Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 10/93/04. The contractual start date was in March 2013. The draft report began editorial review in July 2015 and was accepted for publication in January 2016. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2016. This work was produced by Free et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
Younger people bear the heaviest burden of sexually transmitted infections (STIs) such as chlamydia and gonorrhoea, which can cause long-term adverse health effects including ectopic pregnancy and subfertility, especially in those with repeated infections. 1,2 Young people are most likely to report having at least two sexual partners in the last year with whom no condom was used. 1,3 The highest prevalence of STIs is in those from socioeconomically deprived areas and those with higher numbers of sexual partners. 1 Reinfection rates following treatment are high, with reinfection rates of 30% for chlamydia and 12% for gonorrhoea at 1 year. 4,5 Those with a STI are more likely to acquire human immunodeficiency virus (HIV), if exposed.
Safer sex behaviours such as condom use, notifying partner(s) about an existing STI and STI testing reduce the risk of STIs but young people can lack the knowledge, confidence and skills needed to adopt these behaviours. Existing interventions delivered face to face or in the media are limited in their appeal or effects or are too costly for widespread application. 6,7 Strategies to increase partner notification that can be delivered in primary care settings have been elusive. 8
Mobile phones provide a broad-reach delivery mechanism for effective, low-cost health behaviour support. 9–11 Support via text message is likely to be acceptable to young people and might increase safer sexual health behaviours. Mobile phones are able to provide confidential and non-judgemental support, which is essential for a sexual health intervention. 12 Interactive support can be delivered at any time and in any location, ensuring privacy, which is especially important for young people. Behaviour change techniques (BCTs) used in effective face-to-face interventions can be modified for delivery via text message. 13,14 The content can be personalised for different genders and ethnic groups.
The effects of safer sex support delivered by text message are not reliably known. We searched six databases (MEDLINE, EMBASE, Global Health, Web of Science, PsycINFO and The Cochrane Library) from January 1990 to November 2014 to identify trials of mobile phone-based support to increase safer sex behaviours. We identified seven trials. 15–21 Interventions were limited; they included up to three BCTs and did not address partner notification. 22 None of the trials had a low risk of bias. Two trials reported statistically significant increases in testing for STIs. 17,18 Lim et al. 17 reported that mobile phone-based sexual health interventions can increase discussion of sexual health with a health-care professional threefold and lead to over a doubling of STI testing. Although some trial results look promising, the effects of text messaging on key safer sex behaviours, including telling your partner about your infection, correctly following treatment advice, obtaining STI testing for yourself and your partner(s) prior to unprotected sex and condom use, have not been reliably established.
The National Institute for Health Research (NIHR) Health Technology Assessment (HTA) programme commissioned us to develop a mobile phone-based intervention to promote safer sex behaviour in young people in the UK aged 16–24 years and conduct a pilot randomised controlled trial of the intervention. The HTA programme commissioning brief was to:
-
develop the intervention
-
determine the acceptability of the package
-
determine the feasibility of a main trial
-
determine the parameters for a main trial.
In Chapter 2 we describe the development of the intervention based on evidence of factors influencing safer sex behaviours, theory, evidence-based BCTs, the content of existing effective face-to-face support, information technology (IT) expertise and user and provider views. Trials can fail to reliably establish the effects of interventions when they under-recruit or achieve low rates of follow-up. In the area of sexual health research low follow-up rates have been a particular issue. Therefore, in Chapter 3 we describe research conducted to develop our follow-up procedures based on evidence, testing prototype procedures and user views. In Chapter 4 we describe the pilot randomised controlled trial of the intervention. Outcomes for judging the success of the pilot trial were the recruitment rate and completeness of the postal chlamydia test follow-up. We also tested the intervention’s acceptability and appropriateness, evaluated all trial procedures and materials and obtained prevalence estimates for sexual risk behaviours and chlamydia reinfection rates to inform the sample size calculation for the main trial. In Chapter 5 we describe the qualitative interviews with participants conducted to explore their experiences and the acceptability of the intervention.
Chapter 2 Intervention development
In this chapter we describe the formative research that we conducted to develop a text message intervention informed by theory, evidence and expert and user views to increase safer sex behaviours. Participants were young people attending services who either were diagnosed with chlamydia or reported sex unprotected by a condom with more than one partner in the last year.
Objective
To develop an acceptable intervention designed to increase safer sex behaviours based on behavioural theory, evidence and expert and user views.
Methods
The theoretical basis of our intervention
The intervention was informed by the capability, opportunity and motivation model of behaviour (COM-B). 23 This is linked to a comprehensive model of behaviour change, the behaviour change wheel, which aims to capture the full range of intervention functions involved in behaviour change. 23 These include education, persuasion, environmental restructuring (encouraging people to change their environment to support the behaviour), training and enablement. Each intervention function can be implemented by a wide range of BCTs. 22
In the case of sexual behaviour, knowledge, beliefs, self-efficacy and skills as well as social and interpersonal influences have important effects on motivation, capability and opportunity. 24,25 Our intervention aimed to influence these factors to reduce sexual risk behaviour. It aimed to support participants in correctly following treatment instructions, by correctly taking their prescribed treatment, telling partner(s) about their infection and avoiding sex for a week after taking treatment. The intervention aimed to encourage participants to use condoms with new or casual partners and obtain testing for STIs for themselves and their sexual partner(s) prior to unprotected sex (see Figure 2 and Appendix 1).
Generating content
We identified factors influencing safer sex behaviours using evidence from systematic reviews of the literature. 24,26 We generated messages, selecting intervention functions23 and BCTs that might be employed to influence these factors.
We identified trials of interventions promoting safer sex behaviours that reported STI outcomes in a systematic review6 and obtained the protocols, the content of which was coded using Abraham and Michie’s14 and Michie et al. ’s27 2011 taxonomy of BCT. We computed the inter-rater reliability (Cohen’s kappa and percentage agreement) for the scoring of the presence/absence of BCTs. We described the BCTs identified in face-to-face interventions reporting statistically significant reductions in STI infection at follow-up. Messages were drafted to include all those BCTs that we had identified in effective face-to-face interventions and additional BCTs shown to be effective in changing other behaviours. We adapted them for delivery by text message where necessary.
To ensure that the intervention content was informed by technical experts and those experienced in working with young people on safer sex behavioural support, a sexual health counsellor (Melanie Otterwill) generated messages. Experts in sexual and reproductive health service delivery, research and public health (PB, KW, RF, JB, KD, CF) reviewed the messages and were asked to identify additional content that they considered should be included in the intervention.
Generating the automated information technology system for delivering the messages
An IT programmer developed an automated text messaging system to deliver the intervention, which had an automated link to the randomisation system and database.
Testing and refining the messages: obtaining user views in focus group discussions
We convened focus groups of people aged 16–24 years to seek their preferences regarding the intervention and modify the messages based on their views regarding their acceptability. We recruited participants attending community sexual and reproductive health services in an inner city in the south of England (south-east London), a city in the north of England (Greater Manchester) and a rural area (Cambridgeshire). Clinic staff invited participants to join the focus group discussions. A researcher provided verbal and written study information. Groups were single sex, including teenagers and those in their 20s. We obtained informed written consent from participants. We explored the participants’ preferences regarding the intervention and sought their comments on the preliminary messages, specifically with regard to their acceptability, and suggestions for improvement. A second facilitator made notes during the meeting regarding their views and suggestions for improving messages and, with participants’ agreement, recorded the meeting. Participants received £20 in thanks for their time. Data were stored confidentially and anonymised in publications or reports. According to the feedback received in the initial focus groups, we retained, discarded or modified messages and retested them in subsequent focus groups or by e-mail. We continued refining the messages and conducting focus groups until participants reported that the messages were acceptable, comprehensible and appropriate.
Testing and refining the messages based on feedback obtained in a survey
The messages modified by the focus group participants were then tested in a survey and adapted based on survey responses. We recruited young people from community sexual and reproductive health services located in south-east London and rural Cambridgeshire. The eligibility criteria for the survey were age 16–24 years, ownership of a personal mobile phone and either testing positive for chlamydia or reporting unsafe sex in the last year (more than one partner and at least one occasion of unprotected sex). The researcher working in the clinic provided written and verbal information and sought informed written consent. We offered participants a private room in which to complete the questionnaire.
We selected any messages for which the feedback had been ambiguous in the focus groups and a random selection of other messages for testing. The questionnaire asked participants to score each of the messages using a 3-point scale on how relevant they considered them to be (relevant, unsure or not relevant). They were asked to identify messages that were hard to understand or that they did not like and to provide suggestions as to how the messages could be improved. Participants received £5 for completing the questionnaire. We conducted a descriptive analysis reporting the scores for each message using Microsoft Excel® 2013 (Microsoft Corporation, Redmond, WA, USA). We removed or adapted messages that achieved low scores for perceived relevance.
Testing and refining the messages based on feedback regarding the intervention when delivered to participants’ mobile phones
The resultant messages were delivered to participants’ mobile phones and final adaptations were made based on their feedback about the intervention obtained in telephone interviews. Clinic staff identified potential men and women in their teens and early 20s who had been diagnosed with chlamydia. If they agreed to take part their details were passed to OM. OM recruited participants by phone and provided verbal and written information by e-mail to potential participants and asked them to text their consent. After obtaining informed consent, the text messages were sent to participants from our automated computer-based delivery system.
Seven days after enrolment, OM contacted the participants by phone and asked them for further feedback regarding the intervention. OM asked participants about the appropriateness of the timing, frequency and content of the messages and their experiences when trying to implement the advice in the messages. Based on their feedback we made further modifications to the intervention. We continued to recruit participants until no new data regarding how the intervention should be modified emerged from the interviews. Participants received £20 in thanks for their time.
Results
Content derived from evidence on barriers to safer sexual behaviours
In Table 1 we describe key evidence-based barriers to safer sexual behaviour and how our intervention addressed these and which BCTs and which functions from the COM-B behavioural theory we employed. The principles informing the content of the intervention based on evidence on factors associated with safer sex are also reported in Table 1.
| Target behaviour | Factors associated with or influencing sexual behaviour | Intervention functions | BCTs and other implications for the intervention |
|---|---|---|---|
| Partner notification and correct treatment of a STI | Capability | ||
| Lack of knowledge regarding how to prevent infection/reinfection (partner notification) | Education | Provides information about the consequences of behaviour (partner notification and correct treatment) (5.1) | |
| Lack of knowledge regarding how to correctly treat a STI | Education | Provides instruction on how to treat STIs (4.1) | |
| Lack of skills in how to start a conversation and how to tell a partner | Education | Demonstrates how others told a partner about a STI (6.1) | |
| Opportunity | |||
| Social attitudes that STIs are associated with stigma impede partner notification | Creates an enabling environment for partner notification | Provides non-judgemental, non-stigmatising information (e.g. about how common STIs are and social support) (3.1) | |
| Models non-stigmatising ways of telling a partner about a STI (6.1) | |||
| Motivation | |||
| Lack of knowledge that you may not have symptoms of a STI and so you may not know that you are infected | Education | Provides information about the health consequences of partner notification (if you don’t tell them they may not be aware) (5.1) | |
| Sexual reputations are important and people act to protect them.24 As STIs are associated with stigma, telling a partner about a STI can have a negative impact on the reputation of both | Creates an enabling environment for partner notification | Reframes partner notification as responsible (rather than having a negative impact on identity) (13.2) | |
| Models telling a partner about a STI (6.1) (without this impacting on his or her reputation) | |||
| Condom use | Capability | ||
| Young people report problems using condoms (splitting, coming off) | Education | Provides examples of how others avoided common condom use problems (4.1) | |
| Provides a link to a web page that demonstrates how to use condoms correctly (6.1) | |||
| Young people report problems initiating condom use | Creates an enabling environment for condom use | Encourages problem solving (1.2) | |
| Encourages the creation of action plans (1.4) (BCT adapted so that examples of action plans are provided) | |||
| Young women can lack assertiveness and communication skills to negotiate condom use | Creates an enabling environment for condom use | Models how others negotiated condom use (6.1) | |
| Opportunity | |||
| Young people report not using condoms as they are not immediately available | Creates an enabling environment for condom use | Encourages young people to carry condoms (12.5) | |
| Motivation | |||
| Lack of knowledge about how you cannot tell if someone is infected; young people assess partners’ STI risk according to how well they know them or appearance | Education | Provides education about STIs and health consequences of UPI (5.1) | |
| Condom use is associated with a lack of trust in the relationship | Creates an enabling environment for condom use | Reframes condom use as demonstrating respect (13.2) | |
| Young people report negative attitudes towards condoms (reduced sensation, reduced pleasure, discomfort) | Creates an enabling environment for condom use | Emphases positive aspects of condom use and provides instruction about how to reduce the negative effects of condom use (4.1) | |
| Carrying condoms can affect a woman’s sexual reputation | Creates an enabling environment for condom use | Models women carrying condoms (6.1) | |
| STI testing | Capability | ||
| Lack of confidence in using services for testing | Creates an enabling environment for testing | Encourages testing and provides non-judgemental information about STIs | |
| Opportunity | |||
| STIs are associated with stigma and being ‘unclean’ | Creates an enabling environment for testing | Provides non-judgemental, non-stigmatising information about STIs | |
| Motivation | |||
| Lack of knowledge of how to prevent STIs by getting tested (lack of knowledge that STIs are common and that you may not know if you have one) | Education | Provides information about the health consequences of getting tested before UPI with a new partner (5.1) | |
| Evokes anticipated regret if not tested prior to UPI with a new partner (5.5) | |||
| Provides non-specific incentives (10.6) | |||
| Provides social rewards for testing (10.4) | |||
| Young people assess new partners’ STI risk according to how well they know them or appearance | Health consequences of getting tested before UPI with a new partner (5.1) | ||
Content derived from behaviour change techniques in effective face-to-face interventions promoting safer sexual behaviours
The BCTs identified in face-to-face interventions reporting statistically significant reductions in STI infection at follow-up are reported in Table 2. 27 The agreement in coding the BCTs in trials of all behaviour change interventions reporting STI outcomes was 100% except for goal-setting (kappa 0.74, agreement 90%), demonstrating condom communication (kappa 0.74, agreement 90%) and encouraging practice of condom communication (kappa 0.74, agreement 90%). In our intervention we included 21of the 25 BCTs found in effective face-to-face interventions when coded according to Abraham and Michie’s taxonomy of BCTs. 14
| Component | No. of effective face-to-face interventions with the component | Implication for intervention delivered by text message |
|---|---|---|
| You cannot assess risk according to how well you know someone socially or by their appearance | 3 | Included |
| Gender roles | 1 | Removed based on focus group feedback |
| Sexual pleasure | 1 | Removed based on focus group feedback |
| Relationships | 1 | Removed based on focus group feedback |
| Information on consequences of behaviour in general | 3 | Included |
| Information on personal risk | 4 | Included |
| Others’ approval | 2 | Included |
| Normative information about others’ behaviour | 2 | Included |
| Goal-setting – behaviour | 2 | We included action planning as this incorporates goal-setting |
| Goal-setting – outcome | 2 | We included action planning as this incorporates goal-setting |
| Action planning – barriers to reduce risk | 1 | Included but modified based on focus group feedback |
| Barrier identification/problem solving – strategies to reduce risk | 3 | Included |
| Set graded tasks | 0 | Not included |
| Prompt review of behavioural goals | 2 | Not included because of participant views that this was ‘too intrusive’ |
| Prompt review of outcome goals | 1 | Not included (as above) |
| Rewards contingent on progress towards goals | 1 | Automated interactive elements of intervention were not able to provide this |
| Rewards contingent on successful behaviour | 1 | Included in relation to getting tested |
| Shaping – providing rewards for an approximation to target behaviour | 0 | Not included |
| Prompt generalisation of a target behaviour | 1 | Not included |
| Prompt self-monitoring of behaviour | 0 | Not included |
| Prompt self-monitoring of behavioural outcome | 0 | Not included |
| Prompt focus on past success | 1 | Included |
| Provide feedback on performance | 1 | Included |
| Information on where and when to perform the behaviour | 2 | Included |
| Instruction on how to perform the behaviour | 3 | Included |
| Model/demonstrate condom use | 4 | Included via website link |
| Model/demonstrate communication | 4 | Included |
| Teach to use prompts/cues | 1 | Not included |
| Environmental restructuring | 0 | Included in relation to carrying condoms |
| Agree behavioural contract | 1 | Not included |
| Prompt practice – condom use | 3 | Included |
| Prompt practice – communication | 2 | Included |
| Use of follow-up prompts | 0 | Not included |
| Facilitate social comparison – intervention draws attention to others’ performance | 0 | Included |
| Plan social support/social change | 1 | Included |
| Prompt identification as role model/position advocate | 0 | Not specifically included but participants reported adopting this role (see Chapter 5) |
| Prompt anticipated regret | 0 | Included |
| Fear arousal | 1 | Not included – considered inappropriate by expert group |
| Prompt self-talk | 0 | Not included |
| Prompt use of imagery | 0 | Not included |
| Relapse prevention/coping planning | 2 | Included |
| Stress management | 0 | Not included |
| Emotional control training | 0 | Not included |
| Motivational interviewing | 0 | Not included |
| Time management | 0 | Not included |
| General communication skills training | 1 | Included |
Content derived from expertise
To ensure that the intervention content, tone and style were informed by technical experts and those experienced in communicating with young people regarding safer sexual behaviours, a sexual health counsellor (Melanie Otterwill) generated messages. Experts in sexual and reproductive health service delivery, research and public health (PB, KW, RF, JB, KD, CF) reviewed the messages and were asked to identify additional content that they considered should be included in the intervention.
Content derived from focus group discussions
We convened eight focus groups with 82 participants (nine of whom attended two focus groups). The focus groups included 32 men and 50 women and the median age of participants was 17 years. In total, 39 participants were from London, eight were from Manchester and 35 were from rural Cambridgeshire (Table 3).
| Characteristic | n (%) |
|---|---|
| Age (years) | |
| 16–19 | 45 (55) |
| 20–24 | 15 (18) |
| No data | 22 (27) |
| Sex | |
| Female | 50 (61) |
| Male | 32 (39) |
| Sexual orientation | |
| Heterosexual | 30 (37) |
| Bisexual | 3 (4) |
| Gay/lesbian | 1 (1) |
| No data | 48 (59) |
| Ethnicity | |
| White British/white other | 45 (55) |
| Black/black British | 18 (22) |
| Asian British | 1 (1) |
| Mixed | 6 (7) |
| Other | 1 (1) |
| No data | 11 (13) |
| Education/work | |
| School | 2 (2) |
| College/university | 37 (45) |
| Working | 6 (7) |
| Unemployed | 5 (6) |
| Long-term sick | 1 (1) |
| No data | 31 (38) |
Participants’ views regarding the messages informed the tone, style, language, punctuation, frequency and duration of the messages, the content of the messages and the way that BCTs were operationalised. Young people wanted messages in a non-judgemental, credible tone that they ‘could relate to’. The preferred style of messages was those containing practical information about what needs to be done, why and how, for example:
You can make sure you don’t get another infection by (1) getting the person you are having sex with treated, (2) using condoms every time you have sex, (3) you and your partner getting tested before sex without a condom and (4) having another test in 3 months.
They identified messages that were too negative, for example ‘I was shocked when I was told I had it’.
