Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 12/137/05. The contractual start date was in September 2014. The draft report began editorial review in June 2017 and was accepted for publication in October 2017. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Eleanor McGee was the manager of the First Steps children’s weight management programme (the programme on which this study is based). Peymane Adab is a member of the National Institute for Health Research (NIHR) Public Health Research Funding Board. Jayne Parry undertakes committee work for the NIHR that attracts a small stipend, which is paid directly to the University of Birmingham where she is employed full-time.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2019. This work was produced by Pallan et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2019 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
Epidemiology of childhood overweight and obesity
In England, 9% of 4- and 5-year-olds are classified as obese and a further 13% are classified as overweight. By age 10 and 11 years, the prevalence significantly increases, with 20% being obese and 14% being overweight. 1 Ethnic differences in childhood obesity prevalence exist, with the prevalence in 10- to 11-year-old South Asian children (those originating from the Indian subcontinent, including Pakistan and Bangladesh) at 25% compared with 18% in white children. 1 Specifically, Pakistani and Bangladeshi children have higher obesity levels than white British children; at ages 10 and 11 years, 28% and 33% of Pakistani and Bangladeshi boys were classified as obese in 2014/15 compared with 19% of white British boys, and 22% of Pakistani and Bangladeshi girls were classified as compared with 16% of white British girls. 2
Obesity is associated with a range of physical, psychological and social consequences in childhood,3 and up to 80% of obese children will remain obese in adulthood. 4 Obesity in adulthood is a risk factor for a variety of health consequences, including certain cancers, cardiovascular disease and type 2 diabetes mellitus;5,6 thus, it is a major contributor to morbidity and premature mortality. The economic costs associated with overweight and obesity-related ill-health are considerable. Costs to the NHS in England were estimated to be £5.1B in 2006/7. 7 In addition, there are societal costs associated with a reduction in years of disability-free life, increased absences from work and early retirement, increased morbidity for those of working age and reductions in productivity. 8
South Asians are the largest minority ethnic population in the UK and are particularly susceptible to the health consequences of obesity. South Asians have higher levels of body fat and central obesity than white European populations9 and are more vulnerable to the cardiometabolic consequences of obesity than other ethnic groups in the UK. 10 Markers of increased cardiovascular risk are seen in South Asians, even in childhood. 11 Thus, South Asians represent an important target group for obesity intervention, particularly in childhood, given the disparity in obesity prevalence in children.
Effectiveness of current programmes addressing overweight and obesity in children
Evidence to date for effective childhood obesity behavioural treatment programmes is limited. In the Cochrane review conducted by Luttikhuis et al. 12 in 2009, a meta-analysis of a small subset of high-quality studies showed that behavioural intervention programmes have a small but clinically significant effect on weight status at 6 months post intervention [a reduction in body mass index (BMI) z-score of 0.06 and 0.14 compared with standard care in preadolescents and adolescents, respectively]. However, the review highlighted a range of methodological issues within the included studies, such as insufficient power, lack of allocation concealment, high attrition rates and lack of intention-to-treat analysis. Therefore, it was difficult to draw firm conclusions. Clinically meaningful effects on anthropometric measures have been reported in more recent randomised controlled trials (RCTs) of behavioural intervention programmes13–16 and in a comprehensive evidence review that informed the 2013 National Institute for Health and Care Excellence (NICE)’s guidance on children’s weight management [public health guideline (PH) number 47],17 which included meta-analyses to estimate the pooled intervention effect of behavioural programmes targeting children and their parents or families. A 0.2 reduction in BMI z-score at the end of the intervention and a 0.1 reduction at the 6-month follow-up compared with standard care was estimated from 8 and 11 studies, respectively. 17 Evidence from studies suggests that even such small reductions in BMI z-score could lead to clinical improvements. 18 The absence of data on the cost-effectiveness of childhood obesity behavioural treatment interventions and the lack of data on longer-term outcomes have been highlighted. 12,19
Critical elements of effective programmes
Owing to limitations of the evidence, the most effective intervention components of behavioural child weight management programmes are, as yet, undetermined. In most studies to date, the measurement of processes and an assessment of the fidelity of programme delivery have not been undertaken or reported,12,20 which limits the interpretation of outcomes and assessment of which elements of the programme are likely to have had the most influence. However, the available evidence suggests that, in the preadolescent age group, interventions that address both diet and physical activity, include behavioural elements and involve parents are the most promising,12,20,21 although the specific nature of this parental engagement still needs to be determined. 21,22
Evidence of the clinical effectiveness of overweight and obesity management programmes in minority ethnic children
Evidence evaluating the clinical effectiveness of childhood obesity treatment programmes in minority ethnic populations is also limited and studies were undertaken mainly in the USA. 23–26 Existing studies have evaluated programmes with adaptations such as the delivery of materials in different languages, the tailoring of nutritional content and the ethnic matching of programme providers. Two RCTs that evaluated culturally adapted interventions, one targeting Chinese American children aged 8–10 years24 and the other targeting a mixed population of Hispanic, black and white children aged 8–16 years,25 have reported small to moderate reductions in BMI z-score in the intervention compared with the control groups (controls received no intervention and a low-intensity clinic-based intervention, respectively). Effects appeared to be sustained for at least 8 months. Another uncontrolled study in a Latino community in the USA reported positive effects on dietary and physical activity behaviours but no effect on BMI. 26 Furthermore, there is evidence to suggest that interventions delivered in multiethnic populations may have a differential effect; a recent RCT of a multidisciplinary intervention targeting obese adolescents in the Netherlands reported a 0.35 reduction in BMI z-score over 18 months in participants of Western descent but no BMI z-score reduction in participants of other ethnicities. 27
In the UK, one small RCT (n = 72) has been undertaken to evaluate the clinical effectiveness of a family-based behavioural treatment programme targeting obese children in an ethnically and socioeconomically diverse community of 8- to 12-year-old children (of whom 43% were non-white European). The programme, originally developed in the USA,28 was not culturally adapted and, although acceptable to the target population,29 it did not have a significant effect on weight. 30
Retention in children’s weight management programmes
Previous studies suggest that there is an association between better programme attendance and the weight loss achieved in children’s weight management programmes;14 however, retention of participants has been highlighted as a problem. Programme characteristics that are associated with greater dropout include having large group sizes and logistical barriers to attendance. 31,32 Lower retention in programmes has also been reported to be associated with socioeconomic disadvantage32 and ethnicity. 33,34
Development of culturally adapted children’s weight management programmes
To date, theoretical approaches to the cultural adaptation of child weight management programmes have been lacking,23 and little has been done in the way of evaluating the success of cultural adaptation of obesity treatment and health promotion programmes in general. In a comprehensive evidence synthesis review on the adaptation of health promotion programmes for minority ethnic groups, Liu et al. 35 stated the requirement for future trials to compare culturally adapted programmes with standard programmes.
Provision of childhood obesity treatment services in the UK
Although in the last 15 years there has been widespread provision of children’s weight management services across the UK,36 no programmes have been specifically designed to meet the needs of ethnically and culturally diverse communities, such as those living in many large cities in the UK. In Birmingham, the UK’s second largest city, 42% of the total population and 59% of the 0- to 15-year-old population are from minority ethnic communities. More than half of these residents are of South Asian ethnicity, although the great majority were born in the UK. 37
Since 2010, a child weight management programme, First Steps (a weekly programme delivered over a school half-term that targets parents), has been available in Birmingham. Participants are referred through health professionals, schools or the National Child Measurement Programme (NCMP) or are self-referred. Over one-third of the referrals received by the service have been for children and families from Pakistani and Bangladeshi communities, but an analysis of routine service data has highlighted differences in completion rates between different ethnic groups. Pakistani and Bangladeshi families are as likely to start attending the programme as other families but are less likely to complete the programme, which suggests that it is less well suited to families from these communities. Of those starting the First Steps programme, 40% of Pakistani and Bangladeshi families completed it compared with 65% of white British and African-Caribbean families.
Although there may be a number of reasons for this difference in completion, it may imply that aspects of the current programme are not culturally relevant to Pakistani and Bangladeshi families. The existing weight management programme in Birmingham has developed over time, based on research evidence and service provider experience, to try to make it more acceptable to the community that it serves. Prior to the introduction of First Steps in Birmingham, established and evidence-based child weight management programmes, such as Mind, Exercise, Nutrition . . . Do it! (MEND)13 and Watch It,38 had been commissioned. However, the intensity and duration of the courses resulted in very low uptake rates and high attrition, and service providers identified that there was a lack of flexibility to tailor the programmes to accommodate cultural and language requirements. The First Steps programme was designed to be more suited to the local population by placing a greater focus on parental engagement, increasing the visual programme content, including culturally appropriate foods in the programme materials and providing interpreters. Elements of the Watch It and MEND programmes that were observed to have worked in the local population were retained in First Steps (specific behaviour change strategies, and some nutrition content). Other elements that were incorporated were consistent with the evidence base. Routinely collected data at the first and last sessions of First Steps indicated that those who completed the programme achieved an average reduction in BMI z-score of 0.1 at programme end, which is comparable to effect sizes reported in clinical trials. 12 Given the evolution of the First Steps programme in the local ethnically diverse population, it provided a good foundation on which to develop a new programme that incorporated further cultural adaptations.
Rationale for the CHANGE study
The focus of the Child weigHt mANaGement for Ethnically diverse communities (CHANGE) study was to further develop and culturally adapt the current First Steps programme, using a theoretically informed approach, such that it better met the needs of the Pakistani and Bangladeshi communities within Birmingham. However, a programme delivered to families from only these communities would not address the needs of the wide range of cultural communities found in a city such as Birmingham. Communities across Birmingham provide an example of super-diversity, a term used to characterise the complexity of modern communities in Britain, in which there are dynamic relationships between multiple variables, including country of origin, ethnicity, language, religion, regional/local identities, migration history and experience, and immigration status. 39,40 This complexity creates a challenge to health-care providers to meet the health needs of all members of society. Thus, this study aimed to develop a programme that was culturally adapted to meet the needs of Pakistani and Bangladeshi families but that would also be flexible enough to accommodate the needs of all families and could be transferred to communities with a different cultural and ethnic composition. To ensure that the developed programme was suitable for all, we evaluated it in a feasibility study involving families from different ethnic and cultural backgrounds.
Chapter 2 Study design
Aims and objectives
Study aims
The CHANGE study was designed in two phases. In the first phase, we aimed to adapt a weight management programme for children aged 4–11 years and their families, and to make it culturally relevant to Pakistani and Bangladeshi communities but also appropriate for families from all communities. In the second phase, we aimed to undertake a feasibility study of the culturally adapted intervention programme, using a cluster randomised design to compare the culturally adapted programme with the standard weight management programme.
Phase I objectives
-
To explore factors that promote or discourage engagement with, and completion of, existing childhood obesity treatment programmes among Pakistani and Bangladeshi families in the UK.
-
To use this information, together with existing research evidence and theoretical frameworks for cultural adaptation and complex intervention development, to design a theoretically informed childhood obesity treatment programme that is appropriate for all families but is culturally adapted to meet the particular needs of Pakistani and Bangladeshi families.
Phase II objectives
-
To assess the proportion of Pakistani and Bangladeshi families and the proportion of all families completing the adapted programme.
-
To assess the acceptability of the programme to Pakistani and Bangladeshi families and families from other ethnic groups.
-
To assess the feasibility of delivery of the adapted programme.
-
To assess the feasibility of participant recruitment, randomisation and follow-up.
-
To assess the feasibility of the collection of cost data from both a health and societal perspective to inform a future trial that evaluates intervention clinical effectiveness and cost-effectiveness.
-
To collect data on recruitment, attrition and other relevant measures to inform the parameters of any future trial.
Design and setting
Study design
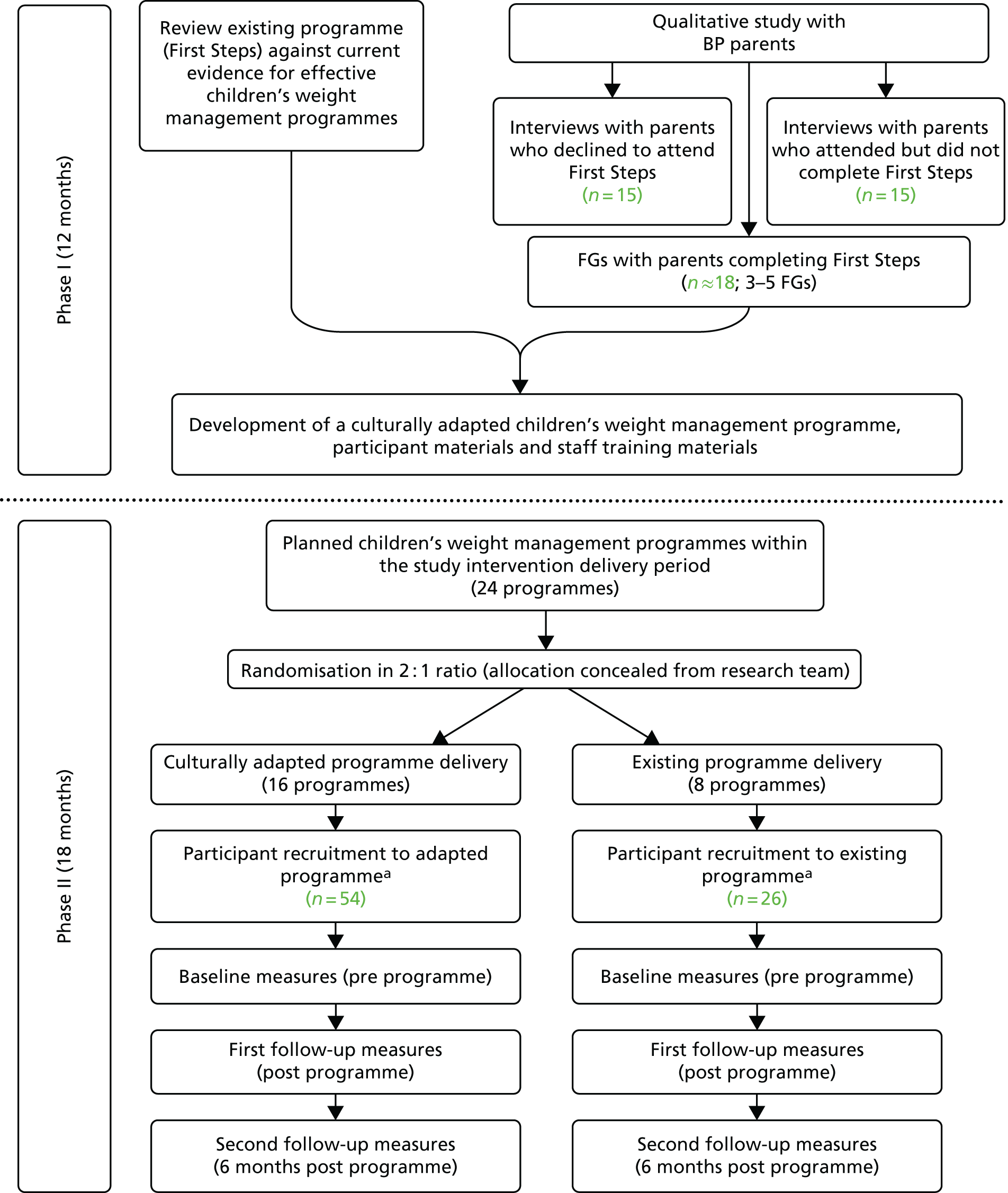
The first phase addressed the theoretical and modelling stages of the UK Medical Research Council’s framework for the development and evaluation of complex health interventions. 41,42 It involved adaptation of the current children’s weight management programme delivered in Birmingham, UK (First Steps). The adaptation process was informed by research evidence relating to the clinical effectiveness of childhood obesity treatment programmes and the experiences and view points of Pakistani and Bangladeshi families who had participated, or initially agreed but then declined to participate, in the current programme. The intervention adaptation process was guided by theoretical frameworks for complex intervention development and for adaptation of health promotion programmes for minority ethnic groups. 35,43 The second phase addressed the feasibility stage of the Medical Research Council’s complex health intervention framework. We conducted a two-arm cluster randomised feasibility study that compared the culturally adapted programme with the existing programme. Programmes were randomised to be delivered as either the adapted or the standard programme in a 2 : 1 ratio. This ratio was used to ensure that there were a sufficient number of families in the intervention arm to enable calculation of the primary outcome of the proportion of Pakistani and Bangladeshi families completing the adapted programme. Data were collected from participants at three time points: before programme attendance, after programme completion and 6 months after programme completion. The study design is summarised in Figure 1.
FIGURE 1.
The CHANGE study flow chart: study design and participants. a, Participants are blind to the allocation of the programme that they are attending. BP, Bangladeshi or Pakistani; FG, focus group.
The study took place in Birmingham, which is the UK’s second largest city and has a population of nearly 1.1 million. Of this population, 16.5% are from Pakistani and Bangladeshi communities. Pakistani and Bangladeshi children constitute 26% of the Birmingham population that is aged 0–15 years. 37
At the time of the study, all families resident in Birmingham with a child aged 4–11 years who had a BMI over the 91st centile of the UK’s 1990 growth reference charts44 were eligible to attend the First Steps children’s weight management programme (the programme that was adapted in this study). First Steps was commissioned by Birmingham City Council and delivered by Birmingham Community Healthcare NHS Trust (BCHCT). Children could be referred to the programme through several different routes: via health professionals, schools, the NCMP or self-referral. First Steps was a group-based programme delivered as weekly 1-hour sessions over 5–7 weeks in community venues. Session content included nutrition education, physical activity promotion and the promotion of positive lifestyle behaviour changes. The programme was aimed at parents/carers and children attended only the first and last sessions, at which their height and weight were measured. Participants for both phases of the study were identified through the existing children’s weight management services in Birmingham.
Public and patient involvement
A panel of parents of primary school-aged children from Bangladeshi and Pakistani communities was convened for the duration of the study. The Parent Advisory Panel was consulted at specific stages of the study to enable them to bring their values to the project and ensure that the development of the programme, outcome measures and research procedures were culturally appropriate. Input from the panel was sought for the planning of the qualitative studies in both phases I and II, the adapted intervention design, the planning of data collection procedures in the phase II feasibility study, the plans for disseminating the study findings and the preparation of the Plain English summary of the report. There was also a public member of the Study Steering Committee from the Pakistani community in Birmingham.
Study management
The study was overseen by an externally appointed, independent Study Steering Committee comprising three subject experts (two public health specialists with an interest in childhood obesity prevention and management and an expert on equality and diversity in relation to health and social care) and a public representative. A study management group, comprising the principal investigator, the study co-ordinator and two co-investigators, met regularly to guide the conduct of the study.
Ethics approval and study registration
Ethics approval was obtained in July 2014 from Edgbaston NHS Research Ethics Committee, West Midlands, UK (reference number 14/WM/1036). The study was registered with the International Standard Randomised Controlled Trial Register as reference number ISRCTN81798055. The original study protocol was sent to and was approved by the National Institute for Health Research (NIHR) Health Technology Assessment programme on 31 July 2014. A number of revisions and additions were made to the protocol during the course of the study and these are shown in Appendix 1. The final protocol was published as a journal article in 2016. 45
Chapter 3 Phase I: intervention design
Methods
Information from three main sources was used in the adaptation process: (1) data from a qualitative study conducted with Pakistani and Bangladeshi parents/carers of children with excess weight, who had previously had some contact with the First Steps programme; (2) local information from the First Steps programme that was being delivered at the time; and (3) existing children’s weight management literature.
The information collected was then used in the adaptation process that was guided by two theoretical frameworks. The behaviour change wheel (BCW)43,46 ensured that the pathways to change and how these were addressed in the adapted intervention were clearly articulated. The typology of cultural adaptation and health promotion programme theory proposed by Liu et al. 35 ensured that appropriate cultural adaptations across all aspects of the programme were considered for inclusion in the adapted intervention.
The methods for obtaining data to inform intervention adaptation and the process of adaptation itself are described in detail in the following sections.
Qualitative study with Pakistani and Bangladeshi parents
Community researchers
Researchers from Pakistani and Bangladeshi communities in Birmingham with qualitative research experience were recruited for this part of the study [community researchers: Aisha Ahmad (of Pakistani heritage), and Minara Bibi and Salma Khan (of Bangladeshi heritage)]. The community researchers received bespoke training to work alongside the study research team (Tania Griffin and Laura Griffith; both of white British heritage) to recruit participants and undertake interviews and focus groups (FGs). The community researchers were able to communicate in Urdu, Bengali, Mirpuri or Sylheti, when necessary, and to understand the cultural context of participating families.
Participants
The BCHCT identified all families that had been invited to take part in the First Steps programme from September 2013 to July 2014 (1 school year). The eligibility criteria for family participation in the First Steps programme were having a child aged 4–11 years with a BMI z-score on the 91st percentile or above and the ability of the child to attend and participate in a group setting. The families were categorised as (1) attended ≥ 60% of the First Steps programme (‘completers’); (2) started the First Steps programme but attended < 60% (‘non-completers’); or (3) did not attend the programme (‘non-attenders’). The BCHCT contacted families to explain the CHANGE study and confirm whether or not the family agreed for their details to be forwarded to the CHANGE study research team. Parents who did not speak English were contacted by the BCHCT in their preferred language. The university research team received contact details for families that had verbally agreed for their information to be passed on.
The research team sent a study invitation letter with a parent and child information sheet to all potential participants for whom they had contact details. These documents were reviewed by the Parent Advisory Panel (comprising Pakistani and Bangladeshi parents) to make sure that they conveyed information clearly and appropriately. To make provision for parents who did not speak English, a cover letter, translated into Urdu and Bengali, was included with the study information. This explained that they were being invited to take part in a research study relating to children’s weight management and that they would receive a telephone call in the next few days in which the study would be explained to them in detail in their preferred language. Within 7 days, potential participants were contacted by telephone and asked if they had any questions about the study and whether or not they would like to participate. If they were happy to participate, ‘non-completers’ and ‘non-attenders’ were asked if they would be willing to participate in a face-to-face interview or, if this was not possible, a telephone interview. ‘Completers’ were asked whether or not they would be willing to attend a FG in a community venue. FGs were the preferred method of data collection, as they explicitly use group interaction as a way of stimulating discussion. 47 However, to maximise participation, individual interviews were deemed to be more appropriate for participants in the first two groups, as they had not fully engaged with the First Steps programme and were, therefore, less likely to engage with FGs. We aimed to recruit 15 ‘non-completers’ and 15 ‘non-attenders’ to participate in interviews and to hold 3–5 FGs with ‘completers’. If a participant who had completed First Steps was unable to attend a FG but wanted to provide feedback, they were offered a one-to-one interview as an alternative. All participants received a £10 shopping voucher. The recruitment process is summarised in Figure 2.
FIGURE 2.
The CHANGE study phase I participant recruitment.

Data collection
Interviews took place in the participants’ homes. FG locations were selected to be as convenient as possible, based on the postcodes of potential participants. Along with the information sheets, potential participants were also sent an invitation card detailing their closest FG, location date and time. Before the interview or FG commenced, participants were asked to give written informed consent and to complete a short questionnaire asking for demographic information about themselves and their family (see Appendix 2). Interviews and FGs were conducted by either a CHANGE study researcher or a community researcher with the relevant language skills. At the FGs, an observer was present in addition to the facilitator.
All researchers conducting interviews and FGs were trained in qualitative data collection and analysis and had attended CHANGE study-specific training and so were aware of the context of the study for follow-up questions. Semistructured interview and FG schedules were developed, which were informed by literature and input from the study Parent Advisory Panel. In addition to a general exploration of participants’ experiences of the First Steps programme, the specific research questions that were explored are shown in Box 1. The full interview and FG schedules can be found in Appendix 3.
-
What are the barriers to, and facilitators of, participating in and completing the programme?
-
Which aspects of the structure, content and delivery of the programme are perceived as problems?
-
Which aspects of the structure, content and delivery of the programme are valued?
-
What information, content or format would increase the appeal of the programme?
-
What might need to change about the current programme to ensure its cultural relevance?
Reproduced with permission from Pallan et al. 48 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/.
Researchers recorded their observations and reflections after each interview or FG to provide context to local and cultural understandings and references and assist in interpretation at the data analysis stage.
Interviews and FGs recorded in English were transcribed verbatim and anonymised by an external transcription company (Clayton Research Support, Old Stratford, UK). Those conducted in a different language were translated and transcribed by the community researchers. A sample of translated transcripts was checked against the audio-recording by an independent researcher who understood the relevant language to check for accuracy. If a participant requested that an interview was not recorded, the researcher wrote notes summarising the interview content.
Data analysis
Data analysis was guided by thematic analysis approaches and used similar techniques to those developed by the Health Experiences Research Group at the University of Oxford. 49 Two researchers (Tania Griffin and Laura Griffith) reviewed the transcripts independently (approximately 50% each) and identified themes and codes to apply to the data. The researchers discussed their allocated codes, especially when differences occurred, and agreed on a final coding framework, which was then applied to all transcripts using NVivo version 10 (QSR International, Warrington, UK). Overarching themes from the data were then identified. Particular attention was given to the identification of whether or not there were differences between the three participant groups.
Review of children’s weight management literature
A comprehensive guideline on managing overweight and obesity in children was published in 2013 by NICE. 17 Two evidence reviews were undertaken to support the development of this guideline: one was a review of the clinical effectiveness and cost-effectiveness of interventions to manage children’s weight50 and the other was a review of the barriers to, and facilitators of, implementing weight management programmes for children. 51 These reviews, together with more recent evidence on effective children’s obesity interventions, were referred to when planning the adapted intervention to ensure that it was coherent with the established evidence base on children’s weight management intervention. A systematic review of behaviour change techniques that are effective in influencing obesity-related behaviours in children was also identified52 and, again, it was ensured that the planning of the intervention was consistent with information from this evidence synthesis.
Information from the existing children’s weight management service
Direct observation of the current children’s weight management programme was undertaken to assess how the structure, content and delivery worked in practice. Observations were undertaken by a researcher (Tania Griffin), who made notes on the delivery of the programme by the facilitator, and the response and engagement of the participants who were present. In addition, the service managers were consulted so that a clear picture of the existing infrastructure and processes was gained, and current concerns with the programme were highlighted.
Process of intervention development
Application of the behaviour change wheel
The BCW framework,43,46 shown in Figure 3, was used to guide the adaptation process. This framework for intervention development has been developed from 19 behaviour change frameworks and incorporates a broad range of drivers of behaviour (e.g. individual perceptions and beliefs, unconscious biases and the social environment). The first step in the BCW is the identification of target behaviours requiring change. We identified that there are two different levels of family engagement with a children’s weight management programme; the first is continuing attendance at the programme sessions and the second is the change in health behaviours in response to the programme content. Therefore, three target behaviours requiring change were identified: (1) programme attendance, (2) dietary intake and (3) physical activity.
FIGURE 3.
The behaviour change wheel. Reproduced with permission from Michie et al. 46 Copyright © Susan Michie, Lou Atkins and Robert West 2014. All rights reserved.
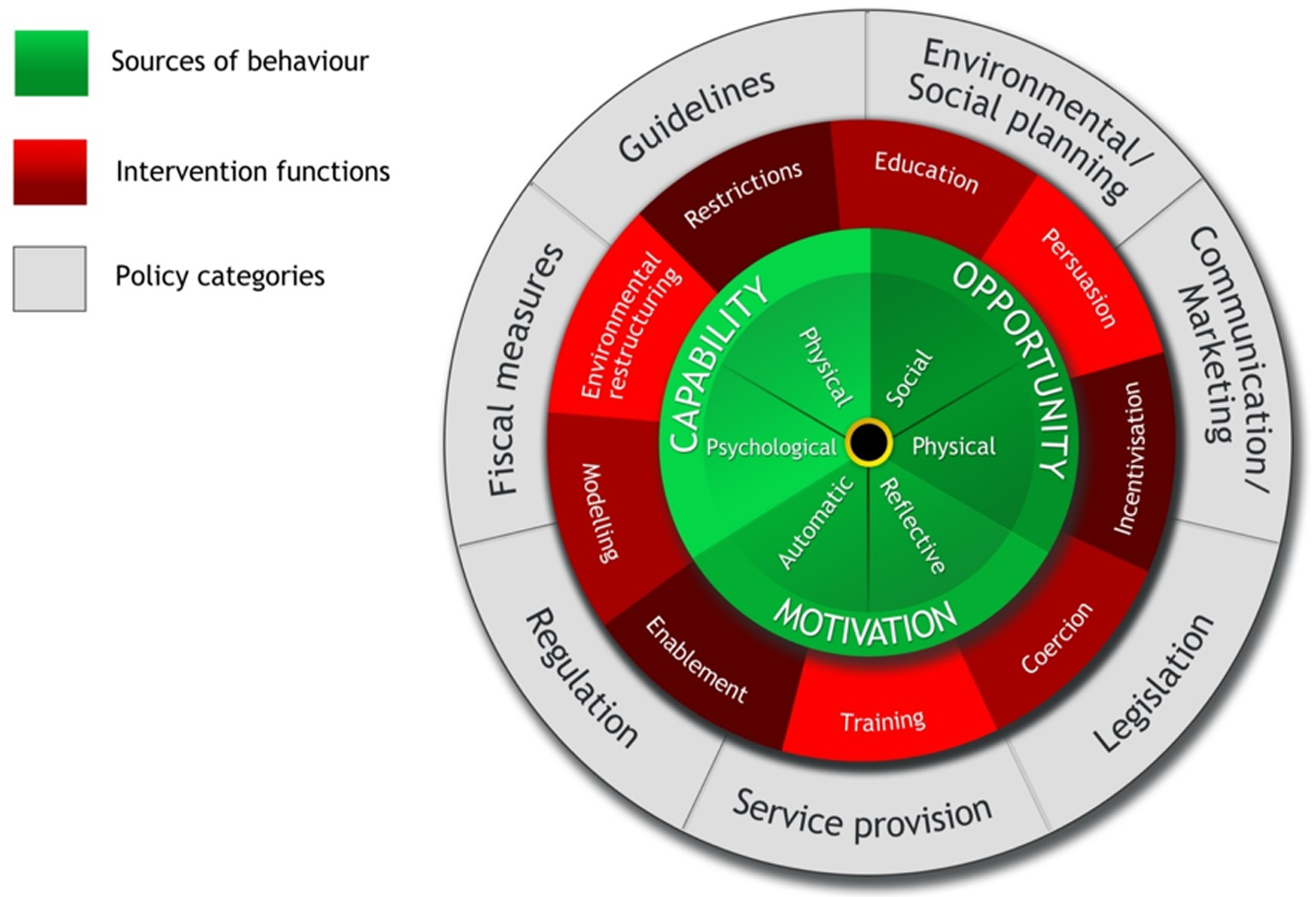
The capability, opportunity, motivation and behaviour (COM-B) model at the centre of the BCW is a diagnostic tool to help understand the factors preventing improvement in the target behaviours. The three elements of this model are further broken down into physical capability (physical skill, strength and stamina), psychological capability (psychological skills to engage in the necessary mental processes), physical opportunity (opportunity provided by the environment, involving time, resources, locations, etc.), social opportunity (opportunity provided by interpersonal influences, social cues, cultural norms, etc.), reflective motivation (reflective processes, involving planning and evaluation) and automatic motivation (automatic processes involving emotional reactions, desires, impulses, inhibitions, etc.). We mapped the qualitative data from parents to the different elements of the COM-B model to gain a theoretical understanding of the factors preventing Pakistani and Bangladeshi families from adopting the desired behaviours. The BCW outlines nine different intervention functions (i.e. categories of mechanisms by which interventions may have their effects; see Figure 3). For each aspect of capability, opportunity and motivation, there are corresponding intervention functions that have been identified as being the most likely to achieve change. Once we had an understanding of which drivers of behaviour needed to change, we identified the corresponding intervention functions. This informed the detailed intervention planning.
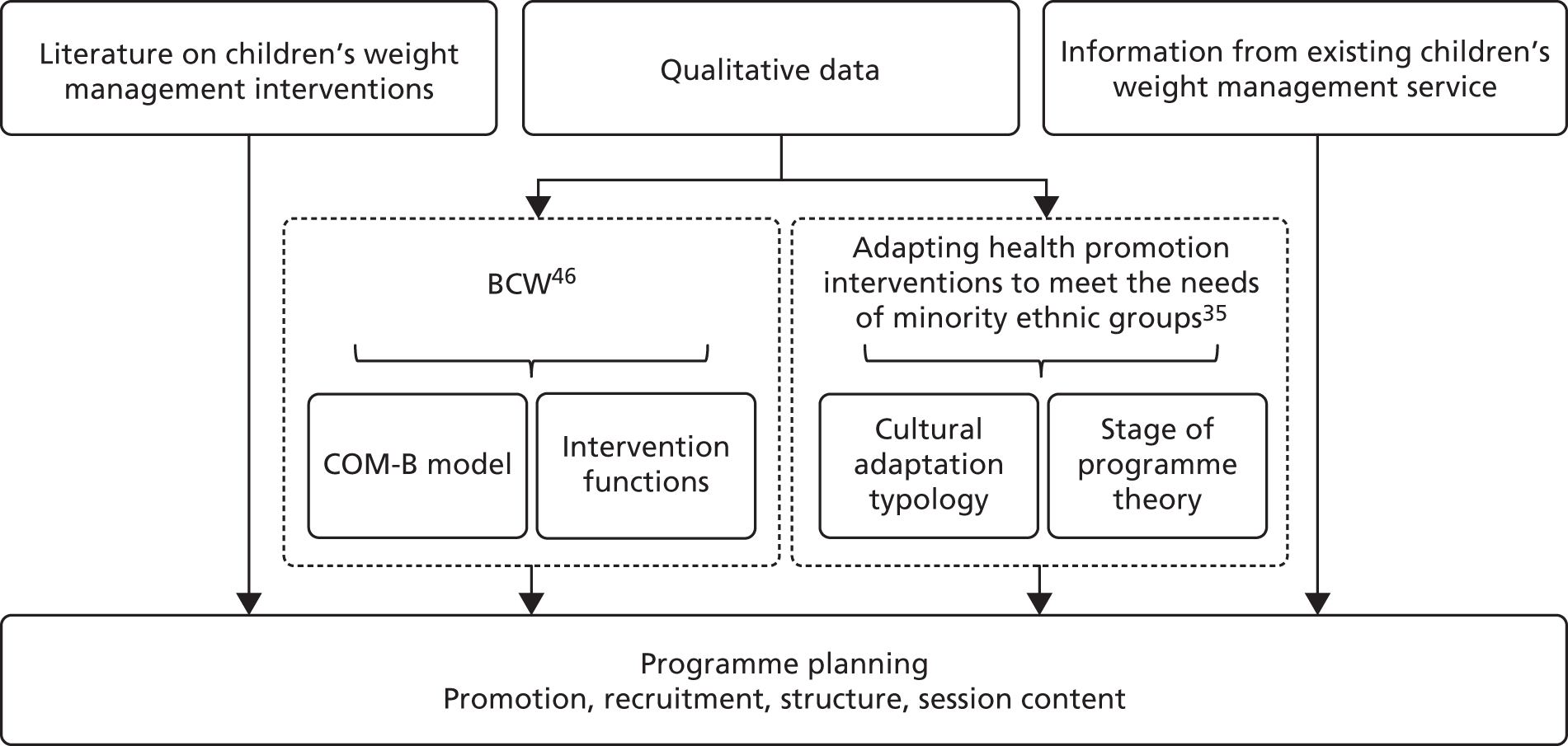
Cultural adaptation using the typology of cultural adaptation and health promotion programme theory
In parallel with the BCW, another theoretical adaptation process was employed specifically to address adaptation of the programme to make it more culturally acceptable to Pakistani and Bangladeshi families. In 2012, Liu et al. 35 published a comprehensive report that explored the adaptation of health promotion programmes targeting smoking, diet and physical activity for minority ethnic groups. As part of this report the authors undertook a systematic review of health promotion programmes adapted for minority ethnic groups, which included international research. From this work, they constructed a 46-item typology of cultural adaptation approaches. They also highlighted the importance of a systematic approach to cultural adaptation and recommended a generic theory of the health promotion programme cycle (Figure 4) to be used by those adapting programmes in conjunction with the typology of adaptation, thus ensuring that all aspects of the programme are considered during the adaptation process.
As part of our intervention programme adaptation process, we mapped relevant types of adaptation from Liu’s cultural adaptation typology to the themes identified from the qualitative data from Pakistani and Bangladeshi parents and determined which stages of the programme theory these adaptation types would need to be applied to. In this way, we identified how the standard programme needed to change to make it more culturally relevant to Pakistani and Bangladeshi families.
Detailed intervention planning
Identification of intervention functions to change target behaviours and cultural adaptation types at the relevant point in the programme cycle provided the foundations on which to plan the detailed structure, content and delivery of the adapted programme. Information gained from reviewing the children’s weight management literature, consultation with the local service providers and directly observing the local programme fed into the intervention adaptation process at this point. The detailed planning process was iterative, ensuring that all adaptations and additions to the programme were coherent with (1) the identified intervention functions and adaptation types, (2) the qualitative data, (3) local service information and (4) the existing evidence on children’s weight management.
During this process, we also gave consideration to designing the programme so that there was enough flexibility in delivery that it was appropriate for children of different ages and was coherent with current guidelines. During the adaptation process, there was continuing consultation with the children’s weight management service managers to ensure that the programme could be feasibly delivered. Figure 5 summarises the intervention adaptation process.
FIGURE 5.
The process of cultural adaptation of a child weight management programme. Reproduced with permission from Pallan et al. 48 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/.
