Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 09/91/16. The contractual start date was in July 2011. The draft report began editorial review in June 2014 and was accepted for publication in November 2014. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Dr Steve Cunningham has the following potential competing interests: (1) current chair of the National Institute for Health and Care Excellence Bronchiolitis Guideline Group; (2) past chair of the Scottish Intercollegiate Guideline Network Bronchiolitis Guideline Group; (3) principal investigator for Alios Pharmaceuticals Phase 1 investigational medicine for treatment of infants with bronchiolitis; and (4) consultancy work on behalf of NHS Lothian for Ablynx Pharmaceuticals Phase 1 product development for treatment of infants with bronchiolitis.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2015. This work was produced by Cunningham et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
Bronchiolitis is a common self-limiting viral illness generally affecting children under 12 months of age. The illness is marked by acute inflammation of the mucous membranes of the nasal cavities (a coryzal illness) with a subsequent viral infection of the lower airway, associated with poor feeding, cough, increased work of breathing and hypoxaemia (low blood oxygen levels).
Normoxaemia and hypoxaemia
Normoxaemia is the range of oxygen levels within the blood of healthy individuals. An oxygen saturation of 94% or more is seen in 97.5% of the population up to 1500 m altitude, and 94% is commonly accepted as defining the lower limit of normoxaemia. 1
Hypoxaemia (an oxygen saturation of < 94%) is common, particularly in respiratory disease, and results from poor ventilation or perfusion or both.
Clinical approach to hypoxaemia in respiratory disease
Cyanosis has been a core clinical sign of hypoxaemia for over three centuries. With ready supply of supplemental oxygen from the 1950s, cyanosis was corrected during disease. The clinical availability of arterial pulse oximetry in the 1980s, becoming ubiquitous in the 1990s, has enabled clinicians to have a more finely tuned understanding of arterial oxygenation. This precision, however, has vexed clinicians about how to interpret safely small changes in oxygen saturation. Clinical cyanosis is distinguishable at approximately 85% oxygen saturation, so what is the clinical impact of increments in oxygen saturation between 85% and 94%? Since the early 1990s, clinicians have grown accustomed to interpreting changes in oxygen saturation without an evidence base on which to do so; in acute bronchiolitis the rate of admission to hospital would double when clinicians were provided with scenarios depicting only a 2% difference in oxygen saturation (from 94% to 92%). 2
Clinical response to supplemental oxygen in those with hypoxaemia
Supplemental oxygen is provided for both acute and chronic respiratory disease to treat hypoxaemia. There are different recommendations for oxygen saturation targets from which to supplement oxygen in developed and developing health-care settings. The evidence for recommendations is limited or absent.
In developed health-care settings, in adults with acute respiratory disease, it is recommended that a target oxygen saturation of 94–98% be maintained;3 however, supplemental oxygen has no effect on acute respiratory symptoms,4,5 and there is no evidence that it has any effect on duration of illness. Among adults with chronic respiratory disease (chronic obstructive pulmonary disease), domiciliary oxygen supplementation confers a survival benefit on those who are severely hypoxaemic but not on those with mild or moderate hypoxia. 6 At the other end of the age spectrum, it has been found that preterm infants managed to a target oxygen saturation of 84–89% (median oxygen saturation attained 89%) were significantly more likely to die than those managed to a target oxygen saturation of 90–95% (median oxygen saturation attained 92%). 7 The small differences in median oxygen saturation observed in this study highlight the potential for significant health implications from minor variance of oxygen saturation in vulnerable populations.
In developing health-care settings, it is recommended that a target oxygen saturation of ≥ 90% be maintained in those with acute respiratory disease. 8 Provision of supplemental oxygen to meet this recommendation is associated with reduced mortality in children with acute respiratory infection. 9 The World Health Organization has recommended that the oxygen saturation target in acute respiratory infection be derived from expert interpretation of oxygen dissociation dynamics combined with a pragmatic wish to optimise resource allocation for maximal reduction of mortality in resource-poor settings. 10
Before the present study, there were no randomised studies assessing the role of oxygen supplementation in acute respiratory infection in children.
Hypoxaemia in acute viral bronchiolitis
One in five infants develops symptomatic bronchiolitis in the first year of life, and approximately 3% of all infants require hospital admission to receive supportive care,11 predominantly for help with feeding and to receive supplemental oxygen for hypoxaemia. Oxygen saturation below 92% leads to oxygen supplementation being provided in 70% of infants admitted to hospital with acute viral bronchiolitis. 12 In 57% of infants admitted to hospital, hypoxaemia will prolong length of stay after all issues have resolved (i.e. feeding). Length of stay for all infants with bronchiolitis is a mean of 72 hours, but in those requiring supplemental oxygen the mean is 96 hours. 12
Controversies in approach to hypoxaemia in bronchiolitis
Hypoxaemia is common in bronchiolitis; however, the majority of infants do not have clinical cyanosis. The controversies lie in how to address oxygen saturation values just below the limit of normoxaemia. Could there be clinical benefit from elevating oxygen saturation in this region to normoxaemia (as is suggested by adult recommendations for acute respiratory disease)? What harm may come from accepting oxygen saturation in this region during acute respiratory disease (because small changes in oxygen saturation targets cause significant harms in preterm infants)?
Since the early 1990s, the number of admissions to hospital with bronchiolitis have increased, while mortality from the condition has remained the same. 13 Death occurs in approximately 0.9% of hospital patients with bronchiolitis, mostly in those with pre-existing conditions. 14 Some have questioned whether or not the increase in admissions may be (in part) because of the increased use of oxygen saturation monitoring. 15
Two recent evidence-based guidelines have considered oxygen saturation in bronchiolitis. The Scottish Intercollegiate Guidelines Network (SIGN) guideline No. 9116 considered that, with no evidence available, current practice should prevail and infants should be considered ready for discharge once normoxaemia (oxygen saturation ≥ 94%) has been restored. The American Academy of Pediatrics (AAP) Guideline on Bronchiolitis,17 published in the same year, also accepted that there was no evidence but considered (by expert opinion of the group) that infants could be discharged home once they are clinically stable with an oxygen saturation ≥ 90%. The recommendation of an oxygen saturation at discharge below normal ranges has been controversial. 18 Since publication of these two evidence-based guidelines, there continues to be variation in practice and recommendations, possibly highlighting clinician uneasiness at the interpretation of oxygen saturation in sick infants. There are a variety of recommended oxygen saturation targets present within national guideline portals in the USA,19 the UK,20 Spain21 and Australia. 22 In addition, guidelines have recommended a lower target for starting supplemental oxygen than for stopping, typified by current guideline synthesis provided by the Agency for Healthcare Research and Quality at the US Department for Health and Human Services. 23 The clinical logic for the different targets to start and stop supplemental oxygen is not clear, particularly the lower oxygen saturation target for commencing supplemental oxygen at a time when infants are typically clinically less stable.
Potential health-care impact of clinical response to hypoxaemia in bronchiolitis
We performed a pilot study in 62 infants admitted to hospital with bronchiolitis who were provided with supplemental oxygen for low oxygen saturation. 24 Nursing observations noted oxygen saturation in air and amount of supplemental oxygen (if required) every 2 hours during the hospital stay. The median time for infants to improve from 90% to 94% oxygen saturation in air was 33 hours (stability for 4 hours at each level was required). In some infants, oxygen saturation was stable at ≥ 90% before feeding had been re-established. Taking feeding into account identified that a move from discharge at ≥ 94% saturation to ≥ 90% could facilitate discharge 22 hours earlier (30%) than currently is the case. If projected to the 70% of infants with bronchiolitis requiring oxygen during their admission, this would be equivalent to 18,434 bed-days per year gained for the UK NHS (an equivalent US value would be 95,608 bed-days per year). This represents substantial cost savings to the UK NHS, and, hence, assuming no significant cost increases through implementation of this changed regime and equal or improved health benefits, this would represent a highly cost-effective intervention.
There is a significant pressure to improve hospital logistics and costs associated with bronchiolitis. In the USA, an estimated 149,000 infants were admitted in 2002, for an average of 3.3 days, at a total cost of US$543M. Paediatric hospitals are logistically challenged each winter, particularly during the 6-week peak of respiratory syncytial virus (RSV) infection, as infants who are clinically stable remain in hospital for oxygen supplementation. In response, some centres now provide short-term supplemental oxygen at home, using primary care (USA)25 or secondary care home nursing teams (Australia). 26 The burden on primary care services and families of home oxygen is significant. 27 Studies have not provided a health-economic perspective on this service development. 28
Study aims
Bronchiolitis has no effective treatment. 16,17 Care is supportive to those who need it. In Scotland, approximately 2000 children under 12 months of age are admitted each year with bronchiolitis. 16 In the UK, in 2007, an estimated 28,728 infants under 12 months of age were admitted to hospital with bronchiolitis, similar to the number of all children (aged 0–14 years) admitted each year with acute asthma.
If the AAP recommendation of an oxygen saturation target of ≥ 90% were widely adopted and used as a target for both starting and stopping supplemental oxygen, this could reduce time in hospital for infants. To be acceptable to clinicians, however, the practice would need to be demonstrated to be safe, without clinical detriment and without undue additional burden on primary care or families caring for children at home during an earlier part of their illness. To answer this clinical question we performed a double-blind, randomised controlled, equivalence trial in children with acute viral bronchiolitis to determine whether or not a target oxygen saturation of ≥ 90% would be equivalent to ≥ 94% for resolution of illness and also to compare clinical, safety and parental outcomes.
Chapter 2 Methods
Trial design
This was a multicentre, parallel-group, double-blind, randomised controlled, equivalence trial conducted in the UK (eight sites). Infants were allocated 1 : 1 to trial intervention.
The trial was completed to the same methods throughout with one exception. In season 1, infants were met at 28 days for measurement of oxygen saturation. An unblinded review of the data by the independent Data Monitoring Committee (DMC) at the end of season 1 identified satisfactory oxygen saturation and no significant difference in oxygen saturation between groups. As a consequence, in season 2, there was no further measurement of oxygen saturation at day 28, and this meeting was replaced by a telephone call to parents to gather the same information that had previously been collected at the day-28 meeting.
Participants
Participants were infants aged ≥ 6 weeks and ≤ 12 months (corrected for prematurity) presenting to a participating hospital emergency department (ED)/acute assessment area (AAA) [either by general practitioner (GP) referral or by spontaneous attendance] who had a clinical diagnosis of bronchiolitis (consistent with SIGN guideline No. 9116) made by acute receiving medical staff and who required admission to hospital for supportive care. The clinical decision to admit an infant with bronchiolitis prompted informed consent and randomisation to the study.
The following inclusion and exclusion criteria were used:
-
Inclusion criteria
-
Infants with a corrected age of ≥ 6 weeks and ≤ 12 months of age admitted to hospital with a clinical diagnosis of bronchiolitis made by a medically qualified practitioner in ED/AAA.
-
-
Exclusion criteria
-
Preterm infant (< 37 weeks’ gestation) who received oxygen therapy in the previous 4 weeks.
-
Cyanosis/haemodynamically significant heart disease.
-
Cystic fibrosis or interstitial lung disease.
-
Documented immune function defect.
-
Direct admission to high-dependency unit (HDU)/paediatric intensive care unit (PICU) from ED/AAA.
-
Previously recruited to Bronchiolitis of Infancy Discharge Study (BIDS).
-
Infants were recruited only from 6 weeks of age, as infants below this age are often considered at higher risk and present more frequently with apnoea, often without significant desaturation. The generalisation of results to infants in this age group is covered in the discussion.
Identifying participants
The study aimed to recruit and randomise only during the historic peaks for bronchiolitis in two northern hemisphere winters. Infants who were eligible were identified by clinicians and research/specialist nurses in the ED/AAA. The clinical decision to admit an infant with bronchiolitis prompted consent for the study.
Settings and locations where the data were collected
The study took place in the ED/AAA and paediatric wards of eight paediatric hospitals in the UK (in Aberdeen, Bristol, Dundee, Edinburgh, Exeter, Glasgow, Kilmarnock and Truro). In season 1, randomisation was open from 3 October 2011 to 30 March 2012 in the five Scottish sites only. In season 2, randomisation was open from 1 October 2012 to 29 March 2013 in all eight sites.
Interventions
The intervention was to a randomly allocated standard or modified pulse oximeter. Therapeutic options for the treatment of acute viral bronchiolitis are very limited, and, in general, infants are admitted to hospital for supportive care only. 16,17 Supportive care includes feeding support (with nasal suction, nasogastric or intravenous fluids) and supplemental oxygen for oxygen desaturation. Oxygen saturation monitors are ubiquitous in the care of infants admitted to hospital with acute bronchiolitis and guide supplementation of oxygen and decision-making for discharge.
Eighty oxygen saturation monitors were provided by Masimo (Rad-8® with LNC 10 patient cable; Masimo Corporation Limited, CA, USA). Standard oximeters measured and displayed oxygen saturation in a standard way as usual care. The modified oximeters measured arterial oxygen saturation as per standard oximeters but manufacturer-altered internal algorithms provided a non-standard display: in the oxygen saturation measured range of 85–90%, the display was within the range of oxygen saturation of 85–94%. In this way infants with modified oximeters would appear to have a more rapid improvement with regard to oxygen requirement and, consequently, could stop supplemental oxygen at a displayed 94% oxygen saturation level when the actual oxygen saturation level was 90%. Figure 1 demonstrates the algorithmic relationship of measured (true) to displayed (altered) oxygen saturation. From a clinical perspective, study pulse oximeters were of identical appearance and function, identified only by a study number (Figure 2). In the study, infants received supplemental oxygen to maintain oxygen saturation of ≥ 94% (actual 90% on modified oximeters). As we expected that infants on modified oximeters might go home sooner, with an associated faster turnaround of oximeters, there were 43 standard oximeters and 37 modified oximeters in the oximeter pool.
FIGURE 1.
Adjusted algorithm for modified oximetry (true vs. altered).

FIGURE 2.
Masimo Rad-8 study oximeter.

Infants remained on their study oximeter for the duration of their admission. Infants who suffered post-randomisation deterioration and required admission to a HDU/PICU were transferred to a standard non-study pulse oximeter during the HDU/PICU stay and recommenced on the same blinded study oximeter on transfer back to the ward for the remainder of their stay until discharge.
Outcomes
Primary outcome
The primary outcome was equivalent time to no cough (collected by phone calls at follow-up). The primary outcome was assessed by the primary caregiver.
Secondary outcomes (admission questionnaires, clinical data, parental phone calls, home visit)
We were looking for equivalence between treatment groups in the following secondary outcomes:
-
time to re-established feeding (approximately 75% normal)
-
parental perspective of ‘time to back to normal’
-
oxygen saturation at 28 days post randomisation (season 1 only).
We were looking for a difference between treatment groups in the following secondary outcomes:
-
time to fit for discharge (oxygen saturation ≥ 94% for 4 hours including a period of sleep and adequate feeding at ≥ 75% usual)
-
time to discharge
-
health-care reattendance (primary care, ED, readmission)
-
change in anxiety score
-
time to return to work/usual activities for parent(s)/nursery for infants
-
family and societal costs incurred
-
health-care costs related to discharge time and subsequent health-care utilisation.
There were no major changes to trial outcomes following trial commencement. As above, oxygen saturation was measured at 28 days in season 1 with the agreement of the DMC when no significant differences were identified between the groups.
Measurements
Demographic information was collected by research nurses within 24 hours of admission. Data related to the hospital stay were collected progressively during the period of hospitalisation and at discharge.
Parents were contacted by the study team on four occasions, at 7, 14 and 28 days and at 6 months following randomisation. Standardised interview questions were asked to obtain study-related data. In season 1, infants and parents were met in person at 28 days for measurement of oxygen saturation and parents were asked day-28 information at this visit. In season 2, the same information was obtained by telephone call.
We could not identify a validated measure of parental anxiety during an acute illness of a child. The anxiety section of the Hospital Anxiety and Depression Scale (HADS) was therefore used without the depression section (as the depression questions were not relevant). 29
Sample size
The sample size was determined for the primary outcome of time to resolution of cough following randomisation. An estimate of 544 participants was made by assuming that there would be no difference between the treatment groups, with a common standard deviation of 8.3 days. 30 The standard deviation of 8.3 days was calculated by dividing the interquartile range by 1.35. 31 This used a two-sided test (overall alpha 0.05), with power of 80% and limits of equivalence of 2 days (i.e. the difference between the two arms could be up to 2 days in either direction). To allow for skewness in the outcome measure, as well as any dropouts and non-compliance, the recruitment target was 600 infants. Every effort was made to minimise dropout and non-compliance.
There is no published evidence to support the limit of equivalence for cough resolution. We therefore sampled the expert opinion of consultant paediatricians who contribute to the general paediatric service at the Royal Hospital for Sick Children, Edinburgh (and who provide clinical management of infants with bronchiolitis), and identified a variance of 2 days as being clinically meaningful with adequate safety. The same equivalence limit of 2 days in either direction was used for time to return to normal. For time to return to satisfactory feeding we used a typical infant feed interval of 4 hours as equivalence.
Although the number of infants admitted to these hospitals during the study would be more than 600, the sample size estimate included an allowance for infants with exclusion criteria, infants admitted on more than one occasion and parents who did not wish to participate (all exclusions estimated at 25%).
The epidemic and variable nature of seasonal bronchiolitis made it difficult to plan exact recruitment rates. The goal was to achieve recruitment of 75% of admissions, and centres provided monthly Consolidated Standards of Reporting Trials (CONSORT)-style infant outcome feedback32 to identify centre mismatch in recruitment rates and to enable re-evaluation and optimisation of study recruitment if poorer than expected. The chief investigator and trial manager, together with the principal investigator and lead clinical research facility nurse at each centre, held monthly teleconferences to discuss the project, problems encountered and difficulties in recruitment and to share experiences of how these issues may be addressed.
Following the outline proposal, we were asked to confirm that parents would, in principle, consent to a study as proposed. In a short survey carried out at the Royal Hospital for Sick Children, Edinburgh, in spring 2010, a group of parents whose infants had been admitted to or recently discharged from hospital with bronchiolitis were provided with the study scenario and asked if they would be willing for their infant to take part in the study. Fifteen parents were approached. The children of two parents were < 6 weeks of age at the time of admission and both parents said that they would decline to participate in the study because of their child’s age, confirming that a 6-week age minimum was reasonable. A further parent declined because their child had been admitted to hospital with bronchiolitis on numerous occasions. Of the remaining 12 parents, 11 said that they would have agreed to take part in the study (92% of those eligible), with one parent considering and requiring more information before making a decision.
Interim analyses and stopping guidelines
An independent DMC reviewed the efficacy and safety data after season 1. There were no safety concerns. A review of oxygen saturation data measured at 28 days revealed no differences, so these data were not collected for season 2.
The following criteria for stopping the trial were in the DMC charter (09.05.11 Version 1.0) (see Appendix 5):
The DMC should inform the Chair of the steering committee if, in their view:
(i) the results are likely to convince a broad range of clinicians, including those supporting the trial and the general clinical community, that one trial arm is clearly indicated or contraindicated, and there was a reasonable expectation that this new evidence would materially influence patient management; or
(ii) it becomes evident that no clear outcome would be obtained.
Randomisation
Sequence generation
Randomisation was by central internet-based secure password-protected randomisation database. Patient identifiers and some clinical details were entered to confirm eligibility (inclusion and exclusion criteria) and to prevent re-recruitment. The random allocation sequence was generated by the programmers at the Edinburgh Clinical Trials Unit (ECTU).
Type of randomisation
Randomisation was by blocks of varying length (four and six) without stratification.
Allocation concealment mechanism
The person randomising the infant did not know the allocation until the infant was definitely enrolled into the study via the system.
Implementation
Infants were enrolled by clinicians and research/specialist nurses in the ED/AAA. Clinicians (mostly nursing staff) attached either a standard or a modified pulse oximeter in accordance with the computer-generated randomisation code. The administering clinician removed non-study oximeters from infants and, with an interval of 1 minute, reapplied the appropriate study oximeter, typically at a time when the infant was preparing to move between departments in the hospital (i.e. ED to a ward area).
Blinding
The monitors were identical in appearance and general function, with the exception of the study number (see Figure 2). All study staff involved in day-to-day running of the trial, hospital staff and parents were blind to study intervention and could not tell what the randomised group was from the study numbers on the machines. To further reduce the opportunity for accidental unblinding, study numbers on oximeters were changed in the period between season 1 and season 2. Those assessing outcomes were blind to the assigned intervention. The blind was not broken for any infant during the study.
Statistical methods
General statistical methods
All analyses were by intention to treat (ITT) unless otherwise specified. The ITT population included all infants randomised into the BIDS study. Infants were analysed in the group to which they were randomised, regardless of treatment received. Where a per-protocol analysis was performed, infants were analysed in the group of the treatment they actually received: any use of standard pulse oximeter versus any use of modified pulse oximeter. The group of infants in which no pulse oximeter was used were excluded from the per-protocol population. No infants received both types of oximeter. All applicable statistical tests were two-sided using a 5% significance level. Ninety-five per cent (two-sided) confidence intervals (CIs) were presented. The primary analysis was an unadjusted analysis. Where there were missing data for an outcome variable, in the first instance, those records were removed from any formal statistical analysis, unless otherwise specified.