They also wanted to know how to carry out behaviours, for example starting a conversation about having a STI was seen as particularly challenging. Messages needed to avoid ‘patronising’ content or ‘telling people what to do’. They wanted exclamation marks to be avoided, as these were also experienced as patronising, for example ‘Having a test can feel like a big step. You did it!’
In terms of other aspects of language and punctuation, participants wanted messages to be easy to understand. They wanted slang terms to be avoided and some phrases or terms such as ‘your man’ were considered overfamiliar and to be ‘trying too hard’ to identify with youth culture, for example ‘Not sure how to convince your man to wear a condom? Text 3 for some tips’.
Focus group participants identified messages that did not meet these criteria and made suggestions about how they could be altered or improved. An acceptable frequency of messages was up to four a day, with message frequency reducing within the first 2 weeks.
When asked to give feedback regarding the messages, participants reported particularly liking short, positive and non-judgemental messages, for example:
If you make it a habit for you and your partner(s) to get tested before you have sex, you can avoid a lot of hassle and regret later.
They identified messages that were supportive and reassuring, for example:
You made the right decision to get a test. Getting treated quickly means you are less likely to have any problems.
They liked messages describing other people’s experiences of how they told a partner about an infection or how they dealt with other sexual health issues such as condom use problems:
Some people say they didn’t use a condom because their partner didn’t want to use one. If you’d like to hear how other people convinced their partner to use one text 3.
Here is an example of how others told their partner: ‘I said I don’t really want to tell you this but I have to – I found out I have chlamydia. It’s awkward to tell people but it’s not right not to, is it? They may not know. You can’t just let them walk round with an infection’.
‘I just couldn’t tell some partners so the clinic offered to do it for me. They gave me the option of keeping my name out of it’. Text 7 to hear more.
Although the intervention content that we developed based on the content of effective face-to face interventions was mostly appreciated, some content had to be adapted or removed, such as messages in which the content did not resonate with participants’ experience or messages that were ‘unrealistic’, for example:
One possible benefit of knowing that you’re safe is that you might enjoy sex more.
Participants reported that the text message designed to ‘review participants’ behavioural goals’ by asking if participants had told their partner about an infection was ‘too intrusive’. Some messages involving ‘action plans’ that encouraged participants to consider when, where and how they would carry out a behaviour were also considered ‘too intrusive’ and these were mainly reframed as suggestions regarding when, where and how a behaviour could be carried out, for example:
A lot of the time, sex isn’t planned. So it’s best to always have a condom on you. Find a time to put a few in your wallet. You could also keep a supply in places where you have sex (bedroom, partner’s house, car).
Men and women reported that messages covering gender roles, relationships and sexual pleasure were ‘too personal’ and ‘intrusive’ when delivered by text message and so this content was removed from the intervention.
Heterosexual men and women found messages about sexual pleasure without sexual intercourse ‘unrealistic’ and felt that this content reduced the credibility of the intervention, for example:
There are other ways of having safer sex without having intercourse. This might include kissing, fantasising, touching and mutual masturbation.
There were no clear differences in feedback on the content of the messages according to urban or rural residence. Men reported that they were able to negotiate condom use and so this content was included only for women.
Adapting the content based on a survey
In total, 100 participants were recruited and completed the questionnaire, of whom 74 were women and 26 were men (Table 4). The data set was 98% complete, with five instances of missing data.
| Characteristic | n (%) |
|---|---|
| Age (years) | |
| 16–18 | 43 (43) |
| 19–24 | 57 (57) |
| No data | 0 (0) |
| Sex | |
| Female | 74 (74) |
| Male | 26 (26) |
| Sexual orientation | |
| Heterosexual | 92 (92) |
| Bisexual | 5 (5) |
| Gay/lesbian | 0 (0) |
| No data | 3 (3) |
| Ethnicity | |
| White British/white other | 53 (53) |
| Black/black British | 31 (31) |
| Asian British | 1 (1) |
| Mixed | 14 (14) |
| Other | 1 (1) |
| No data | 0 (0) |
| Education/work | |
| School | 6 (6) |
| College/university | 59 (59) |
| Working | 18 (18) |
| Training | 1 (1) |
| Unemployed | 13 (13) |
| No data | 3 (3) |
Of the 19 messages tested in women, there were three that < 40% of women scored as relevant and > 30% of women scored as not relevant (see Appendix 6, Table 12). One of these messages had received mixed feedback in the focus groups and was discarded from the message set. The other two messages were modified based on feedback obtained from the focus groups. For each of the remaining messages, the number of respondents reporting that the message was relevant ranged from 36 out of 74 (49%) to 66 out of 74 (89%), a median of 51 out of 74 respondents (69%).
Of the 17 messages tested in men, there were four messages that < 40% of men scored as relevant (see Appendix 6, Table 12). Two of these had received ambiguous feedback in the focus groups and were discarded. One received positive feedback in the focus group and was considered to be important and so was retained (‘You made the right decision to get a test. Getting treated quickly means you are less likely to have any problems. Text 2 to hear about how others felt when they found out that their test was positive’). One was modified based on further feedback obtained from participants: ‘You might be thinking about how they’ll react when you tell them. It might help by warming up the conversation and easing into it’ was changed to ‘You might be thinking about how they’ll react when you tell them. You could try practising what you’re going to say’. For each of the remaining messages, the number of respondents reporting that the message was relevant ranged from 12 out of 26 (46%) to 24 out of 26 (92%), a median of 18 out of 26 respondents (69%). No messages were considered ‘hard to understand’ or were ‘disliked’.
Testing and adapting the content based on telephone interviews with users after sending the text messaging intervention to users’ mobile phones
The eight participants who took part in the interview study, six women and two men, had a median age of 20 years (average 19 years). Six participants were from south-east London and two were from Cambridgeshire and participants were from a range of ethnic backgrounds (including white British, black British African, black British Afro-Caribbean and mixed ethnicity).
Participants were positive about the intervention content and delivery. In general, participants found the information in the messages useful and relevant to someone who has just received a positive chlamydia test result. They thought that the messages made them more aware of what chlamydia is and how to prevent it.
I think in general it was really good, like it was really helpful, it helps you know everything and gave you all the right information.
ID6
A few participants expressed a strong engagement with the messages, with one reporting that she discussed the information in the messages with friends and another saying that she kept the messages on her mobile phone because she valued the information in them and was planning to share them with her younger cousins:
I think I will keep it on my phone because I think it’s good information. I’ve got like younger cousins and stuff and now I have more information that I can tell them, I think I’m going to use it in that way.
ID5
It’s in my mind now.
ID2
You send me messages, I speak with friends or many people about chlamydia this week because it’s good information.
ID7
One participant commented that she was disappointed when it ended and that she goes through the messages in her room at night when she thinks a lot more:
I go back through my texts, say I was reading them . . . like when I’m in my room at night, I think a lot more, so when I go through my texts, they did kind of make me think a lot more.
ID3
A few comments were less complimentary. One found the message that ‘chlamydia is a common bacterial infection’ a bit ‘scary’ (ID1). An older participant (aged 23 years) said that he thought that some of the messages were a bit ‘silly’ (ID4). One participant indicated that some people might have trouble understanding the messages:
Well, some people are not going to understand because some people, like it’s difficult for them.
ID1
All but one participant reported that they told their partner about their infection. However, the participant who had not yet told her partner expressed an intention to tell him:
It might change his view on me, so it’s kind of scary, but I realise that I do need to do it. It would be better for me and him if I tell him.
ID3
One said that she would have told her partner anyway:
I was planning on telling him but I think it just gave me a push.
ID2
Two participants told their partner about their infection before they started to receive the messages. Four participants attributed telling their partner about their infection directly to the messages:
I forgot, innit, because I don’t want . . . like if I have sex with a girl that I don’t know, yeah, it’s just like maybe that just that one night, yeah, it’s over, I don’t want to know you again, like so . . . well, obviously I’ve got on my BlackBerry thing, so I pinged that, I was like ‘uh, you need to go check out yourself in the clinic, innit’. I didn’t tell her what I got.
Do you think if you didn’t get the text messages that you would have told her?
Well, I wouldn’t because the day I came here, you just gave me the pill then, I forgot about everything.
Another said that he ended up telling his partner about his infection because the texts were making him feel guilty for not doing so:
And how did you tell them?
I said um [laughs] I kind of ripped it off, you know like a plaster, like I just ripped it off, just ripped the plaster off. It just made me feel guilty, made me feel guilty for not telling so I had to tell someone.
One participant said that she did not know that chlamydia could be treated. She said that the clinic told her that it is treatable but she only realised that the infection was not too serious after receiving the messages:
I thought that Chlamydia was like, once you get it, you don’t get rid of it.
But, even though they told you that, what was the difference of receiving the text?
Because it was more than one person telling me, I felt, ‘OK, well, maybe it’s not that bad’ because I was a bit down and, yeah.
She said that she used a condom during the week after she was treated because the clinic had given her condoms and the messages reinforced the advice not to have unprotected sex during this time:
It was because of everything, really, like the texts and what the clinic told me. But, I guess, if the clinic didn’t give me condoms and you just texted me, then I probably wouldn’t have, but because they gave me condoms and they told me, and the text told me, it was like, it made things more serious and I realised like I don’t want to infect anybody I know.
ID3
Most thought that the tone of the messages was appropriate, although one participant thought that the messages sounded too automated and could have sounded more ‘humany’ (ID3).
Some participants gave feedback about the length of the messages and the timing and frequency of message delivery. Five recipients were happy with the frequency and one wanted more messages. Two recipients reported that there were too many messages, one of whom said that he was enjoying the messages at first but that it became too much after five or six messages and he wanted them to stop.
At what point did you want it to stop, like how far into it?
Like when obviously like five or six messages, I was like ‘oh, that’s too much now’ but it’s like the same thing, they’re saying the same thing but different words over and over again, so that’s kind of annoying.
Most thought that the length of the messages was about right:
I think they are not too long and they usually have the most important thing in the first sentence so they don’t try to say more, they just said what is important and I think that is great.
ID8
Most participants were unconcerned about keeping the messages confidential. Those who were concerned reported being confident about knowing how to protect their mobile phone and prevent others reading messages.
Participants reported that they especially liked the messages giving examples of how others had told their partner about having an infection. Based on this feedback we included the content about how others had told a partner about their infection in the core message set, rather than as part of the optional messages. An older male participant pointed out that the message ‘That’s great if you’ve told your partner . . .’ would make someone who has not told their partner feel bad. As a result we removed this message. No new issues were emerging in interviews and so no further participants were enrolled. We also ensured that information was included in the intervention that simply replying ‘stop’ to any messages would result in no further messages being sent.
Final intervention content
Intervention content for the pilot trial
The final message set was tailored according to sex and infection status at enrolment [no infection, chlamydia, gonorrhoea or non-specific urethritis (NSU)]. The message sets for those diagnosed with a STI were similar to each other except that the information provided was specific to the STI diagnosed. The number of messages targeting each behaviour and the number of messages employing specific intervention functions and BCTs are described (see Table 6).
For those diagnosed with a STI, messages over the first 3 days focused on engaging with the study, getting treatment, taking treatment and providing information about the infection. Over the next week messages targeted telling partner(s) about an infection. The messages provided non-judgemental, non-stigmatising information covering how common infections are; that an individual may not have symptoms and so may be unaware that they have a STI; that many people diagnosed with a STI have had only one sexual partner in the previous year; and that infections are easy to treat. Messages provided information about how to prevent infections. They provided suggestions about when, where and how to tell a partner about an infection and examples of how others told their partners, covering a range of different types of relationship (e.g. casual, long term). The messages then provided links to services that could inform partners and links to support for anyone concerned about violence in their relationship after telling a partner about an infection. Messages also aimed to provide social support, acknowledging people’s experiences.
For those diagnosed with an infection, after day 14 the messages targeted condom use and testing for STIs before having unprotected sex with a new partner. Participants who had not been diagnosed with an infection were sent the messages about safer sex behaviours (condom use and testing for STIs) starting on day 1. Over the following 30 days messages were sent providing information on how to prevent infections and how you cannot assess risk according to how well you know someone or by their appearance. Messages included instructions on how to use condoms, emphasised positive aspects of condom use and provided tips on preventing condom problems and examples of how others resolved condom use problems. Participants were prompted to think about risks that they had taken and what they could do differently in the future and also to consider how they had carried out safer sex behaviours in the past. Text messages included advice about getting tested before unprotected sex with a new partner. Participants were sent links to further web-based information about contraception, alcohol and sexual risk, how to use a condom and general communication about sex. Women were sent messages covering how other women had negotiated condom use. The messages were designed to provide social support for safer sex behaviours.
Control
The set of control messages consisted of 13 messages in total, which were spaced 30 days apart starting from the point of randomisation (see Table 6). The control messages contained no BCTs or information regarding sexual health. The messages were intended to help keep participants engaged in the study and to remind them of their participation, for example ‘Young people can experience health inequalities. Taking part in the texting study can help things to be equal. Thanks for taking part’. The messages expressed our appreciation of participants’ involvement in the study and suggested that participation in research can be personally beneficial: ‘Taking part in the texting study is a way to help you be actively involved in things that affect your life. Thank you for taking part’.
The information technology system delivering the messages
The IT system developed for message delivery was designed to be automated and to deliver different content according to allocation (intervention or control) and, for those receiving the intervention, according to participant characteristics (STI status and sex). Interactive messages could be sent in response to key words sent to the system from participants’ mobile phones requesting more content on specific topics. The system is held on a secure server with secure access. The system was fully tested with ‘dummy’ participants and the research team members’ mobile phones to check that the correct set of messages was delivered according to participant characteristics (STI status and sex) and the prescheduled time frame and to test that interactive content sent in response to key words was sent in accordance with the intervention protocol.
Discussion
Key findings
We have described the development of a theoretically informed intervention designed to address barriers to safer sex behaviours and increase safer sex behaviours in those aged 16–24 years diagnosed with a STI or reporting unprotected sex with more than one partner in the last year. We have described how the intervention content was derived from theory, evidence-based BCTs identified in effective face-to-face safer sex interventions, evidence regarding barriers to safer sex and expert and user views. Focus group discussions, a survey and telephone interviews with users informed and refined the intervention to ensure that it was acceptable to young people. In the survey participants reported that all of the messages were easy to understand and none was disliked.
Strengths and weakness of the intervention development work
Our work on intervention development has some weaknesses: although the intervention content associated with increased self-reported condom use is known,28 it remains unclear which BCTs are associated with increased effectiveness at reducing the incidence of STIs. We therefore included all of the BCTs in face-to-face interventions evaluated by randomised controlled trial and reporting reductions in the incidence of STIs at follow-up. To develop an intervention that was acceptable we excluded content that participants found to be unacceptable or irrelevant. Some evidence-based BCTs were modified based on feedback from young people and the effectiveness of the ‘acceptable’ but modified content is not yet known. Although the current intervention is tailored by infection status and sex, it is not tailored according to specific personal issues with regard to adopting safer sex behaviours. Thus, messages sent may not all be directly relevant to every participant. During the conduct of our work a new internationally agreed taxonomy of BCTs was published. 14,22 We included BCTs defined according to an older taxonomy in our intervention, but coded the final intervention using the new internationally agreed taxonomy. The intervention requires further adaptation to ensure that the content is appropriate for men who have sex with men and women who have sex with women.
Discussion in relation to existing research
In keeping with current guidance29 we used theory, evidence and testing to develop our complex intervention. The approach that we used to develop our behaviour change intervention based on theory, evidence regarding barriers to behaviours, evidence regarding the content of effective interventions and user views is not new. 30 There is no evidence that the content of interventions delivered by text message targeting safer sex has previously been based on a process designed to identify and then target documented barriers to safer sex behaviours. No previous intervention delivered by mobile phone informed by the COM-B comprehensive model of behaviour change has been reported. The recent development of validated taxonomies of BCTs allowed us to code the content of face-to-face interventions using a valid and reproducible methodology. There are no reports of previous interventions being developed based on empirical evidence regarding the content and BCTs employed in effective face-to-face interventions targeting safer sex behaviours. Our intervention includes content addressing attitudes, information and behavioural skills, which are found in the most effective interventions promoting condom use. 28 Our intervention includes a larger number of BCTs than previous interventions. No previous trials of interventions delivered by mobile phone have targeted the correct treatment of existing STIs, including providing support for telling partners about a STI. We ensured that the content of the text messages is consistent with the British Association for Sexual Health and HIV current safer sex advice,31 which recommends focusing on increasing motivation, skill acquisition (including communication skills) and provision of information about safer sexual practices.
Implications for the research project
The intervention was used in the pilot trial (see Chapter 4).
Chapter 3 Development of the trial materials and procedures
The importance of maximising follow-up responses
Any loss to follow-up (> 0%) in randomised controlled trials can represent an important threat to the validity of the trial results as participants lost are likely to be different from participants retained. The potential for bias is increased when the loss to follow-up is different in the intervention and control groups (differential loss to follow-up) because this further reduces the comparability of the results. 32 Although there are no universally agreed criteria with which to categorise the risk of such bias, some researchers have suggested that ≤ 5% loss to follow-up introduces minimal bias and ≥ 20% introduces significant bias. 33
Despite the importance of minimising loss to follow-up, many trials fall short of achieving their targets. A review of participant recruitment and retention in six high-quality journals found that 48% of trials reporting a sample size calculation did not meet their target at outcome assessment and analysis. 34 The authors suggest that their review may even overestimate the degree of retention because such journals are less likely to publish trials with poor retention.
Achieving high follow-up rates for collecting sensitive data such as sexual health data is particularly challenging. In sexual health research, response rates for self-reported data and STI testing kits have been relatively low in both RCTs and surveys. The National Survey of Sexual Attitudes and Lifestyles (Natsal) study in the UK achieved a 57.7% response rate for face-to-face interviews and a 60% response rate for urine samples requested. 35 A UK cross-sectional population-based study reported an uptake of chlamydia postal screening of 31.5% in young people aged 16–24 years [the Chlamydia Screening Studies (ClaSS) project]. 36 A pilot trial of a sexual health website intervention for young people (Sexunzipped) achieved a 45% follow-up rate using chlamydia postal test kits and a 72% for self-reported data at 3 months. 37
A key criterion for progressing to a main trial in our HTA programme-commissioned research was demonstrating the feasibility of a main trial. We aimed to demonstrate in the pilot trial that a response rate of ≥ 80% at 12 months for chlamydia sample test kits was achievable. To achieve this we developed and tested all of our follow-up procedures prior to the pilot trial.
Objective
To develop follow-up procedures and materials to use in the trial to achieve > 80% follow-up.
Methods
Our approach for developing follow-up procedures consisted of three main steps.
