Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 06/43/05. The contractual start date was in May 2009. The draft report began editorial review in January 2014 and was accepted for publication in September 2014. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Simon Gilbody is a Health Technology Assessment Clinical Evaluation and Trials Board Member. Michael Barkham is a developer of the Clinical Outcomes in Routine Evaluation – Outcome Measure, which was used as a secondary outcome measure in the trial. Peter Bower reports personal fees from paid consultancy for the British Association of Counselling and Psychotherapy, outside the submitted work. Karina Lovell is a Non-Executive Director for Manchester Mental Health and Social Care Trust and is paid a salary.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2015. This work was produced by Littlewood et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Background
Depression
Depression is the most common mental health disorder in community settings and is estimated to become the second largest cause of global disability by 2020. 1 It is one of the most common reasons for consulting a general practitioner (GP), and is associated with significant personal and economic burden. 2
Psychological therapy for depression
Antidepressant medication is an important treatment option for depression; however, many patients and health-care professionals would like to access psychological therapy as an alternative or adjunct to medication. 3 A leading evidence-supported form of brief psychological therapy for people with depression is cognitive behaviour therapy (CBT). 4,5 However, given that patient demand for CBT cannot be met from existing therapist resources,6 there is a need to increase patient access to psychological therapy. One potential way of achieving this might be the provision of CBT delivered via computer. 7 In recent years, a number of interactive programs have been developed which enable CBT to be delivered by computer. The provision of computerised CBT (cCBT) is now recommended in the National Institute for Health and Care Excellence (NICE) guidelines as an initial lower-intensity treatment for depression as part of a ‘stepped care’ approach in primary care. 5 cCBT, if shown to be effective, has the potential to expand the provision of psychological therapy in primary care and, as such, may represent an efficient and effective form of care for depression. 8
There are a number of interactive internet-based products that are available for those who decide to use (or commission the provision of) cCBT. Some of these cCBT products are commercially produced whereas others are free to use. 7 A number of commercial products have been marketed to bodies such as the NHS and have also been made available for patients to purchase directly. The free-to-use products have been developed by the public sector or by research institutes and can be accessed at no direct purchase cost to patients or health-care providers, although there may be costs associated with their support and use in the NHS.
Evidence for computerised cognitive behaviour therapy
Computerised CBT represents an alternative form of therapy delivery that has the potential to enhance access to psychological care. Existing research into cCBT has been summarised by Kaltenthaler and colleagues in their 2006 Health Technology Assessment (HTA) review of clinical effectiveness and cost-effectiveness. 6 With respect to depression, three commercially produced computerised packages available to the NHS were considered: Beating the Blues® (Ultrasis, London, UK), COPE and Overcoming Depression. Of these, only one, Beating the Blues, had been evaluated in a randomised controlled trial (RCT); the program was shown to be effective at reducing symptoms of depression. 7 However, this research was conducted by those who owned and held the intellectual copyright to Beating the Blues. Among internet-based free-to-use packages, only one, MoodGYM (National Institute for Mental Health Research, Australian National University, Canberra, Australia), has been evaluated in a randomised trial, which was also conducted by the package developers. 8 MoodGYM was found to be effective at reducing depressive symptomatology. 8 The overall conclusion of the HTA review was that ‘the efficacy but not effectiveness of Beating the Blues had been established in comparison with treatment as usual’. 6
Recommendations for further research on the effectiveness of computerised cognitive behaviour therapy
At the time of the commissioning and design of the REEACT (Randomised Evaluation of the Effectiveness and Acceptability of Computerised Therapy) trial, several caveats applied and specific recommendations for further research were made that are important with respect to the present trial.
-
Computerised CBT had been shown to be effective in the short term, but trials rarely examined the longer-term impact on depression compared with usual care. Trials with longer periods of follow-up are needed.
-
The cost-effectiveness of computerised packages is as yet unknown. More importantly, the cost-effectiveness from the perspective of the UK NHS has not been sufficiently established and the longer-term cost-effectiveness beyond the brief time horizon of existing trials is essentially unknown. This is important, as commercial packages (such as Beating the Blues) will need to be purchased by the NHS.
-
Existing trials are based on populations who have been referred to specialist cCBT services and are necessarily comfortable with information technology and willing to be offered computerised therapy as a treatment option. Computer-delivered CBT uses a computer rather than a trained CBT therapist, and the acceptability of the replacement of the therapist with a machine interface is largely unknown. Patients with depression might show a strong preference for or against computer therapy, and this might, in turn, be related to uptake and effectiveness. The acceptability and effectiveness of cCBT among patients who are representative of people treated for depression in NHS primary care services has not yet been established. There is, therefore, a need for pragmatic evaluations of cCBT based in UK primary care that examine real-world effectiveness and the issue of patient preference.
-
There are no trials of free-to-use cCBT packages versus pay-to-use cCBT packages. This is important, as the effectiveness of free-to-use cCBT would need to be comparable to pay-to-use CBT if it were to be a viable alternative within a stepped care pathway. 9
-
Evaluations of all the commercially available and free-to-use packages of cCBT have been conducted by researchers responsible for their development. Although this does not invalidate the results, it does raise concerns that a truly independent evaluation of the clinical effectiveness and cost-effectiveness of cCBT is needed to inform NHS decision-making. In their 2006 HTA report, Kaltenthaler and colleagues make this a core research recommendation and state that ‘Research needs to be carried out by independent researchers. It should be carried out by those who are not associated with commercial or product gains’. 6
The present trial was designed to address these recommendations. A subsequent meta-analysis has demonstrated that cCBT can be effective for depression, but there remains a need for longer-term pragmatic studies and evaluations by researchers other than the product developers. 10
The REEACT study represents a pragmatic evaluation of cCBT in a trial that is adequately controlled and has appropriate statistical power.
Research objectives
This was a fully randomised patient preference trial of usual GP care for depression versus the addition of one of two cCBT packages to usual GP care. The REEACT study included a concurrent economic and qualitative evaluation to meet the following specific aims:
-
to establish the clinical effectiveness and cost-effectiveness of the addition of cCBT to usual GP care compared with usual GP care alone over a 2-year trial follow-up period
-
to establish the acceptability (to patients and health professionals) of cCBT
-
to establish the differential clinical effectiveness and cost-effectiveness of a free-to-use computerised package, in comparison with a commercial pay-to-use cCBT package over a 2-year and longer-term time horizon.
Some of this text has been reproduced from Gilbody et al. 11 © BMJ 2015. This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/.
Chapter 2 Methods
Trial design
The REEACT trial was a pragmatic, multicentre, open, three-armed parallel RCT with simple randomisation. The design included a fully randomised patient preference approach. 12 Participants with depression [defined as a score of ≥ 10 on the Patient Health Questionnaire-9 (PHQ-9) depression severity instrument]13 were randomised (1 : 1 : 1) to receive:
-
a commercial pay-to-use cCBT program (Beating the Blues) plus usual GP care or
-
a free-to-use cCBT program (MoodGYM) plus usual GP care or
-
usual GP care alone.
Approvals obtained
The Leeds (East) Research Ethics Committee (REC) approved the study on 10 July 2008 and approved the substantial amendment to revise the trial design following advice from the funder on 22 September 2008 (see Chapter 3 for details of this substantial amendment). The details of the REC and Research and Development Department approvals are provided in Appendix 1. The trial was registered as ISRCTN91947481; EudraCT number 2007-007645-12; and UK Clinical Research Network Study Portfolio (UKCRN) identification number 4115.
Trial sites
The trial was conducted in nine UK sites. Five sites were involved from the commencement of the trial, and the remaining four sites were recruited throughout the duration of the trial. Details of the study sites are provided in Appendix 2.
Participant eligibility
People with depression were eligible to take part in the trial. Both prevalent and incident cases of depression were included.
Inclusion criteria
Potential participants were eligible for inclusion in the trial if they met the following criteria:
-
They met the inclusion threshold of a score of ≥ 10 on the PHQ-9 depression severity instrument. 13 This cut-off point is known to detect clinical depression (major depression) in a UK primary care population with sensitivity of 91.7% and specificity of 78.3%. 14
-
They were not currently in receipt of cCBT or specialist psychological therapy (including therapy from a psychologist), and were not currently under care from a local Improving Access to Psychological Therapies (IAPT) service.
-
They were aged 18 years or over.
Potential participants who met the above inclusion criteria were not excluded if:
-
They had a comorbid physical illness (such as diabetes).
-
They had a comorbid non-psychotic functional disorder (such as anxiety).
-
They were in receipt of antidepressant medication.
-
They had previous treatment experience of CBT.
Exclusion criteria
Potential participants were excluded if they met any one of the following criteria:
-
They were actively suicidal.
-
They were suffering a psychotic illness (as ascertained by the GP).
-
They had recently suffered bereavement (bereavement was classed as having lost a mother, father, partner, husband, wife, son or daughter in the last year).
-
They were depressed in the postnatal period (the postnatal period was classed as having had a baby in the last year).
-
They were suffering from psychotic depression (this decision was based on NICE guidance in which computerised therapy is not recommended for people with psychotic depression). 15
-
They had a primary diagnosis of alcohol or drug abuse.
-
They were not able to read and write in English.
Recruitment into the trial
All researchers participating in the study received training in all aspects of the trial including trial recruitment, eligibility criteria, trial protocol, adverse event reporting procedures, participant risk assessment and reporting procedures, trial database and trial documentation. Each researcher received a researcher manual detailing these procedures in order to standardise the running of the study across researchers and trial sites. All researchers also undertook Good Clinical Practice training.
Potential participants were referred to the trial through GP practices. All GP practices were provided with a GP practice manual. This provided details of key trial contacts and site information, information about cCBT and the trial intervention cCBT programs, a GP information sheet (see Appendix 3), and procedures and forms for recruiting participants via the various recruitment routes (described in Recruitment routes) and for reporting serious adverse events (SAEs). The manual also contained copies of trial documentation including the trial protocol, participant information sheet and patient consent form (see Appendix 4). GP practices were also provided with participant study information packs containing a study invitation/cover letter, a participant information sheet and a permission form for release of personal details (see Appendix 4).
In line with recommendations from a HTA-funded primary care depression trial by Peveler and colleagues,16 GP practices were reimbursed for the additional time involved in recruitment of patients to the trial via service support costs. An additional GP practice incentive was the use of the Quality and Outcomes Framework (QOF). 17 As the PHQ-9 was a validated assessment measure incentivised for the Depression 2 indicator in the QOF during the trial’s recruitment period, all GPs were provided with participants’ PHQ-9 scores at recruitment.
Recruitment routes
Potential participants were identified through one of four main recruitment routes:
General practitioner-initiated recruitment (direct referral)
General practitioners identified potential participants who presented with depression during patient consultations (both prevalent and incident cases of depression). GPs were asked to introduce the study to potential participants. For patients who were immediately interested in the trial, GPs completed a referral form stating that the patient matched the study criteria and provided the patient with a study cover letter and the participant information sheet. Patients were asked to complete a ‘permission for release of personal details form’ which included their contact details. The GP or a member of the GP practice staff would then fax the referral form and permission form to the local research team. For those patients who expressed a wish to consider the study over a longer period, GPs were asked to provide the patient with a study information pack which included an invitation letter explaining how to contact the research team. Patients interested in taking part in the study completed the ‘permission for release of personal details form’ and sent this back to the local research team. Patients were advised by their GP that they should expect to hear from a study researcher within 2 working days of the research team receiving their permission form.
Recruitment initiated by health professionals attached to a general practitioner practice (direct referral)
Practice-attached nurses and primary care mental health workers identified potential participants who presented with depression during patient visits. These health professionals were asked to introduce the study to potential participants and provide interested patients with the study information pack. They were also able to complete a referral form, ask patients to complete the ‘permission for release of personal details form’ and fax these forms to the local research team in the same way that a GP would. They would then notify the patient’s GP that a referral to the trial had been made.
Record screening (database screening)
General practitioner practice staff, with agreement from the lead research GP, reviewed patient records in accordance with a pre-specified protocol to identify a list of potential study participants (presenting prevalent cases of depression). This protocol contained a list of read codes which described a range of inclusion and exclusion criteria to search for over pre-specified time frames. GPs reviewed the list of potential participants and identified any patients who they felt were not suitable to take part in the trial. GP practices were supplied with study information packs to send out to potential participants on this list; alternatively, the GP could consider the patient for the trial at their next GP appointment. The frequency of these record searches was agreed between individual GP practices and the REEACT research team. Interested participants who received the study information pack in the post completed the ‘permission for release of personal details form’ and sent this back to the local research team.
Waiting room screening
Where a GP practice agreed, REEACT researchers would screen patients in the GP practice waiting room with a simple two-question screening instrument. 18 GPs were immediately notified of any patients who screened positive for possible depression so that the GP could consider introducing the study to them during their appointment. Although this recruitment route was available it was not implemented in any of the recruiting GP practices.
The number of participants recruited to the trial via direct referral and database screening recruitment routes is detailed in Appendix 5.
Researcher contact following trial referral
See Appendix 6 for a summary of participant involvement in the trial.
Following receipt of a completed ‘permission for release of personal details form’, the REEACT researcher would contact the patient to discuss the study and to pre-screen for eligibility using the PHQ-9 depression instrument. Initial contact was made within 1 or 2 working days of receiving the permission form, to allow the patient a minimum of 24 hours to read the information sheet and consider participation. If the patient scored ≥ 10 on the PHQ-9 during the pre-screen, the researcher arranged a face-to-face visit with the patient, at which the researcher would confirm the patient’s eligibility after obtaining written informed consent (part 1) by readministering the PHQ-9. If the patient scored ≥ 10 at this point, the researcher would obtain the patient’s written informed consent (part 2) to participate in the trial, administer the baseline measurements and ascertain treatment preference. The researcher would then ascertain and inform the patient of treatment allocation and make arrangements to initiate cCBT if this was the allocation. Arrangements would be made for the researcher to collect follow-up measures after 4 months. Following recruitment, participants’ GPs (and referrers, if the referrer was not their GP) were notified of the outcome of the referral, including treatment allocation and PHQ-9 score for participants who had been randomised to the study.
Baseline assessment
After written informed consent (parts 1 and 2) had been obtained, baseline data were collected on participants prior to randomisation using several self-report baseline questionnaires. The following data were collected.
Depression severity and symptomatology
Participants completed the PHQ-9 self-report questionnaire13 to confirm their eligibility to participate in the trial and to assess baseline depression severity and symptomatology.
Participants also completed a diagnostic gold standard lay-administered computer-based interview [Clinical Interview Schedule – Revised, (CIS-R)],19 which assesses depression severity and diagnosis and other common mental health disorders, such as anxiety, according to the International Classification of Diseases, Tenth Edition (ICD-10) criteria. 20
Biographical data
Participants completed a bespoke biographical questionnaire which recorded data on ethnicity, education, employment status, marital status, living arrangements, previous episodes of depression and treatment preference.
Ethnicity
The ethnicity of participants was recorded.
Education
Participants were asked to indicate their highest educational qualification.
Employment status
Information relating to participants’ current employment status was recorded. Participants who classed themselves as employed or self-employed indicated if they were currently off work sick because of their depression. Participants who described themselves as unemployed were asked to record the duration of their unemployment. Participants also indicated the type of position held in their most recent job.
Marital status
The marital status of participants was recorded.
Living arrangements
Married participants were asked to indicate if their spouse lived with them. The number of other people living with each participant, including the number of people under the age of 18 years, was recorded.
Previous episodes of depression
Whether or not participants had experienced a previous episode of depression for which they had sought help was recorded. Further information was recorded for those participants who indicated that they had experienced a previous episode of treated depression; this included the number of previous episodes of treated depression, if antidepressants had been prescribed, if participants had ever seen anyone for help with their depression other than their GP and, if so, who they had seen.
Treatment preference
The participant’s treatment preference was recorded on the biographical questionnaire (see Appendix 7) to allow us to explore the influence of patient preference prior to randomisation and the differential impact of preference on the relative effectiveness of cCBT versus usual GP care.
Generic and global mental health
Participants completed the Clinical Outcomes in Routine Evaluation – Outcome Measure (CORE-OM) questionnaire21,22 to assess their baseline generic and global mental health.
Health-related quality of life
Participants completed two self-report questionnaires to assess baseline health-related quality of life (HRQoL) and health-state utility. These were the Short Form questionnaire-36 items Health Survey® version 2 (SF-36v2)23,24 (QualityMetric Incorporated, Lincoln, RI, USA) and the European Quality of Life-5 Dimensions (EQ-5D). 25,26
Resource use data
Participants completed an adapted version of the Client Service Receipt Inventory (CSRI)27 to assess baseline resource utilisation.
Randomisation
Participants were randomised 1 : 1 : 1 between the three trial arms: cCBT (Beating the Blues) plus usual GP care; cCBT (MoodGYM) plus usual GP care; and usual GP care alone. In view of the large number of participants to be recruited to the study, stratification by depression severity was not required. Randomisation was simple and, therefore, not restricted in any way. Simple randomisation reduces the risk of any possible subversion associated with restricted randomisation methods and has been shown to produce equally precise results28 as stratified randomisation, which improves treatment precision in trials with fewer than 50 participants. However, simple randomisation can lead to unequal group sizes by chance alone. To maintain allocation concealment, the generation of the randomisation sequence and subsequent treatment allocation were performed by an independent, secure, remote telephone or web-based randomisation service. The computerised randomisation sequence was checked periodically during the trial following standard operating procedures. Owing to the nature of the trial design and the intervention, it was not possible to conceal treatment allocation from either the participant or the REEACT researcher.
Sample size
We needed to know if cCBT represented a clinically effective addition to usual GP care and whether or not the free-to-use computerised program (MoodGYM) represented a less effective (non-inferior) choice of therapy for patients compared with the commercial pay-to-use computerised program (Beating the Blues). We therefore powered our trial both to capture any benefit of cCBT over usual GP care alone and to test the non-inferiority of free-to-use cCBT. We based our sample size calculation on the usual care arm of our own primary care trial of collaborative care for depression, where the proportion of patients responding to usual care was in the region of 0.6;29 a response rate similar to that found in a UK HTA trial of antidepressants in primary care16 and a US pragmatic depression trial. 30 We regarded a response rate of not more than 0.15 below this rate as being acceptable, given the additional care options that are available to patients who do not initially respond to cCBT within a stepped care framework. Our original sample size calculation of 600 participants (200 participants in each of the three arms) gave us in excess of 80% power to detect non-inferiority using the percentage success in both groups as 60%, with a non-inferiority margin of 15% and allowing for 25% attrition. However, the sample size was re-estimated as, despite better levels of recruitment than anticipated, levels of attrition were slightly higher than originally expected (see Chapter 3). In order to retain similar levels of power to detect non-inferiority between the free-to-use and commercial cCBT packages with 5% probability, while allowing for 35% attrition, 690 participants were recruited (230 participants in each of the three arms). The trial also retained 80% power to detect a difference of 15% between the usual GP care arm and either of the two cCBT arms using a conventional power analysis (α = 0.05; two-sided significance).
Trial interventions
Participants were randomised to receive a commercial pay-to-use cCBT program (Beating the Blues) plus usual GP care, a free-to-use cCBT program (MoodGYM) plus usual GP care, or usual GP care alone.
Experimental interventions
Participants randomised to either of the two intervention arms each received cCBT (Beating the Blues or MoodGYM) in addition to usual GP care. Given that this was a pragmatic trial design, we imposed no restrictions on usual GP care, including the use of antidepressant drugs or the addition of drug treatment to cCBT in the two intervention arms.
Location of computerised cognitive behaviour therapy access
In order to maximise participant accessibility and flexibility, while respecting the importance of patient choice, cCBT was offered in one of three locations, according to patient choice and local availability: (1) in the participant’s own home (if the participant already had a computer and a broadband connection at home); (2) in a central location close to the participant’s home – this could be in a psychotherapy department, a local library or a large GP practice (where a standalone computer in a private room operating on a weekly booking system would be provided); or (3) in the GP practice (provided the participant’s GP practice was able to provide a broadband-connected computer in a private room on a fixed weekly basis).
Telephone support calls
All participants in the two intervention arms were provided with support in the form of regular (weekly) telephone calls, conducted by telephone support staff. The purpose of these telephone calls was to provide participants with technical support with using the cCBT programs (such as how to access the cCBT programs and resetting passwords) and to encourage them to engage with the cCBT programs. The supportive telephone calls were not intended to offer any form of psychotherapy. The telephone support staff completed each of the two cCBT programs in order to familiarise themselves with the nature and content of these programs. As a way of ensuring standardisation of the telephone support calls, telephone support staff worked to specific and standardised instructions regarding what should be covered during each telephone call to ensure delivery of ‘support’ rather than ‘therapy’. Telephone support staff were provided with the skills required to respond to common questions which would inevitably arise during the telephone calls. The option of support e-mails was offered to those participants who specifically requested contact via e-mail or who found it difficult to respond to telephone calls. A record was made of all participant contacts, including a brief summary of the content of the contact and an estimate of the duration of the telephone calls. In order to supervise the telephone support staff, and as a means of ensuring quality control, the telephone calls were recorded. All participants were asked for their verbal informed consent to record each telephone call and participants were not excluded from the trial if they withheld their consent to the recording. Telephone support staff were aware that calls were being recorded, where participant consent had been given. Telephone support staff underwent regular supervision with the chief investigator or other senior study co-investigators.
Experimental group: Beating the Blues (pay-to-use computerised cognitive behaviour therapy program) plus usual general practitioner care
Beating the Blues (www.ultrasis.com) is an interactive, multimedia, cCBT program developed by Ultrasis comprising a 15-minute introductory video followed by eight therapy sessions of approximately 50 minutes’ duration each, with homework exercises between sessions. It was used via the internet. Beating the Blues has been shown to be effective in reducing symptoms of depression. 7 In addition, all participants were offered usual GP care, and no restrictions were placed on GPs in their ability to prescribe medication or refer participants to other forms of psychological therapy (including IAPT services).
Experimental group: MoodGYM (free-to-use computerised cognitive behaviour therapy program) plus usual general practitioner care
MoodGYM (http://moodgym.anu.edu.au) is a free-to-use, internet-based, interactive CBT program for depression developed and copyrighted at the National Institute for Mental Health Research of the Australian National University. It consists of five interactive modules of approximately 30–45 minutes’ duration, with revision of all aspects of the program in the sixth session. The program includes a personal workbook containing exercises and assessments, and ‘characters’ to represent patterns of ‘dysfunctional’ thinking, and provides patients with CBT techniques to overcome this. 31 MoodGYM has been shown to be effective in reducing symptoms of depression in a developer-led trial. 8 At the commencement of the study, MoodGYM was being used in the UK, with 20.5% of the registrants on MoodGYM being from the UK. In addition, all participants were offered usual GP care, and no restrictions were placed on GPs in their ability to prescribe medication or refer participants to other forms of psychological therapy (including IAPT services).
Control group: usual general practitioner care
Participants randomised to the control arm received usual care by their GP. In line with the overall pragmatic approach of the trial, we replicated ‘usual GP care’ by making no specific patient-level recommendation or requirement to alter usual GP care by participating in the trial. However, GPs were reminded of the existence of NICE guidance on the management of depression,15 including the prescription of antidepressants, where this is indicated. Participants in the control arm were given no specific encouragement to access cCBT but this remained an option if the GP chose to suggest this treatment or if it was offered in the context of a local IAPT service.
Participant follow-up
Participants were followed up at three time points following randomisation: 4 months, 12 months and 24 months. During the first 6 months of the trial follow-up period, participants completed their follow-up questionnaires with a REEACT researcher during face-to-face interviews or telephone interviews, according to participant preference. In order to improve follow-up rates, participants were later given the additional option of completing and returning follow-up questionnaires in the post (see Chapter 3). The participant information sheet was revised to reflect this additional method of follow-up completion, and participants already recruited to the trial were advised of this option and received a copy of the revised participant information sheet at their next scheduled follow-up. As a further means of improving our retention rates, participants received an unconditional £5 voucher with their follow-up as an acknowledgement for their taking part in the study and completing the questionnaires. The £5 voucher either accompanied their appointment letter for face-to-face or telephone interviews, or was sent along with postal questionnaires.
Trial completion
Participants were deemed to have exited the trial when:
-
The participant had completed the 24-month follow-up.
-
The participant wished to exit the trial fully.
-
The participant’s GP withdrew him or her from the trial.
-
The participant died.
Instead of withdrawing fully from the trial, participants had the option of:
-
withdrawing only from receiving the trial intervention (applicable only to participants randomised to receive either of the two cCBT programs).
Participants who elected to withdraw from the trial intervention (cCBT programs) and follow-ups were deemed to be full withdrawals (trial exit). REEACT researchers were able to indicate any change in the patient’s level of participation by registering this information on the trial database, which immediately notified the co-ordinating centre (University of York) of this change. REEACT researchers notified the patient’s GP when a participant elected to withdraw fully from the trial.
Measurement and verification of primary outcome
The primary outcome measure was depression severity and symptomatology as measured by the PHQ-913 questionnaire at 4 months. Participants completed the primary outcome measure during face-to-face interviews or telephone interviews with REEACT researchers, or as a postal questionnaire, according to their preference.
The PHQ-9 is a nine-item self-report questionnaire which records the core symptoms of depression based on the Diagnostic and Statistical Manual of Mental Disorders diagnostic criteria for major depressive disorder. 32 Each item is rated on a scale of 0 to 3 based on the frequency of depressive symptoms (0 = ‘not at all’ to 3 = ‘nearly every day’). Scores range from 0 to 27, with higher scores indicating a greater degree of depression severity. It has the added advantage that it can be reliably administered over the telephone. 33
There are extensive US and non-US validation and sensitivity to change data using the PHQ-9. It has been validated in a UK primary care population14 and has become the instrument of choice in the management of depression in UK primary care, including monitoring symptom change,34,35 and in the fulfilment of QOF routine depression measurement. 36 It has also been shown to be sensitive to change over time. 37,38
Measurement and verification of secondary outcomes
A variety of disease-specific and generic outcome measures were administered to ascertain clinical effectiveness. Cost-effectiveness was determined by obtaining measures of HRQoL and resource utilisation using self-report questionnaires, along with objective data collection from participants’ GP medical records.
Outcome measures completed by participants were administered at each follow-up – 4 months, 12 months and 24 months – and were completed during face-to-face interviews or telephone interviews with REEACT researchers, or as a postal questionnaire, according to participant preference. Objective data from participants’ GP medical records were obtained after participants had completed their 24-month follow-up.
The following data were collected.
Depression severity and symptomatology
Participants completed the PHQ-913 self-report questionnaire to assess depression severity and symptomatology at each follow-up (see section on Measurement and verification of primary outcome for detailed information on this instrument).
Global and generic mental health
The CORE-OM21 questionnaire was completed by participants at each follow-up. The CORE-OM is a 34-item generic instrument which measures common mental health problems (including four items measuring depression), subjective well-being, functional capacity and risk. 21,22 It has been validated in a UK primary care population14 and is a widely used outcome measure for psychological therapies21,39 and in research. 40,41 It shows reliable sensitivity to change over time. 39
Health-related quality of life
Participants completed two generic questionnaires about their HRQoL (SF-36v2) and health-state utility (EQ-5D) at each follow-up in order to measure participants’ perceptions of health outcome during the study. Generic instruments of health status are useful for comparing different groups of participants, while also having a broad capacity for use in economic evaluations. Their generic nature also makes them potentially responsive to side effects or unforeseen effects of treatment.
Each participant’s perception of his or her general health was assessed using the SF-36v223,24 and the EQ-5D. 25,26 The SF-36v2 is a reliable and well-validated generic HRQoL measure. It has been validated for use in UK primary care42,43 and has been used as an outcome measure in a wide variety of patient groups, including patients with depression. 44 It measures health on eight dimensions covering functional status, well-being and overall evaluation of health, with scores ranging from 0 (worst HRQoL) to 100 (best HRQoL). It also yields two summary scores assessing physical and mental components, which have been shown to be reliable and valid measures of HRQoL. 45 It can also be used to generate a Short Form questionnaire-6 Dimensions (SF-6D) score, which is a preference-based generic HRQoL measure suitable to be used as an outcome in economic evaluation. 46,47
The EQ-5D is a generic preference-based measure of health state that covers five dimensions: mobility, self-care, usual activity, pain/discomfort and anxiety/depression. 25 Patients indicate their health state by rating each dimension according to three possible levels of severity: no problems, some problems and major problems. This response will identify one among the 243 mutually exclusive health states defined by the combination of dimensions and levels, plus two additional health states referring to ‘death’ and ‘unconsciousness’, yielding a total of 245 health states. 26 HRQoL weights for these health states have been previously elicited by Dolan et al. 48 using a time trade-off technique from a representative sample of the UK population. A score of 1 represents perfect health and a score of 0 represents death. The EQ-5D has been validated in UK populations and has been used to measure HRQoL in patients with depression in primary care. 49–51
Resource use data
Information relating to participants’ resource utilisation was obtained via two measures: completion of a self-report questionnaire (an adapted CSRI) and objective data collection from GP medical records. Resource use data were used in the assessment of cost-effectiveness and allowed us to assess whether or not participants randomised to the two cCBT arms experienced differing levels of resource use from the usual GP care alone group. Given the significant overlap between the content of the adapted CSRI and service use data collected from GP medical records, preference was given to the use of GP record data to inform resource use, as GP records were considered the more consistent and reliable source of data. At the outset of the trial, the logistical issues of collecting data from GP medical records were not clear and so the adapted CSRI was retained and was planned to be used in the event of difficulties in accessing these records. In the final analysis, only resource data from GP medical records were used because of the high proportion of patients in whom service records were obtained and the degree of completeness.
Questionnaire data
The CSRI is a self-report questionnaire which asks participants about their use of health and social care services and employment. 27
Participants completed an adapted version of the CSRI at each follow-up (see Appendix 7). Participants were asked about their use of services in the previous 6 months (including inpatient and outpatient hospital services, community-based day services and primary and community care contacts) and whether or not they had incurred any additional costs associated with their depression in the previous 6 months (e.g. medication or drug costs, child-care costs, travel costs). Participants were asked about their current occupational status, including information about type of occupation, weekly hours worked, days absent from work and reason and duration for unemployment. Participants were also asked to record their use of any medication to help with their depression, including medication name, dose and duration taken (however, participants were asked this medication question only at the 24-month follow-up, as it was not included on previous versions of the questionnaire).
In addition, participants were asked to indicate their use of any cCBT since their last REEACT follow-up, allowing us to determine self-reported level of engagement with the two cCBT programs, or any other cCBT packages, for those participants randomised to the two intervention arms, and to examine whether or not participants in the control arm (usual GP care alone) made use of any cCBT packages. Participants were also asked to record their use of other self-help materials (such as self-help books for depression) since their last REEACT follow-up.
Data collected from general practitioner medical records
A range of data were obtained directly from participants’ GP medical records, provided participants had given their informed consent for us to access this information. Data were collected from 2 months before randomisation until the 24-month follow-up, or the date the participant was de-registered from his or her recruiting GP practice, if this occurred before their 24-month follow-up. The data were obtained across three time frames: (1) from 2 months before randomisation to the date of randomisation (representing a 2-month period); (2) from the date of randomisation to 12-month follow-up (‘year 1’, representing a 12-month period); and (3) from 12-month follow-up to 24-month follow-up (‘year 2’, representing a 12-month period).
Data were not collected for those participants who had withdrawn fully from the trial before completion of their 24-month follow-up (see section on Trial completion). Data were recorded by either REEACT researchers or GP practice staff using a data collection form.
Data were collected on the following.
General practitioner consultations
The number of consultations with a GP (including face-to-face, telephone and home consultations) was recorded. The number of these consultations that were clearly related to depression was also recorded.
Nurse appointments
The number of appointments with a practice nurse was recorded, along with the type of nurse seen, if known (e.g. practice nurse, treatment nurse, midwife, health-care assistant).
Health problems
Information about participants’ health problems was recorded. This included mental health problems (specifically depression and anxiety/panic), chronic illness (e.g. diabetes, hypertension, asthma), myocardial infarction, accident/life events (e.g. bereavement, divorce, birth of a baby), drug/alcohol disorders and any other health conditions.
Medication
Information about prescribed depression-related medication was recorded, including medication type, dosage, and prescription start and end dates. Medication type included antidepressants, antipsychotics, mood stabilisers, sleeping tablets and anxiety medication.
Referrals
General practitioner referrals were recorded. This included referrals to various mental health services [e.g. inhouse counsellor, community mental health teams (CMHTs), IAPT, psychologist and psychiatry services] and ‘other’ referrals for all other conditions. The date of referral was recorded, along with the number of sessions received for any mental health services accessed, if known.
Hospital stays
Hospital inpatient stays were recorded, including number of inpatient nights, area of specialty and reason for admission.
Hospital outpatient appointments
Hospital outpatient appointments were recorded, including the appointment date, specialty and reason.
Emergency contacts
The date and reason for visits to accident and emergency departments (for mental health concerns and ‘other’ concerns) and contacts made with out-of-hours services were recorded.
Adverse events
An adverse event was defined as ‘any undesirable clinical occurrence in a subject, whether it is considered to be caused by or related to treatment or not’.
Adverse events were identified during participant recruitment and follow-up by REEACT researchers or at any point during the participant’s involvement in the trial by the participant’s GP. In addition, participants completed a Health Events Questionnaire at each follow-up (see Appendix 7). This asked participants if they had experienced any health problems since their last follow-up, with particular reference to any problems or events that may be related to their depression. Participants were asked to describe their health problems, including when the problem or event happened. Adverse events were also identified via the adapted CSRI questionnaire, which was administered at each follow-up and asked participants about their use of inpatient hospital services during the previous 6 months.
Adverse events were categorised as serious or non-serious. A serious adverse event (SAE) was defined as an event that resulted in death, was life-threatening, required inpatient hospitalisation or prolonging of existing hospitalisation, resulted in persistent or significant disability or incapacity, resulted in a congenital anomaly or birth defect or was deemed medically significant by the reporter.
Adverse events that were felt to be serious were reported to the trial co-ordinating team either by REEACT researchers or by the participant’s GP. The reporter was asked to complete a ‘serious adverse event/reaction form’ (see Appendix 7) for all those adverse events he or she judged to be serious, indicating why, in the reporter’s opinion, the event was considered to be serious and the relationship of the adverse event to treatment. Reporters were asked to report any SAEs to the trial co-ordinating team within 24 hours of the event occurring, or within 24 hours of becoming aware of the event. All adverse events judged to be serious were reviewed by at least two members of the Trial Management Group. SAEs felt to be related to treatment in some way were reviewed by the Data and Ethics Monitoring Committee (DMEC) and the Trial Steering Committee (TSC). SAEs that were felt to be unrelated to treatment were reviewed by the DMEC and TSC at the next scheduled meeting.
The trial co-ordinating team regularly reviewed participant outputs reported on the Health Events Questionnaire. A SAE/reaction form was completed for any reported health problems/events considered to be serious and/or related to treatment. Health problems/events reported by participants that were felt to be non-serious by the trial co-ordinating team were reviewed by the DMEC and the TSC at the next scheduled meeting.
Statistical analysis of the REEACT clinical effectiveness data
All analyses were conducted on an intention-to-treat basis, including all participants in the groups to which they were randomised. For superiority comparisons, two-sided significance tests at the 5% significance level were used. Analyses were conducted in Stata version 13 (StataCorp LP, College Station, TX, USA).
Overview of analyses
All outcome measures were assessed separately among the following groups of participants:
-
Beating the Blues versus usual GP care alone (superiority)
-
MoodGYM versus usual GP care alone (superiority)
-
MoodGYM versus Beating the Blues (non-inferiority).
For each group comparison, similar analyses were applied depending on the type of comparison (superiority or non-inferiority) and the inclusion of potentially important covariates. It was aimed to minimise the number of models applied to each outcome to avoid issues arising from multiple comparisons. The non-inferiority comparison was undertaken only for the dichotomised PHQ-9 scores, with the primary outcome being at 4 months. To assess non-inferiority between Beating the Blues and MoodGYM, we computed two-sided 90% confidence intervals (CIs). Using this method, the free-to-use cCBT program MoodGYM was not inferior to the commercial pay-to-use cCBT program Beating the Blues at the 5% level if the upper boundary was below the pre-specified margin of non-inferiority [0.15 difference in proportions, which translated to 1.44 for the odds ratio (OR)].
Baseline data
All baseline data were summarised by treatment group and described descriptively. No formal statistical comparisons were undertaken. Continuous measures were reported as means and standard deviations (SDs; with medians and minimum and maximum values where appropriate), whereas the categorical data were reported as counts and percentages.
Primary analysis
The primary outcome was depression status at 4 months using a cut-off point of 10 on the PHQ-9. The PHQ-9 was scored if at least eight out of the nine questions were completed. If there was a missing response for one item, then the mean of the other eight responses was imputed. Groups were compared using a logistic regression model with adjustments for gender, age, baseline depression severity, depression duration and level of anxiety. From this model, we obtained ORs and corresponding 95% CIs.
Secondary analyses
Patient Health Questionnaire-9 dichotomised
The primary analysis was repeated for the 12- and 24-month dichotomised PHQ-9 data using the same methods as described above. In addition, all time points were analysed in a single model rather than individual analyses at each time point, using a repeated measures multilevel logistic regression model. The outcome measures were the values at 4, 12 and 24 months, and baseline PHQ-9 score, age, gender, depression duration, level of anxiety, treatment group and time were included as fixed effects. The model also included an interaction between treatment and time. Participants were treated as random effects (to allow for clustering of data within individual participants). Different covariance patterns were calculated for the repeated measurements within participants: unstructured, independent, exchangeable and identity. Models were compared and the model with the smallest Akaike information criterion (AIC) value was selected for the final model for each comparison. Model assumptions for the final models were checked for all comparisons. Overall ORs and corresponding 95% (or 90% for non-inferiority) CIs and individual ORs at each time point (4, 12 and 24 months) were estimated from these models.
Subgroup analyses
An a priori subgroup analysis was performed for the dichotomised PHQ-9 scores at 4 months only. The primary analysis was repeated, including an interaction term between the baseline factor and treatment comparison as described in the previous section. As this study has not been powered to detect interactions, a statistical significance level of 10% (p < 0.10) was used. The subgroup analysis was based on baseline pre-randomised patient preference in relation to cCBT.
Patient Health Questionnaire-9 continuous
The PHQ-9 outcome was also analysed in its continuous form using a repeated measures multilevel linear mixed model following a similar procedure to those outlined above for the dichotomised PHQ-9 scores. The model made adjustments for the same covariates.
Clinical Outcomes in Routine Evaluation – Outcome Measure
The CORE-OM was analysed using a repeated measures multilevel linear mixed model following a similar procedure to that outlined above for the dichotomised PHQ-9 scores. The model adjusted for the same covariates but included the baseline CORE-OM score and not the baseline PHQ-9 score. If there was a missing response for no more than three items, then the overall score was still calculated by summing the valid responses and dividing by the number of valid responses.
Short Form questionnaire-36 items Health Survey version 2
The HRQoL was measured using the SF-36v2 questionnaire at baseline and 4, 12 and 24 months. The scores for the individual SF-36v2 health components (physical functioning, role-physical, bodily pain, general health, role-emotional, vitality, social functioning and mental health) were summarised at each time point by group. For statistical analysis purposes, only the physical component summary (PCS) scores and mental component summary (MCS) scores were analysed to prevent problems caused by multiple testing. The SF-36v2 PCS and MCS scores were analysed using a repeated measures multilevel linear mixed model following a similar procedure to that outlined above for the dichotomised PHQ-9 scores. The model adjusted for the same covariates but included the baseline SF-36v2 score and not the baseline PHQ-9 score.
Adverse events
The number of adverse events and the number of participants experiencing those events were summarised overall and by group for non-serious adverse events (NSAEs) and SAEs separately. No statistical comparisons were undertaken.
Economic analysis of the REEACT cost-effectiveness data
Overview
A within-trial economic analysis was conducted to evaluate the cost-effectiveness of cCBT programs when added to usual GP care in patients with depression. Costs and health benefits expressed in terms of quality-adjusted life-years (QALYs) were estimated over a time horizon of 2 years for each treatment group. Incremental analyses of costs and QALYs were then performed to provide estimates of the incremental cost-effectiveness of a commercial pay-to-use cCBT program (Beating the Blues) plus usual GP care and a free-to-use cCBT program (MoodGYM) plus usual GP care compared with usual GP care alone. The analysis was conducted on an intention-to-treat basis from the perspective of the UK NHS and Personal Social Services, in line with current UK guidelines for a cost-effectiveness analysis. 52 All costs were considered at a 2011–12 price base. Main analyses were conducted on multiply imputed data sets because of the presence of missing data in the trial. 53 A sensitivity analysis was performed to explore and quantify uncertainty in the cost-effectiveness results. The sensitivity analysis included: (1) scenario analyses testing different assumptions in terms of costs, HRQoL and missing data; and (2) a probabilistic sensitivity analysis. 54 Similar to the clinical analyses, a subgroup analysis was performed. The planned subgroup analysis aimed to assess the influence of participants’ treatment preference for treatment allocation on outcomes. Finally, exploratory analyses were conducted to integrate trial findings on a wider evidence base, and to include other psychological therapies as comparators in the cost-effectiveness analyses. All analyses were undertaken in Stata version 12.0 (StataCorp LP, College Station, TX, USA).
Health-care resource use
Health-care resource use data were based on GP medical records. Data were collected for the following periods: 2 months prior to randomisation, from randomisation to 12 months after randomisation and from 12 to 24 months after randomisation. Use of health care was recorded for the following categories (see earlier section on Resource use data for a detailed description): GP visits (including telephone call appointments), including the number of GP contacts that were specifically related to depression; nurse visits (including telephone call appointments); out-of-hours GP services; hospital inpatient stays; hospital outpatient visits; other community services visits (including counsellors, psychologists, psychiatrists, CMHT and IAPT services); and depression-related medication (including antidepressants, antipsychotics, mood stabilisers, sleeping tablets and anxiety medication).
Costs
