Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 12/150/04. The contractual start date was in November 2014. The draft report began editorial review in May 2017 and was accepted for publication in August 2018. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Stephen Morris is a member of the National Institute for Health Research Health Services and Delivery Research Board and the Public Health Research Research Funding Board.
Disclaimer
This report contains transcripts of interviews conducted in the course of the research and contains language that may offend some readers.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2019. This work was produced by St James-Roberts et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2019 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
Background
There is evidence that around 20% of 1- to 4-month-old infants in Western countries cry for long periods without an apparent reason. 1–3 Much of this evidence comes from parents’ reports, but objective measurements have confirmed that most parents are accurate in judging that their baby cries substantially more than others of the same age. 4,5
Early studies of the cause of this crying assumed that it was attributable to gastrointestinal disturbance and pain, leading to the use of the word ‘colic’ (from the Greek word for the intestine) to describe it. 6,7 However, evidence has accumulated that most such infants are healthy and grow and develop normally,8,9 that many infants have a crying ‘peak’ at around 1 to 2 months of age3,10 and that this crying peak and the ‘unsoothable’ crying bouts that distress parents usually resolve spontaneously by 5 months of age. 11 Studies have concluded that only about 5% of infants cry a lot because of organic disturbances;2,12 in most cases, the crying is attributable to normal developmental processes. 13,14
Although most infants who cry a lot are well, the crying can distress some parents15,16 and disrupt their ability to provide care. This has encouraged a focus not only on the crying but on parents’ responses and subsequent outcomes. One reason for that focus is that parental worries and concerns, not infant behaviour, are responsible for health service contacts and costs. These costs are considerable. For instance, a 2001 estimate was that the time professionals spent advising parents about infant crying and unsettled behaviour in the first 3 months costs the NHS > £65M per year. 17 There is evidence, too, that the crying that parents judge to be excessive can trigger premature termination of breastfeeding,18 overfeeding,19 parental distress and depression,15,16 poor parent–child relationships20 and, in a small number of cases, infant abuse. 21 Although most infants who cry a lot in early infancy develop normally, parental vulnerabilities have been implicated when serious long-term disturbances are seen at school age. 22
The distinction underlying this recent research is between infant crying and its evaluation by, and impact on, parents. Crying has been described as a ‘biological siren’ that compels parents to respond to it. 23 As well as its loud and aversive sound, it is easy to understand why a feature particular to crying in the first 4 months – bouts that resist soothing techniques that are usually effective – triggers feelings of frustration in many parents. 24 However, its impact on parental emotions and actions depends partly on how parents cope with it, which depends on parental vulnerabilities, resources and circumstances. For instance, parental characteristics, such as depression, anxiety and high levels of arousal, have been found to influence how parents interpret and respond to infant crying. 25–28 Social isolation, although less studied, may also increase its impact. The implication for clinical practice is that assessments need to take account of parental vulnerabilities and supports, as well as infant crying. Equally, the findings imply that health services need to form a bridge between paediatric concern regarding infant crying and services for adult well-being and mental health. By bringing these two traditionally distinct scientific and professional areas together, interventions that support parenting have the potential to help parents, enhance parent–infant interactions and infant development and improve health services.
Against this background, it is striking that there are no evidence-based NHS practices for supporting parents in managing infant crying. Instead, parents turn to popular books, magazines or websites, which give conflicting advice,29 or take babies to clinicians or hospital accident and emergency (A&E) departments,12 adding to the burden and cost of infant crying to the NHS.
By developing evidence-based services that support parents, the Surviving Crying study, described in this report, was designed to take the first steps towards the provision of routine health-care services that improve the coping and well-being of parents whose babies excessively cry, their infants’ outcomes and how NHS money is spent.
To reduce terminological confusion, the phrase ‘excessive infant crying’ is used throughout this report to refer to a parent’s judgement that an infant is crying too much, often accompanied by a concern that the crying is a sign that something is wrong with the baby. The phrase ‘prolonged infant crying’ refers to a measure of crying duration.
Aims and objectives
This was a preliminary study to develop a novel intervention package of materials and services that support parents of excessively crying babies and to examine the feasibility of delivering and evaluating the package in the NHS. The aims included preparing for a possible future large-scale controlled trial and advising on the form it might take. The study comprised two stages:
-
the development of an intervention package
-
a feasibility study of package implementation in the NHS.
Stage 1 aims:
-
Update a 2011 systematic review2 in order to identify existing examples of support packages.
-
Allow parents to advise on the supports needed for parents whose babies are excessively crying. Parents were also asked to rate four example support packages identified by the literature review. Because the package needed to be accepted by parents in order to be effective, parents and NHS staff were closely involved in its development.
Stage 2 aims:
-
Assess parents’ and NHS health visitors’ (HVs’) or community public health nurses’ (SCPHNs’) willingness to enter and complete a study of the support package.
-
Measure parental use and parental and HV/SCPHN evaluation of the package components.
-
Identify measures for estimating package clinical effectiveness and cost.
-
Identify barriers to and facilitators of the research.
-
Assess the feasibility and design parameters for a future large-scale trial of the intervention package’s clinical effectiveness and cost, and establish whether or not parents would be willing to participate in such a trial.
Figure 1 is a flow chart showing the timetable for the study as a whole.
FIGURE 1.
The planned Surviving Crying study timetable. NIHR, National Institute for Health Research.

Ethics approval and governance
The study was registered on the International Standard Randomised Controlled Trial Number (ISRCTN) database (registration number ISRCTN84975637). Ethics approval was granted by De Montfort University (DMU) (reference number 13450) and the National Research Ethics Service Committee East Midlands (Nottingham) (project ID 152836, National Research Ethics Service reference 14/EM/1202). Leicestershire Partnership NHS Trust (LPT) provided local research and development approval (reference PAED0706). The study protocol can be accessed on the National Institute for Health Research (NIHR) Journals Library website (www.journalslibrary.nihr.ac.uk/programmes/hta/1215004/#/; accessed 6 December 2018). Approvals for a series of non-substantial and substantial amendments were obtained at various stages in order to conduct and progress the study, details of which are provided in Report Supplementary Material 1.
The study was regulated by a NIHR-appointed steering committee and co-ordinated by a management group, including the research team, senior LPT HVs, a paediatrician, a general practitioner (GP), a health economist, members of the Leicester Clinical Trials Unit and National Childbirth Trust (NCT), members of the charity Cry-Sis and parent representatives.
Patient and public involvement
The involvement of key stakeholders, particularly parents, was integral to the design and delivery of the feasibility study at all stages, and is described throughout the report. In summary, parents contributed in the following ways:
-
Twenty parents whose babies had cried excessively attended focus groups to describe their experience and provide information on what resources and support might have been beneficial. The support package was then developed to include these resources and information.
-
Most of these parents consented for aspects of their experience to be included in the website and information booklet developed as part of the intervention. These took the form of quotations from the focus groups and written or video accounts of their experiences and suggestions.
-
The focus group parents reviewed the draft intervention materials and made suggestions for improvements, which were included in the final version.
-
One of the focus group parents joined the Study Management Group and presented their experience as part of the Surviving Crying conference to disseminate the findings.
-
In stage 2 of the study, 52 parents provided feedback on the package components they had used, including what had been most valuable and suggestions for improvement.
An evaluation of the impact of patient and public involvement on the study is included in Chapter 14, Evaluation of patient and public involvement.
Structure of the report
Because the feasibility study was divided into two distinct stages, this report is arranged to reflect these stages and the elements of them. Thus, Chapters 2–6 provide an overview of the methods and results from stage 1 (the development of the intervention) and Chapters 7–13 describe the methods and results from stage 2 (the evaluation of the intervention). Chapter 14 then summarises the findings and identifies conclusions from the study, including making recommendations for future research.
Chapter 2 Stage 1: development of an intervention package – overview
Stage 1 had three key aims, which are described in detail in the following chapters:
-
Update a 2011 systematic review2 in order to identify existing examples of support packages (see Chapter 3).
-
To allow parents to advise on the supports needed for parents whose babies are excessively crying, parents of previously excessively crying babies were invited to focus groups to share their experiences and identify what resources or support would have helped them to cope. Parents also rated four example support packages identified by the literature review (see Chapters 4–5).
-
Develop a package of support materials to test in stage 2. Because the package needed to be accepted by parents in order to be effective, parents and NHS staff were closely involved in its development (see Chapter 6).
Chapter 3 Stage 1 literature review
Aims
As part of the process of developing the intervention for this study, a focused literature review was undertaken with three specific aims:
-
identify recent evidence of existing interventions to support parents of babies considered to be excessively crying
-
select a number of these interventions to show to parents attending focus groups in order to gain their feedback
-
search for evidence of interventions that were effective in supporting parents’ mental health, particularly in the postpartum period.
Method
Identification and selection of interventions to show to focus group parents
As set out in the study protocol, the review was based on an update of the 2011 systematic review by Douglas and Hill2 concerning the causes of excessive crying and interventions to manage term infants who cry excessively in the first few months of age. For the purposes of this review, ‘excessive crying’ was taken to mean any crying behaviour that was considered problematic by parents.
Full details of the inclusion criteria and search strategies are provided in Appendix 2. The materials identified through the initial search were reviewed against additional criteria to identify a selection of interventions that could be viewed and rated by focus group parents to inform the development of the intervention for this study. These criteria were:
-
intervention materials available in a published and exportable form
-
delivery costs that enabled the potential adoption of the intervention within the NHS
-
at least provisional evidence of clinical effectiveness
-
offering a variety of styles of presentation.
Contracts with the organisations involved in producing these interventions were arranged to allow the website and supplementary materials to be reviewed by the focus group participants.
Identifying evidence for interventions that support parents experiencing postpartum distress
As noted in Aims, the literature review also aimed to review recent evidence for interventions found to be effective in supporting parental coping and mental health, particularly during the postpartum period. This was based on the premise that, as noted in Chapter 1, Background, infant crying can be viewed as a stressor and its impact on parents is, therefore, partly attributable to how parents evaluate and cope with it and, consequently, to parents’ underlying vulnerabilities, circumstances and resources. The strategies described above were used to identify relevant research in this area.
Results
Appendix 2 provides full details of the literature review process and results. Once the initial screening process was completed, a total of 19 relevant articles remained, which referred to 11 different interventions (more than one article having been published in relation to some interventions). These interventions, details of which are provided in Report Supplementary Material 2, were reviewed against the additional criteria to consider their appropriateness within the context of this study. Three relevant packages were identified, together with one further intervention programme30 that met the inclusion criteria but was omitted by Douglas and Hill. 2 A programme that required a multiprofessional clinic31 was excluded because it was costly and difficult to export. Therefore, a total of four example packages that met the study inclusion criteria were identified:
-
Period of PURPLE Crying® (http://purplecrying.info/; accessed 6 December 2018)
-
What Were We Thinking! (www.whatwerewethinking.org.au; accessed 6 December 2018)
-
Coping with Crying (www.copingwithcrying.org.uk; accessed 6 December 2018)
-
Cry Baby (http://raisingchildren.net.au/newborns/behaviour/crying-colic/cry_baby_program; accessed 15 January 2019).
A brief description of each package is given in Table 1.
| Name | Origin | Format |
|---|---|---|
| Coping with Crying | UK | A film and website aimed at preventing parents from harming their babies because of crying. Includes videos of parents and experts discussing their experiences and advice, and one specifically highlighting the risks from shaken baby syndrome |
| Cry Baby | Australia | A web-based resource for parents with babies with crying or sleep problems. Presented in visual, written and audio format, with downloadable checklists and tips (shown in focus groups) |
| Period of PURPLE Crying | USA | A website with an accompanying DVD (not shown in focus groups) aimed at preventing parents from harming their babies because of crying. Includes comprehensive text on a range of relevant topics, plus short videos of experts and role-played scenarios |
| What Were We Thinking! | Australia | A website and workbook (sample pages shown in focus groups) as part of a course aimed at supporting new parents to cope with and negotiate their changed roles and responsibilities |
In relation to identifying evidence about support for parents experiencing postpartum distress, the review highlighted multiple randomised controlled trials (RCTs) indicating the effectiveness of cognitive–behavioural therapy (CBT) programmes in helping adults, including parents in the postpartum period, to cope with stressful conditions and moderate psychological distress. 32–35 As these findings were also supported by the recommendations of the UK National Institute for Health and Care Excellence (NICE),36,37 this was considered sufficient evidence to adopt this approach for the intervention developed for this study.
Chapter 4 Stage 1 focus group methodology
Introduction
This chapter and Chapter 5 report the second part of stage 1, in which a series of small focus group discussions were held with parents who had previously had a baby who had excessively cried when < 6 months of age. Using a mixed-methods approach, the aim was to gather qualitative and quantitative information about parents’ experiences, their preferred methods for accessing information and ratings of example package components. This chapter describes the recruitment to and delivery of the focus groups, and Chapter 5 reports the findings from them.
Method
Participants
A purposive sample of 20 parents participated in stage 1. The eligibility criteria for parents were:
-
living in the LPT area
-
previously had a healthy baby whose excessive crying in the first 6 months of age had caused concern for either parent
-
their baby was no longer excessively crying
-
English speaking or supported by an English speaker.
Parents whose baby was still crying or was judged to be ill at the time of crying by their HV/SCPHN or another qualified professional were excluded from participating. Parents who lived outside the LPT area were also excluded.
Participants were recruited to the study by two routes:
-
They were referred to the study team via their HV/SCPHN, having previously spoken with them about their baby’s crying.
-
They contacted the study team directly after seeing the call for eligible parents on the NCT website or on flyers distributed to local children’s centres in which HVs/SCPHNs were based. An example recruitment flyer can be accessed at www.journalslibrary.nihr.ac.uk/programmes/hta/1215004/#/ (accessed 6 December 2018).
All parents received high-street shopping vouchers in acknowledgement of their participation; one was given at the end of the focus group session and another was given when they reviewed the developed package.
Table 2 shows the sociodemographic profile of participants, noting that complete information was not available for two parents. The two male parents attended with partners. Most parents were white British, had an undergraduate or postgraduate degree and were married or living with a partner at the time when their baby cried excessively.
| Sociodemographic characteristics | n (%) |
|---|---|
| Sex (N = 20) | |
| Female | 18 (90.0) |
| Male | 2 (10.0) |
| Age (years) (N = 19)a | |
| Mean (range) [SD] | 31.0 (19–42) [6.0] |
| Ethnicity (N = 19)a | |
| English/Welsh/Scottish/Northern Irish/British | 14 (73.7) |
| Indian/Bangladeshi/Pakistani | 3 (15.8) |
| White/black Caribbean mixed | 1 (5.3) |
| Other (not specified) | 1 (5.3) |
| Highest education level (N = 19)a | |
| Postgraduate degree/qualification | 6 (31.6) |
| Undergraduate degree/qualification | 6 (31.6) |
| Higher post-A-level vocational qualification | 1 (5.3) |
| A level/NVQ level 3/BTEC diploma | 4 (21.0) |
| GCSE/O level/NVQ level 2/completed secondary school education | 2 (10.5) |
| Employment status when baby was crying (N = 19)a | |
| Maternity leave | 7 (36.8) |
| Employed part time | 5 (26.3) |
| Self-employed | 2 (10.5) |
| Unemployed and looking for work | 2 (10.5) |
| Not in paid employment | 3 (15.8) |
| Marital/living status (N = 18)a | |
| Married/cohabiting | 16 (88.8) |
| Living alone but supported by partner | 1 (5.5) |
| Single and living alone | 1 (5.5) |
Materials
A short participant demographic questionnaire was devised to obtain participant sociodemographic details prior to the focus groups. The questionnaire can be accessed at www.journalslibrary.nihr.ac.uk/programmes/hta/1215004/#/ (accessed 6 December 2018). A brief semistructured topic guide was also developed (see Appendix 3), dividing the focus groups into two parts. Part 1 involved explaining the group aims and procedures, and introductions (participants could use pseudonyms if they wished to maintain anonymity). Participants were asked to describe their experience of having a baby who cried excessively: what was most challenging?; what helped?; what sorts of support would they have liked to have received at the time?; and their thoughts on what should be included as part of routine NHS care.
Part 2 involved parents completing rating scales to establish the best way of delivering a package of support (i.e. website, leaflet, direct and/or telephone contact with a professional) and which electronic devices they used to access information and support. Materials from the four example support packages identified by the literature review were evaluated by participants, using five 5-point rating scales, with an opportunity for participants to make written comments on features that they felt were important, they disliked or they felt could be improved. These questionnaires can be accessed at www.journalslibrary.nihr.ac.uk/programmes/hta/1215004/#/ (accessed 6 December 2018). All four example packages included a website, together, in some cases, with supplementary materials. Sample materials from each package were shown to parents with a changed presentation order for each session to reduce order effects. Appendix 1 provides details of the materials shown and how these were sampled from the example packages.
Safeguarding procedures
Together with LPT’s safeguarding officers, HVs/SCPHNs and the study paediatrician, the research team developed safeguarding protocols to ensure the safety of parents and babies involved in the study (see Appendix 4).
Procedure
Health visitor involvement
In the UK, HVs/SCPHNs provide universal primary care for parents with young babies and are the obvious choice for delivering the intended service within the NHS. With support from the LPT managers collaborating on the study, HVs/SCPHNs from five health-visiting teams within Leicester, Leicestershire and Rutland attended briefing meetings about the study. A total of 55 HVs/SCPHNs gave written agreement to collaborate in stage 1 by referring eligible parents to the research team. All HVs/SCPHNs were given an information pack containing details about the study and how to approach and refer eligible parents.
All HV/SCPHN teams were revisited when the draft package was developed in order to obtain their overall views regarding its suitability.
Parent recruitment
The HVs/SCPHNs approached parents whom they knew to have previously had a healthy baby whose excessive crying in the first 6 months of life had caused concern for either parent. They provided brief details about the study in order to seek expressions of interest for researchers to contact them. To supplement HV/SCPHN contacts with parents, information about the study was also circulated via the NCT network, through researcher attendance at local parent and baby groups and through flyers that were distributed to local children’s centres, HV/SCPHN bases and local parenting/baby groups. An example recruitment flyer can be accessed at www.journalslibrary.nihr.ac.uk/programmes/hta/1215004/#/ (accessed 6 December 2018).
On receipt of an expression of interest, the researchers contacted each parent by telephone to fully explain the study and assess eligibility. Eligible parents were sent a formal letter of invitation to participate from the principal investigator (PI) and an information sheet and consent form if their HV/SCPHN had not already provided them. Parents were invited to attend a pre-arranged focus group discussion, bringing their babies and/or older children with them if need be, and were invited to provide feedback on the draft.
Parent involvement
Participants were invited to attend pre-arranged focus groups over a 5-month period (April to August 2015), held at venues and locations convenient for parents. Seven arranged groups were cancelled or rearranged owing to a lack of parent availability. Focus groups continued when only one parent attended, provided the parent was happy for this to happen, and the structure and format remained the same. In effect, these sessions became interviews. Parental written consent was obtained prior to the focus group/interview sessions. In total, 10 focus groups/interview sessions were held.
Two researchers who were experienced in focus groups and interview methods facilitated each session and two others made observational notes or provided informal childcare. When only one parent attended, two researchers shared the duties. All sessions were audio-recorded for later verbatim transcription. Each session lasted approximately 2.5–3 hours. Parents were asked to revisit the example packages following the focus groups and were recontacted when possible by the researchers to establish if they had done so and whether or not this more extensive exposure had changed their initial opinions and ratings. At this point, parents were invited to further contribute to the development of the package by consenting to the inclusion of their stories and experiences in one of three ways:
-
permitting the use of anonymous direct quotations from the audio recording of the sessions
-
providing more detailed information about their experiences in a written format
-
appearing in video recordings talking about their experiences.
Analysis
Parent qualitative discussions
All sessions were digitally recorded and transcribed verbatim. Data analysis and its interpretation were informed by hermeneutic phenomenology38 and Ricoeur’s theory of interpretation. 39,40 Analysis was undertaken at three levels; an initial reading of transcripts with the identification of themes was progressed to an explanation and naive understanding of meaning facilitated by the clustering of related themes. This then progressed back and forth between explanation and understanding to assist deeper interpretation and understanding, reminiscent of Gadamer’s hermeneutic circle41 or hermeneutic arc. 40 Analysis was supported by the use of NVivo 10 qualitative data analysis software (QSR International, Warrington, UK). All transcripts were read and reread several times and a line-by-line analysis of content was undertaken and grouped under themed headings that emerged from the data. To enhance credibility, these themed headings were shared and agreed with the researchers present at the focus groups. Initially, a large number of themes were identified; these were refined by grouping similar themes together under new overarching themes. This process was repeated until the following conceptual themes emerged: (1) disrupted experiences of parenthood, (2) feeling different and social isolation, (3) reluctance to seek support and (4) validation of experience and seeking help (see Appendix 5). Participant codes were assigned and potential identifiers removed in order to protect the anonymity and confidentiality of participants. One parent accompanied his partner and did not contribute to discussions, so only his partner’s data were included in the qualitative analysis.
Parent-completed questionnaires
Simple univariate descriptive analyses were conducted on data from the parent-completed questionnaires and a content-analysis approach was used to analyse the free-text comments. Some data were specific to the example package materials and these were summarised as a whole in order to maintain confidentiality of the providers of those packages.
Chapter 5 Focus group quantitative and qualitative results
Focus group quantitative data
Demographic data relating to focus group parents were presented in Table 2.
Baby characteristics
The 20 study participants had 19 excessively crying infants; one parent had experienced excessive crying with both her first and second child and two couples participated in the study (their baby’s data have been included only once). Table 3 presents the babies’ characteristics.
| Descriptive particulars | Total, n (%) |
|---|---|
| Baby’s sex | |
| Male | 9 (47.4) |
| Female | 10 (52.6) |
| Baby’s birth order | |
| Firstborn | 10 (52.6) |
| Secondborn | 8 (42.1) |
| Thirdborn | 1 (5.3) |
| Baby’s feeding method when excessive crying started | |
| Breast milk only | 7 (36.8) |
| Breast plus formula milk | 6 (31.6) |
| Formula milk only | 6 (31.6) |
| Baby’s health in the period when he/she cried excessively | |
| Baby had a fever | 0 (0) |
| Baby seemed unwell | 2 (10.5) |
| Concerns about baby’s weight gain | 1 (5.3) |
| Baby had feeding problems | 11 (57.8) |
| Baby’s feeding checked by a health professional | 17 (89.5) |
| Baby’s weight checked by a health professional | 19 (100) |
| Baby’s age when the excessive crying started and stopped (weeks) | |
| Started, median (range) | 1 (0–9) |
| Stopped, median (range) | 19 (8.5–104) |
| Length of excessive crying, median (range) | 18 (4–100) |
Noticeably, only 10 of the babies were firstborn. Eight of the 18 families had other children who had not cried excessively. The babies were equally likely to be boys or girls, and they were almost equally divided between breastfeeding, formula feeding and mixed feeding when the crying started. None had a fever and only two seemed unwell. Although 11 of the babies (58%) were reported by their parents as having had problems with feeding, all the babies had been checked by clinicians for weight gain and 17 (89%) for feeding problems.
The median age at which parents reported that the babies started excessively crying was 1 week (range from birth to 9 weeks). However, there was a substantial variation in the age at which the crying stopped, ranging from 8.5 to 104 weeks (median 19 weeks). In line with this, the excessive crying duration ranged from 4 to 100 weeks (i.e. 1 month to just under 2 years), with a median length of crying of 18 weeks (i.e. 4 months).
Sources of information and support
Participants completed questionnaires about the sources of information that they used and would have found useful when their baby was excessively crying and which formats they felt were the best for presenting information about crying babies to parents (Table 4).
| Sources of information and support | Total, n (%) |
|---|---|
| Sources used by participants when their baby cried excessively (n = 20) | Used this source |
| Leaflets | 9 (45.0) |
| Magazines | 4 (20.0) |
| Books | 7 (35.0) |
| Websites | 16 (80.0) |
| Mobile phone apps | 5 (25.0) |
| Telephone conversations with HV/SCPHN, doctor or other health professional | 17 (85.0) |
| Visits to speak with HV/SCPHN, doctor or other health professionala | 10 (58.8) |
| Online discussion boards | 4 (20.0) |
| Other sources of information or support | 0 (0.0) |
| Sources participants would have found most helpful when their baby cried excessively (n = 18) | Would have liked this a lot |
| Extra visits from HVs/SCPHNs | 14 (77.7) |
| Extra telephone calls from HVs/SCPHNs | 11 (61.1) |
| Leaflets | 13 (72.2) |
| Websites | 18 (100.0) |
| Online activities to completeb | 4 (25.0) |
| Online discussion boardsa | 10 (58.8) |
| Facebook (Facebook, Inc., Menlo Park, CA, USA; www.facebook.com) | 11 (64.7) |
| Group to meet other parents | 18 (100.0) |
| Best format for presenting information to parents (n = 18) | Rated this as effective or highly effective |
| Leaflets from HV/SCPHN, doctor or hospitala | 13 (76.5) |
| Websites | 16 (88.9) |
| Mobile phone appsa | 14 (82.3) |
| Telephone conversation with HV/SCPHN, doctor or other health professionala | 13 (76.5) |
| Visit to speak with HV/SCPHN, doctor or other health professional | 16 (88.9) |
| Preferred device for accessing the internet (n = 18) | Preferred this device |
| Desktop computer, laptop or workbook | 3 (16.7) |
| Tablet computer | 8 (44.4) |
| Telephone | 14 (77.8) |
Noticeably, 10 parents (53%) had attended extra visits with a HV/SCPHN, doctor or other health professional about their baby’s crying and 14 (78%) reported that they would have found an extra visit with their HV/SCPHN helpful when their baby was excessively crying. Furthermore, 16 participants (89%) felt that a visit with a HV/SCPHN, GP or other health professional would be an effective format for presenting information about crying babies to parents, stating that this would give reassurance, advice and explanation for the infants’ crying.
Half of parents also had a telephone conversation about their baby’s crying with a HV/SCPHN, doctor or other health service professional. Eleven participants (61%) reported that they would have liked extra telephone calls from a HV/SCPHN when their baby was excessively crying and 13 (76%) reported that a telephone call with a HV/SCPHN, doctor or other health professional would be an effective way to present information to parents. The high usage of visits and telephone support from HVs/SCPHNs, doctors or other health professionals, particularly given that such a high proportion of parents rated them as effective, supports the qualitative finding that participants felt a need for more personal support rather than simply having more information available.
All parents stated that they would have found a group helpful when their baby was excessively crying, with 10 (59%) stating that online discussion boards and 11 (65%) stating that Facebook sessions would have been helpful sources of information; this emphasises the importance of contact with other parents.
Websites were used by 16 respondents (80%), although none reported using a crying-specific website. All 18 said that they would have found a website helpful and 16 (89%) said that websites were an effective format for presenting information. These parents felt that websites were effective sources of information owing to their accessibility in various situations and availability 24 hours a day.
Leaflets were identified by 13 parents (72%) as a resource they would have found helpful and as an effective format for presenting information, although only nine (45%) had used leaflets when their baby was excessively crying. Participants felt that leaflets made good reference material that could be perused in their own time; however, they expressed concern about the number of leaflets already given to new parents and felt that it would be easy to lose a leaflet or not have it available when needed.
Support sessions
All participants stated that they would have wanted support sessions with a professional if they had been offered to them at the time when their baby was excessively crying. Only one parent wanted one-to-one sessions only, with most parents (55%) wanting group sessions or a mix of both. Most parents would have preferred between four and five sessions, with a range from two to six sessions.
Parents’ feedback on four example packages
Parents completed rating scales on all four of the example packages, giving detailed, package-specific information on which aspects they did and did not like. All parents reported that it was important that materials such as those shown in the focus groups were included as part of routine NHS care.
In order to protect the identities of the packages used in the focus groups (and because the aim was to identify which features parents judged to be needed in future packages, rather than comparing existing packages), overall information is reported about the features of the packages that parents did and did not like, as summarised in Figure 2. This shows that parents positively rated all of the researcher-identified aspects of the packages, such as the practical suggestions for parents, the reliability of the information for parents, reassurance for parents and that the information was aimed at both parents and easy to access when needed.
FIGURE 2.
Aspects of the four sample packages that parents liked (n = 20). 1, Practical suggestions; 2, reassurance that I wasn’t doing anything wrong/it wasn’t my fault; 3, that I could trust what they said; 4, other parents’ experiences and ideas; 5, expert opinion and advice; 6, that the information is aimed at both parents; 7, videos; 8, workbooks; 9, interactive materials – responsive to your interests and concerns; 10, that the materials are easy to access when you need them.

Table 5 provides the reasons parents gave for their preference for certain materials. These largely echo the researcher-identified features of the packages and also reflect the wider discussion that took place in the focus groups. However, some of the participants’ comments went on to clarify what in particular they had liked, providing useful information for the development of the intervention package. For example, participants’ comments made it clear that they liked information that was ‘clearly explained’, ‘relevant’ and in ‘bite-size chunks’. The information and websites needed to be able to be ‘read and understood within a few minutes’, ‘clear’, ‘easy to navigate and find [the] information you are looking for’. Parents valued the reassurance, saying that the packages ‘seemed to “normalise” the crying more and helps you to feel better in yourself’. Participants were positive about other parents’ stories, with one explaining that it ‘gave a realistic situation which I could identify with’. Information aimed at the couple together was also valued; as one parent explained, ‘if your relationship is strengthened, workload shared and baby-related issues discussed and problem-solving done together then I think crying would be easier to deal with’.
| Website features | Number (%) of parents |
|---|---|
| Information: relevant, easily accessible and not too in depth | 11 (55.0) |
| Clear and easy format: clear, simple and easy-to-use format, able to find and understand information when needed | 10 (50.0) |
| Practical: practical tips, advice and suggestions of strategies for soothing the baby and coping tips for parents | 9 (45.0) |
| Gave reassurance: materials that took the crying seriously and acknowledged that sometimes babies do just cry | 7 (35.0) |
| Includes other parents’ experiences: other parents’ experiences, as they could identify with them (e.g. case studies) | 4 (20.0) |
| Dads and mums: information that was relevant to dads as well as mums | 3 (15.0) |
| Couples: parents liked the fact that the materials gave information for couples and ways for parents to support each other and work together | 2 (10.0) |
| Items specific to certain packages: specific items in the materials that parents liked included coping skills, videos, audio files and websites that were interactive | 8 (40.0) |
| Focused: specifically focused on uncontrollable, unsoothable crying | 1 (5.0) |
Twelve of the 20 parents were successfully recontacted after the focus groups. Eight had revisited one or more of the example websites. None of the parents wished to amend their responses given within the focus groups.
Focus group qualitative data
In the focus groups, participants reported what it was like to be the parent of an infant who cried excessively for no apparent reason. They described how they tried to make sense of what was happening, how they dealt with feelings of inadequacy, physical and mental exhaustion and concerns for their baby’s well-being. Data analysis identified four themes: (1) disrupted experience of parenthood, (2) feeling different and social isolation, (3) reluctance to seek support and (4) validation of experience and seeking help.
Disrupted experience of parenthood
Parent participants indicated that their expectations of parenthood were positive and that they had little prior awareness that some babies could cry excessively for prolonged periods:
I think the, the expectation that you have after you have been carrying your unborn child and then you have your baby and then this whole feeling of this is going to be wonderful, and you can’t wait to hold your baby and nurture and look after and everything else – and the screaming just doesn’t stop, it just seemed to go on in a bit of an endless cycle and you think to yourself ‘it’s going to stop, it will just be the first week’ and it, for me it didn’t, it didn’t for a long, long, time.
P1P19
Consequently, they were shocked by the experience of having an excessively crying baby and they gave accounts of the many strategies they adopted to comfort their babies. However, their inability to soothe the babies made parents feel that they were somehow responsible for the crying. This, subsequently, led to feelings of inadequacy, frustration and anxiety, which seriously eroded their confidence in their ability to parent these babies:
I would say it made you feel like you are no good at it, like you are helpless really, because you try everything . . . But when she carried on crying you try and feed them, you change them, there is nothing wrong with them you just feel like useless.
P1P7
The crying often resulted in parents feeling exhausted and sleep deprived. This tiredness reduced their ability to cope, and even daily tasks, such as eating and attending to basic personal needs, were compromised for some:
I wasn’t looking after myself, I wanted to but I just couldn’t because, everything was so consumed with the crying that I just didn’t, I just almost neglected myself.
P1P13
Many mothers perceived that their partners did not fully understand their experience of being at home all day with a baby who cried incessantly. They often felt that their experiences were invalidated and dismissed as an exaggeration, creating tension between couples:
I don’t think he really understood what it was like to be at home all day on your own with a crying baby. And whilst he never came home and said ‘well it’s a mess, where is my dinner?’ you still have to do those things. He’d come in and be, ‘oh I am so tired, I have been at work’, and expect to have a chill out and she would be there screaming the place down. I started to resent him . . . a complete breakdown in communication there.
P1P16
However, there were several examples of a positive shared parental approach:
He would do all the night feeds. I went to bed at 10 [p.m.] and then he would do the night feeds and then I would get up at 6 [a.m.]. With the crying to be fair he never lost his temper once, he didn’t shout. In the middle of the night he would wake up and say ‘oh give her to me’. And he slept downstairs for 3 months with her so that I got sleep.
P1P5
Feeling different and social isolation
Parents perceived that both they and their baby were somehow ‘different’ to families with ‘normal babies’:
The year I had my baby there were five of us that all went to school that all had our babies within a few months. All of their babies were happy, they never particularly cried. So we were very much the odd ones out.
P1P16
Negative comparisons between their situation and that of others increased their sense of isolation and loneliness. Parents recognised that meeting friends or attending groups could be beneficial, but physical exhaustion and the all-consuming nature of trying to soothe their babies made getting out of the house both physically and mentally challenging:
I went to them baby massage classes but I only went for one . . . because he was crying the whole time we were there. I couldn’t do a lot with him because I just thought it’s just gonna be embarrassing. Especially cos you’d have all the mums there and they’d be like ‘oh my baby is like so’, ‘he’s brilliant, sleeps 8 hours, happy to just sit there’, but that don’t make you feel better.
P1P17
Reluctance to seek support
These feelings, together with a wish not to impose on others, appeared to inform parents’ initial reluctance to seek professional support, even from partners or close family members in some cases:
It’s sort of like admitting defeat isn’t it . . . you feel like you have been defeated by this little child and it’s actually admitting that to your family. Even my other half I never told him how bad I actually felt.
P1P5
More worryingly still, reluctance to seek help appeared to be fuelled by fears of being judged by others, particularly health-care professionals, who some parents feared would take their baby away:
But you do think that don’t you? ‘Oh my god they [health-care professionals] are going to come round and take her off me.’
P1P1
A reluctance to seek support from others led parents to look for reasons for the excessive crying and self-help strategies from sources such as the internet. However, they reported difficulty with finding information specific to excessive infant crying and how to cope with it, and several questioned the quality of the advice on offer:
Yeah, [I used the internet] a lot, when I was trying to look on Google [Google Inc., Mountain View, CA, USA], some stuff came up but it wasn’t stuff that gave you proper advice or anything on what to do.
P1P10
Parents indicated that they found online parent forums valuable and were reassured to find that they were not the only parents dealing with an excessively crying baby:
[I was] looking for information. I was just looking for what other people had been through and what they’d said; the whole act of finding and reading what other parents have been through helped me – I felt like I wasn’t on my own.
P1P18
As well as providing reassurance, online forums also provided the opportunity to interact with other parents who were sharing the same experience and, as a consequence, participants felt less isolated.
