Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number NIHR127810. The contractual start date was in July 2019. The draft report began editorial review in May 2021 and was accepted for publication in September 2021. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2023 Wright et al. This work was produced by Wright et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2023 Wright et al.
Chapter 1 Background
Attachment
Attachment theory, originally developed by John Bowlby, focuses on understanding the functional significance of the distress that infants experience when alarmed, frightened or very uncomfortable and how they deal with that distress. Attachment, then, refers to the proximity-seeking of an attachment figure by the infant when they are alarmed or frightened, with the anticipation that they will receive a caregiving response. Bowlby conceptualises it as the ‘lasting psychological connectedness between human beings’. 1 An attachment figure tends to be the primary caregiver of an infant, someone the infant can seek out when they are distressed.
Bowlby’s attachment took an explicitly evolutionary perspective when seeking to understand these phenomena; Bowlby suggested that infants are born with an innate instinct to form attachments with their caregiver. 2 The proximity that infants seek is thought of as a mechanism that increases fitness and improves the chances of survival; they produce behaviours to gain attentive responses and protection from their caregiver, particularly pertinent at times of threat.
Two concepts are particularly central to attachment theory: a secure attachment develops as the product of interactions between infant and caregiver. These interactions are the result of care-seeking and caregiving behaviours. It is thought that caregiving behaviours also serve a biological function, that of protecting the attached individual from psychological and physical harm. 3 Care-seeking (i.e. attachment) behaviours are apparent in the first few months of an infant’s life and become most clearly apparent at around 7–9 months of age. Prior to this, attachment behaviours initially encourage proximity in general, but in the second half of the first year these behaviours become directed towards individual attachment figures,4 and it is at this point that selective attachments can be unambiguously identified.
A second key concept is that the quality of a child’s attachment underpins, in part, their later development. An infant’s instinct to seek a recognised caregiver for safety and security is vital in promoting healthy social and emotional development. 1 Although attachment acts as a predictor of later individual differences in socioemotional development, and is thought of as a cause of these differences, there is no evidence to suggest that attachment relationships cannot be altered. 2 For example, an insecure attachment relationship at 12 months can later change to a secure one, and this is likely to be associated with better outcomes subsequently.
Attachment patterns
The quality of an infant–caregiver attachment relationship is assessed by observing their attachment behaviours, and these can be categorised as attachment patterns. 5 To assess attachment patterns, the Strange Situation Procedure (SSP), proposed by Mary Ainsworth, was developed, which initially identified three attachment patterns present in infants. 6 These patterns represent the ways in which infants behave when they are anxious and search for protection, which are believed to be innate but are shaped partly by the infant’s history of interactions with the caregiver, and particularly by how the caregiver has responded to the infant’s bids for comfort and contact. ‘Secure attachment (B)’ refers to infants who actively seek proximity to their caregiver, and although they may be distressed during separation they seek contact actively when the caregiver returns, and, once settled, they are happy to return to exploring on their own. 7 This attachment pattern is likely the result of sensitive and consistent caregiver responses. By contrast, ‘insecure avoidant (A)’ infants may cry little during separation and do not seek proximity on reunion. This is thought to be a consequence of previous emotional unavailability at the moment when the child has signalled emotional need. Last, an infant with an ‘insecure resistant (C)’ pattern constantly seeks reassurance and tends to cry and resist comfort, this pattern occurring largely as a result of unpredictable caregiving behaviour. 7 The term ‘disorganised attachment pattern’ was introduced by Main and Solomon8 to describe infants who do not fall into one of the A, B and C categories. Instead, these infants show distorted, conflicted and contradictory behaviours in the strange situation. 9 This attachment pattern and, to a lesser extent, ‘insecure’ attachment patterns have been associated with psychopathology later in life10 and act as significant predictors of mental ill-health. 11
In normative populations across different countries, the majority of children have a secure attachment pattern. 12 The distribution of insecure patterns in normative samples varies with culture.
‘Severe attachment problems’ can be defined as disorganised attachment patterns or attachment disorders. 13 In recent policy guidance, disorganised attachment and attachment disorders [e.g. reactive attachment disorder (RAD)] have been referred to as ‘severe attachment problems’ to indicate their clinical significance and differentiate them from more normative patterns of avoidance and resistance. According to the National Institute for Health and Care Excellence (NICE) guidelines,14 attachment disorders include RAD, or a disinhibited attachment disorder, which is now termed ‘disinhibited social engagement disorder’ (DSM-5). 15 Children with RAD often do not seek proximity when they feel distressed and do not acknowledge comforting caregiving behaviours, often behaving in a withdrawn manner. 14 These children also show a lack of positive interaction with and emotions towards others. The diagnosis of RAD requires evidence of experiences of severe neglect or multiple different caregivers, with the behaviours being present before the age of 5 years. 14 Disinhibited attachment disorder in DSM-IV has been replaced by ‘disinhibited social engagement disorder’ in DSM-5. 15 The main characteristics of this disorder are active approaches towards and overfamiliar interaction with unfamiliar adults, with reduced or absent reticence; diminished or absent checking back with an adult caregiver after venturing away, even in unfamiliar settings; and willingness to go off with an unfamiliar adult with minimal or no hesitation. This is thought to be based on the lack of development of stranger awareness due to early extreme neglect or care by multiple different caregivers, similar to RAD.
Attachment and maladaptation
Research has found a significant association between early attachment classification and children’s developmental outcomes. 16 For instance, a longitudinal study from infancy to childhood found that a higher rate of antisocial behaviour in preschool was seen in children with an insecure attachment pattern than in those with a secure attachment pattern. 17 Insecure/disorganised attachment patterns are associated with more common major mental health disorders such as depression and personality disorders. 10,18,19 Early studies provided evidence that insecure attachment, specifically insecure avoidant attachment, is a predictor of later antisocial behaviour and anxiety disorders. 20
Meta-analyses have revealed significant and robust but modest associations between avoidant attachment and lower social competence, higher levels of internalising problems and higher levels of externalising problems; and between resistant attachment and lower social competence. 16 Fearon et al. 21 have shown a significant association between insecure and disorganised attachment patterns in infancy and later externalising behaviour problems. Disorganised attachment has associations with specific maladaptive behaviours later in life. Some infants with disorganised attachment develop controlling behaviour, either punitive or caregiving, towards their parents in middle childhood. 11,22 Disorganised attachment is specifically linked to internalising and externalising behaviour problems in early school years and at 6 years old. 23,24 Similarly, a large-scale longitudinal Minnesota study25 found that disorganisation was linked to internalising behaviour problems in middle childhood and psychopathology at 17 years of age.
Secure attachment is accompanied by more positive outcomes across the lifespan, including better peer relationships, more independence and fewer behaviour problems. 16,21,26–28
Influences on attachment patterns
The quality of care during the first years of life and the continuity of this care are predictors of adaptation through childhood and adolescence. 29
A vital factor found to affect attachment is whether or not the caregiver provides consistent and attuned interactions when the infant requires them. Inconsistent responses can affect the quality of attachment relationships. Maternal sensitivity as a response to infant cues has been found to be a predictor of a secure attachment classification globally. 30,31 Parenting practices such as maternal responsiveness and sensitivity are associated with reduced severe attachment difficulties. 32,33
The opportunity for secure attachment is reduced in a number of populations, especially those who have been maltreated and/or are living in alternative care. Those living in alternative care such as foster care or institutions differ in terms of attachment pattern from those living with non-maltreating biological or adoptive families. 34
Assessing attachment
Strange Situation Procedure
Attachment patterns can be assessed through observational procedures such as the SSP. 6 The SSP was the first assessment of attachment patterns, developed by Ainsworth and Wittig. 6 The procedure involves a direct observation of the interaction between an infant, their caregiver and a stranger. In an eight-episode sequence, the infant interacts with the caregiver while an experimenter is in the room; the infant and caregiver are left alone; a stranger then walks in; the caregiver leaves the infant alone with the stranger; the caregiver returns to the room and the stranger leaves; the caregiver exits and leaves the infant on their own; the stranger returns; and finally the stranger leaves and the caregiver enters. During the sequence, the interactions between the infant and the caregiver are observed partly in terms of how the infant responds to separation from the caregiver, but mainly when reunited with the caregiver. The interaction between the infant and stranger is not measured; the stranger is there purely to act as a stressor. Ainsworth and Wittig described three attachment patterns resulting from these observations: secure attachment, insecure resistant attachment and insecure avoidant attachment. A fourth pattern, as described previously, is ‘disorganised attachment’,9 which appears to be a predictor of psychopathology. 13,25
The validity of the SSP has been found to be similar among western cultures; however, there are potentially cross-cultural differences in less westernised populations. 12
Attachment Q-Sort
The Attachment Q-Sort (AQS) is also used to assess attachment security. The AQS was developed to better define secure base behaviour in a non-stressful environment at home. This assessment can also be used with preschool children. 35 There are two AQS assessments: observer and self-reported. A meta-analytic study36 has established that the observer AQS shows convergent validity with the SSP and predictive validity with measurements of maternal sensitivity.
Other assessments
Interviews such as the Child Attachment Interview have been used to capture a child’s account of their relationship with their parents; this is an adaptation of the Adult Attachment Interview for use with children aged 7–11 years. 37 The Disturbances of Attachment Interview is administered to caregivers and is used to assess attachment disorders in children. 38
Other questionnaires are also used in attachment research. 13 For example, the Randolph Attachment Questionnaire (RADQ)39 assesses the presence of symptoms related to attachment disorders,40 although it includes several questions that are not directly related to the construct of attachment and so lacks specificity. 41
As mentioned previously, the most consistent predictor of attachment is caregiver sensitivity. 42 A large number of instruments are designed to assess sensitivity. The original sensitivity assessment was developed by Mary Ainsworth. 5 Since then, numerous similar instruments have been developed and validated. For example, the Infant Care Index has a similar format to other observational methods, whereby a play interaction between infant and caregiver is coded and caregiver sensitivity is one construct that is measured. 43 This is not, however, designed to assess attachment. Similarly, the Emotional Availability Scale is used to code caregiver sensitivity during infant–caregiver interaction. 44
Current treatment approaches
Interventions largely focused on improving caregiver sensitivity have been developed to reduce disorganised attachment and promote secure attachment. 45 Research has shown that attachment-focused interventions are effective. 13,46–48 Interventions focusing on parental sensitivity are found to be effective in reducing disorganised and insecure attachment, more so than broader interventions. 49 The NICE guidelines on attachment, published in 2015, recommend video feedback as an intervention. This involves video-recording the parent–child interaction, with feedback about the interaction and then further guidance on improving caregiver sensitivity, for example Video Feedback to improve Positive Parenting (VIPP) or Video Interaction Guidance (VIG). 14 It is important to thoroughly examine the evidence behind recommended interventions to inform practice.
Study summary
The present study comprises both a national survey and two comprehensive systematic reviews. First, a survey was utilised to map the UK services currently delivering attachment interventions to families and then a scoping of the literature was conducted to identify common and effective interventions for attachment problems in infants and young children, which was followed by two systematic reviews. The study encompasses three stages. The first involved preparatory work to establish a stakeholder group and Expert Reference Group (ERG) to advise us throughout the study. This group included patient and public involvement (PPI) representatives, those working directly with families with lived experience, researchers, academics, teachers, clinicians and charities and third-sector organisations. Second, a large-scale national survey was distributed to establish the attachment treatments used currently in UK services. In stage 3, a systematic review on interventions for children with or at risk of attachment problems was conducted and evidence for the commonly used interventions was sought.
Study rationale
It is essential that UK services employ the most effective interventions to improve child–caregiver attachment. There is a need for clarification about which manualised interventions are currently used to improve attachment in infancy and to explore the evidence base for their effectiveness. This is a complex area to review, because there are significant problems with the usage of attachment terms and concepts in routine practice, and diverse interventions are used for a wide range of children with the stated aim of promoting security of attachment. We also note that there is poor availability of evidence-based interventions in UK health and social care, which suggests both the need to identify and disseminate evidence-based approaches and the need to evaluate interventions that have a strong foundation in current services but for which good evidence is lacking.
The lack of evidence supporting interventions for attachment is a significant problem because resources in child mental health services are already limited. 50 Without thorough research, we do not know whether existing interventions are clinically effective, safe or used in appropriate population groups, and they may not be cost-effective if they are time-consuming and/or ineffective. This could cause a potential waste in resources or, even worse, harm to the well-being of children and their families. Therefore, it is important that interventions showing a good research evidence base are utilised to provide the most effective services. There are also challenges in the appropriate assessment of attachment for supporting referrals and for routine outcome monitoring, with few evidence-based, reliable and valid tools that clinicians can use. This research also investigates which assessment tools clinicians/practitioners working with children with attachment difficulties use to assess attachment security and attachment disorders.
Study aims and objectives
This research aims to:
-
conduct a large-scale survey of the structured interventions that are routinely used across UK services to improve child attachment to their caregiver
-
carry out a systematic review to carefully assess the research that supports these manualised interventions and other parenting interventions for children with (or at risk of) severe attachment problems aged 0–13 years
-
develop recommendations for carrying out future clinical trial research on the effectiveness of those commonly used interventions that have not been properly tested in the past.
Chapter 2 Methods
Survey
Overview
We undertook an online survey to identify the interventions that services currently deliver to support children with or at risk of disorganised attachment patterns or attachment disorders in the UK (aim 1). This survey focused on relevant UK services [including local authorities (LAs), child and adolescent mental health services (CAMHS), voluntary agencies, education services, fostering and adoption agencies and health visiting services] and collected details about the interventions used for these attachment problems. The results from the survey informed the systematic review. This allowed the research team to robustly evaluate the existing evidence behind routinely used attachment interventions.
Ethics considerations
The survey was conducted in accordance with the University College London Code of Conduct for Research and was approved by the University College London Research Ethics Committee prior to data collection (project ID 16687/001; approval granted 18 November 2019). Only the research team could access the data, which were held on a secure server. Informed consent was obtained from all respondents. The information necessary to make informed consent was included in an information sheet (see Report Supplementary Material 1), which details the survey aims and the content and length of the survey, and gives data protection and storage information. Respondents were able to begin the survey only once they had read the information sheet. Respondents had to indicate their consent online to be able to complete the survey. Those respondents who had not indicated that they had read the information sheet and/or given their consent skipped to the end of the survey and provided no data for the survey results. All data were provided anonymously, and all respondents were given careful instructions not to reveal any personally identifying information concerning themselves or their client(s). All free-text responses were checked by the research team to ensure that no individuals had been inadvertently identified in participant responses.
Questionnaire development
Methods for designing survey
The survey was designed in consultation with the ERG and subject to modification after an initial pilot study. The questionnaire is in Report Supplementary Material 2, and it has the following section headings:
-
section 1 – consent
-
section 2 – about your work
-
where you work (nature of service setting)
-
your work supporting attachment (summary of children seen, referrers)
-
section 3 – therapeutic practice to support secure attachments (use of cross-package therapeutic techniques for promoting attachment)
-
section 4 – specific attachment intervention packages.
Development of general survey structure
A checklist was created to capture information about commonly used attachment interventions and techniques. When planning this work, we were aware of two significant problems that may affect the interpretation of the survey results. The first is that clinicians vary in their understanding of what an attachment problem is and what (if any) reliable tool they use for assessment; some therapists may also use eclectic practice rather than manualised interventions, combining treatment elements from several different approaches. A simple list of interventions on its own might therefore miss important elements of practice. Following the work of Chorpita et al. ,51 the research team drew on a taxonomy of common treatment elements of attachment interventions, cross-referenced against intervention manuals. We used this knowledge of treatment elements identified within those therapies to help design the survey to capture routine practice on the ground beyond, or in addition to that captured by, named intervention programmes. We also provided respondents with an opportunity to describe, in their own words, what the term attachment meant in terms of their practice.
Generation of intervention list
The survey listed a set of attachment-focused interventions identified by the ERG, by representatives from the research team’s network of partner organisations working in the attachment domain and from previous systematic reviews of attachment-focused interventions. Interventions had to be used for work directly with children and/or work with parents and caregivers. The research team took advice from the ERG, tapping into extensive links and networks with families, voluntary agencies, clinicians, services and experts, and scoping of published research, to identify interventions used to address attachment problems with families. Advice was sought from those who attended the first ERG meeting to inform the survey design. The survey itself also included open-text fields for services to specify any interventions they were using that were not already listed.
Detailed information about interventions and techniques
For each intervention that the respondent endorsed having used in the previous year to address attachment-related difficulties, the survey requested information concerning the number of children, approximately, to whom they had provided the intervention, what training they received, whether supervision was provided to deliver the intervention, any changes to the approach and how the outcome of the work was assessed. We were guided by the Template for Intervention Description and Replication checklist. 52 This included information regarding:
-
the typical number of sessions
-
core practice procedures and materials
-
mode of delivery (individual child face to face, individual parent face to face, working jointly with parent and child, parent or child groups, telephone contact with parent).
The common elements that were used to identify attachment-focused techniques (beyond any named interventions) were modelling sensitivity; supporting parent–child interaction; exploring mental representations of attachment; education and guidance; and ‘other’. Sixteen individual practice elements were identified within these five themes. For example, ‘in vivo feedback of attachment interactions’, ‘video-feedback of positive interactions’ and ‘tools to stimulate reflection on own parenting history’ were subsumed under the parent–child interaction theme. Each of these elements was accompanied by a textual description of what the intervention element consists of, and respondents were asked to endorse whether or not this element formed part of their practice with children who have attachment difficulties. For example, the element referred to as ‘raising attachment awareness’ was accompanied by the following text from the review manual:
The therapist provides suggestions/recommendations/guidance to the parent on attachment-related constructs. Attachment-related constructs would include matters relating to the parent’s sensitivity and responsiveness to the child’s cues and needs. This includes joint observation of the child/infant during intervention sessions, and raising the parent’s awareness of the importance of attachment, and healthy parent-child relationships.
Inclusion criteria
The study was designed to capture a broad range of practice and, therefore, the sole inclusion criterion for the survey was that UK-based practitioners had to work therapeutically with children (aged 0–13 years) with or at risk of attachment difficulties and/or their caregivers. The age range for children was selected as 0–13 years as this study was a follow-up to previous work that involved children in this range. 13 The age range was relatively wide to capture all children and child groups of interest in clinical practice. The survey asked respondents to base their responses on therapeutic work they had carried out in the last 12 months. There was no minimum number of children with whom practitioners were required to have worked across this timescale. In addition, respondents had to do only some proportion of their therapeutic work with children who have attachment difficulties. The survey focused only on face-to-face working and excluded online provision as a result of discussion with the ERG.
Ethics-informed questionnaire development
Ethics approval was obtained prior to commencement of the research. As per this approval, the information collected was kept in accordance with the Data Protection Act 2018,53 GDPR (General Data Protection Regulation) and University College London standard operating procedures. 54 Information was stored and archived by University College London. Survey responses were anonymous. We requested in the information sheet that respondents did not supply any personal information or information that could identify another person. In addition to this, the research team reviewed the data in open-text fields to ensure that no personal information had been supplied inadvertently. The survey asked respondents to select the type of organisation and service they worked in, as well as their role, using predefined dropdown lists. Respondents could also specify and write this information in open-text fields if the appropriate response had not been included in the predefined lists. The survey asked respondents for their service location in order to geographically map service provision. Respondents could include the name of the service(s) they worked in, but this was not mandatory.
Respondent pathway
The survey was built online using the secure data platform REDCap (Research Electronic Data Capture, version 8.5.27). 55 The questions were ordered to follow two pathways: one for respondents who worked in only one service and one for respondents who worked in multiple services (a respondent could describe up to two services they worked in). The survey was distributed over six screen pages. Respondents had to answer the majority of questions, in turn, in order to progress, although some questions did not require an answer and respondents were given the option to write ‘not applicable’. Respondents were able to review and change their answers using ‘previous’ and ‘next’ buttons, and monitor their progress through the questionnaire with a ‘page 1 of 6’ page indicator display.
Pilot
A small-scale pilot was conducted with the project team members, colleagues and practitioners to assess the survey’s usability and technical functionality, and minor changes to the survey format and wording were implemented as a result.
Survey distribution
Generation of list of services/providers to be surveyed
The draft survey was reviewed by the ERG before it was deployed in the pilot study and the final large-scale mail-out. In addition, after a consultation with the ERG, a comprehensive contact list of services and providers to be surveyed was generated based on previous work that mapped intervention delivery in services and organisations across the UK.
Modes of distribution
After refinements, the survey was delivered online using REDCap, with optional paper fill-in and face-to-face meetings if requested by respondents. The survey was distributed as an open survey link via e-mail invitation that included information about the study and promotional materials such as flyers in addition to information regarding social media. Flyers were also distributed at conferences and events.
Survey procedure
Participation was voluntary and no incentives were offered or passwords required to complete the survey. The first distribution e-mail and post on social media were conducted in January 2020; reminder e-mails and social media posts were sent after distribution and the survey was closed in June 2020. The research team judged that the 625 responses received by the end of June 2020 provided sufficient data to meet the aim of this phase of work.
Types of providers and services covered
The survey covered a substantial range of providers supporting children with attachment difficulties in the UK. Furthermore, the data collected from the survey were supplemented by service-level responses from managers in both services and Clinical Commissioning Groups. We wanted to reach all types of services that work with children aged 0–13 years with or at risk of attachment problems and/or their caregivers. Attachment interventions occur in a range of organisations, and so the following were contacted: NHS, LA, voluntary sector (including organisations specialising in relevant areas such as attachment and perinatal mental health working with children, parents, mothers, and families), education (including schools and virtual schools), private provider organisation, individual private practice and social enterprise. In addition to this, we contacted a large array of service types in these organisations, including general practitioner/primary care, CAMHS, child health disability service, looked-after children’s service, adoption/fostering service, parent advice/information service, child safeguarding team/service, perinatal mental health service, health visiting service, midwifery service, specialist education (e.g. teacher of the deaf, specialist preschool/nursery service), counselling service, and parent–child support service/family centre/children’s centre. Numerous roles were covered, including clinical psychologist, counselling psychologist, educational psychologist, psychiatrist, nurse, health visitor, social worker, family therapist, psychotherapist and other therapist (e.g. art, drama, play, music). Respondents also had the opportunity, using open-text boxes, to specify any other relevant organisation, service type and role in relation to the service they worked in.
Survey dissemination
The survey was circulated to relevant practitioners including a large Learning Network at the Anna Freud National Centre for Children and Families (AFNCCF) linking professionals and stakeholders (including families) with an interest in child mental health. The AFNCCF is also home to the Children and Young People Improving Access to Psychological Therapies (CYP IAPT) collaborative of collaboratives, consisting of all CYP IAPT CAMHS. CAMHS services were also contacted via the Anna Freud Centre’s Youth Well-being Directory. We also contacted a range of other networks identified through our Expert Reference Group, including the DDP Network, Attachment Parenting UK, iHV and The Fostering Network. In addition to this, we worked closely with Parent-Infant Partnership UK, which has recently undertaken its own mapping exercises in relation to partially overlapping parent–infant services for children, which was used to supplement our initial longlist.
All NHS UK trusts and social care/LAs were mapped, identifying senior managers in services and contacts including NHS England and its Clinical Commissioning Groups in England, Health Boards in Scotland and Wales, and the Health and Social Care Board in Northern Ireland. We worked directly with service leads, who distributed the e-mail invitation to all practitioners working with children aged 0–13 years. In addition to this, directories such as the National Directory of NHS Research Offices and the Contact, Help, Advice and Information Network (CHAIN), an online network for people working in health and social care, were used to supplement our list. Furthermore, we contacted the heads of communication teams in NHS trusts to ask them to disseminate the survey to key departments and workers and include the survey e-mail invitation in internal communications such as newsletters and intranets. The e-mail invitation was also distributed through professional organisations to their members via mailing lists and newsletters such as relevant professional bodies/groups, including (but not exclusive to) the British Psychological Society, Royal College of Psychiatrists, the Royal College of Nursing, the British Association of Social Workers, the Association for Family Therapy and Systemic Practice, the Association of Child Psychotherapists, the British Association of Art Therapists, the British Association of Play Therapists, the Association of Directors of Children’s Services Ltd, the Consortium of Voluntary Adoption Agencies and the Consortium of Adoption Support Agencies. This was especially important for reaching private providers.
Social media coverage
To ensure widespread coverage, social media platforms were used to reach potential respondents who would be missed by these sampling methods (e.g. if the services were relatively new or less well known or networked private providers). We used feeds via Twitter (Twitter, Inc., San Francisco, CA, USA, www.twitter.com), Facebook (Facebook, Inc., Menlo Park, CA, USA, www.facebook.com) and Instagram (Facebook, Inc., Menlo Park, CA, USA, www.instagram.com) to raise awareness of the project, explain the research methods being used and promote practitioners’ involvement in the survey. Social media was also used to raise awareness that the survey was live. This was followed up with reminders and messages about the value and importance of receiving responses from as many different practitioners as possible. The project-specific account was set up as Attachment Matters Study @Attachment2020 across Twitter, Facebook and Instagram. Tweets and posts were sent to followers to encourage their involvement in the study and provided information about the different elements of the project as these progressed. Social media accounts ‘followed’ relevant individuals and charitable and professional organisations to raise visibility and encourage reciprocal links and followers. Details of the social media accounts was sent to relevant networks, organisations and charities as well as being featured on flyers for the project for general awareness-raising. Shortly after the closure of the survey, the Twitter account had gained 771 followers, the Facebook account 222 followers and the Instagram account 162 followers. After the initial wave of survey promotion, the social media posts focused on the next steps after the closure of the survey. The social media accounts remained live after the survey ended as they formed part of the dissemination strategy for the final results. In addition to this, the survey was publicised on a large number of relevant organisation websites/blogs/newsletters, Facebook groups, and Twitter and Instagram accounts, for example newsletters, websites and social media platforms for AIMH, Home-Start UK, Family Action, and PANDAS Foundation.
Data collection and modes of analysis
Analysis of results overall
Quantitative data from the online survey were analysed using Microsoft Excel, the primary purpose of which was to produce descriptive statistics relating to the background information of respondents and interventions offered. Qualitative data from the survey’s free-text sections were subject to thematic analyses. Free-text comments were placed under the headings of the original questions. These were then grouped into clusters of thematically related topics and distinct topic clusters for further analysis. A narrative summary was drafted related to each cluster of topics. In this way, the themes presented in Chapters 3 and 4 were defined and the findings were drafted. Once the results had been analysed, a report was created detailing the UK services providing interventions; where these services were located, both geographically and organisationally; and the number of children practitioners had worked with over the last year.
The thematic analysis process involved six phases: familiarisation with the data, coding, generation of the initial themes, a review of themes, defining and naming themes and drafting the findings. There was movement back and forth between the phases. These phases facilitated the rigorous process of data interrogation and arrangement.
Familiarisation with the data
The research team underwent the process of familiarisation to obtain a thorough overview of all of the qualitative data collected before the analysis of individual items, which involved reading through the text and taking initial notes.
Coding
The free-text survey responses were placed under the headings of the original questions. The data were coded to identify key sections in the text to describe the content. Once all text had been coded, the research team collated all of the data into groups identified by code, allowing a condensed overview of the main points and common meanings that recurred throughout. The data were grouped into clusters of thematically related topics and distinct topic clusters for further analysis. A narrative summary was drafted of each cluster of topics.
Generating initial themes
The research team then reviewed the codes that had been created, identifying patterns among them, and initiated the generation of themes.
Reviewing themes
Once the themes had been generated, the research team compared the original data set against the themes to ensure that these were accurate representations of the data.
Defining and naming themes
Once the final list of themes had been created, the research team named and defined each, developing a detailed analysis and determining the narrative for each. This involved formulating exactly what was meant by each theme to enable a good understanding of the data, with clear and comprehensible names for each.
Drafting the findings
The findings were drafted and presented with data extracts and the analysis was contextualised in relation to existing literature.
Generating routinely used interventions
We quantitatively reported the frequency of different intervention types, and estimates of the numbers of children receiving these different types of therapy, across geographical areas to identify routinely used interventions for improving attachment in infants and young children. This information was presented to the ERG. We identified the 10 most commonly used interventions (based on the number of respondents who reported using each intervention) and these were included in the systematic review search strategy.
Systematic review (reviews 1 and 2)
The systematic review phase was split into two separate reviews to allow us to capture both the existing randomised controlled trial (RCT) evidence for all attachment parenting interventions (review 1) and the best available research evidence to support each of the most commonly used interventions in current practice, as identified by the survey (review 2).
Review 1 is an update of a previous systematic review conducted by the team in the same field. This systematic review was originally conducted as part of a National Institute for Health and Care Research (NIHR) Health Technology Assessment (HTA) project to assess the clinical effectiveness and cost-effectiveness of parenting interventions for children with or at risk of an attachment disorder or disorganised attachment patterns. 13 Part of this review was previously updated and published in 2017 as a systematic review47 of the effectiveness of parenting interventions aiming to reduce disorganised attachment in children at risk of attachment problems. The research team used the same searches and processes to update this review to include all RCT evidence for parenting interventions that aim to either reduce disorganised attachment or promote secure attachment in children at risk of an attachment disorder or disorganised attachment patterns. The results of this review (review 1) were then combined with those results from 2015 and the 2017 updates to provide a comprehensive overview of published RCT literature in this field. Where possible, this also included meta-analyses.
Review 2 is focused on the available evidence for the named interventions identified in the survey as the ‘most commonly used’ (based on the frequency with which respondents reported using the intervention). Chapter 3 contains further information on how the most commonly used interventions were identified from the survey results. We included all available study designs, including, but not limited to, RCTs, non-randomised comparisons, pre and post studies and case series. To maximise the breadth and informativeness of the second review, we also included studies that assessed parental sensitivity and not only those studies assessing child attachment.
Both reviews were registered on PROSPERO (CRD42019137362) at study set-up, and this record was updated in June 2020 to reflect the finalisation of the PICOS criteria and search strategy after the survey results became available and after discussion with the ERG. Both reviews followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist to ensure that they adhered to the PRISMA guidelines.
Search strategy (reviews 1 and 2)
The search strategy was drafted by the research team with the ERG. For review 1, we used the same search strategy as for the previous reviews (2015, 2017), and this strategy was modified for review 2. 13,47 It was finalised with an information specialist, who ran the searches in June 2020. Databases searched for both review 1 and review 2 were ASSIA, Cochrane Central Register of Controlled Trials (CENTRAL), CDSR, Conference Proceedings Citation Index – Science, Conference Proceedings Citation Index Social Science & Humanities, EMBASE, ERIC, MEDLINE, PsycINFO, Science Citation Index, Social Care Online, Social Policy & Practice, Social Science Citation Index and Social Services Abstracts. The two independent reviewers also conducted thorough reference checking and grey literature searching. The search strategy is in Appendix 4.
For review 1, we searched for records published after 2016, to line up with the previous update (2017). 47 For review 2, there was no limit on publication date. Both published and unpublished records were included for both reviews.
PICOS criteria
Review 1
The final PICOS for review 1 were as follows.
Population
Parents/caregivers of young children 0–13 years who had a disorganised classification of attachment or were identified as at high risk of developing severe attachment problems (attachment disorders or disorganised attachment patterns).
Intervention
Any parenting intervention that aimed to reduce disorganised attachment, improve secure attachment or treat attachment disorders was included. This included any interventions targeted at developmental trauma that sought to improve attachment. It included interventions involving the parent with or without the child, with parent or caregiver, in groups or one to one, with or without video feedback, and interventions involving a range of strategies or models, such as behavioural advice, provision of information, environmental change advice, activities, or support for the development of parental sensitivity. Interventions were included that were aimed at parents or caregivers, including foster carers. Interventions involving only teachers or teaching assistants (without parents or caregivers) were excluded.
Comparator
Comparators included no intervention, an alternative intervention, an attention control, and treatment or care as usual.
Outcome
The outcome was change in attachment (e.g. increase in secure attachment, decrease in disorganised attachment, or post-intervention comparisons between groups), measured using a validated attachment instrument that enables the classification of child attachment style.
Study design
Studies that did not use a true RCT design were excluded. Both published and unpublished papers from 2016 until present were included, as were foreign-language papers. We matched the PICOS criteria to those of the previous review to enable the results to be combined.
Review 2
The final PICOS for review 2 were as follows.
Population
Parents/caregivers of young children or children themselves aged 0–13 years who had disorganised classification of attachment or were identified as high risk of developing attachment problems (attachment disorders or disorganised attachment patterns).
Intervention
Interventions identified in the national survey as being most commonly used in the UK (based on frequency of respondents reporting using the intervention), aimed at reducing disorganised attachment, improving secure attachment, treating attachment disorders or improving parental sensitivity were included. This included interventions involving the parent with or without the child, the child with or without the parent and with either parent/caregiver.
Comparator
Where the study is a RCT we included any comparator (including control conditions or other active comparators). We included other designs and applied the same comparator criteria for any study using a comparison group (e.g. non-randomised controlled designs). Other empirical designs such as pre–post designs were included in the absence of a comparator.
Outcome
Change in attachment (increase in secure attachment or decrease in disorganised attachment), measured using a validated attachment instrument (either measuring attachment classification or a continuous attachment measure) or a change in parental sensitivity measured using a validated tool. This latter was chosen as a proxy indicator for attachment because of research showing strong associations between child attachment and parental sensitivity. 42
Study design
Studies including the 10 specific identified interventions were carefully scrutinised for available research evidence, including cohort studies, observational studies, case–control and case series evidence. Both published and unpublished papers were included, with no restrictions on years since publication, and foreign-language papers were included.
Review strategy: review 1
Screening
Sifting was conducted by two independent reviewers, both of whom screened all papers at all sift stages. Agreement was consistently above a baseline of a pre-agreed 80%. Where there was a disagreement, the paper was pulled through to full-paper screening and discussed together with input from an independent reviewer. Authors were contacted to clarify details and provide raw results where necessary. Translation services and library services were accessed as needed.
Record title and abstracts were screened in an initial phase against the PICOS criteria. If they met the inclusion criteria at this stage, the full paper was screened against the PICOS criteria. All records in the full-paper sift were reference checked, and books, systematic reviews and meta-analyses were checked for any additional relevant papers. Records that met the criteria at this stage were data extracted by the same two reviewers working independently. We ensured to follow the same process as for the previous review and update.
One paper discovered that met the inclusion criteria was dated pre 2016. 56 Although the study had been conducted pre 2016, it was made available only post 2016 and therefore had not been identified in the searches for the previous reviews. As the paper met the inclusion criteria, it was subsequently included.
Data extraction
Child attachment classifications were extracted as the primary outcome and information was collected on the demographics of the sample and the characteristics of the interventions. The data extraction was structured using the framework of intervention descriptions provided by the Template for Intervention Description and Replication (TIDieR) checklist. 52 Many interventions are poorly described in publications, limiting their replicability. The checklist covers the rationale for or theoretical basis of the intervention, materials and procedures, who delivered its main components, where it was delivered and the frequency and duration of delivery. The data extracted were the same as in the previous reviews and update to allow data to be combined in the meta-analysis, and to allow for the same exploratory analyses to be conducted. The data extraction tables are in Appendix 2. These show the headings used to extract detailed information about the intervention and study design based on the TIDieR checklist, including participants, sample risk, intervention focus, intervention duration, intensity, delivery, control group, measure of attachment and attachment outcomes.
The data resulting from the extraction were split into outcome data for increasing secure attachment and outcome data for reducing disorganised attachment. All papers provided data for both of these, except for one. The authors of one paper that provided data on secure attachment did not respond to multiple requests within the required time frame to provide results for disorganised attachment and so the paper was included in the secure analyses only. 57
One paper met the inclusion criteria but did not provide enough information to allow data extraction for the meta-analyses. 58 The authors reported a change in attachment but did not provide the raw numbers of children in either group, and so the paper could not be included in the meta-analysis. The paper was excluded because the authors did not respond to multiple requests for these additional data within an appropriate timeframe.
Risk-of-bias assessment
A risk-of-bias assessment was conducted of all included papers by two independent reviewers using the Revised Risk of Bias Tool for Randomised Trials (ROB-2). 59
Meta-analyses methods
Statistical heterogeneity was assessed using Cochran’s Q through the chi-squared test and was quantified using the I2-test. If there was statistical heterogeneity, a fixed-effects model was not appropriate and a random-effects model was used. Publication bias was assessed by examining the asymmetry of the funnel plot and the Harbord regression-based test was used. 60 Statistical analysis was performed using Review Manager 5.3. The results were considered statistically significant when the two-sided p-value was < 0.05. Cohen’s d effect sizes were calculated61 to make comparisons with previous meta-analyses on attachment interventions.
The included studies were stratified into groups based on their characteristics, and subgroup analyses were undertaken on the number of sessions, use of video feedback, age of child and whether or not a male caregiver was included.
Review strategy: review 2
Screening
Sifting was conducted by two independent reviewers, both of whom screened all papers at all sifts. Agreement was consistently above a pre-agreed baseline of 80%. When there was a disagreement, a paper was pulled through to full-paper screening and discussed, with input from an independent reviewer if necessary. Authors were contacted to clarify details and provide raw results where necessary. Translation services were used if needed and we used library access services for those records we were unable to access directly.
The titles and abstracts of records were screened in an initial phase against the PICOS criteria. If they met the criteria, the full paper was screened against the PICOS criteria. We conducted significant reference and grey literature checking. All records in the full-paper sift were reference checked, and books, attachment systematic reviews and meta-analyses were checked for any additional relevant papers. Records that met the criteria at this stage were data extracted by the same two reviewers each working independently.
Data extraction
Child attachment and/or parental sensitivity outcomes were extracted as the primary outcome and information was collected on the demographics of the sample and the characteristics of the interventions. This was structured using the framework of intervention descriptions provided by the TIDieR checklist and based on characteristics used in previous reviews. 52 Research has shown strong associations between child attachment and parental sensitivity,42 and parental sensitivity is also recommended as an attachment outcome in NICE guidelines. 14 The data extraction table for review 2 is in Appendix 2 (see Table 23). This shows the headings used to extract detailed information about the intervention and study design based on the TIDieR checklist, including participants, sample risk, name of manualised intervention focus, study design, control group, measure of attachment, attachment outcomes, measure of parental sensitivity and parental sensitivity outcomes.
Chapter 3 Survey results
Introduction
The current survey was intended to inform the design of a systematic review of interventions for severe attachment problems by identifying which interventions are routinely used in practice in the UK.
In this chapter we first summarise the completion rate of the survey from different parts of the UK and organisational characteristics relating to the services that responded to the survey. Following this, the findings from the quantitative components of the survey are explored and the most commonly reported interventions are described.
Completion rate
The survey was circulated to 1279 respondents. The actual number of individuals or organisations in receipt of survey invitations is likely to be greater than this number as survey participation was also encouraged through social media, flyers and conferences. A total of 2656 practitioners initially agreed to participate in the survey, that is, they clicked into the survey questionnaire via the link in the e-mail invitation or on social media and consented to taking part in the survey (however, note that an unknown proportion of these may have realised they did not meet the inclusion criteria or may have logged into the survey site more than once). A total of 625 respondents completed the survey. The overall completion rate in terms of the number of respondents who finished the survey (n = 625)/the number of respondents who agreed to participate in the survey (n = 2656) was 23.5% (although the denominator here is likely to have been inflated by individuals returning to the survey site more than once prior to completion, or by those who looked at the survey and then decided they did not meet the survey criteria). The completion rate in terms of the number of respondents who completed the survey (n = 625)/the number who began the survey (by completing the first question) (n = 965) was 64.8%. The 625 respondents completed the survey with respect to 734 different services.
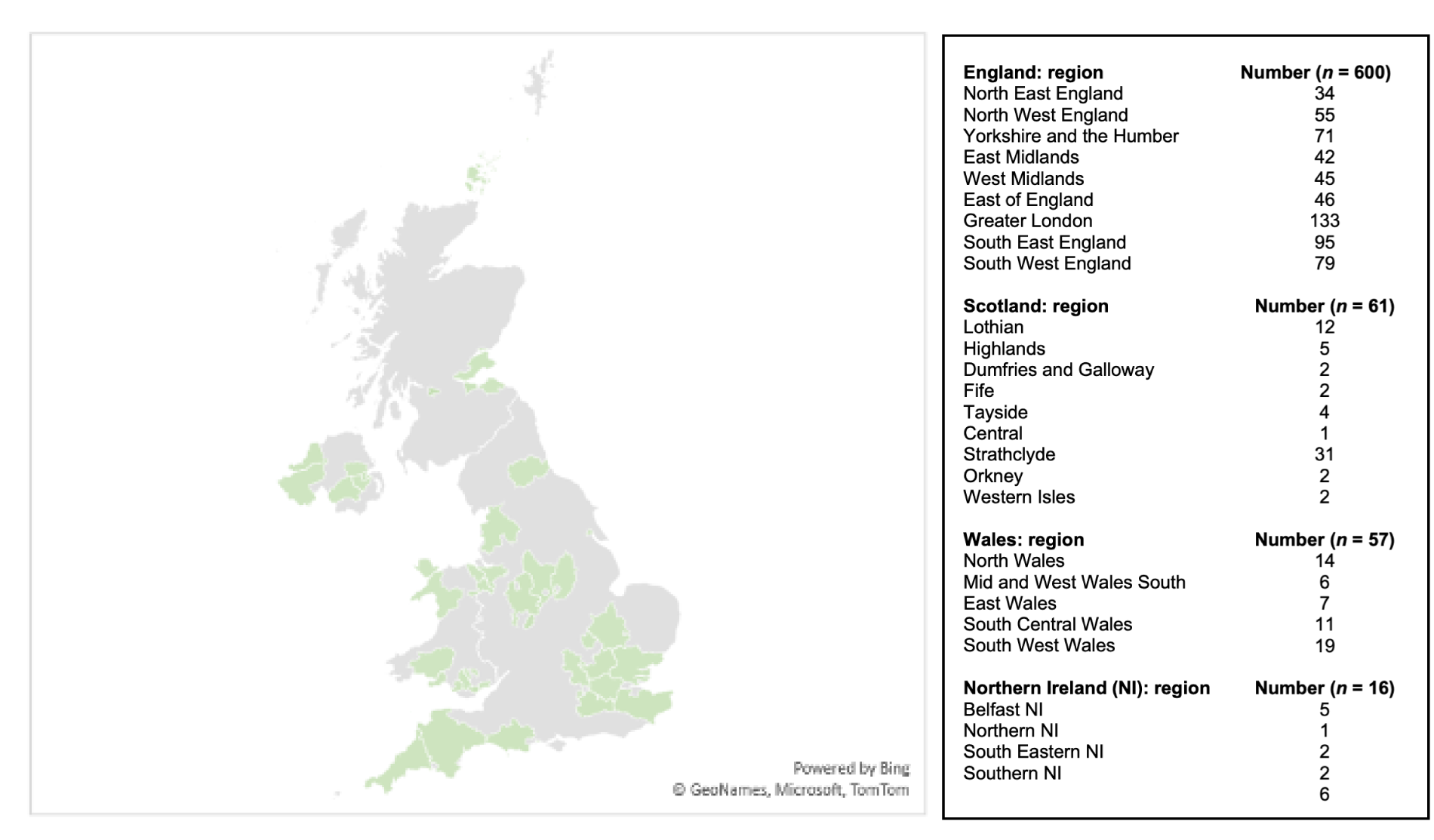
Scope of the survey
Descriptive statistics regarding the pattern of responses to this survey are presented by service as well as by practitioner. Respondents were asked where the service they worked in was located in terms of region and town. Responses were received from all four UK nations (Figure 1). The majority of services were in England (n = 600), with a significant number based in southern England (n = 353) and northern England (n = 160) and a small proportion located in central England (n = 87). A smaller proportion of services were based in Scotland (n = 60), Wales (n = 58) and Northern Ireland (n = 16).
FIGURE 1.
Map showing the geographical distribution of survey responses across the UK. Microsoft product screenshot reprinted with permission from Microsoft Corporation.
Organisational characteristics
Respondents were asked about the type of organisation in which they worked. The most common services were in the NHS (41.6%, n = 305); 17.8% of respondents were from LAs (n = 131), 10.9% (n = 80) were from the voluntary sector, 8.3% (n = 61) were from a private provider organisation, 7.6% (n = 56) were from individual private practice, 6.8% (n = 50) were from an educational organisation and 1.8% (n = 13) were from a social enterprise (Table 1).
| Organisation type | Responses, n (%) |
|---|---|
| NHS | 305 (41.6) |
| LA | 131 (17.8) |
| Voluntary sector | 80 (10.9) |
| Educational | 50 (6.8) |
| Private provider | 61 (8.3) |
| Individual private practice | 56 (7.6) |
| Social enterprise | 13 (1.8) |
| Other | 38 (5.2) |
Thirty-eight (5.2%) organisations were identified as an ‘other’ type; this included a university department (n = 1); an adoption/regional adoption agency (n = 4); another type of voluntary sector (including a children’s charity and a mental health charity) (n = 14); commercial manufacturing (n = 1); a community interest company (n = 1); counselling (n = 1); Department of Justice (n = 1); a grant-aided special school (n = 1); a parent (n = 1); self-employed (n = 2); an independent organisation (n = 1); NHS and LA collaboration (n = 4); mental health (n = 1); multiagency − NHS, LA, voluntary (n = 2); NSPCC (n = 2); and training − play therapy (n = 1).
Respondents were asked about the type of service(s) they worked in within their organisation. The most common was CAMHS (23.7%, n = 174). Similar proportions of service types were from looked-after children’s services (8.4%, n = 62), adoption/fostering services (8.7%, n = 64), counselling services (7.6%, n = 56), parent–child support service/family centre/children’s centres (7.5%, n = 55), health visiting services (6.0%, n = 44), perinatal mental health services (5.4%, n = 40) and specialist education (e.g. teacher of the deaf, specialist preschool/nursery service) (4.4%, n = 32). A smaller proportion were from child safeguarding team/services (2.5%, n = 18) and general practitioner/primary care (1.0%, n = 7). In addition, the same proportion in terms of service type (0.7%, n = 5) were from child health disability services, parent advice/information services and midwifery services (Table 2).
| Service type | Responses, n (%) |
|---|---|
| General practitioner/primary care | 7 (1.0) |
| CAMHS | 174 (23.7) |
| Child health disability | 5 (0.7) |
| Looked-after children’s | 62 (8.4) |
| Adoption/fostering | 64 (8.7) |
| Parent advice/information | 5 (0.7) |
| Child safeguarding team/service | 18 (2.5) |
| Perinatal mental health | 40 (5.4) |
| Health visiting | 44 (6.0) |
| Midwifery | 5 (0.7) |
| Specialist education (e.g. teacher of the deaf, specialist preschool/nursery service) | 32 (4.4) |
| Counselling service | 56 (7.6) |
| Parent–child support service/family centre/children’s centre | 55 (7.5) |
| Other (please specify) | 167 (22.8) |
A total of 22.8% (n = 167) services were reported as an ‘other’ type. These services were organised into the following groups; children’s care service (1.9%, n = 14), combined/collaboration service (i.e. various combinations of the following: looked-after children, adoption, fostering, CAMHS, education, LA and CAMHS provider collaborative) (1.0%, n = 7), education service (2.3%, n = 17), other family/parental service (2.9%, n = 21), general health service (0.7%, n = 5), mental health service (1.5%, n = 11), other therapy/psychological treatment service (10.5%, n = 77) and training service (1.1%, n = 8).
Roles and occupations of respondents
Respondents were asked about their role in the service. A sizeable proportion of respondents were clinical psychologists (n = 123, 16.8%). A considerable proportion were social workers (n = 58, 7.9%), psychotherapists (n = 57, 7.8%), health visitors (n = 41, 5.6%) and nurses (n = 34, 4.6%). A smaller proportion comprised 21 family therapists (2.9%), 19 educational psychologists (2.6%), 17 psychiatrists (2.3%) and 10 counselling psychologists (1.4%) (Table 3).
| Role | Responses, n (%) |
|---|---|
| Clinical psychologist | 123 (16.8) |
| Counselling psychologist | 10 (1.4) |
| Educational psychologist | 19 (2.6) |
| Psychiatrist | 17 (2.3) |
| Nurse | 34 (4.6) |
| Health visitor | 41 (5.6) |
| Social worker | 58 (7.9) |
| Family therapist | 21 (2.9) |
| Psychotherapist | 57 (7.8) |
| Other therapist (e.g. art, drama, play, music) | 122 (16.6) |
| Other (please specify) | 232 (31.6) |
A total of 31.3% (n = 230) of roles were identified as ‘other’. These were characterised into groups: other psychologist (n = 18, 2.5%), other psychotherapist (n = 14, 1.9%), other education practitioner (n = 33, 4.5%), other nurse (n = 14, 1.9%), other social worker (n = 7, 1.0%), other therapeutic clinician (n = 15, 2.0%), other family/parental related role (n = 26, 3.5%), other child-related role (n = 9, 0.8%), advisory role (n = 5, 0.7%), other allied health professionals (n = 12, 1.6%: speech and language therapist, n = 5, 0.7%; and occupational therapist, n = 7, 1.0%), senior management role (n = 39, 5.3%), other mental health specific role (n = 8, 1.1%), midwife (n = 5, 0.7%), foster carer/parent (n = 9, 1.2%), well-being/support worker (n = 11, 1.5%), medical doctor (n = 5, 0.7%) and trainer (n = 3, 0.4%).
Age of children practitioners work with
Respondents were asked the age range of the children with whom they worked. There was no predominant age range: practitioners worked with children from 0–3 years (56.0%, n = 350), 4–6 years (65.3%, n = 408), 7–9 years (68.0%, n = 425), 10–11 years (65.9%, n = 412) and 12–13 years (58.4%, n = 365) (Table 4).
| Age range (years) | Responses, n (%) |
|---|---|
| 0–3 | 350 (56.0) |
| 4–6 | 408 (65.3) |
| 7–9 | 425 (68.0) |
| 10–11 | 412 (65.9) |
| 12–13 | 365 (58.4) |
Tools and measures for assessing attachment difficulties
Respondents were asked to use an open-text field to list any measures or tools used to assess attachment difficulties or the parent–child relationship; 581 (93.0%) respondents completed this field. Of those 581, 37 commented ‘N/A/none’. Table 5 shows a selection of the types of measures and tools reported (only those reported at least three times are presented).
| Measures | |||
|---|---|---|---|
|
Parent Attachment AAI (n = 20) Attachment Style Interview (n = 4) Dynamic-Maturational Model (n = 4) Mental health Edinburgh Postnatal Scale (n = 9) Hospital Anxiety and Depression Scale (n = 4) General Anxiety Disorder (n = 7) Clinical Outcomes in Routine Evaluation (n = 8) Clinical Interview (n = 14) Warwick–Edinburgh Mental Well-being Scale (n = 5) |
Child Emotional/behavioural ASQ (n = 21) SDQ (n = 77) Behaviour Rating Inventory of Executive Function (n = 6) Boxall Profile (n = 14) Child Behaviour Checklist (n = 4) Mental health/well-being Adverse Childhood Experiences (n = 7) Trauma Symptom checklist (n = 11) Children’s Revised Impact of Event Scale (n = 3) Assessment Checklist (n = 38 – 14 Assessment Checklist for Children (ACC), 10 Assessment Checklist for Adolescents (ACA), 2 Assessment Checklist for Children plus (ACC+), 1 The Assessment Checklist (Tarren Sweeney), 11 Brief Assessment Checklist (3 BAC, 4 Brief Assessment Checklist for Children BAC-C and 4 Brief Assessment Checklist for Adolescents BAC-A)). Levels of Adaptive Functioning (n = 4) Revised Child Anxiety and Depression Scale (n = 19; 17 children and 2 parent version) Children’s Global Assessment Scale (n = 4) |
Relationship Parent report PSI (n = 24) Brief Parental Efficacy Scales (n = 3) Tool to Measure Parenting Self-Efficacy (n = 6) Parental Reflective Functioning Questionnaire (n = 9) MORS (n = 35) Postpartum Bonding Questionnaire (n = 7) Observation Keys to Interactive Parenting Scale (n = 6) COS (n = 3) Theraplay (n = 23) MIM (n = 50) WWW (n = 3) Care Index (n = 16) SSP (n = 8) Parent–Infant Interaction Observation Scale (n = 11) Newborn Behavioural Observations (n = 11) |
Other Goal-setting (n = 13) BERRI (n = 3) CORC (n = 3) Sensory Attachment Intervention (n = 3) Social Responsiveness Scale (n = 4) Child Attachment and Play Assessment (n = 7) Coventry Grid (n = 21) DDP (n = 11) Family Relations Test (n = 10) Dyadic assessment of naturalistic caregiver–child experiences Dance (n = 7) VIG (n = 20) Meaning of Child Interview (n = 4) Solihull (n = 8) Playfulness, Acceptance, Curiosity and Empathy (n = 3) SCORE Index of Family Functioning and Change SCORE-15 score 15 (n = 10) Kim Golding (n = 16) – 6 Carers Questionnaire, 1 Attachment Observation Schedule and Being a Parent Questionnaire, 7 Thinking about your child, 1 Attachment profiles (Kim Golding/Louise Bomber books) Story Stem (n = 28) Thrive (n = 6) Observation (general) (n = 153) |
The most commonly used measure was the Strengths and Difficulties Questionnaire (SDQ) (n = 77) (Table 6). A large proportion of respondents also mentioned the Marschak Interaction Method (MIM) (n = 50). Many respondents noted using the Mothers’ Object Relations Scales (MORS) (n = 35). In addition, respondents reported using variations of the Assessment Checklist (n = 38). Frequently reported measures also included the Parenting Stress Index (n = 24), Story Stem (n = 28), Adult Attachment Interview (n = 20), Ages and Stages Questionnaire (ASQ) (n = 21) and Coventry Grid (n = 21). Many respondents also noted using general observation to measure attachment (n = 153).
| Intervention | Respondents, n (%) | Services, n (%) |
|---|---|---|
| Other | 368 (58.9) | 436 (59.4) |
| Dyadic Developmental Psychotherapy | 150 (24.0) | 173 (23.6) |
| Individual Child Psychotherapy | 147 (23.5) | 168 (22.9) |
| Theraplay | 137 (21.9) | 151 (20.6) |
| VIG | 96 (15.4) | 108 (14.7) |
| Child–Parent Psychotherapy | 75 (12.0) | 86 (11.7) |
| Parent–Infant Psychotherapy | 74 (11.8) | 89 (12.1) |
| Circle of Security | 64 (10.2) | 72 (9.8) |
| Watch, Wait and Wonder | 50 (8.0) | 58 (7.9) |
| Video Feedback to Promote Positive Parenting | 26 (4.2) | 28 (3.8) |
| Attachment and Biobehavioral Catch-up | 10 (1.6) | 11 (1.5) |
Generally speaking, two measures are considered the ‘gold standard’ for assessing attachment in infants and toddlers: the SSP and the AQS. It is interesting that no respondents reported using the AQS and a very small number (n = 8) of respondents reported using the SSP, each of whom worked in only one service, meaning that eight services used the SSP. Of these eight respondents, three stated that they did not explicitly carry out the SSP: one noted that they used informal observation that mirrored the SSP, one said that they used the Crowell Procedure and then incorporated elements of the SSP, and one reported that they used the psychoanalytically based State of Mind Assessment of the child, including some aspects of the SSP.
Findings: routinely used interventions
Based on initial discussion with the ERG, and previous reviews of the attachment interventions literature, the survey included several named attachment interventions that respondents could report having used. These were Attachment and Biobehavioral Catch-up (ABC), Individual Child Psychotherapy (ICP), Parent–Infant Psychotherapy (PIP), Child–Parent Psychotherapy (CPP), Dyadic Developmental Psychotherapy (DDP), Circle of Security (COS), Video Feedback to Promote Positive Parenting (VIPP), VIG, Theraplay and Watch, Wait and Wonder (WWW). We included manualised parenting interventions only, with the exception of ICP; the ERG strongly advised including ICP as it is very commonly used in this context.
Respondents were also asked to list any other attachment interventions that they used when working with children and/or caregivers. Respondents could list up to three other interventions (see Appendix 1, Table 21, for the list of other interventions). The most common response was ‘other’ (n = 368, 58.9%), indicating that respondents used interventions not in our initial list. This set of ‘other’ interventions included a wide range of interventions, and no individual interventions were reported more frequently than any of those in the named set presented in Table 6. Therefore, we refer to this set of 10 named interventions as ‘routinely used interventions’ for attachment as identified by this survey.
Out of the list of named interventions prespecified by the ERG, a substantial number of respondents (24.0%, n = 150) reported using DDP, 23.5% (n = 147) reported using ICP, and 21.9% (n = 137) reported using Theraplay. In addition to this, a similar proportion reported using VIG (15.4%, n = 96), CPP (12.0%, n = 75), PIP (11.8%, n = 74), COS (10.2%, n = 64) and WWW (8.0%, n = 50). A smaller proportion of the sample reported using VIPP (4.2%, n = 26) and ABC (1.6%, n = 10).
Outcome measures
For each reported intervention, respondents were asked how they assessed the outcome of work with a particular child or caregiver; the responses were given in an open-text box. Table 7 shows the outcome measures that respondents reported using to assess work for each of the routinely used interventions with a particular child or caregiver. Responses were varied, with respondents noting multiple outcome measures; these were subsequently categorised by the research team. Assessments often included a variety of self-report measures (e.g. SDQ, MIM, ASQ). Below, we summarise the assessments used for each of the most commonly reported interventions.
| Informal clinical feedback | Observation | Assessments | Goal-setting | Reviews | Report writing | Other | None | |
|---|---|---|---|---|---|---|---|---|
| ABC | 3 | 1 | 2 | 0 | 0 | 0 | 0 | 4 |
| Individual Child Psychotherapy | 48 | 14 | 95 | 16 | 34 | 9 | 10 | 10 |
| PIP | 20 | 11 | 47 | 11 | 6 | 3 | 2 | 7 |
| CPP | 20 | 11 | 41 | 5 | 13 | 5 | 7 | 8 |
| DDP | 46 | 13 | 75 | 13 | 32 | 5 | 11 | 22 |
| COS | 15 | 6 | 30 | 3 | 3 | 1 | 5 | 13 |
| VIPP | 3 | 2 | 7 | 0 | 2 | 1 | 2 | 11 |
| VIG | 26 | 14 | 55 | 14 | 10 | 3 | 8 | 8 |
| Theraplay | 45 | 25 | 65 | 14 | 15 | 6 | 13 | 26 |
| WWW | 20 | 10 | 24 | 10 | 2 | 1 | 5 | 2 |
A large proportion (n = 95, 64.6%) of respondents who work with ICP reported using some form of assessment to assess the outcome with a particular child or caregiver. A similar proportion stated that they used informal clinical feedback (n = 48, 32.7%) and reviews (n = 34, 23.1%). A smaller proportion of respondents used observation (n = 14, 9.5%), goal-setting (n = 16, 10.9%) and report writing (n = 9, 6.1%), and a similar number of respondents (n = 10, 6.8%) noted that they use no outcome measures or chose ‘other’, which included internal work targets (n = 1, 0.7%), multidisciplinary team meetings (n = 1, 0.7%), improvement in target child behaviour, carer attunement and the parent–infant relationship (n = 5, 3.4%), expressing feelings verbally to therapist (n = 1, 0.7%), and through CAMHS (n = 1, 0.7%).
