Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 09/163/02. The contractual start date was in September 2012. The draft report began editorial review in July 2014 and was accepted for publication in March 2015. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
John Norrie is a member of the National Institute for Health Research Health Technology Assessment (HTA) and Efficacy and Mechanism Evaluation Editorial Board and HTA Commissioning Board.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2015. This work was produced by Blyth et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Background
The menisci are two semilunar, fibrocartilaginous discs located between the medial and lateral articular surfaces of the femur and tibia in each knee. 1 Although both menisci are crescent shaped, the medial meniscus appears comma shaped, with larger separation between the anterior and posterior horns, and the lateral meniscus is ‘C’ shaped with less separation between the horns (see Figures 1 and 2). 1 Lateral menisci are reported to show greater variation in size, shape and mobility than medial mensci. 2 The anatomy of the menisci is unique, being made up of circumferentially and radially oriented collagen fibres that provide resistance to ‘hoop’ stress and shear forces respectively. 3 The meniscal microstructure of fibrochondrocytes situated in the inner portion and fibroblasts situated on the outer portion enable the key properties of these structures. The fibrochondrocytes synthesise extracellular matrix and the fibroblasts produce collagen and proteoglycans. 3
The meniscus is a relatively avascular structure; at maturity 10–25% of the peripheral meniscal tissue is supplied by the popliteal artery. 4 Three regions can be described, dividing the meniscus by its vascular supply. The ‘red zone’ is located in the peripheral third of the meniscal body and is heavily vascularised, the ‘red–white zone’ comprises the central third of the meniscal body and the ‘white zone’ is located in the inner third of the body of the meniscus and has no vascular supply (Figure 1). 4,5 The healing capacity of each area of the meniscus is directly related to its vascularisation, with the white zone susceptible to permanent damage and degenerative lesions. 4 The peripheral red zone is a thick, convex structure attached to the joint capsule whereas the inner white zone tapers to a thin edge. 6 To allow effective articulation with the convex femoral condyles the superior surface of the menisci are concave. The inferior surfaces of the menisci are flat to match the tibial plateau. 6
FIGURE 1.
Blood supply to the menisci.
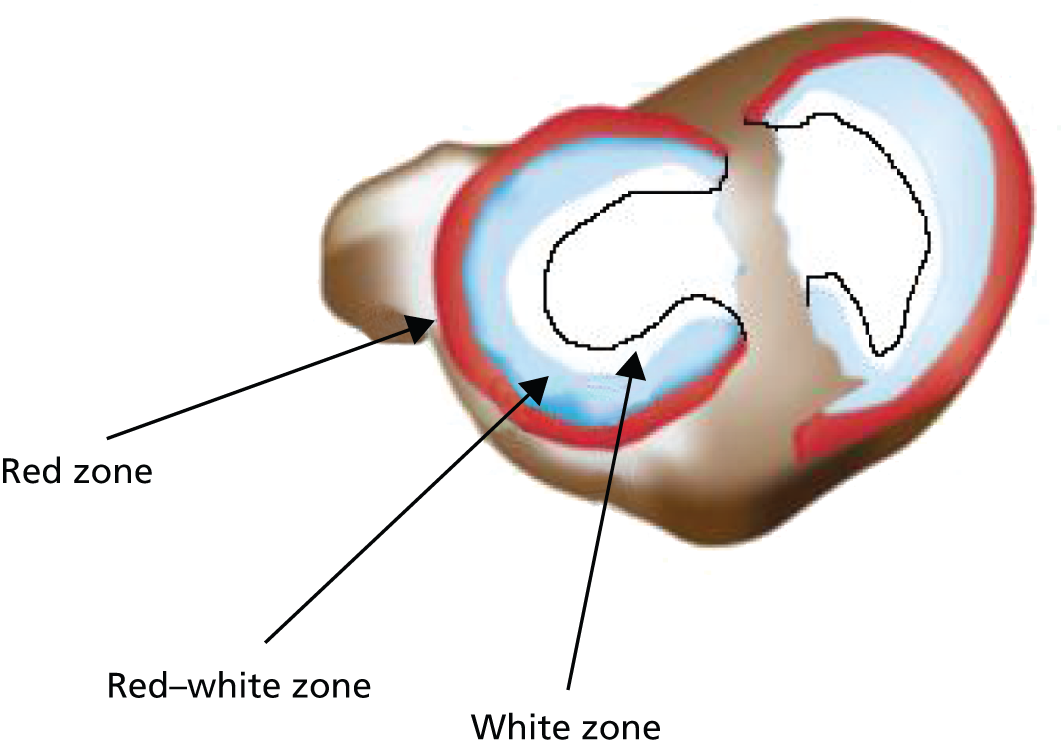
The ‘red zone’ is heavily vascularised, the ‘red–white zone’ constitutes the central third of the meniscal body and has limited vascularity, and the ‘white zone’ is located in the inner third of the body of the meniscus and has no vascular supply.
The menisci play an important role in the knee, providing multiple complex functions including load bearing, stress distribution and shock absorption. Loads transmitted through the joint to the cartilage are partially borne by the menisci, giving them an important role in both the protection of the cartilage and the subsequent development of degenerative osteoarthritis of the knee should the menisci become damaged.
Damage to the menisci commonly occurs in two different scenarios. In young active individuals the menisci are often damaged during sporting activity. Acute tears of the menisci occur secondary to a rotational and compressive load placed on the knee during movement from a flexed position (knee bent) to an extended position (knee straight). Sport participants often describe knee pain after twisting their leg while the foot is planted on the ground with the affected limb bearing their full weight. The combination of compression and rotation that occurs during this movement results in shear stresses that can tear the meniscal tissue. At the time of injury there is often pain and swelling of the knee joint, with twisting or pivoting movements often exacerbating the pain. The pain and swelling subside over a period of weeks after an acute injury, but patients can present weeks later with typical symptoms including intermittent localised pain, locking or catching, giving way, difficulty with deep knee bending and kinesiophobia or fear of movement.
During a 10-year epidemiological study in Switzerland and Germany 17,397 patients with 19,530 sports injuries were documented: 40% of injuries related to the knee joint; 10.8% had a medial meniscus lesion with a further 3.7% having a lateral meniscus lesion. 7 Degenerative meniscal tears are more common in older people. Tears in this age group usually result from long-term degeneration of the meniscus itself and cause joint swelling, joint line pain and mechanical locking. 8–10 The presence of meniscal tears has been identified as an important risk factor in the development of knee osteoarthritis. 10,11 Degenerative meniscal tears are associated with articular cartilage defects, loss of articular cartilage volume and prevalence of radiographical osteoarthritis. 12 Individuals with osteoarthritis of the knee are twice as likely to have a meniscal tear as age-matched individuals without osteoarthritis. 13
A number of different patterns of meniscal tear have been reported including vertical or longitudinal (bucket-handle), flap or oblique, radial or transverse, torn horn and complex degenerative tears (Figure 2).
FIGURE 2.
Menisci of the knee and common tear patterns.

Reliable non-invasive diagnosis of meniscal tears is difficult. Magnetic resonance imaging (MRI) is often referred to as the gold standard for non-invasive diagnosis of meniscal tears. However, incidental meniscal findings by MRI of the knee are common in the general population. These incidental findings increase with age and are often not associated with pain. 13 The only completely accurate way to diagnose meniscal tears is to perform an arthroscopy of the knee in order to image the menisci directly. However, this is an invasive procedure and therefore carries risks for the patient. Infection is a rare complication of arthroscopy, but septic arthritis may have devastating consequences and therefore every procedure should be well justified. 14 Reported rates in the literature are low and vary from 0.08% to 0.42%. 15,16 Several systematic reviews taking arthroscopy findings as ‘gold standard’ compared with MRI results have shown that MRI is both sensitive and specific. 17,18 MRI is reported to be better at identifying patients with medial meniscal tears rather than lateral tears. 17 Sensitivity of 93.3% [95% confidence interval (CI) 91.7% to 95.0%] and specificity of 88.4% (95% CI 85.4% to 91.4%) have been reported for medial meniscal tears by MRI. 18 For lateral meniscal tears sensitivity and specificity are 79.3% (95% CI 74.3% to 84.2%) and 95.7% (95% CI 94.6% to 96.8%) respectively. 18 We believe that performing unnecessary arthroscopy procedures cannot be ethically justified in this patient group and that MRI is an acceptable surrogate for diagnosis of meniscal tears.
However, meniscal damage is also a frequent finding on MRI of the osteoarthritic knee, limiting the value of this diagnostic tool for meniscal tears in this section of the population. 19 Among patients with clinical and radiographic findings of osteoarthritis of the knee the prevalence of meniscal tears has been reported to be as high as 68–90%. 20,21 It is therefore essential that a detailed history, including mechanism of injury, onset of symptoms and a physical examination, is carried out prior to MRI scanning for meniscal tear. 22
In addition to imaging tests, there are a number of physical examination tests described for the diagnosis of meniscal tears. However, a meniscal tear can be difficult to diagnose as symptoms are often non-specific and associated injuries can disguise a tear in the meniscus. 23 The most commonly used physical tests include the joint line tenderness Test, McMurray’s Test and Apley’s Test. These tests have been in use for many years, but are widely acknowledged to have limited specificity and sensitivity, particularly in the presence of other knee pathologies, such as anterior cruciate ligament rupture. 24
Although limited in diagnostic accuracy compared with MRI scanning or arthroscopy, these physical tests have the advantage of being relatively easy to perform and also to incur no additional cost. More recently Karachalios et al. 25 have described a new physical test to detect meniscal tears – the Thessaly Test. When performed at 20° of knee flexion the Thessaly Test is reported to have a high diagnostic accuracy for detecting both lateral and medial meniscal tears. Table 1 summarises the current literature with respect to the diagnostic capabilities of the Thessaly Test, McMurray’s Test, Apley’s Test and the joint line tenderness Test.
| Test | Sensitivity (95% CI) | Specificity (95% CI) | Reference (n) | Diagnostic ‘gold standard’ |
|---|---|---|---|---|
| McMurray’s Test | 70.5% (67.4% to 73.4%) | 71.1% (69.3% to 72.9%) | Hegedus et al.26 (meta-analysis pooled data) | Mixed arthroscopy and MRI |
| Apley’s Test | 60.7% (55.7% to 65.5%) | 70.2% (68.0% to 72.4%) | Hegedus et al.26 (meta-analysis pooled data) | Mixed arthroscopy and MRI |
| Joint line tenderness Test | 63.3% (60.9% to 65.7%) | 77.4% (75.6% to 79.1%) | Hegedus et al.26 (meta-analysis pooled data) | Mixed arthroscopy and MRI |
| Thessaly Test (original paper) | 89%a [medial] | 97%a [medial] | Karachalios et al.25 (n = 213 symptomatic and 197 asymptomatic) | Arthroscopy |
| Thessaly Test (original paper) | 92%a [lateral] | 96%a [lateral] | Karachalios et al.25 (n = 213 symptomatic and 197 asymptomatic) | Arthroscopy |
| Thessaly Test | 90%a | 98%a | Harrison et al.27 (n = 116) | Arthroscopy |
| Thessaly Test | 59% (47% to 71%) [medial] | 67% (45% to 83%) [medial] | Konan et al.28 (n = 109) | Arthroscopy |
| Thessaly Test | 31% (15% to 54%) [lateral] | 95% (87% to 98%) [lateral] | Konan et al.28 (n = 109) | Arthroscopy |
| Thessaly Test in ACL-deficient patients | 79%a | 40%a | Mirzatolooei et al.29 (n = 80) | Arthroscopy |
Summary description of physical tests for meniscal tears
The joint line tenderness Test involves palpation of the joint line with the knee in 90° of flexion. The test is considered positive when there is pain along the joint line on palpation (Figure 3).
FIGURE 3.
Joint line tenderness Test.

The McMurray’s Test (Figure 4) was originally described in 1940 and designed to detect tears in the posterior portion of the meniscus. A test is considered positive when a click can be heard and/or felt on joint line palpation when the knee is bent beyond 90° flexion and the tibia is rotated on the femur into full internal rotation then full external rotation (to test the lateral and medial meniscus respectively).
FIGURE 4.
McMurray’s Test.

Apley’s Test is carried out with the patient prone and the knee flexed to 90° (Figure 5). The tibia is then compressed onto the knee joint while being externally rotated. If this manoeuvre produces pain, this constitutes a positive test. 30,31
FIGURE 5.
Apley’s Test.

The Thessaly Test was first described in 2005 by Karachalios et al. 25 as a novel clinical examination used to detect meniscal tears in the knee. When performed at 20° of knee flexion it is reported to have a high diagnostic accuracy rate for detecting both lateral and medial meniscal tears. 28 The Thessaly Test is a dynamic reproduction of joint loading in the knee. The examiner supports the patient by holding the patient’s outstretched hands while he/she stands flatfooted on the floor. The patient then rotates his or her knee and body, internally and externally, three times, keeping the knee in slight flexion (20°) (Figure 6). Patients with a suspected meniscal tear will experience medial or lateral joint line pain if the test is positive.
FIGURE 6.
Thessaly Test.

The aim of this prospective study was to determine the diagnostic accuracy of the Thessaly Test and to determine if the Thessaly Test (alone or in combination with other tests) can obviate the need for further investigation by MRI or arthroscopy for patients with suspected meniscal tears.
Chapter 2 Study design/methods
This study was a single-centre diagnostic accuracy study comparing two cohorts of patients with and without knee pathology, assessed by two groups of clinicians – primary care clinicians and musculoskeletal clinicians. The primary goal was to assess the diagnostic accuracy of the Thessaly Test for meniscal tears; however, the diagnostic accuracy of three other physical tests and a standardised clinical history were also analysed.
Musculoskeletal clinicians included both orthopaedic specialist knee surgeons and extended scope physiotherapists with specialist knee interest (operating in a secondary care orthopaedic setting). Primary care clinicians were either general practitioner- (GP-) or community-based physiotherapists.
The study protocol was developed in response to a call for proposals from the National Institute for Health Research Heath Technology Assessment (HTA) programme. Funding was provided by HTA.
Ethical approval was obtained from the West of Scotland Research Ethics Committee (reference 12/WS/0225) prior to initiation of the study. The study was registered on the International Randomised Controlled Trial Number registry (ISRCTN 43527822).
The study was performed as a collaboration between the Orthopaedic Research Unit at Glasgow Royal Infirmary and the Robertson Centre for Biostatistics at the University of Glasgow.
Study objectives
-
To determine the diagnostic accuracy of the Thessaly Test for meniscal tears in the knee and whether or not this test can obviate the need for further investigation by arthroscopy or MRI.
-
To determine how the Thessaly Test compares with clinical history and to other commonly used physical examinations (McMurray’s Test, Apley’s Test and the joint line tenderness Test) in diagnosing meniscal tears.
-
To determine if the presence of arthritis or other knee pathologies influences the accuracy of the Thessaly Test.
-
To determine if the use of combinations of physical tests (such as the Thessaly Test, McMurray’s Test, Apley’s Test and the joint line tenderness Test) provides better specificity and sensitivity than a single test alone in the diagnosis of meniscal tears.
-
To determine the ability of non-specialist GPs to use the Thessaly Test in comparison with specialist knee clinicians.
