Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 11/97/01. The contractual start date was in March 2013. The draft report began editorial review in February 2015 and was accepted for publication in July 2015. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2015. This work was produced by Adams et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
This project involved three linked components:
-
A systematic review of existing research evidence on the effectiveness, acceptability, cost and efficiency of parental incentives and quasi-mandatory schemes for increasing the uptake of vaccinations in preschool children.
-
A qualitative study undertaken with a range of stakeholders (including parents, health and other relevant professionals, and policy-makers) exploring what is and is not acceptable about these schemes and what can be done to improve acceptability.
-
A discrete choice experiment (DCE) exploring the relative preferences of parents and carers of preschool children for approaches to delivering vaccination programmes, including parental incentives and quasi-mandatory schemes, and the predicted uptake rates of these.
These three pieces of work aimed to answer three overarching research questions, respectively. These questions were:
-
According to existing published and unpublished evidence, what is the effectiveness, acceptability and balance of costs and effects to society of using parental incentives and quasi-mandatory schemes to increase the uptake of vaccinations in preschool children in high-income countries?
-
According to key stakeholders in England (including parents, health and other relevant professionals, and policy-makers), what is and is not acceptable about parental incentives and quasi-mandatory schemes for increasing uptake of vaccinations in preschool children? Can anything be done to improve acceptability?
-
What are the relative preferences of English parents and carers of preschool children for a range of characteristics associated with schemes designed to encourage uptake of vaccinations, including parental incentives and quasi-mandatory schemes?
Chapter 2 provides a general introduction to preschool vaccinations and financial incentive interventions, both in general and as applied to preschool vaccinations. The three pieces of work mentioned above are then described in turn in Chapters 3–5. Chapter 6 provides an integrated discussion of findings and conclusions.
Project team and steering group
The work was guided by a project team, a wider steering committee and a lay Parent Advisory Group. Members of the project team, along with their roles, are listed in Chapter 9. In addition, the steering committee included Professor Shona Hilton (Glasgow University), Dr Monique Lhussier (Northumbria University) and Mr Rodolfo Hernandez (Aberdeen University). The steering committee and full project team formally met on three occasions, each time making a number of useful contributions to data interpretation and future directions for the work.
Parent Advisory Group (public involvement)
The Parent Advisory Group consisted of around eight members of an existing parent committee based at a Children’s Centre in North Tyneside. Participants were mothers and grandmothers of children using the centre. The Parent Advisory Group met on four occasions. The first meeting provided an opportunity for researchers and members of the group to get to know each other, and to introduce the project and reflect on findings of the systematic review. In the second meeting, preliminary attributes and levels for the DCE were discussed. The third meeting was used to discuss and ‘sense-check’ early results from the qualitative work. During the final meeting, the full findings from the project were considered and methods for dissemination discussed. The specific contributions made by the Parent Advisory Group are reported in Chapters 3–5.
Chapter 2 Background
Childhood vaccination programmes form a core component of public health strategies worldwide. Nationally and globally, childhood vaccinations have been highly effective in reducing the incidence of, and associated morbidity and mortality from, a range of infectious diseases. 1
Preschool vaccinations in England
The current schedule of recommended vaccinations offered by the NHS for low-risk, preschool children is shown in Table 1. The full schedule involves 14 injections (11 excluding the new influenza programme) plus two orally administered vaccines given at a minimum of eight visits between 2 and 60 months of age (five excluding the new influenza programme). Further vaccinations are recommended for ‘at-risk’ infants and for all children in school years. We refer to the full schedule described in Table 1 as ‘preschool vaccinations’ throughout.
| Vaccine | Recommended age | Coverage (all relevant doses) July–September 2014 (%) | ||
|---|---|---|---|---|
| At 12 months | At 24 months | At 60 months | ||
| DTaP, IPV and Hib, combined 5-in-1; primary course | 2, 3 and 4 months | 93.9 | 95.9 | 95.7 |
| PCV; primary course | 2 and 4 months | 93.5 | – | – |
| MenC; primary course | 3 months | N/A | 94.8 | – |
| Hib/MenC booster | 12–13 months | – | 92.2 | 92.6 |
| MMR; primary course | 12–13 and 40–60 months | – | 92.2 (one dose) | 94.5 (one dose); 88.5 (two doses) |
| PCV booster | 12–13 months | – | 92.3 | – |
| DTaP/IPV booster | 40–60 months | – | – | 88.6 |
| Rotavirusa | 2 and 3 months | 86–88 | – | – |
| Influenzaa | 2, 3 and 4 years | – | – | – |
Vaccination ‘coverage’ is defined as the percentage of those eligible for each primary course of vaccinations, or booster, who receive it. The World Health Organization (WHO) has set a goal of 90% coverage for all vaccinations, with 95% coverage for measles and diphtheria. 1,3 This high level of coverage is recommended both to protect as many vaccinated individuals as possible, and to achieve ‘herd immunity’, where the reservoir of people who can harbour infection is minimised to the extent that unvaccinated individuals are also effectively protected.
Table 1 shows coverage rates in England in 2014. Although coverage rates approach or exceed the WHO targets for most vaccinations, some show much lower rates, in particular both doses of measles, mumps and rubella (MMR) and the diphtheria, tetanus and pertussis (DTaP)/inactivated polio virus booster. Furthermore, coverage rates vary geographically with, for example, coverage of all three doses of the primary course of DTaP/inactivated polio virus/ Haemophilus influenzae type B (Hib) varying between 88.7% (Surrey and Sussex) and 97.1% (Cumbria, Northumberland, and Tyne and Wear). 4
Factors associated with uptake of preschool vaccinations
Systematic reviews have identified a range of factors associated with low uptake of preschool vaccinations. 5–8 These can be grouped into three categories: sociodemographic factors, attitudinal factors and health-care factors.
Sociodemographic factors associated with non-vaccination include being a child of a single, or younger, mother;7 being a younger child in a large family;5,7 and being a child of a family living in more deprived socioeconomic circumstances. 5,7 The association with lower socioeconomic position is not entirely consistent with some evidence that negative publicity around the MMR vaccine had a larger detrimental effect on coverage rates in children living in more affluent circumstances. 9 Looked-after children, those with physical and learning difficulties, those not registered with a general practitioner (GP), those from non-English speaking families, and asylum seekers have also been identified as being at greater risk of not being fully vaccinated. 10,11
Non- or suboptimal vaccination does not necessarily represent a simple omission. Overall, around 50% of UK parents and carers of children who have not received the full schedule of vaccinations have made a conscious decision not to vaccinate. 5 Evidence from systematic reviews suggests that attitudes related to low uptake of vaccinations map closely to the components of the Protection Motivation Theory model. 12 This suggests that behaviour change (e.g. taking a child for vaccination) in response to persuasive communications (e.g. a letter from a general practice surgery) is determined by both a threat appraisal (i.e. the perceived severity of the disease that could be prevented by vaccination and perceived vulnerability to that disease) and a coping appraisal (i.e. perceived efficacy of the vaccination and perceived self-efficacy, or self-confidence, of being able to take the child for the vaccination). 12 Parents who are less likely to have their children immunised are less likely to believe the diseases that vaccines protect against are serious5,6 and less likely to believe that their child is at risk of contracting them. 5,7 They are also less likely to believe that vaccines are effective5,6 and more likely to be concerned about potential side effects. 5–7
In terms of health-care factors, those who have experienced poor relationships with health-care professionals, forget appointments or are unaware of the vaccination schedule are also less likely to have their children vaccinated. 5,6 Parents who have not had their children immunised also tend to have less trust in health professionals. 5,6
It is important to note that these factors are not necessarily independent. For example, mothers living in more deprived circumstances are more likely to have larger families. 13 Furthermore, parents often hold mixed views about vaccination and do not always act in line with their attitudes and beliefs.
Current guidance on increasing vaccination coverage and decreasing differences in coverage
In 2009 the National Institute for Health and Care Excellence (NICE) published guidance on reducing the differences in the uptake of vaccinations among children and young people. 11 This adds to the existing Department of Health strategy on reducing inequalities in uptake of vaccinations. 10 Both of these documents stress the importance of good information recording systems; appropriate training of all relevant health-care professionals; culturally specific parental information provided in a variety of formats; flexible access to vaccination services provided in a range of settings; and repeated, opportunistic checking of children’s vaccination status by a range of professionals. 10,11
The NICE guidance notes that there is little UK research on the effect of parental incentives and quasi-mandatory schemes for increasing vaccination uptake, but that evidence from other countries suggests that these may be effective. 11,14
Definition of parental incentives and quasi-mandatory schemes for increasing uptake of preschool vaccinations
Defining incentives in the context of preschool vaccinations is challenging. In general, behavioural incentives have been defined as motivating rewards which are provided contingent on behavioural performance. 15 However, this definition could be interpreted as including any reward (e.g. a sticker or praise) and not just those with real material value. Furthermore, this definition specifically excludes the converse of motivating rewards: penalties.
Briss et al. 16 identify incentives as interventions that increase demand for vaccinations. These are likely to include both rewards for immunising and penalties for not immunising.
Although rewards that do not have real material value may also increase demand for vaccinations, it is highly likely that in advanced societies, interventions offering rewards with real material value are conceptually different from those offering rewards with social, emotional or tokenistic value. As such, and following Briss et al. ,16 we restrict our definition of incentives to interventions that increase demand for vaccinations by offering contingent rewards with real material value (whether or not these are offered in the form of cash), but widen this to include interventions imposing contingent penalties with real material value (again, whether or not these are imposed in the form of cash).
One form of contingent non-cash penalty with real material value is withholding a universal service from those who do not engage in particular behaviours. If mandatory behaviours are those that are universally required by law, quasi-mandatory ones are those that are almost universally required by law. In the context of vaccinations, quasi-mandatory schemes are generally operationalised as programmes that make access to what would normally be considered a universally provided good or service contingent on either vaccination or a valid reason for non-vaccination, such as religious objections. The most common example is school enrolment programmes, where children must provide vaccination certificates (or evidence of exemption) in order to enrol in school. 17,18 Here, the universally provided service is education. The intervention is only quasi-mandatory as parents can, theoretically, choose not to send their children to a state-funded school. As such, quasi-mandatory interventions can be considered to be a particular type of incentive, that is contingent penalties that restrict access to ‘universal’ goods or services.
Thus, henceforth, we use the term ‘parental incentive scheme’ to describe both rewards and penalties with real material value that are contingent on having, or not having, a preschool child immunised.
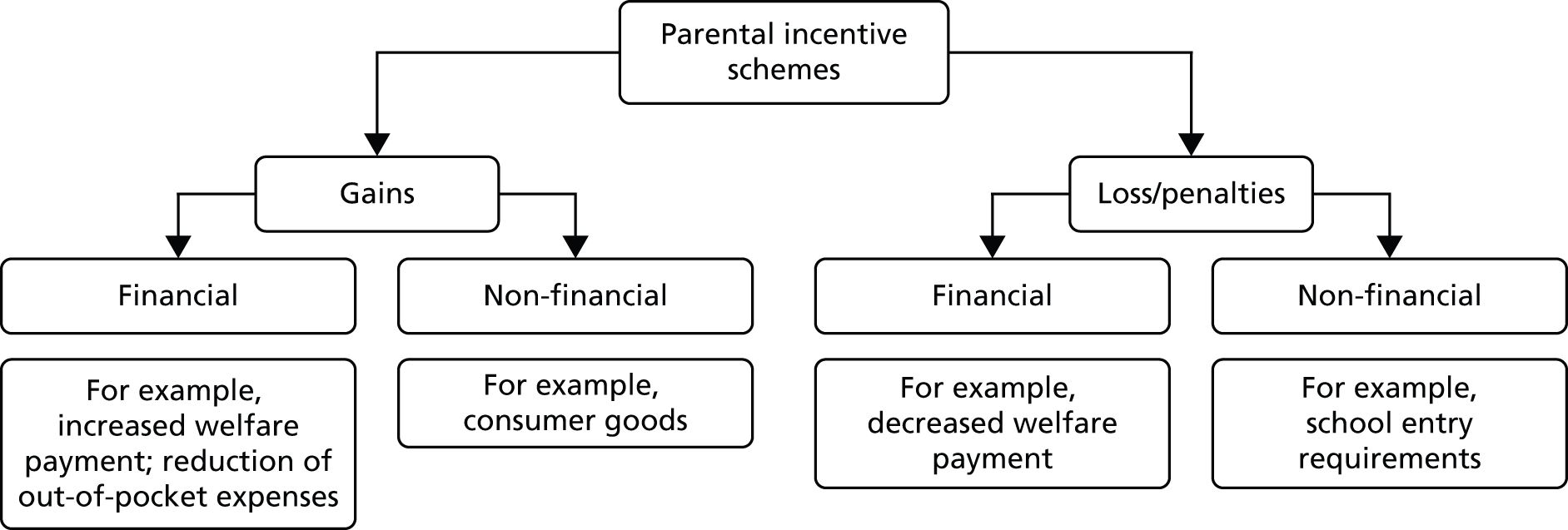
Parental incentive schemes can be further conceptualised using the framework in Figure 1.
FIGURE 1.
Conceptual framework of parental incentive schemes for encouraging the uptake of preschool vaccinations.
Theory of health-promoting incentives and parental incentive schemes for preschool vaccinations
Parental incentive schemes are grounded in both psychological and economic theory.
Operant learning theory describes how behaviours can be modified by association of behaviour with rewarding and punishing stimuli. 19 A rewarding incentive that is provided contingent on performance of a behaviour, such as vaccination, would be expected to increase the behaviour by acting as a positive reinforcement. Similarly, a penalty that is associated with behavioural non-performance would also be expected to increase behaviour.
However, as has been previously described, incentive schemes may be more complex than ‘simply’ providing positive and negative behavioural reinforcers. 20 For example, in order for an incentive to be given (or imposed), there must be clear monitoring of behaviours to ensure that the conditions for receiving the incentive have been met. This monitoring could be self-monitoring, or it could be done by professionals – a process which would be expected to increase contact with professionals. Both self-monitoring and increased contact with professionals might be expected to have a positive impact on behaviour, independent of any effect of the incentive itself. 20,21
The economic concept of ‘time preference’ and the related psychological concept of ‘time perspective’ suggest that one important reason for not engaging in health-promoting behaviours is that the rewards and benefits of these behaviours are often delayed and uncertain, while the costs and harms are immediate and certain. 22 When this is coupled with the consistent human preference for immediate (vs. delayed) rewards and benefits, or cost and harm avoidance, the result is that many healthy behaviours are avoided. 23,24 For example, taking a young child to be immunised often involves a certain outcome of inflicting pain on the child today (i.e. a harm) for a gain in health, through disease avoidance (i.e. a benefit) that is uncertain and may be realised only after many years. Most parents, when temporally distant from both options, will value the long-term health benefit of avoiding life-threatening diseases in their children more than the pain avoided by not taking them for the vaccination. However, when faced with the immediate choice between inflicting pain and not, the immediate benefit, or harm avoided, is preferred and the vaccination is avoided. This suggests that one way of promoting healthier behaviours would be to change the temporal pattern of benefits and harms associated with them, for example by attaching an immediate reward, or incentive, to behavioural performance. 25,26
A number of theoretical concerns with the use of health-promoting incentives have also been raised. It has been suggested that providing extrinsic motivators, such as incentives, for behaviour change erodes internal motivation. The driver of behaviour becomes the incentive, rather than any personal desire to perform the behaviour or achieve the health outcome. 25,27 The expected effect of this is that any behaviour change achieved by introduction of an incentive would be unlikely to persist after the incentive is withdrawn. Incentives may also erode self-efficacy:28 an individual’s belief in their ability to perform a behaviour. This is a well-documented determinant of successful behaviour change. 29 It is possible that attaching an incentive to successful behaviour change substantially increases the costs of failure, making those who have failed on one occasion less likely to believe they can successfully achieve the change and so less likely to try again. Both of these issues may be less important for behaviours like vaccination that do not require sustained behaviour change.
Previous research on the effectiveness of health-promoting incentives
Despite this theoretical support for the use of incentive schemes, empirical evidence of their effectiveness is mixed.
Conditional cash transfer schemes that require performance of health-promoting behaviours are widespread in low- and middle-income countries. These schemes can supplement household income by up to 20%,30 are generally targeted at families with young children, and require behaviours such as regularly attending antenatal care, vaccination of children and regular school attendance. A recent Cochrane review reported that such conditional cash transfer schemes in low-income countries are generally successful in improving clinic attendance and the uptake of vaccinations. 31 This has prompted interest in health-promoting incentives in high-income countries. 32–34
One systematic review and meta-analysis described ‘overwhelming evidence of positive effect’ for financial incentives for abstinence among substance users,35 and this is supported by a further systematic review and meta-analysis. 36 However, both analyses highlight that the long-term effects of such incentives are not clear and that there is evidence of effects decreasing over time and after incentives are withdrawn – although it should be noted that this is the case with many public health and behaviour-change interventions. This conclusion is supported by a Cochrane review on the use of incentives to promote smoking cessation. 37 Similarly, two systematic reviews found short-term effects of financial incentives in promoting weight loss, but less evidence of long-term benefits. 38,39
The benefits of incentives are clearer when they are used to promote shorter-term, or one-off, behaviours such as attendance for screening, or supervised treatment. 28,40 A number of authors have concluded that, in high-income countries, incentives may be useful in promoting ‘simple’ one-off behaviours, but that their use in achieving more ‘complex’, long-term behaviour change may be minimal. 25,28,30,34
Attendance for preschool vaccinations is a series of discrete behaviours over a time-limited period. As such, it is the type of behaviour that would be expected to be responsive to incentives.
Previous research on the effectiveness of parental incentive schemes for preschool vaccinations
Previous research on the effectiveness of parental incentive schemes for increasing uptake of preschool vaccinations is considered according to the conceptual framework in Figure 1.
Financial and non-financial gains
In practice it can be difficult to separate financial and non-financial gains, as these have often been used in combination. For example, in 1998, Australia introduced legislation linking two welfare payments to preschool vaccinations. The Maternity Vaccination Allowance is a means-tested payment of AU$200 (£132; 75% of mothers are eligible) provided conditionally on children’s vaccinations being up to date by their second birthday. This is a direct financial gain. All families in Australia are also eligible for Child Care Benefit of AU$22–130 (£15–86) per week, which is given in part payment for child care costs dependent on children having up-to-date vaccinations. 41 As the benefit is child care costs, rather than straightforward cash-in-hand, this can be considered a non-financial gain. Within 2 years of the introduction of both payments, coverage among 2-year-olds in Australia increased from 80% to 94%. However, it is difficult to separate the differential effects of the two components of this programme.
In the USA, one study found that giving tickets for a lottery to win a US$50 (£32) grocery voucher in exchange for vaccination increased uptake in preschool children. Another study found that tickets for a lottery to win cash prizes of up to US$100 (£65) also had a small positive effect. 42 However, US$10 (£6) gift certificates for nappies and shoes given in exchange for attendance for vaccinations did not lead to statistically significant increases in coverage. 43
It would be expected that larger value and more certain rewards (e.g. cash) would be more effective than smaller and less certain ones (e.g. a lottery ticket). However, few, if any, studies in this area have justified the value, or type, of incentive offered or explored the relative effectiveness of different values, or types, of incentive. Similarly, it might be expected that financial incentives would be more effective in individuals living in more deprived circumstances. Again, few studies have explored the differential effect of incentives according to socioeconomic position.
Financial losses
Two studies have explored the use of welfare-linked financial penalties for failing to keep children’s vaccinations up to date. One study in Maryland, USA, imposed a US$25 (£16) monthly penalty on parents receiving welfare payments who did not vaccinate their children. 44 The intervention had no effect on coverage rates, but this may be because other benefits increased in response to the penalty, resulting in an average overall loss of only US$10 (£6) per month. In Georgia, USA, a similar intervention, where all benefits relating to the child in question were lost (value not stated), had a significant positive impact on coverage rates. 45 It is possible that these divergent findings are explained by differences in the actual value of the loss incurred in the different programmes. But, as above, the minimum level of effective loss has not been justified or explored by any authors.
Non-financial losses
The only non-financial loss incentives that have been studied in relation to preschool vaccinations are school enrolment requirements. In their systematic review of studies from industrialised countries, Briss et al. 16 concluded that ‘sufficient scientific evidence exists that vaccination requirements for child care, school and college attendance are effective in improving vaccination coverage and in reducing rates of disease’. This is supported from findings from an evidence analysis commissioned by NICE. 46 Both reviews included studies with a range of both vaccination and disease outcomes suggesting that the conclusion is not limited to any one type of vaccination. However, except for one study based in Canada, all of the studies were conducted in the USA, making them of limited relevance to a UK setting. There is also some evidence that such programmes can reduce inequalities in the uptake of vaccinations. 18
Previous research on acceptability of health-promoting incentives
The acceptability of health-care interventions has a number of dimensions and must be considered from the viewpoint of a number of stakeholder groups, particularly the target population, professionals involved in intervention delivery, and policy-makers responsible for intervention implementation. In order for any health-promoting intervention to be effective in practice, members of all stakeholder groups must be both willing and able to engage with it. 47
The best overall measure of acceptability of an intervention is probably take-up of that intervention (i.e. revealed acceptability). 48 However, this requires that interventions are already in place and is unable to distinguish between acceptability among different stakeholder groups. Thus, uptake might be low because the target population are unwilling to engage with an intervention, or because professionals are unwilling to deliver it. Overall uptake rates may also be confounded by factors that limit access to services and have little to do with acceptability. In a context where interventions have yet to be implemented, and in order to differentiate between acceptability among the different stakeholders, the views (i.e. stated acceptability) of relevant stakeholders must be captured. This can be done using in-depth qualitative methods or quantitative survey methods. Both are likely to yield important insights.
Health-promoting incentives have been described as ‘coercive’. 49 This is seen by some not only as ethically questionable but also, given that poorer individuals may be more receptive to financial incentives, as socially divisive. 50 There is also a potential and, in some cases, actual, risk of incentives designed to promote healthy behaviours perversely creating incentives to pursue less healthy behaviours. 25 For instance, the introduction of a cash transfer, conditional on attendance for antenatal care, in Honduras was associated with an increase in the birth rate. 30
In one study exploring stated acceptability of financial incentives versus hypothetical injections or tablets of equal effectiveness, incentives were rated as universally less acceptable and less fair by respondents in both the UK and the USA. 51 However, media coverage of health-promoting incentives in the UK is generally more positive, with only 13% of articles published in the popular and medical press on this topic during 2005–10 being entirely unfavourable. 52
Previous research on acceptability of parental incentive schemes for preschool vaccinations
Few studies have explored views around acceptability of parental incentive schemes for increasing uptake of preschool vaccinations. One study in the early 1990s (before the MMR controversy53 began) found that the majority of a small sample of UK primary school head teachers would be willing to ask about vaccination status at school enrolment and to recommend that children were fully immunised. 54 The issue of making enrolment contingent on full vaccination was not explored. A more recent study, conducted after the MMR controversy, found that parents and health visitors from the London area were not generally supportive of linking welfare payments to vaccination or restricting school entry to those who were fully immunised, as they felt that this undermined parental choice. 55
Conclusions and unanswered questions
There are empirical and theoretical reasons to believe that parental incentives may be effective as a method of increasing uptake of preschool vaccinations. Fewer studies have explored acceptability, and evidence on this is more mixed. Although a number of reviews have explored the use of parental incentives for increasing uptake of preschool vaccinations,16,40,46 no recent systematic review has explored the effectiveness, acceptability, and economic costs and consequences of such interventions in high-income countries. Furthermore, little attention has been paid to how both effectiveness and acceptability of parental incentives varies according to the characteristics of these schemes and their recipients – including incentive value (both absolute or relative to income), incentive type (e.g. cash or voucher, certain or uncertain reward), how such incentive schemes are organised and delivered (e.g. what other behavioural-change techniques are used alongside incentives) – or how acceptability and effectiveness interact. For example, it is possible both that more effective incentive schemes are more acceptable, and that the value of incentive required to make a scheme effective is considered unacceptably large and coercive.
This project comprised three distinct, but interlinked, stages: a systematic review of existing work exploring the effectiveness, acceptability and balance of economic costs and effects of parental incentive schemes for increasing uptake of vaccinations in preschool children; a qualitative study further exploring the stated acceptability of such schemes among a range of key stakeholders, including particular components that are and are not acceptable and what can be done to improve acceptability; and a DCE to establish the relative preferences for, and likely uptake of, a range of different vaccination strategies among parents and carers of preschool children. The results of the systematic review informed the qualitative study, and the results of both the systematic review and qualitative study informed the DCE.
Chapter 3 Systematic review
A systematic review of existing research evidence on the effectiveness, acceptability and economic costs and consequences of parental incentive and quasi-mandatory schemes for increasing uptake of vaccinations in preschool children in high-income countries, compared with usual care or no intervention, was conducted.
Research questions
The systematic review aimed to answer the following research questions:
-
What is the existing evidence on parental incentive and quasi-mandatory schemes for increasing uptake of vaccinations in preschool children in high-income countries, compared with usual care or no intervention, in terms of:
-
effectiveness
-
acceptability
-
economic costs and consequences?
-
This work has been described in a manuscript published in Pediatrics. 56 A condition of the licence for reproduction of substantial components of that article is that the full manuscript is reproduced, word for word, in full. This chapter is, therefore, reproduced with permission from Pediatrics, Vol. 134, Pages e1117–28, Copyright © 2014 by the American Academy of Pediatrics.
Introduction
Childhood vaccination programmes form a core component of public health strategies worldwide, and have been highly effective in reducing the incidence of, and morbidity and mortality from, a range of infectious diseases. 57
The WHO has a goal of 90% coverage for all vaccinations, with 95% coverage for measles and diphtheria. Coverage rates in the UK and USA approach or exceed the WHO targets for most preschool vaccinations. 58 However, coverage rates also vary substantially within countries with high overall coverage. For example, DTaP coverage at 19–35 months in the USA varies from 77% in Idaho to 91% in Connecticut. 59
Factors identified as contributing to variation in vaccination coverage fall into the categories of sociodemographic, attitudinal and health care. Parents living in less affluent circumstances, who lack trust in health-care professionals, have limited access to health care or believe that the disease protected against is not serious, are less likely to have vaccinated children. 5,6,8 Other factors related to uptake include concerns over pain, safety and side effects; access to transport and child care; and a lack of familiarity with vaccination schedules. 5,6
Financial incentives have been successfully used to promote uptake of vaccinations in developing countries,31,60 but are not always viewed as acceptable. Criticisms include that they are socially divisive and coercive. 49 However, recent work has found that financial incentives can be acceptable given that the problems addressed are perceived to be serious, other interventions ineffective, and the behaviours required particularly difficult to achieve. 51,52 Quasi-mandatory policies, such as requiring vaccinations for school enrolment (‘quasi’ because parents can exempt their child on e.g. philosophical or religious grounds), are widely implemented in some countries (e.g. the USA), and have the potential to have large impacts on families and communities, in terms of both vaccination rates achieved and education lost. They have also been reported to be effective in some cases. 61
However, to date, no existing systematic review has comprehensively explored the effectiveness of parental financial incentive and quasi-mandatory interventions in high-income countries. Similarly, there is a lack of existing review-level evidence on the cost-effectiveness and acceptability of these interventions.
One existing systematic review explored the effectiveness of financial incentives for the uptake of all healthy behaviours, including vaccinations, in low- and middle-income countries. 31 Given the substantially different resource and health-care settings in high- and middle- versus low-income countries, findings cannot be assumed to be generalisable. Two previous reviews on methods for increasing vaccination uptake have included sections on financial incentives, but neither focused on preschool children in particular. 16,62 There are many reasons why individuals may act differently for themselves than for their children, and findings on offering incentives to adults to vaccinate themselves are not necessarily generalisable to the context of offering incentives to parents to vaccinate their children. Furthermore, only one of these previous reviews was systematic and studies were included only up to 1997 – more than 15 years ago. 16
In order to fill this evidence gap, a systematic review of existing research evidence on the effectiveness, acceptability and economic costs and consequences of parental incentive and quasi-mandatory schemes for increasing uptake of vaccinations in preschool children in high-income countries, compared with usual care or no intervention, was conducted.
Methods
The review was registered with PROSPERO (International Prospective Register of Systematic Reviews) before searches commenced (registration number CRD42012003192). There were no substantive deviations from protocol. The review is presented in accordance with PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidance. 63
Inclusion criteria
One systematic review was performed, which had three parallel components: effectiveness, acceptability and economic. Studies that met the criteria for either the effectiveness or the acceptability components were screened for inclusion in the economic component. Throughout, parental incentive and quasi-mandatory schemes were defined as ‘interventions that increase demand for vaccinations by offering contingent rewards or penalties with real material value; or that restrict access to universal goods or services’. The inclusion criteria for all three components are summarised in Table 2. No studies were excluded on the basis of language. Relevant articles were translated locally as required.
| Component | Effectiveness component | Acceptability component | Economic component |
|---|---|---|---|
| Population | Parent of preschool children living in high-income countriesa | Member of any relevant stakeholder group living in high-income countriesa | Included in either of the other components |
| Intervention | Interventions that increase demand for vaccinations by offering contingent rewards or penalties with real material value; or quasi-mandatory schemes that restrict access to ‘universal’ goods or services | Interventions that increase demand for vaccinations by offering contingent rewards or penalties with real material value; or quasi-mandatory schemes that restrict access to ‘universal’ goods or services | Included in either of the other components |
| Comparator | Usual care or no intervention | Usual care or no intervention | Included in either of the other components |
| Outcome | Uptake of preschool vaccinations | Acceptability of the intervention | Economic costs and consequences of the intervention to parents or society |
| Study design | RCTs, cluster RCTs, controlled before-and-after studies, time series analysesb | Any study design | Included in either of the other components |
Information sources
The following databases were searched: Cumulative Index to Nursing and Allied Health Literature, Applied Social Science Index and Abstracts, International Bibliography for the Social Sciences, PsycInfo, MEDLINE, Web of Science, EMBASE, Education Resources Information Center, Health Economic Evaluations Database and The Cochrane Library (see Appendix 1 for an example search strategy). The reference lists of studies meeting the inclusion criteria, and relevant reviews16,40,62 were searched for additional publications, and citation searches of studies meeting the inclusion criteria were run in the Science and Social Science Citation Indices. Grey literature was searched via e-mails sent to relevant online discussion groups and entry of the formal search strategy terms into GoogleTM (Mountain View, CA, USA; www.google.com). When both an internal report and a peer-reviewed paper on the same study were retrieved, peer-reviewed findings were favoured, but additional information from reports was used where relevant. Searches were carried out in February 2013, with no limits on earliest date of searches (i.e. database inception to February 2013).
Study selection
The initial screening of titles and abstracts was conducted by SW. Full texts were screened independently by two researchers (SW and JA) against the inclusion criteria. Discrepancies were resolved by discussion. Where publications lacked the details required for a decision, the authors were contacted for further details.
Data collection and data items
A data extraction form was developed to record data on nature and location of study participants, age and gender of children involved, time period, socioeconomic status of participants, type of intervention, study design, comparator, vaccination and results. Data were extracted independently by two reviewers (SW and JA), with consensus reached by discussion. To allow comparisons, values of financial incentive were converted to their equivalent commodity real-price value in US$ in 2012, the latest date for which data were available when searches were conducted. 66
Information on economic costs and consequences in all papers was assessed by a health economist (LT). This focused on whether or not studies reported the cost of delivering the incentive and the consequences of undertaking, or not undertaking, the desired activity. Methods for the review of the economic evidence followed those set out by the Cochrane and Campbell Collaborations. 67
Risk of bias
The quality and risk of bias of all studies meeting the inclusion criteria were independently assessed by two researchers (SW and JA). Quantitative studies were assessed using the Quality Assessment Tool for Quantitative Studies, which has acceptable test-retest and construct validity. 68 Qualitative studies were assessed using the Critical Appraisal Skills Programme checklist. 69 Methods derived from Campbell and Cochrane Economic Methods Group were used to assess the quality of studies in the economic component. 67 Quality ratings were used to inform the approach to synthesis.
Synthesis of results
A narrative synthesis was performed throughout. Within the narrative synthesis, interventions were described using an existing framework. 70 A meta-analysis was considered for all three components. In the effectiveness component, two studies could, theoretically, have been meaningfully combined in a meta-analysis. 44,45 However, one was at high risk of bias,44 leaving any sensitivity analysis with only one included study. Thus, meta-analysis was not considered appropriate for the effectiveness component.
Studies in the acceptability component were more heterogeneous in design, and meta-analysis was inappropriate. Following recommendations of the Cochrane and Campbell Collaborations, the economic data were not quantitatively synthesised; rather, a narrative synthesis was adopted.
Results
Four studies were identified that met the criteria for inclusion in the effectiveness component,42,44,45,71 six studies were identified for inclusion in the acceptability component72–77 and one study was identified for inclusion in the economic component (Figure 2). 76
FIGURE 2.
Flow diagram showing the identification, inclusion and exclusion of studies.

Studies included in the effectiveness component consisted of one cluster randomised controlled trial (RCT),42 two non-clustered RCTs44,45 and one time series analysis. 71 Studies included in the acceptability component were primarily surveys,72,76 including one survey that made use of discrete choice modelling methods,75 with one qualitative study using semistructured interviews77 (Table 3).
| Study | Country | Population | n | Interventiona | Comparator | Outcome(s) | Study design | Results |
|---|---|---|---|---|---|---|---|---|
| Effectiveness component | ||||||||
| Yokley and Glenwick (1984)42 | USA | Preschoolers (aged < 5 years) registered at public health clinic not UTD with vaccinations Mean (SD) age of children = 37.3 (18.2) months; 50% male |
Intervention children, n = 183; control children, n = 191 | Parents sent tickets for cash lottery that could be entered when attended vaccination clinic, with prizes from US$55.20–221 | Usual care | n attending clinic for any reason n attending for vaccination n vaccinations given |
Cluster RCT clustered at family level with follow-up at 2 weeks, 2 months and 3 months | At each follow-up time point, the intervention was associated with significantly more attendance for any reason, attendance for vaccination and number of vaccinations |
| Minkowitz et al. (1999)44 | USA | Welfare claimants from Maryland Children aged 3–24 months; 51% male |
Intervention children, n = 911; control children, n = 864 | Loss of US$38.70 welfare benefits for failing to verify children’s vaccinations | Usual care | UTD for DTaP, polio and MMR | RCT with follow-up at 1 and 2 years | No difference in UTD rates for any vaccinations at 1- or 2-year follow-up |
| Kerpelman et al. (2000)45 | USA | Welfare claimants from Georgia Mean age of intervention children = 3.22 years; 50% male. Mean age of control children = 3.34 years; 48.5% male |
Intervention children, n = 1725; control children, n = 1076 | Loss of welfare benefit, with amount depending on family size and child’s age | Usual care | UTD for DTaP, MMR, polio, Hib and HBV UTD for full series at age 2 years |
RCT with follow-up at 1, 2, 3 and 4 years | At 1, 2, 3 and 4 years, intervention associated with greater uptake of all vaccinations. This difference was significant except for HBV at 1 year and Hib at 1 and 2 years At age 2 years, the intervention was associated with higher series completion |
| Abrevaya and Mulligan (2011)71 | USA | State- and individual-level data on parents from National Vaccination Surveys, 1996–2007 Children aged 19–35 months; 51% male |
324,553 children | Day-care or school entry restricted to those with varicella vaccination | Usual care | Varicella vaccination | Time series analysis from 1 year pre intervention to 7 years post intervention | At state level, mandate effective from introduction to 6 years post introduction, peaking at 2 years post introduction At individual level, mandate was effective from introduction to 5 years post introduction, peaking at 1 year post introduction |
| Acceptability components | ||||||||
| Schaefer Center (1997)76 | USA | Recipients and staff of incentive programme | 1331 | Penalty of loss of US$38.70 from welfare benefits for failing to verify children’s vaccinations | Usual care | Views on interventions | Survey | 73% of recipients thought that the penalty was fair 66.7% of recipients thought that the penalty would motivate parents 73.5% of staff thought that behaviour could be changed by penalties Majority of staff believed that both the threat and the imposition of penalty were effective |
| Freed et al. (1998)74 | USA | District and county health department directors | 75 | State laws allowing school or day-care entry to be restricted, criminal misdemeanour charges to be brought, or injunctions to be filed against parents for not keeping children’s vaccinations UTD | No comparator | Experience of, and views on, intervention | Survey | 100% were aware of their authority to enforce school and day-care restrictions; 83% were aware of criminal misdemeanour charges; 65% were aware that they could file injunctions 99% believed that non-vaccinated children should be restricted from school or day care 83% believed that misdemeanour charges should be brought 5% reported that misdemeanour charges had been brought; 24% had threatened to do so 83% believed injunctions should be filed; none had done so |
| Bond et al. (1999)73 | Australia | Parents of children regularly attending council-run day care in metropolitan area Children aged < 3 years (except 62 who were older); 50% male |
1722 families with 1779 eligible children | Additional welfare payments of AU$29.30–175 per week for child care; plus one off payment of AU$307 if UTD for all vaccinations | No comparator | Views on intervention | Survey | 30% believed that incentives should be given to parents for immunising their child, although ‘many’ believed that the child’s health and not monetary reasons should be the motivator ‘About 30%’ believed that the decision to immunise would not be affected by intervention |
| Bond et al. (2002)72 | Australia | Parents of children regularly attending council-run day care in metropolitan area Children aged < 3 years |
1706 families with 1793 eligible children | Additional welfare payments of AU$29.30–175 per week for child care; plus one off payment of AU$307 if UTD for all vaccinations | No comparator | Views on intervention | Survey | ‘About 30%’ believed that intervention had not influenced their decision to immunise 4% reported that they had kept their children’s vaccinations UTD because they relied on related payments |
| Hall et al. (2002)75 | Australia | Parents of children aged < 12 years 50% aged < 5 years |
50 | School entry restricted to those UTD for all vaccinations | Range of other interventions to promote vaccination | Stated preference for vaccination uptake | Survey; DCM | Most respondents preferred vaccination under most scenarios; 31% chose not to vaccinate in all scenarios. Requiring vaccination for school entry increased vaccination preference from 75% to 92% |
| Tarrant and Thomson (2008)77 | Hong Kong | Parents of children aged 6 months to 3 years receiving secondary health care | 15 | Day-care and school entry restricted to those UTD for all vaccinations | No comparator | Views on intervention | Semistructured person-centred interviews | Day-care and school entry restriction identified as contributing to high vaccination rates, within a system of other contributory factors |
Interventions in included studies comprised proof of vaccination for school or day-care entry,71,75,77 loss of welfare benefits44,45,72,73,76 or the imposition of criminal misdemeanour charges74 for non-vaccination, and entry into a cash lottery for attending for vaccination (Table 4). 42
| Study | Direction | Form | Magnitude (US$ 2012) | Certaintya | Target | Frequency | Immediacy | Schedule | Recipient |
|---|---|---|---|---|---|---|---|---|---|
| Effectiveness component | |||||||||
| Yokley and Glenwick (1984)42 | Positive reward | Cash lottery | US$55.20–221 | Uncertain chance | Clinic attendance and vaccination uptake | Once | No more than 2 months | Fixed | Parent |
| Minkowitz et al. (1999)44 | Avoidance of penalty | Welfare benefits | US$38.70 | Certain | Vaccination uptake | Reassessed 6-monthly | Written warning prior to sanction | Fixed | Parent |
| Kerpelman et al. (2000)45 | Avoidance of penalty | Welfare benefits | Variable | Certain | Vaccination uptake | Reassessed 6-monthly | Oral or written warning prior to sanction | Fixed | Parent |
| Abrevaya and Mulligan (2011)71 | Avoidance of penalty | Day-care or school entry | Loss of education | Certain | Vaccination uptake | Unclear | Unclear | Fixed | Parent and child |
| Acceptability component | |||||||||
| Schaefer Center (1997)76 | Avoidance of penalty | Welfare benefits | US$38.70 | Certain | Vaccination uptake | Reassessed 6-monthly | Written warning prior to sanction | Fixed | Parent |
| Freed et al. (1998)74 | Avoidance of penalty | Day-care or school entry; criminal charges; parental injunctions | Loss of education, loss of parental freedom | Certain | Vaccination uptake | Unclear | Written warning prior to sanction | Fixed | Parent and child |
| Bond et al. (1999)73 | Avoidance of penalty | Welfare benefits | AU$29.30–175, plus one-off payment of AU$307 | Certain | Vaccination uptake | Weekly | Unclear | Fixed | Parent |
| Bond et al. (2002)72 | Avoidance of penalty | Welfare benefits | AU$29.30–175, plus one-off payment of AU$307 | Certain | Vaccination uptake | Weekly | Unclear | Fixed | Parent |
| Hall et al. (2002)75 | Avoidance of penalty | School entry | Loss of education | Certain | Vaccination uptake | Unclear | Unclear | Fixed | Parent and child |
| Tarrant and Thomson (2008)77 | Avoidance of penalty | Day-care or school entry | Loss of education | Certain | Vaccination uptake | Unclear | Unclear | Fixed | Parent and child |
Risk of bias within studies
Of the studies in the effectiveness component, three were at a low risk of bias,42,45,71 while the fourth was at a strong risk of bias. 44 All of the quantitative studies in the acceptability component were at a strong risk of bias, and, in particular, were weak on study design and on data collection methods (Table 5). The qualitative study in the acceptability component77 lacked details of recruitment and assignment of patients to intervention groups, justification of data collection methods, and adequate discussion of reflexivity and how data saturation and contradictory data were dealt with.
| Author | Selection bias | Study design | Confounders | Blinding | Data collection | Withdrawals | Global rating |
|---|---|---|---|---|---|---|---|
| Effectiveness component | |||||||
| Yokley and Glenwick (1984)42 | |||||||
| Minkowitz et al. (1999)44 | N/A | ||||||
| Kerpelman et al. (2000)45 | |||||||
| Abrevaya and Mulligan (2011)71 | N/A | ||||||
| Acceptability component | |||||||
| Schaefer Center (1997)76 | |||||||
| Freed et al. (1998)74 | N/A | N/A | |||||
| Bond et al. (1999)73 | N/A | N/A | |||||
| Bond et al. (2002)72 | N/A | ||||||
| Hall et al. (2002)75 | N/A | N/A | |||||
Effectiveness component
All studies in the effectiveness component were set in the USA.