As for PIP, a substantial proportion of respondents stated that they used assessments (n = 47, 63.5%), whereas a smaller number used feedback (n = 20, 27%), reviews (n = 6, 8.1%), report writing (n = 3, 4.1%) and no outcome measures (n = 7, 9.5%). The same number of respondents (n = 11, 14.9%) stated that they used observation and goal-setting. Two respondents chose ‘other’, namely improvement in parent–infant relationship and lessening of symptoms in child (n = 1, 1.4%) and multiagency care plans usually related to placement stability (n = 1, 1.4%).
In relation to CPP, respondents frequently noted assessments (n = 41, 54.7%). A similar proportion was noted for feedback (n = 20, 27%), observation (n = 11, 14.7%) and reviews (n = 13,17.3%). Five respondents stated that they used goal-setting and report writing, and a small number worked with no outcome measures. Seven chose ‘other’, namely informal increased reflective capacity of the caregivers and attunement in the relationship and positive change in child’s presentation (n = 3, 2.3%), multidisciplinary team meetings (n = 1, 1.3%), ongoing process of supervision, case supervision and individual reflective practice (n = 1, 1.3%), monitoring interaction and responsiveness against pre-agreed outcomes (n = 1, 1.3%) and using CPP forms (n = 1, 1.3%).
As for DDP, a large proportion of respondents used assessment (n = 75, 50%), with a significant proportion also using clinical feedback and reviews (n = 46, 30.7%). Eleven chose ‘other’, namely clinical judgement (n = 1, 0.7); any success achieved (n = 1, 0.7); ability to show positive distance travelled (n = 1, 0.7); positive outcome for the family, which they felt really improved their communication with one another (n = 1, 0.7); parent reflective capacity and parents felt a sense of relationship (n = 1, 0.7); case supervision with clinical psychologist, reflection – improvement in carer child relationships and behaviour or actions on referral forms (n = 1, 0.7%); increased attunement with the child and understanding and use of the attitude and approaches of PACE (playfulness, acceptance, curiosity and empathy) to connect with and other commentary about the child’s inner emotional world (n = 1, 0.7%); positive outcome (n = 1, 0.7%); child feels listened to and validated, improvement in emotional regulation and caregiver relationship (n = 1, 0.7%); placement stability, discharge (n = 1, 0.7%); and improvement in parent–child relationship as reported by dyad (n = 1, 0.7%).
Most of the respondents who used COS used assessments (n = 30, 46.9%). Five chose ‘other’, namely progress of family (n = 1, 1.6%), engagement with school and educational outcomes (n = 1, 1.6%), psychoeducation for caregivers (n = 1, 1.6%), mother’s understanding of the concept of COS and examples of her supporting exploration (n = 1, 1.6%), and ongoing process of supervision, case supervision and individual reflective practice (n = 1, 1.6%). VIPP respondents were found to mostly use assessments (n = 7, 26.9%). Two chose ‘other’: changes in carer management, feelings and the relationship, child more regulated/feeling more contained and held and behaviours reflecting this (n = 1, 3.8%); and generally the intervention being well received by parents (n = 1, 3.8%).
In addition to this, respondents who worked with VIG report using assessments (n = 55, 57.3%). Eight chose ‘other’: improvements, trust and attachments growing (n = 1, 1.04%); changes in carer management, feelings and the relationship, child more regulated/feeling more contained and held and behaviours reflecting this (n = 1, 1.04%); outcomes negotiated with the caregiver and indicators of change from third parties such as school; also in some cases if the child is taken into care or not (n = 1, 1.04%); ongoing process of supervision, case supervision and individual reflective practice (n = 1, 1.04%); positive outcome (n = 1, 1.04%); in the community every 2 or 3 weeks (n = 1, 1.04%); VIG outcome measures (n = 1, 1.04%); and supportive family (n = 1, 1.04%).
A substantial number of respondents who used Theraplay used assessments (n = 65, 47.4%), with a significant proportion of these being clinical feedback (n = 45, 32.9%) and observation (n = 25, 18.3%). Thirteen chose ‘other’, namely child’s behaviour (n = 1, 0.7%); quality of interactions between the child, peers and adults in school (n = 1, 0.7%); improvement in attachment to main caregiver, their confidence in working with their child and way the relationship develops in terms of increased responsiveness and enjoyment of the child (n = 1, 0.7); improvement in child’s behaviour and relationship between caregiver and child (n = 1, 0.7%); game with a child and therapist or with a caregiver with the child, where communication would be the focus of the game and co-operation is needed to achieve the end goal, assessing the ability of the child to remain focused and listen and promoting caregivers’ ability to lead the game and remain in control (n = 1, 0.7%); clinical supervision, reflection, case management, improvement in behaviours and child carer interactions (n = 1, 0.7%); placement stability (n = 1, 0.7%); facilitating play sessions with parent to child and, over time, seeing if there is a difference (n = 1, 0.7%); no assessment diagnostically, therapeutic alliance built on holding space and time and trust, which allows child to work through and express emotionally in a safe and boundaried play space (n = 1, 0.7%); reflective practice and supervision (n = 1, 0.7%); quality of interaction between the caregiver and the child (n = 1, 0.7%); and use alongside other modalities (n = 1, 0.7%).
A notable number of respondents who used WWW used assessments (n = 24, 48%). Five chose ‘other’, including progress made (n = 1, 2%), recordings and photographs (n = 1, 2%), documentation within electronic clinical records (n = 1, 2%), and therapeutic alliance allowing child to work through and express emotionally in play space (n = 1, 2%).
Geographical location of the most common interventions
Respondents were asked to use a redefined drop-down list to select the region in which they worked. They were then asked to use an open-text box to name the town in which their service or services were located (some respondents mentioned multiple towns in their response). The research team were then able to cross-reference the location with the routinely used interventions.
A fairly even distribution of use of ABC was recorded in services across the UK, including in southern England, with services using this intervention in Greater London (n = 2) in addition to northern England (North West England, n = 2; North East England, n = 1), Wales (n = 2), Scotland (n = 2), Northern Ireland (n = 1) and central England including the West Midlands (n = 1). Figure 2 shows this geographical distribution, with darker colours indicating higher frequency of use.
FIGURE 2.
Maps showing the geographical location of the 10 named interventions identified in the survey: (a) ABC; (b) ICP; (c) PIP; (d) CIP; (e) DDP; (f) COS; (g) VIPP; (h) VIG; (i) Theraplay; and (j) WWW. Approximate distribution of children in receipt of interventions by age.









The majority of services (n = 94) using ICP were in southern England (Greater London, n = 41; South East England, n = 23; East of England, n = 17; South West England, n = 13). A substantial proportion of services using CP (n = 39) were in Northern England (Yorkshire and the Humber, n = 17; North West England, n = 13; North East England, n = 9). A smaller proportion of services (n = 19) were based in central England (West Midlands, n = 12; East Midlands, n = 7). In addition to this, 16 services were based in Scotland, 12 were based in Wales and six were based in Northern Ireland.
A significant number (n = 55) of services that reported using PIP were located in southern England (Greater London, n = 30; South West England, n = 13; South East England, n = 10; East of England, n = 2). A considerable number of services (n = 21) were located in northern England (Yorkshire and the Humber, n = 14; North West England, n = 5; North East England, n = 2). A smaller number of services were located in central England (n = 12, comprising six in each of West and East Midlands). Furthermore, six services were based in Wales, three were based in Northern Ireland and one was based in Scotland.
Most commonly (n = 42), CPP was reported as being used in services in southern England (Greater London, n = 25; South East England, n = 11; East of England, n = 6). Services were also based in northern England (n = 24: Yorkshire and the Humber, n = 11; North West England, n = 9; North East England, n = 4). Ten services were located in Central England (West Midlands, n = 5; East Midlands, n = 5), six were in Scotland, five were in Wales and three were in Northern Ireland.
By contrast, services reporting the use of DDP were fairly evenly spread across regions, with 65 services based in southern England (South West England, n = 27; South East England, n = 16; Greater London, n = 12; East of England, n = 10) and a similar proportion based in northern England (n = 48: Yorkshire and the Humber, n = 22; North West England, n = 15; North East England, n = 11) and central England (n = 43: West Midlands, n = 28; East Midlands, n = 15). A considerable 21 services were found to be in Wales, whereas a smaller number were found to be in Scotland (n = 11) and Northern Ireland (n = 5).
No services that responded to our survey reported using COS in Northern Ireland. A smaller number of services reported using COS in Wales (n = 9) and Scotland (n = 5). The vast majority (n = 41) of services that reported using COS were in southern England (Greater London, n = 21; East of England, n = 9; South West England, n = 9; South East England, n = 2). A similar proportion were in northern England (n = 14: Yorkshire and the Humber, n = 7; North East England, n = 4; North West England, n = 3) and 12 services were based in central England (West Midlands, n = 9; East Midlands, n = 3).
The majority of services (n = 24) that reported using VIPP were located in southern England (Greater London, n = 11; South West England, n = 8; South East England, n = 4; East of England, n = 1). A smaller proportion of services were in northern England, with five in North East England and two in Central England: one each in East and West Midlands. Two services were in Scotland and one was in Wales. No services were in Northern Ireland.
A significant number (n = 72) of services reporting the use of VIG were located in Southern England (Greater London n = 22; South West England, n = 22; South East England, n = 17; East of England, n = 11). A considerable number (n = 21) of services were located in Northern England (North West England, n = 9; Yorkshire and the Humber, n = 6; North East England, n = 6). Nine services were also recorded in Central London (West Midlands, n = 5; East Midlands, n = 4). In addition to this, seven services were based in Wales and nine were in Scotland; no services were in Northern Ireland.
Sixty-three services that reported using Theraplay were based in Southern England (South West England, n = 25; Greater London, n = 19; South East England, n = 10; East of England, n = 9). A similar number were located in Central England (n = 42: East Midlands, n = 23; West Midlands, n = 19) and Northern England (n = 37 services); of these, 18 were in Yorkshire and the Humber, 11 were in North West England and eight were in North East England. Furthermore, 19 services were in Wales, 10 were in Scotland and none were recorded in Northern Ireland.
Of those services reporting the use of WWW, these were most often found in parts of Southern England (n = 38), including 16 services in Greater London, 9 in both South East and South West England and 4 in East of England. A considerable number of services were based in Northern England (n = 14). Of these, nine were based in Yorkshire and the Humber and five were based in North West England. In addition, six services were in Central England (West Midlands, n = 5; East Midlands, n = 1). Additionally, five services were in Wales and two were in Northern Ireland. No services that reported using WWW were found to be in Scotland.
We asked respondents to estimate the overall approximate number of children with attachment difficulties (and/or their caregivers) with whom they had used some form of therapeutic intervention for across all work settings in the past year and we used this to estimate the number of children who respondents work with annually for each routinely used intervention.
The largest proportion of children were estimated to be receiving DDP (16.7%, n = > 5078 of children), followed by Theraplay (13.5%, n = > 4091 of children), ICP (12.8%, n = > 3889 of children), WWW (9.4%, n = > 2839 of children), CPP (7.8%, n = > 2375 of children), PIP (6.2%, n = > 1868 of children), and COS (5.0%, n = > 1503 of children). We estimate that the smallest proportion of children and/or caregivers were receiving VIPP (2.8%, n = > 842 of children) and ABC (0.4%, n = 119 of children) (Table 8).
| Intervention | Respondents, n (%) |
|---|---|
| DDP | > 5078 (16.7) |
| Theraplay | > 4091 (13.5) |
| ICP | > 3889 (12.8) |
| WWW | > 2839 (9.4) |
| CPP | > 2375 (7.8) |
| PIP | > 1868 (6.2) |
| COS | > 1503 (5.0) |
| VIG | > 1422 (4.7) |
| VIPP | > 842 (2.8) |
| ABC | 119 (0.4) |
Table 9 shows the age ranges of children with whom practitioners using each of the 10 named interventions commonly worked. Respondents who work with ABC reported that they work with a fairly even proportion of children across the age range of 0–13 years (see Table 9). The age range reported by respondents of children who practitioners work with for the remaining routinely used interventions was as to be expected. Respondents who work with ICP reported that the majority of children who they work with were aged ≥ 4 years. As for practitioners working with PIP, the vast majority of children who they work with were aged 0–3 years. Practitioners using CPP reported that they work with children aged 4–11 years. In addition, respondents that work with DDP were found to work mainly with children aged ≥ 4 years. Practitioners using COS and VIPP were found to mostly work with children aged 0–6 years. Practitioners working with VIG reported that they predominantly work with children aged 0–3 years. Practitioners using Theraplay reported working with children aged 4–13 years, whereas those using WWW were found to work mostly with children aged 0–3 years.
| Age range (years), n (%) of responses | |||||
|---|---|---|---|---|---|
| 0–3 years | 4–6 years | 7–9 years | 10–11 years | 12–13 years | |
| ABC | 6 (60.0) | 6 (60.0) | 5 (50.0) | 5 (50.0) | 5 (50.0) |
| ACP | 64 (43.5) | 107 (72.8) | 127 (86.4) | 124 (84.4) | 107 (72.8) |
| PIP | 66 (89.2) | 41 (55.4) | 35 (47.3) | 33 (44.6) | 29 (39.2) |
| CPP | 45 (60.0) | 63 (84.0) | 62 (82.7) | 60 (80.0) | 51 (68.0) |
| DDP | 80 (53.3) | 125 (83.3) | 137 (91.3) | 138 (92.0) | 127 (84.7) |
| COS | 47 (73.4) | 45 (70.3) | 36 (56.3) | 35 (54.7) | 31 (48.4) |
| VIPP | 22 (84.6) | 21 (80.8) | 18 (69.2) | 17 (65.4) | 16 (61.5) |
| VIG | 80 (83.3) | 59 (61.5) | 45 (46.9) | 42 (43.8) | 35 (36.5) |
| Theraplay | 70 (51.1) | 111 (81.0) | 119 (86.9) | 118 (86.1) | 99 (72.3) |
| WWW | 44 (88.0) | 21 (42.0) | 18 (36.0) | 15 (30.0) | 16 (32.0) |
Referrals
We asked respondents to provide service-level information on the percentage of children who were referred from various sources and the type of family arrangement the service served [e.g. cared for by biological parent(s), children who are adopted, children in foster care]. We used this information to gain a picture of the contexts in which services were delivering the different types of routinely used interventions.
A substantial proportion of respondents who used ABC reported receiving referrals from social workers (40.5%), with the education sector (24.2%) being another significant source. With regard to services providing ICP, a similar proportion of referrals were from social workers (32.8%) and the education sector (24.1%). Most commonly, services providing PIP received referrals from social workers (26.2%), health visitors (24.8%) and mental health services (20.7%), and 36.3% of referrals to services using CPP were from social workers. Respondents who used DDP stated that their referrals were predominantly from social workers (54.0%). Services providing COS reported that over one-third (33.5%) of their referrals were from social workers. With regard to VIPP-providing services, 35.4% of their referrals were from social workers and 23.8% were from education. Of those services using VIG, a considerable number of their referrals were from social workers (29.9%). Respondents who used Theraplay reported that almost half of their referrals were from social workers (45.5%), with a significant number also being from the education sector (20.9%). Most of the referrals for services using WWW practitioners were from health visitors (29.5%) and social workers (23.6%) (Table 10).
| Type of respondent, % | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| General practitioner | Social worker | Self-referral | Voluntary sector | Health visitor | Education | Mental health service | Paediatrics | Other | |
| ABC | 6.2 | 40.5 | 12.3 | 6.2 | 18.2 | 24.2 | 15.3 | 9.2 | 21.2 |
| ICP | 12.0 | 32.8 | 12.5 | 5.0 | 4.6 | 24.1 | 10.5 | 6.7 | 5.2 |
| PIP | 15.6 | 26.2 | 10.4 | 5.2 | 24.8 | 8.9 | 20.7 | 10.7 | 7.4 |
| CPP | 12.2 | 36.3 | 12.4 | 3.8 | 4.9 | 17.0 | 14.3 | 9.5 | 8.5 |
| DDP | 7.2 | 54.0 | 10.9 | 1.9 | 3.3 | 10.8 | 6.5 | 6.5 | 6.2 |
| COS | 8.6 | 33.5 | 14.7 | 5.0 | 13.6 | 15.4 | 9.7 | 13.8 | 14.7 |
| VIPP | 7.5 | 35.4 | 16.0 | 5.6 | 12.9 | 23.8 | 14.9 | 7.9 | 6.7 |
| VIG | 9.6 | 29.9 | 9.4 | 4.5 | 19.6 | 14.1 | 15.6 | 5.2 | 13.7 |
| Theraplay | 7.1 | 45.5 | 13.1 | 3.4 | 4.7 | 20.9 | 10.8 | 7.2 | 6.7 |
| WWW | 13.7 | 23.6 | 8.5 | 7.0 | 29.5 | 15.0 | 18.5 | 9.4 | 10.6 |
Children with whom practitioners worked
The majority of ABC practitioners worked with children who were cared for by biological parent(s) (53.5%), with almost one-quarter of children being in foster care (21.4%). Almost half of the children with whom ICP practitioners worked were cared for by biological parent(s) (41.4%), with a substantial number being adopted (21.0%). With regard to PIP practitioners, a large majority of children with whom they worked were cared for by biological parent(s) (64.9%). A considerable proportion of the children with whom CPP practitioners worked were cared for by biological parent(s) (39.6%), while 22.6% were in foster care and 20.2% were adopted. Most commonly, respondents who used DDP worked with children who were adopted (32.5%); in addition to this, a significant proportion were children in foster care (24.3%) and children cared for by biological parent(s) (22.5%). COS practitioners predominantly worked with children cared for by biological parent(s) (49.9%), as well as with those in foster care (21.1%). Respondents who used VIPP were found to work with a considerable number of children cared for by biological parent(s) (41.1%), with a substantial number being children in foster care and children who were adopted (28.2% and 23.9%, respectively). VIG practitioners reported that the majority of children with whom they worked were cared for by biological parent(s) (57.4%). Theraplay practitioners noted that a similar proportion of children with whom they work were adopted (30.0%), cared for by biological parent(s) (29.0%) and in foster care (23.2%). Respondents who worked with WWW reported that they worked with a large proportion of children cared for by biological parent(s) (61.6%) (Table 11).
| Care context, % | |||||
|---|---|---|---|---|---|
| Children cared for by biological parent(s) | Children who are adopted | Children who are cared for by kinship or friends and family care | Children in foster care | Children in residential care | |
| ABC | 53.5 | 8.4 | 14.4 | 21.4 | 8.2 |
| ICP | 41.4 | 21.0 | 13.1 | 16.9 | 8.1 |
| PIP | 64.9 | 12.8 | 10.9 | 13.0 | 3.4 |
| CPP | 39.6 | 20.2 | 14.9 | 22.6 | 6.7 |
| DDP | 22.5 | 32.5 | 13.1 | 24.3 | 10.7 |
| COS | 49.9 | 13.3 | 11.6 | 21.1 | 5.5 |
| VIPP | 41.1 | 23.9 | 9.2 | 28.2 | 8.7 |
| VIG | 57.4 | 9.7 | 12.1 | 16.8 | 3.3 |
| Theraplay | 29.0 | 30.0 | 12.4 | 23.2 | 7.9 |
| WWW | 61.6 | 10.5 | 10.3 | 17.3 | 3.3 |
Training and supervision
Respondents were asked to comment in an open-text field on the type of training they had received for the routinely used interventions. These responses were immensely varied and were sorted into a set of general categories. For the purposes of analysis, training was considered as formal training that related directly to the routinely used intervention that may have been provided within their organisation or externally.
Almost three-quarters of respondents who worked with ABC reported that they had received formal training (70.0%, n = 7). The vast majority of respondents who reported working with ICP had been formally trained (93.2%, n = 137). A large proportion of respondents who worked with PIP had been formally trained (89.2%, n = 66). Of the 10.8% (n = 8) who had received no formal training in PIP, two mentioned informal training, including a training event-related observation course, reading and on-the-job training.
A substantial number of respondents who worked with CPP were formally trained (86.7%, n = 65). Of the 13.3% (n = 10) who were not formally trained, two were informally trained, which included learning through experience and drawing on psychodynamic psychotherapy training. The vast majority of respondents who worked with DDP were formally trained (94.0%, n = 141). Of the 6.0% (n = 9) who had no formal training, two mentioned informal training, including attending training where DDP was recommended and learning through experience and supervision.
The majority of respondents who worked with COS were formally trained (73.4%, n = 47). Just over one-quarter of respondents did not report having any formal training (26.6%, n = 17). Among these, one noted that they used elements of COS in psychoeducation, and five reported informal training including research, reading, videos handouts, accessing resources and becoming familiar with some useful elements via other training and supervision.
A large proportion of respondents who worked with VIPP (76.9%, n = 20) had formal training; 23.1% (n = 6) were not formally trained and three reported receiving informal on-the-job training. Almost all respondents who worked with VIG were formally trained (94.8%, n = 91). A significant proportion of respondents who used Theraplay were formally trained (83.9%, n = 115). Of the 15.3% (n = 21) who had no formal training, 12 mentioned informal training, including supervision, reading, on-the-job training, attending workshops and shadowing. In addition, the majority of respondents who worked with WWW (78.0%, n = 39) were formally trained, whereas almost one-quarter had no formal training (22.0%, n = 11) and six mentioned informal training, including reading and supervision (Table 12).
| Intervention | Training, n (%) of responses |
|---|---|
| ABC | 7 (70.0) |
| ICP | 137 (93.2) |
| PIP | 66 (89.2) |
| CPP | 65 (86.7) |
| DDP | 141 (94.0) |
| COS | 47 (73.4) |
| VIPP | 20 (76.9) |
| VIG | 91 (94.8) |
| Theraplay | 115 (83.9) |
| WWW | 39 (78.0) |
In addition to training, approximately half of the respondents who worked with ABC (50.0%, n = 5) and just over half of respondents who worked with COS (54.7%, n = 35) reported receiving ‘regular supervision to deliver this intervention’. Just under half of respondents who worked with WWW (44.0%, n = 22) received supervision. The vast majority of respondents who worked with ICP and CPP reported having received supervision (ICP − 90.5%, n = 133; and CPP − 93.3%, n = 70). A similar proportion of respondents who worked with VIPP 65.4% (n = 17) and Theraplay 63.5% (n = 87) also reported having received supervision. In addition to this, the majority of respondents who worked with PIP (85.1%, n = 63), VIG (83.3%, n = 80) and DDP (74.7%, n = 112) reported having received supervision (Table 13).
| Intervention | Supervision, n (%) of responses |
|---|---|
| ABC | 5 (50.0) |
| ICP | 133 (90.5) |
| PIP | 63 (85.1) |
| CPP | 70 (93.3) |
| DDP | 112 (74.7) |
| COS | 35 (54.7) |
| VIPP | 17 (65.4) |
| VIG | 80 (83.3) |
| Theraplay | 87 (63.5) |
| WWW | 22 (44.0) |
Adaptations made to interventions
Respondents were asked to use an open-text field to record if they had made any important changes or modifications to the way the routinely used interventions were delivered (compared with the original manual or training). Adaptations identified were categorised in the following: integrating models and/or approaches (the intervention was modified to incorporate additional models and/or approaches); tailoring to the client(s) [the intervention was modified to be tailored around the client(s) needs]; setting (the intervention was modified in terms of the setting, i.e. face to face/online, individually/group, location); timings (the intervention was modified due to timings, i.e. number of times the intervention was delivered and over what period of time, including the number and duration of sessions); practice informed by the approach (the intervention was modified in terms of being delivered as an informed approach as opposed to being guided by the manual); video procedure/materials (video procedure – intervention modified through changes to the video procedure, materials – intervention modified through changes to the materials delivered); and other.
Two manuals are available to those receiving training and supervision in the unpublished document ‘Attachment and biobehavioral catch-up’ by Dozier. 63 The first provides the content of the intervention and the second details the procedures and rules for coding ‘in the moment commenting’. 64 Of the respondents who reported working with ABC, only one (10.0%) commented that they had made modifications to the way the intervention was delivered, with a comment of ‘not many’, and did not elaborate on how the intervention had been modified (Table 14).
| Intervention | Adaptations overall | Integrating other models and/or approaches | Tailoring to the client(s) | Setting | Timings | Practice informed by the approach | Video procedure/materials | Other |
|---|---|---|---|---|---|---|---|---|
| ABC | 1 (10.0) | − | − | − | − | − | − | 1 (10.0) |
| ICP | 65 (44.2) | 32 (21.8) | 22 (15.0) | 3 (2.0) | 1 (0.7) | − | 1 (0.7) | 6 (4.1) |
| PIP | 32 (43.2) | 15 (20.3) | 4 (5.4) | 3 (4.1) | 2 (2.7) | 1 (1.4) | 2 (2.7) | 5 (6.8) |
| CPP | 30 (40.0) | 10 (13.3) | 10 (13.3) | 2 (2.7) | − | 1 (1.3) | 2 (2.7) | 5 (6.7) |
| DDP | 62 (41.3) | 30 (20.0) | 11 (7.3) | 1 (0.7) | 3 (2.0) | 10 (6.7) | − | 7 (4.7) |
| COS | 31 (48.4) | 8 (12.5) | 4 (6.3) | 8 (12.5) | 1 (1.6) | 6 (9.4) | 2 (3.1) | 2 (3.1) |
| VIPP | 6 (23.1) | 2 (7.7) | − | − | − | − | 1 (3.8) | 3 (11.5) |
| VIG | 17 (17.7) | 6 (6.3) | 4 (4.2) | − | 1 (1.0) | 3 (3.1) | 1 (1.0) | 2 (2.1) |
| Theraplay | 62 (45.3) | 35 (25.5) | 10 (7.3) | 4 (2.9) | 3 (2.2) | 3 (2.2) | − | 7 (5.1) |
| WWW | 19 (38.0) | 7 (14.0) | 4 (8.0) | 4 (8.0) | 1 (2.0) | − | − | 3 (6.0) |
There is no one specific manual for ICP, as the term is a broad description of a therapeutic approach with various theoretical underpinnings and models of delivery. It was included in the survey on the strong advice of the ERG. In addition, although it is not specifically manualised for attachment, numerous papers and books describe its use. In the UK, the ACP and UKCP have different training requirements. A significant proportion of respondents stated that they had modified the intervention by integrating other models and/or approaches (21.8%, n = 32). A small proportion changed the intervention by tailoring it to the client(s) (15.0%, n = 22). 2.0% (n = 3) or changing the setting. Another respondent reported modifying the intervention by adapting timings and the video procedure/materials and six (4.1%) respondents made modifications categorised as ‘other’.
PIP has two manuals: one from the Parent Infant Project at the Anna Freud Centre and the other detailing the approach of the School of Infant Mental Health. 65 Fewer than half of respondents who worked with PIP made changes to the original manual (43.2%, n = 32). Among these respondents, modifications included integrating other models and/or approaches (20.3%, n = 15), tailoring to the client(s) (5.4%, n = 4) and setting (4.1%, n = 3). The same proportion (2.7%, n = 2) made modifications to timings and to video procedure/materials. Five (6.8%) were categorised as ‘other’.
CPP has two published manuals available. The first can be used when working with very young children who have been traumatised66 and the second is used to work with children who have experienced the death of a parent or primary caregiver. 67 These are supplemented by an online version from the New Mexico Children, Youth and Families Department. 65 A total of 40.0% (n = 30) of practitioners that reported using CPP reported they had made changes to the way the intervention is delivered. Modifications included 13.3% (n = 10) integrating of other models and/or approaches and tailoring to the client(s), 2.7% (n = 2) setting, 1.3% (n = 1) practice informed by the approach and 2.7% (n = 2) video procedure/materials. Five (6.7%) was categorised as other.
There are some key texts for DDP that accompany the core training in the approach: Attachment-Focused Family Therapy Workbook68 (2011) and Healing Relational Trauma with Attachment-focused Interventions: Dyadic Developmental Psychotherapy. 69 In addition, there are manuals that accompany Kim Golding’s DDP-informed therapeutic parenting programmes for parents/carers of care-experienced children Nurturing Attachments and Foundations for Attachment. 70 A total of 41.3% (n = 62) of respondents who worked with DDP had made modifications to the intervention, including integrating other models and/or approaches (20.0%, n = 30), tailoring to the client(s) (7.3%, n = 11), setting (0.7%, n = 1), timings (2.0%, n = 3), and using the intervention as a practice informed by the approach (6.7%, n = 10). Seven (4.7%) respondents were categorised as ‘other’.
COS does not have a published manual, and a practitioner needs to train before they can become a facilitator; however, there are two COS books, one for professionals and one for parents. 71 Around half of respondents who work with COS (48.4%, n = 31) reported that they had made changes to the original programme, including integrating other models and/or approaches (12.5%, n = 8), tailoring to the client(s) (6.3%, n = 4), setting (12.5%, n = 8), timings (1.6%, n = 1), and used the intervention as a practice informed by the approach (9.4%, n = 6), and the same proportion (3.1%, n = 2) made changes to the video procedure/materials and were categorised as other.
VIPP has different versions for different circumstances, for example the Video-feedback intervention (version 3.0) to promote Positive Parenting and Sensitive Discipline (VIPP-SD) manual by Juffer et al. 72 Almost one-quarter (23.1%, n = 6) of respondents made changes to the original manual or training, including integrating other models and/or approaches (7.7%, n = 2). One respondent modified the intervention by changing the video procedure. Three (11.5%) respondents were categorised as ‘other’.
The Skills Development Scale is used as the VIG manual. 73 A total of 17.7% (n = 17) of practitioners who used VIG made modifications to this intervention, including integrating other models and/or approaches (6.3%, n = 6) and tailoring to the client(s) (4.2%, n = 4). One respondent made modifications to the timings and video procedure. Three (3.1%) respondents made modifications in terms of using the intervention as a practice informed by the approach and were categorised as ‘other’.
There are three texts for Theraplay74–76 and the last two form the manual. 77 Just under half (45.3%, n = 62) of Theraplay practitioners made modifications to the intervention, including integrating other models (25.5%, n = 35), tailoring to the client(s) (7.3%, n = 10) and setting (2.9%, n = 4). Three (2.2%) respondents reported that they had made changes to timings and used the intervention as a practice informed by the approach. Seven (5.1%) respondents were categorised as ‘other’.
A published manual is available for WWW. 78 Among respondents who worked with WWW, 38.0% (n = 19) made changes to the intervention, including integrating other models and/or approaches (14.0%, n = 7), and 8.0% (n = 4) made changes in terms of tailoring the intervention to the client(s) and setting. One respondent made changes to timings. Three (6.0%) were categorised as ‘other’.
Therapeutic techniques
Although no single intervention type was reported to be used by > 25.0% of practitioners or services, large proportions of respondents reported using one or more of the common techniques used in attachment interventions. Table 15 lists descriptions of these therapeutic techniques. A large proportion of the respondents reported using the technique ‘modelling sensitivity’ (84.2%, n = 526), reflecting on being a caregiver (86.4%, n = 540) and reflecting on the caregiver’s past (82.2%, n = 514). Around three-quarters of the sample reported using speaking for the child (77.4%, n = 484) and attachment psychoeducation (74.6%, n = 466). A substantial number of respondents reported using live feedback (59.8%, n = 374) and facilitating interaction (62.4%, n = 390), and a significant number of respondents used skin-to-skin (37.3%, n = 233) and video feedback (31.7%, n = 198).
| Therapeutic techniques | Respondents, n (%) | Number (%) of children and/or caregivers |
|---|---|---|
| Promoting sensitive caregiving | ||
|
Modelling sensitivity The therapist directly models or demonstrates sensitive parenting, showing by example how one responds to a child’s attachment cues, provides sensitive comfort, etc. |
526 (84.2) | > 23,714 (> 78.2) |
|
Video feedback Using video recordings of the caregiver’s own interactions with the child to highlight sensitive (or insensitive) behaviours by replaying the video, and providing opportunity for reflection and feedback |
198 (31.7) | > 9737 (> 32.1) |
|
Live feedback Providing in-the-moment feedback to caregivers during spontaneous live interactions with the child to highlight sensitive or insensitive behaviours (Note: this does not refer to feedback provided only during a specific structured activity arranged by the therapist, which would be scored in the next item) |
374 (59.8) | > 17,879 (> 58.9) |
|
Facilitating interaction During intervention sessions, the therapist encourages the caregiver to play or interact with the child for a discrete period of time (e.g. using some provided toys, or a feeding) and provides verbal comments and encouragement to promote sensitive interactions with the child |
390 (62.4) | > 15,001 (> 49.5) |
|
Speaking for the child The therapist voices what the baby or young child might be thinking or feeling, as if in the child’s own words. Or, the therapist encourages the caregiver to verbalise what they think the child might be thinking or feeling |
484 (77.4) | > 18,939 (> 62.4) |
| Attachment-related therapeutic support for caregivers | ||
|
Reflecting on the caregiver’s past The therapist facilitates the caregiver’s exploration of their own experiences of attachment or past traumas and facilitates the making of connections between their past and the caregiver’s relationship with the baby or young child |
514 (82.2) | > 20,032 (> 66.0) |
|
Reflecting on being a caregiver Here-and-now-focused discussion of how caregivers find looking after a baby or young child, or therapeutic discussion about how the caregiver thinks about the child |
540 (86.4) | > 23,597 (> 77.8) |
|
Attachment psychoeducation Providing information (e.g. in a presentation, or via leaflets, handouts) about attachment and/or sensitive caregiving |
466 (74.6) | > 25,668 (> 84.6) |
|
Skin-to-skin Promoting skin-to-skin contact between caregiver and infant, including kangaroo mother care or baby massage |
233 (37.3) | > 10,545 (> 34.8) |
Conclusions and discussion
Patient and public involvement: stakeholder workshops and focus groups
We included PPI throughout the research. The PPI group included PPI representatives, those working directly with families with lived experience, researchers, academics, teachers, clinicians and charities and third-sector organisations.
We held three PPI meetings throughout the study, and updated members by e-mail between these meetings. The first meeting was held at the start of the study, to introduce the overall aims as well as to gather specific feedback on the survey. The members advised us on the questions to include and which organisations to circulate the survey to. The second meeting was held once we had gathered the survey results, the purpose of which was to provide an update on these findings and to gather advice on the search strategy for the systematic review. Members supported us with the selection of the search criteria and helped us to refine the PICOS. The third and final meeting was held after the completion of the systematic review, to provide a summary of the findings of the study. The members provided advice in terms of interpreting the findings and recommendations for dissemination and future work.
We also held a specific PPI workshop at the end of the study to share our findings. During this workshop, we gave members a summary of the findings. Members provided information about their current experiences in practice and how they related to the findings in our study, as well as the barriers they faced in both practice and research. The members advised us on future research directions and ideas around dissemination.
Completion rates
The completion rate for the survey was low, at 23.5% (n = 625) of the 2656 professionals who had initially agreed to participate. The reasons for this are unclear, but it might have been that professionals were daunted by the number of questions. We also heard from a number of professionals that, where more than one professional had been approached from any service, they agreed among themselves who would represent that service. The number of responses and the reasonable geographical distribution of responses across England and Wales and Northern Ireland (albeit with a smaller proportion in Scotland) nevertheless permit conclusions to be reached.
Types of organisation, services and professional roles
A wide range of services were named as working with children with attachment difficulties and their families. This included staff in social care, education services, LA services, a variety of voluntary organisations and private practitioners both individually and within organisations. A substantial proportion of services (41.6%) were from the NHS. The most common type of service was CAMHS (23.7%), but perinatal services, health visiting, midwifery and primary care were also included. This suggests that the NHS and CAMHS may dominate provision. The ages of children with whom practitioners worked were fairly evenly distributed across the whole age range of 0–13 years. In younger age groups, the target of the intervention is often attachment security/disorganisation, whereas in older age groups the target of the intervention is often severe attachment problems. This explains why DDP, which targets severe attachment problems, is often used in older age groups, up to the teenage years.
Clinical psychologists were the commonest professional role (16.8%), followed by social workers (7.9%) and psychotherapists (7.8%). Other diverse professions included other therapists, education practitioners, other psychologists, health visitors and other nurses and allied health professionals.
Referral sources
The commonest referrers were social workers, followed by education, health visitors and mental health services. Some were self-referrals. Reports of referral source varied to some extent by the mode of intervention used by the practitioners.
Procedures and tools used for assessing attachment difficulties or parent–child relationships
A wide variety of instruments was reported by 581 responders. Some of these related directly to attachment, whereas many were measures of a range of child mental health or other outcomes. The most commonly used (13%) was the SDQ. The MIM was reported by 9%, variations of the Assessment Checklist 6% and the MORS 6%. Many respondents also noted using general observation to assess attachment (26%) and 6% reported using none. Of the two procedures considered the ‘gold standard’ of attachment in infants, the SSP was reported as being used, often with modifications, in a small number of services (n = 8) and the AQS was not used at all. This may reflect the challenges in administering the SSP and the need to undergo strict training and validation. The administration of and training for the AQS is not as demanding but this measure was still not used by any of the respondents (this is discussed further in Chapter 6).
It is of concern that most services are not using outcomes that can give them detailed information about attachment. Given that this is the main purpose of these interventions, there is an expectation that more services would be using at least one main measure of attachment to monitor outcomes. This is particularly pertinent in the younger age groups where attachment is the construct targeted in therapy, whereas in older age groups some clinicians were targeting alternative outcomes such as behaviour. Intervention targets in older age children are often related to severe attachment problems (including attachment disorders) and therefore it may be that for these children alternative measures are needed, and the SSP or AQS are less appropriate.
Therapeutic techniques
Most respondents reported using one or more of the common techniques in attachment interventions. Video feedback and promoting skin-to-skin contact between the caregiver and infant were the least commonly used techniques. Overall, these various therapeutic techniques were used in a range of geographical locations and services.
Routinely used interventions and modifications made to them
Between them, respondents had used all the 10 named therapies, packages of, or manualised interventions in the questionnaire. However, the rate of use varied, the order from most to least common being DDP (24%), ICP (23.5%), Theraplay (22%), VIG (15%), CPP (12%), PIP (12%), COS (10%), WWW (8%), VIPP (4.2)%, and ABC (1.6%). Importantly, 59% professionals used ‘other’ interventions. Of these, the commonest were various psychotherapies/talking therapies (11%), play therapies (7.5%) and family therapies (6.5%). This wide variety may be a reflection of the wide range of what professionals regarded as attachment difficulties.
Although most of these interventions were manualised, considerable modifications were made to the way these interventions were delivered compared with the original manual or training. These modifications included integrating other models and/or approaches; tailoring the intervention to the particular needs of the client(s); and changing the setting, timings and materials, which included delivering the intervention on an individual basis rather than in a group setting, using the home rather than a clinical setting and undertaking the intervention online. Some respondents mentioned that, owing to COVID-19 restrictions, they had had to adapt the intervention for delivery online. Some interventions were informed by the particular intervention’s approach but did not follow the manual. Fewer adaptations were made to VIPP and no adaptations were made to ABC (this is further discussed in Chapter 6).
Other outcome measures
The outcome was measured in a variety of ways, including informal clinical feedback, observation, assessments, goal-setting, reviews and report-writing. The choice of measures varied with the mode of intervention. ICP most commonly was followed by an outcome assessment. The commonest interventions for which no outcome measure was used were Theraplay and DDP. However, both of these interventions were often followed by an assessment.
There was not one consistently used instrument used as an outcome measure. The SDQ was used by practitioners who worked with all of the routinely used interventions, with the exception of those working with ABC (this is discussed further in Chapter 6).
Geographical distribution of interventions
There is a disparity in what is on offer in different parts of the UK. The majority of services using the routinely used interventions were found in England. ABC recorded a fairly even distribution of usage within services across the UK. DDP was found to have a fairly even distribution of coverage across parts of England. Furthermore, a fairly similar proportion of services were found to use Theraplay across England. Usage of the routinely used interventions was found in parts of Scotland, Wales and Northern Ireland. However, no services in Scotland were found to use WWW. In addition, no services in Northern Ireland were found to use VIPP, VIG, COS or Theraplay.
The differences in the use of interventions across geographical locations are likely to be related to differences in local training availability, disciplinary training programmes, commissioning preferences, provider preferences and available local therapeutic resources. Further research would need to be undertaken to disentangle this complex picture, which is beyond the scope of this current survey.
Which children received which interventions?
Children with whom practitioners worked were most often being cared for by their biological parent(s), with the exception of DDP and Theraplay, as the children using this were most commonly adopted. The commonest interventions for children living with their biological parent(s) were PIP, WWW and VIG. For children who were living in foster care, VIPP was the most common intervention. Children being cared for by kinship or family friends received an even distribution of all the interventions. There was thus some selection of intervention for children in particular living circumstances, although the basis on which this choice was made is not clear. Adoptive parents may have particular preferences for interventions for their children. In England, the Adoption Support Fund is available for helping parents to access interventions.
In terms of the proportion of children receiving the various interventions, this mostly reflected the frequency of interventions used by respondents, with DDP, Theraplay and ICP being the commonest, while the fewest children received VIPP and ABC.
Training
The majority of respondents had received training in the intervention(s) that they were using. Of those using VIG, DDP, ICP, PIP and CPP the rate of training was 95–87%. Of those using Theraplay, WWW, VIPP, COS and ABC the rate was 84–70%. Others attended informal training. However, some training was part of general professional training rather than formal training in the particular intervention. The majority of practitioners had completed professional formal training for DDP, Theraplay, VIG and WWW. Although the high rate of training for some interventions is good, there must be concern that some untrained or only relatively trained professionals are providing treatment. Availability, duration and cost for training in the various interventions varies. It is clearly important for training to be more available and affordable, at least for evidence-based interventions.
Supervision
The rate of supervision was more variable. The highest rates of supervision were for CPP (93%), ICP (91%), PIP (85%) and VIG (83%). The lowest was for WWW, at 44%. These variable results are of concern, particularly as 25% of those working with DDP and 36% of those working with Theraplay, two out of the three commonest interventions, received no ‘supervision to deliver this intervention’. Although this shows low rates of intervention-specific supervision, it may be that practitioners also received general supervision as part of their role.
Chapter 4 Understanding of attachment difficulties
Overview
As part of the survey on common interventions, respondents were invited to use a free-text section of the questionnaire to describe the kinds of difficulties they considered to fall under the heading of attachment difficulties. As there was a very wide range of responses to this question, this aspect of the results is presented here as a separate chapter.
Qualitative data collected in this free-text section of the questionnaire were analysed according to thematic analysis. The thematic analysis process involved six phases – familiarisation with the data, coding, generation of the initial themes, a review of themes, defining and naming themes and drafting the findings – with movement back and forth between the phases. More detail regarding this process can be found in Chapter 2 (see Data collection and modes of analysis).
The themes emerging from the free-text data could be understood as falling under two main headings, each containing several subthemes. In the first, many of the comments left by respondents reflected a perception of attachment difficulties as relating to certain kinds of ‘cause’ or ‘origin’ of attachment difficulties. Respondents particularly drew attention to the importance of considering early developmental trauma, severe family adversity and insensitive or disrupted caregiving. The second major theme focused on the ‘features’ of a child’s behaviour that indicated difficulties with attachment directly, including signs and symptoms relating to difficulties with general functioning, neurodevelopmental difficulties, mental health problems and disturbances in relationships with others. These themes and their inter-relations are organised schematically in Figure 3.
FIGURE 3.
Schematic representation of respondents’ perceptions of attachment difficulties, organised by theme.
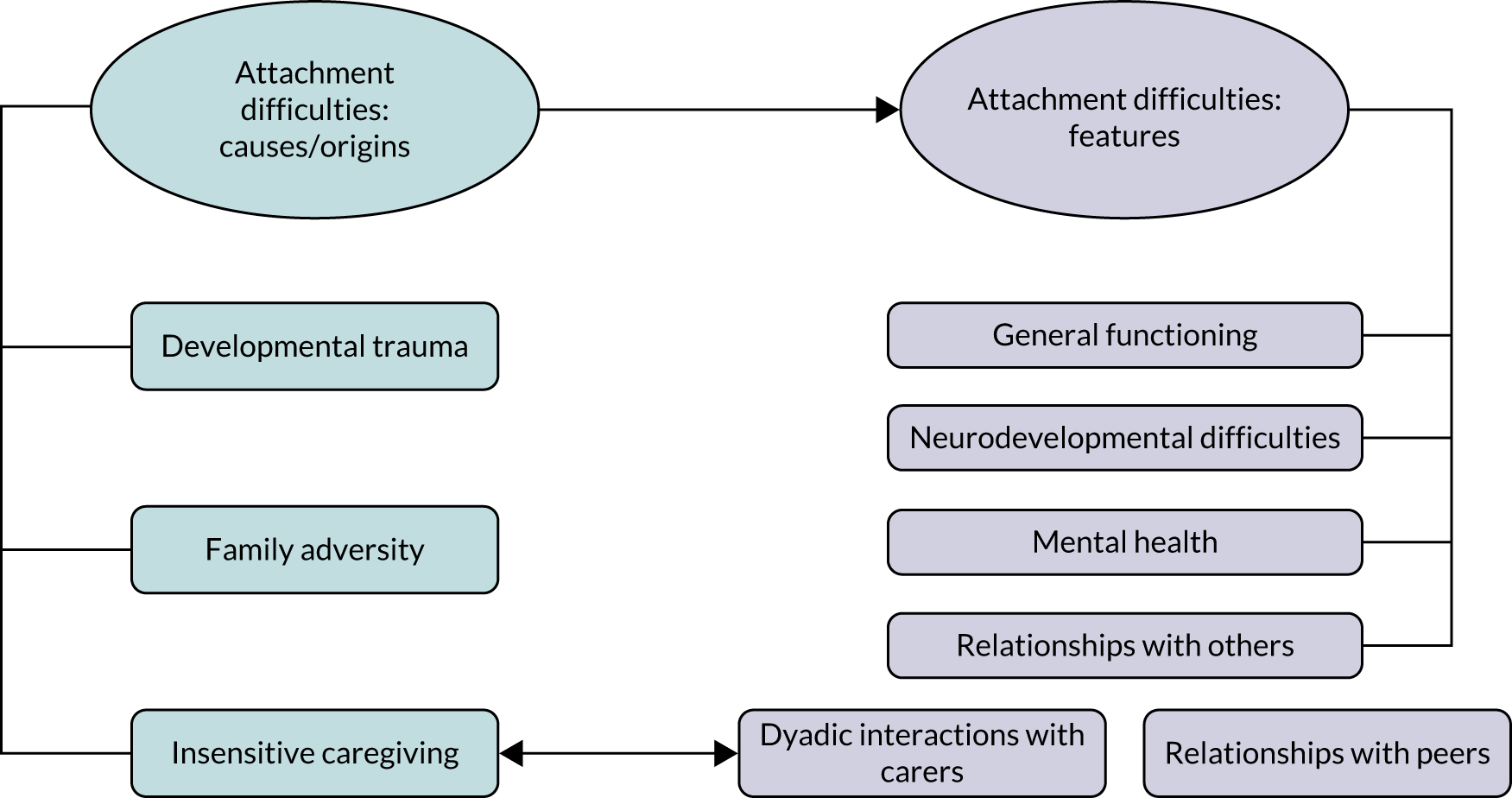
Theme 1: causes or origins of attachment difficulties
Developmental trauma
Some respondents highlighted the importance of trauma occurring during pregnancy and postnatally as a key factor that could have an impact on attachment. Often, this focus on traumatic causes was linked particularly to neurodevelopmental difficulties within the second theme of Presentations and Features:
Children who have marked difficulties the sensory attachment regulation, those who tend become emotionally dysregulated . . . difficulties with executive functioning (esp. impulse control, reasoning) and possible underdeveloped cognitive skills, educational delay. These difficulties are just the start but occur because of early attachment trauma/significant neglect from neglect whilst either in utero or in the crucial formative years of childhood.
383
Children with developmental disorders including ASC, as well as social, psychological, emotional and behavioural difficulties that have arisen in response to family circumstances and breakdown. Also, children who are adopted and cared for and are therefore coping with complex trauma.
517
Children who have experienced trauma, abuse or neglect. They may have cross-over symptoms to children with ADHD [attention deficit hyperactivity disorder]/ASD [autism spectrum disorder]: poor concentration, disruptive behaviour, unable to cope with change, attention seeking/avoidant . . . explosive/impulsive behaviour.
169
Behavioural issues eating difficulties, trauma, complex presentations which on first glance appear ADHD/ASD.
556
In relation to trauma, a number of respondents also commented that many parents seek a diagnosis of developmental disabilities such as ASD and ADHD:
Often parents seeking ASD or ADHD diagnosis but are diagnosed with attachment difficulties. Most or all of these relate to trauma.
098
Many respondents reported that attachment difficulties are impacted by early life experiences and disruptions in early childhood that can have an impact on the child’s behaviour. A number of respondents said that developmental trauma can lead to attachment difficulties that present in many ways, for example in violent behaviour or lying and stealing. Respondents reported how traumatic events or experiences such as neglect and abuse can have a profound impact on development and are associated with attachment difficulties:
Developmental trauma and early trauma can lead to attachment difficulties which look like: oppositional behaviour, lying, stealing, running away, climbing on things (roofs), smearing of faeces, clinginess, bed wetting, nightmare.
582
Children who have experienced trauma, abuse and neglect in their early lives may not have been able to form close relationships with their parents/carers. As such they may not have been provided with sufficient nurturing for their social, emotional and intellectual development . . . This early adversity affects brain development and skills such as cause and effect thinking, logical and abstract thinking, anticipation skills, memory, impulse control and emotion regulation may be affected. Consequently, a child may be unable to do as you ask, rather than deliberately ignoring requests.
330
Children whose earliest parenting experiences were neglectful and/or traumatic resulting in compromised early development particularly in children’s capacity to develop self-regulatory skills, emotional awareness and competence, empathy, impulse control and management of shame. These difficulties often result from impaired attachment experiences.
039
A number of respondents thought that children with attachment difficulties may experience reduced trust in adults and their peers due to trauma in their early childhood, especially children who have been adopted or are in care:
A lack of security and consistent parenting in the early stages of their life will often have reduced their language development and ability to trust other adults and they may feel distress and anxiety in social situations. Additional trauma or continued stress will further impact . . . with consequent impacts on language development, executive functioning and academic achievement.
312
Children who have experienced trauma in their early childhood which is inhibiting their ability to form trusting safe relationships with their adoptive parents and others.
097
We support a lot of children and their families who have experienced early trauma, losses, separations and disrupted attachments. Primarily our children are living in foster care or have been adopted but I also work with children who have been very sick and spent time in hospital in other parts of the country and who live in a residential school setting. Many of the difficulties these children face centre around feeling safe and secure and being able to trust the grownups around them.
622
Respondents reported that emotional regulation has an impact on children’s internal working model and that this can be affected by trauma:
Children with impaired attachment security due to separation and loss and trauma in early life, who as a result are unable to form trusting and nurturing relationships with others. These children frequently have behaviour difficulties relating to their insecurity and impaired sense of self-worth (negative internal working model).
185
Clients are typically children who have experienced very significant attachment disruption in the context of abuse/neglect/maltreatment/adversity/interpersonal/early development/complex trauma. This can present as significant difficulties with emotion recognition or regulation . . . very negative internal working model of self/others . . . Significant issues with trust.
187
In addition to this, developmental trauma may often become a barrier to care and caregivers as a result of emotional dysregulation; many respondents commented that these barriers affect children who have been adopted or are in care. This difficulty can manifest in a strategy for survival, which caregivers find challenging:
I look for and expect signs of attachment difficulties in children with developmental or early childhood trauma, including children in care or adopted children. Parental attachment style, often parents with attachment difficulties pass this on to their child as they struggle to form a healthy attachment . . . a strong disengagement with services/home support and a lack of motivation to change.
294
Children experiencing historical or ongoing trauma, abuse, or neglect affecting their relationship with their primary caregiver and potentially further relationships in their life. Other barriers to forming a relationship with caregivers such as other childhood adversity . . . that may impair the child and parent’s ability and bond.
546
We think about attachment under the umbrella of developmental trauma – as one aspect of a constellation of difficulties. We think about attachment alongside: emotional dysregulation, mistrust . . . For us, Attachment difficulties captures the parts of the presentation that leave the child reliant on rigid ways of conveying and getting their needs met, ways which may have served them well in the past such as avoidance or preoccupation.
013
Particularly with post-adoption clients . . . developmental trauma symptoms; impacts their ability to engage with therapy also – particularly has an impact on breaks and endings.
511
Developmental trauma difficulty with relationships and regulation resulting in developing strategies for survival which can be hard for parents/carers/teachers to manage.
121
Many respondents indicated that developmental trauma can affect a family as a whole, with a child showing a ‘miscuing’ of their needs:
Child being unable to express needs, child’s need not being recognised and responded to, child miscuing, child’s expression of distress (not expressed, not able to be soothed), evidence of emotional dysregulation or trauma symptoms.
596
Miscuing needs, role reversal, intergenerational trauma, avoidant/anxious/maladjusted attachment behaviours.
597
In relation to developmental trauma, many respondents also noted that inconsistent care affects attachment:
Children who have experienced complex trauma, children who have been removed from the care of their birth parents and places in the care of foster carers. Children who have been adopted and moved from birth parents to foster carers to adoptive parents. Children who live with parents who are not emotionally available, or who are unable to protect and keep them safe. Children who live in homes where there is violence or coercion. Children who move between numerous family members. Children who experience inconsistent care.
308
Trauma, young person having experienced multiple placements, several changes in social workers, changes of schools, care givers, lack of contact, contact that is not going well with parents etc, abuse from past, any traumatic past events, in a young person’s life.
324
Respondents also reported that attachment difficulties could arise because parents and caregivers have experienced trauma:
When a parent has neglected or abused their child in the past, and/or has their own difficulties with relationships and experiences of trauma impacting on their emotional wellbeing and how they interact with their child . . . can be defiant or withdrawn in placement or back at home with parents we would assume some attachment difficulties while also trying not to exclude additional influences such as neuro-developmental or physical health issues; try and make sense of the complex interaction of difficulties.
407
Parent not being responsive to child’s emotional needs sometimes due to trauma themselves.
147
Some respondents reported that trauma was not always recognised or acknowledged in children with attachment difficulties:
Children with attachment difficulties that we support have issues with historic, developmental and current trauma . . . Services and parents tend to externalise these issues . . . rather than acknowledging the trauma.
563
If there was trauma/neglect in the history attachment difficulties might be expressed in behaviour . . . cognitive functioning, ADHD like signs, ASD like signs . . . The trauma/neglect may not be obvious.
604
Family adversity
In addition to experiences of developmental trauma, many respondents pointed to attachment difficulties being linked to severe family adversity such as financial difficulties, domestic violence, parental substance misuse and ill health:
Multiple stressors impacting parental availability and mental health (housing, finance, domestic violence) . . . parental disengagement.
037
Attachment disorders . . . attachment problems brought about by dv [domestic violence], mental health, substance misuse. Often working with challenging behaviour that stems from attachment.
494
Adoption, separation . . . loss, grief . . . parental mental ill health . . . disability and illness, single parent family life, enmeshment, economic stressors, isolation and marginalisation where they may impact on attachment bonds within the family.
502
I also work with siblings who are often feeling invisible or spend periods of separation from family in hospital. We work also with parents who are preoccupied by the stress of cancer the impact on either the relationships or family dynamics.
444
Maternal/parental mental health
A number of respondents linked attachment difficulties with the caregiver’s mental health and the impact that this can have on maternal and paternal sensitivity and the ability to respond to a baby’s cues:
Cases where the maternal mental health problem is interfering with the mother’s ability to appropriately and sensitively respond to her baby’s cues.
004
In parents: difficulties in bonding, parental responsivity/sensitivity (impacted by mental health, for example).
454
Mothers with mental health illness often struggle to form an attachment.
021
Antenatal referrals usually centre around a woman being unable to ‘bond with her bump’ for a multitude of reasons, usually pertaining to her own mental health or life issues. These may include previous loss of a baby whereby there is a fear of a further loss with the current baby. Between 0–18 months the difficulties might be around a persistence of the difficulties during pregnancy or may be exacerbated by postnatal depression or anxiety, either pre-existing or triggered by becoming a mother (or father) due to early trauma or relationship difficulties with the parents’ own parents, for example. These examples are not exhaustive but account for many of our referrals.
419
Some respondents thought about attachment issues when serious mental or physical health problems or substance misuse had an impact on a caregiver’s ability to look after a child:
Mother or infant being ill and hospitalised. Mother’s mental health. Mother experiencing extreme tiredness, overwhelmed. Feeding problems. Crying babies (colic, cow’s milk protein allergy etc).
085
Families being separated for mental health treatments, mothers unable to hold their babies in mind as very focused on their own needs.
254
I work with children aged 0–12 months only. Difficulties I see are usually related to maternal low mood e.g. baby withdrawn/passive/not easily consoled by mother/unsettled infant due to mother’s changeable mental state/difficulty with self-soothing etc. Mother may have difficulty separating from baby even when still in the same room.
133
Mother–infant relationship difficulties impacted by mother emotional regulation difficulties, lack of confidence with parenting, depression, anxiety, OCD [obsessive–compulsive disorder], PTSD [post-traumatic stress disorder].
072
Mother insecure or ambivalent attachment. Same for father. Parental depression and other MH [mental health] conditions. Drug and alcohol abuse.
515
Children under a child protection plan for all different kinds of abuse. Children whose parents are substance misuse difficulties. Parents that experience mental health or learning difficulties, and so many more.
562
Attachment disorders . . . attachment problems brought about by dv [domestic violence, mental health, substance misuse. Often working with challenging behaviour that stems from attachment.
494
In addition, respondents often mentioned the connection between parents’ mental health problems and bonding difficulties:
Only work with children up to 1 year of age so mums reporting difficulties with bonding – saying their baby doesn’t like them or prefers other people. Mum’s mental health may be an influencing factor on this which the baby picks up on.
060
Mothers mental health impacting ability to parent and therefore form bond.
063
Difficulty with bonding between mother and baby due to mental and parental illness.
205
Lack or relationship between mother or father and their baby. Unhappy or troubled relationship between parent and baby. Parental ill health, poverty, isolation, displacement, vulnerability in the parent such as complex route to conception . . . Previous mental or physical health problems.
036
New mothers bonding with babies. Postnatal depression. Anxiety. Poverty. Lack of support. poor housing.
071
Inability to create a bond with baby in antenatal or postnatal period. Maternal mental health concerns . . . Lack of support. Lack of rooming in.
078
A number of neonatal practitioners said that parental depression also plays a part in attachment difficulties, which can occur when the baby is placed away from the parent in a neonatal intensive care unit (NICU):
Parental depression impacting on relationship with infant. Maternal ambivalence impacting on the child. Separation following birth in NICU.