Validation of experience and seeking help
Parents described trying to find a way of relieving their baby’s crying, often going through a mental checklist of things that may be causing the baby distress, such as their nappy, feeding, temperature, etc. When they had exhausted these options, they became concerned that their baby was unwell and sought advice and reassurance from health-care professionals. As no physical cause was found and the crying continued, many parents spoke of repeated appointments as they were convinced, despite reassurance, that there was something seriously wrong.
It [crying] went on and on for 2 weeks straight it was, he just cried so much. I remember going to the doctors and then the midwife was coming round and I asked, ‘what’s he crying for?’. And I just kept looking at him and thought ‘what’s wrong with him?’, ‘why is he crying?’.
P1P12
However, despite frequent contact with health professionals, some parents felt that their concerns were not taken seriously or that professionals thought that they were exaggerating. This increased their frustration at not being heard and added to their distress:
You are banging your head against a brick wall, you are knocking on everyone’s door and you are not getting anywhere. So not only did I feel undervalued from a mother’s point of view [and] feel that what I was doing was wrong, but as an individual, as an adult I felt like nobody was listening to me, nobody cared, nobody is taking me seriously, it was a nightmare.
P1P11
Other parents found health professionals to be sympathetic and helpful; however, they questioned their level of experience in relation to excessively crying babies and their knowledge and skills in the area:
I found that the health visitor was helpful, she was quite sympathetic. She didn’t have the answers that I felt that I needed, and she didn’t have probably the experience of babies that cry. But it just made it just nicer to talk to somebody who was sympathetic to talk to.
P1P8
Parents valued acknowledgement of their concerns. Moreover, when there was continuity of care, and they were able to build up a relationship with health-care professionals, parents felt more able to share their concerns:
My health visitor was really supportive; even now she’s really supportive. She was really nice, really good, even like now she is really good, and she always like rings me to see how I am. She has given me her number and said if you ever feel down, if you ever want to talk to anyone ring me and, I go to the groups and she is there sometimes and she has a chat and she is really helpful.
P1P9
The importance of continuity and the quality of the relationship with health professionals in supporting parents was evident:
It’s a lot of work, because we have had so many health visitors it’s like starting from scratch all over again. He has three already, he’s only 15 months old and not one of them knows him. So when they ring I just say ‘yes I am fine’. I just don’t bother now.
P1P5
Although parents used a variety of means to access information about crying babies, a home visit from a HV was particularly valued. Parents felt that these visits allowed HVs to see first-hand how the baby was crying, and in doing so supported validation of the parent experience:
I used to think she [HV] should come to my house and see what I am going through. She never came to my house, she’d ring me and she was just trying to tell me things to do over the phone.
P1P7
Implications of these findings
In the opinion of parents who have experienced an excessively crying baby, the supports available for parents in this position can be improved in several ways:
-
Parent education prenatally or in the first few postnatal weeks should include information about excessive infant crying, including signposting of parents towards resources and sources of help.
-
Training resources in how to support parents should be developed for health-care professionals involved with the care of parents before and after their baby’s birth.
-
Care models that provide continuity of care and allow parents to develop relationships that support disclosure of their concerns and anxieties should be promoted.
-
There is a need to promote awareness of excessive infant crying more widely to the general public using a number of media, including television, radio and articles in popular magazines.
Parents who have had an excessively crying baby have reported that it is a bewildering and anxiety-provoking experience that undermined their confidence in their skills and aptitude to be proficient parents and shattered their expectations of parenthood. Participants felt that they might have been able to cope better if they had more information prior to the birth of their baby or even in the early days of parenthood. Understanding the parent experience of excessive crying and the perceived stigma associated with this enables the identification of how to better support parents. For the parents of excessively crying infants, this would need to include enhancing the education and training of the health-care professionals who support them. It is important to bear in mind that few fathers and parents from ethnic minority groups were involved in this study, so the findings need to be generalised with care. Nevertheless, the findings highlight an unmet need in the NHS and identify the sorts of support services that parents would like to see developed.
Chapter 6 Stage 1 development of parental support materials
Note: please contact the corresponding author to request access to the practitioners’ manual.
Reflecting the literature review and focus group data, three package elements were developed: a Surviving Crying website, a printed version of the website materials and a programme of CBT-based support sessions delivered directly to parents by a qualified practitioner, together with a programme manual.
Website
Following an invitation to tender and a competitive selection process, a marketing and communications agency, Consider Creative (London, UK), was appointed to assist in developing the website and study materials. Its brief included:
-
developing the imagery, templates and required features of the website
-
testing the website to ensure compatibility with different devices and operating systems
-
setting up Google Analytics (Google Inc., Mountain View, CA, USA) to enable monitoring of usage of the website by different user groups – parents, HVs/SCPHNs and other visitors
-
hosting and maintaining the website
-
developing a set of template documents to enable production of the information booklet in the same style and appearance as the website.
Once the website structure had been designed and approved, the content was developed and uploaded by the study team, using an iterative process of drafting and revision.
As noted in Chapter 5, Focus group qualitative data, feedback from the focus groups had highlighted the importance for parents of knowing that their experience was not an isolated one and that other people had survived having a crying baby. As a result, in addition to providing expert information and advice, efforts were made to ensure that parents’ experiences were included throughout the website. As described in Chapter 4, Parent involvement, focus group parents were recontacted to obtain their consent for inclusion of their experiences within the website. All of those whom it was possible to contact (n = 16) gave consent for the inclusion of their quotations from the focus group transcripts, and 14 parents also consented to provide written or video accounts of their experiences, leading to the production of five written stories and three videos. Videos were filmed in parents’ homes and edited by DMU staff with expertise in this field. Names were changed throughout to protect anonymity. In addition, videos of three professionals providing information and guidance were produced.
To ensure ease of reading, information was presented using bullet points and subheadings, and all text was adjusted to a reading age of 9–12 years. Care was taken to ensure that all advice given on the website was evidence based, with the text checked by the study paediatrician for accuracy. Focus group parents were asked to comment on a draft version of the website and 16 of them provided feedback; HVs/SCPHNs and members of the Study Management Group also provided input, leading to some minor revisions. In consultation with DMU legal advisers, information regarding copyright, the use of cookies and terms of use, including a disclaimer, were drawn up and added to the website.
Once the content had been finalised, Consider Creative and the research team completed the testing of the website, including ensuring its suitability for a range of electronic devices (personal computers, tablet computers and mobile phones), and provided a mechanism to enable the study team to issue individual user names and passwords to parents and others accessing the website. They also created templates, based on the website imagery, to enable other elements of the package to be produced in a consistent style.
Figure 3 shows the home page of the resulting Surviving Crying website, as it appears on mobile phone, tablet computer, desktop computer and laptop computer screens.
FIGURE 3.
The Surviving Crying website home page displayed on a range of devices. Reproduced with permission from De Montfort University.

The home page of the website was deliberately kept simple and focused, with text stating that:
This website is for parents who are worried about their baby’s excessive crying. Here you’ll find:
Drawing on the expert knowledge of the PI, the findings from focus groups and the literature review, the website was designed with four main sections: ‘Expert Help and Advice’, ‘Your Stories’, ‘News and Research’ and ‘About Us’. In addition, prominently highlighted on each page was a link to a section entitled ‘Need Help Now’, which provided advice and information to parents who might be in crisis.
The website contained a mixture of content, including written information and advice, quotations and videos from parents and experts and downloadable checklists and tips. Relevant parent quotations and/or videos were selected to support each section topic. A more detailed description of the website layout and content is provided in Appendix 6. DMU holds the copyright for the website and log-in details are required to access it.
Information booklet
The finalised website text was used to form the content of the information booklet. Some adjustments were necessary to enable the material to be accessible in paper format, including the addition of an introduction and a contents page. All of the written content of the website was included in the booklet, but it was not possible to incorporate any of the content of the videos. The booklet was then produced in an A4 format, with spiral binding and plastic covers for ease of use. It was printed in colour using the templates created by Consider Creative to create a consistent image across the resources.
Support session resources and practitioners’ manual
Based on CBT studies identified through the literature review,36,37,42,43 and the longitudinal course of infant crying, a programme of practitioner CBT support was designed by the study team in collaboration with a CBT-qualified counselling psychologist with extensive experience in supporting adult mental health in the NHS. The resources underwent several iterative revisions, were piloted and then were reviewed by parent and HV/SCPHN members of the Study Management Group.
The programme was designed to include up to five sessions, each lasting 60–90 minutes, delivered to parents in person or by telephone within a 4- to 6-week period. The sessions were designed for delivery at home or at another location of the parents’ choosing. Depending on the availability of other parents, parents could choose whether to take part in one-to-one or small-group sessions. Three key topics were included in each practitioner-delivered session:
-
assessing infant crying and well-being, making arrangements to obtain any other information or support needed and providing parents with information and reassurance
-
monitoring the soothing and baby-care methods parents were using
-
supporting parents in developing coping strategies that helped them to manage their own emotions and actions and ensure their well-being.
Each support session was based on core CBT principles, which were introduced in session 1, entitled ‘Introduction to thoughts and emotions’. The materials for this session, plus an introduction to the sessions as a whole, were in the folder when it was given to parents. Materials for a range of other topics were also provided, to be delivered flexibly in response to parents’ needs over subsequent sessions. These were:
-
how to stay feeling good when you have a new baby
-
managing the stress of a baby who cries excessively
-
looking after yourself – getting support, asking for help and saying no
-
relaxation and diaphragmatic breathing
-
getting good-enough sleep.
Each session included home activities for parents to undertake between sessions and review at the next meeting.
The resources for the support sessions were provided in a plastic folder with clear pockets into which the information could be slotted over the course of the sessions. The materials used a template based on the website and booklet imagery and also included a large amount of full-colour graphics to illustrate the various topics.
In addition to the resources for parents, a practitioners’ manual was developed to enable the materials to be delivered by the CBT practitioner (please contact the corresponding author to request access to the practitioners’ manual). This manual provided an introduction to the study and an overview of the sessions, together with guidance on how to use the resources to facilitate the sessions, including a plan of activities and session notes. Record sheets for the practitioner to log their activities and the outcome of the individual sessions were also included.
Methods for evaluating the package materials
Measures of participation and cost, questionnaires assessing infant crying, feeding and health, parental well-being and crying knowledge, together with rating scales to evaluate each element of the support package, were developed. To avoid duplication, these methods will be described together with the evaluation findings in the following sections.
Chapter 7 Stage 2: feasibility study of package implementation in the NHS – overview
The aims of stage 2 were to:
-
assess parents’ and HVs’ (HVs/SCPHNs) willingness to enter and complete a study of the support package
-
measure parental use and parental and HV/SCPHN evaluation of the package components
-
identify measures for assessing package clinical effectiveness and cost-effectiveness
-
identify barriers to and facilitators of the research
-
assess the feasibility and design parameters for a future large-scale trial of the intervention package’s clinical effectiveness and cost-effectiveness, and find out whether or not parents would be willing to participate in such a trial.
Reporting of stage 2 is divided into the following sections:
-
methods of recruitment and data collection (see Chapter 8)
-
baseline findings for parents and babies (see Chapter 9)
-
outcome measures and changes for parents and babies (see Chapter 10)
-
parental evaluation of the Surviving Crying materials (see Chapter 11)
-
the HV/SCPHN evaluation of the Surviving Crying materials (see Chapter 12).
Chapter 8 Stage 2 methods
Introduction
This section reports the methods used to recruit parents to the study, the process of data collection and the methods employed to analyse the quantitative and qualitative data. A series of structured questionnaires and rating scales, at baseline and outcome assessments, were used to show changes over time, to provide information about the uptake of each package component and to record parents’ and HVs’/SCPHNs’ evaluations of their suitability for use in the NHS. Data were also collected to indicate the extent to which a future large-scale trial would be worthwhile and to identify the intervention package components and methods for that trial.
Additional ethics approvals
Because stage 1 of the study developed a novel intervention package, ethics approval for its use and evaluation in stage 2 could not be applied for until the end of stage 1. Ethics approval was subsequently granted by DMU and the National Research Ethics Committee East Midlands (Nottingham). In addition, as in stage 1, a substantial amendment was obtained in order to widen recruitment using flyers.
Participants
From May to October 2016, participants were recruited to one of two groups:
-
The ‘referred crying group’ – parents who sought HV/SCPHN help because of their baby’s current excessive crying or parents who contacted the research team directly after seeing the call for eligible parents on the NCT website or from information distributed locally. Based on LPT birth numbers and an incidence of 20%, allowing for attrition, we expected to recruit one or two parents to this group each week, allowing the target of 30 parent cases to be recruited.
-
The ‘new birth visit group’ – HVs/SCPHNs invited parents to enter the study at the statutory primary home visit within 10–14 postnatal days. Ten parents per week were expected to give informed consent to be followed up to 8 weeks following birth, and screened for excessive infant crying by researchers, giving a total of 150 recruited parents, of whom 30 were expected to be parents of excessively crying infants.
The new birth visit group would provide figures for the incidence of excessive infant crying, allow us to ask these parents if they had any reservations about accessing NHS services for infant crying, might enable earlier detection and intervention and would indicate differences between the two recruitment groups. The two recruitment methods would indicate potential numbers and recruitment methods for a future RCT and allow adjustment of the recruitment strategy if the expected numbers were not forthcoming. The total of 60 cases was judged to be sufficient for the purposes of the feasibility study. Table 6 shows the expected recruitment figures and stage 2 timetable, including providing the support package and follow-up assessments.
| Week in year 2 | Group 1: referred crying group cases (n = 30) | Group 2: new birth visit group cases (n = 150) | Excessive crying cases selected from new birth visit group when infants are 5 weeks old (20% prevalence) (n = 30) | Parents offered package | Outcome measures 4 weeks later | ||
|---|---|---|---|---|---|---|---|
| Group | Group | ||||||
| 1 (n = 30) | 2 (n = 30) | 1 (n ≥ 30) | 2 (n = 30) | ||||
| 1 | 1 | 10 | 1 | ||||
| 2 | 2 | 10 | 2 | ||||
| 3 | 1 | 10 | 1 | ||||
| 4 | 2 | 10 | 2 | ||||
| 5 | 1 | 10 | 2 | 1 | 2 | 1 | |
| 6 | 2 | 10 | 2 | 2 | 2 | 2 | |
| 7 | 1 | 10 | 2 | 1 | 2 | 1 | |
| 8 | 2 | 10 | 2 | 2 | 2 | 2 | |
| 9 | 1 | 10 | 2 | 1 | 2 | 1 | 2 |
| 10 | 2 | 10 | 2 | 2 | 2 | 2 | 2 |
| 11 | 1 | 10 | 2 | 1 | 2 | 1 | 2 |
| 12 | 2 | 10 | 2 | 2 | 2 | 2 | 2 |
| 13 | 1 | 10 | 2 | 1 | 2 | 1 | 2 |
| 14 | 2 | 10 | 2 | 2 | 2 | 2 | 2 |
| 15 | 1 | 10 | 2 | 1 | 2 | 1 | 2 |
| 16 | 2 | 2 | 2 | 2 | 2 | 2 | |
| 17 | 1 | 2 | 1 | 2 | 1 | 2 | |
| 18 | 2 | 2 | 2 | 2 | 2 | 2 | |
| 19 | 1 | 2 | 1 | 2 | 1 | 2 | |
| 20 | 2 | 2 | 2 | 2 | |||
| 21 | 1 | 2 | |||||
| 22 | 2 | 2 | |||||
| 23 | 1 | 2 | |||||
| 24 | 2 | ||||||
| 25 | |||||||
| 26 | |||||||
| 27 | |||||||
| 28 | |||||||
A total of 154 parents were recruited and consented to participate in stage 2, of whom 57 received the Surviving Crying support materials. To be eligible to participate, parents were required to have a healthy baby aged ≤ 6 months, be English speaking or supported by an English speaker and live within Leicester, Leicestershire or Rutland. Parents were eligible to receive the support materials if they had a baby who they judged to be excessively crying. Parents whose baby was older than 6 months, or was judged to be ill at the time of crying by their HV/SCPHN or another qualified professional, were excluded from participating. Parents who lived outside the LPT area were also excluded.
Thirty participants in group 1 received the support materials. In group 2, out of 124 parents who consented to take part in the study, 27 reported their baby to be excessively crying and subsequently received the support package (Table 7), with an incidence of 21.7%. Recruitment to this group proved more resource- and time-consuming than expected and it fell just short of the target of 30 cases.
| Participant consents | Group | All parents receiving support materials | All parents | |||
|---|---|---|---|---|---|---|
| Referred crying | New birth visit | |||||
| Excessively crying baby | No excessively crying baby | Total | ||||
| Number of parents consented | 30 | 27 | 97 | 124 | 57 | 154 |
Table 8 shows the sociodemographic profile of participants in both groups. There were no statistically significant differences between them.
| Sociodemographic characteristics | Group | All parents with an excessively crying baby | All parents | ||
|---|---|---|---|---|---|
| Referred crying | New birth visit | ||||
| Excessively crying baby | No excessively crying baby | ||||
| Parental sex, n (%) | |||||
| Female | 24 (80.0) | 27 (100.0) | 94 (96.9) | 51 (89.5) | 145 (94.1) |
| Male | 6 (20.0) | 0 (0.0) | 3 (3.1) | 6 (10.5) | 9 (5.9) |
| Parental age (years) | |||||
| Mean age | 31.5 | 29.6 | 30.7 | 30.6 | 30.7 |
| SD (minimum–maximum) | 5.7 (20–43) | 4.7 (21–38) | 5.2 (16–42) | 5.3 (20–43) | 5.2 (16–43) |
| Parental ethnicity, n (%) | |||||
| White | 24 (80.0) | 23 (85.2) | 86 (88.7) | 47 (82.4) | 133 (86.4) |
| Mixed | 0 (0.0) | 1 (3.7) | 2 (2.1) | 1 (1.7) | 3 (1.9) |
| Asian | 5 (16.7) | 2 (7.4) | 5 (5.1) | 7 (12.3) | 12 (7.8) |
| Black | 0 (0.0) | 1 (3.7) | 3 (3.1) | 1 (1.7) | 4 (2.6) |
| Other | 1 (3.3) | 0 (0.0) | 1 (1.0) | 1 (1.7) | 2 (1.3) |
| Highest education level, n (%) | |||||
| Postgraduate degree | 5 (16.7) | 6 (22.2) | 22 (22.7) | 11 (19.3) | 33 (21.4) |
| Undergraduate degree | 6 (20.0) | 7 (25.9) | 21 (21.6) | 13 (22.8) | 34 (22.0) |
| Higher post-A-level vocational qualification | 4 (13.3) | 3 (11.1) | 8 (8.2) | 7 (12.3) | 15 (9.7) |
| A level/NVQ level 3 | 8 (26.7) | 6 (22.2) | 19 (19.6) | 14 (24.6) | 33 (21.4) |
| GCSE/NVQ level 2 | 3 (10.0) | 2 (7.4) | 10 (10.3) | 5 (8.8) | 15 (9.7) |
| Secondary school education | 0 (0.0) | 0 (0.0) | 3 (3.1) | 0 (0.0) | 3 (1.9) |
| Primary school education | 2 (6.7) | 1 (3.7) | 1 (1.0) | 3 (5.3) | 4 (2.6) |
| Other | 2 (6.7) | 2 (7.4) | 13 (13.4) | 4 (7.0) | 17 (11.0) |
| Employment status, n (%) | |||||
| Full time | 6 (20.0) | 0 (0.0) | 2 (2.1) | 6 (10.5) | 8 (5.2) |
| Part time | 2 (6.7) | 0 (0.0) | 0 (0.0) | 2 (3.5) | 2 (1.3) |
| Maternity/paternity leave | 15 (50.0) | 18 (66.7) | 74 (76.3) | 33 (57.9) | 107 (69.5) |
| Self-employed | 0 (0.0) | 2 (7.4) | 3 (3.1) | 2 (3.5) | 5 (3.3) |
| Unemployed, looking for work | 2 (6.7) | 2 (7.4) | 1 (1.0) | 4 (7.0) | 5 (3.3) |
| Not in paid employment | 4 (13.3) | 5 (18.5) | 14 (14.4) | 9 (15.8) | 23 (14.9) |
| Student | 0 (0.0) | 0 (0.0) | 3 (3.1) | 0 (0.0) | 3 (1.9) |
| Full-time carer | 1 (3.3) | 0 (0.0) | 0 (0.0) | 1 (1.7) | 1 (0.7) |
| Marital/living status, n (%) | |||||
| Married/cohabiting | 28 (93.3) | 22 (81.5) | 92 (94.8) | 50 (87.7) | 142 (92.2) |
| Living alone but supported by partner | 2 (6.7) | 2 (7.4) | 1 (1.0) | 4 (7.0) | 5 (3.2) |
| Living with parents/friends | 0 (0.0) | 0 (0.0) | 2 (2.1) | 0 (0.0) | 2 (1.3) |
| Single parent living alone | 0 (0.0) | 3 (11.1) | 2 (2.1) | 3 (5.3) | 5 (3.3) |
Measures
Parent questionnaires
A short participant demographic questionnaire was developed and was completed with all participants at the time of obtaining consent. It can be accessed at www.journalslibrary.nihr.ac.uk/programmes/hta/1215004/#/ (accessed 6 December 2018).
Participants with an excessively crying baby completed baseline questionnaires to rate their baby’s crying problem severity, feeding and health and well-being, using items from previous studies. 44 The questionnaires can be accessed at www.journalslibrary.nihr.ac.uk/programmes/hta/1215004/#/ (accessed 6 December 2018). They also completed four validated rating scales to measure parental well-being: the EuroQol-5 Dimensions (EQ-5D),45 the Edinburgh Postnatal Depression Scale (EPDS),46 the Generalised Anxiety Disorder-7 (GAD-7) anxiety scale47 and the Maternal Confidence Questionnaire. 48,49
These measures were repeated at the outcome stage to indicate potential improvements and were supplemented with measures of length of breast-milk feeding and crying knowledge. Parents provided ratings of each package component (see Appendix 7) and their suitability for use in the NHS. They were also asked about their willingness to participate in a RCT to evaluate the package components.
Participant take-up of the study support package and the extent of use of each component was recorded. To permit future cost-effectiveness analyses, measures of costs of each component, together with crying-related NHS costs, were also developed; these are discussed in detail in Chapter 13.
Health visitor questionnaire
A HV/SCPHN questionnaire was developed in order to obtain feedback about their involvement in stage 2, their opinions as to how helpful the materials were for parents and the extent to which they were suitable for inclusion in the NHS and their views on the provision of training in supporting parents with excessively crying babies. This questionnaire can be accessed at www.journalslibrary.nihr.ac.uk/programmes/hta/1215004/#/ (accessed 6 December 2018).
Cognitive–behavioural therapy practitioner questionnaire
A ‘session form’ to enable the CBT practitioners to record information about the CBT sessions was developed, detailing type, length and location of sessions, child attendance at the sessions and homework completion, and included free-text comments to capture information relating to the extent to which the sessions went as planned and the success of the sessions. This form can be accessed at www.journalslibrary.nihr.ac.uk/programmes/hta/1215004/#/ (accessed 6 December 2018).
Procedure
Health visitor involvement
The HVs/SCPHNs from the health visiting teams involved in stage 1 attended briefing meetings about stage 2 of the study. Six further health visiting teams were approached to collaborate in the study after initial participant referrals to the study team were slower than anticipated. All HVs/SCPHNs were given an information pack containing details about stage 2 of the study and how to refer eligible parents.
A total of 124 HVs/SCPHNs from 12 HV/SCPHN teams within Leicester, Leicestershire and Rutland gave written agreement to collaborate with the study team by identifying eligible parents.
Following the close of recruitment and follow-up of parents, HVs/SCPHNs were recontacted and asked to complete the HV/SCPHN questionnaire. Over a 3-week period, a total of 124 questionnaires were returned in one of the following ways:
-
hand-delivered to HVs/SCPHNs to complete and immediately return to the researcher
-
completed over the telephone with HVs/SCPHNs because of the pressures on their time
-
left at HV/SCPHN bases with a pre-paid envelope, for HVs/SCPHNs to complete and return in the post to the study team.
Of the 124 questionnaires delivered to HVs/SCPHNs, 96 (77%) were returned completed.
Parent recruitment and involvement
The Consolidated Standards of Reporting Trials (CONSORT) flow diagram in Appendix 8 shows the flow of participants’ involvement throughout stage 2 of the study. A total of 503 parents were considered for the study, of which 259 (51.5%) declined to participate or were considered to be unsuitable or ineligible to participate by their HVs/SCPHNs. In total, 47 parents were referred to the referred crying group and 197 were referred to the new birth visit group.
The HVs/SCPHNs referred both groups of parents to the study team. As in stage 1, HVs/SCPHNs provided parents with brief written details about the study in order to seek parental expressions of interest to enable researchers to contact them. Information about the study was also circulated via the NCT network and flyers were distributed to local children’s centres, HV/SCPHN bases, GP surgeries and venues where parents of young children might attend (e.g. libraries). Parents were thus able to self-refer to the referred crying group.
On receipt of an expression of interest, the researchers contacted each parent by telephone to fully explain the study, assess eligibility and formally invite parents to participate. In instances when the study team were unable to contact the parent using the telephone number given, attempts were made to contact those parents by e-mail, if an e-mail address was available, and telephone conversations were then had with those parents. Appendix 8 shows the number of parents for both groups who were no longer eligible to participate at this point, declined to participate or could not be contacted.
Group 1: referred crying group
During initial telephone contacts, appointments to obtain written consent and to conduct demographic and baseline measures were arranged with parents. Appointments took place at participants’ homes and the study support package developed in stage 1 was offered following the completion of the baseline measures. The package information booklet was handed to participants who chose that element of the package, the study website address and individual participant log-in details were given to parents and, for those parents who chose the CBT sessions, the contact details of the CBT practitioner were given to parents and parent contact details were given to the CBT practitioner following the baseline appointment.
Group 2: new birth visit group
Parents referred to this group were asked to return the written consent form to the study group in a pre-paid envelope provided and the demographic form was completed over the telephone. If any babies were excessively crying at this point, appointments were made to obtain participant written consent and to conduct the demographic and baseline measures. The procedure for arranging and conducting baseline appointments and the offering of the support package mirrored that of the referred crying group.
Participants whose babies were not excessively crying at the time of initial telephone contact received follow-up screening telephone calls from the study team at approximately 6 weeks and then 8 weeks after their baby’s birth. If excessive crying had developed by either of the follow-up contacts, the same procedures for arranging baseline appointments and the offering of the support package were followed. If by the 8-week follow-up contact no excessive crying had developed, parents were thanked for their participation in the study and were closed to follow-up. At this point, a high-street shopping voucher was delivered to participants in acknowledgement of their participation in the study.
Outcome appointments
All participants who received the support package, regardless of which group they were referred to, were recontacted to arrange an appointment to conduct the outcome measures. The length of time to follow-up depended on the support package components that participants chose, with an average of 5 weeks and 5 days from the baseline appointment to the follow-up outcome appointment (range 1 week and 6 days to 13 weeks and 6 days). Five participants could not be recontacted despite repeated attempts. At the final outcome appointment, participants received a high-street shopping voucher in acknowledgement of their participation.
Analysis
Parent questionnaires
Summary scores for questionnaires were treated as continuous variables. Confidence intervals (CIs) for the summary scores were calculated from linear regression models, which adjusted for the baseline score of the respective questionnaire. CIs calculated were for the follow-up score and the change from baseline, both overall and by group. In addition, differences in the outcomes between the referred crying group and the new birth visit group were investigated, with the results expressed as 95% CIs.
This was a feasibility study with two intervention groups, defined by two different methods of recruitment, and there was no control group. As this was a feasibility study, it was not powered to detect differences between the two groups. Therefore, the findings must be interpreted with caution and further investigation with a full trial would be necessary to evaluate the clinical effectiveness of the intervention. Although some statistical findings are reported when informative, for the most part the data are considered in relation to their implications for further, large-scale studies in the future.
Parent evaluations
Simple univariate and bivariate descriptive analyses were conducted and free-text comments were summarised using a simple thematic or content-analysis-style approach.
Health visitor and specialist community public health nurse feedback
Descriptive statistics (i.e. counts and percentages) were generated using IBM SPSS Statistics version 22 (IBM Corporation, Armonk, NY, USA) and free-text comments were summarised, highlighting key themes in HV/SCPHN responses.
Cognitive–behavioural therapy practitioner feedback
Simple univariate descriptive analyses were conducted and free-text comments were summarised; NVivo 10 was used to review and identify key themes in the data.
Chapter 9 Baseline findings
Parents occasionally omitted answers to some questions; therefore, tables in the remainder of this report include the group sizes for each item of information. Percentage figures are calculated from cases providing data. Owing to the nature of this study (i.e. assessing feasibility), it was not designed, nor powered, to allow statistical testing. Although some statistical findings are reported when informative, for the most part the data have been considered in relation to their implications for further, large-scale studies in the future.
Baseline measures of parents
Demographic data
Basic demographic information for the study participants is presented in Table 8. Noticeably, there were few, if any, demographic differences between the groups and cases with and without excessively crying infants. The majority of participants were mothers (80–100% across the two groups) and were married or cohabiting (81.5–95%). They were predominantly white, but small numbers of Asian, black, mixed-ethnicity and other-ethnicity parents took part. Around 40% had university degrees and a further 10% had post-Advanced-level vocational qualifications. Many (50–76%) were on maternity or paternity leave when their baby cried excessively.
Pregnancy complications and general health
Parents gave information about any complications during their pregnancy and most recent childbirth and their physical and mental health in the year prior to taking part in the study. These are shown in Table 9 and suggest that, when comparing those in the new birth visit group who have an excessively crying baby with those who do not, those in the former group were more likely to report complications during their most recent pregnancy (mean difference 1.50, 95% CI 0.82 to 2.73), labour and childbirth (mean difference 1.51, 95% CI 1.01 to 2.25). These data require careful interpretation but indicate a need to include measures of parental health, including medical data if possible, in a future study.
| Health data | Group | All parents with an excessively crying baby | All parents | |||
|---|---|---|---|---|---|---|
| Referred crying | New birth visit | |||||
| Excessively crying baby | No excessively crying baby | Total | ||||
| Pregnancy complications, n (%) | 14 (46.7) | 10 (37.0) | 24 (24.7) | 34 (27.4) | 24 (42.1) | 48 (31.2) |
| Labour/childbirth complications, n (%) | 16 (54.3) | 16 (59.3) | 38 (39.2) | 54 (43.6) | 32 (56.1) | 70 (45.5) |
| Number of GP appointments in last year (because of illness) | ||||||
| n | 30 | 27 | 97 | 124 | 57 | 154 |
| Mean (SD) | 3.8 (7.5) | 3.7 (10.1) | 1.0 (2.6) | 1.6 (5.3) | 3.7 (8.7) | 2.0 (5.8) |
| Range | 0–30 | 0–52 | 0–24 | 0–52 | 0–52 | 0–52 |
| Median | 1 | 1 | 0 | 0 | 1 | 1 |
| Number of hospital visits in last year (because of illness) | ||||||
| n | 29 | 27 | 97 | 124 | 56 | 153 |
| Mean (SD) | 1.9 (4.7) | 2.7 (7.8) | 0.1 (0.3) | 0.7 (0.8) | 2.3 (6.4) | 0.9 (3.9) |
| Range | 0–18 | 0–40 | 0–2 | 0–40 | 0–40 | 0–40 |
| Median | 0 | 0 | 0 | 0 | 0 | 0 |
| Number of times seen by other health professionals in last year (because of illness) | ||||||
| n | 28 | 27 | 97 | 124 | 55 | 152 |
| Mean (SD) | 0.1 (0.2) | 3.1 (10.9) | 0.1 (0.5) | 0.8 (5.2) | 0 (0.0) | 0.6 (4.7) |
| Range | 0–1 | 0–52 | 0–4 | 0–52 | 0–52 | 0–52 |
| Median | 0 | 0 | 0 | 0 | 0 | 0 |
| Number of GP appointments in last year (because of stress) | ||||||
| n | 29 | 27 | 97 | 124 | 56 | 153 |
| Mean (SD) | 0.1 (0.3) | 1.0 (2.1) | 0.2 (1.3) | 0.4 (1.5) | 0.6 (1.3) | 0.4 (1.4) |
| Range | 0–1 | 0–6 | 0–12 | 0–12 | 0–6 | 0–12 |
| Median | 0 | 0 | 0 | 0 | 0 | 0 |
| Number of hospital visits in last year (because of stress) | ||||||
| n | 28 | 27 | 97 | 124 | 55 | 152 |
| Range | 0 | 0 | 0 | 0 | 0 | 0 |
| Number of times seen by other health professionals in last year (because of stress) | ||||||
| n | 28 | 27 | 97 | 124 | 55 | 152 |
| Mean (SD) | 0.3 (1.4) | 2.7 (8.7) | 0.01 (0.1) | 0.6 (4.2) | 1.5 (6.2) | 0.6 (3.8) |
| Range | 0–7 | 0–35 | 0–1 | 0–35 | 0–35 | 0–35 |
| Median | 0 | 0 | 0 | 0 | 0 | 0 |
Parental well-being and mental health
Table 10 presents the baseline psychometric measures of parental well-being and mental health for parents with excessively crying babies. As there were no significant differences between the referred crying group and the new birth visit group, the overall findings are reported. Changes in these measures at outcome assessment, which are of particular interest, are examined in Chapter 10, Parental well-being and mental health. In addition, the aim was to evaluate the sensitivity and suitability of the measures for use with these parents, both in this study and for a possible future large-scale trial.
| Baseline measures | Group | All parents | |
|---|---|---|---|
| Referred crying | New birth visit | ||
| EQ-5D TTO value set | |||
| n | 30 | 27 | 57 |
| Mean | 0.88 | 0.84 | 0.86 |
| SD | 0.16 | 0.24 | 0.20 |
| Minimum | 0.36 | –0.23 | –0.23 |
| Median | 0.92 | 0.90 | 0.92 |
| Maximum | 1 | 1 | 1 |
| Missing | 0 | 0 | 0 |
| EPDS total score | |||
| n | 30 | 27 | 57 |
| Mean | 10.2 | 10.2 | 10.2 |
| SD | 5.1 | 4.8 | 4.9 |
| Minimum | 1 | 1 | 1 |
| Median | 9.5 | 10 | 10 |
| Maximum | 22 | 19 | 22 |
| Missing | 0 | 0 | 0 |
| GAD-7 anxiety scale total score | |||
| n | 30 | 27 | 57 |
| Mean | 6.8 | 5.8 | 6.3 |
| SD | 5.3 | 4.3 | 4.8 |
| Minimum | 0 | 0 | 0 |
| Median | 5.5 | 5 | 5 |
| Maximum | 18 | 15 | 18 |
| Missing | 0 | 0 | 0 |
| Maternal Confidence Questionnaire total score | |||
| n | 30 | 27 | 57 |
| Mean | 55.8 | 57.2 | 56.5 |
| SD | 5.5 | 6.5 | 6.0 |
| Minimum | 44 | 45 | 44 |
| Median | 56 | 58 | 56 |
| Maximum | 69 | 67 | 69 |
| Missing | 0 | 0 | 0 |
| Maternal Confidence Questionnaire mean score | |||
| n | 30 | 27 | 57 |
| Mean | 1.9 | 2.0 | 2.0 |
| SD | 0.2 | 0.2 | 0.2 |
| Minimum | 1.6 | 1.6 | 1.6 |
| Median | 2 | 2.1 | 2 |
| Maximum | 2.5 | 2.4 | 2.5 |
| Missing | 0 | 0 | 0 |
The EQ-5D45 is widely used to provide quality-of-life measures, particularly by health economists, and was included partly for that reason (see Chapter 13 for this study’s health economic data). Total scores on the EQ-5D vary from 0 to 1, such that a score near to 1 indicates an excellent quality of life. The scale is designed for use across a variety of physical and mental health areas, including for people with severe disabilities, so that low scores were not expected here. In practice, as Table 10 shows, the mean parental score of 0.86 [standard deviation (SD) 0.20] indicates a good general quality of life at the baseline stage.