Individual- and state-level data from the US National Vaccination Survey were used to conduct an interrupted time series study of the effects of school and day-care entry mandates on uptake of varicella vaccination in preschool children. 71 Significant effects were seen in the year of mandate introduction at both individual and state level. At both state and individual level, mandates were associated with a 2.6%-point increase in vaccination uptake in the first year. The effects at the state level peaked 2 years after introduction and were extinguished by 6 years. At the individual level, the effects peaked at 2 years post mandate and were extinguished by 5 years.
A cluster RCT of children who were not up to date with DTaP, polio or MMR vaccinations compared a cash lottery ticket incentive (combined with a vaccination prompt) with a no-intervention control. 42 The cash lottery ticket incentive (US$55.20–221 in 2012 USD), and postal prompt advising that the lottery could be entered on attendance at the clinic, was associated with a significant 21% increase in numbers of vaccinations received, compared with control. The effect persisted to at least 3 months after the incentive expired, with a 31.6% increase in number of vaccinations received, compared with control.
In a RCT of families in receipt of welfare benefits, no effect was found from a penalty of US$38.70 (in 2012 USD) for failing to have a child vaccinated for DTaP, polio and MMR. 44 However, those who were penalised tended to have more children, qualifying them for extra welfare benefits, and this may have reduced the financial impact of the penalty. 44,76
A RCT found significant effects of cutting welfare benefits when children were not up to date for five preschool vaccinations. 45 Significantly more of the intervention (72.4%) than the control (60.6%) group achieved vaccination series completion. The authors note that parents rarely lost benefits and the threat, rather than the imposition, of the penalty appeared to be sufficiently incentivising.
Acceptability component
Of the six studies included in the acceptability component, three were conducted in Australia,72,73,75 two in the USA74,76 and one in Hong Kong. 77
Two studies were based on the Australian government’s incentive schemes introduced in 1998 linking child care subsidies to vaccination, collecting data before and after introduction of the scheme. 72,73 Prior to the introduction of the scheme, only 30% of respondents said that incentives should be given to parents for immunising their children, with many saying that health promotion rather than finance should be the motivation for vaccination, and that education could encourage this. 73 In the follow-up study, only 4% of parents reported child care benefits as motivating them to keep their children’s vaccinations up to date. 72
Hall et al. 75 used stated preference discrete choice modelling to predict the optimal characteristics of a preschool varicella vaccination programme. Survey data collected from parents indicated that requiring vaccination for school entry was associated with a greater preference for vaccination uptake.
Freed et al. 74 describe North Carolina’s statute requiring age-appropriate vaccination for school and day-care entry that allows criminal misdemeanour charges and injunctions to be brought against non-compliant parents. County health directors, whose decision it was to implement criminal statutes, were interviewed on their attitudes towards the statute. Most respondents (83%) believed that criminal charges should be brought, but only 5% were aware of this ever being done, and none had filed an injunction themselves. Most respondents (99%) agreed that children should be excluded from school or day care if they were not up to date with vaccinations. There was some belief that using a criminal law in this context was too expensive, excessively punitive and politically inadvisable, and that this explained the low enforcement rates. Some felt that clarification of the charges and process of parent warnings would help enforcement.
Only one qualitative study was included in the acceptability component. 77 Parents in Hong Kong, where vaccination uptake is high, were interviewed to identify factors which encourage this high uptake. Content analysis identified mandatory vaccination for child care and school entry as one important factor in a system of other vaccine-related services. Cultural and contextual factors found to be important included the relative importance of society versus individualism, trust of health professionals, and the high population density of Hong Kong increasing perceived susceptibility to infectious diseases.
In a survey of administrators and staff involved in delivery of a welfare benefit penalty for non-compliance with health behaviours, including vaccination of preschool children,76 70% agreed that behaviour could be changed by the intervention. Of these, 14% said that the penalties were very powerful and 28% said they were effective only when imposed, rather than just threatened. Recipients of the intervention reported that the penalty was fair (73%) and would motivate parents to meet health requirements (67%).
Economic component
Of the four studies included in the effectiveness component, none provided detailed information on the consequences of undertaking, or not undertaking, the desired activity. No study conducted a formal economic evaluation of the incentive scheme.
Only one of the studies included in the acceptability component included economic information on costs and consequences in the format of a cost–benefit framework. 76 As no evidence of effectiveness of the programme was found, the authors concluded that the costs of implementing the programme outweighed the benefits.
Discussion
Summary of findings
To our knowledge, this is the first systematic review to explore the effectiveness, acceptability and economic costs and consequences of parental incentive and quasi-mandatory schemes for increasing uptake of preschool vaccinations in high-income countries. Few studies were found that met the inclusion criteria. There was substantial heterogeneity across studies in terms of both interventions and methods.
There was insufficient evidence to conclude whether or not parental financial incentives and quasi-mandatory interventions are effective for encouraging the uptake of preschool vaccinations. Interventions and evaluation were heterogeneous and results were inconsistent. One study at a low risk of bias did find short-term effects of quasi-mandatory interventions linking vaccinations to education, but the effects were extinguished by 6 years after introduction of mandates. Studies also found that these mandates were particularly acceptable, although the risk of bias in relevant studies was high and they were conducted in contexts where such interventions were the norm. There was insufficient evidence to draw generalised conclusions on the economic costs and consequences of these interventions.
Comparison of results to previous reviews
Previous reviews that have included work on these topics have had much wider scopes in terms of interventions, outcomes and populations considered. A systematic review commissioned by NICE explored the effectiveness and cost-effectiveness of all types of interventions for increasing the uptake of preschool vaccinations. 62 Only two studies included in the current review44,45 overlapped with studies in the NICE review. Other studies identified in the NICE review as ‘incentives’ did not meet our definition, as they either involved changing the frequency of attendance for welfare benefits but not the level of benefit itself78–80 or did not involve incentives with real material value. 81 Similar to the current review, the NICE review concluded that incentives could be effective but that the strength and quality of the evidence varied and cost-effectiveness data were insufficient.
Briss et al. 16 reviewed a range of interventions to improve vaccination coverage across all ages using non-systematic methods. Similar to the current work, they concluded that there was some evidence to support the effectiveness of day-care and school entry mandates across all ages (not just preschool children), but insufficient evidence for the effectiveness of family incentives. Economic evidence was also limited.
Kane et al. 40 conducted a structured, but not systematic, review of the effectiveness of financial incentive interventions for uptake of a range of preventative health behaviours. She reported that these were most effective for short-term goals, such as vaccinations. However, this included vaccinations across all ages, not just in preschool children. It is possible that the effects of financial incentive interventions on uptake of vaccinations are different when considering incentives given directly to adults for receiving a vaccination themselves, compared with incentives given to parents for having their child vaccinated.
Strengths and limitations of included studies
Studies included in the effectiveness component tended to be at a low risk of bias, while those in the acceptability component were at a higher risk of bias. This reflects the cross-sectional survey designs in the acceptability component.
There was a lack of reported theory underpinning the design of interventions in included studies. Given the complexity of financial incentive interventions,70 more consideration of behaviour-change theory may help to guide the development of effective interventions.
There were a number of reports in included studies of threatened penalties not being imposed and belief that the threat of a penalty is sufficient for behaviour change. 76 This raises a number of important questions concerning intervention fidelity, and the effective component(s) or financial incentive interventions that should be explored further.
This is the first systematic review we are aware of that considered the acceptability of financial incentive and quasi-mandatory interventions. Only one of six included studies used qualitative methods. Further, in-depth, exploration of the acceptability of financial incentive, and quasi-mandatory, interventions to a range of stakeholders is required.
Those studies which found school entry mandates to be acceptable were conducted in settings in which these mandates were already common. The threat of withholding education from children may be less acceptable in other settings and this should be explored further. 55
Strengths and limitations of the review
Throughout, established criteria and protocols were used to inform methods and reporting. 63,65 This led to the exclusion of a number of studies that have been included in previous reviews. 16,40,62 In particular, we excluded uncontrolled before-and-after studies that are relatively straightforward to carry out using routine data. However, the lack of a control group makes it particularly difficult to infer causation from these studies.
A clear definition of parental incentive and quasi-mandatory interventions was also used,70 leading to the exclusion of interventions that have previously been considered incentives. In particular, we excluded studies related to the Special Supplemental Nutrition Programme for Women, Infants and Children in the USA,78–80 which offers low-income families vouchers that can be exchanged for nutritious food. Normally, enough vouchers for 3 months are provided per attendance at the programme. Under a vaccination initiative, families received only 1 month of vouchers at a time until their children’s vaccinations were up to date. As the absolute number of vouchers families were eligible to receive did not change, we did not consider this a financial incentive. Although it is always possible that studies that met the inclusion criteria were not found, this is unlikely given the exhaustive searching process used.
There was considerable heterogeneity across studies included in the effectiveness component in terms of intervention and methodology such that a meta-analysis was not considered appropriate. 44,45 This highlights the potential heterogeneity of financial incentive and quasi-mandatory interventions. 70 A more considered approach to intervention design may be required to begin to establish what configurations of financial incentive interventions are likely to be most effective in a range of different circumstances.
We attempted to describe the characteristics of interventions used in included studies. However, some details were missing and unobtainable from study authors. Such description of the complex components of incentives has been missing in previous research and this limits meaningful comparisons across studies. 70
Interpretation of findings and implications for policy, practice and research
Any interventions to increase the uptake of health-promotion behaviours need to be both effective and acceptable for widespread implementation. Consistent evidence that parental financial incentive and quasi-mandatory interventions are effective in encouraging uptake of preschool vaccinations was not found; the available evidence base was small, with substantial heterogeneity in both interventions and methods. Thus, it is not clear whether or not these interventions are effective and, if so, in what circumstances.
Despite this absence of evidence, quasi-mandatory schemes limiting school entry to those children who are up to date with required vaccinations are common in some countries, particularly the USA. Although such programmes may be effective, without robust evaluation it is difficult to conclude this, or justify any associated cost, or advocate for the expansion of such programmes to other vaccinations or countries.
Parental financial incentives and quasi-mandatory interventions for encouraging the uptake of preschool vaccinations are likely to be implemented on a large scale. This can make evaluation difficult. Creative evaluation strategies such as natural experiments and step-wedge designs may be most useful in these contexts. 82
Intervention development work, taking into account existing behaviour-change theory, may also be useful to develop more effective incentive interventions. This should involve further consideration of the effective component, or components, of financial incentive interventions. Strategies such as multiphase optimisation strategy may be particularly helpful in this context. 83
All of the studies included in the review were conducted in countries that tend to achieve overall high coverage of preschool vaccinations. Although pockets of poor coverage exist in these countries, population-wide interventions such as parental incentives and quasi-mandatory interventions may not be adequately targeted to those families that require the most assistance. Furthermore, these interventions may not adequately address the reasons for non-vaccination – including mistrust of health-care professionals, limited access to health care, chaotic lifestyles and low perceived susceptibility to and severity of vaccinated diseases. 5,6,8 Further consideration of reasons for non-vaccination should be taken into account when designing new interventions for promoting vaccination.
Overall, these interventions were not considered to be clearly unacceptable by any stakeholders. However, neither did parents report that financial incentives were particularly motivating in this context, and quasi-mandatory policies appeared to be considered more appropriate. However, only one study used an in-depth qualitative approach. 77 Furthermore, few studies appeared to make specific attempts to capture the views of parents with unvaccinated children. Further, in-depth, qualitative analysis is required to explore what aspects of these interventions are and are not acceptable, to whom, and why.
In addition, it is likely that acceptability is, at least partly, dependent on perceptions of effectiveness. This suggests that if high-quality evidence of effectiveness is generated, and then effectively communicated to the public, good levels of acceptability are likely to follow. Better understanding of how to effectively communicate research findings to the public would be valuable.
Although the acceptability of restricting day-care or school entry to vaccinated children appeared to be high, all studies reporting this were conducted in settings where these restrictions are already the norm. Only one study of the effectiveness of such quasi-mandatory policies was included in the effectiveness component, finding that these policies were effective for up to 5 years after introduction. 71 Such policies clearly have potential in countries where they do not currently exist. But effectiveness, cost-effectiveness and acceptability in new contexts need to be considered further across a range of stakeholders, using both qualitative and quantitative methods. Discrete choice experimental methods may be particularly useful.
Conclusions
This systematic review of the effectiveness, acceptability and economic costs and consequences of parental financial incentives and quasi-mandatory interventions to increase the uptake of preschool vaccinations identified a very limited evidence base in all areas. There is insufficient evidence to conclude whether or not these interventions are effective, although mandates limiting access to education to vaccinated children may be effective for up to 6 years post intervention. There was some evidence that quasi-mandatory interventions linking vaccinations to education were also the most acceptable interventions considered, although the risk of bias in these studies was high and this finding may be specific to contexts where such interventions are widespread. There was insufficient evidence to draw conclusions on the economic costs and consequences of these interventions.
Chapter 4 Qualitative study
A series of qualitative focus groups and individual interviews was conducted with a range of stakeholders (including parents, health and other relevant professionals, and policy-makers). This work drew on the systematic review by discussing with participants examples of parental incentives schemes identified in the review and focusing on issues of acceptability identified as understudied.
Research questions
The qualitative study aimed to answer the following questions:
-
What are stakeholders’ views, wants and needs concerning interventions to promote the uptake of preschool vaccination programmes?
-
Would parental incentive or quasi-mandatory schemes for encouraging uptake of preschool vaccinations be viewed as acceptable?
-
If not, why not?
-
If not, what, if anything, could be done to make such schemes more acceptable?
-
This study is presented in accordance with COREQ (Consolidated Criteria for Reporting Qualitative Research) guidance. 84
Methods
In this phase of the study we were keen to build on the results of the systematic review (much of which relied on non-UK studies) by exploring the acceptability of introducing financial incentives schemes or quasi-mandatory schemes for preschool vaccinations in a UK context. This part of the study used a qualitative approach to gather data about the views, wants and needs of parents as well as health and other professionals in relation to preschool vaccinations and their uptake; and the theoretical introduction of financial incentives or quasi-mandatory schemes to increase uptake of preschool vaccinations. A mixture of focus groups (parents) and semistructured individual interviews (health and other professionals) was undertaken to gather data for analysis.
We sought to answer two primary research questions, as described above. The research questions were both informed by extensive engagement with empirical literature and UK policy guidance.
Inclusion criteria
We attempted to capture the views of stakeholders, who we defined either as people who would be in receipt of such schemes (parents and carers of preschool children) or as those who would have a role either in creating such policies or commissioning and implementing the schemes (health and other professionals).
Parents and carers of preschool children
Parents and carers of preschool children would be the intended recipients of any parental incentives scheme. It is therefore crucial to capture their views in order to determine the acceptability of any proposed scheme. We were interested in hearing the views of both immunisers and partial or non-immunisers.
Health and other professionals
It is important to pay attention to the views of those professionals who could be involved in developing, commissioning and delivering preschool vaccinations and any change to the current system. These professionals include policy-makers, practice nurses, health visitors, GPs, community paediatricians and school teaching staff. Although, in England and Wales, preschool vaccinations are normally administered by practice nurses at a GP practice, other professionals have a role in the success (or otherwise) of the vaccination programme. Health visitors, GPs and community paediatricians have a key role in advising parents about the benefits of vaccinations and could have a role in administering any parental incentive scheme. Similarly, primary school staff may be required to administer any parental incentive scheme that is based around school enrolment. If any such scheme is not acceptable to those who deliver and administer it, it is unlikely that the scheme would be delivered to a high standard.
Sampling
Parents and carers of preschool children
No sociodemographic factors were found to be particularly associated with parental acceptability or effectiveness of parental incentive schemes in the systematic review. Accordingly, these were not specifically used to guide purposive sampling of parents and carers of preschool children. Instead, factors known to be associated with uptake of preschool vaccinations more generally5,7,10,11 were used to guide purposive sampling. A sampling frame was devised to capture the views of a demographic mix of parents and also, on the advice of the steering group, to include the views of parents both from a geographical subarea that had experienced a measles outbreak in 2012–13 and another which had not. We identified these areas in consultation with several members of the steering group and after perusal and discussion of the epidemiological data. We were interested to see whether or not greater familiarity with a recent disease outbreak would affect responses. We hoped to recruit both immunisers and partial or non-immunisers in these community samples. Parents were all resident in the north-east of England, with the no-measles-cases area being located in the northern end of the region and the measles outbreak area being located in the south of the region.
In each location, north and south, four focus groups were carried out in children’s centres, which served populations living in areas of relatively high deprivation, and one focus group was carried out in a baby and toddler group that drew a population of parents living in more affluent areas. Deprivation was assessed using the 2010 Indices of Multiple Deprivation85 quintile for the location of the group setting. Ten focus groups were carried out in total.
Owing to ethical constraints on the access to vaccination status data, it was not possible to obtain details of parents and carers who had refused vaccination or had only partially immunised their child. It was hoped that targeting recruitment in some of the most deprived and some of the most affluent areas would uncover some parents and carers who were partial or non-immunisers.
Health and other professionals
These participants were identified purposively, and through discussion with key stakeholders, because of their job role and current responsibility for developing, commissioning and delivering vaccination services. In the main, these were staff already employed in various levels of the health service, both strategic (n = 6) and operational (practice nurses, health visitors and GPs) (n = 13), but we also extended the sample to other professional groups (community paediatricians, school nurses and primary school head teachers) (n = 5) who might become involved if quasi-mandatory schemes were to be introduced.
Recruitment
Different recruitment strategies were used for each of the stakeholder groups.
Parents and carers of preschool children
Parents were recruited through children’s centres and baby and toddler groups in each of the two localities. Children’s centre area managers were sent an e-mail asking for permission to approach parents who used their centre’s facilities. A copy of the project information sheet was included in the initial contact. All area managers who were approached responded positively and a meeting was set up between the researcher (RM) and the area manager. Each children’s centre hosted regular meetings and groups for parents who were resident within their catchment area. Children’s centre staff handed out information sheets and posters about the research to parents. The staff then arranged a convenient time for the researcher to carry out a focus group with those parents who were interested in taking part. Participants were, essentially, a self-selecting sample.
Eight children’s centres recruited parents to focus groups, four in each locality (north and south of the region). Table 6 shows the demographic make-up of each of the groups.
| Focus group number(s) | Descriptor |
|---|---|
| 1 | South of region. Lower deprivation. Lower rates of childhood vaccination. High incidence of measles 2012–13 |
| 4, 5, 7, 8 | South of region. Higher deprivation. Lower rates of childhood vaccination. High incidence of measles 2012–13 |
| 10 | North of region. Lower deprivation. Higher rates of childhood vaccination. Low incidence of measles 2012–13 |
| 2, 3, 6, 9 | North of region. Higher deprivation. Higher rates of childhood vaccination. Low incidence of measles 2012–13 |
For all participants, any costs of transport to and from focus groups were reimbursed, or taxis were arranged. For parents and carers of preschool children, the cost of child care, arranged through parents’ normal providers, was reimbursed if required. All parent/carer participants were offered a £20 high-street shopping voucher as a ‘thank you’ for taking part.
Health and other professionals
These were recruited through a variety of approaches. The professional networks of the research team and wider steering group were exploited to identify key stakeholder individuals, who were then contacted via e-mail, with a copy of the study information sheet. The North of England Commissioning Support Unit (NECS) also recruited health professionals on our behalf, as we anticipated a poor response rate from GP practices to cold calling. Research-active health professionals were approached by NECS, along with the approved study information, and the contact details of those who responded positively were passed to the research team, who then made contact.
Letters confirming individual interview appointments were sent at least 1 week prior to appointment, and reminder telephone calls were made, or text messages sent, the day before.
Participants were asked at the end of the interview if they had contact with other professionals in the field onto whom they could pass the study information, and so a degree of snowball sampling was also employed in the study. Table 7 shows the number of participants recruited from each stakeholder group.
| Professional group | Number of interviews completed |
|---|---|
| National and regional policy and commissioners | 6 |
| GP, practice nurses and practice managers | 9 |
| Health visitors | 4 |
| School nurses | 1 |
| Community paediatricians | 2 |
| Primary school head teachers | 2 |
Data collection
Parents and carers of preschool children
Data collection with parents and carers took place in focus group settings. Focus groups were chosen as a method over individual interviews as it was felt that parental decision-making is often the result of social interaction and sharing of views. Focus groups encourage interaction between participants as well as between participant and researcher and the flow between participants can often encourage the challenge and justification of views, which would be helpful in this instance. An interview schedule (see Appendix 2) with six vignettes (see Appendix 3) was developed. The vignettes were based on the different incentives and quasi-mandatory schemes that were identified through the systematic review phase of this project. Each vignette covered a different type of incentive scheme:
-
a universal gift of money upon completion of a full course of vaccinations
-
a targeted gift of money for non-/partially immunising parents to bring their child’s vaccinations up to date
-
a cash penalty for those unable to demonstrate a full record of child vaccination
-
removal of child care contributions from those unable to demonstrate a full record of child vaccination
-
entry into preschool, nursery or day-care settings restricted to those able to demonstrate a full record of child vaccination, or acceptable reason for exemption (e.g. on religious, moral or medical grounds)
-
entry into school restricted to those able to demonstrate a full record of child vaccination, or acceptable reason for exemption (e.g. on religious, moral or medical grounds).
Children’s centres and parent and toddler groups allowed us to use their facilities to carry out the focus groups. In the majority of cases child care was provided on-site to allow parents to attend the focus group, except in three cases. One was a breastfeeding support group, where babies and toddlers were present with their mothers. The two other occasions were toddler groups where the mothers requested that their children be present.
Focus groups began with introductions from the researchers and a brief recap on the purpose of the study and ground rules for participation. Participants were asked to sign the consent form and complete a brief demographic questionnaire covering their age; sex; marital status; educational attainment; employment status; and the number, ages and vaccination status (including any vaccinations refused) of their children. Once discussion started, parents were asked to introduce themselves to the group and then activities began. First, parents were asked to name as many childhood diseases as possible; these responses were captured on a flip chart. This acted as an icebreaker to get parents talking within the group. Next, parents were presented with flashcards on which names of childhood diseases had been written. Parents were asked to form small groups or pairs and sort the various diseases into two piles, one for illnesses for which they believed a vaccine was available for and one for those where there was no vaccine. These answers were then fed back to the wider group. After the card-sorting exercise, discussions centred on the semistructured guide and vignettes. The order in which vignettes were presented to participants was varied in each of the focus groups to mitigate any bias effects produced by the sequencing.
Focus groups were digitally recorded with the consent of all participants and these recordings were subsequently transcribed, verbatim, in preparation for data analysis. One of the focus groups, group 10, had many more parents in attendance than had been anticipated (n = 23) and these parents were accompanied by their 26 babies and toddlers. In order to carry out the discussions these parents were broken into smaller discussion groups, which were recorded. However, these tapes were too noisy to transcribe and researchers relied on the notes that had been made during the discussions to inform analysis. So, although the discussions contributed to our understanding and interpretation of the data, no direct quotes are used in the report from group 10.
RM, a full-time research associate, carried out the fieldwork with parents and carers. One other researcher was present during focus group discussions to take notes. Both researchers were female and had no prior relationships with any of the participants. Data collection took place in the autumn and winter of 2013–14.
Health and other professionals
Interviews with health and other professionals took place at participants’ places of work. These discussions followed a similar format to focus group discussions, exploring the six possible scenarios, but without the use of the icebreaker exercises or formal use of the vignettes (see Appendix 8).
All individual interviews were carried out by RM and were digitally recorded and, as before, these recordings were subsequently transcribed, verbatim, in preparation for data analysis.
Ethical approval and conduct
The protocol for the qualitative phase of work was scrutinised and approved by Teesside University’s School of Health and Social Care Research Ethics and Governance Committee (study number 105/13). The study was adopted to the National Institute for Health Research portfolio, to facilitate research and development approval to recruit professionals employed by the NHS. Approval to begin recruiting staff was granted by most north-east sites at the end of February 2014.
All participants were provided with a written information sheet that included details of the purpose of the study, what their involvement would entail and what would happen to the data collected from them (see Appendices 9 and 10). All participants were informed that the research team would keep any personal information confidential and would ensure that their anonymity would be maintained in any written reports or presentation made based on the data collected. For some participants, particularly policy-makers and commissioners, it was considered possible that colleagues could identify them by the very nature of their job role. These participants were asked specifically to bear this in mind when agreeing to take part in the study.
Details from the information sheet were reiterated verbally before the commencement of the focus groups or interviews. All participants were provided with contact details of the primary researcher, prior to interview, in case they wished to ask any questions or seek clarification of any issues. Each participant was asked to complete a written consent form if they agreed to participate in either a focus group or an interview.
Sample size
The sample size for qualitative studies is not determined by considerations of statistical power. Instead, sample size is intended to explore the range of views that members of stakeholder groups hold. Qualitative analyses do not impose sample size restrictions, and even traditionally ‘small’ samples can yield large amounts of data and insightful findings. 86
We conducted 10 focus group discussions with parents, generally with 8–12 participants per group, giving 91 participants in total. In addition, we conducted 18 interviews with health and other professionals, and six interviews with policy-makers and commissioners, as described in Table 7.
Although the focus groups allowed us to achieve thematic ‘saturation’ – whereby new focus groups were no longer raising new issues – the small number of individual interviews did not achieve this. Instead, these were a more pragmatic undertaking, designed to give implementation context to the main focus on parents and carers.
Analysis
Framework analysis was used to analyse the focus group and individual interview transcripts. This method involved developing an initial coding framework based on preliminary analyses of concepts of importance to participants, iteratively applying the framework to code the data, and refining the framework in light of insights that emerged. 87 Framework analysis provides a procedural structure for qualitative analysis that enables a systematic approach to the data, while also allowing some flexibility in interpretation. It has been identified as a suitable method for analysing data where the objectives of the research have been set in advance, and for policy-focused research. 86,88
Initially, a subset of transcripts, selected to reflect a range of participant demographics, were read by the researchers (RM and JS) to identify recurrent concepts. These were then organised into higher-order categories to produce a thematic coding framework. RM then applied the framework to the full data corpus to identify and code pertinent extracts. NVivo 10 (QSR International, Warrington, UK) was used to facilitate the management of the large number of data during the coding stages of the analysis. Extracts that reflected concepts insufficiently, identified by the coding framework, were used to modify the coding framework. Thus, the framework was iteratively refined in response to the data until a definitive framework was established capturing all concepts and offering a coherent, structured and cohesive account of stakeholders’ views. Explanatory conceptual accounts of views expressed in the data were developed using constant comparison methods to identify properties inherent in similarly coded extracts. 89 Once higher-order themes had been established, data were scrutinised across groups to explore any commonalities or themes arising in particular contexts (e.g. in terms of incidence of measles in the area in recent past and deprivation). These are highlighted throughout the findings and discussion sections.
Although coding of the full data set was undertaken by one researcher (RM), frequent discussions took place between this researcher and the more experienced project leader (JS), as well as the wider project team, ensuring that interpretations and conceptualisations of the data were credible, valid and shared. 90 Both RM and JS contributed to the reporting of the data.
Themes were also presented to the Parent Advisory Group, a group of parents who gave their views on the project’s development, to check that themes were not overstated and bore resemblance to their experiences. Emerging themes were also presented to the wider research team, to the steering group and at an academic conference to ensure that they were reasonable reflections of the data.
RM was responsible for drafting the qualitative part of the report and JS was responsible for refining the drafts.
Results
In this section, the results from the parent and carer focus groups are presented first, followed by the results from the individual interviews with practice and policy partners. Within each of these subsections, we look first at reaction to the suggestion of the introduction of financial incentives, followed by penalties and, finally, quasi-mandatory schemes. In both participant groups, there were various suggestions as to how existing schemes could be changed to improve vaccine uptake, regardless of the introduction of incentives, and these, too, are summarised in each subsection.
Parents and carers of preschool children: financial incentives
The parent/carer sample comprised males (n = 7) and females (n = 84) and included mothers, fathers and primary carers (grandparents) of preschool children. Focus groups were purposely held in locations that would attract parents from across the socioeconomic spectrum. The majority of parents were either living with a partner (n = 37) or married (n = 35), with a few stating that they were single (n = 14) or living separately from their partner (n = 1).
Parents had, on average, two children (n = 34); however, the number did range from one to six children. The majority of parents stated that their children were up to date with their vaccinations (n = 83). Only one mother stated that she had refused a vaccination, but she did not state on the demographic capture form which vaccination had been refused. Five parents opted not to answer that question.
The introduction of financial incentives (universal and targeted)
We explored, through the use of scenarios, the introduction of two distinct ways of offering a financial incentive to parents. The first explored the introduction of a universal incentive and the second a targeted incentive to parents who had either not immunised their child or only partially immunised their child. Overwhelmingly, parents described financial incentives as inappropriate and displayed dismay that this type of incentive scheme would be under consideration.
I think it’s disgusting.
Right, we’ve got one person who’s grasping their head.
I think it’s shocking.
Quite a lot of shocked faces.
£50 is a lot of money. If you think of all them children that have their injections, £50 for each one [child], they could use it for research, they could use it for extra hospital equipment, and it’s not, it’s just for lazy parents who can’t do something that they should already be doing for their children.
Mothers, focus group 9
Parents were asked, after their initial reactions, to try to think about the positive and negative impacts of each scenario. When probed about financial incentives, parents could recognise two potential advantages to the programme; first, the equity of the universal scheme and, second, the potential for cash payments to encourage disadvantaged parents to immunise.
Equitable treatment
When discussions turned to the universal incentive, the fact that this type of scheme would be offered to all, regardless of vaccination status of the child or socioeconomic status of the parent, was noted as the overwhelming positive of this particular scenario. However, it was noted that a small financial incentive may not be attractive to more affluent parents.
I think it’s all-inclusive because everyone’s going to get the same thing. I do think, despite what you’re saying though, if it’s just a small nominal amount, then again, the rich will say, well I don’t need that £20.
Mother, focus group 1
Parents felt that, if this financial reward were to be introduced, there would have to be a nationwide roll-out to ensure fairness to all UK parents, from all backgrounds.
Well I don’t know. And if it’s just in this area, what if you were just out of the catchment area, then they’d feel hard done by wouldn’t they?
So do you think to work it would have to be all parents?
Universal.
Universal and the whole.
Mother, focus group 2
Payments could encourage ‘disadvantaged’ few
The other advantage that parents cited for the introduction of financial incentives was that this type of reward might help to encourage parents who did not otherwise prioritise vaccinations for whatever reason, for example time or forgetfulness. However, all parents, regardless of socioeconomic status, felt that this incentive would serve only to attract really disadvantaged parents. As two mothers commented:
Some people probably literally can’t be bothered, which is horrible but . . .
So actually giving them money would get the child there. It’s about the child at the end of the day, not the means.
Mothers, focus group 3
Financial gain, it was suggested, would be very attractive to many parents who were living in disadvantaged circumstances. It was anticipated that, among this group of parents, financial rewards would certainly lead to increased vaccination uptake.
You think it might make it a little bit more attractive to ‘certain’ people?
To ‘certain’ people.
If you’re getting £50, yes of course it will. It will make some people get off their backside and take them [children] to the doctors.
Mothers, focus group 4
It was discussed that financial incentives would be seen positively in these disadvantaged groups as a way of supplementing income from work or benefits:
There’d be a big queue for it.
Do you think some people would take advantage of it?
Oh yes, of course they would.
Like people who’ve got nothing.
People would have their kids immunised three or four times wouldn’t they?
Yes.
There’d be a way of making sure that you weren’t getting them done every week.
It could be a good little earner couldn’t it really. You could have like more and more kids to get more and more vaccinations.
Fathers, focus group 5
There were concerns, mainly from the parents from more affluent areas, that the introduction of financial incentives, regardless of how they were implemented, could create a divide between rich and poor. Parents who were financially stable could still make a conscious decision to immunise their child or not, as they could afford to disregard a nominal payment. This became more evident when parents were presented with scenarios that included a financial penalty, such as the removal of certain benefits or government contributions to child care.
It will bring a divide amongst the, between the rich and the poor, because like I can afford not to [not immunise my child].
Mother, focus group 1
This point was reiterated by another mother:
I think it’s all-inclusive because everyone’s going to get the same thing [universal incentive]. I do think, despite what you’re saying though, if it’s just a small nominal amount, then again, the rich will say, well I don’t need that.
Mother, focus group 1
Rewarding ‘bad’ behaviour and encouraging people to ‘play the system’
The introduction of a financial transaction into the vaccinations programme was generally viewed negatively. Parents felt that this was a way of rewarding parents for what was perceived as ‘bad’ parenting behaviour:
There’s people who just can’t be bothered to take their kids to get it done. And then they’re the kids that end up catching it and it starts building up as like a more common disease again. So to get them to go, I suppose [financial incentives are a good idea], but then why should they be rewarded with money because they couldn’t be bothered to take their kids in the first place?
Mother, focus group 6
These feelings of unfairness emerged more vehemently when discussions turned to the possibility of a targeted catch-up approach to incentivising vaccination:
It’s just irritating isn’t it? It’s just saying, we’re going to reward the people who are rubbish. I mean I can get that you are then targeting the people who are the problem, or the people that you know about are the problems, but I still think it’s better to go round and say, receive the letter saying, the nurse will be popping round on Tuesday afternoon [to immunise at home].
Mother, focus group 1
Another mother noted how this approach would actually be penalising parents who had fulfilled their obligations to immunise their child on time:
I don’t think anyone should get the cash bonus, I’d feel like, as a parent that took my child to all of his appointments, I’m being penalised because of it.
Mother, focus group 6
These feelings of injustice led parents to think that that the introduction of a targeted incentive would actually have unintended consequences. It was suggested that parents would begin to ‘play the system’ by delaying vaccination to ensure that they were eligible for the incentive:
People would wait longer on purpose to get the vaccinations. And the ones who’ve done it on time would feel as if they were penalised.
Father, focus group 5
Another mother noted how she would play the system and delay vaccination to become eligible for the money, while still feeling that she had fulfilled her role as a responsible parent:
The funny thing is though, that’s the sort of thing that, I think people would do that [delay vaccination]. I’m not being horrible but . . . I would if somebody was going to give me £50 that I could spend on my children, I would. I know it sounds horrible and a horrible thing to do but yes I would. I know that the children aren’t going to suffer in the long run.
Mother, focus group 7
Thresholds or time limits before a targeted incentive was made available
Parents were concerned that if a targeted approach were to be implemented there would have to be clear guidance about who was and was not eligible for payments, as many noted that they had taken their children to be immunised but, for one reason or another, the health professional had not done it at the appropriate time, usually because of the child’s temporary ill health. In cases like this, parents who would have immunised as a matter of course would become eligible for the targeted incentive.
You see if, like [child’s name] didn’t get his on time and I would have, if that was me I would have found it unfair. Obviously, because if it was me, it would be that they’d be chasing up and offering me the cash bonus, but [child’s name] was delayed because of his illness. He wasn’t delayed because I’d forgotten or anything.
Mother, focus group 7
Incentives viewed as bribery
The possibility of a financial incentive being introduced to ‘encourage’ uptake of vaccinations, regardless of it being implemented via a targeted or universal approach, was commonly identified by parents as ‘bribery’. Parents felt that a cash reward was not the way to encourage an activity that they thought was part of their duty as a responsible parent and a routine behaviour that they should want to do for the health and protection of their child. It was suggested that the introduction of financial incentives would actually have a negative effect on this link between understood concepts of parental responsibility and social duty.
Why should you have to be paid or bribed to take your kids to the doctor’s for their needs to be met? I just don’t understand why?
Father, focus group 5
Parents were adamant that money should not be a factor in the decision-making process to encourage them to perform behaviours that were ultimately for the protection of a child:
I think it’s wrong.
It’s wrong, why is it wrong?
Well why would you bribe someone to get your kid’s needles done?
They should want to.
It’s your duty to protect your children.
Mothers, focus group 7
Likelihood of ‘conscientious objectors’ changing their mind
There were concerns that the introduction of financial incentives would not act as a catalyst to immunise for all parents. As noted previously, it was felt that these types of incentives might entice parents from the lower ends of the economic spectrum as a way of obtaining money to supplement their income. However, it was not felt that these incentives would entice parents who had made a conscious decision, for whatever reason, to change their minds. The reasons given for this were that these ‘conscientious objectors’ had made decisions based on morals, beliefs or research, rather than because they had failed to prioritise vaccinations because of fecklessness, difficulty of access to services or lack of understanding of disease:
I’m not sure that everyone that doesn’t get their child immunised would be kind of swayed by having £50, because, with people I know that won’t have their children immunised, it’s because they’ve done research and they’ve decided. But that £50 is not going to make any difference to their decision.
Mother, focus group 6
Another parent noted:
It depends on the individual I suppose, doesn’t it? You might get people who come [to have their children immunised] by paying them, probably as you would, but then not the ones that are just against them [vaccinations], because some people genuinely believe that they’re no good for them, for their children, don’t they?
Mother, focus group 4
Parents sometimes described friends who did not immunise their children, or accept medical intervention, as being very steadfast in their beliefs. It was stated that these parents would not be swayed by the offer of financial inducement.
I’ve got a friend who has two little [children], a little boy and a little girl, and she doesn’t immunise. And she’s very educated and she has made a conscious decision she’s not going to immunise. No matter what the rules were, she wouldn’t immunise. I don’t think anything would work on her.
Do you know why she feels so strongly about it?
She doesn’t do medication either. They don’t do antibiotics, they do everything herbal, so they think there’s too many toxins in the vaccines, so they don’t want to use them.
Mothers, focus group 1
Costs of incentive schemes
There were great concerns, from parents, about where the money would come from to pay for financial incentive schemes, regardless of whether they were universal or targeted. It was felt that, in a time of austerity, this type of scheme would be a frivolous use of money. Again, parents noted that vaccinations were already offered free of charge and that that, in itself, should be sufficient to incentivise parents:
Well no, they’re being paid, the vaccinations cost a fortune in themselves. That is like, every child that’s immunised is getting that, you know. In other countries, you know, people would have to be finding the money to get their children immunised, wouldn’t they, against illnesses.
But then that comes back to where are they [the government] going to find the money from to pay for this scheme?
Mothers, focus group 3
There were concerns that taxes would be utilised to cover the cost of implementation, which some parents did not feel was fair:
Where does the money come from? That’s my first thought.
From the government?
So through taxes?
Out of which pot?
I don’t know, I don’t know which pot it would come out of. Would it matter to you which pot it came out of?
I would say it would for me because a lot of people go to work and, like, you work really hard for your money. And people are getting all sorts of benefits for doing things that everybody else is just doing for free.
Mother, focus group 1
Parents felt that they would prefer to see public funds used to improve the quality of life for children in sustainable, physical ways, rather than spent on financial incentive schemes:
Put the money to better use, build parks for the kids to go and play. Don’t pay a parent to vaccinate.
Mother, focus group 8
Alongside concerns about financing such programmes, parents raised concerns about the wider costs and benefits of such an incentive scheme. Introducing a universal system would mean paying a percentage of parents to do something that they would have done as a matter of course, which seemed like a waste of resources to many.
Acceptability of a cash penalty
In line with the findings from the systematic review, we explored scenarios around the introduction of a financial penalty, rather than a reward. Discussions showed that the removal of quasi-universal benefits, such as Child Benefit (not actually feasible within the rules that currently govern this type of benefit), was the most acceptable solution to all groups of parents in our study. Framing the incentive as a penalty, rather than as a reward, was most acceptable to parents.
It’s not giving them anything additional. Like everyone’s entitled to that £20.30 a week, aren’t they? We’re all entitled to it, whether we work or whether we don’t, whether we’re [married] or single. So you’re not giving me anything additional to take my child to get, but you’re taking away something, just to give a bit of a kick up the backside.
It’s not like a cash, yes it’s not a cash bonus that time. It’s just something you’re getting took away that you’re entitled to. So it’s not a hand-out.
You’re not getting an extra £20 to do it, they’re just stopping your money, aren’t they?
Give them a kick up the backside to think, well I will get it or I won’t get it, I won’t get that money but we’re all entitled to it anyway, no one gets anything extra.
Mothers, focus group 7
It was felt that removal of benefits would act as a push to immunise (or even as a punishment) for those who were simply lax about keeping up to date with vaccinations, rather than for those who had made a conscious decision against vaccination:
I think the only way to get people that have decided, not because of any medical reason, but have decided not to immunise, the only way you’re going to get them to do it is this. Because I think they’re not going to take the incentive of: I’ll give you money. They’ll say, well I just won’t take the money. But if you penalise them by not giving them money . . .
Mother, focus group 6
Another group of parents noted that it seemed more realistic to penalise than to reward:
That’s more like the real world.
If you’re at work and you don’t do something right at work, you get told off don’t you; you get a kick. And I know that if I don’t get a kick, you know, I need a kick every, I do need a kick! Do you know what I mean? I’m not saying I enjoy a kick but . . .
Fathers, focus group 5
It was noted, however, that many families do rely heavily on Child Benefit to supplement their wages or benefits and that the removal of it could push already struggling families into severe hardship:
Some people rely on Child Benefit though, don’t they, and some families really do rely on it. So if they say, look if you’re not going to pay, if you’re going to take that away from me, how am I going to survive without it if I’m not. . ? But then it goes back to their beliefs.