Primary outcome
The primary outcome was the number of days from randomisation until resolution of cough. The difference in median number of days until cough resolution between the two treatment groups was estimated along with a 95% CI for the difference. The treatment arms were considered equivalent with respect to this outcome if this 95% CI lay entirely within the equivalence limits of ± 2 days. For the primary analysis, the difference between the medians and the 95% CI for this difference were estimated as described by Altman et al. 33 The large-sample formula for derivation of the confidence limits was used. The main primary outcome analysis was conducted on an ITT basis. A per-protocol analysis was also performed. The study would lead to firm conclusions only if the findings from the main analysis and the per-protocol analysis were in agreement.
Missing data
If a date of cough resolution was known, it was used. If it was known that the cough resolved but the precise date was unknown, a random value was chosen between the date that the cough was last known to be present and the date of the follow-up when it was found that the cough had stopped. The random value was chosen from infants in the same treatment group whose cough stopped in a similar time frame. If it was known that the cough had not resolved by 6 months, the date of cough was predicted by taking a random value from a uniform distribution capped from 180 days to 200 days (upper cap based on the observations by Shields and Thavagnanam34). If it was known that the cough had not stopped by the last follow-up but the infant was not followed to 6 months, then a random value was chosen from a uniform distribution with the lower cap pegged to the last known follow-up time (i.e. 7, 14 or 28 days) instead of 180 days. This process was repeated 100 times, and the analysis done on each data set. The mean values for the estimate of the median and the estimates of the CI limits were used. If 100 repetitions did not produce a stable estimate, then this number was to be increased, but this was not necessary. As a sensitivity analysis, a complete-case analysis was also done.
Secondary outcomes
Secondary outcome measures were tested for a difference between the two arms of the trial.
For the outcome measures, the times, split by treatment group, were presented using a Kaplan–Meier plot. Cox proportional hazards regression was used to estimate the treatment effect: time from randomisation to (1) fit for discharge and (2) actual discharge for all infants admitted with acute viral bronchiolitis; (3) time to no supplemental oxygen; (4) time to readmission to hospital. We considered whether or not the season-1 data for Glasgow (Yorkhill) should be removed from the analysis of time to fit for discharge, as this variable was not recorded consistently at this centre in season 1. However, this made no difference to the results so these data were left in.
The results are presented at multiple time points, and due allowance would be made for this if any of them proved to be statistically significant. The effect of the intervention was estimated using binary logistic regression and reported as an adjusted odds ratio and 95% CI for the proportion of infants with at least one health-care reattendance (primary care, ED, hospital readmission) at days 7, 14 and 28 and at 6 months. The effect of the intervention was estimated using Poisson regression for the number of health-care reattendances (primary care, ED, hospital readmission) at days 7, 14 and 28 and at 6 months. The effect of the intervention was estimated using analysis of covariance models with the baseline score as a covariate for parental anxiety score (anxiety questions from HADS questionnaire at admission, at 7, 14 and 28 days’ follow-up and at 6 months’ follow-up).
For the outcome measures, the mean difference in times between the two trial arms was estimated from a normal linear model, and presented with a 95% CI: heart rate at discharge; respiratory rate at discharge.
We tested for equivalence between the two arms of the trial for the secondary outcome measures. The same method as the primary outcome was used for time in hours from randomisation to re-established feeding (equivalence limits of ± 4 hours), and time in days from randomisation to parental perspective of back to normal (equivalence limits of ± 2 days). For time to re-establish adequate feeding, no imputations for missing data were performed, as the data were recorded only at the end of discharge and they were almost complete. The difference in mean oxygen saturation measurements between the two trial arms was estimated with its corresponding 95% CI for awake oxygen saturation at 28 days after randomisation (equivalence limits of ± 1.0% oxygen saturation – season-1 data collection only).
Subgroup analyses
Primary outcome
The difference in median time from randomisation until resolution of cough between the two treatment groups was estimated along with a 95% CI for the difference, by subgroup, using the same method as for the primary outcome. As the two treatment groups were expected to be equivalent, subgroup analyses were unlikely to be informative, as qualitative subgroup effects were not expected. No formal analyses between subgroup comparisons were made, and the significance or non-significance of within-subgroup effects will not be discussed. The subgroups to be presented are length of illness prior to randomisation (0–3 days vs. ≥ 4 days), use of antibiotics before and/or during admission (any vs. none) and parental smoking (any vs. none).
Other outcomes
The effect of treatment allocation on time from randomisation to (1) fit for discharge and (2) actual discharge from hospital was evaluated separately in infants with/without an oxygen requirement during their stay. Formal evidence of a differential subgroup effect was based on the statistical significance of the regression coefficient for the interaction between treatment allocation and oxygen requirement.
Economic evaluation methods
Overview of economic evaluation
This trial investigated whether or not a 90% oxygen saturation discharge protocol (modified) is cost-effective compared with the standard 94% oxygen saturation discharge procedure. The research question the economic evaluation therefore addressed was: is the modified discharge procedure a cost-effective alternative to the standard discharge procedure? The economic evaluation measured the costs to the NHS and social care and combined this with the main outcome measure, time to cough resolution, within a cost-effectiveness analysis (CEA) framework. CEA is a form of economic evaluation in which both the costs and effects of two or more health interventions are compared, and the results report the incremental difference between the alternatives under consideration as an incremental cost-effectiveness ratio (ICER). The economic evaluation was undertaken alongside the trial, capturing individual resource-use data collected via economic data-collection questions integral to the trial forms. The analysis reported the incremental cost per reduction in time to cough resolution. The economic evaluation also took into consideration the seasonality of the disease by outlining the opportunity cost of hospital bed displacement during peak winter seasons. Individual patient-level data on outcomes and information on resource use were identified and measured during the trial and used in the economic evaluation.
Outcome measure for cost-effectiveness analysis
The primary endpoint in the trial is time to cough resolution (measured at 6 months). The economic evaluation used mean time to cough resolution, by measuring the area under the curve. 35,36 The area under the curve method permits comparison of the mean difference between treatment arms based on the entire survival curve, or in this case the entire time to cough resolution curve. 36,37 This is standard practice for an economic evaluation for determining the primary endpoint in time to event/survival analysis, where censored and skewed data are prevalent. The economic analysis considered the joint distribution of costs and effects. Therefore, the economic analysis used the mean time to cough resolution and accompanying standard errors for each arm of the trial to undertake probabilistic analysis, using bootstrapping38 to account for uncertainty around this primary outcome measure and how this affects the cost-effectiveness outcomes. The economic analysis explored the impact that baseline variables have on the mean time to cough resolution. It was hypothesised that variables such as sex, child gestation at birth, length of illness prior to onset, parental smoking status, antibiotics on arrival at accident and emergency (A&E), oxygen saturation and GP visits prior to onset might affect the time to cough resolution. In addition, the quality of life of parents was measured using the anxiety component of the HADS. 29
Resource use data collection
The base-case analysis was undertaken from the perspective of the UK NHS and personal social services. That is, the costs relevant to the economic analysis are those incurred by the NHS and social services. In a sensitivity analysis, the patient perspective was also incorporated, adding the costs incurred by the parent in terms of both financial costs (such as travel to and from hospital) and time lost from normal activities because of the illness.
There are five main resource categories of relevance: initial hospitalisation costs, medication, readmission costs, follow-up care and, in the sensitivity analysis, costs to parents. The base-case total cost (CT) is a function of the cost of hospital days (or hours) (Chosp), medication (Cmed), readmission (Creadmit) and any follow-up care (CFUcare). In the sensitivity analysis, the cost to parents is also included (Cparents). Equation 1 illustrates the main components of total cost.
Patient-level resource-use data were collected within trial, for example days (or hours) in an acute paediatric ward, days (or hours) in the HDU, tests and scans undertaken, medication prescribed, hospital readmissions and any additional follow-up care, that is GP appointments, referrals, etc. Parent time was also collected. Resource-use quantities and mean patient cost values are reported separately as per recent recommendations [Consolidated Health Economic Evaluation Reporting Standards (CHEERS) guidelines]. 39
Health-economic analysis methods
Stata version 12 (StataCorp LP, College Station, TX, USA) was used to carry out regression analysis exploring the effect that baseline variables have on the cost of each intervention, such as sex, child gestation at birth, length of illness prior to onset, parental smoking status and antibiotics on arrival at A&E. Potential non-normality in the cost data was explored and, if the cost data were found to be skewed, a generalised linear model (GLM) was employed. It was hypothesised that the cost data were likely to be highly skewed because of the very high costs associated with cases that are referred on to HDU or are readmitted. The GLM for cost regressions, described by Glick et al. ,40 was used in this case, and 95% CIs around the cost estimates were also calculated. 41 If, however, the cost data were found to be normally distributed, then standard parametric tests were used. In line with recent CHEERS guidelines,39 resource-use values, ranges references and probability distributions are reported for all resources. Mean values for the main categories of costs, as well as mean differences between the comparator groups (modified compared with standard), are reported.
Additional analyses were undertaken to explore the effect that baseline variables, such as sex, duration of illness before randomisation, parent smoking, GP visits prior to admission, had on the cost and time to cough resolution of each intervention. Potential non-normality in the cost and time to cough resolution data was explored and a GLM was employed. 40
Outcomes were analysed using multivariate logistic regression, adjusting for child age and sex, parental age left full-time education and heaviness of smoking index. 42 GLM regression was used for analysis of costs if they were skewed. GLM regression for cost was adjusted for treatment group, parental smoking and GP visits prior to admission. The other specified variables in the analysis plan (protocol) had no significant impact. A variety of families and various links for each family were investigated and tested using modified Park tests; gamma was found to be best fit, with a power link of –1. We ran GLM using gamma family and link power –1. GLM regression was used for the time-to-cough-resolution variable, given that the mean is skewed. GLM regression for time to cough resolution was adjusted for treatment group, season, sex, preterm birth, cost (total NHS cost), parental smoking, GP visits prior to admission and antibiotics prior to admission.
All within-trial analyses were performed using Stata version 12.
Unit costs
Unit cost information was combined with the resource-use data collected and the mean cost per patient per arm estimated. Valuing the resource use using the unit costs provided an estimate of the total cost for each resource. These were aggregated to estimate total patient costs within each arm, and the mean cost per patient per arm. The difference in average costs (and significance) between the two trial arms was estimated. All unit costs were collected in UK pounds sterling for the base year 2012/13. Cost information was collected from routine sources such as the British National Formulary (BNF) 63,43 Personal Social Services Research Unit44 and NHS Reference Costs. 45 Some unit costs were collected specifically from the trial/hospital financial records, such as the cost of specific lab tests that are not available on the BNF.
Handling missing cost and outcome data
Missing data were handled through the use of multiple imputation (for both cost and outcome data). The multiple imputation approach has been widely recommended by most experts in biomedical literature. 40 The key dependent variables used to base the imputations on were sex, child gestation at birth, length of illness prior to onset of cough, parental smoking status, antibiotics on arrival at A&E, oxygen saturation and number of GP visits prior to admission. Sensitivity analysis was undertaken to determine the influence of missing data at follow-up (resource-use data and primary outcome) on study conclusions, to assess the strength of association between time to cough resolution and ‘missingness’ (i.e. whether or not data are missing) and to allow for individual, sampling and imputation variation using multiple imputation.
Reporting and presenting of results
Appropriate consideration was given to the distribution of the cost and effect data in the economic evaluation. In order to explore the variation around the costs and effects generated by the trial data, stochastic variance around the cost–effect pairs was estimated using non-parametric bootstrapping methods. The incremental costs and the incremental benefits were reported within an ICER format where appropriate. The 95% CI for each ICER was estimated using Fieller’s theorem, a technique that includes any correlation between cost and outcome. 46 Sample uncertainty was explored using non-parametric bootstrapping to generate 1000 ICER values which are plotted on a cost-effectiveness plane in order to represent graphically uncertainty. 47 The result for the CEA was expressed in terms of positioning on the cost-effectiveness plane as well as translated into cost-effectiveness acceptability curves, indicating the likelihood that the results fall below any given cost-effectiveness ceiling ratio, where appropriate. Cost differences were reported between the arms as standard; however, in a departure from typical ‘treatment minus comparator’ differences for reporting purposes, the cost-effectiveness plane reported the differences as ‘standard minus modified’ to reflect the fact that this trial tested for equivalence in costs and effects.
Adjustment of timing of costs and benefits
Allowance for differential timing of costs and benefits was made using the recommended discount rate of 3.5% (National Institute for Health and Care Excellence Methods Guidance). 48 Data within this trial were collected over two consecutive winter periods, and costs and benefits were estimated for the baseline year, 2012/13.
Sensitivity analyses
A detailed sensitivity analysis of key parameters was undertaken. In addition to this the patient perspective was incorporated to the analysis, adding the costs incurred by the parent (in terms of financial costs such as travel to and from hospital and time lost from normal activities because of the illness) to the NHS and social services costs.
Seasonality impacts
The economic analysis also took into consideration the seasonality of the disease and the economic impact of this with regard to availability of ward space/beds during peak hospital times. Information was collected on the type of ward in which patients were being cared for. It may be that during peak times infants have to be cared for in, say, surgical wards and this will have cost consequences. Further to this, the capacity of wards during such busy times was explored by obtaining hospital attendance information from the business managers at trial centres to allow a more precise costing (saving) in terms of opportunity cost of hospital stay as a result of bronchiolitis. This additional information will allow the economic analysis to provide further relevant policy implications for the potential hospital stay reductions arising through implementation of the 90% oxygen saturation protocol.
Publication policy
To safeguard the integrity of the trial, data from this study were not presented in public or submitted for publication without requesting comments and receiving agreement from the National Institute for Health Research Health Technology Assessment programme. The success of the trial was dependent on the collaboration of many people. The results were, therefore, presented first to the trial local investigators. A summary of the results of the trial will be made available on the Scottish Children’s Research Network website (www.scotcrn.org) and the research sites can provide these to parents of participating children on request.
Organisation
A Trial Steering Committee (TSC; see Appendix 4) and a DMC were established (see Appendix 5). Day-to-day management of the trial was overseen by a Trial Management Group (see Appendix 6). Each participating centre identified a paediatric consultant as a principal investigator (see Acknowledgements). Each participating centre was reimbursed on a per-patient fee from the core trial grant. The Medicines for Children Research Network and/or local Comprehensive Local Research Networks supported research nursing time, and employed or reallocated a research nurse to support all aspects of the trial at the local centres.
Confidentiality
Patients were identified by their trial number to ensure confidentiality. However, as the main caregivers to the patients in the trial were contacted during the follow-up, the caregivers’ names and contact details were recorded on the data collection forms in addition to the allocated trial number. Stringent precautions were taken to ensure confidentiality of names and addresses at ECTU and the sites. The chief investigator and local investigators ensured conservation of records in areas to which access is restricted.
Audit
No audit of BIDS was carried out. The trial manager monitored all the sites at least once to verify that the site staff had sufficient knowledge of the trial protocol and procedures, that the site file was being properly maintained and that the site adhered to local requirements for consent.
Termination of the study
Before termination of recruitment, ECTU contacted all sites by telephone or e-mail in order to inform sites of the final date for recruitment. Once the recruitment period had expired, the internet-based randomisation database was disabled to prevent further recruitment. After all recruited patients had been followed up until 6 months after randomisation, a declaration of the end of trial form was sent to the Multicentre Research Ethics Committee. The following documents will be archived in each site file and kept for at least 10 years: original consent forms, data forms, trial-related documents and correspondence. The trial master files at ECTU will be archived for at least 10 years.
Funding
The costs for the study itself were covered by a grant from the National Institute for Health Research Health Technology Assessment programme. See the Health Technology Assessment programme website for further project information. Clinical costs were met by the NHS under existing contracts.
Indemnity
If there was negligent harm during the clinical trial, then the NHS body owes a duty of care to the person harmed. NHS indemnity covers NHS staff, medical academic staff with honorary contracts and those conducting the trial. NHS indemnity does not offer no-fault compensation. The cosponsors were responsible for ensuring proper provision was made for insurance or indemnity to cover their liability and the liability of the chief investigator and staff.
Chapter 3 Results
Participant flow
A CONSORT diagram for recruitment is provided in Figure 3. In total, 615 infants were randomised in two seasons, meeting the recruitment target. Fifty-two per cent of eligible infants were randomised to the study, with 9% of parents declining to take part.
FIGURE 3.
Consolidated Standards of Reporting Trials diagram: seasons 1 and 2.

Study recruitment by country, centre and season is provided in Table 1, demonstrating no important differences in allocation of oximeters by centre or season.
| Parameter | Category | Allocated intervention | Overall, N = 615 | |
|---|---|---|---|---|
| Standard pulse oximeter, n = 308 | Modified pulse oximeter, n = 307 | |||
| Distribution by country, n (%) | Scotland | 247 (80.2) | 260 (84.7) | 507 (82.4) |
| England | 61 (19.8) | 47 (15.3) | 108 (17.6) | |
| Distribution by centre, n (%)a | Aberdeen | 22 (7.1) | 22 (7.2) | 44 (7.2) |
| Dundee | 56 (18.2) | 54 (17.6) | 110 (17.9) | |
| Edinburgh | 100 (32.5) | 95 (30.9) | 195 (31.7) | |
| Glasgow | 45 (14.6) | 55 (17.9) | 100 (16.3) | |
| Kilmarnock | 24 (7.8) | 34 (11.1) | 58 (9.4) | |
| Bristol | 33 (10.7) | 26 (8.5) | 59 (9.6) | |
| Exeter | 14 (4.5) | 11 (3.6) | 25 (4.1) | |
| Truro | 14 (4.5) | 10 (3.3) | 24 (3.9) | |
| Distribution by season, n (%)b | 1 | 113 (36.7) | 112 (36.5) | 225 (36.6) |
| 2 | 195 (63.3) | 195 (63.5) | 390 (63.4) | |
Patient disposition and changes post randomisation
Tables 2 and 3 provide information on patient disposition. See Table 2 for the number of infants who reached the end of the study with > 90% of data [N = 584 (95%)]. Thirty-one infants did not reach 6-month follow-up: there were two deaths, one infant was withdrawn by the clinician, 21 infants were lost to follow-up and the parents declined further contact in another seven cases. Breakdown by group is provided in Table 2. Table 3 gives details of those in whom the primary outcome was directly obtained and the number in whom the primary outcome was estimated [standard care 43 (14.0%); modified care 38 (12.3%)].
| Parameter | Category | Allocated intervention | Overall, N | |
|---|---|---|---|---|
| Standard pulse oximeter, n | Modified pulse oximeter, n | |||
| Reached end of studya | Reaching 6-month assessment | 293 | 291 | 584 |
| Reason not reached end of study | Deceased | 2 | 0 | 2 |
| Withdrawn by clinician | 1 | 0 | 1 | |
| Lost to follow-up | 8 | 13 | 21 | |
| Participant declined – no further contact | 4 | 3 | 7 | |
| Parameter | Category | Allocated intervention | Overall, N | |
|---|---|---|---|---|
| Standard pulse oximeter, n | Modified pulse oximeter, n | |||
| Patients in database | All patients | 309 | 308 | 617 |
| Not treated | Randomised in error | 1 | 1 | 2 |
| Randomised and consented (ITT population) | Treated | 308 | 307 | 615 |
| In primary outcome | Data obtained | 296 | 293 | 589 |
| In primary outcome split by estimation | Yes | 43 | 39 | 82 |
| No | 253 | 254 | 507 | |
| Reason primary outcome not obtained | Deceased | 1 | 0 | 1 |
| Withdrawn by clinician | 1 | 0 | 1 | |
| Lost to follow-up | 7 | 12 | 19 | |
| Participant declined – no further contact | 3 | 2 | 5 | |
Protocol deviations and classification are provided in Table 4. There were similar numbers and categories in each group.
| Parameter | Category | Allocated intervention | Overall, N = 615 | |
|---|---|---|---|---|
| Standard pulse oximeter, n = 308 | Modified pulse oximeter, n = 307 | |||
| Patients with a recorded deviation, n (%) | Yes | 34 (11.0) | 42 (13.7) | 76 (12.4) |
| No | 274 (89.0) | 265 (86.3) | 539 (87.6) | |
| Deviation categories (n)a | Attached late | 5 | 13 | 18 |
| Removed early | 15 | 9 | 24 | |
| Never attached | 6 | 9 | 15 | |
| Discharge criteria not met | 5 | 9 | 14 | |
| Other | 3 | 9 | 12 | |
Recruitment
Infants were recruited within two winter seasons. For the first season, recruitment was between 3 October 2011 and 30 March 2012 in the five Scottish sites only. For the second season, randomisation was from 1 October 2012 to 29 March 2013 in eight sites. The addition of three sites in south-west England was in response to a quieter RSV season than expected in season 1. An analysis of season-1 peak oximeter use enabled a redistribution of study oximeters across eight sites for season 2.
The trial completed recruitment on schedule and to target on 29 March 2013.