Step 1: identifying evidence-based effective strategies to increase follow-up in trials
We searched for existing systematic reviews of trials of interventions designed to increase follow-up in research and contacted Public Health England’s Chlamydia Screening Programme team to identify any unpublished trials of interventions designed to increase response rates to postal STI test kits. We identified methods in systematic reviews for which there was there was good evidence (p ≤ 0.05) of success in increasing response to postal follow-up requests in trials. We developed prototype follow-up procedures incorporating the effective strategies identified (Table 5).
| Steps | Key findings | Implications for follow-up design |
|---|---|---|
| 1. Identify effective strategies to increase follow-up38–44 | Providing monetary incentives: OR 1.99 (95% CI 1.81 to 2.18);38 RR 1.18 (95% CI 1.09 to 1.28);39 RR 1.12 (95% CI 1.04 to 1.22) (£10 vs. £20);39 OR 2.02 (95% CI 1.79 to 2.27)44 | We included £5 cash with the initial postal request for the questionnaires and samples. We sent £20 cash to each participant on receipt of the sample |
| Sending post by recorded delivery: OR 2.04 (95% CI 1.60 to 2.61);38 RR 2.08 (95% CI 1.11 to 3.87);39 OR 2.21 (95% CI 1.51 to 3.25)44 | We did not send study materials by recorded delivery as this may have compromised confidentiality. However, we sent all materials using first class postage and included a first class stamp on the self-addressed return envelope | |
| Adding a ‘teaser’ comment on the envelope: OR 3.08 (95% CI 1.27 to 7.44)38 | We did not add a teaser comment on the envelope as this may have compromised confidentiality | |
| Pre-notifying participants to expect the questionnaire or postal test kit: OR 1.50 (95% CI 1.29 to 1.74);38 OR 1.54 (95% CI 1.24 to 1.92)44 | We notified participants before we sent the initial questionnaires and postal test kits | |
| Personalised letters: OR 1.16 (95% CI 1.06 to 1.28)44 | We addressed participants by their first name in letters, e-mails and text messages | |
| Coloured ink: OR 1.39 (95% CI 1.16 to 1.67)38,44 | Questionnaires were printed on white paper, had a light blue colour scheme and used black ink | |
| Following up with participants after the initial request: OR 1.44 (95% CI 1.25 to 1.65);38 RR 1.43 (95% CI 1.22 to 1.67);39 OR 3.71 (95% CI 2.30 to 5.97)41 | We contacted questionnaire non-responders and test kit non-responders | |
| Using a short questionnaire: OR 1.86 (95% CI 1.55 to 2.24);44 OR 1.73 (95% CI 1.47 to 2.03);38 OR 1.35 (95% CI 1.19 to 1.54)41 | We designed the questionnaire to be as short as possible by collecting only essential data | |
| Providing unconditional incentives: OR 1.61 (95% CI 1.27 to 2.04);38 OR 1.71 (95% CI 1.29 to 2.26)44 | We included £5 cash with the initial postal request for the questionnaires and samples | |
| Providing a second questionnaire and test kit: OR 1.51 (95% CI 1.13 to 2.00);38 OR 1.41 (95% CI 1.02 to 1.94)44 | We posted the questionnaire four times and sent the website questionnaire link twice. We sent the test kit four times and continued to send one each month to non-responders | |
| Mentioning an obligation to respond: OR 1.61 (95% CI 1.16 to 2.22)38 | We considered mentioning an obligation to respond in the letters but decided against it because our sexual health expert group thought that the target group may respond negatively | |
| Stamped return envelopes: OR 1.29 (95% CI 1.18 to 1.42);38 OR 1.26 (95% CI 1.13 to 1.41)44 | We sent self-addressed, stamped return envelopes for participants to return the questionnaire. Postal test kits included a prepaid box | |
| Assurance of confidentiality: OR 1.33 (95% CI 1.24 to 1.42)38 | We included the study identification number only on the questionnaire and included a statement about confidentiality on both the questionnaire and in the letter | |
| First class outward mailing: OR 1.12 (95% CI 1.02 to 1.23)44 | We sent all materials using first class postage | |
| Beginning questionnaires with general questions: OR 0.80 (95% CI 0.67 to 0.96)38 | We listed the key questions about treatment and sexual behaviour first | |
| Offering the opportunity to opt out: OR 0.76 (95% CI 0.65 to 0.89)38 | We did not include a statement about opting out in the letter | |
| Mentioning university sponsorship: OR 1.32 (95% CI 1.13 to 1.54);38 OR 1.31 (95% CI 1.11 to 1.54)44 | We included OM’s University of London address on all letters | |
| 2. Identify barriers to follow-up completion by testing the process | Test kits | |
| Some test kits do not fit through letter boxes | We selected a test kit that could fit through the smallest letter box | |
| The test kit included potentially distracting and non-essential components | We removed the following components from the test kit: the pen, condom, business promotional card, chlamydia information leaflet, urine sample tube (for women) and personal details form | |
| Most people could not open or broke the urine collection pouch that was included in the test kit | We removed the urine pouch and tested alternatives such as a urine collection cone and collecting urine directly in the sample tube | |
| The test kit included an instruction slip that was divided into two columns, one blue for the male urine sample and one pink for the female swab, and included non-essential graphics and information | We simplified and shortened the instruction slip. The revised slip was separated into two, one for the urine sample and one for the swab. The slips were plain white and included only the basic steps: three steps for the urine sample and four for the swab | |
| The test kit required the person to apply a laboratory tracking label | We applied the laboratory tracking label before we sent the test kits | |
| The test kit required the person to tick whether they were providing a urine or swab sample | We ticked a urine sample for men and a swab for women before we sent the test kits | |
| The pouch for urine collection included in the test kit was unnecessary | We did not include a pouch or any other container for urine collection | |
| Providing only a swab rather than a choice between a swab and a urine sample was acceptable for women | We included only a swab in the test kit for women | |
| Questionnaire and letters: | ||
| It is unappealing to list the less relevant questions first | We listed the key questions about treatment and sexual behaviour first | |
| A long questionnaire is unappealing | We included necessary questions only | |
| Including personal identifiable information on the postal questionnaire could cause confidentiality concerns | We included the study identification number only on the questionnaire and included a statement about confidentiality on both the questionnaire and in the letter | |
| Letters should include a statement about the importance of participating | We included a statement about how participants are helping to improve the health of young people | |
| The questionnaire should be short | We included necessary questions only | |
| 3. Consult with the target group | Young people wanted to be contacted before we sent the kits and questionnaire so that they knew to expect it | We contacted participants before we sent them any study materials |
| The envelopes should be identifiable to participants but not to anyone else | We sent all study materials in blue envelopes. We alerted participants to this when we contacted them before sending the materials | |
| Sending materials by recorded delivery could compromise confidentiality | We sent self-addressed, stamped return envelopes for participants to return the questionnaire | |
| Providing only a swab rather than a choice between a swab and a urine sample was acceptable for women | We included only a swab in the test kit for women | |
| The simplified and shortened instruction slip that we wrote was clear and acceptable | We included the simplified and shortened instruction slip rather than the pink and blue graphical instruction slip | |
Step 2: testing prototype follow-up procedures and materials
Sample postal testing kits routinely used in Cambridgeshire, Manchester and south-east London (our trial recruitment sites) and STI test kits used in NHS chlamydia postal testing services were obtained by OM. Successful receipt of the postal STI testing kit depended on the kit fitting through participants’ letterboxes. OM measured a range of London letterboxes on central London streets and measured the test kits to identify those that would fit through the smallest letterboxes measured. OM and CF attempted to complete all prototype follow-up procedures to identify barriers to follow-up completion and refine procedures to make follow-up as easy as possible.
Two researchers (OM and CF) attempted to follow the instructions for providing urine and swab samples that were included in postal STI testing kits that fit through the smallest letterboxes and completed the forms. Based on this experience, we generated ideas on how to make the follow-up processes easier. OM generated prototype test kits including combinations of the original materials and the newly generated materials (a choice of a vaginal swab or urine collection tube for women, a urine collection tube only for women and men and a swab only for women; a cone or pouch urine collection tube; a blue or brown envelope). OM provided volunteers from the London School of Hygiene & Tropical Medicine’s (LSHTM) Clinical Trials Unit (CTU) with test kits and asked them to provide samples (which were disposed of) and feedback regarding their experience of completing the test. We consulted with experts in sexual health regarding the questionnaire design and follow-up procedures.
Step 3: consulting with users
See Chapter 2 for focus group methods.
We held one participant representative group to obtain the views of participants regarding the trial questionnaires and follow-up procedures and also asked participants for their views regarding trial follow-up procedures during focus group discussions convened to inform the development of the intervention. People aged 16–24 years who owned a mobile phone were eligible to take part. We asked for participants’ views on the pilot trial questionnaires, level of incentive offered and the acceptability of postal follow-up and materials (e.g. chlamydia test kit, envelopes).
Follow-up interviews
As part of the main trial we conducted interviews with participants seeking their views on the acceptability of the intervention. 45 We conducted follow-up interviews with these participants after sending the 3-month postal STI testing kits. The interviews followed a semistructured topic guide, which explored participants’ views on the trial materials and follow-up procedures.
Results
Effective strategies to increase postal follow-up
The follow-up strategies for which there is good evidence of increasing the odds of response according to systematic review and trial evidence38–44 are reported in Table 5. We employed all except four of the strategies. We did not send post by recorded delivery as users reported that recorded delivery would be unacceptable to them as they were concerned that it would draw parents’ attention to the package. 38,39,44 For the same reason we did not add a ‘teaser’ on the envelope (mentioning that there may be a benefit to opening). 38 We did not include a statement about an obligation to respond to the request because our sexual health expert group thought that our particular target group might respond negatively to this. 38
Testing the prototype follow-up procedures
The smallest London letterbox that OM measured was approximately 19 cm × 2.5 cm. The most appropriately sized postal testing kit that we found was provided by a laboratory diagnostic company and contained prepackaged components. The test kit included nine items: a urine sample tube and urine collection pouch (males and females), a vaginal swab tube (females only), a laboratory request form, a sample instruction leaflet, a chlamydia information leaflet, a business promotional card, a condom and a pen.
It was found by OM and CF that the components in the postal testing kit included many non-essential items. When CF opened the box all of the items fell out. Based on this experience we removed all but the essential content. CF broke the urine collection pouch when she attempted to open it and OM was unable to open it. Volunteer staff in the CTU (n = 12) were asked to provide a urine sample in the pouch. Only one person successfully used the pouch. The others broke it when they opened it, could not open it or did not know what it was for so did not use it. As an alternative four people were provided with a urine collection cone. No one reported difficulties in using the cone to collect urine or urinating directly into the urine sample bottle (men only).
The two sets of instructions were found to be overly complicated by OM and CF. The instructions for women could be confusing because they received a postal testing kit with both the swab and the urine tube but were required to provide only one sample. We provided the CTU volunteers with the original instructions or simplified instructions and found that they preferred the shorter instructions. Female CTU staff volunteers did not express a preference for providing a urine sample or a vaginal swab. CTU staff suggested that we include a statement in the postal letter to participants about the importance of their participation so that they would feel ‘proud’ about doing something good.
Experts in sexual health questionnaire design suggested that we list the key questions – those on treatment and sexual health behaviour – first.
User views
The focus group participant demographics are provided in Table 3. Participants wanted the questionnaires to be as short as possible. They had no objections to the prototype questionnaire design or content. They reported that the envelope used to send postal follow-up materials should be identifiable only to them. They suggested using a coloured envelope so that they would know what it was without others knowing. They reported that the short version of the sample STI test kit instructions was clear and acceptable. Participants asked to receive a text or phone call before we sent the questionnaire and STI test kit so that they would know to look out for them. They were concerned that sending follow-up materials by recorded delivery could call attention to the post and possibly compromise the confidentiality of their participation in the study. Some were concerned about parents asking questions about the content of a recorded delivery parcel. Women thought that it was acceptable to include a vaginal swab only in the kit rather than providing a choice between a swab or a urine sample, partly because it was what they were used to doing at the clinic.
Final follow-up procedures
The results of steps 1–3 informed the final follow-up procedures.
Materials
Questionnaires
Our follow-up questionnaire was two pages long. Research evidence38,40–42,44 and feedback from the target group suggested that the questionnaire should be as short as possible. We used a light blue colour scheme. 44 In accordance with guidance from our consultation with experts in sexual health questionnaire design and evidence from Edwards et al. 38 that the response rate is lowered when questionnaires begin with general questions, we ordered the key questions on treatment and sexual behaviour first. We did not include any participant-identifiable information on the questionnaire and included a statement about confidentiality. 38 We offered an online questionnaire as an alternative to postal completion. Participants had the opportunity to reply to key questions by text and e-mail.
Postal testing kit
We selected a postal testing kit that could fit through the smallest letterbox that we measured. Based on the findings of OM, CF and the volunteer testing of the kits, the kits contained only essential components (we removed the urine collection pouch, chlamydia information leaflet, business promotional card, condom and pen). We included only a swab for women and used the short, basic instruction slips. We used a pared-down laboratory slip that did not ask participants for personal details and included only the laboratory number and date that the sample was collected. We also filled out the laboratory form (ticked whether it was a urine or a swab sample) so that the participants would not be required to do it themselves. Participants had the option of providing their test sample at the clinic.
Letters
We kept the letters as short as possible. 38,40–42,44 The template was formal but the tone was casual, for example we addressed participants by their first name and used ‘Hi [name]’ instead of ‘Dear [name]’. 44 The letters included a statement saying that by completing the questionnaire and providing a sample participants were helping to improve the health of young people (a suggestion from our consultation with the CTU); a NHS/NIHR logo; and the trial co-ordinator’s University of London address. 38 All of the letters were from and hand signed by the trial co-ordinator.
Envelopes and postage
We sent all correspondence in blue envelopes, handwrote the addresses and used first class outward and incoming postage. 38,44 We did not send the post by recorded delivery or add a ‘teaser’ on the envelope (mentioning that there may be a benefit to opening) because of its potential to call attention to participants’ participation in the study, which could compromise confidentiality. 38
Mailings and incentives
We notified all participants by phone, e-mail or text before the initial mailing of both the questionnaire and the postal testing kit. 38,44 All initial mailings of the questionnaire and postal testing kit included a £5 unconditional cash incentive (subsequent mailings to non-responders did not). 38,40,43 Additionally, we sent £20 cash to all participants who returned the chlamydia test sample. 38,39,43,44 After the initial follow-up request, we contacted non-responders by phone, text message and e-mail, unless they opted out of further follow-up at any stage. 38,39,41,44
Month 1 questionnaire
The initial questionnaire posting included a £5 unconditional cash incentive. 38,40,43 We sent an e-mail message that included a link to the online questionnaire within a week of the initial questionnaire posting. 38,39,41,44 We posted the questionnaire again around 2–3 weeks later and sent a second e-mail within a week of this. 38,44 The third paper mailing included a statement in the letter saying that we would send £10 if we received the questionnaire within 2 weeks. 38,39,43,44 The fourth paper mailing included a statement in the letter that we would enter participants into a £50 prize draw if they returned the questionnaire within 2 weeks. 38,39,43,44 Finally, we e-mailed, texted and posted one or two key outcome questions to non-responders (according to their chlamydia status at enrolment). 38,39,41,44
Month 3 chlamydia test
The initial postal testing kit included a £5 unconditional cash incentive. 38,40,43 All letters mentioned that participants would receive £20 if they returned the sample. 38,39,43,44 We sent the testing kit to non-responders a further three times. 38,44 The fourth mailing included a statement in the letter saying that participants would be entered into a prize draw for £50 if we received the questionnaire within 2 weeks. 38,39,43,44 After each mailing we followed up with participants by telephone and e-mail. 38,39,41 We sent the testing kit to non-responders once a month. 38,44
Month 12 questionnaire and chlamydia test
We sent the initial 12-month questionnaire and testing kit together with £10 unconditional cash incentives. 38,40,43 All letters mentioned that participants would receive £20 if they returned the sample. 38,39,43,44 The initial letter included a statement saying that we would enter participants into a £50 prize draw if they returned both the questionnaire and the test. 38,39,43,44 We telephoned and sent an e-mail message that included a link to the online questionnaire around 3 weeks after the initial mailing. 38,39,41,44 We sent the questionnaire and testing kit to non-responders a further three times. 38,39,41,44 At each mailing we followed up with participants by phone and e-mail. 38,39,41 We sent the testing kit to non-responders once a month. 38,39,41 We e-mailed, texted and posted one or two key outcome questions to questionnaire non-responders (according to their chlamydia status at enrolment). 38,39,41,44
User views of the final follow-up procedures
We interviewed 17 of the original 20 main trial interview participants (we were unable to reach three) (R French, 2015, manuscript in review). None of the participants had any significant criticisms of the materials or the procedures and they found them acceptable. They thought that the pre-notification served as a reminder to look in the post. Similarly, participants mentioned that the blue envelopes helped them to recognise the study materials. One participant said that the letters were polite in that we were not telling participants that they had to send the questionnaires and samples back and another appreciated that the letters were short and to the point. Most participants thought that the instructions were clear and easy to follow and most did not have any problems with or criticisms of the postal testing kit. One participant said that initially he was not clear whether or not he should post the box on its own. Another participant said that it would have been easier if we had provided a pouch to collect the urine to pour it into the tube. One participant said that she initially had difficulty opening the swab but worked out how to do it. Another participant suggested that we include a condom in the kit.
Most participants said that they would have returned the questionnaire and chlamydia sample if they were not offered an incentive, with some indicating that the motivating factor was their health not the money. A few participants mentioned that the unconditional £5 motivated them to return the questionnaire and sample and another wanted to return them because we ‘treated’ him and said he would have procrastinated without it. Women preferred the swab sample collection method and none of the participants mentioned that they would rather have had a choice (swab or urine sample).
Discussion of the development of our follow-up procedures
Key findings
We have described the stepwise approach that we used to develop our follow-up procedures for this trial.
The approach involved using evidence-based methods to increase follow-up, testing prototype procedures and obtaining potential participant views on the procedures.
Strengths and limitations
To the best of our knowledge this is the first description of a systematic approach to developing follow-up procedures. The approach has resulted in a follow-up package. In the single case study of our pilot trial it will not be possible to determine the effectiveness of the ‘follow-up package’ in isolation from other factors such as the management style and experience of the CTU and researchers conducting the pilot trial. It is not possible to determine which elements of the follow-up package are most important.
Discussion in relation to the existing literature
The approach mirrors methods used to develop behaviour change interventions, for example consulting with the user group, identifying barriers to performing behaviours and choosing techniques to enable the behaviours. 30,46 We used a similar approach to the approach used to develop follow-up procedures in the txt2stop pilot and main trial. The pilot trial achieved a 96% response rate for self-reported data collected by mobile phone or e-mail at 1 month and a 92% response rate at 6 months. 13 The main trial achieved a 95% (5524/5800) response rate for self-reported data collected by post, mobile phone or study website at 6 months and an 81% (542/666) response rate for postal salivary cotinine tests at 6 months. 10 An earlier trial achieved only a 74% response rate for self-reported data collected using voice and text messaging at 6 months and experienced differential follow-up between the intervention group and the control group (69% in the intervention group and 79% in the control group). 47
Implications for this research project
The follow-up procedures that we developed were used in the pilot trial (see Chapter 4).
Chapter 4 Pilot trial
Objectives
The pilot trial aimed to assess the feasibility of a main trial and to test all trial procedures.
The objectives were to:
-
recruit 200 participants within 3 months
-
successfully deliver ≥ 93% of messages from the aggregator to participants’ mobile phones (data provided by the aggregator)
-
complete follow-up of ≥ 80% for the proposed primary outcome for the main trial (the cumulative incidence of chlamydia).
Methods
Description of trial design
This was a pilot, parallel-arm randomised controlled trial with an allocation ratio of 1 : 1, conducted in multi-geographical areas of the UK.
Important changes to methods after trial commencement
There were no changes to the methods after the trial commenced.
Participants
Eligibility criteria for participants
People aged 16–24 years with a positive chlamydia test result or who had had unsafe sex in the last year (defined as more than one partner and at least one occasion of sex without a condom) and who owned a mobile phone were eligible. People who satisfied these requirements were ineligible if they were non-English-language speakers or were unable to provide informed consent (e.g. people with severe learning difficulties).