Results
Findings from the qualitative study with parents/carers
Participant characteristics
In total, 31 parents/carers participated in interviews and 12 participated in FGs. Of these, 36 were Pakistani and seven were Bangladeshi. This broadly reflects the proportion of families from these communities who are referred to the Birmingham children’s weight management service. The great majority of participants were female (37/43) and all participants were Muslim. We recruited 15 participants from each of the ‘non-completer’ and ‘non-attender’ groups; however, during the course of the interviews, it was identified that several participants who were initially identified as ‘non-completers’ were ‘non-attenders’. Therefore, nine participants were ‘non-completers’ and 21 were ‘non-attenders’. There were 13 participants in the ‘completer’ group. The average age of the participants’ children at the time of the study was 11 years and more participants had female children who had been referred to the service than male children. The majority of families had been referred to the service following identification that their child has excess weight through the NCMP. Participant characteristics are shown in Table 1.
| Participant characteristic | Participant type | All participants (N = 43) | ||
|---|---|---|---|---|
| Completers (N = 13) | Non-completers (N = 9) | Non-attenders (N = 21) | ||
| Sex, n (%) | ||||
| Male | 3 (23.1) | 2 (22.2) | 1 (4.8) | 6 (14.0) |
| Female | 10 (76.9) | 7 (77.8) | 20 (95.2) | 37 (86.0) |
| Age of child (years),a median (IQR) | 11.0 (2.0) | 11.5 (3.0) | 11.0 (6.0) | 11.0 (3.0) |
| Sex of child referred to the programme (n)a | ||||
| Male | 7 | 5 | 8 | 20 |
| Female | 7 | 5 | 14 | 26 |
| Relationship to the child, n (%) | ||||
| Mother | 10 (76.9) | 7 (77.8) | 20 (95.2) | 37 (86.0) |
| Father | 3 (23.1) | 2 (22.2) | 1 (4.8) | 6 (14.0) |
| Ethnicity, n (%) | ||||
| Pakistani | 12 (92.3) | 8 (88.9) | 16 (76.2) | 36 (83.7) |
| Bangladeshi | 1 (7.7) | 1 (11.1) | 5 (23.8) | 7 (16.3) |
| Referral method, n (%b) | ||||
| Doctor | 0 (0.0) | 2 (22.2) | 1 (4.8) | 3 (7.0) |
| School nurse | 2 (15.4) | 0 (0.0) | 3 (14.3) | 5 (11.6) |
| NCMP | 9 (69.2) | 4 (44.4) | 12 (57.1) | 25 (58.1) |
| Hospital/dietitian referral | 1 (7.7) | 1 (11.1) | 2 (9.5) | 4 (9.3) |
| Leaflet/self-referral | 1 (7.7) | 2 (22.2) | 3 (14.3) | 6 (14.0) |
| Method of discussion, n (%) | ||||
| Interview | 1 (7.7) | 9 (100.0) | 21 (100.0) | 31 (72.1) |
| FG | 12 (92.3) | 0 (0.0) | 0 (0.0) | 12 (27.9) |
Interviews and focus groups
Of the 31 interviews, 27 were face to face and four were conducted by telephone. The average length was 28 minutes, ranging from 15 to 47 minutes. The average interview length was slightly longer for ‘completers’ than for ‘non-completers’ (27 vs. 30 minutes). Three interviews were conducted in Bengali and six in Urdu. The remainder of the interviews were conducted in English.
There were seven FGs arranged; however, despite agreement from participants and attendance reminders being sent out the day before, no participants attended three of the FGs. Two of the FGs were conducted in English and each was attended by four participants; the remaining two FGs were each attended by two participants. The last two FGs were conducted in Urdu. The FG duration ranged from 35 to 50 minutes of discussion.
Qualitative data
The interviews and FGs were conducted so that they were free-flowing, to enable participants to raise any issues that were important to them. Several different themes emerged from the resulting data. The themes identified from the three participant groups were broadly coherent with each other; therefore, this section presents themes emerging from the data across all participants. Any differences that were found between ‘completers’, ‘non-completers’ and ‘non-attenders’ are reported within the themes. The participant’s identification number, sex, ethnicity and programme attendance status is shown after each quotation.
Logistical issues with programme attendance
Several practical issues were highlighted as barriers to families attending sessions. Almost all participants wanted the location to be closer to them. A location that was some distance away was a particular concern for parents who had to take other siblings to the programme or collect them from school:
Well, it shouldn’t be too far away, it’s better if it’s closer because sometimes the car isn’t available and then I could walk too.
Interviewee 154, female, Pakistani, non-attender (interview conducted in Urdu)
If it’s closer, then it’s better because it saves time; because sometimes we have to collect the children, and both mother and father needed to attend, so we both went.
FG3, participant 2, male, Pakistani, completer (FG conducted in Urdu)
They did send out appointment but it was quite far in the distance; then I couldn’t actually travel ’cause I had the small children, as well.
Interviewee 114, female, Pakistani, non-attender
The reason why I couldn’t make it is because I’m not driving, so having to travel to the place and then coming back with another small child, at the time I think she was a baby, was really difficult for me . . . It was just that really, I really want to go as well.
Interviewee 144, female, Pakistani, non-attender
Many participants, regardless of whether or not they had attended, thought that their local school would be a convenient and familiar venue and would, therefore, encourage families to attend. However, this was not universal and some participants thought that a new environment might be more stimulating for children.
From FGs 1 and 2 came the following opinions:
I think if you go through the school it’s better. Everybody has to take their children to school. So if in the morning, when they’ve gone to school to drop their child off or in the afternoon, if the teachers come forward and talk to the parents then like ‘this is what’s happening and if you would like to attend’ maybe they would be, because everybody takes their kids to school and that would be a good way of catching them.
FG1, participant 3, female, Bangladeshi, completer
But the lady that said about the school that was really good like, that just clicked onto my brain and there should be more sessions in school I think and you will get more turn out like with the parents and stuff.
FG1, participant 1, female, Pakistani, completer
I think it should be in different areas, because they get bored in their own schools, because the children develop their confidence going to a new setting, because they know why they’re attending, this is a better idea.
FG2, participant 4, female, Pakistani, completer
The timing of the programmes was often difficult, with participants commenting on other commitments that could prevent families from attending. Of note was the daily attendance at the mosque after school for some children from these communities, which would prevent them from attending sessions at this time. The suggestion of running programmes at the weekends was made by many participants. It was generally felt that this would be more convenient for families:
I think that it’s about timing because some people have young children and others are older so they need to pick them up from school, others are in college so they need to collect them, so I think it’s about timing.
FG3, participant 1, female, Pakistani, completer (FG conducted in Urdu)
. . . the timing and, you know, it’s not – and town is like, you know, busy and . . . so . . . especially after 4. It’s really hard. They have, like, their own activity. Mosque and everything. Tuition. This and that. So that’s why I couldn’t.
Interviewee 133, female, Pakistani, non-attender
Weekends, because after school they go to school and mosque, all Muslims, even Indian or Bengali or Pakistani, every Asian, children attend mosque after school.
Interviewee 139, female, Pakistani, non-attender
Well, you know this weekend, it would be better, the children would be home and you could take them instead of missing them and they’re taking time off from school.
FG1, participant 1, female, Pakistani, completer
Several participants spoke about running the programme during school time and the need for children to take time away from school to attend. Generally, this was felt to be something that was important enough for a child to miss school for and that schools would allow it. However, in some cases it was a deterrent to attending, even though schools allow absence for health-care appointments:
I’m sure if it’s a school day, the school would give him an hour or so just to go into, it’s regarding health isn’t it, so I’m sure school would allow him to go for an hour or do the programme in the weekend like Saturday/Sunday.
Interviewee 129, male, Bangladeshi, non-completer
Yeah, I was just saying that, they need to go to every session, even though I know it’s school time.
FG1, participant 1, female, Pakistani, completer
I was upset because I couldn’t go. I couldn’t have the time, I couldn’t take my – especially with schools now where they’re strict on the children, you know, attending school and not missing days. So it was hard for me.
Interviewee 104, female, Pakistani, non-attender
The requirement to attend to siblings was also raised. Some parents reported that having very young children in the family prevented them from attending; however, some participants in the completer group reported that younger siblings were present in the sessions and this did not cause any problems:
When I started receiving letters and phone calls from yourselves then I realised that there might be support. My daughter says to me that ‘mamma I want to go for exercise’ . . . I told her that I couldn’t go with her because I have other children. I have small children, my youngest is 2 years old.
Interviewee 109, female, Pakistani, non-attender (interview conducted in Urdu)
I didn’t have younger children but other families had young children with them. And they sat too, it wasn’t that the younger ones couldn’t sit and listen too.
FG2, participant 4, female, Pakistani, completer
Finally, parking near the venue was raised as an issue by some participants and, in some cases, was a deterrent to attending further sessions:
It’s not far but it’s like finding parking is the worst problem, that was the biggest problem for me not attending. The first day when we went, we were going round and round and then we managed to find a little space. The second time when I went I couldn’t find a space and I just said ‘oh enough’.
Interviewee 129, male, Bangladeshi, non-completer
Language barriers and programme attendance
Some parents who were unable to speak English reported difficulties in communication at the first contact, and for some this prevented them from attending:
Someone rang on my home phone speaking English and inviting me to attend the programme but I was asking her if I needed to take my daughter with me, because my English is not very good; but she could not understand what I was trying to ask her. I was asking if I needed to take my daughter with me. She couldn’t understand me so she said she will call me back but we never heard from her again.
Interviewee 150, female, Bangladeshi, non-attender (interview conducted in Bengali)
English-speaking participants also reported observing difficulties experienced by the non-English-speaking parents who attended the programme. However, some participants who completed the programme felt that non-English-speaking parents were able to understand the programme content, either because of the way the information was delivered or because they had brought a family member to interpret for them:
Yes, because I’ve seen some parents there that are, like, it was hard for them to understand and I was doing a lot of explaining to them as well.
Interviewee 123, female, Pakistani, non-completer
I don’t know English, they were English, but I understood everything because of the way they explained it, with gestures and all the information so that we could understand.
FG2, participant 2, male, Pakistani, completer (FG conducted in Urdu)
So was there a translator there?
No. Because at first I didn’t really mention it because my daughter was with me and so I didn’t have any problems because my daughter would speak for me and she’d translate what I was saying back to them about what to do, etc.
FG3, participant 1, female, Pakistani, completer (FG conducted in Urdu)
In general, participants felt that the availability of interpreters (which were provided in the First Steps programme) would overcome the barriers to participation that were related to language:
If it’s local and an interpreter is available. We would like to attend because it will help our child. I know I can get advice and help on diet and exercise.
Interviewee 150, female, Bangladeshi, non-attender (interview conducted in Bengali)
My niece had taken her son to First Steps programme, but she herself didn’t understand English, right? . . . She told me what was there, but she felt left out, as a parent – saying that, you know, ‘If there’s enough information for me, because I can’t read,’ she said, ‘and I can’t understand, then it would have been easier if there was somebody to explain to me’.
Interviewee 113, female, Pakistani, non-attender
And language difficulties. Not for yourself but was there any ladies in the class that you think language was a barrier?
Well they brought someone along with them or they got the children to interpret for them.
Interviewee 1036, female, Pakistani, completer
Programme structure and delivery
The course duration of 5–7 weeks was generally thought to be appropriate by most families, although a few participants thought that more sessions would be helpful. The session duration of 1 hour was raised as an important consideration among some families, especially if they were required to travel some distance. It was felt that if they had made the effort to attend, the session duration should be longer:
It’s not reasonable for me going and going back and coming back, so that is an issue, as well. So if the hours were extended, like an hour and a half or 2 hours, that would be reasonable.
Interviewee 113, female, Pakistani, non-attender
I think 7 weeks is OK, to be honest, yeah. That’s not a problem. I think that’s just about right to be honest, yeah. Because if you make it too long, probably get a bit boring wouldn’t it.
Interviewee 143, female, Pakistani, non-attender
Aspects of the programme that deterred families from participation were the didactic nature of the programme sessions and the presence of too much paperwork. Participants disliked just sitting in sessions being given information and wanted a much more interactive format:
I thought it was going to be like kind of activities where they actually show you what kind of activities you can do with your children, what kind of sports and obviously get them interested in them [sic.] kind of activities. But obviously it was like just basically information just sit there and obviously giving us information about what kind of nutrition and diet and exercise and everything but I thought it was going to be more physical than obviously classroom based.
Interviewee 142, female, Pakistani, non-completer
I think there was a bit too much paperwork and what it is, she was giving out the information, yes she was trying her best, but I think the way she was delivering it everyone was like going half asleep . . . because some parents don’t take it in as that, and it’s like they need to get up and do.
Interviewee 107, female, Pakistani, non-completer
Those who attended or completed the programme valued messages being presented in a visual way, and participants’ experiences of interactive activities were viewed very positively:
The visual, it was the visual things really that she all brought the visual things and that really like makes it more better understanding then like you know.
FG1, participant 1, female, Pakistani, completer
I was quite impressed with that because four spoons of sugar, I will just, in my head it’s four spoons of sugar, but when you actually see it in a packet it’s got four spoons in it, then you think my life it’s that much sugar, you know?
Interviewee 129, male, Bangladeshi, non-completer
[Participant talking about a related workshop that was not delivered as part of the main programme] It wasn’t really cooking it was just ready-made wraps, and you would just put salad in it, and we needed to cut it and put it in and whatever you need to put in there like butter they had brought along with them. So we cut it up, and the children cut it up and made them and then you have a look. In this way I think the children enjoy it too, so they understand that this is happening for them, so it sinks into their minds that if they do this then it will be of benefit to them.
FG3, participant 1, female, Pakistani, completer (FG conducted in Urdu)
The great majority of parents across all three participant groups felt that the programme would be more valuable if children attended all sessions:
It would have been a bit more ideal if the kids were more involved. That’s what I would – because then yes we need to have that understanding, but I believe the kids need to understand what they should have and the intake and how it’s with their body.
Interviewee 107, female, Pakistani, non-completer
I realised it was only first and last session that he has to attend, so I wasn’t really pleased with that, because I was thinking he needs to go there like to other sessions.
Interviewee 103, female, Pakistani, non-completer
They also felt that their children would take more notice if messages were given by an ‘outsider’ rather than their parents:
Because sometimes children don’t listen to their mum or dad but they listen to the teacher or outsider.
FG4, participant 1, male, Pakistani, completer (FG conducted in Urdu)
. . . although my daughter does listen to me. I think getting the information first-hand would make a big difference. So it’s important for both mother and child to attend.
Interviewee 150, female, Bangladeshi, non-attender (interview conducted in Bengali)
There was also the view that the children need to understand why it was important to eat healthily or do physical activity, as this would be more likely to lead to a change in their behaviour. One participant felt that children in the group who lost weight would provide motivation for other children:
I think children should go [to] every session because then, you know, well how I look at [it] is if the children don’t go and then we’re telling [them] ‘oh you’ve got to do this, this’, they probably think we just sometimes, most kids, they will think oh just my parents being horrible to me, my parents, but when they go into classes and they see these other people they don’t know who are actually telling them, then they will listen more because they will think: hang on if I don’t know the chap there was telling me, so I think my dad is right, so yeah OK I’ll try that.
Interviewee 129, male, Bangladeshi, non-completer
If the children are involved then they will take notice of how hard they have worked, and if that child’s weight reduces then the other children are listening too so it will benefit them too.
FG2, participant 4, female, Pakistani, completer
They [children] need to go to every session, even I know it’s school time.
FG1, participant 1, female, Pakistani, completer
So if like you know if like if these sessions are done but then it’s explained to the kids a little bit more about ‘this is what you need to do because it’s your life, you’re going to be affected in the future’ and stuff like that then it might help them.
FG1, participant 3, female, Bangladeshi, completer
Participants were generally positive about attending a group programme with other families and sharing experiences. Some really valued the sense of community that they gained from attending the group sessions:
I think this is a really good idea like when you go to a talk then you get to hear the views of others and that has an effect on you.
Interviewee 109, female, Pakistani, non-attender (interview conducted in Urdu)
There was [sic.] different community families, and friendly, Indian, Bengali, English, Sikh, and children mix up, and share their experiences.
FG2, participant 4, female, Pakistani, completer
Because it was the same lady [facilitator] for all five sections, and she nicely laughs and you know and mostly my son was happy you know and when different communities people sit and talk and like it was like a challenge between everyone and she used to push them to compete.
FG2, participant 4, female, Pakistani, completer
Programme content: weight status
The programme’s focus on weight loss was a barrier to some families’ participation. Some parents who never attended the programme did not identify their child as being overweight or that their weight was something that needed to be addressed but they were interested in helping their children to become more active:
I don’t see it as overweight, ’cause I know what they eat. I know they’re not eating the wrong food. Yes, they’re less active, but what do you do?
Interviewee 108, female, Pakistani, non-attender
My daughter, she’s not really overweight, it’s just that her weight has gone a bit over the mark.
Interviewee 104, female, Pakistani, non-attender
I mean, if you look at my son, he’s not overweight, I mean, he’s quite, for his age, he looks bigger than his age, I mean, he doesn’t look like really big or anything but he is quite heavy.
Interviewee 144, female, Pakistani, non-attender
Some parents who attended some or all of the programme reported that their children were sensitive about their weight and did not like being weighed. One parent who completed the programme reported that she did not have the support to attend from other family members:
I know it was weigh in and there was less time but with the kids I think if they approach them a bit differently because nowadays kids are very, very sensitive and every sort of thing just sticks in their head and I think, you know, ‘oh God, mum’ and then in school they’ll have that – because they had to come out of school and then it’s them like ‘oh, we’re going for the weigh in’ and she was embarrassed to even tell her brother and sisters what she was going for.
Interviewee 107, female, Pakistani, non-completer
My family members say that what’s the point of you going to the programme, and how it takes a lot of time and that there aren’t going to be any benefits. I said that they may not see the benefits but I do, because I can get my daughter’s weight down about 2/3 kg in 1 week if I focus on this information.
FG3, participant 1, female, Pakistani, completer (FG conducted in Urdu)
Programme content: nutrition
Participants, particularly non-attenders and non-completers, reported that they felt that the course offered no new insights for them. Several parents thought that their knowledge of what a healthy diet consisted of was good, and they already knew or had been previously told what their children should be eating. However, among the completers, some participants felt that their knowledge of the nutritional content of foods had significantly improved, and they particularly valued when they were also advised how to address nutritional content in their children’s diets:
I thought it would be just like talking through healthy and unhealthy but myself, I always look on the internet for healthy options, healthy meals and you know what’s good for me, what’s not good for me. So I’m constantly on the internet, right? So I thought I probably know it anyway.
Interviewee 104, female, Pakistani, non-attender
We went on the first session. The minute that plate came up and those sugary – you know, those little packets and everything, we thought, ‘Oh, we’ve been there, done that. Forget this.’
Interviewee 121, female, Pakistani, non-completer
What they were telling us on that first day, it’s like more or less we know it, you know, doctors and the nurses and surgery, they’re telling us what to do.
Interviewee 129, male, Bangladeshi, non-completer
But the way they explained everything it was very interesting. I didn’t know just a bottle of water with lemon juice had like so many rounds of sugar in there and all that stuff and like they said biscuits you think that’s the healthy option, actually it isn’t. You know like so it was quite an eye opener.
FG1, participant 3, female, Bangladeshi, completer
Because they brought a lot of material about foods with them, like sweet packets, crisps, sugar, etc., all these things were there and how much sugar was in them. How much salt is in things and how to swap these things and it will be effective. And I did this 100% and it took effect.
FG3, participant 1, female, completer (interview conducted in Urdu)
The relevance of the programme content to the food that families typically consumed was explored with the participants. Participants reported that they and their children ate both Western and South Asian food and that there needs to be a focus on both in the programme:
I think they should talk about both [South Asian and Western food]. We do eat Asian food a lot but my children like both so it would be beneficial to get advice on both.
Interviewee 150, female, Bangladeshi, non-attender (interview conducted in Bengali)
We do eat fish and we do eat baked beans and stuff, but we do eat our own food as well, so we need education on our own food.
Interviewee 113, female, Pakistani, non-attender
We eat a range of foods and my daughter likes eating food like this. They eat Pakistani food too but also English foods that are vegetarian.
Interviewee 109, female, Pakistani, non-attender (interview conducted in Urdu)
From FG1 the following was noted:
And what sort of foods would you like to learn about in cooking, westernised or traditional or a bit of both?
A bit of both, yeah.
A bit of – the children do have both.
FG1, participants 1 and 4, female, Pakistani, completer
They get to have, they get bored with this type of food all the time, they want to try something different. So that would be like a mixture really.
FG1, participant 4, female, Pakistani, completer
There was a concern among several participants that related to the consumption of ‘junk’ foods and takeaways:
She eats a lot of chocolates, sweets and crisps, she eats a lot of takeaways, like burgers, drinks a lot of fizzy drinks, she eats a lot of this stuff. Stuff like chapatti and curry, she eats less of.
Interviewee 154, female, Pakistani, non-attender (interview conducted in Urdu)
But, the temptation in this area is that we have cheap takeaways, and they are very tempting. You know, you think, ‘Why cook?’ And, you know, we’re tempted to, you know, just, ‘Oh, it’s an easier option. We’ll get chicken and chips. It’s only £1.50.’ So, you know, that’s why the weight is creeping up with children.
Interviewee 113, female, Pakistani, non-attender
Some participants commented that they would like to learn how to cook South Asian foods in a healthier way. However, one participant who had completed the programme commented that although she could change certain aspects of her child’s diet, she was not going to change the way she prepared traditional foods:
I want to know, if I’m making a chapatti, how many calories are in there? You know. If I’m making a curry – it’s really hard to – how many calories – you know, hand-size or, you know, it’s hard – in reality, it’s really, really hard. Maybe do a cooking session; say, ‘This is a portion.’ You know. ‘It’s right.’ Maybe do it that way . . . or even, like, give recipes on maybe even healthier Asian food, rather than – fair enough, do the English food, as well. OK, we have it once a week or whatever. And that’s ovenly – oven-made or it’s grilled. But help us with the type of food that we’re eating. Where are we going wrong?
Interviewee 108, female, Pakistani, non-attender
Yeah, because if I change using less oil, I can’t taste my curry without oil, since I was 3 and have grown up, I can’t change that but I can swap other things, fat milk with semi skimmed and white with wholemeal breads but I can’t change my curries.
FG2, participant 1, female, Pakistani
Some participants identified that shopping for healthy food was an issue, and that education about food labelling and purchasing healthy food options was required:
When you buy the shopping, more labelling, more information, because I understand what they say sometimes there’s energy and then the parents, some get confused because obviously and some English is not even there, so if they can like give a bit more which is more better and which is more healthy, like [drink brand], because I didn’t pick it up from there, [drink brand] does have a lot more sugar than we thought.
Interviewee 107, female, Pakistani, non-completer
Programme content: physical activity
Participants almost universally wanted some physical activity content in the programme. It was acknowledged that the facilitators spoke about physical activity but parents felt that the children should be doing physical activity in the programme sessions:
They should do more activities like, you know, physical activities to help them and not just concentrate on the food side.
Interviewee 123, female, Pakistani, non-completer
If they could like have a meeting for half an hour and then integrate like another half an hour to do the sports, I think that would be good as well.
FG1, participant 3, female, Bangladeshi, completer
I think that if you are doing this programme then you need to put some exercise sessions in it too, whatever is best for children . . . if you have the space then you should have exercise programmes in it too.
FG3, participant 1, female, Pakistani, completer (FG conducted in Urdu)
In response to the above: it’s exactly like what the sister [other participant] is saying. In terms of food, there’s calories and how much you should eat but besides this exercise is really important.
FG3, participant 2, male, Pakistani, completer (FG conducted in Urdu)
Several barriers to children undertaking physical activity were identified, including busy families lacking time, a lack of local opportunities and the perception of dangerous environments, particularly in terms of outdoor activities. Some participants suggested that practical advice about physical activity that children could do at home would be useful, which would overcome several of the identified barriers:
We rarely get to go to the park unless it’s a hot summer’s day. It’s just busy.
Interviewee 108, female, Pakistani, non-attender
There’s just nowhere for us to send them where they can get exercise. Whether they can play football or cricket or anything, they should do something. And I would enrol them there.
Interviewee 155, female, Pakistani, non-completer
I want to ride a bike . . . and my husband goes ‘can you see how dangerous it is, the cars out there’.
Interviewee 112, female, Pakistani, non-attender
And you can’t let them go to the parks alone. And it’s just round the corner but you just can’t . . . You just can’t let them out, ’cause a lot has been, you know, happening around here.
Interviewee 108, female, Pakistani, non-attender
And you can do something at home as well, children sitting down, it’s better to tell them to walk like 10 times on the stairs, up and down. That’s a good exercise for them.
FG2, participant 1, female, Pakistani, completer
Several participants also identified that they used cars when they felt that they should be walking with their children:
My sister gets into the car and drops them off to the secondary school, you see. But they need that exercise. They need to learn how to walk, as well. You know, the car is very convenient, but it’s really bad for the kids.
Interviewee 121, female, Pakistani, non-completer
Parents’ influence over their children
Among the parents who had completed part or all of the programme, a common theme was that even when they implemented changes in the home to try and encourage a more healthy diet, children would find ways of circumventing this. In some cases, parents also admitted to ‘treating’ their children to something unhealthy:
I’ve tried to cut down. You know they showed us a certain plate of vegetables, that’s how much and all that stuff and I’ve tried doing that, I’ve really tried getting into it but I find that he sneaks behind me, he goes in the kitchen and helps himself.
FG1, participant 3, female, Bangladeshi, completer
When he goes to my mum’s house, he helps himself a lot and then when we go to family, like, he doesn’t listen, he helps himself a lot.
Interviewee 103, female, Pakistani, non-completer
But the drink wise, he does drink sometimes fizzy drink and I’m not going to deny that I do bring sometimes, I feel bad, they like it, right, so just drink a bottle and give it to them, I say ‘look hide it’.
Interviewee 129, male, Bangladeshi, non-completer
Summary of the qualitative findings
A key set of barriers to attending a community weight management programme is logistical considerations. Families reported that they require a close, familiar location and a programme run at a convenient time. Language barriers to participation did exist for parents from Pakistani and Bangladeshi communities who do not speak English. A particular linguistic barrier comes at the recruitment stage, and so this part of a programme needs careful attention. Once participants attend the programme, language barriers do not present so much of a problem, particularly if interpreters are provided (as they are in the First Steps programme). The focus of the programme was on weight loss; therefore, parents who did not identify that their child had a weight problem did not engage as much or felt that there was nothing that they could do about it. However, the data suggest that these parents still recognised the value of healthy lifestyles and wished to encourage their children to adopt healthy behaviours.
There was strong support for a programme that involved children in all the sessions, as it was felt that they need to learn how to change their behaviour first hand, and would respond differently to messages given by someone other than their parents. It was also emphasised by many participants that physical activity should be included in the programme. The group environment and being able to share experiences and ideas with other families was generally valued highly by participants who had attended the programme, but there was a feeling among participants who had not attended much or all of the programme that they were not going to gain anything new from it, and that they already knew what was ‘good’ and ‘bad’ for their children. Although the First Steps programme includes South Asian foods, some parents felt that the nutritional content could be made more relevant to traditional South Asian diets, but many acknowledged the importance of also talking about Western foods, as typically their children’s diets consisted of a mixture of foods. Finally, there was a feeling that parents had difficulty ensuring that their children adhered to changes they made in the home, particularly regarding food, and, therefore, help with addressing this issue would be valued. Apart from language and dietary considerations, there were no other themes that related explicitly to Pakistani and Bangladeshi culture that emerged from the data. However, what emerged more prominently were the restrictions within which the families lived their lives (e.g. the competing demands of younger siblings, busy family lives and the perceived lack of safety in the local environments) and the impact of these on the families being able to undertake healthy behaviours.
Findings from a review of children’s weight management evidence
The NICE guideline on managing overweight in children and young people (PH47)17 presents a series of recommendations for the provision of children’s weight management services. These are listed in Box 2. Each recommendation was considered in the adapted intervention planning to ensure consistency with this evidence-based guideline (Table 2). The importance of parental involvement in interventions for childhood weight management was strongly emphasised in this guideline and other children’s weight management literature,17,53 as was the importance of combining both diet and physical activity elements into programmes rather than focusing on one element alone. 54,55 Therefore, these important aspects of the standard children’s weight management programme were retained in the adapted programme. In addition, behaviour change techniques, identified as being effective in a systematic review of behaviour change techniques in obesity interventions for children,52 were considered for inclusion in the adapted intervention design at the appropriate points. These behaviour change techniques included the provision of information on the consequences of behaviour to the individual, environmental restructuring, prompting practice, prompting the identification of role models or advocates, stress management/emotional control training and general communication skills training.
Lifestyle weight management programmes for overweight/obese children should:
-
be multicomponent and focus on diet, healthy eating habits, physical activity, reducing time spent sedentary and strategies for changing behaviour of the child and their family
-
include behaviour change techniques to increase confidence and motivation in ability to make changes
-
include parent skills training
-
provide a tailored plan to meet the needs of the child and family, taking into account factors such as child age, family social and economic circumstances, ethnicity and cultural background
-
incorporate learning of practical skills, such as reading nutrition labels
-
help identify and signpost families to opportunities to build physical activity into their daily lives
-
introduce simple physical activity opportunities within the programme
-
provide support materials and information that can be shared with other family members not in attendance
-
provide a form of ongoing support following the end of the course
-
be delivered in comfortable locations where the participants feel at ease
-
when possible provide continuity, in that the course facilitator should remain through the whole programme
-
be provided at flexible times to meet the needs of the community.
Reproduced from NICE. 17 © NICE 2013. Weight Management: Lifestyle Services for Overweight or Obese Children and Young People. Available from www.nice.org.uk/guidance/PH47. All rights reserved. Subject to Notice of rights.
| Factors to address identified from qualitative data | BCW | Cultural adaptation | NICE guidelines17 | Intervention adaptation | ||
|---|---|---|---|---|---|---|
| COM-B element | Intervention function | aTypology of adaptation35 | Programme theory stage | |||
| Behaviour target 1: improve session attendance and completion of the programme | ||||||
|
Convenient programme location Ease of travel and parking Convenient timing of programme |
Physical opportunity | Environmental restructuring |
25. Consider target populations employment/home situations 29. Utilise appropriate incentives and timing of programme 33. Located in ethnically/culturally appropriate/familiar location |
|
Programmes should be provided at flexible times to meet the needs of the community |
Increase opportunity for Saturday sessions Identify convenient programme locations (e.g. schools, good transport links) |
| Parental responsibility for other siblings |
Physical opportunity Psychological capability |
Environmental structuring Enablement |
24. Intervention delivered in a culturally appropriate or preferred format 39. Address structural barriers to participation |
|
Allow siblings to attend Ensure that siblings are made welcome and included in sessions |
|
| Facilitate children attending in school hours | Psychological capability | Enablement | 38. Address emotional barriers and stressors |
|
Programmes should provide a tailored plan to meet the needs of the child and family (such as child age, family social and economic circumstances, ethnicity and cultural background) | Improve knowledge of authorisation for children to have time out of school |
| Language barriers at initial recruitment and language requirements in programme sessions |
Psychological capability Social opportunity Reflective motivation Automatic motivation |
Enablement | 14. Reflect target population’s language |
|
Provide high-quality language support at recruitment stage and within programme | |
| Increase duration of programme sessions | Physical opportunity | Environmental restructuring | 24. Intervention delivered in a culturally appropriate or preferred format |
|
– | Increase session length from 60 to 90 minutes |
Weight not perceived as:
|
Reflective motivation Automatic motivation Psychological capability |
Education Persuasion Enablement |
22. Intervention content targets population’s social and cultural values 23. Intervention goals and outcomes are culturally appropriate |
|
Programmes should be multicomponent and focus on diet, healthy eating habits, physical activity, reducing time spent being sedentary and strategies for changing behaviour of the child and their family |
Focus on the benefits of healthy behaviours for good health outcomes at recruitment and throughout the programme (vs. focus on weight) Inclusion of effective behaviour change techniques |
| Sensitivity of children to being weighed | Automatic motivation | Enablement | 38. Address emotional barriers and stressors |
|
Focus on healthy behaviours to influence health outcomes, rather than weight | |
| Interactive format better received than didactic format |
Social opportunity Automatic motivation |
Enablement |
16. Reflect target population’s preferred method of communication 24. Intervention delivered in a culturally appropriate or preferred format |
|
Programmes should include behaviour change techniques and parent skills training and should incorporate learning of practical skills and introduce simple physical activity opportunities within the programme |
Inclusion of more interactive activities More opportunities to socialise and share experiences to encourage peer support |
| Visual materials are important to communicate messages |
Psychological capability Automatic motivation |
Education Persuasion |
|
Inclusion of visual materials with clear educational messages | ||
| Parents prefer less ‘paperwork’ (handouts) |
Psychological capability Automatic motivation |
Education Environmental restructuring |
15. Match reading level and literacy 16. Reflect target population’s preferred method of communication |
|
Programmes should provide a tailored plan to meet the needs of the child and family (such as child age, family social and economic circumstances, ethnicity and cultural background) | Reduce the number of handouts; make them attractive and visual, with less written information |
| Children should attend all sessions to interact directly with programme facilitators |
Physical opportunity Social opportunity |
Environmental restructuring | 24. Intervention delivered in a culturally appropriate or preferred format |
|
Children attend all sessions with parents Session content appropriate for children aged 4–11 years |
|
| Encourage social interaction and peer support |
Social opportunity Automatic motivation |
Enablement | 41. Encourage/involve social support |
|
Inclusion of more interactive activities More opportunities to socialise and share experiences to encourage peer support |
|
| Perceived value of the programme; parents feel that they have enough knowledge about healthy lifestyles | Reflective motivation |
Education Persuasion Incentivisation |
19. Material/guidance based on preferences of target population 23. Intervention goals and outcomes are culturally appropriate |
|
Include parent skills training, behaviour change techniques and learning of practical skills |
Increased focus on how to change dietary and physical activity behaviours Inclusion of effective behaviour change techniques Attractive recruitment materials, emphasising relevance of programme to families |
| Behaviour target 2: improve physical activity behaviours | ||||||
| Physical activities should be included in the sessions | Physical opportunity |
Training Enablement |
19. Material/guidance based on preferences of target population 36. Provide ethnically/culturally appropriate food/activities |
|
Programmes should introduce simple physical activity opportunities within the programme | Incorporate fun physical activities into all programme sessions |
| Lack of local physical activity opportunities, lack of time for physical activity and reliance on sedentary transport |
Physical opportunity Psychological capability |
Education Training |
22. Intervention content targets population’s social and cultural values 24. Intervention delivered in a culturally appropriate or preferred format 25. Consider target population’s employment/home situations 36. Provide ethnically/culturally appropriate food/activities 39. Address structural barriers to participation |
|
Programmes should provide a tailored plan to meet the needs of the child and family (such as child age, family social and economic circumstances, ethnicity and cultural background) |
Include a range of physical activities throughout, led by the facilitator, encouraging simple movement patterns and aerobic exercise opportunities that can be performed in the home and require little time Address cultural norms resulting in perceived limitations to physical activity Discuss active transport and other walking opportunities |
| Perceived dangers of undertaking physical activity |
Psychological capability Automatic motivation |
Training Modelling |
38. Address emotional barriers and stressors 39. Address structural barriers to participation |
|
Programmes should introduce simple physical activity opportunities within the programme | Undertake fun and safe physical activities that can be done at home |
| Parents’ perceived ability to effectively influence their child’s physical activity behaviours | Psychological capability |
Enablement Training |
23. Intervention goals and outcomes are culturally appropriate 26. Intervention addresses health behaviour patterns found in target populations 38. Address emotional barriers and stressors 41. Encourage/involve social support |
|
Programmes should include behaviour change techniques to increase confidence and motivation in ability to make changes and also include parent skills training |
Improved social support to encourage self-belief Encourage parental physical activity Incorporate parenting skills training Set achievable targets and rewards |
| Behaviour target 3: improve dietary habits | ||||||
| A need to address both Asian and Western foods in sessions focusing on diet |
Reflective motivation Social opportunity |
Education Enablement |
19. Material/guidance based on preferences of target population 27. Dietary issues unique to their context 36. Provide ethnically/culturally appropriate food/activities 43. Maintaining cultural significance of food |
|
Programmes should provide a tailored plan to meet the needs of the child and family (such as child age, family social and economic circumstances, ethnicity and cultural background) |
Nutrition education content to include traditional and Western food examples Sensitivity to the social importance of food in different cultures Encourage sharing of skills and experiences through social interactivity and support |
| A need to know how to prepare healthier food | Physical capability | Training |
24. Intervention delivered in a culturally appropriate or preferred format 36. Provide ethnically/culturally appropriate food/activities 43. Maintaining cultural significance of food |
|
Programmes should incorporate learning of practical skills such as reading nutrition labels |
Include content on healthier ways to prepare traditional foods, alongside Western foods Education regarding portion sizes Hands-on healthy food preparation and tasting session |
| Address excessive consumption of ‘junk food’ and takeaways |
Psychological capability Physical opportunity |
Training Enablement |
19. Material/guidance based on preferences of target population 26. Intervention addresses health behaviour patterns found in target populations |
|
Programmes should include behaviour change techniques to increase confidence and motivation in ability to make changes and also include parent skills training |
Incorporate training on parenting skills, cut down on undesirable behaviours and change food availability in the home Set achievable targets and rewards |
| Difficulty understanding food labelling and purchasing healthy foods | Physical capability | Training |
19. Material/guidance based on preferences of target population 36. Provide ethnically/culturally appropriate food/activities |
|
Programmes should incorporate learning of practical skills such as reading nutrition labels |
Educational interactive activities on food labelling Hands-on healthy food preparation and tasting session |
| Parents’ perceived ability to influence their children’s eating behaviours | Psychological capability |
Enablement Training |
23. Intervention goals and outcomes are culturally appropriate 26. Intervention addresses health behaviour patterns found in target populations 38. Address emotional barriers and stressors 41. Encourage/involve social support |
|
Programmes should include behaviour change techniques to increase confidence and motivation in ability to make changes and also include parent skills training |
Improved social support to encourage self-belief Incorporate parenting skills training Set achievable healthy eating targets and rewards |
Findings from observation of the First Steps standard programme and consultation with the programme managers
Direct observations of the First Steps standard programme were undertaken during phase I. A study researcher (Tania Griffin) observed all sessions of one programme, which was delivered on weekday afternoons, and two sessions of a programme that was delivered on Saturdays by a different member of staff from the weekday sessions. Findings from the direct observation were coherent with the qualitative findings: the sessions were noted to be didactic, leading to the disengagement of participants towards the end of sessions, and a copious number of handouts were given, mostly black and white photocopies, which were very word heavy and which participants did not appear to value. The content of the sessions was heavily weighted towards nutrition, with a focus on increasing nutritional knowledge. There was some focus on behaviour change, with goal-setting incorporated into the programme; however, this was not well implemented in the observed sessions.
The programme managers also identified similar difficulties with the standard programme, especially with respect to the classroom style of delivery and the number of handouts. We attempted to address these identified issues in the adapted intervention design. This consultation also ensured that the planned adapted intervention was feasible to deliver within the existing service infrastructure. The children’s weight management service providers had some degree of flexibility to allow structural changes to the programme.
