Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 10/98/05. The contractual start date was in March 2013. The draft report began editorial review in July 2015 and was accepted for publication in October 2015. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Dr Emma Clark is a member of the Health Technology Assessment Elective and Emergency Specialist Care Panel. Dr Howard Thom has undertaken consulting work for Novartis Pharmaceuticals, ICON plc and Eli Lilly and Company. The work had no connection to joint hypermobility or Ehlers–Danlos syndrome. To our knowledge the organisations have no commercial interests in these areas.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2016. This work was produced by Palmer et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
Joint hypermobility syndrome
Musculoskeletal problems represent some of the most common reasons for seeking primary health care. 1 Joint hypermobility syndrome (JHS) is a heritable connective tissue disorder, characterised by excessive joint range of motion and symptoms of pain, fatigue, proprioception difficulties, soft-tissue injury and joint instability. 2 Many experts now consider JHS to be indistinguishable from Ehlers–Danlos syndrome – hypermobility type (EDS-HT),3 although this report uses the term JHS. Asymptomatic generalised joint laxity (often described as being ‘double jointed’) is very common and generally asymptomatic, occurring in 10–20% of Western populations, with higher prevalence in Indian, Chinese, Middle Eastern and African populations. 4–6 However, symptomatic JHS is reported to be under-recognised, poorly understood and poorly managed in clinical practice. 7–9 Symptomatic joint hypermobility has been reported to affect approximately 5% of women and 0.6% of men. 10 It should be acknowledged, however, that there is currently a lack of good-quality epidemiological evidence for the true prevalence of JHS in the general population.
The revised (Brighton 1998) criteria (see Table 1) are now recommended for the diagnosis of JHS,11 although a range of other diagnostic criteria has been used historically. A key component of the Brighton criteria is the Beighton score, a 9-point score of joint mobility that has been in clinical use for many years. 5 One point is awarded for being able to place the hands flat on the floor while keeping the knees straight. One point is also awarded for each hypermobile peripheral joint as follows: 10° knee hyperextension; 10° elbow hyperextension; 90° extension of the fifth finger metacarpophalangeal joint; and opposition of the thumb to touch the forearm (points are awarded for the left and right limbs as appropriate). The Brighton criteria incorporate a number of other clinical features to confirm a diagnosis of JHS and exclude other differential diagnoses. Diagnosing JHS is often challenging, as symptoms may easily be attributed to other causes. Patients report a wide range of fluctuating symptoms in addition to pain, and it has been suggested that many patients presenting in primary care with everyday musculoskeletal conditions may have unrecognised JHS. 12 Indeed, the use of the Brighton criteria has revealed a very high prevalence of JHS in musculoskeletal clinics, with rates of 46% of women and 31% of men referred to one rheumatology service,13 30% of those referred to a musculoskeletal triage clinic in the UK14 and 55% of women referred to physiotherapy services in Oman. 15 However, the diagnosis of generalised joint laxity and JHS is contentious. Clinch et al. ,16 for example, suggested that a traditional cut-off value of 4/9 on the Beighton score was unlikely to be clinically meaningful, with 19.2% of 6022 14-year-old children meeting that criterion. A more stringent cut-off value of 6/9 reduced prevalence to 4.2% which seemed more discriminative. Remvig et al. 17 also found little agreement between clinicians on the criteria that should be used to diagnose JHS. Indeed, the median importance ratings were zero for Marfanoid habitus, skin signs, eye signs and varicose veins, hernias and rectal/uterine prolapse (minor criteria 5–8 in Table 1), suggesting that these are often not considered. This lack of consensus on diagnosis perhaps explains why JHS is often under-recognised in clinical practice. 7–9
| Major criteria | Minor criteria |
|---|---|
|
|
When compared with healthy control subjects, JHS has been shown to have a significant impact on a wide range of outcomes, such as exercise endurance, gait, pain, proprioception, strength, function and quality of life in both children20–23 and adults. 24–27 A recent systematic review and meta-analysis has also confirmed the impact of JHS on a range of psychological variables such as fear, agoraphobia, anxiety, depression and panic disorders. 28
Physiotherapy, particularly exercise, is generally considered the mainstay of treatment,2,8,9,15,29–31 and professionals in a number of centres in the UK have developed a specialist interest in treating people with JHS. It should be recognised that ‘physiotherapy’ is not an intervention in itself but describes professional practice in which a range of interventions is often employed in complex treatment ‘packages’. 32 Exercise therapy seems to be ‘core’ to physiotherapy practice,32 but professional autonomy in the UK allows individual physiotherapists to assess, diagnose and treat using the best available evidence and their own professional judgement. Keer and Simmonds31 reported that pain relief and preventing the recurrence of joint pain are the main aims of treatment of JHS, with exercise key to achieving these aims. They reported research evidence supporting the importance of interventions targeting posture, proprioception, strength and motor control, in conjunction with education, physical activity and fitness. However, there is little empirical evidence supporting the efficacy of exercise or physiotherapy. Two recent systematic reviews included only a handful of eligible trials of physiotherapy and occupational therapy interventions for JHS, and found limited evidence for their clinical effectiveness and cost-effectiveness. 33,34 Although there is some evidence that people with JHS who receive exercise interventions improve over time, there is little convincing evidence for the effectiveness of different forms of exercise or for exercise being more effective than a control condition. 33 The current lack of evidence on the most effective management options for JHS may contribute to anecdotally reported negative experiences of management. 7,35 Higher-quality multicentre trials are clearly required to investigate the clinical effectiveness and cost-effectiveness of physiotherapy for JHS. The following section will consider the existing research evidence in more detail.
Evidence for the effectiveness of physiotherapy
Although physiotherapy is considered the mainstay of treatment for JHS, there is currently little evidence related to its effectiveness. The research evidence is at a very early stage of development, with a recent systematic literature review conducted by this research team33 identifying only three exercise studies in adults that met the inclusion criteria. 26,35,36 One further study was conducted in children. 37
Barton and Bird36 conducted a cohort study to investigate the effects of exercise in 25 hypermobile adults. They implemented a 6-week exercise intervention, which included warm-up exercises, specific joint exercises and proprioception exercises (the selection of exercises and number of repetitions were tailored to each individual). Patients were asked to perform the exercises three times per week. Outcome measures included a questionnaire developed for the project, the Beighton score and the range of movement of major joints. The results showed that the maximum distance walked and pain on movement improved significantly (both from the questionnaire). Range of motion in the knee joints also improved significantly, but there were no significant changes in any other outcome measure.
Ferrell et al. 35 also conducted a cohort study with 20 adults with joint hypermobility (18 completed the study and were analysed). Their intervention and outcome measures focused specifically on the knee joints, although they did also include the Short Form questionnaire-36 items (SF-36) to assess general health perceptions. The exercise intervention included a range of closed kinetic chain exercises and a static hamstring strengthening exercise. Exercises were performed on 4 out of 7 days of the week for 8 weeks. A clear progression of the type of exercises and number of repetitions was described, although this did not seem to have been individualised. Also included as outcome measures were knee joint proprioception, balance, knee flexor and extensor muscle strength and knee joint pain. The results showed significant improvements over time in proprioception, balance, muscle strength, physical functioning and mental health.
Sahin et al. 26 conducted a randomised controlled trial (RCT) in 40 adults diagnosed with JHS. It seems that 15 patients were randomly selected to receive proprioception exercises for 8 weeks and 25 received no exercise intervention, although there is some uncertainty about patient numbers. For example, in the text the control arm is said to have comprised 3 men and 17 women (n = 20 rather than 25) and one of the tables reported 15 participants in each of the exercise and control arms. Exercise was performed three times per week for 8 weeks, supervised by a doctor in a clinic. Unfortunately, the method of randomisation is not reported, nor are any details of assessor blinding provided. Proprioceptive acuity, pain and the occupational activity subscale of the Arthritis Impact Measurement Scale – 2 (AIMS-2) questionnaire all significantly improved over time in the arm that received proprioception exercises. No other subscale of the AIMS-2 improved (physical status, emotional status, symptoms or social activity). No outcome changed over time in the control arm. Unfortunately, no direct statistical comparison of trial arm data after treatment was reported, so the significance of differences between arms cannot be determined.
The only other randomised trial of exercise in joint hypermobility included in the review by Palmer et al. 33 was conducted in children. 37 This study did not include a ‘no or minimal intervention’ arm but instead compared the effects of targeted (n = 30) with a more generalised exercise approach (n = 27). Treatment was received for half an hour per week for 6 weeks and exercises were progressed on an individual basis. Home exercises were also given, to be performed daily. Outcomes included pain (both child and parent reports), global evaluation of the impact of hypermobility (parent report), functional impairment (the child Health Assessment Questionnaire) and a 6-minute shuttle test. When both arms were combined, there were significant improvements in pain (both child and parent reported) and the child Health Assessment Questionnaire. Parental global assessment and the shuttle test did not improve significantly. There were no differences between arms, except for parental global assessment (in favour of the targeted intervention).
Subsequent to the census date used in the review by Palmer et al. ,33 a further randomised trial of exercise was conducted in children with knee pain and JHS. 38 It also compared two different types of exercise: one using exercise to neutral knee extension (n = 14) and one using exercise into the full hypermobile range (n = 12). Exercises were performed for 8 weeks. The primary outcome measure was knee pain, with secondary outcome measures of muscle strength, function and parent-reported quality of life. When the arms were combined, there was a significant improvement in knee pain, patient global impression of change, strength and parent-reported quality of life (in both physical and psychosocial health components). There was a difference between arms only in the parent-reported quality of life, in favour of the neutral exercise arm for physical health and in favour of the exercising into the hypermobile range for psychosocial health. No other differences were observed and there were no adverse events.
These studies seem to suggest that patients with JHS might improve over time with exercise, but it is important to note that only Sahin et al. 26 included an appropriate no-treatment control arm. The other papers were either uncontrolled cohort studies or comparative trials of different forms of exercise. Unfortunately, Sahin et al. 26 failed to report any direct head-to-head statistical analysis of between-arm differences and fundamental methodological details are unclear. Another systematic review of occupational therapy and physiotherapy interventions for JHS34 independently identified a high risk of bias in the study by Sahin et al. 26 and did not identify any additional RCTs of physiotherapy in this area. Also of note is that three of the five studies26,35,38 focused on the knee joint in what is a multiple-joint condition and all assessed a relatively brief intervention of ≤ 8 weeks. So, the true effectiveness of physiotherapy (including exercise) in JHS remains unknown. Observed improvements over time could be explained by the natural history of the condition, positive interactions with therapists or other unknown factors. Therefore, an appropriately controlled study is urgently required.
The commissioned research
The research commissioned by the National Institute for Health Research Health Technology Assessment (HTA) programme called for proposals to answer the following question: does physiotherapy improve outcomes in adults with musculoskeletal pain associated with hypermobility syndrome? It specifically asked for assessment of a ‘whole-body’ physiotherapy intervention, with examples of proprioception, muscle strengthening, pain management strategies and hydrotherapy. The commissioning brief (HTA 10/98/05: whole-body physiotherapy package for hypermobility) requested a feasibility study in preparation for a possible RCT in outpatients or other specialist care settings. The comparator requested was no active physiotherapy, with clarification that advice on joint care could be given. Important outcomes of the feasibility study were specified as follows: the number of potential eligible patients with hypermobility syndrome; feasibility of recruitment; development and piloting of the intervention; and acceptability to patients in terms of quality of life. An estimate of the value of information (VOI) from a subsequent RCT was also specified. Outcomes requested for a later trial were function, musculoskeletal pain, quality of life, adverse events (e.g. dislocations and susceptibility to injury), range of movement, strength, proprioception and psychological well-being.
The study team carefully considered the commissioning brief when developing the research project, which is described in The research project.
The research project
The study team designed a study that aimed to develop and evaluate a complex physiotherapy intervention. The lack of research in this area meant that it was difficult to provide firm recommendations for what the physiotherapy intervention should look like. Therefore, preliminary work was planned to determine patient and health professional perspectives on physiotherapy, and to use this information to help design the intervention package. A number of broad guiding principles were agreed in advance. It was agreed that the intervention should include one-to-one patient–therapist interaction because of the complexity of individual patient needs. It was also agreed that the devised physiotherapy intervention should be easily implementable across the NHS, meaning that very specialist interventions or those requiring specialist facilities (such as hydrotherapy) would be excluded. The team was also mindful of trying to ensure that the frequency and duration of sessions and overall duration of treatment was broadly in line with usual care at the two NHS trusts taking part in the research (approximately six 30-minute sessions over 4 months). A subsequent UK-wide survey conducted by the research team has revealed that this pattern of care fits very well with what is delivered by physiotherapists nationally. 39 By agreeing such broad guiding principles, the research team wanted to ensure that the physiotherapy intervention package developed stood the best chance of being adopted in practice, should it ultimately prove to be beneficial.
As part of the commissioning process there was discussion with the funding committee about the identity of the comparator arm, with the study team initially preferring a delayed intervention arm. This preference was because of concerns about the ethics of delivering an advice-only control that was less than ‘usual care’ at the two centres involved, and the potential negative impact this would have on study recruitment. The funding committee asserted that a delayed intervention arm would cause problems for long-term follow-up in any future trial (as all patients would have received treatment) and that genuine equipoise was present because of the lack of robust evidence for the effects of physiotherapy. The study team therefore agreed to deliver an advice-only control intervention.
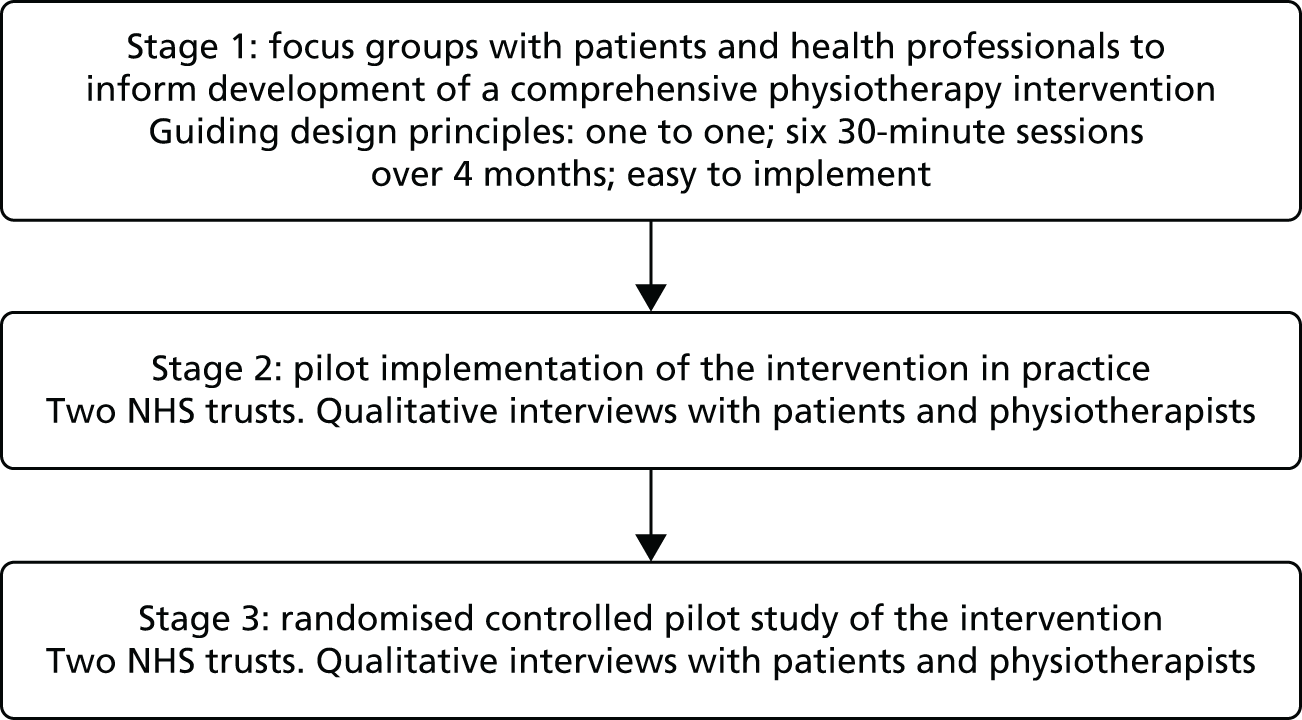
The commissioned study was, therefore, designed in three stages (Figure 1). Stage 1 aimed to understand the physiotherapy management of JHS, from patient and health professional perspectives. This information was used by a working group of researchers, health professionals and patient research partners to develop the physiotherapy intervention package. Stage 2 aimed to pilot the intervention in practice so that it could be adapted and refined as necessary before moving on to stage 3, which was a pilot RCT of the intervention, compared with an advice-only control arm. Full details of each stage of the research are contained in subsequent chapters.
FIGURE 1.
Flow diagram illustrating the overall study design.
Chapter 2 Stage 1: Hypermobility – Perspectives On Physiotherapy study and development of a complex physiotherapy intervention
Aims
The aims of this first stage of the research included examining the views and experiences of individuals with JHS and health professionals of physiotherapy for the management of JHS (component 1). This was to inform the development of a comprehensive physiotherapy intervention for adults with JHS (component 2).
Component 1: focus groups with patients and health professionals to determine their perspectives on physiotherapy for joint hypermobility syndrome and the proposed trial
Introduction
In order to examine the views and experiences of physiotherapy for JHS, we conducted a series of focus groups with patients and health professionals. Qualitative methods were chosen as the most appropriate means of gathering data regarding beliefs, experiences and perceptions of physiotherapy interventions. 40,41 Qualitative methods are also valuable in the pretrial development phase both to help develop and refine the trial and to improve understanding of the experiences of patients receiving, and staff delivering, interventions. 42–44 Such use of qualitative methods in RCTs as part of preintervention development is well established. 45–48 Focus groups permit sharing and comparing of ideas among group members, which then facilitates the evaluation and interpretation of those ideas and the exploration of areas of consensus and disagreement. This component of the study was conducted under the name Hypermobility: Perspectives on Physiotherapy (HPoP). Findings from this component have previously been published as peer-reviewed journal articles. 49,50
Objectives
The specific objectives were as follows:
-
to investigate the lived experiences of individuals with JHS
-
to explore patients’ and health professionals’ views on current ‘usual care’ physiotherapy management of JHS
-
to examine what would be considered the optimal content and delivery of a physiotherapy intervention for adults with JHS
-
to investigate how to measure success of a physiotherapy intervention
-
to describe the attitudes and opinions of individuals with JHS and health professionals to facilitate the design of a pilot RCT of a physiotherapy intervention.
Methods
Seven focus groups were conducted with people with JHS and health professionals with a special interest in managing patients with JHS between January and February 2013 in four UK locations. Participants were recruited via mailed invitations to health professionals and patients from physiotherapy services at two NHS trusts, as well as to local members of the Hypermobility Syndromes Association (HMSA) and patients who had previously expressed an interest in assisting with research activity at two university locations.
Eligible patient participants were aged ≥ 18 years, had previously received a diagnosis of JHS, had attended physiotherapy within the preceding 12 months and were able to speak English. Individuals with other known musculoskeletal pathology causing pain, particularly osteoarthritis and inflammatory musculoskeletal disease, such as rheumatoid arthritis, were excluded. Eligibility criteria for health professionals were that they should be post qualification and should have had some interest or involvement in treating people with JHS. The purposive sampling strategy aimed for diversity with regard to age, sex, socioeconomic situation and geographical location to capture maximum variation in views and experiences. Ethical approval was obtained from the North East NHS Research Ethics Committee (reference number 12/NE/0307) and all participants gave written consent. There was a substantial delay to securing appropriate NHS approvals for this stage of the research, which ultimately shortened the recruitment period available for the later pilot RCT (stage 3) by 4 months.
Separate focus groups were conducted with patients and health professionals. All focus groups were conducted in non-clinical settings. The focus groups were facilitated by two researchers (SP and JH). One researcher led the discussion using open-ended questioning techniques to elicit participants’ own experiences and views, and to ensure that all participants had an opportunity to take part. The other researcher summarised the discussion, audio-recorded the session and noted down who was speaking to aid transcription. Focus groups lasted between 71 and 100 minutes.
Topic guides were used to facilitate discussions and, in line with an inductive approach, were revised in light of emerging findings (see Appendices 1 and 2). Topic guides explored experiences of physiotherapy for JHS and views regarding physiotherapy treatment for JHS, including the optimal content and delivery of education, advice, exercises and support packages. In addition, focus groups explored attitudes to the proposed trial design and views on the most appropriate outcomes for the intervention.
In addition to the focus groups, patient participants were asked to complete a Physiotherapy Outpatient Satisfaction questionnaire51 to capture information about their last course of physiotherapy. Patients are asked to indicate their agreement to a total of 38 statements on a 5-point Likert scale, with higher scores indicating higher levels of satisfaction. An average score out of 5 was produced for six subscales: expectations, therapist, communication, organisation, clinical outcome and satisfaction.
Analytic procedures
With written informed consent from participants, all focus groups were audio-recorded, fully transcribed and anonymised, checked for accuracy and then imported into the NVivo qualitative data analysis software (version 10, QSR International Pty Ltd, Doncaster, VIC, Australia) to aid data analysis. Analysis began in parallel with data collection and was ongoing and iterative. Thematic analysis,52 using the constant comparison technique,53 was used to scrutinise the data to identify and analyse patterns across the data set. Transcripts were examined on a line-by-line basis, with codes being assigned to segments of the data and an initial coding frame developed. An inductive approach was used to identify participants’ perceptions of their experiences. To enhance analysis and enable team discussion and interpretation, team members (RT and JH) independently coded transcripts; any discrepancies were discussed to achieve a coding consensus and maximise rigour. Scrutiny of the data showed that data saturation had been reached at the end of analysis, such that no new themes were arising from the data. 54 All participants were assigned a letter as a pseudonym.
Findings
In total, four focus groups were conducted with 25 patients (three men and 22 women; aged 19–60 years) and three focus groups were conducted with 16 health professionals (three men and 13 women; 0–30 years post qualification; 14 physiotherapists and two podiatrists) (Table 2).
| Characteristic | n (%) |
|---|---|
| Patients (N = 25) | |
| Age (years) | |
| 18–29 | 8 (32) |
| 30–39 | 7 (28) |
| 40–49 | 6 (24) |
| 50–59 | 2 (8) |
| > 60 | 3 (12) |
| Mean, (median) | 33 (36) |
| Sex | |
| Female | 22 (88) |
| Male | 3 (12) |
| Ethnicity | |
| White | 23 (92) |
| Other | 2 (8) (both self-reported as British white and Chinese) |
| Socioeconomic statusa | |
| 1 (affluent) | 8 (32) |
| 2 | 8 (32) |
| 3 | 4 (16) |
| 4 | 3 (12) |
| 5 (most deprived) | 1 (4) |
| Education | |
| Schooling to 16 years | 3 (12) |
| College diploma/equivalent | 6 (24) |
| University degree/equivalent | 10 (40) |
| Postgraduate degree | 6 (24) |
| Employment | |
| Employed full-time | 7 (28) |
| Employed part-time | 8 (32) |
| Student full-time | 4 (16) |
| No paid job | 5 (20) |
| Retired | 1 (4) |
| Health professionals (N = 16) | |
| Sex | |
| Female | 13 (81) |
| Male | 3 (19) |
| Role | |
| Physiotherapists | 14 (88) |
| Podiatrists | 2 (13) |
| Years since qualifying | |
| Newly qualified (< 1 year) | 1 (6) |
| 1–4 years | 1 (6) |
| 6–20 years | 7 (44) |
| > 20 years | 7 (44) |
Out of 25 patient participants, 24 completed the Physiotherapy Outpatient Satisfaction questionnaire. Table 3 presents the median scores for each of the subscales.
| Subscales | Median rating (IQR = Q3 – Q1) (maximum = 5) |
|---|---|
| Expectations | 2.80 (0.80) |
| Therapist | 4.17 (1.33) |
| Communication | 3.60 (2.00) |
| Organisation | 3.50 (0.88) |
| Clinical outcome | 2.33 (0.33) |
| Satisfaction | 3.00 (1.57) |
Table 3 suggests that, in general, satisfaction with physiotherapy was rather neutral (median rating 3.00/5), with median ratings of clinical outcome (2.33/5) and expectations (2.80/5) of treatment tending towards negative ratings. More positively rated were the therapist (median rating 4.17/5), communication (3.60/5) and organisation (3.50/5). So, the expectations of physiotherapy and the perceived outcome of treatment were rated as lowest of the six subscales.
Six themes, developed from the qualitative analysis, related to (1) the impact of JHS; (2) JHS as a difficult to diagnose, chronic condition; (3) physiotherapy to manage JHS; (4) optimising physiotherapy as an intervention for JHS; (5) measuring success, and managing expectations, of physiotherapy; and (6) patients’ and health professionals’ views on the proposed physiotherapy trial design.
Theme 1: the impact of joint hypermobility syndrome
Figure 2 illustrates the subthemes related to this main theme.
FIGURE 2.
Subthemes associated with theme 1: the impact of JHS.

All patients reported JHS symptoms including fatigue, pain, proprioception problems, recurring joint dislocation and ‘cycles’ of injury and recovery (Table 4), although there was wide agreement that the impact and consequences of these symptoms were different for each patient. The diverse nature of the symptoms was also noted by both patients and health professionals.
All of us are probably so different yet we’re categorised as the same.
Female patient A, 60 years old, focus group 2
It’s the heterogeneous group that makes it very interesting.
Female health professional D, 22 years post qualification, focus group 4
| Feature of JHS | Illustrative quotation |
|---|---|
| Pain | Most days I’m in some sort of pain, it’s always there, it never actually goesFemale patient A, 35 years old, focus group 5Every second, that’s the ankle, the knee, the back, the headFemale patient B, 32 years old, focus group 1 |
| Repeated cycles of injury, pacing or activity restriction and recovery | . . . it’s difficult to know how much to push yourself because then you are worried about injuring and then you’re setting yourself back, well it’s a vicious cycle reallyFemale patient B, 27 years old, focus group 5I find that I get to a level with exercise and then I’ll have a bad day or I’ll injure myself and so you kind of step back, you have to go backwards, and you never seem to go that far forwardFemale patient G, 42 years old, focus group 5 |
| Impact of JHS on activity | I will only go out if I know that we’re going somewhere where I can sit downFemale patient D, 32 years old, focus group 5I think it was one of the questions in there, it was about how much how much pain have you been in, well loads, has it stopped you doing anything, no, because we all sort of pushed through it and we still do it anywayFemale patient D, 21 years old, focus group 1 |
| Fatigue | You’re managing your pain and it’s a lot of pain, it’s a dull ache and it makes you sleepy and it makes you tired and you’re exhaustedFemale patient G, 30 years old, focus group 1 |
| Proprioception issues | It’s on your mind the whole time, because I’m constantly thinking about where my hands and feet areFemale patient G, 48 years old, focus group 2 |
Patients described difficulties in making the distinction between chronic and acute pain, and that it was challenging for them to understand how, or if, injuries had occurred:
Well, how do we know whether we’ve injured something, because we’ve got pain all the time?
Female patient C, 40 years old, focus group 1
However, patients also observed that their pain thresholds appeared to be unusually high and that their perception and interpretation of pain is somehow altered:
That would be the first problem, I can’t feel pain. I snapped some bones in my wrist, and up here somewhere, and it was ‘oh that’s not quite right’ and the doctor went ‘aren’t you screaming’, and I was like ‘why?’, and he said ‘that should really hurt’, oh OK, it’s a bit of a whinge, until he took me through into the hospital and he was going ‘painkillers’, no, don’t take them, doesn’t hurt that much, he did the operation and came through OK and they said ‘you can have the morphine if you want it’, and I didn’t bother, it didn’t hurt.
Male patient A, 50 years old, focus group 1
Repeated injuries were common and patients frequently talked about cycles of injury and recovery in which periods of injury required participants to pace and restrict activity. Consequently, some participants found living with JHS to be ‘very debilitating’, limiting the type of activities they could engage in and severely impacting on their engagement with the social world. Patients also described how prior experiences of repeated injuries led to heightened levels of anxiety and catastrophising about future injuries, or extrapolating their current or prior experiences to an imagined future (Table 5).
| Psychosocial impact | Illustrative quotation |
|---|---|
| Anxiety | I feel like I’m in a constant state of anxiety, waiting for the next injury and trying to pre-empt anything that’s going to cause itFemale patient G, 48 years old, focus group 2 |
| Catastrophising | I think also there’s an element of fear, I worry dreadfully and I’m frightened of what will come next [. . .] There’s all these ‘what ifs’ that boil up into this massive pile of anxiety inducing terror. What’s happened in reality is you’ve got a slightly aching wrist, but what’s actually happened is it’s gone from if that’s gone the next thing’s going to go, what if this and what if this, and what if I let everyone down and this sort of awful . . .Female patient E, 34 years old, focus group 2 |
| Fear of the future | Oh my god is this going to be like this for the next 60 years of my lifeFemale patient B, 27 years old, focus group 5I’m going to have it forever and it’s never going to get betterFemale patient E, 19 years old, focus group 6 |
Theme 2: joint hypermobility syndrome as a difficult to diagnose, chronic condition
A number of subthemes were associated with this main theme (Figure 3).
FIGURE 3.
Subthemes associated with theme 2: JHS as a difficult to diagnose, chronic condition.
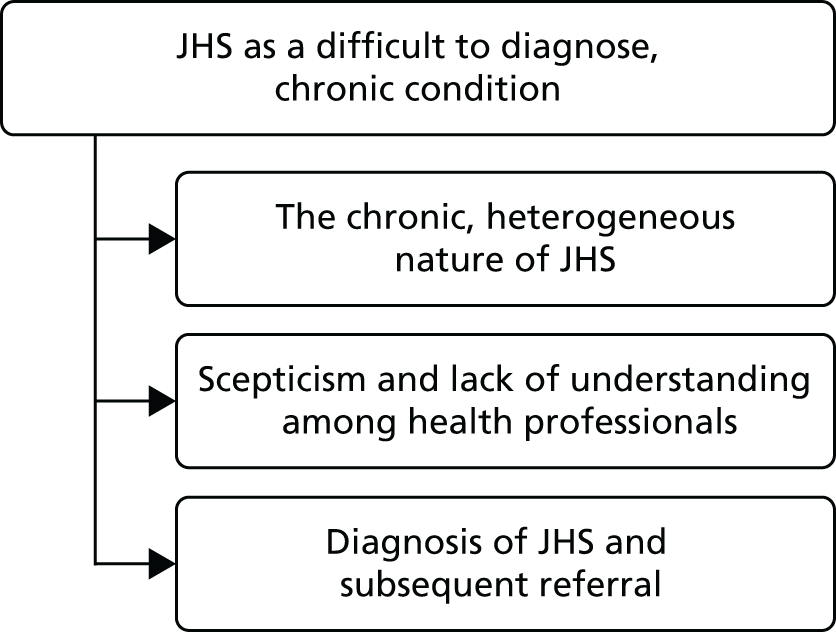
The chronic, heterogeneous nature of joint hypermobility syndrome
Both patients and health professionals described the chronicity of JHS and its symptoms. Patients recognised that they were ‘going to have it forever’ (female patient E, 19 years old, focus group 6) and that ‘you won’t be fine, not completely’ (female patient C, 40 years old, focus group 1). Similarly, one health professional described having JHS as ‘almost like a recovering alcoholic, you are always a recovering hypermobility person’ (female health professional B, 28 years post qualification, focus group 4).
Scepticism and lack of understanding among health professionals
Both patients and health professionals felt that JHS is not a widely understood condition and sometimes not recognised as a syndrome among health professionals. Patients described a lack of understanding of JHS in health settings and reported feeling that sometimes their symptoms were not believed or understood by health professionals:
I think I was described as a biomechanical conundrum by one of the physiotherapists I saw . . . and this is what I found repeated over and over again, that hypermobility shouldn’t be causing pain, it’s just the way you are . . . you shouldn’t be in pain because you have mobility.
Female patient C, 53 years old, focus group 2
When I went back to physio[therapy] for strengthening exercises to help my joints after the hypermobility diagnosis, there was . . . I got that a little bit, ‘I’m not sure about this hypermobility . . .’.
Female patient B, 34 years old, focus group 2
I work in a rheumatology department who don’t recognise joint hypermobility as an entity and in fact, probably a lot of people tend to get diagnosed with things like fibromyalgia more than normal.
Female health professional E, 30 years post qualification, focus group 3
As joint laxity often causes no problems, and JHS symptoms vary, the unpredictable, diverse, evolving and fluctuating nature of their symptoms exacerbated others’ misunderstanding of the nature of JHS and patients’ reports of problematic symptoms to health professionals were often met with scepticism:
And if you’re inconsistent as well, they sort of go, she was alright with that last week, why is it this week she’s saying that, you know, that’s going to be difficult for her today.
Female patient C, 53 years old, focus group 2
Consequentially, health professionals perceived ‘a lot of mismanagement’ (female health professional E, > 20 years post qualification, focus group 4) of JHS by health professionals and that patients may be given erroneous information by some health professionals. One patient described a rheumatologist who had said ‘in his opinion, his professional opinion, that hypermobility doesn’t cause pain’ (female patient C, 53 years old, focus group 2). JHS-trained health professionals felt that they were required to ‘undo misconceptions, other health professionals’ understanding and what they have taught or implied to the patient about their condition. So for us we sort of have to unravel an onion so to speak, and it’s quite hard, yeah challenging I think’ (female health professional E, > 20 years post qualification, focus group 4).
Patients felt that JHS does not generally fit with health professionals’ models of acute injury and recovery, and that this may be a source of frustration for health professionals:
[Physiotherapists] get frustrated because their model of physiotherapy and what they’re taught and how joints move and how they get better, hypermobility is totally the opposite of what they’re expecting and they can’t understand that. I’ve had physio[therapist]s before say well stop the shoulder dislocating.
Female patient B, 32 years old, focus group 1
Diagnosis of joint hypermobility syndrome and subsequent referral
The heterogeneous nature of JHS symptoms, lack of recognition of the syndrome among health professionals and subjective diagnostic criteria were seen to contribute to often slow and convoluted diagnostic trajectories. Patients commonly remarked that ‘it takes so many years to get diagnosed’ (male patient E, 36 years old, focus group 5). Patients felt that education for health professionals was required, particularly, in order to facilitate timely diagnosis and referral:
I think it sounds like we’ve all been passed from pillar to post where people don’t recognise it or they just attribute the pain to something else, when a kind of snap diagnosis just comes out of the air and you know you progress from there, I don’t know, I mean there’s lots of things I still need to know about hypermobility but on the flip side I do think it’s the health professionals that need to know more.
Female patient G, 42 years old, focus group 5
Health professionals highlighted the difficulties in diagnosing JHS using the criteria available:
I think it’s the diagnostic criteria for hypermobility syndrome that’s actually part of the problem [. . .] So it’s almost going right back to the start, finding a slightly more sensitive diagnostic criteria that can help us to then manage it.
Female health professional F, 11 years post qualification, focus group 7
Both physiotherapists and patients recognised that, if JHS remained undiagnosed, chronic pain may develop that may be less likely to be responsive to physiotherapy. The biopsychosocial impact of living with untreated or inappropriately treated symptomatic hypermobility may lead to a more multidisciplinary approach being required:
And you see by the time – for me they come with quite a lot of psychological baggage, and you know, they are difficult patients. And then you’re trying to unravel what’s the primary and secondary issue here, is it that your mental health is actually what’s driving your hypermobility, or is it the fact you have such debilitating joints is making you mentally unwell. But by the time they get to us that’s so hard to deal with, [. . .] and they almost then, it’s a cry for help. So they’re desperate to get help so the psychological side comes out because the physical manifestation of what they’re suffering with is just so severe.
Female health professional E, > 20 years post qualification, focus group 4
Actually, there’s some that do quite well [with physiotherapy] as well in terms of . . . especially I think if you catch them early, really the key is, before they develop a lot of the chronic pain.
Male health professional B, 8 years post qualification, focus group 7
Patients also recognised that delays in diagnosis may result in the development of maladaptive responses to JHS, for example, compensatory postures, which are then difficult to rectify:
I was 15 when I was diagnosed and that was even too late really for me because the way I stand, the way I move, everything, my Pilates teacher – her grandson was 3 when he was diagnosed and he has Pilates, and physiotherapy now so he will get into habits of a life time.
Female patient G, 30 years old, focus group 1
For patients, receiving a diagnosis was considered to be essential in order to access appropriate treatment and patients felt that ‘the sooner you get the treatment the less likely it is that it is going to have such a great impact on your life’ (male patient E, 36 years old, focus group 5). However, physiotherapists felt that care pathways for JHS were not well defined and intimated that, as a result, patients may develop more complex problems or chronic pain issues:
I see the other end. I think we don’t have a structured pathway of care for hypermobiles, which is what I’m interested in developing, but we don’t have it. So there’s no rheumatologist in the trust that has a special interest in hypermobility, and my god I’ve tried to find one [. . .] So there isn’t a defined pathway of care for someone with generalised – with hypermobility syndrome, so . . .
Female health professional C, 25 years post qualification, focus group 4
So for me I feel that’s a key problem because I think we end up getting them too late, and if [name] had the support I feel to get these pathways better earlier.
Female health professional E, > 20 years post qualification, focus group 4
A diagnosis of JHS was considered to be necessary in order to access appropriate care pathways, for example, to be referred to secondary care for JHS rather than for a single-joint problem. Once patients had been diagnosed and referred to JHS-trained physiotherapists, many participants reported that their treatment was beneficial:
I found that once I was diagnosed with hypermobility the physio[therapy] I received [has] been really good.
Female patient G, 42 years old, focus group 5
I was originally seen by a physio[therapist] who hadn’t diagnosed with the hypermobility and then went back to a musculoskeletal specialist who then put me forward to specialist hypermobility physiotherapist and since then it’s been amazing; I feel like it’s been worthwhile and it felt like the right thing to do and I’ve been really enjoying it.
Female patient B, 27 years old, focus group 5
Theme 3: physiotherapy to manage joint hypermobility syndrome
Both patients and physiotherapists emphasised that physiotherapy would not be effective if individual joints were being treated in isolation and described difficulties in treating JHS within some NHS constraints, for example, where patients are generally referred for a single problematic joint:
Because of, I think, the way – at least in my experience – that the NHS seems to approach things, they have a sort of, ‘you’re here for one joint’ approach, which is quite difficult, because you go: ‘Well, I’m floopy all over’. And then you have to have the conversation about ‘Well, which is the most difficult?’ You’re like ‘Well, it’s kind of all related’, so if, like, if my knee is stronger and I’m doing less weird things with my knee, then my hip will feel better because – and I can say that, and to me it’s obvious, that if you fix – just because it’s your hip that hurts it doesn’t mean that it is actually the problem. It could well be that your knee is the issue, making you do weird things with your hip, but there’s this, ‘This is the joint, and we will deal with this joint,’ when that isn’t really . . .
Female patient C, 53 years old, focus group 2
Patients and health professionals reported that in the NHS, ‘usual care’ was normally up to six physiotherapy sessions to treat a specific joint. However, it was felt that this specific number of sessions was not necessarily appropriate for treating JHS.
They’ve got us as their clinical leads telling them to look at people globally, pick up this diagnosis, but then they’ve got their managers telling them you have to do six sessions [. . .] I should really be saying ‘I know you’ve got hypermobility, I know it’s all related, but actually I need six sessions with your back, I need six sessions with your shoulder and I need six sessions with your knee, and we need to negotiate that with your PCT [primary care trust] because otherwise [place name] is not going to get paid.
Female health professional E, 30 years post qualification, focus group 4
In all focus groups, the need for continuous, ongoing access to physiotherapy was highlighted, whether or not the patient was experiencing problematic symptoms. One patient felt:
The difficulty is, it’s a chronic condition and the only time you are actually able to access any care in the NHS is when you have an acute incident from it.
Female patient G, 48 years old, focus group 2
Health professionals, unless practicing privately, were equally frustrated by the lack of flexibility in the number of treatment sessions that could be offered:
And I think the limitations of, like, if you were receiving NHS treatment, then you’re only going to get so many sessions.
Female health professional D, newly qualified, focus group 3
In addition to the perceived limited number of sessions, physiotherapy may also be unsuitable and exacerbate symptoms if it ignores the complexity of JHS symptoms:
Then, as you say, being given some more exercises that weren’t helpful because they did seem to cause more pain which then sets you back even more and then you seem to get into the cycle of never sort of making any progress and then the treatment’s over because you only get a few sessions.
Female patient G, 48 years old, focus group 2
Theme 4: optimising physiotherapy as an intervention for joint hypermobility syndrome
Figure 4 illustrates the subthemes associated with this theme.
FIGURE 4.
Subthemes associated with theme 4: optimising physiotherapy as an intervention for JHS.