Costs were estimated in UK pounds sterling based on the financial year 2011–12. Unit costs were obtained from routinely published national cost sources, namely the British National Formulary,55 the Personal Social Services Research Unit (PSSRU) Unit Costs of Health and Social Care56 and the NHS reference costs. 57 Costs accrued from 12 to 24 months were discounted at a 3.5% discount rate, in line with current UK guidance. 52
Appendix 8 provides sources and details of key unit costs. Total costs include the costs of cCBT, GP visits, nurse visits, out-of-hours GP services, hospital inpatient stays, outpatient visits, other community services and depression-related medication. Mental health services included visits to counsellors, psychologists, psychiatrists, CMHT and IAPT services.
Mean total costs were estimated per treatment group using regression analysis to control for patients’ covariates, including costs incurred in the 2 months prior to randomisation (henceforth referred to as baseline costs), and used as a primary outcome measure in the economic analysis.
An alternative costing scenario was considered, in which only costs related to depression were included in the cost analysis. Total depression-related costs included depression-related costs of GP and nurse visits, other community services attendances and depression-related medication costs. As depression-related nurse visits were not collected in this trial, this cost category was estimated by assuming that the proportion of nurse visit costs which were depression related was the same as for GP visits. Depression-related nurse visits costs per time period were estimated by applying to total nurse visits costs the ratio between mean depression-related GP visit costs and mean total GP visit costs. It was not possible to identify which hospital services costs were related to depression and, therefore, they were excluded entirely from the depression-related costs analysis.
Costs of computerised cognitive behaviour therapy
The costs associated with the provision of cCBT are shown in Table 1. These costs include the licence fee (applicable only to Beating the Blues) and the cost of support in the form of telephone calls to provide technical support and to encourage participants to engage with the computerised therapy. All costs related to the provision of cCBT were assumed to be incurred in the first year of follow-up.
| cCBT package | Licence fee cost per patient (£) | Support cost | |||
|---|---|---|---|---|---|
| Mean duration (minutes) | Mean number of calls | Unit cost per hour (£) | Details | ||
| Beating the Blues | 50 | 6.2 | 0.2 | 21 | Based on clinical support worker nursing hour (Community – Band 2) |
| MoodGYM | Free software | 6.5 | 0.3 | 21 | |
The licence fee for Beating the Blues was obtained from the software website, and corresponds to £250 per five treatments. 58 The cost of the Beating the Blues licence per patient can be a maximum of £250 (if only one patient takes the treatment) and a minimum of £50 (if all five treatments are used by five patients). This is in contrast with a previous HTA report,6 where the cost of the Beating the Blues licence fee was a fixed cost per purchase at the GP practice level, with cost per patient depending on assumptions of the patient throughput at the practice. For the purpose of this evaluation, the cost of £50 per patient was used, as it was considered plausible that all five treatments permitted under each licence purchase were taken, given that the previous HTA estimated an annual patient throughput of 25 to 50 per practice. 6
The cost of telephone support calls was estimated based on mean duration and mean number of support calls recorded as part of the study and assuming the support was provided by a clinical support worker. The support calls aimed to provide technical support and to encourage participants to engage with the cCBT programs. In the REEACT trial, support was mostly provided by telephone support staff (grade 4).
Hardware and overhead costs associated with the provision of the computerised therapies at the GP practice were not included in the cost of any of the two interventions. Although the trial protocol allowed the use of the cCBT programs at the GP practice, only nine patients accessed the cCBT programs at their GP practice throughout the 2 years of trial follow-up. Therefore, it was assumed that use of the cCBT programs at the GP practice is likely to be minimal and that the exclusion of related costs was unlikely to affect the results of the cost-effectiveness analysis.
Health-related quality of life
The HRQoL was assessed using responses to the EQ-5D questionnaire applied at baseline, 4, 12 and 24 months. The EQ-5D is a generic preference-based measure of health state that covers five dimensions (mobility, self-care, usual activities, pain/discomfort and anxiety/depression) that can be rated according to three levels of severity to define unique health states. 25 HRQoL weights for these health states have been previously elicited by Dolan et al. 48 using a time trade-off technique from a representative sample of the UK population. A score of 1 represents perfect health and a score of 0 represents death.
The SF-6D was used as an alternative instrument to obtain estimates of HRQoL. SF-6D scores were estimated from responses to the SF-36v224,59 applied at baseline, 4, 12 and 24 months. The SF-6D instrument uses the participant’s responses to 11 items from the SF-36v2 to identify one health state from the 18,000 possible health states. Health states are defined by the different combinations of six attributes (physical functioning, role limitations, social functioning, pain, mental health and vitality) and four to six levels. 46,47 The classification score was based on standard gamble utility measurements on a representative sample of the UK population. 46,60
The EQ-5D scores were used to estimate patient-specific QALYs using the area under the curve method. 61 Mean QALYs measured by EQ-5D were estimated per treatment group using regression analysis to control for patients’ covariates, including baseline EQ-5D score,62 and were used as a primary outcome measure in the economic analysis. QALYs were also estimated using the SF-6D scores as an alternative to EQ-5D scores. Regression analysis was used in a similar way to estimate mean QALYs measured by SF-6D per treatment group, controlling for baseline SF-6D score and the same patient covariates as in the analysis with EQ-5D estimated QALYs. QALYs accrued from 12 to 24 months were discounted at a 3.5% discount rate, in line with current UK guidance. 52
Missing data
The existence of missing data is a common problem when economic evaluation relies on patient-level data. The use of complete case analysis not only can reduce the power of the analysis, but may also lead to biased estimates if there is an underlying relationship between missing values and any observed or unobserved variables, that is if values are not missing completely at random. 63 Available case analysis will only partially address the problem. Despite not reducing the power of the analysis like complete case analysis, in available case analysis sample size will vary across analysis, reducing comparability. 63
Alternative ways to deal with missing data include imputation techniques, where missing values are replaced by estimates based on observable variables. 63 Multiple imputation by chained equations (MICE) was selected to handle missing data in this analysis. 53,64,65 This method’s central assumption is that data are missing at random, conditional on the values of observed variables in the data set and not on other unobserved variables. Another important feature of this method is that it allows incorporation of the uncertainty associated to the imputation method in the estimates that replace the missing values. 66
As complete case analysis requires stricter assumptions regarding the nature of missing data and is more likely to yield biased and less efficient estimates, and given the previously discussed advantages of multiple imputation, it was decided prior to the analysis that MICE would be used to handle missing data.
Multiple imputation by chained equations was performed for a total of 10 imputations (m), as previous research has suggested that three to five m are sufficient to provide adequate estimates but that increasing m improves efficiency. 67 EQ-5D and SF-6D scores were imputed at every follow-up time point (baseline, 4, 12 and 24 months), while costs were imputed for the same time intervals as resource use was collected (the 2 months prior to randomisation, from randomisation to 12 months, and from 12 to 24 months) for each resource use category that was collected on the trial. The independent variables specified in the imputation were baseline EQ-5D score, baseline SF-6D score, age, gender, anxiety level at baseline, depression level at baseline and depression duration at baseline.
Costs and utility scores distributions can accrue some difficulties to the analysis, as the former are bounded at 0 and tend to be positively skewed, whereas the latter are bounded between –0.594 and 1 for EQ-5D and between 0 and 1 for SF-6D. Failure to account for this while imputing the data sets can lead to predicting values that lie outside the bounds for each variable. To overcome this difficulty, predictive mean matching was used. In predictive mean matching, observed data are used to estimate a predictive model (using the MICE-specified covariates), but, instead of replacing missing values with the model predicted values, the nearest observed value is used to fill the missing value. Imputed values are, thus, sampled from values in the original data set and will not lie outside the bounds of the original data distribution. 66
Cost-effectiveness analysis
The cost-effectiveness of the two cCBT programs, Beating the Blues and MoodGYM, when added to usual GP care in patients with depression, was assessed by comparing costs and QALYs in each cCBT treatment arm with costs and QALYs in the usual GP care alone arm, while controlling for baseline patient covariates. Costs and QALYs accrued from 12 to 24 months were discounted at a 3.5% discount rate, in line with current UK guidance. 52
All categories of health-care costs were included in the base-case analysis and QALYs estimated from EQ-5D scores were considered. Incremental estimates of costs and QALYs were obtained through regression methods, adjusting for the baseline characteristics of age, anxiety level, baseline depression severity, depression duration and gender (in accordance with the statistical analysis plan). Difference in QALYs measured by EQ-5D was also controlled for baseline EQ-5D, as it is likely to be a strong predictor of follow-up QALYs, and failure to adjust for this covariate may bias estimates in the presence of a EQ-5D baseline score imbalance between the treatment groups. 62 Similarly, differences in costs were also adjusted for baseline costs.
The regression model selected for the analysis of costs in the base case was a generalised linear model (GLM). This type of model was preferred to an ordinary least squares (OLS) regression, as cost data tend to be heavily skewed and follow a non-normal distribution,68 which leads to violations of the OLS assumptions. GLM models impose a specific distribution function (F) on the dependent variable, to account for the relation between its mean and variance conditional on the covariates, and a link function (g(.)) to define the relationship between the mean (µi) and covariates (xji). 69 This allows the selection of a distribution that better fits cost data and enables issues with heteroscedasticity (i.e. non-constant variance of the error term in a regression) to be addressed, as mean and variance are modelled simultaneously. The model is described by the equation(1)g(µi)=β0+Σ1Jβjxji,yi∼F69,
where j is the total number of independent covariates in the model. For the analysis of costs (and also in subsequent scenario and subgroup analysis), a gamma family distribution was selected. Selection of the family distribution was based on the modified Park’s test70 performed on each imputed data set and complete case data set. An identity link function was selected, thus assuming an additive effect of covariates on costs. 69 The model was adjusted for the patient characteristics of age, gender, anxiety level at baseline, depression severity at baseline and depression duration at baseline. Adjustment was also made for baseline costs.
Incremental QALYs estimation was performed through OLS regression, as this method has been recommended for the estimation of QALYs in economic evaluation. 71 The distribution of QALYs was also inspected through histograms to assess distribution shape. QALYs distribution appeared to resemble normal distributions for both EQ-5D- and SF-6D-calculated QALYs (the latter used on scenario analyses). The regression model was adjusted for age, gender, anxiety level at baseline, depression severity at baseline and depression duration at baseline, as well as EQ-5D score at baseline (or the SF-6D score at baseline for the SF-6D scenario analysis).
Seemingly unrelated regressions (SURs; a bivariate regression model)72 of costs and QALYs were also considered as an alternative regression model to jointly estimate outcomes. In this bivariate model, incremental costs and QALYs were simultaneously estimated from two separate OLS regressions, assuming correlation between the error terms in each regression. The bivariate model was adjusted using the same covariates for costs and QALYs as in the main analysis. Although the bivariate approach allows the simultaneous estimation of costs and QALYs, and can increase the precision of estimates if there is a correlation between outcomes, it assumes an underlying normal distribution of error terms. 73 As the modified Park’s test suggested that a gamma distribution, rather than the normal distribution, is likely to provide a better fit for the error terms in the costs regression, SUR was not the preferred model.
Standard decision rules74 were used to evaluate the incremental cost-effectiveness of the two cCBT programs, Beating the Blues and MoodGYM, when added to usual GP care, compared with GP usual care alone. An intervention that generates greater mean QALYs and lower mean costs can be considered dominant. Where no dominance arises, the interventions can be compared by calculating the ratio between incremental costs and QALYs to establish the incremental cost-effectiveness ratio (ICER) between each cCBT intervention plus usual GP care and usual GP care alone. The cost-effectiveness of the interventions was assessed by comparing ICERs against a cost-effectiveness interval ranging from £20,000 to £30,000 per QALY, in line with NICE cost-effectiveness thresholds for the UK. 52
Uncertainty surrounding the decision was assessed using probabilistic sensitivity analysis and presented through cost-effectiveness acceptability curves (CEACs) which graphically represent the probability of an intervention being cost-effective across a range of cost-effectiveness thresholds. 75 CEACs do not aim to identify which is the optimal strategy for a particular decision problem. 75 The estimation of probabilities of cost-effectiveness is nevertheless important to quantify the uncertainty surrounding the decision, and whether or not it is worth conducting further research to reduce this uncertainty. 75,76 In order to plot the CEAC, the variance–covariance matrices from the costs and QALYs regressions (one matrix for each, except in the SUR model) were extracted and the corresponding Cholesky decompositions used to obtain correlated draws from a multivariate normal distribution. 54 This approach is commonly used to ensure that parameters taken from a regression framework remain correlated when the probabilistic sensitivity analysis is performed (and CEACs are plotted), but it has the disadvantage of imposing normality on the sampling distribution.
Sensitivity analyses
Sensitivity analyses were conducted by performing a number of alternative scenario analyses, where assumptions underlying the base-case analysis were varied. The aim of the sensitivity analyses was to assess the robustness of base-case results to alternative assumptions in terms of costs, HRQoL and nature of missing data. Table 2 illustrates which elements were varied in each scenario analysis.
| Scenario | Element | Base case | Variation for the sensitivity analysis |
|---|---|---|---|
| 1 | Source of HRQoL | EQ-5D instrument used to estimate QALYs | SF-6D instrument used to estimate QALYs |
| 2 | Costs | All cost categories included | Only depression-related costs included |
| 3 | Missing data | Data assumed to be missing at random; analysis therefore conducted on imputed data | Data assumed to be missing completely at random; therefore, analysis conducted on the complete case data |
| 4 | Missing data and source of HRQoL | Data assumed to be missing at random. EQ-5D instrument used to estimate QALYs | Data assumed to be missing completely at random; therefore, analysis conducted on the complete case data. SF-6D instrument used to estimate QALYs |
| 5 | Missing data and costs | Data assumed to be missing at random. All cost categories included | Data assumed to be missing completely at random; therefore, analysis conducted on the complete case data. Only depression-related costs included in the analysis |
The use of EQ-5D to measure HRQoL is recommended by NICE as part of the preferred base case for HTA52 and, therefore, EQ-5D-estimated QALYs were included in the base-case analysis. NICE also accepts the use of alternative instruments to measure HRQoL, such as the SF-6D, when EQ-5D-measured utilities are not available. 52 Nevertheless, it has been demonstrated that, despite the convergence of measurements by EQ-5D and SF-6D, the two instruments are not interchangeable. 60 As the data collected in the REEACT trial allowed estimating QALYs as measured by SF-6D data, it was possible to explore in scenario 2 how sensitive the results of the base-case analysis were to the choice of HRQoL instrument. Similar to the base-case analysis, incremental QALYs were estimated through an OLS regression adjusted for age, gender, anxiety level at baseline, depression severity at baseline and depression duration at baseline, as well as SF-6D score at baseline.
In principle, only costs that differ as a result of the treatments being considered should be included, so as not to introduce additional variability in the analysis that will make relevant differences in costs more difficult to detect. 77 Nevertheless, the identification of which costs are relevant can be difficult, and it may be preferable to include a wider range of costs in the analysis. Uncertainty regarding which costs are relevant can be explored by testing the impact on cost-effectiveness analysis results of including a more restricted set of costs. In scenario 1, the categories of costs included in the estimation of total costs per treatment group was limited to those considered to be related to depression, that is depression-related GP and nurse visits, other community service attendances and depression-related medication. The regression model used to estimate incremental costs for scenario 2 was similar to the base case, that is, a GLM model with a gamma distribution and identity link function, adjusted for age, gender, anxiety level at baseline, depression level at baseline and depression duration at baseline. Adjustment was also made for baseline depression-related costs.
In scenario 3, the base-case analysis is performed on an alternative data set, obtained by excluding from the available case data set all observations for which data on costs, EQ-5D scores, age, gender, anxiety level at baseline, depression level at baseline and depression duration at baseline were missing (i.e. the complete case data set). Analyses on the complete case data set assume that data are missing completely at random and not conditional on any covariates (observable or unobservable). 63 Scenarios 4 and 5 are parallel to scenarios 1 and 2, respectively, assuming, similarly to scenario 3, that data are missing completely at random. These two scenarios aim to verify whether or not varying costs and HRQoL assumptions on complete case data set impact similarly on cost-effectiveness results when these variations were performed on the imputed data sets. Regression models corresponding to those fitted to the imputed data sets were used in the complete case data sets scenario. It should be noted that the complete case data set (n = 265) for scenario 4 is not an exact match to the complete case data set (n = 290) in scenarios 3 and 5, given that questionnaire rate of completion was lower at each time point for the SF-36v2 than for EQ-5D.
Subgroup analyses
Heterogeneity of treatment impact on costs and QALYs was explored through a subgroup analysis based on participant preference for allocation to a cCBT treatment group. The aim of the subgroup analysis was to identify whether or not the cost-effectiveness of the cCBT treatments plus usual GP care compared with usual GP care alone in the overall patient population is likely to change for specific patient subgroups.
The preference subgroup analysis explored the influence of participants’ treatment preference for allocation to a cCBT treatment group on outcomes. This analysis was conducted by including participant’s treatment preference as a covariate and an interaction term (between treatment allocation and participant’s treatment preference) on both the base-case costs and QALYs’ regression models.
Extrapolation and evidence synthesis
The within-trial economic evaluation has been criticised by Sculpher and colleagues78 as a limited framework to inform decision-making. Duration of trial follow-up is frequently insufficient to capture the time over which all relevant costs and benefits may differ between the competing interventions and has been identified as one of the reasons for lack of appropriateness to inform decision-making in within-trial analyses. Decision-analytic models are used to overcome this (and other) limitation(s), allowing the extrapolation of trial results over longer and potentially more relevant time horizons. However, it is worth noting that there are circumstances under which any within-trial cost-effectiveness results are unlikely to change regardless of how long the time horizon is extended. For example, if no difference between treatment arms in terms of HRQoL is detected for the duration of the trial, there is no basis for inferring that these changes will occur in the future. Another circumstance where extrapolation will be unnecessary is when a given intervention is dominated by the comparator (i.e. is more costly and less effective) and extending the time horizon will only make that dominance more evident. Similarly, if no changes in costs and QALYs are plausibly expected to occur past the trial period, then extrapolation would be redundant.
The within-trial analysis traditional framework is also not amenable to the incorporation of other relevant sources of evidence, nor does it usually allow the comparison of all relevant comparators. 78 The incorporation of other sources of evidence in cost-effectiveness can be accomplished with decision-analytic models, where parameters are informed from multiple studies or evidence synthesis outputs. However, modelling would require imposing a formal decision model structure which may not be consistent with the within-trial analyses and result. Therefore, to maintain consistency with the trial analyses, a novel approach to evidence synthesis has been used here. Estimates of the impact of changes in depression severity from the trial on costs and QALYs of patients are combined with estimates of the impact of alternative treatment on changes in depression from the wider literature to estimate what the incremental difference would be of these alternative treatments on costs and QALYs in patients from the REEACT study.
In this evidence synthesis approach, regression analyses similar to those outlined previously were used to determine the impact of changes in depression, measured by change in PHQ-9 from baseline, rather than treatment arm on costs and excluding intervention costs, and QALYs measured in the trial. The coefficients on the change in PHQ-9 from the regression equations estimate the impact of changes in PHQ-9 on costs and QALYs for patients within the trial. Two meta-analyses were identified, one on the effectiveness of internet-based treatments for depression in adults10 and another on other psychological therapies for patients with depression. 79 These reported the effect of the interventions compared with usual care in terms of a standardised mean difference (SMD). SMD is calculated as the difference between the average scores on the depression severity measurement instrument of the control group and treatment group at post-test divided by the pooled SDs of the two groups. These SMDs can be converted back onto the scale of change in PHQ-9 (ΔPHQ-9) by multiplying them by the standard deviation (SD) in ΔPHQ-9 observed in the trial, so as to estimate the incremental impact of the two interventions on costs and QALYs in the trial population compared with usual GP care alone.
The above analyses can then be combined along with estimates of the intervention specific costs to estimate the cost-effectiveness of cCBT and other psychological therapies compared with usual GP care in patients from the REEACT study.
Qualitative study of the acceptability to patients and health professionals of computerised therapy
A concurrent qualitative study was undertaken to examine the acceptability and experiences of patients and health professionals in relation to computerised therapy.
Design of qualitative study
Patient interviews
We explored patient experience of cCBT in a sample of trial participants who were randomised to receive either of the two cCBT programs (Beating the Blues or MoodGYM). Informed by prior literature on engagement and uptake, we aimed to explore the:
-
experience of using the program, including perceptions of the content, accessibility and perceived effectiveness
-
reported barriers to engagement and perceived limitations of the cCBT intervention, particularly in comparison with face-to-face interventions
-
experience of using the cCBT programs in routine care, specifically if primary care staff were involved in providing support or follow-up.
Sampling and recruitment for the qualitative study
We had originally planned to conduct 10 focus groups each consisting of 7–10 participants, with participant sampling based on expressed preference for cCBT prior to randomisation; on randomisation to Beating the Blues, usual GP care alone, or MoodGYM; and on whether cCBT was accessed at home or from a central location. However, a number of factors (e.g. pragmatic difficulties in arranging the focus groups, but, furthermore, the fact that individual interviews may be more appropriate given the individual nature of the cCBT programs and initial follow-up data indicating that participants struggled to complete the cCBT programs, and also that the majority of participants were accessing the cCBT programs from home independently rather than working in any group or social format – see Chapter 3) led us to revise our design and sampling framework. In addition, in order to explore whether or not treatment refusal may relate to perceived unacceptability or unsuitability of the cCBT program, we received ethical approval to recruit participants who declined to take part in the trial before randomisation (see Chapter 3).
We therefore aimed to conduct individual semistructured interviews with 30–40 participants, sampling for expressed preference for cCBT prior to randomisation (assessed by one question in the Biographical Questionnaire, which asked participants if they would prefer to receive cCBT – see Appendix 7) and self-reported engagement with the cCBT program (assessed by the number of sessions of cCBT completed as reported on the adapted CSRI – see Appendix 7). We also aimed to conduct individual semistructured interviews with participants who indicated that their primary reason for refusal to participate in the trial prior to randomisation was concern over using cCBT. We aimed to recruit 8–10 participants in this group.
Although we wished to consider preference and engagement, we adopted a convenience sampling method to ensure adequate recruitment rather than using an a priori sampling theme, and instead attended to preference and engagement in the topic guides and in the analysis. The first 80 participants to complete their 4-month follow-up at each of the four main trial sites (including the additional five trial sites recruited through the University of York) were invited by letter to participate (320 participants in total). Participants who responded to the invitation letter (see Appendix 9) were contacted by telephone to discuss taking part. Participants who opted to take part in the qualitative study received a participant information sheet and completed a consent form (see Appendix 9). Face-to-face interviews were then arranged with a qualitative researcher at a time and location convenient to participants. Interviews were conducted separately from any outcome assessments to avoid bias and to ensure that the interaction felt open and exploratory (in contrast to the pre-defined nature of the outcome assessments.) We assessed completed analysis of the interviews for data saturation in order to decide whether or not to initiate a second round of recruitment (which was agreed to be unnecessary). Owing to a slowing in overall trial recruitment, we were unable to recruit any participants to the qualitative study who had declined participation to the trial on the expressed basis of an unwillingness to try cCBT.
Patient interviews were conducted by three research associates, one based at the University of Manchester (SK) and two based at the University of Bristol (HT, EA). The researchers were all experienced in qualitative interviewing and had backgrounds in psychology. The topic guides were adapted iteratively as the study progressed to ensure that emergent themes were attended to and that interviews were sensitive to new areas or topics being discussed (see Appendix 10). Within the interviews, topic guides were used to suggest areas of discussion but we avoided using them as a definite framework to limit or explicitly focus conversations.
Health professional interviews
We explored health professionals’ views of referring patients for computerised therapy as part of the REEACT trial. We aimed to explore:
-
the degree to which health professionals targeted referral or ‘matched’ the interventions to particular patients, exploring perceptions about which patients cCBT would be most suitable for
-
if cCBT could be implemented within GP practices
-
if health professionals provided support or structured follow-up for patients using cCBT and whether or not this was considered feasible.
Sampling and recruitment for the qualitative study
In the original protocol, we aimed to conduct individual semistructured interviews with a purposive sample of up to 25 health professionals (GPs and practice managers) in order to explore perceptions of implementing cCBT within GP practices. However, given that GP practices involved in the trial did not provide on-site access to the cCBT programs, and as a result of patient reports indicating that GPs did not play a significant part in monitoring or supporting their use of the cCBT programs, we aimed instead to interview a minimum of 10 GPs to explore perceptions of referring patients to cCBT (with the intention of extending recruitment if GPs reported, contrary to the patient interviews, that they had been significantly involved with the cCBT programs. However, GPs confirmed that they had minimal input into patients’ experience of the cCBT programs, as further discussed in Chapter 5). We specifically attended to whether or not data saturation was achieved in this smaller sample, however, in order to determine whether further interviews were necessary.
Once participant trial recruitment was completed, invitation letters (see Appendix 11) were sent to all those GP practices that had recruited participants to the trial via the Universities of Manchester, York and Bristol (70 GP practices in total). GP practices that recruited participants via the University of Sheffield (13 GP practices in total) were not included because of local NHS restructuring, delaying the necessary study approvals. Health professionals who responded to the invitation were sent an information sheet about the qualitative study and completed a consent form (see Appendix 11).
Interviews were conducted by a qualitative researcher based at the University of Manchester (SK). All interviews were conducted by telephone and followed a topic guide (see Appendix 10). GP practices were offered reimbursement for their time participating in the interviews.
Qualitative analysis
Patient interviews
Patient interviews and subsequent analyses were undertaken before the clinical results of the study were known. Interviews were conducted face to face and were transcribed verbatim.
Data were analysed using the constant comparative method as described by Boeije. 80 One researcher (SK) analysed all the transcripts and three co-investigators (PB, KL and HL) analysed a subset of 16 interview transcripts. Significant phrases in the transcripts were noted and used to generate initial codes, which were then discussed to reach consensus on themes. Analysis consisted of two key processes, fragmenting and connecting. 80 Fragmenting refers to exploring the separate themes that emerge within each interview, to code items relevant to the individual research questions. Connecting emphasises the interview as a whole, to understand the themes together in context. These processes were conducted first within single interviews, then between interviews in the same group and finally across the sample as a whole. Disagreements on themes were discussed until agreement was reached.
In the original protocol we stated our aim to use Normalisation Process Theory (NPT) to guide analysis in order to understand barriers and facilitators of cCBT being embedded within practices (which was an initial plan prior to the trial commencing). As very few practices provided on-site access and most participants accessed the packages alone from home, we decided to reconsider if NPT was appropriate. We aimed instead to conduct an inductive analysis (as previously described) and then consider if NPT was still valuable in adding understanding to the emergent themes. Consensus was reached within the qualitative team that NPT did not add significantly to the primary analysis in this case.
Professional interviews
Interviews with health professionals were conducted by telephone and were transcribed verbatim.
Data were analysed using the constant comparative method as previously described. 80 All transcripts were analysed by a qualitative researcher (SK) and emergent themes discussed and clarified with two of the study co-investigators (PB and KL). Analysis was also informed by the thematic findings from the patient interviews to enable cross-comparison and to identify consistencies or differences between patient and professional reports.
Patient and public participation
The REEACT trial received patient and public participation input at the design, conduct, analysis and interpretation stages. We received input from those with lived experience of depression in the design of all research materials. The REEACT trial received oversight via committee membership from members with lived experience of common mental health problems and a representative of a user-led self-help organisation. A user-led organisation (Anxiety UK and Self-Help Services via its Chief Executive) acted as co-applicant and collaborator on the REEACT trial.
Some of this text has been reproduced from Gilbody et al. 11 © BMJ 2015. This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/.
Chapter 3 Protocol changes
Research objectives/trial design
In the original protocol the primary research objective was to establish the clinical effectiveness and cost-effectiveness of two cCBT programs – Beating the Blues and MoodGYM – versus antidepressant medication over a 2-year follow-up period. All participants were to receive usual GP care, with the key comparison being in the selection of initial treatment for depression, where the comparison would be between antidepressants and a non-drug alternative in the form of cCBT. Participants who were randomised to either of the two cCBT programs would receive computerised therapy rather than medication in the first instance, with the addition of drug treatment to cCBT if the participant’s GP felt that the patient was failing to respond to computerised therapy. Participants randomised to the control group – usual GP care alone – would be prescribed antidepressants by their GP. Although no specific patient-level recommendations were to be made about which medication to prescribe or the dosage, GPs were asked to follow the NICE recommendations on the prescription of antidepressants15 and the British National Formulary dosage recommendations. 55
Following ethical approval of our original protocol (10 July 2008), we received notification from the Medicines and Healthcare products Regulatory Agency that our design qualified our trial as a clinical trial of an investigational medicinal product. We sought advice from our funders, who advised against using this trial design and recommended that all participants receive ‘care as usual’ and that participants’ medication use should not in any way be altered by participating in the trial.
In light of this advice, the basic design of the trial was revised. The revised design maintained the original structure of a three-armed trial but with slight changes to the content of each arm. The control arm was revised to be usual GP care. The two intervention arms were amended to include the addition of usual GP care to one of two cCBT programs (usual GP care plus Beating the Blues and usual GP care plus MoodGYM). The revised trial design now meant that all participants would receive usual GP care. Usual GP care might include antidepressant medication but also might not. As a result, the original exclusion criterion that participants already in receipt of antidepressants would be ineligible to participate in the trial was removed. This change in trial design meant our primary research objective was now to establish the clinical effectiveness and cost-effectiveness of the addition of cCBT to usual GP care over a 2-year follow-up period.
On the basis that all participants would be receiving care as usual, the trial was no longer classified as a clinical trial of an investigational medicinal product but as a non-interventional trial. We received ethical approval (22 September 2008) for this revised trial design before the study commenced.
Outcome measures
Primary outcome measure
In our original protocol we had defined our primary outcome measure as depression severity and symptomatology as measured by the PHQ-913 and a self-report computer-administered diagnostic interview (CIS-R)19 at 4 months. However, we were advised by the study co-investigators that participants in other studies they were involved in had found the CIS-R interview prohibitively onerous. In the light of this we decided that the burden of the CIS-R interview was not justified by its usefulness as a follow-up measure and therefore removed this measure from each of the follow-up time points, although it remained as a baseline measure. The primary outcome measure was, therefore, measured by only the PHQ-9 at 4 months.
Telephone support calls
During early trial meetings (and prior to the first participant being randomised) we decided to introduce regular telephone support calls to those participants who were randomised to use either one of the two cCBT programs in order to ensure uptake and to be in line with good clinical practice. These telephone calls were undertaken by telephone support staff who would deal with any technical problems the participants might experience and would try to encourage them to engage with the cCBT programs. The telephone calls were not intended to offer any form of psychotherapy. This protocol change was implemented following information that cCBT interventions are usually implemented in practice with this kind of support, and so this change allowed us to reflect current practice and maintain the pragmatic design of the trial.
In addition, the protocol was adapted to include supervision of the telephone support staff. Telephone support staff were required to work to specific and standardised instructions on what should be covered during each telephone call to ensure the delivery of ‘support’ rather than ‘therapy’ and to provide the telephone support staff with the skills needed to respond to the common questions that would inevitably arise during the telephone calls. Therefore, as a means of ensuring standardisation and quality control, we gained ethical approval to record the telephone calls. All participants were asked for their informed consent to record each telephone call and participants were not excluded from the trial if they withheld their consent to the recordings. All telephone support staff were aware that telephone calls were being recorded where participant consent was given. Regular supervision with the chief investigator or other senior study co-investigators was provided to the telephone support staff.
These protocol changes were implemented before the first participant was randomised.
Exclusion criteria
It was decided to add two additional exclusion criteria when considering potential trial participants. It was felt by the study investigators that patients who have a primary diagnosis of alcohol or drug abuse and patients who are not able to read and write in English would be highly unlikely to benefit from cCBT. This protocol change was implemented before the first participant was randomised.
Trial referrals
In our original protocol, direct referrals to the trial could be made only by a patient’s GP. Practice nurses could identify potential participants with depression but would need to advise the patient to make an appointment with his or her GP and notify the GP of the patient’s potential eligibility for the trial. However, during the first 3 months of recruitment we received numerous requests from those health professionals attached to a GP practice (primary care-based mental health workers and practice-attached nurses) participating in REEACT to allow them to directly refer patients to the trial. Following discussions with GPs, practice-attached nurses and members of the primary care mental health team, we decided it was reasonable to allow the latter two groups of staff to check participant eligibility and refer directly to the trial, with the understanding that the referrer would need to inform the patient’s GP of the trial referral. The REEACT researcher would then need to inform both the referrer and the patient’s GP of the outcome of the referral. This method of direct referral was permitted only following discussions with and agreement from individual GP practices and all practice staff involved. This recruitment method was available from November 2009.
Pre-screening for trial eligibility
Problems with the process of REEACT researchers confirming trial participant eligibility led us to change our protocol. During the first 4 months of trial recruitment, we were finding that approximately 40% of participants who had provided their permission for us to contact them had a depression score below the inclusion threshold (PHQ-9 ≥ 10) when assessed for eligibility during face-to-face visits. This meant that, because of the large geographical areas covered by each centre, researchers were travelling long distances to see ineligible patients. In addition, there seemed to be a level of disappointment among otherwise willing participants when they were told they were ineligible to take part in the trial following a face-to-face meeting.
We therefore extended the eligibility protocol to allow REEACT researchers to administer the PHQ-9 over the telephone to pre-screen for baseline eligibility before arranging a face-to-face meeting. The PHQ-9 has been shown to be reliable when administered over the telephone. 33 Those participants who scored ≥ 10 on the PHQ-9 during the pre-screen would receive a face-to-face meeting where the PHQ-9 eligibility check would be repeated to confirm eligibility at the actual point of entry into the trial. Those participants who proved to be ineligible following the pre-screen were advised that their symptoms did not match the symptoms under investigation in the trial and were advised to continue to see their GP as normal. This process of pre-screening for trial eligibility was implemented from November 2009.
Postal questionnaires
During the first 6 months of the follow-up period it became apparent that our current retention rate of approximately 65% at 4-month follow-up – the point at which our primary outcome measure was collected – was falling below our target retention rate of 75%. REEACT researchers were finding it difficult to contact participants to arrange follow-up interviews. It was felt that this might in part be a result of participants having returned to their normal daily activities following their recruitment into the trial, as they might find it more difficult to spare the additional time required to be interviewed.
In an attempt to improve our retention rates, we gained ethical approval to give participants the option of completing and returning follow-up questionnaires by post, in the hope that this method might make it easier for participants to fit completing the questionnaires into their daily lives. The participant information sheet was revised to reflect the additional option of postal questionnaire completion. Participants were still provided with the option of completing their follow-up through a face-to-face or telephone interview as described in the original participant information sheet. Participants already in the trial were given the option of postal questionnaire completion at their next follow-up and received a copy of the updated participant information sheet. The suicide protocol was also revised to describe the procedure to follow if a potential suicide risk was identified on return of a postal questionnaire. Participants recruited to the trial following implementation of this protocol change were asked to provide their consent to us informing their GP about potential risk if this was deemed necessary. The addition of postal questionnaires as a completion method was implemented in August 2010.
Qualitative study
We revised our plans for evaluating the acceptability of cCBT from those detailed in our original protocol. The original protocol stated that the qualitative data would be collected during 10 focus groups each with 7–10 participants. However, because of pragmatic difficulties in arranging group sessions across the four recruitment centres, our qualitative researcher was concerned that participants might be excluded from the qualitative study if they were unable to find convenient times to attend the focus groups. We also considered that individual interviews might be more appropriate given the individual nature of the intervention and might better enable us to explore how the individual patients experienced the independent computerised therapy. Therefore, in order to increase the accessibility of the study, and in the light of considerations about the nature of the individual experience, we decided instead to collect the qualitative data through individual semistructured interviews, which could be arranged at times and locations to suit each participant.
We also revised our patient-sampling frame. In the original protocol, we planned to sample participants based on expressed preference for cCBT prior to randomisation; on randomisation to Beating the Blues, usual GP care, or MoodGYM; and on whether cCBT was accessed at home or from a central location. However, data collected from participants during the first 8 months of the follow-up period indicated that many participants were struggling to complete the cCBT programs and that the majority of participants were accessing the cCBT programs at home. Treatment completion is a significant issue in patient acceptability and we felt it was important to explore reasons for discontinuing or continuing treatment. As a result, the patient sampling frame was changed so that participants would be sampled based on their expressed preference for cCBT prior to randomisation and on whether they completed the course of cCBT or not. This allowed us to identify both positive and negative experiences of the treatment. We planned to recruit between 30 and 40 participants, with the group reflecting a roughly equal balance of preference and completion.
In the original protocol we were not able to explore the views of participants who did not think computerised therapy was acceptable and who did not wish to be randomised into one of the trial groups. Non-acceptability – refusal to begin treatment – is a noted problem in the literature on cCBT81 and it is likely to be especially relevant in routine primary care, where not all individuals are likely to be willing to try cCBT. 82 We therefore revised our original protocol to allow us to explore reasons for treatment refusal in an attempt to understand perceived barriers to using cCBT and to identify how treatment uptake can be improved. We thus amended the original protocol. Participants who spontaneously expressed an unwillingness to try cCBT as the reason why they did not wish to join the trial would be asked if they would consider being interviewed. Those participants who agreed would be sent an information sheet before being contacted again. We aimed to recruit between 8 and 10 participants in this group.
Finally, in the light of the finding that the majority of participants did not access the cCBT programs in their GP practices as previously expected, we revised the interview topic guides and information sheet to be used in the planned qualitative interviews with health professionals. However, data would still be collected on professionals’ opinions of the feasibility of providing cCBT on site and their perceptions of the acceptability of home and central access for patients.
These protocol changes were implemented from September 2010.
Sample size
Early in the trial we noticed lower than expected follow-up rates at 4-month follow-up (the point at which our primary outcome was measured). This led us to increase our recruitment target from 600 (200 participants in each of the three groups) to 690 participants (230 participants in each of the three groups). In our original protocol we had allowed for a loss to follow-up of 25% to retain 80% power to detect superiority between the usual GP care group and either of the two cCBT groups and non-inferiority between commercial (Beating the Blues) and free-to-use (MoodGYM) cCBT.
To calculate the most effective sample size we modelled the effects of follow-up rates on power. We subsequently gained ethical approval to over-recruit by 30 participants in each arm (an overall increase of 90 participants), which allowed for a loss to follow-up of 35% while retaining 80% power to detect superiority between the usual GP care group and either of the two cCBT groups, and non-inferiority between commercial and free-to-use cCBT. This protocol change was implemented from September 2010.
Questionnaire response rates
As previously mentioned, we experienced lower than expected follow-up rates. As a way of improving our follow-up response rate, we received ethical approval to send a £5 voucher as a token ‘thank you’ payment to participants at each follow-up time point. This token payment was not mentioned in the participant information sheet so that the risk of this being interpreted as a financial incentive to take part in, or continue with, the study was minimised. Receipt of a £5 voucher at follow-up was not conditional on participants completing their follow-up questionnaires. For follow-ups completed during face-to-face visits or telephone interviews, participants received a £5 voucher with their appointment letter. Follow-up questionnaires that were posted out to participants for them to complete and return were accompanied by a £5 voucher. This approach was based on the findings of a systematic review investigating ways of increasing response rates to postal questionnaires. 83 This protocol change was implemented from February 2011.
Long-term follow-up
Given that this study allowed us to assemble one of the largest groups of people with depression in UK primary care, we took the opportunity to investigate the impact of depression and treatment over the longer term. We therefore gained ethics approval to develop a primary care depression cohort of trial participants over a follow-up period of 10 years, with additional follow-ups taking place at 3, 5, 7 and 10 years. Participants were provided with information about these additional follow-ups and those interested were asked to provide their consent to take part. Although the development of a primary care depression cohort represented an extension of our original research objectives, it was not an objective for which we received funding. Therefore, although the primary care depression cohort is referred to in the protocol, it will not be discussed within this report.
Chapter 4 Clinical results
This chapter presents the statistical analysis of the clinical results of REEACT. In the first section of the chapter the trial recruitment, baseline participant characteristics and clinical data are summarised in tables and narratively described. In the second section the outcome data are summarised and results from the statistical models fitted to the data are presented.
Trial recruitment
Four main sites across the UK co-ordinated recruitment to the study. These were the University of Bristol, the University of Manchester, the University of Sheffield and the University of York. In addition, the University of York site was responsible for co-ordinating recruitment at an additional five sites (Durham and Darlington, Gateshead, Hull, North of Tyne and South of Tyne). Table 3 shows the number of participants recruited at each site. Participants were recruited through GP practices, with each site recruiting between 4 and 21 GP practices. Eighty-three out of 100 participating GP practices recruited at least one trial participant (recruitment of participants per GP practice ranged from 1 to 56). Recruitment was staggered, with GP practices participating at different time points during the course of the study. Further details of recruiting sites and GP practices are presented in Appendix 12.
| Site | Beating the Blues (n = 210) | MoodGYM (n = 242) | Usual GP care alone (n = 239) | Total (n = 691) |
|---|---|---|---|---|
| University of Bristol | 51 (24.29) | 68 (28.10) | 64 (26.78) | 183 (26.48) |
| University of Manchester | 32 (15.24) | 37 (15.29) | 32 (13.39) | 101 (14.62) |
| University of Sheffield | 30 (14.29) | 33 (13.64) | 36 (15.06) | 99 (14.33) |
| University of York | 38 (18.10) | 41 (16.94) | 38 (15.90) | 117 (16.93) |
| Durham and Darlington | 8 (3.81) | 9 (3.72) | 7 (2.93) | 24 (3.47) |
| Gateshead | 8 (3.81) | 11 (4.55) | 12 (5.02) | 31 (4.49) |
| Hull | 28 (13.33) | 30 (12.40) | 29 (12.13) | 87 (12.59) |
| North of Tyne | 11 (5.24) | 11 (4.55) | 15 (6.28) | 37 (5.35) |
| South of Tyne | 4 (1.90) | 2 (0.83) | 6 (2.51) | 12 (1.74) |
Recruitment of participants began in August 2009 and ended in March 2011. In total, 1273 individuals were screened as potential participants and, of these, 691 (54.3%) were randomised. The overall rate of recruitment is shown in Figure 1. Figure 2 shows the Consolidated Standards of Reporting Trials (CONSORT) flow chart of participants through the trial. The follow-up period began in December 2009 and ended in April 2013.
FIGURE 1.
Trial recruitment rate.

