2295) (Programmes Director, BirthRights) contributed to research concept and protocol development, contributed to analysis of findings and contributed to study write-up.
Julie Hartley (https://orcid.org/0000-0002-6873-2748) (Research Associate, Social Science and Maternity Service Research) contributed to realist data collection, contributed to primary data collection and contributed to analysis of findings and study write-up.
Alexander Edward Heazell (https://orcid.org/0000-0002-4303-7845) (Senior Clinical Lecturer in Obstetrics and Clinical Director of the Tommy’s Stillbirth Research Centre, Manchester) contributed to research concept and protocol development, contributed to analysis of findings and study write-up.
Elsa Montgomery (https://orcid.org/0000-0002-4193-1261) (Senior Lecturer, Midwifery) contributed to primary data collection, contributed to analysis of findings and contributed to study write-up.
Natalie Sanford (https://orcid.org/0000-0003-2650-1818) (Research Associate and Doctoral Researcher, Florence Nightingale Faculty of Nursing, Midwifery, and Palliative Care) co-led the policy review, contributed to data analysis, co-designed and co-led the interpretive forums with primary data collection and co-drafted study write-up.
Maureen Treadwell (https://orcid.org/0000-0001-7531-7553) (Research Officer and Project Lead, Birth Trauma Association) contributed to research concept and protocol development, contributed to analysis of findings and contributed to study write-up.
Jane Sandall (https://orcid.org/0000-0003-2000-743X) (Professor of Social Science and Women’s Health) co-led research concept and protocol development, co-led research study, contributed to analysis of findings and contributed to study-write up.
Disclosure of interest
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, are available in the toolkit on the NIHR Journals Library report publication page at https://doi.org/10.3310/YTDF8015.
Primary conflicts of interest: None declared.
Patient data statement
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it is important that there are safeguards to make sure that they are stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Data-sharing statement
This is a qualitative study on a sensitive subject and therefore the data generated are not suitable for sharing beyond that contained within the report. Further information can be obtained from the corresponding author mary.adams@kcl.ac.uk.
Ethics statement
Three ethical approvals were obtained for the study. University ethical approvals were granted by the ethics committee at King’s College London Biomedicinal Sciences, Dentistry, Medicine and Natural and Mathematical Sciences (BDM RESC) Ref 11174 and BDM RESC Ref 22033) for the research conducted outside of the NHS. National ethical approval approvals were granted from the Health Research Authority (HRA) Research Ethics Committee (REC), London Bridge [REC reference 20/LO/1152; Integrated Research Application System (IRAS) Project ID: 262197] for research conducted in the NHS. Approval was also obtained from the HRA CAG (20/CAG/0121) on the grounds that patient confidentiality might be breached during the fieldwork observations. After favourable opinion from the REC and the Confidentiality Advisory Group (CAG), we obtained research and development (R&D) permissions from our study sponsors and local R&D permissions to allow access to the case-study services and to interview families and staff.
Information governance statement
King’s College, London is committed to handling all personal information in line with the UK Data Protection Act (2018) and the General Data Protection Regulation (EU GDPR) 2016/679. Under the Data Protection legislation, King’s College, London is the Data Controller, and you can find out more about how we handle personal data, including how to exercise your individual rights and the contact details for our Data Protection Officer here https://www.kcl.ac.uk/hscwru/research/mrc-data-protection.
Department of Health and Social Care disclaimer
This publication presents independent research commissioned by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by the interviewees in this publication are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, MRC, NIHR Coordinating Centre, the Health and Social Care Delivery Research programme or the Department of Health and Social Care.
This monograph was published based on current knowledge at the time and date of publication. NIHR is committed to being inclusive and will continually monitor best practice and guidance in relation to terminology and language to ensure that we remain relevant to our stakeholders.
Disclaimers
This article presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- Harrison R, Birks Y, Bosanquet K, Iedema R. Enacting open disclosure in the UK National Health Service: a qualitative exploration. J Eval Clin Pract 2017;23:713-8.
- Myren B, de Hullu J, Bastiaans S, Koksma J, Hermens R, Zusterzeel P. Disclosing adverse events in clinical practice: the delicate act of being open. Health Commun 2022;37:191-20.
- Manser T, Staender S. Aftermath of an adverse event: supporting health care professionals to meet patient expectations through open disclosure. Acta Anaesthesiol Scand 2005;49:728-34.
- Allan A, McKillop D. The health implications of apologizing after an adverse event. Int J Qual Health Care 2010;22:126-31.
- Manser T. Managing the aftermath of critical incidents: meeting the needs of health-care providers and patients. Best Pract Res Clin Anaesthesiol 2011;25:169-79.
- Larizgoitia I, Bouesseau MC, Kelley E. Who efforts to promote reporting of adverse events and global learning. J Public Health Res 2013;2:jphr.2013.e29-74.
- Garbutt J, Brownstein DR, Klein EJ, Waterman A, Krauss MJ, Marcuse EK, et al. Reporting and disclosing medical errors: pediatricians’ attitudes and behaviors. Arch Pediatr Adolesc Med 2007;161:179-85.
- Gallagher TH, Garbutt JM, Waterman AD, Flum DR, Larson EB, Waterman BM, et al. Choosing your words carefully: how physicians would disclose harmful medical errors to patients. Arch Intern Med 2006;166:1585-93.
- Iedema RAM, Mallock NA, Sorensen RJ, Manias E, Tuckett AG, Williams AF, et al. The National Open Disclosure Pilot: Evaluation of a policy implementation initiative. Med J Aust 2008;188:397-400.
- Dingley C, Daugherty K, Derieg MK, Persing R. Advances in Patient Safety: New Directions and Alternative Approaches. Vol 3: Performance and Tools. Rockville: Agency for Healthcare Research and Quality; 2008.
- Wu AW, McCay L, Levinson W, Iedema R, Wallace G, Boyle DJ, et al. Disclosing adverse events to patients: international norms and trends. J Patient Saf 2017;13:43-9.
- Birks Y, Harrison R, Bosanquet K, Hall J, Harden M, Entwistle V, et al. Health Services and Delivery Research. Southampton, UK: NIHR Journals Library; 2014.
- Vincent C. Understanding and responding to adverse events. N Engl J Med 2003;348:1051-6.
- Iedema R, Allen S, Britton K, Piper D, Baker A, Grbich C, et al. Patients’ and family members’ views on how clinicians enact and how they should enact incident disclosure: the ‘100 patient stories’ qualitative study. BMJ 2011;343.
- Vincent C, Amalberti R. Safer Healthcare: Strategies for the Real World. Cham, CH: Springer Nature; 2016.
- Wu AW, Boyle DJ, Wallace G, Mazor KM. Disclosure of adverse events in the United States and Canada: an update, and a proposed framework for improvement. J Public Health Res 2013;2.
- Dekker S, Bergström J, Amer-Wåhlin I, Cilliers P. Complicated, complex, and compliant: best practice in obstetrics. Cogn Technol Work 2013;15:189-95.
- McVeety J, Keeping-Burke L, Harrison MB, Godfrey C, Ross-White A. Patient and family member perspectives of encountering adverse events in health care: a systematic review. JBI Evid Synth 2014;12:315-73.
- Prentice JC, Bell SK, Thomas EJ, Schneider EC, Weingart SN, Weissman JS, et al. Association of open communication and the emotional and behavioural impact of medical error on patients and families: state-wide cross-sectional survey. BMJ Qual Saf 2020;29:883-94.
- Berlinger N. After Harm: Medical Error and the Ethics of Forgiveness. Baltimore, MD: Johns Hopkins University Press; 2005.
- Harrison R, Lawton R, Perlo J, Gardner P, Armitage G, Shapiro J. Emotion and coping in the aftermath of medical error. J Patient Saf 2015;11:28-35.
- Bell SK, Moorman DW, Delbanco T. Improving the patient, family, and clinician experience after harmful events: the ‘when things go wrong’ curriculum. Acad Med 2010;85:1010-7.
- Piper D, Iedema R. Literature Review: Incident Disclosure Policy, Legal Reform and Research Since 2008. Sydney, Australia: Centre for Health Communication (University of Technology Sydney) and Australian Commission on Safety and Quality in Health Care; 2011.
- Terry D, Kim J-A, Gilbert J, Jang S, Nguyen H. ‘Thank you for listening’: an exploratory study regarding the lived experience and perception of medical errors among those who receive care. Int J Health Serv 2022;52:292-30.
- Dhawale T, Zech J, Greene SM, Roblin DW, Brigham KB, Gallagher TH, et al. We need to talk: provider conversations with peers and patients about a medical error. J Patient Saf Risk Manag 2019;24:140-6.
- Hågensen G, Nilsen G, Mehus G, Henriksen N. The struggle against perceived negligence. A qualitative study of patients’ experiences of adverse events in Norwegian hospitals. BMC Health Serv Res 2018;18:1-11.
- Robbennolt JK. Apologies and medical error. Clin Orthop Relat Res 2009;467:376-82.
- Glasper A. Duty of candour: can nurses lead the way in implementation?. Br J Nurs 2011;20:1318-9.
- Holmes A, Bugeja L, Ranson D, Griffths D, Ibrahim JE. The potential for inadvertent adverse consequences of open disclosure in Australia: when good intentions cause further harm. MedSci Law 2019;59:265-74.
- O’Connor E, Coates HM, Yardley IE, Wu AW. Disclosure of patient safety incidents: a comprehensive review. Int J Qual Health Care 2010;22:371-9.
- O’Dowd A. Doctors increasingly practise ‘defensive’ medicine for fear of litigation, says regulator. BMJ 2015;350.
- Perez B, Knych SA, Weaver SJ, Liberman A, Abel EM, Oetjen D, et al. Understanding the barriers to physician error reporting and disclosure. J Patient Saf 2014;10:45-51.
- Wu AW. BMJ. 2000.
- Bunting RF, Groszkruger DP. From to err is human to improving diagnosis in health care: the risk management perspective. J Healthc Risk Manag 2016;35:10-23.
- Iedema R, Jorm C, Wakefield J, Ryan C, Sorensen R. A new structure of attention?: open disclosure of adverse events to patients and their families. J Lang Soc Psychol 2009;28:139-57.
- Quick O. Regulating and Legislating Safety: The Case for Candour. London: BMJ Publishing Group Ltd; 2014.
- Iedema R, Sorensen R, Manias E, Tuckett A, Piper D, Mallock N, et al. Patients’ and family members’ experiences of open disclosure following adverse events. Int J Qual Health Care 2008;20:421-32.
- Martin GP, Chew S, Dixon-Woods M. Senior stakeholder views on policies to foster a culture of openness in the English National Health Service: a qualitative interview study. J R Soc Med 2019;112:153-9.
- Kraman SS, Hamm G. Risk management: extreme honesty may be the best policy. Ann Intern Med 1999;131:963-7.
- Berlinger N, Wu AW. Subtracting insult from injury: addressing cultural expectations in the disclosure of medical error. J Med Ethics 2005;31:106-8.
- Saying Sorry When Things Go Wrong: Being Open: Communicating Patient Safety Incidents with Patients, Their Families and Carers. London: The Stationery Office: National Patient Safety Agency; 2009.
- The Health and Social Care Act 2008 (Regulated Activities). London: Care Quality Commission; 2014.
- Francis R. Independent Inquiry into Care Provided by Mid Staffordshire NHS Foundation Trust January 2005–March 2009. London: The Stationery Office; 2010.
- The Duty of Candour: Guidance for Team Managers and RCA Chairs 2015. www.whatdotheyknow.com/request/349547/response/865169/attach/5/The%20Duty%20of%20Candour%20Guidance%20for%20Staff.pdf?cookie_passthrough=1 (accessed 27 January 2023).
- Care Quality Commission . Regulation 20: Duty of Candour 2022. www.cqc.org.uk/guidance-providers/all-services/regulation-20-duty-candour (accessed 14 July 2022).
- Gardiner S, Morrison D, Robinson S. Integrity in public life: reflections on a Duty of Candour. Public Integr 2021;24:217-28.e.
- Care Quality Commission . The duty of candour: guidance for providers 2021. https://www.cqc.org.uk/guidance-providers/all-services/regulation-20-duty-candour (accessed 14 January 2024).
- Hawkes N. Seeing things from the patients’ view: what will it take?. BMJ 2015;350.
- Care Quality Commission . Learning, Candour and Accountability: A Review of the Ways That NHS Trusts Review and Investigate the Deaths of Patients in England 2016. https://www.cqc.org.uk/sites/default/files/20161213-learning-candour-accountability-full-report.pdf (accessed 14 January 2024).
- Blythe H. Regulating the Duty of Candour: A Report by Action Against Medical Accidents on CQC Inspection Reports and Regulation of the Duty of Candour (AvMA2016), 2016. n.d.
- Francis A. Breach of the Duty of Candour: First Time Prosecution. JMW; 2020.
- Quick O. Duties of Candour in healthcare: the truth, the whole truth, and nothing but the truth?. Med Law Rev 2022;30:324-47.
- House of Commons . The coroner service: government response to the committee’s first report. House of Comons Justice Committee, Third Special Report of Session 2021–22 2021.
- Kirkup B. The Report of the Morcambe Bay Investigation. London: The Stationery Office; 2015.
- Magro M. Five Years of Cerebral Palsy Claims: A Thematic Review of NHS Resolution Data. London: NHS Resolution; 2017.
- NHS Resolution . Annual Report and Accounts 2021 22 2022.
- Department of Health . A rapid resolution and redress scheme for severe avoidable birth injury: government summary and consultation response. Department of Health: Resolution PE, and Maternity Team 2017. https://assets.publishing.service.gov.uk/media/5a82df8aed915d74e3403ffb/RRR_consultation_response.pdf (accessed 14 January 2024).