An ‘ideal’ physiotherapy service
All focus groups were able to provide descriptions of an ‘ideal’ physiotherapy intervention or suggested improvements which were based upon their own previous experiences of giving or receiving treatment. Health professionals’ and patients’ descriptions of ideal physiotherapy were notably similar (Table 6). Both felt that it was important to have continuity of therapist who was trained in JHS and who provided reassurance to the patient. Both patients and health professionals described the importance of flexible treatment, ensuring that the treatment is patient led, meeting and managing goals and expectations, taking a holistic, long-term approach and treating JHS rather than acute manifestations of the syndrome. The importance of ongoing, ‘maintenance’ physiotherapy for patients was also highlighted.
| Suggested improvements | Illustrative quotation from patient | Illustrative quotation from health professional |
|---|---|---|
| Therapist | ||
| Continuity of therapist to improve patient–therapist interaction/relationship | They get to know you as well, don’t they, and they know your lifestyle and they know what you do day in day out and therefore they can start to understand any trigger . . . they get to know you as a personFemale patient G, 30 years old, focus group 1 | For everybody, all patients, is continuity. But it’s especially difficult [for JHS patients] because they have so many different problemsMale health professional A, 6 years post qualification, focus group 3 |
| Therapist should be JHS expert | . . . the two physiotherapists I’ve had who’ve known about [erm] hypermobility have been a lot better than ones I’ve had in the past where they obviously haven’t had a clueFemale patient C, 60 years old, focus group 6 | . . . if they see somebody who hasn’t had an interest in that then they’re learning along with the patient at the same time. . . . So that’s quite difficult. It’s much better, isn’t it, to be seen by a specialist straight away who has got a broader knowledge base to be able to tap into their tools and skillsFemale health professional E, 30 years post qualification, focus group 3 |
| Therapists should provide reassurance and encouragement | quite often I’ll come out of the next physio[therapy] feeling much happier because they’ve reassured me that it’s not the end of the world and you know sometimes you have a bad week but it doesn’t mean that you won’t then have a good weekFemale patient F, 44 years old, focus group 1 | I think you’ve got to set achievable goals, then you’ve got to give a lot of reassurance and positive feedbackFemale health professional B, 28 years post qualification, focus group 4 |
| Physiotherapy | ||
| Flexibility in treatment, (e.g. number of sessions, content, specific techniques, mode of delivery, structure and focus) | . . . Or consider the person’s life style, . . . and that sort of flexibility, not just on what they’re asking the patient to do, even being flexible on the times of day or you know when these things can happen, you know make it interesting, you know we can’t all get in at 11 o’clock in the morning or 2 o’clock in the afternoon, we do need the half past 7’s the 8 o’clock in the morning, and the evening appointmentsFemale patient C, 40 years old, focus group 1 | Ideally, you’d want to have a service offer where they could tap into the service where they wanted to. If they suddenly got a flare up of something, say their hands started to give way or become more of a problem, then they could come back to youFemale health professional E, 30 years post qualification, focus group 3 |
| Patient-led treatment, while managing and understanding patient expectations | I think being patient led, . . . what it is that they want to achieve out of it and how the best way they can do that, and you know with a bit of guidance, like . . .Female patient B, 32 years old, focus group 1 | You try and tease out, you know, what are your expectations? No idea. So your hopes? No idea. I don’t know what I’m supposed to be doing . . . Forget that, what would you like to be doing? . . . Then you start to offer things and start to treat or start to address . . .Male health professional D, 5 years post qualification, focus group 7 |
| Meeting individual goals, to manage rather than cure | Or consider the person’s life style, you know consider what is going to be feasible, what they need to be able to get to in terms of achievement and you know and that sort of flexibility not just on what they’re asking the patient to do . . .Female patient C, 40 years old, focus group 1 | Because we’re very good at having goals, but you know, it’s making sure that the patients, they are the patients’ as wellFemale health professional G, 23 years post qualification, focus group 4 |
| Holistic, long-term approach | It’s not just your joints, it is all the other bits around it and that sort of slightly bigger picture, you’re probably going to be like this always, you need to think of different ways to manage different thingsFemale patient E, 34 years old, focus group 2 | . . . obviously if there’s a mechanical element to it we’d have to go into that, but as I say, the hypermobility is something that needs to be addressed more holisticallyFemale health professional E, 19 years post qualification, focus group 7 |
| Recognition of the need to treat multiple joints for JHS rather than individual problematic joints | I think they need to take notice that it is a full body condition rather than just individual, rather than just like one area, it is individual parts but they often concentrate on one area and then forget that the rest of the body hurts as well and that the pain can be interlinkedMale patient E, 36 years old, focus group 5 | If it was classified as a condition, [unclear 31:00] spondylitis or all those other rheumatological conditions which are, extend beyond one section, it’s treated differently isn’t it, so it’s got to do with its recognition presumably. It’s multi systemic, therefore you can treat multiple sites and therefore it may take longer in the endFemale health professional D, 22 years post qualification, focus group 4 |
| Focus on core strengthening and ‘correct’ movement | basically you’ve really got to give them a comprehensive set of useful exercises that will cover a whole range of joints, you know because most of our joints are affected, but particular core stabilityFemale patient E, 44 years old, focus group 1 | but really just concentrating on . . . on kind of core, and . . . good posture . . . concentrate on how they’re exercising, what they’re doing, technique rather than just exercising. Because a lot of them just . . . they find the most bizarre ways of doing things that I could never do in a million yearsMale health professional B, 8 years post qualification, focus group 7 |
| Maintenance physiotherapy for a chronic condition rather than acute problems arising from JHS | If it’s like say the diabetic clinic, where you get called every year to see them. . . . So could they not do a package where you actually went back every 6 months to see somebody regardless of how you were feelingFemale patient A, 60 years old, focus group 2 | So what we’ve tried to do is . . . a sort of self-referral back into the service, so they’re not having to go round the houses, and we pick them up quickly when they’re starting to get a flare up or a deteriorationFemale health professional E, > 20 years post qualification, focus group 4 |
Central role of education in managing joint hypermobility syndrome
Education for patients and health professionals and raising awareness of JHS within society as a whole was seen to be a key issue for participants in this study. Both patients and health professionals considered education to be a key underlying requirement to optimise the viability of physiotherapy for JHS. Because of the lack of understanding that patients perceived to be common among health professionals, patients felt that health professionals required more training in JHS. Some patients felt that they faced a situation in which they were providing education for the health professionals, and felt that this was not necessarily beneficial for them:
There’s lots of things I still need to know about hypermobility but on the flip side I do think it’s the health professionals that need to know more.
Female patient G, 42 years old, focus group 5
So there’s this odd situation where I’m explaining how it works to them and I think that it is not ideal and I think there does need to be better education for the physio[therapist]s because I think that is quite important that they tell you how and why things are happening to you, rather than vice versa because that’s unhelpful.
Female patient E, 21 years old, focus group 2
Health professionals also highlighted the need for education among health professionals and suggested a variety of educational sources, including websites, special interest and support groups and further professional training. One health professional highlighted the value of evidence-based guidelines:
Because if you get a patient in front of you, you need to be able to think, OK, what can I look at? What is the most effective? So guidelines that you were talking about, or maybe you can do, would be very helpful.
Female health professional E, 30 years post qualification, focus group 3
Health professionals felt that education was necessary for patients in order to facilitate a greater understanding of the condition:
I think a large part of it, as well, is to the education. To think that the patients don’t necessarily understand the condition. [. . .] Sometimes they don’t actually, nobody has never actually sat down and explained to them what that is and the implications. And what can actually be done to help them. So I think that’s a large part of it.
Female health professional D, newly qualified, focus group 3
Health professionals felt that education is necessary for patients develop realistic expectations of treatment and a better understanding of the rationale for particular treatment plans:
A lot of . . . I think what is . . . is education, ‘this is why I’m doing it’, and making sure they understand why I’m getting them to do these exercises . . . even if it doesn’t work and goes horrendously wrong, that’s fine, we can change that, but they’ve got to have an understanding of what we’re asking them to do and why we’re asking them to do it.
Male health professional B, 8 years post qualification, focus group 7
Patients similarly recognised that education helped them to fully engage with a prescribed treatment:
I think probably a third of my physio[therapy] session is me quizzing my physio[therapist] about what it is that’s hurting and why and what I can do about it and the way forwards, how I can perhaps do things slightly differently. So I think I get a huge amount of enlightenment from her . . . So I think education is really important and it needs to be part of what’s delivered to the hypermobile patient.
Female patient D, 54 years old, focus group 2
Theme 5: measuring success, and managing expectations, of physiotherapy
All participants recognised that the aim of physiotherapy was to manage, rather than cure, the symptoms of JHS, that ‘successful’ therapy did not mean the patient would be pain free; rather, the aim was for the patient to be able to manage their pain:
I think measuring success should be more about reaching a point of continuity where you know you might not be great all the time or you might not be really bad all the time but you’re manageable.
Female patient G, 30 years old, focus group 1
. . . you may not be expecting to get them pain free, but if they’re happy and if they’re managing the problem better, you know what to do to manage it, then you’re there.
Female health professional C, 19 years post qualification, focus group 3
Some health professionals raised concerns about patient expectation, that patients were expecting to gain more than the treatment could realistically offer. For example, one health professional felt that some patients often wanted, and expected, a ‘cure’:
I don’t want them to go away and think, well, she’s done nothing, when they expected me to fix it. So I have to say from the beginning, well, I can’t fix it, but this is what I can do. And to a point, that’s all you can do, isn’t it, really?
Female health professional E, 19 years post qualification, focus group 7
Some patients considered that physiotherapy would be successful if it resulted in some reduction in pain intensity, in some parts of their body. But contrary to some health professionals’ perceptions, patients did not appear to hold unrealistic expectations about the treatment that was being offered to them:
You can measure it [the success of physiotherapy] by parts of body I guess because I, although I don’t feel remotely better in many parts I still say that my last physiotherapy was a success because it significantly helped me with my shoulders so that I, I like suffer a lot less pain in that area of the body now, so I call it a success but when you get to my knees and ankles and neck and back it did do that much, the neck surgery was a success because that significantly reduced the neck pain although I still get probably more muscular now than any joints but that’s still again one part of it, so there’s lots of other areas that are still very bad, so erm I guess that in order to say that I’m better every bit would have to have improved significantly to say that they didn’t affect my day-to-day life, but to have individual parts improve is still a success.
Female patient F, 19 years old, focus group 5
Both patients and health professionals considered physiotherapy would be successful if it resulted in patients having a positive attitude, increased confidence and the ability to cope with daily activities relevant to the individual:
. . . whether that is feeling better equipped to handle your body going forwards, feeling like you’ve got the tools or feeling like you actually physically can do more, but I think it’s a little bit . . . it’s so subjective and almost impossible to measure. I think feeling better about your situation and your body, because I’m never going to feel brilliant. I think there are definitely ways you do feel better, whether that’s feeling better equipped or feeling you actually can now, I don’t know, walk 200 yards rather than one hundred without having to stop, or whatever, the feeling that you can or the feeling that you will be able to.
Female patient E, 34 years old, focus group 2
Because you may not be expecting to get them pain free, but if they’re happy and if they’re managing the problem better, you know what to do to manage it, then you’re there.
Female health professional C, 19 years post qualification, focus group 3
I feel more able to cope with my condition than I did before, and be able to measure that. Some kind of functional measure that might be patient specific – a functional scale.
Female health professional D, 22 years post qualification, focus group 4
Theme 6: patients’ and health professionals’ views on the proposed physiotherapy trial design
During the focus groups, patients and health professionals were presented with a proposed design of a physiotherapy intervention RCT (an assessment and advice session compared with an assessment and advice session plus six 30-minute physiotherapy sessions) as a means of creating debate to examine the range of opinions expressed on issues salient to the acceptability and feasibility of the proposed trial.
Views of proposed trial design
Trial inclusion/exclusion criteria and the implications of these were discussed by health professionals, in particular the potentially heterogeneous nature of the patient group which may include chronic pain comorbidities:
My thought is something that might skew the kind of outcome is if they were . . . if they’d come through a consultant pathway into this trial quite a lot of them are referred with dual diagnosis of hypermobility and fibromyalgia, and if they are referred with, you know . . . hypermobility may be the diagnosis, but if they’re referred for their fibromyalgia and they end up on a fibromyalgia coping skills programme they’ll get an awful lot of kind of input in that respect on how to manage a long-term condition, so it may not be that the input they’ve had for hypermobility is what’s been affected. So I don’t know how you would screen that, if you make that an exclusion criteria?
Female health professional A, 12 years post qualification, focus group 7
A minority of patients felt that the control arm, which consisted of a one-off advice session with a physiotherapist, would be acceptable to some patients because of the lack of current advice and information available:
I think it is a little bit of a case of . . . anything that makes you feel like you’re not on your own or anything that gives you any more information, or any more tips, or any ideas of things that might help. It’s that thing of feeling that you’ve got tools to help yourself, because you don’t want to be dependent on having to go and see a physio[therapist] every week or every month or however. I mean having someone who you can go back to check up on you and make sure everything is OK, that I think is ideal, but obviously difficult funding-wise in the NHS.
Female patient E, 34 years old, focus group 2
The majority of patient and health professionals, however, highlighted a number of concerns with the content of the control arm. Some health professionals felt that patients would require more than just advice:
I don’t think people generally like, what they would term, as being talked to. So if the advice was just talking, information giving but no hands-on or assessment of looking or something specific to their problem, I don’t think they would buy into that.
Female health professional B, 29 years post qualification, focus group 3
Some patients felt that they would not be willing to take part in the trial if they were randomised to the control arm because of the lack of ongoing physiotherapist support to ensure exercises are done correctly:
You then think ‘OK, I can do this’, and whatever you do, you could be doing it completely wrong which could be then be making you even worse, so then without, obviously you’ll then know that but you’ve just then wasted all that time just to know, OK, that was wrong. So I know with the physio[therapist]s that can happen as well but at least they got some sort of background to maybe steer you in the right place, so I think just straight out physio[therapy]’s going to be better.
Female patient D, 21 years old, focus group 1
I definitely would go no thanks I’m going to go down the physio[therapy] route because like you said you want constantly reassuring that you’re doing things the right way because someone would say that the diagrams with you know lean on the side, do this, do that, you could be doing it, but not doing it right, so you do need someone to say you’re doing it wrong and show you how to do it right, so I would definitely say no.
Female patient B, 27 years old, focus group 5
Patients felt that the control arm may not be viewed as equitable treatment in comparison with a physiotherapy intervention arm. Patients felt that those who were in enough pain to seek health care would require an active intervention to treat their symptoms and, therefore, may be reluctant to consent to the trial if the arms were not seen to be balanced:
I still think to leave everyone, if you told in that group ‘right half of you are going to go to physio[therapy] and half advice.’ I think wouldn’t you feel a little bit jipped, knowing ‘wait a minute how come I’m not going to get anything’?
Female patient A, 36 years old, focus group 5
If you’re in that much pain to actually go to the GP [general practitioner] to be referred. You need something . . .
Female patient B, 27 years old, focus group 5
Yeah, I think you definitely need something there that’s an alternative but obviously isn’t physio[therapy] but is something otherwise people are generally not going to be interested because they want to have something that they think might help them.
Female patient D, 32 years old, focus group 5
Patients and health professionals stated that if patients had specific problems that they felt needed treatment, they may be likely to withdraw from the trial if randomised to the control arm.
The only thing I would say is if I got . . . I would sign up, but if I got referred for the advice session and usual GP care I may well go back to my GP and ask for another referral. Because if you had a problem, you’d want some physio[therapy] . . . Depending on what level I was at when I . . . you know, if I felt I really needed it then obviously I’d be like, well, that’s a bit annoying.
Female patient A, 30 years old, focus group 6
See, because I think you might get people dropping out. Because if I had a problem and I was only being talked to and my problem wasn’t being identified and it was just general knowledge, I would soon seek somebody else, if I had the ability to do that.
Female health professional E, 30 years post qualification, focus group 3
Both patients and health professionals felt that the willingness of individuals to participate in the trial would be influenced by patients’ severity of symptoms and personal requirements and treatment expectations:
I think it depends on how bad you are and your symptoms are at the moment and myself is relatively manageable at the moment so I’d be willing to do that, I’d be happy to do that.
Female patient D, 32 years old, focus group 5
It depends on the individual to, wouldn’t it? If you’ve got somebody who’s got good feelings of self-ethnicity [sic] and internal locus for control, they might well go for it, because they think that’s fine, all I need is some good advice. For those who were thinking they might be getting treatment, they might well drop out if you were to allocate them.
Female health professional C, 19 years post qualification, focus group 3
Although more preferable to many patients than the control arm of the trial, some felt that the intervention arm of six physiotherapy sessions would not be enough to be beneficial:
I think you’ve also got to be realistic about what success you can get out of the group that had the physio[therapy] on just 6 half hour session because I don’t think in a 4-month period you will get much success I think you will be needing to look at it on a much longer term.
Female patient F, 44 years old, focus group 1
That is very quick, I mean even by the standards of what I’ve had into them, so . . . when I felt rushed with 10 sessions.
Female patient G, 30 years old, focus group 1
Suggested changes to trial design
Patients and health professionals offered a number of suggestions for augmenting the content of the control arm, including providing ongoing support through group meetings, gym membership and the provision of general, not targeted, exercises, so the two arms were perceived as more equitable:
So I think it has to, something else has to be, whether you do just get offered a holistic approach so they only, you meet with someone, the same number of sessions and talk about it or you just go to groups about it.
Female patient A, 36 years old, focus group 5
Can you give them six sessions of Pilates instead of the, with the advice leaflets and then they can come back to physio[therapy], you know does just going off and doing a Pilates class on your own help you manage it better than a physio[therapist].
Female patient B, 32 years old, focus group 1
What about one group has the specific one to one intervention and another group, basically, referred with exercise prescription to a gym? They’re still exercising, but it’s non-targeted, isn’t it?
Female health professional C, 19 years post qualification, focus group 3
I think if you gave an advice session plus like a free gym pass that you can use somewhere, I think that might be more of an incentive.
Female patient B, 32 years old, focus group 1
Both patients and health professionals suggested that having a delayed intervention for the control arm may be seen as more acceptable and could possibly encourage trial participation:
Maybe you could encourage more people, I think they’d be willing to do it anyway, ‘I’m not getting physio[therapy] right away although I was expecting to have some, at some point fairly soon’, you could try and get over the objections by saying that after this has completed then the people that were sent down the not doing anything route will just get referred onto physiotherapy anyway so they still get the physiotherapy they require.
Female patient D, 21 years old, focus group 1
Would they be able to receive, if you approve that having the six sessions [of physiotherapy] is beneficial, would they be then guaranteed to receive that at a later date?
Female health professional D, newly qualified, focus group 3
Conclusion
Both patients and health professionals described JHS as a painful, chronic condition with heterogeneous, fluctuating and evolving symptoms. Patients and health professionals reported a lack of recognition and understanding about JHS, and even some scepticism. Patients reported difficulties in being diagnosed and how they had encountered health professionals who they felt did not believe or understand their descriptions or their experiences of JHS. 49 The data indicate the importance of a timely diagnosis of JHS and referral for specialist care in order to facilitate effective treatment of JHS. Physiotherapy was viewed as beneficial if used to manage JHS holistically rather than to treat acute injuries in isolation. Patients valued physiotherapy when delivered by therapists who had an understanding of the chronic nature of JHS, as appropriate management could be delivered. The aim of physiotherapy should be considered to be long-term injury prevention and symptom amelioration. 50 Education for health professionals and patients, and raising awareness of the condition was seen as essential in order to optimise physiotherapy provision for JHS.
In relation to the proposed trial design, both patients and health professionals felt that the content of the control arm, consisting of a one-off advice session, may not be perceived as equitable to the physiotherapy intervention arm and concerns were raised that this may impact on trial recruitment and retention.
Strengths and limitations
The use of a qualitative methodology is a key strength in the current study, which is the first to our knowledge to undertake an in-depth investigation of the day-to-day experiences of managing JHS from both patients’ and health professionals’ perspectives. Employing focus group methodology allowed consensus to be gained regarding physiotherapy treatment, although it is recognised that using focus groups as a method of data collection did not permit as much in-depth exploration of some of the issues raised as other forms of data collection, for example, one-to-one interviews. The congruence between patients’ and health professionals’ descriptions and perceptions of JHS was notable.
Our participants were recruited from four different geographical locations in the UK and, therefore, had experiences of different health-care services. A diverse range of individuals in terms of demographics participated and analysis showed commonality in views and experiences. However, the research findings may be limited by the fact that our patient participants were already using the health system and the health professionals in these focus groups were experts in the field, providing specialist care for JHS.
The authors recognised that the participants cannot provide accounts of their experiences that are not influenced by the research act (the focus group) and that this represents a particular kind of social interaction, which plays a role in shaping the participants’ dialogue. The researchers were aware of this issue and it is hoped that any negative effects were ameliorated where possible, for example by the fact that multiple authors, from diverse methodological backgrounds, were involved in the data analysis.
Component 2: development of the physiotherapy intervention
Aim
Using the findings from component 1, the overall aim of this component of the study was to develop a comprehensive physiotherapy intervention package and associated training materials.
Methods
Development of the advice intervention
The research team were very conscious of some of the feedback from patients and health professionals as part of the HPoP study regarding the design of the control intervention. There was a concern that an advice-only intervention would have a negative impact on recruitment and retention. The initial preferred design of the study was to include a delayed intervention control arm. However, the HTA funding committee convincingly argued that this would cause problems for establishing the long-term effectiveness of the physiotherapy intervention in any future definitive RCT. In the absence of any convincing research evidence for the effectiveness of physiotherapy, the research team agreed that there was an argument for clinical equipoise between physiotherapy and an advice-only control. It was therefore agreed that all patients would receive a one-off advice session, supplemented by advice booklets from the HMSA56 and Arthritis Research UK. 57 It was also agreed that some specific key issues from the Arthritis Research UK booklet would be discussed in detail, but that all participants would also be given the opportunity to ask for specific advice related to their own circumstances. The research team agreed that the key topics for discussion from the Arthritis Research UK booklet57 should be as follows:
-
What is hypermobility? (p. 5).
-
How is hypermobility diagnosed? (p. 10).
-
Drugs (pp. 11–13) – although patients would also be advised to consult their GP if they wanted a review of their medication.
-
Self-help and daily living (p. 14).
This one-off advice session and the advice booklets would act as the control intervention for those patients randomised to the control arm of the trial in the later pilot RCT (stage 3) but would be piloted as part of stage 2.
Development of the physiotherapy intervention
A comprehensive whole-body physiotherapy intervention was developed using a working group of researchers, health professionals and patient research partners. The group included three physiotherapists, a consultant rheumatologist, a clinical psychologist and two patient research partners with JHS.
Discussion took place within the context of a number of guiding principles. These were related primarily to the resource context within which most physiotherapy services operate39 but also mirrored best practice as conducted at North Bristol NHS Trust. First, it was agreed that the intervention would be delivered on a one-to-one basis, as the needs of individual patients were considered to be so varied. Second, it was agreed that the intervention should be easy to implement in any outpatient department (and would therefore exclude complex or resource-intensive interventions such as hydrotherapy). Third, it was agreed that the intervention should include a maximum of six 30-minute treatment sessions over 4 months.
Two half-day meetings were held, the first of which reviewed the findings from component 1 of the research (the HPoP study) and discussed the implications of these data for the design of the intervention. At this meeting it was also agreed to adapt an existing supported self-management intervention with proven clinical effectiveness and cost-effectiveness, rather than starting from scratch. The Enabling Self-management and Coping with Arthritic knee Pain through Exercise (ESCAPE) programme58 was originally developed for chronic knee pain and is based on a self-efficacy theory of behaviour change. 59 The theory of self-efficacy is central to Bandura’s social cognitive theory,60 with self-efficacy describing the confidence one has is one’s ability to complete tasks or reach goals. The premise is that increased self-efficacy makes it more likely that one can successfully achieve one’s goals. In the context of JHS, goals might include being more active and managing the condition more successfully. There are a number of key factors that regulate self-efficacy, with learning by results a crucial component (i.e. past successful experiences can enhance self-efficacy). Also important are attitudes and subjective norms (from vicarious experience and social persuasion), and these drive intentions and behaviour. Experience of the outcomes from that behaviour then inform further self-efficacy judgements. 59 Both the ESCAPE programme and the new physiotherapy intervention for JHS therefore aim to enhance self-efficacy by positively influencing attitudes, subjective norms, intentions and behaviour.
The research team already had experience of using an adapted version of the ESCAPE programme’s intervention package61 in a previous sham-controlled RCT of exercise and transcutaneous electrical nerve stimulation. 62 We are also currently investigating its adaptation and application to a wider population of patients with chronic knee, hip and lower back pain in a cluster RCT. 63 The general approach is to help patients to become more physically active through developing the knowledge, understanding and skills to better manage their condition. This is achieved through a process of education, problem-solving, reflection and planning, along with gaining experience of exercise and learning from accomplishments. A key component of the original ESCAPE programme is learning through vicarious experience and social persuasion by conducting group education and group exercise. This is a key difference between the ESCAPE programme and the current intervention (which was conducted on a one-to-one basis) and, for this reason, we are careful not to draw too many comparisons. However, it was agreed that the broad approach and patient materials were considered to be an excellent starting point.
Following the first meeting the chief investigator drafted a patient handbook. This was adapted from that used for our previous transcutaneous electrical nerve stimulation study62 and involved a process of mapping content against some of the key themes raised in the HPoP study, removing topics irrelevant to JHS, developing new sections to address issues specific to JHS and generally reviewing and refining the handbook so that it was specific to JHS rather than chronic knee pain. Ongoing advice was taken from members of the working group through e-mail and telephone consultation.
The draft patient handbook was then discussed in depth at a second working group meeting where further changes and amendments were recommended. Patient research partner input was particularly important in ensuring that the language and layout was as user-friendly as possible. Following this meeting, the requested changes were made and a final draft of the patient handbook was agreed by e-mail. A key new section was developed relating to ‘taking control’ and this addressed many of the psychological issues raised by participants in the focus groups. This section was developed in close consultation with our clinical psychologist. Posture and Movement quality were also developed as new sections, led by physiotherapy colleagues. The Medication section was completely revised by our consultant rheumatologist and a further section on Sleep hygiene was added on the advice of our clinical psychologist to address some of the issues related to fatigue reported by focus group participants. A ‘menu’ of exercises was developed in consultation with physiotherapy colleagues. Other sections, such as Aims, Benefits of exercise, Goal setting, Pacing of activity, Long-term management, Staying active and the tools to support reflection and planning remained very similar, but the content and wording was updated to make them specific to JHS. A section related to diet was removed as this was not raised by focus group participants.
The handbook was designed to support the face-to-face physiotherapy sessions. To maximise the use of time within the physiotherapy sessions, the handbook encouraged patients to reflect following sessions and to read information and prepare in advance of the next session. Time was allocated at the beginning of each session to allow participants to discuss any specific issues that they might have in relation to the educational topics. The majority of the session was then dedicated to exercise, with the physiotherapist selecting specific exercises from the ‘menu’ available at the end of the booklet. Exercises were selected on the basis of findings from the initial clinical assessment and were adapted as necessary over time. Space was provided for notes to be added regarding exercise adaptations or progressions. Patients were also encouraged to increase their general physical activity, choosing an activity that they enjoyed and that could form part of their daily routine. A physical activity action plan and activity diary was included in the handbook to assist with planning and self-monitoring. Reflection encouraged problem-solving in relation to the topics, exercises and physical activity.
The final draft handbook was prepared as an A5 booklet. It included six sections, one for each session, covering the following topics:
-
Session 1: aims, benefits of physical activity, posture, movement quality and pain relief.
-
Session 2: medication, sleep hygiene, goal-setting, exercise and physical activity.
-
Session 3: pacing of activity, exercise and physical activity.
-
Session 4: dealing with set-backs, exercise and physical activity.
-
Session 5: taking control, exercise and physical activity.
-
Session 6: long-term management and staying active.
A training package for physiotherapists was also subsequently developed by the chief investigator, comprising a slideshow presentation addressing the following areas: definition, diagnosis and prevalence of JHS; an overview of the impact of JHS and its management, including theoretical aspects and evidence for the effectiveness of physiotherapy; patient and health professional perspectives on physiotherapy; the process of developing the physiotherapy intervention package and its guiding principles; an introduction to JHS assessment; an overview of the advice intervention; and a session-by-session overview of the physiotherapy intervention. This was followed by an introduction to the design of stage 2 of the research (the pilot of the intervention) and relevant study procedures including screening of referrals, assessment and consent, treatment and questionnaire administration. The training was designed to be delivered in 5 hours, which included a 15-minute break for coffee and 45 minutes for lunch.
This final draft intervention and training package was evaluated as part of stage 2 of the research and will be reported in Chapter 3. The draft patient handbook and training package are not included in this report, as they underwent further revision after stage 2. The final versions are reported later in this report.
Strengths and limitations
The process of developing the interventions had a number of strengths, including being very collaborative and informed by findings from the patient and health professional focus groups. The design of the physiotherapy intervention was underpinned by the theory of self-efficacy and built on an existing intervention package with proven clinical effectiveness and cost-effectiveness in another musculoskeletal condition. It is recognised, however, that the decision to deliver the physiotherapy intervention on a one-to-one basis as opposed to a group format might limit the proposed effectiveness of socialisation. 59 The advice intervention made use of existing resources developed by a major charity and a patient organisation56,57 and, again, this was seen as a strength.
Conclusions and implications
Overall, stage 1 of the research provided an important insight into patients’ lived experiences. It also provided important patient and health professional perspectives on the physiotherapy management of JHS. This information was instrumental in informing the development of a draft physiotherapy intervention and associated training package.
The findings also informed the design of the subsequent pilot RCT. Of note were the concerns from patients and health professionals about the proposed use of an advice-only control arm. On discussion, the research team decided to maintain this study arm but to ensure that there was an opportunity for patients to receive personally tailored advice in addition to issuing advice booklets. Patients could, therefore, generate their own questions that could be addressed by the physiotherapist. However, the potential impact on recruitment and retention of a perceived lack of equipoise between study arms remained a concern.
Chapter 3 Stage 2: pilot of the physiotherapy intervention
Aims and objectives
The primary aim of this stage of the research was to evaluate the physiotherapy intervention by implementing it with a small sample of patients from two NHS trusts (North Bristol NHS Trust and the Royal National Hospital for Rheumatic Diseases NHS Foundation Trust). A qualitative evaluation from the perspectives of patients who received the intervention and physiotherapists who received training and delivered the intervention was therefore the main focus. Secondary aims included gathering information related to patient referrals, application of the inclusion and exclusion criteria, recruitment rates and acceptability of the study questionnaires.
Specific objectives were to:
-
deliver a comprehensive physiotherapy intervention for adults with JHS in two NHS trusts
-
interview patients about their views and experiences of receiving the intervention and the acceptability of the study questionnaires
-
interview physiotherapists about their experiences of receiving training and delivering the intervention
-
gather information about referral rates, application of the inclusion and exclusion criteria and recruitment rates
-
refine the intervention package, training and study procedures for the forthcoming pilot RCT.
Methods
The physiotherapy intervention was delivered to people with JHS referred to the rheumatology physiotherapy services within the two NHS trusts. Recruitment took place across a 1-month period (August 2013), with subsequent treatment lasting 4 months (until the end of December 2013). Qualitative interviews were undertaken with physiotherapists and patients to determine the issues involved with the content and delivery of the intervention and its acceptability, and to help refine the design and content of the pilot RCT. This study and the subsequent pilot RCT were conducted under the name ‘Physiotherapy for Hypermobility Trial’ and received ethical approval from the National Research Ethics Service Committee South West – Exeter (reference number 13/SW/0083).
Physiotherapist recruitment
Four physiotherapists (two from each NHS trust; one man and one woman at each site) were trained to deliver the intervention. All physiotherapists had extensive experience and a particular interest in treating JHS patients. A principal investigator (the lead physiotherapist) was appointed at each site.
Patient recruitment
Patients referred for physiotherapy within the two NHS trusts who had a suspected diagnosis of JHS were invited to participate. Both NHS trusts had rheumatology physiotherapy services with expertise in managing JHS and received referrals mainly from GPs and rheumatology consultants. Potential participants were identified by the principal investigator from their referrals (looking for specific reference to hypermobility) and were sent a study information pack and a reply slip to be returned if they were interested in taking part. An initial physiotherapy assessment was then arranged, during which the inclusion and exclusion criteria were confirmed. Those eligible and consenting to take part then received the physiotherapy intervention. Participants included both those with a new and more established JHS diagnosis.
Inclusion criteria
-
Aged > 18 years.
-
Able to give informed consent.
-
Able to understand and communicate in English (with the assistance of an interpreter as necessary).
-
Fulfil the Brighton criteria for JHS (see Table 1).
Exclusion criteria
-
Other known musculoskeletal pathology causing pain, particularly osteoarthritis and inflammatory musculoskeletal disease such as rheumatoid arthritis.
-
Other serious pathology including malignancy.
-
Conditions affecting ability to exercise, for example uncontrolled cardiovascular disease.
-
Recent physiotherapy for JHS (within the last year).
-
Pre-existing psychological distress or psychiatric conditions.
Quantitative aspects
A screening proforma, assessing the Brighton diagnostic criteria and the other inclusion and exclusion criteria, was completed by the physiotherapist at the baseline assessment (see Appendix 3). The baseline study questionnaires were also piloted with patient participants. This included a biographical questionnaire (see Appendix 4); a questionnaire booklet (see Appendix 5) containing the Multidimensional Health Assessment Questionnaire (MDHAQ), a draft version of the Bristol Impact of Hypermobility (BIoH) questionnaire, pain visual analogue scales (VASs), the Exercise Self-efficacy (ESE) scale and the European Quality of Life-5 Dimensions-5 Levels (EQ-5D-5L); and the Measure Yourself Medical Outcome Profile (MYMOP) (see Appendix 6). The biographical questionnaire and questionnaire booklet were mailed to potential participants prior to the baseline assessment and they were asked either to complete and return them in advance or to bring them to their appointment. Completed questionnaires were returned to the chief investigator using prepaid return envelopes.
The MDHAQ is a rheumatology-specific outcome measure64 that has been used successfully in a wide range of other rheumatological conditions, including Behçet syndrome, cutaneous lupus erythematosus, fibromyalgia, gout, osteoarthritis, psoriatic arthritis, rheumatoid arthritis, scleroderma, spondyloarthropathy, systemic lupus erythematosus and vasculitis. It has demonstrated good test–retest reliability and face validity. 64 It contains items related to physical function (scored 0–10), pain (scored 0–10), patient global rating (scored 0–10), fatigue (scored 0–10) and self-reported joint count (scored 0–10). The function, pain and global rating scores can be summed to provide a Routine Assessment of Patient Index Data 3 (RAPID3) score (scored 0–30), which has been shown to compare favourably with other scores such as the Disease Activity Score and Clinical Disease Activity Index. 65 The self-reported joint count item is also known as the Rheumatoid Arthritis Disease Activity Index (RADAI). Higher scores on all MDHAQ items represent increasing condition severity. Although the MDHAQ has not previously been used in JHS patients, it was considered potentially useful by the research team because of its focus on multiple-joint pathology.
The BIoH questionnaire is the first condition-specific outcome measure developed for JHS. It was still undergoing development by the research team at the time of this pilot. The version administered to participants as part of the pilot had 104 items, 94 of which were scored. It has since undergone a process of item reduction and the final version has 55 scored items, this version was administered as part of stage 3 of the present research. It incorporates the Bristol Rheumatoid Arthritis Fatigue numerical rating scales, which have demonstrated good reliability and responsiveness. 66 The final version of the BIoH questionnaire has been shown to validate very well against the SF-36, particularly the physical function component score. 67 The final BIoH questionnaire produces a score out of 360, with higher scores representing a more severe impact of JHS. The questionnaire is currently undergoing further testing with patients and health professionals to determine its test–retest reliability, sensitivity, appropriateness, validity, acceptability, feasibility and interpretability.
The wording of the anchors for the four pain VASs was adapted very slightly from those used in a previous study of exercise for JHS. 36 VASs are generally considered to be valid, reliable and responsive instruments for the measurement of pain, although they are unidimensional. 68 Each scale was measured on a 0- to 100-mm horizontal line, with higher scores representing higher pain intensity.
Bandura’s ESE scale69 was the version adapted by Everett et al. 70 It has been well validated in patients undergoing cardiac rehabilitation and we have previously successfully used this scale to assess self-efficacy for exercise in knee osteoarthritis. 62 The scale asks participants to rate how confident they are (on a 0–10 scale) that they can exercise regularly in 18 different circumstances. The scale is converted to a score out of 100, with higher scores representing higher exercise self-efficacy.
The EQ-5D-5L is an established health outcome measure applicable to a wide range of health conditions and treatments that can be used to produce health economic estimates. It produces a single summary index on the basis of responses to five dimensions related to (1) mobility, (2) self-care, (3) usual activities, (4) pain/discomfort and (5) anxiety/depression. Its validity and responsiveness has been well established in a range of chronic pain conditions. 71
The MYMOP aims to assess the outcomes that each individual patient identifies as being most important to them72 and was adopted to address the comments of some focus group participants that the success of physiotherapy might be very individual. The MYMOP was completed with the patient as part of the baseline assessment.
Owing to the substantial delay to the start of the research reported in Chapter 2, Methods, follow-up questionnaires were not administered in an attempt to recoup some lost time. Data are presented using descriptive statistics. Owing to the ongoing development of the BIoH, those results have not been reported in this chapter.
Qualitative aspects
During the pilot implementation of the intervention, face-to-face interviews were conducted with patients 4 months after starting treatment to consider their experiences of JHS and physiotherapy. We also sought to gather the views and experiences of physiotherapists and of patients who did not complete the intervention.
Procedure
All patients and physiotherapists participating in the physiotherapy intervention were asked if they were willing to be contacted about taking part in an interview at the time of consent. All participants provided written, informed consent prior to the interview. Topic guides were used to facilitate the interviews and, in line with an inductive approach, were revised in light of emerging findings. Patient interview topic guides (see Appendix 7) focused on their experiences of the advice and physiotherapy interventions; changes experienced or made following participation; what worked well; and any aspects of the intervention where improvements could be made. Physiotherapist topic guides (see Appendix 8) focused on training; the content, delivery and acceptability of the advice and physiotherapy interventions; and suggestions for improvements. Patient interviews took place in the patients’ home or in the hospital where they were receiving their physiotherapy treatment. Physiotherapist interviews took place in the hospital where the physiotherapist normally worked. Open-ended questioning techniques were used to elicit participants’ own experiences and views. Interviews lasted between 30 and 62 minutes and were conducted by an experienced qualitative researcher (RT) employed on the project.
Data analysis
All interviews were audio-recorded, fully transcribed and anonymised. Transcripts were coded using framework methodology. 73 Analysis began shortly after data collection started and was ongoing and iterative. Each transcript was read, reread and then coded on a line-by-line basis, so that salient content was integrated into the coding framework under predetermined codes or new codes generated by the data. Predetermined codes included patients’ and physiotherapists’ views on the study information, trial recruitment, information/advice session, physiotherapy session, trial information booklet, homework and suggestions for improvements in the trial design. Emergent codes generated by the data included patients’ expectations and comparisons with previous physiotherapy. Coding aimed to classify all of the data so that they could be compared systematically with other parts of the data set. The emergent themes were discussed by the multidisciplinary research team to ensure credibility and confirmability.
Results
Quantitative results
A total of 42 referrals were assessed for eligibility, of which 23 did not meet the inclusion criteria. A further 11 participants did not respond or failed to attend within the recruitment period. The remaining eight participants consented to take part in the pilot of the physiotherapy intervention (19% of all referrals) (Figure 5). One participant withdrew following consent because she was too busy (this participant also did not return a baseline questionnaire). Another participant withdrew after she had received four physiotherapy sessions as she was diagnosed with systemic lupus. This participant was still happy to be interviewed about her experience of being involved with the study and her baseline questionnaire was also analysed. One participant failed to return a baseline questionnaire despite receiving a reminder. A further participant was not able to be contacted to arrange an interview.
FIGURE 5.
An abbreviated Consolidated Standards of Reporting Trials (CONSORT) flow diagram.

The main reason for exclusion was other musculoskeletal conditions (n = 14). Closer analysis of this data showed that six of these were excluded on the basis of fibromyalgia syndrome, which is a common concomitant diagnosis. Of those excluded on the basis of psychological conditions (n = 3), all had received a diagnosis of anxiety or depression.
Table 7 summarises the participant characteristics and baseline outcome measure scores. All participants were female and the mean Beighton score approached 6/9. Pain scores were moderate (in the region of 50%) and the mean RAPID3 score also fell within the ‘moderate severity’ category. Mean exercise self-efficacy was relatively high in this group, approaching 60/100.
| Demographics and baseline characteristics | Values |
|---|---|
| Age (years), mean (SD), n = 8 | 33.5 (7.4) |
| Sex (male-to-female ratio), n = 8 | 0 : 8 |
| Beighton (maximum = 9), mean score (SD), n = 6 | 5.8 (2.0) |
| MDHAQ, mean score (SD), n = 6 | |
| Function (maximum = 10) | 1.2 (1.1) |
| Pain (maximum = 10) | 5.8 (2.1) |
| Patient global (maximum = 10) | 4.0 (3.3) |
| RAPID3 (maximum = 30) | 11.0 (6.0) |
| RADAI (maximum = 10) | 1.9 (1.1) |
| Fatigue (maximum = 10) | 4.3 (3.3) |
| Pain (maximum = 100 mm), mean score (SD), n = 6 | |
| Most affected joint at rest | 56.7 (26.3) |
| Most affected joint on movement | 55.7 (34.3) |
| Joints in general at rest | 51.0 (29.1) |
| Joints in general on movement | 48.2 (33.6) |
| ESE scale (maximum = 100), mean score (SD), n = 6 | 59.7 (26.2) |
| EQ-5D-5L index, mean score (SD), n = 6 | 0.56 (0.29) |
Qualitative findings
Four physiotherapists (two men, two women) were interviewed. At the time of interview, three physiotherapists had treated two patients using the physiotherapy intervention. Two of the physiotherapists had initially recruited three patients, although two patients withdrew later in the study. One therapist had not treated any patients using the trial intervention, but had discussed the booklet and its contents with patients not involved in the trial. All physiotherapists had extensive experience and a particular interest in treating JHS patients. Six JHS patients who had participated in piloting the intervention conducted an interview (Table 8). One patient withdrew from the study as they were too busy and it was not possible to contact another patient regarding participating in an interview. One patient withdrew from treatment as she received a diagnosis of systemic lupus, but she still consented to be interviewed.
| Participant number | Site | Age (years) | Sex | Interviewed | Comment |
|---|---|---|---|---|---|
| 101 | 1 | 22 | Female | No | Unable to contact |
| 102 | 1 | 35 | Female | Yes | – |
| 103 | 1 | 31 | Female | Yes | – |
| 104 | 1 | 42 | Female | No | Withdrew after consent – too busy |
| 106 | 1 | 41 | Female | Yes | – |
| 201 | 2 | 29 | Female | Yes | – |
| 202 | 2 | 27 | Female | Yes | – |
| 203 | 2 | 41 | Female | Yes | Withdrawn after four treatments – diagnosed with systemic lupus. Consented to be interviewed |
Physiotherapists’ views on initial training
Physiotherapists felt that the training was based on the current practice at the two research sites and that it was aimed at physiotherapists who were less experienced in managing JHS:
Yeah, I think that’s the task, is taking the practice from [city name] and from here, and, and also [city name][. . .] generally the practice there is very good and that’s what we built the, the treatment on, which is, which is fine. Um, it’s, I suppose, teaching other people to do that and those sorts of things.
Physiotherapist 102
The focus of the training was on the assessment of JHS, the theoretical background of JHS, the paperwork involved in the trial, the use of the booklet and the content of the physiotherapy intervention:
So it was quite formulated and quite, er, specific with the intervention, ‘cause they didn’t want us to, erm, freestyle too much, because you need to be able to compare and contrast, I guess.