FIGURE 2.
The REEACT trial CONSORT diagram. Reproduced from Gilbody et al. 11 © BMJ 2015. This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/.

Baseline data
Baseline patient characteristics
In total, 691 eligible participants were recruited to the study: 210 were randomised to receive the cCBT program Beating the Blues plus usual GP care (Beating the Blues), 242 were randomised to receive the cCBT program MoodGYM plus usual GP care (MoodGYM) and 239 were randomised to receive usual GP care (usual GP care alone). The baseline demographic characteristics are shown in Tables 4–6. The mean age of the participants in the study was 39.86 years (SD 12.65 years) and randomisation resulted in groups that were well balanced for age, gender, ethnicity, educational qualification, employment variables and marital status. The majority of participants in the study were white British (95.1%), and more females (66.9%) than males were included. The majority of participants in the study were employed: 61.8% of participants were employed on a full-time or part-time basis or were self-employed. Of those participants who were employed, 26.2% were on sick leave because of depression. The proportion of participants who were on sick leave because of depression was well balanced across the three groups.
| Characteristic | Beating the Blues (N = 210) | MoodGYM (N = 242) | Usual GP care alone (N = 239) |
|---|---|---|---|
| Age (years), mean (SD) | 39.61 (12.34) | 39.43 (12.96) | 40.52 (12.64) |
| Gender, n (%) | n = 210 | n = 242 | n = 239 |
| Female | 142 (67.62) | 157 (64.88) | 163 (68.20) |
| Ethnicity, n (%) | n = 210 | n = 242 | n = 239 |
| White – British | 199 (94.76) | 230 (95.04) | 228 (95.40) |
| White – Irish | 0 (0.00) | 0 (0.00) | 1 (0.42) |
| Any other white background | 3 (1.43) | 8 (3.31) | 5 (2.09) |
| Mixed – white and black Caribbean | 2 (0.95) | 1 (0.41) | 0 (0.00) |
| Mixed – white and black African | 1 (0.48) | 0 (0.00) | 0 (0.00) |
| Any other mixed background | 0 (0.00) | 1 (0.41) | 0 (0.00) |
| Asian or Asian British – Indian | 1 (0.48) | 0 (0.00) | 1 (0.42) |
| Asian or Asian British – Pakistani | 0 (0.00) | 1 (0.41) | 0 (0.00) |
| Chinese | 3 (1.43) | 0 (0.00) | 1 (0.42) |
| Other | 1 (0.48) | 1 (0.41) | 3 (1.26) |
| Marital status, n (%) | n = 210 | n = 242 | n = 239 |
| Married | 75 (35.71) | 87 (35.95) | 92 (38.49) |
| Living with a partner | 34 (16.19) | 43 (17.77) | 38 (15.90) |
| Divorced/separated | 30 (14.29) | 37 (15.29) | 36 (15.06) |
| Widowed | 3 (1.43) | 3 (1.24) | 4 (1.67) |
| Single/never married | 65 (30.95) | 71 (29.34) | 67 (28.03) |
| Other | 3 (1.43) | 1 (0.41) | 2 (0.84) |
| Characteristic | Beating the Blues (N = 210) | MoodGYM (N = 242) | Usual GP care alone (N = 239) |
|---|---|---|---|
| Educational qualification, n (%) | n = 210 | n = 242 | n = 239 |
| GCSE/O level | 41 (19.52) | 53 (21.90) | 48 (20.08) |
| GCE A/AS level or Scottish Higher | 31 (14.76) | 21 (8.68) | 31 (12.97) |
| NVQ/SVQ levels 1–3 | 21 (10.00) | 30 (12.40) | 24 (10.04) |
| GNVQ (Advanced) | 6 (2.86) | 5 (2.07) | 2 (0.84) |
| B Tec Certificate | 3 (1.43) | 6 (2.48) | 4 (1.67) |
| B Tec Diploma | 6 (2.86) | 7 (2.89) | 9 (3.77) |
| National Certificate or Diploma (ONC/OND/HNC/HND) | 15 (7.14) | 19 (7.85) | 14 (5.86) |
| Qualified Teacher Status | 3 (1.43) | 3 (1.24) | 11 (4.60) |
| Higher Education Diploma | 7 (3.33) | 6 (2.48) | 17 (7.11) |
| Degree (First Degree/Ordinary Degree) | 27 (12.86) | 46 (19.01) | 32 (13.39) |
| Post Graduate Certificate | 7 (3.33) | 5 (2.07) | 3 (1.26) |
| Post Graduate Diploma | 8 (3.81) | 2 (0.83) | 8 (3.35) |
| Masters Degree | 14 (6.67) | 10 (4.13) | 7 (2.93) |
| Other | 16 (7.62) | 19 (7.85) | 21 (8.79) |
| Don’t know | 1 (0.48) | 2 (0.83) | 3 (1.26) |
| No response | 4 (1.90) | 8 (3.31) | 5 (2.09) |
| Characteristic | Beating the Blues (N = 210) | MoodGYM (N = 242) | Usual GP care alone (N = 239) |
|---|---|---|---|
| Employment, n (%) | n = 210 | n = 242 | n = 239 |
| Employed part-time | 43 (20.48) | 45 (18.60) | 37 (15.48) |
| Employed full-time | 59 (28.10) | 101 (41.74) | 95 (39.75) |
| Self-employed | 21 (10.00) | 12 (4.96) | 14 (5.86) |
| Retired | 10 (4.76) | 11 (4.55) | 21 (8.79) |
| Looking after family or home | 15 (7.14) | 8 (3.31) | 11 (4.60) |
| Not employed but seeking work | 12 (5.71) | 15 (6.20) | 12 (5.02) |
| Not employed but not seeking work because of ill health | 23 (10.95) | 31 (12.81) | 29 (12.13) |
| Not employed but not seeking work for some other reason | 7 (3.33) | 3 (1.24) | 3 (1.26) |
| Full-time student | 16 (7.62) | 14 (5.79) | 15 (6.28) |
| Other | 4 (1.90) | 2 (0.83) | 2 (0.84) |
| Employed but on sick leave because of depression, n (%) | n = 123 | n = 158 | n = 146 |
| Yes | 34 (27.64) | 37 (23.42) | 41 (28.08) |
| No | 89 (72.36) | 120 (75.95) | 105 (71.92) |
| Don’t know | 0 (0.00) | 1 (0.63) | 0 (0.00) |
| Unemployment (duration) , n (%) | n = 42 | n = 49 | n = 44 |
| < 3 months | 7 (16.67) | 10 (20.41) | 9 (20.45) |
| 4–12 months | 11 (26.19) | 12 (24.49) | 13 (29.55) |
| 1–2 years | 7 (16.67) | 4 (8.16) | 6 (13.64) |
| 2–5 years | 8 (19.05) | 7 (14.29) | 6 (13.64) |
| > 5 years | 7 (16.67) | 13 (26.53) | 10 (22.73) |
| No response | 2 (4.76) | 3 (6.12) | 0 (0.00) |
| Job details, n (%) | n = 210 | n = 242 | n = 239 |
| Foreman/supervisor | 13 (6.19) | 8 (3.31) | 11 (4.60) |
| Manager | 37 (17.62) | 44 (18.18) | 41 (17.15) |
| Self-employed with employees | 5 (2.38) | 5 (2.07) | 10 (4.18) |
| Self-employed without employees | 21 (10.00) | 13 (5.37) | 18 (7.53) |
| Other employee | 125 (59.52) | 165 (68.18) | 154 (64.44) |
| Never been in paid employment | 6 (2.86) | 5 (2.07) | 4 (1.67) |
| No response | 3 (1.43) | 2 (0.83) | 1 (0.42) |
Table 7 shows the baseline clinical data for both groups. This demonstrates the nature of depression and anxiety in this population at baseline. Participants experiencing previous episodes of depression for which they sought help were high (n = 491, 71%), with 51% (n = 249) of participants having one or two previous treated episodes of depression and 14% (n = 70) categorising themselves as being chronically depressed. The majority of participants had previously been prescribed antidepressants for their depression (n = 430, 88%) and 365 (74%) had sought help with their depression from someone other than their GP (counsellor 75%, psychiatrist 25% and psychologist 21%). Participants’ current profile of depression and anxiety were obtained at baseline for a total of 685 participants using a diagnostic gold standard (CIS–R). 19 Data for six participants were lost because of file corruption (two in the Beating the Blues group, one in the usual GP care group and three in the MoodGYM group). There were approximately equal numbers of participants in each of the levels of depression (scored from no problem recorded to unable to be cheered up) and anxiety categories (scored from no problem recorded to anxious for more than 3 hours per day). There were two spikes for the duration of anxiety recorded and the duration of depression recorded in the categories of being present for 2 weeks to 6 months and being present for over 2 years. Randomisation resulted in well-balanced groups across all baseline clinical data.
| Characteristic | Beating the Blues (N = 210) | MoodGYM (N = 242) | Usual GP care alone (N = 239) |
|---|---|---|---|
| Previous episodes of depression, n (%) | n = 210 | n = 242 | n = 239 |
| Yes | 144 (68.57) | 169 (69.83) | 178 (74.48) |
| No | 65 (30.95) | 72 (29.75) | 60 (25.10) |
| Don’t know | 1 (0.48) | 1 (0.41) | 0 (0.00) |
| No response | 0 (0.00) | 0 (0.00) | 1 (0.42) |
| Number of episodes of depression, n (%) | n = 144 | n = 169 | n = 178 |
| 1 | 42 (29.17) | 44 (26.04) | 49 (27.53) |
| 2 | 34 (23.61) | 31 (18.34) | 49 (27.53) |
| 3 | 12 (8.33) | 23 (13.61) | 21 (11.80) |
| 4 | 10 (6.94) | 14 (8.28) | 7 (3.93) |
| 5 + | 22 (15.28) | 22 (13.02) | 24 (13.48) |
| Chronically depressed | 19 (13.19) | 30 (17.75) | 21 (11.80) |
| Don’t know | 4 (2.78) | 5 (2.96) | 7 (3.93) |
| No response | 1 (0.69) | 0 (0.00) | 0 (0.00) |
| Previously prescribed antidepressants, n (%) | n = 144 | n = 169 | n = 178 |
| Yes | 129 (89.58) | 149 (88.17) | 152 (85.39) |
| No | 14 (9.72) | 20 (11.83) | 26 (14.61) |
| Don’t know | 1 (0.69) | 0 (0.00) | 0 (0.00) |
| Seen anyone other than GP for depression, n (%) | n = 104 | n = 132 | n = 129 |
| Psychiatrist | 25 (24.04) | 31 (23.48) | 37 (28.68) |
| Psychologist | 21 (20.19) | 35 (26.52) | 21 (16.28) |
| Counsellor | 79 (75.96) | 95 (71.97) | 99 (76.74) |
| Community psychiatric nurse | 15 (14.42) | 19 (14.39) | 26 (20.16) |
| Social worker | 2 (1.92) | 1 (0.76) | 3 (2.33) |
| Citizens Advice Bureau | 2 (1.92) | 2 (1.52) | 1 (0.78) |
| Other statutory/voluntary agency | 11 (10.58) | 9 (6.82) | 17 (13.18) |
| Don’t know | 1 (0.96) | 1 (0.76) | 1 (0.78) |
| Level of anxiety, n (%) | n = 208 | n = 239 | n = 238 |
| 0 (no problem recorded) | 43 (20.67) | 52 (21.76) | 45 (18.91) |
| 1 (+ 1 if anxious for > 3 days in past week) | 32 (15.38) | 38 (15.90) | 41 (17.23) |
| 2 (+ 1 if causes feeling of unpleasantness) | 39 (18.75) | 30 (12.55) | 41 (17.23) |
| 3 (+ 1 if causes physical symptoms) | 39 (18.75) | 43 (17.99) | 43 (18.07) |
| 4 (+ 1 if anxious > 3 hours in any day) | 55 (26.44) | 76 (31.80) | 68 (28.57) |
| Duration of anxiety | n = 208 | n = 239 | n = 238 |
| 0 (no problem recorded) | 31 (14.90) | 33 (13.81) | 33 (13.87) |
| 1 (present for < 2 weeks) | 6 (2.88) | 6 (2.51) | 5 (2.10) |
| 2 (present for 2 weeks to 6 months) | 57 (27.40) | 63 (26.36) | 79 (33.19) |
| 3 (present for 6 months to 1 year) | 32 (15.38) | 34 (14.23) | 41 (17.23) |
| 4 (present for 1 to 2 years) | 24 (11.54) | 32 (13.39) | 21 (8.82) |
| 5 (present > 2 years) | 58 (27.88) | 71 (29.71) | 59 (24.79) |
| Level of depression, n (%) | n = 208 | n = 239 | n = 238 |
| 0 (no problem recorded) | 14 (6.73) | 24 (10.04) | 17 (7.14) |
| 1 (+ 1 if less/no enjoyment with life during past week) | 17 (8.17) | 20 (8.37) | 27 (11.34) |
| 2 (+ 1 depressed for > 3 days in past week) | 43 (20.67) | 45 (18.83) | 46 (19.33) |
| 3 (+ 1 if depressed for > 3 hours in any day of past week) | 50 (24.04) | 64 (26.78) | 56 (23.53) |
| 4 (+ 1 if unable to be cheered up) | 84 (40.38) | 86 (35.98) | 92 (38.66) |
| Duration of depression | n = 208 | n = 239 | n = 238 |
| 0 (no problem recorded) | 9 (4.33) | 14 (5.86) | 13 (5.46) |
| 1 (present for < 2 weeks) | 3 (1.44) | 2 (0.84) | 0 (0.00) |
| 2 (present for 2 weeks to 6 months) | 67 (32.21) | 79 (33.05) | 96 (40.34) |
| 3 (present for 6 months to 1 year) | 49 (23.56) | 43 (17.99) | 46 (19.33) |
| 4 (present for 1 to 2 years) | 24 (11.54) | 37 (15.48) | 30 (12.61) |
| 5 (present > 2 years) | 56 (26.92) | 64 (26.78) | 53 (22.27) |
| Presence of phobia (phobia flag), n (%) | n = 208 | n = 239 | n = 238 |
| Only anxiety | 59 (28.37) | 70 (29.29) | 76 (31.93) |
| Specific fear | 149 (71.63) | 169 (70.71) | 162 (68.07) |
Patient Health Questionnaire-9
To be included in the study participants had to score 10 or more on the PHQ-9 at baseline. A cut-off point of 10 has been shown to detect clinical depression in UK primary care. 14 A cut-off point of 10 was used to categorise participants as depressed or not depressed at 4 months, 12 months and 24 months (PHQ-9 ≥ 10 = depressed, PHQ-9 < 10 = not depressed). The descriptive statistics for the PHQ-9 by group across all time points are presented in Table 8 and displayed in Figure 3.
FIGURE 3.
Bar chart of the proportion of patients who are depressed by group. (a) Beating the Blues; (b) MoodGYM; and (c) usual GP care alone.

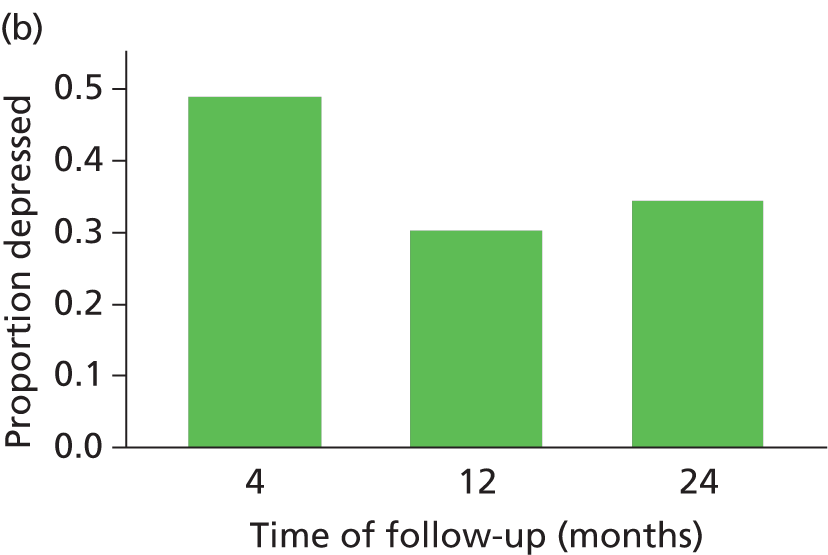

| Characteristic | Beating the Blues | MoodGYM | Usual GP care |
|---|---|---|---|
| Baseline | n = 210 | n = 242 | n = 239 |
| Depressed (PHQ-9 ≥ 10), n (%) | 210 (100.00) | 242 (100.00) | 239 (100.00) |
| 4 months | n = 165 | n = 182 | n = 179 |
| Depressed (PHQ-9 ≥ 10), n (%) | 83 (50.30) | 89 (48.90) | 78 (43.58) |
| 12 months | n = 153 | n = 165 | n = 166 |
| Depressed (PHQ-9 ≥ 10), n (%) | 54 (35.29) | 50 (30.30) | 66 (39.76) |
| 24 months | n = 143 | n = 160 | n = 158 |
| Depressed (PHQ-9 ≥ 10), n (%) | 60 (41.96) | 55 (34.38) | 61 (38.61) |
As previously stated, to be eligible for the study participants had to score 10 or above on the PHQ-9 at baseline. The mean PHQ-9 score at baseline was 16.65 (SD 4.25) and randomisation resulted in balance across the three groups. The mean PHQ-9 score at 4 months was 9.71 (SD 6.35), at 12 months was 7.99 (SD 5.98) and at 24 months was 8.33 (SD 6.19). If we dichotomise the PHQ-9 using a cut-off point of 10, the number of participants depressed at 4 months was 250 (47.53%), at 12 months was 170 (35.12%) and at 24 months was 176 (38.18%).
Primary outcome
At 4 months, 83 of the 165 (50.30%) participants in the Beating the Blues group, 78 of the 179 (43.58%) participants in the usual GP care group and 89 of the 182 (48.90%) participants in the MoodGYM group scored 10 or more on the PHQ-9. The logistic regression results at 4 months highlighted that there was little or no evidence of a difference between Beating the Blues and usual GP care alone (OR 1.19, 95% CI 0.75 to 1.88) or between MoodGYM and usual GP care alone at 4 months (OR 0.98, 95% CI 0.62 to 1.56; Table 9).
| Comparison | OR | 95% CI | p-value | |
|---|---|---|---|---|
| Lower | Upper | |||
| 4 months | ||||
| Beating the Blues vs. usual GP care alone | 1.19 | 0.75 | 1.88 | 0.46 |
| MoodGYM vs. usual GP care alone | 0.98 | 0.62 | 1.56 | 0.95 |
| MoodGYM vs. Beating the Blues | 0.91 | 0.62a | 1.34a | 0.69 |
| 12 months | ||||
| Beating the Blues vs. usual GP care alone | 0.77 | 0.47 | 1.26 | 0.29 |
| MoodGYM vs. usual GP care alone | 0.56 | 0.34 | 0.93 | 0.02 |
| MoodGYM vs. Beating the Blues | 0.77 | 0.50a | 1.18a | 0.31 |
| 24 months | ||||
| Beating the Blues vs. usual GP care alone | 1.00 | 0.60 | 1.68 | 0.99 |
| MoodGYM vs. usual GP care alone | 0.68 | 0.41 | 1.15 | 0.15 |
| MoodGYM vs. Beating the Blues | 0.72 | 0.47a | 1.11a | 0.21 |
The non-inferiority comparison between MoodGYM and Beating the Blues found the OR at 4 months was 0.91 (90% CI 0.62 to 1.34, p = 0.69). The upper limit of the 90% CI for the OR was 1.34, thus satisfying statistical criteria for non-inferiority of MoodGYM compared with Beating the Blues.
Secondary outcomes
Patient Health Questionnaire-9: results from the logistic regression at 12 and 24 months
At 12 months, 54 of the 153 (35.29%) participants in the Beating the Blues group, 66 of the 166 (39.76%) participants in the usual GP care group and 50 of the 165 (30.30%) participants in the MoodGYM group scored 10 or more on the PHQ-9. At 24 months, 60 of the 143 (41.96%) participants in the Beating the Blues group, 61 of the 158 (38.61%) participants in the usual GP care group and 55 of the 160 (34.38%) participants in the MoodGYM group scored 10 or more on the PHQ-9. The logistic regression results revealed that there was little or no evidence of a difference between Beating the Blues and usual GP care across any of the time points (12 months OR 0.77, 95% CI 0.47 to 1.26; 24 months OR 1.00, 95% CI 0.60 to 1.68; Table 9). There was some evidence of a difference between MoodGYM and usual GP care at 12 months (OR 0.56, 95% CI 0.34 to 0.93) but this was no longer evident at 24 months (OR 0.68, 95% CI 0.41 to 1.15; Table 9). For the non-inferiority comparison between MoodGYM and Beating the Blues at 12 months, the OR was 0.77 (90% CI 0.50 to 1.18, p= 0.31) (Table 9 and Figure 4) and at 24 months was 0.72 (90% CI 0.47 to 1.11, p = 0.21) (Table 9 and Figure 4). At both time points, the upper limit of the 90% CI for the OR satisfied statistical criteria for non-inferiority of MoodGYM compared with Beating the Blues. For the non-inferiority comparison between MoodGYM and Beating the Blues at 24 months, the OR was 0.72 (90% CI 0.47 to 1.11, p = 0.21) (Table 9 and Figure 4). The upper limit of the 90% CI for the OR was 1.11, thus satisfying statistical criteria for non-inferiority of MoodGYM and Beating the Blues.
FIGURE 4.
Mean PHQ-9 score over time by trial arm comparison. Means are predicted means and 95% CIs, estimated from the mixed model and adjusted for gender, age, baseline PHQ-9 score, duration of depression and level of anxiety as fixed effects. The model also included an interaction between month and treatment. Raw unadjusted means are presented for baseline. (a) Beating the Blues vs. usual GP care; and (b) MoodGYM vs. usual GP care. Reproduced from Gilbody et al. 11 © BMJ 2015. This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/.