269
I sometimes see attachment difficulties on the side of the parent if they have had a stay in NICU and their baby has been very unwell – PND, PTSD, Anxiety as well as struggles to bond with their baby . . . and this can also impact on the early bonding time. In addition, if younger children have to spend long periods of time in hospital, I often see separation anxiety, reluctance to mix with other children.
540
Furthermore, some commented that birth trauma can cause mental health difficulties, which can also have an impact on secure attachment styles:
Working on a neonatal unit I work with babies that are either born early, sick or following a birth trauma. This means parents are anxious, stressed and worried that can interfere with the development of bonding and attachment. If survival of the baby is in doubt that can also interfere with bonding. Some parents feel that as the neonatal staff are looking after their baby they have no role which can also interfere with bonding.
070
Several respondents commented that parents may have experienced attachment difficulties in their own childhood and from experience of the care system:
We work with parents and children under two who have social care involved (usually child protection). Problems we work with are those that are negatively affecting the parent–children relationship and parenting sensitivity e.g. parental mental health problems, parents who have been in care and experienced attachment difficulties themselves.
595
Mental ill health . . . Experience of being in the care system. I work within a specialist intensive health visiting service . . . 1st time parents from pregnancy till child is 2 (1001 critical day period) . . . impacts on their attachments and can cause difficulties. These attachment difficulties can result in mental health difficulties and/or personality disorder. We work 1 : 1 with families to break the cycle and encourage positive attachments through mentoring.
534
Insensitive caregiving
Many respondents highlighted the importance of difficulties with parenting, caregiver sensitivity and emotional attunement as a key issue in their work with attachment. These can be separated into several subthemes.
Parental difficulties in relating to the child
Many respondents talked about the importance to attachment of difficulties with a parent’s ability to relate appropriately to the child:
Disruption in parent child relationship where parent is unable to support child’s emotional needs and parent consistently . . . Parent feeling negative about their child . . . Parent/child conflict. Low self-esteem and resilience attachment to objects withdrawn/anger/anxiety low self-esteem and resilience if concurrent with poor parental relationship.
126
Parent emotionally unavailable to child, intrusive parenting.
120
Parents struggling to respond to baby’s cues, parents struggling to understand children’s communication, parents speaking negatively about the baby/child.
261
Mother and baby (under 1 year), where mum feels/states she has no attachment to her baby. Observations of mum’s interaction with baby which would indicate lack of attachment i.e. only providing basic cares, no talking to baby, not cuddling baby, not giving appropriate eye contact, no displays of warmth/affection or inappropriate/lack of response to baby’s needs.
009
We typically work with women who are observed to have a difficulty in the attachment with their baby, or feel that they have a difficulty in the attachment with their baby.
616
Mother not bonding with baby following birth.
100
Mothers and fathers and other children not bonding with their unborn (in pregnancy) and newborn baby (postnatally).
069
Mothers and fathers not bonding with the baby in utero and consequently neither after the baby has arrived.
327
Respondents also said that relational difficulties between mother and baby could be characterised by the mother’s unrealistic expectations for the baby:
Parent infant relationship.. not understanding baby states, adjustment difficulties, role adjustment, unrealistic expectations.
029
I generally work with mothers and infants aged 0–12 months. I am usually alerted to potential attachment difficulties when there appears to be a regular mismatch between mother and infant affect and attention, when mothers seem irritated or unaffected by their infants’ distress, and when mothers describe unrealistic expectations of their infants.
396
Misattunement
A number of respondents noted maternal/parental misattunement, with mothers/parents being unresponsive to their infants and children’s needs:
Poor parent child relationship. Parent, usually mother not meeting child’s emotional needs. Parent negative about her child. Parent not in tune, missing her baby’s cues and signals. Little play between adult and child.
579
Eye contact, vocal contact, not recognising cues, how parent feels about baby, how cues are mistaken by parent.
096
Parents not understanding that babies are communicating all the time and therefore not noticing or responding to cues.
101
Children who have experienced primary carers as poorly attuned to their initiations including communications of their distress. This may have been lower than 40% of these communications . . . They have confused experiences of relationships and have not developed an internalised sense of safety with adults . . . High levels of adversity without sufficient attuned adult care, may impact on any or all of these aspects of development, depending on the child’s experiences at different times.
335
0–2 years. Focus on pre-attachment indicators and repairing misattunement, ruptured relationships, parental sensitivity as well as understanding and addressing what might have replaced paternal sensitivity in the care-giver (and why/how).
522
Respondents also noted that caregivers may have difficulties with ‘mind-mindedness’:
We observe attachment behaviours of infants – signalling behaviours like crying or protest, or approach behaviours – and how a parent would respond to these in a consistent way or whether there is inconsistency in terms of warmth, invasiveness, tone of voice, language, teasing etc. We would observe the timings of interactions and whether they are attuned and contingent. We would also note how a parent might refer to their child and use mind-minded comments; or in general conversation how they might refer to their child. We would be alert to thoughts of maternal incompetence or a mother expressing that her baby hated her. We could observe how a parent might position a baby for interaction or play . . . Any of these factors might indicate possible attachment difficulties.
087
Relationship communication and interaction difficulties . . . Parenting misalignment and lack of connection with and mind-mindedness for their child.
226
Where there is a rupture or problem in the relationship between the child and a main caregiver (including nursery staff) meaning that the child does not feel safe and there is a lack of an attuned and mind-minded caregiver, leading to the infant/child being distressed.
316
Some respondents considered attachment difficulties to be related to a lack of warmth and reciprocity in the relationship between caregiver and child:
Problems in the parent-infant relationship – a lack of connection, a lack of warmth, misunderstanding or ignoring communication, a lack of understanding or application of knowledge of child development. Basically, a lack of safety and joy in the parent–baby relationship.
190
I work with under 5’s particularly babies and mothers during the perinatal period. No obvious warmth between the dyad. Little or no eye contact. No reciprocity between the dyad etc.
237
Parental issues of attachment to their children, behavioural issues suggestive of attachment difficulties; sleep, infant feeding, conduct difficulties, reciprocity between children and their parents.
585
Lack of reciprocity; difficulties with emotional and behavioural regulation; high need to control; aversion to physical touch and affection; inability to trust that adults can meet their needs; poor impulse control.
498
Theme 2: features of attachment difficulties
As noted above, the second major theme in practitioners’ responses to the open-text field regarding their understanding of attachment difficulties in clinical practice related to features of attachment problems in children.
General functioning
Many respondents reported that they thought about attachment difficulties in terms of the impact that adverse attachment experiences may have on cognitive, behavioural and emotional functioning. They referred to difficulties and delays in play, learning, attention, regulating emotions, sleeping, feeding, motor skills, speech, language, communication and challenging behaviour:
Difficulties in this area could cause problems with playing, learning, developing . . . Developmental difficulties including neurodevelopment and problems with learning – emotional difficulties including anxiety, mood disorders, serious emotional dysregulation . . . externalising difficulties such as aggression and oppositionality – interruptions or delays in development of young children in areas such as sleeping, feeding, motor development and speech, language and communication.
520
The children are under 2 years. Unsettled infants crying a lot. Delayed development slow to smile. Poor weight gain. Delayed speech development . . . Repetitive behaviours e.g. rocking.
222
I work for the LD [learning disabilities] team within CAMHS and often receive referrals for ‘challenging behaviour’. Attachment is at the centre of my developing an understanding of the presenting difficulty.
413
Many respondents referred to difficulties at school:
Difficulty focusing/attention. A lower developmental age to their chronological age. Academically behind peers. Unable to understand and express how they feel. Underdeveloped executive functioning.
483
Behaviour difficulties, communication both verbal and non-verbal empathy and emotional intelligence weakness as growing older and participating with others and wider networking a limited ability to learn in a coherent way.
564
Neurodevelopmental difficulties
A number of practitioners associated attachment difficulties with having developmental difficulties such as ADHD and ASD. Respondents mentioned that, in some cases, these children receive a misdiagnosis for these conditions when in fact they may have attachment difficulties. Conversely, some also suggested that some of the questionnaires used to assess attachment included a number of questions not directly related to attachment but related to other developmental differences or psychopathology such as oppositional defiant behaviour or callous unemotional traits, and that this may blur the construct of attachment in practitioners’ minds:
I feel that children who often get diagnosed with ADHD are often children who actually have attachment problems. So, difficulties forming relationships, paying attention, low self esteem, often disruptive.
436
I think we have a lot of children who have an ASC diagnosis who may have attachment challenges. Children who are needing attention, children who suddenly erupt, a child who may smile but feeling something complete different . . . Child may find it hard to settle, talk a lot, can find it hard to concentrate . . . children who are aggressive, find it hard to recognise their behaviour, struggles with organising themselves.
544
A developmental history will often show me warning signs that attachment may have been disrupted in early childhood . . . I will often work with parents who present with a child who has challenging behaviour. The parent will suspect ASC or ADHD . . . When I discuss the developmental history I will so often hear a parent say ‘they have been like it since they were 18 months/2 years’ . . . A child will often be described as always on the go, not concentrating, not sitting still, easily dysregulated and the parents suspects ADHD – I listen to these worries and concurrently consider attachment difficulties.
527
Mental health difficulties
Child mental health
A large proportion of respondents considered attachment difficulties in the context of mental health difficulties such as depression, anxiety, eating disorders such as anorexia, self-harm and psychosis:
Especially young people suffering from emerging personality disorder, anorexia, depression, and some aspects of psychosis.
453
Poor mental health, sometimes appearing as self-harm/low mood.
584
Infants displaying attachment difficulties = avoiding parents’ gaze, frozen babies, depressed babies.
197
Behavioural difficulties in child where there is an early history of parental mental ill health, or significant absence that has impacted on child. Attachment difficulties are often significant contributors in anxiety, depression and conduct disorders.
165
Some respondents mentioned that attachment difficulties were at the root of mental health presentations. In addition, some stated that mental health difficulties contributed to a child’s (particularly an infant’s) failure to ‘thrive’, including sleeping and eating:
Children with difficult relationships with parents where attachment difficulties are at the root of their mental health presentation.
521
Mental difficulties such as depression, eating disorders and anxiety often have their roots in attachment difficulties.
462
In infants poor feeding and sleeping, persistent crying, difficulties in toilet training, failure to thrive. Difficulties in weaning. In older children and young adolescents . . . suicidality, risky acting out, self-harm. Low mood and depression.
603
Our team works with infants in foster/kinship care and their primary caregivers (including birth parents and foster/kinship caregivers). All the infants we work with have experienced maltreatment or have siblings who have experienced maltreatment. We consider that mental health issues emerging in this context are related to and mediated by the infant’s attachment experiences.
594
Difficulties which have an effect on the relationship between parent and child . . . can cause attachment difficulties for the child . . . and often resulting in SEMH [social, emotional and mental health] difficulties.
547
Many respondents reported that they considered attachment difficulties when they observed separation anxiety:
Difficulties with relationships with parents/carers/other adults. Trouble separating from known adults . . . High levels of anxiety and distress around separation or transitions and boundaries.
181
Children refusing to go to school. Anxiety in children. Anxiety in parents so they need their children close.
358
Prolonged distress when away from a caregiver – e.g. difficulty attending school, avoidance of peer/social events in which a parent won’t attend, avoidance of extra-curricular activities – negative thinking patterns/expressions when discussing being away from a caregiver.
350
Some respondents mentioned adverse childhood experiences (ACEs) as a cause of mental health problems:
There have been Adverse Childhood Experiences (ACEs). There may or may not be associated mental health difficulties in addition to the behaviours.
162
Relational difficulties
Inability to form and maintain relationships
Many respondents reported that they considered attachment issues when children struggled to form and maintain relationships with family members, adults and peers:
Maladjusted behaviours relational challenges – with authority and peers.
452
Children who use behaviour to meet an internal need, whether that sparks a negative or positive response from care giver. Children who are hypervigilant, struggle to maintain friendships, who lash out.
568
Regular arguments, disagreements and dysfunction between parent and child, a child who needs to be around the parent and is unable to function in school.
571
Intense relationships with peers. Inability to maintain friendships.
625
Challenges building and maintaining relationships with teachers and significant adults.
023
Struggles to accept guidance from teaching staff, difficulties with peer relationships.
025
I consider attachment in terms of a child’s ability to build and sustain healthy (secure) relationships. Attachment difficulties therefore are any problems children encounter in relationships with parents, carers, siblings, teachers, friends, etc. This might manifest in the child acting in or out, bullying or being bullied, suffering from loneliness . . . social isolation, causing disruption at home or at school, becoming dependent on social media, etc.
046
Difficulty forming/maintaining relationships or trusting, seeming to arise from non-secure attachment patterns . . . challenging/non-functioning parent–child relationships seeming to be based in early attachment patterns.
050
Parents and child, birth, foster and adopted children where lack of connection impinges on secure bond.
490
In our service the connection between the parent and the child is often disrupted. Some of the children find it difficult to express their emotions in regards to what they are or have experienced in the past . . . In very young babies they are finding it difficult to settle after feeding, and do not want to be held close, non-responsive to birth mother/father. Children 2–6 age range do not seem to notice when their parent leaves the room, some have exhibited self-soothing techniques. This is also apparent when the child has fallen over they do not exhibit any emotions. Within the teen years some have demonstrated defiance and anger towards their parent in an attempt to hold in their anger. Avoidance of attending school thus affecting their education ability.
215
Fractured or at risk of relationship fractures in the relationship between the parent and the infant.
612
Rejection/sabotage/control
Some respondents said that attachment problems may be indicated when an element of rejection is observed, for example when children present rejecting behaviours and sabotage healthy relationships with those with whom they interact out of fear of rejection, which may lead to controlling behaviour:
Difficulties making and maintaining healthy relationships. Unhealthy proximity seeking or rejecting behaviours that impact on accessing and managing day to day life and learning.
122
Difficulties making and maintaining relationships, difficulties understanding and labelling emotions, frequent attempts at sabotaging potentially healthy relationships to avoid rejection, difficulties understanding social situations, difficulties with engagement and participation . . . controlling play in others, repetition in play, repetitive questioning.
506
Forming and maintaining relationships including friendships. Fear of rejection.
478
Children with social emotional and behavioural difficulties who display aggressive or anxious behaviours with adults and peers. Children who demonstrate resistance to relationship with others, demonstrate distancing and rejecting behaviours to others . . . inability to acknowledge or express feelings, fearfulness of anger, anticipation of rejection, unable to respond appropriately to social situations.
439
Complex difficulties with managing and sustaining relationships. Patterns of rejection and loss which push away close relationships. An extreme need to take control of situations and relationships.
103
Numerous respondents noted that children with attachment problems may not accept nurturance from caregivers:
Difficulty accepting nurture and care, overly independent, difficulties in peer relationships, struggling to separate, struggling to regulate.
282
Aggressive behaviours towards parents, siblings, peers. Difficulty accepting parents nurture. Controlling behaviour of parents. Parents struggling to feel confident in their parenting . . . School difficulties with behaviour and learning and relationships.
053
Inability to accept nurture from caregiver. Controlling, coercive and manipulative behaviour . . . Avoidant or coercive/reactive attachment patterns.
509
Difficulty with boundaries
Many respondents reported relational difficulties that are often seen in school, where a child may also experience difficulties with boundaries:
Many behavioural presentations in children where they don’t respond in the ‘normal’ manner. So reject or sabotage supporting relationships. Begin to respond to a strategy but then reject it. Not motivated at all by typical school ‘reward’ structures.
619
Attachment difficulties effect the child’s sense of self, ability to focus and achieve educational goals, the ability to understand social interactions and maintain friendships with peers. It may also contribute to the child’s ability to emotionally regulate by themselves, and the reliance on parents or caregivers. Parent-child relationship may be strained, there may be behaviour from the child perceived as chaotic and explosive at times, or as overly compliant at others.
220
Difficulties with family relations, Challenging behaviours at school and home . . . School and family not understanding where the child is coming from and how to manage distress.
247
Problems with family relationships – usually identified by parent/professionals. Unhelpful patterns of interaction between parent/s and child. Hypervigilance – often whole family Child finding it hard to learn/respond to correction or teaching.
256
Contradictory behaviour
Many respondents thought that extremely contradictory behaviours or emotions or hyper-reactivity were indicative of attachment difficulties, with some overlap (either explicit or implicit) with features of attachment disorders (e.g. reactive attachment disorder):
Poor peer relationships, trying to please, extreme feelings of love and hate.
590
When the child has special needs e.g. disruptive behaviour in class, extreme quietness.
465
Children frequently present as hyper vigilant with sensory hyper-sensitivities, they present with hyper or hypoarousal levels and suggest high levels of dissociation . . . Children present with pseudo maturity in some responses and immaturity in others.
302
Attachment disorder either overly anxious or non-responsive to carers presence.
081
When interacting with a parent displaying clusters of behaviours, particularly if observed on a few occasions, and considered not due to physical health problems, or not merely temperamental features, for example: Inhibited affect, looking away/avoiding eye contact, Withdrawn, Reduced vocalisation. Not easily soothed when upset and older child – disinhibited, overly clingy to the parent, or clingy to strangers, or not interacting etc.
532
The child’s predictions about parent/caregiver behaviour (in relation to the desire for comfort, and the need to feel safe) are of nil or minimal response, or unpredictable response, or frightening response. Behaviourally this may present as not-seeking proximity or having a tendency to organise only from the child’s own resources, or an intense set of displays which are viewed as being geared towards engaging the caregiver, or confusion and bewilderment in relation to caregiver actions and intentions. Emotionally, the child’s responses can vary from minimal to intense and/or discordant.
228
Unexplained emotions and behaviours. Confusing and unpredictable relationship building. Not knowing how to respond to comfort . . . Not knowing how to interact with self and others. Inability to play.
526
Early relationship difficulties between care-giver and infant/child . . . Behavioural concerns resulting from inconsistent patterns of relating.
460
Many respondents described attachment difficulties as relational difficulties due to a ‘push/pull’ relational behaviour seen in children:
Complex relational needs or push/pull attitudes.
567
Difficulties in relationships to carers . . . reactive attachment disorder, push-pull with carer, clingy unable to safely explore.
466
Need to be in control, rejecting of nurture, push-pull dynamics with carers, difficulty allowing adults to look after and care for them.
523
Difficulty building trusting relationships, push-pull relationships. Lack of preference for a caregiver/appears to be no attachment relationship. Need for control over environment and others behaviour. Difficulty turn taking and sharing. Dissociation and fight/flight behaviours.
558
Difficulties with relationships with carers, difficulties forming friendships with peers, significant emotion regulation difficulties, apparently ‘angry’ outbursts, hypervigilance to changes in their environment and in caring strategies, stuck in a bind both yearning for relationships yet finding them too intense and pushing them away somehow.
276
Some respondents also considered overly self-reliant and independent behaviour to be indicative of attachment difficulties:
Children who are . . . over self-reliant and overly distrustful of others, children whose behaviour is unpredictable and inconsistent with key figures in their lives.
400
Overfamiliarity with/indiscriminate attachments to strangers
Furthermore, some respondents said that they considered attachment difficulties, along the lines of disinhibited social engagement disorder or disinhibited attachment, when a child was overfamiliar with and formed indiscriminate attachments to strangers:
Children who present as overfamiliar and not recognising boundaries with strangers.
073
Going to unfamiliar people, excessive friendliness. Not looking for a familiar adult when in new environments.
267
Child seeking out care and soothing from a wide range of adults, not always their parents/caregivers.
086
Child: indiscriminately seeking contact with random adults, lacking awareness of strangers, muting expressions of need to the point of appearing independent of career or maximising expression of need to the extent that preoccupation with maintaining proximity impacts on play, learning, peers’ relationships.
129
Insecure attachments and associate behaviours, children can have no boundaries or fear of strangers and go to anyone, not able to seek support when they have a problem etc.
220
Low self-esteem
A number of respondents mentioned children’s low self-esteem:
Difficulty experiencing relational joy. Low self-esteem. Feeling of little worth or value in the world.
528
Difficulties forming positive relationships with peers. Problems with self-esteem and feeling different or not special. Difficulties relating to others and developing empathy.
510
Issues concerning relationships (with self, others and the social world); preferred coping styles . . . and in respect of risk (to self, others and from others).
623
The child blaming themselves for their behavior – as the child becomes a young person the shift to autonomy where they manage their own behavior and relationships can be difficult – Specifically in a school setting some children struggle to have a positive enough relational frame to allow them to seek competence in something challenging – The child feeling caught between the behavior they ‘know’ they should do and the behavior their body knows how to do – Children (particularly LAC [looked-after children]) who are still involved in systems that don’t offer the relationships they need to change. So if you are in a system that you can accurately describe as not loving you, why should you attach.
379
Chapter 5 Systematic review results
Results (review 1)
Review 1 is an update of a previous systematic review to include all randomised controlled trial (RCT) evidence for parenting interventions that aim to either reduce disorganised or promote secure attachment in children at risk of attachment problems.
PRISMA diagram (review 1)
A total of 2516 records were identified through searches; 2216 were excluded at the initial sift based on title and abstract screening. Thirty-one could not be accessed initially, but 19 of these were found in library searches and so 12 were excluded because they could not be accessed and one additional record was identified through reference checks. A total of 289 records were pulled through to full-paper screening, at which stage the majority were excluded because of a lack of use of a validated measure that would allow an attachment classification to be measured. Seven papers were data extracted and assessed for risk of bias. All of these papers included secure attachment outcomes, and six of these included disorganised attachment outcomes. Figure 4 shows the PRISMA flow diagram. A list of the excluded studies is in Appendix 5.
FIGURE 4.
The PRISMA diagram showing the numbers of included and excluded papers at each stage of the systematic review for review 1.

Study characteristics (review 1)
Different interventions were identified, including The Healthy Families Durham programme, Circle of Security – Parenting/Intensive, baby massage classes, Minding the Baby, Baby Wearing and Mothering from the Inside Out. All interventions had a similar focus to reduce the rates of disorganised attachment and increase the rates of secure attachment. Two studies look at the COS intervention but with different adaptations. Circle of Security – Parenting focuses on sensitive responding to child distress as opposed to times of no distress, and consists of 10 sessions. Circle of Security – Intensive is a 20-session intervention that allows for an individualised procedure. Mothering from the Inside Out is a metallisation-based therapy, delivered weekly over 12 weeks, that focuses heavily on parental reflective functioning, enabling the mother to cope better with her child’s emotional distress. Similarly, Minding the Baby is an intensive weekly home visiting service consisting of developmental guidance, supporting attachment, signposting and support with basic supplies, and once again focusing on parental reflective functioning. Baby-wearing is a high physical contact intervention in which mothers are encouraged and instructed to use a baby-wearing carrier for 1 hour per day, focusing on using skin-to-skin contact to improve attachment. Baby massage involves six 1-hour sessions that allow the parent to learn about their infant and their cues and signals. Healthy Families Durham is a home visiting programme consisting of weekly visits for 12 months aimed at encouraging and supporting parent and child interaction.
All interventions were delivered to families who were at higher risk of developing attachment problems for many different reasons. This included mothers who had a history of substance abuse or mental ill health. Two samples included young mothers, with one of these samples including adolescent mothers and the one including young mothers from poor, underserved communities. Another sample looked at all mothers in low socioeconomic status communities. Last, one sample were at risk if parents met one of six risk factors; younger than 16 years old, history of childhood maltreatment, mental health symptoms, concerns about addictive behaviours, history of or current concerns about domestic violence or low support. Sample sizes ranged from 33 to 136 participants, with a variety of ethnicities in each sample. Two samples were majority Caucasian, one sample was majority Hispanic/Latino and one study reported both Hispanic/Latino and Caucasian as being the majority ethnicity. Another two studies reported the majority ethnicity to be African American. One study did not specify ethnicity. Five samples were based in the USA, one sample in the UK and the other in Germany. All interventions were delivered to mothers and infants; no studies included a male caregiver.
Four studies used the SSP to measure attachment, while two studies used a modified version of SSP for preschool children. One study used the Global Rating Scales used to classify attachment type from the Still Face Paradigm. These outcome measures all include observation of child behaviour, which was then coded to provide an attachment classification. As discussed in Chapter 2, Meta-analyses methods, we used the frequencies of children being classified as showing either secure attachment or disorganised attachment for the meta-analyses. See Appendix 2, Table 22, for further study characteristics of the seven studies included in this update. 56,57,79–83
Meta-analysis findings (review 1)
We conducted a random-effects model meta-analysis by combining the studies from this review with those from the original HTA report and the subsequent updates. The analyses separately address intervention effects on disorganised attachment outcomes,47 and those reporting secure attachment outcomes (currently unpublished).
Harbord regression-based tests were used to investigate whether or not the small-study effect (or funnel-plot asymmetry) was present. Statistical heterogeneity was assessed using Cochran’s Q through the chi-squared test and was quantified using the I2-test. Statistical analysis was performed using Review Manager 5.3. The results were considered statistically significant when the two-sided p-value was < 0.05 (see Chapter 2, Data extraction, and Meta-analyses methods, for detail).
Reducing disorganised attachment
Figure 5 shows the meta-analysis of the 20 included studies over the three reviews. Eight papers were from the original 2015 HTA report, six were from the 2017 update and six were from the current update. The overall meta-analysis results show statistically significant intervention effects (p < 0.001). The pooled odds ratio (OR) is 0.54 [95% confidence interval (CI) 0.39 to 0.77]. Hence, there is evidence that attachment-focused parenting interventions decrease disorganised attachment.
FIGURE 5.
Results of the disorganised meta-analysis, including ORs.
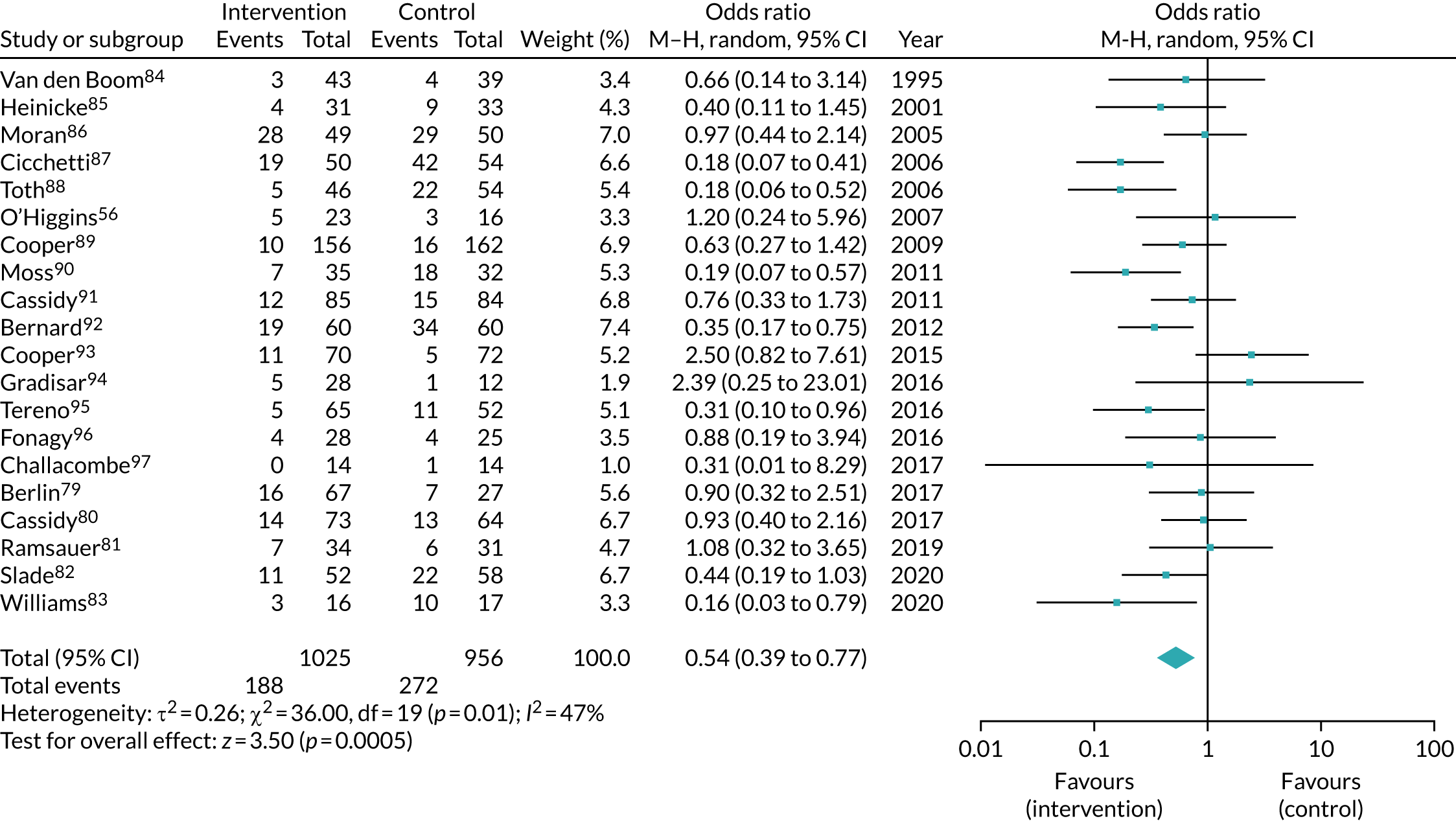
Publication bias was assessed by examining the asymmetry of the funnel plot (Figure 6). There was no indication of publication bias (Harbord test statistic = 0.51; p = 0.609).
FIGURE 6.
Funnel plot of the studies included in the disorganised meta-analysis.
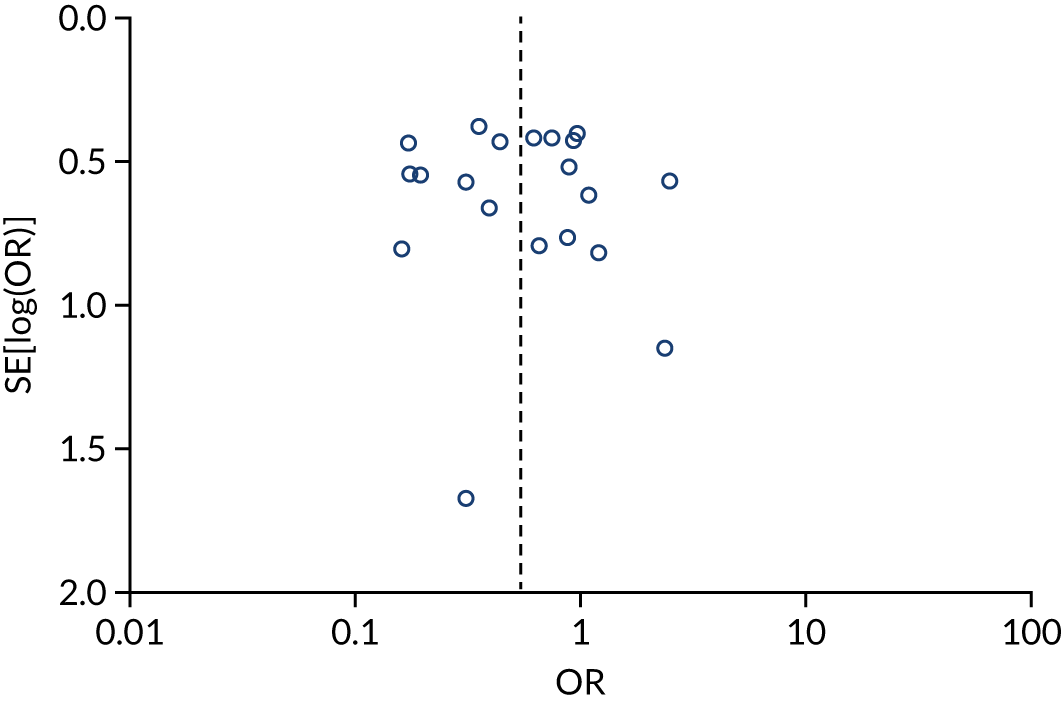
Increasing secure attachment
Figure 7 shows the meta-analysis of the 26 included studies over the three reviews. This comprises 13 studies from the original review, six studies from the first update (conducted in 2017) and seven studies from the current update. The overall meta-analysis results show statistically significant intervention effects (p < 0.001), and the pooled OR is 1.85 (95% CI 1.36 to 2.52). Hence, there is evidence that parenting intervention increases secure attachment.
FIGURE 7.
Results of the secure meta-analysis, including ORs.

Publication bias was assessed by examining the asymmetry of the funnel plot (Figure 8). There was no indication of publication bias (Harbord test statistic = 0.02; p = 0.9864).
FIGURE 8.
Funnel plot of the studies included in the secure meta-analysis.
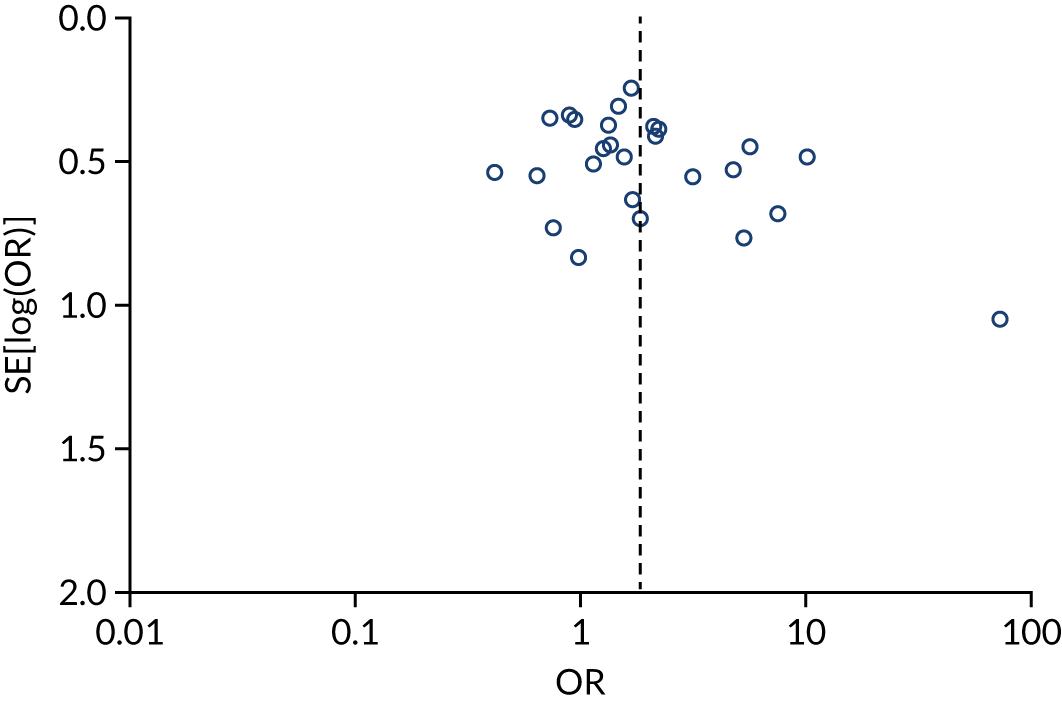
Exploratory analyses
The included studies for both disorganised and secure analyses were stratified into groups based on the characteristics of the studies: number of sessions, video feedback, age of child and whether or not a male caregiver was included. The results of these are to be interpreted with caution as no study compared each of these directly.
Reducing disorganised attachment
Figure 9 demonstrates the subgroup meta-analysis by the number of sessions. There was no significant difference (p = 0.14). The biggest effect was seen in the 16+ group (0.38, 95% CI 0.24 to 0.62; p < 0.001).
FIGURE 9.
Disorganised subgroup analysis for number of sessions.
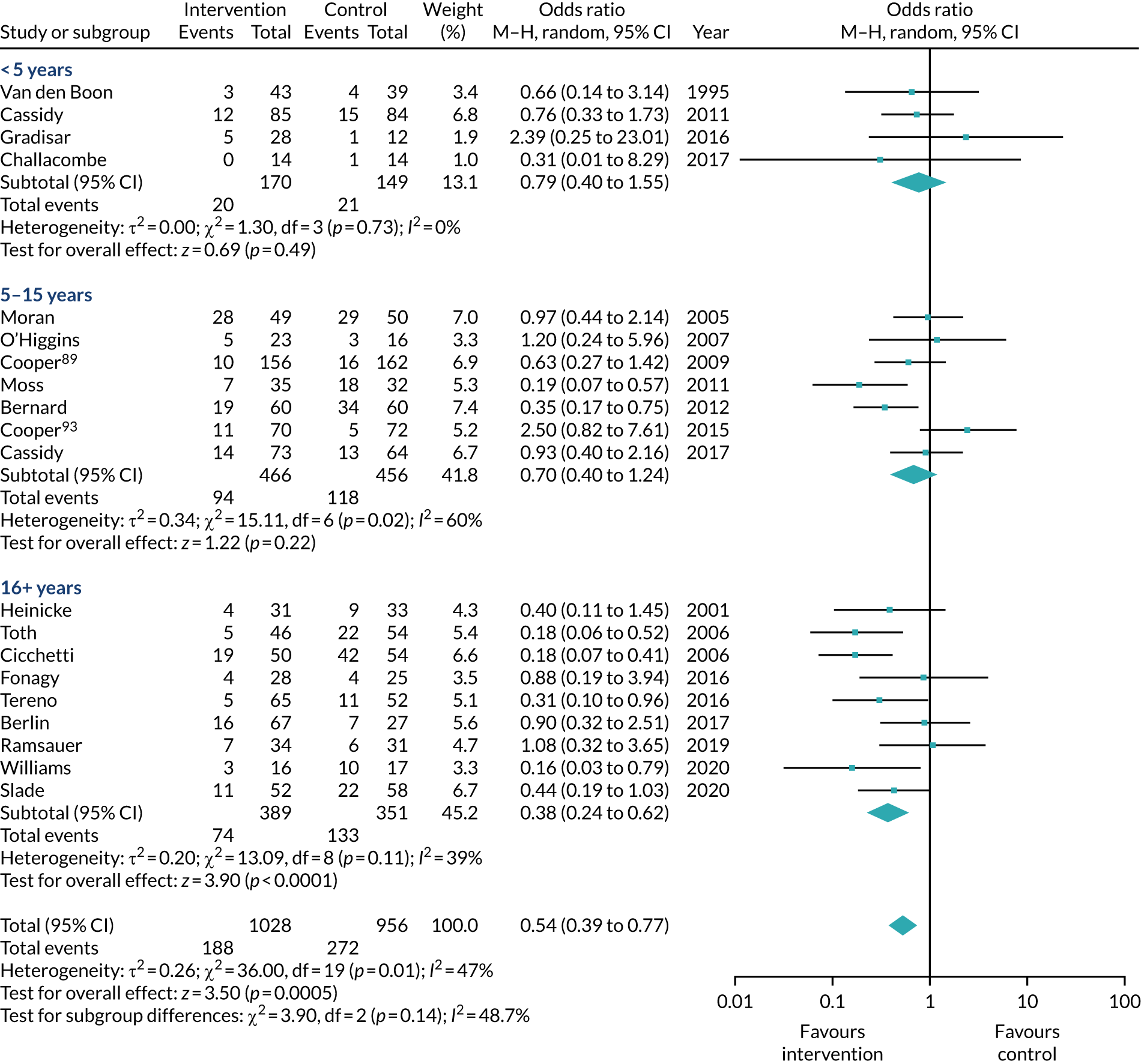
Figure 10 shows the analysis by whether or not video feedback was used, and there was no significant difference (p = 0.51).
FIGURE 10.
Disorganised subgroup analysis for use of video feedback.

Figure 11 shows the analysis by age of child and there was no significant difference (p = 0.14). The biggest effect was seen in the group where the children were > 6 months (0.39, 95% CI 0.22 to 0.69; p = 0.001).
FIGURE 11.
Disorganised subgroup analysis for age of child.

Figure 12 shows the analysis by whether or not a male caregiver was included, and there was no significant difference (p = 0.63).
FIGURE 12.
Disorganised subgroup analysis for inclusion of male caregiver.

Increasing secure attachment
Figure 13 demonstrates the subgroup meta-analysis by the number of sessions. There was no significant difference (p = 0.07); however, the highest OR was observed in the < 5 sessions group (2.05, 95% CI 1.12 to 3.75; p = 0.02).
FIGURE 13.
Secure subgroup analysis for number of sessions.
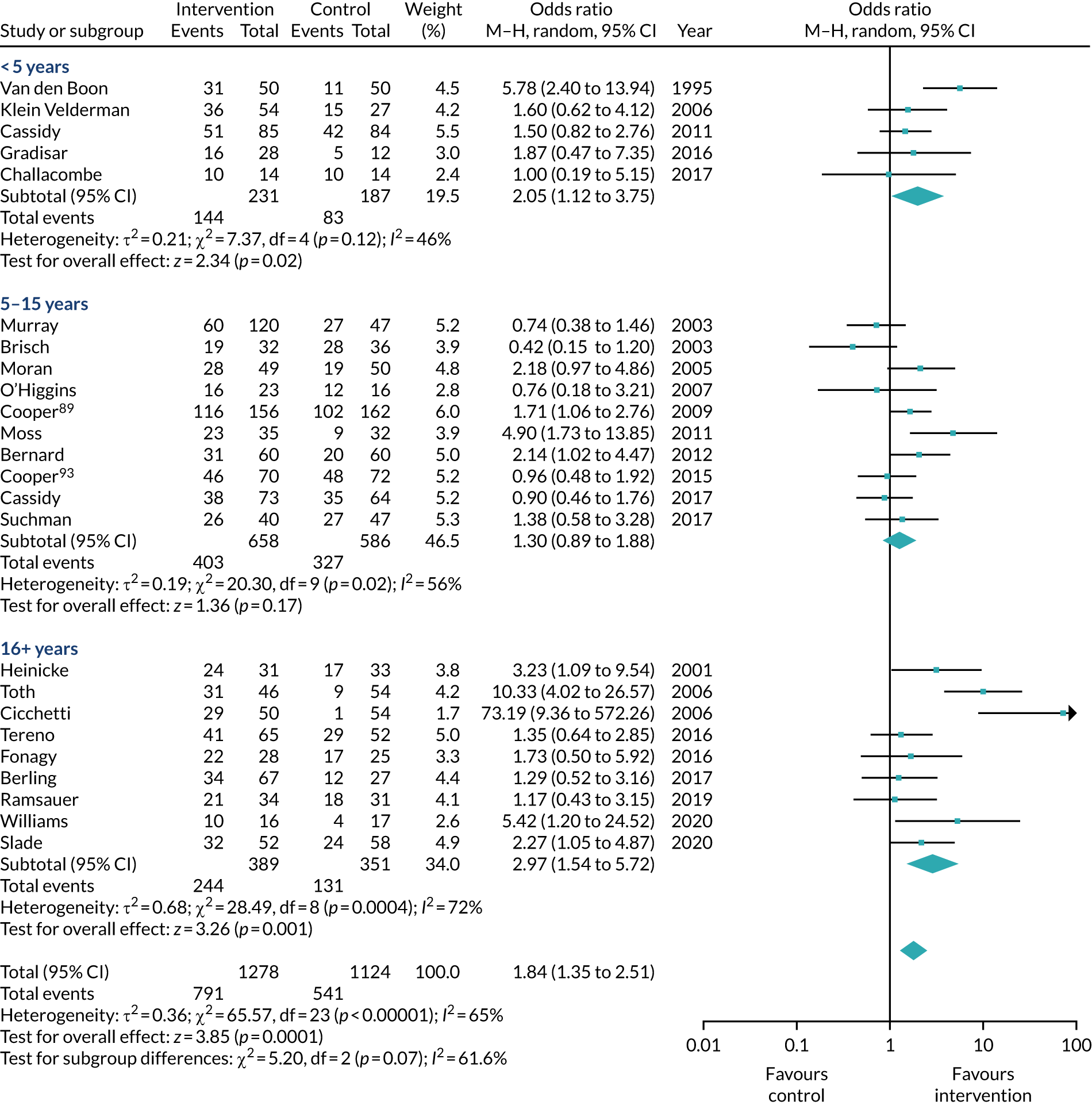
Figure 14 shows the analysis by whether or not video feedback was used, and there was no significant difference between studies that did and studies that did not (p = 0.55).
FIGURE 14.
Secure subgroup analysis for use of video feedback.
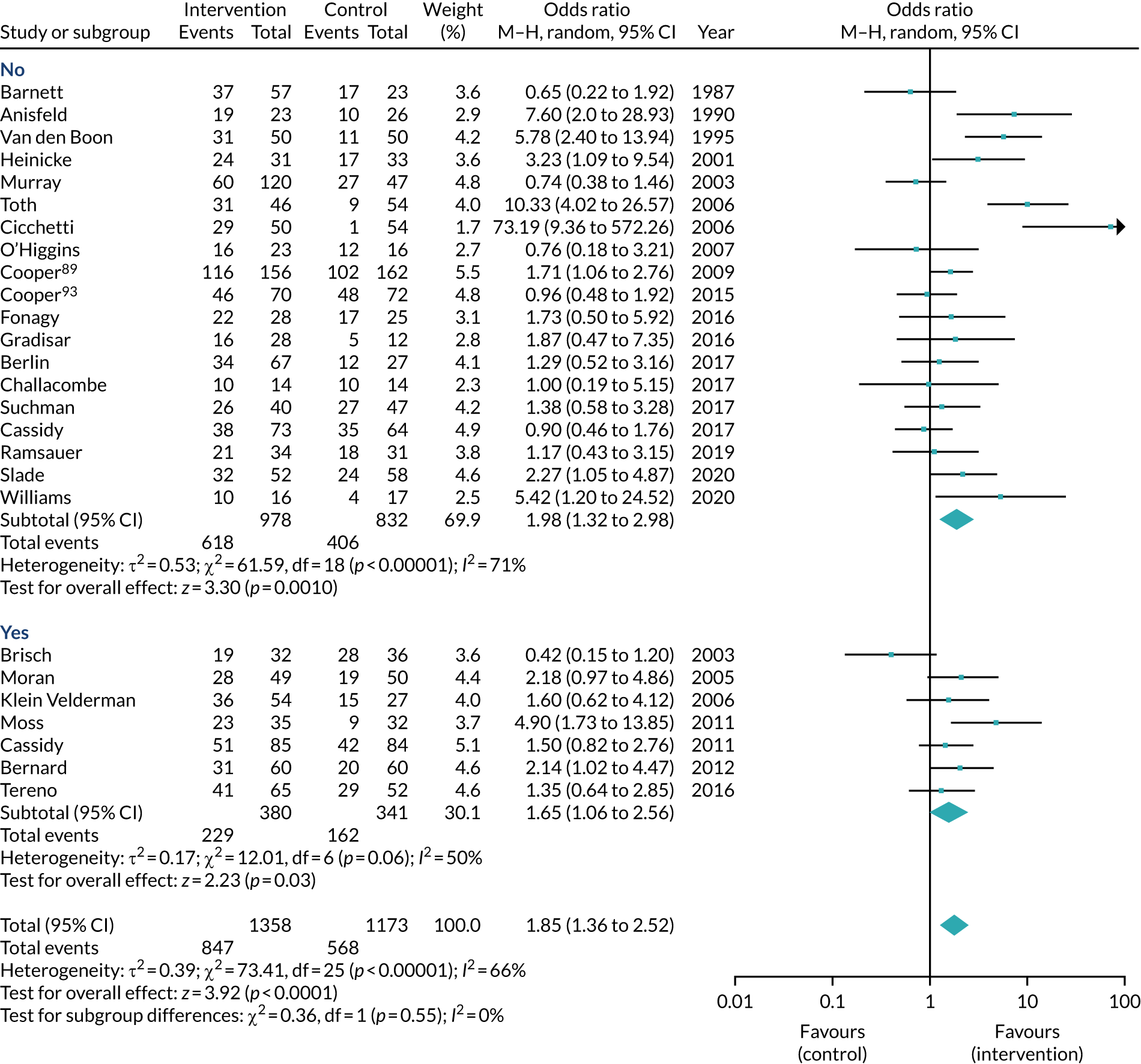
Figure 15 shows the analysis by age of child and there was no significant difference (p = 0.43).
FIGURE 15.
Secure subgroup analysis for age of child.

Figure 16 shows the analysis by whether or not a male caregiver was included, and there was no significant difference (p = 0.30).
FIGURE 16.
Secure subgroup analysis for inclusion of male caregiver.

Risk-of-bias assessment (review 1)
Table 16 shows the results of the risk-of-bias assessment of the seven studies included in this update, which was carried out using the ROB-2. 59 Most studies were rated as being at low risk of bias, with one showing some concerns due to the lack of information provided about the randomisation procedures or analyses accounting for dropouts. Studies could be classified as being at low risk of bias despite having attrition when the authors account for this in the analyses, as specified in the ROB-2 guidance. We include the risk-of-bias assessment outcomes for the included studies from the previous systematic review13 and update47 in Appendix 3, Table 24.
| Authors, year | Randomisation process | Deviations from the intended interventions | Missing outcome data | Measurement of outcome | Selective reporting of results | Overall risk-of-bias judgement |
|---|---|---|---|---|---|---|
| Berlin et al., 201779 | Low risk | Low risk | Low risk | Low risk | Low risk | Low |
| Cassidy et al., 201780 | Low risk | Low risk | Low risk | Low risk | Low risk | Low |
| O’Higgins, 200756 | Some concerns | Some concerns | Low risk | Low risk | Low risk | Some concerns |
| Ramsauer et al., 201981 | Low risk | Low risk | Low risk | Low risk | Low risk | Low |
| Slade et al., 202082 | Low risk | Low risk | Low risk | Low risk | Low risk | Low |
| Williams and Turner, 202083 | Low risk | Low risk | Low risk | Low risk | Low risk | Low |
| Suchman et al., 201757 | Low risk | Low risk | Low risk | Low risk | Low risk | Low |
Results (review 2)
Review 2 focused on the available evidence for the 10 named interventions identified in the survey as ‘most commonly used’. We included all available study designs, including, but not limited to, RCTs, non-randomised comparisons, pre and post designs and case series. Parental sensitivity was included as an outcome in addition to attachment.
PRISMA diagram
A total of 1198 papers were screened in this initial search. We excluded 442 at the first sift based on title and abstract; 756 were pulled through to the full-paper screen in sift 2. The PRISMA diagram in Figure 17 shows the reasons for exclusion at this stage. Although the number of records we were unable to access was fairly large, this was because large numbers of book chapters were identified in the searches. Owing to the extensive grey literature searching the reviewers carried out, we can be confident that all relevant records were identified. We had 182 records for a further full-paper screen in sift 3. Again, reasons for exclusion are provided in the PRISMA diagram. After this third sift, there were 48 records that we were unable to access despite the help of library services, and 29 papers were excluded as they reported the same results from a sample that was already included. We included 61 papers87,88,91,92,96,102–155 across all of the named interventions to data extraction and assessment of risk of bias. Figure 17 shows the PRISMA flow diagram, and a list of excluded studies is in Appendix 4.
FIGURE 17.
The PRISMA diagram showing the numbers of included and excluded papers throughout each stage of the systematic review for review 2.

Study characteristics
Table 17 shows the evidence available for each of the 10 named interventions in terms of number of included papers, their study design and how many papers reported either child attachment and attachment disorder outcomes, parental sensitivity outcomes or both of these outcomes. Interventions were included if they followed the manualised intervention or were a close adaptation of one of the named interventions (e.g. COS-I, VIPP-FC, VIPP-SD).
| Named intervention | Number of studies | Study designs | Outcomes, n | ||
|---|---|---|---|---|---|
| Child attachment | Parental sensitivity | Both child attachment and parental sensitivity | |||
| VIPP | 17 | RCT, n = 15; NRSI, n =2; case study, n = 0 | 5 | 17 | 5 |
| ABC | 14 | RCT, n = 11; NRSI, n = 2; case study, n = 1 | 4 | 10 | 0 |
| COS | 10 | RCT, n = 4; NRSI, n = 3; case study, n = 3 | 10 | 1 | 1 |
| PIP | 8 | RCT, n = 6; NRSI, n = 2; case study, n = 0 | 6 | 4 | 2 |
| VIG | 6 | RCT, n = 2; NRSI, n = 2; case study, n = 2 | 0 | 6 | 0 |
| CPP | 3 | RCT, n = 3; NRSI, n = 0; case study, n = 0 | 3 | 0 | 0 |
| DDP | 2 | RCT, n = 0; NRSI, n = 2; case study, n = 0 | 2 | 0 | 0 |
| WWW | 2 | RCT, n = 0; NRSI, n = 2; case study, n = 0 | 2 | 0 | 0 |
| Theraplay | 1 | RCT, n = 0; NRSI, n = 1; case study, n = 0 | 0 | 1 | 0 |
| ICP | 0 | RCT, n = 0; NRSI, n = 0; case study, n = 0 | 0 | 0 | 0 |
Thirty of the included papers reported child attachment outcomes (most commonly the SSP, but also through coded observations, AQS and Kern’s Security Scale) and 39 used parental sensitivity measures. This was mainly measured through coded observations, using the Emotional Availability Scales, CARE-index, Maternal Behaviour Q-sort, Ainsworth’s Sensitivity Scales and Observational Ratings of the Caregiving Environment scales). We use the term parental sensitivity throughout this report, although it should be noted that many of the papers referred to this as maternal sensitivity, with main outcomes for sensitivity usually being taken from the mother only. Across all included studies, only eight included both child attachment outcomes and parental sensitivity outcomes. Table 18 shows the age range that each of the included studies targeted, for each of the 10 named interventions. One study reported child’s age at follow-up, which was 9 years, but children received the intervention at approximately 10 months old. 124 Two studies that looked at the effectiveness of VIG did not report the age of the child. 88,150 Most studies reported the mean age of the child or the age at which the child started the intervention.
| Intervention | Age range (years) | ||||
|---|---|---|---|---|---|
| 0–3 | 4–6 | 7–9 | 10–11 | 12–13 | |
| VIPP | 17 | 0 | 0 | 0 | 0 |
| ABC | 13 | 1 | 0 | 0 | 0 |
| COS | 6 | 4 | 0 | 0 | 0 |
| PIP | 8 | 0 | 0 | 0 | 0 |
| VIG | 4 | 0 | 0 | 0 | 0 |
| CPP | 3 | 0 | 0 | 0 | 0 |
| DDP | 0 | 0 | 2 | 0 | 0 |
| WWW | 2 | 0 | 0 | 0 | 0 |
| Theraplay | 1 | 0 | 0 | 0 | 0 |
| ICP | 0 | 0 | 0 | 0 | 0 |
The aim of review 2 was to enable a comprehensive overview of the current literature for each of the named interventions; therefore, when setting the criteria the priority was to be broad and inclusive to avoid excluding relevant studies. The aim was to identify the available evidence for each of the interventions, and not to compare them in terms of efficacy. Owing to the varying numbers of papers for each of the 10 named interventions, and the diverse outcome measures used, it was not felt to be appropriate to conduct meta-analyses as not all studies or interventions would have been able to be included.
See Appendix 2, Table 23, for the characteristics of each of the studies included in review 2.
Risk-of-bias assessment
Tables 19 and 20 show the risk-of-bias assessment results for each of the studies, split by named interventions and study design. ROB-2 was used for the RCTs, and ROBINS-I was used for non-randomised comparison group designs. Some studies used case series designs and therefore did not allow for a meaningful risk-of-bias assessment to be conducted for comparison with studies that had other designs.
| Intervention | Authors and year | Randomisation process | Deviations from the intended interventions | Missing outcome data | Measurement of outcome | Selective reporting of results | Overall risk-of-bias judgement |
|---|---|---|---|---|---|---|---|
| VIPP | Alsancak-Akbulut et al., 2021103 | Low | Low | Low | Low | Low | Low |
| Barone and Lionetti, 2019104 | Low | Low | Low | Low | Low | Low | |
| Casonato et al., 2017105 | Low | Some concerns | Low | Low | Some concerns | Some concerns | |
| Kalinauskiene et al., 2009108 | Some concerns | Some concerns | Low | Low | Some concerns | Some concerns | |
| Klein et al., 2006102 | Some concerns | Some concerns | Low | Low | Some concerns | Some concerns | |
| Klein Velderman et al., 2006109 | Low | Low | Low | Low | Low | Low | |
| Negrão et al., 2014110 | Low | Low | Low | Low | Low | Low | |
| Platje et al., 2018111 | Low | Low | Low | Low | Low | Low | |
| Poslawsky et al., 2015112 | Low | Low | Low | Low | Low | Low | |
| Shoemaker et al., 2020113 | Low | Low | Low | Some concerns | Low | Some concerns | |
| Van Zeijl et al., 2006114 | Low | Low | Low | Some concerns | Low | Some concerns | |
| Whitehouse et al., 2019115 | Low | Low | Low | Low | Low | Low | |
| Yagmur et al., 2014116 | Low | Some Concerns | Low | Low | Low | Some concerns | |
| Green et al., 2015117 | Low | Low | Low | Low | Low | Low | |
| Paula Oliveira et al. (University College London; 08.12.2020) | Low | Low | Low | Low | Low | Low | |
| ABC | Berlin et al., 2014118 | Low | Low | Low | Low | Low | Low |
| Berlin et al., 2018119 | Low | Low | Low | Low | Low | Low | |
| Yarger et al., 2016120 | Low | Low | Low | Low | Low | Low | |
| Yarger et al., 2020121 | Low | Low | Low | Low | Low | Low | |
| Lind et al., 2020122 | Low | Low | Low | Low | Low | Low | |
| Bernard et al., 201292 | Low | Low | Low | Low | Low | Low | |
| Bernard et al., 2015123 | Low | Some concerns | Low | Some concerns | Low | Some concerns | |
| Zajac et al., 2020124 | Low | Low | Low | Some concerns | Some concerns | Some concerns | |
| Dozier et al., 2009125 | Low | Some Concerns | Low | High | Low | High | |
| Raby et al., 2019126 | Low | Low | Low | Low | Low | Low | |
| Perrone et al., 2020129 | Low | Low | Low | Low | Low | Low | |
| COS | Cassidy et al., 201780 | Low | Low | Low | Low | Low | Low |
| Hanlon-Dearman et al., 2017133 | Some concerns | Some concerns | Low | Low | Low | Some concerns | |
| Ramsauer et al., 202081 | Low | Low | Low | Low | Low | Low | |
| Cassidy et al., 201191 | Low | Low | Low | Low | Low | Low | |
| PIP | Fonagy et al., 201696 | Low | Low | Low | Low | Low | Low |
| Cicchetti et al., 200687 | Low | Low | Low | Low | Low | Low | |
| Lieberman et al., 1991138 | Some concerns | Some concerns | Low | Some concerns | Some concerns | Some concerns | |
| Robert-Tissot et al., 1996139 | Some concerns | Some concerns | Low | Low | Some concerns | Some concerns | |
| Salomonsson and Sandell, 2011140 | Low | Low | Low | Low | Low | Low | |
| Salomonsson et al., 2015141,142 | Low | Low | Low | Low | Low | Low | |
| VIG | Barlow et al., 2016145 | Low | Low | Low | Low | Low | Low |
| Hoffenkamp et al., 2015146 | Low | Low | Low | Low | Low | Low | |
| CPP | Cicchetti et al., 1999151 | Some concerns | Some concerns | Low | Some concerns | Low | Some concerns |
| Toth et al., 200688 | Low | Low | Low | Low | Low | Low | |
| Stronach et al., 2013152 | Low | Low | Low | Low | Low | Low |
| Intervention | Authors, year | Bias due to confounding | Bias in selection of participants into the study | Bias in classification of interventions | Bias due to deviation from intended interventions | Bias due to missing data | Bias in measurement of outcomes | Bias in selection of reported result | Overall risk of bias |
|---|---|---|---|---|---|---|---|---|---|
| VIPP | Cassibba et al., 2015106 | Low | Low | Low | Low | Low | Low | Low | Low |
| Iles et al., 2017107 | Moderate | Low | Low | Low | Low | Moderate | Low | Moderate | |
| ABC | Caron et al., 2016127 | Moderate | Low | Low | Low | Low | No information | Low | Moderate |
| Roben et al., 2017128 | Moderate | Low | Low | Low | Low | Moderate | Low | Moderate | |
| COS | Hoffman et al., 2006134 | Moderate | Low | Low | Low | Low | Low | Low | Moderate |
| Huber et al., 2015135 | Moderate | Low | Low | Low | Moderate | Low | Low | Moderate | |
| Page and Caine, 2010137 | Low | No Information | No information | No Information | Low | No Information | No information | No information | |
| VIG | James, Wadnerkar-Kamble and Lam-Cassettari, 2013147 | Low | Low | Low | Low | Low | Low | Low | Low |
| Kennedy et al., 2010148 | Moderate | Low | Low | Moderate | Low | Moderate | Low | Moderate | |
| WWW and PIP | Cohen et al., 1999143 | Low | Low | Low | Low | Low | Low | Low | Low |
| Cohen et al., 2002144 | Low | Low | Low | Low | Low | Low | Low | Low | |
| DDP | Becker-Weidman, 2006153 | Moderate | Moderate | Low | Moderate | Low | Moderate | Low | Moderate |
| Becker-Weidman, 2006154 | Moderate | Moderate | Low | Moderate | Low | Moderate | Low | Moderate | |
| Theraplay | Salo et al., 2020155 | Moderate | Low | Low | Low | Low | Low | Low | Moderate |
Commonly identified issues include a lack of blinded coders, a lack of information on analysis procedures (including how the authors overcome challenges around attrition and missing data) and limited information on processes used for recruiting and allocating participants to groups. Studies may still be classified as low risk of bias despite having attrition when the authors account for this in the analyses, as specified in the risk-of-bias tool guidance.