Physiotherapist 202
It was suggested that the training package could be enhanced, particularly for less-experienced physiotherapists, by the addition of more practical training and a greater focus on JHS assessment:
And it’s, um, necessarily getting them comfortable treating hypermobility. [. . .] I think, again, a little bit more in terms of, sometimes, teaching on practical aspects of teaching of, of hypermobility and common things they do, and how they do it, and exactly what we’re looking for. Um, I, that’s what I want, depending on who else was in the trial [. . .] but I think we do need to, probably, in terms of assessment wise, apart from hypermobility, what are we looking at muscle control wise [. . .] And sometimes that’s the bit, if I didn’t have any experience of treating hypermobility and came in, and I had one of our junior physio[therapist]s and said, ‘There you go, do this’. That’s the bit I’d be slightly concerned they don’t necessarily do so well.
Physiotherapist 102
One physiotherapist felt that a particularly positive aspect of the training was the opportunity to revisit the evidence base for the use of physiotherapy to treat JHS:
I think it was good to have the recap of the evidence base, and obviously the reason why we’re there and things like that, that’s always good as a reminder more than anything else.
Physiotherapist 101
The training may have been influenced by the assumption that those undergoing training were already experienced in treating JHS patients:
Well, there was an assumption that we already knew quite a bit about it. Erm, because this is a pilot trial, I think they want to know if we cannot deliver it, then somebody who has no experience of hypermobility might really struggle.
Physiotherapist 202
Patient feedback relating to the study information
Patients had a clear understanding of the aims of the trial from the information provided. Participants described the information positivity and appreciated that JHS was being recognised and the topic of empirical investigation:
Yes it [the information] was really useful. It was fine, really clear. [. . .] it was really good. It was just really helpful. I think it was just that initial thing of it being recognised. The idea that something was happening for that and that was, you know – yes, it was really good.
Patient 102
One participant, however, found the information provided and the completion of the questionnaires ‘a bit depressing’ on realising the extent to which JHS had impacted on her life. Nonetheless, the information also made her realise that things were not as bad for her as they could be:
Yes, I think for me it was a bit depressing because I didn’t really realise how much this impacted on my life when I filled it in. Then I thought oh OK, yes, it does impact a bit. I was glad I could do my buttons up and things like that. It would give you a context of other people and their issues. But then realising, I suppose it made me realise it was a good visual demonstration, variations, because when you’re in the middle of a really bad flare up, you kind of forget that it’s not always that bad. If you’ve had 6 weeks of feeling awful, you’re just ‘Oh, it’s always like this, it’s terrible’. Then it isn’t.
Patient 106
Trial recruitment
Patient views
Potential patient participants were informed about the study via their GP, rheumatologist or JHS specialist physiotherapist. All who took part were happy to participate in the study, keen to be involved in research and to try something that they felt might help their symptoms or that they could learn from:
I did kind of jump at the chance for a trial ‘cause I knew it would be much more focused in its approach.
Patient 203
One participant described feeling frustrated by previous physiotherapy and, therefore, keen to be involved in a trial of specialist JHS care:
I think because it was frustration that [physiotherapist’s name] was probably the only person that’s ever actually paid attention to what I was saying and appreciate it, and had seen other people with the same problems. She knew it was an issue, and they’d been researching it, it made me want to partake in it more than maybe just going to see a different physio[therapist] who didn’t, necessarily, think hypermobility was an issue and that it was just achy joints.
Patient 103
Physiotherapist views
Therapists felt that patients most likely to benefit from the intervention were those without comorbidities such as chronic pain or depression and felt that the inclusion/exclusion criteria were therefore appropriate:
I actually think the inclusion/exclusion criteria are very good. Um, in terms of, um, actually purely getting the hypermobile type people that will, will benefit. Um, what they’re probably is, is there’s a, in terms of the ones that are depressed, have other surgery and other particular problems that aren’t going to do so well. Um, there is a group of those that aren’t really covered by this and they will take longer and those sorts of things. So in a way probably the exclusion criteria are probably slightly biased to showing, getting the people that we will help.
Physiotherapist 102
Initial information/advice session
Patient views
The topic guide aimed to ask patients to distinguish between the first advice session and subsequent sessions. However, it may have been difficult for some participants to dissociate recollections of the first session having then undergone subsequent physiotherapy sessions. Generally, the advice session was recalled positively and patients appreciated the opportunity to discuss their experiences in some depth with a health professional:
It was very thorough as well, so it meant, even though I was pointing out 100 things that were causing me grief, it was nice to have that time to be able to go through everything knowing that’s what would actually help with the solution and the physio[therapy] afterwards. So it wasn’t daunting or anything like that. It was just quite nice to sit down with someone who knew what I was talking about. When I was saying, ‘I click all the time’ it wasn’t like, ‘Well stop clicking’.
Patient 103
One participant described feeling ‘optimistic’ after the first session:
And, actually, I think I came away thinking, probably, more optimistic because again, because I think I know under, essentially I do know the underpinning stuff, I know I need to keep myself well, which is core strength. Actually it’s all the other bits that I need somebody to unpick my life and actually go, ‘You’re doing too much here . . . You’re doing too much one day, so no wonder you don’t feel that great’. And actually take a, take a step back kind of thing. Um, but also speaking to somebody who’s doing that research who actually understands, that actually life doesn’t work like that.
Patient 203
Physiotherapist views
Physiotherapists felt that there was a lot to cover in the first session. They felt that although 1.5 hours was probably realistic, there may be a slight danger of ‘losing’ patients if physiotherapists tried to cover too much in this session:
So, time wise, it’s not too bad, just a lot of content and I think slight danger of losing people at the opening stage.
Physiotherapist 202
One therapist suggested splitting the initial session into two, although it was recognised that this would result in repeated journeys for the patient:
I think practically speaking, that’s almost like bringing them back twice to do the same thing. So you could be considered to be replicating, but, erm, I think that would be the thing that would be easiest, to be able to either, um, break it up into trial related paperwork and questions and erm, physio[therapy] intervention, assessment and treatment, really. Erm, but I don’t think there’s a way around it. I think it’ll have to be done in one session. I think it’s going to take a long time.
Physiotherapist 202
It was also felt that the delivery of this first session improved as physiotherapists became more familiar with the trial requirements:
I think maybe, definitely, the more I did, the slicker I got at it.
Physiotherapist 202
One physiotherapist noted that patients were not ‘just trial candidates’ – that the patients still required treatment if they did not meet the trial inclusion criteria:
Erm, there’s also pressure that even if they don’t, you still have to treat the session as though it was a normal assessment session, because in case they don’t meet the trial, you’ve still got to do something with them. So, erm, you’re still treating them as a person, not just a trial candidate.
Physiotherapist 202
Trial information booklet
Patient views
Patients valued the booklet and each participant used the booklet in a slightly different way. For example, some valued the activity diary, whereas others commented positively on the different topics in the book. Patients felt that the booklet was clear to follow and well laid out, and that it could be adapted to suit their individual needs. Others valued having the booklet to refer to as-and-when needed and used it to help explain the nature of JHS to others. Thus, the booklet helped to validate patients’ experiences and provided them with information that could be shared with others:
It was good. It was very informative. The booklet is really good. Not that anyone else really understands, but when I do talk to them about hypermobility if I show them the book, they kind of in a way get it a little bit more. Hypermobility is not so well known they do kind of understand a little bit more once they read it.
Patient 201
Patients felt that the information in the booklet was appropriately pitched. However, participants also noted that it did not contain a lot of information that was new to them:
So whilst we kind of went through it, a lot of the stuff wasn’t new to me, it wasn’t anything I had to learn, it wasn’t stuff to read through. But at the same time it just clarified in my mind that, ‘OK, they get it’ . . . But to me I needed a bit more because I’m obviously doing all those things and it’s not making any difference. So whilst all that is great and I appreciate it pinpoints what’s wrong, I still need something else.
Patient 103
The booklet provided patients with a reminder of strategies to manage their symptoms, and of previously held information, and helped them to develop a deeper understanding of JHS:
I think it was certainly useful, it was more of an affirmation of the things that I knew already. But some of it was really useful to connect the dots, if that make sense? So things that I’d thought about quite separately it was quite interesting to see them together in one thing. That was really positive actually.
Patient 102
Participants were prompted to think about whether or not any other sort of media might be helpful. One participant suggested mobile technology while another felt that visual reminders of exercises was important:
Because sometimes it’s all well and good going along to your physio[therapy] sessions and going, ‘Oh yes, exercises, oh great’. But actually if you’ve got nothing to follow it up with it can leave you feeling a bit lost. [. . .] I’ve realised what I need to have is like a wall chart, like an A4 sheet of paper with my exercises on. Because I find with the booklet I’m flicking and then missing a page, so I was finding it quite difficult to work out what I should be doing in order [. . .] Because then I can stick it up on the wall. While she’s having dinner I can go, ‘Oh I’ll do 20 of those now’. A visual reminder works much better for me.
Patient 102
Physiotherapists’ views
Physiotherapists felt that the booklet helped to provide a focus and structure for the intervention and that this would be particularly valuable for new members of staff:
They said it was quite good, coming in, fairly new to the department; it was quite nice to follow that structure. It was quite nice for them as therapists to follow something. So, I suppose that’s quite a good tool in terms of you wanting continuity with therapy interventions.
Physiotherapist 201
The requirement to adhere to the structure of booklet may have potentially resulted in therapists spending less time addressing specific patient needs. Working through the booklet could, for example, have resulted in rushing or truncating the hands-on physiotherapy component of the session. Although physiotherapists conceded that whether or not this was problematic depended upon the individual patient, they nonetheless did report occasions when providing patient-led care and following the booklet proved to be a difficult dichotomy:
I’m a little bit undecided. I thought it was very useful in terms of it did provide some structure, um, and it gave, in terms of some other stuff to do, and it talked through a lot of the education. Often without that you would, kind of, sometimes miss a little bit here or there. Um, on the flip side I kind of ended up, I found that I working through the workbook and I’d, ‘Op . . . I’ll go back’. And it, kind of, then took me less away from actually assessing the patient, looking at the patient and those sorts of things.
Physiotherapist 102
Moreover, this participant felt that the booklet could potentially be ‘dangerous’ without adequate training, to both patients and physiotherapists:
As it stands now, as we’re doing it, if we were just to give therapists a booklet, I think it could be dangerous in the wrong hands and without the knowledge.
Physiotherapist 102
Along the same lines, therapists felt that it was important to demonstrate the correct way of doing exercises and one physiotherapist felt that the booklet did not provide comprehensive explanations relating to why a particular exercise was required:
It would give them, yes, the starting blocks, but it doesn’t give them huge amounts of reasoning, um, and as I say, more information about the quality. And obviously a lot of our work is correcting the compensations and things like that, and they would never get any of that in a booklet.
Physiotherapist 101
Although the information in the booklet was generally considered to be adequate, it was remarked upon that the information could be expanded on in treatment sessions as required:
I think the booklet errs on basic and so is not going into huge amounts of detail for patients. I think the idea is that it’s the basic information that then we can expand on in the treatment sessions and things like that.
Physiotherapist 101
One physiotherapist felt that, even if patients initially considered that the information in the booklet was not of relevance to them, adhering to its structure allowed topics to be discussed that may have otherwise been circumvented, and, as a result, improved outcomes:
Sometimes you can see them rolling their eyes a little bit, with, ‘Why are we discussing it?’ But, actually, it’s really relevant and really important that by the end of discussing it, you’ve had another breakthrough, or, erm, you’ve gained some insight into what’s causing a lot of their problems, which you may not have done if you picked up off their verbal clues that they didn’t really want to talk about it and you’re thinking, ‘I didn’t really think it’s very high on the agenda either’, and then you’ll just park it, perhaps to go into later, whereas this makes you do it.
Physiotherapist 202
Some changes to the booklet were recommended, for example font size; a slightly larger booklet that would allow making notes easier; and making the booklet more like a diary. Patients with additional needs were also discussed:
I mean, for the average person, I think it’s fine. It’s not too complicated. I think the other thing I guess you need to take into account is – but then, they’re probably excluded – is often you get your ADHD [attention deficit hyperactivity disorder] patients or dyslexia. Whether there are alternate formats. We don’t often see ethnic minorities here, so that’s probably not an issue in terms of language and stuff. The size of the print’s probably – maybe here needs to be a little bit bigger, just for, you know, so you take into account people’s eyesight. It could be slightly bigger, maybe, the booklet, so that they’ve got a bit more space. I don’t know what [colleague’s name] says, but I guess what might be quite nice is you have a slightly bigger one that they can put their own notes to it. So it becomes their own proper little diary that they can . . . Rather than being too small, that’s a possibility, maybe.
Physiotherapist 201
Physiotherapy sessions
Patient views
Patients generally felt that there was scope to adjust the method and pace of the sessions to meet their individual needs and felt that physiotherapists were willing to do this:
They’d tailor exercises to suit where my flexibility and my problems were.
Patient 102
One patient valued seeing the same physiotherapist at each appointment:
. . . by seeing the physio[therapist], the same person, that was really important. Um, because they were able to see the, my changes. I think that’s so crucial. Um, and I think, again, emotionally how he saw me through, he could tell from the moment I stood up in the waiting room to walking through what had happened, what happened in that week preceding.
Patient 203
Although another felt that they may benefit from seeing different physiotherapists:
It’s good having the same one because you don’t have to go through, from start to finish. I suppose you lose the knowledge that they have of everything you’ve been through or what you’ve done before. So it’s good to have the same person, but it might just be nice . . . I felt the benefit from having someone else come in on the session.
Patient 103
The importance of ‘hands-on’ physiotherapy was highlighted by both patients and physiotherapists, in addition to, or in combination with, the educational aspects of the intervention:
So he would spend the first bit talking and then the second bit doing. Um, and yeah that, that worked really well actually.
Patient 203
Patients’ expectations and comparisons to previous physiotherapy
Most patients felt that the intervention met their expectations. One thought the intervention would involve more ‘hands-on’ physiotherapy. One described wondering if they might not be in pain at the end of the intervention sessions, but, like other patients and therapists, accepted that this would be a longer-term goal. Patients felt that previous experiences of physiotherapy, which was not specifically for JHS, tended to be of more limited value:
I had some prior to this when I originally went into the doctors and was saying about joint pain. But the physio[therapist] there didn’t, kind of, really . . . He was giving me stuff to do which was actually causing me more pain . . .
Patient 103
Physiotherapists’ views
Because of the individual nature of JHS, physiotherapists felt that there was a need to tailor the treatment to meet the patient’s needs:
I think it will give a structure to the basics, like a rehab programme, yes; there will be components of it, but within that you still need to have an individual approach. You can’t be too generic with these people, because each person’s really different. So I think it helps like you would if you did a rehab programme, you’re going to have basic information that will be generic throughout the whole, which I guess that does address. In terms of the exercises, that’s very individual, so I don’t think you could really, necessarily put people into a generic programme like that.
Physiotherapist 201
A lack of time to complete all aspects of the physiotherapy sessions was highlighted by some therapists. They recognised the need to balance the information content with the hands-on physiotherapy to meet the patient’s needs:
Personally speaking proportions wise I tend to spend a lot of time going through the booklet as I’m supposed to do and then kind of rushing through the physio[therapy] session bit at the end. Erm, and, I think that’s, it depends what kind of patient you have, so some of the participants are basically nodding their heads, waiting to get the booklet out of the way, to get on to the hands-on other bit. Whereas some are all about the booklet. So, I think that reflects the different types of learners and the different types of patients that you have, really.
Physiotherapist 202
However, one physiotherapist felt that this would improve with practice:
I think it’s probably something that would improve with practice and getting to know the book better, and those sorts of stuff. Um, but, yeah, sometimes found that I was getting through everything in the workbook and, you know, which was great and, again, standardised their treatment a little bit more. But then, actually, the individual bits of tailoring exercises and stuff to them and sometimes that is at risk of getting lost a little bit.
Physiotherapist 102
Homework
Patients’ views
All patients described a busy lifestyle; one participant who had previously worked full time had recently given up work and felt that otherwise it would have been too difficult to focus on the demands of the intervention and that any benefit from participation may have been compromised. Patients were more able to incorporate exercises into their lifestyle that were not over and above their normal routine, such as correcting posture or movement patterns. One patient appeared to be daunted by the prospect of achieving set goals:
I think I found, like the goals section of the book I was getting a bit stressed about it because I was a bit worried about, ‘Well I don’t really know what is achievable, because I want to go back to swimming and circuit training, but at the moment I can barely walk for 20 minutes’. So actually going into the session and him going, ‘We can just look at you walking to work, that can be a goal’, it was like, ‘Oh, OK’. So it made it much more achievable. [. . .] So the thing I’ve had difficulty with is fitting the exercises in my day. I’m not doing very well at putting in a routine, and I know that I need to do that. Actually realising that I need to do this daily, or at least every other day, and I still haven’t found balance of that yet.
Patient 102
Some patients found that even though they were able to do exercises correctly during the physiotherapy session, they were less confident to continue these at home, or needed encouragement to continue doing the exercises:
Obviously the physiotherapist is an encouragement to you. At home when you’re doing those things you don’t have that person going ‘Go on’, that encouragement. You’ve kind of got your own head saying ‘That hurts, just stop’. So yes, in a way you do it, it’s kind of bit of both really, it just depends on how much you’re willing to push yourself.
Patient 201
It was noted that having appointments already booked helped to motivate patients to do their homework:
It was quite motivating in terms of thinking, ‘Oh God I’ve got to see him again on Thursday, if I haven’t done it then, I know . . .’ kind of thing. Um, so yeah, so again I think again that’s where the structured thing comes in. If you know you’re going back to somebody they’re going to know if you haven’t done something and all the rest of it.
Patient 203
Physiotherapists’ views
Therapists felt that patients’ engagement with homework was mixed. They reported that some of their patients had read ahead, engaged, reflected and made notes in the booklet, while others had not. One therapist reported that, although the booklet was useful, the amount of homework actually done may not be reflected in what patients had written in the booklet. Some felt that just having an awareness of the next session was helpful:
They come with awareness of what we’re going to talk about, the conversation flows really freely.
Physiotherapist 202
One physiotherapist felt that the outcome of the intervention may be affected by the participant’s level of engagement with homework:
I think we could still advise them and things like that, and give them the information. But it’s structured in a way, especially with the, the continuing what they should be filling in and things like that. I think you’re going to get a much better outcome if the patients are on board and completing it.
Physiotherapist 101
Summary
Patients’ views of what worked well
The intervention helped to raise patients’ awareness of posture, core strength and ‘correct’ movements:
I’m aware now. So when, I always set myself, um, because I can’t, literally, sit with my feet on the floor like you’re supposed to, I set my goals so that during my breakfast when I sit up to the table I sit up straight, I have my feet on the floor, and I eat my breakfast.
Patient 202
Patients valued this even if they were not always able to put their knowledge into practice:
It’s made me think more about my posture, and the way that I’m sitting and standing differently. I’m trying to correct that. When I’m picking up [child’s name] and playing with her, and things like that. But I found it difficult to adapt.
Patient 102
Patients’ awareness of exacerbating and ameliorating behaviours, such as adopting the correct posture, analgesic use and pacing, was greatly enhanced:
Um, it’s been brilliant in that way, it has brought much more awareness of what I’m doing with my body, um, and how that is affecting [. . .] And so then to be aware of what that’s doing to me now, and then to physically feel the change . . .
Patient 202
Patients were particularly pleased that JHS was being recognised and the topic of research:
I thought it was really good and really positive. Part of it is simply having it recognised.
Patient 102
Patients felt that the information they had been given could be used to help others to understand their experiences, as they had often met with a lack of understanding regarding their symptoms:
Um, I feel like, by doing it my family is much more aware of it and I get much less hassle from them about everything and they’re then being a, really supportive.
Patient 202
As described above, patients valued the combination of hands-on physiotherapy and educational components of the intervention.
Physiotherapists’ views of what worked well
The intervention was thought to be useful in that it gave structure to the treatment for JHS and helped to focus on particular issues; the therapist was required to cover topics that they might otherwise have steered away from:
I think it’s really nice to have a structured intervention that you stick . . . So you’ve got some, so people are saying the same thing and you’re not missing anything. I think that will be really nice. People are able to reflect on their intervention and if they find a structured way of . . . If they find this structured way more useful, then maybe that will help to change our practice as all.
Physiotherapist 201
One physiotherapist felt that the treatment intervention could potentially be very helpful for a particular group of patients:
I think this treatment, tailored to the right people at the right time works very well.
Physiotherapist 102
One physiotherapist felt that the education aspect of the intervention was particularly important:
. . . this is an interesting part of the intervention because, historically, people with musculoskeletal pains and joint pains were treated with exercise or hands-on physio[therapy], whereas the intervention that’s been chosen for the trial is much more about discursive, erm . . . management, so it’s lots of talking therapy and education, ‘cause without the understanding you’ve got no chance of managing your condition.
Physiotherapist 202
Patients’ views on challenges
Patients described challenges that were specific to their circumstances, such as postnatal depression. However, finding time to do exercises at home, and to attend the sessions, was the greatest barrier to adherence.
I think the problems with it were my time and my life, nothing to do with the trial.
Patient 106
Physiotherapists’ views on challenges
One physiotherapist felt that patients, in general and prior to the trial pilot, often had negative expectations of physiotherapy and did not expect physiotherapy to be beneficial:
Some of the main challenges we had were that patients had been treated in lots of different places and all been told lots of different things. That they couldn’t be helped. There was nothing to benefit them. They were preventing their own rehab. All sorts of things like that really, more than anything else. So the patients were coming in extremely negative, expecting physio[therapy] not to work.
Physiotherapist 101
It was suggested that for some patients, completing the delivery of the intervention within a 4-month period may be difficult. Sessions may be scheduled too closely together or patients may need more than six sessions. One physiotherapist noted that standard practice at one hospital is to offer between 2 and 20 sessions to suit patients’ needs:
With some of those that, again, are slower and things like that, with the study we haven’t got the time scales to make the time frames longer, to, to give them that time to adapt and progress a little bit more and things with it.
Physiotherapist 101
The ability to be flexible and to tailor the intervention to the individual patient was considered to be a key issue; on the one hand this constituted a potential challenge, and yet the structure of the intervention was also appreciated and valued:
He was able to use that [the booklet] as a tool, but not, but able to work with it . . . It was very much tailored to where I was, to where I was at the moment.
Patient 203
When we’re seeing patients, everything is a little bit more fluid. You might jump backwards and forwards a little bit, whereas that probably can help you to be a bit more focused, maybe, if you follow through a booklet. I think, from people who are quite new here, so the inpatients have tried it out, even though they’re not in the trial. I’ve asked them just to trial the booklet with the patients, just to see what, you know, how they’ve found it. They said it was quite good, coming in, fairly new to the department; it was quite nice to follow that structure.
Physiotherapist 201
Suggestions for improvements
One patient participant felt that the provision of more information before enrolling on to the trial may have been beneficial:
I guess information coming into it. I came in a bit blind. But I don’t know what. Maybe like a, a full breakdown of what, you know, like, a, with a letter with the appointment, you know, ‘you’re seeing [physiotherapist’s name] at 3.15. And this is what we’ll be doing . . .’ You know – so an introduction into what’s wrong with you, or, you know, like what you’re symptoms are. ‘Then we’ll do an assessment for such and such. Then we will discuss these topics . . .’ I don’t know, just to give me a bit more information as to what was happening, the structure within that first session.
Patient 202
Patients either did not make any suggestions for improvements or recognised that it may be difficult to suggest generic improvements, and made suggestions specific to them. For example, access to additional information on specific aspects (e.g. medication) was suggested by one patient (patient 201). Other suggestions relating to the individual’s needs are reported below as More detailed advice on exercises, The opportunity to see other health professionals and More structured or detailed programme of advice.
More detailed advice on exercises
It’s difficult to say because I can only reference it to my situation really. I think that it would’ve been useful – I think that comes from me, it would’ve been useful to look into the exercises in more precision, for me. But we did in the last session, but I think that’s only something I’ve really thought about in retrospect really [. . .] I think, maybe, my situation didn’t really help, going back to work and walking every day has knocked me back a few stages. I think if that hadn’t been the case I probably would’ve asked, we would’ve got more into the exercises and I would’ve then been able to ask more questions . . . I don’t know about other people with hypermobility, but for me specifically the exercises are about the finer points. Because sometimes I can do it, but just because I can doesn’t mean I should.
Patient 102
The opportunity to see other health professionals
I think having more opportunities within the programme to possibly see different specialists.
Patient 103
More structured or detailed programme of advice
Um . . . I guess it depends on who, individual, um, how you like things. And I think, for a lot of people, that book would work very well. What came out of all of it for me is I am somebody, and again I guess whether it’s because I spend my life telling other people what to do, I wanted to be told, myself, what to do. Unlike what, what did come out of it was I very much like an ordered programme of events, ‘Do this, this, this, this and this’. And whether that can be, sort of, developed within that programme a bit more really?
Patient 203
Personal changes arising from taking part in the intervention
Patients reported a greater awareness of the importance of posture and correct movement:
The physio[therapist]’s kind of helped my head home in on what’s causing the pain, more than anything. So I’m a bit more aware as to what could, possibly, stop it.
Patient 103
Patients reported being more aware or more ‘in tune’ with their body and more accepting of their limitations:
I think I’ve probably been slightly more in tune with my body when it’s knackered and in pain. I haven’t beaten myself up for not doing a lot.
Patient 106
The long-term nature of the condition was recognised. Neither patients nor physiotherapists expected quick results.
He was quite clear and I was quite clear that this wasn’t going to change overnight and that’s why the doing too much and then giving up was an unhelpful strategy. It’s playing the long game, really.
Patient 106
I think a lot of it is just giving myself a break and just realising that it is real and that it is manageable. Also that it’s long term, this is something that I’m going to be managing for the rest of my life and I don’t have to do it all now.
Patient 102
It doesn’t all end here, you’ve got to keep working at it. And you will go up and down, we’re on the end of the phone if you go down. But otherwise keep going and finding out what is out there that you can . . . what is out there that you can go and enjoy to continue exercising and looking after yourself long term?
Physiotherapist 101
Overall conclusions
The strength of this part of the research lay in determining the acceptability of the physiotherapy intervention to patients and therapists, and in gathering information related to recruitment. Unfortunately, all of the patients recruited were women and two were unavailable for interview. This might be seen as a limitation, particularly if the experiences of men or those who were not interviewed were at variance with the data collected. Nevertheless, the study generated very useful information.
The consent rate was relatively low, at 19% (8/42) of the referrals screened. A large number of referrals (23, 55%) were found to be ineligible based on the inclusion and exclusion criteria. Closer analysis of those excluded suggested that slight refinement of the inclusion and exclusion criteria might be helpful; for example, those with a concomitant diagnosis of fibromyalgia or those with mild anxiety or depression should not be specifically excluded.
Patients were generally positive about the advice and physiotherapy interventions and pleased that JHS treatment was being recognised, researched and ‘taken seriously’, as JHS patients often met with a lack of understanding regarding their symptoms by health professionals and lay people.
The study patient handbook was rated highly by patients. Having written information in this format provided validation and something that could be shared with others. Some valued the activity diary, others valued just having something to refer to as and when needed.
The physiotherapy programme raised patients’ awareness of posture, core strength, pacing of exercise and ‘correct’ movements. Patient participants appreciated seeing the same physiotherapist and that the therapist was able to tailor the intervention programme to suit their personal needs.
Amendments
A number of changes were made to the design of the pilot RCT on the basis of interview data, additional observations during the conduct of the pilot and discussions with the research team. Where appropriate, these changes were approved by substantial amendment to the ethical approval for the PHyT (13/SW/0083).
Refinement of the physiotherapy intervention
Following data collation at the end of stage 2, a number of minor changes were made to the intervention and training package.
-
The flexibility of the delivery of the intervention was seen as an important feature by both patients and physiotherapists. Minor changes were therefore made to enhance the ability of patients and therapists to use the intervention in a flexible manner. Session numbers were removed from the patient handbook to enhance the perceived flexibility of the intervention. The flexibility of delivery was also reiterated and encouraged in the introduction section of the patient handbook, and was further reinforced in the training package.
-
The patient handbook was increased in size from A5 to A4 to make it easier to handle and to provide more space for making notes. The exercise ‘menu’ was printed in landscape format to also provide more space for patients and physiotherapists to add notes.
-
The patient handbook incorporated ideas for videoing movements using patients’ own mobile devices, an idea suggested by our patient research partners.
-
Some additional figures about pacing of activity were incorporated to clarify this concept.
-
The training package was revised to include practical training. Detailed ‘speaker notes’ to supplement the training slides were developed. The training package was refocused to emphasise diagnosis and to incorporate findings from our UK-wide survey of physiotherapy practice39 and findings from the stage 2 pilot of the intervention.
Refinement of the pilot trial design
Some further minor amendments were made to the study procedures for the subsequent pilot RCT. These were in an attempt to boost referrals, to prevent unnecessary exclusions from the study and to streamline study procedures. Specific changes were as follows:
-
The minimum age of participants was reduced from 18 to 16 years. Three potential participants had been excluded on the basis of being < 18 years, but 16- to 18-year-olds are commonly seen within the adult rheumatology services and JHS is common in this age group.
-
The wording of the inclusion and exclusion criteria was refined to ensure that those with a concomitant diagnosis of fibromyalgia and those with mild anxiety or depression were not unnecessarily excluded from taking part. The revised wording is detailed in Chapter 4.
-
A local clinical service agreement was reached with another local NHS trust (University Hospitals Bristol NHS Foundation Trust), so that referrals of people with JHS were forwarded to North Bristol NHS Trust in order for them to be considered for the study. Patients were given a choice as to which service they accessed.
-
The reply slip was amended to encourage potential participants to respond both positively (‘I am interested in taking part’) and negatively (‘I am NOT interested in taking part’). If a reply slip was not received after 2 weeks, one further recruitment pack would be sent.
-
The questionnaire burden on participants was reduced. The MYMOP was removed as this was incomplete in many cases. Therapists reported that it was extremely difficult to complete the MYMOP effectively in the time available for the baseline assessment. The second page of the EQ-5D-5L (the vertical VAS) was removed on the advice of our health economists as it would not be used later for the health economics evaluation. The final shortened version of the BIoH was used.
-
Questionnaire return would be closely monitored, with written and telephone reminders at 2 and 4 weeks in the event of non-return.
Chapter 4 Stage 3: Physiotherapy for Hypermobility Trial – quantitative and economic evaluation
Aims and objectives
The overall aim of this stage of the research was to conduct a pilot RCT of a comprehensive physiotherapy intervention to determine if it was feasible to conduct a future definitive RCT. 74
A number of objectives related to determining the acceptability of the research design and the physiotherapy intervention to patients and physiotherapists and these are addressed in the following chapter (Chapter 5). The current chapter will therefore concentrate on reporting quantitative aspects of the pilot RCT. Specific objectives reported in this chapter were to determine the number of potentially eligible patients with JHS; assess the rates of patient recruitment and retention; explore the practicalities of collecting the proposed cost and outcome measures; and explore the VOI of a subsequent, larger RCT.
Methods
Overview of the pilot randomised controlled trial
The pilot study was conducted within the same two NHS trusts that took part in the pilot of the intervention (stage 2; see Chapter 3). The study was designed as a parallel two-arm RCT, comparing an advice control with advice plus physiotherapy. Figure 6 summarises the study design.
FIGURE 6.
Flow diagram illustrating the design of the pilot RCT. (The shaded area represents the initial physiotherapy assessment and advice session.)
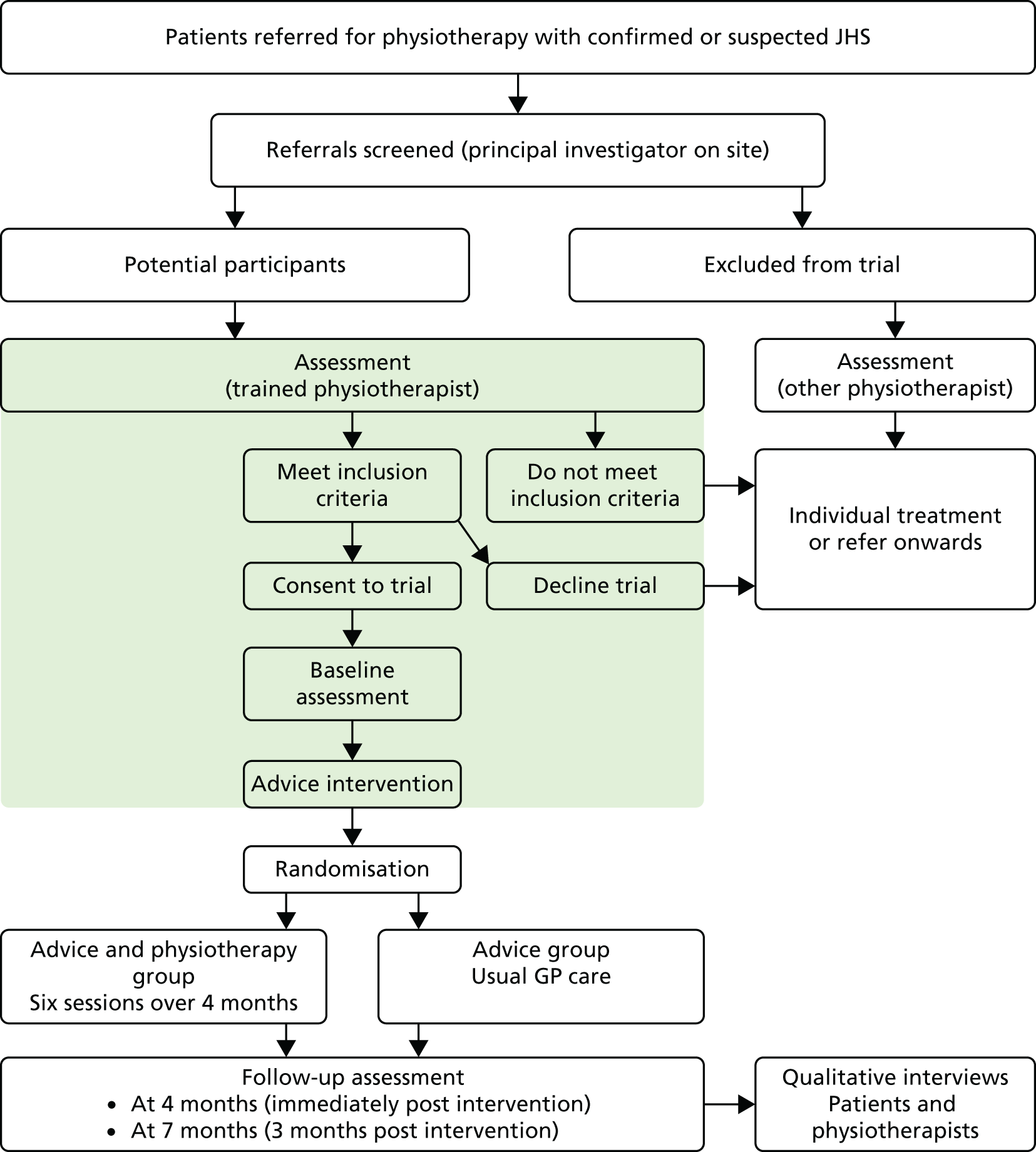
Following an assessment and advice session, participants were randomly allocated to receive the physiotherapy intervention or to continue with usual GP care. Further details of the interventions and other study procedures are given in subsequent sections (from Physiotherapist recruitment to Data analysis).
Physiotherapist recruitment
The same physiotherapists who took part in stage 2 were invited and agreed to take part in the pilot RCT. All four physiotherapists were retrained in the assessment of JHS, the revised intervention package and the study processes (see Appendix 9 for training materials). Training was conducted at the University of the West of England, Bristol by the chief investigator (SP) and one of the principal investigators (RL). To determine the feasibility of conducting in-service training of the intervention package, the trained physiotherapists were asked to train at least one other physiotherapist within their NHS trust. This meant that a minimum of three physiotherapists with a variety of experience were available within each NHS trust to implement the intervention.
Patient recruitment
The process of identifying and approaching people with JHS was similar to that described in stage 2. The principal investigator within each NHS trust screened all referrals to their rheumatology physiotherapy service and sent a participant information sheet (see Appendix 10) and reply slip to all potentially eligible patients. Those responding positively were then scheduled for an initial assessment to confirm eligibility, to provide an opportunity for further discussion and explanation and, should they agree to take part, to provide signed, informed consent. A formal patient screening proforma was completed for all patients (see Appendix 11). A full baseline study assessment was then conducted with those consenting to the study (see Baseline physiotherapy assessment).
Some minor changes were made to the inclusion and exclusion criteria between stage 2 (feasibility of the intervention) and stage 3 (pilot RCT) because of unintended exclusions and in an attempt to boost recruitment. This included reducing the minimum age from 18 years to 16 years; clarifying that fibromyalgia and EDS-HT were not exclusion criteria; and clarification of wording regarding multiple-joint osteoarthritis and psychological treatment. A local service agreement was also made with another local NHS trust (University Hospitals Bristol NHS Foundation Trust) to forward JHS referrals to North Bristol NHS Trust so that those patients could be offered the opportunity to take part in the study. The final inclusion and exclusion criteria were as follows:
-
Inclusion criteria:
-
Exclusion criteria:
-
other known musculoskeletal pathology causing pain, particularly multiple-joint osteoarthritis and inflammatory musculoskeletal disease such as rheumatoid arthritis (fibromyalgia and EDS-HT are not exclusion criteria)
-
other serious pathology including malignancy
-
conditions affecting ability to exercise, for example uncontrolled cardiovascular disease
-
recent physiotherapy for JHS (within the last year)
-
pre-existing significant psychological distress or psychiatric conditions
-
referred for or currently undergoing psychological treatment, such as cognitive–behavioural therapy.
-
Baseline physiotherapy assessment
Following eligibility screening, a full physiotherapy clinical assessment was carried out for all patients consenting to take part in the study. This included taking a subjective medical history and history of their present complaints, followed by an objective examination of elements such as posture, joint range, strength, gait and movement, focusing on identification of relevant signs and symptoms associated with the patient’s condition. The format of the assessment was not prescribed and followed each individual physiotherapist’s usual practice. Baseline study questionnaires were completed either in advance of the initial physiotherapy assessment or immediately following consent and these were posted back to the chief investigator using prepaid envelopes.
Advice intervention
At the end of the baseline physiotherapy assessment all participants received advice booklets produced by the HMSA56 and Arthritis Research UK. 57 These contain information and advice on a range of factors such as physical activity and joint protection. The physiotherapist discussed in particular the following sections from the Arthritis Research UK57 booklet: What is joint hypermobility? (p. 5), How is joint hypermobility diagnosed? (p. 10), Drugs (pp. 11–13; with advice to discuss further with their GP) and Self-help and daily living (p. 14). All patients were also given an opportunity to ask the physiotherapist for additional advice specific to their own circumstances. Physiotherapists were instructed to provide any additional advice to patients according to information contained within the advice booklets.
Usual practice within the rheumatology services at the two NHS trusts was for a 1-hour initial appointment. As part of this research, an additional 20 minutes was allocated for consent and delivering the advice intervention.
Randomisation
Following the baseline physiotherapy assessment and delivery of the advice intervention, and after the patient had left the department, all patients were randomised using an automated randomisation service devised specifically for the study. This was developed and administered by the Bristol Randomised Trials Collaboration and could be accessed by telephone or computer, ensuring that treatment allocation was concealed from the clinician and participant. The principal investigator on each site contacted the randomisation service to determine treatment allocation. The system asked for the principal investigator’s unique identification code, a study centre code, and the date of birth and sex of the study participant. The system then randomly generated a treatment allocation of ‘advice’ or ‘advice and physiotherapy’ and a unique study identification number for the participant. Automatic notification was also e-mailed to the principal investigator. Allocation to the study arms was in the ratio 1 : 1, with a block size of four. There was no stratification by study site or other factors.
Owing to the nature of the interventions, it was not possible to blind clinicians or participants to the treatment allocation. All patients were contacted by the principal investigator on each site by telephone to advise them of their treatment allocation. Those randomised to the advice control were asked to follow the advice given during the baseline physiotherapy appointment and advice intervention, supported by the HMSA and Arthritis Research UK booklets. No additional physiotherapy sessions were scheduled for these patients. Those randomised to receive advice and physiotherapy were given an initial appointment to attend for physiotherapy.
Physiotherapy intervention
A comprehensive whole-body physiotherapy intervention was developed by the research team as described in Chapter 2. This was subsequently amended slightly as described in Chapter 3. The accompanying training materials for physiotherapists and the patient handbook are available in Appendices 9 and 12. The physiotherapy intervention built on information already delivered to patients as part of the advice intervention, supplemented by the HMSA56 and Arthritis Research UK57 advice booklets. As already described, the intervention aimed to enhance the ability of people with JHS to manage their condition and to be physically active. It included advice on a range of topics, tools to aid reflection and planning, and a ‘menu’ of exercises that could be selected as appropriate. The intervention is described fully in Chapter 3 and the associated patient handbook is included as Appendix 12. The intervention was delivered over a maximum of six 30-minute sessions across a 4-month period. A 30-minute follow-up appointment reflected usual practice within the two trusts and is also typical of that delivered across the UK. 39 The spacing of the sessions was agreed with each patient on an individual basis, allowing some flexibility in delivery.
Primary outcomes
As this was a pilot trial, the primary outcomes were to determine:
-
the number of potentially eligible patients with JHS referred to the two NHS trusts
-
the rate of patient recruitment and retention
-
an estimate of the VOI of a subsequent, larger, RCT.
Secondary outcomes
One purpose of the pilot trial was to pilot the potential primary and secondary outcome measures for a definitive trial, examine the completeness of data, estimate the variability of potential outcome measures and obtain an idea of feasible effect sizes.
All patients completed questionnaires at the start of the study prior to randomisation, at 4 months and, again, at 7 months post randomisation. All questionnaires were administered by post, with prepaid return envelopes. Baseline questionnaires were posted to all patients who indicated a potential interest in taking part in the study in advance of their baseline assessment. The consenting therapist checked verbally with the patient whether or not the baseline questionnaire had been completed and, if not, these were completed following consent. A participant database was used to monitor questionnaire return and to schedule the posting of 4- and 7-month questionnaires. Participants who failed to return questionnaires within 2 weeks of the relevant due date were sent a reminder pack and were also contacted by telephone. A second reminder pack was sent after a further 2 weeks and further telephone contact made. No further attempts were made following this point. As this was a pilot study, all available questionnaires were included in analysis, regardless of when they were returned. The process of questionnaire administration is commented upon later. The 7-month follow-up was considered satisfactory for the pilot study to assess participant retention post treatment but also ensure timely completion of the study.