- NHS Resolution . Maternity Incentive Scheme – Year Four 2022. https://resolution.nhs.uk/wp-content/uploads/2022/05/MIS-year-4-relaunch-guidance-May-2022-converted.pdf (accessed 14 January 2024).
- Bakhbakhi D, Siassakos D, Lynch M, Timlin L, Storey C, Heazell A, et al. Parents Collaborative Group . PARENTS 2 study: consensus report for parental engagement in the perinatal mortality review process. Ultrasound Obstet Gynecol 2019;54:215-24.
- Bakhbakhi D, Burden C, Storey C, Heazell AE, Lynch M, Timlin L, et al. PARENTS 2 Study: a qualitative study of the views of healthcare professionals and stakeholders on parental engagement in the perinatal mortality review – from ‘bottom of the pile’ to joint learning. BMJ Open 2018;8.
- NHS Resolution . Maternity Incentive Scheme – Year Two 2018. https://resolution.nhs.uk/wp-content/uploads/2018/12/maternity-incentive-scheme-year-two.pdf (accessed 14 January 2024).
- Kurinczuk JJ, Boby T, Prince S, Johnston T, Neves M, Smith P, et al. Learning from Standardised Reviews When Babies Die. National Perinatal Mortality Review Tool: Second Annual Report. Oxford: National Perinatal Epidemiology Unit; 2020.
- Chepkin S, Prince S, Johnston T, Boby T, Neves M, Smith P, et al. MNe. Learning from Standardised Reviews When Babies Die. National Perinatal Mortality Review Tool: First Annual Report. Oxford: National Perinatal Epidemiology Unit; 2019.
- Kurinczuk JJ, Smith P, Bevan C, Burden C, Draper ES, Fenton A, et al. Learning from Standardised Reviews When Babies Die: National Perinatal Mortality Review Tool Fourth Annual Report. Oxford: National Perinatal Epidemiology Unit; 2022.
- Sands . In Their Own Words: Parents’ Experiences of the Hospital Review of Their Care 2021. www.sands.org.uk/professionals/reviews-and-investigations/their-own-words-parents-experiences-review (accessed 14 January 2024).
- Health Safety Investigation Branch . Summary of Themes Arising from the Health Safety Investigation Branch Maternity Programme (NLR) 2020. www.hssib.org.uk/patient-safety-investigations/summary-of-themes-arising-from-the-hsib-maternity-programme/ (accessed 14 January 2024).
- Health Safety Investigation Branch . What We Investigate n.d. www.hsib.org.uk/what-we-do/maternity-investigations/what-we-investigate/ (accessed 29 January 2022).
- Healthcare Safety Investigation Branch . Giving Families a Voice: HSIB’s Approach to Patient and Family Engagement During Investigations: Independent Report by the Healthcare Safety Investigation Branch 2020. www.hssib.org.uk/patient-safety-investigations/giving-families-a-voice/investigation-report/ (accessed 15 January 2024).
- NHS Resolution . The Second Report: The Evolution of the Early Notification Scheme 2022. https://resolution.nhs.uk/resources/the-second-report-the-evolution-of-the-early-notification-scheme/ (accessed 15 January 2024).
- Robertson-Hayes L. The NHS Early Notification Scheme – Successes, Concerns and Your Rights. Bolt Burdon Kemp; 2020.
- NHS Resolution . Support for Patients, Families or Carers n.d. https://resolution.nhs.uk/services/claims-management/clinical-schemes/clinical-negligence-scheme-for-trusts/early-notification-scheme/support-for-patients-families-or-carers/ (accessed 25 January 2022).
- Pawson R, Manzano-Santaella A. A realist diagnostic workshop. Evaluation 2012;18:176-91.
- Adams M, Iedema R, Heazell AE, Treadwell M, Booker M, Bevan C, et al. Protocol: investigation of the critical factors required to improve the disclosure and discussion of harm with affected women and families: a study protocol for a qualitative, realist study in NHS maternity services (the DISCERN study). BMJ Open 2022;12.
- Pawson R. Evidence-based Policy: A Realist Perspective. Thousand Oaks, CA: SAGE Publications Ltd; 2006.
- Wong G, Greenhalgh T, Westhorp G, Buckingham J, Pawson R. RAMESES publication standards: realist syntheses. BMC Med 2013;11:1-14.
- Wong G, Westhorp G, Pawson R, Greenhalgh T. RAMESES Training Materials. London: The RAMESES Project; 2013.
- Kirst M, O’Campo P. Methods for Community Public Health Research. New York: Springer; 2014.
- Wong G. Doing Realist Research. London: SAGE Publications Ltd; 2018.
- Astbury B. Doing Realist Research. London: SAGE Publications Ltd; 2018.
- Rycroft-Malone J, McCormack B, Hutchinson AM, DeCorby K, Bucknall TK, Kent B, et al. Realist synthesis: illustrating the method for implementation research. Implement Sci 2012;7:1-10.
- Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci 2010;5.
- Emmel N, Greenhalgh J, Manzano A, Monaghan M, Dalkin S. Doing Realist Research. SAGE Publications Ltd; 2018.
- Adams M, Sanford N, Hartley J, Heazell AE, Iedema R, Bevan C, et al. Strengthening open disclosure after incidents in maternity care: a realist synthesis of international research evidence. BMC Health Serv Res 2023;23.
- Manzano A. The craft of interviewing in realist evaluation. Evaluation 2016;22:342-60.
- Baxter R, Lawton R. The Positive Deviance Approach. Cambridge: Cambridge University Press; 2022.
- Stake RE. Multiple Case Study Analysis. New York: Guilford Press; 2013.
- Jagosh J. Realist synthesis for public health: building an ontologically deep understanding of how programs work, for whom, and in which contexts. Annu Rev Public Health 2019;40:361-72.
- Mukumbang FC. Retroductive theorizing: a contribution of critical realism to mixed methods research. J Mix Methods Res 2021;17:93-114. https://doi.org/10.1177/15586898211049847.
- Ockenden D. Emerging Findings and Recommendations from the Independent Review of Maternity Services at Shrewsbury and Telford Hospital NHS Trust 2020. www.gov.uk/government/publications/ockenden-review-of-maternity-services-at-shrewsbury-and-telford-hospital-nhs-trust (accessed 15 January 2024).
- Ockenden D. Summary of Findings, Conclusions, and Essential Actions from the Independent Review of Maternity Services at the Shrewsbury and Telford Hospital NHS Trust 2022. www.gov.uk/government/publications/final-report-of-the-ockenden-review/ockenden-review-summary-of-findings-conclusions-and-essential-actions (accessed 15 January 2024).
- Royal College of Obstetricians and Gynaecologists . Review of Maternity Services at Cwm Taf Health Board. Gynaecologists RCoOa, Midwives RCo 2019. https://www.gov.wales/sites/default/files/publications/2019-04/review-of-maternity-services-at-cwm-taf-health-board_0.pdf (accessed 15 January 2024).
- Bakhbakhi D, Siassakos D, Burden C, Jones F, Yoward F, Redshaw M, et al. Learning from deaths: Parents’ Active Role and ENgagement in The review of their Stillbirth/perinatal death (the PARENTS 1 study). BMC Preg Childbirth 2017;17:1-6.
- Royal College of Obstetricians and Gynaecologists . Each Baby Counts Progress Report 2020. https://www.rcog.org.uk/media/a4eg2xnm/ebc-2020-final-progress-report.pdf (accessed 15 January 2023).
- Royal College of Obstetricians and Gynacologists . Each Baby Counts Progress Report 2018 2018. https://www.rcog.org.uk/media/dswjqyin/each-baby-counts-report-2018-11-12.pdf (accessed 15 January 2024).
- Care Quality Commission . Guidance for NHS Bodies on the Fit and Proper Person Requirement for Directors and the Duty of Candour 2014. https://www.cqc.org.uk/sites/default/files/20140725_nhs_fppr_and_doc_consultation_final.pdf (accessed 15 January 2023).
- Healthcare Improvement Scotland . Being Open NHS Scotland: Guidance on Implementing the Being Open Principles 2015. www.healthcareimprovementscotland.org/our_work/governance_and_assurance/learning_from_adverse_events/being_open_guidance.aspx (accessed 15 January 2023).
- Department of Health . Culture Change in the NHS: Applying the Lessons of the Francis Inquiries 2015.
- NHS England, Patient Safety Domain . Serious Incident Framework: Supporting Learning to Prevent Recurrence 2015. https://www.england.nhs.uk/wp-content/uploads/2020/08/serious-incidnt-framwrk.pdf (accessed 15 January 2024).
- Nursing and Midwifery Council, General Medical Council . Openness and Honesty When Things Go Wrong: The Professional Duty of Candour 2015. https://www.nmc.org.uk/globalassets/sitedocuments/nmc-publications/openness-and-honesty-professional-duty-of-candour.pdf (accessed 15 January 2023).
- NHS Resolution . Saying Sorry Poster 2017. https://resolution.nhs.uk/wp-content/uploads/2017/04/NHS-Resolution-Saying-Sorry-2017.pdf (accessed 15 January 2024).
- Dalton D, Williams N. Building a Culture of Candour: A Review of the Threshold for the Duty of Candour and of the Incentives for Care Organisations to Be Candid. Royal College of Surgeons of England; 2014.
- Care Quality Commission . Regulation 5: Fit and Proper Persons Requirement 2015. https://www.cqc.org.uk/sites/default/files/20150324_guidance_providers_meeting_regulations_01.pdf (accessed 15 January 2024).
- House of Commons . The Safety of Maternity Services in England 2021.
- Rose L. Better Leadership for Tomorrow: NHS Leadership Review. Department of Health and Social Care; 2015.
- Manktelow BN, Smith LK, Evans TA, Hyman-Taylor P, Kurinczuk JJ, Field DJ, et al. Perinatal Mortality Surveillance Report: UK Perinatal Deaths for Births from January to December 2013. Leicester: Department of Health Sciences, University of Leicester; 2015.
- Department of Health . Learning Not Blaming 2015.
- UK Government . New Ambition to Halve Rate of Stillbirths and Infant Deaths 2015. www.gov.uk/government/news/new-ambition-to-halve-rate-of-stillbirths-and-infant-deaths#:~:text=Government%20announces%20new%20commitment%20to,world%20to%20have%20a%20baby.&text=The%20Health%20Secretary%2C%20Jeremy%20Hunt,England%20by%2050%25%20by%202030 (accessed 15 January 2024).
- National Health Service . Better Births: Improving Outcomes of Maternity Services in England – A Five Year Forward View for Maternity Care 2016. https://www.england.nhs.uk/wp-content/uploads/2016/02/national-maternity-review-report.pdf (accessed 15 January 2024).
- National Quality Board . National Guidance on Learning from Deaths 2017. https://www.england.nhs.uk/wp-content/uploads/2017/03/nqb-national-guidance-learning-from-deaths.pdf (accessed 15 January 2024).
- NHS Improvement . Implementing Learning from Deaths: Key Requirements for Trust Boards 2017. https://www.england.nhs.uk/wp-content/uploads/2021/07/170921-Implementing-LfD-information-for-boards.pdf (accessed 15 January 2024).
- Royal College of Obstetricians and Gynaecologists . Each Baby Counts: 2015 Full Report 2017.
- Department of Health . Safer Maternity Care: The National Maternity Safety Strategy – Progress and Next Steps 2017.
- NHS England . Implementing Better Births: Continuity of Carer 2017. https://www.england.nhs.uk/wp-content/uploads/2017/12/implementing-better-births.pdf (accessed 15 January 2024).
- NHS Improvement . A Guide to Support Maternity Safety Champions 2018.
- NHS Improvement . Spoken Communication and Patient Safety in the NHS 2018. www.england.nhs.uk/publication/spoken-communication-and-patient-safety-in-the-nhs/ (accessed 15 January 2024).
- Royal College of Obstetricians and Gynaecologists . Each Baby Counts 2018 Progress Report 2018.
- Coroners B, Cremation, and Inquires Policy Team . Consultation on Coronial Investigations of Stillbirths 2019. https://consult.justice.gov.uk/digital-communications/coronial-investigations-of-stillbirths/ (accessed 15 January 2024).
- Care Quality Commission . Learning from Deaths. A Review of the First Year of NHS Trusts Implementing the National Guidance 2019. www.cqc.org.uk/publications/themed-work/learning-deaths (accessed 15 January 2024).
- NHS England . Saving Babies’ Lives – Version Two: A Care Bundle for Reducing Perinatal Mortality 2019. www.england.nhs.uk/publication/saving-babies-lives-version-two-a-care-bundle-for-reducing-perinatal-mortality/ (accessed 15 January 2024).
- NHS England and NHS Improvement . National Patient Safety Strategy 2019. www.england.nhs.uk/patient-safety/the-nhs-patient-safety-strategy/2019 (accessed 15 January 2024).
- NHS Resolution . The Early Notification Scheme Progress Report: Collaboration and Improved Experience for Families 2019. https://resolution.nhs.uk/wp-content/uploads/2019/09/NHS-Resolution-Early-Notification-report.pdf (accessed 15 January 24).
- NHS Resolution . Maternity Incentive Scheme Year 3 2020. https://resolution.nhs.uk/wp-content/uploads/2021/03/Maternity-Incentive-Scheme-year-3-March-2021-FINAL.pdf (accessed 15 January 2024).
- NHS England, NHS Improvement . Better Births – Four Years On: A Review of Progress 2020. https://www.england.nhs.uk/wp-content/uploads/2020/03/better-births-four-years-on-progress-report.pdf (accessed 15 January 2023).