But that means a rich family would have choice and a poor family wouldn’t have a choice.
Mothers, focus group 3
As Child Benefit is now means tested, parents who were not eligible to receive it reflected that once again it could cause inequity, in as far as affluent parents could afford to ‘choose’ not to immunise because they would be no worse off financially, leaving only disadvantaged parents with a choice between losing money they were entitled to (and were, in many cases, reliant on) and conscientiously objecting to vaccinations.
But at the same time I think it would be seen as only people whose incomes are going to be affected by it and it’s, so it’s possibly not people who are on lower incomes who are the ones who choose not to immunise anyway, so [it] almost looks like an attack on those people who are receiving benefit.
Yes and it becomes something, well-off people don’t immunise because they can afford not to.
Mothers, focus group 1
Parents from areas of both higher and lower deprivation were concerned about the equity and equality of any incentive scheme to increase vaccination. However, although these themes were common across groups, parent’s concerns in each group were quite different. Parents from areas of least deprivation noted that the introduction of such a scheme would be neither equitable nor equal for them, as they could afford to ‘opt out’ of such a scheme, and thus their decision would not be influenced by the introduction of a financial transaction. Parents from areas of higher deprivation, however, were concerned with how the introduction of a financial incentive might be construed as rewarding those parents who had acted irresponsibly by not immunising their child. Likewise, differences were found between deprivation groups when discussing the introduction of a financial penalty. Many of the parents from the areas of least deprivation were not in receipt of Child Benefit as they earned over the threshold for entitlement, meaning that the introduction of such a scheme would, essentially, not affect them, leading again to inequalities in parents’ ability to make informed decisions.
Summary: parents and carers of preschool children – financial incentives
In summary, the responses of parents and carers of preschool children to the suggestion of using financial incentives (and penalties) for preschool vaccinations were as follows:
-
The introduction of financial incentives could encourage some parents, especially those experiencing financial hardship, to immunise their children.
-
Financial incentives offered universally were more acceptable, as they were seen as more equitable.
-
Financial penalties were more acceptable than financial rewards.
-
The introduction of a financial penalty could act as a timely reminder to immunise a child.
-
Financial incentives were seen as a mechanism that might encourage socially undesirable behaviour.
-
Financial incentives were seen as bribery for carrying out a behaviour that should be an integral part of being a responsible parent.
-
A targeted incentive system could lead to ‘gaming the system’, with parents delaying vaccination to become eligible for the reward.
-
Financial incentives could be very costly within the context of an already overstretched financial system.
-
Financial incentives could be ineffective at changing the views of parents who had made a conscientious decision not to immunise their child.
Parents and carers of preschool children: quasi-mandatory schemes
Parents noted many advantages to the introduction of quasi-mandatory schemes to increase uptake and coverage of preschool vaccinations. There was a consensus that mandating vaccinations was preferable to financial incentives and, most importantly, seemed like the sensible choice to make. As one mother noted:
You’re not allowed to walk your dog in public until you’ve had its injections, so why should it be different for children to be allowed to visit a park even if they haven’t been immunised? You’re not allowed to walk your dog in the public park if they haven’t had their first lot of injections, so why is it different for children?
Mother, focus group 7
All parents felt that this type of scheme was preferable to the introduction of financial incentives for vaccination, and many felt that it was a much fairer option.
I prefer this idea to the last one [financial incentive], I think it’s more inclusive. And OK, yes fair enough it’s implying that if you don’t have the vaccinations your child can’t go to the school, but I think it’s probably fair from the school’s point of view that they should be able to exclude people who are at risk of transmitting these diseases through the school. So, in that respect, I think it is fairer than the other one.
Mother, focus group 1
There was a general feeling that unimmunised children should be excluded from interacting with other children in a day-care setting as they would pose a risk of passing infectious diseases on to the wider community of children attending the setting.
I don’t think the kids should be allowed to come, like I know you can’t, but like visit playgroups or Sure Start Centres or even be allowed at school nursery if they haven’t been immunised. Because then they could be carrying something and passing it on to other kids.
Exactly, I agree with that.
Do you know what I mean, I don’t think they should be allowed around any other kids if they haven’t been immunised.
Mothers, focus group 7
The ‘shared nature’ of child care settings was also raised. In a day-care environment, children crawl on the floor and play with communal toys, making it a perfect situation for the transmission of infectious disease. This was another reason that parents felt it preferable to mandate vaccinations for entry into that environment.
It’s just the fact of, that’s actually like, you’re thinking in a sense that that’s protecting your child, by everybody having their vaccinations because, obviously, the infections or diseases will go round quicker. So if everybody’s had it, but it’s like just saying, if somebody hasn’t got it, it’s like using a public toilet isn’t it?
Mother, focus group 3
A mandate feels ‘normal’
There was a general feeling that mandates were fair in nature and made good sense when the intention was to normalise behaviour. Parents discussed the view that if vaccination for entry into either day care or school was the routine requirement for entry then this would be accepted by the majority as being ‘just the way it is’. One mother expressed herself thus:
And also to start parents early with the idea that this is how it is. You know, if you know from the beginning, if you get your child all the way to 4 or 5 [years old] and then someone says, have they had all their vaccinations, they say, no I don’t agree with it and they say, well they can’t go to primary school, you’d think, oh, oh dear. But if you know from the beginning that they’re not going to be able to [get entry to nursery without vaccination], because we put our name down for nursery when I was pregnant with my first, and if I’d known, if they said then, oh you will be getting the vaccines, then you would, from the beginning.
Mother, focus group 1
Parents noted that they had been asked about the vaccination status of their child before using other services, such as ear piercing. Had her child’s vaccinations not been up to date, one mother affirmed that she would have been refused the service. Likewise, people felt that if vaccination was a requirement for education it would act as a timely reminder to other parents to keep their child’s vaccinations up to date.
When I took [child’s name] to get her ears pierced, the place I took her, I had to take her red book to prove she’d been immunised, otherwise they wouldn’t do it. It should be the same for the nurseries; they should have to prove that they’ve got them [vaccinations], otherwise . . . If I have to do it to get her ears pierced, then I expect to have to do it if she’s going into a child care place.
Mother, focus group 4
Parents relied to a certain extent on child care provision and felt that mandates would just become normalised – another one of those things done to access the services.
It should be that way instead. It should be made, [that] if you need child care for your child, you’re going in there with all these children who have already been immunised, if you want your child in that placement, you need to have your child immunised before it starts and that’s the rule. And if they don’t have it done, you can’t have the child care.
Mother, focus group 8
A mandate system would protect my own child
Parents discussed how mandating vaccinations for entry into day care or school would provide them with peace of mind when making decisions about taking their own children into the setting.
It wouldn’t bother me if they did. I’d be quite happy if they did. And I’d be quite happy to know that they’ve asked the other parents in there, because you’re right, they do pick up everything at nursery, [child’s name] gets absolutely everything . . . so it wouldn’t bother me to be asked that and I’d probably get more comfort in knowing that everybody else is being asked that question.
Mother, focus group 4
Parents felt that immunising a child was the right thing to do in the interests of protecting their child and, therefore, it was acceptable to mandate this behaviour in order to apply pressure on other parents who were not making the ‘right’ decision on behalf of their child:
What the problem is, there’s too many lazy parents that can’t be arsed to get off their arses and take their kids to the doctors to go and get them done, because they’ll cry or they’ll do this or they’ll do that. They prefer to sit in the house instead. So I think they [vaccinations] should be made law, so I have to have it done. And it’s protecting them, the children, it’s not protecting yourself, it’s protecting your children.
Mother, focus group 9
It was felt that immunising one’s own child was a major step towards protecting the child from serious infectious diseases but that, as a parent, one was also reliant on other parents performing this behaviour in order to better protect everyone:
I mean, as a parent, as well I think, like if they hadn’t been done and they go into a nursery . . . As you know, as soon as your kids start school, nursery or anything like that, they pick everything up. I’d be more worried about sending them to a day-care setting if they hadn’t had their vaccinations [in relation] to what they were going to pick up.
Mother, focus group 7
Another parent noted:
But I mean I think that’s good because [child’s name] started going to nursery at 8 months old and she’d only had, obviously, her first lot of injections, and some of them she hasn’t had. And she’s in touch with . . . that nursery is up to the age of 8. So there’s older kids there that she’s going to be in contact with, and if they’ve got anything that she’s not been . . .
Protected against.
Yes, then she could run the risk of being very ill. So I’d much rather know that all the kids that are going to that nursery have to have all their things up to date.
Mothers, focus group 6
The fear of one’s own child being unprotected against something that could be passed on by other children was expressed by one mother:
This is completely off the wall, but when dogs go in kennels, they’ve got to be immunised . . . so children should be the same if they’re going in care where there’s other children around them.
Mother, focus group 8
Protecting others, as well as your own child
Parents were not only concerned with protecting their own children, but also mindful about protecting others in their community – both children and adults. There was concern that, as a parent, one would not want other people’s children to suffer because of one’s own decisions. It was felt that mandating vaccination could reduce the risk of infections ‘doing the rounds’:
Because, obviously, you’re more strongly [concerned] about your own child but obviously, you still want to protect other children. You don’t want to see someone else go through something that you wouldn’t want to go through yourself.
Mother, focus group 4
Another mother also commented:
It [illness] puts everybody at risk; it [vaccination] protects everybody doesn’t it?
Mother, focus group 2
Day-care settings bring together children of many ages, from small babies who are too young for certain vaccinations to older toddlers, who are, potentially, not fully immunised. Parents raised concerns that these older, partially immunised or unimmunised children posed a significant risk to young babies who, owing to their age, could not be fully immunised. It was felt that, as a result of these issues, making vaccination mandatory for entry into such universal services should be encouraged.
They [unimmunised children] are in contact with all the little babies that can’t be immunised.
All the ones that can’t be immunised because they’ve not reached the right age yet, or just the fact that there are a lot of 3-year-olds and like 2-year-old, and a baby is a lot more susceptible to complications than older kids.
Mothers, focus group 6
Parents raised the importance of protecting not only other children in an educational setting, such as day care or children’s centres, but also the staff who worked in these settings. Adults, they knew, were also capable of contracting infectious diseases brought in by unimmunised children, which could also lead to the spread of disease throughout families.
I mean some of these adults can catch them can’t they, you know, it’s not just children, you know, it’s not just, when you were just saying there about a day worker, you know, comes into your home or whatever, they’re going to go to other people’s houses and everything. And it’s the same as the nursery teachers, they’re going to go home to their own families.
Mother, focus group 5
Encouraging people to prioritise
Parents felt that framing vaccinations as a requirement for entry into day care or school could encourage the group of those parents who, for whatever reason, had not prioritised vaccination. Parents felt that there was a cohort of parents who did not actively choose not to immunise their child; they just did not prioritise it. It was felt that mandating could actively engage these parents:
Yes, incentive wise I agree that will work . . . it depends on what the overall outcome is trying to be. If it’s trying to get that number up to 100% of children, then I don’t think it would work for that. However, if it’s to sweep up and to make people think about vaccinations more, from that side of it, to spread, stop spreading disease between, well before school age, it would work in that respect.
Mother, focus group 1
Another mother noted:
If the nursery turned round and said, you can’t come in unless you get immunised, that inspires you to go to the doctor’s [surgery], doesn’t it?
Then it seems like a rule – not just being forced to do it.
Mothers, focus group 2
Parents felt that some ‘other’ parents would be encouraged to immunise their children for entry into school because they were the sort of parents who were keen to put their children into day care to give themselves a break. These parents, who were described as ‘lazy’, were the type of parents that a quasi-mandatory scheme would particularly encourage.
You’d be [encouraging] the type of parents that are too lazy to get the injections or the type of parents that are like, [to their children] ‘go to school, go to school’.
Yes, get out of my way.
The parents that are like lazy and don’t get them done for that reason, they’d be like, right, let’s get them done, they can go to school. I mean everybody like gets to that stage when it’s like, oh 5 minutes to myself, do you know what I mean? But like, yes them type of parents are like, I don’t know anything about the injections, I can’t be bothered, they’re not getting them. They’re going to be, them type of parents are like, get away.
Mothers, focus group 9
One father commented:
If you’ve got parents who are lazy, who are not taking the kids for their injections, they’re going to want rid of the kids, aren’t they, to school.
Father, focus group 5
Children’s rights to a normal life interrupted?
A child’s right to socialise in either day-care or school settings was seen as important to many parents. Many felt that the threat that a child would not be allowed to partake in such activities, as a result of incomplete vaccination coverage, would be a motivating factor for parents to participate in the childhood vaccination programme:
Maybe that might be an incentive for a parent to get it done then, because then their children won’t be able to lead a normal life like that might they?
Yes, no school or nothing.
Mothers, focus group 7
Moreover, a child who was refused entry into school would be missing out on educational opportunities, which, again, could motivate parents to keep vaccinations up to date. On the other hand, however, it was felt that this approach could be seen as punishing the child and jeopardising his or her future as a result of a decision that had been made for them by their parent:
Surely you’d want your child to have the best education. You don’t want them to miss out on that year, just because you haven’t had your vaccination.
It’s not just an education, it’s a social life, you want them to socialise, wouldn’t you really, definitely.
Mothers, focus group 7
Another mother commented:
Lots of children could be affected by that, couldn’t they? It’s the parent making the decision that a child can’t make. [Child’s name] can’t make a decision as to whether she gets her vaccinations or not, that’s something that I have to make. She doesn’t have that choice. So if I just don’t give her them, then I’m affecting her future aren’t I? Whether she goes to school to get educated or I educate her at home, and it won’t be nowhere near the standard as a school would. You don’t have time to educate the child at home.
Mother, focus group 4
Parents also raised concerns that they could be prosecuted if their child was unable to attend school because they refused vaccinations, as education is compulsory in the UK.
Yes, I suppose yes, because then if you don’t put your child in, it’s like, that’s it. You’ll be the one that’s going to get prosecuted for it. So it’s going to make you want to do it.
It’s going to make you do it.
Mothers, focus group 3
There was a tendency among participants to focus on the legalities of a quasi-mandatory system to increase vaccination. For example, parents were unsure if, in the UK, a parent could be penalised through fines or imprisonment for failing to send their child to school or for taking them out of school for family excursions. They were concerned that, if this were true, it would also apply to parents opting their child out of the vaccination programme.
You can’t really reprimand some parents for not taking their children in and say, well you’ll be facing imprisonment if they don’t go to school, and then say, but if they’re not immunised they’re not allowed to go to school. So then, do they face imprisonment for their child not going to school because they’re not immunised?
Mother, focus group 6
The need for legitimate exceptions
The possibility of introducing a vaccination mandate for school entry raised the issue of being able to gain an exemption from the vaccination programme for a child, either on medical grounds or because the parent had made a conscious decision based on, for example, religious beliefs or their own research. Many parents were unsure about what exactly a valid reason for exemption should be; some believed that members of certain religious groups could not receive vaccinations:
I was going to say, it’s Muslims isn’t it that don’t have pork, and a lot of medicines have got stuff like the pigs’ trotters in them . . . because the chemist I used to work in, they used to come in and say, has it got this in it, has it got, and we had to look at the ingredients and make sure it did or it didn’t have something else.
Mother, focus group 6
The exemption of so-called ‘conscientious objectors’ on the basis of their beliefs was acknowledged by many parents as valid:
I think it’s really controversial really because if people have very strong beliefs, for whatever their reason is for their beliefs, they obviously have a very strong belief for not wanting to do something. And that’s different from just not being bothered and that’s then penalising someone for something they believe in.
Mother, focus group 3
Others acknowledged that parents might seek exemption because they were fearful about side effects from the vaccinations themselves, especially when faced with a decision to immunise with the MMR vaccine.
The thing is, forget about the money side of it, some parents are frightened about the injections because they’re thinking the bairns are going to get something else. They’re frightened that that injection’s going to cause autism or something else.
Father, focus group 5
Another parent noted:
Well some people believe that the vaccines are going to cause damage. And actually, the scientific research is, there’s always a, there is a chance with all of the vaccines, that yes they could do. You know, it’s a case of weighing up the risk factors and some people aren’t prepared to take that risk. And, obviously, then feel very strongly about, because they’ve heard of someone who’s had a reaction or they’ve read something and they really believe in that culture that they believe in. But yes, I guess, unless they can’t say 100% certain when you go for an vaccination, there’s absolutely no chance this vaccination is going to affect your child negatively.
Mother, focus group 3
Removing ‘choice’
Some parents felt that mandating vaccination for entry into day care and school would be interpreted as a removal of parental choice, which they felt was one of parents’ main rights. There was fear that this type of scheme might lead to a severe reaction in some quarters.
I don’t agree with paying, but I think like, if you make it mandatory, then they’re going to be like, oh human rights, you know, you’re taking away our choice.
Mother, focus group 8
Another mother noted:
Like that’s not how our, that isn’t actually how our country works. And as much as I’ve got my child immunised, and I believe in vaccination, I don’t think you can start telling people they don’t have the choice for their options.
Mother, focus group 3
Mandating vaccination was likened to being forced into other ‘socially acceptable’ behaviours, such as breastfeeding.
If it was something else though that they were telling you to do, like they were saying you have to breastfeed otherwise you’d lose it [the baby], you wouldn’t like that though would you? So it’s like it’s your choice isn’t it? It’s like forcing you into something. That’s what I don’t like.
Mother, focus group 6
Questions were also raised about the feasibility of introducing such a mandate in the UK, where education is compulsory.
That would be hard to do though.
Hard to do, what do you mean?
Because you have to educate your kids and the government, they have to provide them with education. So for them to stop your [child’s education], through having the vaccinations, I don’t think they’d be able to do that.
Father, focus group 5
The wealthy could opt out of mandates
It was noted that even mandating vaccination for entry into school would not necessarily result in 100% coverage of children (although it would probably ensure that there was sufficient coverage to achieve herd immunity), as some parents would have the resources to opt their children out of formal education by educating them at home.
It’s better than the taking away the Child Benefit, but I still think there’d be people who would say, well I’ll home school or I’ll send my children to this special homeopathic school down the road because I can afford to pay. I can get out of this, it doesn’t apply to me.
Mother, focus group 1
Another mother commented:
The two people I know that don’t immunise, they’re both home schooled as well, but out of choice. So I’m wondering whether it’s kind of that kind of psyche that, them kind of people, not in a horrible way.
Mother, focus group 6
A degree of vaccination surveillance at day-care entry is already happening
Some parents reported that childhood vaccination status was already monitored through day-care facilities and many had accepted this without questioning why staff had requested this information.
I had to prove when my oldest went into nursery, I had to take my red book and prove that everything was up to date . . .
Would they have refused you a place if you weren’t up to date?
I don’t know. They [vaccinations] were up to date, so I didn’t really have to take the chance, but I had to take the red book and prove it all.
Mothers, focus group 4
Health-care staff confirmed that it was common practice in some local areas to ask parents to show their ‘red book’ (personal child health record), so that rates of vaccination in each facility could be assessed by local health authorities, who would then know where the likely ‘hotspots’ were in the event of an epidemic ‘flare’.
It was felt that, although mandating vaccination for entry into day care would be acceptable to parents, it might not catch all eligible children, as not all children access such services and may be cared for within the family. In that respect parents felt that mandating vaccinations for entry into school might be more effective, as the great majority of children access school.
I don’t think it would work because a lot of parents actually don’t work, don’t put their children in child care. So like grandparents and things look after them while they’ve gone to do their shopping or whatever. There’s a lot of kids that don’t even go.
So you’re missing a lot of people there?
Yes, a lot of people they’ll be missing more than the school one.
Mothers, focus group 1
Across deprivation groups, parents agreed that the introduction of a quasi-mandatory scheme would be most inclusive; however, it was acknowledged that some more affluent parents would still have the financial resources to opt out and potentially home-school their children or put them into private education.
Summary: parents and carers of preschool children – quasi-mandatory schemes
In summary, the responses of parents and carers of preschool children to the suggestion of restricting entry to child care or school based on vaccination status were as follows:
-
Quasi-mandatory schemes were felt to be preferable to financial incentives; they were described as fairer and more acceptable.
-
Mandating vaccinations for entry into universal services was seen as preferable, as this:
-
offered protection for children who were too young to be immunised (day care)
-
offered protection to all children in the shared setting
-
offered greater protection to staff who work in the setting.
-
-
Mandating vaccinations would act as a reminder to immunise for those parents who did not prioritise vaccination.
-
Refusing entry into universal preschool services or, ultimately, into school itself would punish children for a decision made by their parents.
-
It may not be acceptable to remove people’s ‘free choice’ to engage or not engage with a health-related behaviour.
-
There would have to be a clear opt-out process for those who had legitimate reasons for non-vaccination.
Parents and carers of preschool children: alternatives
Parents proposed a number of alternative methods for encouraging the uptake of preschool vaccinations during the discussion of financial incentives and quasi-mandatory interventions.
Vaccination should be the incentive
There was a feeling from some parents that a shift was needed when thinking about incentivising vaccinations. The offer of protection for your child, free of charge, should be viewed as incentive enough, without the need for bonuses. Promoting the vaccination as being, in itself, a gift that holds a monetary value was suggested as a way of promoting vaccination to those who did not prioritise it.
Maybe people need to know how much it costs, what it does and all the facts about it. This costs the government x amount of money and you’re being given it for free. This is a fantastic opportunity, your child will be better because they won’t have this illness, which could do this to them.
Mother, focus group 3
Another mother noted:
It’s costing the government loads of money to give this to people for free, and because we’re getting it for free, we all get a bit blasé, people are more casual about it.
Mother, focus group 1
Providing accessible services
There was a call for more accessible services, for example out-of-hours clinics or a health professional visiting parents at home, to do some of the ‘mopping up’ among those who had failed to attend the vaccination sessions at their GP practice:
It depends on people’s circumstances doesn’t it? But if you were thinking, right, I’m going to go at 1 o’clock, and we’ve all been there, where you’re still sitting at half past three and thinking, what am I going to do? I’ve got to pick such-and-such up from school. So is it more about making it convenient or at the house, have an appointment time, where you just go in, get the injections.
Mother, focus group 2
One father noted:
I think you’re right, having surgeries open longer and having more people, more flexibility of staff to go around on an evening, that sort of thing.
Father, focus group 5
Another alternative to offering financial incentives was the suggestion of providing transportation to vaccination clinics for those who found it difficult to access them:
Or like the offer of a free taxi or the offer of, do you know people who haven’t got no money, who have to walk everywhere, you see people pushing kids, five and six kids at a time, lone parents, I don’t know, incentives that way, maybe that would work.
Father, focus group 5
Education
Parents also felt that increases in vaccination rates could be achieved through better education, as one parent expressed:
You can’t force people to do something, you need to educate them to make the decision themselves, rather than force them.
Mother, focus group 6
All parents acknowledged that they had been provided with a wealth of written materials about the childhood vaccination programme, although none had read this information in its entirety.
Yes, you just need that, well for me personally, you just need, for those people that need persuading, they need a push to get their children immunised. I think there needs to be so much more information, rather than a little booklet that you, you’ve just came home with a baby, you don’t want to sit and flick through. Well I didn’t want to sit and flick through all the leaflets when I bought my kids home.
Mother, focus group 9
Parents felt that they did not really understand what they were protecting their child against and had trouble weighing up the risks of the vaccination against the risks of the disease should a child become infected:
I think better education about it as well, because I mean I know with having four [children], you don’t really know anything about half of these illnesses, but I know they’ve got, you know, they’ve got the vaccinations. And I know that, or I’ve been told, that the risk of them getting a reaction to one of those, is not as bad as getting one of those [illnesses] if they didn’t have the vaccination. But other than knowing what they are and how bad they can be and things like that, I wouldn’t know.
Mother, focus group 3
There was a call for clear and concise information, and not necessarily in a written format. Parents wanted to see pictures of the consequences of the diseases that vaccination protected against, as, for example, many had never seen a child with diphtheria. Diseases such as this were no longer part of people’s lived experience.
The information should be clear and people friendly.
Mother, focus group 3
Another mother noted:
More of the risks should be highlighted, more of what could happen if you don’t have it done, more of these like horrible pictures, you know what I mean, should be concentrated on and sent to all parents, yes.
Mother, focus group 7
Another mother noted:
I think a lot of the problem as well though, is because of all the vaccinations, most people do have it, you don’t hear about people day to day having had polio or diphtheria and stuff like that. So it’s just a word and it’s, I have a vague idea of what those things are, but you just think, oh it will never happen to us, it’s just a word. Whereas I think, if people knew what they were and what it involved if the child had them [diseases], you might [reconsider].
Mother, focus group 1
Education during pregnancy was highlighted as an ideal opportunity to discuss vaccination and provide education about disease and its consequences. Again, parents favoured being shown, pictorially, what the results of being infected could mean for their child:
And if they’re new parents, like first-time parents, you know, and during antenatal classes or, you know, something, some kind of like course that, like pre-course before actually the baby’s born, you know, to let you know that, you know, these are the vaccinations, this is what age they have them at, you know, the benefits, the pros and cons. Like what [names participant] said, hit home hard with like visual aids, you know.
Mother, focus group 7
The mother went on to note:
Well like [names participant] has just said, maybe it’s one of the midwifery sessions that you attend, should be concentrated around vaccination. And the midwife showing you these horrible statistics and horrible pictures and saying, this is why it’s done.
Mother, focus group 7
The use of a television advertising campaign was suggested as a way of communicating messages about the severity of childhood diseases for unimmunised children who could become infected:
An advert. The amount of adverts that stop people from smoking and things like that these days. So an advert. You’d have to have a family where they’ve regretted, like something’s happened and they’ve not made the right decision to have their child protected against these things, or even, like something that’s the truth, because an advert’s just fiction isn’t it?
Mother, focus group 9
Summary: parents and carers of preschool children – alternatives to financial incentives or quasi-mandatory interventions
Parents and carers of preschool children identified a number of alternative methods to financial incentives and quasi-mandatory interventions for increasing uptake of preschool vaccinations. In summary, these were:
-
provision of accessible services
-
out-of-hours clinic appointments
-
appointments available outside baby clinics
-
outreach services
-
-
accessible information about childhood diseases and their consequences
-
effective communication through the media.
Health and other professionals: financial incentives
The following section presents findings from interviews with health and other professionals. As described in Table 7, our sample comprised GPs, practice nurses, practice managers, community paediatricians, health visitors, school nurse, head teachers (primary school), commissioners and national policy representatives.
Mixed feelings were expressed about the introduction of financial incentives to the vaccination programme.
Incentives have been successful in some circumstances
It was acknowledged that incentives had been introduced into different areas of health care. Cited examples included incentivising mothers to breastfeed their babies or providing a financial reward in smoking cessation and weight management programmes. Participants identified a local area in which financial incentives had been introduced into non-childhood vaccination programmes, with some success.
You could look at is as being a way of getting people engaged in preventative health care that they might not have considered before. And we have done it with hepatitis B vaccinations, by way of giving an incentive for completing the whole course. And it increased the uptake by about 45%, which was excellent and, obviously, you’re then protecting the individual and it becomes less of a public health issue if that person’s undertaken the vaccination. I suppose you could apply that to [childhood] vaccines as well.
Commissioner 1
However, even though it was acknowledged that incentives can be and have been successful in certain areas of health-care provision, it was postulated that the introduction of any universal incentive might be met with opposition from certain sectors of the population.
Certainly, financial incentives, I mean my understanding is it can work with weight loss . . . so we already do that with certain groups. But it’s one of these things, which the public would probably see as, you know, just giving money out to ‘chavs’ [derogatory term for less affluent people] and blah, blah, blah, you can just see the stories.
GP 1
Parental responsibility to protect children
Although it was acknowledged that financial incentives had the potential to attract certain sections of the population to engage with preventative medicine, these statements were always followed by statements of uncertainty about paying money in exchange for engagement with what many health professionals (and parents, previously) felt was the ‘morally right’ thing for a parent to do to protect their child.
I mean having worked in lots of different places, I do think that it probably would motivate some people, you know, whether that’s right or whether that’s wrong, I don’t know. Personally, I think it’s wrong but I think it probably would motivate some people, if they thought they were going to get a fiver [£5] or something.
Practice nurse 1
However, it was expressed, on occasion, that incentives could have a future in preventative care. A societal shift was noted, whereby individuals expect that they will be reimbursed for or profit from engaging in what are seen to be socially responsible behaviours.
We don’t often think about giving patient incentives, but more and more we might have to. Because there’s an old thought, you know, in previous generations everybody did stuff because it was their duty and, you know, the community thing and they knew what was right and what was wrong and did it because they knew they should. But now we’re in a community where people more and more, well you’re feeling people more and more need to be reimbursed for doing what might, in the past, have been accepted as normal.
GP 2
Many professionals, however, described the introduction of financial incentives as distasteful, as they held steadfast to the belief that immunising a child was one of the obligations of a responsible parent.
I mean at the end of the day, I just think having children and making sure that they’re vaccinated against all these diseases, should not be down to cash, at the end of the day. I think they’ve got a responsibility, they bring these little ones into the world and they should look after them as best as they can.
Practice nurse 3
Another practice nurse commented:
You shouldn’t actually have to be paid to do, what I consider, to be the right thing for your child’s health. You should inherently have that because you’re their mum and you want the best for them.
Practice nurse 1
The introduction of incentives for health care was viewed as something that could erode the notion of the parent having the responsibility for protecting his or her child:
You know, actually having your child vaccinated is something that we, I don’t think we should reward them with money. I think, again, it would, I think it will have unintended consequences. But I don’t know what, I don’t know what they are, but they kind of distort our view of health care and our view of responsibility for our children’s health care.
Community paediatrician 1
Parental responsibility was described as what should be the main motivating factor for accepting vaccination.
As a parent myself, I think no [financial incentives should not be offered]. I think sometimes we spoon feed parents too much and, ultimately, the responsibility is with parents. As a professional, I think I hold the same opinion, in that, you know, parents have to be responsible. And I know some parents aren’t, but I think we’re just playing into their hands again, in that you’re giving them an incentive. And the incentive should be they want the best for their children.
Head teacher 2
In many cases, professionals felt that the introduction of a financial incentive was unnecessary and that it equated to bribery.
It’s a really difficult question, isn’t it? Because I think, I think we should be working harder to accommodate those patients who, for whatever reason, don’t bring their children in, not a financial incentive per se . . . it doesn’t sit very well with me. I think it’s coercion really, bribery and corruption. It doesn’t sit well with me and I just think there are other things that we could be doing, working harder to do.
Practice nurse 2
Governance issues and cash alternatives
In some localities, commissioning teams had previously considered introducing financial incentives to try to encourage health-related behaviours. They had, however, been faced with local governance issues that restricted the types of incentive they could offer.
Having some experience of looking at financial incentives as a provider, and then incentivising, you know, an example, smoking in pregnancy, for a financial incentive you hit a lot of financial governance issues around how you track that finance. When you pay it out, was it used by that person, what was it used for? So, you know, you might pay them a fiver [£5] for a vaccination, but are they then spending that fiver on fags [cigarettes], which is then your public health [issue] . . . we didn’t do it in the end.
Commissioner 3
Concerns about how, where and on what cash incentives could be spent were paramount in participants’ minds. There were fears that such money would be spent inappropriately.
If you’re giving cash, you don’t know where that money’s going to. It might not be spent on anything that would benefit the family or the child.
Commissioner 1
Alternatives to cash were suggested as a way of working around the issues posed by directly paying parents, in cash, to immunise their children.
If it was morally repugnant just to give money, then it could be, you know, it could be health vouchers, which could only be spent on children, you know, so be it baby food or milk or, you know, clothing or whatever it is.
GP 1
Another participant noted:
If we gave them something that was good for them, like books or fruit and vegetables or child care vouchers or something, actually we are giving them something that’s good for them. But I think to politically sell it would be really difficult.
Community paediatrician 1
However, it was also noted that vouchers might not be a foolproof option, as they could be sold or exchanged for products that health professionals deemed inappropriate, thus invalidating efforts to offer voucher alternatives.
Where I used to work in [locality], a lot of the mums would take the Healthy Start vouchers [which can be exchanged for fruit, vegetables and milk] and things into the shop and sell £10 worth of Healthy Start vouchers for a 10-pack of Lambert and Butler [cigarette brand], which is what, about £3.80.
Health visitor 3
Health services have finite resources
Participants noted that UK health services are currently working within tight budgets, especially in the current economic climate where budgets are being cut and closely and publicly scrutinised. To commit money to incentivising parents to immunise their children was seen as unsustainable, and probably something that could be offered for a limited time only.
It can’t be continuous [offering incentives] because it’s a lot of money that is being given out. Then [when you stop offering incentives] you’ll find vaccination rates dropping and then you find again, the diseases coming up and then again, the government having to step in with extra resources to kind of top up this vaccination again.
Community paediatrician 2
Another participant noted:
It’s a big issue if you’re going to give cash, especially in today’s NHS culture of working smarter and leaner and, obviously, the cash issues to the NHS at the moment, so we’ve got to look at that.
Commissioner 1
If incentives were to be introduced as a long-term plan to increase the uptake of vaccinations, and money was to be raised through an increase in taxes, it was postulated that this could cause an outcry in the general population.
I think, I don’t think, in these times of economic constraints as well . . . actually, if you were to say to a community, your taxes are point 1% higher because we’re paying families to immunise their kids, that would have a, not only would it have an unintended consequence on parenting, I think it wouldn’t have a good community impact either.
Community paediatrician 1
Incentives would not change the minds of ‘conscientious objectors’
Mirroring the findings from the parent focus groups, professionals raised concerns that the introduction of financial incentives would not encourage parents to immunise their children if they had already made a conscious decision to refuse vaccination. This point was often made at the same time as expressing a belief that financial incentives might encourage a small section of the population who were living in disadvantage:
The monetary incentive would work for the lower socioeconomic class and there are quite a few in that particular class who either just couldn’t be bothered, because they’ve too many things and their lives are very, not easy, discordant and lots of other things going on. So for them I think if there was a monetary incentive it might work in kind of attracting that class of people. But, as I said, the other class [who have made a conscious decision] is very unique and I don’t think monetary incentive would work in them.
Community paediatrician 2
Parents’ beliefs around vaccination and immunity, it was believed, would not be affected by the offer of a small financial reward.
It depends upon what kind of beliefs you have about the vaccination. For example, the mother that I was talking to you about, she believed in getting kind of natural immunity. For her, even if you give £10, I don’t think that would kind of change her opinion in any way. So I’m not entirely sure about the financial incentivisation.
GP 3
Another participant added:
I think it’s terrible, I really do [offering a financial incentive] . . . I think the choices that the majority of patients have made are informed choices. And for all, you know, from my perspective, a financial incentive will not change that parent’s mind. Because they believe that the vaccine is going to affect their child in a, you know, in a clinical way.
Practice nurse 2
Summary: parents and carers of preschool children – financial incentives
In summary, health and other professionals raised the following issues in relation to offering financial incentives for preschool vaccinations:
-
Financial incentives have been successful in some circumstances in encouraging healthy behaviours.
-
Introducing a financial transaction into vaccination may break the bonds of social responsibility.
-
There are finite resources for funding health services and providing financial incentives to parents may not be the most appropriate use of these.
Health and other professionals: quasi-mandatory schemes
The suggestion of introducing quasi-mandatory schemes, such as financial incentives, to increase the uptake of vaccinations was met with mixed opinions among health and other professionals about how and if they could work.
Could be a good way of increasing coverage rates
Reflecting responses from parents, health and other professionals generally thought that the prospect of introducing quasi-mandatory schemes restricting day-care and school entry to immunised children was preferable to providing financial incentives. The importance of children being fully immunised before they entered shared settings, where they could pick up infections, was acknowledged, and many professionals thought that mandating vaccinations made good sense for this reason.
Yes and I do think that it’s important that these children are vaccinated before they attend toddler groups, playgroups, you know, and school. I do think that that should, you know, it should be, well I’m sorry, your children can’t attend if you haven’t had their vaccinations.
Practice nurse 1
From a perspective of protecting the health of the population, quasi-mandatory schemes made sense to participants as a mechanism to promote uptake.
I think there is a lot to be said for mandatory requirement, you know, for entry into a day care or, you know, a preschool setting, be it, you know, for the under-twos, yes nursery or, yes child care nursery or educational nursery. And I think from a population health point of view and protection, and the great and the good, I think mandatory is something that we should be looking at.
Commissioner 3
Many mandatory schemes have been introduced in the UK to protect the health of the public with great success and general acceptance. Thus, it was seen as plausible that the introduction of a quasi-mandatory scheme for preschool vaccinations could have a positive impact on uptake rates. However, there are subtle differences between these schemes and the introduction of a mandate for vaccinations.
But on the whole, that would be a simpler way forward. And simpler, relative to all the ethical complexities elsewhere. We’ve had seatbelts, we’ve had smoking environmental, all of those have worked better than hundreds of different ways of helping people to change behaviour.
Commissioner 4
How could quasi-mandatory schemes work in practice?
Although quasi-mandatory schemes were deemed to have the potential to positively affect vaccination rates for preschool children, some concerns were raised about how such a scheme would work on a practical level. Head teachers were adamant that the administration of such a scheme should not be the responsibility of an educational institution and, rather, that the responsibility should lie directly with the health sector.
Who polices that then? Say, for instance, we accept children into our nursery or into school, we notice they haven’t been immunised . . . it’s then office time or our parent support advisor who will be doing that chasing up, I’d think. And I don’t think that’s a school responsibility. Again, that’s a parent responsibility, or a health professional’s responsibility.
Head teacher 2
If such a scheme were to be introduced, it was suggested that to reduce the impact on school administration, the process of identifying unimmunised children could be carried out during the application process, at the relevant local authority.
So is that going to be something Civic Centre do then? That’s where all our admissions go. So they apply to the Civic Centre, they don’t apply to school direct. Who is going to do that workload? . . . Because I don’t think my office staff are the most appropriate to do that, to chase up parents. Again, you’re almost just passing the buck to another service, aren’t you, another professional. It hasn’t worked for us or we haven’t had the uptake say within the health, so we’ll pass that on to education, or we’ll pass that to somewhere else.
Head teacher 2
Moreover, it was highlighted that identification of partial or unimmunised children was a complex process. The vaccination schedule is constantly evolving. Health professionals involved in the process of vaccination were felt to be the most competent at reading and interpreting vaccination records. If this task were to be devolved to other professions, specific training would be required to ensure competence and consistency in interpretation.
If a parent wants a child [to get] into nursery, [and] their policy is your child must be up to date with vaccinations and you must have evidence of that [vaccination record]. What the evidence is, is another matter. You know, who can scrutinise a red book? Who can read a list of vaccinations? Does it need to be a health professional reading it? Can you train somebody in the nursery group to do that? So there’s those issues to consider as well.
Commissioner 1
There were also concerns that, although parents have a hand-held record of their child’s vaccination history (in the ‘red book’), this can be easily lost or may not always be up to date. Those working in general practice highlighted that the sharing of data about children may be difficult, as each parent would have to consent to sharing vaccination records with outside organisations, such as the local authority or school, if these organisations became responsible for administering the vaccination programme.
To share the child’s information, we wouldn’t just be able to, you know, County Hall wouldn’t just be able to say, we need vaccination histories on these 30 children. We would, you know [have to get consent], and that consent thing would be the time-consuming thing and I think that that would have to be not, the practice shouldn’t be responsible for getting the consent.
Practice manager
Those involved in the school nursing side of health provision also raised the issue that they would struggle to obtain accurate information about the vaccination status of a child, without the introduction of a robust system that was synchronised to GP records.
I don’t think we’d be able to identify the children who haven’t [been immunised], we haven’t got the information in front of us . . . the information that a parent has, information that’s on our database, and the database a GP practice has, is often not the same . . . and that is a big stumbling block I think.
School nurse
Removal of choice has ethical implications
Along with the practical difficulties in administering a quasi-mandatory scheme, professionals grappled with the ethical implications of such a change to the way vaccinations are offered. All of the professionals we spoke to raised concerns about the ethical implications of this type of scheme. Although quasi-mandatory schemes could be deemed as preferable from a public health point of view, it was felt that these might be perceived as a step too far for many citizens.
It’s a kind of communist kind of principle isn’t it? That you have to have it, otherwise you can’t do it [enter into universal services]. It’s just the ethics of it and what, some people would argue that it’s, you know, human rights and, you know, I have a right to do what I think is best for my child . . . so though I agree with it in principle, I think that there would be a lot of argument against it as well, particularly in the kind of society we live in.
Community paediatrician 2
Professionals, like parents, felt that it was a parent’s right to choose vaccination for his or her child, and that being able to make an informed choice was one of the prerogatives of living in a democratic society. Refusing a child access to education based on vaccination status did not sit well with this concept.
The ethical aspect, the morality of it . . . It’s like, you know, making a nanny kind of a state and we are a democratic county and, you know, everybody’s beliefs and opinions are kind of respected. But then we are sort of saying; your child is not going to have education if you don’t immunise.
GP 3
Another participant added:
I think there probably should be some free choice left in our country about what we do and what we don’t do. And I, as long, you know, I think you should have the choice not to immunise your children. That, you know, I think health interventions, which do carry a risk, as a parent or as a citizen, we should be able to choose whether or not we want that health intervention.
Community paediatrician 1
Those who worked closely with families in disadvantage felt that that the introduction of quasi-mandatory schemes could actually undermine the work they were doing with those families to promote better health outcomes, essentially going against their professional ethos.
In a way I think that’s nonsense because, for a lot of our families who we would want mandatory nursery places for, our harder to reach families, where there is social need, so if we’re saying they potentially might be the ones that are highest non-uptake of vaccinations, that becomes a nonsense. Because the thought beyond that then is, you’re excluding the excluded . . . And quite often we want them in nursery because that allows parents maybe to access some parenting courses . . . then if we’re to exclude those from nursery because they’re not up to date with their vaccinations, that’s a nonsense to me unfortunately.