Summary of findings (review 2)
We found the largest number of studies for VIPP and ABC; however, despite this, the survey results indicated that in routine practice these were the least commonly used of the top 10 named interventions (see Appendix 2, Table 23, for further study characteristics).
VIPP
We identified 17 papers that investigated the effectiveness of VIPP. Nearly all of the 17 included adaptations of VIPP, including VIPP-SD (Sensitive Discipline); VIPP-FC (Foster Carers); VIPP-R (Discussions on the Representational Level); VIPP-V (Visual or visual-and-intellectual disabilities); VIPP-AUTI (Children with Autism); VIPP-TM (Turkish Minorities); iBASIS-VIPP (Intervention within the British Autism Study of Infant Siblings); and VIPP-CO (Community). Fifteen of these were RCTs, 14 of which measured paternal sensitivity using a range of measures including the Ainsworth Sensitivity Scale;5 Emotional Availability Scale (EAS);156 Maternal Behaviour Q-Set;157 National Institute of Child Health and Human Development Scales;158 Seven-point rating scales for Supportive presence and Intrusiveness;159 and Manchester Assessment of Caregiver–Infant interaction. 160 Of the 14 RCT studies measuring parental sensitivity, six102–104,108,114,116 showed an increase in sensitivity after the intervention compared with the control group. One study102 established that intervention group mothers were more sensitive than control group mothers, although the follow-up found no long-term effects in terms of improved maternal sensitivity. 109 A further seven105,110–113,115,117 RCTs found no evidence to suggest that VIPP improves parental sensitivity. Among the 15 RCTs, only four reported attachment outcomes, using the SSP5 and the Attachment Q-Set161 and AQS. 162 Three of these studies102,108,109 reported no intervention effects on attachment security, although one study found no long-term effects of improved attachment security. 109 The other study has not yet coded for the SSP and therefore has not drawn any conclusions (Oliveira et al. , University College London, 8 December 2020, unpublished data).
Two of the 17 papers included non-randomised studies;106,107 both of these measured parental sensitivity using the EAS156 and an adapted version of the Global Ratings Scale. 163 Both papers indicated that VIPP-R and VIPP-CO are effective in enhancing maternal sensitivity. One of these studies106 also measured attachment security using the SSP5 and, once again, showed that VIPP-R is effective in enhancing infant attachment security. However, only mothers who had an insecure attachment pattern benefited from VIPP-R. 106 One paper that used a RCT design also included a case series using the Disturbances of Attachment Interview38 and SSP5 at follow-up; however, group differences were not reported because of the small sample size (Oliveira et al. , University College London, 8 December 2020, unpublished data).
ABC
We identified 14 papers for ABC; 11 of these included RCTs with one adaptation of the intervention being ABC-T (aimed at toddlers). Eight of these 11 RCT studies measure a change in maternal sensitivity using mainly two measures: Maternal Behaviour Q-sort157 and Observational Ratings of the Caregiving Environment Sensitivity Scales164–166 and adaptations of the Observational Ratings of the Caregiving Environment scales. All eight RCTs found that parents who received the ABC intervention displayed higher sensitivity scores than those in the control group, providing a good evidence base on the effectiveness of ABC in regards to improving parental sensitivity. 92,118–122,126,129 Three RCTs measured attachment using the SSP5 Parent attachment diaries,167 which were validated against the SSP and The Kerns Security Scale. 168 These studies found that ABC was effective in reducing rates of disorganised attachment,92 reducing rates of an avoidant attachment pattern125 and increasing perceived attachment security. 124 Of the 14 identified studies, two were non-randomised studies, both of which used a pre–post design. Both studies used the Observational Ratings of the Caregiving Environment scales164 as a measure of sensitivity and found that parents showed higher levels of sensitivity post intervention than pre intervention. 127,128 One of the 14 studies130 was a case study design to measure attachment using the SSP. 5 The authors found that ABC positively changed the attachment between mother and infant.
COS
The number of studies focusing on the effectiveness of COS in improving attachment or maternal sensitivity was 10. Four of these were RCTs using different adaptations of COS, including COS-I (intensive), COS-HV4 (home visiting) and COS-P (parenting). All four RCT studies measured attachment using the SSP5 or adaptations/measures based on the strange situation such as the MacArthur Preschool Strange Situation169 and the Secure Base-Safe Haven coding procedure. 133 Three of these RCT studies found no effect of the intervention on attachment security or disorganisation. 80,81,91 One RCT found a change in attachment classification in 25% of cases; however, the sample consisted of only 12 dyads and so drawing reliable conclusions may be difficult because of the small sample size. 133 One RCT also looked at the effects of COS-I on caregiver sensitivity using the Mini-Maternal Behaviour Q-Sort (Mini-MBQS-V)170 but found no statistical differences between the intervention and control groups in terms of change in sensitivity. 81 Three non-randomised studies134,135,137 investigating the effectiveness of COS all found some improvements in attachment classifications after the intervention, with one showing significant changes from disorganised to organised attachment classifications. 134 A further three studies131,132,136 all found some evidence for COS improving attachment security, although these were case studies and so come with many limitations.
PIP
Eight studies, six RCTs and two non-randomised studies were identified for PIP. Two included Mother–Infant Psychoanalytic treatment, two included Psychodynamic Psychotherapy and another included Psychodynamic Mother–Infant Psychotherapy. Four of the six RCTs measured attachment as an outcome and five also measured parental sensitivity. The attachment studies used the SSP,5 AQS162 and the Story Stem Assessment profile171 as measures of attachment. Two of the RCTs88,151 that measured attachment showed that children receiving PIP had substantial increases in secure attachment. The other three studies96,138,141 using attachment as an outcome found that infant attachment did not differ between the intervention and control groups. The five RCTs measuring parental sensitivity used the EAS,156 the Maternal Behaviour Q-set157 and a 5-point sensitivity scale. 172 Four of these RCTs87,139,140,142 found increased improvements in maternal sensitivity in the PIP groups. A preliminary report of Robert-Tissot139 was conducted by Cramer,173 providing initial findings of a subsample of 35 cases from the 75 reported in the most up-to-date paper139 and so was not included in the final numbers because of the overlap in samples. One study96 did not find any treatment-group effects for parental sensitivity. The two non-randomised studies compared PIP with WWW. They showed that those in the PIP group were less likely to move to a secure attachment than those in WWW. 143 However, at the 6-month follow-up the authors found no difference between the groups in terms of retaining or moving towards a secure attachment. 144 The SSP5 was used to measure attachment classifications.
CPP
We identified three RCT studies investigating the effects of CPP on attachment. The measures used were the Attachment Q-Set158 and the SSP. 5 All three studies found that secure attachment increased in the intervention group, and one study also confirmed that the intervention group had lower rates of disorganised attachment than the control groups. 88,151,152
VIG
Six studies using VIG were identified, two RCT studies, two non-randomised studies and two case studies/case series, all measuring parental sensitivity using scales such as the EAS,156 CARE Index43 or coding based on Biemans’ hierarchy of attuned interactions. 174 Both RCTs examined the effects of VIG on parental sensitivity: one found that VIG proved to be effective in enhancing sensitivity,146 whereas the other found a large but non-significant difference in sensitivity across the groups. 145 Both non-randomised studies also used parental sensitivity as an outcome and both found increases in sensitivity post intervention compared with the non-treatment groups. 148,149 One case study found a slight increase in sensitive interactions. 147 The final study was a case series; all cases showed improvements in sensitivity. 150
DDP
DDP was reported as commonly used in the UK to reduce severe attachment problems, such as improving the child’s ability to signal attachment needs to adoptive or foster parents (RAD) and to accept care/nurture/help from them (RAD), improving emotional regulation (RAD), reducing indiscriminate behaviours (disinhibited social engagement disorder) and improving the directedness of attachment behaviours towards adoptive and foster carers (disinhibited social engagement disorder). However, we identified only two studies, and both were non-randomised. Using the Randolph Attachment Disorder Questionnaire,39 the authors found that those in the DDP group had significantly decreased RAD-Q scores. 153 At the follow-up 4 years later, the RAD-Q scores had decreased significantly in the treatment group. 154
WWW
We identified only two studies that evaluated WWW; both were non-randomised and were mentioned previously in the PIP section. Cohen et al. 143 found that infants in the WWW group were significantly more likely to move to a secure attachment pattern than infants in the mother–infant psychotherapy group. At the 6-month follow-up, they found no difference between the groups in terms of retaining or moving towards a secure attachment. 144 Both the original and the follow-up study used the SSP5 to measure attachment classifications.
Theraplay
Theraplay was another intervention reported in the survey as being commonly used in the UK. However, we identified only one (non-randomised) study that investigated its effects on attachment and maternal sensitivity. Using the EAS156 with both parents (mother and father) pre and post intervention, this study showed an increase in parental sensitivity post intervention. 155
ICP
We found no studies that tested the effectiveness of ICP on attachment or parental sensitivity, even though the survey identified that ICP is one of the most commonly used interventions among the top 10.
It is important to bear in mind that there may be some overlap between types of intervention in the review presented. For example, although survey responses suggested that PIP and CPP are separate, in the literature there were large amounts of overlap between the two. There were cases in which an original sample was included in a paper and described as receiving CPP, and then a later follow-up study was published following the same sample that was then described as receiving parent–infant psychotherapy. The differences between these two approaches are evidently not clear-cut. In addition, some interventions were excluded, such as perinatal dyadic psychotherapy, because, although likely to be very similar to parent–infant psychotherapy, they are described as a separate manualised intervention.
There were some early video feedback interventions that were not described as one of the manualised interventions and therefore were excluded. However, these are likely to be early testing of VIPP or VIG, which then went on to develop into either VIG or VIPP. 33,175–177
Systematic review discussion
The main findings from the systematic reviews are that attachment-focused parental interventions can significantly decrease disorganised attachment with a small effect size61 [OR 0.54, 95% CI 0.39 to 0.77, effect size (d) = −0.15; see Figure 5] and improve rates of secure attachment in children with or at risk of developing attachment difficulties or children with attachment problems [OR 1.85, 95% CI 1.36 to 2.52, effect size (d) = 0.15; see Figure 7]. This confirms previous systematic review and meta-analysis findings. 13,46,47,178–180
The strengths of this work include the fact that we were able to maintain a focus on the highest levels of research evidence (e.g. RCTs). This has meant that several recent high-quality studies have been included in the present review with a low risk of bias, suggesting improvement in methodologies over time. This work also builds on previous reviews in which relatively small numbers of studies were found. By following the same methodology and processes, we were able to combine the results from these reviews, leading to a comprehensive overview of the literature. More research has been, and is being, commissioned in this field.
This specific focus of the review criteria could also cause potential limitations. For example, our criteria excluded any studies that were not focused on parent or caregiver interventions. Interventions that involve a change in caregiver such as adoption,181,182 or studies examining the effects of institutionalisation and foster care, such as the Bucharest Early Intervention Project, are not included in this review. 183,184
We also excluded research without attachment outcome measures in review 1. We recognise that much good work is being done outside this delineation but we cannot quantify it or understand its relevance to attachment if an attachment measure, or a measure for RAD and/or disinhibited social engagement disorder, is not included.
In review 2, we included measures of parental sensitivity as a proxy measure outcome based on research to gather as much research as possible about commonly used manualised interventions. 42 This second review was also inclusive of study design, which led to large numbers of included papers with diverse study types and outcome measures. As such, we did not conduct meta-analyses for this review, which could be seen as a potential weakness. However, the inclusive criteria allowed us to meet our aim for this review, by providing a comprehensive overview of the range of studies that have been carried out for each of the routinely used named interventions. Further work focusing specifically on the effectiveness of each intervention may be a potential avenue of future research.
Although we created a comprehensive search strategy, some identified papers did not include the name of the manualised intervention in either the title or the abstract. A potential limitation is that a fairly large number of papers could not be accessed, especially for this second review. This may be due to the lack of restrictions on the date. As a result, the reviewers conducted extensive reference checking and grey literature reviews to ensure that no relevant papers were missed.
When considering the analysis from review 1, the categories in the exploratory subgroup analyses need to be interpreted with caution as they include a relatively small numbers of studies. We presented the results here to encourage debate about which parameters to examine in future research.
Previous research has shown mixed results regarding the value of video feedback in improving insecure attachment. The review by Bakermans-Kranenburg et al. 46 found that interventions were more effective for child attachment outcomes when they did not use video feedback. The review in 201513 showed that interventions were more effective than a control, whether or not they made use of video feedback. The current review shows no apparent differences in effect depending on whether or not video feedback was used. Video feedback is a commonly used intervention with a focus on parental sensitivity. It allows parents to explore ways to review their infant’s behaviours and needs, and reflect on their responses.
Our study showed robust effect sizes where therapy was conducted in the 6–12 months age group. Most of the included studies focused on interventions that were delivered in the early years (0–6 months). There is a significant gap in the research for interventions targeting attachment in children post pre-school. There is a need for research in older age groups to identify what works best for them.
We found that attrition rates were high across studies. This is a general problem in child mental health clinical provision185 and needs to be given more thought in planning of research, dissemination, cost-effectiveness and sustainability.
The overall finding that several manualised interventions have little or no RCT evidence is concerning, and this is discussed further in the main discussion section alongside the survey findings.
Chapter 6 Discussion
The study
The project was undertaken in response to a call to address the following objectives: to conduct a national survey of what structured treatments are routinely used across UK services to improve infant attachment to their caregiver(s) and reduce severe attachment problems; to carry out a systematic review to assess the evidence base that supports these treatments and other parenting interventions for children with (or at risk of) severe attachment problems aged 0–13 years; and to develop recommendations for future clinical trial research on the effectiveness of those commonly used treatments that have not been properly tested in the past.
Main findings
Our main findings in answer to these key questions are as follows.
Are attachment interventions clinically effective?
In an up-to-date systematic review, interventions for children at risk of severe attachment problems show clinical effectiveness with small to medium effect sizes at statistically significant levels when considered in meta-analyses examining interventions to promote secure attachment or interventions to reduce disorganised attachment (the highest risk group for future psychopathology). Most of these interventions are targeted at promoting sensitive, nurturing parenting among main caregivers. These findings confirm previous systematic review and meta-analysis research in this field. 13,46,47,180
What does our survey tell us about clinical practice in the UK?
Our survey of clinical practice highlighted a number of important issues that were reported in Chapter 3, which we discuss here where they are relevant to our overall conclusions. We found that there was a wide range of services for attachment across the UK from a range of providers; the broadest range of available provision was in London and the South East. The survey of practice highlighted four main areas of concern:
-
varied perspectives on and understanding of attachment and severe attachment problems among those in therapeutic practice
-
inconsistent recognition and assessments of children for severe attachment problems and parent–child relationship
-
varied assessment of outcome/evaluation of attachment-related interventions
-
variety of interventions used with limited evidence base for those most commonly used.
Variable understanding of attachment and severe attachment problems
It was clear that there were some very high-quality services integrated into care pathways with good training and supervision opportunities and providing evidence-based interventions. However, when viewed overall, there was a wide range of presentations that responding professionals would consider as falling under the heading of attachment difficulties. Based on these professionals’ responses, there appeared to be several ways in which the construct of attachment was being used as a less precise term than originally intended, with other issues often conflated. The following misunderstandings regarding attachment difficulties appeared in more than a minority of practitioners. (1) The respondents did not distinguish clearly between aspects that could be regarded as risk factors for, or influences on, attachment difficulties and actual attachment difficulties themselves. (2) Many of the indicators mentioned were describing caregivers’ (often mothers’) difficulties and past experiences rather than focusing on difficulties in the child’s attachment behaviours expressed towards current caregivers. (3) Although many of the difficulties reported with which children presented may be associated with attachment difficulties (perhaps as consequences), they were not necessarily attachment difficulties themselves. (4) The concept of trauma was used in very broad ways and often treated as being the same construct as attachment. Practitioners commonly referred to traumas occurring within past attachment relationships (i.e. what is often referred to as developmental trauma) and considered their impact on current functioning as reflecting ‘attachment difficulties’, without necessarily considering whether or not the child’s current attachment behaviour towards his or her caregivers is problematic. This conflation of cause (in the previous example) or consequence (in the latter) with the construct itself blurs the meaning of attachment in ways that we believe are unhelpful and potentially confusing. 186 These various misunderstandings or ‘overstretch’ of terms and concepts among practitioners was common. Such misunderstandings would have the potential to impact on client report writing, offers of interventions and decision-making in important areas of a child’s life. We take the view that there is a clear need for more rigorous training and sources of reliable information about attachment for practitioners so that their use of findings, assessments and interventions from this field is done in a way that is accessible and clinically useful, but also consistent with the underpinning research. Clear and accurate understanding of attachment theory should be incorporated into the curricula of the professional training of child and adolescent mental health professionals, social workers, midwives and health visitors.
Inconsistent recognition and assessments of children for severe attachment problems and parent–child relationship
As reported in the results section of Chapter 3, a number of instruments and procedures were used in assessments by practitioners for addressing attachment problems. There are challenges in the assessment of attachment and attachment problems. Two measures are considered the ‘gold-standard’ of attachment in infants and toddlers: the SSP and the AQS. 187 The AQS is considered a valid measure alongside the SSP. 188 Although the SSP was designed for infants aged 11–20 months, there are also modifications that can be used for preschool children, although these are less well developed. The AQS can be utilised across a larger age range than the SSP. 188 However, practitioners who took part in this study worked with children across a wide age range, from 0 to 13 years old. A number of other validated instruments have been developed for older children. They include the narrative stem assessments (McArthur; Hodges; Manchester Child Attachment Story Task (MCAST)189 and the Child Attachment Interview. 37 For children who may have attachment disorders, the Disturbances of Attachment Interview can be used. 38 There are also several validated assessments of parent–child interactions, in particular caregiver sensitivity. They include the CARE Index43 for infants and toddlers, the NICHD sensitivity assessment and the AMBIANCE, of which a brief version has recently been developed. 190 These instruments were generally not used by the practitioners who responded to our survey. A very small proportion (n = 8) of respondents reported using the SSP (although some of these respondents were using only aspects and adaptations), and no respondents reported using the AQS or any of the other instruments noted above. Many services reported using instruments such as the SDQ, which, although helpful for exploring a child’s overall mental health functioning and a range of potential consequences related to attachment, does not measure attachment itself. Although the SDQ is easy to use and has very good validity as a screening instrument of child and adolescent mental health, severe attachment difficulties are a far more specific problem than generic mental health problems. It is important to acknowledge that there are serious barriers to the routine use of validated attachment instruments in terms of cost, complexity and time. Many of these assessments require training in administering and coding them, some of which are not easily accessible and are costly in terms of time and money. A number of recently developed tools are undergoing validation research, including the Reactive Attachment Disorder and Disinhibited Social Engagement Disorder Assessment,191 that no practitioners reported using at the time of the survey.
Clinical observations may well be helpful and have the advantage of a degree of ecological validity (when conducted thoroughly). However, the lack of structure and validation means that there is inevitably considerable doubt about what is actually being assessed, and whether or not there are reasonable levels of consistency across practitioners who have different prior assumptions and training.
Given the lack of formal assessments or attachment measures, another potential concern is the finding that interventions are offered without a rigorous formulation and delineation of the problem or diagnostic assessment. Whether the medical model of establishing as accurate an assessment of a patient’s problem as possible before offering treatment is the appropriate approach requires further discussion, but certainly practitioners need better support in conducting consistent and valid assessments of attachment in routine practice that inform the best interventions.
Varied assessment of outcome/evaluation of interventions
No single instrument was consistently used in terms of outcome measures. The variation was to some extent related to the particular intervention used.
Practitioners may prefer to use short and simple measures. This is in line with literature that suggests that SDQ, CORE (Clinical Outcomes In Routine Evaluation), MORS, Care Index, ASQ and PRFQ (Parental Reflective Functioning Questionnaire) are brief and acceptable measures. 192–197 A substantial proportion of the survey sample worked in the NHS, with a significant number working in CAMHS. The majority of CAMHS casework is time limited or brief. 192
In addition, SDQ, CORE, MORS, ASQ, MIM and PRFQ are self-report measures. This suggests that self-report measures may be preferred by respondents. This finding concurs with the findings of Shemmings’ study in 2004, which found that one group of attachment practitioners prefer self-report methods of data collection, in part because of their low cost, convenience and ability to survey large samples. 198 In addition, many services find it helpful to either send out the SDQ to clients and families prior to a first appointment or ask the client and/or family to complete the questionnaires in clinics prior to the first meeting (the questionnaires may also be subsequently given out again after 6 months). 192
It appears that respondents focused primarily on using outcome measures to address parenting, maternal mental health, child mental health and development and less so on attachment itself. Further work is required to achieve consensus between practitioners to ensure the use of a common set of outcome measures in the field of attachment. Any future research must consider how best to measure the impact of attachment work supporting a particular child and/or caregiver and any adverse effects and can focus on brief, convenient and easy-to-administrator measures that can be used across attachment-focused services. Adequate training is also needed to use attachment tools appropriately.
Variety of interventions used with the most common ones having limited or no evidence base and evidence-based interventions being rarely used
Perhaps the most important finding was that many different interventions are being used by professionals to treat attachment difficulties. These included both the 10 named most commonly used interventions we focused on in our second systematic review and a great many others. The survey results indicate that one of the most commonly named interventions was ICP, of which we identified no good evidence base fitting our PICOS criteria. Although this does not mean that the intervention is not helpful, it does mean that the evidence base on which to make this judgement is limited. It was clear that, in the same way that the term attachment was used in different ways by our survey practitioners, many described child psychotherapy with reference to psychodynamic psychotherapy,199 but some used the term more generally to include a range of individual psychotherapies with children, such as creative arts and play therapies. 200 The finding of limited research may be because psychoanalytic child psychotherapy as a field has traditionally been less likely to be subjected to RCTs for a variety of reasons and there have been calls for more research. 199,201 The next two most commonly used interventions were DDP and Theraplay, for which we also found limited studies, two and one, respectively, and no RCTs. There is, however, at least one RCT under way into the clinical effectiveness of DDP. Furthermore, DDP is described in the literature as both a therapy and a practice model. There may therefore be some ‘DDP informed’ parenting interventions that may not be manualised or that did not meet the inclusion criteria, and, although we are not aware of any RCTs, there may be other research relating to these. 202 By contrast, we found a substantial number of studies for VIPP and ABC. These also included the largest number of RCTs, at 15 and 11, respectively. Despite this, VIPP and ABC were at the bottom of our list of the top 10 most commonly used interventions. The low uptake of ABC in the UK in particular is noteworthy, given the robust evidence of its efficacy for improving both caregiving sensitivity and attachment security and reducing disorganised attachment. It would be helpful to investigate the barriers to the implementation of this programme in the UK and to conduct robust trials for key target groups of children at risk of severe attachment problems in the UK context.
There is a clear mismatch between current evidence and practice. This is not to say that the more commonly used interventions are not clinically effective or cost-effective, but that there is limited evidence to support their use in addressing attachment problems or to ensure that they cause no harm. The NICE guidelines recommend that children with or at risk of severe attachment problems should be offered an evidence-based intervention to support caregivers to enhance their sensitive responsiveness. The results of the current survey and systematic review suggest that more work needs to be done to achieve this across the UK.
The findings from this study indicate an urgent need for the commonly used interventions to be assessed for clinical effectiveness and cost-effectiveness.
Strengths
This study has provided an up-to-date snapshot of current practice across the UK while at the same time mapping this against the best current available evidence for the interventions in the field of attachment. It does what few studies do, which is to connect information from real-world practice and the latest research evidence base to inform service providers, commissioners and policy-makers.
Weaknesses
Although we received responses in our survey from 734 services across the four UK nations, we had more responses from England than from other countries in the UK. It is not clear if this represents a greater availability of provision in England or different response rates. This study made no attempt to map practice in other countries, which could have informed the findings by reporting on localities of good practice. Although the survey focused on the UK, the systematic review criteria were broad and inclusive of different study types and studies conducted in other countries. This allowed a wide range of findings to be captured that may be relevant to current practice, given that the field remains at the early stages of building a strong evidence base.
In the systematic reviews, it is possible that many interventions that had good clinical effectiveness were not included because they did not measure attachment outcomes in any way. This was one of our inclusion criteria to allow a degree of precision about the findings related to this field. This will have excluded some potentially helpful interventions. Another weakness is that a large number of papers could not be accessed for review 2. We used library searching services and conducted extensive grey literature searches to ensure that we did not miss relevant papers as far as possible.
Implications for practice
As discussed in detail above, a number of things would help practice. There needs to be improved training for practitioners in the concept of attachment and its relation to the parent child relationship, as well as increased training for delivery of the interventions. Appropriate training is important, especially given the potentially vulnerable populations with whom practitioners may be working.
It would also be helpful if researchers and practitioners collaborated to develop standardised guidelines and training curricula in relation to attachment concepts and interventions to reduce the variability in their use in order to support best practice and consistent care.
Pre-intervention assessment and routine assessment of intervention outcome also require improvements in practice. Outcome measurement in the field of child mental health is well recognised as difficult to achieve in general,203 but the attachment domain in particular suffers from significant challenges in terms of routine outcome assessment. More research is needed to develop and test valid assessment tools that can be used in routine clinical practice, following the lead of Cooke et al. on the AMBIENCE-brief. 190 In addition to research into, and provision of, routine tools for assessing attachment, the widespread adoption of improved assessment practices requires systemic change in practice, an acknowledgement of the importance of these aspects of practice and also the provision of more resources and support. In addition to the use of routine outcome measures, more structured training and resources should be available to ensure that routine clinical observation regarding attachment is undertaken with relative consistency and rigour.
Many stakeholders highlighted that after identifying infants and children at risk or with severe attachment problems there were no clear pathways to treatment, that these pathways were often complex and varied by locality or that they were not aware of them. Many practitioners also feared that the focus had moved away from prevention and that only children with severe problems were being treated in many places. Some work on improved streamlining and clarity around commissioning of care and improved care pathways will be important.
Future research priorities
The main research recommendation emanating from this report is the commissioning of RCTs for the most commonly used interventions (e.g. DDP and Theraplay). These interventions are used very commonly for supporting children at risk of severe attachment problems and lack a robust evidence base. It is, therefore, encouraging that there is currently at least one RCT under way for DDP. It is vital to provide this evidence base for these interventions and robustly test their clinical effectiveness, cost-effectiveness and safety. We would also recommend the commissioning of a pragmatic trial of ABC, which has good evidence from studies in the USA but has not been delivered in the UK setting.
The systematic review highlighted a gap in the evidence base for children aged ≥ 4 years. There is a need for more research to focus on attachment interventions in this older age group to identify what works best for this population.
Some exploration of why practitioners do not follow NICE guidelines would be of interest in terms of knowledge transfer and implementation science and would yield a better understanding of the barriers to and facilitators of achieving high-quality practice that is available and accessible to all in real-world day-to-day practice.
A further key research priority is the development of valid and reliable assessment tools that are readily accessible and can be used by clinicians to rigorously assess attachment. There is also a need for improved clinical and academic consensus on the best outcome measures to use in research to measure attachment and other outcomes in clinical trials so that we have better evidence in future by which to judge the impact of attachment on outcomes. This requires research investment as most current tools used in research are not suitable for use by practitioners. The development of a core outcomes data set for attachment could benefit clinicians as well as researchers, especially when planning future research, including RCTs.
Conclusions
In summary, there is good evidence that attachment interventions do work for children at risk of or experiencing severe attachment problems. However, there is a need to better integrate research findings with clinical practice in terms of both sharing up-to-date information and informing next steps in improved practice and research. There is also a need to develop improved and clear evidence-based protocols for the assessment and measurement of outcomes.
For any future work to improve clinical practice and research design, it is critical that PPI be incorporated. Our study has shown a gap between research and practice, and bringing in the views and advice of professionals working in the field and members of the public with lived experience can help to reduce this. Researchers studying the basic phenomenon of attachment and developing interventions to promote security of attachment also need to engage more comprehensively with practitioners, so that there is greater cross-talk between science and practice, so that terms, assessments tools and interventions are used more consistently and to allow for the improved provision of relevant training.
Chapter 7 Project management
Ethics approval
The survey was conducted according to the University College London Code of Conduct for Research and was approved by the University College London Research Ethics Committee (REC) prior to collecting the data (project ID 16687/001, approval granted 18 November 2019).
Project registration
The systematic review was registered on PROSPERO (CRD42019137362) at study set-up, and this record was updated in June 2020.
Data handling
Data handling and record-keeping
All data were collected and retained in accordance with the Data Protection Act 2018, General Data Protection Regulation and University College London Standard Operating Procedures.
Data storage and archiving
After study completion, all documentation and study data will be stored securely for 5 years. Anonymised digital data from the survey and systematic review will be retained indefinitely according to the policies of the sponsor, and these can be made available if requested.
Changes to protocol after start of trial
There were no major changes to the protocol after the start of the trial (version 1.1). The protocol was updated before the start of the study to reflect the ethics approval obtained for the survey. The protocol was also updated to reflect staff changes; Dr Catarina Teige took the role of Danielle Varley, who left the research team.
Conflict of interest statement
There are no conflicts of interest to declare.
Acknowledgements
We would like to thank the ERG for their contribution at all stages of this report. The ERG was made up of the following members: Danya Glaser, Sheila Redfern, Kim Golding, Doug Simkiss, Kevin Williams, Helen Minnis, Cheryll Adams, Esther Mugweni, Maureen Giles, Matthew Woolgar, Alison O’Sullivan, Michelle McHale and Michael Brown.
We would also like to thank all co-applicants for their support throughout the research, including Professor Peter Fonagy, Dr Danya Glaser, Dr Matthew Woolgar, Professor Paul Ramchandani, Dr Victoria Allgar, Mrs Alison O’Sullivan, Ms Michelle McHale, Mr Michael Brown, Professor Rachel Churchill, Dr Dean McMillan and Dr Catarina Teige.
We thank all of the practitioners who participated in the survey and those who assisted with survey recruitment. We thank Kath Wright at the University of York, Centre for Reviews and Dissemination, who ran the searches for the systematic reviews.
Contributions of authors
Professor Barry Wright (https://orcid.org/0000-0002-8692-6001) (Professor, Child Mental Health) was joint chief investigator for the study.
Professor Pasco Fearon (https://orcid.org/0000-0003-1847-8443) (Professor, Developmental Psychopathology) was joint chief investigator for the study.
Ms Megan Garside (https://orcid.org/0000-0001-5250-2326) (Research Fellow, Child Mental Health) conducted the systematic review and prepared the results for publication.
Ms Eleni Tsappis (https://orcid.org/0000-0003-2432-5881) (Research Assistant, Child Mental Health) conducted the systematic review and prepared the results for publication.
Ms Elaine Amoah (https://orcid.org/0000-0003-3497-2695) (Research Assistant, Child Mental Health) conducted the survey and prepared the results for publication.
Dr Danya Glaser (https://orcid.org/0000-0002-8786-1377) (Professor, Child and Adolescent Psychiatry) was chair of the ERG and prepared the results for publication.
Professor Victoria Allgar (https://orcid.org/0000-0002-5228-2623) (Professor, Medical Statistics) conducted the statistical analyses.
Professor Helen Minnis (https://orcid.org/0000-0002-2377-8945) (Professor, Child and Adolescent Psychiatry) was involved in the ERG, PPI workshops and contributed to the publication.
Dr Matthew Woolgar (https://orcid.org/0000-0002-3618-0395) (Consultant Clinical Psychologist, Developmental Research) was involved in the ERG and contributed to the publication.
Professor Rachel Churchill (https://orcid.org/0000-0002-1751-0512) (Professor, Evidence Synthesis) supported the design of systematic review and contributed to the publication.
Professor Dean McMillan (https://orcid.org/0000-0002-2901-8410) (Professor, Clinical Psychology) supported the design of systematic review and contributed to the publication.
Professor Peter Fonagy (https://orcid.org/0000-0003-0229-0091) (Director, Child Psychotherapy) supported the design of the study and contributed to the publication.
Ms Alison O’Sullivan (https://orcid.org/0000-0002-9464-6755) (Association of Directors of Children’s Services, Child Services) was involved in the ERG and contributed to the publication.
Miss Michelle McHale (https://orcid.org/0000-0002-5294-1094) (Director of Attachment Parenting UK, child attachment) was involved in the ERG and contributed to the publication.
Ethics statement
The survey was conducted in accordance with the University College London Code of Conduct for Research. It was approved by the University College London Research Ethics Committee prior to data collection (project ID 16687/001, approval granted 18 November 2019).
Data-sharing statement
Data sharing information can be obtained from the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HTA programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HTA programme or the Department of Health and Social Care.
References
- Bowlby J. Attachment: Attachment and Loss Volume 1. London: Hogarth Press; 1969.
- Draper P, Beisky J. Personality development in evolutionary perspective. J Personality 1990;58:141-61. https://doi.org/10.1111/j.1467-6494.1990.tb00911.x.
- Bretherton I. Attachment theory: retrospect and prospect. Mon Soc Res Child Dev 1985:3-5. https://doi.org/10.2307/3333824.
- Stayton DJ, Ainsworth MD, Main MB. Development of separation behavior in the first year of life: protest, following, and greeting. Dev Psychol 1973;9. https://doi.org/10.1037/h0035090.
- Ainsworth M, Blehar M, Waters E, Wall S. Patterns of Attachment: A Psychological Study of the Strange Situation. Hillsdale, NJ: Lawrence Erlbaum Associates; 1978.
- Ainsworth M, Wittig B, Foss BM. Determinants of Infant Behavior. London: Methuen; 1969.
- Sroufe LA. Attachment classification from the perspective of infant-caregiver relationships and infant temperament. Child Dev 1985;56:1-14. https://doi.org/10.1111/j.1467-8624.1985.tb00080.x.
- Main M, Solomon J. Discovery of an Insecure-Disorganized Disoriented Attachment Pattern 1986.
- Main M, Solomon J, Greenberg MT, Cicchetti D, Cummings EM. Attachment in the Preschool Years: Theory, Research, and Intervention. Chicago, IL: University of Chicago Press; 1990.
- Carlson EA. A prospective longitudinal study of attachment disorganization/disorientation. Child Dev 1998;69:1107-28. https://doi.org/10.1111/j.1467-8624.1998.tb06163.x.
- Lyons-Ruth K, Jacobvitz D, Cassidy J, Shaver PR. Handbook of attachment: Theory, Research, and Clinical Applications. New York, NY: Guilford Press; 2016.
- Van Ijzendoorn MH, Kroonenberg PM. Cross-cultural patterns of attachment: a meta-analysis of the strange situation. Child Dev 1988:147-56. https://doi.org/10.1111/j.1467-8624.1988.tb03202.x.
- Wright B, Barry M, Hughes E, Trépel D, Ali S, Allgar V, et al. Clinical effectiveness and cost-effectiveness of parenting interventions for children with severe attachment problems: a systematic review and meta-analysis. Health Technol Assess 2015;19. https://doi.org/10.3310/hta19520.
- National Institute for Health and Care Excellence . Children’s Attachment. Attachment in Children and Young People Who Are Adopted from Care, In Care or at High Risk of Going Into Care 2015. www.nice.org.uk/guidance/NG26/documents/childrens-attachment-full-guideline2 (accessed 5 February 2021).
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders 2013:5-25. https://doi.org/10.1176/appi.books.9780890425596.
- Groh AM, Fearon RP, van IJzendoorn MH, Bakermans-Kranenburg MJ, Roisman GI. Attachment in the early life course: meta-analytic evidence for its role in socioemotional development. Child Dev Perspect 2017;11:70-6. https://doi.org/10.1111/cdep.12213.
- Erickson MF, Sroufe LA, Egeland B. The relationship between quality of attachment and behavior problems in preschool in a high-risk sample. Monogr Soc Res Child Dev 1985;50:147-66. https://doi.org/10.2307/3333831.
- Solomon J, George C. Disorganized Attachment and Caregiving. New York, NY: Guilford Press; 2011.
- Carlson EA, Egeland B, Sroufe LA. A prospective investigation of the development of borderline personality symptoms. Dev Psychopathol 2009;21:1311-34. https://doi.org/10.1017/S0954579409990174.
- Green J, Goldwyn R. Annotation: attachment disorganisation and psychopathology: new findings in attachment research and their potential implications for developmental psychopathology in childhood. J Child Psychol Psychiatry 2002;43:835-46. https://doi.org/10.1111/1469-7610.00102.
- Fearon RP, Bakermans-Kranenburg MJ, van Ijzendoorn MH, Lapsley AM, Roisman GI. The significance of insecure attachment and disorganization in the development of children’s externalizing behavior: a meta-analytic study. Child Dev 2010;81:435-56. https://doi.org/10.1111/j.1467-8624.2009.01405.x.
- Lyons-Ruth K, Jacobvitz D, Cassidy J, Shaver P. Handbook of Attachment: Theory, Research, and Clinical Applications. Guilford Press; 2008.
- Lyons-Ruth K. Attachment relationships among children with aggressive behavior problems: the role of disorganized early attachment patterns. J Consult Clin Psychol 1996;64:64-73. https://doi.org/10.1037//0022-006x.64.1.64.
- Lyons-Ruth K, Easterbrooks MA, Cibelli CD. Infant attachment strategies, infant mental lag, and maternal depressive symptoms: predictors of internalizing and externalizing problems at age 7. Dev Psychol 1997;33:681-92. https://doi.org/10.1037//0012-1649.33.4.681.
- Carlson V, Cicchetti D, Barnett D, Braunwald K. Disorganized/disoriented attachment relationships in maltreated infants. Dev Psychol 1989;25:525-31. https://doi.org/10.1037/0012-1649.25.4.525.
- Sroufe LA. Attachment and development: a prospective, longitudinal study from birth to adulthood. Attach Hum Dev 2005;7:349-67. https://doi.org/10.1080/14616730500365928.
- Groh AM, Roisman GI, van Ijzendoorn MH, Bakermans-Kranenburg MJ, Fearon RP. The significance of insecure and disorganized attachment for children’s internalizing symptoms: a meta-analytic study. Child Dev 2012;83:591-610. https://doi.org/10.1111/j.1467-8624.2011.01711.x.
- Groh AM, Fearon RP, Bakermans-Kranenburg MJ, van Ijzendoorn MH, Steele RD, Roisman GI. The significance of attachment security for children’s social competence with peers: a meta-analytic study. Attach Hum Dev 2014;16:103-36. https://doi.org/10.1080/14616734.2014.883636.
- DeKlyen M, Greenberg MT, Cassidy J, Shaver PR. Handbook of Attachment: Theory, Research, and Clinical Applications. New York, NY: Guilford Press; 2008.
- Grossmann K, Grossmann KE, Spangler G, Suess G, Unzner L. Maternal sensitivity and newborns’ orientation responses as related to quality of attachment in northern Germany. Monogr Soc Res Child Dev 1985;50:233-56. https://doi.org/10.2307/3333836.
- Maslin CA, Bates JE. Precursors of Anxious and Secure Attachments: A Multivariate Model at Age 6 Months. Detroit, MI: Biennial meeting of the Society for Research in Child Development; 1983.
- Stams GJ, Juffer F, van IJzendoorn MH. Maternal sensitivity, infant attachment, and temperament in early childhood predict adjustment in middle childhood: the case of adopted children and their biologically unrelated parents. Dev Psychol 2002;38:806-21. https://doi.org/10.1037//0012-1649.38.5.806.
- Juffer F, Bakermans-Kranenburg MJ, van IJzendoorn MH. The importance of parenting in the development of disorganized attachment: evidence from a preventive intervention study in adoptive families. J Child Psychol Psychiatry 2005;46:263-74. https://doi.org/10.1111/j.1469-7610.2004.00353.x.
- Garcia Quiroga M, Hamilton-Giachritsis C. Attachment styles in children living in alternative care: a systematic review of the literature. Child Youth Care Forum 2016;45:625-53. https://doi.org/10.1007/s10566-015-9342-x.
- Teti DM, Nakagawa M, Das R, Wirth O. Security of attachment between preschoolers and their mothers: relations among social interaction, parenting stress, and mother’s sorts of the Attachment Q-Set. Dev Psychol 1991;27. https://doi.org/10.1037/0012-1649.27.3.440.
- van IJzendoorn MH, Vereijken CM, Bakermans-Kranenburg MJ, Riksen-Walraven JM. Assessing attachment security with the Attachment Q Sort: meta-analytic evidence for the validity of the observer AQS. Child Dev 2004;75:1188-213. https://doi.org/10.1111/j.1467-8624.2004.00733.x.
- Target M, Fonagy P, Shmueli-Goetz Y. Attachment representations in school-age children: the development of the Child Attachment Interview (CAI). J Child Psychother 2003;29:171-86. https://doi.org/10.1080/0075417031000138433.
- Smyke A, Zeanah C. ‘Disturbances of Attachment Interview’ 1999.
- Randolph E. Manual for the Randolph Attachment Disorder Questionnaire. Evergreen, CO; 2000.
- Ogilvie AM. The Assessment of Children With Attachment Disorder: The Randolph Attachment Disorder Questionnaire, the Behavioral and Emotional Rating Scale, and the Biopsychosocial Attachment Types Framework 1999. https://doi.org/10.15760/etd.6023.
- Cappelletty GG, Brown MM, Shumate SE. Correlates of the Randolph Attachment Disorder Questionnaire (RADQ) in a sample of children in foster placement. Child Adolescent Soc Work J 2005;22:71-84. https://doi.org/10.1007/s10560-005-2556-2.
- De Wolff MS, van Ijzendoorn MH. Sensitivity and attachment: a meta-analysis on parental antecedents of infant attachment. Child Dev 1997;68:571-91. https://doi.org/10.1111/j.1467-8624.1997.tb04218.x.
- Crittenden PM. CARE-Index Infant and Toddlers. Miami, FL: Family Relations Institute; 2001.
- Biringen Z, Altenhofen S, Aberle J, Baker M, Brosal A, Bennett S, et al. Emotional availability, attachment, and intervention in center-based child care for infants and toddlers. Dev Psychopathol 2012;24:23-34. https://doi.org/10.1017/S0954579411000630.
- O’Connor TG, Zeanah CH. Attachment disorders: assessment strategies and treatment approaches. Attach Hum Dev 2003;5:223-44. https://doi.org/10.1080/14616730310001593974.
- Bakermans-Kranenburg MJ, van IJzendoorn MH, Juffer F. Less is more: meta-analyses of sensitivity and attachment interventions in early childhood. Psychol Bull 2003;129:195-21. https://doi.org/10.1037/0033-2909.129.2.195.
- Wright B, Hackney L, Hughes E, Barry M, Glaser D, Prior V, et al. Decreasing rates of disorganised attachment in infants and young children, who are at risk of developing, or who already have disorganised attachment. A systematic review and meta-analysis of early parenting interventions. PLOS ONE 2017;12. https://doi.org/10.1371/journal.pone.0180858.
- Facompré CR, Bernard K, Waters TEA. Effectiveness of interventions in preventing disorganized attachment: a meta-analysis. Dev Psychopathol 2018;30:1-11. https://doi.org/10.1017/S0954579417000426.
- van Ijzendoorn MH, Bakermans-Kranenburg MJ. Attachment disorders and disorganized attachment: similar and different. Attach Hum Dev 2003;5:313-20. https://doi.org/10.1080/14616730310001593938.
- Mental Health Taskforce . The Five Year Forward View for Mental Health 2016. www.england.nhs.uk/mental-health/taskforce/ (accessed April 2021).
- Chorpita BF, Daleiden EL, Weisz JR. Identifying and selecting the common elements of evidence based interventions: a distillation and matching model. Ment Health Serv Res 2005;7:5-20. https://doi.org/10.1007/s11020-005-1962-6.
- Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;348. https://doi.org/10.1136/bmj.g1687.
- Great Britain . Data Protection Act 2018 2018.
- University College London . UCL Data Protection Policy. Information Security Policy n.d. www.ucl.ac.uk/legal-services/sites/legal-services/files/data-protection-policy.pdf (accessed 15 November 2022).
- REDCap . Redcap.slms.ucl.ac.Uk. 2020. https://redcap.slms.ucl.ac.uk/.
- O’Higgins M. Improving Mother-Infant Outcomes After Postnatal Depression 2007.
- Suchman NE, DeCoste CL, McMahon TJ, Dalton R, Mayes LC, Borelli J. Mothering From the Inside Out: results of a second randomized clinical trial testing a mentalization-based intervention for mothers in addiction treatment. Dev Psychopathol 2017;29:617-36. https://doi.org/10.1017/S0954579417000220.
- Knight RM, Albright JJ, Huth-Bocks A, Morris NK, Mills L, Klok K, et al. Impact of behavioral feeding intervention on child emotional and behavioral functioning, parenting stress, and parent-child attachment. J Pediatr Gastroenterol Nutr 2019;69:383-7. https://doi.org/10.1097/MPG.0000000000002382.
- Higgins JP, Savović J, Page MJ, Elbers RG, Sterne JA, Higgins JPT, et al. Cochrane Handbook for Systematic Reviews of Interventions. Chichester: John Wiley & Sons; 2019.
- Harbord RM, Egger M, Sterne JA. A modified test for small-study effects in meta-analyses of controlled trials with binary endpoints. Stat Med 2006;25:3443-57. https://doi.org/10.1002/sim.2380.
- Borenstein M, Hedges L, Higgins J, Rothstein H. Converting Among Effect Sizes, in Introduction to Meta-Analysis. Chichester: John Wiley; 2009.
- Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016;355. https://doi.org/10.1136/bmj.i4919.
- The National Child Traumatic Stress Network . ABC: Attachment and Biobehavioral Catch-Up: General Information 2012. www.nctsn.org/sites/default/files/interventions/abc_fact_sheet.pdf.
- The National Child Traumatic Stress Network . Training Guidelines Attachment and Biobehavioral Catch-up (ABC) 2016. www.nctsn.org/sites/default/files/interventions/abc_training_guidelines.pdf.
- School of Infant Mental Health n.d. www.infantmentalhealth.com/the-school/ (accessed September 2022).
- Lieberman AF, Ippen CG, Van Horn. 'Don't Hit My Mommy!': A Manual for Child-parent Psychotherapy with Young Children Exposed to Violence and Other Trauma. Washington, DC: Zero to Three; 2015.
- Lieberman AF, Compton NC, Van Horn P, Ippen CG. Losing a Parent to Death in the Early Years: Guidelines for the Treatment of Traumatic Bereavement in Infancy and Early Childhood. Washington, DC: Zero to Three; 2003.
- Hughes D. Attachment-focused Family Therapy Workbook. New York, NY: WW Norton & Co; 2011.
- Hughes DA, Golding KS, Hudson J. Healing Relational Trauma with Attachment-focused Interventions: Dyadic Developmental Psychotherapy with Children and Families. New York, NY; 2019.
- DDP Network – The Home of Dyadic Developmental Psychotherapy 2020. https://ddpnetwork.org/ (accessed 6 May 2021).
- Connected Lives n.d. www.connectedlives.org.uk (accessed 6 May 2021).
- Juffer F, Bakermans-Kranenburg MJ, van IJzendoorn MH. Manual VIPP-SD Video-feedback Intervention to Promote Positive Parenting and Sensitive Discipline (VIPP-SD) (Version 3.0). Centre for Child and Family Studies, Leiden University; 2015.
- Gibson H, Marczak M. Video Interaction Guidance – Skill Development Scale (VIG-SDS). 2018. https://videointeractionguidance.net/resources/Documents/2018%20New%20Training%20Route/C.2%20VIG-SDS%20v5%20reduced%20-%20detailed%20scale%20removed.pdf (accessed 5 May 2021).
- Jernberg AM, Booth PB. Theraplay: Helping Parents and Children Build Better Relationships Through Attachment-based Play. Hoboken, NJ: John Wiley & Sons; 2009.
- Norris V, Lender D. Theraplay® – The Practitioner’s Guide. London: Jessica Kingsley Publishers; 2020.
- Booth P. Theraplay® – Theory, Applications and Implementation. London: Jessica Kingsley Publishers; 2020.
- Theraplay 2021. https://theraplay.org (accessed 6 May 2021).
- Watch, Wait and Wonder 2020. https://watchwaitandwonder.com (accessed 6 May 2021).
- Berlin LJ, Martoccio TL, Appleyard Carmody K, Goodman WB, O’Donnell K, Williams J, et al. Can typical US home visits affect infant attachment? Preliminary findings from a randomized trial of Healthy Families Durham. Attach Hum Dev 2017;19:559-79. https://doi.org/10.1080/14616734.2017.1339359.
- Cassidy J, Brett BE, Gross JT, Stern JA, Martin DR, Mohr JJ, et al. Circle of Security-Parenting: a randomized controlled trial in Head Start. Dev Psychopathol 2017;29:651-73. https://doi.org/10.1017/S0954579417000244.
- Ramsauer B, Mühlhan C, Lotzin A, Achtergarde S, Mueller J, Krink S, et al. Randomized controlled trial of the Circle of Security-Intensive intervention for mothers with postpartum depression: maternal unresolved attachment moderates changes in sensitivity. Attach Hum Dev 2020;22:705-26. https://doi.org/10.1080/14616734.2019.1689406.
- Slade A, Holland ML, Ordway MR, Carlson EA, Jeon S, Close N, et al. Minding the Baby®: Enhancing parental reflective functioning and infant attachment in an attachment-based, interdisciplinary home visiting program. Dev Psychopathol 2020;32:123-37. https://doi.org/10.1017/S0954579418001463.
- Williams LR, Turner PR. Infant carrying as a tool to promote secure attachments in young mothers: comparing intervention and control infants during the still-face paradigm. Infant Behav Dev 2020;58. https://doi.org/10.1016/j.infbeh.2019.101413.
- Van den Boom DC. Do first-year intervention effects endure? Follow-up during toddlerhood of a sample of Dutch irritable infants. Child Dev 1995:1798-816.
- Heinicke CM, Fineman NR, Ruth G, Recchia SL, Guthrie D, Rodning C. Relationship‐based intervention with at‐risk mothers: outcome in the first year of life. Infant Ment Health J 1999;20:349-74. https://doi.org/10.1002/(SICI)1097-0355(199924)20:4<349::AID-IMHJ1>3.0.CO;2-X.
- Moran G, Pederson DR, Krupka A. Maternal unresolved attachment status impedes the effectiveness of interventions with adolescent mothers. Infant Ment Health J 2005;26:231-49. https://doi.org/10.1002/imhj.20045.
- Cicchetti D, Rogosch FA, Toth SL. Fostering secure attachment in infants in maltreating families through preventive interventions. Dev Psychopathol 2006;18:623-49. https://doi.org/10.1017/s0954579406060329.
- Toth SL, Rogosch FA, Manly JT, Cicchetti D. The efficacy of toddler-parent psychotherapy to reorganize attachment in the young offspring of mothers with major depressive disorder: a randomized preventive trial. J Consult Clin Psychol 2006;74:1006-16. https://doi.org/10.1037/0022-006X.74.6.1006.
- Cooper PJ, Tomlinson M, Swartz L, Landman M, Molteno C, Stein A, et al. Improving quality of mother-infant relationship and infant attachment in socioeconomically deprived community in South Africa: randomised controlled trial. BMJ 2009;338. https://doi.org/10.1136/bmj.b974.
- Moss E, Dubois-Comtois K, Cyr C, Tarabulsy GM, St-Laurent D, Bernier A. Efficacy of a home-visiting intervention aimed at improving maternal sensitivity, child attachment, and behavioral outcomes for maltreated children: a randomized control trial. Dev Psychopathol 2011;23:195-210. https://doi.org/10.1017/S0954579410000738.
- Cassidy J, Woodhouse SS, Sherman LJ, Stupica B, Lejuez CW. Enhancing infant attachment security: an examination of treatment efficacy and differential susceptibility. Dev Psychopathol 2011;23:131-48. https://doi.org/10.1017/S0954579410000696.
- Bernard K, Dozier M, Bick J, Lewis-Morrarty E, Lindhiem O, Carlson E. Enhancing attachment organization among maltreated children: results of a randomized clinical trial. Child Dev 2012;83:623-36. https://doi.org/10.1111/j.1467-8624.2011.01712.x.
- Cooper PJ, De Pascalis L, Woolgar M, Romaniuk H, Murray L. Attempting to prevent postnatal depression by targeting the mother–infant relationship: a randomised controlled trial. Primary Health Care Res Dev 2015;16:383-97. https://doi.org/10.1017/S1463423614000401.
- Gradisar M, Jackson K, Spurrier NJ, Gibson J, Whitham J, Williams AS, et al. Behavioral interventions for infant sleep problems: a randomized controlled trial. Pediatrics 2016. https://doi.org/10.1542/peds.2015-1486.
- Tereno S, Guedeney N, Dugravier R, Greacen T, Saïas T, Tubach F, et al. Sécurité de l’attachement des jeunes enfants dans une population française vulnérable. L'Encéphale 2017;43:99-103. https://doi.org/10.1016/j.encep.2015.11.006.
- Fonagy P, Sleed M, Baradon T. Randomized controlled trial of parent-infant psychotherapy for parents with mental health problems and young infants. Infant Ment Health J 2016;37:97-114. https://doi.org/10.1002/imhj.21553.
- Challacombe FL, Salkovskis PM, Woolgar M, Wilkinson EL, Read J, Acheson R. A pilot randomized controlled trial of time-intensive cognitive–behaviour therapy for postpartum obsessive–compulsive disorder: effects on maternal symptoms, mother–infant interactions and attachment. Psychol Med 2017;47:1478-88. https://doi.org/10.1017/S0033291716003573.
- Barnett B, Blignault I, Holmes S, Payne A, Parker G. Quality of attachment in a sample of 1-year-old Australian children. J Am Acad Child Adolesc 1987;26:303-7. https://doi.org/10.1097/00004583-198705000-00003.
- Anisfeld E, Casper V, Nozyce M, Cunningham N. Does infant carrying promote attachment? An experimental study of the effects of increased physical contact on the development of attachment. Child Dev 1990;61:1617-27. https://doi.org/10.1111/j.1467-8624.1990.tb02888.x.
- Brisch KH, Bechinger D, Betzler S, Heinemann H. Early preventive attachment-oriented psychotherapeutic intervention program with parents of a very low birthweight premature infant: results of attachment and neurological development. Attach Hum Dev 2003;5:120-35. https://doi.org/10.1080/1461673031000108504.
- Murray L, Cooper PJ, Wilson A, Romaniuk H. Controlled trial of the short- and long-term effect of psychological treatment of post-partum depression: 2. Impact on the mother–child relationship and child outcome. Br J Psychiatry 2003;182:420-27.
- Klein Velderman M, Bakermans-Kranenburg MJ, Juffer F, van IJzendoorn MH. Effects of attachment-based interventions on maternal sensitivity and infant attachment: differential susceptibility of highly reactive infants. J Fam Psychol 2006;20:266-74. https://doi.org/10.1037/0893-3200.20.2.266.
- Alsancak-Akbulut C, Sahin-Acar B, Sumer N. Effect of video-feedback intervention on Turkish mothers’ sensitivity and physical intrusiveness: a randomized control. Attach Hum Dev 2021;23:795-813. https://doi.org/10.1080/14616734.2020.1753085.
- Barone L, Ozturk Y, Lionetti F. The key role of positive parenting and children’s temperament in post-institutionalized children’s socio-emotional adjustment after adoption placement. A RCT study. Soc Dev 2019;28:136-51. https://doi.org/10.1111/sode.12329.
- Casonato M, Nazzari S, Frigerio A. Feasibility and efficacy of an attachment-based intervention in a maltreatment sample in residential care: a pilot study. Clin Child Psychol Psychiatry 2017;22:561-71. https://doi.org/10.1177/1359104517719115.
- Cassibba R, Castoro G, Costantino E, Sette G, Van Ijzendoorn MH. Enhancing maternal sensitivity and infant attachment security with video feedback: an exploratory study in Italy. Infant Ment Health J 2015;36:53-61. https://doi.org/10.1002/imhj.21486.
- Iles JE, Rosan C, Wilkinson E, Ramchandani PG. Adapting and developing a video-feedback intervention for co-parents of infants at risk of externalising behaviour problems (VIPP-Co): a feasibility study. Clin Child Psychol Psychiatry 2017;22:483-99. https://doi.org/10.1177/1359104517704025.