A copy of the 4-month questionnaires is included in Appendix 13. These were identical to the baseline and 7-month questionnaires except that resource use and adverse events were not assessed at baseline. In addition, in the 7-month questionnaire the resource use and adverse events sections asked about the previous 3 months rather than 4 months. The biographical questionnaire administered at baseline was identical to that used in stage 2 (see Appendix 4).
Outcomes that were considered as candidates for the primary outcomes in a definitive trial were:
-
RAPID364 – a score between 0 and 30 (30 being the most severe) obtained from the MDHAQ
-
a new condition-specific physical function questionnaire developed by the research team (the BIoH)67 (see Appendix 13) – a score between 0 and 360 (360 being the most severe).
Outcomes considered as secondary outcomes for a definitive trial were:
-
physical function, pain, global status, fatigue and self-reported joint count (MDHAQ)64
-
pain at rest and on movement (VASs; see Appendix 13)
-
health-related quality-of-life preference score (EQ-5D-5L)75
-
the ESE scale70
-
resource-use questionnaires to measure health-care use and costs (see Appendix 13)
-
adverse events (e.g. dislocations or other injury; see Appendix 13).
Sample size
A formal sample size calculation was not carried out for this pilot study. We aimed to randomise a total of 60 patients in the pilot RCT over a 12-month recruitment period in the expectation that this would provide sufficient data on likely recruitment and retention rates. We also estimated this sample size would yield sufficiently precise estimates of outcome variability and between-group differences to inform sample size calculations for a future RCT. Owing to delays in study approval prior to stage 1, a reduced 8-month recruitment period was used in this pilot RCT.
Data analysis
It was not the intention of this pilot study to formally test hypotheses related to group differences. All analyses are therefore descriptive and exploratory in nature. Analyses are performed on an intention-to-treat basis, and point estimates and confidence intervals (CIs) are reported.
Economic analyses
We tracked the use of NHS staff time and expenses in developing the training materials and in delivering the training sessions prior to the pilot trial to provide context about the fixed set-up costs of the intervention. NHS resource use (including medications, community, primary and secondary care) was collected using patient-completed resource-use questionnaires administered at 4 and 7 months.
Resource use was valued using national unit costs. Physiotherapist and other primary care visits (e.g. GP, podiatrist) were valued using estimates from the Unit Costs of Health and Social Care 2014. 76 Hospital care, including admissions, accident and emergency, urgent care and outpatient visits, was costed based on the most relevant health-care resource group codes in NHS Reference Costs 2013 to 2014. 77 Medication costs, based on the drug name and dose reported by the patient, were estimated using the net price recorded in the British National Formulary. 78 Based on this information we estimated the NHS cost of physiotherapy, other primary care, hospital care and medications at 4 and 7 months, summarising these costs using descriptive statistics.
We estimated utilities (a single index summary of health-related quality of life) and quality-adjusted life-years (QALYs) based on the EQ-5D-5L79 administered before randomisation and at 4 and 7 months. EQ-5D-5L responses were weighted and aggregated to a summary score using the value set for England. 80 EQ-5D-5L results were summarised using descriptive statistics.
Value-of-information analysis
We use VOI methods81 to explore the potential value of a future larger RCT with the same interventions as included in the pilot RCT. VOI requires a decision model that captures the health benefits and resource-use costs arising from adoption of the interventions being compared into clinical practice. This model should be based on all currently available information, however sparse (in our case results from the feasibility study). The important point is that all uncertainty in the available evidence is reflected, so small samples will have correspondingly wide CIs that are propagated through the decision model. The key idea is that further evidence will reduce uncertainty in the inputs to the decision model (i.e. the CIs will be narrower), which in turn may change the optimal decision. If the optimal decision changes then we can work out the gain in net monetary benefit (health-care benefits minus costs) resulting from using the ‘new’ rather than the ‘current’ optimal intervention. VOI measures what, on average, we would expect this net monetary benefit gain from collection of new evidence to be. The expected value of perfect information (EVPI) measures the expected gain in net monetary benefit resulting from elimination of uncertainty in all model parameters. The expected value of partial perfect information (EVPPI) measures the expected gain in net monetary benefit resulting from elimination of uncertainty in a subset of model parameters (e.g. utility, cost or natural history parameters). The expected value of sample information measures the expected gain in net monetary benefit from reducing uncertainty in a set of model parameters through the collection of new evidence using a specific study design. The expected value of sample information can be compared between different types of research to establish priorities. We report here EVPI and EVPPI for a variety of model parameters, but note that these give an upper bound on the expected returns from a new RCT, the actual value will be less than this depending on sample size and other design factors.
Our pilot trial provides evidence on QALYs, intervention costs and resource-use costs over a 7-month time period from a small number of patients. We fit statistical models for total costs and EQ-5D-5L, adjusting for baseline EQ-5D-5L score,82 to obtain estimates of mean total costs and mean EQ-5D-5L for the two interventions. EQ-5D-5L was assumed to have a normal distribution and costs were assumed to have a log-normal distribution (see Appendix 14 for model details). We considered a bivariate model that accounts for correlation between costs and EQ-5D-5L; however, scatterplots of EQ-5D-5L scores versus costs indicated no evidence of such correlations. Results are therefore presented from the model without correlation. We estimated QALYs using the ‘area under the EQ-5D-5L curve’ approach, where a piecewise linear trend is assumed for the two time periods (0–4 months and 4–7 months). We report the mean total costs and mean EQ-5D-5L score at 4 and 7 months. We also report mean total costs and mean QALYs over the 7-month time period, and the expected net benefit for a range of willingness-to-pay per QALY thresholds. The expected net benefit is equal to the mean QALYs multiplied by willingness-to-pay per QALY minus mean total costs. A Bayesian approach is taken to estimate the statistical models, evaluated using WinBUGS (version 1.4.3; MRC Biostatistics Unit, Cambridge, UK)83 (see Appendix 14 for the code). To identify all the available relevant evidence to inform the decision, we used a recently published systematic review33 to identify other relevant intervention studies on JHS patients. We conducted a rapid review of journal articles listed in PubMed estimating utility scores or health-care costs in patients with JHS (Table 9). We consulted with the project team to identify long-term natural progression studies and information on annual incidence of new JHS patient referrals. The results of these searches are given in Results, Economic analysis.
| Group | PubMed search terms |
|---|---|
| Synonyms for cost | Cost OR resource use |
| OR synonyms for utility scores | Quality of life OR utility OR EQ-5D OR EQ5D OR SF36 OR SF-36 |
| AND synonyms for JHS | Ehlers danlos OR hypermobility |
The net monetary benefit depends on the monetary value (willingness to pay) that we give to changes in health outcomes (in QALYs). We plot EVPI and EVPPI for a range of willingness to pay per QALY thresholds. We also present population-level EVPI and EVPPI given the annual incidence of new JHS referral, assuming a lifetime of the intervention of T = 1, 5 and 10 years, and discounting at 3.5%. 84
The lifetime of the intervention represents the time until the intervention becomes obsolete, for example by being superseded by a new intervention.
The decision model is evaluated using Markov chain Monte Carlo simulation in WinBUGS, so that all uncertainty in the model parameters is propagated directly into the model, and allows a probabilistic model to be evaluated. 85 EVPI is computed in WinBUGS directly86 for a range of willingness-to-pay thresholds. EVPPI for subsets of parameters (costs, efficacy and baseline utilities) were computed using a generalised additive model approach87 evaluated using the Sheffield Accelerated Value of Information web application. 88
Results
Recruitment and retention
Figure 7 provides the Consolidated Standards of Reporting Trials (CONSORT) flow chart detailing recruitment and retention of patients for the primary clinical and economic outcomes. The intention was to recruit patients with hypermobility over a 12-month period; however, because of the delays reported previously (see Chapter 2, Methods) this recruitment period was reduced to 8 months. In total, 121 patients were referred to the two physiotherapy units between January and August 2014. An initial assessment of eligibility was carried out and 107 patients were found to be potentially eligible and were contacted about the study. Of these, 55 (51%) attended for baseline assessment and, of these, 29 (53%) gave consent and were randomised. The proportions of men referred and recruited were 7.6% and 10.3%, respectively. Figure 8 illustrates recruitment during the 8 months. Within the first 2 months recruitment was slow, followed by nearly one-third of the final sample being recruited in month 3. Recruitment in months 4–8 was reasonably consistent, with four patients recruited in each month with the exception of month 5 (where only one was recruited). Of the 29 randomised, 14 (48%) and 15 (52%) were allocated to the ‘advice-only’ and the ‘advice and physiotherapy’ arms, respectively.
FIGURE 7.
The CONSORT diagram.
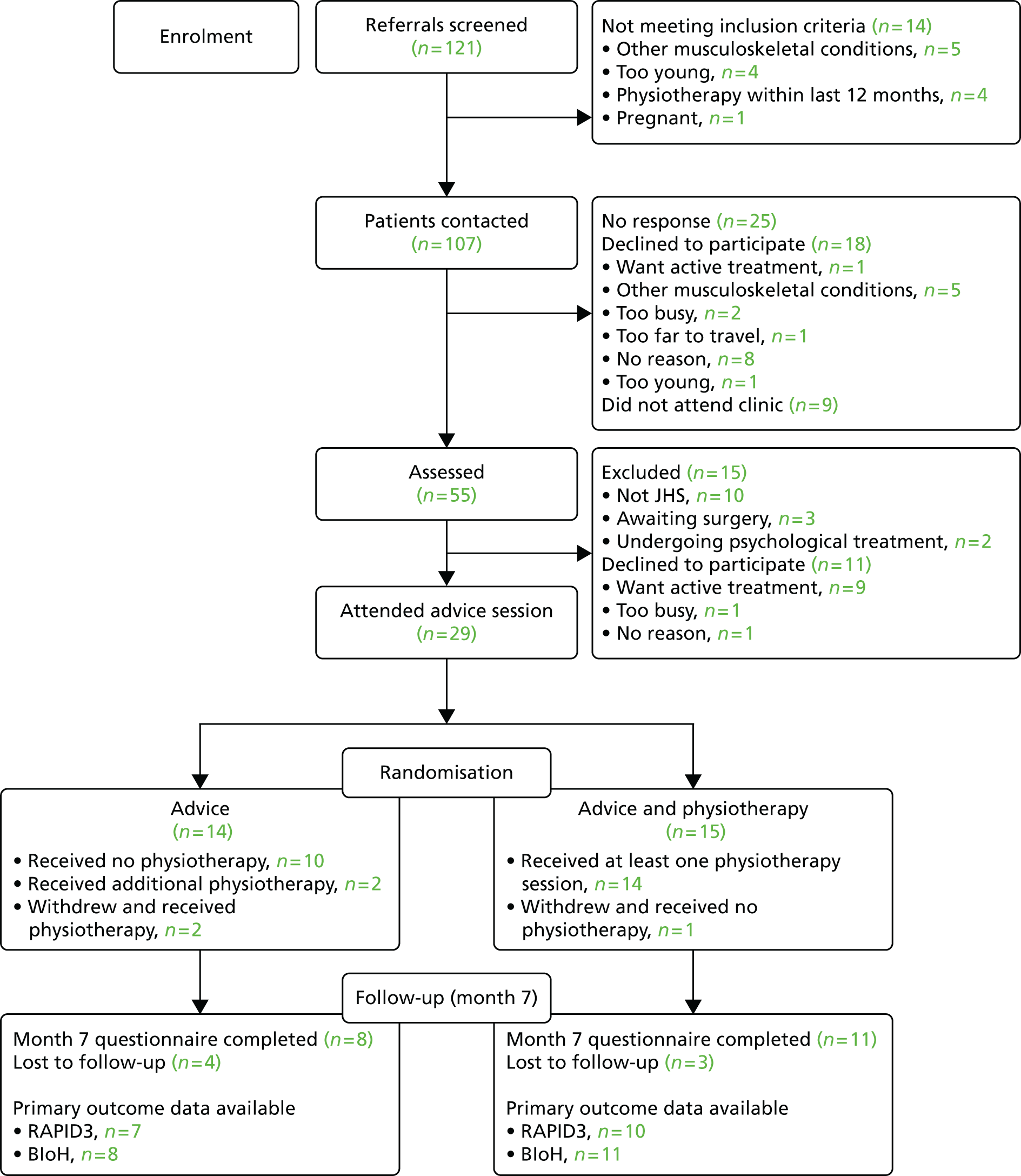
FIGURE 8.
Cumulative frequency of recruitment during the 8-month period.
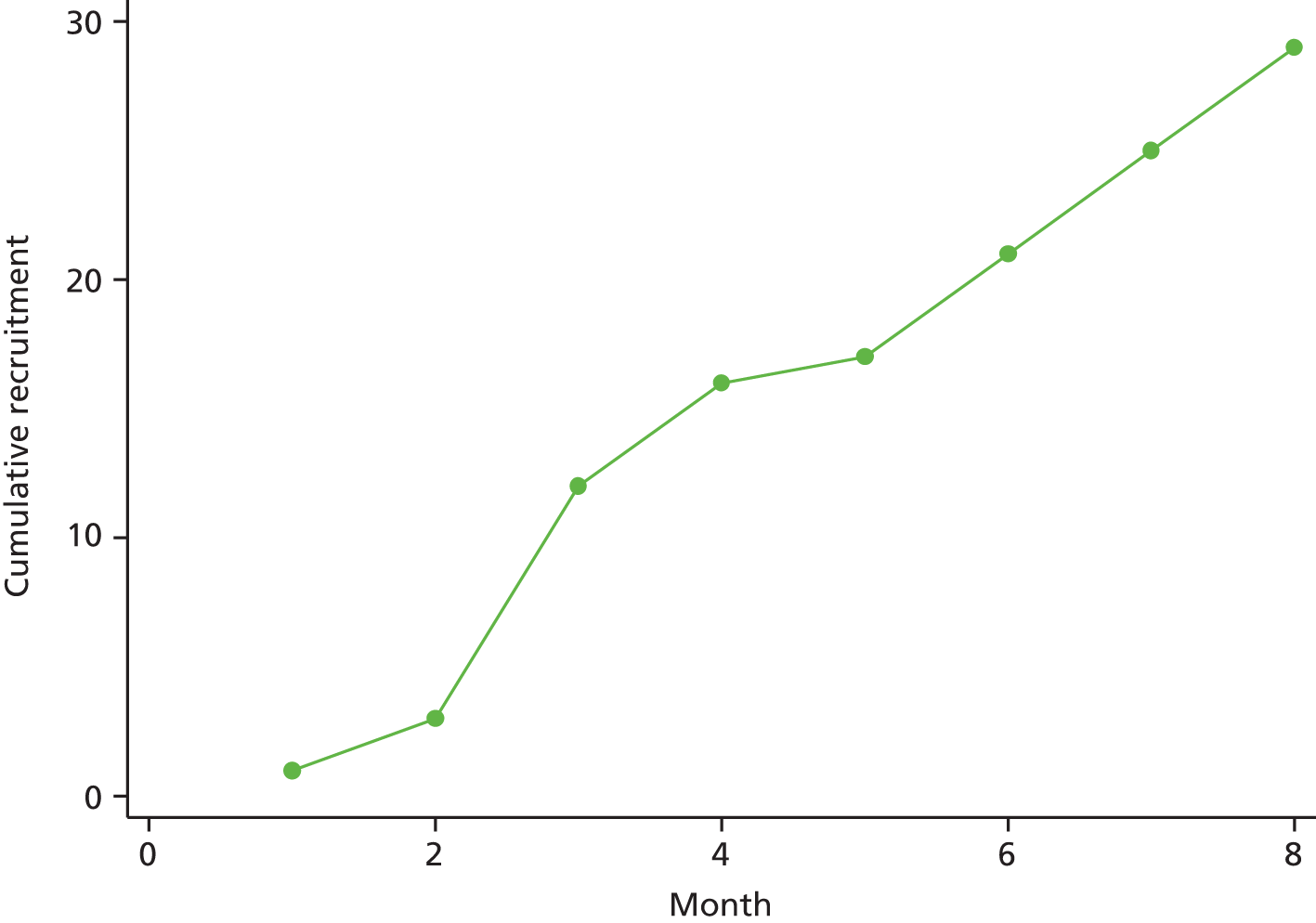
All baseline and outcome data were collected using a single patient-reported questionnaire at each time point. Two patients did not complete any of the questionnaires (one in the ‘advice-only’ arm and one in the ‘advice and physiotherapy’ arm). At baseline, the questionnaire was completed by 24 of the 29 (83%) participants. Before the 4-month follow-up, two patients allocated to the ‘advice-only’ arm withdrew from the study (both requesting active physiotherapy treatment) and one patient in the ‘advice and physiotherapy’ arm (unable to fit appointments around work) also withdrew. Of the remaining 26 patients, 17 (65%) completed the 4-month questionnaire and 19 (73%) completed the 7-month questionnaire. Completion rates were consistently higher among those randomised to the ‘advice and physiotherapy’ arm than the advice arm for each of the three time points (Table 10).
| Time point | Arm | Overall (N = 29)a,b | |
|---|---|---|---|
| Advice only (n = 14)a | Advice and physiotherapy (n = 15)b | ||
| Baseline | 10 (71) | 14 (93) | 24 (83) |
| Month 4 | 7 (58) | 10 (71) | 17 (65) |
| Month 7 | 8 (67) | 11 (79) | 19 (73) |
Adherence to randomised treatment
All patients in both treatment arms attended their advice session at which consent was taken. Among those allocated to advice and physiotherapy, the patient who withdrew from the study after randomisation did not receive any physiotherapy sessions. For one patient, the number of sessions attended was not recorded. The remaining 13 patients randomised to advice and physiotherapy attended a total of 63 sessions equating to an overall 80.7% compliance (mean number of sessions was 4.8; range 1–6 sessions). These patients completed a mean of 14.1 (range 3–18) of the topics covered in the intervention package.
Two patients in the advice-only arm reported visiting a physiotherapist at either the 4- or the 7-month follow-up.
Baseline characteristics
With the exception of age and sex, which was collected for all patients, baseline demographic and symptom data were available only for those patients who completed a baseline questionnaire. The advice-only and advice and physiotherapy arms were comparable at baseline in terms of their sociodemographic details (Table 11) and their baseline symptoms and problems (Table 12). The only exceptions to this were in relation to sex, age, marital status and current joint pain (RADAI). Patients allocated to the advice and physiotherapy arm were more likely to be older, single female and experience more joint pain than the advice-only arm. Given the small sample size these differences at baseline are likely to have occurred by chance despite randomisation. There is a lack of good epidemiological evidence for prognostic indicators in JHS, but it is generally understood that joint hypermobility is more prevalent in women and declines with age. 2 Joint pain is predictive of functional outcome in other conditions such as rheumatoid arthritis89 and osteoarthritis,90 so it seems reasonable to assume that it might also be predictive in JHS. There is no evidence to suggest that marital status is prognostic. Given the sparsity of data, marital status was not adjusted for in the initial analyses, but was considered in auxiliary analyses.
| Sociodemographic variable | Arm | |
|---|---|---|
| Advice (n = 14) | Advice and physiotherapy (n = 15) | |
| Female, n (%) | 11 (78.6) | 15 (100) |
| Age, mean (SD) | 33.3 (9.71) | 37.2 (14.13) |
| Ethnicity (white), n (%)a | 10 (100) | 13 (92.9) |
| Marital status, n (%)a | ||
| Single | 3 (30.0) | 5 (35.7) |
| Married/partner | 7 (70.0) | 7 (50.0) |
| Divorced/separated | 0 | 2 (14.3) |
| Widowed | 0 | 0 |
| Other | 0 | 0 |
| Years of education, median (IQR)a,b | 13 (12–13) | 13 (12–13) |
| Further education, n (%) | 9 (90) | 11 (84.6) |
| Paid employment, n (%)a | 9 (90) | 14 (100)a |
| Measure | Arm | |
|---|---|---|
| Advice only (n = 10) | Advice and physiotherapy (n = 14) | |
| Beighton score, mean (SD) | 5.7 (2.3) | 5.8 (1.8) |
| MDHAQ, mean (SD) | ||
| Functiona | 2.21 (1.81) | 1.69 (1.35) |
| Pain | 5.85 (1.72) | 5.93 (2.01) |
| Global | 4.45 (3.00) | 4.89 (1.68) |
| RAPID3a | 12.52 (5.77) | 12.49 (4.67) |
| RADAI | 9.70 (5.25) | 16.43 (9.28) |
| Other symptoms | 13.64 (11.28) | 17.13 (10.84) |
| Fatigueb | 5.67 (3.29) | 5.89 (3.31) |
| BIoH questionnaire, mean score (SD) | 200.77 (49.19) | 199.05 (58.34) |
| BRAF scale, mean score (SD) | ||
| Average fatigue | 5.5 (2.55) | 5.14 (2.80) |
| Effect of fatigue | 4.9 (2.88) | 5.36 (3.15) |
| Coping with fatigue | 4.1 (1.91) | 3.64 (2.50) |
| Pain in . . . , mean (SD) | ||
| Most affected joint at rest | 47.10 (26.28) | 49.43 (22.34) |
| Most affected joint on movement | 53.70 (29.99) | 61.07 (25.42) |
| All joints in general at rest | 33.40 (20.92) | 41.93 (22.62) |
| All joints in general on movement | 45.20 (28.17) | 52.29 (24.14) |
| ESE scale,c mean (SD) | 43.17 (13.86) | 48.99 (17.51) |
| EQ-5D-5L, mean score (SD) | 0.65 (0.30) | 0.72 (0.12) |
Completers and non-completers
Baseline data were also compared between those for whom 7-month outcome data were available and those who withdrew or were lost to follow-up (Table 13). Baseline values were compared for age, sex, RADAI score (potential prognostic factors) and the following primary outcomes: RAPID3, BIoH and EQ-5D-5L scores. Of the 24 with a completed baseline questionnaire, seven withdrew or were lost to follow-up and gave no 7-month outcome data. Age and sex were known for the remaining five patients who returned no baseline questionnaire; of these, two completed the 7-month questionnaire, one withdrew and two were lost to follow-up.
| Measure | Completers (n = 19) | Non-completers (n = 10) |
|---|---|---|
| Female, n (%) | 18 (94.74) | 8 (80.00) |
| Age (years), mean (SD) | 37.79 (12.93) | 30.60 (9.32) |
| RADAI,a mean score (SD) | 13.76 (8.41) | 13.29 (9.12) |
| RAPID3,a,b mean score (SD) | 12.95 (5.11) | 11.44 (3.90) |
| BIoH questionnaire,a mean score (SD) | 197.48 (57.34) | 205.32 (46.79) |
| EQ-5D-5L,a,c mean score (SD) | 0.70 (0.24) | 0.68 (0.16) |
Primary and secondary patient-reported outcomes
As described previously, the analyses of patient-reported outcomes are only exploratory; it was not the intention of this pilot study to estimate the effect of physiotherapy, only to pilot the potential primary and secondary outcome measures for a full trial, examine the completeness of data, estimate the variability of potential outcome measures and obtain an idea of feasible effect sizes. The RAPID3 score (calculated from items relating to difficulties, pain and global measure of how the patient is, within the MDHAQ) and the BIoH score were measured as potential primary outcomes for a definitive trial.
Number of missing data
The RAPID3 score is an amalgamation of 12 items within the MDHAQ; if one or more items are missing for an individual, then the overall RAPID3 score cannot be calculated (although missing data can be imputed: see Ancillary analyses). Of those completing questionnaires, data were present for missing (17%) participants at baseline, for one (6%) participant at month 4 and for two (10%) participants at month 7. The BIoH score is an amalgamation of 55 items and the scoring system automatically incorporates imputation (using the patient’s average value in that section) for missing values. Before imputation, of those completing questionnaires, the number of participants with missing data was four (17%) at baseline, three (18%) at month 4 and one (5%) at month 7. With the exception of one patient at baseline who had 10 missing values, patients had between 1 and 3 items missing, so imputation is unlikely to have had major impact on the final score. For all secondary outcomes, the proportion of missing data was very low: < 5% for all and, in the majority of cases, 0%.
Change between baseline and follow-up
Although a future definite RCT would compare RAPID3 and BIoH scores at follow-up adjusting for baseline, change scores from baseline to follow-up are also reported here for completeness. Table 14 presents the mean change in participant RAPID3 and BIoH scores from baseline to the 4- and 7-month follow-ups. Caution is needed in any interpretation as the number of patients included is very small because of different patients having missing data at different time points.
| Outcome measure | Arm | |
|---|---|---|
| Advice only | Advice and physiotherapy | |
| RAPID3 | n = 4 | n = 8 |
| Mean score change: baseline to 4 months (SD) | 2.79 (5.11) | –4.79 (3.38) |
| Mean score change: baseline to 7 months (SD) | –2.21 (0.71) | –4.88 (2.77) |
| BIoH questionnaire | n = 6 | n = 10, 11a |
| Mean score change: baseline to 4 months (SD) | 14.51 (27.80) | –31.72 (36.75) |
| Mean score change: baseline to 7 months (SD) | 1.70 (14.44) | –34.26 (36.57) |
Table 14 suggests that, although reductions were seen in RAPID3 and BIoH mean score changes at 4 and 7 months in the advice and physiotherapy arm, among the few participants with sufficient data receiving advice only, there was, on average, an initial increase in symptoms by 4 months followed by a reduction in RAPID3 score to just below that at baseline and just above the baseline score for the BioH questionnaire.
Between-group comparisons
Figure 9 displays the mean RAPID3 and BioH questionnaire scores at baseline, and at 4 and 7 months among the two treatment arms. Looking at the mean scores across patients at each time point, a different picture is seen to that in Table 14. Both groups demonstrated an improvement from baseline to 4 months in terms of RAPID3 and BioH questionnaire scores. Values in the advice-only group returned back towards baseline between 4 and 7 months, and this was more marked for the BIoH questionnaire scores. Values in the advice and physiotherapy group continued to improve between 4 and 7 months. These different interpretations based on change scores or actual scores at months 4 and 7 are a result of the fact that different individuals are included in the two analyses. Additional patients are included in the last analysis.
FIGURE 9.
Mean (95% CI) RAPID3 and BIoH questionnaire scores at baseline and at the 4- and 7-month follow-ups. (a) RAPID3 scores; and (b) BIoH scores.
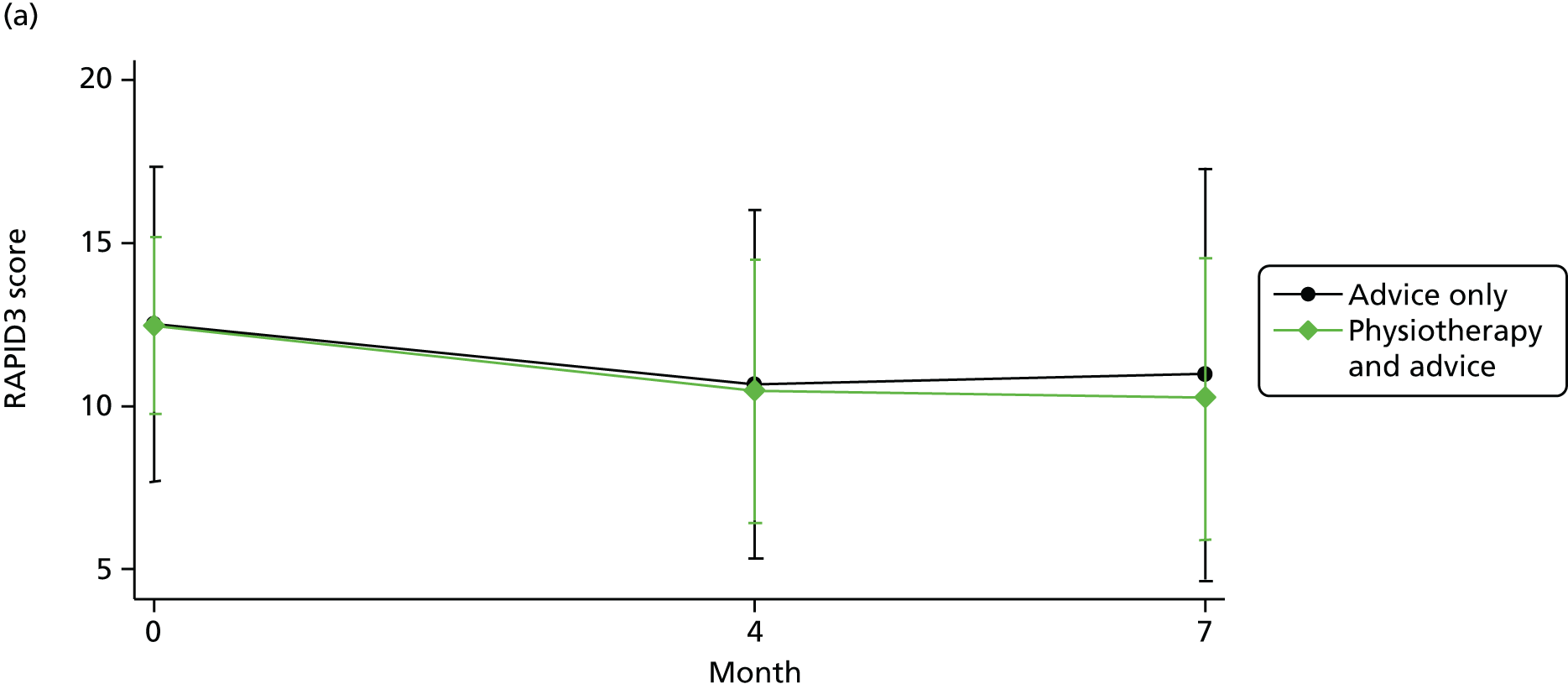
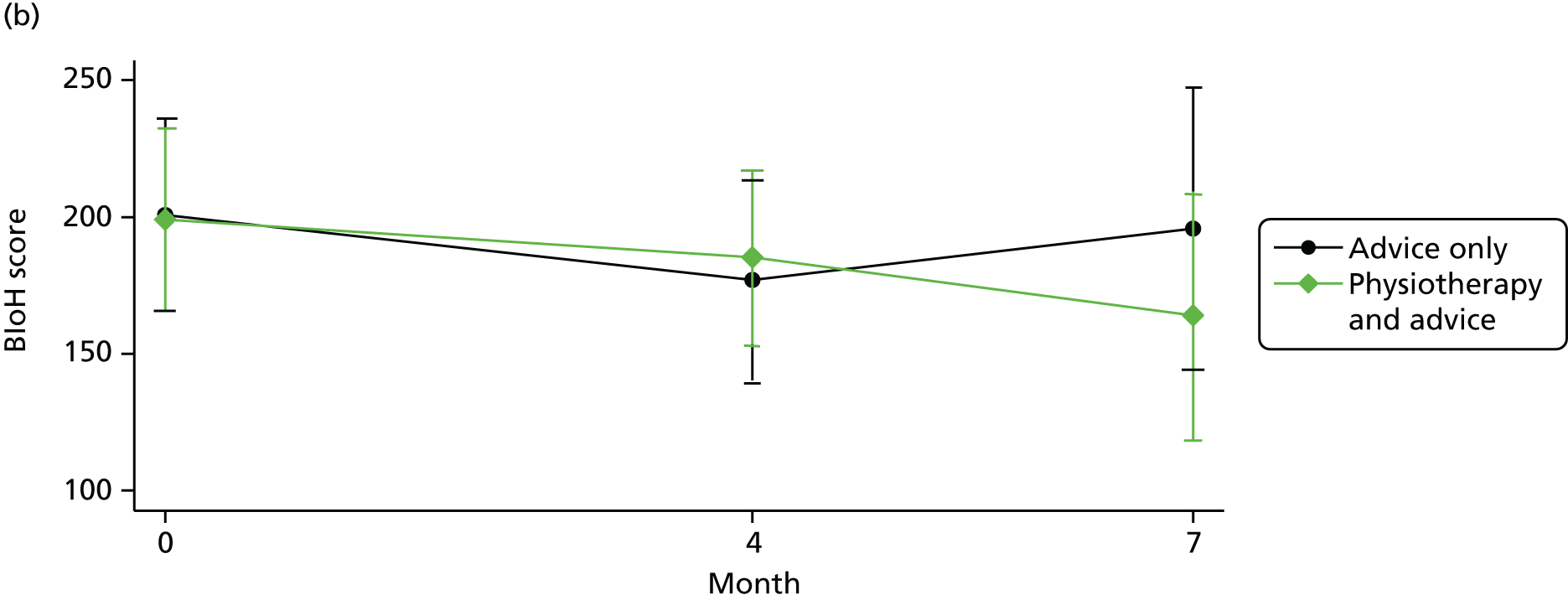
Linear regression models
Linear regression models reported in this section first considered the unadjusted association between treatment group and outcome at 7 months, and, second, the association adjusted for baseline measure, age, sex and RADAI score. Participants are analysed in the arms to which they were randomised with missing data ignored, with the exception of the BIoH questionnaire scores, for which missing data were imputed as part of the scoring system (see Appendix 15).
Table 15 presents the difference in mean scores at 7 months between the two treatment arms. Both the unadjusted and adjusted analyses for RAPID3 and BIoH are consistent with a potential beneficial effect of the advice and physiotherapy arm. If the addition of physiotherapy is beneficial, then the results in Table 14 also suggest that the new outcome measure, BIoH, may be more sensitive to change than the RAPID3 score. In terms of RAPID3 score, the observed difference in means is in the region of 0.3 standard deviations (SDs) compared with 0.5 SDs for the BIoH questionnaire. Of course, given the small sample size and exploratory nature of these analyses, although the CIs are consistent with large beneficial effects of the advice and physiotherapy intervention, they are also consistent with no difference between the groups, or indeed a moderate detrimental effect.
| Outcome measure | Arm | Unadjusted difference in means (95% CI) | Adjusteda difference in means (95% CI) | |
|---|---|---|---|---|
| Advice only (n = 7), mean score (SD) | Advice and physiotherapy (n = 11), mean score (SD) | |||
| RAPID3b | 11.00 (6.82) | 10.27 (6.05) | –0.73 (–7.42 to 5.95) | –1.26 (–5.60 to 3.08) |
| BIoH questionnaire | 195.83 (61.79) | 163.99 (67.39) | –31.85 (–95.71 to 32.01) | –28.57 (–75.97 to 18.84) |
The results of linear regression models examining differences between the groups in terms of secondary outcomes are presented in Table 16. For the majority of outcomes, the 95% CIs demonstrate that a moderate benefit of advice plus physiotherapy is plausible and that a beneficial effect of advice only of the same magnitude is less likely. Exceptions relate to the RADAI score relating to pain in all joints and the visual analogue questions relating to pain in the most affected joint at rest and on movement. The CIs for these three outcomes suggest that it is also plausible that the addition of physiotherapy may cause more pain; of course, all CIs are also consistent with no real difference between the groups, as we would expect in this small pilot trial.
| Outcome measure | Arm | Unadjusted difference in means (95% CI) | Adjusteda difference in means (95% CI) | |
|---|---|---|---|---|
| Advice only (n = 7), mean score (SD) | Advice and physiotherapy (n = 11), mean score (SD) | |||
| MDHAQ | ||||
| Function | 2.14 (2.54) | 2.17 (1.64) | 0.02 (–2.13 to 2.18) | 0.52 (–0.69 to 1.74) |
| Pain | 5.07 (2.05) | 4.36 (2.68) | –0.71 (–3.23 to 1.82) | –0.81 (–4.47 to 2.85) |
| Global | 3.79 (2.60) | 3.55 (2.78) | –0.24 (–3.02 to 2.54) | –0.78 (–4.54 to 2.97) |
| RADAI | 8.71 (10.39) | 12.60 (8.53) | 3.89 (–5.90 to 13.67) | 3.01 (–3.83 to 9.84) |
| Fatigue | 4.71 (3.99) | 3.77 (3.08) | –0.94 (–4.47 to 2.59) | –0.04 (–4.15 to 4.07) |
| BRAF scale | ||||
| Average fatigue | 5.13 (3.14) | 3.73 (2.87) | –1.40 (–4.32 to 1.52) | –0.65 (–4.31 to 3.01) |
| Effect of fatigue | 4.88 (3.48) | 3.36 (3.53) | –1.51 (–4.95 to 1.93) | –1.68 (–6.61 to 3.26) |
| Coping with fatigue | 3.63 (2.97) | 2.36 (2.34) | –1.26 (–3.83 to 1.30) | –2.49 (–5.84 to 0.86) |
| Pain in . . . | ||||
| Most affected joint at rest | 38.50 (30.02) | 51.45 (29.26) | 12.95 (–16.04 to 41.95) | 5.90 (–30.88 to 42.68) |
| Most affected joint on movement | 45.13 (26.46) | 61.82 (31.94) | 16.69 (–12.53 to 45.92) | 6.64 (–29.98 to 43.26) |
| All joints in general at rest | 35.29 (26.74) | 26.64 (20.60) | –8.65 (–32.32 to 15.02) | –18.37 (–51.57 to 14.84) |
| All joints in general on movement | 42.57 (25.71) | 38.64 (26.89) | –3.94 (–31.05 to 23.18) | –14.34 (–49.21 to 20.52) |
| ESE scale | 47.04 (30.02) | 60.28 (21.69) | 13.24 (–8.81 to 35.29) | 7.03 (–18.59 to 32.65) |
In summary, the exploratory results of this pilot trial provide evidence of promise for the advice and physiotherapy intervention, which needs to be evaluated in a definitive trial.
Ancillary analyses
Missing items within the BIoH questionnaire were imputed for the primary analysis described above (see Primary and secondary patient-reported outcomes) following the user scoring guidelines (see Appendix 15). Consideration was subsequently given to single imputation of missing items within specific sections of the questionnaire, which contributed to an overall score – this included the 10-item function score (used also to generate RAPID3 score) in the MDHAQ; and the 18-item ESE scale. Multiple imputation and cases with complete missing data were not considered in the analysis of this pilot trial. Table 17 presents the findings for the outcomes with imputed data and demonstrates little impact on the findings.
| Outcome measure | Arm | Unadjusted difference in means (95% CI) | Adjusteda,b difference in means (95% CI) | |
|---|---|---|---|---|
| Advice only (n = 7), mean score (SD) | Advice and physiotherapy (n = 11), mean score (SD) | |||
| Function | 2.14 (2.54) | 2.05 (1.61) | –0.10 (–2.16 to 1.96) | 0.19 (–0.96 to 1.20) |
| RAPID3 | 11.00 (6.82) | 9.95 (5.83) | –1.05 (–7.42 to 5.33) | –1.46 (–8.63 to 5.71) |
| ESE scale | 41.45 (17.72) | 61.86 (21.23) | 20.41 (0.93 to 39.88) | 10.55 (–15.00 to 36.09) |
Adverse events
The baseline, month 4 and month 7 questionnaires contained an open-text question asking participants to tell the research team about any ‘untoward event, particularly if you feel it has been related to taking part in the research or which was unexpected’. Table 18 presents events that were reported at months 4 and 7.
| Participant | Allocation | 4-month questionnaire | 7-month questionnaire |
|---|---|---|---|
| 112 | Advice only | I was diagnosed with depression (again) soon after filling out the first questionnaire and put on sertraline. While on this my pain has improved in my legs somewhat, but as at the same time I changed my contraceptive pill I cannot be sure which (if either) effected [sic] this. Following reading the material on hypermobility I was given, I asked my Doctor to change my contraceptive pill from oestrogen-based yasmin to oestrogen-free mini-pill | Fractured my wrist in September by falling over. Appears that I hyperextended my wrist |
| 113 | Advice only | Withdrawn (requested treatment) | Withdrawn (requested treatment) |
| 114 | Advice only | Have to undergo physio[therapy] due to hip pain | Questionnaire not returned |
| 117 | Advice only | Withdrawn (requested treatment) | Withdrawn (requested treatment) |
| 121 | Advice only | Questionnaire not returned | Questionnaire not returned |
| 122 | Advice only | Questionnaire not returned | Questionnaire not returned |
| 126 | Advice only | Questionnaire not returned | Still breastfeeding and carry around 12 kg child a lot usually in a slingb |
| 212 | Advice only | I have had a painful Achilles tendon in my left ankle for several weeks. Worse after swimming and cycling and aches at night. Seen podiatrist for insoles – said left Achilles tendon appears swollen compared to right. Have been doing stretches and ice pack application but not really helping | Have had pain in mid back for past 2 weeks – feels like pulled muscles around vertebrae. Have been managing with pain relief, massager and trying to keep mobile – swimming and gentle stretching and walking. Used ice packs and rest for 1 day. Have not yet sought help as seems to be getting better slowly |
| 213 | Advice only | I badly sprained my left ankle about 6½ weeks ago. It’s a high ankle sprain, above the ankle bone. Has been very slow to heal and I’m still in pain. There was no specific twist/trip/fall, just came on after a running session | Experiencing severe migraines last 6 weeks, probably stress related |
| 215 | Advice only | Nil reported | Nil reported |
| 216 | Advice only | Questionnaire not returned | Problems with nerve root in my lumber [sic] spine, I had bad muscle spasms and pains in leg and groin. Pains in leg and groin have gone but muscles spasm’s remain very bad |
| 218 | Advice only | Nil reported | Questionnaire not returned |
| 219 | Advice only | Nil reported | Questionnaire not returned |
| 220 | Advice only | Questionnaire not returned | My shoulder blade had been feeling like it was coming away from my chest for a few days causing pain and then out of nowhere (at rest) my whole chest went into spasm (intercostal muscles, I guess) and it was a 9/10 pain and it felt like someone was sitting on my chest and it was agony to breathe. Paramedic came and gave me i.v. [intravenous] paracetamol on top of all the morphine (oral) and diazepam I had taken. Nothing was helping so I went to A&E [accident and emergency] to get i.v. morphine (what usually works) and have chest X-ray and heart monitoring. My heart was fine. This happened before when they thought I was having a heart attack but it turned out to be a really high up gut spasm. It’s very hard to find the actual problem because the hypermobility can masquerade as something else or cover the real problem |
| 111 | Advice and physiotherapy | Doctors halved my pain medication so was unable to do as many exercises given, physio[therapist] phoned and left messages to my doctor saying to keep me on the same dose until physio[therapy] finished, Doctor got back to physio[therapist] and they agreed to half my dose! Miscommunication | Questionnaire not returned |
| 115 | Advice and physiotherapy | Questionnaire not returned | Questionnaire not returned |
| 116 | Advice and physiotherapy | Nil reported | Nil reported |
| 118 | Advice and physiotherapy | Questionnaire not returned | Nil reported |
| 119 | Advice and physiotherapy | Nil reported | Nil reported |
| 120 | Advice and physiotherapy | Nil reported | Questionnaire not returned |
| 123 | Advice and physiotherapy | Seen by: [name removed] (orthopaedic surgeon) 29/9/14 Diagnosis bilateral patellofemoral joint arthritis; Dr [name removed] (clinical psychologist) 4/8/14 Self management; Dr [name removed] 7/11/14 Pain management | Nil reported |
| 124 | Advice and physiotherapy | Questionnaire not returned | Nil reported |
| 125 | Advice and physiotherapy | Questionnaire not returned | Nil reported |
| 127 | Advice and physiotherapy | Nil reported | Nil reported |
| 128 | Advice and physiotherapy | Nil reported | Nil reported |
| 211 | Advice and physiotherapy | Dislocated knee half way through trial during Aqua Aerobics. Knee has been in brace and taken a while to heal. Physio[therapy] has been helpful and has improved quicker this time than previous incidents | Nil reported |
| 214 | Advice and physiotherapy | Withdrawn (too busy) | Withdrawn (too busy) |
| 217 | Advice and physiotherapy | Nil reported | I am about to move house again which I seem to be doing every 18 months/2 years – each time it gets more and more painful physically and after each move there appears to be a considerable deterioration which does not come back to the level it was before pre the moveb |
| 221 | Advice and physiotherapy | Have recently had a sickness bug and a cough making back pain and spasms worse | Nil reported |
Adverse events were discussed on an ongoing basis with the study Data Monitoring and Ethics Committee (DMEC), which, at the end of the study, produced the analysis presented in Table 19. Events classified by two members of the DMEC as possibly being a result of the treatment or lack of treatment, including withdrawing from the study to seek additional treatment, were included in the analysis. Events were examined using chi-squared and Fisher’s exact tests, as appropriate.
| Type of comparison | Arm | p-value | |
|---|---|---|---|
| Advice, % | Advice and physiotherapy, % | ||
| 4-month questionnaire results | 0.236 | ||
| No event | 28.6 (4/14) | 60.0 (9/15) | |
| Event (including withdrawn) | 35.7 (5/14) | 20.0 (3/15) | |
| Questionnaire not returned | 35.7 (5/14) | 20.0 (3/15) | |
| Percentage with event (excluding incomplete) | 55.6 (5/9) | 25.0 (3/12) | 0.203 |
| 7-month questionnaire results | 0.002 | ||
| No event | 14.3 (2/14) | 80.0 (12/15) | |
| Event (including withdrawn) | 50.0 (7/14) | 6.7 (1/15) | |
| Questionnaire not returned | 35.7 (5/14) | 13.3 (2/15) | |
| Percentage with event (excluding incomplete) | 77.9 (7/9) | 7.7 (1/12) | 0.001 |
| 4- and 7-month questionnaire results combined | 0.022 | ||
| Event (including withdrawn) | 76.7 (8/12) | 20.0 (3/15) | |
Table 20 presents odds ratios and 95% CIs for an event in the advice-only arm compared with the advice and physiotherapy arm. Having an event appears far more likely in the advice-only arm. Despite the small numbers, this finding is unlikely to have occurred by chance alone. It should be noted, however, that this analysis includes all events potentially related to treatment; in reality, the number as a result of treatment may be far lower.
| Time point | Odds ratio | 95% CI |
|---|---|---|
| 4-month event | 3.74 | 0.59 to 23.8 |
| 7-month event | 41.7 | 3.19 to 500 |
| Event at any time | 8.00 | 5.72 to 45.5 |
Sample size calculation
Given the nature of the intervention, it is envisaged that randomisation in a definitive trial would be at the level of the patient not the physiotherapy unit. At the time of conducting this pilot RCT, the anticipated outcomes that would be primary outcome measures in a definitive trial are RAPID3 (calculated from the MDHAQ) and the BIoH questionnaire score from the newly developed BIoH.