Settings and locations where the data were collected
This trial identified potential participants through sexual health services in six geographical locations in the UK: London, Cambridgeshire (rural and urban), Manchester, East Anglia, Kent and Hull. Research staff recruited participants on site at the London and Manchester services. Staff at the Cambridgeshire, East Anglia, Kent and Hull services identified eligible potential participants and referred them to the trial centre (LSHTM) for recruitment.
Intervention
Intervention delivery and timing
The bespoke texting software delivered the intervention messages automatically, directly to the mobile phone number given by each participant at enrolment. The messages were tailored according to sex and infection status at enrolment. Additional tailoring enabled participants to choose a daily time period when they did not want the messages delivered (‘embargoed time’). We collected embargoed time preference data at enrolment, which were automatically fed into the texting software during baseline data entry (see Data collection and entry). The automatic embargoed time was from 2300 to 0900. Each day, the system delivered the messages from the start of the non-embargoed period, every 4 hours. For shorter non-embargoed periods, the system delivered the messages in proportionally shorter intervals. The computer automated mode of delivery ensured standardisation of the intervention.
Message frequency and spacing
For men and women testing positive for chlamydia the intervention included four messages per day for the first 3 days, reducing to one to two messages per day for the first 2 weeks. The number of messages was then reduced to one per day for the first month followed by between one and nine per month until 12 months. For men and women who tested negative for chlamydia the intervention included one to two messages per day for 1 month and then one to three messages per week for up to 12 months.
Intervention for chlamydia-, non-specific-urethritis- and gonorrhoea-positive participants
The intervention for female participants who received a chlamydia-, NSU- and gonorrhoea-positive result at the time of enrolment (‘positive participants’) consisted of 63 text messages sent over 1 year, starting from the point of randomisation. The intervention for positive male participants consisted of 61 text messages sent over 1 year, starting from the point of randomisation.
The message set was tailored according to sex and infection status at enrolment (no infection, chlamydia, gonorrhoea or NSU). The message sets for those diagnosed with a STI were similar to each other, except that the information provided was specific to the STI diagnosed. The numbers of messages targeting each behaviour and the numbers of messages employing specific intervention functions and BCTs are described in Table 6.
| Number of messages | ||||
|---|---|---|---|---|
| Tested positive for chlamydia, gonorrhoea (or men diagnosed with NSU) | Without a STI, but reporting unprotected sex with more than one partner in the last year | |||
| Women | Men | Women | Men | |
| Target behaviour | ||||
| Engagement with the trial | 3 | 2 | 3 | 2 |
| Getting treated | 1 | 2 | 0 | 0 |
| Telling partner about an infection | 7 | 8 | 0 | 0 |
| Linking with services (partner notification, concerns about violence and pregnancy) | 3 | 2 | 1 | 1 |
| Engage with intervention | 3 | 6 | 1 | 3 |
| Condom use | 25 | 23 | 24 | 22 |
| Contraception | 3 | 2 | 3 | 2 |
| Testing for STI | 7 | 7 | 5 | 6 |
| Communication about sex | 2 | 2 | 2 | 2 |
| Intervention function according to the COM-B theory | ||||
| Education | 16 | 17 | 10 | 11 |
| Enablement | 33 | 28 | 25 | 19 |
| Incentivisation | 4 | 5 | 4 | 5 |
| Behaviour change technique22 | ||||
| 1.2 Problem-solving | 7 (+1 optional message) | 6 (+1 optional message) | 6 (+1 optional message) | 6 (+1 optional message) |
| 1.4 Action planning | 3 | 3 | 2 | 1 |
| 3.3 Social support (emotional) | 2 (+1 optional message) | 3 (+2 optional messages) | 0 | 1 |
| 4.1 Instruction on how to perform behaviour | 8 (+2 optional messages) | 9 (+2 optional messages) | 7 (+2 optional messages) | 4 (+2 optional messages) |
| 5.1 Information about health consequences | 10 | 13 | 5 | 7 |
| 5.5 Anticipated regret | 2 | 1 | 2 | 1 |
| 6.1 Demonstrating behaviour | 5 (+7 optional messages) | 1 (+1 optional message) | 3 (+3 optional messages) | 0 |
| 10.4 Social reward | 1 | 1 | 0 | 0 |
| 10.6 Non-specific incentive | 4 | 6 | 4 | 6 |
| 12.5 Adding objects to the environment | 1 | 1 | 1 | 1 |
| Other technique | ||||
| Reward study involvement with thanks, emphasise credibility and importance of study | 1 | 1 | 1 | 1 |
| Provide non-judgemental information/correct misconceptions | 11 | 15 | 7 | 11 |
| Traditional action planning adapted so that the text message provides ideas on how to perform a behaviour | 2 | 2 | 0 | 0 |
| Facilitate link to services for additional support | 9 | 7 | 8 | 7 |
| Validate experience | 2 | 1 | 2 | 1 |
For those diagnosed with a STI, messages over the first 3 days focused on engaging with the study, getting treatment, taking treatment and providing information about the infection. Over the next week messages targeted telling partner(s) about an infection. The messages provided non-judgemental, non-stigmatising information covering how common infections are, that an individual may not have symptoms and so therefore be unaware that they have a STI; that many people diagnosed with a STI have had only one sexual partner in the previous year, and that infections are easy to treat. Messages provided information about how to prevent infections. They also provided suggestions about when, where and how to tell a partner about an infection and examples of how others had told partners, covering a range of different types of relationship (e.g. casual, long term). The messages then provided links to services that could inform partners and links to support for anyone concerned about violence in their relationship after telling a partner about an infection. Messages also aimed to provide social support, acknowledging people’s experiences.
For those diagnosed with an infection, after day 14 the messages targeted condom use and testing for STIs before having unprotected sex with a new partner, employing the same messages as for those who were not diagnosed with an infection.
Intervention for chlamydia-, non-specific-urethritis- and gonorrhoea-negative participants
The intervention for female participants who did not have a positive test result at the time of enrolment (‘negative participants’) consisted of 51 text messages, starting from the point of randomisation (see Table 6). The intervention for negative male participants consisted of 49 text messages, starting from the point of randomisation. Participants who had not been diagnosed with an infection were sent the messages about safer sexual behaviours (condom use and testing for STI) starting on day 1. Over the following 30 days messages were sent providing information on how to prevent infections and how you cannot assess risk according to how well you know someone or by their appearance. Messages included instructions on how to use condoms, emphasised positive aspects of condom use and provided tips on preventing condom problems and examples of how others resolved condom use problems. Participants were prompted to think about risks that they had taken and what they could do differently in the future and also to consider how they had carried out safer sexual behaviours in the past. Text messages included advice regarding getting tested before unprotected sex with a new partner. Participants were also sent links to further web-based information regarding contraception, alcohol and sexual risk, how to use a condom and general communication about sex. Women were sent messages covering how other women had negotiated condom use. The messages were designed to provide social support for safer sexual behaviours.
Control
Control messages were also delivered through the bespoke texting software, that is, during the chosen non-embargoed time period. All participants (including participants randomised to the intervention) received the control messages. The set of control messages consisted of 13 messages in total, which were spaced 30 days apart starting from the point of randomisation (see Table 6). The control messages contained no BCTs or information regarding sexual health. The messages were intended to help keep participants engaged in the study and to remind them of their participation, for example ‘Young people can experience health inequalities. Taking part in the texting study can help things to be equal. Thanks for taking part’. The messages expressed our appreciation of their involvement in the study and suggested that participation in research can be personally beneficial: ‘Taking part in the texting study is a way to help you be actively involved in things that affect your life. Thank you for taking part’.
Recruitment
We identified participants from seven sexual health services located in inner-city Manchester, south-east London, Cambridgeshire, Norfolk, Maidstone, Hull and London Brook services. Recruitment staff recruited participants on site at the service or staff referred eligible participants to OM at LSHTM for telephone recruitment.
Recruitment staff on site assessed potential participants for eligibility, provided detailed verbal and written information and gave potential participants the opportunity to ask any questions. Those who agreed to participate were asked to provide written informed consent by filling out a paper-based version of the consent form.
Staff at other services identified eligible participants (aged 16–24 years and who had recently received a positive chlamydia test result) and asked those who were interested in participating for their permission to pass their mobile phone number to OM. OM telephoned the referrals and provided detailed verbal information. She then texted or e-mailed the link to the online participant information sheet [see https://text4health.lshtm.ac.uk/registration/information_sheet.aspx (accessed 15 March 2016)] and gave participants the opportunity to ask any questions. Participants who agreed to participate provided informed consent through the secure online trial consent form [see https://text4health.lshtm.ac.uk/registration/Consent_Form.aspx (accessed 15 March 2016)].
Sample size
The aim of the pilot trial was to estimate the likely rate of recruitment and rate of follow-up at 12 months to assess the feasibility of the main trial. With a pilot sample size of 200, we would be able to estimate a loss to follow-up rate of 20% to within a 95% confidence interval (CI) of ± 6% (i.e. a 95% CI of 14% to 26%). The width of the CI was calculated by 1.96 × [p × (1 – p)/n], where p is the percentage dropout that we expect to see and n is the intended sample size. If the loss to follow-up was 10%, this would be within 4% of the true rate (i.e. a 95% CI of 6% to 14%).
Interim analyses and stopping rules
There were no interim analyses. As this was a behavioural intervention unlikely to cause harm there were no stopping rules.
Outcomes
Primary outcomes
The primary outcomes for the pilot trial were the recruitment rates and completeness of follow-up for the proposed primary outcome for the main trial (cumulative incidence of STIs at 12 months).
Our target was to recruit 200 participants over 3 months and to achieve an 80% response rate at each follow-up point. We assessed the numbers recruited by the number randomised during the 3-month time period. We assessed the follow-up response by the numbers completing the questionnaire at months 1 and 12 and returning a chlamydia test sample at months 3 and 12.
Secondary outcomes
Secondary outcomes were:
-
the proportion of messages successfully delivered (measured using the IT system metrics)
-
at month 1 we assessed:
-
process outcomes:
-
number of text messages read (all/some/none)
-
Knowledge of someone else who took part in the study (yes/no) – if yes: if the other person read the messages we sent the participant; how many they read; if the participant read the messages we sent the other person and how many they read
-
If anyone read messages sent to the participant and if yes, how the participant felt about this
-
-
behavioural outcomes:
-
for participants testing positive for chlamydia, gonorrhoea or NSU at the time of recruitment: if they took the treatment (yes/no); if they avoided sex for 7 days after treatment (yes/no/unsure); if they told the last person they had sex with before the test that they needed to get treatment (yes/no/sort of); if they avoided sex with this person for 7 days after they took the treatment (yes/no/not applicable); and if there was someone else they were having sex with around the time they tested positive, if they told this person to get treatment (yes/no/there wasn’t anyone else)
-
condom use at last sex (yes/no/unsure)
-
sex with someone new since joining the study (yes/no/unsure)
-
condom use at last sex with someone new (yes/no/unsure)
-
STI testing for self prior to sex with someone new (yes/no/unsure)
-
participant’s report whether their last new partner was tested for STIs prior to sex with them (yes/no/unsure)
-
number of sexual partners since joining the study (0/1/2+)
-
-
-
at month 3 we assessed:
-
infection (urine test for men and self-taken vulvovaginal swab for women, according to their preference) (positive/negative)
-
-
at month 12 we assessed:
-
infection (urine test for men and self-taken vulvovaginal swab for women, according to their preference) (positive/negative)
-
behavioural outcomes:
-
for participants testing positive for chlamydia, gonorrhoea or NSU after joining the study: if they took the treatment (yes/no); if they avoided sex for 7 days after treatment (yes/no/unsure); if they told the last person they had sex with before the test that they needed to get treatment (yes/no/sort of); if they avoided sex with this person for 7 days after they took the treatment (yes/no/not applicable); and if there was someone else they were having sex with around the time they tested positive, if they told this person to get treatment (yes/no/there wasn’t anyone else)
-
condom use at last sex (yes/no/unsure)
-
sex with someone new since joining the study (yes/no/unsure)
-
condom use at last sex with someone new (yes/no/unsure)
-
STI testing for self prior to sex with someone new (yes/no/unsure)
-
participant’s report whether their last new partner was tested for STIs prior to sex with them (yes/no/unsure)
-
number of sexual partners since joining the study (0/1/2+)
-
number of text messages read (all/some/none)
-
car accident in which the participant was the driver in the past 12 months (yes/no).
-
-
We also report participants’ views regarding the intervention messages (agree/unsure/disagree):
-
the text messages made me take action
-
the text messages made me think
-
the text messages were from someone I could trust
-
the text messages were respectful
-
the text messages talked down to me
-
the text messages were easy to understand
-
there were too few text messages each day
-
there were too many text messages each day
-
I would have liked the text messages to stop sooner
-
the text messages came at the right time of day.
There were no changes to the trial outcomes after the trial commenced.
Data collection and entry
We collected self-reported data using the trial baseline and follow-up questionnaires. Participants recruited on site completed a paper version of the baseline questionnaire with the recruitment staff. Participants who were enrolled by telephone referral provided baseline data to OM over the telephone. If participants had a positive chlamydia or gonorrhoea test result or NSU diagnosis at enrolment, recruiting staff at the clinic entered the baseline data onto the secure online trial database system within 24 hours. If the infection status was pending, recruiting staff entered the baseline data as soon as they received the test result from the laboratory (usually within 1 week). All participants enrolled by telephone referral had received a positive chlamydia test result and OM entered their data on the day that they were recruited.
In addition to sexual behaviour data, the baseline questionnaire also collected the following contact information: first name; surname; main mobile phone number; alternative phone number; e-mail address; alternative e-mail address; primary postal address; alternative postal address; and name and contact details of someone to contact if the participant could not be reached and his or her relationship with this person (optional) (see Appendix 5). We also collected the following demographic data: date of birth, sex, ethnicity and sexual orientation. Finally, the baseline questionnaire collected data on participants’ preferences regarding message delivery times and whether they preferred to test for chlamydia using a postal test kit or by attending the clinic.
Randomisation
Sequence generation
An independent online randomisation system [see www.sealedenvelope.com/ (accessed 22 July 2016)] generated the 1 : 1 allocation sequence, stratified by site, using random permuted block sizes of 2, 4 and 6. Staff were not aware of the block sizes.
Allocation concealment
The online randomisation system generated the allocation sequence, which meant that staff enrolling participants into the trial could not have known in advance which treatment allocation the next participant would receive.
Implementation
The online randomisation system randomised participants immediately after the recruiting staff entered their baseline data onto the online trial database system (see Recruitment and Data collection and entry).
Masking
Because of the nature of the intervention, participants could have been aware of their treatment allocation; they would have expected frequent text messages (intervention) or one text message a month (control). Thus, the participants were unmasked. The trial manager (OM) required access to treatment allocation to monitor the incoming texts and identify intervention participants for the qualitative interviews. However, the risk of bias associated with this unmasking is low as the intervention was prescribed and delivered by the bespoke texting software, directly to participants’ mobile phones; OM was not involved in the delivery of the intervention. Laboratory staff assessing chlamydia infection and researchers assessing the outcomes were masked to treatment allocation. Staff performing the statistical analysis were also masked to treatment allocation. Data were double entered with one researcher masked to allocation. The treatment allocation variable in the data set was coded 1 or 2 and this was kept undisclosed until the full analysis was complete.
Statistical methods
We estimated the follow-up rate for the primary outcome proposed for the main trial (cumulative incidence of chlamydia at 12 months) with a 95% CI. For all other outcome measures we estimated the relative risk with a 95% CI and a p-value using log binomial regression with robust standard errors. We analysed by randomised arm and conducted a complete case analysis only. This is a behavioural intervention unlikely to produce adverse effects and so the analysis by the research team was undertaken once, at the end of the trial.
Pooling of sites
Data were pooled across all sources of recruitment.
Time points for analysis
This is a behavioural intervention unlikely to produce adverse effects and so the analysis by the research team was undertaken once, at the end of the trial and after the data set had been locked.
Methods for dealing with missing data
We conducted a complete-case analysis only.
Adjustments for covariates
We did not adjust for covariates in the primary analysis.
Multiple comparisons
We did not adjust for multiple comparisons.
Examination of subgroups
We did not conduct a subgroup analysis.
Analysis of primary and secondary end points
The primary outcomes were the recruitment rate and completeness of follow-up for the proposed primary outcome for the main trial and the proportion of messages successfully delivered to participants’ mobile phones. We report the cumulative incidence rate of chlamydia infection in the control group to inform the sample size calculation for the main trial. For each binary outcome we report relative risks with 95% CIs and give a two-sided p-value for statistical significance.
Adverse events
Involvement in a road traffic accident is the only plausible adverse event that might be caused by a mobile phone-based texting intervention. We also report the proportion of participants who experienced someone else reading their text messages and the participants’ response to this (happy/unhappy/unsure).
Results
We assessed 470 people for eligibility (Figure 1) of whom 270 were excluded (n = 169 did not meet the inclusion criteria, n = 101 declined to participate); therefore, 200 participants were recruited within 3 months. In total, 66% (n = 131) of participants were recruited face to face at the Camberwell Sexual Health Centre at King’s College Hospital in London (see Appendix 7, Table 13), 4% (n = 8) were recruited from the Palatine Contraception and Sexual Health Service in Manchester, 6% (n = 11) were recruited face to face at Cambridge Regional College and Huntingdonshire Regional College and 25% (n = 50) were recruited by telephone referral. Recruitment stopped once we had achieved our target recruitment number. Participants were randomised from 9 September 2013 to 29 November 2013 and were followed up between October 2013 and the end of February 2015. In total, 99 participants were allocated to the intervention and 101 were allocated to the control (see Figure 1).
FIGURE 1.
Pilot trial Consolidated Standards of Reporting Trials (CONSORT) diagram.