The EPDS scores are screening measures that require careful interpretation. There is some variation in the cut-off score used to identify possible depression symptoms and the need for further assessment. Although a score of ≥ 13 is often used for clinical purposes, an influential review50 recommended a score of ≥ 10 as a sensitive indicator of postpartum depression. Because it is important to include all possible cases at this stage, we have adopted this cut-off score of ≥ 10 here. As Table 10 shows, the average parental score at baseline exceeded this cut-off score (mean 10.2, SD 4.9). Using a simple head count, 30 of 57 parents of excessively crying babies were depressed at baseline in accordance with this criterion.
Scores on the GAD-7 anxiety scale can be interpreted to indicate level of anxiety, with total scores of 5, 10 and 15 indicating mild, moderate and severe anxiety, respectively. 47 As Table 10 shows, the study mean GAD-7 score of 6.3 (SD 4.8) indicates that parents in this study were, on average, at least mildly anxious. More specifically, 16 parents were mildly anxious, 11 were moderately anxious and four were severely anxious at baseline.
The Maternal Confidence Questionnaire scores are presented as a total score (which can range from 14 to 70) and a mean score (which can range from 1 to 5). 49 A higher score on the Maternal Confidence Questionnaire indicates higher perceived confidence; a mean score of 2.0 suggests that parents were relatively low in confidence. However, without a comparison group (without excessive crying) it is unclear whether or not this is typical for all parents with babies of this age.
Sleep adequacy
Table 11 provides baseline figures and ratings for sleep adequacy among parents of excessively crying babies. These are chiefly of interest so far as they change at outcome assessment, and the lack of a comparison group without excessively crying babies hampers this interpretation. That said, it is noteworthy from Figure 4 that about half of the parents in both study groups judged their sleep quality to be fairly or very bad at this stage. The average of 5.9 hours of sleep per 24 hours is less than the recommended daily adult sleep range of 7–9 hours for 26- to 64-year-old adults published by the American National Sleep Foundation. 51 The implication is that future studies should include measures of parental sleep adequacy.
| Sleep adequacy | Group | All parents | |
|---|---|---|---|
| Referred crying | New birth visit | ||
| Hours of sleep per night | |||
| n | 30 | 27 | 57 |
| Mean | 5.5 | 5.1 | 5.3 |
| SD | 1.5 | 1.0 | 1.3 |
| Minimum | 3 | 2 | 2 |
| Median | 5.5 | 5 | 5 |
| Maximum | 8 | 7 | 8 |
| Missing | 0 | 0 | 0 |
| Hours of sleep per 24 hours | |||
| n | 28 | 24 | 52 |
| Mean | 6.0 | 5.9 | 5.9 |
| SD | 1.5 | 0.9 | 1.3 |
| Minimum | 3 | 4 | 3 |
| Median | 6 | 6 | 6 |
| Maximum | 10 | 8 | 10 |
| Missing | 2 | 3 | 5 |
FIGURE 4.
Overall sleep quality in previous 2 weeks, at baseline by group. (a) Referred crying group (n = 30); and (b) new birth visit group (n = 27).


Social support
Parents’ reports of the support they received from partners and friends/family are shown in Figures 5–7. Here, too, inclusion of a comparison group with typically crying babies would enhance interpretation. However, notably, the vast majority of parents (about 70%) judged these supports to be enough and few reported that they often needed support but could not get it. Even so, around one-quarter of the parents considered that partner and family/friend support was inadequate. Although this is a concern for a minority of parents, it will be worth including measures of social support in future studies, particularly if they are designed to improve parental well-being. Seven parents (12.2%) stated that they did not have enough/any support from either their partner or their family/friends. These parents may be a particularly vulnerable group in coping with an excessively crying infant.
FIGURE 5.
Support from partner, at baseline by group. (a) Referred crying group (n = 29); and (b) new birth visit group (n = 27).
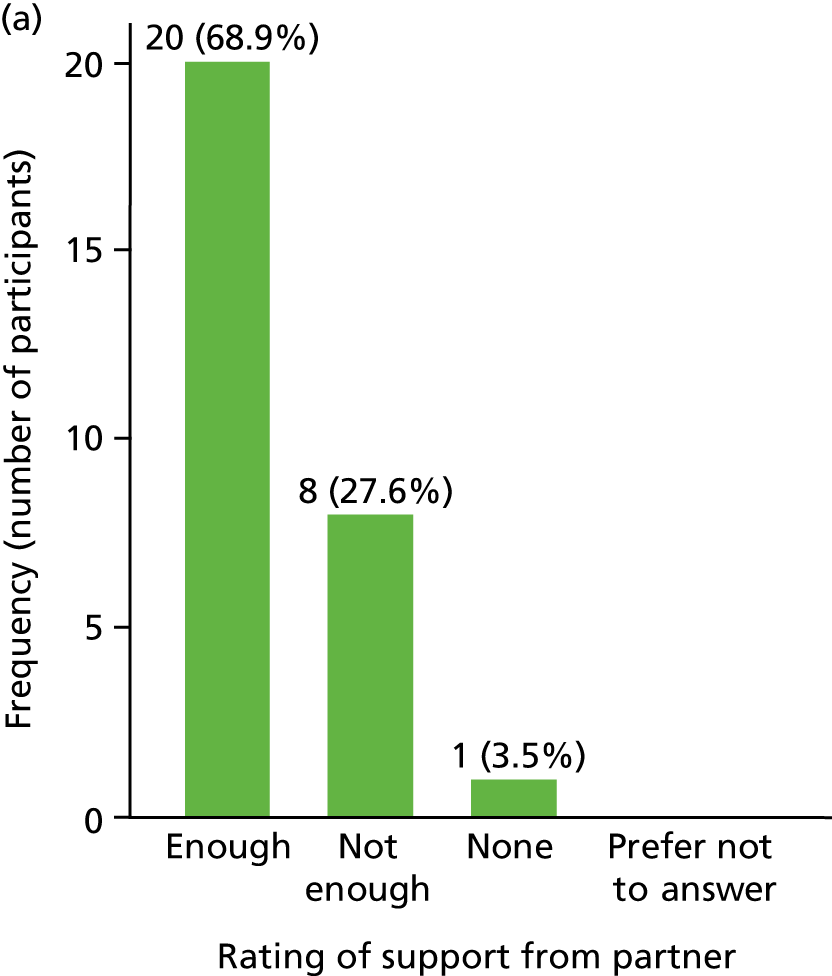
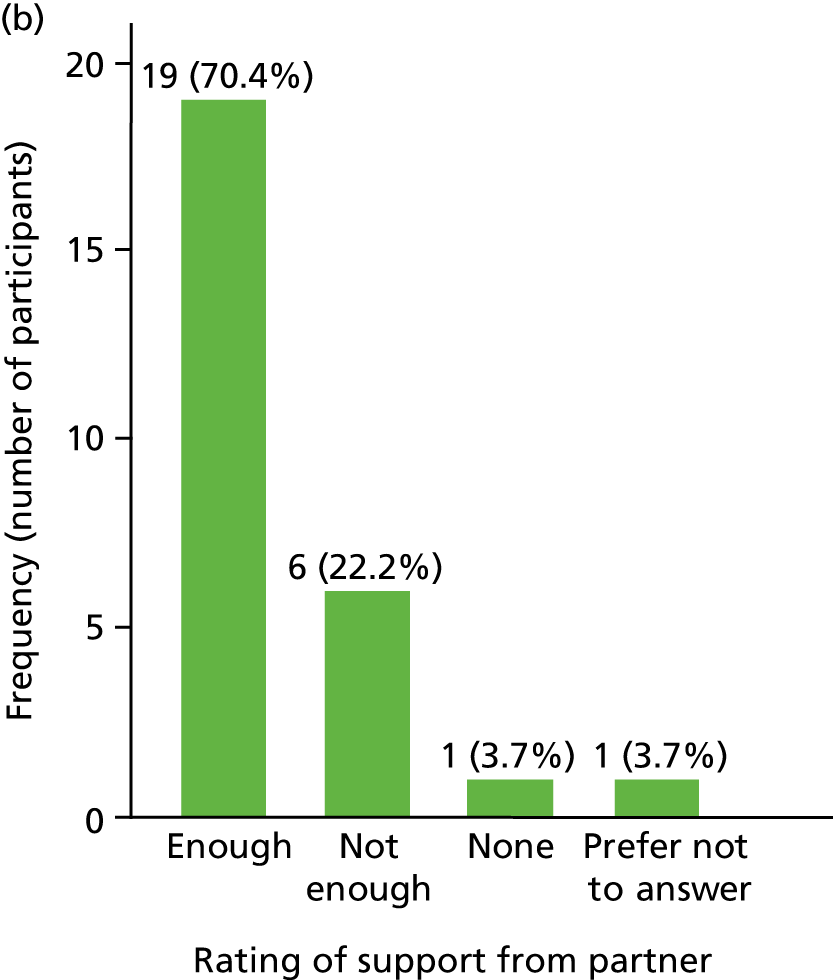
FIGURE 6.
Support from family and friends, at baseline by group. (a) Referred crying group (n = 30); and (b) new birth visit group (n = 27).


FIGURE 7.
Parents needing support but unable to get it, at baseline by group. (a) Referred crying group (n = 30); and (b) new birth visit group (n = 27).
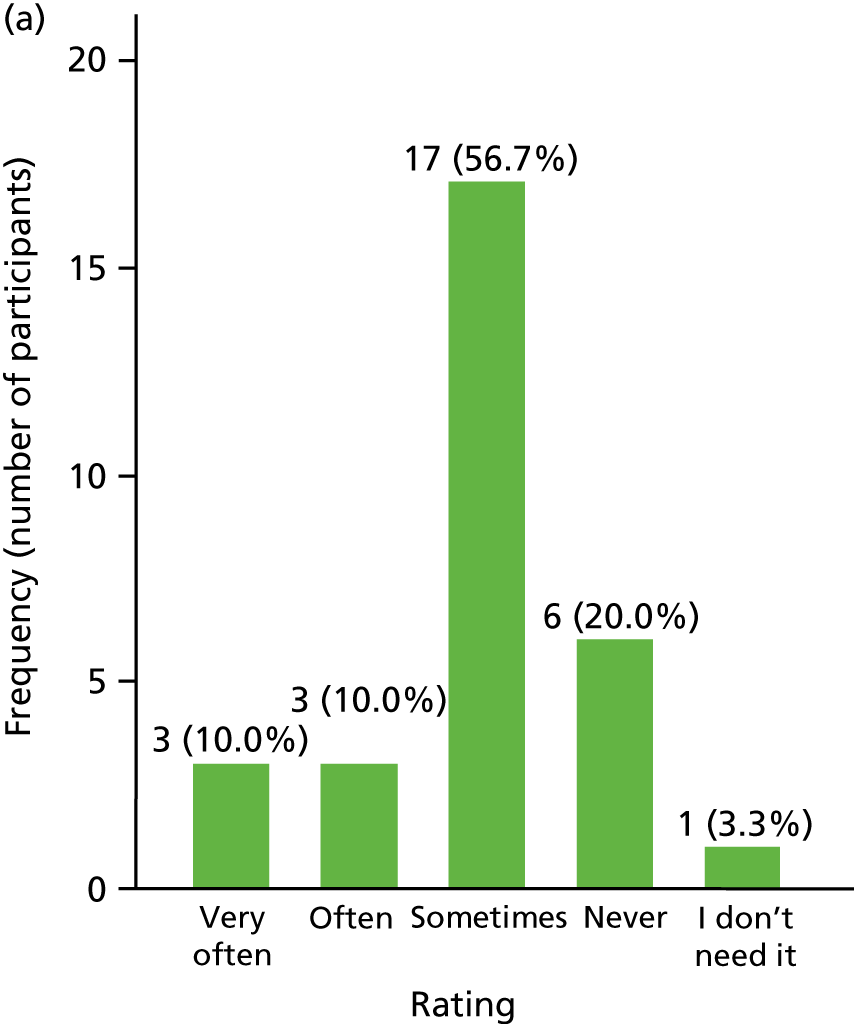

Baseline measures of babies
Babies’ sex and birth order
As shown in Table 12, baseline information was available for 52 babies (five couples participated in the study). There were similar proportions of male and female babies (47% were male and 53% were female). Noticeably, fewer than half of the babies were firstborns, with 40% being secondborn or later-born infants.
| Babies’ sex and birth order | Group, n (%) | All excessively crying cases, n (%) (N = 57) | All cases, n (%) (N = 154) | |||
|---|---|---|---|---|---|---|
| Referred crying (N = 30) | New birth visit | |||||
| Excessively crying baby (N = 27) | No excessively crying baby (N = 97) | Total (N = 124) | ||||
| Sex of excessively crying baby | ||||||
| Male | 20 (66.7) | 14 (51.8) | 39 (40.2) | 53 (42.7) | 34 (59.7) | 73 (47.4) |
| Female | 10 (33.3) | 13 (48.2) | 58 (59.8) | 71 (57.3) | 23 (40.4) | 81 (52.6) |
| Baby’s birth order | ||||||
| Firstborn | 15 (50.0) | 12 (44.4) | 42 (43.3) | 54 (43.6) | 27 (47.4) | 69 (44.8) |
| Secondborn | 14 (46.7) | 10 (37.0) | 38 (39.2) | 48 (38.7) | 24 (42.1) | 62 (40.3) |
| Thirdborn | 0 (0.0) | 1 (3.7) | 3 (3.1) | 4 (3.2) | 1 (1.8) | 4 (2.6) |
| Fourthborn or later | 1 (3.3) | 1 (3.7) | 2 (2.1) | 2 (1.6) | 2 (3.5) | 4 (2.6) |
Crying patterns and impact on parents
In keeping with existing evidence, the infant’s excessive crying typically began at 2–3 weeks of age (Table 13). The mean age of new birth visit group babies on entering the study at baseline (6.6 weeks) was significantly lower than that of referred crying group babies (12.8 weeks), indicating that the new birth visit group recruitment method identified excessive crying cases at a younger age (mean difference 6.13 weeks, 95% CI 3.50 to 8.77 weeks). On average, across both groups, the babies were reported to cry for 6.9 hours per day, and up to 17 hours in one case. The daily crying pattern showed the typical afternoon and evening peak found at this age. Most parents (77%) judged the crying to be a moderate or large problem for them, but 17% rated it a severe problem. Similarly, most parents (73%) had been moderately or very frustrated by the crying and 15% had been extremely frustrated.
| Babies’ crying and its impact | Group | All cases | |
|---|---|---|---|
| Referred crying | New birth visit | ||
| Age of baby at baseline (weeks) | |||
| n | 25 | 27 | 52 |
| Mean | 12.8 | 6.6 | 9.6 |
| SD | 6.6 | 1.6 | 5.6 |
| Minimum | 4 | 3 | 3 |
| Median | 11 | 7 | 7 |
| Maximum | 24 | 10 | 24 |
| Missing | 0 | 0 | 0 |
| Age of baby at the start of excessive crying (weeks) | |||
| n | 25 | 27 | 52 |
| Mean | 2.8 | 3.4 | 3.1 |
| SD | 3.6 | 1.8 | 2.8 |
| Minimum | 0 | 0 | 0 |
| Median | 2 | 3 | 3 |
| Maximum | 16 | 7 | 16 |
| Missing | 0 | 0 | 0 |
| Total number of hours of fuss/crying in a typical day | |||
| n | 25 | 27 | 52 |
| Mean | 6.9 | 6.9 | 6.9 |
| SD | 3.5 | 4.0 | 3.7 |
| Minimum | 1.3 | 1.8 | 1.3 |
| Median | 6.5 | 5.5 | 5.7 |
| Maximum | 13.0 | 17.0 | 17.0 |
| Missing | 0 | 0 | 0 |
| Crying pattern: number of hours spent crying in each period of a typical day, mean (%) | |||
| n | 25 | 27 | 52 |
| Morning | 1.6 (21.5) | 1.5 (18.8) | 1.6 (20.1) |
| Afternoon | 2.2 (34.9) | 1.7 (24.4) | 2.0 (29.5) |
| Evening | 2.2 (32.6) | 2.4 (38.9) | 2.3 (35.9) |
| Night | 0.9 (10.9) | 1.3 (19.3) | 1.1 (15.3) |
| How much of a problem has your baby’s crying been for you?, mean (%) | |||
| n | 25 (100) | 27 (100) | 52 (100) |
| Severe | 6 (24.0) | 3 (11.1) | 9 (17.3) |
| Large | 11 (44.0) | 7 (25.9) | 18 (34.6) |
| Moderate | 7 (28.0) | 15 (55.6) | 22 (42.3) |
| Minor | 0 (0.0) | 1 (3.7) | 1 (1.9) |
| None | 1 (4.0) | 1 (3.7) | 2 (3.9) |
| How frustrated have you felt about your baby’s crying?, mean (%) | |||
| n | 25 (100) | 27 (100) | 52 (100) |
| Extremely | 5 (20.0) | 3 (11.1) | 8 (15.4) |
| Very | 12 (48.0) | 10 (37.0) | 22 (42.3) |
| Moderately | 6 (24.0) | 10 (37.0) | 16 (30.8) |
| A little | 1 (4.0) | 2 (7.4) | 3 (5.8) |
| Not at all | 1 (4.0) | 2 (7.4) | 3 (5.8) |
Babies’ feeding
Table 14 provides descriptive figures for the infants’ feeding at baseline.
| Feeding method | Group, n (%) | All cases, n (%) | |
|---|---|---|---|
| Referred crying | New birth visit | ||
| Feeding at the time excessive crying started | 25 (100) | 27 (100) | 52 (100) |
| Breast milk | 16 (64.0) | 21 (77.8) | 37 (71.2) |
| Formula milk | 11 (44.0) | 10 (37.0) | 21 (40.4) |
| Baby solid foods | 1 (4.0) | 0 (0.0) | 1 (1.9) |
| Family foods | 1 (4.0) | 0 (0.0) | 1 (1.9) |
| Feeding at baseline | 25 (100) | 27 (100) | 52 (100) |
| Breast milk | 11 (44.0) | 16 (59.3) | 27 (51.9) |
| Formula milk | 15 (60.0) | 13 (48.2) | 28 (53.9) |
| Baby solid foods | 2 (8.0) | 0 (0.0) | 2 (3.9) |
| Family foods | 1 (4.0) | 0 (0.0) | 1 (1.9) |
| Baby’s feeding checked by a professional | 14 (56.0) | 16 (59.3) | 30 (57.7) |
| Baby’s weight checked by a professional | 25 (100.0) | 26 (96.3) | 51 (98.1) |
As Table 14 shows, most babies (71%) were breast-fed when the excessive crying started, 40% were formula-fed and 11.5% were a mixture of breast- and formula-fed. On study entry, 52% were breast-fed, in keeping with other evidence that excessive crying is associated with stopping breastfeeding. Infant weight gain had been checked by a professional in all but one case and feeding had been checked in most cases (58%). Measures of breastfeeding continuation and precise medical record and diagnostic information (when available) should be included in future studies.
Remedies given for crying, contacts with professionals and babies’ health
Tables 15 and 16 describe the remedies that parents had tried for their excessively crying babies, their contacts with professionals regarding the crying and the infants’ baseline health more generally.
| Remedies | Group, n (%) | All cases, n (%) | |
|---|---|---|---|
| Referred crying | New birth visit | ||
| Remedies for crying | |||
| Number of parents who used this | 25 | 27 | 52 |
| Remedy prescribed by a doctor | |||
| Number of parents who used this | 12 (48.0) | 5 (18.5) | 17 (32.7) |
| Number of times used | |||
| 0 | 13 (52.0) | 22 (81.5) | 35 (67.3) |
| 1–20 | 2 (8.0) | 1 (3.7) | 3 (5.8) |
| 21–100 | 4 (16.0) | 3 (11.1) | 7 (13.5) |
| > 100 | 6 (24.0) | 1 (3.7) | 7 (13.5) |
| Change of formula feed | |||
| Number of parents who used this | 13 (52.0) | 6 (22.2) | 19 (37.3) |
| Number of times used | |||
| 0 | 12 (48.0) | 21 (77.8) | 32 (62.8) |
| 1/2 | 8 (32.0) | 4 (14.8) | 12 (23.5) |
| > 2 | 5 (20.0) | 2 (7.4) | 7 (13.7) |
| Colic drops | |||
| Number of parents who used this | 20 (80.0) | 18 (66.7) | 38 (73.1) |
| Number of times used | |||
| 0 | 5 (20.0) | 9 (33.3) | 14 (26.9) |
| 1–20 | 1 (4.0) | 5 (18.5) | 6 (11.5) |
| 21–100 | 6 (24.0) | 1 (3.7) | 7 (13.5) |
| > 100 | 13 (52.0) | 12 (44.4) | 25 (48.1) |
| Herbal remedies | |||
| Number of parents who used this | 4 (16.0) | 3 (11.5) | 7 (13.7) |
| Number of times used | |||
| 0 | 21 (84.0) | 23 (88.5) | 44 (86.3) |
| 1/2 | 2 (8.0) | 1 (3.9) | 3 (5.9) |
| > 2 | 2 (8.0) | 2 (7.7) | 4 (7.8) |
| Chiropractor | |||
| Number of parents who used this | 1 (4.0) | 0 (0.0) | 1 (2.0) |
| Number of times used | |||
| 0 | 24 (96.0) | 27 (100.0) | 51 (98.1) |
| Other remedies | |||
| Number of parents who used this | 20 (83.3) | 11 (47.8) | 31 (66.0) |
| Number of times used | |||
| 0 | 4 (16.7) | 12 (52.2) | 16 (34.0) |
| 1–20 | 6 (25.0) | 5 (21.7) | 11 (23.4) |
| 21–100 | 4 (16.7) | 5 (21.7) | 9 (19.2) |
| > 100 | 10 (41.7) | 1 (4.4) | 11 (23.4) |
| Type of contact | Group, n (%) | All cases, n (%) (N = 52) | |
|---|---|---|---|
| Referred crying (N = 25) | New birth visit (N = 27) | ||
| HV visited at home | |||
| Number of parents who had visits | 21 (84.0) | 17 (63.0) | 38 (73.1) |
| Number of times | |||
| 0 | 4 (16.0) | 10 (37.0) | 14 (26.9) |
| 1/2 | 8 (32.0) | 13 (48.2) | 21 (40.4) |
| > 2 | 13 (52.0) | 4 (14.8) | 17 (32.7) |
| Went to HV clinic | |||
| Number of parents who did this | 8 (32.0) | 2 (7.4) | 10 (19.2) |
| Number of times used | |||
| 0 | 17 (68.0) | 25 (92.6) | 42 (80.8) |
| 1/2 | 6 (24.0) | 1 (3.7) | 7 (13.5) |
| > 2 | 2 (8.0) | 1 (3.7) | 3 (5.8) |
| HV telephone call | |||
| Number of parents who did this | 17 (68.0) | 7 (25.9) | 24 (46.2) |
| Number of times used | |||
| 0 | 8 (32.0) | 20 (74.1) | 28 (53.9) |
| 1/2 | 11 (44.0) | 7 (25.9) | 18 (34.6) |
| > 2 | 6 (24.0) | 0 (0.0) | 6 (11.5) |
| HV e-mail/internet contact | |||
| Number of parents who did this | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Number of times used | |||
| 0 | 25 (100.0) | 27 (100.0) | 52 (100.0) |
| GP visit at home | |||
| Number of parents who did this | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Number of times used | |||
| 0 | 25 (100.0) | 27 (100.0) | 52 (100.0) |
| Went to GP surgery | |||
| Number of parents who did this | 17 (68.0) | 9 (33.3) | 26 (50.0) |
| Number of times used | |||
| 0 | 8 (32.0) | 18 (66.7) | 26 (50.0) |
| 1/2 | 11 (44.0) | 7 (25.9) | 18 (34.6) |
| > 2 | 6 (24.0) | 2 (7.4) | 8 (15.4) |
| GP telephone call | |||
| Number of parents who did this | 4 (16.0) | 3 (11.1) | 7 (13.5) |
| Number of times used | |||
| 0 | 21 (84.0) | 24 (88.9) | 45 (86.5) |
| 1/2 | 4 (16.0) | 3 (11.1) | 7 (13.5) |
| GP e-mail or internet contact | |||
| Number of parents who did this | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Number of times used | |||
| 0 | 25 (100.0) | 27 (100.0) | 52 (100.0) |
| Other home visitor | |||
| Number of parents who did this | 4 (16.0) | 2 (7.4) | 6 (11.5) |
| Number of times used | |||
| 0 | 21 (84.0) | 25 (92.6) | 46 (88.5) |
| 1/2 | 3 (12.0) | 1 (3.7) | 4 (7.7) |
| > 2 | 1 (4.0) | 1 (3.7) | 2 (3.9) |
| Visited other | |||
| Number of parents who did this | 10 (40.0) | 3 (11.1) | 13 (25.0) |
| Number of times used | |||
| 0 | 15 (60.0) | 24 (88.9) | 39 (75.0) |
| 1/2 | 8 (32.0) | 2 (7.4) | 10 (19.2) |
| > 2 | 2 (8.0) | 1 (3.7) | 3 (5.8) |
| Other telephone call | |||
| Number of parents who did this | 4 (16.0) | 0 (0.0) | 4 (7.7) |
| Number of times used | |||
| 0 | 21 (84.0) | 27 (100) | 48 (92.3) |
| 1/2 | 3 (12.0) | 0 (0.0) | 3 (5.8) |
| > 2 | 1 (4.0) | 0 (0.0) | 1 (1.9) |
| Other e-mail or internet contact | |||
| Number of parents who did this | 0 (0.0) | 1 (3.7) | 1 (1.9) |
| Number of times used | |||
| 0 | 25 (100.0) | 26 (96.3) | 51 (98.1) |
| 1/2 | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| > 2 | 0 (0.0) | 1 (3.7) | 1 (1.9) |
| Other internet resources | |||
| Number of parents who did this | 20 (80.0) | 21 (77.8) | 41 (78.9) |
| Number of times used | |||
| 0 | 5 (20.0) | 6 (22.2) | 11 (21.2) |
| 1–20 | 13 (52.0) | 12 (44.4) | 25 (48.1) |
| 21–100 | 4 (16.0) | 7 (25.9) | 11 (21.2) |
| > 100 | 3 (12.0) | 2 (7.4) | 5 (9.6) |
Consistent with previous research, a substantial number of parents had tried various remedies, including prescriptions from their doctor, changes of formula and the use of ‘colic drops’. Most (73%) had received HV/SCPHN visits at home and 50% had visited their GP. Websites other than the study website had been accessed by 79% of parents who provided data. Even allowing for parents who did not answer this question, this finding clearly illustrates the importance of internet resources for these parents.
Vomiting and feeding problems accompanied the crying in 40–50% of cases, parents judged around one-quarter of infants to be unwell and half of the infants had been seen by their GP in the last fortnight for reasons other than their crying (Table 17). These figures all involve parental subjective judgements that are hard to interpret; for instance, vomiting is known to be common in healthy babies at this age. 52 Nonetheless, so far as these measures indicate the source of parents’ concerns, it will be worthwhile to include them in future studies, particularly in studies involving the clinical effectiveness of interventions. The values in Table 17 highlight the cost of excessive infant crying for families and health services, a topic that will receive detailed attention in Chapter 13.
| Additional health problems | Group, n (%) | All cases (N = 52), n (%) | |
|---|---|---|---|
| Referred crying (N = 25) | New birth visit (N = 27) | ||
| Additional health problems | |||
| Fever | 1 (4.0) | 3 (11.1) | 4 (7.7) |
| Seemed unwell | 6 (24.0) | 6 (22.2) | 12 (23.1) |
| Concerns about weight gain | 3 (12.0) | 4 (14.8) | 7 (13.5) |
| Feeding problems | 9 (36.0) | 12 (44.4) | 21 (40.4) |
| Vomiting | 12 (48.0) | 14 (51.9) | 26 (50.0) |
| Overall health and well-being | |||
| Admitted to a hospital specialist care unit in the first week after being born | 3 (12.0) | 1 (3.7) | 4 (7.7) |
| Any other signs of illness in the last fortnight? | 6 (24.0) | 12 (44.4) | 18 (34.6) |
| Seen GP or other doctor in the last fortnight for anything other than crying? | 9 (36.0) | 17 (63.0) | 26 (50.0) |
Chapter 10 Outcome measures and changes since baseline
Parents
All parents who received the support package were recontacted to arrange an appointment to conduct the outcome measures. Length of time to follow-up depended on the support package component they chose; the average time from the baseline appointment to the follow-up outcome appointment was 5 weeks and 5 days (range 1 week and 6 days to 13 weeks and 6 days; CBT cases involved longer intervals). Five participants could not be recontacted despite repeated attempts.
Parental well-being and mental health
Table 18 presents the outcome scores and changes from baseline in psychometric measures of well-being and mental health for parents with excessively crying babies. Standardised change measures and CIs are also given. As noted previously, no formal hypothesis tests were conducted because this feasibility study is not powered for such tests. However, the CIs provide an indication of the findings that are likely to be repeated in an adequately powered study.
| Psychometric measures | Group | All cases (n = 51a) | |
|---|---|---|---|
| Referred crying (n = 26a) | New birth visit (n = 25a) | ||
| EQ-5D TTO value set | |||
| Baseline, mean (SD) | 0.88 (0.15) | 0.84 (0.25) | 0.87 (0.20) |
| Follow-up, mean (SD) | 0.91 (0.082) | 0.89 (0.22) | 0.90 (0.16) |
| Adjusted mean at follow-up (95% CI)b | 0.90 (0.86 to 0.93) | 0.90 (0.87 to 0.93) | 0.90 (0.88 to 0.92) |
| Change from baseline, adjusted mean (95% CI)c | 0.030 (–0.00068 to 0.061) | 0.036 (0.0040 to 0.067) | 0.033 (0.011 to 0.055) |
| Difference vs. referred crying group (95% CI)d | 0.00531 (–0.039 to 0.050) | ||
| Adjusted for change in crying (95% CI)e | 0.00532 (–0.40 to 0.050) | ||
| EPDS | |||
| Baseline, mean (SD) | 10.23 (5.19) | 9.92 (4.73) | 10.08 (4.93) |
| Follow-up, mean (SD) | 7.19 (4.43) | 7 (4.67) | 7.10 (4.50) |
| Adjusted mean at follow-up (95% CI)b | 7.11 (5.62 to 8.61) | 7.08 (5.56 to 8.60) | 7.10 (6.03 to 8.16) |
| Change from baseline, adjusted mean (95% CI)c | –2.97 (–4.46 to –1.47) | –3.00 (–4.52 to –1.47) | –2.98 (–4.05 to –1.92) |
| Difference vs. referred crying group (95% CI)d | –0.031 (–2.16 to 2.10) | ||
| Adjusted for change in crying (95% CI)e | 0.031 (–2.14 to 2.20) | ||
| GAD-7 anxiety questionnaire | |||
| Baseline, mean (SD) | 7.35 (5.48) | 5.56 (4.05) | 6.47 (4.87) |
| Follow-up, mean (SD) | 4.27 (4.38) | 3.56 (3.32) | 3.92 (3.87) |
| Adjusted mean at follow-up (95% CI)b | 3.89 (2.57 to 5.21) | 3.95 (2.61 to 5.30) | 3.92 (2.99 to 4.86) |
| Change from baseline, adjusted mean (95% CI)c | –2.58 (–3.90 to –1.26) | –2.52 (–3.86 to –1.17) | –2.55 (–3.48 to –1.61) |
| Difference vs. referred crying group (95% CI)d | 0.063 (–1.84 to 1.97) | ||
| Adjusted for change in crying (95% CI)e | –0.065 (–2.01 to 1.88) | ||
| Maternal Confidence Questionnaire total score | |||
| Baseline, mean (SD) | 55.69 (5.07) | 57.40 (6.44) | 56.53 (5.78) |
| Follow-up, mean (SD) | 58.65 (5.28) | 61.64 (4.99) | 60.12 (5.31) |
| Adjusted mean at follow-up (95% CI)b | 59.15 (57.61 to 60.87) | 61.12 (59.56 to 62.69) | 60.12 (59.03 to 61.20) |
| Change from baseline, adjusted mean (95% CI)c | 2.62 (1.08 to 4.16) | 4.60 (3.03 to 6.16) | 3.59 (2.50 to 4.68) |
| Difference vs. referred crying group (95% CI)d | 1.98 (–0.23 to 4.18) | ||
| Adjusted for change in crying (95% CI)e | 1.90 (–0.36 to 4.16) | ||
| Maternal Confidence questionnaire mean score | |||
| Baseline, mean (SD) | 1.99 (0.19) | 2.05 (0.23) | 2.02 (0.21) |
| Follow-up, mean (SD) | 2.09 (0.19) | 2.20 (0.18) | 2.15 (0.19) |
| Adjusted mean at follow-up (95% CI)b | 2.11 (2.06 to 2.17) | 2.18 (2.13 to 2.24) | 2.15 (2.11 to 2.19) |
| Change from baseline, adjusted mean (95% CI)c | 0.094 (0.039 to 0.15) | 0.16 (0.11 to 0.22) | 0.13 (0.089 to 0.17) |
| Difference vs. referred crying group (95% CI)d | 0.071 (–0.0083 to 0.15) | ||
| Adjusted for change in crying (95% CI)e | 0.068 (–0.13 to 0.15) | ||
The EQ-5D findings showed modest improvements in quality of life between the baseline and outcome assessment points. These small improvements are to be expected, given the broad nature of quality-of-life measurements and the lack of severe physical and mental health disabilities in the parents involved in this study. A key reason for including these measures was their utility for health economic analyses, which are examined in Chapter 13. After adjusting for the baseline EQ-5D score and for the change in crying, the change in the quality-of-life scores from baseline in the referred crying group was not significantly different from the change in the new birth visit group (mean difference 0.0053, 95% CI –0.40 to 0.05).
The observed EPDS summary scores indicated that postnatal depression was lower in both groups at follow-up. The summary scores for the GAD-7 anxiety questionnaire and the Maternal Confidence Questionnaire also showed that both groups had lower anxiety and greater parenting confidence, respectively, at follow-up. The mean scores at outcome assessment [EPDS mean score of 7 (SD 4.6); GAD-7 mean score of 3.3 (SD 3.3)] no longer approximated to the clinical cut-off scores. Expressed as a head count, the number of parents with an EPDS criterion score for depression (≥ 10) halved (from 30 to 15 parents) between the baseline and outcome assessments. Similarly, the number of parents with mild, moderate and severe anxiety reduced from 16, 11 and 4 parents, respectively, at baseline, to 12, 2 and 2 parents, respectively, at outcome assessment. These findings are in keeping with the notion that the impact of infant crying on parents (and vice versa) involves parental mental health and well-being in particular. The associated CIs indicate that similar changes are likely to be found in a future large-scale study with adequate statistical power.
The figures also showed modest increases in parental confidence scores. Although not as substantial as the improvements in anxiety and depression, they are encouraging in so far as the aim is to increase parents’ confidence as part of enhancing parental coping skills and interactions with infants. There is some evidence of an inverse relationship between parental confidence and depression,49 which can be assessed more thoroughly in a future large-scale trial.