Routine Assessment of Patient Index Data 3 score
As discussed in Chapter 3, Quantitative aspects, although the MDHAQ and its RAPID3 subscale has not been used before in JHS, it has been successfully employed with a very wide range of other rheumatological conditions and was attractive because of its multijoint approach to assessment. Response criteria for the RAPID3 score have been proposed as a decrease in score of 3.6 units or more for a ‘good’ response, and 1.8 units or more for a ‘moderate’ response. 65 In terms of high, moderate and low severity, and near remission for RAPID3, scores of > 12, 6–12, 3–6, and ≤ 3 are proposed, respectively. 65 Within the pilot trial the mean baseline RAPID3 score was just over 12 units (50% classified as high severity), with a SD of ≈ 5 units. At 7 months, the SDs were ≈ 6 units and 6.8 units for the advice and physiotherapy group and within the advice-only group, respectively. There is currently no published literature reporting variability in RAPID3 score among JHS patients following an intervention. Table 21 illustrates the required sample size for 80%, 85% and 90% power, a two-sided 1% and 5% alpha level for a difference in means analogous to a ‘moderate’ and ‘good’ response. As the primary outcome for a definitive trial is likely to be 12 months (for which we do not have data), a conservative estimate for SD of 7 units has been used to inform sample size in Table 21.
| Minimally important difference (unit difference in means) | Two-sided alpha | Sample size, n (per arm) | ||
|---|---|---|---|---|
| 80% power | 85% power | 90% power | ||
| 1.8 | 0.01 | 354 | 395 | 451 |
| 0.05 | 238 | 272 | 318 | |
| 3.6 | 0.01 | 89 | 99 | 113 |
| 0.05 | 60 | 68 | 80 | |
Attrition rate
Overall attrition within the pilot trial was approximately 35% (higher in the advice-only group than in the physiotherapy group); therefore, to allow for this degree of attrition the above sample sizes would need to be inflated by a factor of 1.54 (1/0.65). Strategies to improve the attrition rate are discussed in Chapter 6, Recruitment rates.
Recruitment time
As an example, if a definitive trial was powered to detect a difference in mean RAPID3 scores of 3.6 units, with 90% power and a two-sided 5% alpha, 80 patients would be required for each arm of the trial. Incorporating a factor of 1.54 for a potential loss to follow-up rate of 35% this would require 122 patients to be allocated to each treatment group. Within the pilot trial, on average, two patients were recruited and randomised each month from each of the two units. If, in a definitive trial, patients could be recruited from six units and it is assumed that all have similar referral rates to those within the pilot trial, it would take approximately 20 months to recruit sufficient patients to the trial.
Making the same assumptions, a 5-year recruitment period would be required to detect a difference of 1.8 (more within the region of the difference observed within the pilot trial), to ensure 80% power, 5% alpha and an attrition rate of 35%. Unless the eligibility criteria for a definitive trial are dramatically widened, the rate of consent improved or the attrition rate diminished, a definitive trial to detect this magnitude of difference appears unlikely.
Bristol Impact of Hypermobility questionnaire score
Full validation of the BIoH questionnaire is ongoing and will be completed before any definitive trial takes place. It is anticipated that part of this validation will include discussion and consensus as to the minimally clinically important difference to be detected in any future trial. Table 22 illustrates the required sample size for a range of minimally important differences for 80%, 85% and 90% power, and a two-sided 1% and 5% alpha level. As this is a new measure there is no previously published data in terms of the variability in BIoH questionnaire score. At the 7-month follow-up the SDs were approximately 62 and 67 units in the advice-only and advice plus physiotherapy groups, respectively. As the primary outcome for a definitive trial is likely to be 12 months (for which we do not have data), a conservative estimate for SD of 70 units has been used to inform sample size in Table 22.
| Minimally important difference (unit difference in means) | Two-sided alpha | Sample size, n (per arm) | ||
|---|---|---|---|---|
| 80% power | 85% power | 90% power | ||
| 10 | 0.01 | 1145 | 1279 | 1459 |
| 0.05 | 770 | 880 | 1030 | |
| 20 | 0.01 | 287 | 320 | 365 |
| 0.05 | 193 | 220 | 258 | |
| 30 | 0.01 | 163 | 143 | 128 |
| 0.05 | 74 | 85 | 99 | |
| 40 | 0.01 | 72 | 80 | 92 |
| 0.05 | 42 | 48 | 56 | |
The highlighted section of Table 22 illustrates the sample sizes required to detect a difference of the same magnitude as that observed within the pilot trial – a plausible real size of effect. As the BIoH questionnaire score can take a value between 0 and 360, a difference in means between two interventions of anything < 30 (a jump of 8.3% on the total scale) is unlikely to be clinically significant.
Recruitment time
As an example, if a definitive trial was powered to detect a difference in mean BIoH questionnaire scores of 30 units, with 90% power and a two-sided 5% alpha, 99 patients would be required for each arm of the trial. Incorporating a factor of 1.53 for a potential loss to follow-up rate of 35%, this would require 152 patients to be allocated to each treatment group. In the pilot trial, on average, two patients were recruited and randomised each month from each of the two units. If, in a definitive trial, patients could be recruited from six units and it is assumed that all have similar referral rates of those within the pilot trial, it would take approximately 25 months to recruit sufficient patients to the trial.
In terms of RAPID3, recruiting 152 per arm would provide 85% power to detect a difference of 3.6 units with a two-sided alpha of 1% or a difference of 3.0 units with a two-sided alpha of 5%.
Economic analysis
Results: descriptive statistics
The set-up and training resource use and costs in preparation for the pilot RCT included 5 days of chief investigator (SP) time to develop and refine the training materials; 1 day for the chief investigator (SP) to train four physiotherapists (one band 7, three band 6) in intervention delivery; and two 5-hour sessions for three of these physiotherapists to train four additional colleagues (three band 6, one band 7) and one student in train-the-trainer events. Additional expenses included staff travel to training events. Graphic design, printing and purchase cost of HMSA booklets (used by patients in both arms of the RCT) totalled £520.
The absolute EQ-5D-5L scores in the advice-only and advice and physiotherapy groups were similar at both 4 and 7 months (Table 23). However, the advice and physiotherapy group had higher mean EQ-5D-5L scores at baseline and lower variability than the advice-only group, and this remains the case throughout follow-up. The changes in EQ-5D-5L scores from baseline were also very similar (Table 24), although the mean change in the advice and physiotherapy group was higher at 4 months and lower at 7 months. There is a high degree of uncertainty in these estimates because of the low numbers. One patient (patient 216) had a large negative EQ-5D-5L score at baseline, which led to unusually high increases in EQ-5D-5L at 7 months in the advice-only arm. Omitting this patient, the absolute EQ-5D-5L scores are similar across the arms, including at baseline, and the variability in the advice-only arm is reduced (Table 25). Change from baseline at 7 months becomes similar between the two arms when the outlier is omitted (Table 26).
| Time point | Arm | |||||
|---|---|---|---|---|---|---|
| Advice only | Advice and physiotherapy | |||||
| n | Mean score (95% CI) | SD | n | Mean score (95% CI) | SD | |
| Baseline | 10 | 0.65 (0.44 to 0.87) | 0.30 | 14 | 0.72 (0.65 to 0.79) | 0.12 |
| 4 months | 7 | 0.72 (0.50 to 0.94) | 0.24 | 10 | 0.76 (0.69 to 0.83) | 0.10 |
| 7 months | 8 | 0.69 (0.47 to 0.90) | 0.26 | 11 | 0.74 (0.64 to 0.85) | 0.15 |
| Time point | Arm | |||||
|---|---|---|---|---|---|---|
| Advice only | Advice and physiotherapy | |||||
| n | Mean change in score (95% CI) | SD | n | Mean change in score (95% CI) | SD | |
| 4 months | 6 | –0.12 (–0.42 to 0.18) | 0.29 | 10 | 0.07 (–0.04 to 0.17) | 0.15 |
| 7 months | 6 | 0.06 (–0.13 to 0.25) | 0.18 | 11 | 0.01 (–0.11 to 0.12) | 0.17 |
| Time point | Arm | |||||
|---|---|---|---|---|---|---|
| Advice only | Advice and physiotherapy | |||||
| n | Mean score (95% CI) | SD | n | Mean score (95% CI) | SD | |
| Baseline | 9 | 0.74 (0.64 to 0.84) | 0.14 | 14 | 0.72 (0.65 to 0.79) | 0.12 |
| 4 months | 7 | 0.72 (0.50 to 0.94) | 0.24 | 10 | 0.76 (0.69 to 0.83) | 0.10 |
| 7 months | 7 | 0.75 (0.55 to 0.94) | 0.21 | 11 | 0.74 (0.64 to 0.85) | 0.15 |
| Time point | Arm | |||||
|---|---|---|---|---|---|---|
| Advice only | Advice and physiotherapy | |||||
| n | Mean change in score (95% CI) | SD | n | Mean change in score (95% CI) | SD | |
| 4 months | 6 | –0.12 (–0.42 to 0.18) | 0.29 | 10 | 0.07 (–0.04 to 0.17) | 0.15 |
| 7 months | 5 | –0.01 (–0.10 to 0.08) | 0.07 | 11 | 0.01 (–0.11 to 0.12) | 0.17 |
We compared the baseline EQ-5D-5L scores in patients who dropped out of the study and those who did not in the advice-only and advice and physiotherapy arms (Table 27). In the advice arm, baseline mean EQ-5D-5L scores were higher in the dropouts than in those that continued in the trial, whereas in the advice and physiotherapy group baseline mean EQ-5D-5L scores were lower in the dropouts. However, as expected, omitting the outlier patient 216, the two arms show comparable baseline mean EQ-5D-5L scores that are lower in those who drop out than in those who continue with the trial (see Table 27).
| Status | Arm | |||||
|---|---|---|---|---|---|---|
| Advice only | Advice and physiotherapy | |||||
| n | Mean score (95% CI) | SD | n | Mean score (95% CI) | SD | |
| Drop-out | 4 | 0.69 (0.38 to 0.99) | 0.19 | 3 | 0.67 (0.29 to 1.05) | 0.15 |
| Non-dropout | 6 | 0.63 (0.24 to 1.02) | 0.38 | 11 | 0.74 (0.66 to 0.82) | 0.12 |
| Non-dropout, omitting patient 216 | 5 | 0.78 (0.70 to 0.87) | 0.07 | 11 | 0.74 (0.66 to 0.82) | 0.12 |
Total costs had a skewed distribution. We provide the observed mean total costs in Table 28, with the median and interquartile range. The point estimates indicated higher total costs in the advice and physiotherapy arm than in the advice-only arm at 4 months and lower costs at 7 months. As to be expected given the sample sizes and skewed distributions, there is a high degree of uncertainty around these estimates. The largest contributor to the costs was primary care visits, followed by community costs. The pattern also persisted when an outlier (patient 216, who visited their GP 26 times in the second time period, and reported a negative EQ-5D-5L score result at baseline) was removed from the advice group, although total costs for the advice group were substantially lower at 7 months when this outlier was removed (Table 29).
| Time point | Advice only | Advice and physiotherapy | ||||
|---|---|---|---|---|---|---|
| n | Mean cost, £ | Median cost, £ (IQR) | n | Mean cost, £ | Median cost, £ (IQR) | |
| 4 months | 7 | 192.0 | 128 (78.75–248.61) | 10 | 342.8 | 279 (129.78–470.76) |
| 7 months | 8 | 556.1 | 162 (13.88–701.66) | 11 | 122.6 | 32 (3.525–131.66) |
| Time point | Advice only | Advice and physiotherapy | ||||
|---|---|---|---|---|---|---|
| n | Mean cost, £ | Median cost, £ (IQR) | n | Mean cost, £ | Median cost, £ (IQR) | |
| 4 months | 7 | 192.0 | 128 (78.75–248.61) | 10 | 342.8 | 279 (129.78–470.76) |
| 7 months | 7 | 289.2 | 71 (9.25–407.88) | 11 | 122.6 | 32 (3.525–131.66) |
Value-of-information analysis
Pilot trial results: statistical model, adjusting for baseline European Quality of Life-5 Dimensions-5 Levels scores
Statistical models are used to estimate the mean costs and QALYs under the two interventions. EQ-5D-5L scores are assumed normally distributed, and a piecewise linear model is assumed on the intervals 0–4 months and 4–7 months, and adjusted for baseline EQ-5D-5L score. Costs are assumed to be log-normally distributed and adjusted for baseline EQ-5D-5L score. Because the model predicts total costs and QALYs for a given baseline EQ-5D-5L score, we integrate over the estimated distribution of baseline EQ-5D-5L scores to obtain a population average for total costs and total QALYs (see Appendix 14 for details).
As previously noted, patient 216 in the advice arm was identified as having an unusually high cost at 7 months (26 GP visits), and also a negative EQ-5D-5L score at baseline leading to an unusually high improvement in EQ-5D-5L at 7 months. Model fit improved by omitting this outlier and, although the estimates changed, none of the conclusions changed. This outlier is therefore omitted in the results presented in Table 30.
The effect of adjusting for baseline utility scores is that for those patients with lower EQ-5D-5L scores, utilities increase over time, whereas for those with higher EQ-5D-5L scores, utilities decrease over time. However, for all baseline EQ-5D-5L scores, advice only has higher EQ-5D-5L than advice and physiotherapy.
Table 30 presents the cost-effectiveness analysis results from the statistical modelling. Compared with advice only, advice and physiotherapy has lower expected costs (£242.9 vs. £399.0), but lower expected QALYs (0.41 vs. 0.45). At both £20,000 and £30,000 willingness to pay per QALY thresholds advice only is the most cost-effective intervention, as seen by the negative expected incremental net benefit. There is a high degree of uncertainty in these results, so that it is plausible that advice and physiotherapy is the most cost-effective intervention.
| Estimates | Arm | |
|---|---|---|
| Advice only, posterior mean (95% CrI) | Advice and physiotherapy, posterior mean (95% CrI) | |
| Expected costs, £ | 399.00 (33.60 to 1797.00) | 242.90 (32.80 to 947.20) |
| Expected QALYs | 0.45 (0.40 to 0.50) | 0.41 (0.36 to 0.45) |
| Expected incremental net benefit (£) advice and physiotherapy vs. advice only | £20,000 threshold, posterior mean (95% CrI) | £30,000 threshold, posterior mean (95% CrI) |
| –675.7 (–2309.0 to 1189.0) | –1092.0 (–3318.0 to 1315.0) | |
Previous relevant literature to inform the value-of-information analysis
Our rapid review of studies reporting utilities or costs identified 149 potentially relevant articles on PubMed. Based on a review of titles and abstracts we found six papers35,38,91–94 reporting generic health-related quality of life in patients with JHS (Table 31). These studies typically were cross-sectional surveys with small numbers of patients with JHS (range 20–115). All of the studies used quality-of-life measures (e.g. SF-36 or the Pediatric Quality of Life Inventory™) which were not designed to calculate utility scores. We did not find any articles describing the costs of treating JHS. We did not identify any economic models for JHS patients.
| Study name | Design | Condition | Setting | Participant characteristics | Sample size | Outcomes |
|---|---|---|---|---|---|---|
| Pacey et al., 201338 | Survey | JHS | Children aged 6–16 years with JHS from a specialised clinic in Sydney, Australia. Private paediatricians and paediatric rheumatologists recruited additional patients | Mean age 11.55 years (SD 2.95 years); 39 females and 50 males | 89 | PedsQL reported by children and parents |
| Albayrak et al., 201591 | Survey with controls | BJHS | Konya Research and Educational Hospital, Turkey. Patients aged 18–50 years with BJHS and severe pain. Not clear if these were patients at the Konya hospital. Control group were age-matched healthy volunteers | In BJHS group, mean age 30.17 years (SD 7.47 years); 13 males and 102 females | 115 with BJHS and 114 healthy controls | SF-36 and VAS for pain |
| De Wandele et al., 201492 | Survey with controls | EDS-HT | Patients with EDS-HT recruited by Centre for Medical Genetics at Ghent University Hospital, Belgium | In EDS-HT group, mean age 40.7 years (SD 12.17 years); 5 males and 75 females | 80 with EDS-HT, 43 healthy controls | SF-36 and other questionnaires related to autonomic symptoms |
| Ferrell et al., 200435 | Cohort study | JHS | JHS patients aged 16–49 years recruited from hypermobility clinic at Glasgow Royal Infirmary, Scotland, UK | Mean age 27.3 years (SD 10.4 years); 2 males and 16 females | 20 baseline, 18 completed intervention | SF-36, knee pain VAS |
| Rombaut et al., 201093 | Survey with controls | EDS-HT | Women with EDS-HT recruited by Centre of Medical Genetics at Ghent University Hospital, Belgium | In EDS-HT group, median age 38 years (range 25–67 years); all female | 32 with EDS-HT, 32 healthy controls | SF-36 for QoL |
| Berglund et al., 201594 | Survey with controls | All EDS | Postal survey of members, aged > 18 years, of the Swedish National EDS Association. Swedish population study used as control | Mean age 46.1 years (95% CI 44.5 to 47.7 years) | 250 any EDS, 76 (30%) hypermobility type. 250 matched healthy controls | SF-36 and HADS (for mental health) |
The systematic review of interventional studies for JHS33 identified only four studies26,35–37 despite no restrictions on study design. Of these, Kemp et al. 37 included only children; Sahin et al. 26 focused on knee exercises, rather than a whole-body approach; Ferrell et al. 35 was a cohort study that measured quality of life with the SF-36 (also identified in our rapid review; see Table 30); and Barton and Bird36 was a cohort study that did not report enough detail to know the age of participants nor to calculate an effect size. None of the studies had a follow-up > 5 months; therefore, the 7-month follow-up from our pilot trial represents the most mature evidence of efficacy of therapeutic exercise interventions in JHS patients and, consequently, it is this evidence that is used to define our uncertainty in intervention efficacy (the range of potential benefits/harms) for use in the decision model.
In the absence of any existing models, and no evidence on intervention efficacy or natural history of JHS patients beyond the 7-month follow-up of our pilot trial, we restrict our model to a 7-month time horizon. This assumes that all differential costs and benefits between advice only and advice and physiotherapy will have been accrued by 7 months. The model is identical to that presented in the previous section (see Appendix 14 for details), estimated using the data collected in the pilot trial (omitting the outlier patient 216).
Population measures of VOI require an estimate of the incidence of new patients who will be eligible for the intervention. We estimate the population of England and Wales aged ≥ 16 years to be 46,161,703. 95 Based on a recent survey of physiotherapy services,96 we estimate the average annual rate of new physiotherapy referrals as 0.033. Connelly et al. 14 estimated that 30% of referrals to a musculoskeletal triage service receive a diagnosis of JHS. Under these assumptions then we estimate the annual incidence of new hypermobility patients referred to physiotherapy services to be:
The 30% of referrals receiving a diagnosis of JHS reported by Connelly et al. 14 is likely to be an overestimate because the authors specifically applied the diagnostic criteria to all patients referred to the triage clinic where they were, and many of those patients might not otherwise have been diagnosed with JHS and problems associated with JHS may not have been the primary reason for referral. We therefore also present results for an incidence estimate based on a much more conservative estimate of 10% of referrals receiving a diagnosis of JHS:
Value-of-information results
The population EVPI is plotted against willingness-to-pay per QALY for three different lifetimes of the intervention (1, 5 and 10 years) and for the two different estimates of incidence (Figure 10). These figures represent the potential health gains (in net monetary units) from knowing the best intervention to use (based on the range of plausible values predicted from our pilot study), multiplied by the population eligible to benefit over different time horizons. As expected, the value of new research increases with the lifetime of the intervention and with estimates incidence. The curves have a peak around the threshold where the optimal decision changes (from advice and physiotherapy for low willingness to pay to advice for high willingness to pay). There appears to potentially be a high value of new research if it were to eliminate all uncertainty in the model, reflecting in part the number of individuals likely to benefit and also the plausible health benefits/harms that are consistent with the results from our small pilot study (i.e. the range of values given by the confidence limits).
FIGURE 10.
Population EVPI is plotted against willingness to pay per QALY for three different lifetimes of the intervention (1, 5 and 10 years) and for (a) incidence: 457,000; and (b) incidence: 152,334.


Table 32 shows for a willingness to pay of £20,000 per QALY the population EVPPI for eliminating uncertainty in all inputs to the decision model (EVPI) and for three different subsets of parameters: cost parameters alone, efficacy parameters alone and baseline EQ-5D-5L distribution parameters alone. This is helpful to identify which model inputs the decision is most sensitive to and identify where future research efforts may be most worthwhile. It can be seen that the decision is most sensitive to uncertainty in the cost parameters, and further research to understand the differences in costs between the interventions is likely to be of value. This is the case even if incidence of JHS referrals is only 152,334 per year and the lifetime of the intervention is only 1 year. There is also value in reducing uncertainty in the efficacy (EQ-5D-5L) parameters, especially if the lifetime for the intervention is likely to be long and incidence of JHS referrals is large.
| Population EVPPI parameters | Incidence: 457,000 | Incidence: 152,334 | ||
|---|---|---|---|---|
| 1 year | 5 years | 1 year | 5 years | |
| All (EVPI) | £58.00M | £271.20M | £19.30M | £90.40M |
| Cost parameters | £49.40M | £231.00M | £16.50M | £77.00M |
| Efficacy parameters | £19.00M | £88.90M | £6.30M | £29.60M |
| Baseline EQ-5D-5L distribution | £1.40M | £6.40M | £0.50M | £2.10M |
Discussion
In conclusion, the results of the pilot RCT seem to support the feasibility of conducting a definitive RCT of physiotherapy for JHS. The pilot raised a number of important issues which will be briefly identified here. Many of these are discussed in more detail in Chapter 6.
First, recruitment was challenging throughout the recruitment period, despite strategies being implemented to clarify the inclusion and exclusion criteria and to enhance referrals. The rate of recruitment was < 4 recruits per month across two sites. In a future RCT, close attention needs to be made to the number of patients in exclusion categories such as ‘no response’, ‘want active treatment’ and ‘did not attend clinic’ in the CONSORT diagram (see Figure 4). Specific strategies to deal with these are discussed in Chapter 6.
Another consideration is whether or not identifying patients at the point of referral for physiotherapy is the right point at which to try to recruit. There may be more patients in primary care that could be identified and offered treatment earlier in the referral pathway. However, there are likely to be major problems in trying to effectively identify such patients, given the reported lack of recognition of the condition by many health professionals.
The retention rate was also an issue in the pilot RCT. Although only three participants officially withdrew from the study (two from the advice-only arm and one from the advice and physiotherapy arm), questionnaire return was incomplete at all time points. Both of the withdrawals from the advice-only arm cited that the reason was to access active treatment, suggesting a lack of satisfaction with the advice intervention. Questionnaire return was also consistently lower for the advice-only arm, again suggesting dissatisfaction with this intervention. Face-to-face completion might be much better, coupled with a redesign of the advice intervention to make it more credible. Analysis of the dropouts is potentially informative, indicating that patients with low baseline utilities were more likely to drop out of the advice-only arm. This might indicate that this format of control intervention is not acceptable to patients with low quality of life. Additional information related to these issues has been gained from the qualitative research findings to be reported in Chapter 5.
Adherence to physiotherapy was generally very good. The one withdrawal from this treatment arm cited lack of time as being a reason, suggesting that for some attending six sessions could be a large commitment. On the whole, however, attendance was very good and there seems to have been a strong effect of the physiotherapy intervention on improving exercise self-efficacy when compared with the advice intervention. This would seem to indicate some support for self-efficacy being an important mediator in realising positive effects on clinical outcomes.
There is a lack of evidence on any long-term outcomes, meaning that there is uncertainty as to what the long-term effects of the advice and physiotherapy arm may be. Follow-up in this study was only to 7 months (3 months post treatment). Any future definitive trial should include longer-term follow-up, such as to 12 months.
For a future definitive RCT we have assumed that the control arm will be the same (or has the same costs and benefits) as the control in the pilot RCT. If not, then the results might not extend and this would be a limitation of the analysis presented in this chapter.
Training costs of the intervention might be considered part of continuing professional development and would obviously diminish if spread out among more patients. The economic results suggest that the advice-only arm is most likely to be cost-effective if willingness to pay is over £3000 per QALY. This is because it has higher quality of life, but also higher costs. This suggests that the physiotherapy intervention may have cost-saving benefits, rather than improvements in quality of life. This seems conflicting with the results seen on the majority of the clinical measures and it may be that the EQ-5D-5L may fail to reflect the benefits that the clinical measures do. It might also be that the higher joint pain scores reported in the advice and physiotherapy arm had a disproportionate effects on the EQ-5D-5L scores. Johnsen et al. 97 compared the EQ-5D with the Short Form questionnaire-6 Dimensions (SF-6D; derived from the SF-36) in a population with chronic low back pain. The authors found that the EQ-5D had less similarity to a condition-specific outcome measure (the Oswestry Disability Index) in terms of sensitivity, specificity and responsiveness. The SF-6D performed better on these indices. Therefore, it is possible to see divergence in outcome between the EQ-5D and different clinical scores.
Chapter 5 Stage 3: Physiotherapy for Hypermobility Trial – patients’ and physiotherapists’ evaluation
Aims
This chapter reports the qualitative evaluation of the pilot RCT. The broad aims of this part of the research were to determine the:
-
acceptability of the research design and physiotherapy intervention to patients in terms of quality of life
-
acceptability and feasibility of the physiotherapy intervention to physiotherapists in terms of training and implementation.
Introduction
The overall design of the pilot RCT has already been described in detail in Chapter 4. This chapter will therefore focus specifically on aspects related to the qualitative evaluation of patients’ and physiotherapists’ experiences of this complex intervention. Complex interventions are often difficult to assess quantitatively, and qualitative assessment can provide nuanced and comprehensive information about the value, acceptability and clinical effectiveness of the treatment in question. The qualitative component of this pilot trial has allowed the researchers to explore the processes and the context within which the intervention was evaluated, as well as expectations of the intervention and outcomes that have meaning to those with JHS. It has also allowed a deeper understanding of how the physiotherapy intervention can be incorporated into the life of someone living with JHS. As discussed previously (see Chapter 2), qualitative methods are valuable and well established in the pretrial development phase of research to both help develop and refine the trial and to improve our understanding of the experiences of patients receiving, and staff delivering, an intervention. 42–48 Such methods are recommended in the development and evaluation of complex interventions. 98
This chapter will firstly report the methodology and findings related to patients’ experiences, followed by physiotherapists’ experiences.
Patients’ experiences
Objectives
Specific objectives related to exploring patients’ experiences were as follows:
-
To explore participants’ experiences of living with JHS, events leading to diagnosis and subsequent referral for physiotherapy (in order to contextualise their experience of the trial); and to explore their experiences of, and attitudes towards, the use of physiotherapy to manage JHS.
-
To ascertain the acceptability of the trial design for participants, including treatment aims and randomisation, and their preferences for treatment.
-
To develop an understanding of the participants’ experiences of the advice and physiotherapy treatment interventions. More specifically, to ascertain participants’ perception of the value, acceptability and clinical effectiveness of both trial arms and to develop an understanding of any barriers and facilitators to participant compliance, and to understand the acceptabity of data collection.
-
For each of the trial arms, to ascertain whether or not participants perceived any changes had been made or experienced in terms of their health, behaviour and well-being. Also, to develop a deeper understanding of which outcomes or changes are considered to be meaningful by the patients.
-
To explore participants’ suggestions for improvements to the trial design and to each of the interventions (advice and physiotherapy arm).
-
To explore the views and experiences of participants who did not complete the intervention and patients who did not wish (or were unable) to take part.
Methods
Eighteen of the 29 participants recruited to the trial were interviewed between July 2014 and March 2015, either in person or by telephone. Interviews took place at the end of the physiotherapy intervention and at a corresponding time point for those randomised to receive the advice intervention (i.e. at 4 months following randomisation for both arms). The participant information sheet and consent form for the pilot RCT included information regarding the interviews. This information was reiterated verbally to interviewees and verbal consent sought before each interview, supplementing the informed written consent given earlier in the study. Nine of the 18 participants recruited at site 1 and nine of the 11 participants recruited at site 2 agreed to take part in an interview. Interviews lasted between 18 and 90 minutes and were conducted by an experienced qualitative researcher (RT) employed on the project. Topic guides were used to facilitate the interviews and, in line with an inductive approach, were revised in light of emerging findings (see Appendix 16). The interviews focused on trial recruitment, acceptability of the trail, the acceptability of the physiotherapy and advice intervention (including content and delivery), changes experienced or made following participation, and suggestions for improvements. Six of the 23 decliners also agreed to be contacted by a researcher to describe their reasons for being unable or unwilling to participate.
All interviews were audio-recorded, fully transcribed, anonymised, checked for accuracy and then imported into a qualitative software package (NVivo 10) to aid data analysis. Thematic analysis,52 using the constant comparison technique,53 was used to scrutinise the data to identify and analyse patterns across the data set. Transcripts were examined on a line-by-line basis, with codes being assigned to segments of the data and an initial coding frame developed. An inductive approach was used to identify participants’ perceptions of their experiences. To enhance analysis and enable team discussion and interpretation, team members (RT and JH) independently coded 10% of the transcripts; any discrepancies were discussed to achieve a coding consensus and maximise rigour. Scrutiny of the data showed that data saturation had been reached at the end of analysis, such that no new themes were arising from the data. 54
Results
Demographic details for the patient participants who were interviewed are reported in Table 33.
| Participant number | Age (years) | Sex | Treatment allocation | Site number |
|---|---|---|---|---|
| 111 | 36 | Female | Advice and physiotherapy | 1 |
| 112 | 30 | Female | Advice only | 1 |
| 113 | 22 | Male | Advice only (withdrawn following advice – wanted active treatment) | 1 |
| 114 | 25 | Female | Advice only | 1 |
| 119 | 33 | Female | Advice and physiotherapy | 1 |
| 121 | 35 | Female | Advice only | 1 |
| 123 | 23 | Female | Advice and physiotherapy | 1 |
| 127 | 66 | Female | Advice and physiotherapy | 1 |
| 128 | 56 | Female | Advice and physiotherapy | 1 |
| 211 | 27 | Female | Advice and physiotherapy | 2 |
| 212 | 46 | Female | Advice only | 2 |
| 215 | 38 | Female | Advice only | 2 |
| 216 | 38 | Male | Advice only | 2 |
| 217 | 52 | Female | Advice and physiotherapy (withdrawn following advice – too busy) | 2 |
| 218 | 18 | Male | Advice only | 2 |
| 219 | 42 | Female | Advice only | 2 |
| 220 | 24 | Female | Advice only | 2 |
| 221 | 47 | Female | Advice and physiotherapy | 2 |
Living with joint hypermobility syndrome (objective 1)
Symptoms
Participants suffered from a wide range of joint pain, including pain in the hips, knees, shoulders, wrists, ankles, hands and toes. Alongside joint problems, participants described other diverse, long-term symptoms which they attributed to JHS, including fatigue, problems with the effectiveness of local anaesthetics, sleep disruption, irritable bowel syndrome, depression and anxiety. Participants described days when:
You wake up and just ‘oh, please, not today, I really can’t face it’ but you haven’t got a choice you’ve just gotta get going, especially when you’ve got kids and things, it’s – you’ve just got to keep going.
Patient 121 (advice only)
They also described how these symptoms often limited their lifestyle and behaviour choices:
Otherwise I would say that I’m fit and healthy, apart from these annoying discomforts, and I feel that it limits me in the exercise that I want to do because I’ve always been a very sporty person.
Patient 215 (advice only)
Diagnosis trajectory
Although many participants were newly diagnosed with JHS, participants usually described experiencing symptoms of joint hypermobility for many years. Although not always problematic, most noted the onset of symptoms much earlier, often in childhood:
At first they called it like ‘clumsy child syndrome’.
Patient 216 (advice only)
When I was younger, it always used to be like ‘oh, it’s just growing pains’.
Patient 123 (physiotherapy and advice)
Some participants had been previously told that they were hypermobile, but were not given further information about how or what symptoms may develop:
When I went and had my knee operation, they just said ‘oh, you’re hypermobile’, that’s it. This is why we’re putting you in a brace. That’s it.
Patient 121 (advice only)
Factors prompting diagnosis and referral for physiotherapy
A specific injury or symptom that had become increasingly problematic was what usually prompted participants to seek health care. For example, participants often found they had become unable to participate in activities that they had previously engaged in. Usually, however, diagnosis was slow and often difficult:
I’ve always been busy, what’s changed? And they just ran full bloods and said, ‘Oh they’ve come back fine’ and I said ‘but that’s not giving me the answers to why I’m feeling like this’.
Patient 121 (advice only)
I had all sorts of misdiagnoses.
Patient 216 (advice only)
The meaning of diagnosis
As in stages 1 and 2 of this research, participants in stage 3 reported that a diagnosis was extremely important in helping participants to ‘make sense’ of their symptoms:
I literally when [the physiotherapist] told me I said, I burst into tears [. . .] especially when I read through that leaflet, it was just literally my entire life, and I was just like ‘all this time I’ve been going to the doctors and being told that it’s all in my mind‘.
Patient 121 (advice only)
All the things, like when you’re a kid, being clumsy, and things like that, not being able to do PE [physical education], and these little things, it’s, it all adds up.
Patient 111 (physiotherapy and advice)
Pretrial symptom management
Participants described a number of ways in which they managed their symptoms prior to taking part in the trial, typically through the use of painkillers and avoiding exacerbating behaviours. Prior to the trial, many participants were unclear about how best to manage the condition and which behaviours might exacerbate or ameliorate their symptoms:
I just avoided, avoided exercise I suppose, and avoided, sort of, exacerbating it.
Patient 119 (physiotherapy and advice)
I had been going to the gym for a while, you know, under the probably mistaken belief that [. . .] lots of heavy lifting would sort of, you know, strengthen the muscles and therefore the tendons and then it would improve the situation, although actually it had been making I worse, I think.
Patient 113 (advice only – withdrawn to physiotherapy)
Prior experiences of physiotherapy
Most participants had received physiotherapy for specific joint injuries in the past. Experiences and attitudes to physiotherapy were mixed; some had received physiotherapy for an injury or specific problem and found it to be helpful:
When it’s like, specific joints that I know will flare up [. . .] it helps it massively physio[therapy] I find.
Patient 218 (advice only)
However, others’ attitudes to physiotherapy were ‘pretty negative’ [patient 219 (advice only)]. Participants felt that their bodies did not behave or respond in the same ways as those without JHS and that physiotherapy that did not take JHS into account was not appropriate:
I’m not a normal person, I don’t have the joints of a normal person, so that isn’t actually relevant to me.
Patient 220 (advice only)
Thus, even where physiotherapy had been helpful in the resolution of a specific joint problem, its effectiveness was limited if JHS was not recognised as an underlying factor contributing to their joint problems:
I had a fantastic knee physio[therapy] specialist, who, erm, really helped me, erm, and I had a really great shoulder specialist [. . .]. I think she got to the point where she said ‘you know, I can only give you so many exercises. I can’t change your physiology’.
Patient 220 (advice only)
Many felt that the physiotherapists who had treated them in the past had eventually ‘given up’.
I felt a little disappointed that she, this physio[therapist] had kind of given up in a sense saying, you know ‘I, there’s only so much I can do’ and, erm, that kind of thing.
Patient 220 (advice only)
Attitude to the use of physiotherapy to treat joint hypermobility syndrome
In spite of the ambivalent views regarding the value of previous physiotherapy, and sometimes negative experience of physiotherapy, many felt that physiotherapy had the potential to treat their symptoms and participants were open to the possibility that there may be a form of physiotherapy which they would find helpful to manage their symptoms:
If somebody said to me the question ‘do you think it would help’ I would say ‘yes’. I don’t have any knowledge, you know, any evidence to base that on.
Patient 219 (advice only)
I was hoping there may be some exercises that I wasn’t doing, I thought actually it might make things – improve things a little bit.
Patient 127 (physiotherapy and advice)
Acceptability of the trial for patients (objective 2)
Recruitment and attitudes to participation
Participants were usually referred for physiotherapy (and subsequently informed about the trial) for ongoing, progressively worsening or recurring joint problems and pain. Participants had a clear understanding of the aim of the research and what would be involved when taking part and none felt the need to discuss the study with anybody else to help them decide whether or not to participate. Most participants who took part in the trial were keen to be involved in research investigating JHS, to help augment the evidence base and develop an understanding of JHS. Participants were also keen that JHS should be better understood within wider society. Quotations relating to participants’ attitudes to participation in the trial are show in Table 34.
| Participant number | Treatment allocation | Attitude to participating |
|---|---|---|
| 111 | Advice and physiotherapy | Glad really, I think. So people can sort of realise [. . .] people think it’s all in the mind and things like that |
| 112 | Advice only | Excited actually. I thought it sounded really interesting. I always quite liked the idea of being involved in a study [. . .] I thought ‘oh, how wonderful. It would be really interesting to be involved in more of an understanding about what it is that has caused me so much pain for so many years’ |
| 113 | Advice only (then treatment) | Wanted to be a part of it |
| 114 | Advice only | Happy to [take part] [. . .] if I can help anyone or, help out, as much as I can, knowing how it feels [. . .] so we could help other people with the same situation |
| 119 | Advice and physiotherapy | I think it’s important that people do these things, you know, and I was in the, the right place at the right time [. . .] I just think it’s important to do |
| 121 | Advice only | kind of way forward for people in the future that have been diagnosed with it, which is why I agreed to do it, because I spent years with nothing |
| 123 | Advice and physiotherapy | I was more than happy to take part cause I just see it as if, erm, because I’ve struggled so much with like understanding what’s wrong with me and stuff, I just think I was all for to, you know, see if anything could be done or to help others or anything |
| 127 | Advice and physiotherapy | I’m always quite happy to do these things, if they’re going to be of benefit to the, to other [other] people |
| 128 | Advice and physiotherapy | Well, I thought it would be quite interesting cause I feel as though there hasn’t been anything [. . .] really. So, erm, and I thought it, you know, it would be a good thing to do |
| 211 | Advice and physiotherapy | I was quite pleased to be asked really, yes, quite happy to take part in things that help other people |
| 212 | Advice only | I was in a bit of a dilemma I suppose that the time, because at that time I was still working. I was trying to get my head around whether I should be having more input, physiotherapy-wise or whether this was going to be enough for me, with advice and being left to get on with it, so to speak |
| 215 | Advice only | I wanted to see whether I was going to, erm, answer positive for some of them [. . .] so part of me I think was a way of finding out was I or wasn’t I [suffering from JHS] |
| 216 | Advice only | It was useful [. . .] I mean I’ve done medical studies before [. . .] I was taking part in other medical studies, [. . .]. I’m erm, studied human biology. I’m interested in that, I’m doing everything I – it’s interesting |
| 217 | Advice and physiotherapy | If there’s any way that I can erm, do something that will assist people to, to have a better quality of life – and particularly in view of my daughter, erm, and understand what’s going on, then I’d be very happy to take part |
| 218 | Advice only | Well, I find it’s quite interesting [. . .] and I thought, well, it’d be a great opportunity for me, er, not only help myself, but you know, see how it works [. . .] I thought it was an amazing idea |
| 219 | Advice only | I thought it was really important like that. Because, erm, you need to know whether physiotherapy actually does help people, but I don’t know that from evidence, [. . .] research into anything is important so that you can understand things more [. . .] Even if it doesn’t help me it might help somebody else |
| 220 | Advice only | I was very interested to. I think it’s you know, any, any research into something that’s you know, not well understood is, is good |
| 221 | Advice and physiotherapy | Oh I was really thrilled to take part because, erm, I’m very interested in finding out more about my own body. [. . .] I’m a movement teacher myself. So, erm, I try and help others with their pain a little bit. So, erm, I’m very interested in, in what pain can do to your body. Don’t know enough about it, so it, it was ideal for me to find out about my body. To try and sort of pass it onto others and try and help others a little bit |
Study information and treatment equipoise
Participants understood the principles of equipoise:
The thing is, the study didn’t know whether or not physiotherapy helped. And I can understand why, OK, because of the nature of the disorder. Er, it made sense.