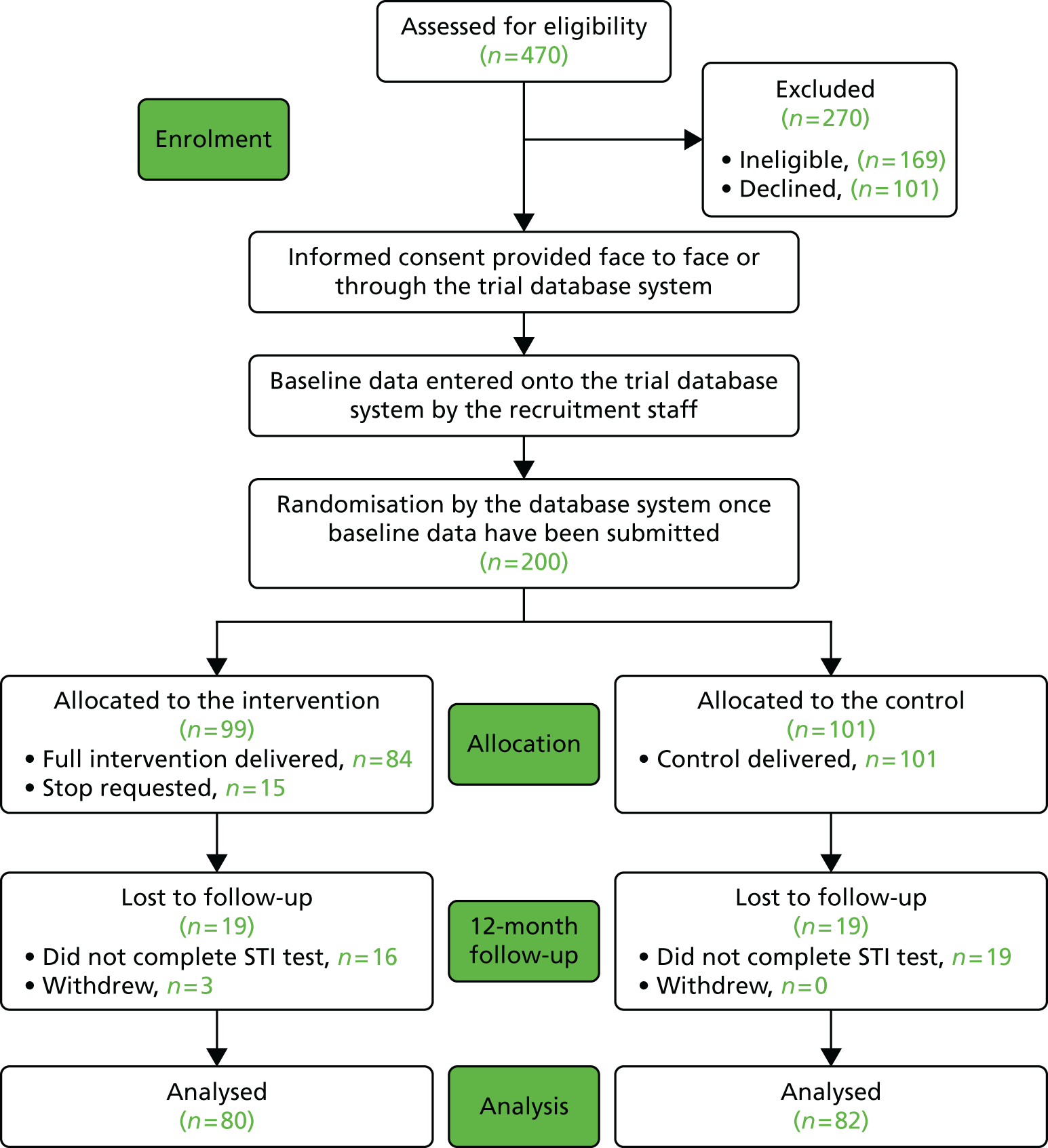
The baseline demographic and sexual behaviour data of the randomised participants are presented in Table 7.
| Baseline characteristics | Group | |
|---|---|---|
| Control, n/N (%) | Intervention, n/N (%) | |
| Sex | ||
| Male | 31/101 (30.69) | 29/99 (29.29) |
| Female | 70/101 (69.31) | 70/99 (70.71) |
| Age | ||
| Mean (SD) | 20.60 (2.39) | 20.39 (2.42) |
| 16–19 years | 33/101 (32.67) | 36/99 (36.36) |
| 20–24 years | 68/101 (67.33) | 63/99 (63.64) |
| Ethnicity | ||
| White | 55/101 (54.46) | 59/99 (59.60) |
| Black | 32/101 (31.68) | 21/99 (21.21) |
| Asian | 0/101 (0.0) | 2/99 (2.0) |
| Chinese | 0/101 (0.0) | 0/99 (0.0) |
| Other | 14/101 (13.86) | 17/99 (17.17) |
| Refused/missing | 0/101 (0.0) | 0/99 (0.0) |
| Sexual orientation | ||
| Heterosexual | 83/101 (82.18) | 88/99 (88.89) |
| Gay or lesbian | 5/101 (4.95) | 3/99 (3.03) |
| Bisexual | 10/101 (9.90) | 5/99 (5.05) |
| Refused/missing | 3/101 (2.97) | 3/99 (3.03) |
| STI infection at baseline | ||
| No infection | 53/101 (52.48) | 58/99 (58.59) |
| Chlamydia positive | 42/101 (41.58) | 35/99 (35.35) |
| Gonorrhoea/NSU | 5/101 (4.95) | 5/99 (5.05) |
| Chlamydia/gonorrhoea/NSU diagnosis | 1/101 (0.99) | 1/99 (1.01) |
| Sexual behaviour | ||
| Condom use at last sex | 35/101 (34.65) | 32/99 (32.32) |
| Condom use at last sex with someone new | 52/101 (51.49) | 48/99 (48.48) |
| Last time participant had sex with someone new participant was tested prior to sex | 37/101 (36.63) | 32/99 (32.32) |
| Last time participant had sex with someone new partner was tested prior to sex | 12/101 (11.88) | 11/99 (11.11) |
| Number of sexual partners in last 12 months | ||
| 0 | 0/101 (0.0) | 0/99 (0.0) |
| 1 | 9/101 (8.91) | 6/99 (6.06) |
| 2+ | 92/101 (91.09) | 93/99 (93.94) |
Primary outcomes
Our primary outcomes were full recruitment within 3 months and follow-up rate for our proposed primary outcome for the main trial. We fully recruited within 3 months and 97% of messages were successfully delivered. We obtained an 81.0% (162/200) follow-up rate for the cumulative incidence rate of chlamydia, with a rate of 81.2% (82/101) in the control group and 80.8% (80/99) in the intervention group (Table 8).
| Follow-up at 12 months for: | Group | Follow-up, n/N (%, 95% CI) | |
|---|---|---|---|
| Control, n/N (%) | Intervention, n/N (%) | ||
| Cumulative incidence of chlamydia (trial test kits + clinic data) | 82/101 (81.19) | 80/99 (80.81) | 162/200 (81.0, 74.86 to 86.19) |
| Trial test kits | 80/101 (79.21) | 80/99 (80.81) | 160/200 (80.0, 73.78 to 85.31) |
In total, 92% (183/200) provided questionnaire outcome data at 1 month. Of the 183 providing data, 80% (146/183) returned the postal questionnaire, 13% (23/183) completed the questionnaire online, 4% (7/183) completed the questionnaire at the clinic, 0.5% (1/183) responded to the key questions by e-mail and 3% (6/183) responded to the key questions by text message. In total, 86% (171/200) provided a chlamydia test sample at 3 months. Of the 171, 98% (167/171) returned the sample by post and 2% (4/200) provided the sample at the clinic. In total, 82% (163/200) provided questionnaire outcome data at 12 months. Of the 163, 94% (153/163) returned the postal questionnaire, 3% (5/163) completed the questionnaire online, 2% (3/163) completed the questionnaire at the clinic, 0% (0/163) responded to the key questions by e-mail and 1% (2/163) responded to the key questions by text message. Finally, 80% (160/200) provided a chlamydia test sample at 12 months (see Table 8). Of the 160, 98% (157/160) returned the sample by post and 2% (3/160) provided the sample at the clinic.
Withdrawals and requests to stop the intervention
Three participants withdrew from the study, all of whom were randomised to the intervention arm. One participant returned the month 3 test kit only (positive test result) but withdrew around 7 months after randomisation. Another participant returned the month 1 questionnaire only and requested to be withdrawn 3.5 months after randomisation. The third participant withdrew 11.5 months after randomisation, never requested that the messages stop and did not respond at any follow-up point. Of the 99 participants receiving the intervention, 15 participants (15%) requested that the messages stop; two of these also withdrew from the study (both stopped the messages 1 day after enrolment).
Secondary outcomes
Process outcomes
At 1 month 82% (72/88) of respondents in the intervention group had read all messages and at 12 months 74% of respondents in the intervention group (56/76) had read all messages (Table 9). There were three documented cases at 12 months in which participants in the control group reported reading messages sent to other trial participants.
| Outcome | Group | |
|---|---|---|
| Control, n/N (%) | Intervention, n/N (%) | |
| Number of text messages read at 1 month | ||
| All | 69/83 (83.13) | 73/89 (82.02) |
| Some | 10/83 (12.05) | 10/89 (11.24) |
| None | 4/83 (4.82) | 6/89 (6.74) |
| Number of text messages read at 12 month | ||
| All | 65/80 (81.25) | 57/77 (74.03) |
| Some | 12/80 (15.0) | 18/77 (23.38) |
| None | 3/80 (3.75) | 2/77 (2.60) |
| At 1 month | ||
| Did anyone read messages sent to the participant? | 19/91 (20.88) | 24/92 (26.09) |
| If yes, how did the participant feel about this? | ||
| Happy | 6/19 (31.58) | 7/24 (29.17) |
| Unhappy | 0/19 (0.0) | 2/24 (8.33) |
| OK | 11/19 (57.89) | 15/24 (62.50) |
| Did the participant know someone else who took part in the study? | 5/91 (5.49) | 6/92 (6.52) |
| If yes, if the other person read the messages we sent the participant? | 2/5 (40.0) | 5/6 (83.33) |
| How many did they read? | ||
| All | 1/2 (50.0) | 2/5 (40.0) |
| Some | 0/2 (0.0) | 3/5 (60.0) |
| None | 0/2 (0.0) | 0/5 (0.0) |
| Missing | 1/2 (50.0) | 0/5 (0.0) |
| If yes, did the participant read the messages that we sent to the other person? | 0/5 (0.0) | 2/6 (33.33) |
| How many did they read? | ||
| All | 1/2 (50.0) | |
| Some | 1/2 (50.0) | |
| None | 0/2 (0.0 | |
| Missing | 0/2 (0.0) | |
| At 12 months | ||
| Did anyone read messages sent to the participant? | 19/83 (22.89) | 19/80 (23.75) |
| If yes, how did the participant feel about this? | ||
| Happy | 6/19 (31.58) | 8/19 (42.11) |
| Unhappy | 0/19 (0.0) | 2/19 (10.53) |
| OK | 13/19 (68.42) | 9/19 (47.37) |
| Did the participant know someone else who took part in the study? | 7/83 (8.43) | 6/80 (7.50) |
| If yes, if the other person read the messages we sent the participant? | 2/7 (28.57) | 3/6 (50.0) |
| How many did they read? | ||
| All | 1/2 (50.0) | 1/3 (33.33) |
| Some | 1/2 (50.0) | 2/3 (66.67) |
| None | 0/2 (0.0) | 0/3 (0.0) |
| Missing | 0/2 (0.0) | 0/3 (0.0) |
| If yes, did the participant read the messages that we sent to the other person? | 2/7 (28.57) | 5/6 (83.33) |
| How many did they read? | ||
| All | 0/2 (0.0) | 1/5 (20.0) |
| Some | 2/2 (100) | 4/5 (80.0) |
| None | 0/2 (0.0) | 0/5 (0.0) |
| Missing | 0/2 (0.0) | 0/5 (0.0) |
Intervention group participant views regarding the messages at month 1 are presented in Table 10. Over 80% of intervention recipients reported that the text messages ‘made me think’, were ‘respectful’ and were ‘easy to understand’. Just over one-third of recipients reported that the messages ‘made me take action’. A significant minority thought that the messages talked down to them (11/85; 13%); of these, seven out of 11 did not have an infection at the outset of the trial. About two-thirds of participants reported that the messages ‘were from someone they could trust’ and ‘came at the right time of day’. About one-fifth of respondents thought that there were too many messages and about one-fifth thought there were too few.
| View | Agree, n/N (%) | Unsure, n/N (%) | Disagree, n/N (%) |
|---|---|---|---|
| The text messages made me take action | 32/85 (37.65) | 32/85 (37.65) | 21/85 (24.71) |
| The text messages made me think | 71/86 (82.56) | 7/86 (8.14) | 8/86 (9.30) |
| The text messages were from someone I could trust | 57/86 (66.28) | 21/86 (24.42) | 8/86 (9.30) |
| The text messages were respectful | 76/86 (88.37) | 8/86 (9.30) | 2/86 (2.33) |
| The text messages talked down to me | 11/85 (12.94) | 15/85 (17.65) | 59/85 (69.41) |
| The text messages were easy to understand | 81/85 (95.29) | 3/85 (3.53) | 1/85 (1.18) |
| There were too few text messages each day | 17/85 (20.0) | 18/85 (21.18) | 50/85 (58.82) |
| There were too many text messages each day | 20/85 (23.53) | 17/85 (20.0) | 48/85 (56.47) |
| I would have liked the text messages to stop sooner | 12/86 (13.95) | 25/86 (29.07) | 49/86 (56.98) |
| The text messages came at the right time of day | 56/86 (65.12) | 21/86 (24.42) | 9/86 (10.47) |
There were 11 behavioural outcomes collected for all participants and 16 collected for participants testing positive for a STI at the start of the trial. There were no statistically significant changes in behaviour or infection using a cut-off of 0.005 (which uses a Bonferroni correction for multiple comparisons). The secondary behavioural and STI outcomes are reported in Appendices 8–10.
Contact problems
Losses to follow-up were mainly the result of mobile phone numbers no longer being current. Six out of the 17 non-responders to the month 1 questionnaire had a problematic mobile phone number. Three mobile phone numbers went straight to voicemail and two numbers were not in service after many attempts. We could not reach one participant at the number provided. Five of the 29 non-responders to the month 3 chlamydia test had a problematic mobile phone number. Two mobile phone numbers went straight to voicemail, two numbers were not in service and we could not reach one participant at the number provided.
Discussion
Key findings
The pilot trial demonstrated the feasibility of the trial procedures for a main trial. We fully recruited early and achieved an 81% follow-up rate for our proposed primary outcome of cumulative incidence of chlamydia at 12 months. There was no differential follow-up between groups. The IT system delivering the messages was effective, with 97% of messages sent being successfully delivered to participants’ mobile phones. Participant views of the intervention suggest that it is acceptable to the majority of participants. Some participants shared messages with friends and there were three cases of control group participants (3%) reporting reading other participants’ messages.
Strengths and weakness
In the pilot trial we achieved a high follow-up rate, allocation was concealed and laboratory staff and those analysing data were blind to allocation. Only one of the researchers double entering data was masked to allocation; however, in a main trial there would be sufficient staff for all staff entering follow-up data to be masked to allocation. Given the small sample size and the large number of variables assessed, the baseline characteristics of participants were reasonably well balanced. There were some differences in baseline infections and ethnicity between groups. Nonetheless, as the primary outcomes for the pilot were recruitment and follow-up, the allocation balance would not impact on this. Although the response rate overall was high, the response rate for some questions, such as partner notification, was low. A larger sample size in a main trial would allow for better balance between the arms. The pilot trial was not powered for behavioural or STI outcomes and so 95% CIs for these outcomes were large and it is unsurprising that no outcomes were statistically significant when the multiple comparisons were taken into account.
Discussion in relation to the existing literature
This pilot trial’s follow-up response rate for return of the chlamydia test samples was considerably higher that that seen in similar trials, screening initiatives and surveys. 37 The Natsal study in the UK achieved a 57.7% response rate for face-to-face interviews and a 60% response rate for urine samples requested. 35 The ClaSS project reported an uptake of chlamydia postal screening of 31.5% in people aged 16–24 years,36 whereas the Sexunzipped trial achieved a 45% follow-up rate using chlamydia postal test kits and a 72% follow-up rate for self-reported data at 3 months. 37
The ClaSS project36 employed some elements of our approach to follow-up described in Chapter 3, such as choosing a postal testing kit that fit through a ‘standard’ letterbox and testing the kit with the target group. 48 In the ClaSS project the researchers evaluated interventions to increase follow-up after the project commenced and later adopted pre-notification in the form of an invitation letter sent in advance of the kits. Adopting our approach would have identified methods known to increase postal follow-up before the study commenced, which may have increased the response. Our response rate may be higher than that achieved by the ClaSS project because our participants had agreed to provide follow-up data when they were recruited, we offered unconditional incentives and we included only essential test kit components.
Generalisability
The pilot trial was designed to demonstrate the feasibility of a main trial. It was not designed to generate reliable estimates of the intervention effect and thus the intervention effects are neither accurately estimated nor generalisable. The proportion of eligible participants agreeing to take part was 66% (200/301). The intervention has been designed to be accessible across socioeconomic and ethnic groups.
The implications of the pilot trial results for the design of the main trial are discussed in Chapter 6.
Chapter 5 Qualitative interviews
Objectives
The objectives of the qualitative interviews were to:
-
explore young people’s views and experiences of the text message intervention
-
explore their experiences of the follow-up procedures.
Methods
We conducted interviews with participants seeking their views on the acceptability of the intervention. 45 The main trial consent form included a tick box asking if participants would be willing to be contacted about participating in an interview. Of those indicating that they were willing to be contacted, we purposively sampled participants to ensure variation according to age, sex, STI test result at enrolment and treatment group. Control group participants were included as we wanted to explore young people’s experiences of participation in the pilot trial. We selected participants from two of the study sites, London and Cambridgeshire, to ensure representation from inner-city and suburban/rural settings.
Participants were telephoned by OM, who provided detailed verbal information, texted or e-mailed the link to the online participant information sheet [see https://text4health.lshtm.ac.uk/registration/information_sheet.aspx (accessed 15 March 2016)] and gave participants the opportunity to ask any questions. Participants who agreed to participate provided informed consent through the secure online trial consent form [see https://text4health.lshtm.ac.uk/registration/Consent_Form.aspx (accessed 15 March 2016)].
Interviews
Qualitative interviews were conducted by RF with 20 participants by telephone 2–3 weeks after enrolment to the pilot trial. One interview was conducted by OM. Interviews took place between October 2013 and January 2014. The interviews followed a semistructured topic guide, which aimed to find out about participants’ views and experiences of the intervention and their recommendations for improvements. Questions were included on the tone and frequency of the text messages, the message content and sexual behaviour since enrolment, such as condom use and partner notification. Participants were each given £20 for completing the interview. The interviews were audio recorded and transcribed verbatim.
Follow-up interviews
Follow-up interviews with participants were conducted by OM after sending the 3-month postal test kits, asking for participants’ views on the acceptability of the follow-up materials and procedures. We interviewed 17 of the original 20 participants (we were unable to reach three participants). The follow-up interviews followed a semistructured topic guide, which explored participants’ views on the trial materials and follow-up procedure.
Thematic analysis
Data were managed and transcripts coded thematically using NVivo 10 (QSR International, Warrington, UK). After familiarisation with the data, RF generated an initial coding framework (with OM). RF coded all of the interviews according to the framework and these were checked by and agreed with CF. Each theme was described and subthemes identified by RF and CF. RF searched for deviant or atypical cases.
Results
At enrolment, 84% of participants (n = 167) indicated that they were willing to be contacted regarding an interview; 20 interviews were conducted. None of those contacted declined to be interviewed. One participant who agreed to be interviewed did not answer calls at the prearranged interview time. The characteristics of the participants interviewed are provided in Table 11. Seven of the female participants and four of the male participants were diagnosed with chlamydia infection at enrolment.
| Age group (years) | London (ID01), n | Cambridgeshire (ID03), n | Allocation, n | ||
|---|---|---|---|---|---|
| Male | Female | Male | Female | ||
| 16–18 | 2 | 1 | 0 | 3 | Intervention: 16; control: 4 |
| 19–21 | 1 | 3 | 2 | 3 | |
| 22–24 | 2 | 0 | 1 | 2 | |
Engagement with text messages
Most young people were positive about the intervention. Five key themes relating to user engagement with the text messages were identified: the importance of tone, the frequency and timing of texts, convenience, saving messages for reflection and the sharing of messages.