Baseline data
Baseline demographic and clinical characteristics are provided by group in Table 5. The modified care group had slightly fewer males and more preterm infants, though all other demographics and characteristics were similar.
| Parameter | Standard | Modified | All |
|---|---|---|---|
| N | 308 | 307 | 615 |
| Age (weeks), median (IQR) | 21.3 (12.6–31.1) | 21.1 (11.1–32.0) | 21.3 (11.7–31.6) |
| Male sex, n (%) | 186 (60.4) | 166 (54.1) | 352 (57.2) |
| Preterm (< 37 weeks), n (%) | 28 (10.1) | 45 (16.1) | 73 (13.1) |
| Eczema, n (%) | 51 (16.7) | 44 (14.5) | 95 (15.6) |
| Food allergy, n (%) | 8 (2.6) | 11 (3.6) | 19 (3.1) |
| Household smoking, n (%) | 133 (43.9) | 130 (42.8) | 263 (43.3) |
| Siblings (≥ 1), n (%) | 221 (72.7) | 211 (69.4) | 432 (71.1) |
| Number of primary care attendances in previous 4 weeks, median (IQR) | 1 (1–2) | 1 (0–2) | 1 (1–2) |
| Heart rate on arrival at ED, median (IQR) | 159 (146–173) | 158 (148–172) | 159 (147–172) |
| Respiratory rate on arrival at ED, median (IQR) | 50 (44–58) | 49 (42–58) | 50 (42–58) |
| Antibiotics on arrival at ED, n (%) | 24 (7.9) | 23 (7.6) | 47 (7.7) |
| Bronchodilator on arrival at ED, n (%) | 17 (5.6) | 16 (5.3) | 33 (5.4) |
| Length of illness (days) on arrival at ED, median (IQR) | 4 (3–5) | 4 (3–5) | 4 (3–5) |
| Apnoea on arrival at ED, n (%) | 3 (1) | 3 (1) | 6 (1) |
| SpO2 on arrival at ED, median (IQR) | 95 (93–97) | 95 (93–97) | 95 (93–97) |
| SpO2 on arrival at ED ≤ 94%, n (%) | 121 (39.8) | 119 (39.3) | 240 (39.5) |
Virology test data
Laboratory virology testing was performed in 81.9% of infants, with near-patient testing in 40.0% of infants (Table 6). The proportion of infants who were RSV positive (either laboratory or near-patient testing) was 69.8% in the standard care group and 76.3% in the modified care group. Laboratory testing identified a positive result for a virus other than RSV in 27.2% of standard care infants and 22.0% of modified care infants.
| Parameter | Standard | Modified | All |
|---|---|---|---|
| N | 308 | 307 | 615 |
| Laboratory virology testing | 250/302 (82.7) | 245/303 (80.9) | 495/605 (81.8) |
| Laboratory: any virus positive | 204/250 (81.6) | 217/245 (88.6) | 421/495 (85.1) |
| Laboratory: RSV positive | 167/250 (66.8) | 181/245 (73.9) | 348/495 (70.3) |
| Laboratory: non-RSV virus positive | 68/250 (27.2) | 54/245 (22.0) | 122/495 (24.6) |
| Near-patient testing | 121/305(39.7) | 122/303 (40.3) | 243/608 (40.0) |
| Near-patient testing: RSV positive (of those with result) | 79/101 (78.2) | 91/108 (84.3) | 170/209 (81.3) |
| RSV positive on laboratory or near-patient testing (of those with result) | 194/278 (69.8) | 213/279 (76.3) | 407/557 (72.9) |
Numbers analysed
The treatment offered versus allocated is given in Table 7. In eight instances the incorrect treatment was allocated (by staff attaching the wrong oximeter): in seven instances a modified oximeter was provided to an infant randomised to standard care and in one instance a standard oximeter was attached to an infant randomised to modified care. These infants are included in the group to which they were allocated as per ITT. In 44 instances treatment was interrupted, the majority per protocol during an admission to the HDU, with treatment restarted on discharge from the HDU.
| Parameter | Category | Allocated intervention | Overall, N = 615 | |
|---|---|---|---|---|
| Standard pulse oximeter, n = 308 | Modified pulse oximeter, n = 307 | |||
| Treatment allocated, n (%) | Standard | 308 (100) | 0 | 308 (50.1) |
| Modified | 0 | 307 (100) | 307 (49.9) | |
| Treatment offered, n (%) | Standard | 307 (99.7) | 7 (2.3) | 314 (51.1) |
| Modified | 1 (0.3) | 300 (97.7) | 301 (48.9) | |
| Treatment given, n (%) | Standard | 301 (97.7) | 7 (2.3) | 308 (50.1) |
| Modified | 1 (0.3) | 291 (94.8) | 292 (47.5) | |
| Never treated | 6 (1.9) | 9 (2.9) | 15 (2.4) | |
| Treatment interrupted,a n (%) | Yes | 22 | 22 | 44 |
Protocol deviation
Seventy-six participants had a protocol deviation, 34 (11.0%) in the standard care group and 42 (13.7%) in the modified care group. The deviation categories are provided in Table 4 and are similar between groups.
Outcomes and estimation
Primary outcome
Our primary outcome was time to cough resolution (days) (Table 8). From the primary ITT analysis, the median time to no cough was 15.0 days in the standard care group and in the modified care group, with a median difference of 1.0 day (shorter for modified care). The upper and lower CIs for the median difference were –1 and 2 days. This interval falls within the prespecified equivalence limits of –2 to 2 days. We specified that perprotocol analysis must be in agreement with the ITT protocol for equivalence. In the per-protocol analysis, median difference in time to no cough was 0 days (95% CI –1 to 2 days). This interval falls within the prespecified equivalence limits of –2 to 2 days and is consistent with the ITT analysis. We performed a complete-case analysis for the ITT population, which showed very similar results (difference between groups of 0 days, 95% CI –1 to 2 days). The groups are considered equivalent for the primary outcome.
| Parameter | Standard care, median (IQR), n | Modified care, median (IQR), n | Median differencea | Upper and lower 95% CI | All, median (IQR) |
|---|---|---|---|---|---|
| Time to cough resolution (days). Equivalence defined as ± 2 days | 15.0 (10.0–42.5), n = 296 | 15.0 (10.0–41.0), n = 293 | 1.0 | –1 to 2 | 15.0 (10.0–42.0) |
| Time feeding returned to ≥ 75% normal (hours). Equivalence defined as ± 4 hours | 24.1 (6.5–62.1), n = 304 | 19.5 (6.3–47.2), n = 296 | 2.7 | –0.3 to 7.0 | 21.8 (6.3–53.9) |
| Time to return to normal (days). Equivalence defined as ± 2 days | 12.0 (7.0–25.0), n = 296 | 11.0 (6.0–20.0), n = 293 | 1.0 | 0 to 3 | 11.0 (7.0–23.0) |
| Subgroup analyses | |||||
| Time to cough resolution: smoking household (days) | 15.0 (10.0–35.0), n = 129 | 13.0 (9.0–34.0), n = 125 | 1.0 | –2 to 3 | 14.0 (10.0–35.0) |
| Time to cough resolution: non-smoking household (days) | 15.5 (10.0–47.0), n = 166 | 16.0 (10.0–44.0), n = 168 | 0 | –2 to 2 | 16.0 (10.0–45.0) |
| Time to cough resolution: illness duration ≤ 3 days (days) | 13.0 (10.0–32.0), n = 143 | 14.0 (10.0–33.0), n = 134 | 0 | –2 to 2 | 14.0 (10.0–32.0) |
| Time to cough resolution: illness duration ≥ 4 days (days) | 18.0 (10.0–48.0), n = 153 | 16.0 (9.9–44.0), n = 157 | 1.0 | –1 to 3 | 17.0 (10.0–47.0) |
| Time to cough resolution: antibiotics yes (days) | 12.0 (9.0–65.0), n = 57 | 15.0 (10.0–43.0), n = 52 | 0 | –4 to 5 | 13.0 (10.0–55.0) |
| Time to cough resolution: antibiotics no (days) | 16.0 (10.0–39.0), n = 239 | 15.0 (9.0–40.0), n = 241 | 1 | –1 to 2 | 15.5 (10.0–39.5) |
Subgroup analysis of primary outcome
We specified an assessment of subgroups of the primary outcome for the number of days of illness prior to randomisation (would any effect be influenced by the degree of airway inflammation present?), household smoking (would an early discharge to a smoking household prolong symptoms?) and use of antibiotics. Between-subgroup comparisons did not show any evidence of a difference in the magnitude of the treatment effect between subgroups.
Secondary outcomes
Equivalence outcomes
Three further outcomes were assessed for equivalence: (1) time to return to adequate feeding (≥ 75% normal) in hospital, (2) time until parents considered that the infant was back to normal and (3) oxygen saturation measured at 28 days after randomisation.
Median time to return to adequate feeding was 24.1 hours in the standard care group and 19.5 hours in the modified care group. The median difference was 2.7 hours (95% CI –0.3 to 7.0 hours). This falls outside the prespecified equivalence limits of ± 4.0 hours, so we cannot infer equivalence. The 95% CI overlaps zero, so we cannot conclude that there is a difference either.
Figure 4 provides a survival curve for time to return to adequate feeding. A post-hoc analysis (Table 9) gave a hazard ratio of 1.22 (95% CI 1.04 to 1.44; p-value = 0.015), demonstrating some evidence that the modified care group returned to feeding faster than the modified care group, and the survival curve indicates that any difference between the groups was in the time period following the median time to return to adequate feeding. Thus, we have not proved equivalence. If any difference does exist, it goes in favour of the modified care group.
FIGURE 4.
Time to return to adequate feeding.

| Parameter | Standard care, median (IQR) | Modified care, median (IQR) | Hazard ratio estimate | Upper and lower 95% CI | p-value |
|---|---|---|---|---|---|
| Time feeding returned to ≥ 75% normal | 24.1 (6.5–62.1) | 19.5 (6.3–47.2) | 1.22 | 1.04 to 1.44 | 0.015 |
| Time back to normal (days) | 12.0 (7.0–25.0) | 11.0 (6.0–20.0) | 1.19 | 1.01 to 1.41 | 0.043 |
Parents were asked in standardised telephone interviews when they considered their child had returned back to normal. This was a median of 12.0 days in the standard care group and 11.0 days in the modified care group. The median difference was 1.0 day (95% CI 0.0 days to 3.0 days). The 95% CI of the median difference fall outside the prespecified limits of ± 2 days and so we cannot infer equivalence. The 95% CI just touches zero, so there is some evidence that there was a small difference in favour of the modified care group.
Figure 5 provides a survival curve for time until parents considered their infant back to normal. A post-hoc analysis (see Table 9) gave a hazard ratio of 1.19 (95% CI 1.00 to 1.41; p-value = 0.043), providing some evidence that, in the parents’ perception, infants in the modified care group returned to normal faster than infants in the standard care group, and the survival curve indicates that any difference between the groups occurred after the median time it took for infants to return to normal. Thus, we have not proved equivalence. If any difference does exist, it is in favour of the modified care group. The benefit to the modified care group was not expected and is a modest overall difference.
FIGURE 5.
Time to return to normal (days).

These data were only collected for season 1, following unblinded review by the DMC at the end of the season. The median peripheral capillary oxygen saturation (SpO2) value was 99% in both groups. At 28 days there was a mean absolute difference between the treatment groups in oxygen saturation of 0.11% (95% CI –0.35% to 0.57%). We prespecified equivalence limits of 1% in either direction. Oxygen saturation at 28 days was equivalent in the two groups.
Differences outcomes
Infants could be considered fit for discharge from hospital once they had achieved adequate feeding (≥ 75% normal) and had been observed to have stable oxygenation in air with continuous oxygen saturation monitoring for a period of hours including a period of sleep. Infants in the standard care group were fit for discharge at 44.2 hours, compared with 30.2 hours in the modified care group (Table 10). The hazard ratio was 1.46 (95% CI 1.23 to 1.73; p-value < 0.001) (Figure 6).
| Parameter | Standard care, median (IQR), n | Modified care, median (IQR), n | Hazard ratio estimate | 95% CI | All, median (IQR), n | p-value |
|---|---|---|---|---|---|---|
| Time to fit for discharge (hours) | 44.2 (18.6–87.5), n = 283 | 30.2 (15.6–59.7), n = 276 | 1.46 | 1.23 to 1.73 | 38.4 (16.9–69.7), n = 559 | < 0.0001 |
| Time to actual discharge (hours) | 50.9 (23.1–93.4), n = 303 | 40.9 (21.8–67.3), n = 301 | 1.28 | 1.09 to 1.50 | 44.5 (22.2–78.4), n = 604 | 0.003 |
| Time to no further supplemental oxygen (hours) | 27.63 (0–68.1), n = 305 | 5.65 (0–32.4), n = 304 | 1.37 | 1.12 to 1.68 | 14.44 (0–54.5), n = 609 | 0.002 |
| Time to readmission to hospital (days) | 17 (7–22), n = 23 | 11 (2–21), n = 12 | 0.925 | 0.433 to 1.977 | 15 (3–22), n = 35 | 0.84 |
FIGURE 6.
Time to fit for discharge.

The time at which infants were actually discharged from hospital could be influenced by local practice and logistics. Infants in the standard care group were discharged after a median of 51.0 hours, compared with 40.9 hours in the modified care group (see Table 10). The hazard ratio was 1.28 (95% CI 1.09 to 1.50; p-value = 0.027) (Figure 7).
FIGURE 7.
Time to discharge.

We measured the time from randomisation to the time that infants in each group last received supplemental oxygen prior to discharge. In the standard care group this was a median of 27.6 hours, and in the modified care group 5.7 hours (see Table 10). The hazard ratio was 1.37 (95% CI 1.12 to 1.68; p-value = 0.0021) (Figure 8).
FIGURE 8.
Time to no supplemental oxygen.

There was no significant difference in time to readmission to hospital in those infants who were subsequently readmitted to hospital following discharge (see Table 10). Median difference was 0.9 days (95% CI 0.4 days to 2.0 days; p-value = 0.8410). Median duration of readmission was 3.0 days in both the modified and standard care groups.
Safety outcomes
It was expected that infants on modified oximeters would be managed on monitors that would report higher oxygen saturation than was actually the case and that reducing oxygen delivery could lead to an increase in the number of adverse events (AEs). It was also expected that infants on modified oximeters would be discharged home sooner than infants on standard monitors and that this might result in increased morbidity.
Deaths from bronchiolitis are infrequent, and we did not consider that the intervention would result in more deaths. Two deaths were recorded during the study period; both were in the standard care group and were unrelated to the study intervention.
The study did not recruit infants who were directly admitted to a high-dependency area at admission (n = 56; see Figure 3). There were eight HDU admissions (in eight infants) in the standard care group and 13 (in 12 infants) in the modified care group.
Tachycardia and tachypnoea are characteristic clinical features of infants admitted to hospital with bronchiolitis. We wished to determine if infants who were discharged home sooner in the course of their illness (as expected in the modified care group) had significantly higher heart and respiratory rates at discharge. Clinical observations of heart rate and respiratory rate were measured every 8 hours and the final measurement prior to discharge was used for discharge measurement. Contrary to expectation, there were no significant differences between standard and modified care groups in either heart rate (hazard ratio –1.16; p-value = 0.37) or respiratory rate (hazard ratio 0.09; p-value = 0.88) at discharge.
Readmission to hospital was reported as a serious adverse event (SAE) during the first 28 days following randomisation. In the first 7 days after randomisation there were eight readmissions to hospital in six infants in the standard care group and five readmissions in five infants in the modified care group. By 28 days there had been 26 readmissions in 23 infants in the standard care group and 12 readmissions in 12 infants in the modified care group. It was not expected that there would be fewer admissions in the modified care group, as this group was expected to be discharged sooner in the course of their illness than those in the standard care group. The absolute reduction of three readmissions (relative reduction 38%) at 7 days is not a clinically important difference, but an absolute difference of 14 readmissions (relative reduction 54%) at 28 days could be considered a clinically important difference (a 5% absolute reduction in readmission rate for infants in the modified care group).
An earlier discharge from hospital may have been associated with a greater number of contacts with health care after discharge. The numbers of heath-care contacts at 7, 14 and 28 days and at 6 months after randomisation were similar between groups (Table 11). There were no significant differences in the number of infants with a health-care contact at 7 days after randomisation (see Table 11). Infants in the modified care group did not experience a higher number of health-care contacts up to 6 months following randomisation.
| Parameter | Standard care | Modified care | All | Mean difference (95% CI) | Odds ratio (95% Cl) | p-value |
|---|---|---|---|---|---|---|
| Deaths | 2 | 0 | 2 | – | – | – |
| High-dependency care (episodes) | 8 | 13 | 21 | – | – | – |
| Heart rate at discharge, median | 133 (IQR 122–144) | 135 (IQR 123–147) | 134 (IQR 122–145) | –1.16 (–3.70 to 1.37) | – | 0.37 |
| Respiratory rate at discharge, median | 38 (IQR 34–41) | 38 (IQR 34–42) | 38 (IQR 34–42) | 0.09 (–1.05 to 1.23) | – | 0.88 |
| Readmission to hospital within 7 days (episodes) | 8 | 5 | 13 | – | – | – |
| Readmission to hospital within 7 days (infants) | 6 | 5 | 11 | – | – | – |
| Readmission to hospital within 28 days (episodes) | 26 | 12 | 38 | – | – | – |
| Readmission to hospital within 28 days (infants) | 23 | 12 | 35 | – | – | – |
| Reattendance at health care within 7 days (episodes) | 41 | 43 | 84 | – | – | – |
| Reattendance at health care within 7 days (infants) | 39 (14.4%) (n = 270) | 34 (12.7%) (n = 267) | 73 (13.6%) (n = 537) | – | 0.98 (0.65 to 1.49) | 0.94 |
| Reattendance at health care within 14 days (episodes) | 92 (n = 270) | 88 (n = 267) | 180 (n = 537) | – | – | – |
| Reattendance at health care within 14 days (infants) | 76 (28.5%) (n = 267) | 70 (27.1%) (n = 258) | 146 (27.8%) (n = 525) | – | 1.07 (0.73 to 1.57) | 0.73 |
| Reattendance at health care within 28 days (episodes), n | 199 (n = 290) | 188 (n = 288) | 387 (n = 578) | – | – | – |
| Reattendance at health care within 28 days (infants) | 127 (46.4%) (n = 274) | 128 (48.9%) (n = 262) | 256 (47.6%) (n = 536) | – | 0.90 (0.64 to 1.27) | 0.56 |
| Reattendance at health care within 6 months (episodes) | 802 (n = 295) | 774 (n = 293) | 1576 (n = 588) | – | – | – |
| Reattendance at health care within 6 months (infants) | 214 (84.6%) (n = 253) | 209 (80.1%) (n = 261) | 423 (82.3%) (n = 514) | – | 1.37 (0.87 to 2.16) | 0.18 |
| Antibiotics after discharge | 24 (7.8%) (n = 305) | 10 (3.3%) (n = 304) | 34 (5.5%) (n = 609) | – | – | – |
| SpO2 measured at 28 days (season 1 only) | 99 (IQR 97–100) (n = 94) | 99 (IQR 97–100) (n = 101) | 99 (IQR 97–100) (n = 195) | 0.111 (–0.350 to 0.572) | – | 0.64 |
An earlier discharge from hospital and attendance at primary care in an earlier part of disease recovery might be associated with a higher level of antibiotic prescribing after discharge in the modified care group. Infants in the modified care group received fewer courses of antibiotics in the 28 days after discharge than the standard care group (see Table 11; a 58% relative reduction).
Hospital treatments
The hospital treatments received by both treatment groups are shown in Table 12. Use of intravenous fluids, antibiotics and bronchodilator (salbutamol) was similar in both groups.
| Parameter | Standard, n (%) | Modified, n (%) | All, N (%) |
|---|---|---|---|
| Need for supplemental oxygen | 223 (73.1) | 169 (55.6) | 392 (64.4) |
| Use of nasogastric tube feeding | 141 (46.2) | 125 (41.3) | 266 (43.8) |
| Use of intravenous fluids | 29 (9.5) | 28 (9.2) | 57 (9.4) |
| Use of antibiotics | 44 (14.4) | 39 (12.8) | 83 (13.6) |
| Use of salbutamol | 25 (8.2) | 21 (6.9) | 46 (7.6) |
Supplemental oxygen was provided to 73.1% of infants in the standard care group and 55.6% of those in the modified care group. It was understood that there could be a difference between the groups, as oxygen saturation measured in the ED may decline following admission to hospital (in association with disease progression and continuous monitoring). The difference (17.5%) should approximate to those infants in the modified care group in whom oxygen saturation fell below 94% but remained above 90%, so the monitor would display at ≥ 94% and they would not have been commenced on supplemental oxygen. In other words, approximately one in six infants admitted to hospital who would receive oxygen at a target oxygen saturation of 94% would not do so at a target oxygen saturation of 90%.
The proportion of infants receiving nasogastric tube feeding was lower in the modified care group (41.3%) than in the standard care group (46.2%).
Anxiety scores
We wished to understand whether or not earlier discharge from hospital at an earlier stage of disease recovery might be associated with greater anxiety for parents looking after their child at home.