Patient 216 (advice only)
Moreover, most participants also recognised that physiotherapy had not necessarily been helpful in the past, and potentially may exacerbate their symptoms.
The pain levels, and the, the constant sort of stiffness of everything [. . .]. And that’s what I thought it would sort of help with. Erm, but again, I’m not entirely sure ‘cause, you know, what I’ve received is basically a 5-minute appointment with a physiotherapist before, where they’ve given me a list of ‘do these exercise and come back in a month’, that’s all I’ve had before.
Patient 218 (advice only)
Treatment preference
Regardless of their prior experiences and understanding of equipoise, many participants still hoped to be randomised into the advice and physiotherapy arm, hoping that ‘something’ rather than ‘nothing’ would be more beneficial. The preference to access physiotherapy was particularly strong among those participants who were experiencing pain.
I think when you’re in that situation and you’re, you’re in pain you want something to help [. . .]. I think I was very keen to be in the physiotherapy group.
Patient 119 (physiotherapy and advice)
A preference for physiotherapy was also expressed when they felt that they needed ongoing health guidance and support.
I would have preferred to have the physiotherapy, but I didn’t have it [. . .] like so when I do have a flare up, I’m not sure if I am actually doing the correct thing by taking my weight of it, or if I should be keeping it moving and things like that [. . .] it would have been nice to, er, find out, erm actually more into [. . .] what the correct kind of thing to do is.
Patient 114 (advice only)
On the other hand, others felt that, although they would have preferred physiotherapy, they also felt that taking part in the trial was important and thought that:
Well, I’ve lasted this long, I might as well just carry on the way I am.
Patient 121 (advice only)
Some had no preference for either treatment arm and were ‘just happy to go with whatever really’ [patient 215 (advice only)], or willing to participate knowing that it would be possible to withdraw from the study and access physiotherapy if necessary, or to access physiotherapy once the trial was over:
I’d have preferred to go in [i.e. have physiotherapy], for being so long without anything, to the point where I’d kind of just rip my hair out, and then finding out I was in the control group, I was like, ‘Well, I’ve lasted this long, I might as well just carry on the way I am’ but I also said to him, ‘So what happens if I do have an issue or a flare-up or something like that?’ He said, ‘If, at any point, it becomes too much, we can take you out of the study and we can help you, you know, you’re on our radar and we can’.
Patient 121 (advice only)
When I first saw the physio[therapist], he said, ‘Well, when the trial is over, I will see you anyway’, so it wasn’t going to make that much difference.
Patient 127 (physiotherapy and advice)
Those quotations might also suggest an issue with equipoise on behalf of the physiotherapists involved with the trial. Others were willing to take part because the evidence to suggest that physiotherapy is effective in treating JHS is lacking:
I can understand how it could do more harm than good, if you don’t really know, then I’m probably, probably best off not trying it, I’d say.
Patient 216 (advice only)
Nonetheless, when randomised to the control arm, some reported feeling ‘a bit disappointed’ [patient 219 (advice only)], or frustrated:
I guess I was slightly, well, not disappointed, cause as I said, I now it’s not, you know, the be all and end all, and you know it h – it has its purpose for the study, erm but I thought ‘Ah, it’s not going to work. This is erm, er kind of frustrating. That puts me back’.
Patient 220 (advice only)
Others, although disappointed, took a longer-term view and were more circumspect:
I was quite disappointed actually [. . .] but I thought ‘I don’t care if I’m not’. It was disappointing because I was quite looking forward to getting the physiotherapy especially if it helped reduce my pain. On the other hand, I sat there and thought at the end of the day I can have physiotherapy afterwards.
Patient 112 (advice only)
Participants’ experiences of the trial (objective 3)
Pace, format, content and delivery of the advice session
Interviews with patient participants were carried out 4 months after their advice session. Some participants therefore reported difficulties in recalling details of this session. For some, the advice session was recalled as an opportunity to discuss in more depth more generic information they had previously accessed from different sources, such as the internet, and provided an opportunity to ask questions about JHS relevant to their personal circumstances. Generally, patients found the advice session helpful and informative. Some felt that, owing to time restrictions, particular aspects of JHS were not discussed in enough depth:
It was helpful but it just really touched, just touched upon the subject [. . .]. I mean some things weren’t even, you know, gone into ‘cause there just was not enough time, I mean, for somebody else it might have been enough, but not me.
Patient 219 (advice only)
Athough some participants would have liked more information, most felt that the advice session was pitched at about the right level, and could be tailored to meet the needs of the individual patient.
One participant randomised to the advice and physiotherapy arm felt that advice alone would have been an inferior treatment:
I don’t think I’d have been that – um, it wouldn’t, well, it wouldn’t have been that good really, if that was all I was going to get, then I wouldn’t have been that impressed with it, really.
Patient 127 (physiotherapy and advice)
Written literature: Hypermobility Syndromes Association and Arthritis Research UK booklets
The participants’ evaluation of the HMSA56 and Arthritis Research UK57 booklets was mixed. Some could not recall being given booklets. Others felt that the booklets were very useful and could be used as a starting point for finding out more about JHS, and one participant passed the booklet on to their GP:
I think the one I found particularly, personally, I found particularly helpful and very informative [. . .] this is the one I actually gave to my GP who, as I say, has a particular interest in this.
Patient 217 (physiotherapy and advice)
What worked well: ‘active ingredients’ of the advice intervention
Most participants valued the opportunity of discussing JHS with somebody who was an expert in the field:
Basically, talking to someone about it and understanding it more made me even feel a little better.
Patient 114 (advice only)
One participant described the physiotherapist’s explanation of JHS and the use of a model skeleton to demonstrate movement as being ‘amazingly invaluable’ and that the physiotherapist ‘explained properly [. . .] like no other person has before, how it actually affects me, and the reason why I get the pain and the best way to avoid it’ [patient 218 (advice only)].
The information provided was another important aspect of the advice session:
From that, you know, couple of hours session; receiving all that advice I found more invaluable than anything else.
Patient 220 (advice only)
Many felt that the information booklets given during the advice session were helpful to support the information given verbally by the physiotherapist:
He delivered it really well, and it was really helpful having the leaflet [. . .] it is quite a lot to take in, especially ‘cause I was in a bit of a state.
Patient 121 (advice only)
Understanding about JHS provided a lot of reassurance, and in turn allowed participants to understand and therefore mange their symptoms:
The fact that I just didn’t feel like I was going mad anymore, which, it was a huge, huge thing that I’m not going insane [laughter], that I’m not imagining things. [. . .] the relief in not knowing I’m going mad was a huge thing [. . .] whereas now I just think, ‘Well that’s what the matter is, this is what helps’.
Patient 121 (advice only)
Many participants valued the contact with the physiotherapist in order to ensure exercises are carried out properly:
I needed, before I even started the exercises I needed to be in, I needed my body to be in the correct position. And I think that’s something that other physio[therapist]s haven’t, er, picked up on. A lot of them are just like, ‘Do a load of exercise’ [. . .] but you’re not, you know, dealing with the underlying physiological, erm, you know, where your bones are supposed to be and where your joints are supposed to be [. . .] So it was, erm, it, the advice was really great for me because I needed to not really do any exercises at that point I just needed to change the way I stood, the way I sat, the way I, you know.
Patient 220 (advice only)
Participants described the holistic approach to the advice session, taking into account personal circumstances and lifestyle, as being a valuable aspect of the advice session:
The 50% of talking about your lifestyle, your sleeping, erm, was something that really made me sit back and think, ‘Oh hang on a minute. I really need to get my life in order a bit more, and I need my sleeping pattern to be better so that it doesn’t make the pain worse’. I hadn’t even thought about that.
Patient 221 (advice only)
Were expectations of the advice intervention met?
Many participants reported that they did not know what to expect, or went ‘with an open mind’ or did not have any expectations:
If I’d had the physiotherapy then maybe I would have expected it to help me.
Patient 219 (advice only)
Some patients had low expectations; one participant felt that they would have expected physiotherapy to help, but did ‘not really’ have any expectations of the advice treatment arm:
I did not really have any expectations. Just hope I suppose [. . .] I do not think you can really say if anything met your expectations until it’s all over and done with and you have the findings.
Patient 112 (advice only)
For others, their expectations were met or exceeded, because of their prior experience of physiotherapy:
Because my expectations were it was just going to be another physio[therapy] and it would probably help a bit [. . .] but I wasn’t, er, expecting to get the results that I got, at all.
Patient 220 (advice only)
One participant felt that the study did not meet their expectations because they were hoping for physiotherapy, but had been randomised to the advice intervention arm.
Global evaluation of the advice intervention
Information related to individuals’ global evaluation of treatment is shown later in Table 35. Those who went on to have the physiotherapy still felt that the advice session was of value:
It was very, you know, very, it made, I definitely felt very positve afterwards.
Patient 119 (physiotherapy and advice)
Others were less positive and did not feel that the advice arm was helpful:
I didn’t really feel that I got much out of it.
Patient 219 (advice only)
However, some were very happy with the advice provided and felt that it empowered them to self-manage their JHS:
I think he was really thorough. And so no, I don’t think anything could have improved it. I think he did what he had to.
Patient 215 (advice only)
Participants’ experiences of the physiotherapy intervention
Participants generally felt that the physiotherapy sessions were flexibile enough to be tailored to meet their specific needs:
I found that there was some things where some of it wasn’t so relevant and so we just moved on and then the other bits that were we could focus on it in more detail.
Patient 211 (physiotherapy and advice)
She’d often sort of change an exercise slightly, because she knew that I was struggling to do it. So she’d change it slightly to adapt it for me.
Patient 111 (physiotherapy and advice)
I think, I think we talked about changing them and then we ended up doing them more or less in the order they were in the book. They actually, kind of, they flowed nicely.
Patient 119 (physiotherapy and advice)
The physiotherapy patient handbook
Generally, the patient handbook was very well received:
The information, the booklet, look at your lifestyle plus the physio[therapy], er, I think it was fantastic.
Patient 221 (physiotherapy and advice)
Erm, I found it nice and easy to read. [. . .] I’ve kept it because it was such a good booklet. I want to revisit it at some point. I don’t think there’s anything I’d particularly change about it. It was very easy to understand. Erm, and I think most people would understand it.
Patient 221 (physiotherapy and advice)
The booklet reinforced the work done in the physiotherapy sessions.
I think the tendency is, as I said, you go in, you do your exercise, you have a discussion, you walk away, you leave it. [. . .] and I think it [the booklet] almost stimulates you to make sure that you do try and do some of the things you’ve discussed in there because you think, ‘Ooh yeah, no we did talk about that, maybe I ought to try doing that then’. [. . .] Whereas, I think sometimes if you haven’t got something like that, then erm you, then, then you don’t bother in quite the same way. You, you think you’re going to, and you mentally, you know ‘Oh yeah I’ll do that, I will do that’. But you just don’t do it – in the same way. And I think actually having a booklet makes you do it more. You know you think, at the start, you think, ‘Why have I got a booklet, why am I being, you know, why am I doing this?’. And that’s why I said it’s part of a process. It doesn’t become clear until you’re actually in the process of doing it and you’re actually in the process of using the book and then it starts to become a point to it, if that makes sense?
Patient 217 (physiotherapy and advice)
Well it’s good really, ‘cause sometimes you forget what exercises you’ve done, and she’d tick the boxes, so then you could sort of come home and have a look through it. And then at your own pace, you can sort of do the exercises at home. And then you’re not forgetting which one’s which, and so it’s good. It’s showing the actual pictures as well, so just in case you forgot what it was.
Patient 111 (physiotherapy and advice)
Although the book was considered by many to be important, some felt that there was not enough time in the session to work through the booklet and then ‘hands-on’ exercises and physiotherapy:
I think we both felt that it would have been nicer to have a longer period of time to not just go through the booklet but to actually go through the actual exercises in, you know – in more detail.
Patient 217 (physiotherapy and advice)
A minority did not feel that the booklet was of value:
I felt the booklet was useless really. And even if I had written in it, it wasn’t even looked at anyway.
Patient 217 (physiotherapy and advice)
What worked well: ‘active ingredients’ of the physiotherapy intervention
The flexibility of the physiotherapy sessions allowed the intervention to be tailored to meet the individual needs of the participant. In effect then, the intervention was slightly different for each patient. For example, participants felt that taking their individual circumstances into account, physiotherapists could appropriately tailor their treatment:
It was actually focusing on what was going to do best for me. It was what was different with this session to anything else I’ve done.
Patient 127 (physiotherapy and advice)
Other aspects of the advice with physiotherapy intervention were also highlighted as working particularly well, as illustrated in the following examples.
As with the advice session, participants valued the holistic approach to the physiotherapy.
It was very nice to actually be seen as a whole person, rather than individual bits and pieces.
Patient 127 (physiotherapy and advice)
I think maybe one of the reasons that doing the actual physio[therapy] helps is that, you know, it’s, it’s a hell of a lot easier to remember all the advice when you kind of, you know that you’re going to go back to a physio[therapist] in a couple of weeks and have to prove that you’ve actually been following the advice.
Patient 113 (advice only – withdrawn to physiotherapy)
I can’t think of anything specific, other than, you know, the accumulation of, of the different sessions all worked to improve it.
Patient 128 (physiotherapy and advice)
Showing you how to do it and then watching you saying ‘oh no, you need to put your arm there, or your leg there’. That helps massively [. . .] ‘cause a lot of exercises I was doing and I was doing it completely wrong and I was like ‘well this is easy’.
Patient 111 (physiotherapy and advice)
Were expectations of the physiotherapy intervention met?
I had very low expectations, and, and they certainly exceeded my expectations because I didn’t really have any. I, I, I didn’t really expect much. [. . .] I thought, ‘Oh here we go. I’m going to find some physio[therapist] that doesn’t really understand me, doesn’t know much about it’ and I, I, I didn’t have any expectations and I was pleasantly surprised.
Patient 221 (physiotherapy and advice)
Trial questionnaires
Views regarding the questionnaires were mixed:
If I’m being honest, they were very repetitive questions. And I understand why they’re repetitive. But I just felt a bit annoyed.
Patient 218 (advice only)
Looking forward to writing down in it. I think it’s going to be quite therapeutic.
Patient 112 (advice only)
Changes following participation in the trial (objective 4)
Most participants felt that participation in the trial, in both arms, led to some changes being made or experienced. A summary of these changes is shown in Table 35. A notable change reported by both treatment arms was the increased feeling of being able to cope with and understand the symptoms of JHS. Similarly, many felt that changes arose from developing a deeper understanding of the condition and, therefore, being able to implement behavioural changes to deal with their symptoms.
Changes following the advice session
One participant reported it was like ‘weights dropping off’ [patient 112 (advice only)] as the physiotherapist explained the symptoms of JHS. Like others, this participant found that during the advice session ‘everything just fell into place’. However, physically, few changes could be identified:
Mobility [. . .] that has not changed [. . .]. Fatigue, that has not changed as a result of the advice session because all is has done is made me understand it more. I do not feel like a waste of space, is probably the best way of putting it, I have a bit more understanding for why I am always tired so therefore, it has become more acceptable and I have lived with it better rather than always worrying that there is something wrong with me [. . .]. At the end of the day, I am not going to magically stop being tired all the time from a bit of advice.
Patient 112 (advice only)
Rather, the advice allowed the participant to self-manage the condition:
Really, just through all the information, I made myself a bullet point list of all the things that I could do to make a start on making myself feel better.
Patient 112 (advice only)
I felt more positive about things that I, because I – it was allowing me to, to look at things more and research it myself, it, it, it was making it, it was giving me a much better understanding of the whole thing.
Patient 221 (physiotherapy and advice)
It was very nice to actually be seen as a whole person rather than bits and pieces.
Patient 127 (physiotherapy and advice)
Participants in the advice intervention arm reported making number of changes following the advice session. Behavioural changes included modifiying exersice regimes (e.g. stopping weightlifting and running or increasing exercise levels). Others felt less able to make informed changes:
I didn’t really, erm, know what to do, or anything like that, erm, so I just, erm, I did start swimming more so – I thought that would be quite good.
Patient 114 (advice only)
In spite of making behavioural change and being more aware of activities which could ameliorate or exacerbate JHS symptoms, many participants still experienced considerable amounts of pain:
You know, I’m still feeling the pain [. . .] and still feeling the same as I have before. It’s just now I understand why I’m feeling it [. . .] it’s not like – there isn’t any magical way to get rid of all the pain – it’s just the understanding of why I think that’s the reason why it’s changed. I think, yeah, massively.
Patient 218 (advice only)
For others, even though their knowledge and understanding of the condition had improved, making changes was difficult:
It’s very difficult to make the changes that I needed to make just like that. Erm, It’s without really going back and asking somebody ‘what – am I doing this right’ and things like that.
Patient 219 (advice only)
Changes following the physiotherapy intervention
As shown in Table 35 most of the participants reported positive changes following the physiotherapy sessions. Behaviour changes included changes to their exercise regime and changes to posture, pacing and sleep. In addition, participants reported making changes to their work patterns or environments. As a result, participants noticed changes to pain levels, ability to cope with pain, along with changes to sleep and fatigue.
| Participant number | When diagnosed and reason for referral | Attitude to intervention arm | Overall evaluation or experience of treatment | Changes made or experienced |
|---|---|---|---|---|
| Advice-only participants | ||||
| 112 | < 3 months. Pain after 10 years of problems. No specific current joint injury | Preference for physiotherapy. Disappointed, wanted physiotherapy, but participated as knew physiotherapy was a later option. Recognised that physiotherapy may not help | Positive: like a massive weight had been liftedSomeone saying ‘This is what the problem is’ changed my life really | Has a greater understanding of the condition, now more acceptable to live with. Very positive psychological changes, ‘just knowing I’m not crazy’. Helps validate to others. No behaviour changes from literature, but from seeing a podiatrist |
| 114 | Approximately 10 years ago, aged 16 years. Hip problems | Preference for physiotherapy. Would have preferred physiotherapy as is unsure whether or not she is ‘doing the correct thing’ (e.g. restricting movement). But happy to take part to help others | Positive: just given a better understandingTalking to someone about it and understanding it more, made me even feel a little better | Nothing specific. Did not really know what to do. No difference to health (e.g. pain, fatigue) |
| 121 | ‘Recently’ (now aged mid-30s). Following knee surgery and joint problems | Preference for physiotherapy | Positive:I was a blethering wreck by the end of it, just a relief really, that I wasn’t going mad, you know, there is something that all these things relate to | Hard to make any changes but has taken painkillers more frequently, taken more regular rest breaks and say ‘no’ when necessary. No changes to sleep. Pain has been betterI am in control of how I can help myself [. . .] I feel a lot happier now in, that I’m not going mad and there are things that I can do to help [. . .]. You know, it’s really really made a difference |
| 212 | < 1 year ago | Ambivalent:It looks like it might not work anyway [. . .] so perhaps it’s just enough to have the information and do it myself | Positive:To speak to someone who does understand it does help. From that point of view, it was a really good thing | Tried pacing exercises differently, greater awareness of posture. Improved sleep if exercise is better. More accepting of JHS symptoms a as result of having a greater understanding of the condition. Psychological improvements |
| 215 | < 1 year ago. Recent onset of hip and knee pains. History of a lot of sport. Childhood dislocations | No preference: happy with either treatment arm, as ‘didn’t really think the diagnosis of hypermobility was correct’ | Positive:Great to have information to read around a subject when you’re a bit unsure of whether you have that condition or notTherapist ‘was really thorough’ | Some postural changes and changes to exercise regime. Has not noticed any physiological changes or improvements |
| 216 | < 1 year ago. Lower back pain after car stopped working. Pain started aged 20 years, diagnosis at 37 years old (now 38 years old) | No preference:can understand how it [physiotherapy] can do more harm than good | Positive:Really really interesting | No behaviour changes. Was an informative session, nice to talk to someone about it. The diagnosis made a lot of difference |
| 218 | 3 years ago | Preference for physiotherapy | Positive:. . . the advice that I received you know, was more invaluable than I can ever imagine. From that, you know, couple-of-hour session; receiving all that advice, I found that more invaluable than anything else | Changes to posture, walking and moving. Purchased knee brace. No changes to pain |
| 219 | 6 months ago | Preference for physiotherapy | Negative:I felt disappointed, and to be fair I felt like it was a bit of a waste of a, waste of time [. . .] there wasn’t enough time as I was newly diagnosed and I was wanting to know this, you know, lots of different things. There was just not enough time to give as much advice as I feel I would really have liked | Yes, but owing to other, unrelated, lifestyle changes. Has tried to make changes but difficult without really going back and asking somebody ‘What – am I doing this right?’ |
| 220 | 14 years ago. Diagnosed following hip pain aged 11 years (now 25 years old) | Preference for physiotherapy initially. Very interested realising the JHS is not well understood. Initially wanted physiotherapy, but realised it is not the be all and end all. Intrigued but worried it might cause a set back | Positive:But, [erm], it worked out very well for me having the one off session [. . .] it genuinely has made a dramatic difference [. . .] I think, [erm], to sum it up [. . .] the physio[therapist] looked at me and how my body behaved. Erm, and looked at, yeah, instead of, erm, talking about how the human body should behave or the average human body should behave. [. . .] And he took the time to, erm, you know, research into my lifestyle [. . .] of what it’s really like day to day to live with those kinds of joints | Postural and other behavioural changes, resulted in physical improvements. Less tired, lifted mood, more ‘alive’ |
| Advice and physiotherapy participants | ||||
| 111 | < 1 year. Hip pain/diagnosis of fibromyalgia | Hoped to have physiotherapy | Positive:Erm, I’m glad it happened. ‘Cause it has definitely made a difference | [. . .] exercise seemed to help. If I was doing the right exercises, strengthening exercises. So I joined the gym. So yeah, it’s sort of given me a better attitude towards exercise [. . .] I’m still going to the gym. And I think that does help, definitely. And the slowing down, I’m still trying that . . . make the kids do more [. . .]. Still tired [. . .] Not aching as much when I’m waking up in the morning |
| 119 | ≤ 1 year ago. Knee problems following symptom flare up | Preference for physiotherapy | Positive:You know, I, I feel pretty much better. It’s a good feeling [. . .] I think a lot of people find it difficult to appreciate actually you being in pain all the time, it’s really, really hard to deal with it emotionally and psychologically. [. . .] I think having, having had the physiotherapy helped me get over that. But also knowing that if the pain comes back I have the coping mechanisms to deal with it. Erm, more generally it’s just all improved, it’s you know, I’ve, it’s, it’s now, for me, a managed condition [. . .] I don’t even think about it every day, you know, I, I think about it when I get the odd twinge or when, you know, when my joints click or whatever. It’s, it’s, it’s just become part of my life rather than ruling my life | More aware of pacing, setting time aside to do exercises, increased awareness of movement, posture. Has had workplace assessment. Changes to sleep position, resulting in improved sleepThe improvement to my health is, is, has been fairly remarkable, I mean I’ve gone from being in pain, pretty much, all the time to some degree to, I mean like right now I’m not in pain and I haven’t been, I haven’t been regularly in pain for a few months now. [. . .] the fatigue has, has pretty much vanished |
| 123 | < 1 year ago. Knee surgery after a long history of symptoms since about the age of 4 years | Did not understand the choice available | Negative: pointless, felt not listened to. But information session good in one way as an ‘answer to all my pains and problems’ | First session helped with lots of symptoms like sleeping. Feels a bit more energetic. Learned to pace |
| 127 | Start of trial. Very loose joints, frequent sprains. Rheumatology visit for osteoarthritis | Preference for physiotherapy | Two therapists seen; positive with one physiotherapist, negative with the otherIt was very nice to actually be seen as a whole person rather than bits and pieces | Subtle changes to exercise regime, which made a big difference, particularly core stability |
| 128 | Approximately 10 years ago. Hip problem | Preference for physiotherapy, but would have accepted either | Positive:Generally when I’ve had physio[therapy] before, amongst other things, it has helped to a degree, so I was hoping it would have the same effect. And I’ve got to be honest, it has, it has improved | Pain reduction, less joint dislocation |
| 211 | Approximately 6 years ago. Huge flare up of symptoms and pain | Preference for physiotherapy, but interesting to see if advice only would be beneficial | Positive:The most useful thing I’ve taken part in since being diagnosed | Completely changed from where I was before the trial . . . life-changing really |
| 217 | > 1 year ago. Ongoing symptoms | ‘Sort of hoped’ for physiotherapy, but also would have accepted advice | Advice session: ‘Very positive’ that somebody else actually could explain symptoms and that there was an explanation for them. Sessions not long enough to ensure exercises were done properly | Pacing or resting rather than ‘push on’, saying ‘no’ to other people, not to ‘go 100 miles an hour all the time’. Changes to medication use, taking painkillers before pain becomes too severe, using different shoes Quality of life ‘slightly better’, less ‘boom and bust’. ‘A lot more sustainable and on the whole, not hitting those walls of extreme, extreme pain’ |
| 221 | Recently diagnosed. Hip instability | No preference | Positive:I’ve seen lots of people in the past about things and injuries. And you just think sometimes, ‘Do people really understand me? Maybe not’. You know? [laughter] And then, then you, when I went there, I, I found people that were just brilliant | Has made practical changes for example buying a new mattress which has improved sleep ‘So totally made me think about things . . .’ Learned to ‘slow it down and think about me a bit more and calm down a bit’. ‘Totally’ changed quality of life |
| 113 (originally advice only; withdrawn – received physiotherapy) | ≤ 1 year ago | Very strong preference for physiotherapy | Advice session was not enough to help with specific symptoms. But if not experiencing symptoms:I think I wouldn’t have dropped out. [. . .] I just couldn’t, you know, I just couldn’t do nothing about it, you know | Advice only was:Probably, you know, it’s probably better than nothing [. . .] the advice is definitely a good thing to give people, but then you know, depending on the severity of the problems [. . .] that was the main reason that I wanted to drop out, in that I could actually get some help, ‘cause it was – I, I don’t think it was going to go away on, you know, just with the advice |
Suggested improvements (objective 5)
Participants described a number of ways in which their experiences of the trial may have been improved.
Suggested improvements to trial design
Although participants understood the notion of equipoise and that there was no evidence that physiotherapy was more beneficial than advice, participants still, by and large, felt that advice only was ‘less’ of an intervention than advice and physiotherapy. Participants described the advice-only arm as being in the ‘wrong’ arm or as ‘not being part of it’.
I suppose, as I said, I was a bit dissapointed that I wasn’t gonna get any physiotherapy or any further advice [. . .] the control group or however you like to put it that I was in. [Erm] felt like you were sort of not really part of it anyway. Because you’d have that session at the beginning and then that was it.
Patient 219 (advice only)
Suggested improvements to the advice intervention
A number of suggestsions were put forward to augment the advice intervention arm, including additional information sessions, pain management advice and alternative or complementary therapies. However, there was no consensus as to what would augment the advice-only treatment arm. For example, some participants felt that two advice sessions would be beneficial, whereas others felt that the single advice session worked well, minimising travel time and expenses. The suggestions for improvements to the advice-only intervention are summarised in Table 36.
| Suggested improvement | Illustrative quotation |
|---|---|
| Additional pain management course | He did explain to me the best way to avoid pain and when I do get pain how to hold my knee and all that. So that was addressed [. . .] I think the, the only thing for me was, erm, obviously sort of pain managementPatient 118 (advice only) |
| Gym membership, alternative treatments and heat therapy | Erm, the likes of that gym membership idea, that’s a fantastic idea, because not only does it give that, that person access to that gym, I think, yeah, it probably, you know, give them more chance to goPatient 218 (advice only)what I found invaluable for me, is a lot of alternative treatments, which are like reflexology [erm] going for a massage on my back, that really does helpPatient 218 (advice only) |
| Ongoing telephone support | Not necessarily face-to-face advice but perhaps when others received their physiotherapy and then more advice then that would come hand in hand. But the people in the other group should have had advice by phonePatient 219 (advice only) |
| Ongoing check ups | I reckon kind of a rolling check-up every now and again would be a good ideaPatient 113 (advice only – withdrawn to physiotherapy)It’s literally, it’s all there. Yeah, so, yeah, maybe, just so you could have a, even if it was like a phone call conversation that you could have with somebody, so that you know, erm, that it would be a, you know, that if you needed somebody, or they’re saying, ‘How are you getting on?’ or whatever, or if you’d had a fall, or something like that, then they’d kind of be aware of that ongoing thingPatient 121 (advice only) |
| Group interventions | I don’t know whether they do it, but anything like erm, any groups or anything, like not only like information sessions or something, like something you can go to and erm, have more – proper, a proper talk to you, if you get me? Something like that would have been a lot more helpful as well. [. . .] meeting other people, or someone just like fully explaining, ‘cause I never really got fully explained by someone, it’s only from what I’ve read from like a few of the booklets and online, like about hypermobility, so I’ve never actually got personally told what it is and what it’s about and the symptoms or anythingPatient 123 (physiotherapy and advice)It would nice to erm, speak to other people, erm, with the, the condition, just to know that you’re not by yourself and that there are other people, and have a common thingPatient 114 (advice only) |
| Advice session split into two sessions | I think it was done well, but I think it would be better spread out over maybe two. I know you can’t do the full thing, but maybe two, because for half of it my head was spinning with all the, you know, you know, ‘I’m not going mad I’m not’, but then I’m trying to focus on the information side of things, umm, or maybe you do one and we get shown the exercises and everything then, perhaps a month later, you went back and then you could check that, you know, it’s right or you’re doing it right or, you know, ‘cause it is quite a lot of things to try and remember, I’m rubbish at trying to remember things, erm, just so that you know you’ve, you’re doing it all properlyPatient 121 (advice only)I think maybe just presented in smaller sections, yes, more bit sized sections so that you can just do a bit and think about it a do a bit and think about itPatient 121 (physiotherapy and advice) |
| More comprensive advice regarding JHS from physiotherapist to support reading material | Perhaps the session could have involved a bit more of sitting down and going through what normally happens with somebody who has this. Perhaps not everybody would have been like me and gobbled up every bit of reading material because I am an avid reader so I am, I suppose, probably quite different to other people in that way. Not everyone obviously. So perhaps that could have been some way of improving it because there are people who would not read it allPatient 112 (advice only) |
Suggested improvements for the physiotherapy sessions
Most of the participants who were randomised to the advice and physiotherapy arm evaluated the intervention positively. These participants offered a range of suggestions for improvements that were usually very specific and related to the individual participants’ circumstances and interaction with the physiotherapist. It was apparent that the sessions were flexible enough to be tailored to meet the needs of the individual participant and it was therefore unsurprising that the issues raised by some participants as being problematic were not experienced as such by others. For example, several participants felt that ongoing contact with physiotherapists or ‘maintenance’ physiotherapy would be desirable:
I reckon kind of a rolling check up every now and again would be a good idea [. . .] like every 6 months or so, just to make sure you’re still keeping up with stuff.
Patient 113 (advice only – withdrawn to physiotherapy)
However, others felt that ongoing contact with a physiotherapist may not be required:
I think that’s debatable. I think if you carry on and, and do what you’re supposed to be doing, then possibly not [. . .] if you have a relapse then maybe you might.
Patient 128 (physiotherapy and advice)
Similarly, some participants felt that group physiotherapy sessions might be valuable:
I think a group session would’ve been helpful, erm, also because I’ve never met anyone else who has hypermobility syndrome [. . .] it would’ve been good to sort of get to know other people and you know, have a bit more of a – a sort of feeling of how other people are, are dealing with it, and you know, what, what’s going on for them.
Patient 119 (physiotherapy and advice)
But others preferred one-to-one physiotherapy:
I don’t mind group information but group physiotherapy I wouldn’t want, no. I think it’s quite a personal thing.
Patient 128 (physiotherapy and advice)
Two participants specifically noted the complexity of the intervention and, in particular, the potential for differences between physiotherapists:
You’re doing a, a trial, you know, with lots of different people, with lots of different physiotherapists, but the outcome could be so different, depending on which physiotherapist you have.
Patient 127 (physiotherapy and advice)
Sometimes there’s some very good ones and sometimes there’s some not quite so good [laughter] but that’s the only, I can only base it on what I’ve seen on that side of things.
Patient 121 (advice only)
Other, more practical, issues were raised. For example, one participant felt that getting to the hospital for the physiotherapy sessions was ‘a bit of a pain’ [patient 111 (physiotherapy and advice)] and others suggested physiotherapy sessions could be held in easier to access locations:
Somewhere with better, easier access and easier parking, so that I could have actually done it on my own without actually having to have somebody drive me and be responsible for the parking, because it’s very, very difficult now to actually know that you’re going to be able to get parked and get to your appointment on time. And, the distances involved are too far for me to walk now.
Patient 217 (physiotherapy and advice)
One participant as a means of contacting others with JHS suggested the use of social media:
I’ve only recently gone online through Facebook I found people with the same conditions and it’s been really interesting, I just talk to them. Sometimes it’s difficult to find people, or you don’t know where to start, so the possibility of people getting together or a group of people that can talk together I found that really helpful.
Physiotherapy 211 (physiotherapy and advice)
Non-completers and decliners (objective 6)
Three participants withdrew from the study. One was randomised to advice and physiotherapy and withdrew owing to a lack of time for being involved in the trial. The other two participants to withdraw had been randomised to advice only and withdrew from the study in order to access specific treatment. One of these participants was interviewed. This participant [patient 113 (advice only – withdrawn to received physiotherapy)] felt that they were given too much information about the physiotherapy intervention and felt disadvantaged by not being allocated to that treatment arm, but did not cite this as a reason for withdrawing. Table 37 summarises data related to decliner interviews.
| Topic | Decliner 1 | Decliner 2 | Decliner 3 | Decliner 4 | Decliner 5 | Decliner 8 |
|---|---|---|---|---|---|---|
| Time of diagnosis | < 1 year ago | When aged about 11 years | < 1 year ago | Not interviewed; brief telephone conversation. D4 felt they would ‘rather not risk it’ | Within the last 2 years | 8–9 years ago for EDS-HT |
| Reason for physiotherapy referral | For JHS that was causing chronic problems. Felt physiotherapy was now needed | Part of ongoing treatment, including a pain management course | For JHS | Hip problems, referred for JHS, by chance | Only just seen a specialist. Has been pushing for physiotherapy following own research | |
| Prior physiotherapy | No (not specifically asked but inferred from other responses) | Yes, for years | Yes, for other things – acute, one-off things. Not for JHS per se | Since the age of about 14 years. Physiotherapists ‘did not know what to do’ | Extensive physiotherapy, also knee surgery. Not at all useful | |
| Reason for declining | Did not want to risk being in the non-physiotherapy arm. Had already waited a long time | Thought it was a good idea. Already on a pain management course preventing participation | Was not in a position to participate owing to other life events | Wanted to participate but could not because of a lack of time. Too busy: ‘The busiest year of my life’ | Distance to physiotherapist in Bath. Not practical | |
| Understanding of study aim | All understood clearly | To help manage JHS | To understand about EDS side of things and the hypermobility and finding out about what physiotherapy could help or not help with | To understand whether physiotherapy itself makes more of a difference than just the knowledge or whether the knowledge itself is powerful enough | How to treat JHS/EDS better. Understanding of aim and what would be involved was not clear. Felt that it would be extra trips to hospital if involved in the trial | |
| Understanding of what would be involved | A ‘risk’ of:. . . just receiving stuff to read about or self-manage, ‘cos I thought ‘I’d already tried all that’ | To an extent, but further explanation was not given as she was currently on a pain management course. Therefore, ‘Not entirely sure’ what would be involved | Probably going to physiotherapy sessions and doing either exercises to help with JHS or not having anything done, whether or not you have any extra problems | I think at the time I did not know what it involved as such, so I just said, ‘Yes I’m up for it and I’ll read about it’ | ||
| Understanding of treatment allocation | Yes, but had ‘already selected out of it’ | The two arms were explained. No explanation of how allocation would work | That it would ‘just be random’ | Believes details were in the letter but could not recall details | Unclear | |
| Treatment preference | Physiotherapy, as above | Rather have the physiotherapy | No, not if I could have done them, no | Physiotherapy if not so busy | Advice and physiotherapy. Would have been ‘devastated’ not to have physiotherapy | |
| Anything that would encourage participation | Different approach to having ‘advice only’ arm | No, but did not have a clear idea of what the study entails | No, personal situation prevented participation | No | No, felt it would be far to travel | |
| Further information required? | No, very clear that she did not want to participate and risk not getting physiotherapy | Do not know, as was not going ahead with the study | No, think it was very very informative | No, felt it was well written and very self-explanatory | More information about medication | |
| Other comments | Cannot understand rationale for not having any physiotherapy. Cannot envisage anyone would participate in something preventing access to treatment | Thinks it is quite a good idea. Lack of research in JHS, limited mobility research. Wishes a study of this kind had been running when she was a teenager. Would like to take part after pain management course | Would be interested in receiving a summary of research findings | Just want to say thank you, I’m very happy that there is someone doing a study with joint hypermobility, I know it’s very difficult to get people to do that, so thank you | Focus group, group intervention would be valuable. There is a lack of understanding about the condition |
Discussion: patient participants’ experiences of the trial
The interviews with patient participants during stage 3 of the study allowed for a detailed exploration of patients’ experiences of being involved in the trial. As in stages 1 and 2, participants described diverse symptoms of JHS, often experiencing many years of individual joint problems, often during childhood. Although historically these symptoms were ‘not necessarily problematic’, for some, symptoms were often severe. Diagnosis was slow, and participants were often misdiagnosed with eventual diagnosis usually following repeated injury or pain in a particular joint (most frequently hip, knee or ankle). Most participants had previously experienced physiotherapy, but this had focused on a single joint rather than the holistic approach employed in the trial, and the outcome of physiotherapy was mixed. Most participants had been keen to try a form of physiotherapy that they thought may be different from their previous experiences.
Participants were told about the trial after referral to secondary care to either a rheumatologist or a physiotherapist. All participants who subsequently participated in the trial reported being keen to do so and fully understood the aims of the trial. Although some conceded that if physiotherapy was of no value their time would potentially be wasted in having physiotherapy, and they understood the notion of equipoise, for many ‘something rather than nothing’ was preferable. Most participants felt that the advice intervention was ‘less’ of an intervention than physiotherapy. A number of those who declined to participate did so because they wanted to ensure they received physiotherapy. Recruiting participants earlier in the referral trajectory may have resulted in participants having a different attitude to participation, although given the lengthy delays in securing a diagnosis expressed by many patients, adequately identifying JHS patients in primary care might prove extremely difficult. Having waited for a referral for what they believed would be physiotherapy, it is understandable that a patient may not want to accept the alternative advice-only intervention. In terms of the acceptability of the treatment arms, the perceived lack of equipoise between advice only and advice and physiotherapy may have had wide-reaching implications.
Only one person having physiotherapy reported that it was a generally negative experience and that the treatment was a ‘waste of time’. Most benefited from the physiotherapy in some way.
Key findings in relation to study objectives
The strength of this part of the research lay in strong recruitment of participants. The majority of patient participants in the pilot RCT were interviewed, as were six patients who declined to take part in the trial. Participants were broadly representative of those recruited to the pilot RCT in terms of sex, trial arm and clinical site. This helped to generate extensive data. A potential limitation lies in the possibility that those who declined to take part in interviews varied in their experiences and that these experiences were therefore not captured. The key findings in relation to the study objectives are summarised below.
Objective 1: to contextualise participants’ experience of the trial, to explore their experiences of living with joint hypermobility syndrome, events leading to diagnosis and subsequent referral for physiotherapy. Also to explore participants’ experiences of, and attitudes to, the use of physiotherapy to manage joint hypermobility syndrome
Numerous and diverse symptoms experienced by the participants had a varying effect on their quality of life. Prior to diagnosis, many had experienced problems for many years, often in childhood, and an important finding was the need for greater recognition among health professionals that JHS can cause problems. One of the most important outcomes of obtaining a diagnosis for the participant was the validation of their symptoms, the reassurance that their experiences were ‘real’ and they were ‘not going mad’.
Objective 2: to ascertain the acceptability of the trial design for participants, including treatment aims and randomisation, and their preferences for treatment
Participants all felt that the trial was important and valued the recognition of JHS as a condition with diverse, complex and often problematic symptoms. Participants found it to be a valuable opportunity to learn about JHS. Although participants understood the notion of equipoise and that the evidence suggesting the effectiveness of physiotherapy to treat JHS was lacking, many felt that the two arms were unequal, and that those in the advice and physiotherapy arm obtained ‘more’ treatment that those ‘only’ receiving advice. This may have impacted on the participants’ retrospective evaluation and attitude to participating in the trial and the outcomes.