- Kalinauskiene L, Cekuoliene D, Van Ijzendoorn MH, Bakermans-Kranenburg MJ, Juffer F, Kusakovskaja I. Supporting insensitive mothers: the Vilnius randomized control trial of video-feedback intervention to promote maternal sensitivity and infant attachment security. Child Care Health Dev 2009;35:613-23. https://doi.org/10.1111/j.1365-2214.2009.00962.x.
- Klein Velderman M, Bakermans-Kranenburg MJ, Juffer F, Van Ijzendoorn MH, Mangelsdorf SC, Zevalkink J. Preventing preschool externalizing behavior problems through video-feedback intervention in infancy. Infant Mental Health J 2006;27:466-93. https://doi.org/10.1002/imhj.20104.
- Negrão M, Pereira M, Soares I, Mesman J. Enhancing positive parent-child interactions and family functioning in a poverty sample: a randomized control trial. Attach Hum Dev 2014;16:315-28. https://doi.org/10.1080/14616734.2014.912485.
- Platje E, Sterkenburg P, Overbeek M, Kef S, Schuengel C. The efficacy of VIPP-V parenting training for parents of young children with a visual or visual-and-intellectual disability: a randomized controlled trial. Attach Hum Dev 2018;20:455-72. https://doi.org/10.1080/14616734.2018.1428997.
- Poslawsky IE, Naber FB, Bakermans-Kranenburg MJ, van Daalen E, van Engeland H, van IJzendoorn MH. Video-feedback Intervention to promote Positive Parenting adapted to Autism (VIPP-AUTI): a randomized controlled trial. Autism 2015;19:588-603. https://doi.org/10.1177/1362361314537124.
- Schoemaker NK, Juffer F, Rippe RC, Vermeer HJ, Stoltenborgh M, Jagersma GJ, et al. Positive parenting in foster care: testing the effectiveness of a video-feedback intervention program on foster parents’ behavior and attitudes. Children Youth Serv Rev 2020;110. https://doi.org/10.1016/j.childyouth.2020.104779.
- Van Zeijl J, Mesman J, Van IJzendoorn MH, Bakermans-Kranenburg MJ, Juffer F, Stolk MN, et al. Attachment-based intervention for enhancing sensitive discipline in mothers of 1- to 3-year-old children at risk for externalizing behavior problems: a randomized controlled trial. J Consult Clin Psychol 2006;74:994-1005. https://doi.org/10.1037/0022-006X.74.6.994.
- Whitehouse AJO, Varcin KJ, Alvares GA, Barbaro J, Bent C, Boutrus M, et al. Pre-emptive intervention versus treatment as usual for infants showing early behavioural risk signs of autism spectrum disorder: a single-blind, randomised controlled trial. Lancet Child Adolesc Health 2019;3:605-15. https://doi.org/10.1016/S2352-4642(19)30184-1.
- Yagmur S, Mesman J, Malda M, Bakermans-Kranenburg MJ, Ekmekci H. Video-feedback intervention increases sensitive parenting in ethnic minority mothers: a randomized control trial. Attach Hum Dev 2014;16:371-86. https://doi.org/10.1080/14616734.2014.912489.
- Green J, Charman T, Pickles A, Wan MW, Elsabbagh M, Slonims V, et al. Parent-mediated intervention versus no intervention for infants at high risk of autism: a parallel, single-blind, randomised trial. Lancet Psychiatry 2015;2:133-40. https://doi.org/10.1016/S2215-0366(14)00091-1.
- Berlin LJ, Shanahan M, Appleyard Carmody K. Promoting supportive parenting in new mothers with substance-use problems: a pilot randomized trial of residential treatment plus an attachment-based parenting program. Infant Ment Health J 2014;35:81-5. https://doi.org/10.1002/imhj.21427.
- Berlin LJ, Martoccio TL, Jones Harden B. Improving early head start’s impacts on parenting through attachment-based intervention: a randomized controlled trial. Dev Psychol 2018;54:2316-27. https://doi.org/10.1037/dev0000592.
- Yarger HA, Hoye JR, Dozier M. Trajectories of change in attachment and biobehavioral catch-up among high-risk mothers: a randomized clinical trial. Infant Ment Health J 2016;37:525-36. https://doi.org/10.1002/imhj.21585.
- Yarger HA, Bernard K, Caron EB, Wallin A, Dozier M. Enhancing parenting quality for young children adopted internationally: results of a randomized controlled trial. J Clin Child Adolesc Psychol 2020;49:378-90. https://doi.org/10.1080/15374416.2018.1547972.
- Lind T, Bernard K, Yarger HA, Dozier M. Promoting compliance in children referred to child protective services: a randomized clinical trial. Child Dev 2020;91:563-76. https://doi.org/10.1111/cdev.13207.
- Bernard K, Simons R, Dozier M. Effects of an attachment-based intervention on child protective services–referred mothers’ event-related potentials to children’s emotions. Child Dev 2015;86:1673-84. https://doi.org/10.1111/cdev.12418.
- Zajac L, Raby KL, Dozier M. Sustained effects on attachment security in middle childhood: results from a randomized clinical trial of the Attachment and Biobehavioral Catch-up (ABC) intervention. J Child Psychol Psychiatry 2020;61:417-24. https://doi.org/10.1111/jcpp.13146.
- Dozier M, Lindhiem O, Lewis E, Bick J, Bernard K, Peloso E. Effects of a foster parent training program on young children’s attachment behaviors: preliminary evidence from a randomized clinical trial. Child Adolesc Social Work J 2009;26:321-32. https://doi.org/10.1007/s10560-009-0165-1.
- Raby KL, Freedman E, Yarger HA, Lind T, Dozier M. Enhancing the language development of toddlers in foster care by promoting foster parents’ sensitivity: results from a randomized controlled trial. Dev Sci 2019;22. https://doi.org/10.1111/desc.12753.
- Caron EB, Weston-Lee P, Haggerty D, Dozier M. Community implementation outcomes of Attachment and Biobehavioral Catch-up. Child Abuse Negl 2016;53:128-37. https://doi.org/10.1016/j.chiabu.2015.11.010.
- Roben CKP, Dozier M, Caron EB, Bernard K. Moving an evidence-based parenting program into the community. Child Dev 2017;88:1447-52. https://doi.org/10.1111/cdev.12898.
- Perrone L, Imrisek SD, Dash A, Rodriguez M, Monticciolo E, Bernard K. Changing parental depression and sensitivity: randomized clinical trial of ABC’s effectiveness in the community. Dev Psychopathol 2020;1. https://doi.org/10.1017/S0954579420000310.
- Puckering C, Webster J, Wilson P. Secure mother-infant attachment and the ABC programme: a case history. Community Pract 2011;84:35-7.
- Andrews E, Coyne J. Travelling the circle together, solo: an individual protocol for the Circle of Security intensive intervention. J Clin Psychol 2018;74:1333-45. https://doi.org/10.1002/jclp.22644.
- Fardoulys C, Coyne J. Circle of security intervention for parents of children with autism spectrum disorder. Aus N Z J Family Ther 2016;37:572-84. https://doi.org/10.1002/anzf.1193.
- Hanlon-Dearman A, Malik S, Wellwood J, Johnston K, Gammon H, N Andrew K, et al. A descriptive study of a community-based home-visiting program with preschool children prenatally exposed to alcohol. J Popul Ther Clin Pharmacol 2017;24:e61-e71. https://doi.org/10.22374/1710-6222.24.2.3.
- Hoffman KT, Marvin RS, Cooper G, Powell B. Changing toddlers’ and preschoolers’ attachment classifications: the Circle of Security intervention. J Consult Clin Psychol 2006;74:1017-26. https://doi.org/10.1037/0022-006X.74.6.1017.
- Huber A, McMahon CA, Sweller N. Efficacy of the 20-week Circle of Security intervention: changes in caregiver reflective functioning, representations, and child attachment in an Australian clinical sample. Infant Ment Health J 2015;36:556-74. https://doi.org/10.1002/imhj.21540.
- Page T, Koren-Karie N. Evidence of attachment disorganization and growth in one mother’s descriptions of her son: a case study. J Infant Child Adolesc Psychother 2013;12:100-17. https://doi.org/10.1080/15289168.2013.791185.
- Page TF, Caine DS. A Pilot Application of the Circle of Security Parenting Intervention to Child Welfare-Involved Mothers n.d.
- Lieberman AF, Weston DR, Pawl JH. Preventive intervention and outcome with anxiously attached dyads. Child Dev 1991;62:199-20. https://doi.org/10.2307/1130715.
- Robert-Tissot C, Cramer B, Stern DN, Serpa SR, Bachmann JP, Palacio-Espasa F, et al. Outcome evaluation in brief mother-infant psychotherapies: report on 75 cases. Infant Mental Health J 1996;17:97-114. https://doi.org/10.1002/(SICI)1097-0355(199622)17:2<97::AID-IMHJ1>3.0.CO;2-Y.
- Salomonsson B, Sandell R. A randomized controlled trial of mother-infant psychoanalytic treatment: I. Outcomes on self-report questionnaires and external ratings. Infant Ment Health J 2011;32:207-31. https://doi.org/10.1002/imhj.20291.
- Salomonsson MW, Sorjonen K, Salomonsson B. A long-term follow-up of a randomized controlled trial of mother-infant psychoanalytic treatment: outcomes on the children. Infant Ment Health J 2015;36:12-29. https://doi.org/10.1002/imhj.21478.
- Salomonsson MW, Sorjonen K, Salomonsson B. A long-term follow-up study of a randomized controlled trial of mother-infant psychoanalytic treatment: outcomes on mothers and interactions. Infant Ment Health J 2015;36:542-55. https://doi.org/10.1002/imhj.21536.
- Cohen NJ, Muir E, Lojkasek M, Muir R, Parker CJ, Barwick M, et al. Watch, wait, and wonder: testing the effectiveness of a new approach to mother–infant psychotherapy. Infant Ment Health J 1999;20:429-51. https://doi.org/10.1002/(SICI)1097-0355(199924)20:4<429::AID-IMHJ5>3.0.CO;2-Q.
- Cohen NJ, Lojkasek M, Muir E, Muir R, Parker CJ. Six-month follow-up of two mother–infant psychotherapies: convergence of therapeutic outcomes. Infant Ment Health J 2002;23:361-80. https://doi.org/10.1002/imhj.10023.
- Barlow J, Sembi S, Underdown A. Pilot RCT of the use of video interactive guidance with preterm babies. J Reproductive Infant Psychol 2016;34:511-24. https://doi.org/10.1080/02646838.2016.1217404.
- Hoffenkamp HN, Tooten A, Hall RA, Braeken J, Eliëns MP, Vingerhoets AJ, et al. Effectiveness of hospital-based video interaction guidance on parental interactive behavior, bonding, and stress after preterm birth: a randomized controlled trial. J Consult Clin Psychol 2015;83:416-29. https://doi.org/10.1037/a0038401.
- James DM, Wadnerkar-Kamble MB, Lam-Cassettari C. Video feedback intervention: a case series in the context of childhood hearing impairment. Int J Lang Commun Disord 2013;48:666-78. https://doi.org/10.1111/1460-6984.12039.
- Kennedy H, Landor M, Todd L. Video Interaction Guidance as a method to promote secure attachment. Educ Child Psychol 2010;27.
- Lam-Cassettari C, Wadnerkar-Kamble MB, James DM. Enhancing parent-child communication and parental self-esteem with a video-feedback intervention: outcomes with prelingual deaf and hard-of-hearing children. J Deaf Stud Deaf Educ 2015;20:266-74. https://doi.org/10.1093/deafed/env008.
- Pethica S, Bigham K. ‘Stop talking about my disability, I am a mother’: adapting video interaction guidance to increase sensitive parenting in a young mother with intellectual disability. Br J Learning Disabil 2018;46:136-42. https://doi.org/10.1111/bld.12215.
- Cicchetti D, Toth SL, Rogosch FA. The efficacy of toddler-parent psychotherapy to increase attachment security in offspring of depressed mothers. Attach Hum Dev 1999;1:34-66. https://doi.org/10.1080/14616739900134021.
- Stronach EP, Toth SL, Rogosch F, Cicchetti D. Preventive interventions and sustained attachment security in maltreated children. Dev Psychopathol 2013;25:919-30. https://doi.org/10.1017/S0954579413000278.
- Becker-Weidman A. Treatment for children with trauma-attachment disorders: dyadic developmental psychotherapy. Child Adolesc Soc Work J 2006;23:147-71. https://doi.org/10.1007/s10560-005-0039-0.
- Becker-Weidman A, Sturt, Stanley M. New Developments in Child Abuse Research. Hauppauge, NY: Nova Science Publishers; 2006.
- Salo S, Flykt M, Mäkelä J, Lassenius-Panula L, Korja R, Lindaman S, et al. The impact of Theraplay® therapy on parent-child interaction and child psychiatric symptoms: a pilot study. Int J Play 2020;9:331-52. https://doi.org/10.1080/21594937.2020.1806500.
- Biringen Z, Derscheid D, Vliegen N, Closson L, Easterbrooks MA. Emotional availability (EA): theoretical background, empirical research using the EA Scales, and clinical applications. Dev Rev 2014;34:114-67. https://doi.org/10.1016/j.dr.2014.01.002.
- Pederson DR, Moran G. Appendix B: Maternal behavior Q-set. Monographs of the Society for Research in Child Development 1995:247-54. https://doi.org/10.1111/j.1540-5834.1995.tb00215.x.
- Egeland B, Hiester M. Teaching Task Rating Scales. Institute of Child Development, University of Minnesota; 1993.
- Egeland B, Erickson MF, Clemenhagen-Moon JC, Hiester MK, Korfmacher J. 24 Months Tools Coding Manual. Project STEEP Revised 1990 from Mother–child Project Scales. Minneapolis, MN: University of Minnesota; 1990.
- Elsabbagh M, Bruno R, Wan MW, Charman T, Johnson MH, Green J. BASIS Team . Infant neural sensitivity to dynamic eye gaze relates to quality of parent-infant interaction at 7-months in infants at risk for autism. J Autism Dev Disord 2015;45:283-91. https://doi.org/10.1007/s10803-014-2192-9.
- Waters E, Waters E, Vaughn BE, Posada G, Kondo-Ikemura K. Caregiving Culture, and Cognitive Perspectives on Secure Base Behaviour and Working Models: New Growing Points of Attachment Theory and Research (Monographs of the Society for Research in Child Development). Chicago, IL: University of Chicago Press; 1995.
- Waters E, Deane KE. Defining and assessing individual differences in attachment relationships: Q-methodology and the organization of behavior in infancy and early childhood. Monographs Soc Res Child Dev 1985:41-65. https://doi.org/10.2307/3333826.
- Murray L, Fiori-Cowley A, Hooper R, Cooper P. The impact of postnatal depression and associated adversity on early mother-infant interactions and later infant outcome. Child Dev 1996;67:2512-26. https://doi.org/10.2307/1131637.
- NICHD Early Child Care Research Network . Child care and mother–child interaction in the first three years of life. Dev Psychol 1999;35:1399-413. https://doi.org/10.1037/0012-1649.35.6.1399.
- NICHD Early Child Care Research Network . Early child care and mother–child interaction from 36 months through first grade. Infant Behav Dev 2003;26:345-70. https://doi.org/10.1016/S0163-6383(03)00035-3.
- Vandell DL. Characteristics of infant child care: Factors contributing to positive caregiving: NICHD early child care research network. Early Childhood Res Q 1996;11:269-306. https://doi.org/10.1016/S0885-2006(96)90009-5.
- Stovall-McClough KC, Dozier M. Forming attachments in foster care: infant attachment behaviors during the first 2 months of placement. Dev Psychopathol 2004;16:253-71. https://doi.org/10.1017/S0954579404044505.
- Kerns KA, Klepac L, Cole A. Peer relationships and preadolescents’ perceptions of security in the child-mother relationship. Dev Psychol 1996;32. https://doi.org/10.1037/0012-1649.32.3.457.
- Cassidy J, Marvin R. the MacArthur Consortium on Attachment in the Preschool Years 1989–1992. Attachment Organization in Three- and Four-Year-Olds: Coding Guidelines 1992.
- Moran G, Pederson DR, Bento S. Mini-MBQS-V Revised Mini-MBQS 25 Item for Video Coding 2009. http://works.bepress.com/gregmoran/4 (accessed 21 September 2021).
- Hodges J, Steele M, Hillman S, Henderson K, Kaniuk J. Changes in attachment representations over the first year of adoptive placement: narratives of maltreated children. Clin Child Psychol Psychiatry 2003;8:351-67. https://doi.org/10.1177/1359104503008003006.
- Ainsworth MD, Bell SM, Stayton DF, Richards MPM. The Integration of a Child into the Social World. London: Cambridge University Press; 1974.
- Cramer B, Robert-Tissot C, Stern DN, Serpa-Rusconi S, De Muralt M, Besson G, et al. Outcome evaluation in brief mother-infant psychotherapy: a preliminary report. Infant Ment Health J 1990;11:278-300. https://doi.org/10.1002/1097-0355(199023)11:3<278::AID-IMHJ2280110309>3.0.CO;2-H.
- Biemans H. International Seminar for Innovative Institutions. Rijswijk: Ministry of Welfare, Health and Culture; 1990.
- Bakermans-Kranenburg MJ, Juffer F, Van Ijzendoorn MH. Interventions with video feedback and attachment discussions: does type of maternal insecurity make a difference?. Infant Ment Health J 1998;19:202-19. https://doi.org/10.1002/(SICI)1097-0355(199822)19:2<202::AID-IMHJ8>3.0.CO;2-P.
- Juffer F, Hoksbergen RA, Riksen-Walraven JM, Kohnstamm GA. Early intervention in adoptive families: supporting maternal sensitive responsiveness, infant-mother attachment, and infant competence. J Child Psychol Psychiatry 1997;38:1039-50. https://doi.org/10.1111/j.1469-7610.1997.tb01620.x.
- Rosenboom LG. Mixed Families, Mixed Feelings? Attachment and Competence of Adopted Babies in Families With Biological Children 1994.
- van IJzendoorn MH, Juffer F, Duyvesteyn MG. Breaking the intergenerational cycle of insecure attachment: a review of the effects of attachment-based interventions on maternal sensitivity and infant security. J Child Psychol Psychiatry 1995;36:225-48. https://doi.org/10.1111/j.1469-7610.1995.tb01822.x.
- Mountain G, Cahill J, Thorpe H. Sensitivity and attachment interventions in early childhood: a systematic review and meta-analysis. Infant Behav Dev 2017;46:14-32. https://doi.org/10.1016/j.infbeh.2016.10.006.
- Bakermans-Kranenburg MJ, Van IJzendoorn MH, Juffer F. Disorganized infant attachment and preventive interventions: a review and meta-analysis. Infant Ment Health J 2005;26:191-216. https://doi.org/10.1002/imhj.20046.
- O’Connor TG, Bredenkamp D, Rutter M. English and Romanian Adoptees (ERA) Study Team. Attachment disturbances and disorders in children exposed to early severe deprivation. Infant Ment Health J 1999;20:10-29. https://doi.org/10.1002/(SICI)1097-0355(199921)20:1<10::AID-IMHJ2>3.0.CO;2-S.
- Jaffari-Bimmel N, Juffer F, van Ijzendoorn MH, Bakermans-Kranenburg MJ, Mooijaart A. Social development from infancy to adolescence: longitudinal and concurrent factors in an adoption sample. Dev Psychol 2006;42:1143-53. https://doi.org/10.1037/0012-1649.42.6.1143.
- Boris NW, Hinshaw-Fuselier SS, Smyke AT, Scheeringa MS, Heller SS, Zeanah CH. Comparing criteria for attachment disorders: establishing reliability and validity in high-risk samples. J Am Acad Child Adolesc Psychiatry 2004;43:568-77. https://doi.org/10.1097/00004583-200405000-00010.
- Zeanah CH, Berlin LJ, Boris NW. Practitioner review: clinical applications of attachment theory and research for infants and young children. J Child Psychol Psychiatry 2011;52:819-33. https://doi.org/10.1111/j.1469-7610.2011.02399.x.
- de Haan AM, Boon AE, de Jong JT, Hoeve M, Vermeiren RR. A meta-analytic review on treatment dropout in child and adolescent outpatient mental health care. Clin Psychol Rev 2013;33:698-711. https://doi.org/10.1016/j.cpr.2013.04.005.
- Woolgar M, Scott S. The negative consequences of over-diagnosing attachment disorders in adopted children: the importance of comprehensive formulations. Clin Child Psychol Psychiatry 2014;19:355-66. https://doi.org/10.1177/1359104513478545.
- Cadman T, Belsky J, Pasco Fearon RM. The Brief Attachment Scale (BAS-16): A short measure of infant attachment. Child Care Health Dev 2018;44:766-75. https://doi.org/10.1111/cch.12599.
- Cadman T, Diamond PR, Fearon P. Reassessing the validity of the attachment Q-sort: an updated meta-analysis. Infant 2018;27. https://doi.org/10.1002/icd.2034.
- Green J, Stanley C, Smith V, Goldwyn R. A new method of evaluating attachment representations in young school-age children: the Manchester Child Attachment Story Task. Attach Hum Dev 2000;2:48-70. https://doi.org/10.1080/146167300361318.
- Cooke JE, Eirich R, Racine N, Lyons-Ruth K, Madigan S. Validation of the AMBIANCE-brief: an observational screening instrument for disrupted caregiving. Infant Ment Health J 2020;41:299-312. https://doi.org/10.1002/imhj.21851.
- Lehmann S, Monette S, Egger H, Breivik K, Young D, Davidson C, et al. Development and examination of the reactive attachment disorder and disinhibited social engagement disorder assessment interview. Assessment 2020;27:749-65. https://doi.org/10.1177/1073191118797422.
- Law D, Wolpert M. Guide to Using Outcomes and Feedback Tools 2014.
- Evans John Mellor-Clark, Margison Frank, Barkham Michael, Audin Kerry, Connell Janice, McGrath C Graeme. CORE: clinical outcomes in routine evaluation. J Ment Health 2000;9:247-55. https://doi.org/10.1080/713680250.
- Simkiss DE, MacCallum F, Fan EE, Oates JM, Kimani PK, Stewart-Brown S. Validation of the Mothers Object Relations scales in 2-4 year old children and comparison with the Child-Parent Relationship Scale. Health Qual Life Outcomes 2013;11. https://doi.org/10.1186/1477-7525-11-49.
- Szaniecki E, Barnes J. Measurement Issues: Measures of infant mental health. Child Adolesc Ment Health 2016;21:64-7. https://doi.org/10.1111/camh.12105.
- Kerstjens JM, Bos AF, ten Vergert EM, de Meer G, Butcher PR, Reijneveld SA. Support for the global feasibility of the Ages and Stages Questionnaire as developmental screener. Early Hum Dev 2009;85:443-7. https://doi.org/10.1016/j.earlhumdev.2009.03.001.
- Luyten P, Mayes LC, Nijssens L, Fonagy P. The parental reflective functioning questionnaire: development and preliminary validation. PLOS ONE 2017;12. https://doi.org/10.1371/journal.pone.0176218.
- Shemmings D. Researching relationships from an attachment perspective: the use of behavioural, interview, self-report and projective measures. J Soc Work Pract 2004;18:299-31. https://doi.org/10.1080/0265053042000314393.
- Midgley N, O’Keeffe S, French L, Kennedy E. Psychodynamic psychotherapy for children and adolescents: an updated narrative review of the evidence base. J Child Psychother 2017;43:307-29. https://doi.org/10.1080/0075417X.2017.1323945.
- Malchiodi CA, Crenshaw DA. Creative arts and play therapy for attachment problems. Guilford Publications; 2015.
- Fonagy P. The research agenda: the vital need for empirical research in child psychotherapy. J Child Psychother 2003;29:129-36. https://doi.org/10.1080/0075417031000138406.
- Hughes DA, Golding KS, Hudson J. Healing relational trauma with attachment-focused interventions: dyadic developmental psychotherapy with children and families. WW Norton & Company; 2019.
- Kilbourne AM, Beck K, Spaeth-Rublee B, Ramanuj P, O’Brien RW, Tomoyasu N, et al. Measuring and improving the quality of mental health care: a global perspective. World Psychiatry 2018;17:30-8. https://doi.org/10.1002/wps.20482.
Appendix 1 List of other interventions
| Interventions | Identified in survey, n |
|---|---|
| Massage therapy | 11 |
| Baby massage | 8 |
| Infant massage | 3 |
| Psychotherapy/talking therapies | 69 |
| Art psychotherapy | 6 |
| Art therapy | 4 |
| CPP | 1 |
| Gestalt therapy | 1 |
| Interpersonal psychotherapy | 2 |
| Psychotherapy | 1 |
| Cognitive analytic therapy (CAT) | 3 |
| Developmental CAT | 1 |
| CBT | 2 |
| Talking therapy | 2 |
| Trauma-focused CBT | 5 |
| Systematic psychotherapy | 3 |
| Parent–child therapy | 2 |
| Narrative attachment therapy | 2 |
| Neurophysiological psychotherapy (NPP) | 1 |
| EMDR (eye movement desensitisation and reprocessing) | 9 |
| Mentalisation-based therapy | 13 |
| Children and Parents DBT Skills | 2 |
| Adult psychotherapy | 1 |
| Short-term psychoanalytic psychotherapy | 1 |
| Therapeutic life story work | 7 |
| Mentalisation-based therapy | 13 |
| Mentalisation-based therapy (MBT) | 7 |
| Mentalisation-based therapy for children (MBT-C) | 2 |
| Mentalisation-based therapy parenting group | 1 |
| Adaptive mentalisation based therapy (AMBIT) | 1 |
| Mentalisation-based art therapy group | 1 |
| Mentalisation-based therapy for families | 1 |
| Trauma informed/focused therapy | 14 |
| Trauma recovery model (ECM) | 1 |
| Trauma focused CBT | 5 |
| Trauma informed approach (Beacon House Polyvagal Theory) | 3 |
| Trauma informed schools | 1 |
| Mellow Babies/Parenting | 3 |
| Neurophysiological psychotherapy | 1 |
| Family therapy/interventions | 41 |
| Family therapy | 7 |
| Systematic family therapy | 2 |
| Partners in Parenting Education (PIPE) | 5 |
| Mellow Babies/Parenting | 4 |
| Mind-Mindedness intervention | 1 |
| Incredible Years | 7 |
| Dandelion Time Model | 6 |
| Narrative Attachment Therapy | 2 |
| Collaborative Problem Solving approach | 4 |
| Attachment based family therapy | 1 |
| Nurturing Families Programme | 1 |
| Parenting interventions | 21 |
| Non-Violent Resistance (NVR) | 5 |
| Foundations for Attachment | 2 |
| Incredible Years Parenting Programme | 2 |
| Triple P (Positive Parenting Programme) | 1 |
| Family First Parenting Groups | 1 |
| WFT Parenting Work | 1 |
| Reflective Parenting | 3 |
| Therapeutic Parenting | 6 |
| Play therapy | 47 |
| Individual Play Therapy | 1 |
| Life Story Play Therapy | 1 |
| Non-directive Play Therapy | 4 |
| Parent–Child Attachment Play (PCAP) | 3 |
| Play Therapy | 11 |
| Therapeutic Play | 1 |
| Watch me play | 3 |
| Group Filial Therapy | 2 |
| Filial Therapy | 10 |
| Here’s Looking at you Baby | 1 |
| Letting the future in (NSPCC post abuse programme) | 1 |
| Ball Throwing/Game Play | 1 |
| Child Parent Relationship Model (Filial Model) | 3 |
| Child Centred Integrative Approach | 1 |
| Play and interaction groups | 1 |
| Parent in the playroom | 1 |
| Individual play therapy | 1 |
| Attending or special play | 1 |
| Art therapy | 21 |
| Art Psychotherapy | 6 |
| Art Therapy | 4 |
| Drawing and Talking | 5 |
| Using art and play | 1 |
| Mandala | 1 |
| Puppet/Acting out | 1 |
| Ball Throwing/Game Play | 1 |
| Dramatherapy | 2 |
| Music therapy | 9 |
| Music Therapy | 8 |
| Watch videos of Music Therapy | 1 |
| Sensory interventions | 28 |
| Sensory attachment intervention | 10 |
| Sensory integration | 7 |
| Sensory attachment work | 1 |
| Underdeveloped sensory systems | 1 |
| Eye movement desensitisation and reprocessing (EMDR) | 9 |
| School interventions | 17 |
| ARC (The attachment Research Community) | 2 |
| Nurtured Heart Approach | 1 |
| Nurturing Attachments Course | 4 |
| Nurture Groups | 1 |
| Neurosequential Model | 1 |
| Partners in Parenting Education (PIPE) | 3 |
| NESSie (Parent training forums) | 1 |
| Trauma Informed Schools | 1 |
| Fagus | 1 |
| Training Schools in Attachment Aware | 1 |
| Collaborative Problem Solving approach | 1 |
| Approaches | 16 |
| Solihull Approach | 10 |
| Thrive Approach | 6 |
| Remote/online interventions | 10 |
| BABY BEATS Advanced Bionics | 3 |
| Baby Bonding | 1 |
| Gordon Neufeld Approach | 1 |
| Gro Brain | 2 |
| Hand in Hand Parenting | 3 |
Appendix 2 Tables of included study characteristics for systematic reviews
| Study | Participants | Sample risk | Intervention focus | Intervention/duration/intensity/delivery | Control group | Attachment measure | Attachment outcomes |
|---|---|---|---|---|---|---|---|
| Berlin et al., 201779 |
n = 94 Mean age Child 16.5 months; mother 20.1 years Ethnicity 68.1% black, 27.7% Hispanic |
Parents met one of the six risk factors: maternal age < 16 years, history of childhood maltreatment, mental health symptoms, concerns about use of alcohol or other addictive substances, history of or current concerns about domestic violence and/or low social support | Attachment security and targeting disorganised attachment |
The Healthy Families Durham programme Weekly visits for 1 year and then reduced in frequency depending on family needs. Delivered by social work and counselling professionals with a master’s degree |
Yearly check-up control group not receiving any Healthy Family services | Secure and disorganised; measured post intervention; SSP | There were no significant programme group differences in the likelihood of an infant being classified secure or disorganised |
| Cassidy et al., 201780 |
n = 141 Mean age IG: child 50.68 months; mother 28.21 years; CG: child 51.5 months; mother 31.07 years Ethnicity IG: African American (81%); white (11%); other (5%); CG: African American (68%); white (14%); other (11%) |
Recruited from Head Start centres in low-socioeconomic status communities | Caregiving sensitivity; insecure and disorganised attachment | Circle of Security: parenting – 90-minute sessions for 10 weeks delivered by four clinicians (three master’s level and one doctorate level) | Waitlist control | Secure and disorganised; post intervention only; Preschool Attachment Classification System from modified SSP |
There were no main effects of intervention on continuous attachment outcomes (i.e. security or avoidance) Rates of disorganised attachment were not found to differ between the treatment and control |
| O’Higgins, 200756 |
n = 62 Child median age IG: 9 weeks; CG: 10 weeks Mother age range IG: 17–40+ years; CG: 20–40+ years Ethnicity 77.08% white, 12.5% black, 5.21% Asian, 5.21% mixed/other/unstated |
Postnatally depressed mothers | Learning about their infant and their cues and signals; maternal sensitivity | Baby massage 1-hour classes run at a hospital by trained instructors from the International Association of Infant Massage. Social discussion, instruction and practical work. Aim to attend six sessions, with telephone contact weekly from the research team to keep track of progress |
Support group sessions Hourly sessions run by an experienced member of the research team at an outpatient department. Groups of up to eight; discuss and share experiences. Aim to attend six sessions, with telephone contact weekly from the research team to keep track of progress |
Secure and disorganised; post intervention; SSP | Attachment status did not vary by intervention; no significant differences found between groups, indicating that the rates of secure, avoidant, resistant and disorganised attachment were equivalent for each group |
| Ramsauer et al., 201981 |
n = 72 Mean age IG: child 6.03 months; mother 32.79 years; CG: child 6.33 months; mother 31.63 years Ethnicity NR |
Mothers with DSM-IV diagnosis of depression | Maternal sensitivity |
Circle of Security – intensive 20 group sessions, once per week for 90 minutes. Six mothers in the group, facilitated by two trained COS therapists |
Treatment as usual Case management service, occasional dyadic mother–infant psychotherapy, usually approximately 50 minutes |
Secure and disorganised; post intervention; SSP | No significant overall treatment group differences in rates of infant attachment security and disorganisation were found at follow-up |
| Slade et al., 202082 |
n = 156 Mean age Child: prenatal baseline measures, intervention delivered through first 2 years Mother: IG: 20.1 years; CG: 20.0 years Ethnicity IG: 3.9% white/non-Hispanic, 75.3% Hispanic/Latino, 15.6% African American, 5.2% other CG: 5.1% white/non-Hispanic, 60.8% Hispanic/Latino, 31.6% African American, 2.5% other |
Young first-time mothers living in underserved, poor, urban communities | Maternal reflective functioning and affective communication between mother and child |
Minding the Baby intervention Intensive weekly home visiting service (developmental guidance, supporting attachment, signposting, and support with basic supplies) from start of third trimester until child is 12 months, and then biweekly home visits until child is 24 months. Continued to receive routine care from community health centre. Minding the Baby practitioners completed training and regular supervision |
Care as usual Routine prenatal and postnatal well-woman health visits and well-baby health-care visits. Families were sent quarterly information from Healthy Steps |
Secure and disorganised; post intervention; SSP | Infants in the Minding the Baby group were significantly more likely to be securely attached and significantly less likely to be disorganised than infants in the control group |
| Williams and Turner, 202083 |
n = 33 Mean age Child 2–4 weeks; mother 19.1 years Ethnicity White 45.3%, Hispanic 44%, black 2.7%, American Indian 2.7%, other 5.3% |
Adolescent mothers | Skin-to-skin contact and the link to improving maternal sensitivity and attachment |
Baby-wearing – high-physical-contact intervention A certified educator in baby-wearing instructed mothers how to use a baby-wearing carrier and encouraged they to use for at least 1 hour per day |
Reading – low physical contact intervention Mothers were given four high-contrast baby books and encouraged to read to their babies |
Secure and disorganised; post intervention only; Global Rating Scales used to classify attachment type from the Still Face Paradigm at 7 months | Infants in the intervention group were more likely to be secure and less like to be disorganised than those in the control condition at 7 months |
| Suchman et al., 201757 |
n = 87 Mean age Child 27.62 months; mother 29.68 years Ethnicity 77% Caucasian, 13.8% African American, 3.4% Hispanic/Latina, 5.7% mixed race |
Mothers enrolled in addiction treatment for substance abuse | Parental mentalisation and reflective functioning to develop maternal caregiving sensitivity | Mothering from the Inside Out; manualised 12 weekly 1-hour sessions of individual therapy, delivered by therapist | Parent education 12-session individual psychoeducational comparison intervention in which developmental guidance and parenting strategies were provided by an individual counsellor | Secure only; SSP at baseline and post intervention; MacArthur Preschool SSP | There were no significant group differences in the percentage of children whose attachment status either remained secure or became more secure at post treatment |
| Study | Participant details (number/age/ethnicity) | Sample risk | Intervention focus | Manualised intervention | Study design | Control group | Attachment measure | Attachment outcomes | Parental sensitivity measure | Parental sensitivity outcomes |
|---|---|---|---|---|---|---|---|---|---|---|
| Alsancak-Akbulut et al., 2020103 |
n = 68 Age Child’s mean age 20.04 months (6.62 months); mother’s mean age 29.29 years (5.20 years) Ethnicity Not specified but mainly Turkish |
Low-SES area, disadvantaged mothers | Maternal sensitivity | VIPP-SD | RCT | Dummy intervention – received four telephone calls | N/A | N/A | Ainsworth Sensitivity Scale | VIPP-SD proved effective in promoting maternal sensitivity among Turkish mothers, with a moderate effect size for intervention effect |
| Barone and Lionetti, 2019104 |
n = 83 Age Child’s mean age 43.3 months (15.9 months); mother’s mean age 42.6 years (3.9 years) Ethnicity Caucasian |
Adoptive mothers, internationally adopted children | Caregiver sensitivity | VIPP-SD, VIPP-FC/A | RCT | Dummy intervention – received six telephone calls | N/A | N/A | Emotional Availability Scale | There was a higher increase in caregiver sensitivity for those in the intervention group than for those in the control group |
| Casonato et al., 2017105 |
n = 12 Age Child’s mean age 19.58 months (9.51 months); mother’s mean age 26.83 years (9.52 years) Ethnicity Not specified |
Placed in parental residential care | Maternal sensitivity | VIPP-SD | RCT | Received six telephone calls | N/A | N/A | Maternal Behaviour Q-set | No significant improvements in maternal sensitivity |
| Cassibba et al., 2015106 |
n = 32 Age Child age 7 months; mother mean age 33.03 years (4.37 years) Ethnicity Italian sample |
Categorised according to mother’s attachment classification | Maternal sensitivity | VIPP-R | Non-randomised study | Two dummy visits | SSP |
Children of insecure mothers were assessed as more secure than the comparison children of insecure mothers Children of secure mothers who received the intervention did not show significant changes of attachment security |
Emotional Availability Scale |
VIPP-R appeared to enhance the sensitivity of only insecure mothers compared with insecure mothers without intervention At the same time, the VIPP-R was ineffective in secure mothers, as the sensitivity of secure mothers after intervention was not significantly higher than that of secure mothers in the comparison group |
| Iles et al., 2017107 |
n = 5 Age Child mean age 16 months (3.4 months); mother mean age 35 years (4.3 years); father mean age 36 years Ethnicity 100% white |
Families who reported to be struggling with their infant’s behaviour | Parental sensitivity | VIPP-Co | Non-randomised study | No control group | N/A | N/A | Adapted Global Rating Scale | Preliminary outcome data indicated positive changes in parental sensitivity |
| Kalinauskiene et al., 2009108 |
n = 54 Age Child’s mean age: 6 months 12 days (0.07) Mother’s mean age: 26.4 years (2.94) Ethnicity 77.8% Lithuanian |
Considered ‘insensitive mothers’ scoring below mid-point of 5 on Ainsworth’s rating scale | Maternal sensitivity | VIPP | RCT | Dummy intervention – contacted by telephone monthly for 5 months | AQS | Attachment security was not enhanced in the VIPP group compared with controls | Ainsworth Security Scale | Intervention mothers improved sensitive responsiveness (d = 0.78) |
| Klein Velderman et al., 2006102 |
n = 81 Age Child mean age 6.83 months (1.03 months); mother mean age 27.8 years (3.63 years) Ethnicity Not specified |
Mothers with insecure attachment | Maternal sensitivity; attachment |
VIPP VIPP-R |
RCT | No intervention | SSP at T2 | The number of secure infants in both intervention groups was not significantly higher than in the control group | Ainsworth Sensitivity Scale | After the intervention, intervention mothers were more sensitive than control mothers |
|
Klein Velderman et al. , 2006109 Follow-up of Klein Velderman et al. , 2006102 |
n = 77 Age Child mean age 6.83 (1.03); mother mean age 27.83 years (3.63 years) Ethnicity Not specified |
Mothers with insecure attachment | Maternal sensitivity; attachment |
VIPP VIPP-R |
RCT | No intervention | AQS at T3 | No long-term intervention effects on children’s AQS security scores were found either | Ainsworth Sensitivity Scale | At T3, no significant long-term intervention effects were found on EAS sensitivity among all three groups |
| Negrão et al., 2014110 |
n = 43 Age Child mean age 29.07 months (10.49 months); mother mean age 29.98 years (6.19 years) Ethnicity Not specified |
Poor families of toddlers screened for professional’s concerns about the child’s caregiving environment | Maternal sensitivity; attachment | VIPP-SD | RCT | Six telephone calls at the same time intervals as the VIPP-SD sessions | N/A | N/A | Emotional Availability Scales | Intervention group showed higher post-test sensitivity scores; however, effects failed to reach significance |
| Platje et al., 2008111 |
n = 86 Child mean age Intervention 3.36 years; control 3.22 years Parent mean age Intervention 34.50 years; control 35.65 years Ethnicity (Dutch) Intervention group 35 (91%); control group 31 (86%) |
Visual or visual-and-intellectual disability | Parental sensitivity | VIPP-V | RCT | Care as usual | N/A | N/A | The boxes procedure coded using the National Institute of Child Health and Human Development Scales | The parents receiving VIPP-V did not show increased parental sensitivity |
| Poslawsky et al., 2015112 |
n = 78 Child mean age Intervention group 42.16 months; control group 43.80 months Caregiver mean age Intervention group 36.8 years old; control group 36.42 years old Ethnicity Not reported |
Children with autism spectrum disorder | Parental sensitivity | VIPP-AUTI | RCT | Care as usual | N/A | N/A | Emotional Availability Scale | No significant effects for parental sensitivity |
| Shoemaker et al., 2020113 |
n = 60 Child mean age Intervention group 3.63 years old; control group 3.67 years old Foster parent mean age Intervention group 46.04 years old; control group 44.81 years old Ethnicity Dutch |
Foster children | Parental Sensitivity | VIPP-FC | RCT | Dummy intervention – six telephone calls | N/A | N/A | Adapted Ainsworth Sensitivity Scales | No evidence that VIPP-FC was more effective in improving foster parents’ sensitive parenting behaviour than control group |
| Van Zeijl et al., 2006114 |
n = 237 Mother mean age Intervention group 33 years; control group, 44.81 years old Child age range: 1–3 years old Ethnicity Dutch |
Children with relatively high levels of behaviour problems and parents facing relatively high levels of stress | Maternal sensitivity | VIPP-SD | RCT | Control group | N/A | N/A | 7-point scales drawn from Egeland et al.159 | VIPP-SD was effective in promoting sensitive discipline interactions in the intervention group as compared with the control group |
| Whitehouse et al., 2019115 |
n = 98 Child mean age Intervention group 12.40 months; control group 12.38 months Parent/caregiver age: not specified Ethnicity Australian sample |
Foster children | Parental sensitivity | iBASIS-VIPP | RCT | Community treatment as usual | N/A | N/A | Manchester Assessment of Caregiver–Infant interaction | No significant differences on secondary outcomes measuring caregiver sensitive responding |
| Yagmur et al., 2014116 |
n = 76 Age Child’s mean age: 30.83 months Mother’s mean age: 29.96 years Ethnicity 100% Turkish |
Turkish immigrant families with toddlers at risk for the development of externalising problems | Maternal sensitivity | VIPP-TM | RCT | Dummy intervention | N/A | N/A | Emotional Availability Scale | The VIPP-TM was effective in increasing maternal sensitivity |
| Green et al., 2015117 |
n = 54 Child mean age Control group 276.58 days (24.25 days); intervention group 267.14 days (20.93 days) |
Infants at risk of autism | Parental sensitivity | iBASIS-VIPP | RCT | No treatment group | N/A | N/A | Manchester Assessment of Caregiver–Infant interaction | The intervention did not show any effect on caregiver sensitive-responding |
| Oliveira et al. (University College London; 8 December 2020, personal communication) |
n = 30 Age Child mean age: 47.37 months Carer mean age: 49.87 years Ethnicity Carer ethnicity: 22 (73%) White British Child ethnicity 14 (47%) White British 2 (7%) Caribbean 3 (10%) White/Caribbean mixed 11 (36%) other ethnicities 9 (29%) |
Foster children | Parental sensitivity | VIPP-FC | RCT | Care as usual | SSP | Results are not yet published as the SSP is still being coded | N/A | N/A |
| Berlin et al., 2014118 |
n = 21 Age Child’s mean age: 9.55 months (6.8) Mother’s mean age: 33 years (7) Ethnicity: 85% white |
Mothers and their infant living in residential substance abuse treatment | Maternal sensitivity | ABC | RCT | Light, 10-session ‘intervention’ book of the week – brief, home-based appointments | N/A | N/A | Maternal behaviour Q-sort | There was an effect of the intervention on observed sensitive parenting behaviour favouring the ABC group |
| Berlin et al., 2018119 |
n = 202 Age Child’s mean age: 13 months (4 months) Mother’s mean age: 31 years (6.5 years) Ethnicity: 87% Latino, 8% black, 5% other |
Early Head Start eligible, low SES | Maternal sensitivity | ABC | RCT | Early Head Start, plus book of the week, 10 developmentally appropriate books sent weekly, and three telephone calls | N/A | N/A | Coded observations, overall sensitivity score | Following the intervention, ABC mothers were rated as significantly more sensitive. The effect on overall sensitivity was medium (d = 0.47) |
| Yarger et al., 2016120 |
n = 24 Mother mean age IG: 24.70 years; CG 28.2 years Child mean age IG 13.18 months; CG 15.14 months Ethnicity IG: African American 46.2%, European American 38.5, biracial 7.7%, other 7.7% CG: African American 63.6%, European American 36.4% |
Families had an unsubstantiated report of neglect in the state of Delaware | Maternal sensitivity | ABC | RCT | DEF | N/A | N/A | The ORCE Sensitivity scale | Mothers who participated in ABC were significantly more sensitive than were mothers who participated in DEF, and mothers in ABC showed a steeper rate of change in sensitivity than mothers in DEF |
| Yarger et al., 2019121 |
n = 120 dyads Age Parent mean age: 39.7 years Children mean age: 21.9 months Ethnicity White/non-Hispanic: 95.0% |
Adopted children | Parental sensitivity | ABC | RCT | DEF | N/A | N/A | Adapted ORCE scales | Parents who participated in ABC were significantly more sensitive than parents who participated in DEF. Furthermore, parents in ABC showed a steeper rate of change in sensitivity than parents in DEF |
| Lind et al., 2020122 |
n = 101 Child age at intervention IG: 9.3 months (5.9 months); CG: 9.4 months (6.3 months) Mother age at intervention IG: 27.4 years (7.4 years); CG: 25.1 years (7.3 years) Ethnicity IG: 11.1% white, 68.9% African American, 11.1% Hispanic, 8.9% biracial; CG: 7.1% white, 71.4% African American, 16.1% Hispanic, 5.4% biracial |
Child protective services involvement | Maternal sensitivity | ABC | RCT | DEF | N/A | N/A | A global 5-point scale of sensitivity adapted from ORCE scales | Parents who received ABC demonstrated significantly higher sensitivity than parents who received the control intervention at the 1-month post-intervention assessment (d = 0.47). Parents who received the ABC intervention engaged in sensitive behaviour for more of the interaction than parents who received the control intervention, although the difference was not statistically significant (d = 0.40) The correlation between parent sensitivity at the 1-month post-intervention assessment and parent sensitivity at 36-month-old follow-up assessment was moderate but non-significant (r = 0.20) |
| Bernard et al., 201292 |
n = 120 children Age Child mean age: 10.1 months (6.0 months) Parent mean age: 28.4 years (7.8 years) Ethnicity 61% African American, 9% biracial, 15% white/Hispanic |
Young children who have experienced early adversity | Parental sensitivity | ABC | RCT | DEF | SSP | Children in the ABC intervention group showed lower rates of disorganised attachment than those in the control group | N/A | N/A |
|
Bernard et al. , 2015123 Follow-up of Bernard et al. , 201292 |
n = 70 Age Mother mean age: 31.6 years Child mean age IG: 4.94; CG: 4.83 (0.56) Ethnicity IG: 74% African American, 16% white, 11% biracial; CG 81% African American, 5% white, 14% Hispanic |
CPS referred mothers | Maternal sensitivity | ABC | RCT | DEF | N/A | N/A | ORCE Scales | There were significant group differences in maternal sensitivity. Those in the DEF group scored significantly lower sensitivity scores than those in the ABC group |
|
Zajac et al. , 2020124 9-year follow-up of Bernard et al. , 2012122 |
n = 129 Age Child age at follow-up: 9.46 years Mother age at follow-up: IG: 38.71 years; CG: 37.14 years |
Families were initially referred for the study by child welfare agencies as part of a foster care diversion programme | Perceived attachment security | ABC | RCT | DEF | Kerns Security Scale | Children who received the ABC intervention had higher perceived attachment security ratings than children who received the DEF intervention | N/A | N/A |
| Dozier et al., 2009125 |
n = 46 Age Child mean age: 18.9 months Parent age: not reported Ethnicity 63% African American, with 26% non-Hispanic white, 3% Hispanic, and 7% biracial |
Foster children | Attachment security | ABC | RCT | DEF | Parent attachment diaries | Children whose parents had received ABC showed significantly less avoidance than children whose parents had received the educational intervention | N/A | N/A |
| Raby et al., 2019126 |
n = 88 Age Child age range: between 24 and 36 months Parent age: not reported Ethnicity IG: 50% Caucasian, 43.2% African American; CG: 33.3% Caucasian, 50% African American |
Parents with foster children | Maternal sensitivity | ABC-T | RCT | DEF | N/A | N/A | ORCE Scales | Foster parents who received ABC-T interacted with their children in a more sensitive manner |
| Caron et al., 2016127 |
n = 78 dyads Age Child mean age: 12.2 months (7.4 months) Parent mean age: 28.6 years (6.8 years) Ethnicity 50% mixed racial background, 13% white/non-Hispanic, 5% white/Hispanic, 1% African American, 9% Asian American, 10% native Hawaiian, 6% other Pacific Islander |
Referred to needing services (e.g. CPS involvement, observed difficulties) | Parental sensitivity | ABC | Non-randomised study | No control group | N/A | N/A | Adapted ORCE Scales | Improvements were observed in parent–child interaction |
| Roben et al., 2017128 |
n = 108 Age Child age: 6 months Parent age: not reported Ethnicity Not reported |
Referred to needing services (e.g. CPS involvement, observed difficulties) | Parental sensitivity | ABC | Non-randomised study | No control group | N/A | N/A | Adapted ORCE scales | Parents showed higher levels of sensitivity at post intervention than at pre intervention |
| Perrone et al., 2020129 |
n = 200 Age Child mean age: 11.82 months Parent mean age: 29.85 years Ethnicity 64.5% African American, 15% Hispanic or Latin |
Recruited through community-based organisations (e.g. family-based homeless shelters, community fairs, health service providers) | Parental sensitivity | ABC | RCT | Waitlist | N/A | N/A | Adapted ORCE scale | On average parents who completed ABC displayed greater increases in sensitivity |
| Puckering et al., 2011130 |
n = 1 Participant characteristics: not reported |
Mother with history of moderate depression and referred to local infant mental health services by their general practitioner | Attachment | ABC | Case study | No control group | SSP | ABC changed the attachment between mother and infant | N/A | N/A |
| Andrews and Coyne, 2018131 |
n = 1 Age Child: 5 years old Mother: ‘early 40s’ Ethnicity Not reported |
Child referred by a psychologist | Attachment | COS-I | Case study | No control group | SSP | The relationship was moving towards security, although it was not formally coded | N/A | N/A |
| Cassidy et al., 201780 |
n = 141 mothers Child mean age IG: 50.68 months (5.94 months); CG: 51.15 months (6.01 months) Mother mean age IG: 28.21 years (5.39 years); CG: 31.07 years (7.14 years) Ethnicity IG: 81% African American, 11% white, 5% other; CG: 68% African American, 14% white, 11% other |
Attending Head Start/Early Head Start | Parental sensitivity | COS-P | RCT | Waitlist control | Preschool Attachment Classification System, from modified SSP | There were no main effects of intervention on continuous outcomes. Rate of disorganised attachment were not found to differ between treatment and control groups | N/A | N/A |
| Fardoulys and Coyne, 2016132 |
n = 2 Age Child: 3.5 years Mother: 33 years Ethnicity 1 Australian–Japanese household, 1 Australian |
Children with ASD diagnosis | Attachment | COS | Case series | No control group | SSP coded with MacArthur Preschool Attachment Coding System | Results found one dyad shifted from avoidant to secure while the other dyad remained secure over time | N/A | N/A |
| Hanlon-Dearman, 2017133 |
n = 12 Age Child mean age: 4.1 years Parent/caregiver age: not reported Ethnicity Not reported |
Children with fetal alcohol spectrum disorder and affected by prenatal alcohol exposure; foster children | Attachment | COS | RCT | Waitlist or treatment as usual | Secure Base-Safe Haven coding procedure based on SSP | In 25% of the cases, COS treatment resulted in a shift to secure attachment at post-intervention and follow-up | N/A | N/A |
| Hoffman et al., 2004134 |
n = 65 dyads Age Child mean age: 32 months (12.6 months) Caregiver mean age: 23.8 years (6.8 years) Ethnicity 86% white/Caucasian |
Significantly high risk – violent neighbourhood, caregivers experienced childhood trauma | Attachment | COS | Non–randomised study | No control group | MacArthur Preschool Strange Situation for children | There were significant within-subject changes from disorganised to organised attachment classifications, with a majority changing to the secure classification | N/A | N/A |
| Huber et al., 2015135 |
n = 83 Age Child age: 47.80 months (17.48 months) Caregiver age: not reported Ethnicity 4% Aboriginal or Torres Strait Islander, 24% other culturally or linguistically diverse backgrounds |
Referred to a community-based infant and early childhood mental health service | Attachment | COS | Non-randomised study | No control group | SSP | Level of child attachment security increased after the intervention, and level of attachment disorganisation decreased for those with high baseline levels but not a significant change | N/A | N/A |
| Page and Koren-Karie, 2013136 |
n = 1 Age Parent: 21 years old Child: 3 years old Ethnicity Not reported |
Characteristics consistent with attachment disorganisation | Attachment | COS | Case study | No control group | SSP | Attachment changed from disorganised to secure | N/A | N/A |
| Ramsauer et al., 202081 |
n = 72 Child mean age IG: 6.03 months; CG: 6.33 months Parent mean age IG: 32.79 years; CG: 31.63 years Ethnicity Not reported |
Mothers with post-partum depression | Attachment and maternal sensitivity | COS-I | RCT | Treatment as usual | SSP | No significant overall treatment group differences in rates of infant attachment security and disorganisation were found at follow-up | Mini-Maternal Behaviour Q-Sort for Video Coding | No statistical differences of treatment effects between treatment as usual and COS-I intervention groups on changes in maternal sensitivity across time |
| Cassidy et al., 201191 |
n = 220 Age Infant age: 1 month Ethnicity 43.2% African American/black, 20.5% white, 18.6% more than one race, 14.1% Hispanic |
Irritable infants and economically stressed mothers | Attachment | COS- HV4 | RCT | Control group – three 1-hour psychoeducational sessions | Strange situation assessed when infants were 12 months old (post intervention) | There was no main effect of treatment | N/A | N/A |
| Page and Caine, 2010137 |
n = 8 Age Child mean age: 48 months Mother mean age: 25 Ethnicity 7 Caucasian, 1 Hispanic |
Referred for parenting services by a local child welfare agency | Attachment | COS | Non-randomised study | No control group | Preschool SSP | Half of participants showed some improvements in children’s attachment security | N/A | N/A |
| Fonagy et al., 201696 |
n = 76 Age Child: 3.85 months Parent: 31.1 years Ethnicity 63% white |
Parental mental health problems and social adversity | Attachment and parental sensitivity | PIP | RCT | Treatment as usual | SSP | Infant attachment classifications did not differ between the groups | Emotional Availability Scale | There was no demonstrated treatment group effects for parental sensitivity |
| Cicchetti et al., 200687 |
n = 137 Age Child mean age: 13.3 months old Mother mean age: 26.87 years old Ethnicity Not reported |
All infants known to have been maltreated and or who were living in maltreating families with their biological mothers | Attachment and maternal sensitivity | Infant–parent psychotherapy (IPP) | RCT | Psychoeducational parenting intervention and community standard controls and low-income normative comparison | SSP | Children in the IPP and psychoeducational parenting intervention groups demonstrated substantial increases in secure attachment, whereas increases in secure attachment were not found for the community standard and normative comparison groups | Maternal behaviour Q-set | Processes that were expected to change as a result of IPP included improvements in maternal representations of her own mother and increases in maternal sensitivity |
| Lieberman et al., 1991138 |
n = 100 Age Child mean age: 12 months Mother mean age: 25.08 years |
Low SES; anxiously attached dyads | Attachment security | Infant–parent psychotherapy | RCT |
Secure attachment control group Anxious attachment control group |
AQS at 24 months | There were no group differences on the AQS post intervention | N/A | N/A |
| Robert-Tissot et al., 1996139 |
n = 75 Age Child mean age: 15.6 months Father mean age: 33.9 years Mother mean age: 31.1 years |
Children referred to Child Guidance Clinic for sleep, feeding, and behavioural disorders | Maternal sensitivity | Psychodynamic Mother–Infant Psychotherapy | RCT | No control group | N/A | N/A | Ainsworth Sensitivity Scale | Maternal sensitivity to the infant’s signals increased after treatment |
| Salomonsson and Sandell, 2011140 |
n = 75 Child mean age IG: 4.4 months; CG: 5.9 months Mother mean age IG: 34.0 years; CG: 32.3 years Father mean age IG: 35.1 years; CG: 34.0 years |
Previously reported diagnoses of eating disorders, depression, or anxiety disorders | Maternal sensitivity | MIP | RCT | Routine care at child health centres | N/A | N/A | EAS | MIP treatment improved maternal sensitivity |
|
Salomonsson et al. , 2015141,142 Follow-up of Salomonsson and Sandell, 2011140 |
n = 66 | Previously reported diagnoses of eating disorders, depression or anxiety disorders | Attachment representations | MIP | RCT | Routine care at child health centres | Story Stem Assessment Profile | Between-group differences were non-significant | Emotional Availability Scale | There was no difference in sensitivity scores between groups at the 4.5-year follow-up |
| Cohen et al., 1999143 |
n = 67 WWW Child mean age 21.5 months (6.5 months) Mother mean age: 32.2 years (5.6 years) PPT Child mean age: 19.2 months (6.1 months) Mother mean age: 32.4 years (4.1 years) Ethnicity Not reported |
Referred to child mental health clinic | Maternal sensitivity and attachment | WWW, PPT | Non-randomised study | PPT (care as usual) | SSP | Infants in the WWW group were significantly more likely than infants in the PPT group to move towards either a secure or organised attachment relationship | N/A | N/A |
|
Cohen et al. , 2002144 Follow-up of Cohen et al. , 1999143 |
n = 58 WWW Child mean age: 21.7 months (6.7 months) Mother mean age: 32 years (4.8 years) PPT Child mean age: 19.4 months (6.2 months) Mother mean age: 32.4 years (3.9 years) Ethnicity Not reported |
Referred to child mental health clinic | Maternal sensitivity and attachment | WWW, PPT | Non-randomised study | PPT (care as usual) | SSP | In the WWW group, eight infants showed either retained or moved towards a secure attachment pattern (32%), and in the PPT group nine infants (36%) did so. There was no difference between groups | N/A | N/A |
| Barlow et al., 2016145 |
n = 31 Age Child mean age: ≤ 32 weeks’ gestation Mother mean age: 32 years (6.1 years) Ethnicity 67% white British, 33% mixed ethnic origin |
Parents of preterm infants | Maternal sensitivity | VIG | RCT | Care as usual | N/A | N/A | CARE index | There was a large (d = 0.86) but non-significant difference in sensitivity between the two groups, with intervention parents scoring above the cut-off point used to indicate the need for intervention, and parents in the control group scoring below the cut-off point |
| Hoffenkamp et al., 2015146 |
n = 150 Age Child age: birth Mother mean age: IG: 31.1 years (4.9 years); CG: 30.8 years (5.4 years) Father mean age: IG: 34.1 years (5.4 years); CG: 33.6 years (5.5 years) Ethnicity Mainly Dutch |
Infants born preterm | Maternal sensitivity | VIG | RCT | Treatment as usual | N/A | N/A | 15-minute recordings observed and coded | VIG proved to be effective in enhancing sensitive behaviour |
| James et al., 2013147 |
n = 3 Age Child age: A: 1, 11 years, B: 3, 10 years, C: 9 months Parent age: not reported Ethnicity Not reported |
Children congenitally profoundly deaf and pre-lingual, born to hearing mothers | Parental sensitivity | VIG | Case series | No control group | N/A | N/A | Emotional Availability Scale | Results for each case showed that there were some improvements in EAS sensitivity after the intervention and were maintained at follow-up |
| Kennedy et al., 2010148 |
n = 23 Age Child: NR Parent: NR Ethnicity Not reported |
Families places in a residential treatment centre with their children for 3 months | Parental sensitivity | VIG | Non-randomised study | Treatment as usual | N/A | N/A | CARE – index | The mean post-CARE-Index score went down slightly for the control group whereas it went up for the VIG intervention group. This result shows a significant effect size (d = 0.5) |
| Lam-Cassettar et al., 2015149 |
n = 14 Age Child mean age: 2 years 8 months Mother age: not reported Ethnicity 13 British, 1 Latvian |
Deaf/hard of hearing children | Maternal sensitivity | VIG | Non-randomised study | No control group | N/A | N/A | Emotional Availability Scale | There was a significant difference in scores of parental sensitivity according to the assessment visit with an increase from pre to post intervention |
| Pethica and Bigham, 2018150 |
n = 1 Participant characteristics: not reported |
Mother has intellectual disability Children were on the child protection register for emotional abuse |
Maternal sensitivity | VIG | Case study | No control group | N/A | N/A | Coding based on Biemans’ hierarchy of attuned interactions (1990) | There was an increase in sensitive interactions |
| Cicchetti et al., 1999151 |
n = 108 Age Child mean age: 20.40 months Mother mean age: 31.70 years Ethnicity Not reported |
Mothers with major depressive disorder | Attachment | Toddler–parent psychotherapy | RCT | Non-depressed mothers (control group) | Attachment Q-Set | Children in the intervention group reached rates of secure attachment that were comparable with those in the non-depressed control group | N/A | N/A |
| Toth et al., 200688 |
Depressed mothers: n = 130 Non-depressed mothers: n = 68 Age Mean child age: 20.34 months Mean mother age: 31.68 years Ethnicity Not reported |
Mothers who had experienced major depressive disorder since their child’s birth | Attachment | Toddler–parent psychotherapy | RCT | Control group and non-depressed comparison group (n = 68) | SSP | The rate of secure attachment increased substantially in the Intervention group and was higher than that for the control group and the non-depressed comparison group | N/A | N/A |
|
Stronach et al. , 2013152 Follow-up of Cicchetti et al. , 200687 |
n = 189 Age Child mean age: 13.31 months Mother mean age: 26.98 years Ethnicity 74.6% minority race |
Maltreated infants identified through Child Protective Service | Attachment | CPP | RCT | Psychoeducational parenting intervention or community standard | SSP | At follow-up, children in the CPP group had higher rates of secure and lower rates of disorganised attachment than did children in the psychoeducational parenting intervention or community standard group | N/A | N/A |
| Becker-Weidman, 2006153 |
n = 64 Age Child mean age: IG: 9.4 years (2.6); CG: 11.7 years (4) Mother age: not reported Ethnicity of child 88% Caucasian, 4% African American, 8% Asian |
Children had significant history of physical abuse, physical or psychological neglect, sexual abuse or institutional care and were experiencing PTSD | Attachment | DDP | Non-randomised study | Usual care | RADQ | RADQ scores decreased significantly for the treatment group, increased non-significantly for the control group | N/A | N/A |
|
Becker-Weidman, 2006154 Follow-up of Becker-Weidman, 2006153 |
n = 44 Follow-up: 4 years later |
Children had significant history of physical abuse, physical or psychological neglect, sexual abuse or institutional care and were experiencing PTSD | Attachment | DDP | Non-randomised study | Usual care | RADQ measures taken 4 years after children in the treatment group ended therapy | RADQ scores decreased significantly for the treatment group; the control group showed statistically significant deterioration in behaviour | N/A | N/A |
| Salo et al., 2020155 |
n = 18 Age Child mean age: 4.42 months Parent mean age: 34.90 years |
Children from outpatient psychiatric clinics with a diagnosis | Parental sensitivity | Theraplay | Non-randomised study | No control group | N/A | N/A | Emotional Availability Scale | There were improvements in parental sensitivity post intervention |
Appendix 3 Risk-of-bias assessment
| Authors and year | Random sequence | Allocation concealment | Blinding performance | Incomplete outcome | Selective reporting | Other sources of bias |
|---|---|---|---|---|---|---|
| Anisfeld et al., 1990 | Unclear | Unclear | Low | High | High | High |
| Barnett et al., 1985, 1987 | Unclear | Unclear | Low | High | Unclear | High |
| Bernard et al., 2012 | Unclear | Unclear | Low | Low | Low | Low |
| Brisch et al., 2003 | Unclear | Unclear | High | High | High | High |
| Cassidy et al., 2011 | Unclear | Unclear | Low | High | Unclear | High |
| Challacombe et al., 2017 | Low | Low | Low | High | Unclear | High |
| Cooper et al., 2009 | Low | Low | Low | High | Low | Low |
| Cooper et al., 2015 | Low | Low | Low | High | High | High |
| Fonagy et al., 2016 | Low | Low | Low | High | Low | High |
| Gradisar et al., 2016 | Low | Unclear | Low | Unclear | Low | High |
| Heinicke et al., 1999, 2000, 2001 | Low | Low | Low | Unclear | Unclear | High |
| Klein Velderman et al., 2006a, 2006 | Unclear | Unclear | Unclear | Low | High | High |
| Moran et al., 2005 | Unclear | Unclear | Unclear | Low | Low | Low |
| Moss et al., 2011 | Low | Unclear | Low | High | Unclear | High |
| Murray et al., 2003; Cooper et al., 2003 | Low | Unclear | Unclear | High | Unclear | High |
|
Stronach et al. , 2013 Cicchetti et al. , 2006 |
Unclear | Unclear | Low | High | Unclear | High |
| Tereno et al., 2016 | Low | Low | Low | Low | High | High |
| Toth et al., 2006; Cicchetti et al., 1999 | Low | Unclear | Low | High | High | High |
| van den Boom, 1994, 1995 | Unclear | Unclear | Low | Unclear | High | High |
Appendix 4 Search strategy for systematic reviews
Appendix 5 Reference list of excluded studies for systematic reviews
Review 1
World Health Organisation. A Randomised Controlled Trial to Evaluate ‘SAFE® - Basic Trust’, an Intervention to Support Attachment Security and Parental Mentalization. 2019. URL: https://trialsearch.who.int/Trial2.aspx?TrialID=DRKS00013099 (accessed 21 September 2021).