Parents’ levels of anxiety were similar at the time of their child’s admission to hospital, but the intervention did not result in parents experiencing greater levels of anxiety and there were no significant differences in anxiety scores at 7, 14 and 28 days or at 6 months (Table 13).
| Parameter | Standard care, median (IQR) | Modified care, median (IQR) | All, median (IQR) | Mean difference (95% CI) | p-value |
|---|---|---|---|---|---|
| Anxiety score at admission | 7 (4–10) | 7 (4–11) | 7 (4–11) | – | – |
| Anxiety score at 7 days | 4 (2–8) | 4 (2–7) | 4 (2–7) | –0.18 (–0.75 to 0.39) | 0.53 |
| Anxiety score at 14 days | 3 (1–6) | 3 (1–5) | 3 (1–5) | 0.00 (–0.57 to 0.56) | 0.99 |
| Anxiety score at 28 days | 3 (1–7) | 3 (1–6) | 3 (1–6) | –0.27 (–0.88 to 0.34) | 0.39 |
| Anxiety score at 6 months | 4 (1–7) | 3 (1–6) | 4 (1–7) | –0.16 (–0.82 to 0.49) | 0.62 |
Family life
Discharging a child from hospital earlier in the course of their illness could have an impact on family life, with lead carers having to give up time to care for the child, secondary carers taking additional time off work and children returning later to paid and unpaid child care than they otherwise would have done (Table 14). Lead carers were generally mothers (94.4% overall), and mothers of infants in the modified care group lost fewer hours to usual activities, with 23% fewer hours lost at 7 days, 28% at 14 days, 25% at 28 days and 21% at 6 months. In contrast, levels of activity lost by secondary carers (typically fathers) were similar regardless of intervention group, and most of this time was lost in the first 7 days. Relatively few children had childcare placements and the time to return to child care was similar between groups.
| Parameter | Standard | Modified | All |
|---|---|---|---|
| Lead carer (= mother), n (%) | 288 (95.4) | 283 (93.4) | 571 (94.4) |
| Lead carer work status (= employed), n (%) | 43 (14.2) | 39 (12.9) | 82 (13.5) |
| Lead carer hours missed, 0–7 days, median (IQR) | 58.3 (25.1–96.5) | 44.8 (24.6–72.0) | 49.3 (24.8–85.5) |
| Lead carer hours missed, 0–14 days, median (IQR) | 62.3 (25.7–97.3) | 45.0 (25.3–72.7) | 50.9 (25.6–85.5) |
| Lead carer hours missed, 0–28 days, median (IQR) | 63.4 (27.5–101.2) | 47.3 (25.7–76.4) | 53.4 (26.3–89.3) |
| Lead carer hours missed, 0–6 months, median (IQR) | 67.6 (28.1–114.8) | 53.2 (30.4–86.2) | 59.0 (29.0–97.8) |
| Secondary carer work status (= employed), n (%) | 233 (83.3) | 251 (89.6) | 484 (86.5) |
| Secondary carer hours missed, 0–7 days, median (IQR) | 15.0 (8.0–24.0) | 16.0 (8.0–27.0) | 15.0 (8.0–24.0) |
| Secondary carer hours missed 0–14 days, median (IQR) | 15.0 (8.0–27.5) | 16.0 (8.3–30.5) | 16.0 (8.0–30.0) |
| Secondary carer hours missed 0–28 days, median (IQR) | 16.0 (8.0–33.8) | 17.3 (8.5–34.0) | 16.5 (8.0–34.0) |
| Secondary carer hours missed 0–6 months, median (IQR) | 22.0 (10.0–43.0) | 18.0 (9.0–36.0) | 20.0 (9.5–40.0) |
| Child well enough to return to child care by 7 days, n (%) | 24 (48.0) | 18 (52.9) | 42 (50.0) |
| Child well enough to return to child care by 14 days, n (%) | 28 (54.9) | 22 (62.9) | 50 (58.1) |
Prespecified subgroup analyses of secondary outcomes
Time to fit for discharge by oxygen requirement is demonstrated in Figure 9. We have already shown that, overall, infants in the modified care group were fit for discharge earlier than those in the standard care arm (hazard ratio 1.46, 95% CI 1.23 to 1.73). There was a significant difference (p-value = 0.04) in the magnitude of this treatment effect between those who received oxygen supplementation (hazard ratio 1.37, 95% CI 1.11 to 1.69) and those who did not (hazard ratio 0.95, 95% CI 0.71 to 1.26). Among those who received oxygen supplementation, infants in the modified care group seemed to do better than those in the standard care group, whereas among those who did not have oxygen supplementation, the groups were similar. These results are difficult to interpret, as some of this oxygen supplementation occurred after randomisation, and will therefore have been affected by the allocated treatment: more infants in the standard care group were given oxygen supplementation, as we would expect.
FIGURE 9.
Time to fit for discharge by oxygen required.

Time to discharge by oxygen requirement is demonstrated in Figure 10. We have already shown that, overall, infants in the modified care group were discharged earlier than those in the standard care arm (hazard ratio 1.28, 95% CI 1.09 to 1.50). There was a significant difference (p-value = 0.002) in the magnitude of this treatment effect between those who received oxygen supplementation (hazard ratio 1.22, 95% CI 0.99 to 1.49) and those who did not (hazard ratio 0.71, 95% CI 0.54 to 0.94). Among those who received oxygen supplementation, infants in the modified care group seemed to do better than those in the standard care group, whereas among those who did not received oxygen supplementation, infants in the standard care group seemed to do better than those in the modified care group. These results are difficult to interpret, as some of this oxygen supplementation occurred after randomisation and will therefore have been affected by the allocated treatment: more infants in the standard care group were given oxygen supplementation, as we would expect.
FIGURE 10.
Time to discharge by oxygen requirement.

Serious adverse events
Serious adverse events were recorded up to 28 days and were recorded in 56 participants (Table 15a and 15b). There were 35 SAEs in 32 infants in the standard care group and 25 SAEs in 24 infants in the modified care group. The standard care group had 8 infants with an HDU transfer, 23 with a readmission and one with prolonged hospitalisation. The modified care group had 12 infants with a HDU admission and 12 infants with a readmission to hospital.
| Parameter | Category | Allocated intervention | Overall, N = 615 | |
|---|---|---|---|---|
| Standard pulse oximeter, n = 308 | Modified pulse oximeter, n = 307 | |||
| Number of patients with at least one SAE | Overall | 32 | 24 | 56 |
| Number of patients with SAEs: HDU transfer | Overall | 8 | 12 | 20 |
| Number of patients with SAEs: readmission | Overall | 23 | 12 | 35 |
| Number of patients with SAEs: hospital prolongation for ‘other’ | Overall | 1 | 0 | 1 |
| Parameter | Category | Allocated intervention | Overall, N = 615 | |
|---|---|---|---|---|
| Standard pulse oximeter, n = 308 | Modified pulse oximeter, n = 307 | |||
| Number of SAEs | Overall | 35 | 25 | 60 |
| Number of SAEs by classification | HDU transfer | 8 | 13 | 21 |
| Hospital prolongation for ‘other’ | 1 | 0 | 1 | |
| Readmission | 26 | 12 | 38 | |
| Number of SAEs by severity | Mild | 11 | 1 | 12 |
| Moderate | 17 | 15 | 32 | |
| Severe | 7 | 9 | 16 | |
| Number of SAEs by outcome | Recovered | 34 | 25 | 59 |
| Death | 1 | 0 | 1 | |
Adverse events
Adverse events were recorded to 28 days and were recorded in 144 infants (Table 16a and 16b). An AE was recorded at least once for each SAE. Overall, there were 173 AEs recorded in 144 infants. There were 89 AEs in 75 infants in the standard care group and 84 AEs in 69 infants in the modified care group. No important differences between groups were noted in terms of subcategory (respiratory, gastrointestinal, other) or severity of AEs.
| Parameter | Category | Allocated intervention | Overall (N = 615) | |
|---|---|---|---|---|
| Standard pulse oximeter (n = 308) | Modified pulse oximeter (n = 307) | |||
| Number of patients with at least one AE | Overall | 75 | 69 | 144 |
| Number of patients with respiratory AEs by severity | Mild | 26 | 23 | 49 |
| Moderate | 17 | 18 | 35 | |
| Severe | 6 | 9 | 15 | |
| Number of patients with gastrointestinal AEs by severity | Mild | 7 | 7 | 14 |
| Moderate | 0 | 5 | 5 | |
| Number of patients with other AEs by severity | Mild | 19 | 12 | 31 |
| Moderate | 6 | 2 | 8 | |
| Severe | 2 | 0 | 2 | |
| Parameter | Category | Allocated intervention | Overall (N = 615) | |
|---|---|---|---|---|
| Standard pulse oximeter (n = 308) | Modified pulse oximeter (n = 307) | |||
| Number of AEs | Overall | 89 | 84 | 173 |
| Number of respiratory AEs by severity | Mild | 28 | 25 | 53 |
| Moderate | 17 | 20 | 37 | |
| Severe | 7 | 9 | 16 | |
| Number of gastrointestinal AEs by severity | Mild | 7 | 8 | 15 |
| Moderate | 0 | 5 | 5 | |
| Number of other AEs by severity | Mild | 19 | 12 | 31 |
| Moderate | 8 | 2 | 10 | |
| Severe | 2 | 0 | 2 | |
Chapter 4 Economic evaluation
Economic evaluation results
The cost data were analysed using GLM regression because of skewness in the data. GLM regressions were adjusted for treatment group, parental smoking and GP visits prior to admission (other specified variables in the data analysis plan had no significant impact). The GLM regression used gamma family and link power –1 as this was the best fit. GLM regression was also used for time to cough resolution and for time to cough resolution adjusted for treatment group, season, sex, preterm birth, cost (total NHS cost), parental smoking, GP visits prior to admission and antibiotics prior to admission.
Table 17 outlines the unit costs for all resources identified in the study. Table 18 presents mean resource quantities per participant per arm and Table 19 presents these resource differences as mean cost differences between the arms. Table 18 shows that the majority of resource-use categories are equivalent in the two arms; however, supplemental oxygen time during hospital stay was significantly longer in the standard protocol arm, with a mean difference of 16 hours (p-value = 0.002). Table 18 also shows that paediatric inpatient stay was also longer in the standard protocol arm, with hospital stay in this arm being 0.46 more days (p-value = 0.046). The results from Table 19 reflect the resources outlined in Table 18 with unit costs attached. Table 19 shows that there is an overall cost saving for the NHS in the modified protocol group compared with the standard protocol group.
| Cost item | Description | Unit cost (£) | Source |
|---|---|---|---|
| GP visit | Average 11.7-minute consultation | 36.00 | Curtis, 2012 (Personal Social Services Research Unit)44 |
| A&E | Emergency medicine, category 2 | 184.00 | DH Reference Costs 2012–1345 |
| Outpatient attendance | Paediatric – general use – outpatient attendance | 187.00 | DH Reference Costs 2012–1345 |
| Inpatient paediatric cost/night | PA15B Acute bronchiolitis (£3433 mean five nights) | 686.60 | DH Reference Costs 2012–1345 |
| Inpatient paediatric cost/night | Hotelling cost – 55.8%a variable cost from NAUC | 373.08 | DH Reference Costs 2012–1345 |
| HDU paediatric cost per bed-day | Paediatric critical care, high dependency | 886.00 | DH Reference Costs 2012–1345 |
| Laboratory tests: total cost | Overall cost of laboratory tests | 144.70 | BIDS team, NHS Lothian 2013 |
| Laboratory tests: RSV | Cost per screen (respiratory virus screen) | 25.95 | BIDS team, NHS Lothian 2013 |
| Laboratory tests: adenovirus | Cost per screen (respiratory virus screen) | 25.95 | BIDS team, NHS Lothian 2013 |
| Laboratory tests: rhinovirus | Cost per screen (respiratory virus screen) | 25.95 | BIDS team, NHS Lothian 2013 |
| Laboratory tests: coronavirus | Cost per sample | 14.95 | BIDS team, NHS Lothian 2013 |
| Laboratory tests: parainfluenza | Cost per screen (respiratory virus screen) | 25.95 | BIDS team, NHS Lothian 2013 |
| Laboratory tests: metapneumovirus | Cost per screen (respiratory virus screen) | 25.95 | BIDS team, NHS Lothian 2013 |
| Laboratory tests: near patient testing RSV | Cost per screen (respiratory virus screen) | 25.95 | BIDS team, NHS Lothian 2013 |
| Blood culture | Cost per sample | 20.60 | BIDS team, NHS Lothian 2013 |
| Urine culture | Cost per sample | 9.60 | BIDS team, NHS Lothian 2013 |
| Chest radiograph | Net cost per examination | 56.13 | ISD 2012, R120x49 |
| Oxygen (by nasal or mask) | Supplementary oxygen cost per hourb | 0.80 | BIDS team, NHS Lothian 2013 |
| Supplemental oxygen | Supplementary oxygen cost per hourb | 0.80 | BIDS team, NHS Lothian 2013 |
| Oximeter probes | Cost per probec (approx. 1.5 probes every 3 days) | 3.70 | BIDS team, NHS Lothian 2013 |
| Oximeter | Assume fixed cost of inpatient cost/cared | NA | NA |
| Intravenous fluids | Assume fixed cost of inpatient cost/care | NA | NA |
| Ng feeding | Assume fixed cost of inpatient cost/care | NA | NA |
| Prescription antibiotics | Cost per day based on average dosage advice | 1.01 | Average of antibiotics |
| Co-amoxiclav (Augmentin®, GSK) | Cost per day based on average dosage advice | 0.27 | BNFC 2012–1350 |
| Amoxicillin (Amoxil®, GSK) | Cost per day based on average dosage advice | 1.43 | BNFC 2012–1350 |
| Clarithromycin (Klaricid®, Abbott Healthcare) | Cost per day based on average dosage advice | 1.89 | BNFC 2012–1350 |
| Erythromycin (Tiloryth®, Tillomed Laboratories) | Cost per day based on average dosage advice | 3.66 | BNFC 2012–1350 |
| Bronchodilator: salbutamol | Cost per day based on average dosage advice | 3.00 | BNFC 2012–1350 |
| Bronchodilator: ipratropium bromide | Cost per day based on average dosage advice | 1.05 | BNFC 2012–1350 |
| Corticosteroids (inhale)e | Cost per day based on average dosage advice | 3.70 | BNFC 2012–1350 |
| Parent costs | |||
| Travel expense | Expense estimated by parents | NA | BIDS trial data |
| Cost missed work/usual activities | National minimum wage rate ≥ 21 years, 2012 | 6.19 | UK Government 201451 |
| Cost child care | National minimum wage rate ≥ 21 years, 2012 | 6.19 | UK Government 201451 |
| Mean resource use | n (observations) | Standard care | Modified care | Incremental | p-value |
|---|---|---|---|---|---|
| Before admission resource use | |||||
| Antibiotics on arrival: duration (days) | – | 3.63 | 5.14 | 1.51 | 0.746 |
| GP visits | 500 | 1.80 | 1.65 | –0.15 | 0.124 |
| A&E visits | 502 | 0.43 | 0.41 | –0.02 | 0.765 |
| Inpatient paediatric nights | 501 | 0.06 | 0.09 | 0.03 | 0.609 |
| Outpatient attendance | 502 | 0.16 | 0.14 | –0.02 | 0.696 |
| Hospital treatmenta | |||||
| Oxygen: supplemental (hours) given on arrival | 609 | 4.59 | 3.76 | –0.84 | 0.257 |
| Oxygen: supplemental (hours) during stay | 609 | 59.22 | 42.66 | –16.56 | 0.002 |
| Nebulised saline (hours) during stay | 385 | 44.11 | 23.38 | –20.73 | 0.205 |
| Salbutimol (hours) during stay | 609 | 7.41 | 36.38 | 28.97 | 0.067 |
| Oximeter probes duration (days) | 604b | – | – | – | – |
| Antibiotics (days) during stay | 609 | 6.43 | 5.57 | –0.86 | 0.252 |
| Hospital tests | |||||
| Laboratory virology tests | 609 | 0.98 | 0.93 | –0.05 | 0.403 |
| Blood culture | 608 | 0.75 | 0.76 | 0.00 | 0.982 |
| Urine culture | 608 | 0.05 | 0.05 | 0.00 | 0.845 |
| Chest radiograph | 608 | 0.17 | 0.13 | –0.04 | 0.420 |
| Near patient testing virology test | 608 | 0.40 | 0.40 | 0.01 | 0.882 |
| Hospital stay | |||||
| Inpatient paediatric duration (mean days) | 604 | 2.83 | 2.37 | –0.45 | 0.046 |
| HDU duration (mean days) | 612 | 0.14 | 0.15 | 0.01 | 0.943 |
| Follow-up (mean difference)a | |||||
| GP visits at 7 days (mean number) | 500 | 0.77 | 0.71 | –0.05 | 0.639 |
| GP visits at 14 days (mean number) | 516 | 0.93 | 0.77 | –0.16 | 0.1659 |
| GP visits at 28 days (mean number) | 520 | 1.05 | 1.04 | –0.01 | 0.9309 |
| GP visits at 6 months (mean number) | 476 | 2.84 | 2.59 | –0.25 | 0.3919 |
| A&E visits at 7 days (mean number) | 500 | 0.26 | 0.46 | 0.20 | 0.156 |
| A&E visits at 14 days (mean number) | 516 | 0.16 | 0.23 | 0.07 | 0.4237 |
| A&E visits at 28 days (mean number) | 520 | 0.26 | 0.33 | 0.07 | 0.09 |
| A&E visits at 6 months (mean number) | 476 | 0.60 | 0.55 | –0.05 | 0.67 |
| Inpatient visits at 7 days (mean number) | 500 | 0.51 | 0.26 | –0.26 | 0.39 |
| Inpatient visits at 14 days (mean number) | 516 | 0.20 | 0.07 | –0.14 | 0.265 |
| Inpatient visits at 28 days (mean number) | 520 | 0.45 | 0.11 | –0.34 | 0.0348 |
| Inpatient visits at 6 months (mean number) | 476 | 0.74 | 0.56 | –0.18 | 0.52 |
| Outpatient visits at 7 days (mean number) | 500 | 0.03 | 0.06 | 0.03 | 0.4994 |
| Outpatient visits at 14 days (mean number) | 516 | 0.07 | 0.02 | –0.05 | 0.3116 |
| Outpatient visits at 28 days (mean number) | 520 | 0.08 | 0.01 | –0.06 | 0.106 |
| Outpatient visits at 6 months (mean number) | 476 | 0.27 | 0.30 | 0.03 | 0.784 |
| Number antibiotics at 6 months follow up | 145 | 2.04 | 1.80 | –0.24 | 0.3538 |
| Extra medication duration | 379 | 17.88 | 11.04 | –6.84 | 0.252 |
| Costs (mean per arm) | Standard care (£) | Modified care (£) | Incremental | p-value | 95% CI (£) |
|---|---|---|---|---|---|
| Before admission costs | |||||
| Antibiotics on arrival | 0.42 | 1.83 | 1.41 | 0.343 | –1.53 to 4.35 |
| GP visit | 66.33 | 59.56 | –6.77 | 0.124 | –15.42 to 1.86 |
| A&E | 79.06 | 75.55 | –3.51 | 0.765 | –26.71 to 19.68 |
| Inpatient stay | 21.86 | 31.98 | 10.12 | 0.609 | –287.71 to 48.95 |
| Outpatient attendance | 29.95 | 25.85 | –4.10 | 0.691 | –24.73 to 16.52 |
| Total cost before admission | 199.09 | 195.10 | –3.99 | 0.882 | –56.83 to 48.84 |
| Hospital costs | |||||
| Oxygen on arrival | 1.01 | 0.77 | –0.24 | 0.212 | –0.63 to 0.69 |
| Supplemental oxygen | 34.17 | 18.74 | –15.43 | 0.000 | –21.58 to –9.28 |
| Nebulised saline | 0.28 | 0.12 | –0.16 | 0.176 | –0.38 to 0.07 |
| Salbutimol | 0.06 | 0.23 | 0.17 | 0.159 | –0.06 to 0.40 |
| Oximeter probes | 6.68 | 5.54 | –1.14 | 0.028 | –2.16 to 0.12 |
| Antibiotics during stay | 0.78 | 0.62 | –0.16 | 0.367 | –0.51 to 0.19 |
| Tests: virology, cultures, radiographs | 161.01 | 152.10 | –8.92 | 0.326 | –26.74 to 8.91 |
| Hospital inpatient stay | 1055.27 | 885.96 | –169.31 | 0.046 | –335.72 to –2.90 |
| Hospital HDU stay | 126.57 | 132.76 | 6.19 | 0.943 | –158 to 170 |
| Total cost hospital | 1298.16 | 1159.64 | –138.53 | 0.227 | –363 to 86 |
| Follow-up | |||||
| Total cost GP visits | 71.53 | 67.43 | –4.11 | 0.586 | –18.93 to 10.72 |
| Total cost A&E visits | 80.65 | 86.31 | 5.66 | 0.712 | –24.45 to 35.76 |
| Total cost inpatient paediatric | 410.18 | 259.43 | –150.75 | 0.186 | –374 to 73 |
| Total cost outpatient | 33.39 | 33.50 | 0.11 | 0.990 | –17.78 to 17.56 |
| Antibiotics at 6 months | 0.47 | 0.44 | –0.02 | 0.785 | –0.20 to 0.15 |
| Extra medication | 7.45 | 5.55 | –1.90 | 0.566 | –8.41 to 4.61 |
| Total cost follow-up | 603.67 | 452.66 | –151.01 | 0.236 | –400 to 99 |
| Total costs for NHS | 1901.83 (IQR 1631–2172) | 1612.30 (IQR 1363–1862) | –289.53 | 0.122 | –657 to 78 |
Hospital costs are significantly higher in the standard protocol group because of hospital inpatient stay, supplemental oxygen and oximeter probes. Table 19 reveals that hospital inpatient stay costs are significantly higher in the standard care arm than in the modified care arm (difference £169.31), and this accounts for the majority of the cost difference between the arms. The NHS costs during the 6-month follow-up period are £151 higher in the standard protocol group than the modified protocol group; however, this difference is not statistically significant. Taken together, the total hospital and NHS follow-up costs are £290 higher in the standard protocol arm than the modified protocol arm; however, this is not a statistically significant difference. Table 20 reports the mean differences in primary and secondary outcomes, time to cough resolution in infants and HADS scores for parents. There are no statistically significant differences revealing equivalence in outcomes; however, the multiple-imputed analysis, taking into consideration missing outcomes data, does increase the size of the difference in time to resolution of cough from –0.78 days to –3.17 days.