Objective 3: to develop an understanding of the participants’ experiences of the advice-only intervention and the advice and physiotherapy intervention. More specifically, to ascertain participants’ perception of the value, acceptability and effectiveness of the treatments and develop an understanding of any barriers and facilitators to participant compliance. Also to understand the acceptability of data collection
The provision of information and guidance about managing JHS in the advice session (including the two information booklets provided at the advice session) was highly beneficial for many participants, regardless of whether or not they were subsequently randomised to receive the physiotherapy intervention. Equally, many felt that the advice-only intervention would be of limited benefit if they were suffering from an acute problem related to JHS which required physiotherapy input. Many felt that physiotherapy, or at least contact with a physiotherapist, was required for ongoing support, reassurance and for the treatment of an acute or specific injury or problem. The patient handbook used to support the six physiotherapy sessions was generally rated positively, as a useful resource that is user friendly and could be referred back to at a later date and used to reinforce what had been learned during the physiotherapy sessions.
Objective 4: for both intervention arms, to ascertain if participants perceived any changes had been made or experienced, to participants’ health, behaviour and well-being. Also to develop a deeper understanding of which outcomes or changes are considered to be meaningful by the patients
The majority of participants reported making or experiencing some changes following the advice intervention and the physiotherapy intervention. Some found the information ‘life-changing’, while, for others, the information was a reiteration of information they had already accessed independently. For the participants who did feel the intervention had been beneficial, it was psychological benefits stemming from an enhancing feeling of being able to cope with the symptoms of JHS, to know how best to manage symptoms. Some participants also reported physiological changes including improvements in pain, sleep and mobility.
Objective 5: to explore participants’ suggestions for improvements to the trial design and to each of the interventions (advice and physiotherapy components)
There is no ‘one size fits all’ physiotherapy or advice intervention. This was reflected in the design of the trial which allowed for considerable flexibility within the treatment and advice sessions. Suggestions for improvements reflected the individual’s personal experience of the trial and individual circumstances and none of the suggestions could be considered unanimous.
Objective 6: to explore the views and experiences of participants who did not complete the intervention and patients who did not wish (or were unable) to take part
Wanting to access physiotherapy and lack of time were the primary reasons for not participating in the trial.
Physiotherapists’ experiences
Introduction
Physiotherapists were interviewed at the beginning and at the end of stage 3 (the pilot RCT) to explore their views relating to the practicalities and clinical effectiveness of the intervention as well as their experiences of participating in the pilot RCT.
Aims and objectives
Interviews were carried out in order to develop a deeper understanding of physiotherapists’ views and experiences of being involved in the pilot trial. Specifically, the topic guides (see Appendices 8 and 16) were designed to address the following objectives:
-
To evaluate the format and delivery of the training for the pilot RCT. To ascertain trainer and trainee physiotherapists’ training needs and requirements and obtain trainees’ views on their ability to carry out the trial post training.
-
To understand the experiences of the physiotherapists delivering the trial interventions.
-
To evaluate the format, content, design and usability of the patient handbook.
-
To explore physiotherapists’ views regarding the trial design, recruitment, randomisation and equipoise.
-
To ascertain physiotherapists’ views on how the trial intervention arms could be improved in future trials or as part of standard care, and what improvements could be made and how physiotherapists can be supported in their role when delivering the physiotherapy intervention.
The initial study protocol indicated an intention to also interview physiotherapists who had not been directly involved with the trial to determine the feasibility of rolling out the physiotherapy package. In hindsight, the research team felt that this would only generate hypothetical data as the physiotherapists would lack the context of familiarity with the intervention. It was therefore decided to concentrate on interviewing those who had experienced training and those who had delivered the intervention as part of the trial.
Methods
In-depth semistructured face-to-face or telephone interviews were carried out with JHS-trained physiotherapists who were already involved in the trial and with therapists (‘trainees’) who had received the JHS training delivered by the trained therapists (‘trainers’). All participants received a participant information sheet and gave signed informed consent. Interviews were carried out immediately after training (within 4 weeks of being trained; see Appendix 16) and at the end of the trial (within 4 weeks of the last trial participant being seen; see Appendix 17). Interviews lasted between 23 and 76 minutes, were digitally recorded and professionally transcribed. Transcripts were analysed using a thematic approach. Broad themes were assigned to the data which reflected both the main research questions and key issues which emerged in the interviews. The process of data analysis was similar to that already described for the patient interviews.
In total, seven physiotherapists (three trained and four trainees) participated in the interviews prior to trial commencement. Four physiotherapists (band 6) were trained to deliver the hypermobility training to therapists who had not previously been involved in the study. At site 1, one trainee was a band 5, with little previous experience in treating JHS, one was a band 6 with limited experience of JHS and one was a student physiotherapist (second year undergraduate). At site 2, one JHS specialist (band 6) trained one other band 6 therapist, who had prior experience of treating inpatient JHS patients.
Results
Table 38 summarises the physiotherapists who were interviewed at each site.
| Physiotherapist | Site 1 | Site 2 | Total |
|---|---|---|---|
| Trainer (post-training interview) | 2 | 1 | 3 |
| Trainee (post-training interview) | 3 | 1 | 3 |
| Trainer (end-of-study interview) | 2 | 1 | 3 |
| Trainee (end-of-study interview) | 1 | 0 | 1 |
Training for the Physiotherapy for Hypermobility Trial (objective 1)
Training was delivered by the trial chief investigator (SP) and one of the principal investigators (RL) to the physiotherapists already involved in the trial. Approximately 2 months later, the same training package was delivered at site 1 by the trained physiotherapists to three additional therapists. The study chief investigator (SP) observed this training day. At site 2, one physiotherapist was trained over two sessions, separated by a number of weeks.
General evaluation of training package format and delivery
Overall, all participants viewed the JHS training positively and felt that the level of training was appropriate. Experienced trainees valued it as a ‘refresher’, as well as identifying information that was new to them. Less experienced trainees, including a physiotherapist undergraduate student, also found the information to be pitched at the right level, and reported that ‘all the information was really good’ (trainee D, post training).
Trainers, who were delivering the training for the first time, expected that the delivery of the training may evolve and improve over time:
I think, again, because we weren’t 100% OK with each bit, probably I didn’t deliver it as best as I could do, to my own standards.
Trainer C, post training
One trainer felt that the training was limited from a general lack of empirical knowledge about JHS:
The difficulty is that we don’t really know exact answers on the theoretical approach. There is no evidence based on it, we haven’t got it there, that’s why we’re doing the study.
Trainer B, post training
Although the benefits of allowing some flexibility in the training content to suit the trainee needs was recognised, it was also recognised that the training package was able to demonstrate a standardised approach to assessing and treating JHS. However, one therapist cautioned against making the package of training too inflexible:
We thought it was a good way of standardising information; however, there’s also the recognition that these are very complex patients who you can’t always be quite so – not rigid, but you can’t be quite so prescriptive in what you’re going to say to them because of how you’re going to manage them, because each one’s going to be a bit individual; there are going to be other aspects.
Trainer F, post training
The training was delivered using a mixture of hands-on, interactive sessions and more formal lecture-style presentations. Some felt that the training session was quite lengthy:
I think it got a bit long and drawn out at the end.
Trainer C, post training
Trainees also reported that a lot of information was provided during the course and that this could be overwhelming:
It was good. Um, it, it explained everything that needed to be done. Um, so it, it was all in depth. But I just came out of it thinking, ‘There’s a lot that I need to remember’.
Trainee A, post training
However, trainees generally did not feel that the training day was rushed and generally reported that the course was delivered well. At site 2, training was delivered over two sessions, although the trainer felt that it would have been better to deliver the training in one session:
It’s probably better to try and do it all in one, while it’s all familiar, really, rather than having a big gap and then it’s trying to recall what you’ve already gone through. Yes, I think it’s probably better, because you’re going through the information, then you can go and say, ‘Let’s go and have a look at the practical side of it a little bit’.
Trainer F, post training
Some trainees felt that it may be a good idea to have two training sessions:
. . . because I think that helps with your learning; then you’ve got a chance to consolidate in between.
Trainee G, post training
Some physiotherapists highlighted the need to reread, refer back or refresh their memory of what they had learned on the course, for example, to reread the booklets that they had been given.
Training for the advice session
Trainer physiotherapists recognised that the delivery of the advice session may be difficult for newly trained physiotherapists and were careful not to ‘overload’ the trainees. They noted that the trainees appeared to be anxious about this session, even though a lot of the content of this session would be considered to be ‘normal care’:
None of it was completely alien or different, and I was happy with delivering all of it. It was just an awful lot to do and a lot of it, and the questions around it, were, ‘What do I do in assessments?’ I think that a lot of their concern was that there was so much to do, but actually a lot of it they do in their normal assessment, they would’ve already covered it. I think it’s a lot to do [. . .] when you’re not necessarily quite so au fait with the paperwork [. . .] that can take a bit of time. That was really their main concern, how much there was to fit in.
Trainer B, post training
One trainer reported that the trainees initially lacked confidence in their knowledge and ability to treat patients with JHS but that trainees subsequently gained the confidence in their clinical skills:
I think we were going through in quite a lot of detail and I think they thought, ‘Oh my God, this is quite a lot to take on board’, but when you reassure them that actually, you have all these clinical skills and you would do this anyway, they were like, ‘Oh, yes, we do actually, don’t we’.
Trainer C, post training
Training for the physiotherapy sessions
The standardisation of the training relating to the physiotherapy sessions was highlighted. One participant felt that different physiotherapists could potentially deliver the training quite differently and, therefore, that it was important to ensure the theoretical aspects of the training were standardised:
I think the difference comes in, it’s not saying treating differently, but I suppose it’s the theoretical thinking about, ‘Why am I doing this particular exercise or those?’ [. . .] As I say, a lot of physio[therapist]s do work in different ways, and therefore, I don’t know, my one thing, now thinking about it is, in terms of thinking about that exercise and how it’s being delivered. Some people may take a more general exercise route, some people are more specific. A lot of it would depend in their training, what they’ve done previously and how they view it. [. . .] actually within terms of exercise and those specific exercises they do, it’s just being aware of that really and making sure that it gets delivered the same
Just to make sure that’s standardised?
Well yes, the theoretical approach at least
Trainer B, post training
One trainee reported feeling daunted by the prospect of the physiotherapy sessions following the training:
. . . that was the one that kind of freaked me out a little bit. Because we basically, the way that we done it, is we done the, kind of, what is hypermobility and the criteria, in the morning. And then they basically said, they gave us this handbook kind of just before lunchtime and said, ‘This is the handbook that they get, but we’re going to cover this, um, in the afternoon’. And that booklet just looks very detailed. And, then when it came to that part, and talking about what you need to get done in your half an hour follow-ups, seems quite a lot to do. And even, and even [physiotherapist’s name] was saying, ‘You’ll, you’ll literally just be talking and talking and talking’. So I’m thinking, ‘If, if she, as a manager and a specialist in hypermobility is saying it’s, you’re going at quite a speed, someone like me, who has a limited experience’. Seems, seems a bit frightening.
Trainee A, post training
Training relating to the physiotherapy patient handbook
One therapist felt that delivering the training on the workbook was ‘boring’ and that it was necessary to make it more interesting for the trainees:
From a workbook perspective, I found it a bit dull and boring, actually. I was working from the text that we got given and it was quite repetitive. I was trying to go through and jazz it up and the idea was to keep it quite bland, so that you’re not bringing in a lot of patient information and different things as well, or patient history, I suppose.
Trainer C, post training
The patient handbook was generally rated positively, although the exercises included in the booklet met with a more a mixed response from trainers and trainees:
I think the booklet’s really good and I think that covers what we normally do in terms of the different sessions, like taking control [. . .] I think that’s really good. I just think it’s the exercises at the back that probably aren’t quite what I would normally do. But I understand, we’ve been told we can add our own in, anyway.
Trainee G, post training
One therapist felt that the rationale for including specific exercises required further explanation:
Maybe a little bit more on some of the reasoning behind some of the exercises we give, a little bit.
Trainer C, post training
One participant was unclear how to use the booklet in each of the physiotherapy sessions:
They obviously said this is the booklet the patient’s going to have, but I was a bit confused as to how we were supposed to use the booklet with our treatment, if you see what I mean? I had to ask [colleague name] and when I had my follow-up and came back in, I was a bit like, ‘Am I supposed to actually go through everything in this book with her?’ She was like, ‘No, they’re supposed to go away and read that and they’re supposed to just come in and ask you questions about it and then your treatment is what I would normally do, so you’d just assess someone and you treat them how I would normally treat a patient’. Obviously, I was a bit confused as to how these six things in the booklet were going to feed into my treatment and assessment. I was a bit confused about that; I’m still a bit confused about that. I think I need to go away and actually read the booklet back to back.
Trainee D, post training
Additional training requirements
Trainee and trainer physiotherapists described possible additional training requirements (Table 39). A number of suggestions for changes may have reflected individual preferences rather than a consensus.
| Area of training | Suggested change | Illustrative excerpt |
|---|---|---|
| Information session | Allow more time for training | ‘Cause in that part particularly, the advice part and the handbook, there’s a lot of information and also it’s a case of the logi- you know, just gave us these leaflets and said, ‘You have to refer to page eight’, or whatever. Um, so yeah. Probably, probably just to slow the pace down at that pointTrainee A, post training |
| Physiotherapy session | Use of a JHS model patient | I think one thing that I would have found more useful in going through the assessment was actually having a patient here who had hypermobility, so that you could have, as they were going through the assessment, you would actually have seen someone who had hypermobilityTrainee D, post training |
| Patient handbook | Clarify use and content of written information | I think maybe just a bit more about how they would have expected us to go through the booklet with patients would be goodTrainee D, post trainingI think, if it was training for physio[therapist]s that hadn’t done any hypermobility before, there’d perhaps need to be a bit more about what exercise therapy, what way to approach thatTrainee G, post training |
| General | Education for health professionals | A lot of the clinicians won’t recognise what they’re seeing. So, it’s getting that information over. The Hypermobility Association does do their own treatment and training packages. We could be using it in conjunction with them a lot more as well. People with an interest would already be there. Maybe that might be a better way forward, I don’t knowTrainer C, post training |
| Provision of background information | If I was doing more a teaching on hypermobility, I’d probably go perhaps a little bit more detail into perhaps why people get pain – we don’t really know why, but what are the things that we might look at? – so, in terms of objective assessment, might explore that a little bit moreTrainer F, post training | |
| Interactive training | I think I’d make it very interactive. I think what you’ve got to do is probably have lots of examples. You might want either someone, a model, coming in or you’ve got videos [. . .] so people are aware of how people might compensate on the assessment side of itTrainer F, post training | |
| Distinguish between trial training and training related to JHS | I’d probably almost separate it out a little bit from that training from hypermobility syndrome. And the trouble is then when you come to doing the trial of making sure everybody’s clear on what needs to happen when and, and how and those sorts of bits of stuff, are the bits that, I think, got a bit confused. Er, I mean, yeah, I think I’d just try and probably be clearer from my point of view. And I don’t – I probably don’t think that’s – I would, yeah, I think just delivering it clearer. I think we kind of went through the workbook and those sorts of things, and, and what was supposed to happen. But being clearer with, er, exactly what was going to happenTrainer B, end of study | |
| Standardising training | We all do things in a slightly different way. But I think in terms of, of really trying to make that training as standardised as, as possible is quite key because there are a number of things within hypermobility that are open to interpretation. Erm, and I, I think that, again, doing a wider study, that has to be probably, erm, made quite kind of clear and, and defined to, to make it repeatable – and accurate as possible – across the sitesTrainer B, end of study | |
| Ongoing support for ‘new’ physiotherapists | We can probably offer some telephone support and things like that, or whether we give them another back-up hour, perhaps for a session, or something, for case studies, or something like that to give them something. I think a lot of it is that they don’t know what they don’t knowTrainer C, post training | |
| Training materials to be available to refer to | I said that I’d wanted to take a couple of the booklets home and the patient booklet home, but I gathered that we’ve not got that many of them. We don’t really get time in work to read through them and recap and stuff. Obviously, I just wanted to take a couple of them home so I’d have them to read through the night before. Trying to read through them in work doesn’t really work for me anywayTrainee D, post training |
Trainees’ ability to carry out the trial post training
Three trainee therapists who had not worked with JHS patients before were apprehensive about delivering the intervention after the course. However, all realised that their confidence would grow as they saw more patients. One participant who had previously expressed anxiety about conducting the trial reported ‘well, now I’ve seen a patient I feel better’ (trainee A, post training).
Timing of the training was important; too large a time period between training and recruiting a patient with JHS to the trial meant that what was learnt may have been forgotten:
I would have preferred to have done the training day and then know that I had a patient booked in the following week. For me, I felt like I had that training and then didn’t have a patient for 5 weeks . . . Then I just felt that I didn’t then get that chance to consolidate everything you’ve learned and then you were trying to dig it back out of your brain from 5 weeks ago, trying to remember exactly what you were doing and trying to follow all of the information sheets I had. I think if I’d done the training and known I had a patient booked in the following week, that would have been better for me, I think.
Trainee D, post training
Conversely, one trainee noted ‘when I saw that I had that patient a few days afterwards that kind of freaked me out a little bit’ (trainee A, post training).
One trainer felt that while the course provided basic knowledge and skills, hands-on practical experience was essential:
What we’re going to be giving them is the basics; really, they’re not going to have the detail. We’re never going to be able to deliver that without having patients to work on. We’ve learned through patient mileage, unfortunately, like most things, they will probably learn through their own errors.
Trainer C, post training
Although participants were concerned that there was a lot to fit into each treatment and/or advice session, one therapist recognised that the intervention did not differ greatly from current standard care. One trainee therapist who routinely worked with inpatient JHS patients at site 2 felt confident to treat as per the trial protocol.
Trial training for trainee physiotherapists
Trainee therapists did not have much prior experience of carrying out trials. Although sometimes daunting – this was an area where trainees often felt they learned a lot – it was also a valued part of the training.
So, in terms of the hypermobility part, I was fairly OK with. It, it was then, you know, when it moved onto the study part, it was really thinking about what I need to do.
Trainee A, post training
Some felt that providing training about the trial and about delivering the intervention per se was problematic. Trainers felt that it was difficult for the trainees to take this information on board:
When we were just delivering the training element, and that should be fine, because we would do the assessment and then we could say, ‘Right, now to consent the patient, do this and this and this’ whereas, in the normal training, they wouldn’t have asked to do that. I think it’s that extra add-on that made them more jumpy about it all.
Trainer C, post training
Physiotherapists providing the training were asked about the practicalities of training physiotherapists with little or no prior experience of treating JHS. Most felt that JHS-naive physiotherapists would require additional training and support:
The difficulty with it is, it’s a lot to cover – in a very short space of time. I think we probably need to maybe be a bit clearer on study protocol and things that, erm, are the actual criteria and what happens and, and, from there and there and there. [. . .] I also, I think, erm, having that probably ongoing support and back-up. [. . .] And, as I say, it is the experience of treating these sorts of patients because if you’re not used to treating them, any physio[therapist] would find that, I guess, a little bit difficult.
Trainer B, end of study
Possible changes to the training were discussed, for example providing separate training on the workbook from training on hypermobility.
I’d probably almost separate it out a little bit from that training from hypermobility syndrome.
Trainer B, post training
In summary, trainees and trainers felt that there was a lot of information to deliver in order to equip physiotherapists to deliver the trial intervention. Trainers felt that only in hindsight did it become apparent which aspects of the training course were not clear.
But being clearer with, er, exactly what was going to happen. [. . .] And it’s probably easier being clearer once you do it and you realise the bits that aren’t quite clear. [. . .] So as we got experience of actually running it and, ‘How does this work in?’ and those sorts of things. And, erm, so I think that kind of, that could be clearer. But that probably comes from the experience of, of running it as well and realising what – doesn’t work so well and what does work well.
Trainer B, end of study
Physiotherapists’ experiences of delivering the trial treatment (objective 2)
Four physiotherapists (three trainers and one trainee) were interviewed at the end of the trial period, having gained experience of delivering the intervention to at least one patient. Participants were asked about their experiences of the trial and about their experiences of both of the intervention arms.
Advice-only intervention
Physiotherapists described the format of the advice session, of assessing the patient, exploring their particular problems, describing the trial to the patient and presenting the advice based on the HMSA56 and Arthritis Research UK57 booklets. Most physiotherapists felt that the advice session, although it shared aspects of normal care, was rushed. Participants felt that there was a lot of information to provide and administration to undertake in the time allocated:
You’ve got to recruit them and then you’ve gotta give them the information quick.
Trainer C, end of study
Physiotherapists felt that, although the session was lengthy, by and large, patients did engage well with the session:
Did you find that the patients were engaged throughout that session?
Yeah. I mean, I think it was a long session. But it’s – for a patient-wise, the normal session, that’s fine and the explanation bit, erm, which was the bit they really paid attention was – was, was relatively good.
Trainer B, end of study
The standardisation of the advice session was considered to be potentially problematic in terms of its inflexibility:
Some people might need some information not the other . . . It makes it very generic then.
Trainer F, end of study
However, on the other hand, the standardisation of this session was also potentially valuable.
. . . I think probably for someone who perhaps isn’t so used to seeing lots of hypermobility maybe it’s a good way of keep making sure that you’re giving consistent information.
Trainer F, end of study
Physiotherapists felt that the advice intervention was acceptable – and potentially valuable – for a certain subgroup of patients, who did not have a current issue which needed to be addressed, or who had been experiencing manageable symptoms for some time. For example, some participants had been given a prior diagnosis of JHS but had not been provided with information about what it was or how it could be managed. For these patients, physiotherapists highlighted the potential value of the advice intervention.
. . . particularly working in rheumatology I have thought, ‘Actually just, just advice could play . . . quite a big part’. [. . .] But for them, for you to actually, kind of, see them early on to say, ‘This is what it is. You’re not doing it any harm. But we need just to control what you’re doing a bit better and make you generally fitter’ I think is, is quite a, quite a big factor really.
Trainee A, post training
On the other hand, participants felt that many who were experiencing problems wanted to access physiotherapy treatment, or would have benefited from some form of additional treatment.
I mean, I think if you’re picking up a general kind of population of, of hypermobility patients that necessarily aren’t struggling that’s an easier. But actually when you’ve got people that are struggling, they do kind of want that treatment.
Trainer B, end of study
It just felt to us that they were getting a sho – a short shrift of a package really.
Trainer C, end of study
Physiotherapists felt that for some people, the advice arm was not an acceptable intervention:
Would have like to have done something more with those people, or, or, or something else with them rather than absolute just one-off treat- information session. ‘Cause they weren’t even – we weren’t even allowed to give them exercises and send them away, it was literally, ‘This is the booklet, this is what hypermobility is now go away and get on with it’.
Trainer C, end of study
As described in Participants’ experiences of the trial (objective 3), What worked well: ‘active ingredients’ of the advice intervention, the provision of information about JHS was very valuable for some participants:
It sort of calms them down about the whole situation, I suppose, sort of giving them a reason for their pain and things like that, I think, has a massive effect and, um, I think that’s one of the main differences, often, working in rheumatology, to normal outpatients, that you’re actually giving, the majority of the time, you’re giving people an explanation for their pain, which they can understand . . . whereas, I think a lot of the things that we do in rheumatology, well, for hypermobility and the inflammatory conditions, is there’s a very clear explanation as to what’s happening and why it’s happening and the reasons behind it. I think that makes a massive impact on how people manage that mentally.
Trainee E, end of study
It’s just really making sure that their understanding of what hypermobility syndrome is really and, and why that – and that reassurance that it isn’t, erm, necessarily anything bad or anything disastrous. Or anything like that. And, erm, erm, I think that’s probably the key element to get across into, yes, ‘Yes, you have got this. But it’s not a terrible thing. It’s not a particularly serious thing. We have to manage it and we have to manage it well’. But then giving them the confidence to go in and, and do a bit more and not necessarily be, be worried about their pain all the time.
Trainer B, end of study
Physiotherapy intervention
Physiotherapists described the outline of the physiotherapy sessions. Some felt that it was necessary to adjust the order or content of the sessions in order to respond to individual patients’ specific needs:
Erm, I was a bit happier to kind of address the bits a bit earlier if they were having things with them, and, and, and moved it round to sort – to help me really with their current problems. Rather than kind of stick too rigidly.
Trainer B, end of study
Lack of time was always an issue:
I think it’s just being aware of timing. And, and getting them in within the 4 months. I tend to not be very good at necessarily thinking about that.
Trainer B, end of study
Well, I feel it was quite deliverable. You were always running at a pace, you had to keep going with the exercises and doing the talking while you’re exercising and reiterating things all of the time like that. That was quite hard. I also found that I found, six sessions, in some ways we were going at pace to follow what was in the booklet for that week or whatever and to give them their exercises, but by about the fifth session we, we were probably there.
Trainer C, end of study
One physiotherapist identified that patients often experienced improvements from the first physiotherapy sessions, but that more difficult-to-treat issues may have required further sessions or a longer duration of treatment.
I think they were surprised how much information they were given. And I think also a lot of them felt very much better very quickly. They would come back with, not major, not massively different, but one part of them had felt that much better. That they felt really quite, erm, motivated by that I think really. So then, then once you got through some of those initial really good progressions then you’re left with the more difficult slower things to recover – ‘Well, now, these things are going to take longer to improve and this is we’re teaching you how to look after you so you sort of stick with the programme and you should continue to improve more’. So in some way they’re having to fit it in in 4 months, would have been – if we could have had a bit longer, we could have maybe got that a bit more, so it was trying to squeeze it into that 4 months’ time as well.
Trainer C, end of study
. . . we had a few coming through with multiple other issues going on, which would have taken a bit longer, which would have taken, potentially, some of the time away at the end. Um, that, but I guess would have had an affect on their education side of things.
Trainee E, end of study
Physiotherapists felt that increasing postural awareness was an important ‘active ingredient’ of the physiotherapy sessions.
It’s that postural awareness. And that is, is increasing their awareness of their posture which is a lot of work that I do with through exercises and, and how they’re moving and how they’re doing stuff. Along with keeping that general activity up really.
Trainer B, end of study
She [the patient] said ‘Oh, I’ve really changed how I work now and I don’t get pain from wor-working in a bad posture’. Things like that. So one of the big things is probably their posture more than anything else that improved.
Trainer C, end of study
It’s the fact that these patients don’t know at times, um, they can’t sort of see the compensations they do and the fact that they haven’t got the ability to selectively move [. . .] it’s highlighting sort of those aspects in them and they’re so used to moving and behaving in that way, that trying to see that and change it is actually really difficult for them. So, by having that sort of regular input, you’re sort of there, sort of showing them whether they’re doing it right or correct, you know, and trying to help them find ways to, to get the right muscles to facilitate and, and switch on to, sort of, that idea of selective movement and control of their movement. Um, I would say is that is the main thing and that’s really what they need. To help identify and working towards.
Trainee E, end of study
Trained physiotherapists, because of their previous experience of delivering the intervention, felt that they were able to deliver the intervention in a way that followed the protocol and yet tailor it to the needs of the participant.
I think having the experience of work and working with it before and not necessarily feeling you have to stick to that structure, so much of that book. So I did use the book. But I felt I could do probably more of my – I wasn’t just doing the book. I was doing a bit more of my normal kind of treatment bit as well. Whereas before when we did it, I got a bit too much of doing the book and not enough of looking at the patient.
Trainer B, end of study
The use of the workbook accompanying the physiotherapy sessions for the duration of the trial was thought to be valuable for patients [see also To explore physiotherapists’ views regarding the trial design, randomisation, equipoise and recruitment (objective 4)].
Most of the patients I have, they come back having read the booklet, sort of, actually, they’ll know it all completely. It makes sense then. Um, ‘That completely explains my symptoms’, I suppose. So, I think the added benefit of having that longer period of time with them meant that you could explain everything in the booklet prior to them reading it. Which hopefully helped with their understanding.
Trainee E, end of study
The really positive thing I think I would take from it is the booklet itself. And the reflection in the booklet.
Trainer F, end of study
To evaluate the trial booklet (objective 3)
Physiotherapists felt that the workbook accompanying the physiotherapy sessions was of value and rated it positively.
And it was great to have the booklet, the booklet made quite a bit of difference. They could go away, read about it and come back. And the exercises were all in there readymade, so it gave us more time to spend with the patients and things as well rather than having to print more stuff off.
Trainer C, end of study
The opportunity given by the booklet for reflection, for both the patient and the physiotherapist, was considered to be valuable:
I think the booklet was really good. It’s really – it’s information that we normally cover. But to have it written down in a booklet format was really helpful. ‘Cause often what we do is give them bits of paper. It’s not always in one piece. [. . .] and the feedback from patients was that they, it was really nice to, we talked about it, they were able to go back through and think, ‘Oh yeah, I remember going through that’. Er, and the reflection bit was really helpful for both therapist and the patient I think. So I, I think on both camps it was really helpful.
Trainer F, end of study
However, one physiotherapist felt that the patients would have benefited from engaging in more reflection:
It [the booklet] also gave patients something, a hard copy to take away with them, so in the future they would always have something to look back on. And, I think the self-reflections, although, [unclear] my patients’ booklets, very few did that. Um, but I think if they had, that would have been useful as well.
Trainee E, end of study
The need for the workbook to be used by a trained physiotherapist, who could ensure the movements were carried out correctly, was highlighted:
The positions that you might get someone in isn’t actually maybe the position that you would teach them, so the picture doesn’t always reflect what you might actually show them to do. Or you might not show them any of the exercises in that booklet; we might show them something different.
Trainer G, post training
However, it was felt by some that the workbook may be of limited use if not employed to accompany the physiotherapy sessions, and could be potentially restrictive:
We both agreed that the workbook isn’t very useful on its own, because obviously you’re going to have to give someone an exercise for that individual, and some of the positions in – generally, actually, we don’t like physio[therapy] tools anyway, because it restricts us quite a bit [laughter].
Trainer F, post training
Although others felt that such restrictions were minimal.
Most of them [patients] were quite happy just to go through the sections as they were put in the book.
Trainee E, end of study
Because of time constraints, one physiotherapist felt that it was not possible to fully utilise the exercises at the back of the workbook.
I don’t think the exercises at the back of the booklet were particularly – I think they were good to be there. Erm, but you, you didn’t really have time to go through a lot of exercises. So you might have to give them one or two to do.
Trainer F, end of study
To explore physiotherapists’ views regarding the trial design, randomisation, equipoise and recruitment (objective 4)
Trial inclusion and exclusion criteria, recruitment and randomisation
Physiotherapists discussed at some length issues surrounding recruitment to the trial, in relation to equipoise, randomisation and the acceptability of the treatment arms. Physiotherapists generally felt that there were distinct groups of patients: (1) those who required treatment for a specific, often acute, problem; and (2) those who had been living with JHS for a long period of time and were willing to take part in the research and to potentially accept the advice intervention, to find out more about the condition, raise awareness and for altruistic purposes – ‘to help others’. Some of these individuals may have been unable to attend a course of six physiotherapy sessions. One physiotherapist described the different groups of patients in some detail:
. . . I’ve struggled to recruit because people were in too much pain. [. . .] People were in fear of moving and didn’t – a lot of people didn’t want to go on a trial and not get treatment.
. . . there were some that were definitely borderline and they said, ‘No, I definitely want treatment’. And there were a couple that were in really bad pain. And I sort of said, ‘We have got this study going’, erm, ‘It’s up to you which way you go’ and professionally you think they need to be treated. And we wholeheartedly agree together they needed to get on with treatment, we didn’t recruit . . .
Trainer C, end of study
On the other hand:
. . . They want a diagnosis and though – and then they can’t afford the time to come in – and the – that would fit the bill for some of them. And then for others, they need that real looking at the quality of how they move and changing it and things like that [. . .]
There was one lot of people that said, ‘I’ve had this for years, I’m gonna cope for another 7 months and then come back. [. . .] I just want things changed for the people in the future [. . .] and I don’t care what I get and I’ll pick up the pieces in 7 months after the questionnaires have gone out’, kind of thing. There was that kind of group [. . .].
There was another group that was in a lot of pain and they said, erm, and they were very fearful of doing things, that they definitely needed someone there to support them through it, and they didn’t want to wait for that and they wanted to have treatment immediately. And so we couldn’t recruit them. And then there were another batch that were sort of, ‘Well, erm, [unclear] and obviously if I do hit problems there’s a backup system that the service is there if we need it’. [. . .] Some people are very strongly, erm, very much – that they want something changed for the future, that they don’t want other people going through what they’ve been through.
Trainer C, end of study
Physiotherapists felt that patients understood the trial and the implications of participation. One physiotherapist reported that patients had sometimes asked their opinion regarding whether or not they should enrol into the trial:
I tried to stay out – kind of not guide them as much as I can really. But there was kind of bit of, ‘Do you think I should do it?’ ‘Do you not think I should do it?’ Erm, as I say, I tried to not answer that question as best I could. [Laughter.] To not influence it.
Trainer B, end of study
Physiotherapists felt that patients who did not want or require treatment at that particular time were happy to enrol on to the trial, whereas patients who had been referred to physiotherapy were less willing to accept the possibility of an advice-only intervention.
People that have been referred for physio[therapy] for management of their – in terms of hypermobility syndrome, then they, they come in expecting something and wanting something. And, and they’ve already kind of selected themselves for that in a way, I guess.
Trainer B, end of study
One participant felt that if individuals with JHS without current problems were asked to take part in the trial, recruitment rates may have been better.
If you’re have a just a group of hypermobility patients that you sent out a random and said, ‘Would you like to come and see if we can manage your hypermobility syndrome better’ then you’d get people that probably are a lot more happier doing one or the other. [. . .] if they’re just diagnosed and they want to learn more about it but don’t have a specific problem, then they’re happier to – to, to try, to try both.
Trainer B, end of study
Equipoise
Although physiotherapists understood the rationale and aim of the trial, and that the lack of empirical evidence indicating the efficacy of physiotherapy to treat JHS justified the trial design, they anticipated that it may be difficult to ‘persuade’ patients that clinical equipoise existed:
I think it’s easy to convince a physiotherapist that the trial is worth doing because we don’t know if the treatment is or isn’t beneficial. But to convince a member of the general public, I think, would be much harder . . . the problem that you have is that you tell a patient that they’re either going to have treatment or not have treatment. But I think that immediately that a puts a barrier for them because they need to get over the option where they’re thinking, ‘Well, if I don’t accept to join the trial, I will get a treatment. If I do go to the trial, then I might potentially not’. That was the only thing I felt on the day that confused me a little. I don’t know if that’s something that would be able to be dealt with at all.
Trainee E, post training
Participants felt strongly that they had a responsibility to their patients to provide optimum level of care and considered that the advice intervention could not provide this for some patients.
That whole of, ‘We’ll just let you get on with it’, as I say, I found slightly difficult to – [erm], well, not ‘sell’, but in terms of – I think that’s a big, big ask of, of patients. Particularly when they’re, they’re struggling and not so good. I mean, I think if you’re picking up a general kind of population of, of hypermobility patients that necessarily aren’t struggling that’s an easier. But actually when you’ve got people that are struggling, they do kind of want that treatment.
Trainer B, end of study
I think we always didn’t want a no treatment arm – but that was what we ended up having to have.
Trainer C, end of study
One participant felt that although the two intervention arms provided a way to help clarify the benefits of physiotherapy, the advice intervention would not be as beneficial to patients as advice and physiotherapy.
Obviously, being a physio[therapist], I believe in what we’re doing, so it feels a bit harsh for the patients who are obviously only getting the advice, I feel that they’re not getting, um, the best out of their treatments, I suppose. But, then, you know, like I said, for research purposes, then that’s the best way of doing sort of a control group, isn’t it?
Trainee E, end of study
Generally, physiotherapists found the issue of equipoise in this study difficult, and felt that this was an issue related to recruitment. One participant alluded to the advice-only intervention being ‘no treatment’ and felt that it was difficult to ‘sell’ the trial to patients.
OK. Do you think the patients believe there was equipoise?
Erm – very difficult to say. Erm, [laughter] I would guess probably not. Erm, kind of that that they’d been referred. I mean, I would – well I don’t know even if they believe that – I think they believed that there was no evidence one way or the other. Erm, if it was me coming as a patient – I’d rather try something than nothing. That is, is, I think, is generally – how a lot of them viewed it. [. . .] probably at least 50% of the people I’ve assessed, erm, or have responded saying they’re interested in the trial have probably decided not to do the trial. For the sake of, of the risk of having – not having treatment essentially. So, from – I think that’s the hardest point with it is selling the no-treatment side of the arm. And, and, and that there is that 50/50 per cent chance that they might get nothing.
Trainer B, end of study
Randomisation
Physiotherapists felt that patients would prefer to be randomised to the treatment, rather than to advice condition:
Most people were quite positive, in the sense that they were very keen. Anything that they could contribute to increase understanding, awareness of their condition. You know, they were really happy to participate in a trial of any sort. However, when they, some people who found out that they then may not get any input, then felt that actually that wasn’t really what they wanted. So they were really keen to participate in a trial. But they didn’t want to then be on a trial that meant they might not actually have any input. Or they agreed and then some, we had a couple who then said, ‘Actually, I’ve gone off and had some . . . ’ So they might’ve been on the advice arm and then they wanted to actually have some physio[therapy] anyway.
Trainer F, end of study
Future recommendations and requirements (objective 5)
Physiotherapists’ views were gathered on how the trial intervention arms could be improved in future trials or as part of standard care, and what improvements could be made and how physiotherapists can be supported in their role when delivering the physiotherapy intervention. Suggestions are summarised in Table 40.
| Issue | Suggested improvement | Illustrative quotation |
|---|---|---|
| Advice-only intervention arm | Reduce the ‘information load’ for the patient and improve delivery of information in the advice session, for example by delivering the advice in two sessions | When we were doing that advice session, we weren’t necessarily sure which arm they, that they’ll go down. So we tried to give them any – everything. I personally would prefer people to come back. I would prefer, but, I mean, again, it’s logistics of asking people to come back just for an advice session [. . .] all the logistics behind getting here, difficulties of getting here, getting time off work, parking here, etc. But, I would have personally found it better to almost, um, have done the assessment, introduced the idea of the trial to people, let people go away, think about that. And then booked them in for their first treatment after thatTrainee E, end of studyUm, I just think it’s a lot of information for people to take on board, you’re coming in, you’re assessing them, you’re telling them, ‘You’re hypermobile’, you’re then explaining a trial to them, which, probably most of them aren’t very familiar with how things like that work. And then on top of that, you’re then asking them to listen to you while you explain what hypermobility isTrainee E, end of study |
| Provide additional ‘treatments’ to augment advice session | The other thing I wanted to include but I don’t think costing would allow it and wasn’t available for equipoise around the country would be some, like, hydrotherapy as well. As another arm, or maybe they just get given a one-off set of home exercises. Rather than nothing at all. If they were just told to go and do Tai Chi, go and do Pilates and see how you get on. But maybe we could have given them, ‘This is a generic exercise programme, carry on with it and see’Trainer C, end of study | |
| Allow more time for the advice session | No time was the main one, more than anything else. [. . .] time was really the only thing that you were fighting againstTrainer C, end of study | |
| Suggest to patients that they come accompanied to the advice/assessment session | Erm, I suppose things like you could always say to them they could have brought a carer with them and things like thatTrainer C, end of study | |
| Advice and physiotherapy arm | Group sessions | I think they missed out on the group session. We have a lot more time to describe things and the peer support and things, and they can look at other people and see what they’re doing better than we – ‘cause I can’t show them the things that they’re doing, I think they find that much betterTrainer C, end of study |
| Longer/flexible trial duration | So in some way they’re having to fit it in in 4 months, would have been – if we could have had a bit longer – we could have maybe got that a bit more, so it was trying to squeeze it into that 4 months’ time as wellTrainer C, end of study | |
| Trial workbook | Reorganisation/modification of exercises | For example, all the hand ones might be better to all be on one place and all the hip ones were a little bit, sort of, er, intermittentTrainer F, end of study |
| Diagnosis | Standardising or addressing limitations of diagnosis | And while the Brighton criteria does help, erm, a lot of those, those sorts of thing is – that, again, is open to a degree of interpretationTrainer B, end of study |
| Inclusion/exclusion criteria | Reconsider/clarify inclusion/exclusion criteria | Think we need to make sure that we exclude, and, and be a little bit clearer on people with other inflammatory arthropathies. Erm, because there was a little bit of confusion with some peopleTrainer B, end of studyAnd actually some people that are, are quite active and, and, and quite keen can actually go through it in less sessions than they do. . . . and I think so catching them early is, is, is quite, quite important in, in terms of prompt treatment, er, and those sorts of things and before they’ve had too much other surgery. So that’s too many other problems that will limit their exerciseTrainer B, end of study |
Discussion and recommendations
A particular strength of this part of the research lay in strong recruitment to the interviews. All therapists who were trained and/or were directly involved with the trial were also interviewed. The strong recruitment generated extensive data. The decision not to interview physiotherapists who were not involved with the study (see justification in Physiotherapists’ experiences, Aims and objectives) might be seen as a limitation as there are limited data on potential issues with rolling out the intervention. However, the data generated were based on direct experience of training and/or delivering the intervention rather than hypothetical projections on the behalf of therapists.
Trainees and trainers were generally satisfied with both the 1-day training sessions and the training which took place at study site 2 over 2 non-consecutive days. Combining training on the advice and physiotherapy interventions for JHS with training specific to the trial in one session meant that there was a lot for new physiotherapists to take on board. Some therapists felt that the training day was ‘too long’, but generally it was felt that this was preferable to splitting the course into more sessions. However, one training session for the trial and one session for the intervention may be preferable. Flexibility in training delivery and content is a ‘double-edged sword’. Although this flexibility was necessary to respond to the needs of the trainees, it also may reduce standardisation. ‘Take-home’ training literature for the trainee physiotherapists was required, to support their confidence and allow them to refer back. Hands-on experience and contact with JHS patients are necessary soon after training. A JHS model patient would help trainees new to treating JHS to understand the nature of the syndrome and its manifestations.
Trainers and trainees felt that the volume of information in the advice session may be overwhelming. There was some agreement that the advice session, while acceptable to some, left some patients requiring more input.
The patient handbook was helpful in many ways, but physiotherapists’ attitudes to the exercises included at the end of the booklet were more ambivalent. The workbook was rated positively as an adjunct to the physiotherapy sessions. It was felt, however, that physiotherapy input was also required. The physiotherapy sessions were regarded positively. Time and duration were raised as issues which may have impacted upon the clinical effectiveness of the intervention. Being treated for JHS and simply having the condition recognised was considered by physiotherapists to be a very important component of the intervention.
Inclusion and exclusion criteria were discussed at length in relation to clinical equipoise and recruitment issues. It was felt that there may be distinct groups of patients who may differentially benefit from each of the intervention arms.