Patient Health Questionnaire-9 dichotomised: results from the mixed model
We also fitted a repeated measures multilevel logistic regression model to the PHQ-9 scores, and Table 10 shows the results of this analysis. The values at 4, 12 and 24 months were the outcome measures, and the baseline PHQ-9 score, age, gender, depression duration, level of anxiety, treatment group and time were included as fixed effects; an interaction between treatment and time was also included in the model. Different covariance patterns were assessed for the repeated measurements within participants and, as the results were similar, the model with the smallest AIC was chosen for each comparison (independent for all comparisons). For the Beating the Blues versus usual GP care and MoodGYM versus usual GP care comparison there was no evidence of an overall difference between the two groups (p = 0.96 and p = 0.11, respectively). The results are similar to those from the logistic regression models at each individual time-point presented in Table 9. However, the results did change for the non-inferiority comparison between MoodGYM and Beating the Blues at 4 months: the OR was 0.94 (90% CI 0.57 to 1.55, p = 0.84). The upper limit of the 90% CI for the OR was 1.55, thus no longer satisfying statistical criteria for non-inferiority of MoodGYM and Beating the Blues (Figure 5).
FIGURE 5.
Results from the logistic regression and mixed models for the non-inferiority comparisons between MoodGYM and Beating the Blues.
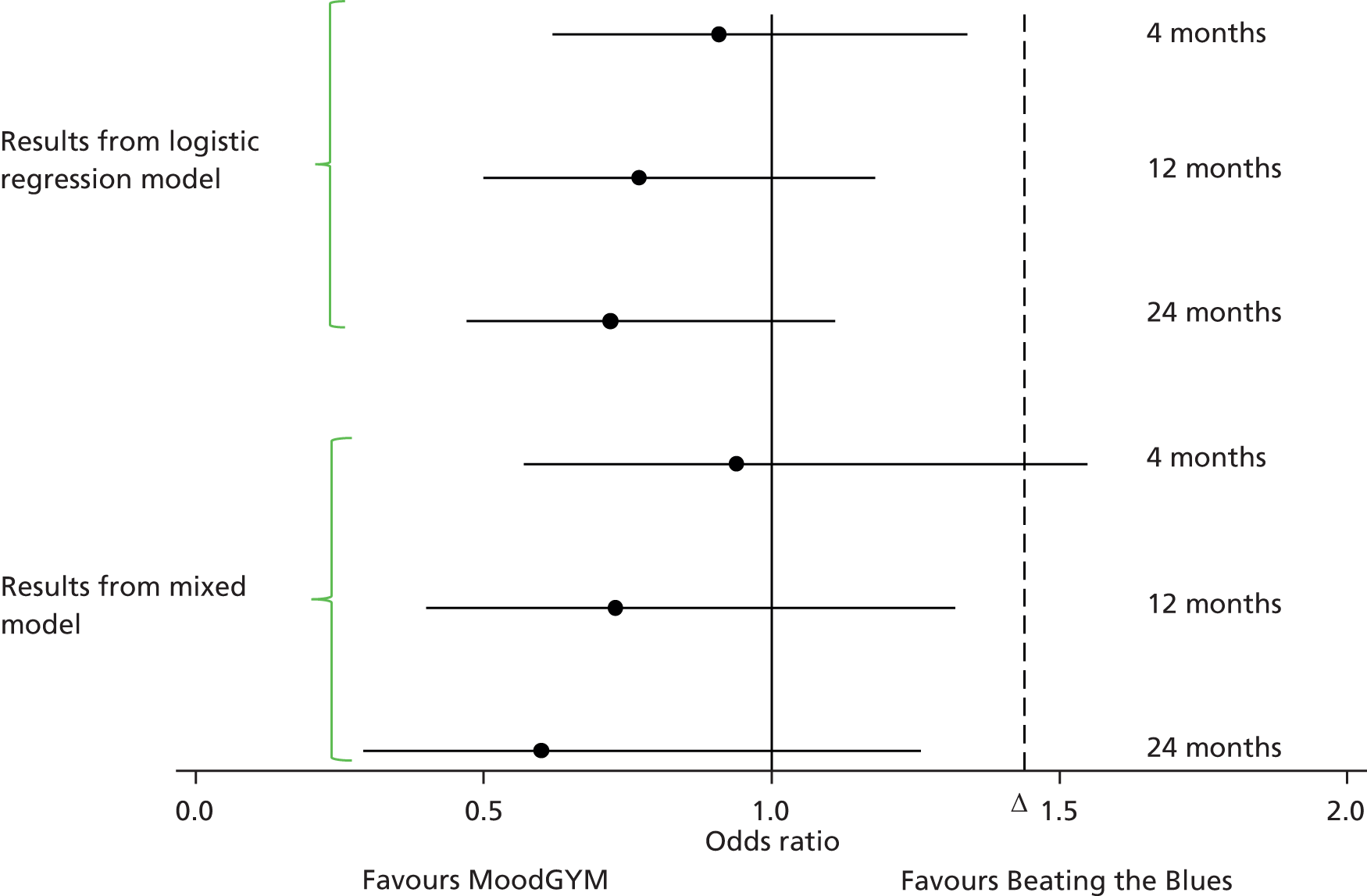
| Comparison | OR | 95% CI | p-value | |
|---|---|---|---|---|
| Lower | Upper | |||
| 4 months | ||||
| Beating the Blues vs. usual GP care alone | 1.27 | 0.70 | 2.28 | 0.43 |
| MoodGYM vs. usual GP care alone | 1.13 | 0.61 | 2.10 | 0.70 |
| MoodGYM vs. Beating the Blues | 0.94 | 0.57a | 1.55a | 0.84 |
| 12 months | ||||
| Beating the Blues vs. usual GP care alone | 0.66 | 0.32 | 1.34 | 0.24 |
| MoodGYM vs. usual GP care alone | 0.44 | 0.22 | 0.88 | 0.02 |
| MoodGYM vs. Beating the Blues | 0.73 | 0.40a | 1.32a | 0.39 |
| 24 months | ||||
| Beating the Blues vs. usual GP care alone | 1.16 | 0.44 | 3.05 | 0.77 |
| MoodGYM vs. usual GP care alone | 0.62 | 0.30 | 1.29 | 0.20 |
| MoodGYM vs. Beating the Blues | 0.60 | 0.29a | 1.26a | 0.26 |
Subgroup analysis
Patient preference
Treatment preferences and the strength of these preferences were recorded at baseline in advance of randomisation and are summarised in Tables 11 and 12. Approximately two-thirds of the participants had a preference for the cCBT interventions, and less than 2% of participants did not know if they had a preference to be randomised to receive cCBT. Of the participants who expressed a preference to be randomised to receive cCBT, 12.92% had an extremely strong preference, 20.04% had a very strong preference, 44.77% had a quite strong preference and 22.05% had a not particularly strong preference.
| Prefer to be randomised to receive cCBT | Beating the Blues (n = 210) | MoodGYM (n = 242) | Usual GP care (n = 239) | Total (n = 691) |
|---|---|---|---|---|
| Yes | 133 (63.33) | 163 (67.36) | 153 (64.02) | 449 (64.98) |
| No/Don’t mind | 74 (35.24) | 75 (30.99) | 80 (33.47) | 229 (33.14) |
| Don’t know | 3 (1.43) | 4 (1.65) | 6 (2.51) | 13 (1.88) |
| Strength of preference | Beating the Blues (n = 133) | MoodGYM (n = 163) | Usual GP care alone (n = 153) | Total (n = 449) |
|---|---|---|---|---|
| Not particularly strong | 23 (17.29) | 37 (22.70) | 39 (25.49) | 99 (22.05) |
| Quite strong | 61 (45.86) | 75 (46.01) | 65 (42.48) | 201 (44.77) |
| Very strong | 35 (26.32) | 27 (16.56) | 28 (18.30) | 90 (20.04) |
| Extremely strong | 14 (10.53) | 23 (14.11) | 21 (13.73) | 58 (12.92) |
The primary analysis was repeated with the addition of patient preference measured at baseline and its interaction with trial arm as additional covariates. There was no evidence of an interaction between patient preference and allocated treatment across any of the comparisons (Beating the Blues vs. usual GP care, p = 0.47; MoodGYM vs. usual GP care, p = 0.35).
Patient Health Questionnaire-9 scores: results from the mixed model
The PHQ-9 questionnaire was used to assess depression severity at baseline and at 4, 12 and 24 months. Descriptive statistics of the PHQ-9 scores are presented in Table 13. The minimum, and best, score possible was 0 and the maximum was 27. The mean PHQ-9 score decreased over time across all trial arms but increased slightly at 24 months in the two cCBT groups.
| Characteristic | Beating the Blues | MoodGYM | Usual GP care alone |
|---|---|---|---|
| Baseline | n = 210 | n = 242 | n = 239 |
| Mean (SD) | 16.78 (4.21) | 16.87 (3.99) | 16.32 (4.52) |
| Median (minimum to maximum) | 17 (10 to 27) | 17 (10 to 26) | 16 (10 to 27) |
| 4 months | n = 165 | n = 182 | n = 179 |
| Mean (SD) | 10.30 (6.35) | 9.70 (6.36) | 9.17 (6.34) |
| Median (minimum to maximum) | 10 (0 to 26) | 9 (0 to 26) | 9 (0 to 27) |
| 12 months | n = 153 | n = 165 | n = 166 |
| Mean (SD) | 8.13 (6.13) | 7.39 (5.51) | 8.45 (6.28) |
| Median (minimum to maximum) | 7 (0 to 27) | 6 (0 to 24) | 7 (0 to 25) |
| 24 months | n = 143 | n = 160 | n = 158 |
| Mean (SD) | 8.93 (6.09) | 7.75 (5.81) | 8.36 (6.62) |
| Median (minimum to maximum) | 8 (0 to 25) | 7 (0 to 26) | 7 (0 to 25) |
We fitted a repeated measures multilevel linear regression model to the PHQ-9 scores. The values at 4, 12 and 24 months were the outcome measures, and the baseline value, treatment group and time were included as fixed effects; an interaction between treatment and time was also included in the model. Different covariance patterns were assessed for the repeated measurements within participants and, as the results were similar, the model with the smallest AIC was chosen for each comparison (independent for Beating the Blues vs. usual GP care and unstructured for MoodGYM vs. usual GP care). For the Beating the Blues versus usual GP care comparison there was no evidence of an overall difference between the two groups (p = 0.81) and the mean PHQ-9 score (over all follow-up assessments) was 8.06 (95% CI 6.92 to 9.20) for Beating the Blues and 7.93 (95% CI 6.74 to 9.13) for usual GP care. For the MoodGYM versus usual GP care comparison there was no evidence of an overall difference between the two groups (p = 0.09) and the mean PHQ-9 score (over all follow-up assessments) was 8.49 (95% CI 7.26 to 9.72) for MoodGYM and 9.30 (95% CI 8.00 to 10.60) for usual GP care. Table 14 and Figure 4 display the results of the mixed model for each time point individually.
| Comparison | Intervention, mean (95% CI) | Usual GP care, mean (95% CI) | Difference (95% CI) | p-value |
|---|---|---|---|---|
| 4 months | ||||
| Beating the Blues vs. usual GP care alone | 9.18 (7.94 to 10.42) | 8.46 (7.18 to 9.73) | 0.72 (– 0.46 to 1.90) | 0.23 |
| MoodGYM vs. usual GP care alone | 9.86 (8.55 to 11.18) | 9.80 (8.42 to 11.18) | 0.06 (– 1.09 to 1.22) | 0.91 |
| 12 months | ||||
| Beating the Blues vs. usual GP care alone | 7.20 (5.94 to 8.46) | 7.83 (6.53 to 9.13) | – 0.63 (– 1.87 to 0.62) | 0.33 |
| MoodGYM vs. usual GP care alone | 7.63 (6.31 to 8.95) | 9.22 (7.83 to 10.60) | – 1.59 (– 2.75 to –0.42) | 0.008 |
| 24 months | ||||
| Beating the Blues vs. usual GP care alone | 7.79 (6.47 to 9.12) | 7.52 (6.16 to 8.88) | 0.28 (– 1.10 to 1.65) | 0.69 |
| MoodGYM vs. usual GP care alone | 7.97 (6.61 to 9.33) | 8.88 (7.45 to 10.30) | – 0.91 (– 2.16 to 0.35) | 0.16 |
Clinical Outcomes in Routine Evaluation – Outcome Measure
The CORE-OM questionnaire was measured at baseline and at 4, 12 and 24 months. Descriptive statistics of the CORE-OM scores are presented in Table 15. The mean CORE-OM scores decreased over time across all trial arms but increased slightly at 24 months in the two cCBT groups.
| Characteristic | Beating the Blues | MoodGYM | Usual GP care alone |
|---|---|---|---|
| Baseline | n = 209 | n = 242 | n = 237 |
| Mean (SD) | 19.23 (5.22) | 18.65 (5.75) | 18.63 (5.59) |
| Median (minimum to maximum) | 19.12 (7.94 to 34.12) | 18.97 (4.41 to 32.94) | 18.53 (4.12 to 34.41) |
| 4 months | n = 155 | n = 170 | n = 167 |
| Mean (SD) | 13.81 (7.19) | 12.85 (7.37) | 13.03 (8.28) |
| Median (minimum to maximum) | 13.82 (0.88 to 33.24) | 11.91 (0.59 to 30.00) | 12.94 (0.29 to 34.41) |
| 12 months | n = 137 | n = 155 | n = 150 |
| Mean (SD) | 11.07 (7.42) | 10.10 (6.72) | 11.75 (7.99) |
| Median (minimum to maximum) | 10.59 (0.29 to 31.18) | 9.12 (0 to 31.47) | 10.58 (0 to 31.47) |
| 24 months | n = 124 | n = 143 | n = 139 |
| Mean (SD) | 12.76 (7.68) | 10.57 (6.97) | 11.48 (8.05) |
| Median (minimum to maximum) | 11.76 (0.29 to 32.65) | 9.41 (0 to 30.59) | 10.29 (0 to 33.24) |
We fitted a repeated-measures multilevel linear regression model to the CORE-OM scores. The values at 4, 12 and 24 months were the outcome measures, and the baseline value, treatment group and time were included as fixed effects; an interaction between treatment and time was also included in the model. Different covariance patterns were assessed for the repeated measurements within participants and, as the results were similar, the model with the smallest AIC was chosen for each comparison (independent for both comparisons). For the Beating the Blues versus usual GP care comparison there was little or no evidence of an overall difference between the two groups (p = 0.50) and the mean CORE-OM score (over all follow-up assessments) was 11.74 (95% CI 10.27 to 13.21) for Beating the Blues and 12.18 (95% CI 10.64 to 13.71) for usual GP care. For the MoodGYM versus usual GP care comparison there was some evidence of an overall difference between the two groups (p = 0.05) and the mean CORE-OM score (over all follow-up assessments) was 11.98 (95% CI 10.47 to 13.50) for MoodGYM and 13.14 (95% CI 11.55 to 14.73) for usual GP care. Table 16 and Figure 6 display the results of the mixed model for each time point individually.
| Comparison | Intervention, mean (95% CI) | Usual GP care, mean (95% CI) | Difference (95% CI) | p-value |
|---|---|---|---|---|
| 4 months | ||||
| Beating the Blues vs. usual GP care alone | 12.87 (11.31 to 14.43) | 12.75 (11.14 to 14.36) | 0.12 (– 1.33 to 1.57) | 0.87 |
| MoodGYM vs. usual GP care alone | 13.61 (12.01 to 15.20) | 13.69 (12.02 to 15.36) | – 0.09 (– 1.44 to 1.27) | 0.90 |
| 12 months | ||||
| Beating the Blues vs. usual GP care alone | 10.51 (8.91 to 12.11) | 12.00 (10.34 to 13.66) | – 1.49 (– 3.04 to 0.06) | 0.06 |
| MoodGYM vs. usual GP care alone | 10.87 (9.25 to 12.48) | 12.98 (11.28 to 14.68) | – 2.12 (– 3.54 to – 0.69) | 0.004 |
| 24 months | ||||
| Beating the Blues vs. usual GP care alone | 11.84 (10.13 to 13.55) | 11.78 (10.05 to 13.51) | 0.06 (– 1.68 to 1.80) | 0.95 |
| MoodGYM vs. usual GP care alone | 11.48 (9.80 to 13.16) | 12.74 (11.00 to 14.49) | – 1.27 (– 2.80 to 0.27) | 0.11 |
FIGURE 6.
Mean CORE-OM scores over time by trial arm comparison. (a) Beating the Blues vs. usual GP care; and (b) MoodGYM vs. usual GP care.
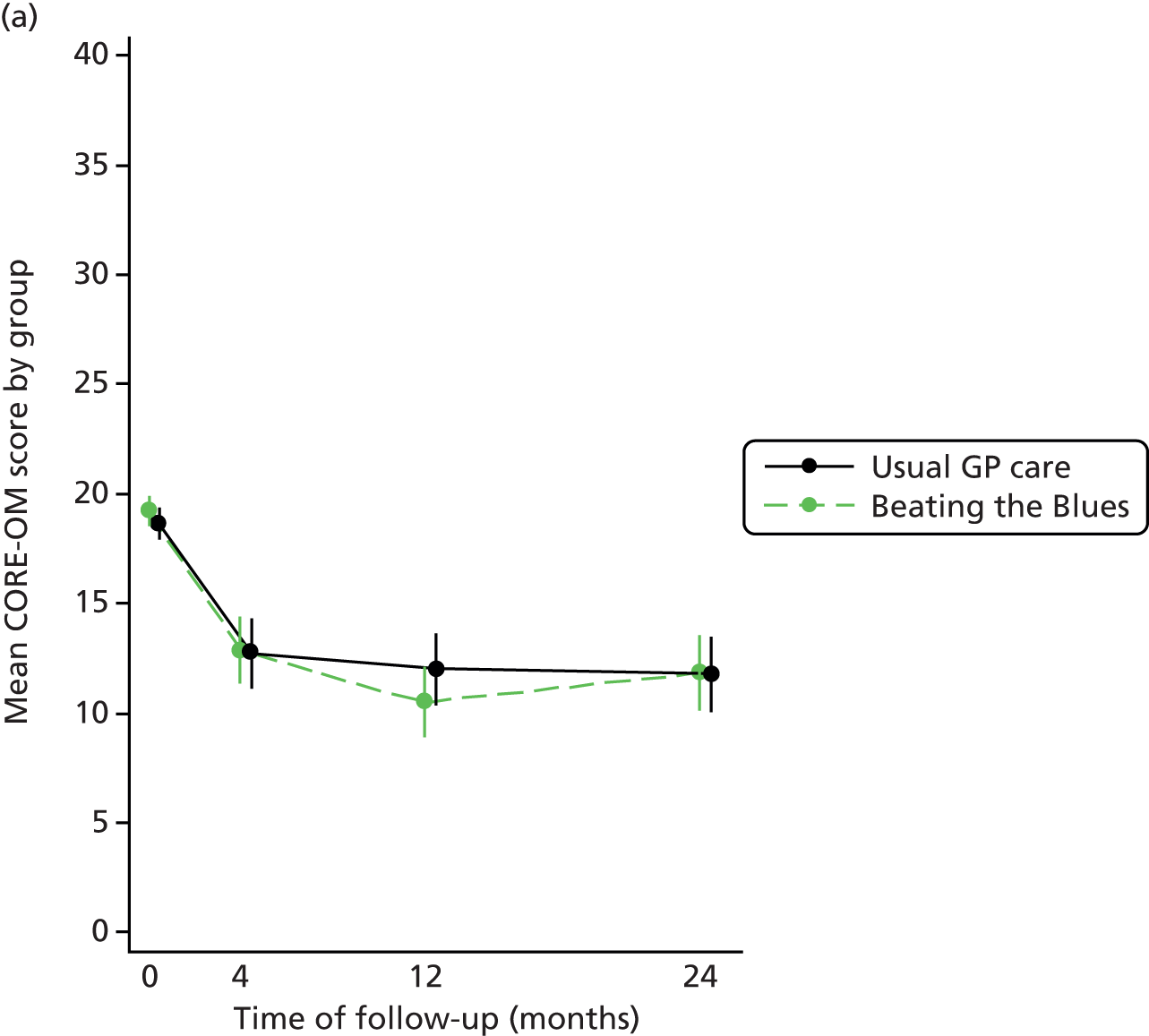

Short Form questionnaire-36 items Health Survey version 2
The SF-36v2 questionnaire was used to assess self-reported HRQoL at baseline and at 4, 12 and 24 months. Descriptive statistics of the domain scores and the PCS scores and MCS scores are presented in Tables 17 and 18. Only the PCS scores and MCS scores have been analysed, all other components are presented descriptively. Figures 7 and 8 show the mean MCS scores and PCS scores (and 95% CI) by trial arm, over time. This shows that, for the PCS, there was little difference between the treatment groups at any time and no clear pattern of improvements over time. For the MCS, the mean scores for Beating the Blues increased between 4 and 12 months and then decreased slightly at 24 months, but this score was still higher than at 4 months. For MoodGYM the scores increased between 4 and 12 months and then remained constant, whereas for usual GP care scores remained similar over all time points.
| Characteristic | Beating the Blues | MoodGYM | Usual GP care alone | |||
|---|---|---|---|---|---|---|
| n | Mean score (SD) | n | Mean score (SD) | n | Mean score (SD) | |
| Physical functioning | ||||||
| Baseline | 210 | 48.39 (9.90) | 242 | 49.25 (9.32) | 239 | 49.55 (9.78) |
| 4 months | 155 | 48.06 (10.65) | 170 | 49.53 (10.02) | 167 | 49.86 (9.41) |
| 12 months | 137 | 48.51 (10.77) | 156 | 49.53 (10.34) | 151 | 49.69 (10.27) |
| 24 months | 123 | 47.23 (11.77) | 143 | 47.61 (12.13) | 139 | 49.78 (9.87) |
| Role-physical | ||||||
| Baseline | 210 | 43.17 (11.94) | 242 | 42.85 (12.67) | 239 | 45.24 (12.35) |
| 4 months | 155 | 44.37 (11.31) | 170 | 45.56 (11.95) | 167 | 46.35 (11.59) |
| 12 months | 137 | 45.82 (11.38) | 156 | 45.91 (11.75) | 151 | 45.45 (11.92) |
| 24 months | 124 | 44.75 (12.84) | 143 | 44.97 (12.41) | 139 | 46.19 (11.11) |
| Bodily pain | ||||||
| Baseline | 210 | 43.29 (10.95) | 242 | 43.89 (10.70) | 239 | 44.48 (10.52) |
| 4 months | 155 | 45.00 (11.94) | 170 | 46.77 (11.67) | 167 | 47.14 (11.41) |
| 12 months | 137 | 46.94 (12.05) | 156 | 46.92 (12.49) | 151 | 47.84 (11.26) |
| 24 months | 123 | 45.45 (12.95) | 142 | 46.30 (13.02) | 137 | 47.81 (12.04) |
| General health | ||||||
| Baseline | 210 | 37.84 (10.43) | 242 | 39.49 (11.08) | 239 | 39.47 (10.20) |
| 4 months | 155 | 39.63 (11.74) | 169 | 41.93 (11.55) | 167 | 41.48 (11.65) |
| 12 months | 136 | 42.39 (12.53) | 156 | 44.04 (12.07) | 150 | 43.27 (11.18) |
| 24 months | 124 | 40.17 (13.18) | 141 | 43.93 (12.75) | 139 | 42.80 (11.41) |
| Vitality | ||||||
| Baseline | 210 | 32.01 (8.10) | 242 | 32.39 (7.70) | 239 | 33.61 (8.05) |
| 4 months | 155 | 38.60 (10.63) | 170 | 40.55 (11.49) | 166 | 40.36 (10.92) |
| 12 months | 137 | 41.77 (11.24) | 156 | 42.58 (11.67) | 151 | 41.51 (11.23) |
| 24 months | 124 | 40.13 (12.05) | 143 | 42.91 (11.81) | 139 | 41.51 (11.57) |
| Social functioning | ||||||
| Baseline | 209 | 30.39 (10.47) | 242 | 29.47 (10.83) | 238 | 31.05 (10.00) |
| 4 months | 155 | 36.37 (12.68) | 170 | 38.18 (12.11) | 167 | 39.21 (11.91) |
| 12 months | 136 | 41.69 (13.22) | 156 | 41.43 (12.64) | 151 | 40.96 (12.29) |
| 24 months | 123 | 38.71 (13.53) | 143 | 41.02 (13.25) | 137 | 41.32 (12.23) |
| Role-emotional | ||||||
| Baseline | 210 | 28.34 (11.26) | 242 | 28.57 (12.12) | 239 | 29.79 (11.07) |
| 4 months | 155 | 36.49 (13.12) | 170 | 37.31 (13.13) | 167 | 38.10 (13.06) |
| 12 months | 137 | 43.00 (12.06) | 156 | 42.55 (12.75) | 151 | 40.02 (14.02) |
| 24 months | 124 | 39.08 (13.88) | 143 | 41.82 (12.47) | 139 | 40.86 (13.18) |
| Mental health | ||||||
| Baseline | 210 | 28.73 (7.98) | 242 | 28.11 (9.01) | 239 | 29.05 (8.78) |
| 4 months | 155 | 36.15 (11.31) | 170 | 38.15 (12.45) | 166 | 38.25 (13.19) |
| 12 months | 137 | 41.11 (12.05) | 156 | 42.67 (11.88) | 151 | 40.17 (13.18) |
| 24 months | 124 | 38.55 (12.81) | 143 | 42.19 (12.16) | 139 | 40.32 (13.08) |
| Characteristic | Beating the Blues | MoodGYM | Usual GP care alone |
|---|---|---|---|
| Baseline | n = 209 | n = 242 | n = 238 |
| PCS score, mean (SD) | 50.31 (11.55) | 51.20 (10.08) | 51.94 (10.40) |
| MCS score, mean (SD) | 22.81 (9.96) | 22.22 (10.55) | 23.51 (9.64) |
| 4 months | n = 155 | n = 169 | n = 166 |
| PCS score, mean (SD) | 48.45 (11.72) | 50.08 (11.22) | 50.29 (10.39) |
| MCS score, mean (SD) | 32.85 (13.27) | 34.50 (14.20) | 34.79 (14.01) |
| 12 months | n = 135 | n = 156 | n = 150 |
| PCS score, mean (SD) | 48.24 (12.46) | 48.80 (11.91) | 49.80 (10.88) |
| MCS score, mean (SD) | 39.56 (12.59) | 40.16 (13.05) | 37.28 (14.93) |
| 24 months | n = 122 | n = 140 | n = 137 |
| PCS score, mean (SD) | 47.45 (13.19) | 47.96 (12.99) | 49.92 (10.70) |
| MCS score, mean (SD) | 36.11 (13.95) | 40.36 (13.04) | 37.79 (14.07) |
FIGURE 7.
Short Form questionnaire-36 items Health Survey version 2 MCS scores over time trial arm comparison. (a) Beating the Blues vs. usual GP care; and (b) MoodGYM vs. usual GP care.
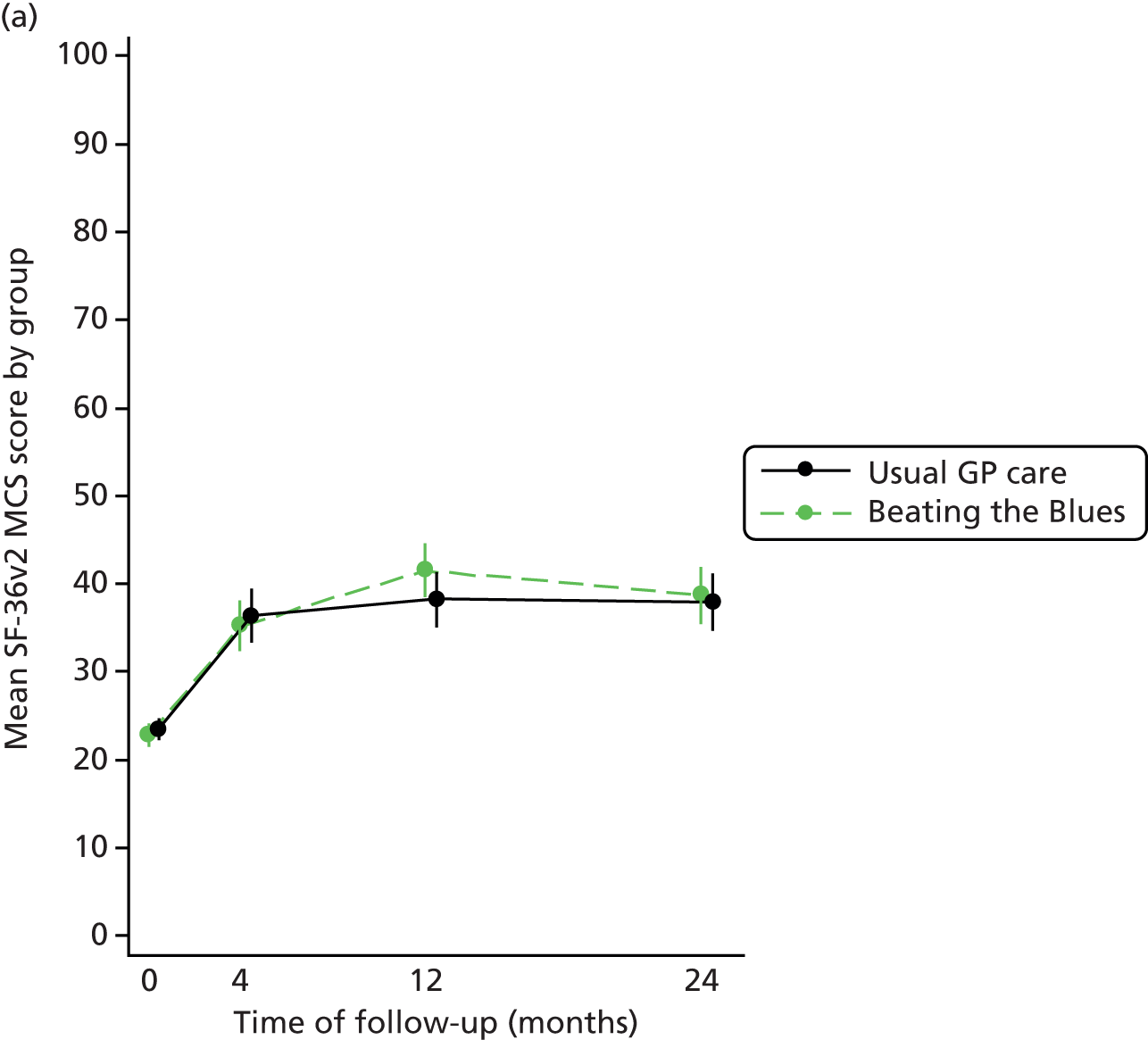

FIGURE 8.
Mean SF-36v2 PCS scores over time trial arm comparison. (a) Beating the Blues vs. usual GP care; and (b) MoodGYM vs. usual GP care.