Patient selection
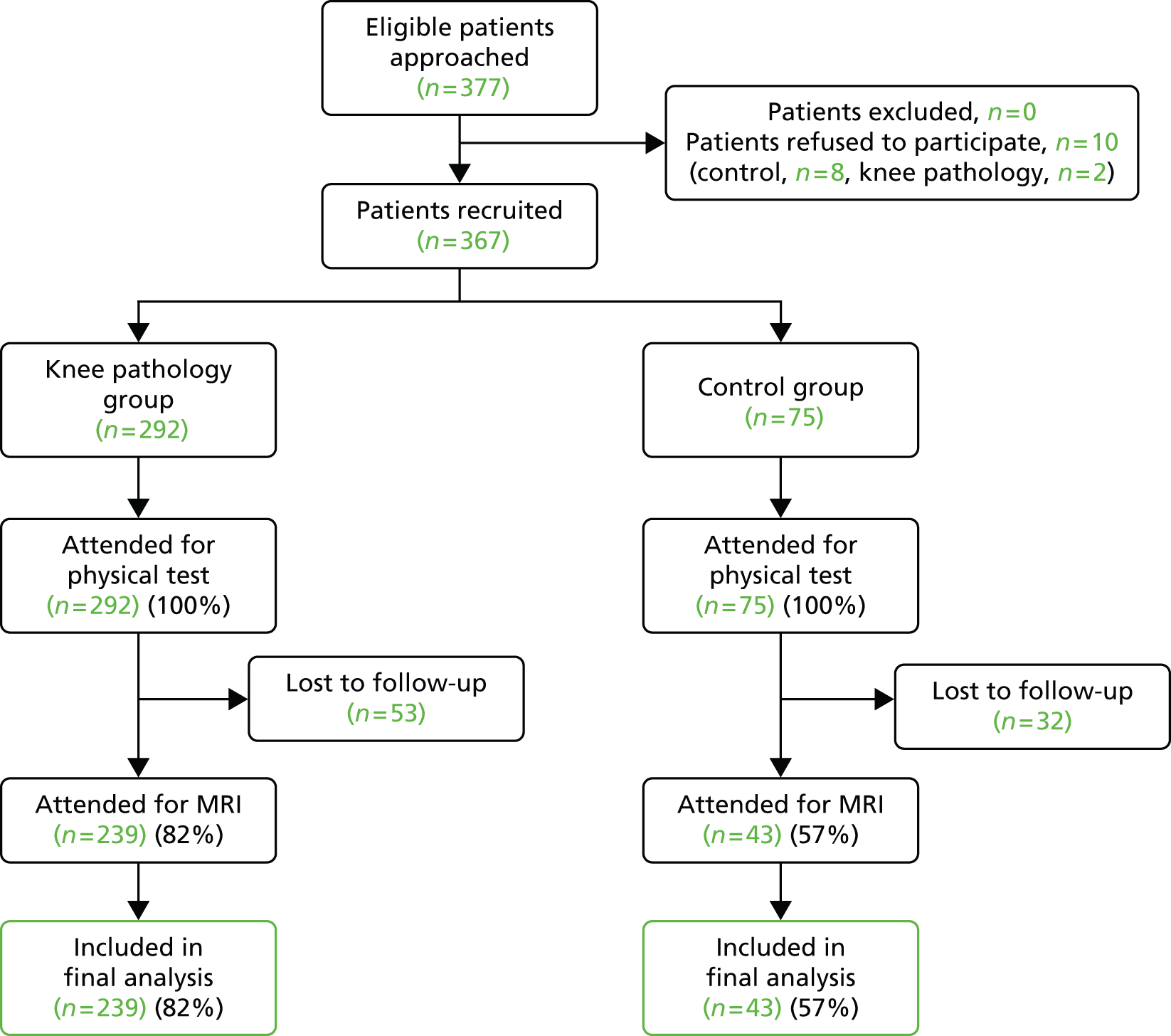
Two cohorts of patients were recruited to the study between October 2012 and March 2014 (Figure 7). The first group had unspecified knee pathology and were typical of the target patient group that a primary care clinician may wish to assess using the Thessaly Test. These patients were primarily drawn from patients referred to a specialist knee clinic at Glasgow Royal Infirmary by GPs and other primary care clinicians. A proportion of this group were recruited directly from a single GP practice (n = 11). This group were used as an internal control to verify that subjects recruited at Glasgow Royal Infirmary were representative of the target population of patients who attend general practice with knee pain. The second control group consisted of patients with no current or recent knee pathology. These subjects were included in order to test the specificity of the Thessaly Test. Control subjects were recruited from two sources – from the hand injury clinic at Glasgow Royal Infirmary and from advertisement posters placed within Glasgow Royal Infirmary and local universities.
FIGURE 7.
Study flow diagram. Note: patients who did not attend for a MRI scan were classed as lost to follow-up.
Only one knee from any one individual was included in the study.
Written informed consent was obtained from each patient.
As all patients attending the knee clinic were essentially eligible for the study, there were no screening failures from the knee clinic. Similarly, patients in the control group responding to our advert were effectively self-screened and therefore there were no screen failures from this source either.
Knee pathology group
Inclusion criteria
-
Patients referred to the knee clinic at Glasgow Royal Infirmary.
Exclusion criteria
-
Age < 18 years.
-
Unable to give informed consent.
-
Previous knee replacement surgery.
Control group
Inclusion criteria
-
Patients attending the hand clinic at Glasgow Royal Infirmary or responding to advertisement posters placed within Glasgow Royal Infirmary.
Exclusion criteria
-
Age < 18 years.
-
Unable to give informed consent.
-
Previous knee replacement surgery.
-
A history of knee pain in the last 6 months.
-
Osteoarthritis.
-
Rheumatoid arthritis.
Sample size
Sample size calculation was based on the following assumptions. Assuming the sensitivity of the Thessaly Test is around 75%, the study would need around 300 subjects to estimate the sensitivity to within ± 5%. A similar calculation for the width of the CI for a binomial proportion is appropriate for the specificity (e.g. if the specificity was around 90%, the required sample size to estimate the specificity to within ± 8% would be n = 50 participants). The power for the pairwise comparison of tests, or combinations of tests, will depend on the degree of disagreement between the tests [e.g. with around 220 pairs of measurements the study would have 90% power to detect a difference in proportions of 0.10 when the proportion of discordant pairs is expected to be 0.15 (using McNemar’s Test)].
Patient assessment
Patients were examined by two types of independent practitioners: a trained orthopaedic musculoskeletal specialist (n = 11) and a primary care clinician (n = 12). The orthopaedic musculoskeletal specialist was either an orthopaedic consultant knee surgeon (n = 3) or an orthopaedic extended scope physiotherapist with a specialist interest in the knee (n = 8). Primary care clinicians were either a GP (n = 4) or a community physiotherapist (n = 8). There was a broad range of experience within the primary care clinician group ranging from newly qualified practitioners to a practitioner with more than 30 years of experience. We believe that the diverse mix of experience reflects reality in the primary care setting.
Each clinician performed the following physical tests: the Thessaly Test, McMurray’s Test, Apley’s Test and the joint line tenderness Test. In addition, each clinician took a clinical history from the patient. The order in which physical tests were carried out was randomised to avoid bias in knowledge gained from performing any previous test. This was achieved using a random sequence generator to determine the order that each test should be performed in. The sequences were generated in advance and printed on study data collection forms. The forms were handed out in the order they were printed by the study co-ordinator (KB) to sequential examiners.
All patients in both groups were asked to attend for a MRI scan of their knee, any patient not attending for MRI was excluded from the final analysis. MRI diagnosis of meniscal tears was used as the gold standard reference for each of the physical tests examined in this study. All MRI scans were reported by radiologists who were not linked to the study and who were blind to the patients’ status with regard to clinical history and examination findings. MRI scans for the knee pathology patients were carried out within 6 weeks of assessment.
Magnetic resonance imaging scan sequences are detailed below:
-
T1 spin-echo Sagittal
-
T2 fl2d Sagittal (flash-gradient ECHO)
-
proton-density turbo-spin echo fat saturation transverse.
-
proton-density turbo-spin echo fat saturation coronal.
In order to determine if the presence of osteoarthritis of the knee influenced the outcome of physical tests for meniscal tears, knee radiography was performed on all patients with knee pathology. No radiography was performed on control patients as it was deemed unethical to expose control patients to unnecessary X-rays. Degree of osteoarthritis of the knee was graded from knee radiography using the Kellgren and Lawrence system. 32 Kellgren and Lawrence grading was undertaken by a single-blinded examiner (AP).
A proportion of patients with a knee pathology subsequently had a routine arthroscopy as part of their treatment/diagnosis of their knee condition. In these patients we recorded the presence of any meniscal tears at the time of arthroscopy. Arthroscopy was normally carried out within 6 weeks of the MRI scan. These data were then correlated with the diagnosis of meniscal tears obtained from MRI images of the patient, in order to verify the accuracy of MRI imaging for meniscal tears by computing specificity, sensitivity, negative and positive predictive values (NPVs and PPVs) for MRI, with arthroscopy as the gold standard.
Physical tests
The Thessaly Test was carried out as described by Karachalios et al. 25 The Thessaly Test, McMurray’s Test, Apley’s Test and the joint line tenderness Test were all carried out as described in Chapter 1.
Standardised clinical history
A simple standardised clinical history was developed for this study (see Standardised minimal clinical history data set). Our concept was that any test that proved successful in this study required to be simple enough for national roll-out without requiring an extensive training programme. All clinicians were therefore given basic instruction in the use of the standardised clinical history in Standardised minimal clinical history data set and asked to use this as a minimum in their diagnosis.
Standardised minimal clinical history data set
-
History of knee injury?
-
Was this a sports injury?
-
-
Past history of anterior cruciate ligament (ACL) injury?
-
Past history of arthritis?
-
Previous surgery to the knee?
-
Past history of medial meniscal tear?
-
Past history of lateral meniscal tear?
-
Presence of associated patella–femoral symptoms?
Primary outcome measures
-
Sensitivity and specificity of the Thessaly Test in determining the presence of meniscal tears when employed by primary care clinicians.
Secondary outcomes measures
-
Sensitivity and specificity of the Thessaly Test in determining the presence of meniscal tears when employed by specialist musculoskeletal clinicians.
-
Sensitivity and specificity of McMurray’s Test, Apley’s Test, the joint line tenderness Test and clinical history in determining the presence of meniscal tears.
-
Determination of the influence of osteoarthritis on the sensitivity and specificity of the Thessaly Test, McMurray’s Test, Apley’s Test and the joint line tenderness Test.
-
Determination of the influence of other knee pathologies such as ACL damage or patellofemoral instability on the sensitivity and specificity of the Thessaly Test, McMurray’s Test, Apley’s Test and the joint line tenderness Test.
-
Determination of the optimal combination of tests for most accurate diagnosis of meniscal tears.
Statistical analysis
The full statistical analysis plan is described in detail in Appendix 1. In brief, we calculated the specificity, sensitivity, PPV and NPV for each of the following individual tests: Thessaly Test, McMurray’s Test, Apley’s Test, the joint line tenderness Test and clinical history. We have used evidence of meniscal tear on MRI as our ‘gold standard’ reference for diagnosis. We have compared the relative rates between each individual test. These results are reported separately for specialist musculoskeletal clinicians and for primary care clinicians.
The following subanalysis was also performed:
-
Patients with and without osteoarthritis of the knee were compared to determine if osteoarthritis influences the outcome of the Thessaly Test or any of the other physical tests. Other patient factors were also considered [body mass index (BMI), sex, age and previous surgery].
-
A comparison of results of all four physical tests between specialist musculoskeletal clinicians and primary care clinicians was performed to determine if specialised training influences the outcome of test results.
-
We have examined whether or not a combination of physical tests can produce greater diagnostic accuracy than a single test alone.
-
In a subset of patients, we have compared the accuracy of MRI scan diagnosis of meniscal tears to that achieved using arthroscopy.
Statistical tests applied to data
A chi-squared test was used for comparisons between musculoskeletal clinicians and primary care clinicians for each physical test and clinical history, as well as to compare the sensitivity or specificity of the four physical tests along the different bins of the categorical (or categorised) covariates.
McNemar’s Test was used to for comparisons between musculoskeletal clinicians and primary care clinicians for each physical test and clinical history. McNemar’s Test assesses the significance of the difference between two correlated proportions, where the two proportions are based on the same sample of subjects. In this study we wished to determine the difference between the proportion of successful diagnoses obtained by the two groups of observers; hence, the choice of McNemar’s Test over intraclass correlation.
Logistic regression was used to assess the influence of different covariates on the sensitivity or specificity of the four physical tests for musculoskeletal clinicians and primary care clinicians (all patients or knee patients).
Logistic regression using a stepwise procedure from the covariates and the four physical tests to build a model to predict MRI.
Guide to likelihood ratio graphs
The diagnostic abilities of two or more diagnostic tests are traditionally compared by their respective sensitivities and specificities. Comparison is relatively simple if both tests have similar sensitivity, but one has a superior specificity. However, comparison is more complicated when the specificities and sensitivities are both different and a trade-off of one over the other is required.
Likelihood ratio graphs are a simple graphic that readily facilitates comparison between two or more diagnostic tests, allowing an assessment of whether or not a decrease in specificity may be offset by a sufficient gain in sensitivity to yield a test that, nevertheless, has superior diagnostic ability.
For all likelihood ratio graphs in this report, the Thessaly Test is plotted as the reference test (solid black lines). Any comparator test plotted in zone I is superior in all aspects to the Thessaly Test. Comparators plotted in zone II are superior at detecting the absence of a meniscal tear, but inferior at detecting the presence of a tear. Comparators plotted in zone III are superior at detecting the presence of a tear, but inferior at detecting the absence of a tear. Any comparator plotted in zone IV is inferior to the Thessaly Test (Figure 8).
FIGURE 8.
Likelihood ratio graph.

Chapter 3 Study cohort demographics and description
Demographics
The study cohort demographics are displayed in Tables 2 and 3.
| Age (years)a | BMI (kg/m2)a | ||
|---|---|---|---|
| All patients | n (NA) | 367 (0 or 0%) | 345 (22 or 6%) |
| Mean (SD) | 41.6 (13.7) | 27.5 (4.7) | |
| Min.–max. | 18–71 | 18–47 | |
| Knee pathology group | n (NA) | 292 (0 or 0%) | 276 (16 or 5.5%) |
| Mean (SD) | 42.6 (13.4) | 27.8 (4.8) | |
| Min.–max. | 18–71 | 18–47 | |
| Control group | n (NA) | 75 (0 or 0%) | 69 (6 or 8%) |
| Mean (SD) | 37.9 (14.3) | 26.2 (4.2) | |
| Min.–max. | 18–71 | 20.4–41.7 | |
| p-value | t-test | 0.011 | 0.008 |
| Knee pathology group | Control group | |
|---|---|---|
| Female, n | 104 | 38 |
| Male, n | 188 | 37 |
| % male | 64 | 49 |
The control group were on average 4.7 years younger than the knee pathology group with the same age range for both groups (see Table 2). Forty-nine per cent of the control group were male compared with a significantly higher proportion of 64% in the knee pathology group (see Table 3). Although the mean ages and sex distribution were statistically significantly different we do not believe that this is important in the context of this particular study. Furthermore, our logistic regression models have adjusted for variables such age and sex.
The control group were included to allow us to test the specificity of the Thessaly Test in a group with no knee pathologies and not to provide a direct comparison with the knee pathology group. The specificity of a test indicates how often the test correctly predicts negative results. As increasing age is associated with meniscal tears a younger control cohort are less likely to have meniscal tears and therefore should allow more accurate assessment of the specificity of the test.