Health visitor 2
As in the focus groups with parents, professionals noted differences in parents’ ability to make health decisions based on their socioeconomic status, with wealthy parents being able to afford to opt their children out of vaccinations and pay for private education or day care.
The only thing that would fall down on that is parents that are able to, you know, private nursery and private education. And most of those parents do immunise and if they don’t, they’re the ones that you’re not going to persuade because they will have done their own research for their own slant on it.
Health visitor 3
Summary: health and other professionals – quasi-mandatory interventions
In summary, health and other professionals’ views concerning quasi-mandatory interventions restricting entry to child care or school based on vaccination status were as follows:
-
Quasi-mandatory schemes were viewed by professional staff as more acceptable than financial incentives.
-
Quasi-mandatory schemes could facilitate the normalisation of vaccination.
-
Entry into school could be an ideal time to monitor vaccination and provide catch-up.
-
Schools were reluctant to take over the administration and monitoring of a mandated scheme.
-
Data sharing between health and educational sectors around vaccination status could be problematic.
-
Professionals were uncomfortable with the idea of the removal of personal choice and free will in relation to this particular health-related behaviour.
Health and other professionals: alternatives
While the professionals in our sample discussed the pros and cons of the introduction of either financial incentives or quasi-mandatory schemes, like parents, they all offered alternatives which they felt could have a greater impact on the uptake of vaccinations. Building trusting relationships with families, providing timely and relevant information about vaccination and childhood diseases and facilitating access to vaccination clinics were all seen as ways in which uptake could be encouraged without the need for incentives or mandates.
Building trusting relationships with families
Health visitors felt that an ongoing part of their role was to support parents in their decisions about vaccination. In one area of the north-east, which boasts the highest vaccination uptake in the region, health visitors prided themselves on working closely with parents to educate them and facilitate decisions about vaccination.
[uptake can be influenced by] . . . better systems and processes, more joined up working, more transparency and ownership of professionals to have accountability. I think to demonise and to chastise and to punish families, isn’t the first option and shouldn’t be the first option.
It should be at more of a sort of organisational level?
I think it should be an organisational level. It should be professionals’ accountability to demonstrate what they’ve done to support the families.
Health visitor 1
Supporting families by providing timely and appropriate education was seen as imperative to facilitating parents’ readiness to accept vaccination:
It’s about the readiness for that change. And that’s, I think, what we probably do with our families, is work with our families, informing them, giving them the information, for that readiness to make that decision . . . some parents, you know, who are, you know, professionals themselves, might want a certain level of detail. There are sheets . . . they’re very wordy, very detailed, analytically talking about the research backing, you know, and that’s what some parents do want. And it’s an understanding of the population that you’re working with isn’t it?
Health visitor 1
Raising awareness of preventable childhood illnesses was suggested as particularly important given that, owing to the success of the vaccination programme, many such illnesses are now a distant memory.
Most people, if you sit down and explain it, are not conscientiously objecting to being immunised. In my anecdotal evidence and some of the evidence I’ve read, it’s more, sometimes there’s a lack of awareness of the benefit of the vaccines. Vaccinations are a victim of its own success, because people aren’t seeing those diseases any more and may need that explaining, or there’s myths around the vaccine that you need a professional to talk to.
Commissioner 2
Education
The act of persuading parents to immunise their children through education was deemed more acceptable to professionals, as parents could then make an informed decision about how to proceed.
I think PHE [Public Health England] . . . [are] quite clear that, you know, vaccinations, when it comes down to it, are voluntary. So there is a lot to be said about persuading people to [immunise] but not kind of forcing people to.
National policy representative 2
The way in which information is presented to parents could have an impact on their decision process. It was acknowledged, as it was in our parent sample, that parents receive a vast amount of written material, but that this may not be an effective method of communication:
Parents get so much information. They don’t read any of it . . . but I don’t know, if the medium is leaflets because there’s so many leaflets . . . they get quite a lot and most of it just gets left. So I don’t know and it may be back to that having somebody as a trusted person knowing about vaccination or be able to ask anything about myths and the barriers.
Commissioner 2
The way in which information is consumed and used has also changed greatly over the past decade or so. The rise of social media sites and internet forums provides an opportunity to interact with parents and provide information in new ways.
There’s a changing world and social media again, can be useful, sort of viral ads or, you know, stories that are bound to go, get spread around Facebook or Mumsnet and those sorts of things, could, you know, may have a more direct impact.
GP 1
School head teachers, although reluctant to take on responsibility for the organisation and delivery of a quasi-mandatory vaccination programme, suggested that introductory days and parents’ evenings could be utilised as occasions to communicate with and educate parents about the benefits of vaccination, especially prior to their children entering school:
I mean is it not more feasible to use our sort of hub, if you like, our school, as a promotion [location]. So do sessions with parents, talk to parents about vaccinations, the facts, you know, the fors, the againsts? So parents are educated, you know, use our school for things like that, rather than using us as the police.
Head teacher 2
Another head teacher reiterated:
They meet the class teacher and they have like sort of half a day [induction day] . . . so, you know, that would be a perfect opportunity, you know, there and then, if we’re doing that and we’ve got the parents in.
Head teacher 1
Access to clinic services
In confirmation of the views of parents, problems in accessing vaccination clinics were acknowledged by professionals as one of the greatest barriers to achieving better vaccination rates. All of the health and other professionals included in the study raised the issue of access to vaccination services as one that required attention before financial incentives or a quasi-mandatory scheme could be considered.
Especially in areas where the uptake isn’t fantastic, are we actually making the vaccines accessible? Could we do with more people going out and talking about the vaccines, more children’s groups, things like that?
Commissioner 1
Accessibility is massive to families, you know. If the surgery’s on two bus routes, they’re not going to come. You’re looking at extending hours, you’re looking at people in the practice being able to give vaccinations.
Commissioner 2
It was noted that access issues played a part for parents across a broad socioeconomic range, but for very different reasons.
For a working parent, it might be difficult to get your child out of nursery to be immunised, especially if you’ve got a couple of kids and you’re working 9 to 5.
Commissioner 2
The same participant noted:
Families who are in disadvantaged areas and who are a little bit chaotic . . . they tended to be the ones, in my experience as a health visitor, who didn’t come. But if you took it to them or managed to catch them at any odd time, when they’ve come in for something else, you could get it done. But they were very poor at making appointments or meeting appointments.
Commissioner 2
It was acknowledged that for families living in disadvantage, especially those with multiple needs, it could be more beneficial to provide practical support to access services than to provide a financial incentive. One head teacher noted that his or her school tried to provide support for their families by accompanying parents to hospital appointments and offering interpreter services, as the majority of their families did not speak English.
Often, when they’ve got doctor’s appointments, hospital appointments, we actually take them and actually physically take them in the car and get them there. Because their understanding . . . and then we act as interpreter as well. So in terms of education, we have to go that extra mile really. And it is, it’s, you know, we’ve been ferrying children up and down to the hospital this morning and supporting with that, because parents just don’t understand what’s going on really.
Head teacher 1
Some GP practices and health visitors evidenced how they worked closely with families to understand the barriers to accessing services and aimed to work with families to overcome these barriers. One practice manager described how a GP practice had worked in conjunction with their children’s centre to help a local family to access vaccinations for their children:
We worked with the children’s centre in the village. And they actually, because they [the family] didn’t have transport, so the bus that they used for the children’s centre, we actually kind of worked quite closely with them and they actually bussed them all into the surgery to get vaccinated. And then we got them all up to date.
Practice manager 1
It was felt that it could be appropriate to offer vaccination clinics outside normal practice hours. There are instances where these services are offered, for example for the seasonal influenza vaccination, so it was felt that appropriate systems were already in place for this sort of initiative.
I know certainly around the ‘flu [influenza] campaign, some practices even open on a Saturday morning for that, you know, cohort, to get their ‘flu vaccinations in. Yes, they’ll stay open later on an evening, they’ll run sessions on a Saturday. So why can’t we do it for childhood vaccinations?
Commissioner 3
However, offering these extended clinic hours would necessitate a change to the way in which GP practices are commissioned to deliver the vaccination programme. Remuneration would need to make any changes to the Local Enhanced Service Agreement attractive to GP practices.
We have more flexibility over LESs [Local Enhanced Service Agreements]. We could do a local enhanced service, so we could maybe ask a GP to open longer. They all get paid for enhanced hours; then they can open certain times, but not directed what they can do in it. So the GP might stay late for their patients but they say the money doesn’t cover getting the practice nurse in.
Commissioner 2
It was noted that the best way to engage with those families who are not prioritising vaccination is to try to engage with them in different ways from those used currently, for example offering vaccinations in different locations and by different health professionals, utilising all contacts with families to promote and deliver vaccination.
The only way I think it will increase in them areas, is by doing things differently. They’ve got to find other ways. And be it a practice, be it a health visitor, school nursing, you know, NHS Service, has got to play the part and do it differently. You know, I think it’s got to be everybody’s business, it’s not just one area. It’s not just a GP practice or parent responsibility.
Commissioner 3
Summary: parents and carers of preschool children – alternative to financial incentives or quasi-mandatory interventions
Health and other professionals suggested a number of alternative methods for maximising the uptake of preschool vaccinations that were unrelated to financial incentives of quasi-mandatory interventions. In summary, these were:
-
Building trusting relationships with parents and consistently providing education at each contact, which has been shown to facilitate the uptake of vaccinations.
-
Educating parents about the importance of vaccination and understanding parent fears can facilitate the uptake of vaccinations.
-
Offering accessible clinic times can facilitate the uptake of vaccinations.
-
Multidisciplinary working can facilitate the uptake of vaccinations.
Discussion
Summary of findings
On the basis of the evidence collected as part of the qualitative study, both parents and professional staff based in the north-east of England felt that offering cash payments in exchange for immunising a child was inappropriate. It was felt that financial incentives might encourage families who were living in disadvantage to prioritise vaccination. However, this advantage would be outweighed by the unintended consequences of turning a behaviour that is generally engaged in willingly in order to achieve protection for children, out of a sense of altruism and social responsibility, into a cash transaction. It was feared that monetising this behaviour might break down these bonds of social responsibility and lead to parents gaming or playing the system – especially if the scheme was a targeted one based on the vaccination status of the child. For that reason (as well as for reasons of equity), most respondents felt that if a financial incentive was to be used, it would have to be introduced on a universal basis.
Financial incentives are usually suggested in situations in which policy-makers wish to overcome a level of inertia or ‘fecklessness’ or where they wish to ‘nudge’ people over the boundary from lack of interest or a ‘can’t be bothered’ state into a state of acceptance. There was concern from all participant groups, however, that the introduction of financial incentives would create inequity between parents on different ends of the socioeconomic spectrum. Although it was supposed that financial incentives would be attractive to those families living in disadvantage, thus perhaps over-riding any serious qualms about the procedure, those parents who had the power and resources to ignore a monetary incentive would remain able make a health decision based on their belief systems. Those parents who did not have such resources would be less able to make an informed decision, creating an ethical quandary.
It was also considered by most interviewees that the offer of a financial incentive would do nothing to change the mind of a parent who had made a moral or ethical decision to refuse vaccination for their child. In a democratic society it was suggested that these parents needed to be given impartial information and counselling about vaccination and disease, but, if they still chose not to immunise and were prepared to take the consequences, they should not be penalised in any way that disadvantaged them or their child.
The roll-out of a penalty scheme (e.g. reducing family benefits) was seen by parents as superficially more attractive than a financial reward scheme, as it avoided some of the potential disadvantages caused by financial incentivisation, such as game-playing, the undermining of social norms by their monetisation and any accusation that people were being bribed to undergo a procedure. However, parents acknowledged that the most disadvantaged families were very reliant on this aspect of their income and that children might suffer as a consequence of a parent’s decision if this were implemented.
The introduction of a quasi-mandatory scheme, whereby vaccination would be a requirement for entry into universal services such as nursery or ultimately school, was met with mixed opinions. For many, it seemed like an appropriate option that was fair and equitable, regardless of the socioeconomic status of the family. However, the suggestion that a child could be refused entry into education based on their vaccination status seemed immoral to some, as ultimately this would be punishing a child for a decision made by the parent – a punishment that would have far-reaching implications in that child’s life. For this reason, participants believed that there would have to be robust procedures in place for parents to legitimately opt out of vaccinations for moral, religious or health reasons without punishment. Again, it was noted that those families who were able to could opt their children out of such a scheme and either home or privately educate their children, once again suggesting that not all families would have the power or economic resources to make the same decision for their children.
A number of parents thought that quasi-mandatory schemes felt more natural and emphasised the fact that vaccination was important protection for all children. Parents tended to be very aware of the ways in which preschool and primary school children passed ‘germs’ around and easily became infected. Some parents noted that it was already customary for nurseries to ask to see children’s ‘red book’ personal health record to note their vaccination status.
Although both parents and health professionals considered the relevant pros and cons of introducing changes to the ways in which vaccination could be offered to enhance uptake, these discussions always came back to one factor: the need to strengthen delivery of the existing programme.
Both parents and professionals felt that vaccinations should be offered primarily through GP practices. These were seen as a tried and tested delivery scheme, with systems in place for monitoring uptake. However, there was interest in opening up vaccination provision to other providers. Parents tended to want vaccinations to be offered in community-based settings such as children’s centres, not least because these are accessible but also because they are seen as child-friendly. Professionals discussed the possibility of opening up vaccinations to providers such as community pharmacies, much like recent pilots for the seasonal influenza vaccination. If childhood vaccinations were extended to other providers, extending child health record systems to those providers would also have to be considered.
Professionals from every group represented in the research noted many missed opportunities for both health promotion activity and opportunistic vaccination. The lack of a single vaccination recording system, accessible across multiple sites, was highlighted as a barrier to this. Many professionals who came into contact with families felt that they would be happy to promote vaccination to families and, in many cases, would be happy to deliver the vaccination, should they be confident that the child had not already received it. Of course, there would be issues around the availability and safe storage of the vaccines, the complexity of the vaccination schedule and professionals being trained and competent to deliver the injection. However, there was a distinct feeling that opportunities were regularly missed.
The two head teachers in our sample were reluctant to allow schools to become an integral part of the administration or policing of the childhood vaccination programme; this was seen as a responsibility of Public Health England and the NHS rather than the education system. Head teachers did, however, acknowledge that schools offered opportunities to promote child health, and even to deliver vaccinations. For example, parents often attend an open day in the summer before their child enters full-time education. School nursing teams could attend these events to discuss the importance of children being fully immunised before school entry and even to offer vaccination.
All participants felt that education was central to facilitating decisions about vaccination. Parents often felt overwhelmed by the written information that was presented to them and highlighted how often this information was inappropriate to answer their needs. Although, rightly, information often focused on the safety of vaccinations, parents often had no clear concept of the diseases against which vaccinations were intended to protect. The childhood vaccination programme has been highly successful in reducing the prevalence of childhood diseases, and, in this respect, the programme has become a victim of its own success. Contemporary parents have, for the most part, never seen a child with polio, diphtheria or, until the recent outbreaks, measles. Inevitably, this means that parental focus is on vaccination rather than on the diseases it protects against.
Strengths and limitations of methods
This qualitative study serves to strengthen evidence about the introduction of both financial incentives and quasi-mandatory schemes to increase the uptake of vaccinations for preschool children in a UK context and provided a basis for the DCE work described in the third phase of this study. This small qualitative study allows us to triangulate findings between stakeholder groups to assess the acceptability and feasibility of introducing such schemes, further strengthening the evidence base.
There are, however, several limitations to the study. There is only low representation from partial and non-vaccinating parents in our parent sample. Therefore, their views are largely absent from the analysis, and future work should prioritise their inclusion. Likewise, there were only two head teachers who agreed to take part in interviews, so caution should be exercised when interpreting the findings from this sector. GPs and staff from GP practices were recruited with assistance from NECS from a list of practices known to be research friendly. Their views may not be representative of all GP practices.
The focus groups were well attended, with some very large groups, and it was, at times, difficult to engage all participants in discussions. Every effort was made to ask for the opinions of quieter members of the group and to include them in discussions. Inevitably, on occasion two or three voices were more forceful. However, the parents in these groups all knew one another prior to taking part in the fieldwork and on many occasions would monitor the quieter members of the group automatically. Icebreaker activities helped to facilitate this. The use of vignettes also allowed parents to reflect on their opinions while not having to offer their own personal experiences to the group (although they often did).
Babies and toddlers were present in some focus groups. In some cases, parents accepted the offer of child care while the focus groups were conducted. On other occasions, especially with younger babies, parents refused this offer. Generally, children were occupied with toys while the focus groups took place and were very well behaved. Some parents did have to dual task by feeding their children while engaging in discussions. Each focus group had two researchers present and they helped to occupy some of the children. Overall, we do not feel that having children present during the fieldwork was a negative experience.
This work focuses on a pragmatic definition of ‘acceptability’ in terms of what various stakeholders believe to be appropriate behaviour and policies within the context of the early twenty-first century NHS in England. We have not focused on the more theoretical issue of the moral and ethical ‘rightness’ of financial incentive and quasi-mandatory interventions for encouraging the uptake of preschool vaccinations. Although we believe that the pragmatic approach we have taken is particularly important in terms of influencing policy and any policy changes, other work has explored the theoretical morality and ethics of financial incentives in other contexts. It could be useful to extend this to preschool vaccinations. 91
In addition, we asked participants to reflect on hypothetical interventions that few, if any, would have had any personal experience of. This may have limited their ability to give informed opinions.
This study focused specifically on offering financial incentives to parents whose children either had completed the full programme of preschool vaccinations, described in Table 1, or were fully up to date with this programme for their age. The same is true of quasi-mandatory programmes; these were described only in terms of children who were fully up to date with vaccinations for their age. Although the partial completion of vaccination programmes does offer children some protection over total non-completion, the examples of incentives and quasi-mandatory interventions used in the qualitative study were based on examples from the systematic review – all of which focus on full completion or children being up to date for their age.
Comparison with previous work
Financial incentives have been found to be effective in some circumstances to encourage health-related behaviours,31,35,36,38,39 and the suggestion has been made that they may be more effective in encouraging one-off, short-term behaviours such as vaccination than in improving sustained behaviour change over a long period, such as that required for weight loss and weight maintenance. 25,28,30,34 However, in the UK in particular, childhood vaccination has (because of well-rehearsed historical incidents)92 become a loaded and contested area that must be carefully negotiated. The association of vaccination with bribery or coercion thus raises moral and ethical implications, which, for both groups of participants, seemed to potentially outweigh the hypothesised benefits of financial incentives.
Studies have shown the benefit of introducing a financial penalty for the non-vaccination of preschool children41,45 and this scenario was also deemed the most acceptable of the financial incentives discussed in this study. Health professionals did suggest that non-cash incentives, for example shopping vouchers, might be more acceptable, while still having the potential to increase vaccination uptake. Similar results have been reported in relation to financial incentives for other healthy behaviours. 93 However, governance and ethical issues were raised relating to the potential for vouchers to be used to facilitate unhealthy behaviours, such as buying alcohol or cigarettes, which would sit in contrast to the work being undertaken to promote healthy behaviours generally. Findings from both stakeholder groups provide strong support for previous research, where a variety of stakeholders across a range of clinical and public health settings have described health-promoting financial incentives as coercive, divisive and akin to bribery. 49,50,91,93–96 However, unlike previous work in other settings, in which stakeholders have challenged the potential effectiveness of health promoting financial incentives in general (sometimes as a way of avoiding discussion of acceptability altogether),93–96 there was, overall, an acceptance that financial incentives could be effective in encouraging the uptake of preschool vaccinations for some parents. A more detailed understanding of what aspects of acceptability of health-promoting financial incentives are common across all settings and which are context-specific – as well as what determines context-specific differences – would be helpful. Our results support findings from US studies and the current systematic review around the acceptability of quasi-mandatory schemes for increasing the uptake of vaccination,56 suggesting that the introduction of such schemes, with the inclusion of an opt-out system, would be acceptable to parents and professionals, and could encourage the normalisation of vaccination while being equitable for parents across the socioeconomic spectrum.
One particularly interesting finding was the frequency with which alternative approaches to encouraging the uptake of preschool vaccinations were spontaneously offered by participants without any prompting. This appears to be a common phenomenon in qualitative work on the acceptability of health-promoting financial incentives. 96,97 It is not clear exactly what this reflects: perhaps that participants dislike the idea of incentives so much that they would rather not talk about them, or perhaps that they dislike them but find it hard to articulate specifically why, choosing instead to move the conversation to easier ground. Furthermore, many of the alternative approaches to maximising vaccination uptake proposed by participants reflect existing guidance and good practice11 and known attitudes of parents to vaccination. 5
Interpretation of findings and implications for policy, practice and research
There was evidence that the introduction of financial incentives for childhood vaccination would not be acceptable to parents or to health and other professionals. There was also some indication that such incentives may do unintended social and health harm, by monetising good parenting behaviours and encouraging ‘gaming’ of the system. There was some preference among parent stakeholders for the use of financial penalties, but there were also concerns that these may also cause unintended harms and increase inequalities.
There was most support for the introduction of quasi-mandates at preschool and school entry and some indication that the parent-held child health record could be an acceptable instrument for enforcing this. However, it would be advisable to examine how this ‘red book’ system could be maintained more consistently and how any issues about data sharing and the competence of staff in interpreting its contents could be overcome.
In the interim, it is evident that a comprehensive review and the improvement of existing systems and resources may be as effective as, or more effective than, any new incentive or quasi-mandatory scheme. Attention to making services as accessible as possible needs to be accompanied by an acknowledgement that a parent’s decision to vaccinate is a process and not an event, and one which, therefore, must be supported across a range of time points and professional encounters.
Conclusions
Our findings suggest that the introduction of parental financial incentives for preschool vaccination may not be acceptable in a UK context. There is a potential harm from associating vaccination with the need for bribery and coercion, which may outweigh any positive impact of these types of schemes. Applying financial penalties by reducing benefits was seen as more acceptable by some parents, but it is unlikely that this would be feasible in a UK setting, given that the removal of child-related benefits could result in poor outcomes for children themselves from a decision made by their parents, and would almost certainly increase inequalities. Mandating vaccination for entry into universal settings such as day care and school was the most acceptable option discussed and seen by both parents and professionals as contributing to a normalising of vaccination at a point where it was easiest to demonstrate the benefits of herd immunity. Further work would be needed to assess how such a scheme could be implemented in reality.
Among all participant groups there was consensus that there was still much that could be done to improve vaccination service delivery, access and joined-up working before considering monetising vaccination or imposing mandates. The importance of professionals in building trusting relationships with parents to understand their needs and provide appropriate education and decision support was identified as being both acceptable and appropriate.
Chapter 5 Discrete choice experiment
A DCE was undertaken to estimate the value parents place on key attributes and associated attribute levels of preschool vaccination programmes. DCEs describe a service or intervention in terms of a number of characteristics, or ‘attributes’ (e.g. where vaccinations are delivered, who delivers the vaccination and what information is provided). The extent to which an individual values a service or an intervention would be expected to vary as a function of the ‘levels’ of the attributes (e.g. one attribute could be the location in which vaccinations are administered, with levels being a local surgery or a community clinic).
Discrete choice experiments allow us to explore the relative importance of each attribute of the vaccination service that may influence a parent’s decision to vaccinate their child and allow uptake of services configured in different ways to be predicted. 98 DCEs are a well-established methodology in health economics to elicit preferences on health-care products, programmes and in the valuation of preference for health states99–101 and offer an additional approach to investigating service acceptability.
Discrete choice experiments involve three inter-related components: (i) an experimental design used to implement a choice survey and generate choice data; (ii) a quantitative statistical analysis to estimate preferences from choice data; and (iii) the use of the resulting model to either derive welfare measures or construct other policy analyses. 98
Financial attributes/levels can also be incorporated into a DCE. Therefore, it is possible to determine a population’s willingness to pay (WTP) for, or accept, an intervention. The marginal willingness to accept (WTA) is defined here as the minimum monetary value that would be required to compensate for a change in the level of a certain attribute,102 that is, when individuals face a reduction in utility derived from moving from one scenario to another.
A DCE was designed for the following: (i) to establish the preferences of parents and carers of preschool-aged children for vaccination programmes with differing attributes and levels; (ii) to provide policy-relevant information on parental preferences on the configuration of vaccination programmes in England; (iii) to establish the likely minimum level of effective parental incentives; and (iv) to predict uptake levels of the different configurations of vaccination programmes.
Methods
We adhered to published guidance for undertaking a DCE study. 98,103 In accordance with good practice, the DCE adhered to the four stages:
-
stage 1 – identification of attributes and levels
-
stage 2 – experimental design
-
stage 3 – data collection
-
stage 4 – data analysis and interpretation.
These are described in turn.
Stage 1: identification of attributes and levels
The results from published systematic reviews,5–7,16 the systematic review (see Chapter 3), the qualitative study (see Chapter 4) and a focused search of the general literature were used to develop a comprehensive list of potential attributes for inclusion in the DCE. This assessed the literature around immunisation services and programmes available for preschool children in England. Twelve studies identified that preferences for specific health professionals, parental education and perceived effectiveness of vaccinations are important factors influencing parental decision-making. An expert panel (comprising the project team and steering group members) deliberated these attributes and associated levels in a series of discussions. This process generated a provisional list of attributes and associated levels that may influence the uptake of preschool vaccination programmes. In all cases, attributes and levels had to be plausible in both clinical and policy terms. 98 Information from all sources available to us informed the identification of maximum and minimum attribute levels, where relevant.
In addition to service configuration attributes, parental incentive attributes were included so that WTA could be indirectly estimated from the DCE. 6 Incentive attributes were framed as financial rewards, which would be offered to parents for immunising their child as either a universal (all parents) or a targeted reward (targeted at parents highly unlikely to immunise their children). These attributes were included to arrive at an estimate of the minimum incentive (if any) that the population would be willing to accept in exchange for having a child immunised, and enabled the likely value of effective incentives to be established.
This process resulted in a list of nine attributes and associated levels (Table 8).
| Attributes | Levels |
|---|---|
| Type of health-care professional administering vaccinations | Practice nurse at local GP surgery |
| Community nurse at vaccination service | |
| Health visitor in the community or vaccination service | |
| Number of visits to complete the full vaccination programme | 7 (minimum for current UK programme; > 1 injection per visit) |
| 15 (maximum for current UK programme; 1 injection per visit) | |
| Method of conveying information on net benefit from vaccination | No preference |
| Numerical (natural frequencies ‘out of 100 children’ as denominator) | |
| Graphical display (pictograph) | |
| Graphical display (clustered bar graphs) | |
| Mode of information provision prior to appointment | Written (post) |
| Electronic (internet) | |
| Availability of appointments | Normal hours (8 a.m. to 5 p.m. on weekdays) |
| Normal hours plus out of hours (weekday evenings and normal hours on Saturdays) | |
| Parental incentive type | No incentive |
| Cash reward for ‘complete’ vaccinations | |
| Additional child care benefits for ‘complete’ vaccinations | |
| Parental incentive value immediately payable at first vaccination, with claw-back for future non-compliance | £0 |
| £75 | |
| £100 | |
| £150 | |
| £200 | |
| Type of incentive | Universal: same incentive value for all parents |
| Targeted: only for parents considered high-risk of non-compliance | |
| Waiting time at each appointment | < 5 minutes |
| 5–15 minutes | |
| > 15 minutes |
Establishing acceptability of the provisional list of attributes and levels
The Parent Advisory Group [see Chapter 1, Parent Advisory Group (public involvement)], comprising eight parents and guardians of preschool children, was consulted on the comprehensiveness and acceptability of the provisional list of attributes and levels. This took the form of an interactive workshop, which was facilitated by JA, RM and LT. Participants were presented with a hand-out (see Appendix 4) of the list of attributes and levels in Table 8 and their views on each were elicited. In addition, for attribute 3 (method of conveying information on net benefit from vaccination) participants were presented with examples of natural frequencies, clustered bar graphs and pictographs.
Participants reported mixed preferences for type of health-care professional administering vaccinations. With regard to location of vaccinations services, there was a dominant preference for community settings (e.g. Sure Start Centres). Participants also suggested additional locations for the provision of vaccinations, such as a vaccination bus, to be situated outside schools, and local pharmacies.
Few participants expressed a preference for vaccination services within a GP surgery; this was because of protracted waiting times and a lack of choice of appointment times, with several intimating that they had received a letter stating the date and time when they were required to attend their GP surgery. Extended waiting periods were considered particularly problematic, owing to a lack of child-friendly spaces and activities in GP surgeries. When participants were asked about the maximum time they would wait for an appointment, there was a general consensus that up to 60 minutes would be acceptable. Participants also reported difficulties in attending afternoon appointments, owing to the necessity of collecting other children from school at around 3 p.m.
The attribute of ‘method of conveying information on net benefit from vaccination’ elicited strong preferences for numerical presentation alone or the use of clustered bar graphs. Contrary to expectations, pictographs attracted largely negative comments and were considered to be unclear. Participants were in general agreement that receipt of information on benefits and risks was desirable to inform their decisions about immunising their children. However, those present in the workshop reported that they had received very little information on the benefits of vaccination. Indeed, the majority of participants would have preferred to have received balanced information on benefits and risks of vaccination presented to them verbally by a health-care professional (e.g. a health visitor) prior to appointments (e.g. 7 days before a scheduled appointment).
With regard to parental incentives, there was initially a strong opposition to any type of incentives being offered for immunising children. However, several participants conceded that £10–20 per visit (assuming seven visits) would be acceptable, with the caveat that this ‘reward’ should be universal (as opposed to targeted at those parents unlikely to immunise their children).
The workshop also identified very strong preferences for as few visits as possible, and it was unlikely that including this as a variable attribute in the DCE would yield any meaningful data.
Changes made to the provisional list of attributes and levels
These findings guided additional expert panel discussions to refine the provisional list of attributes and levels. Number of appointments was designated as a fixed factor and amended in accordance with recent NHS guidance (published in July 2014) that proposes five visits for the routine components of the child programme plus three visits (aged 2, 3 and 4 years for the influenza vaccination), with up to three injections per visit. 104 Consequently, this fixed attribute reads as follows: ‘Number of appointments to complete the full vaccination programme = eight (with up to three injections per appointment).’
The type of health-care professional administering vaccinations was intrinsically linked to location. Therefore, this attribute was amended to capture preferences on a range of health-care professionals administering vaccinations at specific locations.
The members of the expert panel were in agreement that balanced information needs to be presented on the probabilities of disease and its consequences alongside absolute risk reduction in disease from vaccination. Taking into account feedback on the range of parental information needs on the benefits and risks of vaccination, the attribute ‘Method of conveying information on net benefit from vaccination’ was replaced with the following two attributes:
-
Mode of information provision about vaccinations (benefits, risks and consequences) prior to appointment. This reflects the provision of ‘balanced’ information in terms of benefits, risks and consequences of a parent’s decisions to vaccinate or not vaccinate his or her child prior to the first appointment. The level was via the post, and, in order to demarcate the different methods of electronic information provision, a further two levels were included (e-mail and multimedia via the internet).
-
Method of conveying information on consequences of disease, including absolute risk reduction in probability of disease from vaccination. There is good evidence that pictographs can effectively support the communication of balanced probabilistic information to people irrespective of their health literacy level. 105 However, the examples of pictographs presented to participants in the workshop were not well received and were not considered clear or valuable. Furthermore, the graphical methods used in the workshop were illustrative examples, and a separate research project is warranted to identify the optimal mode, form and information content of graphical risk presentations in this case context. Therefore, the decision was made to omit illustrative examples of graphical display. To enable elicitation of preferences on generic methods of communicating probabilistic information, the following levels were presented textually: numerical (percentages and frequencies ‘out of 100 children’); graphical methods such as bar graphs; and both numerical and graphical methods.
Given the value that workshop participants placed on verbal information provided by trusted health-care professionals, the levels of the attributes related to benefit and risk information, and method of probabilities on consequences and risk reduction from vaccination, were all suffixed with ‘plus verbal information at time of appointment’.
The phrase ‘normal hours’ was replaced with ‘working hours during school term times (9 a.m. to 5 p.m.)’ in the levels of the attribute ‘Availability of appointments’.
References to quasi-mandatory schemes were raised during the expert panel discussion. However, these were not deemed to be prudent for inclusion in the DCE, as exploring mandates and incentives within the same DCE would be counterintuitive and impose too many design constraints; that is, inclusion of a mandate in a choice scenario would prohibit the inclusion of levels related to parental incentives (form, type and value). However, an item to assess preferences for no reward (current practice), targeted versus universal rewards, and mandatory schemes was given in the questionnaire included with the DCE.
The terms ‘reward’ and ‘incentive’ were used interchangeably in the descriptions of DCE attributes and the associated levels. Expert panel discussions emphasised the need for consistency (and interpretation, as there are qualitative differences between the two terms); the term ‘reward’ was deemed to be more accessible to parents and any references to incentive were replaced with ‘reward’ in the DCE attributes and levels and other survey items. Levels for the parental reward attribute were also amended based on discussions with the Parent Advisory Group.
For the attribute ’waiting time at each appointment’, the three levels were amended in accordance with the maximal value identified from the workshop (60 minutes), with a capped value (up to 120 minutes) to facilitate interpretation of the parameter estimates.
The revised list of eight attributes and levels for inclusion in the DCE are shown in Table 9, with number of visits to complete the full vaccination programme designated as a ninth, fixed attribute.
| Attributes | Levels |
|---|---|
| Type of health-care professional administering vaccinations and location of appointments | Practice nurse at local GP surgery |
| Community nurse at local clinic or children’s centre | |
| Health visitor in the community at local clinic or children’s centre | |
| Health visitor at neonatal visits at home | |
| Community nurse in vaccination bus stationed at schools | |
| How information about vaccinations (benefits, risks and consequences) is provided prior to the appointment | Written (post) plus verbal information at time of appointment |
| Electronic (e-mail) plus verbal information at time of appointment | |
| Electronic [multimedia (film clips, words and pictures) via the internet] plus verbal information at time of appointment | |
| How information on how vaccinations reduce the risk of children getting diseases is provided prior to the appointment | Provided in the form of numbers |
| Provided in the form of charts or pictures | |
| Provided in the form of numbers and charts or pictures | |
| Availability of appointments | During working hours (9 a.m. to 5 p.m.) |
| During working hours (9 a.m. to 5 p.m.) plus out of hours [weekday evenings and Saturday (9 a.m. to 5 p.m.)] | |
| Type of parental reward | No reward |
| Cash reward for ‘complete’ vaccinations | |
| Additional child care benefits for ‘complete’ vaccinations | |
| Parental reward value (received when the full schedule of vaccinations is completed) | £0 |
| £70 | |
| £140 | |
| £210 | |
| £280 | |
| Which parents would receive a reward | Targeted reward (given to parents considered unlikely to have their child immunised) |
| Universal reward (given to all parents) | |
| Current practice – no reward | |
| Waiting time at each appointment | Up to 30 minutes |
| Up to 60 minutes | |
| Up to 120 minutes |
Stage 2: experimental design
The DCE experimental design followed guidelines for best practice. 106 All possible combinations of attributes and levels described in Table 9 would generate a prohibitively large number of choice scenarios, namely 12,150 (the total number of possible combinations can be calculated as 35 × 52 × 2, i.e. five attributes with three levels, two attributes with five levels and one attribute with two levels). Therefore, we used a D-efficient design to identify the most efficient combination of choice sets while still being able to estimate the main effects and all higher-order interactions. 98,107
The D-efficient design was generated using Ngene design software (version 1.1.1, ChoiceMetrics Pty Ltd, Sydney, NSW, Australia) with input from an expert in the design and analysis of DCEs and following guidelines for best practice. 106 The best design generated by Ngene was chosen with the aim of minimising the standard errors. 108
Not all attributes and level combinations were plausible (e.g. if type of reward was ‘no reward’ then value of reward must be ‘£0’). Design constraints were utilised to ensure plausibility and reduce hypothetical bias (where the hypothetical nature of the questions result in biased responses). Excluding implausible combinations of attribute levels affected level balance and statistical efficiency (a good choice design is level balanced where all levels of an attribute occur with equal frequency across the total number of choice sets included in all versions of a questionnaire). Levels were unbalanced with regard to type of reward, with ‘no reward’ appearing less frequently; and incentive amount, with ‘£0’ appearing less frequently. For respondents with strong preferences for those under-represented attribute levels of ‘no reward’ and ‘£0’ incentive value, the opt-out option was assumed to present a valid alternative choice. Therefore, following guidelines for best practice, level balance (and hence some statistical efficiency) was sacrificed in favour of a practical and plausible design with the aim of increasing in overall response efficiency.
In order to minimise respondents’ cognitive burden, each participant was presented with 18 choice questions. The design allowed for four blocks of 18 choice scenarios to maximise variance in the data. Each respondent was assigned to one block randomly.
Questionnaire design
A paper-based questionnaire survey (see Appendix 5 for the final version) was designed, with reference to published guidance on good survey design. 109
The questionnaire survey instrument included the following sections:
-
Study information: what the work is aiming to achieve, what participation would involve, the estimated time to complete the survey and the purpose of the research, including obtaining consent to participate.
-
Screening questions, based on inclusion criteria.
-
Respondents’ (and, where applicable, their partners’) demographics, socioeconomic status (household income, highest level of education, employment status, ethnicity) and self-assessed health status.
-
Details of the respondents’ children (number, age, gender, presence of disability).
-
Introduction and explanation of the choice task with an illustrative example of pairwise choice scenario (choice set), followed by presentation of choice sets based on the Ngene design in the format shown in Table 10.
-
Questions to assess how difficult the respondents found the DCE task to complete.
-
Questions on the influence of financial incentives on decisions to immunise, including for those individuals who stated that they would require an incentive to vaccinate, the minimum value of that incentive (their WTA), and, for those who would not require an incentive, the maximum level at which they believed an incentive should be set (including £0). Questions also included whether cash or vouchers would be preferable and the reasons underpinning the minimum acceptable incentive value they stated (if applicable).
-
Questions about preferences for organisation of vaccination services (universal, targeted, mandatory or current practice).
-
Information on vaccinations, including mode information, was received, extent information needs were fulfilled and alternative sources of information were consulted.
-
Intentions for immunising participants’ youngest child, followed by a series of attitudinal questions designed to assess attitudes towards the safety, importance/value and efficacy of vaccinations.
-
A ranking exercise in which respondents were asked to rank order the eight attributes in the choice sets.
-
An open-ended question asking for any further information on the topic of vaccination in preschool age children.
| Scenario A | Scenario B |
|---|---|
| Practice nurse at a local GP surgery administering vaccinations | Community nurse at local clinic or children’s centre administering vaccinations |
| Information about vaccinations (benefits and risks) is provided in written (via post) form prior to appointments (plus verbal information at time of appointment) | Information about vaccinations (benefits and risks) is provided in electronic (e-mail) prior to appointments (plus verbal information at time of appointment) |
| Information on reducing the risk of your child getting the disease by them having the vaccination is provided in the form of numbers | Information on reducing the risk of your child getting the disease by them having the vaccination is provided in the form of charts or pictures |
| Appointments available during working hours (9 a.m. to 5 p.m.) | Appointments available during working hours (9 a.m. to 5 p.m.) and out of hours [evenings (weekdays) and Saturday (9 a.m. to 5 p.m.)] |
| Parents receive a cash reward for completing the full schedule of vaccinations | Parents do not receive any reward for completing the full schedule of vaccinations |
| Reward value payable is £70 (received when the full schedule of vaccinations is completed) | No reward |
| Targeted reward – only given to parents considered unlikely to have their child immunised | Current practice – no reward |
| Waiting time at each appointment is up to 30 minutes | Waiting time at each appointment is up to 60 minutes |
Paper piloting the discrete choice experiment and questionnaire
Paper piloting was undertaken with five parents or guardians of preschool-aged children (one male and four female) using a ‘think-aloud’ approach110 to test respondents’ understanding of the wording of questionnaire survey items, the DCE choice task, the definitions of attributes and levels; and identification of salient ‘missing’ attributes and levels. The sample size for this aspect was determined by data saturation – that is, we continued conducting additional interviews until no new issues were raised.
The first two participants took considerable time to read text in both columns of the choice sets (i.e. they were experiencing excessive cognitive burden that prohibited an expeditious and valid comparison of attribute levels between the pairwise scenarios). Therefore, the format of presenting the pairwise choice sets shown in Table 11 was used to reduce cognitive burden in subsequent pilot participants.
| Characteristic | Scenario A | Scenario B |
|---|---|---|
| Type of health-care professional administering vaccinations and location | Practice nurse at a local GP surgery | Community nurse at local clinic or children’s centre |
| How information about vaccinations (benefits and risks) is provided prior to the appointment | Provided in written (via post) form | Provided in electronic (e-mail) form |
| How information on reducing the risk of your child getting diseases due to having the vaccinations is provided prior to the appointment | Provided in the form of numbers | Provided in the form of charts or pictures |
| Availability of appointments | Working hours (9 a.m. to 5 p.m.) | Working hours (9 a.m. to 5 p.m.) plus out of hours [evenings (weekdays) and Saturday (9 a.m. to 5 p.m.)] |
| Type of parental reward for completing the full schedule of vaccinations | Cash reward | Parents do not receive any reward |
| Reward value payable to parents (received when the full schedule of vaccinations is completed) | £70 | No reward |
| Which parents would receive a reward | Only those considered unlikely to have their child immunised | Current practice – no reward |
| Waiting time at each appointment | Up to 30 minutes | Up to 60 minutes |
Based on responses during the paper piloting, participants expressed a desire to know why information on demographics and socioeconomic status was being sought. In response, we included the following information: ‘the following questions ask about the characteristics of the parents responding to the survey (so we can demonstrate that we have collected information from a representative cross section of parents living in England) and to explore how characteristics of parents could help us to design better vaccination services’. An option of ‘prefer not to say’ was also added to items in this section.