Adeli M, Aradmehr M. A comparative study of maternal-neonate abdominal and kangaroo (skin-to-skin) skin contact immediately after birth on maternal attachment behaviors up to 2 months. J Educ Health Promot 2018;7:42.
US National Library of Medicine. Affective Touching on Poststroke Depression. 2018. URL: https://clinicaltrials.gov/show/NCT03789994 (accessed 21 September 2021).
Akbarzadeh M, Dokuhaki A, Joker A, Pishva N, Zare N. Teaching attachment behaviors to pregnant women: a randomized controlled trial of effects on infant mental health from birth to the age of three months. Ann Saudi Med 2016;36:175–83. https://doi.org/10.5144/0256-4947.2016.175
Alghali H. Professionals’Perception of the Process of Change During an Attachment Based Parenting Intervention (Video Interaction Guidance) with Parents with Intellectual Disabilities. PhD thesis. London: Royal Holloway, University of London; 2019.
Alsancak-Akbulut C, Sahin-Acar B, Sumer N. Effect of video-feedback intervention on Turkish mothers’ sensitivity and physical intrusiveness: a randomized control trial [published online ahead of print April 20 2020]. Attach Hum Dev 2020. https://doi.org/10.1080/14616734.2020.1753085
Alto ME, Petrenko CLM. Fostering secure attachment in low- and middle-income countries: suggestions for evidence-based interventions. Eval Program Plann 2017;60:151–65.
Anis L, Letourneau N, Benzies K, Ewashen C, Hart MJ. Effect of the attachment and child health parent training program on parent-child interaction quality and child development. Can J Nurs Res 2020;52:157–68. https://doi.org/10.1177/0844562119899004
Bailhache M, Doyle O, Salmi LR, McDonnell T. Does maternal attachment to her infant mediate the link between perceptions of infant crying at 6 months and parenting stress at 24 months? A structural equation modelling approach. Child Care Health Dev 2019;45:540–50. https://doi.org/10.1111/cch.12676
Bakermans-Kranenburg MJ, van IJzendoorn MH, Juffer F. Disorganized infant attachment and preventive interventions: a review and meta-analysis. InfantMentHealthJ 2005;26:191–216.
Balakrishna R, Teixeira M, Meyrick J, Hart R. Can infant massage programmes improve attachment between mother and baby? Community Pract 2019;92:45–7.
Balldin S, Fisher PA, Wirtberg I. Video feedback intervention with children: a systematic review. Res Soc Work Pract 2018;28:682–95.
Bark C, Georg A, Taubner S. Infant/toddler-parent psychotherapy (SKEPT). Treatment of early childhood regulatory disorders. Psychotherapeut 2018;63:367–72.
Barlow J, Bennett C, Midgley N, Larkin SK, Wei Y. Parent-infant psychotherapy for improving parental and infant mental health. Cochrane Database Syst Rev 2015;1:CD010534. https://doi.org/10.1002/14651858.CD010534.pub2
Barlow J, Herath NI, Bartram Torrance C, Bennett C, Wei Y. The Neonatal Behavioral Assessment Scale (NBAS) and Newborn Behavioral Observations (NBO) system for supporting caregivers and improving outcomes in caregivers and their infants. Cochrane Database Syst Rev 2018;3:CD011754. https://doi.org/10.1002/14651858.CD011754.pub2
Barlow J, Schrader-McMillan A, Axford N, Wrigley Z, Sonthalia S, Wilkinson T, et al. Review: attachment and attachment-related outcomes in preschool children – a review of recent evidence. Child Adolesc Ment Health 2016;21:11–20. https://doi.org/10.1111/camh.12138
Bergström M, Gebreslassie M, Hedqvist M, Lindberg L, Sarkadi A, Hjern A. Narrative review of interventions suitable for well-baby clinics to promote infant attachment security and parents’ sensitivity. Acta Paediatr 2020;109:1745–57. https://doi.org/10.1111/apa.15212
Berlin LJ, Martoccio TL, Bryce CI, Jones Harden B. Improving infants’ stress-induced cortisol regulation through attachment-based intervention: a randomized controlled trial. Psychoneuroendocrinology 2019;103:225–32.
Berlin LJ, Martoccio TL, Jones Harden B. Improving early head start’s impacts on parenting through attachment-based intervention: a randomized controlled trial. Dev Psychol 2018;54:2316–27. https://doi.org/10.1037/dev0000592
Bernard K, Frost A, Jelinek C, Dozier M. Secure attachment predicts lower body mass index in young children with histories of child protective services involvement. Pediatr Obes 2019;14:e12510. https://doi.org/10.1111/ijpo.12510
Bernard K, Simons R, Dozier M. Effects of an attachment-based intervention on child protective services–referred mothers’ event-related potentials to children’s emotions. Child Dev 2015;86:1673–84.
Bindt C. Infant colic, persistent fuzziness and bonding experiences: widening the scope beyond attachment theory. Monatsschrift Kinderheilkunde 2018;166:912–4.
Blizzard AM, Barroso NE, Ramos FG, Graziano PA, Bagner DM. Behavioral parent training in infancy: what about the parent-infant relationship? J Clin Child Adolesc Psychol 2018;47(Suppl. 1):S341–53. https://doi.org/10.1080/15374416.2017.1310045
Borelli JL, Smiley PA, Kerr ML, Hong K, Hecht HK, Blackard MB, et al. Relational savoring: an attachment-based approach to promoting interpersonal flourishing. Psychotherapy 2020;57:340–51. https://doi.org/10.1037/pst0000284
Boris NW, Renk K. Beyond reactive attachment disorder: how might attachment research inform child psychiatry practice? Child Adolesc Psychiatr Clin N Am 2017;26:455–76.
Bosmans G. Cognitive behaviour therapy for children and adolescents: can attachment theory contribute to its efficacy? Clin Child Fam Psychol Rev 2016;19:310–28. https://doi.org/10.1007/s10567-016-0212-3
Brennan J. The Circle of Security intervention: enhancing attachment in early parent-child relationships. J Reprod Infant Psychol 2017;35:207–8. https://doi.org/10.1080/02646838.2016.1277193
Browne JV. Recorded Maternal Voice, Recorded music, or live intervention: a bioecological perspective. In Filippa M, Kuhn P, Westrup B, editors. Early Vocal Contact and Preterm Infant Brain Development. Cham: Springer; 2017. pp. 183–201.
Bryson SA, Gauvin E, Jamieson A, Rathgeber M, Faulkner-Gibson L, Bell S, et al. What are effective strategies for implementing trauma-informed care in youth inpatient psychiatric and residential treatment settings? A realist systematic review. Int J Ment Health Syst 2017;11:36. https://doi.org/10.1186/s13033-017-0137-3
Buckwalter KD, Reed D. Attachment Theory in Action: Building Connections Between Children and Parents. Lanham, MD: Rowman & Littlefield; 2017.
Byrne G, Sleed M, Midgley N, Fearon P, Mein C, Bateman A, Fonagy P. Lighthouse Parenting Programme: description and pilot evaluation of mentalization-based treatment to address child maltreatment. Clin Child Psychol Psychiatry 2019;24:680–93. https://doi.org/10.1177/1359104518807741
Camoirano A. Mentalizing makes parenting work: a review about parental reflective functioning and clinical interventions to improve it. Front Psychol 2017;8:14. https://doi.org/10.3389/fpsyg.2017.00014
Carr A. Family therapy and systemic interventions for child-focused problems: the current evidence base. J Fam Ther 2019;41:153–213.
Carr A. Family therapy for adolescents: a research-informed perspective. Aust N Z J Fam Ther 2016;37:467–79.
Casonato M, Nazzari S, Frigerio A. Feasibility and efficacy of an attachment-based intervention in a maltreatment sample in residential care: a pilot study. Clin Child Psychol Psychiatry 2017;22:561–71. https://doi.org/10.1177/1359104517719115
Cavett AM. Integrative attachment informed cognitive behavioral play therapy (IAI-CBPT) for children with medical trauma. In Rubin LC, editor. Handbook of Medical Play Therapy and Child Life: Interventions in Clinical and Medical Settings. New York, NY: Routledge; 2017. pp. 131–53.
Challacombe FL, Salkovskis PM, Woolgar M, Wilkinson EL, Read J, Acheson R. A pilot randomized controlled trial of time-intensive cognitive-behaviour therapy for postpartum obsessive-compulsive disorder: effects on maternal symptoms, mother-infant interactions and attachment. Psychol Med 2017;47:1478–88. https://doi.org/10.1017/S0033291716003573
Chamberlain C, Gee G, Harfield S, Campbell S, Brennan S, Clark Y, et al. Parenting after a history of childhood maltreatment: a scoping review and map of evidence in the perinatal period. PLOS ONE 2019;14:e0213460. https://doi.org/10.1371/journal.pone.0213460
Chen EM, Gau ML, Liu CY, Lee TY. Effects of father-neonate skin-to-skin contact on attachment: a randomized controlled trial. Nurs Res Pract 2017;2017:8612024. https://doi.org/10.1155/2017/8612024
Cierpka M. Treatment approaches for regulatory disorders. In Cierpka M, editor. Regulatory Disorders in Infants: Assessment, Diagnosis, and Treatment. Cham: Springer International Publishing; 2016. pp. 181–200.
Cohen JA. Trauma-Focused CBT for Preschool Children. Paper presented at the 66th Annual Meeting of the American Academy of Child & Adolescent Psychiatry, Chicago, IL, USA, 14–19 October 2019.
Cohen JA. Trauma-Focused Psychotherapies for Early Interpersonal Trauma. Paper presented at the 65th Annual Meeting of the American Academy of Child & Adolescent Psychiatry, Seattle, WA, USA, 22–27 October 2018.
Colegrove VM, Havighurst SS. Review of nonverbal communication in parent–child relationships: assessment and intervention. J Child Fam Stud 2017;26:574–90.
Compitus K. Traumatic pet loss and the integration of attachment-based animal assisted therapy. J Psychother Integr 2019;29:119.
World Health Organisation. Confidence in Care Evaluation. 2017. URL: https://trialsearch.who.int/Trial2.aspx?TrialID=ISRCTN19090228 (accessed September 2021).
Cooper PJ, De Pascalis L, Woolgar M, Romaniuk H, Murray L. Attempting to prevent postnatal depression by targeting the mother-infant relationship: a randomised controlled trial. Prim Health Care Res Dev 2015;16:383–97. https://doi.org/10.1017/S1463423614000401
US National Library of Medicine. COS-P for Parents of Children Referred to Child Psychiatric Services. 2018. URL: https://clinicaltrials.gov/show/NCT03578016 (accessed 21 September 2021).
Cowan PA, Cowan CP, Pruett MK, Pruett K. Fathers’ and mothers’ attachment styles, couple conflict, parenting quality, and children’s behavior problems: an intervention test of mediation. Attach Hum Dev 2019;21:532–50. https://doi.org/10.1080/14616734.2019.1582600
Cozza SJ. 4.4 Childhood adversity, trauma, and psychiatric disorders: developmental outcomes and effective interventions. J Am Acad Child Adolesc Psychiatry 2016;10(Suppl.):S91.
Creighton AL. Play Songs and Lullabies: Features of Emotional Communication and Developing Mother-Infant Attachment. PhD thesis. Sydney, NSW: University of Western Sydney; 2014.
Crugnola CR, Ierardi E, Albizzati A, Downing G. Promoting responsiveness, emotion regulation, and attachment in young mothers and infants: an implementation of video intervention therapy and psychological support. In Steele H, Steele M, editors. Handbook of Attachment-based Interventions. New York, NY: Guilford Press; 2017. pp. 441–65.
Cyr C, Alink LR. Child maltreatment: the central roles of parenting capacities and attachment. Curr Opin Psychol 2017;15:81–6.
Cyr C, Poulin C, Losier V, Michel G, Paquette D. [Assessing parenting capacity in child protection cases (0–5 years old): an attachment-based assessment and intervention protocol.] Revuede Psychoeducation 2012;41:155–77.
De Oliveira C, Rahioui H, Smadja M, Gorsane MA, Louppe F. [Mentalization based treatment and borderline personality disorder.] Encephale 2017;43:340–5.
Deans CL. Maternal sensitivity, its relationship with child outcomes, and interventions that address it: a systematic literature review. Early Child Dev Care 2020;190:252–75.
Dehghani-Arani F, Besharat MA, Fitton VA, Aghamohammadi A. Efficacy of an attachment-based intervention model on health indices in children with chronic disease and their mothers. Adm Policy Ment Health 2018;45:900–10. https://doi.org/10.1007/s10488-018-0873-y
Dennis CL, Grigoriadis S, Zupancic J, Kiss A, Ravitz P. Telephone-based nurse-delivered interpersonal psychotherapy for postpartum depression: nationwide randomised controlled trial. Br J Psychiatry 2020;216:189–96. https://doi.org/10.1192/bjp.2019.275
Diamond DJ, Diamond MO. Parenthood after reproductive loss: how psychotherapy can help with postpartum adjustment and parent-infant attachment. Psychotherapy 2017;54:373–9. https://doi.org/10.1037/pst0000127
Diamond G, Russon J, Levy S. Attachment-based family therapy: a review of the empirical support. Fam Process 2016;55:595–610. https://doi.org/10.1111/famp.12241
Donato S, Bertoni A. Positive parenting as responsible care: risks, protective factors, and intervention evaluation. J Prev Interv Community 2017;45:151–5.
Donelan-McCall D. The Nurse-Family Partnership: theoretical and empirical foundations. In Steele H, Steele M, editors. Handbook of Attachment-based Interventions. New York, NY: Guilford Press; 2018. pp. 79–103.
Dong S, Liang X, Zhang Y, Wang Z. Maternal positive parenting behaviors and toddler’s compliance: prediction from maternal sensitivity in infancy and bidirectional effects of autonomy encouragement in toddlerhood. Acta Psychol Sin 2017;49:460–71.
Doyle C, Cicchetti D. From the cradle to the grave: the effect of adverse caregiving environments on attachment and relationships throughout the lifespan. Clin Psychol 2017;24:203–17. https://doi.org/10.1111/cpsp.12192
Dozier M, Bernard K. Attachment and Biobehavioral Catch-up: addressing the needs of infants and toddlers exposed to inadequate or problematic caregiving. Curr Opin Psychol 2017;15:111–17. https://doi.org/10.1016/j.copsyc.2017.03.003
Dozier M, Bernard KR, Roben CK. Attachment and biobehavioral catch-up. In Steele H, Steele M, editors. Handbook of Attachment-based Interventions. New York, NY: Guilford Press; 2017. pp. 27–49.
Dozier M, Roben CKP, Caron E, Hoye J, Bernard K. Attachment and Biobehavioral Catch-up: an evidence-based intervention for vulnerable infants and their families. Psychother Res 2018;28:18–29. https://doi.org/10.1080/10503307.2016.1229873
World Health Organisation. Efficacy of Parent Infant Psychotherapy by Children with Regulatory Disorders as Part of the SKKIPPI Study. 2019. URL: https://trialsearch.who.int/Trial2.aspx?TrialID=DRKS00017008 (accessed September 2021).
Dubois-Comtois K, Cyr C, Tarabulsy GM, St-Laurent D, Bernier A, Moss E. Testing the limits: extending attachment-based intervention effects to infant cognitive outcome and parental stress. Dev Psychopathol 2017;29:565–74. https://doi.org/10.1017/S0954579417000189
Dumesnil J. The contagion of trauma: exploring attachment through the book Love Lessons. In Baker M, Ford J, Canfield B, Grabb T, editors. Identifying, Treating, and Preventing Childhood Trauma in Rural Communities. Hershey, PA: IGI Global; 2016. pp. 225–47.
Eckstein M, Zietlow AL, Gerchen MF, Schmitgen MM, Ashcroft-Jones S, Kirsch P, Ditzen B. The NeMo real-time fMRI neurofeedback study: protocol of a randomised controlled clinical intervention trial in the neural foundations of mother-infant bonding. BMJ Open 2019;9:e027747. https://doi.org/10.1136/bmjopen-2018-027747
Eckstein-Madry, T.A., Lieselotte. [Children from socially disadvantaged families - how attachment deficits and behaviour problems can be reduced through child care attendance.] Familiendynamik 2016:41:304–11.
World Health Organisation. Effect of Maternal Attachment Behaviors on the Health of Premature Infants. 2018. URL: https://trialsearch.who.int/Trial2.aspx?TrialID=IRCT20180718040513N1 (accessed September 2021).
World Health Organisation. Effect of Training on Acceptance of Maternal Role. 2018. URL: https://trialsearch.who.int/Trial2.aspx?TrialID=IRCT20171026037022N3 (accessed September 2021).
US National Library of Medicine. Effects of Baby Massage on Parenting Stress and Attachment in Premature. 2020. URL: https://clinicaltrials.gov/show/NCT04255797 (accessed 21 September 2021).
US National Library of Medicine. Effects of Father-Neonate Skin-to-Skin Contact on Attachment. 2018. URL: https://clinicaltrials.gov/show/NCT02886767 (accessed 21 September 2021).
US National Library of Medicine. Efficacy of Family Programs for Improving Child and Family Health and Development. 2018. URL: https://clinicaltrials.gov/show/NCT03367845 (accessed 21 September 2021).
World Health Organisation. Efficacy of Parent Infant Psychotherapy by Mothers with Postpartum Psychopathological Disorders as Part of the SKKIPPI Study. 2019. URL: https://trialsearch.who.int/Trial2.aspx?TrialID=DRKS00016353 (accessed September 2021).
Espinet SD, Motz M, Jeong JJ, Jenkins JM, Pepler D. ‘Breaking the Cycle’ of maternal substance use through relationships: a comparison of integrated approaches. Addict Res Theory 2016;24:375–88.
US National Library of Medicine. Evaluating the Efficacy of ABC for High-Risk Parent and Infants. 2016. URL: https://clinicaltrials.gov/show/NCT02647463 (accessed 21 September 2021).
World Health Organisation. Evaluation of the Exploring Together Program for Primary School Children with Behavioural and Emotional Problems. 2017. URL: https://anzctr.org.au/Trial/Registration/TrialReview.aspx?ACTRN=12617001523392 (accessed September 2021).
Evans T, Boyd RN, Colditz P, Sanders M, Whittingham K. Mother-very preterm infant relationship quality: RCT of baby triple P. J Child Fam Stud 2017;26:284–95.
Ewing ESK, Levy SA, Scott SA, Diamond GS. Attachment-based family therapy for adolescent depression and suicide risk. In Steele H, Steele M, editors. Handbook of Attachment-based Interventions. New York, NY: Guilford Press; 2018. pp. 79–103.
Facompré CR, Bernard K, Waters TEA. Effectiveness of interventions in preventing disorganized attachment: a meta-analysis. Dev Psychopathol 2018;30:1–11. https://doi.org/10.1017/S0954579417000426
Field T. Postnatal anxiety prevalence, predictors and effects on development: a narrative review. Infant Behav Dev 2018;51:24–32.
Filippa M. Early Vocal Contact: Direct talking and singing to preterm infants in the NICU. In Filippa M, Kuhn P, Westrup B, editors. Early Vocal Contact and Preterm Infant Brain Development. Cham: Springer; 2017. pp. 133–50.
Fisher PA, Gunnar MR, Dozier M, Bruce J, Pears KC. Effects of therapeutic interventions for foster children on behavioral problems, caregiver attachment, and stress regulatory neural systems. Ann N Y Acad Sci 2006;1094:215–25.
Fisher PA, Skowron EA. Social-learning parenting intervention research in the era of translational neuroscience. Curr Opin Psychol 2017;15:168–73.
Fonagy P, Sleed M, Baradon T. Randomized controlled trial of parent–infant psychotherapy for parents with mental health problems and young infants. Infant Ment Health J 2016;37:97–114. https://doi.org/10.1002/imhj.21553
Fonagy P. What makes a difference? Supporting families in caring for children. In Leach P, editor. Transforming Infant Wellbeing: Research, Policy and Practice for the First 1001 Critical Days. London: Routledge; 2017. pp. 129–38.
Foulon S, Greacen T, Pasquet B, Dugravier R, Saïas T, Guedeney N, et al. Predictors of study attrition in a randomized controlled trial evaluating a perinatal home-visiting program with mothers with psychosocial vulnerabilities. PLOS ONE 2015;10:e0142495. https://doi.org/10.1371/journal.pone.0142495
Fox NA, Nelson CA, Zeanah CH. The effects of psychosocial deprivation on attachment: lessons from the Bucharest Early Intervention Project. Psychodyn Psychiatry 2017;45:441–50. https://doi.org/10.1521/pdps.2017.45.4.441
Gardiner E, Iarocci G, Moretti M. Integrative care for adolescents with dual diagnosis: considering trauma and attachment within an innovative model for clinical practice. J Ment Health Res Intellect Disabil 2017;10:321–44.
Girard EI, Wallace NM, Kohlhoff JR, Morgan SS, McNeil CB. Parent-Child Interaction Therapy with Toddlers. Improving Attachment and Emotional Regulation. Cham: Springer International Publishing; 2018.
Glibota LC, Lindaman S, Coleman A. Theraplay as a treatment for children with selective mutism: integrating the polyvagal theory, attachment theory, and social communication. In Drewes AA, Schaefer CE, editors. Play-based Interventions for Childhood Anxieties, Fears, and Phobias. New York, NY: Guilford Press; 2018. pp. 124–43.
Golding KS. The development of DDP-informed parenting groups for parents and carers of children looked after or adopted from care. Adopt Foster 2019;43:400–12.
Gradisar M, Jackson K, Spurrier N, Gibson J, Whitham J, Sved-Williams A, Dolby R, Kennaway D. A Randomised Controlled Trial of Behavioural Treatments for Infant Sleep Problems: Effects on Sleep, Infant and Maternal Stress, and Attachment. Paper presented at the 23rd Congress of the European Sleep Research Society, Bologna, Italy, 13–16 September 2016.
Gradisar M, Jackson K, Spurrier NJ, Gibson J, Whitham J, Williams AS, et al. Behavioral interventions for infant sleep problems: a randomized controlled trial. Pediatrics 2016;137:e20151486. https://doi.org/10.1542/peds.2015-1486
Graffi J, Moss E, Jolicoeur-Martineau, Moss G, Lecompte V, Pascuzzo K, et al. The dopamine D4 receptor gene, birth weight, early maternal care, maternal depression over the postnatal time period and the prediction of disorganized attachment at 36 months of age: a prospective gene x environment analysis. Infant Behav Dev 2018;50:64–77.
Granqvist P, Sroufe LA, Dozier M, Hesse E, Steele M, van IJzendoorn M, et al. Disorganized attachment in infancy: a review of the phenomenon and its implications for clinicians and policy-makers. Attach Hum Dev 2017;19:534–58. https://doi.org/10.1080/14616734.2017.1354040
Grecucci A, Messina I, Dadomo H. Decoupling internalized dysfunctional attachments: a combined ACT and Schema Therapy approach. Front Psychol 2018;9:2332. https://doi.org/10.3389/fpsyg.2018.02332
Green E, Baggerly J, Myrick A. Play Therapy with Preteens. Lanham, MD: Rowman & Littlefield; 2018.
Gregory M, Kannis-Dymand L, Sharman R. A review of attachment-based parenting interventions: recent advances and future considerations. AustJPsychol 2020;72:109–22.
Guild DJ, Alto ME, Toth SL. Preventing the intergenerational transmission of child maltreatment through relational interventions. In Teti DM, editor. Parenting and Family Processes in Child Maltreatment and Intervention. Cham: Springer; 2017. pp. 127–37.
Guild DJ, Toth SL, Handley ED, Rogosch FA, Cicchetti D. Attachment security mediates the longitudinal association between child-parent psychotherapy and peer relations for toddlers of depressed mothers. Dev Psychopathol 2017;29:587–600. https://doi.org/10.1017/S0954579417000207
Guild DJ. Affective Expression and Relationship Cohesion Between Depressed Mothers and Their Offspring: A Longitudinal Examination of the Effects of Child-Parent Psychotherapy. PhD thesis. Rochester, NY: University of Rochester; 2017.
Guyon-Harris KL, Humphreys KL, Degnan K, Fox NA, Nelson CA, Zeanah CH. A prospective longitudinal study of Reactive Attachment Disorder following early institutional care: considering variable- and person-centered approaches. Attach Hum Dev 2019;21:95–110. https://doi.org/10.1080/14616734.2018.1499208
Guyon-Harris KL, Humphreys KL, Fox NA, Nelson CA, Zeanah CH. Course of disinhibited social engagement disorder from early childhood to early adolescence. J Am Acad Child Adolesc Psychiatry 2018;57:329–35.e2.
Haley M. Attachment-based approaches. In Vossler A, Havard C, Pike G, Barker M, Raabe B, editors. Mad or Bad?: A Critical Approach to Counselling and Forensic Psychology. 19th edn. Thousand Oaks, CA: SAGE Publications Inc; 2017. pp. 189–203.
Handley ED, Michl-Petzing LC, Rogosch FA, Cicchetti D, Toth SL. Developmental cascade effects of interpersonal psychotherapy for depressed mothers: longitudinal associations with toddler attachment, temperament, and maternal parenting efficacy. Dev Psychopathol 2017;29:601–15. https://doi.org/10.1017/S0954579417000219
Haslbeck F, Hugoson P. Sounding together: family-centered music therapy as facilitator for parental singing during skin-to-skin contact. In Filippa M, Kuhn P, Westrup B, editors. Early Vocal Contact and Preterm Infant Brain Development Cham, Springer; 2017. pp. 217–38.
Heckman JJ, Karapakula G. The Perry Preschoolers at Late Midlife: A Study in Design-Specific Inference. Cambridge, MA: National Bureau of Economic Research; 2019.
Hendry A. The imprint of another life: assessment and dyadic parent child art psychotherapy with an adoptive family. In Meyerowitz-Katz J, Reddick D, editors. Art Therapy in the Early Years: Therapeutic Interventions with Infants, Toddlers and Their Families. London: Routledge; 2016.
Hermenau K, Goessmann K, Rygaard NP, Landolt MA, Hecker T. Fostering child development by improving care quality: a systematic review of the effectiveness of structural interventions and caregiver trainings in institutional care. Trauma Violence Abuse 2017;18:544–61. https://doi.org/10.1177/1524838016641918
Hocson SM, Sacayan RL. OR0380 Resiliency, attachment style, and sex role orientation among children of overseas Filipino workers: implications for a proposed Cosp intervention program. Int J Psychol 2016;51:266–94.
Hornor G. Attachment disorders. J Pediatr Health Care 2019;33:612–22.
Hughes DA, Golding KS, Hudson J. Healing Relational Trauma with Attachment-Focused Interventions: Dyadic Developmental Psychotherapy with Children and Families. New York, NY: WW Norton & Company; 2019.
US National Library of Medicine. Intervening Early: Key Adolescent Outcomes. 2019. URL: https://clinicaltrials.gov/show/NCT04168684 (accessed 22 September 2021).
Isobel S, Goodyear M, Furness T, Foster K. Preventing intergenerational trauma transmission: a critical interpretive synthesis. J Clin Nurs 2019;28:1100–13. https://doi.org/10.1111/jocn.14735
Ispanovic VI, Ignjatovic M. Enhancing mother child interaction in neonatal period. J Perinat Med 2017;45(Suppl. 2):138.
Jahnke-Majorkovits AC, Buchheim A. [Attachment based short intervention during inpatient treatment of adolescents.] Prax Kinderpsychol Kinderpsychiatr 2018;67:367–85.
Jarvis P. Attachment theory, cortisol and care for the under-threes in the twenty-first century: constructing evidence-informed policy. Early Years 2020;15:1–5.
Jonkman CS, Schuengel C, Oosterman M, Lindeboom R, Boer F, Lindauer RJL. Effects of Multidimensional Treatment Foster Care for Preschoolers (MTFC-P) for young foster children with severe behavioral disturbances. J Child Fam Stud 2017;26:1491–503. https://doi.org/10.1007/s10826-017-0661-4
World Health Organisation. Investigating the Effects of Parent Training for Mothers of Children with ADHD and its Effect on Parental Stress – A Randomised Control Trial. 2019. URL: https://trialsearch.who.int/Trial2.aspx?TrialID=JPRN-UMIN000038693 (accessed September 2021).
Juffer F, Bakermans-Kranenburg MJ, van IJzendoorn MH. Pairing attachment theory and social learning theory in video-feedback intervention to promote positive parenting. Curr Opin Psychol 2017;15:189–94.
Juffer F, Struis E, Werner C, Bakermans-Kranenburg MJ. Effective preventive interventions to support parents of young children: illustrations from the Video-feedback Intervention to promote Positive Parenting and Sensitive Discipline (VIPP-SD). J Prev Interv Community 2017;45:202–14. https://doi.org/10.1080/10852352.2016.1198128
Julal FS. Holding the baby: using the Leiden Infant Simulator Sensitivity Assessment to examine attachment theory’s sensitivity hypothesis. Psychol Learn Teach 2018;17:229–41.
Julian MM, McCall RB, Groark CJ, Muhamedrahimov RJ, Palmov OI, Nikiforova NV. Development of children adopted to the United States following a social-emotional intervention in St. Petersburg (Russian Federation) institutions. Appl Dev Sci 2019;23:273–93. https://doi.org/10.1080/10888691.2017.1420480
Kasparian NA, Kan JM, Sood E, Wray J, Pincus HA, Newburger JW. Mental health care for parents of babies with congenital heart disease during intensive care unit admission: systematic review and statement of best practice. Early Hum Dev 2019;139:104837.
Katzman J, Del Fabbro A. Attachment in the psychiatric curriculum. Psychodyn Psychiatry 2017;45:564–87. https://doi.org/10.1521/pdps.2017.45.4.564
Keller H. Universality claim of attachment theory: children’s socioemotional development across cultures. Proc Natl Acad Sci U S A 2018;115:11414–19. https://doi.org/10.1073/pnas.1720325115
Kelly D, Paul M. Veterans-by-proxy: a conceptual framework of ambiguous loss among children of combat veterans. J Fam Soc Work 2018;21:255–70.
Kemmis-Riggs J, Dickes A, McAloon J. Program components of psychosocial interventions in foster and kinship care: a systematic review. Clin Child Fam Psychol Rev 2018;21:13–40. https://doi.org/10.1007/s10567-017-0247-0
Kennedy H, Underdown A. Video interaction guidance: promoting secure attachment and optimal development for children, parents and professionals. In Leach, P, editor. Transforming Infant Wellbeing. London: Routledge; 2017. pp. 224–37.
Kim AR, Kim SY, Yun JE. Attachment and relationship-based interventions for families during neonatal intensive care hospitalization: a study protocol for a systematic review and meta-analysis. Syst Rev 2020;9:61. https://doi.org/10.1186/s13643-020-01331-8
Kim S, Kochanska G. Relational antecedents and social implications of the emotion of empathy: evidence from three studies. Emotion 2017;17:981–92. https://doi.org/10.1037/emo0000297
Kindler H. [Child maltreatment and new morbidity in pediatrics: consequences for early child support and child protective interventions.] Bundesgesundheitsbl 2016;59:1332–6. https://doi.org/10.1007/s00103-016-2428-2
Kingsley K, Sagester G, Weaver LL. Interventions supporting mental health and positive behavior in children ages birth-5 Yr: a systematic review. Am J Occup Ther 2020;74:7402180050p1–29. https://doi.org/10.5014/ajot.2020.039768
Kissgen R, Franke S. An attachment research perspective on ADHD. Neuropsychiatr 2016;30:63–8. https://doi.org/10.1007/s40211-016-0182-1
Kleinbub JR. State of the art of interpersonal physiology in psychotherapy: a systematic review. Front Psychol 2017;8:2053.
Knight RM, Albright JJ, Huth-Bocks A, Morris NK, Mills L, Klok K, et al. Impact of behavioral feeding intervention on child emotional and behavioral functioning, parenting stress, and parent-child attachment. J Pediatr Gastroenterol Nutr 2019;69:383–7. https://doi.org/10.1097/MPG.0000000000002382
Kobak RR, Kerig PK. Introduction to the special issue: attachment-based treatments for adolescents. Attach Hum Dev 2015;17:111–18. https://doi.org/10.1080/14616734.2015.1006382
Koehn AJ, Kerns KA. Parent-child attachment: meta-analysis of associations with parenting behaviors in middle childhood and adolescence. Attach Hum Dev 2018;20:378–405. https://doi.org/10.1080/14616734.2017.1408131
Kondili E, Duryea DG. The role of mother-infant bond in neonatal abstinence syndrome (NAS) management. Arch Psychiatr Nurs 2019;33:267–74.
Landers AL, McLuckie A, Cann R, Shapiro V, Visintini S, MacLaurin B, et al. A scoping review of evidence-based interventions available to parents of maltreated children ages 0–5 involved with child welfare services. Child Abuse Negl 2018;76:546–60.
Lanktree CB, Briere JN. Treating Complex Trauma in Children and Their Families: An Integrative Approach. New York, NY: SAGE Publications Ltd; 2015.
Larkin F, Oostenbroek J, Lee Y, Hayward E, Meins E. Proof of concept of a smartphone app to support delivery of an intervention to facilitate mothers’ mind-mindedness. PLOS ONE 2019;14:e0220948. https://doi.org/10.1371/journal.pone.0220948
Lauren, S. Parental Substance Misuse and Social Worker Intervention. Glasgow: IRISS; 2017.
Lescalier-Grosjean I, Vander Vorst C. Therapeutic groups for children: between singularity and bond(s). Psychothérapies 2016;36:35–46.
Levy KN, Johnson BN. Attachment and psychotherapy: implications from empirical research. Can Psychol 2019;60:178–93.
Lien F, Jolly K, Noonan N. A critical response to Jean Mercer’s article: conventional and unconventional perspectives on attachment and attachment problems: comparisons and implications. The Institute for Attachment and Child Development Model. Child Adolesc Soc Work J 2019;36:111–7.
Lind T, Bernard K, Yarger HA, Dozier M. Promoting compliance in children referred to Child Protective Services: a randomized clinical trial. Child Dev 2020;91:563–76. https://doi.org/10.1111/cdev.13207
Longhi E, Murray L, Hunter R, Wellsted D, Taylor-Colls S, MacKenzie K. The NSPCC UK Minding the Baby®(MTB) home visiting programme, supporting young mothers (aged 14-25) in the first two years of life: study protocol for a randomized controlled trial. Trials 2016;17:486.
Losinski M, Katsiyannis A, White S, Wiseman N. Addressing the complex needs of students with attachment disorders. Interv Sch Clin 2016;51:184–7.
Louca EP, Kyriakides S. Attachment, trust, love and personality development. In Zamosteanu A, editor. Theoretical and Applied in Psychology. Bologna: Medimond; 2016. pp. 135–8.
Lovelock H, Eisenbruch M. Forced adoption: clinical implications and treatment guidelines. Aust N Z J Psychiatr 2016;50:117.
Luby JL. The primacy of parenting. J Child Psychol Psychiatr 2020;61:399–400.
Lumsden V. Does the evidence support parent-infant psychotherapy? Commentary on… Cochrane Corner. BJ Psych Adv 2017;23:217–21.
Mahmoudi P, Elyasi F, Nadi A, Shirvani MA. Effect of maternal–fetal/neonatal attachment interventions on perinatal anxiety and depression: a narrative review. J Nurs Midwifery Sci 2020;7:126.
Mathews S, Onwumere J, Bissoli S, Ruggeri M, Kuipers E, Valmaggia L. Measuring attachment and parental bonding in psychosis and its clinical implications. Epidemiol Psychiatr Sci 2016;25:142–9. https://doi.org/10.1017/S2045796014000730
Matos I, Tereno S, Wendland J, Guédeney N, Panaccione E, Fuentealba L. [Maternal sensitivity and attachment security in an early intervention project.] Neuropsychiatr Enfance Adolesc 2017;65:219–24.
Maya J, Hidalgo V, Jiménez L, Lorence B. Effectiveness of Scene-based Psychodramatic Family Therapy (SB-PFT) in adolescents with behavioural problems. Health Soc Care Community 2020;28:555–67. https://doi.org/10.1111/hsc.12888
Maya J, Lorence B, Hidalgo V, Jiménez L. The role of psychosocial stress on a family-based treatment for adolescents with problematic behaviors. Int J Environ Res Public Health 2018;15:1867.
McKenzie R, Dallos R, Stedmon J, Hancocks H, Vickery PJ, Ewings P, et al. SAFE, a new therapeutic intervention for families of children with autism: study protocol for a feasibility randomised controlled trial. BMJ Open 2019;9:e025006. https://doi.org/10.1136/bmjopen-2018-025006
McNamara J, Townsend ML, Herbert JS. A systemic review of maternal wellbeing and its relationship with maternal fetal attachment and early postpartum bonding. PLOS ONE 2019;14:e0220032. https://doi.org/10.1371/journal.pone.0220032
Mellenthin C. Attachment-centered play therapy with middle school students. In Green E, Baggerly J, Myrick A, editors. Play Therapy with Preteens. Lanham, MD: Rowman & Littlefield. 2018. pp. 35–48.
Mercer J. Conventional and unconventional perspectives on attachment and attachment problems: comparisons and implications, 2006–16. Child Adolesc Soc Work J 2019;36:81–95.
Milligan K, Meixner T, Tremblay M, Tarasoff LA, Usher A, Smith A, et al. Parenting interventions for mothers with problematic substance use: a systematic review of research and community practice. Child Maltreat 2020;25:247–62. https://doi.org/10.1177/1077559519873047
US National Library of Medicine. Modified ABC: A Home-based Parenting Program for Opioid-dependent Mothers and Their Infants. 2019. URL: https://clinicaltrials.gov/show/NCT03891628 (accessed 22 September 2021).
Moretti M, Spieker S. Adolescence, Trauma, and Attachment: Translating Research into Practice. Paper presented at the 65th Annual Meeting of the American Academy of Child & Adolescent Psychiatry, Seattle, WA, 22–27 October 2018.
Morgan B, Kumsta R, Fearon P, Moser D, Skeen S, Cooper P, et al. Serotonin transporter gene (SLC6A4) polymorphism and susceptibility to a home-visiting maternal-infant attachment intervention delivered by community health workers in South Africa: reanalysis of a randomized controlled trial. PLOS Med 2017;14:e1002237. https://doi.org/10.1371/journal.pmed.1002237
Mountain G, Cahill J, Thorpe H. Sensitivity and attachment interventions in early childhood: a systematic review and meta-analysis. Infant Behav Dev 2017;46:14–32.
Nadali H, Besharat MA, Rostami R, Bahrami EH. The effectiveness of mother-child attachment-based intervention in enhancing preschoolers’ attachment security. J Dev Psychol 2016;12:354–43.
Narvaez D, Wang L, Cheng A, Gleason TR, Woodbury R, Kurth A, Lefever JB. The importance of early life touch for psychosocial and moral development. Psicol Reflex Crit 2019;32:16. https://doi.org/10.1186/s41155-019-0129-0
Navarro J, Martínez M. The establishment of an early intervention programme using parent–infant psychotherapy in South America. Infant Obs 2017;20:161–74.
Nelson BW, Bernstein R, Allen NB, Laurent HK. The quality of early infant-caregiver relational attachment and longitudinal changes in infant inflammation across 6 months. Dev Psychobiol 2020;62:674–83. https://doi.org/10.1002/dev.21940
Nelson CA, Fox NA, Zeanah CH. The effects of early psychosocial deprivation on brain and behavioral development: findings from the Bucharest Early Intervention Project. In Cicchetti D, editor. Developmental Psychopathology. Hoboken, NJ: John Wiley & Sons; 2016. pp. 1–37.
World Health Organization. Neurobiological Mechanisms of Early Mother-Infant-Bonding. 2018. URL: https://trialsearch.who.int/Trial2.aspx?TrialID=DRKS00014570 (accessed September 2021).
Matos I, Tereno S, Wendland J, Guédeney N, Panaccione E, Fuentealba L, et al. [Maternal sensitivity and attachment security in an early intervention project.] Neuropsychiatr Enfance Adolesc 2017;65:219–24.
Ní Chobhthaigh S, Duffy F. The effectiveness of psychological interventions with adoptive parents on adopted children and adolescents’ outcomes: a systematic review. Clin Child Psychol Psychiatry 2019;24:69–94. https://doi.org/10.1177/1359104518786339
Niccols A, Smith A, Benoit D. The working model of the child interview: stability of the disrupted classification in a community intervention sample. Infant Ment Health J 2015;36:388–98. https://doi.org/10.1002/imhj.21522
Nikitiades, A. An Exploration of Relational Patterns of Mothers and Their Children Exposed to Domestic Violence and Observed Changes Following Group-attachment Based Intervention (GABI). PhD thesis. New York, NY: The New School; 2020.
O’Hara L, Smith ER, Barlow J, Livingstone N, Herath NI, Wei Y, et al. Video feedback for parental sensitivity and attachment security in children under five years. Cochrane Database Syst Rev 2019;11:CD012348. https://doi.org/10.1002/14651858.CD012348.pub2
Metin-Orta I, Sümer N. [Maternal sensitivity and attachment-based parenting support and intervention programs.] Turk Psikoloji Yazilari 2016;19:54–73.
Parolin M, Simonelli A. Attachment theory and maternal drug addiction: the contribution to parenting interventions. Front Psychiatry 2016;7:152. https://doi.org/10.3389/fpsyt.2016.00152
Pasalich DS, Fleming CB, Oxford ML, Zheng Y, Spieker SJ. Can parenting intervention prevent cascading effects from placement instability to insecure attachment to externalizing problems in maltreated toddlers? Child Maltreat 2016;21:175–85. https://doi.org/10.1177/1077559516656398
Pasalich DS, Fleming CB, Spieker SJ, Lohr MJ, Oxford ML. Does parents’ own history of child abuse moderate the effectiveness of the Promoting First Relationships® intervention in child welfare? Child Maltreat 2019;24:56–65. https://doi.org/10.1177/1077559518809217
Pasalich DS, Fleming CB, Spieker SJ, Lohr MJ, Oxford ML. Does parents’ own history of child abuse moderate the effectiveness of the Promoting First Relationships® intervention in child welfare? Child Maltreat 2019;24:56–65. https://doi.org/10.1177/1077559518809217
Piá Santelices M, Zapata J, Fischersworring M, Pérez F, Mata C, Barco B, et al. [Mentalization based interventions for parents and educators: a systematic review.] Terapia Psicológica 2016;34:71–80.
Pillhofer M, Spangler G, Bovenschen I, Kuenster AK, Gabler S, Fallon B, et al. Pilot study of a program delivered within the regular service system in Germany: effect of a short-term attachment-based intervention on maternal sensitivity in mothers at risk for child abuse and neglect. Child Abuse Negl 2015;42:163–73. https://doi.org/10.1016/j.chiabu.2014.07.007
Platje E, Sterkenburg P, Overbeek M, Kef S, Schuengel C. The efficacy of VIPP-V parenting training for parents of young children with a visual or visual-and-intellectual disability: a randomized controlled trial. Attach Hum Dev 2018;20:455–72. https://doi.org/10.1080/14616734.2018.1428997
Plokar A, Bisaillon C. Assessing for dissociation in maltreated children: the theoretical and clinical relevance of narrative story stems. J Child Adolesc Trauma 2016;9:305–14.
Popo E, Kenyon S, Dann SA, MacArthur C, Blissett J. Effects of lay support for pregnant women with social risk factors on infant development and maternal psychological health at 12 months postpartum. PLOS ONE 2017;12:e0182544. https://doi.org/10.1371/journal.pone.0182544
Prendiville E. Neurobiology for psychotherapists. In Prendiville E, Howard J, editors. Creative Psychotherapy. London: Routledge. 2016. pp. 21–34.
Purvis K, Howard ARH, Call C. Trust-based relational intervention. In Buckwalter KD, Reed D, editors. Attachment Theory in Action: Building Connections Between Children and Parents. Lanham, MD: Rowman & Littlefield; 2018. pp. 143–56.
Garcia Quiroga M, Hamilton-Giachritsis C. Attachment styles in children living in alternative care: a systematic review of the literature. Child Youth Care Forum 2016;45:625–53. https://doi.org/10.1007/s10566-015-9342-x
Raby KL, Freedman E, Yarger HA, Lind T, Dozier M. Enhancing the language development of toddlers in foster care by promoting foster parents’ sensitivity: results from a randomized controlled trial. Dev Sci 2019;22:e12753. https://doi.org/10.1111/desc.12753
Rawatlal N, Pillay B, Kliewer W. OR0179 The role of insecure attachment on emotion dysregulation in a South African adolescent cohort. Int J Psychol 2016;51:114.
Rayce SB, Rasmussen IS, Klest SK, Patras J, Pontoppidan M. Effects of parenting interventions for at-risk parents with infants: a systematic review and meta-analyses. BMJ Open 2017;7:e015707. https://doi.org/10.1136/bmjopen-2016-015707
US National Library of Medicine. Relationships in Good Hands - Clinical and Cost-effectiveness of Dyadic Developmental Psychotherapy. 2019. URL: https://clinicaltrials.gov/show/NCT04187911 (accessed 22 September 2021).
Renaud M. Evaluation of a Structured Programme of Group Intervention with Families Experiencing Parenting Difficulties. PhD thesis. Guilford: University of Surrey; 1997.
Renk K, Boris NW, Kolomeyer E, Lowell A, Puff J, Cunningham A, et al. The state of evidence-based parenting interventions for parents who are substance-involved. Pediatr Res 2016;79:177–83. https://doi.org/10.1038/pr.2015.201
Richter L, Slemming W, Norris SA, Stein A, Poston L, Pasupathy D. Health Pregnancy, Healthy Baby: testing the added benefits of pregnancy ultrasound scan for child development in a randomised control trial. Trials 2020;21:25. https://doi.org/10.1186/s13063-019-3924-0
Riva Crugnola C, Ierardi E, Albizzati A, Downing G. Effectiveness of an attachment-based intervention program in promoting emotion regulation and attachment in adolescent mothers and their infants: a pilot study. Front Psychol 2016;7:195. https://doi.org/10.3389/fpsyg.2016.00195
Riva Crugnola C, Ierardi E, Peruta V, Moioli M, Albizzati A. Video-feedback attachment based intervention aimed at adolescent and young mothers: effectiveness on infant-mother interaction and maternal mind-mindedness. Early Child Dev Care 2021;191:475–89.
Roben CKP, Dozier M, Caron EB, Bernard K. Moving an evidence-based parenting program into the community. Child Dev 2017;88:1447–52. https://doi.org/10.1111/cdev.12898
Rose J, O’Reilly B. A systematic review of attachment-based psychotherapeutic interventions for adopted children. Early Child Dev Care 2017;187:1844–62.
Rosenblum K, Lawler J, Alfafara E, Miller N, Schuster M, Muzik M. Improving maternal representations in high-risk mothers: a randomized, controlled trial of the Mom Power parenting intervention. Child Psychiatry Hum Dev 2018;49:372–84. https://doi.org/10.1007/s10578-017-0757-5
Rowe AC, Gold ER, Carnelley KB. The effectiveness of attachment security priming in improving positive affect and reducing negative affect: a systematic review. Int J Environ Res Public Health 2020;17:968.
Sachdeva S, Donson N. Application of Advances in Developmental Research in Infants to Psychotherapeutic Work with Children and Adolescents. Paper presented at the 64th Annual Meeting of the American Academy of Child & Adolescent Psychiatry, Washington, DC, 23–28 October 2017.
Saghaei M, Omidi P, Dehkordi EH, Safavi P. The effectiveness of cognitive-function stress management training in glycemic control in children and in mental health of mother caring for child with type 1 diabetes mellitus. Diabetes Metab Syndr 2017;11(Suppl. 2):S925–8.
Saltzman J, Cole N, Bost KK, Fiese BH, Donovan S. Responsive feeding and breastfeeding moderate the association between maternal attachment security and overeating in 18-month old infants in the STRONG Kids 2 Cohort. FASEB J 2017;31:169.
Sanderson K, Preedy P. Supporting parents of preschool children to develop strategies for schema-based play activities to enhance attachment and well-being: a preliminary study in the United Arab Emirates. FIRE 2016;3:25–40.
Schacht R, Meins E, Fernyhough C, Centifanti LC, Bureau JF, Pawlby S. Proof of concept of a mind-mindedness intervention for mothers hospitalized for severe mental illness. Dev Psychopathol 2017;29:555–64. https://doi.org/10.1017/S0954579417000177
Schäfer N, Karutz H, Schenk O. [The need for psychosocial support of parents of children in neonatal care.] Z Geburtshilfe Neonatol 2017;221:217–25. https://doi.org/10.1055/s-0043-110056
Schechter DS. Integrating Exposure Therapy, Interaction Guidance, and Psychodynamic Principles to Address Mutual Emotional Dysregulation in Traumatized Parent-Child Relationships. Paper presented at the 64th Annual Meeting of the American Academy of Child & Adolescent Psychiatry, Washington, DC, 23–28 October 2017.
Schoemaker NK, Jagersma G, Stoltenborgh M, Maras A, Vermeer HJ, Juffer F, Alink LRA. The effectiveness of Video-feedback Intervention to promote Positive Parenting for Foster Care (VIPP-FC): study protocol for a randomized controlled trial. BMC Psychol 2018;6:38. https://doi.org/10.1186/s40359-018-0246-z
Schoemaker NK, Juffer F, Rippe RC, Vermeer HJ, Stoltenborgh M, Jagersma GJ, et al. Positive parenting in foster care: testing the effectiveness of a video-feedback intervention program on foster parents’ behavior and attitudes. Child Youth Serv Rev 2020;110:104779.
Setodeh S, Sharif F, Akbarzadeh M. The impact of paternal attachment training skills on the extent of maternal neonatal attachment in primiparous women: a clinical trial. Fam Med Prim Care Rev 2018;20:47–54.
Shafi RMA, Bieber ED, Shekunov J, Croarkin PE, Romanowicz M. Evidence based dyadic therapies for 0- to 5-year-old children with emotional and behavioral difficulties. Front Psychiatry 2019;10:677. https://doi.org/10.3389/fpsyt.2019.00677
Shah N, Stewart-Brown S. Parenting and health: a call for action. Paediatr Child Health 2018;28:120–5.
Shariat M, Abedinia N. The effect of psychological intervention on mother-infant bonding and breastfeeding. Iran J Neonatol 2017;8:7–15.
Shirvanian N, Michael T. Implementation of attachment theory into early childhood settings. Int Educ J Comp Perspect 2017;16:97–115.
Shoghi M, Sohrabi S, Rasouli M. The effects of massage by mothers on mother-infant attachment. Altern Ther Health Med 2018;24:34–9.
Skoblo GV, Trushkina SV. [Mental health disorders in the first years of life: disorders mostly related with psychogenic factors.] Zh Nevrol Psikhiatr Im S S Korsakova 2016;116:130–6. https://doi.org/10.17116/jnevro2016116121130-136
Slade P, Weeks A, West H. STRAWB2 (Stress and Wellbeing After Childbirth): a trial of targeted self-help materials to prevent PTSD following childbirth. BJOG 2019;126:13–13.
Stein A, Netsi E, Lawrence PJ, Granger C, Kempton C, Craske MG, et al. Mitigating the effect of persistent postnatal depression on child outcomes through an intervention to treat depression and improve parenting: a randomised controlled trial. Lancet Psychiatry 2018;5:134–44.
Stephenson LA, Beck K, Busuulwa P, Rosan C, Pariante CM, Pawlby S, Sethna V. Perinatal interventions for mothers and fathers who are survivors of childhood sexual abuse. Child Abuse Negl 2018;80:9–31.
St George JM, Wroe JK, Cashin ME. The concept and measurement of fathers’ stimulating play: a review. Attach Hum Dev 2018;20:634–58. https://doi.org/10.1080/14616734.2018.1465106
Suchman NE, DeCoste C, Borelli JL, McMahon TJ. Does improvement in maternal attachment representations predict greater maternal sensitivity, child attachment security and lower rates of relapse to substance use? A second test of Mothering from the Inside Out treatment mechanisms. J Subst Abuse Treat 2018;85:21–30.