In summary, these psychometric findings indicate that measures of parental mental health and well-being should have a central role in future research in this area. They also identify methods that are suitable for such a study. In addition, the findings have implications for theoretical understanding and for health service practice. On the theoretical side, the association between excessive infant crying and maternal depression and anxiety is well known, but there is little consensus about the direction of causation. For example, a recent study27 concluded that maternal anxiety during pregnancy predicted excessive infant crying. The present study was not designed to provide causal information and the absence of a control group, in particular, prevents a conclusion regarding whether the reductions in parental anxiety and depression that were observed between baseline and outcome measurements were attributable to the study’s parental support package, to reductions in infant crying that would be expected with infant development or to the passage of time. What the findings indicate is that levels of parental depression and anxiety, as measured, did reduce in substantial numbers of parents during this relatively short period of postnatal experience. The implication is that, if similar findings emerge from an adequately powered RCT, the findings will increase our knowledge of causation. One plausible theoretical viewpoint is that excessive infant crying provides a stressor that triggers the onset of anxiety and depression, and reduces coping, in vulnerable parents. To examine this theory, a future study would need to track infant crying and parental well-being over time, at least until the crying subsides, in treated (i.e. website, booklet and CBT programme) and control groups. A specified model of change, which sets out how the processes involved are expected to work and includes, for instance, measures of parental coping behaviours, parent–infant interaction and relational measures, such as attachments, could be used to provide evidence to advance scientific knowledge still further.
Equally, the findings from this part of the study have implications for health services. There is reliable evidence that CBT programmes can help to reduce postnatal depression and anxiety in some parents. For the most part, programmes of this type target parental cognitive, emotional and behavioural processes, but do not take environmental factors, such as excessive infant crying, into account. For at least a subgroup of parents, the promise of the findings here is that support programmes that include coping with infant crying will be particularly effective in enhancing parental mental health.
Sleep adequacy
Table 19 provides outcome and change measures of sleep adequacy for parents of excessively crying babies. Both groups of parents reported increased sleep, amounting to an average increase of 1 hour and 6 minutes per 24 hours at the outcome measurement. Both groups also improved their sleep quality, so that the number reporting fairly bad or bad sleep quality halved at the outcome assessment point. These figures reinforce the conclusion that measures of parental sleep amount and quality should be included in future studies.
| Sleep adequacy | Group | All cases | |
|---|---|---|---|
| Referred crying | New birth visit | ||
| Number of hours of parental sleep per night | |||
| Baseline/outcome assessment (n) | 30/26 | 27/24 | 57/50 |
| Baseline, mean (SD) | 5.5 (1.5) | 5.1 (1.0) | 5.3 (1.3) |
| Outcome, mean (SD) | 6.3 (1.5) | 6.4 (1.0) | 6.4 (1.3) |
| Number of hours of parental sleep per 24 hours | |||
| Baseline/outcome assessment (n) | 28/25 | 24/25 | 52/50 |
| Baseline, mean (SD) | 6.0 (1.5) | 5.9 (0.9) | 5.9 (1.3) |
| Outcome, mean (SD) | 6.5 (1.3) | 6.9 (1.2) | 6.7 (1.3) |
| Parental sleep quality rating | |||
| Baseline/outcome assessment (n) | 29/27 | 27/25 | 56/52 |
| Rating, n (%) | |||
| Baseline very good | 2 (6.7) | 0 (0) | 2 (3.6) |
| Outcome very good | 4 (14.8) | 3 (12.0) | 7 (13.5) |
| Baseline fairly good | 12 (40.0) | 14 (51.9) | 26 (46.4) |
| Outcome fairly good | 16 (59.3) | 19 (76.0) | 35 (67.3) |
| Baseline fairly bad | 12 (40.0) | 10 (37.0) | 22 (39.3) |
| Outcome fairly bad | 5 (18.5) | 3 (12.0) | 8 (15.4) |
| Baseline very bad | 4 (13.3) | 3 (11.1) | 7 (12.5) |
| Outcome very bad | 2 (7.4) | 0 (0) | 2 (3.9) |
Social support
Figures for the support that partners and friends gave to parents of excessively crying babies at the outcome assessment, together with changes since the baseline measures, are shown in Table 20. As at baseline, the majority of parents in both groups reported receiving enough support from partners (70–83%) and family and friends (72–74%). The figures indicate small but consistent reductions of around 10% in the number of parents who judged that these supports were not enough and who sometimes needed support but could not get it. However, the smaller overall numbers of parents at the outcome assessment complicate this interpretation. The findings’ main implication is to add to the proposal that social support measures need to be included in future controlled studies with large-enough numbers to allow firm conclusions.
| Support measures | Group | All cases | |
|---|---|---|---|
| Referred crying | New birth visit | ||
| Support from partner | |||
| Baseline/outcome assessment (n) | 29/27 | 27/24 | 56/51 |
| Rating, n (%) | |||
| Baseline, enough | 20 (68.9) | 19 (70.4) | 39 (69.6) |
| Outcome, enough | 19 (70.4) | 20 (83.3) | 39 (76.5) |
| Baseline, not enough | 8 (27.6) | 6 (22.2) | 14 (7.1) |
| Outcome, not enough | 5 (18.5) | 3 (12.5) | 8 (15.7) |
| Baseline, none | 1 (3.5) | 1 (3.7) | 2 (3.6) |
| Outcome, none | 0 (0.0) | 1 (4.2) | 1 (2.0) |
| Baseline, do not need | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Outcome, do not need | 3 (11.1) | 0 (0.0) | 3 (5.9) |
| Baseline, prefer not to answer | 0 (0.0) | 1 (3.7) | 1 (1.8) |
| Outcome, prefer not to answer | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Support from family and friends | |||
| Baseline/outcome assessment (n) | 30/27 | 27/25 | 57/52 |
| Rating, n (%) | |||
| Baseline, enough | 21 (70.0) | 19 (70.4) | 40 (70.2) |
| Outcome, enough | 20 (74.1) | 18 (72.0) | 38 (73.1) |
| Baseline, not enough | 7 (23.3) | 7 (25.9) | 14 (24.6) |
| Outcome, not enough | 4 (14.8) | 5 (20.0) | 9 (17.3) |
| Baseline, none | 2 (6.7) | 0 (0.0) | 2 (3.5) |
| Outcome, none | 1 (3.7) | 2 (8.0) | 3 (5.8) |
| Baseline, do not need | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Outcome, do not need | 1 (3.7) | 0 (0.0) | 1 (1.9) |
| Baseline, prefer not to answer | 0 (0.0) | 1 (3.7) | 1 (3.7) |
| Outcome, prefer not to answer | 1 (3.7) | 0 (0.0) | 1 (1.9) |
| How often need support but cannot get it | |||
| Baseline/outcome assessment (n) | 30/27 | 27/25 | 57/52 |
| Rating, n (%) | |||
| Baseline, very often | 3 (10.0) | 0 (0.0) | 3 (5.3) |
| Outcome, very often | 1 (3.7) | 0 (0.0) | 1 (1.9) |
| Baseline, often | 3 (10.0) | 3 (11.1) | 6 (10.5) |
| Outcome, often | 1 (3.7) | 4 (16.0) | 5 (9.6) |
| Baseline, sometimes | 17 (56.7) | 16 (59.3) | 33 (57.9) |
| Outcome, sometimes | 13 (48.2) | 10 (40.0) | 23 (44.2) |
| Baseline, never | 6 (20.0) | 8 (29.6) | 14 (24.6) |
| Outcome, never | 10 (37.0) | 9 (36.0) | 19 (36.5) |
| Baseline, do not need | 1 (3.3) | 0 (0.0) | 1 (1.7) |
| Outcome, do not need | 2 (7.4) | 2 (8.0) | 4 (7.7) |
| Baseline, prefer not to answer | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Outcome, prefer not to answer | 0 (0.0) | 0 (0.0) | 0 (0.0) |
Infants
Crying patterns and impact on parents
Table 21 shows the figures for infant crying, its impact on parents at the outcome assessment, as well as changes in these measures since baseline. Fourteen infants were reported to still be excessively crying at the outcome assessment. However, for those that had stopped crying, on average, the crying lasted for 8 weeks and 3 days. Those infants who were still excessively crying at the outcome assessment had an average age of 15 weeks and 6 days, which implies a need for longer follow-up in future studies. The total time that infants spent fussing and crying per 24 hours halved from the baseline assessment to the outcome assessment, from 6.9 to 2.6 hours.
| Descriptive statistics | Group | All cases | |
|---|---|---|---|
| Referred crying | New birth visit | ||
| Age of baby at baseline/outcome assessment (weeks) | |||
| Baseline/outcome (n) | 25/22 | 27/25 | 52/47 |
| Baseline/outcome mean | 12.8/18.1 | 6.6/12.8 | 9.6/15.3 |
| Baseline/outcome SD | 6.6/6.6 | 1.6/2.7 | 5.6/5.6 |
| Baseline/outcome minimum | 4/9 | 3/9 | 3/9 |
| Baseline/outcome median | 11/16.5 | 7/12 | 7/13 |
| Baseline/outcome maximum | 24/30 | 10/20 | 24/30 |
| Age of baby when excessive crying started/stopped (weeks) | |||
| Baseline/outcome (n) | 25/13 | 27/16 | 52/29 |
| Started/stopped mean | 2.8/14.5 | 3.4/9.6 | 3.1/11.8 |
| Started/stopped SD | 3.6/6.9 | 1.8/2.1 | 2.8/5.4 |
| Started/stopped minimum | 0/7 | 0/7 | 0/7 |
| Started/stopped median | 2/11 | 3/10 | 3/10 |
| Started/stopped maximum | 16/26 | 7/14 | 16/26 |
| Not stopped (n) | 8 | 6 | 14 |
| Total number of hours of fuss/crying in a typical day | |||
| Baseline/outcome (n) | 25/22 | 27/25 | 52/47 |
| Baseline/outcome mean | 6.9/3.0 | 6.9/2.2 | 6.9/2.6 |
| Baseline/outcome SD | 3.5/2.9 | 4.0/1.5 | 3.7/2.3 |
| Baseline/outcome minimum | 1.3/0.3 | 1.8/0.4 | 1.3/0.3 |
| Baseline/outcome median | 6.5/2.1 | 5.5/2.0 | 5.7/2.1 |
| Baseline/outcome maximum | 13.0/13.0 | 17/5.5 | 17.0/13.0 |
| Crying pattern: hours (%) of fuss/crying in each period of a typical day | |||
| Baseline/outcome (n) | 25/22 | 27/25 | 52/47 |
| Morning | |||
| Baseline | 1.6 (21.5) | 1.5 (18.8) | 1.6 (20.1) |
| Outcome | 0.7 (26.3) | 0.6 (24.7) | 0.7 (25.5) |
| Afternoon | |||
| Baseline | 2.2 (34.9) | 1.7 (24.4) | 2.0 (29.5) |
| Outcome | 1.0 (37.5) | 0.7 (30.1) | 0.8 (33.5) |
| Evening | |||
| Baseline | 2.2 (32.6) | 2.4 (38.9) | 2.3 (35.9) |
| Outcome | 0.9 (27.5) | 0.9 (58.1) | 0.9 (43.8) |
| Night | |||
| Baseline | 0.9 (10.9) | 1.3 (19.3) | 1.1 (15.3) |
| Outcome | 0.3 (6.2) | 0.1 (7.6) | 0.2 (6.9) |
Figure 8 demonstrates that the number of parents reporting crying to be a severe or large problem reduced from 27 parents (47%) to three parents (6.5%) at the outcome assessment. Strikingly, this was matched by a drop in the number of parents feeling extremely or very frustrated by the crying from 30 (58%) at baseline to none at the outcome assessment (Figure 9). If frustration is the trigger for infant abuse, as studies indicate,24 this substantial reduction is a particularly promising and encouraging finding. Broadly, across the groups and findings as a whole, the tendency was for parents to report a reduction in the degree of frustration they felt because of their baby’s crying, rather than a complete elimination. These findings emphasised the importance of longer follow-up. In addition, they indicate the need for a larger-scale study with control groups and sufficient numbers, so that the contribution of the support package, and each of its components, can be distinguished from the reductions that happen with time and age.
FIGURE 8.
Impact of babies’ crying on parents at baseline (n = 57) and outcome assessment (n = 52).
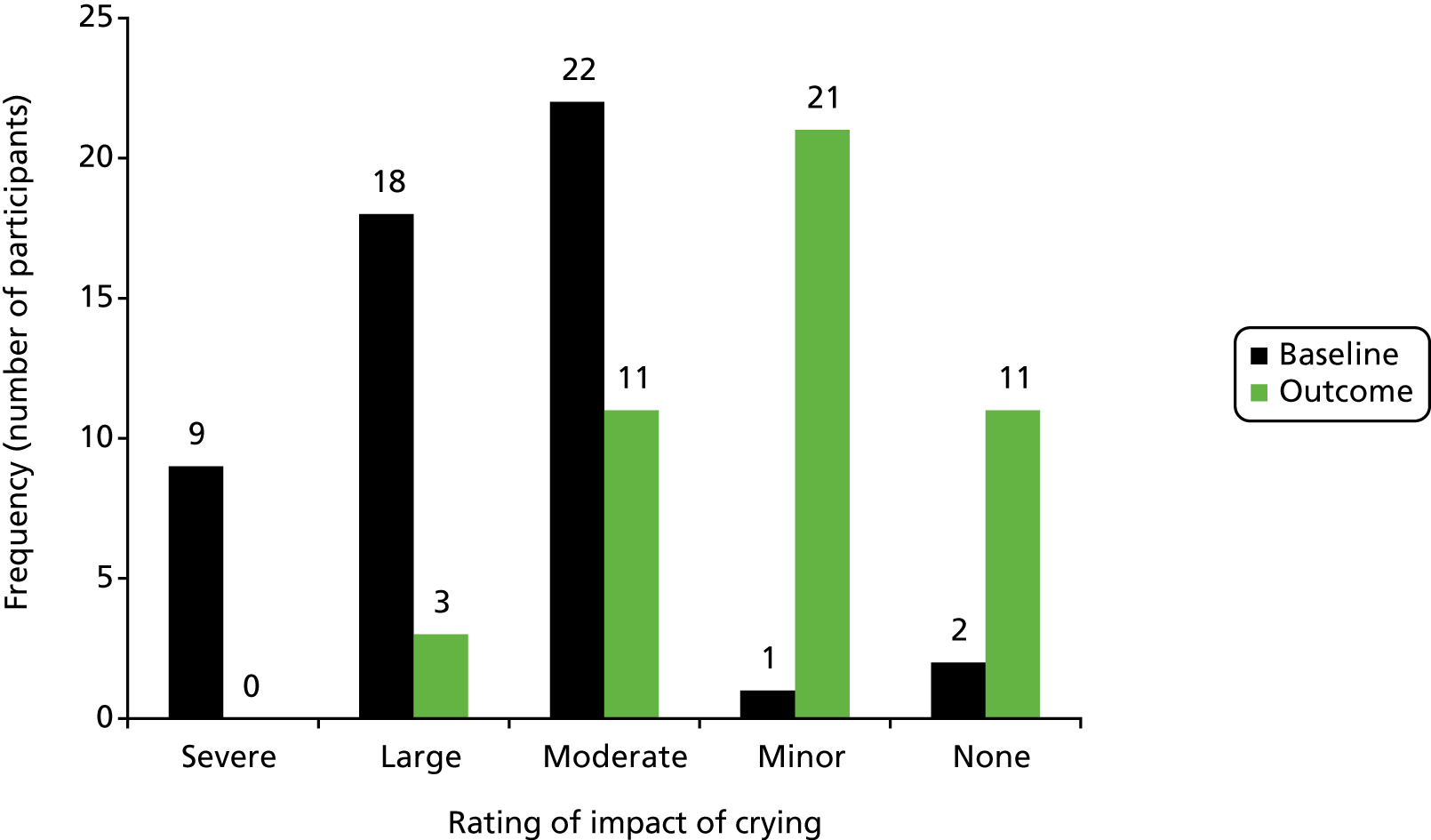
FIGURE 9.
Parents’ frustration at babies’ crying at baseline (n = 57) and outcome assessment (n = 52).
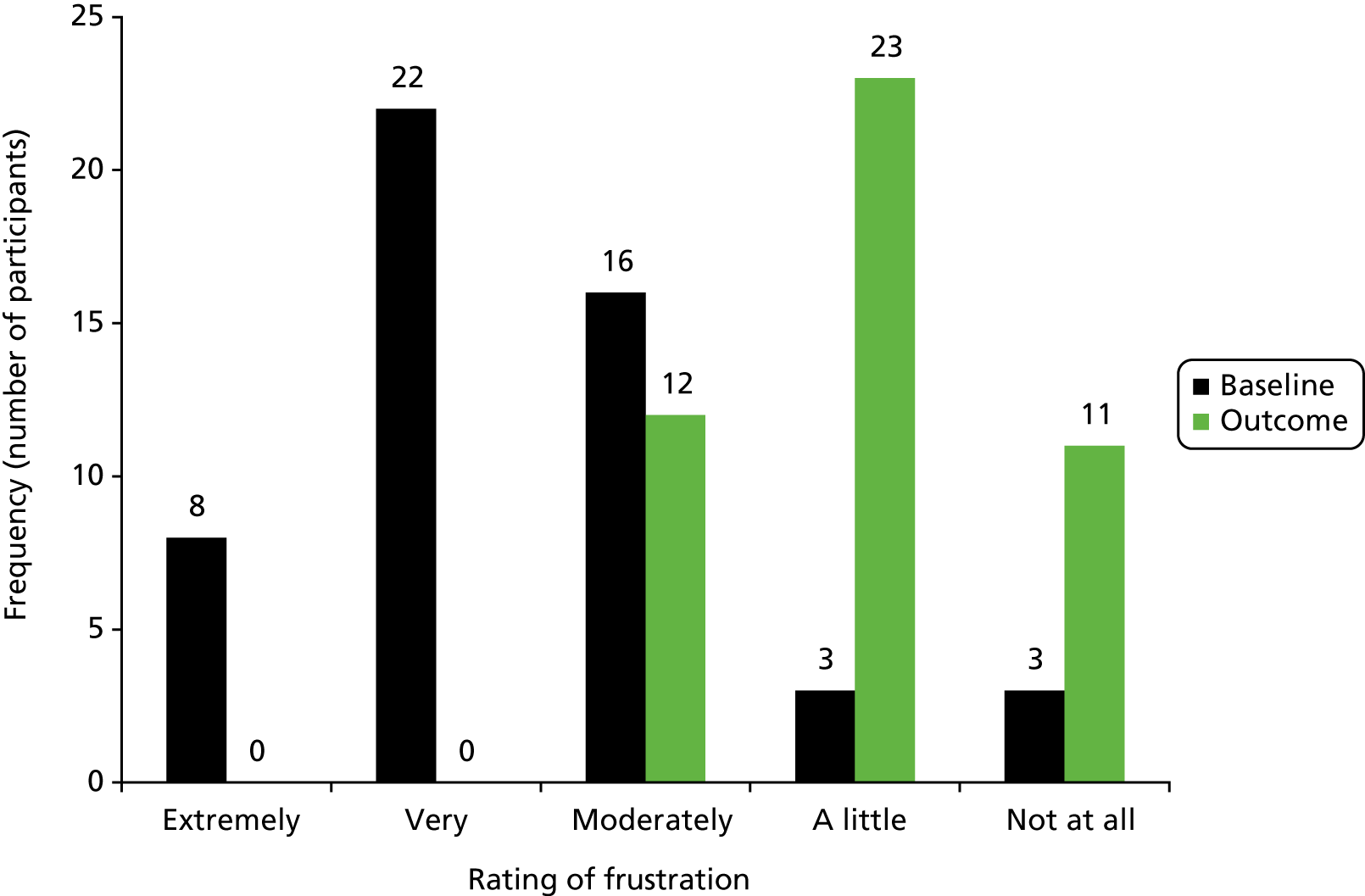
Babies’ feeding
Table 22 shows the figures for babies’ feeding at the outcome assessment, together with changes since baseline. It is worth noting that very little change in breastfeeding and formula-feeding rates was seen between the baseline and outcome assessments. In the 21 cases in which parents reported stopping breastfeeding, the median infant age at this point was 2 weeks. It follows that any effects of infant crying on breastfeeding appeared to happen predominantly at an early age.
| Feeding methods | Group | All cases | |
|---|---|---|---|
| Referred crying | New birth visit | ||
| Feeding method at baseline and outcome assessment, n (%) | |||
| Baseline/outcome (n) | 25/22 | 27/25 | 52/47 |
| Breast milk | |||
| Baseline | 11.0 (44) | 16 (59.3) | 27 (51.9) |
| Outcome | 10 (45.5) | 15 (60.0) | 25 (53.2) |
| Formula milk | |||
| Baseline | 15 (60.0) | 13 (48.2) | 28 (53.9) |
| Outcome | 14 (63.3) | 11 (44.0) | 25 (53.2) |
| Baby solid foods | |||
| Baseline | 2 (8.0) | 0 (0.0) | 2 (3.9) |
| Outcome | 3 (13.6) | 0 (0.0) | 3 (6.4) |
| Family foods | |||
| Baseline | 1 (4.0) | 0 (0.0) | 1 (1.9) |
| Outcome | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Age of baby when breastfeeding stopped (weeks) | |||
| n | 11 | 10 | 21 |
| Mean (SD) | 3.9 (5.5) | 3.3 (1.9) | 3.6 (4.1) |
| Not stopped (n) | 11 | 15 | 26 |
| Missing (n) | 3 | 2 | 5 |
Remedies given, contacts with professionals and babies’ health
Measures of infant health and well-being at the outcome assessment, as well as changes, are shown in Tables 23–25. Parents were asked to provide outcome details solely for the period between the baseline and outcome assessments, that is, to omit instances included in the baseline measures. Measures of HV/SCPHN and GP e-mail or internet contact and GP home visits have been omitted from the table because no parent reported these at baseline or outcome. Notably, the length of the period from birth to baseline assessment and from baseline to outcome assessment is different (a mean interval of 9 weeks and 4 days between birth and baseline and 5 weeks and 5 days between baseline and outcome assessment), so changes in the values given in these tables need to be interpreted with caution.
| Remedies | Group | All cases | |
|---|---|---|---|
| Referred crying | New birth visit | ||
| Remedies for crying | |||
| Baseline/outcome (n) | 25/22 | 27/25 | 52/47 |
| Remedy prescribed by a doctor, n (%) of parents who used this | |||
| Baseline | 12 (48.0) | 5 (18.5) | 17 (32.7) |
| Outcome | 8 (36.4) | 4 (16.0) | 12 (25.5) |
| Number of times used, n (%) | |||
| Baseline: 0 | 13 (52.0) | 22 (81.5) | 35 (67.3) |
| Outcome: 0 | 14 (63.6) | 21 (84.0) | 35 (74.5) |
| Baseline: 1–20 | 2 (8.0) | 1 (3.7) | 3 (5.8) |
| Outcome: 1–20 | 3 (13.6) | 0 (0) | 3 (6.4) |
| Baseline: 21–100 | 4 (16.0) | 3 (11.1) | 7 (13.5) |
| Outcome: 21–100 | 3 (13.6) | 1 (4.0) | 4 (8.5) |
| Baseline: > 100 | 6 (24.0) | 1 (3.7) | 7 (13.5) |
| Outcome: > 100 | 2 (9.1) | 3 (12.0) | 5 (10.6) |
| Change of formula feed, n (%) of parents who used this | |||
| Baseline | 13 (52.0) | 6 (22.2) | 19 (37.3) |
| Outcome | 3 (13.6) | 5 (20.0) | 8 (17.0) |
| Number of times used, n (%) | |||
| Baseline: 0 | 12 (48.0) | 21 (77.8) | 32 (62.8) |
| Outcome: 0 | 19 (86.4) | 20 (80.0) | 39 (83.0) |
| Baseline: 1/2 | 8 (33.3) | 4 (14.8) | 12 (23.5) |
| Outcome: 1/2 | 3 (13.6) | 3 (12.0) | 6 (12.8) |
| Baseline: > 2 | 5 (20.8) | 2 (7.4) | 7 (13.7) |
| Outcome: > 2 | 0 (0) | 2 (8.0) | 2 (4.3) |
| Colic drops, n (%) of parents who used this | |||
| Baseline | 20 (80.0) | 18 (66.7) | 38 (73.1) |
| Outcome | 3 (13.6) | 5 (20.0) | 8 (17.0) |
| Number of times used, n (%) | |||
| Baseline: 0 | 5 (20.0) | 9 (33.3) | 14 (26.9) |
| Outcome: 0 | 19 (86.4) | 20 (80.0) | 39 (83.0) |
| Baseline: 1–20 | 1 (4.0) | 5 (18.5) | 6 (11.5) |
| Outcome: 1–20 | 1 (4.6) | 1 (4.0) | 2 (4.3) |
| Baseline: 21–100 | 6 (24.0) | 1 (3.7) | 7 (13.5) |
| Outcome: 21–100 | 0 (0) | 2 (8.0) | 2 (4.3) |
| Baseline: > 100 | 13 (52.0) | 12 (44.4) | 25 (48.1) |
| Outcome: > 100 | 2 (9.1) | 2 (8.0) | 4 (8.5) |
| Herbal remedies, n (%) of parents who used this | |||
| Baseline | 4 (16.0) | 3 (11.5) | 7 (13.7) |
| Outcome | 2 (9.1) | 2 (8.0) | 4 (8.5) |
| Number of times used, n (%) | |||
| Baseline: 0 | 21 (84.0) | 23 (88.5) | 44 (86.3) |
| Outcome: 0 | 20 (90.9) | 23 (92.0) | 43 (91.5) |
| Baseline: 1/2 | 2 (8.0) | 1 (3.9) | 3 (5.9) |
| Outcome: 1/2 | 1 (4.6) | 1 (4) | 2 (4.3) |
| Baseline: > 2 | 2 (8.0) | 2 (7.7) | 4 (7.8) |
| Outcome: > 2 | 1 (4.6) | 1 (4.0) | 2 (4.3) |
| Chiropractor, n (%) of parents who used this | |||
| Baseline | 1 (4.0) | 0 (0.0) | 1 (2.0) |
| Outcome | 0 (0) | 0 (0) | 0 (0) |
| Number of times used, n (%) | |||
| Baseline: 0 | 24 (96.0) | 27 (100.0) | 51 (98.1) |
| Outcome: 0 | 22 (100) | 25 (100) | 47 (100) |
| Other, n (%) of parents who used this | |||
| Baseline | 20 (83.3) | 11 (47.8) | 31 (66.0) |
| Outcome | 8 (38.1) | 11 (45.8) | 19 (42.2) |
| Number of times used, n (%) | |||
| Baseline: 0 | 4 (16.7) | 12 (52.2) | 16 (34.0) |
| Outcome: 0 | 13 (61.9) | 13 (54.2) | 26 (57.8) |
| Baseline: 1–20 | 6 (25.0) | 5 (21.7) | 11 (23.4) |
| Outcome: 1–20 | 4 (19.1) | 6 (25.0) | 10 (22.2) |
| Baseline: 21–100 | 4 (16.7) | 5 (21.7) | 9 (19.2) |
| Outcome: 21–100 | 2 (9.5) | 4 (16.7) | 6 (13.3) |
| Baseline: > 100 | 10 (41.7) | 1 (4.4) | 11 (23.4) |
| Outcome: > 100 | 2 (9.5) | 1 (4.2) | 3 (6.7) |
| Contacts | Group | All cases | |
|---|---|---|---|
| Referred crying | New birth visit | ||
| Contacts with health-care professionals because of excessive infant crying | |||
| Baseline/outcome (n) | 25/22 | 27/25 | 52/47 |
| HV visited at home, n (%) of parents who had visits | |||
| Baseline | 21 (84.0) | 17 (63.0) | 38 (73.1) |
| Outcome | 1 (4.6) | 4 (16.0) | 5 (10.6) |
| Number of times, n (%) | |||
| Baseline: 0 | 4 (16.0) | 10 (37.0) | 14 (26.9) |
| Outcome: 0 | 21 (95.5) | 21 (84.0) | 42 (89.4) |
| Baseline: 1/2 | 8 (32.0) | 13 (48.2) | 21 (40.4) |
| Outcome: 1/2 | 1 (4.6) | 3 (12.0) | 4 (8.5) |
| Baseline: > 2 | 13 (52.0) | 4 (14.8) | 17 (32.7) |
| Outcome: > 2 | 0 (0) | 1 (4.0) | 1 (2.1) |
| Went to HV clinic, n (%) of parents who did this | |||
| Baseline | 8 (32.0) | 2 (7.4) | 10 (19.2) |
| Outcome | 3 (13.6) | 4 (16.0) | 7 (14.9) |
| Number of times used, n (%) | |||
| Baseline: 0 | 17 (68.0) | 25 (92.6) | 42 (80.8) |
| Outcome: 0 | 19 (86.4) | 21 (84.0) | 40 (85.1) |
| Baseline: 1/2 | 6 (24.0) | 1 (3.7) | 7 (13.5) |
| Outcome: 1/2 | 3 (13.6) | 4 (16.0) | 7 (14.9) |
| Baseline: > 2 | 2 (8.0) | 1 (3.7) | 3 (5.8) |
| Outcome: > 2 | 0 (0) | 0 (0) | 0 (0) |
| HV telephone call, n (%) of parents who had this | |||
| Baseline | 17 (68.0) | 7 (25.9) | 24 (46.2) |
| Outcome | 3 (13.6) | 2 (8.0) | 5 (10.6) |
| Number of times used | |||
| Baseline: 0 | 8 (32.0) | 20 (74.1) | 28 (53.9) |
| Outcome: 0 | 19 (86.4) | 23 (92.0) | 42 (89.4) |
| Baseline: 1/2 | 11 (44.0) | 7 (25.9) | 18 (34.6) |
| Outcome: 1/2 | 3 (13.6) | 1 (4.0) | 4 (8.5) |
| Baseline: > 2 | 6 (24.0) | 0 (0) | 6 (11.5) |
| Outcome: > 2 | 0 (0) | 1 (4.0) | 1 (2.1) |
| Went to GP surgery, n (%) of parents who did this | |||
| Baseline | 17 (68.0) | 9 (33.3) | 26 (50.0) |
| Outcome | 5 (22.7) | 5 (20.0) | 10 (21.3) |
| Number of times used, n (%) | |||
| Baseline: 0 | 8 (32.0) | 18 (66.7) | 26 (50.0) |
| Outcome: 0 | 17 (77.3) | 20 (80.0) | 37 (78.7) |
| Baseline: 1/2 | 11 (44.0) | 7 (25.9) | 18 (34.6) |
| Outcome: 1/2 | 4 (18.2) | 4 (16.0) | 8 (17.0) |
| Baseline: > 2 | 6 (24.0) | 2 (7.4) | 8 (15.4) |
| Outcome: > 2 | 1 (4.6) | 1 (4.0) | 2 (4.3) |
| GP telephone call, n (%) of parents who did this | |||
| Baseline | 4 (16.0) | 3 (11.1) | 7 (13.5) |
| Outcome | 1 (4.6) | 1 (4.0) | 2 (4.3) |
| Number of times used, n (%) | |||
| Baseline: 0 | 21 (84.0) | 24 (88.9) | 45 (86.5) |
| Outcome: 0 | 21 (95.5) | 24 (96.0) | 45 (95.7) |
| Baseline: 1/2 | 4 (16.0) | 3 (11.1) | 7 (13.5) |
| Outcome: 1/2 | 1 (4.6) | 0 (0) | 1 (2.1) |
| Baseline: > 2 | 0 (0) | 0 (0) | 0 (0) |
| Outcome: > 2 | 0 (0) | 1 (4.0) | 1 (2.1) |
| Other home visitor, n (%) of parents who did this | |||
| Baseline | 4 (16.0) | 2 (7.4) | 6 (11.5) |
| Outcome | 2 (9.1) | 1 (4.0) | 3 (6.4) |
| Number of times used, n (%) | |||
| Baseline: 0 | 21 (84.0) | 25 (92.6) | 46 (88.5) |
| Outcome: 0 | 20 (90.9) | 24 (96.0) | 44 (93.6) |
| Baseline: 1/2 | 3 (12.0) | 1 (3.7) | 4 (7.7) |
| Outcome: 1/2 | 1 (4.6) | 1 (4.0) | 2 (4.3) |
| Baseline: > 2 | 1 (4.0) | 1 (3.7) | 2 (3.9) |
| Outcome: > 2 | 1 (4.6) | 0 (0) | 1 (2.1) |
| Visited other, n (%) of parents who did this | |||
| Baseline | 10 (40.0) | 3 (11.1) | 13 (25.0) |
| Outcome | 4 (18.2) | 3 (12.0) | 7 (14.9) |
| Number of times used, n (%) | |||
| Baseline: 0 | 15 (60.0) | 24 (88.9) | 39 (75.0) |
| Outcome: 0 | 18 (81.8) | 22 (88.0) | 40 (85.1) |
| Baseline: 1/2 | 8 (32.0) | 2 (7.4) | 10 (19.2) |
| Outcome: 1/2 | 3 (13.6) | 2 (8.0) | 5 (10.6) |
| Baseline: > 2 | 2 (8.0) | 1 (3.7) | 3 (5.8) |
| Outcome: > 2 | 1 (4.6) | 1 (4.0) | 2 (4.3) |
| Other telephone call, n (%) of parents who did this | |||
| Baseline | 4 (16.0) | 0 (0) | 4 (7.7) |
| Outcome | 0 (0) | 1 (4.0) | 1 (2.1) |
| Number of times used, n (%) | |||
| Baseline: 0 | 21 (84.0) | 27 (100.0) | 48 (92.3) |
| Outcome: 0 | 22 (100) | 24 (96.0) | 46 (97.9) |
| Baseline: 1/2 | 3 (12.0) | 0 (0) | 3 (5.8) |
| Outcome: 1/2 | 0 (0) | 1 (4.0) | 1 (2.1) |
| Baseline: > 2 | 1 (4.0) | 0 (0) | 1 (1.9) |
| Outcome: > 2 | 0 (0) | 0 (0) | 0 (0) |
| Other e-mail or internet contact, n (%) of parents who did this | |||
| Baseline | 0 (0) | 1 (3.7) | 1 (1.9) |
| Outcome | 0 (0) | 0 (0) | 0 (0) |
| Number of times used, n (%) | |||
| Baseline: 0 | 25 (100) | 26 (96.3) | 51 (98.1) |
| Outcome: 0 | 22 (100) | 25 (100) | 47 (100) |
| Baseline: 1/2 | 0 (0) | 0 (0) | 0 (0) |
| Outcome: 1/2 | 0 (0) | 0 (0) | 0 (0) |
| Baseline: > 2 | 0 (0) | 1 (3.7) | 1 (1.9) |
| Outcome: > 2 | 0 (0) | 0 (0) | 0 (0) |
| Other internet resources, n (%) of parents who did this | |||
| Baseline | 20 (80.0) | 21 (77.8) | 41 (78.9) |
| Outcome | 9 (40.9) | 8 (32.0) | 17 (36.2) |
| Number of times used, n (%) | |||
| Baseline: 0 | 5 (20.0) | 6 (22.2) | 11 (21.2) |
| Outcome: 0 | 13 (59.1) | 17 (68.0) | 30 (63.8) |
| Baseline: 1–20 | 13 (52.0) | 12 (44.4) | 25 (48.1) |
| Outcome: 1–20 | 4 (18.2) | 6 (24.0) | 10 (21.3) |
| Baseline: 21–100 | 4 (16.0) | 7 (25.9) | 11 (21.2) |
| Outcome: 21–100 | 5 (22.7) | 2 (8.0) | 7 (14.9) |
| Baseline: > 100 | 3 (12.0) | 2 (7.4) | 5 (9.6) |
| Outcome: > 100 | 0 (0) | 0 (0) | 0 (0) |
| Infant health measures | Group, n (%) | All cases, n (%) | |
|---|---|---|---|
| Referred crying | New birth visit | ||
| Additional problems | |||
| Baseline/outcome (n) | 25/22 | 27/25 | 52/47 |
| Fever | |||
| Baseline | 1 (4.0) | 3 (11.1) | 4 (7.7) |
| Outcome | 1 (4.6) | 1 (4.0) | 2 (4.3) |
| Seemed unwell | |||
| Baseline | 6 (24.0) | 6 (22.2) | 12 (23.1) |
| Outcome | 4 (18.2) | 2 (8.0) | 6 (12.8) |
| Weight gain concerns | |||
| Baseline | 3 (12.0) | 4 (14.8) | 7 (13.5) |
| Outcome | 3 (13.6) | 5 (20.0) | 8 (17.0) |
| Feeding problems | |||
| Baseline | 9 (36.0) | 12 (44.4) | 21 (40.0) |
| Outcome | 4 (18.2) | 8 (32.0) | 12 (25.5) |
| Vomiting | |||
| Baseline | 12 (48.0) | 14 (51.9) | 26 (50.0) |
| Outcome | 7 (31.8) | 12 (48) | 19 (40.4) |
| Any other signs of illness in the previous fortnight | |||
| Baseline | 6 (24.0) | 12 (44.4) | 18 (34.6) |
| Outcome | 8 (36.4) | 10 (40.0) | 18 (38.3) |
| Seen a GP or other doctor in the previous fortnight for anything other than crying | |||
| Baseline | 9 (36.0) | 17 (63.0) | 26 (50.0) |
| Outcome | 9 (40.9) | 8 (32.0) | 17 (36.2) |
With a few exceptions, the figures indicated improved infant health, reduced contacts with professionals and reduced use of remedies at outcome assessment, compared with baseline (see Tables 23–25). The reductions in the number of HV/SCPHN home visits (from 73% to 11% of parents) and telephone contacts (from 46% to 11% of parents) because of excessive infant crying are substantial, as is the reduced number of visits to GP surgeries (from 50% to 21% of parents) for this reason (see Table 24). Potentially, these figures identify worthwhile benefits and cost savings for families and health services because of the intervention package. However, the figures are difficult to interpret because of differences in the periods of time addressed by the baseline and outcome measures, the reduced numbers providing outcome measures, the dependency on parental reports and the lack of a control group or groups needed to distinguish the effects of the support package from the effects of time and infant age. The implication is to point to the need for a future large-scale controlled trial that enables these factors to be distinguished. Because the figures in both these and the previous tables suggested that excessive infant crying and its impact on parents were continuing, albeit at reduced levels, at the outcome assessment point, an extended follow-up duration until after the crying resolves should also be included in future studies.