Approximately half of the study cohort had a meniscal tear identified by MRI (Table 4), these tears were predominantly medial (Table 5). In the knee pathology group 56% of patients (n = 130) had a meniscal tear compared with just 12% in the control group (n = 5). All patients in the control cohort who had meniscal tears diagnosed by MRI were asymptomatic (n = 5) and four of these five patients had osteoarthritis of the knee. In the knee pathology group 71.4% of those with meniscal tears had medial tears, 28.6% lateral tears and 11% had meniscal cysts (note some patients had more than one pathology). A total of 18.3% of the knee pathology cohort had an ACL injury and 27% had grade II or worse osteoarthritis of the knee on X-ray (Table 6). Other major knee pathologies observed in both groups are detailed in Table 7.
| MRI observation | Knee pathology | Control | |||
|---|---|---|---|---|---|
| Yes | No | Yes | No | ||
| Meniscal tear | n | 130 | 100 | 5 | 38 |
| % | 56.5 | 43.5 | 11.6 | 88.4 | |
| Arthritis | n | 81 | 148 | 9 | 34 |
| % | 35.4 | 64.6 | 20.9 | 79.1 | |
| ACL injury | n | 42 | 187 | 1 | 42 |
| % | 18.3 | 81.7 | 2.3 | 97.7 | |
| Medial | Lateral | |
|---|---|---|
| % | 71.4 | 28.6 |
| Grade | 0 | I | II | III | IV |
|---|---|---|---|---|---|
| n | 109 | 83 | 35 | 29 | 8 |
| % | 41.3 | 31.4 | 13.3 | 11 | 3 |
| Other knee pathologies | Knee pathology | Control group |
|---|---|---|
| Previous knee surgery, % | 15 | 0 |
| History of knee pain (last 6 months), % | 100 | 0 |
| Rheumatoid arthritis, % | 0 | 0 |
| Ligament instabilities, % | 21 | 2 |
| Tendonitis, % | 3 | 0 |
| Patellofemoral disorders, % | 16 | 0 |
Chapter 4 Diagnostic accuracy of the Thessaly Test and other tests for diagnosis of meniscal tear
STAndards for the Reporting of Diagnostic accuracy studies (STARD) diagrams are provided in Appendix 2 for each of the following tests: the Thessaly Test, the joint line tenderness Test, McMurray’s Test, Apley’s Test and clinical history. These figures give the exact number of patients assessed using each test and their respective test outcomes.
Accuracy of the Thessaly Test when used by primary care clinicians
When the study tests were performed by primary care clinicians, significant differences were found between the tests with respect to sensitivity and specificity of the tests, but not with NPVs and PPVs (Table 8).
| Statistical test | Thessaly Test | McMurray’s Test | Apley’s Test | Joint line tenderness Test | Recorded clinical history | p-value |
|---|---|---|---|---|---|---|
| Sensitivity | 0.66 (0.57 to 0.74) | 0.58 (0.49 to 0.67) | 0.53 (0.44 to 0.62) | 0.77 (0.68 to 0.84) | 0.65 (0.56 to 0.74) | 0.001 |
| Specificity | 0.39 (0.29 to 0.50) | 0.56 (0.45 to 0.66) | 0.53 (0.42 to 0.63) | 0.26 (0.18 to 0.36) | 0.43 (0.33 to 0.54) | < 0.001 |
| LR+ | 1.08 (0.88 to 1.33) | 1.33 (1.01 to 1.75) | 1.12 (0.85 to 1.46) | 1.04 (0.89 to 1.21) | 1.16 (0.93 to 1.43) | – |
| LR– | 0.87 (0.61 to 1.25) | 0.74 (0.56 to 0.98) | 0.90 (0.69 to 1.17) | 0.89 (0.57 to 1.41) | 0.80 (0.57 to 1.11) | – |
| OR | 1.24 (0.71 to 2.18) | 1.79 (1.04 to 3.09) | 1.24 (0.73 to 2.12) | 1.16 (0.63 to 2.13) | 1.45 (0.84 to 2.49) | – |
| PPV | 0.47 (0.40 to 0.55) | 0.53 (0.45 to 0.62) | 0.50 (0.41 to 0.58) | 0.45 (0.38 to 0.51) | 0.48 (0.40 to 0.55) | 0.598 |
| NPV | 0.47 (0.35 to 0.58) | 0.50 (0.40 to 0.60) | 0.45 (0.35 to 0.55) | 0.46 (0.33 to 0.60) | 0.49 (0.39 to 0.60) | 0.96 |
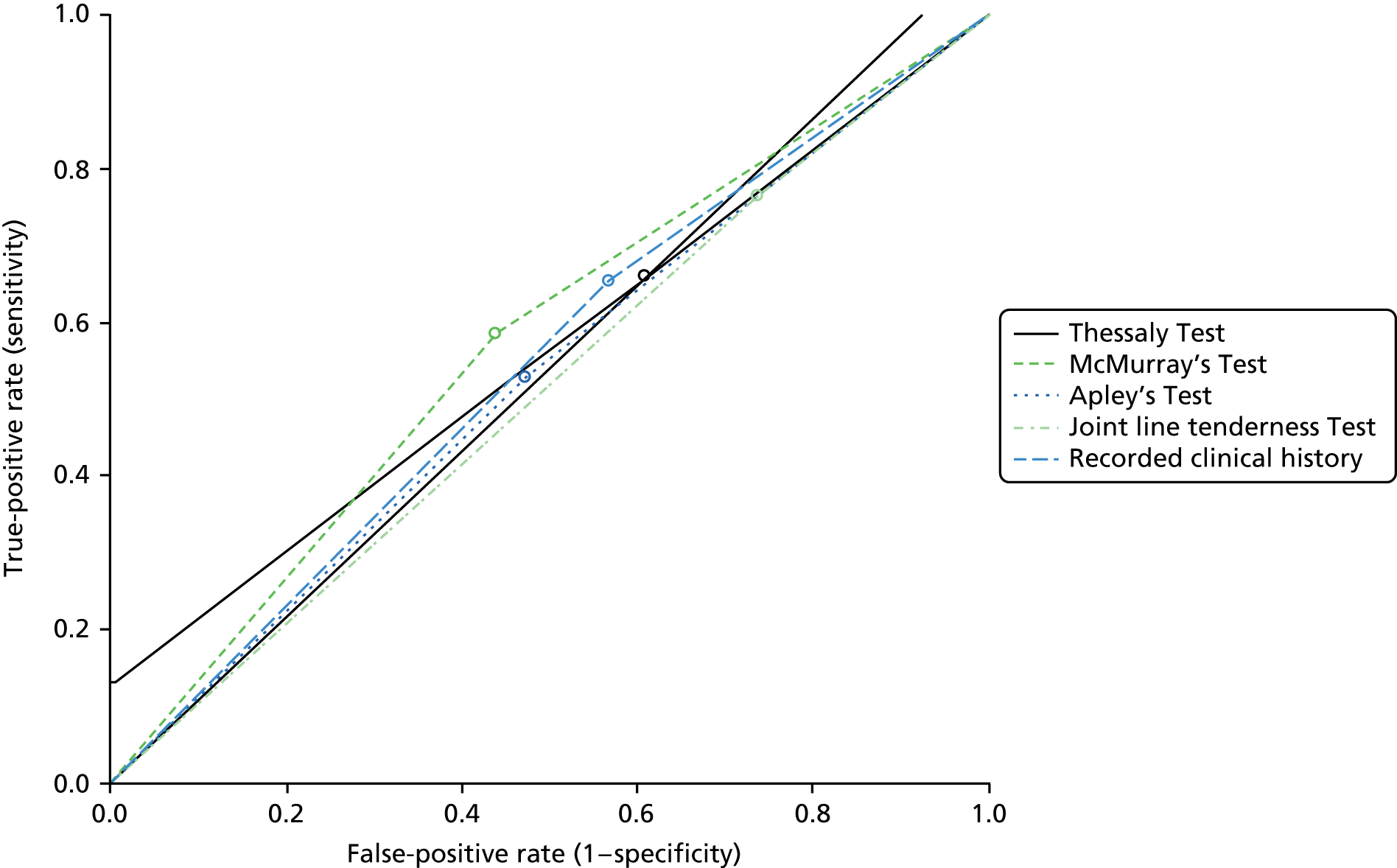
The most sensitive test was the joint line tenderness Test [0.77 (95% CI 0.68 to 0.84)]; however, this test also had the lowest specificity in the hands of primary care clinicians [0.26 (95% CI 0.18 to 0.36)]. Figure 9 shows a likelihood ratio graph for each test with the Thessaly Test set as the reference line (solid black). The graph shows slight superiority for McMurray’s Test over the Thessaly Test when used by primary care clinicians. No single test was identified as being an appropriate surrogate for MRI diagnosis of meniscal tears by primary care clinicians (see Table 9). All tests including clinical history had a diagnostic accuracy of 55% or lower (Table 9).
FIGURE 9.
Likelihood ratio graph, primary care clinicians vs. MRI (knee pathology patients only).
| Diagnostic test | In every 100 patients how many will have a MRI-positive meniscal tear? | In every 100 patients how many patients with a tear would be correctly sent for a MRI scan? | In every 100 patients how many patients with a tear would be missed? | In every 100 patients how many patients without a tear would be wrongly referred for a MRI scan? | Diagnostic accuracya |
|---|---|---|---|---|---|
| Thessaly Test | 56/100 | 37 | 19 | 27 | 54% |
| McMurray’s Test | 56/100 | 33 | 23 | 19 | 54% |
| Apley’s Test | 56/100 | 30 | 26 | 21 | 53% |
| Joint line tenderness Test | 56/100 | 43 | 13 | 33 | 54% |
| Clinical history | 56/100 | 36 | 20 | 25 | 55% |
For guidance on the interpretation of likelihood ratio graphs, see Chapter 2, Guide to likelihood ratio graphs.
We examined the influence of subject characteristics (age, sex and BMI), arthritis, presence of knee injury, ACL injury on the sensitivity and specificity of the Thessaly Test as performed by primary care clinicians. When examining the entire cohort, only the presence of a knee injury influenced sensitivity of the Thessaly Test (Table 10). Specificity was influenced by both the presence of an injury and the report of a sports injury. These results are intuitive and fit with the accepted pathogenesis of meniscal tear, at least in younger patients.
| Subject characteristic | Sensitivity | Specificity | |
|---|---|---|---|
| Sex | Female | ||
| Male | 0.807 (0.306 to 2.127); p = 0.664 | 1.18 (0.449 to 3.103); p = 0.737 | |
| Age (years) | 0.986 (0.945 to 1.029); p = 0.526 | 1.001 (0.957 to 1.046); p = 0.976 | |
| BMI (kg/m2) | Low (< 27.5 kg/m2) | ||
| High (≥ 27.5 kg/m2) | 0.808 (0.336 to 1.940); p = 0.633 | 0.546 (0.214 to 1.393); p = 0.205 | |
| Arthritis | Yes | ||
| No | 0.638 (0.217 to 1.877); p = 0.414 | 2.312 (0.639 to 8.363); p = 0.201 | |
| Knee injury | No injury | ||
| Other injury | 0.139 (0.028 to 0.681); p = 0.015 | 0.088 (0.021 to 0.368); p < 0.001 | |
| Sports injury | 1.982 (0.749 to 5.242); p = 0.168 | 0.242 (0.08 to 0.729); p = 0.012 | |
| ACL | Yes | ||
| No | 0.844 (0.102 to 6.983); p = 0.875 | Not estimable | |
| Past arthritis | Yes | ||
| No | 1.098 (0.164 to 7.350); p = 0.923 | 0.703 (0.098 to 5.052); p = 0.726 | |
| Previous surgery | Yes | ||
| No | 1.128 (0.283 to 4.494); p = 0.865 | 6.836 (0.533 to 87.635); p = 0.14 | |
The STARD diagram for the Thessaly Test when carried out by primary care clinicians (see Appendix 2) shows that in 35 patients the clinician was unable to perform the Thessaly Test. This was due to pain in the knee at the time of the examination. In order to ensure that this effect has not biased the overall results we have compared the rate of meniscal tears diagnosed by MRI for the group of patients in whom the test was unable to be performed with the remaining study cohort. Eight of the 35 patients did not attend for a MRI scan and we therefore have no knowledge of their meniscal status. The results for the remaining 27 patients are detailed in Table 11. A statistical comparison of the two groups of patients, using Fisher’s exact test, revealed no significant difference between the two groups (p = 0.224).
| MRI diagnosis of meniscal tear | Thessaly not performed | Thessaly performed |
|---|---|---|
| Yes, n | 10 | 125 |
| No, n | 17 | 121 |
Accuracy of the Thessaly Test when used by musculoskeletal specialists
When the study tests were performed by specialist musculoskeletal clinicians, significant differences were found between the tests with respect to sensitivity and specificity and NPV of the tests, but not PPVs (Table 12).
| Location | Test | Recorded clinical history | p-value | |||
|---|---|---|---|---|---|---|
| Thessaly Test | McMurray’s Test | Apley’s Test | Joint line tenderness Test | |||
| Sensitivity | 0.62 (0.52 to 0.71) | 0.63 (0.53 to 0.72) | 0.43 (0.34 to 0.52) | 0.83 (0.75 to 0.89) | 0.76 (0.67 to 0.83) | < 0.001 |
| Specificity | 0.55 (0.44 to 0.66) | 0.63 (0.53 to 0.73) | 0.72 (0.61 to 0.80) | 0.39 (0.29 to 0.49) | 0.60 (0.50 to 0.70) | < 0.001 |
| LR+ | 1.38 (1.05 to 1.81) | 1.72 (1.26 to 2.33) | 1.52 (1.04 to 2.21) | 1.36 (1.14 to 1.62) | 1.89 (1.46 to 2.46) | – |
| LR– | 0.69 (0.51 to 0.93) | 0.50 (0.44 to 0.78) | 0.80 (0.65 to 0.97) | 0.44 (0.28 to 0.69) | 0.40 (0.29 to 0.57) | – |
| OR | 2.00 (1.14 to 3.50) | 2.93 (1.66 to 5.19) | 1.91 (1.08 to 3.38) | 3.08 (1.67 to 5.67) | 4.69 (2.66 to 8.29) | – |
| PPV | 0.55 (0.46 to 0.64) | 0.57 (0.48 to 0.66) | 0.59 (0.48 to 0.69) | 0.50 (0.43 to 0.57) | 0.62 (0.54 to 0.69) | 0.227 |
| NPV | 0.52 (0.41 to 0.62) | 0.57 (0.47 to 0.67) | 0.49 (0.41 to 0.58) | 0.64 (0.51 to 0.76) | 0.66 (0.55 to 0.76) | 0.075 |
The most sensitive test was the joint line tenderness Test [0.83 (95% CI 0.75 to 0.89)]; however, this test also had the lowest specificity [0.39 (95% CI 0.29 to 0.49)]. The test with the highest sensitivity was Apley’s Test [0.72 (95% CI 0.61 to 0.81)], but Apley’s Test had low specificity [0.43 (95% CI 0.34 to 0.52)]. Figure 10 shows a likelihood ratio graph for each test with the Thessaly Test set as the reference line (solid black). The graph shows slight superiority for both clinical history and McMurray’s Test over the Thessaly Test when used by musculoskeletal clinicians.
FIGURE 10.
Likelihood ratio graph, musculoskeletal clinicians vs. MRI (knee pathology patients only).