Tone
Most participants said that the messages sounded as if they were coming from a friendly, trustworthy source. Participants liked the fact that the messages were simple, avoided slang and were not too long. They described the messages as easy to understand and stated that the messages did not make them feel as if they were being lectured:
they didn’t use like too many big words, where if it had been a load of words that I didn’t really know what they meant I’d have probably not read like the first one and then I’d have probably not read any of the others after that.
ID030012, male, 24 years, intervention, chlamydia positive
Some described how it was important for them to relate to and trust the messages. They did not feel pressured, told off or lectured – the messages were ‘on their side’ and enabling:
It was kind of like coming from a friend ‘cos it’s like it’s not speaking down to you, it’s like speaking to you, they’re like not trying to make you feel like little, they’re trying to like help you kind of thing.
ID03003, female, 20 years, intervention, chlamydia positive
I didn’t feel like I was pressured into it. It was my choice if I wanted to either carry on doing the text message, if I wanted to find out the stories. It was very friendly, very user friendly.
ID03002, female, 21 years, intervention, chlamydia positive
However, one 22-year-old man who had previously had genital warts felt that the messages were ‘patronising and ‘dumbed down’. He said that he would have preferred more statistical facts.
Frequency and timing
All of the participants thought that the frequency of the texts, one or two a day, was just right. Their view was that they would have felt bombarded had there been any more, but less would not have been enough to reinforce the messages:
It’s been really helpful . . . not too much, like they don’t text too much and it gives you like information, like just little bits of information and it kind of sticks in your head so it’s been good yeah.
ID03006, female, 18 years, intervention, chlamydia positive
One participant was impressed that the messages continued to arrive at the weekend. It was possible to request the time of day that messages would be sent, but none of the participants had chosen to do this. A few mentioned the merit in sending messages out on Friday evenings when young people may be going out drinking, for example to remind them to carry condoms before going out.
Convenience
Delivery by mobile phone was felt to be appropriate for young people as ‘kids are always on the phone’. Participants described the convenience of receiving texts on their mobile phone: being easily accessible and not taking up much time or attention, unlike having to go somewhere after work or trying to read through pages on the internet:
it’s nothing like sitting on the internet and reading all different things about it, just kind of getting some text messages every now and again.
ID03006, female, 18 years, intervention, chlamydia positive
‘cos it’s just a text, so even if you can’t read it right then you’d go back to read it later, it doesn’t cause any problems.
ID03013, female, 22 years, intervention, chlamydia positive
Saving messages for reflection
Most intervention participants described having saved the messages that they had received. Some said that they returned to, and reflected on, the messages or kept them for future reference:
I’ve got all of them on my phone so like sometimes I’m going through my text messages . . . and then I go back through and read the stuff that’s come through and I do find it very helpful . . . but sometimes you want to go back on stuff, . . . if you are thinking about where your situation’s gonna be, you’re meeting a new partner and you’re like, right, we’re gonna have to have this conversation, . . . then you have a look and then you kind of, it helps you, it builds your confidence a bit with the tips and it’s the reassurance.
ID03002, female, 21 years, intervention, chlamydia positive
The fact that the messages were not personal allayed fears connected to their discovery by other people. Some participants locked their mobile phone so that it could not be accessed by anyone else and some set their phones to prevent messages popping up on the screen. A couple of participants deleted their messages, one saying that he had done this as he did not want anyone else coming across them.
Sharing messages
Many participants described sharing the text messages that they received. For some this was to pass on information to younger siblings or friends. One young woman had kept her messages so that she could forward them to friends if they had any ‘problems’ in the future. Another, in the control group, read the intervention messages sent to her friend in the intervention group. She was particularly enthusiastic about the messages and reported that she would not have been able to tell her partner about her test result had it not been for the support and tips provided through the texts. Sharing was not always intentional. One young woman said that her mother had seen the texts and, although her mother was initially angry on learning that her daughter had had a positive chlamydia test, after talking through the texts with her daughter she felt that the texts were a good idea.
For some, an important aspect of sharing messages was to help initiate a conversation, usually with a partner. For example, messages were used by some women to support or back up negotiations on condom use:
I’ve shown him a few [messages] about condoms and that but he wasn’t listening to me and I was like oh my God . . . then show him the messages, yeah . . . he’s like well, I’m not fussed about it. I’m so like worried about it and like I know a lot about it now he’s kind of said ‘Oh yeah, I’d rather’ . . . I told him about that oh if I caught this again . . . I’d rather have a condom than catch an infection again. At first he was just like ‘Oh, like I really don’t like it’ but after he’s seen the get pregnant or something in the future [reference to texts relating to infection and risk to infertility] which made him think as well. So I think like when you look into it deeper it helps a lot.
ID03006, female, 18 years, intervention, chlamydia positive
However, not all partners were as responsive:
He didn’t really pay any attention, he was just like, ‘Oh you’ve got one of them texts again’, you know.
ID03024, female, 17 years, intervention, chlamydia negative
Impact on knowledge
Topics reported to be particularly helpful included how to put a condom on, how to prevent condom breakages (e.g. not using oil-based lubricants), STI testing and how to talk to a partner as well as building confidence and reducing the stigma and worry related to the chlamydia test result.
Participants’ reports regarding the impact of the intervention on knowledge varied. At one end of the spectrum there were those who reported that they knew little about STIs or how to use a condom:
Well, there was this one, yeah, that said how to put a condom on, the best . . . [laughs]. The quick and fresh way to put a condom on . . . [laughs]. Because I didn’t know that much about condoms so I followed the link [to obtain further information] and I’m like, oh and it feels good when I learned how to put it on, you don’t have to use something that got oil, yeah, you don’t have to use it because the condom might burst and something like that . . . oh I didn’t know that’s how you get it [chlamydia], I didn’t know, I was like, oh I need to be more careful then, I need to use a condom mostly when I meet someone new.
ID01002, female, 23 years, intervention, chlamydia positive
Although some of the participants reported that they already knew most of the information, they said that the messages reminded them of what they had learnt in the past, reinforced this information or helped them reflect on what they knew:
Most of the stuff I knew but it kind of gave me a thought, because you don’t really think about it sometimes at the time that you’re getting into anything, you just kind of do what you’re doing, but because of the texts it kind of keeps it in your mind so you know what you’re doing really before you get into anything.
ID01043, male, 18 years, intervention, chlamydia negative
I think everyone should have this texting thing come out to them every day because sometimes you do forget little things that obviously you should be doing.
ID03013, female, 22 years, intervention, chlamydia positive
Some participants had not found the texts helpful, describing the messages as ‘common sense’. They tended to be older and/or chlamydia negative at enrolment. However, they generally felt that the advice was good but would be better targeted at those aged 16–18 years. Participants had the option to text ‘Stop’ if they wanted to discontinue receiving the messages. One had done this and he explained that he would have preferred more ‘scary facts . . . to make kids think’ (ID01042, male, 22 years, intervention, chlamydia negative). One of the female participants who had sexual relationships solely with women felt that some of the messages, for example those on condom use and contraception, were not relevant for her.
Reported impact on behaviour
Partner notification and treatment
Nearly all of those diagnosed with a STI in the intervention and control groups reported feeling able to notify their sexual partners of their test result. The exception was one young woman who had no contact details for a casual partner. Some of those in the intervention group said that they had notified their partners before receiving the texts, but others said that the texts about talking to your partner had helped them to have this discussion.
Participants reported lacking confidence in how to tell a partner about an infection and it was particularly helpful to receive messages about how others had done so. The mode of delivery was compared favourably with the approach adopted in health-care settings, which was described as more didactic:
When they told me first, yeah, at the hospital you have to tell him, I’m like no, I’m not going to tell him and they’re like, do you want us to call him? I’m like, no, I’m not going to give you his number and they’re like, well you have to [laughs], you know, you have to tell him. I’m like, no, I don’t know how to, anyway, you have to, just find a way to tell him. So I wasn’t that confident . . . but when I start this group and they start telling me about chlamydia, that it’s not that dangerous, you can cure it, . . . you have to get tested and all that so it actually helped me a lot.
D01002, female, 23 years, intervention, chlamydia positive
All participants diagnosed with chlamydia said that they and their main partner had been treated and that they had not had sexual intercourse in the week following treatment.
Reassurance and reduction of stigma
The information received in text messages that chlamydia is common, that you may not know you have it and that it is easily curable was said to have reduced concerns and stigma, which in turn increased confidence in telling a partner. Some described being distressed after receiving a positive chlamydia result and the text messages were able to give them some reassurance. They reported being able to tell partners about an infection without blaming them or being blamed:
It basically said like not to blame him kind of thing ‘cos, so . . . it made it easier for me to handle the fact that I had it as well as the fact that obviously I needed to tell him so it was more comfortable like ‘cos I wasn’t like angry or whatever.
ID03003, female, 20 years, intervention, chlamydia positive
The texts were also seen as helping to manage their own or their partner’s anger and reinforce that they had ‘done the right thing’ in telling their partner:
Well I got the text and it was like ‘Best way to tell your partner, sit down and explain it, and just say “Look, we both need to get treated” ’. So I did, I told him, he kicked off first of all, he weren’t very happy, and he was like ‘You’ve cheated on me’. I was like ‘No I haven’t, you blatantly know’. Then we stopped speaking for a couple of days, and then he said ‘Yeah, it’s cool, I’ve been treated’ . . . but yeah, that was basically it.
ID03007, female, 16 years, control (read the texts of a friend in the intervention group), chlamydia positive
I probably would of [notified her partner] because even though I don’t like him and even though I think that this whole problem is caused from him . . . I wouldn’t want it to be passed onto anyone else, . . . but then this sort of study has shown me that that’s the right thing to do and really you should just tell someone.
ID03013, female, 22 years, intervention, chlamydia positive
Condom use and sexually transmitted infection testing
Some young people in the intervention group said that they were now using condoms following their chlamydia test result and receiving the texts:
I’ve been with him for 8 months, it’s like before I met him I didn’t use like condoms and stuff and then obviously when I found out I had chlamydia I’ve used one every single time, like ‘cos obviously I know how to put them on now . . . I don’t have a problem using them now, so it’s helped me in that sense as well.
ID03003, female, 20 years, intervention, chlamydia positive
When asked whether their behaviour change was a result of their positive chlamydia result or the texts, some interviewees felt that the texts had helped improve their use of condoms:
And do you think that’s more to do with the texts or was that because you got diagnosed with chlamydia?
ID 03007 [female, 16 years, control (read the texts of a friend in the intervention group), chlamydia positive]: No, the texts, the slogans. One of the texts were . . . ‘use a condom’ or something like that, and I thought ‘Yes, I’m doing that!’
,
One woman was of the view that the text messages would not be sufficient for her to change behaviour as it would not be possible to introduce condoms if a partner refused:
My partner don’t like them so I’ve never used them before, yeah. Whenever I tell him to use them, he’s like no, you’re my wife, I’m not going to use them. You know how . . . [laughs] . . . African men are like, no [laughs] . . . they’re like, you’re my wife so I’m not going to use it. We’re not married but that’s what he always says, oh you’re going to be my wife so there’s no point of you using them. Yeah, so and I like him, I love him, so I’m like, okay, I’m not going to use it then.
ID01002, female, 23 years, intervention, chlamydia positive
Some in established relationships said that they would not be using condoms with their current partner, but their intention would be to use them with any future partners and to go for chlamydia screening:
But beforehand I didn’t really think about it, I just used to go ‘yeah, that’ll be fine, it’ll never happen to me’ . . . cos I don’t really use, well I only ever had one one-night stand anyway but, I’ve got a missus now anyway, but we don’t use a condom now, but if I did sleep with someone else now, if I split up and then see someone else I would definitely use a condom now.
ID03012, male, 24 years, intervention, chlamydia positive
Some expressed the intention to go for screening and to ask their partners to do so in the future. Participants reporting behaviour change were more often younger, had received a positive STI test result and were not living in an inner-city setting.
Mechanism of action
Coding and analysing the interviews led to the development of a theoretical framework for the mechanism of action, that is, how the intervention is hypothesised to work at increasing safer sexual behaviours. Figure 2 illustrates the prerequisites for content and delivery and the mechanism of action. The findings from the interviews suggest that the intervention could work by providing information and skills to young people via a channel that is convenient and acceptable to them. For example, the texts appeared to help by providing new knowledge on how to put a condom on or facilitating condom use and breaking down assumptions about how chlamydia infection is transmitted. The messages could also work by allowing recipients to reflect on their behaviour and/or by helping them talk to their partner about the importance of protecting themselves against STIs, such as giving them the words that could be used when having these discussions or sharing the actual texts. The fact that this was done in a way that reduced stigma and was not pressured or judgemental assisted in communication with others.
FIGURE 2.
Prerequisites and mechanism of action from participants’ perspectives.

There was less suggestion from the interviews that attitudes had shifted. The one exception was in relation to stigma. Stigma associated with STIs can result in young people not accessing appropriate care and services16 and therefore its inclusion in health promotion interventions addressing sexual health is key.
Follow-up interviews
In total, 17 of the original 20 main trial interview participants (we were unable to reach three) were interviewed by OM. The participants found the materials and the procedure acceptable and none had any significant criticisms. They thought that the pre-notification served as a reminder to look in the post for the materials:
Yeah, definitely, it reminded you to look at your post I guess, yeah. Otherwise it tends to just pile up at our house, so it was better.
ID01005, female, 21 years, intervention, chlamydia negative
Similarly, participants mentioned that the blue envelopes helped them recognise that the contents were study materials and did not call attention to what was in them:
Yeah, I thought that was, it was fine, it’s like it’s not got anything suspicious you wouldn’t even think that there was a chlamydia test in there.
ID01067, female, 18 years, intervention, chlamydia negative
One participant said that the letters were polite in that we were not telling participants that they had to send back the tests and questionnaires and another appreciated that they were short and to the point:
They were clear as well, yeah, it’s like really, they were like really polite as well so it’s not just like, it’s telling you, you have to do it, like it’s speaking to you like an actual person so.
ID03003, female, 20 years, intervention, chlamydia positive
Most participants thought that the test instructions were clear and easy to follow and most did not have any problems or criticisms of the postal testing kit. One participant said that he initially was not clear whether or not he should post the box on its own:
No, about right, kind of not too informative but what you need to know, but when I received the test I can’t lie to you, like that was over in there and I was thinking, okay, I’ll follow the instructions but I was thinking, do I just send it in the box, or do I have to wait for something else to send it, put a stamp on it or something but then I thought, then I just thought yeah I think it’s just a box, I just put that in the postbox.
ID01043, male, 18 years, intervention, chlamydia negative
Another participant said it would have been easier if we had provided a pouch to collect the urine to pour it into the tube. One participant said that initially she had had difficulty opening the swab but worked it out. Another suggested that we include a condom in the kit.
Most participants said that they would have returned the questionnaire and chlamydia sample whether they were offered an incentive or not, with some indicating that the motivating factor was their health, not the money:
like obviously I was happy to receive it, like for doing the minimal thing, like I piss every day, you know . . . It was piss in a pot and you get twenty pound for it, obviously I was happy to receive it but it wasn’t really, it wasn’t really.
ID01042, male, 22 years, intervention, chlamydia negative
the test is like your health so you’re going to do it anyway.
ID03009, male, 20 years, control, chlamydia positive
A few participants mentioned that the unconditional £5 motivated them to return the questionnaire and test kit and another wanted to return them because we ‘treated’ him and said that he would have procrastinated without it. Women preferred the swab sample collection method and none of the participants mentioned that they would rather have had a choice of test (swab or urine).
Discussion of the qualitative interviews
Principal findings
The majority of young people who we interviewed were positive about the mobile phone texting intervention to promote safer sex, particularly as it was convenient and took little of their time. The frequency, timing and tone of the texts were appropriate for most. Receiving information and support in simple ‘bite-size’ messages was reported to help participants retain information. The text message medium also enabled participants to save and reflect on messages in their own time and share messages. Sharing texts provided participants with the opportunity to ‘educate’ friends and siblings and acted as a prompt for discussions about sexual health and safer sex behaviours with partners. Text messages reportedly improved knowledge and confidence and had a positive effect on safer sex behaviours, including condom use, STI testing and notification of partners about a positive STI test result and/or hastening notification of partners. Participants were happy with the follow-up procedures used, although there were a couple of suggestions regarding adding back in package content that we had removed to simplify follow-up procedures.
Strengths and weaknesses of the qualitative interviews
As far as we are aware this is the first study to describe recipients’ perspectives on how the mode of text messaging facilitated communication about sexual health. The nature of the short content and method of delivery may have made the messages more acceptable than traditional methods of health promotion such as printed leaflets. The content was designed to address attitudes, information and behaviour skills, rather than induce fear, which has been found to be ineffective. 10,17,18 The formative work carried out with the target group on the development of the messages was key to the intervention’s acceptability. Interviews were conducted shortly after participants had received the messages to minimise problems with recall. Our sampling strategy ensured that there was representation of different age groups, sexes and settings, so that a broad range of views could be included.
There are challenges in conducting research by telephone, for example telephone interviewing may have resulted in more superficial and briefer responses to questions than would have been the case if the interviews had been conducted face to face. 49 However, given the nature of the intervention this was an appropriate method that allowed us to interview geographically dispersed individuals. We were reliant on young people’s self-reports, which may differ from actual behaviour, and we were unable to explore the extent to which any behaviour change might be sustained. Young people may have provided responses that they felt would be desirable for the interviewer to hear and they may have also felt that they needed to be positive about the intervention itself. We tried to minimise this effect by having a member of the team (RF) conduct the interviews who was not directly involved with recruiting participants or the day-to-day running of the project.
Discussion of qualitative interviews in relation to the existing literature
In keeping with other research, participants viewed the mobile phone as an essential everyday item that is owned by most people, with easy-to-use technology. 19,20 The fact that messages are sent to participants rather than retrieved by them20 makes this a convenient, low-commitment way to receive and share information and gain support. The ‘always on you’ nature of the mobile phone21,22 enabled the mobile phone and the text messages to act as reminders and maintain the salience of sexual health behaviours. This is consistent with previous work, which reported that text messages in a smoking cessation intervention acted as reminders and maintained the importance of quitting. 23 Previous research in sexual health has also reported that text messages provided and reminded people of information. 24 The technology allowed participants to easily retain messages. 25 This enabled recipients to absorb information at their own pace and refer back to messages and reflect on them in relation to their own experiences and behaviour. Rereading messages has been reported in previous research in which a text message intervention was used to support smoking cessation. 23 In this case rereading messages was used as a tool to sustain motivation for quitting rather than for reflecting on past and current behaviour. Retaining messages also facilitated discussions with friends and family and partners. Retained messages were shown to partners to support participants in negotiating condom use and in telling partners about being diagnosed with a STI. This is in keeping with previous research, which has reported that women receiving text messages regarding contraception retained and shared messages to initiate conversations with partners about contraception. 26 The perception of the mobile phone as a highly personal object,25,27 combined with messages written in a non-judgemental tone, may have underpinned participants’ experiences of the intervention as providing support and increasing confidence. As others have shown, concern about ‘reputation’ and perceived social expectations can inhibit communication50 but, by increasing confidence and allaying fears, our findings suggest that a text messaging intervention has the potential to provide young people with skills to overcome some of the barriers to partner notification.