Application of the behaviour change wheel and cultural adaptation theory
Themes from the qualitative data were mapped to the COM-B components46 to identify which aspects that determine the three identified target behaviours (programme attendance, dietary intake and physical activity) needed to change. The intervention functions that corresponded to the identified COM-B component, and were also deemed to be appropriate to include in a children’s weight management programme, were then identified. Enablement featured as a prominent intervention function across the three target behaviours, with environmental restructuring emerging as important to address programme attendance and training and persuasion emerging as important to address physical activity and healthy eating. Less prominent intervention functions identified were education (to address all three behaviours), persuasion and incentivisation (to address programme attendance) and modelling (to address physical activity).
From the parallel process of mapping the 46-item cultural adaptation typology35 to the qualitative data, a variety of cultural adaptation types were identified, which could be applied at various stages in the programme cycle. This process ensured that, during the detailed planning of the adapted intervention programme based on the identified intervention functions, there was explicit consideration of how to make each aspect of the programme culturally appropriate to the target population. However, throughout the whole process, it was kept in mind that the programme needed to be appropriate for a diverse community, and not exclusively Pakistani and Bangladeshi communities.
The qualitative themes, mapped COM-B components, intervention functions, cultural adaptations and programme cycle stage, and corresponding NICE recommendations, are shown in Table 2.
Detailed planning of the adapted intervention programme
Following the application of the two guiding frameworks to the qualitative themes, specific adaptations were planned. These are outlined in column 7 of Table 2. The NICE guideline recommendations,17 other information gained from the literature, direct observation of the standard programme and consultation with the children’s weight management service managers also informed this planning process.
The adaptation process was undertaken by two members of the research team (Tania Griffin and Miranda Pallan). An example of how the process was undertaken is as follows. We identified, through the qualitative data, that parents perceived that they lacked the ability to positively influence their children to undertake physical activity. We used the COM-B model to identify that we needed to address parents’ psychological capability and the BCW to identify that this could best be achieved through the intervention functions of enablement and training. In parallel, using the typology of cultural adaptation,35 we identified that the types of adaptations that we should consider to address this were making intervention goals culturally appropriate, addressing health behaviour patterns found in target populations, addressing emotional barriers and stressors and encouraging social support. We also identified that we should consider adaptations at various stages in the programme cycle (e.g. planning, implementation, retention and outcome stages). In addition, we incorporated the following NICE guideline recommendation17 into our adaptation planning: programmes should include behaviour change techniques to increase confidence and motivation in ability to make changes and also include parent skills training. From this point, we developed specific adaptations, taking into account information from our direct observation and consultation with the weight management providers. We also ensured that we incorporated evidence-based behaviour change techniques at this point. This resulted in planning the following adaptations: increasing social support to encourage self-belief (enablement), encouraging parental physical activity (enablement), incorporating parenting skills training (training) and setting and reviewing achievable and culturally appropriate targets (enablement).
When the detailed planning was completed, the planned intervention programme was presented to the Parent Advisory Panel for feedback and refined accordingly.
Final intervention design
The key changes to the programme can be divided into three sections: (1) programme promotion and recruitment, (2) programme structure and delivery and (3) programme content.
Programme promotion and recruitment
During the theoretical intervention adaptation process, key messages were identified to be conveyed to potential participants at the promotion and recruitment stage. The initial written and verbal contacts with families who were referred into the service were modified to reflect this; for example, parents who are non-English-speaking were to receive a telephone call in a language that they could understand as a follow-up to the initial invitation letter. In addition, the promotion and recruitment materials were adapted to place an emphasis on changing eating and physical activity behaviours to improve health rather than focusing on weight.
Programme structure and delivery
The major adaptations to the programme structure and delivery were an increase in session length from 60 to 90 minutes, the provision of more programmes at the weekend and the inclusion of the children in all programme sessions. In addition, throughout all programme sessions, there is a focus on tailoring so that the programme is able to address the issues faced by the individual families attending the programme. This was achieved by developing interactive activities that allowed families to think about their own situation and by building in time for the facilitators to have informal discussions with families about any particular issues they had.
Session content
Sessions were adapted to include many more interactive components, including physical activity opportunities, throughout the programme. Content was also designed to encourage interaction between the families attending and to foster the sharing of experiences and peer support. Behaviour change techniques were incorporated into each session, with the addition of a specific session to help parents consider how they can best support their child to change their behaviours. More detail on the content of each session is included in Table 3.
| Item number | Item |
|---|---|
| 1. Name | First Steps. The name of the current child weight management programme in Birmingham was retained, ensuring that the comparator and intervention programmes had identical titles in the feasibility study so that participants would be unaware of whether they were attending a standard or adapted programme |
| 2. Why? |
The primary aim of adapting the intervention programme was to increase the acceptability and value of the programme to families from Pakistani and Bangladeshi communities in order to increase their likelihood of completing the programme, while maintaining acceptability of the programme to families of other ethnicities. In addition, the adaptation process was an opportunity to ensure that the programme was consistent with current evidence The adaptation process was informed by data from Pakistani and Bangladeshi families of overweight children, current literature and local programme provider experience and was guided by two theoretical frameworks (the BCW46 and typology of cultural adaptation and health promotion programmes35). The frameworks ensured that factors influencing behaviour that required change were identified and targeted and that the adaptations made were culturally appropriate to the Pakistani and Bangladeshi communities. Adaptations were made to the structure, delivery and content of the programme |
| 3 and 4. Materials and Procedures |
Families referred to the children’s weight management service are sent a letter inviting them to attend their nearest children’s weight management programme. This initial invitation letter was redesigned to be more engaging and emphasise the aims and benefits of the programme. All families receiving an initial invitation letter will also have a follow-up telephone call and this should be in their preferred language The intervention programme consists of six 90-minute sessions that are delivered over 6 weeks. Both children and their parents/carers attend all sessions. Programmes run on weekdays (50% of programmes) or on Saturdays (50% of programmes). A step-by-step programme delivery guide was developed for the programme facilitators (see Report Supplementary Material 1), with a training programme alongside, comprising a 2.5-hour session and a follow-up 1.5-hour session Attractive programme materials were developed for use within the programme, including visual display boards and materials for the interactive components. At the first session, participants receive a First Steps-branded ring binder in which to keep their goal sheets and the activity sheets that are given each week. Non-English-speaking participants are accompanied by an interpreter. Attendance at each programme session is rewarded by a gold star on the participant’s attendance sheet. Progress towards behavioural goals are also rewarded with gold stars. A website was developed for use by participants, which provides a variety of resources, including recipe and physical activity ideas, frequently asked questions, worksheets and games, and links to other relevant resources. Aims and outlines of the six programme sessions are as follows: Week 1: welcome Aims Provide a welcoming, friendly, supportive environment Improve knowledge on why a healthy lifestyle is important Collect baseline height and weight data OutlineWeek 2: healthy eatingOutlineWeek 3: making changes AimsOutlineWeek 4: physical activity AimsOutlineWeek 5: give it a go AimsOutlineWeek 6: review and celebrate AimsOutline |
| 5. Who provided? | Two BCHCT employees were trained to deliver the adapted programme. The BCHCT employees both had a minimum of 12 months’ experience of delivering a children’s weight management programme. A third BCHCT employee was trained to assist in delivery, in particular supporting the interactive activities, running the children’s physical activity session in week 3, and collecting height and weight data. The facilitators were provided with a detailed delivery guide (see Report Supplementary Material 1) and attended two training sessions, which were run by the CHANGE study research team |
| 6. How? | The programme is designed to be delivered to a group of families (optimum group size is 10 families) |
| 7. Where? | The programme is designed to be delivered in local community venues (e.g. community centres or primary schools) |
| 8. When and how much? | The programme is delivered through six 1.5-hour sessions over 6 weeks. Compared with the standard programme, a higher proportion of programmes was planned to be delivered on Saturdays than in the standard programme |
| 9. Tailoring | Throughout the programme, there is provision for tailoring to individual family needs. This is built into the planned interactive components and the facilitator delivery guide (see Report Supplementary Material 1) |
| 10. Modifications | The adapted programme was delivered in a feasibility study (see Chapter 4). During the first 8 weeks of the intervention delivery period, minor modifications were made to intervention delivery (session 2 was streamlined, as there was too much material to deliver in 90 minutes, and in session 5 options for healthy food preparation activities were modified to make delivery more feasible) |
| 11. How well programme was delivered: planned? | In the feasibility study, delivery of intervention sessions was directly observed and facilitators debriefed with the research team after each session (see Chapter 4). This information was used to refine the delivery guide and verbally feedback to the facilitators to improve implementation fidelity when the corresponding session in the next programme was delivered |
| 12. How well programme was delivered: actual? | Fidelity of intervention delivery is described in the feasibility study findings in Chapter 4 |
Developed resources
The attractive and attention-grabbing display materials were recognised as important tools in engaging families; therefore, colourful visual display boards and resources for the interactive activities were developed for use within the sessions. Folders with visual inserts were also designed to be given to families in the first week, and then further inserts were given in subsequent weeks. All materials were designed to have minimal writing and more pictorial representations. A website was also developed as an additional resource for families. This contained a variety of resources relating to healthy eating and physical activity.
To support facilitators in delivering the programme, a detailed intervention delivery guide (see Report Supplementary Material 1) was developed. A two-session training programme for facilitators was also developed.
More detail of the adapted intervention programme is found in the Template for Intervention Description and Replication (TIDieR) checklist in Table 3 and Report Supplementary Material 1.
Discussion
The aim of the first phase of the CHANGE study was to adapt Birmingham’s child weight management programme to encourage attendance and completion by Bangladeshi and Pakistani families, while ensuring that it was appropriate for all ethnic groups. The intervention adaptation process was multifaceted and iterative, informed by participants’ and service providers’ experiences of the current programme and the current available evidence.
The use of the BCW46 alongside the typology of cultural adaptation35 enabled development of the theoretical underpinning of the programme and clear articulation of how the programme was designed to positively influence the target behaviours.
The adaptation process was centrally driven by the qualitative data obtained from Pakistani and Bangladeshi parents of overweight children who had experience of the standard children’s weight management programme. This, together with the use of the cultural adaptation typology, enabled a focus on cultural needs throughout the adaptation process. However, as we progressed through the process, it became clear that of the adaptations that were required, very few addressed factors that are specific to only these cultural groups. We also identified that there is a need for flexibility in the delivery of a programme to suit not only different ethnic groups but each individual family, as there is a high degree of variation from family to family in terms of their needs, customs and lifestyles, regardless of their ethnicity. Thus, the final intervention design incorporated flexibility and responsiveness so that it could best meet the needs of all participants and it fulfilled our aim of developing the programme to be inclusive of all participating families. Our approach is also coherent with the identified need for a conceptual shift by researchers and policy-makers from a traditional focus on ‘ethnic groups’ to a more nuanced understanding of diversification of the population in terms of a range of complex and dynamic factors that are linked to migration (so-called super-diversity). 56
The adaptation process also ensured that the programme incorporated the most up-to-date children’s weight management research evidence. Although we undertook a literature review, in reality this added very little to NICE’s guidelines,17 which were published in November 2013 and were underpinned by two extensive systematic literature reviews. 50,51 Therefore, we ensured that NICE’s recommendations were taken into account in the adaptation process and detailed intervention planning.
Literature on cultural adaptation defines two levels of adaptation: deep and surface structure adaptation. Adaptations at the surface structural level are those that address observable or ‘superficial’ characteristics of a minority ethnic group, for example making adaptations to address language needs or providing materials with culturally matched food, images, etc. Deep structural adaptations address aspects such as core values, beliefs and other aspects that contribute to a person’s world view. 57,58 The adaptations that we made to the children’s weight management programme incorporated both of these levels. In particular, the design of the programme to be responsive to each individual family context, the focus on health and the encouragement of peer support are all examples of deep structural adaptation.
Research into the cultural adaptation of health promotion programmes is still relatively sparse. A comprehensive review on the adaptation of programmes for minority ethnic groups was published in 2012, which brought together the literature on adapted health promotion programmes targeting smoking, physical activity and diet. 35 They highlighted that most research into culturally adapted health promotion interventions has taken place in the USA, focusing on African-American communities, and, thus, these intervention have limited generalisability to the UK. This is certainly true in childhood obesity intervention research, in which culturally targeted interventions have mainly focused on US minority ethnic communities. Systematic reviews of these targeted interventions have explored the level of cultural adaptation and often this is minimal or confined to surface-level adaptation, although there are some examples of deep structural adaptation within the included studies. 23,59 An additional issue is the lack of reporting of the adaptation strategies used,59 which precludes an understanding of the theoretical underpinning of the adaptations, even when researchers have undertaken formative research (as we have done) to inform the adaptation process. Thus, as well as the use of formative research, a further strength of this study is the detailed description of our processes of adaptation and use of theoretical frameworks to guide these.
Challenges
There were several challenges to undertaking the methodology described. The qualitative study in particular presented several practical problems. The multistage recruitment process meant that it took time to recruit participants. The reliance on telephone calls proved problematic, as often people would not answer the telephone. This was in part resolved by ensuring that telephone calls from the university did not display as ‘private number’. However, on several occasions, the university research team was unable to contact a person, despite initial contact being made by telephone by BCHCT staff. Undertaking home visits for the interviews also proved challenging on occasions, as participants were sometimes not at home, despite the research team making prior arrangements with them. A system of postal, telephone and text reminders was developed and implemented to minimise these issues.
We were successful in achieving recruitment of non-English-speaking participants in the qualitative study, which was critical as this phase of the study focused on UK Pakistani and Bangladeshi communities. Such recruitment is notoriously challenging but the use of community researchers who not only had the appropriate language skills but also had a full understanding of the participants’ cultural context enabled the inclusion of these participants in the study. The process of informed consent with these participants needed particular attention, as the information in the participant information sheet and on the consent form needed to be carefully communicated to them verbally by the community researchers. To ensure that this was a robust process, initial training was provided for the community researchers and this was followed up with regular training updates.
The recruitment of participants to attend the FGs was not successful. The research team made many efforts to make the FGs as accessible as possible, setting them up in convenient, well-known locations based on the participant’s postcodes (such as local libraries, community centres or schools), sending bright, appealing laminated invitation cards and making several telephone call reminders on the days before the FGs. Despite participants confirming their attendance on the telephone, they often failed to turn up. Given this pattern of attendance, we amended the protocol for phase II so that we undertook only interviews as part of our evaluation rather than FGs.
When undertaking interviews and FGs, the university research team took great care to explain to participants that they were independent of the children’s weight management service providers. Despite this, some participants seemed convinced that the research team were also part of the provider organisation, which may have influenced the data obtained from these participants, particularly in terms of their willingness to be critical of the programme.
Despite the challenges described, we successfully achieved the objectives of phase I of the study by developing a culturally adapted, manualised and theoretically underpinned children’s weight management programme that was ready to be evaluated in a feasibility study.
Chapter 4 Phase II: feasibility study
Objectives
The objectives of the feasibility phase, as stated in Chapter 2, were to:
-
assess the proportion of Pakistani and Bangladeshi families and the proportion of all families completing the adapted programme
-
assess the acceptability of the programme to Pakistani and Bangladeshi families and families from other ethnic groups
-
assess the feasibility of delivery of the adapted programme
-
assess the feasibility of participant recruitment, randomisation and follow-up
-
assess the feasibility of the collection of cost data from both a health and societal perspective to inform a future trial evaluating intervention clinical effectiveness and cost-effectiveness
-
collect data on recruitment, attrition and other relevant measures to inform the parameters of any future trial.
Design
The feasibility study was designed as a small-scale, two-arm cluster RCT, with the weight management programmes as the clusters. This enabled an estimation of the proportion of families completing the adapted intervention programme and the standard programme, an evaluation of the feasibility of intervention programme delivery and processes to be used in a future clinical effectiveness and cost-effectiveness trial and the collection of key data to inform a future trial. All programmes that were planned to be delivered across Birmingham within the study period (September 2015 to April 2016, n = 24) were randomised to be delivered as either the adapted First Steps programme (intervention) or the standard First Steps programme (comparator). Families who were referred to the weight management service in this time period were invited to attend the programme that was most convenient for them, regardless of whether or not they consented to participate in the CHANGE study. Therefore, both intervention and comparator programmes contained a mix of CHANGE study participants and non-CHANGE study participants. The families participating in the children’s weight management programmes within the study period were not aware of whether the programme was the standard or the adapted intervention.
Community researchers
Community researchers (individuals from local Pakistani and Bangladeshi communities with relevant language skills) were again recruited to assist with the feasibility study. They worked alongside the core research team and undertook informed consent procedures, collection of outcome data and evaluation interviews and also provided language support when required.
Researcher training
All community researchers and the CHANGE study research team completed the NIHR e-learning courses on good clinical practice and informed consent in paediatric research. In addition, they completed a 1-day training course on child protection (‘Child Protection Level 2 Recognition & Referral’ run by the BCHCT). Community researchers received two bespoke training sessions on data collection procedures, run by the study research team. The community researcher undertaking interviews (Meanaz Akhtar, of Pakistani heritage) had prior qualitative research experience and received additional training from the research team.
Methods
Study arm allocation
Randomisation of the weight management programmes was conducted by a member of Birmingham Primary Care Clinical Research & Trials Unit (Andrea Roalfe) before the start of the feasibility study to enable service providers to plan delivery of the programmes within the study period. The 24 programmes planned in the study period were randomised to intervention and comparator arms using a 2 : 1 ratio, so that 16 programmes were delivered as the adapted programme and eight were delivered as the standard programme. This randomisation ratio ensured that there was a sufficient number of Pakistani and Bangladeshi families in the intervention arm to enable calculation of the primary outcome of completion (see Sample size). The randomisation was conducted in Stata® version 13 (StataCorp LP, College Station, TX, USA). The 24 programmes were planned to be delivered over four school half-terms (six programmes per school half-term), and so randomisation was stratified by school half-term (i.e. for each half-term the six planned programmes were randomised with a 2 : 1 ratio). The name ‘First Steps’ was retained for both the standard and the adapted programmes, so that participants remained unaware of which study arm they were in. Programme allocation was communicated to the BCHCT service providers but concealed from the research team who were, therefore, unaware of the allocations at the time of baseline data collection.
Participant recruitment
Families in Birmingham with a child aged 4–11 years who had excess weight (defined as > 91st centile for BMI on the 1990 UK growth reference charts44) and who were referred to the existing children’s weight management service within the study recruitment period were eligible to participate. An additional eligibility criterion was the ability of the child to attend and participate in a group setting. We aimed to recruit 80 children and their families to participate in data collection within the study period (approximately 20% of all families referred to the children’s weight management service). As the intervention was adapted primarily to be more suited to Pakistani and Bangladeshi families, we prioritised recruitment of these families. We aimed for Pakistani and Bangladeshi families to comprise 60% of the study sample so that the success of the programme adaptation could be explored from the perspective of these families.
For families referred to the weight management service, the BCHCT service providers identified the First Steps programme that was closest to their home postcode and wrote to the families to confirm that they had been booked onto a programme. A CHANGE study invitation letter and parent and child information sheets were included with this booking confirmation. A cover letter, translated into Urdu and Bengali, was also included with the study information, which explained that families were being invited to take part in a research study relating to children’s weight management and that they would shortly receive a telephone call in which the study would be explained to them in their preferred language.
Within 3 days of receipt of the booking letter, BCHCT staff conducted follow-up telephone calls to check each family’s intention of attending a programme and to ask if they would be happy for their contact details to be forwarded to the CHANGE study research team. Parents who did not speak English were contacted by telephone in their preferred language. The contact details of those who verbally agreed were then passed to the CHANGE researchers.
The CHANGE research team contacted the families by telephone to ask if they had any questions and if they were happy to take part in the study. If they agreed to participate, an appointment at their home was arranged to obtain informed consent to participate and to undertake baseline assessments. For parents who did not speak English, the telephone calls and measurement appointments were conducted by a community researcher with the appropriate language skills. If required, participant information sheets were verbally translated by the community researchers before consent was obtained.
Consent
At the initial home visit, parental consent was obtained for all children taking part in the CHANGE study. Additional consent and assent were obtained for family members who were present at the home visit. Consent to conduct height, weight and body fat percentage measures was requested from any family members aged ≥ 16 years. Parental consent was requested for family members aged < 16 years. Written assent was obtained from children aged ≥ 8 years and verbal assent was obtained from younger children.
Follow-up
After the initial visit to obtain consent and baseline data (time point 0; T0), study participants received two further home visits to collect outcome data: within 1 month of the end of the programme (time point 1; T1) and 6 months after the end of the programme (time point 2; T2). Participants were telephoned to arrange the follow-up appointments and were then sent a letter of confirmation. They also received a reminder telephone call or text on the day of the appointment. All participants who provided data at T1 were given a shopping voucher worth £10. A flow diagram of the process of participant recruitment and assessment during the study is shown in Figure 6.
FIGURE 6.
Flow diagram of feasibility study participant recruitment and assessment. a, Language support available.
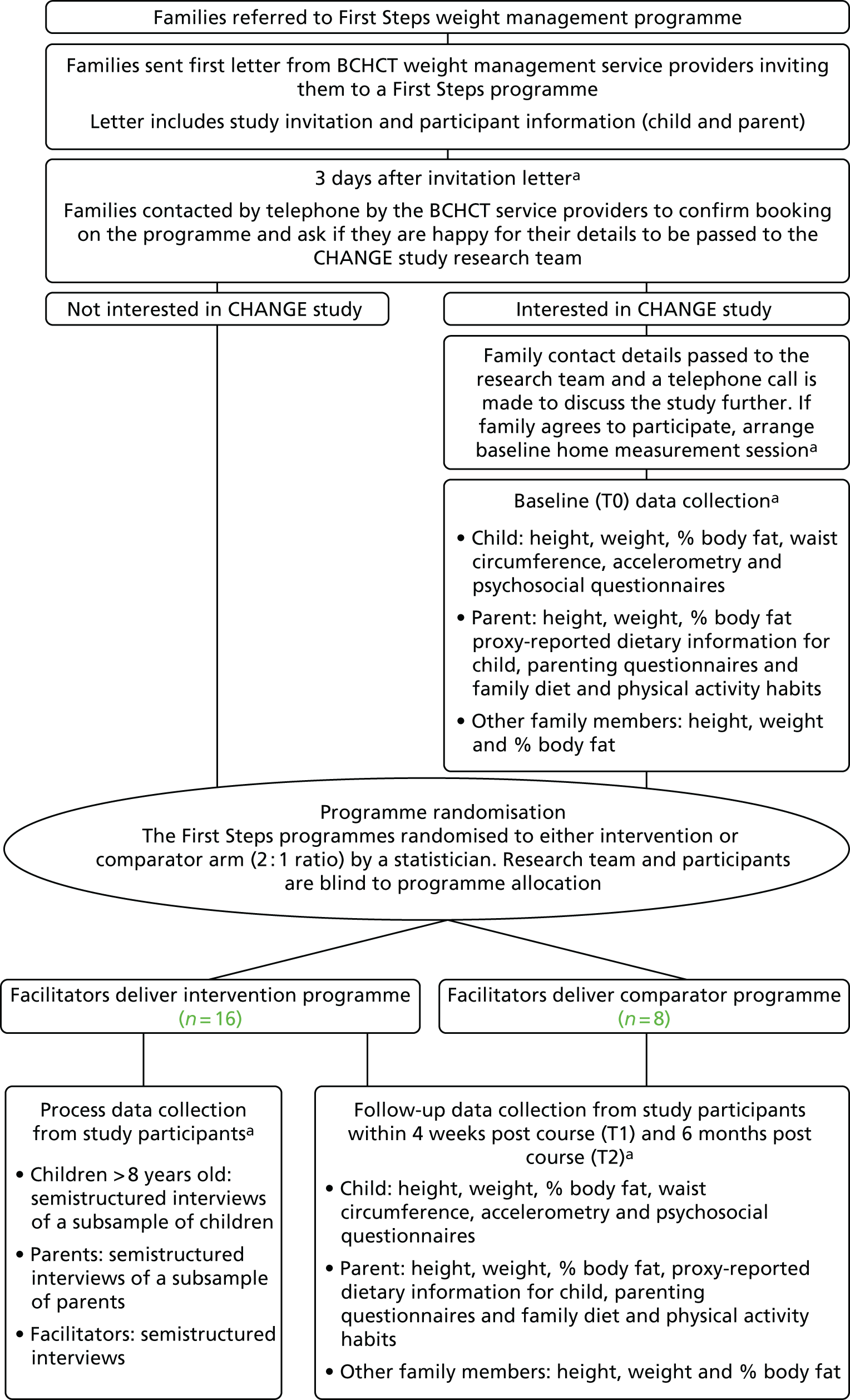
Safeguarding
If, during the study, the researchers had any concerns regarding the safety or well-being of a child or family member, they were required to document these on a safeguarding incident report form and submit these to the BCHCT. The BCHCT staff then followed their standard safeguarding procedures.
Intervention
The adapted intervention programme was delivered over 6 weeks and is described in detail in Chapter 1 (see Table 3 and Report Supplementary Material 1). Parents and children attended all sessions. Owing to school term time constraints, there were only 5 weeks available for the delivery of some of the programmes. In these instances, session plans for weeks 4 and 5 of the programme were combined to be delivered in one session. Details of how they were combined are in the facilitator’s manual in Report Supplementary Material 1. The study intervention period ran over four school half-terms. Four intervention programmes were run during each school half-term (16 programmes delivered in the intervention arm in total).
Facilitator training
Two intervention facilitators and a third assistant facilitator from the BCHCT children’s weight management service were trained to deliver the adapted First Steps programme. Two training sessions (of 2.5 hours and 1.5 hours) were provided by the CHANGE study co-ordinator and principal investigator, which were completed 1 week prior to the start of the courses (September 2015). The children’s weight management service operational manager also attended the training. The first session introduced the new materials and discussed the plan for each week in detail. The second session was delivered 3 days later to allow the facilitators to review the material. At this session, there was further discussion of the programme and the opportunity for the facilitators to raise any queries or concerns, which were then discussed and resolved. Facilitators were asked to adhere to the session plans and not to make any changes without first discussing them with the CHANGE research team. During the programme delivery period, facilitators were asked to feedback their experiences to the study co-ordinator, which enabled ongoing refinement of the programme sessions and the provision of further support to the facilitators.
Comparator
The standard First Steps programme was delivered for all programmes that were randomised to the comparator arm within the study period. Another facilitator from the BCHCT children’s weight management service delivered this programme over 5–7 weeks (depending on school term constraints), with parents attending all sessions and children attending the first and last sessions. More detail on the comparator programme is given in a TIDieR checklist in Appendix 4. Two comparator programmes were run during each of the four school half-terms within the study period (eight programmes in total).
To avoid contamination between the two arms, the facilitators delivering the adapted programme did not deliver the standard programme during the study period and were asked to refrain from discussing programme content with the facilitator who was delivering the standard programme during this time.
Evaluation of the adapted programme’s acceptability and the feasibility of its implementation
Programme completion
The primary outcome, to evaluate success of the programme adaptation to increase its suitability for Pakistani and Bangladeshi families, was calculated as an estimation of the proportion of these families completing the adapted programme and 95% confidence intervals (CIs). We also aimed to estimate the proportion of families of all ethnicities that completed the adapted programme and the proportion of families that completed the comparator programme. Completion was defined as attending at least 60% of the programme. To enable more precise estimates of these proportions to be made, we used routinely collected, anonymised attendance data from all programmes within the study period. This enabled us to use data from all programme participants, regardless of whether or not they were CHANGE study participants.
Family attendance at the programmes was recorded via parental signature at each session. Attendance information was collated and anonymised by the BCHCT weight management team and provided to the CHANGE study team once all programmes within the study period had been completed. Families were categorised into three groups: (1) completers (attended ≥ 60% of sessions), (2) non-completers (attended < 60% of sessions) and (3) non-attenders (did not attend any sessions).
Observation of programme delivery and facilitator feedback
Direct observations of programme sessions were undertaken by the research team to evaluate implementation and participant engagement and response. Specifically, observers took note of whether or not the programme was delivered as planned, which aspects were more challenging to deliver and how well the various parts of the programme engaged the families attending. We aimed to observe each facilitator delivering each programme session at least once across the study intervention period. Observers also made note of how the context influenced delivery and response (e.g. size of group, the facilitator, the venue, etc.). Facilitators were also asked to feed back their experiences to the study co-ordinator after each week of delivery of the programme, which provided valuable information on the feasibility of delivery of the sessions and the engagement of participants. The information gained from observations and feedback was used to refine further the adapted programme in the first 8 weeks of the study intervention period.
Interviews with programme facilitators, parents and children
At the end of the study intervention period, interviews were conducted with the two facilitators who delivered the adapted programme, with the aim of exploring their experiences of programme delivery, their perceptions of how participants responded to the programme and how this compared with their previous experience of delivering the standard programme.
Interviews were also undertaken with parents/carers who attended the adapted programme to explore their experiences, which parts of the programme they valued most and least and whether or not they were able to make positive behaviour changes as a result of attending the programme. We aimed to recruit 15 parents to participate in interviews, purposively sampling to ensure that approximately half were Pakistani or Bangladeshi and that we included a mix of programme completers and non-completers. We developed the interview schedules to include specific prompts to explore participants’ views of the adaptations made to the programme. Interviews were undertaken by the CHANGE research team (Tania Griffin and Kiya L Hurley, both of white British heritage), or by a community researcher (Meanaz Akhtar, of Pakistani heritage) if a participant required the interview to be in another language. In addition, nine children aged ≥ 8 years who had completed the programme were recruited to participate in interviews in which their experiences of the programme were explored. Again, we purposively sampled to include Pakistani and Bangladeshi children. Participating parents and children each received a shopping voucher worth £10. The interview schedule included participatory techniques that are designed to assist with interaction and recall. 60–62 The interview schedules for facilitators, parents and children are shown in Appendix 5. Written consent/assent was obtained from all interview participants.
The interviews were audio-recorded, translated into English (when required) and transcribed verbatim. The interviews that were recorded in English were transcribed by an external transcription company (Clayton Research Support), whereas those conducted in a different language were translated and transcribed by the community researchers and back translated by an independent researcher to check for accuracy.
Data analysis for all participants was guided by the framework approach. 63 This more deductive analysis approach was selected, as we were seeking to evaluate the adapted programme and to explore specific aspects of the adaptations that were made. Two researchers (Tania Griffin and Kiya L Hurley) reviewed the transcripts independently and identified codes to apply to the data. The researchers discussed their allocated codes and agreed on a final coding framework that was then applied to all transcripts using NVivo 10. The data were charted and mapped and overarching themes were identified. For the interviews with parents, differences were explored between those who completed the programme and those who did not.
Measurement of outcomes to be assessed in a future trial to evaluate intervention clinical effectiveness and cost-effectiveness
Data on a range of outcome measures were collected from study participants at three time points (T0, T1, T2; see Figure 6). The main purposes of this data collection were to (1) assess the feasibility of collecting these data from participants, (2) assess the completeness of the data collected and (3) gain estimates of parameters to be used in a sample size calculation of a future trial. In addition, we aimed to use the data to explore the direction of effect of the intervention and comparator programmes on these outcomes.
Assessments were undertaken with children, parents and other family members who were available and gave consent at the data collection visits to their homes. Assessments with children included measures of adiposity, an assessment of pubertal status and objectively measured physical activity and psychosocial measures, which included a quality-of-life utility measure (a key outcome measure in cost–utility analysis). Usual eating patterns of the children were assessed through parental report. Assessments with parents and other family members included anthropometric measures, an assessment of family eating and physical activity behaviours, parenting styles, parental feeding practices and parental self-efficacy. Anthropometric measures on parents and other family members and the measure of family behaviours were included because, in a future economic evaluation of the adapted children’s weight management programme, it would be important to try and measure any benefits of the programme to the wider family.
The complete list of outcome measures collected is shown in Table 4. The assessments were undertaken by trained researchers in the participants’ homes.
| Assessment | Data collection method |
|---|---|
| Child assessments | |
| Sex | Obtained from BCHCT records, verified by child |
| Date of birth | Obtained from BCHCT records, verified by parent/carer |
| Postcode | Obtained from BCHCT records, verified by parent/carer |
| Ethnicity | Reported by parent/carer |
| Religion | Reported by parent/carer |
| Language | Reported by parent/carer |
| Height | Leicester Height Measure HM-250P (Marsden Weighing Machine Group Limited, Rotherham, UK) (two measures taken) |
| Weight and percentage of body fat | Body Composition Analyzer BC-420MA (Tanita®, Yiewsley, UK) |
| Waist circumference | Lufkin® W606PM flexible steel tape measure (Apex Tool Group, Sparks, MD, USA) (two measures taken) |
| Pubertal status | Simplified visual assessment of breast development in girls, facial hair in boys. Parent report of whether or not girls had started menstruating |
| Objective 7-day physical activity record | Wrist-worn GENEActiv© (Activinsights Limited, Kimbolton, UK) or waist-worn ActiGraph© GT3X+ (ActiGraph, Pensacola, FL, USA) on non-dominant side of body for 7 days |
| Health-related quality of life | PedsQL64,65 (aged 5–7 or 8–12 years) |
| CHU-9D66–68 | |
| Body image questionnaire | Figure Rating Scale69,70 |
| Child dietary patterns | Children’s Dietary Questionnaire71 (completed by parent/carer) |
| Parent assessments | |
| Ethnicity | Reported by parent/carer |
| Religion | Reported by parent/carer |
| Language | Reported by parent/carer |
| Place of birth and when moved to UK | Reported by parent/carer |
| Age when left full-time education | Reported by parent/carer |
| Highest educational qualification | Reported by parent/carer |
| Employment status | Reported by parent/carer |
| Family diet and activity habits | FNPA survey72 |
| Authoritative parenting style | The authoritative parenting dimension of the Parenting Styles and Dimensions questionnaire73 |
| Parental self-efficacy | Parental Locus of Control Scale74 |
| Parental feeding practices | CFPQ75 |
| Height | Leicester Height Measure HM-250P (two measures taken) |
| Weight and percentage of body fat | Tanita® BC-420MA body composition scales |
| Assessments with other family members | |
| Date of birth | Self-reported (or proxy reported by parent for younger children) |
| Height | Leicester Height Measure HM-250P (two measures taken) |
| Weight and percentage of body fat | Body Composition Analyzer BC-420MA |
Collection of child outcome data
Anthropometric assessments
Height, weight and body fat percentage measurements were collected following standard operating procedures (see Appendix 6). Participants were measured in light clothing without socks and shoes and any headwear was removed. If the participant was wearing religious headwear that they did not wish to remove, it was measured and then deducted from the height measure. Child height measurements were taken on inspiration, and in duplicate, using a Marsden Weighing Group© Leicester Height Measure (HM-250P). To allow for measurement error, a third measurement was taken when the difference between the two measurements was > 0.4 cm. The two closest of the readings were averaged to give the definitive measurement.
Weight and body fat percentage measurements were taken using Tanita® body composition scales (Tanita® BC-420MA body composition scales). Participants were asked to pass urine before stepping on to the scales to minimise the effect that a full bladder could have on the fat percentage measurement. BMI was calculated by dividing weight (kg) by height squared (m). BMI z-scores were calculated for BMI and fat percentage using the lambda–mu–sigma (LMS) method and UK reference data. 44,76
Waist circumference was measured 4 cm above the umbilicus (a measurement point identified to be the most valid and pragmatic in overweight children77) using a flexible steel tape measure. Children were asked to raise their clothing to access the waist; however, if they refused, an option was given to take the waist measure over thin clothing. Waist measurements were taken at the end of a normal expiration and were taken in duplicate. When the difference between measurements was > 0.4 cm, a third measurement was taken. The two closest of the readings were averaged to give the definitive measurement. The LMS method and UK reference data78 were used to produce an age- and sex-specific waist z-score from the definitive waist circumference measurement value.
Questionnaire assessments
The researchers verbally administered a number of questionnaires to children and recorded the responses (see Appendix 7). Quality of life was assessed using two instruments: the Pediatric Quality of Life Inventory (PedsQL) Generic Core Scales version 4.0 and the Child Health Utility 9D (CHU-9D) questionnaire. PedsQL is a validated questionnaire consisting of subscales measuring physical, emotional, social and school functioning. 64,65 These aspects of quality of life are considered separately and all four are combined to assess overall quality of life. Age-specific versions of the PedsQL were used according to the child’s current age. Items were read to the children and responses were obtained either verbally or by using pictorial scales with younger children. PedsQL Likert scales were converted to 0- to 100-point scales, in which higher scores indicate a better quality of life.
The CHU-9D is a validated quality-of-life measure,66–68 which is administered for use in health economic analyses. It is a preference-based measure of health-related quality of life for use in children. It comprises a descriptive system and a set of preference weights, allowing the calculation of quality-adjusted life-years for use in a cost–utility analysis.
A figure rating scale, developed by Collins,69 and adapted by Rand and Resnick,70 was used to assess body image. This scale consists of sex-specific drawings of nine prepubescent figures ranging from very underweight (value = 1) to very overweight (value = 9). Two versions (light skinned and dark skinned) were developed for use in the study. Researchers used the version that was most appropriate for the child’s skin colour. Children were asked ‘Which picture looks the most like you look?’ and ‘Which picture shows the way you want to look?’ to assess ‘self’ and ‘ideal self’, respectively. To calculate children’s body dissatisfaction, the ‘ideal self’ score was subtracted from the ‘self’ score, giving a value of between –8 and +8. A score of 0 indicated body satisfaction, negative values indicated that the child would like to be larger and positive values indicated that the child would like to be thinner.
To assess children’s patterns of food intake, the Children’s Dietary Questionnaire was used (see Appendix 8). This parent/carer-completed 28-item questionnaire is a measure of intake patterns of a variety of healthy and unhealthy foods and is validated for assessment of intake patterns in children aged 4–16 years. 71 Four food group scores are calculated from the items: fruit and vegetables, fat from dairy, non-core foods and sugar-sweetened beverages. As the questionnaire was originally developed in Australia, minor adaptations were made, with input from the Parent Advisory Panel and the co-investigator team, to ensure applicability to the diets of the UK-based ethnically diverse study population. Parents were asked to complete the questions independently unless language or literacy support was required. In these cases, the researchers completed the questions with the parents.