No diagnostic physical test was better at diagnosing a meniscal tear than a well-trained musculoskeletal clinician taking a clinical history (Figure 10 and Table 13). McMurray’s Test was a better overall test than the Thessaly Test with a better compromise of sensitivity and specificity (see Figure 10).
| Diagnostic test | In every 100 patients how many will have a MRI-positive meniscal tear? | In every 100 patients how many patients with a tear would be correctly sent for a MRI scan? | In every 100 patients how many patients with a tear would be missed? | In every 100 patients how many patients without a tear would be wrongly referred for a MRI scan? | Diagnostic accuracya |
|---|---|---|---|---|---|
| Thessaly Test | 56/100 | 35 | 21 | 20 | 59% |
| McMurray’s Test | 56/100 | 35 | 21 | 16 | 63% |
| Apley’s Test | 56/100 | 24 | 32 | 10 | 58% |
| Joint line tenderness Test | 56/100 | 47 | 9 | 27 | 64% |
| Clinical history | 56/100 | 43 | 13 | 18 | 69% |
There were only subtle differences in the ability of each test to diagnose medial and lateral tears (Table 14).
| Test | Thessaly Test | McMurray’s Test | Apley’s Test | Joint line tenderness Test | Recorded clinical history | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Location | Medial | Lateral | Medial | Lateral | Medial | Lateral | Medial | Lateral | Medial | Lateral |
| Sensitivity | 0.63 (0.52 to 0.74) | 0.59 (0.41 to 0.75) | 0.62 (0.50 to 0.73) | 0.66 (0.48 to 0.81) | 0.44 (0.33 to 0.55) | 0.41 (0.25 to 0.58) | 0.82 (0.72 to 0.89) | 0.84 (0.68 to 0.94) | 0.76 (0.66 to 0.85) | 0.73 (0.56 to 0.86) |
| Specificity | 0.51 (0.42 to 0.60) | 0.46 (0.38 to 0.54) | 0.55 (0.46 to 0.64) | 0.51 (0.44 to 0.59) | 0.68 (0.60 to 0.76) | 0.64 (0.57 to 0.71) | 0.33 (0.25 to 0.41) | 0.29 (0.23 to 0.36) | 0.51 (0.42 to 0.60) | 0.43 (0.36 to 0.50) |
| LR+ | 1.3 (1.02 to 1.66) | 1.09 (0.80 to 1.50) | 1.38 (1.07 to 1.80) | 1.35 (1.02 to 1.80) | 1.38 (0.98 to 1.96) | 1.13 (0.73 to 1.76) | 1.22 (1.05 to 1.42) | 1.18 (1.00 to 1.40) | 1.56 (1.27 to 1.92) | 1.28 (1.01 to 1.61) |
| LR– | 0.71 (0.51 to 1.00) | 0.89 (0.58 to 1.38) | 0.69 (0.50 to 0.95) | 0.67 (0.41 to 1.08) | 0.82 (0.66 to 1.03) | 0.93 (0.69 to 1.23) | 0.55 (0.33 to 0.91) | 0.56 (0.26 to 1.20) | 0.46 (0.31 to 0.69) | 0.63 (0.36 to 1.10) |
| OR | 1.82 (0.31 to 0.97) | 1.22 (0.39 to 1.72) | 2.01 (0.28 to 0.88) | 2.03 (0.23 to 1.05) | 1.69 (0.34 to 1.04) | 1.23 (0.4 to 1.68) | 2.23 (1.17 to 4.27) | 2.12 (0.84 to 5.37) | 3.38 (1.87 to 6.12) | 2.02 (0.93 to 4.42) |
| PPV | 0.39 (0.31 to 0.48) | 0.15 (0.09 to 0.22) | 0.38 (0.30 to 0.47) | 0.18 (0.12 to 0.26) | 0.41 (0.31 to 0.52) | 0.17 (0.10 to 0.26) | 0.34 (0.28 to 0.41) | 0.15 (0.10 to 0.20) | 0.43 (0.35 to 0.51) | 0.17 (0.12 to 0.24) |
| NPV | 0.67 (0.57 to 0.77) | 0.85 (0.76 to 0.91) | 0.70 (0.60 to 0.79) | 0.88 (0.80 to 0.94) | 0.66 (0.57 to 0.74) | 0.84 (0.77 to 0.90) | 0.74 (0.61 to 0.84) | 0.90 (0.80 to 0.96) | 0.77 (0.67 to 0.85) | 0.89 (0.81 to 0.95) |
Interestingly, the specificity and NPV was greater for all tests in the control group when analysed separately (Table 15). This indicates that the tests actually work well in differentiating a normal knee from a knee with a meniscal tear. However, all of the physical tests have limited ability to differentiate between a painful knee with a meniscal tear and painful knee due to any other cause. Table 16 lists the diagnosis and clinical findings in patients who were positive for the Thessaly Test, but did not have a meniscal tear on MRI scan. This demonstrates the range of common conditions that affect the knee which are poorly differentiated by both the Thessaly Test and the other physical tests assessed in this study.
| Statistical test | Thessaly Test | McMurray’s Test | Apley’s Test | Joint line tenderness Test | Recorded clinical history | p-value |
|---|---|---|---|---|---|---|
| Specificity | 1.00 (0.83 to 1.00) | 1.00 (0.83 to 1.00) | 1.00 (0.82 to 1.00) | 0.95 (0.75 to 1.00) | 1.00 (0.83 to 1.00) | 0.407 |
| NPV | 0.80 (0.59 to 0.93) | 0.83 (0.63 to 0.95) | 0.83 (0.61 to 0.95) | 0.83 (0.61 to 0.95) | 0.80 (0.59 to 0.93) | 0.997 |
| n = 39 | Yes | No |
|---|---|---|
| Primary osteoarthritis, % | 43.6 | 56.4 |
| Patellofemoral disorders, % | 17.9 | 82.1 |
| Ligament instabilities, % | 7.7 | 92.3 |
| Osteochondritis dissecans, % | 2.6 | 97.4 |
| Tendonitis, % | 2.6 | 97.4 |
| Seronegative arthritis, % | 2.6 | 97.4 |
For guidance on the interpretation of likelihood ratio graphs, see Chapter 2, Guide to likelihood ratio graphs.
Comparison between primary care clinicians and specialist musculoskeletal clinicians using physical tests and clinical history to diagnose meniscal tears
Comparison between the two clinician groups (specialist musculoskeletal clinicians and primary care clinicians) showed significant differences in the results obtained using both the Thessaly Test and Apley’s Test to diagnose meniscal tears (Table 17). Better agreement was found with McMurray’s Test and the joint line tenderness Test. Note that this analysis only assesses whether or not the two clinicians agreed and if they were correct. Assessment of diagnostic accuracy shows that specialist musculoskeletal clinicians were consistently better at diagnosing meniscal tears based on both physical tests and on clinical history (Table 18).
| Clinical test | p-value |
|---|---|
| Thessaly Test | 0.001 |
| McMurray’s Test | 0.91 |
| Apley’s Test | < 0.001 |
| Joint line tenderness Test | 0.525 |
| Recorded clinical history | 0.076 |
Influence of the presence of osteoarthritis and other patient factors on the accuracy of the Thessaly Test (and other physical tests)
We have examined the influence of the following patient characteristics on the sensitivity and specificity of all four physical tests in the hands of both musculoskeletal and primary care clinicians: sex, age, BMI, osteoarthritis, sports injury, knee injury, ACL tear and previous surgery on the affected knee.
The sensitivity of the Thessaly Test when performed by primary care clinicians was influenced by age and presence of sports injuries (Table 19). The sensitivity of Apley’s Test was influenced by age and other knee injuries. The specificity of McMurray’s Test was also influenced by age and other injuries.
| Subject characteristic | Musculoskeletal clinicians | Primary care clinicians | ||||||
|---|---|---|---|---|---|---|---|---|
| Thessaly Test | McMurray’s Test | Apley’s Test | Joint line tenderness Test | Thessaly Test | McMurray’s Test | Apley’s Test | Joint line tenderness Test | |
| Sex | 0.671 | 0.655 | 0.441 | 0.855 | 0.42 | 0.915 | 0.886 | 0.086 |
| Age (years) | 0.022 | 0.194 | 0.132 | 0.023 | 0.009 | 0.214 | 0.01 | 0.073 |
| BMI (kg/m2) | 0.892 | 0.27 | 0.936 | 0.591 | 0.82 | 0.561 | 0.355 | 0.635 |
| Arthritis | 0.563 | 0.923 | 0.366 | 0.047 | 0.109 | 0.808 | 0.082 | 0.739 |
| Other injury | 0.023 | 0.017 | 0.028 | 0.02 | 0.112 | 0.083 | 0.016 | 0.304 |
| Sports injury | 0.245 | 0.064 | 0.279 | 0.301 | 0.004 | 0.796 | 0.122 | 0.399 |
| ACL | 0.99 | 0.326 | 0.274 | 1 | 0.383 | 0.604 | 0.892 | 0.944 |
| Past arthritis | 0.899 | 0.8 | 0.495 | 0.126 | 0.094 | 0.996 | 0.463 | 0.9 |
| Previous surgery | 0.971 | 0.347 | 0.913 | 0.994 | 0.422 | 0.413 | 0.825 | 0.696 |
The presence of an injury influenced the sensitivity of all tests performed by musculoskeletal clinicians. In addition, the joint line tenderness Test was also influenced by age (Table 20). No factors influenced specificity.
| Subject characteristic | Musculoskeletal clinicians | Primary care clinicians | ||||||
|---|---|---|---|---|---|---|---|---|
| Thessaly Test | McMurray’s Test | Apley’s Test | Joint line tenderness Test | Thessaly Test | McMurray’s Test | Apley’s Test | Joint line tenderness Test | |
| Sex | 0.636 | 0.823 | 0.564 | 0.188 | 0.216 | 0.095 | 0.281 | 0.052 |
| Age (years) | 0.275 | 0.09 | 0.291 | 0.384 | 0.91 | 0.05 | 0.159 | 0.485 |
| BMI (kg/m2) | 0.39 | 0.752 | 0.118 | 0.222 | 0.319 | 0.576 | 0.873 | 0.911 |
| Arthritis | 0.549 | 0.478 | 0.839 | 0.253 | 0.696 | 0.015 | 0.643 | 0.978 |
| Other injury | 0.072 | 0.494 | 0.607 | 0.487 | 0.101 | 0.01 | 0.113 | 0.085 |
| Sports injury | 0.481 | 0.377 | 0.305 | 0.552 | 0.836 | 0.78 | 0.836 | 0.853 |
| ACL | 0.095 | 0.237 | 0.74 | 0.573 | 0.294 | 0.652 | 0.646 | 0.377 |
| Past arthritis | 0.571 | 0.92 | 0.576 | 0.447 | 0.646 | 0.44 | 0.76 | 0.486 |
| Previous surgery | 0.366 | 0.94 | 0.39 | 0.515 | 0.993 | 0.906 | 0.868 | 0.422 |
The presence of osteoarthritis of the knee did not significantly influence the sensitivity or specificity of any of the tests, performed by either group of clinicians.
Comparison of patient subgroup recruited directly from a general practitioner practice compared with patients recruited from within an orthopaedic department
Eleven patients were recruited directly from their GP (PD) in order to allow us to verify that the cohort of patients recruited through the orthopaedic department at Glasgow Royal Infirmary were representative of the overall target population (patients attending GP with knee pathologies). The patient groups were well matched for age and BMI (Table 21), with only minimal differences that were not of statistical clinical relevance. There was a lower proportion of females in the group recruited directly from the GP practice (18% vs. 37%), but this was not statistically significant (p = 0.338). The proportion of patients in each group that had a meniscal tear diagnosed by MRI was almost the same, 57% for the group recruited directly from the GP practice and 55% for the group recruited through the orthopaedic department (p = 1.0).
| Patient source | Age (years) | BMI (kg/m2) | |
|---|---|---|---|
| All patients (n = 292) | Mean (SD) | 42.6 (13.4) | 27.8 (4.8) |
| Min.–max. | 18–71 | 18–47 | |
| Recruited from a GP practice (n = 11) | Mean (SD) | 44 (15.4) | 26 (2.8) |
| Min.–max. | 21–71 | 21.5–31.5 | |
| Not recruited from a GP practice (n = 281) | Mean (SD) | 42.7 (13.3) | 27.9 (4.9) |
| Min.–max. | 18–71 | 18–47 | |
| p-value | t-test | 0.794 | 0.069 |
Although the overall proportion of patients recruited directly from their GP was smaller than we had anticipated (4% vs. 10%), the group demographics and final diagnoses are very similar indicating that our main cohort is representative of the target population.
Do combinations of physical tests provide better specificity and sensitivity than a single physical test?
Analysis of individual tests for primary care clinicians is given in Table 22. Only McMurray’s Test, when performed by a primary care clinicians, was predictive of MRI outcome, no other test or the clinical history taken by a primary care clinician was a significant predictor. Nor was the order that the tests were performed in significant (see Table 22). In contrast, all physical tests and the clinical history taken by musculoskeletal clinicians were significant predictors of MRI (see Table 23). The order that the tests were performed in was not found to be significant (Table 23).
| Statistical test | Thessaly Test | McMurray’s Test | Apley’s Test | Joint line tenderness Test | Recorded clinical history | |
|---|---|---|---|---|---|---|
| Effect p-value | Test | 0.366 | 0.018 | 0.280 | 0.489 | 0.154 |
| Order | 0.138 | 0.874 | 0.711 | 0.956 | 0.528 | |
| AUC | 0.644 | 0.671 | 0.660 | 0.654 | 0.668 | |
| Statistical test | Thessaly Test | McMurray’s Test | Apley’s Test | Joint line tenderness Test | Recorded clinical history | |
|---|---|---|---|---|---|---|
| Effect p-value | Test | 0.009 | < 0.001 | 0.019 | < 0.001 | < 0.001 |
| Order | 0.210 | 0.920 | 0.257 | 0.670 | 0.514 | |
| AUC | 0.621 | 0.649 | 0.611 | 0.644 | 0.71 | |
The simple analysis of individual test fails to take account of any potential covariates and therefore logistic regression was undertaken. We have used a logistic regression model including all relevant factors and their interactions with a stepwise procedure to remove unimportant variables. Logistic regression analysis including all four tests, the clinical history and relevant covariates (BMI, age, sex, osteoarthritis and previous surgery) reveal a different result to the individual analyses. When all relevant factors are taken into account the only factors for primary care clinicians that are predictive of a MRI result are age and a past history of osteoarthritis (Table 24). Although this may be beneficial in aiding diagnosis of meniscal tears in the elderly that are associated with degenerative disease of the knee, neither of these factors are helpful in diagnosing acute traumatic injuries in young individuals participating in sports. As degenerative tears tend to be associated with knee conditions such as osteoarthritis, few degenerative tears are ever treated. In contrast, treatment is regularly offered for young patients with acute traumatic or sporting injuries.
| Factor | Multivariable analysis: all factors included | Stepwise analysis | |
|---|---|---|---|
| Effect p-value | Thessaly Test | 0.486 | |
| McMurray’s Test | 0.268 | ||
| Apley’s Test | 0.427 | ||
| Joint line tenderness Test | 0.545 | ||
| Clinical history | 0.283 | ||
| Age | < 0.001 | 0.002 | |
| BMI | 0.652 | ||
| Knee injury | 0.437 | ||
| Past arthritis | 0.037 | 0.041 | |
| Previous surgery | 0.325 | ||
| Sex | 0.128 | ||
| Arthritis | 0.126 | ||
| AUC | 0.722 | 0.651 | |
A variety of different clinicians of participated in this study and we had originally intended to include experience of the clinician undertaking the assessment within our models. However, classifying or grading clinician experience is not a simple process. It cannot simply be based on years since qualification as this takes no count of part-time working, maternity leave, training quality, or the number of appropriate cases each clinician has been previously exposed to. We were unable to produce a reliable method of classifying clinicians to include in our models. Instead, within the logistic regression models we included clinician as a random effect to take account of the variability between clinicians. However, this could not be specified with the stepwise regression models, where this factor was left unspecified and therefore included by default in the residual variability not accounted for by the model.