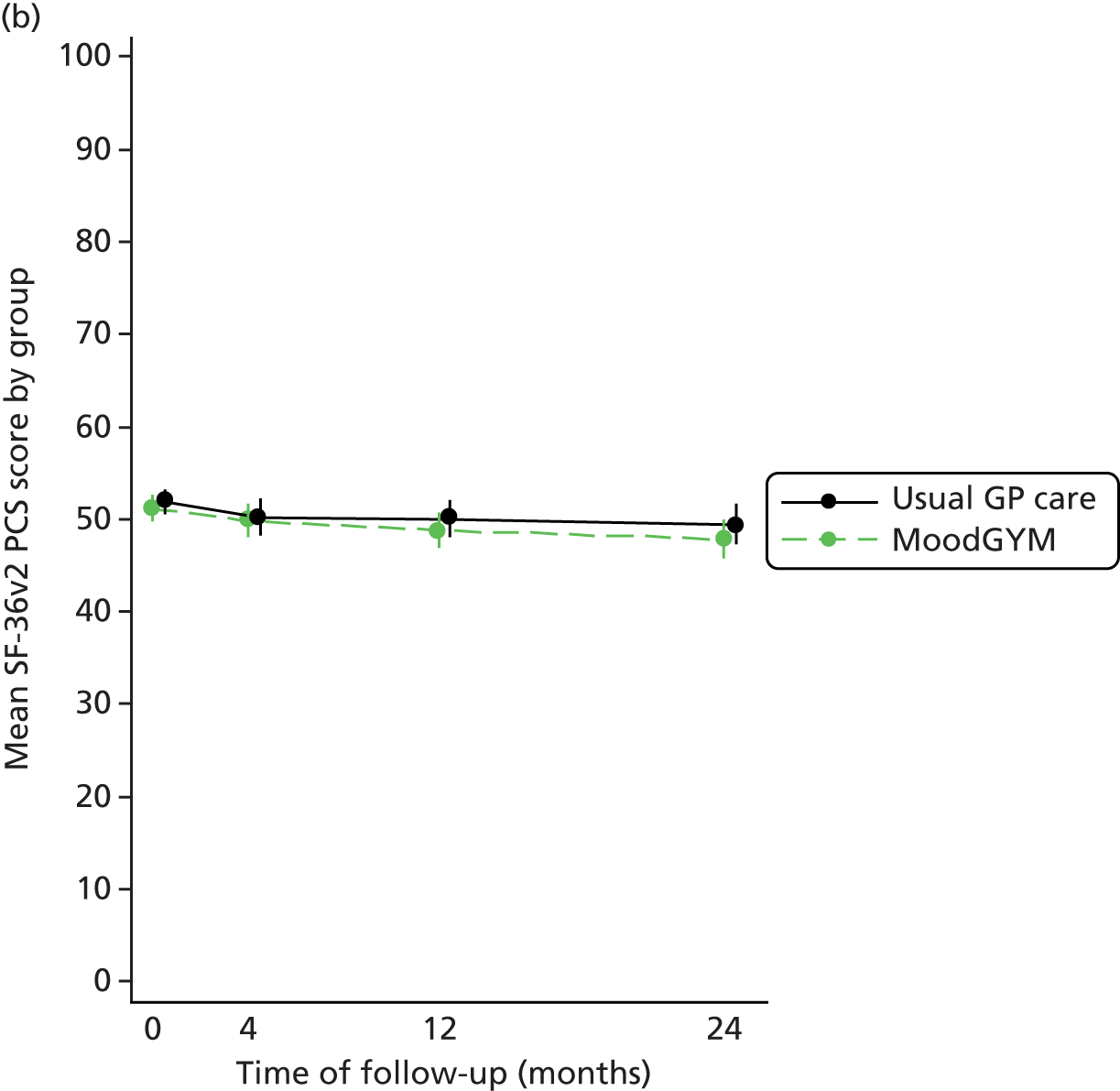
We fitted a repeated measures multilevel regression model to the PCS scores and MCS scores. The values at 4, 12 and 24 months were the outcome measures, and the baseline value, treatment group and time were included as fixed effects. An interaction between treatment and time was also included in the model. Different covariance patterns were assessed for the repeated measurements within participants and, as the results were similar, the model with the smallest AIC was chosen for each component score and comparison (independent for Beating the Blues vs. usual GP care alone and unstructured for MoodGYM vs. usual GP care alone for both component scores). For the Beating the Blues versus usual GP care comparison, there was little or no evidence of an overall difference between the two groups for the MCS (p = 0.40) or for the PCS (p = 0.22), and the mean SF-36v2 MCS score (over all follow-up assessments) was 38.52 (95% CI 35.77 to 41.27) for Beating the Blues and 37.50 (95% CI 34.62 to 40.38) for usual GP care and for the PCS was 48.66 (95% CI 47.05 to 50.28) for Beating the Blues and 49.55 (95% CI 47.86 to 51.23) for usual GP care. For the MoodGYM versus usual GP care comparison, there was evidence of an overall difference between the two groups for the MCS (p = 0.009) but little or no evidence for the PCS (p = 0.14). The mean SF-36v2 MCS score (over all follow-up assessments) was 38.98 (95% CI 36.03 to 41.92) for MoodGYM and 35.99 (95% CI 32.88 to 39.11) for usual GP care and for the PCS was 48.87 (95% CI 47.11 to 50.63) for MoodGYM and 49.91 (95% CI 48.05 to 51.76) for usual GP care. Tables 19 and 20 and Figures 7 and 8 display the results of the mixed model for each time point individually.
| Comparison | Intervention, mean (95% CI) | Usual GP care, mean (95% CI) | Difference (95% CI) | p-value |
|---|---|---|---|---|
| 4 months | ||||
| Beating the Blues vs. usual GP care alone | 35.23 (32.28 to 38.17) | 36.33 (33.29 to 39.37) | – 1.10 (– 3.85 to 1.64) | 0.43 |
| MoodGYM vs. usual GP care alone | 35.07 (31.90 to 38.23) | 34.87 (31.54 to 38.20) | 0.20 (– 2.60 to 2.99) | 0.89 |
| 12 months | ||||
| Beating the Blues vs. usual GP care alone | 41.58 (38.55 to 44.60) | 38.25 (35.11 to 41.39) | 3.32 (0.37 to 6.28) | 0.03 |
| MoodGYM vs. usual GP care alone | 40.91 (37.77 to 44.05) | 36.66 (33.33 to 40.00) | 4.25 (1.47 to 7.02) | 0.003 |
| 24 months | ||||
| Beating the Blues vs. usual GP care alone | 38.76 (35.52 to 41.99) | 37.92 (34.62 to 41.22) | 0.84 (–2.49 to 4.17) | 0.62 |
| MoodGYM vs. usual GP care alone | 40.95 (37.68 to 44.23) | 36.44 (33.03 to 39.86) | 4.51 (1.51 to 7.51) | 0.003 |
| Comparison | Intervention, mean (95% CI) | Usual GP care, mean (95% CI) | Difference (95% CI) | p-value |
|---|---|---|---|---|
| 4 months | ||||
| Beating the Blues vs. usual GP care alone | 49.18 (47.44 to 50.92) | 49.85 (48.05 to 51.64) | – 0.67 (– 2.33 to 0.99) | 0.43 |
| MoodGYM vs. usual GP care alone | 49.86 (47.97 to 51.75) | 50.21 (48.23 to 52.19) | – 0.35 (– 2.04 to 1.33) | 0.68 |
| 12 months | ||||
| Beating the Blues vs. usual GP care alone | 48.61 (46.80 to 50.43) | 49.73 (47.86 to 51.61) | – 1.12 (– 2.95 to 0.71) | 0.23 |
| MoodGYM vs. usual GP care alone | 48.85 (46.96 to 50.73) | 50.06 (48.07 to 52.05) | – 1.21 (– 2.91 to 0.49) | 0.16 |
| 24 months | ||||
| Beating the Blues vs. usual GP care alone | 48.19 (46.17 to 50.22) | 49.06 (47.02 to 51.10) | – 0.87 (– 3.06 to 1.32) | 0.44 |
| MoodGYM vs. usual GP care alone | 47.89 (45.82 to 49.97) | 49.45 (47.30 to 51.60) | – 1.56 (– 3.61 to 0.50) | 0.14 |
Adverse events
A total of 745 NSAEs were reported from 302 participants: 264 events (from 93 participants) in the Beating the Blues group, 240 events (from 99 participants) in the MoodGYM group and 241 events (from 110 participants) in the usual GP care alone group. Table 21 summarises the NSAEs by trial arm and Table 22 summarises the SAEs by trial arm. There were 49 SAEs reported from 39 participants. Of these SAEs, 39 events were classified as unrelated to treatment and nine were classified as unlikely to be related to treatment, with the final event being unable to classify. Five of the reported SAEs were referred to the DMEC for further discussion and two were referred to the REC. Of the 49 SAEs reported, 40 (81.6%) involved inpatient hospitalisation, seven were deemed life-threatening and two resulted in participants dying.
| Summary | Beating the Blues (n = 210) | MoodGYM (n = 242) | Usual GP care alone (n = 239) | Total (n = 691) |
|---|---|---|---|---|
| Total number of NSAEs | 264 | 240 | 241 | 745 |
| Number of participants with one or more NSAEs | 93 (44.3) | 99 (40.9) | 110 (46.0) | 302 (43.7) |
| NSAEs per patient | ||||
| 1 | 27 (29.0) | 36 (36.4) | 49 (44.5) | 112 (37.1) |
| 2 | 30 (32.3) | 21 (21.2) | 31 (28.2) | 82 (27.2) |
| 3 | 14 (15.1) | 22 (22.2) | 13 (11.8) | 49 (16.2) |
| 4 | 6 (6.5) | 12 (12.1) | 7 (6.4) | 25 (8.3) |
| 5 | 5 (5.4) | 6 (6.1) | 6 (5.5) | 17 (5.6) |
| 6 or more | 11 (11.8) | 2 (2.0) | 4 (3.6) | 17 (5.6) |
| Summary | Beating the Blues (N = 210) | MoodGYM (N = 242) | Usual GP care (N = 239) | Total (N = 691) |
|---|---|---|---|---|
| Total number of SAEs | 19 | 11 | 19 | 49 |
| Number of participants with one or more SAEs | 15 (7.1) | 9 (3.7) | 15 (6.3) | 39 (5.6) |
| Events per patient | ||||
| 1 | 12 (80.0) | 7 (77.8) | 11 (73.3) | 30 (76.9) |
| 2 | 2 (13.3) | 2 (22.2) | 4 (26.7) | 8 (20.5) |
| 3 | 1 (6.7) | 0 (0.0) | 0 (0.0) | 1 (2.6) |
| Relationship to treatment | ||||
| Unrelated | 18 (94.7) | 6 (54.5) | 15 (78.9) | 39 (79.6) |
| Unlikely to be related | 0 (0.0) | 5 (45.5) | 4 (21.1) | 9 (18.4) |
| Possibly related | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Probably related | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Definitely related | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Unable to assessa | 1 (5.3) | 0 (0.0) | 0 (0.0) | 1 (2.0) |
| Number of SAEs referred to DMEC | 0 (0.0) | 2 (18.2) | 3 (15.8) | 5 (10.2) |
| Number of SAEs referred to REC | 0 (0.0) | 0 (0.0) | 2 (10.5) | 2 (4.1) |
| Event details | ||||
| Involved inpatient hospitalisationb | 17 (89.5) | 10 (90.9) | 13 (68.4) | 40 (81.6) |
| Life-threateningb,c | 0 (0.0) | 1 (9.1) | 6 (31.6) | 7 (14.3) |
| Patient died | 2 (10.5) | 0 (0.0) | 0 (0.0) | 2 (4.1) |
| Involved persistent or significant disability or incapacityc | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Resulted in a congenital anomaly or birth defect | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
Data on computerised cognitive behaviour therapy usage
Data were obtained on participants’ engagement with the two cCBT programs. This included data relating to participants’ progression through the cCBT programs on a session-by-session basis. Following randomisation, a total of 175 (83%) Beating the Blues participants and 186 (77%) MoodGYM participants went on to access the programs at least once.
In terms of progression through the programs, the median number of Beating the Blues sessions completed was two [interquartile range (IQR) 0–5] and the most frequent number of sessions was one. The median number of sessions completed for MoodGYM was one (IQR 0–2) and the most frequent number of sessions was one. Of the 175 participants who started Beating the Blues, 31 (18%) participants completed all eight sessions of the program; and of the 186 participants who started MoodGYM, a total of 29 (16%) participants completed all six sessions of the program. The average length of time spent using the cCBT programs (from initial access to last session accessed) was 67 days (median 40 days, IQR 1–98 days) for Beating the Blues and 34 days (median 8 days, IQR 1–50 days) for MoodGYM participants.
Data on technical support telephone calls and contacts
Information relating to technical support telephone calls and contacts was recorded for each participant. The default mode of contact was by telephone call, with e-mails and/or texts sent if this alternative mode of communication was specifically requested by the participant. Contact attempts (which included telephone calls, e-mails and texts) were made to participants irrespective of their progression through the cCBT program, meaning that participants could be contacted on a number of separate occasions while still working through the same cCBT session.
A median of 13 contact attempts were made to both Beating the Blues (IQR 11–16) and MoodGYM (IQR 10–16) participants. A total mean of 6.0 (IQR 3–8) technical telephone support calls were made to participants allocated to Beating the Blues. A total mean of 6.8 (IQR 4–9) technical telephone support calls were made to MoodGYM participants. Of the technical telephone support calls made, the mean number of calls answered by participants allocated to Beating the Blues was 3.1 (IQR 1–5), with a mean per call duration of 1.8 minutes (IQR 1–2 minutes). For MoodGYM participants, the mean number of technical telephone support calls answered by participants was 3.3 (IQR 1–5), with a mean per call duration of 2.0 minutes (IQR 1–2 minutes). The total mean number of minutes of technical support calls delivered to participants was 6.2 minutes (IQR 2–8 minutes) for participants allocated to Beating the Blues and 6.5 minutes (IQR 2–9 minutes) for participants allocated to MoodGYM. The mean number of e-mails sent was 5.3 (IQR 2–8) and 5.0 (IQR 1–8) for Beating the Blues and MoodGYM participants, respectively. Few texts were sent (mean of < 0.1 texts sent to both Beating the Blues and MoodGYM participants).
Summary
There was little or no evidence of statistically significant effects of Beating the Blues on the proportion of participants who are depressed across all time points when compared with usual GP care alone. There was some evidence of a statistically significant effect of MoodGYM on the proportion of participants who are depressed when compared with usual GP care at 12 months but this was no longer evident at 24 months and was not present at 4 months. The free-to-use cCBT program MoodGYM was found to be non-inferior to the commercial pay-to-use cCBT program Beating the Blues across all time points. There was no evidence of statistically significant effects of the interactions between patient preference and allocated treatment across any of the comparisons.
There was no evidence of statistically significant effects on the overall (including all time points) mean depression scores, CORE-OM scores and MCS and PCS quality of life scores of Beating the Blues when compared with usual GP care alone; however, there was evidence of a statistically significant effect of Beating the Blues on MCS scores at 12 months. There was no evidence of statistically significant effects on overall (including all time points) mean depression scores and PCS quality of life scores of MoodGYM when compared with usual GP care alone; however, there was evidence of a statistically significant effect of MoodGYM on the mean depression scores at 12 months when compared with usual GP care. There was evidence of statistically significant effects on the overall (including all time points) mean CORE-OM scores and MCS quality of life scores of MoodGYM when compared with usual GP care alone, with highly statistically significant effects of MoodGYM on CORE-OM scores at 12 months and MCS quality of life scores at 12 and 24 months when compared with usual GP care alone.
Participant engagement with the cCBT programs was low for both Beating the Blues and MoodGYM, with the majority of participants not completing the series of sessions. Participants were offered and received similar levels of technical telephone support across Beating the Blues and MoodGYM programs.
Some of this text has been reproduced from Gilbody et al. 11 © BMJ 2015. This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/.
Chapter 5 Economic evaluation results
Health-care resource use
Descriptive statistics (mean, SD, median and IQR) of health-care resource use by resource category per time period during trial follow-up, and aggregated for the full duration of the trial, are shown in Tables 23–25. The unit costs applied to resource use items to calculate total costs are also presented within the tables. The results presented are based on the available case data set, as multiple imputation was performed for total costs as opposed to individual resource use items.
| Service | Beating the Blues (n = 173) | MoodGYM (n = 205) | Usual GP care alone (n = 202) | Unit | Unit cost or range (£) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean (SD) | Median (IQR) | Used by (%) | Mean (SD) | Median (IQR) | Used by (%) | Mean (SD) | Median (IQR) | Used by (%) | |||
| Primary care | |||||||||||
| GP | 7.66 (5.48) | 7.0 (7.0) | 96.49 | 6.98 (4.62) | 6.00 (7.00) | 97.51 | 6.94 (4.82) | 6.00 (5.74) | 95.92 | Contact | 26.00–110.00 |
| Nurse | 1.60 (2.31) | 1.00 (2.00) | 57.89 | 2.03 (3.86) | 1.00 (3.00) | 61.19 | 1.86 (2.85) | 1.00 (2.50) | 62.76 | Contact | 2.10–32.54 |
| Out of hours | 0.09 (0.33) | 0.00 (0.00) | 8.19 | 0.06 (0.26) | 0.00 (0.00) | 5.47 | 0.07 (0.31) | 0.00 (0.00) | 5.61 | Contact | 61.14 |
| Hospital | |||||||||||
| Inpatient | 0.23 (1.08) | 0.00 (0.00) | 6.10 | 0.12 (1.63) | 0.00 (0.00) | 6.53 | 0.18 (0.84) | 0.00 (0.00) | 6.19 | Length of stay | 206.89–430.14 |
| Outpatient | 1.07 (2.62) | 0.00 (1.00) | 37.87 | 0.99 (2.09) | 0.00 (1.00) | 38.86 | 0.77 (1.20) | 0.00 (1.00) | 40.21 | Attendance | 14.00–459.00 |
| Other community services | |||||||||||
| IAPT | 0.25 (1.23) | 0.00 (0.00) | 5.29 | 0.33 (1.46) | 0.00 (0.00) | 6.97 | 0.41 (1.25) | 0.00 (0.00) | 12.76 | Visit | 70.35 |
| CMHT | 0.20 (1.58) | 0.00 (0.00) | 5.26 | 0.08 (0.41) | 0.00 (0.00) | 4.48 | 0.14 (0.70) | 0.00 (0.00) | 6.12 | Visit | 44.84 |
| Counsellor | 0.28 (1.65) | 0.00 (0.00) | 5.29 | 0.13 (0.86) | 0.00 (0.00) | 3.48 | 0.04 (0.29) | 0.00 (0.00) | 2.04 | Visit | 59.00 |
| Psychiatric | 0.17 (1.16) | 0.00 (0.00) | 4.68 | 0.11 (0.88) | 0.00 (0.00) | 1.99 | 0.13 (0.82) | 0.00 (0.00) | 3.06 | Visit | 174.64 |
| Psychological | 0.46 (2.95) | 0.00 (0.00) | 4.09 | 0.01 (0.21) | 0.00 (0.00) | 0.50 | 0.37 (2.26) | 0.00 (0.00) | 4.08 | Visit | 70.08 |
| Medication | |||||||||||
| Depression-related | NA | NA | 81.55 | NA | NA | 76.77 | NA | NA | 83.94 | Item | Various |
| Service | Beating the Blues (n = 173) | MoodGYM (n = 205) | Usual GP care alone (n = 202) | Unit | Unit cost or range (£) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean (SD) | Median (IQR) | Used by (%) | Mean (SD) | Median (IQR) | Used by (%) | Mean (SD) | Median (IQR) | Used by (%) | |||
| Primary care | |||||||||||
| GP | 6.31 (5.41) | 5.00 (7.00) | 90.74 | 5.41 (5.14) | 4.00 (6.00) | 86.15 | 5.13 (4.62) | 4.00 (7.00) | 85.86 | Contact | 26.00–110.00 |
| Nurse | 1.89 (3.08) | 1.00 (3.00) | 58.28 | 1.82 (3.29) | 1.00 (2.50) | 50.51 | 1.88 (3.57) | 1.00 (3.00) | 54.45 | Contact | 2.10 – 32.54 |
| Out of hours | 0.15 (0.61) | 0.00 (0.00) | 9.20 | 0.06 (0.26) | 0.00 (0.00) | 5.61 | 0.07 (0.29) | 0.00 (0.00) | 5.76 | Contact | 61.14 |
| Hospital | |||||||||||
| Inpatient | 0.12 (0.69) | 0.00 (0.00) | 4.49 | 0.07 (0.45) | 0.00 (0.00) | 3.09 | 0.17 (1.08) | 0.00 (0.00) | 4.23 | Length of stay | 206.89–430.14 |
| Outpatient | 0.98 (1.81) | 0.00 (1.00) | 41.61 | 0.89 (1.75) | 0.00 (1.00) | 34.22 | 0.79 (1.26) | 0.00 (1.00) | 38.80 | Attendance | 14.00–459.00 |
| Other community services | |||||||||||
| IAPT | 0.08 (0.60) | 0.00 (0.00) | 1.85 | 0.04 (0.43) | 0.00 (0.00) | 1.02 | 0.07 (0.44) | 0.00 (0.00) | 2.62 | Visit | 70.35 |
| CMHT | 0.00 (0.00) | 0.00 (0.00) | 0.00 | 0.02 (0.21) | 0.00 (0.00) | 1.53 | 0.15 (1.18) | 0.00 (0.00) | 4.19 | Visit | 44.84 |
| Counsellor | 0.14 (1.12) | 0.00 (0.00) | 3.09 | 0.06 (0.56) | 0.00 (0.00) | 1.02 | 0.06 (0.48) | 0.00 (0.00) | 2.09 | Visit | 59.00 |
| Psychiatric | 0.07 (0.86) | 0.00 (0.00) | 0.61 | 0.01 (0.07) | 0.00 (0.00) | 0.51 | 0.03 (0.32) | 0.00 (0.00) | 1.05 | Visit | 174.64 |
| Psychological | 0.03 (0.39) | 0.00 (0.00) | 0.61 | 0.01 (0.10) | 0.00 (0.00) | 1.02 | 0.18 (1.31) | 0.00 (0.00) | 3.14 | Visit | 70.08 |
| Medication | |||||||||||
| Depression-related | NA | NA | 68.75 | NA | NA | 65.80 | NA | NA | 69.68 | Item | Various |
| Service | Beating the Blues (n = 173) | MoodGYM (n = 205) | Usual GP care alone (n = 202) | Unit | Unit cost or range (£) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean (SD) | Median (IQR) | Used by (%) | Mean (SD) | Median (IQR) | Used by (%) | Mean (SD) | Median (IQR) | Used by (%) | ||||
| Primary care | ||||||||||||
| GP | 13.91 (9.23) | 12.00 (15.00) | 98.15 | 12.24 (8.55) | 10.00 (11.00) | 98.46 | 12.03 (8.15) | 11.00 (10.00) | 96.34 | Contact | 26.00–110.00 | |
| Nurse | 3.56 (4.45) | 2.00 (4.00) | 75.46 | 3.88 (5.85) | 2.00 (5.00) | 72.96 | 3.76 (5.14) | 2.00 (5.00) | 74.87 | Contact | 2.10–32.54 | |
| Out of Hours | 0.24 (0.70) | 0.00 (0.00) | 16.56 | 0.12 (0.41) | 0.00 (0.00) | 9.18 | 0.14 (0.49) | 0.00 (0.00) | 10.47 | Contact | 61.14 | |
| Hospital | ||||||||||||
| Inpatient | 0.36 (1.55) | 0.00 (0.00) | 9.62 | 0.66 (5.29) | 0.00 (0.00) | 9.28 | 0.36 (1.36) | 0.00 (0.00) | 10.05 | Length of stay | 206.89–430.14 | |
| Outpatient | 2.10 (3.68) | 1.00 (3.00) | 12.43 | 1.84 (2.99) | 1.00 (2.00) | 10.36 | 1.54 (1.96) | 1.00 (2.00) | 8.47 | Attendance | 14.00–459.00 | |
| Other community services | ||||||||||||
| IAPT | 0.31 (1.35) | 0.00 (0.00) | 6.79 | 0.38 (1.53) | 0.00 (0.00) | 8.16 | 0.45 (1.27) | 0.00 (0.00) | 14.66 | Visit | 70.35 | |
| CMHT | 0.21 (1.62) | 0.00 (0.00) | 5.52 | 0.11 (0.46) | 0.00 (0.00) | 6.12 | 0.30 (1.36) | 0.00 (0.00) | 10.47 | Visit | 44.84 | |
| Counsellor | 0.33 (1.51) | 0.00 (0.00) | 8.02 | 0.19 (1.02) | 0.00 (0.00) | 4.59 | 0.10 (0.56) | 0.00 (0.00) | 4.19 | Visit | 59.00 | |
| Psychiatric | 0.24 (2.01) | 0.00 (0.00) | 4.91 | 0.12 (0.90) | 0.00 (0.00) | 2.55 | 0.17 (0.89) | 0.00 (0.00) | 4.19 | Visit | 174.64 | |
| Psychological | 0.51 (3.34) | 0.00 (0.00) | 4.29 | 0.03 (0.24) | 0.00 (0.00) | 1.53 | 0.56 (2.83) | 0.00 (0.00) | 6.28 | Visit | 70.08 | |
| Medication | ||||||||||||
| Depression-related | NA | NA | 83.13 | NA | NA | 82.38 | NA | NA | 85.64 | Item | Various | |
Regarding the completeness of data, resource use data were available for 83.9% (n = 580) of all trial participants during the 2 years of follow-up. In general, differences between treatment groups in resource use appeared small, and resource use estimates appeared considerably variable with large SDs. Regarding the dispersion of the results, median estimates were smaller than means for all resource categories, treatment groups and follow-up periods. Medians were equal to zero for all treatment groups and resource use categories, except GP and nurse visits in both follow-up periods. This suggests that the distributions were skewed to the right.
Costs
Mean costs from baseline to 12 months and from 12 months to 24 months by treatment arm are shown in Table 26. The results are presented by type of services, namely primary care, hospital and other community services. Costs of depression-related medication and cCBT are also shown. Table 27 reports undiscounted and discounted costs aggregated for the full 24-month duration of the trial. All costs results were estimated from the multiple imputed data sets.
| Costs | Period covered: Baseline to 12 months | Period covered: 12 to 24 months | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Beating the Blues | MoodGYM | Usual GP care alone | Beating the Blues | MoodGYM | Usual GP care alone | |||||||
| Mean cost (£) (SE) | % of total | Mean cost (£) (SE) | % of total | Mean cost (£) (SE) | % of total | Mean cost (£) (SE) | % of total | Mean cost (£) (SE) | % of total | Mean cost (£) (SE) | % of total | |
| Primary care services | 348.12 (18.17) | 48.34 | 319.20 (15.45) | 45.90 | 320.05 (16.78) | 54.42 | 290.26 (19.40) | 60.14 | 252.93 (17.82) | 60.55 | 245.10 (16.70) | 54.73 |
| Hospital services | 179.22 (30.97) | 24.89 | 272.50 (112.47) | 39.18 | 148.92 (25.71) | 25.32 | 127.70 (27.28) | 26.46 | 115.38 (19.09) | 27.71 | 132.94 (24.80) | 29.69 |
| Other community services | 103.42 (31.58) | 14.36 | 62.13 (15.68) | 8.93 | 82.56 (18.04) | 14.04 | 27.03 (11.86) | 5.60 | 10.32 (5.66) | 2.48 | 29.94 (8.46) | 6.69 |
| Depression-related medication | 38.91 (5.36) | 5.40 | 40.95 (6.38) | 5.89 | 36.55 (5.52) | 6.22 | 37.65 (7.55) | 7.80 | 38.57 (7.12) | 9.26 | 39.85 (8.43) | 8.90 |
| cCBT | 50.43 (0.00) | 7.00 | 0.66 (0.00) | 0.09 | 0.00 (0.00) | 0.00 | 0.00 (0.00) | 0.00 | 0.00 (0.00) | 0.00 | 0.00 (0.00) | 0.00 |
| Total | 720.11 (50.13) | 100.00 | 695.43 (120.00) | 100.00 | 588.08 (38.74) | 100.00 | 482.64 (41.33) | 100.00 | 417.21 (32.29) | 100.00 | 447.82 (37.93) | 100.00 |
| Costs | Period covered: Baseline to 24 months – undiscounted | Period covered: Baseline to 24 months – discounted | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Beating the Blues | MoodGYM | Usual GP care alone | Beating the Blues | MoodGYM | Usual GP care alone | |||||||
| Mean (SE) (£) | % of total | Mean (SE) (£) | % of total | Mean (SE) (£) | % of total | Mean (SE) (£) | % of total | Mean (SE) (£) | % of total | Mean (SE) (£) | % of total | |
| Primary care services | 638.39 (32.90) | 53.08 | 572.13 (28.99) | 51.42 | 565.15 (29.09) | 54.56 | 628.58 (32.32) | 52.98 | 563.58 (28.45) | 51.30 | 556.86 (28.61) | 54.55 |
| Hospital services | 306.92 (43.78) | 25.52 | 387.88 (116.25) | 34.86 | 281.85 (36.13) | 27.21 | 302.60 (43.20) | 25.51 | 383.98 (116.07) | 34.95 | 277.36 (35.54) | 27.17 |
| Other community services | 130.45 (31.58) | 10.85 | 72.45 (17.36) | 6.51 | 112.49 (21.01) | 10.86 | 129.53 (31.28) | 10.92 | 72.10 (17.27) | 6.56 | 111.48 (20.86) | 10.92 |
| Depression-related medication | 76.55 (11.94) | 6.36 | 79.52 (13.10) | 7.15 | 76.40 (12.77) | 7.38 | 75.28 (11.70) | 6.35 | 78.22 (12.86) | 7.12 | 75.05 (12.51) | 7.35 |
| cCBT | 50.43 (0.00) | 4.19 | 0.66 (0.00) | 0.06 | 0.00 (0.00) | 0.00 | 50.43 (0.00) | 4.25 | 0.66 (0.00) | 0.06 | 0.00 (0.00) | 0.00 |
| Total costs | 1202.75 (79.97) | 100.00 | 1112.64 (134.63) | 100.00 | 1035.90 (61.58) | 100.00 | 1186.43 (78.79) | 100.00 | 1098.53 (134.04) | 100.00 | 1020.76 (60.56) | 100.00 |
Primary care services represented the largest share of health-care expenditure for all treatment groups in both trial follow-up periods, constituting over 50% of total costs for all groups. The second largest category of costs was hospital services, which varied from 25% to 35% across the groups.
Total (discounted) costs for the 24 months were £1186 for Beating the Blues plus usual GP care, £1121 for usual GP care alone and £1098 for MoodGYM plus usual GP care group. There is limited value in interpreting differences in mean costs across time periods and for different treatment groups at this level, as the results shown in Table 27 are unadjusted for baseline costs and participant covariates. The adjusted mean differences for each cCBT treatment versus usual GP care alone and corresponding 95% CIs, obtained through regression analysis, are reported within the cost-effectiveness results section (see Cost-effectiveness analysis).
Health-related quality of life
Table 28 shows the extent to which EQ-5D questionnaires were completed at each time point during trial follow-up. Table 29 shows the corresponding information for SF-6D scores.
| Treatment group | Time point (month), n | Time point (month), % | ||||||
|---|---|---|---|---|---|---|---|---|
| 0 | 4 | 12 | 24 | 0 | 4 | 12 | 24 | |
| Beating the Blues | 210 | 157 | 144 | 129 | 100.00 | 74.7 | 68.57 | 61.43 |
| MoodGYM | 242 | 170 | 159 | 144 | 100.00 | 70.25 | 65.70 | 59.50 |
| Usual GP care alone | 239 | 167 | 156 | 143 | 100.00 | 69.87 | 65.27 | 59.83 |
| Treatment group | Time point (month), n | Time point (month), % | ||||||
|---|---|---|---|---|---|---|---|---|
| 0 | 4 | 12 | 24 | 0 | 4 | 12 | 24 | |
| Beating the Blues | 209 | 155 | 132 | 117 | 99.52 | 73.81 | 62.86 | 55.71 |
| MoodGYM | 242 | 170 | 155 | 139 | 100.00 | 70.25 | 64.05 | 57.44 |
| Usual GP care alone | 237 | 165 | 147 | 135 | 99.16 | 69.04 | 61.51 | 56.49 |
There was a steady decrease in completed EQ-5D questionnaires throughout trial follow-up. The rate of questionnaire return was slightly higher for the Beating the Blues plus usual GP care treatment group but, in general, it was similar for all treatment groups.
The pattern of response to SF-6D is similar to that of EQ-5D, with the response rate decreasing over time. Tables 30 and 31 summarise the unadjusted HRQoL scores and QALY estimates obtained from EQ-5D and SF-6D, respectively, from the multiple imputed data sets.
| Outcome | Beating the Blues, mean (SE) | MoodGYM, mean (SE) | Usual GP care alone, mean (SE) |
|---|---|---|---|
| Baseline | 0.6162 (0.0173) | 0.6111 (0.0173) | 0.6256 (0.0174) |
| 4 months | 0.6854 (0.0204) | 0.6851 (0.0211) | 0.7275 (0.0184) |
| 12 months | 0.6914 (0.0225) | 0.7186 (0.0203) | 0.7081 (0.0210) |
| 24 months | 0.6677 (0.0234) | 0.6734 (0.0250) | 0.7093 (0.0216) |
| QALYs | 1.3325 (0.0337) | 1.3564 (0.0330) | 1.3888 (0.0328) |
| Outcome | Beating the Blues, mean (SE) | MoodGYM, mean (SE) | Usual GP care alone, mean (SE) |
|---|---|---|---|
| Baseline | 0.5702 (0.0054) | 0.5705 (0.0050) | 0.5790 (0.0050) |
| 4 months | 0.6223 (0.0084) | 0.6359 (0.0080) | 0.6540 (0.0087) |
| 12 months | 0.6528 (0.0114) | 0.6668 (0.0088) | 0.6666 (0.0087) |
| 24 months | 0.6360 (0.0137) | 0.6368 (0.0080) | 0.6580 (0.0102) |
| QALYs | 1.2464 (0.0177) | 1.2810 (0.0135) | 1.2856 (0.0144) |
Mean QALYs estimated through EQ-5D over 24 months (discounted at 3.5% rate for QALYs accrued in the last 12 months of follow-up) were 1.3325 for Beating the Blues plus usual GP care, 1.3888 for usual GP care alone and 1.3564 for MoodGYM plus usual GP care. Mean QALYs estimated through SF-6D over 24 months (discounted at 3.5% rate for QALYs accrued in the last 12 months of follow-up) were 1.2464 for Beating the Blues plus usual GP care, 1.2856 for usual GP care alone and 1.2810 for MoodGYM plus usual GP care.
As for total costs, HRQoL scores and QALYs estimates shown here are unadjusted means, and, therefore, there is limited value in interpreting differences between treatments. Mean differences for each cCBT treatment versus usual GP care alone and corresponding 95% CIs, adjusted for patient covariates by regression analysis, are shown in the following section.
Cost-effectiveness analysis
Table 32 shows the results for the differences in mean costs and QALYs adjusted for patient covariates, between each cCBT treatment group and usual GP care alone. In general, differences in costs and QALYs between both cCBT groups and usual GP care alone were small with wide CIs and were not statistically significant at a 5% significance level.
| Comparison | Adjusted difference in means | 95% confidence limits | |
|---|---|---|---|
| Lower | Upper | ||
| QALYsa (n = 691) | |||
| Beating the Blues vs. usual GP care alone (n = 210 and n = 239, respectively) | – 0.0435 | – 0.1167 | 0.0297 |
| MoodGYM vs. usual GP care alone (n = 242 and n = 239, respectively) | – 0.0153 | – 0.0919 | 0.0613 |
| Total costsb (n = 691) | |||
| Beating the Blues vs. usual GP care alone (n = 210 and n = 239, respectively) | £104.24 | – £66.77 | £275.26 |
| MoodGYM vs. usual GP care alone (n = 242 and n = 239, respectively) | – £106.07 | – £261.65 | £49.52 |
Results for the SUR models, where incremental QALYs and costs are estimated simultaneously, are presented in Appendix 13. The estimates from the SUR model are very similar to those estimated for the base-case analysis. The results lack statistical significance (5% level of significance) and CIs on both models are wide (and overlap between models).
Base-case cost-effectiveness results
Table 33 presents the fully incremental cost-effectiveness estimates and probability that each intervention is cost-effective at a threshold of £20,000 per QALY.
| Treatment group | Δ costsa (£) | Δ QALYsa | ICERa (£ per QALY) | Probability cost-effective at £20,000/QALY |
|---|---|---|---|---|
| Beating the Blues | 104.24 | – 0.0435 | Dominated | 0.038 |
| MoodGYM | – 106.07 | – 0.0153 | 6933b | 0.417 |
| Usual GP care alone | – | – | – | 0.545 |
Beating the Blues plus usual GP care is dominated by usual GP care alone, with higher mean costs and lower QALYs. As both mean costs and QALYs were lower for MoodGYM plus usual GP care than for usual GP care alone, the ICER estimated falls within the south-west quadrant of the cost-effectiveness plane. In this quadrant, the interpretation of the ICER is estimated using the difference in costs and QALYs between the lower-cost intervention (in this case, MoodGYM) and the higher-cost intervention (usual GP care alone). Consequently, the ICER of £6933 per additional QALY actually represents the ICER of usual GP care alone versus MoodGYM. As this falls within the £20,000 per QALY threshold, the conclusion is that usual GP care alone is cost-effective when compared with MoodGYM plus usual GP care. Consequently, these main results do not provide evidence supporting the cost-effectiveness of either Beating the Blues or MoodGYM compared with usual GP care alone.
Table 33 also reports probabilities of cost-effectiveness for each of the treatments under comparison at a cost-effectiveness threshold of £20,000 per QALY. The corresponding CEACs, showing the probability of each treatment being cost-effective across a range of cost-effectiveness thresholds, are shown in Figure 9. At a £20,000 per QALY threshold, usual GP care alone is the treatment most likely to be cost-effective (0.545 probability of cost-effectiveness), followed by MoodGYM plus usual GP care (0.417 probability of cost-effectiveness) and Beating the Blues plus usual GP care (0.038 probability of cost-effectiveness).
FIGURE 9.
Base case cost-effectiveness acceptability curve.

Figures 10 and 11 present the incremental cost and effectiveness estimates of the comparator (Beating the Blues or MoodGYM) compared with usual GP care alone taken from the probabilistic sensitivity analysis. Each point represents the incremental costs and effectiveness given one particular realisation of uncertainty. The £20,000 per QALY line represents the cost-effectiveness threshold. All points south-east of this line represent realisations of uncertainty when the comparator (Beating the Blues or MoodGYM) is cost-effective compared with usual GP care alone at a cost-effectiveness threshold of £20,000 per QALY.
FIGURE 10.
Distribution of incremental costs and QALYs of Beating the Blues vs. usual GP care alone.