Physical activity assessment
Objectively measured free-living individual physical activity was assessed using triaxial accelerometers. At each assessment period, during the home data collection visit, children were asked to wear an accelerometer continuously for 7 days on their non-dominant side, except when sleeping. Two types of accelerometers were used in the study: the wrist-worn GENEActiv© (Activinsights Limited, Kimbolton, UK) and the waist-worn ActiGraph© GT3X+ (ActiGraph, Pensacola, FL, USA). The purpose of including two different accelerometer types was to assess which gave the greatest level of participant compliance and data completeness. GENEActiv monitors are typically worn on the wrist and provide raw acceleration data. ActiGraphs are typically worn on the waist, have been commonly used in research with children and have been validated for use in this age group. 79–83 They can also provide raw acceleration data. At the baseline assessments, researchers assigned children either a GENEactiv or ActiGraph monitor at random. The children were then fitted with the same monitor type at the follow-up time points.
Both devices were set to record at 100 Hz in 60-second epochs. Data were analysed using the GGIR version 1.4 package developed in R version 3.3.1 (The R Foundation for Statistical Computing, Vienna, Austria; www.r-project.org; accessed 9 May 2016) through the University of Birmingham BlueBEAR High Performance Computing Service (www.birmingham.ac.uk/bear; accessed 9 May 2016). This package autocalibrates the raw triaxial accelerometer signals (x, y and z) to produce one omnidirectional value, the gravity-subtracted signal vector magnitude (SVMg; mg), using the Euclidean norm minus one (ENMO) formula [i.e. SVMg = √(x2 + y2 + z2) – 1]. Further information on the GGIR package is detailed at the following web page: (https://cran.r-project.org/web/packages/GGIR/GGIR.pdf; accessed 9 May 2016). A valid day’s wear was defined as > 10 hours of wear time in a 24-hour period. Device- and location-specific ENMO cut-off points were employed to estimate minutes spent in moderate activity (equivalent of four metabolic equivalents), vigorous physical activity (equivalent of six metabolic equivalents) and moderate to vigorous activity (activity at intensity levels over four metabolic equivalents). These were 359.7 mg (moderate activity) and 695.8 mg (vigorous physical activity) for GENEActiv monitors and 249.9 mg (moderate activity) and 464.6 mg (vigorous physical activity) for ActiGraph monitors. 84–86
Other data collection
In children aged ≥ 8 years, pubertal status was assessed using a simplified version of the Tanner scale. 87 Researchers were asked to indicate if there was any sign of breast development (females) or facial hair (males). In addition, parents were discreetly asked if menstruation had begun for female children. The Parent Advisory Panel was consulted on this approach to ensure its acceptability to participating children and parents.
The BCHCT children’s weight management team provided information on date of birth, sex and postcode for the participating children. This information was verified at the initial home visit. Parent/carers reported their child’s ethnicity, religion and language spoken. The postcodes were converted to the Index of Multiple Deprivation (IMD)88 2015 scores, a measure of small-area deprivation, which was used as a proxy for socioeconomic status. Participants were categorised into five groups using quintile cut-off points for England, so that group 1 included all individuals living in an area that is classified as being in the 20% most deprived areas in England, and group 5 included all those living in areas that are classified as being in the 20% least deprived areas in England.
Collection of parent outcome data
Anthropometric assessments
Height, weight and body fat percentage measurements were conducted with parents and carers who gave consent using the previously described measurement protocols (see Appendix 6). The BMI score was calculated by dividing weight (kg) by height squared (m).
Questionnaire assessments
Parents were given a questionnaire booklet and asked to complete it (see Appendix 8). Researchers provided assistance to parents when necessary. If a parent did not speak English, it was ensured that a community researcher with relevant language skills undertook the data collection visit so that they could verbally translate and complete the questionnaire with the parent. If participants spoke a language that was not spoken by the community researchers, an interpreter accompanied the researcher and verbally translated questions and participant responses, which were then recorded by the researcher.
At baseline, questionnaires included a range of questions to collect sociodemographic information, including parental ethnicity, religion, first language, place of birth (and when they moved to the UK if applicable), age when leaving full-time education, highest educational qualification and employment status.
At all time points, a number of questionnaire subscales relating to aspects of parenting style, self-efficacy and feeding practices were included in the parent questionnaire booklet. Parenting style was assessed using the authoritative parenting dimension of the Parenting Styles and Dimensions Questionnaire. 73 This dimension consists of three subscales: connection (five items), regulation (five items) and autonomy (five items). Subscale scores were calculated individually and summed to give a total authoritative parenting score. Higher scores represent a more authoritative parenting style.
Parental self-efficacy was measured using the Parental Locus of Control scale. 74 This scale consists of 10 items, which were summed to create a total self-efficacy score. Higher scores represent lower parental self-efficacy.
Nine subscales of the Comprehensive Feeding Practices Questionnaire (CFPQ) were used to measure a selection of parental feeding practices. The CFPQ has been shown to be valid in children up to 12 years of age and in varied cultural contexts. 75,89 However, to keep respondent burden to a minimum, only selected subscales of the CFPQ were included in the parent questionnaire. These were: (1) child control, (2) encourage balance and variety, (3) environment, (4) modelling, (5) monitoring, (6) restriction for health, (7) restriction for weight control, (8) teaching about nutrition and (9) involvement. Each subscale contains between three and eight items, totalling 39 items. Higher scores represent greater use of each practice.
All items from the three questionnaire instruments described above were answered on Likert scales from 1 to 5 points. Items indicated as needing to be reverse-scored by the relevant instrument instructions were reversed accordingly. For ease of interpretation, scores for all items in each subscale were summed and divided by the number of items, creating a score range of 1–5 points for each subscale. If one (3- to 5-item subscales) or two items (6- to 15-item subscales) were missing for any responder, the subscale was standardised using the number of items answered as the denominator. When more than 1 or 2 items were missing, a score was not calculated.
Collection of family outcome data
Anthropometric assessments
Height, weight and body fat percentage measurements were taken for any other consenting/assenting family members aged > 4 years who were present at the data collection visits. The previously described measurement protocols were used to conduct these measurements (see Appendix 6).
Family behavioural assessment
The Family Nutrition and Physical Activity (FNPA) questionnaire is designed to assess family behaviours and environments related to children’s nutrition and physical activity. 72 The questionnaire has 20 items overall and 10 subscales (two items each). The subscales are (1) family meals, (2) family eating practices, (3) family food choices, (4) family beverage choices, (5) restriction and reward, (6) screen time, (7) creating a healthy environment, (8) family activity, (9) child activity and (10) family schedule/sleep routine. All items of the FNPA were included in the questionnaire booklet for completion by parents/carers.
Collection of data on costs associated with the intervention
Within the feasibility study, we explored methods to measure costs from a societal perspective, including intervention-specific costs, parent productivity costs (e.g. time off work to attend the intervention sessions), associated child-care costs and changes to the family’s weekly food bill.
Intervention costs
For both the intervention and the comparator programmes, resource use data were collected prospectively by the BCHCT staff delivering the programmes and by the study research staff. Methods were developed to capture the resource use and costs associated with the development and production of programme materials for both intervention and comparator programmes. This included costs relating to the development and production of manuals, additional information provided and any other materials used within the programmes. In addition, the costs associated with training the facilitators in the intervention arm were also captured, as were the staffing costs associated with delivering the programmes. Data were also collected on the costs associated with the hiring of premises, with the resources used to promote the programmes and project manage the programmes and with the time spent assembling the materials used within the programmes. Costs associated with travel for staff to and from the venues were also captured.
Costs to families
Spending time attending a weight management programme and spending further time putting the learning into practice leads to a cost being incurred by families. This includes a cost linked to the time spent attending the programme, any associated child-care costs and changes to the family’s weekly food bill. A questionnaire survey was designed to capture this information (see Appendix 9). Specifically, the questionnaire asked parents what they would have been doing if not attending the programme, what arrangements they had made if they had needed time off work, whether or not they had paid for child care for other children when attending the programme, how long their journey to the venue was and how they had travelled, and whether or not their weekly food bill had changed since attending the programme. The questionnaire was administered by the facilitators to all programme participants (regardless of whether or not they were CHANGE study participants) at the final session.
Collection of anonymised outcome data from all children attending the intervention or comparator weight management programmes in the study period
To assist in exploring the direction of effect of the adapted children’s weight management programme on BMI z-score, the BCHCT team provided the research team with routinely collected, anonymised data on sex, ethnicity and pre- and post-programme height and weight measurements from all children who attended the weight management programmes within the study period. This provided a larger sample size for the exploratory analysis of the outcome of BMI z-score in the intervention and comparator groups. The measurement protocols used for the routine programme data collection were different from the study protocols, so the analyses of the study data and the routinely collected data were undertaken separately.
Sample size
We used routinely collected, anonymised data on programme completion to calculate the primary outcome (the proportion of Pakistani and Bangladeshi families completing the adapted programme and 95% CIs). An analysis of existing service data showed that the mean group size when a programme commenced was 11; therefore, it was expected that approximately 176 families would attend the 16 adapted programmes delivered in the intervention period, 40% of which would be Pakistani or Bangladeshi (approximately 70 families). We calculated that this sample size would allow an estimation of the proportion of Pakistani and Bangladeshi families completing the programme to within 26% precision. For example, if 65% of Pakistani and Bangladeshi families completed the adapted programme, the 95% CI of the estimate of completion would be 52% to 78%. For this calculation, we inflated the variance that we would expect under individual randomisation by the variance inflation factor for cluster trials (with an additional inflation of 11% to account for the varying cluster size90) and assumed a mean cluster size of five. As there were no specific data to inform the estimate of the intracluster correlation coefficient (ICC), we used patterns of ICCs from other sources to inform our calculation. 91 We expected a moderate to high prevalence of our outcome (programme completion), which is associated with lower ICCs, but our outcome was a process measure and we had small cluster sizes, both of which factors are associated with higher ICCs. 92 Therefore, we assumed a moderate ICC of 0.05.
We planned to recruit at least 80 participants into the study to undergo data collection at the three time points. This number of participants was deemed to be sufficient to test recruitment and data collection methods, and to enable estimation of the key parameters required for a sample size calculation of a future trial. 93
Statistical analysis
As the feasibility study was a cluster randomised design, methods were employed throughout the analysis to account for the clustered nature of the data. In accordance with the Consolidated Standards of Reporting Trials (CONSORT) guidelines,94 an intention-to-treat approach was used for all outcome analyses. Outcomes were considered significant at the 5% level. Statistical analysis was conducted in Stata version 13.
Estimation of programme completion
The primary outcome was the estimate of the proportion of Pakistani and Bangladeshi families that would complete the adapted programme and the 95% CIs (using routinely collected, anonymised programme data). Completion was defined as attending at least 60% of the programme. We adjusted the CIs using robust standard errors to account for the effect of clustering. To implement this calculation, we used the proportion function, with adjustment for cluster, in Stata version 13.
The same methods of analysis were performed to estimate the secondary outcomes to assess programme acceptability: (1) the proportion of all families completing the adapted programme, (2) the proportion of Pakistani and Bangladeshi families completing the comparator programme and (3) the proportion of all families completing the comparator programme.
Participant characteristics
Routinely collected individual child data (age, sex and ethnicity) were summarised at baseline for the CHANGE study participants and non-CHANGE study participants (i.e. children attending a weight management programme but not participating in the CHANGE study). The baseline characteristics of the CHANGE study participants were summarised by intervention and comparator arm. Categorical data are presented as numbers and percentages. Normality of continuous variables was assessed by comparison of the mean and median values and the distribution of values in a histogram plot. When normally distributed, continuous data are presented by their mean and standard deviation. Medians and interquartile ranges (IQRs) are presented for variables that exhibited non-normality.
Completeness of outcome data
To assess completeness of the outcome data collected from participants, the number and proportion of participants completing each measure are presented for each data collection time point.
Intervention and comparator costs
An exploratory analysis was undertaken to refine the focus for the methods for an economic evaluation within a future trial. In line with good practice for economic evaluation, we assessed the incremental costs. Therefore, costs that were common to both arms (i.e. the comparator and the intervention), such as costs associated with staff travelling to and from venues, programme promotion costs, project management and costs associated with assembling materials, were excluded from this analysis. Only the costs that were different between the two arms (i.e. the costs linked to the adaptation) were included in the analysis.
Estimation of parameters to inform a sample size calculation of a future trial
In addition to study attrition, other parameters required for the sample size calculation of a future cluster RCT are estimations of the ICC for the primary outcome and the correlation between baseline and follow-up measures of the primary outcome. Therefore, we used anonymised BMI z-score data routinely collected at the end of the programme to estimate the ICC, and we estimated correlation between baseline and post-intervention BMI z-score using the routinely collected programme data and outcome data from the CHANGE study participants. We also estimated the correlation between baseline and 6-month post-intervention BMI z-scores in the CHANGE study participants.
Exploratory analysis of participant outcome data by intervention and comparator arms
For each study arm, outcome data from children and parents at T1 and T2 were summarised using their means and standard deviations, when normally distributed, and medians and IQRs otherwise.
To explore the direction of effect of the adapted and standard programmes on the outcomes studied, mean differences between T0 and T1 (end-of-programme follow-up), and T0 and T2 (6-month follow-up) were calculated for both study arms, taking into account clustering.
Although an evaluation of intervention effectiveness was not an aim of the feasibility study and it was not sufficiently powered to detect minimum clinical differences in outcomes between intervention and comparator arms, we performed exploratory analyses to estimate differences in outcomes between the study arms. The purpose of undertaking these analyses was twofold: first, to develop methods of analysis for use in a future trial and, second, to explore the direction of effect of the adapted programme compared with the standard programme. Mixed-effects linear regression models were developed, adjusting for clustering and baseline measures. Ninety-five per cent CIs were reported and differences deemed significant at the 5% level. For each outcome, two models are presented. First, a model was developed with the T1 or T2 outcome as the dependent variable, adjusted for the baseline value of the outcome and clustering. Then, a second model was developed, further adjusting for child age, sex, ethnicity and IMD score. In addition, models were developed with the anonymised BMI z-score data routinely collected from all programme participants as the outcome, first, adjusting for clustering and baseline BMI z-score and then, second, further adjusting for child age, sex and ethnicity.
When necessary, data were transformed for use within the models. The following method was used to identify outcome variables that required transformation. First, the mean and median values of each outcome variable were compared to identify data skew. For those outcomes with an obvious skew, a Tukey’s Ladder of Powers plot was generated using the gladder command in Stata version 13. 95 When a particular transformation was undertaken, two models were tested: one with the data in their raw form and another with the transformed data. The residuals from each model were calculated, plotted and compared for normality. When transformation of the outcome variable did not improve the normality of the model residuals, the untransformed data were used in preference to aid interpretation of the results. Transformations for a particular outcome were used for all models with that outcome to improve comparability. Outputs of all transformed models were back-transformed.
For the main analyses, only participants with complete data were included in the models. The number of participants included in each model is presented by study arm to allow full consideration of missing data.
Sensitivity analyses
For a variety of reasons (incomplete data collection, attrition, etc.) the numbers of participants included in the models to explore differences in outcomes between intervention and comparator arms were lower than the total number of study participants. For some outcomes, the number of missing data was substantial. Therefore, to explore further the differences between study arms, two imputation techniques were employed. First, the baseline observation carried forward technique was utilised, in which the missing follow-up value is replaced with the observed baseline value. 96 This technique allows a conservative effect estimate to be generated. However, concern has been raised over the ability of single-imputation methods, such as baseline observation carried forward, to produce unbiased estimates of variance96 and there is an overconservative assumption that study non-completion is synonymous with no effect. 97 Therefore, we used multiple imputation techniques in a second sensitivity analysis. Imputation was conducted for each outcome separately. For the anthropometric and physical activity outcomes at T1 and T2, the following items were included in the imputation process: the outcome of interest, the baseline (T0) value of the outcome (when available), other anthropometric and physical activity measures taken at the relevant time point (i.e. T1 or T2), completion status, pubertal status, age, sex, ethnicity and IMD score. For the questionnaire-based outcomes at T1 and T2, the following items were included in the imputation process: the outcome of interest, the baseline (T0) value of the outcome (when available), completion status, pubertal status, age, sex, ethnicity and IMD score.
We allowed for clustering in the multiple imputation procedure. The procedure involves fitting a conditional model for each variable with missing data in which the variable is linearly regressed on all other variables using mixed-effects linear regression (those with and without missing data). It then uses a Gibbs sampling approach (100 iterations), updating each set of parameters in turn, conditional on the others. A mixed-effect linear regression model was used to analyse each continuous outcome variable conditional on the imputed data. Rubin’s rule is used to pool the effect estimates of 10 sets of imputed data. 98 We transformed any variables that showed marked non-normality. Transformations used in the imputation process were consistent with the main analysis. These multiple imputation models were implemented in Stata and REALCOM-Impute (Centre for Multilevel Modelling, Bristol, UK).
Results
Families participating in the First Steps weight management programmes within the study period
In the study intervention period (September 2015 to April 2016), a total of 536 families were referred to the children’s weight management service and invited to attend a programme. In total, 49% of referrals were made through the NCMP, 27% were self-referrals, 13% of families were referred by their general practitioner and 11% were referred by their school nurse. Of the 536 families invited, 243 families (45.3%) attended at least one programme session. This was consistent across the intervention and comparator arms. Forty per cent of all families who were invited to attend were Pakistani or Bangladeshi, with a slightly higher proportion in the intervention arm than in the comparator arm (42% vs. 35%). Of all Pakistani and Bangladeshi families invited, 48.1% (103/214) attended at least one programme session, with a slightly higher proportion attending in the intervention arm than in the comparator arm (51% vs. 41%). The flow of programme participants in the intervention and comparator programmes is shown in Figure 7.
FIGURE 7.
Flow diagram of First Steps programme participants. BP, Bangladeshi or Pakistani.
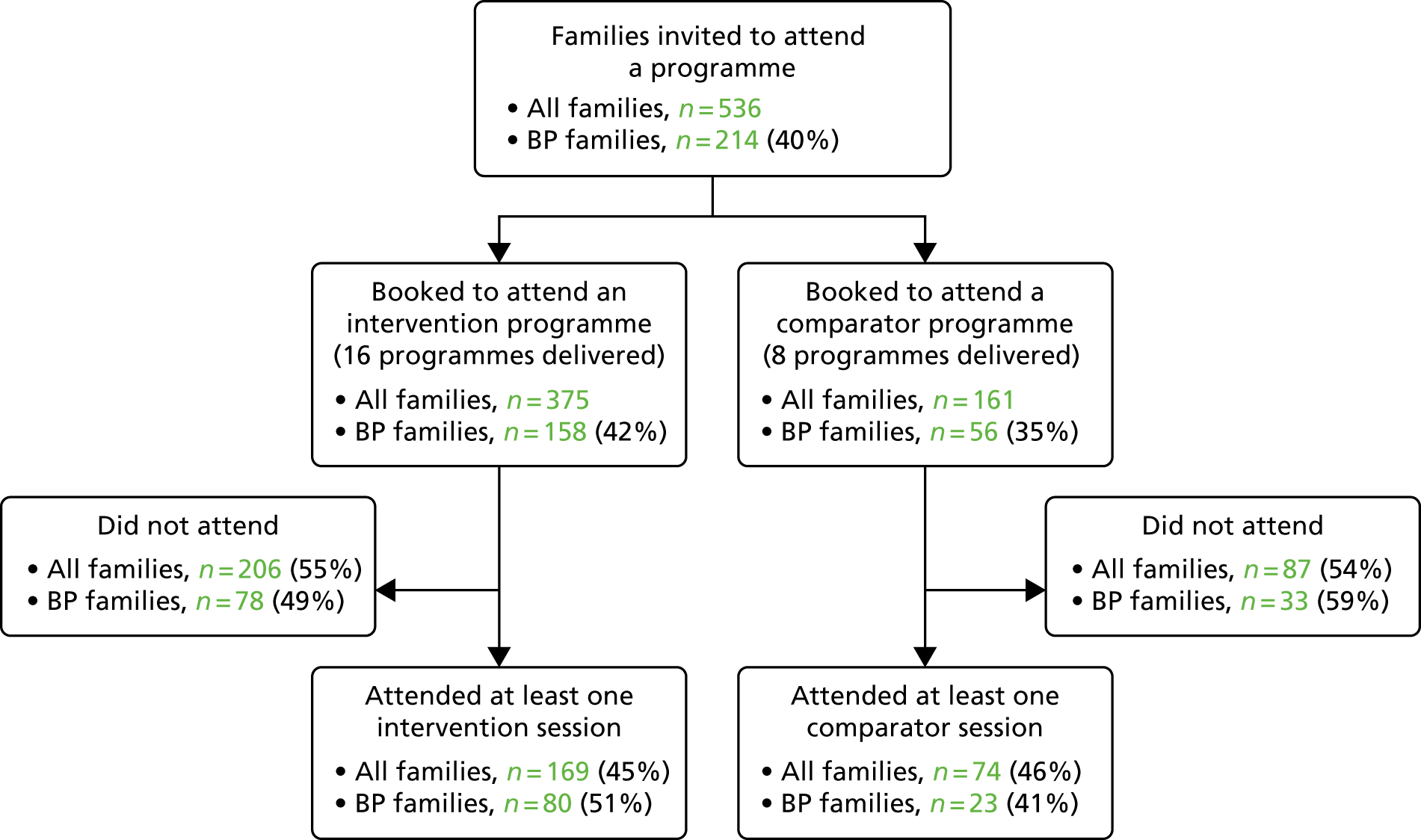
Anonymised attendance data from all families who attended at least one session of a programme during this period were used to calculate the proportion of families completing the programmes.
The CHANGE study participant recruitment and follow-up
A total of 92 children and their families consented to participate in the CHANGE study between September 2015 and April 2016. During this period, BCHCT provided contact details for 157 families. Details for 14 families were received once the recruitment target of 80 had been surpassed; therefore, these families were sent a letter explaining that recruitment was complete but that if they were interested to hear more about the research they were welcome to contact the study team. Therefore, 62.9% (92/143) of participants approached by the research team consented to participate in the study.
Of the 92 participating families, 75 (81.5%) received a home data collection visit at T0 (baseline). We were unable to arrange a T0 data collection visit with the remaining 17 families (see Recruitment difficulties). We attempted to contact all participants at T1 and T2. If we were unable to make contact at T1, we still attempted to contact families at T2. Of the 92 families, 82 had outcome assessments at T1 (end of programme, 89.1%) and 60 had outcome assessments at T2 (6 months post intervention, 65.2%). Participant recruitment and follow-up is shown in Figure 8. A total of 19 families participating in the CHANGE study (20.7%) did not attend any programme sessions (14 families, 20.3%, in the intervention arm; five families, 21.7%, in the comparator arm).
FIGURE 8.
Flow diagram of the CHANGE study participants. a, Attempts were still made to contact families at T2.
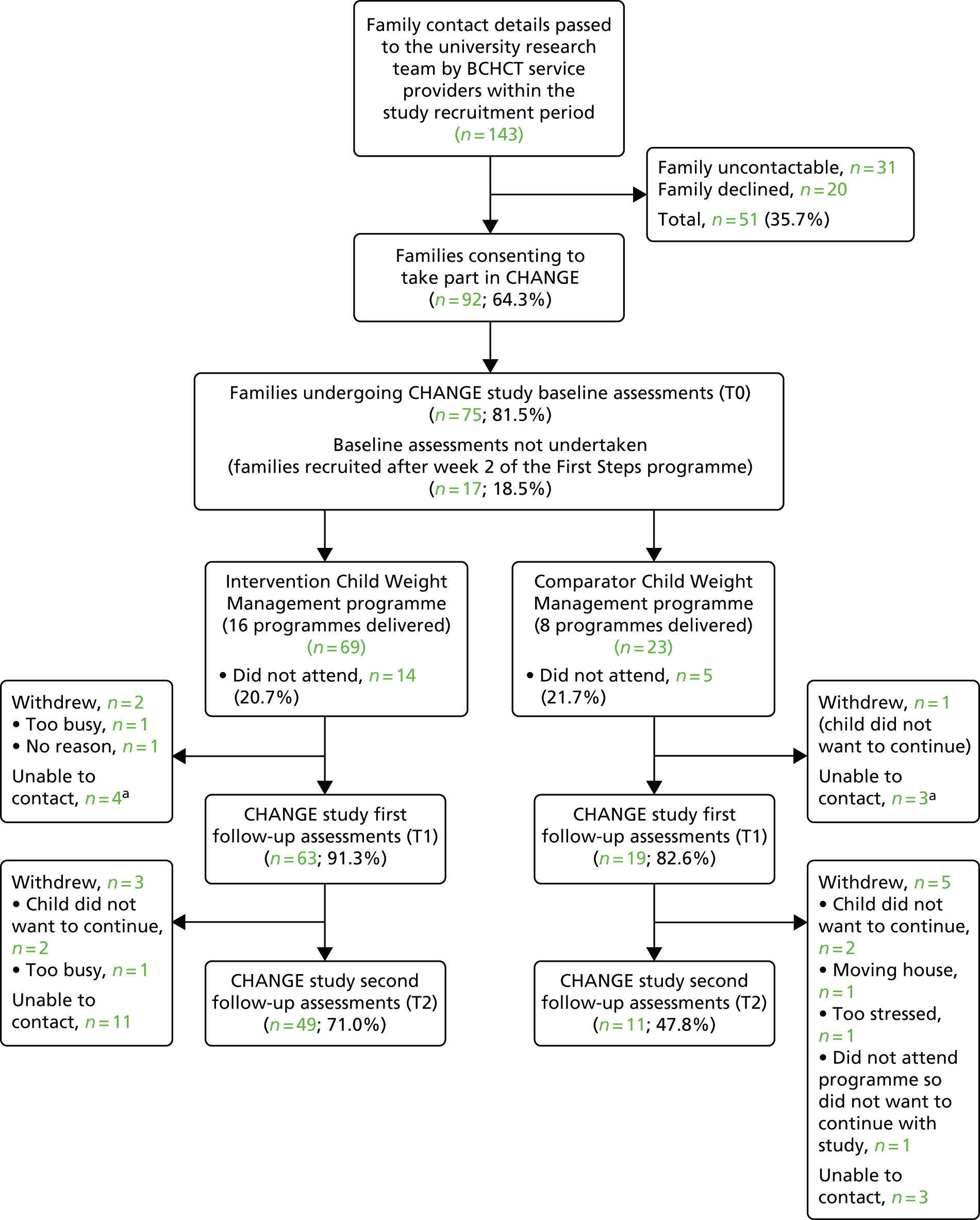
Recruitment difficulties
A multistage recruitment process was developed (see Figure 6), which was designed to be implemented by the BCHCT children’s weight management service team and the CHANGE study research team on a continuous basis throughout the study recruitment period, so that all families invited to attend a programme were also invited to participate in the study. However, in reality, not all families were invited to take part in the CHANGE study. This was a result of several factors. During the study period, the BCHCT team had significant administrative staffing issues, which resulted in delays in calling families and incomplete recording of whether or not participation in the CHANGE study had been discussed with the families. In addition, not all families received a telephone call as a follow-up to their programme invitation letter.
The second stage of recruitment also proved problematic. The research team experienced some difficulties in contacting people, even though the BCHCT team had successfully been able to contact them by telephone. Telephone calls were made at different times of the day to optimise the chances of making contact but for some families contact was still not achieved. In some cases, the telephone numbers were no longer active. If contact was not achieved after multiple attempts, a letter was sent to the family asking them to contact us should they be interested in taking part in the study.
Contact details were often received by the study research team either just before participants started a programme or after the programme had started, which posed logistical difficulties in arranging the collection of baseline data. In addition, the study researchers and community researchers encountered multiple delays when attempting to gain the necessary permissions to take consent and collect data from participants. This meant that, particularly at the beginning of the study, the number of researchers able to undertake the initial visits to take consent and collect baseline data (T0) was less than expected. The impact of both of these factors was that it became difficult or impossible for the research team to arrange the baseline (T0) appointment prior to the families starting their programme. A pragmatic decision was made to allow T0 appointments to be undertaken up until the families had attended their second session so that baseline data collection feasibility and acceptability could be tested. However, we were unable to arrange T0 visits to collect baseline data for 17 out of the 92 families who consented to participate, as they had already had the opportunity to attend at least two programme sessions. These families received a first data collection visit at T1 (i.e. after the end of the programme), and their baseline data were recorded as missing. Recruitment to a future trial would need careful planning with all partners involved to ensure that baseline data are collected from participants before they receive the intervention.
Attrition
There was a high level of attrition in this study, with only 65% of participants followed up at 6 months (T2). Of the 32 participants who were not followed up at T2, one-third actively withdrew from the study and the rest were lost to follow-up, despite multiple attempts to contact them by telephone and letter. There was greater attrition in the comparator arm than in the intervention arm (52.2% vs. 29.0%; see Figure 8). There was also a difference in the proportion of participants actively withdrawing between the two study arms, with a greater proportion of participants withdrawing in the comparator arm than in the intervention arm (26.1% vs. 7.2%). Participant characteristics of those who were followed up compared with those who were not followed up were broadly similar (Table 5). A higher proportion of Pakistani and Bangladeshi participants were followed up than not followed up. We also explored programme attendance and completion by study arm in those who could not be followed up. In the intervention arm, 7 out of the 20 participants (35%) who were not followed up at T2 did not attend any weight management programme sessions and three (15%) attended but did not complete the programme. In the comparator arm, 3 out of the 12 participants (25%) who were not followed up at T2 did not attend any programme sessions and four (33.3%) attended but did not complete the programme.
| Participant characteristics | Participants, n (%a) or mean (SD) | |
|---|---|---|
| Followed up to end of study (N = 60) | Withdrew or lost to follow-up (N = 32) | |
| Sex of the child | ||
| Male | 27 (45.0) | 17 (53.1) |
| Female | 33 (55.0) | 15 (46.9) |
| Age at the start of the programmeb (years) | 9.8 (1.9) | 10.5 (4.4) |
| Ethnicity (N = 91c) | ||
| White | 8 (13.3) | 6 (19.4) |
| Black | 6 (10.0) | 3 (9.7) |
| Bangladeshi or Pakistani | 32 (53.3) | 12 (38.7) |
| Indian | 3 (5.0) | 4 (12.9) |
| Mixed or other ethnicities | 11 (18.3) | 6 (19.4) |
| IMD quintile (N = 90d) | ||
| 1 (most deprived) | 46 (78.0) | 25 (80.7) |
| 2 | 6 (10.2) | 4 (12.9) |
| 3 | 4 (6.8) | 2 (6.5) |
| 4 | 3 (5.1) | 0 (0.0) |
| 5 (least deprived) | 0 (0.0) | 0 (0.0) |
| Baseline BMI z-score (N = 75e) | 2.5 (0.5) | 2.6 (0.8) |
Participant characteristics
Characteristics of the CHANGE study and non-CHANGE study participants
The characteristics of children invited to attend a First Steps programme in the study period by the CHANGE study consent status are shown in Table 6. Overall, child characteristics of the families consenting to participate in the CHANGE study were broadly similar to those who did not consent to participate. When comparing the characteristics of the CHANGE study participants with those of the non-CHANGE study participants by programme type, for the group allocated to receive the adapted programme (the intervention arm), there was a higher proportion of Pakistani and Bangladeshi families who consented to be in the study than did not consent. However, in the group allocated to receive the standard programme (i.e. the comparator arm), the proportion of these families who consented was lower than those who did not consent. Mean pre-programme BMI z-scores were similar across the CHANGE study participants and non-CHANGE study participants in the two study arms, with a slightly lower mean in the CHANGE study participants than in the non-CHANGE study participants in the intervention arm (2.76 vs. 2.93). There are a large number of missing BMI data for the non-CHANGE study participants, as more than half of those invited to attend a programme did not attend and, therefore, their height and weight measurements were not taken.
| Participant characteristics | Trial arm | Total (N = 536) | ||||
|---|---|---|---|---|---|---|
| Intervention (N = 375) | Comparator (N = 161) | |||||
| CHANGE participants (n = 69) | Non-CHANGE participants (n = 306) | CHANGE participants (n = 23) | Non-CHANGE participants (n = 138) | CHANGE participants (n = 92) | Non-CHANGE participants (n = 444) | |
| Sex of the child, n (%b) (n = 531a) | ||||||
| Male | 32 (46.4) | 164 (54.5) | 12 (52.2) | 67 (48.6) | 44 (47.8) | 231 (52.6) |
| Female | 37 (53.6) | 137 (45.5) | 11 (47.8) | 71 (51.5) | 48 (52.2) | 208 (47.4) |
| Age at start of programme (years), median (IQR) (n = 533c) | 10 (2.0) | 10 (3.0) | 10 (2.0) | 10 (3.0) | 10 (2.0) | 10 (2.0) |
| Ethnicity, n (%b) (n = 461d) | ||||||
| White | 8 (11.8) | 58 (22.7) | 6 (26.1) | 20 (17.5) | 14 (15.4) | 78 (21.1) |
| Black | 6 (8.8) | 20 (7.8) | 3 (13.0) | 9 (7.9) | 9 (9.9) | 29 (7.8) |
| Bangladeshi or Pakistani | 36 (52.9) | 122 (47.7) | 8 (34.8) | 48 (42.1) | 44 (48.4) | 170 (46.0) |
| Indian | 5 (7.4) | 15 (5.9) | 2 (8.7) | 10 (8.8) | 7 (7.7) | 25 (6.8) |
| Mixed or other ethnicities | 13 (19.1) | 41 (16.0) | 4 (17.4) | 27 (23.9) | 17 (18.9) | 68 (18.4) |
| Pre-programme BMI z-score, mean (SD) (n = 235e) | 2.71 (0.65) | 2.93 (0.87) | 2.90 (0.60) | 2.87 (0.72) | 2.76 (0.64) | 2.91 (0.83) |
CHANGE study participant characteristics
The baseline characteristics of children in the intervention and comparator arms are shown in Table 7. In total, almost half of the study participants were of Pakistani or Bangladeshi ethnicity, with a higher proportion of Pakistani and Bangladeshi children in the intervention arm. Nearly 80% were in the most deprived quintile and this was consistent across the study arms. Mean anthropometric measures were marginally higher in the comparator arm.
| Participant characteristics | Trial arm, n (%a) or mean (SD) | Total (n = 92), n (%a) or mean (SD) | |
|---|---|---|---|
| Intervention (N = 69) | Comparator (N = 23) | ||
| Sex of the child (n = 92) | |||
| Male | 32 (46.4) | 12 (52.2) | 44 (47.8) |
| Female | 37 (53.6) | 11 (47.8) | 48 (52.2) |
| Age at start of programme (years) (n = 92) | 10 (2.0) | 10 (2.0) | 10 (2.0) |
| Ethnicity (n = 91) | |||
| White | 8 (11.8) | 6 (26.1) | 14 (15.4) |
| Black | 6 (8.8) | 3 (13.0) | 9 (9.9) |
| Pakistani or Bangladeshi | 36 (52.9) | 8 (34.8) | 44 (48.4) |
| Indian | 5 (7.4) | 2 (8.7) | 7 (7.7) |
| Mixed or other ethnicities | 13 (19.1) | 4 (17.4) | 17 (18.7) |
| IMD quintile (n = 90) | |||
| 1 (most deprived) | 53 (79.1) | 18 (78.3) | 71 (78.9) |
| 2 | 9 (13.4) | 1 (4.4) | 10 (11.1) |
| 3 | 2 (3.0) | 4 (17.4) | 6 (6.7) |
| 4 | 3 (4.5) | 0 (0.0) | 3 (3.3) |
| 5 (least deprived) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| First language (n = 89) | |||
| English | 58 (86.6) | 19 (86.4) | 77 (86.5) |
| Urdu | 4 (6.0) | 0 (0.0) | 4 (4.5) |
| Mirpuri | 1 (1.5) | 1 (4.6) | 2 (2.3) |
| Sylheti | 1 (1.5) | 0 (0.0) | 1 (1.1) |
| Bengali | 1 (1.5) | 1 (4.6) | 2 (2.3) |
| Other | 2 (3.0) | 1 (4.6) | 3 (3.4) |
| Religious identity (n = 82) | |||
| Muslim | 42 (65.6) | 8 (44.4) | 50 (61.0) |
| Sikh | 1 (1.6) | 2 (11.1) | 3 (3.7) |
| Hindu | 1 (1.6) | 1 (5.6) | 2 (2.4) |
| Christian | 7 (10.9) | 5 (27.8) | 12 (14.6) |
| Other | 1 (1.6) | 0 (0.0) | 1 (1.2) |
| No religion | 12 (18.8) | 2 (11.1) | 14 (17.1) |
| BMI z-score (n = 75) | 2.5 (0.6) | 2.7 (0.7) | 2.5 (0.6) |
| Body fat percentage z-score (n = 73) | 2.2 (0.4) | 2.3 (0.4) | 2.2 (0.4) |
| Waist circumference z-score (n = 69) | 2.8 (0.7) | 3.1 (0.5) | 2.9 (0.6) |
| Puberty commenced (n = 65) | 13 (28.3) | 8 (42.1) | 21 (32.3) |
| Average accelerationb (SVMg; mg), (n = 64) | 32.1 (14.7) | 32.0 (12.1) | 32.1 (14.0) |
| Moderate to vigorous physical activityb (minutes/24 hours), (n = 64) | 14.5 (11.2) | 11.0 (22.7) | 13.6 (12.2) |
| PedsQL scoreb (n = 71) | 76.1 (23.9) | 70.63 (28.1) | 75.2 (24.2) |
| Physical functioning scoreb (n = 72) | 81.25 (15.7) | 81.25 (21.9) | 81.3 (17.2) |
| Emotional functioning scoreb (n = 74) | 80.0 (40.0) | 75.0 (30.0) | 77.5 (35.0) |
| Social functioning scoreb (n = 75) | 75.0 (30.0) | 60.0 (40.0) | 70.0 (40.0) |
| School functioning scoreb (n = 75) | 75.0 (25.0) | 70.0 (45.0) | 75.0 (30.0) |
| Body dissatisfaction scoreb (n = 73) | 2.0 (2.0) | 2.0 (2.0) | 2.0 (2.0) |
| CHU-9D score (n = 75) | 0.85 (0.12) | 0.89 (0.09) | 0.86 (0.11) |
| Children’s Dietary Questionnaire (scores) | |||
| Fruit and vegetables (n = 67) | 5.9 (2.9) | 4.6 (3.0) | 5.5 (3.0) |
| Dairyb (n = 61) | 2.0 (2.0) | 1.0 (2.0) | 2.0 (2.0) |
| Sugar-sweetened beveragesb (n = 68) | 1.3 (1.9) | 1.4 (2.1) | 1.3 (1.9) |
| Non-core foodsb (n = 63) | 2.4 (1.5) | 2.0 (2,6) | 2.3 (1.6) |
| FNPA (n = 53) | 57.4 (5.5) | 54.8 (7.2) | 56.6 (6.1) |
| Authoritative parenting (n = 47) | 4.3 (0.6) | 4.2 (0.3) | 4.3 (0.6) |
| Parenting efficacy (n = 50) | 2.2 (0.6) | 2.1 (0.6) | 2.2 (0.6) |
| Parent feeding practices scores | |||
| Child control (n = 42) | 1.7 (0.7) | 2.2 (0.7) | 1.8 (0.8) |
| Encouraging balance and varietyb (n = 42) | 3.5 (0.8) | 3.3 (1.5) | 3.5 (1.0) |
| Environmentb (n = 42) | 3.0 (1.3) | 3.0 (1.8) | 3.0 (1.3) |
| Modelling (n = 42) | 2.6 (0.9) | 2.4 (1.4) | 2.5 (1.0) |
| Monitoring (n = 42) | 2.7 (0.8) | 2.9 (1.1) | 2.7 (0.9) |
| Restriction for healthb (n = 42) | 3.0 (1.0) | 3.5 (1.0) | 3.3 (1.0) |
| Restriction for weight control (n = 42) | 2.5 (0.7) | 2.0 (1.0) | 2.4 (0.8) |
| Teaching about nutrition (n = 42) | 2.8 (0.8) | 2.7 (0.8) | 2.8 (0.8) |
| Involvement (n = 42) | 2.2 (0.7) | 2.4 (0.7) | 2.2 (0.7) |
Programme completion
The proportions of families that completed the programme in the intervention and comparator arms, estimated from anonymised attendance data from all families attending at least one session of a programme during the study period, are shown in Table 8. The primary outcome, the proportion of Pakistani and Bangladeshi families completing the adapted programme, was estimated to be 78.8% (95% CI 64.8% to 88.2%). The proportion of all families who completed the adapted programme was 76.3% (95% CI 67.0% to 83.6%), which was higher than the estimated proportion of all families completing the standard programme (58.1%; 95% CI 46.5% to 68.8%).
| Family | Trial arm | |||||
|---|---|---|---|---|---|---|
| Intervention | Comparator | |||||
| Families attending at least one session (n) | Families completing programmea (n) | % (95% CIb) | Families attending at least one session (n) | Families completing programmea (n) | % (95% CIb) | |
| BP | 80 | 63 | 78.8 (64.8 to 88.2) | 23 | 14 | 60.9 (48.5 to 72.0) |
| Non-BP | 83 | 62 | 74.7 (65.0 to 82.4) | 45 | 26 | 57.8 (40.9 to 73.4) |
| Allc | 169 | 129 | 76.3 (67.0 to 83.6) | 74 | 43 | 58.1 (46.5 to 68.8) |
The analysis of programme completion was repeated for only the CHANGE study participants (see Appendix 10), and a broadly similar pattern of completion in the intervention and comparator arms was seen, although the 95% CIs of the estimates are very wide because of the small numbers of participants included in the analysis.