Participants also noted that knowledge of the full vaccination schedule was a prerequisite for responding to the questionnaire items. Consequently, in the introduction section a link to details of the vaccination schedule currently recommended by the NHS was included.
Other comments that resulted in amendments were that participants wanted to know whether or not pharmacists would have received specific training on vaccinations in order to consider this attribute as a valid option. In the section on WTA, one participant queried the locations at which shopping vouchers could be redeemed (this item was subsequently amended to state that shopping vouchers would be accepted in most high-street shops and supermarkets). The paper pilot identified no other salient issues (other than minor typographical errors and clarification of potentially ambiguous definitions in the demographic and socioeconomic status items).
The findings of the paper-pilot, along with additional expert panel discussions, informed the development of a revised list of attributes and levels (Table 12) along with a final paper-based version of the questionnaire survey for electronic piloting.
| Attribute (code) | Levels |
|---|---|
| Type of health-care professional administering vaccinations and location of appointments (WHO_WHERE) | Practice nurse at local GP surgery |
| Community nurse at local clinic or children’s centre | |
| Health visitor in the community at local clinic or children’s centre | |
| Health visitor at neonatal visits at home | |
| Community nurse in vaccination bus stationed at schools | |
| Pharmacist who has received specific training on vaccination at local pharmacy | |
| How information about vaccinations (benefits and risks) is provided prior to the appointment (INFO) | Written (post) plus verbal information at time of appointment |
| Electronic (e-mail) plus verbal information at time of appointment | |
| Electronic (multimedia film clips, words and pictures via the internet) plus verbal information at time of appointment | |
| How information on reducing the risk of your child getting diseases by having the vaccinations is provided prior to the appointment (RISK) | Provided in the form of numbers |
| Provided in the form of charts or pictures | |
| Provided in the form of numbers and charts or pictures | |
| Availability of appointments (AVAILABLITY) | During working hours (9 a.m. to 5 p.m.) |
| During working hours (9 a.m. to 5 p.m.) plus out of hours [evenings (weekdays) and Saturday (9 a.m. to 5 p.m.)] | |
| Type of parental reward (REWARD) | No reward |
| Cash reward for ‘complete’ vaccinations | |
| Shopping voucher as a reward for ‘complete’ vaccinations | |
| Parental reward value (received when the full schedule of vaccinations is completed) (VALUE) | £0 |
| £70 | |
| £140 | |
| £210 | |
| £280 | |
| Which parents would receive a reward (TARGETED) | Targeted reward (given to parents considered unlikely to have their child immunised) |
| Universal reward (given to all parents) | |
| Current practice – no reward | |
| Waiting time at each appointment (TIME) | Up to 30 minutes |
| Up to 60 minutes | |
| Up to 120 minutes |
Electronic piloting of the discrete choice experiment questionnaire
A market research company (ResearchNow.com) converted the amended paper-based questionnaire into an online survey. The survey was then subjected to an initial ‘soft launch’ with 40 respondents to establish usability of the survey, as well as to assess response fatigue (time taken to complete) and understanding of the DCE choice sets and WTA questions. This identified an issue with the WTA question, whereby several respondents entered a minimum incentive value of £0 after stating that they would require an incentive in order to vaccinate their child. Only positive values were considered to be valid responses to this question. This section of the survey was redesigned to minimise this type of response. The original wording of the WTA question was:
Would you be willing to accept a financial reward for immunising your child? (Y/N)
Please state the minimum amount you would be willing to accept.
This was amended to:
Would you require a financial reward to immunise your child? (Y/N)
If Yes:
What is the minimum amount you would require?
If No:
If offered a financial reward on completion of vaccinations would you take it? (Y/N)
What do you think should be the maximum financial reward offered to parents for immunising their child?
A second ‘soft launch’ was undertaken with the revised WTA questions (n = 37). In addition to the tests conducted as part of the first soft launch, further data analysis was undertaken at this stage. This included running preliminary regression analyses (n = 77) and analysing data relating to participants’ understanding of the DCE questions. The majority (82%) of respondents stated that they fully understood the questions, while 17% partially understood and around 1% reported that they did not understand the DCE questions. This high level of understanding of the DCE was deemed satisfactory and no further changes were made to the DCE design or survey questionnaire.
Stage 3: data collection
Ethical approval for all aspects of this study (piloting and main study data collection) was granted from Newcastle University Ethics Committee (reference 00748).
Recruitment and data collection was subcontracted to the market research company (ResearchNow.com), who adhere to the highest standards of market research ethics, as described in the Market Research Society’s Code of Conduct. 111 ResearchNow use a number of methods to recruit individuals onto their panels, including e-mail, online marketing and website targeting. ‘By invitation’ methods are also used, where individuals with known characteristics are directly targeted. Small (£1–2) incentives in the form of shopping vouchers were paid to participants, as per their normal procedures. Data were returned to the research team in an anonymised format. The research team did not receive contact details or any personal identifier information from survey participants.
The first soft-launch data collection started in November 2014. Final survey data collection commenced in December 2014, with the final data set available in early January 2015.
Inclusion criteria
Two samples were included in the study: relative to the likelihood of not having their children fully vaccinated, parents were identified as either ‘at high risk’ or ‘not at high risk’ of not having their children fully vaccinated. It is particularly important to explore the preferences of parents ‘at high risk’, as this subgroup would probably be the primary target of any parental incentive scheme. It was also important to explore the preferences of parents who were ‘not at high risk’ in order to determine the wider impact of population-wide changes in the configuration of vaccination services.
Individuals who met the following criteria were eligible to complete the survey:
-
a parent or guardian of one or more children aged under 5 years
-
currently residing in England
-
a member of an online research panel held by the subcontracting market research company ResearchNow.com.
Respondents who additionally met the following criteria were included in the ‘at high risk’ sample:5–7,10,11
-
living in one of the 20% most deprived areas of England – as identified by Index of Multiple Deprivation 201085 score of lower super output area of residence, calculated from postcode of residence
-
the parent or guardian of a child aged under 5 years old who has a physical or mental disability
-
a single parent or guardian
-
aged under 20 years
-
a parent or guardian of more than three children (of any age).
Respondents who did not meet any of the above criteria were assigned to the ‘not at high risk’ sample.
Sample size
Lancsar and Louviere98 highlight the complexities and problems of performing sample size calculations for DCEs and the need for further research in this area. Previous studies using DCEs for exploring experience factors in health-care settings have included samples ranging from fewer than 50112 to almost 4000,113 and robust choice models have been estimated from sample sizes of between 50 and 100 respondents. 114 Optimal sample size requirements for DCEs depend on knowledge of the true choice probabilities, which are not known prior to undertaking the research115 and, therefore, DCE sample size estimates are generally based on rules-of-thumb and budget constraints. Given the number of attributes included in the DCE, it was estimated that a minimum sample size of 400 [i.e. 200 ‘at high risk’ (50 per block) plus 200 ‘not at high risk’ parents (50 per block)] would provide sufficient statistical power based on a rule of thumb of a minimum of 10 observations per parameter estimate plus an additional 50.
Stage 4: data analysis and interpretation
Descriptive statistical techniques were used to describe the sociodemographic profile and characteristics of parents and their children of the full sample, and the subgroups ‘at high risk’ and ‘not at high risk’ of incompletely vaccinating their children. Appropriate tests of differences (chi-squared tests and t-tests) were used to establish any statistically significant differences between the subsamples as a function of sociodemographic and child variables.
The DCE approach allows an analysis of individual stated preferences in response to hypothetical choices and enables the quantification of the relative importance of each attribute/level during the decision-making process. 103,107 When presented with hypothetical options (i.e. choice scenarios) that describe alternative specifications of a vaccination service, respondents are assumed to choose the scenario they prefer. The higher a respondent’s preference for certain attribute levels, the more likely they are to choose that scenario over any alternative.
Appendix 6 provides a technical description of the data analytic strategy applied to the choice scenario data. In short, the initial analysis employed a conditional logit model116 which is based on three assumptions: (i) independence of irrelevant alternatives (IIAs) (i.e. the ratio of probabilities for any two alternatives is assumed to be independent of the attribute levels in a third alternative); (ii) error terms are independent and identically distributed across observations; and (iii) no preference heterogeneity (i.e. homogeneous preferences across respondents).
As the number of observations for the opt-out option was too small (around 5% of chosen options) to perform the appropriate Hausman test, we assumed a violation of the IIA assumption, which would result in biased parameter estimates. Therefore, mixed-effects logistic regression models were considered more appropriate to analyse the choice set data. Mixed logit models counteract any violations in the assumptions of conditional logit models and permit the investigation of unobserved preference heterogeneity, that is, varying model estimates across individuals.
Mixed logit models were, therefore, used to establish whether or not the eight attributes presented in the choice scenarios were statistically significant predictors of parents’ preferences. Positive coefficients in the models represent a positive preference (utility) associated with a particular level of an attribute, whereas negative coefficients represent a negative preference (disutility) associated with a particular level of an attribute compared with the reference level. p-Values < 0.05 indicate whether positive or negative preferences are statistically significantly different from zero. Mixed logit models were undertaken using choice set data from the full sample and the two subgroups.
For all models the intercepts [alternative specific constants (ASCs)] and time attribute are assumed to be random and normally distributed [means and standard deviations (SDs) reported]; all other parameters in the model remain fixed (mean estimates reported only). For all mixed logit models, positive values for the intercepts (ASCs for options A and B) would indicate a general parental preference for vaccinating their children. Attributes capturing ‘time’ and ‘value’ were included in the analysis as linear variables. Effects coding was used for all categorical attributes (using +1, 0 and –1 to represent different attribute levels) to facilitate estimation of main effects across all categorical attributes and levels. 117 The level ‘no reward’ in the attribute ‘type of reward’ was omitted in these analyses owing to multicollinearity; the no-reward situation was already coded by the according category in the type of reward attribute and additionally included in the choice sets descriptions only for plausibility.
Marginal WTA values for all statistically significant attributes in the mixed logit models were also calculated for the full sample and subgroups in the form of a minimum monetary value that would be required as ‘compensation’ for any change in the level of an attribute associated with gains or losses in utility. 102 This enables an estimate of the trade-offs between attribute levels and the magnitude of the coefficient in the mixed logit models (i.e. the WTA values can be compared to determine the relative strength of preferences). The estimated WTA values, therefore, represent the amount of financial incentive (in £) that parents would need to receive in order to compensate for accepting a level of an attribute of a vaccination service that is associated with a negative preference (disutility).
We did not check for internal inconsistency, as a number of studies have now shown their DCEs are internally consistent and valid. The qualitative work and pre-testing of different versions of the questionnaire during the development stage further helped to reduce the risk of internal inconsistencies. 118–121
Responses to the following questions presented after the respondents had completed the choice task (DCE) were analysed using appropriate descriptive statistics for the full sample and two subgroups: parents’ preferences for organisation of vaccination services (universal, targeted, mandatory or current practice); influence of financial incentives on decisions to immunise, including for those individuals who stated that they would require an incentive to vaccinate, the minimum value of that incentive (their WTA), and, for those who would not require an incentive, the maximum value they thought an incentive should be (their WTP); preferences for cash or voucher rewards and the reasons underpinning the minimum acceptable incentive value (if applicable); information received on vaccinations, including the way that information was received, the extent their information needs were fulfilled and alternative sources of information consulted; and the rank order assigned to the eight attributes presented in the DCE choice task.
Items used to assess parents’ intentions for immunising their youngest child, and attitudes on safety, importance/value and efficacy of vaccinations, were analysed using overall means and SDs for each subscale in accordance with the factor structure reported in Kennedy et al. 122 Differences between subgroups were analysed using independent t-tests and chi-squared statistics.
Observed and predictive uptake rates for vaccination services were calculated for the full sample. Observed uptake rates were based on responses to the 18 choice questions. Predictive uptake rates were based on findings of the mixed logit models and used to produce estimated probabilities that control for all levels included in the 72 choice sets in the DCE across all respondents.
Uptake rates were also calculated for vaccination services based on the most and least preferred choice scenarios (as defined by the DCE results) and were compared with predicted uptake rates based on the scenario that represents current practice and an ‘opt-out option’. These statistics are expressed as percentages and capture the variation in uptake rates associated with different configurations of vaccination services based on preferences across the sample.
Results
Sample characteristics
Table 13 presents a summary of the sociodemographic profile and characteristics of the study respondents in the overall sample (n = 521) and subgroups of respondents classified to be ‘at high risk’ (n = 259, 49.7%) of not fully vaccinating their children and ‘not at high risk’ (n = 262, 50.3%).
| Variables | Full sample, N = 521 | ‘At high risk’ of incomplete vaccination (n = 259) | ‘Not at high risk’ of incomplete vaccination (n = 262) | |||
|---|---|---|---|---|---|---|
| Mean (SD) | n (%) | Mean (SD) | n (%) | Mean (SD) | n (%) | |
| Number of completed questionnaires | ||||||
| Version 1/DCE block 1 | 129 (25) | 64 (25) | 65 (25) | |||
| Version 2/DCE block 2 | 131 (25) | 65 (25) | 66 (25) | |||
| Version 3/DCE block 3 | 131 (25) | 65 (25) | 66 (25) | |||
| Version 4/DCE block 4 | 130 (25) | 65 (25) | 65 (25) | |||
| Age (years) | 34.1 (6.0) | 33.8 (6.9) | 34.3 (5.1) | |||
| Female | 370 (71) | 204 (79) | 166 (63)a | |||
| Relationship status | ||||||
| Married/cohabiting/civil partnership | 395 (76) | 137 (53) | 258 (99)a | |||
| Single | 95 (18) | 92 (36) | 3 (1)a | |||
| Separated/divorced/widowed | 31 (6) | 30 (12) | 1 (< 1)a | |||
| Annual household income (pre-tax) | ||||||
| < £15,000 | 83 (16) | 64 (25) | 19 (7)a | |||
| £15,000 to < £26,000 | 106 (20) | 60 (23) | 46 (18) | |||
| £26,000 to < £35,000 | 88 (17) | 40 (15) | 48 (18) | |||
| £35,000 to < £50,000 | 121 (23) | 51 (20) | 70 (27) | |||
| £50,000 to < £70,000 | 58 (11) | 23 (9) | 35 (13) | |||
| ≥ £70,000 | 49 (9) | 14 (5) | 35 (13)a | |||
| Prefer not to say | 16 (3) | 7 (3) | 9 (3) | |||
| Highest level of education | ||||||
| GCSE/O-level/CSE/NVQ | 127 (24) | 72 (28) | 55 (21) | |||
| A-level or equivalent | 128 (25) | 68 (26) | 60 (23) | |||
| Degree/master’s/PhD | 251 (48) | 106 (41) | 145 (55)a | |||
| No formal qualifications | 7 (1) | 6 (2) | 1 (< 1) | |||
| Other | 5 (1) | 4 (2) | 1 (< 1) | |||
| Prefer not to say | 3 (1) | 3 (1) | 0 (0) | |||
| Employment status | ||||||
| Employed/maternity leave | 381 (73) | 179 (69) | 202 (77)a | |||
| Unemployed | 11 (2) | 9 (4) | 2 (1)a | |||
| Not in labour force | 117 (23) | 65 (25) | 52 (20) | |||
| Other | 8 (2) | 5 (2) | 3 (1) | |||
| Prefer not to say | 4 (1) | 1 (< 1) | 3 (1) | |||
| Ethnicity | ||||||
| White | 448 (86) | 229 (88) | 219 (84) | |||
| Asian | 43 (8) | 16 (6) | 27 (10) | |||
| Black | 17 (3) | 5 (2) | 12 (5) | |||
| Other | 5 (1) | 3 (1) | 2 (1) | |||
| Prefer not to say | 8 (2) | 6 (2) | 2 (1) | |||
| Self-reported health over the past 12 months | ||||||
| Excellent | 116 (22) | 52 (20) | 64 (24) | |||
| Good | 274 (53) | 118 (46) | 156 (60)a | |||
| Fair | 105 (20) | 73 (28) | 32 (12)a | |||
| Poor | 21 (4) | 12 (5) | 9 (3) | |||
| Very poor | 3 (1) | 3 (1) | 0 (0) | |||
| Prefer not to say | 2 (< 1) | 1 (< 1) | 1 (< 1) | |||
| n children | 2.0 (1.2) | 2.5 (1.4) | 1.5 (0.6)a | |||
| n children with disability | 20 (4) | 20 (8) | 0 (0)a | |||
Respondents had a mean age of 34 years. The majority of respondents were white (86%); female (71%); employed or on maternity leave (73%); and in a relationship (76%). The modal annual income was £35,000 to < £50,000 (23%). Almost half had a degree or post-graduate education (48%). The majority of the sample reported ‘good’ health (53%) over the past 12 months and had an average of two children (4% of whom were reported to have a physical or mental disability).
Many of the differences between subgroups reflect the criteria for allocation to groups. There were significantly more female and single or separated/divorced/widowed respondents, with, on average, more children and children with disabilities in the ‘at high risk’ group. A significantly smaller proportion of respondents in the ‘at high risk’ group reported good health over the past 12 months. The ‘at high risk’ group also had significantly greater and smaller proportions of respondents in the lowest (< £15,000) and highest (> £70,000) annual household income ranges, respectively. Significantly larger proportions of respondents in the ‘not at high risk’ group had a degree or post-graduate education and were employed or on maternity leave, with significantly greater numbers of unemployed respondents in the ‘at high risk’ group. Patterns of ethnicity were approximately equivalent across subgroups.
Regression model results (discrete choice experiment data)
Model 1 results (full sample)
The results of the mixed logit models for the full sample are presented in Table 14. The ASCs for options A and B are both positive and statistically significant, indicating that there is a general preference for vaccinations, compared with not vaccinating (option C). Indeed, only 5% of all respondents chose the opt-out option, ‘I would not vaccinate my child’.
| Attribute | Level | Coefficient | SE | p-value | WTAa |
|---|---|---|---|---|---|
| Health-care professional | Practice nurse | 0.1842 | |||
| Community nurse | 0.0253 | 0.0394 | 0.521 | ||
| Health visitor | 0.0505 | 0.0463 | 0.275 | ||
| Health visitor: home visit | 0.0232 | 0.0467 | 0.619 | ||
| Community nurse: bus | –0.0915 | 0.0447 | 0.041* | 67.96 | |
| Pharmacist | –0.1918 | 0.0493 | < 0.001** | 142.40 | |
| Format of information received | Written: post | –0.0015 | |||
| Electronic: e-mail | 0.0409 | 0.0349 | 0.241 | ||
| Electronic: internet | –0.0394 | 0.0258 | 0.126 | ||
| Information on risks and benefits | Numbers | 0.0621 | |||
| Charts/pictures | –0.0747 | 0.0304 | 0.014* | 55.45 | |
| Both | 0.0126 | 0.0265 | 0.635 | ||
| Availability of appointments | Working hours | –0.0236 | |||
| Working hours and out of hours | 0.0236 | 0.0144 | 0.102 | ||
| Type of reward | No reward | –0.0850 | |||
| Cash | 0.0840 | 0.0317 | 0.008** | –62.37b | |
| Voucher | 0.0010 | 0.0295 | 0.973 | ||
| Value of reward (£) | Amount | 0.0013 | 0.0002 | < 0.001** | N/Ac |
| Parents receiving reward | Universal reward | 0.2618 | |||
| Targeted reward | –0.2618 | 0.0155 | < 0.001** | 194.40 | |
| Maximum waiting time at each appointment (minutes) | |||||
| Duration | Mean (SD) | –0.0109 (–0.0194) | 0.0010 (0.0011) | < 0.001** | 8.08 |
| < 0.001** | |||||
| Alternative-specific constants | |||||
| Option A | Mean (SD) | 2.9409 (0.4230) | 0.0790 (0.0616) | < 0.001** | |
| < 0.001** | |||||
| Option B | Mean (SD) | 2.9420 (0.4302) | 0.0785 (0.0547) | < 0.001** | |
| < 0.001** | |||||
The SDs for all random coefficients, namely ASCs and time variables, are statistically significant, indicating the existence of preference heterogeneity among respondents for the characteristics of vaccination services in the DCE choice sets.
Given the use of effects coding, the reported results for each of the attribute levels indicate the distance from average utility (specified as the negative sum of coefficients for all but the reference level) derived from a specific attribute. According to equation (2) (see Appendix 6), positive coefficients indicate a positive preference (utility) and negative coefficients indicate a negative preference (disutility) associated with a specific attribute level compared with the reference category. Non-significant attribute levels indicate respondents’ indifference between the specific level and the reference level of each attribute.
There were statistically significant negative preferences (disutility) for pharmacists delivering vaccination in a local pharmacy (WTA = £142.40) and community nurses delivering vaccinations in a community bus stationed at schools (WTA = £67.96); for use of charts or pictures to convey information on risks and benefits (WTA = £55.45); use of targeted rewards (WTA = £194.40); and for longer waiting times at each appointment (WTA = £8 per minute of additional wait after having waited for 30 minutes).
On the other hand, there was a statistically significant positive preference (utility) for cash rewards. Higher-value rewards were associated with a statistically significant increase in utility.
Models 2 and 3 results (subgroup analyses)
Results of the mixed logit models for the subgroups of respondents classified as ‘at high risk’ and ‘not at high risk’ are presented in Table 15. There was a general preference for vaccinations in both subgroups as well as the existence of preference heterogeneity for the characteristics of vaccination services in the DCE choice sets. This result is consistent with the full sample (model 1), in which only 5% of all respondents use the opt-out option ‘I would not vaccinate my child’. In the subgroup analyses, 6% of the ‘at high risk’ group and 4% of the ‘not at high risk’ group use the opt-out option.
| Attribute | Level | ‘At high risk’ (model 2; n = 259) | ‘Not at high risk’ (model 3; n = 262) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Coefficient | SE | p-value | WTAa | Coefficients | SE | p-value | WTA | ||
| Health-care professional | Practice nurse | 0.0967 | 0.2686 | ||||||
| Community nurse | 0.0765 | 0.0546 | 0.162 | –0.0570 | 0.0577 | 0.323 | |||
| Health visitor | –0.0236 | 0.0644 | 0.713 | 0.1405 | 0.0678 | 0.038 | –66.03 | ||
| Health visitor: home visit | 0.0067 | 0.0637 | 0.916 | 0.0578 | 0.0699 | 0.408 | |||
| Community nurse: bus | 0.0427 | 0.0616 | 0.488 | –0.2217 | 0.0659 | 0.001** | 104.17 | ||
| Pharmacist | –0.1989 | 0.0687 | 0.004 | 356.84 | –0.1882 | 0.0721 | 0.009** | 88.44 | |
| Format of information received | Written: post | 0.0091 | –0.0169 | ||||||
| Electronic: e-mail | 0.0250 | 0.0488 | 0.609 | 0.0376 | 0.0510 | 0.460 | |||
| Electronic: internet | –0.0341 | 0.0359 | 0.343 | –0.0208 | 0.0376 | 0.581 | |||
| Information on risks and benefits | Numbers | 0.0566 | 0.0832 | ||||||
| Charts/pictures | –0.1037 | 0.0439 | 0.018 | 186.12 | –0.0446 | 0.0427 | 0.296 | ||
| Both | 0.0471 | 0.0361 | 0.192 | –0.0386 | 0.0396 | 0.330 | |||
| Availability of appointments | Working hours | –0.0007 | –0.0485 | ||||||
| Working hours and out of hours | 0.0007 | 0.0205 | 0.971 | 0.0485 | 0.0206 | 0.018* | –22.81 | ||
| Type of reward | No reward | –0.1754 | –0.0063 | ||||||
| Cash | 0.1364 | 0.0449 | 0.002 | –244.68 | 0.0433 | 0.0454 | 0.340 | ||
| Voucher | 0.0390 | 0.0411 | 0.342 | –0.0370 | 0.0431 | 0.391 | |||
| Value of reward (£) | Amount | 0.0006 | 0.0003 | 0.086 | N/Ab | 0.0021 | 0.0003 | < 0.001** | N/Ab |
| Parents receiving reward | Universal reward | –0.2573 | 0.2687 | ||||||
| Targeted reward | –0.2573 | 0.0222 | < 0.001 | 461.65c | –0.2687 | 0.0218 | < 0.001** | 126.28c | |
| Maximum waiting time (minutes) | |||||||||
| Duration | Mean (SD) | –0.0124 (0.0230) | 0.0016 (0.0019) | < 0.001 | 22.22 | –0.0097 (–0.0168) | 0.0012 (0.0013) | < 0.001** | 4.55 |
| < 0.001 | < 0.001** | ||||||||
| Alternative-specific constants | |||||||||
| Option A | Mean (SD) | 2.9784 (–0.4832) | 0.1136 (0.0772) | < 0.001 | 2.9408 (0.3434) | 0.1117 (0.0805) | < 0.001** | ||
| < 0.001 | < 0.001** | ||||||||
| Option B | Mean (SD) | 2.9972 (0.4648) | 0.1132 (0.0810) | < 0.001 | 2.9269 (0.3627) | 0.1104 (0.0813) | < 0.001** | ||
| < 0.001 | < 0.001** | ||||||||
There were statistically significant negative preferences (disutility) for pharmacist-delivered vaccinations in both the ‘at high risk’ and ‘not at high risk’ groups; although this disutility was substantially stronger in the former than the latter group (WTA = £356.84 and £88.44, respectively). In the ‘not at high risk’ group there was a statistically significant disutility for vaccinations provided by community nurses in a school-based vaccination bus (WTA = £104.17) and utility for vaccinations provided by health visitors in the community.
Parents in the ‘at high risk’ group also had statistically significant disutility for receipt of information on the benefits and risks of vaccinations in the form of charts and pictures (WTA = £186.12). Furthermore, only the ‘not at high risk’ group had a statistically significant positive preference (utility) for additional flexibility around availability of appointments.
Both subgroups expressed significant disutility for targeted rewards (WTA = £461.65 and £126.28 in the ‘at high risk’ and ‘not at high risk’ group, respectively), whereas only respondents at high risk of not fully vaccinating their children had a statistically significant utility for cash rewards. Increased value of rewards was statistically significant only in the ‘not at high risk’ group.
Finally, increased waiting times were associated with significant disutility in both subgroups (WTA values for each additional minute waiting after 30 minutes was £22.22 and £4.55 in the ‘at high risk’ and ‘not at high risk’ group, respectively).
Additional questions on attitudes towards preschool vaccination service organisation
Individual attitudes towards the organisation of vaccination services and attitudes towards financial rewards for preschool vaccinations were captured using the questionnaire which followed the DCE. The questionnaire also included open-ended WTA and WTP questions using the contingent valuation method. Results of these additional questions are presented in Table 16.
| Variables | Full sample (N = 521) | ‘At high risk’ (n = 259) | ‘Not at high risk’ (n = 262) | |||
|---|---|---|---|---|---|---|
| Mean (SD) | n (%) | Mean (SD) | n (%) | Mean (SD) | n (%) | |
| Require reward to vaccinate | n = 481 | n = 259 | n = 222 | |||
| Yes | 122 (25) | 79 (31) | 43 (19)a | |||
| No | 359 (75) | 180 (70) | 179 (81)a | |||
| Minimum reward amount (£) | n = 122 £109.57 (135.92) |
n = 79 £112.49 (130.89) |
n = 43 £104.19 (146.15) |
|||
| Influences on minimum amount | n = 122 | n = 79 | n = 43 | |||
| Time to complete course | 68 (54) | 40 (51) | 28 (65) | |||
| Compensation (time off work) | 63 (52) | 40 (51) | 23 (53) | |||
| Compensation (travel) | 46 (38) | 30 (38) | 16 (37) | |||
| Other | 5 (4) | 4 (5) | 1 (2) | |||
| Reward preference | n = 122 | n = 79 | n = 43 | |||
| Cash | 103 (84) | 67 (85) | 36 (84) | |||
| Voucher | 19 (16) | 12 (15) | 7 (16) | |||
| Accept reward if offered | n = 359 | n = 180 | n = 179 | |||
| Yes | 287 (80) | 148 (82) | 139 (78) | |||
| No | 72 (20) | 32 (18) | 40 (22) | |||
| Maximum reward amount (£) | n = 359 £69.41 (196.88) |
n = 180 £81.34 (246.66) |
n = 179 £57.41 (128.39) |
|||
| Influences on maximum amount | n = 359 | n = 180 | n = 183 | |||
| Time | 79 (22) | 40 (22) | 39 (21) | |||
| Compensation (time) | 90 (25) | 42 (23) | 48 (26) | |||
| Compensation (travel) | 76 (21) | 43 (24) | 33 (18) | |||
| Other | 27 (8) | 13 (7) | 14 (8) | |||
| Preferred organisation of vaccination services | ||||||
| Reward: universal | 226 (43) | 122 (47) | 104 (40) | |||
| Reward: targeted | 53 (10) | 32 (12) | 21 (8) | |||
| Mandatory | 142 (27) | 61 (24) | 81 (31) | |||
| Current situation | 100 (19) | 44 (17) | 56 (21) | |||
One-quarter of respondents stated that they would require a financial incentive to vaccinate their child, with a higher proportion of respondents in the ‘at high risk’ group than ‘not at high risk’ groups indicating this (31% vs. 19%). Of those who stated that they would require an incentive, the average ‘minimum’ WTA was £110 (greater in the ‘at high risk’ than in the ‘not at high risk’ group) and the most frequently cited reason was compensation for their time, followed by time off work.
Consistent with the results of the logit models, there was a generic preference for cash as opposed to voucher rewards as well as for universal as opposed to targeted rewards.
Although a large majority of respondents stated that they would not require a financial incentive to vaccinate their child, approximately 80% would accept one if offered. The maximum value of any incentive (for an unspecified vaccination programme) on average was £69.41 and was substantially larger in the ‘at high risk’ subgroup (£81.34) than in the ‘not at high risk’ group (£57.41). Again, the most common reason influencing these values was compensation for time to attend appointments.
Worthy of note is that approximately one-fifth of respondents expressed a preference for current organisation of vaccination services and a further one-fifth for mandatory schemes. Preference for the latter was greater in the ‘not at high risk’ subgroup (31% vs. 24%), but this difference was not statistically significant.
Intentions and attitudes towards the safety, importance, value and efficacy of preschool vaccinations
On average, the majority (76%) of respondents in the full sample stated an intention for their youngest child to receive all of the recommended vaccinations. Respondents in the ‘at high risk’ subgroup were significantly less likely to express an intention for their children to receive all the recommended vaccinations (69%) than those in the ‘not at high risk’ subgroup (83%).
Attitudes towards importance, value and efficacy of preschool vaccinations were also generally positive, with mean values of ≈4 for all items (Table 17). However, attitudes were significantly more positive in the ‘not at high risk’ subgroup, compared with the ‘at high risk’ group for 9 out of the 12 attitudes items (related to value/importance and safety of vaccinations). Significant differences in proportions of responses ‘strongly disagree/not at all likely’ were found between subgroups, with greater numbers of respondents in the ‘at high risk group’ stating ‘strongly disagree/not at all likely’ for items on perceived susceptibility of their child, other children and family members to serious disease if children are not immunised.
| Item | Categories | Full sample (N = 521), n (%) | ‘At high risk’ of incomplete vaccination (n = 259), n (%) | ‘Not at high risk’ of incomplete vaccination (n = 262), n (%) |
|---|---|---|---|---|
| Having my children immunised is the right thing to do | Mean (SD) | 4.31 (1.06) | 4.14 (1.17) | 4.47 (0.91)a |
| 1 – strongly disagree | 21 (4) | 15 (6) | 6 (2)a | |
| 2 | 16 (3) | 12 (5) | 4 (2)a | |
| 3 | 63 (12) | 36 (14) | 27 (10) | |
| 4 | 103 (20) | 55 (21) | 48 (18) | |
| 5 – strongly agree | 318 (61) | 141 (54) | 177 (68)a | |
| Importance of vaccinations for keeping children healthy | Mean (SD) | 4.39 (0.88) | 4.27 (0.97) | 4.50 (0.76)a |
| 1 – not at all important | 10 (2) | 8 (3) | 2 (1) | |
| 2 | 4 (1) | 3 (1) | 1 (< 1) | |
| 3 | 67 (13) | 39 (15) | 28 (11) | |
| 4 | 134 (26) | 71 (27) | 63 (24) | |
| 5 – very important | 306 (59) | 138 (53) | 168 (64)a | |
| Importance of vaccinations in order to prevent spread of disease in community | Mean (SD) | 4.38 (0.94) | 4.22 (1.05) | 4.54 (0.78)a |
| 1 – not at all important | 12 (2) | 11 (4) | 1 (< 1)a | |
| 2 | 11 (2) | 7 (3) | 4 (2) | |
| 3 | 61 (12) | 32 (12) | 29 (11) | |
| 4 | 119 (23) | 72 (28) | 47 (18)a | |
| 5 – very important | 318 (61) | 137 (53) | 181 (69)a | |
| Vaccinations recommended by NHS are safe | Mean (SD) | 4.24 (0.99) | 4.06 (1.10) | 4.42 (0.83)a |
| 1 – strongly disagree | 14 (3) | 13 (5) | 1 (< 1)a | |
| 2 | 16 (3) | 9 (3) | 7 (3) | |
| 3 | 74 (14) | 44 (17) | 30 (11) | |
| 4 | 143 (27) | 76 (29) | 67 (26) | |
| 5 – strongly agree | 274 (53) | 117 (45) | 157 (60)a | |
| General safety of vaccinations for children | Mean (SD) | 4.15 (0.95) | 4.03 (1.02) | 4.27 (0.86)a |
| 1 – not safe at all | 10 (2) | 8 (3) | 2 (1) | |
| 2 | 18 (3) | 10 (4) | 8 (3) | |
| 3 | 88 (17) | 54 (21) | 34 (13)a | |
| 4 | 174 (33) | 82 (32) | 92 (35) | |
| 5 – very safe | 231 (44) | 105 (41) | 126 (48) | |
| Confidence in safety of routine childhood vaccinations | Mean (SD) | 4.14 (0.96) | 4.02 (1.06) | 4.26 (0.85)a |
| 1 – not at all confident | 13 (3) | 11 (4) | 2 (1)a | |
| 2 | 15 (3) | 10 (4) | 5 (2) | |
| 3 | 87 (17) | 45 (17) | 42 (16) | |
| 4 | 175 (34) | 89 (34) | 86 (33) | |
| 5 – very confident | 231 (44) | 104 (40) | 127 (48) | |
| If some children do not receive vaccinations, other children may be ill with the disease | Mean (SD) | 3.92 (1.10) | 3.89 (1.11) | 3.94 (1.09) |
| 1 – strongly disagree | 20 (4) | 12 (5) | 8 (3) | |
| 2 | 33 (6) | 13 (5) | 20 (8) | |
| 3 | 120 (23) | 64 (25) | 56 (21) | |
| 4 | 146 (28) | 72 (28) | 74 (28) | |
| 5 – strongly agree | 202 (39) | 98 (38) | 104 (40) | |
| How likely are children to get diseases, if they are not immunised against them? | Mean (SD) | 3.84 (0.97) | 3.85 (1.04) | 3.84 (0.90) |
| 1 – not at all likely | 12 (2) | 10 (4) | 2 (1)a | |
| 2 | 21 (4) | 11 (4) | 10 (4) | |
| 3 | 157 (30) | 70 (27) | 87 (33) | |
| 4 | 177 (34) | 85 (33) | 92 (35) | |
| 5 – very likely | 154 (30) | 83 (32) | 71 (27) | |
| My children could get a serious disease if they are not immunised | Mean (SD) | 4.07 (0.98) | 3.95 (1.08) | 4.20 (0.85)a |
| 1 – strongly disagree | 12 (2) | 10 (4) | 2 (1)a | |
| 2 | 21 (4) | 15 (6) | 6 (2)a | |
| 3 | 96 (18) | 52 (20) | 44 (17) | |
| 4 | 179 (34) | 83 (32) | 96 (37) | |
| 5 – strongly agree | 213 (41) | 99 (38) | 114 (44) | |
| Other children could get a serious disease if my child is not immunised | Mean (SD) | 3.94 (1.03) | 3.86 (1.09) | 4.01 (0.96) |
| 1 – strongly disagree | 15 (3) | 11 (4) | 4 (2) | |
| 2 | 29 (6) | 17 (7) | 12 (5) | |
| 3 | 115 (22) | 57 (22) | 58 (22) | |
| 4 | 177 (34) | 86 (33) | 91 (35) | |
| 5 – strongly agree | 185 (36) | 88 (34) | 97 (37) | |
| My child could get a serious disease if other children are not immunised | Mean (SD) | 3.90 (1.04) | 3.82 (1.10) | 3.98 (0.96) |
| 1 – strongly disagree | 16 (3) | 12 (5) | 4 (2)a | |
| 2 | 24 (5) | 11 (4) | 13 (5) | |
| 3 | 140 (27) | 79 (31) | 61 (23) | |
| 4 | 158 (30) | 67 (26) | 91 (35)a | |
| 5 – strongly agree | 183 (35) | 90 (35) | 93 (36) | |
| Other family members could get a serious disease if other children are not immunised | Mean (SD) | 3.89 (1.04) | 3.85 (1.12) | 3.94 (0.96) |
| 1 – strongly disagree | 17 (3) | 14 (5) | 3 (1)a | |
| 2 | 26 (5) | 11 (4) | 15 (6) | |
| 3 | 133 (26) | 67 (26) | 66 (25) | |
| 4 | 165 (32) | 75 (29) | 90 (34) | |
| 5 – strongly agree | 180 (35) | 92 (36) | 88 (34) |
Information about vaccinations
The majority of respondents (55%) stated that they had not received any information regarding vaccinations in the past 3 months, with similar proportions in both subgroups (Table 18). Of those who had received information, the majority reported that they had received this by post (67%). Respondents were also asked ‘to what extent would you agree the information you received for your youngest child in the last 3 months addressed all your information needs about vaccination?’. Overall, 63% (n = 148) of the full sample responded strongly agreed or agreed with the statement.
| Questionnaire item | Full sample (N = 521), n (%) | At high risk of incomplete vaccination (n = 259), n (%) | Not at high risk of incomplete vaccination (n = 262), n (%) |
|---|---|---|---|
| Received information on vaccination for youngest child in past 3 months | |||
| Yes | 235 (45) | 113 (44) | 122 (47) |
| No | 286 (55) | 146 (56) | 140 (53) |
| Information received | n = 235 | n = 113 | n = 122 |
| Verbally | 62 (26) | 32 (28) | 30 (25) |
| Post | 158 (67) | 77 (68) | 81 (66) |
| Other | 15 (6) | 4 (4) | 11 (9) |
| Information received met needs | n = 235 | n = 113 | n = 122 |
| 1 – strongly disagree | 8 (3) | 5 (4) | 3 (2) |
| 2 | 22 (9) | 13 (12) | 9 (7) |
| 3 | 57 (24) | 28 (25) | 29 (24) |
| 4 | 87 (37) | 38 (34) | 49 (40) |
| 5 – strongly agree | 61 (26) | 29 (26) | 32 (26) |
| Additional information sought | n = 235 | n = 113 | n = 122 |
| Yes | 101 (43) | 55 (49) | 46 (38) |
| No | 134 (57) | 58 (51) | 76 (62) |
| Additional information sought via | n = 101 | n = 113 | n = 122 |
| Internet | 58 (57) | 33 (29) | 25 (20) |
| Friends/family | 42 (42) | 24 (21) | 18 (15) |
| GP/family doctor | 43 (43) | 24 (21) | 19 (16) |
| Other | 6 (6) | 3 (3) | 3 (2) |
Additional information regarding vaccinations was sought by 43% of respondents, including 49% of parents ‘at high risk’ of incompletely vaccinating their children and 37% of those ‘not at high risk’. Information sources consulted by the full sample included the internet (57%), GP (43%) and friends or family (41%). There were no statistically significant differences between subgroups for any of the responses to the questions about vaccination information.
Ranking exercise
The rank order (highest to lowest) of importance for each of the eight attributes in the DCE based on mean scores for the overall sample was:
-
location type of health-care professional administering vaccinations (mean score 2.81, SD 1.82)
-
how information is received prior to vaccination (mean score 3.10, SD 1.85)
-
availability of appointments (mean score 3.10, SD 1.53)
-
how information on risks and benefits is communicated (mean score 3.26, SD 1.73)
-
waiting times (mean score 4.59, SD 2.00)
-
value of rewards (mean score 6.05, SD 1.69)
-
type of reward – cash or voucher (mean score 6.25, SD 1.45)
-
who receives the reward, for example universal or targeted (mean score 6.84, SD 1.32).
Predictive uptake rates
Appendix 7 presents the percentages of respondents choosing specific options from the 72 choice sets presented in the DCE as well as the predicted probability of uptake estimated from the mixed logit models.
Predicted uptake rates for a vaccination incentive scheme (i.e. options A or B) ranged from 13% (choice situation 27, option B; observed, 22%) to 85% (choice situation 27, option A; observed, 70%). Conversely, predicted uptake for the no vaccination scheme (i.e. opt-out option C) ranged from 2% (choice situation 4; observed, 3%) to 7% (choice situation 52; observed, 11%).
Predicted uptake rates, based on a hypothetical choice set forcing respondents to choose between the most preferred scenario [health visitor in the community at local clinic or children’s centre; vaccination information: electronic (e-mail); risk information: numbers and charts/pictures; during working hours and out of hours; cash reward; value (£280); universal reward; waiting time (up to 30 minutes); ASC] and a current practice alternative [practice nurse; vaccination information: written (post); risk information: numbers; during working hours; type of reward: no reward; value (£0); parents receiving reward: no reward; waiting time (up to 30 minutes); ASC], were 66% for the most preferred scenario in the total sample (60% in the ‘at high risk’ sample, 55% in the ‘not at high risk’ sample), 32% for the current practice scenario in the total sample (38%; 44%) and 2% for the opt-out option (2%; 2%).