- NHS England . National Health Service Improvement 2021. www.england.nhs.uk/patient-safety/incident-response-framework (accessed 1 June 2021).
- NHS England, NHS Improvement . Maternity and Neonatal Safety Champions Toolkit 2020. https://www.england.nhs.uk/wp-content/uploads/2021/02/Feb-2021-Maternity-and-Neonatal-Safety-Champions-Toolkit-July-2020.pdf (accessed 15 January 2024).
- NHS England . Saving Babies Lives: A Care Bundle for Reducing Stillbirth 2016.
- NHS England . Spotlight on Maternity: Contributing to the Government’s National Ambition to Halve the Rates of Stillbirths, Neonatal, and Maternal Deaths and Intrapartum Brain Injuries by 2030 2016. https://www.england.nhs.uk/signuptosafety/wp-content/uploads/sites/16/2015/11/spotlight-on-maternity-guide.pdf (accessed 15 January 2024).
- Department of Health . Safer Maternity Care: Next Steps Towards the National Maternity Ambition 2016.
- Department of Health . Preventing Avoidable Harm in Maternity Care: Department of Health Capital Fund 2015–16 2016.
- Grimwood T, Snell L. The Maternity Safety Training Fund: An Evaluation. Health Education England; 2018.
- Health Safety Investigation Branch . Detection of Retained Vaginal Swabs and Tampons Following Childbirth 2019. https://www.england.nhs.uk/north-west/wp-content/uploads/sites/48/2020/02/HSIB-full-report-Detection-of-Retained-Vaginal-Swabs-and-Tampons-Following-Childbirth-Report.pdf (accessed 15 January 2024).
- Health Safety Investigation Branch . East Kent Hospitals University NHS Foundation Trust 2020. https://assets.publishing.service.gov.uk/media/5e8c5097e90e07077048040e/HSIB_East_Kent_report.pdf (accessed 15 January 2024).
- NHS Resolution . Maternity Incentive Scheme Year Three – Summary of Changes 2020. https://resolution.nhs.uk/wp-content/uploads/2020/02/Materity-incentive-scheme-year-three-changes-to-safety-actions.pdf (accessed 15 January 2024).
- Health Safety Investigation Branch . National Learning Report: Sever Brain Injury, Early Neonatal Death, and Intrapartum Stillbirth Associated With Group B Streptococcus Infection 2020. www.hssib.org.uk/patient-safety-investigations/severe-brain-injury-early-neonatal-death-and-intrapartum-stillbirth-associated-with-group-b-streptococcus-infection/investigation-report/ (accessed 15 January 2024).
- Health Safety Investigation Branch . National Learning Report Neonatal Collapse Alongside Skin-to-Skin Contact 2020. www.mnsi.org.uk/publications/neonatal-collapse-alongside-skin-to-skin-contact/ (accessed 15 January 2024).
- Health Safety Investigation Branch . Delays to Intrapartum Intervention Once Fetal Compromise Is Suspected 2020. www.hssib.org.uk/patient-safety-investigations/delays-to-intrapartum-intervention-once-fetal-compromise-is-suspected/investigation-report/ (accessed 15 January 2024).
- Iedema R, Greenhalgh T, Russell J, Alexander J, Amer-Sharif K, Gardner P, et al. Spoken communication and patient safety: a new direction for healthcare communication policy, research, education and practice?. BMJ Open Quality 2019;8.
- Pawson R, Greenhalgh T, Harvey G, Walshe K. Realist review – a new method of systematic review designed for complex policy interventions. J Health Serv Res Policy 2005;10:21-34.
- Jagosh J, Macaulay AC, Pluye P, Salsberg J, Bush PL, Henderson J, et al. Uncovering the benefits of participatory research: implications of a realist review for health research and practice. Milbank Q 2012;90:311-46.
- Quinn AM. The 3Rs program: the Colorado experience. Clin Obst Gynaecol 2008;51.
- Stanford SER, Bogod DG. Failure of communication: a patient’s story. Int J Obstet Anesth 2016;28:70-5.
- Ellis A, Chebsey C, Storey C, Bradley S, Jackson S, Flenady V, et al. Systematic review to understand and improve care after stillbirth: a review of parents’ and healthcare professionals’ experiences. BMC Pregn Childbirth 2016;16.
- Scholefield H. Embedding quality improvement and patient safety at Liverpool Women’s NHS Foundation Trust. Best Pract Res Clin Obstet Gynaecol 2007;21:593-607.
- Sakala C, Yang YT, Corry MP. Maternity care and liability: most promising policy strategies for improvement. Women’s Health Issues 2013;23:e25-37.
- Bonnema RA, Gosman GG, Arnold RM. Teaching error disclosure to residents: a curricular innovation and pilot study. J Grad Med Ation 2009;1:114-8.
- Karkowsky CE, Landsberger EJ, Bernstein PS, Dayal A, Goffman D, Madden RC, et al. Breaking Bad News in obstetrics: a randomized trial of simulation followed by debriefing or lecture. J Matern Fetal Neonatal Med 2016;29:3717-23.
- Raemer DB, Locke S, Walzer TB, Gardner R, Baer L, Simon R. Rapid learning of adverse medical event disclosure and apology. J Patient Saf 2016;12:140-7.
- Sauvegrain P, Zeitlin J. Investigating the benefits and challenges of including bereaved women in research: a multifaceted perinatal audit in a socially disadvantaged French district. BMJ Open 2020;10.
- Bennett J, Hacking B, Murdoch E. Being Open: Communicating Well With Patients and Families About Adverse Events 2016. https://ihub.scot/media/2186/rights-and-responsibilities-in-providing-safe-care-jbennett-emurdoch_d593c9.pdf (accessed 15 January 24).
- N. H. S. Lothian, Healthcare Improvement Scotland, Effective Communication for Healthcare, Simpsons Special Care Babies . Communicating well with parents and families about adverse events and significance adverse events (SAE) reviews: checklists and resources for staff 2016. www.healthcareimprovementscotland.org/our_work/governance_and_assurance/learning_from_adverse_events/learning_report_2016.aspx (accessed 15 January 2024).
- Hendrich A, McCoy CK, Gale J, Sparkman L, Santos P. Ascension health’s demonstration of full disclosure protocol for unexpected events during labor and delivery shows promise. Health Aff (Millwood) 2014;33:39-45.
- Gluyas H, Alliex S, Morrison P. Do inquiries into health system failures lead to change in clinical governance systems?. Collegian J Royal Coll Nurs 2011;18:147-55.
- Sorensen R, Iedema R, Piper D, Manias E, Williams A, Tuckett A. Health care professionals’ views of implementing a policy of open disclosure of errors. J Health Serv Res Policy 2008;13:227-32.
- Make Birth Better CIC . The Make Birth Better Survey 2019: The Circle of Trauma for Parents and Professionals: Make Births Better CIC 2020. https://static1.squarespace.com/static/5ed8a1b746cc235b44a50be1/t/5f58c377a3e7714b418e00e5/1599652751027/MBB+2019+Survey+Report_FINAL.pdf (accessed 15 January 2024).
- Coughlan B, Powell D, Higgins MF. The second victim: a review. Eur J Obstet Gynecol Reprod Biol 2017;213:11-6.
- Heazell AEP, Leisher S, Cregan M, Flenady V, Frøen JF, Gravensteen IK, et al. Sharing experiences to improve bereavement support and clinical care after stillbirth: report of the 7th annual meeting of the international stillbirth alliance. Acta Obstet Gynecol Scand 2013;92:352-61.
- Downe S, Schmidt E, Kingdon C, Heazell AEP. Bereaved parents’ experience of stillbirth in UK hospitals: a qualitative interview study. BMJ Open 2013;3.
- Bakhbakhi D, Burden C, Storey C, Siassakos D. Care following stillbirth in high-resource settings: latest evidence, guidelines, and best practice points. Semin Fetal Neonatal Med 2017;22:161-6.
- Redshaw M, Rowe R, Henderson J. Listening to Parents After Stillbirth or the Death of Their Baby After Birth. Oxford: University of Oxford; 2014.
- Burden C, Bakhbakhi D, Lynch M, Timlin L, Storey C, Heazell A, et al. All parents should be offered the opportunity to engage with the review of their baby’s death. PolicyBristol 2018. www.bristol.ac.uk/media-library/sites/policybristol/PolicyBristol-report-oct18-engaging-parents-baby-loss.pdf (accessed 15 January 2024).
- NHS Improvement . The Future of NHS Patient Safety Investigation: Engagement Feedback 2018. www.pslhub.org/learn/investigations-risk-management-and-legal-issues/the-future-of-nhs-patient-safety-investigation-engagement-feedback-november-2018-r116/ (accessed 15 January 2024).
- Kenyon S, Cross-Smith F, Keegan C, Johnston T. MBRRACE-UK 2017 Perinatal Confidential Enquiry: Term, Singleton, Intrapartum Stillbirth and Intrapartum-related Neonatal Death. Leicester: The Infant Mortality and Morbidity Studies, Department of Health Sciences, University of Leicester; 2017.
- Pillinger J. State Claims Agency. Ireland: Health Service Executive; 2016.
- Santos P, Ritter GA, Hefele JL, Hendrich A, McCoy CK. Decreasing intrapartum malpractice: targeting the most injurious neonatal adverse events. J Healthc Risk Manag 2015;34:20-7.
- Boyle F, Horey D, Siassakos D, Burden C, Bakhbakhi D, Silver RM, et al. Parent engagement in perinatal mortality reviews: an online survey of clinicians from six high-income countries. BJOG Int J Obstet Gynaecol 2021;128:696-703.
- Iedema R, Allen S. Anatomy of an incident disclosure: the importance of dialogue. Jt Comm J Qual Patient Saf 2012;38:435-42.
- Kok J, Leistikow I, Bal R. Patient and family engagement in incident investigations: exploring hospital manager and incident investigators’ experiences and challenges. J Health Serv Res Policy 2018;23:252-61.
- Harrison R, Walton M, Smith-Merry J, Manias E, Iedema R. Open disclosure of adverse events: exploring the implications of service and policy structures on practice. Risk Manag Healthcare Policy 2019;12:5-12.
- Mazor KM, Greene SM, Roblin D, Lemay CA, Firneno CL, Calvi J, et al. More than words: patients’ views on apology and disclosure when things go wrong in cancer care. Patient Educ Couns 2013;90:341-6.
- Wolk SW, Sine DM, Paull DE. Institutional disclosure: promise and problems. J Healthc Risk Manag 2014;33:24-32.
- Berg M. Problems and promises of the protocol. Soc Sci Med 1997;44:1081-8.
- Hannawa AF. Medical error disclosure: a pressing agenda for Public Health researchers. J Public Health Res 2012;1:214-5.
- Sims S, Leamy M, Davies N, Schnitzler K, Levenson R, Mayer F, et al. Realist synthesis of intentional rounding in hospital wards: exploring the evidence of what works, for whom, in what circumstances and why. BMJ Qual Saf 2018;27:743-57.
- Wong G, Westhorp G, Manzano A, Greenhalgh J, Jagosh J, Greenhalgh T. RAMESES II reporting standards for realist evaluations. BMC Med 2016;14:1-18.
- Keenan B, Pottage A. Ethics in rehearsal. JR Anthropol Inst 2017;23:153-65.
- Heimer CA, Gazley JL. Performing regulation: transcending regulatory ritualism in HIV clinics. Law Soc Rev 2012;46:853-87.
- Calnan M, Rowe R. Trust relations in a changing health service. J Health Serv Res Policy 2008;13:97-103.
- The Duty of Candour: Guidance for Team Managers and RCA Chairs 2015. www.cqc.org.uk/guidance-providers/regulations (accessed 15 January 2024).
- Diamond-Brown L. ‘It can be challenging, it can be scary, it can be gratifying’: obstetricians’ narratives of negotiating patient choice, clinical experience, and standards of care in decision-making. Soc Sci Med 2018;205:48-54.
- Luxford K, Safran DG, Delbanco T. Promoting patient-centered care: a qualitative study of facilitators and barriers in healthcare organizations with a reputation for improving the patient experience. Int J Qual Health Care 2011;23:510-5.
- Slade P, Sheen K, Goodfellow L, Rymer J, Spiby H, Weeks A. Authors’ reply re: work-related post-traumatic stress symptoms in obstetricians and gynaecologists: findings from INDIGO, a mixed-methods study with a cross-sectional survey and in-depth interviews. BJOG Int J Obstet Gynaecol 2020;127.
- Slade P, Balling K, Sheen K, Goodfellow L, Rymer J, Spiby H, et al. Work-related post-traumatic stress symptoms in obstetricians and gynaecologists: findings from INDIGO, a mixed-methods study with a cross-sectional survey and in-depth interviews. BJOG Int J Obstet Gynaecol 2020;127:600-8.
- Hindmarsh J. Organization, Interaction and Practice: Studies in Ethnomethodology and Conversation Analysis. 2010.
- McNamara K, Meaney S, O’Connell O, McCarthy M, Greene R, O’Donoghue K. Healthcare professionals’ response to intrapartum death: a cross-sectional study. Arch Gynecol Obstet 2017;295:845-52.
- Schroder K, Bovil T, Jorgensen JS, Abrahamsen C. Evaluation of ‘the Buddy Study’, a peer support program for second victims in healthcare: a survey in two Danish hospital departments. BMC Health Serv Res 2022;22.
- O’Riordan S, O’Donoghue K, McNamara K. Interventions to improve wellbeing among obstetricians and midwives at Cork University Maternity Hospital. Ir J Med Sci 2020;189:701-9.
- Waring J, Currie G, Crompton A, Bishop S. An exploratory study of knowledge brokering in hospital settings: facilitating knowledge sharing and learning for patient safety?. Soc Sci Med 2013;98:79-86.