| Mean resource use | n (observations) | Standard care | Modified care | Incremental | 95% CI | p-value |
|---|---|---|---|---|---|---|
| Time to cough resolution (days) | 507 | 23.13 | 22.35 | –0.78 | –5.25 to 3.69 | 0.732 |
| Time to cough resolution (days)a | 589 | 39.65 | 36.48 | –3.17 | –11.18 to 4.84 | 0.4375 |
| Anxiety score (mean at 6 months) | – | 4.7 | 4.5 | –0.16 | – | 0.624 |
Table 21 outlines the cost and outcome summary. Both the t-test and the GLM analysis, adjusting for covariates, reveals that with reduced costs and improved outcome the modified protocol arm dominates the standard protocol arm and would be deemed the cost-effective option for this comparison. Figure 11 plots the results of 1000 bootstrapped cost–effect pairs from these base-case analyses on a cost-effectiveness plane. The cost-effectiveness plane illustrates the uncertainty around the mean cost saving of £274 and the mean gain in effectiveness (reduction in time to cough resolution) of 1.58 days from the modified care intervention in comparison with standard care. The mean difference in time to cough resolution is within the statistical equivalence boundary of ± 2 days. The outcomes from the probabilistic sensitivity analysis illustrated in Figure 11 show little uncertainty regarding the likelihood of the modified care protocol being cost saving compared with the standard care protocol; however, there is considerable uncertainty regarding any improvement or reduction in days to cough resolution. Given this uncertainty, the modified protocol is most likely to be cost-effective compared with the standard care intervention over a wide range of willingness-to-pay thresholds for the value for a 1-day reduction in time to resolution of cough. If society is not willing to pay anything extra (£0) per reduced day to cough resolution, the modified intervention is the optimal choice, with a likelihood of being cost-effective of 91.5%; even if society were willing to pay £20,000 per reduced day to cough resolution, the modified protocol still remains the optimal choice, with a likelihood of being the cost-effective choice of 63.5%.
| Results table: within trial cost, outcome and ICER (modified care vs. standard care) | |||||||
|---|---|---|---|---|---|---|---|
| Arm | Total cost (£) | 95% CI (£) | Mean days to cough resolution (95% CI) | ICER | Probability modified cost-effectivea | ||
| WTP £0 | WTP £25 | WTP £50 | |||||
| Standard care | 1902 | 1631 to 2172 | 23.13 (19.84 to 26.42) | – | – | – | – |
| Modified care | 1612 | 1363 to 1862 | 22.35 (19.30 to 25.40) | – | – | – | – |
| Differenceb | –290 | –657 to 78 | –0.78 (–5.25 to 3.69) | Modified care dominatesc | – | – | – |
| Bootstrapped differenced | –274 | –684 to 130 | –1.58 (–13 to 10) | Modified care dominatesc | 91.5% | 90.3% | 86.5% |
FIGURE 11.
Cost-effectiveness plane: modified minus standard.

Sensitivity analysis results
Table 22 reports the sensitivity analyses outlined in the economics method section in Chapter 2 (incorporation of patient costs for a societal perspective) and Table 23 provides a summary of the ICER results for this sensitivity analysis as well as the effect on the ICER of incorporating the multiply imputed outcomes data from Table 20. Table 22 reveals that incorporating patient travel costs, time off work and leisure costs within a societal perspective sensitivity analysis only serves to strengthen the dominance of the modified protocol group, with the total cost difference between the arms increasing to £321. Table 23 explores the impact of these sensitivity analyses on the ICER and reveals that both scenarios retain the modified arm as being the dominant option.
| Total costs | Standard care (£) | Modified care (£) | Incremental (£) | 95% CI (£) |
|---|---|---|---|---|
| Preadmissiona | 199 | 195 | –4 | –57 to 49 |
| Hospital | 1298 | 1160 | –139 | –363 to 86 |
| Follow-up | 604 | 453 | –151 | –400 to 99 |
| Total NHS cost | 1902 | 1612 | –290 | –657 to 78 |
| Preadmissiona travel expense | 8.05 | 6.27 | –1.78 | –3.87 to 0.31 |
| Follow-up travel expense | 7.90 | 9.10 | 1.19 | –3.03 to 5.43 |
| Follow-up missed work both carers | 84.31 | 71.07 | –13.24 | –40.33 to 13.86 |
| Follow-up missed normal activities | 118.64 | 98.95 | –19.69 | –57.82 to 18.45 |
| Total parent cost | 211 | 179 | –32 | –85 to 22 |
| Total cost societal perspective | 2113 | 1791 | –321 | –719 to 77 |
| Analysis | Difference in mean cost (£) | 95% CI (£) | Difference mean days to cough resolution | 95% CI | ICER |
|---|---|---|---|---|---|
| Base-case analysis | –274 | –684 to 130 | –1.58 | –13 to 10 | Modified care dominatesa |
| (1) Societal costs | –321 | –719 to 77 | –1.58 | –13 to 10 | Modified care dominates |
| (2) Multiple imputation on days to cough resolution | –274 | –684 to 130 | –3.72 | –12 to 5 | Modified care dominatesa |
Seasonality analysis
For the purpose of the seasonality analysis, data have been collected from the Edinburgh site, with analysis of data for the following variables under way: elective admissions, emergency admissions, ward transfers in, ward transfers out, discharges, complement bed-days, midnight-occupied bed-days, day cases in, day cases out, inpatient days, admissions and transfers in, discharges and transfers out, patient count, bed complement, beds available, beds occupied, bed occupancy rate and average ward stay (days). These data have been collected for all wards likely to be affected by the peak seasonality effects to explore displacement impacts and reveal the true opportunity cost of increased admissions due to BIDS during peak times. Work is ongoing to track the extent to which seasonality impacts give rise to overcapacity. This reflects months where a ward is operating over capacity and a hospital has had to make use of 'unfunded beds', i.e. the hospital doesn’t have capacity and have had to hire or utilise bank nurses and extra beds, which is a direct additional cost to the health board. In such a case the effects of seasonality take them over their budget. Sensitivity analysis applied a direct cost to the health board for each bed-day above capacity. This was costed at £686 per night (using the NHS reference unit costs) and overcapacity was estimated for the months September to March (although hospitals actually operate on a 6-month winter duration). Figure 12 provides initial insight as to the patient count impact, where months 8 and 9 are November and December.
FIGURE 12.
Seasonality analysis: patient count for months 1–9 (April–December) at Edinburgh site.

Chapter 5 Discussion
The BIDS study protocol prespecified that equivalence would be met if the time to resolution of cough was within the CIs of ± 2 days. The median difference in the time to resolution of cough was 1 day with a lower 95% confidence limit of –1 day and an upper 95% confidence limit of 2 days. The outcome of infants with acute viral bronchiolitis within hospital to a modified target oxygen saturation of ≥ 90% is therefore considered similar to management to a standard target oxygen saturation of ≥ 94%, for resolution of cough.
In addition to our primary outcome, we aimed to demonstrate safety and other measures of clinical comparability. We did not prove equivalence for time to parent perspective of return to normal and time to return to adequate feeding; however, the treatment effect was in the direction of favouring the modified care group.
Overall, there were no safety concerns (number of admissions to the HDU, readmissions to hospital, reattendances at health services) and no additional burden on parents from the intervention and earlier discharge home.
The economic analysis shows that the modified therapy dominates the standard therapy when using conventional economic evaluation cost-effectiveness criteria. The economic analysis revealed that total NHS costs are £290 (95% CI –£657 to £78) lower in the modified care arm. Although this total cost difference is not significant, this is likely due to the large variance around the many individual components making up the total cost variable. However, the hospital inpatient stay cost difference comprises the largest individual component of this total NHS cost difference and, accounting for almost 60% of the total cost variable, represents a statistically significant difference in favour of the modified arm. This difference in favour of the modified care arm further increases when patient costs are included within a societal perspective. The economic analysis shows little uncertainty regarding the likelihood of the modified care protocol being cost saving compared with the standard care protocol; however, there is greater uncertainty regarding any improvement or reduction in days to cough resolution. The modified protocol is the dominant option, with a likelihood of being cost-effective of 91.5%, even when society is willing to pay zero for the health improvements. We consider the management of infants with acute viral bronchiolitis to a target oxygen saturation of ≥ 90% to be safe and as clinically effective as an oxygen saturation target of ≥ 94%.
Limitations
Exclusion of infants under 6 weeks of age
Our exclusion criteria were kept to a minimum, as we wished, if successful, for this study to be widely applicable to acute bronchiolitis admissions; however, we did exclude infants under 6 weeks of age. The reasons for this were twofold. First, in our recruitment feasibility assessment in the season prior to the study, parents of children in this age group indicated that they would decline consent to the study because of concerns about the age of their child and their first acute illness. Second, infants in this age group frequently present with apnoea and, although we accommodated this within the protocol, the clinical and parental anxiety associated with infant apnoea may have provided an undue skew to greater length of stay in this age range. We consider that infants under 6 weeks of age will require a higher degree of personalisation of oxygen saturation targets depending on their disease course. Although there are some who may be stable and able to be managed at an oxygen saturation target of ≥ 90%, there will be others who will require a higher target for management and discharge (particularly those with apnoea) and this will be as is clinically appropriate.
Measures of concurrent symptom relief
Supplemental oxygen is provided in hypoxaemia for both tissue oxygenation and perceived symptom relief. In adults, there is no demonstrable effect of supplemental oxygen on relief of respiratory symptoms. 4,5 We used proxy measures of symptom relief, assessing heart and respiratory rate as indicators of comfort in acute respiratory disease. At time of discharge, heart rate and respiratory rate were similar in the two groups, suggesting that stopping supplemental oxygen sooner in the modified care group was not associated with an increase in discomfort reflected by an increase in respiratory or heart rate.
Measurement of clinical scores
The study did not use a bronchiolitis clinical score. A range of clinical scores are reported in studies, some specific for bronchiolitis, others adapted from asthma scores. Our reason for not using a bronchiolitis score was threefold. First, bronchiolitis scores are not used clinically in the majority of UK hospitals, in particular in our study site partners, as they have not been demonstrated to be of greater value than routine clinical decision-making. Second, there is no agreed best clinical score. Third, agreement between observers tends to be poor unless the number of trained observers is limited. 54 To have study staff available 24 hours per day for scoring would have been expensive for measurement of single outcome. The alternative approach of training clinical staff across all sites to clinical score accurately and precisely for bronchiolitis may have changed behaviour with regard to routine care (which we wished to observe) and still have been associated with unacceptable variance in scoring with corresponding concerns for data surety.
Measures of neurocognitive development
Neurocognitive delay has been associated with hypoxaemia in children, with most anxieties stemming from observation of lower school attainment in children with obstructive sleep apnoea. 54 Such children experience recurrent, variable, hypoxaemia with obstructed breathing while asleep. Hypoxaemia in acute respiratory illness tends to be less variable, and often less severe, and with a pattern of resolution over a significantly shorter period of time. Longer periods of hypoxaemia than that experienced by infants with bronchiolitis may have no associated neurocognitive impact. Preterm infants maintained at an oxygen saturation target of 91–94% had no neurocognitive deficit at 2 years compared with those maintained at an oxygen saturation target of 95–98%. 55 Neurocognitive scores in children with mild/moderate obstructive sleep apnoea observed for a period of 6 months were no different from scores in children who had undergone immediate tonsillectomy. 56 These studies support the perspective that children may be neurocognitively tolerant of short-term borderline hypoxia.
Compliance with study protocol
It could be considered a limitation of the study that we did not collect and download the time-matched ‘true’ oxygen saturation of the modified oximeters; this was predominantly for logistic and cost reasons, and we considered that the additional study resource would not have proportionally added to the study outcome or understanding of the effects of oxygen in borderline hypoxia. The differences noted for use of oxygen and time to stopping supplemental oxygen in each of the groups suggest good compliance to the study protocol in those who received the intervention. We were not aware of any episodes of unblinding associated with the study protocol; hospital oximeters were removed and a study oximeter applied after an interval of 1 minute. The average difference between the hospital and study oximeter display was 2% SpO2 and, as a consequence, to our knowledge, there were no instances of accidental unblinding.
Strengths
This study was sufficiently large to answer this important clinical question, with very good follow-up of infants to 6 months (95%) and data completeness. It can, therefore, provide strong evidence to support recommendations for clinical practice, in a topic area without current evidence and with significant practice variation.
Reducing variance in clinical practice
This is the first study of oxygen saturation targets for acute respiratory infection in children in a developed health-care setting. The recommendation of the AAP that an oxygen saturation of ≥ 90% is acceptable in acute bronchiolitis has not been widely adopted, with varying practice and continued debate. 19,57 The AAP recommendation has, however, led to a drift in clinical practice without sufficient evidence, with clinicians now managing bronchiolitis to a range of oxygen saturation targets even within the same hospital. The risks of practice drift are well demonstrated by recent studies in preterm infants, in which a progressive clinical acceptance of lower oxygen saturation targets58 was only subsequently shown to be associated with increased risk of death in exposed infants. 7 The results of this study therefore enable the range of oxygen saturation targets currently in use to be coalesced into a clear oxygen saturation target of ≥ 90%.
Unifying oxygen management strategy for acute bronchiolitis
Debate in oxygen management in acute respiratory disease focuses on target oxygen saturations, whether or not oxygen saturation monitoring should be continuous or intermittent and for how long oxygen saturation should be observed to be stable prior to discharge. The debate on oxygen saturation targets is presented in the rationale for the study in Chapter 1, Controversies in approach to hypoxaemia in bronchiolitis, but important within this is the differential approach to starting and stopping oxygen supplementation. In guidelines for respiratory disease, target oxygen saturation for commencing supplemental oxygen is typically lower than that for stopping. In children with respiratory infection, lower oxygen saturation early in the course of the illness often represents clinical instability and the clinical logic for a higher threshold at these times is unclear. A strength of our study was the use of a single target oxygen saturation for starting and stopping supplemental oxygen.
There are concerns that continuous oxygen saturation monitoring leads to clinical overinterpretation of minor physiological and artefactual brief and self-correcting desaturation. Such minor desaturation is considered to delay patient progress to management in air and, consequently, discharge. Unfortunately, there is no agreement on the frequency or duration of intermittent monitoring, and, as a consequence, we considered it safest to provide continuous monitoring over a short period of time.
There is also no agreement on the length of time that infants should be observed to have stable oxygen saturation in room air prior to discharge, with 8–24 hours considered appropriate by over two-thirds of clinicians and 24–48 hours considered appropriate by nearly one-fifth (Clare van Miert, University of Liverpool, 2012, personal communication).
In developing our protocol, while acknowledging these concerns, we hoped to provide a pragmatic, sensible and safe approach that would not miss important desaturation events in acutely infected infants but also would not inappropriately prolong admissions. We therefore elected to have a shorter period of continuous monitoring. The results of this study, by combining these three issues of debate, provide an evidence-based structure for clinical decision-making at discharge.
Context
The study addresses oxygen saturation targets for infants admitted to hospital with acute bronchiolitis. The results will prompt consideration of the generalisability of these results to other inpatient and outpatient health-care settings and also to other acute respiratory diseases in children.
Applicability within UK hospitals and beyond
In general, the care in each of the paediatric units within the BIDS study team was similar and we would consider that the results are generalisable to the care of infants with bronchiolitis in UK paediatric hospitals. We have no reason to believe that the study results would not be applicable to other similar health-care settings across the world. Infants living at higher altitudes have lower oxygen saturation in health and may be managed at lower oxygen saturation limits during disease. 1 This study was performed at sea level and, therefore, is widely applicable to most urban areas, in line with recent requests for evidence at sea level. 59
Although the study protocol was for infants admitted to hospital, we deliberately chose a more intense (continuous monitoring) but shorter period of observation (4 hours) than most current practice. The debate of continuous or intermittent oxygen saturation monitoring is discussed above; however, our shorter period of observation was intended to capture infants with important prolonged episodes of desaturation during a short period of observation, such that the results could be applicable to acute paediatric observation areas (short stay, acute assessment units, etc.) and negate the need for admission if the criteria for safe discharge were fulfilled. Such acute observation areas typically have fewer time pressures than EDs and therefore provide a better safety net for sick infants.
Use of oxygen saturation target ≥ 90% in emergency departments and primary care
The study did not address appropriate oxygen saturation targets for primary care and EDs. Infants in the first year of life with an acute respiratory infection are a vulnerable patient group. Our study boundary when considering the ethical approach to this research question was the knowledge of a greater risk of death in children with acute respiratory infection managed below an oxygen saturation of 90%,9 a finding recently also seen in infants born preterm. 7 Bronchiolitis typically has good outcomes, with few deaths, under current management strategies. Although there is some evidence that infants recovering from bronchiolitis have temporary dips below 90% at home,60 we did not consider it ethical or appropriate to devise a protocol that would lead to a sustained period below the 90% oxygen saturation threshold, and therefore we restricted the trial to those who would be observed in hospital.
In infants with bronchiolitis presenting to an ED with an oxygen saturation of ≤ 92% there is a high probability that oxygen saturation will fall below 90% during the observation period. 61 Among ED physicians, the threshold for admitting an infant with an oxygen saturation of 92% is much lower than that for admitting those with an oxygen saturation of 94%. 2 These studies, together with the wish to provide a sufficient safety net to young infants, persuaded us that a study of a 90% oxygen saturation target in EDs may not be in the best interests of infants with acute viral bronchiolitis, and a better understanding of the safety and clinical impact of target oxygen saturations during a typically longer period of observation would be most appropriate. The same reasoning would be applicable to primary care.
Applicability of oxygen saturation target ≥ 90% in other acute respiratory disease in childhood
The generalisability of targeting oxygen saturation ≥ 90% in other acute respiratory conditions has not been tested in this study. Our population was infants under 1 year of age with acute respiratory infection, who could be considered potentially more vulnerable than many older children with acute respiratory infection. In children recovering from acute pneumonia (viral or bacterial) or acute virus-induced wheeze, oxygen saturation often follows a pattern of a long tail of recovery (particularly during sleep), during which time the child’s clinical status may have significantly improved, and with no or stable chest signs on auscultation, and with hospitalisation needed only for the provision of supplemental oxygen. Clinicians caring for children who are recovering from such illnesses and who are cardiovascularly stable may consider targeting to a lower threshold of ≥ 90% oxygen saturation for hospital care and discharge. Until appropriately tested, children with acute pneumonia and acute asthma/wheeze at presentation should continue to receive supplemental oxygen according to current guideline recommendations (typically a target of ≥ 92%) because of the risk of acute change in symptoms and tissue hypoxia in these conditions during the acute phase of the illness.
Potential risks not explored within this study
The principal risk not explored by this study methodology was that children who present with clinical bronchiolitis may have an alternative diagnosis. Many conditions masquerading as bronchiolitis would typically be picked up as current (e.g. congenital heart disease). Possible exceptions are rare lung diseases in children, which may present a similar clinical picture similar to bronchiolitis. Children with such conditions (e.g. neuroendocrine hyperplasia of infancy or bronchiolitis obliterans) often struggle to maintain oxygen saturation in air ≥ 90%, and in some cases the presentation will resemble that of recurrent bronchiolitis with oxygen saturation maintained at ≥ 90% but < 94%. Clinicians should be educated that any infant presenting with a second episode of bronchiolitis should be assessed for lack of chest signs and normal oxygen saturation at discharge or follow-up.
Unanticipated findings
The study was not anticipated or designed to identify differences in the outcomes considered for equivalence. Nor did we expect to see the modest but additional benefit to the modified intervention for readmissions to hospital and carer time lost. Post-hoc analyses are discussed further here.