Parents’ knowledge of infant crying
To establish whether or not parents’ knowledge of infant crying had been increased by the support package, parents were asked about information included in the package materials, using five questions adapted from the study by Barr et al. 53 Table 26 shows the questions and parents’ answers. Some parents (10–56%) knew some answers before taking part in the study, whereas others (0–14%) reported that this was new information for them, despite its inclusion in the study support materials. The implication that some parents did not access or retain some of the package information is supported by the website access figures shown below. Parents gained some knowledge about infant crying from HVs/SCPHNs. However, 32–64% of parents acquired this knowledge from the support package materials, substantially more than those who acquired it from HVs/SCPHNs (6–14%). The implication is that it will be worthwhile to include these questions, and possibly to assess parents’ knowledge in other ways, in future studies. Whether or not the website and other package elements can be improved to deliver this information more effectively also needs to be considered.
| Measures | Response, n (%) | |||
|---|---|---|---|---|
| This is new to me | Learned in study | Learned from HV/SCPHN | Already knewa | |
| Referred crying group (N = 26) | ||||
| Infant crying reaches a peak in the first 2 or 3 months before getting less | 3 (11.5) | 12 (46.2) | 6 (23.1) | 5 (19.2) |
| Infants of this age cry more often in the late afternoon and evening | 1 (3.9) | 9 (34.6) | 4 (15.4) | 12 (46.2) |
| Even healthy infants sometimes cry unexpectedly or without a clear reason | 1 (3.9) | 11 (42.3) | 2 (7.7) | 12 (46.2) |
| Even good parents are sometimes unable to soothe their crying infant | 0 (0.0) | 15 (57.7) | 1 (3.9) | 10 (38.5) |
| It is OK to walk away from a crying infant when his/her crying becomes very frustrating, providing that the baby is in a safe place | 1 (3.9) | 11 (42.3) | 3 (11.5) | 11 (42.3) |
| New birth visit group (N = 24) | ||||
| Infant crying reaches a peak in the first 2 or 3 months before getting less | 4 (16.7) | 20 (83.3) | 0 (0.0) | 0 (0.0) |
| Infants of this age cry more often in the late afternoon and evening | 1 (4.2) | 15 (62.5) | 2 (8.3) | 6 (25.0) |
| Even healthy infants sometimes cry unexpectedly or without a clear reason | 0 (0.0) | 5 (20.8) | 3 (12.5) | 16 (66.7) |
| Even good parents are sometimes unable to soothe their crying infant | 0 (0.0) | 6 (25.0) | 2 (8.3) | 16 (66.7) |
| It is OK to walk away from a crying infant when his/her crying becomes very frustrating, providing that the baby is in a safe place | 3 (12.5) | 10 (41.7) | 4 (16.7) | 7 (29.2) |
| All parents (N = 50) | ||||
| Infant crying reaches a peak in the first 2 or 3 months before getting less | 7 (14.0) | 32 (64.0) | 6 (12.0) | 5 (10.0) |
| Infants of this age cry more often in the late afternoon and evening | 2 (4.0) | 24 (48.0) | 6 (12.0) | 18 (36.0) |
| Even healthy infants sometimes cry unexpectedly or without a clear reason | 1 (2.0) | 16 (32.0) | 5 (10.0) | 28 (56.0) |
| Even good parents are sometimes unable to soothe their crying infant | 0 (0.0) | 21 (42.0) | 3 (6.0) | 26 (52.0) |
| It is OK to walk away from a crying infant when his/her crying becomes very frustrating, providing that the baby is in a safe place | 4 (8.0) | 21 (42.0) | 7 (14.0) | 18 (36.0) |
Chapter 11 Parental use of the Surviving Crying materials
Parents could choose which of the support package materials they used and how often they used them. Fifty-five participants chose the website, 32 chose CBT sessions with the study practitioner and 27 chose to have the information in the form of a printed booklet. Of the 57 participants who opted to receive the support package, 49 (86%) reported using at least one of the three study components (i.e. website, information booklet and CBT programme). There were no statistically significant differences in the package components used between the two participant groups so the data are presented combined.
The website, accessed on a computer/tablet computer and mobile phone, was the most commonly used package component, accessed by 30 individual participants: four participants had accessed the website on both a computer/tablet computer and a mobile phone, 15 used just a computer/tablet computer to access it and 11 used just their mobile phone to access the website.
Detailed Google Analytics data for website access
Google Analytics software automatically monitors website access and gives detailed figures for website usage. Data for the period from 12 April to 21 December 2016 (the period when participants were active in the study) were examined. A limitation of this software is that figures are kept anonymously for parents as a whole – they do not allow individual use to be tracked, for instance, to measure how often an individual parent revisited the website or how their visits varied.
As Table 27 shows, 34 parents accessed the website and, in total, they had 54 sessions, indicating that some parents visited the website on more than one occasion. (Google Analytics defines a session as a group of interactions that take place on a website within a given time frame. If a user remains logged into the website but is inactive for > 30 minutes then the session ends. If they then return to looking at the website after 30 minutes has passed, this will count as a new session. In addition, a session is considered to end at midnight, so if a user is logged into the website as midnight passes then this will be considered as two sessions.) Over the 54 sessions, parents viewed 325 unique pages, giving an average of 6.02 unique page views per session.
| Measures of use | Usage values |
|---|---|
| Number of users | 34 |
| Number of sessions | 54 |
| Number of page views | 425 |
| Mean number of page views per session | 7.87 |
| Number of unique page views | 325 |
| Mean number of unique page views per session | 6.02 |
| Mean length of session | 6 minutes and 1 second |
| Mean length of page view | 1 minute and 27 seconds |
Table 28 shows the 10 pages that had the most unique page views within a session. Noticeably, many of the pages that were designed to give parents information are in the top 10 pages.
| Page | Unique number of page views within a session, n (%) |
|---|---|
| Log-in page | 74 (22.8) |
| Home page | 46 (14.2) |
| Settling and Soothing Your Baby | 26 (8.0) |
| Your Stories | 18 (5.5) |
| News and Research | 16 (4.9) |
| Health Checklist | 18 (5.5) |
| Why Do Babies Cry Excessively | 17 (5.2) |
| Is it Colic | 15 (4.6) |
| Coping Tips for Parents | 14 (4.3) |
| Can Parents Stop the Crying | 8 (2.5) |
The average time parents spent viewing one page was 1 minute 27 seconds; however, some pages were viewed for substantially longer. Table 29 provides details for the 10 pages with the highest average time spent on a page. Noticeably, three of the pages with the longest average viewing time were parent stories.
| Page | Average length of view (minutes) |
|---|---|
| Need Help Now | 10.22 |
| Mina’s Story (video) | 9.20 |
| Coping Tips | 3.38 |
| Surviving as a Family | 3.02 |
| Alison’s Story | 2.33 |
| Can Parents Stop the Crying | 2.31 |
| Settling and Soothing | 2.17 |
| Is it Colic | 2.11 |
| Waking and Crying at Night | 2.06 |
| Suzanne’s Story | 2.02 |
Devices used to access the website
The Google Analytics data showed that parents mostly used mobile phones (n = 31, 57.4%) and tablet computers (n = 17, 31.5%) to access the website, with a small number (n = 6, 11.1%) using a desktop/laptop computer.
Detailed figures for parental use of the practitioner cognitive–behavioural therapy support sessions
A total of 32 parents originally requested support from the CBT practitioner. Seven parents did not actually see the CBT practitioner for various reasons (Figure 10). Twenty-five parents went on to book a support session (21 females and 4 males), although one parent did not attend any sessions; thus, 24 parents actually received support sessions from a CBT practitioner.
FIGURE 10.
Support sessions take-up rates.

Although the original intention had been to offer group sessions when possible, in practice, owing to the large geographical area covered and the rate at which parents consented to the study, it was not possible to set up any group sessions. All sessions were delivered either one to one or to couples, with some parents having a mix of one-to-one and couple sessions.
A total of 40 sessions were delivered to participants in the study. Most sessions (n = 38) were provided by the study CBT practitioner, and two were provided by her colleague, a trainee counselling psychologist. Table 30 shows the number of sessions parents received. Parents were able to have up to five sessions. In practice, most opted to have one or two and none opted to have five sessions. On average, participants in the study received 1.8 sessions with a range of 1 to 4 sessions (SD 0.91). Sessions were planned to last for 1 hour but in practice some were longer than this. The mean session length was 1 hour and 6 minutes (range 45 minutes to 1 hour and 45 minutes, SD 0.2 hours). All sessions took place in the parents’ homes.
| Number of sessions | Type of session (number of parents) | |
|---|---|---|
| One to one | Couple | |
| 1 | 10 | 2 |
| 2 | 6 | 4 |
| 3 | 3 | 0 |
| 4 | 1 | 0 |
Couples and family members
Five couples requested CBT support. Six sessions were planned to be delivered as couple sessions to participants, both of whom consented to take part in the study. One parent did not attend their only booked couple session, but their partner did go on to receive one-to-one sessions. Two couples (four parents) were seen only as a couple, whereas the other two couples had a combination of both couple and one-to-one sessions. Noticeably, males only attended couple sessions; no males requested or received one-to-one sessions. In addition, family members who were not participants in the study were unexpectedly present at five further sessions that were planned as one-to-one sessions (four were participants’ partners, but in one case a participant’s mother and sister also attended).
Most sessions (93%) had at least one child in attendance, with 22% of sessions having two or more children in attendance and, as mentioned above, five sessions included other adults who were not study participants. These figures highlight the complications involved in delivering an intervention in a family home. However, in spite of this, the CBT practitioners delivering the support sessions reported that the sessions largely went as planned.
Although the first two support sessions were planned to cover pre-set topics to establish the core CBT ideas and techniques underpinning the intervention, parents were able to choose which (if any) supplementary topics they would like to be covered. For parents who already had some understanding of the core CBT ideas and techniques, the CBT practitioners were able to cover supplementary topics in the parents’ first session. Table 31 shows which supplementary topics parents received. The majority of parents chose the relaxation and diaphragmatic breathing and more than half of parents chose arranging social supports and asking for help when needed.
| Topic | Parents, n (%) |
|---|---|
| How to manage the stress of a baby’s unsoothable crying | 11 (46) |
| Arranging social supports and asking for help when needed | 13 (54) |
| Relaxation and diaphragmatic breathing | 18 (75) |
| Getting good-enough sleep and exercise | 2 (8) |
| Others | |
| Self-care | 2 (8) |
| Planning for mum’s return to work | 1 (4) |
| Unknown | 1 (4) |
Parents who attended more than one support session were given activities to practise the work that had been covered by the CBT practitioner in between sessions. Of the 21 parents who went on to attend more than one session, 18 had completed their home activities, two had tried but been unable to complete their home activities and one parent had not carried out any home activities.
Cognitive–behavioural therapy practitioners’ views on the sessions
The CBT practitioners rated 97% of the sessions as highly or moderately successful and wrote free-text comments to highlight key aspects of the sessions. They reported that, in a few instances, some early clarification and discussion with participants about the sessions was necessary. One couple initially had ‘a lot of questions and concerns’, and two parents had expectations that the session would focus on the baby’s crying. For one parent, the practitioners reported that this affected the session outcome to some degree, and the other was ‘happy to focus on herself once explained’.
The CBT practitioners noted that parents generally seemed to engage well with the sessions and the material, and were highly motivated and open to making changes in their lives (17 of 24 parents). Parents reportedly focused on the session content, although in a few instances this was a considerable challenge owing to the distraction of their baby or other children:
Whilst the baby cried throughout the session, both parents listened and contributed to the session. Both appeared very motivated to make changes.
When parents were introduced to the CBT model, practitioners reported that parents appeared to be able to understand this readily and to relate it to their own thoughts and experiences (18 of 24 parents). In two instances, parents had prior knowledge of CBT that they could draw on, and two others were already using some of the recommended strategies without describing this as CBT. In addition to general observations relating to taking the theory on board, the practitioners sometimes noted specifically how parents were able to identify negative thinking patterns (five parents), the importance of self-care and support (three parents) and the need to be more assertive (two parents):
. . . understood the theory and talked about wanting help to say ‘no’ or direct others’ help.
They had previous experience/understanding of CBT. We talked of the principles and looked at the importance of self-care and how to restart strategies which were helpful to [participant] in the past.
The issue of self-care and parents trying to focus on their own needs was highlighted frequently by the practitioners (15 of 24 parents). As a result, for a number of parents, the sessions included relaxation techniques or looking at how to get the right support from others. In two instances, a tension between housework and self-care was identified, with parents struggling to be kind to themselves as a result of trying to be ‘perfect’. For a few others, the sessions explored the challenges of trying to manage the balance between meeting their partner’s needs and their own:
Discussed how to support each other in a different way as both seem so keen on supporting the other they are not wanting to take time for themselves, or if they do they feel very guilty.
In addition to offering strategies for change, the CBT practitioners reported that for a few parents the sessions provided a valuable space to talk about how they were feeling. A number were struggling with low mood or feeling overwhelmed, and this was affecting their motivation to make changes. In two instances, this led to the CBT practitioner encouraging the parents to access further support for their mental health; one parent took action as a result of this and the other was planning to do so in their last session:
. . . talked about things which she said she hadn’t talked to anyone about and found it very useful.
. . . able to identify that she was struggling with her emotions and may benefit from further support. Will contact her GP.
In later sessions, the CBT practitioners’ impression was that many parents (n = 11) reported benefits arising from having made changes in their thinking and behaviour, even though in some instances their babies continued to cry excessively. Some had shared their learning with their partner or both partners had made changes as a result of their sessions together. Others were finding ways of taking time for themselves and for relaxation, and were planning further changes:
Relaxation/breathing exercises working. Has changed how she thinks and is more relaxed. Discussed how she can get the best support from mum and sister.
[Participant] had spent some time for herself, and her mum had looked after children so she and her partner could have an evening together. Could see the benefits and will continue.
Parental evaluation of the usefulness of the Surviving Crying materials
The following sections provide feedback on parents’ ratings of the Surviving Crying materials as a whole, followed by their evaluation of the individual elements of the support package.
As well as their use of the support package materials, parents were asked to provide overall opinions about their usefulness. These findings, which take the form of ratings, are shown in Tables 32 and 33.
| Usefulness | Rating, n (%) | N | |||
|---|---|---|---|---|---|
| Very useful | A bit useful | No opinion | Not useful | ||
| Referred crying group | |||||
| Website accessed by computer/tablet computer | 2 (22.2) | 7 (77.8) | 0 (0) | 0 (0) | 9 |
| Website accessed on mobile phone | 4 (44.4) | 5 (55.6) | 0 (0) | 0 (0) | 9 |
| Spoke face to face with CBT practitioner | 11 (73.3) | 4 (26.7) | 0 (0) | 0 (0) | 15 |
| Spoke on the telephone with CBT practitioner | 4 (80.0) | 0 (0) | 1 (20.0) | 0 (0) | 5 |
| Internet correspondence with a CBT practitioner | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 |
| Read printed materials | 7 (58.3) | 5 (41.7) | 0 (0) | 0 (0) | 12 |
| New birth visit group | |||||
| Website accessed by computer/tablet computer | 4 (40.0) | 6 (60.0) | 0 (0) | 0 (0) | 10 |
| Website accessed on mobile phone | 5 (83.3) | 1 (16.7) | 0 (0) | 0 (0) | 6 |
| Spoke face to face with CBT practitioner | 9 (100) | 0 (0) | 0 (0) | 0 (0) | 9 |
| Spoke on the telephone to CBT practitioner | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 |
| Internet correspondence with a CBT practitioner | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 |
| Read printed materials | 9 (75.0) | 3 (25.0) | 0 (0) | 0 (0) | 12 |
| All parents | |||||
| Website accessed by computer/tablet computer | 6 (31.6) | 13 (68.4) | 0 (0) | 0 (0) | 19 |
| Website accessed on mobile phone | 9 (60.0) | 6 (40.0) | 0 (0) | 0 (0) | 15 |
| Spoke face to face with CBT practitioner | 20 (83.3) | 4 (16.7) | 0 (0) | 0 (0) | 24 |
| Spoke on the telephone to CBT practitioner | 4 (80.0) | 0 (0) | 1 (20.0) | 0 (0) | 5 |
| Internet correspondence with a CBT practitioner | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 |
| Read printed materials | 16 (66.7) | 8 (33.3) | 0 (0) | 0 (0) | 24 |
| Materials to be routinely included in the NHS | Rating, n (%) | N | |||
|---|---|---|---|---|---|
| Strongly agree | Agree | No opinion | No | ||
| Referred crying group | |||||
| Website accessed by computer/tablet computer | 2 (22.2) | 7 (77.8) | 0 (0) | 0 (0) | 9 |
| Website accessed on mobile phone | 8 (88.9) | 1 (11.1) | 0 (0) | 0 (0) | 9 |
| Spoke face to face to CBT practitioner | 12 (80.0) | 3 (20.0) | 0 (0) | 0 (0) | 15 |
| Spoke on the telephone to CBT practitioner | 4 (80.0) | 1 (20.0) | 0 (0) | 0 (0) | 5 |
| Internet correspondence with a CBT practitioner | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 |
| Read printed materials | 9 (75.0) | 3 (25.0) | 0 (0) | 0 (0) | 12 |
| New birth visit group | |||||
| Website accessed by computer/tablet computer | 8 (80.0) | 2 (20.0) | 0 (0) | 0 (0) | 10 |
| Website accessed on mobile phone | 5 (83.3) | 1 (16.7) | 0 (0) | 0 (0) | 6 |
| Spoke face to face to CBT practitioner | 8 (88.9) | 1 (11.1) | 0 (0) | 0 (0) | 9 |
| Spoke on the telephone to CBT practitioner | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 |
| Internet correspondence with a CBT practitioner | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 |
| Read printed materials | 8 (66.7) | 4 (33.3) | 0 (0) | 0 (0) | 12 |
| All parents | |||||
| Website accessed by computer/tablet computer | 15 (79.0) | 4 (21.1) | 0 (0) | 0 (0) | 19 |
| Website accessed on mobile phone | 13 (86.7) | 2 (13.3) | 0 (0) | 0 (0) | 15 |
| Spoke face to face with CBT practitioner | 20 (83.3) | 4 (16.7) | 0 (0) | 0 (0) | 24 |
| Spoke on the telephone to CBT practitioner | 4 (80.0) | 1 (20.0) | 0 (0) | 0 (0) | 5 |
| Internet correspondence with a CBT practitioner | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 |
| Read printed materials | 17 (70.8) | 7 (29.2) | 0 (0) | 0 (0) | 24 |
All but one of the parents who reported using the package components rated them positively in terms of their usefulness. Furthermore, as Table 34 shows, all participants agreed that the Surviving Crying materials should be routinely included in the NHS.
| Materials to be routinely included in the NHS | Opinion, n (%) | N | |||
|---|---|---|---|---|---|
| Strongly agree | Agree | No opinion | No | ||
| Website | 28 (82.3) | 6 (17.6) | 0 (0) | 0 (0) | 34 |
| Printed booklet | 17 (70.8) | 7 (29.2) | 0 (0) | 0 (0) | 24 |
| Practitioner CBT sessions | 20 (83.3) | 4 (16.7) | 0 (0) | 0 (0) | 24 |
These findings highlight the fact that parents with excessively crying babies identify support services as an unmet need in the NHS. The Surviving Crying support materials examined here were considered by parents to be suitable for this purpose. That is not to say that there is no room for improvement. Parents who used the materials provided more detailed feedback on each of the support package materials and suggested what sort of improvements could be made.
Overall, participants were positive about the extent to which they felt that the package components met their needs, particularly noting that the materials offered reassurance and hope and also practical help, advice and information. The timing of using the materials was important for some participants, reporting that they would have benefited more had they accessed the materials when their baby’s crying was at its peak. One participant reported that the materials were particularly good for first-time parents. Consequently, most participants rated the materials as a success in terms of meeting their needs (Figure 11).
FIGURE 11.
Parental view of the overall success of Surviving Crying support materials (n = 51). N/A, not applicable.

Overall, there was strong agreement that the Surviving Crying support materials should be routinely included in the NHS (see Table 34).
Parental feedback on the Surviving Crying website
The website was considered clear, helpful and relevant by all but two of the 30 participants who provided these judgements and over half rated its attractiveness highly (Table 35).
| Characteristic | Overall opinion of website, n (%) | N | ||||
|---|---|---|---|---|---|---|
| Very | Yes | Adequate | No | Not at all | ||
| Attractive | 4 (13.3) | 13 (43.3) | 12 (40.0) | 1 (3.3) | 0 (0) | 30 |
| Clear | 20 (66.7) | 8 (26.6) | 2 (6.7) | 0 (0) | 0 (0) | 30 |
| Helpful and relevant | 13 (43.3) | 15 (50.0) | 2 (6.7) | 0 (0) | 0 (0) | 30 |
The website was rated particularly highly for (1) ease of access, (2) giving other parents’ experiences and ideas and (3) making participants feel that they could trust the information supplied, as shown in Table 36. Participants liked the simple design and layout of the website, with one appreciating that they were able to access it on their mobile phone. Almost half of the participants who rated the website highlighted the videos and the sharing of other parents’ experiences as being particularly helpful and reassuring, with some liking that the website also included practical tips and demonstrations. Only one participant reported that they were not interested in hearing about other parents’ experiences. A few participants noted that they particularly liked that the website included a section on research, as they felt that this gave the website credibility and, consequently, they felt that they could trust the information that was given. One participant reported that, as a result, they had looked at the suggested research in more detail.
| Website strengths and weaknesses | Rating, n (%) | N | |||||
|---|---|---|---|---|---|---|---|
| Very strong | Strong | Adequate | Weak | Very weak | N/A | ||
| Practical suggestions | 10 (33.3) | 15 (50.0) | 4 (13.3) | 0 (0) | 1 (3.3) | 0 (0) | 30 |
| Reassurance | 16 (53.3) | 11 (36.7) | 3 (10.0) | 0 (0) | 0 (0) | 0 (0) | 30 |
| Could trust it | 17 (56.7) | 9 (30.0) | 4 (13.3) | 0 (0) | 0 (0) | 0 (0) | 30 |
| Gave other parents’ experiences and ideas | 17 (56.7) | 9 (30.0) | 3 (10.0) | 0 (0) | 0 (0) | 1 (3.3) | 30 |
| Expert opinion and advice | 13 (43.3) | 12 (40.0) | 4 (13.3) | 1 (3.3) | 0 (0) | 0 (0) | 30 |
| Aimed at both parents | 12 (40.0) | 10 (33.3) | 6 (20.0) | 1 (3.3) | 0 (0) | 1 (3.3) | 30 |
| Videos | 9 (30.0) | 10 (33.3) | 6 (20.0) | 0 (0) | 0 (0) | 5 (16.7) | 30 |
| Easy to access | 17 (56.7) | 11 (36.7) | 1 (3.3) | 0 (0) | 1 (3.3) | 0 (0) | 30 |
| Other | 2 (6.7) | 28 (93.3) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 30 |
Around one-third of those who had rated the website gave suggestions for its improvement. Most of those suggested a parent forum section in which parents could share advice and information, as well as offer support to each other. Two participants wanted more information, advice and practical tips from other parents on, for example, alternative soothing techniques and practices, for single parents in particular. One participant thought that the parent videos were too long when they needed immediate reassurance but that they were ‘perfect’ to look at when their baby was asleep.
Parental feedback on the printed information booklet
The printed information booklet was considered to be clear, helpful and relevant by all of the 23 participants who provided these judgements, with most rating its attractiveness highly (Table 37).
| Characteristic | Overall opinions of booklet, n (%) | N | ||||
|---|---|---|---|---|---|---|
| Very | Yes | Adequate | No | Not at all | ||
| Attractive | 5 (21.7) | 15 (65.2) | 3 (13.0) | 0 (0) | 0 (0) | 23 |
| Clear | 15 (65.2) | 8 (34.8) | 0 (0) | 0 (0) | 0 (0) | 23 |
| Helpful and relevant | 13 (56.5) | 10 (43.5) | 0 (0) | 0 (0) | 0 (0) | 23 |
Overall, the information booklet was rated particularly highly on being aimed at both parents, the practical suggestions and ease of access, as shown in Table 38. Participants explained that the fact that the information booklet was in a printed format meant that it was easily and readily accessible and available to both parents and that it could easily be read, for example when feeding a baby, taking a bath, or at times when parents needed some instant reassurance. Some participants liked that it provided reassurance by including other parents’ experiences, in the form of quotations, stories, advice and practical tips. Only two participants suggested improvements to the information booklet: one was to produce it in an A5 format, so that it could be portable, and the other suggestion was to include more information, for example advice for older children trying to cope with a crying baby.
| Booklet strengths and weaknesses | Rating, n (%) | N | |||||
|---|---|---|---|---|---|---|---|
| Very strong | Strong | Adequate | Weak | Very weak | N/A | ||
| Practical suggestions | 14 (60.9) | 8 (34.8) | 1 (4.3) | 0 (0) | 0 (0) | 0 (0) | 23 |
| Reassurance | 13 (56.5) | 8 (34.8) | 2 (8.7) | 0 (0) | 0 (0) | 0 (0) | 23 |
| Could trust it | 11 (47.8) | 10 (43.5) | 2 (8.7) | 0 (0) | 0 (0) | 0 (0) | 23 |
| Gave other parents’ experiences and ideas | 14 (60.9) | 6 (26.1) | 3 (13.0) | 0 (0) | 0 (0) | 0 (0) | 23 |
| Expert opinion and advice | 11 (47.8) | 8 (34.8) | 4 (17.4) | 1 (4.3) | 0 (0) | 0 (0) | 23 |
| Aimed at both parents | 16 (69.6) | 7 (30.4) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 23 |
| Easy to access | 16 (69.6) | 5 (21.7) | 2 (8.7) | 0 (0) | 0 (0) | 0 (0) | 23 |
| Other | 2 (8.7) | 21 (91.3) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 23 |
Parental feedback on the practitioner-delivered sessions
Information provided as part of the CBT practitioner-delivered session was considered to be clear, helpful and relevant by almost all of the 24 participants who provided judgements (Table 39).
| Characteristic | Overall opinions of CBT practitioner sessions, n (%) | N | ||||
|---|---|---|---|---|---|---|
| Very | Yes | Adequate | No | Not at all | ||
| Clear | 20 (83.3) | 2 (8.3) | 2 (8.3) | 0 (0) | 0 (0) | 24 |
| Helpful and relevant | 19 (79.2) | 2 (8.3) | 3 (12.5) | 0 (0) | 0 (0) | 24 |
Overall, the sessions were rated particularly highly on convenience of the session location, convenience of session times and trust in the practitioner, as shown in Table 40, and were rated ‘weak’ by only two participants in the areas of practical suggestions given, expert advice, helpfulness for both parents and convenience of session times.
| CBT practitioner sessions’ strengths and weaknesses | Rating, n (%) | N | |||||
|---|---|---|---|---|---|---|---|
| Very strong | Strong | Adequate | Weak | Very weak | N/A | ||
| Practical suggestions | 15 (62.5) | 6 (25.0) | 1 (4.2) | 2 (8.3) | 0 (0) | 0 (0) | 24 |
| Reassurance | 16 (66.7) | 5 (20.8) | 3 (12.5) | 0 (0) | 0 (0) | 0 (0) | 24 |
| Expert advice | 15 (62.5) | 6 (25.0) | 1 (4.2) | 2 (8.3) | 0 (0) | 0 (0) | 24 |
| Could trust them | 17 (70.8) | 5 (20.8) | 2 (8.3) | 0 (0) | 0 (0) | 0 (0) | 24 |
| Helpful for both parents | 11 (45.8) | 5 (20.8) | 3 (12.5) | 2 (8.3) | 0 (0) | 3 (12.5) | 24 |
| Convenient times | 17 (70.8) | 6 (25.0) | 0 (0) | 1 (4.2) | 0 (0) | 0 (0) | 24 |
| Convenient place | 18 (75.0) | 6 (25.0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 24 |
| Other | 1 (4.2) | 23 (95.8) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 24 |
Participants liked that the practitioners provided general practical information and personal advice, that they were non-judgemental, made parents feel supported and gave them time to talk. Some participants liked that the sessions took place in their own homes, where they felt relaxed, and that there was some degree of flexibility around the times of the sessions, although one participant explained that such flexibility resulted in her not giving the sessions priority like she would have done if they were fixed appointments. A couple of participants liked that the sessions were face to face and one to one; in addition, one participant found it helpful that the sessions could involve their partner too. A few participants liked knowing that they were able to contact the practitioners outside the planned sessions if they felt that they were struggling and needed their reassurance.
The breathing and relaxation exercises were highlighted by some participants as being particularly helpful; others highlighted the coping with crying tips and strategies, as well as the written information that could be read and referred to outside the sessions. Some participants felt that the CBT approach was particularly helpful for them in dealing with the crying, for example in changing their thought processes, as well as more broadly, for example in dealing with other people’s unwanted advice and opinions and with their own postnatal depression.
One participant felt that it was particularly important that the CBT practitioner was, as they described, ‘completely independent from health visitors’, but they also stated ‘I would urge the NHS to give this kind of support to all mothers’ (P2C03).
Twenty-three of the 24 participants identified possible improvements to the CBT practitioner-delivered sessions, as shown in Table 41, with a large proportion wanting to see more small-group sessions.
| Suggested improvements | Parents, n (%) |
|---|---|
| More one-to-one contact | 2 (8.7) |
| More small-group sessions | 9 (39.1) |
| More telephone contact | 3 (13.0) |
| More internet contact | 1 (4.3) |
| More sessions | 2 (8.7) |
| Longer sessions | 3 (13.0) |
| Additional materials | 0 (0) |
| Did not meet my needs | 1 (4.3) |
| Other | 3 (13.0) |
Other suggestions for improvements were more practical advice on helping a crying baby and more evidence-based support, longer sessions (possibly with goal-setting targets), leaflets listing soothing techniques that could be referred to when needed and the timing of the sessions (so that they happened when the crying was at its worst). In keeping with our stage 1 findings, suggestions for improvement included the need for small-group sessions, which proved impractical at this stage because too few parents were available at the same time in nearby locations. Other, possibly online, methods of contact can be considered in the future.
The findings reinforce the need for a large-scale study to evaluate the study support package more rigorously and for the package materials to be revised before and during the next evaluation.
Parental willingness to take part in a randomised controlled trial
As part of the outcome assessments, parents were asked whether or not, at the time when their baby was excessively crying, they would have been willing to take part in a RCT to provide a more rigorous and controlled evaluation of the Surviving Crying materials. The randomisation process and the possibility that they would be assigned to the control group was explained to them, together with the option of entering a waiting list control group. The findings are shown in Figure 12. Overall, 69% of parents said that they would be willing to take part, rising to 85% if the option of a waiting list control group is offered. The implication is that such a RCT should be feasible, particularly if it includes a waiting list control group.
FIGURE 12.
Parents’ willingness to participate in a RCT (n = 52).

Chapter 12 Health visitor evaluation of the Surviving Crying package materials
This chapter presents the findings from the questionnaires completed by 96 HVs/SCPHNs at the conclusion of the study, as described in Chapter 8, Health visitor/specialist community public health nurse feedback. As not all questions were completed by all HVs/SCPHNs, the number of respondents is indicated for each table.