The results for musculoskeletal clinicians are potentially more clinically relevant than those observed for primary care clinicians (Table 25). In this clinician group the predicative factors are clinical history (history taken from the patient regarding recent symptoms and, if relevant, injury and mechanism of injury) and age.
| Factor | Multivariable analysis – all factors included (p-value) | Stepwise analysis (p-value) | |
|---|---|---|---|
| Effect p-value | Thessaly Test | 0.702 | |
| McMurray’s Test | 0.322 | ||
| Apley’s Test | 0.793 | ||
| Joint line tenderness Test | 0.073 | ||
| Clinical history | 0.004 | < 0.001 | |
| Age | 0.025 | 0.019 | |
| BMI | 0.629 | ||
| Knee injury | 0.207 | ||
| Past arthritis | 0.986 | ||
| Previous surgery | 0.655 | ||
| Sex | 0.088 | ||
| Arthritis | 0.788 | ||
| AUC | 0.762 | 0.761 | |
The area under the curve (AUC) for the stepwise logistic regression (where clinician variability is accounted for in residual variability) is nearly the same as the logistic regression model with all the effects included and clinician specified as random effect (AUC 0.762 vs. 0.761), suggesting that there was nearly no difference between the different musculoskeletal clinicians. This was not the case for the primary care clinicians (AUC 0.722 vs. 0.651), suggesting a higher degree of variability between clinicians in this group.
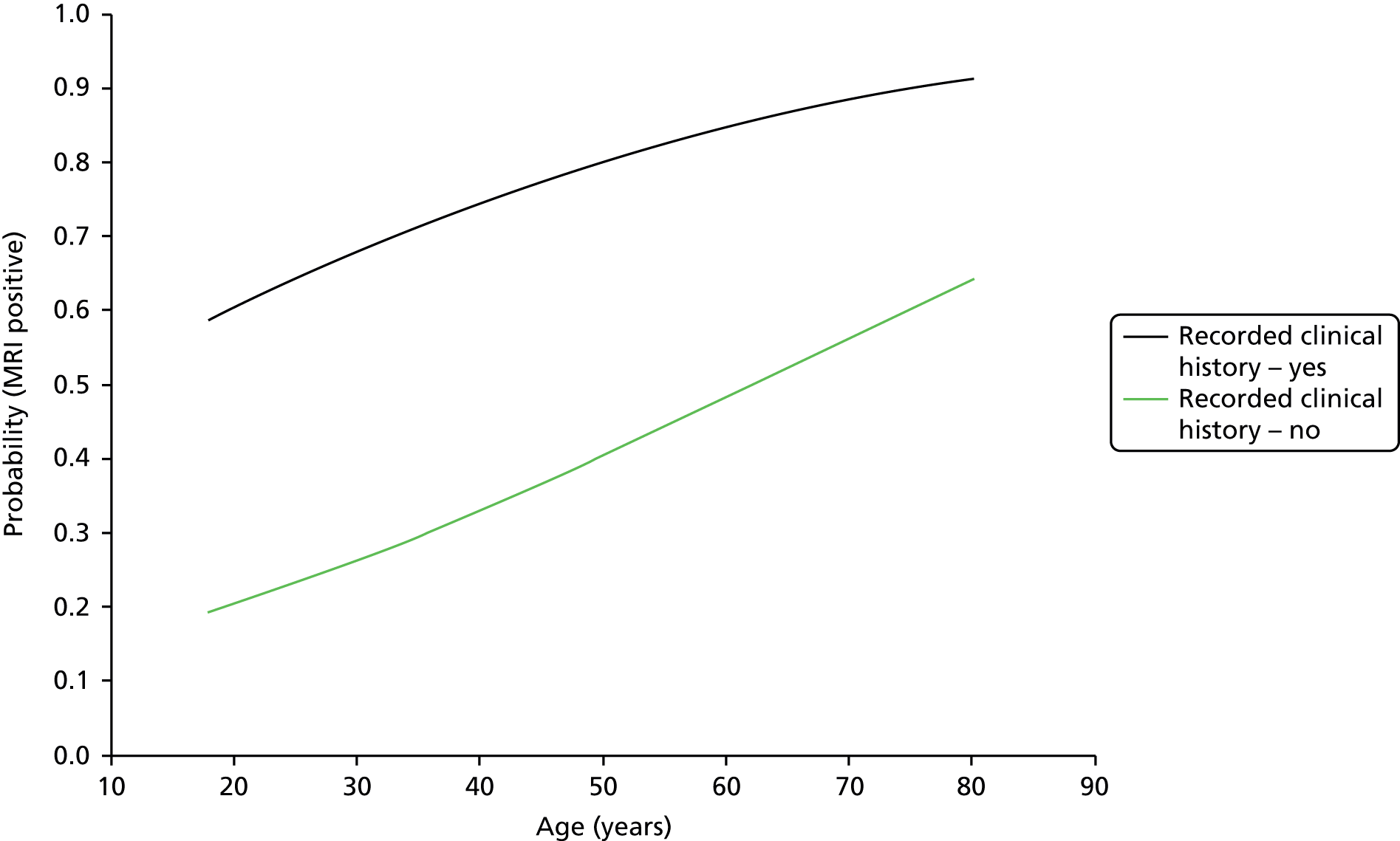
Odds ratio for musculoskeletal clinicians diagnosis of meniscal tear based on taking a clinical history, and also for the influence of age, have been calculated and are presented in Table 26. A graphical representation of these probabilities for standard adult age range is shown in Figure 11.
| Effect | Point estimate | 95% Wald confidence limits | |
|---|---|---|---|
| Clinical history taken by a musculoskeletal clinician: no vs. yes | 5.910 | 2.954 | 11.826 |
| Age | 0.968 | 0.943 | 0.995 |
FIGURE 11.
Influence of age on the probability of a meniscal tear diagnosis by MRI when a musculoskeletal clinician diagnoses a meniscal tear based on a clinical history.
Validation of magnetic resonance imaging diagnosis for meniscal tears using knee arthroscopy
Seventy-seven patients had an arthroscopy as part of their routine clinical care. When arthroscopic diagnosis of meniscal tears is taken as the gold standard and compared with results obtained with MRI, the sensitivity of MRI was 1.0, whereas the specificity was 0.53 (Table 27).
| Statistical test | MRI/arthroscopy |
|---|---|
| Sensitivity | 1.00 (0.93 to 1.00) |
| Specificity | 0.53 (0.28 to 0.77) |
| LR+ | 2.12 (1.28 to 3.52) |
| LR– | 0 (not estimable) |
| OR | Not estimable |
| PPV | 0.40 (0.32 to 0.49) |
| NPV | 1.00 (0.66 to 1.00) |
The specificity of 0.53 (95% CI 0.28 to 0.77) is lower than reported in the literature for MRI diagnosis of meniscal tears. Only eight patients had a disagreement between their MRI diagnosis and their arthroscopic findings. In three patients the radiologist’s report of the MRI scan reported a ‘possible’ meniscal tear. We have included in the analysis any patient with these ‘possible’ meniscal tears, because this reflects the real life situation where diagnosis, even on MRI scan, is not clear cut. Diagnosis on MRI is an interpretation of scan findings and although the results tend to be reported using a binary approach, MRI itself is certainly not binary and is highly dependent on the experience of the radiologist reporting the scan.
In a further three cases the patients had previously received meniscal knee surgery. We believe that the explanation for the discordant results in these patients is that the MRI scan still shows an abnormal signal in the areas of the knee that previously underwent surgery; however, on arthroscopic visualisation any previous meniscal damage appears to have been repaired and therefore a result of no meniscal tear was recorded. Removing patients who have had previous knee surgery improved the specificity from 0.53 to 0.60 (95% CI 0.32 to 0.84). Similarly, including only those patients who were classified as not having a meniscal tear based on diagnosis by a musculoskeletal clinician improved the specificity to 0.67. This suggests that indiscriminate use of MRI to diagnose meniscal injuries is unlikely to be beneficial and a more targeted approach to use of MRI will yield more accurate and beneficial data.
Patient and public involvement
Patients were not directly involved in the design or analysis of the study. We had intended to recruit a suitable patient to the trial management group prior to initiation of the study. However, we were unable to recruit a candidate with appropriate patient feedback, and opinion was sought on the individual physical tests used within the study. Each patient who underwent examination was asked to give their view on the tests (the Thessaly Test, McMurray’s Test, Apley’s Test and the joint line tenderness Test), particularly in relation to the pain experienced during the test.
Overall, 72% of patients said that one or more tests were painful when performed. In particular the joint line tenderness Test (57.1% of patients) and the Thessaly Test (50.5%) were found to cause pain during the test procedure. In comparison McMurray’s Test and Apley’s Test were reported as causing pain less frequently, 37.7% and 33.3% respectively.
Chapter 5 Discussion
In the UK approximately 30% of GP appointments are for musculoskeletal complaints, with knee problems being one of the most common problems. 33 Complicated forces are exerted through the knee during various activities, making it susceptible to a range of acute and chronic injuries. The mean annual incidence of meniscal tears in the knee may be as high as 60–70 per 1000 population, with a 2.5 to 4 times male to female predominance. 3 The age distribution of patients with meniscal tears shows a bimodal peak with acute injuries peaking in young active patients in their mid-to-late twenties and chronic degenerative injuries becoming more prevalent in old age. Patients with meniscal tears present both acutely to the emergency department at the time of injury, but also commonly post injury to their GP. The latter scenario usually occurs if the initial injury has failed to settle and symptoms remain.
This study was designed to evaluate whether or not the Thessaly Test, alone or in combination with other physical tests, could be used by primary care clinicians (GPs, community physiotherapists, etc.) to rule out a meniscal tear in patients presenting with knee pain. This would allow targeted onward referral to secondary care and minimising the utilisation of expensive and overburdened diagnostic imaging such as MRI scanning.
Several previous studies have examined the diagnostic accuracy of the Thessaly Test since the original publication by Karachalios et al. 25 In a retrospective study of 116 patients, Harrison et al. 27 validated the Thessaly Test against arthroscopy concluding that the Thessaly Test is a valid a reproducible test for diagnosis of meniscal tears. Harrison et al. 27 found a sensitivity of 90% and a specificity of 98%. However, the study patient group was preselected by an experienced musculoskeletal clinician and all patients enrolled in the study were classified as having a suspicion of a meniscal tear and were on a waiting list for arthroscopic surgery. Importantly, this study group is therefore not comparable with our desired target group which encompasses all knee patients likely to be encountered by a non-specialist primary care clinician.
In a similar study, Konan et al. 28 reviewed 121 patients and used both MRI imaging and arthroscopy, with arthroscopy set as the ‘gold standard’. Sensitivity and specificity for medial meniscal tears was 83% and 76%, respectively, though specificity dropped in the presence of ACL injury to just 56%. They conclude that the Thessaly Test alone is not beneficial in diagnosis of meniscal tears, but that in combination with McMurray’s Test it may be useful. As with the cohort of patients selected for Harrison et al. ’s study,27 the cohort used by Konan et al. 28 were preselected by an experienced musculoskeletal clinician and all patients enrolled in the study were classified as having a high suspicion of a meniscal tear.
Finally, Mirzatolooei et al. 29 have examined the specificity and sensitivity of the Thessaly Test in diagnosing meniscal tears in a cohort of patients with ACL injuries (n = 80). They found a sensitivity of 79%, but low specificity of just 40%. They conclude that low specificity of the Thessaly Test renders it unsuitable for this cohort of patients with significant additional knee pathology.
There are several limitations to our study. The use of MRI as the diagnostic ‘gold standard’ has limitations as diagnostic accuracy of MRI for meniscal tears is not 100%. The only truly accurate method of diagnosing meniscal tears is to perform an arthroscopy, but for obvious ethical reasons it was not feasible to perform an invasive arthroscopy of the knee on all patients with suspected knee pathology. The data generated during this study suggest that when MRI is used to detect meniscal tears in a diverse group of knee pathology patients the accuracy of MRI is lower than is often reported in the literature. Other authors have also commented on this issue with Mirzatolooei et al. 29 estimating that relying blindly on MRI to determine surgical intervention could result in inappropriate treatment in up to 35% of the cases.
Although the recruitment to the study reached its target, there were a significant number of patients who did not attend for MRI of the knee resulting in us being unable to include their data in the final analysis. The dropout rate for the knee pathology group was just 18%, but the control group had a dropout rate of 43%. In order to compensate for this we recruited an additional 25 control subjects, giving us usable data on 43 subjects, which was close to the target value of 50 control subjects. We believe that there were two reasons for the large discrepancy in the dropout rate between the two study groups. First, the control group were unlikely to derive any personal benefit from attending for their MRI scan and therefore were more likely to dropout. Second, around a third of our control subjects had their MRI scan delayed due to a lack of capacity in imaging reporting. This undoubtedly affected the willingness of volunteers to attend for scanning when appointments were rearranged. Although the number of patients with data available for final analysis was below our target, post-hoc power calculations have demonstrated that the study is still appropriately powered.
We had originally intended to recruit our control group from only an orthopaedic hand clinic. However, recruitment rates were slower than anticipated and so we utilised local adverts in order to increase the recruitment rate for control subjects. We did not undertake any comparison between those recruited through the clinics and those responding to the adverts.
The final potential weakness of the study was undertaking the study in a secondary care setting when the target population was patients in primary care. Although our study was set in a secondary care environment, we have attempted to replicate the typical patient group that a primary care clinician might encounter (i.e. a diverse cohort of patients with multiple knee pathologies in whom a non-specialist may struggle to differentiate meniscal tears). This methodology was chosen in order to allow us to recruit sufficient numbers of patients to perform the study and to avoid the need for a large network of GP practices to participate in the study, each of whom would only have contributed a few patients. In order to validate that our cohort was representative of the types of patients who a typical GP may encounter, we asked one GP to directly recruit all patients who presented to him during the study period with soft tissue knee pain. This group represented just under 5% of the overall cohort and were well matched to the main cohort recruited from the orthopaedic department at Glasgow Royal Infirmary indicating that the main group recruited in secondary care were representative of the target population. Although we recruited fewer patients directly from GP practices than we had specified in the original study protocol, it is unlikely that this influenced the overall study results. This element of the study was simply to ensure that demographics of patients recruited in secondary care matched those that would have been recruited from primary care had the study been run in this setting. If anything, the lower than anticipated number of patients recruited from GP practice vindicates the decision to run the study in secondary care and serves to highlight the issues that would have been encountered if we had opted to use a large network of primary care units for recruitment rather than a secondary care setting.
Our results have demonstrated that the Thessaly Test used in isolation is not superior to existing physical tests for diagnosing meniscal tears. None of the physical tests examined is sufficiently sensitive or specific to use as a routine alternative to MRI, or referral to a musculoskeletal specialist. We found that no combination of tests, when used by primary care clinicians, was suitable as an alternative to MRI diagnosis or referral to a musculoskeletal clinician for assessment. Our data demonstrates that even in the hands of experienced musculoskeletal clinicians, physical tests for meniscal tears have limited value if used indiscriminately.
Interestingly, there was a large disparity between the two groups of clinicians with respect to the proportion of patients classified as being too painful to perform the test on. Primary care clinicians opted not to perform the Thessaly Test on 10% of patients compared with 17% for musculoskeletal clinicians. The reason that the test was not completed was not formally recorded as part of the study, but anecdotally it was most commonly secondary to knee pain. We can speculate that experience levels in dealing with musculoskeletal complaints influenced the threshold for stopping the test due to pain. We hypothesise that more experienced clinicians realise that little value will be gained from performing the test in patients with high levels of knee pain. It is also possible that the primary care clinicians who were brought in specifically to undertake study assessments, rather than providing direct clinical care, may have been more likely to adhere to the study protocol. The relatively high rate of ‘test unable to be performed’ further limits the usefulness of the Thessaly Test as a generic tool.