Parents of children in the modified care group reported that their infants had returned to normal 1 day sooner (median 11 days) than parents of children in the standard care group (median 12 days), with the 95% CI of 0 to 3 days falling outside the prespecified limits of –2 to 2 days. When this difference was explored with hazard ratios, the estimate of difference was 1.2 (95% CI 1.0 to 1.4; p-value = 0.0434). Differences between the groups in time to return to normal are more evident in those returning to normal at a time longer than the median value (see Figure 5). This difference may represent a relationship between the return to a sense of health and well-being of a child from a parent perspective and the time since hospital discharge. Alternatively, a shorter period in hospital receiving supplemental oxygen may have conferred health benefits that were not captured by cough duration, for example a lower potential risk of nosocomial infection in those discharged home sooner or a reduced viral replication rate as a result of oxygen restriction. Parents appeared to consider their infant ‘back to normal’ even when there was residual cough (as cough took longer to resolve), suggesting that cough is only a component of parents’ perspectives of their child’s health status as normal and does not define it.
Median time to return to adequate feeding (≥ 75% normal) was 2.7 hours shorter in the modified care group (24.1 hours) than in the standard care group (19.5 hours), with the 95% CI of –0.3 to 7.3 hours falling outside the prespecified limits of –4 to 4 hours. When this difference was explored with hazard ratios, the estimate of difference was 1.2 (95% CI 1.0 to 1.4; p-value = 0.0147). Across the whole group of infants, this is a clinically important difference. It may represent altered behaviour by nursing staff to resolve feeding issues sooner in those with apparently better oxygen saturation. However, we also note that fewer infants in the modified care group required nasogastric tube feeding (see Table 12; typically provided for respiratory distress rather than for low oxygen saturation levels). Although speculative, there could be merit in further exploring whether or not supplementation with dry oxygen gas exacerbates nasal obstruction in acute bronchiolitis, compounding feeding difficulties and prolonging hospitalisation, particularly where nasal cannulae increase airflow resistance in obligate nasal breathers.
Medical therapies, including bronchodilators,16 adrenaline,62 corticosteroids30,63 and possibly hypertonic saline, are of limited or no benefit in the treatment of acute bronchiolitis. 64 The data from this study pose two further issues. The first is whether or not there is a risk/benefit to supplemental oxygen use in mild/moderate bronchiolitis. Infants in the modified care group appeared to recover sooner. Emerging evidence that RSV replication may be boosted in an enhanced oxygen environment65 suggests that risk–benefit implications of supplemental oxygen should be considered more actively. The second is that the trend for benefits in this study was in favour of the modified care group, who spent less time in hospital with fewer interventions. This concurs with recent evidence that fewer interventions in bronchiolitis result in faster recovery. 66 Is less more in the management of acute bronchiolitis in hospital?
Patient and public involvement
In the study set-up stages we engaged with a parent representative to guide protocol development. Unfortunately, that link was lost early in the study and we were unable to engage appropriate patient and public involvement, possibly as acute bronchiolitis is a relatively short-duration illness for many and is often not given a labelled diagnosis in primary care.
In our prestudy feasibility assessment, we were fortunate to be able to meet the parents of children during an admission to hospital with acute bronchiolitis, to gauge their perspective on our proposed trial at a similar time point as that in which we would be engaging with parents of children enrolled to the study. Parents were more positive than we had expected and the discussions gave valuable guidance for study exclusions, parent information sheets and appropriate use of language when conveying potential risks and benefits of the study.
Chapter 6 Conclusions
Implications for health care
This project has demonstrated that infants with acute viral bronchiolitis may be managed to an oxygen saturation target of ≥ 90% in air when observed for a period of 4 hours, including a period of sleep, and continuously monitored. The implications for health care are that:
-
Starting and stopping points for oxygen supplementation in acute bronchiolitis could be around a single oxygen saturation target of 90% – streamlining and coalescing care across all health-care settings. The study does not identify an oxygen saturation point at which infants require health-care observation (but notes a previous recommendation of ≤ 92%).
-
Infants could be safely discharged once they attain a stable oxygen saturation of ≥ 90% in air for 4 continuous hours, including a period of sleep, and are feeding adequately and clinically stable. This could take place in any health-care setting with the facility to provide this level of evaluation. In many cases this should result in earlier discharge home with benefits demonstrated for infants and parents in addition to cost savings for health-care providers.
Recommendations for research
Is 90% oxygen saturation an appropriate target threshold for supplementing oxygen in acute respiratory infection in children?
This study demonstrates that, in infants with bronchiolitis, management to a target oxygen saturation of 90% confers some modest benefits compared with management to 94%. A reasonable question is whether or not this benefit would be further extended at a target SpO2 of < 90%. This inflection point for the oxyhaemoglobin dissociation curve would require careful ethical consideration, as it has been associated with increased deaths in preterm infants managed below this target. Exploring the clinical effectiveness of oxygen supplementation at an SpO2 target of < 90% may be considered ethically more appropriate in health-care settings at altitude and/or with limited resources to supply supplemental oxygen in acute lower respiratory tract infection.
What is the clinical effectiveness and cost-effectiveness of community-based supplemental oxygen provision at home for infants with acute bronchiolitis who have been discharged home from hospitals that have adopted a target oxygen saturation of 90%?
In the past 10 years, with increasing pressure on paediatric inpatient beds, there has been a move to provide supplemental oxygen to infants with bronchiolitis at home once they are clinically stable. Although most reports come from the USA and Australia, there are some reports in the UK. The infrastructure to provide home care oxygen has involved primary care physicians and dedicated nursing teams. This has required financial expenditure due to the associated costs of home-based oxygen delivery and monitoring. To date there has been no published comprehensive cost-effectiveness analysis of this. Assuming that hospitals will adopt a 90% target for administration of supplemental oxygen in bronchiolitis (with fewer infants receiving supplemental oxygen for a shorter duration), a reasonable research question would be to gauge the clinical effectiveness and cost-effectiveness of home care oxygen-delivery systems in acute bronchiolitis.
What is the clinical effectiveness and cost-effectiveness of continuous or intermittent oxygen saturation monitoring on outcomes in acute bronchiolitis managed to a target oxygen saturation of 90%?
Measured oxygen saturation varies over time and with movement and sleep state. Minor dips in oxygen saturation are not considered to be of clinical significance but are thought to influence clinician behaviour unduly with respect to starting and stopping supplemental oxygen. Intermittent monitoring is understood to identify only important changes in baseline oxygen saturation. Some clinicians monitor oxygen saturation intermittently as infants improve, but typically to a higher baseline target than the 90% SpO2 recommended by this study. There are no agreed standards for frequency or duration of intermittent monitoring. A reasonable question, therefore, could be to identify whether or not intermittent monitoring to a target oxygen saturation of 90% could be clinically effective and cost-effective.
What are safe oxygen saturation targets for management of infants with acute bronchiolitis in primary care and emergency department discharge?
This report provides evidence for patients observed as inpatients. The majority of patients with bronchiolitis, however, are managed in primary care. Infants with bronchiolitis in the community may be maintaining adequate feeding but have an oxygen saturation of < 94% but > 90%. Currently, they would be referred to hospital and may be admitted (in most, SpO2 is at or below 92%), but a reasonable question arising from our study is whether or not such infants could safely remain in the community under primary care review.
Acknowledgements
The BIDS was funded by the National Institute for Health Research Health Technology Assessment programme (project reference 09/91/16).
We would like to thank all the parents and guardians of participating children. We gratefully acknowledge the help of the following people:
*The BIDS Collaborators Group.
Trial Steering Committee
Dr Clare Murray* (Independent Clinician), Senior Lecturer and Paediatric Respiratory Consultant, University of Manchester.
Dr Colin Powell* (Independent Clinician), Senior Lecturer in Child Health and Honorary Consultant Paediatrician, University of Cardiff.
Professor Mike Shields* (Chairperson), Professor of Child Health, Queen’s University Belfast.
Data Monitoring Committee
Professor Carrol Gamble* (DMC Statistician), Professor of Medical Statistics, University of Liverpool.
Dr Mike McKean* (Independent Member), Consultant in Respiratory Paediatrics, Newcastle upon Tyne Hospitals.
Dr Sheila McKenzie* (Chairperson), Community Paediatrician, NHS Highland.
Data Management Group
Dr Kathleen A Boyd, Dr Isabella Butcher, Dr Steve Cunningham, Dr Steff C Lewis, Dr Morag MacLean, Dr Emma McIntosh, Ms Aryelly Rodriguez, Dr Sharon Tonner and Mrs Fiona Wee (née Sloan).
Economic evaluation
Dr Kathleen A Boyd and Dr Emma McIntosh.
Recruiting centres [collaborating doctors and nurses (the principal investigators listed first and italicised)]
Royal Aberdeen Children’s Hospital, Aberdeen: Dr Steve Turner,* Ms Lindsay Cameron, Ms Donna Nelson, Ms Jill Paxton and Ms Victoria Thomson.
Bristol Royal Hospital for Children, Bristol: Dr Huw Thomas,* Ms Tracey Bingham, Ms Helen Clark, Ms Laura Clifford, Dr Mark Lyttle, Ms Alice Parham, Ms Sarah Potter (née Jelly), Ms Nicola Robinson and Ms Hannah Spires.
Tayside Children’s Hospital, Dundee: Dr Jonathan McCormick,* Ms Susan MacFarlane and Ms Fiona Treanor.
Royal Hospital for Sick Children, Edinburgh: Dr Steve Cunningham, Ms Emma Carson, Ms Vikki Gould, Ms Debbie Miller, Ms Orla Duncan and Mrs Kay Riding.
Royal Devon and Exeter Hospital, Exeter: Dr Beth Enderby,* Ms Caroline Harrill and Ms Suzanne Wilkins.
Royal Hospital for Sick Children, Yorkhill, Glasgow: Dr Jack Beattie,* Dr James Paton*, Dr Claire Milne and Ms Elizabeth Waxman.
University Hospital Crosshouse, Kilmarnock: Dr Tim Adams,* Ms Claire Bell and Ms Margo Henry.
Knowledge Spa Royal Cornwall Hospital, Truro: Dr Chris Williams,* Dr Anne Prendiville, Ms Gill Craig, Ms Hannah Solomon and Ms Nina Worrin.
Database programming and data management
Mr Ronald Harkness, Ms Samantha Thomas and Mr Allan Walker.
Masimo Corporation Limited.
Dr Mark Holody.
South West Medicines for Children Local Research Network
Professor Adam Finn.
Scottish Children’s Research Network
Professor Peter Helms and Dr Pamela Dicks.
National Institute for Health Research Health Technology Assessment
Mrs Lesley Dodd.
Contributions of authors
Dr Steve Cunningham* (Consultant and Honorary Reader in Paediatric Respiratory Medicine, Department of Respiratory and Sleep Medicine, Royal Hospital for Sick Children, Edinburgh) Chief investigator. He devised the study, was involved in the design and conduct of research and was a member of the trial development group, the project management group and the TSC. He was also involved in the development and refinement of the trial protocol, the conduct of the research interpretation and the reporting of results and he revised the manuscript for important intellectual content.
Aryelly Rodriguez* (Statistician, ECTU, University of Edinburgh, Edinburgh) Study statistician. Wrote the statistical analysis plan and undertook end of study analysis. She prepared the final study statistical report and was involved in the interpretation and reporting of results and the draft and revision of this manuscript for important intellectual content.
Dr Kathleen A Boyd* (Lecturer in Health Economics, Health Economics and Health Technology Assessment, Institute of Health and Wellbeing, University of Glasgow, Glasgow) Undertook the majority of the health economics analysis and was involved in the study design, the data management team, the interpretation and reporting of results and the draft and revision of the manuscript for important intellectual content.
Dr Emma McIntosh* (Reader in Health Economics of Public Health, Health Economics and Health Technology Assessment, Institute of Health and Wellbeing, University of Glasgow, Glasgow) Led the health-economic evaluation and was involved in the study design, the data management group, the health economics analysis and the interpretation and reporting of results. Dr McIntosh wrote the economic evaluation sections of the report and revised the manuscript for important intellectual content.
Dr Steff C Lewis* (Reader in Medical Statistics, Centre for Population Health Sciences, University of Edinburgh, Edinburgh) Lead study statistician. Involved in the design and conduct of research, the TSC, the interpretation and reporting of results and the draft and revision of the manuscript for important intellectual content.
Other contributors
Mrs Kay Riding* (Lead Paediatric Research Nurse, Children’s Clinical Research Facility, Royal Hospital for Sick Children, Edinburgh) Involved in the set-up, conduct and acquisition of data of this research and assisted with TSC meetings.
Mrs Fiona Wee* (née Sloan) (Trial Manager for this trial until January 2012, ECTU, University of Edinburgh, Edinburgh) and Dr Morag MacLean* (Trial Manager for this trial from January 2012, ECTU, University of Edinburgh, Edinburgh) Involved in the day-to-day trial management, data management and were members of the Trial Management Group.
Publications
Cunningham S, Rodriguez A, Adams T, Boyd KA, Butcher I, Enderby B, et al. , for the Bronchiolitis of Infancy Discharge Study (BIDS) group. Oxygen saturation targets in infants with bronchiolitis (BIDS): a double-blind, randomised, equivalence trial. Lancet 2015;386:1041–8.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health.
References
- Subhi R, Smith K, Duke T. When should oxygen be given to children at high altitude? A systematic review to define altitude-specific hypoxaemia. Arch Dis Child 2009;94:6-10. http://dx.doi.org/10.1136/adc.2008.138362.
- Mallory MD, Shay DK, Garrett J, Bordley WC. Bronchiolitis management preferences and the influence of pulse oximetry and respiratory rate on the decision to admit. Pediatrics 2003;111:e45-51. http://dx.doi.org/10.1542/peds.111.1.e45.
- O’Driscoll BR, Howard LS, Davison AG. BTS guideline for emergency oxygen use in adult patients. Thorax 2008;63:vi1-68. http://dx.doi.org/10.1136/thx.2008.102947.
- Cranston JM, Crockett A, Currow D. Oxygen therapy for dyspnoea in adults. Cochrane Database Syst Rev 2008;3. http://dx.doi.org/10.1002/14651858.cd004769.pub2.
- Abernethy AP, McDonald CF, Frith PA, Clark K, Herndon JE, Marcello J, et al. Effect of palliative oxygen versus room air in relief of breathlessness in patients with refractory dyspnoea: a double-blind, randomised controlled trial. Lancet 2010;376:784-93. http://dx.doi.org/10.1016/S0140-6736(10)61115-4.
- Cranston JM, Crockett AJ, Moss JR, Alpers JH. Domiciliary oxygen for chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2005;4. http://dx.doi.org/10.1002/14651858.cd001744.pub2.
- Stenson BJ, Tarnow-Mordi WO, Darlow BA, Simes J, Juszczak E, Askie L, et al. Oxygen saturation and outcomes in preterm infants. N Engl J Med 2013;368:2094-104. http://dx.doi.org/10.1056/NEJMoa1302298.
- Shann F, Dobson MB, Peel D. Oxygen Therapy for Acute Respiratory Infections in Young Children in Developing Countries. Geneva: World Health Organization Press; 1993.
- Duke T, Wandi F, Jonathan M, Matai S, Kaupa M, Saavu M, et al. Improved oxygen systems for childhood pneumonia: a multihospital effectiveness study in Papua New Guinea. Lancet 2008;372:1328-33. http://dx.doi.org/10.1016/S0140-6736(08)61164-2.
- Duke T. The Clinical Use of Oxygen in Hospitals With Limited Resources. World Health Organization 2011. http://video.rch.org.au/cich/The_Clinical_Use_of_Oxygen_November_2011.pdf (accessed 10 April 2015).
- Deshpande SA, Northern V. The clinical and health economic burden of respiratory syncytial virus disease among children under 2 years of age in a defined geographical area. Arch Dis Child 2003;88:1065-9. http://dx.doi.org/10.1136/adc.88.12.1065.
- Unger S, Cunningham S. Effect of oxygen supplementation on length of stay for infants hospitalized with acute viral bronchiolitis. Pediatrics 2008;121:470-5. http://dx.doi.org/10.1542/peds.2007-1135.
- Mansbach JM, Emond JA, Camargo CA. Bronchiolitis in US emergency departments 1992 to 2000: epidemiology and practice variation. Pediatr Emerg Care 2005;21:242-7. http://dx.doi.org/10.1097/01.pec.0000161469.19841.86.
- Thorburn K. Pre-existing disease is associated with a significantly higher risk of death in severe respiratory syncytial virus infection. Arch Dis Child 2009;94:99-103. http://dx.doi.org/10.1136/adc.2008.139188.
- Shay DK, Holman RC, Newman RD, Liu LL, Stout JW, Anderson LJ. Bronchiolitis-associated hospitalizations among US children, 1980–1996. JAMA 1999;282:1440-6. http://dx.doi.org/10.1001/jama.282.15.1440.
- Bronchiolitis in Children (SIGN 91). NHS Quality Improvement Scotland; 2006.
- American Academy of Pediatrics (AAP) . Diagnosis and management of bronchiolitis. Pediatrics 2006;118:1774-93. http://dx.doi.org/10.1542/peds.2006-2223.
- Bass JL, Gozal D. Oxygen therapy for bronchiolitis. Pediatrics 2007;119. http://dx.doi.org/10.1542/peds.2006-3002.
- Evidence-Based Care Guideline for Management of Bronchiolitis in Infants 1 Year of Age or Less with a First Time Episode. Cincinnati, OH: Cincinnati Children’s Hospital Medical Center; 2010.
- National Institute for Health and Care Excellence (NICE) n.d. www.evidence.nhs.uk/Search?q=bronchiolitis+guideline (accessed 10 April 2015).
- Clinical Practice Guideline on Acute Bronchiolitis. Barcelona: Catalan Agency for Health Technology Assessment and Research; 2010.
- Australian Government National Health and Medical Research Council n.d. www.clinicalguidelines.gov.au/browse.php?treePath=C.D012140.D001982.D001991&showResults=true&pageType=1& (accessed 10 April 2015).
- Guideline Synthesis: Prevention, Diagnosis and Treatment of Pediatric Bronchiolitis. Rockville, MD: Agency for Healthcare Research and Quality; 2012.
- Cunningham S, McMurray A. Observational study of two oxygen saturation targets for discharge in bronchiolitis. Arch Dis Child 2012;97:361-3. http://dx.doi.org/10.1136/adc.2010.205211.
- Bajaj L, Turner CG, Bothner J. A randomized trial of home oxygen therapy from the emergency department for acute bronchiolitis. Pediatrics 2006;117:633-40. http://dx.doi.org/10.1542/peds.2005-1322.
- Tie SW, Hall GL, Peter S, Vine J, Verheggen M, Pascoe EM, et al. Home oxygen for children with acute bronchiolitis. Arch Dis Child 2009;94:641-3. http://dx.doi.org/10.1136/adc.2008.144709.
- Flett KB, Breslin K, Braun PA, Hambidge SJ. Outpatient course and complications associated with home oxygen therapy for mild bronchiolitis. Pediatrics 2014;133:5769-775. http://dx.doi.org/10.1542/peds.2013-1872.
- Cunningham S. ‘A hospital is no place to be sick’ Samuel Goldwyn (1882–1974). Arch Dis Child 2009;94:565-6. http://dx.doi.org/10.1136/adc.2009.160218.
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67:361-70. http://dx.doi.org/10.1111/j.1600-0447.1983.tb09716.x.
- Plint AC, Johnson DW, Patel H, Wiebe N, Correll R, Brant R, et al. Epinephrine and dexamethasone in children with bronchiolitis. N Engl J Med 2009;360:2079-89. http://dx.doi.org/10.1056/NEJMoa0900544.
- Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions 2009.
- Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ 2010;340. http://dx.doi.org/10.1136/bmj.c332.
- Altman DG, Machin D, Bryant TN, Gardner MJ. Statistics with Confidence. London: BMJ Books; 1989.
- Shields MD, Thavagnanam S. The difficult coughing child: prolonged acute cough in children. Cough 2013;9. http://dx.doi.org/10.1186/1745-9974-9-11.
- Manca A, Hawkins N, Sculpher M. Estimating mean QALYs in trial-based cost-effectiveness analysis: the importance of controlling for baseline utility. Health Econ 2005;14:487-96. http://dx.doi.org/10.1002/hec.944.
- Ramsey S, Willke R, Briggs AH, Brown R, Buxton M, Chawla A, et al. Good Research Practices for Cost-Effectiveness Analysis Alongside Clinical Trials: The ISPOR RCT-CEA Task Force Report. Value Health 2005;8:521-33. http://dx.doi.org/10.1111/j.1524-4733.2005.00045.x.
- Davies A, Briggs AH, Schneider J, Levy A, Ebeid O, Wagner S, et al. The ends justify the mean: outcome measures for estimating the value of new cancer therapies. Health Outcomes Res Med 2012;3:e25-36. http://dx.doi.org/10.1016/j.ehrm.2012.01.001.
- Fenwick E, Claxton K, Sculpher M. Representing uncertainty: the role of cost-effectiveness acceptability curves. Health Econ 2001;10:779-87. http://dx.doi.org/10.1002/hec.635.