Observation of programme delivery and facilitator feedback
The CHANGE research team directly observed delivery of 12 of the adapted programme sessions. One facilitator was observed delivering all six sessions. The other facilitator was observed delivering all but the first session and was observed twice when delivering session 2 (healthy eating). The facilitators also communicated with the study co-ordinator by e-mail or telephone to feed back on their experiences of programme delivery each week. Overall, the facilitator feedback of session delivery was positive and the facilitators reported a high level of enjoyment when running the sessions.
In the first school half-term of programme delivery, the research team used the observation and facilitator feedback to refine programme materials further. Refinements to the programme and other actions undertaken in response to the observations and feedback are shown in Table 9. After the first school half-term, the intervention materials and the facilitator’s manual were finalised.
| Programme session | Issue identified | Changes made/actions taken |
|---|---|---|
| Week 2: healthy eating | Visual aids that were used in the standard programme and had been deliberately not included in the adapted programme were used by the facilitators | Researchers went through the week 2 session plan with the facilitators again and reminded them that the visual aids from the standard programme had been purposely removed during the adaptation process |
| There was too much material to deliver within 90 minutes and the facilitators struggled to cover it all | The number of activities in the session was reduced to ensure that the key messages about nutrition were delivered | |
| Some of the nutrition messages were not clearly delivered and it was noted that participants became confused on occasions | The content of the nutrition session was streamlined to ensure more focus on the core nutrition and healthy living messages. The key nutrition concepts were discussed again with the facilitators and additional notes were included in the facilitator’s handbook | |
| Week 4: physical activity | Delivery of this session did not require the full 90 minutes | Facilitators were encouraged to revisit nutrition messages in this week to allow the group to ask questions |
| Week 5: give it a go | This was noted to be very difficult to deliver with only one facilitator, especially with larger group sizes | Children’s weight management service agreed to provide an extra facilitator for this session. A plan for setting up the materials in advance of the session was also developed and the participant worksheets were simplified to enable families to complete them with less input from the facilitators |
| The ‘make a healthy snack’ activity was too messy | The number of healthy snack-making options was reduced from four to two, retaining the least messy options | |
| The recipe planning activity did not work well | Recipe planning was removed from the session and the group were provided with a number of recipes to take home with them if they wanted to | |
| All sessions | The setting of weekly goals was sometimes missed out or only very hurriedly covered at the end of a session. The review of goals at the beginnings of sessions was also sometimes rushed and not adequately covered. The beginnings of sessions were challenging for facilitators, as participants often arrived late, which interrupted the flow of the session | The content of week 2 was reduced to allow adequate time for review and setting of goals. The study co-ordinator also explained to the facilitators that the goal-setting and subsequent review in the following week was a key behaviour change technique within the intervention programme and, therefore, it was essential that these were focused on in each session |
| Week 6: review and celebrate | Facilitators felt uncomfortable singling out particular participants for the ‘star achiever’ certificate | It was agreed that all children would receive a completion certificate and no child would be singled out for being a top performer |
Further observations and feedback continued throughout the study intervention period to determine whether or not the programme was being delivered as intended and to identify ongoing difficulties with programme delivery. No major concerns were identified and, in general, the facilitators delivered the programme materials in the way that they were directed to in the manual and training sessions. However, contextual challenges in delivering the programme remained throughout the intervention period. Particular issues were the disruptions caused by families arriving late, which happened at almost all sessions, and the logistical challenges of large group sizes (e.g. when there were > 12 families or when there were many siblings accompanying the children). The presence of interpreters for non-English-speaking participants worked well and the participants who required interpreters were observed to be included and engaged in the sessions.
Interviews with programme facilitators
Both intervention facilitators were interviewed (F01 was female, of Pakistani ethnicity and delivered 12 adapted programmes, and F02 was female, of white British ethnicity and delivered four adapted programmes within the study). One interview took place face to face in the facilitator’s workplace and the other took place via the telephone because of the facilitator’s availability. The interviews were 46 minutes and 41 minutes in length.
Facilitator views of the adapted intervention
Overall experiences
Both facilitators reported that they enjoyed delivering the adapted programme, which was consistent with the feedback they gave during the running of the programmes. They both acknowledged that the programme was very different from the standard programme that they had previously delivered. Much of the facilitators’ praise for the new programme focused on the more interactive and flexible delivery, which was a significant change from the standard programme (although there were interactive elements in the standard programme; see Appendix 4). The facilitators also felt that the families attending responded well to the interactive nature of the programme:
I think a lot of the aspects of the course worked brilliantly and I really enjoyed the interaction of it so overall I enjoyed it and I much prefer it as a course.
F02
It was a nice refreshing change to see that we could facilitate rather than actually talk, erm, some of the families to death at times so it was, it was I would say nice. Erm, and as I, like I said it was a refreshing change to sort of try and deliver something new. Erm, and to be honest I, I would say that it was, erm, a pleasant I would say response from a lot of the families as well.
F01
With the new programme I would say that there was a lot more opportunity for the families to get involved so a lot more sort of, erm, I would say practical activities that we could get them involved into as well, so that was nice. Although we did have some practical things in the old programme, erm, I would say that maybe some of the things we didn’t sort of hit the nail on the head with certain things which you guys [researchers] did.
F01
Both facilitators highlighted that the programme sessions provided a good environment for social interaction between participants and that parents would share experiences and support one another in sessions. This meant that their role was much more facilitatory and less directive than previously:
There, erm, a better I would say, erm, social environment between I would say the participants because we gave them I think more opportunities as well though in this course. Although they still had opportunities in the older course, I would say they did have a few more extra ones here where we’d bring in the games and things as well. So I think it was a, it was a nice chance for them to, I would say more chances for them to actually gel together and, and, and speak to one another.
F01
What tended to happen was one parent would say ‘from last week do you remember talking about this? And blah, blah, can you tell me a bit more about it?’ And then another parent would join in and go ’you know my daughter does that and then for me when . . .’ it worked brilliantly. I could just sit back and let them do it and for the most part a lot of good discussion was had. Certainly in that when the children were removed and they went off to play in the physical activity session when it’s just me and the parents and that’s when it works beautifully. If one parent does pipe up with something and then they all start talking and I liked that because it took it away from me going ‘right, do you do this or do you do that?’.
F02
The provision of new, high-quality printed materials (display boards, participant folders, etc.) was well received by the facilitators. They felt that it gave the programme a more professional edge and helped the families feel that they were important, thus encouraging their engagement with the programme. The facilitator delivery guide was also highly valued:
I think because the [display] boards themselves which I love, the materials and everything fantastic, the boards are brilliant . . . and just the whole fact that they’re getting materials you know the ones that we were giving [in the standard programme] were very good but these were of a quality that’s kind of far in excess of the ones that we were giving previously and I think that kind of gives them a sense of ownership and importance and they’re coming to something and a little bit of excitement and involvement for the children.
F02
We’ve loved the resources, colour copies and the folders. We’ve been enjoying all of that part.
F01
And for me to have my guide, my facilitator guide so I’m sitting there with that one guide constantly and making notes and thinking about it, um, I like that as well, that’s a big help.
F02
Challenges of delivering the new course were also discussed. Difference in delivery style (i.e. from ‘classroom’ to a more interactive style) and running all sessions with both parents and children present were raised by one facilitator as big challenges:
Wow, massively challenging because it was very different, the course previously was only involving the parents and it was a very much classroom-based type thing, ‘you listen to me, this is what I would like you to do’ kind of thing. We met the children only at the beginning and at the end, so we didn’t really have to interact with the children as much, um, we only took their weight and height, you know their weights and measures at the beginning and the end, we were trying basically to persuade the parents that this is how they should be adapting their lifestyle to suit their children and to improve the health of their children, but it was very much more weight focused as well, so we had to think of a way to approach the subject because they were there because their children were overweight and that was always there. So the focus I think, and the delivery was very different, so when this course came along it was a lot more involved on our part and because the children were going to be there . . . the big difference is that the method of delivering it was going to have to be very different, so that I liked, um, and then delivering it I enjoyed.
F02
Saturday programmes
One of the adaptations of the new programme was more availability of programmes on a Saturday. With the standard programme, 25% of sessions were delivered on a Saturday, but with the adapted programme this proportion was increased to 50%. Both facilitators recognised that this had a positive impact on the success of the adapted programmes, as they believed that it enabled the parents to be more relaxed, outside the pressures of the working week, and allowed them to bring other family members along and, therefore, to embed the behaviour change messages more firmly into the family:
Families are, are very relaxed about Saturdays and, and I would say that they have been very successful . . . I think it’s the same as any of us though ‘cause on a weekday I just, on my working days oh God, I can’t take any extra on, you know. So I can see that for, for some families although they’re still doing it they might be quite stretched and then quite stressed out by the time they’re there, they’re not really concentrating. So I don’t know . . . they’re just, you know, a bit more relaxed and they’re probably just in a better mind frame, erm, to concentrate on something, something that’s gonna benefit their family.
F01
It does make a massive difference because the family can come, the whole family can come, whereas during the week you know even some adults find it difficult to take that hour and a half you know they’re working or you know they’re at home but they’ve got other you know commitments . . . but an hour or so on a Saturday morning before the weekend starts if they’re motivated to come to it, which most of them are it has to be said, it seems like the obvious time to do it and you do get, you get siblings along and the messages apply to them just as much as it applies to the person who’s been nominated to come.
F02
Children in attendance
A key adaptation was the presence of parents and children at all programme sessions (children attended only the first and last sessions of the standard programme). The facilitators were clear that this had a positive impact on the programme for a number of reasons. From a delivery perspective, they felt that the delivery needed to focus on engaging the children to keep them interested, and this would have a positive impact by removing the spotlight from parents and lessening the perception that their parenting was being criticised. They also felt that the children motivated the parents to keep attending the programme sessions, and they valued the opportunity to witness interactions between parents and children, as this helped to shape the support they gave the families:
. . . the children were going to be there, and if you can engage the children then you stand a lot more chance of engaging the parents because sometimes it’s very difficult to persuade an adult not that they’re doing something wrong but you’re always treading that line between you’re kind of not being a very good parent are you?. . . but when the children are there you can approach it in a very different way, so when we were given this course it was obvious that that was going to be, the big difference is that the method of delivering it was going to have to be very different, so that I liked.
F02
The children drive it. If the children can drive it, ‘I want to go, I want to go, I want to go’ then the parents will bring them, they just will whereas if the parent is going ‘do you know, I can’t be bothered to go’ they just won’t but if the child is there going ‘you, I want to go’ so having the children there I think it has made the whole course has made a difference to attendance I think, definitely.
F02
Erm, and also as a, get, having the kids involved was such a big plus for us because like I said, there were lots of reasons why we’re, it was, you know, it was good to see them with their parent and what their relationship was like and act with them. We’re there, you’d act, you’d know whether they’re doing the, the targets or not which was hilarious because you’d just see in their faces they weren’t.
F01
However, the facilitators identified that having younger children in the group was a big challenge. They felt that the content of the programme was beyond the comprehension of 4- and 5-year-old children and this sometimes resulted in them losing interest and disrupting the session:
We had very young children there so I think we need to think about it in terms of the age of the children and age appropriateness, which I don’t think we thought about at all, any of us, when you’ve got 4- and 5-year-olds there they’re not interested because they’re 4 and 5, whereas when they’re kind of 6 and 7 they can sit and talk to you and listen.
F02
In actual fact, talking age of children, some of the age groups we did realise . . . that we found that the 5-year-olds were losing interest very quickly . . . It was that the very young ones were so in, in reflection to what I’ve just said, because some of the content was still quite, I would say, I would say quite hard for them to understand when we’re talking about things like carbohydrates and things for a 5-year-old that’s just gonna go straight past them. They would lose interest but it became sort of a bit of challenging.
F01
Programme content
Both facilitators expressed concerns about the ‘healthy eating’ session (week 2). There was a feeling that all the nutrition messages were packed into this session, whereas with the standard programme this content was spread throughout all sessions. This session had been revised so that the content was reduced but the facilitators remained concerned about its delivery. One facilitator highlighted that trying to give the planned amount of information to the participants in this session created a conflict with the programme’s ethos of listening to, and being responsive to, participants:
. . . but we only had about an hour to deliver what we were previously delivering in 6 weeks, and it’s a lot of information for anyone to take in. Even as a nutrition professional there was a lot of information to kind of get in for an hour so to deliver it to parents, and for them to go away. It was kind of they were reeling from all the information that we were trying to give them.
F02
Erm, but that was the only thing that I really struggled with was week 2 to actually get that, all that information across and it didn’t really, then it kind of went against what we were trying to do, which was giving them a chance to sort of interact with us, because there was so much.
F01
One facilitator felt that the programme was imbalanced in terms of having too great a focus on physical activity and not enough of a focus on nutrition. However, this was in contrast to the views expressed by the parents and children:
I think that’s my biggest frustration about the course itself is that we’ve moved too far in down the road to saying physical activity is key, and it is key but they need to go hand in hand and we are losing the practical food tips, so that’s my frustration I think, um, with the course because overall I love it and I much prefer delivering this one than I did the previous one which was a lot more stilted and a lot more formal but the balance has shifted . . . we should talk about the food again and the physical activity and try and marry them both together.
F02
The same facilitator also expressed her frustration at the shift in focus of the adapted programme away from weight management and towards healthy behaviours. In contrast to the findings from the qualitative study in phase I, she felt that a focus on weight was necessary and led to better outcomes in terms of weight loss:
So [on the standard programme] we were giving them practical [advice] – look at this, did you realise, no I didn’t, I’m going to change it for that, and it was like a peg, they could grab onto that one and do something about it whereas [on the adapted programme] we always veered away from the words weight, overweight, and it was healthy lifestyle, which is fine but the results at the end anecdotally I don’t think were as good in that regard.
F02
Although they preferred the adapted programme overall, both facilitators clearly identified aspects of the standard programme that they valued highly but that had been omitted in the nutrition content in week 2 of the adapted programme. In particular, the use of visual props, such as showing the actual amount of sugar in a fizzy drink, was felt to be of great value in delivering key messages. In addition, one facilitator felt that the messages on how to implement changes were less clear to participants than in the standard programme, and some of the more practical tips had been lost in the adapted programme:
Everybody is astounded when they see those kinds of sugar, it just, something just drops, the penny drops even though they think they know until they actually see it physically and I think we missed that massively and the plate, the portion plate, not the Eatwell plate but there’s a portion plate, because when you look at the size of the plate as well and I think visually, props-wise, we needed to incorporate more of that stuff . . . The parents all know cans of coke have got sugar in them, but until you pick up the sugar bag and put it alongside it, that’s when the shock registers as to exactly how much there is.
F02
The only thing that I would say is that when it came to sort of the nutrition side of things, I still found that things were a little bit vague . . . when we talk about carbohydrates and things, I still think they needed a little bit more direction as to how, you know, like how many portions they should be having or just that staying a little bit clinical, erm, with what we’re expecting them to do, which we didn’t really, in the new programme we didn’t really go into, which is the only thing that I was a bit, er, sceptical about.
F01
Both facilitators reported that many parents returned to discussing nutrition and healthy eating in the third session when their children were not present (‘making changes’, week 3). One facilitator found this very helpful as the parents themselves were bringing up points from the previous session and it gave her an opportunity to tie in healthy eating messages with changing behaviours. In contrast, the other facilitator felt that this was a sign that the messages were not covered in enough detail and that parents were frustrated:
. . . and they would say [in week 3], you know, ‘Oh’, you know, ‘This is the issue that we’re having with food again’, so they’d bring that back up and it was kind of nice because although we were, we were discussing and delivering behaviour change, it kind of brought in stuff from the previous session and an opportunity for them to ask questions without their children being there . . . it was nice for them because they sort of felt like there was a bit of a break, you know, a breakout for them where they’d actually have a chance to, to ask us, you know, ‘This is what we’re struggling with’, or, you know, not necessarily just behaviour, just in general all their habits and how to break them.
F01
I have found in my behaviour, the behaviour session [week 3] when the children go away and I’ve got the parents there we tend to spend the first half of that session talking about food, portion size, tell me about how many meals they should be having a day and it’s kind of well we did cover that last week but they’re frustrated that we didn’t cover it in enough detail or give them something like, I’m going to show you my hand, this is the size of the plate, you know the fist, any kind of practical tips as to how much they should eat, when they should be serving their children.
F02
Programme website
The facilitators had differing opinions on the value of the website. One was very positive about the website as a resource for families, whereas the other felt that there were barriers to its use among the programme participants, although she acknowledged that it was a good resource for older children who may have more information technology skills than their parents:
Apart from the fact it had my face in I loved it, no I think it’s great because we’d always been asking for a resource that we could give them um anyway, so I think it’s a great idea and I do like it, and I think it’s easy to get around, um, because the courses are so short I think sometimes they’re left hanging and go well, what do we do without seeing you every week now? And to be able to say to them you’ve got your website, you’ve got my number, both those things, everything is there and if you can’t find the answer there then you can phone us and we can support you because that’s you know that’s what they want, they want some support, and having that is brilliant.
F02
Erm, I would say that some of them were a little bit sort of not, erm, what’s the word, sort of computer whizz, so some of the parents like, well who had language barriers and things wouldn’t really, I would say, go onto a website . . . But some of the kids that were, I would say, at an age where they understood ‘cause kids, you know, kids are computer whizzes so they knew what they were doing, they, they would say they’ve been on, erm, some of them had looked at recipes.
F01
Interviews with parents and children attending the adapted programme
Participant characteristics
Fifteen interviews with sixteen parents who attended the intervention were conducted. One mother and father, from the same family, were interviewed together. There was a mix of mothers and fathers, ethnicities and levels of programme attendance, with 11 participants classed as programme completers and five as non-completers. Unfortunately, we were unable to recruit any Bangladeshi parents to participate in an interview. Three participants were interviewed in another language (two in Urdu, one in Mirpuri). Nine children were interviewed, seven of whom were children of parents who were also interviewed. All children had completed the programme and were between the ages of 10 and 12 years at the time of interview. Participant characteristics are summarised in Table 10. The average length of the interviews with parents was 20 minutes, ranging from 14 to 29 minutes. The average length of the interviews with children was 19 minutes, ranging from 12 to 28 minutes.
| Participant characteristics | Participant type | |
|---|---|---|
| Completers | Non-completers | |
| Number of parents/carers (n = 16) | 11 | 5 |
| Relationship to the child | ||
| Mother | 7 | 3 |
| Father | 4 | 2 |
| Ethnicity | ||
| Pakistani | 4 | 2 |
| Indian | 1 | |
| Black | 3 | 1 |
| White | 2 | |
| Mixed | 1 | 2 |
| Number of children (n = 9) | 9 | |
| Sex | ||
| Male | 4 | |
| Female | 5 | |
| Mean age (years), (range) | 11 (10–12) | |
| Ethnicity | ||
| Pakistani | 2 | |
| Indian | 1 | |
| Black | 1 | |
| White | 2 | |
| Mixed | 3 | |
Parent and child views of the adapted programme
Overall experiences
In general, parents and children reported attending the programme as a positive experience and felt that it had encouraged them to make behavioural changes. Several participants discussed the wider impact that the programme had within the family, with many reporting behavioural changes that had occurred in other family members. These wider impacts were not confined to families who completed the programme, with some participants who had only partially attended reporting that there were behavioural changes within the family as a result of attending sessions:
. . . the whole thing it was delivered so softly it was just about making sensible choices, informed choices, you know, and I think that we got all the tools that we needed to do that, you know, we were told everything and the way it was delivered was superb, I can’t say that enough it was just from start to finish it was a really good course. Er, and yeah we’ve continued doing it and we’ve made changes and we’re continuing to make changes.
P2148, father, black, completer
All I can say is it was a brilliant experience for my daughter because she’s made a major change in her life and I think as she grows older she will realise, you know, how to keep on going that was instead of going the other way she was doing, that’s the only other thing I can really say.
P2079, mother, Pakistani, non-completer
. . . it was really good, it helped a lot, erm . . . I enjoyed going to it because it was fun, yeah.
C2148, child, mixed/other ethnicity, completer
. . . but I think whatever we learnt, we will actually stick to it erm, in our family, her dad is one that he loves his food and drink, so changing him was quite hard, but even like, if he has a choice with a meal he might actually chose a water instead of the fizzy drink now, whereas before that wouldn’t have even been an option . . . I think you know, even whilst I was doing the course I was mostly focusing on my daughter, but after the course I thought I don’t actually have any physical activity implemented on myself so I’ve started doing my walks, going to the gym, doing a bit of aerobics.
P2025, mother, Pakistani, completer
I think all of it was because I could see her weight and I could see what I could do as a parent to help her and all my family. And my husband made a few changes in his diet as well, like he picked up that, because he used to eat unhealthy and now he’s eating healthily and he’s going to the gym as well, so I think so it has worked for us.
P2079, mother, Pakistani, non-completer
Er, I’ve sort of, er, changed portion size as well for the 2 year old and I haven’t changed the size of the plates yet, but portion size I’ve changed, er, fruit and vegetables, they eat a lot more fruit, they’ve always even before we started the programme they really love their fruit but the vegetables with the two younger ones was a problem, but with [child name] he eats almost all vegetables.
P2124, mother, black, completer
Some parents felt that they already knew some of the information presented within the programme, but they acknowledged that they also acquired new knowledge:
They explained quite well, I mean what to eat and what should be avoided. Although I already knew about this but it is common when we attend such events we always learn some new information, so this helped me a lot.
P2017, mother, Pakistani, non-completer
But the stuff was pretty much a lot of stuff we’d already knew, you know, and we picked up and stuff already, so – but there was a – quite a few beneficial things, like stuff like, erm, for instance, erm, like the [brand name] jars, like we didn’t – we knew they had sugar but we didn’t know how much and stuff like that, and then the sugar stuff smart [application] and stuff like that.
P2112, mother Pakistani, completer
The group-based aspect of the course was generally well received by both parents and children. Parents valued the support they gained through sharing experiences with and learning from other parents, and children enjoyed the opportunity to make new friends:
It was nice to be around other people that had the same like issues with weight management stuff with their children, because the support was good, as in, you know, to be around other parents and, you know, just generally when you talk to the parents and stuff, you kind of like – it makes you realise that you’re not the only family with this issue and stuff, so the support helped and stuff.
P2112, mother, Pakistani, completer
It was brilliant because I’ve, good idea, because for me, it’s just I’m learning things and I learned through other parents as well, if I listen to them I get some ideas as well and they learned something from me as well.
P2079, mother, Pakistani, completer
OK, so let’s go through the things that you liked, so [child wrote] ‘the course helped me doing things which I enjoyed’, fantastic, so what do you mean around that, what did you enjoy?
The things that I enjoyed was like, I got to make new friends and everything.
C2091, child, Indian, completer
In line with the facilitators, parents found the session in which the children undertook activities separately (week 3) to be very beneficial, as it allowed more opportunity to develop relationships with other parents:
The week that [name of child] went off to do her stuff, I think you [talking to child] really enjoyed it. And it was quite a – it was quite useful as well – it was quite useful as well to have an opportunity to talk about things while [name of child] was busy doing something else.
P2115a, mother, white, completer
Programme timing
Programmes delivered on Saturdays were generally well received. One parent expressed concern at taking her child out of school on a weekday during an important school year and so chose a programme on a Saturday that was much further away. Some parents and children reported that a 9.00 a.m. start on a Saturday morning was challenging for them:
It was [the Saturday programme], oh gosh it was at [place name] which is two bus rides away so . . .
Oh it was quite a way then.
The other one was in, er, [place name] but because it was on, er, Tuesday afternoon at 1 o’clock I didn’t want him to go to that because he’d miss 2 hours, not even 2 hours, half a day of school because he’d have to leave school early.
P2124, mother, black, completer
Fantastic. OK, so things you did not like. You [child wrote] ‘had to go early in the morning and it feels difficult’, was it a really early start?
We like started, like, I used to go there at 9 o’clock . . .
OK, was that on a Saturday . . .?
Yeah . . .
So that’s a bit early for a Saturday . . .
Yeah . . .
So you’d like it to be a bit later . . .
Like go at 10, 10 o’clock . . .
C2091, child, Indian, completer
Programme structure
Parents were mostly happy with the six 90-minute programme sessions delivered over 6 weeks. A minority of parents commented that they would prefer a different structure, either a more intensive programme with sessions close together (e.g. over the summer holidays) or a programme delivered over a longer time period:
Maybe that it was just once a week basically. Maybe, yeah. ‘Cause now that we’ve got a 6 week [school holiday] that could take place now and the children off – off school.
P2026, mother, Pakistani, completer
I think personally that there should be a programme for overweight children that they should be in touch with them regularly, rather than, you know, just a session – like a few sessions clustered together, or you – do you know what I mean? Like a longer time period to kind of lengthen that.
P2112, mother, Pakistani, completer
Barriers to programme attendance
Parents who did not complete the programme generally recalled logistical reasons for not attending. This was consistent with the findings in the phase I qualitative study. However, one parent felt that his child was uncomfortable with being identified as overweight and that he did not identify himself as being the same as the other children who were attending the group:
I wanted to join again but my car broke down. However, they said if you want to come please let us know, though I wanted to go but I had this issue so I said I will try to come . . . In the beginning I attended two sessions and then one more, but then I could not go. I wanted to go with my friend but I could not go in the last three sessions.
P2017, mother, Pakistani, non-completer
Because of getting from school to go it was – and because going to college and stuff, it’s kind of – was kind of impossible to attend every session.
P2055, mother, black, non-completer
. . . from first impression I find all of them they’re fat kids and this kind of – this, erm, first impression, it can affect him. He thought, ‘Am I one of them? I’m not fat. I’m a sportsman’. So from that side I think that can affect him saying, ‘No, I’m not the one to attend this kind of course.’
P2047, father, mixed/other ethnicity, non-completer
Children in attendance
The inclusion of children at all programme sessions was generally very well received. Parents valued the fact that children were directly hearing messages relating to healthy eating and physical activity from a professional, and some also felt that it provided an opportunity for them to start conversations around weight management with their child:
It was actually quite useful because most of the time children won’t listen to parents, but when they see a professional explaining they take on board. And I think it was actually tool for me to reach him, so it’s literally opened our communications between us so it was quite useful really.
P2092, mother, black, completer
. . . I thought you know, we might as well go for it and see what happens and when we did go, finally when they finished, I thought it really, really helped, I think that bit of encouragement from somebody else rather than the mum saying to the child, I think it really helps.
P2025, mother, Pakistani, completer
Parents also identified some difficulties with having children present at the sessions. In line with the facilitators’ views, some parents felt that the wide age range of children presented a difficulty, with younger children becoming disengaged and older children becoming bored:
I definitely think, it probably didn’t have the same, er, the same accessibility or the same outcome with the younger children, I felt that they were you know they weren’t engaged in it, they were more playing with toys and all of that, so it didn’t really benefit them too much. And as a result because they were getting into mischief and the parents were being drawn away from it and possibly missing key points, er, but yeah for the older children, I’d probably say 9 upwards they were fully engaged and they were listening to what was going on, you know, and they were taking it in. I don’t think it was much use for the younger, if anything it was more of a hindrance.
P2148, father, black, completer
Erm, I think a little bit, because [child’s name] was one of the, I’m not really sure if she was one of the eldest but she was a Year 6 child and she’s quite bright anyway so a little bit of it was too basic for her, so she found that, like occasionally you know once the main part of it, she found it a little bit boring so maybe if you were to do it again, split it up into the age groups.
P2025, mother, Pakistani, completer
They just got a bit bored, didn’t they, after it? It’s quite – it was about an hour and a half, and I think it was just too long for some of the little ones to sit and listen.
P2115a, mother, white, completer
Pitching the sessions at the right level to engage both the children and the parents was also identified as a challenge, particularly around more complex concepts such as food labelling. This activity in particular evoked differing responses from participants, ranging from those who found it challenging but learned from it to those who felt that it was too complex for the children to grasp:
To be honest with you we both learned, it’s whatever applicable to the children was also applicable to the parent as well. And I think one of the useful things which I never really pay attention initially was the food labelling, was that fat and how many grams salt, it’s not something I normally pay attention, I just grab them.
P2092, mother, black, completer
I think she didn’t really pick on it that much, for her if you put a package in front of her it’s still going to be a package. She did sort of understand that if she had too much it’s bad for her, that’s it, but I think it was more for adults.
P2079, mother, Pakistani, non-completer
Erm, it was quite fun at first. Err, it was quite fun altogether because we had to go round the room and we had to find the different foods. Then you had to find out how much they were labelled in, err how much sugar and fats are there in there.
C2025, child, Pakistani, completer
Um, I didn’t like the food labelling activity because you didn’t get to write the um, you had to quickly write the words down and um, you had to like, you would get muddled up and things. And uh, you would get confused. But with the sheets I’ve got in my folder, I know which is a healthy snack and which is not.
C2063, child, Pakistani, completer
Physical and other activities
In contrast to the facilitators’ views, parents felt that there was still not enough focus on physical activity, despite the incorporation of physical activity into each session and a dedicated physical activity session for children. Children really enjoyed the physical activities, along with the food-making activity. Some parents and children reported that there was too much sitting and listening for children, despite the increased interactive content:
I think it was really good although I think they could have done a bit more in sort of 1 day, like if she went the next week they could have done a bit more, I think that would have been, now she’s picked up on it anyway she does exercise but I think if they increased that a little bit more . . .
A bit more activity?
Yeah a bit more activity, as well as the food and diet, but more activity as well.
P2079, mother Pakistani, non-completer
Yeah, but I thought there’d be more like activities for the kids and stuff, I think they only had activities on 1 day and the other time they had, that’s when they had to make snacks, so the rest of the time they were sitting there and [child’s name] would say, do we have to go because it’s so boring just sitting there.
P2124, mother, black, completer
Like, erm, when you got to do some exercise for only 1 week, and sitting down, that’s not much fun, it was supposed to be fun but it wasn’t that fun . . .
C2124, child, black, completer
Right, OK, for the second [sticky note] you’ve mentioned [child wrote] ‘I would like to do more active activities there’. So do you want to explain?
Well I would have liked to, um, in the course I would like to like be more active, like run around and stuff like, they’d only, I think on like the last or two lessons [hmm-hmm], I was there for the course and they were active and you were playing games and things.
C2063, child, Pakistani, completer
Some parents suggested that local community facilities could be used, such as the park or local leisure centre:
I think it was good, erm, I think at the time the weather didn’t really support us so we couldn’t really go out but, erm, if you were to do it again, maybe one of the sessions could have been at the park or at a leisure centre or something to actually, erm; they did go into the playground for a while, but if you were to do like a full session outside with the parents, maybe that would have helped, but we learnt that the children need, the amount of exercise they need each day which is quite a lot if you think about it.
P2025, mother, Pakistani, completer
You know, it was in the morning, weekend morning, was I think my son also plays with his friends, er, and I think if he can – you know, I’m thinking if they can – if they can do that the same activities in the park, the student with the kids always playing there, some kind of – some activities, they always, erm, start that kind of, erm, erm, er, activities in the park. So if they can move the place to the park maybe.
P2047, father, mixed/other ethnicity, non-completer
Programme website
All participants were asked about their use of the website. Only one parent and some of the children reported having used the website; however, it is possible that there was some confusion between the programme website, developed as part of the adapted intervention, and the nationally available Change4Life website (https://registration.change4life.co.uk; accessed 20 April 2017). This suggests that this may have been a less useful aspect of the programme and possibly signposting to existing online resources, such as Change4Life, may be a more cost-effective option:
Yes, but not as much as I should have if I’m honest, I used it three or four times and we did use it, er, we did use it every now and again just to look at food, the sugar content and the fat content because of the items on the site because some of the – some of the cards and things like that.
P2148, father, black, completer
Summary of findings from interviews with facilitators, parents and children
The experiences of all those who were interviewed were generally very positive. Participants reported behaviour change within their families, even if they did not attend all programme sessions, and facilitators valued the flexibility of programme delivery. In keeping with the findings of the qualitative study in phase I, the weekend delivery of the programmes generally worked well for families, and the adaptation of children attending all programme sessions was felt to be of value by the facilitators and the participating parents. As in phase I, parents acknowledged the value of children hearing messages directly from an authoritative figure. However, both parents and facilitators drew attention to the fact that having such a wide age range of children attending presented difficulties. In particular, it was felt that the programme content did not keep the younger children engaged. Facilitators, parents and children all welcomed the interactive elements and valued the social and peer support aspects of the programme, both of which had been highlighted as important elements in the phase I qualitative study. Parents and children especially liked the physical activity and food-making activities but wanted more of these. Again, this is consistent with the phase I findings, in which parents identified that they wanted physical activities within the programme. However, these findings in phase II imply that the adaptation of introducing physical activity content into the programme did not go far enough and that families felt that there should be even more opportunity to undertake physical activity within the sessions. In contrast, the facilitators felt that there needed to be more content in relation to nutrition, especially practical advice when preparing food for the family. Contrary to the findings in phase I, one of the facilitators felt that the shift in the focus of the programme away from weight management was unhelpful. However, this viewpoint was not articulated by any parents or children. The programme website was not well used. Overall, the programme was valued by those delivering and participating.
Feasibility and completeness of outcome measurements
Feasibility of data collection
Data collection in the participant’s home
A number of difficulties were experienced with the data collection visits to the participant’s home. The home visit appointments were made by telephone a few days in advance, with a follow-up confirmation letter and a reminder text or telephone call on the day of the appointment. Despite this, on several occasions the families were not at home when the researcher arrived. Some participants gave reasons (e.g. unplanned hospital trips, unexpected school commitments); others did not give an explanation. It was possible to rearrange some of these data collection appointments, but some families were lost to follow-up as repeated attempts to contact the family and rearrange the visit failed.
Initially, data collection home visits were planned to be undertaken by one researcher and a lone-working policy was implemented. Following the first few visits, concerns were raised by researchers, as many appointments were during hours of darkness and often they had to park their car some distance from the home and walk with heavy equipment in unfamiliar areas. Therefore, it was agreed that first visits to a home should be attended by two researchers and that a risk assessment should be undertaken for lone researchers to make the subsequent visits.
Participant burden
At the start of data collection, the baseline home visits lasted a median length of 60 minutes, ranging from 40 to 90 minutes. In some cases this was too long, with participants becoming fatigued before data collection was completed. Researchers noted early on that the number of questionnaire items was too high for the adult participants. In response to this, the data collection process was modified in January 2016. The questionnaire booklet was divided into two. One contained core data questions (sociodemographic information, Children’s Dietary Questionnaire, FNPA questionnaire) and was completed at the appointment and the other (containing questions on parenting style, parental self-efficacy and parental feeding practices) could be completed by parents at the measurement appointment, or at a later date, and returned to the research team in a Freepost envelope.
For non-English-speaking participants, community researchers (or, when necessary, accompanying interpreters) translated all the questionnaires. Therefore, these participants did not have the option of completing the second questionnaire booklet at a later time. The data collection appointments took even longer for these families to allow for translation time and for all questionnaires to be completed. This remained an unresolved issue in the study.
Concealment of study arm allocation from researchers undertaking data collection
Programme allocation was unknown to the study team at the time of baseline measurements. However, once participants had started a programme, it became apparent to the study team which arm they were in through conversation with the participants and the presence of the programme materials within the home. This was less of a problem with the community researchers, as they were unaware of the differences between the intervention and comparator programmes. In a future trial, study arm could be concealed from the researchers undertaking the measurements if they are separate from the researchers who are co-ordinating the study and undertaking process evaluation of the intervention.