- Braithwaite J, Runciman WB, Merry AF. Towards safer, better healthcare: harnessing the natural properties of complex sociotechnical systems. Qual Saf Health Care 2009;18:37-41.
- Bishop S, Waring J. A Socio-cultural Perspective on Patient Safety. Boca Raton: CRC Press; 2017.
- Martin G, Chew S, McCarthy I, Dawson J, Dixon-Woods M. Encouraging openness in health care: policy and practice implications of a mixed-methods study in the English National Health Service. J Health Serv Res Policy 2022;28:14-2. https://doi.org/10.1177/13558196221109053.
- Fletcher J. Morals and Medicine. The Moral Problems of: The Patient’s Right to Know the Truth, Contraception, Artificial Insemination, Sterilization, Euthanasia. Princeton: Princeton University Press; 1979.
- Bok S. Lying: Moral Choice in Public and Private Life. New York: Vintage; 1999.
- Scheirton LS. Proportionality and the view from below: analysis of error disclosure. HEC Forum 2008;20:215-41.
- Robinson S, Doody O. Nursing & Healthcare Ethics-E-Book. Oxford: Elsevier Health Sciences; 2021.
- Sullivan E, Segers M. Handbook of Public Policy Analysis. New York: Routledge; 2017.
- Fainzang S. An Anthropology of Lying: Information in the Doctor–Patient Relationship. London: Routledge; 2016.
- Mannion R, Davies H. Understanding organisational culture for healthcare quality improvement. BMJ 2018;363.
- Iedema R, Sandal J, Adams M. Legally protecting apologies shrinks the clinician-patient relationship. BMJ 2019;366.
- Schwappach DL, Boluarte TA. The emotional impact of medical error involvement on physicians: a call for leadership and organisational accountability. Swiss Med Wkly 2008;138:9-15.
- Scott SD, Hirschinger LE, Cox KR, McCoig M, Brandt J, Hall LW. The natural history of recovery for the healthcare provider ‘second victim’ after adverse patient events. BMJ Qual Saf 2009;18:325-30.
- Sheen K, Spiby H, Slade P. Exposure to traumatic perinatal experiences and posttraumatic stress symptoms in midwives: prevalence and association with burnout. Int J Nurs Stud 2015;52:578-87.
- Mendel P, Bate P, Robert G. Organizing for Quality: Inside the ‘Black Box’ of Health Care Improvement in Europe and the United States 2008. www.rand.org/pubs/research_briefs/RB9329.html (accessed 15 January 2024).
- Waring J, Currie G. A Socio-cultural Perspective on Patient Safety. London: CRC Press; 2017.
- Sanford N, Lavelle M, Markiewicz O, Reedy G, Rafferty AM, Darzi A, et al. Capturing challenges and trade-offs in healthcare work using the pressures diagram: an ethnographic study. Appl Ergon 2022;101.
- Cohen S. States of Denial: Knowing about Atrocities and Suffering. New York: John Wiley & Sons; 2013.
- Morgan R. States of denial: knowing about atrocities and suffering. By Stanley Cohen (Cambridge: Polity Press, 2001. 344 pp. {pound}15.99 pb). Br J Criminol 2002;42:807-9.
- Cubellis L. Gestures of care and recognition: an introduction. Cult Anthropol 2020;35:1-5.
- Lister R. Social Justice and Public Policy: Seeking Fairness in Diverse Societies. Bristol: Policy Press; 2008.
- Care Quality Commission . Regulation 20 Duty of Candour 2015. https://www.cqc.org.uk/sites/default/files/2022-12/20220722-duty-of-candour-pdf-version-FINAL-2.pdf (accessed 15 January 2024).
- Robertson L, Knight H, Snelling EP, Petch E, Knight M, Cameron A, et al. Seminars in Fetal and Neonatal Medicine. Elsevier; 2017.
- O’Hara JK, Lawton RJ. At a crossroads? Key challenges and future opportunities for patient involvement in patient safety. BMJ Qual Saf 2016;25:565-8.
- Frank AW. The Wounded Storyteller: Body, Illness, and Ethics. Chicago: University of Chicago Press; 2013.
- Carel H, Kidd IJ. The Routledge Handbook of Epistemic Injustice. New York: Routledge; 2017.
- Duclos CW, Eichler M, Taylor L, Quintela J, Main DS, Pace W, et al. Patient perspectives of patient–provider communication after adverse events. Int J Qual Health Care 2005;17:479-86.
- Fricker M. The Routledge Handbook of Epistemic Injustice. New York: Routledge; 2017.
- Fricker M. Epistemic Injustice: Power and the Ethics of Knowing. New York: Oxford University Press; 2007.
- Aveling E-L, Jovchelovitch S. Partnerships as knowledge encounters: a psychosocial theory of partnerships for health and community development. J Health Psychol 2014;19:34-45.
- Ocloo J, Garfield S, Franklin BD, Dawson S. Exploring the theory, barriers and enablers for patient and public involvement across health, social care and patient safety: a systematic review of reviews. Health Res Policy Syst 2021;19.
- Ocloo JE. Harmed patients gaining voice: challenging dominant perspectives in the construction of medical harm and patient safety reforms. Soc Sci Med 2010;71:510-6.
- Ocloo J, Matthews R. From tokenism to empowerment: progressing patient and public involvement in healthcare improvement. BMJ Qual Saf 2016;25:626-32.
- Mackintosh N, Rance S, Carter W, Sandall J. Working for patient safety: a qualitative study of women’s help-seeking during acute perinatal events. BMC Preg Childbirth 2017;17.
- Rutten R. Uncertainty, possibility, and causal power in QCA. Sociol Methods Res 2021;52:1707-36. https://doi.org/10.1177/00491241211031268.
- Barnes M, Cotterell P. Critical Perspectives on User Involvement. Bristol: Policy Press; 2012.
- Cordey S, Moncrieff G, Cull J, Sarian A, Group A-CC. ‘There’s only so much you can be pushed’: magnification of the maternity staffing crisis by the 2020/21 COVID-19 pandemic. BJOG 2022;129:1408-9.
- Jardine J, Relph S, Magee LA, von Dadelszen P, Morris E, Ross-Davie M, et al. Maternity services in the UK during the coronavirus disease 2019 pandemic: a national survey of modifications to standard care. BJOG 2021;128:880-9.
- Homer CSE, Leisher SH, Aggarwal N, Akuze J, Babona D, Blencowe H, et al. Counting stillbirths and COVID 19: there has never been a more urgent time. Lancet Glob Health 2021;9:e10-1.
- Hui L, Marzan MB, Potenza S, Rolnik DL, Pritchard N, Said JM, et al. Increase in preterm stillbirths in association with reduction in iatrogenic preterm births during COVID-19 lockdown in Australia: a multicenter cohort study. Am J Obstet Gynecol 2022;227:491.e1-491.e17.
- Baker T. Restorative Just Culture in Practice. New York: Productivity Press; 2022.
- House of Commons Department of Health and Social Care . Health and Care Act 2022 n.d. https://bills.parliament.uk/bills/3022 (accessed 15 January 2024).
- Chantler C. Placing the Ockenden report in context. AIMS J 2022;34:50-2.
- Booth A, Sutton A, Clowes M, Martyn-St James M. Systematic Approaches to a Successful Literature Review. London: Sage Publications; 2021.
- Health Research Authority . Confidentiality Advisory Group 2022. www.hra.nhs.uk/approvals-amendments/what-approvals-do-i-need/confidentiality-advisory-group/ (accessed 12 July 2022).
Appendix 1 Further details of policy scoping and realist review methods
Section A: stages of the policy scoping literature review
-
A search was performed to identify key documents for analysis in the Care Quality Commission Database, UK government policy papers and consultations database, Health Safety Investigation Branch investigation and report database, NHS Resolution website, and the NHS Improvement Publications database. Combinations of the search terms ‘Incident’, ‘Clinical Incident’, ‘Serious Incident’, ‘Harm’, ‘Death’, ‘Mortality’, ‘Review’, ‘Investigation’, ‘Duty of candour’, ‘Maternity’ and ‘Maternity Services’ were used. Documents related to maternity safety and harm, openness, incidents, reviews or investigations in the UK were included. Academic papers, essays, conference presentations and research studies were excluded. Documents were excluded if they were published before 1 January 2014, or if they were not related to safety, incidents, reviews or investigations in maternity services in the UK. The search was considered an iterative process and was completed by authors JH and NS between July 2020 and July 2022. Reference lists were snowballed to identify additional documents relevant to the research question. Although the Kirkup report was published in March 2015, documents published in 2014 were included so that a baseline for family involvement recommendations, immediately prior to the landmark report, could be established.
-
Second, after initial data immersion, the documents were scanned to identify segments of text pertaining to family involvement or recommendations for family involvement. These areas were identified by searching the documents for key words and phrases such as ‘family involvement’, ‘parent involvement’, ‘parental involvement’, ‘family’ and ‘parent’.
-
Next, we extracted and mapped key features from these segments using a data extraction table. The data extraction table was developed by author NS and reviewed by author MA to ensure relevance to the research question. Data extracted included: title, author/publishing body, date, sections in the document explicitly discussing family involvement, language/terminology used, described priorities/justification for family involvement and any explicit recommendations related to family involvement. The documents were sorted chronologically in the data extraction table. As data analysis progressed, the data extraction table was thematically split into two smaller tables based on overall document content. The first included all documents related to the statutory DoC and the second included all other included documents, which were related to maternity safety more generally.
-
Finally, the data in the extraction tables were thematically analysed using inductive, open coding. We collated and thematically summarised the extracted data, reporting on the shifts in the conceptualisation of and recommendations for family involvement between 2014 and 2022.
Section B: stages of the realist literature review
-
First, a two-stage literature search of key clinical and social science bibliographic databases was conducted using search terms developed with a subject specialist (RI). Sources published in English and after year 2000 were included; no predetermined exclusion criteria on research methods were applied; however, only studies reporting primary data or systematically reviewing primary data were included. In early 2019, initial scoping searches and consultations with a subject specialist led to the identification of key words, synonyms and spelling variations. A search term strategy was developed for MEDLINE (OvidSP) and adapted for other databases (CINAHL, HMIC, PsycINFO and EMBASE) to establish an initial overview of available international interventions (national, organisational and individual/team-based) to improve OD. Inclusion criteria were ‘maternity services’ and ‘disclosure and discussion of incidents’. Following guidance on realist data gathering, no predetermined exclusion criteria on research methods were applied. 78 Grey literature, including policy reports, service guidance and pubic and professional commentary, was also retrieved. ProQuest and British Library EThOS were searched for relevant theses. Citation searches and reference lists of included studies supplemented the database searches. The search was limited to English language documents published from 2000 onwards. In total, 993 sources were identified (see Figure 3). For quality assurance, MEDLINE, CINAHL and ProQuest searches were repeated in August 2019 with no additional papers identified for inclusion. In August 2019, a key word search was conducted within the full text of the 993 sources to identify evidence of OD in maternity care settings. This search included two phases. In phase one, free text, mapped terms operators and limiters, together with the stage one limiters, were applied 64 of the 993 sources were identified. This search enabled us to identify papers that included analysis of organisational and national interventions that explicitly included maternity services, but that may have been missed by exclusively using maternity and disclosure search terms. 9,37,49,118,143,153,161,163 On the advice of our PAG, our final full-text review excluded 30 studies that did not include primary data, apart from systematic reviews which were retained. In stage two, a further five recent documents (published in 2020) that met our stage two inclusion criteria were identified in consultation with subject experts.
-
Second, using a tailored appraisal tool, and following realist principles, two researchers (MA and JH) assessed the documents for ‘fitness for purpose’ (relevance75 and rigour231).
-
Third, a guided discussion of data and initial retroductive theorisation was conducted at a 2-hour meeting with our PAG (14 subject experts). This discussion guided the focus of data extraction (where multiple propositions might be embedded in single statements). This meeting began to identify the relevance of different OD improvement issues to families, clinicians and services.
-
Fourth, the two researchers (MA and JH) extracted data from each paper using a tailored template. The template was for documentation of explicit or implicit rationales for OD improvement, with evidence of the context and proposed and evidenced outcomes of interventions. These rationales, documented as a series of EAs based on ‘if/then’ statements, enable to identification of full or partial C–M–Os. Reflective notes on emergent programme theories were kept informing the synthesis.
-
Fifth, one researcher (MA) consolidated the extracted data into more general EAs addressing the question of ‘what worked, when and why’. These EAs were mapped for three different interest groups (families, clinicians and services). Researchers twice consulted the project CIG (n = 5) for advice on the prioritisation and consolidation of the extracted data and the EAs into a series of more generalisable programme theories. Final theories were selected for their relevance; their scope and breadth within different service delivery situations; and because they could be ‘tested’ during the case-study research.
FIGURE 3.
Diagram illustrating the literature search, screening and synthesis.