Similarly, for a choice set including the least preferred scenario [pharmacist; vaccination information: electronic (internet); risk information: charts/pictures; during working hours; shopping voucher; value (£0); targeted reward; waiting time (up to 120 minutes); ASC] current practice scenario and an opt-out option, the predicted uptake rates were estimated as 15% for the least preferred scenario in the total sample (36% in the at high risk sample, 33% in the not at high risk sample), 80% for the current practice scenario in the total sample (61%; 63%) and 5% for the opt-out option (3%; 3%).
Discussion
Summary of results
This is the first DCE to investigate the differential configuration of vaccination services and their potential impact on parents’ decisions to vaccinate their children in accordance with the full programme recommended by the NHS, including the efficacy of incentive-based schemes on service acceptability and uptake rates.
Analysis of choice set data from the DCE (hypothetical vaccination services described in the choice scenarios) revealed that ≈95% of parents had strong preferences for vaccinating their children and we found evidence of statistically significant preference heterogeneity for different characteristics of vaccination services.
In terms of type of health-care professional administering vaccinations and their location, there was a strong negative preference for pharmacists. Statistically significant negative preferences (disutility) were identified for vaccination services with three characteristics. In descending rank order of WTA these were (i) pharmacists with specialist training (compared with practice nurses within GP practices), with stronger disutility for this characteristic in the ‘at high risk’ group; (ii) targeted rewards to parents who are ‘at high risk’ of not adhering to the full vaccination programme (as opposed to universal rewards for all parents), which was stronger in the group ‘at high risk’ of incompletely vaccinating their children; and (iii) longer waiting times for each appointment with greater disutility, as indicated by WTA values in the ‘at high risk’ group per additional minute after 30 minutes had expired.
We also found evidence of differences in preferences for characteristics of vaccination services as a function of a parent’s risk status. In those ‘at high risk’ of incompletely vaccinating their children, there were significant positive preferences (utility) for cash rewards for completing the full vaccination schedule (as opposed to no reward), and a significant disutility associated with presenting information on the risks and benefits of vaccinations using graphical methods (compared with only numerical presentation).
In those ‘not at high risk’ of incompletely vaccinating their children, there were significant positive preferences (utility) for provision of vaccinations by health visitors in the community and strong negative preferences for community nurses in a school-based vaccination bus. This group also preferred more flexible appointment times (out of hours). They also assigned greater utility to increasing reward values.
There were no statistically significant positive or negative preferences for mode of information provision about vaccinations (benefits and risks) prior to appointment (written vs. electronic).
Consistent with the results of the logit models, there was a generic preference for cash as opposed to voucher rewards as well as universal as opposed to targeted rewards in the attitudinal questionnaire. We also found evidence of a ‘gift horse attitude’ being adopted towards the issue of incentives. The majority of parents reported that they did not require a reward (the ≈20% who did reported an average ‘minimum’ WTA value of £110), but the majority would accept a financial reward for completion of the vaccination programme if it was offered to them (maximum value ranged from £57.41 in the ‘not at high risk’ group to £81.34 in the ‘at high risk’ group). Compensation for time to attend appointments was the factor that most influenced the rationale underpinning the minimum and maximum values suggested by parents.
There was minority support (≈20%) for current practice and for mandatory schemes, should they be rolled out, with support for the latter greater in those ‘not at high risk’ of incomplete vaccination (31%).
Responses to items about the intentions of parents for their youngest child to receive all of the recommended vaccinations were high, but not maximal (i.e. 76% overall), and there was a statistically significant lower rate of expressed intentions in the subgroup ‘at high risk’ of incomplete vaccination (69% vs. 83% in the ‘not at high risk’ group). In the full sample, attitudes towards the safety, importance/value and efficacy of immunisations was positive across both subgroups, although statistically significantly greater numbers of respondents in the ‘at high risk’ group stated ‘strongly disagree/not all likely’ for items on the perceived susceptibility of their child, other children and family members to serious disease if children are not vaccinated.
Approximately 50% of parents in both subgroups had not received any information about vaccinations in the past 3 months. Although the majority (63%, n = 148) were satisfied that the information they had received fulfilled all of their information needs, substantial numbers of respondents (43%) sought additional information, most frequently via the internet.
Interpretation of results in relation to the literature
Differences in expressed preferences for organisational and incentive characteristics of vaccination services between the subgroups of parents can largely be explained by the criteria used to classify them. As would be expected, respondents classified as ‘at high risk’ of incompletely vaccinating their children had statistically significantly more children, more children with a disability, lower household income levels, higher rates of unemployment, lower educational attainment and were poorer self-assessed than parents classified as ‘not at high risk’. Respondents ‘at high risk’ of incompletely vaccinating their children were also more likely to be female and single or separated, divorced or widowed. These sociodemographic characteristics have previously been reported to strongly influence parental intentions, attitudes and decision-making about childhood vaccination. 5,7
Strong opposition to pharmacists delivering vaccinations may be a result of concerns around safety and perceived adequacy of training. This is supported by comments to this effect from the Parent Advisory Group workshop in the development phase of this study. Disutility in parents ‘not at high risk’ of incompletely vaccinating their children for vaccinations provided by community nurses in vaccination buses located at schools may be attributable to these parents placing a greater value on flexibility. This is reflected in this subgroup having significant utility for health visitor-administered vaccinations in the community, and the availability of out-of-hours appointments.
It is not surprising that cash rewards were preferred by parents in the ‘at high risk’ group, given the lower-income status of these parents. However, increasing the value of a reward was associated with significant utility only in the subgroup of parents who were ‘not at high risk’ of incomplete vaccination. Therefore, cash and higher-value non-financial incentives may be more effective depending on the parents’ inherent risk status.
Disutility for targeted rewards was found in the DCE logit regression models, the survey responses and in the discussions with the Parent Advisory Group. Reasons provided by Parent Advisory Group members were that some parents may be susceptible to ‘game playing’ in the form of strategically delaying vaccinations if they thought that a reward might be given. Furthermore, targeted rewards were considered by some parents in the Parent Advisory Group to represent a reward for ‘bad behaviour’ (i.e. not vaccinating children). The finding that parents ‘at high risk’ of incompletely vaccinating would be less willing to wait at vaccination appointments than those ‘not at high risk’ may be related to the former group experiencing greater difficulties with arranging child care or cover at work as well as other practical considerations while they are waiting for appointments (e.g. having more children to manage).
There is robust evidence that graphical displays such as bar graphs and pictographs can effectively support the communication of balanced probabilistic information to people irrespective of their health literacy level. 105 However, parents ‘at high risk’ assigned disutility to this method of information provision. This was reflected in the Parent Advisory Group workshop, where examples of graphical display (pictographs and bar graphs) were not well received. This finding for disutility of graphical methods in the DCE may be an artefact created by presenting these options using textual descriptions as opposed to mocked-up examples.
The high proportion of parents reporting non-receipt of information within the past 3 months may be influenced by recall bias. It will also be influenced by the specific age of their children and whether or not the children were due vaccinations in the previous 3 months. However, this finding provides some further evidence that quality information provision is currently suboptimal, and this was supported by comments made in the Parent Advisory Group.
The use of the internet is common to investigate issues relating to health. However, not all sites are reputable and there is a risk of parents being exposed to inaccessible, unbalanced and unreliable information that may impact on their decisions about vaccinating their children.
Suboptimal intentions to vaccinate their youngest child were more pronounced in those identified as ‘at high risk’ of incompletely vaccinating their children. This may in part be related to disutility associated with long waiting times for appointments, suboptimal information provision and lower perceived susceptibility of their child, other children and family members to serious disease if children are not vaccinated.
Strengths and weaknesses
A major strength of our approach to eliciting preferences for different characteristics of vaccination services is the use of a DCE embedded within an online survey. We adhered to best practice guidelines for design and development of DCEs (with a clear audit trail and engagement of an expert Parent Advisory Group) and survey questionnaires to maximise internal validity and external validity.
The strength of the DCE approach is that it permits an examination of multiple factors influencing decision-making and that all choices involve trade-offs between levels of multiple factors, which cannot be readily elucidated, rank ordered or quantified using other methods. The increased internal and external validity of the DCE approach is evidenced by findings of the ranking exercise that does not account for preferences as a function of different levels of attributes or their complex trade-offs with levels of other attributes. Moreover, we incorporated WTA terms into the DCE analyses to facilitate the interpretation of results in terms of the strength of positive or negative preferences.
Discrete choice experiments have been criticised as difficult for participants to understand. To minimise the risk of this we conducted substantial development work. The overwhelming majority of respondents indicated a good understanding of the DCE.
We acknowledge that the sample recruited by the research company is effectively a non-random (convenience) sample that may not be representative of the target population. Furthermore, by using the recruitment method we did, it is not possible to determine response rates to the survey. However, we asked ResearchNow to recruit a national sample of parents that fulfilled our inclusion criteria, which were stratified into groups according to pre-defined criteria in order to maximise representativeness. Previous DCE research suggests that alternative methods of recruitment and data collection in this context, such as random postal or telephone surveys, achieve very low response rates, which also threatens representativeness. 123 By using a stratified sampling matrix we were at least able to ensure a degree of representativeness in the sample.
We combined health-care professional delivering immunisations and the place of delivery of immunisations into one attribute. Although these may be seen as separate constructs, they are inextricably linked, and separating them out would have imposed a prohibitive number of design constraints, which would have had negative implications for the model parameters and conclusions that could be drawn from the results.
As with the qualitative study, we were primarily asking participants to reflect on interventions that few, if any, of them would have had any personal experience of. This may have limited their ability to give fully informed opinions.
Furthermore, and as with the qualitative study, we restricted the DCE to consideration of incentives for parents of children who had fully completed the preschool vaccination schedule described in Table 1. This was both to reflect existing practice, as described in the systematic review, and because partially rewarding partial immunisation would have introduced significant complexity into the design of the DCE.
Implications of findings for research
Respondents desired probabilistic information about the benefits and risks of vaccination and expressed strong preferences for numerical presentation of these data. Natural frequencies using consistent denominators (out of 100 children aged under 5 years) are likely to impact positively on parents’ understanding and perceptions of the benefits of vaccination. It is also important to ensure that parents receive this information prior to appointments. There is also a pressing need to evaluate the impact of probabilistic information on perceptions of benefit from vaccination and uptake rates. More research is needed to engage parents in an iterative codesign process to design optimally acceptable and usable information that conveys robust and balanced data on the consequences of disease and the benefits and risks of vaccinations.
According to our findings, incentive-based schemes are likely to be optimal in future vaccination service design. However, the cost of rolling out incentive-based schemes may be prohibitive and may prove difficult to justify. Mandatory schemes may, therefore, be the next best alternative for increasing uptake rates for vaccination services, although in this study only a minority of parents preferred these. The factors that may increase acceptance of mandatory schemes warrant further research and additional DCEs could be conducted to explore parental preferences for how a mandate for vaccination might be imposed.
Implications of findings for policy and practice
Differences in predicted uptake rates for the most and least preferred scenarios in the DCE show that the specification of a financial incentive scheme is essential when aiming to effectively increase vaccination rates among the population in general or across specific subgroups. According to our findings, any policy that specifically targets specific groups using incentives would meet significant resistance, as there were strong negative preferences for targeted incentives.
Furthermore, taking into account similarities and differences in preferences expressed by parents ‘at high risk’ and ‘not at high risk’ of completing the full programme could be valuable for any policy directive at improving uptake rates. This will serve to maintain uptake rates in parents who are likely to complete the full programme and potentially increase uptake rates in the high-risk group.
Findings from the DCE suggest that universal rewards would be acceptable and could be made available as a cash payment or voucher (with the latter at an increased monetary value). A public education campaign may also be warranted, given suboptimal intentions to vaccinate, low perceived susceptibility to serious disease if children are not vaccinated and issues related to information provision. However, such campaigns are expensive and frequently do not impact on the actual behaviour of the public. An alternative would be to review and update the information currently provided to include robust, probabilistic information on the consequences of disease and the net benefit from vaccination.
Conclusion
This is the first use of a DCE to elicit parental preferences for the optimal organisation of vaccination services and the relative importance of different service configurations. We found that universal ‘high-value’ rewards, in the form of cash payments for parents, are likely to increase uptake rates within populations ‘at high risk’ of incomplete vaccination without any negative impact on current high uptake rates of those ‘not at high risk’ of incomplete vaccination. The cost of incentives could be offset to some extent by offering additional flexibility in terms of alternative community settings for vaccinations and out-of-hours appointments. The provision of robust and balanced information on consequences of disease and the benefits and risks of vaccination in numerical format prior to appointments is also likely to increase uptake rates. Further research to optimise the provision and quality of such information is warranted. Mandatory schemes may be more acceptable alternatives to incentives, and further research should investigate parental preferences for the organisation of such schemes.
Chapter 6 Triangulation and integration of results
Background
Triangulation is a general approach whereby the convergence, complementarity and dissonance of results on related research questions, obtained from different methodological approaches, sources, theoretical perspective, or researchers are explored. It has been proposed that the validity of conclusions is enhanced if different approaches produce convergent findings.
Four types of triangulation have been described:124
-
methodological triangulation, where more than one methodological approach is used to collect data
-
data triangulation, where data are collected from more than one data source or respondent group
-
investigator triangulation, where two or more researchers take part in integrative analysis
-
theoretical triangulation, where different theoretical perspectives or interpretative frameworks are adopted.
‘Triangulation’ is primarily used to describe the process of comparing concurrently collected qualitative findings. The term ‘integration’ has been used to describe the ‘interaction and conversation between’ findings from quantitative and qualitative components of a research programme, often conducted in series, to produce the proverbial ‘whole greater than the sum of its parts’. 125
This research programme was specifically designed to allow earlier phases to inform the development of later phases. Thus, the results of the effectiveness component of the systematic review were used to help to develop vignettes for the qualitative study, and those from the acceptability component helped to guide the focus of the qualitative study. Similarly, both the systematic review and the qualitative study informed the development of attributes and levels for the DCE. Thus, there was a degree of integration built into the programme from the start. However, an integrated consideration of the results adds further value to the programme.
Although the systematic review was the only aspect of the research that addressed the question of the effectiveness of parental financial incentives and quasi-mandatory interventions for increasing uptake of preschool vaccinations, all three studies addressed the question of the acceptability of these interventions. The triangulation and integration of findings, therefore, focuses primarily on the issue of acceptability, but this is not to the exclusion of other issues.
The first three types of triangulation listed above are particularly relevant to the present programme. A range of both quantitative (DCE, and systematic searching in the systematic review) and qualitative (focus groups with parents and carers, individual interviews with health and other professionals, and narrative synthesis in the systematic review) methods were used in the research. This diversity of methods allows methodological triangulation of the diverse perspectives provided by the three different research methods used.
As data were collected from more than one participant group (parents and carers, and health and other professionals, in the qualitative study; parents and carers who were and were not at high risk of not vaccinating their children in the DCE), data triangulation can also take place. Finally, as described below, a number of researchers took part in triangulation, leading to investigator triangulation.
Methods
The complex and problematic nature of triangulation and integration, and the absence of detailed information on how to perform them, has been identified by a number of authors. 125,126 We base our approach to triangulation and integration on Farmer et al. ’s ‘triangulation protocol’. 126 This involves identifying themes from each data source and method and then sorting these into similar categories. These are then ‘convergence coded’ to identify where there is agreement, silence and dissonance in terms of data from different sources and methods. Initially, this coding was performed by the lead researcher (JA). Preliminary results were then discussed, virtually, among the full research team, and the convergence coding was refined based on these discussions.
Results
Table 19 shows a summary of the main themes identified in the research, sorted into three overall groups (financial incentives and penalties, quasi-mandatory interventions and alternative interventions to increase vaccination uptake), and then ordered to bring related themes near to each other. ‘✗’ in relevant columns indicates that a theme was identified in that research component. For this exercise, we divided the qualitative study into two components: results from parents and carers, and results from health and other professionals. Similarly, the DCE is split into two components: results from the formal DCE, and results from the wider questionnaire that supported and incorporated the DCE choice sets.
| Theme | Systematic review | Qualitative study: parents | Qualitative study: professionals | DCE | Questionnaire |
|---|---|---|---|---|---|
| Financial incentives and penalties | |||||
| Financial incentives have been successful in some circumstances in encouraging healthy behaviours | ✗a | ✗ | |||
| ≈25% of participants would require a financial incentive to vaccinate their children | ✗ | ||||
| Financial incentives could encourage parents experiencing financial hardship to vaccinate | ✗ | ||||
| Universal financial incentives are more equitable than/preferred to targeted incentives | ✗ | ✗ | ✗ | ||
| Targeted financial incentives could lead to parents ‘gaming the system’ and delaying vaccination to become eligible | ✗ | ||||
| Financial penalties are more acceptable than financial rewards | ✗ | ||||
| Financial penalties could act as a timely reminder to vaccinate a child | ✗ | ||||
| Financial incentives are a bribe for being a responsible parent and may break the bonds of social responsibility | ✗ | ✗ | |||
| Financial incentives may not be the most efficient use of resources | ✗ | ✗ | |||
| Financial incentives would not change the mind of parents who have made a conscious decision not to vaccinate | ✗ | ||||
| Cash rewards are preferable to vouchers | ✗ | ||||
| Higher-value rewards are preferable | ✗ | ||||
| Quasi-mandatory interventions | |||||
| Quasi-mandatory interventions are more acceptable than any financial incentives | ✗ | ✗ | ✗ | ||
| Quasi-mandatory interventions are preferable to targeted, but not universal, financial incentives | ✗ | ||||
| Quasi-mandatory interventions offer protection for all children and staff in a shared setting | ✗ | ||||
| Quasi-mandatory interventions would act as a reminder to vaccinate | ✗ | ||||
| Quasi-mandatory interventions would punish children for a decision made by their parents | ✗ | ||||
| Quasi-mandatory interventions remove valued choice to engage with a health-related behaviour | ✗ | ✗ | |||
| Quasi-mandatory interventions would have to incorporate clear opt-out processes | ✗ | ||||
| Quasi-mandatory interventions could normalise vaccination | ✗ | ||||
| School entry is an ideal time to monitor vaccination status and provide catch-up vaccinations | ✗ | ||||
| Schools should not become responsible for administration of a quasi-mandatory intervention | ✗ | ||||
| Alternative interventions to increase vaccination uptake | |||||
| More flexibility is required in the timing and location of where vaccinations are delivered, with less waiting time | ✗ | ✗ | ✗ | ||
| Information and education about vaccination and related diseases needs to be more accessible to parents | ✗ | ✗ | |||
| Information on risks and benefits provided in numerical format is preferable to that in chart or pictorial format | ✗ | ||||
| Professionals must build trusting relationships with parents and listen to their fears | ✗ | ||||
| Better multidisciplinary working and information sharing is required | ✗ | ||||
| Vaccinations provided by pharmacists are less preferred than those provided by practice nurse at GP surgery | ✗ | ||||
| Vaccinations provided by community nurses in a mobile bus are less preferred those provided by practice nurse at GP surgery | ✗ | ||||
In Table 19, where a theme was not identified in a particular research component, there was silence on that theme in that component. We did not identify any clear instances of dissonance with disagreement on a theme between research components. However, there are themes that could be interpreted as potentially contradictory. These are placed near each other in Table 19 and discussed further below.
Relative preferences for universal and targeted financial incentives, and quasi-mandatory interventions
There was a consistent finding across the systematic review, and both components of the qualitative study, that quasi-mandatory interventions tended to be more acceptable than parental financial incentives. Although this was not specifically tested in the DCE, the questionnaire found that quasi-mandatory interventions were more acceptable than targeted parental financial incentives, but that universal financial incentives were preferred to both quasi-mandatory and targeted incentives. The qualitative study also found that universal incentives were more acceptable than targeted incentives. It is possible that ordering effects influenced DCE participants’ responses; all participants were invited to consider quasi-mandatory interventions after having considered financial incentives interventions. However, the order in which participants in the qualitative study were invited to consider interventions varied, although preference did not. Ordering effects was not relevant to the systematic review. Overall, it seems unlikely that ordering effects are responsible for the consistent finding that quasi-mandatory interventions were preferred to parental financial incentives.
To summarise, the order of preference found for these interventions in the different research components was:
-
systematic review – quasi-mandatory > financial incentives (distinction between targeted and universal financial incentives not explored)
-
qualitative study (both components) – quasi-mandatory > universal financial incentives > targeted financial incentives
-
DCE questionnaire component – universal financial incentives > quasi-mandatory interventions > targeted financial incentives.
The preference for universal, compared with targeted, financial incentives found in both the qualitative work and the DCE questionnaire may be related to issues of equity. The qualitative study identified that there was a general belief that any intervention should be ‘fair’, in the sense that it should be available to all. Targeting financial incentives to particular groups was considered ‘unfair’, as this would mean that only some parents would be eligible for a reward. As discussed in Chapter 5, the idea that those parents who had delayed vaccination (i.e. acted irresponsibly) would become eligible for a financial reward under the targeted scenario was considered particularly inequitable.
The difference in relative preference for universal incentives compared with quasi-mandatory interventions found in the qualitative study and the DCE questionnaire may reflect differences in the way questions were asked, or in the setting in which preferences were elicited. The DCE questionnaire was conducted anonymously online. In contrast, although data from the qualitative study was anonymised at the analysis stage, data collection took place in a social context with an interviewer and, in the case of focus groups, other participants, present. This hints, but does not confirm, that universal parental incentives may be more acceptable than qualitative data suggest, but that people find it difficult to express this in social spaces. This could be interpreted as a form of ‘social desirability’ bias, where participants report what they feel is socially acceptable in the context, rather than their ‘true’ beliefs and attitudes. Furthermore, open and non-judgemental discussion of the acceptability of financial incentives and quasi-mandatory interventions in wider public forums (e.g. the media) may enable people to more honestly express their views about financial incentives for health behaviours in general and about preschool vaccinations in particular.
Responsible parenting, freedom to choose and ‘appropriate’ motivations for vaccination
Both parents and carers, and health and other professionals expressed concern that financial incentives could interfere with normal social expectations of ‘responsible parenting’, and that quasi-mandatory interventions might remove parents’ freedom to choose whether or not to vaccinate. The findings that parents should both be responsible and have the freedom to choose not to be responsible could, superficially, be interpreted as contradictory. However, the latter theme reflects the obvious respect that participants had for the conscious decision of some parents not to vaccinate their children. Although rarely, if ever, overtly agreeing with such a decision, participants appeared to believe that such decisions tended to be well thought through and strongly adhered to.
Furthermore, these apparently contradictory themes suggest that there is a general belief that the motivation for having one’s children vaccinated should be the desire to protect them, and others, and to act as a responsible citizen and parent. The motivation should not be the achievement of a financial reward or the avoidance of a penalty. This belief in what ‘appropriate’ motivations for health behaviours should be could be an important fundamental barrier to the widespread implementation of financial incentive and quasi-mandatory interventions. This is not a barrier that could be addressed by designing or communicating these interventions differently, but is, instead, inherent to the nature and intention of such interventions. Financial incentives and quasi-mandatory interventions are expressly designed to alter the motivation for behaviours in order to increase the likelihood they will take place.
Potential effectiveness
Previous work has found that perceived (lack of) effectiveness appears to be one important reason why financial incentive interventions are not considered acceptable. 94–97 However, this was not a strong finding in the current work. The systematic review was not able to draw generalisable conclusions concerning effectiveness, but did find some instances in which financial incentives were effective at encouraging uptake. Participants in the qualitative work also believed that financial incentive interventions could be effective – particularly for some specific groups of parents.
The DCE found that parents preferred financial incentives with higher values, and the questionnaire identified that 80% of those who would not require a financial incentive to vaccinate their children would, nevertheless, accept one if it was offered. Thus, although there may be a general perception that gaining financial rewards should not be the appropriate motivation for vaccination, this does not mean that people would not accept such rewards, or that rewards would not be effective in some cases. Indeed, around one-quarter of DCE questionnaire respondents stated that they would require a financial incentive to fully vaccinate their children. The potential effectiveness of financial incentives in some groups was also acknowledged in both components of the qualitative study.
Cost and cost-effectiveness
Both parents and carers, and health and other professionals expressed concerns about the cost of financial incentives and whether or not resources might be more efficiently used in other ways. Although no explicit references to cost-effectiveness were made, concerns about cost and efficiency certainly reflect this concept. In contrast, although quasi-mandatory interventions would also require substantial resources for their development and implementation, the issue of the cost and cost-effectiveness of these was not raised by participants.
Concerns about cost were not explicitly sought in the DCE or questionnaire. However, the questionnaire identified that the minimum effect level (WTA) among the minority (around one-quarter) of parents who stated that they would require a financial incentive was around £110. Most parents who would not require a financial reward to vaccinate would still accept one. The maximum acceptable level among these parents was around £70.
Cost-effectiveness may be particularly salient when considering financial incentives because of the explicit financial element in the intervention. 96 As identified in the systematic review, the cost-effectiveness of financial incentive and quasi-mandatory interventions has been very poorly studied and is not yet known. However, previous research indicates that the great majority of public health interventions meet NICE’s criteria for cost-effectiveness. 127
Alternative approaches to encouraging uptake of preschool vaccination
Participants in both components of the qualitative study made a variety of suggestions for other methods of increasing vaccination rates. Although these suggestions were spontaneous and unprompted by the researcher, they were common. In particular, both groups of participants suggested that more flexibility in the timing and location of where vaccinations were delivered and improvements in the accessibility of information and education about vaccinations and vaccine-preventable diseases would be useful.
A preference for greater flexibility in appointments was also expressed in the DCE, where out-of-hours appointments were associated with a gain in utility, but only in those parents ‘not at high risk’ of incompletely vaccinating their children. Longer waiting times were associated with a loss of utility across the board, but particularly in those parents ‘at high risk’ of incompletely vaccinating their children. Reducing waiting times during normal clinic hours may, therefore, be particularly important for increasing preschool vaccination uptake. Providing extended-hours appointments would certainly be preferred by many parents, but would be unlikely to increase uptake among those ‘at high risk’ of incomplete vaccination and so may be lower priority. One particular approach to avoid, identified in the qualitative study, was issuing ‘block’ appointments, in which a group of parents are all given the same appointment time and then made to wait until a slot is available.
Although the qualitative study found a general preference for wider availability of vaccinations, the DCE revealed a significant disutility of vaccination delivery by pharmacists and by community nurses in mobile buses, compared with vaccination provided by practice nurses in GP surgeries. This suggests that any changes to vaccination personnel and location would have to be carefully considered. It appears that parents will not trust ‘just any’ trained individual to vaccinate their children, and that some locations (e.g. pharmacies and mobile buses) are not considered appropriate. Professionals in the qualitative study also raised considerable concerns about how data on vaccination status could be shared between those working in different sectors. These issues would need to be overcome before professionals working in non-health sectors are trained to offer vaccinations. Parents in the qualitative study showed an interest in vaccination delivery in children’s centres. In the DCE, preference for vaccination delivery in children’s centres did not differ from preference for practice nurses delivering vaccinations at GP surgeries, and this could be explored further.
Although participants in the qualitative study acknowledged that substantial information on vaccinations is currently provided to new parents, there was widespread recognition that the information was not provided in a format that parents found easy to access. The DCE found a preference for information about the risks and benefits of vaccinations to be provided in numerical format rather than in charts and pictures. This preference was particularly strong in parents ‘at high risk’ of incompletely vaccinating their children. Presenting information in a range of different formats, and being sensitive to the different information needs of different parents, may help all parents to feel that their information needs are met.
Discussion
This brief chapter has attempted to integrate, and triangulate, findings from the three different components of this project. By using an adapted version of the triangulation protocol method,126 we have identified areas of overlap, as well as difference, in results from the three components. Although there were no areas of specific disagreement in the results from the different components, there were some apparent contradictions.
The use of a triangulation protocol also serves to highlight the strengths and limitations of the different methods used. The results in Table 19 indicate some of the differences in the depth and scope of the methods used. The systematic review focused on a limited number of specific questions and was able to generate evidence only on these. The small evidence base identified in the systematic review further limited the conclusions that could be drawn. In contrast, the qualitative study had a wider scope and was able to generate evidence on relevant topics not specified a priori. As in the systematic review, the DCE was able to generate evidence only on the specific a priori aims. By including a range of supporting questions in addition to the formal DCE choice set, some context and colour could be added to the DCE results. By combining these three methods, we were able to overcome some of the limitations of each individual method and provide a more holistic and nuanced understanding of the topic than if we had focused on one particular method, or disciplinary perspective, alone.
Chapter 7 Recommendations for future research
Recommendations for future research have been considered in the discussion sections of Chapters 3–5 and are summarised here for ease of reference. We have attempted to place these in priority order.
-
Further evidence is required on the effectiveness and cost-effectiveness of parental financial incentive and quasi-mandatory interventions for encouraging the uptake of preschool vaccinations. As such, interventions are likely to be implemented on a large scale; evaluation strategies such as natural experiments and step-wedge designs may be most useful in generating such evidence. 82
-
Further evidence is required on the most effective and cost-effective configuration of any parental financial incentive and quasi-mandatory interventions for encouraging the uptake of preschool vaccinations. Intervention development work, taking account of existing behaviour-change theory, may be useful to maximise the potential effectiveness of incentive interventions. This should involve further consideration of the effective component, or components, of financial incentive interventions.
-
Further consideration of reasons for non-vaccination should be incorporated into new interventions for promoting the uptake of preschool vaccinations. Parental financial incentive and quasi-mandatory interventions for encouraging uptake of preschool vaccinations may not adequately address the reasons for non-vaccination in high-income countries that tend to achieve overall high coverage of preschool vaccinations.
-
Further consideration of how a quasi-mandatory intervention for encouraging the uptake of preschool vaccinations could be designed and implemented is required. Particular issues requiring further consideration include data sharing of vaccination status between health-care providers and schools, responsibilities of different sectors and staff, and how provision would be made for legitimate opt-out.
-
If high-quality evidence of effectiveness of parental financial incentive and quasi-mandatory interventions for encouraging uptake of preschool vaccinations is generated, further evidence is required on how to effectively communicate this information to all stakeholders. As acceptability is linked to perceived effectiveness, further evidence on the impact of well-communicated effectiveness evidence on perceived acceptability is also required.
-
The factors that may increase acceptance of mandatory schemes warrant further research, and additional DCEs could be conducted to explore parental preferences on how a mandate for vaccination might be imposed.
-
Further consideration may be required of how existing systems and resources for encouraging the uptake of preschool vaccinations can be optimised. In particular, further evidence may be required on how to provide accessible information and education, and how to deliver accessible vaccination services. However, although these issues were raised in the present work, we did not conduct a systematic review on these topics and, as such, cannot make definitive recommendations for future research.
-
Research engaging parents in an iterative codesign process to design optimally acceptable and usable information that conveys robust and balanced data on the consequences of disease and the benefits and risks of vaccinations is required.
Chapter 8 Conclusions
There is a limited existing evidence base on the effectiveness, acceptability and economic costs and consequences of parental financial incentive and quasi-mandatory interventions for encouraging the uptake of preschool vaccinations.
There is a consistent preference for universal over targeted parental financial incentives for encouraging the uptake of preschool vaccinations among UK parents and stakeholders.
There is a consistent preference for quasi-mandatory interventions over targeted parental financial incentives for encouraging the uptake of preschool vaccinations among UK parents and stakeholders.
Relative preferences for universal parental financial incentives compared with quasi-mandatory interventions were inconsistent. This inconsistency may reflect ‘social desirability’ bias, where participants report what they believe to be the socially acceptable response, particularly in social settings in which other people are present, such as focus groups. Further opportunities for open and non-judgemental discussion of these interventions in public settings may lead to people feeling more able to express their views and to an apparent increase in acceptability.
There was consistent recognition that universal financial incentives may be effective in encouraging a small group of parents to vaccinate. Around one-quarter of parents stated that they would require a reward, of at least around £110, to vaccinate. Most parents who would not require a reward would still accept one if it was offered. Higher-value incentives provided as cash, rather than as vouchers, were preferred.
A range of methods for optimising the configuration and delivery of existing services was identified. Reducing waiting times, avoiding block appointments and providing information about the risks and benefits of vaccinations using numbers, rather than charts and pictures, were identified as potentially valuable. Offering vaccinations in pharmacies or community buses was not valued.
Acknowledgements
During this work, FFS was funded in full, and JA was funded in part by Fuse (the Centre for Translational Research in Public Health), a UK Clinical Research Collaboration Public Health Research Centre of Excellence. Latterly, JA was funded in part by the Centre for Diet and Activity Research (CEDAR), a UK Clinical Research Collaboration Public Health Research Centre of Excellence. Funding for both Fuse and CEDAR from the British Heart Foundation, Cancer Research UK, Economic and Social Research Council, Medical Research Council, the National Institute for Health Research and the Wellcome Trust, under the auspices of the UK Clinical Research Collaboration, is gratefully acknowledged. The funders had no role in the study design, data analysis, report writing or choice of publication. The views and opinions expressed herein are those of the authors and do not necessarily reflect those of the HTA programme, National Institute for Health Research, the NHS or the Department of Health.
Contributions of authors
Jean Adams (senior research fellow, public health) conceived the idea for the research, developed the protocol and acted as second reviewer for the systematic review, contributed to data interpretation across all components, and led the drafting of the report.
Belinda Bateman (consultant in paediatrics) contributed to the study design and data interpretation across all components.
Frauke Becker (research associate, health economics) led the data analysis and contributed to the interpretation and reporting of the DCE.
Tricia Cresswell (consultant in public health) contributed to the study design and data interpretation across all components.
Darren Flynn (senior research associate, health psychology) managed the data collection, contributed to the data analysis, and contributed to the interpretation and reporting of the DCE.
Rebekah McNaughton (research associate, public health) conducted the data collection and data analysis, organised the service user groups that advised the study and led the reporting of the qualitative work.
Yemi Oluboyede (senior research associate, health economics) developed the protocol, and contributed to the data analysis and the reporting of the DCE.
Shannon Robalino (information scientist) developed and ran the search strategies for the systematic review.
Laura Ternent (senior lecturer, health economics) acted as economics reviewer for the systematic review; conceived the idea, developed the protocol, and contributed to data analysis and the reporting of the DCE.
Benjamin Gardner Sood (lecturer, health psychology) contributed to the study design and data interpretation across all components.
Susan Michie (professor, health psychology) contributed to the study design and data interpretation across all components.
Janet Shucksmith (professor, public health) conceived the idea, developed the protocol, and contributed to the data interpretation and reporting for the qualitative work.
Falko F Sniehotta (professor, behavioural medicine and health psychology) contributed to the study design and data interpretation across all components.
Sarah Wigham (research associate, public health) conducted and led the reporting of the systematic review and meta-analysis.
Publications
To date, the scientific outputs from this research are as follows.
Publication of the systematic review
Wigham S, Ternent L, Bryant A, Robalino S, Sniehotta FF, Adams J. Parental financial incentives for increasing preschool vaccination uptake: systematic review. Pediatrics 2014;134:e1117–28.
Presentation of the qualitative study
McNaughton R, Shucksmith J. Persuading the last 15%: do we need sticks or carrots to achieve full infant immunisation? A mixed methods study of parental incentives and quasi-mandatory schemes for increasing uptake of vaccinations in preschool children. UKCRC Public Health Research Centres of Excellence, 5th Annual Scientific Meeting, Leeds, UK, 19–20 June 2014.
Presentation of the qualitative study
Shucksmith J, McNaughton R. Persuading the last 15%: do we need sticks or carrots to achieve full infant vaccination? Early results from a study of parental incentives and quasi-mandatory schemes for increasing uptake of vaccinations in pre-school children. BSA Medical Sociology Group Annual Conference, Aston University, Birmingham, UK, 10–12 September 2014.
Data sharing statement
Data from the systematic review can be obtained from the corresponding author. We did not obtain ethical approval, or informed consent from participants, for the sharing of data from the qualitative study or DCE beyond the study team. Subject to additional ethical approval, anonymised data from the qualitative study and DCE can be obtained from the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health.
References
- Immunization Coverage. Geneva: WHO; 2010.
- Public Health England . Coverage. Health Protection Report 2014;8.
- Begg N. Manual for the Management and Control of Diphtheria in the European Region. Copenhagen: WHO; 1994.
- The NHS. NHS Immunisation Statistics England: 2010–11. London: The NHS Information Centre; 2011.
- Brown KF, Kroll JS, Hudson MJ, Ramsay M, Green J, Long SJ, et al. Factors underlying parental decisions about combination childhood vaccinations including MMR: a systematic review. Vaccine 2010;28:4235-48. http://dx.doi.org/10.1016/j.vaccine.2010.04.052.
- Mills E, Jadad AR, Ross C, Wilson K. Systematic review of qualitative studies exploring parental beliefs and attitudes toward childhood vaccination identifies common barriers to vaccination. J Clin Epidemiol 2005;58:1081-8. http://dx.doi.org/10.1016/j.jclinepi.2005.09.002.
- Falagasa M, Zarkadouliaa E. Factors associated with suboptimal compliance to vaccinations in children in developed countries: a systematic review. Curr Med Res Opin 2008;24:1719-41. http://dx.doi.org/10.1185/03007990802085692.
- Mindlin M, Jenkins R, Law C. Maternal employment and indicators of child health: a systematic review in pre-school children in OECD countries. J Epidemiol Community Health 2009;63:340-50. http://dx.doi.org/10.1136/jech.2008.077073.
- Middleton E, Baker D. Comparison of social distribution of immunisation with measles, mumps, and rubella vaccine, England, 1991–2001. BMJ 2003;326. http://dx.doi.org/10.1136/bmj.326.7394.854.
- Vaccination Services: Reducing Inequalities in Uptake. London: Department of Health; 2005.
- Reducing Differences in the Uptake of Immunisations (Including Targeted Vaccines) among Children and Young People Aged Under 19 Years. London: NICE; 2009.
- Rogers R, Cacioppo J, Petty R. Social Psychophysiology. New York, NY: Guilford Press; 1983.
- Birth Statistics: Review of the Registrar General on Births and Patterns of Family Building in England and Wales, 2005. London: Office for National Statistics; 2006.
- Reducing Differences in the Uptake of Immunisations: Revised Analysis of the Evidence. London: NICE; 2010.
- Abraham C, Michie S. A taxonomy of behaviour change techniques used in interventions. Health Psychol 2008;27:379-87. http://dx.doi.org/10.1037/0278-6133.27.3.379.
- Briss P, Rodewald L, Hinman A, Shefer A, Strikas R, Bernier R, et al. Reviews of evidence regarding interventions to improve vaccination coverage in children, adolescents, and adults. Am J Prevent Med 2000;18:97-140. http://dx.doi.org/10.1016/S0749-3797(99)00118-X.
- Shah S, Raman S, Moreira C, MacIntyre C. School immunisation certificates – a review over time in a disadvantaged community. Aust N Z J Public Health 2001;25:534-8. http://dx.doi.org/10.1111/j.1467-842X.2001.tb00319.x.
- Moria J, Ramirez E, Trick W. Effect of a school-entry vaccination requirement on racial and ethnic disparities in Hepatitis B immunization coverage levels among public school students. Pediatrics 2008;121:e547-52. http://dx.doi.org/10.1542/peds.2007-0799.
- Skinner B. Science and Human Behavior. New York, NY: Macmillan; 1953.
- Johnston M, Sniehotta F. Financial incentives to change patient behaviour. J Health Serv Res Policy 2010;15:131-2. http://dx.doi.org/10.1258/jhsrp.2010.010048.
- Michie S, Abraham C, Whittington C, McAteer J, Gupta S. Effective techniques in healthy eating and physical activity interventions: a meta-regression. Health Psychol 2009;28:690-701. http://dx.doi.org/10.1037/a0016136.
- Adams J, White M, Babones S. Social Inequality and Public Health. Bristol: Policy Press; 2009.
- Ariely D, Zakay D. A timely account of the role of duration in decision making. Acta Psychol (Amst) 2001;108:187-20. http://dx.doi.org/10.1016/S0001-6918(01)00034-8.
- Bleichrodt H, Gafni A. Time preference, the discounted utility model and health. J Health Econ 1996;15:49-66. http://dx.doi.org/10.1016/0167-6296(95)00031-3.
- Marteau TM, Ashcroft RE, Oliver A. Using financial incentives to achieve healthy behaviour. BMJ 2009;338. http://dx.doi.org/10.1136/bmj.b1415.
- Le Grand J. The giants of excess: a challenge to the nation’s health. J R Stat Soc Series A 2008;171:843-56. http://dx.doi.org/10.1111/j.1467-985X.2008.00549.x.
- Deci E, Koestner R, Ryan R. A meta-analytic review of experiments examining the effects of extrinsic rewards on intrinsic motivation. Psychol Bull 1999;125:627-68. http://dx.doi.org/10.1037/0033-2909.125.6.627.
- Sutherland K, Christianson JB, Leatherman S. Impact of targeted financial incentives on personal health behavior: a review of the literature. Med Care Res Rev 2008;65:36S-78. http://dx.doi.org/10.1177/1077558708324235.
- Salazar MK. Comparison of four behavioral theories. A literature review. AAOHN J 1991;39:128-35.
- Forde I, Zeuner D. Financial incentives to promote social mobility. BMJ 2009;339. http://dx.doi.org/10.1136/bmj.b3219.
- Lagarde M, Haines A, Palmer N. Conditional cash transfers for improving uptake of health interventions in low- and middle-income countries: a systematic review. JAMA 2007;298:1900-10. http://dx.doi.org/10.1001/jama.298.16.1900.
- Antenatal Care: Routine Care for the Healthy Pregnant Woman. London: NICE; 2008.