In addition to testing the accuracy of diagnosis of meniscal tears using physical tests, our protocol also included an assessment of the accuracy of diagnosis based on a standardised clinical history. We developed a simple minimal data set to be collected as part of the routine clinical history, which was designed to aid the correct diagnosis. The design was deliberately kept simple so that if it was successful in the hands of primary care clinicians it could easily be utilised nationally with no need for an expensive educational programme to support the roll out of the concept.
Although both groups of clinicians received basic training in the use of this diagnostic tool our multivariate analysis showed that it was either more effective in the hands of specialist knee clinicians or that it was insufficient on its own as a surrogate for specialist experience.
We have validated our MRI findings in a subset of patients using arthroscopy as the ‘gold standard’. Our initial validation of MRI against arthroscopy revealed high sensitivity (1.0), but low specificity (0.53). This was surprising given the good specificity of MRI reported in the literature. 18 The Thessaly Test validation study by Konan et al. 28 used both MRI and arthroscopy. Konan et al. 28 found that MRI detected 96% of tears which is in line with other reports validating MRI against arthroscopy. 18,28 However, this was in a preselected group of patients with a high suspicion of meniscal tears, rather than the more general group that we have studied. We believe that our study cohort is more representative of the patient cohort that an average primary care clinician may encounter and that our results are of greater relevance to this group of clinicians than previous studies of highly selected patient groups.
We are not the first group to document the lack of specificity of MRI for diagnosis of meniscal tears in the presence of concomitant knee pathology. Several other authors have reported reduced accuracy in the presence of acute ACL rupture. 24,34
Although MRI accuracy is clearly influenced by multiple knee pathologies, it is also influenced by patient age. England et al. 13 have reported high rates of incidental meniscal findings on MRI of the knee in the general population and that these findings tend to increase with age. In middle-aged and elderly patients a lower threshold of suspicion should be applied for meniscal tears as they tend to follow minor trauma and MRI signal changes are significantly higher in the elderly population.
Few studies have examined diagnostic accuracy of MRI in a community-based setting; however, Hardy et al. ,35 in the USA, have reported community-based recording of MRI for diagnosis of meniscal tears to have a sensitivity of 73% and specificity of 68%, which suggests that this imaging modality is of less use in a diverse poorly stratified cohort and perhaps corroborates our data.
Our study data shows that the most accurate non-imaged method of diagnosing meniscal tears is to use a clinical history taken by an experience musculoskeletal clinician. Mohan and Gosal36 have reported similar findings suggesting that the accuracy of clinical diagnosis by an experienced musculoskeletal clinician based on examination and history is 88% for medial meniscal tears and 92% for lateral meniscal tears, with similar results reported by Ercin et al. 37 These results are comparable with that achieved by MRI, suggesting that MRI should be reserved for use in more doubtful, difficult or complex knee injuries. 36
The data generated by this study suggest that the Thessaly Test is no better at diagnosing meniscal tears than other established physical tests. We found that neither the Thessaly Test alone or in combination with other physical tests could be reliably used by primary care clinicians as an alternative, or surrogate, for MRI scanning to diagnose meniscal tears in the knee.
We have also found that MRI diagnosis of meniscal tears in comparison with arthroscopic diagnosis was less accurate than is commonly reported in the literature. This was particularly true when MRI is used indiscriminately rather than in targeted populations of patients with specific ‘suspected’ knee pathologies. Further well-defined studies are required to determine the true accuracy of MRI for the diagnosis of meniscal tears.
The findings of this study have implications for primary care clinicians who may wish to consider referral of patients with significant knee pain and injuries to a specialist clinician for assessment and treatment rather than automatic referral for MRI of the knee. This approach is likely to maximise the benefit from MRI and minimise the cost of unnecessary or inappropriate imaging, though further cost-effectiveness studies are required to validate this assumption.
Chapter 6 Conclusion
The data generated by this study suggest that the Thessaly Test is no better at diagnosing meniscal tears than other established physical tests. We found that neither the Thessaly Test alone or in combination with other physical tests could be reliably used by primary care clinicians as an alternative, or surrogate, for MRI scanning to diagnose meniscal tears in the knee.
We have also found that MRI diagnosis of meniscal tears in comparison with arthroscopic diagnosis was less accurate than is commonly reported in the literature. This was particularly true when MRI is used indiscriminately rather than in targeted populations of patients with specific ‘suspected’ knee pathologies. Further well-defined studies are required to determine the true accuracy of MRI for the diagnosis of meniscal tears.
The findings of this study have implications for primary care clinicians who may wish to consider referral of patients with significant knee pain and injuries to a specialist clinician for assessment and treatment rather than automatic referral for MRI of the knee. This approach is likely to maximise the benefit from MRI and minimise the cost of unnecessary or inappropriate imaging.
Recommendation for further research
Further research is required to determine the true accuracy and cost-effectiveness of MRI for the detection of meniscal tears, in a cohort of patients who has not been highly selected by experienced specialists.
Acknowledgements
We gratefully acknowledge the funding received for this study from the National Institutes of Health Research HTA programme, grant reference 09/163/02.
We would like to acknowledge the help and support provided by Miss Sinead O’Donnell and Sister Emma Sharp (Orthopaedic Department, Glasgow Royal Infirmary), Mr Alun Bevan (Medical Illustration Department at Glasgow Royal Infirmary) and the Extended Scope Physiotherapy Team at Glasgow Royal Infirmary (Linda Mercer, Jenny Love, Val Forgie, John O’Toole, Alan Krawcyzk, Brenda Danks, Margot Cohen, Lynn Smyth and Jo Chambers).
We would also like to acknowledge all of the primary care clinicians who participated in this study.
Contributions of authors
Mr Mark Blyth (Consultant Orthopaedic Surgeon, Glasgow Royal Infirmary), as chief investigator had overall responsibility for the study.
Dr Iain Anthony (Senior Clinical Research Manager, Glasgow Royal Infirmary) wrote the initial grant application, wrote the final report and was responsible for study co-ordination and set-up.
Dr Bernard Francq (Statistician, Robertson Centre for Biostatistics, University of Glasgow) conducted the statistical analysis of the study.
Dr Katriona Brooksbank (Research Assistant, Glasgow Royal Infirmary) was responsible for patient recruitment and data collection.
Dr Paul Downie (General Practitioner) was responsible for recruitment of patients directly from GP practice, he also undertook study clinician assessments.
Mr Andrew Powell (Orthopaedic Surgical Trainee, Glasgow Royal Infirmary) was responsible for undertaking osteoarthritis grading of X- ray images.
Mr Bryn Jones (Consultant Orthopaedic Surgeon, Glasgow Royal Infirmary) aided in editing of the final report.
Mr Angus MacLean (Consultant Orthopaedic Surgeon, Glasgow Royal Infirmary) aided in editing of the final report.
Dr Alex McConnachie (Assistant Director of Biostatistics, Robertson Centre for Biostatistics, University of Glasgow) contributed to the development of the statistical analysis plan and supervised the statistical analysis.
Professor John Norrie (Director of the Centre for Randomised Health Care Trials, University of Aberdeen) generated the original statistical analysis plan and aided in report editing.
Data sharing statement
Data can be obtained from the corresponding author on request.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health.
References
- Messner K, Gao J. The menisci of the knee joint. Anatomical and functional characteristics, and a rationale for clinical treatment. J Anat 1998;193:161-78. http://dx.doi.org/10.1046/j.1469-7580.1998.19320161.x.
- Greis PE, Bardana DD, Holmstrom MC, Burks RT. Meniscal injury: I. Basic science and evaluation. J Am Acad Orthop Surg 2002;10:168-76.
- Maffulli N, Longo UG, Campi S, Denaro V. Meniscal tears. Open Access J Sports Med 2010;1:45-54. http://dx.doi.org/10.2147/OAJSM.S7753.
- Arnoczky SP, Warren RF. Microvasculature of the human meniscus. Am J Sports Med 1982;10:90-5. http://dx.doi.org/10.1177/036354658201000205.
- de Albornoz PM, Forriol F. The meniscal healing process. Muscles Ligaments Tendons J 2012;2:10-8.
- Fox AJ, Bedi A, Rodeo SA. The basic science of human knee menisci: structure, composition, and function. Sports Health 2012;4:340-51. http://dx.doi.org/10.1177/1941738111429419.
- Majewski M, Susanne H, Klaus S. Epidemiology of athletic knee injuries: a 10-year study. Knee 2006;13:184-8. http://dx.doi.org/10.1016/j.knee.2006.01.005.
- Barrett GR, Field MH, Treacy SH, Ruff CG. Clinical results of meniscus repair in patients 40 years and older. Arthroscopy 1998;14:824-9. http://dx.doi.org/10.1016/S0749-8063(98)70018-0.
- Englund M, Niu J, Guermazi A, Roemer FW, Hunter DJ, Lynch JA, et al. Effect of meniscal damage on the development of frequent knee pain, aching, or stiffness. Arthritis Rheum 2007;56:4048-54. http://dx.doi.org/10.1002/art.23071.
- Englund M, Roos EM, Lohmander LS. Impact of type of meniscal tear on radiographic and symptomatic knee osteoarthritis: a sixteen-year followup of meniscectomy with matched controls. Arthritis Rheum 2003;48:2178-87. http://dx.doi.org/10.1002/art.11088.
- Hunter DJ, Zhang YQ, Niu JB, Tu X, Amin S, Clancy M, et al. The association of meniscal pathologic changes with cartilage loss in symptomatic knee osteoarthritis. Arthritis Rheum 2006;54:795-801. http://dx.doi.org/10.1002/art.21724.
- Ding C, Martel-Pelletier J, Pelletier JP, Abram F, Raynauld JP, Cicuttini F, et al. Meniscal tear as an osteoarthritis risk factor in a largely non-osteoarthritic cohort: a cross-sectional study. J Rheumatol 2007;34:776-84.
- Englund M, Guermazi A, Gale D, Hunter DJ, Aliabadi P, Clancy M, et al. Incidental meniscal findings on knee MRI in middle-aged and elderly persons. N Engl J Med 2008;359:1108-15. http://dx.doi.org/10.1056/NEJMoa0800777.
- Allum R. Complications of arthroscopy of the knee. J Bone Joint Surg Br 2002;84:937-45. http://dx.doi.org/10.1302/0301-620X.84B7.13637.
- DeLee JC. Committee on Complications of Arthroscopy Association of North America . Complications of arthroscopy and arthroscopic surgery: results of a national survey. Committee on Complications of Arthroscopy Association of North America. Arthroscopy 1985;1:214-20. http://dx.doi.org/10.1016/S0749-8063(85)80086-4.
- Armstrong RW, Bolding F, Joseph R. Septic arthritis following arthroscopy: clinical syndromes and analysis of risk factors. Arthroscopy 1992;8:213-23. http://dx.doi.org/10.1016/0749-8063(92)90039-E.
- Crawford R, Walley G, Bridgman S, Maffulli N. Magnetic resonance imaging versus arthroscopy in the diagnosis of knee pathology, concentrating on meniscal lesions and ACL tears: a systematic review. Br Med Bull 2007;84:5-23. http://dx.doi.org/10.1093/bmb/ldm022.
- Oei EH, Nikken JJ, Verstijnen AC, Ginai AZ, Myriam Hunink MG. MR imaging of the menisci and cruciate ligaments: a systematic review. Radiology 2003;226:837-48. http://dx.doi.org/10.1148/radiol.2263011892.
- Englund M, Guermazi A, Lohmander LS. The meniscus in knee osteoarthritis. Rheum Dis Clin North Am 2009;35:579-90. http://dx.doi.org/10.1016/j.rdc.2009.08.004.
- Bhattacharyya T, Gale D, Dewire P, Totterman S, Gale ME, McLaughlin S, et al. The clinical importance of meniscal tears demonstrated by magnetic resonance imaging in osteoarthritis of the knee. J Bone Joint Surg Am 2003;85:4-9.
- Kornaat PR, Bloem JL, Ceulemans RY, Riyazi N, Rosendaal FR, Nelissen RG, et al. Osteoarthritis of the knee: association between clinical features and MR imaging findings. Radiology 2006;239:811-17. http://dx.doi.org/10.1148/radiol.2393050253.
- Kocabey Y, Tetik O, Isbell WM, Atay OA, Johnson DL. The value of clinical examination versus magnetic resonance imaging in the diagnosis of meniscal tears and anterior cruciate ligament rupture. Arthroscopy 2004;20:696-700. http://dx.doi.org/10.1016/j.arthro.2004.06.008.
- Rossi R, Dettoni F, Bruzzone M, Cottino U, D’Elicio DG, Bonasia DE. Clinical examination of the knee: know your tools for diagnosis of knee injuries. Sports Med Arthrosc Rehabil Ther Technol 2011;3. http://dx.doi.org/10.1186/1758-2555-3-25.
- Fowler PJ, Lubliner JA. The predictive value of five clinical signs in the evaluation of meniscal pathology. Arthroscopy 1989;5:184-6. http://dx.doi.org/10.1016/0749-8063(89)90168-0.
- Karachalios T, Hantes M, Zibis AH, Zachos V, Karantanas AH, Malizos KN. Diagnostic accuracy of a new clinical test (the Thessaly test) for early detection of meniscal tears. J Bone Joint Surg Am 2005;87:955-62. http://dx.doi.org/10.2106/JBJS.D.02338.
- Hegedus EJ, Cook C, Hasselblad V, Goode A, McCrory DC. Physical examination tests for assessing a torn meniscus in the knee: a systematic review with meta-analysis. J Orthop Sports Phys Ther 2007;37:541-50. http://dx.doi.org/10.2519/jospt.2007.2560.
- Harrison BK, Abell BE, Gibson TW. The Thessaly test for detection of meniscal tears: validation of a new physical examination technique for primary care medicine. Clin J Sport Med 2009;19:9-12. http://dx.doi.org/10.1097/JSM.0b013e31818f1689.
- Konan S, Rayan F, Haddad FS. Do physical diagnostic tests accurately detect meniscal tears?. Knee Surg Sports Traumatol Arthrosc 2009;17:806-11. http://dx.doi.org/10.1007/s00167-009-0803-3.
- Mirzatolooei F, Yekta Z, Bayazidchi M, Ershadi S, Afshar A. Validation of the Thessaly test for detecting meniscal tears in anterior cruciate deficient knees. Knee 2010;17:221-3. http://dx.doi.org/10.1016/j.knee.2009.08.007.
- Apley AG. The diagnosis of meniscus injuries; some new clinical methods. J Bone Joint Surg Am 1947;29:78-84.
- Chivers MD, Howitt SD. Anatomy and physical examination of the knee menisci: a narrative review of the orthopedic literature. J Can Chiropr Assoc 2009;53:319-33.
- Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis 1957;16:494-502. http://dx.doi.org/10.1136/ard.16.4.494.
- Department of Health . The Musculoskeletal Services Framework 2006. http://webarchive.nationalarchives.gov.uk/20130107105354/http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4138413 (accessed 8 June 2015).
- Nam TS, Kim MK, Ahn JH. Efficacy of magnetic resonance imaging evaluation for meniscal tear in acute anterior cruciate ligament injuries. Arthroscopy 2014;30:475-82. http://dx.doi.org/10.1016/j.arthro.2013.12.016.
- Hardy JC, Evangelista GT, Grana WA, Hunter RE. Accuracy of magnetic resonance imaging of the knee in the community setting. Sports Health 2012;4:222-31. http://dx.doi.org/10.1177/1941738111434396.
- Mohan BR, Gosal HS. Reliability of clinical diagnosis in meniscal tears. Int Orthop 2007;31:57-60. http://dx.doi.org/10.1007/s00264-006-0131-x.