- Husereau D, Drummond M, Petrou S, Carswell C, Moher D, Greenberg D, et al. Consolidated health economic evaluation reporting standards (CHEERS) – explaination and elaboration: a report of ISPOR health economic evaluation publication guidelines good reporting task force. Value Health 2013;16:231-50. http://dx.doi.org/10.1016/j.jval.2013.02.002.
- Glick H, Doshi J, Sonnad S, Polsky D. Economic Evaluation in Clinical Trials. Oxford: Oxford University Press; 2007.
- Glick H. Stata Programs: Sampling Uncertainty for Cost-Effectiveness – Bsceaprogs.Do 2011. www.uphs.upenn.edu/dgimhsr/stat-cicer.htm (accessed 6 March 2014).
- Petrou S, Gray A. Economic evaluation alongside randomised controlled trials: design, conduct, analysis, and reporting. BMJ 2011;342:1069-73. http://dx.doi.org/10.1136/bmj.d1548.
- British National Formulary. London: BMJ Group and Pharmaceutical Press; 2012.
- Curtis L. Unit Costs of Health and Social Care 2012. Canterbury: Personal Social Services Research Unit, University of Kent; 2012.
- NHS Refererence Costs: Financial year 2012–2013. London: DH; 2013.
- Fieller EC. Some problems in interval estimation. J R Stat Soc Series B Stat Methodol 1954;16.
- Briggs AH. Statistical approaches to handling uncertainty in health economic evaluation. Eur J Gastroenterol Hepatol 2004;16:551-61. http://dx.doi.org/10.1097/00042737-200406000-00007.
- Guide to the Methods of Technology Appraisal: 2013. London: NICE; 2013.
- Information Services Division (ISD) . Scottish Health Service Costs Book 2012: R129x 2012. www.isdscotland.org/Health-Topics/Finance/Costs/ (accessed February 2014).
- BNF for Children. London: BMJ Group, Pharmaceutical Press and RCPCH Publications; n.d.
- UK Government . The National Minimum Wage 2012. www.gov.uk/national-minimum-wage (accessed February 2014).
- Geue C, Lewsey J, Lorgelly P, Goven L, Hart C, Briggs A. Spoilt for choice: implications of using alternative methods of costing hospital episode statistics. Health Econ 2012;21:1201-16. http://dx.doi.org/10.1002/hec.1785.
- McCallum GB, Morris PS, Wilson CC, Versteegh LA, Ward LM, Chatfield MD, et al. Severity scoring systems: are they internally valid, reliable and predictive of oxygen use in children with acute bronchiolitis?. Pediatr Pulmonol 2013;48:797-803. http://dx.doi.org/10.1002/ppul.22627.
- Gozal D, Pope DW. Snoring during early childhood and academic performance at ages thirteen to fourteen years. Pediatrics 2001;107:1394-9. http://dx.doi.org/10.1542/peds.107.6.1394.
- Askie LM, Henderson-Smart DJ, Irwig L, Simpson JM. Oxygen-saturation targets and outcomes in extremely preterm infants. N Engl J Med 2003;349:959-67. http://dx.doi.org/10.1056/NEJMoa023080.
- Marcus CL, Moore RH, Rosen CL, Giordani B, Garetz SL, Taylor HG, et al. A randomized trial of adenotonsillectomy for childhood sleep apnea. N Engl J Med 2013;368:2366-76. http://dx.doi.org/10.1056/NEJMoa1215881.
- Wagner T. Bronchiolitis. Pediatr Rev 2009;30:386-95. http://dx.doi.org/10.1542/pir.30-10-386.
- Tin W, Milligan DW, Pennefather P, Hey E. Pulse oximetry, severe retinopathy, and outcome at one year in babies of less than 28 weeks gestation. Arch Dis Child Fetal Neonatal Ed 2001;84:F106-10. http://dx.doi.org/10.1136/fn.84.2.F106.
- Teach SJ. Progress toward a new tool for the toolbox: supplemental home oxygen for viral bronchiolitis. Pediatrics 2014;133:913-14. http://dx.doi.org/10.1542/peds.2014-0512.
- Wong JYW, Moon S, O’Callaghan C. Arterial oxygen desaturation in infants recovering from acute bronchiolitis: hypoxic infants coughed more. Am J Respir Crit Care Med 2003;167.
- Parker MJ, Allen U, Stephens D, Lalani A, Schuh S. Predictors of major intervention in infants with bronchiolitis. Pediatr Pulmonol 2009;44:358-63. http://dx.doi.org/10.1002/ppul.21010.
- Wainwright C, Altamirano L, Cheney M, Cheney J, Barber S, Price D, et al. A multicenter, randomized, double-blind, controlled trial of nebulized epinephrine in infants with acute bronchiolitis. N Engl J Med 2003;349:27-35. http://dx.doi.org/10.1056/NEJMoa022226.
- Corneli HM, Zorc JJ, Mahajan P, Shaw KN, Holubkov R, Reeves SD, et al. A multicenter, randomized, controlled trial of dexamethasone for bronchiolitis. N Engl J Med 2007;357:331-9. http://dx.doi.org/10.1056/NEJMoa071255.
- Wu S, Baker C, Lang ME, Schrager SM, Liley FF, Papa C, et al. Nebulized hypertonic saline for bronchiolitis: a randomized clinical trial. JAMA Pediatr 2014;168:657-63. http://dx.doi.org/10.1001/jamapediatrics.2014.301.
- Gladwell W, Middleton L, Cook D, Ciencewicki J, Kleeberger SR. Susceptibility and response to respiratory syncytial virus infection enhanced by exposure to hyperoxic conditions. Am J Respir Crit Care Med 2014;189.
- Skjerven HO, Hunderi JO, Brugmann-Pieper SK, Brun AC, Engen H, Eskedal L, et al. Racemic adrenaline and inhalation strategies in acute bronchiolitis. N Engl J Med 2013;368:2286-93. http://dx.doi.org/10.1056/NEJMoa1301839.
Appendix 1a Bronchiolitis of Infancy Discharge Study Parent/Carer Consent Form Version 2.0, 16 May 2011
Appendix 1b Bronchiolitis of Infancy Discharge Study Parent/Carer Consent Form Version 3.0, 30 May 2012
Appendix 1c Bronchiolitis of Infancy Discharge Study Parent Information Sheet Version 2.0, 16 May 2011
Parent Information Sheet
Bronchiolitis of Infancy Discharge Study (BIDS)
We would like to invite you to take part in our research study. Before you decide we would like you to understand why the research is being done and what it would involve for you and your child. One of our team will go through the information sheet with you and answer any questions you have.
Quick summary
Your child has been diagnosed with a common chest infection, ‘bronchiolitis’, and needs to come into hospital for help with feeding and/or breathing. Children admitted to hospital with bronchiolitis go home once they improve and are able to breathe and feed OK. At present we keep them in hospital until their blood oxygen has reached a normal level (more than 93% oxygen saturation), even though otherwise they would be fit to go home.
Children’s doctors in the USA have been advised that infants with bronchiolitis who have improved feeding and breathing can be managed without being given extra oxygen once blood oxygen levels are nearly normal (90% oxygen saturation or higher). Many doctors in the UK also think this is sensible as children recovering from bronchiolitis often have mildly low blood oxygen levels despite looking much better and feeding well. At present these children would need to stay in hospital, but we think that this time in hospital does not help recovery and could be time spent at home with family. This study is to investigate whether children going home from hospital, once breathing and feeding have improved, continue their recovery just as quickly as those who stay a little longer.
Our study doesn’t involve any additional tests. Apart from filling in a questionnaire at the start of the study, there will be no need for further contact with you by the study team until a week from now.
Part 1 tells you the purpose of this study and what will happen to you if you take part. Part 2 gives you more detailed information. Ask if there is anything that is not clear. The study diagram summarises what will happen to your child in the study.
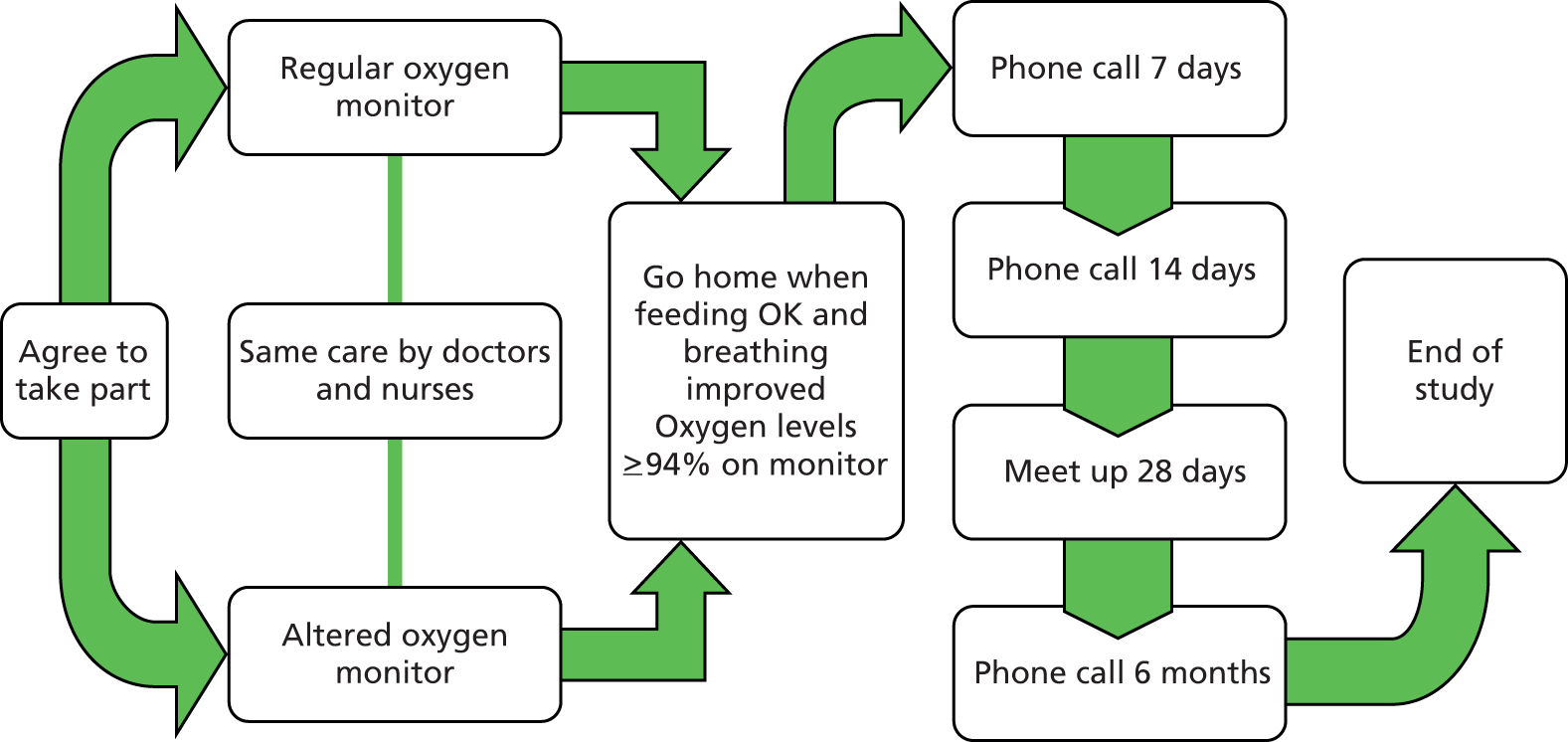
Part 1
What is the purpose of the study?
People with chest infections can have lower blood oxygen levels. As the chest infection gets better the blood oxygen levels go back to normal. Sometimes the improvement in blood oxygen levels is slower than improvements in how people feel. This can happen with bronchiolitis, the condition your child has been diagnosed with. If oxygen levels are very low then we know that giving extra oxygen helps – that question is not being studied in this project. The American Academy of Pediatrics (which advises all children’s doctors in the USA) considers that it would be OK to stop giving extra oxygen earlier than is current practice in the UK. We want to know if we should change UK practice to that recommended in the USA.
Do I have to take part?
It is up to you to decide to let your child join the study. If you agree, we will ask you to sign a consent form. You are free to withdraw your child at any time, without giving a reason. This would not affect the standard of care your child receives.
What will happen to my child if we take part?
As now, your child will go home once they are feeding and breathing comfortably and look improved.
In the UK, children usually stop being given extra oxygen to breathe when their oxygen saturation monitor levels read more than 93%. The American Academy of Pediatrics (which advises all children’s doctors in the USA) considers that it would be OK to stop giving extra oxygen to breathe when oxygen saturation has reached 90%. We think this small difference won’t affect how quickly children get better once they get home, but we want to make sure with this study. In hospital we use oxygen saturation monitors to monitor blood oxygen levels in children with bronchiolitis.
To answer this question we will use two types of blood oxygen (saturation) monitoring machines. An important part of good studies is that no-one knows which monitor is which (until the end of the study). This makes sure that the only difference in the study is the type of oxygen monitor. In this study there is no choice as to which oxygen saturation monitor is given to each child, it is ‘random’.
The oxygen saturation monitors will look the same from the outside. One type will be just the same as all other types seen in hospital. The other type changes the display seen by doctors and nurses (and you) so that the numbers appear slightly higher than they really are when blood oxygen levels are just near healthy levels (once they measure 90% they will actually display 94%). Your child would remain on the oxygen saturation monitor they are randomised to until they leave hospital.
A small number of children need to go to high dependency or intensive care during their stay. These children would switch to a regular non-study oxygen saturation monitor while they were in high dependency or intensive care, and go back onto their original study oximeter once they return to the ward.
How often would we be contacted?
We want to understand how long it takes for your child to get completely better following this illness, how you feel about your child’s illness and how quickly family life takes to get completely back to normal (so that we understand the economic implications for you as a family as well as the health costs of the study).
To understand this we will contact you on just four occasions: at 7 and 14 days from now by phone (if not still in hospital); in 28 days we want to ask similar questions, but at that time we also want to meet with you to check your child’s oxygen saturation levels to make sure they are now normal as we expect: that meeting can be here at the hospital (we will reimburse reasonable expenses) or at your home; in 6 months we will contact you one final time by phone to see how your child has been over that period (some infants with bronchiolitis can have problematic cough and chestiness for some weeks).
What are the possible risks of taking part?
We don’t expect any important risks for children from this study, but will monitor for them. Even now, some children with bronchiolitis need to revisit medical services (GP/Hospital/Out of Hours) once they have gone home from hospital, but we want to make sure that doesn’t happen more often in this study. We will ensure all children have completely healthy oxygen levels by meeting with you and your child 28 days following admission to hospital.
What are the possible benefits of taking part?
If a child can go home safely at an earlier stage then this has benefits for the hospital (which can use the bed for another child), the child (who is able to go back home with its family) and the family (who can look after the child at home rather than having to come to hospital).
This completes Part 1
If the information in Part 1 has interested you and you are considering participation, please read the additional information in Part 2 before making any decision.
Part 2
What will happen if I don’t want my child to continue in the study?
The study team will ask if information collected up to that time could be used, or whether you would like the information to be destroyed. If your child were still in hospital, they would transfer to a regular oxygen saturation monitor. A study doctor/nurse would discuss with you whether or not you would be happy to continue to have contact from the study team after going home.
Complaints
If you have a concern about any aspect of this study, you should ask to speak to the researchers, who will do their best to answer your questions [local contact number]. If you remain unhappy and wish to complain formally, you can do this [insert details e.g. NHS Complaints Procedure or Private Institutional arrangements]. Details can be obtained from [insert local details].
Harm
In the event that something does go wrong and your child is harmed during the research and this is due to someone’s negligence then you may have grounds for a legal action for compensation against Lothian Health Board/University of Edinburgh but you may have to pay your legal costs. The normal National Health Service complaints mechanisms will still be available to you (if appropriate).
Will information collected about my child during this study be kept confidential?
All information that is collected about you and your child during the course of the research will be kept strictly confidential, and any information about you that leaves the hospital/surgery will have your child’s name and address removed so that they cannot be recognised. To make sure information stays confidential we give each child in the study a unique number and only that number appears in the main study computer database.
We will store your child’s initials and CHI number (a unique health number for your child incorporating their date of birth and a four digit number) in the randomisation database to ensure that children do not enter the study on two occasions.
Researchers and those monitoring the research (to make sure it is done safely) will be able to see data with your child’s name, address and date of birth. All have a duty to ensure data confidentiality.
The data will be kept for 10 years in a secure place and then disposed of securely.
Informing your GP
If you agree, we will inform your General Practitioner, by letter, that your child is taking part in this study.
What will happen to the results of the research study?
We will publish the results in a medical journal, hopefully in 2014. Participants wishing to be notified of this publication should let the study team know.
Who is funding the research?
The research is funded by the UK National Institute for Health Research (NIHR) HTA programme (www.hta.ac.uk). The Sponsor of the research is University of Edinburgh/Lothian Health Board.
Who has reviewed the research?
All research in the NHS is looked at by an independent group of people, called a Research Ethics Committee, to protect your interests. This study has been reviewed and given favourable opinion by Lothian Research Ethics Committee.
Further information about the research
The lead for the research in your area who can provide more information about the research or discuss any problems you have with the research is:
Dr [insert name]
[insert address]
Tel: [insert number]
The lead for the study as a whole is:
Dr Steve Cunningham
Consultant Respiratory Paediatrician
Royal Hospital for Sick Children
Sciennes Road
Edinburgh
EH9 1LF
Tel: [insert number]
Should you wish to discuss the study with someone not associated with the study please contact:
Dr Don Urquhart
Consultant Respiratory Paediatrician
Royal Hospital for Sick Children
Sciennes Road
Edinburgh
EH9 1LF
Tel: [insert number]
Appendix 1d Bronchiolitis of Infancy Discharge Study Parent Information Sheet Version 3.0, 30 May 2012, Scottish sites
Parent Information Sheet
Bronchiolitis of Infancy Discharge Study (BIDS)
We would like to invite you to take part in our research study. Before you decide we would like you to understand why the research is being done and what it would involve for you and your child. One of our team will go through the information sheet with you and answer any questions you have.
Quick summary
Your child has been diagnosed with a common chest infection, ‘bronchiolitis’, and needs to come into hospital for help with feeding and/or breathing. Children admitted to hospital with bronchiolitis go home once they improve and are able to breathe and feed OK. At present we keep them in hospital until their blood oxygen has reached a normal level (more than 93% oxygen saturation), even though otherwise they would be fit to go home.
Children’s doctors in the USA have been advised that infants with bronchiolitis who have improved feeding and breathing can be managed without being given extra oxygen once blood oxygen levels are nearly normal (90% oxygen saturation or higher). Many doctors in the UK also think this is sensible as children recovering from bronchiolitis often have mildly low blood oxygen levels despite looking much better and feeding well. At present these children would need to stay in hospital, but we think that this time in hospital does not help recovery and could be time spent at home with family. This study is to investigate whether children going home from hospital once breathing and feeding have improved continue their recovery just as quickly as those who stay a little longer.
Our study doesn’t involve any additional tests. Apart from filling in a questionnaire at the start of the study, there will be no need for further contact with you by the study team until a week from now.
Part 1 tells you the purpose of this study and what will happen to you if you take part. Part 2 gives you more detailed information. Ask if there is anything that is not clear. The study diagram summarises what will happen to your child in the study.
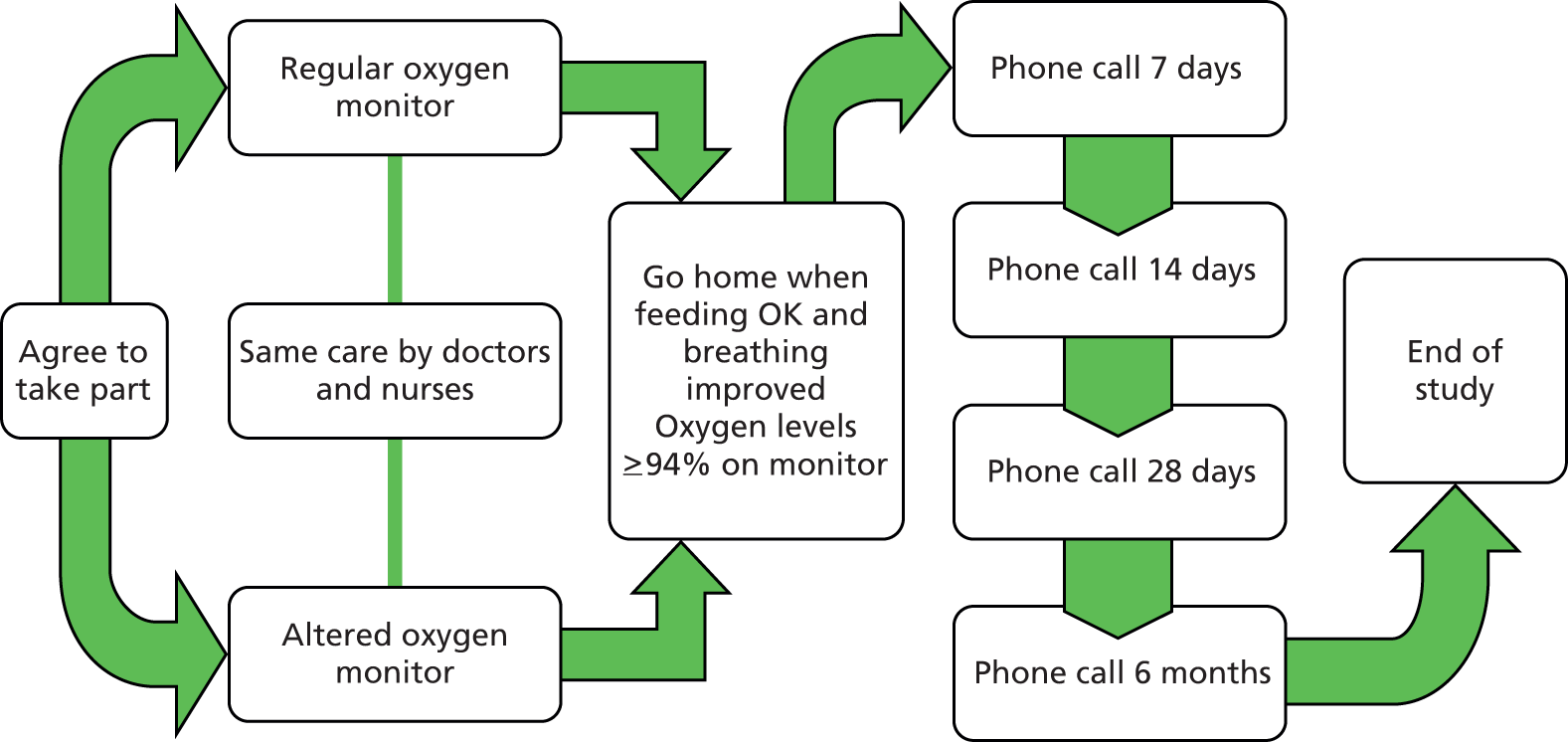
Part 1
What is the purpose of the study?
