Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number NIHR129388. The contractual start date was in March 2020. The draft report began editorial review in February 2022 and was accepted for publication in July 2022. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2023 Cooper et al. This work was produced by Cooper et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – Journals Library, and the DOI of the publication must be cited.
2023 Cooper et al.
Chapter 1 Introduction
Tendinopathy
Definition
Tendinopathy is the term used to describe a spectrum of changes in damaged or diseased tendons that lead to pain and functional impairment. 1 It is primarily a degenerative condition related to overuse and is characterised by dysfunction and localised pain with loading that is variably associated with a range of altered tendon structural features. 1 Tendinopathy can affect any muscle-tendon unit in the body; however, it is most reported in the Achilles, patellar, lateral elbow, rotator cuff (RC) and hip tendons. 2
Epidemiology
Tendinopathy is prevalent in many sports and at all levels of participation but also affects non-athletic populations. Children, adolescents and adults of all ages can be affected by tendinopathies, many of which have a chronic or recurrent course,2 with adults aged 18–65 most affected. Lower-limb tendinopathy has a reported incidence of 10.52 per 1000 person-years, which is greater than the incidence of osteoarthritis (8.4 per 1000 person-years). 3–5 The prevalence of upper-limb tendinopathies has been estimated between 1.3% and 21%. 6,7 Prevalence of tendinopathy increases with age and women are more likely to be affected than men. Tendinopathy is therefore a common, painful and functionally limiting condition for which those affected by it seek support from healthcare professionals. It is therefore essential that healthcare professionals have the best available evidence on which to base their management of tendinopathy.
Aetiology
The aetiology of tendinopathy is multifactorial and complex, with the exact pathogenesis unclear. 1 However, excessive repetitive loading without adequate recovery is widely recognised as a contributing factor to its onset and progression. 8 These increases in load are thought to make tendons susceptible to pathological changes and degeneration, where tendon capacity is insufficient to cope with the mechanical demand. Other risk factors are associated with specific genetic factors, drug reactions, inflammatory conditions and a range of cardiometabolic co-morbidities. 1 Therefore, treatment options for tendinopathy typically focus on reducing pain and improving function by managing load demand and improving capacity through exercise. There is evidence that heavy, slow, progressive loading remodels tendon tissue over the medium term. 9 Changes to structural outcomes such as neovascularisation and tendon morphology (cross-sectional area of tendon) have been reported as a response to therapeutic exercise. 10 However, there is a mismatch between tendon structure and the degree of tendinopathic function and associated pain as improvements in observable structural change do not necessarily translate to clinical outcomes. Additional modalities are often deployed in an attempt to improve outcomes,11 which are partial at best, as reflected in the lack of studies demonstrating long-term effectiveness.
Exercise therapy
Exercise therapy is the mainstay of conservative management of tendinopathy, often used as a first- or second-line intervention, with only a small proportion of individuals seeking surgery to alleviate pain. Exercise therapy frequently includes resistance exercise, which can be classified by training variables such as contraction mode (isotonic-eccentric,12 isotonic-concentric,13 isometric,12) or load intensity scaled relative to a maximum (e.g. moderate load or heavy load), or by a combination of factors (e.g. time under tension14). However, other types of exercise, including flexibility, proprioception and balance, and whole-body vibration, with varying dosage and intensity, have also been reported. 8,15,16 In experimental studies, the success of exercise therapy is often measured against alternative exercise types, or splinting, bracing, electro-therapy modalities, manual therapies, injection therapies or, less commonly, a control situation (placebo, sham or wait-and-see).
Exercise therapy comprises the bulk of the tendinopathy management research to date, with much of that research focussed on eccentric resistance training,8 reported to be effective primarily in the management of Achilles and patellar tendinopathies. Several exercise therapy protocols have been investigated, including the Alfredson protocol, which comprises eccentric-only action,17 and more mixed or combined protocols18–20 that emphasise eccentric work but also involve concentric exercise with a focus on power and progression by speed and load to simulate the mechanism of injury, which often occurs at higher velocities. 19 However, at present no single protocol appears to have demonstrated superiority.
Other types of resistance training, including isotonic, combined and heavy slow resistance exercise,18,21 have also been recommended for management of some tendinopathies (e.g. patellar12). In addition to contraction mode and intensity, other factors including overall dosage (e.g. intensity, volume and frequency) and contextual factors such as supervision may also play a role in efficacy of exercise for tendinopathy and have also been studied. 22–24
Range of movement and flexibility exercises are often incorporated within strengthening regimes to facilitate improvements in the early phase of rehabilitation. 8 In the rehabilitation of shoulder-related tendinopathies, proprioceptive exercise including movement retraining and sensing of force and joint position have been used to retrain normal patterns of muscle recruitment, with supportive evidence provided in trials and systematic reviews. 25,26 Similarly, balance and core stabilisation exercises have been recommended for patients presenting with lumbo-pelvic instability associated with patellar and Achilles tendinopathies. 15
Depending on the complexity of the tendinopathy involved, exercise may be used in isolation or as part of a multi-component intervention, where it is often combined with modalities including the use of extracorporeal shockwave therapy (ESWT),27 laser therapy28 or corticosteroid injections or following regenerative procedures such as prolotherapy, platelet-rich plasma (PRP) or stem-cell injection therapies. 29 This approach reflects current expert opinion and evidence syntheses that recommend exercise-based physiotherapy as the first-line management for tendinopathy with the addition of other interventions in recalcitrant cases. 2,11
Education is typically deployed alongside exercise and other interventions but is variably reported and has not had extensive intervention development and testing. There are encouraging indications of efficacy,30 indicating the need to establish the link with treatment adherence and outcome, particularly as adherence is often considered the main challenge to effectiveness of exercise interventions. 31
Rationale for the evidence synthesis
This body of work aimed to examine the evidence base on exercise therapy for tendinopathies, specifically evaluating the effectiveness of exercise therapies to make recommendations for practice and future research. Tendinopathy intervention studies can be placed on a continuum, with progression from efficacy (performance under ideal and controlled circumstances) to effectiveness (performance under ‘real-world’ conditions), in keeping with intervention studies in any field. 32 Most of the tendinopathy intervention research appears to comprise efficacy, rather than true effectiveness studies such as large simple or pragmatic trials. 31,33 The focus appears to have been on comparisons between interventions and the moderating effects of dosage,22 and contextual factors such as supervised versus unsupervised exercise,34 with highly selected, homogeneous populations, trained providers and standardised interventions. 32 This has inevitably impacted on the body of work reported here and scope of the practice recommendations that are made. Whilst the first contingent synthesis employed ‘effectiveness review methodologies’, it was expected that the synthesis would investigate efficacy given the composition of the included research.
Previous systematic reviews on exercise for tendinopathy have typically focussed on individual tendinopathies35 and where meta-analyses were deemed appropriate, these have generally focussed on small numbers of homogeneous studies of specific intervention types, compared specific exercise modes (e.g. eccentric vs. concentric), or considered exercise as a single entity. This approach does not offer comparative efficacy of the wide range of exercise interventions, leading to a lack of established hierarchy of tendinopathy interventions. This project aimed to address that gap, that is, to explore which exercise therapies are most effective across all tendinopathies and, where possible, within relevant subgroups.
With increasing pressure and demands on healthcare services, the need for clear evidence-based practice guidance is increasingly important. To synthesise evidence in such a way that it is optimally relevant to real-world clinical practice, it is important to consider the factors that may moderate exercise therapy efficacy, for example the feasibility of delivering, and acceptability of undertaking, specific exercise interventions. This project therefore incorporated synthesis of evidence in these domains alongside synthesis of evidence of efficacy.
Due to the heterogeneity of tendinopathy sites, target populations and exercise protocols, and the focus on efficacy, feasibility and acceptability, a broad and comprehensive evidence synthesis was essential. This body of work therefore comprises two main phases. Firstly, a large scoping review was undertaken to map the tendinopathies and exercise interventions that have been studied, and the outcomes that have been reported. This informed the design of the second phase, in which several efficacy reviews were undertaken, alongside a mixed-method review on feasibility and acceptability of exercise for tendinopathy.
The novel approach for the efficacy reviews was to combine exercise-related research across all tendinopathies and to identify commonalities and heterogenic treatment effects, whilst also considering relevant variables and participant characteristics. We employed the use of a range of meta-analysis models including network meta-analyses (NMA) and meta-regressions where possible to best synthesise complex and heterogeneous data to compare the efficacy of different interventions across a range of tendinopathies and outcomes to better establish a treatment hierarchy. This extensive modelling approach was adopted to enhance existing knowledge regarding the most effective type of exercise therapy across multiple tendinopathy outcomes. This body of work is also novel in its simultaneous inclusion of evidence on efficacy, feasibility and acceptability of exercise therapy for tendinopathy. By conducting such a comprehensive evidence synthesis, it is possible to make some clear recommendations with direct implications for practice and service commissioners. Inevitably, findings from this synthesis have also identified gaps in the evidence base and recommendations are made that will guide future high-quality primary research and the prioritisation of research needs.
Structure of the report
The aim and specific review questions are outlined next (see Chapter 2), followed by the overall design for the body of work (see Chapter 3). The specific methods and findings of phase 1 (scoping review) are presented in Chapter 4. Thereafter, the specific methods and findings of phase 2 are presented in Chapter 5 (efficacy reviews) and Chapter 6 (mixed-method feasibility and acceptability review). Findings are discussed in each chapter, with a final synthesis and interpretation presented in Chapter 7 (discussion), along with recommendations for policy, practice, and research.
Chapter 2 Aim and objectives
The aim of this mixed-methods evidence synthesis was to examine the evidence base on exercise therapy for tendinopathies in order to make recommendations for clinical practice and future research. The specific review questions were as follows:
-
What exercise interventions have been reported in the literature and for which tendinopathies?
-
What outcomes have been reported in studies investigating exercise interventions for tendinopathies?
-
Which exercise interventions are most effective across all tendinopathies?
-
Does type/location of tendinopathy or other specific covariates affect which are the most effective exercise therapies?
-
How feasible and acceptable are exercise interventions for tendinopathies?
Review questions 1 and 2 were addressed by an initial scoping review. Thereafter, contingent systematic reviews were undertaken to address questions 3, 4 (effectiveness reviews) and 5 (mixed-method review).
Chapter 3 Overall design
Methodology
A mixed-method evidence synthesis was conducted in two phases in order to address the review questions (see Figure 1). This approach was informed by previous published work,36 which demonstrated its suitability for addressing clearly defined objectives and assimilating evidence according to relevance, rather than research design alone. This approach had also been employed by several of the review team members in a recent evidence synthesis workstream. 37
FIGURE 1.
Overall approach to the evidence synthesis, illustrating how the scoping review preceded the four contingent syntheses.
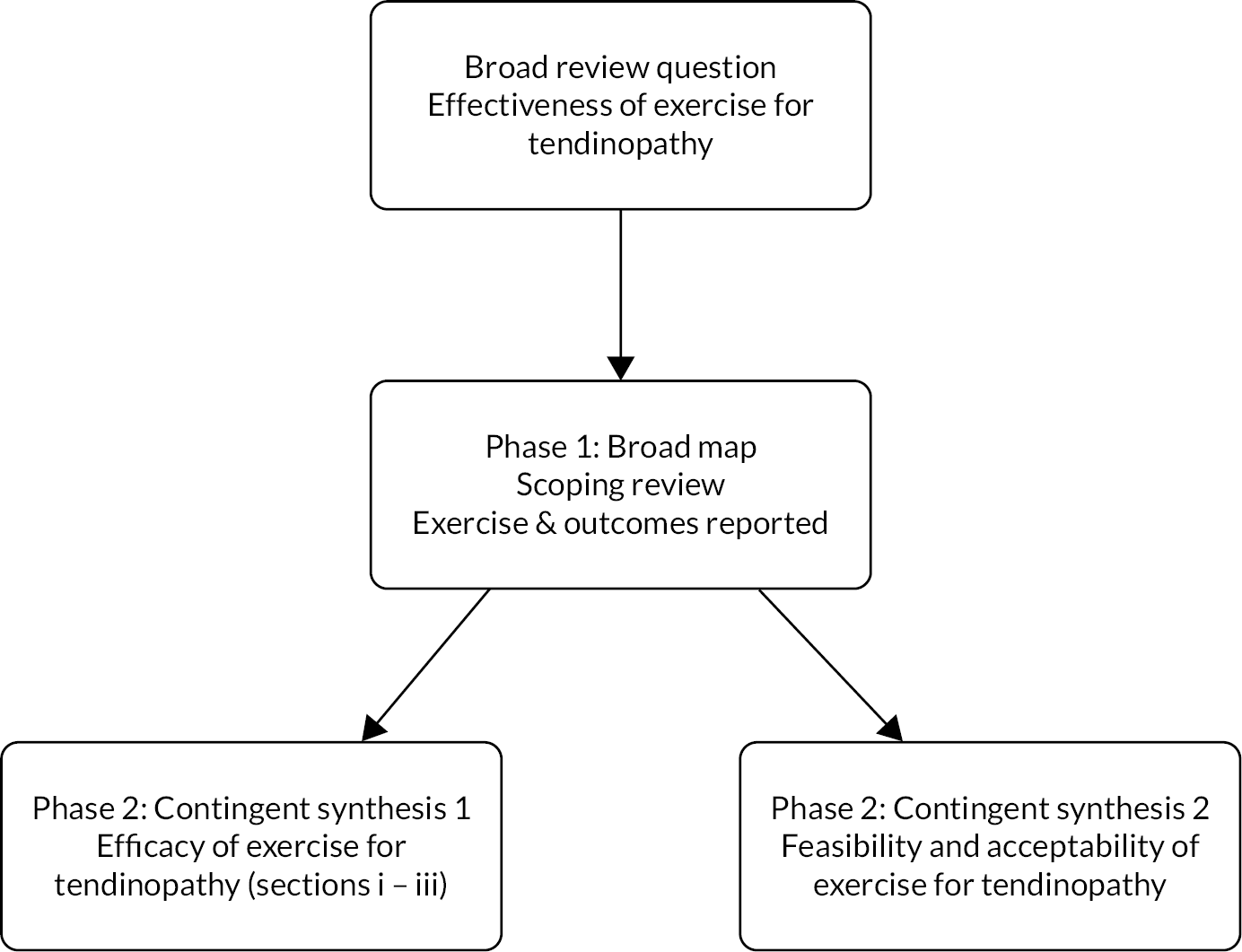
In phase 1 we conducted a comprehensive scoping review to map the tendinopathies, exercise interventions and outcomes reported in the exercise for tendinopathy literature. This enabled us to understand and describe the research field and informed the conduct of the contingent reviews by establishing the nature of the evidence, identifying domains that could be explored. Furthermore, it ensured we did not duplicate pre-existing high-quality syntheses. Few true effectiveness studies were identified, with most being conducted under controlled circumstances. Therefore, efficacy, rather than effectiveness, was explored in the contingent reviews. In phase 2 we conducted two workstreams: (i) efficacy of exercise for tendinopathy (consisting of three reviews) and (ii) feasibility and acceptability of exercise for tendinopathy (mixed-method review). Each review was informed by an a priori protocol and is reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement38 and extension for scoping reviews (PRISMA-ScR). 39 Specific methods used in each review are reported in Chapters 4–6.
Population
The population for both phases of this evidence synthesis was people of any age or sex with a diagnosis of tendinopathy of any severity or duration and at any of the common anatomical locations. The terminology adopted for shoulder tendinopathy in the reviews was rotator cuff-related shoulder pain (RCRSP) as defined by Lewis (2016). 40 RCRSP describes the signs and symptoms of pain and impaired movement and function of the shoulder that may arise from one or more structures, and encompasses subacromial pain/impingement syndrome, RC tendinopathy and subacromial bursitis. 41 We have used the term RCRSP in this review in recognition of the difficulty in diagnosing the patho-anatomical cause of shoulder pain,40,41 and due to exercise therapy being the intervention of choice for its management. 42,43 We included studies where participants were described as having tendinopathy, subacromial impingement syndrome (as the terms have been used interchangeably in previous literature), or RCRSP. Therefore, participants with shoulder pain in our review may have tendinopathy with or without involvement of other structures. In keeping with previous research, we excluded large, full-thickness tears (for the shoulder and all other tendinopathies), and samples where tear size could not be determined. 44 We also excluded plantar heel pain as this is not considered to be a true tendinopathy and may respond differently to exercise compared to true tendinopathies. 45 We excluded hand and wrist tenosynovitis for the same reason.
The health technology
The health technology being evaluated was any type or format of exercise therapy for the treatment of any tendinopathy of any aetiology or duration. For the purpose of this review, exercise therapy was defined as any plan of physical activities designed to facilitate recovery or support longer-term self-management. Since physical activity is defined as ‘any bodily movement produced by skeletal muscles that requires energy expenditure’,46 we included a broad range of exercise therapies, in isolation or combination. These included but were not limited to eccentric, concentric, heavy slow resistance, stretching, proprioceptive, cardiovascular and whole-body exercise. The exercise therapy could be used as a first- or second-line intervention for tendinopathy and could be delivered in isolation or with adjunct therapies including but not limited to manual therapies, ESWT, laser therapy, taping and splinting and various types of injection. The exercise therapy could be delivered in any setting including primary care, secondary care, community locations and in people’s own homes as a home exercise programme (HEP). A range of health or exercise professionals or support workers could be involved in delivering the exercise therapy, including but not limited to physiotherapists, medical doctors, strength and conditioning coaches and personal trainers. We included exercise therapy delivered in a supervised or unsupervised (self-management) manner in any setting, using any mode or delivery.
Stakeholder involvement
We involved stakeholders in two ways. Firstly, an individual with lived experience of exercise for tendinopathy who had previously contributed to developing the proposal was an active member of our project management group and study steering committee. She participated in meetings, reviewed public-facing materials and assisted us with interpreting findings from the lived experience viewpoint. An NHS specialist musculoskeletal physiotherapist with an interest in tendinopathy also contributed to the project management group. She contributed to meetings, reviewed output and assisted with interpreting findings from the practitioner’s viewpoint. We had anticipated recruiting more than one person with lived experience and one professional to be involved in the management of the review. However, recruitment coincided with the start of the COVID-19 pandemic, when many professionals were advised to cease non-essential activities. This and the move to exclusively online communication were undoubtedly limiting factors. Nonetheless, the two stakeholders provided valuable input to the design and delivery of the review.
We held stakeholder workshops towards the end of phase 1 (scoping review), to inform the design of the contingent reviews. These were originally intended to be face-to-face events held in Aberdeen and London but were instead delivered online via Microsoft Teams due to COVID-19 restrictions on gatherings. People with lived experience of receiving exercise for tendinopathy (general population and performance athletes), strength and conditioning professionals and health professionals took part in two workshops, which provided valuable insight to assist interpretation of the scoping review findings and informed planning of the contingent syntheses. In addition to the workshops, largely due to the success of the online environment for widening participation, we also used an electronic survey as an additional means of involving additional stakeholders, particularly those based in different countries and time-zones for whom workshop participation would have been challenging. In this way we were able to approach internationally recognised authors in the field of tendinopathy and combine their views with those from the stakeholder workshops, providing a comprehensive interpretation of the findings. We also asked these internationally recognised authors to share the survey using their social media channels, thereby increasing its reach. Full details of the workshops and survey are provided in Chapter 4.
We are in the process of planning dissemination workshops for late 2022, which will be held via a combination of online and face-to-face delivery methods. We will invite participants from the workshops, and will recruit additional participants from NHS, private practice, performance sport, academia and the public to a series of workshops where we will present the findings of the contingent syntheses and seek participants’ views on implementation of the findings into practice and future research. This will ensure that we translate the findings of this evidence synthesis across the research-practice gap.
Stakeholder involvement in this review was therefore commensurate with recommendations specific to systematic reviews,47 with varying levels of involvement at various stages throughout the review. Table 1 maps user involvement in this review to the Authors and Consumers Together Impacting on Evidence (ACTIVE) framework48 and reporting of user involvement has been guided by the GRIPP2 checklist (Guidance for Reporting Involvement of patients and the Public 2). 49
| Framework constructs | Involvement in this evidence synthesis |
|---|---|
| Who was involved? |
|
| How were they recruited? | Advertised via
|
| Approach | Combined approach
|
| Methods | Direct and indirect methods used, dominated by direct
|
| Stage and level of involvement |
|
Chapter 4 Phase I: Exercise therapy for tendinopathy: a scoping review
Review 1 summary
This chapter reports on phase 1, which aimed to map the tendinopathy exercise interventions and outcomes reported in the literature via a Joanna Briggs Institute (JBI) scoping review. Eligibility criteria included Participants (any age or gender with any tendinopathy), Concept (supervised or unsupervised exercise of any type or format, delivered by any professional with any outcome evaluated) and Context (any setting in any highly developed country). A comprehensive search strategy identified 22,550 sources of evidence. Following screening, 555 studies were included representing 25,490 participants from 31 countries. A range of exercise interventions were reported including strengthening, flexibility, aerobic, proprioceptive and motor control exercises; we mapped intervention reporting to the template for intervention description and replication (TIDieR) checklist. The main tendinopathies reported were RCRSP, Achilles, patellar and lateral elbow. A range of outcome measurement tools were reported; we mapped these to the International Scientific Tendinopathy Symposium Consensus (ICON) health-related domains for tendinopathy. The scoping review results, combined with the stakeholder workshops and survey that followed, directly informed the focus and methods of the Phase 2 contingent syntheses.
This chapter has informed the following manuscript:
Alexander, L.A., et al. Exercise therapy for tendinopathy: A scoping review mapping interventions and outcomes. SportRxiv preprint doi: https://osf.io/a8ewy/.
Methods
This scoping review was conducted in accordance with JBI scoping review methodology50 and an a priori protocol was published in JBI Evidence Synthesis. 51 JBI scoping review methodology is the most up-to-date guidance for the conduct of scoping reviews. It is based on the foundational framework proposed by Arksey and O’Malley52 and further developed by Levac, Colquhoun and O’Brien. 53 JBI methodology50 built upon the previous approaches and developed comprehensive guidance for reviewers who are planning and conducting a scoping review. This scoping review is reported in accordance with the PRISMA-ScR. 39
The aim of this scoping review was to comprehensively map the existing evidence on exercise for the management of tendinopathies, addressing the first and second review questions:
-
What exercise interventions have been reported in the literature and for which tendinopathies?
-
What outcomes have been reported in studies investigating exercise interventions for tendinopathies?
The results of this scoping review subsequently informed the contingent systematic reviews reported in Chapters 5 and 6.
Inclusion criteria
The inclusion criteria were defined for this scoping review using the ‘PCC’ mnemonic relating to the Participants, Concept and Context, and informed by the definitions of participants and health technology provided in Chapter 3.
Participants
As described in Chapter 3, we included sources of evidence where participants were people of any age or gender with a diagnosis of tendinopathy of any severity or duration and at any anatomical location.
Concept
As described in Chapter 3, exercise interventions that could be categorised as one or more of strengthening, flexibility, aerobic, proprioception or motor control were included. They could be first- or second-line interventions and could be used in isolation or in combination with other interventions. Studies focussing on exercise following surgical repair were excluded as the review concerned non-surgical management of tendinopathy. Exercise interventions delivered by any health, exercise professional or support worker, either supervised or unsupervised, were included. Any outcomes used to evaluate exercise interventions for tendinopathy were included.
Context
Any setting including primary care, secondary care, community locations, clinics or people’s homes in any nation classified as having very high human development (defined as the top 62 ranked countries in the 2019 Human Development Index (HDI))54 at the time of conducting the review were included. The top 62 HDI countries were categorised as having ‘very high human development’ and included the UK, therefore findings from studies conducted in any of these 62 countries could be considered for generalising to the UK setting.
Search strategy
Following the JBI three-step search strategy, an initial search using exercise and tendinopathy terms was conducted in CINAHL and MEDLINE (step 1). Review of the titles, abstracts and index terms from the initial search results informed the development of a full search strategy that was constructed using a combination of subject headings and keywords which was then tailored to each database (step 2). The full search strategies for all databases and grey/unpublished literature were developed by the review team, which comprised experienced reviewers (n = 4), subject experts (n = 5) and a specialist information scientist. The search strategies were piloted and amended by the team before the final searches were conducted to ensure specificity and sensitivity. The following databases were searched: MEDLINE, CINAHL, AMED, SPORTDiscus (all EBSCOhost), EMBase (Ovid), Cochrane library (Controlled trials, Systematic reviews), JBI Evidence Synthesis, PEDRo and Epistemonikos. Grey and unpublished literature was searched using trial registries (ClinicalTrials.gov, ISRCTN Registry, The Research Registry, EU-CTR [European Union Clinical Trials Registry], ANZCTR [Australia and New Zealand Clinical Trials Registry]), Open Grey, MedNar, The New York Academy Grey Literature Report, Ethos, CORE, and Google Scholar using modified search terms. All searches were conducted in April 2020 and the full search strategies are presented in Appendix 1.
Sources of evidence published in any language where a translation was accessible via Google Translate or the review team’s international networks were included. The seminal publication of Alfredson et al. ’s17 eccentric protocol for Achilles tendinopathy (AT) marked the start of a proliferation of high-quality research on the efficacy and explanatory mechanisms of well-described exercise interventions for tendinopathy. Therefore, databases were searched from 1 January 1998 onwards.
Step 3 usually involves hand-searching the reference lists of included studies. However, due to the comprehensive search strategy and volume of studies located and in consultation with our steering committee, it was decided not to conduct this step for the scoping review. Instead, we employed citation tracking using Scopus and hand-searching of reference lists of studies included in the scoping review as part of the efficacy review search strategy. The citation analysis enabled the review team to understand where articles were published (which journals and country), who was using the articles as well as identifying collaborative work between countries.
A range of study designs were included in this scoping review to ensure a comprehensive map was produced. The included study designs were experimental, quasi-experimental, observational, pilot, mixed-methods, qualitative and systematic review. The inclusion of systematic reviews enabled previous evidence syntheses to be mapped in order to avoid replication in the contingent reviews. Other designs including opinion, narrative or other non-systematic reviews, protocols and case studies were excluded.
Screening for inclusion
Following the search, all results were uploaded into ProQuest® RefWorks and duplicates were removed. Sources were then imported to Covidence (Melbourne, Australia) systematic review management software for two-level screening, following the identification and removal of remaining duplicates identified by Covidence. Firstly, titles and abstracts were screened independently by two reviewers with conflicts identified by Covidence and resolved by a third reviewer. The full-text copies of all sources included following title and abstract screening were uploaded to Covidence. The full texts were then screened by two reviewers independently and all conflicts were resolved by a third reviewer. Training for all reviewers using the inclusion criteria was conducted in Covidence prior to the start of title and abstract screening. Ongoing communication occurred between reviewers throughout the screening stage via weekly team meetings and posts in Microsoft Teams. This enabled all queries around screening to be addressed in a timely manner. All sources excluded at full-text screening stage and the reasons for exclusion are available as supplementary material (Supplementary Material 1). Following full text screening, four tendinopathy experts external to the review team also reviewed the included study list for completeness.
Data extraction
A bespoke data-extraction tool (Supplementary Material 2) was developed for this review in Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA). The tool was used to extract study demographic details as well as data related to the review questions.
The following demographic information was extracted from the included primary studies: author(s), year of publication, country, study title, aims/purpose, study design, participant details (age, gender, ethnicity, comorbidities and other characteristics), inclusion criteria, setting and tendinopathy diagnosis method. Extracted data relating to the review questions included: body area affected, tendinopathy type, the author’s focus on exercise, that is, primary (exercise as the novel intervention being studied), secondary (exercise as the control arm to another novel intervention) or neutral (exercise being compared with other intervention/s where neither is the novel intervention or main focus of study); exercise intervention details including reporting and monitoring; treatment adjuncts; primary and secondary outcomes including health domains and tools used to evaluate interventions, and key findings.
Data extraction from included systematic reviews was limited to demographic information including year of publication, author(s), country, aims/purpose, study type, number of included studies, inclusion criteria, settings, body area affected and tendinopathy type, as information on interventions and outcomes was extracted from the primary studies.
Piloting and iterative development of the data-extraction tool was conducted by the review team over ten rounds prior to commencing final extraction. Ten per cent of data extraction was replicated in an informal assessment of consistency that was identified as appropriate and reflected the extensive piloting and discussions among the review team. As per the screening process, data extraction was supported by the weekly team meetings and regular Microsoft Team chat. In accordance with scoping review methodology, critical appraisal was not conducted in this review. 50
Data synthesis
The extracted data were synthesised and integrated into a series of visual outputs to answer the review questions and present a comprehensive map of exercise interventions and outcomes; data are presented alongside an accompanying narrative in the Results section.
Extracted exercise intervention component data were mapped against the TIDieR checklist55 to identify if full and accurate reporting of interventions had occurred. The review team modified the TIDieR checklist for the purposes of this scoping review. The TIDieR template requires one to identify and note the location of each criterion in the study and supporting detail. The review team added to each criterion a grading of ‘Fully reported’ (if criterion was fully described), ‘Partially reported’ (if some components of the criterion were described but lacked detail) and ‘Not reported’ (if there was not enough detail to satisfy a partially reported definition). An additional criterion was then added by the team to reflect overall reproducibility of the intervention which reflected ‘Fully reproducible’ (all criteria fully reported to enable replication of the intervention), ‘Partially reproducible’ (if exercise components were described (what, when and how much) but other components were not reported (e.g. where, who)) and ‘Not reproducible’ if there was not enough detail to satisfy a partially reproducible definition. This allowed an evaluation of overall reproducibility of each intervention as a whole to facilitate reporting and clearer interpretation. For the ‘When and How much’ criterion, the intervention details were extracted on how often the intervention was delivered, over what time period, number of sessions in total, duration, intensity, dose and volume. For the ‘Tailoring’, ‘Modification’, and ‘How well’ criteria, details were extracted for each (including what, when, why and how the intervention was tailored or modified during the study, how adherence or fidelity was assessed, by whom, and strategies to improve and the actual adherence or fidelity reported).
The outcomes were recorded as domains informed by the ICON health-related domains. 56 For completeness, we adopted the 24 candidate domains identified at stage one of the ICON Delphi process to fully map all domains reported in the included sources, rather than the nine core domains finally recommended by Vicenzino et al. 56
All data were imported from the MS Excel spreadsheet and analysed in the R programming environment (v.4.1.2; R Core Team 2021). 57 A citation analysis was also conducted using citation, bibliographical, author and keyword information obtained from Scopus and Bibliometrix. 58
Results
Description of included studies
The search identified 22,550 sources, of which 1994 were obtained in full text following deduplication and title and abstract screening. A further 1439 sources were excluded following full-text screening, leaving 548 studies from a total of 555 total sources, as seven studies were reported in more than one source. The main reasons for exclusion at full-text screening were wrong study design (n = 600, 42%), duplicate study (n = 351, 24%), wrong population (n = 150, 10%), wrong concept (n = 101, 7%) or not originating from a very highly developed country (n = 99, 7%) (see Supplementary Material 1). The study selection process is presented in Figure 2 and a table of included studies is presented in Table 33, Appendix 2.
FIGURE 2.
Study selection process – PRISMA flowchart.
From: Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. https://doi.org/10.1136/bmj.n71.

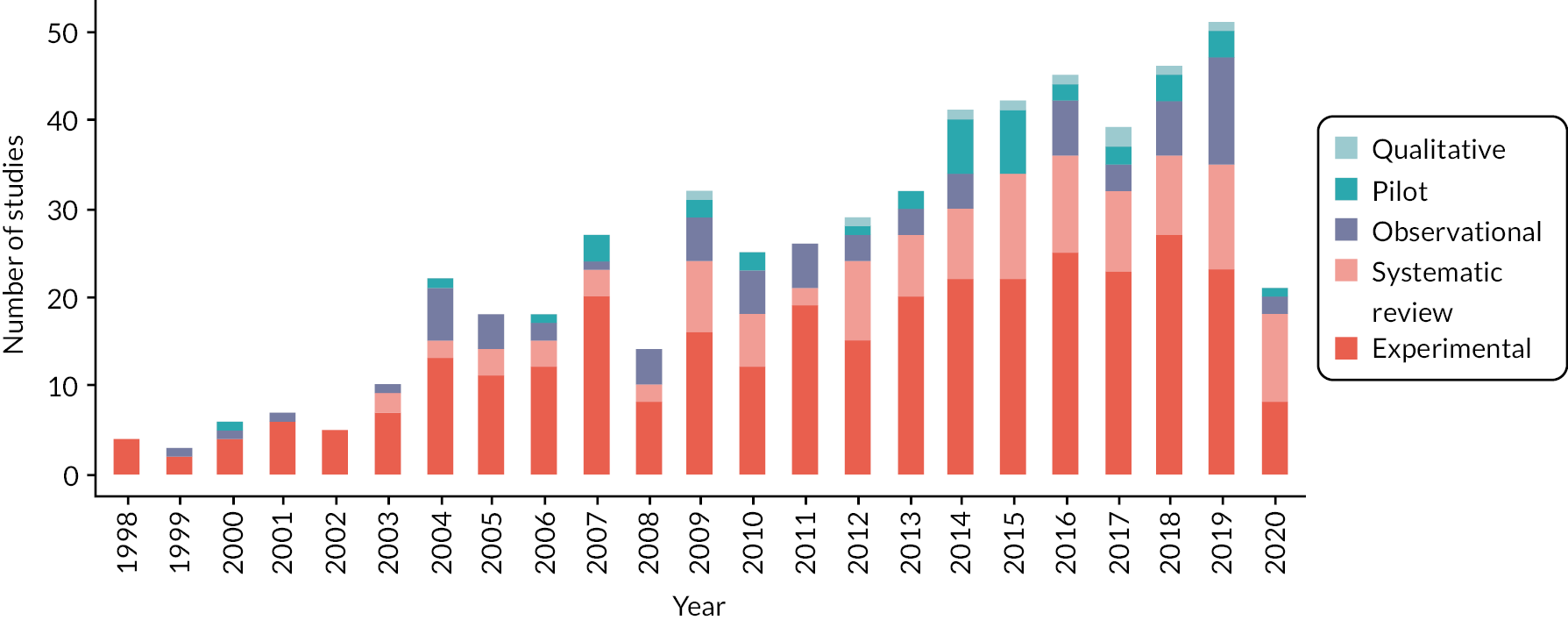
The 555 included sources comprised 119 (21%) systematic reviews and 436 (79%) primary studies. Sources were mostly published in English (n = 539; 97%), with 3% published in German (n = 6), Turkish (n = 5), Spanish (n = 3), Italian (n = 1) and Norwegian (n = 1). Automated translation was used for five sources, with the remainder being translated by colleagues of the review team. Assessment of the included studies’ publication dates identified a consistent increase in the volume of research from 1998, reaching a peak of 50 studies published in 2019 and an average of 37 studies published each year between 2010 and 2019 (see Figure 3).
FIGURE 3.
Number of included studies published over time and their study design.
Citation analysis
A citation analysis was conducted on the Scopus information obtained from 450 (81%) of the included sources, generating 14,860 references. The full citation analysis is available in Appendix 3. Of the 450 citations used to complete the analysis, they were published in: British Journal of Sports Medicine (n = 39, 9%), American Journal of Sports Medicine (n = 28, 6%), Journal of Orthopaedic and Sports Physical Therapy (n = 15, 3%), Clinical Journal of Sports Medicine (n = 14, 3%) and Knee Surgery Sports Traumatology Arthroscopy (n = 14, 3%). Based on citations per year, the top-ranked studies included De Vos et al. (49 citations per year),59 Alfredson et al. (30 citations per year),17 De Jonge et al. (21 citations per year),60 Malliaras et al. (21 citations per year)61 and Thanasas et al. (20 citations per year). 62 Across the 14,860 references identified, they were obtained from the American Journal of Sports Medicine (n = 655, 4%), British Journal of Sports Medicine (n = 628, 4%), Journal of Orthopaedic Sports Physical Therapy (n = 304, 2%) and British Medical Journal (n = 262, 2%). A country collaboration network diagram of the included references is available in Appendix 3, Figure 23, and illustrates extensive collaborations across many countries particularly the UK, USA and Australia. Figure 24 (see Appendix 3) illustrates the rise in exercise for tendinopathy research from the early 1980s, reaching a peak in 2009.
Systematic reviews
There were 119 systematic reviews included in this scoping review. The reviews were classified by the review team as 72 (61%) systematic reviews without meta-analysis, 45 (37%) systematic reviews with meta-analysis and two (2%) umbrella/review of reviews. The number of studies included across the systematic reviews ranged from two to 84 with a median of 12 (IQR: 8–19). Four main tendinopathy types were the focus of the reviews, with 43 (36%) investigating RCRSP, 26 (22%) Achilles, 14 (12%) lateral elbow and 14 (12%) patellar tendinopathy. Five (4%) systematic reviews related to both Achilles and patellar tendinopathies, three (3%) focussed on gluteal or posterior tibial tendinopathies, two (2%) on hamstring or medial elbow tendinopathies and one (1%) on quadriceps. Most of the reviews were conducted by teams based in four countries: UK (n = 28; 23%), Australia (n = 17; 14%), USA (n = 14; 12%) and the Netherlands (n = 13, 11%). Exercise was the primary focus in 46 (38%) systematic reviews, a secondary focus (e.g. the control) in 49 (42%), and a neutral focus (i.e. equivalence between exercise and other interventions) in 24 (20%). Exercise was more commonly the primary focus of systematic reviews investigating lower-limb tendinopathy [Achilles (46%) and patellar (43%)), compared to upper-limb tendinopathy (RCRSP (34%) and lateral elbow (29%)].
The remainder of the results section and analysis relates only to the primary studies.
Primary studies
Study demographics
The predominant design for the 436 included primary studies was randomised controlled trial (RCT) (n = 236; 54%), followed by quasi-experimental (n = 81; 19%), observational (n = 75; 17%), pilot (n = 35; 8%) and qualitative (n = 9; 2%). The studies comprised information obtained from 25,490 participants (male = 10,463; female = 10,734), with study mean age ranging from 15 to 65 years. Most studies were conducted in a mixed setting (n = 116; 27%), with clinic (n = 91; 21%) and home settings (n = 61; 14%) also reported. A total of 31 countries were identified, with most studies conducted in four countries: Turkey (n = 60; 14%), USA (n = 48; 11%), UK (n = 43; 10%) and Australia (n = 32; 7%).
A range of additional participant characteristics were recorded across 362 studies (83%), with the most frequently reported characteristic being symptom duration (n = 253; 70%). Other less frequently reported characteristics included weight (n = 115; 32%), height (n = 113; 31%), affected side (including bilateral) (n = 105; 29%), body mass index (BMI) (n = 102; 28%), hand/limb dominance (n = 86; 24%), physical activity level (n = 82; 23%), employment status (n = 50; 14%), previous treatment (n = 34; 9%), number of physical activity sessions (hours of sport/week, mileage/week, or training/week) (n = 28; 7%), education level (n = 22; 6%), co-morbidities (n = 21; 6%), smoking status (n = 18; 5%), analgesic/nonsteroidal anti-inflammatory drug NSAID use (n = 16; 4%), mechanism of injury/causation (n = 15; 4%), previous history/episodes (n = 14; 4%), sports participation interference (n = 13; 4%), location of symptoms (n = 13; 4%), manual occupation (n = 11; 3%) and ethnicity (n = 9; 2%). Of the nine studies reporting ethnicity, European/Caucasian participants were included in all, with African American (four studies), Hispanic/Latino (three studies), Asian (one study) and Māori (one study) also reported. Sixty studies (17%) did not report any additional characteristics for participants.
Which tendinopathies were reported?
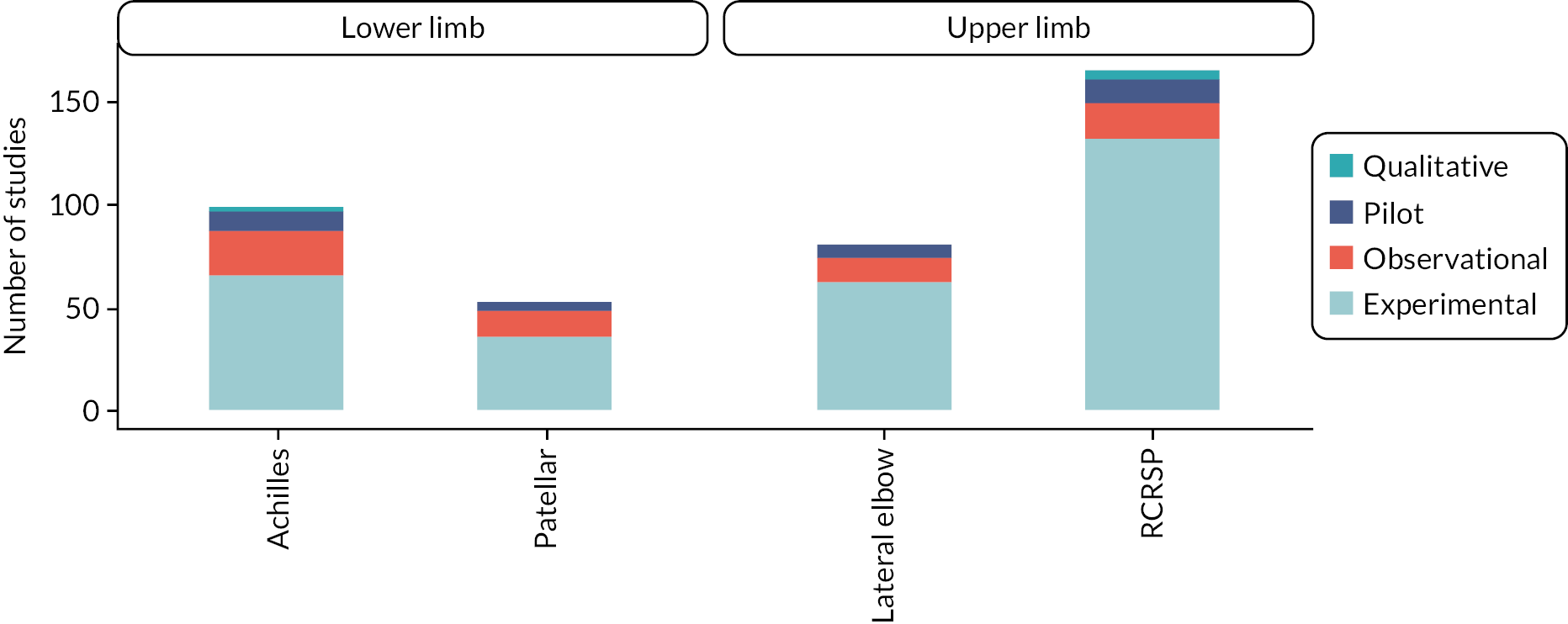
Four tendinopathy types accounted for over 90% of the results, with 167 (38%) studies focussing on RCRSP, 103 (23%) on Achilles, 82 (19%) on lateral elbow and 53 (12%) on patellar tendons. Less frequently investigated tendinopathies included gluteal, tibialis posterior and hamstring, which were the focus of 9 (2%), 7 (2%) and 3 (1%) studies, respectively. The breakdown of study design for the four most common tendinopathy types is illustrated in Figure 4. Experimental studies were the most commonly reported study design compared to the far smaller number of qualitative studies conducted across all the common tendinopathies.
FIGURE 4.
Primary study designs across main tendinopathy types.
Exercise interventions investigated
Exercise therapy interventions were reported as the primary focus of 161 (37%) studies, the secondary focus of 188 (43%) studies, and a neutral focus in 87 (20%) studies. The different exercise interventions were categorised as strengthening, flexibility (including dynamic range of motion (ROM) exercises), aerobic, proprioception or motor control and determined by the authors’ stated purpose. A mapping of the different exercise intervention components and subcomponents across different tendinopathy types is presented in Table 2.
| All (n = 436) |
RC (n = 165) |
Achilles (n = 99) |
Lateral elbow (n = 81) |
Patellar (n = 53) |
Other (n = 38) |
|
|---|---|---|---|---|---|---|
| Strengthening | 367 (84%) | 128 (78%) | 92 (93%) | 62 (77%) | 53 (100%) | 32 (84%) |
| Eccentric | 205 (47%;56%) | 21 (13%;16%) | 88 (89%;96%) | 36 (44%;58%) | 45 (85%;85%) | 15 (39%;47%) |
| Concentric | 37 (8%) | 12 (7%) | 4 (4%) | 5 (6%) | 9 (17%) | 7 (18%) |
| Eccentric + Concentric | 49 (11%;13%) | 32 (19%;25%) | 1 (1%;1%) | 6 (7%;10%) | 2 (4%;4%) | 8 (21%;25%) |
| Isometric | 68 (16%;19%) | 34 (21%;27%) | 5 (5%;5%) | 11 (14%;18%) | 10 (19%;19%) | 8 (21%;25%) |
| Progressive strength | 28 (6%;8%) | 19 (12%;15%) | 0 (0%;0%) | 5 (6%;8%) | 1 (2%;2%) | 3 (8%;9%) |
| Isotonic | 15 (3%;4%) | 11 (7%;9%) | 1 (1%;1%) | 2 (2%;3%) | 1 (2%;2%) | 0 (0%;0%) |
| Isokinetic | 17 (4%;5%) | 6 (4%;5%) | 1 (1%;1%) | 1 (1%;2%) | 3 (6%;6%) | 6 (16%;19%) |
| HSRT | 4 (1%;1%) | 0 (0%;0%) | 0 (0%;0%) | 1 (1%;2%) | 3 (6%;6%) | 0 (0%;0%) |
| Plyometric | 12 (3%3%) | 2 (1%;2%) | 4 (4%4%) | 3 (4%;5%) | 1 (2%;2%) | 2 (5%;6%) |
| Flexibility | 208 (48%) | 103 (62%) | 20 (20%) | 53 (65%) | 14 (26%) | 18 (47%) |
| Traditional stretching | 95 (22%;46%) | 42 (25%;41%) | 6 (6%;30%) | 30 (37%;57%) | 6 (11%;43%) | 11 (29%;61%) |
| Dynamic ROM | 72 (17%;35%) | 63 (38%;61%) | 0 (0%;0%) | 5 (6%;9%) | 1 (2%;7%) | 3 (8%;17%) |
| PNF | 14 (3%;7%) | 8 (5%;8%) | 0 (0%;0%) | 4 (5%;8%) | 0 (0%;0%) | 2 (5%;11%) |
| No detail | 75 (17%;36%) | 32 (19%;31%) | 12 (12%;60%) | 17 (21%;32%) | 7 (13%;50%) | 7 (18%;39%) |
| Proprioception | 21 (5%) | 10 (6%) | 2 (2%) | 2 (2%) | 2 (4%) | 5 (13%) |
| Motor control | 73 (17%) | 66 (40%) | 0 (0%) | 1 (1%) | 1 (2%) | 5 (13%) |
| Aerobic | 24 (6%) | 4 (2%) | 6 (6%) | 0 (0%) | 9 (17%) | 5 (13%) |
The most common exercise type reported across all tendinopathies was strengthening (84%), followed by flexibility (48%). When investigated individually, there were some differences in exercise types between different tendinopathies. All patellar tendinopathy studies (100%) reported the use of strengthening exercise, compared to 77–93% of studies for other tendinopathies. There was also greater use of aerobic exercise (17%) reported in patellar tendinopathy studies compared to other tendinopathies (0–13%).
While eccentric was the most common strengthening exercise reported for Achilles (89%), patellar (85%) and lateral elbow tendinopathy (44%), RCRSP studies reported isometric (21%) followed by a combination of eccentric and concentric (19%) as the most common. For flexibility exercise, upper-limb tendinopathies reported this more often (RCRSP 62%; lateral elbow 65%) than lower-limb tendinopathies (patellar 25%; Achilles 20%).
Flexibility exercise was poorly described across all tendinopathies, with 17% of studies not providing sufficient detail to categorise the type of flexibility exercise included. Where flexibility was well described, dynamic ROM was the most common form of flexibility exercise used for RCRSP (38%), with static sustained stretching most common for all other tendinopathies (6–37%). Motor control exercise interventions were mainly reported for RCRSP.
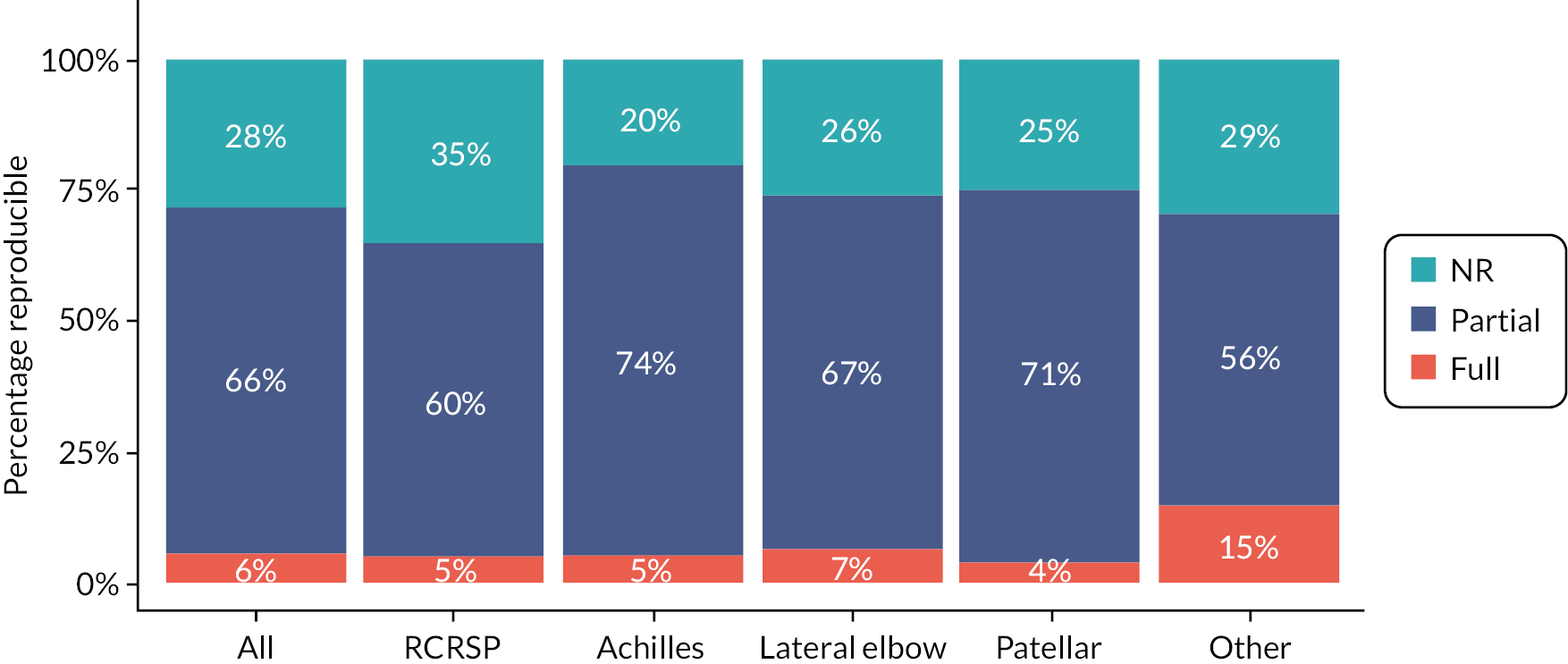
Exercise intervention reporting
All exercise interventions were mapped to the TIDieR checklist55 and are presented for all tendinopathies in Figure 5 and for the four main tendinopathies in Figure 6. The intervention setting was often not reported (51%) or only partially reported (19%). Additionally, over one-third of studies did not report the how (mode of delivery, 38%), who (intervention provider expertise, 37%), why (rationale, theory, or goal, 36%) or what (physical or informational materials used, 35%) components of interventions. Data from the TIDieR checklist were used by the review team to categorise study interventions as fully reproducible (all details reported to enable reproduction of the exercise), partially reproducible (some but not all details of exercise reported to enable partial reproduction of the exercise) or not reproducible (see Figures 5 and 6). Reproducibility was assessed across different tendinopathies, with most exercise interventions (56–74%) categorised as partially reproducible, and only a minority (4–15%) categorised as fully reproducible.
FIGURE 5.
Exercise therapy reporting across all tendinopathy types using the TIDieR checklist.