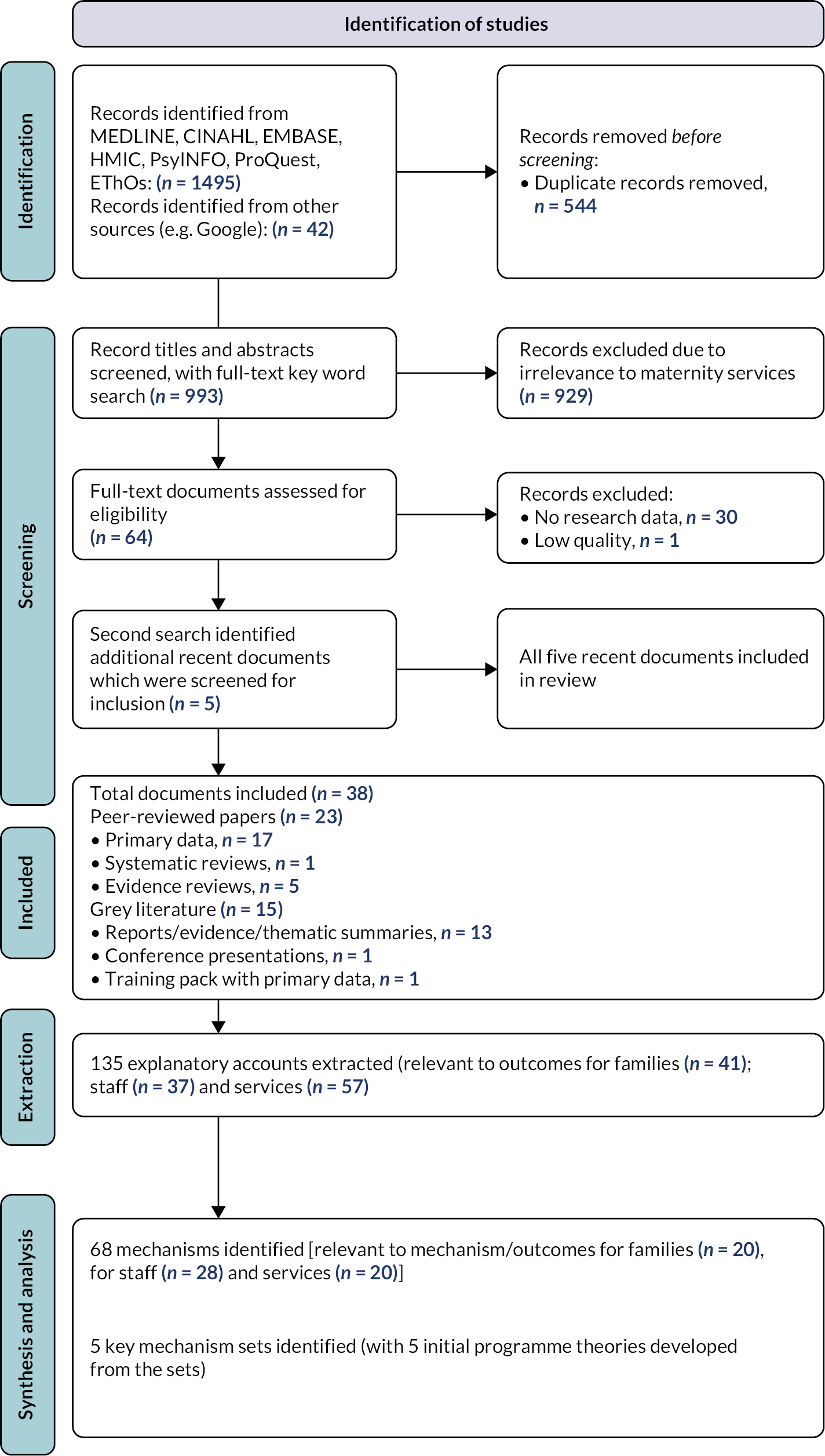
Appendix 2 Further details of research process, study adjustments, and research ethics and management
Data collection process (study phases 2 and 3)
During the case-study research, formal meeting observations were conducted after informed written consent from meeting chairs and verbal consent from all meeting participants. Written informed consent was also acquired from families if their identifiable data were to be discussed during the meeting. Consent practices were more challenging during online meetings, as many participants’ attendance was transient. In these situations, potential attendees were also informed of the researchers’ presence when the online invitations were circulated by administrators. At the close of meetings, attendees were invited to contact the research team, in confidence, if they wanted their contribution to meeting discussion to be withdrawn from the data set. For ethnographic observations, informed, written consent was obtained from shift leads or from meeting chairs. The presence of researchers was explained to all other participants, along with an option for them to request their withdrawal of any findings relevant to them. Given the sensitivity of the study topic, all participants at panel meetings were invited to ask for the researchers to leave the meeting at any time and without having to explain why. During the research, no participant requested that researchers leave a meeting or an event that they were observing. Additionally, under Health Research Authority (HRA) Confidentiality Advisory Group (CAG) regulations,232 the researchers always sought to ensure that they were not present in any situations where identifiable patient data were exposed without prior patient consent. As with SP1, all participants interviewed and directly observed were given a unique code to protect their anonymity and confidentiality. Documents such as meeting minutes, action plans, organisational and service bulletins, quality and safety improvement reports, CG papers, family communication templates, and informal team guidance diagrams were collected, in a redacted form, to assist the researchers with the construction of different aspects of disclosure in each case-study service.
Staff and family interviews were audio-recorded and transcribed verbatim and took place over the phone or in-person, based on the preferences of the interviewee. Interviews were conducted by MA and JH. We were only able to approach families from one of the case-study sites (site A). Trust corporate staff requested that their interviews were not audio-recorded, but the researcher was permitted to make notes during the interview. Most often, the verbatim transcripts and interview notes were read by both researchers while field research was ongoing with any notable issues arising from the interview agreed between the researchers to be explored in subsequent observations and interviews. Reflective notes on clinician and family interviews were also recorded by each researcher; these were used during weekly research meetings and to assist with the development of in-case and cross-case findings. Participant information can be found in Tables 3 and 4.
| Participant type | Interviews (n) |
|---|---|
| National leads for maternity quality and safety improvement initiatives | 18 |
| Independent associations/charities | 6 |
| Medicolegal representatives | 6 |
| Leads of professional bodies | 2 |
| Clinicians with national roles in quality and safety improvement initiatives | 12 |
| Families working in national, regional or Trust-level quality and safety improvement | 14 |
| Families not working in quality and safety improvement | 9 |
| Total national stakeholder interviews | 67 |
| Participant type | Site A (n) | Site B (n) | Site C (n) | Cross sites B and C (n) | Subtotals |
|---|---|---|---|---|---|
| Families | 4 | 0 | 0 | 0 | 4 |
| Family representatives | 1 | 0 | 0 | 2 | 3 |
| Specialist midwives and matrons | 8 (plus 3 return) | 3 | 4 | 5 | 20 (plus 3 return) |
| Service leads (midwifery, clinical risk, QI) | 5 | 2 | 4 | 1 | 12 |
| Front-line clinicians (consultants, senior registrars and midwives) | 9 | 2 | 4 | 1 | 16 |
| Corporate services (claims and general management) | 7 | 0 | 0 | 3 | 10 |
| Trust leads and directors | 4 | 0 | 0 | 3 | 7 |
| Non-Trust staff (counsellors) | 1 | 0 | 0 | 2 | 3 |
| Independent investigators (HSIB and coroner) | 0 | 0 | 0 | 2 | 2 |
| Total interviewees per site | 39 | 7 | 12 | 17 | N = 75 |
| Total interviews | N = 78 |
Whenever possible, the two researchers (MA and JH) conducted ethnographic observations together. Their social and physical positioning in meetings, unit and office events varied depending on the nature of that event; on the presence of a key informant (particularly during ward shift observations); and on the degree of social familiarity with participants. The types of meetings observed by the research team are detailed in Table 5. Each researcher drafted independent and in-depth fieldnotes immediately after the observation period. Fieldnotes were compared and discussed between the two researchers at least twice weekly, with an ongoing record kept of significant agreements and differences in fieldnotes and their interpretation. During this time, personal reflections on responses to observed events and informant situations and attitudes were encouraged, including reflection on distressing events. Emergent findings, agreements and differences were discussed with the wider research team monthly, with further questions or ongoing discrepancies explored during ongoing or return interviews. The two researchers identified that the most significant disparity in data collected from all case-study services to be that individual clinicians who planned to leave their service spoke more about the challenges and insufficiencies in OD and patient safety in that service than those who remained highly invested in this organisational work and who intended to remain at their service.
| Meeting type | Site A (n) | Site B (n) | Site C (n) | Cross sites B and C (n) | Subtotal |
|---|---|---|---|---|---|
| Risk | 8 | 3 | 7 | 0 | 18 |
| PMRT | 3 | 0 | 2 | 0 | 5 |
| SI panel (internal and external) | 2 | 0 | 2 | 0 | 4 |
| Learning | N/A | 5 | 9 | 0 | 14 |
| Family debriefings (in person) | 0 | 3 | 2 | 0 | 5 |
| Quality assurance | 1 | 0 | 0 | 2 | 3 |
| LMNS insight group | 0 | 0 | 0 | 1 | 1 |
| Family representatives | 1 | 0 | 0 | 1 | 2 |
| Total meetings observed per site | 15 | 11 | 22 | 4 | N = 52 |
| Total observation time | 93 hours |
As agreed with our ethics committees and explained to families, each family was debriefed after interview and, if required, further advice on contacts for family support was given by the research team. All families were contacted for a debriefing within a few days of interview; additionally, the researchers initiated debriefing calls with three clinicians who became distressed at interview. No families or clinicians chose to terminate or withdraw their interviews. Families and case-study site participants reported that the use of a staged debriefing process was appreciated. No families or clinicians were known to have sought further support after the forums, although contact details of support services were announced before and after each forum. No managers employed as corporate staff agreed to audio-recorded interviews, so one researcher (MA) agreed to taking interview notes that were then checked with the participant.
For the interpretive forums, two members of research team (NS and MA) prepared a standard set of introductory slides, organised around the initial programme theories. Anonymised, illustrative quotations from SP1 and SP2 interviews were used to illustrate and contrast emerging theories. The slide set was adjusted to accommodate the time available for each forum. The forums varied in duration from 2 hours at the national forum to 90 minutes at the FF, and to between 20 and 60 minutes for the three site forums. Informed, written consent was obtained for the national and parents forum (where meetings were audio-recorded) and from the chairs of the site forum meetings (where hand-written observation notes were taken). In total, 69 people attended the interpretive forum (see Table 6).
| Forum type | Location | Staff participants (n) | Family participants (n) | Duration |
|---|---|---|---|---|
| PAG | Online | 8 (national policy leads, professional leads, academics) | 6 | 90 minutes |
| Family | Online | – | 5 | 60 minutes |
| Site forums (× 3) | (Online × 2; face-to-face × 1) | 50 (doctors, midwives, service and clinical managers, specialist midwives) | – | 20–60 minutes per forum |
| Total forum participation: N = 69 | ||||
Study adjustments
As stated in our protocol Version 4 (www.fundingawards.nihr.ac.uk/award/17/99/85), we set out to spend 12 weeks at each case-study service and to conduct an estimated 25 hours of focused observations at each site. 73 In the context of COVID-19-related staffing pressures, instead, the researchers (MA and JH) spent 36 weeks across the three case-study services to enable flexibility in response to shifting staff schedules. According to our protocol, we also intended to conduct return interviews with key clinicians. We conducted three return interviews with staff who expressed a particular commitment to OD improvement in two services. We did not conduct more return interviews due to work pressures within services at the time of the research, and because we found expertise and interest in OD to be more distributed that we originally anticipated.
We had anticipated that interviews and focused observations of external investigations (notably HSIB investigations) and their interface with in-service processes were acceptable and feasible. Senior HSIB staff had indicated this in SP1. However, in SP2 there was limited engagement of HSIB teams in the study (n = 1 interviewee) and no opportunity to observe HSIB investigation processes or feedback meetings in the case-study services.
We did not originally set out to recruit any families from the case-study services because we anticipated that services would object to this. However, necessary CAG procedures opened R&D permissions for family recruitment with site PI agreement. In total, four families were recruited from Site A.
Coronavirus disease 2019 study adjustments
A series of adjustments to the study protocol were required in response to two waves of the COVID-19 pandemic (March 2020–February 2022). Adjustments were required because of delays in R&D permissions due to Tier-1 research studies prioritisation and ongoing staffing pressures within the three maternity services. Adjustments were possible because of a 9-month extension to the study, with a 3-month costed extension, granted by the National Institute for Health and Care Research (NIHR) Health and Social Care Delivery Research (HSDR) Panel.
The following adjustments were made to the study timeline, methods and recruitment:
-
SP1 extension: (1) expansion of literature scoping to an international realist synthesis; (2) addition of a scoping review of policy documents to identify patterns for engaging with families post incident; and (3) increasing the national stakeholder interviews from n = 18–22 to n = 67. This extension enabled us to capture a wider range of stakeholder interests, including those of less senior organisational representatives, of front-line clinicians, and of families without organisationally prescribed safety improvement roles while awaiting R&D approvals.
-
SP2: A revision of the number of case-study services from four Trusts, services, or networks to two Trusts with three services. We were able to make some compensations to this loss of comparative data during the SP3 national and family interpretive forums, where the research team directly enquired about the generalisability of key findings and implications from research of case studies selected for positive deviance.
-
Finally, some of the in-person SP2 and SP3 research was conducted virtually. At the choice of study participants, three of the four interpretive forums were conducted on-line. In-person ethnography was conducted for 30 of the total 93 hours of observations across the three case-study services. On-line ethnography (63 hours) was conducted when meetings and other staff events were scheduled as on-line for all participants.
Patient and public involvement
Following the 2019 standards of public involvement, our PPI strategy supported meaningful representation of families across all SPs, through direct involvement and third-sector organisation representation. Research and policy leads (including one harmed parent) from three third-sector organisations were involved throughout the research cycle from the inception and development of the study as study co-applicants. They worked with the research team to develop research tools, identify emerging research issues and questions, analyse data, and draft and present study findings. One family representative was part of the SSG, and eight harmed families (two leading black maternity associations) were active members of the PAG. As PAG members, they advised on the relevance of our emerging programme theories as well as on our project dissemination and impact plans. At one PAG meeting, four families presented and discussed findings from our SP1 interviews with families to the wider PAG and later contributed to the PAG Interpretive Forum. Five families, recruited through SP1, participated in a national Family Interpretive Forum, advising on the interpretation of our primary research findings. Reflections on the impact of PPI on the study are detailed in Chapter 9.