Suchman NE, DeCoste CL. Substance abuse and addiction: implications for early relationships and interventions. Zero Three 2018;38:17–22.
Suess GJ, Bohlen U, Carlson EA, Spangler G, Frumentia Maier M. Effectiveness of attachment based STEEP™ intervention in a German high-risk sample. Attach Hum Dev 2016;18:443–60. https://doi.org/10.1080/14616734.2016.1165265
Suess GJ, Bohlen U, Carlson EA, Spangler G, Frumentia Maier M. Effectiveness of attachment based STEEP™ intervention in a German high-risk sample. Attach Hum Dev 2016;18:443–60. https://doi.org/10.1080/14616734.2016.1165265
World Health Organisation. Supporting Foster Carers to Improve Mental Health Outcomes of Young Children in Foster Care: A Feasibility Study. 2017. URL: https://trialsearch.who.int/Trial2.aspx?TrialID=ISRCTN18374094 (accessed September 2021).
Suskind DL, Leung CYY, Webber RJ, Hundertmark AC, Leffel KR, Fuenmayor Rivas IE, Grobman WA. Educating parents about infant language development: a randomized controlled trial. Clin Pediatr 2018;57:945–53. https://doi.org/10.1177/0009922817737079
Swedish Council on Health Technology Assessment. Interventions to Improve Foster Children’s Mental and Physical Health: A Systematic Review and Assessment of the Economic, Social and Ethical Aspects. Stockholm: Swedish Council on Health Technology Assessment; 2017.
Tang E, Bleys D, Vliegen N. Making sense of adopted children’s internal reality using narrative story stem techniques: a mixed-methods synthesis. Front Psychol 2018;9:1189.
Tereno S, Guedeney N, Dugravier R, Greacen T, Saïas T, Tubach F, et al. [Infants’ attachment security in a vulnerable French sample.] L’Encephale 2017;43:99–103.
Tereno S, Madigan S, Lyons-Ruth K, Plamondon A, Atkinson L, Guedeney N, et al. Assessing a change mechanism in a randomized home-visiting trial: reducing disrupted maternal communication decreases infant disorganization. Dev Psychopathol 2017;29:637–49. https://doi.org/10.1017/S0954579417000232
Tereno S, Savelon SV, Guedeney A. Preventive parent-young child interaction interventions to promote optimal attachment. Curr Opin Psychiatry 2019;32:542–8. https://doi.org/10.1097/YCO.0000000000000552
World Health Organization. The Effect of a Mindfulness-based Stress Reduction (MBSR) Program on Coping Behaviors, and Attachment of Mothers of Neonates with Congenital Diseases in the Selected Hospitals Affiliated to Shahid Beheshti University of Medical Sciences. 2019. URL: https://trialsearch.who.int/Trial2.aspx?TrialID=IRCT20190123042471N1 (accessed September 2021).
World Health Organization. The Effect of Body Massage on the Attachment Behaviors of Premature Infants’ Mothers. 2019. URL: https://trialsearch.who.int/Trial2.aspx?TrialID=IRCT20180621040184N1 (accessed September 2021).
World Health Organization. The Effect of Educational Support based on Parenting Self-Efficacy on Attachment and Self-Efficacy of Mothers of Newborns in NICU. 2018. URL: https://trialsearch.who.int/Trial2.aspx?TrialID=IRCT20150928024239N3 (accessed September 2021).
US National Library of Medicine. The Effectiveness of Minding the Baby in a Danish Community Sample. 2018. URL: https://clinicaltrials.gov/show/NCT03495895 (accessed 22 September 2021).
World Health Organization. The Effects of Teaching Maternal Attachment Behavior on Perceived Stress, Parental Expectations, and Mother-Infant Bonding. 2016. URL: https://trialsearch.who.int/Trial2.aspx?TrialID=IRCT2015092124108N1 (accessed September 2021).
World Health Organization. The Karitane ‘My Toddler and Me’ study: a Randomised Controlled Trial comparing Parent-Child Interaction Therapy with Toddlers (PCIT-T), Circle of Security-Parenting (COS-P) and Waitlist Controls in the Treatment of Disruptive Behaviours in Children aged 14-24 Months. 2018. URL: https://anzctr.org.au/Trial/Registration/TrialReview.aspx?ACTRN=12618001554257 (accessed September 2021).
Thompson RA. On what is read, shared, and felt: parent-child conversation about stories. Attach Hum Dev 2020;22:85–9. https://doi.org/10.1080/14616734.2019.1589064
Toosi M, Akbarzadeh M, Ghaemi Z. The effect of relaxation on mother’s anxiety and maternal-fetal attachment in primiparous IVF mothers. J Natl Med Assoc 2017;109:164–71.
Tucker C, Smith-Adcock S. Theraplay: the evidence for trauma-focused treatment for children and families. In Steen RL, editor. Emerging Research in Play Therapy, Child Counseling, and Consultation. Hershey, PA: IGI Global; 2017. pp. 42–59.
Twohig A, Figuerdo R, Byrne F, Underdown A, McNicholas F, Molloy E. Evaluation of the effects of an early attachment focused intervention for parents of very preterm infants in the NICU (PIPPA Study). Eur J Pedriatr 2016;175:1574.
Twohig A, Segurado R, McCarthy A, Underdown A, Smyke A, McNicholas F, Molloy E. GP81 Early intervention to support preterm infant-parent interaction and development: results of a randomised controlled trial on maternal sensitivity, social-emotional development and parental mental health. Arch Dis Child 2019;104(Suppl. 3):A62.3–63.
Væver MS, Smith-Nielsen J, Lange T. Copenhagen infant mental health project: study protocol for a randomized controlled trial comparing Circle of Security -parenting and care as usual as interventions targeting infant mental health risks. BMC Psychol 2016;4:57. https://doi.org/10.1186/s40359-016-0166-8
Vahdati M, Mohammadizadeh M, Talakoub S. Effect of kangaroo care combined with music on the mother-premature neonate attachment: a randomized controlled trial. Iran J Nurs Midwifery Res 2017;22:403–7. https://doi.org/10.4103/ijnmr.IJNMR_50_16
van Andel H, Post W, Jansen L, van der Gaag RJ, Knorth E, Grietens H. Optimizing foster family placement for infants and toddlers: a randomized controlled trial on the effect of the foster family intervention. Am J Orthopsychiatry 2016;86:332–44. https://doi.org/10.1037/ort0000162
van den Broek EGC, van Eijden AJPM, Overbeek MM, Kef S, Sterkenburg PS, Schuengel C. A systematic review of the literature on parenting of young children with visual impairments and the adaptions for Video-feedback Intervention to promote Positive Parenting (VIPP). J Dev Phys Disabil 2017;29:503–45. https://doi.org/10.1007/s10882-016-9529-6
van Zeijl J, Mesman J, van IJzendoorn MH, Bakermans-Kranenburg MJ, Juffer F, Stolk MN, et al. Attachment-based intervention for enhancing sensitive discipline in mothers of 1- to 3-year-old children at risk for externalizing behavior problems: a randomized controlled trial. J Consult Clin Psychol 2006;74:994–1005.
Vandesande S, Bosmans G, Sterkenburg P, Maes B. A micro-trial intervention approach to foster parent-child attachment in young children with severe or profound intellectual disabilities. J Intellect Disabil Res 2019;63:826–7.
Vogel-Hammen A, Luby J. Parent-Child Interaction Therapy: Emotion Development. Paper presented at the 66th Annual Meeting of the American Academy of Child & Adolescent Psychiatry, Chicago, IL, 14–19 October 2019.
Walter I, Landers S, Quehenberger J, Carlson E, Brisch KH. The efficacy of the attachment-based SAFE® prevention program: a randomized control trial including mothers and fathers. Attach Hum Dev 2019;21:510–31. https://doi.org/10.1080/14616734.2019.1582599
Waterman J, Langley A, Miranda J, Riley D. Theoretical and Empirical Underpinnings of Adoption-Specific Therapy. In Waterman J, Langley A, Miranda J, Riley D, editors. Adoption-Specific Therapy: A Guide to Helping Adopted Children and Their Families Thrive. Washington, DC: American Psychological Association; 2018. pp. 13–26.
Waters SF, Thompson RA. Children’s perceptions of emotion regulation strategy effectiveness: links with attachment security. Attach Hum Dev 2016;18:354–72. https://doi.org/10.1080/14616734.2016.1170051
Weinman ML. A response to controversies in attachment disorders. Child Adolesc Soc Work J 2019;36:107–10.
Welch MG, Ludwig RJ. Calming cycle theory and the co-regulation of oxytocin. Psychodyn Psychiatry 2017;45:519–40. https://doi.org/10.1521/pdps.2017.45.4.519
Werner CD, Vermeer HJ, Linting M, van IJzendoorn MH. Video-feedback intervention in center-based child care: a randomized controlled trial. Early Child Res Q 2018;42:93–104.
Wiebe SA, Johnson SM. A review of the research in emotionally focused therapy for couples. Fam Process 2016;55:390–407. https://doi.org/10.1111/famp.12229
Woodhouse S, Miah A, Rutter M. A new look at the supposed risks of early institutional rearing. Psychol Med 2018;48:1–10. https://doi.org/10.1017/S0033291717001507
Woodhouse SS. Attachment-based interventions for families with young children. J Clin Psychol 2018;74:1296–9. https://doi.org/10.1002/jclp.22640
Wray W. A Tele-Coaching Intervention to Support Families in the NPP+: An Experimental Mixed Method Design. PhD thesis. Loma Linda, CA: Loma Linda University; 2016.
Wright B, Edginton E. Evidence-based parenting interventions to promote secure attachment: findings from a systematic review and meta-analysis. Glob Pediatr Health 2016;3:2333794X16661888. https://doi.org/10.1177/2333794X16661888
Wright B, Hackney L, Hughes E, Barry M, Glaser D, Prior V, et al. Decreasing rates of disorganised attachment in infants and young children, who are at risk of developing, or who already have disorganised attachment. A systematic review and meta-analysis of early parenting interventions. PLOS ONE 2017;12:e0180858. https://doi.org/10.1371/journal.pone.0180858
Wright B, Barry M, Hughes E, Trépel D, Ali S, Allgar V, et al. Clinical effectiveness and cost-effectiveness of parenting interventions for children with severe attachment problems: a systematic review and meta-analysis. Health Technol Assess 2015;19(52). https://doi.org/10.3310/hta19520
Yarger HA, Bronfman E, Carlson E, Dozier M. Intervening with Attachment and Biobehavioral Catch-up to decrease disrupted parenting behavior and attachment disorganization: the role of parental withdrawal. Dev Psychopathol 2020;32:1139–48. https://doi.org/10.1017/S0954579419000786
Yarger HA, Hoye JR, Dozier M. Trajectories of change in Attachment and Biobehavioural Catch-up among high-risk mothers: a randomised clinical trial. Infant Ment Health J 2016;37:525–36. https://doi.org/10.1002/imhj.21585
Yarger HA. Investigating Longitudinal Pathways to Dysregulation: The Role of Anomalous Parenting Behavior. PhD thesis. Newark, DE: University of Delaware; 2018.
Zajac L, Raby KL, Dozier M. Sustained effects on attachment security in middle childhood: results from a randomized clinical trial of the Attachment and Biobehavioral Catch-up (ABC) intervention. J Child Psychol Psychiatry 2020;61:417–24. https://doi.org/10.1111/jcpp.13146
Zayde A, Prout TA, Kilbride A, Kufferath-Lin T. The Connecting and Reflecting Experience (CARE): theoretical foundation and development of mentalizing-focused parenting groups. Attach Human Dev 2020;23:293–309.
Zeanah CH Jr. Handbook of Infant Mental Health. New York, NY: Guilford Press; 2018.
Zeanah CH, Fox NA, Nelson CA. Attachment at the extremes: lesson from the Bucharest Early Intervention Project. In Gojman-de-Millán S, Herreman C, Sroufe LA, editors. Attachment Across Clinical and Cultural Perspectives: A Relational Psychoanalytic Approach. London: Routledge; 2016. pp. 142–62.
Zeanah CH, Fox NA, Nelson CA. Recovery from severe deprivation: the Bucharest Early Intervention Project. Zero Three 2018;22:60.
Zeraati H, Nasimi F, Shahinfar J, Milan Delaiee M, Momenizadeh A, Barfidokht A. The effect of family-centered care program on maternal attachment in mothers of premature infants. J Babol Univ Med Sci 2017;19:22–7
Zwönitzer A, Ziegenhain U, Bovenschen I, Bressem K, Pillhofer M, Fegert JM, et al. Effects of early intervention in children at risk: short-term and long-term findings from an attachment-based intervention program. Ment Health Prev 2015;3:98–102.
Review 2
Aarestrup AK, Skovgaard Væver M, Petersen J, Røhder K, Schiøtz M. An early intervention to promote maternal sensitivity in the perinatal period for women with psychosocial vulnerabilities: study protocol of a randomized controlled trial. BMC Psychol 2020;8:41. https://doi.org/10.1186/s40359-020-00407-3
Aguayo J, Salomonsson B. The study and treatment of mothers and infants, then and now: Melanie Klein’s ‘Notes on Baby’ in a contemporary psychoanalytic context. Psychoanal Q 2017;86:383–408. https://doi.org/10.1002/psaq.12144
Alghali H. Professionals’ Perception of the Process of Change During an Attachment Based Parenting Intervention (Video Interaction Guidance) with Parents with Intellectual Disabilities. PhD thesis. London: Royal Holloway, University of London; 2019.
Allen B. The use and abuse of attachment theory in clinical practice with maltreated children, part I: diagnosis and assessment. Trauma Violence Abuse 2011;12:3–12. https://doi.org/10.1177/1524838010386811
Ammen S. A Play-based teen parenting program to facilitate parent-child attachment. In Kaduson HG, Schaefer CE, editors. Short-term Play Therapy for Children. New York, NY: Guilford Press; 2000. pp. 345–69.
Amos J, Furber G, Segal L, Cantor C. When wounds from infancy collide. Parallel Parent and Child Therapy (P-Pact): a dyadic psychotherapy for mothers and their children aged 3-12 years caught in intergenerational cycles of neglect and abuse. Aust N Z J Psychiatry 2015;49(Suppl. 1):94. https://doi.org/10.1177/0004867415578344
World Health Organization. An Innovative Early Intervention for Antisocial Children with Callous-Unemotional Traits. 2011. URL: https://trialsearch.who.int/Trial2.aspx?TrialID=ISRCTN62822052 (accessed September 2021).
Andrew E, Williams J, Waters C. Dialectical Behaviour Therapy and attachment: vehicles for the development of resilience in young people leaving the care system. Clin Child Psychol Psychiatry 2014;19:503–15. https://doi.org/10.1177/1359104513508964
Andrews E. A parenting intervention for middle childhood: an expansion of a Circle of Security intensive individual protocol. Educ Dev Psychol 2019;36:27–31.
Aparicio EM, Denmark N, Berlin LJ, Jones Harden B. First-generation Latina mothers’ experiences of supplementing home-based early head start with the Attachment and Biobehavioral Catch-up Program. Infant Ment Health J 2016;37:537–48.
Arons J. ‘In a black hole’: the (negative) space between longing and dread: home-based psychotherapy with a traumatized mother and her infant son. Psychoanal Study Child 2005;60:101–27. https://doi.org/10.1080/00797308.2005.11800748
Atkinson N. Theraplay used in a multi-cultural environment. In Munns E, Atkinson N, Bettendorf C, editors. Applications of Family and Group Theraplay. Lanham, MD: Jason Aronson, Inc; 2009. pp. 137–57.
Bacon H. Book review: Alicia F. Lieberman and Patricia Van Horn, Psychotherapy with infants and young children: repairing the effects of stress and trauma on early development. Clin Child Psychol Psychiatry 2009;14:459–60.
Bain K, Frost K, Esterhuizen M. ‘The mothers have mercy for me’: change in parent-infant relationships through group psychotherapy. Psychoanal Psychother South Africa 2012;20:33–68.
Bain K. ‘New beginnings’ in South African shelters for the homeless: piloting of a group psychotherapy intervention for high-risk mother-infant dyads. Infant Ment Health J 2014;35:591–603. https://doi.org/10.1002/imhj.21457
Bakermans-Kranenburg MJ, Juffer F, van IJzendoorn MH. Interventions with video feedback and attachment discussions: does type of maternal insecurity make a difference? Infant Ment Health J 1998;19:202–19.
Bakermans-Kranenburg MJ, van IJzendoorn MH, Mesman J, Alink LR, Juffer F. Effects of an attachment-based intervention on daily cortisol moderated by dopamine receptor D4: a randomized control trial on 1- to 3-year-olds screened for externalizing behavior. Dev Psychopathol 2008;20:805–20. https://doi.org/10.1017/S0954579408000382
Bakermans-Kranenburg MJ, van IJzendoorn MH, Pijlman FT, Mesman J, Juffer F. Experimental evidence for differential susceptibility: dopamine D4 receptor polymorphism (DRD4 VNTR) moderates intervention effects on toddlers’ externalizing behavior in a randomized controlled trial. Dev Psychol 2008;44:293–300. https://doi.org/10.1037/0012-1649.44.1.293
Baradon T, Gerhardt S, Tucker J. Working with the hidden obstacles in parent–infant relating: two parent–infant psychotherapy projects. In Barlow J, Svanberg PO, editors. Keeping The Baby In Mind. London: Routledge; 2009. pp. 159–172.
Baradon T, Target M. Mothers and babies in prison: a psychoanalytic approach supporting attachment. In Lemma A, Patrick M, editors. Off the Couch: Contemporary Psychoanalytic Applications. London: Routledge; 2010. pp. 66–81.
Baradon T. Psychotherapeutic work with parents and infants – psychoanalytic and attachment perspectives. Attach Hum Dev 2002;4:25–38. https://doi.org/10.1080/14616730210123143
Barlow J, Bennett C, Midgley N, Larkin SK, Wei Y. Parent-infant psychotherapy for improving parental and infant mental health. Cochrane Database Syst Rev 2015;1:CD010534. https://doi.org/10.1002/14651858.CD010534.pub2
Barlow J, Bennett C, Midgley N, Larkin SK, Wei Y. Parent-infant psychotherapy for improving parental and infant mental health. J Reprod Infant Psychol 2016;34:464–82.
Barlow J, McMillan AS, Kirkpatrick S, Ghate D, Barnes J, Smith M. Health-led interventions in the early years to enhance infant and maternal mental health: a review of reviews. Child Adolesc Ment Health 2010;15:178–85. https://doi.org/10.1111/j.1475-3588.2010.00570.x
Barlow J, Schrader-McMillan A, Axford N, Wrigley Z, Sonthalia S, Wilkinson T, et al. Review: attachment and attachment-related outcomes in preschool children – a review of recent evidence. Child Adolesc Ment Health 2016;21:11–20. https://doi.org/10.1111/camh.12138
Barlow J, Sembi S, Underdown A. A pilot randomised controlled trial of the use of video-interaction guidance with preterm babies. J Reprod Infant Psychol 2015;33:E2.
Barlow J. AIMH UK Best Practice Guidance (BPG) No. 2. 2021. URL: https://aimh.uk/best-practice-guides-infant-mental-health/bpg-2-improving-attachment-in-babies-what-works/ (accessed 23 September 2021).
Barone L, Barone V, Dellagiulia A, Lionetti F. Testing an attachment-based parenting intervention-VIPP-FC/A in adoptive families with post-institutionalized children: do maternal sensitivity and genetic markers count? Front Psychol 2018;9:156.
Barrell JN. Holding the baby – community based therapeutic intervention for the earliest relationship. The International Marcé Society for Perinatal Mental Health Biennial Scientific Conference, Swansea University, Swansea, Wales, UK. Arch Womens Ment Health 2015;18:2–340.
Barron CC, Brown S. Building relational possibilities: theoretical roots of infant mental health practice in the case of Alycia. J Soc Work Pract 2018;32:73–85.
Barrows P. Fathers in parent–infant psychotherapy. Infant Ment Health J 1999;20:333–45.
Barrows P. [Fathers in parent-infant psychotherapy.] Prax Kinderpsychol Kinderpsychiatr 2000;49:596–610.
Barrows P. Parent-infant psychotherapy: a review article. J Child Psychother 1997;23:255–64.
Baubet T, Gaboulaud V, Grouiller K, Belanger F, Vandini PP, Salignon P, et al. [Psychological factors in malnourished infants in a post-conflict context. Evaluation of a therapeutic program for infants and mothers in Hebron (Palestinian territories).] Annales Médico-Psychologiques 2003;161:609–13.
Becker AL, de Souza PH, de Oliveira MM, Paraguay NL. [Child protection network and the intersector implementation of the Circle of Security as alternatives to medication.] Rev Paul Pediatr 2014;32:247–51. https://doi.org/10.1590/0103-0582201432316
Becker-Weidman A. Dyadic Developmental psychotherapy: effective treatment for complex trauma and disorders of attachment. Illinois Child Welf 2012;6:119–29.
Becker-Weidman A, Hughes D. Dyadic developmental psychotherapy: an evidence-based treatment for children with complex trauma and disorders of attachment. Child Fam Soc Work 2008;13:329–37.
Becker-Weidman A, Hughes D. Dyadic Developmental psychotherapy: an effective and evidence-based treatment – comments in response to Mercer and Pignotti. Child Fam Soc Work 2010;15:6–11.
Becker-Weidman A, Shell D. Beginnings. In Becker-Weidman A, Shell D, editors. Attachment Parenting: Developing Connections and Healing Children. Lanham, MD: Jason Aronson, Inc; 2010. pp. 21–46.
Becker-Weidman A, Shell D. End notes. In Becker-Weidman A, Shell D, editors. Attachment Parenting: Developing Connections and Healing Children. Lanham, MD: Jason Aronson, Inc; 2010. pp. 261–80.
Becker-Weidman A. Dyadic Developmental Psychotherapy: An Effective Treatment for Children with Trauma-Attachment Disorders. 2004. URL: www.Center4familyDevelop.com (accessed 10 May 2005).
Becker-Weidman A. Treatment for children with reactive attachment disorder: dyadic developmental psychotherapy. Child Adolesc Ment Health [published online ahead of print November 21 2006]. [Retraction published in Child Adolesc Ment Health 2008;13:52.] https://doi.org/10.1111/j.1475-3588.2006.00428.x
Becker-Weidman A. Assessment session – exploration begins. In Becker-Weidman A, Casswell G, Clark C. The Dyadic Developmental Psychotherapy Casebook. Lanham, MD: Jason Aronson; 2011.
Becker-Weidman A. Components and phases of dyadic developmental psychotherapy. In Becker-Weidman A, Casswell G, Clark C. The Dyadic Developmental Psychotherapy Casebook. Lanham, MD: Jason Aronson; 2011.
Becker-Weidman A. Introduction. In Becker-Weidman A, Casswell G, Clark C. The Dyadic Developmental Psychotherapy Casebook. Lanham, MD: Jason Aronson; 2011.
Becker-Weidman A. The girl who becomes aggressive. In Becker-Weidman A, Casswell G, Clark C. The Dyadic Developmental Psychotherapy Casebook. Lanham, MD: Jason Aronson; 2011.
Beeber LS, Chazan-Cohen R, Squires J, Jones Harden B, Boris NW, Heller SS, Malik NM. The early promotion and intervention research consortium (E-PIRC): five approaches to improving infant/toddler mental health in Early Head Start. Infant Ment Health J 2007;28:130–50. https://doi.org/10.1002/imhj.20126
Bellak L. On some limitations of dyadic psychotherapy and the role of group modalities. Int J Group Psychother 1980;30:7–22. https://doi.org/10.1080/00207284.1981.11491665
Belsky J, Campbell SB, Cohn JF, Moore G. Instability of infant–parent attachment security. Dev Psychol 1996;32:921.
Belt R, Punamäki RL. Mother–infant group psychotherapy as an intensive treatment in early interaction among mothers with substance abuse problems. J Child Psychother 2007;33:202–20. https://doi.org/10.1080/00754170701437096
Belt RH, Kouvo A, Flykt M, Punamäki RL, Haltigan JD, Biringen Z, Tamminen T. Intercepting the intergenerational cycle of maternal trauma and loss through mother-infant psychotherapy: a case study using attachment-derived methods. Clin Child Psychol Psychiatry 2013;18:100–20. https://doi.org/10.1177/1359104512444116
Benzies KM, Magill-Evans J, Kurilova J, Nettel-Aguirre A, Blahitka L, Lacaze-Masmonteil T. Effects of video-modeling on the interaction skills of first-time fathers of late preterm infants. Infants Young Child 2013;26:333–48.
Berg A. Beyond the dyad: parent–infant psychotherapy in a multicultural society – reflections from a South African perspective. Infant Ment Health J 2003;24:265–77.
Berg A. Infant-parent psychotherapy at primary care level: establishment of a service. S Afr Med J 2012;102:582–4. https://doi.org/10.7196/samj.5772
Berg A. Reflective practice in infant mental health – a South African perspective. Infant Ment Health J 2016;37:684–91. https://doi.org/10.1002/imhj.21605
Bergeron MA. Factors that support the use of child–parent psychotherapy as an intervention for child–parent dyads exposed to pediatric medical traumatic stress. Clin Soc Work J 2017;45:77–87.
Berlin LJ, Martoccio TL, Bryce CI, Jones Harden B. Improving infants’ stress-induced cortisol regulation through attachment-based intervention: a randomized controlled trial. Psychoneuroendocrinology 2019;103:225–32.
Berlin LJ. Interventions to enhance early attachments: the state of the field today. In Berlin LJ, Ziv Y, Amaya-Jackson L, Greenberg MT, editors. Enhancing Early Attachments: Theory, Research, Intervention, and Policy. New York, NY: Guilford Press; 2005. pp. 178–94.
Bernard K, Dozier M, Bick J, Gordon MK. Intervening to enhance cortisol regulation among children at risk for neglect: results of a randomized clinical trial. Dev Psychopathol 2015;27:829–41. https://doi.org/10.1017/S095457941400073X
Bernard K, Frost A, Jelinek C, Dozier M. Secure attachment predicts lower body mass index in young children with histories of child protective services involvement. Pediatr Obes 2019;14:e12510. https://doi.org/10.1111/ijpo.12510
Bernard K, Hostinar CE, Dozier M. Intervention effects on diurnal cortisol rhythms of Child Protective Services-referred infants in early childhood: preschool follow-up results of a randomized clinical trial. JAMA Pediatr 2015;169:112–19. https://doi.org/10.1001/jamapediatrics.2014.2369
Bernard K, Lee AH, Dozier M. Effects of the ABC intervention on foster children’s receptive vocabulary: follow-up results from a randomized clinical trial. Child Maltreat 2017;22:174–9. https://doi.org/10.1177/1077559517691126
Bernard K, Meade EB, Dozier M. Parental synchrony and nurturance as targets in an attachment based intervention: building upon Mary Ainsworth’s insights about mother-infant interaction. Attach Hum Dev 2013;15:507–23. https://doi.org/10.1080/14616734.2013.820920
Bernard K, Simons R, Dozier M. Effects of an attachment-based intervention on child protective services–referred mothers’ event-related potentials to children’s emotions. Child Dev 2015;86:1673–84.
Bernstein RE, Timmons AC, Lieberman AF. Interpersonal violence, maternal perception of infant emotion, and child-parent psychotherapy. J Fam Violence 2019;34:309–20.
Bick J, Bernard K, Dozier M. Attachment and biobehavioral catch-up: an attachment-based intervention for substance using mothers and their infants. In Suchman NE, Pajulo M, Mayes LC, editors. Parenting and Substance Abuse: Developmental Approaches to Intervention. Oxford: Oxford University Press; 2013.
Bick J, Dozier M, Moore S. Predictors of treatment use among foster mothers in an attachment-based intervention program. Attach Hum Dev 2012;14:439–52. https://doi.org/10.1080/14616734.2012.706391
Bick J, Dozier M. A review of ‘Promoting Positive Parenting: An Attachment-based Intervention’. Adopt Q 2009;12:53–4.
Bick J, Dozier M. The effectiveness of an attachment-based intervention in promoting foster mothers’ sensitivity toward foster infants. Infant Ment Health J 2013;34:95–103. https://doi.org/10.1002/imhj.21373
Bidonde J, Meneses J. The Effect of Interventions for Children Who Have Experienced Violence in Close Relationships: An Overview of Reviews. Oslo: The Norwegian Institute of Public Health; 2017.
Blome WW, Bennett S, Page TF. Organizational challenges to implementing attachment-based practices in public child welfare agencies: an example using the Circle of Security® model. J Public Child Welf 2010;4:427–49.
Blos P. Intergenerational separation-individuation. Treating the mother-infant pair. Psychoanal Study Child 1985;40:41–56.
Blumberg ML. Review of Trad PV, editor. Short-term Parent-infant Psychotherapy. New York, NY: Basic Books; 1994.
Blumenthal A. Child Neglect II: Prevention and Intervention. Montreal, QC: McGill Centre for Research on Children and Families; 2015.
Bojanowski JJ, Ammen S. Discriminating between pre-versus post-theraplay treatment Marschak Interaction Methods using the Marschak Interaction Method Rating System. Int J Play Ther 2011;20:1–11.
Bojanowski JJ. Discriminating Between Pre-Versus Post-Theraplay® Treatment Marschak® Interaction Methods using the Marschak® Interaction Method Rating System. PhD thesis. Fresno, CA: Alliant International University; 2005.
Bond AH. New aspects of infantile trauma. PsycCRITIQUES 2010;55.
World Health Organization. Boosting Baby Behaviour and Bonding for Parents with Enduring Difficulties in Managing Emotions and Relationships. 2017. URL: https://trialsearch.who.int/Trial2.aspx?TrialID=ISRCTN10052006 (accessed September 2021).
Booth PB, Jernberg AM. Theraplay: Helping Parents and Children Build Better Relationships Through Attachment-based Play. Hoboken, NJ: John Wiley & Sons; 2009.
Booth PB, Winstead ML-R. Theraplay: creating secure and joyful attachment relationships. In O’Connor KJ, Schaefer CE, Braverman LD, editors. Handbook of Play Therapy. Hoboken, NJ: John Wiley & Sons; 2016.
Bovingdon T, Fabian K. Relinquishment visits: saying goodbye is an unnatural process. In Munns E, Atkinson N, Bettendorf C, editor. Applications of Family and Group Theraplay. Lanham, MD: Jason Aronson; 2009. pp. 211–24.
Bray JH. Neuroscience and attachment in helping maltreated children and adolescents. PsycCRITIQUES 2017;62(5).
Brennan J. The Circle of Security intervention: enhancing attachment in early parent-child relationships. J Reprod Infant Psychol 2017;35:207–8. https://doi.org/10.1080/02646838.2016.1277193
Brewer TA. Building Bridges: A Trauma-informed Relational Intervention for Parents Experiencing Homelessness. Palo Alto, CA: Palo Alto University; 2019.
Buckwalter KD, Finlay AL. Theraplay: the powerful catalyst in residential treatment. In Munns E, Atkinson N, Bettendorf C, editor. Applications of Family and Group Theraplay. Lanham, MD: Jason Aronson; 2009. pp. 81–96.
US National Library of Medicine. Building Healthy Children. 2013. URL: https://clinicaltrials.gov/show/NCT01888809 (accessed 23 September 2021).
Bundy-Myrow S, Booth PB. Theraplay: supporting attachment relationships. In O’Connor KJ, Braverman LD, editors. Play Therapy Theory and Practice: Comparing Theories and Techniques. Hoboken, NJ: John Wiley & Sons; 2009.
Bundy-Myrow S. Theraplay for children with self-regulation problems. In Schaefer C, McCormick J, Ohnogi A, editors. International Handbook of Play Therapy: Advances in Assessment, Theory, Research and Practice. Lanham, MD: Jason Aronson; 2010.
Calebi M, Carr-Hopkins R. Video interaction guidance and the family courts [published online ahead of print July 2019]. Seen Heard J –Nagalro 2019.
Campbell D, Trowell J. Narrative perspectives on childhood depression. In Vetere A, Dowling E, editors. Narrative Therapies with Children and Their Families: A Practitioner’s Guide to Concepts and Approaches. New York, NY: Taylor & Francis; 2016.
Carel A. [Parents-infant’ psychotherapy. Research on the autistic process.] Neuropsychiatr Enfance Adolesc 1982;30:209–15.
Carlberg GO. Multiperspective views of factors underlying change in psychoanalytic individual child psychotherapy. Int J Psychol 2000;35:307.
Carlsson T, Tuomi K. When individual therapy is not enough – Theraplay as a treatment for traumatized children. Eur Child Adolesc Psychiatry 2011;20:S86.
Caron EB, Bernard K, Dozier M. In vivo feedback predicts parent behavior change in the Attachment and Biobehavioral Catch-up intervention. J Clin Child Adolesc Psychol 2018;47(Suppl. 1):S35–46. https://doi.org/10.1080/15374416.2016.1141359
Casanueva C, Harris S, Carr C, Burfeind C, Smith K. Evaluation in multiple sites of the safe babies court team approach. ChildWelf 2019;97:85–107.
Cassano K. Introducing video enhanced reflective practice into CYC education. Relat Child Youth Care Pract 2018;6:28–32.
Cassidy J, Shaver PR. Handbook of Attachment: Theory, Research, and Clinical Applications. New York, NY: Guilford Press; 2002.
Cassidy J, Ziv Y, Stupica B, Sherman LJ, Butler H, Karfgin A, et al. Enhancing attachment security in the infants of women in a jail-diversion program. Attach Hum Dev 2010;12:333–53. https://doi.org/10.1080/14616730903416955
Celebi M, Cox F, Hinds C, Suppiah C, Taylor D. Training peer supporters in Video Interaction Guidance (VIG). Int J Birth Parent Educ 6.
Chaffin M, Hanson R, Saunders BE, Nichols T, Barnett D, Zeanah C, et al. Report of the APSAC task force on attachment therapy, reactive attachment disorder, and attachment problems: reply to letters. Child Maltreat 2006;11:76–89.
Chen H, Lee T. The maternal infant dyadic relationship – looking beyond postpartum depression. ASEAN J Psychiatry 2013;14:161–9.
US National Library of Medicine. Child-Parent Psychotherapy for Preschooler Witnesses of Domestic Violence Program. 2005. URL: https://clinicaltrials.gov/show/NCT00187772 (accessed 23 September 2021).
Chinitz S, Guzman H, Amstutz E, Kohchi J, Alkon M. Improving outcomes for babies and toddlers in child welfare: a model for infant mental health intervention and collaboration. Child Abuse Negl 2017;70:190–8.
Cicchetti D, Rogosch FA, Toth SL, Sturge-Apple ML. Normalizing the development of cortisol regulation in maltreated infants through preventive interventions. Dev Psychopathol 2011;23:789–800. https://doi.org/10.1017/S0954579411000307
Cicchetti D, Rogosch FA, Toth SL. The effects of child maltreatment and polymorphisms of the serotonin transporter and dopamine D4 receptor genes on infant attachment and intervention efficacy. Dev Psychopathol 2011;23:357–72. https://doi.org/10.1017/S0954579411000113
Cicchetti D, Toth SL, Rogosch FA. The efficacy of toddler-parent psychotherapy to increase attachment security in offspring of depressed mothers. Attach Hum Dev 1999;1:34–66. https://doi.org/10.1080/14616739900134021
Clark R, Tluczek A, Wenzel A. Psychotherapy for postpartum depression: a preliminary report. Am J Orthopsychiatry 2003;73:441–54. https://doi.org/10.1037/0002-9432.73.4.441
Claudon P, Lighezzolo-Alnot J, de Tychey C, Dekkoumi S, Roche G. Evaluating parent-infant psychotherapy: about bodily mobilizations and bodily interactions. Infant Ment Health J 2011;32:216.
Cohen JA. 12.4 Trauma-focused CBT for preschool children. Clinical Perspectives 2019;58(Suppl.):S18.
Cohen JA. Trauma-Focused Psychotherapies for Early Interpersonal Trauma. Paper presented at the 65th Annual Meeting of the American Academy of Child & Adolescent Psychiatry, Seattle, WA, USA, 22–27 October 2018.
Cohen N. Workshop: Watch, Wait and Wonder: a child-led parent-child psychotherapy: theory and practice. Infant Ment Health J 2010;31:145–6.
Cohen NJ, Muir E, Lojkasek M. The first couple: using watch, wait, and wonder to change troubled infant-mother relationships. In Johnson SM, Whiffen VE, editors. Attachment Processes in Couple and Family Therapy. New York, NY: Guilford Press; 2003.
Cohen NJ, Muir E, Lojkasek M, Muir R, Parker CJ, Barwick M, Brown M. Watch, Wait, and Wonder: testing the effectiveness of a new approach to mother–infant psychotherapy. Infant Ment Health J 1999;20:429–51.
Cohen NJ, Muir E, Lojkasek M, Muir R, Parker CJ, Barwick M, Brown M. Watch, Wait, and Wonder: testing the effectiveness of a new approach to mother–infant psychotherapy. Infant Ment Health J 1999;20:429–51. [Erratum published in Infant Ment Health J 2000;21:131.]
Coleman R. Research findings that support the effectiveness of Theraplay. In Booth PB, Jernberg AM, editors. Theraplay: Helping Parents and Children Build Better Relationships Through Attachment-based Play. Hoboken, NJ: John Wiley & Sons; 2009.
Colley B. Video interaction guidance: a relationship-based intervention to promote attunement, empathy and wellbeing. Emot Behav Diffic 2013;18:347–9.
Colmer K, Rutherford L, Murphy P. Attachment theory and primary caregiving. Australas J Early Child 2011;36:16–20.
Connerty TJ, Roberts R, Sved Williams A. Managing life, motherhood and mental health after discharge from a mother-baby unit: an interpretive phenomenological analysis. Community Ment Health J 2016;52:954–63.
Cooper G, Hoffman K, Powell B, Marvin R. The Circle of Security intervention: differential diagnosis and differential treatment. In Berlin LJ, Ziv Y, Amaya-Jackson L, Greenberg MT, editors. Enhancing Early Attachments: Theory, Research, Intervention, and Policy. New York, NY: Guilford Press; 2007. pp. 127–51.
US National Library of Medicine. Copenhagen Infant Mental Health Project: Enhancing Parental Sensitivity and Attachment (CIMHP). 2015. URL: https://clinicaltrials.gov/show/NCT02497677 (accessed 23 September 2021).
Cort L, Rowley E. A case study evaluation of a group Theraplay intervention to support mothers and their preschool children following domestic abuse (research in brief). In Cornish U, editor. DECP Debate 156 September 2015. Leicester: British Psychological Society; 2015.
US National Library of Medicine. COS-P for Parents of Children Referred to Child Psychiatric Services. 2018. URL: https://clinicaltrials.gov/show/NCT03578016 (accessed 23 September 2021).
Coyne J. Parenting from the outside-in: reflections on parent training during a potential paradigm shift. Aust Psychol 2013;48:379–87.
Cramer B. Psychodynamic perspectives on the treatment of postpartum depression In Murray L, Cooper PJ, editors. Postpartum Depression and Child Development. New York, NY: Guilford Press; 1997. pp. 237–61.
Cramer B, Robert-Tissot C, Stern DN, Serpa-Rusconi S, De Muralt M, Besson G, et al. Outcome evaluation in brief mother-infant psychotherapy: a preliminary report. Infant Ment Health J 1990;11:278–300.
Cramer B. [Child as a therapist.] System Familie-Forschung Und Therapie 1995;8:226–33.
Cramer B. Infant creativity. Infant Ment Health J 1995;16:21–7.
Cramer B. Mother—infant psychotherapies: a widening scope in technique. Infant Ment Health J 1998;19:151–67.
Cramer B. [Mother-infant relations: beginnings of the psychological structure.] Prax Kinderpsychol Kinderpsychiatr 1994;43:345–9.
Crenshaw D. Play therapy approaches to attachment issues. In Malchiodi CA, Crenshaw DA, editors. Creative Arts and Play Therapy for Attachment Problems. New York, NY: Guilford Press; 2014.
Cunningham A, Renk K. I’m uncomfortable, you’re uncomfortable, we’re uncomfortable: an integrative family approach to the treatment of Tourette’s disorder and separation anxiety disorder in a young child. Clin Case Stud 2017;16:446–63.
Daws D. Child psychotherapy in the baby clinic of a general practice. Clin Child Psychol Psychiatry 1999;4:9–22. https://doi.org/10.1177/1359104599004001002
Daws D. Parent-infant psychotherapy: remembering the Oedipus complex. Psychoanal Inq 1999;19:267–78.
Dawson H. Watch, Wait, and Wonder: a dyadic infant-led approach to problems in infancy and early childhood as described by Elizabeth Muir, Mirek Lojkasek and Nancy Cohen. Infant Obs 2008;11:228–30.
de Rementeria A. How the use of transference and countertransference, particularly in parent–infant psychotherapy, can inform the work of an education or childcare practitioner. Psychodyn Pract 2011;17:41–56.
de Rementeria A. Relational trauma in infancy. Psychoanalytic, attachment and neuropsychological contributions to parent–infant psychotherapy. PsychodynPract 2013;19:91–6.
de Sousa DD, Prado LC, Piccinini CA. [Representations concerning motherhood in postpartum depression context.] Psicol Reflex Crit 2011;24:335.
Debray R. [A case of paroxystic crying in a 4 month-old baby-conjoint mother-child psychotherapy.] Neuropsychiatr Enfance Adolesc 1985;33:135–7.
Dehghani A, Malekpour M, Abedi A, Amiri S. The efficacy of Circle of Security on attachment and well-being in preschool children. Manag Sci Lett 2014;4:607–12.
Di Lascio R, Stefani A, [Mother-infant psychology: the specificity of the first encounter.] Richarde Piggle: Studi Psicoanaliticidel Bambinoedell’Adolexcente 2001;9:312–28.
Doherty N. Psychotherapy with infants and young children: repairing the effects of stress and trauma on early attachment. J Reprod Infant Psychol 2012;30:217–18.
Donato S, Bertoni A. Positive parenting as responsible care: risks, protective factors, and intervention evaluation. J Prev Interv Community 2017;45:151–5. https://doi.org/10.1080/10852352.2016.1198120
Doria MV, Kennedy H, Strathie C, Strathie S. Explanations for the success of Video Interaction Guidance (VIG) an emerging method in family psychotherapy. Fam J 2014;22:78–87.
Dozier M, Bernard K, Roben CKP. Attachment and biobehavioural catch-up. In Steele H, Steele M, editors. Handbook of Attachment-based Interventions. New York, NY: Guilford Press; 2017.
Dozier M, Bernard K. Attachment and Biobehavioral Catch-up: addressing the needs of infants and toddlers exposed to inadequate or problematic caregiving. Curr Opin Psychol 2017;15:111–17. https://doi.org/10.1016/j.copsyc.2017.03.003
Dozier M, Bick J, Bernard K. Intervening with foster parents to enhance biobehavioral outcomes among infants and toddlers. Zero Three 2011;31:17–22.
Dozier M, Lindhiem O, Ackerman JP. Attachment and biobehavioral catch-up: an intervention targeting empirically identified needs of foster infants. In Berlin LJ, Ziv Y, Amaya-Jackson L, Greenberg MT, editors. Enhancing Early Attachments: Theory, Research, Intervention, and Policy. New York, NY: Guilford Press; 2005.
Dozier M, Meade E, Bernard K. Attachment and biobehavioral catch-up: an intervention for parents at risk of maltreating their infants and toddlers. In Timmer S, Urquiza A, editors. Evidence-based Approaches for the Treatment of Maltreated Children. New York, NY: Springer; 2014.
Dozier M, Peloso E, Lewis E, Laurenceau JP, Levine S. Effects of an attachment-based intervention on the cortisol production of infants and toddlers in foster care. Dev Psychopathol 2008;20:845–59. https://doi.org/10.1017/S0954579408000400
Dozier M, Roben CKP, Caron E, Hoye J, Bernard K. Attachment and Biobehavioral Catch-up: an evidence-based intervention for vulnerable infants and their families. Psychother Res 2018;28:18–29. https://doi.org/10.1080/10503307.2016.1229873
Drewes AA, Schaefer CE. School-based Play Therapy. Hoboken, NJ: John Wiley & Sons; 2010.
Drewes AA. Working with Asian families in Theraplay: understanding cultural differences. Psychother Res 2008;28:18–29.
World Health Organization. Efficacy of Parent Infant Psychotherapy by Mothers with Postpartum Psychopathological Disorders as Part of the SKKIPPI Study. 2019. URL: https://trialsearch.who.int/Trial2.aspx?TrialID=DRKS00016353 (accessed September 2021).
du Toit Q. Four approaches to individual psychotherapy with the child. Southern African J Child Adolesc Psychiatry Allied Prof 1992;4:17–21.
Dugmore N. Flexing the frame: contemplating the use of multiple ports of entry in parent-infant psychotherapy. Infant Ment Health J 2014;35:366–75. https://doi.org/10.1002/imhj.21452
Dugmore N. The grandmaternal transference in parent–infant/child psychotherapy. J Child Psychother 2013;39:59–75.
US National Library of Medicine. Efficacy of Family Programs for Improving Child and Family Health and Development. 2017. URL: https://clinicaltrials.gov/show/NCT03367845 (accessed 29 September 2021).
World Health Organization. Efficacy of Parent Infant Psychotherapy by Children with Regulatory Disorders as Part of the SKKIPPI Study. 2019. URL: https://trialsearch.who.int/Trial2.aspx?TrialID=DRKS00017008 (accessed September 2021).
Elicker J, Georgescu O, Bartsch E. Increasing the sensitivity of childcare providers: applying the video-feedback intervention in a group care setting. In Juffer FE, Bakermans-Kranenburg MJ, van IJzendoorn MH, editors. Promoting Positive Parenting: An Attachment-based Intervention. London: Routledge; 2008.
Elliott A. Every Child. Vol 12, Number 1. 2006.
Enebrink P, Danneman M, Mattsson VB, Ulfsdotter M, Jalling C, Lindberg L. ABC for parents: pilot study of a universal 4-session program shows increased parenting skills, self-efficacy and child well-being. J Child Fam Stud 2015;24:1917–31.
Erickson N, Julian M, Muzik M. Perinatal depression, PTSD, and trauma: impact on mother-infant attachment and interventions to mitigate the transmission of risk. Int Rev Psychiatry 2019;31:245–63. https://doi.org/10.1080/09540261.2018.1563529
Eskin V. Ladies in waiting: a group intervention for families coping with deployed soldiers. Int J Group Psychother 2011;61:414–37. https://doi.org/10.1521/ijgp.2011.61.3.414
Euser S, Bakermans-Kranenburg MJ, van den Bulk BG, Linting M, Damsteegt RC, Vrijhof CI, et al. Efficacy of the Video-feedback Intervention to promote Positive Parenting and Sensitive Discipline in Twin Families (VIPP-Twins): study protocol for a randomized controlled trial. BMC Psychol 2016;4:33. https://doi.org/10.1186/s40359-016-0139-y
US National Library of Medicine. Evaluating the Efficacy of ABC for High-Risk Parent and Infants. 2016. URL: https://clinicaltrials.gov/show/NCT02647463 (accessed 29 September 2021).
Faustman WOW. Part C: service applications. In Jensen RE, editor. Standards and Ethicsin Clinical Psychology. Lanham, MD: University Press of America; 1992. pp. 141–214.
Feindler E, Belfiore L. Everything you ever wanted to know about treatment of conduct disordered children… almost. Psyc CRITIQUES 1992;37:872–3.
Feliciano F, Santos P, Silva C. Strengths, depression symptoms at risk children families’ under Video Home Training and Video Interaction Guidance (VHT/VIG) intervention. Procedia Soc Behav Sci 2012;69:1059–66.
Fenichel E. Agents of change in foster care for infants and toddlers. Zero Three 2002;22:n5.
Fenichel E. Perinatal mental health: supporting new families through vulnerability and change. Zero Three 2002;22:n6.
Fenichel E. Working with infants, toddlers, and families in rural areas. Zero Three 1995;15:n5.
Ferguson KG. Review of Experiential psychotherapy: basic practices. Can Psychol 1984;25:147–9.
Frame L, Ivins B, Wong L, Cantrell S. Therapeutic guidance for infants and families: using multi-family groups as an extension of child–parent psychotherapy. Zero Three 2015;35:2–9.
Francis YJ, Bennion K, Humrich S. Evaluating the outcomes of a school based Theraplay® project for looked after children. Educ Psychol Pract 2017;33:308–22.
Franke U. [Theraplay – a direct communication play therapy.] Prax Kinderpsychol Kinderpsychiatr 1990;39:12–17.
Frauman DC. Featured review: mother-to-infant trauma transmission: assessment and treatment. Psychoanal Soc Work 2012;19:144–50.
Baradon T. Relational Trauma in Infancy: Psychoanalytic, Attachment, and Neuropsychological Contributions to Parent-Infant Psychotherapy. London: Routledge; 2010.
Frauman DC. Featured review: mother-to-infant trauma transmission: assessment and treatment. Psychoanal Soc Work 2012;19:144–50.
Freedman WA. Patterns of Behavior in Delta Caregiving and Intervention-related Changes. PhD thesis. Charlottesville, VA: University of Virginia; 2003.
French N. Learning to wonder together: a group approach to work with parents and infants in a community setting. Infant Obs 2011;14:75–88.
Friend J. Mitigating intergenerational trauma within the parent-child attachment. Aust N Z J Fam Ther 2012;33:114–27.
Fukkink R. [Effects of video interaction analysis in a childcare context.] Pedagogische Studien 2016;93:316–31.
Fukkink RG, Tavecchio LW. Effects of Video Interaction Guidance on early childhood teachers. Teach Teach Educ 2010;2:1652–9.
Fukkink RG, Trienekens N, Kramer L. [Video feedback in education and training: learning portrayed.] Amsterdam: University of Amsterdam; 2010.
Fukkink RG. Video feedback in widescreen: a meta-analysis of family programs. Clin Psychol Rev 2008;28:904–16. https://doi.org/10.1016/j.cpr.2008.01.003
Garez V, Genet MC, Heroux C, Valente M, Carlberg E, Richerd D, et al. Pounce and prevent! Eur Child Adolesc Psychiatry 2011;20:S91–2.
Gates B. Domestic violence, psychotropic medication, families, consent and health: recurring themes in learning disabilities. Br J Learn Disabil 2018;46:71–3.
Geddes H. Attachment theory in clinical work with children bridging the gap between research and practice. Psychodyn Pract 2012;18:387–91.
Gençer AA, Aksoy, Ayşe B. [A different approach to mother and child interaction: Theraplay play therapy.] Psikiyatride Guncel Yaklasimlar 2016;8:244–54.
Georg A, Kress S, Taubner S. Strengthening mentalizing in a depressed mother of an infant with sleep disorders. J Clin Psychol 2019;75:859–73. https://doi.org/10.1002/jclp.22762
Gibson KA. Appreciating the world of autism through the lens of video interaction guidance: an exploration of a parent’s perceptions, experiences and emerging narratives on autism. Disabil Soc 2014;29:568–82.
Gibson KA. Appreciating the world of autism through the lens of video interaction guidance: an exploration of a parent’s perceptions, experiences and emerging narratives on autism. Disabil Soc 2014;29:568. [Erratum published in Disabil Soc 2014;29:VI.]
Gill EH, Thorød AB, Vik K. Marte Meo as a port of entry to parental sensitivity - a three-case study. BMC Psychiatry 2019;19:5. https://doi.org/10.1186/s12888-018-1959-5
Golden BR. How theraplay facilitates healthy narcissism. J Child Adolesc Psychother 1986;3:99–104.
Golding KS. The development of DDP-informed parenting groups for parents and carers of children looked after or adopted from care. Adopt Foster 2019;43:400–12.
Gomes AG, Piccinini C, Prado LC. [Parent-infant psychotherapy in the context of malformation: implications on the mother’s perception about the baby’s development.] Revistade Psiquiatriado Rio Grandedo Sul 2009;31:95–104.
Gomez AM. EMDR Therapy and Adjunct Approaches with Children: Complex Trauma, Attachment, and Dissociation. New York, NY: Springer Publishing Company; 2012.
Goncalves M-J. [Identification and countertransference in mother-infant psychotherapies.] Revue Francaisede Psychanalyse 1994;58:669–1673.
Goodlin-Jones BL, Anders TF. Relationship disturbances and parent-child therapy. Sleep problems. Child Adolesc Psychiatr Clin N Am 2001;10:487–99.
Goodman JH, Guarino AJ, Prager JE. Perinatal dyadic psychotherapy: design, implementation, and acceptability. J Fam Nurs 2013;19:295–323. https://doi.org/10.1177/1074840713484822
Goodman JH, Guarino AJ, Prager JE. Perinatal dyadic psychotherapy: design, implementation, and acceptability. J Fam Nurs 2013;19:295–323. https://doi.org/10.1177/1074840713484822
Goodman JH, Prager J, Goldstein R, Freeman M. Perinatal Dyadic Psychotherapy for postpartum depression: a randomized controlled pilot trial. Arch Womens Ment Health 2015;18:493–506. https://doi.org/10.1007/s00737-014-0483-y
Goodman JH, Prager J, Goldstein R, Freeman M. Perinatal Dyadic Psychotherapy for postpartum depression: a randomized controlled pilot trial. Arch Womens Ment Health 2015;18:493–506. https://doi.org/10.1007/s00737-014-0483-y
Gorski C, Minnis H. Feeding forward to a ‘miracle day’ – a pilot study of video feedforward in reactive attachment disorder. Clin Child Psychol Psychiatry 2014;19:384–91. https://doi.org/10.1177/1359104513488376
Grant RJ. Play therapy for children with autism spectrum disorder. In Kaduson HG, Cangelosi D, Schaefer CE, editors. Prescriptive Play Therapy: Tailoring Interventions for Specific Childhood Problems. New York, NY: Guilford Publications; 2020.
Grasso DJ. Clinical Exercises for Treating Traumatic Stress in Children and Adolescents: Practical Guidance and Ready-to-use Resources. Philadelphia, PA: Jessica Kingsley Publishers; 2014.
Gravener-Davis J. Representations of Toddler, Self, and Caregiver in Mothers With and Without Major Depressive Disorder and Their Relation to Child Socioemotional Functioning Over a One-year Follow-up Period. Dissertation Abstracts International: Section B: The Sciences and Engineering; 2014.
Groeneveld MG, Vermeer HJ, van IJzendoorn MH, Linting M. Enhancing home-based child care quality through video-feedback intervention: a randomized controlled trial. J Fam Psychol 2011;25:86–96. https://doi.org/10.1037/a0022451
Groeneveld MG, Vermeer HJ, van IJzendoorn MH, Linting M. Randomized video-feedback intervention in home-based childcare: improvement of children’s wellbeing dependent on time spent with trusted caregiver. Child Youth Care Forum 2016;45:587–606. https://doi.org/10.1007/s10566-015-9344-8
Grube WA, Liming KW. Attachment and biobehavioral catch-up: a systematic review. Infant Ment Health J 2018;39:656–73. https://doi.org/10.1002/imhj.21745
Guedeney A, Guedeney N, Wendland J, Burtchen N. Treatment – mother–infant relationship psychotherapy. Best Pract Res Clin Obs Gynaecol 2014;28:135–45.
Guild DJ, Alto ME, Toth SL. Preventing the intergenerational transmission of child maltreatment through relational interventions. In Teti DM, editor. Parenting and Family Processes in Child Maltreatment and Intervention. New York, NY: Springer; 2016.
Guild DJ, Toth SL, Handley ED, Rogosch FA, Cicchetti D. Attachment security mediates the longitudinal association between child-parent psychotherapy and peer relations for toddlers of depressed mothers. Dev Psychopathol 2017;29:587.
Guild DJ. Affective Expression and Relationship Cohesion Between Depressed Mothers and Their Offspring: A Longitudinal Examination of the Effects of Child-Parent Psychotherapy. Rochester, NY: University of Rochester; 2017.
Hagan MJ, Browne DT, Sulik M, Ippen CG, Bush N, Lieberman AF. Parent and child trauma symptoms during child-parent psychotherapy: a prospective cohort study of dyadic change. J Trauma Stress 2017;30:690–7. https://doi.org/10.1002/jts.22240
Halasz G. Book review: The baby as subject: new directions in infant–parent psychotherapy from the Royal Children’s Hospital, Melbourne. Aust N Z J Psychiatry 2009;38:851–2.
Hamby S. Psychotherapy with infants and young children, by AF Lieberman and P. Van Horn. J Trauma Dissociation 2011;12:110–12.
Hare-Mustin RTM. Therapy and other forms of intervention. In Bersoff DN, editor. Ethical Conflicts in Psychology. Washington, DC: American Psychological Association; 2008.
Harley EK, Williams ME, Zamora I, Lakatos PP. Trauma treatment in young children with developmental disabilities: applications of the Child-Parent Psychotherapy (CPP) model to the cases of’ James’ and’ Juan’. Pragmat Case Stud Psychother 2014;10:156–95.
World Health Organization. Healthy Start, Happy Start: Helping Parents with Children’s Behaviour. 2015. URL: https://trialsearch.who.int/Trial2.aspx?TrialID=ISRCTN58327365 (accessed 29 September 2021).
Hegarty K, Tarzia L, Hooker L, Taft A. Interventions to support recovery after domestic and sexual violence in primary care. Int Rev Psychiatry 2016;28:519–32. https://doi.org/10.1080/09540261.2016.1210103
World Health Organization. Helping Parents with Mental Health Problems to Parent Young Infants: A Randomised Controlled Trial of Parent-Infant Psychotherapy and Counselling. 2006. URL: https://trialsearch.who.int/Trial2.aspx?TrialID=ISRCTN38741417 (accessed September 2021).
Hepworth AD, Berlin LJ, Martoccio TL, Cannon EN, Berger RH, Harden BJ. Supporting infant emotion regulation through attachment-based Intervention: a randomized controlled trial. Prev Sci 2020;21:702–13. https://doi.org/10.1007/s11121-020-01127-1
Herve M, Maury M. Predictors of outcome in infant functional or behavioral disorders and mother anxious-depressive symptoms after a brief parent-infant psychotherapy. Infant Ment Health J 2011;31:217–18.
Hervé MJ, Paradis M, Rattaz C, Lopez S, Evrard V, White-Koning M, Maury M. Predictors of outcome in infant and toddlers functional or behavioral disorders after a brief parent-infant psychotherapy. Eur Child Adolesc Psychiatry 2009;18:737–46. https://doi.org/10.1007/s00787-009-0032-9
Herzog JM. ‘Polarity, Paradox and the Organizing Process in Development’; parent-infant psychotherapy and child analytic technique: in honor of Louis Sander. Psychoanal Inq 2019;39:98–108.