Other issues
Ramadan is a period of fasting during daylight hours that is observed by many Muslim families, and in 2016 it was within the planned T1 measurement time period. It became clear during the study that the participating Muslim families did not want a data collection appointment during Ramadan. Therefore, we delayed the appointments with these families until after the end of this period.
Data completeness: sociodemographic data
The completeness of sociodemographic data collection from participating children and parents/carers is shown in Table 11. Most sociodemographic data that were requested were provided. Data on parental education level and employment status were less complete, with approximately 85% of participants providing these data. Data completeness for birth place was high, but data completeness for the age at which parents moved to the UK was lower (74.5% of those born outside the UK provided this information).
| Sociodemographic data | Participants | |||||
|---|---|---|---|---|---|---|
| Child | Parent/carer completing the questionnaire | |||||
| Potential total (n) | Number collected (n) | Completed (%) | Potential total (n) | Number collected (n) | Completed (%) | |
| Ethnicity | 92 | 90 | 97.8 | 92 | 85 | 92.4 |
| Education level | – | – | – | 92 | 79 | 85.9 |
| Employment | – | – | – | 92 | 78 | 84.8 |
| Employment type | – | – | – | 29 | 29 | 100.0 |
| Religion | 92 | 82 | 89.1 | 92 | 86 | 93.5 |
| Main language | 92 | 89 | 96.7 | 92 | 90 | 97.8 |
| Birth place | 92 | 89 | 96.7 | 92 | 90 | 97.8 |
| Age when came to the UK | 11 | 10 | 90.9 | 51 | 38 | 74.5 |
Data completeness: outcome measurements
Table 12 shows the number and proportion of families who provided valid data and the average score/value for each outcome.
| Outcome measure | Time point | |||||
|---|---|---|---|---|---|---|
| T0 (n = 75) | T1 (n = 82) | T2 (n = 60) | ||||
| n (%) | Mean (SD) or median (IQR) | n (%) | Mean (SD) or median (IQR) | n (%) | Mean (SD) or median (IQR) | |
| BMI z-score, mean (SD) | 75 (100.00) | 2.52 (0.61) | 82 (100.00) | 2.45 (0.66) | 60 (100.00) | 2.34 (0.60) |
| Body fat percentage z-score, mean (SD) | 73 (97.33) | 2.25 (0.41) | 80 (97.56) | 2.24 (0.46) | 58 (96.67) | 2.05 (0.54) |
| Waist z-score, mean (SD) | 64 (85.33) | 2.92 (0.67) | 68 (82.93) | 2.77 (0.70) | 43 (71.67) | 2.96 (0.65) |
| Average acceleration (SVMg; mg), median (IQR) | 64 (85.33) | 32.07 (14.01) | 67 (81.71) | 32.23 (20.75) | 44 (73.33) | 34.32 (12.40) |
| Moderate to vigorous physical activity (minutes), median (IQR) | 64 (85.33) | 13.61 (12.18) | 67 (81.71) | 16.58 (15.02) | 44 (73.33) | 15.93 (13.89) |
| PedsQL (maximum = 100), median (IQR) | 71 (94.67) | 75.16 (24.22) | 77 (93.90) | 83.75 (18.44) | 52 (86.67) | 83.67 (21.02) |
| Physical functioning score | 72 (96.00) | 81.25 (17.19) | 78 (95.12) | 87.50 (25.00) | 56 (93.33) | 92.19 (15.63) |
| Emotional functioning score | 74 (98.67) | 77.50 (35.00) | 80 (97.56) | 87.50 (25.00) | 58 (96.67) | 87.50 (35.00) |
| Social functioning score | 75 (100.00) | 70.00 (40.00) | 80 (97.56) | 85.00 (30.00) | 58 (96.67) | 87.50 (25.00) |
| School functioning score | 75 (100.00) | 75.00 (30.00) | 79 (96.34) | 80.00 (25.00) | 60 (100.00) | 80.00 (20.00) |
| Body dissatisfaction score, median (IQR) | 73 (97.33) | 2.00 (2.00) | 78 (95.12) | 2.00 (2.00) | 59 (98.33) | 2.00 (1.00) |
| CHU-9D score (maximum = 1.0), mean (SD) | 75 (100.00) | 0.86 (0.11) | 78 (95.12) | 0.90 (0.09) | 58 (96.67) | 0.92 (0.06) |
| Children’s Dietary Questionnaire (score) | ||||||
| Fruit and vegetables (maximum = 28), mean (SD) | 67 (89.33) | 5.55 (3.00) | 75 (91.46) | 6.08 (2.99) | 58 (96.67) | 6.54 (3.46) |
| Dairy (maximum = 15), median (IQR) | 61 (81.33) | 2.00 (2.00) | 69 (84.15) | 1.00 (3.00) | 56 (93.33) | 2.00 (2.00) |
| Sugar-sweetened beverages (maximum = 5.9), median (IQR) | 68 (90.67) | 1.29 (1.86) | 77 (93.90) | 1.29 (2.14) | 57 (95.00) | 1.29 (2.00) |
| Non-core foods (maximum = 10.3), median (IQR) | 63 (84.00) | 2.29 (1.57) | 70 (85.37) | 2.00 (1.57) | 47 (78.33) | 2.57 (1.14) |
| FNPA (maximum = 80), mean (SD) | 53 (70.67) | 56.60 (6.12) | 51 (62.20) | 59.60 (6.03) | 44 (73.33) | 60.25 (6.76) |
| Standardised authoritative parenting (maximum = 5), mean (SD) | 47 (62.67) | 4.26 (0.58) | 45 (54.88) | 4.34 (0.66) | 26 (43.33) | 4.27 (0.48) |
| Standardised parental efficacy (maximum = 5), mean (SD) | 50 (66.67) | 2.16 (0.60) | 47 (57.32) | 2.19 (0.63) | 27 (45.00) | 2.12 (0.68) |
| Standardised parent feeding practices scores (maximum = 5) | ||||||
| Child control, mean (SD) | 42 (56.00) | 1.81 (0.78) | 41 (50.00) | 1.80 (0.77) | 29 (48.33) | 1.54 (0.57) |
| Encouraging balance and variety, median (IQR) | 42 (56.00) | 3.50 (1.00) | 42 (51.22) | 3.50 (1.00) | 29 (48.33) | 3.50 (0.75) |
| Environment, median (IQR) | 42 (56.00) | 3.00 (1.25) | 42 (51.22) | 3.00 (1.00) | 29 (48.33) | 3.25 (1.50) |
| Modelling, mean (SD) | 42 (56.00) | 2.52 (1.04) | 42 (51.22) | 2.79 (0.76) | 29 (48.33) | 2.88 (0.71) |
| Monitoring, mean (SD) | 42 (56.00) | 2.72 (0.90) | 41 (50.00) | 3.01 (0.92) | 29 (48.33) | 2.99 (0.84) |
| Restriction for health, median (IQR) | 42 (56.00) | 3.52 (1.00) | 42 (51.22) | 3.38 (1.00) | 29 (48.33) | 3.25 (0.75) |
| Restriction for weight control, mean (SD) | 42 (56.00) | 2.36 (0.76) | 41 (50.00) | 2.41 (0.77) | 29 (48.33) | 2.13 (0.57) |
| Teaching about nutrition, mean (SD) | 42 (56.00) | 2.81 (0.80) | 41 (50.00) | 3.06 (0.67) | 29 (48.33) | 2.91 (0.78) |
| Involvement, mean (SD) | 42 (56.00) | 2.24 (0.70) | 41 (50.00) | 2.39 (0.85) | 29 (48.33) | 2.39 (0.91) |
Anthropometric measurements: children
All children consented to height and weight measurements being taken and, therefore, a BMI z-score was calculated for all children. At each time point, two children had invalid body fat percentage measurements (e.g. the child did not want to remove their socks); therefore, the number of children with body fat percentage z-scores is marginally lower. Of the anthropometric measurements, waist circumference had the lowest compliance at each time point, with 15–28% of children declining this measurement. Children were asked to raise their clothing to access the waist; however, if they refused, an option was given to take the waist measure over thin clothing. When utilised, this was noted on the case report form (T0, n = 4; T1, n = 2; T2, n = 1).
Questionnaires
All child-completed questionnaires (the PedsQL, the Figure Rating Scale and CHU-9D) were completed at the home visit appointment and had good completion rates [ranging from 87% (T2, PedsQL score) to 100% (T0, CHU-9D score)].
Parent-completed questionnaires were split between those that were completed at the home visit appointment (the Children’s Dietary Questionnaire and the FNPA) and those for which parents had the option to complete after the home visit and return by post (from January 2016; the authoritative dimension of the Parenting Styles and Dimensions Questionnaire, Parental Self-efficacy scale and various subscales of the CFPQ). Completion rates for those questionnaires completed at a home visit ranged from moderate (62%, T1, FNPA score) to good (97%, T2, Children’s Dietary Questionnaire: fruit and vegetables score). However, those questionnaires that could be completed later and returned by post had substantially lower completion rates, ranging from poor (43%, T2, the authoritative parenting score) to moderate (67%, T0, parental self-efficacy score).
Physical activity measurements
Two types of accelerometer were tested: the wrist-worn GENEActiv and the hip-worn ActiGraph. The aim of using both accelerometer types in this feasibility study was to determine whether or not there was a difference in compliance between the two monitor types. GENEActiv monitors are less established in the literature than the hip-worn ActiGraphs; therefore, it was planned to use the GENEActiv monitors on approximately 75% of participants. Table 13 highlights the difference between the monitor types at each time point. At T0, the return rate and proportion of children who wore a monitor for at least 1 valid day (> 10 hours) were similar between monitors. However, at T1 and T2, both were lower for the hip-worn ActiGraph. For those who wore a monitor, the number of valid days of wear time recorded was similar between monitor types (Figure 9).
| Physical activity data | Time point | |||||
|---|---|---|---|---|---|---|
| T0 (n = 75)a | T1 (n = 82)b | T2 (n = 60)c | ||||
| GENEActiv (n = 66) | ActiGraph (n = 9) | GENEActiv (n = 68) | ActiGraph (n = 14) | GENEActiv (n = 50) | ActiGraph (n = 10) | |
| Number of extracted files, n (%) | 58 (87.9) | 8 (88.9) | 62 (93.9) | 11 (70.0) | 42 (84.0) | 8 (80.0) |
| Number with > 1 day of wear recorded, n (%) | 56 (84.8) | 8 (88.9) | 57 (86.4) | 10 (62.5) | 36 (72.0) | 6 (60.0) |
| Valid days of wear (if worn), median (IQR) | 5.0 (2.0) | 6.0 (1.5) | 5.0 (2.0) | 4.5 (4.0) | 6.0 (2.0) | 5.0 (2.0) |
| Average acceleration (SVMg; mg), median (IQR) | 32.9 (10.8) | 14.7 (3.0) | 33.7 (16.3) | 13.3 (5.8) | 35.2 (11.1) | 11.9 (9.9) |
| Moderate vigorous physical activity (minutes/24 hours), median (IQR) | 16.0 (13.3) | 9.9 (5.1) | 18.6 (15.0) | 8.1 (12.2) | 16.4 (13.2) | 4.8 (10.9) |
FIGURE 9.
Physical activity monitor: median valid days of wear at each time point.
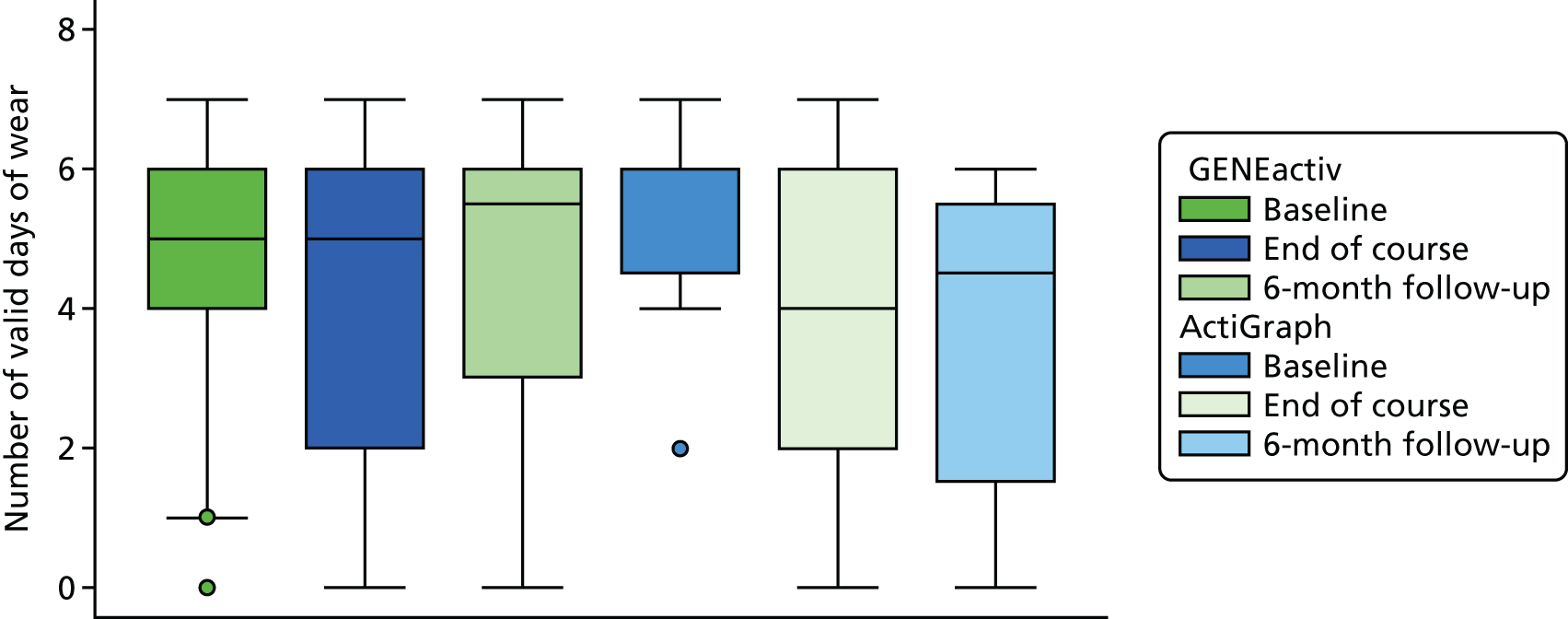
Anthropometric measurements: parents and other family members
The purpose of undertaking anthropometric measurements (height, weight and percentage of body fat) with parents and other family members was to assess the feasibility of collecting data that would enable evaluation of the impact that the intervention had on the wider family. The collection of these data proved problematic. At baseline (T0), of the 75 families who had a data collection home visit, 64 (85%) had at least one other family member and 37 (49%) had at least two family members who consented to measurements. These proportions reduced to 78% and 34% for T1 and 60% and 28% for T2, respectively. A major issue was that the family members who consented to be measured at each time point were often not the same, that is, one sibling was measured at T0 and another sibling was measured at T1, etc. The implication of this is that it would not be possible to use these data to evaluate the impact that the intervention had on the BMI or percentage of body fat of other family members, as the data are so incomplete.
Costs associated with the intervention programme
Development of the facilitator manual
A manual for facilitators delivering the adapted programme was designed in phase I of the study. Small refinements to the manual will be made in response to the findings of the feasibility study, but the cost of doing so will be minimal and will be classed as a programme development cost, so will not contribute any further cost to the intervention if ‘scaled up’. Therefore, these costs were not included in the overall costs of the intervention.
Programme set-up costs
To deliver the intervention programme, two training sessions were held with the facilitators. This involved introducing the new materials and discussing the plan for each week. The costs associated with the training of facilitators were classed as set-up costs, as staff received training at the start of the programme but this was not ongoing. Hence, if the programme was rolled out more widely, some initial staff training would be needed but this would not be required on a regular basis.
For both the intervention and comparator programmes, items of equipment were purchased for use during the sessions. These equipment costs were also classed as set-up costs, as the equipment was then used at each subsequent session. Table 14 presents the set-up costs for both the intervention and comparator programmes. The total set-up costs were £178 for the comparator arm and £940 for the intervention arm. The additional costs for the intervention arm are mainly related to staff training and the production of display boards.
| Training and equipment | Unit cost (£) | Resource use | Total cost (£) | Total incremental cost (£) for the intervention arm | |
|---|---|---|---|---|---|
| Comparator arm | Intervention arm | ||||
| Training of two main facilitators (two sessions: 1 × 2.5 hours and 1 × 1.5 hours)a | 10.80a (hourly rate) | 8 hours | – | 86.40 | – |
| Training of one assistant facilitator (two sessions of 2.5 and 1.5 hours, respectively)a | 10.80b (hourly rate) | 4 hours | – | 43.20 | – |
| Display boardsc | 395.00 | 2 | – | 790.00 | – |
| Card gamec | 18.93 | 1 | – | 18.93 | – |
| Floor mata | 39.00 | 1 | 39.00 | – | – |
| Photocarda | 6.00 | 1 | 6.00 | – | – |
| Stomach modela | 60.00 | 1 | 60.00 | – | – |
| Fat modela | 73.00 | 1 | 73.00 | – | – |
| Total cost | – | – | 178.00 | 938.53 | 760.53 |
Delivery costs
There were several elements that were common to both the intervention and comparator arms, relating to the promotion of the programmes, project management and assembling materials. However, our focus was on collecting costs that were different between the intervention and comparator arms. These included the provision of adapted materials, the hire of premises and staffing costs.
Both the intervention and the comparator participants received printed materials. With the exception of the BMI charts, these were different for each arm. For the intervention arm, resource use linked to the provision of the materials was successfully collected. For the comparator arm, however, the resource use linked to the participant materials was challenging to collect, as this represented ‘routine practice’ for the BCHCT children’s weight management team. For example, it was challenging to separate out resource use that was linked to providing photocopied information for the comparator sessions with other routine photocopying undertaken by the team. As a consequence, the material costs for the comparator arm were estimated based on feedback from the BCHCT staff alongside analysis of the comparator session plans.
For both the intervention and the comparator arms, average resource use was estimated based on an assumed full attendance of families at each session. In other words, once a family had signed up to at least one session, it was assumed that materials would be prepared for them for each subsequent session. For the intervention arm, 169 families attended at least one session; this number was 74 families for the comparator arm. The session materials provided to the families in each arm, and the incremental cost associated with the provision of these materials for the intervention arm, are detailed in Table 15.
| Items given to families | Cost (£) per item | Number of participants requireda | Total cost (£) | Incremental costs (£) for the intervention arm | ||
|---|---|---|---|---|---|---|
| Intervention arma | Comparator arma | Intervention armb | Comparator armb | |||
| Folders | 4.00 | 169 | 74 | 676.00 | Freec | – |
| Inserts for the cover of the folder | 0.45 | 169 | 0 | 76.05 | – | – |
| Folder dividers | 1.23 | 169 | 0 | 207.87 | – | – |
| Food labelling sheets | 0.27 | 169 | 0 | 45.63 | – | – |
| Certificates | 0.72 | 169 | 0 | 121.68 | – | – |
| Single-sided worksheets | 0.10 | 1859 | 0 | 185.90 | – | – |
| Double-sided sheets (colour) | 0.20 | 1014 | 0 | 202.80 | – | – |
| Double-sided sheets (black and white) | 0.04d | 0 | 7400 (100 per participant) | – | 296.00 | – |
| Healthy portion plates | 1.88 | 0 | 74 | – | 139.12 | – |
| BMI charts | 0.55 | 169 | 74 | 92.95 | 40.70 | – |
| Total cost | – | – | – | 1608.88 | 475.82 | – |
| Average cost per session | – | – | – | 100.56 | 59.48 | 41.08 |
| Average cost per attendere | – | – | – | 9.52 | 6.43 | 3.09 |
The cost of materials for the intervention arm was higher than that for the comparator arm. This was because the materials for the intervention arm were printed in colour and were bespoke products. Families in the comparator arm were given folders that had no cost for BCHCT, and all handouts were printed in black and white. Additional incremental costs for the intervention arm were attributable to the additional venue hire and staffing costs for the intervention compared with the comparator. The intervention involved additional support from an assistant and increased provision at the weekends. Details of these incremental costs are shown in Table 16.
| Cost category | Unit cost (£)a | Resource use | Additional resource use for the intervention | Incremental cost (£) for the intervention | |
|---|---|---|---|---|---|
| Intervention arm | Comparator arm | ||||
| Assistant | 10.80 (hourly rate) | 5 weeks for 2.5 hours | 3 weeks for 2 hours | 6.5 hours (×16) | 1123.20 |
| Venue hire | 580.00 (average weekend rate) | Seven weekend sessions | One weekend session | Six courses at weekends | 3480.00 |
| Total incremental cost | 4603.20 | ||||
| Average incremental cost per sessionb | 287.70 | ||||
| Average incremental cost per attenderc | 27.24 | ||||
Table 17 summarises the additional costs associated with the intervention, compared with the standard weight management programme. Costs are presented in terms of average additional (incremental) costs per session and per attender (family).
| Cost category | Average incremental cost (£) (per session) | Average incremental cost (£) (per attender) |
|---|---|---|
| Materials | 41.08 | 3.09 |
| Additional staffing costs | 70.20 | 6.65 |
| Additional venue hire costs | 217.50 | 20.59 |
| Average incremental cost | 328.78 | 30.33 |
Costs borne by families
We attempted to capture the costs incurred by those attending the intervention and comparator programmes via a questionnaire survey delivered at the end of the programme. However, the questionnaire was completed by all those who attended the final session, including by parents who were not participating in the CHANGE study. The questionnaire was completed by 96 parents, 13 of whom had attended a comparator programme and 83 of whom had attended an intervention programme. Respondents were asked about the main activity they would be engaged in, if they had not attended the First Steps programme. This question was completed by 66% of respondents. Overall, the highest number stated that they would be looking after the home or family (n = 37 respondents) and only four people stated that they would otherwise have been in paid employment (all from the intervention group). Just one of the respondents who had taken time out of paid employment stated that alternative arrangements had been made to cover their work. None of the respondents stated that they had paid someone to look after dependants while they attended the programme.
As part of the questionnaire survey, data were collected on whether or not participants had noted a change in their weekly food bill since they started the programme. This question was completed by 53% of respondents. Of those who completed the question, a slightly higher number stated that they had noticed a change in their food bill (n = 28 respondents) than stated that there had not been a change (n = 23 respondents). Of those who noticed a change in the amount of their food bill, the numbers saying that the bill had increased (n = 8 respondents) and decreased (n = 10 respondents) were similar. The amount of change to families’ weekly food bills was cited as ranging from an increase in the weekly shopping bills of £25 to a decrease of £5.
Parameters to inform sample size estimation for a future trial to evaluate intervention effectiveness
Using the anonymised data on BMI z-score from the children’s weight management programme providers (n = 154), we estimated the ICC to be 0.03 (95% CI 0.002 to 0.40) at the end of the programme, and the correlation between start-of-programme and end-of-programme BMI z-score to be 0.98. Using data from only the CHANGE study participants, the correlation between baseline (T0) and end-of-programme (T1) BMI z-scores was 0.97 and between baseline and 6 months post intervention (T2) was 0.91.
Exploratory analysis of the effect of the adapted programme on outcome measures
Mean changes (and standard deviation) in outcome scores by study arm allocation are presented in Table 18. In both arms, the mean changes of all anthropometric outcomes were in a favourable direction at the end of the programme (T1) and at 6 months after the end of the programme (T2). Only very marginal changes were seen in physical activity indicators, with the average acceleration decreasing in both study arms and moderate to vigorous physical activity decreasing by 1 minute per 24 hours at 6 months in the intervention arm and increasing by just over 2 minutes per 24 hours in the comparator arm. The PedsQL scores increased in both study arms, as did the CHU-9D utility scores. Body dissatisfaction scores decreased in both arms (indicating a favourable direction of effect). The direction of change of dietary indicators was mixed in both study arms, but changes were marginal. The FNPA scores increased in both arms and there was a mixed picture of changes of the authoritative parenting style, parental self-efficacy and parental feeding practices scores (low numbers of participants completed these questionnaire items). The mean changes seen in the comparator arm were generally slightly larger than in the intervention arm. However, there are a number of issues that need to be taken into account when considering these findings. First, the feasibility study was not designed to evaluate programme clinical effectiveness. The intervention was refined during delivery and, because of the logistical issues we encountered at T0, some participants had their baseline measurements taken when they had already commenced the programme. In addition, there were very small numbers in the comparator arm and, of particular note, there was differential attrition across the two study arms (29% and 52% at 6 months in the intervention and comparator arms, respectively). The combination of these factors makes it impossible to draw any meaningful conclusions from the differences in mean changes in outcomes seen across the two study arms. In addition, regression to the mean may, in part, explain the changes seen.
| Outcome | Trial arm | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention (N = 69) | Comparator (N = 23) | |||||||||||
| End of programme (T1) | 6-month follow-up (T2) | End of programme (T1) | 6-month follow-up (T2) | |||||||||
| n | Mean change | SD | n | Mean change | SD | n | Mean change | SD | n | Mean change | SD | |
| BMI z-score | 48 | –0.09 | 0.13 | 40 | –0.12 | 0.23 | 17 | –0.13 | 0.13 | 11 | –0.18 | 0.21 |
| Waist z-score | 32 | –0.06 | 0.31 | 29 | 0.05 | 0.43 | 14 | –0.17 | 0.21 | 9 | –0.21 | 0.19 |
| Body fat percentage z-score | 47 | –0.07 | 0.17 | 38 | –0.19 | 0.30 | 15 | –0.10 | 0.14 | 11 | –0.17 | 0.27 |
| Average acceleration (SVMg; mg) | 52 | –0.68 | 16.95 | 28 | –0.63 | 15.14 | 14 | –0.68 | 1.70 | 8 | 4.85 | 10.60 |
| Moderate to vigorous physical activity (minutes/24 hours) | 38 | 0.55 | 13.39 | 28 | –1.06 | 12.76 | 14 | 1.96 | 14.49 | 8 | 2.33 | 12.71 |
| PedsQL score | 43 | 4.95 | 12.36 | 35 | 6.24 | 13.36 | 16 | 11.17 | 9.64 | 10 | 9.50 | 11.07 |
| Physical functioning score | 44 | 5.82 | 17.27 | 37 | 5.07 | 15.19 | 17 | 6.80 | 8.36 | 11 | 12.50 | 10.64 |
| Emotional functioning score | 45 | 9.22 | 21.97 | 39 | 9.74 | 21.61 | 16 | 11.88 | 16.92 | 10 | 9.50 | 20.74 |
| Social functioning score | 46 | 4.02 | 17.18 | 39 | 7.56 | 16.93 | 17 | 15.88 | 16.89 | 11 | 10.00 | 17.61 |
| School functioning score | 46 | 0.76 | 14.83 | 40 | 2.50 | 18.54 | 16 | 10.94 | 16.35 | 11 | 13.64 | 18.99 |
| Body dissatisfaction score | 44 | –0.20 | 1.36 | 38 | –0.27 | 1.01 | 17 | –0.41 | 0.94 | 11 | –0.26 | 1.83 |
| CHU-9D score | 45 | 0.05 | 0.12 | 39 | 0.04 | 0.12 | 17 | 0.03 | 0.09 | 11 | 0.07 | 0.09 |
| Children’s Dietary Questionnaire (score) | ||||||||||||
| Fruit and vegetables | 39 | 0.34 | 3.28 | 32 | 1.00 | 3.09 | 15 | 0.76 | 3.30 | 11 | 1.48 | 3.94 |
| Dairy | 33 | 0.30 | 2.67 | 30 | 0.10 | 2.93 | 15 | –0.13 | 2.00 | 9 | 0.00 | 0.94 |
| Sugar-sweetened beverages | 40 | 0.09 | 1.54 | 35 | 0.31 | 1.67 | 16 | 0.21 | 1.23 | 10 | –0.45 | 1.83 |
| Non-core foods | 34 | –0.16 | 1.52 | 26 | 0.09 | 1.15 | 14 | –0.26 | 1.26 | 9 | 0.95 | 0.17 |
| FNPA | 21 | 1.62 | 6.55 | 23 | 1.91 | 5.76 | 7 | 3.71 | 4.79 | 7 | 5.57 | 10.24 |
| Authoritative parenting | 25 | 0.11 | 0.36 | 16 | –0.07 | 0.49 | 5 | –0.06 | 0.19 | 3 | 0.30 | 0.15 |
| Parenting efficacy | 26 | 0.01 | 0.42 | 16 | –0.06 | 0.53 | 7 | 0.30 | 0.66 | 4 | 0.30 | 0.55 |
| Parent feeding practices scores | ||||||||||||
| Child control | 20 | –0.18 | 0.71 | 16 | –0.28 | 0.50 | 6 | –0.17 | 0.61 | 3 | –0.33 | 0.42 |
| Encouraging balance and variety | 20 | 0.01 | 0.63 | 16 | 0.15 | 0.42 | 6 | 0.01 | 0.77 | 3 | 0.25 | 0.50 |
| Environment | 20 | 0.10 | 1.06 | 16 | 0.27 | 1.03 | 6 | –0.01 | 0.94 | 3 | 0.36 | 0.35 |
| Modelling | 20 | 0.33 | 0.63 | 16 | 0.47 | 0.62 | 6 | 0.71 | 1.27 | 3 | 1.00 | 1.75 |
| Monitoring | 20 | 0.69 | 1.14 | 16 | 0.59 | 0.87 | 6 | 0.50 | 1.26 | 3 | 1.25 | 1.30 |
| Restriction for health | 20 | –0.01 | 0.83 | 16 | 0.27 | 0.92 | 6 | –0.08 | 0.66 | 3 | 0.50 | 1.15 |
| Restriction for weight control | 20 | 0.08 | 0.53 | 16 | –0.31 | 0.59 | 6 | –0.04 | 0.99 | 3 | 0.08 | 0.80 |
| Teaching about nutrition | 20 | 0.18 | 1.08 | 16 | –0.22 | 0.99 | 6 | 0.00 | 0.52 | 3 | 0.11 | 0.51 |
| Involvement | 20 | 0.24 | 0.87 | 16 | 0.25 | 0.63 | 6 | 0.22 | 0.40 | 3 | 0.67 | 0.58 |
We also undertook exploratory analyses to compare outcomes in intervention and comparator arms at T1 and T2 by developing mixed-effects linear regression models (using intention-to-treat analysis). The models are presented in Tables 19 and 20. At both time points, the point estimates of the mean differences were of small magnitude. In the adjusted models, all CIs of the estimates included a value of zero at T1. This was also the case at T2, with the exception of the quality-of-life physical functioning score and the CHU-9D score. Again, it is not possible to draw meaningful conclusions from these models because of the feasibility study design, issues with timing of the baseline data collection, small sample size and differential level of attrition in the two study arms.
| Outcome | Model number | |||||
|---|---|---|---|---|---|---|
| 1a | 2b | |||||
| n | Mean difference | 95% CI | n | Mean difference | 95% CI | |
| BMI z-scorea | 65 | 0.04 | –0.04 to 0.11 | 63 | 0.03 | –0.04 to 0.10 |
| Waist z-scorea | 46 | 0.06 | –0.13 to 0.26 | 45 | 0.07 | –0.14 to 0.27 |
| Body fat percentage z-scorea | 62 | –0.02 | –0.05 to 0.11 | 60 | –0.02 | –0.12 to 0.08 |
| Average accelerationc | 52 | 0.76 | –6.13 to 7.66 | 51 | –0.92 | –7.55 to 5.71 |
| Moderate to vigorous physical activityc | 52 | 0.37 | –5.57 to 6.31 | 51 | –2.23 | –13.55 to 9.09 |
| PedsQL score | 59 | –5.35 | –11.36 to 0.66 | 58 | –4.57 | –11.12 to 1.97 |
| Physical functioning score | 61 | –0.73 | –8.49 to 7.02 | 60 | –1.51 | –9.51 to 6.49 |
| Emotional functioning score | 62 | –2.83 | –11.62 to 5.95 | 60 | –0.57 | –8.24 to 9.37 |
| Social functioning score | 63 | –8.86 | –17.50 to -0.22 | 61 | –7.63 | –16.57 to 1.31 |
| School functioning score | 62 | –7.69 | –15.12 to -0.27 | 61 | –6.23 | –13.90 to 1.43 |
| Body dissatisfaction score | 61 | 0.26 | –0.39 to 0.90 | 59 | –0.02 | –0.70 to 0.66 |
| CHU-9D score | 62 | 0.01 | –0.04 to 0.05 | 60 | 0.01 | –0.03 to 0.06 |
| Children’s Dietary Questionnaire (score) | ||||||
| Fruit and vegetables | 54 | 1.00 | –1.31 to 3.31 | 53 | 0.56 | –1.90 to 3.02 |
| Dairyc | 48 | 0.42 | –0.35 to 1.19 | 47 | –0.23 | –1.50 to 1.03 |
| Sugar-sweetened beveragesc | 56 | –0.25 | –0.83 to 0.32 | 55 | 0.32 | –0.42 to 1.07 |
| Non-core foodsc | 48 | 0.03 | –0.52 to 0.58 | 47 | 0.09 | –0.44 to 0.62 |
| FNPA | 28 | –1.37 | –5.99 to 3.24 | 27 | 0.15 | –4.26 to 4.56 |
| Authoritative parenting | 32 | 0.18 | –0.10 to 0.38 | 25 | 0.13 | –0.09 to 0.35 |
| Parenting efficacyc | 34 | –0.18 | –0.42 to 0.06 | 33 | –0.16 | –0.34 to 0.02 |
| Parent feeding practices scores | ||||||
| Child control | 26 | –0.16 | –0.74 to 0.42 | 25 | –0.53 | –1.39 to 0.33 |
| Encouraging balance and variety | 26 | –0.18 | –0.64 to 0.28 | 25 | –0.11 | –0.60 to 0.37 |
| Environment | 26 | 0.31 | –0.40 to 1.01 | 25 | 0.22 | –0.38 to 0.82 |
| Modelling | 26 | –0.39 | –0.91 to 0.14 | 25 | –0.42 | –0.99 to 0.16 |
| Monitoring | 26 | 0.39 | –0.35 to 1.13 | 25 | 0.31 | –0.28 to 0.89 |
| Restriction for health | 26 | 0.07 | –0.57 to 0.72 | 25 | 0.20 | –0.43 to 0.84 |
| Restriction for weight control | 26 | 0.23 | –0.34 to 0.80 | 25 | –0.04 | –0.52 to 0.44 |
| Teaching about nutrition | 26 | 0.13 | –0.36 to 0.62 | 25 | 0.09 | –0.21 to 0.40 |
| Involvementc | 26 | –0.15 | –0.73 to 0.43 | 25 | –0.08 | –0.59 to 0.44 |
| Outcome | Model number | |||||
|---|---|---|---|---|---|---|
| 1a | 2b | |||||
| n | Mean difference | 95% CI | n | Mean difference | 95% CI | |
| BMI z-scorea | 51 | 0.06 | –0.08 to 0.21 | 50 | 0.001 | –0.15 to 0.16 |
| Waist z-scorea | 31 | 0.11 | –0.19 to 0.39 | 30 | –0.07 | –0.32 to 0.18 |
| Body fat percentage z-scorea | 49 | –0.02 | –0.21 to 0.17 | 49 | –0.07 | –0.26 to 0.12 |
| Average accelerationc | 36 | –4.96 | –12.80 to 2.88 | 36 | –4.86 | –17.79 to 8.06 |
| Moderate to vigorous physical activityc | 36 | –1.25 | –8.12 to 5.62 | 36 | –1.03 | –24.38 to 22.32 |
| PedsQL score | 45 | –2.68 | –10.22 to 4.86 | 44 | –3.70 | –11.35 to 3.96 |
| Physical functioning score | 48 | –7.70 | –15.37 to -0.02 | 47 | –8.43 | –16.23 to –0.63 |
| Emotional functioning score | 49 | –1.09 | –12.65 to 10.47 | 48 | –1.79 | –13.74 to 10.16 |
| Social functioning score | 50 | 0.25 | –9.69 to 10.20 | 49 | –0.08 | –10.83 to 9.22 |
| School functioning score | 51 | –5.59 | –15.60 to 4.43 | 50 | –5.71 | –16.09 to 4.67 |
| Body dissatisfaction score | 49 | –0.06 | –1.60 to 1.48 | 48 | –0.34 | –1.86 to 1.19 |
| CHU-9D score | 50 | –0.05 | –0.09 to –0.01 | 49 | –0.07 | –0.11 to –0.03 |
| Children’s Dietary Questionnaire (score) | ||||||
| Fruit and vegetables | 43 | –0.03 | –2.19 to 2.12 | 43 | –1.05 | –3.12 to 1.03 |
| Dairyc | 39 | 0.20 | –0.91 to 1.31 | 39 | 1.70 | –2.95 to 6.34 |
| Sugar-sweetened beveragesc | 45 | 0.42 | –0.24 to 1.08 | 45 | 0.66 | –0.73 to 2.06 |
| Non-core foodsc | 35 | 0.06 | –0.52 to 0.64 | 35 | 0.73 | –0.53 to 1.99 |
| FNPA | 30 | –3.35 | –8.08 to 1.37 | 30 | –4.06 | –8.42 to 0.30 |
| Authoritative parenting | 17 | –0.40 | –1.03 to 0.23 | 17 | –0.52 | –1.05 to 0.03 |
| Parenting efficacyc | 20 | –1.59 | –7.52 to 4.34 | 20 | –0.01 | –0.07 to 0.06 |
| Parent feeding practices scores | ||||||
| Child control | 19 | 0.01 | –0.49 to 0.50 | – | Model did not converge | |
| Encouraging balance and variety | 19 | –0.08 | –0.56 to 0.40 | – | Model did not converge | |
| Environment | 19 | 0.15 | –0.85 to 1.15 | – | Model did not converge | |
| Modelling | 19 | –0.45 | –1.17 to 0.26 | 19 | –0.76 | –1.99 to 0.46 |
| Monitoring | 19 | –0.40 | –1.05 to 0.25 | 19 | –0.42 | –0.97 to 0.13 |
| Restriction for health | 19 | 0.13 | –0.64 to 0.91 | 19 | 0.07 | –0.57 to 0.70 |
| Restriction for weight control | 19 | –0.13 | –0.84 to 0.59 | 19 | –0.27 | –0.92 to 0.38 |
| Teaching about nutrition | 19 | –0.39 | –1.36 to 0.57 | 19 | –0.19 | –0.94 to 0.55 |
| Involvementc | 19 | –0.30 | –0.82 to 0.21 | 19 | –0.21 | –0.78 to 0.37 |
Sensitivity analyses
Two imputation methods were undertaken to estimate missing values at T1 and T2: (1) baseline observation carried forward and (2) multiple imputation techniques. The sensitivity analyses for T1 and T2 are presented in Appendix 11 but, in brief, the mean differences in outcomes remained very small.