FIGURE 11.
Distribution of incremental costs and QALYs of MoodGYM vs. usual GP care alone.
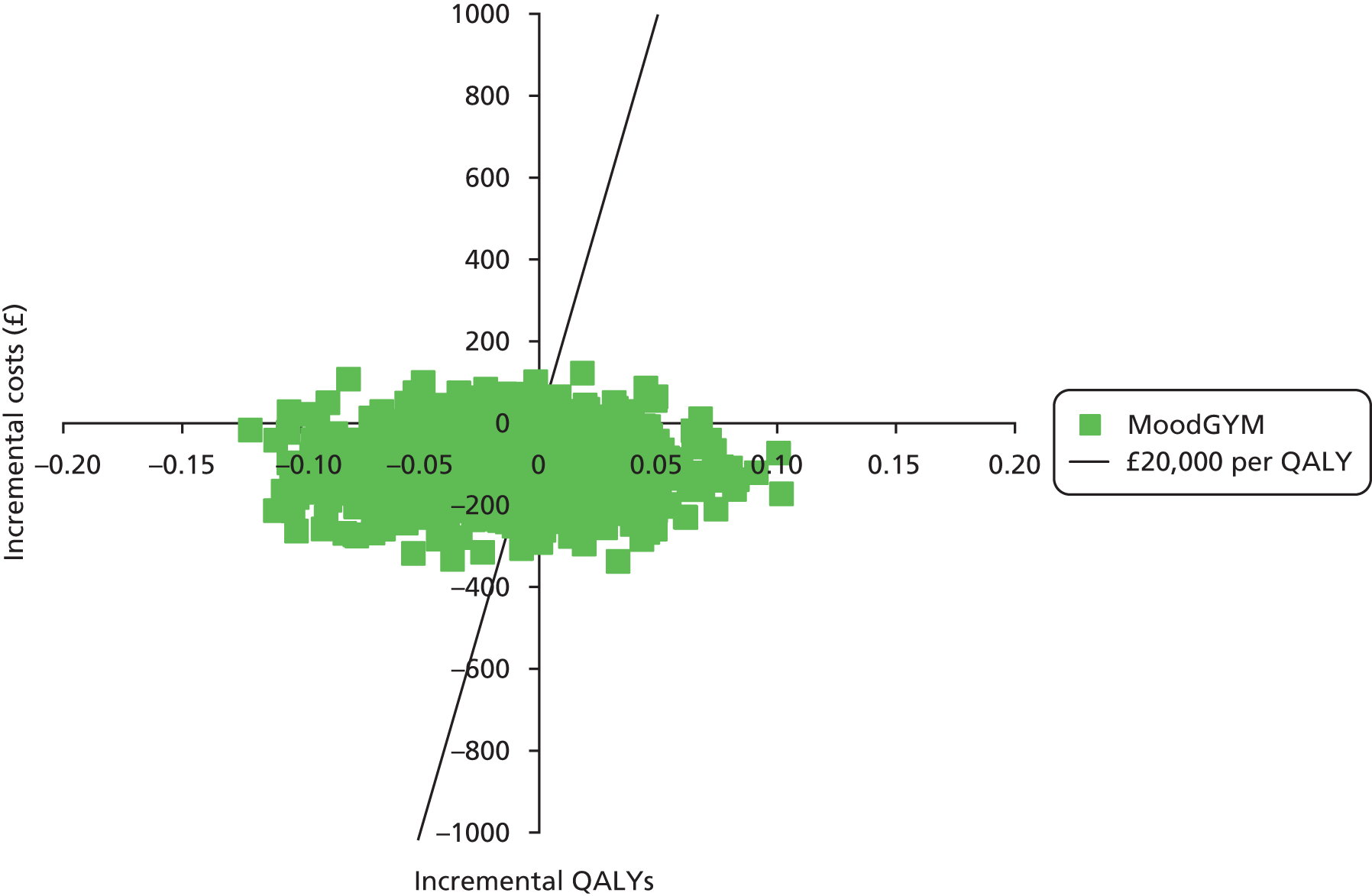
Sensitivity analysis
A series of scenario analyses were conducted to test the robustness of the base-case results to alternative assumptions, as previously described in Chapter 2. Tables 34 and 35 show the results for scenario 1, where SF-6D scores were used to calculate QALYs instead of EQ-5D scores. Difference in means for QALYs (SF-6D estimated) between each cCBT treatment group compared with usual GP care alone (adjusted for participant covariates) are presented in Table 34.
| Comparison | Adjusted difference in means | 95% confidence limits | |
|---|---|---|---|
| Lower | Upper | ||
| QALYs – SF-6Da (n = 691) | |||
| Beating the Blues vs. usual GP care alone (n = 210 and n = 239, respectively) | – 0.0277 | – 0.0672 | 0.0118 |
| MoodGYM vs. usual GP care alone (n = 242 and n = 239, respectively) | 0.0058 | – 0.0294 | 0.0409 |
| Treatment group | Δ costs (£) | Δ QALYs | ICER (£ per QALY) | Probability of CE at £20,000/QALY |
|---|---|---|---|---|
| Beating the Blues | 104.24 | – 0.0277 | Dominated | 0.007 |
| MoodGYM | –106.07 | 0.0058 | Dominant | 0.756 |
| Usual GP care alone | – | – | – | 0.237 |
Consistent with the main analysis, Beating the Blues plus usual GP care was less effective, on average, than usual GP care alone (– 0.0277 QALYs). In contrast to the main analysis, when QALYs were generated using SF-6D values, MoodGYM plus usual GP care had a positive, albeit small, QALY increment (0.0058). Nevertheless, the estimates were not statistically significant at a 5% significance level for comparison of either cCBT program against usual GP care alone.
Table 35 reports the cost-effectiveness results for scenario 1. Although Beating the Blues remains dominated compared with usual GP care alone, MoodGYM now appears cost-effective, resulting in lower mean costs and higher mean QALYs compared with usual GP care alone. At a £20,000 per QALY threshold, MoodGYM has a 0.756 probability of being the optimal intervention in terms of cost-effectiveness.
Although the results appear sensitive to the choice of whether EQ-5D or SF-6D was used to estimate QALYs, with different conclusions reached concerning the cost-effectiveness of MoodGYM, it should be noted that the differences between all three groups were relatively minor in terms of both costs and QALYs in both sets of analyses. Therefore, minor differences in the assumptions can lead to different cost-effectiveness interpretations because of relatively small impacts on the mean incremental estimates of costs and QALYs.
Table 36 shows the results for scenario 2, where only depression-related treatment costs are considered (in contrast to all health-care costs in the base case). The estimated impact of each cCBT treatment group compared with usual GP care alone (adjusted for participant covariates) on depression-related costs is presented. In this scenario, the results for the incremental costs were consistent with the main analysis, albeit the magnitude of the differences between the cCBT groups and usual GP care was reduced.
| Comparison | Adjusted difference in means | 95% confidence limits | |
|---|---|---|---|
| Lower | Upper | ||
| Depression-related costsa (n = 691) | |||
| Beating the Blues vs. usual GP care alone (n = 210 and n = 239, respectively) | £52.55 | – £45.48 | £150.58 |
| MoodGYM vs. usual GP care alone (n = 242 and n = 239, respectively) | – £57.15 | – £142.98 | £28.67 |
Scenarios 3–5 relax the base-case assumption that data are missing at random and assume, instead, that data are missing completely at random and analyses are, therefore, conducted on a complete case data set. Scenario analysis 3 replicated the base-case analysis on the complete case data set. In scenario 4, HRQoL was sourced on the SF-6D questionnaire and the analysis was performed on the correspondent complete case data set. Finally, in scenario 5 only depression-related costs were included in the analysis which was also conducted on the complete case data set. Results for the adjusted differences in mean QALYs and/or costs between each cCBT treatment group compared with usual GP care are presented in Tables 37–39.
| Comparison | Adjusted difference in means | 95% confidence limits | |
|---|---|---|---|
| Lower | Upper | ||
| QALYs – EQ-5Da (n = 290) | |||
| Beating the Blues vs. usual GP care alone (n = 89 and n = 101, respectively) | – 0.0485 | – 0.1488 | 0.0518 |
| MoodGYM vs. usual GP care alone (n = 100 and n = 101, respectively) | – 0.0295 | – 0.1264 | 0.0674 |
| Total costsb (n = 290) | |||
| Beating the Blues vs. usual GP care alone (n = 89 and n = 101, respectively | – £23.62 | – £247.75 | £200.51 |
| MoodGYM vs. usual GP care alone (n = 100 and n = 101, respectively) | – £176.54 | – £386.44 | £33.37 |
| Comparison | Adjusted difference in means | 95% confidence limits | |
|---|---|---|---|
| Lower | Upper | ||
| QALYs – SF-6Da (n = 265) | |||
| Beating the Blues vs. usual GP care alone (n = 77 and n = 92, respectively) | – 0.0297 | – 0.0791 | 0.0196 |
| MoodGYM vs. usual GP care alone (n = 96 and n = 92, respectively) | 0.0028 | – 0.0436 | 0.0491 |
| Total costsb (n = 265) | |||
| Beating the Blues vs. usual GP care alone (n = 77 and n = 92, respectively) | £25.96 | – £214.87 | £266.80 |
| MoodGYM vs. usual GP care alone (n = 76 and n = 92, respectively) | – £157.92 | – £372.00 | £56.16 |
| Comparison | Adjusted difference in means | 95% confidence limits | |
|---|---|---|---|
| Lower | Upper | ||
| QALYs – EQ-5Da (n = 290) | |||
| Beating the Blues vs. usual GP care alone (n = 89 and n = 101, respectively) | –0.0485 | – 0.1488 | 0.0518 |
| MoodGYM vs. usual GP care alone (n = 100 and n = 101, respectively) | –0.0295 | – 0.1264 | 0.0674 |
| Depression-related costsb (n = 290) | |||
| Beating the Blues vs. usual GP care alone (n = 89 and n = 101, respectively) | – £42.27 | – £173.21 | £88.67 |
| MoodGYM vs. usual GP care alone (n = 100 and n = 101, respectively) | – £115.35 | – £234.08 | £3.37 |
Table 40 reports the incremental cost-effectiveness results for these three scenarios. CEACs for each scenario are reported in Appendix 14. The results of all scenarios based on complete case data were consistent with the findings based on the imputed data.
| Scenario | Δ costs (£) | Δ QALYs | ICERa (£ per QALY) | Probability of CE at £20,000/QALY |
|---|---|---|---|---|
| Scenario 3 – complete case | ||||
| Beating the Blues | – 23.62 | – 0.0485 | 487b | 0.109 |
| MoodGYM | – 176.54 | – 0.0295 | 5984b | 0.290 |
| Usual GP care alone | – | – | – | 0.601 |
| Scenario 4 – complete case and SF-6D as HRQoL sources | ||||
| Beating the Blues | 25.96 | – 0.0297 | Dominated | 0.017 |
| MoodGYM | – 157.92 | 0.0028 | Dominant | 0.662 |
| Usual GP care alone | – | – | – | 0.321 |
| Scenario 5 – complete case and depression-related costs | ||||
| Beating the Blues | – 42.27 | – 0.0485 | 872b | 0.100 |
| MoodGYM | – 115.35 | – 0.0295 | 3910b | 0.281 |
| Usual GP care alone | – | – | – | 0.619 |
Subgroup analysis
Preference subgroup analysis
The cost-effectiveness estimates for the preference subgroup analysis are shown in Table 41.
| Analysis | Δ costsa (£) | Δ QALYsa | ICERa (£ per QALY) | Probability of CE at £20,000/QALY |
|---|---|---|---|---|
| Base case | ||||
| Beating the Blues | 104.24 | – 0.0435 | Dominated | 0.038 |
| MoodGYM | – 106.07 | – 0.0153 | 6933b | 0.417 |
| Usual GP care alone | – | – | – | 0.545 |
| No preference | ||||
| Beating the Blues | 295.26 | – 0.0599 | Dominated | 0.124 |
| MoodGYM | 89.41 | 0.0117 | 7615 | 0.560 |
| Usual GP care alone | – | – | – | 0.440 |
| Preference | ||||
| Beating the Blues | – 4.62 | – 0.0341 | 135b | 0.124 |
| MoodGYM | – 210.87 | – 0.0285 | 7390b | 0.303 |
| Usual GP care alone | – | – | – | 0.573 |
In line with the corresponding subgroup analysis reported in Chapter 4, there was little evidence of an actual interaction effect between preference and treatment allocation on treatment outcomes (costs and QALYs), with coefficients on the interaction terms for each treatment both being non-significant at 5% significance level.
Extrapolation
No strong evidence of difference between the treatments arms in terms of clinical effectiveness, HRQoL or costs was found in the trial. Given the lack of difference between arms, there is no basis for inferring that any differences might occur in the future and, therefore, that conclusions might be altered if extrapolation was conducted. Thus, no extrapolation of the trial results has been conducted.
Evidence synthesis
External evidence was used to facilitate the inclusion of additional trial evidence on the effectiveness of cCBT and also to incorporate additional comparators which were not included within the REEACT study. This was undertaken as an exploratory analysis to determine the robustness of the results to external evidence and to ascertain the generalisability of the findings to a broader decision problem which included additional comparators. Regression analyses were used to determine the impact of changes in depression, measured by change in PHQ-9 from baseline, rather than treatment arm on costs, excluding intervention costs, and QALYs measured in the trial. The coefficients on the change in PHQ-9 from the regression equations estimate the impact of changes in PHQ-9 on costs and QALYs for participants within the trial. This approach allowed external evidence on the changes in PHQ-9 to be related to expected changes in total costs and QALYs for a range of different comparators.
As this analysis was exploratory in nature, we did not undertake a formal systematic search of individual RCTs. Instead we restricted our approach to including external evidence published in recent meta-analyses of internet-based and face-to-face psychological therapies for adult patients with depression. Two meta-analyses were identified, one on the effectiveness of internet-based treatments for depression in adults,10 in which there was some evidence of effect for therapist-guided cCBT, and another on the effectiveness of brief face-to-face psychological therapies for patients with depression managed in primary care settings. 79 These reported the effect of the interventions compared with usual care in terms of a SMD. These SMDs can be converted back onto the change in PHQ-9 (ΔPHQ-9) scale by multiplying them by the SD in ΔPHQ-9 observed in the trial, so as to estimate the incremental impact of the two interventions on costs and QALYs in the trial population compared with usual GP care. These analyses were then combined with estimates of the intervention-specific costs to estimate the cost-effectiveness of cCBT and other psychological therapies compared with usual GP care alone in participants from the REEACT study.
As shown in Tables 42 and 43, a one-point reduction in PHQ-9 from baseline to 12 months resulted in a 0.02927 increase in QALYs over the trial period and a £7.07 reduction in costs over the trial period. For cCBT, the meta-analysis10 showed supported cCBT to be the most effective, with a SMD of 0.61, which, when converted onto the change in PHQ-9 scale, resulted in a reduction of 4.32 on the PHQ-9 score. Unsupported cCBT had a SMD of 0.25, which resulted in a reduction of PHQ-9 score of 1.771, whereas all cCBT had a SMD of 0.41, which resulted in a reduction of PHQ-9 score of 2.905. Costs for cCBT treatment were based on the REEACT trial, assuming that 50% of participants would use Beating the Blues and 50% MoodGYM and that supported cCBT would involve 1 hour’s support from a community support worker per patient.
| Parameters | Mean | SE | Source |
|---|---|---|---|
| From trial analysis | |||
| Incremental impact of one point reduction in PHQ-9 from baseline to 12 months on QALYs | 0.02927 | 0.002249 | REEACT trial |
| Incremental impact of one point change in PHQ-9 from baseline to 12 month on costs (excluding cCBT costs) | – £7.07 | £6.7926 | REEACT trial |
| SD of change in PHQ | 7.084 | – | REEACT trial |
| Treatment effects | |||
| SMD of unsupported cCBT | 0.25 | 0.05102 | Andersson and Cuijpers (2009)10 |
| SMD of supported cCBT | 0.61 | 0.08163 | Andersson and Cuijpers (2009)10 |
| SMD of all cCBT | 0.41 | 0.06120 | Andersson and Cuijpers (2009)10 |
| SMD of other psychological therapy (including face-to-face CBT) | 0.31 | 0.07142 | Cuijpers et al. (2009)79 |
| Corresponding change in PHQ-9 compared with usual care | |||
| Unsupported cCBT | 1.771 | – | – |
| Supported cCBT | 4.321 | – | – |
| All cCBT | 2.905 | – | – |
| Other psychological therapy | 2.196 | – | – |
| Treatment costs | Mean (£) | Source | Assumptions |
|---|---|---|---|
| Cost of unsupported cCBT | 25 | REEACT trial | 50% split between Beating the Blues and MoodGYM |
| Cost of supported cCBT | 46 | REEACT trial | As above but assuming one hour of clinical support from a community support worker (based on Kaltenhaler et al.6) |
| Cost of all cCBT | 35.50 | REEACT trial | Average of above two assuming 50% split |
| Cost of other psychological therapies | 1160 | National Clinical Practice Guideline 9084 | Assuming same cost as for 18 sessions of CBT |
Other psychological therapies, which included face-to-face CBT, had a SMD of 0.3179 which resulted in a reduction in PHQ-9 score of 2.196. Treatment costs for other psychological therapies were based on the cost of face-to-face CBT from a previous economic evaluation. 84
Table 44 presents the results of the evidence synthesis analysis. As can be seen from the table, all treatments, when compared with usual care, resulted in increased costs but also increased QALYs. Supported cCBT was the most effective option and extendedly dominated or dominated all the other cCBT and other psychological treatment options. Supported cCBT compared with usual care generated an ICER of £126 per QALY and a probability of being cost-effective at a £20,000 per QALY cost-effectiveness threshold of 0.9747.
| Comparison | Incremental cost | Incremental QALY | ICER | Probability cost-effective at £20,000 per QALY |
|---|---|---|---|---|
| Usual care | 0 | 0 | – | – |
| Unsupported cCBT vs. usual care | £12.67 | 0.05193 | Extendedly dominated | 0 |
| All cCBT vs. usual care | £15.33 | 0.08508 | Extendedly dominated | 0.0253 |
| Supported cCBT vs. usual care | £15.99 | 0.12664 | £126 per QALY | 0.9747 |
| Other psychological treatments vs. usual care | £1144.70 | 0.06435 | Dominated | 0 |
The evidence synthesis analysis results suggested that, based on external evidence of effectiveness and the impact of changes in PHQ-9 from baseline to 12 months on costs and QALYs (observed in the REEACT trial), therapist-guided cCBT is the most cost-effective treatment option compared with usual GP care alone, unsupported cCBT and other psychological therapies. These findings are based on exploratory analyses and, as such, the findings should be considered tentative, as they are not based on directly randomised evidence. Furthermore, although we sought to include evidence from published meta-analyses, we did not attempt to critically appraise or quality assess their findings.
Summary
The within-trial results of the economic analysis suggest that neither Beating the Blues nor MoodGYM appeared cost-effective compared with usual GP care alone. In the base-case results, Beating the Blues was dominated by usual GP care alone (higher mean costs and lower QALYs), and mean costs and QALYs were lower for MoodGYM than for usual GP care alone, resulting in an ICER of £6933 per additional QALY for usual GP care alone versus MoodGYM. Usual GP care alone, compared with either cCBT intervention, was also the cost-effective intervention in the majority of scenario analyses, and it was the intervention most likely to be cost-effective at a £20,000 per QALY threshold (probabilities ranging across scenarios from 0.545 and 0.619). The exceptions to this were scenarios where SF-6D scores were used to estimate QALYs. In these scenarios, MoodGYM dominated usual GP care alone (lower mean costs and higher QALYs) and was the intervention most likely to be cost-effective at a £20,000 per QALY threshold (probabilities ranging across scenarios from 0.662 to 0.756).
Although the cost-effectiveness conclusions appear sensitive to the choice of whether EQ-5D or SF-6D is used to estimate them, the magnitude of the differences between all three groups was relatively low (and non-significant) for both cost and QALY estimates across all the scenarios. Hence, minor differences in the assumptions can lead to different cost-effectiveness interpretations because of relatively small impacts on the mean incremental estimates of costs and QALYs and, therefore, some caution should be exercised when interpreting these results. Results for the patient subgroup analysis were broadly consistent between the overall population and patient preference subgroups. There was little evidence of interaction effects between treatment allocation and patient preference.
Chapter 6 Results from the qualitative study on the acceptability to patients and health professionals of computerised cognitive behaviour therapy
Patient interviews
A total of 320 trial participants were sent an invitation to take part in the qualitative study. Of these, 39 (12%) participants responded to the invitation letter and were contacted by telephone to discuss participating in the study. A total of 36 participants were subsequently recruited to the study from across the four main trial sites, sampling for expressed preference for cCBT prior to randomisation and self-reported engagement with the cCBT program. Owing to a slowing in overall trial recruitment, no participants were recruited who indicated that their primary reason for refusal to participate in the main trial prior to randomisation was concern over using cCBT. All recruited participants received a participant information sheet about the qualitative study and completed a consent form. Individual semistructured patient interviews were conducted face to face in participants’ homes, except for three patient interviews with participants recruited via the University of Sheffield, which were conducted by telephone. Patient interviews were conducted by three qualitative researchers from the Universities of Manchester and Bristol (SK, HT, EA). Participants were interviewed between January and October 2011, at which point data saturation was judged complete.
Participant characteristics
Details of the study participants are given in Table 45. In summary, 10 (28%) of the participants were male. The mean age of participants was 51 years, with ages ranging from 29 to 69 years. Thirty-four (94%) of the participants were white British, with the two remaining participants reporting any other white background. The mean PHQ-9 score at baseline was 19, with scores ranging from 12 to 27. The participant sample was, therefore, representative of the wider trial population regarding gender and ethnicity but the average age of participants in the interview sample was older (51 years compared with 40 years in the trial overall). Ten of the participants reported that they would not prefer to receive cCBT, 22 participants indicated that they would prefer to receive cCBT and four participants gave no response. Only four participants reported during the qualitative interview that they completed all modules of computerised therapy (all four of whom had used the Beating the Blues program). Two-thirds of participants used the MoodGYM program (six males, 17 females).
| Transcript code | Patient acceptability | cCBT program | Trial site | Baseline PHQ-9 score | Gender | Age (years) | Ethnicitya | Treatment preference at baselineb | Number of times cCBT program usedc |
|---|---|---|---|---|---|---|---|---|---|
| DS0026 | Ambivalent | Beating the Blues | York | 26 | Male | 57 | 1 | No | 4 |
| DS0018 | Ambivalent | Beating the Blues | York | 17 | Female | 53 | 1 | No | 7 |
| DS0023 | Ambivalent | Beating the Blues | York | 19 | Female | 46 | 1 | Yes | 6 |
| DS0014 | Ambivalent | Beating the Blues | York | 13 | Male | 54 | 1 | Yes | 8 |
| DSB16.5 | Ambivalent | Beating the Blues | Bristol | 15 | Female | 50 | 1 | NR | 2 |
| DSB0906 | Ambivalent | Beating the Blues | Bristol | 22 | Female | 50 | 1 | Yes | 4 |
| DS0019 | Ambivalent | Beating the Blues | York | 16 | Male | 55 | 1 | Yes | 8 |
| DS0024 | Ambivalent | MoodGYM | York | 26 | Female | 43 | 3 | Yes | 6 |
| DS0043 | Ambivalent | MoodGYM | Sheffield | 17 | Male | 66 | 1 | Yes | 6 |
| DS0015 | Ambivalent | MoodGYM | York | 19 | Male | 48 | 1 | Yes | 18 |
| DS007 | Ambivalent | MoodGYM | Manchester | 17 | Female | 43 | 1 | Yes | 8 |
| DS0013 | Ambivalent | MoodGYM | York | 21 | Female | 48 | 1 | Yes | 1 |
| DS0020 | Ambivalent | MoodGYM | York | 21 | Female | 56 | 1 | Yes | 6 |
| DSB2505 | Ambivalent | MoodGYM | Bristol | 23 | Female | 32 | 1 | Yes | 6 |
| DSB200511 | Ambivalent | MoodGYM | Bristol | 25 | Female | 52 | 1 | Yes | 10 |
| DS0012 | Ambivalent | MoodGYM | Manchester | 16 | Male | 58 | 1 | Yes | 5 |
| DS0025 | Ambivalent | MoodGYM | Manchester | 22 | Male | 59 | 1 | Yes | 10 |
| DS0029 | Negative | Beating the Blues | York | 13 | Female | 54 | 1 | Yes | 2 |
| DS003 | Negative | Beating the Blues | Manchester | 26 | Male | 45 | 1 | Yes | 0 |
| DS25511 | Negative | MoodGYM | Bristol | 12 | Female | 65 | 1 | No | 8 |
| DS004 | Negative | MoodGYM | Manchester | 25 | Female | 29 | 1 | No | 5 |
| DS008 | Negative | MoodGYM | Manchester | 14 | Male | 32 | 3 | Yes | 1 |
| DS0021 | Negative | MoodGYM | York | 15 | Female | 56 | 1 | No | 4 |
| DS006 | Negative | MoodGYM | Manchester | 24 | Male | 59 | 1 | Yes | 2 |
| DSB23.05 | Negative | MoodGYM | Bristol | 16 | Female | 69 | 1 | No | 2 |
| DSB0706 | Negative | MoodGYM | Bristol | 16 | Female | 58 | 1 | No | 8 |
| DS0011 | Negative | MoodGYM | Manchester | 21 | Female | 59 | 1 | Yes | 0 |
| DS0017 | Positive | Beating the Blues | York | 17 | Female | 60 | 1 | Yes | 12 |
| DS044 | Positive | Beating the Blues | Sheffield | 17 | Female | 44 | 1 | Yes | 8 |
| DS0016 | Positive | Beating the Blues | York | 24 | Female | 48 | 1 | No | 5 |
| DS0031 | Positive | Beating the Blues | Manchester | 15 | Female | 40 | 1 | No | 8 |
| DSB24.5 | Positive | MoodGYM | Bristol | 16 | Female | 49 | 1 | No | 10 |
| DS038 | Positive | MoodGYM | Bristol | 25 | Female | 53 | 1 | Yes | 15 |
| DSB240511 | Positive | MoodGYM | Bristol | 27 | Female | 54 | 1 | NR | 10 |
| DSB0906 | Positive | MoodGYM | Bristol | 20 | Female | 52 | 1 | Yes | 8 |
| DS0045 | Positive | MoodGYM | Sheffield | 12 | Female | 37 | 1 | Yes | 5 |
Main themes from patient interviews
We did not observe any specific differences in themes between the two cCBT programs (Beating the Blues and MoodGYM). Differences in patient experience did not appear to be due to any specific features of a particular program, but related to the broader experience of therapy delivered by computer.
Three key themes emerged from the data: acceptability; engagement and adherence; and absence of support. Although participants varied in their reported acceptability, common issues relating to adherence and support were reported across the whole sample.
Patient acceptability: perceived benefits and barriers
We observed in the data that participants could be classified as ‘positive’, ‘negative’ or ‘ambivalent’ based on their perceptions of cCBT, referring to the fact that the participants’ perceptions could be clearly and consistently grouped under the headings of positive, negative or ambivalent and particularly noting how opinions on the same aspect of the program (e.g. its flexibility) could be seen to vary across these dimensions. Examples of this, presented in the classifications, are shown in Figure 12. These classifications were found to conceptualise differences usefully and were exhaustive (all participants could be clearly defined within the groupings). It is not typical to assign qualitative data into formal groups in this manner, but the categories are useful in the context of this pragmatic trial to understand experience and uptake of the health technology. Seventeen participants were categorised as ‘ambivalent’ (Beating the Blues, n = 7; MoodGYM, n = 10 ), 10 were categorised as ‘negative’ (Beating the Blues, n = 2; MoodGYM, n = 8) and nine as ‘positive’ (Beating the Blues, n = 4 ; MoodGYM, n = 5). These classifications were reached through consensus among the qualitative team, based on the rereading of the transcripts and the identification of consistent differences that could be classified as positive, negative or ambivalent. However, it is notable that these categorisations did not map clearly onto expressed prior preference for cCBT. There was no consistent relationship between prior expressed preference at baseline and whether the participant reported being positive or negative after they had personal experience of the programs. Although numbers are too small to draw any definitive conclusions, this may indicate that patients are not able to anticipate if computerised therapy would be appropriate for them based on initial preferences alone.
FIGURE 12.
Subthemes and extracts relating to perceived benefits and barriers. (a) Flexibility and autonomy; and (b) relational and connectedness. Reproduced from Knowles et al. 85 © BMJ Open 2015. This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/.