The favourable reception of our text messaging intervention among the young people who we interviewed resonates with findings from qualitative studies in Australia and the USA, which have found that sexual health promotion interventions delivered by text messaging are an acceptable and convenient way to deliver potentially sensitive information and support to young people. 16,51 In accordance with our findings, they found that young people favoured simple messages, they reflected on the content and they shared messages with friends. The Australian study reported no change in condom use. 52
In summary, our qualitative research found that a mobile phone texting intervention was acceptable to young people and the interviews suggested that it helped promote safer sexual behaviours, including increased condom use and partner notification. No changes were made to the follow-up procedures based on these interviews.
Chapter 6 Summary discussion
Key findings
We have described the development of a theoretically informed intervention designed to address barriers to safer sexual behaviours and increase safer sexual behaviours in young people aged 16–24 years diagnosed with a STI or reporting unprotected sex with more than one partner in the last year. Our formative research and qualitative interviews have demonstrated the acceptability of the intervention and our pilot trial has demonstrated the feasibility of delivery of the intervention and the feasibility of conducting a main trial.
Patient and public involvement
Before developing the intervention we discussed possible safer sex interventions with young people based in a further education college. They were enthusiastic about receiving information and support by mobile phone. They reported that this mode of delivery was more private than other modes of delivery such as the internet, which is often monitored by parents.
Patients have been involved in designing the content of the intervention. The views of the target audience were collected in eight focus groups, which informed the tone, style, frequency, duration and content of the intervention (see Chapter 2).
King’s College Hospital, London, has an active user group of young people wishing to contribute to sexual and reproductive health research. We met with a group of 14 patient representatives to seek their views on the trial design. Their views influenced our follow-up procedures. They asked for materials to be posted by normal (not recorded) delivery in a coloured envelope and wanted a text message saying that materials had been posted so that they could look out for any packages. Most people were happy to provide urine or vaginal swabs by post, but a few wanted a clinic-based option and so this was included in the trial design. We modified the patient information, questionnaires and consent procedures based on feedback from this group and Keanu Taylor, our patient representative on the steering committee.
Adverse events
We collected data on car accidents as these are the only documented harm of text messaging.
There was no evidence of any differences in car accidents between the intervention group and the control group (control 1/80 vs. intervention 2/77; relative risk 2.08, 95% CI 0.19 to 22.6; p = 0.548).
Some participants deliberately shared messages but there were two instances in which participants reported that someone else had read their messages and that they were unhappy about this.
Strengths and weaknesses of the research
A key strength of the research was the use of multiple methods and a multidisciplinary team to address the challenges involved in the development and piloting research. We have shown that it is feasible to develop an intervention targeting safer sexual behaviours based on theory, known barriers to safer sexual behaviours, empirical evidence regarding the BCTs employed in effective face-to-face interventions and expert and user views, which recipients report is acceptable, comprehensible and relevant. The team was able to demonstrate the acceptability of the intervention in qualitative interviews, in a survey and in intervention recipients in the trial. We were able to conduct a successful pilot trial, which demonstrates the feasibility of delivery of the intervention and the feasibility of a main trial (recruitment and follow-up). Further work is needed to reliably establish the effectiveness of the intervention.
Strengths and weaknesses of the intervention development work
Our work on intervention development has some weaknesses: although the content associated with increased self-reported condom use is known,28 it remains unclear which BCTs are associated with increased effectiveness in reducing STIs. We therefore included all of the BCTs in face-to-face interventions evaluated by randomised controlled trial and reporting reductions in STIs at follow-up. To develop an intervention that was acceptable we excluded content that participants found to be unacceptable or irrelevant. Some evidence-based BCTs were modified based on feedback from young people and the effectiveness of the ‘acceptable’ but modified content is not yet known.
Although the current intervention is tailored by infection status and sex, it is not tailored according to specific personal issues with regard to adopting safer sex behaviours. Thus, messages sent may not all be directly relevant to every participant. During the conduct of our work a new internationally agreed taxonomy of BCTs was published. We included BCTs defined according to an older taxonomy in our intervention but coded the final intervention using the new internationally agreed taxonomy. The intervention requires further adaptation to ensure that the content is appropriate for men who have sex with men and women who have sex with women. We have received funding from the NIHR for a main trial and are carrying out these adaptations prior to starting the main trial.
Strengths and weaknesses of the development of the follow-up procedures work
To the best of our knowledge this is the first description of a systematic approach to developing follow-up procedures. The approach has resulted in a follow-up package. In the single case study of our pilot trial it was not possible to determine the effectiveness of the ‘follow-up package’ in isolation from other factors such as the management style and experience of the CTU and researchers conducting the pilot trial. It was not possible to determine which elements of the follow-up package are most important.
Strengths and weakness of the pilot trial
In the pilot trial we achieved high follow-up rates, allocation was concealed and laboratory staff and those analysing data were blind to allocation. Only one of the researchers double entering data was masked to allocation, whereas in a main trial there would be sufficient staff for all staff entering follow-up data to be masked to allocation. Given the small sample size and the large number of variables assessed, the baseline characteristics of the participants were reasonably well balanced. There were some imbalances between groups in the baseline characteristics of participants (ethnicity and infection status at recruitment). Nonetheless, as the primary outcomes for the pilot were recruitment and follow-up, the allocation balance would not impact on this. Although the response rate overall was high, the response rate for some questions, such as partner notification, was low. A larger sample size in a main trial would allow for better balance between the arms. The pilot trial was not powered for behavioural or STI outcomes and so 95% CIs for these outcomes were large and it is unsurprising that no outcomes were statistically significant when the multiple comparisons were taken into account.
Interpretation
A main trial to establish the effects of the intervention on STIs at 12 months should be conducted. In Chapter 2 we have provided a transparent description of the intervention content. Based on evaluations of the effectiveness and mechanism of action of the intervention we will be able to build on this work. BCTs may be added or removed to refine the intervention with the aim of enhancing its effectiveness. In Chapter 3 we have described an easy stepwise approach to developing trial follow-up procedures, which we have used to achieve a high follow-up rate in our pilot trial. Other researchers could adopt this approach to develop their trial follow-up procedures.
Potential implications for health care
The suggestion in our qualitative research is that the text messages had a positive effect on the promotion of safer sexual behaviours, particularly with reference to providing encouragement, support and skills relating to partner notification, with strong implications for infection control. Mathematic modelling suggests that the expected probability of chlamydial reinfection without partner notification is 19.4%; however, if a partner receives treatment within 3 days of the patient being treated this is reduced to 4.2%. 53 It is estimated that only around 40–60% of sexual contacts are notified by patient referral28,30 and so new strategies are needed to help improve the partner notification process. If the difficulties of notifying a partner can be lessened by giving young people the necessary skills to expedite the process, as described in our study, and reduce the time to treatment, the number of contacts informed through patient referral is likely to increase.
If our trial shows that the intervention is effective, it will be low cost and could be integrated with electronic systems so that it is automatically sent to patients when they receive their test results.
Implications of our research for the main trial
A number of factors have been identified in the pilot work that should influence the design of the intervention for the main trial and the design of the main trial.
Based on the findings from our qualitative research we have made changes to the intervention for the main trial. We have refined the message content so that it is relevant to men who have sex with men and women who have sex with women, for example by ensuring that pronouns used are gender neutral. We have included additional content providing examples of how others negotiated condom use in ongoing sexual relationships. We will include an option for more messages for those who want this and send additional messages regarding how to stop messages for those who would like to stop receiving messages.
A number of issues have informed the main trial design. There was a small amount of contamination (sharing messages) between the intervention group and the control group, which should be taken into account in the sample size calculation for the main trial. Only two of the infections at 12 months’ follow-up occurred in those who did not have an infection at baseline. Conducting a main trial including only those with an infection at the outset would provide a higher incidence of STIs at follow-up and allow for a smaller sample size than using the current inclusion criteria employed in the pilot trial. Our overall follow-up rate was high but the response rate to the question about partner notification was low. It may be that this question appeared to be optional as it was not relevant to all participants. In the main trial, a response to this question will be clearly requested from all participants and the main trial will also include an objective measure of partner notification. Services will search clinic records to identify whether named partners attended for treatment.
Digital technology is rapidly evolving and young people are often among the first to adopt new innovations and novel means of communication. Although young people continue to communicate by short written messages, these can now be delivered by instant messaging or by social media messaging as well as by text message. It is likely that novel means of delivering messages may be developed in the future. The way that messages are received (directly flashing up on the screen on a private device with the ability to reread content in your own time) is similar for text messages, instant messages and private social media messages. The NIHR has funded a main trial to reliably establish the effect of our safer sex intervention on STIs at 1 year. Our trial will reliably establish the effect of the written content of the intervention, which may in the future be delivered using different delivery mechanisms (instant messaging, private social media messaging).
Potential implications for other similar interventions
It is feasible for videos and other visual content to be delivered by mobile phone. We focused our intervention on written messages as in earlier pilot work employing videos (conducted prior to this research) we found that young people’s engagement with the video intervention was highly dependent on whether they related to the specific person (people) portrayed. This in turn depended on the style of clothes (and whether these were the very latest trends), accent, perceived socioeconomic background, gender and ethnicity of the person (people) involved. Thus, young people considered that video content went out of date rapidly, whereas written messages were not easily dated. We found that written content could be generated that was considered more socioeconomically, gender and ethnic group neutral. In our view the written content of the intervention would not need to be frequently updated, although checks would need to be carried out regularly to ensure that the links to websites provided remained current. Future research could consider using animated content in videos within interventions.
Our intervention and research focuses on high-risk groups attending services. We and other researchers have used text messages and social media to encourage high-risk groups to use existing and novel internet-based services. 16,54 In this research we have demonstrated that content delivered by IT targeting safer sex can be developed so that it is acceptable to young people. A range of social media and mobile IT could also be used to encourage high-risk people who are not currently service users to adopt safer sexual practices.
Conclusion
We have shown that it is feasible to develop an intervention targeting safer sexual behaviours based on theory, known barriers to safer sexual behaviours, empirical evidence regarding the BCTs employed in effective face-to-face interventions and expert and user views, which recipients report is acceptable, comprehensible and relevant. A full-scale randomised controlled trial is required to establish the effects of the intervention on the acquisition of STIs.
Protocol
The pilot trial protocol is in the appendices.
Acknowledgements
We would like to thanks the following services for their support in recruitment to the trial: Camberwell Sexual Health Centre, Cambridge Regional College, Palatine Contraception and Sexual Health Service Manchester, Maidstone Sexual and Reproductive Health Services and Huntingdonshire Regional College. We would also like to thank Melanie Otterwill for writing the first draft of the messages.
This study was funded by the NIHR HTA programme. The funders had no role in the design or execution of the pilot trial or the analysis or writing up of the results.
Contributions of authors
Caroline Free conceived the idea for the project, which was refined in discussion with Paula Baraitser.
Caroline Free took overall responsibility for the design, conduct, analysis and writing up of the project, and designed the studies drawing on intervention design methodologies developed by Susan Michie and with input from Ian Roberts on the randomised controlled trial design. All authors provided comments on the design of the studies. Caroline Free also generated additional messages selecting BCTs to address the factors known to influence safer sex behaviours.
Caroline Free reviewed the existing literature regarding factors influencing safer sex behaviours and, alongside Karen Devries, coded the content of existing face-to-face interventions according to the BCTs employed in interventions.
Ona McCarthy took responsibility for the day-to-day management of the pilot trial.
Ona McCarthy, Jonathan Syred and clinic staff organised the focus groups.
Caroline Free, Rebecca S French and Karen Devries reviewed the protocols of existing effective face-to-face interventions.
Caroline Free, Ona McCarthy and Rebecca S French ran the focus groups with young people and Caroline Free and Ona McCarthy worked with focus group participants to refine the intervention content.
Caroline Free, Rebecca S French, Kaye Wellings, Karen Devries, Julia Bailey and Paula Baraitser reviewed the preliminary content of the intervention and generated additional content.
Susan Michie provided advice regarding behaviour change and reviewed the behaviour change content of the intervention.
Karen Devries conducted the analysis of the intervention coding.
Ona McCarthy and Sujit Rathod each separately conducted the trial analysis.
Caroline Free, Ona McCarthy, Rebecca S French, Karen Devries and Sujit Rathod prepared the tables and figures.
Jonathan Syred and clinic staff recruited participants to the questionnaire study and Ona McCarthy analysed the data.
Ona McCarthy, Jonathan Syred and the clinic staff recruited patients to the pilot trial; Ona McCarthy conducted the pilot trial follow-up.
Phil Edwards provided statistical advice.
Caroline Free, Ona McCarthy, Rebecca S French and Ian Roberts developed the follow-up procedures with input from staff based in the LSHTM CTU and drawing on Phil Edwards’ previous research.
Caroline Free, Ona McCarthy, Rebecca S French, Kaye Wellings, Susan Michie, Ian Roberts, Karen Devries, Sujit Rathod, Julia Bailey, Jonathan Syred, Phil Edwards, Graham Hart, Melissa Palmer and Paula Baraitser commented on the writing up of the project.
Melissa Palmer prepared the lists of tables and figures.
Caroline Free, Ona McCarthy, Rebecca S French and Paula Baraitser wrote the report.
Publications
Published
French R, McCarthy O, Baraitser P, Wellings K, Bailey J, Free C. Young people’s views and experiences of a mobile phone texting intervention to promote safer sex behaviour. JMIR Mhealth Uhealth 2016:4;e26.
McCarthy O, French R, Roberts I, Free C. Simple steps to improve trial follow up procedures. Trials 2016;17:28.
Submitted
Burns K, Keating P, Free C. A systematic review of randomised control trials of sexual health interventions delivered by mobile technologies. BMC Public Health; submitted.
Free C, McCarthy O, French R, Devries K, Michie S, Wellings K, et al. Safetxt: The development of an intervention delivered by text message to increase safer sex behaviours. BMJ Open; submitted.
McCarthy O, French R, Baraitser P, Roberts I, Rathod S, Devries K, et al. Safetxt: a pilot randomised controlled trial of a mobile phone-based intervention to increase safer sex behaviours in young people. BMJ Open; submitted.
Data sharing statement
All data will be archived and anonymised data will be made available to other researchers on request to Ona McCarthy (Ona.mccarthy@lshtm.ac.uk).
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health.
References
- Sonnenberg P, Clifton S, Beddows S, Field N, Soldan K, Tanton C, et al. Prevalence, risk factors, and uptake of interventions for sexually transmitted infections in Britain: findings from the National Surveys of Sexual Attitudes and Lifestyles (Natsal). Lancet 2013;382:1795-806. http://dx.doi.org/10.1016/S0140-6736(13)61947-9.
- Cates W, Wasserheit JN. Genital chlamydial infections: epidemiology and reproductive sequelae. Am J Obstet Gynecol 1991;164:1771-81. http://dx.doi.org/10.1016/0002-9378(91)90559-A.
- Mercer CH, Tanton C, Prah P, Erens B, Sonnenberg P, Clifton S, et al. Changes in sexual attitudes and lifestyles in Britain through the life course and over time: findings from the National Surveys of Sexual Attitudes and Lifestyles (Natsal). Lancet 2013;382:1781-94. http://dx.doi.org/10.1016/S0140-6736(13)62035-8.
- Connell P, McKevitt C, Low N. Investigating ethnic differences in sexual health: focus groups with young people. Sexually Transm Infect 2004;80:300-5. http://dx.doi.org/10.1136/sti.2003.005181.
- Hosenfeld CB, Workowski KA, Berman S, Zaidi A, Dyson J, Mosure D, et al. Repeat infection with Chlamydia and gonorrhea among females: a systematic review of the literature. Sex Transm Dis 2009;36:478-89. http://dx.doi.org/10.1097/OLQ.0b013e3181a2a933.
- Free C, Roberts IG, Abramsky T, Fitzgerald M, Wensley F. A systematic review of randomised controlled trials of interventions promoting effective condom use. J Epidemiol Community Health 2009;65:100-10. http://dx.doi.org/10.1136/jech.2008.085456.
- French RS, Bonell C, Wellings K, Weatherburn P. An exploratory review of HIV prevention mass media campaigns targeting men who have sex with men. BMC Public Health 2014;14. http://dx.doi.org/10.1186/1471-2458-14-616.
- Estcourt C, Sutcliffe L, Mercer C, Copas A, Muniia P, Rait G, et al. Can accelerated partner therapy (APT) improve outcomes of partner notification for women diagnosed with genital chlamydia in primary care settings: a pilot randomized controlled trial in general practice and community sexual health services. Sex Transm Dis 2014;41:S32-3.
- Free C, Phillips G, Galli L, Watson L, Felix L, Edwards P, et al. The effectiveness of mobile-health technology-based health behaviour change or disease management interventions for health care consumers: a systematic review. PLOS MED 2013;10. http://dx.doi.org/10.1371/journal.pmed.1001362.
- Free C, Knight R, Robertson S, Whittaker R, Edwards P, Zhou W, et al. Smoking cessation support delivered via mobile phone text messaging (txt2stop): a single-blind, randomised trial. Lancet 2011;378:49-55. http://dx.doi.org/10.1016/S0140-6736(11)60701-0.
- Guerriera C, Cairns J, Roberts I, Rodgers A, Whittaker R, Free C. Txt2stop: a randomised controlled trial of a mobile phone based smoking cessation intervention: cost-effectiveness analysis. Eur J Health Econ 2012;14:789-97. http://dx.doi.org/10.1007/s10198-012-0424-5.
- Thomas N, Murray E, Rogstad KE. Confidentiality is essential if young people are to access sexual health services. Int J STD AIDS 2006;17:525-9. http://dx.doi.org/10.1258/095646206778145686.
- Free C, Whittaker R, Knight R, Abramsky T, Rodgers A, Roberts IG. Txt2stop: a pilot randomised controlled trial of mobile phone-based smoking cessation support. Tob Control 2009;18:88-91. http://dx.doi.org/10.1136/tc.2008.026146.
- Abraham C, Michie S. A taxonomy of behavior change techniques used in interventions. Health Psychol 2008;27:379-87. http://dx.doi.org/10.1037/0278-6133.27.3.379.
- de Tolly K, Skinner D, Nembaware V, Benjamin P. Investigation into the use of short message services to expand uptake of human immunodeficiency virus testing, and whether content and dosage have impact. Telemed J E Health 2012;18:18-23. http://dx.doi.org/10.1089/tmj.2011.0058.
- Gold J, Aitken CK, Dixon HG, Lim MSC, Gouillou M, Spelman T, et al. A randomised controlled trial using mobile advertising to promote safer sex and sun safety to young people. Health Educ Res 2011;26:782-94. http://dx.doi.org/10.1093/her/cyr020.
- Lim MS, Hocking JS, Aitken CK, Fairley CK, Jordan L, Lewis JA, et al. Impact of text and e-mail messaging on the sexual health of young people: a randomised controlled trial. J Epidemiol Community Health 2012;66:69-74. http://dx.doi.org/10.1136/jech.2009.100396.
- Downing SG, Cashman C, McNamee H, Penney D, Russell DB, Hellard ME. Increasing chlamydia test of re-infection rates using SMS reminders and incentives. Sex Transm Infect 2013;89:16-9. http://dx.doi.org/10.1136/sextrans-2011-050454.
- Suffoletto B, Akers A, McGinnis KA, Calabria J, Wiesenfeld HC, Clark DB. A sex risk reduction text-message program for young adult females discharged from the emergency department. J Adolesc Health 2013;53:387-93. http://dx.doi.org/10.1016/j.jadohealth.2013.04.006.