Who: intervention provider expertise; What(M): informational materials used; What(P): physical materials used; How: mode of delivery; Where: intervention setting; Why: rationale, theory or goal; NR: not reported; Partial: partially reported; Full: fully reported; Other: refers to all other tendinopathy types.

FIGURE 6.
Reproducibility of exercise therapies across tendinopathy types using the TIDieR checklist.
NR: not reported; Partial: partially reported; Full: fully reported; Other: refers to all other tendinopathy types.
Monitoring exercise adherence was planned by authors in 152 studies and the main method consisted of exercise diaries (71% of reported methods). Other methods included summary records from therapist (8%), self-report (7%), therapist individual session records (6%), follow-up phone calls to monitor attendance (4%), follow-up appointments to monitor adherence (3%) and adherence reported by family member (1%). Whilst exercise adherence was planned in 152 studies, adherence data were only reported in 89 (59%) of those studies, representing 20% of all primary studies in the review.
Reported adherence means ranged from 16% to 100% in individual studies and were 77% across all studies. Authors used varied grading of adherence from subjective terms such as ‘high’, ‘good’ and ‘adherent’ to aligning frequencies to rankings of poor to excellent (e.g. >75% ‘good’, 70% ‘good/excellent’, 25–75% ‘moderate to excellent’, 50% ‘good’, 27% ‘moderate to poor’). Studies also reported a reduction in adherence over time with 12-week adherence ranging from 27% to 94.2% and two-year adherence ranging from 41% to 87.4%.
Reporting of modifications (any modifications to the intervention during the study) and tailoring (planned personalisation, titration or adaptations) of exercise interventions were also recorded. Tailoring was reported in 247 (56%) studies and involved personalised progression of exercise interventions via increasing: sets, number of sessions per day, repetitions, resistance/load, speed, duration of muscle contraction, time spent on exercise, ROM, difficulty (up to 13–15 rating of perceived exertion), addition of new exercises, reducing base of support/stability, gradual increase in other physical and sporting activities, and progression from low to higher impact activities. Progressions were determined by the physiotherapist/exercise professional, improved quality of movement control, full range of movement, ratings of participant-perceived effort (e.g. less than 7, up to 11–14), fatigue, the absence of pain, pain rated as no more than 3–5/10 on a pain scale, or as ‘pain allowed’.
Tailoring also involved decrements in exercise via reduced loading and ROM due to participant-reported pain, typically including pain greater than 4–5/10 on a visual or verbal analogue scale or pain that did not rapidly subside (e.g. within 10–15 minutes post exercise). Modifications were reported in only 20 (5%) studies. Modifications included participants being withdrawn and referred for further investigation, follow-up appointments as required to facilitate self-management or for any difficulties, and alternative planes of motion or training technique modifications that were more comfortable for participants or due to additional musculoskeletal problems occurring during the study.
Exercise therapy adjuncts
Treatment adjuncts (non-exercise treatments in addition to the exercise component of interventions) were included in 140 studies (44%) and were not present in 109 (67 were not applicable due to study design). The main treatment adjuncts were injection, laser, ESWT, manual therapy (MT) and splinting/taping. Additionally, of the 316 experimental studies included, 49 (16%) included a specific non-exercise arm (whereby one or more of the groups were not prescribed any exercise as part of their intervention) whilst 184 did not include a non-exercise arm (83 were not applicable).
Health domains
To answer the second review question on what outcomes have been reported, outcomes were broken down into health domains and the outcome measurement tools used for each domain. Primary and secondary health domains were extracted across all tendinopathy types and are presented in Table 3. Disability was the most common primary health domain (n = 282) for RCRSP (n = 123), Achilles (n = 67) and patellar (n = 40) tendinopathies (see Table 2). For lateral elbow, physical function capacity (PFC) was most common (n = 40). Secondary health domains also varied across tendinopathies, with Achilles and patellar both reporting participant rating of overall condition most frequently (n = 15 and n = 8 respectively), with disability the most common secondary domain for RCRSP (n = 27), and PFC (n = 14) for lateral elbow. Across tendinopathies, adverse effects or cost effectiveness were rarely the primary or secondary outcome.
| ICON domain Description (where required) |
Primary or secondary outcome | All (n = 436) |
RC (n = 165) |
Achilles (n = 99) |
Lateral elbow (n = 81) |
Patellar (n = 53) |
Other (n = 38) |
|---|---|---|---|---|---|---|---|
| Adverse effects/events Unintended treatment effect |
Primary | 11 | 1 | 6 | 1 | 2 | 1 |
| Secondary | 13 | 4 | 2 | 2 | 5 | 0 | |
| Clinical examination findings e.g. clinical examination tests |
Primary | 19 | 10 | 1 | 2 | 0 | 6 |
| Secondary | 6 | 5 | 0 | 1 | 0 | 0 | |
| Disability Composite scores of patient-rated pain and disability due to pain, usually tendon-specific |
Primary | 282 | 123 | 67 | 35 | 40 | 17 |
| Secondary | 53 | 27 | 5 | 11 | 6 | 4 | |
| Drop out or discontinued treatment | Primary | 7 | 1 | 1 | 3 | 2 | 0 |
| Secondary | 0 | 0 | 0 | 0 | 0 | 0 | |
| Economic impact costs | Primary | 4 | 3 | 0 | 1 | 0 | 0 |
| Secondary | 2 | 1 | 0 | 1 | 0 | 0 | |
| Function Patient-rated – not referring to pain intensity |
Primary | 21 | 7 | 1 | 7 | 2 | 4 |
| Secondary | 13 | 6 | 3 | 2 | 0 | 2 | |
| Medication use | Primary | 9 | 2 | 4 | 2 | 1 | 0 |
| Secondary | 10 | 5 | 0 | 2 | 3 | 0 | |
| Other | Primary | 24 | 6 | 8 | 7 | 3 | 0 |
| Secondary | 17 | 5 | 6 | 3 | 2 | 1 | |
| Pain – clinician-applied stress/examination | Primary | 8 | 1 | 1 | 4 | 1 | 1 |
| Secondary | 5 | 0 | 1 | 3 | 1 | 0 | |
| Pain on loading/activity Pain during tendon-specific provocation |
Primary | 108 | 42 | 21 | 18 | 21 | 6 |
| Secondary | 34 | 18 | 5 | 5 | 6 | 0 | |
| Pain over a specified time Pain intensity over e.g. 24 hours, 7 days |
Primary | 63 | 30 | 5 | 19 | 4 | 5 |
| Secondary | 38 | 21 | 6 | 8 | 2 | 1 | |
| Pain without further specification Pain without reference to specified time or activity |
Primary | 90 | 41 | 13 | 18 | 10 | 8 |
| Secondary | 16 | 5 | 4 | 3 | 2 | 2 | |
| Palpation | Primary | 9 | 0 | 4 | 2 | 2 | 1 |
| Secondary | 1 | 0 | 1 | 0 | 0 | 0 | |
| Participant/patient rating overall condition Single numerical assessment |
Primary | 66 | 15 | 20 | 17 | 8 | 6 |
| Secondary | 46 | 13 | 15 | 6 | 8 | 4 | |
| Participation Patient rating e.g. level of/return to sport |
Primary | 25 | 8 | 6 | 5 | 4 | 2 |
| Secondary | 18 | 8 | 5 | 3 | 2 | 0 | |
| Physical activity Self-report or wearables |
Primary | 6 | 0 | 5 | 0 | 0 | 1 |
| Secondary | 4 | 0 | 2 | 0 | 0 | 2 | |
| PFC Physical tasks e.g. hops, squat tests |
Primary | 100 | 30 | 13 | 40 | 8 | 9 |
| Secondary | 44 | 18 | 7 | 14 | 4 | 1 | |
| Psychological factors e.g. self-efficacy, kinesiophobia |
Primary | 5 | 4 | 1 | 0 | 0 | 0 |
| Secondary | 9 | 5 | 2 | 0 | 0 | 2 | |
| QoL General well-being |
Primary | 17 | 10 | 3 | 4 | 0 | 0 |
| Secondary | 26 | 11 | 3 | 7 | 2 | 3 | |
| ROM | Primary | 56 | 44 | 3 | 4 | 1 | 4 |
| Secondary | 18 | 14 | 3 | 1 | 0 | 0 | |
| Sensory modality specific pain e.g. quantitative sensory testing |
Primary | 11 | 3 | 3 | 4 | 1 | 0 |
| Secondary | 6 | 1 | 1 | 4 | 0 | 0 | |
| Structure (tendon tissue characteristics) e.g. imaging/biopsy |
Primary | 56 | 9 | 32 | 4 | 10 | 1 |
| Secondary | 18 | 5 | 10 | 1 | 2 | 0 |
Outcome measurement tools
An extensive range of primary and secondary outcome tools were reported across tendinopathies. A comprehensive map of the tools relative to health domains and tendinopathy types is provided here: Primary outcomes: http://www2.rgu.ac.uk/nhir/tendinopathy-primary-outcomes-interactive-table.html Secondary outcomes: http://www2.rgu.ac.uk/nhir/tendinopathy-secondary-outcomes-interactive-table.html. The most frequently reported tools included visual analogue scales (VAS) (RCRSP n = 73, lateral elbow n = 44, Achilles n = 29, patellar n = 22); Victorian Institute of Sport Assessment questionnaires (Achilles VISA-A n = 59, patellar VISA-P n = 39); Shoulder Pain and Disability Index (SPADI) (RCRSP n = 45); dynamometer (lateral elbow n = 39, RCRSP n = 17); Goniometer (RCRSP n = 39); Constant Murley Score (CMS) (RCRSP n = 36); Disabilities of the Arm, Shoulder and Hand questionnaire (DASH/Quick DASH) (RCRSP n = 35); ultrasonography (Achilles n = 20, patellar n = 11); patient-rated tennis elbow evaluation questionnaire (lateral elbow n = 17) and numerical pain rating scale (NPRS) (RCRSP n = 14).
The main secondary outcome tools were dynamometer (lateral elbow n = 15, RCRSP n = 13), VAS (RCRSP n = 15, Achilles n = 10, lateral elbow n = 8, patellar n = 8), NPRS (RCRSP n = 13, Achilles n = 5), ultrasonography (Achilles n = 11), goniometer (RCRSP n = 9), DASH (RCRSP n = 8), 36-item short-form survey (SF-36) (RCRSP n = 7), EQ-5D (gluteal n = 6), CMS (RCRSP n = 6), Western Ontario Rotator Cuff Index (RCRSP n = 6) and algometer (lateral elbow n = 5).
Of the nine qualitative studies included, the majority were on RCRSP (five studies) followed by Achilles (n = 2), tibialis posterior (n = 1) and a mixed tendinopathy group (n = 1: Achilles/patellar/RCRSP). These studies represented 114 participants (people with tendinopathy and physiotherapists), of whom 59 were female and 36 male. The studies reported participants’ barriers and facilitators to exercise interventions, which included psychosocial impact, treatment burden, motivation, confidence, coping, pain, socialisation, and benefits of group exercise, recognising the challenges of exercise interventions and self-management. They also reported on a range of physiotherapist-related factors including views, clinical reasoning, perceived barriers and facilitators, and treatment awareness.
Discussion
This is the first scoping review to comprehensively map existing evidence on exercise therapy interventions and outcomes for the treatment of tendinopathies. A total of 555 sources were included, demonstrating the abundance of research, the need for it to have been mapped in this review, and also the need for a taxonomy of exercise interventions and reporting standards to allow comparisons of efficacy to be made. This review guided the subsequent contingent evidence syntheses reported in Chapters 5 and 6. It also identified research gaps which can inform future research and evidence syntheses. Finally, the review identified potential areas of improvement in clinical practice which will need to be explored further.
Although the number of RCTs in this field has increased recently, there were large numbers of quasi-experimental and observational studies identified by this review. The mapping of all these study designs directly informed the efficacy reviews reported in Chapter 5.
This review also identified a small number of qualitative studies which can contribute to understanding feasibility and acceptability of exercise for tendinopathy. These are reported, along with relevant quantitative designs exploring these phenomena, in the mixed-method review reported in Chapter 6. The small number of qualitative studies identified, compared with the volume of quantitative research, identifies a need for further primary research to fully understand patients’ and practitioners’ perceptions and experiences of exercise therapy interventions for tendinopathy in order to guide intervention development and assist with real-world implementation of findings from trials.
Exercise for tendinopathy
The findings that strengthening exercise was the most reported exercise type across all tendinopathies, particularly the lower limb, and that eccentric strengthening exercise was most common for three tendinopathies (Achilles, patellar, lateral elbow) are in keeping with previous evidence. 63 However, due to the variable levels of reporting, it would be difficult to determine whether many interventions described as strengthening would in fact achieve the required overload for strengthening to occur. This has implications for practice, and improved quality of reporting of exercise interventions in future studies is urgently required, along with better clarity about the definitions of terms such as ‘strength’ compared to ‘muscle activation’ or ‘endurance exercise’.
The findings related to RCRSP demonstrated the most clinical heterogeneity, with greater variation in strengthening exercise type, and exercise type per se, with flexibility, motor control and proprioceptive exercise reported in addition to strengthening. Dynamic ROM exercise for flexibility was more frequently reported than traditional active or passive stretching for RCRSP. This varied approach to the management of RCRSP suggests that there is, as yet, no consensus in the literature on how best to manage this complex tendinopathy. 64,65
Reporting of interventions was highly variable, with the TIDieR checklist classifying 15% or fewer included interventions as fully reproducible. This finding has implications for practice, as it would be challenging, if not impossible, for practitioners to adopt interventions demonstrated as efficacious in research studies, possibly resulting in suboptimal exercise prescription and patient outcomes. This identification of variable and typically inadequate reporting further supports the need for the development of minimum standards of reporting, using available guidelines such as TIDieR to assist the process. 66,67
Only 20% of included primary studies reported adherence, despite the planned intention to collect adherence measures in 35% of studies, which is similar to previous adherence reports three decades ago. 68 Adherence monitoring relied primarily on a range of participant self-report instruments with wide variation in scoring methods, and a lack of objective monitoring. These issues are further explored in Chapter 6 (mixed-method review of feasibility and acceptability).
Around half of the studies included personalised tailoring of exercise guided by pain, in keeping with the evidence that adherence to interventions that require exercising into or through pain (e.g. Alfredson protocol) will typically be lower. 69 The small body of included qualitative studies suggest that there may be several barriers to adherence (e.g. treatment burden, pain, psychosocial factors, motivation, confidence and coping). These are likewise further explored in Chapter 6.
Proposed initial reporting criteria for exercise interventions for the management of tendinopathy
Having mapped the exercise interventions on the management of tendinopathy, the review team produced initial criteria to inform the reporting of tendinopathy exercise interventions to ensure consistency and allow easier comparisons in the future. The proposed initial criteria (see Box 1) combined the results from the mapping of the type of exercise interventions during the scoping review and the recommendations in the TIDieR checklist. The initial reporting criteria identified in this scoping review require further funding and development with all relevant stakeholders to create a comprehensive taxonomy to guide exercise reporting in tendinopathy practice and research.
Including information on the place and method of delivery of exercise interventions is important to allow cost-effectiveness analyses. The increasing delivery of medical interventions remotely or in group settings presents opportunities for efficiencies, but currently there is lack of evidence on the cost-effectiveness of such approaches.
Information to be collected
-
Anatomical location of tendinopathy (e.g. RCRSP)
-
Exercise therapy class/treatment
-
Dominant therapy class (e.g. strength/resistance)
-
Exercise treatment (e.g. eccentric exercise)
-
-
Complete therapy class (e.g. strength/resistance + flexibility + proprioception)
-
Complete exercise treatment (e.g. eccentric exercise + static stretching + movement pattern retraining)
-
-
-
Exercise dose
-
Intensity (e.g. load (kg))
-
Volume (e.g. sets × repetitions)
-
Frequency (e.g. number of times per week)
-
Duration (length of time intervention delivered)
-
-
Non-exercise intervention class (e.g. electro-therapy)
-
Intervention (e.g. Shockwave) and delivery information
-
-
Intervention delivery
-
Intervention setting (e.g. primary/secondary care)
-
Delivered by whom (e.g. physiotherapist)
-
Delivered how (e.g. supervised one-to-one)
-
-
Exercise fidelity and adherence
-
Exercise fidelity and adherence measures used (e.g. proportion of exercise sessions completed)
-
Exercise attendance data (e.g. attendance [the number of sessions attended over the follow-up period])
-
Participant responsiveness (e.g. self-report of how far participants respond to, or are engaged by, an intervention)
-
-
Outcome domain – primary and secondary (e.g. disability)
-
Outcome measurement tools for primary and secondary domains (e.g. SPADI)
-
-
Demographic information
-
Patient characteristics (e.g. age, BMI, sex, ethnicity, activity levels, comorbidities, occupation)
-
Symptom duration
-
Reporting of participant characteristics
Reporting of participant demographics was also highly variable across studies, with very low reporting rates for some potentially important comorbidities and confounders such as age, gender, cardiovascular conditions, diabetes and non-Caucasian ethnicities. For example, low- to moderate-quality evidence has demonstrated a link between metabolic syndrome, obesity and RCRSP but this was not well reported in studies. 70 This has limited the ability to pool findings, evident in the small number of previous systematic reviews that have conducted meta-analyses. This limitation also influenced the meta-analyses that could be conducted in the efficacy reviews presented in Chapter 5. There is therefore an urgent need for full and transparent reporting of patient characteristics in tendinopathy research66,71,72 and to continue the development of the ICON standards for such reporting. 73 The wide age range reported across included studies and the lack of reporting of co-morbidities (particularly in older populations) lend support to demographic sub-grouping of participants to lessen the impact of confounders and to identify different responses to exercise across groups.
Outcomes
The finding that numerous primary (n = 335) and secondary (n = 194) outcomes were reported across a range of 22 health domains highlights the lack of consensus to date on outcome measurement for tendinopathy. The work of the ICON group led by Vicenzino et al. 56 demonstrates that there is a difference between outcomes reported in the evidence base and those currently recommended. For example, ROM was the second most commonly reported domain for RCRSP yet it is not considered a core domain by ICON. 56 Of the six core ICON domains agreed on by healthcare professionals and patients, only two (rating of condition and PFC) were reported as primary or secondary domains in this review. This may reflect the differences between researchers’ focus and what health professionals and patients feel are important in practice,56 also indicated by low reporting of quality-of-life outcomes. Adverse events and cost-effectiveness outcomes were also rarely reported.
Numerous outcome measurement tools were used across each health domain, highlighting the need for core outcome sets to be agreed for both research and practice. The ongoing international work on developing core outcome sets for Achilles, gluteal, lateral elbow and proximal hamstring tendinopathies74–77 and shoulder disorders78 will enhance standardisation of outcomes and enable future pooling of findings in systematic reviews. Outcomes reported for RCRSP in this review were not congruent with the core set endorsed by the Outcome Measures in Rheumatoid Arthritis Clinical Trials (OMERACT) network;78 only pain was common to both OMERACT and this review. The health domains and outcome measures identified in this scoping review informed the domains that could be included in the efficacy reviews (Chapter 5).
The finding that physical outcomes (e.g. pain, disability) were dominant, with infrequent reporting of psychosocial outcomes (e.g. psychological factors), conflicts with clinical tendinopathy management, where the long duration and impact on peoples’ lives mean that those more severely affected may experience more fear avoidance, kinesiophobia, anxiety and depression. 79,80 This finding further emphasises the need for qualitative research, and the use of more holistic, patient-centred outcomes in tendinopathy research. 81,82 This scoping review clearly demonstrates that research to date is skewed towards physical interventions and outcomes and has neglected the social and psychological aspects of presentation and management.
Limitations
There are some inevitable limitations to this scoping review. We were unable to locate 56 articles. The use of the HDI54 ensured that the international evidence gathered is compatible with the UK context; however, it is possible that some pertinent evidence may have been excluded as a result. Nonetheless, we are confident that including studies from countries ranked as having lower HDI would not significantly affect the results of this review, as a comprehensive search was conducted and translations were sourced for all included non-English-language studies. It should also be noted that this scoping review has comprehensively mapped what has been conducted in the field of research. Although practice is informed by the evidence base, there are well-documented evidence-practice gaps,83 and it is therefore not known to what extent the findings represent what is done in the practice setting.
Conclusions
This scoping review provides the first comprehensive map of exercise therapy interventions and outcomes for tendinopathy research. Several important recommendations for future research and its reporting have emerged from this review, and are itemised below. Practice recommendations are limited from scoping reviews, due to the lack of methodological quality assessment of included studies. The results from this scoping review directly informed the remainder of this body of work, reported in Chapters 5 and 6.
Recommendations for research
Research study types
-
There is a need for adequately powered and methodologically sound studies that can truly demonstrate the effectiveness of interventions.
-
To achieve (a) we recommend that intervention development studies are conducted prior to moving to adequately powered trials, including feasibility and acceptability studies. Qualitative studies (stand-alone or embedded within other designs) should explore participants’ perceptions and experiences of exercise for tendinopathy. There is an urgent need for cost-effectiveness analyses and for studies on the implementation of effective interventions in practice.
-
Future evidence synthesis should focus on conducting high-quality systematic reviews (such as quantitative, qualitative, mixed-method and cost-effectiveness) and combining high-quality reviews into umbrella reviews. For these to add meaningful findings, there is an urgent need for further high-quality primary studies that address the limitations identified in this review.
Research reporting
-
The description of exercise interventions for tendinopathy needs to follow minimum standards to ensure consistency and allow comparisons. For this purpose, the initial reporting criteria proposed by this review could be helpful but require further development and investment to create a comprehensive taxonomy and guidance.
-
Full reporting of participant characteristics including psychological factors, ethnicity, co-morbidities and activity level is required in future tendinopathy research.
-
Future research should consider sub-groups such as those based on gender age, sedentary/active/performance populations and ethnicity.
-
Future research should apply the ICON core health domains to ensure collection and reporting of all relevant biopsychosocial outcomes.
-
Future research should carefully consider adequate monitoring and reporting of adherence to exercise. This will require refinement of data-collection methods, and we recommend considering objective monitoring.
Patient and practitioner lived experience
-
There is a need for research on participants’ views and experiences of exercise interventions across tendinopathies and populations. There is also a need for research on practitioners’ views of management approaches for different tendinopathies, how to navigate the research-practice gap and address barriers to exercise intervention implementation.
Stakeholder engagement with scoping review findings
Two workshops were initially planned to be held in Aberdeen and London to discuss the results of the scoping review with people who had received exercise for tendinopathy, people who manage tendinopathy and academics/researchers with an interest in tendinopathy. The outcome from the workshops was intended to inform the conduct of the subsequent contingent reviews conducted in phase 2 of this body of work. The impact of COVID-19 led to the workshops occurring online via Microsoft Teams in September–October 2020. One workshop was held with people who had experience of receiving exercise as a treatment for tendinopathy and one with people involved in tendinopathy management and/or research.
Following initial introductions and an overview of the scoping review results, the workshops were designed to:
-
consult with stakeholders on what information they would like the project to provide, and
-
discuss what stakeholders thought the findings were saying, what was of interest to them, and discussing their thoughts on what the subsequent syntheses should focus on.
Participants were recruited via social media (including Twitter and Facebook accounts for the project and the project team members’ personal accounts, Council for Allied Health Professions Research Twitter, Robert Gordon University [RGU] School of Health Sciences Twitter and Facebook accounts), RGU volunteer patient group, NHS Grampian physiotherapy staff email, NHS Grampian Involve Facebook page, and snowball recruitment via word of mouth and through personal and professional contacts of the review team.
Nine people who deliver exercise therapy for tendinopathy or have an academic or research interest in the topic attended the first workshop. This represented four physiotherapists (from the NHS, sportscotland institute of sport and private practice), one podiatrist, two PhD students focussed on RCRSP and patellar tendinopathy, and two physical preparation coaches. There were five female and four male professionals. Four females with experience of exercise therapy for tendinopathy attended the second workshop. They had experience of RCRSP (n = 2) and recurrent patellar tendinopathy (n = 1), with one identifying as a high-performance athlete.
To augment the workshop findings, a short online survey (incorporating the same questions used in the workshops) was distributed via Jisc online surveys using the same recruitment methods as for the workshops, with emphasis on the review team’s professional networks. This enabled the views of non-UK-based clinicians and researchers to be considered, as they could provide feedback in an asynchronous manner. Twenty-six survey responses were obtained and the findings were combined with those from the workshops. We did not obtain demographic details of workshop or survey participants. They represented a convenience sample of people willing to engage with the review team and can therefore not be considered representative of the lay, clinical or scientific population. Nonetheless, their contribution was helpful in refining the direction of the project.
The outcome of the workshops and survey identified what was important to stakeholders and can be summarised as follows:
People with experience of exercise for tendinopathy
-
wanted to know what type of exercise they should do, at what dosage and how hard they should push themselves
-
said that key factors to consider in the exercise intervention include self-management, trust in the professional delivering the exercise, being motivated by the professional delivering the exercise, monitoring of exercise and individually tailored prescription of exercise
-
told us that important treatment outcomes are pain, function and sleep: the last-named particularly for people with RCRSP.
Exercise for tendinopathy practitioners/researchers
-
were interested in how the scoping review data could be used as a resource
-
wanted exercise guidance for tendinopathy subgroups (including different populations, tendons, exercise types, co-morbidities, BMI, age, gender)
-
wanted clear clinical messages for specific exercises that work
-
for those working with performance athletes, they wanted to know how hard to push into pain (guidance for the ‘sweet spot’)
-
wanted progression guides for active and sedentary populations
-
recommended the following to be considered in the contingent syntheses
-
age and chronicity-related subgroups
-
performance- related outcomes such as training load, rating of perceived exertion, training duration, activity tracking using global positioning system (GPS) or heart rate data
-
general population (NHS patients) outcomes should include QoL, return to previous activity, global rating of change, patient acceptance of symptoms, expectations for improvement, and sleep (especially gluteal and RCRSP)
-
analysis of exercise intensity, volume, frequency, and training progression
-
rating the quality of interventions
-
effect of adjunct therapies
-
adherence and supervision.
-
The workshops and survey therefore provided insight into what was considered important by people with tendinopathy and people who manage tendinopathy. We gave due consideration to all suggestions, some of which could be taken forward in the contingent syntheses, and some of which we were unable to consider, due to the nature of the available research. We have further workshops planned to assist with dissemination of the contingent review findings.
Chapter 5 Phase II: Contingent synthesis 1: efficacy of exercise therapy for the management of tendinopathy
Contingent synthesis 1 summary
This part of the evidence synthesis investigated the efficacy of exercise therapy for the management of tendinopathies. The contingent synthesis sought to quantify efficacy of exercise therapies and address review questions 3 (Which exercise interventions are most effective across all tendinopathies?) and 4 (Does type/location of tendinopathy or other specific covariates affect which are the most effective exercise therapies?) of the project. To address these questions, a series of large meta-analysis models were conducted employing ‘effectiveness review’ methodologies.
The review was split into three sections, with the first (efficacy review 1) quantifying efficacy through calculation of a range of effect sizes from exercise-only interventions. Sections 2 and 3 investigated comparative efficacy. A hierarchical approach was used to categorise interventions so that comparisons could be made. Interventions were initially categorised according to their therapy class. The broadest categorisation of therapy classes comprised demarcations including exercise, non-exercise and non-active. More specific therapy classes further partitioned these categories (e.g. exercise to: resistance, flexibility and proprioception). Interventions were then categorised according to their therapy treatment (e.g. eccentric-only, static stretching and joint position sense). Interventions frequently comprised multiple therapy classes and multiple therapy treatments. Where this was the case, the dominant therapy class and treatment based on the relative contributions and/or the focus of the study was identified.
In the second section of this review (efficacy review 2), comparative efficacy was assessed between different exercise therapies based on their dominant therapy class and their dominant therapy treatment. In the third section of this review (efficacy review 3), comparative efficacy was assessed between exercise-only therapies, non-exercise therapies (e.g. surgery, injection, and MT) and combined therapies to quantify comparative efficacy across a range of therapy classes frequently used in the management of tendinopathy.
A total of 204 studies comprising 467 TAs and 12,081 participants were identified that met the inclusion criteria to be included in at least one section of the review. Additionally, a total of 125 studies were identified featuring 188 TAs that comprised exercise-only therapies. Efficacy review 1 identified that, in general, exercise-only therapies can be considered efficacious across the most common tendinopathy locations and outcome domains measured. Whilst large variation in response to exercise-only therapies can be expected, in general, substantive improvements are frequently reported based on standardised changes from baseline measurements. Analyses identified consistency in improvements across RCRSP, Achilles, patellar and lateral elbow tendinopathies. However, substantive differences were identified across outcome domains, with QoL and objective outcomes including ROM and physical functional capacity demonstrating smaller relative improvements compared with subjective outcomes measuring disability, function and pain. In addition, exercise-only therapies were found to generate low numbers of adverse events and scored well on patient rating outcomes, with most patients reporting they were satisfied and perceived moderate to strong recovery. Resistance exercise was used more frequently than any other exercise class and analyses demonstrated dose-response relationships corresponding with perspectives of the importance of higher mechanical loads. Evidence was obtained to indicate less frequent loading with greater resistance is more efficacious, particularly with tendinopathies of the lower body. However, review of the resistance exercise therapies identified that most were likely to employ relatively low resistances and instead focus on high frequencies.
In efficacy review 2, analyses were conducted on 21 studies comparing different classes of exercise-only therapy, and 34 studies comparing different exercise-only treatments. Separate analyses were conducted across different outcome domains and tendinopathy locations where possible. Low-quality evidence was obtained for a small but consistent increase in efficacy where flexibility was the dominant class of exercise therapy. Most of the research contributing to these comparisons was obtained for the shoulder, where the pathoetiology is multifactorial and guidelines for therapies often focus on flexibility and proprioceptive exercises. When investigating dominant treatments, most of the available data compared therapies comprising different resistance contraction modes, with the most popular being eccentric-only. Evidence was obtained indicating that eccentric-only therapies were superior to concentric-only or isometric therapies; however, evidence was also obtained indicating that the combination of eccentric and concentric actions was superior to eccentric-only. These results may be influenced by the findings in efficacy review 1 highlighting that most resistance exercise therapies are unlikely to apply substantive loads and therefore any potential benefits of the potential to apply higher load during eccentric actions may not be realised.
In efficacy review 3, analyses were conducted on 201 studies, with comparisons made between broad therapy classifications and dominant classes of therapy. Analyses were pooled across all tendinopathy locations and separated according to outcome domain. The single most popular class was resistance exercise, followed by electro-therapy, flexibility, injections and MT. Inconsistent results were obtained when comparing dominant classes across outcome domains. As a result, no hierarchy of therapy class could be created. Broad comparisons of therapy classifications comparing exercise-only, non-exercise-only and combined therapies identified that combining exercise and non-exercise therapies appeared more efficacious. Further analyses identified that the strongest evidence was obtained for combining exercise with either electro-therapy, injections or kinetics (e.g. immobilisation or altered loading through taping and braces).
Overarching methods
Search strategy
The comprehensive search strategy for this review comprised: (1) identifying potentially relevant systematic reviews, RCTs and quasi-experimental trials from the original search conducted for the scoping synthesis (see Chapter 4); (2) obtaining all references and citations from the 130 systematic reviews and 317 primary studies (236 RCTs and 81 quasi-experimental trials) using Scopus and hand-searching and adding to the overall search results for screening; (3) updating the original search conducted for the scoping synthesis (update search on 21 January 2021).
Screening for inclusion
Proquest® Refworks was used to manage references and remove duplicates before importing to Covidence (Melbourne, Australia) to facilitate screening and initiate a second deduplication process. Titles/abstracts were reviewed, independently, by two members of the research team. Full text copies of all studies included at title/abstract screening stage were retrieved and screened independently by two members of the research team. Each record was screened and determined if it met the inclusion criteria for any of the three review sections. Conflicts were resolved by discussion or by input from a third reviewer.
Inclusion criteria
Distinct inclusion criteria were adopted for each review section. However, some features were common to all sections and are therefore presented here to avoid duplication. To be included in any review, at least one TA in the investigation was required to include an exercise component. In addition, we required studies to report sufficient information regarding the exercise intervention to enable appropriate identification of the exercise class (resistance, flexibility, proprioception, plyometric or vibration) and the exercise dose. In clinical settings it has been recommended that exercise dose is determined by duration, frequency and intensity. 84 To be included in the review we required studies to provide sufficient information to describe at least two of the three parameters describing exercise dose. Where sufficient information was not presented in the main text of a study, a search was made of the publisher’s website to check for supplementary files that may include relevant information. To reflect the broad range of exercise therapies used in the management of tendinopathy, we included exercise therapies delivered in a range of settings (e.g. primary care, secondary care, community, people’s homes) and delivered by a range of health or exercise professionals (e.g. physiotherapists, strength and conditioning coaches, personal trainers) or support workers. We also included both supervised and unsupervised exercise therapies.
Inclusion based on tendinopathy location differed across the review sections. However, for all sections we accepted trial authors’ diagnoses where a clearly verifiable group of clinical features is reported including: pathognomonic location of pain; a symptom-altering response to applied load and/or stretch, with there being a specific test for most tendinopathies; strategies to rule out differential diagnoses; ultrasound or magnetic resonance imaging confirmation of structural change. We included studies with mixed groups where there was clear reporting of the tendinopathic group, or those participants comprised >90% of the investigated cohort.
We only included data from RCTs or quasi-experimental trials. In addition, studies were required to meet the overall context of the reviews which included primary care, secondary care or community locations in any developed nation (defined as the top 62 countries in the HDI). 54 Given the modelling focus of the efficacy reviews and the aims of quantitatively synthesising data across many sources, only those studies that included data that could be incorporated into meta-analyses were included. As for the scoping review, bespoke data-extraction forms were created for each of the three reviews (Supplementary Materials 3–5).
Inclusion results
The search strategy identified a total of 9246 potential studies, with 4635 remaining following removal of duplicates. After title and abstract screening 4210 studies were removed, leaving 425 studies obtained for full text screening. Of these studies, a further 221 were excluded (NIHR129388 Supplementary Material 6) leaving a total of 204 studies that were included throughout the different parts of the efficacy review (see Figure 7). The reasons for exclusion on full text screening included: insufficient information regarding exercise therapy: 116, wrong study design, 35; wrong HDI rank, 22; duplicates, 17; wrong concept, 14; wrong outcomes, 13; wrong population, 2; and not tendinopathy specific, 2 (see Figure 7).
FIGURE 7.
PRISMA chart describing study selection for overall efficacy review.
From: Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. https://doi.org/10.1136/bmj.n71.

Data extraction
Data were extracted independently by eight members of the review team (PS/KC/LA/RM/LG/EP/JS/AP) into pre-piloted excel sheets. Separate extraction sheets were developed for the three different review sections (Supplementary Materials 4–6). Each entry was then double-checked by a different member of the review team. Where pre-post intervention data were not presented in text but in figures, data were extracted using digitisation software (PlotDigitizer Version 2.6.8).
Risk of bias
We used Cochrane’s Risk of Bias tool85 and six outcome domains: (1) selection bias (random sequence generation and allocation concealment); (2) performance bias (blinding of participants); (3) detection bias (blinding of outcome assessors); (4) attrition bias (incomplete outcome data); (5) reporting bias (selective reporting); and (6) other bias, to assess risk of bias for RCTs and domains 2 to 6 for non-randomised trials. Risk of bias was recorded for each outcome and time point within each study. When obtaining a summary risk of bias for each domain within a study, the mode category across all outcomes and timepoints was selected. The Cochrane’s Risk of Bias tool85 was selected as a recent review of popular risk of bias tools in tendinopathy management highlighted none was superior86 and Cochrane’s Risk of Bias tool85 could be semi-automated with RobotReviewer,87 a machine-learning system software. RobotReviewer was used to make initial assessments on selection bias and performance bias domains, with manual validation made on the relevant free texts extracted to support the final selection of low, high or unclear risk of bias. This semi-automated process was more efficient and pragmatic given the large number of included studies and provided an additional element of consistency in the review process.
Confidence in cumulative evidence
The strength of evidence was assessed using the Grading of Recommendations Assessment Development and Evaluation (GRADE) guidelines88,89 and transparent reporting recommended in a recent review of how to improve reporting of evidence in tendinopathy management. 90 Assessments were made at the outcome level, with strength of evidence assessed according to overall risk of bias, inconsistency, imprecision, indirectness and small-study effects (e.g. publication bias and other biases associated with small number of studies). Overall risk of bias was identified by the mode rating across all outcome data included in the analysis, with a ranking of high, low or unclear risk of bias. Inconsistency was assessed based on meta-analysis results and comparison of central and variance parameter estimates. Imprecision was judged based on the number of data points available (number of studies, TAs and outcome measures) and width of credible intervals (CrIs) for central estimates. Based on inclusion criteria that were developed from the scoping review and stakeholder workshops it was determined that indirectness for all outcomes would be identified as low risk. Small-study effects were assessed using visual inspection of the distribution of effect sizes and their sampling variance. Overall strength of evidence was categorised as high/moderate/low/very low. Assessments began with a categorisation of high strength of evidence and were downgraded one level for each of the domains that were not judged low risk. Potential upgrading factors included the presence of large effects or evidence of dose-response. 88,89
Data synthesis overview
Distinct data synthesis approaches were adopted across the three review sections. Full details of each analysis approach are presented in the review-specific sections; however, the following provides brief overviews.
Efficacy review section 1
Data synthesis approaches for efficacy review 1 were separated into three parts (A, B, C) based primarily on the distinct analysis approaches and the research questions targeted. The primary aim of efficacy review 1A was to quantify effect size distributions describing change in continuous outcomes measured at baseline and at subsequent time points. Therefore, a data synthesis approach was adopted to describe the overall effect size distributions, estimating threshold values that could be used to describe ‘small’, ‘medium’ and ‘large’ effect thresholds. This approach enabled a more detailed exploration of the efficacy of exercise therapies, quantifying the distribution of improvements that should be expected. These distributions were then compared across different tendinopathy locations and outcome domains to assess if these factors acted as modifiers and to address objective 4 of the project (Does type/location of tendinopathy or other specific covariates affect which are the most effective exercise therapies?). Similarly, the effect of intervention and participant characteristics on expected effect sizes was also investigated by quantifying the extent to which exercise supervision and symptom duration of patients influenced effect sizes. In addition to continuous outcome measures, a smaller number of binary and ordinal level data were collected post-intervention quantifying, in the main, patient satisfaction, perceived change and number of adverse events. Data were synthesised for these outcomes in efficacy review 1B estimating the central tendency expressed primarily as proportions (e.g. mean proportion satisfied or experiencing an adverse event, or mean satisfaction of perceived change expressed a proportion of maximum). Finally, based on the results of the scoping review and workshops conducted with clinicians and exercise professionals, it was evident that most exercise therapies comprised resistance exercise and that this exercise mode was the most amenable to quantification of exercise dose and therefore exploration of dose–response relationships. Therefore, efficacy review 1C comprised meta-analyses and meta-regressions performed on intervention data obtained from treatments where resistance exercise was identified as the dominant class. Meta-regressions explored relationships between dosing variables (e.g. frequency, intensity and volume) and mean effect sizes.
Efficacy review section 2
The data synthesis approach in efficacy review 1 enabled a large amount of exercise data to be modelled and the distributions of effect sizes from exercise therapies to be quantified and potential moderators explored. However, effect sizes are likely to be influenced by a range of factors, for many of which appropriate data are not available to control for statistically. Therefore, the purpose of the analysis approach in efficacy review 2 was to calculate and synthesise pairwise effect sizes quantifying comparative efficacy of two or more exercise therapies on the same population. Similar to the analyses of review section 1, investigations were restricted to exercise-only therapies, with the addition of other treatments such as electro-therapy or injection excluded. Comparisons were made on the therapy class (e.g. resistance, flexibility, proprioception) and treatments (e.g. resistance: eccentric-only, isometric; flexibility: static, dynamic; proprioception: movement pattern retraining and sense of joint position and force). Analyses quantifying comparative efficacy were conducted first by fitting direct pair-wise effect sizes between different class and treatment levels, then by network meta-analyses (NMAs) enabling direct and indirect effect sizes to be combined.
Efficacy review section 3
The purpose of the analysis approach in the efficacy review 3 was to calculate and synthesise pairwise effect sizes to investigate comparative efficacy of exercise therapies, non-exercise therapies, and the combination of exercise and non-exercise therapies on the same populations. Similar approaches to efficacy review 2 were included, with both direct pair-wise comparisons and NMAs used to synthesis results and identify a treatment hierarchy.
Efficacy review 1
The purpose of efficacy review 1 was to quantify the efficacy of exercise-only therapies across a range of outcome domains and tendinopathy locations. The potential for efficacy to be influenced by a range of factors including exercise and patient characteristics was also explored. The review was split into three parts to account for the wide range of outcomes and data types collected across the evidence base. Parts A and B focussed on the core health-related outcome domains,51 including those typically measured by continuous measures (pain, function, PFC, disability, QoL, participation) and those typically measured by binary or ordinal measures (patient rating and adverse events), respectively. Part C of the review focussed on investigating the dose–response of therapies where resistance exercise was the dominant exercise class.
Review-specific methods
The following sections describe the specific inclusion criteria, data extraction and statistical analyses employed across the three parts of efficacy review 1. The inclusion criteria were influenced by the project aims, the results of our initial scoping review mapping the exercise and tendinopathy literature as well as stakeholder workshops.
Participants
This meta-analysis included people of any age or gender with a diagnosis of any tendinopathy for part B, and a diagnosis of RCRSP, lateral elbow, patellar, Achilles or gluteal tendinopathy for parts A and C. Any severity or duration of tendinopathy was included.
Intervention
The intervention being assessed is exercise therapy. Based on the scoping review and stakeholder workshops, it was decided that components of exercise therapies could be categorised into five different classes: (1) resistance; (2) plyometric; (3) vibration; (4) flexibility and (5) proprioception. Definitions for each exercise class are presented in Appendix 4 (see Tables 34 and 35). For efficacy review 1 parts A and B, exercise interventions comprising any of the five therapy classes were included. For part C, only exercise interventions where resistance exercise was classified as the dominant class were included. Interventions combining exercise with other therapies (e.g. laser, shockwave, MT or injection) were not included in any of the review parts.
Comparator
No head-to-head comparators were included, and all effect sizes were derived from the data obtained from exercise-only interventions.
Outcomes
Based on the results of our initial scoping review and subsequent stakeholder workshops, in parts A and C we included outcomes that quantified six domains: disability, pain (either on loading, over a specified time, or without further specification), PFC, function, quality of life (QoL) and ROM (for RCRSP only). For part B, we included outcomes that quantified adverse events, participation, patient satisfaction and perception of change. Definitions of each domain and example tools are presented in Appendix 4 (see Table 36).
Statistical analysis overview
All meta-analyses conducted in this report were generated under a Bayesian framework. This approach was selected over a traditional frequentist approach as the former provides a more flexible modelling approach and enables meta-analysis results to be interpreted intuitively through reporting of subjective probabilities91 focussing on strength and direction of evidence, rather than over-reliance on dichotomous interpretations of results (e.g. with null hypothesis significance testing). In general, weakly informative default priors were used for model parameters. However, where model constraints or sufficient external information existed, informative priors were used to generate more accurate estimates. Inferences from all analyses were performed on posterior samples generated using the Hamiltonian Markov Chain Monte Carlo method. Interpretations were based on the median value (SMDpre0.5: 0.5-quantile) and CrIs with 95% widths set for intercept parameters and 75% widths set for variance parameters. Where meta-regressions were conducted, interpretations were also based on probabilities calculated from the posterior sample and quantifying the chance that the pooled mean effect size of one level of the covariate was greater than another. Meta-analyses were conducted using the R wrapper package brms interfaced with Stan to perform sampling. 91,92 Convergence of parameter estimates was obtained for all models with Gelman-Rubin R-hat values below 1.1. 93
Statistical analysis efficacy review 1A
To synthesise effects across different measurement outcomes within each domain, standardised mean difference (SMDpre) effect sizes were calculated by dividing the relevant mean difference by the pre-intervention standard deviation and including a small sample bias correction. 94 Where required, SMDpre values were reflected by multiplying by −1 to ensure that positive values represented an improved clinical effect. Where outcomes were assessed at multiple time-points following baseline measurement, all possible SMDpre values were calculated and included in the meta-analysis models. Where means and standard deviations were not presented but included combinations of the median, range or interquartile range, the values were estimated by the calculations presented by Wan et al. (2014)95 Where sufficient information was not available to estimate standard deviations (e.g. based on confidence intervals), these were imputed through simple linear regression of the log-transformed standard deviations and means obtained from all other studies. 96 Separate regressions were performed for pre- and post-intervention data.
All meta-analyses were conducted using a nested four-level mixed-effects meta-analytic model. 97 The series of nestings included the individual study (level 4), the outcome (level 3), the measurement occasion (level 2) and the sampling variance (level 1). The sampling variance of SMDpre values was calculated using standard distributional assumptions. However, these values require an estimate of the pre-post correlation, which is rarely reported in studies. To account for uncertainty in the sampling variance, values within the model were allowed to vary and were estimated by including an informative Gaussian prior approximating correlation values centred on 0.7 and ranging from 0.5 to 0.9. To quantify small, medium and large threshold values, parameters from the respective model were used to generate posterior predictions and the 0.25-, 0.5- and 0.75-quantiles calculated, respectively. It was determined a priori to assess the influence of tendinopathy type, outcome domain, assessment duration, training status (performance, sporting and other) and supervised versus non-supervised exercise on effect size and threshold values. This was achieved by subset analysis for training method and outcome type, and meta-regressions for assessment duration, training status and supervision. Meta-regressions were presented by selecting one level of the factor as a reference to make comparisons with the median and 95% CrI given (βReference:Comparison = Median [95% CrI: lower bound to upper bound], such that β > 0 indicates an increased effect of the comparison relative to the reference). The initial meta-analysis model combining the entire data set was fitted with a normal distribution, a skew normal distribution and a t-distribution. No substantive improvements in model fit were obtained with the skew normal or t-distributions based on the Watanabe–Akaike information criterion. Consequently, a normal distribution was used throughout all analyses. Due to the large number of outcomes and the potential for outliers to influence estimates,98 outlier SMDpre values were identified by adjusting the distribution by a Tukey g-and h- distribution and obtaining the 0.0035- and 0.9965-quantiles, with values beyond these points removed prior to further analysis. 99
Statistical analysis efficacy review 1B
A series of meta-analyses were conducted to synthesise results from reporting of adverse events, participation, patient satisfaction and patient rating (perception of condition and recovery) following exercise therapy for the management of tendinopathy. Adverse events and patient satisfaction measures comprised binary post-intervention data such that the proportion of adverse events or patients stating satisfaction with the exercise therapy was calculated from each study. The logit transformation was used on proportional data and sampling variances calculated using standard distributional assumptions. 100 Continuity correction factors were applied for proportions equal to 0 or 1. After pooling data and obtaining uncertainty estimates, values were back-transformed and expressed as proportions. 100 Where large numbers of proportions were equal to 0 or 1, exact binomial meta-analysis models were conducted. 101
Post-intervention data quantifying patient ratings of condition and recovery were standardised by scaling group means relative to their maximum values. For outcomes restricted to positive values, items were shifted to have zero as the lowest value and the group mean was divided by the shifted maximum such that effect sizes ranged from 0 to 1. That is, if the item was scored on a 2 to 10 scale, 2 was subtracted from the group mean and this shifted value divided by 8. In contrast, for outcomes already centred on zero between two symmetric positive and negative maximum values, the group mean was divided by the positive maximum such that effect sizes ranged from −1 to 1. Sampling variances for both sets of outcomes were calculated using group standard deviations and the number of patients in each group.
All meta-analyses were conducted within a Bayesian framework employing three-level hierarchical models to enable inclusion of multiple data points from the same study where available. In general, weakly informative Student-t prior and half-t priors with 3 degrees of freedom and scale parameter equal to 2.5 were used for intercept and variance parameters. 102 However, informative flat priors were used for the intercept parameter of outcomes that were scaled relative to their maximum value (e.g. uniform 0 to 1, or uniform −1 to 1). It was identified a priori that moderator analyses investigating the effects of assessment duration (length of time from baseline to follow-up measurement) and tendinopathy type on outcome variables would be included. Assessment duration was categorised as short (≤12 weeks), medium (13–52 weeks) and long (>52 weeks). Moderator analyses were only performed where at least 10 data points were available for each category, and where required tendinopathy types were grouped into upper- and lower-body tendinopathies.
Statistical analysis efficacy review 1C
The purpose of the meta-analyses conducted in part of the review was to explore which exercise-related factors of the therapy influenced efficacy. Based on results from the scoping review and discussions with stakeholders, analyses were limited to resistance exercise. This decision was made due to resistance exercise being shown to be the most popular exercise modality in the management of tendinopathy, and it was identified that resistance exercise provided the best opportunity to appropriately characterise and quantify exercise dose. For each study and outcome extracted, attempts were made to quantify exercise intensity, volume and frequency. For exercise intensity it was identified whether the study prescribed loads based on absolute loading criteria (e.g. newtons when using elastic resistance and kilograms when using isoinertial loads) or relative criteria (e.g. percentage of the maximum load that could be lifted). The actual loads prescribed were also recorded where available. Exercise intensity was also categorised using a binary structure comprising body mass only (entire body mass or mass of a limb) or addition of external resistance (e.g. in the form of a loaded backpack, dumbbell or elastic resistance). Exercise volume was calculated by recoding the number of sets and repetitions, and the number of resistance exercises prescribed. Exercise frequency was calculated by recording the number of sessions prescribed per week. Where multiple resistance exercises were prescribed, the exercise intensity and volume calculated by the multiplication of sets and repetitions were calculated for the primary resistance exercise only.
Due to the use of different outcome domains and different tests within the same outcome domain, pooling of data required standardisation. This was achieved using the standardised mean difference (SMDpre) effect size, dividing the mean group change by the pre-intervention standard deviation. Where required, SMDpre values were reflected by multiplying by −1 to ensure that positive values represented an improved clinical effect. Where multiple outcomes were reported from the same study (different outcomes and/or the same outcome at multiple time points), all possible SMDpre values were calculated and included in the meta-analysis models. To account for covariances created, all meta-analyses were conducted using a nested four-level model. 97 The series of nestings included the individual study (level 4), the outcome (level 3), the measurement occasion (level 2) and the sampling variance (level 1). The relative contributions of variance sources were described by variance partition coefficients (VPCs) calculated by dividing each estimated variance level by the total sum. The meta-analysis was conducted within a Bayesian framework providing additional flexibility in the handling of within-study variances and enabled model estimates to be interpreted more intuitively through reporting of subjective probabilities. 91
To assess the effects of dose variables, meta-regressions were performed with intensity (limb/bodyweight versus additional external) and volume (lower volume: less than 45 repetitions versus 45 or more repetition) comprising a binary categorisation, and frequency (less than once a day versus once per day and more than once per day) comprising a trinary categorisation. Meta-regressions were presented by selecting one level of the factor as a reference to make comparisons (βReference:Comparison = Median [95% CrI: LB to UB], such that β > 0 indicates an increased effect of the comparison relative to the reference). Meta-regressions were only performed in cases where at least 10 outcomes from two or more TAs were available for each level of the potential moderator.