- Healthy Weight, Healthy Lives: A Cross-Government Strategy for England. London: HM Government; 2008.
- Jochelson K. Paying the Patient: Improving Health using Financial Incentives. London: The King’s Fund; 2007.
- Lussier J, Heil S, Mongeon J, Badger G, Higgins S. A meta-analysis of voucher-based reinforcement therapy for substance use disorders. Addiction 2006;101:192-203. http://dx.doi.org/10.1111/j.1360-0443.2006.01311.x.
- Prendergast M, Podus D, Finney J, Greenwell L, Roll J. Contingency management for treatment of substance use disorders: a meta-analysis. Addiction 2006;101:1546-60. http://dx.doi.org/10.1111/j.1360-0443.2006.01581.x.
- Cahill K, Perera R. Competitions and incentives for smoking cessation. Cochrane Database Syst Rev 2008;4. http://dx.doi.org/10.1002/14651858.cd004307.pub3.
- Paul-Ebhohimhen V, Avenell A. Systematic review of the use of financial incentives in treatments for obesity and overweight. Obes Rev 2008;9:355-67. http://dx.doi.org/10.1111/j.1467-789X.2007.00409.x.
- Wall J, Ni Mhurchu C, Blakely T, Rodgers A, Wilton J. Effectiveness of monetary incentives in modifying dietary behavior: a review of randomized, controlled trials. Nutr Rev 2006;64:518-31. http://dx.doi.org/10.1111/j.1753-4887.2006.tb00185.x.
- Kane R, Johnson P, Town R, Butler M. A structured review of the effect of economic incentives on consumers’ preventive behavior. Am J Prev Med 2004;27:327-52. http://dx.doi.org/10.1016/j.amepre.2004.07.002.
- Lawrence G, MacIntyre C, Hull B, McIntyre P. Effectiveness of the linkage of child care and maternity payments to childhood immunisation. Vaccine 2004;22:2345-50. http://dx.doi.org/10.1016/j.vaccine.2003.10.038.
- Yokley J, Glenwick D. Increasing the immunization of preschool children: an evaluation of applied community interventions. J Appl Behav Anal 1984;17:313-25. http://dx.doi.org/10.1901/jaba.1984.17-313.
- Browngoehl K, Kennedy K, Krotki K, Minzer H. Increasing immunization: a Medicaid managed care model. Pediatrics 1997;99. http://dx.doi.org/10.1542/peds.99.1.e4.
- Minkovitz C, Holt E, Hughart N, Hou W, Thomas L, Dini E, et al. The effect of parental monetary sanctions on the vaccination status of young children. Arch Pediatr Adolesc Med 1999;153:1242-7. http://dx.doi.org/10.1001/archpedi.153.12.1242.
- Kerpelman L, Connell D, Gunn W. Effect of a monetary sanction on immunization rates of recipients of aid to families with dependent children. JAMA 2000;284:53-9. http://dx.doi.org/10.1001/jama.284.1.53.
- Tuckerman J, Rajesh S, Oeppen C, Balachander N, Bancsi A, Jacklin P, et al. Reducing Difference in the Uptake of Immunisations: Revised Analysis of the Evidence. London: National Collaborating Centre for Women’s and Children’s Health; 2008.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337. http://dx.doi.org/10.1136/bmj.a1655.
- Buehler J, Hopkins R, Overhage J, Sosin D, Tong V. Framework for evaluating public health surveillance systems for early detection of outbreaks: recommendations from the CDC Working Group. Morbidity Mortality Weekly Rep 2004;53:1-11.
- Oliver A, Marteau TM, Ashcroft RE. Can financial carrots improve health?. J Health Serv Res Policy 2009;14:1-2. http://dx.doi.org/10.1258/jhsrp.2008.008132.
- Gardner B, Davies A, McAteer J, Michie S. Beliefs underlying UK parents’ views towards MMR promotion interventions: a qualitative study. Psychol Health Med 2010;15:220-30. http://dx.doi.org/10.1080/13548501003623963.
- Promberger M, Brown R, Ashcroft R, Marteau T. Acceptability of financial incentives to improve health outcomes in UK and US samples. J Med Ethics 2011;37:682-7. http://dx.doi.org/10.1136/jme.2010.039347.
- Parke H, Ashcroft R, Brown R, Marteau T, Seale C. Financial incentives to encourage healthy behaviours: an analysis of UK media coverage. Health Expect 2013;16:292-304. http://dx.doi.org/10.1111/j.1369-7625.2011.00719.x.
- Casiday R. Children’s health and the social theory of risk: insights from the British measles, mumps and rubella (MMR) controversy. Soc Sci Med 2007;65:1059-70. http://dx.doi.org/10.1016/j.socscimed.2007.04.023.
- Bedford HE, Masters JI, Kurtz Z. Immunisation status in inner London primary schools. Arch Dis Child 1992;67:1288-91. http://dx.doi.org/10.1136/adc.67.10.1288.
- Gardner B, McAteer J, Davies A, Michie S. Views towards compulsory MMR vaccination in the UK. Arch Dis Child 2010;95:658-9. http://dx.doi.org/10.1136/adc.2009.169813.
- Wigham S, Ternent L, Bryant A, Robalino S, Sniehotta FF, Adams J. Parental financial incentives for increasing preschool vaccination uptake: systematic review. Pediatrics 2014;134:e1117-28. http://dx.doi.org/10.1542/peds.2014-1279.
- Ehreth J. The global value of vaccination. Vaccine 2003;21:596-600. http://dx.doi.org/10.1016/S0264-410X(02)00623-0.
- NHS Immunisation Statistics, England 2012–13. Leeds: Health and Social Care Information Centre; 2012.
- Centers for Disease C, Prevention . National, state, and local area vaccination coverage among children aged 19-35 months – United States, 2009. Morbidity Mortality Weekly Rep 2010;59:1171-7.
- Giles EL, Robalino S, McColl E, Sniehotta FF, Adams J. The effectiveness of financial incentives for health behaviour change: systematic review and meta-analysis. PLOS ONE 2014;9. http://dx.doi.org/10.1371/journal.pone.0090347.
- Davis MM, Gaglia MA. Associations of daycare and school entry vaccination requirements with varicella immunization rates. Vaccine 2005;23:3053-60. http://dx.doi.org/10.1016/j.vaccine.2004.10.047.
- Tuckerman J, Rajesh S, Oeppen C, Balachander N, Bancsi A, Jacklin P, et al. Review of the Evidence of the Effectiveness and Cost Effectiveness of Interventions to Address Differences in the Uptake of Immunisations (Including Targeted Vaccines) in People Younger than 19 Years. London: National Collaborating Centre for Women’s and Children’s Health; 2008.
- Liberati A, Altman D, Tetzlaff J, Mulrow C, Gøtzsche P, . The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of studies that evaluate health care interventions: explanation and elaboration. PLOS Med 2009;6. http://dx.doi.org/10.1371/journal.pmed.1000100.
- The World Bank . World Development Indicators 2013 n.d. http://data.worldbank.org/about/country-classifications (accessed 6 December 2013).
- Resources for Review Authors. Oslo: Norwegian Knowledge Centre for the Health Services; 2013.
- Officer L, Williamson S. Purchasing Power of Money in the United States from 1774 to Present 2013 n.d. www.measuringworth.com/ppowerus/ (accessed 6 December 2013).
- Shemilt I, Byford S, Drummond M, Eisenstein E, Knapp M, Mallender J, et al. Cochrane Handbook for Systematic Reviews of Interventions. Chichester: John Wiley & Sons; 2008.
- Thomas B, Ciliska D, Dobbins M, Micucci S. A process for systematically reviewing the literature: providing the research evidence for public health nursing interventions. Worldviews Evid Based Nurs 2004;1:176-84. http://dx.doi.org/10.1111/j.1524-475X.2004.04006.x.
- 10 Questions Developed by the National CASP Collaboration for Qualitative Methodologies. Milton Keynes: Public Health Resource Unit, Primary Care Trust; 2002.
- Adams J, Giles E, McColl E, Sniehotta F. Carrots, sticks and health behaviours: a framework for documenting the complexity of financial incentive interventions to change health behaviours. Health Psychol Rev 2013;8:286-95. http://dx.doi.org/10.1080/17437199.2013.848410.
- Abrevaya J, Mulligan K. Effectiveness of state-level vaccination mandates: evidence from the varicella vaccine. J Health Econ 2011;30:966-76. http://dx.doi.org/10.1016/j.jhealeco.2011.06.003.
- Bond L, Davie G, Carlin JB, Lester R, Nolan T. Increases in vaccination coverage for children in child care, 1997 to 2000: an evaluation of the impact of government incentives and initiatives. Aust N Z J Public Health 2002;26:58-64. http://dx.doi.org/10.1111/j.1467-842X.2002.tb00272.x.
- Bond L, Nolan T, Lester R. Immunisation uptake, services required and government incentives for users of formal day care. Aust N Z J Public Health 1999;23:368-76. http://dx.doi.org/10.1111/j.1467-842X.1999.tb01277.x.
- Freed GL, Freeman VA, Mauskopf A. Enforcement of age-appropriate immunization laws. Am J Prevent Med 1998;14:118-21. http://dx.doi.org/10.1016/S0749-3797(97)00023-8.
- Hall J, Kenny P, King M, Louviere J, Viney R, Yeoh A. Using stated preference discrete choice modelling to evaluate the introduction of varicella vaccination. Health Econ 2002;11:457-65. http://dx.doi.org/10.1002/hec.694.
- Maryland’s Primary Prevention Initiative Final Report. Primary Prevention Initiative Evaluation. Baltimore, MD: Schaefer Centre for Public Policy; 1997.
- Tarrant M, Thomson N. Secrets to success: a qualitative study of perceptions of childhood immunisations in a highly immunised population. J Paediatr Child Health 2008;44:541-7. http://dx.doi.org/10.1111/j.1440-1754.2008.01334.x.
- Hoekstra E, LeBaron C, Johnson-Partlow T. Does reminder-recall augment the impact of voucher incentives on immunization rates among inner-city infants enrolled in WIC?. J Pediatr 1999;135:261-3. http://dx.doi.org/10.1016/S0022-3476(99)70033-8.
- Hoekstra EJ, LeBaron CW, Megaloeconomou Y, Guerrero H, Byers C, Johnson-Partlow T, et al. Impact of a large-scale immunization initiative in the special supplemental nutrition program for Women, Infants, and Children (WIC). JAMA 1998;280:1143-7. http://dx.doi.org/10.1001/jama.280.13.1143.
- Hutchins SS, Rosenthal J, Eason P, Swint E, Guerrero H, Hadler S. Effectiveness and cost-effectiveness of linking the special supplemental program for Women, Infants, and Children (WIC) and immunization activities. J Public Health Policy 1999;20:408-26. http://dx.doi.org/10.2307/3343128.
- Kreuter MW, Caburnay CA, Chen JJ, Donlin MJ. Effectiveness of individually tailored calendars in promoting childhood immunization in urban public health centers. Am J Public Health 2004;94:122-7. http://dx.doi.org/10.2105/AJPH.94.1.122.
- Craig P, Cooper C, Gunnell D, Haw S, Lawson K, Macintyre S, et al. Using Natural Experiments to Evaluate Population Health Interventions: Guidance for Producers and Users of Evidence. London: Medical Research Council; 2011.
- Collins L, Baker T, Mermelstein R. The multiphase optimization strategy for engineering effective tobacco use interventions. Ann Behav Med 2011;41:208-26. http://dx.doi.org/10.1007/s12160-010-9253-x.
- Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 2007;19:349-57. http://dx.doi.org/10.1093/intqhc/mzm042.
- Department of Communities and Local Government . The English Indices of Deprivation 2010 2011. www.communities.gov.uk/publications/corporate/statistics/indices2010 (accessed 15 October 2012).
- Pope C, Ziebland S, Mays N. Analysing qualitative data. BMJ 2000;320:114-16. http://dx.doi.org/10.1136/bmj.320.7227.114.
- Ritchie J, Spencer L, O’Connor W, Ritchie J, Lewis J. Qualitative Research Practice. London: Sage; 2003.
- Bryman A, Burgess R, Ritchie J, Spencer L, Bryman A, Burgess R. Analysing Qualitative Data. London: Routledge; 1993.
- Strauss A, Corbin J. Basics of Qualitative Research: Grounded Theory Procedures and Techniques. Newbury Park: Sage; 1990.
- Elliott R, Fischer C, Rennie D. Evolving guidelines for publication of qualitative research studies in psychology and related fields. Br J Clin Psychol 1999;38:215-29. http://dx.doi.org/10.1348/014466599162782.
- Ashcroft RE. Personal financial incentives in health promotion: where do they fit in an ethic of autonomy?. Health Expectations 2011;14:191-200. http://dx.doi.org/10.1111/j.1369-7625.2011.00664.x.
- Burgess DC, Burgess MA, Leask J. The MMR vaccination and autism controversy in United Kingdom 1998–2005: inevitable community outrage or a failure of risk communication?. Vaccine 2006;24:3921-8. http://dx.doi.org/10.1016/j.vaccine.2006.02.033.
- Giles E, Robalino S, McColl E, Sniehotta F, Adams J. Acceptability of financial incentives and penalties for encouraging uptake of healthy behaviours: a critical review using systematic methods. Prevent Med 2015;73:145-58. http://dx.doi.org/10.1016/j.ypmed.2014.12.029.
- Priebe S, Sinclair J, Burton A, Marougka S, Larsen J, Firn M, et al. Acceptability of offering financial incentives to achieve medication adherence in patients with severe mental illness: a focus group study. J Med Ethics 2010;36:463-8. http://dx.doi.org/10.1136/jme.2009.035071.
- Sinclair JMA, Burton A, Ashcroft R, Priebe S. Clinician and service user perceptions of implementing contingency management: a focus group study. Drug Alcohol Depend 2011;119:56-63. http://dx.doi.org/10.1016/j.drugalcdep.2011.05.016.
- Giles EL, Sniehotta FF, McColl E, Adams J. Acceptability of financial incentives and penalties for encouraging uptake of healthy behaviours: focus groups. BMC Public Health 2015;15. http://dx.doi.org/10.1186/s12889-015-1409-y.
- Giles E, Holmes M, McColl E, Sniehotta F, Adams J. Acceptability of financial incentives for breastfeeding: thematic analysis of readers’ comments to UK online news reports. BMC Pregn Childbirth 2015;15. http://dx.doi.org/10.1186/s12884-015-0549-5.
- Lancsar E, Louviere J. Conducting discrete choice experiments to inform healthcare decision making. Pharmacoeconomics 2008;26:661-77. http://dx.doi.org/10.2165/00019053-200826080-00004.
- Ryan M, Netten A, Skatun D, Smith P. Using discrete choice experiments to estimate a preference-based measure of outcome – an application to social care for older people. J Health Econ 2006;25:927-44. http://dx.doi.org/10.1016/j.jhealeco.2006.01.001.
- Flynn T, Louviere J, Marley A, Coast J, Peters T. Rescaling quality of life values from discrete choice experiments for use as QALYs: a cautionary tale. Population Health Metrics 2008;6. http://dx.doi.org/10.1186/1478-7954-6-6.
- Coast J, Flynn T, Natarajan L, Sproston K, Lewis J, Louviere J, et al. Valuing the ICECAP capability index for older people. Social Sci Med 2008;67:874-82. http://dx.doi.org/10.1016/j.socscimed.2008.05.015.
- O’Brien B, Gertsen K, Willan A, Faulkner L. Is there a kink in consumers’ threshold value for cost-effectiveness in health care?. Health Econ 2002;11:175-80. http://dx.doi.org/10.1002/hec.655.
- Ryan M, Gerard K, Amaya-Amaya M. Using Discrete Choice Experiments to Value Health and Health Care. Dordrecht: Springer; 2008.
- NHS Choices . The NHS Vaccination Schedule 2014 n.d. www.nhs.uk/Conditions/vaccinations/Pages/vaccination-schedule-age-checklist.aspx (accessed 24 November 2014).
- Hawley S, Zikmund-Fisher B, Ubel P, Jancovic A, Lucas T, Fagerlin A. The impact of the format of graphical presentation on health-related knowledge and treatment choices. Patient Educ Couns 2008;73:448-55. http://dx.doi.org/10.1016/j.pec.2008.07.023.
- Reed Johnson F, Lancsar E, Marshall D, Kilambi V, Mühlbacher A, Regier DA, et al. Constructing experimental designs for discrete-choice experiments: report of the ISPOR conjoint analysis experimental design good research practices task force. Value Health 2013;16:3-13. http://dx.doi.org/10.1016/j.jval.2012.08.2223.
- De Bekker-Grob E, Ryan M, Gerard K. Discrete choice experiments in health economics: a review of the literature. Health Econ 2010;21:145-72. http://dx.doi.org/10.1002/hec.1697.
- Bliemer M, Rose J. Construction of experimental designs for mixed logit models allowing for correlation across choice observations. Transport Res Part B 2010;44:720-34. http://dx.doi.org/10.1016/j.trb.2009.12.004.
- McColl E, Jacoby A, Thomas L, Soutter J, Bamford C, Steen N. Design and use of questionnaires: a review of best practice applicable to surveys of health staff and patients. Health Technol Assess 2001;5. http://dx.doi.org/10.3310/hta5310.
- Willis G. Cognitive Interviewing: A ‘How To’ Guide. Rockville, MD: Research Triangle Institute; 1999.
- Code of Conduct. London: Market Research Society; 2010.
- Dwight-Johnson M, Lagomasino I, Aisenberg E, Hay J. Using conjoint analysis to assess depression treatment preferences among low-income Latinos. Psychiatr Serv 2004;55:934-6. http://dx.doi.org/10.1176/appi.ps.55.8.934.
- Scott A, Watson M, Ross S. Eliciting preferences of the community for out of hours care provided by general practitioners: a stated preference discrete choice experiment. Soc Sci Med 2003;56:803-14. http://dx.doi.org/10.1016/S0277-9536(02)00079-5.
- King M, Hall J, Lancsar E, Fiebig D, Hossain I, Louviere J, et al. Patient preferences for managing asthma: results from a discrete choice experiment. Health Econ 2007;16:703-17. http://dx.doi.org/10.1002/hec.1193.
- Louviere J, Hensher D, Swait J. Stated Choice Methods Analysis and Application. Cambridge: Cambridge University Press; 2000.
- McFadden D, Zarembka P. Frontiers in Econometrics. New York, NY: Academic Press; 1973.
- Bech M, Gyrd-Hansen D. Effects coding in discrete choice experiments. Health Econ 2005;14:1079-83. http://dx.doi.org/10.1002/hec.984.
- Whitty JA, Walker R, Golenko X, Ratcliffe J. A think aloud study comparing the validity and acceptability of discrete choice and best worst scaling methods. PLOS ONE 2014;9. http://dx.doi.org/10.1371/journal.pone.0090635.
- Kenny P, Hall J, Viney R, Haas M. Do participants understand a stated preference health survey? A qualitative approach to assessing validity. Int J Technol Assess Health Care 2003;19:664-81. http://dx.doi.org/10.1017/S026646230300062X.
- Cheraghi-Sohi S, Bower P, Mead N, McDonald R, Whalley D, Roland M. Making sense of patient priorities: applying discrete choice methods in primary care using ‘think aloud’ technique. Fam Pract 2007;24:276-82. http://dx.doi.org/10.1093/fampra/cmm007.
- Xie F, Pullenayegum E, Gaebel K, Oppe M, Krabbe PF. Eliciting preferences to the EQ-5D-5L health states: discrete choice experiment or multiprofile case of best-worst scaling?. Eur J Health Econ 2014;15:281-8. http://dx.doi.org/10.1007/s10198-013-0474-3.
- Kennedy A, Basket M, Sheedy K. Vaccine attitudes, concerns, and information sources reported by parents of young children: results from the 2009 HealthStyles survey. Pediatrics 2011;127:92-9. http://dx.doi.org/10.1542/peds.2010-1722N.
- Watson V, Porteous T, Ryan M. Survey Mode Effects when Eliciting Public Preferences for Health Care: A Pilot Discrete Choice Experiment Study. Coventry: Health Economists’ Study Group, University of Warwick; 2013.
- Denzin N. The Research Act: A Theoretical Introduction to Sociological Methods. New York, NY: McGraw Hill; 1978.
- O’Cathain A, Murphy E, Nicholl J. Three techniques for integrating data in mixed methods studies. BMJ 2010;341. http://dx.doi.org/10.1136/bmj.c4587.
- Farmer T, Robinson K, Elliott SJ, Eyles J. Developing and implementing a triangulation protocol for qualitative health research. Qual Health Res 2006;16:377-94. http://dx.doi.org/10.1177/1049732305285708.
- Owen L, Morgan A, Fischer A, Ellis S, Hoy A, Kelly MP. The cost-effectiveness of public health interventions. J Public Health 2012;34:37-45. http://dx.doi.org/10.1093/pubmed/fdr075.
Appendix 1 Example search strategy from MEDLINE
Date range searched: from inception to first week in March 2013.
Date searched: March 2013.
Search strategy
-
exp Immunization/
-
exp immunization programs/
-
exp Immunization Schedule/
-
exp Vaccination/
-
influenza vaccines/ or measles-mumps-rubella vaccine/ or measles vaccine/ or mumps vaccine/ or poliovirus vaccines/ or rubella vaccine/ or exp Vaccines, Combined/ or exp Pertussis Vaccine/ or Diphtheria-Tetanus Vaccine/ or Diphtheria-Tetanus-Pertussis Vaccine/ or chickenpox vaccine/
-
Health Promotion/mt [Methods]
-
Child Welfare/
-
or/1-7
-
immuni*.ti,ab.
-
“vaccin*”.ti,ab.
-
((measles* or mumps* or rubella or MMR or diphtheria* or polio* or pertussis* or tetanus* or whooping cough or varicella* or influenza*) adj5 (immuni* or vaccin* or injection*)).ti,ab.
-
or/8-11
-
Child, Preschool/
-
School Admission Criteria/
-
Child Day Care Centers/st [Standards]
-
or/13-15
-
(kindergarten or preschool or preschool or day-care or day care or nursery or pre-matriculation or prematriculation).af.
-
((immuni* or vaccin*) adj3 (requirement* or law?)).af.
-
(school adj3 (immuni* or vaccin*)).af.
-
or/16-19
-
12 and 20
-
(Conditional adj2 (cash or payment$)).af.
-
(contingency adj2 management).af.
-
(financial adj2 incentive$).af.
-
(gift adj2 certificate$).af.
-
(tax adj2 credit$).af.
-
(award$ or benefit$ or competition$ or contest$ or coupon$ or discount or discounts or disincentiv$ or forfeit$ or incentiv$ or lotter$ or monetary or nonmonetary or payment).af.
-
(penalt$ or prize$ or reinforcement or relinquish$ or reward$ or taxation or taxes or token$ or voucher$).af.
-
(pay$ adj2 deduction$).af.
-
P4P4P.af.
-
(Pay-For-Performance adj3 Patients).af.
-
(penalisation or penalization or penalise or penalize).af.
-
or/22-32
-
exp reward/ or Gift Giving/ or *Punishment/ or *Motivation/ or *achievement/ or *goals/ or *intention/
-
or/33-34
-
21 and 35
-
limit 36 to humans
-
or/12,14-15
-
or/13,17-19
-
38 and 39 and 35
-
or/13,17
-
or/12,14-15,18-19
-
41 and 42 and 35
-
40 or 43
-
limit 44 to humans
-
(immuni* or vaccin*).mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept, rare disease supplementary concept, unique identifier]
-
14 and 46
-
School Health Services/
-
46 and 48
-
15 and 46
-
47 or 49 or 50
-
51 and 35
-
(parent* or carer* or guardian*).mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept, rare disease supplementary concept, unique identifier]
-
51 and 53
-
52 and 53
-
54 not 55
-
or/1-6,9-11
-
or/13,17
-
or/22-32,34
-
and/57-59
-
60 and 53
-
60 not 61
-
(Moral or ethicality or ethical or coercion or motivation$ or fairness or acceptability or inducement or controvers$ or ethics or coercive or reinforcement or unethical).af.
-
morals/ or ethics/ or exp social responsibility/ or exp principle-based ethics/ or Coercion/
-
or/63-64
-
and/57-59,65
-
60 not 66
-
66 not 60
-
60 or 66
-
and/57,59,65
-
or/60,70
-
70 not 60
-
and/57-58,65
-
and/53,57-58,65
-
73 or 74
-
73 not 72
-
or/1-5,9-11
-
or/13,17
-
77 and 78 and 35
-
77 and 78 and 65
-
77 and 78 and 53
-
79 or 81
-
or/79-81
-
79 or 80
-
77 and 78 and (35 or 53) and 80
-
77 and 78 and ((35 and 53) or 80)
-
77 and 78 and (35 or 80)
-
77 and 78 and (53 or 80)
-
77 and 78 and (35 or 65)
-
remove duplicates from 89
Appendix 2 Interview schedule for focus groups with parents and carers
Introductions (5 minutes)
-
Introduce researcher(s).
-
Give overview of what is about to happen.
-
– Group discussion.
-
– Set ground rules.
-
Only one person to speak at a time.
-
Respect each other’s opinion, even if you don’t agree with it.
-
Value each other’s right to privacy - only share what you feel comfortable sharing.
-
Keep the discussions confidential.
-
-
-
Check everyone has read and understood the information.
-
Collect consent forms – turn on tape.
-
Get everyone to introduce themselves to the group.
-
No right or wrong answers.
State that while we are talking about different ways to encourage more parents to immunise their children, the vast majority of parents already do that. 89–98% depending on which vaccination you look at.
Knowledge (10–15 minutes)
-
Can you name some childhood diseases? (FLIP CHART).
-
Flash cards – ask participants to group by:
-
– Vaccination available.
-
– Vaccination not available.
-
-
Discuss results. Are there any illnesses that are a surprise? i.e. for which you thought there is a vaccine but there isn’t or vice versa?
-
Which of the childhood diseases we have discussed are serious/ dangerous/life-threatening to children? Relate back to cards and flip chart.
Financial incentives/mandates (5–10 minutes)
Introduce the concept of incentives and mandates (use prop) to sensitise the parents to what is to come.
-
Do you think that parents should be offered incentives to immunise their child?
-
– What are incentives?
-
– Financial/non-financial gains?
-
– Facilitating access to vaccinations?
-
-
What kind of incentives do you think might make parents want to immunise their child?
-
Do you think that vaccination should be made mandatory, so everyone HAS to immunise their child?
-
– How would this work?
-
Scenarios (up to 25 minutes)
Moving on to set of scenarios to introduce different possible incentive schemes aimed at increasing vaccination rates. Introduce each scenario in turn and ask:
-
What do you think about this scheme?
-
Are there any advantages to offering this type of scheme?
-
– to parents
-
– for the children being immunised
-
– to other children
-
– to family
-
– to the health service
-
– to communities
-
-
Are there any disadvantages to this type of scheme?
-
– As above but also: would people begin to delay vaccination just to get the money as a bonus?
-
-
Do you think this type of scheme would encourage more people to immunise their child?
Finisher (3–5 minutes)
-
Thinking about financial incentives and mandates do you think either method would help to increase vaccination rates?
-
– Any?
-
– None?
-
– Why?
-
– Which would be (un)acceptable? Why?
-
-
What else could be done to increase vaccination rates, for the few who do not immunise their children?
Other possible questions
-
Do you think there are any benefits of having a child immunised? If so, what are they?
-
– Good for the child? Absence of disease? Saves time off school? Stops adults getting the disease? Stops other children in family getting the disease?
-
– Good for society?
-
-
Are there any disadvantages of having a child immunised?
-
– Pain? Vaccine overload? Possibility of catching a disease from vaccine? Other contents of the vaccine?
-
-
Where would you try and get information that you trust about vaccinations?
-
– Media, internet (which sites in particular?), health professionals (GPs/nurses)? Which are most approachable/are you likely to turn to? Why? Family, friend, nursery staff? Sure Start staff?
-
-
Which of those sources do you think is the most helpful? Reliable?
-
– Reliable, trustworthy, accessible . . .
-
-
What do you think influences decisions to immunise/ not immunise child?
-
– Family, friends, media, professionals, government, access, religion . . .
-
-
Why do you think most parents decide to immunise their child?
-
Why do you think some parents decide not to immunise their child?
Thank for time and close group.
Appendix 3 Vignettes for focus groups with parents and carers
Scenario 1: gift of money (universal)
Anna is a mum of two. Her youngest child, Alfie, is only a couple of months old.
A new scheme has just started in Anna’s area that means she will receive a cash payment for each completed course of vaccinations that Alfie receives. All parents with children in Anna’s area are eligible for this new scheme.
For example, once Alfie has had both of his measles, mumps and rubella vaccinations, Anna will be paid £50.
Anna will be paid for only vaccinations that are on the NHS list of recommended routine vaccinations.
Scenario 2: gift of money (targeted)
Emma has a son, Joshua, who is 1 year old. Joshua has had some of his vaccinations, but not all of them are up to date.
A new scheme has been introduced to make sure that children have received all their vaccinations on time. That means that all children that either have not had any vaccinations or have not had them all are being chased up.
Emma received a letter saying that if she brings Joshua into her GP practice and gets all of his vaccinations up to date she will be paid a cash bonus.
Parents that have already had their child immunised are not eligible for the cash bonus.
Scenario 3: receipt of universal benefits (child benefit)
Jonathan and his partner get the standard £20.30 child benefit each week for their daughter Amelia. But there has been a change to the way it is paid.
Now, Jonathan and his partner will get their child benefit only if they keep up to date with Amelia’s vaccinations. This means that they are asked to prove that Amelia has had her vaccinations, or provide an exemption letter from a GP, or their child benefit will be stopped until Amelia has had them.
Scenario 4: removal of child care contributions
Gemma puts Charlie into child care while she goes to work.
Gemma gets help toward paying for child care from the government. However, she has to send proof to the government that Charlie has had all of his vaccinations or an exemption letter from a GP – otherwise her help with payment will stop.
Scenario 5: mandatory for entry into registered day-care
Edward is 3 years old and goes to day care 3 days a week. So that Edward can go to day care his parents had to prove that he had had all of his vaccinations, or show a letter of exemption, before he could attend.
Edward’s parents have to do this every year to show that he is up to date with his vaccinations. If they don’t, Edward is not allowed into day care.
Scenario 6: mandatory for school entry
Blake starts primary school this year. However, to be able to enrol in school his parents have to prove Blake has had all of his vaccinations, or have a letter from the GP to say that he is exempt.
If Blake is not up to date with his vaccinations or exempt from having them he cannot start primary school.
Appendix 4 Materials used in Parental Advisory Group workshop for discrete choice experiment
Appendix 5 Final questionnaire used in discrete choice experiment
Note: the DCE was administered on-line. The content is reproduced here, but the on-screen format cannot be captured.
Thank you for your interest in this study. We are inviting you to take part in a research project that is exploring how to increase the number of children who receive a full programme of recommended vaccinations before they start school. This research has been funded by the National Institute for Health Research (NIHR) Health Technology Assessment (HTA) programme. The project is being carried out by a team of researchers from Newcastle University and Teesside University.
What is the research about?
Childhood vaccinations are very effective in protecting children from diseases such as measles, polio and mumps. The recent measles outbreaks have shown how these childhood diseases can return if children do not have all their vaccinations, but many parents have legitimate reasons for not having their children immunised. We are looking into the different factors that may influence parents’ decisions about immunising their children.
Further details of the vaccination schedule currently recommended by the NHS can be found at the following website: http://www.nhs.uk/Conditions/vaccinations/Pages/vaccination-schedule-age-checklist.aspx
We would like to explore parents’ thoughts on the different aspects of vaccination services for children in the UK. Many factors have been found to influence parents’ decisions about childhood vaccinations such as: the individual who administers the vaccinations (e.g., nurse or health visitor); where the vaccinations are given (e.g., clinic or local GP surgery); and the number of visits required to complete the full vaccination programme. We are also interested in your views on whether the introduction of rewards (such as financial rewards for immunising their children) would be acceptable to parents.
What will it involve and what happens to the information that is collected?
If you decide to take part in this study, we will ask you to complete a survey. We anticipate that it will take approximately 30–45 minutes to complete the survey. The survey will ask questions about you (e.g., where you live, your age, household income etc.) and about your children such as how many children you have and their ages. You will then be presented with a series of scenarios that describe different vaccination services, and we will ask you to choose which one that you would prefer. The scenarios will differ in terms of specific characteristics of vaccination services, which allows us to explore peoples’ preferences on different aspects of healthcare services.
We will also ask you questions about the use of financial rewards such as cash money or shopping vouchers to encourage parents to immunise their children. Finally, we will ask you about your intentions and attitudes towards immunising your own children.
All of the information that you provide in the survey will be strictly confidential and your data will be stored safely on a secure computer network owned by Research Now (the company managing the survey). Your individual responses to the survey questions will be anonymous as they will be grouped together with the responses provided by all the parents who complete the survey. You can withdraw from the study at any time while you are completing it by closing the browser window.
By ticking the box below ‘I agree to participate in this study’ and continue to the survey, you are indicating your agreement with the following:
-
I have read the information about this study.
-
I understand that my participation in this study is voluntary.
-
I understand that I am free to withdraw my participation at any time during completion of the survey by closing the browser window.
-
I understand that responses I provide to the survey questions will be anonymous, and that no personally identifiable information about me will appear in any report or article based on the findings of this study.
Please choose one of the following options:
-
I agree to participate in this study
-
I do not agree to participate in this study
Part 1: about your eligibility to participate in the survey
Are you a parent or guardian of a child aged less than 5 years old? Please select one answer
-
Yes
-
No
Do you live in England?
-
Yes
-
No
[If response is NO to 1 or 2 then NOT eligible to participate.] Thank you for considering taking part in this survey. Based on the responses you provided you are not eligible to participate.
[If response is YES to 1 or 2 then eligible to participate.] We have invited you to take part in a survey about vaccination services because you are a resident of England and a parent/guardian of a child under 5 years of age.
What is your postcode?
Part 2: about you
The following questions ask about the characteristics of the parents responding to the survey (so we can be sure that we have collected information from a representative cross section of parents living in England).
What is your relationship status? Please select one answer
-
Married/cohabiting/civil partnership
-
Single
-
Separated (but still legally married or in a civil partnership)
-
Divorced (including formerly in a civil partnership which is now legally dissolved)
-
Widowed (including surviving partner from a civil partnership)
-
Other (please specify):
-
Prefer not to say
Please state your age in years
Are you male or female? Please select one answer
-
Male
-
Female
Could you please provide an estimate of your annual household income from all sources, before tax / and including your partner or spouse if you have one)? Please select one answer
-
Less than £15,000
-
More than or equal to £15,000 and less than £26,000
-
More than or equal to £26,000 and less than £35,000
-
More than or equal to £35,000 and less than £50,000
-
More than or equal to £50,000 and less than £70,000
-
More than or equal to £70,000
-
Prefer not to say
What is the highest level of education you and your partner (if applicable) have completed? Please select one answer for you, and one answer for your partner (if applicable)
-
GCSE/O-level/CSE/NVQ
-
A-level or equivalent
-
Degree/Masters/PhD
-
No formal qualifications
-
Other (please specify)
-
Prefer not to say
Are you or your partner currently: Please select all that apply for you, and all that apply for your partner (if applicable)
-
In full-time paid employment
-
In part-time paid employment
-
In full-time self-employment
-
In part time self-employment
-
Unemployed and seeking work
-
In full-time education
-
In part-time education
-
On maternity leave
-
On a government scheme for employment training
-
Temporarily sick/disabled (If temporarily on sick leave from job – code as employed)
-
Permanently sick/disabled
-
Looking after home/family
-
Full-time carer
-
Part-time carer
-
Retired from work
-
Other (please specify)
-
Prefer not to say
What is your ethnicity? Please select one answer
-
English/ Welsh/ Scottish/ Northern Irish/ British
-
Irish
-
Gypsy, Traveller or Irish Traveller
-
Any other White background
-
White and Black Caribbean
-
White and Black African
-
White and Asian
-
Any other Mixed/ Multiple ethnic background
-
Indian
-
Pakistani
-
Bangladeshi
-
Chinese
-
Any other Asian background
-
African
-
Caribbean
-
Any other Black/ African/ Caribbean background
-
Arab
-
Any other ethnic group
-
Prefer not to say
Overall, how would you rate your health during the past 12 months? Please select one answer
-
Excellent
-
Good
-
Fair
-
Poor
-
Very Poor
-
Prefer not to say
Part 3: about your children
How many children (of any age) do you have, including step and adopted children?
Please state the gender and age of each child living in your household
Do you consider any of your children to have a disability? Please select one answer for each child
-
No
-
Yes (please specify)
-
Prefer not to say
Part 4: introduction to scenario section
In the questions that appear in the next section you will be presented with two imaginary "scenarios". Each scenario describes vaccination services for preschool children. We would like you to think about each scenario as if you were making a decision between them in the real world. Then we will ask you to tell us which scenario A or B that you most prefer. You can state that you do not prefer either scenario by choosing ‘Neither’ (I would not have my child immunised). If you choose Neither as your preferred option then we would still like you to indicate whether scenario A and B would be the most preferable to you (i.e., the least bad) if vaccination was mandatory.
Each scenario is made up of 8 different characteristics of an vaccination service:
-
Type of healthcare professional administering vaccinations and location of appointments
-
The way you receive information about vaccinations prior to the appointment (e.g., post or email)
-
How information about the risks and benefits of vaccinations is provided prior to the appointment
-
Availability of appointments
-
Type of parental reward (none, cash or voucher)
-
Parental reward value received when the full schedule of vaccinations is completed
-
Which parents would receive a reward (given to all parents, only parents who are considered unlikely to immunise their children or current practice [no reward])
-
Waiting time at each appointment or scheduled appointment time
When reading the scenarios, the number of appointments to complete the full vaccination programme will always be 8. An example of a scenario is shown below.
| Characteristic | Scenario A | Scenario B |
|---|---|---|
| Type of healthcare professional administering vaccinations and location | Practice nurse at a local GP surgery | Community nurse at local clinic or children’s centre |
| The way you receive information about vaccinations prior to the appointment, plus verbal information at time of appointment | Provided in written form sent by post | Provided in electronic form in an email |
| How information about the risks and benefits of vaccinations is provided prior to the appointment. | Provided in the form of numbers | Provided in the form of charts or pictures |
| Availability of appointments | Working hours (9am to 5pm) | Working hours (9am to 5pm) + out of hours weekday evenings and Saturday 9am–5pm |
| Type of parental reward for completing the full schedule of vaccinations | Cash reward | Parents do not receive any reward |
| Reward value payable to parents received when the full schedule of vaccinations is completed | £70 | No reward |
| Which parents would receive a reward | Only those considered unlikely to have their child immunised | Current practice - no reward |
| Waiting time at each appointment or scheduled appointment time | Up to 30 minutes | Up to 60 minutes |
Which scenario do you prefer?
-
Scenario A
-
Scenario B
-
Neither (do not like either option – I would not have my child immunised) [If this option is chosen – then display the following question: We would still like you to indicate whether scenario A and B is most preferable to you (i.e., the least bad) if vaccination was mandatory - which would you choose?]
Part 5: scenarios
Eighteen choice sets presented as in part 4.
How difficult did you find answering the questions in the previous section? Please select one answer
-
Very difficult
-
Quite difficult
-
Nether difficult or easy
-
Fairly easy
-
Very easy
To what extent did you understand the questions in the previous section? Please select one answer
-
Fully understood the questions
-
Partially understood the questions
-
Did not understand the questions at all
Part 6: preschool vaccination and financial rewards
We are interested in the minimum level of a financial reward that people are willing to accept in exchange for having their child immunised (if this policy were to go ahead). This information will help us to determine the value at which a financial reward might increase the rate of preschool vaccinations.
Would you require a financial reward (cash or voucher) to vaccinate your child? Please select one answer
-
Yes
-
No
If yes to “Would you require a financial reward (cash or voucher) to vaccinate your child?”, please explain briefly why
Please write the minimum amount you would be willing to accept for immunising your child.
Would you prefer a cash payment or shopping voucher? Please select one answer
-
Cash
-
Shopping voucher (accepted in most high street shops and supermarkets)
Please state the reason(s) that influenced the amount you stated. Please select all that apply
-
Time required to complete the full course of vaccinations
-
Compensation for time off work needed to attend appointments
-
Compensation for travel costs to attend appointments
-
Other: please specify:
If no to “Would you require a financial reward (cash or voucher) to vaccinate your child?” please explain briefly why
If you were offered a financial reward on completion of vaccinations would you take it? Please select one answer
-
Yes
-
No
What do you think should be the maximum financial reward offered to parents for immunising their child. If you do not believe that a reward should be given please enter 0.
Please state the reason(s) that influenced the amount you stated. Please select all that apply
-
Time required to complete the full course of vaccinations
-
Compensation for time off work needed to attend appointments
-
Compensation for travel costs to attend appointments
-
Other: please specify:
All respondents: What is your preference on how vaccination services should be organised? Please select one answer
-
Reward: universal – reward is given to all parents
-
Reward: targeted – reward is only given to parents considered unlikely to have their child immunised
-
Mandatory - full course of vaccination required for entry into nursery/school (unless there is a medical reason or a strongly held ethical belief for the child not being immunised)
-
Current situation - relying on parents’ decisions only (no reward or mandate)
If you would like to explain the reasons related to your preference on how vaccination services should be organised, please do so below
For your youngest child, have you received any information about vaccinations in the last 3 months? Please select one answer
-
Yes
-
No
If yes to “For your youngest child, have you received any information about vaccinations in the last 3 months?” answer following four questions, if no skip to “What best describes your intentions for immunising your youngest child?”