- Ercin E, Kaya I, Sungur I, Demirbas E, Ugras AA, Cetinus EM. History, clinical findings, magnetic resonance imaging, and arthroscopic correlation in meniscal lesions. Knee Surg Sports Traumatol Arthrosc 2012;20:851-6. http://dx.doi.org/10.1007/s00167-011-1636-4.
Appendix 1 Statistical analysis plan
Appendix 2 STAndards for the Reporting of Diagnostic accuracy studies diagrams for the Thessaly Test, the joint line tenderness Test, McMurray’s Test, Apley’s Test and clinical history
Each patient who was examined had four physical tests performed and a clinical history taken. In some patients the injured knee was too painful to perform all of the tests. The STARD diagrams (Figures 12–21) report the number patients assessed for each test by each clinician.
FIGURE 12.
STAndards for the Reporting of Diagnostic accuracy studies diagram for the Thessaly Test: primary care clinicians. MSK, musculoskeletal clinician; PCC, primary care clinician.
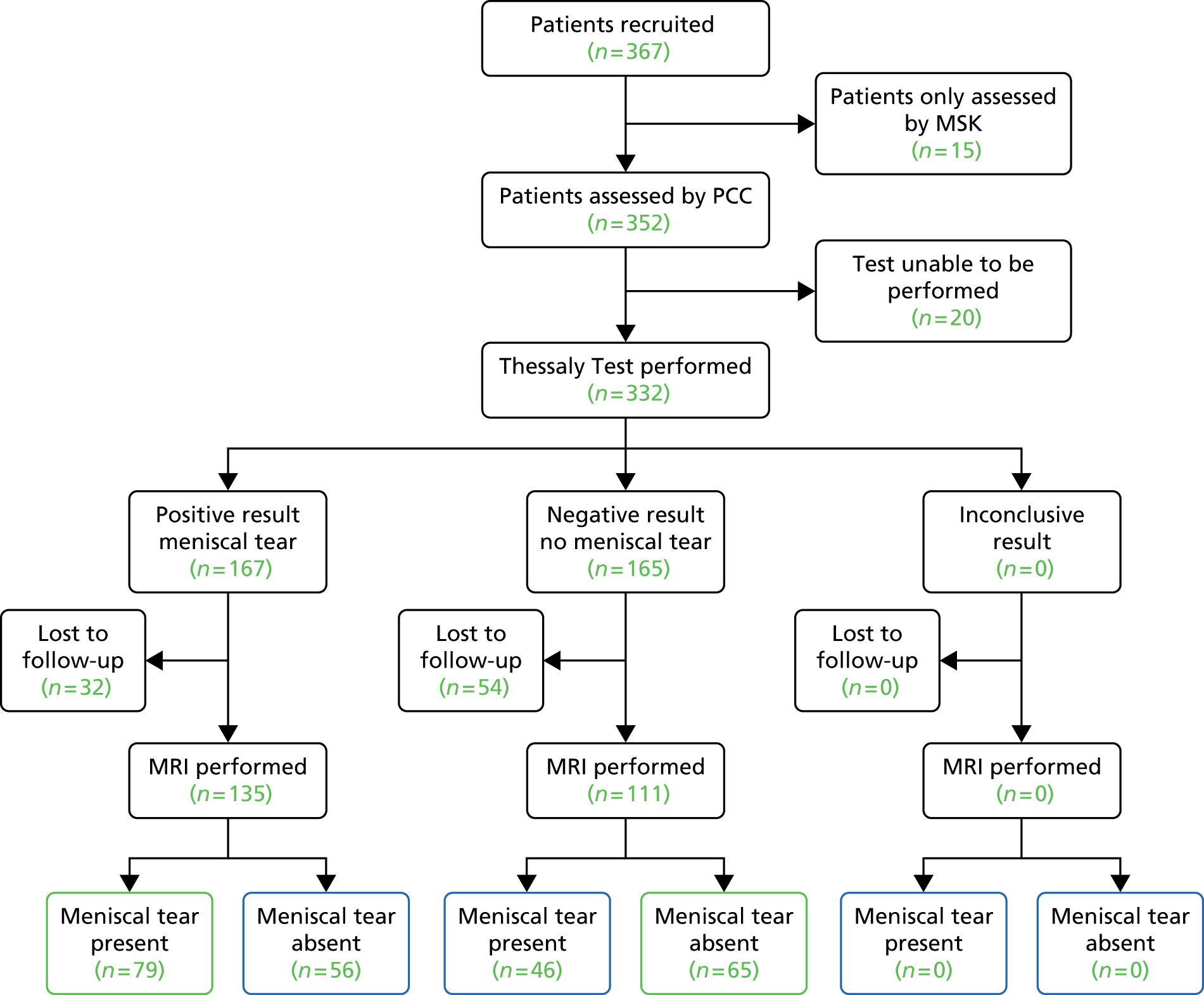
FIGURE 13.
STAndards for the Reporting of Diagnostic accuracy studies diagram for the Thessaly Test: musculoskeletal clinicians.
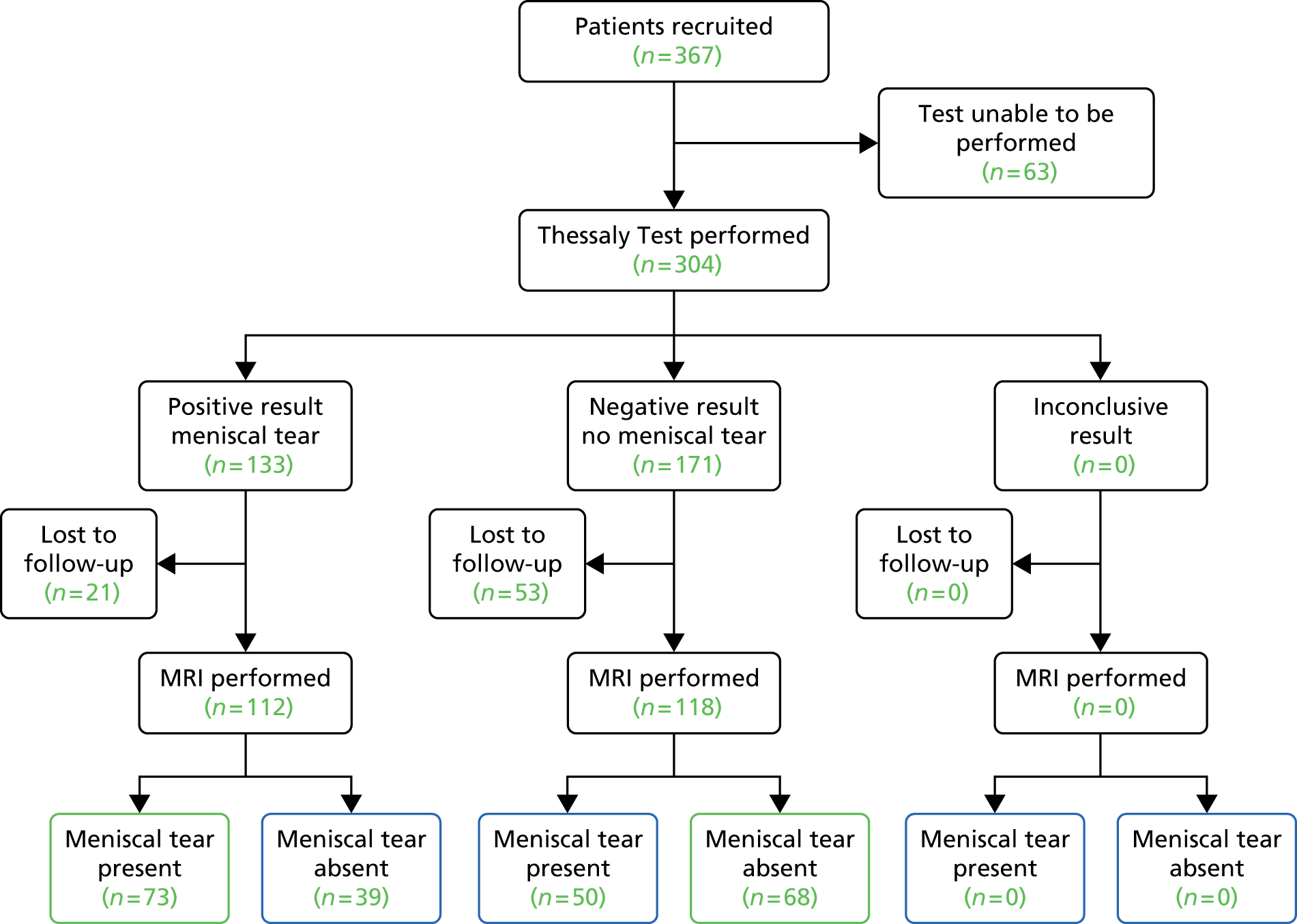
FIGURE 14.
STAndards for the Reporting of Diagnostic accuracy studies diagram for McMurray’s Test: primary care clinicians. MSK, musculoskeletal clinician; PCC, primary care clinician.
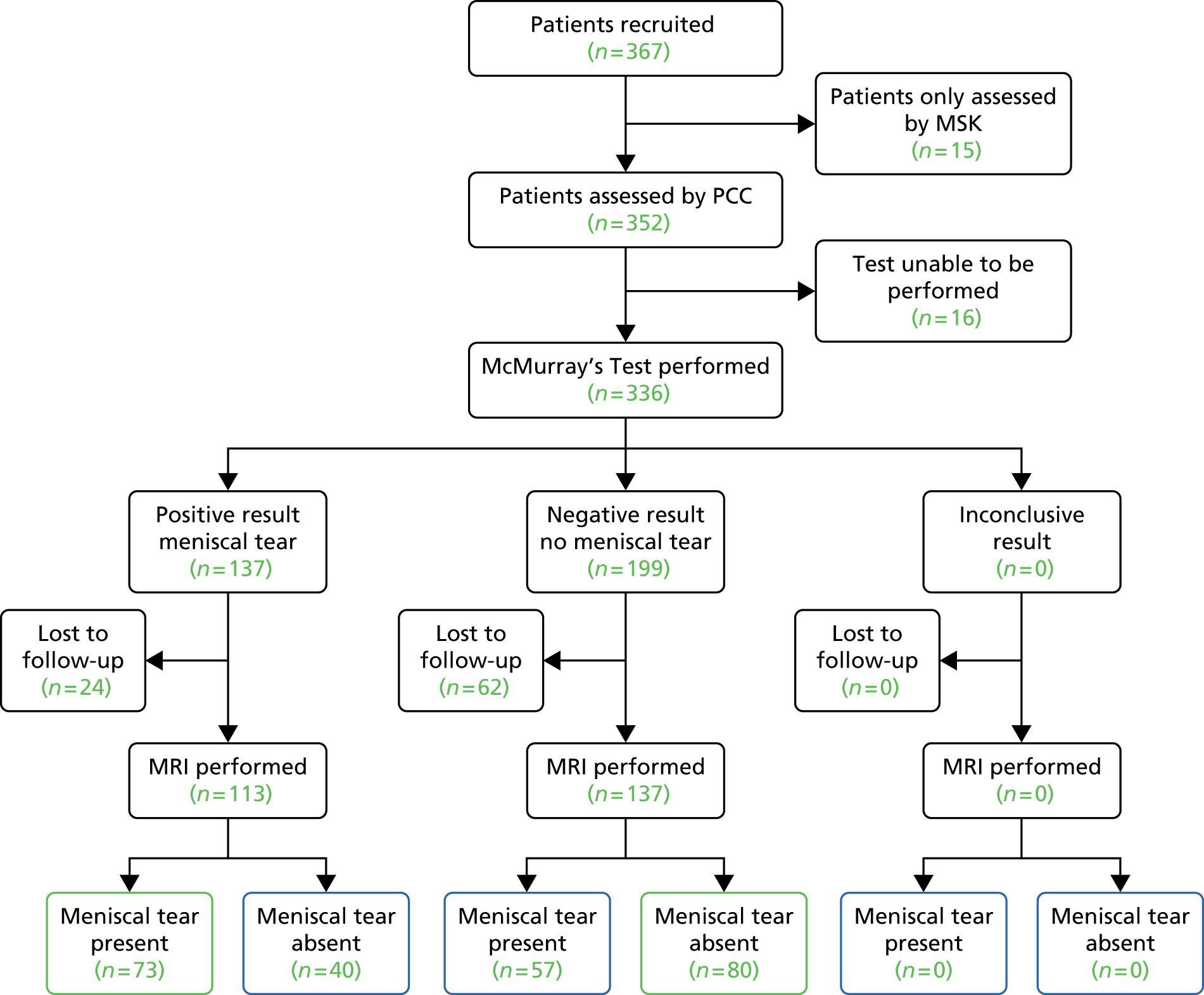
FIGURE 15.
STAndards for the Reporting of Diagnostic accuracy studies diagram for McMurray’s Test: musculoskeletal clinicians.

FIGURE 16.
STAndards for the Reporting of Diagnostic accuracy studies diagram for Apley’s Test: primary care clinicians. MSK, musculoskeletal clinician; PCC, primary care clinician.

FIGURE 17.
STAndards for the Reporting of Diagnostic accuracy studies diagram for Apley’s Test: musculoskeletal clinicians.

FIGURE 18.
STAndards for the Reporting of Diagnostic accuracy studies diagram for the joint line tenderness Test: primary care clinicians. MSK, musculoskeletal clinician; PCC, primary care clinician.
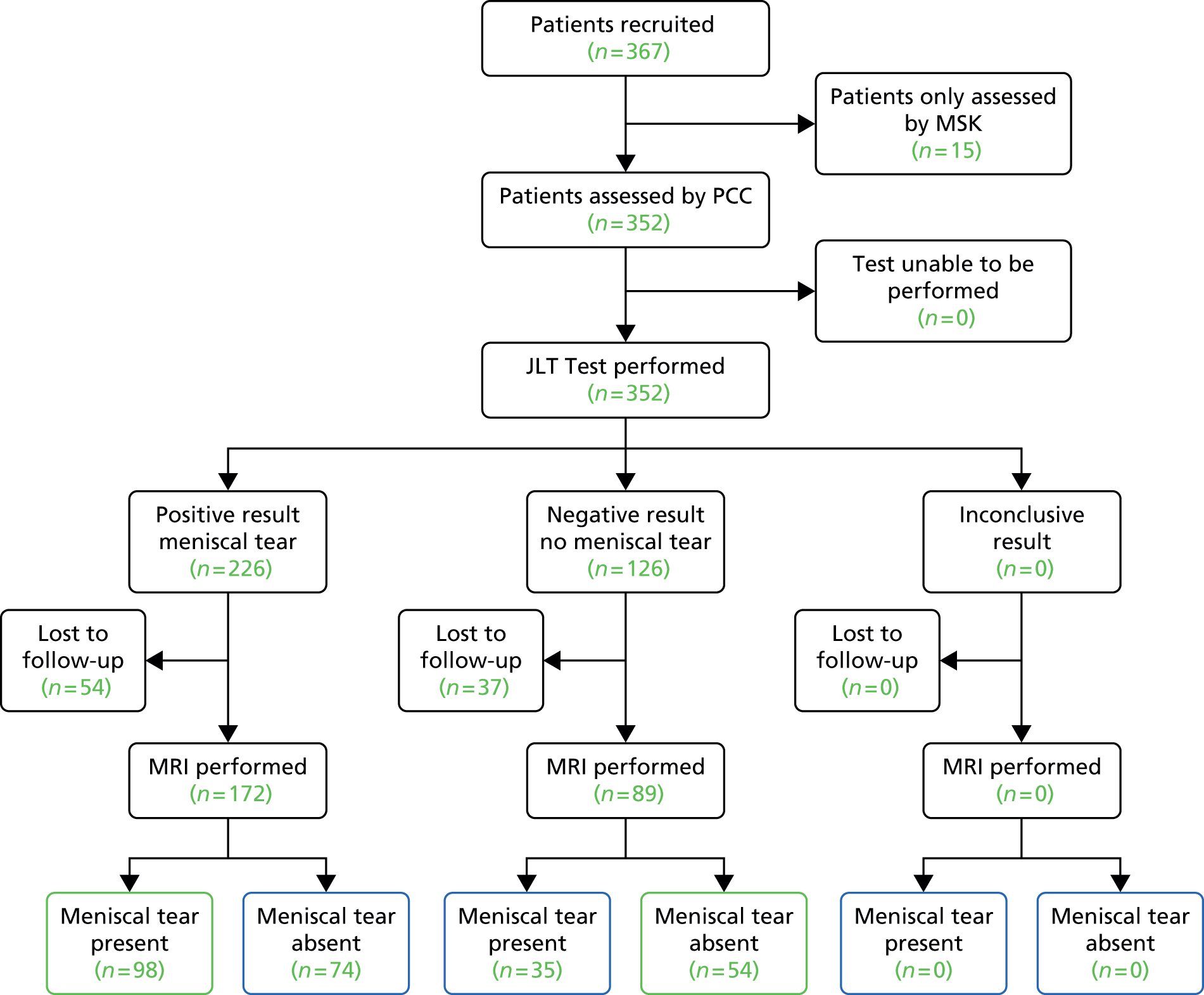
FIGURE 19.