Chapter 6 Conclusions and recommendations
Main findings
The focus group data demonstrated that JHS is a complex and unpredictable condition with a wide impact on physical and psychological well-being. Diagnosis is often delayed and this may make the condition more difficult to manage. Patients and health professionals with experience of managing JHS shared many key notions of what a good physiotherapy intervention should look like. Essentially JHS needs to be treated holistically as a long-term multijoint condition, rather than treating individual acutely painful joints in isolation.
A comprehensive user-informed physiotherapy intervention and associated training package was developed, which was generally evaluated positively by patients and physiotherapists. Training could be improved to incorporate patient models and more practical hands-on teaching, including early clinical experience of treating JHS patients following training. The advice intervention and the patient handbook and general structure and content of the physiotherapy intervention were generally commented upon favourably.
The pilot RCT provided evidence of promise that the physiotherapy intervention may produce moderate clinical effects on outcome measures that are specific to rheumatological conditions (RAPID3) and JHS (BIoH questionnaire) over and above advice alone. The qualitative interviews with patients and physiotherapists supported the potential effectiveness of both the advice intervention and the physiotherapy intervention and generated clear recommendations concerning the design and conduct of any future RCT. There were no clear trends in terms of cost-effectiveness, although the VOI estimates were supportive of the likely benefit of conducting a future definitive RCT. Taken as a whole, the data generated in the current project suggest that a future definitive RCT is warranted.
There were some specific challenges in conducting the pilot RCT and these would need to be addressed in any future RCT. Further consultation with people with JHS and with health professionals with regards to these issues would be crucial in refining the final design of a future definitive trial. Specific lessons are discussed in Specific lessons from the Physiotherapy for Hypermobility Trial.
Specific lessons from the Physiotherapy for Hypermobility Trial
Clinical equipoise
Conducting the pilot RCT was challenging because of the perceived lack of equipoise between the advice intervention and the physiotherapy intervention. Qualitative data suggested that this was an issue both for patients and physiotherapists involved with the study, and is likely to have negatively impacted on recruitment and retention. The lack of adequate control groups has been highlighted in the literature as a major issue in convincingly demonstrating the effectiveness of physiotherapy for JHS. 33 Only one previous RCT included a no-treatment control group,24 but unfortunately those authors failed to report a direct statistical comparison of trial arms following treatment. The only other controlled studies were conducted with children and employed different types of exercise as comparator groups. 37,38 So, there is an argument that the existing research evidence (or lack thereof) supports a notion of clinical equipoise in terms of if physiotherapy is better than advice or indeed doing nothing. The qualitative data seems to support the notion that this was largely understood by patients and physiotherapists in the present study. It is clear, however, that this collective understanding of clinical equipoise did not translate to personal equipoise on behalf of patients and physiotherapists, with many believing that the advice intervention was inferior. This conflict between clinical and personal equipoise has been recognised in other areas of physiotherapy research, such as manual therapy. 99
Any future RCT in this area will need to ensure robust training and monitoring of trial personnel to ensure that notions of equipoise are delivered and reinforced consistently. This might include openly eliciting and discussing treatment preferences with patients as part of the informed consent process. 100 Revision of the wording of participant information sheets should also be undertaken with the assistance of patient research partners to reinforce messages related to equipoise.
Design of the comparator trial arm
An issue closely related to equipoise was the design of the advice-only control intervention in this pilot RCT. Some patients clearly benefited from the one-off advice intervention and booklets, reporting that the information helped them to understand their condition better and that it acted as a catalyst for change. Other patients and physiotherapists, however, were clearly not convinced that it represented a credible alternative to the physiotherapy intervention. Patients had been referred for physiotherapy and, therefore, many felt that advice was ‘less’ of an intervention. Another important consideration in this was that the advice session deviated from ‘usual care’ at the two study centres involved in the research, both of which have particular expertise in the management of JHS. Patients and physiotherapists provided some useful suggestions for how the comparator intervention might be redesigned for any future study. In considering these suggestions, the research team was mindful of striking a balance between creating a credible comparator trial arm and diluting the potential difference in effectiveness between trial arms, should one exist.
It was felt that the principles of the advice intervention used in the present pilot RCT were probably sound – aiming to respond to questions and issues generated by individual patients, supported by advice literature. The data suggested that there was insufficient time in the one-off advice session to do this effectively, however. The strategies of using telephone support and additional face-to-face sessions suggested by study participants would seem to allow the opportunity to maintain the existing principles of the advice intervention but allow additional time to listen to and respond to individuals’ issues. It is therefore recommended that a future RCT employs additional telephone and face-to-face contact to support participants randomised to the advice control arm. The participant information sheet should again be revised with the assistance of patient research partners to ensure that the advice arm is portrayed positively.
Recruitment rates
A further inter-related issue was the lower than expected rate of recruitment to the pilot RCT. An initial target was 60 participants over 12 months (equivalent to five per month). Owing to delays in NHS approvals, a shorter 8-month recruitment period was available, over which 29 participants consented to the study (equivalent to 3.6 per month). The recruitment period also coincided with a move of one of the physiotherapy services into a new hospital building which caused a hiatus of recruitment activity at that site. A range of strategies was implemented to boost referrals and enhance consent rates but recruitment remained disappointing.
Issues related to perceived equipoise between study arms and the design of the control intervention have already been discussed and attention to those factors is likely to improve recruitment rates to a future RCT. It is also worth noting, however, that some 28% (34/121) of referrals either failed to respond or did not attend for assessment during the recruitment period. A ‘did not attend’ has been defined as ‘a wasted appointment slot, caused by a patient who does not attend an appointment (whether they cancel or do not turn up on the day) and the appointment slot is unused’. 96 The average did not attend rate for musculoskeletal physiotherapy outpatient services has been reported to be 9.45% across the UK. 96 Although many of the 28% of referrals in the present study simply did not respond and would not officially be classified as ‘did not attends’, this still represents a sizeable group of potential participants who were not available for assessment of eligibility. A future RCT should ensure that resources are in place to follow up all potential participants to maximise recruitment.
Another potential strategy would be to try to identify participants earlier in the referral pathway, for example in primary care. Given the difficulties in recognising and diagnosing JHS reported by participants throughout this research, however, this is likely to be extremely difficult and would require concerted education and awareness-raising in primary care. It would likely be more productive to concentrate on adequately identifying those with JHS from referrals to musculoskeletal outpatient physiotherapy services. Connelly et al. 14 found that 30% of all referrals to a musculoskeletal triage service met the diagnostic criteria for JHS. Although not all of those patients would have been referred for symptoms directly attributed to JHS, it does suggest that there is a large population of potential JHS patients being referred to physiotherapy services. Clark et al. 101 reported that JHS is accompanied by a wide range of concomitant diagnoses such as chronic widespread pain (86%), chronic fatigue syndrome (31%) and fibromyalgia (19%), each of which might form the basis for a referral for physiotherapy. It might therefore be possible to screen all referrals to physiotherapy services to help identify participants with JHS. A simple five-item screening questionnaire for identifying those with JHS was developed by Hakim and Grahame102 and has been shown to have 84% sensitivity. Such a tool could help to identify patients with other concomitant diagnoses who are hypermobile and who might be likely to receive benefit from the advice and/or physiotherapy intervention package. A diagnosis of JHS could then be confirmed clinically before recruitment to the trial. As a minimum, a future RCT should aim to train all musculoskeletal physiotherapists within participating organisations to recognise those patients likely to have JHS so that they could help to identify potential trial participants.
Recruitment of men was roughly proportionate to expected rates. It has been reported that symptomatic joint hypermobility affects 5% of women and 0.6% of men,10 equating to a ratio of 88 : 12 women to men (if the populations are roughly equal). Men comprised 12% (3/25) of those recruited to stage 1 and 10.3% (3/29) of those recruited to stage 3 of the current research. Stratification by sex should be employed as part of the randomised allocation to trial arms in any future RCT as, by chance, all three men were allocated to the advice-only intervention in stage 3 of the current project.
It is clear that a future RCT should be multicentre to maximise recruitment. Sample size calculations for a future RCT have been conducted on the basis of a similar recruitment and attrition rate as was experienced in the pilot RCT, although there are clear opportunities to improve on these. Recruiting six centres of a similar size to those participating in the pilot RCT seems realistic and it is estimated that recruitment would take 20 months (based on RAPID3 as the primary outcome measure) or 25 months (based on the BIoH questionnaire). Again, this seems feasible.
Questionnaire return
The proportion of pilot RCT questionnaires completed was 83%, 65% and 73% at baseline, 4 and 7 months, respectively. The rate of completion was consistently lower in the advice-only arm than the advice and physiotherapy arm, which may indicate an element of disengagement from the study on behalf of those randomised to receive the advice intervention in isolation. Administration of questionnaires was by mail and, despite mail and telephone reminders, it was very difficult to secure completion and return of questionnaires. A future RCT should schedule a face-to-face review to ensure completion and return (or complete over the telephone). If the advice intervention was redesigned it might be possible to schedule face-to-face advice sessions with outcome assessment.
Adverse events
The rate of adverse events was higher in the advice-only arm than in the advice and physiotherapy arm. It was extremely difficult to attribute events directly to treatment (or the lack thereof), particularly when a baseline of adverse events had not been established. It is known that this patient group is prone to events such as trips and falls, joint subluxation and dislocation, and a range of soft-tissue conditions2 and one interpretation may be that the physiotherapy intervention reduced the incidence relative to the advice intervention. However, because the advice intervention deviated from ‘usual care’ at the two NHS trusts involved with the trial, the DMEC asserted that all participants in the advice-only arm should be offered physiotherapy at the end of the trial and this was enacted. It is recommended that a future RCT should record adverse event rates at baseline to better inform judgements about changes in rates over time and between trial arms.
Recommendations for future research
Based on a wide range of quantitative and qualitative data generated as part of this research, it is recommended that a future definitive RCT is warranted. Some specific lessons to inform a future RCT have been identified in Specific lessons from the Physiotherapy for Hypermobility Trial and are summarised as follows:
-
Train and monitor trial personnel to ensure notions of equipoise are delivered and reinforced consistently.
-
Offer additional telephone and face-to-face contact to support participants randomised to the advice-only control arm.
-
Screen all referrals to physiotherapy services to identify those with JHS.
-
Stratify randomisation to trial arms by sex.
-
Employ multicentre recruitment.
-
Schedule face-to-face review to complete study outcome measures.
-
Record adverse event rates at baseline.
The lack of high-quality epidemiological evidence on the incidence and prevalence of JHS remains a barrier to the development of research in this area. Future epidemiological research should also aim to identify prognostic indicators, which might form the focus for refinement of management interventions.
Future research is required to understand the extent to which any changes are maintained in the longer term. A minimum of 12-month follow-up would be useful to determine long-term benefits of treatment.
Participants and physiotherapists talked of the potential benefit of ongoing review and support, and it might be useful to explore whether or not the addition of such review enhances long-term management. This might be difficult within the constraints of a RCT but it is worth investigating in the future whether or not ongoing access to treatment and advice is effective in the long term.
It would be helpful to determine if there are subgroups of patients who might have different requirements, for example those recently diagnosed and those who have lived with the condition for a number of years. De Wandele et al. 103 found evidence for three distinct subtypes of patients with EDS-HT, with non-musculoskeletal symptoms acting as an important distinction between subgroups. If subgroups of patients are verified, then future research could determine what their specific needs might be and if more tailored physiotherapy interventions might enhance effectiveness. Future research should also endeavour to recruit wider ethnic and sex diversity than was reflected in the current research.
Barriers to physiotherapy treatment effectiveness also need to be explored in more depth. This could include future research exploring factors affecting treatment adherence and the extent to which participants did adhere to the advice given by the physiotherapists. As numbers in the advice and physiotherapy arm were small, it was difficult to assess the extent to which the intervention was adhered to.
Both therapists and patients in this study reported that difficulties in diagnoses often stem from primary care, so recognition and diagnosis needs to be improved. There are obvious implications for the education and training of GPs and other health professionals. Research should be conducted to identify the educational needs of primary care health professionals with regards to JHS diagnosis.
Conclusion
The present research has developed and evaluated a comprehensive user-informed physiotherapy intervention. The findings demonstrate that a future definitive RCT of physiotherapy for JHS is feasible in the UK.
Acknowledgements
The authors would like to thank our patient research partners Alison Cossons and Jennifer Elvin for their invaluable insights at every stage of the design and conduct of the research and interpretation of the findings.
We would also like to thank the HMSA for their support for recruitment to stage 1 of the research. The contributions of Jane Simmonds and Carol Clark for their support for recruitment to stage 1 of the research and for their assistance with interpretation and publication of the stage 1 findings are very much appreciated.
Thank you to Tim Jenkinson for his support in developing the original grant application.
The Study Steering Committee (SSC) and DMEC provided invaluable advice throughout the conduct of the research. We are very thankful to the chairpersons (SSC chairperson, Elizabeth White; DMEC chairperson, Francis Fatoye) and committee members (SSC members: Carol Clark, Melissa Domaille and Jennifer Elvin; DMEC members: Alison Cossons, Rosemary Greenwood and Carey McClellan).
Thank you to all those who took part in the research: patient and health professional focus group participants (stage 1) and patient and physiotherapist participants (stages 2 and 3).
The huge contribution of the principal investigators at each site is duly acknowledged: Rachel Lewis and Sin-ti Towlson. Thank you also to the physiotherapists involved with delivery of the interventions and to the clinical managers who supported staff engagement with the study.
The MDHAQ has been used under license from Corporate Translations, Inc., East Hartford, CI, USA.
A final thank you goes to members of the relevant National Research Ethics Service Research Ethics Committees; NHS Research and Development Departments; University Finance Departments; University Research Departments; and to the National Institute for Health Research HTA programme staff for their support throughout the planning and conduct of the research.
Contributions of authors
Shea Palmer (Professor of Musculoskeletal Rehabilitation) was the principal grant applicant, led the development of the study protocol, led preparation of the report, was responsible for the overall conduct of the study and is guarantor of the study.
Fiona Cramp (Associate Professor in Musculoskeletal Health) contributed to the development of the study design, development of the physiotherapy intervention, was a member of the study management group and assisted in preparation of the report.
Emma Clark (Consultant Senior Lecturer in Rheumatology) contributed to the development of the study design, development of the physiotherapy intervention, was a member of the study management group and assisted in preparation of the report.
Rachel Lewis (Clinical Specialist Physiotherapist in Rheumatology) contributed to the development of the study design, development of the physiotherapy intervention and training package, acted as principal investigator at one of the clinical sites, was a member of the study management group and assisted in the wider preparation of the report.
Sara Brookes (Senior Lecturer in Medical Statistics) contributed to the development of the study design, led on statistical analysis aspects of the study, was a member of the study management group and assisted in the wider preparation of the report.
William Hollingworth (Professor of Health Economics) contributed to the development of the study design, led on the health economics aspects of the study, was a member of the study management group and assisted in the wider preparation of the report.
Nicky Welton (Reader in Evidence Synthesis) contributed to the development of the study design, led on the value of information analysis, was a member of the study management group and assisted in the wider preparation of the report.
Howard Thom (Research Associate in Health Economics Modelling) assisted with the health economics aspects of the study and assisted in the wider preparation of the report.
Rohini Terry (Research Associate) conducted and analysed the interviews as part of stages 2 and 3 of the research, was a member of the study management group and assisted in the wider preparation of the report.
Katharine A Rimes (Senior Lecturer) helped to refine the focus group topic guides as part of stage 1 of the research, advised on the development of the physiotherapy intervention (particularly aspects related to clinical psychology), was a member of the study management group and assisted in the wider preparation of the report.
Jeremy Horwood (Senior Research Fellow in Ethnography/Qualitative Social Science) contributed to the development of the study design, was responsible for the day-to-day management of the qualitative aspects of the study, led on the writing of the qualitative components of the report, was a member of the study management group and assisted in the wider preparation of the report.
Publications
Terry R, Palmer S, Rimes K, Clark C, Simmonds J, Horwood J. Living with joint hypermobility syndrome: patient experiences of diagnosis, referral and self-care. Fam Pract 2015;32:354–8.
Palmer S, Terry R, Rimes KA, Clark C, Simmonds J, Horwood J. Physiotherapy management of joint hypermobility syndrome – a focus group study of patient and health professional perspectives. Physiotherapy 2016;102:93–102.
Data sharing statement
All available data can be obtained from the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health.
References
- Jordan K, Clarke AM, Symmons DP, Fleming D, Porcheret M, Kadam UT, et al. Measuring disease prevalence: a comparison of musculoskeletal disease using four general practice consultation databases. Br J Gen Pract 2007;57:7-14.
- Grahame R, Keer R, Grahame R. Hypermobility Syndrome: Recognition and Management for Physiotherapists. Edinburgh: Butterworth Heinemann; 2003.
- Tinkle BT, Bird HA, Grahame R, Lavallee M, Levy HP, Sillence DL. The lack of clinical distinction between the hypermobility type of Ehlers–Danlos syndrome and the joint hypermobility syndrome (a.k.a. hypermobility syndrome). Am J Med Genet A 2009;149:2368-70. http://dx.doi.org/10.1002/ajmg.a.33070.
- Al Rawi Z, Al-Aszawi AJ, Al-Chalabi T. Joint hypermobility among university students in Iraq. Br J Rheumatol 1982;24:326-31. http://dx.doi.org/10.1093/rheumatology/24.4.326.
- Beighton PH, Solomon L, Soskolne CL. Articular mobility in an African population. Ann Rheum Dis 1973;32:413-7. http://dx.doi.org/10.1136/ard.32.5.413.
- Birrell FN, Adebajo A, Hazleman BL, Silman AJ. High prevalence of joint laxity in West Africans. Br J Rheumatol 1994;33:56-9. http://dx.doi.org/10.1093/rheumatology/33.1.56.
- Grahame R. Hypermobility – not a circus act. Int J Clin Pract 2000;54:314-15.
- Hakim AJ, Grahame R. Non-musculoskeletal symptoms in joint hypermobility syndrome. Indirect evidence for autonomic dysfunction?. Rheumatology 2004;43:1194-5. http://dx.doi.org/10.1093/rheumatology/keh279.
- Simmonds JV, Keer RJ. Hypermobility and the hypermobility syndrome: part 2. Assessment and management of hypermobility syndrome. Illustrated via case studies. Man Ther 2008;13:e1-1. http://dx.doi.org/10.1016/j.math.2007.11.001.
- Simpson MR. Benign joint hypermobility syndrome: evaluation, diagnosis, and management. J Am Osteopath Assoc Clin Pract 2006;106:531-6.
- Grahame R, Bird HA, Child A. The revised (Brighton 1998) criteria for the diagnosis of benign joint hypermobility syndrome (BJHS). J Rheumatol 2000;27:1777-9.
- Ross J, Grahame R. Joint hypermobility syndrome. BMJ 2011;342. http://dx.doi.org/10.1136/bmj.c7167.
- Grahame R, Hakim A. High prevalence of joint hypermobility syndrome in clinic referrals to a north London community hospital. Rheumatology 2004;43.
- Connelly E, Hakim A, Davenport HS, Simmonds JV. A study exploring the prevalence of joint hypermobility syndrome in patients attending a musculoskeletal triage clinic. Physiother Pract Res 2015;36:43-5.
- Clark CJ, Simmonds JV. An exploration of the prevalence of hypermobility and joint hypermobility syndrome in Omani women attending a hospital physiotherapy service. Musculoskeletal Care 2011;9:1-10. http://dx.doi.org/10.1002/msc.184.
- Clinch J, Deere K, Sayers A, Palmer S, Riddoch C, Tobias JH, et al. Epidemiology of generalized joint laxity (hypermobility) in fourteen-year-old children from the UK. A population-based evaluation. Arthritis Rheum 2011;63:2819-27. http://dx.doi.org/10.1002/art.30435.
- Remvig L, Flycht L, Christensen KB, Juul-Kristensen B. Lack of consensus on tests and criteria for generalized joint hypermobility, Ehlers–Danlos syndrome: hypermobile type and joint hypermobility syndrome. Am J Med Genet A 2014;164A:591-6. http://dx.doi.org/10.1002/ajmg.a.36402.
- De Paepe A, Devereux RB, Dietz HC, Hennekam RC, Pyeritz RE. Revised diagnostic criteria for the Marfan syndrome. Am J Med Genet 1996;62:417-26. http://dx.doi.org/10.1002/(SICI)1096-8628(19960424)62:4%3C417::AID-AJMG15%3E3.0.CO;2-R.
- Beighton P, De Paepe A, Steinmann B, Tsipouras P, Wenstrup RJ. Ehlers–Danlos syndromes: revised nosology, Villefranche, 1997. Ehlers–Danlos National Foundation (USA) and Ehlers–Danlos Support Group (UK). Am J Med Genet 1998;77:31-7.
- Engelbert RH, van Bergen M, Henneken T, Helders PJ, Takken T. Exercise tolerance in children and adolescents with musculoskeletal pain in joint hypermobility and joint hypomobility syndrome. Pediatrics 2006;118:e690-6. http://dx.doi.org/10.1542/peds.2005-2219.
- Fatoye F, Palmer S, Macmillan F, Rowe P, van der Linden M. Proprioception and muscle torque deficits in children with hypermobility syndrome. Rheumatology 2009;48:152-7. http://dx.doi.org/10.1093/rheumatology/ken435.
- Fatoye F, Palmer S, Macmillan F, Rowe P, van der Linden M. Gait kinematics and passive knee joint range of motion in children with hypermobility syndrome. Gait Posture 2011;33:447-51. http://dx.doi.org/10.1016/j.gaitpost.2010.12.022.
- Fatoye F, Palmer S, Macmillan F, Rowe P, van der Linden M. Pain intensity and quality of life perception in children with hypermobility syndrome. Rheumatol Int 2012;32:1277-84. http://dx.doi.org/10.1007/s00296-010-1729-2.
- Mallik AK, Ferrell WR, McDonald A. Impaired proprioceptive acuity at the proximal interphalangeal joint in patients with the hypermobility syndrome. Br J Rheumatol 1994;33:631-7. http://dx.doi.org/10.1093/rheumatology/33.7.631.
- Hall MG, Ferrell WR, Sturrock RD, Hamblen DL, Baxendale RH. The effect of the hypermobility syndrome on knee joint proprioception. Br J Rheumatol 1995;34:121-5. http://dx.doi.org/10.1093/rheumatology/34.2.121.
- Sahin N, Baskent A, Cakmak A, Salli A, Ugurlu H, Berker E. Evaluation of knee proprioception and effects of proprioception exercise in patients with benign joint hypermobility syndrome. Rheumatol Int 2008;28:995-1000. http://dx.doi.org/10.1007/s00296-008-0566-z.
- Sahin N, Baskent A, Ugurlu H, Berker E. Isokinetic evaluation of knee extensor/flexor muscle strength in patients with hypermobility syndrome. Rheumatol Int 2008;28:643-8. http://dx.doi.org/10.1007/s00296-007-0493-4.
- Smith T, Easton V, Bacon H, Jerman E, Armon K, Poland F, et al. The relationship between benign joint hypermobility syndrome and psychological distress: a systematic review and meta-analysis. Rheumatology 2014;53:114-22. http://dx.doi.org/10.1093/rheumatology/ket317.
- Simmonds JV, Keer RJ. Hypermobility and the hypermobility syndrome. Man Ther 2007;12:298-309. http://dx.doi.org/10.1016/j.math.2007.05.001.
- Tinkle BT. Issues and Management of Joint Hypermobility. A Guide for the Ehlers–Danlos Syndrome Hypermobility Type and the Hypermobility Syndrome. Niles, IL: Left Paw Press; 2008.
- Keer R, Simmonds J. Joint protection and physical rehabilitation of the adult with hypermobility syndrome. Curr Opin Rheumatol 2011;23:131-6. http://dx.doi.org/10.1097/BOR.0b013e328342d3af.
- Turner PA, Whitfield TWA. A multidimensional scaling analysis of the techniques that physiotherapists use. Physiother Res Int 1997;2:233-50. http://dx.doi.org/10.1002/pri.109.
- Palmer S, Bailey S, Barker L, Barney L, Elliott A. The effectiveness of therapeutic exercise for joint hypermobility syndrome: a systematic review. Physiotherapy 2014;100:220-7. http://dx.doi.org/10.1016/j.physio.2013.09.002.
- Smith TO, Bacon H, Jerman E, Easton V, Armon K, Poland F, et al. Physiotherapy and occupational therapy interventions for people with benign joint hypermobility syndrome: a systematic review of clinical trials. Disabil Rehabil 2014;36:797-803. http://dx.doi.org/10.3109/09638288.2013.819388.
- Ferrell WR, Tennant N, Sturrock RD, Ashton L, Creed G, Brydson G, et al. Amelioration of symptoms by enhancement of proprioception in patients with joint hypermobility syndrome. Arthritis Rheum 2004;50:3323-8. http://dx.doi.org/10.1002/art.20582.
- Barton LM, Bird HA. Improving pain by the stabilization of hyperlax joints. J Orthop Rheumatol 1996;9:46-51.
- Kemp S, Roberts I, Gamble C, Wilkinson S, Davidson JE, Baildam EM, et al. A randomized comparative trial of generalized vs targeted physiotherapy in the management of childhood hypermobility. Rheumatology 2010;49:315-25. http://dx.doi.org/10.1093/rheumatology/kep362.
- Pacey V, Tofts L, Adams RD, Munns CF, Nicholson LL. Exercise in children with joint hypermobility syndrome and knee pain: a randomised controlled trial comparing exercise into hypermobile versus neutral knee extension. Pediatr Rheumatol 2013;11. http://dx.doi.org/10.1186/1546-0096-11-30.
- Palmer S, Cramp F, Lewis R, Muhammad S, Clark E. Diagnosis, management and assessment of adults with joint hypermobility syndrome: a UK-wide survey of physiotherapy practice. Musculoskeletal Care 2015;13:101-11. http://dx.doi.org/10.1002/msc.1091.
- Dowswell G, Dowswell T, Lawler J, Green J, Young J. Patients’ and caregivers’ expectations and experiences of a physiotherapy intervention 1 year following stroke: a qualitative study. J Eval Clin Pract 2002;8:361-5. http://dx.doi.org/10.1046/j.1365-2753.2002.00302.x.
- Galvin R, Cusack T, Stokes E. Physiotherapy after stroke in Ireland: a qualitative insight into the patients’ and physiotherapists’ experience. Int J Rehabil Res 2009;32:238-44. http://dx.doi.org/10.1097/MRR.0b013e32832b083c.
- Campbell M, Fitzpatrick R, Haines A, Kinmonth AL, Sandercock P, Spiegelhalter D, et al. Framework for design and evaluation of complex interventions to improve health. BMJ 2000;321:694-6. http://dx.doi.org/10.1136/bmj.321.7262.694.
- Donovan J, Mills N, Smith M, Brindle L, Jacoby A, Peters T, et al. Improving the design and conduct of randomised trials by embedding them in qualitative research: ProtecT (prostate testing for cancer and treatment) study. BMJ 2002;325:766-70. http://dx.doi.org/10.1136/bmj.325.7367.766.
- Lewin S, Glenton C, Oxman A. Use of qualitative methods alongside randomised controlled trials of complex healthcare interventions: methodological study. BMJ 2009;339. http://dx.doi.org/10.1136/bmj.b3496.
- Finch T, May C, Mair F, Mort M, Gask L. Integrating service development with evaluation in telehealthcare: an ethnographic study. BMJ 2003;327:1205-9. http://dx.doi.org/10.1136/bmj.327.7425.1205.
- Flottorp S, Havelsrud K, Oxman AD. Process evaluation of a cluster randomized trial of tailored interventions to implement guidelines in primary care-why is it so hard to change practice?. Fam Pract 2003;20:333-9. http://dx.doi.org/10.1093/fampra/cmg316.
- Sandelowski M. Focus on qualitative methods: using qualitative methods in intervention studies. Res Nurs Health 1996;19:359-64. http://dx.doi.org/10.1002/(SICI)1098-240X(199608)19:4%3C359::AID-NUR9%3E3.0.CO;2-H.
- Toroyan T, Oakley A, Laing G, Roberts I, Mugford M, Turner J. The impact of day care on socially disadvantaged families: an example of the use of process evaluation within a randomized controlled trial. Child Care Health Dev 2004;30:691-8. http://dx.doi.org/10.1111/j.1365-2214.2004.00481.x.
- Terry R, Palmer S, Rimes K, Clark C, Simmonds J, Horwood J. Living with joint hypermobility syndrome: patient experiences of diagnosis, referral and self-care. Fam Pract 2015;32:354-8. http://dx.doi.org/10.1093/fampra/cmv026.
- Palmer S, Terry R, Rimes K, Clark C, Simmonds J, Horwood J. Physiotherapy management of joint hypermobility syndrome – patient and health-professional perspectives. Physiotherapy 2015;101. http://dx.doi.org/10.1016/j.physio.2015.03.2086.
- Hills R, Kitchen S. Satisfaction with outpatient physiotherapy: a survey comparing the views of patients with acute and chronic musculoskeletal conditions. Physiother Theory Pract 2007;23:21-36. http://dx.doi.org/10.1080/09593980601147876.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. http://dx.doi.org/10.1191/1478088706qp063oa.
- Glaser B, Strauss A, Glaser B, Strauss A. The Discovery of Grounded Theory: Strategies for Qualitative Research. Chicago, IL: Aldine Publishing Company; 1967.
- Sandelowski M. Sample size in qualitative research. Res Nurs Health 1995;18:179-83. http://dx.doi.org/10.1002/nur.4770180211.
- Lad M. The English Indices of Deprivation 2010. London: Department for Communities and Local Government; 2011.
- A Guide to Living with Hypermobility Syndrome. Plymouth: HMSA; 2011.
- Joint Hypermobility. Chesterfield: Arthritis Research UK; 2011.
- Hurley MV, Walsh NE, Mitchell HL, Pimm TJ, Patel A, Williamson E, et al. Clinical effectiveness of a rehabilitation program integrating exercise, self-management, and active coping strategies for chronic knee pain: a cluster randomized trial. Arthritis Rheum 2007;57:1211-19. http://dx.doi.org/10.1002/art.22995.
- Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev 1977;84:191-215. http://dx.doi.org/10.1037/0033-295X.84.2.191.
- Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice-Hall; 1986.
- Domaille M, Mascarenhas R, Dayal N, Kirwan J. Evaluation of the Bristol Royal Infirmary physiotherapy programme for the management of patients with osteoarthritis of the knee. Musculoskeletal Care 2006;4:78-87. http://dx.doi.org/10.1002/msc.80.
- Palmer S, Domaille M, Cramp F, Walsh N, Pollock J, Kirwan J, et al. Transcutaneous electrical nerve stimulation as an adjunct to education and exercise for knee osteoarthritis: a randomised controlled trial. Arthritis Care Res 2014;66:387-94. http://dx.doi.org/10.1002/acr.22147.
- Walsh N, Pollock J, Cramp F, Palmer S, Hampson L, Gooberman-Hill R, et al. Exercise and self-management for people with chronic knee, hip or lower back pain: a cluster randomised controlled trial of clinical and cost-effectiveness. Study protocol. Physiotherapy 2013;99:352-7. http://dx.doi.org/10.1016/j.physio.2012.09.002.
- Pincus T, Swearingen C, Wolfe F. Toward a multidimensional health assessment questionnaire (MDHAQ). Arthritis Rheum 1999;42:2220-30. http://dx.doi.org/10.1002/1529-0131(199910)42:10%3C2220::AID-ANR26%3E3.0.CO;2-5.
- Pincus T, Furer V, Keystone E, Yazici Y, Bergman MJ, Luijtens K. RAPID3 (Routine Assessment of Patient Index Data 3) severity categories and response criteria: similar results to DAS28 (Disease Activity Score) and CDAI (Clinical Disease Activity Index) in the RAPID 1 (Rheumatoid Arthritis Prevention of Structural Damage) clinical trial of certolizumab pegol. Arthritis Care Res 2011;63:1142-9. http://dx.doi.org/10.1002/acr.20481.
- Dures EK, Hewlett SE, Cramp FA, Greenwood R, Nicklin JK, Urban M, et al. Reliability and sensitivity to change of the Bristol Rheumatoid Arthritis Fatigue scales. Rheumatology 2013;52:1832-9. http://dx.doi.org/10.1093/rheumatology/ket218.
- Palmer ST, Cramp F, Lewis R, Gould G, Clark E. Development and Initial Validation of the Bristol Impact of Hypermobility Questionnaire n.d. http://dx.doi.org/10.13140/RG.2.1.3622.6080.
- Waterfield J, Sim J. Clinical assessment of pain by the visual analogue scale. BJTR 1995;3:94-7.
- Bandura A, Pajares F, Urdan T. Self-Efficacy Beliefs of Adolescents. Greenwich, CT: Information Age Publishing; 2006.
- Everett B, Salamonson Y, Davidson PM. Bandura’s exercise self-efficacy scale: validation in an Australian cardiac rehabilitation setting. Int J Nurs Stud 2009;46:824-9. http://dx.doi.org/10.1016/j.ijnurstu.2009.01.016.
- Obradovic M, Lal A, Liedgens H. Validity and responsiveness of EuroQol-5 dimension (EQ-5D) versus Short Form-6 dimension (SF-6D) questionnaire in chronic pain. Health Qual Life Out 2013;11. http://dx.doi.org/10.1186/1477-7525-11-110.
- Paterson C. Measuring outcome in primary care: a patient-generated measure, MYMOP, compared to the SF-36 health survey. BMJ 1996;312:1016-20. http://dx.doi.org/10.1136/bmj.312.7037.1016.
- Ritchie J, Spencer L, Bryman A, Burgess RG. Analyzing Qualitative Data. London: Routledge; 1994.
- Lancaster GA. Pilot and feasibility studies come of age!. Pilot Feasibility Stud 2015;1. http://dx.doi.org/10.1186/2055-5784-1-1.
- Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res 2011;20:1727-36. http://dx.doi.org/10.1007/s11136-011-9903-x.
- Curtis L. Unit Costs of Health and Social Care 2014. Canterbury: Personal Social Services Research Unit, University of Kent; 2014.
- NHS Reference Costs 2013 to 2014. London: Department of Health; 2014.
- British National Formulary. London: BMA and RPS; 2015.
- Devlin NJ, Krabbe PFM. The development of new research methods for the valuation of EQ-5D-5L. Eur J Health Econ 2013;14:S1-3. http://dx.doi.org/10.1007/s10198-013-0502-3.
- Devlin N, van Hout B. An EQ-5D-5L Value Set for England 2014. www.ohe.org/news/ohe-seminar-launches-eq-5d-5l-value-set-england (accessed July 2015).
- Claxton K, Posnett J. An economic approach to clinical trial design and research priority-setting. Health Econ 1996;5:513-24. http://dx.doi.org/10.1002/(SICI)1099-1050(199611)5:6%3C513::AID-HEC237%3E3.0.CO;2-9.
- Manca A, Hawkins N, Sculpher M. Estimating mean QALYs in trial-based cost-effectiveness analysis: the importance of controlling for baseline utility. Health Econ 2005;14:487-96. http://dx.doi.org/10.1002/hec.944.
- Lunn DJ, Thomas A, Best N, Spiegelhalter D. WinBUGS – a Bayesian modelling framework: concepts, structure, and extensibility. Stat Comput 2000;10:325-37. http://dx.doi.org/10.1023/A:1008929526011.
- Guide to the Methods of Technology Appraisal 2013. London: National Institute for Health and Care Excellence; 2013.
- Cooper NJ, Sutton AJ, Abrams KR, Turner D, Wailoo A. Comprehensive decision analytical modelling in economic evaluation: a Bayesian approach. Health Econ 2003;13:203-26. http://dx.doi.org/10.1002/hec.804.
- Welton NJ, Sutton AJ, Cooper NJ, Abrams KR, Ades AE. Evidence Synthesis for Decision Making in Healthcare. Chichester: Wiley; 2012.
- Strong M, Oakley JE, Brennan A. Estimating multiparameter partial expected value of perfect information from a probabilistic sensitivity analysis sample. A nonparametric regression approach. Med Decis Making 2014;34:311-26. http://dx.doi.org/10.1177/0272989X13505910.
- SAVI – Sheffield Accelerated Value of Information. Sheffield: University of Sheffield; 2015.
- Jansen LMA, van Schaardenburg D, van der Horst-Bruinsma IE, Bezemer PD, Dijkmans BAC. Predictors of functional status in patients with early rheumatoid arthritis. Ann Rheum Dis 2000;59:223-6. http://dx.doi.org/10.1136/ard.59.3.223.
- Creamer P, Lethbridge-Cejku M, Hochberg MC. Factors associated with functional impairment in symptomatic knee osteoarthritis. Rheumatology 2000;39:490-6. http://dx.doi.org/10.1093/rheumatology/39.5.490.
- Albayrak I, Yimaz H, Akkurt HE, Salli A, Karaca G. Is pain the only symptom in patients with benign joint hypermobility syndrome?. Clin Rheumatol 2015;34:1613-19. http://dx.doi.org/10.1007/s10067-014-2610-6.
- De Wandele I, Calders P, Peersman W, Rimbaut S, De Backer T, Malfait F, et al. Autonomic symptom burden in the hypermobility type of Ehlers–Danlos syndrome: a comparative study with two other EDS types, fibromyalgia, and healthy controls. Semin Arthritis Rheum 2014;44:353-61. http://dx.doi.org/10.1016/j.semarthrit.2014.05.013.
- Rombaut L, Malfait F, Cools A, De Paepe A, Calders P. Musculoskeletal complaints, physical activity and health-related quality of life among patients with the Ehlers–Danlos syndrome hypermobility type. Disabil Rehabil 2010;32:1339-45. http://dx.doi.org/10.3109/09638280903514739.
- Berglund B, Pettersson C, Pigg M, Kristiansson P. Self-reported quality of life, anxiety and depression in individuals with Ehlers–Danlos syndrome (EDS): a questionnaire study. BMC Musculoskelet Disord 2015;16. http://dx.doi.org/10.1186/s12891-015-0549-7.
- Population Estimates by Age and Sex. London: ONS; 2015.
- A Survey of NHS Physiotherapy Waiting Times, Workforce and Caseloads in the UK 2010–2011. London: Chartered Society of Physiotherapy; 2011.
- Johnsen LG, Hellum C, Nygaard ØP, Storheim K, Brox JI, Rossvoll I, et al. Comparison of the SF6D, the EQ5D, and the oswestry disability index in patients with chronic low back pain and degenerative disc disease. BMC Musculoskelet Disord 2013;14. http://dx.doi.org/10.1186/1471-2474-14-148.
- Developing and Evaluating Complex Interventions: New Guidance. London: Medical Research Council; 2008.
- Cook C, Sheets C. Clinical equipoise and personal equipoise: two necessary ingredients for reducing bias in manual therapy trials. J Man Manip Ther 2011;19:55-7. http://dx.doi.org/10.1179/106698111X12899036752014.
- Mills N, Donovan JL, Wade J, Hamdy FC, Neal DE, Lane JA. Exploring treatment preferences facilitated recruitment to randomized controlled trials. J Clin Epidemiol 2011;64:1127-36. http://dx.doi.org/10.1016/j.jclinepi.2010.12.017.
- Clark C, Khattab A, Carr E. Chronic widespread pain and neurophysiological symptoms in joint hypermobility syndrome (JHS). Int J Ther Rehabil 2014;21:60-7. http://dx.doi.org/10.12968/ijtr.2014.21.2.60.
- Hakim AJ, Grahame R. A simple questionnaire to detect hypermobility: an adjunct to the assessment of patients with diffuse musculoskeletal pain. Int J Clin Pract 2003;57:163-6.
- De Wandele I, Rombaut L, Malfait F, De Backer T, De Paepe A, Calders P. Clinical heterogeneity in patients with the hypermobility type of Ehlers–Danlos syndrome. Res Dev Disabil 2013;34:873-81. http://dx.doi.org/10.1016/j.ridd.2012.11.018.
Appendix 1 Stage 1 patient focus group topic guide
Appendix 2 Stage 1 health professional focus group topic guide
Appendix 3 Stage 2 patient screening proforma
Appendix 4 Stages 2 and 3 biographical details
Appendix 5 Stage 2 baseline questionnaires
Appendix 6 Stage 2 Measure Yourself Medical Outcome Profile questionnaire
Appendix 7 Stage 2 patient topic guide
Appendix 8 Stage 2 and 3 physiotherapist topic guide (post training)
Appendix 9 Slides for Physiotherapy for Hypermobility Trial physiotherapist training
Appendix 10 Stage 3 patient information sheet
Appendix 11 Stage 3 patient screening proforma
Appendix 12 Physiotherapy for Hypermobility Trial patient handbook
Appendix 13 Stage 3 month 4 questionnaire
Appendix 14 Model to estimate expected quality-adjusted life-years and costs
Appendix 15 Bristol Impact of Hypermobility questionnaire scoring guidance
© University of the West of England, Bristol (2013).
Appendix 16 Stage 3 patient topic guide
Appendix 17 Stage 3 physiotherapist topic guide (post trial)
List of abbreviations
- AIMS-2
- Arthritis Impact Measurement Scale – 2
- BIoH
- Bristol Impact of Hypermobility questionnaire
- CI
- confidence interval
- CONSORT
- Consolidated Standards of Reporting Trials
- DMEC
- Data Monitoring and Ethics Committee
- EDS-HT
- Ehlers–Danlos syndrome – hypermobility type
- EQ-5D-5L
- European Quality of Life-5 Dimensions-5 Levels
- ESCAPE
- Enabling Self-management and Coping with Arthritic knee Pain through Exercise programme
- ESE
- Exercise Self-Efficacy scale
- EVPI
- expected value of perfect information
- EVPPI
- expected value of partial perfect information
- GP
- general practitioner
- HMSA
- Hypermobility Syndromes Association
- HPoP
- Hypermobility: Perspectives on Physiotherapy
- HTA
- Health Technology Assessment
- JHS
- joint hypermobility syndrome
- MDHAQ
- Multidimensional Health Assessment Questionnaire
- MYMOP
- Measure Yourself Medical Outcome Profile
- QALY
- quality-adjusted life-year
- RADAI
- Rheumatoid Arthritis Disease Activity Index
- RAPID3
- Routine Assessment of Patient Index Data 3
- RCT
- randomised controlled trial
- SD
- standard deviation
- SF-36
- Short Form questionnaire-36 items
- SF-6D
- Short Form questionnaire-6 Dimensions
- SSC
- Study Steering Committee
- VAS
- visual analogue scale
- VOI
- value of information