Efficacy review 1 overall results
Study selection
Of the 204 studies identified for the overall review, a total of 125 studies were included across the three parts of efficacy review 1 (see Appendix 5, Table 37) after 75 studies were removed for not including an exercise-only TA. The 125 studies comprised 188 TAs and a total of 4612 patients. Descriptions of the age, BMI, gender proportions, training status and symptom duration of the patients are presented in Table 4. Similarly, a summary of the tendinopathies, outcome domains and dominant exercise classes investigated across the 188 TAs is presented in Table 4.
| Characteristic | Median (IQR) | Percentage unavailable |
|---|---|---|
| Age (mean) | 47.0 (42.6–49.2) | 1.6% |
| Age (SD) | 9.0 (7.1–11.1) | 17.6% |
| BMI (mean) | 25.8 (24.7–27.9) | 64.0% |
| BMI (SD) | 4.1 (3.1–4.5) | 72.8% |
| Percentage female | 47.3 (34.5–61.4) | 4.8% |
| Symptom duration months (mean) | 14.5 (6.3–25.9) | 35.2% |
| Symptom duration months (SD) | 11.0 (4.2–27.7) | 59.2% |
| Training status | 4.8% Performance athlete 11.3% Recreational athlete 83.9% Other |
0.8% |
|
Outcome domain
( N ; % TAs) |
Tendinopathy location ( N ; % TAs) | Exercise therapy class ( N ; % TAs) |
| Disability (470; 26.2%) | RCRSP (81; 43.1%) | Resistance (136; 72.3%) |
| Pain (452; 25.2%) | Achilles (47; 25.0%) | Flexibility (29; 15.4%) |
| PFC (354; 19.7%) | Elbow (32; 17.0%) | Proprioception (21; 11.2%) |
| ROM (166; 9.3%) | Patellar (20; 10.6%) | Vibration (2; 1.1%) |
| Patient rating (102; 5.7%) | Gluteal (4; 2.1%) | |
| Participation (61; 3.4%) | Hamstring (2; 1.1%) | |
| Function (85; 4.7%) | Biceps (1; 0.5%) | |
| QoL (65; 3.6%) | Tibialis posterior (1; 0.5%) | |
| Adverse events (39; 2.2%) |
Distribution of outcome domains and dominant exercise classes across the five most studied tendinopathies is illustrated in Figures 8 and 9. The distribution of outcome domains was relatively consistent across tendinopathy types, with disability and pain outcomes measured most frequently. In addition, ROM was commonly measured in studies investigating RCRSP. In contrast, clear differences were identified in the distribution of dominant therapy classes across tendinopathies. Resistance exercise featured as the dominant class in more than 90% of TAs across all tendinopathies except RCRSP, where resistance exercise comprised approximately 50% of the distribution combined with relatively equal numbers of TAs where flexibility or proprioception were the dominant exercise classes.
FIGURE 8.
Relative distributions of outcome domains across the five most studied tendinopathy locations.
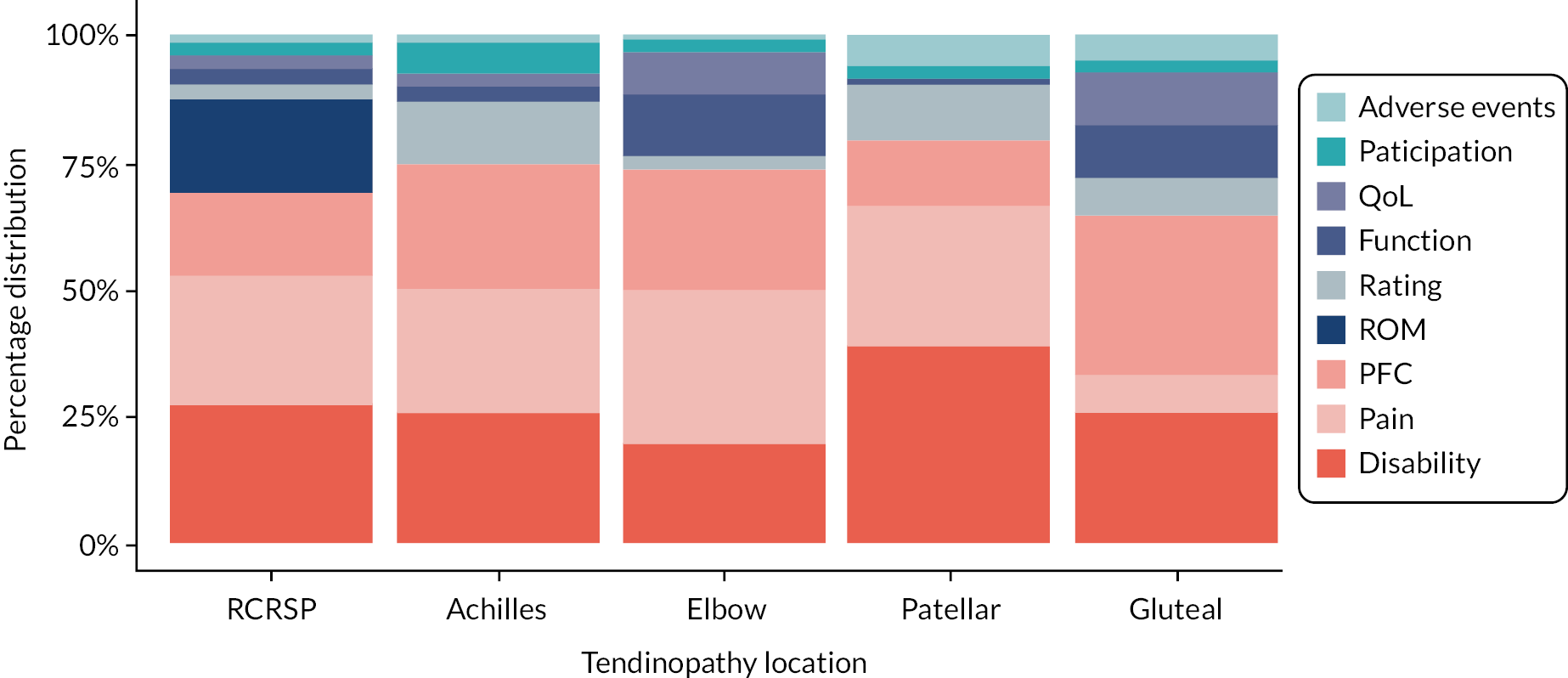
FIGURE 9.
Relative distributions of dominant exercise therapy class across the five most studied tendinopathy locations.

Risk of bias
Risks of bias expressed for each individual study included across the different parts of efficacy review 1 are presented in Appendix 6. A summary of the risk of bias assessment across the studies expressed in percentages is presented in Table 5. For RCTs risk of bias was highest for ‘other bias’ (48% high risk of bias), blinding (participants: 40% high risk of bias; outcome assessors: 22% high risk of bias) and incomplete outcome bias (13% high risk of bias). For quasi-experimental trials, risk of bias was also highest for ‘other bias’ (79% high risk of bias) and reporting quality was also lower, with high percentages of unclear risk of bias identified for selective reporting (86% unclear risk of bias) and blinding (participants: 38% unclear risk of bias; outcome assessors: 54% unclear high risk of bias).
Efficacy review 1A results: exercise-only continuous health-related measurements
Study characteristics, tendinopathies and outcomes
Across the 125 studies comprising at least one exercise-only TA, data from 115 studies were included in efficacy review 1A. Studies were excluded based on the wrong tendinopathy (n = 3), wrong outcome domain (n = 2), and for not including sufficient data to meet the requirements of the meta-analysis models (n = 5). In total, the 115 included studies comprised 173 TAs and 4161 participants. Descriptions of the study characteristics, tendinopathy types and outcome domains are presented in Table 6. Outcomes obtained from studies investigating gluteal tendons were not included in the analysis based on the number of effect sizes falling below the a priori threshold set to generate accurate estimates of the population effect size distribution. Risk of bias results for individual studies are presented in Appendix 6, Table 38.
| Study characteristic | 0% | 10% | 20% | 30% | 40% | 50% | 60% | 70% | 80% | 90% | 100% |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Participants per group | 5 | 10 | 13 | 16 | 19 | 20 | 24 | 29 | 31 | 44 | 70 |
| Mean age | 22.5 | 28.0 | 39.8 | 42.6 | 44.0 | 46.0 | 47.9 | 48.6 | 49.9 | 51.8 | 62.1 |
| Mean symptom duration (months) | 0.85 | 4.5 | 6.0 | 7.4 | 11.0 | 17.5 | 19.5 | 23.8 | 28.9 | 36.6 | 98.5 |
| Publication year | 1998 | 2005 | 2007 | 2009 | 2012 | 2014 | 2015 | 2017 | 2017 | 2019 | 2020 |
| Intervention length (weeks) | 2 | 4 | 4 | 4 | 6 | 8 | 12 | 12 | 12 | 12 | 21 |
| Measurement duration (weeks) |
0.7 | 3 | 4 | 4 | 5 | 6 | 6 | 11 | 12 | 13 | 104 |
| Tendinopathy type | Number of TA (%) |
Number of effects
(%) |
Outcome
domain |
Number of TA (%) |
Number of effects
(%) |
||||||
| RC | 77 (44.5) | 817 (55.7) | Disability | 142 (82.1) | 447 (30.5) | ||||||
| Achilles | 45 (26.0) | 321 (21.9) | Pain | 124 (71.7) | 410 (28.0) | ||||||
| Lateral elbow | 31 (17.9) | 239 (16.3) | |||||||||
| Patellar | 20 (11.6) | 89 (6.1) | PFC | 61 (35.3) | 324 (22.1) | ||||||
| RC | 77 (44.5) | 817 (55.7) | Disability | 142 (82.1) | 447 (30.5) | ||||||
| Achilles | 45 (26.0) | 321 (21.9) | Pain | 124 (71.7) | 410 (28.0) | ||||||
| Lateral elbow | 31 (17.9) | 239 (16.3) | |||||||||
| Patellar | 20 (11.6) | 89 (6.1) | PFC | 61 (35.3) | 324 (22.1) | ||||||
| Dominant exercise class | Number of TA (%) |
Number of effects
(%) |
ROM | 30 (17.3) | 159 (10.8) | ||||||
| Resistance | 126 (72.8) | 1026 (70.0) | Function | 31 (17.9) | 72 (4.9) | ||||||
| Flexibility | 25 (14.5) | 215 (14.7) | |||||||||
| Proprioception | 21 (12.1) | 223 (15.2) | QoL | 12 (6.9) | 54 (3.7) | ||||||
| Vibration | 1 (0.6) | 2 (0.1) | |||||||||
Description of effect size distributions
From the initial 1466 outcomes extracted, a total of 44 outliers were removed from the analysis, with a lower bound threshold of −0.82 (6 effect sizes below) and an upper bound threshold of 7.0 (38 effect sizes above). Across all outcomes and tendinopathy types, direct calculation of the 0.25- (small), 0.5- (medium) and 0.75-quantiles (large) from the complete empirical data returned the following SMDpre values: 0.37, 0.77 and 1.31, respectively. Application of the meta-analysis model across this complete data set with borrowing of information across studies resulted in similar but shrunken estimates (0.25-quantile0.5 = 0.34 [95% CrI 0.31 to 0.37]; 0.5-quantile0.5 = 0.73 [95% CrI 0.70 to 0.77]; and 0.75-quantile0.5 = 1.22 [95% CrI 1.17 to 1.27]).
Analysis of effect size distributions across the different tendinopathy locations is illustrated in Figure 10 with numerical values presented in Table 7. Analysis of the modelled small, medium and large thresholds showed considerable overlap in small and medium thresholds across all tendinopathy locations (0.25-quantile0.5 ranged from 0.30 to 0.38; 0.5-quantile0.5 ranged from 0.70 to 0.85). However, greater divergence was identified for large threshold estimates, with the greatest values estimated for elbow tendinopathy (0.75-quantile0.5 ranged from 1.18 to 1.62).
FIGURE 10.
Effect size distributions across tendinopathy locations with identification of small, medium and large thresholds.
Black curve represents density plot of empirical effect size distribution. Diamonds with intervals represent small, medium and large thresholds with CrIs (black: all outcomes; red: tendinopathy specific).
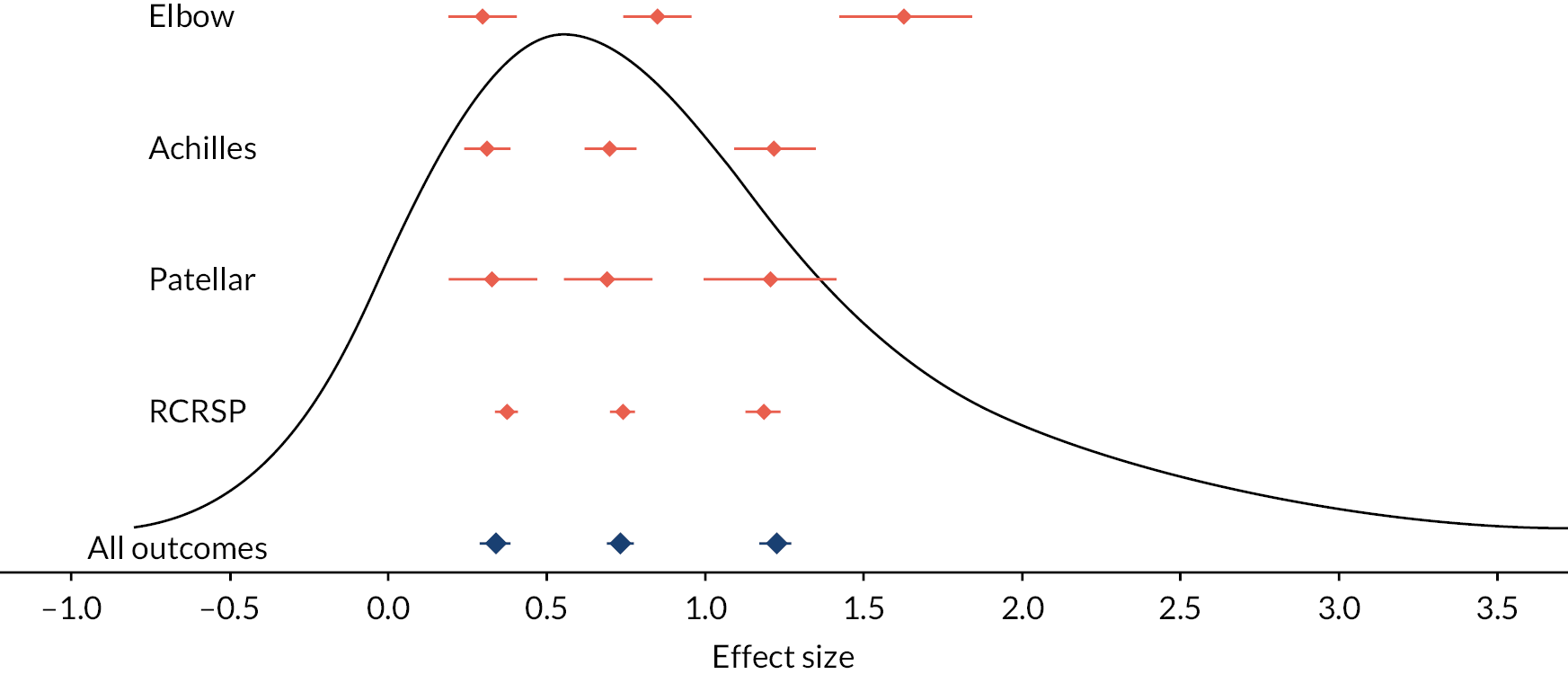
FIGURE 11.
Effect size distributions across outcome domains with identification of small, medium and large thresholds.
Black curve represents density plot of empirical effect size distribution. Diamonds with intervals represent small, medium and large thresholds with CrIs (black: all outcomes; red: tendinopathy specific).
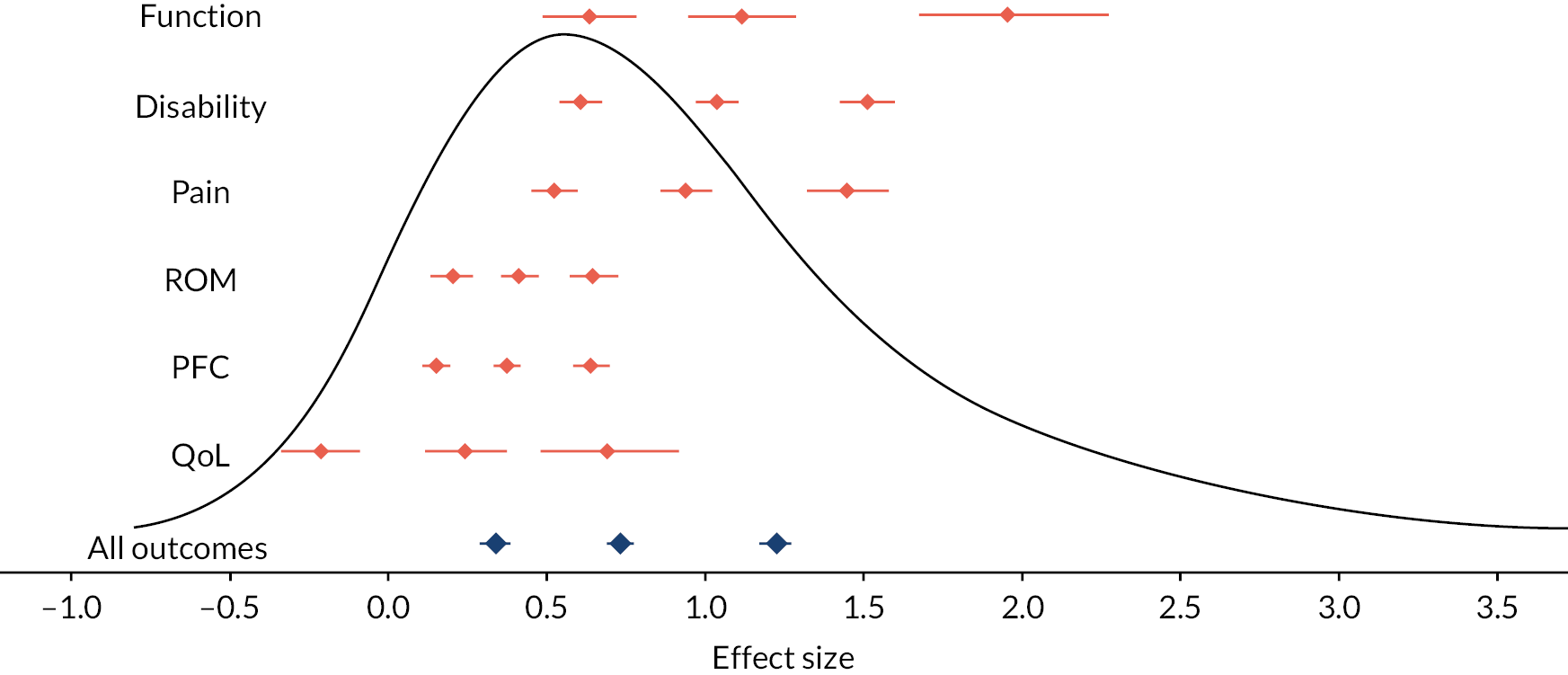
| Tendinopathy location |
Small [95% CrI] |
Medium [95% CrI] |
Large [95% CrI] |
Study VPC [75% CrI] |
Outcome VPC [75% CrI] |
Measurement VPC [75% CrI] |
|---|---|---|---|---|---|---|
| All | 0.34 [0.31 to 0.37] |
0.74 [0.71 to 0.77] |
1.23 [1.18 to 1.28] |
0.74 [0.69 to 0.78] |
0.26 [0.22 to 0.31] |
0.01 [0.00 to 0.02] |
| RCRSP | 0.38 [0.34 to 0.41] |
0.74 [0.70 to 0.78] |
1.18 [1.12 to 1.24] |
0.55 [0.48 to 0.62] |
0.45 [0.37 to 0.52] |
0.01 [0.00 to 0.02] |
| Achilles | 0.32 [0.25 to 0.39] |
0.70 [0.62 to 0.78] |
1.22 [1.10 to 1.35] |
0.71 [0.59 to 0.81] |
0.27 [0.18 to 0.39] |
0.01 [0.00 to 0.03] |
| Elbow | 0.30 [0.20 to 0.41] |
0.85 [0.75 to 0.96] |
1.62 [1.43 to 1.84] |
0.87 [0.81 to 0.92] |
0.12 [0.07 to 0.18] |
0.01 [0.00 to 0.02] |
| Patellar | 0.33 [0.19 to 0.47] |
0.69 [0.56 to 0.84] |
1.21 [1.00 to 1.42] |
0.57 [0.26 to 0.75] |
0.41 [0.23 to 0.71] |
0.01 [0.00 to 0.05] |
Analysis of the effect size distributions across outcome domains is presented in Figure 11 with numerical values presented in Table 8. A clear split was identified between the domains of QoL and the objective measures of PFC and ROM, versus the subjective measures of function, disability and pain. The lowest threshold values were estimated for QoL, physical functional capacity and ROM, with the small threshold for QoL estimated to be below zero (0.25-quantile0.5 = −0.21 [95% CrI −0.33 to −0.08]). In contrast, the greatest effect sizes values were obtained for outcomes measuring disability, pain and function, with the reduced amount of data for function resulting in wider CrIs. Central estimates indicated that small threshold estimates for domains with the greatest effect sizes were situated between the medium and large threshold estimates for domains with the lowest effect sizes (see Figure 11).
| Outcome domain | Small [95% CrI] |
Medium [95% CrI] |
Large [95% CrI] |
Study VPC [75% CrI] |
Outcome VPC [75% CrI] |
Measurement VPC [75% CrI] |
|---|---|---|---|---|---|---|
| All | 0.34 [0.31 to 0.37] |
0.74 [0.71 to 0.77] |
1.23 [1.18 to 1.28] |
0.74 [0.69 to 0.78] |
0.26 [0.22 to 0.31] |
0.01 [0.00 to 0.02] |
| Function | 0.65 [0.49 to 0.79] |
1.11 [0.95 to 1.30] |
1.95 [1.68 to 2.28] |
0.51 [0.04 to 0.85] |
0.47 [0.13 to 0.94] |
0.01 [0.00 to 0.04] |
| Disability | 0.61 [0.55 to 0.68] |
1.04 [0.97 to 1.11] |
1.51 [1.43 to 1.60] |
0.78 [0.68 to 0.88] |
0.15 [0.08 to 0.24] |
0.05 [0.00 to 0.13] |
| Pain | 0.53 [0.45 to 0.61] |
0.94 [0.87 to 1.02] |
1.45 [1.33 to 1.59] |
0.26 [0.06 to 0.46] |
0.71 [0.51 to 0.90] |
0.02 [0.00 to 0.07] |
| ROM | 0.21 [0.14 to 0.27] |
0.42 [0.36 to 0.48] |
0.65 [0.58 to 0.73] |
0.88 [0.79 to 0.94] |
0.10 [0.04 to 0.18] |
0.01 [0.00 to 0.05] |
| PFC | 0.16 [0.11 to 0.20] |
0.38 [0.34 to 0.43] |
0.64 [0.59 to 0.70] |
0.73 [0.61 to 0.82] |
0.27 [0.18 to 0.38] |
0.01 [0.00 to 0.02] |
| QoL | −0.21 [−0.33 to −0.08] |
0.25 [0.12 to 0.38] |
0.68 [0.49 to 0.93] |
0.84 [0.65 to 0.93] |
0.14 [0.05 to 0.33] |
0.01 [0.00 to 0.04] |
Moderator analyses
Moderator analyses investigating potential changes in the mean effect size across all outcomes and tendinopathies are presented in Table 9. Composition of outcome domains and tendinopathy locations across the levels of each moderator are presented in Appendix 6 (see Table 39) along with individual domains for the strength of evidence assessment (see Appendix 6, Table 40). Evidence of a moderator effect was identified for assessment duration (short: ≤12 weeks; medium: 13–52 weeks; long duration: >52 weeks), with results showing a hierarchy and greater mean estimate with increased time from baseline assessment (short duration (βShort:Medium0.5 = 0.28 [95% CrI 0.23 to 0.32]; βShort:Long0.5 = 0.37 [95% CrI 0.27 to 0.47]). These estimates remained consistent after meta-regressions were controlled for tendinopathy location and outcome domain (βShort:Medium0.5 = 0.28 [95% CrI 0.23 to 0.32]; βShort:Long0.5 = 0.38 [95% CrI 0.27 to 0.48]). Consistent evidence of a moderating effect was also obtained for supervision, with greater mean estimate for supervised exercise therapies (βUnupervised:Supervised0.5 = 0.43 [95% CrI 0.09 to 0.78]), which increased in estimate after controlling for tendinopathy location and outcome domain (βUnupervised:Supervised0.5 = 0.70 [95% CrI 0.39 to 1.0]). Finally, some evidence was obtained indicating a hierarchy of effects with regard to symptom duration and greater mean estimates with patients reporting shorter durations (βMedium:Short0.5 = 0.47 [95% CrI −0.01 to 0.95]; βLong:Short0.5 = 0.67 [95% CrI 0.19 to 1.1]). However, differences between the symptom duration levels were close to zero after controlling for tendinopathy location and outcome domain (βMedium:Short0.5 = 0.02 [95% CrI −0.41 to 0.45]; βLong:Short0.5 = 0.07 [95% CrI −0.35 to 0.50]). Strength of evidence was judged between low and moderate for assessment duration and supervision. Downgrading was due to imprecision from wide CrIs based on imbalances in trial numbers and consistent small-study effects highlighting a strong skew and relatively high frequency of very large positive effect sizes. Strength of evidence was consistently low for analysis of assessment duration also based on imprecision and small-study effects.
| Moderator | Estimate of mean [95% CrI] |
Probabilities | Strength of evidence | Study VPC [75% CrI] |
Outcome VPC [75% CrI] |
Measurement VPC [75% CrI] |
|
|---|---|---|---|---|---|---|---|
| Assessment duration | Short (≤ 12 weeks) 931 outcomes from 147 trials |
1.0 [0.87 to 1.1] | p (Medium > Short) > 0.999 |
Moderate | 0.72 [0.67 to 0.76] |
0.26 [0.22 to 0.31] |
0.02 [0 to 0.03] |
| Medium (13–52 weeks) 460 outcomes from 24 trials |
1.3 [1.1 to 1.4] | p (Medium < Long) = 0.980 |
Moderate | ||||
| Long (> 52 weeks) 51 outcomes from 2 trials |
1.4 [1.2 to 1.6] | p (Long > Short) > 0.999 |
Low | ||||
| Symptom duration | One year or less 314 outcomes from 46 trials |
1.5 [1.2 to 1.8] | p (1yr > 2yr) = 0.973 |
Low | 0.82 [0.77 to 0.85] |
0.16 [0.13 to 0.20] |
0.02 [0.00 to 0.04] |
| Two years or less 258 outcomes from 30 trials |
1.1 [0.73 to 1.4] | p (2yr > +2yr) = 0.775 | Low | ||||
| Over two years 381 outcomes from 33 trials |
0.89 [0.55 to 1.1] | p (1yr > +2yr) > 0.999 | Low | ||||
| Supervision | Supervised 356 outcomes from 36 trials |
1.4 [1.1 to 1.7] | p (Supervised > Unsupervised) = 0.994 | Low | 0.78 [0.74 to 0.82] |
0.19 [0.16 to 0.23] |
0.03 [0.00 to 0.05] |
| Unsupervised 918 outcomes from 113 trials |
1.0 [0.84 to 1.2] | Moderate | |||||
Efficacy review 1B results: exercise-only patient adverse events and patient rating outcomes
Study characteristics, tendinopathies and outcomes
Of the 125 studies including exercise-only therapies, a total of 52 studies (48 RCTs and 4 quasi-experimental trials) comprising 72 TAs and 1957 participants were identified to include adverse event or patient rating data (see Appendix 5, Table 37). A summary of the extracted data including study numbers and the specific tendinopathy locations investigated is presented in Table 10. Risk of bias results for individual studies are presented in Appendix 6, Table 41.
FIGURE 12.
Proportion of adverse events reported across included studies.
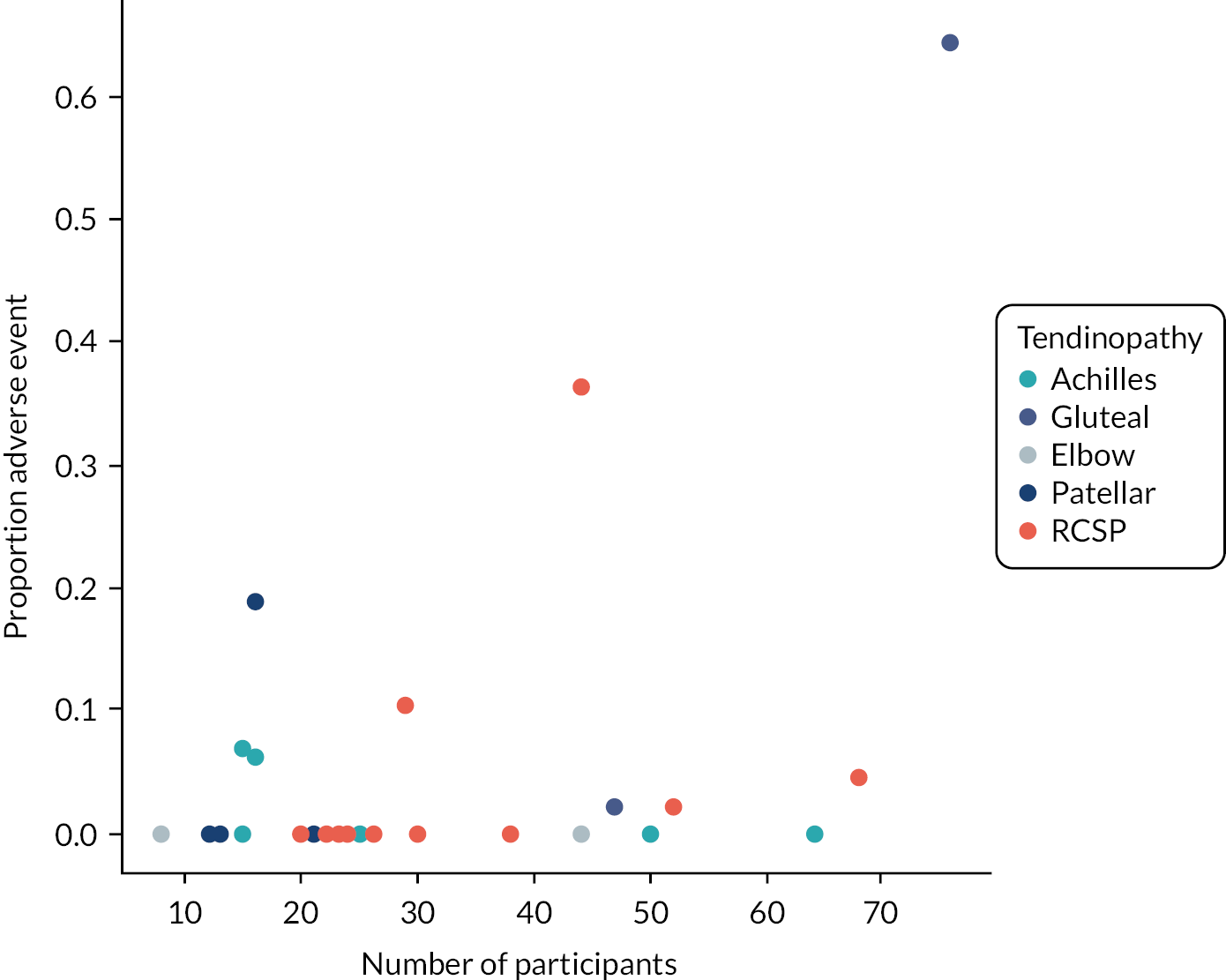
| Patient rating | Adverse events | |
|---|---|---|
| Number of studies | 35 | 30 |
| Number of TAs | 50 | 39 |
| Number of participants | 1265 | 1173 |
| Total number of outcomes | 102 | 39 |
| Total Achilles outcomes | 51 (50.0%) | 8 (20.5%) |
| Total RCRSP outcomes | 28 (27.5%) | 17 (43.6%) |
| Total patellar outcomes | 13 (12.7%) | 7 (17.9%) |
| Total elbow outcomes | 7 (6.9%) | 5 (12.8%) |
| Total gluteal outcomes | 3 (2.9%) | 2 (5.1%) |
Adverse events
Across the 39 TAs that reported the number of adverse events, 29 (74.4%) reported no adverse events, six reported adverse events between 0% and 10% of the patients, and two TAs reported relatively high percentages of adverse events of 36.4% and 64.0% (see Figure 12). Due to the large number of TAs reporting zero adverse events, only the exact binomial model was used to estimate the expected proportion of adverse events, which was equal to 0.002 [95% CrI 0.000 to 0.010]. The strength of evidence for the outcome was assessed as high (see Appendix 6, Table 42)
Patient satisfaction and rating
A range of measurement tools and scales were used to report the 102-patient rating outcomes across the 50 TAs. The most common outcomes reported included a binary rating of patient satisfaction (satisfied or not satisfied with treatment: 19 outcomes from 14 TAs) and the global rating of change (GROC) scales (17 outcomes from 7 TAs). The GROC scales used zero as a neutral point with values below and above this point representing negative and positive ratings of change, respectively. To enable appropriate synthesis, meta-analyses were restricted to these outcomes only. For the binary satisfaction data, the breakdown of the tendinopathy locations included seven outcomes for the Achilles, six outcomes for the patellar, four outcomes for the elbow and two outcomes for RCRSP. The pooled estimate of the proportion of patients reporting satisfaction was ES0.5 = 0.72 [95% CrI 0.55 to 0.88]. For the GROC scales, the breakdown of the tendinopathy locations included 12 outcomes for RCRSP and 5 outcomes for the patellar. The pooled estimated of patients’ perception of change was ES0.5 = 0.52 [95% CrI 0.39 to 0.65], indicating that patients tended to rate their change approximately half-way up the positive scale. The strength of evidence assessment for both patient satisfaction (see Appendix 6, Table 43) and GROC outcomes were high (see Appendix 6, Table 44).
Efficacy review 1C results: resistance exercise moderation
Study characteristics, tendinopathies and outcomes
Of the 125 studies including exercise-only therapies, sufficient information was obtained from 93 studies including resistance exercise as the dominant therapy class to be included in efficacy review 1C meta-analyses (see Appendix 5, Table 37). The studies comprised 130 TAs and 3040 participants. Risk of bias results for individual studies are presented in Appendix 6, Table 45. Descriptions of the tendinopathy locations, outcome domains and exercise therapies are presented in Table 11. Seventy-one of the TAs comprised resistance exercise only, with most multi-exercise therapies comprising resistance and flexibility classes (45 TAs). The most common dominant treatment was eccentric-only (62 TAs), followed by concentric and eccentric (43 TAs) then isometric (16 TAs). Resistance was frequently prescribed using the mass of the limbs or whole-body (40 TAs) and was infrequently prescribed based on a percentage of the maximum (11 TAs) resistance that could be overcome. The distribution of training frequency, number of exercised performed and number of repetitions performed are presented in Table 12. The results showed that the most common training frequency was twice per day, and that most TAs performed one to two exercises each with approximately 45 repetitions (most frequently 3 sets of 15 repetitions).
| Tendinopathy type | Number of TA (%) |
Number of effects (%) | Outcome domain |
Number of TA (%) |
Number of effects (%) |
|---|---|---|---|---|---|
| RCRSP | 39 (30.0) | 430 (40.6) | Disability | 99 (76.2) | 308 (29.1) |
| Achilles | 41 (31.5) | 292 (27.6) | Pain | 91 (70.0) | 299 (28.2) |
| Lateral elbow | 27 (20.8) | 217 (20.5) | |||
| Patellar | 19 (14.6) | 87 (8.2) | PFC | 47 (36.2) | 262 (24.7) |
| Gluteal | 4 (3.1) | 33 (3.1%) | |||
| Dominant exercise | Number of TA (%) |
Number of effects
(%) |
ROM | 14 (10.8) | 78 (7.4) |
| Eccentric-only | 62 (47.7) | 467 (44.1) | Function | 27 (20.8) | 65 (6.1) |
| Concentric and eccentric | 43 (33.1) | 408 (38.5) | |||
| Isometric | 16 (12.3) | 82 (7.7) | QoL | 10 (7.7) | 47 (4.4) |
| Concentric-only | 7 (5.4) | 58 (5.5) | |||
| Isokinetic | 2 (1.5) | 44 (4.2) |
| Study characteristic | 0% | 10% | 20% | 30% | 40% | 50% | 60% | 70% | 80% | 90% | 100% |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Training frequency | 2 | 3 | 4 | 5 | 7 | 7 | 7 | 14 | 14 | 14 | 21 |
| Number of exercises | 1 | 1 | 1 | 2 | 2 | 2 | 3 | 5 | 5 | 6 | 10 |
| Number of repetitions | 3 | 12.5 | 27.8 | 30 | 32.5 | 45 | 45 | 45 | 45 | 45 | 200 |
Analysis of exercise dose parameters
Based on the results of efficacy review 1A and the substantive difference in effect size distributions with a clear split between two sets of outcome domains, analyses were split into two categories described as small effects (QoL, physical functional capacity and ROM) and large effects (function, disability and pain). In addition, tendinopathy locations were categorised as upper-body (RCRSP and elbow) or lower-body (Achilles, patellar and gluteal) to increase the amount of data available for sub-analyses. Overviews of the tendinopathy locations and outcome domains included in each moderator analysis are presented in Appendix 6, Tables 46, 48, 50 and 52.
Exercise intensity
An analysis of exercise intensity was conducted comparing pooled mean effect sizes from a binary classification of TAs comprising body mass only resistance, or additional external resistance using, for example, TheraBands or isoinertial loads. A total of 119 TAs provided sufficient information for intensity to be coded, with 84 prescribing additional external resistance and 35 restricted to the mass of a limb or the whole body. In general, evidence was obtained for greater pooled mean values with resistance training prescribing additional external resistance (see Table 13), with point estimates indicating an increase of 0.2 to 0.5 for large effects. However, for analyses of small effects, values were closer and point estimates indicated increased mean values for body mass only resistance for the upper body and addition of external resistance for the lower body (see Table 13). Strength of evidence was generally low to moderate, with consistent evidence of small-study effects and frequent occurrences of imprecision (see Appendix 6, Table 47).
| Moderator | Estimate of mean [95% CrI] |
Probability | Strength of evidence | |
|---|---|---|---|---|
| Large effects (all tendinopathies) |
Body mass 35 TAs 193 outcomes |
1.0 [0.65 to 1.4] |
p (Additional > Body mass) = 0.989 | Low |
| Additional external 80 TAs 432 outcomes |
1.5 [1.2 to 1.7] |
Moderate | ||
| Large effects (lower body) |
Body mass 24 TAs 125 outcomes |
0.83 [0.54 to 1.1] |
p (Additional > Body mass) = 0.988 | High |
| Additional external 34 TAs 133 outcomes |
1.3 [1.0 to 1.6] |
Moderate | ||
| Large effects (upper body) |
Body mass 11 TAs 68 outcomes |
1.4 [0.67 to 2.2] |
p (Additional > Body mass) = 0.659 | Low |
| Additional external 46 TAs 299 outcomes |
1.6 [1.2 to 2.0] |
Low | ||
| Small effects (all tendinopathies) |
Body mass 13 TAs 98 outcomes |
0.53 [0.29 to 0.76] |
p (Body mass > Additional) = 0.723 | Moderate |
| Additional external 36 TAs 266 outcomes |
0.44 [0.30 to 0.58] |
High | ||
| Small effects (lower body) |
Body mass 8 TAs 83 outcomes |
0.51 [0.04 to 0.92] |
p (Additional > Body mass) = 0.851 | Moderate |
| Additional external 9 TAs 61 outcomes |
0.73 [0.30 to 1.1] |
Low | ||
| Small effects (upper body) |
Body mass 5 TAs 15 outcomes |
0.56 [0.20 to 0.95] |
p (Body mass > Additional) = 0.803 | Moderate |
| Additional external 27 TAs 205 outcomes |
0.38 [0.23 to 0.53] |
Low | ||
Exercise volume
Exercise volume was quantified based on the total number of resistance exercises prescribed each session, and the total repetitions prescribed (e.g. sets × repetitions) for the primary resistance exercise. Based on the distributions obtained (see Table 12) both variables were discretised into binary classifications characterising lower volume (<45 repetitions; two or fewer resistance exercises) and higher volume (≥45 repetitions; more than two resistance exercises).
Results were generally inconsistent for both volume variables, with no clear patterns identified across the different outcome domain and tendinopathy location groupings (see Tables 14 and 15). Similar point estimates were obtained for analyses conducted across the large effect outcome domains. For the small effect outcome domains some evidence was identified indicating greater effects for lower volume resistance exercise in the lower body and higher volume resistance exercise in the upper body (see Tables 14 and 15). However, strength of evidence assessment was frequently low due to consistent small-study effects, imprecision and some occurrences of indirectness (see Appendix 6, Tables 49 and 51).
| Moderator | Estimate of mean [95% CrI] |
Probability | Strength of evidence | |
|---|---|---|---|---|
| Large effects (all tendinopathies) |
Lower volume 51 TAs 271 outcomes |
1.5 [1.2 to 1.8] |
p (Lower volume > Higher volume) = 0.736 | Moderate |
| Higher volume 59 TAs 322 outcomes |
1.4 [1.1 to 1.7] |
Moderate | ||
| Large effects (lower body) |
Lower volume 11 TAs 54 outcomes |
1.0 [0.49 to 1.4] |
p (Higher volume > Lower volume) = 0.758 | Low |
| Higher volume 43 TAs 176 outcomes |
1.2 [0.92 to 1.4] |
High | ||
| Large effects (upper body) |
Lower volume 40 TAs 217 outcomes |
1.6 [1.2 to 2.0] |
p (Higher volume > Lower volume) = 0.518 | Low |
| Higher volume 16 TAs 146 outcomes |
1.7 [1.0 to 2.3] |
Low | ||
| Small effects (all tendinopathies) |
Lower volume 24 TAs 169 outcomes |
0.56 [0.36 to 0.75] |
p (Lower volume > Higher volume) = 0.885 | High |
| Higher Volume 21 TAs 173 outcomes |
0.38 [0.18 to 0.59] |
Low | ||
| Small effects (lower body) |
Lower volume 3 TAs 21 outcomes |
1.1 [0.38 to 1.9] |
p (Lower volume > Higher volume) = 0.938 | Low |
| Higher volume 13 TAs 114 outcomes |
0.53 [0.17 to 0.91] |
Low | ||
| Small effects (upper body) | Lower volume 21 TAs 148 outcomes |
0.47 [0.31 to 0.66] |
p (Lower volume > Higher volume) = 0.921 | High |
| Higher volume 8 TAs 59 outcomes |
0.23 [−0.04 to 0.51] |
Low | ||
| Moderator | Estimate of mean [95% CrI] |
Probability | Strength of evidence | |
|---|---|---|---|---|
| Large effects (all tendinopathies) |
Two or fewer 73 TAs 332 outcomes |
1.5 [1.2 to 1.7] |
p (Lower volume > Higher volume) = 0.797 | Moderate |
| More than two 43 TAs 293 outcomes |
1.3 [0.95 to 1.6] |
Moderate | ||
| Large effects (lower body) |
Two or fewer 50 TAs 206 outcomes |
1.1 [0.86 to 1.3] |
p (Higher volume > Lower volume) = 0.670 | Moderate |
| More than two 8 TAs 50 outcomes |
1.2 [0.68 to 1.7] |
Moderate | ||
| Large effects (upper body) |
Two or fewer 23 TAs 126 outcomes |
2.2 [1.7 to 2.7] |
p (Lower volume > Higher volume) = 0.997 | Low |
| More than two 35 TAs 243 outcomes |
1.3 [0.87 to 1.7] |
Low | ||
| Small effects (all tendinopathies) |
Two or fewer 25 TAs 160 outcomes |
0.44 [0.26 to 0.62] |
p (Higher volume > Lower volume) = 0.604 | Low |
| More than two 23 TAs 197 outcomes |
0.48 [0.29 to 0.66] |
High | ||
| Small effects (lower body) |
Two or fewer 12 TAs 72 outcomes |
0.65 [0.27 to 1.0] |
p (Lower volume > Higher volume) = 0.614 | Low |
| More than two 6 TAs 73 outcomes |
0.57 [0.05 to 1.1] |
Low | ||
| Small effects (upper body) |
Two or fewer 13 TAs 88 outcomes |
0.29 [0.08 to 0.52] |
p (Higher volume > Lower volume) = 0.876 | Low |
| More than two 17 TAs 124 outcomes |
0.46 [0.27 to 0.65] |
High | ||
Exercise frequency
Exercise frequency was quantified based on the number of resistance exercise sessions prescribed per week and, based on the distribution obtained (see Table 12), frequency was discretised into a trinary classification (less than daily, once per day or more than once per day). Meta-regressions performed comparing mean effect sizes across these categorisations are presented in Table 16. A consistent pattern was obtained, with the greatest pooled means generally obtained for the lowest frequency, and central estimates up to 1.1 greater for large effect outcomes and 0.59 greater for small effect outcome domains. Strength of evidence was frequently assessed as low to moderate based on consistent small-study effects and imprecision (see Appendix 6, Table 53).
| Moderator | Estimate of mean [95% CrI] |
Probability | Strength of evidence | |
|---|---|---|---|---|
| Large effects (all tendinopathies) |
Less than daily 37 TAs 194 outcomes |
2.0 [1.6 to 2.2] |
p (Less than daily > Once per day) > 0.999 p (Once per day > More than once per day) = 0.645 |
Moderate |
| Once per day 29 TAs 160 outcomes |
1.2 [0.89 to 1.5] |
Moderate | ||
| More than once per day 48 TAs 259 outcomes |
1.1 [0.71 to 1.5] |
p (Less than daily > More than once per day) > 0.999 | Moderate | |
| Large effects (lower body) | Less than daily 12 TAs 38 outcomes |
1.2 [0.71 to 1.6] |
p (Less than daily > Once per day) = 0.590 p (More than once per day > Once per day) = 0.530 |
Low |
| Once per day 10 TAs 33 outcomes |
1.1 [0.61 to 1.6] |
Low | ||
| More than once per day 36 TAs 187 outcomes |
1.1 [0.84 to 1.3] |
p (Less than daily > More than once per day) = 0.589 | Moderate | |
| Large effects (upper body) |
Less than daily 25 TAs 156 outcomes |
2.2 [1.7 to 2.8] |
p (Less than daily > Once per day) > 0.999 p (More than once per day > Once per day) = 0.752 |
Low |
| Once per day 19 TAs 127 outcomes |
1.1 [0.50 to 1.6] |
Low | ||
| More than once per day 12 TAs 72 outcomes |
1.4 [0.68 to 2.1] |
p (Less than daily > More than once per day) = 0.966 | Low | |
| Small effects (all tendinopathies) |
Less than daily 15 TAs 134 outcomes |
0.75 [0.56 to 0.95] |
p (Less than daily > Once per day) > 0.999 | Moderate |
| Once per day 17 TAs 137 outcomes |
0.24 [0.05 to 0.43] |
p (More than once per day > Once per day) = 0.908 | Low | |
| More than once per day 16 TAs 88 outcomes |
0.43 [0.24 to 0.61] |
p (Less than daily > More than once per day) = 0.992 | Moderate | |
| Small effects (lower body) |
Less than daily 5 TAs 44 outcomes |
0.90 [0.67 to 1.2] |
p (Less than daily > Once per day) > 0.999 | Very low |
| Once per day 4 TAs 50 outcomes |
0.31 [0.03 to 0.63] |
p (More than once per day > Once per day) = 0.547 | Low | |
| More than once per day 9 TAs 51 outcomes |
0.35 [0.04 to 0.66] |
p (Less than daily > More than once per day) = 0.989 | Very low | |
| Small effects (upper body) |
Less than daily 13 TAs 87 outcomes |
0.55 [0.33 to 0.79] |
p (Less than daily > Once per day) = 0.981 | Moderate |
| Once per day 29 TAs 160 outcomes |
0.22 [0.02 to 0.43] |
p (More than once per day > Once per day) = 0.948 | Low | |
| More than once per day 7 TAs 37 outcomes |
0.50 [0.23 to 0.78] |
p (Less than daily > More than once per day) = 0.618 | High | |
Efficacy review 1 discussion
The purpose of efficacy review 1 was to quantify the efficacy of exercise-only therapies across a range of outcome domains and tendinopathy locations, and explore the extent to which efficacy was influenced by exercise and patient characteristics. In contrast to many previous systematic reviews and meta-analyses that have investigated effectiveness or efficacy of exercise therapies for the management of tendinopathies,103 a more broad and large-scale modelling approach was adopted, combining large numbers of heterogeneous studies with regard to the exercise content, populations investigated and the tendinopathy locations and outcome domains measured. The review was split into three parts to account for the wide range of outcomes and data types collected. Parts 1 and 2 focussed on the core health-related outcome domains,56 including those typically measured by continuous measures (pain, function, PFC, disability, QoL) and those typically measured by binary or ordinal measures (patient rating and adverse events). Part 3 of the review focussed on investigating the dose–response of therapies where resistance exercise was the dominant exercise class, which comprised most therapies. Collectively, the mixture of meta-analysis models and approaches explored the heterogeneity in the studies, generating several key and novel findings.
Efficacy review 1A main findings
It was shown that exercise therapies create a response distribution that is relatively diffuse, reflecting the large number of potential factors that are likely to exert systematic effects. The bulk of the distributions, however, identify that, in general, individuals should expect to experience substantive improvements as quantified by standardised change scores from baseline in key outcome domains including function, disability, pain, ROM, PFC, QoL, patient satisfaction and patient rating. It was also shown that the distributions of responses are likely to be similar among the most common tendinopathies, including RCRSP, Achilles, patellar and lateral elbow tendinopathies. In contrast, another key and novel finding of this review is the substantive difference in effect size distributions across commonly measured outcome domains. It was identified that lower responses should be expected in QoL and objective measurement tools commonly used to quantify physical functional capacity and ROM. Indeed, the results of the analyses demonstrated that quality-of-life assessments may decrease following over 25% of exercise therapies (QoL 0.25-quantile small threshold: −0.21 [−0.32 to −0.09]). It is not clear whether these quality-of-life measures necessarily relate to health-related QoL as they are often used interchangeably in the literature. The former construct is a broader concept which covers all aspects of life and therefore may not necessarily correlate with the impact of the treatment. As such, the effect of exercise therapy on global QoL remains equivocal. 104 In stark contrast, efficacy for outcome domains that generally feature patients’ subjective assessment of more specific tendinopathy outcomes, for example pain, function, or disability, may be very large, with median standardised effect sizes close to 1, and the most efficacious exercise therapies (e.g. 0.75-quantile) generating standardised effect sizes closer to 1.5. Further research is required to better understand the reasons for the different effect size magnitudes across the outcome domains, the mechanisms of improvement and their relation to potential changes at the tendon.
Efficacy review 1A moderator analyses
As identified in the scoping review, reporting of patient and exercise characteristics is frequently limited in primary studies investigating exercise therapies. A lack of clear, consistent and stratified reporting of patient demographics, including age, race and sex, meant that these factors could not be used in moderator analyses. The most frequently reported characteristics that could be used to explore differences in overall response across the large data set included the duration of assessment from baseline, whether the therapy was supervised or not, and the symptom duration of patients. For assessment duration (time relative to baseline measurement), moderator analyses demonstrated an ordered effect, with the smallest mean pooled effect size obtained for short durations (1.0 [95% CrI 0.87 to 1.1]), and evidence of greater pooled means for medium (1.3 [95% CrI 1.1 to 1.4]) and subsequently long durations (1.4 [95% CrI 1.2 to 1.6]). Whilst the absolute magnitudes of the differences were relatively small and in keeping with previous research investigating differences between short and long-term follow-up,105 the results provide support that exercise therapies generate lasting improvements. Given the finding that almost all exercise therapies were of short duration (≤12 weeks) and the regenerative time of tendon repair is long106 it is possible that maintained and even continued improvement over long periods is due to patients maintaining exercise beyond treatment. Since the final stage of tendon repair does not start until 1–2 months after injury and can last over a year,106 self-management may play an important role in continuing the rehabilitation process through the long tendon remodelling phase once an intervention is finished. Although several barriers to implementation and adherence have been reported, studies suggest that self-management for tendinopathy is feasible with the right support. 107,108 Further exploration of issues surrounding self-management is continued in the mixed-methods review presented in Chapter 6.
Moderator analyses also identified an increased efficacy of supervised compared with unsupervised (βUnupervised:Supervised0.5 = 0.43 [95% CrI 0.09 to 0.78]) therapies, with the estimated difference increasing after controlling for tendinopathy location and outcome domain (βUnupervised:Supervised0.5 = 0.73 [95% CrI 0.41 to 1.1]). A recent systematic review by Hopewell (Hopewell S, Keene DJ, Marian IR, Dritsaki M, Heine P, Cureton L, Dutton SJ, Dakin H, Carr A, Hamilton W, Hansen Z. Progressive exercise compared with best practice advice, with or without corticosteroid injection, for the treatment of patients with rotator cuff disorders (GRASP): a multicentre, pragmatic, 2 × 2 factorial, RCT. The Lancet 2021;398(10298):416–28) investigating RCRSP rehabilitation identified that most (6/7) studies showed no differences between supervised and unsupervised exercise. One large RCT found that physiotherapist-led supervised exercise for subacromial pain resulted in greater improvements in pain and disability compared with unsupervised exercise. 109 However, their unsupervised exercise was facilitated only with a leaflet comprising no individualisation or progression. As such, the format of the supervised and unsupervised therapies may influence the results of any comparison. Issues surrounding supervision of exercise therapies are explored in greater depth in the mixed-methods review presented in Chapter 6.