STAndards for the Reporting of Diagnostic accuracy studies diagram for the joint line tenderness Test: musculoskeletal clinicians.
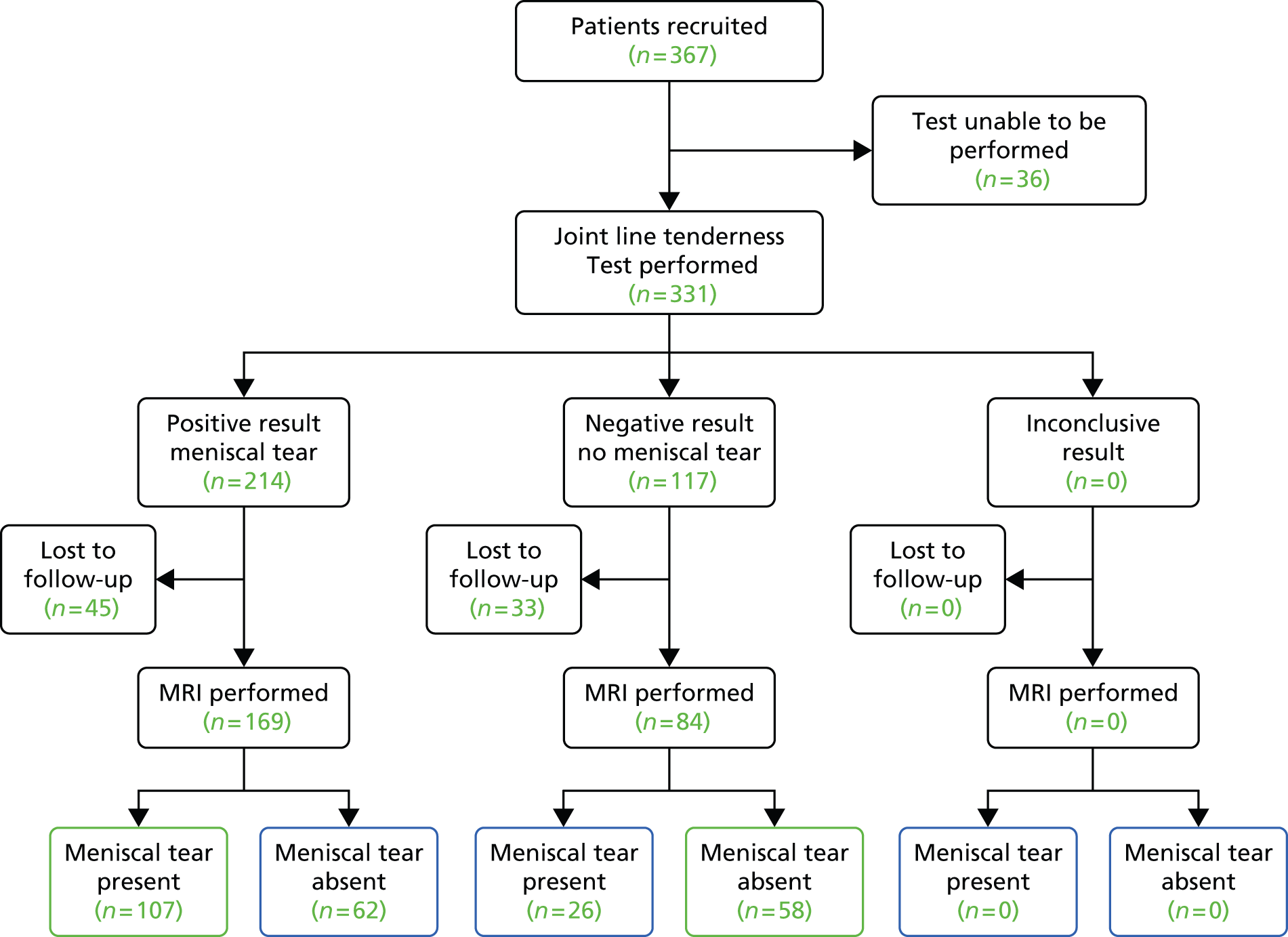
FIGURE 20.
STAndards for the Reporting of Diagnostic accuracy studies diagram for clinical history: primary care clinicians. MSK, musculoskeletal clinician; PCC, primary care clinician.
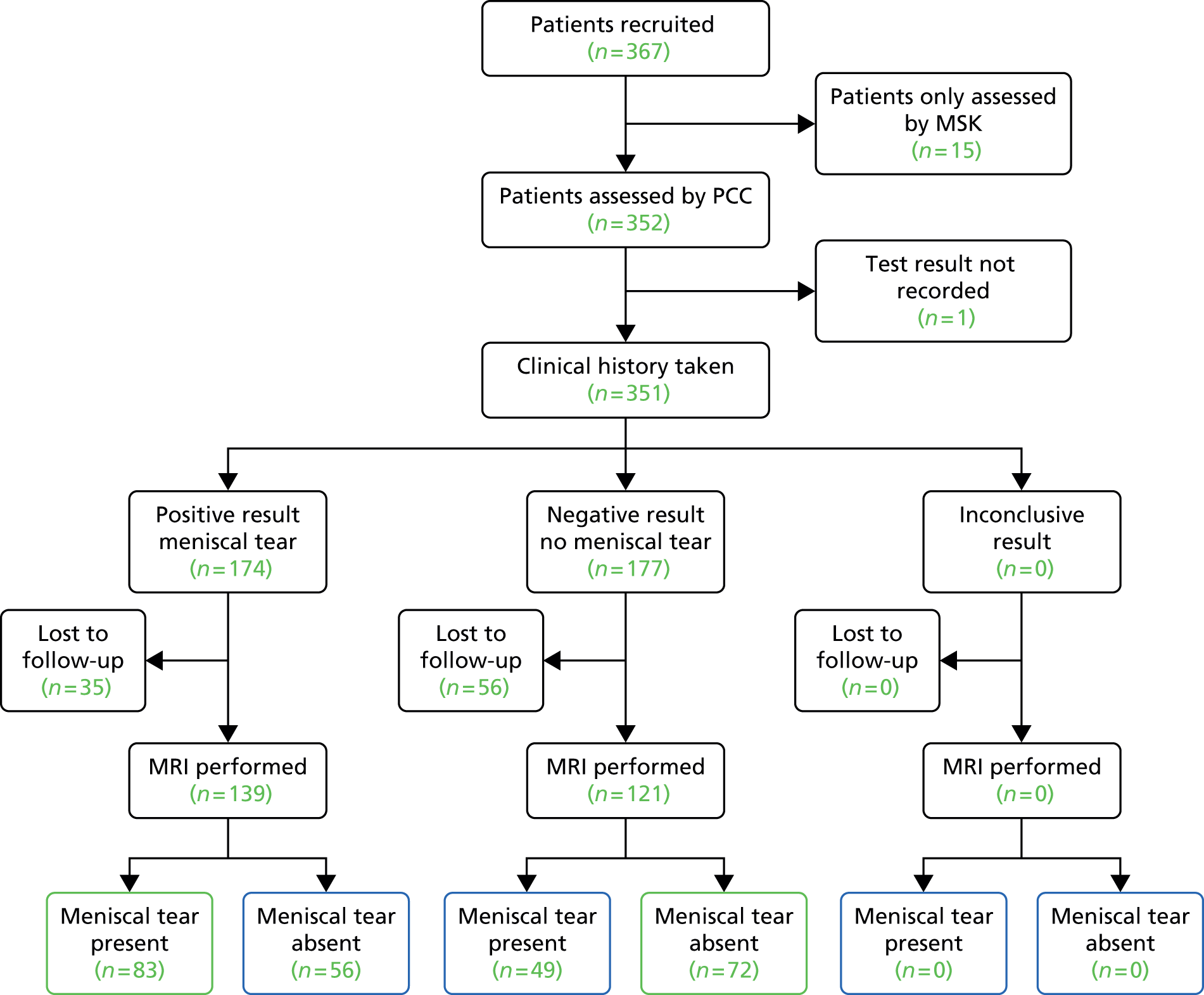
FIGURE 21.
STAndards for the Reporting of Diagnostic accuracy studies diagram for clinical history: musculoskeletal clinicians.
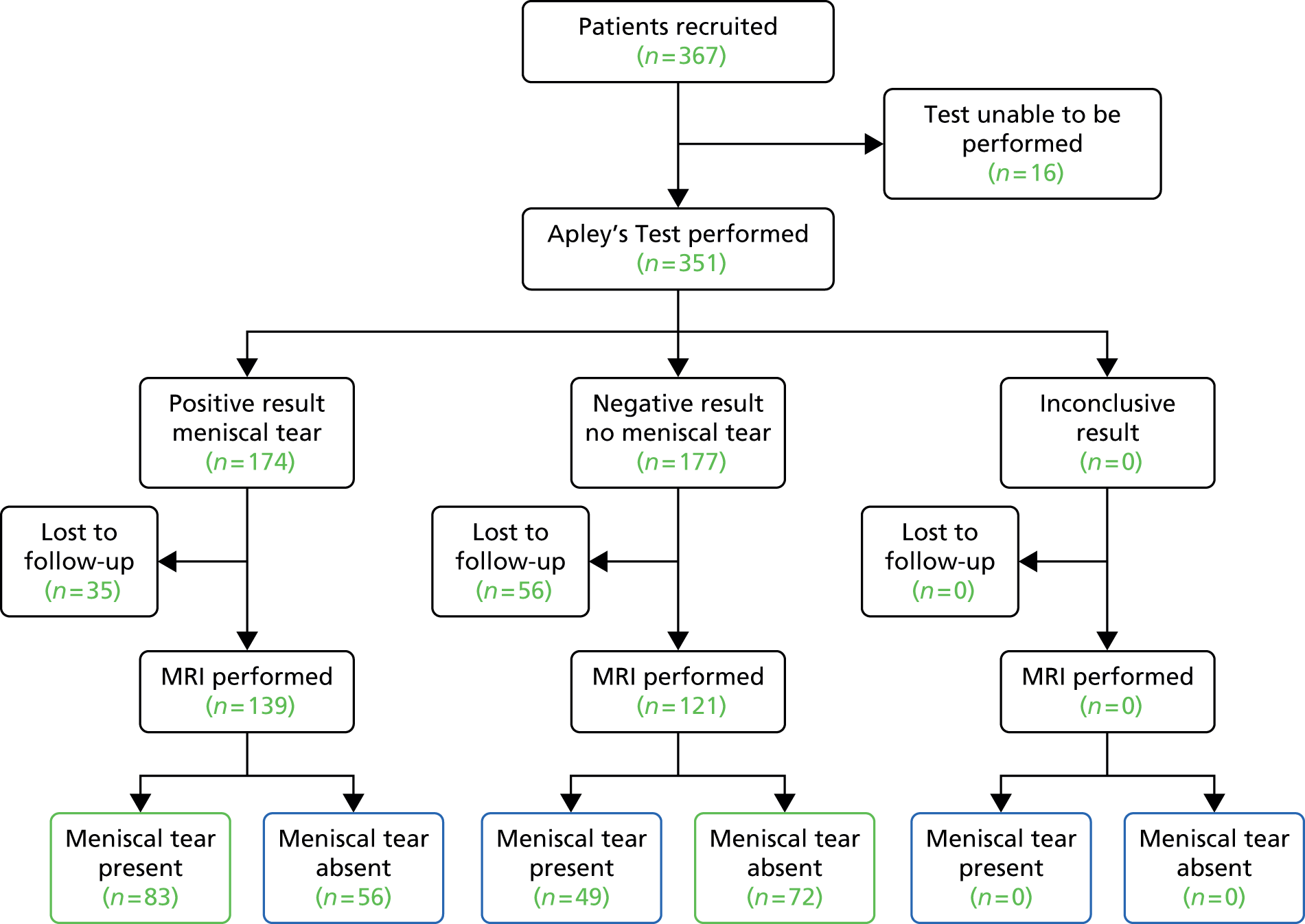
Appendix 3 Deviations from the statistical analysis plan
Logistic regressions actually performed in this report in comparison to those specified in the statistical analysis plan:
Core model Not performed, unnecessary.
Model level 1 Five models (four physical tests + clinical history); includes effect of the test and its order.
Model level 2 One model; includes all covariates + GP as random effect.
Model level 3 Five models (four physical tests + clinical history); model level 2 + effect of the test.
Model level 4 Not performed, as data not available (GP characteristics).
Model level 5 One model; model level 2 + effects of all tests.
Model level 6 One model, derived by backwards stepwise selection; starting model is model level 5 plus all interactions.
Appendix 4 Patient referral pathway for knee pain
Appendix 5 Control patient recruitment poster
Glossary
- Likelihood ratio for negative test
- How many times more likely you are to not have a meniscal tear if you have a negative test compared with someone who has a positive test.
- Likelihood ratio for positive test
- How many times more likely you are to have a meniscal tear if you have a positive test compared with someone who has a negative test.
- Musculoskeletal clinician
- Orthopaedic specialist knee surgeon or extended scope physiotherapist with specialist knee interest (operating in a secondary care orthopaedic setting).
- Negative predictive value
- The proportion of patients with a negative test who do not have a meniscal tear.
- Odds ratio
- Diagnostic odds ratio of a test is the ratio of the odds of positivity in subjects with a tear relative to the odds in subjects without a tear. It is calculated according to the formula: odds ratio = (true positive/false negative)/(false positive/true negative).
- Positive predictive value
- The proportion of patients with a positive test who actually have a meniscal tear.
- Primary care clinician
- General practitioner- or community-based physiotherapist.
- Sensitivity
- The proportion of those patients with a meniscal tear who are correctly identified as positive by the test. Low sensitivity indicates a high rate of false-negative tests.
- Specificity
- The proportion of those patients without a meniscal tear who are correctly identified as negative by the test. Low specificity indicates a high rate of false-positive tests.
List of abbreviations
- ACL
- anterior cruciate ligament
- AUC
- area under the curve
- BMI
- body mass index
- CI
- confidence interval
- GP
- general practitioner
- HTA
- Health Technology Assessment
- MRI
- magnetic resonance imaging
- NPV
- negative predictive value
- PPV
- positive predictive value
- STARD
- STAndards for the Reporting of Diagnostic accuracy studies