Health visitor and specialist community public health nurse contact with parents regarding stage 2 of the study
As shown in Table 42, HVs/SCPHNs were asked to indicate what contact they had had with parents in relation to stage 2 of the study. Thirty-six (37.5%) had referred one or more parents to the study team, and 43 (50%) had spoken with parents, either by telephone or in person, but had not referred them, either because they were not suitable or they were unwilling to take part. The remaining HVs/SCPHNs (n = 35, 36.5%) indicated that they had not had any contact with parents about the study.
| HV/SCPHN contact with parents | n (%)a |
|---|---|
| Referred one or more parents for inclusion | 36 (37.5) |
| Spoken by telephone but not referred | 9 (9.4) |
| Spoken in person but not referred | 39 (40.6) |
| No contact with parents about the study | 35 (36.5) |
Health visitor and specialist community public health nurse experience and opinion of the study support materials
The HVs/SCPHNs were asked if they had seen or heard about the support package components: the website, information booklet and CBT support sessions. Just over two-thirds (n = 65, 68%) indicated that they had seen or heard about one or more of the materials, although a relatively small proportion (just under one-third for the website and booklet, and < 10% for the CBT sessions) had actually seen the materials directly rather than being told about them by someone else, predominantly colleagues (Table 43).
| Study materials | Type of contact, n (%) | Missing, n (%) | |||
|---|---|---|---|---|---|
| Seen directly by HV/SCPHN | Told about by parents | Told about by colleagues | Not seen or heard about | ||
| Website | 29 (30.2) | 4 (4.2) | 25 (26.0) | 36 (37.5) | 6 (6.3) |
| Booklet | 27 (28.1) | 3 (3.1) | 23 (24.0) | 45 (46.9) | 2 (2.1) |
| CBT sessions | 8 (8.3) | 12 (12.5) | 17 (17.7) | 54 (56.3) | 5 (5.2) |
Because of their lack of direct contact with the materials, feedback on their helpfulness to parents and suitability for inclusion in the NHS was only given by a proportion of the HVs/SCPHNs. Fifty-one HVs/SCPHNs (53%) provided feedback on some aspects of the package components, with 39 (41%) giving feedback on their suitability for inclusion in NHS provision. Data relating to ratings for the different materials are presented in Tables 44 and 45. Overall, HVs/SCPHNs were strongly positive in their feedback on the materials, with > 90% of those completing this section rating each component as either ‘very helpful’ or ‘a bit helpful’ to parents. Ratings regarding suitability for NHS use were also high for the 39 HVs/SCPHNs who completed this section; at least one component was rated by > 85% of this group as either ‘very suitable’ or ‘a bit suitable’.
| Study materials | HVs/SCPHNs providing rating data, n (%) of forms completed | Rating scores for completed forms, n (%) | ||
|---|---|---|---|---|
| Very helpful | A bit helpful | Not helpful | ||
| Website | 43 (44.8) | 30 (69.8) | 11 (25.6) | 2 (4.7) |
| Booklet | 42 (43.8) | 26 (61.9) | 14 (33.3) | 2 (4.8) |
| CBT sessions | 38 (39.6) | 28 (73.7) | 8 (21.1) | 2 (5.3) |
| Study materials | HVs/SCPHNs providing rating data, n (%) of forms completed | Rating scores for completed forms, n (%) | ||
|---|---|---|---|---|
| Very suitable | A bit suitable | Not suitable | ||
| Website | 33 (34.4) | 23 (69.7) | 8 (24.2) | 2 (6.1) |
| Booklet | 34 (35.4) | 20 (58.8) | 11 (32.4) | 3 (8.8) |
| CBT sessions | 28 (29.2) | 17 (60.7) | 7 (25.0) | 4 (14.3) |
Specific feedback, either on the package as a whole or its components, was offered by nine HVs/SCPHNs. The website received specific positive comments about the information it provided and its accessibility: ‘Excellent at 2 a.m. when nothing else available’. One recommended that the resources be shared with HVs/SCPHNs, suggesting that the booklet could be provided antenatally or as part of the HV/SCPHN services, and the website offered to parents at their universal visits. However, concerns were raised by a few HVs/SCPHNs, particularly in relation to their unsuitability for non-English-speaking clients. These points were predominantly made by HVs/SCPHNs in areas where non-English-speaking parents formed the majority of their caseload. One HV/SCPHN recommended that the booklet should be very visual, possibly in response to this concern. Other particular points made were in relation to the lack of internet access for some parents and a concern that it may not be possible to meet the demand for the CBT support.
Although two HVs/SCPHNs observed that they had received little feedback from parents they had referred to the study, four reported positive comments, and no negative comments from parents were noted. Two were in relation to the website: one commenting that it had been really useful and the other appreciating other parents’ stories. Positive feedback had been received in relation to the CBT sessions from one parent, and one comment regarding all the package elements simply noted ‘the family I referred found the service very helpful’.
Barriers to inclusion of study materials in NHS services
The HVs/SCPHNs were asked for their views on whether or not they foresaw any barriers to including the study materials in routine NHS services and to suggest any ways of overcoming these barriers. Although some HVs/SCPHNs did not complete this section owing to their lack of familiarity with the materials, 73 (76%) provided feedback (Figure 13). Although just over half of those completing the forms (n = 40, 55%) did not identify any problems, a substantial minority considered that there were barriers to the introduction within the NHS of some or all elements of the support package.
FIGURE 13.
The HVs/SCPHNs identifying barriers to inclusion of materials in NHS provision (n = 73). Figures do not total 100% as HVs/SCPHNs could tick as many boxes as applied.

Forty HVs/SCPHNs provided additional comments regarding barriers to the implementation of the materials. Language barriers were identified as the main impediment to implementing the resources equally with all clients (27 HVs/SCPHNs), with some parents neither speaking nor reading English. Wider cultural and communication issues were also mentioned, with literacy problems highlighted by a few. One HV/SCPHN also observed that ‘most parents don’t identify themselves as in the booklets or website’, which had made recruitment difficult. In addition, financial barriers were emphasised, meaning that some parents did not have access to the internet for viewing the website.
Other barriers related to the resources available to HVs/SCPHNs to enable delivery of the service, with financial and time pressures being noted by a number of respondents. One HV/SCPHN noted that the mobility of her clients presented a challenge, as the service would need to be provided very quickly or they would no longer be available. The amount of information HVs/SCPHNs already need to communicate to parents was also mentioned as making it difficult to ensure that these new resources were accessible. Few suggestions were made as to how these barriers could be overcome. One HV/SCPHN suggested linking the website to a new 0–5 website under development, and the need for regular staff training was mentioned by another.
Training for health visitors and specialist community public health nurses in supporting parents with excessively crying babies
The HVs/SCPHNs gave their views on whether or not their training should include information on how to support parents concerned about their baby’s excessive crying. There was very strong support for this kind of training, either as part of routine training or as special training for those who want it (Figure 14).
FIGURE 14.
The HVs’/SCPHNs’ views regarding the provision of training to support parents with crying babies (n = 96). Figures do not total 100% as some HVs/SCPHNs ticked more than one box.

Additional comments were provided by 41 HVs/SCPHNs. Almost all of these welcomed the idea of training, with the impact of the crying on parents and the need to provide better support being explicitly acknowledged:
This is an issue that is often raised with parents and has implications for assessment of both parental and infant mental health.
. . . it would enhance our care to parents and their children affected by this subject . . .
There were a range of views on when and to whom the training should be offered. Inclusion within routine training was felt to be important by some, with one HV/SCPHN observing that they were ‘recently qualified and feel this would have been an excellent part of training as fits with so many modules’. Others additionally emphasised the need to also offer the training to qualified HVs/SCPHNs, who would miss out if it was only available as part of initial training. Providing the training as an ‘extra’ was also seen as important in opening it up to other relevant staff, particularly community nursery nurses, a number of whom had filled in the questionnaire and emphasised its relevance to their work: ‘. . . most prob[ably] the advice and support would be one of my duties’.
A few HVs/SCPHNs felt that the training should only be an additional specialism, noting that not all would be interested in it and that their training and workload were already at capacity with existing commissioned work. Particularly in relation to the CBT skills, a number recognised the specialist nature of this work and suggested that it would be better to have a few practitioners who would then use their skills more, with one suggesting that ‘each area could have a Crying Baby Champion’. However, a contrasting view was expressed by a few HVs/SCPHNs, who felt that the lack of CBT techniques was a significant gap in their knowledge, which ‘could also help parents cope with other situations that arise’.
Other comments
In this section, HVs/SCPHNs were invited to offer any further comments, and 35 contributed their thoughts. These covered a variety of themes, with some reiterating points made earlier, including the need to address language barriers and the importance of specific training and knowledge on this topic. A few also observed how either their role or joining the study late had prevented them from fully engaging with the study. Further comments were made about the value of the study to both parents and professionals, with a particular concern for first-time parents being noted:
As a HV/SCPHN I found info [information], help and support very helpful to me and the family I referred.
First-time parents especially need assistance. They often suffer in silence and feel ashamed to admit having problems.
It has been very interesting to be involved in this study and anything that can further help parents and their children is very welcome.
A number of HVs/SCPHNs made specific comments about the process of being engaged in the study, which had been a positive experience for most, with one observing that ‘the research was very professionally carried out in an appropriate manner and by very informed professionals’. However, a few challenges were identified, including finding the time to engage fully with the process and to obtain feedback on parents referred, and one HV/SCPHN emphasised the need to rule out any medical reasons for the crying. A few HVs/SCPHNs also highlighted issues relating to recruitment, particularly at the primary visit, partly owing to the amount of other information to cover at that time, but also owing to parents’ reluctance to consider the possibility of their baby developing excessive crying:
. . . no parent likes to think they will get [a] crying baby.
Parents not happy to participate just in case their baby became ‘crying baby’. Much easier to discuss once crying baby identified.
Another HV/SCPHN suggested the use of a DVD (digital versatile disc) to recruit parents and to give further explanation of what the research would involve. For the future, HVs/SCPHNs recommended widely publicising the support available to parents, through both local media and children’s centres.
Chapter 13 Costs of routine services and the support package elements
Background and scope
In this section, we describe the economic analysis that accompanied the main study. This was designed to inform a future economic evaluation of the intervention package from a NHS perspective. Based on recommendations for health economics input into feasibility studies,54 the aim was not to undertake an economic evaluation of the intervention package, but to identify what measures to collect in a future economic evaluation and how best to collect them.
We undertook a review of the NHS Economic Evaluation Database, Google Scholar (Google Inc., Mountain View, CA, USA) and PubMed using the search terms “infant” OR “baby” AND “crying” AND “cost” in any field (searches last conducted on 7 May 2017). We found a single economic evaluation assessing a behavioural and educational intervention aimed at reducing infant crying and sleeping problems relative to usual services using a three-armed RCT. 17 The outcome measure was interruption-free nights, defined as a night in which parents reported that their baby remained asleep continuously for ≥ 5 hours between 22.00 and 06.00. The perspective taken was that of the NHS. The cost components included were the cost of each intervention and the cost of all contacts with health-care professionals in which infant crying and sleeping problems were discussed. These were measured over the first 12 weeks from birth. Mothers were asked to keep prospective logs of the number of contacts that wholly or partly concerned their baby’s crying and sleeping problems every week across the 12-week period. Contacts included HV, midwife and GP contacts (i.e. mother visits HV at clinic or surgery, HV or midwife visits mother at home, mother telephones HV or midwife, mother visits GP at surgery or GP visits mother at home). Medications used for babies prompted by their crying and unsettled behaviour included colic-relieving remedies, infant paracetamol, antibiotics and herbal remedies. These were not included in the economic evaluation because > 99% were purchased over the counter at no cost to the NHS. The mean costs per baby for the behavioural intervention, educational intervention and control groups were £92.45 (SD £116.92), £98.96 (SD £127.88) and £90.64 (SD £123.30) (1997/8 prices), respectively. The largest cost component, comprising > 60% of the costs in each group, was ‘mother visits HV at clinic or surgery’. The incremental cost per interruption-free night gained for the behavioural intervention relative to the control was £0.56. For the educational intervention relative to the control, the cost was £4.13. The authors also calculated the annual total cost to the NHS of infant crying and sleeping problems in the first 12 weeks. The mean cost per baby of NHS contacts for infant crying and sleeping problems in the control group was multiplied by the number of live births in the UK to produce a value of £65M in 1997.
The future economic evaluation for the intervention package developed in the present study is likely to take the form of a cost-effectiveness or cost–utility analysis. For the cost-effectiveness analysis, outcomes could be measured in accordance with the assessments for babies and/or parents described in Chapter 8. For infants, these measures included baby fussing and crying patterns and baby feeding patterns. For parents, they include health-related quality of life measured using the EQ-5D, five-level version, postnatal depression measured using the EPDS, anxiety measured using the GAD-7 anxiety questionnaire, parenting confidence measured using the Maternal Confidence Questionnaire, parental sleep patterns and quality and parental social support. As shown in Chapter 8, all of these measures had high completion rates at baseline and outcome assessments and were completed accurately with few errors or missing data. To undertake a cost–utility analysis, the recommended outcome is quality-adjusted life-years (QALYs), with health-related quality of life measured using a generic measure such as the EQ-5D. 45 Unfortunately, deriving QALYs for infants during the first weeks of life is problematic, given their physical and cognitive ability at such a young age, their dependence on parents and other family members and the lack of appropriate and relevant generic quality-of-life measures. 55 Therefore, measurement of utilities for cost–utility analyses is likely to focus on the measurement of utilities among parents, which, as shown in Chapter 8, appears to be feasible in the present context.
In this chapter, we focus on the measurement of costs and explore (1) crying-related NHS costs and (2) the intervention costs associated with the Surviving Crying intervention package (i.e. website, printed booklet and CBT programme).
Cost of routine services
Methods
We collected data on the costs of routine services associated with excessive crying in order to inform a future economic evaluation. We focused on what items of resource use to collect from a NHS and Personal Social Services (PSS) perspective, as this perspective is likely to be relevant for economic evaluations for decision-making bodies such as NICE. 56 Potential cost components using this perspective could include NHS and PSS contacts and medications. Based on the study by Morris et al. ,17 we created a resource questionnaire that was given to participants at the baseline and outcome assessments. This questionnaire can be accessed at www.journalslibrary.nihr.ac.uk/programmes/hta/1215004/#/ (accessed 6 December 2018). Given the results of the study by Morris et al. ,17 the questionnaire specifically itemised NHS contacts, but participants were invited to record any contacts because of a concern about their baby’s crying, which could have included social care. For example, postnatal depression (e.g. related to excessive infant crying) could be related to the increased use of social care services. 57 We also collected data on the use of remedies for infant crying, including those prescribed by a doctor, although based on the findings of Morris et al. ,17 costs associated with NHS medications were expected to be negligible.
At the baseline assessment, the questionnaire asked about contacts since birth. At the outcome assessment, the questionnaire asked about contacts since the baseline assessment.
As noted, at the baseline and outcome assessments parents were asked to record other remedies they used for their baby’s crying. As well as remedies prescribed by a doctor, these included change of formula feed, use of colic drops and herbal remedies, treatment by a chiropractor and other remedies. The costs of these remedies are likely to be borne by families; therefore, we quantified the proportion of families using these remedies but did not include them in the following preliminary cost calculations.
Other non-NHS/PSS costs that might be included if a societal perspective to cost measurement was taken are travel costs for families going to and from NHS visits and days taken off work by parents because of excessive infant crying. We did not include either of these costs in the analysis given the perspective of our analysis. With regard to travel costs for families, we note that most of the NHS contacts are either at home or by telephone, thereby negating the need for travel. We also did not collect data on days off work given the fact that many parents with babies at this age are on maternity/paternity leave, making the measurement of days off work difficult.
For the non-zero cost components identified using the resource use questionnaire, we identified potential unit costs that could be used in a future economic evaluation. These were mainly derived from Curtis and Burns58 and are reported in 2015/16 Great British pounds (GBP). For HV contacts, we based the cost per contact on the cost per hour reported by Curtis and Burns. 58 It was felt that in the case of HV/SCPHN contacts, it was unlikely that a whole contact would be exclusively devoted to discussing infant crying problems; therefore, we quantified the amount of time spent discussing these problems during a visit. To do this, HVs/SCPHNs from the LPT teams participating in the study recorded the time spent discussing infant crying problems in contacts (all types) in which these were discussed. Across 445 contacts, the mean time was 17.3 minutes (range < 1 minute to 120 minutes). As this figure related to all HV/SCPHN contacts in which infant crying problems were discussed, it was used as the mean duration of all these contacts. For all other contacts (e.g. with a GP), we assumed that the whole contact was used to discuss infant crying problems and that the duration of each contact was as stated by Curtis and Burns. 58
The additional contacts included as free text in the questionnaire were classified into six categories based on the responses received:
-
nurse home visit
-
midwife home visit
-
A&E department visit
-
outpatient visit
-
walk-in centre visit
-
health centre visit.
No details were recorded on the type and grade of nurse and the grade of midwife; these were monetised using the same unit costs for HVs, described previously in this section. No additional details were provided for A&E, outpatient, walk-in centre and health centre visits. Therefore, A&E visits were monetised using the national average unit cost for all consultant-led outpatient attendances reported by Curtis and Burns. 58 Outpatient visits were monetised using the national average unit cost for all outpatient attendances reported by Curtis and Burns. 58 Walk-in centre visits were monetised using the national average unit cost for all non-consultant-led outpatient attendances reported by Curtis and Burns. 58 Health centre visits were monetised using the unit cost of a practice nurse visit with a duration of 17.3 minutes reported by Curtis and Burns. 58
We calculated the mean NHS cost per family of excessive crying for three time periods (i.e. birth to baseline measurement, baseline measurement to outcome measurement and birth to outcome measurement) by summing the different cost components. It should be noted that there was a difference in the duration of the first and second time periods. It should also be noted that the cost estimates for the period from baseline measurement to outcome measurement may be affected by any impact of the study interventions on NHS contacts.
Results
Useable resource use data were collected for 98% of respondents at baseline assessment (56/57 respondents) and 91% of respondents (52/57 respondents) at outcome assessment. Across the whole study period, resource use data were available for 89% of respondents (51/57 respondents). The mean age of babies at the baseline assessment was 9.3 weeks (range 3 to 24 weeks) (Table 46); at the outcome assessment, the mean age was 15.0 weeks (range 9 to 30 weeks) (Table 47).
| Contact | Units | Number of observations | Mean | SD | Minimum | Maximum |
|---|---|---|---|---|---|---|
| Age of baby | Weeks | 56 | 9.3 | 5.5 | 3 | 24 |
| HV home visit | Number of contacts | 56 | 2.1 | 2.0 | 0 | 8 |
| HV clinic visit | Number of contacts | 56 | 0.4 | 1.1 | 0 | 5 |
| HV contact by telephone | Number of contacts | 56 | 1.0 | 1.4 | 0 | 6 |
| HV contact by e-mail or internet | Number of contacts | 56 | 0 | 0 | 0 | 0 |
| GP home visit | Number of contacts | 56 | 0 | 0 | 0 | 0 |
| GP surgery visit | Number of contacts | 56 | 1.6 | 4.1 | 0 | 30 |
| GP contact by telephone | Number of contacts | 56 | 0.2 | 0.5 | 0 | 2 |
| GP contact by e-mail or internet | Number of contacts | 56 | 0 | 0 | 0 | 0 |
| Access website, chat room or social media | Number of contacts | 57 | 36.9 | 90.3 | 0 | 616 |
| Other contacts | ||||||
| Nurse home visit | Number of contacts | 57 | 0.1 | |||
| Midwife home visit | Number of contacts | 57 | 0.04 | |||
| A&E visit | Number of contacts | 57 | 0.04 | |||
| Outpatient visit | Number of contacts | 57 | 0.1 | |||
| Walk-in centre visit | Number of contacts | 57 | 0.1 | |||
| Health centre visit | Number of contacts | 57 | 0.1 | |||
| Contact | Units | Number of observations | Mean | SD | Minimum | Maximum |
|---|---|---|---|---|---|---|
| Age of baby | Weeks | 52 | 15.0 | 5.4 | 9 | 30 |
| HV home visit | Number of contacts | 52 | 0.3 | 0.8 | 0 | 4 |
| HV clinic visit | Number of contacts | 52 | 0.2 | 0.5 | 0 | 2 |
| HV contact by telephone | Number of contacts | 52 | 0.5 | 1.9 | 0 | 10 |
| HV contact by e-mail or internet | Number of contacts | 52 | 0 | 0 | 0 | 0 |
| GP home visit | Number of contacts | 52 | 0 | 0 | 0 | 0 |
| GP surgery visit | Number of contacts | 52 | 0.7 | 2.3 | 0 | 12 |
| GP contact by telephone | Number of contacts | 52 | 0.3 | 1.6 | 0 | 8 |
| GP contact by e-mail or internet | Number of contacts | 52 | 0 | 0 | 0 | 0 |
| Access website, chat room or social media | Number of contacts | 53 | 2.1 | 4.0 | 0 | 22 |
| Other contacts | ||||||
| Nurse home visit | Number of contacts | 53 | 0.1 | |||
| Midwife home visit | Number of contacts | 53 | 0.02 | |||
| A&E visit | Number of contacts | 53 | 0 | |||
| Outpatient visit | Number of contacts | 53 | 0.02 | |||
| Walk-in centre visit | Number of contacts | 53 | 0.1 | |||
| Health centre visit | Number of contacts | 53 | 0.1 | |||
Across the whole period, there were non-zero contacts for excessive crying for the following items collected in the resource use questionnaire (Tables 46–48):
-
HV home visit
-
HV clinic visit
-
HV contact by telephone
-
GP surgery visit
-
GP contact by telephone.
There were zero contacts for the following items:
-
HV contact by e-mail or internet
-
GP home visit
-
GP contact by e-mail or internet.
| Contact | Units | Number of observations | Mean | SD | Minimum | Maximum |
|---|---|---|---|---|---|---|
| Age of baby | Weeks | 52 | 15.0 | 5.4 | 9 | 30 |
| HV home visit | Number of contacts | 51 | 2.4 | 2.1 | 0 | 8 |
| HV clinic visit | Number of contacts | 51 | 0.6 | 1.2 | 0 | 5 |
| HV contact by telephone | Number of contacts | 51 | 1.5 | 2.3 | 0 | 11 |
| HV contact by e-mail or internet | Number of contacts | 51 | 0 | 0 | 0 | 0 |
| GP home visit | Number of contacts | 51 | 0 | 0 | 0 | 0 |
| GP surgery visit | Number of contacts | 51 | 2.4 | 5.4 | 0 | 33 |
| GP contact by telephone | Number of contacts | 51 | 0.5 | 1.6 | 0 | 8 |
| GP contact by e-mail or internet | Number of contacts | 51 | 0 | 0 | 0 | 0 |
| Access website, chat room or social media | Number of contacts | 52 | 39.9 | 93.7 | 0 | 616 |
| Other contacts | ||||||
| Nurse home visit | Number of contacts | 51 | 0.1 | |||
| Midwife home visit | Number of contacts | 51 | 0.1 | |||
| A&E visit | Number of contacts | 51 | 0.04 | |||
| Outpatient visit | Number of contacts | 51 | 0.1 | |||
| Walk-in centre visit | Number of contacts | 51 | 0.1 | |||
| Health centre visit | Number of contacts | 51 | 0.2 | |||
| Contacts | Unit cost (£) | Period | |||||
|---|---|---|---|---|---|---|---|
| Birth to baseline measurement (mean 9.3 weeks) (n = 56) | Baseline measurement (mean 9.3 weeks) to outcome measurement (mean 15.0 weeks) (n = 52) | Birth to outcome measurement (mean 15.0 weeks) (n = 51) | |||||
| Mean number | Total cost (£) | Mean number | Total cost (£) | Mean number | Total cost (£) | ||
| HV home visit | 37 | 2.1 | 76 | 0.3 | 11 | 2.4 | 89 |
| HV clinic visit | 22 | 0.4 | 9 | 0.2 | 4 | 0.6 | 12 |
| HV contact by telephone | 22 | 1.0 | 22 | 0.5 | 11 | 1.5 | 32 |
| GP surgery visit | 44 | 1.6 | 72 | 0.7 | 30 | 2.4 | 105 |
| GP contact by telephone | 27 | 0.2 | 4 | 0.3 | 9 | 0.5 | 14 |
| Other contacts | 0 | 0 | |||||
| Nurse home visit | 37 | 0.1 | 3 | 0.1 | 2 | 0.1 | 5 |
| Midwife home visit | 37 | 0.04 | 1 | 0.02 | 1 | 0.1 | 3 |
| A&E visit | 118 | 0.04 | 4 | 0 | 0 | 0.04 | 5 |
| Outpatient visit | 112 | 0.1 | 6 | 0.02 | 2 | 0.1 | 9 |
| Walk-in centre visit | 91 | 0.1 | 5 | 0.1 | 5 | 0.1 | 11 |
| Health centre visit | 16 | 0.1 | 2 | 0.1 | 1 | 0.2 | 3 |
| Total cost | 206 | 75 | 287 | ||||
| Remedy | Parents using this remedy, n/Na (%) | |
|---|---|---|
| Birth to baseline measurement (mean 9.3 weeks) | Baseline measurement (mean 9.3 weeks) to outcome measurement (mean 15.0 weeks) | |
| Remedy prescribed by a doctor | 19/56 (34) | 16/52 (31) |
| Change of formula feed | 21/55 (38) | 10/52 (19) |
| Colic drops | 41/56 (73) | 9/52 (17) |
| Herbal remedy | 8/55 (15) | 6/52 (12) |
| Chiropractor | 1/56 (2) | 0/52 (0) |
| Other remedies | 39/56 (70) | 24/62 (46) |
The most common type of contact for excessive crying was with the HV/SCPHN. In the period from birth to baseline assessment (mean 9.3 weeks), the most common HV/SCPHN contact was a home visit, with a mean number of visits per family of 2.1 (range 0 to 8 visits) (see Table 46). In the period from baseline to outcome assessment (mean 5.7 weeks), the most common HV/SCPHN contact was by telephone, with a mean number of calls per family of 0.5 (range 0 to 10 calls) (see Table 47). Across the whole period (mean 15.0 weeks), the most common HV/SCPHN contact was a home visit (mean number of visits per family 2.4, range 0 to 8 visits) (see Table 48).
When respondents were asked to record other types of contact they had made, these were categorised into:
-
nurse home visit
-
midwife home visit
-
A&E visit
-
outpatient visit
-
walk-in centre visit
-
health centre visit.
The mean number of contacts of each of these types was small (i.e. ≤ 0.2 contacts per family across the whole period) (see Table 48).
The total mean NHS cost per family for excessive crying was £206 in the period from birth to baseline measurement (mean 9.3 weeks), £75 in the period from baseline measurement to outcome measurement (mean 9.3 weeks to mean 15.0 weeks) and £287 across both periods combined (see Table 49). It should be noted that there is a difference in duration between the first and second time periods. It should also be noted that the figures of £75 in the period from baseline measurement to outcome measurement and £287 across both periods combined include any impact of the study interventions on NHS contacts.
Thirty-four per cent of parents reported using a remedy prescribed by a doctor for infant crying during the period from birth to baseline measurement, compared with 31% in the period from baseline measurement to outcome measurement (see Table 50). Remedies recorded as prescribed by the doctor were:
-
allergy milk
-
amoxicillin
-
Gaviscon® [Reckitt Benckiser Healthcare (UK) Ltd]
-
Simeticone (Infacol®, Purna Pharmaceuticals)
-
ranitidine
-
hydrolysed milk formulation (Aptamil Pepti®, Nutricia Ltd; Nutramigen®, Mead Johnson Nutrition)
-
cream for eczema
-
lactulose
-
nose drops
-
chlorphenamine maleate (Piriton®, GlaxoSmithKline).
Data on whether the medication was for the infant or the parent were not recorded. The majority of these items are available over the counter. Data on the dosage and duration of the remedy were not recorded, although this could be measured in a future economic evaluation.
The most commonly used remedy in the first period was colic drops (73%) (see Table 50). Other remedies that were recorded were:
-
baby massage
-
changing bottles
-
foot manipulation
-
gripe water
-
Gaviscon
-
lactulose
-
an osteopath
-
ranitidine
-
Rescue Remedy® (A Nelson & Co Ltd)
-
cool water
-
laxatives
-
a hot water bottle
-
nose drops
-
teething gel
-
paracetamol.
Cost burden
In this section, we use the data described in Results to calculate the potential annual burden of excessive crying problems in infants to the NHS in the UK, associated with ‘usual care provision’. We do this by multiplying (1) the mean NHS cost per excessively crying infant by (2) the number of excessively crying infants each year in the UK. The first element (1) was taken from estimates calculated in the present study. We calculated that from birth to 9.3 weeks of age, the mean NHS cost per excessively crying infant was £206. We also calculated that from birth to 15.0 weeks of age, the mean NHS cost per excessively crying infant was £287. It should be noted that the latter figure is calculated over a longer period and includes the period during which parents in the study received the intervention package. Therefore, the costs during this period may be depressed because of the impact of the intervention. We observe in our data that the costs during the second period were lower than in the first period (£206 vs. £75). This is partly attributable to the difference in the time periods (mean 9.3 weeks vs. 5.7 weeks), but the costs per week during the two periods were also different [£22 for the first period (£206/9.3) and £13 for the second period (£75/5.7)]. This difference may be attributable to a reduction in excessive crying over time, a reduction in the propensity to contact health services about excessive crying over time or the impact of the intervention. The first two of these are legitimate sources of lower costs for the cost burden calculation during the second period but the last is not, because we wish to estimate the cost burden in the absence of the intervention. Hence, we estimate the cost burden using both estimates, recognising that the first covers a shorter time period and the latter may be contaminated by the impact of the intervention.
The second element (2) was based on the total number of live births in the UK and the incidence of excessive crying in infants. In 2015, there were 777,165 live births in the UK. 59 There is considerable uncertainty surrounding the incidence of excessive crying, with estimates varying in accordance with the definition of excessive crying and the age of the baby when these are measured. We used five estimates. The first is the incidence found in the new birth visit group in the present study (21.7%; see Chapter 8). The other measures were the maxima and minima reported in previous reviews of this topic (1.5% and 5%, 11.9% and 32.1%). 60,61
Using this approach and these figures, the total annual UK NHS cost of excessively crying infants is estimated to be in the range of £2.4M to £51.4M during the period from birth to 9.3 weeks and £3.3M to £71.7M during the period from birth to 15 weeks (Table 51).
| Source | Incidence of excessive crying (%) | Total cost (£M) | |
|---|---|---|---|
| Birth to 9.3 weeksa | Birth to 15.0 weeksb | ||
| New birth visit group | 21.8 | 34.8 | 48.6 |
| St James-Roberts (2012)60 | |||
| Lower estimate | 5 | 8.0 | 11.2 |
| Upper estimate | 32.1 | 51.4 | 71.7 |
| Reijneveld et al. (2001)61 | |||
| Lower estimate | 1.5 | 2.4 | 3.3 |
| Upper estimate | 11.9 | 19.1 | 26.6 |
Intervention costs
Introduction
In this section, we calculate the intervention costs associated with the Surviving Crying intervention package (i.e. website, printed booklet and CBT programme). We only include the costs of delivering the intervention package, not of developing it. The development costs comprise the costs of the research undertaken during stage 1 of the research study and are not included here. For the website and booklets, the costs reported in the following sections were based on market prices incurred in the production of these materials. The costs of the CBT programme were based on the resource use for the provision of the programme, which were recorded by the practitioner.
Website
The costs of the website include the one-off costs to set the website up, the costs of maintaining the website and the cost of registering new users to it. The one-off cost to produce the website by the developers was £12,296. The annual cost to maintain the website had two elements. First, there was an annual fee of £525.75 for the cost of the website domain and of hosting the website. Second, there were costs associated with maintaining the content of the website. This was estimated to require three person-days’ input per year at a total cost of £957 per year. Combining both elements, the annual cost to maintain the website was £1482.75. Registering new users to the website required approximately 15 minutes of administration time per family to create the new registration and communicate the log-in details and information about the website. This was estimated to incur an additional cost per new registration of £32.33.
Booklet
The second component of the intervention package was the printed booklet, which was designed to match the layout and content of the website as far as possible. The cost to produce each booklet (the cost per family) was £6.46.
The cognitive–behavioural therapy programme
The third component of the intervention package was the CBT programme. This included the following cost components:
-
therapist time spent undertaking the following activities –
-
face-to-face CBT sessions
-
telephone contacts with participating families
-
text, e-mail or internet contacts with participating families
-
preparation for the CBT sessions
-
administration
-
travel to the participants’ homes
-
-
costs to travel to the participants’ homes
-
printed information booklet.
The therapist providing the CBT sessions recorded the total time spent on each task across all 21 participating families. These totals were monetised and divided by the number of families participating in the CBT programme to calculate the mean cost per family. The cost of therapist time was valued at £105.82 per hour, based on the total cost per hour of CBT therapist time reported by Curtis and Burns. 58 The mean therapist time input per family was 3.92 hours, giving a total cost of £415 per family (Table 52). The therapist also recorded the distance travelled to each home (in miles) to enable the calculation of travel costs. These were valued at a cost of £0.56 per mile. 62 The mean distance travelled per family was 24.38 miles and, therefore, the mean travel cost per family was £14. All participating families received a printed booklet; the cost to produce each booklet (the cost per family) was £7.83. Note that this is different to the cost of the booklet based on the Surviving Crying website, which was £6.46. Combining each cost component, the mean cost per family participating in the CBT programme was £437.
| Activity | Input | Cost (£) | ||||
|---|---|---|---|---|---|---|
| Unit | Totala | Per family | Per unit | Totala | Per familyb | |
| Face-to-face CBT session | Hours | 23 | 1.10 | 105.82 | 2434 | 116 |
| Telephone contact | Hours | 9 | 0.43 | 105.82 | 952 | 45 |
| Text, e-mail or internet contact | Hours | 7.5 | 0.36 | 105.82 | 794 | 38 |
| Preparation | Hours | 7.5 | 0.36 | 105.82 | 794 | 38 |
| Administration | Hours | 11.5 | 0.55 | 105.82 | 1217 | 58 |
| Travel (time) | Hours | 23.9 | 1.14 | 105.82 | 2531 | 121 |
| Subtotal | Hours | 82.4 | 3.92 | 105.82 | 8721 | 415 |
| Travel (distance) | Miles | 512 | 24.38 | 0.56 | 287 | 14 |
| Booklet | Booklets | 21 | 1 | 7.83 | 164 | 8 |
| Total | 9172 | 437 | ||||
Conclusions from the health economic analyses
Summary
The aim of this analysis was to undertake preliminary research to inform a future economic evaluation of the Surviving Crying intervention package from a NHS perspective. We focused on the measurement of costs, explored crying-related NHS costs and the intervention costs associated with the Surviving Crying intervention package. We asked study participants to retrospectively record data on NHS and other contacts related to their baby’s excessive crying and achieved high response rates. We collected data on the frequency of different types of NHS contact, which can be used to identify which contacts ought to be included in future resource use questionnaires and which are likely to be less important. We calculated the cost burden associated with excessive crying and found that this varied considerably, mainly in accordance with variations in the incidence of excessive crying. We calculated the intervention costs associated with the Surviving Crying intervention package (i.e. website, printed booklet and CBT programme). The website incurred a one-off cost to be produced of £12,296 and an annual cost to maintain of £1482.75. In addition, it incurred an additional cost per new registration of £32.33. The cost per family for each printed booklet was £6.46. The mean cost per family participating in the CBT programme was £437.
Lessons learned
The following is a list of lessons learned from the economic analysis, which may be useful in planning future economic evaluations:
-
Based on the data collected in this study, especially the high response rates, it is likely to be feasible to undertake an economic evaluation of an intervention to manage infant crying problems alongside a RCT.
-
Retrospective resource use questionnaires to collect cost data are feasible in this population group, at least over the period considered in the present study (birth to 15 weeks).
-
When collecting resource use data, it is important to specify whether the contacts relate to all contacts or just those relating to crying problems. This is because, especially in the case of HV/SCPHN contacts, it is unlikely that a whole contact will be exclusively devoted to discussing crying problems. It is important to quantify the amount of time spent discussing these problems during a visit.
-
Resource use questionnaires should include the following items: (1) HV/SCPHN home visits, (2) HV/SCPHN clinic visits, (3) HV/SCPHN contacts by telephone, (4) GP surgery visits and (5) GP contacts by telephone. The following items had no contacts in the present study and so may not be required: (1) HV/SCPHN contacts by e-mail or internet, (2) GP home visits and (3) GP contacts by e-mail or internet. No PSS contacts were recorded. In addition, it may be worth delineating specific contacts for midwife visits, other nurse visits and contacts with secondary care (e.g. A&E, outpatient and walk-in centre contacts) and health centre visits, although the total number of contacts of these types is likely to be small.
-
Resource use questionnaires could also include medications prescribed by the GP and whether these are for the infant or for the parent. If these items are to be costed, then data ought to be collected on the name of the drug and the dosage and duration of treatment.
-
If non-NHS/PSS costs are to be included in a cost analysis using a societal perspective, then these could include remedies for excessive crying paid for by families, including colic drops and herbal remedies.
-
Future economic evaluations could comprise both cost-effectiveness analyses and cost–utility analyses. The former can include both infant and parent outcomes; the latter is likely to be restricted to parent QALYs only, given the difficulties in measuring QALYs in infants.
-
Further research to evaluate the cost of excessive crying would be useful, and such analyses could be based on resource use in a control group of a RCT, provided treatment in this group reflected usual care. The total cost burden depends on the incidence of excessive crying, and there are a wide range of available estimates. A reliable measure of this incidence is needed to produce an accurate cost burden estimate.