- Jones R, Hoover DR, Lacroix LJ. A randomized controlled trial of soap opera videos streamed to smartphones to reduce risk of sexually transmitted human immunodeficiency virus (HIV) in young urban African American women. Nurs Outlook 2013;61:205-15. http://dx.doi.org/10.1016/j.outlook.2013.03.006.
- Odeny TA, Bailey RC, Bukusi EA, Simoni JM, Tapia KA, Yuhas K, et al. Effect of text messaging to deter early resumption of sexual activity after male circumcision for HIV prevention: a randomized controlled trial. J Acquir Immune Defic Syndr 2014;65:e50-7. http://dx.doi.org/10.1097/QAI.0b013e3182a0a050.
- Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med 2013;46:81-95. http://dx.doi.org/10.1007/s12160-013-9486-6.
- Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci 2011;6. http://dx.doi.org/10.1186/1748-5908-6-42.
- Marston C, King E. Factors that shape young people’s sexual behaviour: a systematic review. Lancet 2006;368:1581-6. http://dx.doi.org/10.1016/S0140-6736(06)69662-1.
- Michie S, Johnston M, Abraham C, Lawton R, Parker D, Walker A, et al. Making psychological theory useful for implementing evidence based practice: a consensus approach. Qual Saf Health Care 2005;14:26-33. http://dx.doi.org/10.1136/qshc.2004.011155.
- Sheeran P, Abraham C, Orbell S. Psychological correlates of heterosexual condom use: a meta analysis. Psychol Bull 1999;125:90-132. http://dx.doi.org/10.1037/0033-2909.125.1.90.
- Michie S, Ashford S, Sniehotta FF, Dombrowski SU, Bishop A, French DP. A refined taxonomy of behaviour change techniques to help people change their physical activity and healthy eating behaviours: the CALO-RE taxonomy. Psychol Health 2011;26:1479-98. http://dx.doi.org/10.1080/08870446.2010.540664.
- Albarracin D, Gillette JC, Earl AN, Glasman LR, Durantini MR, Ho MH. A test of major assumptions about behavior change: a comprensive look at the effects of passive and active HIV prevention interventions since the beginning of the epidemic. Psychol Bull 2005;131:856-97. http://dx.doi.org/10.1037/0033-2909.131.6.856.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337. http://dx.doi.org/10.1136/bmj.a1655.
- Bartholomew LK, Parcel GS, Kok G, Gottlieb NH, Fernandez ME. Planning Health Promotion Programs. An Intervention Mapping Approach. San Francisco, CA: Jossey-Bass; 2011.
- Clutterbuck DJ, Flowers P, Barber T, Wilson H, Nelson M, Hedge B, et al. UK National Guidelines On Safer Sex Advice. Cheshire: The Clinical Effectiveness Group of the British Association for Sexual Health and HIV, The British HIV Association; 2012.
- Schulz KF, Grimes DA. Sample size slippages in randomised trials: exclusions and the lost and wayward. Lancet 2002;359:781-5. http://dx.doi.org/10.1016/S0140-6736(02)07882-0.
- Sackett D, Straus SE, Richardson WS, Rosenberg W, Haynes RB. Evidence-Based Medicine: How to Practice and Teach EBM. New York, NY: Churchill Livingstone; 2000.
- Toerien M, Brookes ST, Metcalfe C, de Salis I, Tomlin Z, Peters TJ, et al. A review of reporting of participant recruitment and retention in RCTs in six major journals. Trials 2009;10. http://dx.doi.org/10.1186/1745-6215-10-52.
- Erens B, Phelps A, Clifton S, Hussey D, Mercer CH, Tanton C, et al. The Third National Survey of Sexual Attitudes and Lifestyles (Natsal-3): Technical Report. London: Natsal; 2013.
- Low N, McCarthy A, Macleod J, Salisbury C, Horner PJ, Roberts TE, et al. The chlamydia screening studies: rationale and design. Sex Transm Infect 2004;80:342-8. http://dx.doi.org/10.1136/sti.2003.006197.
- Bailey JV, Pavlou M, Copas A, McCarthy O, Carswell K, Rait G, et al. The sexunzipped trial: optimizing the design of online randomized controlled trials. J Med Internet Res 2013;15. http://dx.doi.org/10.2196/jmir.2668.
- Edwards P, Roberts I, Clarke M, DiGuiseppi C, Pratap S, Wentz R, et al. Methods to increase response rates to postal questionnaires. Cochrane Database Syst Rev 2009;2.
- Brueton VC, Tierney J, Stenning S, Harding S, Meredith S, Nazareth I, et al. Strategies to improve retention in randomised trials. Cochrane Database Syst Rev 2013;12. http://dx.doi.org/10.1002/14651858.mr000032.pub2.
- Edwards P. Questionnaires in clinical trials: guidelines for optimal design and administration. Trials 2010;11. http://dx.doi.org/10.1186/1745-6215-11-2.
- Nakash RA, Hutton JL, Jørstad-Stein EC, Gates S, Lamb SE. Maximising response to postal questionnaires – a systematic review of randomised trials in health research. BMC Med Res Methodol 2006;6. http://dx.doi.org/10.1186/1471-2288-6-5.
- Edwards P, Roberts I, Sandercock P, Frost C. Follow-up by mail in clinical trials: does questionnaire length matter?. Controlled Clin Trials 2004;25:31-52. http://dx.doi.org/10.1016/j.cct.2003.08.013.
- Edwards P, Cooper R, Roberts I, Frost C. Meta-analysis of randomised trials of monetary incentives and response to mailed questionnaires. J Epidemiol Community Health 2005;59:987-99. http://dx.doi.org/10.1136/jech.2005.034397.
- Edwards P, Roberts I, Clarke M, DiGuiseppi C, Pratap S, Wentz R, et al. Increasing response rates to postal questionnaires: systematic review. BMJ 2002;324. http://dx.doi.org/10.1136/bmj.324.7347.1183.
- French R, McCarthy O, Baraitser P, Wellings K, Bailey J, Free C. Young people’s views and experiences of a mobile phone texting intervention to promote safer sex behaviour. JMIR Mhealth Uhealth 2016;4. http://dx.doi.org/10.2196/mhealth.4302.
- Michie S, Atkins L, West R. The Behaviour Change Wheel: a Guide to Designing Interventions. London: Silverback Publishing; 2014.
- Rodgers A, Corbett T, Bramley D, Riddell T, Wills M, Lin RB, et al. Do u smoke after txt? Results of a randomised trial of smoking cessation using mobile phone text messaging. Tob Control 2005;14:255-61. http://dx.doi.org/10.1136/tc.2005.011577.
- Low N, McCarthy A, Macleod J, Salisbury C, Campbell R, Roberts TE, et al. Epidemiological, social, diagnostic and economic evaluation of population screening for genital chlamydial infection. Health Technol Assess 2007;11. http://dx.doi.org/10.3310/hta11080.
- Herrmann B, Törner A, Low N, Klint M, Nilsson A, Velicko I, et al. Emergence and spread of Chlamydia trachomatis variant, Sweden. Emerg Infect Dis 2008;14:1462-5. http://dx.doi.org/10.3201/eid1409.080153.
- Boyer CB, Shafer MA, Shaffer RA, Brodine SK, Pollack LM, Betsinger K, et al. Evaluation of a cognitive-behavioral, group, randomized controlled intervention trial to prevent sexually transmitted infections and unintended pregnancies in young women. Prev Med 2005;40:420-31. http://dx.doi.org/10.1016/j.ypmed.2004.07.004.
- Perry RC, Kayekjian KC, Braun RA, Cantu M, Sheoran B, Chung PJ. Adolescents’ perspectives on the use of a text messaging service for preventive sexual health promotion. J Adolesc Health 2012;51:220-5. http://dx.doi.org/10.1016/j.jadohealth.2011.11.012.
- Kamb ML, Fishbein M, Douglas JM, Rhodes F, Rogers J, Bolan G, et al. Efficacy of risk-reduction counseling to prevent human immunodeficiency virus and sexually transmitted diseases: a randomized controlled trial. Project RESPECT Study Group. JAMA 1998;280:1161-7. http://dx.doi.org/10.1001/jama.280.13.1161.
- National Institute of Mental Health . The NIMH Multisite HIV Prevention Trial: reducing HIV sexual risk behavior. The National Institute of Mental Health (NIMH) Multisite HIV Prevention Trial Group. Science 1998;280:1889-94. http://dx.doi.org/10.1126/science.280.5371.1889.
- Wilson E, Free C, Morris TP, Kenward MG, Syred J, Baraitser P. Can internet-based sexual health services increase diagnoses of sexually transmitted infections (STIs)? Protocol for an evaluation of an internet-based STI testing and results service. JMIR Res Protoc 2016;5. http://dx.doi.org/10.2196/resprot.4094.
Appendix 1 Theoretical model
FIGURE 3.
Theoretical model.

Appendix 2 Topic guide for panels/focus groups
Part A
We are developing text messages for young people aged 16–24 years at risk of getting chlamydia.
-
What do you think we should cover in the messages?
-
What kind of messages should we send?
We are developing text messages to support young people who have been diagnosed with chlamydia.
-
What do you think we should cover in the messages?
-
What kind of messages should we send?
-
Are there any types of messages we shouldn’t send?
-
Is there anything else you would like to suggest about the messages and how we send them?
Prompts if not raised:
Should we cover examples of how other people have told their partner/condom use instructions/good and bad relationships or other/information about safer sex/negotiation skills – example of how other people negotiated safe sex or condom use/sexual pleasure?
Should the tone be jokey/like a friend/serious/like a doctor/nurse/counsellor/none of these?
Part B
Here are some messages that we have written. Please can you tell us what you think about each of them.
The whole group will be shown each message.
Prompts if not raised:
Are they easy to understand/relevant/helpful/irritating? Would you be happy to receive them? How would you improve them? Are there any you particularly like/dislike? Why?
Appendix 3 Texting sexual health study questionnaire
Version 4, Questionnaire (women).
Appendix 5 Pilot trial baseline questionnaire
Appendix 6 Questionnaire study results
| Sex | Message | % thought relevant | % thought not relevant | Outcome | Rationale |
|---|---|---|---|---|---|
| Female | Think about what you’re going to say. You could stick to facts, such as: it’s easy to treat and you can have it without knowing, so no one can really tell who had it first | 30 | 24 | Modified | Focus groups gave feedback on how to improve this message |
| Talking about sex with your partner can be awkward and embarrassing but the more you do it, the more comfortable and confident you feel | 32 | 34 | Discarded | < 40% reported relevant; > 30% reported not relevant | |
| Being light-hearted but sensitive can make your partner feel more encouraged rather than criticised | 32 | 42 | Modified | Focus groups found this message helpful | |
| Male | You made the right decision to get a test. Getting treated quickly means you are less likely to have any problems. Text 2 to hear about how others felt when they found out that their test was positive | 37 | 11 | Retained | Focus group feedback was favourable; may not have been relevant to survey participants who did not test positive for chlamydia |
| You might be thinking about how they’ll react when you tell them. It might help by warming up the conversation and easing into it | 37 | 48 | Modified | Focus groups gave feedback on how to improve this message | |
| Try rehearsing what you’re going to say. Plan when and where you’ll tell them. Text 2 to hear how others told their partner(s) | 33 | 30 | Discarded | < 40% reported relevant | |
| Talking about sex with your partner can be awkward and embarrassing but the more you do it, the more comfortable and confident you feel | 33 | 26 | Discarded | < 40% reported relevant |
Appendix 7 Pilot trial recruitment by enrolment mode
| Site | Assessed for eligibility, n | Not eligible, n | Eligible, n | Eligible but declined enrolment, n | Enrolled, n | Acceptance rate (by site), % (n/N) | Acceptance rate (by recruitment mode), % (n/N) |
|---|---|---|---|---|---|---|---|
| Camberwell Sexual Health Centre at King’s College Hospital, London | 305 | 139 | 166 | 35 | 131 | 79 (131/166) | Face to face: 69 (150/216) |
| Palatine Contraception and Sexual Health Service, Manchester | 48 | 10 | 38 | 30 | 8 | 21 (8/38) | |
| Cambridge Regional College | 15 | 5 | 10 | 1 (said yes, then left and never enrolled) | 9 | 90 (9/10) | |
| Huntingdonshire Regional College | 10 | 8 | 2 | 0 | 2 | 100 (2/2) | |
| LSHTM telephone referral | 92 | 7 | 85 | 35 (includes 10 who said yes but never enrolled) | 50 | 59 (50/85) | Telephone: 59 (50/85) |
| Overall: 66 (200/301) |
Appendix 8 Pilot trial secondary outcomes for participants with a sexually transmitted infection at baseline
| Outcome at month 1 | Group | Risk Ratio (95% CI) | p-value | |
|---|---|---|---|---|
| Control, n/N (%) | Intervention, n/N (%) | |||
| Took the treatment | 19/19 (100) | 18/19 (94.74) | 0.50 | |
| Avoided sex for 7 days | 16/19 (84.21) | 17/18 (94.44) | 1.12 (0.89 to 1.40) | 0.324 |
| Told the last person they had sex with to take treatment | ||||
| Yes | 19/21 (90.48) | 15/19 (78.95) | 0.84 (0.68 to 1.04) | 0.116 |
| No | 1/21 (4.76) | 3/19 (15.79) | Ref. | |
| Sort of | 1/21 (9.1) | 1/19 (5.26) | ||
| Avoided sex with this person for 7 days | ||||
| Yes | 17/19 (89.47) | 13/17 (76.47) | 1.02 (0.82 to 1.28) | 0.862 |
| No | 1/19 (5.26) | 0/17 (0.00) | Ref. | |
| Unsure | 1/19 (5.26) | 4/17 (23.53) | ||
| If there was someone else the participant was having sex with around the time they were diagnosed with a STI, did they tell this person to get treatment? | ||||
| Yes | 8/20 (40.0) | 9/21 (42.86) | 1.22 (0.65 to 2.31) | 0.763 |
| No | 1/20 (5.0) | 2/21 (9.52) | Ref. | |
| There wasn’t anyone else | 11/20 (55.0) | 10/21 (47.62) | ||
Appendix 9 Pilot trial secondary outcomes collected for all participants
| Outcome | Group | Risk ratio, (95% CI) | p-value | |
|---|---|---|---|---|
| Control, n/N (%) | Intervention, n/N (%) | |||
| Month 1 | ||||
| Condom use at last sex | 37/90 (41.11) | 29/92 (31.52) | 0.77 (0.52 to 1.13) | 0.183 |
| Sex with someone new since joining the study | ||||
| Yes | 27/84 (32.14) | 27/90 (30.0) | 0.93 (0.60 to 1.46) | 0.761 |
| No | 56/84 (66.67) | 63/90 (70.0) | Ref. | |
| Unsure | 1/84 (1.19) | 0/90 (0.0) | ||
| If sex with someone new since joining the study | ||||
| Condom use at last sex with someone new | 16/27 (59.26) | 15/27 (55.56) | 0.94 (0.59 to 1.49) | 0.785 |
| Participant took a STI test prior to first sex with someone new | 13/27 (48.15) | 16/27 (59.26) | 1.23 (0.74 to 2.04) | 0.421 |
| Partner took a STI test prior to first sex with them | 10/27 (37.04) | 2/27 (7.41) | 0.20 (0.05 to 0.84) | 0.028 |
| Sexual partners since joined the study | ||||
| 0 | 16/83 (19.28) | 17/89 (19.10) | Ref. | 0.081 |
| 1 | 47/83 (56.63) | 60/89 (67.42) | ||
| 2+ | 20/83 (24.10) | 12/89 (13.48) | 0.56 (0.29 to 1.07) | |
| Month 3 | ||||
| Chlamydia infection | 3/89 (3.37) | 6/82 (7.32) | 2.17 (0.56 to 8.43) | 0.263 |
| Month 12 | ||||
| Cumulative incidence of chlamydia | 15/101 (14.85) | 9/99 (9.09) | 0.61 (0.28 to 1.34) | 0.218 |
| Condom use at last sex | 23/83 (27.71) | 29/80 (36.25) | 1.30 (0.83 to 2.06) | 0.247 |
| Sex with someone new since joining the study | ||||
| Yes | 57/79 (72.15) | 50/78 (64.10) | 0.89 (0.71 to 1.10) | 0.283 |
| No | 21/79 (26.58) | 28/78 (35.90) | Ref. | |
| Unsure | 1/79 (1.27) | 0/77 (.00) | ||
| If sex with someone new since joining the study | ||||
| Condom use at last sex with someone new | 22/57 (38.60) | 18/50 (36.0) | 0.93 (0.57 to 1.53) | 0.783 |
| Participant took a STI test prior to first sex with someone new | 33/57 (57.89) | 19/50 (38.0) | 0.66 (0.43 to 0.99) | 0.049 |
| Partner took a STI test prior to first sex with them | 13/57 (22.81) | 8/50 (16.0) | 0.70 (0.32 to 1.56) | 0.384 |
| Sexual partners since joined the study | ||||
| 0 | 0/80 (0.00) | 2/77 (2.60) | Ref. | 0.812 |
| 1 | 41/80 (51.25) | 36/77 (46.75) | ||
| 2+ | 39/80 (48.75) | 39/77 (50.65) | 1.04 (0.76 to 1.42) | |
| Car accident where participant was the driver | 1/80 (1.25) | 2/77 (2.60) | 2.08 (0.19 to 22.62) | 0.548 |
Appendix 10 Pilot trial secondary outcomes for participants testing positive for a sexually transmitted infection after randomisation
| Outcome | Group | Risk ratio (95% CI) | p-value | |
|---|---|---|---|---|
| Control, n/N (%) | Intervention, n/N (%) | |||
| Took the treatment | 12/12 (100) | 15/15 (100) | ||
| Avoided sex for 7 days | 9/12 (75.0) | 14/15 (93.33) | 1.24 (0.87 to 1.78) | 0.234 |
| Told last person to take treatment | ||||
| Yes | 13/13 (100) | 15/17 (88.24) | 0.492 | |
| No | 0/13 (0/0) | 1/17 (5.88) | ||
| Sort of | 0/13 (0.0) | 1/17 (5.88) | ||
| Avoided sex with this person for 7 days | ||||
| Yes | 9/12 (75.0) | 14/14 (100) | 0.91 (0.65 to 1.28) | 0.597 |
| No | 1/12 (8.33) | 0/14 (0.00) | Ref. | |
| Unsure | 2/12 (16.67) | 0/14 (0.00) | ||
| If there was someone else the participant was having sex with around the time they were diagnosed with a STI, did they tell this person to get treatment? | ||||
| Yes | 3/10 (30.0) | 4/14 (28.57) | 0.95 (0.26 to 3.44) | 0.941 |
| No | 0/10 (0.0) | 1/14 (7.14) | Ref. | |
| There wasn’t anyone else | 7/10 (70.0) | 9/14 (64.29) | ||
List of abbreviations
- BCT
- behaviour change technique
- CI
- confidence interval
- ClaSS
- Chlamydia Screening Studies
- COM-B
- capability, opportunity and motivation model of behaviour
- CTU
- Clinical Trials Unit
- HIV
- human immunodeficiency virus
- HTA
- Health Technology Assessment
- IT
- information technology
- LSHTM
- London School of Hygiene & Tropical Medicine
- Natsal
- National Survey of Sexual Attitudes and Lifestyles
- NIHR
- National Institute for Health Research
- NSU
- non-specific urethritis
- STI
- sexually transmitted infection