Research ethics
Three ethical approvals were obtained for the study. For SP1, approvals were granted by the ethics committee at King’s College London (BDM RESC Ref 11174 and BDM RESC Ref 22033 for additional family interviews). SP2 and 3 approvals were obtained from the HRA Research Ethics Committee (REC) London Bridge (REC reference 20/LO/1152; IRAS Project ID: 262197). Approval was also obtained from the HRA CAG (20/CAG/0121) on the grounds that patient confidentiality might be breached during the fieldwork observations. After favourable opinion from the REC and the CAG, we obtained R&D permissions from our study sponsors and local R&D permissions from the two Trusts where data were collected. Researchers had research passports as well as letters of access before start of research in each study site.
Study management
The project was co-led and co-managed by a senior and a junior PI at King’s College London. Study co-investigators met at least monthly with the PIs and researchers. During the study period, three PAG meetings were held and three SSG meetings were held. See (www.fundingawards.nihr.ac.uk/award/17/99/85) for roles of PAG members and SSG minutes.
Appendix 3 Flow diagram of case study selection
FIGURE 4.
Case-study sampling approach to identify the case-study services.
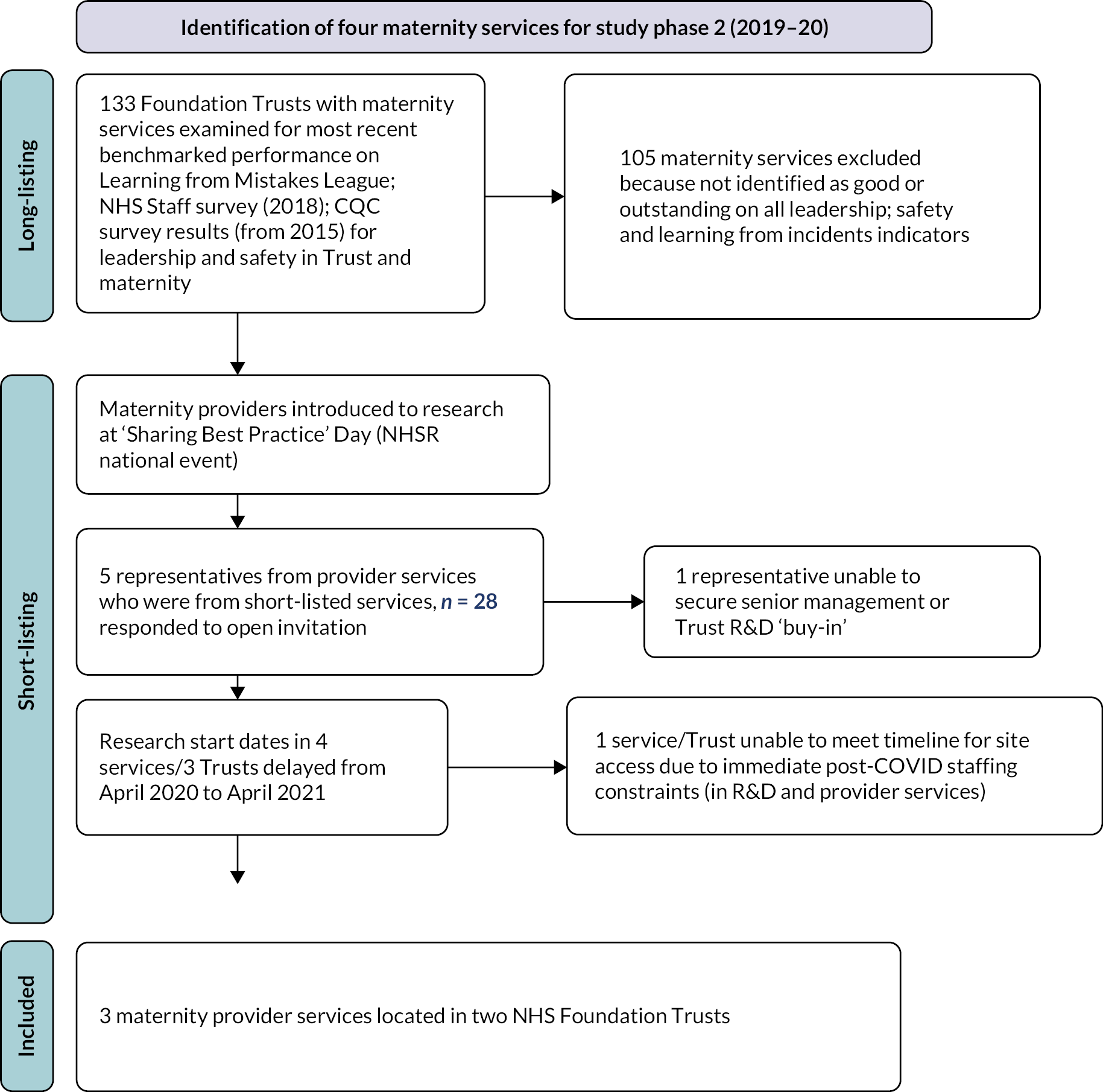
Appendix 4 General and topic-relevant features of the selected case-study services
| Trust-level context | TRUST A | TRUST B | ||
|---|---|---|---|---|
| Service-level context | TRUST A, SITE A | TRUST B, SITE B | TRUST B, SITE C | |
| 2019–20 CQC Ratings |
Well-led | Outstanding | Good | |
| Safe | Requires improvement | Good | ||
| Caring | Outstanding | Outstanding | ||
| 2016 Learning from Mistakes League | Outstanding levels of openness and transparency | Significant concerns about openness and transparency | ||
| Items in Board minutes | 2017: DoC noted as requiring improvement in all services 2018: Trust-wide, clinical debrief programme of meetings to encourage MD review of quality and performance in a ‘no blame’ environment |
2014: importance of DoC noted 2016 on: all SIs, and SIs specific to maternity, have been published in Board minutes (are publicly available) 2018: adherence to DoC and ‘Being Open’ guidance as a CG outcome |
||
| Service provision | Acute and community; Consultant-Led Care and Midwifery-Led Birth Centre Local Facility (50%) and Tertiary Centre; Midwifery-Led Birth Centre; Home Birth Options. Walk-in Medical Admissions Unit (MAU) for pregnancies over 18 weeks; Level 3 (Neonatal Intensive Care Unit) | Consultant-Led Care and Midwifery-Led Birth Centre; Local Facility and Tertiary Centre; Home Birth Options; ‘Out of Guidelines’ Care Supported; 24-hour walk-in MAU for pregnancies over 18 weeks. Level ½ (Special Care Baby Unit) |
Acute and community; Consultant-Led Care and Midwifery-Led Birth Centre; Local Facility (40%) and Tertiary Centre; Home Birth Options; ‘Out of Guidelines’ Care Supported; Walk-in MAU for pregnancies over 18 weeks; Specialist fetal medicine service; Level 3 (Neonatal Intensive Care Unit) | |
| Service size (deliveries a year 2020) | 7000 | 5000 | 6000 | |
| Service location | Inner city | Suburban | Inner city | |
| 2019–20 Care Quality Commission (CQC) Ratings |
Overall | Good | Good | Good |
| Well-led | Good | Good | Good | |
| Safe | Good | Good | Requires improvement | |
| Caring | Good | Good | Good | |
| Service-level context | TRUST A, SITE A | TRUST B, SITE B | TRUST B, SITE C | |
| 2020 NHS Staff Survey Results (for Safety Culture) | 7.2 (Best performing Trust: 7.4; worst performing Trust: 6.1) |
6.9 (Best performing Trust: 7.4; worst performing Trust: 6.1) |
||
| Additional items | 2019 CQC maternity inspection reported:
|
2019 CCQ maternity inspection:
|
From 2019 CQC maternity inspection:
|
|
|
|
|
||
|
|
|||
Appendix 5 Summary of realist data extraction findings in relation to the five identified programme theories
| Mechanism for strengthening OD | Contexts | Improvement programmes, interventions and infrastructure | Resources, constraints and opportunities shaping this element | Reasons, responses and assumptions involved in this element | Immediate outcomes | Long-term outcomes |
|---|---|---|---|---|---|---|
| Meaningful acknowledgement | Circumstances where harm is identified by a clinician or family member (irrespective of whether this is avoidable) |
|
|
|
|
|
|
|
|
|
|||
|
|
|
||||
| Involvement of family |
|
|
|
|
|
|
|
|
|
|
|||
| Finding a way to make sense of the event |
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|||
| Skill of clinicians and safety of clinicians |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|||||
| Seeing that changes have been made after the event to prevent reoccurrence |
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
Appendix 6 Overview of open disclosure practices and processes in the case-study services
When an incident that might have a serious outcome occurs, it was usual for an initial conversation (and apology) with the family to be initiated by a senior shift lead. This conversation is followed by two processes of family communication, that are organisationally different and that sometimes overlapped in practice.
If the incident is expected to meet the various criteria for rapid review or for internal or external investigation (see Chapter 1), the clinical governance or 'risk team' (a risk midwife or clinical risk lead) begins a formal DOC process (with spoken apology, explanation of forthcoming processes and timelines, information documents and contact numbers for enquiries). This formal process is completed when the final investigation report was shared with the family by post or one or more 'risk' or 'report' debriefings. These are the 'two steps' for meeting the statutory Duty of Candour by the organisation.
If the incident is catastrophic or is expected to lead to significant family harm or upset, the family's link consultant, possibly with a clinical manager, will often also initiate a meeting with them to discuss the event (answer questions, offer apologies) and plan ongoing and additional care needs. If the family is quickly discharged, this meeting happens as a later debriefing appointment. Post-incident care includes a scheduled 'obstetric debriefing' and, possibly, a midwifery-led debrief with a midwifery consultant or independent Professional Midwifery Advocate (PMA). Referrals might also be made to in-service or outsourced trauma or emotional care clinical specialists or counsellors. Depending on the incident and family situation, post-incident care may begin, or be continued, when the family enters the service when expecting another child.
Where governance teams and clinical teams can collaborate, communication with the family, and the organisation of care, might be aligned to reduce confusion for families. Heads of Midwifery, Clinical Governance Leads or acting risk midwives manage these alignments. In these situations, for example, ongoing conversations with a family might be led by a clinician who already knows the family and who they feel more comfortable with. The risk midwife completes the reporting of the mandated procedure. She may also assume ongoing responsibility for ongoing involvement of a family in the incident review/investigation. Incidents might also be identified after the event – by routine risk assessments of Datix reports or by families themselves through matrons, PALS or complaints teams. In these circumstances, it is most common for the risk midwife to establish first contact with the family.
Across the study sites, risk teams or clinical leads anticipated that conversations with injured families would be ongoing, at least for the duration of the incident investigation and final reporting and that engagement in investigation processes and clinical debriefings would be varied and variable for each family. They also expected that this involvement work was highly varied between families. While the tasks of clinical governance were clearly distinct from those of ongoing clinical care, members of both teams were actively involved in disclosure with some families that extended beyond postal and e-mail correspondence.
FIGURE 5.
Family involvement in incident reviews/investigation process. Blue indicates usual family involvement in decision-making process in the case-study sites.