People with chest infections can have lower blood oxygen levels. As the chest infection gets better the blood oxygen levels go back to normal. Sometimes the improvement in blood oxygen levels is slower than improvements in how people feel. This can happen with bronchiolitis, the condition your child has been diagnosed with. If oxygen levels are very low then we know that giving extra oxygen helps – that question is not being studied in this project. The American Academy of Pediatrics (which advises all children’s doctors in the USA) considers that it would be OK to stop giving extra oxygen earlier than is current practice in the UK. We want to know if we should change UK practice to that recommended in the USA.
Do I have to take part?
It is up to you to decide to let your child join the study. If you agree, we will ask you to sign a consent form. You are free to withdraw your child at any time, without giving a reason. This would not affect the standard of care your child receives.
What will happen to my child if we take part?
As now, your child will go home once they are feeding and breathing comfortably and look improved.
In the UK, children usually stop being given extra oxygen to breathe when their oxygen saturation monitor levels read more than 93%. The American Academy of Pediatrics (which advises all children’s doctors in the USA) considers that it would be OK to stop giving extra oxygen to breathe when oxygen saturation has reached 90%. We think this small difference won’t affect how quickly children get better once they get home, but we want to make sure with this study. In hospital we use oxygen saturation monitors to monitor blood oxygen levels in children with bronchiolitis.
To answer this question we will use two types of blood oxygen (saturation) monitoring machines. An important part of good studies is that no-one knows which monitor is which (until the end of the study). This makes sure that the only difference in the study is the type of oxygen monitor. In this study there is no choice as to which oxygen saturation monitor is given to each child, it is ‘random’.
The oxygen saturation monitors will look the same from the outside. One type will be just the same as all other types seen in hospital. The other type changes the display seen by doctors and nurses (and you) so that the numbers appear slightly higher than they really are when blood oxygen levels are just near healthy levels (once they measure 90% they will actually display 94%). Your child would remain on the oxygen saturation monitor they are randomised to until they leave hospital.
A small number of children need to go to high dependency or intensive care during their stay. These children would switch to a regular non-study oxygen saturation monitor while they were in high dependency or intensive care, and go back onto their original study oximeter once they return to the ward.
How often would we be contacted?
We want to understand how long it takes for your child to get completely better following this illness, how you feel about your child’s illness and how quickly family life takes to get completely back to normal (so that we understand the economic implications for you as a family as well as the health costs of the study).
To understand this we will contact you on just four occasions: at 7, 14 and 28 days from now by phone (if not still in hospital); in 6 months we will contact you one final time by phone to see how your child has been over that period (some infants with bronchiolitis can have problematic cough and chestiness for some weeks).
What are the possible risks of taking part?
We don’t expect any important risks for children from this study, but will monitor for them. Even now, some children with bronchiolitis need to revisit medical services (GP/Hospital/Out of Hours) once they have gone home from hospital, but we want to make sure that doesn’t happen more often in this study.
What are the possible benefits of taking part?
If a child can go home safely at an earlier stage then this has benefits for the hospital (which can use the bed for another child), the child (who is able to go back home with its family) and the family (who can look after the child at home rather than having to come to hospital).
This completes Part 1
If the information in Part 1 has interested you and you are considering participation, please read the additional information in Part 2 before making any decision.
Part 2
What will happen if I don’t want my child to continue in the study?
The study team will ask if information collected up to that time could be used, or whether you would like the information to be destroyed. If your child were still in hospital, they would transfer to a regular oxygen saturation monitor. A study doctor/nurse would discuss with you whether or not you would be happy to continue to have contact from the study team after going home.
Complaints
If you have a concern about any aspect of this study, you should ask to speak to the researchers who will do their best to answer your questions [local contact number]. If you remain unhappy and wish to complain formally, you can do this [insert details e.g. NHS Complaints Procedure or Private Institutional arrangements]. Details can be obtained from [insert local details].
Harm
In the event that something does go wrong and your child is harmed during the research and this is due to someone’s negligence then you may have grounds for a legal action for compensation against Lothian Health Board/University of Edinburgh but you may have to pay your legal costs. The normal National Health Service complaints mechanisms will still be available to you (if appropriate).
Will information collected about my child during this study be kept confidential?
All information that is collected about you and your child during the course of the research will be kept strictly confidential, and any information about you that leaves the hospital/surgery will have your child’s name and address removed so that they cannot be recognised. To make sure information stays confidential we give each child in the study a unique number and only that number appears in the main study computer database.
We will store your child’s initials, date of birth and CHI number (a unique health number for your child incorporating their date of birth and initials and a four digit number) in the randomisation database to ensure that children do not enter the study on two occasions.
Researchers and those monitoring the research (to make sure it is done safely) will be able to see data with your child’s name, address and date of birth. All have a duty to ensure data confidentiality.
The data will be kept for 10 years in a secure place and then disposed of securely.
Informing your GP
If you agree, we will inform your General Practitioner, by letter, that your child is taking part in this study.
What will happen to the results of the research study?
We will publish the results in a medical journal, hopefully in 2014. Participants wishing to be notified of this publication should let the study team know.
Who is funding the research?
The research is funded by the UK National Institute for Health Research (NIHR) HTA programme. (www.hta.ac.uk). The Sponsor of the research is University of Edinburgh/Lothian Health Board.
Who has reviewed the research?
All research in the NHS is looked at by an independent group of people, called a Research Ethics Committee, to protect your interests. This study has been reviewed and given favourable opinion by Lothian Research Ethics Committee.
Further information about the research
The lead for the research in your area who can provide more information about the research or discuss any problems you have with the research is:
Dr [insert name]
[insert address]
Tel: [insert number]
The lead for the study as a whole is:
Dr Steve Cunningham
Consultant Respiratory Paediatrician
Royal Hospital for Sick Children
Sciennes Road
Edinburgh
EH9 1LF
Tel: [insert number]
Should you wish to discuss the study with someone not associated with the study please contact:
[insert name]
[insert address]
Tel: [insert number]
Appendix 1e Bronchiolitis of Infancy Discharge Study Parent Information Sheet Version 3.0, 30 May 2012, English sites
Parent Information Sheet
Bronchiolitis of Infancy Discharge Study (BIDS)
We would like to invite you to take part in our research study. Before you decide we would like you to understand why the research is being done and what it would involve for you and your child. One of our team will go through the information sheet with you and answer any questions you have.
Quick summary
Your child has been diagnosed with a common chest infection ‘bronchiolitis’, and needs to come into hospital for help with feeding and/or breathing. Children admitted to hospital with bronchiolitis go home once they improve and are able to breath and feed OK. At present we keep them in hospital until their blood oxygen has reached a normal level (more than 93% oxygen saturation), even though otherwise they would be fit to go home.
Children’s doctors in the USA have been advised that infants with bronchiolitis who have improved feeding and breathing can be managed without being given extra oxygen once blood oxygen levels are nearly normal (90% oxygen saturation or higher). Many doctors in the UK also think this is sensible as children recovering from bronchiolitis often have mildly low blood oxygen levels despite looking much better and feeding well. At present these children would need to stay in hospital, but we think that this time in hospital does not help recovery and could be time spent at home with family. This study is to investigate whether children going home from hospital once breathing and feeding have improved continue their recovery just as quickly as those who stay a little longer.
Our study doesn’t involve any additional tests. Apart from filling in a questionnaire at the start of the study, there will be no need for further contact with you by the study team until a week from now.
Part 1 tells you the purpose of this study and what will happen to you if you take part. Part 2 gives you more detailed information. Ask if there is anything that is not clear. The study diagram summarises what will happen to your child in the study.

Part 1
What is the purpose of the study?
People with chest infections can have lower blood oxygen levels. As the chest infection gets better the blood oxygen levels go back to normal. Sometimes the improvement in blood oxygen levels is slower than improvements in how people feel. This can happen with bronchiolitis, the condition your child has been diagnosed with. If oxygen levels are very low then we know that giving extra oxygen helps – that question is not being studied in this project. The American Academy of Pediatrics (which advises all children’s doctors in the USA) considers that it would be OK to stop giving extra oxygen earlier than is current practice in the UK. We want to know if we should change UK practice to that recommended in the USA.
Do I have to take part?
It is up to you to decide to let your child join the study. If you agree, we will ask you to sign a consent form. You are free to withdraw your child at any time, without giving a reason. This would not affect the standard of care your child receives.
What will happen to my child if we take part?
As now, your child will go home once they are feeding and breathing comfortably and look improved.
In the UK, children usually stop being given extra oxygen to breathe when their oxygen saturation monitor levels read more than 93%. The American Academy of Pediatrics (which advises all children’s doctors in the USA) considers that it would be OK to stop giving extra oxygen to breathe when oxygen saturation has reached 90%. We think this small difference won’t affect how quickly children get better once they get home, but we want to make sure with this study. In hospital we use oxygen saturation monitors to monitor blood oxygen levels in children with bronchiolitis.
To answer this question we will use two types of blood oxygen (saturation) monitoring machines. An important part of good studies is that no-one knows which monitor is which (until the end of the study). This makes sure that the only difference in the study is the type of oxygen monitor. In this study there is no choice as to which oxygen saturation monitor is given to each child, it is ‘random’.
The oxygen saturation monitors will look the same from the outside. One type will be just the same as all other types seen in hospital. The other type changes the display seen by doctors and nurses (and you) so that the numbers appear slightly higher than they really are when blood oxygen levels are just near healthy levels (once they measure 90% they will actually display 94%). Your child would remain on the oxygen saturation monitor they are randomised to until they leave hospital.
A small number of children need to go to high dependency or intensive care during their stay. These children would switch to a regular non-study oxygen saturation monitor while they were in high dependency or intensive care, and go back onto their original study oximeter once they return to the ward.
How often would we be contacted?
We want to understand how long it takes for your child to get completely better following this illness, how you feel about your child’s illness and how quickly family life takes to get completely back to normal (so that we understand the economic implications for you as a family as well as the health costs of the study).
To understand this we will contact you on just four occasions: at 7, 14 and 28 days from now by phone (if not still in hospital); in 6 months we will contact you one final time by phone to see how your child has been over that period (some infants with bronchiolitis can have problematic cough and chestiness for some weeks).
What are the possible risks of taking part?
We don’t expect any important risks for children from this study, but will monitor for them. Even now, some children with bronchiolitis need to revisit medical services (GP/Hospital/Out of Hours) once they have gone home from hospital, but we want to make sure that doesn’t happen more often in this study.
What are the possible benefits of taking part?
If a child can go home safely at an earlier stage then this has benefits for the hospital (which can use the bed for another child), the child (who is able to go back home with its family) and the family (who can look after the child at home rather than having to come to hospital).
This completes Part 1
If the information in Part 1 has interested you and you are considering participation, please read the additional information in Part 2 before making any decision.
Part 2
What will happen if I don’t want my child to continue in the study?
The study team will ask if information collected up to that time could be used, or whether you would like the information to be destroyed. If your child were still in hospital, they would transfer to a regular oxygen saturation monitor. A study doctor/nurse would discuss with you whether or not you would be happy to continue to have contact from the study team after going home.
Complaints
If you have a concern about any aspect of this study, you should ask to speak to the researchers who will do their best to answer your questions [local contact number]. If you remain unhappy and wish to complain formally, you can do this [insert details e.g. NHS Complaints Procedure or Private Institutional arrangements]. Details can be obtained from [insert local details].
Harm
In the event that something does go wrong and your child is harmed during the research and this is due to someone’s negligence then you may have grounds for a legal action for compensation against Lothian Health Board/University of Edinburgh but you may have to pay your legal costs. The normal National Health Service complaints mechanisms will still be available to you (if appropriate).
Will information collected about my child during this study be kept confidential?
All information that is collected about you and your child during the course of the research will be kept strictly confidential, and any information about you that leaves the hospital/surgery will have your child’s name and address removed so that they cannot be recognised. To make sure information stays confidential we give each child in the study a unique number and only that number appears in the main study computer database.
We will store your child’s initials and date of birth in the randomisation database to ensure that children do not enter the study on two occasions.
Researchers and those monitoring the research (to make sure it is done safely) will be able to see data with your child’s name, address and date of birth. All have a duty to ensure data confidentiality.
The data will be kept for 10 years in a secure place and then disposed of securely.
Informing your GP
If you agree, we will inform your General Practitioner, by letter, that your child is taking part in this study.
What will happen to the results of the research study?
We will publish the results in a medical journal, hopefully in 2014. Participants wishing to be notified of this publication should let the study team know.
Who is funding the research?
The research is funded by the UK National Institute for Health Research (NIHR) HTA programme. (www.hta.ac.uk). The Sponsor of the research is University of Edinburgh/Lothian Health Board.
Who has reviewed the research?
All research in the NHS is looked at by an independent group of people, called a Research Ethics Committee, to protect your interests. This study has been reviewed and given favourable opinion by Lothian Research Ethics Committee.
Further information about the research
The lead for the research in your area who can provide more information about the research or discuss any problems you have with the research is:
Dr [insert name]
[insert address]
Tel: [insert number]
The lead for the study as a whole is:
Dr Steve Cunningham
Consultant Respiratory Paediatrician
Royal Hospital for Sick Children
Sciennes Road
Edinburgh
EH9 1LF
Tel: [insert number]
Should you wish to discuss the study with someone not associated with the study please contact:
[insert name]
[insert address]
Tel: [insert number]
Appendix 2 Summary of protocol amendments
Protocol v1.1 (18 March 2011): initial ethics approval 26 April 2011
Initial approval.
Protocol v2.0 (16 May 2011): non-substantial amendment
Administrative changes.
Protocol v3.0 (29 August 2011): non-substantial amendment
Clarification of safety reporting requirements and change in number of study devices for each site. The changes to the parent card are formatting changes and ability to record the date of scheduled follow-up call.
Protocol v4.0 (12 September 2011): non-substantial amendment
Clarified that study research nurses can take consent.
Protocol v5.0 (7 October 2011): amendment 1 – approved 28 October 2011
Clarification of inclusion/exclusion criteria. It is now explicit that the corrected age of infant determines eligibility. Exclude infants who are admitted directly to HDU/PICU. Addition of guidance for action to be taken at day-28 visit depending on SpO2 measurement. Corrected formatting and typos throughout protocol.
Protocol v6.0 (30 May 2012): amendment 2 – approved 12 June 2012
The day-28 visit will changed to a telephone call (SpO2 was measured at the day-28 visit). The SpO2 data collected in season 1 will be analysed as part of the secondary outcomes. Use text messages to remind parents of the details of scheduled follow-up calls.
Appendix 3a Admission case report form version 1
Appendix 3b Admission case report form version 2
Appendix 3c Pertussis notification case report form
Appendix 3d Discharge case report form version 1
Appendix 3e Discharge case report form version 2
Appendix 3f Discharge case report form version 4: Scottish sites
Appendix 3g Discharge case report form version 4: English sites
Appendix 3h 7-day follow-up case report form
Appendix 3i 14-day follow-up case report form
Appendix 3j 28-day follow-up case report form version 1
Appendix 3k 28-day follow-up case report form version 2
Appendix 3l 6-month follow-up case report form version 1
Appendix 3m 6-month follow-up case report form version 4
Appendix 4 Trial Steering Committee: terms of reference and membership
Terms of reference
-
To provide overall independent supervision of the trial.
-
To monitor the progress of and conduct, in particular, the timely progress of the trial, adherence to the protocol and patient safety.
-
To provide clinical and professional advice relating to the trial design, where relevant.
Roles and responsibilities of the Trial Steering Committee
-
To provide consultation regarding the trial design.
-
To approve substantial amendments (where appropriate) to the trial design and protocol during the course of the trial.
-
To monitor recruitment and follow-up rates and review reports from the trial management committee.
-
To consider new information relevant to the trial, including reports from the DMC (where applicable) and the results of other studies, particularly if the results may have a direct bearing on the future conduct of the trial.
-
On consideration of new information relevant to the trial, make recommendations for appropriate action to the Sponsor/Funder. For example, changes to the trial protocol, additional patient information or stopping or extending the study, to ensure that the rights, safety and well-being of the trial participants are the most important considerations and prevail over the interests of science and society.
-
Attend TSC meetings and provide availability for future TSC meetings.
-
To ensure that appropriate efforts are made to ensure that the results of the trial are adequately disseminated and that due consideration is given to the implementation of the results into clinical practice.
-
To ensure that the trial is conducted in accordance with the principles of Good Clinical Practice.
Frequency of meetings
The TSC met before the trial started, three times during the recruitment period and again at the conclusion of the study. The TSC reports were sent to the Sponsor and Funder.
Membership
-
Professor Mike Shields (chair), Professor of Child Health, Queen’s University Belfast, Belfast.
-
Dr Clare Murray (independent clinician), Senior Lecturer and Paediatric Respiratory Consultant, University of Manchester, Manchester.
-
Dr Colin Powell (independent clinician), Senior Lecturer in Child Health and Honorary Consultant Paediatrician, University of Cardiff, Cardiff.
-
Kay Riding, Lead Paediatric Research Nurse, Children’s Clinical Research Facility, Royal Hospital for Sick Children, Edinburgh.
-
Dr Steve Cunningham (chief investigator), Consultant Respiratory Paediatrician, Department of Respiratory and Sleep Medicine, Royal Hospital for Sick Children, Edinburgh.
-
Dr Steff C Lewis (lead study statistician), Reader in Medical Statistics, Centre for Population Health Sciences, University of Edinburgh, Edinburgh.
-
Fiona Wee/Dr Morag MacLean, ECTU Trial Manager, University of Edinburgh, Edinburgh.
Appendix 5 Data Monitoring Committee
Appendix 6 Trial management
The day-to-day management of the trial was performed by a trial manager in ECTU. During the recruitment phases the trial manager was in direct contact with the sites and chief investigator at least once a week and the chief investigator and trial manager held a monthly telephone conference when all the sites provided participated. The trial manager was responsible for study oversight, overseeing data entry, data quality control and site monitoring.
A Trial Management Group was established and comprised the chief investigator, the trial statisticians, the trial health economists and the trial manager. The group met regularly in person and by telephone. The responsibilities of the group included:
-
producing a statistical analysis plan
-
producing a health economics analysis plan
-
ensuring the statistical and health economics analyses were comprehensive and compatible
-
providing input for and support the chief investigator in preparing the NIHR final study report
-
participating in preparing articles to be submitted to peer-review journals.
List of abbreviations
- A&E
- accident and emergency
- AAA
- acute assessment area
- AAP
- American Academy of Pediatrics
- AE
- adverse event
- BIDS
- Bronchiolitis of Infancy Discharge Study
- CEA
- cost-effectiveness analysis
- CHEERS
- Consolidated Health Economic Evaluation Reporting Standards
- CI
- confidence interval
- CONSORT
- Consolidated Standards of Reporting Trials
- DMC
- Data Monitoring Committee
- ECTU
- Edinburgh Clinical Trials Unit
- ED
- emergency department
- GLM
- generalised linear model
- GP
- general practitioner
- HADS
- Hospital Anxiety and Depression Scale
- HDU
- high-dependency unit
- ICER
- incremental cost-effectiveness ratio
- ITT
- intention to treat
- PICU
- paediatric intensive care unit
- RSV
- respiratory syncytial virus
- SAE
- serious adverse event
- SIGN
- Scottish Intercollegiate Guideline Network
- SpO2
- peripheral capillary oxygen saturation
- TSC
- Trial Steering Committee