How did you receive information about vaccinations for your youngest child in the last 3 months? Please select one answer
-
Verbally
-
Post
-
Other, please specify
To what extent would you agree the information (you received for your youngest child in the last 3 months) addressed all your information needs about vaccination? Please select one answer
-
1 strongly disagree
-
2
-
3
-
4
-
strongly agree
Did you seek additional information about vaccinations for your youngest child in the last 3 months? Please select one answer
-
Yes
-
No
If no to “Did you seek additional information about vaccinations for your youngest child in the last 3 months?” skip to “What best describes your intentions for immunising your youngest child?”
Where did you seek additional information about vaccinations for your youngest child in the last 3 months? Please select all that apply
-
Internet
-
Friends/family
-
General practitioner/family doctor
-
Other, please specify
What best describes your intentions for immunising your youngest child? Please select one answer
-
My child to receive all of the recommended vaccinations
-
My child to receive some but not all of the recommended vaccinations
-
My child to receive none of the recommended vaccinations
-
Not applicable - my child has already received all of the recommended vaccinations
Part 7: attitudinal statements to explain and/or predict parents’ self-reported child vaccination behaviours
The following questions are a measure of your personal beliefs so there are no right or wrong answers – please try to give as honest answers as you can, as this will help the research. Each question has a scale with numbers (1–5) which represents the extent to which you agree with what is stated in the question. For example, the more you agree with what is stated in the question, you would select a higher number. The more you disagree with what is stated in the question, you would select a lower number. Please select one answer per question.
Having my children immunised is the right thing to do
-
1 strongly disagree
-
2
-
3
-
4
-
5 strongly agree
How important do you think vaccinations are for keeping children healthy?
-
1 not at all important
-
2
-
3
-
4
-
5 very important
It is important to immunise my children in order to prevent the spread of disease in my community.
-
1 strongly disagree
-
2
-
3
-
4
-
5 strongly agree
I believe that vaccinations recommended by the NHS are safe for my children.
-
1 strongly disagree
-
2
-
3
-
4
-
5 strongly agree
In general, how safe do you think vaccinations are for children?
-
1 not safe at all
-
2
-
3
-
4
-
5 very safe
How confident are you in the safety of routine childhood vaccinations?
-
1 not at all confident
-
2
-
3
-
4
-
5 very confident
I believe that if some children do not receive vaccinations, then this may cause other children to be ill with the disease
-
1 strongly disagree
-
2
-
3
-
4
-
5 strongly agree
If children in England are not immunised, how likely do you think they are to get diseases that vaccination can prevent?
-
1 not at all likely
-
2
-
3
-
4
-
5 very likely
My children could get a serious disease if they are not immunised
-
1 strongly disagree
-
2
-
3
-
4
-
5 strongly agree
Other children could be ill with a serious disease if I choose not to immunise my child
-
1 strongly disagree
-
2
-
3
-
4
-
5 strongly agree
My child could be ill with a serious disease if other children are not immunised
-
1 strongly disagree
-
2
-
3
-
4
-
5 strongly agree
Older family members could be ill with a serious disease if other children are not immunised
-
1 strongly disagree
-
2
-
3
-
4
-
5 strongly agree
Please rank order the importance of the following characteristics for the organisation of vaccination services (8 = lowest importance and 1 highest importance); for example if you consider availability of appointments to be most important then you would assign this a rank of 1.
-
Type of healthcare professional administering vaccinations and location
-
The way you receive information about vaccinations prior to the appointment (plus verbal information at time of appointment)
-
How information on the benefits (reducing the risk of your child getting diseases due to having the vaccinations) and risks is provided prior to the appointment
-
Availability of appointments
-
Type of parental reward for completing the full schedule of vaccinations
-
Reward value payable to parents (received when the full schedule of vaccinations is completed)
-
Which parents would receive a reward
-
Waiting time at each appointment or scheduled appointment time
Is there anything else you would like to tell us about how vaccination services should be organised for children aged under 5 years?
-
Yes – please describe
-
No
The survey is now complete and your responses have been submitted!
Thank you for taking the time to complete this survey.
Appendix 6 Discrete choice experiment analysis
The DCE approach follows random utility maximisation theory, whereby an individual n is assumed to choose the utility-maximising option i when presented with a choice set Cn containing alternative scenarios following:
where v is systematic component (information generated by means of the questionnaire, that is, utility derived from any alternative, observable), α is ASCs, β is vector of coefficients, X is vector of attributes k and εin is random component (unobservable). A respondent is assumed to choose the scenario j among all alternatives J if the utility derived from that alternative is greater than the utility from any other alternative j in the choice set Cn: Uj > UJ – 1, or the opt-out option.
The probabilistic model will estimate the probability of a chosen alternative j as a function of the attributes k, and establish the trade-off between attributes via the estimation of marginal rates of substitution. The utility derived from the chosen option is described by:
where the ASC captures the mean effect of unobserved factors in the error terms for each of the alternatives.
The logit specification of the probability for an individual choosing alternative j over any other alternative J – 1 in choice set Cn is expressed as:
Different regression models were employed to analyse the effect of attribute levels on individual preferences for the organisation of vaccination services and financial incentives. The opt-out option ‘I would not vaccinate my child’ (i.e. option C) was included as an ASC to account for any latent or unobserved factors when choosing the alternative of no vaccination. Effects coding was used for all options, with the exception of time and value, which were assumed to be linear. It allowed for the effects of each attribute to be uncorrelated with the constant and to calculate the effect of a reference category as the negative sum of the estimated coefficients for remaining attribute levels. 117 Reference levels for the DCE attributes used in the regression models were practice nurse delivering vaccinations at GP surgery, written information on benefits and risks, information on reductions in risk provided in the form of numbers, availability of appointments during working hours only and no reward. Where rewards were offered, universal rewards were used as the base level.
As each respondent was forced to choose from three alternatives, the initial analysis employed a conditional logit model,116 which is based on three assumptions: (i) IIAs (i.e. the ratio of probabilities for any two alternatives is assumed to be independent of the attribute levels in a third alternative); (ii) error terms are independent and identically distributed across observations; and (iii) no preference heterogeneity (i.e. homogeneous preferences across respondents).
Assuming a violation of the IIA assumption, which could result in biased predictions, the utility equation (2) was estimated using a mixed logit model. It allowed the investigating of unobserved preference heterogeneity, that is, varying model estimates across individuals. The mixed logit model is a more general approach to a subgroup analysis as no assumptions are required regarding how individual characteristics may influence individual preferences. Different model specifications allowed for selected model parameters to vary. ASCs and the time variable were considered random, normally distributed parameters, while all other model parameters remained fixed. Model goodness of fit was assessed using the likelihood ratio test statistic.
Willingness to accept
The marginal WTA is defined as the minimum monetary value that is required as compensation for a change in the level of a certain attribute,102 that is, when individuals face a reduction in utility derived from moving from one scenario to a less preferred one.
Given that a price proxy was included (total maximum amount of the incentive), WTA could be calculated for a marginal change in all statistically significant attributes by dividing the regression coefficient of each attribute k by the regression coefficient of the amount attribute, thereby estimating trade-offs between attribute levels:
In order to assess the impact of different risk groups on average WTA, subgroup analyses were run for both the ‘at high risk’ and ‘not at high risk’ subgroups.
In addition, WTP and WTA were estimated directly using the contingent valuation, open-ended method, estimating minimum WTA and maximum WTP for a vaccination incentive scheme.
Appendix 7 Predicted uptake rates of preschool vaccinations
| Choice situation | Block | Option | Choice set specifications | Utility | Probability for uptake | % of respondents (chosen option) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| WHO_WHERE | INFO | RISK | AVAILABILITY | REWARD | VALUE | TARGETED | TIME | ||||||
| 1 | 3 | A | Pharmacist | Written (post) | Numerical and graphical | Out of working hours | Cash | 210 | Universal | 60 | 2.76 | 61.35 | 55.10 |
| 1 | 3 | B | Community nurse, local | Electronic (internet) | Numerical and graphical | Working hours | Voucher | 140 | Targeted | 60 | 2.19 | 34.77 | 33.67 |
| 1 | 3 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 3.89 | 11.22 |
| 2 | 4 | A | Pharmacist | Electronic (internet) | Numerical | Out of working hours | Voucher | 280 | Universal | 60 | 2.78 | 64.69 | 56.25 |
| 2 | 4 | B | Practice nurse at local GP surgery | Written (post) | Numerical | Working hours | Cash | 280 | Targeted | 120 | 2.06 | 31.30 | 36.16 |
| 2 | 4 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 4.00 | 7.59 |
| 3 | 3 | A | Health visitor, local | Graphical | Working hours | Cash | 70 | Universal | 120 | 2.07 | 41.35 | 45.92 | |
| 3 | 3 | B | Health visitor, home | Graphical | Out of working hours | Voucher | 210 | Targeted | 60 | 2.32 | 53.42 | 45.92 | |
| 3 | 3 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 5.23 | 8.16 |
| 4 | 4 | A | Health visitor, local | Numerical and graphical | Working hours | Cash | 280 | Universal | 30 | 3.42 | 67.15 | 62.50 | |
| 4 | 4 | B | Health visitor, home | Numerical | Working hours | No reward | 0 | No reward | 30 | 2.63 | 30.64 | 34.38 | |
| 4 | 4 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 2.20 | 3.13 |
| 5 | 2 | A | Community nurse, vaccination bus | Numerical and graphical | Working hours | No reward | 0 | No reward | 30 | 2.47 | 56.32 | 48.51 | |
| 5 | 2 | B | Community nurse, local | Numerical | Working hours | Voucher | 70 | Universal | 120 | 2.10 | 38.90 | 46.53 | |
| 5 | 2 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 4.78 | 4.95 |
| 6 | 3 | A | Health visitor, home | Written (post) | Numerical | Working hours | Cash | 140 | Targeted | 30 | 2.69 | 61.99 | 39.80 |
| 6 | 3 | B | Health visitor, local | Written (post) | Numerical and graphical | Out of working hours | Voucher | 70 | Universal | 120 | 2.08 | 33.78 | 53.06 |
| 6 | 3 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 4.23 | 7.14 |
| 7 | 4 | A | Community nurse, local | Written (post) | Numerical | Out of working hours | Cash | 70 | Targeted | 120 | 1.66 | 24.14 | 37.95 |
| 7 | 4 | B | Community nurse, vaccination bus | Electronic (internet) | Graphical | Working hours | Voucher | 70 | Universal | 30 | 2.74 | 71.27 | 58.93 |
| 7 | 4 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 4.59 | 3.13 |
| 8 | 2 | A | Health visitor, home | Numerical | Working hours | Voucher | 140 | Targeted | 30 | 2.64 | 70.43 | 60.40 | |
| 8 | 2 | B | Health visitor, local | Graphical | Out of working hours | No reward | 0 | No reward | 120 | 1.59 | 24.56 | 34.65 | |
| 8 | 2 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 5.00 | 4.95 |
| 9 | 3 | A | Practice nurse at local GP surgery | Numerical | Working hours | No reward | 0 | No reward | 120 | 1.81 | 25.73 | 26.53 | |
| 9 | 3 | B | Pharmacist | Written (post) | Numerical and graphical | Out of working hours | Voucher | 70 | Universal | 30 | 2.82 | 70.08 | 67.35 |
| 9 | 3 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 4.20 | 6.12 |
| 10 | 3 | A | Community nurse, vaccination bus | Written (post) | Numerical and graphical | Working hours | Voucher | 70 | Targeted | 120 | 1.36 | 13.60 | 18.37 |
| 10 | 3 | B | Community nurse, local | Electronic (internet) | Numerical and graphical | Out of working hours | Cash | 140 | Universal | 30 | 3.17 | 82.92 | 75.51 |
| 10 | 3 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 3.48 | 6.12 |
| 11 | 1 | A | Health visitor, home | Written (post) | Graphical | Out of working hours | Voucher | 140 | Universal | 30 | 3.04 | 78.70 | 74.49 |
| 11 | 1 | B | Community nurse, local | Electronic (internet) | Graphical | Working hours | Cash | 140 | Targeted | 120 | 1.53 | 17.52 | 20.41 |
| 11 | 1 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 3.78 | 5.10 |
| 12 | 4 | A | Health visitor, home | Numerical | Out of working hours | Cash | 140 | Targeted | 120 | 1.80 | 25.86 | 34.38 | |
| 12 | 4 | B | Health visitor, home | Graphical | Working hours | Cash | 140 | Universal | 60 | 2.79 | 69.85 | 61.61 | |
| 12 | 4 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 4.29 | 4.02 |
| 13 | 1 | A | Community nurse, vaccination bus | Electronic (internet) | Graphical | Out of working hours | Voucher | 140 | Universal | 60 | 2.56 | 53.43 | 52.04 |
| 13 | 1 | B | Community nurse, local | Written (post) | Numerical | Working hours | Cash | 210 | Universal | 120 | 2.33 | 42.43 | 44.90 |
| 13 | 1 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 4.14 | 3.06 |
| 14 | 1 | A | Community nurse, vaccination bus | Written (post) | Numerical | Out of working hours | Cash | 210 | Targeted | 30 | 2.71 | 60.43 | 54.08 |
| 14 | 1 | B | Health visitor, local | Electronic (internet) | Numerical and graphical | Working hours | Voucher | 210 | Universal | 120 | 2.18 | 35.55 | 39.80 |
| 14 | 1 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 4.01 | 6.12 |
| 15 | 4 | A | Community nurse, vaccination bus | Electronic (internet) | Numerical and graphical | Out of working hours | Voucher | 70 | Targeted | 120 | 1.37 | 17.88 | 20.98 |
| 15 | 4 | B | Practice nurse at local GP surgery | Numerical | Out of working hours | No reward | 0 | No reward | 30 | 2.84 | 77.60 | 75.45 | |
| 15 | 4 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 4.53 | 3.57 |
| 16 | 2 | A | Health visitor, local | Graphical | Working hours | Voucher | 280 | Targeted | 120 | 1.74 | 17.50 | 25.74 | |
| 16 | 2 | B | Health visitor, home | Graphical | Out of working hours | Cash | 210 | Universal | 30 | 3.26 | 79.44 | 67.33 | |
| 16 | 2 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 3.06 | 6.93 |
| 17 | 4 | A | Community nurse, local | Numerical and graphical | Out of working hours | Cash | 280 | Targeted | 120 | 1.94 | 38.84 | 47.77 | |
| 17 | 4 | B | Pharmacist | Written (post) | Numerical | Working hours | Voucher | 70 | Targeted | 30 | 2.29 | 55.55 | 45.54 |
| 17 | 4 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 5.60 | 6.70 |
| 18 | 2 | A | Practice nurse at local GP surgery | Written (post) | Numerical | Working hours | Cash | 210 | Targeted | 60 | 2.61 | 59.41 | 55.45 |
| 18 | 2 | B | Community nurse, vaccination bus | Numerical and graphical | Working hours | Voucher | 210 | Universal | 120 | 2.12 | 36.24 | 35.64 | |
| 18 | 2 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 4.35 | 8.91 |
| 19 | 2 | A | Community nurse, vaccination bus | Electronic (internet) | Graphical | Out of working hours | Cash | 210 | Universal | 60 | 2.73 | 38.99 | 40.59 |
| 19 | 2 | B | Practice nurse at local GP surgery | Written (post) | Graphical | Working hours | Cash | 70 | Universal | 30 | 3.14 | 58.48 | 50.50 |
| 19 | 2 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 2.53 | 8.91 |
| 20 | 4 | A | Health visitor, local | Written (post) | Graphical | Working hours | Voucher | 210 | Targeted | 60 | 2.26 | 50.62 | 54.46 |
| 20 | 4 | B | Health visitor, local | Electronic (internet) | Numerical and graphical | Working hours | Voucher | 70 | Targeted | 60 | 2.12 | 44.10 | 40.63 |
| 20 | 4 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 5.28 | 4.91 |
| 21 | 3 | A | Community nurse, local | Written (post) | Numerical and graphical | Out of working hours | Voucher | 70 | Universal | 60 | 2.70 | 46.72 | 44.90 |
| 21 | 3 | B | Community nurse, vaccination bus | Electronic (internet) | Numerical and graphical | Working hours | Cash | 210 | Universal | 60 | 2.78 | 50.15 | 46.94 |
| 21 | 3 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 3.13 | 8.16 |
| 22 | 4 | A | Pharmacist | Numerical | Working hours | Cash | 140 | Universal | 30 | 3.04 | 64.96 | 62.95 | |
| 22 | 4 | B | Community nurse, local | Graphical | Out of working hours | Voucher | 210 | Targeted | 60 | 2.33 | 31.93 | 33.93 | |
| 22 | 4 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 3.12 | 3.13 |
| 23 | 1 | A | Practice nurse at local GP surgery | Numerical and graphical | Working hours | Cash | 70 | Universal | 60 | 2.94 | 56.27 | 65.31 | |
| 23 | 1 | B | Pharmacist | Numerical | Working hours | Voucher | 280 | Targeted | 30 | 2.62 | 40.76 | 28.57 | |
| 23 | 1 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 2.97 | 6.12 |
| 24 | 2 | A | Health visitor, local | Electronic (internet) | Numerical | Working hours | Voucher | 210 | Targeted | 30 | 2.69 | 59.48 | 57.43 |
| 24 | 2 | B | Community nurse, vaccination bus | Written (post) | Numerical | Out of working hours | No reward | 0 | No reward | 60 | 2.20 | 36.46 | 33.66 |
| 24 | 2 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 4.05 | 8.91 |
| 25 | 3 | A | Community nurse, local | Electronic (internet) | Numerical | Out of working hours | Voucher | 70 | Targeted | 120 | 1.54 | 29.27 | 28.57 |
| 25 | 3 | B | Health visitor, home | Written (post) | Graphical | Out of working hours | Cash | 280 | Universal | 120 | 2.33 | 64.46 | 64.29 |
| 25 | 3 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 6.28 | 7.14 |
| 26 | 1 | A | Pharmacist | Electronic (internet) | Numerical | Out of working hours | Cash | 210 | Targeted | 120 | 1.59 | 16.16 | 24.49 |
| 26 | 1 | B | Practice nurse at local GP surgery | Electronic (internet) | Numerical and graphical | Working hours | Voucher | 140 | Universal | 30 | 3.20 | 80.56 | 71.43 |
| 26 | 1 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 3.28 | 4.08 |
| 27 | 2 | A | Practice nurse at local GP surgery | Graphical | Working hours | Cash | 280 | Universal | 30 | 3.46 | 84.76 | 70.30 | |
| 27 | 2 | B | Pharmacist | Electronic (internet) | Numerical and graphical | Out of working hours | Voucher | 280 | Targeted | 120 | 1.56 | 12.59 | 21.78 |
| 27 | 2 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 2.65 | 7.92 |
| 28 | 2 | A | Health visitor, local | Written (post) | Graphical | Out of working hours | Cash | 210 | Universal | 30 | 3.24 | 72.02 | 74.26 |
| 28 | 2 | B | Health visitor, home | Electronic (internet) | Numerical and graphical | Working hours | Voucher | 140 | Targeted | 60 | 2.19 | 25.16 | 19.80 |
| 28 | 2 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 2.82 | 5.94 |
| 29 | 4 | A | Community nurse, local | Graphical | Out of working hours | Cash | 140 | Targeted | 30 | 2.64 | 59.98 | 51.34 | |
| 29 | 4 | B | Community nurse, vaccination bus | Numerical | Out of working hours | Voucher | 140 | Universal | 120 | 2.12 | 35.74 | 44.20 | |
| 29 | 4 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 4.28 | 4.46 |
| 30 | 4 | A | Community nurse, local | Written (post) | Graphical | Working hours | Voucher | 280 | Targeted | 30 | 2.66 | 57.21 | 62.50 |
| 30 | 4 | B | Community nurse, vaccination bus | Electronic (internet) | Graphical | Out of working hours | Voucher | 70 | Targeted | 30 | 2.27 | 38.77 | 31.70 |
| 30 | 4 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 4.02 | 5.80 |
| 31 | 2 | A | Community nurse, vaccination bus | Written (post) | Numerical and graphical | Working hours | Cash | 210 | Targeted | 120 | 1.64 | 19.45 | 33.66 |
| 31 | 2 | B | Practice nurse at local GP surgery | Written (post) | Numerical | Out of working hours | Voucher | 140 | Universal | 60 | 3.01 | 76.77 | 58.42 |
| 31 | 2 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 3.79 | 7.92 |
| 32 | 3 | A | Health visitor, home | Electronic (internet) | Numerical and graphical | Out of working hours | Voucher | 140 | Targeted | 60 | 2.24 | 55.58 | 53.06 |
| 32 | 3 | B | Practice nurse at local GP surgery | Graphical | Working hours | Cash | 210 | Targeted | 120 | 1.87 | 38.48 | 35.71 | |
| 32 | 3 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 5.94 | 11.22 |
| 33 | 3 | A | Community nurse, local | Electronic (internet) | Numerical | Out of working hours | Voucher | 280 | Universal | 120 | 2.35 | 42.88 | 48.98 |
| 33 | 3 | B | Pharmacist | Numerical and graphical | Working hours | Cash | 210 | Targeted | 30 | 2.56 | 53.02 | 44.90 | |
| 33 | 3 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 4.10 | 6.12 |
| 34 | 2 | A | Community nurse, local | Electronic (internet) | Graphical | Working hours | Voucher | 210 | Universal | 30 | 3.05 | 69.04 | 68.32 |
| 34 | 2 | B | Health visitor, home | Written (post) | Numerical and graphical | Out of working hours | Cash | 70 | Universal | 120 | 2.13 | 27.68 | 25.74 |
| 34 | 2 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 3.28 | 5.94 |
| 35 | 2 | A | Practice nurse at local GP surgery | Written (post) | Numerical and graphical | Out of working hours | Voucher | 140 | Targeted | 120 | 1.78 | 18.79 | 35.64 |
| 35 | 2 | B | Health visitor, home | Numerical | Out of working hours | Cash | 70 | Universal | 30 | 3.21 | 78.05 | 58.42 | |
| 35 | 2 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 3.16 | 5.94 |
| 36 | 2 | A | Practice nurse at local GP surgery | Electronic (internet) | Graphical | Out of working hours | Voucher | 140 | Targeted | 60 | 2.31 | 37.41 | 35.64 |
| 36 | 2 | B | Pharmacist | Written (post) | Numerical | Working hours | Cash | 210 | Universal | 60 | 2.76 | 58.87 | 59.41 |
| 36 | 2 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 3.72 | 4.95 |
| 37 | 1 | A | Practice nurse at local GP surgery | Written (post) | Numerical and graphical | Working hours | Voucher | 280 | Universal | 30 | 3.43 | 84.30 | 83.67 |
| 37 | 1 | B | Pharmacist | Electronic (internet) | Graphical | Out of working hours | Cash | 280 | Targeted | 120 | 1.55 | 12.95 | 11.22 |
| 37 | 1 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 2.74 | 5.10 |
| 38 | 2 | A | Health visitor, home | Written (post) | Graphical | Working hours | Cash | 280 | Targeted | 120 | 1.76 | 18.88 | 35.64 |
| 38 | 2 | B | Health visitor, home | Graphical | Out of working hours | Voucher | 210 | Universal | 30 | 3.17 | 77.86 | 59.41 | |
| 38 | 2 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 3.26 | 4.95 |
| 39 | 4 | A | Pharmacist | Graphical | Out of working hours | Voucher | 140 | Targeted | 60 | 2.01 | 26.93 | 29.91 | |
| 39 | 4 | B | Practice nurse at local GP surgery | Graphical | Working hours | Voucher | 210 | Universal | 60 | 2.96 | 69.48 | 67.41 | |
| 39 | 4 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 3.60 | 2.68 |
| 40 | 1 | A | Pharmacist | Written (post) | Numerical | Out of working hours | Voucher | 70 | Universal | 120 | 1.88 | 27.21 | 37.76 |
| 40 | 1 | B | Practice nurse at local GP surgery | Electronic (internet) | Numerical | Working hours | Cash | 140 | Targeted | 30 | 2.81 | 68.65 | 57.14 |
| 40 | 1 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 4.14 | 5.10 |
| 41 | 2 | A | Community nurse, vaccination bus | Electronic (internet) | Numerical and graphical | Working hours | Voucher | 210 | Universal | 60 | 2.69 | 52.11 | 59.41 |
| 41 | 2 | B | Practice nurse at local GP surgery | Electronic (internet) | Numerical | Out of working hours | Cash | 140 | Targeted | 60 | 2.53 | 44.35 | 33.66 |
| 41 | 2 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 3.53 | 6.93 |
| 42 | 2 | A | Health visitor, local | Written (post) | Numerical | Working hours | Voucher | 280 | Universal | 120 | 2.36 | 37.82 | 37.62 |
| 42 | 2 | B | Community nurse, vaccination bus | Numerical and graphical | Out of working hours | Cash | 280 | Targeted | 30 | 2.80 | 58.62 | 54.46 | |
| 42 | 2 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 3.56 | 7.92 |
| 43 | 2 | A | Pharmacist | Electronic (internet) | Numerical and graphical | Out of working hours | Voucher | 280 | Targeted | 60 | 2.21 | 28.17 | 25.74 |
| 43 | 2 | B | Practice nurse at local GP surgery | Electronic (internet) | Numerical | Working hours | Cash | 210 | Universal | 60 | 3.10 | 68.73 | 69.31 |
| 43 | 2 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 3.09 | 4.95 |
| 44 | 1 | A | Health visitor, home | Graphical | Out of working hours | Cash | 70 | Targeted | 60 | 2.22 | 42.68 | 51.02 | |
| 44 | 1 | B | Health visitor, home | Electronic (internet) | Numerical | Working hours | Voucher | 280 | Targeted | 60 | 2.43 | 52.67 | 38.78 |
| 44 | 1 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 4.65 | 10.20 |
| 45 | 4 | A | Practice nurse at local GP surgery | Graphical | Out of working hours | Voucher | 210 | Targeted | 120 | 1.83 | 30.64 | 39.29 | |
| 45 | 4 | B | Pharmacist | Graphical | Working hours | Cash | 140 | Universal | 60 | 2.57 | 64.44 | 56.70 | |
| 45 | 4 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 4.91 | 4.02 |
| 46 | 3 | A | Health visitor, home | Written (post) | Numerical | Working hours | Voucher | 210 | Universal | 60 | 2.89 | 73.50 | 65.31 |
| 46 | 3 | B | Community nurse, local | Written (post) | Numerical and graphical | Out of working hours | Cash | 140 | Targeted | 120 | 1.71 | 22.43 | 26.53 |
| 46 | 3 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 4.07 | 8.16 |
| 47 | 1 | A | Practice nurse at local GP surgery | Numerical and graphical | Working hours | Voucher | 280 | Targeted | 30 | 2.94 | 65.20 | 54.08 | |
| 47 | 1 | B | Pharmacist | Electronic (internet) | Numerical | Out of working hours | Cash | 280 | Universal | 120 | 2.21 | 31.37 | 41.84 |
| 47 | 1 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 3.43 | 4.08 |
| 48 | 4 | A | Pharmacist | Graphical | Out of working hours | Voucher | 140 | Universal | 30 | 2.86 | 74.66 | 56.25 | |
| 48 | 4 | B | Practice nurse at local GP surgery | Electronic (internet) | Graphical | Working hours | Cash | 70 | Targeted | 120 | 1.60 | 21.08 | 39.29 |
| 48 | 4 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 4.26 | 4.46 |
| 49 | 1 | A | Practice nurse at local GP surgery | Electronic (internet) | Numerical and graphical | Out of working hours | Cash | 210 | Universal | 60 | 3.10 | 73.81 | 78.57 |
| 49 | 1 | B | Pharmacist | Written (post) | Graphical | Working hours | Voucher | 140 | Targeted | 60 | 1.93 | 22.85 | 18.37 |
| 49 | 1 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 3.33 | 3.06 |
| 50 | 1 | A | Community nurse, local | Graphical | Working hours | Voucher | 140 | Universal | 60 | 2.71 | 45.57 | 34.69 | |
| 50 | 1 | B | Community nurse, vaccination bus | Graphical | Out of working hours | Voucher | 280 | Universal | 60 | 2.83 | 51.39 | 62.24 | |
| 50 | 1 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 3.04 | 3.06 |
| 51 | 1 | A | Health visitor, home | Graphical | Working hours | Cash | 280 | Universal | 30 | 3.30 | 72.25 | 72.45 | |
| 51 | 1 | B | Health visitor, local | Graphical | Out of working hours | Cash | 70 | Targeted | 60 | 2.25 | 25.10 | 23.47 | |
| 51 | 1 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 2.66 | 4.08 |
| 52 | 3 | A | Pharmacist | Electronic (internet) | Graphical | Out of working hours | No reward | 0 | No reward | 30 | 2.25 | 65.27 | 50.00 |
| 52 | 3 | B | Community nurse, local | Written (post) | Graphical | Working hours | Voucher | 70 | Targeted | 120 | 1.39 | 27.83 | 38.78 |
| 52 | 3 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 6.90 | 11.22 |
| 53 | 3 | A | Health visitor, local | Electronic (internet) | Numerical | Working hours | Voucher | 70 | Universal | 60 | 2.69 | 39.77 | 32.65 |
| 53 | 3 | B | Community nurse, vaccination bus | Written (post) | Graphical | Working hours | Voucher | 280 | Universal | 30 | 3.06 | 57.54 | 61.22 |
| 53 | 3 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 2.69 | 6.12 |
| 54 | 4 | A | Health visitor, local | Electronic (internet) | Numerical | Working hours | No reward | 0 | No reward | 30 | 2.58 | 31.74 | 32.14 |
| 54 | 4 | B | Health visitor, home | Written (post) | Graphical | Out of working hours | Cash | 280 | Universal | 30 | 3.31 | 65.86 | 65.63 |
| 54 | 4 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 2.41 | 2.23 |
| 55 | 1 | A | Health visitor, local | Written (post) | Numerical | Out of working hours | Cash | 280 | Targeted | 60 | 2.62 | 44.87 | 39.80 |
| 55 | 1 | B | Health visitor, local | Written (post) | Numerical and graphical | Working hours | Cash | 70 | Universal | 60 | 2.77 | 51.87 | 57.14 |
| 55 | 1 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 3.26 | 3.06 |
| 56 | 1 | A | Pharmacist | Electronic (internet) | Numerical and graphical | Out of working hours | Cash | 70 | Targeted | 120 | 1.36 | 13.29 | 20.41 |
| 56 | 1 | B | Practice nurse at local GP surgery | Written (post) | Numerical and graphical | Out of working hours | Voucher | 70 | Universal | 30 | 3.19 | 83.29 | 77.55 |
| 56 | 1 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 3.42 | 2.04 |
| 57 | 3 | A | Community nurse, vaccination bus | Numerical and graphical | Working hours | Cash | 280 | Targeted | 30 | 2.75 | 58.49 | 47.96 | |
| 57 | 3 | B | Community nurse, local | Written (post) | Numerical | Out of working hours | Cash | 70 | Targeted | 60 | 2.31 | 37.78 | 41.84 |
| 57 | 3 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 3.73 | 10.20 |
| 58 | 1 | A | Health visitor, local | Electronic (internet) | Numerical | Working hours | Voucher | 70 | Universal | 120 | 2.04 | 34.07 | 37.76 |
| 58 | 1 | B | Health visitor, home | Numerical and graphical | Out of working hours | Cash | 70 | Targeted | 30 | 2.63 | 61.51 | 57.14 | |
| 58 | 1 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 4.42 | 5.10 |
| 59 | 1 | A | Pharmacist | Electronic (internet) | Numerical | Out of working hours | Cash | 140 | Universal | 120 | 2.02 | 33.39 | 38.78 |
| 59 | 1 | B | Community nurse, local | Numerical and graphical l | Out of working hours | Voucher | 140 | Targeted | 30 | 2.65 | 62.19 | 56.12 | |
| 59 | 1 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 4.41 | 5.10 |
| 60 | 3 | A | Community nurse, local | Written (post) | Numerical | Working hours | Voucher | 70 | Universal | 120 | 2.05 | 30.17 | 35.71 |
| 60 | 3 | B | Community nurse, vaccination bus | Electronic (internet) | Numerical | Working hours | Voucher | 280 | Universal | 60 | 2.84 | 65.96 | 58.16 |
| 60 | 3 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 3.87 | 6.12 |
| 61 | 4 | A | Community nurse, vaccination bus | Graphical | Working hours | Cash | 280 | Universal | 120 | 2.21 | 38.99 | 45.98 | |
| 61 | 4 | B | Health visitor, local | Graphical | Out of working hours | Voucher | 140 | Targeted | 30 | 2.58 | 56.73 | 50.45 | |
| 61 | 4 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 4.28 | 3.57 |
| 62 | 2 | A | Community nurse, vaccination bus | Numerical and graphical | Working hours | Voucher | 70 | Targeted | 30 | 2.39 | 62.96 | 66.34 | |
| 62 | 2 | B | Health visitor, local | Written (post) | Numerical | Out of working hours | No reward | 0 | No reward | 120 | 1.69 | 31.25 | 30.69 |
| 62 | 2 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 5.79 | 2.97 |
| 63 | 4 | A | Practice nurse at local GP surgery | Written (post) | Graphical | Out of working hours | Voucher | 210 | Universal | 60 | 2.97 | 58.92 | 51.34 |
| 63 | 4 | B | Pharmacist | Electronic (internet) | Numerical | Working hours | Cash | 210 | Targeted | 30 | 2.53 | 38.05 | 45.98 |
| 63 | 4 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 3.04 | 2.68 |
| 64 | 4 | A | Health visitor, home | Electronic (internet) | Numerical | Working hours | Voucher | 210 | Targeted | 30 | 2.66 | 54.15 | 48.21 |
| 64 | 4 | B | Health visitor, local | Electronic (internet) | Numerical and graphical | Out of working hours | Cash | 280 | Universal | 120 | 2.41 | 42.06 | 46.88 |
| 64 | 4 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 3.79 | 4.91 |
| 65 | 1 | A | Practice nurse at local GP surgery | Electronic (internet) | Numerical | Out of working hours | Cash | 140 | Targeted | 30 | 2.86 | 68.74 | 60.20 |
| 65 | 1 | B | Pharmacist | Written (post) | Numerical | Working hours | Voucher | 140 | Universal | 120 | 1.93 | 27.31 | 36.73 |
| 65 | 1 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 3.95 | 3.06 |
| 66 | 3 | A | Health visitor, local | Graphical | Out of working hours | Cash | 140 | Universal | 60 | 2.86 | 70.44 | 64.29 | |
| 66 | 3 | B | Community nurse, local | Written (post) | Numerical and graphical | Working hours | Cash | 280 | Targeted | 120 | 1.85 | 25.54 | 31.63 |
| 66 | 3 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 4.02 | 4.08 |
| 67 | 4 | A | Community nurse, local | Written (post) | Numerical and graphical | Out of working hours | Cash | 210 | Universal | 30 | 3.30 | 82.49 | 60.71 |
| 67 | 4 | B | Community nurse, vaccination bus | Electronic (internet) | Numerical and graphical | Out of working hours | Voucher | 210 | Targeted | 120 | 1.56 | 14.48 | 35.27 |
| 67 | 4 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 3.03 | 4.02 |
| 68 | 3 | A | Health visitor, home | Written (post) | Numerical and graphical | Working hours | Cash | 70 | Universal | 120 | 2.09 | 37.83 | 43.88 |
| 68 | 3 | B | Community nurse, local | Written (post) | Numerical | Out of working hours | Cash | 210 | Targeted | 60 | 2.50 | 57.47 | 50.00 |
| 68 | 3 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 4.70 | 6.12 |
| 69 | 3 | A | Health visitor, home | Electronic (internet) | Numerical and graphical | Working hours | Cash | 70 | Universal | 60 | 2.70 | 52.21 | 48.98 |
| 69 | 3 | B | Community nurse, vaccination bus | Graphical | Out of working hours | Voucher | 210 | Targeted | 30 | 2.54 | 44.28 | 44.90 | |
| 69 | 3 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 3.51 | 6.12 |
| 70 | 1 | A | Pharmacist | Written (post) | Numerical and graphical | Out of working hours | Cash | 70 | Targeted | 60 | 2.05 | 30.28 | 28.57 |
| 70 | 1 | B | Health visitor, local | Electronic (internet) | Numerical and graphical | Working hours | Cash | 140 | Universal | 60 | 2.82 | 65.81 | 67.35 |
| 70 | 1 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 3.91 | 4.08 |
| 71 | 2 | A | Community nurse, local | Electronic (internet) | Graphical | Out of working hours | Cash | 140 | Universal | 60 | 2.76 | 55.74 | 58.42 |
| 71 | 2 | B | Health visitor, local | Written (post) | Numerical and graphical | Working hours | Voucher | 280 | Targeted | 60 | 2.44 | 40.72 | 35.64 |
| 71 | 2 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 3.54 | 5.94 |
| 72 | 3 | A | Community nurse, vaccination bus | Numerical and graphical | Working hours | No reward | 0 | No reward | 120 | 1.49 | 27.42 | 19.39 | |
| 72 | 3 | B | Health visitor, local | Electronic (internet) | Numerical | Out of working hours | Voucher | 280 | Universal | 120 | 2.37 | 66.39 | 74.49 |
| 72 | 3 | Neither | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | Unspecified | 0.00 | 6.19 | 6.12 |
Appendix 8 Interview schedule for interviews with health and other professionals
Introductions
-
Introduce researcher(s).
-
Give overview of what the project is about, emphasising that we are interested in preschool vaccinations, not childhood vaccinations for older children.
-
– Will be exploring the use of incentives (i.e. payment for vaccination).
-
– Or quasi-mandatory schemes (such as making vaccination mandatory for school entry).
-
Make clear however, that some children may be exempt from the schemes on health grounds.
-
-
-
Check they have had a copy of the information sheet.
-
Collect consent form – turn on tape.
General
First, I would just like to know about your role and how you are involved with the childhood vaccination programme.
-
Could you give me an overview of your current job role and how that involves you in childhood vaccinations?
-
What are your views about the way vaccinations are co-ordinated (a) at national level and (b) at local level?
-
What are your main concerns about how vaccinations are delivered (a) at national level and (b) at local level?
-
– National level (policy): right vaccinations at right time for right children?
-
– Local level (delivery): are we getting it right on the ground? Implementation
-
-
Are you happy with current uptake rates in your area?
-
– Use uptake data for each locality to spark discussion about where uptake is over or under recommended rates.
-
– Is uptake lower in certain groups? Age of mother/deprivation?
-
– Are they targeted in any way locally/nationally
-
-
Do you think anything could be done to increase vaccination rates?
-
– Linking to previous question. Could strategic decisions be made to increase uptake?
-
– Would any action be likely to up-skittle the apple cart?
-
– Could vaccinations be better organised ‘on the ground’?
-
-
Introduce here the concept of incentives and mandates to sensitise participants to what is to come.
-
What are your views on incentivising parents to immunise their children?
-
What kind of incentives do you think might make parents want to immunise their child?
-
What do you think about making vaccination mandatory, so everyone HAS to immunise their child?
Scenarios
Next the interview will move onto a set of scenarios to introduce different possible incentive schemes aimed at increasing vaccination rates.
Gift of money (universal)
This scenario will explore the use of providing a universal financial incentive to parents, i.e. a cash payment upon the completion of each course of vaccination.
Gift of money (targeted)
This scenario will explore the provision of a cash incentive that is available only to parents who have not completed a full course of vaccinations by the time the child is 5 years old.
Receipt of universal benefits (Child Benefit) dependent on vaccination
This scenario will explore the acceptability of only giving universal benefits (such as Child Benefit) to parents who adhere to the recommended vaccination schedule. Parents of children who are not up to date would have their benefits stopped or capped in some way until such time as they were immunised.
Removal of childcare contributions if child is not immunised
This scenario will explore the acceptability of removing childcare contributions from parents who adhere to the recommended vaccination schedule. Parents of children who are not up to date would have their childcare contributions stopped until such time as they were immunised.
Mandatory for entry to day care (nursery/childminder, etc.)
This scenario will explore the feasibility and acceptability of refusing any child who is not fully immunised entry into formal day-care facilities.
Mandatory for entry into school
This scenario will explore the feasibility and acceptability of refusing any child who is not fully immunised entry into school.
For each scenario ask:
-
What effect, if any, do you think introducing [insert incentive scheme] would have on uptake rates?
-
– Do you think it could increase uptake rates?
-
– Do you think it could have a negative effect on uptake rates?
-
-
Do you think it is feasible to offer [insert incentive scheme]?
-
Do you think it is appropriate to offer [insert incentive scheme]?
-
– Knock-on effects on other vaccination programmes?
-
-
Do you think it could work ‘in practice’?
-
– Would it be possible to implement it?
-
– How would it affect your job?
-
– If not, are there ways to make it workable?
-
-
How much money do you think it would be appropriate to offer?
-
What would the impact be on your role?
-
– Have to police parents.
-
– New systems to develop.
-
Finisher
-
Thinking about financial incentives and mandates do you think either method would help to increase vaccination rates?
-
– Any? None? Why? Which would be (un)acceptable? Why?
-
-
Which, if any, would be better to implement and police?
-
What else could be done to increase vaccination rates?
Close by thanking for their time.
Appendix 9 Participant information sheet for parents and carers
Appendix 10 Participant information sheet for health and other professionals
List of abbreviations
- ASC
- alternative specific constant
- DCE
- discrete choice experiment
- DTaP
- diphtheria, tetanus and pertussis
- GP
- general practitioner
- Hib
- Haemophilus influenzae type B
- IIA
- independence of irrelevant alternative
- MMR
- measles, mumps and rubella
- NECS
- North of England Commissioning Support Unit
- NICE
- National Institute for Health and Care Excellence
- RCT
- randomised controlled trial
- SD
- standard deviation
- WHO
- World Health Organization
- WTA
- willingness to accept
- WTP
- willingness to pay