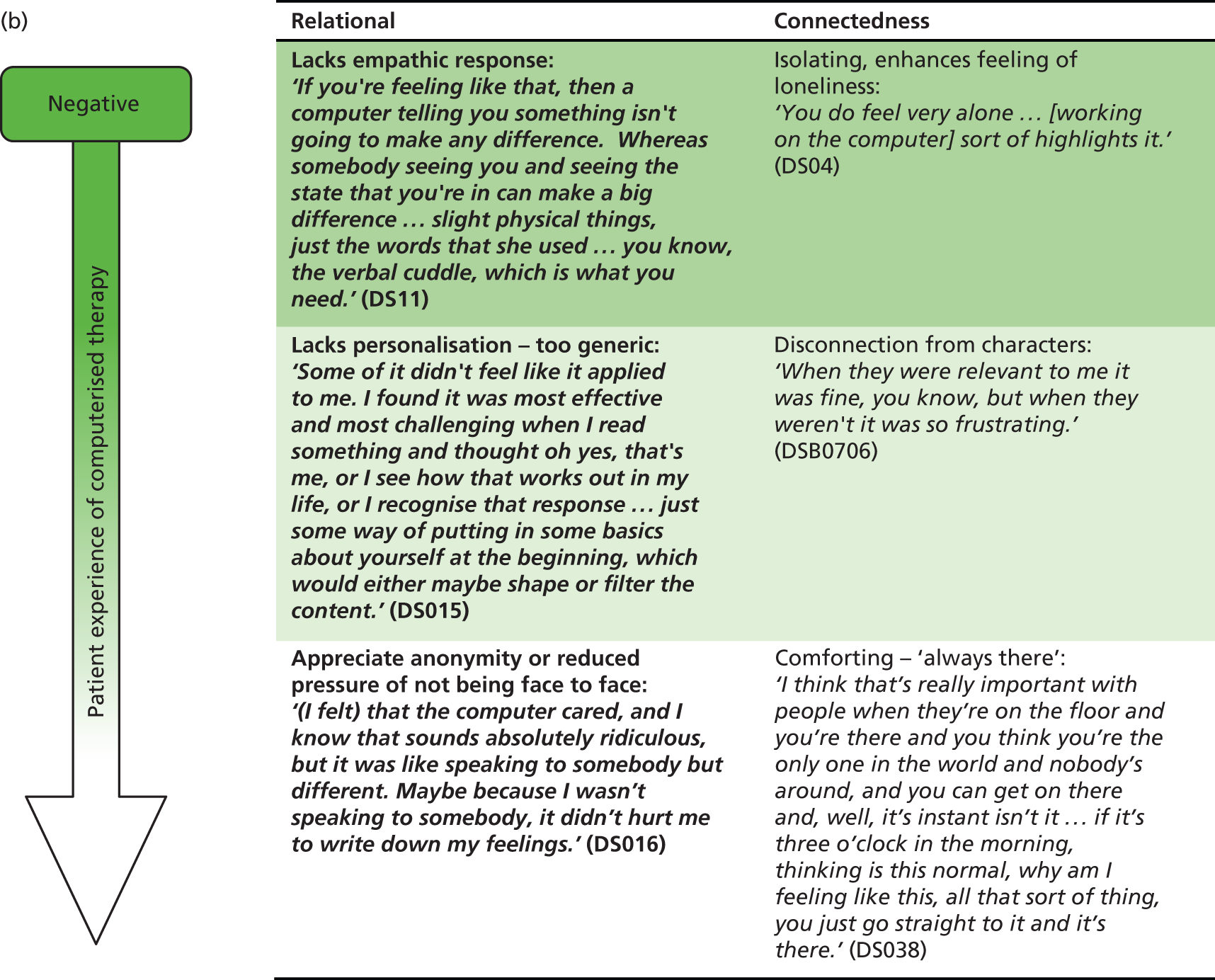
Subthemes and extracts relating to perceived barriers and benefits are shown in Figure 12, which illustrates both the consistency within classifications and also the contrast across the subthemes dependent on classification. Specifically, the four subthemes presented (‘flexibility, ‘autonomy’, ‘relational’, ‘connectedness’) illustrate how the same aspects of cCBT could be perceived both positively and negatively, depending on individual participant experience and preference. The subthemes are further illustrated with quotations within Figure 12.
-
‘Flexibility’ refers to the unstructured, flexible nature of the treatment, which was perceived as advantageous by positive participants, who appreciated the greater accessibility, but as a barrier by negative participants because of the greater responsibility placed on participants to organise and adhere to sessions themselves. Ambivalent participants recognised the potential benefits of this flexibility but reported that additional support or monitoring was necessary to encourage them to engage.
-
‘Autonomy’ refers to how the independence of cCBT was experienced, with negative participants feeling overburdened by the absence of support, in contrast to positive participants, who felt empowered to take control of their recovery. Ambivalent participants occupied a ‘middle ground’, in which they were willing to engage with the program independently but felt that barriers within the content prevented them from doing so.
-
‘Relational’ refers to whether the absence of another person, such as a therapist, was perceived positively (owing to the comfort offered by anonymity) or negatively (with participants struggling without the relational or empathetic input of a therapist). Again, ambivalent participants had a more moderate response, with increased personalisation being felt to be necessary for them to relate to the characters in the program and relate the content to their own lives.
-
‘Connectedness’ refers to the degree of connection that participants experienced with the program, with negative participants feeling that cCBT further isolated them and emphasised their loneliness, in contrast to positive participants, who felt that the program was ‘always there’ for them. Ambivalent participants again seemed instead frustrated by limitations of the content of these particular programs, similar to the ‘Relational’ theme where being able to identify with the material was perceived as important – in this case, the potential for connection with the content was hindered by inappropriate or overly generic material.
The analysis demonstrated that although some participants clearly embraced or rejected computerised therapy, as illustrated in Figure 12, the majority of participants (17 of the sample classed as ‘ambivalent’) fell between these extremes. For these ‘ambivalent’ participants, cCBT was not rejected outright as with the ‘negative’ participants or fully embraced as with the ‘positive’ participants but was considered to require greater external support and greater personalisation of material to enable participants to engage fully with the programs. Barriers relating specifically to experience of technology, such as problems in accessing the program or discomfort using computers, were not observed. This may reflect either that patient populations are increasingly familiar with using technologies, or that only those patients comfortable with technology were willing to enter the trial.
Patient engagement and adherence
All participants reported some difficulties with engaging with the programs, but, consistent with their reported attitudes, there was a trend for ‘positive’ participants to report greater adherence, and three of the four participants who reported completing the programs were in this group. ‘Negative’ participants reported lower levels of engagement than the rest of the sample, suggesting that participant attitudes are associated with behavioural engagement to some extent. On self-reported engagement, positive participants reported using the program an average of 9.1 times in total, ambivalent participants reported using the program 6.7 times in total and negative participants reported an average of 3.2 uses in total.
Participants also reported difficulties maintaining engagement when their depression was more severe and perceived the programs to be inappropriate for patients experiencing severe episodes.
I was feeling so miserable that all those questions did was actually just hold the mirror and show me how miserable I was and, so, I just turned the program off . . . And that was, for me, the first, kind of, 2 months really, 3 months, because I was just feeling so down.
DS025. Reproduced from Knowles et al. 85 © BMJ Open 2015. This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/
If you’re mildly depressed, or if you’ve turned the corner, then I think that’s when it’s appropriate. But I think if you were deeply depressed, and still struggling, then it would be much harder . . . I think you probably would fail and that would make you feel worse. Because the last thing you need is another failure when you’re feeling really down.
DS017. Reproduced from Knowles et al. 85 © BMJ Open 2015. This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/
Despite the provision of regular technical telephone support calls, participants also indicated that a greater level of monitoring or support would have encouraged engagement, which is reflected in the third theme.
Perceived limitations of support
All participants perceived the programs to be unsupported, suggesting that the technical support and encouragement offered via telephone support calls within the trial may not meet patient expectations regarding level or type of support that should be provided. However, although ‘negative’ participants appeared to disengage with the programs deliberately, both ‘positive’ and ‘ambivalent’ participants expressed a desire for greater monitoring and follow-up, providing greater motivational support to help them engage with and complete the programs.
Just someone being aware and sort of either saying ‘oh that’s great, you did another unit! Hey that’s good, keep it up!’ Or ‘you haven’t done a unit for 4 weeks. Only takes an hour, how about it?’.
DSB0906
If I had somebody ringing me up every week, then I would have been more likely to have stuck with it.
DS018
Participants reported that GPs did not tend to monitor their engagement with the programs, and suggested that the support needed to sustain engagement was unlikely to be provided in primary care because of lack of time in consultations and interruptions to continuity of care:
I think if they’d got the time you maybe would, but I think it’s indicative of the world we live in and the system that we live with. The good doctors are always in demand and you go back for your repeat prescription and you see who you see and there are maybe three of them that I would see, but you don’t see the one that suggested this therapy in the first place. So no, I’ve never talked about it to anybody.
DS029. Reproduced from Knowles et al. 85 © BMJ Open 2015. This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/
I wouldn’t have expected a GP to call me. It would have been nice, the family GP practitioner in the countryside but we live in a city and they’ve got what 10,000 patients on their book. So yeah I understand.
DS08. Reproduced from Knowles et al. 85 © BMJ Open 2015. This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/
Summary of main findings from patient interviews
The patient interviews demonstrate the degree of individual difference in experience of cCBT, with a ‘negative’ subset who consider therapy by computer unacceptable because of the absence of interpersonal support, but another subset preferring cCBT to traditional therapy because of the greater accessibility, flexibility and anonymity. However, the majority of participants had a more mixed reaction, appreciating the potential benefits of cCBT but struggling with the content and delivery of the intervention, specifically the lack of personalisation of materials and the partially supported and unstructured delivery of the program. Poor adherence and engagement with cCBT were typical and were attributed to severity of depression and absence of follow-up support to encourage adherence. Even ‘positive’ participants reported that greater monitoring and follow-up would be needed to help sustain their engagement. Although the data suggested that addition of monitoring or supportive follow-up could improve engagement and completion, respondents did not think that this additional follow-up could be provided by GPs in primary care.
There were no obvious differences in attitudes by gender or age, and technological aptitude was not prominently reported, although it is possible that patients who would struggle with computers had already self-selected out of the trial.
Health professional interviews
A total of 70 GP practices that had recruited participants to the main trial were sent invitations to participate in the qualitative study. Fourteen health professionals responded to the invitation and were contacted to discuss the study in more detail. A total of 11 GPs were subsequently recruited to the study from 10 GP practices, across six out of the nine trial sites. No expressions of interest were received from practice managers. All recruited GPs received a participant information sheet about the qualitative study and completed a consent form. Individual semistructured interviews were conducted with GPs by telephone by a qualitative researcher (SK) from the University of Manchester. GPs were interviewed between September 2012 and February 2013.
Health professional participant characteristics
The sample consisted of eight males and three females. Of the 11 participants, nine were white British and two were of Asian origin.
Main themes from health professional interviews
Benefits of computerised cognitive behaviour therapy for patients
The primary benefit of having cCBT as a referral option was the speed of access, even in surgeries supported by local IAPT, where waiting times are relatively short:
For the counselling, even though patient being seen very quickly, usually within . . . now it’s within 14 days, or something like that, there’s no guarantee the next appointment is not 6 weeks, or longer.
GP076 (York site, male)
Yeah, there is a waiting list, our counsellor, usually it’s 4 to 6 weeks, that’s the face to face in the practice, there’s the IAPT service . . . they can be waiting a month, or so for that as well . . . so, yeah, the computerised stuff is the fastest definitely.
GP077 (Bristol site, female)
Computerised CBT was also perceived as particularly useful for patients who might otherwise struggle to access therapy, for example because of time restrictions or job demands:
A few people were very keen on it. That, for example, weren’t able due to work commitments to see someone that works 9 till 5.
GP073 (York site, male)
Young people who have got work commitments that couldn’t get to somewhere, you know, that was useful . . . a pragmatic issue of whether it was, sort of, good to fit in with their work, or their family commitments.
GP077 (Bristol site, female)
‘Matching’ patients to computerised cognitive behaviour therapy
The interviews explored the issue of whether or not GPs referred certain types of patient to cCBT. The primary considerations tended to be practical ones, such as access to a computer and computer literacy, and the GPs also appeared to consider demographic factors which they judged to impact on acceptability and ability to engage:
I think, it also depends on the education of the patient and their ability to use computers and, I guess, their general intelligence.
GP062 (Manchester site, male)
I think younger people are more likely to respond to computer stuff . . . I think that men might be more keen on computerised, I think they’re a bit more IT orientated generally.
GP074 (Bristol site, female)
GPs, similar to the patient interview sample, perceived cCBT as unsuitable for people with more severe depression. However, they justified this on the basis of the level of motivation required to use cCBT, in contrast to the patient interview sample, which reported lack of support and the difficulty of being reminded how depressed they felt as the primary barriers for severely depressed patients:
The extremely unmotivated patients who are severely depressed, I think, I have generally stayed away from, because of the motivation issues.
GP075 (York site, male)
[if they have] difficulty just motivating themselves to get up in the morning, they’re not going to have the ability to engage in a CBT thing.
GP078 (Bristol site, male)
One GP working in a community with a large South Asian population also suggested that differences in attitudes to treatment, particularly self-help based treatments, among ethnic groups could have a role:
I think, for Asian people, explaining that your depression can be helped with an internet program about you helping yourself, I think, a lot of them think the onus of responsibility for their health is on someone else and not on them . . . they won’t participate in something like this, they seem to think it’s an external thing, your health, someone else has to give you medication, it’s not in their control.
GP061 (Manchester site, female)
However, other GPs in the sample also referred to the issue of patients taking responsibility for their own treatment as a deciding factor in their acceptance of cCBT, and they perceived engagement with cCBT as requiring individual initiative:
I think, there’s a subgroup of these patients that want their responsibility taken away . . . some people want to be helped, rather than help themselves.
GP062 (Manchester site, male)
It’s good for somebody who is proactive and wants to get better . . . you have to have the initiative to actually go there every day, or turn the computer on to do the assessment. And I think that in itself shows some life skills that I think is often lacking in people who see me for help.
GP079 (York site, male)
However, these assumptions about responsibility and preference could still be related to overarching perceptions of education and ability, or assumptions about appropriate demographic profiles:
[People who like cCBT] tend to be people that are reasonably literate . . . people that perhaps have an internal locus of control and enough motivation to feel they can contribute to their own recovery . . . whereas some people whose lives are perhaps a bit more chaotic, perhaps less educated, less literate and have a more external locus of control, you know, they don’t necessarily own their own housing, or even pay their own rent . . . that sort of person might not take so much responsibility for their own health care as well, including putting in the effort themselves.
GP073 (York site, male)
The websites, I think, help you, but it’s having the confidence to go for it like that and the intelligence to be analytical like that . . . highly mobile people, intelligent people . . . they need a certain amount of self-confidence to do that, I think.
GP078 (Bristol site, male)
Implementation in primary care
The interviews explored whether or not GPs would consider providing cCBT on site themselves, as this model of provision had been employed in earlier trials of one of the cCBT programs (Beating the Blues). Although some GPs were open to the possibility, they reported a range of barriers in terms of availability of space and concerns about access to protected computer systems:
We’re really pushed for space . . . I can imagine that it would take the managers and partners a little bit of getting their heads round it because you would have people using a system which contained very confidential data.
GP072 (York site, male)
One GP in the sample had set up access on site but reported it was both time-consuming and expensive:
You had to have a room for patients to come and use a computer, we had to create appointment slots for them to book in to use the computer, we then had to get a BT line for internet for that computer, which we ended up paying for two years’ worth, . . . the [primary care trust] said, it has to be a specially set up computer, because patients shouldn’t be able to access anything.
GP061 (Manchester site, female)
The GPs, in fact, reported access from home as a perceived benefit, and reported that public access to cCBT would probably be inappropriate because patients might be unfamiliar with public locations such as libraries or depressed patients might struggle to cope with public access:
I think if you’re depressed, going to a library and logging on in a public place to do something about depression is quite daunting, isn’t it? If they didn’t have their own computer at home . . . that was a very potent discourager from doing it really.
GP074 (Bristol site, female)
Provision of support and follow-up in primary care
The GPs commented that patients in the trial had referred to needing more support to engage with cCBT and suggested that such support could be provided remotely. They perceived barriers to providing such support themselves because of time constraints.
The patients that have spoken to us about it, they talk about wanting a bit more support to engage with it . . . from the perspective of the GP supporting the patient, you’d be concerned how high on the priority of the GP list it would be within the consultation and their knowledge of it as well. So, I think, the support would be better coming from an external, . . . it could just be a five-minute telephone call every couple of weeks, or something, more often just to encourage and motivate somebody.
GP062 (Manchester site, male)
[They’re] probably better off doing IAPT than a GP, just because of the issue of time, we have 10 minutes, by the time we’ve, kind of, reviewed their mental health, then going on to, kind of, reviewing how they’re doing on a computer might be a bit too long.
GP075 (York site, male)
Consistent with the patient interview sample, GPs reported that they did not tend to follow up patients who used the programs and so did not tend to know if experience had been positive or not:
I haven’t got the foggiest what’s happened to them. Probably got better because I haven’t seen them again, or they’re so fed up with what I tried to make them do . . . We come across this sort of situation so often in our work and in research that you just get used to it. When you don’t get hospital discharge letters for three months you get very used to this sort of thing. No news is good news.
GP072 (York site, male)
I don’t know, you know, you wouldn’t know! I mean, the people that I saw who got on well with it, reported positively, but then I might not have seen the people that didn’t get on with it, because they might not have come back.
GP077 (Bristol site, female)
Several of the GPs suggested that providing such follow-up information from the program itself would have been helpful, which is an option for practices that have purchased the Beating the Blues program, but was not provided to GPs within the trial:
I think it would have been nice to have had just a brief discharge summary. What was it, 12 weeks or whenever the final check was, of how that person, how that individual went, just like when I refer to anyone else, it’s nice to get feedback.
GP073 (York site, male)
I think you need to produce some sort of review, report, if the program actually let us know at the end, your patient didn’t complete the program, or completed the program with varying degree of success. Generally, we don’t have any feedback, basically, unless we make the effort ourselves to ask the patient.
GP078 (Bristol site, male)
Summary of main findings from health professional interviews
The GPs interviewed perceived the key benefits of cCBT to be its accessibility, in terms of being the quickest treatment available to access even when IAPT services or on-site counsellors were available and also being more accessible to certain participants because of its flexibility, such as those who work long hours. GPs were sceptical that cCBT could be provided on site and perceived home access to be most appropriate and also preferable for patients. The GPs suggested that cCBT would be inappropriate for patients with more severe depression and most appropriate for patients high in computer literacy who were open to self-help interventions (as opposed to preferring to receive treatment from others). Consistent with the patient interviews, GPs reported that they did not tend to monitor or follow up patients using cCBT, and suggested that incorporating a function within the program to allow them to view patients’ progress would be helpful.
Comparison of the patient and health professional interviews
A core finding from the patient interview transcripts concerned the individual differences in experience of computerised therapy, which related to different preferences around privacy, flexibility and independent working. The GPs tended to consider demographic or pragmatic factors in their referrals such as computer illiteracy or inability to access therapy because of work demands. GPs may be conflating perceptions of ability or education with perceptions of the patient as willing or able to engage with self-help therapies, or assuming certain demographic groups will be more suitable, which contrasts with the findings of the patient qualitative study that did not show consistent differences in age and gender. In fact, the most positive attitudes were reported by female participants, contrary to stereotypes about preference for cCBT among males.
Matching appropriate patients to cCBT treatment may need to be focused more on the individual needs and preferences of the patients, although the lack of congruence between patients’ expressed prior preference and their experience as positive or negative demonstrates the complexity of doing this. This may indicate a need for greater GP follow-up in the early stages of use to identify more rapidly those patients who are now struggling with the intervention, which would be consistent with the principles of stepped care around self-correction9 when patients do not respond to minimal interventions.
Both patients and health professionals reported a lack of follow-up on use of the cCBT program in primary care. GPs suggested that notifications from within the cCBT program about completion and assessment would be helpful to them but did not perceive themselves to have a role in supporting engagement with the program itself. However, patients’ desire for support was specifically related to a higher level of ongoing support while completing the cCBT program, although the patients interviewed also questioned whether or not it was feasible that this could be provided in primary care consultations. This suggests that support for engagement with cCBT in primary care may need to be provided by other health professionals or provided as supplemental remote or face-to-face support as part of the cCBT packages. However, as noted previously, providing earlier feedback to GPs themselves around initial engagement with the cCBT program may be necessary to help them follow the self-correcting principles of stepped care and enable alternative referrals for patients who are unable to complete the computerised intervention.
The majority of GPs were sceptical that computerised therapy could be provided in their practices, demonstrating that in routine primary care it would be unlikely that cCBT would be provided to patients on site. Given that those patients who reported positive experiences with cCBT valued the anonymity and flexibility of access from home, this suggests that attempting to implement cCBT services within general practice sites may lead to barriers for patient engagement as well as creating difficulties for GPs. It is possible that those patients who struggled with the flexibility of the home-accessed treatment would appreciate the greater structure offered by on-site access, but given the reported barriers to implementing this, it may again be the case that more remote support or motivational support built into the intervention would be most feasible and effective.
Limitations of the qualitative study with patients and health professionals
The patient interview sample was predominantly female and all participants were from a white background. This indicates that the sample is representative of the wider trial population (being consistent with the trial population profile); but, nevertheless, further research is necessary to determine whether similar experiences are reported by more diverse patient groups. The finding that technical aptitude was not commonly reported as a prominent issue may be because potential participants with low computer literacy declined to take part in the trial. Interviewing participants who decline should be attempted in future research on computerised interventions to explore if such self-selection occurs.
The GP interview sample was predominantly male, although there did not appear to be any consistent differences between male and female interviewees’ reports. We did not collect data on other factors that may have influenced attitudes, such as numbers of years in practice and specialist training in mental health, although, given the small sample size, it would have been difficult to analyse subgroups within the sample. The reports from GPs regarding follow-up and support may not be representative of how they would respond to patients receiving the intervention who were not part of a larger trial and should be interpreted with caution.
Implications of findings from qualitative study
The combined interviews suggest several approaches for improving engagement and acceptability of cCBT in primary care:
-
identifying factors that impact on patient engagement, specifically personal preferences around working alone or with the support of health professionals
-
improving patient experience and engagement through greater personalisation and provision of motivational support which could involve minimal health professional contact remotely or face to face
-
encouraging early follow-up in primary care to identify which patients find the intervention unsuitable.
Some text has been reproduced from Knowles et al. 85 © BMJ Open 2015. This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/.
Chapter 7 Discussion
The REEACT trial is, to our knowledge, the largest pragmatic evaluation of the clinical effectiveness, cost-effectiveness and acceptability of cCBT in primary care. Hitherto there have been no large-scale trials conducted independently of the developers of cCBT products and the REEACT trial was commissioned following an earlier technology appraisal in this area. 6 At the time of the design of the trial, both cCBT products to be evaluated (MoodGYM and Beating the Blues) were recommended in NICE depression guidelines and both remain NICE-endorsed treatments at the time of publication of this trial. 86 A novel aspect of the REEACT trial is the comparison of a free-to-use cCBT product (MoodGYM) with a commercially available cCBT product (Beating the Blues); a comparison that addresses an important question to commissioners of health services and to policy-makers.
The REEACT trial was unusual in comparison with earlier trial-based evaluations in that it included an extended follow-up to 24 months. Outcomes were measured across a broad range of domains including psychological well-being, quality of life and health state utility. Important aspects of service utilisation were also recorded, and the REEACT trial included concurrent qualitative and economic evaluations. The REEACT trial was also novel in measuring patient preference at baseline, thereby allowing an investigation into the degree to which baseline preference for computer-delivered therapy might influence the effectiveness of this intervention (a fully randomised patient preference trial). 87 The delivery of the cCBT intervention was also supported by weekly technical telephone support calls which offered a general level of motivational enhancement to encourage the uptake of the programs by people with depression and also practical support in the use of computer-based programs. The level of support matched and often exceeded that which might be offered in routine NHS primary care and IAPT services, where cCBT remains a recommended lower-intensity psychological intervention. 86
The main findings of the REEACT study in relation to: (1) trial-based estimates of the clinical effectiveness of cCBT; (2) trial- and model-based estimates of cost-effectiveness; and (3) qualitative examination of acceptability and use of cCBT will now be discussed in turn.
Trial-based estimates of clinical effectiveness for computer-delivered cognitive behaviour therapy
There was little or no evidence of statistically significant effects of Beating the Blues on the proportion of participants who were depressed across all points of follow-up when compared with usual GP care alone. For the free-to-use MoodGYM package, there was no evidence of effect in the primary outcome on the proportion of participants who were depressed at 4 months. There was some evidence of a statistically significant effect of MoodGYM on the proportion of participants who were depressed when compared with usual GP care at 12 months, but this was no longer evident at 24 months. When comparing MoodGYM and Beating the Blues, the free-to-use cCBT program MoodGYM was found to be non-inferior to the commercial pay-to-use cCBT program Beating the Blues across all time points. It is worth noting that, although the target sample size of 230 participants randomised to each trial arm was not achieved in the Beating the Blues arm (n = 210), the actual number of participants required for the analysis (n = 150 per arm) was achieved across all trial arms (Beating the Blues, n = 165; usual GP care alone, n = 179; and MoodGYM, n = 182).
Turning to the broader range of secondary outcomes which were collected in the REEACT trial, there was no evidence of statistically significant effects on the overall (including all time points) mean depression scores, CORE-OM scores and MCS and PCS quality of life scores of Beating the Blues when compared with usual GP care alone; however, there was evidence of a statistically significant effect of Beating the Blues on the MCS scores at 12 months. There was no evidence of statistically significant effects on the overall (including all time points) mean depression scores and PCS quality of life scores of MoodGYM when compared with usual GP care alone; however, there was evidence of a statistically significant effect of MoodGYM on the mean depression scores at 12 months when compared with usual GP care alone. When all time points were considered simultaneously in a mixed model, there was no clinical benefit for either MoodGYM or Beating the Blues when compared with usual GP care.
The clinical significance of the small but statistically significant clinical benefit of MoodGYM at 12 months was not clear. This finding of no benefit at 4 months followed by a small benefit at 12 months for MoodGYM was unexpected and was difficult to interpret. The primary outcome at 4 months is the point where any clinical benefit would most readily have been expected, and this finding is not routinely observed in trial-based evaluations of brief psychological intervention. Based on existing research and systematic reviews, the greatest amount of benefit would have been expected in the short term and any short-term benefits would have been expected to have attenuated by 12 months. 88,89
When baseline preference for treatment allocation was measured prior to randomisation, we found that there was a strong preference in favour of cCBT. This baseline preference did not impact on clinical outcomes within the trial. Computer-delivered CBT was equally ineffective for those with and those without a strong preference for treatment.
When the process of engagement with cCBT was monitored in the trial with reference to computer records it was found that there was low uptake and use of programs. Although the large majority of REEACT participants logged on and used the programs at least once (modal number of sessions = 1 for both programs), further usage was lower than that which has been reported in developer-led trials. Very few participants completed all treatment sessions, and the most common number of sessions for either computer program was just one session. This low usage was apparent despite the provision of regular (weekly) technical telephone support calls.
In summary, the main finding is, therefore, that for the primary outcome of depression severity at 4 months there was no significant additional benefit when participants were offered a technically supported form of computerised therapy in addition to usual GP care. This finding was true for both a free-to-use package (MoodGYM) and commercially produced cCBT (Beating the Blues).
Summary of trial- and model-based estimates of cost-effectiveness
The within-trial results of the economic analysis suggest that neither Beating the Blues nor MoodGYM appeared cost-effective compared with usual GP care alone. In the base-case results, Beating the Blues was dominated by usual GP care alone (with higher mean costs and lower QALYs associated with Beating the Blues), and mean costs and QALYs were lower for MoodGYM versus usual GP care alone, resulting in an ICER of £6933 per additional QALY for usual GP care alone versus MoodGYM. Usual GP care alone compared with either cCBT intervention was also the cost-effective intervention in the majority of scenario analyses, and it was the intervention most likely to be cost-effective at a £20,000 per QALY threshold. The exceptions to this were scenarios where SF-6D scores were used to estimate QALYs. In these scenarios, MoodGYM dominated usual GP care alone (lower mean costs and higher QALYs) and was the intervention most likely to be cost-effective at a £20,000 per QALY threshold.
Although the cost-effectiveness conclusions appear sensitive to the choice of whether EQ-5D or SF-6D is used to estimate them, the magnitude of the differences between all three groups were relatively minor (and non-significant) for both cost and QALY estimates across all the scenarios. Hence, minor differences in the assumptions can lead to different cost-effectiveness interpretations because of relatively small impacts on the mean incremental estimates of costs and QALYs, and some caution should be exercised when interpreting these results.
Results for the patient subgroup analyses were broadly consistent between the overall population and both patient preference subgroups. There was little evidence of interaction effects between treatment allocation and patient preference.
The evidence synthesis analysis results suggested that, based on external evidence of effectiveness and the impact of changes in PHQ-9 from baseline to 12 months on costs and QALYs (observed in the REEACT trial), therapist-guided cCBT may in fact be the most cost-effective treatment option compared with usual GP care alone and less-supported cCBT. These findings are tentative and are not based on directly randomised evidence.
Summary of main findings from qualitative examination of acceptability and use of computerised cognitive behaviour therapy
The qualitative patient interviews demonstrated a level of individual difference in experience of cCBT, with a ‘negative’ subset who consider therapy by computer unacceptable because of the absence of interpersonal therapeutic support, but another subset preferring cCBT to traditional therapy because of the greater accessibility, flexibility and anonymity. However, the majority of participants had a more mixed reaction. While they recognised the potential benefits of cCBT, they struggled with the content and delivery of the intervention, particularly with the lack of personalisation of content and the limited support and unstructured delivery of the program. Poor adherence and engagement were typical and were attributed to severity of depression and absence of follow-up support to encourage adherence. Even ‘positive’ participants reported that greater monitoring and follow-up than was provided in weekly supportive telephone calls would be needed to help sustain their engagement. Although the data suggested that addition of more intensive monitoring or supportive follow-up could improve engagement and completion, respondents did not think that this higher level of follow-up could feasibly be provided by GPs in primary care.
When GPs were interviewed, they perceived the attraction of cCBT to be its accessibility and flexibility, in terms of being the quickest treatment available to access, particularly to certain patients such as those who work long hours. GPs were sceptical that cCBT could ever be provided on site and perceived home access to be most appropriate and also preferable for patients. The GPs suggested that cCBT would be inappropriate for patients with more severe depression and most appropriate for patients high in computer literacy who were open to self-help interventions (as opposed to preferring to receive treatment from others).
Matching appropriate patients to cCBT treatment may need to be focused more on the individual needs and preferences of the patients, although the lack of congruence between patients’ expressed prior preference and their experience as positive or negative demonstrates the complexity of doing this. This may indicate a need for greater GP follow-up in the early stages of use, to more rapidly identify those patients who are now struggling with the intervention, which would be consistent with the principles of stepped care around self-correction9 when patients do not respond to minimal interventions.
The qualitative evaluation also found that support for engagement with cCBT in primary care may need to be provided by health professionals (other than GPs), or provided as supplemental remote or face-to-face support as part of the cCBT packages. Earlier feedback to GPs themselves around initial engagement with the cCBT program may also be necessary to help them follow the self-correcting principles of stepped care and enable alternative referrals for patients who are unable to complete the computerised intervention.
That the majority of GPs were sceptical that computerised therapy could be provided in their own practices demonstrates that in routine primary care it would be impractical and unlikely that cCBT would be provided to patients on site. It is possible that those patients who struggled with the flexibility of the home-accessed treatment would appreciate the greater structure offered by on-site access but, given the reported barriers to implementing this, it may again be the case that more remote support or motivational support built into the intervention would be most feasible and effective.
The combined interviews suggest several approaches for improving engagement and acceptability of cCBT in primary care.
Discussion of main findings
The REEACT trial offered an independent and pragmatic evaluation of cCBT. The clinical results of the trial were shown to be inconsistent with a number of developer-led trials, which have been summarised in systematic reviews90,91 and UK technology appraisals. 6 In addition to the independence of the REEACT trial from trials conducted by the developers of cCBT, there are a number of differences in the trial design of REEACT that are important to acknowledge.
The first difference in design is that the REEACT trial was purposely conducted entirely within primary care, which is the setting in which most cases of depression are managed. This focus on a primary care setting is in contrast with a number of trials which have recruited either from specialist (secondary care) referral centres or from centres that have developed specialist clinics requiring participants to be supervised in their use of the computer package.
The second design difference is the level of support that was offered alongside cCBT. In the REEACT trial, participants were offered regular (weekly) technical support and general encouragement to use the cCBT programs but were purposely not offered structured psychological support over the telephone by a mental health professional. Furthermore, the technical telephone support provided in the REEACT trial did not involve detailed explanations of CBT and did not involve detailed review of homework or between-session tasks. The chosen level of technical and motivational support was, therefore, less intense than other trials where, for example, computer usage has been supervised by therapists on a 1 : 1 basis92 or where a health-care professional has met with the user and has therefore been physically present to ensure the user interacts successfully with the computer. 7 Trials where there has been an intensive level of support have generally demonstrated a greater level of effect than less supported programs. 91 Nevertheless, the pragmatic nature of the REEACT trial meant that the level of support that was offered is one that is at least as intensive as the support offered in many NHS care settings and is in line with (or for MoodGYM exceeds) the level of recommended support. As such, the REEACT trial represents a realistic evaluation of an intervention that replicates the use of cCBT in routine primary care settings. The aim of conducting a pragmatic effectiveness trial of cCBT was, therefore, achieved.
Another important finding in this trial is that there was relatively low uptake of cCBT, despite the provision of technical telephone support. Other lower intensity interventions for depression have similarly shown that dropout and failure to engage are common when such interventions are offered in primary care. 79 The REEACT findings therefore serve to add to this existing evidence. However, the finding of the low uptake of cCBT in REEACT contrasts with other developer-led trials that report good levels of uptake and engagement. 79 Here we note again that REEACT was a pragmatic trial and one which replicated a feasible and representative primary care intervention within the context of a RCT. 7,93 The REEACT trial is a realistic evaluation of computer-delivered CBT, as it is currently offered in the NHS. Within the context of trials, there has been limited investigation of the reasons for poor engagement and barriers to the use of cCBT in routine care, and a concurrent qualitative evaluation in the REEACT trial explored reasons for poor engagement in depth. It was clear that participants with significant levels of depression were not generally motivated to engage in weekly unguided cCBT sessions. The technology was also not one which was sufficiently attractive to ensure that participants returned to further sessions after their initial session.
Conclusion
Computerised CBT forms a core component of stepped psychological care in the UK primary care and other health systems. The overall conclusion of the REEACT trial is that technically supported cCBT conferred modest or no benefit over usual GP care. This finding would therefore suggest that the routine promotion and commissioning of cCBT be reconsidered in the light of the results of this trial. A firm conclusion of the trial is that a commercially developed cCBT product conferred no benefit over a free-to-use product. This finding is particularly important for those who commission services and purchase commercial products on behalf of publicly funded health services. The REEACT trial results suggest that the routine use and purchase of cCBT is likely to be an ineffective low-intensity form of treatment for people with depression and, as such, an inefficient use of finite health-care resources. There are other treatments for depression that might be considered instead of cCBT, which includes telephone-guided self-help, bibliotherapy (unguided or standalone self-help) and therapist-delivered CBT. 86 We would recommend that more large-scale pragmatic trials of these low-intensity forms of guided self-help are conducted within routine NHS primary care services.
Implications for health care
-
In this trial for patients with moderate or severe depression powered to detect non-inferiority, technically supported cCBT in addition to usual GP care was no more effective than usual GP care alone. Practice recommendations such as those offered by NICE and IAPT stepped models of care might usefully be re-examined in the light of these findings.
-
We consider that, where cCBT continues to be offered within the portfolio of low intensity psychological treatment, there should be early follow-up in primary care to identify patients for whom the intervention may be unsuitable.
-
Commissioners of services should take note of our findings that commercially produced products may add little benefit to usual GP care alone.
-
We found no substantial difference in outcomes between the commercially produced product (Beating the Blues), when offered in addition to usual GP care, and the free-to-use product (MoodGYM), which is clearly less costly for the NHS.
-
Free-to-use products such as MoodGYM could be offered in response to patient choice. However, our overall finding of the relative lack of benefit of these programs in addition to usual GP care should also be taken into account in this context.
Recommendations for research
-
There is a clinical and economic need for brief, low-intensity self-help interventions for depression. The finding that computer-based therapies had low uptake and were not well regarded underlines both the need to further understand barriers to uptake of such therapies and the need for trials of alternative forms of guided self-help or brief psychological intervention.
-
Although technically supported cCBT is largely ineffective and inefficient, a more highly supported form of cCBT with therapeutic advice, guidance and psychological support may in fact improve outcomes at an acceptable level of cost. Further trials of more intensively supported computer-delivered guided self-help are, therefore, required to test this hypothesis.
-
Large-scale pragmatic trials of treatments such as bibliotherapy or telephone-based psychological interventions are, therefore, needed.
-
All such studies should be framed in primary care and conducted by researchers other than product developers.
-
In the longer term, if computers are to be used to deliver psychological treatment with minimal therapist input, then there needs to be improved patient experience and engagement through greater personalisation of treatment packages. This requires further research and innovation at the human–computer interface.
Some of this text has been reproduced from Gilbody et al. 11 © BMJ 2015. This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/.
Acknowledgements
Our first thanks are to the REEACT participants for their contribution to this study, the research teams at each site and the Primary Care Research Network for recruiting GP practices to the trial, the GPs, research nurses, GP practice staff, the research teams at each site, the Mental Health Research Network (MHRN) for recruiting participants and completing trial documentation, principal investigators at each site for co-ordinating participant recruitment and the TSC and DMEC members for overseeing the study.
We would specifically like to thank Gwen Brierley, Diane Lee, Sarah Knowles, Debbie Tallon, Anna Thake and David White who were the trial co-ordinators at each main site, and Emma Anderson, Nicola Barclay, David Barker, Sue Bonner, Aimee Card, Lucy Carr, James Coker, Jack Cotter, Tom Devlin, Nathan Filer, Lone Gale, Gemma Hackney, Rebecca Hargate, Susanna Haynes, Terri Hollinghurst, Debbie Johnson, Louise Jones, Deborah Kemp, Amanda Lilley-Kelly, Genevieve Riley, Liz Salter, Lois Savage, Saiqa Shah, Charles Shepherd, Donna Shipley, Fiona Stanton, Angela Swallow, Bridget Telford-Peak, Helen Thorp, Linda Tinkler and Mike Tyldesley for recruiting participants to the study and collecting data. In addition, we would like to thank Phil Andersen and Gwen Brierley for providing telephone support to participants, Sally Brabyn for co-ordinating data collection for the economic evaluation, Ben Cross for developing the trial database and providing data management for the whole trial, Arthur Kang‘ombe for assisting with data preparation for TSC and DMEC meetings and Sarah Mercer for providing administrative trial support. We would also like to thank Simon Douglas and Saffra Knox from the MHRN.
We would also like to extend our gratitude to the developers of MoodGYM and Beating the Blues for providing us with participant logins and usage data. Particular thanks to Helen Christensen and Kylie Bennett from the Centre for Mental Health Research, Australian National University, and Charlie Martin and Charles Elves from Ultrasis.
This trial is dedicated to the memory of Professor Helen Lester (1961–2013), a valued colleague, friend and co-investigator, who contributed time and wisdom at every stage of the REEACT trial.
Collaborators
The REEACT collaborators (current and past) are Phil Andersen (Trial Support Worker, Health Services Research), Professor Ricardo Araya (Professor, Psychiatry), Professor Michael Barkham (Professor, Clinical Psychology), Professor Peter Bower (Professor, Primary Care), Sally Brabyn (Research Fellow, Health Services Research), Gwen Brierley (Study Co-ordinator, Health Services Research), Dr Cindy Cooper (Director, Sheffield Clinical Trials Research Unit, Health Services Research), Dr Ana Duarte (Research Fellow, Health Economics), Professor Linda Gask (Professor, Primary Care Mental Health), Professor Simon Gilbody (Professor, Health Services Research), Dr Catherine Hewitt (Deputy Director, York Trials Unit, Statistics), Dr David Kessler (Consultant Senior Lecturer and GP, Primary Care), Dr Sarah Knowles (Research Fellow, Primary Care), Professor Helen Lester (Professor, Primary Care), Nicola Lidbetter (Chief Executive of Anxiety UK and Self-Help Services), Dr Elizabeth Littlewood (Research Fellow, Health Services Research), Professor Karina Lovell (Professor, Mental Health), Professor Stephen Palmer (Professor, Health Economics), Usman Muhammad (Research Fellow, Statistics), Professor Glenys Parry (Professor, Psychological Therapies), Professor David A Richards (Professor, Mental Health), Rachel Richardson (Senior Research Fellow, Health Services Research), Professor Mark Sculpher (Professor, Health Economics), Debbie Tallon (Trial Co-ordinator, Primary Care Mental Health), Dr Puvan Tharmanathan (Senior Research Fellow, Health Services Research), Professor David Torgerson (Director, York Trials Unit, Clinical Trials), Dr Simon Walker (Research Fellow, Health Economics), David White (Trial Co-ordinator, Clinical Trials).
Contributions of authors
Elizabeth Littlewood, Gwen Brierley, Rachel Richardson and Puvan Tharmanathan were the trial managers (Rachel Richardson between 2009 and 2010, Gwen Brierley between 2010 and 2011, Puvan Tharmanathan in 2011 and Elizabeth Littlewood between 2011 and 2013), monitored the whole trial and contributed to the design of protocol revisions and aquisition of data.
Ana Duarte and Simon Walker conducted the economic analysis.
Catherine Hewitt oversaw the conduct of the clinical analysis.
Sarah Knowles, Peter Bower, Helen Lester and Karina Lovell conducted the qualitative work and analysis.
Stephen Palmer designed and oversaw the conduct of the economic analysis.
Phil Andersen and Gwen Brierley provided technical telephone support to trial participants.
Stephen Palmer, Ricardo Araya, Michael Barkham, Peter Bower, Cindy Cooper, Linda Gask, David Kessler, Helen Lester, Karina Lovell, Glenys Parry, David A Richards, Rachel Richardson and Simon Gilbody were applicants on the HTA application and contributed to the study design.
Sarah Knowles, Sally Brabyn, Debbie Tallon and David White were the site trial co-ordinators and undertook data collection in their sites.
Catherine Hewitt and Usman Muhammad designed and conducted the clinical analysis.
Gwen Brierley was the trial support officer between 2009 and 2010.
Simon Gilbody and Rachel Richardson wrote the original protocol.
Simon Gilbody was the chief investigator, chaired the Trial Management Group and edited and approved the final draft of the report.
The report writing team consisted of Phil Andersen, Sally Brabyn, Ana Duarte, Simon Gilbody, Catherine Hewitt, Sarah Knowles, Elizabeth Littlewood, Stephen Palmer and Simon Walker, who drafted the report.
Contributions of collaborators
Nicola Lidbetter, Mark Sculpher and David Torgerson were co-applicants on the HTA application and contributed to the study design.
Mark Sculpher codesigned the economic analysis.
Statement of independence of researchers
The developers of the MoodGYM (National Institute for Mental Health Research, Australian National University) and Beating the Blues (Ultrasis) cCBT programs used in the study had no role in the design of REEACT or in the collection, analysis and interpretation of data.
Trial Steering Committee members
Professor Joe Reilly (Independent Chair), Professor of Mental Health, Durham University.
Professor Mike Slade (Professor of Health Services Research), Head of Section for Recovery, Health Service and Population Research Department, Institute of Psychiatry, King’s College London.
Professor Shirley Reynolds (Professor of Evidence-Based Psychological Therapies), University of Reading.
Professor Robbie Foy (Professor of Primary Care), Leeds Institute of Health Sciences, University of Leeds.
Dr Lina Gega, Clinical Lead, Northumberland Talking Therapies and Honorary Lecturer at Norwich Medical School.
Mr Nic Seccombe (service-user representative), Informatics and Governance Lead, Self Help Services, Manchester; Anxiety UK, cCBT self-help services.
Data Monitoring and Ethics Committee members
Professor Mike Lucock (Independent Chair), Professor of Clinical Psychology, University of Huddersfield, and Associate Director of Research, South West Yorkshire Partnership NHS.
Professor Chris Roberts (Professor in Biostatistics, Centre for Biostatistics), University of Manchester.
Dr Paul Blenkiron (Consultant Psychiatrist and Honorary Senior Clinical Lecturer), Hull York Medical School.
Publication
Brierley G, Richardson R, Torgerson D. Using short information leaflets as recruitment tools did not improve recruitment: a randomised controlled trial. J Clin Epidemiol 2012;65:147–54.
Gilbody S, Littlewood E, Hewitt C, Brierley G, Tharmanathan P, Araya R, et al. Computerised cognitive behaviour therapy (cCBT) as treatment for depression in primary care (REEACT trial): large scale pragmatic randomised controlled trial. BMJ 2015;351:h5627.
Knowles SE, Lovell K, Bower P, Gilbody S, Littlewood E, Lester H. Patient experience of computerised therapy for depression in primary care. BMJ Open 2015;5:e008581.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health.
References
- The World Health Report (2001): Mental Health: New Understanding, New Hope. Geneva: World Health Organisation; 2001.
- Layard R. The case for psychological treatment centres. BMJ 2006;332:1030-2. http://dx.doi.org/10.1136/bmj.332.7548.1030.
- Roth A, Fonagy P. What Works for Whom? A Critical Review of Psychotherapy Research. New York, NY: Guildford Press; 1996.
- A Review of Strategic Policy on NHS Psychotherapy Services in England. London: HMSO; 1996.
- Lovell K, Richards D. Multiple Access Points and Levels of Entry (MAPLE): ensuring choice, accessibility and equity for CBT services. Behav Cogn Psychother 2000;28:379-91.
- Kaltenthaler E, Brazier J, De Nigris E, Tumur I, Ferriter M, Beverley C, et al. Computerised cognitive behaviour therapy for depression and anxiety update: a systematic review and economic evaluation. Health Technol Assess 2006;10. http://dx.doi.org/10.3310/hta10330.
- Proudfoot J, Goldberg D, Mann A, Everitt B, Marks I, Gray JA. Computerized, interactive, multimedia cognitive-behavioural program for anxiety and depression in general practice. Psychol Med 2003;33:217-27. http://dx.doi.org/10.1017/S0033291702007225.
- Christensen H, Griffiths KM, Jorm AF. Delivering interventions for depression by using the internet: randomised controlled trial. BMJ 2004;328. http://dx.doi.org/10.1136/bmj.37945.566632.EE.
- Bower P, Gilbody S. Stepped care in psychological therapies: access, effectiveness and efficiency: narrative literature review. Br J Psychiatry 2005;186:11-7. http://dx.doi.org/10.1192/bjp.186.1.11.
- Andersson G, Cuijpers P. Internet-based and other computerized psychological treatments for adult depression: a meta-analysis. Cogn Behav Ther 2009;38:196-205. http://dx.doi.org/10.1080/16506070903318960.
- Gilbody S, Littlewood E, Hewitt C, Brierley G, Tharmanathan P, Araya R, et al. Computerised cognitive behaviour therapy (cCBT) as treatment for depression in primary care (REEACT trial): large scale pragmatic randomised controlled trial. BMJ 2015;351. http://dx.doi.org/10.1136/bmj.h5627.
- Torgerson D, Moffett JK. Patient preference and validity of randomized controlled trials: letter to the editor. JAMA 2005;294:41-2.
- Spitzer RL, Kroenke K, Williams JBW. Patient Health Questionnaire Study Group . Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. JAMA 1999;282:1737-44. http://dx.doi.org/10.1001/jama.282.18.1737.
- Gilbody S, Richards D, Barkham M. Diagnosing depression in primary care using self-completed instruments: UK validation of PHQ-9 and CORE-OM. Br J Gen Pract 2007;57:650-2.
- Depression: Core Interventions in the Management of Depression in Primary and Secondary Care. London: HMSO; 2004.
- Peveler R, Kendrick A, Buxton M, Longworth L, Baldwin D, Moore M, et al. A randomised controlled trial to compare the cost-effectiveness of tricyclic antidepressants, selective serotonin reuptake inhibitors and lofepramine. Health Technol Assess 2005;9.
- Revisions to the GMS Contract, 2006/7: Delivering Investment in General Practice. London: British Medical Association; 2006.
- Whooley MA, Avins AL, Browner WS. Case-finding instruments for depression: two questions are as good as many. J Gen Intern Med 1997;12:439-45. http://dx.doi.org/10.1046/j.1525-1497.1997.00076.x.
- Lewis G, Pelosi AJ, Araya R, Dunn G. Measuring psychiatric disorder in the community: a standardized assessment for use by lay interviewers. Psychol Med 1992;22:465-86. http://dx.doi.org/10.1017/S0033291700030415.
- Gruenberg AM, Goldstein RD, Pincus HA, Licinio J, Wong M-L. Classification of Depression: Research and Diagnostic Criteria: DSM-IV and ICD-10. Weinheim: Wiley; 2005.
- Barkham M, Margison F, Leach C, Lucock M, Mellor-Clark J, Evans C, et al. Service profiling and outcomes benchmarking using the CORE-OM: toward practice-based evidence in the psychological therapies. J Consult Clin Psychol 2001;69:184-96. http://dx.doi.org/10.1037/0022-006X.69.2.184.
- Evans C, Mellor-Clark J, Margison F, Barkham M, Audin K, Connell J, et al. CORE: clinical outcomes in routine evaluation. J Ment Health 2000;9:247-55. http://dx.doi.org/10.1080/713680250.
- Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36): I. Conceptual framework and item selection. Med Care 1992;30:473-83. http://dx.doi.org/10.1097/00005650-199206000-00002.
- Ware JE, Kosinski M, Dewey JE. How to Score Version Two of the SF-36 Health Survey (Standard & Acute Forms). Lincoln, RI: QualityMetric Incorporated; 2000.
- The EuroQol Group . EuroQol – a new facility for the measurement of health-related quality of life. Health Policy 1990;16:199-208. http://dx.doi.org/10.1016/0168-8510(90)90421-9.
- Brooks R. EuroQol: the current state of play. Health Policy 1996;37:53-72. http://dx.doi.org/10.1016/0168-8510(96)00822-6.
- Knapp M, Beecham J. Costing mental health services. Psychol Med 1990;20:893-908. http://dx.doi.org/10.1017/S003329170003659X.
- Rosenberger WF, Lachin JM. Randomization in Clinical Trials: Theory and Practice. New York, NY: John Wiley & Sons; 2002.
- King M, Sibbald B, Ward E, Bower P, Lloyd M, Gabbay M, et al. Randomised controlled trial of non-directive counselling, cognitive-behaviour therapy and usual general practitioner care in the management of depression as well as mixed anxiety and depression in primary care. Health Technol Assess 2000;4.
- Simon G, Wagner E, Vonkorff M. Cost-effectiveness comparisons using ‘real world’ randomized trials: the case of new antidepressant drugs. J Clin Epidemiol 1995;48:363-73. http://dx.doi.org/10.1016/0895-4356(94)00141-C.
- Christensen H, Griffiths KM, Korten A. Web-based cognitive behavior therapy: analysis of site usage and changes in depression and anxiety scores. J Med Internet Res 2002;4. http://dx.doi.org/10.2196/jmir.4.1.e3.
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9. J Gen Intern Med 2001;16:606-13. http://dx.doi.org/10.1046/j.1525-1497.2001.016009606.x.
- Pinto-Meza A, Serrano-Blanco A, Penarrubia MT, Blanco E, Haro JM. Assessing depression in primary care with the PHQ-9: can it be carried out over the telephone?. J Gen Intern Med 2005;20:738-42. http://dx.doi.org/10.1111/j.1525-1497.2005.0144.x.
- Clark DM, Layard R, Smithies R, Richards DA, Suckling R, Wright B. Improving access to psychological therapy: initial evaluation of two UK demonstration-sites. Behav Res Ther 2009;47:910-20. http://dx.doi.org/10.1016/j.brat.2009.07.010.
- DeJesus RS, Vickers KS, Melin GJ, Williams MD. A system-based approach to depression management in primary care using the Patient Health Questionnaire-9. Mayo Clin Proc 2007;82:1395-402. http://dx.doi.org/10.4065/82.11.1395.
- Fletcher J, Bower P, Richards D, Saunders T. Enhanced Services Specification for Depression Under the New GP Contract. Manchester: National Institute for Mental Health in England Northwest; 2004.
- Cameron IM, Crawford JR, Lawton K, Reid IC. Psychometric comparison of PHQ-9 and HADS for measuring depression severity in primary care. Br J Gen Pract 2008;58:32-6. http://dx.doi.org/10.3399/bjgp08X263794.
- Löwe B, Kroenke K, Herzog W, Gräfe K. Measuring depression outcome with a brief self-report instrument: sensitivity to change of the Patient Health Questionnaire (PHQ-9). J Affect Disord 2004;81:61-6. http://dx.doi.org/10.1016/S0165-0327(03)00198-8.
- Evans C, Connell J, Barkham M, Margison F, McGrath G, Mellor-Clark J, et al. Towards a standardised brief outcome measure: psychometric properties and utility of the CORE-OM. Br J Psychiatry 2002;180:51-60. http://dx.doi.org/10.1192/bjp.180.1.51.
- Cavanagh K, Shapiro DA, Berg S, Swain S, Barkham M, Proudfoot J. The effectiveness of computerized cognitive behavioural therapy in routine care. Br J Clin Psychol 2006;45:499-514. http://dx.doi.org/10.1348/014466505X84782.
- Richards D, Lovell K, Gilbody S, Gask L, Torgerson D, Barkham M, et al. Collaborative care for depression in UK primary care: a randomized controlled trial. Psychol Med 2008;38:279-87. http://dx.doi.org/10.1017/S0033291707001365.
- Garratt AM, Ruta DA, Abdalla MI, Buckingham JK, Russell IT. The SF-36 health survey questionnaire: an outcome measure suitable for routine use within the NHS?. BMJ 1993;306:1440-4. http://dx.doi.org/10.1136/bmj.306.6890.1440.
- Brazier JE, Harper R, Jones NM, O’Cathain A, Thomas KJ, Usherwood T, et al. Validating the SF-36 health survey questionnaire: new outcome measure for primary care. BMJ 1992;305:160-4. http://dx.doi.org/10.1136/bmj.305.6846.160.
- Cuijpers P, de Graaf R, van Dorsselaer S. Minor depression: risk profiles, functional disability, health care use and risk of developing major depression. J Affect Disord 2004;79:71-9. http://dx.doi.org/10.1016/S0165-0327(02)00348-8.
- Jenkinson C, Layte R, Lawrence K. Development and testing of the medical outcomes study 36-item short form health survey summary scale scores in the United Kingdom: results from a large-scale survey and a clinical trial. Med Care 1997;35:410-16. http://dx.doi.org/10.1097/00005650-199704000-00010.
- Brazier J, Roberts J, Deverill M. The estimation of a preference-based measure of health from the SF-36. J Health Econ 2002;21:271-92. http://dx.doi.org/10.1016/S0167-6296(01)00130-8.
- Brazier J, Usherwood T, Harper R, Thomas K. Deriving a preference-based single index from the UK SF-36 health survey. J Clin Epidemiol 1998;51:1115-28. http://dx.doi.org/10.1016/S0895-4356(98)00103-6.
- Dolan P, Gudex C, Kind P, Williams A. A Social Tariff for EuroQoL: Results from a UK General Population Survey. CHE Discussion Paper. York: Centre for Health Economics; 1995.
- Sobocki P, Ekman M, Ågren H, Krakau I, Runeson B, Mårtensson B, et al. Health-related quality of life measured with EQ-5D in patients treated for depression in primary care. Value Health 2007;10:153-60. http://dx.doi.org/10.1111/j.1524-4733.2006.00162.x.
- Kessler D, Lewis G, Kaur S, Wiles N, King M, Weich S, et al. Therapist-delivered Internet psychotherapy for depression in primary care: a randomised controlled trial. Lancet 2009;374:628-34. http://dx.doi.org/10.1016/S0140-6736(09)61257-5.
- Sapin C, Fantino B, Nowicki M-L, Kind P. Usefulness of EQ-5D in assessing health status in primary care patients with major depressive disorder. Health Qual Life Outcomes 2004;2. http://dx.doi.org/10.1186/1477-7525-2-20.
- Guide to the Methods of Technology Appraisal. London: National Institute for Health and Care Excellence; 2013.
- Royston P. Multiple imputation of missing values. Stata Journal 2004;4:227-41.
- Briggs AH, Claxton K, Sculpher MJ. Decision Modelling for Health Economic Evaluation. Oxford: Oxford University Press; 2006.
- British National Formulary. London: BMA and RPS; 2013.
- Curtis L. Unit Costs of Health Social Care 2012. Canterbury: PSSRU, University of Kent; 2012.
- UK National Health System (NHS) . NHS Reference Costs 2011–12 2012. www.gov.uk/government/uploads/system/uploads/attachment_data/file/127115/NSRC01-2011-12.xls (accessed August 2013).
- The Wellness Shop . Beating the Blues Clinician’s Pack, 2013 n.d. www.thewellnessshop.co.uk/PBSCCatalog.asp?ItmID=12969942 (accessed September 2013).
- Ware JE, Snow KK, Kosinski M, Gandek B. SF-36 Health Survey: Manual and Interpretation Guide. Boston, MA: The Health Institute, New England Medical Centre; 1993.
- Brazier J, Roberts J, Tsuchiya A, Busschbach J. A comparison of the EQ-5D and SF-6D across seven patient groups. Health Econ 2004;13:873-84. http://dx.doi.org/10.1002/hec.866.
- Torrance GW, Feeny D. Utilities and quality adjusted life years. Int J Technol Assess Health Care 1989;5:559-75. http://dx.doi.org/10.1017/S0266462300008461.
- Manca A, Hawkins N, Sculpher MJ. Estimating mean QALYs in trial-based cost-effectiveness analysis: the importance of controlling for baseline utility. Health Econ 2005;14:487-96. http://dx.doi.org/10.1002/hec.944.
- Briggs A, Clark T, Wolstenholme J, Clarke P. Missing . . . presumed at random: cost-analysis of incomplete data. Health Econ 2003;12:377-92. http://dx.doi.org/10.1002/hec.766.
- Royston P. Multiple imputation of missing values: update of ice. Stata Journal 2005;5:527-36.
- Royston P. Multiple imputation of missing values: update. Stata Journal 2005;5:188-201.
- White IR, Royston P, Wood AM. Multiple imputation using chained equations: issues and guidance for practice. Stat Med 2011;30:377-99. http://dx.doi.org/10.1002/sim.4067.
- Graham JW, Olchowski AE, Gilreath TD. How many imputations are really needed? Some practical clarifications of multiple imputation theory. Prev Sci 2007;8:206-13. http://dx.doi.org/10.1007/s11121-007-0070-9.
- Briggs A, Gray A. The distribution of health care costs and their statistical analysis for economic evaluation. J Health Serv Res Policy 1998;3.
- Barber J, Thompson S. Multiple regression of cost data: use of generalised linear models. J Health Serv Res Policy 2004;9:197-204. http://dx.doi.org/10.1258/1355819042250249.
- Manning WG, Mullahy J. Estimating log models: to transform or not to transform?. J Health Econ 2001;20:461-94. http://dx.doi.org/10.1016/S0167-6296(01)00086-8.
- Pullenayegum EM, Tarride J-E, Xie F, Goeree R, Gerstein HC, O’Reilly D. Analysis of health utility data when some subjects attain the Upper Bound of 1: are Tobit and CLAD models appropriate?. Value Health 2010;13:487-94. http://dx.doi.org/10.1111/j.1524-4733.2010.00695.x.
- Zellner A. An efficient method of estimating seemingly unrelated regressions and tests for aggregation bias. J Am Stat Assoc 1962;57:348-68. http://dx.doi.org/10.1080/01621459.1962.10480664.
- Willan AR, Briggs AH, Hoch JS. Regression methods for covariate adjustment and subgroup analysis for non-censored cost-effectiveness data. Health Econ 2004;13:461-75. http://dx.doi.org/10.1002/hec.843.
- Drummond M, Sculpher M, Torrance G, O’Brien B, Stoddart G. Methods for the Economic Evaluation of Health Care Programmes. Oxford: Oxford University Press; 2005.
- Fenwick E, Claxton K, Sculpher M. Representing uncertainty: the role of cost-effectiveness acceptability curves. Health Econ 2001;10:779-87. http://dx.doi.org/10.1002/hec.635.
- Claxton K. The irrelevance of inference: a decision-making approach to the stochastic evaluation of health care technologies. J Health Econ 1999;18:341-64. http://dx.doi.org/10.1016/S0167-6296(98)00039-3.
- Glick H, Doshi J, Sonnad S, Polsky D. Economic Evaluation in Clinical Trials. New York, NY: Oxford University Press; 2007.
- Sculpher MJ, Claxton K, Drummond M, McCabe C. Whither trial-based economic evaluation for health care decision-making?. Health Econ 2006;15:677-87. http://dx.doi.org/10.1002/hec.1093.
- Cuijpers P, van Straten A, van Schaik A, Andersson G. Psychological treatment of depression in primary care: a meta-analysis. Br J Gen Pract 2009;59. http://dx.doi.org/10.3399/bjgp09X395139.
- Boeije H. A purposeful approach to the constant comparative method in the analysis of qualitative interviews. Qual Quant 2002;36:391-409. http://dx.doi.org/10.1023/A:1020909529486.
- Kaltenthaler E, Sutcliffe P, Parry G, Beverley C, Rees A, Ferriter M. The acceptability to patients of computerized cognitive behaviour therapy for depression: a systematic review. Psychol Med 2008;38:1521-30. http://dx.doi.org/10.1017/S0033291707002607.
- Kaltenthaler E, Parry G, Beverley C, Ferriter M. Computerised cognitive behaviour therapy for depression: systematic review. Br J Psychiatry 2008;193:181-4. http://dx.doi.org/10.1192/bjp.bp.106.025981.
- Edwards PJ, Roberts IG, Clarke MJ, DiGuiseppi C, Wentz R, Kwan I, et al. Methods to increase response rates to postal questionnaires. Cochrane Database Syst Rev 2007;2.
- Depression, the Treatment and Management of Depression in Adults – National Clinical Practice Guideline 90. London: The British Psychological Society and the Royal College of Psychiatrists; 2010.
- Knowles SE, Lovell K, Bower P, Gilbody S, Littlewood E, Lester H. Patient experience of computerised therapy for depression in primary care. BMJ Open 2015;5. http://dx.doi.org/10.1136/bmjopen-2015-008581.
- Depression: the Treatment and Management of Depression in Adults (Update). London: National Institute for Health and Care Excellence; 2009.
- Torgerson D, Sibbald B. Understanding controlled trials. What is a patient preference trial?. BMJ 1998;316. http://dx.doi.org/10.1136/bmj.316.7128.360.
- Churchill R, Hunot V, Corney R, Knapp M, McGuire H, Tylee A, et al. A systematic review of controlled trials of the effectiveness and cost-effectiveness of brief psychological treatments for depression. Health Technol Assess 2001;5.
- Bortolotti B, Menchetti M, Bellini F, Montaguti MB, Berardi D. Psychological interventions for major depression in primary care: a meta-analytic review of randomized controlled trials. Gen Hosp Psychiatry 2008;30:293-302. http://dx.doi.org/10.1016/j.genhosppsych.2008.04.001.
- Andrews G, Cuijpers P, Craske MG, McEvoy P, Titov N. Computer therapy for the anxiety and depressive disorders is effective, acceptable and practical health care: a meta-analysis. PLOS ONE 2010;5. http://dx.doi.org/10.1371/journal.pone.0013196.
- Spek V, Cuijpers P, Nyklícek I, Riper H, Keyzer J, Pop V. Internet-based cognitive behaviour therapy for symptoms of depression and anxiety: a meta-analysis. Psychol Med 2007;37:319-28. http://dx.doi.org/10.1017/S0033291706008944.
- Wright JH, Wright AS, Albano AM, Basco MR, Goldsmith LJ, Raffield T. Computer-assisted cognitive therapy for depression: Maintaining efficacy while reducing therapist time. Am J Psychiatry 2005;162:1158-64. http://dx.doi.org/10.1176/appi.ajp.162.6.1158.
- McCrone P, Knapp M, Proudfoot J, Ryden C, Cavanagh K, Shapiro DA, et al. Cost-effectiveness of computerised cognitive behaviour therapy for anxiety and depression in primary care: randomised controlled trial. Br J Psychiatry 2004;185:55-62. http://dx.doi.org/10.1192/bjp.185.1.55.
- Primary Care Foundation . Out of Hours Benchmark – Index and Summary 2013. www.primarycarefoundation.co.uk/benchmark-results-interact-with-data-and-reports.html (accessed September 2013).
- Parry G, Barkham M, Brazier J, Dent-Brown K, Hardy G, Kendrick T, et al. An Evaluation of a New Service Model: Improving Access to Psychological Therapies Demonstration-Sites 2006–2009 2011.
Appendix 1 Regulatory approvals
The REC approval was obtained for the study from the Leeds East REC on 10 July 2008. The relevant Research and Development departments were approached and approval was given for the relevant primary care trust (PCTs)/trusts on the dates shown in Table 46.
| Site | PCT/Trust | Research and development approval |
|---|---|---|
| University of Bristol | Bristol PCT | 21 May 2009 |
| Gloucestershire PCT | 22 June 2009 | |
| North Somerset PCT | 11 November 2009 | |
| Somerset PCT | 16 November 2009 | |
| South Gloucestershire PCT | 21 May 2009 | |
| University of Manchester | Manchester PCT | 22 June 2009 |
| Stockport PCT | 22 June 2009 | |
| University of Sheffield | Barnsley PCT | 27 April 2009 |
| Derbyshire County PCT | 15 October 2009 | |
| Sheffield PCT | 13 May 2009 | |
| University of York | North Yorkshire and York PCT | 27 May 2009 |
| Durham and Darlington | County Durham and Tees Valley PCT | 24 November 2009 |
| Gateshead | Gateshead PCT | 24 April 2009 |
| Hull | NHS East Riding of Yorkshire | 3 February 2010 |
| NHS Hull | 4 November 2008 | |
| North of Tyne | Northumberland Care Trust | 24 April 2009 |
| South of Tyne | Sunderland PCT | 24 April 2009 |
Approval was gained at six additional PCTs/trusts, but these sites did not recruit any participants to the study.
Appendix 2 Details of the study sites
| Site | Recruitment dates |
|---|---|
| University of Bristol | Recruitment via site research team (recruited first patient August 2009, last patient January 2011) |
| University of Manchester | Recruitment via site research team (recruited first patient September 2009, last patient February 2011) |
| University of Sheffield | Recruitment via site research team (recruited first patient September 2009, last patient February 2011) |
| University of York | Recruitment via site research team (recruited first patient August 2009, last patient January 2011) |
| Durham and Darlington | Recruitment via the MHRN (recruited first patient January 2010, last patient November 2010) |
| Gateshead | Recruitment via the Primary Care Mental Health Team (recruited first patient September 2009, last patient January 2011) |
| Hull | Recruitment via University of Hull research nurses (recruited first patient February 2010, last patient March 2011) |
| North of Tyne | Recruitment via the MHRN (recruited first patient October 2009, last patient February 2011) |
| South of Tyne | Recruitment via the MHRN (recruited first patient February 2010, last patient October 2010) |
Appendix 3 Study information for GP practices
Appendix 4 Study information for participants
Appendix 5 Number of participants recruited via direct referrals and database screening methods
| Referral method | Beating the Blues (N = 210) | MoodGYM (n = 242) | Usual GP care alone (n = 239) | Total (n = 691) |
|---|---|---|---|---|
| Direct referral | 153 (72.9) | 163 (67.4) | 170 (71.1) | 486 (70.3) |
| Record screening | 57 (27.1) | 79 (32.6) | 69 (28.9) | 205 (29.7) |
Appendix 6 Summary of participant involvement in the trial