Moderator analyses provide some evidence of ordered effect with symptom duration such that the greatest pooled mean effect sizes were generated for studies including patients with the shortest symptom durations (βMedium:Short0.5 = 0.47 [95% CrI −0.01 to 0.95]; βLong:Short0.5 = 0.67 [95% CrI 0.19 to 1.1]). These results coincide with what would be expected regarding issues of recalcitrant tendinopathies; however, differences were close to zero after controlling for tendinopathy location and outcome domain, suggesting that initial results may have been due to imbalances in these and potentially other covariates. Across the moderator analyses the strength of evidence was judged between low and moderate due to consistent small-study effects creating positive skews to effect size estimates and imprecision in estimates.
Efficacy review 1B main findings
In combination with relatively large changes in commonly measured outcome domains, the findings from efficacy review 1B demonstrated that exercise therapies are generally rated positively on patient-centred and more holistic outcomes. Unlike conventional patient-reported outcomes where the constructs of measurement (such as disability, function, or QoL) can be more easily defined, the measurement of patient satisfaction and perceptions of change are often complex. 110 Patients may have differing levels of satisfaction with the process and outcome of their care based on a range of contextual factors including initial expectations, patient experience and socioeconomic status. 110,111 Additionally, patient experience is likely to reflect a range of aspects of care as perceived by the patient, including accessibility, waiting times and interactions with health workers. In efficacy review 1B, the patient-centred outcomes synthesised included satisfaction and perception of change. Meta-analysis of binary patient satisfaction data taken from studies investigating the Achilles (seven outcomes), patellar (six outcomes), elbow (four outcomes) and RCRSP (two outcomes) generated a pooled estimate indicating that over 70% of patients report positive satisfaction (0.72 [95% CrI 0.55 to 0.88]). The most common scales used to quantify patients’ rating of their overall condition were GROC scales typically comprising 15 integer values ranging from −7 (great deal worse) to +7 (great deal better). Meta-analysis of GROC scales (12 outcomes from RCRSP and 5 outcomes for the patellar) generated a pooled estimate of ES0.5 = 0.52 [95% CrI 0.39 to 0.65], indicating that patients tended to rate their change approximately half-way up the positive scale. The strength of evidence assessment for both patient satisfaction and GROC outcomes was high.
Efficacy review 1C main findings
Analysis across the exercise-only therapies identified that resistance exercise was the dominant class in over 70% of treatments and outcomes extracted. This level of disparity was expected given the results of the scoping review and discussions with stakeholders regarding the predominance of resistance exercise and the focus of many clinicians regarding perspectives around the need to load tendons with a sufficient mechanical stimulus to obtain positive responses. Given this focus on resistance exercise and the potential to more accurately quantify training dose (e.g. intensity, volume and frequency) with this mode compared with for example flexibility or proprioceptive exercises, attempts to investigate dose–response relationships were restricted to therapies where resistance exercise was the dominant class. One of the limitations of this part of the review was the lack of clear reporting of exercise dose in the literature. Exercise volume and frequency were relatively well-reported, but intensity reporting was poor. None of the studies using TheraBands for resistance provided any information on the resistances encountered or detailed progression in intensity. Similarly, many of the studies that used dumbbells or weighted backpacks did not report the actual mass of the loads used. Given these limitations, resistance intensity was categorised based on the use of body mass only resistance (low intensity) or the addition of external sources of resistance (high intensity).
Efficacy review 1C moderator analyses
Despite limitations in the quantity and quality of data describing the exercise dose, the results of the meta-regressions identified plausible trends that align with frequent recommendations of resistance exercise for both the general population and those with tendinopathies. In general, results were consistent in estimating greater pooled means for higher-intensity resistance exercise, with increases of 0.2 to 0.5 for the large effect outcome domains. Performing exercises less frequently throughout the week (less than once per day) was also consistently shown to produce greater pooled mean effect sizes compared with therapies prescribing exercise once per day or more than once per day. Resistance exercise causes microtrauma in the tendon tissue and therefore requires a period of recovery before performing the next session. 112,113 Furthermore, for hypertrophy of the musculotendinous unit the stimulus from resistance exercise requires full activation, which would be optimised with adequate rest between exercise sessions. 112,113 In contrast, comparisons of exercise volume were less consistent, with many comparisons estimating minimal differences between lower- or higher-volume therapies based on the number of exercises performed or the total number of repetitions performed in the primary exercise. Strength of evidence across the moderator analyses was judged between low and moderate due to the existence of consistent small-study effects and a frequent lack of precision.
Summary and limitations of efficacy review 1
This large review and extensive series of meta-analyses were successful in exploring the exercise-only data to investigate the efficacy of exercise therapies for the management of tendinopathy. The results have shown that large changes from baseline should be expected, and that the distribution is likely to be influenced by a range of factors, including the outcome domain measured, the assessment duration, whether the exercise therapy is supervised or not and potentially the length of patients’ symptoms. In addition, the results show that in general patients are satisfied with exercise-only therapies and perceive the changes that occur during therapy to be adequate. It is likely that the efficacy of exercise therapies can be improved by altering the exercise dose and, when using predominantly resistance exercise, by ensuring the intensity is appropriately strenuous and by limiting training frequency. However, with large modelling analyses such as those presented here, there is the potential for substantive findings to be ‘cancelled out’, and for confounding when comparing effects across different levels of potential moderators to bias results. In many cases there were insufficient data and reporting of factors that may have been useful in attempts to control for confounding. In addition, where sufficient data exist to perform moderator analyses, often there are limitations in the selection and categorisation of moderators in representing the construct of interest. For example, in the present review resistance intensity was categorised as either low or high based on whether exercises were performed solely with body mass or the addition of an external resistance, respectively. This simplification was made as most studies did not specify resistances in terms of an absolute magnitude or percentage of maximum, and it was judged that in many instances the addition of an external resistance would decrease the number of repetitions that could be performed and therefore increase the intensity of the exercise. Given the importance of resistance exercise as a therapy for tendinopathy management, it is of great importance that future research provides more detailed accounts of the resistances used so that better understanding can be obtained of the role of intensity and its interaction with other dose components, including training volume and frequency. As a result of these limitations, caution is required when interpreting the results from this review. In addition, the use of exercise-only data in the absence of control groups can introduce bias, as it is possible that similar (or potentially greater) results could have been achieved with no exercise. The strength of evidence assessments frequently highlighted the high risk of bias due to small-study effects and the potential for extremely large and therefore unlikely estimates to bias results.
Efficacy review 2
The purpose of this review was to quantify the comparative efficacy of different exercise therapies and, where possible, develop an efficacy hierarchy while considering factors such as tendinopathy location. Comparative efficacy was established by comparing therapies based on exercise classes and treatments using direct head-to-head comparisons, and where possible combined direct and indirect comparisons using network meta-analyses.
Review-specific methods
The inclusion criteria were influenced by the project aims, the results of our initial scoping review mapping the exercise and tendinopathy literature as well as stakeholder workshops.
Participants
This meta-analysis included people of any age or gender with a diagnosis of RC-related shoulder pain (RCRSP), lateral elbow, patellar, Achilles or gluteal tendinopathy of any severity or duration. Studies that included participants with tendinopathy in the absence of full thickness or large tears were included.
Intervention
The health technology being assessed is exercise therapy for the treatment of any tendinopathy. Exercise therapies considered for inclusion comprised five therapy classes: (1) resistance; (2) plyometric; (3) vibration; (4) flexibility and (5) proprioception (see Appendix 4 for definitions). To enable more detailed comparisons, dominant treatments (see Appendix 4) were also defined by sub-categorising resistance (eccentric-only, concentric-only, concentric and eccentric, isokinetic, isometric), flexibility (static, dynamic, PNF and ballistic) and proprioception (sense of joint position and force, movement pattern retraining and balance). Interventions combining exercise with other therapies (e.g. laser, shockwave, MT or injection) were not included.
Comparator
The review included studies that compared at least two exercise therapies comprising different classes or treatments to enable calculation of comparative pairwise effect sizes.
Outcomes
Based on the results of our initial scoping review and subsequent stakeholder workshops we included outcome measures from six domains including (1) disability; (2) pain (either on loading, over a specified time, or without further specification); (3) physical functional capacity; (4) function; (5) QoL and (6) ROM (for shoulder joint and RCRSP only). Definitions of each domain and example measurement tools are presented in Appendix 4.
Statistical analysis
We fitted class-level and treatment-level Bayesian models. Standardised mean difference pairwise effect sizes were calculated by first identifying a comparator level (e.g. flexibility) and a reference level (e.g. resistance) and subtracting the two change scores. Change scores were calculated by subtracting baseline values from subsequent measurements following the initiation of treatment. Where required, the differences in change scores were reflected by multiplying by −1 to ensure that positive values represented greater improved clinical effect in the comparator compared with the reference. The differences in change scores were then standardised by dividing by the pooled baseline standard deviation (e.g. a value of 0 representing equivalence between comparator and reference). Currently a range of statistical approaches have been developed to best synthesise complex and heterogeneous data including the use of hierarchical models and network meta-analyses (NMA). 110 The use of NMA is increasing due to several potential advantages including the ability to combine direct and indirect estimates of treatment efficacy to enhance precision of estimates. 114 In addition, NMAs may be most effective in areas such as the one considered in the present analysis where there are multiple common treatment options, and an overall hierarchy is unclear. Analyses in this review were first performed by combining all tendinopathies and outcome domains. Subsequent sub-analyses were then performed by isolating tendinopathy locations and outcome domains. To account for the inclusion of multiple data points, hierarchical models were conducted for both direct pair-wise comparisons and NMAs. 115 Analyses were only conducted where at least 10 data points were available116 from a minimum of two studies and for nodes with a minimum of two edges. Results were reported for NMAs only when all parameters converged to appropriate estimates. To summarise potential differences between different classes and different treatments, results from the network meta-analysis (NMA) were used to calculate the surface under the cumulative ranking curve (SUCRA). 117 For each level within the class or treatment models, a SUCRA value expressed as a percentage was calculated representing the likelihood that outcomes were maximised or near maximised relative to other levels. This provided a means of ranking the different classes and treatments. Analyses were performed using the R packages R2WinBUGS.
Results
Study selection
Of the 204 studies identified for the overall review, an additional 167 studies were excluded due to studies not including different exercise-only treatments arms (163 studies), including the wrong outcome (2 studies), including the wrong tendinopathy location (1 study) and not including the required data (1 study). A total of 37 studies were included comprising 24 pairwise comparisons of different dominant exercise classes, 31 pairwise comparisons of different complete exercise classes and 44 pairwise comparisons of different dominant treatments.
Risk of bias
Risks of bias expressed for each of the 37 studies (31 RCTs and 6 quasi-experimental) included in the review are presented in Appendix 6 (see Table 54). Summaries expressed in percentages are presented in Table 17. For RCTs, risk of bias was highest for other biases (29% high risk of bias), blinding of participants (24% high risk of bias) and incomplete outcome bias (11% high risk of bias). For quasi-experimental trials, risk of bias was also highest for other biases (67% high risk of bias). In addition, the clarity of reporting was less effective for quasi-experimental trials with high levels of unclear risk reported for the blinding of outcome assessors (83%) and selective reporting bias (100%).
Dominant exercise class comparison
Fifteen studies comprising 24 head-to-head comparisons of four dominant therapy classes (resistance, flexibility, proprioception and vibration) were identified (see Figure 13 and Table 18). The comparisons included data from 951 participants primarily from studies investigating RCRSP and Achilles tendinopathies, with most comparisons including resistance- and flexibility-dominated exercise classes. Full details of number of studies, tendinopathy locations and outcome domains for each analysis are presented in Appendix 6, Table 55. Based on the available data, meta-analyses were restricted to comparisons between resistance, flexibility and proprioception, with consistent findings obtained between the NMA analysis and direct pairwise comparisons. Pooling data across all tendinopathies and outcomes for the NMA analysis provided stronger evidence of the superiority of flexibility (ESResistance:Flexibility0.5 = 0.18 [95% CrI 0.07 to 0.29], SUCRA = 0.75) and weaker evidence of the superiority of proprioceptive (ESResistance:Proprioceptive0.5 = 0.16 [95% CrI −1.8 to 0.32], SUCRA = 0.50) classes compared to resistance (SUCRA = 0.25) exercise. All direct pairwise comparisons returned median point estimates indicating greater treatment effects for flexibility and proprioceptive classes compared with resistance exercise (see Table 19). Strength of evidence assessments was most frequently low or very low due primarily to consistent risk of imprecision and inconsistency (see Appendix 6, Table 56).
FIGURE 13.
Network diagram illustrating distinct and direct pairwise comparisons between dominant exercise therapy classes.
The size of each node is scaled to the number of pairwise comparisons. Values on each edge quantify the number of direct pairwise comparisons between nodes.

| Tendinopathy location | Treatment comparisons (%) | Outcome domain | Treatment comparisons (%) | Number of outcomes (%) |
|---|---|---|---|---|
| RCRSP | 11 (45.8) | Disability | 24 (100) | 77 (32.6) |
| Achilles | 10 (41.7) | Pain | 17 (70.8) | 72 (30.5) |
| Elbow | 2 (8.3) | PFC | 7 (29.2) | 43 (18.2) |
| Patellar | 1 (3.8) | ROM | 4 (16.7) | 32 (13.6) |
| QoL | 2 (8.3) | 10 (4.2) | ||
| Function | 2 (8.3) | 2 (0.8) |
| Resistance vs. flexibility effect size [95% CrI] |
Strength of evidence |
Resistance vs. proprioception effect size [95% CrI] |
Strength of evidence | Outcome domains | Tendinopathy |
|---|---|---|---|---|---|
| 0.08 [−0.19 to 0.36] 5 studies/6 comparisons/79 outcomes |
Very low | 0.13 [−0.56 to 0.92] 4 studies/4 comparisons/68 outcomes |
Very low | All | RCRSP |
| 0.07 [−0.44 to 0.56] 5 studies/6 comparisons/21 outcomes |
Very low | 0.15 [−0.39 to 0.73] 4 studies/4 comparisons/18 outcomes |
Low | Disability | RCRSP |
| 0.23 [−0.79 to 1.3] 3 studies/3 comparisons/21 outcomes |
Very low | 0.22 [−0.77 to 1.4] 3 studies/3 comparisons/15 outcomes |
Very low | Pain | RCRSP |
| 0.33 [−2.3 to 2.5] 2 studies/2 comparisons/11 outcomes |
Very low | 0.02 [−1.3 to 1.5] 2 studies/2 comparisons/23 outcomes |
Low | PFC | RCRSP |
| 0.15 [−0.47 to 0.77] 2 studies/2 comparisons/16 outcomes |
Very low | Insufficient data | – | ROM | RCRSP |
| 0.27 [0.11 to 0.46] 2 studies/9 comparisons/63 outcomes |
Moderate | Insufficient data | – | All | Achilles |
| 0.28 [0.01 to 0.63] 2 studies/9 comparisons/31 outcomes |
Low | Insufficient data | – | Disability | Achilles |
Complete exercise class comparison
When comparing unique combinations of all exercise classes included in the exercise therapy (complete class), 21 studies comprising 31 head-to-head comparisons were identified (see Figure 14 and Table 20). The comparisons included data from 1210 participants primarily from studies investigating RCRSP and Achilles tendinopathies, with most comparisons between the complete classes of resistance-only, flexibility-only and combined resistance and flexibility. Full details of number of studies, tendinopathy locations and outcome domains for each analysis are presented in Appendix 6 and Table 57. Based on the available data, meta-analyses were restricted to comparisons between these three complete classes, with consistent findings obtained between the NMA analysis and all direct pairwise comparisons. Pooling data across all tendinopathies and outcomes for the NMA analysis provided stronger evidence of the superiority of flexibility (ESResistance:Flexibility0.5 = 0.17 [95% CrI −0.04 to 0.40], SUCRA = 0.72) and weaker evidence of the superiority of combing flexibility and resistance (ESResistance:Flexibility+Resistance0.5 = 0.04 [95% CrI −1.9 to 2.2], SUCRA = 0.50) compared to resistance (SUCRA = 0.28) exercise. All but a single direct pairwise comparison investigating pooled and distinct outcome domains for RCRSP and Achilles tendinopathies returned median point estimates indicating greater treatment effects for flexibility and combined flexibility and resistance exercise compared with resistance-only exercise (see Table 21). Strength of evidence assessments were frequently low or very low due primarily to consistent risk of imprecision and inconsistency (see Appendix 6, Table 58).
FIGURE 14.
Network diagram illustrating distinct and direct pairwise comparisons between complete exercise therapy classes.
The size of each node is scaled to the number of pairwise comparisons. Values on each edge quantify the number of direct pairwise comparisons between nodes.
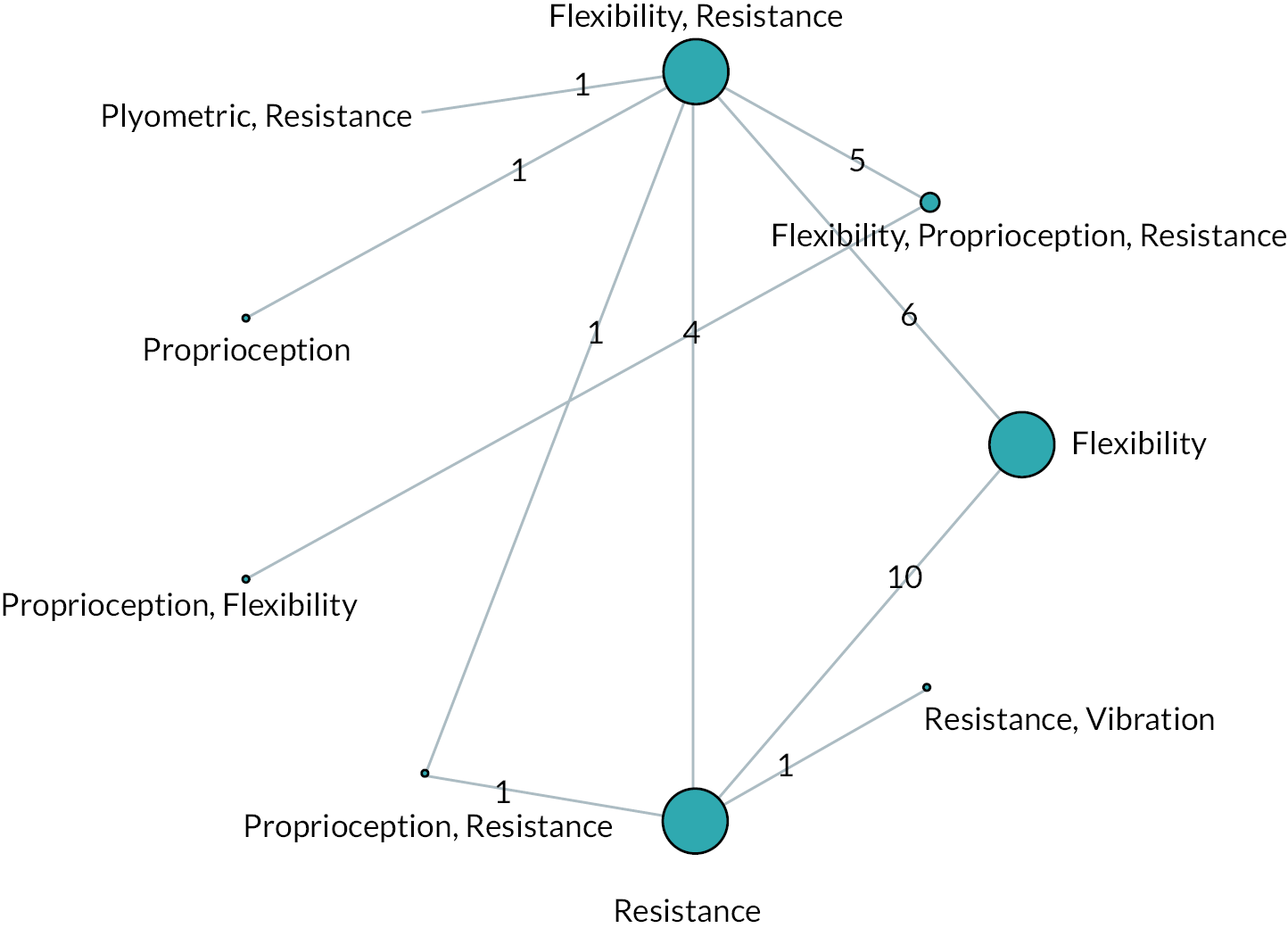
| Tendinopathy location | Treatment comparisons (%) | Outcome domain | Treatment comparisons (%) | Number of outcomes (%) |
|---|---|---|---|---|
| RCRSP | 12 (38.7) | Disability | 26 (83.9) | 84 (30.3) |
| Achilles | 12 (38.7) | Pain | 22 (71.0) | 89 (32.1) |
| Elbow | 4 (12.9) | PFC | 11 (35.5) | 66 (23.8) |
| Patellar | 2 (6.5) | ROM | 3 (9.7) | 20 (7.2) |
| Gluteal | 1 (3.2) | QoL | 2 (6.5) | 10 (3.6) |
| Function | 5 (16.1) | 8 (2.9) |
| Resistance-only vs. flexibility-only Effect size [95% CrI] |
Strength of evidence | Resistance-only vs. resistance + flexibility Effect size [95% CrI] |
Strength of evidence | Outcome domains | Tendinopathy |
|---|---|---|---|---|---|
| 0.23 [0.08 to 0.41] 3 studies/10 comparisons/77 outcomes |
Moderate | 0.14 [−1.4 to 1.4] 3 studies/4 comparisons/26 outcomes |
Very low | All | All |
| 0.22 [−0.04 to 0.59] 3 studies/10 comparisons/35 outcomes |
Low | Insufficient data | – | Disability | All |
| 0.24 [0.03 to 0.45] 2 studies/9 comparisons/3outcomes |
Moderate | Insufficient data | – | Pain | All |
| Insufficient data | – | −0.82 [−2.3 to 0.35] 2 studies/2 comparisons/15 outcomes |
Very low | PFC | All |
| 0.27 [0.11 to 0.46] 2 studies/9 comparisons/63 outcomes |
Moderate | Insufficient data | – | All | Achilles |
| 0.28 [0.00 to 0.63] 2 studies/9 comparisons/31 outcomes |
Low | Insufficient data | – | Disability | Achilles |
Dominant treatment comparison
Thirty-four studies comprising 44 head-to-head comparisons of 11 dominant treatments (resistance: concentric and eccentric, eccentric-only, concentric-only, isokinetic and isometric; flexibility: dynamic, static and PNF; proprioception: movement pattern retraining and joint position sense; and vibration) were identified. The comparisons comprised data from 1769 participants primarily from studies investigating resistance training treatments (see Figure 15 and Table 22). Full details of number of studies, tendinopathy locations and outcome domains for each analysis are presented in Appendix 6, Table 59. Given the data available and the sparsity of the overall network, comparisons were restricted to the resistance exercise treatments (concentric and eccentric, eccentric-only, concentric-only and isometric actions). However, the NMA did not converge, and analyses were restricted to direct pairwise comparisons with eccentric-only treatments, which were most popular, used as the reference. In general, CrIs from effect sizes were wide; however, median estimates across all combinations of outcome domains and tendinopathy types were consistent, indicating greater treatment effects for concentric and eccentric actions compared with eccentric-only (see Table 23), and reduced treatment effects for isometric and concentric-only actions compared with eccentric-only. Strength of evidence assessments were most frequently low or very low due primarily to consistent risk of imprecision and inconsistency (see Appendix 6, Table 60).
FIGURE 15.
Network diagram illustrating distinct and direct pairwise comparisons between dominant exercise therapy treatments.
The size of each node is scaled to the number of pairwise comparisons. Values on each edge quantify the number of direct pairwise comparisons between nodes.
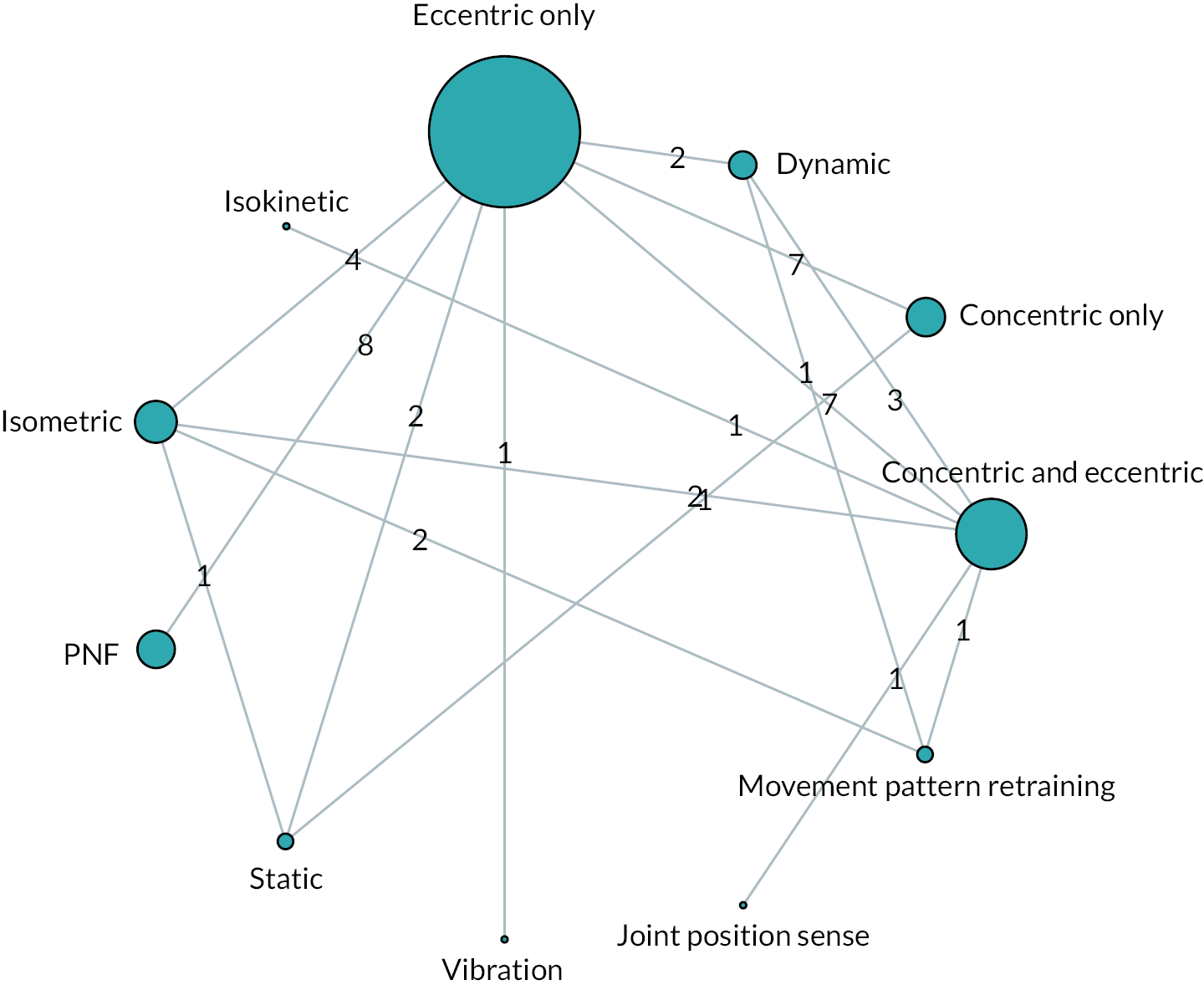
| Tendinopathy location | Treatment comparisons (%) | Outcome domain | Treatment comparisons (%) | Number of outcomes (%) |
|---|---|---|---|---|
| RCRSP | 14 (31.8) | Disability | 38 (86.4) | 108 (28.2) |
| Achilles | 15 (34.1) | Pain | 29 (65.9) | 114 (29.8) |
| Elbow | 8 (18.2) | PFC | 18 (40.9) | 93 (24.3) |
| Patellar | 6 (13.6) | ROM | 6 (13.6) | 37 (9.7) |
| Gluteal | 1 (2.3) | QoL | 3 (6.8) | 19 (5.0) |
| Function | 8 (18.2) | 12 (3.1) |
| Eccentric-only vs. concentric and eccentric Effect size [95% CrI] |
Strength of vidence | Eccentric-only vs concentric-only Effect size [95% CrI] |
Strength of evidence | Eccentric-only vs isometric Effect size [95% CrI] |
Strength of evidence | Outcome domains | Tendinopathy |
|---|---|---|---|---|---|---|---|
| 0.48 [−0.13 to 1.1] 6 studies/7 comparisons/56 outcomes |
Low | −0.76 [−1.7 to 0.15] 7 studies/7 comparisons/57 outcomes |
Very low | −1.7 [−3.2 to −0.05] 4 studies/4 comparisons/16 outcomes |
Very low | All | All |
| 0.18 [−0.45 to 0.67] 5 studies/6 comparisons/14 outcomes |
Low | Insufficient data | – | Insufficient data | – | Disability | All |
| 1.0 [−1.2 to 3.1] 3 studies/4 comparisons/17 outcomes |
Very low | −0.22 [−0.96 to 0.64] 4 studies/4 comparisons/23 outcomes |
Very low | Insufficient data | – | PFC | All |
| 0.62 [0.01 to 1.2] 5 studies/6 comparisons/14 outcomes |
Low | −0.85 [−1.8 to 0.05] 6 studies/6 comparisons/15 outcomes |
Very low | Insufficient data | – | Pain | All |
| Insufficient data | – | −1.0 [−2.8 to 0.60] 3 studies/3 comparisons/17 outcomes |
Low | Insufficient data | – | ALL | Achilles |
| Insufficient data | – | −0.06 [−0.66 to 0.59] 2 studies/2 comparisons/31 outcomes |
Low | Insufficient data | – | ALL | Elbow |
| 0.07 [−0.54 to 1.1] 2 studies/2 comparisons/30 outcomes |
Low | Insufficient data | – | Insufficient data | – | ALL | RCRSP |
| Insufficient data | – | −0.25 [−0.90 to 0.40] 2 studies/2 comparisons/11 outcomes |
Low | Insufficient data | – | Pain | Elbow |
| 0.60 [−0.58 to 1.6] 2 studies/2 comparisons/13 outcomes |
Low | Insufficient data | – | Insufficient data | – | PFC | RCRSP |
Efficacy review 2 discussion
The aim of efficacy review 2 was to synthesise data from studies directly comparing different exercise classes and exercise treatments to quantify comparative efficacy for the management of the most common tendinopathies. Based on this aim, only studies that included TAs featuring exercise in isolation (e.g. not combined with electro-therapy or MT) were included and compared. In addition, to generate pairwise comparisons the TAs within the same study were required to compare different exercise-only therapies with regard to the class or treatment. Whilst this process limited the number of studies that could be included in the analysis, it provided the most effective means of comparing exercise therapies across the research base to identify whether general patterns and a treatment hierarchy could be established.
Therapy class analysis and RCRSP comparisons
The initial broad NMA analysis comparing dominant therapy classes across all tendinopathies and outcomes (24 direct treatment comparisons) provided evidence that flexibility was superior to resistance exercise in the available comparisons. Subsequent analyses comprising direct pairwise comparisons only further supported the NMA results, providing limited but consistent evidence that both flexibility and proprioceptive dominant treatments were superior to resistance when outcome domains were combined or analysed separately. Data for the analyses were taken primarily from studies investigating RCRSP (five studies and six comparisons). The findings of superior efficacy of flexibility and proprioceptive exercise therapies for management of RCRSP should be considered in context of the low and very low quality of evidence used in their generation; however, they do support recent recommendations. 118–122 The pathoetiology of RCRSP is multifactorial and can be attributed to intrinsic, extrinsic or even combined mechanisms. 123,124 Due to this varied nature of the factors involved, RCRSP is not a homogeneous entity and hence may require treatment interventions that consider these specific mechanisms. 124 The primary intervention for RCRSP is generally active exercise therapy, with flexibility treatments, especially those targeting the pectoralis minor commonly prescribed to reduce anterior tilting of the scapula, which decreases the joint space available for the supraspinatus tendon. 125 Additionally, interventions for RCRSP frequently include proprioceptive exercise to restore normal shoulder movement patterns, designed to address degenerated tendons, altered scapular kinematics or abnormal neuromuscular control. 119,126,127 These proprioceptive mechanisms would use the range gained from pectoralis minor stretching to alter scapular kinematics. However, the strength of the evidence for the superiority of flexibility and proprioceptive exercise compared with resistance for RCRSP was judged as low and very low due to high risk of inconsistency, imprecision in estimates and clear evidence of small-study effects with a small number of studies generating very large effect sizes.
Achilles therapy class comparisons
Evidence which must be interpreted with great caution was also obtained indicating superiority of flexibility as the dominant therapy class for AT. The degree of caution is because the evidence comprised only a small amount of data (two studies and nine comparisons) and was judged to be of moderate effect and low quality due to inconsistency and imprecision. Although this finding may seem contrary to the focus and conclusions of research conducted on AT, there remain alternative potential mechanisms of exercise interventions relating to different pathoanatomical diagnosis (e.g. insertional, mid-portion AT) yet to be understood. Studies rarely report the severity and irritability of AT, and therefore the sample population may be at different points along the reactive-degenerative tendon continuum. 128 Flexibility exercises to encourage ROM could be indicated in a painful reactive tendon, where traditional eccentric loading programs might not be tolerated. As such, it is likely that the most beneficial exercise therapies require targeting to the individual, the stage of pathology and functional demands of the patient.
Therapy treatment analysis
When synthesising pairwise comparisons of dominant treatments, data were primarily obtained between resistance modalities including concentric and eccentric, isometric, concentric-only and eccentric-only exercises. The NMA analysis did not converge with the majority of pairwise effect size estimates, returning unfeasibly large CrIs. However, subsequent analyses only comprising direct comparisons provided limited but consistent evidence of a hierarchy where therapies comprising concentric and eccentric repetitions as the dominant treatment were superior to eccentric-only. In addition, therapies comprising eccentric-only repetitions as the dominant treatment were shown to be superior to treatments comprising concentric-only or isometric actions. Most of the studies included in this review recruited patients from the general population. In contrast, much of the previous and influential research demonstrating the efficacy of eccentric-only treatments for tendinopathy management were conducted with performance and recreational athletes. 129–132 The effect of pain and functional outcomes can be conflicting in the literature when comparing eccentric exercise with other exercise modalities. 12 There could be an element of pain tolerance with regard to how well eccentric-only exercises are tolerated in both general and athletic populations, the latter generally more inclined to higher loading and possibly discomfort during activity. Visnes et al. 129 reported poor tolerance of eccentric-only exercises amongst athletes in season with patellar tendinopathy due to excessive loading from sport. Additionally, Bahr et al. 131 reported a 40% drop-out from their eccentric protocol in recreational athletes with chronic tendinopathy, therefore additional factors such as adherence, attendance and fidelity (discussed in Chapter 6) may also influence any differences between treatments.
While it is known that the tendon is responsive to loading and will respond better to an optimum load beyond which further damage can occur,9 there is less certainty that the mode of muscle contraction for a given load can have a differential effect on the biochemical and biomechanical structures (e.g. collagen synthesis) of the tendon. 133,134 Given greater internal forces can be generated during eccentric compared with concentric actions, it is believed that this enhanced force and associated stretching have greater potential for mechanical stimulation. 135–137 However, it has been argued that this potential increase in capacity is rarely applied clinically as rehabilitation exercises seldom perform eccentric 1-repetition maximums but rather involve movements such as eccentric squats and heel drops with resistances targeting 15-repetition maximums. 132,138 In a comparative study of concentric and eccentric contraction on quadriceps and patellar tendon, Farup et al. (2014) found similar magnitudes of tendon hypertrophy irrespective of the mode of contraction. Their findings suggest that if there is sufficient load on the tendon, the mode of action is inconsequential to cellular and tissue response. 139 It is likely, therefore, that when appropriate loadings are used any differences due to mode of action will be small and challenging for individual studies to identify. The benefits of large meta-analyses such as that conducted here include identification of general patterns that may be of use to clinicians and assist in developing future research questions. Under typical constraints associated with resistance exercise therapies for the general population, the results presented here suggest that combined eccentric and concentric repetitions may present fewer challenges and be the most efficacious for management of tendinopathies.
Summary and limitations of efficacy review 2
It is important to highlight that there are many potential limitations with meta-analyses that combine data from studies with diverse populations, interventions and outcomes. Outcomes of analyses may be influenced by imbalances in effect moderators and generate findings that contradict the underlying treatment effects particular to any desired combination of population, intervention and outcomes. In addition, the present analyses have focussed predominantly on identifying dominant therapy classes and treatments that are in practice frequently combined with non-exercise therapies, including electro-therapy, MT, injections and surgery. With these limitations in mind, the findings of broad meta-analyses such as the one conducted here should be viewed with caution.
From a clinical perspective, the findings of the present study acknowledge that there are limitations to perspectives of the superiority of resistance exercise and in particular eccentric-only resistance exercise. The findings prompt the consideration of a broader, more holistic approach to the management of tendinopathy that may be tailored to the functional needs of the individual. The principles of loading are very much still supported; however, clinicians and researchers should consider other paradigms of exercises such as flexibility and proprioception that may yield better improvements in certain circumstances which could also have meaningful impact on overall adherence and patient satisfaction. Where resistance exercise is the dominant treatment, the results of the present meta-analysis identify that eccentric-only modalities may produce greater improvements than other contraction modes such as isometric and concentric-only. However, the combination of concentric and eccentric repetitions may produce the greatest improvements, which requires further investigation and consideration of whether the resistances used in many treatments make use of the additional loading potential with eccentric-only actions.
Efficacy review 3
The purpose of this review was to compare the efficacy of exercise, non-exercise and combined therapies to develop a hierarchy where possible. Comparative efficacy was established by comparing therapies based on their class and treatments using direct head-to-head comparisons and where possible combined direct and indirect comparisons using network meta-analyses.
Review-specific methods
The inclusion criteria were influenced by the project aims, the results of our initial scoping review mapping the exercise and tendinopathy literature as well as stakeholder workshops.
Participants
This meta-analysis included people of any age or gender with a diagnosis of tendinopathy of any severity or duration and at any anatomical location. Studies that included participants with tendinopathy in the absence of full thickness or large tears were included.
Intervention
The primary health technology being assessed is exercise therapy for the treatment of any tendinopathy. Exercise therapies considered for inclusion comprised five classes: (1) resistance; (2) flexibility; (3) proprioception; (4) vibration and (5) plyometric (see Appendix 4 for definitions). No restrictions were placed on the settings in which the exercise therapy was performed or the professionals involved. To be included in the review, studies were required to report sufficient information regarding the exercise intervention to enable appropriate identification of exercise class and quantification of exercise dose.
Comparator
To be included in this review, studies were required to compare at least one exercise TA that met the inclusion criteria with other common therapies used in the management or investigation of tendinopathies. Comparators selected included: (1) non-active (placebo, sham, wait-and-see); (2) electro-therapy (e.g. shockwave, laser, ultrasound, radar); (3) kinetics (e.g. altered loading through taping and braces, or immobilisation through splits); (4) injection therapy (e.g. autologous, drug, volumetric); (5) MT and (6) surgery. Definitions of broad and specific therapy classes for the different therapies are provided in Appendix 4.
Outcomes
Based on the results of our initial scoping review and subsequent stakeholder workshops we included outcome measures from six domains: (1) disability; (2) pain (either on loading, over a specified time, or without further specification); (3) physical functional capacity; (4) function; (5) QoL and (6) ROM (for shoulder joint only). Definitions of each domain and example measurement tools are presented in Appendix 4.
Statistical analysis
We fitted class-level and treatment-level Bayesian models. For continuous data, standardised mean difference pairwise effect sizes were calculated by first identifying a comparator level (e.g. flexibility) and a reference level (e.g. resistance) and subtracting the two change scores. Change scores were calculated by subtracting baseline values from subsequent measurements following the initiation of treatment. Where required, the differences in change scores were reflected by multiplying by −1 to ensure that positive values represented greater improved clinical effect in the comparator compared with the reference. The differences in change scores were then standardised by dividing by the pooled baseline standard deviation. For binary outcomes, proportional odds models were used to compare reference and comparator levels. Analyses in this review were first performed by combining all tendinopathies and outcome domains. Subsequent sub-analyses were then performed by isolating tendinopathy locations and outcome domains. To account for the inclusion of multiple data points, hierarchical models were conducted for both direct pair-wise comparisons and NMAs. 115 Analyses were only conducted where at least 10 data points were available,116 including a minimum of two treatment comparisons and nodes with a minimum of two edges. Results were reported for NMAs only when all parameters converged to appropriate estimates. To summarise potential differences between different classes and different treatments, results from the NMA were used to calculate the SUCRA. 117 For each level within the class or treatment models, a SUCRA value expressed as a percentage was calculated representing the likelihood that outcomes were maximised or near maximised relative to other levels. This provided a means of ranking the different classes and treatments. Analyses were performed using the R packages R2WinBUGS140 and brms. 92 Convergence of parameter estimates was checked with Gelman–Rubin R-hat values. 88,93
Results
Of the 204 studies identified for the overall review, three studies were excluded for not including sufficient data on the required outcomes. A total of 201 studies comprising 460 TAs and 11,888 participants were identified that met the inclusion criteria. A total breakdown of the tendinopathies investigated across the 201 studies and associated 1863 outcomes measured across six outcome domains are presented in Table 24.
| Tendinopathies | Number of studies (%) | Outcome domain | Number of outcomes (%) |
|---|---|---|---|
| RCRSP | 87 (43.3) | Pain | 545 (29.3) |
| Elbow | 43 (21.4) | Disability | 522 (28.0) |
| Achilles | 41 (20.4) | PFC | 385 (20.7) |
| Patellar | 20 (10.0) | ROM | 233 (12.5) |
| Gluteal | 4 (2.0) | Function | 116 (6.2) |
| Tibialis posterior | 4 (2.0) | QoL | 62 (3.3) |
| Hamstring | 1 (0.5) | ||
| Biceps | 1 (0.5) |
Risk of bias
Risks of bias expressed for each of the 201 studies (173 RCTs and 28 quasi-experimental) included in the review are presented in Appendix 6 (see Table 61). Summaries expressed in percentages are presented in Table 25. For RCTs, risk of bias was highest for blinding of participants (37% high risk of bias), other biases (32% high risk of bias) and blinding of outcome assessors (14% high risk of bias). For quasi-experimental trials, risk of bias was also highest for other biases (70% high risk of bias). In addition, the clarity of reporting was less effective for quasi-experimental trials, with high levels of unclear risk reported for all domains other than other bias (52–82% unclear risk).
Broad therapy class
The composition of the broad therapy classifications across the 460 TAs included exercise-only (182/39.6%), non-active (18/3.9%), non-exercise-only (36/7.8%), exercise and non-exercise (224/48.7%). The head-to-head comparisons between the broad therapy classifications are illustrated in Figure 16, with interventions most frequently combining exercise and non-exercise therapies. Full details of the number of trials and outcomes across the different domains are presented in Appendix 6, Table 62. Results obtained from NMAs comparing broad therapy classifications across different outcomes identified a consistent pattern (see Table 26). In all but one model, the SUCRA and pairwise effect sizes indicated the superiority of interventions combining exercise and non-exercise therapies relative to all other classifications. The only exception was in the analysis of QoL, where combined exercise and non-exercise ranked joint top with non-exercise-only based on SUCRA values. Median effect size estimates indicated that the combination of exercise with non-exercise therapies tended to improve outcomes by effect sizes of approximately 0.1 to 0.3. Less consistency was observed in the treatment hierarchy across the remaining broad therapy classes; however, non-active treatments tended to be ranked lowest. Strength of evidence assessments were low or very low due primarily to consistent risk of imprecision and inconsistency (see Appendix 6, Table 63).
FIGURE 16.
Network diagram illustrating distribution of pairwise comparisons between broad therapy classifications.
The size of each node is scaled to the number of pairwise comparisons. Values on each edge quantify the number of direct pairwise comparisons between nodes. A total of 327 pairwise comparisons featured 311 instances of exercise + non-exercise, 252 instances of exercise-only, 62 instances of non-exercise-only and 29 instances of non-active.

| Exercise + non-exercise [95% CrI] | Exercise-only [95% CrI] |
Non-exercise-only [95% CrI] | Non-active [95% CrI] |
Strength of evidence | Outcome domains | Tendinopathy |
|---|---|---|---|---|---|---|
| Reference SUCRA = 0.88 103 trials 909 outcomes |
ES0.5 = −0.09 [−0.22 to 0.04] SUCRA = 0.48 100 trials 1035 outcomes |
ES0.5 = −0.13 [−0.46 to 0.19] SUCRA = 0.40 50 trials 450 outcomes |
ES0.5 = −0.19 [−0.43 to 0.06] SUCRA = 0.23 27 trials 314 outcomes |
Low | All | All |
| Reference SUCRA = 0.81 91 trials 311 outcomes |
ES0.5 = −0.07 [−0.23 to 0.11] SUCRA = 0.59 90 trials 319 outcomes |
ES0.5 = −0.10 [−0.50 to 0.31] SUCRA = 0.53 42 trials 111 outcomes |
ES0.5 = −0.35 [−0.63 to 0.07] SUCRA = 0.07 23 trials 99 outcomes |
Low | Disability | All |
| Reference SUCRA = 0.80 69 trials 282 outcomes |
ES0.5 = −0.13 [−0.30 to 0.03] SUCRA = 0.70 69 trials 295 outcomes |
ES0.5 = −0.03 [−0.40 to 0.37] SUCRA = 0.31 36 trials 132 outcomes |
ES0.5 = −0.21 [−0.51 to 0.09] SUCRA = 0.19 20 trials 69 outcomes |
Low | Pain | All |
| Reference SUCRA = 0.86 32 trials 103 outcomes |
ES0.5 = −0.18 [−0.57 to 0.21] SUCRA = 0.34 32 trials 155 outcomes |
ES0.5 = −0.11 [−0.47 to 0.26] SUCRA = 0.56 20 trials 85 outcomes |
ES0. = −0.20 [−0.68 to 0.29] SUCRA = 0.23 14 trials 75 outcomes |
Low | PFC | All |
| Reference SUCRA = 0.83 24 trials 68 outcomes |
ES0.5 = −0.03 [−0.29 to 0.23] SUCRA = 0.72 24 trials 83 outcomes |
ES0.5 = −0.49 [−1.1 to 0.04] SUCRA = 0.37 13 trials 57 outcomes |
ES0.5 = −0.19 [−0.47 to 0.08] SUCRA = 0.09 9 trials 42 outcomes |
Low | Function | All |
| Reference SUCRA = 0.57 18 trials 71 outcomes |
ES0.5 = −0.05 [−0.28 to 0.18] SUCRA = 0.41 18 trials 71 outcomes |
ES0.5 = 0.09 [−0.37 to 0.54] SUCRA = 0.57 8 trials 25 outcomes |
ES0.5 = −0.11 [−0.52 to 0.31] SUCRA = 0.32 6 trials 17 outcomes |
Very low | QoL | All |
Dominant class
The composition of dominant therapy classes across the 460 TAs included resistance (212/46.1%), electro-therapy (62/13.5%), flexibility (48/10.4%), injection (31/6.7%), proprioception (27/5.9%), MT (28/6.1%), kinetics (20/4.3%), non-active (19/4.1%), surgery (11/2.4%), vibration (1/0.2%) and plyometrics (1/0.2%). The pairwise comparisons between the dominant therapy classifications are illustrated in Figure 17 with interventions most frequently focussing on resistance exercise. For the NMA analysis, comparisons including vibration and plyometrics were removed, and analyses restricted to outcome domains where there were sufficient data across the remaining dominant therapy classes. Distributions of SUCRA values are presented in Figure 18. When assessing the relative rankings of therapy classes across the different outcomes, substantive overlaps were identified, with limited trends emerging. The highest SUCRA values tended to occur for therapies where injection was the dominant class and the lowest SUCRA values for non-active therapies (see Figure 18).
FIGURE 17.
Network diagram illustrating distribution of pairwise comparisons between dominant therapy classes.
The size of each node is scaled to the number of pairwise comparisons. Values on each edge quantify the number of direct pairwise comparisons between nodes. A total of 327 pairwise comparisons that featured 292 instances of resistance, 91 instances of electro-therapy, 69 instances of flexibility, 50 instances of injection, 32 instances of proprioception, 37 instances of MT, 29 instances of non-active, 32 instances of kinetics, 20 instances of surgery, 1 instance of vibration, and 1 instance of plyometrics.
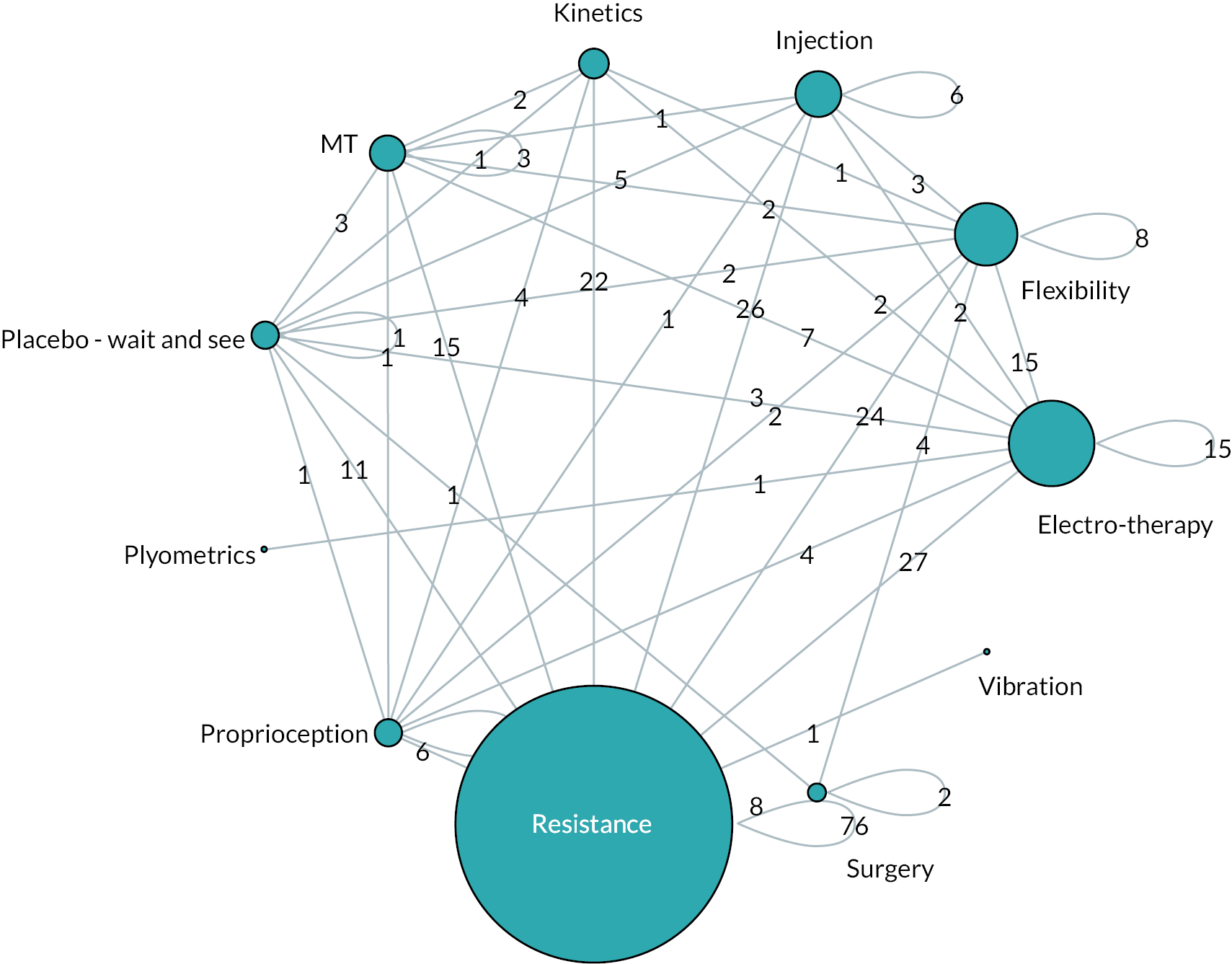
FIGURE 18.