Hewitt O, Gurney-Smith B, Golding K. A qualitative exploration of the experiences of adoptive parents attending ‘Nurturing Attachments’, a dyadic developmental psychotherapy informed group. Clin Child Psychol Psychiatry 2018;23:471–82. https://doi.org/10.1177/1359104517753511
Hiles Howard AR, Lindaman S, Copeland R, Cross DR. Theraplay impact on parents and children with autism spectrum disorder: improvements in affect, joint attention, and social cooperation. Int J Play Ther 2018;27:56.
Hodes MW, Kef S, Meppelder HM, Schuengel C. The effect of VIPP-LD intervention with parents with intellectual disabilities on their children’s behaviour. J Intellect Disabil Res 2012;56:743–8.
Hodes MW, Kef S, Meppelder-de Jong HM, de Moor MH, Schuengel C. Does it work? Vipp-Ld intervention and the effect on parental stress, sensitive responsiveness and sensitive discipline of parents with intellectual disabilities. J Int Disabil Res 2015;59:83–4.
Hodes MW, Meppelder HM, Schuengel C, Kef S. Tailoring a video-feedback intervention for sensitive discipline to parents with intellectual disabilities: a process evaluation. Attach Hum Dev 2014;16:387–401. https://doi.org/10.1080/14616734.2014.912490
Hodes MW, Meppelder M, de Moor M, Kef S, Schuengel C. Alleviating parenting stress in parents with intellectual disabilities: a randomized controlled trial of a video-feedback intervention to promote positive parenting. J Appl Res Intellect Disabil 2017;30:423–32. https://doi.org/10.1111/jar.12302
Hodes MW, Meppelder M, Kef S, Schuengel C. Working with a video-feedback intervention (VIPP-LD): how can parents with intellectual disabilities benefit from it? J Intellect Disabil Res 2016;60:683.
Hoffenkamp HN, Tooten A, Hall RA, Braeken J, Eliëns MP, Vingerhoets AJ, van Bakel HJ. Effectiveness of hospital-based video interaction guidance on parental interactive behavior, bonding, and stress after preterm birth: a randomized controlled trial. J Consult Clin Psychol 2015;83:416–29. https://doi.org/10.1037/a0038401
Hoffman K, Cooper G, Powell B. Raising a Secure Child: How Circle of Security Parenting Can Help You Nurture Your Child’s Attachment, Emotional Resilience, and Freedom to Explore. New York, NY: Guilford Publications; 2017.
Høivik MS, Lydersen S, Drugli MB, Onsøien R, Hansen MB, Nielsen TS. Video feedback compared to treatment as usual in families with parent-child interactions problems: a randomized controlled trial. Child Adolesc Psychiatry Ment Health 2015;9:3. https://doi.org/10.1186/s13034-015-0036-9
Hong R. Practitioners’ Evaluations of Theraplay as an Effective Tool in Serving Foster and Adopted Children and Their Families. PhD thesis. Chicago, IL: Loyola University Chicago; 2014.
Hooker Jones AN. Creating constructs: understanding parental attitudes, comfort, and experiences with play – a Delphi study. Dissertation Abstracts International Section A: Humanities and Social Sciences 2018;79:2–A(E).
Hooker L, Toone E, Raykar V, Humphreys C, Morris A, Westrupp E, Taft A. Reconnecting mothers and children after violence (RECOVER): a feasibility study protocol of child-parent psychotherapy in Australia. BMJ Open 2019;9:e023653. https://doi.org/10.1136/bmjopen-2018-023653
Hopkins J. Failure of the holding relationship: some effects of physical rejection on the child’s attachment and on his inner experience. J Child Psychother 1987;13:5–17.
Hopkins J. The observed infant of attachment theory. Br J Psychother 1990;6:460–70.
Horton E, Murray C. A quantitative exploratory evaluation of the Circle of Security-parenting program with mothers in residential substance-abuse treatment. Infant Ment Health J 2015;36:320–36. https://doi.org/10.1002/imhj.21514
Horton E, Potter D, Sullivan K. Directive filial therapy models with very young children. In Leggett ES, Boswell JN, editors. Directive Play Therapy: Theories and Techniques. New York, NY: Springer Publishing Company; 2016.
Hoye JR, Cheishvili D, Yarger HA, Roth TL, Szyf M, Dozier M. Preliminary indications that the Attachment and Biobehavioral Catch-up intervention alters DNA methylation in maltreated children. Dev Psychopathol 2020;32:1486–94. https://doi.org/10.1017/S0954579419001421
Hoye JR, Dozier M. Implementing attachment and biobehavioral catch-up with birth parents: rationale and case example. J Clin Psychol 2018;74:1300–7. https://doi.org/10.1002/jclp.22641
Huang R, Yang D, Lei B, Yan C, Tian Y, Huang X, Lei J. The short- and long-term effectiveness of mother-infant psychotherapy on postpartum depression: a systematic review and meta-analysis. J Affect Disord 2020;260:670–9.
Huber A, McMahon C, Sweller N. Improved child behavioural and emotional functioning after Circle of Security 20-week intervention. Attach Hum Dev 2015;17:547–69. https://doi.org/10.1080/14616734.2015.1086395
Huber A, McMahon C, Sweller N. Improved parental emotional functioning after Circle of Security 20-week parent–child relationship intervention. J Child Fam Stud 2016;25:2526–40.
Hughes D, Golding KS, Hudson J. Dyadic Developmental Psychotherapy (DDP): the development of the theory, practice and research base. Adopt Foster 2015;39:356–65.
Hughes D. Dyadic Developmental Psychotherapy (DDP): an attachment-focused family treatment for developmental trauma. Aust N Z J Fam Ther 2017;38:595–605.
Hulette AC, Dunham M, Davis M, Gortney J, Lieberman AF. Early Intervention for families exposed to chronic stress and trauma: the Attachment Vitamins program. Zero Three 2016;36:19–25.
Humphreys KL. Early caregiving intervention holds promise for long-term improvements in neural function following adversity. Biol Psychiatry 2019;85:e15–16.
Imrisek SD, Castaño K, Bernard K. Developing self-regulation in a dysregulating world: attachment and biobehavioral catch-up for a toddler in foster care. J Clin Psychol 2018;74:1308–18. https://doi.org/10.1002/jclp.22642
US National Library of Medicine. Intervening Early with Neglected Children. 2014. URL: https://clinicaltrials.gov/show/NCT02093052 (accessed 29 September 2021).
US National Library of Medicine. Intervening Early: Key Adolescent Outcomes. 2019. URL: https://clinicaltrials.gov/show/NCT04168684 (accessed 29 September 2021).
Ippen CG, Noroña CR, Lieberman AF. Clinical considerations for conducting child-parent psychotherapy with young children with developmental disabilities who have experienced trauma. Pragmat Case Studies Psychother 2014;10:196–211.
Ippen GC, Lieberman AF, Osofsky JD. My daddy is a star in the sky: understanding and treating traumatic grief in early childhood. In Cohen P, Sossin KM, Ruth R, editors. Healing After Parent Loss in Childhood and Adolescence: Therapeutic Interventions and Theoretical Considerations. Lanham, MD: Rowman & Littlefield; 2014.
Jernberg A. Theraplay: child therapy for attachment fostering. Psychother Theor Res Pract Train 1984;21:39.
Jones A. How video can bring to view pathological defensive processes and facilitate the creation of triangular space in perinatal parent–infant psychotherapy. Infant Obs 2006;9:109–23.
Jones A. Levels of change in parent–infant psychotherapy. J Child Psychother 2006;32:295–311.
Jonsdottir A, Coyne J. Group processes in the Circle of Security program: a preliminary study. Aust N Z J Fam Ther 2016;37:585–94.
Joyce A. [When the ‘wrong’ baby is born: a case study.] Rivista Di Psicoanalisi 2011;57:681–97.
Juffer F, Bakermans-Kranenburg MJ, van IJzendoorn MH. Pairing attachment theory and social learning theory in video-feedback intervention to promote positive parenting. Curr Opin Psychol 2017;15:189–94.
Juffer F, Bakermans-Kranenburg MJ, van IJzendoorn MH. The importance of parenting in the development of disorganized attachment: evidence from a preventive intervention study in adoptive families. J Child Psychol Psychiatry 2005;46:263–74.
Juffer F, Bakermans-Kranenburg MJ. Working with Video-feedback Intervention to promote Positive Parenting and Sensitive Discipline (VIPP-SD): a case study. J Clin Psychol 2018;74:1346–57. https://doi.org/10.1002/jclp.22645
Juffer F, Hoksbergen RA, Riksen-Walraven JM, Kohnstamm GA. Early intervention in adoptive families: supporting maternal sensitive responsiveness, infant-mother attachment, and infant competence. J Child Psychol Psychiatry 1997;38:1039–50. https://doi.org/10.1111/j.1469-7610.1997.tb01620.x
Juffer F, Struis E, Werner C, Bakermans-Kranenburg MJ. Effective preventive interventions to support parents of young children: illustrations from the Video-feedback Intervention to promote Positive Parenting and Sensitive Discipline (VIPP-SD). J Prev Interv Community 2017;45:202–14. https://doi.org/10.1080/10852352.2016.1198128
Juffer F, van IJzendoorn MH, Bakermans-Kranenburg MJ. Supporting adoptive families with video-feedback intervention. In Juffer F, Bakermans-Kranenburg MJ, van IJzendoorn, editors. Promoting Positive Parenting. London: Routledge; 2012. pp. 159–74.
Juffer FE, Bakermans-Kranenburg MJ, van IJzendoorn MH. Promoting Positive Parenting: An Attachment-based Intervention. London: Routledge; 2008.
Kaduson HG, Schaefer CE. Short-term Play Therapy for Children. New York, NY: Guilford Press; 2006.
Kalinauskiene LK. [Effects of video-feedback correction of infant-mother interaction on two-years-olds’ behaviour.] Psichologija 2009;40:53–65.
ANZCTR. The Karitane ‘My Toddler and Me’ Study: A Randomised Controlled Trial Comparing Parent-Child Interaction Therapy with Toddlers (PCIT-T), Circle of Security-Parenting (COS-P) and Waitlist Controls in the Treatment of Disruptive Behaviours in Children Aged 14–24 Months. 2018. URL: www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=375579 (accessed May 10 2021).
Kennedy H, Angela U. Video interaction guidance: promoting secure attachment and optimal development for children, parents and professionals. In Leach P, editor. Transforming Infant Wellbeing: Research, Policy and Practice for the First 1001 Critical Days. London: Routledge; 2017.
Kennedy H, Ball K, Barlow J. How does video interaction guidance contribute to infant and parental mental health and well-being? Clin Child Psychol Psychiatry 2017;22:500–17.
Kilian D. Relational trauma in infancy: psychoanalytic, attachment and neuropsychological contributions to parent-infant psychotherapy, T. Baradon, editor: book review. Psychoanal Psychother S Africa 2010;18:86–90.
Kirby EK. Parents and Adopted Children Together (PACT): Therapeutic Retreat for Postadoptive Families. Dissertation Abstracts International: Section B: The Sciences and Engineering 2008;68:6968.
Klatzkin A, Lieberman AF, Van Horn P. Child-parent psychotherapy and historical trauma. In Ford JD, Courtois CA, editors. Treating Complex Traumatic Stress Disorders in Children and Adolescents: Scientific Foundations and Therapeutic Models. New York, NY: Guilford Press; 2013.
Klein Velderman M, Bakermans-Kranenburg MJ, Juffer F, van IJzendoorn MH. Effects of attachment-based interventions on maternal sensitivity and infant attachment: differential susceptibility of highly reactive infants. J Fam Psychol 2006;20:266–74. https://doi.org/10.1037/0893-3200.20.2.266
Klein Velderman M, Bakermans-Kranenburg MJ, Juffer F, van IJzendoorn MH, Mangelsdorf SC, Zevalkink J. Preventing preschool externalizing behavior problems through video-feedback intervention in infancy. Infant Ment Health J 2006;27:466–93.
Klein Velderman M. The Leiden VIPP and VIPP-R Study: evaluation of a short-term preventive attachment-based intervention in infancy. PhD thesis. Delft: Delft University of Technology; 2005.
Kobayashi R. Affective communication of infants with autistic spectrum disorder and internal representation of their mothers. Psychiatry Clin Neurosci 2000;54:235–43. https://doi.org/10.1046/j.1440-1819.2000.00664.x
Kofflin PA, Johnson LM, Ameduri RK. Parental role in care of long term hospitalized patients and impact on attachment and development. J Heart Lung Transplant 2015;34:S236.
Kolijn L, Euser S, van den Bulk BG, Huffmeijer R, van IJzendoorn MH, Bakermans-Kranenburg MJ. Which neural mechanisms mediate the effects of a parenting intervention program on parenting behavior: design of a randomized controlled trial. BMC Psychol 2017;5:9. https://doi.org/10.1186/s40359-017-0177-0
Kottman T, Dickinson R, Meany-Walen K. The role of non-directive and directive/focused approaches to play and expressive arts therapy for children, adolescents, and adults. In Prendiville E, Howard J, editors. Creative Psychotherapy: Applying the Principles of Neurobiology to Play and Expressive Arts-based Practice. London: Routledge; 2016.
Kraft RE. Physical activity for the autistic child. Physical Educator 1983;40:33.
Krehbiel G. Review of the newer therapies: a sourcebook. Rehabil Psychol 1986;31:58–9.
Krejcová K. Dynamic assessment in combination with video interaction guidance in preschool education. Int Educ Stud 2015;8:181–90.
Kronenberg M. Book review: psychotherapy with infants and young children: repairing the effects of stress and trauma on early attachment. Infant Ment Health J 2010;31:113–14.
Laava M, Keskitalo M, Kuronen K, Ahola A, Ukura T, Ebeling H. Family therapy in the middle of family life. Eur Child Adolesc Psychiatry 2011;20:S199.
Labella MH, Lind T, Sellers T, Roben CKP, Dozier M. Emotion regulation among children in foster care versus birth parent care: differential effects of an early home-visiting intervention. J Abnorm Child Psychol 2020;48:995–1006. https://doi.org/10.1007/s10802-020-00653-4
Laddipeerla A. Aboriginal perinatal mental health: a South Australian training experience. Aust N Z J Psychiatry 2013;47:84.
Lakatos PP, Matic T, Carson M, Williams ME. Child-parent psychotherapy with infants hospitalized in the neonatal intensive care unit. J Clin Psychol Med Settings 2019;26:584–96. https://doi.org/10.1007/s10880-019-09614-6
Lampi H. Theraplay as an early intervention-a case study of Theraplay in a family with an autistic daughter. Eur Child Adolesc Psychiatry 2011;20:S95.
Lancaster S. Book review: Tessa Baradon (Ed.), Relational trauma in infancy: psychoanalytic, attachment and neuropsychological contributions to parent-infant psychotherapy. Clin Child Psychol Psychiatr 2011;17:476–8.
Larner G. Family therapy with children and adolescents. Aust N Z J Fam Ther 2016;37:439–42.
Larner G. Multifaceted family therapy: systemic-dialogical therapy, Circle of Security parenting, milieu therapy, collaborative foster and kinship care, and more. Aust N Z J Fam Ther 2019;40:173–5.
Lavi I, Gard AM, Hagan M, Van Horn P, Lieberman AF. Child-parent psychotherapy examined in a perinatal sample: depression, posttraumatic stress symptoms and child-rearing attitudes. J Soc Clin Psychol 2015;34:64–82.
Lee L, Griffiths C, Glossop P, Eapen V. The Boomerangs Parenting Program for Aboriginal parents and their young children. Australas Psychiatry 2010;18:527–33. https://doi.org/10.3109/10398562.2010.499435
Lee S, Kim B. The effect of mental health promotion program for adolescent inmates. J Am Acad Child Adolesc Psychiatry 2018;57:S190.
World Health Organization. Leiden Consortium Individual Development. 2015. URL: https://trialsearch.who.int/Trial2.aspx?TrialID=NTR5312 (accessed September 2021).
Lender D, Norris V. Dyadic developmental psychotherapy. In Buckwalter KD, Reed D, editors. Attachment Theory in Action: Building Connections Between Children and Parents. Lanham, MD: Rowman & Littlefield; 2017.
Lenze S, Luby J. A preliminary case series report of a novel intervention for perinatal depression. The Marcé International Society International Biennial General Scientific Meeting ‘Acting Together Around Childbirth’. Arch Womens Ment Health 2013;16:1–146.
Lenze SN, Rodgers J, Luby J. A pilot, exploratory report on dyadic interpersonal psychotherapy for perinatal depression. Arch Womens Ment Health 2015;18:485–91. https://doi.org/10.1007/s00737-015-0503-6
Leung J, Hamilton J. Making a difference for aboriginal families. Women Birth 2018;31:S49–50.
Levant RF, Haffey NA. Forms of Treatment for the Symptomatic Child: A Review and Critique. Paper presented at the 88th Annual Convention of the American Psychological Association, Montreal, QC, Canada, 1–5 September 1980.
Leventhal H. Don’t hit my mommy! A manual for child-parent psychotherapy with young witnesses of family violence, by Alicia F. Lieberman. Attachment: New Directions in Relational Psychoanalysis and Psychotherapy 2019;13:127–9.
Levi S. Silent scream – work with a traumatized immigrant mother and her infant with a severe neurological disorder. In Malberg NT. Raphael-Leff J, editors. The Anna Freud Tradition: Lines of Development-Evolution of Theory and Practice Over the Decades. London: Karnac Books; 2012.
Lewis-Morrarty E, Dozier M, Bernard K, Terracciano SM, Moore SV. Cognitive flexibility and theory of mind outcomes among foster children: preschool follow-up results of a randomized clinical trial. J Adolesc Health 2012;51(Suppl. 2):17–22. https://doi.org/10.1016/j.jadohealth.2012.05.005
Lieberman AF, Bucio GO. When migration separates children and parents. Zero Three 2018;39:55–60.
Lieberman AF, Ghosh Ippen C, Van Horn P. Child-parent psychotherapy: 6-month follow-up of a randomized controlled trial. J Am Acad Child Adolesc Psychiatry 2006;45:913–18.
Lieberman AF, Van Horn P. Child-parent psychotherapy: a developmental approach to mental health treatment in infancy and early childhood. In Zeanah CH Jr, editor. Handbook of Infant Mental Health. New York, NY: Guilford Press; 2009. pp. 439–49.
Lieberman AF, Van Horn P, Grandison CM, Pekarsky JH. Mental health assessment of infants, toddlers, and preschoolers in a service program and a treatment outcome research program. Infant Ment Health J 1997;18:158–70.
Lieberman AF, Van Horn P. Giving voice to the unsayable: repairing the effects of trauma in infancy and early childhood. Child Adolesc Psychiatr Clin N Am 2009;18:707–20. https://doi.org/10.1016/j.chc.2009.02.007
Lieberman AF. Ghosts and angels: intergenerational patterns in the transmission and treatment of the traumatic sequelae of domestic violence. Infant Ment Health J 2007;28:422–39. https://doi.org/10.1002/imhj.20145
Liebermann R, Silverman R, Pawl HJ. Infant-parent psychotherapy: core concepts and current approaches. In Zeanah CH Jr, editor. Handbook of Infant Mental Health. New York: Guilford; 2000. pp. 472–8.
Liggett-Creel K, Barth RP, Mayden B, Pitts BE. The Parent University Program: factors predicting change in responsive parenting behaviors. ChildYouthServRev 2017;81:10–20.
Likierman M. Post natal depression, the mother’s conflict and parent–infant psychotherapy. J Child Psychother 2003;29:301–15.
Lind T, Bernard K, Ross E, Dozier M. Intervention effects on negative affect of CPS-referred children: results of a randomized clinical trial. Child Abuse Negl 2014;38:1459–67. https://doi.org/10.1016/j.chiabu.2014.04.004
Lind T, Lee Raby K, Caron EB, Roben CK, Dozier M. Enhancing executive functioning among toddlers in foster care with an attachment-based intervention. Dev Psychopathol 2017;29:575–86. https://doi.org/10.1017/S0954579417000190
Lind T. Intervening to Enhance Emotion Regulation: Early Childhood Adversity, Parent-child Mutual Positive Affect, and Later Child Regulation Capabilities. PhD thesis. Newark, DE: University of Delaware; 2017.
Linnman J. Play therapy with adolescents. Clin Soc Work J 2006;34:395–6.
Lojkasek M, Muir E, Cohen NJ. Watch, wait, and wonder: infants as agents of change in a play-based approach to mother-infant psychotherapy. In Schaefer CE, Kelly-Zion S, McCormick J, Ohnogi A, editors. Play Therapy for Very Young Children. Lanham, MD: Jason Aronson; 2008.
US National Library of Medicine. Longitudinal, Multi-Dimensional Assessment of Recovery and Added Benefit of a Behavioral Health Intervention for Children With Abusive Head Trauma. 2018. URL: https://clinicaltrials.gov/show/NCT03447899 (accessed 29 September 2021).
Loshak R. Review of The internal and external worlds of children and adolescents: collaborative therapeutic care edited by Lesley Day and Denis Flyn. Psychoanal Psychother 2004;18:238–40.
Luby JL. Handbook of Preschool Mental Health: Development, Disorders, and Treatment. New York, NY: Guilford Press; 2009.
Luci K. Resilient Programs for Resilient Survivors: The Components and Practices of Well-Established Programs for Survivors of Torture. PhD thesis. Harrisonburg, VA: James Madison University; 2010.
Ludwig-Körner C. Parent-infant-psychotherapy and psychoanalytic treatment: contradiction or mutual inspiration? Int Forum Psychoanal 2003;12:252–8.
Lugones M. [The ability to take care of oneself: experience of continuity of being in a child’s psychotherapy.] Richarde Piggle: Studi Psicoanaliticidel Bambinoedell’ Adolexcente 2006;14:108–19.
Lumsden V. Does the evidence support parent-infant psychotherapy? Commentary on … Cochrane Corner. B J Psych Adv 2017;23:217–21.
Lyons-Ruth K, Spielman E. Disorganized infant attachment strategies and helpless-fearful profiles of parenting: integrating attachment research with clinical intervention. Infant Ment Health J 2004;25:318–35. https://doi.org/10.1002/imhj.20008
Maddox AJ, Bettendorf CR. Theraplay in combination with sensory and handling techniques: the body/mind connection in paediatrics. In Munns E, editor. Applications of Family and Group Theraplay. Lanham, MD: Jason Aronson; 2009.
Maestro S, Cesari A, Parrini B, Muratori F. [The treatment of mother-child relationship: a monitoring study.] Minerva Psichiatrica 2003;44:19–27.
Magagna J. Evolving patterns of parental containment of a young child communicating through not eating or speaking. In Magagna J, editor. The Silent Child: Communication Without Words. Nursing Children and Young People. 2012. pp. 77–90.
Mahan MG. Theraplay as an Intervention With Previously Institutionalized Twins Having Attachment Difficulties. Dissertation Abstracts International: Section B: The Sciences and Engineering 2001;62:1089.
Mäkelä J, Vierikko I. From Heart to Heart: Interactive Therapy for Children in Care. Report on the Theraplay Project in SOS Children’s Villages in Finland. Innsbruck: SOS Children’s Villages; 2004.
Mäkelä J. Can Theraplay increase parental sensitivity and child well-being in child psychiatric and foster care families? Eur Child Adolesc Psychiatry 2011;20:S87.
Mann J, Kretchmar MD. A disorganized toddler in foster care: healing and change from an attachment theory perspective. Zero Three 2006;26:29–36.
Many MM, Kronenberg ME, Dickson AB. Creating a “nest” of emotional safety: reflective supervision in a child–parent psychotherapy case. Infant Ment Health J 2016;37:717–27. https://doi.org/10.1002/imhj.21603
Manzano J, Palacio Espasa F, Knauer D. [Problems of therapeutic interventions in infant psychiatry.] Neuropsychiatr Enfance Adolesc 1984;32:443–50.
Marcus SM. Child parent psychotherapy: an evidence-based treatment for traumatized preschoolers. J Am Acad Child Adolesc Psychiatry 2019;58(Suppl.):S18.
Marvin R, Cooper G, Hoffman K, Powell B. The Circle of Security project: attachment-based intervention with caregiver-pre-school child dyads. Attach Hum Dev 2002;4:107–24. https://doi.org/10.1080/14616730252982491
Mascolo MF, Basseches M. An integrative approach to child–parent psychotherapy. J Appl Dev Psychol 2009;30:563–6.
Masur C. Parent-infant psychotherapy. J Am Psychoanal Assoc 2009;57:467–73.
Maupin AN, Samuel EE, Nappi SM, Heath JM, Smith MV. Disseminating a parenting intervention in the community: experiences from a multi-site evaluation. J Child Fam Stud 2017;26:3079–92.
Maxwell N, Rees A. Video Interaction Guidance: a return to traditional values and relationship-based practice? Br J Soc Work 2019;49:1415–33.
May D, Mowthorpe L, Griffiths E. Teetering on the edge of care: the role of intensive attachment-based play therapies. Adopt Foster 2014;38:131–48.
Mayers HA. Treatment of a traumatized adolescent mother and her two-year old son. Clin Soc Work J 2005;33:419–31.
McPheat G. Review of Video Interaction Guidance: a relationship-based intervention to promote attunement, empathy and well-being. Practice: Soc Work in Action 2013;25:369–70.
Menzel B, Rotnem D. Multiple birth and its influence on the mothering experience: a case study of parent/infant psychotherapy with quadruplets. Infant Ment Health J 1990;11:26–36.
Mercer J. Examining Circle of Security™: a review of research and theory. Res Soc Work Pract 2015;25:382–92.
Mercer J. Examining Dyadic Developmental Psychotherapy as a treatment for adopted and foster children: a review of research and theory. Res Soc Work Pract 2014;24:715–24.
Mercer J. Revisiting an article about dyadic developmental psychotherapy: the life cycle of a Woozle. Child Adolesc Soc Work J 2015;32:397–404.
Minde K, Hesse E. The role of the adult attachment interview in parent-infant psychotherapy: a case presentation. Infant Ment Health J 1996;17:115–26.
US National Library of Medicine. MIO-CPP to Improve the Well-being, Permanency, and Safety Outcomes for Young Children At Risk of or in Out-of-home Placement in Philadelphia and Bucks Counties, and Affected by Maternal Substance Use. 2020. URL: https://clinicaltrials.gov/show/NCT04294134 (accessed 29 September 2021).
Moayedoddin A, Moser D, Nanzer N. The impact of brief psychotherapy centred on parenthood on the anxio-depressive symptoms of mothers during the perinatal period. Swiss Med Wkly 2013;143:w13769. https://doi.org/10.4414/smw.2013.13769
US National Library of Medicine. Modified ABC: A Home-based Parenting Program for Opioid-dependent Mothers and Their Infants. 2019. URL: https://clinicaltrials.gov/show/NCT03891628 (accessed 29 September 2021).
Monzo MP. The practice of psychoanalytic parent–infant psychotherapy. Claiming the baby. J Child Psychother 2017;34:295–9.
Morcuende MTB. Circle of Security©, individual protocol: an intervention for the intergenerational transmission of psychopathology. Clin Transl Sci 2010;3:S32.
Moschner SL, Achtergarde S, Ramsauer B. [Treatment satisfaction of mothers with postpartum depression concerning circle of security intervention.] Prax Kinderpsychol Kinderpsychiatr 2018;67:351–67.
Muir E. Watching, Waiting, and Wondering: applying psychoanalytic principals to mother-infant intervention. Infant Ment Health J 1992;13:319–28.
Munns E. Theraplay: Innovations in Attachment-enhancing Play Therapy. Lanham, MD: Jason Aronson; 2000.
Munns E. Filial therapy and Theraplay. In Bowers NR, editor. Play Therapy with Families: A Collaborative Approach to Healing. Lanham, MD: Rowman & Littlefield; 2013.
Munns E, Theraplay with adolescents. In Gallo-Lopez L, Schaefer CE, editors. Play Therapy with Adolescents. Lanham, MD: Jason Aronson; 2005. pp. 30–47.
Munns E. Theraplay with zero to three-year-olds. In Schaefer CE, Kelly-Zion S, McCormick J, Ohnogi A, editors. Play Therapy for Very Young Children. Lanham, MD: Jason Aronson; 2008.
Munns E. Theraplay: attachment-enhancing play therapy. In Schaefer CE, editor. Foundations of Play Therapy. Hoboken, NJ: John Wiley & Sons; 2011.
Muratori FB, Shevchenko J, Lassenius-Panula L, Yule W, Fedor I, Yunes R, Vasen J. Child and adolescent psychiatry. Eleventh International Congress of the European Society for Child and Adolescent Psychiatry, Hamburg, Germany, 1999.
Murray L, Cooper PJ, Wilson A, Romaniuk H. Controlled trial of the short- and long-term effect of psychological treatment of post-partum depression: 2. Impact on the mother-child relationship and child outcome. Br J Psychiatry 2003;182:420–7.
Narayan AJ, Bucio GO, Rivera LM, Lieberman AF. Making sense of the past creates space for the baby: perinatal child-parent psychotherapy for pregnant women with childhood trauma. Zero Three 2016;36:22–8.
National Institute for Health and Care Excellence, Social Care Institute for Excellence. Therapeutic Interventions After Abuse and Neglect: A Quick Guide for Practitioners and Managers Supporting Children, Young People and Families. London: NICE; 2018.
National Scientific Council on the Developing Child. The Science of Neglect: The Persistent Absence of Responsive Care Disrupts the Developing Brain. Working Paper No.12. 2012. URL: https://developingchild.harvard.edu/resources/the-science-of-neglect-the-persistent-absence-of-responsive-care-disrupts-the-developing-brain/ (accessed 29 September 2021).
Navarro J, Martínez M. The establishment of an early intervention programme using parent–infant psychotherapy in South America. Infant Obs 2017;20:161–74.
World Health Organization. Effect of Video Interaction Guidance (VIG) in Parents of Preterm Infants. 2012. URL: www.who.int/trialsearch/Trial2.aspx?TrialID=NTR3423 (accessed 29 September 2021).
Newman L, Stevenson C. Issues in infant–parent psychotherapy for mothers with borderline personality disorder. Clin Child Psychol Psychiatry 2008;13:505–14. https://doi.org/10.1177/1359104508096766
Norsa D. [Connected mother-infant psychotherapies: introductory notes.] Richarde Piggle: Studi Psicoanaliticidel Bambinoedell’Adolexcente 1993;1:149–55.
NSPCC. Spotlight on Preventing Child Neglect. London: NSPCC; 2015.
Nylen KJ, Moran TE, Franklin CL, O’hara MW. Maternal depression: a review of relevant treatment approaches for mothers and infants. Infant Ment Health J 2006;27:327–43.
O’Connor K. Integrating ecosystemic play therapy and theraplay in the treatment of attachment disorders. In Drewes AA, Bratton SC, Schaefer CE, editors. Integrative Play Therapy. Hoboken, NJ: John Wiley & Sons; 2011.
Ogbuagu C. ‘I don’t want to die, I want to feel better’: finding hope through psychoanalytic parent-infant psychotherapy. JChildPsychother 2019;45:257–73.
O’Hara L, Smith ER, Barlow J, Livingstone N, Herath NI, Wei Y, et al. Video feedback for parental sensitivity and attachment security in children under five years. Cochrane Database Syst Rev 2019;11:CD012348. https://doi.org/10.1002/14651858.CD012348.pub2
Oldeschulte R. Relational trauma in infancy: psychoanalytic, attachment and neuropsychological contributions to parent-infant psychotherapy. J Child Psychother 2010;36:194–5.
US National Library of Medicine. Oxytocin and Dyadic Psychotherapy in the Treatment of Post Partum Depression. 2014. URL: https://clinicaltrials.gov/show/NCT02191423 (accessed 29 September 2021).
Page TF, Cain DS. ‘Why don’t you just tell me how you feel?’: a case study of a young mother in an attachment-based group intervention. Child Adolesc Soc Work J 2009;26:333–50.
Palacio-Espasa D. Brief Mother-father-infant psychodynamic psychotherapy: clinical and technical aspects. In Tydeman B, editor. Innovations in Parent-infant Psychotherapy: International Contributions. London: Karnac Books; 2007.
Pally R. Other programs similar to CRP. In Hoffman L, Pally R, Popek P, editors. Clinical Perspectives on Reflective Parenting: Keeping the Child’s Mind in Mind. Lanham, MD: Jason Aronson; 2012.
Papousek M, de Chuquisengo RW. [Integrative parent-infant psychotherapy for early regulatory and relationship disorders.] Prax Kinderpsychol Kinderpsychiatr 2006;55:235–54.
Paradis HA, Sandler M, Manly JT, Valentine L. Building healthy children: evidence-based home visitation integrated with pediatric medical homes. Pediatrics 2013;132(Suppl. 2):174–9. https://doi.org/10.1542/peds.2013-1021R
Pardoe R. Integrating Video Interaction Guidance (VIG) and psychoanalytic psychotherapy in work with parents and infants. Bull Assoc Child Psychother 2016.
Paris R, Spielman E, Bolton RE. Mother–infant psychotherapy: examining the therapeutic process of change. Infant Ment Health J 2009;30:301–19.
Parker P. Safeguarding children with disabilities. In Smith L, editor. Clinical Practice at the Edge of Care: Developments in Working With At-Risk Children and Their Families. New York, NY: Springer; 2016.
Pedrina F. Group therapy with mothers and babies in postpartum crises: preliminary evaluation of a pilot project. Group Anal 2004;37:137–51.
Pedrina F. Parent-infant-psychotherapy with migrants: implications of cultural differences for psychoanalytical technique. Infant Ment Health J 2000;21:308.
Peltz JS, Rogge RD, Rogosch FA, Cicchetti D, Toth SL. The benefits of child-parent psychotherapy to marital satisfaction. Fam Syst Health 2015;33:372–82. https://doi.org/10.1037/fsh0000149
Pereira M, Negrão M, Soares I, Mesman J. Decreasing harsh discipline in mothers at risk for maltreatment: a randomized control trial. Infant Ment Health J 2014;35:604–13. https://doi.org/10.1002/imhj.21464
Perez A. From pathological merger to a reflective, triangular space: parent-infant psychotherapy with a mother with borderline personality disorder. J Infant Child Adolesc Psychother 2018;17:15–27.
Perez LM, Sundheim CJ. Mother-infant psychotherapy informed by polyvagal theory. J Infant Child Adolesc Psychother 2018;17:145–53.
Perez LM. Intergenerational dynamics of trauma. J Infant Child Adolesc Psychother 2009;8:156–68.
Philipp DA. Reflective family play: a model for whole family intervention in the infant and preschool clinical population. Infant Ment Health J 2012;33:599–608. https://doi.org/10.1002/imhj.21342
Phillip M. The Practical Use of Video Interaction Guidance to Improve Communication, Interactions and Knowledge Transfer Between People with PIMD, Staff and Family Members. Paper presented at the Fourth International IASSIDD Europe Regional Congress, Vienna, Austria, 14–17 July 2014.
Pignotti M, Mercer J. Holding therapy and dyadic developmental psychotherapy are not supported and acceptable social work interventions: a systematic research synthesis revisited. Res Soc Work Pract 2007;17:513–9.
Pollak-Cornillot M. [Mother-infant psychoanalytic therapy when mother and baby are depressed.] Neuropsychiatr Enfance Adolesc 2012;5:S120.
World Health Organization. Positive Parenting in Foster Care. 2013. URL: https://trialsearch.who.int/Trial2.aspx?TrialID=NTR3899 (accessed September 2021).
Poslawsky IE, Naber FB, Bakermans-Kranenburg MJ, De Jonge MV, van Engeland H, van IJzendoorn MH. Development of a Video-feedback Intervention to promote Positive Parenting for Children with Autism (VIPP-AUTI). Attach Hum Dev 2014;16:343–55. https://doi.org/10.1080/14616734.2014.912487
Powell B, Cooper G, Hoffman K, Marvin R. The Circle of Security project. In Oppenheim D, Goldsmith D, editors. Attachment Theory in Clinical Work with Children: Bridging the Gap Between Research and Practice. New York, NY: Guilford Press; 2007. pp. 172–202.
Ramchandani PG, O’Farrelly C, Babalis D, Bakermans-Kranenburg MJ, Byford S, Grimas ESR, et al. Preventing enduring behavioural problems in young children through early psychological intervention (Healthy Start, Happy Start): study protocol for a randomized controlled trial. Trials 2007;18:543.
US National Library of Medicine. Promotion of Successful Parenting. 2017. URL: https://clinicaltrials.gov/show/NCT03808987 (accessed 30 September 2021).
Rackett P. Fun with mum: a video interaction group to support mothers with postnatal depression and their relationship with their infants. The International Marcé Society For Perinatal Mental Health Biennial Scientific Conference, Swansea, Wales. Arch Womens Ment Health 2015;18:313.
Rackett P, Macdonald B. Fun with mum: using video interaction guidance to enhance early relationships and diminish maternal postnatal depression. Educ Child Psychol 2014;31:82–92.
Ramsauer B, Lotzin A, Mühlhan C, Romer G, Nolte T, Fonagy P, Powell B. A randomized controlled trial comparing Circle of Security Intervention and treatment as usual as interventions to increase attachment security in infants of mentally ill mothers: study protocol. BMC Psychiatry 2014;14:24. https://doi.org/10.1186/1471-244X-14-24
Rance S. Attending to early relationship difficulties: applying the ‘Watch Wait and Wonder’ approach in a pilot project for babies and parents. Infant Obs 2005;8:125–38.
Ransley R, Sleed M, Baradon T, Fonagy P. ‘What support would you find helpful?’ The relationship between treatment expectations, therapeutic engagement, and clinical outcomes in parent-infant psychotherapy. Infant Ment Health J 2019;40:557–72. https://doi.org/10.1002/imhj.21787
Reck C, Hunt A, Fuchs T, Weiss R, Noon A, Moehler E, et al. Interactive regulation of affect in postpartum depressed mothers and their infants: an overview. Psychopathology 2004;37:272–80.
Reedy AR. Raising a secure child: how Circle of Security parenting can help you nurture your child’s attachment, emotional resilience, and freedom to explore. J Baccalaureate Soc Work 2018;23:311–3.
US National Library of Medicine. Relationship-Based Intervention for Post-Partum Depression. 2019. URL: https://clinicaltrials.gov/show/NCT04193462 (accessed 29 September 2021).
US National Library of Medicine. Relationships in Good Hands - Clinical and Cost-effectiveness of Dyadic Developmental Psychotherapy. 2019. URL: https://clinicaltrials.gov/show/NCT04187911 (accessed 29 September 2021).
Reyes VI, Lieberman AL. Child-parent psychotherapy and traumatic exposure to violence. Zero Three 2012;32:20.
Ribaudo J. Restoring safety: an attachment-based approach to clinical work with a traumatized toddler. Infant Ment Health J 2016;37:80–92. https://doi.org/10.1002/imhj.21549
Risholm Mothander P, Furmark C, Neander K. Adding ‘Circle of Security - Parenting’ to treatment as usual in three Swedish infant mental health clinics. Effects on parents’ internal representations and quality of parent-infant interaction. Scand J Psychol 2018;59:262–72. https://doi.org/10.1111/sjop.12419
Robert-Tissot C. Outcome of brief mother-infant psychotherapies as a function of maternal depression. Eur Psychiatry 2005;20:S212.
Robison M, Lindaman SL, Clemmons MP, Doyle-Buckwalter K, Ryan M. ‘I deserve a family’: the evolution of an adolescent’s behavior and beliefs about himself and others when treated with Theraplay in residential care. Child Adolesc Soc Work J 2009;26:291–306.
Rostad W. Examining the Effectiveness of the Circle of Security Parenting DVD Program. Dissertation Abstracts International: Section B: The Sciences and Engineering 2015;75:10-B(E).
Ryan R, O’Farrelly C, Ramchandani P. Parenting and child mental health. London J Prim Care 2017;9:86–94. https://doi.org/10.1080/17571472.2017.1361630
Sachdeva S, Donson N. Applying Advances in Developmental Research in Infants: Developmentally Informed Psychotherapeutic Work With Children and Adolescents. Paper presented at the 65th Annual Meeting of the American Academy of Child and Adolescent Psychiatry, Seattle, WA, USA, 22–27 October 2018.
Salo FT. Recognizing the infant as subject in infant-parent psychotherapy. Int J Psychoanal 2007;88:961–79.
Salo S. Does Theraplay increase emotional availability among substance-abusing mothers and their infants? Eur Child Adolesc Psychiatry 2011;20:S87.
Salomonsson B, Sandell R. A randomized controlled trial of mother-infant psychoanalytic treatment: II. Predictive and moderating influences of qualitative patient factors. Infant Ment Health J 2011;32:377–404. https://doi.org/10.1002/imhj.20302
Salomonsson B, Sandell R. Maternal experiences and the mother–infant dyad’s development: introducing the Interview of Mother’s Experiences (I-ME). J Reprod Infant Psychol 2012;30:21–50.
Salomonsson B, Winberg Salomonsson M. [Intimacy thwarted and established: following a girl from infancy to child psychotherapy.] Revista Brasileirade Psicanalise 2017;51:133–55.
Salomonsson B. [Mother-infant psychoanalytic treatment: Method and evaluation.] Neuropsychiatr Enfance Adolesc 2012;5:S45.
Salomonsson B. Extending the field: parent–toddler psychotherapy inspired by mother–infant work. J Child Psychother 2015;41:3–21.
Salomonsson B. Mother-infant work and its impact on psychoanalysis with adults. Scand Psychoanal Rev 2009;32:3–13.
Salomonsson B. Psychodynamic therapies with infants and parents: a review of RCTs on mother-infant psychoanalytic treatment and other techniques. Psychodyn Psychiatry 2014;42:617–40. https://doi.org/10.1521/pdps.2014.42.4.617
Salomonsson B. Therapeutic action in psychoanalytic therapy with toddlers and parents. J Child Psychother 2015;41:112–30.
Salomonsson MW, Sorjonen K, Salomonsson B. A long-term follow-up study of a randomized controlled trial of mother–infant psychoanalytic treatment: outcomes on mothers and interactions. Infant Ment Health J 2015;36:542–55. https://doi.org/10.1002/imhj.21536
Santos PC, Feliciano F, Agra S. Highlighting relationships in early intervention with the video home training/video interaction guidance (VHT/VIG) method. Procedia Soc Behav Sci 2011;29:1772–81.
Sayder S. Review of Psychotherapy with infants and young children: repairing the effects of stress and trauma on early attachment. Infant Obs 2010;13:106–12.
Scheftel S. Book essay: psychoanalytic therapy with infants and parents: practice, theory and results. J Am Psychoanal Assoc 2015;63:1269–76.
Schoemaker NK, Jagersma G, Stoltenborgh M, Maras A, Vermeer HJ, Juffer F, Alink LRA. The effectiveness of Video-feedback Intervention to promote Positive Parenting for Foster Care (VIPP-FC): study protocol for a randomized controlled trial. BMC Psychol 2018;6:38. https://doi.org/10.1186/s40359-018-0246-z
Segal L, Amos J, Swift G, McEvoy P. Round and round the mulberry bush no more: disrupting the intergenerational cycle of mental illness. Aust N Z J Psychiatry 2017;51:41.
Selwyn J, Golding K, Alper J, Smith BG, Hewitt O. A Quantitative and Qualitative Evaluation of the Nurturing Attachments Group Programme. Newport Pagnell: Adoptionplus; 2016.
Selwyn J. Post-adoption Support and Interventions for Adoptive Families: Best Practice Approaches. Munich: Deutsche Jugendinstitut; 2017.
Shafi RMA, Bieber ED, Shekunov J, Croarkin PE, Romanowicz M. Evidence based dyadic therapies for 0- to 5-year-old children with emotional and behavioral difficulties. Front Psychiatry 2019;10:677. https://doi.org/10.3389/fpsyt.2019.00677
Shemmings D, Shemmings Y, Cook A. Gaining the trust of ‘highly resistant’ families: insights from attachment theory and research. Child Fam Soc Work 2012;17:130–7.
Sheppard B. Treating a high-risk mother–child relationship. Clin Soc Work J 2006;34:145–60.
Shulman S. Wondering and beyond: discussion of Arietta Slade’s ‘Reflective Parenting Programs’. Psychoanal Inq 2007;26:658–67.
Sidoli M. The little puppet: working with autistic defences in mother-infant psychotherapy. J Anal Psychol 2000;45:159–75. https://doi.org/10.1111/1465-5922.00150
Siksou J. [Joint parent-infant treatment: The place of the third party.] Psychiatrie De L Enfant 1996;39:85–101.
Silverman RC, Lieberman AF. Negative maternal attributions, projective identification, and the intergenerational transmission of violent relational patterns. Psychoanal Dialogues 1999;9:161–86.
Siu AF. Theraplay in the Chinese world: an intervention program for Hong Kong children with internalizing problems. Int J Play Ther 2009;18:1.
Slade A. Reflective parenting programs: theory and development. Psychoanal Inq 2007;26:640–57.
Sleed M, James J, Baradon T, Newbery J, Fonagy P. A psychotherapeutic baby clinic in a hostel for homeless families: practice and evaluation. Psychol Psychother 2013;86:1–18. https://doi.org/10.1111/j.2044-8341.2011.02050.x
Sluckin A. Bonding failure: ‘I don’t know this baby, she’s nothing to do with me’. Clin Child Psychol Psychiatry 1998;3:11–24.
Slutsky J. Review of The Circle of Security intervention: enhancing attachment in early parent–child relationships. Infant Child Dev 2014;23:455–6.
Smillie G. In sync. In Munns E, editor. Applications of Family and Group Theraplay. Lanham, MD: Jason Aronson; 2009.
Stams GJ, Juffer F, van Ijzendoorn MH, Hoksbergen RC. Attachment-based intervention in adoptive families in infancy and children’s development at age 7: two follow-up studies. Br J Dev Psychol 2001;19:159–80.
Steele M, Steele H, Bate J, Knafo H, Kinsey M, Bonuck K, Meisner P, Murphy A. Looking from the outside in: the use of video in attachment-based interventions. Attach Hum Dev 2014;16:402–15. [Corrigendum published in Attach Hum Dev 2014;16:656.]
Steele M, Steele H, Bate J, Knafo H, Kinsey M, Bonuck K, et al. Looking from the outside in: the use of video in attachment-based interventions. Attach Hum Dev 2014;16:402–15. https://doi.org/10.1080/14616734.2014.912491
Steele M, Steele H, Murphy A, The adult attachment interview and relational trauma: implications for parent-infant psychotherapy. In Baradon T, editor. Relational Trauma in Infancy: Psychoanalytic, Attachment and Neuropsychological Contributions to Parent-infant Psychotherapy. London: Routledge; 2009.
Stein A, Woolley H, Senior R, Hertzmann L, Lovel M, Lee J, et al. Treating disturbances in the relationship between mothers with bulimic eating disorders and their infants: a randomized, controlled trial of video feedback. Am J Psychiatry 2006;163:899–906.
Stewart A, Whelan WF, Pendleton C. Attachment theory as a road map for play therapists. In Malchiodi CA, Crenshaw DA, editors. Creative Arts and Play Therapy for Attachment Problems. New York, NY: Guilford Publications; 2014.
Stock L, Spielhofer T, Gieve M. Independent Evidence Review of Post-adoption Support Interventions. London: Department for Education; 2016.
Stronach E. Preventive interventions and sustained attachment security in maltreated children: a 12-month follow-up of a randomized controlled trial. Dissertation Abstracts International: Section B: The Sciences and Engineering 2013;25:919–30.
Stronach EP, Toth SL, Rogosch F, Cicchetti D. Preventive interventions and sustained attachment security in maltreated children. Dev Psychopathol 2013;25:913–30.
Sturm L. Review of clinical work with traumatized young children. J Dev Behav Pediatr 2012;33:655.
Symposium: clinical symposium: psychoanalytic parent–infant- psychotherapy – whose psychic reality or realities are we approaching? Infant Ment Health J 2010;31:125.
Symposium: healing maltreated children: adaptations of the Circle of Security intervention for biological, foster, and adoptive parents. Infant Ment Health J 2010;31:60.
Tabachnick AR, Raby KL, Goldstein A, Zajac L, Dozier M. Effects of an attachment-based intervention in infancy on children’s autonomic regulation during middle childhood. Biol Psychol 2019;143:22–31.
Taylor J, Brandon M, Hodson D, Haynes A. Child neglect: policy, response and developments in England. Policy and planning. J Soc Serv Res Group 2016;32:39–52.
US National Library of Medicine. The Effect of Early Dyadic Psychotherapy for Mothers Suffering From PPD on Oxytocin Level and on Childrens’ Emotional Development. 2019. URL: https://clinicaltrials.gov/show/NCT04138368 (accessed 30 September 2021).
World Health Organization. The Effect of Video Interaction Guidance of Mother-infant Interaction on Stress in Mother. 2018. URL: https://trialsearch.who.int/Trial2.aspx?TrialID=IRCT20170220032693N1 (accessed September 2021).
Overbeek MM, Sterkenburg PS, Kef S, Schuengel C. The effectiveness of VIPP-V parenting training for parents of young children with a visual or visual-and-intellectual disability: study protocol of a multicenter randomized controlled trial. Trials 2015;16:401.
NSPCC. The New Orleans Intervention Model: Testing a New Approach to Looking After Infant Mental Health Through Infant and Family Teams: A Case Study of Practice. London: NSPCC; 2016.
Becker-Weidman A and Hughes D. Dyadic Developmental Psychotherapy: an effective and evidence-based treatment – comments in response to Mercer and Pignotti. Child Fam Soc Work 2010;15:6–11. [Retraction published in Child Fam Soc Work 2010;15:134.]
Thomas PK, Mayes L. The practice of psychoanalytic parent-infant psychotherapy: claiming the baby. In Baradon T, Biseo M, Broughton C, James J, Joyce A, editors. The Practice of Psychoanalytic Parent-Infant Psychotherapy: Claiming the Baby. New York, NY: Routledge; 2005. pp. 215.
Tooten A, Hoffenkamp HN, Hall RA, Winkel FW, Eliëns M, Vingerhoets AJ, van Bakel HJ. The effectiveness of video interaction guidance in parents of premature infants: a multicenter randomised controlled trial. BMC Pediatr 2012;12:76. https://doi.org/10.1186/1471-2431-12-76
Toth SL, Gravener J. Review: bridging research and practice: relational interventions for maltreated children. Child Adolesc Ment Health 2012;17:131–8. https://doi.org/10.1111/j.1475-3588.2011.00638.x
Toth SL, Manly JT. Developmental consequences of child abuse and neglect: implications for intervention. Child Dev Perspect 2019;13:59–64.
Tucker C, Smoth-Adcock S. Theraplay: the evidence for trauma-focused treatment for children and families. In Steen RL, editor. Emerging Research in Play Therapy, Child Counseling, and Consultation. Hershey, PA: IGI Global; 2017.
Tucker J. Using video to enhance the learning in a first attempt at ‘Watch, Wait and Wonder’. Infant Obs 2006;9:125–38.
Tuomi K, Tuulet PL. Supporting interaction in the context of residential child care. Scot J Resid Child Care 2011;10:28–35.
Tuomi K. Enhancing and strengthening the parent–child bond by the means of music therapy and theraplay. Nord J Music Ther 2016;25(Suppl. 1):112.
Turner J. Who are you? Who am I to you? A mother and infant’s experience of difference. J Child Psychother 2018;44:368–80.
Turner-Halliday F, Watson N, Boyer NR, Boyd KA, Minnis H. The feasibility of a randomised controlled trial of Dyadic Developmental Psychotherapy. BMC Psychiatry 2014;14:347. https://doi.org/10.1186/s12888-014-0347-z
Tuters E, Doulis S, Yabsley S. Challenges working with infants and their families: symptoms and meanings-two approaches of infant-parent psychotherapy. Infant Ment Health J 2011;32:632–49. https://doi.org/10.1002/imhj.20323
Twohig A, Segurado R, McCarthy A, Underdown A, Smyke A, McNicholas F, Molloy E. GP81 Early Intervention to Support Preterm Infant-parent Interaction and Development: Results of a Randomised Controlled Trial on Maternal Sensitivity, Social-emotional Development and Parental Mental Health. Paper presented at the Faculty of Paediatrics of the Royal College of Physicians of Ireland, 9th Europaediatrics Congress, Dublin, Ireland, 13–15 June 2019.
Væver MS, Smith-Nielsen J, Lange T. Copenhagen infant mental health project: study protocol for a randomized controlled trial comparing Circle of Security -parenting and care as usual as interventions targeting infant mental health risks. BMC Psychol 2016;4:57. https://doi.org/10.1186/s40359-016-0166-8
Van Horn P, Osofsky JD, Henderson D, Korfmacher J, Thomas K, Lieberman AF. Replication of child-parent psychotherapy in community settings: models for training. Zero Three 2012;33:48–54.
Waters SF, Hagan MJ, Rivera L, Lieberman AF. Improvements in the child-rearing attitudes of Latina mothers exposed to interpersonal trauma predict greater maternal sensitivity toward their 6-month-old infants. J Trauma Stress 2015;28:426–33. https://doi.org/10.1002/jts.22043
Weinman ML. A response to controversies in attachment disorders. Child Adolesc Soc Work J 2019;36:107–10.
Weir KN, Brodzinsky DM. Treatment and therapy considerations for adopted children and their families. Adopt Q 2013;16:153–5.
Weir KN, Lee S, Canosa P, Rodrigues N, McWilliams M, Parker L. Whole family Theraplay: integrating family systems theory and Theraplay to treat adoptive families. Adopt Q 2013;16:175–200.
Weir KN. Playing for keeps: integrating family and play therapy to treat reactive attachment disorder. In Drewes AA, Bratton SC, Schaefer CE, editors. Integrative Play Therapy. Hoboken, NJ: John Wiley & Sons; 2011.
Weir KN. Using integrative play therapy with adoptive families to treat reactive attachment disorder: a case example. J Fam Psychother 2008;18:1–6.
Werner CD, Vermeer HJ, Linting M, van IJzendoorn MH. Video-feedback intervention in center-based child care: a randomized controlled trial. Early Child Res Q 2018;42:93–104.
Wettig HHG, Franke U, Fjordbak BS, Evaluating the effectiveness of Theraplay. In Schaefer CE, Kaduson HG, editors. Contemporary Play Therapy: Theory, Research, and Practice. New York, NY: Guilford Press; 2007.
Whalley P, Williams M. Child Neglect and Video Interaction Guidance: Key Findings and Executive Summary of an NSPCC Service Offered to Parents Where Initial Concerns of Neglect Have Been Noted. London: NSPCC; 2015.
Whittaker A. Video Interaction guidance: a relationship-based intervention to promote attunement. In Kennedy H, Landor M and Todd Liz, editors. Empathy and Wellbeing. London: Jessica Kingsley; 2011. pp. 336.
Willemsen H. Review of Baradon T, editor. Relational trauma in infancy: psychoanalytic, attachment and neuropsychological contributions to parent-infant psychotherapy. JAnal Psychol 2011;56:719–20.
Willheim E. Dyadic psychotherapy with infants and young children: child-parent psychotherapy. Child Adolesc Psychiatr Clin N Am 2013;22:215–39. https://doi.org/10.1016/j.chc.2013.01.003
Williams M. Evaluation of a multi-faceted intervention for women with perinatal mood disorders. The International Marcé Society For Perinatal Mental Health Biennial Scientific Conference, Swansea, Wales. Arch Womens Ment Health 2015;18.
Winberg Salomonsson M, Barimani M. Mothers’ experiences of mother-infant psychoanalytic treatment—a qualitative study. Infant Ment Health J 2017;38:486–98. https://doi.org/10.1002/imhj.21649
Wójtowicz-Dacka M, Miotk-Mrozowska M. Video-feedback Intervention to promote Positive Parenting and Sensitive Discipline as a new psychological method of development support in Poland. Pol Psychol Bull 2016;47:250–7.
Woodhead J. ‘Dialectical process’ and ‘constructive method’: micro-analysis of relational process in an example from parent-infant psychotherapy. J Anal Psychol 2004;49:143–60. https://doi.org/10.1111/j.1465-5922.2004.00450.x
Wright DM, Moelis I, Pollack LJ. The outcome of individual child psychotherapy: increments at follow-up. J Child Psychol Psychiatry 1976;17:275–85. https://doi.org/10.1111/j.1469-7610.1976.tb00403.x
Yaholkoski A, Hurl K, Theule J. Efficacy of the Circle of Security intervention: a meta-analysis. J Infant Child Adolesc Psychother 2016;15:95–103.
Yando R. Play-tonic relationships? PsycCRITIQUES 1981;26:875–6.
Yarger HA, Bronfman E, Carlson E, Dozier M. Intervening with Attachment and Biobehavioral Catch-up to decrease disrupted parenting behavior and attachment disorganization: the role of parental withdrawal. Dev Psychopathol 2020;32:1139–48. https://doi.org/10.1017/S0954579419000786
Yarger HA. Investigating Longitudinal Pathways to Dysregulation: The Role of Anomalous Parenting Behavior. PhD thesis. Newark, DE: University of Delaware; 2018.
Zeanah CH, Berlin LJ, Boris NW. Practitioner review: clinical applications of attachment theory and research for infants and young children. J Child Psychol Psychiatry 2011;52:819–33. https://doi.org/10.1111/j.1469-7610.2011.02399.x
Zeijl JV. Externalizing Problems in 1- to 3-year-old Children. Screening, Intervention, and the Role of Child Temperament. PhD thesis. Leiden: Leiden University; 2006.
List of abbreviations
- ABC
- Attachment and Biobehavioral Catch-up
- ADHD
- attention deficit hyperactivity disorder
- AQS
- Attachment Q-Sort
- ASD
- autism spectrum disorder
- ASQ
- Ages and Stages Questionnaire
- CAMHS
- child mental health services
- CI
- confidence interval
- COS
- Circle of Security
- CPP
- Child–Parent Psychotherapy
- DDP
- Dyadic Developmental Psychotherapy
- EAS
- Emotional Availability Scale
- ERG
- Expert Reference Group
- HTA
- Health Technology Assessment
- ICP
- Individual Child Psychotherapy
- LA
- local authority
- MIM
- Marschak Interaction Method
- MORS
- Mothers’ Object Relations Scales
- NICE
- National Institute for Health and Care Excellence
- NSPCC
- National Society for the Prevention of Cruelty to Children
- OR
- odds ratio
- PICOS
- populations, interventions, comparisons, outcomes, settings
- PIP
- Parent–Infant Psychotherapy
- PPI
- patient and public involvement
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- RAD
- reactive attachment disorder
- RDAQ
- Randolph Attachment Questionnaire
- RCT
- randomised controlled trial
- ROB-2
- Revised Risk of Bias Tool for Randomised Trials
- ROBINS-I
- Risk Of Bias In Non-randomised Studies – of Interventions
- SDQ
- Strengths and Difficulties Questionnaire
- SSP
- Strange Situation Procedure
- TIDieR
- Template for Intervention Description and Replication
- VIG
- Video Interaction Guidance
- VIPP
- Video Feedback to Promote Positive Parenting
- WWW
- Watch, Wait, Wonder
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/IVCN8847).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