Appendix 7 Data collection forms
Appendix 8 Sources and details of key unit costs
| Health-care resource | Unit | Cost per unit (£) | Source | Details |
|---|---|---|---|---|
| Primary care | ||||
| GP | Visit | 43.00 | PSSRU56 | Per surgery consultation lasting 11.7 minutes |
| GP | Telephone contact | 26.00 | PSSRU56 | Per telephone contact lasting 7.1 minutes |
| GP | Home visit | 110.00 | PSSRU56 | Per home visit lasting 23.4 minutes (includes travel time) |
| Practice nurse | Visit | 10.59 | PSSRU56 | Practice nurse (Band 5) cost per appointment. Assumes 15.5 minutes visit duration |
| Practice nurse | Telephone contact | 4.10 | PSSRU56 | Practice nurse (Band 5) cost per appointment. Assumes 6 minutes contact duration, as for nurse advanced telephone consultation (PSSRU) |
| Community nurse | Visit | 12.40 | PSSRU56 | Based on community nurse (Band 6) hour. Assumes 15.5 minutes visit duration |
| Community nurse | Telephone contact | 4.80 | PSSRU56 | Based on community nurse (Band 6) hour. Assumes 6 minutes contact duration, as for nurse advanced telephone consultation (PSSRU) |
| Community nurse | Home visit | 22.00 | PSSRU56 | Based on community nurse (Band 6) hour. Assumes 27.5 minutes visit duration (includes 12 minutes of travel time, as for GP home visit) |
| Specialist nurse | Visit | 12.66 | PSSRU56 | Based on specialist nurse hour (Band 6) hour. Assumes 15.5 minutes visit duration |
| Specialist nurse | Telephone contact | 4.90 | PSSRU56 | Based on specialist nurse hour (Band 6). Assumes 6 minutes contact duration, as for nurse advanced telephone consultation (PSSRU) |
| Senior specialist nurse | Visit | 14.98 | PSSRU56 | Based on nurse advanced hour (Band 7). Assumes 15.5 minutes visit duration |
| Senior specialist nurse | Telephone contact | 5.80 | PSSRU56 | Based on nurse advanced hour (Band 7). Assumes 6 minutes contact duration, as for nurse advanced telephone consultation (PSSRU) |
| Mental health nurse | Visit | 10.33 | PSSRU56 | Based on nurse hour (mental health – Band 5). Assumes 15.5 minutes visit duration |
| Mental health nurse | Telephone contact | 4.00 | PSSRU56 | Based on nurse hour (mental health – Band 5) |
| Health visitor | Visit | 12.66 | PSSRU56 | Based on health visitor hour (Band 6). Assumes 15.5 minutes visit duration |
| Health visitor | Telephone contact | 4.90 | PSSRU56 | Based on health visitor hour (Band 6). Assumes 6 minutes contact duration, as for nurse advanced telephone consultation (PSSRU) |
| Clinical support worker | Visit | 5.43 | PSSRU56 | Based on clinical support worker nursing (community – Band 2) hour. Assumes 15.5 minutes visit duration |
| Clinical support worker | Telephone contact | 2.10 | PSSRU56 | Based on clinical support worker nursing (community – Band 2) hour. Assumes 6 minutes contact duration |
| Out-of-hours service | Visit | 61.14 | Primary Care Foundation Benchmark94 | Average of cost across 84 PCTs in England |
| Hospital services | ||||
| Inpatient | Elective Inpatient excess bed-day | Various | NHS reference costs and PSSRU56 | Per specialty ward, activity weighted average of corresponding health-related group |
| Outpatient | Visit | Various | NHS reference costs56,57 | Activity weighted average per specialty |
| Mental health services | ||||
| IAPT | Visit | 70.35 | Parry et al., 201195 | Cost per visit based on cost per referral and mean number of sessions for the Doncaster cohort. Unit cost estimate uprated to from 2008/09 to 2011/12 cost year |
| CMHT | Visit | 44.84 | PSSRU56 | Based on clinical CMHT member cost per hour. Assumes same relationship as between clinical counsellor cost per consultation and cost per hour |
| Counsellor | Visit | 59.00 | PSSRU56 | Based on clinical counsellor cost per consultation |
| Psychiatrist | Visit | 174.64 | PSSRU56 | Based on psychiatrist (consultant) cost per hour. Assumes same relationship as between clinical counsellor cost per consultation and cost per hour |
| Psychologist | Visit | 70.08 | PSSRU56 | Based on clinical psychologist hour. Assumes same relationship as between clinical counsellor cost per consultation and cost per hour |
| Medication | ||||
| Depression-related | Item | Various | BNF55 | Assumes larger size presentations were used |
Appendix 9 Study information for qualitative study (patients)
Appendix 10 Topic guides for qualitative study (patients and health professionals)
Appendix 11 Study information for qualitative study (health professionals)
Appendix 12 Details of recruiting general practitioner practices
| Site | GP practice | PCT/Trust | Number of patients recruited (n = 691) |
|---|---|---|---|
| University of Bristol | Axbridge and Wedmore Medical Practice | Somerset PCT | 9 |
| Barnwood Medical Practice | Gloucestershire PCT | 4 | |
| Bradley Stoke Surgery | South Gloucestershire PCT | 9 | |
| Brockway | North Somerset PCT | 17 | |
| Campden Surgery | Gloucestershire PCT | 12 | |
| Chipping Surgery | Gloucestershire PCT | 34 | |
| Close Farm Surgery | South Gloucestershire PCT | 7 | |
| Dr Burney & Partners | South Gloucestershire PCT | 5 | |
| Horfield Health Centre | Bristol PCT | 1 | |
| London Road Medical Practice | Gloucestershire PCT | 5 | |
| Longlevens Surgery | Gloucestershire PCT | 3 | |
| Orchard Medical Centre | Gloucestershire PCT | 2 | |
| Painswick Surgery | Gloucestershire PCT | 2 | |
| Portland Practice | Gloucestershire PCT | 1 | |
| Stoke Gifford Medical Centre | South Gloucestershire PCT | 16 | |
| Students’ Health Service | Bristol PCT | 7 | |
| The Cedars Surgery | North Somerset PCT | 5 | |
| The Stokes Medical Centre | South Gloucestershire PCT | 13 | |
| West Walk Surgery | South Gloucestershire PCT | 25 | |
| Yorkley Health Centre | Gloucestershire PCT | 6 | |
| University of Manchester | Adshall Road Medical Practice | Stockport PCT | 3 |
| Arch Medical Practice, Hulme Medical Centre | Manchester PCT | 6 | |
| Barlow Medical Centre | Manchester PCT | 26 | |
| Chadsfield Medical Practice | Stockport PCT | 1 | |
| Eastholme Surgery | Stockport PCT | 1 | |
| Heald Green Health Centre | Stockport PCT | 5 | |
| Heaton Mersey Practice | Stockport PCT | 2 | |
| High Lane Medical Practice | Stockport PCT | 1 | |
| Marple Bridge | Stockport PCT | 1 | |
| Ratcliffe & Chew-Graham | Manchester PCT | 9 | |
| Stockport Medical Group | Stockport PCT | 11 | |
| The Archways Surgery | Stockport PCT | 2 | |
| The Avenue Medical Centre | Manchester PCT | 18 | |
| Wellfield Medical | Manchester PCT | 4 | |
| Woodlands Medical Practice | Manchester PCT | 11 | |
| University of Sheffield | Avondale Surgery | Derbyshire County PCT | 2 |
| Birley Health Centre | Sheffield PCT | 1 | |
| Devonshire Green & Hanover Medical Centres | Sheffield PCT | 8 | |
| Drs M I Kadarsha & M Muthulingaswamy | Barnsley PCT | 9 | |
| Handsworth Grange | Sheffield PCT | 6 | |
| Holywell Medical Group | Derbyshire County PCT | 11 | |
| Mill Road Surgery | Sheffield PCT | 1 | |
| Mosborough Health Centre | Sheffield PCT | 10 | |
| Richmond Medical Centre | Sheffield PCT | 9 | |
| Rotherham Road Medical Centre | Barnsley PCT | 9 | |
| The Old School Medical Centre | Sheffield PCT | 8 | |
| University Health Service | Sheffield PCT | 21 | |
| Whitehouse Surgery | Sheffield PCT | 4 | |
| University of York | Ampleforth Surgery | North Yorkshire and York PCT | 1 |
| Dr Moss & Partners – Kings Rd Harrogate | North Yorkshire and York PCT | 56 | |
| Escrick Surgery | North Yorkshire and York PCT | 9 | |
| Leyburn Medical Group | North Yorkshire and York PCT | 1 | |
| Posterngate Sugery – Selby | North Yorkshire and York PCT | 7 | |
| Spring Vale Medical Centre – Whitby | North Yorkshire and York PCT | 11 | |
| Strensall Medical Group | North Yorkshire and York PCT | 16 | |
| York Medical Group Acomb | North Yorkshire and York PCT | 16 | |
| Durham | Annfield Plain | County Durham and Tees Valley PCT | 7 |
| Harbinson House | County Durham and Tees Valley PCT | 4 | |
| Peaseway Medical Centre | County Durham and Tees Valley PCT | 12 | |
| Station View | County Durham and Tees Valley PCT | 1 | |
| Gateshead | Elvaston Road | Gateshead PCT | 4 |
| Glenpark Medical Centre | Gateshead PCT | 3 | |
| Oxford Terrace Medical Group | Gateshead PCT | 24 | |
| Hull | Beeford & Leven Surgery | NHS East Riding of Yorkshire | 8 |
| Church View Surgery, Hedon | NHS East Riding of Yorkshire | 11 | |
| Cranwell Road Medical Centre | NHS East Riding of Yorkshire | 36 | |
| Dr Cook, Beverley High Road | NHS Hull | 2 | |
| Manor Road HC, Beverley | NHS East Riding of Yorkshire | 2 | |
| Orchard 2000 Medical Centre | NHS Hull | 1 | |
| Springhead Practice | NHS Hull | 20 | |
| St Andrews Group Practice | NHS Hull | 1 | |
| The Marshes, Snaith | NHS East Riding of Yorkshire | 6 | |
| North of Tyne | Belford Medical Practice | Northumberland Care Trust | 1 |
| Bellingham Practice | Northumberland Care Trust | 2 | |
| Coquet Medical Group | Northumberland Care Trust | 12 | |
| Forum Family Practice | Northumberland Care Trust | 5 | |
| Ponteland Medical Group | Northumberland Care Trust | 7 | |
| Sele Medical Practice | Northumberland Care Trust | 10 | |
| South of Tyne | Dr Cloak & Partners, Southwick | Sunderland PCT | 5 |
| Herrington Medical Centre | Sunderland PCT | 2 | |
| Pennywell Medical Centre | Sunderland PCT | 2 | |
| Springwell Medical Group | Sunderland PCT | 2 | |
| Victoria Road Health Centre | Sunderland PCT | 1 |
Appendix 13 Results of the seemingly unrelated regressions model: adjusted mean differences in quality-adjusted life-years and costs between computerised cognitive behaviour therapy and usual general practitioner care – complete regression output for the seemingly unrelated regressions model (base-case assumptions)
| QALYs – EQ-5D (n = 691) | Adjusted difference in means | 95% confidence limits | |
|---|---|---|---|
| Lower | Upper | ||
| Beating the Blues vs. usual GP care alone (n = 210 and n = 239, respectively) | – 0.0435 | – 0.1162 | 0.0291 |
| MoodGYM vs. usual GP care alone (n = 242 and n = 239, respectively) | – 0.0153 | – 0.0914 | 0.0607 |
| Baseline EQ-5D | 0.9557 | 0.8080 | 1.1034 |
| Gender | 0.0199 | – 0.0407 | 0.0806 |
| Age | – 0.0066 | – 0.0090 | – 0.0041 |
| Anxiety level | 0.0022 | – 0.0218 | 0.0261 |
| Depression severity | – 0.0081 | – 0.0151 | – 0.0011 |
| Depression duration | – 0.0378 | – 0.0624 | – 0.0133 |
| Constant | 1.2956 | 1.0630 | 1.5282 |
| Total costs (n = 691) | |||
| Beating the Blues vs. usual GP care alone (n = 210 and n = 239, respectively) | £102.64 | – £92.56 | £297.83 |
| MoodGYM vs. usual GP care alone (n = 242 and n = 239, respectively) | £0.72 | – £202.43 | £203.87 |
| Baseline costs | £2.14 | £1.71 | £2.56 |
| Gender | £22.59 | – £149.07 | £194.26 |
| Age | £12.23 | £5.77 | £18.69 |
| Anxiety level | £27.44 | – £31.33 | £86.21 |
| Depression severity | £19.33 | – £2.03 | £40.68 |
| Depression duration | £8.95 | – £49.41 | £67.31 |
| Constant | –£252.92 | – £729.24 | £223.41 |
Appendix 14 Cost-effectiveness acceptability curves for scenarios 1–5
Scenario 1

Scenario 2

Scenario 3

Scenario 4
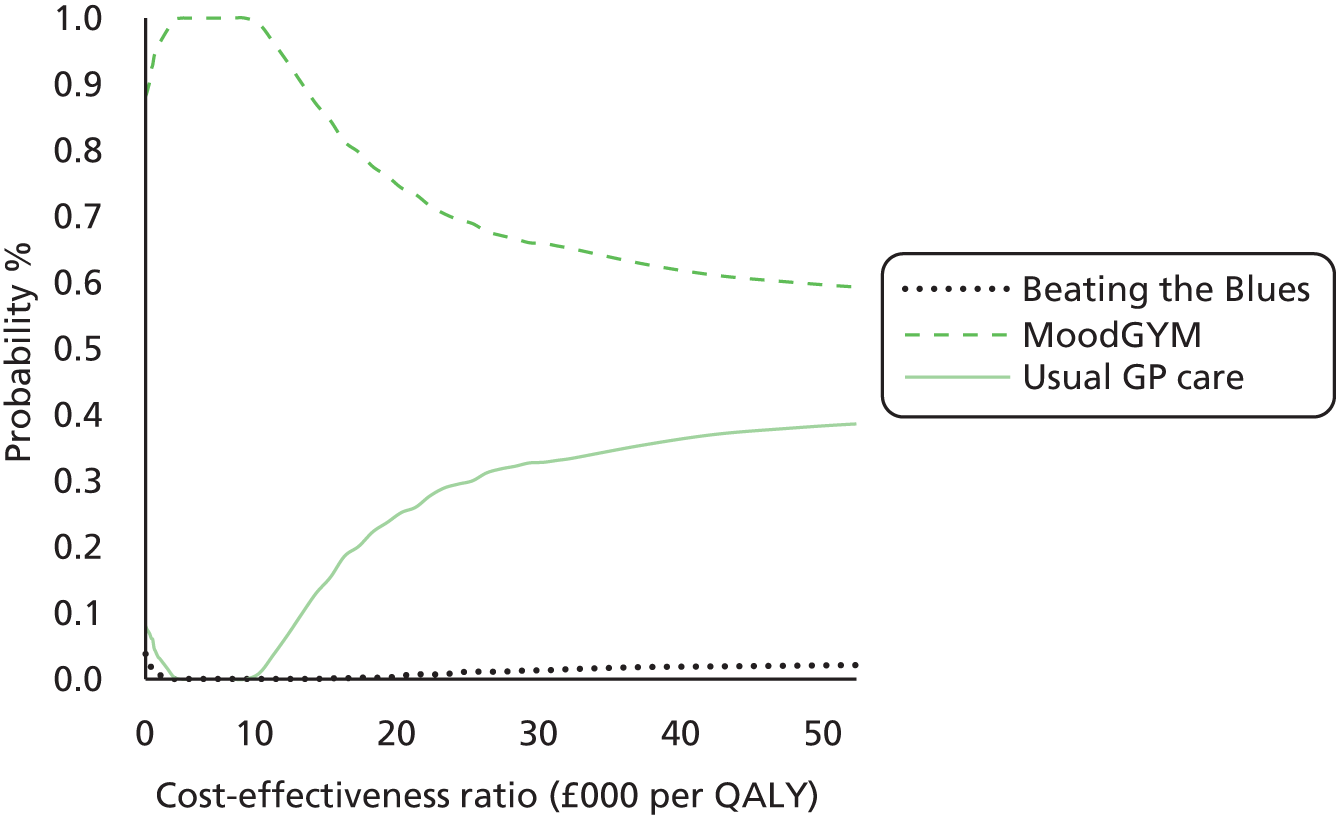
Scenario 5

List of abbreviations
- AIC
- Akaike information criterion
- CBT
- cognitive behaviour therapy
- cCBT
- computerised cognitive behaviour therapy
- CEAC
- cost-effectiveness acceptability curve
- CI
- confidence interval
- CIS-R
- Clinical Interview Schedule – Revised
- CMHT
- Community Mental Health Team
- CONSORT
- Consolidated Standards of Reporting Trials
- CORE-OM
- Clinical Outcomes in Routine Evaluation – Outcome Measure
- CSRI
- Client Service Receipt Inventory
- DMEC
- Data Monitoring and Ethics Committee
- EQ-5D
- European Quality of Life-5 Dimensions
- GLM
- generalised linear model
- GP
- general practitioner
- HRQoL
- health-related quality of life
- HTA
- Health Technology Assessment
- IAPT
- Improving Access to Psychological Therapies
- ICER
- incremental cost-effectiveness ratio
- IQR
- interquartile range
- MCS
- mental component summary
- MHRN
- Mental Health Research Network
- MICE
- multiple imputation by chained equations
- NICE
- National Institute for Health and Care Excellence
- NPT
- Normalisation Process Theory
- NSAE
- non-serious adverse event
- OLS
- ordinary least squares
- OR
- odds ratio
- PCS
- physical component summary
- PHQ-9
- Patient Health Questionnaire-9
- PSSRU
- Personal Social Services Research Unit
- QALY
- quality-adjusted life-year
- QOF
- Quality and Outcomes Framework
- RCT
- randomised controlled trial
- REC
- Research Ethics Committee
- REEACT
- Randomised Evaluation of the Effectiveness and Acceptability of Computerised Therapy
- SAE
- serious adverse event
- SD
- standard deviation
- SF-36v2
- Short Form questionnaire-36 items Health Survey® version 2
- SF-6D
- Short Form questionnaire-6 Dimensions
- SMD
- standardised mean difference
- SUR
- seemingly unrelated regression
- TSC
- Trial Steering Committee