Distribution of rankings (SUCRA values) across outcomes and dominant therapy classes.
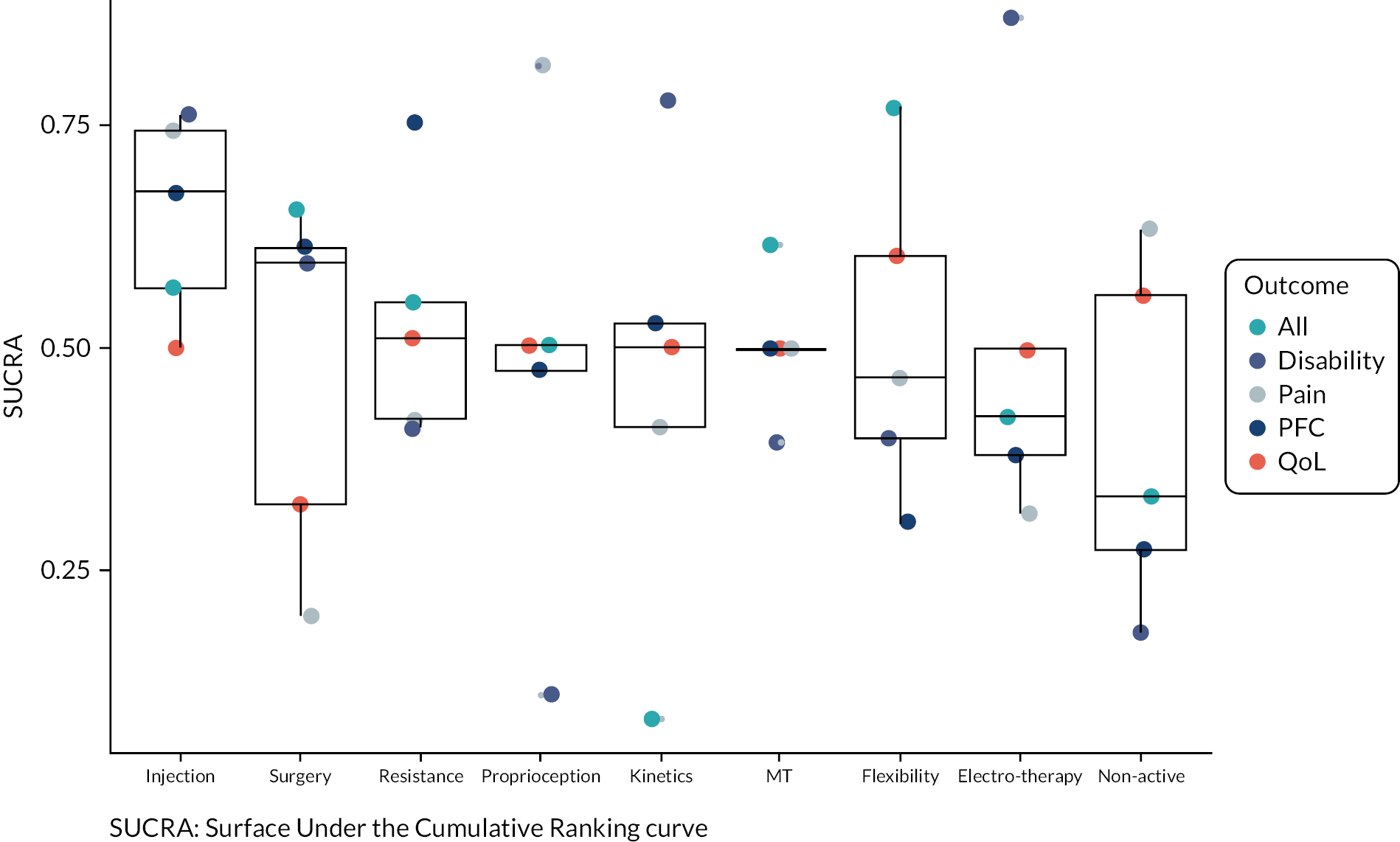
Exercise and non-exercise class combinations
The final analysis was completed across different therapy class combinations (see Figure 19) to determine which produced the greatest improvements and build upon the previous results identifying exercise combined with non-exercise treatments were superior to non-active or exercise and non-exercise therapies in isolation. Due to substantial non-convergence in parameter estimates within the NMA, direct pairwise analyses were completed with exercise-only interventions as the reference (see Table 27). Full details of the number of trials and outcomes across the different domains are presented in Appendix 6, Table 64.Substantive uncertainty was identified across outcomes and domains investigated, with wide CrIs for mean pairwise effect sizes. Median estimates indicated similar efficacy for the combination of exercise with either electro-therapy, injection or kinetics. Strength of evidence assessments across the different comparisons were highly variable, but most frequently categorised as low due primarily to consistent risk of imprecision and inconsistency (see Appendix 6, Table 65).
FIGURE 19.
Network diagram illustrating distribution of pairwise comparisons between complete therapy classes.
The size of each node is scaled to the number of pairwise comparisons. Values on each edge quantify the number of direct pairwise comparisons between nodes. A total of 201 pairwise comparisons that featured 53 instances of non-exercise only, 44 instances of exercise + electro-therapy, 39 instances of resistance, 37 instances of exercise + non-active, 37 instances of flexibility + resistance, 27 instances of non-active, 25 instances of exercise + kinetics, 23 instances of exercise + MT, 21 instances of exercise + injection, 20 instances of exercise + electro-therapy + MT, 13 instances of exercise + surgery, 12 instances of flexibility, 11 instances of flexibility + proprioception + resistance, 7 instances of exercise + electro-therapy + kinetics + MT, 7 instances of exercise + MT + non-active, 4 instances of exercise + kinetics + MT, 4 instances of proprioception + resistance, 3 instances of exercise + electro-therapy + non-active, 3 instances of exercise + injection + kinetics, 2 instances of exercise + electro-therapy + kinetics, 1 instance of exercise + electro-therapy + injection + MT, 1 instance of injection + non-active.
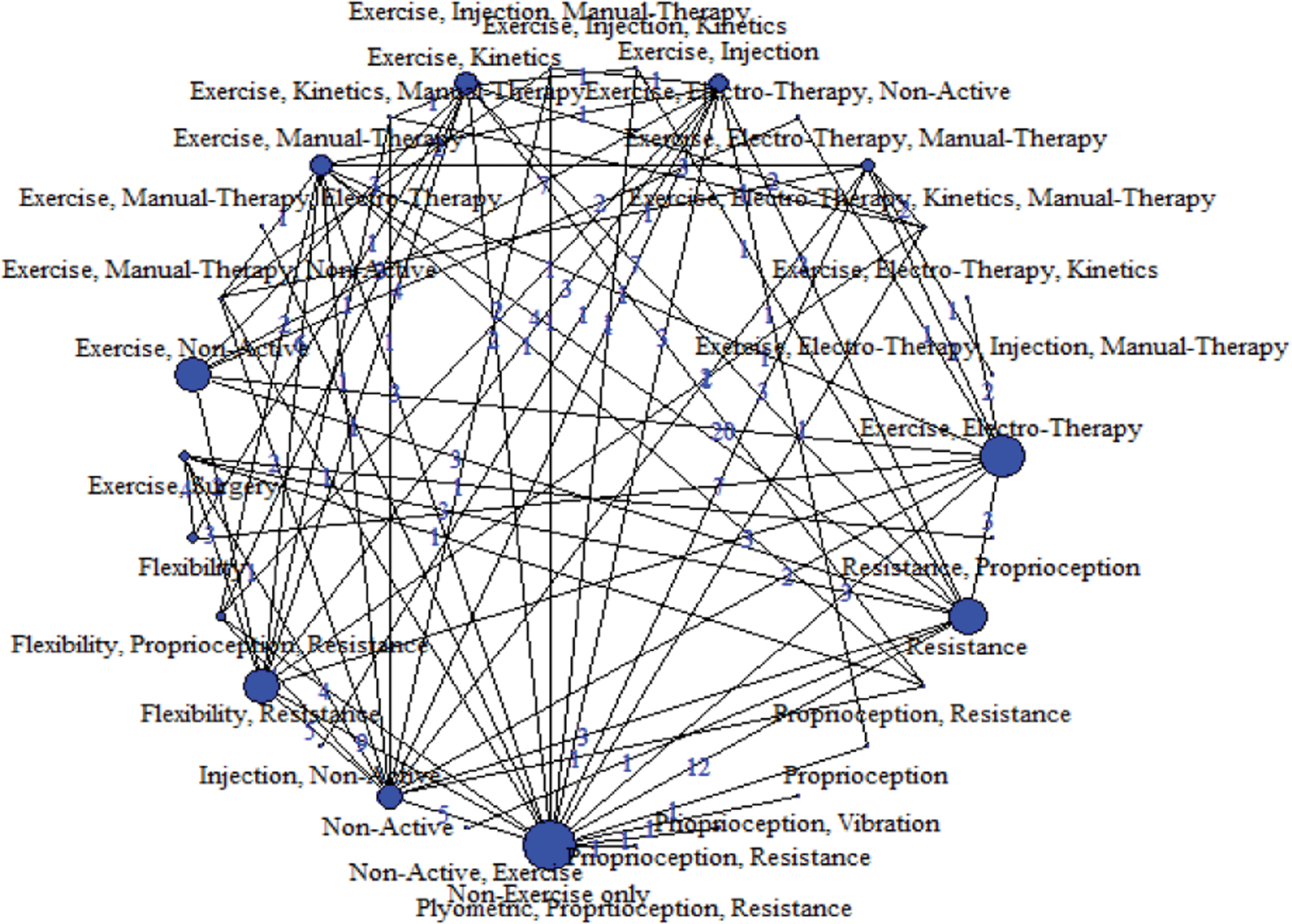
| Exercise + electro-therapy [95% CrI] | Exercise + injection [95% CrI] | Exercise + kinetics [95% CrI] | Exercise + surgery [95% CrI] | Exercise + MT [95% CrI] |
Exercise + non-active [95% CrI] |
Outcome domains | Tendinopathy |
|---|---|---|---|---|---|---|---|
| ES0.5 = 0.31 [−0.21 to 0.88] 12 trials 69 outcomes |
ES0.5 = 0.46 [0.04 to 0.81] 7 trials 67 outcomes |
ES0.5 = 0.19 [−0.02 to 0.39] 16 trials 156 outcomes |
ES0.5 = −0.15 [−0.48 to 0.21] 12 trials 189 outcomes |
ES0.5 = 0.32 [−0.21 to 0.88] 13 trials 110 outcomes |
ES0.5 = 0.16 [−0.59 to 0.64] 5 trials 37 outcomes |
All | All |
| Strength of evidence: low | Strength of evidence: moderate | Strength of evidence: moderate | Strength of evidence: low | Strength of evidence: low | Strength of evidence: low | ||
| ES0.5 = 0.64 [−0.2 to 1.4] 12 trials 32 outcomes |
ES0.5 = 0.67 [−0.11 to 1.5] 5 trials 19 outcomes |
ES0.5 = 0.32 [−0.09 to 0.57] 14 trials 48 outcomes |
ES0.5 = −0.06 [−0.36 to 0.28] 12 trials 63 outcomes |
ES0.5 = 0.64 [−0.20 to 1.4] 10 trials 38 outcomes |
ES0.5 = −0.22 [−0.90 to 0.20] 5 trials 16 outcomes |
Disability | All |
| Strength of evidence: very low | Strength of evidence: moderate | Strength of evidence: high | Strength of evidence: low | Strength of evidence: very low | Strength of evidence: moderate | ||
| ES0.5 = 0.12 [−0.27 to 0.50] 7 trials 20 outcomes |
ES0.5 = 0.71 [−0.78 to 1.8] 5 trials 20 outcomes |
ES0.5 = 0.31 [−0.21 to 0.78] 16 trials 156 outcomes |
ES0.5 = −0.20 [−0.66 to 0.40] 11 trials 80 outcomes |
ES0.5 = 0.12 [−0.26 to 0.50] 9 trials 33 outcomes |
ES0.5 = −0.31 [−2.0 to 1.4] 3 trials 13 outcomes |
Pain | All |
| Strength of evidence: very low | Strength of evidence: moderate | Strength of evidence: very low | Strength of evidence: very low | Strength of evidence: low | Strength of evidence: low | ||
| Insufficient data | Insufficient data | ES0.5 = 0.15 [−0.36 to 0.61] 5 trials 23 outcomes |
Insufficient data | ES0.5 = −0.02 [−1.3 to 1.1.3] 3 trials 12 outcomes |
Insufficient data | PFC | All |
| Strength of evidence: very low | Strength of evidence: low | ||||||
| Insufficient data | Insufficient data | ES0.5 = −0.08 [−1.3 to 0.82] 5 trials 10 outcomes |
ES0.5 = −0.27 [−1.4 to 0.76] 5 trials 18 outcomes |
Insufficient data | Function | All | |
| Strength of evidence: very low | Strength of evidence: low |
Efficacy review 3 discussion
The final efficacy review represents the largest quantitative synthesis and NMA to date investigating the management of tendinopathy. The review included 201 studies, 460 TAs and 11888 participants with data collected over nine different tendinopathies. The largest contribution came from RCRSP tendinopathy (43%), with substantial contributions from elbow (21%), Achilles (20%) and patellar (10%) tendinopathies, across a range of outcome domains, with pain (29%) and disability (28%) the most common. The review provides an overall insight into the efficacy of a range of treatment domains in tendinopathy when compared to exercise therapy. Initial analyses were conducted comparing broad therapy classifications of exercise-only, non-exercise-only, exercise plus non-exercise and non-active. Results were consistent across the pooled analysis and individual outcome domains demonstrating the superiority of combining exercise and non-exercise therapies. The SUCRA values (0.57 to 0.88) were highest for combined exercise and non-exercise in all but one comparison (QoL for all tendinopathies), where a tie was identified with non-exercise-only therapies. Median estimates from the comparative pairwise effect sizes indicated improved efficacy of approximately 0.1 to 0.3. These differences suggest a small to moderate added benefit that is likely to be interpreted as clinically significant. These findings are also in line with previous research comprising NMAs, where both van der Vlist et al. 141 and Rhim et al. 142 ranked exercise training combined with shockwave therapy or injection more favourably than exercise alone for AT.
Following the broadest therapy classifications, analyses were completed comparing dominant exercise and non-exercise classes. Considerable overlap was identified across tendinopathy locations and outcome domains, with non-active therapies tending to rank at the bottom. Considerable overlap may be expected, as many treatments included multiple modalities, and so comparisons based on the dominant class generate substantial heterogeneity over the large data set. When comparing the complete class structure across therapies, it was identified that exercise was most frequently combined with electro-therapy and kinetics. Treatments comprising more than two classes were relatively rare, with the most common including exercise combined with electro-therapy and manual-therapy (21 instances), and a smaller number including four classes (e.g. 7 TAs comprising exercise, electro-therapy, kinetics and MT). Further direct pairwise comparisons in relation to exercise-only interventions suggested that electro-therapy, injection and kinetic (interventions such as taping, brace and orthotics) treatment adjuncts produced similar improvements when combined with exercise. Other systematic reviews have reported similar findings of combined treatments for tendinopathy, although most have conducted standard meta-analysis approaches where appropriate. 27 A recent umbrella review by Irby et al. (2020) evaluated 25 systematic reviews of high quality similarly concluded that exercise therapy is the best treatment option for tendinopathy when combined with the use of other therapeutic modalities. 63 We acknowledge that the findings of these direct pairwise comparisons are limited by some uncertainty as indicated by their wide CrIs. Nevertheless, existing reviews reported small to moderate effect sizes for the combined intervention group compared to monotherapy, which is consistent with our study findings.
Summary and limitations of efficacy review 3
As the evidence currently stands, it is still unclear which treatment is the most efficacious for tendinopathy management. The prescription of exercise therapy to modulate the self-reported symptoms of patients with tendinopathy seems to be a practical and efficacious management approach. Part of the reason for this uncertainty stems from the fact that the pathophysiology of tendinopathy and the working mechanisms of existing treatments are not as yet completely understood. 143,144 Some evidence suggests a failed healing response due to degeneration caused by repetitive overloading where demand exceeds capacity to be the main features, while others suggest an inflammatory process. 137,143,144 However, the absence of strong biomarkers of disease progression and recovery at macro- or micro-structural levels means little is known about the physiological effects of treatments, meaning mechanistic studies are inconclusive. An important limitation of efficacy review 3, especially given the findings of greater efficacy when combining multiple exercise and non-exercise therapies, is the reliance on predominantly short-term data. As many patients experience chronic and recurrent tendinopathy, the additional costs of combining multiple therapies must be considered, and at present there is insufficient information to determine whether use of multiple therapies will be superior over the long term. Finally, it is important to note that even at the most granular level of therapy classification used, amalgamation was required to obtain sufficient data to conduct comparisons. This included combining, for example, different electro-therapies or different types of injection therapies. In each case, the strength of evidence for the individual therapy types within a classification is likely to be different. It is therefore recommended that clinicians adopting the findings from this review and, combining a non-exercise treatment such as electro-therapy or injection therapy with exercise, select the specific adjunct with the strongest evidence base.
Chapter 6 Phase II: Contingent synthesis 2: feasibility and acceptability of exercise for tendinopathy, a mixed-method systematic review
Summary
This part of the evidence synthesis investigated the feasibility and acceptability of exercise for the management of tendinopathy via a convergent segregated mixed-method review using JBI methodology. 145 The review questions were:
-
What is the current knowledge of feasibility of delivering exercise interventions for tendinopathy from the perspective of those delivering and receiving interventions?
-
How feasible is the delivery of exercise therapy in terms of proportions (e.g. of adherence, attendance and fidelity)
-
What are patients’ and healthcare professionals’ perceptions of the feasibility of exercise for tendinopathy?
-
-
What is the current knowledge of acceptability of receiving exercise for tendinopathy?
-
How acceptable is exercise in terms of, for example, tolerability of and willingness to perform exercise therapy?
-
What are patients’ and healthcare professionals’ perceptions of the acceptability of exercise therapy for tendinopathy?
-
Eligibility criteria included Participants (aged 18+, any tendinopathy, any severity; see Chapter 3), Phenomena of interest (feasibility or acceptability of exercise for tendinopathy) and Context (any setting in any country ranked ‘very high’ on the HDI:54 top 62 at the time of conducting the review). A comprehensive search identified 13,070 reports. Following screening, 96 reports from 94 studies (85 quantitative; 11 qualitative) were included, representing 4221 participants from 20 countries. The review identified that exercise therapy for a range of tendinopathies is in general feasible to deliver and acceptable to receive. There is considerable heterogeneity in measurement and reporting of feasibility and acceptability, and an urgent need for clearly agreed definitions. A number of important factors are highlighted that impact on both feasibility and acceptability, and these would benefit from further research, particularly qualitative research to further understand these complex phenomena.
Methods
The review followed JBI guidance for mixed-methods systematic reviews,145 was conducted according to an a priori protocol registered on PROSPERO (CRD42020164641) and is reported according to the PRISMA (2020) statement. 38 We had originally planned a convergent integrated mixed-method review, where quantitative and qualitative data would address the same review questions (quantitative data would be transformed [‘qualitised’], combined with the qualitative data and then all the data would be aggregated to generate synthesised findings). Following the scoping review, however, it became clear that quantitative and qualitative studies addressed different aspects of feasibility and acceptability, meaning that combining data was not appropriate. We updated the PROSPERO record (19 November 2021) to reflect a refinement of the review questions, adding sub-questions ‘a’ and ‘b’ to each review question (1 and 2), with ‘a’ being addressed by quantitative data and ‘b’ being addressed by qualitative data. Separate quantitative and qualitative syntheses were therefore conducted, following which the findings of each single method synthesis were juxtaposed and examined to determine areas of convergence/divergence and where findings from one method may explain findings from the other method.
Search strategy
The comprehensive search strategy for this evidence synthesis comprised: (i) original search conducted for scoping synthesis (Chapter 4), with potentially relevant studies identified during title/abstract and full-text screening; (ii) search update conducted for effectiveness synthesis described in Chapter 5 with potentially relevant studies identified at title/abstract and full-text screening, and (iii) an additional search incorporating keywords specific to feasibility and acceptability, to identify studies that may have been missed by the previous two searches. This additional search was developed with a specialist research librarian (CM) and followed a three-step process: (1) initial limited search of MEDLINE and CINAHL followed by analysis of text words contained in the title and abstract and index terms to construct a full search strategy for each database; (2) applying the full search strategy to each included database, and (3) hand-searching reference lists of included studies for additional publications. The databases searched were MEDLINE, CINAHL, AMED, SPORTDiscus (all EBSCOhost), EmBase (Ovid) and PEDRo. Databases were searched from 1 January 1998, with the last search conducted on 29 March 2021. The full search strategy for each database is available in Appendix 1.
Screening for inclusion
As with syntheses 1 and 2, ProQuest RefWorks® was used to manage duplicates, with screening taking place in Covidence (Melbourne, Australia). Two reviewers independently conducted title/abstract and full-text screening against inclusion and exclusion criteria for the review. Conflicts were resolved by discussion or by a third reviewer where necessary. There were few ‘true’ conflicts, which mainly concerned disagreement on the reason for exclusion, as several studies could be excluded on more than one criterion. Full-text studies that did not meet the inclusion criteria were excluded, and reasons for exclusion are provided as supplementary material on the project website (Supplementary Material 7).
Inclusion criteria
Specific inclusion criteria for the mixed methods synthesis were:
Participants
As reported for syntheses 1 and 2, we included adults (18+) with tendinopathy of any severity, duration and anatomical location. Large, full-thickness or massive tears were excluded, as were studies where tear size could not be determined. Plantar heel pain was also excluded.
Phenomena of interest
The qualitative component of this review considered studies that investigated feasibility of delivering and acceptability of participating in exercise therapy for tendinopathy. Feasibility refers to whether the exercise intervention ‘can’ be delivered and therefore included, but was not limited to, healthcare professionals’ views and perceptions of delivering exercise therapy for tendinopathy. Acceptability refers to the acceptability to patients/carers of receiving exercise therapy for tendinopathy. As such descriptions of the phenomena included, but were not limited to, information such as perceptions, experiences, enjoyment, barriers and facilitators to exercise therapies.
Outcomes
The quantitative component of this review considered studies that included any measure of feasibility or acceptability. Feasibility measures included, but were not limited to, attendance, intervention fidelity and adherence. Due to the variability in reporting of feasibility measures, in order to facilitate synthesis we required numerical data to be presented for them to be included in this portion of the review. The review did not include trial-related feasibility outcomes such as recruitment and retention rates, or completion and return of outcome measures, as the focus of the review was on the feasibility of delivering exercise and not the feasibility of trial processes. Acceptability measures included, but were not limited to, measures of tolerability, willingness and satisfaction (with exercise). The review did not include acceptability of trial-related processes such as randomisation and outcome measurement, for the reasons stated above. Therefore, we did not include all studies that reported drop-outs; drop-outs were only included as a measure of tolerability where they could be directly related to the exercise intervention. The review also did not include satisfaction with treatment outcome or satisfaction per se; this was reported in Chapter 5, effectiveness. Satisfaction was only included as an outcome in this mixed-method review if it was clear that participants were rating satisfaction with the exercise intervention.
Context
As reported for syntheses 1 and 2, the context was any setting in any country ranked ‘very high’ on the HDI54 (top 62 ranked countries at the time of conducting the review).
Types of studies
This review considered quantitative, qualitative and mixed-methods studies. Quantitative studies included both experimental and quasi-experimental study designs, including RCTs, non-RCTs, before and after studies, and interrupted time-series studies. In addition, analytical observational studies including prospective and retrospective cohort studies, case–control studies and analytical cross-sectional studies were considered for inclusion. This review also considered descriptive observational study designs, including case series, individual case reports and descriptive cross-sectional studies for inclusion. Qualitative studies of any philosophical or methodological underpinning were considered for inclusion if they addressed any aspect of the phenomena of interest. Mixed-method studies were considered if data from the quantitative or qualitative components could be clearly extracted.
Methodological quality assessment
Following piloting, eligible studies were critically appraised by two independent reviewers (two out of AP, JS, KC, RM) for methodological quality using relevant JBI checklists for RCTs, quasi-experimental studies, case–control studies, case-series, case reports and qualitative research. 146 Each checklist consisted of 8–10 questions that could receive an answer of Yes, No or Unclear. For ‘Yes’, there had to be clear information in the record to answer the question, for ‘No’ there had to be no mention of this item in the record. Where there was some, but not full, information, an ‘Unclear’ answer was given. Any disagreements that arose between reviewers were resolved through discussion, or with a third reviewer (LA; 10% of reports required one or more items to be moderated). Due to the size of the review, we did not contact authors for missing data. However, we did not exclude any studies based on methodological quality.
Data extraction
For quantitative studies, following piloting, data were extracted from included studies using a data-extraction tool developed in Microsoft Excel for this review (report Supplementary Material 8, 9). Data included specific details about the populations, interventions, methods and outcomes of significance to the review questions. Two rounds of quantitative data-extraction piloting were conducted to ensure reliability; thereafter data were extracted by one reviewer (one of EP, RM).
For qualitative studies (and qualitative components of mixed-methods studies), data were extracted by two independent reviewers (KC, RM) using the qualitative data-extraction tool in JBI SUMARI software. Data extracted included specific details about the population, context, culture, geographical location, study methods and the phenomenon of interest relevant to the review question. Findings with their corresponding illustrations were also extracted and assigned a level of credibility (unequivocal, credible or not supported). Any disagreements that arose between the reviewers were resolved through discussion, or with a third reviewer (LA).
Data synthesis and integration
A convergent segregated approach to synthesis and integration of data was applied, involving an initial independent synthesis of the quantitative and qualitative studies followed by the integration of findings from each synthesis using a comparative analysis approach. 145
Where possible, quantitative data were expressed as mean proportions to describe the relative number of patients that found the intervention feasible or acceptable. For example, with feasibility measures such as attendance and adherence, authors’ reporting of the total number of sessions prescribed and the mean number of sessions attended/adhered was turned into a ratio (mean/total prescribed). Proportion of ‘good’ adherence was calculated where authors provided data on the number of patients who completed a high percentage of the prescribed exercise sessions. Authors’ selection of a high percentage was taken to be an implicit statement of good adherence. Any threshold above 70% was selected as a relevant measure of good adherence and the specific percentage set by the author recorded. Similar calculations of proportions were made for fidelity and the acceptability measures of tolerability, willingness, satisfaction and helpfulness. Where sufficient data were available for meta-analysis, the logit transformation was performed on proportions and sampling variance calculated using standard distributional assumptions. 100
After pooling data and obtaining uncertainty estimates, values were back-transformed and expressed as estimated mean proportions. 100 All meta-analysis models were conducted within a Bayesian framework using hierarchical models where multiple outcomes were obtained from the same study. Posterior estimates of the mean proportion were described by the median value and 95% CrIs (ES0.5 [95% CrI]). Data that could not be included in statistical analyses are reported narratively.
Qualitative synthesis was conducted using the meta-aggregative approach. 147 Meta-aggregation is aligned with the philosophy of pragmatism, focussing on the practicality and usability of the synthesised findings and generation of statements that are useful for informing actions in clinical practice. This involved assembling and aggregating the extracted findings from individual studies, based on similarity in meaning, to generate a set of statements (i.e. categories) that represented that aggregation. These categories were then subjected to meta-synthesis to produce a set of synthesised findings. The development of categories and synthesised findings was initially conducted via a consensus process between two reviewers (KC, RM), followed by review and discussion with two further reviewers (LA, DM), until consensus on the final synthesis was reached.
The results of each single-method synthesis were juxtaposed and examined for convergence/divergence and complementarity. The findings of each single-method synthesis were reviewed to determine whether they were supportive or contradictory, where one method’s findings could explain the other, and to identify which aspects of the quantitative evidence were not explored in the qualitative evidence and vice versa.
Results
Study inclusion
The additional search for this review identified a total of 3824 records (see Figure 20). After removing 1320 duplicates, 2504 reports were screened at title/abstract stage. This resulted in 2359 reports being excluded and 145 sought for retrieval. We were unable to locate four reports, therefore 141 were screened at full-text stage, in addition to 163 reports that had been identified from the scoping (see Chapter 4) and effectiveness (see Chapter 5) searches. Of these 304 reports that were screened at full-text stage, 208 were excluded. There were therefore 96 reports included in the review, representing 94 unique studies. Of these, 85 reports were included in the quantitative synthesis and 11 in the qualitative synthesis. Studies were conducted in Australia (n = 17), UK (n = 15), the Netherlands (n = 9), Denmark (n = 8), Canada (n = 7), USA (n = 7), Germany (n = 6), Sweden (n = 5), Norway (n = 4), New Zealand (n = 3), Ireland (n = 2), South Korea (n = 2), Spain (n = 2), Turkey (n = 2), Finland (n = 1), Iceland (n = 1), Italy (n = 1) and Switzerland (n = 1), with two studies being conducted in both the USA and South Africa and one being conducted in Ireland and Northern Ireland. Study characteristics can be found in Appendix 7 (see Table 66).
FIGURE 20.
PRISMA flow diagram. From: Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. httsp://doi.org/10.1136/bmj.n71.

Characteristics of included studies
Of the 85 quantitative studies, 61 were RCTs evaluating the effectiveness of exercise (with or without co-interventions) compared to another intervention (exercise or another type), and a further seven were pilot and/or feasibility RCTs. Ten studies were quasi-experimental, mostly pre–post designs, two were case–control studies, four were case series reporting on between 5 and 25 patients, and one presented three individual case reports in one paper. 148 Sample sizes ranged from 3148 to 190,149 with a total of 4093 included in the review (see Appendix 7, Table 66 for details of included studies).
The qualitative studies included two interpretive phenomenological analysis (IPA) studies150,151 and two interpretive descriptive studies,152,153 with the remainder being qualitative descriptive in design (either described as such by the authors or determined by the reviewers from information provided in articles),1,2,154–159 with two of these embedded in a pilot and full RCT respectively. 107,156 Studies included 5 to 23 participants, with a total of 128 in the review, and mainly utilised semi-structured interviews (face-to-face or telephone), with one study using focus-group methodology. 155
Participants in seven studies were patients who had recently undergone physiotherapy- (n = 6)150,152–154,156,157 or podiatry- (n = 1)151 led interventions for Achilles (n = 2),152,153 RC (n = 3),154,156,157 mixed tendinopathy (n = 1)149,150 or posterior tibial tendon dysfunction (PTTD) (n = 1). 151 One further study recruited patients with greater trochanteric pain syndrome (GTPS) from a physiotherapy waiting list. 158 Three studies107,154,159 focussed on healthcare professionals’ perceptions and experiences of tendinopathy management, whilst two of the included studies recruited both patients and healthcare professionals. 152,156 Of the 128 participants in the review, 78 were patients and 50 were healthcare professionals, mostly physiotherapists, with one study also including sports medicine physicians and surgeons. 159
The studies (quantitative and qualitative) were focussed on RCRSP (n = 33), Achilles (n = 32), patellar (n = 15), lateral elbow (n = 7), gluteal (n = 4), PTTD (n = 1), hamstring (n = 1) and iliopsoas syndrome (n = 1), with two studies including mixed tendinopathies. A range of exercise types and durations were included (see Appendix 7, Table 66).
Quantitative studies predominantly reported feasibility measures in the form of adherence or attendance, with a small number reporting exercise fidelity. Less than half of the quantitative studies reported acceptability in the form of tolerability, satisfaction (with exercise), willingness to complete, perceived helpfulness and acceptability (of exercise), all being reported in small numbers of studies.
Qualitative studies explored patients’ and/or healthcare professionals’ perceptions and experiences of exercise for tendinopathy. Two studies focussed on adherence,151,157 two on barriers and facilitators to a specific exercise programme being used in an RCT,107,156 three on the lived experience of having a tendinopathy, which included participants discussing exercise,151,153,160 one on the experience of participating in an exercise group,154 one on the experience of gym-based exercise supervised by telehealth152 and two on healthcare professionals’ views of exercise for shoulder tendinopathies. 155,159
Methodological quality
Details of critical appraisal for each study are presented in Appendix 8 (see Tables 67–72). Quantitative studies were moderate to high quality. For the 68 RCTs (see Table 67), methodological quality scores ranged from 5161 to 13 out of 13,59,130,162–164 with most studies (72%) scoring 10 or more. Therefore, most studies could be considered high quality, with 19 moderate quality (5–10 out of 13) and none of low quality (fewer than 5 out of 13). None of the studies scored ‘No’ for question 1: ‘was true randomisation used for assignment of participants to treatment groups?’ Common questions that scored ‘No’ were questions 4: ‘were participants blind to treatment assignment?’, and 5: ‘were those delivering treatment blind to treatment assignment?’ Questions that were commonly either ‘No’ or ‘Unclear’ were question 6: ‘were outcomes assessors blind to treatment assignment?’, 8: ‘was follow up complete and if not, were differences between groups on terms of their follow up adequately described and analysed?’, and 9: ‘were participants analysed in the groups to which they were randomised?’
The ten quasi-experimental studies were scored out of 9, or where there were was only one participant group, they were scored out of 6 as three questions were not relevant to single-cohort studies (see Table 68). All studies scored eight or nine out of nine, or five or six out of six and could therefore be considered high-quality quasi-experimental studies; the most common reason for lower scores (n = 8) was lack of a control group.
The two case–control studies were high quality, scoring 7165 and 8166 out of 8 respectively, with two questions not applicable to these studies (see Table 69). Of the four case series (see Table 70), one was moderate quality (6/10),167 with unclear reporting of participant demographics and study sites, and the other three were high quality (8/10). 168–170 For all four case series it was unclear whether they utilised consecutive and complete inclusion of participants. The one case report (see Table 71) scored 7/8 due to not describing adverse events.
The 11 qualitative studies ranged in scores from 3154,159 to 10,150,151,157 with six scoring above and five scoring below six out of ten (see Table 72). However, the qualitative descriptive study designs (either stand-alone or embedded within RCTs) were the lowest scores, with the more interpretive methodologies (IPA, interpretive description) consistently scoring high. This is not surprising as five questions on the JBI critical appraisal tool relate to congruency between philosophical perspective, methodology and methods, which are often not reported in detail for qualitative descriptive studies. Two further questions had variable reporting for the descriptive studies. There related to a statement locating the researcher culturally or theoretically (question 6) and the influence of the researcher on the research and vice versa being considered (question 7). These dimensions are also arguably not commonly reported in applied qualitative descriptive or mixed-method embedded designs. Therefore, in relation to the design of the included studies, we considered them to be of moderate to high quality.
Measures of feasibility and acceptability: quantitative findings
I: Feasibility
Four feasibility outcomes were reported across 77 of the included studies. Of these, it was possible to include 63 studies in the meta-analyses. For each of the four feasibility outcomes, defined in Box 2, meta-analysis results are presented first, followed by a narrative summary of the remaining studies.
Adherence = Mean proportion of training sessions completed by participants
Good adherence = Mean proportion of training sessions completed beyond a ‘high’ percentage threshold set by authors
Required to be at least 70% to increase consistency
Attendance = Mean proportion of supervised exercise sessions attended
Fidelity = Assessment by study authors of extent to which exercise intervention conducted as intended
Measurement of adherence
Seventy-five studies reported adherence outcomes. Adherence was measured by self-report using exercise diaries/logs (n = 54 studies), telephone calls (n = 1 studies), questionnaires (n = 4 studies) or by questioning participants when they attended for clinical visits (n = 7 studies). Nine studies did not report how they recorded adherence.
Adherence
There were 52 studies that provided data on adherence of training sessions (see Figure 21, top). The estimated mean proportion of adherence was ES0.5 = 0.76 [95% CrI 0.71 to 0.80] (see Figure 21, top).
FIGURE 21.
Bayesian forest plots for proportion of adherence (top) and proportion of good adherence (bottom).
Distributions represent ‘shrunken estimates’ based on all effect sizes obtained from the study, the random-effects model fitted and borrowing of information across studies to reduce uncertainty. Black circles and connected intervals represent the median value and 95% CrIs for the shrunken estimates. Vertical line at 0 represents proportion of 0.5 on the standard scale.
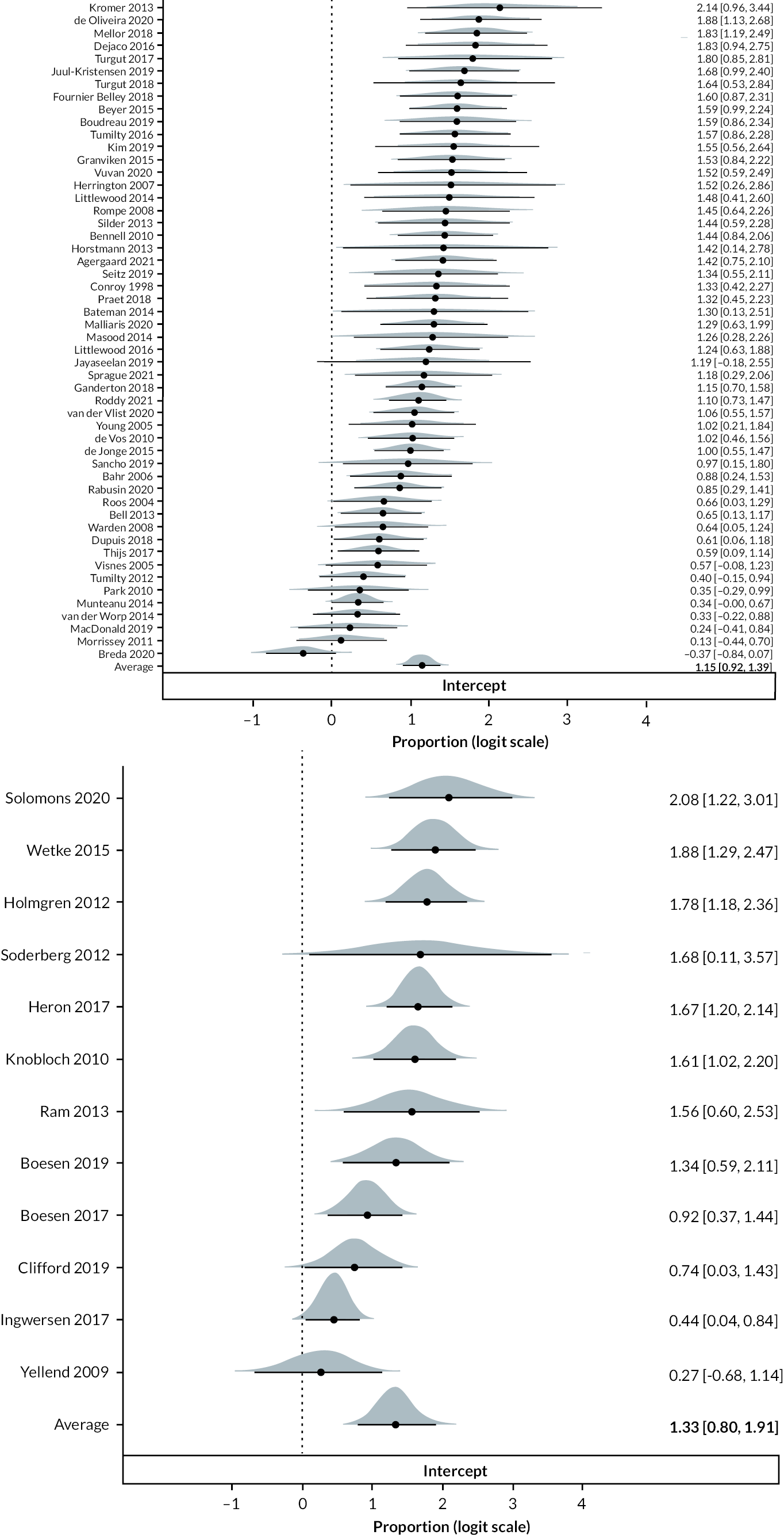
Good adherence
There were 12 studies that provided data on good adherence of training sessions (see Figure 21 bottom). There is no single definition of ‘good’ exercise adherence,171 with included studies using a range of thresholds. In order to extract data that could be synthesised, we required thresholds reported in studies to be 70% or more. Of the 12 studies included in the analysis, two reported the mean proportion of adherence above 70% of sessions, six studies above 75% and four studies above 80%. Combining these data, the estimated mean proportion of good adherence was ES0.5 = 0.79 [95% CrI 0.68 to 0.87] (see Figure 21 bottom).
Adherence data from the 11 studies that could not be included in the meta-analysis are presented in Table 28. It can be seen that most of these studies also reported good adherence, if ‘compliant’172 and ‘mostly’173 are considered good adherence levels. Two studies reported values below the 70% threshold. Luginbuhl et al. (2008)174 reported 67% compliance with a HEP in their lateral epicondylitis strengthening exercise group (without forearm band) compared to 90% with the forearm band, and Stevens et al. (2014)175 reported 62% adherence in their do-as-tolerated Achilles heel-drop group compared to 92% in the standard group. However, participants were told to aim for around 180 repetitions but could alter the number ‘as tolerated’, and notably there were no differences in outcome between the two groups. In Johnston et al. ’s168 iliopsoas rehabilitation program, although a scale was used, it is not possible to determine the threshold used, only that patients did not complete exercises every day.
| Study First author Year Tendinopathy (participants) Intervention |
Outcomes reported | Findings | |||
|---|---|---|---|---|---|
| van Ark 2013170 Patellar (n = 5) PRP injection + graded exercise of 8+ weeks duration |
Self-reported compliance rated 0–10 Assessed by asking ‘to what extent did you comply with the exercise programme?’ |
Mean compliance 7/10 Non-compliance was due to lack of time, lack of motivation, holidays, other injuries |
|||
| Cook 2014172 (n = 68) RCRSP General exercise programme of varied duration |
Compliance with HEP captured at discharge Likert scale (1 highly compliant; 2 compliant, 3 not compliant, 4 extremely not compliant) |
Overall | Shoulder/neck | Shoulder | |
| Highly | 52% | 49% | 55% | ||
| Compliant | 41% | 43% | 39% | ||
| Not | 3% | 0% | 6% | ||
| Extremely not | 4% | 8% | 0% | ||
| Coombes 2013176 Lateral elbow (n = 81) 7-week 2 × day HEP (gripping/concentric/eccentric) + 8-weeks physiotherapy +/− corticosteroid injection |
Compliance Exercise diary |
Mean compliance 70% during at least 5 of 7 weeks | |||
| Dale 2015173 Lateral elbow (n = 17) Pilates-based intervention |
Adherence Exercise diary Reported as always, mostly, sometimes and rarely |
Most participants completed HEP 5–6 × week | |||
| Standard | Standard + Pilates | ||||
| Always | 11% | 38% | |||
| Mostly | 73% | 50% | |||
| Sometimes | 11% | 0 | |||
| Rarely | 0 | 12% | |||
| Ferrer 2018177 RCRSP (n = 5) 6-week supervised and 6-week HEP, strengthening and ROM |
Adherence Daily exercise log |
1/5 patients showed poor compliance | |||
| Johnston 1999168 Iliopsoas syndrome (n = 9) Hip rotation rehabilitation programme |
Adherence Telephone interview using 3-point scale 1 = very compliant; 2 = moderately compliant; 3 = non-compliant |
Mean compliance = 2 (n = 9 patients) Moderately compliant Exercises performed consistently but not daily |
|||
| Luginbuhl 2008174 Lateral elbow (n = 19) Strengthening HEP (2 × day for 3-months) |
Compliance Participants asked at each follow-up |
Strengthening 67% compliant 3 months 11% 3 × week only 11% 2 months only 11% stopped after 3 weeks due to pain |
Strengthening + forearm band 90% compliant 10% stopped one of the exercises |
||
| Rio 2017167 Patellar (n = 25) Double-leg squat using rigid belt 4-week period |
Adherence Self-report |
23/25 reported adherence data Completed exercises median 5 × week |
|||
| Stevens 2014175 Achilles (n = 28) 6-week heel-drop protocols (Alfredson or ‘as tolerated’) |
Adherence Method not reported |
Standard (180 reps) 92% target reps |
Do-as-tolerated 62% target reps, with similar clinical outcomes |
||
| Verrall 2011149 Achilles (n = 190) 6-week progressive eccentric heel-drop programme |
Self-reported compliance Participants asked if they completed the exercise programme |
86% completed programme 8% ceased due to programme failure 6% ceased as they perceived it had been successful |
|||
| de Vos 200759 Achilles (n = 63) 12-week heavy loaded eccentric training |
Daily diary Rated as poor (<25% exercises performed), moderate (25%–50% exercises performed, good (50%–75%), excellent (>75%) |
Excellent/good Moderate/poor |
Eccentric training 72% 28% |
Eccentric training + splint 74% 26% |
|
Therefore, the studies included in this review provide evidence to suggest that self-reported adherence to exercise is good across tendinopathy and exercise types.
Attendance
Thirteen studies provided data on attendance of supervised exercise sessions (see Figure 22). Combining these data, the estimated mean proportion of attendance was ES0.5 = 0.90 [95% CrI 0.82 to 0.96] (see Figure 22).
FIGURE 22.
Bayesian forest plot for proportion of attendance.
Distributions represent ‘shrunken estimates’ based on all effect sizes obtained from the study, the random effects model fitted and borrowing of information across studies to reduce uncertainty. Black circles and connected intervals represent the median value and 95% CrIs for the shrunken estimates. Vertical line at 0 represents proportion of 0.5 on the standard scale.

Fidelity
Three studies reported fidelity measures. It was not possible to combine these in a meta-analysis; therefore, they are reported narratively. Sancho et al. 178 used an exercise diary to assess whether the correct exercises, sets, repetitions, progression and regression criteria had been achieved in their study of pain-guided progressive exercise for AT (n = 15). They used a dichotomous score (achieved or not achieved), with all parameters having to be correct for fidelity to be achieved. They reported fidelity of 50% overall, highest for seated heel-raise (64%) and lowest for double leg jumps (23%). Clifford et al. 179 used a daily diary to evaluate fidelity in their study of progressive home exercise for GTPS (n = 30), reporting that all but one of their participants were able to progress loading intensity and use resistance bands as prescribed. Agergaard et al. 180 assessed fidelity in their study on moderate slow resistance or heavy slow resistance exercise for patellar tendinopathy (n = 42) using an app (InjuryMap), allowing them to evaluate whether the training volume was correctly applied by participants. They reported that the two exercises used in the study (leg press and knee extension) were completed with more than 90% of the prescribed load.
It is not possible to draw conclusions on fidelity of exercise for tendinopathy due to the small number of studies and heterogeneity of measures used.
In conclusion, there is evidence that self-reported adherence and attendance to supervised exercise is good, and that fidelity is seldom reported in studies on exercise for tendinopathy.
II: Acceptability
Twenty-one acceptability outcomes were reported across 17 of the included studies. Due to clinical heterogeneity and limited reporting these findings are reported narratively. Tolerability was most commonly reported (n = 15), with satisfaction (with exercise)109,181 and willingness (to undertake exercise)181,182 reported by two studies and helpfulness (of the exercise) reported in one study. 168 One study reported acceptability as how easy participants found the exercise programme to fit into their daily activities. 184 Details of the outcomes and findings are presented in Table 29.
| Author/year/tendinopathy/intervention | Outcomes reported | Findings |
|---|---|---|
| Bennell et al. 2010188 RCRSP (n = 120) 10-weeks physiotherapy + HEP followed by 12-week HEP |
Treatment tolerability Reporting of events |
10-weeks physiotherapy + HEP period: 12/55 (22%) reported increased pain with home exercise 12-week HEP period: 7/49 (14%) reported short-term pain with home exercise |
| Flores et al. 2017183 RCRSP (n = 84) Supervised exercise with or without hyaluronic acid injection |
Treatment tolerability 4-point scale 0 = ‘very poor’ to 4 = ‘excellent’ |
Patients’ perception of tolerability: Day 7 = >2.5 (same as injection group) Day 15 = 3.0 (same as injection group) Day 30 = >3.0 (injection group higher) Day 90 = >3.0 (injection group higher) |
| Ganderton et al. 2018189 GTPS (n = 94) 12-week GLoBE or sham exercise programme |
Treatment tolerability Adverse events |
1/94 (1.1%) participants reported increased pain attributed to exercises; completed intervention and follow-up outcomes |
| Gual et al. 2016190 Patellar (n = 53) 24-weeks eccentric overload |
Treatment tolerability Drop-outs |
7/53 (13.2%) dropped out due to injury (2 in the ankle and 5 in the knee joint) directly related to the exercise programme |
| Ingwersen et al. 2017191 RCRSP (n = 100) 12-weeks Progressive high load exercise (PHLE) or low load exercise (LLE) Supervised + HEP |
Treatment tolerability At least 1 episode of increased pain >1-hour due to exercise |
13/49 (27%) PHLE group 18/51 (35%) LLE group |
| Jonsson and Alfredson 2005186 Patellar (n = 15) 12-week painful eccentric or concentric quadriceps training programme |
Treatment tolerability Drop-outs |
3/9 (33%) patients (4 tendons) dropped out of concentric group due to severe tendon pain during and after training |
| Johnston et al. 1999168 Iliopsoas (n = 9) Progressive exercise programme; total duration unclear |
Helpfulness Structured telephone interview Treatment tolerability Structured telephone interview |
3/9 (33%) stated exercises with band most beneficial 2/9 (22%) stated stretching and strengthening most effective in combination 2/9 (22%) stated stretches most useful 1/9 (11%) reported the exercises caused pain |
| Knobloch et al. 2007192 Achilles (n = 15) 12-weeks daily painful eccentric HEP |
Acceptability Telephone call |
Participants reported that the daily programme of about 5 minutes was easy to implement into their daily activities (no data reported) |
| Knobloch et al. 2010182 Achilles (n = 75) 12-weeks daily painful eccentric HEP |
Tolerability Reasons for drop-put |
20% non-compliant (n = 12) 25% (4/12) reported drop-off due to overwhelming pain |
| Luginbuhl et al. 2008174 Elbow (n = 19) Forearm support or 2.5-month strengthening programme or combination |
Treatment tolerability Drop-out due to exercise |
Strengthening programme group: 1/9 (11%) stopped after 3-weeks due to increased pain Forearm support + strengthening group: 1/9 (11%) stopped exercise with ball reporting ball to be too hard |
| Mantovani et al. 2020181 Achilles (n = 19) Heavy isometric exercise in plantarflexion (supervised) |
Treatment tolerability 0–10 scale – not at all to very tolerable >5 considered tolerable Willingness to use intervention Participants asked if they would adhere to the intervention in a rehabilitation programme – answer Yes/No Satisfaction with intervention Self-report |
Mean tolerability 6.3 ± 2.2 100% (17 participants) answered Yes No adverse events, discomfort, or inconveniences reported |
| Peterson et al. 2014185 Elbow (n = 120) 12-week graded eccentric or concentric graded HEP |
Treatment tolerability Drop out related to exercise |
1/60 (1.7%) dropped out at 1-month as could not perform intervention |
| Roos et al. 2004193 Achilles (n = 31) 12-week eccentric exercise HEP vs. night splint vs. combination |
Treatment tolerability Reported side-effects |
33% reported muscle soreness with eccentric exercise in first week; no difference between exercise and exercise + splint groups None reported muscle soreness by 6-weeks but 1/16 (6.3%) reported calf stiffness during the day |
| Walther et al. 2004161 RCRSP (n = 40) 12-weeks HEP at least 5 × week for 10–15 minutes |
Treatment tolerability Drop-outs |
No drop-outs from exercise |
| Roddy et al. 2021109 RCRSP (n = 256) 12–16 weeks supervised (physiotherapist-led) or unsupervised (leaflet) exercise with or without corticosteroid injection |
Confidence and satisfaction with intervention Postal questionnaire Treatment tolerability Case report forms, self-report, physician report |
Confidence and satisfaction greater in supervised exercise group compared to unsupervised Exacerbation of shoulder pain after performing exercises 59 (60%) supervised and 60 (59%) unsupervised exercise Improved within couple of hours in 22 (37%) supervised and 21 (36%) unsupervised |
| Stefansson et al. 2019184 Achilles (n = 60) 12-weeks pressure massage, eccentric exercise (Alfredson protocol) or combination |
Treatment tolerability Drop-outs due to exercise |
2/19 (11%) dropped out of eccentric group due to exercises aggravating symptoms 1/21 (4.8%) dropped out of pressure massage and 2/20 (10%) dropped out of combination but no reason provided |
| Vuvan et al. 2020187 Elbow (n = 20) 8-week unsupervised progressive isometric exercise program |
Treatment tolerability Pain intensity during exercise measured on 11-point NRS Length of time for pain to settle after exercise |
Mean 1.9 Median 0–60 seconds |
Treatment tolerability
Tolerability was measured using a scale in two studies. Flores et al. 183 used 0 (very poor) to 4 (excellent) with scores above 3 from day-15 onwards in their supervised exercise intervention for RCRSP. Mantovani et al. 181 used a 0 (not at all tolerable) to 10 (very tolerable) scale, with mean tolerability to a 12-week daily painful eccentric HEP of 6.3 (±2.2).