Chapter 14 Conclusions
This study has been successful in meeting its two main aims: (1) to develop a package of support materials for parents of excessively crying babies and (2) to provide a provisional evaluation of the package and collect evidence to inform decisions about future work. The findings allow the following conclusions:
-
It has proved feasible to recruit and maintain parents and NHS HVs/SCPHNs in the study and to develop and evaluate an evidence-based package of materials to support parents of excessively crying babies. The collaboration provided by LPT and > 120 of its HVs/SCPHNs has been critical to the study’s success. This sustained collaboration is evidence, too, that these NHS professionals value the support package and recognise the need for it.
-
The first stage of the study reviewed the research evidence and worked with parents and HVs/SCPHNs to identify suitable support materials and ways of delivering them. Qualitative and quantitative findings from 20 parents whose babies had previously cried excessively were used to explore their experiences, the needs of parents faced with an excessively crying baby and how best to meet those needs.
-
The resulting ‘Surviving Crying’ support package includes three materials: a website, a printed booklet based on the website and a programme of CBT-based sessions delivered to parents by a qualified practitioner, together with a programme manual.
-
Stage 2 of the study carried out an initial evaluation of these support materials. In total, 57 parents whose babies were currently excessively crying took part. Use of the package materials was associated with substantial reductions in parental frustration, anxiety and depression, together with reductions in reported infant crying, the extent to which parents considered it a problem, and contact with professionals for help with the crying. Parents’ knowledge of infant crying increased. All 52 parents providing outcome data reported that the materials were helpful and would support their inclusion in the NHS. The study was not designed to fully evaluate the clinical effectiveness of the support package and the lack of a control group prevents any conclusions about cause and effect. Nonetheless, the findings at this stage are promising and encouraging. They indicate that a more exhaustive evaluation is worthwhile.
-
Parents of excessively crying infants involved in the study confirmed their willingness to participate in a RCT to provide such an evaluation. Of 52 parents, 69% said that they would be willing to take part, rising to 85% if the option of a waiting list control group is offered. The implication is that a RCT should be feasible, particularly if it includes a waiting list control group.
-
Health economic data collected by the study provided estimates for the cost of excessive infant crying for families and the NHS, together with figures for the cost of each element of the Surviving Crying support package. As expected, the cost of excessive infant crying for the NHS is considerable. The exact figure depends on the incidence, which remains poorly understood. However, based on figures collected in this study, health-care services for excessively crying babies and their parents in the first 15 weeks after birth are estimated to cost the NHS £48.6M per year. Following the NICE stepped model,63 the website was designed to provide inexpensive support suitable for most parents, whereas the CBT programme was expected to be more expensive and suitable for more complex cases. The study findings bore out this expectation. The cost involved in providing and maintaining the study website and written materials, now that they are developed, is small. For example, the total annual cost of the website is estimated to be approximately £1500, plus a registration cost for each new family of £32. The mean cost per family participating in the CBT programme was £437. Because the rate of NHS contacts was found to reduce from the baseline to the outcome assessment points, it is feasible that part or all of these support package costs can be recovered by savings in basic NHS services. However, a full-scale RCT is needed to examine this question.
-
As well as providing evidence about the feasibility of a future trial, this study aimed to develop and examine methods suitable for conducting it. A number of standardised psychometric scales proved to be effective, sensitive to change and viable in use. Future studies should also include measures of parental and infant health, parental sleep, social support and breastfeeding and the reasons for its discontinuation, and a more sustained follow-up of excessive crying cases. Of two recruitment strategies examined, the one that depended on HV/SCPHN referral allowed the planned number of excessive crying cases to be recruited and is suitable for future use. The second strategy, which involved the follow-up and screening of a community cohort, appeared to offer the advantage of identifying cases earlier; however, it was highly resource intensive and unlikely to be feasible in the NHS.
-
The study’s limitations, too, provide lessons for future research. Fathers proved elusive, so that ways of increasing their involvement are needed. Our expectation that non-English-speaking parents would be supported by English-speaking family members or friends proved to be wrong. Although the package materials were set at a low reading level, few parents from minority groups took part. The implication is that the materials need to be translated into one or more other languages, and ways of reaching minority ethnic communities need to be considered more thoroughly in future research. Parental need for contact with other parents, a finding that emerged in both parts of the study, also requires more attention. Although we planned to include small groups in the CBT arm of the study, too few parents were available in the same area at the same time, so all of the CBT sessions were with individual parents or couples. The majority of parents endorsed the use of online discussion boards and social media, so it should be worthwhile to examine their use to promote social contact in future research.
-
A further limitation is that of 124 HVs/SCPHNs recruited into stage 2 of the study, only one-third provided evaluation data. The resulting responses were encouraging: > 90% rated the Surviving Crying materials helpful for parents and > 85% judged them suitable for NHS use. However, these findings cannot be generalised with confidence to HVs/SCPHNs as a whole. This part of the study took place while HV/SCPHN services were being restructured and this and busy HV/SCPHN schedules may have contributed to this weakness, but a future trial will need to support and monitor HV/SCPHN participation more effectively.
-
As well as these implications for future research, the study has raised questions about professional training, policy and practice in the NHS. HVs/SCPHNs provide universal services for UK parents and infants and are the obvious choice for delivering the support package, but current HV/SCPHN training does not include the topic of excessive crying. The involvement of senior HVs/SCPHNs and members of the Institute of Health Visiting in this study highlights their recognition that HV/SCPHN practice should be evidence-based. In the longer term, inclusion of the support materials developed here could enhance HV/SCPHN services. However, these services are currently under pressure, so that their capacity to take on anything new has to be balanced against their resources. Furthermore, although infant crying has traditionally involved paediatric services, CBT and other psychological provisions to support parental well-being in the NHS involve adult mental health services. There is evidence that CBT methods can be taught to other professional groups, but ways to join up these different professional areas need to be developed. Consultations with local and national HV/SCPHN bodies and other groups are currently under way to discuss who might deliver which parts of the support package in the future, when it should be delivered and what it might contain. In the meantime, DMU has invested in this area by providing a short period of funding to develop the Surviving Crying materials into a training module suitable for HVs/SCPHNs and other professionals.
-
A further, policy-related, question is whether or not the evidence collected here might be sufficient for some purposes. Provisional sharing of the findings with our HV/SCPHN, Institute of Health Visiting and NCT collaborators has highlighted that they wish to use these resources, particularly the study website, straight away. Because the ongoing cost of providing the website in the NHS would be small, it could be that some NHS commissioners would consider the evidence reported here as sufficient for making the website universally available. Arguably, this does not apply to the CBT programme, because that is more expensive and requires professional training.
-
Although we are keen to see the materials developed here be made widely available, we do not, on balance, think that they should be made generally available at this stage. Once that is done, it will be impossible to complete a controlled scientific evaluation of their clinical effectiveness and cost-effectiveness. Hence, although a delay is regrettable, we consider that the need to provide scientific evidence should hold sway. That said, there are ethical issues involved in this decision that we hope NIHR will consider. In the meantime, we will make as much progress in preparing for a full trial as possible, so that delays can be kept to a minimum.
In summary, this study has found that support services for parents of excessively crying babies are an unmet need in the NHS and that parents and HVs/SCPHNs consider the materials developed by the study to be suitable for this purpose. The findings indicate that a future large-scale RCT is feasible and identify methods that such a study could use to establish the clinical effectiveness and cost-effectiveness of the support package. Alongside further research, discussions with HVs/SCPHNs and other professionals are needed to establish how the service could be delivered in the NHS. Additional research and consultations are now under way to take these matters forward.
Evaluation of patient and public involvement
As noted in Chapter 1, Patient and public involvement, involving parent stakeholders in the design and conduct of this study was integral to all aspects of the research. It was intended that parents’ experiences and perspectives informed all stages of the study, and this proved both possible and valuable.
Recruitment to stage 1 of the study, the focus groups, took longer than anticipated and required some widening of the recruitment strategy; however, 20 parents were successfully recruited and provided rich and detailed data about the experience of having an excessively crying baby. These parents’ clear message of the importance of knowing about the experience of other ‘real people’ informed the decision to integrate participants’ stories and advice into the stage 2 support package. At this stage in the study, one of the focus group parents also agreed to join the Study Management Group, contributing to subsequent meetings. This parent also gave a presentation at a workshop for study collaborators about their experience of participating in and contributing to the wider study process.
Overall, the intention to involve parents in the study was met and also evolved beyond the original plan as the study progressed.
Dissemination
See Publications and Appendix 9 for lists of outputs and dissemination activities.
Acknowledgements
We are grateful to the parents who took part and to the NIHR Health Technology Assessment programme for its support. LPT provided collaborative assistance throughout the study. In particular, the study could not have taken place without the help of the following LPT staff:
-
Nicy Turney, Fellow of the Institute of Health Visiting, Professional Lead in Health Visiting, Families, Young People and Children Services
-
Joanne Chessman (Clinical Team Leader)
-
Gail Melvin (Research Manager)
-
Joanna McGarr (Trainee Research Assistant)
-
Lynn Hartwell (Research Nurse)
-
the many HVs who took part.
De Montfort University acknowledges the support of the NIHR Clinical Research Network.
We want to thank, too, our other UK collaborators:
-
Dr Elaine Boyle (University of Leicester)
-
Charlie Owen (University College London)
-
Sally Rudge (Counselling Psychologist and CBT Practitioner)
-
Rachel Plachcinski (NCT)
-
Jan Bullen and John Bullen (Cry-Sis)
-
Denise Coster and Peter Richards (National Society for the Prevention of Cruelty to Children)
-
members of our Study Management Group and Study Steering Committee
-
members of Leicester Clinical Trials Unit
-
the many parents who took part
-
the NCT, Institute of Health Visiting and Cry-Sis.
We would also like to thank the staff at Consider Creative, the marketing and communications agency, for the helpful and professional support they provided during the website-development process.
Four university or charity research groups gave permission to evaluate their parental support materials during stage 1 of the study and we are grateful to them and their institutions for this support:
-
Ron Barr and Marilyn Barr for the Period of PURPLE Crying
-
Harriet Hiscock and Fallon Cook, Murdoch Children’s Research Institute, for Cry Baby
-
Jane Fisher and Heather Rowe, Monash University, for What Were We Thinking!
-
Denise Coster and Peter Richards, the National Society for Prevention of Cruelty to Children, for Coping with Crying.
Contributions of authors
Ian St James-Roberts (Emeritus Professor of Child Development) initiated and drafted the design of this study, led the research, wrote first drafts of some sections of this report and approved the final version.
Rosemary Garratt (Senior Lecturer in Midwifery) contributed to the study design, managed the data collection, provided critical review of drafts and approved the final version of this report.
Charlotte Powell (Senior Research Fellow) contributed to the study design, carried out the literature review, collected the data, drafted sections of this report and approved the final version.
Deborah Bamber (Senior Research Fellow) contributed to the study design, carried out the literature review, collected the data, drafted sections of this report and approved the final version.
Jaqui Long (Research Assistant) contributed to the study design, carried out the literature review, collected the data, drafted sections of this report and approved the final version.
Jayne Brown (Professor of Nursing) contributed to the study design, managed the data collection, provided critical review of drafts and approved the final version of this report.
Stephen Morris (Professor of Health Economics) contributed to the study design and methodology, carried out the health economic analyses, wrote sections of the report, provided critical review of drafts and approved the final version of this report.
Sue Dyson (Professor of Nursing) contributed to the study design and administration, provided critical review of drafts and approved the final version of this report.
Tom Morris (Trial Statistician) supervised the processing and analysis of the study’s quantitative data, helped to prepare the results for publication and approved the final report.
Nishal Bhupendra Jaicim (Trial Statistician) supervised the processing and analysis of the study’s quantitative data, helped to prepare the results for publication and approved the final report.
Publications
St James-Roberts I. The Surviving Crying study: progress report for the first stage of research. Community Pract 2016;89:30–1.
Long J, Powell C, Bamber D, Garratt R, Brown J, Dyson S, St James-Roberts I. Development of materials to support parents whose babies cry excessively: findings and health service implications. Prim Health Care Res Dev 2018;19:320–32.
Powell C, Bamber D, Long J, Garratt R, Brown J, Rudge S, et al. Mental health and wellbeing in parents of excessively crying infants: prospective evaluation of a support package. Child Care Health Dev 2018;44:607–15.
Bamber D, Powell C, Long J, Garratt R, Brown J, Rudge S, et al. Parental and health professional evaluations of a support service for parents of excessively crying infants. BMC Health Serv Res 2019;19:592.
Garratt R, Bamber D, Powell C, Long J, Brown J, Turney N, et al. Parents’ experiences of having an excessively crying infant and implications for support services. Journal of Health Visiting 2019;7:132–140.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review. Please contact the corresponding author to request access to the practitioners’ manual.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care.
References
- Alvarez M. Caregiving and early infant crying in a Danish community. J Dev Behav Pediatr 2004;25:91-8. https://doi.org/10.1097/00004703-200404000-00003.
- Douglas P, Hill P. Managing infants who cry excessively in the first few months of life. BMJ 2011;343. https://doi.org/10.1136/bmj.d7772.
- St James-Roberts I, Halil T. Infant crying patterns in the first year: normal community and clinical findings. J Child Psychol Psychiatry 1991;32:951-68. https://doi.org/10.1111/j.1469-7610.1991.tb01922.x.
- Barr RG, Rotman A, Yaremko J, Leduc D, Francoeur TE. The crying of infants with colic: a controlled empirical description. Pediatrics 1992;90:14-21.
- St James-Roberts I, Hurry J, Bowyer J. Objective confirmation of crying durations in infants referred for excessive crying. Arch Dis Child 1993;68:82-4. https://doi.org/10.1136/adc.68.1.82.
- Illingworth RS. Three-months’ colic. Arch Dis Child 1954;29:165-74. https://doi.org/10.1136/adc.29.145.165.
- Wessel MA, Cobb JC, Jackson EB, Harris GS, Detwiler AC. Paroxysmal fussing in infancy, sometimes called colic. Pediatrics 1954;14:421-35.
- Lehtonen L, Barr RG, St James-Roberts I, Keefe M. New Evidence on Unexplained Early Crying: Its Origin, Nature and Management. Skillman, NJ: Johnson & Johnson Pediatric Institute; 2001.
- Stifter CA, Braungart J. Infant colic: a transient condition with no apparent effects. J Applied Dev Psychol 1992;13:447-62. https://doi.org/10.1016/0193-3973(92)90012-7.
- Barr RG. The normal crying curve: what do we really know?. Dev Med Child Neurol 1990;32:356-62. https://doi.org/10.1111/j.1469-8749.1990.tb16949.x.
- Barr RG, Paterson JA, MacMartin LM, Lehtonen L, Young SN. Prolonged and unsoothable crying bouts in infants with and without colic. J Dev Behav Pediatr 2005;26:14-23.
- Freedman SB, Al-Harthy N, Thull-Freedman J. The crying infant: diagnostic testing and frequency of serious underlying disease. Pediatrics 2009;123:841-8. https://doi.org/10.1542/peds.2008-0113.
- Barr R, Gunnar M, Barr RG, Hopkins B, Green JA. Crying as a Sign, a Symptom, and a Signal. Cambridge: Cambridge University Press; 2000.
- St James-Roberts I, Alvarez M, Hovish K. Emergence of a developmental explanation for prolonged crying in 1- to 4-month-old infants: review of the evidence. J Pediatr Gastr Nutr 2013;57:S30-6. https://doi.org/10.1097/01.mpg.0000441932.07469.1b.
- Kurth E, Kennedy HP, Spichiger E, Hösli I, Stutz EZ. Crying babies, tired mothers: what do we know? A systematic review. Midwifery 2011;27:187-94. https://doi.org/10.1016/j.midw.2009.05.012.
- Murray L, Cooper P, Barr RG, St James-Roberts I, Keefe M. New Evidence on Unexplained Early Crying: Its Origin, Nature and Management. Skillman, NJ: Johnson & Johnson Pediatric Institute; 2001.
- Morris S, St James-Roberts I, Sleep J, Gillham P. Economic evaluation of strategies for managing crying and sleeping problems. Arch Dis Child 2001;84:15-9. https://doi.org/10.1136/adc.84.1.15.
- Howard CR, Lanphear N, Lanphear BP, Eberly S, Lawrence RA. Parental responses to infant crying and colic: the effect on breastfeeding duration. Breastfeed Med 2006;1:146-55. https://doi.org/10.1089/bfm.2006.1.146.
- Stifter CA, Anzman-Frasca S, Birch LL, Voegtline K. Parent use of food to soothe infant/toddler distress and child weight status. An exploratory study. Appetite 2011;57:693-9. https://doi.org/10.1016/j.appet.2011.08.013.
- Papousek M, Wurmser H, Von Hofacker N, Barr RG, St James-Roberts I, Keefe M. New Evidence on Unexplained Early Crying: Its Origin, Nature and Management. Skillman, NJ: Johnson & Johnson Pediatric Institute; 2001.
- Barr RG, Trent RB, Cross J. Age-related incidence curve of hospitalized shaken baby syndrome cases: convergent evidence for crying as a trigger to shaking. Child Abuse Negl 2006;30:7-16. https://doi.org/10.1016/j.chiabu.2005.06.009.
- Smarius LJ, Strieder TG, Loomans EM, Doreleijers TA, Vrijkotte TG, Gemke RJ, et al. Excessive infant crying doubles the risk of mood and behavioral problems at age 5: evidence for mediation by maternal characteristics. Eur Child Adolesc Psychiatry 2017;26:293-302. https://doi.org/10.1007/s00787-016-0888-4.
- Hadjistavropoulos HD, Craig KD, Grunau RV, Johnston CC. Judging pain in newborns: facial and cry determinants. J Pediatr Psychol 1994;19:485-91. https://doi.org/10.1093/jpepsy/19.4.485.
- Fujiwara T, Barr RG, Brant R, Barr M. Infant distress at five weeks of age and caregiver frustration. J Pediatr 2011;159:425-30.e2. https://doi.org/10.1016/j.jpeds.2011.02.010.
- Laurent HK, Ablow JC. A cry in the dark: depressed mothers show reduced neural activation to their own infant’s cry. Soc Cogn Affect Neurosci 2012;7:125-34. https://doi.org/10.1093/scan/nsq091.
- Pearson RM, Cooper RM, Penton-Voak IS, Lightman SL, Evans J. Depressive symptoms in early pregnancy disrupt attentional processing of infant emotion. Psychol Med 2010;40:621-31. https://doi.org/10.1017/S0033291709990961.
- Petzoldt J, Wittchen HU, Einsle F, Martini J. Maternal anxiety versus depressive disorders: specific relations to infants’ crying, feeding and sleeping problems. Child Care Health Dev 2016;42:231-45. https://doi.org/10.1111/cch.12292.
- Frodi AM, Lamb ME. Infants at risk for child abuse. Inf Ment Health J 1980;1:240-7. https://doi.org/10.1002/1097-0355(198024)1:4<240::AID-IMHJ2280010407>3.0.CO;2-H.
- Catherine NL, Ko JJ, Barr RG. Getting the word out: advice on crying and colic in popular parenting magazines. J Dev Behav Pediatr 2008;29:508-11. https://doi.org/10.1097/DBP.0b013e31818d0c0c.
- Fisher JR, Wynter KH, Rowe HJ. Innovative psycho-educational program to prevent common postpartum mental disorders in primiparous women: a before and after controlled study. BMC Public Health 2010;10. https://doi.org/10.1186/1471-2458-10-432.
- Twomey JE, High P, Lester BM. Colic: what’s maternal mental health got to do with it?. Infant Ment Health J 2012;33:543-52. https://doi.org/10.1002/imhj.21344.
- Chowdhary N, Sikander S, Atif N, Singh N, Ahmad I, Fuhr DC, et al. The content and delivery of psychological interventions for perinatal depression by non-specialist health workers in low and middle income countries: a systematic review. Best Pract Res Clin Obstet Gynaecol 2014;28:113-33. https://doi.org/10.1016/j.bpobgyn.2013.08.013.
- Dennis CL, Dowswell T. Psychosocial and psychological interventions for preventing postpartum depression. Cochrane Database Syst Rev 2013;2. https://doi.org/10.1002/14651858.CD001134.pub3.
- Morrell CJ, Warner R, Slade P, Dixon S, Walters S, Paley G, et al. Psychological interventions for postnatal depression: cluster randomised trial and economic evaluation. The PoNDER trial. Health Technol Assess 2009;13. https://doi.org/10.3310/hta13300.
- Stein A, Pearson RM, Goodman SH, Rapa E, Rahman A, McCallum M, et al. Effects of perinatal mental disorders on the fetus and child. Lancet 2014;384:1800-19. https://doi.org/10.1016/S0140-6736(14)61277-0.
- National Institute for Health and Care Excellence . Antenatal and Postnatal Mental Health: Clinical Management and Service Guidance CG192 2015.
- National Institute for Health and Care Excellence . Depression in Adults: Recognition and Management CG90 2016.
- Heidegger M. Being and Time. New York, Hagerstown, San Francisco and London: Harper and Row; 1962.
- Ricoeur P. The task of hermeneutics. Philosoph Today 1973;17:112-28. https://doi.org/10.5840/philtoday197317232.
- Ricoeur P, Thompson JB. Hermeneutics and the Human Sciences: Essays on Language, Action and Interpretation. Cambridge: Cambridge University Press; 1981.
- Gadamer H. Philosophical Hermeneutics. Berkeley, CA: University of California Press; 1976.
- Alexander P. Innovation: CBT-based support groups for postnatal depression. Nurs Times 2013;109:12-4.
- Tandon SD, Perry DF, Mendelson T, Kemp K, Leis JA. Preventing perinatal depression in low-income home visiting clients: a randomized controlled trial. J Consult Clin Psychol 2011;79:707-12. https://doi.org/10.1037/a0024895.
- Hiscock H, Cook F, Bayer J, Le HN, Mensah F, Cann W, et al. Preventing early infant sleep and crying problems and postnatal depression: a randomized trial. Pediatrics 2014;133:e346-54. https://doi.org/10.1542/peds.2013-1886.
- EuroQol Group . EuroQol – a new facility for the measurement of health-related quality of life. Health Policy 1990;16:199-208. https://doi.org/10.1016/0168-8510(90)90421-9.
- Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry 1987;150:782-6. https://doi.org/10.1192/bjp.150.6.782.
- Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 2006;166:1092-7. https://doi.org/10.1001/archinte.166.10.1092.
- Parker S, Zahr L. The Maternal Confidence Questionnaire. Boston, MA: Boston City Hospital; 1985.
- Badr LK. Further psychometric testing and use of the Maternal Confidence Questionnaire. Issues Compr Pediatr Nurs 2005;28:163-74. https://doi.org/10.1080/01460860500227572.
- Wisner KL, Parry BL, Piontek CM. Postpartum depression. N Engl J Med 2002;347:194-9. https://doi.org/10.1056/NEJMcp011542.
- National Sleep Foundation . National Sleep Foundation Recommends New Sleep Times 2015. https://sleepfoundation.org/press-release/national-sleep-foundation-recommends-new-sleep-times (accessed 20 April 2017).
- Nurko S, Benninga M, Faure C, Hyman P, Schechter N, St James-Roberts I, et al. Rome IV: The Functional Gastrointestinal Disorders. Raleigh, NC: The Rome Foundation; 2016.
- Barr RG, Barr M, Fujiwara T, Conway J, Catherine N, Brant R. Do educational materials change knowledge and behaviour about crying and shaken baby syndrome? A randomized controlled trial. CMAJ 2009;180:727-33. https://doi.org/10.1503/cmaj.081419.
- Research Design Service London . What Kind of Health Economic Input Is Appropriate in a Feasibility Study? n.d. www.rds-london.nihr.ac.uk/How-to-design-a-study-find-funding/Health-economics/Health-economics-feasibility-study.aspx (accessed 20 April 2017).
- Griebsch I, Coast J, Brown J. Quality-adjusted life-years lack quality in pediatric care: a critical review of published cost–utility studies in child health. Pediatrics 2005;115:e600-14. https://doi.org/10.1542/peds.2004-2127.
- National Institute for Health and Care Excellence . Guide to the Methods of Technology Appraisal PMG9 2013.
- Petrou S, Cooper P, Murray L, Davidson LL. Economic costs of post-natal depression in a high-risk British cohort. Br J Psychiatry 2002;181:505-12. https://doi.org/10.1192/bjp.181.6.505.
- Curtis L, Burns A. Unit Costs of Health And Social Care 2015. London: Personal Social Services Research Unit; 2015.
- Office for National Statistics . Vital Statistics: Population and Health Reference Tables 2016.
- St James-Roberts I. The Origins, Prevention and Treatment of Infant Crying and Sleeping Problems: An Evidence-Based Guide for Healthcare Professionals and the Families They Support. New York, NY: Routledge/Taylor & Francis Group; 2012.
- Reijneveld SA, Brugman E, Hirasing RA. Excessive infant crying: the impact of varying definitions. Pediatrics 2001;108:893-7. https://doi.org/10.1542/peds.108.4.893.
- NHS Employers . Mileage Allowances – Section 17 n.d. www.nhsemployers.org/your-workforce/pay-and-reward/nhs-terms-and-conditions/nhs-terms-and-conditions-of-service-handbook/mileage-allowances (accessed 20 April 2017).
- National Institute for Health and Care Excellence . Common Mental Health Problems: Identification and Pathways to Care CG123 2011.
- Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Res Methodol 2005;8:19-32. https://doi.org/10.1080/1364557032000119616.
Appendix 1 Development of samples of four packages for focus group viewing
Once the packages had been selected, each was reviewed in detail by the team to ensure familiarity with its content. One member of the team then reviewed the packages in further depth to identify a sample of the content that would give an overview of the whole and highlight some of the packages’ key features. Using Microsoft Expression Web (Microsoft Corporation, Redmond, WA, USA), a video capture of the selected elements of each website was created, together with a script to be read out while the video capture was playing. A draft of the videos and scripts was then reviewed by other members of the team for comment and revision. The revised versions were shown to two people who were not part of the study team in order to ensure that they provided a good-enough overview of the websites to enable an informed judgement of them to be made.
Although the study team aimed to ensure that each package was reviewed by parents for the same length of time, the websites contained a considerably varying amount of content. As a result, the video captures were of slightly differing lengths, between approximately 6.5 minutes (Coping with Crying and What Were We Thinking!) and 7.5 minutes (Cry Baby and Period of PURPLE Crying). For one package, What Were We Thinking!, laminated copies of a sample of the accompanying written materials were also circulated to focus group participants, and for another, Cry Baby, some of the downloadable resources were printed off and laminated for viewing.
Once this process was completed, the finished products enabled focus group members to be shown the key features of the websites without the need for an internet connection, and also ensured that all participants were exposed to an identical sample and description of each package. In order to avoid any bias arising from the sequence in which the packages were shown, the order of presentation was varied at each focus group, as shown in Table 53. A brief description of the aspects of each package shown to focus group participants is given in the following sections.
| Order in which packages were shown | Participants viewing this order |
|---|---|
|
Focus group 1 One individual interview Total: 5 |
|
Focus group 2 Total: 5 |
|
Focus groups 3 and 4 One individual interview Total: 6 |
|
Four individual interviews Total: 4 |
Cry Baby
The package was introduced, and it was explained that although the website gave information and advice about managing early infant crying and sleeping, only materials relevant to crying would be shown on this occasion. Having shown the main menu, a section of the introductory video was then played. After this, an overview of some of the topics was given, highlighting how the website offered information on research into crying: the ‘crying curve’ over the first few months, the idea of unsoothable crying that is not because of a problem with the baby or the parents, and the fact that it is not possible to work out the reason for the crying from how it sounds. A section of the website that offers tips to parents on how to check their baby to ensure that nothing is wrong was then shown. The use of various graphic features to give advice and guidance was highlighted to the group. The presentation then moved only to show some of the website section that gave parents advice on how to cope with the crying once they have done what they can to try and stop it.
The presentation showed the other main part of the website resources, which emphasises the importance of parents looking after themselves as well as their baby. A part of the introduction to this section was shown, together with sample aspects of the sections that have been separately developed for mothers and fathers. The resources section was then briefly reviewed, which lists contacts for other organisations and helplines and provides access to the various checklists that can be downloaded from the website. Finally, a section of a page called Baby Myths was introduced, highlighting how it challenges some of the common beliefs that can cause stress among parents. Copies of the three downloadable checklists were then circulated to the group for viewing.
Coping with Crying
The package was introduced, explaining that it consisted of a film, website, DVD and leaflet, but because all the materials are contained within the website, only the website would be shown to the group. The home page was then displayed, and the three sections, Keeping Calm, Soothing Your Baby and Understanding Your Baby, were pointed out. The presentation then moved to the Understanding Your Baby section, explaining how each page included quotations from parents, tips and advice and ideas for where parents can get further help and support. The content of the page was reviewed briefly, explaining how it focused on giving information about babies’ behaviour and learning how to interpret and respond to it – a section listing the kind of things that might trigger a baby to cry was displayed for a short time for the group to read. Other aspects of the page were mentioned, and then the presentation moved to the second section, Soothing Your Baby.
Part of a video on this page was shown to the group, highlighting how it includes content from parents who have had a crying baby and from a parenting adviser. An overview of the information on the page was given, including noting that sometimes none of the soothing strategies will work and, therefore, the importance of parents looking after their own well-being and staying calm. The presentation then moves to the Keeping Calm section of the website, highlighting how this provides advice on strategies to manage stress and information on the potential negative impact of stress on both parents and the baby. An excerpt from a video of parents sharing their experiences and tips was shown, and attention was drawn to the advice offered on what to do if parents are feeling at risk of losing control with the baby.
Finally, the presenter explained that the website contained a further, much longer video that focused on preventing shaken baby syndrome. The content of this video was described to the group, noting that it includes the story of a parent talking about the disability and eventual death of her baby as a result of her partner shaking him. Partly because of this emotive content the research team made the decision not to show this video to the group but to describe its content instead.
The Period of PURPLE Crying
The package was introduced, explaining that the materials consisted of a website, together with a DVD and leaflet given out by health professionals just before or after birth. Only the website was shown to the group, and it was explained that although this contained information about crying and sleeping, only the crying-related content would be described. The home page was displayed, pointing out its six sections: Introduction, Sleeping, Soothing, Crying, Protecting and For Dads. The introductory page was then shown, including an excerpt from a video from a paediatrician explaining the reason for the term ‘PURPLE Crying’, the key features of the crying and that it is neither the baby’s nor the parents’ fault. An overview of the Crying section of the website was then given, showing the information about the research into crying, the advice about responding to people who may not understand it and a caution about ‘foolproof’ solutions to the crying. A section called Real Life Challenges was then introduced, which contained parents’ experiences of having a crying baby, and an excerpt from one of the written stories was read to the group, which described the difficulties a mother had faced and how the situation had been resolved.
A brief overview of the Soothing section was then given, pointing out that it contained information about common features and principles of soothing, together with soothing methods to try and those to avoid. The presentation then moves to the Protecting Children section, noting that there is a large amount of content and showing one page of it, which offers a set of photographic images giving suggestions on how to deal with frustration, followed by some written information that the group is given a short opportunity to read. The presentation then moves to the For Dads section, showing part of a short role-played video illustrating a father’s experience of his baby’s crying. Information about the rest of this section is then given, highlighting how it encourages dads to get involved in parenting their child, the importance of parents working together and the advice on dealing with particular stresses that fathers might face.
What Were We Thinking!
The What Were We Thinking! programme was introduced, explaining that it was not specifically about babies crying, but was designed for first-time parents in general, and that the materials being shown were part of a programme that also includes workbooks and a day workshop that both parents are expected to attend. The presentation began by showing the home page, which introduced the programme, and playing the beginning of a video, which explained the programme using a humorous approach. An overview of the parents’ section was then given, explaining how it starts by discussing the challenges of becoming a parent and adjusting to the changes in relationships; the presentation then describes the worksheets that take up most of the website. An example of one of the worksheets was then displayed, which asks each parent to describe their baby and then to see when they agree and disagree. A demonstration of how to complete the worksheet was given, and the advice given on each page relating to the topic was then highlighted. Another worksheet was then shown and demonstrated, which asks parents to compare how long and when they think that their baby cries and what strategies they have used to soothe them. The accompanying advice was highlighted, and then the presentation moved to a page giving tips on how to settle your baby and an excerpt from one of the short videos demonstrating techniques was shown.
The presentation then highlighted how some of the worksheets are for parents to think about themselves and their experiences. It noted that these include looking at how it feels to be a parent compared with what they thought it would be like, and a brief overview of a section about the losses and gains since becoming a parent is displayed. A section on sharing the workload was then introduced, and part of a role-played video prompting parents to think about their different work responsibilities was shown. Other worksheets, including negotiating support needs, advice for single parents and dealing with criticism, were mentioned but not shown. The presentation then returned to the home page to highlight a blog in which parents can share their experiences. Copies of a number of worksheets were then circulated around the group for viewing.
Appendix 2 Literature review process
Aims
As part of the process of developing the intervention for this study, a focused literature review was undertaken. This review had two aims:
-
identify recent evidence of existing interventions to support parents of babies considered to be excessively crying
-
select a number of these interventions to show to parents attending focus groups in order to gain their feedback.
Strategy
As set out in the study protocol, the review was based on an update of Douglas and Hill’s2 systematic review concerning the causes of excessive crying in the first few months of life in term infants and interventions to manage it. For the purposes of this review, ‘excessive crying’ was taken to mean any crying behaviour that parents considered problematic. Although a full systematic review could not be undertaken within the project’s resources, it was necessary to ensure that all relevant research had been considered. Therefore, a review strategy was drawn up based on Arksey and O’Malley’s64 framework for a scoping study.
The review question was identified as ‘What support is available to parents with an excessively crying baby who is 6 months or under and who is otherwise well?’.
Eligibility criteria
Population
Eligible participants were parents of excessively crying babies aged ≤ 6 months for whom no medical reason for the crying had been identified. Based on the evidence that the term ‘colic’ is often applied to unsoothable crying, babies described as having colic were included.
Parents of babies aged > 6 months were excluded to rule out other issues that arise at older ages. Premature babies or those medically diagnosed as unwell were also excluded because they constitute a different population with a given reason for the crying and potentially different needs. Medically diagnosed feeding problems were excluded for similar reasons.
Interventions supporting parents with diagnosed physical or mental health problems were excluded, apart from those for parents experiencing postnatal depression or anxiety, because these conditions have a known association with excessive crying.
Intervention
All primary studies that had evaluated relevant interventions, using either qualitative or quantitative methods, were included.
Studies only investigating the testing or use of relevant measures of crying were excluded. Protocols for trials of interventions were excluded, as these did not evaluate the relevant intervention.
Methodological quality
The methodological quality of studies was not assessed, as the aim of the review was to identify the range of published material.
Publication type/status
All relevant studies, regardless of publication status, were included.
Owing to time limitations, articles not available in English were excluded. Literature published prior to June 2011 was excluded to avoid duplication of the evidence already reviewed by Douglas and Hill. 2 However, we included an intervention programme evaluated by Fisher et al. 30 that met our criteria but was omitted by Douglas and Hill. 2
Search strategy
During early December 2014, the following databases were searched: MEDLINE, PsycINFO, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Web of Science, the Cochrane Database of Systematic Reviews and the Database of Abstracts of Reviews of Effects. In addition, grey literature was searched via the OpenGrey database.
Search terms were identified pertaining to four key aspects of the review question: (1) babies/infants, (2) parents, (3) crying/distress and (4) parental distress, support and coping (see Table 54 for full details). These terms were applied to each database, although a slightly modified search process was used in OpenGrey because of the database’s more limited capacity.