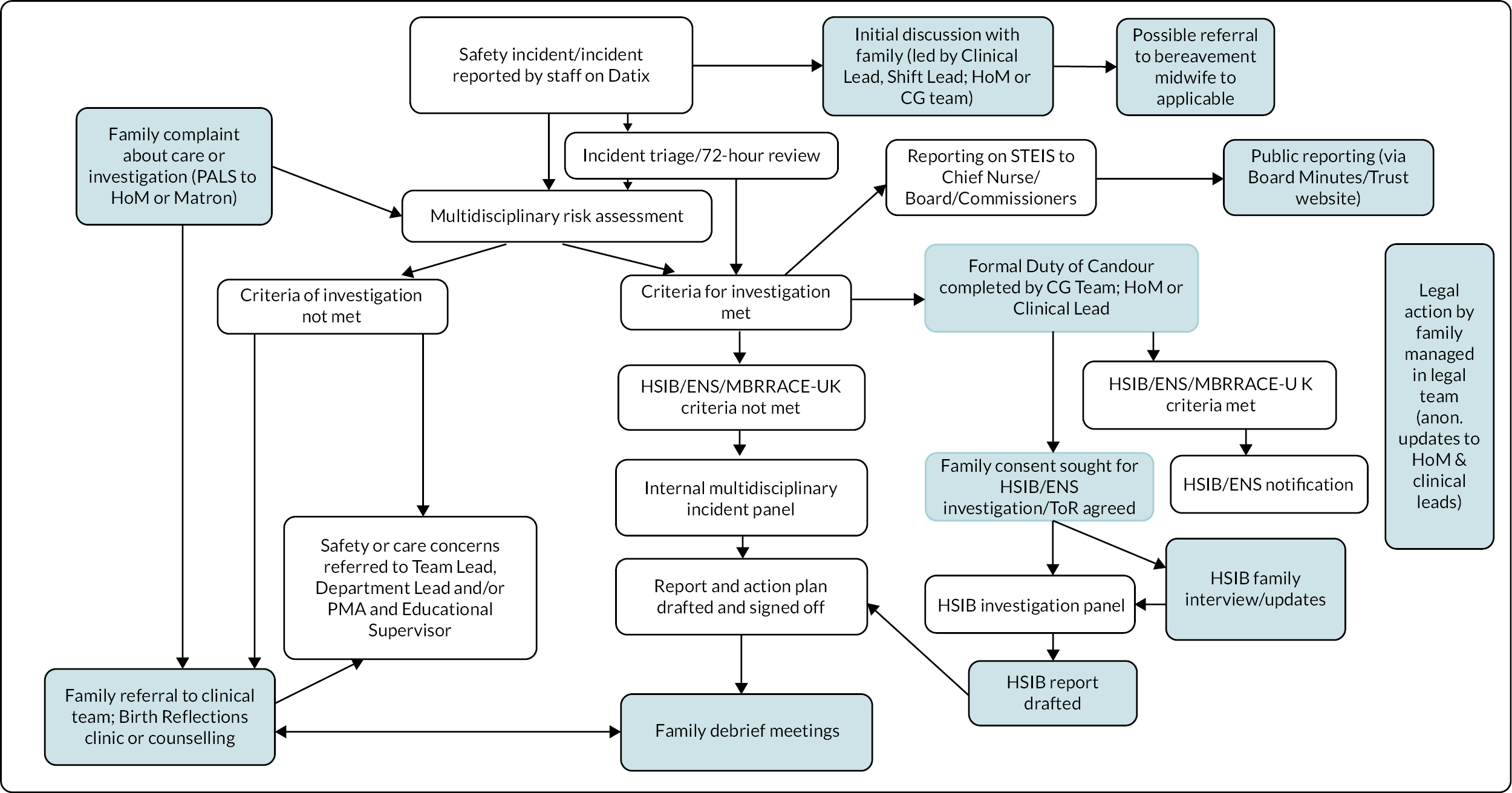
Appendix 7 Organisation and reception of post-incident staff support in the case-study services
| Site | Intervention/resource | Description | Staff group | Reported effects | Summary |
|---|---|---|---|---|---|
| All | External organisations and professional bodies, e.g. the British Medical Association (BMA) | Psychological support (various) | Consultants and trainees | ‘I’m much more likely to come into my office which I share with three other people, talk to them about it and then literally close the book and hope the next time is easier’ (SASi12) ‘You can always tap into things but most are poorly utilised because of the time factor’ (SASi04b) |
Few participants mentioned these resources. The trainee who prepared an inquest statement on an incident of several years previously completed the statement without seeking external professional advice |
| All | Trust psychologist and/or psychotherapist | Self-referral | All staff | ‘Just for people to say we’ll get you a psychologist in one afternoon a week, well, that’s not how it works, it’s a much bigger system change, it’s about resources’ (SDSi04) | Many participants were unaware of this service and some participants felt that this approach individualised and psychologised system-wide organisational difficulties |
| B and C | Service commissioned service (pending initiative) | 1 : 1 staff counselling (self-referral) | All staff | Not known (pending) | Commissioning followed the most recent staff survey that highlighted a self-reported increase in workplace stress |
| A | Service psychologist (group facilitation) | Monthly group reflections for 1 hour (initiated by service matron) | Community midwives | ‘The first ones were just a chance for staff to have a moan up … the later ones were more about specific issues coming up’ (SASi17) ‘We are the only team utilising her expertise like this’ (SASi17b) | Arrangement established by the community service matron (using available service). This team was able to establish shared availability for the meetings |
| A | Service psychologist (individual provision) | Open forum days on different wards | Individual staff | ‘People can just pop in if they have felt affected by something, they can discuss it on a more causal basis. It’s not such a big thing to contact her’ (SASi04b) ‘We’ve had psychological support for a year and she doesn’t get a lot of clinicians approach her’ (SASi37) |
Eight months after the appointment of a dedicated service psychologist (funded by a Trust-acquired charity grant), the forums were infrequently used by service staff, despite many efforts to increase awareness and accessibility of the service. Some senior medical staff were particularly wary of the potential for undermining of more established approaches to trainee support |
| All | Educational supervisors | Not clear | Trainees | ‘They only have time to manage the rotas’ (SASi) ‘It’s hard for all of us to remain present in such a variety of ways’ (SDSi07) |
Across all case-study services, clinicians without sufficiently protected time for educational support marginalised or rushed this work with junior doctors |
| All | Designated SI clinical fellow | To support anyone involved in a SI Role rotates annually (Sites B and C) Short-term appointment (Site A) |
Not known | Not identified or discussed by trainees or junior midwives | Not known |
| All | PMAs (2–3FTE) each service; various Bands (from 6 to 8); at Sites B and C, PMAs on on-call rotas for maternal and neonatal deaths |
|
Midwives | ‘This is the first person you would go to but the question is are midwives doing it? People don’t really have time to do it’ (SASi17) ‘So we are going out into those areas like the birth centre and would know something awful has happened and we see the staff involved or we send an e-mail round to say “if you were involved and want to speak to a PMA then you can do”’ (SASi22) |
The revision of professional midwifery support from a supervisory to advisory approach was cited by longer established midwives as one reason for trauma passing undetected in the profession. PMA availability depended on their levels of access by a diverse workforce, and PMAs could only had limited time available |
|
‘The problem with the PMAs is that staff need to seek them out. The supervisors could say “I’m here” but the PMAs say “please go to your PMA”’ (SASi35) We can go through the notes and help people write their statements, but staff have to put themselves forward, we don’t offer it for every member of staff (PMA SCSi08) |
||||
|
‘The PMAs do a great job with the midwives in their reflective learning and it would be good to extend that to the full multidisciplinary team’ (SDSi12) ‘It’s basically just to given time to people to actually express’ (SASi22) ‘We are trying to make the team aware that they are always there on a Thursday if anyone wants to come to share a case. I think we are not very consistent about it or keep it up because of how much work was are carrying’ (SDSi07) |
||||
| A | Risk midwives | Advice on statement drafting; advice on what to expect during HSIB interviews and inquests Organisation of ‘cool’ debriefs across maternity teams Informal updates to ward/unit staff on SI investigation progress and outcomes |
Individual junior staff (midwives and some junior medical staff) and clinical leads | ‘We have to say if the baby doesn’t survive they’ll be an inquest and it’s best if you write your statement now and keep it on file. These cases are super distressing and you cannot approach them without people thinking you’re insinuating they’re negligent. It is difficult to pitch yourself’ (SASi01) | The development of this staff support and knowledge sharing role of some risk midwives in Site A is distinctive. In Sites B and C, consultant midwives and scheduled learning events were available to meet these post-incident care needs. |
| ‘So I send them a letter saying we need an account of events. Don’t panic. Please do not be alarmed. You can come a speak to us at anytime’ (SASi02) ‘And it’s easier when they know that HSIB are less men in black and more women in cardigans’ (SASi01b) ‘And although we offer support staff may not feel they can access it. They’ll probably go to their peers’ (SCSi08) |
|||||
| B and C | Consultant midwife | Specialist mental health and trauma support for families and staff | Consultants and midwives | ‘I know a lot of staff who are traumatised and it’s fine. I’m a safe space. I’m not a one-stop person’ (SDSi04) ‘My aim with the trauma-informed service is that staff get training because when they understand their own trauma they can understand how to identify it in women’ (SDSi04) |
The seniority of this clinical specialist and long-established role within the Trust enhanced their acceptability to senior medical staff |
| All | Hot debriefs | Meeting initiated by clinical lead before end of shift | Staff team on shift (or staff team directly involved in incident) | ‘A time when you can sit, reflect and debrief together’ (SDSi07) ‘It all really depends on whose doing it’ (SASi35) ‘Not everyone takes to doing these’ (SASi36) |
Across the case-study services, it was expected that there was shift-to-shift variation in the process and effects of ‘hot debriefs’. The researchers dd not identify the use of agreed guidance by shift consultants leading these meetings |
| A?; B and C? | Ongoing debriefs | Series of meetings (where clinical lead feels necessary) | Staff team available | ‘So there is conflicting evidence on hot debriefs and if it’s the right thing to do, I’ve found it really helpful after a vaginal breech delivery where the baby died the staff needed it and then two or three days later we had another one, then another one, because actually there were people who were not at work for the next few months, it had a huge impact' (SASi12). The event took a long time for people ‘to feel safe after that one. There was a lot of blame and the debriefs helped with this’ (Fieldnotes site A 10 June 21) | These interventions were initiated when there was time and space for this ongoing work – the positive impact on individuals and teams of these debriefs and externally facilitated debriefs (see below) were noted by senior clinicians |
| C | Later debriefs | Led by external facilitator (e.g. staff psychologist) | Staff team available | ‘It’s another thing for staff to sort out and access when they are too busy, too tired and its’ not a priority, so it’s how we structure it so that they can do it in their work time’ (SASi13) | The flux of shift work and rotations made it difficult for junior managers to anticipate the degree and extent of post-incident trauma within staff teams |
| ‘Because we don’t have teams that work together regularly and everybody is on different shifts we are not very good at bringing that group back together. Then time marches on and people don’t want to go back to it’ (SASi07) Unless things come through (clinical) governance, it’s really hard to work out who exactly is involved. That sort of thing isn’t written in the notes. Somebody might be feeling really traumatised and we haven’t got the foggiest idea, nobody knows (SASi04b) |
|||||
| A | Case presentations | Clinical presentation of a maternal death (to understand what happened, why and recommendations following learning from case) | Staff team available | ‘It’s not quite a Schwartz Round but it does look at a case and this is a useful way to deal with significant events’ (SASi13) | Some medical staff felt that post-incident clarification and discussion of a clinical scenario was a form of psychological support because it provide some personal reassurance in the management of similar cases in the future |
Appendix 8 Post-incident service communication approaches and their reception at the case-study services
| Case-study services | Approach identified by staff | Content | Reach | Effects discussed | Summary of findings on effects |
|---|---|---|---|---|---|
| All | Routine newsletters, bulletins and infographics |
Short updates on ‘top risks and learning from incidents’ (SASi05); ‘easy wins like staff reminders to complete proformas’ (site A); updates on learning (site C). SI panel learning points; reminders of practice improvement needs (site A); general lessons and changes | 500+ staff | ‘We put in aspects of learning and staff like to read the cases and what happened. We always do a good-news story (too) and “well dones” so that people find it quite positive’ (Risk and Improvement Lead) (SCSi06) ‘You have to be driven to want to go and read it’ (Consultant Midwife) (SDSi07) |
The effectiveness of newsletter and bulletins for sharing learning was widely questioned. Messages about post-incident learning and change could be lost within other correspondence and newsletters themselves |
| Newsletters intended to be engaging, including general staff updates on things that had gone well; congratulations ‘to some people who have done a good job’ (Fieldnotes 29 April 2021) or have ‘handled something difficult well’ (SASi12). Sometimes includes ‘changes to guidelines’ | ‘Unless you are actually part of a QI group how do you really know? Say I’m a band 6 midwife and I do three long days a week, I’m on the go, busy. I’m probably not reading my e-mails or processing them with any great interest … we need to be more innovative about how we hare information’ (Consultant Midwife) (SDSi07) | ||||
| Infographics attached to bulletins condensed information, but this was apparently circulated through same media | ‘Community staff reads out e-mails because we’ve got a laptop, a Trust work phone with e-mail but you don’t really have time for e-mails’ (Matron for Quality and Safety) (SASi17) | ||||
| A risk midwife accidentally pressed ‘send’ on a newsletter that included an extremely offensive comment about incompetence to 748 staff. She received one e-mail reply back, from a matron thanking her for the circular, ‘so now I know that no one reads them’ (Fieldnotes July 2021) | |||||
| ‘it’s more about validations... it’s outlived its welcome’ (PMA) (SASi22) | |||||
| All | E-mail updates specific to a SI updates or update on guideline changes | Updating on learning points or practice or systems change after some SIs | 500+ staff | This correspondence was experienced as ‘coming out on a daily or even hourly basis’ (Consultant Obstetrician) (ASAi12). ‘The Band 5s just don’t receive it’ (Matron for Quality and Safety) (SASi17b) |
Often staff did not read them because of issues of time; access to IT in the workplace; too many messages |
| Site A | Learning events in response to SI panel discussion or report and/or to wider MD intelligence of safety trends (from care issues and patient complaints) from matrons, clinical leads or LMNS discussions | Targeted awareness-raising using a range of local strategies; e-mails sent around to say ‘please do attend when you are available’ (SASi16) | Identified wards and units | A risk midwife and matron organised a ‘Bladder Care week’ that was ‘quite well received because we had a questionnaire and we want round the wards and go people to do the quiz and we had presence and then we incorporated it into mandatory training’ (Matron for Quality and Safety) (SASi17b) | This special learning event at Site A (organised by a matron) was widely welcomed by the CG team and clinical leads. The impact of the event in clinical areas was not evaluated |
| Site A | Teaching afternoons | One-off and very occasional events involving different clinical teams, initiated by a risk midwife who liaises with different teams to generate interest | Senior clinicians and trainees | Not clear | The special learning event in Site A was organised by a risk midwife. Attendance was expected to be limited without clinicians having protected time for learning |
| Site C | Dedicated safety weeks (pre-COVID) | Range of events and documents circulated to all staff (including awareness of SI processes) | All staff | Not clear | The inclusion of post-incident sharing of knowledge and changes made included all cases and was overwhelming for some staff |
| All | CG meetings | Meeting includes audit and risk register updates | Service and clinical managers | ‘Attendance here is higher because all clinics are blocked, so the antenatal clinic midwives should also join us’ (Risk and Improvement Lead) (SCSi06) | CG meetings were focused on the discussion and update of the risk register. At Sites B and C, these meetings were backed onto other risk and improvement meetings that focused on learning from case studies and news of related changes across service and LMNS |
| Sites B and C | Learning meetings | Clinicians (often trainees) invited by safety leads to present on an SI case study; SI case presentations part of a wider learning brief of service and LMNS updates and discussions. SI case studies presented SIs about 8 months after their occurrence |
30–40 clinical staff | ‘Give the clearest view of where learning comes from’ (MVP Lead) (SCSi07) Rarely accessible to front-line staff, ‘such as midwives on the shop floor’ despite CG team walk-arounds to request staff release from matrons or sisters-in-charge because ‘there’s never a quite time or a free member of staff and you probably won’t at up at eight o’clock on your day off’ (Risk and Improvement Lead) (SCSi06). |
See Chapter 7 |
| ‘So who is going to these meetings? Same people every week. It’s just the way it is’ (Clinical Director for Patient Safety) (SCSi05) ‘The way the case is presented maybe we could improve that. Involve the staff involved in the incident so that they can walk away and not feel so awful when they hear it’ (Risk and Improvement Lead) (SCSi06) |
|||||