Drop-outs
As a result of not tolerating exercise interventions were reported in six studies (2 Achilles,182,184 2 lateral elbow,174,185 1 patellar,186 1 RCRSP161) investigating a range of different exercise types. Drop-outs ranged from none (RCRSP; 12-week HEP)161 to 33% (3 participants; 12-week painful quadriceps HEP for patellar tendinopathy),186 with five of the six studies 11% or less.
Seven studies reported adverse events, most commonly increased pain, as a result of exercise. Pain was evaluated by self-report and defined in various ways (e.g. short-term pain, pain due to exercises, at least one episode of pain over 1-hour duration, muscle soreness, pain intensity during exercise). One study187 used a numerical rating scale (NRS) to measure pain during exercise (elbow, HEP, mean pain 1.9), one used a structured telephone interview (Iliopsoas, HEP),168 and the remainder used participant self-report without stating specific methods. The findings (see Table 29) show that exercise is generally associated with some increased short-term pain or muscle soreness, but this appears to be tolerable as the proportion of participants reporting pain (range 1% to 60%) is much higher than the proportion dropping out of exercise studies reported above (range 0 to 33%), although it should be noted that there is a large amount of variance between studies for both measures.
Satisfaction
Two studies reported satisfaction with exercise. Mantovani et al. 181 found no discomfort or inconveniences reported by participants undertaking a heavy isometric HEP for AT, and Roddy et al. 109 reported greater confidence and satisfaction for supervised compared to unsupervised (leaflet) exercise for RCRSP.
Willingness to use the intervention
was reported by Mantovani et al. 181 (Achilles, heavy isometric HEP) with 100% (n = 17) participants reporting that they were willing to adhere to the intervention.
Helpfulness
of specific exercises for iliopsoas tendinopathy was reported by Johnston et al. ,168 with participants reporting various exercises as beneficial.
Acceptability
was briefly reported by Knobloch et al. (2007)192 where they commented that participants reported that the daily 5-minute exercise programme (Achilles, painful eccentric HEP) was easy to implement into daily activities.
Overall, the findings suggest that exercise for tendinopathy is acceptable to participants across a range of tendinopathy and exercise types and formats (supervised, HEP). However, heterogeneity in defining, measuring and reporting the various dimensions of acceptability limit our ability to draw firm conclusions. Furthermore, most of the studies included in the quantitative component of this mixed-method review did not provide acceptability data. Therefore, the findings should be interpreted with some caution.
Patients’ and healthcare professionals’ experiences and perceptions of exercise for tendinopathy: qualitative findings
Eleven qualitative studies explored 78 patients’ and 50 healthcare professionals’ experiences and perceptions of exercise for tendinopathy. The mean age of patients ranged from 40153 to 64.7107 years (mean for n = 7 studies 55.8), with one study not reporting a mean age but including athletes aged 24–38. 150 Both genders were represented, and studies ranged from 10%160 to 67%107 males (one study did not report gender). 152 A total of 68 findings and their illustrations were extracted (see Appendix 9, Table 73). Of the 68 findings, 54 were unequivocal and 14 were credible. The 68 findings were organised into nine categories which were further aggregated into two synthesised findings.
Synthesised finding 1
Patients and healthcare professionals report a range of highly personalised experiences and opinions of exercise therapies along with several barriers and facilitators to adhering to exercise. Therefore, a person-centred, individualised approach should be taken to delivering such interventions to people with tendinopathy.
Seven categories and 51 findings contributed to this synthesised finding (see Table 30), which represents the variability in patients’ and healthcare professionals’ perceptions and experiences of exercise interventions and the way they are delivered. Both patients and healthcare professionals can have conflicting views on the same exercise type and mode of delivery, and healthcare professionals need to be cognisant of this when prescribing therapeutic exercise for individual patients. The majority of findings in this synthesis relate to physiotherapy-delivered exercise interventions and the views of physiotherapists.
| Findings | Categories | Synthesised findings |
|---|---|---|
| Support, motivation, and learning from peers (U) | Category 1.1 Perceptions and opinions of exercise interventions from patients’ and physiotherapists’ perspectives |
Synthesised finding 1
Patients and healthcare professionals report a range of highly personalised experiences and opinions of exercise interventions and their modes of delivery, along with several barriers and facilitators to exercise adherence, indicating the need for a person-centred approach to delivering such interventions to people with tendinopathy |
| Preference for exercise class compared to individual shoulder physiotherapy (U) | ||
| All participants (8/8) found progressive loading exercises to be an effective form of treatment compared to their experience of previous treatment approaches (U) | ||
| The nature of the exercise Several participants (5/8) appreciated the simplicity (i.e. two calf-raise exercises) and how clearly they were explained as part of the trial intervention (U) | ||
| Exercise Several participants (5/8) expressed a feeling of leg discomfort from the pressure of the Smith bar on their thigh during their seated calf raises (U) | ||
| The exercise group was cited as being good fun and helpful by several participants (U) | ||
| Prescription of the self-managed loaded exercise programme was a challenge in terms of what might be regarded as the simplistic and restricted nature of the intervention (C) | ||
| Most of the physiotherapists appreciated the simplicity, particularly from the perspective of the patient, in terms of improving communication and exercise adherence (U) | ||
| This simplicity was not appreciated by all and the physiotherapists considered this from their own perspective and that of the patient (U) | ||
| The physiotherapists felt that most of the patients took longer to achieve a worthwhile clinical outcome than might be expected using other means of treatment (U) | ||
| Some patients still expressed concern about attributes of the intervention (C) | ||
| Disquiet was expressed about the simplicity of the intervention and hence its lack of potential effectiveness (U) | ||
| Whereas some patients had found aspects of the intervention difficult to implement, those patients who reported a successful outcome detailed different experiences (U) | ||
| All participants (8/8) expressed satisfaction with the quality of service they received via telehealth mainly because it was perceived to be efficient (C) | Category 1.2 Barriers and facilitators to the delivery of exercise for tendinopathy |
|
| Usability of the software Nearly all participants (7/8) reported that the telehealth software was easy to use (U) | ||
| Flexibility in arranging an appointment time The flexibility and convenience of telehealth allowed participants to schedule treatment/exercise within convenient times that avoided peak gym-use times (U) | ||
| Several participants (4/8) complained about poor or no Wi-Fi at their gym. There were reservations about having to use their personal phone internet data for the videoconference call. On several occasions, participants reported they were running out of phone battery, which impacted the length of the session (U) | ||
| For a few participants (2/8), assistance was needed to set up the correct camera angle of their phone while they were training on the Smith machine. (U) | ||
| Physiotherapists reflected on the accessibility and convenience of telehealth. Further, physiotherapists felt telehealth enabled more regular contact with participants (U) | ||
| Technology-related Physiotherapists noted multiple technology-related issues during the telehealth sessions, including poor videoconference quality or loss of video conference connection, insufficient participant phone battery life and inability to operate the videoconference video function. Some sessions had to be discontinued due to technology-related issues (U) | ||
| A few physiotherapists discussed the limitations of only having one camera angle to view participants and assist with providing feedback related to calf exercise fidelity. In some cases, physiotherapists experimented with camera angles to improve visualisation (U) | ||
| Gym-based exercise Physiotherapists reported some challenges accessing the Smith machine for some of their participants especially when the local gym had limited equipment (e.g. only one Smith machine). In some cases, sessions had to be rescheduled due to long waiting times (U) | ||
| Motivation (U) | Category 1.3 Facilitators to engaging with/adhering to exercise interventions |
|
| Social support (U) | ||
| All participants (8/8) reported that telehealth was motivating and promoted commitment to their exercise programme (U) | ||
| Accessibility to the gym Several participants [5/8] accessed a 24-h gym in a convenient location, which reportedly assisted with adherence and motivation (U) | ||
| Ability to see progress All participants (8/8) described that the care provided was effective in terms of improvement in symptoms and function. Being able to observe progress and experience less pain was reportedly a key motivator (U) | ||
| Physiotherapists proposed that more encouragement and motivation were needed for participants requiring longer time to complete their sessions (i.e. participants in low-intensity groups who completed 18 repetitions per set rather than six). One of the proposed strategies was a follow-up email post-session (U) | ||
| One patient recognised the role of their partner in providing feedback and stimulating further engagement with the self-managed exercise programme during times when progress was slow (C) | ||
| Patients also described personal traits that indicated self-efficacious individuals who took control of the programme (U) | ||
| Other personal attributes were also described (U) | ||
| Confidence (U) | Category 1.4 Barriers to engaging with/adhering to exercise interventions |
|
| Lack of success with physiotherapy was attributed to many reasons, including lack of belief about the effectiveness, lack of compliance with treatment and the pain caused by exercise (U) | ||
| Time Making time to commit to regular exercise was reported as a barrier by several participants (6/8). This was commonly because of competing commitments, e.g. employment or caregiving (U) | ||
| One patient reflected upon a previous episode of physiotherapy when engagement with a prescribed exercise programme was limited (C) | ||
| What challenges and enablers should be considered in RT education delivery? ‘Maybe we can get better?’ (U) | ||
| Beliefs about pain and exercise (C) | Category 1.5 Influence of patients’ and healthcare professionals’ beliefs about the pain–exercise relationship |
|
| Most of the participants in this cohort experienced some form of treatment burden/fatigue with respect to the prescribed exercises and orthoses. This had psychological consequences when the orthoses or exercises were not having a positive effect in reducing pain or improving function (U) | ||
| Pain (U) | ||
| Most participants remained positive about the potential of exercise therapy to improve their condition and were even happy to tolerate discomfort during it (8/10). This was often caveated with the associated desire to understand when symptoms indicated that exercise was detrimental (U) | ||
| However, not all participants (2/10) would find some discomfort with exercise acceptable, as pain elicited during exercise lingered significantly in some cases (U) | ||
| Discussion around this factor generated a broad range of responses from those who were very comfortable with the notion, those who were very uncomfortable and those who might be regarded as taking more of a middle ground (U) | ||
| However, in contrast participants also discussed their disbelief and lack of confidence in relation to a proposed exercise intervention (C) | Category 1.6 Influence of patients’ and physiotherapists beliefs about exercise (per se and specific intervention components) |
|
| Participants also highlighted the expected role of exercise interventions in the management of their AT (C) | ||
| This illustrates and emphasises the need to find strategies to educate patients regarding expected rehabilitation and recovery times to ensure that their expectations are realistic (U) | ||
| For others with greater experience, it was apparent that their existing belief system served to facilitate for some, but challenge for most, the rationale underpinning the self-managed loaded exercise programme (U) | ||
| This narrative from the patient perspective was in concordance with opinion expressed by one of the physiotherapists, where it can be seen that prior beliefs might impact upon their role in this environment (C) | ||
| Physiotherapists felt able to identify patients who they expected would successfully engage with the self-managed exercise programme (U) | ||
| A key barrier to ongoing engagement appeared to be a lack of an early and appreciable response to the therapy (U) | Category 1.7 Impact of symptomatic response to exercise |
|
| When the symptoms improved to a certain point, although not resolved, the impetus to continue was also challenged (C) | ||
| Following some early reported benefit from the exercise programme, one patient indicated subsequent difficulty as the symptoms failed to respond as the programme progressed. Despite this, they did not consider regressing the programme or seeking advice, indicating an external locus of control as a potential barrier (C) | ||
| Patients experienced a favourable therapeutic response that persuaded them of the potential value of the programme to them (U) |
However, one finding was drawn from podiatry151 and one from a study that included sports medicine physicians and surgeons in addition to physiotherapists. 159
Category 1.1: Perceptions and opinions of exercise interventions from patients’ and physiotherapists’ perspectives
This category concerned patients’ and physiotherapists’ opinions of specific exercise interventions they had experienced receiving and delivering, which included group-based exercise for RCRSP, a self-managed loaded exercise programme for RCRSP consisting of a single exercise performed twice per day, and a gym-based and remotely supervised (telehealth) progressive loading programme for AT. This category was supported by 13 findings. Three unequivocal findings expressed patients’ enjoyment of and preference for group-based exercise (RCRSP), which provided opportunities for peer learning and support:
You’re better off to do it in a group … you’d be more determined to do it … you don’t put the whole 100% effort in at home. (Ben) (p. 467)154
Six unequivocal and two credible findings discussed contrasting views of the ‘simplicity’ of self-managed exercise for both Achilles and RCRSP. Some participants and physiotherapists appreciated programmes with few components:
It was simple and easy to do and straightforward. (P4) (p. 7)
[patient; Achilles]152
it’s been a lot simpler treating the self-management group; keeping the exercise regime simpler, the patients have understood it more, erm the conversation between therapist and patient has been clearer. (P11) (p. 282)
[physiotherapist; RCRSP]107
However, some found even simple exercise programmes could be challenging to implement:
at first it seemed like a big task to do, because it was an additional thing to do through the day. (ID 18) (p. 82)
[patient; RCRSP]156
Whilst others questioned the potential effectiveness of such a simple programme:
to cap it all it’s such a simple exercise. I just came out thinking waste of time. (ID 29) (p. 82)
[patient; RCRSP]156
For my patients, they certainly found it slightly different, especially those that had experienced private physio before, erm they said oh, is that it? They were, well are you not doing anything else? Is it just one exercise? Is that it? (P8) (p. 282)
[physiotherapist; RCRSP]156
The remaining two unequivocal findings demonstrated the individualised nature of the exercise experience, with the same Achilles loading intervention eliciting discomfort in some patients, whilst others rated it positively compared to their previous experiences:
It was suggested that I use like a foam mat or something, but I was up to about 100 odd kilos, it was quite painful to have the bar on. (P5) (p. 7)152
The idea that it is more about of putting it [Achilles tendon] under load for longer has been a lot more effective than all the stretching, warming and icing and everything else that I have tried before. (P8) (p. 4)152
Category 1.2: Barriers and facilitators to the delivery of exercise for tendinopathy
This category comprised eight unequivocal and one credible finding from a single study152 on patients’ and physiotherapists’ perceptions of a gym-based self-managed intervention supervised via telehealth for AT. Notably this study had one of the younger samples (mean age 46.1). Efficiency, convenience and accessibility were reported as facilitators:
I did not have to go and wait in an office or whatever. I could just go to the gym and just get started and if he was not ready or whatever then I could just get into my workout and he [physiotherapist] would join me halfway through sometimes. There was no waiting around. (P4) (p. 4)
[Patient]152
I found that close contact especially with quite anxious type [participants], just being able to reassure them that where their early stages were absolutely fine and appropriate and to be expected, I think that helped them stick to the course. (PT 4) (p. 8)
[Physiotherapist]152
Barriers were related to technology and equipment, with issues such as internet connectivity, mobile phone battery, difficulty positioning mobile phone cameras for physiotherapists to assess exercise performance, and difficulty accessing particular pieces of gym equipment being reported:
It was the longer regimen that I was on [low-intensity group]. A couple of times my battery went out and I was using up all my data because it was an hour and a half session. (P8) (p. 6)
[Patient]152
I think most people have that gym etiquette that someone is using [the machine] then leave them alone and then just keep the workout or do something else, but couple of times I have had to cancel a session because patients could not access the Smith machine for like half an hour or 40 minutes. (PT5) (p. 9)
[Physiotherapist]152
However, most patients reported that the telehealth software itself was easy to use.
Category 1.3: Facilitators to engaging with/adhering to exercise interventions
This category, composed of eight unequivocal and one credible finding, concerned the intrapersonal (e.g. ability to see progress, personality traits, motivation), interpersonal (e.g. social support from others – friends, partners, physiotherapists) and environmental (e.g. aspects of the intervention, exercise setting) factors that can facilitate engagement with/adhering to exercise interventions.
Four unequivocal findings contributed to the role of intrapersonal factors, with motivation seen as a facilitator to exercise, especially if it meant a return to previous activities:
Knowing I would be out of action for three to four months was enough motivation to make me want to stick to my rehabilitation program. My motivation was born out of the fact that I was terribly frustrated with not only being unable to compete, but also missing out on the social side. (Max) (p. 218)
[Athletic rehabilitation, mixed tendinopathies]150
Indeed, ability to see progress in terms of improvement in symptoms and function was also an important facilitator:
I do not have the pain that I used to. I was getting to the stage at times I was quite immobile at work. But I have not had that ever since the programme finished … which is great. (P1) (p. 7)
[Achilles]152
As was the internal motivation to be pain-free:
I was driven to get rid of this pain really, so I thought I’m going to give this a really good go and do it properly. (ID 18) (p. 83)
[RCRSP]156
Personality traits were also considered facilitators, indicating individuals with high levels of self-efficacy were more able to engage with and control their exercise programme:
I kept my diary and I always wrote why I’d not done it so that I could think to myself well how can I fit that in then? (ID 18) (p. 83)
[RCRSP]156
Two unequivocal and one credible finding contributed to the role of interpersonal factors in facilitating engagement and adherence. Social support can come in the form of family and/or friends and can be a source of reassurance for patients:
C: Oh, the support I got from my family and friends was great. My husband has been fantastic watching over me making sure I don’t do anything I shouldn’t. My best friend sometimes came to the rehab centre with me which I really appreciated. (Carol) (p. 221)
[Athletic rehabilitation, mixed tendinopathies]150
My (partner) erm kept saying to me that (they) thought that I was complaining a lot less as time went on. I didn’t feel that but she assured me that I was. (ID 15) (p. 83)
[RCRSP]156
Physiotherapists also play an important role in facilitating engagement. In one study (gym-based, remote monitoring for AT), it was suggested that patients with longer (duration) gym sessions required more motivation and encouragement to complete their sessions and innovative methods of providing that encouragement:
I think other people who got irritated around time at the gym they definitely did longer session … I liked the follow up emails after the session, sort of template kind of idea of what you could send them [to participants] at some point positive things from their session encouraging them for the next week. (PT 3) (p. 8)
[physiotherapist; Achilles]152
The final two unequivocal findings contributed to the role of environmental factors in facilitating engagement with exercise interventions. Environmental factors concerned aspects of the intervention itself, such as the use of audio-feedback during a telehealth exercise programme for AT:
The audio feedback and them [physiotherapists] telling you to go longer, faster, shorter, harder, whatever their instruction happens to be, that is sort of invaluable. (P3) (p. 5)152
Exercise location can also have an impact, and, for the same telehealth exercise programme, access to a 24-hour gym promoted adherence and motivation:
Access to the 24-hour gym was handy for me, because I work in different hours and have got family and young kids, so it’s quite good that I could go at any time I wanted … and having the various gyms and having access to those around the place definitely helped me, because like I said, I travel a fair bit for work, so that was very handy. (P7) (p. 7)152
Category 1.4: Barriers to engaging with/adhering to exercise interventions
This category consists of four unequivocal and one credible finding, and concerns intrapersonal barriers such as confidence, motivation, pain and time.
The personal impact that a lack of confidence can have on performing a sports injury rehabilitation programme was described (unequivocal finding):
Although all the prescribed exercises were new to me, I felt confident performing them in the rehabilitation centre because I knew I was being monitored by the physio, however, I felt much less confident performing exercises at home by myself …. I wasn’t entirely sure I was doing the exercises correctly and, as such, I didn’t want to further injure myself, having this concern made it difficult for me to comply with home-based exercises. (Carol) (p. 218)
[mixed tendinopathies]150
Barriers can also concern internal motivation, with one RCRSP patient (credible finding) describing limited engagement in a previous episode of physiotherapy:
I didn’t do them … I don’t know – because I thought they were doing it for me. So, I came back with the booklet but I didn’t do them. I thought oh well, I’m going back next week. (ID 18) (p. 83)156
Exercise-related pain can be considered a barrier to exercise intervention adherence, with questions posed as to whether the exercises were helping because of the pain (unequivocal finding):
I think I had about three different ones (physiotherapists) … and they were also the ones who did the hydrotherapy and acupuncture as well … but the exercises were just putting me in pain, so it didn’t help. (P10) (p. 4)
[GTPS]160
Most of the patients in Hasani et al. ’s152 study on gym-based exercise for AT noted that time to commit to regular exercise can be a barrier for a variety of reasons:
It was so time-consuming … I did not have much time to do anything else in the gym. (P5) (p. 7)152
The final unequivocal finding in this category involved a physiotherapist reflecting on the challenges and enablers that need to be considered in tendinopathy management:
Work together in a positive pathway with me describing the exercises and illustrating how to do them and motivate patients and have the patients adhere to the program. Because adherence is the key to the success. If they come back and they say, well, I forgot your exercises. I did them once a week instead of every day, then we are not moving forward … so it is a shared responsibility. (P2, Physiotherapist) (p. 3)159
Category 1.5: Influence of patients’ and healthcare professionals’ beliefs about the pain–exercise relationship
Five unequivocal and one credible finding contributed to this category, with a range of views regarding the pain–exercise relationship represented.
Two findings (one credible, one unequivocal) described a positive perspective on the pain–exercise relationship, whereby pain was a motivator for exercising due to the anticipated response:
Still every day I do my exercises and I find that when I feel the pain coming on in my arm, I have a walking stick and I just do exercises with that, I haven’t taken pain killers in I don’t know how long, I am good with pain now. (Margaret) (p. 468)
[RCRSP]154
Whilst patients were positive about the potential for exercise therapy to improve symptoms, and they would tolerate some discomfort, they did want to know how far to ‘push’:
Oh, good Lord yeah. Anything that would help I’d go for …. If they told me that it would help (exercise with discomfort), I would do it. (When asked what information would be useful) Would it be detrimental if I pushed myself that little bit further? (P8) (p. 5)
[GTPS]160
In contrast, two unequivocal findings highlighted that some patients find exercise-induced pain intolerable, particularly if it impacts on daily living:
I wouldn’t do it (put up with discomfort during exercise). And that is purely because if it affects my day to day living … it’s just not worth it. (P6) (p. 5)
[GTPS]160
In some cases, continued pain was considered a treatment burden with associated psychological consequences:
I felt awful, yeah I mean I was doing them (exercises) it was painful, and I was quite regimented, I was like I’ve got to do the physio because I’ve got to make it better … it had been going on a really long time it was just getting worse. (Mila) (p. 6)
[PTTD]151
The final unequivocal finding concerns physiotherapists’ perspectives on the pain–exercise relationship, with physiotherapists expressing varied levels of comfort concerning pushing through pain: for example:
in terms of the training it was always saying, taught that you don’t want to push in to pain that you don’t, you might get associated inhibition and sort of, of the muscles alongside it so, so different from that point of view. But then, like you said, if you have a look at it from the eccentric loading perspective then we do ask people to, to go in to pain when they’re exercising so erm I could see how it might fit.. (P7) (p. 282)
[RCRSP]107
Category 1.6: Influence of patients’ and physiotherapists beliefs about exercise
Three unequivocal and three credible findings contributed to this category, which demonstrates that physiotherapists and patients have a range of beliefs about exercise per se and about different components within exercise interventions, and that these need to be considered when prescribing therapeutic exercise for tendinopathy, as they may have a positive or negative impact.
Three findings (one unequivocal and two credible) provide a patient perspective about beliefs surrounding exercise. Some patients expressed a lack of confidence in relation to the proposed exercise intervention:
but I know there are some exercises you should be doing and things like that. I probably haven’t done as much strength work. I don’t go to the gym. I don’t do any strength work or anything like that. (Participant 1) (p. 110)
[Achilles]153
Other patients with the same tendinopathy seemed to know that exercise would be involved from their prior experience:
There was a therapy that was recommended to me maybe at the start of the year, it was called heel drops or painful heel drops? They’re on the edge of the steps and you basically flex, you basically flex down and flex up …. Was it 10 minutes a night every night for 12 weeks but in my head that was crazy. (Participant 5) (p. 111)153
An important factor for healthcare professionals to consider is educating patients to ensure their expectations are realistic:
At first I expected to see an improvement within a few weeks but it was so small. They tried to encourage me saying it was a long haul and by the end they said it would be six to nine months. I think it might have helped to know the six-to-nine-month time frame at the beginning. (Participant 62) (p. 196)
[RCRSP]157
Three findings (two unequivocal and one credible) provide the physiotherapist perspective, and focus on the impact that their own beliefs can have, such as questioning the rationale underpinning a self-managed loaded exercise programme consisting of one exercise:
to give one exercise … it was more I had a bit of an issue with that more than the patient did to start with. (P11) (p. 281)
[RCRSP]107
Physiotherapists involved in prescribing exercise for RCRSP also felt confident that they could identify whether patients held helpful or unhelpful beliefs about exercise and therefore predict whether or not they would engage with exercise therapy:
I think there are some clients who from interviewing them, doing the examination, that you get an idea of whether they would be compliant and appropriate, and others you just think it’s totally inappropriate and a waste of time. (T1) (p. 82)156
Category 1.7: Impact of symptomatic response to exercise
Two unequivocal and two credible findings contributed to this category, which shows that symptomatic response to exercise is an important factor that impacts on adherence. All four findings relate to one qualitative study155 that included six patients and two physiotherapists involved in a pilot RCT of a self-managed loaded exercise intervention for RCRSP. These findings demonstrate that symptomatic improvement is a key facilitator for continuing with exercise. However, failure to respond, a slow response or a plateau in symptoms could have the opposite effect:
I think that when you find that they’re not making a great deal of improvement, you’re less inclined to erm continue it. (ID 37) (p. 82)156
Synthesised finding 2
Patients and healthcare professionals place value on appropriate and timely patient education facilitated by an effective ‘therapeutic alliance’ between patient and physiotherapist, to promote motivation and confidence in the exercise intervention.
This synthesised finding was generated from 2 categories and 16 findings (13 unequivocal, 3 credible; Table 31) and illustrates the value that patients and healthcare professionals place on self-management and patient education, recognising that it is facilitated by the patient–therapist relationship, which is vital for the motivation and confidence required to adhere to an exercise intervention.
| Findings | Categories | Synthesised finding |
|---|---|---|
| The physiotherapist as an educator and facilitator (U) | Category 2.1 Importance of the patient–therapist relationship |
Synthesised finding 2
Patients and healthcare professionals place value on appropriate and timely patient education facilitated by an effective ‘therapeutic alliance’ between patient and physiotherapist, to promote motivation and confidence in the exercise intervention |
| Coping (U) | ||
| Therapeutic alliance All participants (8/8) acknowledged that despite not being face-to-face with their physiotherapist, they still felt reassured by the telehealth contact with their physiotherapist, especially in the early stages when they were gaining familiarity and confidence with the treatment process (U) | ||
| Regular contact Participants appreciated the ability to have regular contact with a physiotherapist for support and obtain immediate feedback to allow them to progress their exercises (U) | ||
| Therapeutic alliance Although physiotherapists reported that the use of telehealth was an effective method for therapeutic interactions, they also reported some barriers to developing a therapeutic alliance (U) | ||
| The physiotherapists recognised the importance of knowledge translation and the need to ‘sell’ the self-managed exercise intervention, both of which were underpinned by the need to develop a therapeutic relationship (U) | ||
| Additionally, the patients described the role of the physiotherapist which, in some situations, seemed to compound the negative nature of their prior beliefs (C) | ||
| The influence of the physiotherapist was framed in a more positive way (U) | ||
| Additionally, with regard to the pro-active follow-up by the physiotherapist another patient recognised … (U) | ||
| Patient-centred care promotes development of a therapeutic alliance: ‘If a patient trusts you then you are generally going to get much better results’ (U) | ||
| Self-management education All participants (8/8) noted that the one-to-one self-management education they received at the start of the rehabilitation programme was helpful and changed the way they perceive their Achilles symptoms. Specifically, the education improved their self-efficacy and ability to understand acceptable pain limits during activity (U) | Category 2.2 Importance of patient education and self-management |
|
| The importance placed on being able to manage their own condition through improved knowledge and a feeling of increased control was highlighted as a recurrent theme within the participants’ transcripts (U) | ||
| Need for patient education (C) | ||
| Achieving patient education (U) | ||
| With reference to the exercise diary which is used as a key component of the programme as a means of self-monitoring, one patient reflected … (C) | ||
| The need for early, focussed education: ‘Some beliefs can be detrimental to rehabilitation options’ (U) |
Category 2.1: Importance of the patient–therapist relationship
Nine unequivocal and one credible finding contributed to this category. Patients with a range of tendinopathies highlighted the mostly positive aspects of the patient–healthcare professional relationship. Specifically, physiotherapists are seen as educators and facilitators who enable patients to cope with their tendinopathy and exercise programme, providing confidence and motivation to continue:
Performing the rehab exercises can be demanding physically and emotionally …. So to have found a physio who was very supportive was very comforting and reassuring. The physio provided good guidance and frequent feedback about how well I was doing; he seemed to have a lot of time for me in the clinic and had taken a keen interest …. This made me feel valued. He wanted me to get better and this came across well. It is because of this that I didn’t want to let him [the physio] down. (Carol) (p. 220)
[Patient, athletic rehabilitation, mixed tendinopathies]150
Physiotherapists likewise recognise the importance of the therapeutic alliance and its uniqueness:
Some patients might need five minutes of education, another patient may need two or three sessions where it is quite intensive, or they might need to cover different areas, so I think it depends on the patient that you have in front of you similar to what exercise you prescribe. (P1, PT) (p. 3)
[Physiotherapist; RCRSP]159
Motivation provided by the physiotherapist can also be provided effectively via telehealth supervision of exercise, with regular contact being valued:
I think if you did not have to talk to anybody, you might get lazy some days and not bother. Whereas that sort of kept you committed and making sure you will not forget your exercises. (P6) (p. 7)
[Patient, Achilles]152
Physiotherapists agreed with this, but were aware of the potential barriers created by telehealth also:
I was probably a little slower to develop the relationship, so I found a couple of sessions to sort of warm up and get a bit more hold over messages. (PT 1) (p. 9)
[Physiotherapist; Achilles]152
Despite most findings in this category relating to the positive influence of physiotherapists, they need to be aware that they can also have a negative impact on their patients:
well, I think (physiotherapist) felt more or less straight away that it was unfortunate that I’d drawn the short straw in terms of that. (ID 37) (p. 82)
[Patient, RCRSP, referring to single exercise intervention]156
Category 2.2: Importance of patient education and self-management
Four unequivocal and two credible findings were included in this finding, in which patients and healthcare professionals concur on the importance of education so that patients with tendinopathy can self-manage their condition. Patients recognised the value of education and self-management strategies, in order to enhance their self-efficacy, a view that was echoed by physiotherapists:
Having a little bit of pain does not mean to say that you should not be doing the exercises. So as long as it is not getting really bad, that guidance on how to manage the pain aspect of it now that I am thinking about it, was very handy because it gives you framework to decide well is this normal aches and pains or is it something a bit more serious. (P 5) (p. 7)
[Patient; Achilles]152
It’s about trying to reduce anxiety through education or reassurance and to reduce any hypervigilance, which actually may affect their outcome … and ultimately affect their adherence to any exercise intervention. (P1, PT) (p. 3)
[Physiotherapist; RCRSP]159
Integration of quantitative and qualitative evidence
Qualitative findings in this review largely support and explain the quantitative findings (see Table 32) and can be summarised as follows.
| Quantitative findings | Qualitative findings | |
|---|---|---|
| Feasibility | ||
| Adherence | Estimated mean proportions Adherence: 0.76 (95% CrI 0.71 to 0.80] ‘Good’ adherence: 0.79 (95% CrI 0.68 to 0.87) Narrative synthesis 11/13 studies adherence ≥ 70% Lower adherence for 1 upper-limb strengthening programme; adherence > 70% with forearm band and < 70% without, suggesting relationship between pain and adherence Lower adherence for do ‘as tolerated’, suggesting relationship between pain and adherence |
Explanatory A number of reasons why adherence not > 70% Facilitators: motivation, personality, social support, setting and intervention itself Barriers: confidence, motivation, pain, lack of time Beliefs about benefits of exercise Previous experience Importance of patient–therapist relationship for facilitating adherence and self-management through promoting patients’ motivation and confidence; may impact both positively and negatively Importance of education and self-management to enhance self-efficacy for self-management |
| Attendance | Estimated mean proportion 0.90 (95% CrI 0.82 to 0.96) | Explanatory Importance of education and confidence provided by physiotherapist |
| Fidelity | Only reported in 3% of included studies Fidelity ranged from 23% to 90%, but different variables being measured: 90% fidelity for prescribed load 23% to 50% when all exercise parameters included in calculation One study unclear exactly how fidelity was measured |
Explanatory Confidence; less confident for unsupervised exercises that they are conducting them correctly |
| Acceptability | ||
| Tolerability of exercise | Using scales 2 studies used different Likert scales 3/4 for supervised RCRSP 6.3/10 for painful eccentric HEP Achilles Drop-outs due to exercise intolerance Only reported in 7% studies 0 to 33% participants; most studies ≤ 11%; one study 33% drop-outs was small sample (n = 9) and painful quadriceps training for patellar tendinopathy Adverse events related to exercise Only reported in 8% studies Exercise generally associated with some short-term pain or muscle soreness (reported by 1% to 60% of participants) |
Explanatory Most patients will tolerate some discomfort if believe exercise to be beneficial Explanatory Pain response highly individualised – same exercise intervention liked by some patients and disliked by others due to causing pain Pain–exercise relationship; important to know when (not) to push through pain Symptomatic improvement key facilitator to adherence; conversely, failure to respond, slow response or plateau key barrier |
| Satisfaction with exercise | 2 studies (Achilles and RCRSP) Satisfaction good (supervised exercise); however, no details of scale used |
Confirmatory/contradictory Range of individualised views suggesting range of satisfaction levels |
| Willingness to do exercise programme | 1 study 100% willingness to undertake exercise programme (Achilles, supervised) |
Not specifically explored in qualitative studies |
| Helpfulness of exercise | 1 study (iliopsoas) Specific exercises helpful – no clear consensus on which, suggesting individualised experience/preference |
Confirmatory Patients can have conflicting views of the same exercises e.g. ‘simple’ RCRSP exercise liked by some, whilst others questioned efficacy |
| Overall acceptability | 1 study (Achilles) Easy to implement painful eccentric HEP (Achilles) |
Not explored in quantitative studies Environment Group vs. individual exercise – some patients prefer group environment due to peer support, learning and motivation Gym-based telerehabilitation supervised remotely – both barriers and facilitators reported. Potentially important due to changes in healthcare provision during COVID-19 pandemic and ‘new normal’ |
Feasibility
Adherence
Synthesised quantitative findings from 52 studies provide evidence that self-reported adherence to exercise therapy for tendinopathy is good when interpreting ‘good’ as ≥70% adherence. Synthesised findings from 13 quantitative studies show that attendance of supervised exercise therapy sessions (e.g. 1–1 physiotherapy) is excellent (90%). The qualitative findings help to explain why adherence is not even higher than 70% however, as a number of factors including barriers, facilitators, beliefs, previous experience and the ‘therapeutic alliance’ affect adherence in an individualised manner. The qualitative findings also explain adherence to supervised exercise being higher than unsupervised exercise, with patients expressing reduced confidence when unsupervised.
Fidelity
There is a lack of data on fidelity of exercise in the included studies. Quantitative evidence from three studies shows that exercise fidelity is variable. Qualitative findings relating to confidence in supervised more than unsupervised exercise may help to explain this finding.
Acceptability
Tolerability
Quantitative evidence from 15 studies shows that exercise therapy for tendinopathy is tolerated well. Although it is associated with some short-term increase in pain or muscle soreness, it results in relatively few adverse events or drop-outs. Studies with higher drop-outs appear to be those employing pain-inducing exercise. Qualitative findings provide an explanation for the range in tolerability reported in quantitative findings.
Beliefs about the pain–exercise relationship, the individualised response to pain, and the impact of symptomatic response all moderate an individual’s tolerability of therapeutic exercise.
Satisfaction, willingness, helpfulness, overall acceptability
These acceptability measures were reported in one or two quantitative studies each, with few data provided. Findings were positive for all domains. Qualitative evidence confirms the findings from one case-series (n = 9) that individual patients can have conflicting views on the helpfulness of specific exercises. Qualitative evidence provided an understanding of some aspects that were under-reported in the quantitative evidence, including environmental factors such as group and gym-based exercise, and the use of remote supervision via telerehabilitation.
In summary, both the quantitative and qualitative evidence indicates that exercise therapy for tendinopathy is largely feasible and acceptable. The qualitative evidence indicates that an individualised person-centred approach to prescribing exercise therapy, facilitated by a strong therapeutic alliance between patient and healthcare provider, with provision of appropriate and meaningful education, is important for achieving the confidence and motivation required for adherence.
Discussion
To our knowledge, this is the first review to synthesise the available quantitative and qualitative evidence on feasibility and acceptability of exercise therapy for tendinopathy. Feasibility and acceptability are important considerations if exercise interventions are to be conducted outwith controlled experimental settings and adopted in the real-world clinical environment.
The quantitative data showed evidence that self-reported adherence and attendance to supervised exercise are good, and that fidelity is seldom reported in studies on exercise for tendinopathy. It also showed that the acceptability of exercise for tendinopathy is overall good.
The qualitative data highlight a range of factors that impact on feasibility and acceptability of exercise. These include the need for an individualised person-centred approach, facilitated by a strong therapeutic alliance between patient and healthcare provider, with provision of appropriate patient education. These factors need to be considered when designing and delivering services for people with tendinopathies. However, as interventions are increasingly tailored to individual patient needs, the way and rationale for such adaptations will need to be captured and recorded when describing interventions in research studies to allow for comparisons and assessments of effectiveness.
Feasibility
The findings related to adherence can be interpreted in a number of ways. On face value adherence appears to be good across tendinopathies and exercise types, and is congruent with levels reported in previous systematic reviews exploring exercise adherence in a range of health conditions. 194–196 However, we used authors’ own statements of adherence, which at times involved making an assumption that authors were interpreting a particular proportion of exercises completed (e.g. 70%) as being good. Without an agreed definition of ‘good’ adherence however, this remains open to interpretation, and it must be acknowledged that self-report measures are subject to bias. 197 Bailey et al. 171 in their systematic review of 459 studies on adherence to therapeutic exercise for musculoskeletal pain, found proportions of 80–99% to be most commonly used for determining satisfactory adherence; it is therefore possible that our 70% threshold was somewhat generous.
Bailey et al. 171 also found adherence to be variably defined and measured, and recommended that adherence to therapeutic exercise for musculoskeletal pain should be conceptualised in order for a measurement tool to be developed. A Cochrane review on exercise for chronic musculoskeletal pain published more than a decade ago called for a validated measure of exercise adherence to be developed and adopted. 198 The current review shows that work remains to be done in this field, supporting Bailey et al. ’s recommendations. Conceptualising and defining adherence to exercise therapy would enable a common language among clinicians, patients and researchers, and development of a measurement tool (or suite of tools) would facilitate collection of robust and suitably homogeneous data which, if adequately reported, would assist with future primary research and evidence syntheses.
The qualitative findings identified the importance of barriers, facilitators, beliefs, previous experience and the ‘therapeutic alliance’, all of which can impact adherence in a positive or negative manner, adding to the complexity of achieving high levels of adherence to therapeutic exercise. These findings are in keeping with the knowledge that numerous factors influence adherence to exercise interventions, including characteristics of the intervention itself, and factors associated with those delivering and receiving it. 195,199 The findings may assist with the development of strategies to support adherence to exercise for tendinopathy, which might include booster sessions and telephone follow-up, which have shown promising results in people with osteoarthritis. 200 It has been suggested that mobile health interventions may be useful for exercise adherence in musculoskeletal conditions; however, further research on their efficacy is required. 201
The finding of high rates of attendance to supervised exercise may be in contrast to some attendance rates typically seen in the clinical setting, and may be a function of research participation, indicating the need for more pragmatic effectiveness studies to be undertaken. It may also be a function of patients feeling more confident with supervised than unsupervised exercise, as explained by the qualitative findings, and therefore motivated to attend. There is substantive evidence across conditions and populations that supervised exercise is superior to unsupervised,195,202,203 including the efficacy review reported above. However, supervision can be achieved remotely, as demonstrated in this review. 152 Telehealth may therefore provide a cost-effective method of supporting adherence in this population, and is worthy of further research.
The finding of poor reporting of fidelity is important. If we are to truly determine the effectiveness of specific exercise approaches for tendinopathy (and for specific tendinopathies) it is vital to know whether the exercise is being conducted as intended or whether a modified version is in fact proving effective. It will also help, along with further qualitative work, to understand which aspects of exercise programmes or specific exercises patients find acceptable and unacceptable. Fidelity is arguably not easy to assess; however, with the proliferation of exercise tracking and remote monitoring technologies,204 there is scope for this to be greatly enhanced in the future.
Acceptability
The acceptability findings need to be interpreted with caution, with the main finding being limited reporting of acceptability in quantitative studies. The qualitative studies suggest the experience of exercise for tendinopathy to be a highly personalised one, with many factors impacting the patient experience, and the patient–therapist relationship being highly important.
Limitations
There was considerable heterogeneity in reporting of feasibility and acceptability measures. In order to facilitate synthesis of adherence data, which was most commonly reported, we required some form of numerical data to be reported. This did result in the exclusion of some studies on the basis of insufficient data (e.g. those that made general statements about adherence being ‘good’ without providing any quantification). Furthermore, we only reviewed studies which reported adherence, meaning that 347 of 436 potential quantitative studies identified in the scoping review were automatically excluded (i.e. they did not report adherence).
We did not contact authors for missing data. This was a pragmatic decision due in part to the size of the syntheses being undertaken in phase 2 (efficacy and mixed-method reviews), and in part due to the widely acknowledged challenges in collecting feasibility and acceptability data, particularly self-reported exercise adherence, arguably making it unlikely that study authors would be able to provide such data. Our scoping review found that only 59% of studies that intended to collect adherence data actually reported it, and almost 65% did not address adherence at all. Therefore, adherence reporting appears to be variable and selective, and is an important methodological area to address in future research. We also found in this mixed-method review that reporting of other feasibility and acceptability measures was uncommon.
When adherence was reported, there was no consistency on what constitutes ‘good’ adherence, as discussed above. Our findings concur with those of Bailey et al. 171 on the need for a clear definition and robust methods of measuring and reporting adherence. Our findings also concur with views presented recently highlighting the importance of adherence when interpreting the results of exercise interventions. 205
The lack of operational definitions for feasibility and acceptability measures was salient and impacted on our ability to synthesise findings and draw conclusions. Our findings demonstrate that reporting of feasibility and acceptability measures is in general poor within the exercise for tendinopathy literature, suggesting that clear definitions should be agreed for all relevant measures in order to facilitate a common language and understanding, and allow for comparisons and future evidence syntheses to draw firm conclusions.
Methodological quality of quantitative studies was moderate to high. Blinding of participants and those delivering treatments is understandably challenging in exercise studies. However, it should be possible to ensure blinding of outcomes assessors and adequate description and analysis of follow-up. Qualitative studies were likewise moderate- to high-quality, with scores reflecting limitations of the critical appraisal tool rather than individual studies.
We deviated from the original protocol to undertake a segregated rather than integrated synthesis of quantitative and qualitative findings. Following full-text screening it became clear that the quantitative and qualitative studies addressed different aspects of feasibility and acceptability, and therefore required separate syntheses to understand these different aspects. This avoided ‘qualitising’ the quantitative data and allowed us to conduct meta-analyses on the adherence data, prior to integrating findings from the separate quantitative and qualitative syntheses, resulting in confirmatory and explanatory results being presented.
Limiting inclusion to studies ranked ‘very high’ on the HDI may have excluded potentially relevant high-quality studies, as some tendinopathy research is conducted in, for example, Brazil and South Africa. However, the numbers excluded on this basis were not large, and as well as making the review manageable, the findings are arguably more generalisable to the UK.
Heterogeneity of the quantitative data combined with the small number of qualitative studies limits generalisation. We were only able to draw general conclusions and not make recommendations specific to tendinopathy types or other covariates. Some qualitative findings were dominated by one or two studies (e.g. one study on gym-based telerehabilitation and two studies on the same RCRSP intervention generated a large number of findings), therefore these results need to be interpreted with some caution.
Conclusions
The findings show that exercise therapy for tendinopathy is in general feasible to deliver and acceptable to undertake. They also highlight a number of important factors that should be considered when prescribing therapeutic exercise for individuals with tendinopathy. These include: an awareness of potential barriers and facilitators to engaging with exercise, the potential impact of prior experience and beliefs (both patients’ and healthcare professionals’), and the importance of patient education, self-management and the patient–healthcare professional relationship.
There is a need for future research to adequately measure and fully and accurately report feasibility and acceptability of exercise for tendinopathy; that will require definitions and standardised approaches to outcome measurement to be developed and adopted. There is also a need for further high-quality qualitative research to augment the body of knowledge provided here to further understand patients’ and healthcare professionals’ views and experiences across a range of exercise approaches, delivery types and tendinopathies. This will lead to a deeper understanding of this complex phenomenon, providing explanations for the findings of the future pragmatic effectiveness studies that are also urgently required. Finally, future studies should evaluate different modes of delivery of exercise therapy for tendinopathy, including individual, group, supervised, remotely supervised and unsupervised.
Chapter 7 Discussion
To our knowledge, this is the first body of work to provide a comprehensive map of the evidence base for exercise therapy in the management of tendinopathy, and to generate synthesised findings regarding their efficacy, feasibility and acceptability. All reviews conducted in this body of work followed a priori protocols and were conducted in accordance with current methodological guidance.
The scoping review provided a detailed overview of exercise interventions for tendinopathy and the related health domains and outcomes including study design and participant demographics reported. The findings from the scoping review identified recommendations for future tendinopathy research. These included the need for specific high-quality primary research, especially adequately powered and rigorous efficacy studies and qualitative studies of patients’ lived experience, comprehensive reporting and more high-quality evidence syntheses. Importantly, combined with stakeholder engagement activities, the scoping review informed the design and methods used in the contingent efficacy and mixed-method reviews.
Given the extent of previous research investigating different exercise therapies, tendon locations and populations, the contingent efficacy review was split over a series of sub-reviews. The extensiveness of the data obtained provided a unique opportunity to adopt a modelling-based approach to generate novel findings and explore the heterogeneity to address the review questions. Collectively, the sub-reviews and included meta-analyses explored the distribution of effects that should be expected from exercise therapies and the factors likely to influence these across different tendon locations. The efficacy reviews also included comparative meta-analyses attempting to establish which exercise therapies were most beneficial and efficacious in relation to non-exercise and combined exercise and non-exercise therapies. To enhance the clinical relevance of findings from the efficacy reviews, the final mixed-method contingent review provided an understanding of some of the important acceptability and feasibility factors that influence exercise therapy efficacy in the real-world clinical setting. Several recommendations can be made from this body of work. This chapter presents an overview of the main findings, the strengths and limitations of this body of work, and makes recommendations for practice, research and policy.
Main findings
The main findings are presented in relation to the five objectives addressed by this mixed-methods evidence synthesis project.
What exercise interventions have been reported in the literature and for which tendinopathies? (scoping review)
The scoping review identified a range of exercise therapies being used across different tendinopathies (predominantly RCRSP, Achilles, patellar and lateral elbow) in the 555 included reports. Strengthening exercise was the most dominant exercise type reported, with eccentric strengthening most frequently reported for three common tendinopathies (Achilles, patellar, lateral elbow). Flexibility exercise was more commonly reported in the upper limb, and exercise therapy for RCRSP demonstrated the greatest heterogeneity. Reporting of exercise interventions according to the TIDieR checklist55 was highly variable, with few interventions being fully reproducible, and reporting of exercise adherence being infrequent and poor in quality and completeness. These findings in combination with stakeholder workshops directly informed what data were appropriate to extract and synthesise in the contingent reviews.
What outcomes have been reported in studies investigating exercise interventions for tendinopathy? (scoping review)
The scoping review identified that a range of health domains were reported, with disability being the most common primary health domain for RCRSP, Achilles and patellar tendinopathies, and PFC for lateral elbow tendinopathies. For secondary health domains, participant rating of overall condition was most common for Achilles and patellar, disability was most common for RCRSP, and PFC was most common for lateral elbow. Adverse effects/events and cost effectiveness were rarely reported as either primary or secondary health domains.
The scoping review also identified that a range of outcome domains and measurement tools were reported, with lack of consensus between and within tendinopathies being a key finding. Impairment-based outcomes were dominant, with less reporting of psychosocial factors, which are arguably important in any health condition, particularly one requiring adherence to an exercise programme. It is anticipated that this lack of consensus will be addressed in time by the ICON group51 who are working to establish core outcome sets for individual tendinopathies (including Achilles, GTPS, proximal hamstring and lateral elbow) as well as psychological and psychosocial outcomes. The mapping of outcome domains and measurement tools, combined with the views obtained from patients and professionals in the stakeholder engagement activities, directly informed the outcomes for the efficacy reviews.
Another key finding from the scoping review was the limited reporting of participant demographics, including comorbidities and potential confounders, which limited the analyses that could be conducted in phase 2 of the project. We had anticipated that subgroups and covariates such as symptom severity, chronicity, age, sex, activity levels, BMI, comorbidities, health behaviours and medication use might be incorporated within meta-analyses to explain heterogeneity of individual treatment effects. However, this was not possible due to the limited, incomplete, imbalanced or, in many cases, absence of such variables. In many instances adequate reporting of potentially relevant covariates (e.g. BMI, physical activity level, symptom severity or variation in symptom duration) occurred in less than half of the included studies, precluding any relevant analysis. Similarly, a lack of variation in key covariates was identified such as age, with an interquartile range (for mean age) of participants only 43 to 49 years old preventing suitable analysis.
Therefore, the scoping review produced a body of knowledge on the extent and content of the evidence base on exercise for tendinopathy and allowed important design decisions to be made regarding the contingent syntheses, to address the review questions as fully as possible. It also led to a to the development of initial criteria to inform guidance for exercise reporting in tendinopathy research, which can be further developed into a taxonomy beyond this project to ensure consistency in future reporting. Recommendations for research centred on study types, reporting standards, adherence and the need for research on the lived experience of exercise for tendinopathy.
Which exercise interventions are most effective across all tendinopathies? (contingent synthesis 1: efficacy)
and
Does type/location of tendinopathy or other specific covariates affect which are the most effective exercise therapies? (contingent synthesis 1: efficacy)
The scoping review directly informed the extent to which these questions could be addressed, due to the availability of suitable data for inclusion in the meta-analyses conducted for contingent synthesis 1. The key findings of the efficacy reviews are summarised below, indicating that it was possible to address question 3 and to partially address question 4 in relation to location of tendinopathy and a limited number of other specific covariates; however, there were insufficient data to draw conclusions relating to covariates such as age, gender, BMI and training status (e.g. general population, trained athlete, performance athlete), which were identified a priori and from stakeholders as potentially clinically relevant.
The key findings of the efficacy reviews were:
Relative to baseline assessment, a reasonably wide distribution of changes and, in general, improvements should be expected following exercise therapy for tendinopathy. The magnitude of improvement appears somewhat independent of the location of the tendinopathy, but is strongly influenced by the outcome domain, with the greatest improvements measured in subjective patient-reported outcomes (e.g. disability, function, pain) and the smallest improvements measured in QoL and more objective outcomes (e.g. PFC and ROM).