Selection
Retrieved references were reviewed in a number of stages. First, all titles were evaluated against the inclusion and exclusion criteria by two team members, with titles being included for further review when at least one team member considered them relevant. In the second stage, abstracts for all included references were obtained when possible, and these were then reviewed by two team members. When abstracts could not be obtained, a decision regarding inclusion was made on the basis of available information. Finally, the full text of the remaining papers was obtained when possible, and these were then evaluated by two researchers as before. Disagreements were resolved by a third team member at all stages.
Results
Tables 54–57 show the literature review search terms and number of resulting publications identified in each database; the flow chart in Figure 15 sets out the review process.
| Search number | Search terms | Results |
|---|---|---|
| 1 | Parent terms: Parent* OR mother OR maternal OR father OR paternal OR family | 399,122 |
| 2 | Infant terms: bab* OR infant OR neonate OR newborn (age limited to infant or newborn) | 126,546 |
| 3 | Crying terms: cry* OR distress OR excessive crying OR fuss OR irritab* OR unsettled OR colic (age limited to infant or newborn) | 4783 |
| 4 | Mood/coping terms: anxiety OR depression OR *stress OR parenting OR mental illness OR mental health OR expectation OR postnatal/post natal OR postpartum/post partum OR perinatal/peri natal OR sleep deprivation OR fatigue OR support OR coping OR resilience OR vulnerab* | 829,008 |
| 5 | Parent AND Infant terms combined | 30,291 |
| 6 | Parent AND Infant AND Crying terms combined | 1539 |
| 7 | Parent AND Mood/Coping terms combined | 136,602 |
| 8 | Crying OR Mood/Coping terms combined | 830,666 |
| 9 | (Parent AND Infant terms) AND (Crying OR Mood/coping terms) combined | 11,643 |
| 10 | Exported to RefWorks with duplicates automatically removed | 9895 |
| Search number | Search terms | Results |
|---|---|---|
| 1 | Parent terms: Parent* OR mother OR maternal OR father OR paternal OR family | 12,029 |
| 2 | Infant terms: bab* OR infant OR neonate OR newborn | 9273 |
| 3 | Crying terms: cry* OR distress OR excessive crying OR fuss OR irritab* OR unsettled OR colic | 5689 |
| 4 | Mood/coping terms: anxiety OR depression OR *stress OR parenting OR mental illness OR mental health OR expectation OR postnatal/post natal OR postpartum/post partum OR perinatal/peri natal OR sleep deprivation OR fatigue OR support OR coping OR resilience OR vulnerab* | 65,663 |
| 5 | Parent AND Infant terms combined | 3633 |
| 6 | Parent AND Infant AND Crying terms combined | 768 |
| 7 | Parent AND Mood/Coping terms combined | 8682 |
| 8 | Crying OR Mood/Coping terms combined | 66,855 |
| 9 | (Parent AND Infant terms) AND (Crying OR Mood/coping terms) combined | 2692 |
| 10 | Exported to RefWorks | 2692 |
| Search number | Search terms | Results |
|---|---|---|
| 1 | Parent terms: Parent* OR mother OR maternal OR father OR paternal OR family | 350,976 |
| 2 | Parent terms AND Infant terms: bab* OR infant OR neonate OR newborn | 26,265 |
| 3 | Crying terms: cry* OR distress OR excessive crying OR fuss OR irritab* OR unsettled OR colic(age limited to infant or newborn) | 400,522 |
| 4 | Mood/coping terms: anxiety OR depression OR *stress OR parenting OR mental illness OR mental health OR expectation OR postnatal/post natal OR postpartum/post partum OR perinatal/peri natal OR sleep deprivation OR fatigue OR support OR coping OR resilience OR vulnerab* | 993,000 |
| 5 | (Parent AND Infant terms) AND (Crying OR Mood/coping terms) combined | 11,636 |
| 6 | Exported to RefWorks | 11,636 |
| Search number | Search terms | Results |
|---|---|---|
| 1 | Parent terms: Parent* OR mother OR maternal OR father OR paternal OR family (limited to years 2011–14) | 3667 |
| 2 | Infant terms: bab* OR infant OR neonate OR newborn (limited to years 2011–14) | 374 |
| 3 | Crying terms: cry* OR distress OR excessive crying OR fuss OR irritab* OR unsettled OR colic (limited to years 2011–14) | 2150 |
| 4 | Mood/coping terms: anxiety OR depression OR *stress OR parenting OR mental illness OR mental health OR expectation OR postnatal/post natal OR postpartum/post partum OR perinatal/peri natal OR sleep deprivation OR fatigue OR support OR coping OR resilience OR vulnerab* (limited to years 2011–14) | 8197 |
| 5 | Parent terms AND Infant terms combined | 146 |
| 6 | Parent AND Infant AND Crying terms combined | 12 |
| 7 | Parent AND Infant AND Mood/coping terms combined | 69 |
| 8 | 6 and 7 reviewed and copied to RefWorks | 13 |
FIGURE 15.
Flow chart for the literature review process.

The search and selection process for OpenGrey was undertaken slightly differently, owing to the database’s more limited capacity; the results of the final two searches (6 and 7) could not be combined, and the database had no export facility. As a result, the results of these two searches were visually reviewed by one author and all potentially relevant references identified and individually copied into RefWorks (ProQuest LLC, Ann Arbor, MI, USA) for further screening, having first been checked for duplication.
The total numbers of references identified (24,236) were:
-
CINAHL/MEDLINE/PsycINFO (9895)
-
The Cochrane Library (2692)
-
Web of Science (11,636)
-
OpenGrey (13).
Following the removal of duplicates, 18,468 potentially relevant records were identified. Once title and abstract screening were completed, 657 records remained to be assessed for eligibility. On review, it was found that although many articles contained information relating to excessive crying, they did not meet the review criteria; these included studies considering factors that may contribute to the crying, and parents’ experiences of a crying baby. Others explored interventions not specifically targeting support for parents with crying babies, instead focusing on maternal mental health or directly attempting to treat the baby’s crying. Once all these were excluded, a total of 19 relevant articles remained.
The included articles identified a total of 11 different interventions (more than one paper having been published in relation to some interventions), as detailed in Report Supplementary Material 2. These interventions were reviewed in order to consider their appropriateness within the context of this study using the following criteria:
-
intervention materials available in a published and exportable form
-
delivery costs that allowed potential adoption of the intervention within the NHS
-
at least provisional evidence of clinical effectiveness
-
offering a variety of styles of presentation.
Appendix 3 Focus group topic guide
Meet and greet at start of focus group: 10 minutes
-
Meet attendees individually and greet them, let get baby settled.
-
Give name badge/sticker – let parents know OK to use pseudonym if preferred.
-
Give out copies of consent forms.
-
Point attendees in direction of refreshments.
-
Ask parents to complete Q1 on extra questions.
-
Tick names on register of who attended (apologies).
Introduction to group discussion section: 5 minutes
-
Introducing facilitators – including roles of facilitators (e.g. note taker).
-
Housekeeping.
-
Introduction and brief overview of the study – say that we are interested in your experiences, but we need to come away with information to help us develop something that will help other parents in their position.
-
Ground rules for the focus group:
-
Do not share information outside the group.
-
Respect and listen to other people’s views.
-
Groups will be audio-recorded to help us gather an accurate representation of the group.
-
Data will be transcribed and identifiers removed.
-
Information will not be fed back to HVs/SCPHNs unless there is a current immediate risk to yourself or your baby, emphasise current – not judging their behaviour with their baby when distressed.
-
Although babies/children are welcome, we would like to continue if baby cries, please soothe and would you be happy for one of us to entertain/soothe?
-
-
Quick fun icebreaker (one-word) including introductions among parents at the group.
Start audio-recorder here
Group discussion: 20 minutes
-
Tell us, what was it like when your baby was crying a lot?
-
Who did you go to for help?
-
Prompts – HV/SCPHN, GP, online information, family, friends.
-
Support for baby care or for yourself.
-
-
What was most helpful?
-
What else do you think would have helped you?
Ask parents to complete white Q1a of extra questions.
Close this section with a summary followed by:
What research has shown: 5 minutes
(Crying curve – day and months – unsoothable nature of the crying, colic).
Most parents have had to cope with a crying baby but the simple fact is that some babies cry more than others and some parents experience periods when their baby’s crying is prolonged, incessant and unsoothable.
Research has shown that in early infancy, around one in five babies cry for prolonged periods without an apparent reason. This used to be known as ‘colic’ and attributed to indigestion pain. However, recent research has found that only 5–10% of infants taken to the doctor because of their crying are poorly. Most infants who cry a lot are healthy and develop normally.
Research has also shown that many normal babies have a crying peak at around 6 weeks of age, which can tend to be worse in the late afternoon and early evening and this tends to stop at between 5 and 6 months of age. Like all things, no two babies are the same and although most babies seem to follow this pattern some babies just cry more than others while doing it! This and the ‘unsoothable’ nature of the crying, that is the periods of prolonged crying for which no reason can be found, can alarm parents. However, this excessive and unsoothable crying is thought to be normal and linked to normal developmental processes. In other words, research suggests that it is not the parents’ fault – some babies just cry more than others!
So, given that the baby is normally well and there is often nothing that parents or professionals can do to stop the crying, the focus is shifting to look at how parents who are experiencing this can be supported. Currently, there are no tried and tested NHS practices for supporting parents in managing the crying. Instead, parents turn to popular books, magazines or websites, which may give conflicting advice. So, what we are trying to do here today is the first stage in finding out what could be put in place to support parents in that situation.
Developing a package: 10 minutes
Thinking back to what would have been helpful to you at the time, what would you like to include if you were to design something from scratch to support parents who currently have a baby who cries a lot? (Prompts: website/leaflet/support/apps.)
Reviewing existing resources: 15 minutes
We have some examples of packages that have been used with parents either in other countries or focusing on slightly different aspects of infant care and we’d like to get your opinion on these and how you think these would have fit with your needs back when you were trying to deal with your baby’s excessive crying. What we’ll do is show you the packages one at a time and ask for your feedback on each one in turn with discussion afterwards. All four packages are at least partly website based, so we are going to show you a short video tour of each. We will give you the links at the end of the focus group if you want to go away and look at them in more detail.
Four packages to review – Period of PURPLE Crying, NSPCC (National Society for the Prevention of Cruelty to Children), What Were we Thinking!, Cry Baby (order to change for each group).
Show videos with facilitator talking alongside explaining the website (see separate sheet for scripts).
Pause after each package to allow parents to complete rating sheet.
Break – after two/three packages: 10 minutes – toilet/refreshments
Return for last packages: 15 minutes
Having had a brief tour of those four packages, what are your overall thoughts about them?
Which did you prefer and why?
(Hand out separate rating sheet to quantify and qualify individual preferences.)
Our workbook/website: 10 minutes
Introduce our intervention: consists of workbook, worksheets and website, with support with a professional available.
Seeing as we have just been looking at websites I wonder if we could start with that bit of the package. So, if you were hunting the internet late at night with a crying baby in your arms, what information would you like on a website? Is it similar to that which we have seen already or would you like something different?
Show homepage of our wireframe.
This is the website that we are currently working on for this study. Please ignore all of the crosses on the boxes, this is what is called a wireframe, it gives us an idea of how the website might look and work but the content is not all in there at the moment but we have a few pages that we can look at. So I am asking you to kind of see through the work in progress to help us envisage how it could look when it is finished. Firstly though, I want you to look at this opening page, and tell us a little about what you would like to see on an opening page for a website developed to help you deal with your crying baby. So what are your impressions?
(Prompt: image.)
(Prompt: as you can see it gives you some idea of the information that will be on the website, we have the boxes here with topic headings and in the bar along the top it shows that we have other areas on the website giving information from experts, other parents’ stories . . .)
Is there anything you would like to see on this website that is not here?
Discussion about support sessions: 10 minutes
One possible method of supporting parents that we were considering is four sessions with a HV/SCPHN. The sessions would look at, firstly, normalising the crying and reassuring parents that there was nothing wrong with the baby or their parenting and showing understanding of the stresses they are under. We know that parents of excessively crying babies are at risk of developing postnatal depression so the sessions would move on to look at good mental health and how to maintain good mental health and look further into the idea of catching thoughts as was mentioned in the Cry Baby package. To do this they would look at how to cope with the stress, manage emotions and deal with the crying in different ways. These sessions would be based on evidence of what works in practice when faced with extreme stresses like a baby who will not stop crying.
To what extent would you have found some sort of support sessions like these helpful while your baby was crying excessively?
If no, would you have found any sort of support session helpful? What would you like to be included in support sessions?
Would you have preferred these to be on a one-to-one, family basis or even a group of other parents in a similar situation?
If a group, how many people in a group?
How long should these sessions be?
How often should they be?
Face to face or over the phone?
Run by a professional or peer?
Would you travel to attend these sessions?
[Hand out sheet to quantify and qualify (on same sheet as for web material preferences) individual preferences regarding individual/group session, length of session, number of sessions.]
We also have a workbook that would run alongside the support sessions or, if support sessions were not needed, could stand alone. The components in the workbook would be handling stress, problem-solving, relaxation and communication. It would give you information on all of these areas and then give you some work to do on each of the areas. How does this sound to you?
What other resources would they like?: 15 minutes
Out of all of the packages that we have looked at today, what do you really think will be helpful to those in the same situation that you were in with a crying baby?
Prompts: information, content, format.
What didn’t you like?
What could be done differently, if anything?
What else would you have liked that we haven’t covered?
Prompt: phone apps.
A lot of the stuff that we have looked at today is information for once you have a baby that cries excessively. Do you think there is any way that you could have been better prepared for the fact that your baby may cry excessively?
If so – what would have helped you prepare? DVD/leaflet/parentcraft-style talk?
Involving dads and families: 5 minutes
Research shows that dads find excessively crying babies perhaps even harder to handle than mums. Do you think the packages that we have talked about are able to support dads as well as mums or do dads need something else?
How can we involve dads?
How can we involve and support wider family?
Finish up: 5 minutes
To finish up, what is the one key thing out of all of today’s discussions that you think should be in place within the NHS to support parents of crying babies?
Goodbyes and telling about the next stage: 5 minutes
The next stage will be taking away all of the useful information that we have gathered today and trying to use it to develop some sort of package of support. Once we have done that we will get back in touch and arrange a way for you to give your opinions on the package – this may be by phone or e-mail. Again, you will get a voucher for your time.
You will find in your packs the website addresses for the four packages we have looked at today and also our contact details, so please take a look at these and give us any further feedback.
Thanks for time and input.
Give out vouchers and complete voucher receipt form.
Sort any travel expenses.
Collect the packs, ensuring that parents take the relevant paperwork (i.e. our contact details and website addresses).
Appendix 4 Health visitor safeguarding procedure for the Surviving Crying study
FIGURE 16.
Health visitor safeguarding procedure for the Surviving Crying study. ED, emergency department.
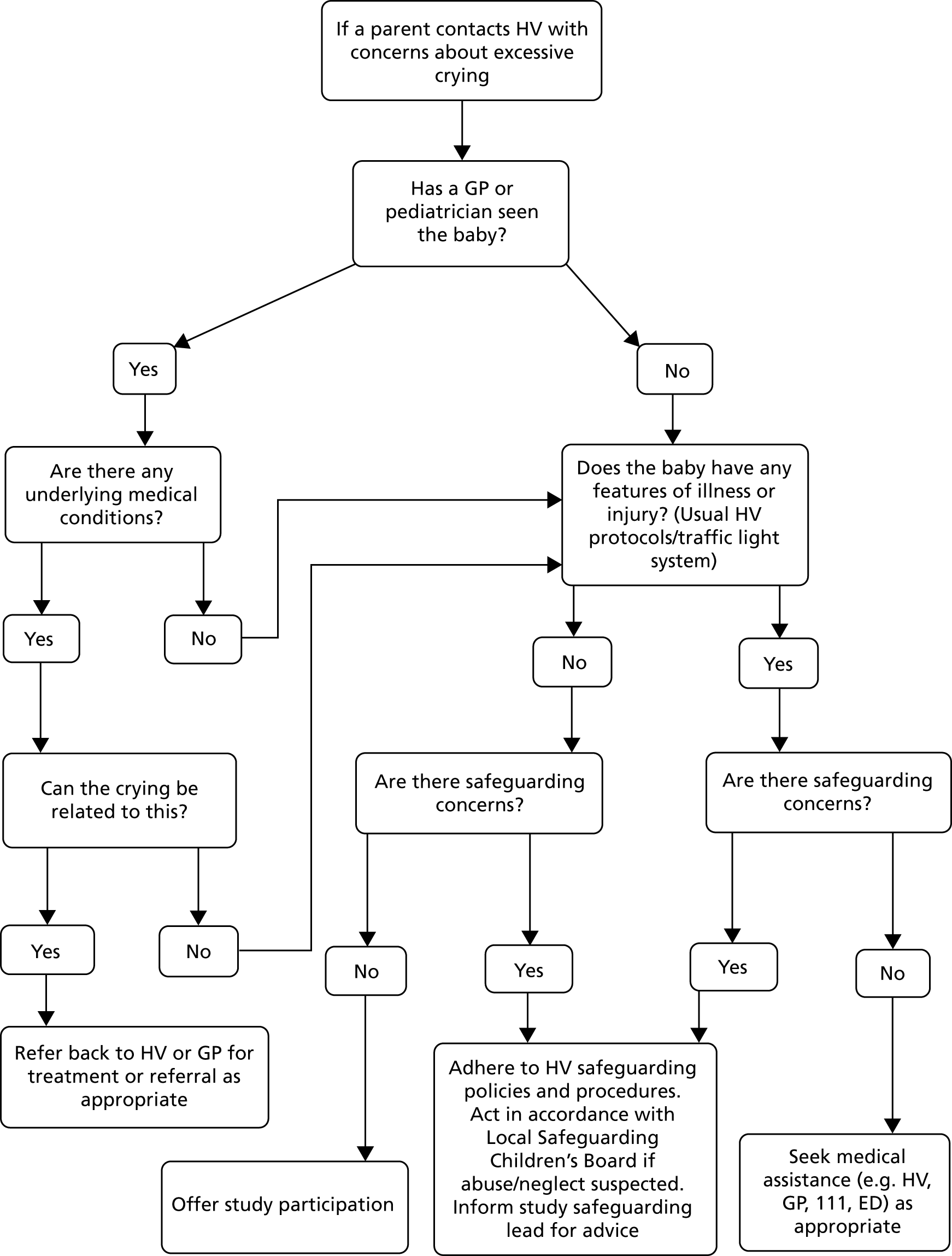
Appendix 5 Focus group analysis: identification of themes and their refinement
| Initial themes | Refined themes | Overarching themes |
|---|---|---|
| Did not expect crying baby | Taken unawares | Expectations of parenthood |
| Not what I expected | ||
| We tried everything | Bad or inadequate parents | |
| Don’t know what to do | ||
| Baby checked and everything fine | ||
| Reaching limit of coping | ||
| My baby does not like me | ||
| Powerless, helpless, useless | ||
| Other parents doing better | ||
| Reaching limit of coping | ||
| Should be able to do this | ||
| Anxious and stressed | ||
| Crying gets to you | ||
| Not like other babies | Comparisons and difference | |
| Not a normal baby | ||
| Not normal to cry so much | ||
| Second or third baby cried, when first and/or second did not | ||
| Coping with another child as well | ||
| Both babies cried | ||
| Our experience different from others | ||
| Exhaustion | Physical effects on parents | |
| Sleep deprivation | ||
| Relentless prolonged crying | ||
| Meeting own basic needs made difficult | ||
| Reaching limit of coping | ||
| Night-time makes it worse | ||
| Reactions of partner | Relationships | |
| Partner not understanding | ||
| Family and friends’ reactions | ||
| Expectations of others (public) | ||
| Difficulty in leaving a crying child | Not going out | Social isolation |
| Experiences of going out to attend groups | ||
| Avoiding going out | ||
| Feelings of loneliness and isolation | ||
| Not wanting to use babysitters | ||
| Cannot get babysitters | ||
| Other people’s reactions to crying | ||
| Should be able to do this | Reluctance to seek support | |
| Other parents coping so much better | ||
| Bad or inadequate parent | ||
| Fears that the baby will be taken away | ||
| Seeking information and reassurance | Self-help strategies | Validation of experience |
| Using the internet | ||
| Using baby-care manuals | ||
| Online peer support | ||
| Concerns dismissed, not believed | Health-care professional support | |
| Experiences seen as exaggeration | ||
| Difficulty in being heard | ||
| Concerns that baby is seriously ill not heard | ||
| Repeated visits/calls to health professionals | ||
| Lack of answers and information | ||
| Conflicting advice | ||
| Lack of continuity of care | ||
| Anxiety labelled as postnatal depression | ||
| Need for information and empathetic support | ||
| Lack of knowledge about excessive crying |
Appendix 6 Overview of the Surviving Crying website
This appendix provides a description of the Surviving Crying website content and layout. As noted in the main report, the booklet content replicated that of the website, with the omission of the content of the parent and expert videos.
The website opened to a line drawing of a couple holding a baby, and a statement explaining that the website is ‘for parents who are worried about their baby’s excessive crying’. In order to access the website, users were required to enter a personal log-in and password provided as part of the study, thus enabling anonymous tracking of individual website usage.
The home page explained that the purpose of the website was to offer information and guidance for parents, access to other sources of support and accounts of parents who have experienced an excessively crying baby. It also provided a brief outline of the crying-related topics covered on the website (see Expert Help and Advice) and information about the research and collaborators on the project. The home page offered access to all the website content through four tabs, labelled Expert Help and Advice, Your Stories, News and Research and About Us. There was also a ‘Need Help Now’ box in the top right of the page and additional legal information was provided at the very bottom of the page. More details of each section are given in the following sections.
Expert Help and Advice
Information regarding a list of eight topics relating to crying could be accessed from this page. Each topic section consisted of a combination of evidence-based information and parents’ experiences. The information was presented in a variety of formats, including a ‘Baby Myths’ box, giving information to help challenge unhelpful assumptions, quotations from focus group parents about their experience of having a crying baby and videos of professionals or parents providing information and advice. Hyperlinks enabled easy navigation between relevant sections of the website.
The eight topics were:
-
Health Checklist. This section provided a list of points for parents to check to ensure that their baby was not ill, and gave suggestions on how to check for these things (e.g. food intolerances). It also highlighted instances in which crying may be a cause for concern and when it would be appropriate to seek help, such as very high-pitched crying. The checklist was downloadable.
-
Settling and Soothing your Baby. This section provided a list of possible reasons why a baby might be crying (e.g. needing comfort) and suggested what to do to address these things. It also featured a video of a lecturer in health visiting demonstrating soothing techniques, plus a downloadable list of suggestions.
-
Can Parents Stop the Crying? This section described research that suggests that babies sometimes cry for no reason and that this crying does not usually continue beyond 6 months. It offered reassurance to parents that the crying is generally not because they are doing anything wrong.
-
Is It Colic? This section discussed the term ‘colic’ and described research challenging the common assumption that excessive crying is because of gut pain. It explained how most new babies show a pattern of crying that peaks in the first few weeks, and that there is nothing physically wrong with most babies who cry in this way.
-
Coping Tips for Parents. This section encouraged parents to think about their own well-being and acknowledged the stress the crying can put on them. It gave advice on what to do to avoid causing any harm to the baby if the crying became overwhelming and also provided coping strategies. A video showed parents talking about how they coped with their baby’s crying, and downloadable tips and suggestions from other parents were also provided.
-
For Dads. This section addressed the fact that fathers can be affected by the crying in a different way from mothers. It discussed the different roles and experiences that the two parents may have and gave suggestions of things that fathers can do to help both themselves and their partner. A video of a father talking about his experiences was included.
-
Surviving as a Family. This section acknowledged the impact that the excessive crying can have on the whole family. It gave advice on how to explain the crying to older siblings and help them to cope. It highlighted the stress that crying can put on couples’ relationships and emphasised that the website is relevant to a diverse range of families, including single parents and same-sex couples.
-
Waking and Crying at Night. This section discussed changing patterns of feeding and sleep in young babies and highlighted the different strategies that parents may adopt in responding to their baby’s crying at night. Downloadable guidelines on managing night-time crying were included.
Your Stories
The information contained on this page focused on parents’ experiences of having an excessively crying baby. It contained accounts of eight parents who took part in the study focus groups who shared what it was like for them when their baby was crying, how they coped and how their baby is now that the crying has stopped. These were presented in a mixture of video and written form. There was also an option for parents using the website to leave comments in response to the stories, with these being reviewed by the study team before they appeared on the website.
News and Research
This page provided more information about the research into crying for those who wanted to explore the topic in more depth, and was presented at a higher reading age than the rest of the website. These articles gave more information on why babies cry excessively, provided references to further research on the topics covered on the website and explained the reason for focusing on supporting parents rather than addressing the baby’s crying. A video of the PI, Professor Ian St James-Roberts, giving further information was included.
About Us
This page gave the background to the research study, including details of the collaborators and research team, including the CBT therapist Sally Rudge. It acknowledged the contribution of HVs and parents to the study, and included a video from LPT’s professional lead for health visiting, Nicy Turney, describing the Health Visiting Service and the role that HVs played in the research. A ‘Contact Us’ box enabled users of the website to e-mail the study team about the research, with a clear direction to visit the ‘Need Help Now’ for any immediate crying-related concerns.
Need Help Now
This section was designed to meet the needs of parents who required more immediate help and support. It could be easily accessed from every page in the body of the website through a prominently coloured box. The page began with information on what to do if feeling overwhelmed by the crying and then gave advice on who to contact about the baby’s health when usual services, such as HVs/SCPHNs or GPs, were not available. It also provided helpline contacts and links to the websites of appropriate organisations, such as Cry-sis (a helpline for parents with crying babies), Family Lives (an organisation providing a range of parenting support and advice) and the Samaritans.
Additional Information
This included the website terms of use and cookies policy, a disclaimer relating to the use of the information on the website and details of copyright and data protection.
Appendix 7 Outcome measures and package ratings
The baseline questionnaires (which can be accessed at www.journalslibrary.nihr.ac.uk/programmes/hta/1215004/#/; accessed 6 December 2018) were completed again at the outcome assessment, together with the following additional forms.
Crying knowledge scale
Parental evaluation of the Surviving Crying materials
Appendix 8 Consolidated Standards of Reporting Trials flow diagram: flow of participants in stage 2
FIGURE 17.
The CONSORT flow diagram: flow of participants in stage 2. Recruitment as of 21 December 2016.
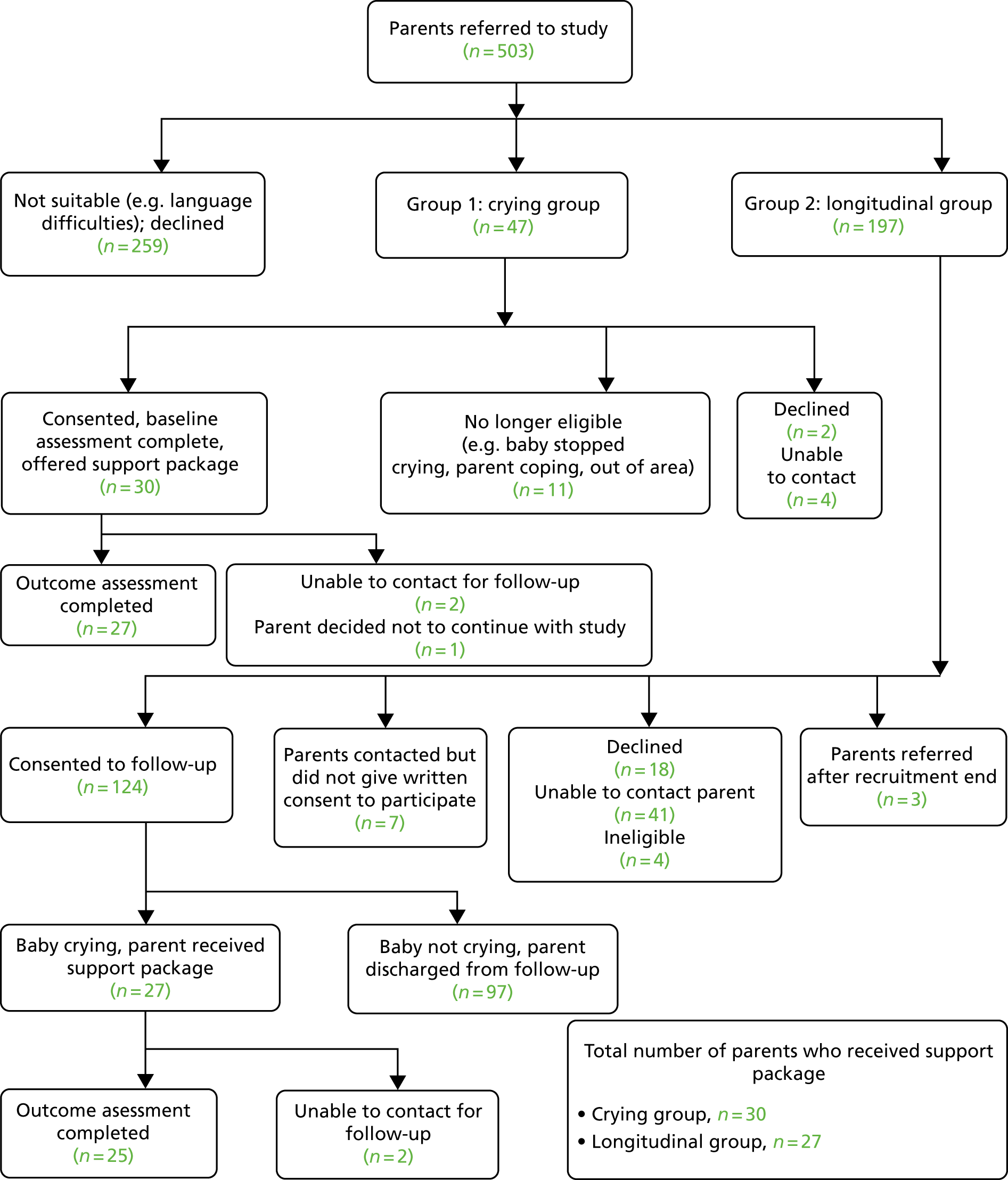
Appendix 9 List of conferences and other dissemination activities
Conferences
| Conference | Date | Title | Presenters | Poster/oral presentation |
|---|---|---|---|---|
| DMU/LPT Symposium: ‘Changing the Mind-set . . . Exploring the Journey from Research to Practice’, DMU, Leicester | 29 April 2015 | The NIHR Surviving Crying Study | Garratt R, Powell C, Bamber D, Long J | Oral presentation |
| NCT Research Advisory Group Conference, King’s College London | 21 October 2015 | Update on The Surviving Crying Study | St James-Roberts I | Oral presentation |
| NCT ‘Babble Live’ Annual Conference, Aston University, Birmingham | 8 October 2016 | The Surviving Crying Study: Evaluation Findings | Bollen A, Roy H, St James-Roberts I, Bamber D | Oral presentation |
| NCT Research Advisory Group Conference, Friends Meeting House, London | 19 October 2016 | The Surviving Crying Study and its Implications for Health Care Practice | St James-Roberts I | Oral presentation |
| DMU Centre for Reproductive Research seminar, DMU, Leicester | 22 February 2017 | The Surviving Crying Study: Development and Preliminary Evaluation of an Intervention Package to Support Parents of Excessively Crying Infants | Bamber D, Powell C, Garratt R | Oral presentation |
| Institute of Health Visiting Conference ‘Mastering Evidence-Based Practice in Health Visiting’, Aston University, Birmingham | 7 March 2017 | Developing Support Services for Parents of Excessively Crying Babies for Inclusion in the NHS | St James-Roberts I, Powell C, Long J, Turney N, Bamber D, Garratt R, Brown J | Oral presentation |
| Leicestershire Partnership Trust Research Forum, Swithland House, Leicester | 5 April 2017 | The Surviving Crying Study: Development and Preliminary Evaluation of an Intervention Package to Support Parents of Excessively Crying Infants | St James-Roberts I, Powell C, Long J, Turney N, Bamber D, Garratt R, Brown J | Oral presentation |
| DMU, Leicester | 27 April 2017 | Surviving Crying Conference: Presentation of Findings of the Study and Discussion of Next Steps | St James-Roberts I, Powell C, Long J, Turney N, Bamber D, Garratt R, Brown J, Morris S, Rumbelow M | Oral presentations |
| Children’s Research Conference, DMU, Leicester | 11 May 2017 | The Surviving Crying Study: Development and Preliminary Evaluation of an Intervention Package to Support Parents of Excessively Crying Infants | Garratt R, Long J | Oral presentation |
Other dissemination activities
| Event/media | Date | Activity |
|---|---|---|
| Twitter (Twitter, Inc., San Francisco, CA, USA; www.twitter.com)/LinkedIn (LinkedIn Corporation, Mountain View, CA, USA; www.linkedin.com)/YouTube (YouTube LLC, San Bruno, CA, USA; www.youtube.com) | 17 October 2014 | Notifications via social media to publicise the launch of the study |
| Leicester Mercury | 14 November 2014 | Press release to publicise the launch of the study |
| Next Steps: 0–19 Healthy Child Programme: Event for Health Visitors and School Nurses | 23 September 2015 | Display stand with members of the team giving information about the study to delegates during breaks and collecting contact details for those wishing to receive further information (Deborah Bamber, Charlotte Powell, Jaqui Long) |
| Webpage | January 2016 | Webpage set up on DMU website to provide information about the research and updates on progress: www.dmu.ac.uk/survivingcryingstudy (accessed 19 December 2018) |
| Child and Maternal Health Knowledge Update | 18 March 2016 | ‘Surviving Crying Study’: item in ‘Reports’ section of this online bulletin, linking to DMU webpage for the study |
| Perinatal and Infant Mental Health eBulletin | April 2016 | ‘Surviving Crying Study’: item in ‘Reports’ section of this online bulletin, linking to DMU webpage for the study |
| Radio Leicester morning programme | 10 October 2016 | Live interview to promote the study and encourage recruitment of parents with excessively crying babies (Deborah Bamber) |
| 11 October 2016 | Tweet to raise awareness of support for parents of persistently crying babies and recruit parents | |
| Leicester Mercury online version | 11 October 2016 | ‘Does your baby cry all the time? There may be a way of coping.’. Online article to promote the study and encourage recruitment of parents with excessively crying babies |
| Leicester Mercury | 13 October 2016 | ‘Parents needed for crying baby study: hopes research will lead to better NHS support’ – article to promote the study and encourage recruitment of parents with excessively crying babies |
| Leicestershire & Rutland Public Health 0–19 Assurance Board | 14 February 2017 | Presentation to give an overview of the study, findings from stage 1 and preliminary information regarding stage 2 (Jayne Brown) |
Glossary
- Baby and infant
- These words are used interchangeably.
- Excessive infant crying
- A parent’s judgement that an infant is crying too much, often accompanied by concern that something is wrong with the baby.
- Prolonged infant crying
- A measure of crying duration.
List of abbreviations
- A&E
- accident and emergency
- CBT
- cognitive–behavioural therapy
- CI
- confidence interval
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- CONSORT
- Consolidated Standards of Reporting Trials
- DMU
- De Montfort University
- DVD
- digital versatile disc
- EPDS
- Edinburgh Postnatal Depression Scale
- EQ-5D
- EuroQol-5 Dimensions
- GAD-7
- Generalised Anxiety Disorder-7
- GBP
- Great British pounds
- GP
- general practitioner
- HV
- health visitor
- ISRCTN
- International Standard Randomised Controlled Trial Number
- LPT
- Leicestershire Partnership NHS Trust
- NCT
- National Childbirth Trust
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- PI
- principal investigator
- PSS
- Personal Social Services
- QALY
- quality-adjusted life-year
- RCT
- randomised controlled trial
- SCPHN
- specialist community public health nurse
- SD
- standard deviation