| Site A | Meetings with midwives | Initiated by newly appointed Quality and Safety Matron to improve midwifery care | Not known | ‘My focus is taking away learning from Datixes and coming up with a plan to then correct what had happened and go back to the midwives and find out how we learn from that and if there are other ways of correcting what happened’ (Matron for Quality and Safety) (SASi17a) | Not known |
| All | Training events | Two MD training days per year (with additional 1 day for midwives) delivered by the PDM team; ongoing obstetric training (weekly event) included generalised learning from complaints and incidents; investigations and reports At Site A learning from family experiences of incidents incorporated into PROMPT training by bereavement midwifery team |
All midwives and trainees | ‘So we include feedback from an incident twice a month and to different groups because you get different team members on each study day’ (PMA) (SDSi08) ‘If I’ve seen a woman and heard her story I can feed it back through the multi-disciplinary mandatory workshops’ (PMA) (SDSi08) |
See Chapter 7 |
| Sites B and C | LMNS learning from incidents meetings | Identification of learning themes from SIs investigated across LMNS and from HSIB reports; sharing guidelines | Cross-Trust; don’t attend every meeting; invited to relevant sections | ‘Our birth outcome data and continuity staff is all there now. It’s like we are watching each other and challenging each other and celebrating each other’s successes across the sector because our dashboard data is shared and on the agenda’ (Consultant Midwife) (SDSi07) | At Sites B and C, LMNS safety meetings were generally seen as beneficial to clinical leads and for service development. Staff were developing ways of collaborating with improvement work (such as draft guidelines). Site A CG team let that the LMNS detracted from their time |
| The idea that units are robustly going to recognise service delivery issues for really investigating care and how we learn from it, it makes me laugh. I know what goes on in the region. It’s what you can get away with a lot of the time (Obstetric Risk Lead) (SDSi19) ‘We pool the learning altogether and it’s a very useful way of displaying joint learning and working together’ (HoM) (SDSi02) |
|||||
| Sites B and C | Ward and unit visits | To update on changes to guidelines (after texts, newsletter entry) | Staff who are present in unit at that time | ‘I think just being present, honestly, like going down every now and again, I walk around every day if there’s anything that’s key that’s changing, just talking to staff, making sure they know they can question you if they are confused about things’ (Guidelines Midwife) (SDSi01) | |
| Site C | Reflection groups | Identifying own learning with case presentations that might include learning from incidents | Community midwives | No data | |
| Site B | Physical media | Whiteboards in units with updates on current learning from incidents | Various units | ‘We asked the LMNS about what other please do and many have returned to actual physical whiteboards’ (Consultant Midwife) (SDSi07) | |
| All | Organised informal spaces | ‘Tea trolly rounds’ or ‘ice cream rounds’ one units and wards by senior midwives | Various units | ‘An opportunity to provide refreshments but also have a conversation, to actually talk to staff and sharing learning and our intentions with improvements on a regular basis’ (Consultant Midwife) (SDSi07) | See discussion Chapter 8 |
| Site A | WhatsApp groups | Learning outcomes | Various WhatsApp groups (several in each unit or service area) | ‘A well-read forum is pockets of groups on WhatsApp. People dive in but it sometimes feels inappropriate to put learning outcomes here. Anyone can create one’ (Matron for Quality and Safety) (SASi17) ‘I’m on [eight] so you get consumed with messages from the WhatsApp groups’ (Matron for Quality and Safety) (SASi17b) |
The growth of WhatsApp staff groups during COVID to deal with more that immediate operational issues (like shift cover) was welcomed by some clinicians as a new means of networked learning. The development of these local communities of practice that differed from formal learning systems was notable in Site A |
| All | Invitations to internal incident review panels | Observing the case presentation, panel review and initial action planning | Band 6 staff | ‘It’s a development opportunity to take some learning forward from whatever it is. They find them interesting. Because these cases that happen on the shopfloor create ripples that go far and wide. And a lot of them don’t have any resolution to it. They don’t have follow-up … at least they are spreading the learning by word of mouth’ (Risk Midwife) (SASi01) | Meetings’ observations at all sites indicated that junior midwives rarely attended these meetings |
| Site A | Coincidental updates | Responses to ongoing questions about an incident | Not known | The risk midwife tells me that her shifts in Labour Ward are important for updating staff there on incidents, many of them ask because they don’t know what’s happened and then issues don’t get opened up like people saying ‘it could be any of us’ (Fieldnotes 29 April 2021) |
Appendix 9 Best practice guidance in development by programme theory (ongoing development with case-study services)
Meaningful acknowledgement of the injury and its effects on the family
-
View disclosure as an ongoing relationship (not a single meeting).
-
Face-to-face disclosure conversations wherever possible, followed by written correspondence.
-
Sensitivity to the setting, tone and timing of meetings.
-
Prompt initial disclosure conversation with a family (including explaining what is not known at that time).
-
Personalised disclosure, guided by families and adapted to meet their needs.
-
Allowing space for family to have initial, wide-ranging conversation about care received.
-
Recognition of family’s harm, especially aspects of harm that might not be immediately obvious to a service (e.g. micro-aggressions, feeling confused by technical language).
-
Clarification of an escalation policy through Trust and Health Service for families who remain dissatisfied with incident report findings, progress of action plans or quality of their post-incident care.
-
Clarification of interunit, interservice and interprofessional responsibilities for initial and ongoing discussions with a family.
Family inclusion in reviews and investigations
-
Initial meeting to identify what families might require from the service in relation to their involvement in likely reviews/investigations.
-
Clarification with families of the primary and secondary purposes of reviews and investigations.
-
Inclusion of families’ views and experiences is aided by an advocate.
-
For families and family representatives involved in reviews and investigations, emotional preparation before and debriefing after the meetings should be available (e.g. Reflections Clinics).
-
Recognition that families have their own perspective of events that might not align with the perspective of the service.
-
Recognition the families’ priorities and desired outcomes from the review may be different than that of the service.
-
Ongoing practical (e.g. navigational advice) and relational care of some families through investigation processes is important (e.g. by an ISA or a trusted member of staff).
-
Proactive updating of families on progress of review or investigation (not simply invite to be contacted).
-
Involvement of family representatives (e.g. MVPs) in some review meetings can ‘humanise’ the process otherwise, embedding completion of parent involvement elements in the context of a wider conversation with a family.
-
Direct involvement of families in panels requires clarification of focus of purpose of discussions (on their case or future cases; on safe practice or even better practise).
Making sense of what happened
-
Invitation to families to contribute to the ToR of a local investigation
-
Time for staff to attend to the production of the report (promoting accessible look and language) and so that it helps the family to make sense of the findings and proposed action plans (these are sometimes drawn from different review/investigation programmes).
-
Reception, discussion and reporting of information offered by families that do not dismiss or marginalise their knowledge over service-defined safety and QI priorities (e.g. inclusion of evidence as central, not marginal, to report findings).
-
Invitation to families to preview and comment on a near-final draft of the investigation report before organisational ‘sign-off’.
-
Each family is offered a prompt, in-person meeting with a clinical lead to discuss their incident investigation report. They may choose to be accompanied by another member of staff and/or an ISA.
-
Co-ordination of this initial family discussion about the report so that this precedes subsequent clinical debriefs.
-
Expectation that more than one, or delayed, meetings about the investigation findings might be required.
-
Opportunities available for a family that is out of contact with the service to revisit the report with a clinical or service lead at a later date.
-
Automatic suggestion for referral of all families affected by moderate/severe injuries to in-service professionals (e.g. birth afterthoughts service and/or PMA) and/or commissioned counselling support at a time suitable for the family (that might be in advance of their receipt of incident report).
Clinical skills and clinician safety
-
Duty of Candour conversations (and initial conversations) should be led by trained, senior clinicians, service or clinical leads where possible.
-
In case of a serious, out-of-hours incident (e.g. maternal death), disclosure conversations should involve senior staff, including a PMA.
-
Training in post-incident communication for all professionals should extend beyond an introduction to the DoC regulations by Trust legal representatives.
-
Clarification on the legal implications of apologising to a family for corporate and clinical teams.
-
Clarification, as far as possible, on the legal status of provisional knowledge that is shared with a family during OD process for corporate and clinical teams.
-
Recognition of skills and time demands of OD work in job descriptions and work plans of senior staff.
-
Preparation time and administrative support for meetings (to be familiar with the case and the family and to ensure that family feels welcome).
-
Senior staff supported to access private meeting rooms that are comfortable for that family, for example not routine clinical rooms, particularly if these evoke memories of care.
-
Tailoring (co-design) of post-incident support for clinicians with clinicians, with recognition of the need for responsive support for staff working out of hours.
-
Specialist training and support for senior staff (prioritising clinical leads and risk midwives) leading on post-incident communication with injured families.
-
Identification of the skills and ongoing (discretionary) work of some clinical leads in OD work and recognition of this training and work plans.
-
Make us of simulation-based training to develop loose scripts to support disclosure conversations that empower staff to personalise and adapted disclosure to meet the needs of the family.
-
Experts in initial disclosure and family debriefings are proactive in encouraging a junior clinician to observe practice (with family consent) and in discussing and teaching on this work.
-
Opportunities for reflection and discussion between clinical experts on ethical challenges of OD and how to resolve in more challenging situations.
-
Development of, and organisational support for, mentoring arrangements for professionals regularly involved in post-incident communication with families.
-
Confidence (though training and local leadership) of non-experts in disclosure to continue care of family without inhibitions.
-
Regular updates for clinicians involved in an incident being investigated and in-person discussion of reported findings and action plan.
Knowing the improvements have been made post incident
-
Proactive updating of families and staff involved in the incident on changes being made following report recommendations and action plan (including explanations of why changes delayed or no longer in progress).
-
Explanation to families that significant changes to practice and service may take more than a few months, but that progress or delays will be explained to them.
-
Discussions within patient safety and governance teams over planning and achievement of ‘quicker wins’ and ‘deeper changes’ (e.g. care pathway development; infrastructure investments; construction projects requiring complex business cases).
-
Families invited to participate in these decisions, or to have a representative participate for them.
-
Recognition of the differing and shifting priorities of families to engage in service improvement.
-
Honing of service communication strategies that ensure learning from incidents communicated to front-line staff (most effective are ongoing multidisciplinary learning forums; regular face-to-face outreach by improvement leads and governance teams).
-
Regular and non-judgemental presentation and discussion of adverse events embedded in ongoing multidisciplinary learning forums.
-
Avenues for injured families to contribute towards service change (through teaching; presentations in Trust or service; involvement in related or unrelated quality and safety improvement programmes) and to be supported for this work.
List of abbreviations
- CAG
- Confidentiality Advisory Group
- CG
- clinical governance
- CIG
- Co-investigator Group
- C–M–O
- context–mechanism–outcome
- CNST
- Clinical Negligence Scheme for Trusts
- CQC
- Care Quality Commission
- CTG
- cardiotocography
- DoC
- Duty of Candour
- DoM
- Director of Midwifery
- EA
- Explanatory Account
- EBC
- Each Baby Counts
- ENS
- Early Notification Scheme
- GP
- general practitioner
- HCP
- healthcare provider
- HoM
- Head of Midwifery
- HRA
- Health Research Authority
- HSDR
- Health and Social Care Delivery Research
- HSIB
- Healthcare Safety Investigation Branch
- ISA
- Independent Senior Advocate
- IT
- information technology
- LMNS
- Local Maternity and Neonatal System
- MDT
- multidisciplinary team
- MST
- Maternity Safety Training
- MVP
- Maternity Voices Partnership
- NHS
- National Health Service
- NHSI
- National Health Service Improvement
- NHSR
- National Health Service Resolution
- NIHR
- National Institute for Health and Care Research
- OD
- open disclosure
- PAG
- Project Advisory Group
- PDM
- Practice Development Midwife
- PI
- principal investigator (site-specific)
- PMA
- Professional Midwifery Advocate
- PMRT
- Perinatal Mortality Review Tool
- PPI
- patient and public involvement
- PSIRF
- Patient Safety Incident Response Framework
- PSS
- Patient Safety Strategy
- QI
- quality improvement
- R&D
- research and development
- RCOG
- Royal College of Obstetricians and Gynaecologists
- REC
- Research Ethics Committee
- Sands
- stillbirth and neonatal death charity
- SI Framework
- serious incident framework
- SP
- study phase
- SSG
- Study Steering Group
- SU
- service user
- ToR
- terms of reference
Note
In this report, the term woman is used to refer to pregnant people, as those involved in the study identified as women. However, the results of this report will be of interest to all child-bearing people.
Notes
-
Realist data extraction: outcomes of improvement in OD for families
-
Realist data extraction: outcomes of improvement in OD for staff
-
Realist data extraction: outcomes of improvement in OD for services
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/YTDF8015).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