In combination with the relatively wide distribution of changes that can be measured, our findings suggest that small but probably clinically relevant systematic shifts in central tendency can be expected from factors such as assessment duration and exercise supervision, with greater improvements as time increases from baseline assessment and with exercise therapies that are supervised.
The findings from the efficacy reviews show that, where reported, the number of adverse events experienced during exercise therapies is extremely low. In addition, most patients report that they are satisfied with exercise-only therapies and that the changes experienced are viewed positively.
As identified by the scoping review, exercise therapies are generally dominated by resistance exercise. However, most therapies appear to prescribe exercise regimes with inadequate intensity to realise the full potential of the unique biomechanical stimulation possible with resistance exercise. Many exercise therapies hardly approached one-repetition maximum contraction and often used only the mass of a limb or the whole body for resistance. Where external resistances were included, these were generally low in intensity, as sets of exercise generally comprised at least 15 repetitions rather than the four to eight which may be required for intense overload training. In addition, most therapies included very high frequencies, with resistance training often prescribed at least twice per day, rather than two to three times per week, which is recognised as the optimum for resistance training and consistent with basic science requirements for improved tendon structure and function. Meta-regressions highlighted that those therapies which featured greater resistances and lower frequencies tended to generate greater mean improvements.
A relatively small number of studies were identified that directly compared exercise-only therapies. In addition, due to the high prevalence of resistance-dominated therapies, comparisons of different exercise therapies were more limited. However, the comparative efficacy reviews identified that for tendinopathies such as RCRSP, therapies that comprise more of a flexibility or proprioceptive focus may be more beneficial than those that focus on resistance exercise. In addition, where resistance exercise was the focus, this frequently comprised eccentric-only exercises. Whilst evidence was identified for increased efficacy of eccentric-only exercises compared with isometric or concentric-only exercises, evidence was also identified for the superiority of standard concentric and eccentric exercises. These findings are potentially influenced by the relatively low resistances and high training frequencies typified by the exercise therapies analysed.
Comparisons of exercise-only, non-exercise only and combined therapies in the final analyses of the efficacy reviews generated several important findings. Firstly, it was identified that non-active therapies (e.g. placebo and wait-and-see) tended to perform worst, highlighting the importance of active therapies. Secondly, evidence was obtained indicating greater improvements when combining exercise and non-exercise therapies compared with either therapy class in isolation. Finally, due to the large amount of heterogeneity present, development of a clear treatment hierarchy was not possible; however, evidence suggested that combining exercise with either electro-therapy, injections or kinetics (e.g. taping, splinting, orthotics) may produce the most effective results.
The efficacy reviews therefore provided evidence that:
-
Exercise therapy is safe and beneficial across the common tendinopathy locations, and patients are generally satisfied with the outcome of exercise interventions and perceived substantive improvements.
-
RCRSP may benefit from exercise interventions that focus on flexibility and proprioception more than strengthening.
-
Resistance training combining both concentric and eccentric repetitions is superior to other contraction modes given the intensities and frequencies commonly adopted.
-
Combining exercise therapy with electro-therapy, injections or kinetics may be most beneficial across tendinopathies and may be considered in the early phase of tendinopathy rehabilitation.
It is important to state that many of the findings of the efficacy reviews were underpinned by low and very low quality of evidence. Whilst overall risk of bias was generally low, frequently there were limitations associated with blinding of both participants and outcome assessors. Additionally, in keeping with the findings of the scoping review, limitations were noted in overall reporting, which introduced further risk of bias, and restricted the capacity of the efficacy reviews to delineate the effects of exercise dose or draw firm conclusions on the superiority of specific exercise types or protocols across tendinopathy per se or its subgroups. This must be rectified in future research, where high-quality, adequately powered studies must be conducted and reported fully and transparently with more detail describing the actual exercise stimulus, including for example the magnitude of the resistances used. Limitations also exist in the ability to make conclusions based on the complexity of the issues and the large number of potentially relevant factors. For example, our finding that combined therapies are more efficacious than any one form of therapy alone may simply be due to the dosage and it is plausible that similar or better results could be achieved with greater doses of a single modality. Nevertheless, increased quality and better reporting in primary studies will enable subsequent evidence syntheses to adopt more robust analyses, improving the overall confidence in findings generated.
How feasible and acceptable are exercise interventions for tendinopathies? (contingent synthesis 2: feasibility and acceptability)
The mixed-method review identified that exercise interventions for tendinopathy can largely be considered feasible and acceptable. However, the findings should be interpreted with some caution as there remains a need for feasibility and acceptability measures to be adequately defined and measured in tendinopathy research, particularly those measures of adherence to therapeutic exercise. It was not possible to identify whether specific intervention types were more or less feasible/acceptable, or for which tendinopathies, due to small amounts of heterogeneous data in the quantitative studies and the small number of qualitative studies.
By integrating quantitative and qualitative findings this review highlighted important patient-centred factors to consider when prescribing exercise for tendinopathy that can influence feasibility and acceptability measures, particularly confidence to adhere to a therapeutic exercise programme. These include an awareness of potential barriers and facilitators to engaging with exercise, the potential impact of prior experience and beliefs (both patients’ and healthcare professionals’), and the importance of patient education, self-management and the patient–therapist professional relationship.
The review identified a need for future research to adequately measure and fully and accurately report feasibility and acceptability of exercise for tendinopathy, requiring definitions and standardised approaches to outcome measurement to be agreed upon by the tendinopathy research community. The review also identified a need for further high-quality qualitative research to explore the complexities of exercise therapy from the perspectives of those experiencing it. Finally, the review identified a need to evaluate different modes of delivery of exercise therapy, as few studies have to date fully explored aspects such as supervision, delivery (including by telehealth) and group dynamics.
Strengths
A strength of this evidence synthesis programme of work is that it included all tendinopathies, and all forms of exercise therapy. Previous systematic reviews have tended to focus on one or a small combination of tendinopathies (e.g. Achilles and patellar) and selected exercise approaches, which does not generate comparative evidence for specific exercise interventions. The inclusive approach adopted here has allowed us to show that approaches generally used to manage different tendinopathies are likely to create similar responses. Additionally, many previous approaches to evidence synthesis have relied on narrative synthesis, meaning that the large amount of previously published data has not been explored as well as could be achieved. The modelling approaches featured in both the efficacy and mixed-methods reviews attempted to synthesise these data, identifying general results and where possible exploring heterogeneity to generate novel and clinically relevant findings. In addition, the inclusive approach with regard to tendinopathies, participants, therapies and outcomes enabled the review to synthesise diverse sets of information from both the clinicians’ and patients’ perspectives to provide the most comprehensive summary of the field to date.
Another strength is the inclusion of studies published in languages other than English, which are frequently excluded from systematic reviews. We used automated translation for some studies and sought translation and assistance with data extraction from the review team’s networks for others; very few studies were excluded due to not being able to secure an English translation.
The results of the mapping of different exercise types, when combined with the proposed criteria in the TIDieR checklist, enabled us to develop initial criteria to guide reporting of exercise for tendinopathy. Further development of this initial guidance is required to establish a comprehensive taxonomy for exercise reporting. The use of a taxonomy to guide consistent reporting of exercise interventions in future tendinopathy research studies will enable better comparisons to be conducted.
Limitations
The use of the HDI was a pragmatic approach that ensured the review was feasible to conduct and that the findings would be relevant to the UK setting. However, the review team acknowledge that some potentially relevant studies were excluded on this basis.
This work identified limitations in the available body of evidence on exercise therapy for tendinopathy. Many key variables lacked clearly agreed definitions and/or methods of measurement, particularly those relating to feasibility and acceptability of exercise therapy. The lack of consensus on outcome domains and measures was clear, and points to the urgent need for core outcome sets not only to be developed but adopted in practice and research. Reporting of exercise interventions themselves lacked clarity, particularly with respect to dosage, and the insufficient reporting of participant factors made it difficult to explore informative heterogeneity and control for confounding in the meta-analyses. There was a lack of qualitative research that explored participants’ and healthcare professionals’ perspectives of exercise for tendinopathy; nonetheless the 11 qualitative studies included in the mixed-method review provided valuable insight to explain some of the findings from the quantitative component of that review and complemented the efficacy review findings.
The modelling of data from heterogeneous studies with regard to interventions, samples and outcomes poses a range of limitations and therefore requires caution when interpreting findings and making recommendations. These limitations are particularly salient in efficacy review 1, where data were extracted and compared from individual exercise-only therapies. It is expected that an extensive range of factors can influence the outcomes of any interventions measured, and that imbalances of these factors across comparisons may influence findings. Attempts were made to explore the heterogeneity through sub-analyses stratifying for factors such as tendinopathy location and outcome domain. In general, sub-analyses tended to show consistent results and match with plausible mechanisms providing some additional support for the findings generated. However, it is possible that imbalances of other relevant factors remained. Additionally, where attempts were made to explore heterogeneity through meta-regressions, it was not always possible to create variables that fully represented the construct of interest, including the use of body mass or additional external resistance to control for resistance intensity. Overall, the strength of analyses would have been improved with greater depth and consistency of reporting enabling more control of factors such as assessment duration and participant and exercise therapy characteristics. However, sufficient data were generally not available to control for these factors based on the number of studies available and the quality of reporting in individual studies.
The quality of evidence underpinning the findings of this review varied across the different sections, with low and very low quality of evidence frequently used for the efficacy reviews. In addition to some concerns with risk of bias, evidence quality was frequently downgraded due to issues of imprecisions, inconsistency and small-study effects. Imprecision and inconsistency reflect the heterogeneous nature of the research base, where not only the patients and therapies differ substantively, but also the focus of authors and the highly specific research questions addressed. There are thus additional limitations when synthesising data and drawing findings such as that multiple therapies are superior to individual therapies, when this is rarely the focus of the individual studies that are amalgamated to build the indirect evidence. The mixed-method review was likewise limited by the variable reporting quality of exercise adherence data, meaning that these results should also be interpreted with some caution. In addition, the well-documented limitations of self-reported measures of adherence should also be acknowledged. Finally, mixed-methods reviews are somewhat complex and may be challenging to replicate. However, we are confident in the rigour of the methods adopted for this component of the synthesis.
Recommendations
Collectively, the findings from the scoping, efficacy and mixed-method reviews contributed to the following recommendations.
Recommendations for practice
-
When setting expectations of what treatment effect to observe in practice, clinicians should consider the outcome domain. Subjective tendinopathy-specific outcomes may result in very large changes compared to objective outcomes. The observed reduction in QoL in some studies requires further exploration.
-
Patient satisfaction appears to be consistently moderate to high. In addition to measuring satisfaction on a binary scale, clinicians may choose to probe reasons for satisfaction or dissatisfaction to better inform practice.
-
Whilst resistance exercise is the most common class of exercise therapy, it appears to be mostly used with limited intensity and high frequencies. Adhering to practices that take advantage of a more optimum exercise stimulus should be encouraged, with lower frequency and higher intensity likely beneficial for lower-limb tendinopathies. Resistances are also infrequently prescribed based on a percentage of maximum; however, this is one of the most effective means of ensuring that resistances are of sufficient magnitude. Practices to achieve loading in line with standard exercise theory which patients can adhere to require development, implementation and investigation.
-
For RCRSP the use of flexibility and proprioceptive regimes may be more effective than using resistance exercise in isolation. There is also some limited evidence that flexibility regimes may be effective in AT.
-
A focus on eccentric resistance exercise above all other treatments does not appear warranted. It is likely that standard resistance exercise practices that combine concentric and eccentric exercise will be superior to eccentric-only and be easier to implement in practice. This requires further investigation.
-
Combining exercise with other therapies such as electro-therapy, injections and kinetics may be more effective than exercise in isolation. It is common for exercise to be the first line and then for additional modalities to be added in recalcitrant cases. Models that include multiple modalities earlier in the therapeutic process could be considered; however, further research, including longer-term follow-ups, is required.
-
In order for the benefits of effective exercise therapy interventions to be realised, clinicians should adopt an individualised, person-centred approach to prescribing exercise therapy. Building a strong therapeutic alliance between patient and healthcare provider is vital, as is the provision of appropriate and meaningful education on tendinopathy and its management, to promote the confidence and motivation required for adherence to and fidelity with exercise therapy interventions and particularly for self-management.
Recommendations for research
Outcome measurement and transparent reporting
-
Reporting needs to be greatly enhanced in studies of exercise therapy for tendinopathy. This includes increased use of reporting checklists such as CONSORT,206 TIDieR55 or CERT207; full and transparent reporting of all outcomes collected (primary, secondary, acceptability); full reporting of participant characteristics and analyses by relevant subgroups (e.g. age, gender, activity level, comorbidities). Detailed reporting of exercise intervention details, particularly where dose can be effectively quantified (e.g. absolute and relative loads), will facilitate greater consistency across future studies and enable dose-response meta-analyses to be more precise. This is essential for translation to clinical practice, with implementation science approaches needed to bridge the research–practice gap. Further development and validation of our proposed outline reporting guidance of exercise for tendinopathy as a comprehensive taxonomy would greatly assist in enhancing reporting, allowing for future comparisons and evidence syntheses.
-
Use of standardised outcome measures that are fully and transparently reported would facilitate future meta-analyses. The observed reduction in QoL in some studies requires further exploration, but an overall measure of well-being and potentially the influence of tendinopathy on an individual’s well-being should be routinely collected in research.
-
Quantification of adherence suggests that it is relatively high, which contrasts with qualitative findings on barriers to adherence and with feedback obtained in stakeholder workshops. A clear definition of adherence needs to be agreed and methods to reliably measure it developed, so that future studies are not reliant on self-report alone.
-
Fidelity to exercise therapy is rarely measured. Whilst adherence may be reasonable, if fidelity is low, particularly with regard to the intensity of activity, exercise therapies are unlikely to be as effective as they can be, synthesised across studies or understandable in terms of biological mechanisms. This should be measured and reported more accurately, and methods for promoting and measuring fidelity are worthy research goals.
Intervention development
-
Exercise therapy interventions should be carefully developed and tested, including establishing feasibility and acceptability, prior to moving to studies of efficacy and effectiveness.
High-quality primary research
-
There is sufficient research to demonstrate the efficacy of exercise therapy. There is still a need for high-quality adequately powered research to continue to better identify the dose parameters and their interactions with patient characteristics to identify best-practice approaches.
-
There is a need for increased true effectiveness studies such as pragmatic trials to better quantify the effectiveness of current and developing therapeutic models.
-
There is a need for increased cost-effectiveness research which may also investigate models that include multiple modalities earlier in the therapeutic process.
-
Further high-quality qualitative research exploring patients’ and healthcare professionals’ perceptions and experiences of exercise for tendinopathy would add to the small body of qualitative work reported here, allowing a greater depth of understanding of the factors that impact on efficacy of exercise therapy and implementation in the real-world clinical setting.
-
Further research may be required to identify why clinicians and researchers are tending to use low-intensity and high-frequency resistance exercise and to explore any barriers from the patient perspective. 55,206,207
Recommendations for policy
-
Research funders and providers of services need to fund and facilitate research within different care settings (including remote and group) to enable cost-effectiveness, acceptability and adherence comparisons between different modes of delivery of exercise therapy interventions for tendinopathy.
-
Service provision may need to be adapted and funded to allow a person-centred approach to care and access to additional non-exercise treatment modalities when appropriate. This could include the need for extended periods of intervention to be available in order that the timescales of physiological tendon change are reflected in interventions.
-
The use of technologies which can facilitate better patient engagement with treatments and more consistent self-reporting of adherence, outcomes and side effects should be explored.
Conclusion
This comprehensive, robust, inclusive mixed-methods evidence synthesis has provided an extensive map of the contemporary research on exercise for tendinopathy, evaluated the efficacy of exercise across the common tendinopathies and identified what is known about the feasibility and acceptability of exercise for tendinopathy from patients’ and providers’ perspectives.
Analysing the results of 555 studies has shown that reporting of exercise therapy in tendinopathy studies needs to improve. The use of common terminology, definitions, outcome sets and reporting guidance is imperative for high-quality evidence to be produced in order for conclusions to be drawn on effectiveness of specific exercise interventions for specific tendinopathies.
It is clear that there is little value in the accumulation of tentative findings from further low-quality studies and instead there is an urgent need for high-quality research that addresses clinical and cost effectiveness. There remains a need for detailed work on mechanisms explaining symptomatic and biological response.
Nonetheless, the findings of this comprehensive set of reviews support the use of exercise therapy combined with non-exercise adjuncts across tendinopathies, the use of flexibility and proprioception exercise for RCRSP, and combining eccentric and concentric exercise in resistance programmes. The findings show that exercise therapy is safe and efficacious across tendinopathies, and that patients are typically satisfied with the delivery and related outcomes. However, these outcomes need further improvement and research to address the identified deficits in the evidence-base. The findings also show that patient and healthcare provider beliefs and prior experience need to be considered, as do barriers and facilitators to engaging with exercise, and the importance of patient education, self-management and the patient–healthcare professional relationship.
Acknowledgements
The review team would like to thank the following people for their support of this project.
The members of our project steering committee for their oversight of the project and expert guidance on methodological and clinical issues:
-
Jo Leonardi Bee (chair), Professor, Division of Epidemiology and Public Health, Faculty of Medicine and Health Sciences, University of Nottingham
-
Morag Andrew, Patient and Public Representative
-
Lorenzo Masci, Sport and Exercise Medicine Consultant, London
-
Seth O’Neill, Associate Professor of Physiotherapy, School of Allied Health Professions, University of Leicester
The stakeholders who contributed to our project management group, supporting the review team throughout the project:
-
Morag Andrew, Patient and Public Representative
-
Catherine Webber, Musculoskeletal Physiotherapist, NHS Grampian
The people with lived experience of receiving or providing exercise therapy for tendinopathy who took part in the stakeholder workshops and online survey for their useful feedback.
The tendinopathy researchers for reviewing the list of systematic reviews identified during the scoping review in order to identify any gaps.
Those individuals who assisted with translation of non-English studies.
Contributions of authors
Kay Cooper (https://orcid.org/0000-0001-9958-2511) (Clinical Professor Allied Health Professions) was the chief investigator, led the mixed-method review and contributed to all phases of the project.
Lyndsay Alexander (https://orcid.org/0000-0003-2437-9150) (Academic Team Lead Research) was a co-applicant, led the conduct of the scoping review and stakeholder workshops and contributed to all phases of the project
David Brandie (https://orcid.org/0000-0003-3624-4130) (Head of Physiotherapy) was a co-applicant, supported recruitment of workshop participants and contributed to all phases of the project
Victoria Tzortziou Brown (https://orcid.org/0000-0001-9819-6395) (Academic GP, Research Lead, Honorary Professor) contributed clinical expertise to all phases of the project and final report
Leon Greig (https://orcid.org/0000-0002-0332-943X) (Research Assistant) supported the conduct of the scoping, effectiveness and mixed-method reviews
Isabelle Harrison (https://orcid.org/0000-0002-0019-6096) (Research Assistant) supported the conduct of the scoping review
Colin Maclean (https://orcid.org/0000-0002-4399-8750) (Liaison librarian) was a co-applicant, and led the development of the search strategies and literature-searching process for the scoping, effectiveness and mixed-method reviews
Laura Mitchell (https://orcid.org/0000-0003-4669-9657) (Senior Physiotherapist) was a co-applicant, supported recruitment of workshop participants and contributed to all phases of the project
Dylan Morrissey (https://orcid.org/0000-0001-7045-3644) (Clinical Professor and Consultant Physiotherapist) was a co-applicant, supported recruitment of workshop participants and contributed to all phases of the project
Rachel Moss (https://orcid.org/0000-0003-4634-2367) (Research Fellow) supported the conduct of the scoping, effectiveness and mixed-method reviews
Eva Parkinson (https://orcid.org/0000-0002-4298-4285) (Research Assistant) supported the conduct of the scoping, effectiveness and mixed-method reviews
Anastasia Pavlova (https://orcid.org/0000-0002-1633-3411) (Research Fellow) was a co-applicant and contributed to the effectiveness and mixed-method reviews
Joanna Shim (https://orcid.org/0000-0001-9438-9640) (Research Fellow) contributed to the conduct of the scoping, effectiveness and mixed-method reviews
Paul Alan Swinton (https://orcid.org/0000-0001-9663-0696) (Reader in Applied Statistics) was a co-applicant, led the conduct of the effectiveness reviews, the quantitative syntheses in the mixed-method review, and contributed to the scoping review
All authors contributed to the overall project, interpretation of findings, drafting, revising and approving the final report. All co-applicants were involved in conceiving and designing the project.
Publications
Alexander LA, Morrissey D, Swinton P, Maclean C, Harrison I, Cooper K. Exercise therapy for the treatment of tendinopathies: a scoping review protocol. JBI evidence synthesis 2021;19(7):1713–9. https://doi.org/10.11124/JBIES-20-00175
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Ethics statement
Ethical approval was not required due to this project being literature-based, with members of the public and healthcare professionals involved in stakeholder engagement and not research activity.
Disclaimers
This report presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HTA programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HTA programme or the Department of Health and Social Care.
References
- Millar NL, Silbernagel KG, Thorborg K, Kirwan PD, Galatz LM, Abrams GD, et al. Tendinopathy. Nat Rev Dis Primers 2021;1. https://doi.org/10.1038/s41572-020-00234-1.
- Fu FH, Wang J–c, Rothrauff BB. Best practice tendinopathy [Internet]. BMJ 2019;2019.
- Riel H, Lindstrøm CF, Rathleff MS, Jensen MB, Olesen JL. Prevalence and incidence rate of lower–extremity tendinopathies in a Danish general practice: a registry–based study. BMC Musculoskelet Disord 2019;20. https://doi.org/10.1186/s12891-019-2629-6.
- Albers IS, Zwerver J, Diercks RL, Dekker JH, Van den Akker–Scheek I. Incidence and prevalence of lower extremity tendinopathy in a Dutch general practice population: a cross sectional study. BMC Musculoskelet Disord 2016;17.
- de Jonge S, van den Berg C, de Vos RJ, van der Heide HJ, Weir A, Verhaar JA, et al. Incidence of midportion Achilles tendinopathy in the general population. Br J Sports Med 2011;45:1026-8. https://doi.org/10.1136/bjsports-2011-090342.
- Shiri R. Prevalence and determinants of lateral and medial epicondylitis: a population study. Am J Epidemiol 2006;164:1065-74.
- Littlewood C, May S, Walters S. Epidemiology of rotator cuff tendinopathy: a systematic review. Shoulder Elbow 2013;5:256-65.
- Abat F, Alfredson H, Cucciarini M, Madry H, Marmott A, Mouton C, et al. Current trends in tendinopathy: consensus of the ESSKA basic science committee. Part I: biology, biomechanics, anatomy and an exercise-based approach. J Exp Orthop 2017;4.
- Bohm S, Mersmann F, Arampatzis A. Human tendon adaptation in response to mechanical loading: a systematic review and meta-analysis of exercise intervention studies on healthy adults. Sports Med Open 2015;1. https://doi.org/10.1186/s40798-015-0009-9.
- Cook JL, Malliaras P, De Luca J, Ptasznik R, Morris ME, Goldie P. Neovascularization and pain in abnormal patellar tendons of active jumping athletes. Clin J Sport Med 2004;14.
- Rowe V, Hemmings S, Barton C, Malliaras P, Maffulli N, Morrissey D. Conservative management of midportion Achilles tendinopathy: a mixed methods study, integrating systematic review and clinical reasoning. Sports Med (Auckland, NZ) 2012;42:941-67. https://doi.org/10.2165/11635410-000000000-00000.
- Lim HY, Wong SH. Effects of isometric, eccentric, or heavy slow resistance exercises on pain and function in individuals with patellar tendinopathy: a systematic review. Physiother Res Int 2018;23.
- Couppé C, Svensson RB, Silbernagel KG, Langberg H, Magnusson SP. Eccentric or concentric exercises for the treatment of tendinopathies?. J Orthop Sports Phys Ther 2015;45:853-63. https://doi.org/10.2519/jospt.2015.5910.
- Toigo M, Boutellier U. New fundamental resistance exercise determinants of molecular and cellular muscle adaptations. Eur J Appl Physiol 2006;97:643-63. https://doi.org/10.1007/s00421-006-0238-1.
- Dimitrios S. Exercise for tendinopathy. World J Methodol 2015;5:51-4.
- Horstmann T, Jud H, Fröhlich V, Mündermann A, Grau S. Whole-body vibration versus eccentric training or a wait-and-see approach for chronic Achilles tendinopathy: a randomized clinical trial. J Orthop Sports Phys Ther 2013;43:794-803. https://doi.org/10.2519/jospt.2013.4762.
- Alfredson H, Pietilä T, Jonsson P, Lorentzon R. Heavy-load eccentric calf muscle training for the treatment of chronic Achilles tendinosis. Am J Sports Med 1998;26:360-6.
- Beyer R, Kongsgaard M, Hougs Kjær B, Øhlenschlæger T, Kjær M, Magnusson SP. Heavy slow resistance versus eccentric training as treatment for Achilles tendinopathy: a randomized controlled trial. Am J Sports Med 2015;43:1704-11.
- Stanish WD, Curwin S, Mandell S. Tendinitis: Its Etiology and Treatment. Oxford University Press; 2000.
- Mellor R, Grimaldi A, Wajswelner H, Hodges P, Abbott JA-O, Bennell K, et al. Exercise and load modification versus corticosteroid injection versus ‘wait and see’ for persistent gluteus medius/minimus tendinopathy (the LEAP trial): a protocol for a randomised clinical trial. BMC Musculoskelet Disord 2016;17. https://doi.org/10.1186/s12891-016-1043-6.
- Kongsgaard M, Kovanen V, Aagaard P, Doessing S, Hansen P, Laursen AH, et al. Corticosteroid injections, eccentric decline squat training and heavy slow resistance training in patellar tendinopathy. Scand J Med Sci Sports 2009;19:790-802.
- Young JL, Rhon DI, Cleland JA, Snodgrass SJ. The influence of exercise dosing on outcomes in patients with knee disorders: a systematic review [with consumer summary]. J Orthop Sports Phys Ther 2018;48:146-61.
- Littlewood C, Malliaras P, Chance-Larsen K. Therapeutic exercise for rotator cuff tendinopathy: a systematic review of contextual factors and prescription parameters. Int J Rehabil Res 2015;38:95-106.
- Meyer A, Tumilty S, Baxter GD. Eccentric exercise protocols for chronic non-insertional Achilles tendinopathy: how much is enough?. Scand J Med Sci Sports 2009;19. https://doi.org/10.1111/j.1600-0838.2009.00981.x.
- Ager AL, Roy JS, Gamache F, Hébert LJ. The effectiveness of an upper extremity neuromuscular training program on the shoulder function of military members with a rotator cuff tendinopathy: a pilot randomized controlled trial. Mil Med 2019;184:e385-93. https://doi.org/10.1093/milmed/usy294.
- Worsley P, Warner M, Mottram S, Gadola S, Veeger HEJ, Hermens H, et al. Motor control retraining exercises for shoulder impingement: effects on function, muscle activation, and biomechanics in young adults. J Shoulder Elbow Surg 2013;22:e11-19. https://doi.org/10.1016/j.jse.2012.06.010.
- Mani-Babu S, Morrissey D, Waugh C, Screen H, Barton C. The effectiveness of extracorporeal shock wave therapy in lower limb tendinopathy: a systematic review. Am J Sports Med 2015;43:752-61.
- Haslerud S, Magnussen LH, Joensen J, Lopes-Martins R, Bjordal JM. The efficacy of low-level laser therapy for shoulder tendinopathy: a systematic review and meta-analysis of randomized controlled trials. Physiother Res Int 2015;20:108-25.
- Sussman WI, Mautner K, Malanga G. The role of rehabilitation after regenerative and orthobiologic procedures for the treatment of tendinopathy: a systematic review. Regen Med 2018;13:249-63.
- Mellor R, Bennell K, Grimaldi A, Nicolson P, Kasza J, Hodges P, et al. Education plus exercise versus corticosteroid injection use versus a wait and see approach on global outcome and pain from gluteal tendinopathy: prospective, single blinded, randomised clinical trial. Br J Sports Med 2018;52:1464-72. https://doi.org/10.1136/bjsports-2018-k1662rep.
- Beedie C, Mann S, Jimenez A, Kennedy L, Lane AM, Domone S, et al. Death by effectiveness: exercise as medicine caught in the efficacy trap!. Sports Med 2015;50:323-4. https://doi.org/doi:10.1136/bjsports-2014-094389.
- Singal AG, Higgins PDR, Waljee AK. A primer on effectiveness and efficacy trials. Clin Transl Gastroenterol 2014;5. https://doi.org/doi:10.1038/ctg.2013.13.
- Ford I, Norrie J. Pragmatic trials. N Engl J Med 2016;375:454-63. https://doi.org/10.1056/NEJMra1510059.
- Littlewood C, Bateman M, Brown K, Bury J, Mawson S, May S, et al. A self-managed single exercise programme versus usual physiotherapy treatment for rotator cuff tendinopathy: a randomised controlled trial (the SELF study). Clin Rehabil 2016;30:686-96. https://doi.org/10.1177/0269215515593784.
- Littlewood C, Ashton J, Chance-Larsen K, May S, Sturrock B. Exercise for rotator cuff tendinopathy: a systematic review. Physiotherapy 2012;98:101-9.
- Pollock A, Campbell P, Struthers C, Synnot A, Nunn J, Hill S, et al. Stakeholder involvement in systematic reviews: a protocol for a systematic review of methods, outcomes and effects. Res Involv Engagem 2017;3. https://doi.org/10.1186/s40900-017-0060-4.
- Cooper K, Pavlova A, Greig L, Swinton P, Kirkpatrick P, Mitchelhill F, et al. Health technologies for the prevention and detection of falls in adult hospital inpatients: a scoping review. JBI Evid Synth 2021;19:2478-658. https://doi.org/10.11124/JBIES-20-00114.
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372. https://doi.org/10.1136/bmj.n71.
- Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 2018;169:467-73. https://doi.org/10.7326/M18-0850.
- Lewis J. Rotator cuff related shoulder pain: assessment, management and uncertainties. Man Ther 2016;23:57-68.
- Requejo-Salinas N, Lewis J, Michener LA, La Touche R, Fernández-Matías R, Tercero-Lucas J, et al. International physical therapists consensus on clinical descriptors for diagnosing rotator cuff related shoulder pain: a Delphi study. Braz J Phys Ther 2022;26. https://doi.org/10.1016/j.bjpt.2022.100395.
- Kukkonen J, Joukainen A, Lehtinen J, Mattila KT, Tuominen EK, Kauko T, et al. Treatment of nontraumatic rotator cuff tears: a randomized controlled trial with two years of clinical and imaging follow-up. J Bone Joint Surg Am 2015;97:1729-37. https://doi.org/10.2106/jbjs.N.01051.
- Haahr JP, Andersen JH. Exercises may be as efficient as subacromial decompression in patients with subacromial stage II impingement: 4-8-years’ follow-up in a prospective, randomized study. Scand J Rheumatol 2006;35:224-8.
- Dejaco B, Habets B, van Loon C, van Grinsven S, van Cingel R. Eccentric versus conventional exercise therapy in patients with rotator cuff tendinopathy: a randomized, single blinded, clinical trial. Knee Surg Sports Traumatol Arthrosc 2017;25:2051-9.
- Morrissey D, Cotchett M, Said J’Bari A, Prior T, Griffiths IB, Rathleff MS, et al. Management of plantar heel pain: a best practice guide informed by a systematic review, expert clinical reasoning and patient values. Br J Sports Med 2021;55:1106-18. https://doi.org/10.1136/bjsports-2019-101970.
- World Health Organization . Physical Activity 2021.
- Pollock A, Campbell P, Synnot A, Smith M, Morley R. Patient and Public Involvement in Systematic Reviews. In GIN Public Toolkit: Patient and Public Involvement in Guidelines 2021. https://g-i-n.net/new-digital-gin-public-toolkit-patient-and-public-involvement-in-guidelines/ (accessed 6 January 2021).
- Pollock A, Campbell P, Struthers C, Synnot A, Nunn J, Hill S, et al. Development of the ACTIVE framework ro describe stakeholder involvement in systematic reviews. J Health Serv Res Policy 2019;24:245-55.
- Staniszewska S, Brett J, Simera I, Seers K, Mockford C, Goodlad S, et al. GRIPP2 reporting checklists: tools to improve reporting of patient and public involvement in research. Res Involv Engagem 2017;3. https://doi.org/10.1186/s40900-017-0062-2.
- Peters M, Godfrey C, McInerney P, Munn Z, Tricco AC, Khalil H. Chapter 11: Scoping Reviews. JBI: Joanna Briggs Institute Reviewer’s Manual; 2020.
- Alexander LA, Morrissey D, Swinton P, Maclean C, Harrison I, Cooper K. Exercise therapy for the treatment of tendinopathies: a scoping review protocol. JBI Evid Synth 2021;19:1713-9. https://doi.org/10.11124/JBIES-20-00175.
- Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol 2005;8:19-32. https://doi.org/10.1080/1364557032000119616.
- Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci 2010;5. https://doi.org/10.1186/1748-5908-5-69.
- Program UND . Human Development Reports [Internet] 2020.
- Hoffmann T, Glasziou P, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;348. https://doi.org/10.1136/bmj.g1687.
- Vincenzino B, de Vos RJ, Alfredson H, Bahr R, Cook JL, Coombes BK, et al. ICON 2019—International Scientific Tendinopathy Symposium Consensus: there are nine core health-related domains for tendinopathy (CORE DOMAINS): Delphi study of healthcare professionals and patients. Br J Sports Med 2019;54:444-51.
- Team RC . R: A Language and Environment for Statistical Computing 2021. www.R-project.org/.
- Aria M, Cuccurullo C. bibliometrix: an R-tool for comprehensive science mapping analysis. J Informetr 2017;11:959-75. https://doi.org/10.1016/j.joi.2017.08.007.
- De Vos RJ, Weir A, Visser RJA, de Winter T, Tol JL. The additional value of a night splint to eccentric exercises in chronic midportion Achilles tendinopathy: a randomised controlled trial. Br J Sports Med 2007;41.
- de Jonge S, de Vos RJ, Weir A, van Schie HT, Bierma-Zeinstra SM, Verhaar JA, et al. One-year follow-up of platelet-rich plasma treatment in chronic Achilles tendinopathy: a double-blind randomized placebo-controlled trial. Am J Sports Med 2011;39:1623-30. https://doi.org/10.1177/0363546511404877.
- Malliaras P, Barton CJ, Reeves ND, Langberg H. Achilles and patellar tendinopathy loading programmes: a systematic review comparing clinical outcomes and identifying potential mechanisms for effectiveness. Sports Med 2013;43:267-86. https://doi.org/10.1007/s40279-013-0019-z.
- Thanasas C, Papadimitriou G, Charalambidis C, Paraskevopoulos I, Papanikolaou A. Platelet-rich plasma versus autologous whole blood for the treatment of chronic lateral elbow epicondylitis: a randomized controlled clinical trial. Am J Sports Med 2011;39:2130-4. https://doi.org/10.1177/0363546511417113.
- Irby A, Gutierrez J, Chamberlin C, Thomas SJ, Rosen AB. Clinical management of tendinopathy: a systematic review of systematic reviews evaluating the effectiveness of tendinopathy treatments. Scand J Med Sci Sports 2020;30:1810-26. https://doi.org/10.1111/sms.13734.
- Clausen MB, Merrild MB, Holm K, Pedersen MW, Andersen LL, Zebis MK, et al. Less than half of patients in secondary care adheres to clinical guidelines for subacromial pain syndrome and have acceptable symptoms after treatment: a Danish nationwide cohort study of 3306 patients. Musculoskelet Sci Pract 2021;52. https://doi.org/10.1016/j.msksp.2021.102322.
- Naunton J, Street G, Littlewood C, Haines T, Malliaras P. Effectiveness of progressive and resisted and non-progressive or non-resisted exercise in rotator cuff related shoulder pain: a systematic review and meta-analysis of randomized controlled trials. Clin Rehabil 2020;34:1198-216. https://doi.org/10.1177/0269215520934147.
- Winters M, Holden S, Lura CB, Welton NJ, Caldwell DM, Vicenzino BT, et al. Comparative effectiveness of treatments for patellofemoral pain: a living systematic review with network meta-analysis. Br J Sports Med 2021;55:369-77. https://doi.org/10.1136/bjsports-2020-102819.
- Major DH, Røe Y, Grotle M, Jessup RL, Farmer C, Småstuen MC, et al. Content reporting of exercise interventions in rotator cuff disease trials: results from application of the Consensus on Exercise Reporting Template (CERT). BMJ Open Sport Exerc Med 2019;5. https://doi.org/10.1136/bmjsem-2019-000656.
- Sluijs EM, Kok GJ, van der Zee J. Correlates of exercise compliance in physical therapy. Phys Ther 1993;73:771-82. https://doi.org/10.1093/ptj/73.11.771.
- Thompson EL, Broadbent J, Bertino MD, Staiger PK. Do pain-related beliefs influence adherence to multidisciplinary rehabilitation?: a systematic review. Clin J Pain 2016;32:164-78. https://doi.org/10.1097/AJP.0000000000000235.
- Burne G, Mansfield M, Gaida JE, Lewis JS. Is there an association between metabolic syndrome and rotator cuff-related shoulder pain? A systematic review. BMJ Open Sport Exerc Med 2019;5. https://doi.org/10.1136/bmjsem-2019-000544.
- Karanasios S, Korakakis V, Whiteley R, Vasilogeorgis I, Woodbridge S, Gioftsos G. Exercise interventions in lateral elbow tendinopathy have better outcomes than passive interventions, but the effects are small: a systematic review and meta-analysis of 2123 subjects in 30 trials. Br J Sports Med 2021;55:477-85. https://doi.org/10.1136/bjsports-2020-102525.
- Clifford C, Challoumas D, Paul L, Syme G, Millar NL. Effectiveness of isometric exercise in the management of tendinopathy: a systematic review and meta-analysis of randomised trials. BMJ Open Sport Exerc Med 2020;6. https://doi.org/10.1136/bmjsem-2020-000760.
- Rio EK, Mc Auliffe S, Kuipers I, Girdwood M, Alfredson H, Bahr R, et al. ICON PART-T 2019-International Scientific Tendinopathy Symposium Consensus: recommended standards for reporting participant characteristics in tendinopathy research (PART-T). Br J Sports Med 2020;54:627-30. https://doi.org/10.1136/bjsports-2019-100957.
- Bateman M, Evans JP, Vuvan V, Jones V, Watts AC, Phadnis J, et al. Protocol for the development of a core outcome set for lateral elbow tendinopathy (COS-LET). Trials 2021;22. https://doi.org/10.1186/s13063-021-05291-9.
- Grimaldi A, Fearon A, Fitzpatrick J, Ladurner A, Mellow R, Vincenzino B. Development of a Core Outcome Set for Clinical Trials in Greater Trochanteric Pain Syndrome (Gluteal Tendinopathy): A Scoping Review and a Delphi Study of Healthcare Professionals and Patients 2021. www.comet-initiative.org/Studies/Details/1468 (accessed 6 January 2021).
- Silbernagel KG, de Vos R, Malliaras P, Vicenzino B. Development of a Core Outcome Set for Clinical Trials in Achilles Tendinopathy 2020. www.comet-initiative.org/Studies/Details/1323 (accessed 6 January 2021).
- Nasser A, Semciw A, Vincenzino B, Grimaldi A, Pizzari T, Rio E. Core outcome set development for proximal hamstring tendinopathy (COS-PHT): a study protocol. Phys Ther Rev 2022. https://doi.org/10.1080/10833196.2022.2077066.
- Ramiro S, Page MJ, Whittle SL, Huang H, Verhagen AP, Beaton DE, et al. The OMERACT core domain set for clinical trials of shoulder disorders. J Rheumatol 2019;46:969-75. https://doi.org/10.3899/jrheum.181070.
- Plinsinga ML, Coombes BK, Mellor R, Nicolson P, Grimaldi A, Hodges P, et al. Psychological factors not strength deficits are associated with severity of gluteal tendinopathy: a cross-sectional study. Eur J Pain 2018;22:1124-33. https://doi.org/10.1002/ejp.1199.
- Lewis R, Gómez Álvarez CB, Rayman M, Lanham-New S, Woolf A, Mobasheri A. Strategies for optimising musculoskeletal health in the 21st century. BMC Musculoskelet Disord 2019;20. https://doi.org/10.1186/s12891-019-2510-7.
- Turner J, Malliaras P, Goulis J, Mc Auliffe S. ‘It’s disappointing and it’s pretty frustrating, because it feels like it’s something that will never go away’. A qualitative study exploring individuals’ beliefs and experiences of Achilles tendinopathy. PLOS ONE 2020;15. https://doi.org/10.1371/journal.pone.0233459.
- McAuliffe S, O’Sullivan K, Whiteley R, Korakakis V. Why do tendon researchers overlook the patient’s psychological state? The review with no papers. Br J Sports Med 2021;55:244-5. https://doi.org/10.1136/bjsports-2020-102359.
- Robinson T, Bailey C, Morris H, Burns P, Melder A, Croft C, et al. Bridging the research–practice gap in healthcare: a rapid review of research translation centres in England and Australia. Health Res Policy Syst 2020;18. https://doi.org/10.1186/s12961-020-00621-w.
- Wasfy MM, Baggish AL. Exercise dose in clinical practice. Circulation 2016;133:2297-313. https://doi.org/10.1161/CIRCULATIONAHA.116.018093.
- Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011;343. https://doi.org/10.1136/bmj.d5928.
- Challoumas D, Millar NL. Risk of bias in systematic reviews of tendinopathy management: are we comparing apples with oranges?. Transl Sports Med 2021;4:21-37. https://doi.org/10.1002/tsm2.196.
- Marshall IJ, Kuiper J, Wallace BC. RobotReviewer: evaluation of a system for automatically assessing bias in clinical trials. J Am Med Inform Assoc 2016;23:193-201.
- Schünemann HJ, Mustafa RA, Brozek J, Steingart KR, Leeflang M, Murad MH, et al. GRADE guidelines: 21 part 1. Study design, risk of bias, and indirectness in rating the certainty across a body of evidence for test accuracy. J Clin Epidemiol 2020;122:129-41. https://doi.org/10.1016/j.jclinepi.2019.12.020.
- Schünemann HJ, Mustafa RA, Brozek J, Steingart KR, Leeflang M, Murad MH, et al. GRADE guidelines: 21 part 2. Test accuracy: inconsistency, imprecision, publication bias, and other domains for rating the certainty of evidence and presenting it in evidence profiles and summary of findings tables. J Clin Epidemiol 2020;122:142-52. https://doi.org/10.1016/j.jclinepi.2019.12.021.
- Challoumas D, Millar NL. Do we need to improve the reporting of evidence in tendinopathy management? A critical appraisal of systematic reviews with recommendations on strength of evidence assessment. BMJ Open Sp Ex Med 2021;7. https://doi.org/10.1136/bmjsem-2020-000920.
- Kruschke JK, Liddell TM. The Bayesian New Statistics: Hypothesis testing, estimation, meta-analysis, and power analysis from a Bayesian perspective. Psychon Bull Rev 2017;25:178-206. https://doi.org/10.3758/s13423-016-1221-4.
- Bürkner PC. brms: an R package for bayesian multilevel models using stan. J Stat Softw 2017;80.
- Gelman A, Carlin JB, Stern HS, Rubin DB. Bayesian Data Analysis. Chapman and Hall/CRC; 1995.
- Morris SB, DeShon RP. Combining effect size estimates in meta-analysis with repeated measures and independent-groups designs. Psychol Methods 2002;7.
- Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 2014;14. https://doi.org/10.1186/1471-2288-14-135.
- Marinho VC, Higgins JP, Sheiham A, Logan S. Fluoride toothpastes for preventing dental caries in children and adolescents. Cochrane Database Syst Rev 2003;1.
- Swinton P, Burgess K, Hall A, Greig L, Psyllas J, Aspe R, et al. A Bayesian approach to interpret intervention effectiveness in strength and conditioning Part 1: a meta-analysis to derive context-specific thresholds. SportRxiv PrePrint 2021. https://doi.org/10.51224/SRXIV.9.
- Swinton P, Burgess K, Hall A, Greig L, Psyllas J, Aspe R, et al. A Bayesian approach to interpret intervention effectiveness in strength and conditioning part 2: effect size selection and application of Bayesian updating. SportRxiv PrePrint 2021. https://doi.org/10.51224/SRXIV.11.
- Verardi V, Vermandele C. Univariate and multivariate outlier identification for skewed or heavy-tailed distributions. Stata J 2018;18:517-32. https://doi.org/10.1177/1536867X1801800303.
- Wang N. How to Conduct a Meta-Analysis of Proportions in R: A Comprehensive Tutorial 2018. https://doi.org/10.13140/RG.2.2.27199.00161.
- Welton NJ, Sutton AJ, Cooper N, Abrams KR, Ades AE. Evidence Synthesis for Decision Making in Healthcare. John Wiley & Sons; 2012.
- Gelman A. Prior distributions for variance parameters in hierarchical models (comment on article by Browne and Draper). Bayesian Anal 2006;1:515-34.
- Alexander LA, Harrison I, Moss RA, Greig L, Shim J, Pavlova AV, et al. Exercise therapy for tendinopathy: a scoping review mapping interventions and outcomes. SportRχiv 2021.
- Awick EA, Wójcicki TR, Olson EA, Fanning J, Chung HD, Zuniga K, et al. Differential exercise effects on quality of life and health-related quality of life in older adults: a randomized controlled trial. Qual Life Res 2015;24:455-62. https://doi.org/10.1007/s11136-014-0762-0.
- Van der Plas A, de Jonge S, de Vos R-J, Van Der Heide HJL, Verhaar JAN, Weir A, et al. A 5-year follow-up study of Alfredson’s heel-drop exercise programme in chronic midportion Achilles tendinopathy. Br J Sports Med 2012;46:214-8.
- Voleti PB, Buckley MR, Soslowsky LJ. Tendon healing: repair and regeneration. Ann Rev Biomed Eng 2012;14:47-71. https://doi.org/10.1146/annurev-bioeng-071811-150122.
- Littlewood C, Mawson S, May S, Walters S. Understanding the barriers and enablers to implementation of a self-managed exercise intervention: a qualitative study. Physiotherapy 2015;101:279-85.
- Major DH, Grotle M, Littlewood C, Brox JI, Matre D, Gallet HV, et al. Adherence to self-managed exercises for patients with persistent subacromial pain: the Ad-Shoulder feasibility study. Pilot Feasibility Stud 2021;31. https://doi.org/10.1186/s40814-021-00767-6.
- Roddy E, Ogollah RO, Oppong R, Zwierska I, Datta P, Hall A, et al. Optimising outcomes of exercise and corticosteroid injection in patients with subacromial pain (impingement) syndrome: a factorial randomised trial. Br J Sports Med 2021;55. https://doi.org/10.1136/bjsports-2019-101268.
- Smith MJ, Choma TJ. Patient satisfaction in musculoskeletal medicine. Curr Rev Musculoskelet Med 2017;10:207-11. https://doi.org/10.1007/s12178-017-9403-x.
- Batbaatar E, Dorjdagva J, Luvsannyam A, Savino MM, Amenta P. Determinants of patient satisfaction: a systematic review. Perspect Public Health 2017;137:89-101. https://doi.org/10.1177/1757913916634136.
- Allison GT, Purdam C. Eccentric loading for Achilles tendinopathy – strengthening or stretching?. Br J Sports Med 2009;43:276-9. https://doi.org/10.1136/bjsm.2008.053546.
- Brumitt J, Cuddeford T. Current concepts of muscle and tendon adaptation to strength and conditioning. Int J Sports Phys Ther 2015;10:748-59.
- ter Veer E, van Oijen MGH, van Laarhoven HWM. The use of (network) meta-analysis in clinical oncology. Front Oncol 2019;9. https://doi.org/10.3389/fonc.2019.00822.
- Dakin HA, Welton NJ, Ades AE, Collins S, Orme M, Kelly S. Mixed treatment comparison of repeated measurements of a continuous endpoint: an example using topical treatments for primary open-angle glaucoma and ocular hypertension. Stat Med 2011;30:2511-35. https://doi.org/10.1002/sim.4284.
- Fu R, Gartlehner G, Grant M, Shamliyan T, Sedrakyan A, Wilt TJ, et al. Conducting quantitative synthesis when comparing medical interventions: AHRQ and the effective health care program. BTI - methods guide for effectiveness and comparative effectiveness reviews. J Clin Epidemiol 2011;64:1187-97.
- Salanti G, Ades AE, Ioannidis JP. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J Clin Epidemiol 2011;64:163-71. https://doi.org/10.1016/j.jclinepi.2010.03.016.
- Kibler WB, Ludewig PM, McClure PW, Michener LA, Bak K, Sciascia AD. Clinical implications of scapular dyskinesis in shoulder injury: the 2013 consensus statement from the ‘scapular summit’. Br J Sports Med 2013;47:877-85. https://doi.org/10.1136/bjsports-2013-092425.
- Ellenbecker TS, Cools A. Rehabilitation of shoulder impingement syndrome and rotator cuff injuries: an evidence-based review. Br J Sports Med 2010;44:319-27. https://doi.org/10.1136/bjsm.2009.058875.
- Lincolnshire Community Health Services NHST . Lincs Physio Service Exercises for Shoulder Impingement Pain n.d. www.lincsphysio.nhs.uk/application/files/1815/9472/1047/Exercises_for_shoulder_impingement.pdf (accessed 6 January 2021).
- Department CP . Self Help for Shoulder Impingement Information for Patients 2018. www.mcht.nhs.uk/EasysiteWeb/getresource.axd?AssetID = 22310&type = full&servicetype = Attachment (accessed 6 January 2021).
- East Lancashire Hospitals NHST . Shoulder Impingement Syndrome (Pinching of the Shoulder When Lifting the Arm) Information and Exercise Leaflet for Patient’s and Carers. Integrated Musculoskeletal Service Physiotherapy Department 2018. https://elht.nhs.uk/application/files/9515/2293/8413/Shoulder_Impingement_Syndrome_-_Patient__Information_and_Exercises_-_PHYSIO_001.pdf (accessed 6 January 2021).
- Lewis JS. Rotator cuff tendinopathy. Br J Sports Med 2009;43:236-41. https://doi.org/10.1136/bjsm.2008.052175.
- Seitz AL, McClure PW, Finucane S, Boardman ND, Michener LA. Mechanisms of rotator cuff tendinopathy: intrinsic, extrinsic, or both?. Clin Biomech 2011;26:1-12. https://doi.org/10.1016/j.clinbiomech.2010.08.001.
- Toliopoulos P, Desmeules F, Boudreault J, Roy J, Frémont P, MacDermid J, et al. Efficacy of surgery for rotator cuff tendinopathy: a systematic review. Clin Rheumatol 2014;33:1373-83. https://doi.org/10.1007/s10067-014-2563-9.
- Lewis JS. Rotator cuff tendinopathy: a model for the continuum of pathology and related management. Br J Sports Med 2010;44. https://doi.org/10.1136/bjsm.2008.054817.
- Ginn KA, Cohen ML. Exercise therapy for shoulder pain aimed at restoring neuromuscular control: a randomized comparative clinical trial. J Rehabil Med 2005;37:115-22. https://doi.org/10.1080/16501970410023443.
- Cook JL, Purdam CR. Is tendon pathology a continuum? A pathology model to explain the clinical presentation of load-induced tendinopathy. Br J Sports Med 2009;43:409-16. https://doi.org/10.1136/bjsm.2008.051193.
- Visnes H, Hoksrud A, Cook J, Bahr R. No effect of eccentric training on jumper’s knee in volleyball players during the competitive season: a randomized clinical trial. Clin J Sport Med 2005;15:227-34. https://doi.org/10.1097/01.jsm.0000168073.82121.20.
- Praet S, Alzyadat T, Purdam C, Welvaert M, Gaida J, Chetty G, et al. Oral supplementation of specific collagen peptides accelerates improvement in Achilles tendon pain and function in combination with a tailored exercise program. J Bodyw Mov Ther 2018;22. https://doi.org/10.1016/j.jbmt.2018.09.048.