Analysis of anonymised body mass index z-score data from programme participants
Anonymised BMI z-scores for all programme participants within the study period were provided by the BCHCT weight management service team. Data were available only for children who attended the first and last sessions of the programmes, as this was when the measurements were undertaken (n = 154; n = 115 in the intervention group and n = 39 in the comparator group). Using these data, the mean changes in BMI z-score at programme end (T1) were –0.09 and –0.13 for the intervention and comparator arms, respectively. The mixed-effects linear regression analysis showed a mean difference of 0.05 (95% CI –0.01 to 0.10) in the model adjusted for baseline BMI z-score and clustering, and 0.04 (95% CI –0.02 to 0.10) in the model that was further adjusted for age, sex and ethnicity. This is similar to the analysis with the CHANGE study participants only (see Table 19). Again, there were differential levels of programme completion, which meant that there were fewer data available at the end of the programme in the comparator group than in the intervention group, which precludes any meaningful conclusions being drawn from this analysis.
Discussion
Summary of the feasibility study findings
Feasibility and acceptability of the adapted programme
The NHS children’s weight management provider service was successfully able to deliver the adapted intervention programme. The delivery structure of six 90-minute sessions over 6 weeks was generally found to be acceptable to participants and feasible in terms of cost and delivery for the service provider. The adaptation of more weekend provision was accommodated by the service providers, although there were higher costs attached to staffing and venue hire at weekends. Weekend sessions seemed to suit the participants who attended them, although some families still identified challenges to attending at weekends.
The facilitators showed a high degree of enthusiasm for the programme and valued the high-quality materials, the interactive and flexible nature of delivery and the inclusion of children in the programme. The participating families also positively viewed these aspects and, in particular, drew attention to the value of becoming connected with other families, sharing experiences and supporting each other in their endeavours to change behaviours within the family. These aspects of the programme were adaptations that were explicitly identified in the theoretical intervention development process in phase I of the study. In contrast to the phase I findings, one facilitator felt that the de-emphasis on weight management in the adapted programme was unhelpful and possibly lessened the impact that the programme had. However, the stigma surrounding overweight has been found to be a barrier to attendance of children’s weight management programmes100 and the need to reframe messages in children’s weight management programmes has been highlighted. 101 This, together with our findings in phase I of the need for an emphasis on healthy lifestyles, rather than weight, supports our approach in the adapted programme.
The views of the programme facilitators and participants diverged when it came to the balance of nutrition and physical activity content. Despite adapting the programme to include physical activity sessions, participating parents and children wanted even more physical activities within the sessions and felt that these and other ‘doing’ activities, such as making healthy snacks, were the ‘fun’ elements of the programme. However, the facilitators felt that the nutritional content and messages had been somewhat lost from the standard programme and that there was too much emphasis on physical activity.
The session that was observed to be most problematic to deliver was the healthy eating session, and this was confirmed by the facilitator feedback. The session was refined in response to this and delivery was improved, although the facilitators still reported difficulties with its delivery at the end of the study period. Thus, further minor refinements to streamline the session may be required in the future.
The interviews with parents and children did not reveal any differences in programme acceptability across different ethnicities and, similarly, direct observation and the views of facilitators were consistent with the universal acceptability of the programme. This evidence supports the underlying principle of having flexibility and responsiveness in the programme, which was identified as important in the adaptation process.
A key indicator of the acceptability of the programme to participants was the estimation of the proportion of families who completed the programme. The definition of 60% attendance was adopted for this study in recognition of the fact that families with children may have other commitments or unexpected events that may prevent them from attending all sessions, even if they intend to. The primary outcome of interest was completion in Pakistani and Bangladeshi families, as the intervention adaptation process focused primarily on increasing programme acceptability for these families. However, a key secondary outcome was to estimate completion rates in families of other ethnicities and, overall, to ensure that in focusing the adaptation process on Pakistani and Bangladeshi communities, the programme had not become less acceptable to other families. The proportion of families who completed the adapted programme was, overall, 76% (79% of Pakistani and Bangladeshi families and 75% of other families). These point estimates of completion were much higher than for the comparator programme (in which 58% of all families completed the comparator programme) and also compare favourably to historical, routinely collected data on attendance (49% of families who attended at least one session completed the programme in the year preceding the study). These findings support the high acceptability of the adapted programme and are consistent with the qualitative data from interviews with programme participants. These levels of programme completion also compare favourably with what is reported in the current children’s weight management literature. A review of 23 studies of child weight management interventions reported a median drop-out rate of 37% (range 4–83%);31 however, these were all clinic-based interventions. In terms of community-based group child weight management programmes, reported programme drop-out rates have frequently been high (> 40%). 102,103 In the UK, the MEND programme has been rolled out on a large scale in the last decade. This is a community-based group programme for 7- to 13-year-old children and their families, comprising 20 sessions. A study of participants, undertaken over a 4-year period, reported that 59% of participants completed the programme (defined as > 75% attendance). 32
Feasibility of trial methods
Study design
The feasibility study was designed as a cluster RCT to enable assessment of the proportion of families that completed the adapted and the standard programmes in the two study arms. We were able to execute this study design within the existing structure of the children’s weight management service. The cluster design enabled participants to attend the most convenient programme for them and was appropriate for a trial in which both the intervention and the comparator are group-based programmes. However, in a future trial to evaluate clinical effectiveness, consideration needs to be given to the comparator arm. The difference in effect size between two programmes that one may expect to see may preclude undertaking such a trial because the sample size would need to be very large. A more feasible approach to a future clinical effectiveness evaluation would involve having a comparator arm that has no active intervention programme. In this scenario, the required study design would be a trial randomised at the individual level. Therefore, using the data generated by this feasibility study, we have undertaken a sample size calculation for a future individually randomised controlled trial that compares the adapted group-based programme with no intervention. One parameter required for this calculation, which we have not been able to estimate in the feasibility study, is the likely difference in effect between a group receiving the intervention and a group with no intervention. We have, therefore, drawn on available literature to determine this parameter. We selected a mean difference in BMI z-score between study arms of 0.15 because, although there are currently no data to support a clinically meaningful threshold for change in BMI z-score,104 significant improvements in a range of cardiovascular disease markers have been reported with this level of BMI z-score reduction. 105
To test a mean difference in BMI z-score of 0.15 in a study population with a BMI z-score standard deviation of 0.6 (as reported in this study) at 90% power and 5% significance, allowing for a correlation between pre- and post-intervention measurements of 0.7 (which is a conservative estimate), 169 participants per study arm would be required. However, the proposed trial, although individually randomised in design, would have clustering in the intervention arm because of the group-based nature of the intervention programme and, therefore, given the findings of this study, attrition also needs to be taken into account in the sample size calculation. Assuming that the programme is delivered to groups of 10 and allowing for 30% attrition, the expected cluster size after attrition would be 7. Therefore, assuming an ICC of 0.03 (as estimated in this study), the sample size in the intervention arm would be 199 [= 169 × 1.18 (= 1 + 6 × 0.03)]. This equates to approximately 199 participants being randomly allocated to the intervention arm across 28 (= 199/7) programme groups and 199 participants being randomly allocated to a control arm.
Participant recruitment and follow-up
We achieved our participant recruitment target of 80 in this study. We did not expect difficulties in recruitment as we were recruiting families that had already agreed to attend a children’s weight management programme. However, the process of recruitment proved problematic for a number of reasons and resulted in difficulties in undertaking baseline assessments with families before they started a programme. In a future trial, it would be necessary to plan carefully with all partners involved in participant recruitment to ensure that there is enough time to gain consent and undertake baseline assessments before the start of the intervention programme. If an individually randomised design was adopted, then randomisation of participants would need to be undertaken after baseline assessments and before the participants start a programme.
Participant attrition was a major issue, with one-third of participants being unable to be followed up at the 6-month time point. The majority of these were lost to follow-up rather than having actively withdrawn from the study, despite multiple attempts to contact them by telephone and letter. The level of attrition seen in this study is within the range of attrition seen in other children’s weight management intervention studies. The Cochrane review12 of 64 studies reported that participant drop out at 6 months ranged from 1% to 42%, with only 31 studies reporting a follow-up of > 80%. The high attrition seen in this study may, in part, be explained by the characteristics of the study population: Birmingham has high levels of population turnover. 106
Attrition poses a major challenge for a future trial to evaluate intervention clinical effectiveness. In this feasibility study, as well as there being a high level of attrition overall, there were differential levels of attrition in the two study arms (29% in the intervention arm vs. 52% in the comparator arm). This makes the interpretation of outcome comparisons between the two arms more complex and necessitates data imputation, as demonstrated in our exploratory outcome analyses. Differential attrition across study arms has been less commonly reported in other studies. 12 There are no obvious solutions to the problem of attrition. We designed our data collection processes to minimise loss to follow-up by offering appointments in the participant’s home, which has been shown to be an effective approach to reduce attrition;107 thus, it was disappointing to retain only two-thirds of the participants until the end of the study. In future research, we would recommend requesting as many contact details as possible, including all telephone numbers and postal and e-mail addresses. Rewards for participants at the final follow-up point should also be considered. In addition, the sample size calculation of a future trial should take into account a significant level of attrition.
Outcome data collection
Overall, the collection of outcome data worked well. The home visits appeared to be acceptable to participants, and they were feasible to undertake. However, the visits were resource intensive, with a great deal of staff time spent travelling to participants’ homes and there being a necessity for two researchers on the first visit. This is a consideration in the design of a future trial.
One issue that arose with the collection of outcome data was the difficulty in concealing the study arm that the participants were allocated to from the researchers undertaking the assessment visits. At baseline, this was in part because some participants had already commenced a weight management programme before the data collection visit took place. In a future trial of similar design to this feasibility study, separation of the research staff undertaking the outcome measures and the core research team responsible for the delivery of the study overall would help in blinding those undertaking the measures. However, in a trial comparing a programme with no intervention, blinding of staff undertaking measurements at follow-up could be challenging.
The feasibility study was planned to enable us to explore the feasibility of collection of a wide range of outcome data. It became clear during the study that the number of questionnaire instruments that we were requiring parents to complete was too much of a burden. In general, home visits lasting for more than 1 hour became wearisome for the families and the researchers. In response to this, we prioritised certain questionnaire instruments to be completed at the visit and asked parents to complete the others at a later time and post them back to the research team. This significantly affected data completeness, with only 43–58% of participants completing the second group of questionnaires at the follow-up time points. The other issue with splitting the collection of questionnaire data in this way was that it did not work for non-English-speaking participants. In these cases, the researchers either stayed to complete all the questionnaires or, if the participant became too fatigued, they left the second group of questionnaires blank. There is also the possibility that the heavy burden on participants at the data collection visits contributed to the high attrition seen in the study. Thus, in a future trial it would be important to consider carefully which outcome data are essential and to resist the temptation to measure too many outcomes.
Overall, sociodemographic and anthropometric data were relatively complete, as were the questionnaire measures that were directly administered to the child participants. Apart from the FNPA questionnaire, the parent questionnaires that were administered during the home visit were relatively well completed. In a future full-scale trial, we would recommend the use of BMI z-score as the primary outcome, given the completeness of data collection; however, it would be important to include other anthropometric measures as secondary outcomes, given the limitations of BMI as a measure of adiposity.
The anthropometric measurements with parents and other family members proved particularly problematic. The number of family members agreeing to be measured reduced over the three time points, and often those agreeing at each time point were different family members. Collection of family data in a future trial would need careful planning with prior agreement at the outset over which family members will be present to be measured at each data collection time point. This would be extremely logistically challenging.
Process evaluation methods
The implementation of the adapted programme was directly observed by researchers, who attended all programme sessions and also observed delivery by both facilitators. In addition, there was contemporaneous feedback from the facilitators on their reflection on delivering the session and how it was received by the participants. We also undertook a series of interviews with facilitators and participants. In this study, these methods were used primarily to assess the feasibility of delivering the adapted programme and how acceptable it was to the participants, as well as enabling refinement of aspects of the intervention during the study intervention period. However, these methods also enabled the collection of key process evaluation data that would be required to assist in the interpretation of the evaluation of outcomes in a future trial. In line with the UK’s Medical Research Council guidance on the process evaluation of complex interventions,108 we clearly articulated the causal assumptions underlying the intervention programme in phase I of this study and have collected data that enable evaluation of intervention fidelity, the degree of tailoring, participant responsiveness to the various elements of the intervention programme and the influence of context on both delivery and participant response. The experience of collecting these process data, together with the previous process evaluation experience of the research team,109 will inform the development of detailed tools to assist in process evaluation in a future trial, such as observation checklists and standardised facilitator feedback forms.
Economic evaluation methods
The economic component of the study aimed to design processes for, and capture data on, the costs and outcomes associated with the intervention and comparator programmes to inform the methods for a future economic evaluation alongside a definitive trial. On the whole, processes were successfully put in place to measure the costs associated with the adapted programme. Data were successfully collected on the costs associated with producing the adapted programme materials. However, some challenges were also encountered. In particular, difficulties were encountered in terms of capturing data on resource use for the comparator programmes. As this represented ‘routine practice’ for staff delivering the programmes, it was difficult to separate out the costs associated with conducting the standard programme from other day-to-day activities. In a future trial, if the same design were adopted, we would recommend having separate processes for capturing the costs associated with producing materials for comparator programmes.
As part of the study, we aimed to collect data on the costs borne by families in attending the weight management programme. These data were collected via a questionnaire distributed at the end of the programmes. Problems were incurred by collecting data in this way. Very few questionnaires were returned by those attending the comparator programmes and the questionnaire was completed by all programme participants at the final session, rather than by only those who had participated in the CHANGE study. We would recommend that, in a future trial, these data are collected alongside the outcome data rather than separately at the end of the programme.
The core outcome data that could be used in a future economic evaluation were collected successfully (see Outcome data collection). This would permit different types of economic evaluation to be conducted in a future definitive trial. First, a cost-effectiveness analysis could be conducted, using the primary clinical outcomes included in the trial, for example estimation of the cost per mean change in BMI z-score. In addition, collection of CHU-9D data would allow a cost–utility analysis to be undertaken as recommended by NICE. However, as discussed (see Outcome data collection), it was not feasible to collect the data to capture the impact that the intervention had on the wider family (anthropometric measurements on parents and other family members). The design of the economic evaluation alongside a future trial would adopt two approaches: a within-trial analysis that would estimate the cost-effectiveness using data generated by only the trial on the basis of an intention-to treat principle and, if appropriate, a longer-term model-based economic evaluation extrapolating both the costs and outcomes over a lifetime. The model-based economic evaluation would need to follow standard guidelines for decision-analytic modelling by adequately capturing the uncertainty with long-term intervention effects, future costs and outcomes linked to disease associated with being overweight and structural uncertainty within the model.
Exploratory analyses of intervention effect on participant outcomes
This feasibility study was not designed to assess intervention clinical effectiveness; however, we undertook exploratory analyses of our outcome data. Although we did show a favourable direction of intervention clinical effect at the end of the programme and at 6 months, the effect size was small. Given the continuing refinement of the intervention programme during its delivery, the high and differential study attrition and the lack of ‘true’ baseline data for some participants (as some T0 measurements were taken after the start of the programme), we cannot draw any conclusions from these analyses, other than that there is a signal that the adapted programme results in some reduction in BMI z-scores and other anthropometric measures.
Strengths and limitations
The cluster randomised design of this feasibility study enabled a detailed evaluation of both the feasibility of delivery and acceptability of the adapted intervention programme and the feasibility of the processes and methods required for a future clinical effectiveness and cost-effectiveness evaluation. Estimation of participant retention gave an indication of overall programme acceptability. The inclusion of a comparator arm gave us the opportunity to directly compare participant retention in the adapted programme with that in the standard programme. In their evidence synthesis on the adaptation of health promotion programmes for minority ethnic groups, Liu et al. 35 highlighted the need for this type of direct comparison. The qualitative evaluation methods that we employed enabled us to explore, in detail, the engagement of programme deliverers and participants and resultant change in behaviours. We were also able to use this information to refine the programme within the feasibility study.
We were able to test recruitment and follow-up over 6 months, as well as the processes involved in the collection of a wide range of outcome measures and cost data that would need to be collected in a future economic evaluation of the programme. We gained valuable insights into the areas that would require particular attention when designing a future trial and what modifications would be required to the methods used in this study.
Although our adaptation was primarily focused on increasing the relevance and acceptability of the children’s weight management programme to families from Pakistani and Bangladeshi communities, we tested its acceptability in an ethnically diverse population, predominantly from socioeconomically disadvantaged areas. This was important, as the adapted programme was designed to be delivered flexibly and to be responsive to families from all ethnic and cultural backgrounds. In addition, we designed the study to be inclusive of participants who did not speak English. The use of community researchers from Pakistani and Bangladeshi communities at the data collection visits was a particular strength, with these community researchers providing language skills to, and having a shared cultural understanding with, families from these communities.
There are limitations to this feasibility study. The programme adaptation process focused specifically on families from Pakistani and Bangladeshi communities. Therefore, we cannot assess whether or not a programme that was adapted with a broader focus would be even more acceptable and relevant to other families. However, the study was designed to focus on Pakistani and Bangladeshi families, as data from the existing weight management service in Birmingham highlighted that families from these communities were more likely to drop out of the programmes than families from other communities. In addition, our findings indicate that all families were more likely to complete the adapted programme than the standard programme, indicating high acceptability across all ethnicities, and this is supported by the qualitative data obtained from the feasibility study participants.
We did not focus on initial attendance at the programme, once a family had been booked to attend. Within this study, some adaptations were made to the programme recruitment materials and processes but these were applied to both intervention and comparator programmes. Despite this, initial programme attendance remained low, with < 50% of the families that were booked to attend actually attending any sessions in both arms of the study. Even of the families who agreed to participate in the CHANGE study, 20% did not attend any First Steps programme sessions. This is clearly another concern for the future provision of children’s weight management services, but it was beyond the scope of this feasibility study and, thus, needs to be a focus of future research.
The cluster randomised design of the study enabled us to assess programme completion in both the adapted and the standard programmes. However, it did not enable us to evaluate the acceptability to study participants of individual randomisation or allocation to a control arm in which no intervention is received, neither did it provide us with an estimate of difference in effect between intervention and control (no intervention) arms to inform the sample size calculation of a future trial. The study design incorporated home visits to collect data from participants in order to minimise attrition. This is a resource-intensive approach and would increase the cost of a future trial. In addition, despite this approach, there were high levels of attrition. During the study, we did consider an alternative and potentially lower cost method: attending the first and last programme sessions to undertake data collection with study participants. However, after discussion with the Study Steering Committee, it was agreed that this approach would present problems in blinding researchers to the study arms that the participants were in and participants who did not attend or complete the programmes would still require home appointments for data collection.
Consideration of progression to a trial to assess clinical effectiveness and cost-effectiveness
Within the CHANGE study protocol, we specified that we would consider the following factors when making the decision to proceed to a full clinical effectiveness and cost-effectiveness trial of the adapted children’s weight management programme:
-
the estimate of the proportion of families completing the modified programme (Pakistani and Bangladeshi families and all families)
-
the feasibility and acceptability of the culturally adapted components of the programme to the ethnically diverse study sample
-
the feasibility and acceptability of trial processes
-
the feasibility and acceptability of outcome measures and other evaluation methods
-
the identification of appropriate methods for an economic evaluation in a full-scale trial.
We have demonstrated increased participant completion of the adapted programme compared with the standard programme, both in the feasibility study and also compared with historical service data. In addition, our qualitative data have shown that the programme is feasible to deliver and highly acceptable to service providers and participants. There was an incremental cost associated with the delivery of the adapted programme, but this was relatively modest (£33 per family attending).
We were able to successfully recruit participants from a pool of families referred to the Birmingham children’s weight management service. However, the number of families that withdrew or were lost to follow-up was high, which has implications for the feasibility of a full-scale trial. We were able to successfully undertake a cluster randomised study design with interventions being delivered in both study arms. However, as previously discussed (see Study design), the likely design of a future trial would involve individual randomisation with no or minimal intervention in the control arm, and this study does not provide data on the acceptability of these trial processes.
Data collection methods overall were feasible; however, in a future trial, fewer outcome data would need to be collected to minimise participant burden. The process evaluation methods that we undertook were both feasible and acceptable and yielded valuable data that would assist in the interpretation of outcomes in a future trial. We also successfully collected cost and outcome data, which would be required for a future economic evaluation of the adapted programme.
We have, therefore, broadly fulfilled our predefined progression criteria. However, we also feel that it is important to consider the changing commissioning landscape of children’s weight management programmes in the UK. In the last 15 years, the commissioning of community-based children’s weight management programmes that address weight-related behaviours has been widespread and the NICE guidelines,17 published in 2013, which were based on extensive and systematic evidence reviews, explicitly recommended the provision of family-based multicomponent lifestyle weight management services for children and young people. However, in the last 2 years, with reductions in public health budgets, a lack of long-term evidence for the effectiveness of programmes and difficulties with uptake,36 anecdotal evidence suggests that the provision of such services has become less widespread. In order to undertake a future trial of our adapted intervention programme, we would require collaboration from commissioners, which may prove challenging in the current climate.
Chapter 5 Conclusions and recommendations
Childhood obesity remains a high-priority issue in the UK and worldwide. The long-term solution is a systems approach to prevention that tackles structural, social, political and economic environments at all levels. 110,111 However, we must also offer effective targeted interventions for children who already have excess weight and, importantly, our intervention approaches must be inclusive of children from all sociocultural backgrounds.
Building on evidence that community-based family interventions can have a positive effect on children’s weight,12,17,21 we sought to culturally adapt a group-based community children’s weight management programme for 4- to 11-year-old children and their families. Although the focus of the cultural adaptation was to increase programme acceptability for families from Pakistani and Bangladeshi communities, the overarching aim was to develop an adapted programme that allowed enough flexibility and tailoring to meet the needs of all families, recognising the complex and fluid diversification that occurs within our communities. Overall, we have successfully achieved this aim and have developed an interactive and responsive programme that incorporates evidence from the children’s weight management literature. The key feature of the programme is the theoretical underpinning of the adaptations, which we achieved through the gathering of qualitative data from Pakistani and Bangladeshi families and the use of two theoretical frameworks, which enabled the articulation of the cultural and behavioural needs of the families and the types of adaptations needed to address these. In contrast with many cultural adaptations of health promotion interventions, our approach resulted in a programme that was adapted at the deep structural level57,58 and was designed to be responsive to the contexts, values and beliefs that differ, not only across different cultural communities, but also from family to family.
Evaluation of the adapted children’s weight management programme in the feasibility study demonstrated that the programme was feasible to deliver and highly acceptable to families from all communities, with increased retention of families in the adapted programme compared with the standard children’s weight management programme. Qualitative evaluation provided an opportunity to explore how the adaptations were received in practice. The feasibility study also highlighted some key areas that would need to be addressed in the design and methodology of a future trial to evaluate the clinical effectiveness and cost-effectiveness of the adapted programme. A major issue that emerged was that of attrition within the study. This would need to be addressed in both the design and sample size in a future trial. Overall, given the high acceptability and feasibility of delivery of the adapted children’s weight management programme, consideration should be given to conducting a clinical effectiveness and cost-effectiveness trial. However, the design of such a trial would need to incorporate the lessons learned from this feasibility study and employ multiple strategies to minimise attrition. In addition, the design of a future trial would differ from the feasibility study design in terms of having randomisation at the individual level and a control arm with no or minimal intervention, the acceptability of which has not been assessed within this study.
Two other broader recommendations have also arisen from this study. The first is the need for consideration of how to practically conduct experimental evaluations of complex interventions to change dietary and physical activity behaviours in a real-world setting where there are constraints on public health resources. The second is the need for further research into the engagement of children and families in weight management or healthy lifestyle interventions, with a particular focus on uptake of these programmes. Future research in this area would complement the findings of this study and enable interventions to be designed so that both uptake and retention are maximised.
Acknowledgements
We wish to acknowledge funding for this study from the NIHR Health Technology Assessment programme (project number 12/137/05). We would like to thank and acknowledge the children, parents and other family members and the NHS delivery staff who participated in the study. We acknowledge the support and collaboration of the BCHCT children’s weight management provider team and the Birmingham City Council Public Health team. We would like to thank all the administrative and research staff who contributed to the study: Andrea Anastassiou, Laura Ocansey, Aisha Ahmad, Minara Bibi, Salma Khan, David Sardar, Meanaz Akhtar, Nafiseh Chalabi Hagkarim, Janice Gunnell and Fyqa Gulzaib. We would also like to thank James Martin for his statistical advice and Andrea Roalfe for undertaking the randomisation.
Study Steering Committee
We would like to thank and acknowledge members of the external Study Steering Committee for overseeing the study: Dr Wendy Robertson (University of Warwick, Warwick, chairperson), Professor Mark Johnson (De Montfort University, Leicester), Dr Ruth Kipping (University of Bristol, Bristol) and Mrs Shahin Ashraf (public representative).
Parent Advisory Panel
We would like to thank and acknowledge members of the Parent Advisory Panel for their advice throughout the study: Mrs Zahida Arif, Mrs Shazia Begum and Mrs Masuma Chaudry.
Contributions of authors
Miranda Pallan (Senior Clinical Lecturer in Public Health) led the study as principal investigator. She led the design and conduct of the study throughout and prepared all chapters in the study report.
Tania Griffin (Research Fellow in Public Health) was the study co-ordinator for 25 months of the study and was a member of the study management team. She substantially contributed to the writing of Chapter 3.
Kiya L Hurley (Research Fellow in Public Health) was the study co-ordinator for the last 7 months of the study, and before this was a research assistant on the study team. She substantially contributed to the writing of Chapter 4 and prepared the results tables for Chapter 4.
Emma Lancashire (Senior Research Fellow in Public Health) was a co-investigator and member of the study management team. She contributed to the design and conduct of the study and the interpretation of the study findings.
Jacqueline Blissett (Professor in Childhood Eating Behaviour) was a co-investigator and contributed to the study design, intervention design, selection of outcome measures and interpretation of the study findings.
Emma Frew (Reader in Health Economics) was a co-investigator and contributed to the design, analysis and writing of the health economic components of the study.
Laura Griffith (Lecturer in the Anthropology of Healthcare) was a co-investigator and contributed to the design and analysis of the qualitative study in phase I.
Karla Hemming (Senior Lecturer in Biostatistics) was a co-investigator. She was the statistical advisor for the study and contributed to the study design and interpretation of the study findings.
Kate Jolly (Professor of Public Health and Primary Care) was a co-investigator and contributed to the study design and interpretation of the study findings.
Eleanor McGee (Public Health Nutrition Lead, BCHCT) was a co-investigator and the main NHS service provider contact. She had overall responsibility for the delivery of the intervention and comparator programmes in phase II and contributed to the study design and interpretation of the study findings.
Janice L Thompson (Professor of Public Health Nutrition and Exercise) was a co-investigator and contributed to the study design, selection of outcome measures and interpretation of the study findings.
Louise Jackson (Research Fellow in Health Economics) undertook the cost data analysis and wrote the health economic components presented in Chapter 4.
Paramjit Gill (Professor of General Practice) was a co-investigator and contributed to the study design and interpretation of the study findings.
Jayne Parry (Professor of Policy and Public Health) was a co-investigator and substantially contributed to the study conception and design.
Peymane Adab (Professor of Chronic Disease Epidemiology and Public Health) was a co-investigator and a member of the study management team. She contributed to the study conception, design, conduct and interpretation of the study findings.
All authors read and approved the final version of the report.
Publications
Pallan M, Griffin T, Lancashire E, Hurley K, Blissett J, Frew E, et al. Cultural adaptation of a children’s weight management programme for Bangladeshi and Pakistani families in the UK: a cluster-randomised feasibility study protocol. Pilot Feasibility Stud 2016;2:48.
Pallan M, Griffin T, Hurley K, Lancashire E, Blissett J, Frew E, et al. Cultural adaptation of a children’s weight management programme: Child weigHt mANaGement for Ethnically diverse communities (CHANGE) study. BMC Public Health 2019;19:848.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care.
References
- National Child Measurement Programme: England, 2015/16 School Year. Leeds: NHS Digital; 2016.
- National Child Measurement Programme – England, 2014–15. Leeds: NHS Digital; 2015.
- Lobstein T, Baur L, Uauy R. IASO International Obesity Task Force . Obesity in children and young people: a crisis in public health. Obes Rev 2004;5:4-104. https://doi.org/10.1111/j.1467-789X.2004.00133.x.
- Singh AS, Mulder C, Twisk JW, van Mechelen W, Chinapaw MJ. Tracking of childhood overweight into adulthood: a systematic review of the literature. Obes Rev 2008;9:474-88. https://doi.org/10.1111/j.1467-789X.2008.00475.x.
- Whitlock G, Lewington S, Sherliker P, Clarke R, Emberson J, Halsey J, et al. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet 2009;373:1083-96. https://doi.org/10.1016/S0140-6736(09)60318-4.
- Ogden CL, Yanovski SZ, Carroll MD, Flegal KM. The epidemiology of obesity. Gastroenterology 2007;132:2087-102. https://doi.org/10.1053/j.gastro.2007.03.052.
- Scarborough P, Bhatnagar P, Wickramasinghe KK, Allender S, Foster C, Rayner M. The economic burden of ill health due to diet, physical inactivity, smoking, alcohol and obesity in the UK: an update to 2006-07 NHS costs. J Public Health 2011;33:527-35. https://doi.org/10.1093/pubmed/fdr033.
- Wang YC, McPherson K, Marsh T, Gortmaker SL, Brown M. Health and economic burden of the projected obesity trends in the USA and the UK. Lancet 2011;378:815-25. https://doi.org/10.1016/S0140-6736(11)60814-3.
- Barba C, Cavalli-Sforza T, Cutter J, Darnton-Hill I. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 2004;363:157-63. https://doi.org/10.1016/S0140-6736(03)15268-3.
- Bhopal R, Unwin N, White M, Yallop J, Walker L, Alberti KGMM, et al. Heterogeneity of coronary heart disease risk factors in Indian, Pakistani, Bangladeshi, and European origin populations: cross sectional study. BMJ 1999;319:215-20. https://doi.org/10.1136/bmj.319.7204.215.
- Whincup PH, Gilg JA, Papacosta O, Seymour C, Miller GL, Alberti KGMM, et al. Early evidence of ethnic differences in cardiovascular risk: cross sectional comparison of British South Asian and white children. BMJ 2002;324. https://doi.org/10.1136/bmj.324.7338.635.
- Oude Luttikhuis H, Baur L, Jansen H, Shrewsbury VA, O’Malley C, Stolk RP, et al. Interventions for treating obesity in children. Cochrane Database Syst Rev 2009;1. https://doi.org/10.1002/14651858.CD001872.pub2.
- Sacher PM, Kolotourou M, Chadwick PM, Cole TJ, Lawson MS, Lucas A, et al. Randomized controlled trial of the MEND program: a family-based community intervention for childhood obesity. Obesity 2010;18:S62-S68. https://doi.org/10.1038/oby.2009.433.
- Kalarchian MA, Levine MD, Arslanian SA, Ewing LJ, Houck PR, Cheng Y, et al. Family-based treatment of severe pediatric obesity: randomized, controlled trial. Pediatrics 2009;124:1060-8. https://doi.org/10.1542/peds.2008-3727.
- Coppins D, Margetts B, Fa J, Brown M, Garrett F, Huelin S. Effectiveness of a multi-disciplinary family-based programme for treating childhood obesity (The Family Project). Eur J Clin Nutr 2011;6:903-9. https://doi.org/10.1038/ejcn.2011.43.
- Collins CE, Okely AD, Morgan PJ, Jones RA, Burrows TL, Cliff DP, et al. Parent diet modification, child activity, or both in obese children: an RCT. Pediatrics 2011;127:619-27. https://doi.org/10.1542/peds.2010-1518.
- Weight Management: Lifestyle Services for Overweight or Obese Children and Young People. London: NICE; 2013.
- Kolsgaard MLP, Joner G, Brunborg C, Anderssen SA, Tonstad S, Andersen LF. Reduction in BMI z-score and improvement in cardiometabolic risk factors in obese children and adolescents. The Oslo Adiposity Intervention Study-a hospital/public health nurse combined treatment. BMC Pediatr 2011;11. https://doi.org/10.1186/1471-2431-11-47.
- Obesity: The Prevention, Identification, Assessment and Management of Overweight and Obesity in Adults and Children. London: NICE; 2006.
- Staniford LJ, Breckon JD, Copeland RJ. Treatment of childhood obesity: a systematic review. J Child and Family Studies 2012;21:545-64. https://doi.org/10.1007/s10826-011-9507-7.
- Upton P, Taylor C, Erol R, Upton D. Family-based childhood obesity interventions in the UK: a systematic review of published studies. Community Pract 2014;87:25-9.
- Faith MS, Van Horn L, Appel LJ, Burke LE, Carson JA, Franch HA, et al. Evaluating parents and adult caregivers as ‘agents of change’ for treating obese children: evidence for parent behavior change strategies and research gaps a scientific statement from the American Heart Association. Circulation 2012;125:1186-207. https://doi.org/10.1161/CIR.0b013e31824607ee.
- Barr-Anderson DJ, Adams-Wynn AW, DiSantis KI, Kumanyika S. Family-focused physical activity, diet and obesity interventions in African–American girls: a systematic review. Obes Rev 2013;14:29-51. https://doi.org/10.1111/j.1467-789X.2012.01043.x.
- Chen J-L, Weiss S, Heyman MB, Lustig RH. Efficacy of a child-centred and family-based program in promoting healthy weight and healthy behaviors in Chinese American children: a randomized controlled study. J Public Health 2009;32:219-29. https://doi.org/10.1093/pubmed/fdp105.
- Savoye M, Nowicka P, Shaw M, Yu S, Dziura J, Chavent G, et al. Long-term results of an obesity program in an ethnically diverse pediatric population. Pediatrics 2011;127:402-10. https://doi.org/10.1542/peds.2010-0697.
- Anderson JD, Newby R, Kehm R, Barland P, Hearst MO. Taking steps together: a family-and community-based obesity intervention for urban, multiethnic children. Health Educ Behav 2015;42:194-201. https://doi.org/10.1177/1090198114547813.
- Hofsteenge GH, Chinapaw MJ, Delemarre-van de Waal HA, Weijs PJ. Long-term effect of the Go4it group treatment for obese adolescents: a randomised controlled trial. Clin Nutr 2014;33:385-91. https://doi.org/10.1016/j.clnu.2013.06.002.
- Epstein L. Family-based behavioural intervention for obese children. Intl J Obes Relat Metab Disord 1996;20:S14-21.
- Edwards C, Nicholls D, Croker H, Van Zyl S, Viner R, Wardle J. Family-based behavioural treatment of obesity: acceptability and effectiveness in the UK. Eur J Clin Nutr 2006;60:587-92. https://doi.org/10.1038/sj.ejcn.1602353.
- Croker H, Viner RM, Nicholls D, Haroun D, Chadwick P, Edwards C, et al. Family-based behavioural treatment of childhood obesity in a UK National Health Service setting: randomized controlled trial. Int J Obes 2012;36:16-2. https://doi.org/10.1038/ijo.2011.182.
- Dhaliwal J, Nosworthy NM, Holt NL, Zwaigenbaum L, Avis JL, Rasquinha A, et al. Attrition and the management of pediatric obesity: an integrative review. Child Obes 2014;10:461-73. https://doi.org/10.1089/chi.2014.0060.
- Fagg J, Cole TJ, Cummins S, Goldstein H, Morris S, Radley D, et al. After the RCT: who comes to a family-based intervention for childhood overweight or obesity when it is implemented at scale in the community?. J Epidemiol Community Health 2015;69:142-8. https://doi.org/10.1136/jech-2014-204155.
- Williams NA, Coday M, Somes G, Tylavsky FA, Richey PA, Hare M. Risk factors for poor attendance in a family-based pediatric obesity intervention program for young children. J Dev Behavl Pediatr 2010;31. https://doi.org/10.1097/DBP.0b013e3181f17b1c.
- Welsby D, Nguyen B, O’Hara BJ, Innes-Hughes C, Bauman A, Hardy LL. Process evaluation of an up-scaled community based child obesity treatment program: NSW Go4Fun®. BMC Public Health 2014;14. https://doi.org/10.1186/1471-2458-14-140.
- Liu JJ, Davidson E, Bhopal RS, White M, Johnson MRD, Netto G, et al. Adapting health promotion interventions to meet the needs of ethnic minority groups: mixed-methods evidence synthesis. Health Technol Assess 2012;16. https://doi.org/10.3310/hta16440.
- National Mapping of Weight Management Services: Provision of Tier 2 and Tier 3 Services in England. London: Royal College of Physicians; 2015.
- 2011 Census in Birmingham: Population and Migration Topic Report. Birmingham: Birmingham City Council; 2013.
- Rudolf M, Christie D, McElhone S, Sahota P, Dixey R, Walker J, et al. WATCH IT: a community based programme for obese children and adolescents. Arch Dis Child 2006;91:736-9. https://doi.org/10.1136/adc.2005.089896.
- Vertovec S. Super-diversity and its implications. Ethn Racial Stud 2007;30:1024-54. https://doi.org/10.1080/01419870701599465.
- Phillimore J. Approaches to health provision in the age of super-diversity: accessing the NHS in Britain’s most diverse city. Crit Soc Policy 2011;31:5-29. https://doi.org/10.1177/0261018310385437.
- Campbell M, Fitzpatrick R, Haines A, Kinmonth AL, Sandercock P, Spiegelhalter D, et al. Framework for design and evaluation of complex interventions to improve health. BMJ 2000;321:694-6. https://doi.org/10.1136/bmj.321.7262.694.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Medical Research Council Guidance . Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337. https://doi.org/10.1136/bmj.a1655.
- Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci 2011;6. https://doi.org/10.1186/1748-5908-6-42.
- Cole TJ, Freeman JV, Preece MA. Body mass index reference curves for the UK, 1990. Arch Dis Child 1995;73:25-9. https://doi.org/10.1136/adc.73.1.25.
- Pallan M, Griffin T, Lancashire E, Hurley K, Blissett J, Frew E, et al. Cultural adaptation of a children’s weight management programme for Bangladeshi and Pakistani families in the UK: a cluster-randomised feasibility study protocol. Pilot Feasibility Stud 2016;2. https://doi.org/10.1186/s40814-016-0089-4.
- Michie S, Atkins L, West R. The Behaviour Change Wheel: A Guide to Designing Interventions. Sutton: Silverback Publishing; 2014.
- Kitzinger J, Holloway I. Qualitative Research in Health Care. Maidenhead: Open University Press; 2005.
- Pallan M, Griffin T, Hurley K, Lancashire E, Blissett J, Frew E, et al. Cultural adaptation of a children’s weight management programme: Child weigHt mANaGement for Ethnically diverse communities (CHANGE) study. BMC Public Health 2019;19. https://doi.org/10.1186/s12889-019-7159-5.
- Pope C, Ziebland S, Mays N. Qualitative research in health care. Analysing qualitative data. BMJ 2000;320:114-16. https://doi.org/10.1136/bmj.320.7227.114.
- Morgan F, Weightman A, Whitehead S, Brophy S, Morgan H, Turley R, et al. Effectiveness and Cost Effectiveness of Lifestyle Weight Management Services for Children and Young People. London: NICE; 2013.
- Turley R, Weightman A, Halstead E, Morgan H, Morgan F, Noyes J, et al. The Barriers and Facilitators to Implementing Lifestyle Weight Management Programmes for Children and Young People. London: NICE; 2013.
- Martin J, Chater A, Lorencatto F. Effective behaviour change techniques in the prevention and management of childhood obesity. Int J Obes 2013;37:1287-94. https://doi.org/10.1038/ijo.2013.107.
- Davison KK, Jurkowski JM, Li K, Kranz S, Lawson HA. A childhood obesity intervention developed by families for families: results from a pilot study. Int J Behav Nutr Phys Act 2013;10. https://doi.org/10.1186/1479-5868-10-3.
- Hung L-S, Tidwell DK, Hall ME, Lee ML, Briley CA, Hunt BP. A meta-analysis of school-based obesity prevention programs demonstrates limited efficacy of decreasing childhood obesity. Nutr Res 2015;35:229-40. https://doi.org/10.1016/j.nutres.2015.01.002.
- Seburg EM, Olson-Bullis BA, Bredeson DM, Hayes MG, Sherwood NE. A review of primary care-based childhood obesity prevention and treatment interventions. Curr Obes Rep 2015;4:157-73. https://doi.org/10.1007/s13679-015-0160-0.
- Meissner F, Vertovec S. Comparing super-diversity. Ethn Racial Stud 2015;38:541-55. https://doi.org/10.1080/01419870.2015.980295.
- Resnicow K, Soler R, Braithwaite RL, Ahluwalia JS, Butler J. Cultural sensitivity in substance use prevention. J Community Psychol 2000;28:271-90. https://doi.org/10.1002/(SICI)1520-6629(200005)28:3<271::AID-JCOP4>3.0.CO;2-I.
- Castro FG, Barrera M, Martinez CR. The cultural adaptation of prevention interventions: resolving tensions between fidelity and fit. Prev Sci 2004;5:41-5. https://doi.org/10.1023/B:PREV.0000013980.12412.cd.
- Bender MS, Clark MJ. Cultural adaptation for ethnic diversity: a review of obesity interventions for preschool children. Calif J Health Promot 2011;9.
- O’Kane C, Christensen P, James A. Research with Children: Perspectives and Practices. London: Falmer Press; 2000.
- Clark A, Moss P. Listening to Young Children: The Mosaic Approach. London: National Children’s Bureau; 2011.
- Punch S. Research with children: the same or different from research with adults?. Childhood 2002;9:321-41. https://doi.org/10.1177/0907568202009003005.
- Ritchie J, Spencer L, Bryman A, Burgess RG. Analysing Qualitative Data. London: Routledge; 1994.
- Varni JW, Seid M, Kurtin PS. PedsQL 4.0: reliability and validity of the Pediatric Quality of Life Inventory version 4.0 generic core scales in healthy and patient populations. Med Care 2001;39:800-12. https://doi.org/10.1097/00005650-200108000-00006.
- Varni JW, Limbers CA, Burwinkle TM. How young can children reliably and validly self-report their health-related quality of life?: An analysis of 8,591 children across age subgroups with the PedsQL 4.0 Generic Core Scales. Health Qual Life Outcomes 2007;5. https://doi.org/10.1186/1477-7525-5-1.
- Stevens K. Developing a descriptive system for a new preference-based measure of health-related quality of life for children. Qual Life Res 2009;18:1105-13. https://doi.org/10.1007/s11136-009-9524-9.
- Stevens KJ. Working with children to develop dimensions for a preference-based, generic, pediatric, health-related quality-of-life measure. Qual Health Res 2010;20:340-51. https://doi.org/10.1177/1049732309358328.
- Stevens K. Assessing the performance of a new generic measure of health-related quality of life for children and refining it for use in health state valuation. Appl Health Econ Health Policy 2011;9:157-69. https://doi.org/10.2165/11587350-000000000-00000.
- Collins ME. Body figure perceptions and preferences among preadolescent children. Int J Eating Disorders 1991;10:199-208. https://doi.org/10.1002/1098-108X(199103)10:2<199::AID-EAT2260100209>3.0.CO;2-D.
- Rand CS, Resnick JL. The ‘good enough’ body size as judged by people of varying age and weight. Obes Res 2000;8:309-16. https://doi.org/10.1038/oby.2000.37.
- Magarey A, Golley R, Spurrier N, Goodwin E, Ong F. Reliability and validity of the Children’s Dietary Questionnaire; a new tool to measure children’s dietary patterns. Int J Pediatr Obes 2009;4:257-65. https://doi.org/10.3109/17477160902846161.
- Ihmels MA, Welk GJ, Eisenmann JC, Nusser SM. Development and preliminary validation of a Family Nutrition and Physical Activity (FNPA) screening tool. Int J Behav Nutr Phys Act 2009;6. https://doi.org/10.1186/1479-5868-6-14.
- Robinson CC, Mandleco B, Olsen SF, Hart CH. Authoritative, authoritarian, and permissive parenting practices: Development of a new measure. Psychol Rep 1995;77:819-30. https://doi.org/10.2466/pr0.1995.77.3.819.
- Campis LK, Lyman RD, Prentice-Dunn S. The parental locus of control scale: development and validation. J Clin Child Psychol 1986;15:260-7. https://doi.org/10.1207/s15374424jccp1503_10.
- Musher-Eizenman D, Holub S. Comprehensive feeding practices questionnaire: validation of a new measure of parental feeding practices. J Ped Psychol 2007;32:960-72. https://doi.org/10.1093/jpepsy/jsm037.
- McCarthy HD, Cole TJ, Fry T, Jebb SA, Prentice AM. Body fat reference curves for children. Int J Obes 2006;30:598-602. https://doi.org/10.1038/sj.ijo.0803232.
- Rudolf MC, Walker J, Cole TJ. What is the best way to measure waist circumference?. Int J Pediatr Obes 2007;2:58-61. https://doi.org/10.1080/17477160601095177.
- McCarthy HD, Jarrett KV, Crawley HF. The development of waist circumference percentiles in British children aged 5.0-16.9 y. Eur J Clin Nutr 2001;55:902-7. https://doi.org/10.1038/sj.ejcn.1601240.
- Evenson KR, Catellier DJ, Gill K, Ondrak KS, McMurray RG. Calibration of two objective measures of physical activity for children. J Sports Sciences 2008;26:1557-65. https://doi.org/10.1080/02640410802334196.
- Hänggi JM, Phillips LR, Rowlands AV. Validation of the GT3X ActiGraph in children and comparison with the GT1M ActiGraph. J Sci Med Sport 2013;16:40-4. https://doi.org/10.1016/j.jsams.2012.05.012.
- Puyau MR, Adolph AL, Vohra FA, Butte NF. Validation and calibration of physical activity monitors in children. Obes Res 2002;10:150-7. https://doi.org/10.1038/oby.2002.24.
- Pate RR, Almeida MJ, McIver KL, Pfeiffer KA, Dowda M. Validation and calibration of an accelerometer in preschool children. Obesity 2006;14:2000-6. https://doi.org/10.1038/oby.2006.234.
- Cain KL, Sallis JF, Conway TL, Van Dyck D, Calhoon L. Using accelerometers in youth physical activity studies: a review of methods. J Phys Act Health 2013;10:437-50. https://doi.org/10.1123/jpah.10.3.437.
- Noonan R, Boddy L, Youngwon K, Knowles Z, Fairclough S. Comparison of children’s free-living physical activity derived from wrist and hip raw accelerations during the segmented week. J Sports Sciences 2017;35:2067-72. https://doi.org/10.1080/02640414.2016.1255347.
- Fairclough S, Noonan R, Rowlands A, Van Hees V, Knowles Z, Boddy L. Wear compliance and activity in children wearing wrist and hip mounted accelerometers. Med Sci Sports Exerc 2016;48:245-53. https://doi.org/10.1249/MSS.0000000000000771.
- Hildebrand M, VAN Hees VT, Hansen BH, Ekelund U. Age group comparability of raw accelerometer output from wrist- and hip-worn monitors. Med Sci Sports Exerc 2014;46:1816-24. https://doi.org/10.1249/MSS.0000000000000289.
- Taylor SJ, Whincup PH, Hindmarsh PC, Lampe F, Odoki K, Cook DG. Performance of a new pubertal self-assessment questionnaire: a preliminary study. Paediatr Perinat Epidemiol 2001;15:88-94. https://doi.org/10.1046/j.1365-3016.2001.00317.x.
- English Indices Of Deprivation. London: Department for Communities and Local Government; 2015.
- Melbye EL, Øgaard T, Øverby NC. Validation of the comprehensive feeding practices questionnaire with parents of 10-to-12-year-olds. BMC Med Res Methodol 2011;11. https://doi.org/10.1186/1471-2288-11-113.
- van Breukelen GJ, Candel MJ, Berger MP. Relative efficiency of unequal versus equal cluster sizes in cluster randomized and multicentre trials. Stat Med 2007;26:2589-603. https://doi.org/10.1002/sim.2740.
- Eldridge SM, Costelloe CE, Kahan BC, Lancaster GA, Kerry SM. How big should the pilot study for my cluster randomised trial be?. Stat Methods Med Res 2016;25:1039-56. https://doi.org/10.1177/0962280215588242.
- Campbell MK, Fayers PM, Grimshaw JM. Determinants of the intracluster correlation coefficient in cluster randomized trials: the case of implementation research. Clin Trials 2005;2:99-107. https://doi.org/10.1191/1740774505cn071oa.
- Lancaster GA, Dodd S, Williamson PR. Design and analysis of pilot studies: recommendations for good practice. J Eval Clin Pract 2004;10:307-12. https://doi.org/10.1111/j. 2002.384.doc.x.
- Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. BMC Med 2010;8. https://doi.org/10.1186/1741-7015-8-18.
- Tukey JW. Exploratory Data Analysis. Reading, MA: Addison-Wesley; 1978.
- Kaiser KA, Affuso O, Beasley TM, Allison DB. Getting carried away: a note showing baseline observation carried forward (BOCF) results can be calculated from published complete-cases results. Int J Obes 2012;36:886-89. https://doi.org/10.1038/ijo.2011.25.
- Liu-Seifert H, Zhang S, D’Souza D, Skljarevski V. A closer look at the baseline-observation-carried-forward (BOCF). Patient Prefer Adherence 2010;4:11-6.
- Rubin DB. Multiple Imputation for Nonresponse in Surveys. Hoboken, NJ: John Wiley & Sons; 2004.
- Winnard G. Agenda for Change Pay 2016 2017 n.d. www.nhsemployers.org/-/media/Employers/Publications/Pay-circulars/Pay-Circular-1-2016.pdf?la=en&hash=453565ED55C61AAE1EDDFD37528038CE2C915749 (accessed 6 March 2017).
- Kelleher E, Davoren MP, Harrington JM, Shiely F, Perry IJ, McHugh SM. Barriers and facilitators to initial and continued attendance at community-based lifestyle programmes among families of overweight and obese children: a systematic review. Obes Rev 2017;18:183-94. https://doi.org/10.1111/obr.12478.
- Puhl RM, Latner JD. Stigma, obesity, and the health of the nation’s children. Psychol Bull 2007;133:557-80. https://doi.org/10.1037/0033-2909.133.4.557.
- Resnicow K, Yaroch AL, Davis A, Wang DT, Carter S, Slaughter L, et al. GO GIRLS! Results from a nutrition and physical activity program for low-income, overweight African American adolescent females. Health Educ Behav 2000;27:616-31. https://doi.org/10.1177/109019810002700507.
- Watson PM, Dugdill L, Pickering K, Owen S, Hargreaves J, Staniford LJ, et al. Service evaluation of the GOALS family-based childhood obesity treatment intervention during the first 3 years of implementation. BMJ Open 2015;5. https://doi.org/10.1136/bmjopen-2014-006519.
- O’Connor EA, Evans CV, Burda BU, Walsh ES, Eder M, Lozano P. Screening for obesity and intervention for weight management in children and adolescents: evidence report and systematic review for the US Preventive Services Task Force. JAMA 2017;317:2427-44. https://doi.org/10.1001/jama.2017.0332.
- Kirk S, Zeller M, Claytor R, Santangelo M, Khoury PR, Daniels SR. The relationship of health outcomes to improvement in BMI in children and adolescents. Obes Res 2005;13:876-82. https://doi.org/10.1038/oby.2005.101.
- People on the Move in England and Wales. London: Office for National Statistics; 2015.
- Peterson JC, Pirraglia PA, Wells MT, Charlson ME. Attrition in longitudinal randomized controlled trials: home visits make a difference. BMC Med Res Methodol 2012;12. https://doi.org/10.1186/1471-2288-12-178.
- Moore GF, Audrey S, Barker M, Bond L, Bonell C, Hardeman W, et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ 2015;350. https://doi.org/10.1136/bmj.h1258.
- Griffin TL, Pallan MJ, Clarke JL, Lancashire ER, Lyon A, Parry JM, et al. Process evaluation design in a cluster randomised controlled childhood obesity prevention trial: the WAVES study. Int J Behav Nutr Phys Act 2014;11. https://doi.org/10.1186/s12966-014-0112-1.
- Lee BY, Bartsch SM, Mui Y, Haidari LA, Spiker ML, Gittelsohn J. A systems approach to obesity. Nutr Rev 2017;75:94-106. https://doi.org/10.1093/nutrit/nuw049.
- Economos CD, Hatfield DP, King AC, Ayala GX, Pentz MA. Food and physical activity environments: an energy balance approach for research and practice. Am J Prev Med 2015;48:620-9. https://doi.org/10.1016/j.amepre.2014.12.007.
Appendix 1 Revisions to the CHANGE study protocol
| Revision/addition to protocol | Date protocol change approved by the Health Technology Assessment programme |
|---|---|
| Phase I | |
| If FGs with parents who completed the First Steps programme were poorly attended and sufficient data were not obtained, a provision was made for running one-to-one interviews | 2 February 2015 |
| Phase II | |
| The original feasibility study design was an individually randomised trial of the adapted children’s weight management programme. Significant concern was raised by the service providers that participants would not attend if they were allocated to a programme that was not convenient to them in terms of timing and location. After discussion with the SSC, we changed the feasibility study design to a cluster randomised trial, whereby the participants could choose the most convenient programme to attend, and the programmes were randomised to intervention or comparator arms. A section on the reporting of adverse events was also added to the protocol at the request of the SSC | 1 May 2015 |
Several minor changes and additions were made to the protocol:
|
16 August 2015 |
| Owing to initial difficulties with recruitment processes in the NHS service provider trust (BCHCT) and in research staff obtaining the relevant permissions to undertake data collection visits, the feasibility recruitment target was revised from 120 to 80 and it was agreed with the SSC that for the primary outcome of intervention completion the routinely collected anonymised service data on attendance would be used | 26 April 2016 |
| In addition to the planned analysis to compare the BMI z-score of the CHANGE study participants in intervention and comparator arms, the co-investigator team agreed that the routine, anonymised BMI data collected by the weight management programme should also be analysed to compare outcomes in the intervention and comparator groups, as this would provide a larger sample size for analysis | 15 July 2016 |
Appendix 2 The questionnaire administered to interview and focus group participants in the phase I qualitative study
Appendix 3 The interview and focus group schedules used in the phase I qualitative study
Appendix 4 The First Steps children’s weight management comparator intervention: the Template for Intervention Description and Replication checklist
| Item number | Item |
|---|---|
| 1. Name | The First Steps programme |
| 2. Why? | The standard First Steps programme was developed by BCHCT, based on research evidence and its own local experiences, and has been delivered in Birmingham since 2010 |
| 3 and 4. Materials and Procedures |
Families referred to the children’s weight management service are sent a letter inviting them to attend their nearest programme. Families receiving an initial invitation letter also have a follow-up telephone call in their preferred language The standard programme consists of seven 1-hour sessions, delivered over 7 weeks. Programmes run either on weekdays in school time (75% of programmes) or on Saturdays (25% of programmes). Programmes are delivered to coincide with school term times. When school terms are short, the programme is delivered over 5 or 6 weeks. Parents attend all sessions and children attend the first and last sessions. Non-English-speaking participants are accompanied by an interpreter Flipcharts and handouts (including Change4Life handouts) are used to assist in delivery of the programme. Games and props are also used for some of the interactive activities. Paper folders to put handouts in are given to the families. Non-English-speaking participants are accompanied by an interpreter Aims and outlines of the seven programme sessions are as follows: Week 1: introductory session AimsOutlineWeek 2: Eatwell plate and 5-a-day AimsOutlineWeek 3: my personal heath plan and the parent’s role AimsOutlineWeek 4: regular meals and snacks AimsOutlineWeek 5: portion sizes and food labelling AimsOutlineWeek 6: physical activity and takeaways AimsOutlineWeek 7: reflection, maintaining behaviour and planning ahead AimsOutline |
| 5. Who provided? | A BCHCT-employed facilitator delivered the standard First Steps programme (a different facilitator from those who delivered the adapted programme). He had experience of delivering the programme since its introduction in 2010. A second BCHCT employee attended the first and last sessions to assist in collecting height and weight data |
| 6. How? | The programme is designed to be delivered to a group of families (optimum group size is 10 families) |
| 7. Where? | The programme is designed to be delivered in local community venues (e.g. community centres or primary schools) |
| 8. When and how much? | The programme is delivered through seven 1-hour sessions over 7 weeks. Approximately 75% of programmes are delivered in school time, with 25% delivered on Saturdays |
| 9. Tailoring | Families are asked to keep behaviour change diaries, which are reviewed by the facilitators. There is also provision for families to attend before the group session starts so they can have one-to-one time with the facilitator |
| 10. Modifications | When there are short school terms the programme content is combined and delivered over 5 or 6 weeks |
Appendix 5 The interview schedules for interviews with programme facilitators, parents and children undertaken as part of the phase II feasibility study
Appendix 6 The standard operating procedures for anthropometric measurements undertaken in the phase II feasibility study
Appendix 7 The questionnaires administered to children in the phase II feasibility study
Pediatric Quality of Life Inventory version 4.064,65
The PedsQL questionnaire can be accessed at:
www.pedsql.org/pedsql12.html (accessed 20 April 2017)
Child Health Utility 9D questionnaire66–68
Information on the CHU-9D questionnaire can be accessed at:
www.sheffield.ac.uk/scharr/sections/heds/mvh/paediatric (accessed 20 April 2017)
Appendix 8 The questionnaires administered to parents in the phase II feasibility study
Ethnicity
Religion
Language
Place of birth
Education
Employment
Children’s dietary questionnaire71 (adapted for use in the CHANGE study)
Family Nutrition and Physical Activity screening tool72
Reproduced with permission from Dr Greg Welk.
Parental Locus of Control Scale74
Reproduced with permission from Campis et al. 74 The parental locus of control scale: development and validation. Journal of Clinical Child Psychology 1986. Reprinted by permission of the publisher (Taylor & Francis Ltd, http://www.tandfonline.com).
Parenting Styles and Dimensions Questionnaire: authoritative dimension73
Reproduced with permission from Professor Craig Hart.
Appendix 9 The questionnaire designed to capture costs incurred by families attending the children’s weight management programmes
Appendix 10 Proportion of CHANGE study participants who completed the First Steps programmes by study arm
| Family | Trial arm | |||||
|---|---|---|---|---|---|---|
| Intervention | Comparator | |||||
| Families attending at least one session (n) | Families completing programmea (n) | % (95% CIb) | Families attending at least one session (n) | Families completing programmea (n) | % (95% CIb) | |
| BP | 28 | 25 | 89.3 (68.1 to 97.0) | 5 | 4 | 80.0 (14.2 to 99.0) |
| Non-BP | 27 | 22 | 81.5 (60.6 to 92.6) | 13 | 6 | 46.2 (9.3 to 87.7) |
| All | 55 | 47 | 85.5 (74.2 to 92.2) | 18 | 10 | 55.5 (19.5 to 86.6) |
Appendix 11 Sensitivity analyses of outcomes in the intervention and comparator arms
| Outcome | Model number | |||||
|---|---|---|---|---|---|---|
| 1a | 2b | |||||
| n | Mean difference | 95% CI | n | Mean difference | 95% CI | |
| BMI z-scorea | 75 | 0.03 | –0.04 to 0.10 | 72 | 0.01 | –0.05 to 0.07 |
| Waist z-scorea | 69 | 0.05 | –0.09 to 0.18 | 67 | 0.03 | –0.12 to 0.18 |
| Body fat percentage z-scorea | 73 | 0.02 | –0.06 to 0.09 | 70 | –0.01 | –0.09 to 0.07 |
| Average accelerationc | 64 | –0.02 | –5.33 to 5.29 | 62 | –0.64 | –5.71 to 4.43 |
| Moderate to vigorous physical activityc | 64 | –0.29 | –4.93 to 4.36 | 62 | –1.59 | –9.10 to 5.92 |
| PedsQL score | 71 | –3.36 | –8.75 to 2.01 | 68 | –2.61 | –8.11 to 2.90 |
| Physical functioning score | 72 | –0.40 | –7.23 to 6.43 | 69 | –1.30 | –8.13 to 5.52 |
| Emotional functioning score | 74 | –1.49 | –9.74 to 6.75 | 71 | –0.15 | –7.89 to 8.18 |
| Social functioning score | 75 | –6.61 | –14.25 to 1.03 | 72 | –5.32 | –12.90 to 2.26 |
| School functioning score | 75 | –4.47 | –10.98 to 2.03 | 72 | –4.07 | –10.64 to 2.49 |
| Body dissatisfaction score | 73 | 0.09 | –0.46 to 0.65 | 70 | –0.14 | –0.70 to 0.43 |
| CHU-9D score | 75 | –0.003 | –0.04 to 0.04 | 72 | 0.003 | –0.04 to 0.05 |
| Children’s Dietary Questionnaire (scores) | ||||||
| Fruit and vegetables | 67 | 0.52 | –1.22 to 2.27 | 65 | 0.09 | –1.80 to 1.98 |
| Dairyc | 61 | 0.33 | –0.26 to 0.93 | 59 | 0.06 | –1.65 to 0.77 |
| Sugar-sweetened beveragesc | 68 | –0.14 | –0.57 to 0.30 | 66 | 0.15 | –0.36 to 0.66 |
| Non-core foodsc | 63 | 0.03 | –0.38 to 0.44 | 61 | 0.05 | –0.35 to 0.45 |
| FNPA | 53 | –0.17 | –2.78 to 2.44 | 51 | 0.37 | –2.35 to 3.09 |
| Authoritative parenting | 47 | 0.12 | –0.07 to 0.30 | 45 | 0.19 | –0.01 to 0.39 |
| Parenting efficacyc | 50 | –0.13 | –0.30 to 0.03 | 48 | –0.13 | –0.28 to 0.01 |
| Parent feeding practices scores | ||||||
| Child control | 42 | –0.18 | –0.59 to 0.23 | 40 | –0.27 | –0.67 to 0.14 |
| Encouraging balance and variety | 42 | 0.02 | –0.31 to 0.36 | 40 | 0.10 | –0.28 to 0.48 |
| Environment | 42 | 0.11 | –0.39 to 0.60 | 40 | 0.11 | –0.39 to 0.61 |
| Modelling | 42 | –0.22 | –0.64 to 0.20 | 40 | –0.39 | –0.86 to 0.08 |
| Monitoring | 42 | 0.25 | –0.25 to 0.75 | 40 | 0.20 | –0.27 to 0.67 |
| Restriction for health | 42 | 0.01 | –0.42 to 0.44 | 40 | 0.02 | –0.44 to 0.48 |
| Restriction for weight control | 42 | 0.16 | –0.21 to 0.54 | 40 | 0.12 | –0.28 to 0.51 |
| Teaching about nutrition | 42 | 0.18 | –0.31 to 0.68 | 40 | 0.14 | –0.38 to 0.67 |
| Involvementc | 42 | –0.05 | –0.18 to 0.13 | 40 | 0.10 | –0.16 to 0.37 |
| Outcome | Model number | |||||
|---|---|---|---|---|---|---|
| 1a | 2b | |||||
| n | Mean difference | 95% CI | n | Mean difference | 95% CI | |
| BMI z-scorea | 75 | 0.01 | –0.09 to 0.11 | 72 | –0.07 | –0.12 to 0.09 |
| Waist z-scorea | 69 | 0.10 | –0.05 to 0.25 | 67 | 0.06 | –0.11 to 0.23 |
| Body fat percentage z-scorea | 73 | –0.03 | –0.16 to 0.10 | 70 | –0.06 | –0.19 to 0.07 |
| Average accelerationc | 64 | –3.91 | –9.43 to 1.61 | 62 | –4.54 | –9.59 to 0.50 |
| Moderate to vigorous physical activityc | 64 | –1.93 | –5.87 to 2.00 | 62 | –5.20 | –11.27 to 0.89 |
| PedsQL score | 71 | 0.71 | –4.55 to 5.97 | 68 | –1.48 | –3.82 to 6.78 |
| Physical functioning score | 72 | –2.79 | –8.59 to 3.00 | 69 | –2.31 | –8.25 to 3.64 |
| Emotional functioning score | 74 | 1.86 | –6.12 to 9.85 | 71 | 3.67 | –4.40 to 11.75 |
| Social functioning score | 75 | 2.13 | –4.92 to 9.20 | 72 | 2.23 | –4.73 to 9.20 |
| School functioning score | 75 | –1.73 | 9.04 to 5.58 | 72 | –2.35 | –9.83 to 5.13 |
| Body dissatisfaction score | 73 | –0.12 | –0.79 to 0.55 | 70 | –0.27 | –0.99 to 0.45 |
| CHU-9D score | 75 | –0.03 | –0.07 to 0.01 | 72 | –0.05 | –0.09 to -0.01 |
| Children’s Dietary Questionnaire (scores) | ||||||
| Fruit and vegetables | 67 | 0.18 | –1.18 to 1.55 | 65 | –0.40 | –1.80 to 1.01 |
| Dairyc | 61 | 0.12 | –0.56 to 0.81 | 59 | 0.46 | –1.07 to 1.98 |
| Sugar-sweetened beveragesc | 68 | 0.23 | –0.14 to 0.60 | 66 | 0.42 | –0.39 to 1.23 |
| Non-core foodsc | 63 | 0.03 | –0.23 to 0.30 | 61 | 0.03 | –0.30 to 0.35 |
| FNPA | 53 | –0.41 | –3.45 to 2.63 | 51 | –1.35 | –4.54 to 1.84 |
| Authoritative parenting | 47 | –0.11 | –0.31 to 0.09 | 45 | –0.13 | –0.35 to 0.09 |
| Parenting efficacyc | 50 | –0.07 | –0.19 to 0.05 | 48 | –0.04 | –0.16 to 0.07 |
| Parent feeding practices scores | ||||||
| Child control | 42 | –0.10 | –0.37 to 0.17 | 40 | –0.19 | –0.46 to 0.07 |
| Encouraging balance and variety | 42 | –0.002 | –0.21 to 0.20 | 40 | 0.04 | –0.20 to 0.28 |
| Environment | 42 | 0.03 | –0.42 to 0.47 | 40 | 0.30 | –0.22 to 0.82 |
| Modelling | 42 | –0.08 | –0.52 to 0.36 | 40 | –0.13 | –0.62 to 0.35 |
| Monitoring | 42 | –0.09 | –0.40 to 0.22 | 40 | –0.08 | –0.41 to 0.24 |
| Restriction for health | 42 | –0.12 | –0.49 to 0.25 | 40 | –0.10 | –0.48 to 0.28 |
| Restriction for weight control | 42 | –0.12 | –0.43 to 0.19 | 40 | –0.18 | –0.50 to 0.15 |
| Teaching about nutrition | 42 | –0.10 | –0.53 to 0.33 | 40 | –0.26 | –0.66 to 0.15 |
| Involvementc | 42 | –0.09 | –0.28 to 0.11 | 40 | 0.03 | –0.16 to 0.22 |
| Outcome | Model number | |||||
|---|---|---|---|---|---|---|
| 1a | 2b | |||||
| n | Mean difference | 95% CI | n | Mean difference | 95% CI | |
| BMI z-scorea | 92 | 0.02 | –0.12 to 0.17 | 92 | 0.02 | –0.13 to 0.17 |
| Waist z-scorea | 92 | 0.04 | –0.27 to 0.36 | 92 | 0.06 | –0.24 to 0.36 |
| Body fat percentage z-scorea | 92 | 0.001 | –0.14 to 0.14 | 92 | 0.01 | –0.14 to 0.15 |
| Average accelerationc | 92 | 0.84 | –11.24 to 9.55 | 92 | –0.51 | –9.33 to 8.30 |
| Moderate to vigorous physical activityc | 92 | 0.82 | –8.60 to 10.24 | 92 | 3.04 | –13.95 to 20.03 |
| PedsQL score | 92 | –0.06 | –7.88 to 7.76 | 92 | –1.18 | –8.37 to 6.01 |
| Physical functioning score | 92 | 0.47 | –10.09 to 11.03 | 92 | –1.40 | –11.25 to 8.45 |
| Emotional functioning score | 92 | 2.12 | –7.18 to 11.42 | 92 | –0.17 | –8.91 to 8.58 |
| Social functioning score | 92 | –6.94 | –16.29 to 2.40 | 92 | –8.20 | –17.15 to 0.75 |
| School functioning score | 92 | –2.63 | –10.68 to 5.42 | 92 | –3.68 | –11.24 to 3.88 |
| Body dissatisfaction score | 92 | 0.38 | –0.53 to 1.28 | 92 | 0.14 | –0.89 to 1.10 |
| CHU-9D score | 92 | 0.02 | –0.03 to 0.07 | 92 | 0.01 | –0.03 to 0.06 |
| Children’s Dietary Questionnaire (score) | ||||||
| Fruit and vegetables | 92 | 1.88 | –0.92 to 4.68 | 92 | 1.66 | –1.33 to 4.66 |
| Dairyc | 92 | 0.47 | –1.40 to 2.34 | 92 | 0.60 | –1.26 to 2.42 |
| Sugar-sweetened beveragesc | 92 | 0.03 | –0.67 to 0.73 | 92 | –0.01 | –0.65 to 0.62 |
| Non-core foodsc | 92 | –0.10 | –0.97 to 0.76 | 92 | –0.04 | –1.10 to 1.01 |
| FNPA | 92 | –0.25 | –6.44 to 5.94 | 92 | –0.40 | –6.90 to 6.11 |
| Authoritative parenting | 92 | 0.68 | –0.68 to 2.03 | 92 | 0.63 | –0.70 to 1.96 |
| Parenting efficacyc | 92 | –0.07 | –0.85 to 0.70 | 92 | –0.07 | –0.74 to 0.60 |
| Parent feeding practices scores | ||||||
| Child control | 92 | –0.62 | –1.88 to 0.65 | 92 | –0.67 | –1.92 to 0.57 |
| Encouraging balance and variety | 92 | –0.21 | –1.08 to 0.67 | 92 | –0.22 | –1.09 to 0.65 |
| Environment | 92 | 0.22 | –1.20 to 1.64 | 92 | 0.16 | –1.32 to 1.64 |
| Modelling | 92 | –0.65 | –2.39 to 1.09 | 92 | –0.69 | –2.46 to 1.07 |
| Monitoring | 92 | 0.01 | –2.91 to 2.93 | 92 | 0.17 | –2.85 to 3.19 |
| Restriction for health | 92 | –0.55 | –2.32 to 1.22 | 92 | –0.58 | –2.45 to 1.28 |
| Restriction for weight control | 92 | –0.34 | –2.73 to 2.05 | 92 | –0.26 | –2.54 to 2.03 |
| Teaching about nutrition | 92 | 0.46 | –1.40 to 2.32 | 92 | 0.46 | –1.34 to 2.27 |
| Involvementc | 92 | 0.004 | –1.41 to 1.42 | 92 | –0.08 | –2.01 to 1.85 |
| Outcome | Model number | |||||
|---|---|---|---|---|---|---|
| 1a | 2b | |||||
| n | Mean difference | 95% CI | n | Mean difference | 95% CI | |
| BMI z-scorea | 92 | 0.08 | –0.97 to 1.12 | 92 | 0.06 | –1.08 to 1.19 |
| Waist z-scorea | 92 | 0.11 | –3.51 to 3.74 | 92 | 0.11 | –3.57 to 3.80 |
| Body fat percentage z-scorea | 92 | –0.20 | –1.42 to 1.03 | 92 | –0.18 | –1.33 to 0.98 |
| Average accelerationc | 92 | 1.45 | –43.80 to 46.71 | 92 | 2.72 | –61.79 to 66.79 |
| Moderate to vigorous physical activityc | 92 | –48.42 | –337.42 to 240.56 | 92 | –59.77 | –406.85 to 287.31 |
| PedsQL score | 92 | –4.44 | –26.33 to 17.46 | 92 | –3.29 | –26.65 to 20.07 |
| Physical functioning score | 92 | –6.35 | –26.17 to 13.47 | 92 | –2.54 | –25.24 to 20.16 |
| Emotional functioning score | 92 | –0.28 | –16.70 to 16.15 | 92 | –0.51 | –17.44 to 16.42 |
| Social functioning score | 92 | –1.20 | –23.42 to 21.02 | 92 | –1.18 | –22.54 to 20.18 |
| School functioning score | 92 | –6.72 | –26.11 to 12.65 | 92 | –7.00 | –28.65 to 14.66 |
| Body dissatisfaction score | 92 | –0.04 | –1.98 to 1.91 | 92 | –0.09 | –2.01 to 1.82 |
| CHU-9D score | 92 | –0.05 | –0.12 to 0.02 | 92 | –0.06 | –0.13 to 0.02 |
| Children’s Dietary Questionnaire (scores) | ||||||
| Fruit and vegetables | 92 | 1.52 | –4.74 to 7.78 | 92 | 1.34 | –4.70 to 7.37 |
| Dairyc | 92 | 0.70 | –1.91 to 3.31 | 92 | 0.62 | –2.06 to 3.30 |
| Sugar-sweetened beveragesc | 92 | 0.15 | –1.61 to 1.92 | 92 | 0.01 | –1.77 to 1.79 |
| Non-core foodsc | 92 | 0.23 | –1.34 to 1.80 | 92 | 0.48 | –2.54 to 3.51 |
| FNPA | 92 | 2.65 | –13.39 to 18.69 | 92 | 2.84 | –13.58 to 19.27 |
| Authoritative parenting | 92 | –0.26 | –4.93 to 4.40 | 92 | –0.24 | –5.04 to 4.56 |
| Parenting efficacyc | 92 | 0.67 | –2.33 to 3.66 | 92 | 0.76 | –4.60 to 6.12 |
| Parent feeding practices scores | ||||||
| Child control | 92 | –0.12 | –3.09 to 2.84 | 92 | –0.12 | –3.20 to 2.97 |
| Encouraging balance and variety | 92 | –0.17 | –1.79 to 1.45 | 92 | –0.30 | –2.05 to 1.46 |
| Environment | 92 | 1.75 | –13.15 to 16.66 | 92 | 1.70 | –13.51 to 16.90 |
| Modelling | 92 | –0.81 | –6.97 to 5.35 | 92 | –0.78 | –7.04 to 5.48 |
| Monitoring | 92 | –2.09 | –7.54 to 3.36 | 92 | –2.47 | –8.28 to 3.33 |
| Restriction for health | 92 | –0.93 | –9.13 to 7.27 | 92 | –1.03 | –8.96 to 6.91 |
| Restriction for weight control | 92 | 1.32 | –4.51 to 7.14 | 92 | 1.08 | –4.82 to 6.99 |
| Teaching about nutrition | 92 | 1.43 | –3.51 to 6.38 | 92 | 1.53 | –3.25 to 6.31 |
| Involvementc | 92 | –0.31 | –6.74 to 6.11 | 92 | –1.64 | –11.59 to 8.31 |
List of abbreviations
- BCHCT
- Birmingham Community Healthcare NHS Trust
- BCW
- behaviour change wheel
- BMI
- body mass index
- CFPQ
- Comprehensive Feeding Practices Questionnaire
- CHANGE
- Child weigHt mANaGement for Ethnically diverse communities
- CHU-9D
- Child Health Utility 9D
- CI
- confidence interval
- COM-B
- capability, opportunity, motivation and behaviour
- ENMO
- Euclidean norm minus one
- FG
- focus group
- FNPA
- Family Nutrition and Physical Activity
- ICC
- intracluster correlation coefficient
- IMD
- Index of Multiple Deprivation
- IQR
- interquartile range
- LMS
- lambda–mu–sigma
- MEND
- Mind, Exercise, Nutrition . . . Do it!
- NCMP
- National Child Measurement Programme
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- PedsQL
- Pediatric Quality of Life Inventory
- PH
- Public Health guideline
- RCT
- randomised controlled trial
- SVMg
- gravity-subtracted signal vector magnitude
- T0
- time point 0
- T1
- time point 1
- T2
- time point 2
- TIDieR
- Template for Intervention Description and Replication