- Bahr R, Fossan B, Løken S, Engebretsen L. Surgical treatment compared with eccentric training for patellar tendinopathy (jumper’s knee): a randomized, controlled trial. JBJS 2006;88:1689-98.
- Young MA, Cook JL, Purdam CR, Kiss ZS, Alfredson H. Eccentric decline squat protocol offers superior results at 12 months compared with traditional eccentric protocol for patellar tendinopathy in volleyball players [with consumer summary]. Br J Sports Med 2005;39:102-5.
- Langberg H, Ellingsgaard H, Madsen T, Jansson J, Magnusson SP, Aagaard P, et al. Eccentric rehabilitation exercise increases peritendinous type I collagen synthesis in humans with Achilles tendinosis. Scand J Med Sci Sports 2007;17:61-6.
- Chaudhry S, Morrissey D, Woledge RC, Bader DL, Screen HRC. Eccentric and concentric exercise of the triceps surae: an in vivo study of dynamic muscle and tendon biomechanical parameters. J Appl Biomech 2015;31:69-78.
- Stanish WD, Rubinovich RM, Curwin S. Eccentric exercise in chronic tendinitis. Clin Orthop Relat Res 1986:65-8.
- Enoka RM. Eccentric contractions require unique activation strategies by the nervous system. J Appl Physiol (Bethesda, Md: 1985) 1996;81:2339-46. https://doi.org/10.1152/jappl.1996.81.6.2339.
- Alfredson H. The chronic painful achilles and patellar tendon: research on basic biology and treatment. Scand J Med Sci Sports 2005;15:252-9.
- Silbernagel KG, Thomeé R, Eriksson BI, Karlsson J. Continued sports activity, using a pain-monitoring model, during rehabilitation in patients with Achilles tendinopathy: a randomized controlled study. Am J Sports Med 2007;35:897-906.
- Farup J, Rahbek SK, Vendelbo MH, Matzon A, Hindhede J, Bejder A, et al. Whey protein hydrolysate augments tendon and muscle hypertrophy independent of resistance exercise contraction mode. Scand J Med Sci Sports 2014;24:788-98.
- Sturtz S, Ligges U, Gelman AE. R2WinBUGS: A Package for Running WinBUGS from R 2005.
- van der Vlist AC, Winters M, Weir A, Ardern CL, Welton NJ, Caldwell DM, et al. Which treatment is most effective for patients with Achilles tendinopathy? A living systematic review with network meta-analysis of 29 randomised controlled trials. Br J Sports Med 2021;55:249-56. https://doi.org/10.1136/bjsports-2019-101872.
- Rhim HC, Kim MS, Choi S, Tenforde AS. Comparative efficacy and tolerability of nonsurgical therapies for the treatment of midportion achilles tendinopathy: a systematic review with network meta-analysis. Orthop J Sports Med 2020;8. https://doi.org/10.1177/2325967120930567.
- Cook JL, Khan KM, Purdam C. Achilles tendinopathy. Man Ther 2002;7:121-30. https://doi.org/10.1054/math.2002.0458.
- Kannus P. Etiology and pathophysiology of chronic tendon disorders in sports. Scand J Med Sci Sports 1997;7:78-85.
- Stern C, Lizarondo L, Carrier J, Godfrey C, Rieger K, Salmond S, et al. Methodological guidance for the conduct of mixed methods systematic reviews. JBI Evid Synth 2020;18:2108-18. https://doi.org/10.11124/JBISRIR-D-19-00169.
- Global J. Critical Appraisal Tools 2021. https://jbi.global/critical-appraisal-tools (accessed 6 January 2021).
- Hannes K, Lockwood C. Pragmatism as the philosophical foundation for the Joanna Briggs meta-aggregative approach to qualitative evidence synthesis. J Adv Nurs 2011;67:1632-42. https://doi.org/10.1111/j.1365-2648.2011.05636.x.
- Jayaseelan DJ, Weber MJ, Jonely H. Potential nervous system sensitization in patients with persistent lower extremity tendinopathies: 3 case reports. J Orthop Sports Phys Ther 2019;49:272-9. https://doi.org/10.2519/jospt.2019.8600.
- Verrall G, Schofield S, Brustad T, Physio D. Chronic Achilles tendinopathy treated with eccentric stretching program. Foot Ankle Int 2011;32:843-9.
- Levy AR, Polman RCJ, Nicholls AR, Marchant DC. Sport injury rehabilitation adherence: perspectives of recreational athletes. Int J Sport Exerc Psychol 2009;7:212-29.
- Campbell RF, Morriss-Roberts C, Durrant B, Cahill S. ‘I need somebody who knows about feet’. A qualitative study investigating the lived experiences of conservative treatment for patients with posterior tibial tendon dysfunction. J Foot Ankle Res 2019;12. https://doi.org/10.1186/s13047-019-0360-z.
- Hasani F, Malliaras P, Haines T, Munteanu SE, White J, Ridgway J, et al. Telehealth sounds a bit challenging, but it has potential: participant and physiotherapist experiences of gym-based exercise intervention for Achilles tendinopathy monitored via telehealth. BMC Musculoskelet Disord 2021;22. https://doi.org/10.1186/s12891-020-03907-w.
- Mc Aulife S, Synott A, Casey H, O’Sullivan K, Purtill H, O’Sullivan K. Beyond the tendon: experiences and perceptions of people with persistent Achilles tendinopathy. Musculoskelet Sci Pract 2017;29:108-14. https://doi.org/10.1016/j.msksp.2017.03.009.
- Barrett E, Hayes A, Kelleher M, Conroy C, Robinson K, O’Sullivan K, et al. Exploring patient experiences of participating in a group exercise class for the management of nonspecific shoulder pain. Physiother Theory Pract 2018;34:464-71. https://doi.org/10.1080/09593985.2017.1422208.
- Hanratty CE, Kerr DP, Wilson IM, McCracken M, Sim J, Basford JR, et al. Physical therapists’ perceptions and use of exercise in the management of subacromial shoulder impingement syndrome: focus group study. Phys Ther 2016;96:1354-63. https://doi.org/10.2522/ptj.20150427.
- Littlewood C, Malliaras P, Mawson S, May S, Walters S. Patients with rotator cuff tendinopathy can successfully self-manage, but with certain caveats: a qualitative study. Physiotherapy 2014;100:80-5.
- Sandford FM, Sanders TAB, Lewis JS. Exploring experiences, barriers, and enablers to home-and class-based exercise in rotator cuff tendinopathy: a qualitative study. J Hand Ther 2017;30:193-9.
- Stephens G, O’Neill S, Fearon A, Grimaldi A, French H, O’Connor L, et al. A Survey of Physiotherapy Practice in the United Kingdom for Patients With Greater Trochanteric Pain Syndrome 2019. https://doi.org/10.1016/j.physio.2018.11.109.
- White J, Auliffe SM, Jepson M, Burstein F, Hopman R, Morrissey D, et al. ‘There is a very distinct need for education’ among people with rotator cuff tendinopathy: an exploration of health professionals’ attitudes. Musculoskelet Sci Pract 2020;45. https://doi.org/10.1016/j.msksp.2019.102103.
- Stephens G, O’Neill S, Mottershead C, Hawthron C, Yeowell G, Littlewood C. ‘It’s just like a needle going into my hip, basically all of the time’. The experiences and perceptions of patients with Greater Trochanteric Pain syndrome in the UK National Health Service. Musculoskelet Sci Pract 2020;47. https://doi.org/10.1016/j.msksp.2020.102175.
- Walther M, Werner A, Stahlschmidt T, Woelfel R, Gohlke F. The subacromial impingement syndrome of the shoulder treated by conventional physiotherapy, self-training, and a shoulder brace: Results of a prospective, randomized study. J Shoulder Elbow Surg 2004;13:417-23. https://doi.org/10.1016/j.jse.2004.02.002.
- Boesen AP, Hansen R, Boesen MI, Malliaras P, Langberg H. Effect of high-volume injection, platelet-rich plasma, and sham treatment in chronic midportion Achilles tendinopathy: a randomized double-blinded prospective study. Am J Sports Med 2017;45. https://doi.org/10.1177/0363546517702862.
- Boesen AP, Langberg H, Hansen R, Malliaras P, Boesen MI. High volume injection with and without corticosteroid in chronic midportion achilles tendinopathy. Scand J Med Sci Sports 2019;29:1223-31. https://doi.org/10.1111/sms.13450.
- Belley AF, Mercier C, Bastien M, Léonard G, Gaudreault N, Roy J-S. Anodal Transcranial direct-current stimulation to enhance rehabilitation in individuals with rotator cuff tendinopathy: a triple-blind randomized controlled trial. J Orthop Sports Phys Ther 2018;48:541-51. https://doi.org/10.2519/jospt.2018.7871.
- Seitz AL, Podlecki LA, Melton ER, Uhl TL. Neuromuscular adaptions following a daily strengthening exercise in individuals with rotator cuff related shoulder pain: a pilot case-control study. Int J Sports Phys Ther 2019;14:74-87. https://doi.org/10.26603/ijspt20190074.
- Masood T, Kalliokoski K, Magnusson SP, Bojsen-Møller J, Finni T. Effects of 12-wk eccentric calf muscle training on muscle-tendon glucose uptake and SEMG in patients with chronic Achilles tendon pain. J Appl Physiol (Bethesda, Md: 1985) 2014;117:105-11. https://doi.org/10.1152/japplphysiol.00113.2014.
- Rio E, Purdam C, Girdwood M, Cook J. Isometric exercise to reduce pain in patellar tendinopathy in-season; is it effective ‘on the road’?. Clin J Sport Med Off J Can Acad Sport Med 2017. https://doi.org/10.1097/JSM.0000000000000549.
- Johnston CAM, Lindsay DM, Wiley JP. Treatment of iliopsoas syndrome with a hip rotation strengthening program: a retrospective case series. J Orthop Sports Phys Ther 1999;29:218-24.
- Skovlund SV, Aagaard P, Larsen P, Svensson RB, Kjaer M, Magnusson SP, et al. The effect of low-load resistance training with blood flow restriction on chronic patellar tendinopathy - a case series. Transl Sports Med 2020. https://doi.org/10.1002/tsm2.151.
- van Ark M, van den Akker-Scheek I, Meijer LTB, Zwerver J. An exercise-based physical therapy program for patients with patellar tendinopathy after platelet-rich plasma injection. Phys Ther Sport 2013;14:124-30.
- Bailey DL, Holden MA, Foster NE, Quicke JG, Haywood KL, Bishop A. Defining adherence to therapeutic exercise for musculoskeletal pain: a systematic review. Br J Sports Med 2020;54:326-31. https://doi.org/10.1136/bjsports-2017-098742.
- Cook C, Learman K, Houghton S, Showalter C, O’Halloran B. The addition of cervical unilateral posterior–anterior mobilisation in the treatment of patients with shoulder impingement syndrome: a randomised clinical trial. Man Ther 2014;19:18-24. https://doi.org/10.1016/j.math.2013.05.007.
- Dale LM, Mikuski C, Miller J. Outcomes of a pilates-based intervention for individuals with lateral epicondylosis: a pilot study. Work (Reading, Mass) 2015;53:163-74.
- Luginbuhl R, Brunner F, Schneeberger AG. No effect of forearm band and extensor strengthening exercises for the treatment of tennis elbow: a prospective randomised study. La Chirurgia Degli Organi Di Movimento 2008;91:35-40. https://doi.org/10.1007/s12306-007-0006-3.
- Stevens M, Tan C-W. Effectiveness of the Alfredson protocol compared with a lower repetition-volume protocol for midportion Achilles tendinopathy: a randomized controlled trial. J Orthop Sports Phys Ther 2014;44:59-67.
- Coombes BK, Bisset L, Brooks P, Khan A, Vicenzino B. Effect of corticosteroid injection, physiotherapy, or both on clinical outcomes in patients with unilateral lateral epicondylalgia: a randomized controlled trial. JAMA 2013;309:461-9. https://doi.org/10.1001/jama.2013.129.
- Ferrer GA, Miller RM, Zlotnicki JP, Tashman S, Irrgang JJ, Musahl V, et al. Exercise therapy for treatment of supraspinatus tears does not alter glenohumeral kinematics during internal/external rotation with the arm at the side. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 2018;26:267-74.
- Sancho I, Morrissey D, Willy RW, Barton C, Malliaras P. Education and exercise supplemented by a pain-guided hopping intervention for male recreational runners with midportion Achilles tendinopathy: a single cohort feasibility study. Phys Ther Sport 2019;40:107-16.
- Clifford C, Paul L, Syme G, Millar NL. Isometric versus isotonic exercise for greater trochanteric pain syndrome: a randomised controlled pilot study. BMJ Open Sport Exerc Med 2019;5.
- Agergaard AS, Svensson RB, Malmgaard-Clausen N, Couppe C, Hjortshoej MH, Doessing S, et al. Clinical outcomes, structure, and function improve with both heavy and moderate loads in the treatment of patellar tendinopathy: a randomized clinical trial. Am J Sports Med 2021. https://doi.org/10.1177/0363546520988741.
- Mantovani L, Maestroni L, Bettariga F, Gobbo M, Lopomo NF, McLean S. Does isometric exercise improve leg stiffness and hop pain in subjects with Achilles tendinopathy? A feasibility study. Phys Ther Sport 2020;46:234-42. https://doi.org/10.1016/j.ptsp.2020.09.005.
- Knobloch K, Schreibmueller L, Kraemer R, Jagodzinski M, Vogt PM, Redeker J. Gender and eccentric training in Achilles mid-portion tendinopathy. Knee Surg Sports Traumatol Arthrosc 2010;18:648-55.
- Flores C, Balius R, Álvarez G, Buil MA, Varela L, Cano C, et al. Efficacy and tolerability of peritendinous hyaluronic acid in patients with supraspinatus tendinopathy: a multicenter, randomized, controlled trial. Sports Med Open 2017;3. https://doi.org/10.1186/s40798-017-0089-9.
- Stefansson SH, Brandsson S, Langberg H, Arnason A. Using pressure massage for achilles tendinopathy: a single-blind, randomized controlled trial comparing a novel treatment versus an eccentric exercise protocol. Orthop J Sports Med 2019;7.
- Peterson M, Butler S, Eriksson M, Svärdsudd K. A randomized controlled trial of eccentric vs. concentric graded exercise in chronic tennis elbow (lateral elbow tendinopathy). Clin Rehabil 2014;28:862-72.
- Jonsson P, Alfredson H. Superior results with eccentric compared to concentric quadriceps training in patients with jumper’s knee: a prospective randomised study. Br J Sports Med 2005;39. https://doi.org/10.1136/bjsm.2005.018630.
- Vuvan V, Vicenzino B, Mellor R, Heales LJ, Coombes BK. Unsupervised isometric exercise versus wait-and-see for lateral elbow tendinopathy. Med Sci Sports Exerc 2020;52:287-95. https://doi.org/10.1249/MSS.0000000000002128.
- Bennell K, Wee E, Coburn S, Green S, Harris A, Staples M, et al. Efficacy of standardised manual therapy and home exercise programme for chronic rotator cuff disease: randomised placebo controlled trial. Br Med J 2010;7763.
- Ganderton C, Semciw A, Cook J, Moreira E, Pizzari T. Gluteal loading versus sham exercises to improve pain and dysfunction in postmenopausal women with greater trochanteric pain syndrome: a randomized controlled trial. J Women Health 2018;27:815-29.
- Gual G, Fort-Vanmeerhaeghe A, Romero-Rodriguez D, Tesch PA. Effects of in-season inertial resistance training with eccentric overload in a sports population at risk for patellar tendinopathy [with consumer summary]. J Strength Cond Res 2016;30:1834-42.
- Ingwersen KG, Jensen SL, Sørensen L, Jørgensen HR, Christensen R, Søgaard K, et al. Three months of progressive high-load versus traditional low-load strength training among patients with rotator cuff tendinopathy: primary results from the double-blind randomized controlled RoCTEx trial. Orthop J Sports Med 2017;5.
- Knobloch K, Kraemer R, Jagodzinski M, Zeichen J, Melier R, Vogt PM. Eccentric training decreases paratendon capillary blood flow and preserves paratendon oxygen saturation in chronic achilles tendinopathy. J Orthop Sports Phys Ther 2007;37:269-76. https://doi.org/10.2519/jospt.2007.2296.
- Roos EM, Engstrom M, Lagerquist A, Soderberg B. Clinical improvement after 6 weeks of eccentric exercise in patients with mid-portion Achilles tendinopathy – a randomized trial with 1-year follow-up [with consumer summary]. Scand J Med Sci Sports 2004;14:286-95.
- Shaw JF, Pilon S, Vierula M, McIsaac DI. Predictors of adherence to prescribed exercise programs for older adults with medical or surgical indications for exercise: a systematic review. Syst Rev 2022;11. https://doi.org/10.1186/s13643-022-01966-9.
- Picorelli AMA, Pereira LSM, Pereira DS, Felício D, Sherrington C. Adherence to exercise programs for older people is influenced by program characteristics and personal factors: a systematic review. J Physiother 2014;60:151-6. https://doi.org/10.1016/j.jphys.2014.06.012.
- Bullard T, Ji M, An R, Trinh L, Mackenzie M, Mullen SP. A systematic review and meta-analysis of adherence to physical activity interventions among three chronic conditions: cancer, cardiovascular disease, and diabetes. BMC Public Health 2019;19. https://doi.org/10.1186/s12889-019-6877-z.
- Kluzek S, Dean B, Wartolowska KA. Patient-reported outcome measures (PROMs) as proof of treatment efficacy. BMJ Evid Based Med 2021. https://doi.org/10.1136/bmjebm-2020-111573.
- Jordan JL, Holden MA, Mason EE, Foster NE. Interventions to improve adherence to exercise for chronic musculoskeletal pain in adults. Cochrane Database Syst Rev 2010;2010. https://doi.org/10.1002/14651858.CD005956.pub2.
- Collado-Mateo D, Lavín-Pérez AM, Peñacoba C, Del Coso J, Leyton-Román M, Luque-Casado A, et al. Key factors associated with adherence to physical exercise in patients with chronic diseases and older adults: an umbrella review. Int J Environ Res Public Health 2021;18. https://doi.org/10.3390/ijerph18042023.
- Cinthuja P, Krishnamoorthy N, Shivapatham G. Effective interventions to improve long-term physiotherapy exercise adherence among patients with lower limb osteoarthritis. a systematic review. BMC Musculoskelet Disord 2022;23. https://doi.org/10.1186/s12891-022-05050-0.
- Agnew JMR, Hanratty CE, McVeigh JG, Nugent C, Kerr DP. An investigation into the use of mhealth in musculoskeletal physiotherapy: scoping review. JMIR Rehabil Assist Technol 2022;9. https://doi.org/10.2196/33609.
- Vemulapalli S, Dolor RJ, Hasselblad V, Schmit K, Banks A, Heidenfelder B, et al. Supervised vs unsupervised exercise for intermittent claudication: a systematic review and meta-analysis. Am Heart J 2015;169:924-37.e3. https://doi.org/10.1016/j.ahj.2015.03.009.
- Gajanand T, Keating SE, Brown WJ, Hordern MD, Fassett RG, Coombes JS. Comparing the efficacy of supervised and unsupervised exercise training on glycaemic control in type 2 diabetes: a systematic review. Curr Diabetes Rev 2020;16:570-9. https://doi.org/10.2174/1573399815666190212120404.
- Francia P, De Bellis A, Iannone G, Sinopoli R, Bocchi L, Anichini R. The role of new technological opportunities and the need to evaluate the activities performed in the prevention of diabetic foot with exercise therapy. Medicines 2021;8. https://doi.org/10.3390/medicines8120076.
- Nagpal TS, Mottola MF, Barakat R, Prapavessis H. Adherence is a key factor for interpreting the results of exercise interventions. Physiotherapy 2021;113:8-11. https://doi.org/10.1016/j.physio.2021.05.010.
- Moher D, Hopewell S, Schulz KF, Montori V, Gøtzsche PC, Devereaux PJ, et al. CONSORT 2010 Explanation and Elaboration: updated guidelines for reporting parallel group randomised trials. BMJ 2010;340. https://doi.org/10.1136/bmj.c869.
- Slade SC, Dionne CE, Underwood M, Buchbinder R. Consensus on Exercise Reporting Template (CERT): explanation and elaboration statement. Br J Sports Med 2016;50:1428-37. https://doi.org/10.1136/bjsports-2016-096651.
- Di Lorenzo L, Pappagallo M, Gimigliano R, Palmieri E, Saviano E, Bello A, et al. Pain relief in early rehabilitation of rotator cuff tendinitis: any role for indirect suprascapular nerve block?. Eura Medicophys 2006;42:195-204.
- Güler H, Turhanoglu AD, Inanoglu K, Inanoglu D, Özer C. Comparison of ketoprofen phonophoresis with ketoprofen and lidocaine-prilocaine phonophoresis in patients with subacromial impingement syndrome. Turk J Rheumatol 2009;24:88-93.
- Abat F, Diesel W-J, Gelber P-E, Polidori F, Monllau J-C, Sanchez-Ibañez J-M. Effectiveness of the Intratissue Percutaneous Electrolysis (EPI®) technique and isoinertial eccentric exercise in the treatment of patellar tendinopathy at two years follow-up. Muscles Ligaments Tendons J 2014;4.
- Abat F, Gelber P-E, Polidori F, Monllau J-C, Sánchez J-M. 1 clinical results after EPI® and eccentric exercise in patellar tendinopathy at 10 years follow-up. Br J Sports Med 2014;48.
- Abat F, Gelber PE, Polidori F, Monllau JC, Sanchez-Ibañez JM. Clinical results after ultrasound-guided intratissue percutaneous electrolysis (EPI®) and eccentric exercise in the treatment of patellar tendinopathy. Knee Surg Sports Traumatol Arthrosc 2015;23:1046-52.
- Abat F, Sanchez-Sanchez J, Martin-Nogueras A, Calvo-Arenillas J, Yajeya J, Mendez-Sanchez R, et al. Randomized controlled trial comparing the effectiveness of the ultrasound-guided galvanic electrolysis technique (USGET) versus conventional electro-physiotherapeutic treatment on patellar tendinopathy. J Exp Orthop 2016;3. https://doi.org/10.1186/s40634-016-0070-4.
- Abdulla SY, Southerst D, Côté P, Shearer HM, Sutton D, Randhawa K, et al. Is exercise effective for the management of subacromial impingement syndrome and other soft tissue injuries of the shoulder? A systematic review by the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration. Man Ther 2015;20:646-56.
- Aceituno-Gómez J, Avendaño-Coy J, Gómez-Soriano J, García-Madero VM, Ávila-Martín G, Serrano-Muñoz D, et al. Efficacy of high-intensity laser therapy in subacromial impingement syndrome: a three-month follow-up controlled clinical trial. Clin Rehabil 2019;33:894-903. https://doi.org/10.1177/0269215518824691.
- Akgün K, Birtane M, Akarirmak U. Is local subacromial corticosteroid injection beneficial in subacromial impingement syndrome?. Clin Rheumatol 2004;23:496-500.
- Akin T, Caglar NS, Burnaz O, Kesmezacar O. Effectiveness of ultrasound in the treatment of subacromial impingement syndrome. Nobel Med 2013;9:104-8.
- Akkaya N, Akkaya S, Gungor HR, Yaşar G, Atalay NS, Sahin F. Effects of weighted and un-weighted pendulum exercises on ultrasonographic acromiohumeral distance in patients with subacromial impingement syndrome. J Back Musculoskelet Rehabil 2017;30:221-8. https://doi.org/10.3233/BMR-160737.
- Akkurt HE, Kocabas H, Yilmaz H, Eser C, Sen Z, Erol K, et al. Comparison of an epicondylitis bandage with a wrist orthosis in patients with lateral epicondylitis. Prosthet Orthot Int 2018;42:599-605. https://doi.org/10.1177/0309364618774193.
- Aktas I, Akgun K, Cakmak B. Therapeutic effect of pulsed electromagnetic field in conservative treatment of subacromial impingement syndrome. Clin Rheumatol 2007;26:1234-9.
- Akyol Y, Ulus Y, Durmus D, Canturk F, Bilgici A, Kuru O, et al. Effectiveness of microwave diathermy on pain, functional capacity, muscle strength, quality of life, and depression in patients with subacromial impingement syndrome: a randomized placebo-controlled clinical study. Rheumatol Int 2012;32:3007-16.
- Al Dajah SB. Soft tissue mobilization and PNF improve range of motion and minimize pain level in shoulder impingement. J Phys Ther Sci 2014;26:1803-5.
- Al-Abbad H, Simon JV. The effectiveness of extracorporeal shock wave therapy on chronic achilles tendinopathy: a systematic review. Foot Ankle Int 2013;34:33-41. https://doi.org/10.1177/1071100712464354.
- Alfredson H, Nordström P, Pietilä T, Lorentzon R. Bone mass in the calcaneus after heavy loaded eccentric calf-muscle training in recreational athletes with chronic achilles tendinosis. Calcif Tissue Int 1999;64:450-5.
- Alfredson Hå, Lorentzon R. Intratendinous glutamate levels and eccentric training in chronic Achilles tendinosis: a prospective study using microdialysis technique. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 2003;11:196-9.
- Alvarez RG, Marini A, Schmitt C, Saltzman CL. Stage I and II posterior tibial tendon dysfunction treated by a structured nonoperative management protocol: an orthosis and exercise program. Foot Ankle Int 2006;27:2-8.
- Andriolo L, Altamura SA, Reale D, Candrian C, Zaffagnini S, Filardo G. Nonsurgical treatments of patellar tendinopathy: multiple injections of platelet-rich plasma are a suitable option: a systematic review and meta-analysis. Am J Sports Med 2019;47:1001-18. https://doi.org/10.1177/0363546518759674.
- Apostolos S. The influence of low level laser and pyrometric exercises in the treatment of patients with tennis elbow. A Pilot Study. (Abstract) n.d. https://cev.org.br/biblioteca/the-influence-of-low-level-laser-and-plyometric-exercises-in-the-treatment-of-patients-with-tennis-elbow-pilot-study/ (accessed 6 January 2021).
- Arias-Buría JL, Fernández-de-Las-Peñas C, Palacios-Ceña M, Koppenhaver SL, Salom-Moreno J. Exercises and dry needling for subacromial pain syndrome: a randomized parallel-group trial. J Pain 2017;18:11-8.
- Arias-Buría JL, Truyols-Domínguez S, Valero-Alcaide R, Salom-Moreno J, Atín-Arratibel MA, Fernández-de-las-Peñas C. Ultrasound-guided percutaneous electrolysis and eccentric exercises for subacromial pain syndrome: a randomized clinical trial. Evid Based Complement Alternat Med 2015;2015.
- Arnal-Gómez A, Espí-López GV, Cano-Heras D, Muñoz-Gómez E, Balbastre Tejedor I, Ramírez Iñiguez-de la Torrez MV, et al. Efficacy of eccentric exercise as a treatment for Achilles Tendinopathy: literature review. Arch Prev Riesgos Labor 2020;23:211-33. https://doi.org/10.12961/aprl.2020.23.02.07.
- Askling CM, Tengvar M, Tarassova O, Thorstensson A. Acute hamstring injuries in Swedish elite sprinters and jumpers: a prospective randomised controlled clinical trial comparing two rehabilitation protocols [with consumer summary]. Br J Sports Med 2014;48:532-9.
- Aytar A, Baltaci G, Uhl TL, Tuzun H, Oztop P, Karatas M. The effects of scapular mobilization in patients with subacromial impingement syndrome: a randomized, double-blind, placebo-controlled clinical trial. J Sport Rehabil 2015;24:116-29. https://doi.org/10.1123/jsr.2013-0120.
- Bae YH, Lee GC, Shin WS, Kim TH, Lee SM. Effect of motor control and strengthening exercises on pain, function, strength and the range of motion of patients with shoulder impingement, syndrome. J Phys Ther Sci 2011;23:687-92.
- Bagcier F, Yilmaz N. The impact of extracorporeal shock wave therapy and dry needling combination on the pain, grip strength and functionality in patients diagnosed with lateral epicondylitis. Turk Osteoporoz Dergisi 2019;25:65-71. https://doi.org/10.4274/tod.galenos.2019.68552.
- Bakkegaard M, Johannsen FE, Højgaard B, Langberg H. Ultrasonography as a prognostic and objective parameter in Achilles tendinopathy: a prospective observational study. Eur J Radiol 2015;84:458-62. https://doi.org/10.1016/j.ejrad.2014.11.028.
- Bal A, Eksioglu E, Gurcay E, Gulec B, Karaahmet O, Cakci A. Low-level laser therapy in subacromial impingement syndrome. Photomed Laser Surg 2009;27:31-6. https://doi.org/10.1089/pho.2007.2222.
- Balius R, Álvarez G, Baró F, Jiménez F, Pedret C, Costa E, et al. A 3-arm randomized trial for Achilles tendinopathy: eccentric training, eccentric training plus a dietary supplement containing mucopolysaccharides, or passive stretching plus a dietary supplement containing mucopolysaccharides. Curr Ther Res 2016;78:1-7.
- Bang MD, Deyle GD. Comparison of supervised exercise with and without manual physical therapy for patients with shoulder impingement syndrome. J Orthop Sports Phys Ther 2000;30:126-37.
- Barr S, Cerisola FL, Blanchard V. Effectiveness of corticosteroid injections compared with physiotherapeutic interventions for lateral epicondylitis: a systematic review. Physiotherapy 2009;95:251-65.
- Barra López ME, López de Celis C, Fernández Jentsch G, Raya de Cárdenas L, Lucha López MO, Tricás Moreno JM. Effectiveness of Diacutaneous Fibrolysis for the treatment of subacromial impingement syndrome: a randomised controlled trial. Man Ther 2013;18:418-24. https://doi.org/10.1016/j.math.2013.02.006.
- Barratt PA, Brookes N, Newson A. Conservative treatments for greater trochanteric pain syndrome: a systematic review. Br J Sports Med 2017;51:97-104. https://doi.org/10.1136/bjsports-2015-095858.
- Barratt PA, Selfe J. A service evaluation and improvement project: a three year systematic audit cycle of the physiotherapy treatment for Lateral Epicondylalgia. Physiotherapy 2018;104:209-16. https://doi.org/10.1016/j.physio.2017.09.001.
- Basas Á, Cook J, Gómez MA, Rafael MA, Ramirez C, Medeiros B, et al. Effects of a strength protocol combined with electrical stimulation on patellar tendinopathy: 42 months retrospective follow-up on 6 high-level jumping athletes. Phys Ther Sport Off J Assoc Chartered Physiother Sports Med 2018;34:105-12. https://doi.org/10.1016/j.ptsp.2018.09.005.
- Baskurt F, Ozcan A, Algun C. Comparison of effects of phonophoresis and iontophoresis of naproxen in the treatment of lateral epicondylitis. Clin Rehabil 2003;17:96-100.
- Başkurt Z, Başkurt F, Gelecek N, Özkan MH. The effectiveness of scapular stabilization exercise in the patients with subacromial impingement syndrome. J Back Musculoskelet Rehabil 2011;24:173-9. https://doi.org/10.3233/BMR-2011-0291.
- Bastia P, Ghirarduzzi P, Schiavi P, Donelli D, Pedrazzini A, Leigheb M, et al. Surgical or conservative treatment in ARGP syndrome? A systematic review. Acta Biomed 2019;90. https://doi.org/10.23750/abm.v90i12-S.8962.
- Bateman M, Adams N. A randomised controlled feasibility study investigating the use of eccentric and concentric strengthening exercises in the treatment of rotator cuff tendinopathy. SAGE Open Med 2014;2.
- Baumer TG, Peltz CD, Drake A, Chan D, Dischler J, Moutzouros V, et al. Effects of Rotator Cuff Pathology and Physical Therapy on Shoulder Motion and Clinical Outcomes in Patients With a Symptomatic Full-Thickness Rotator Cuff Tear 2016. https://doi.org/10.1002/jor.23247.
- Bek N, Simşek IE, Erel S, Yakut Y, Uygur F. Home-based general versus center-based selective rehabilitation in patients with posterior tibial tendon dysfunction. Acta Orthop Traumatol Turc 2012;46:286-92.
- Bell KJ, Fulcher ML, Rowlands DS, Kerse N. Impact of autologous blood injections in treatment of mid-portion Achilles tendinopathy: double blind randomised controlled trial. BMJ (Clin Res Ed) 2013;346. https://doi.org/10.1136/bmj.f2310.
- Bernhardsson S, Hultenheim Klintberg I, Kjellby-Wendt G. Evaluation of an Exercise Concept Focusing on Eccentric Strength Training of the Rotator Cuff for Patients With Subacromial Impingement Syndrome n.d. https://doi.org/10.1016/j.physio.2011.04.002.
- Bianco LC, May JM, Fermin SL, Oates R, Cheatham SW. The effect of positional release therapy on intercollegiate male basketball athletes classified with patella tendinopathy. Int J Athl Ther Train 2019;24:108-14. https://doi.org/10.1123/ijatt.2018-0040.
- Bisset L, Beller E, Jull G, Brooks P, Darnell R, Vicenzino B. Mobilisation with movement and exercise, corticosteroid injection, or wait and see for tennis elbow: randomised trial. Br Med J 2006;333:939-41. https://doi.org/10.1136/bmj.38961.584653.AE.
- Bisset L, Paungmali A, Vicenzino B, Beller E. A systematic review and meta-analysis of clinical trials on physical interventions for lateral epicondylalgia. Br J Sports Med 2005;39:411-22.
- Bisset LM, Coppieters MW, Vicenzino B. Sensorimotor deficits remain despite resolution of symptoms using conservative treatment in patients with tennis elbow: a randomized controlled trial. Arch Phys Med Rehabil 2009;90:1-8.
- Bjordal JM, Lopes-Martins R, Joensen J, Couppe C, Ljunggren AE, Stergioulas A, et al. A systematic review with procedural assessments and meta-analysis of low level laser therapy in lateral elbow tendinopathy (tennis elbow). Database Abstracts Rev Effects (DARE) 2009.
- Hallgren HC, Adolfsson LE, Johansson K, Öberg B, Peterson A, Holmgren TM. Specific exercises for subacromial pain. Acta Orthop 2017;88:600-5. https://doi.org/10.1080/17453674.2017.1364069.
- Blackwood J, Ghazi F. Can the addition of transverse friction massage to an exercise programme in treatment of infrapatellar tendinopathy reduce pain and improve function? A pilot study. Int Musculoskelet Med 2012;34:108-14.
- Blume CL. Comparison of an eccentric exercise intervention to a concentric exercise intervention in adults with subacromial impingement syndrome. Int J Sports Phys Ther 2014;10:441-55.
- Bostrøm K, Mæhlum S, Småstuen MC, Storheim K. Clinical comparative effectiveness of acupuncture versus manual therapy treatment of lateral epicondylitis: feasibility randomized clinical trial. Pilot Feasibility Stud 2019;5.
- Boudreau N, Gaudreault N, Roy JS, Bédard S, Balg F. The addition of glenohumeral adductor coactivation to a rotator cuff exercise program for rotator cuff tendinopathy: a single-blind randomized controlled trial. J Orthop Sports Phys Ther 2019;49:126-35. https://doi.org/10.2519/jospt.2019.8240.
- Bowring B, Chockalingam N. Conservative treatment of tibialis posterior tendon dysfunction – a review. Foot 2010;20:18-26. https://doi.org/10.1016/j.foot.2009.11.001.
- Boyles RE, Ritland BM, Miracle BM, Barclay DM, Faul MS, Moore JH, et al. The short-term effects of thoracic spine thrust manipulation on patients with shoulder impingement syndrome. Man Ther 2009;14:375-80. https://doi.org/10.1016/j.math.2008.05.005.
- Branson R, Naidu K, du Toit C, Rotstein AH, Kiss R, McMillan D, et al. Comparison of corticosteroid, autologous blood or sclerosant injections for chronic tennis elbow. J Sci Med Sport 2017;20:528-33. https://doi.org/10.1016/j.jsams.2016.10.010.
- Braun C, Hanchard NCA. Manual therapy and exercise for impingementrelated shoulder pain. Phys Ther Rev 2010;15:62-83.
- Braun C, Bularczyk M, Heintsch J, Hanchard NCA. Manual therapy and exercises for shoulder impingement revisited. Phys Ther Rev 2013;18:263-84. https://doi.org/10.1179/108331913X13709388114510.
- Brown R, Orchard J, Kinchington M, Hooper A, Nalder G. Aprotinin in the management of Achilles tendinopathy: a randomised controlled trial. Br J Sports Med 2006;40:275-9. https://doi.org/10.1136/bjsm.2005.021931.
- Brox JI, Gjengedal E, Uppheim G, Bøhmer AS, Brevik JI, Ljunggren AE, et al. Arthroscopic surgery versus supervised exercises in patients with rotator cuff disease (stage II impingement syndrome): a prospective, randomized, controlled study in 125 patients with a 2 1/2-year follow-up. J Shoulder Elbow Surg 1999;8:102-11.
- Bury J, West M, ChamorroMoriana G, Littlewood C. Effectiveness of scapula-focused approaches in patients with rotator cuff related shoulder pain: a systematic review and meta-analysis. Man Ther 2016;25:35-42. https://doi.org/10.1016/j.math.2016.05.337.
- Cacchio A, Rompe JD, Furia JP, Susi P, Santilli V, De Paulis F. Shockwave therapy for the treatment of chronic proximal hamstring tendinopathy in professional athletes. Am J Sports Med 2011;39. https://doi.org/10.1177/0363546510379324.
- Cairns G, Owen T, Kluzek S, Thurley N, Holden S, Rathleff MS, et al. Therapeutic interventions in children and adolescents with patellar tendon related pain: a systematic review. BMJ Open Sport Exerc Med 2018;4. https://doi.org/10.1136/bmjsem-2018-000383.
- Calis HT, Berberoglu N, Calis M. Are ultrasound, laser and exercise superior to each other in the treatment of subacromial impingement syndrome? A randomized clinical trial. Eur J Phys Rehabil Med 2011;47:375-80.
- Canbulat N, Seyahi A, Eren SM, Ucak A, Berker E, Demirhan M. The Effect of Core Stabilization Exercises in the Rehabilitation of Patients with Subacromial Impingement Syndrome 2013. https://doi.org/10.4274/tftr.24.59.1.
- Cannell LJ, Taunton JE, Clement DB, Smith C, Khan KM. A randomised clinical trial of the efficacy of drop squats or leg extension/leg curl exercises to treat clinically diagnosed jumper’s knee in athletes: Pilot study. Br J Sports Med 2001;35:60-4. https://doi.org/10.1136/bjsm.35.1.60.
- Carlisi E, Lisi C, Dall’Angelo A, Monteleone S, Nola V, Tinelli C, et al. Focused extracorporeal shock wave therapy combined with supervised eccentric training for supraspinatus calcific tendinopathy. Eur J Phys Rehabil Med 2018;54:41-7.
- Celik D, Anaforoglu Kulunkoglu B. Photobiomodulation therapy versus extracorporeal shock wave therapy in the treatment of lateral epicondylitis. Photobiomodul Photomed Laser Surg 2019;37:269-75. https://doi.org/10.1089/photob.2018.4533.
- Celik D, Atalar AC, Güçlü A, Demirhan M. The contribution of subacromial injection to the conservative treatment of impingement syndrome. Acta Orthop Traumatol Turc 2009;43:331-5. https://doi.org/10.3944/AOTT.2009.331.
- Celik D, Akyüz G, Yeldan I. Comparison of the effects of two different exercise programs on pain in subacromial impingement syndrome. Acta Orthop Traumatol Turc 2009;43:504-9. https://doi.org/10.3944/AOTT.2009.504.
- Cerdán Fabregat FJ. Effectiveness of percutaneous needle electrolysis and eccentric exercise in chronic Achilles tendinopathy. A case series. Revista Fisioterapia Invasiva J Invasive Tech Phys Ther 2019;2.
- Challoumas D, Clifford C, Kirwan P, Millar NL. How does surgery compare to sham surgery or physiotherapy as a treatment for tendinopathy? A systematic review of randomised trials. BMJ Open Sport Exerc Med 2019;5.
- Chan CCH, Li CWP, Hung L, Lam PCW. A standardized clinical series for work-related lateral epicondylitis. J Occup Rehabil 2000;10:143-52.
- Chary-Valckenaere I, Loeuille D, Jay N, Kohler F, Tamisier JN, Roques CF, et al. Spa therapy together with supervised self-mobilisation improves pain, function and quality of life in patients with chronic shoulder pain: a single-blind randomised controlled trial. Int J Biometeorol 2018;62:1003-14. https://doi.org/10.1007/s00484-018-1502-x.
- Chen TW, Huei Su J, Lin TY, Lin CW, Chou PS. Effects of eccentric exercise and extracorporeal shock wave therapy on rehabilitation of patients with noncalcific rotator cuff tendinopathy. Clin Res Foot Ankle 2017;5.
- Chen Z, Baker NA. Effectiveness of eccentric strengthening in the treatment of lateral elbow tendinopathy: a systematic review with meta-analysis. J Hand Ther Off J Am Soc Hand Ther 2020. https://doi.org/10.1016/j.jht.2020.02.002.
- Cheng AS, Hung L. Randomized controlled trial of workplace-based rehabilitation for work-related rotator cuff disorder. J Occup Rehabil 2007;17:487-503.
- Cherry E, Agostinucci J, McLinden J. The effect of cryotherapy and exercise on lateral epicondylitis: a controlled randomised study. Int J Ther Rehabil 2012;19:641-50.
- Chester R, Costa ML, Shepstone L, Cooper A, Donell ST. Eccentric calf muscle training compared with therapeutic ultrasound for chronic Achilles tendon pain--a pilot study. Man Ther 2008;13. https://doi.org/10.1016/j.math.2007.05.014.
- Cho S-I, Shin Y-A. Effect of rehabilitation and prolotherapy on pain and functional performance in patients with chronic patellar tendinopathy. Gazz Med Ital Arch Sci Med 2017;176:330-7. https://doi.org/10.23736/S0393-3660.16.03339-8.
- Chung B, Wiley JP. Effectiveness of extracorporeal shock wave therapy in the treatment of previously untreated lateral epicondylitis: a randomized controlled trial. Am J Sports Med 2004;32:1660-7. https://doi.org/10.1177/0363546503262806.
- Chung B, Wiley JP, Rose MS. Long-term effectiveness of extracorporeal shockwave therapy in the treatment of previously untreated lateral epicondylitis. Clin J Sport Med 2005;15:305-12. https://doi.org/10.1097/01.jsm.0000179137.69598.7e.
- Cioni M, Ristori D, Miele S, Testa M. Impingement, Tendinopatia di cuffia e lesioni slap: efficacia dell’esercizio terapeutico nelle patologie di spalla. Scienza Riabilitativa 2017;19:47-66.
- Citaker S, Taskiran H, Akdur H, Arabaci UO, Ekici G. Comparison of the mobilization and proprioceptive neuromuscular facilitation methods in the treatment of shoulder impingement syndrome. Pain Clinic 2005;17:197-202. https://doi.org/10.1163/1568569053750055.
- Clarke AW, Ahmad M, Curtis M, Connell DA. Lateral elbow tendinopathy: correlation of ultrasound findings with pain and functional disability. Am J Sports Med 2010;38:1209-14. https://doi.org/10.1177/0363546509359066.
- Clarke AW, Alyas F, Morris T, Robertson CJ, Bell J, Connell DA. Skin-derived tenocyte-like cells and exercise based physiotherapy for the treatment of patellar tendinopathy. Am J Sports Med 2011;39:614-23. https://doi.org/10.1177/0363546510387095.
- Cleland JA, Whitman JM, Fritz JM. Effectiveness of manual physical therapy to the cervical spine in the management of lateral epieondylalgia: a retrospective analysis. J Orthop Sports Phys Ther 2004;34:713-24.
- Coghlan JA, Buchbinder R, Green S, Johnston RV, Bell SN. Surgery for rotator cuff disease. Cochrane Database Syst Rev 2008. https://doi.org/10.1002/14651858.CD005619.pub2.
- Conroy DE, Hayes KW. The effect of joint mobilization as a component of comprehensive treatment for primary shoulder impingement syndrome. J Orthop Sports Phys Ther 1998;28:3-14.
- Coombes BK, Connelly L, Bisset L, Vicenzino B. Economic evaluation favours physiotherapy but not corticosteroid injection as a first-line intervention for chronic lateral epicondylalgia: evidence from a randomised clinical trial. Br J Sports Med 2016;50:1400-5. https://doi.org/10.1136/bjsports-2015-094729.
- Crawshaw DP, Helliwell PS, Hensor EMA, Hay EM, Aldous SJ, Conaghan PG. Exercise therapy after corticosteroid injection for moderate to severe shoulder pain: large pragmatic randomised trial. BMJ 2010;340.
- Crill MT, Berlet G, Hyer C. Plantar flexor muscle architecture changes as a result of eccentric exercise in patients with Achilles tendinosis. Foot Ankle Spec 2014;7:460-5. https://doi.org/10.1177/1938640014539812.
- Croisier J, Forthomme B, Foidart-Dessalle M, Godon B, Crielaard J. Treatment of recurrent tendinitis by isokinetic eccentric exercises. Isokinet Exerc Sci 2001;9:133-41.
- Croisier JL, Forthomme B, Foidart-Dessalle M, Godon M, Crielaard JM. Isokinetic eccentric exercises in treating chronic tendinitis. Isokinet Exerc Sci 2002;10:25-6.
- Croisier JL, Foidart-Dessalle M, Tinant F, Crielaard JM, Forthomme B. An isokinetic eccentric programme for the management of chronic lateral epicondylar tendinopathy. Br J Sports Med 2007;41. https://doi.org/10.1136/bjsm.2006.033324.
- Cullinane FL, Boocock MG, Trevelyan FC. Is eccentric exercise an effective treatment for lateral epicondylitis? A systematic review. Clin Rehabil 2014;28:3-19.
- Cumpston M, Johnston RV, Wengier L, Buchbinder R. Topical glyceryl trinitrate for rotator cuff disease. Cochrane Database Syst Rev 2009. https://doi.org/10.1002/14651858.CD006355.pub2.
- Dan M, Phillips A, Johnston RV, Harris IA. Surgery for patellar tendinopathy (jumper’s knee) (Cochrane review) [with consumer summary]. Cochrane Database Syst Rev 2019.
- de Jonge S, Tol JL, Weir A, Waarsing JH, Verhaar JAN, de Vos R-J. The tendon structure returns to asymptomatic values in nonoperatively treated Achilles tendinopathy but is not associated with symptoms: a prospective study. Am J Sports Med 2015;43:2950-8.
- de Jonge S, Tol JL, de Vos R-J, van Schie HTM, Verhaar JAN. One-year follow-up of a randomised controlled trial on added splinting to eccentric exercises in chronic midportion Achilles tendinopathy. Bjsmbmjcom 2008. https://doi.org/10.1136/bjsm.2008.052142.
- de la Fuente A, Valero B, Cuadrado N. Abordaje fisioterápico de la tendinopatía rotuliana: revisión sistemática. Fisioterapia 2019;41:131-42. https://doi.org/10.1016/j.ft.2019.02.007.
- De Mey K, Danneels L, Cagnie B, Cools AM. Scapular muscle rehabilitation exercises in overhead athletes with impingement symptoms: effect of a 6-week training program on muscle recruitment and functional outcome. Am J Sports Med 2012;40:1906-15. https://doi.org/10.1177/0363546512453297.
- de Miguel Valtierra L, Salom Moreno J, Fernández-de-Las-Peñas C, Cleland JA, Arias-Buría JL. Ultrasound-guided application of percutaneous electrolysis as an adjunct to exercise and manual therapy for subacromial pain syndrome: a randomized clinical trial. J Pain Off J Am Pain Soc 2018;19:1201-10. https://doi.org/10.1016/j.jpain.2018.04.017.
- De Reu S. The Immediate Effects of an External Rotation Exercise Program Compared with a General Exercise Program in Patients with Rotator Cuff Tendinopathy and Healthy Controls: A Randomised Controlled Trial. Ghent University; 2018.
- de Vos RJ, Weir A, van Schie HT, Bier-Zeinstra S, Verhaar JA, Weinans H, et al. Platelet-rich plasma injection for chronic Achilles tendinopathy. J Am Med Assoc 2010;303:144-9.
- de Vos RJ, Heijboer MP, Weinans H, Verhaar J AN, van Schie J TM. Tendon structure’s lack of relation to clinical outcome after eccentric exercises in chronic midportion Achilles tendinopathy. J Sport Rehabil 2012;21:34-43.
- de Vos R-J, Weir A, Cobben LPJ, Tol JL. The value of power Doppler ultrasonography in Achilles tendinopathy: a prospective study. Am J Sports Med 2007;35:1696-701.
- de Vos RJ, Weir A, Tol JL, Verhaar JA, Weinans H, van Schie HT. No effects of PRP on ultrasonographic tendon structure and neovascularisation in chronic midportion Achilles tendinopathy. Br J Sports Med 2011;45. https://doi.org/10.1136/bjsm.2010.076398.
- Deans VM, Miller A, Ramos J. A prospective series of patients with chronic Achilles tendinopathy treated with autologous-conditioned plasma injections combined with exercise and therapeutic ultrasonography. J Foot Ankle Surg 2012;51:706-10.
- Desjardins-Charbonneau A, Roy JS, Dionne CE, Desmeules F. The efficacy of taping for rotator cuff tendinopathy: a systematic review and meta-analysis. Int J Sports Phys Ther 2015;10:420-33.
- Desjardins-Charbonneau A, Roy J-S, Dionne CE, Frémont P, MacDermid JC, Desmeules F. The efficacy of manual therapy for rotator cuff tendinopathy: a systematic review and meta-analysis. J Orthop Sports Phys Ther 2015;45:330-50.
- Desmeules F, Minville L, Riederer B, Cote CH, Fremont P. Acromio-humeral distance variation measured by ultrasonography and its association with the outcome of rehabilitation for shoulder impingement syndrome. Clin J Sport Med 2004;14:197-205.
- Desmeules F, Côté CH, Frémont P. Therapeutic exercise and orthopedic manual therapy for impingement syndrome: a systematic review. Clin J Sport Med 2003;13:176-82.
- Desmeules F, Boudreault J, Roy JS, Dionne C, Frémont P, MacDermid JC. The efficacy of therapeutic ultrasound for rotator cuff tendinopathy: a systematic review and meta-analysis. Phys Ther Sport Off J Assoc Chartered Physiother Sports Med 2015;16:276-84. https://doi.org/10.1016/j.ptsp.2014.09.004.
- Desmeules F, Boudreault J, Roy JS, Dionne CE, Frémont P, MacDermid JC. Efficacy of transcutaneous electrical nerve stimulation for rotator cuff tendinopathy: a systematic review. Physiotherapy 2016.
- Desmeules F, Boudreault J, Dionne CE, Frémont P, Lowry V, MacDermid JC, et al. Efficacy of exercise therapy in workers with rotator cuff tendinopathy: a systematic review. J Occup Health 2016;58:389-403.
- Devereaux M, Velanoski KQ, Pennings A, Elmaraghy A. Short-term effectiveness of precut kinesiology tape versus an NSAID as adjuvant treatment to exercise for subacromial impingement: a randomized controlled trial. Clin J Sport Med Off J Can Acad Sport Med 2016;26:24-32. https://doi.org/10.1097/JSM.0000000000000187.
- Díaz JJG. Effectiveness of eccentric exercise in patellar tendinopathy. Literary review. Arch Sports Med 2016;33:59-66.
- Dickens VA, Williams JL, Bhamra MS. Role of physiotherapy in the treatment of subacromial impingement syndrome: a prospective study. Physiotherapy 2005;91:159-64.
- Dilek B, Gulbahar S, Gundogdu M, Ergin B, Manisali M, Ozkan M, et al. Efficacy of proprioceptive exercises in patients with subacromial impingement syndrome: a single-blinded randomized controlled study. Am J Phys Med Rehabil 2016;95:169-82. https://doi.org/10.1097/PHM.0000000000000327.
- Dimitrios S, Pantelis M, Kalliopi S. Comparing the effects of eccentric training with eccentric training and static stretching exercises in the treatment of patellar tendinopathy. A controlled clinical trial. Clin Rehabil 2012;26:423-30.
- Stasinopoulos D, Manias P. Comparing two eccentric exercise programmes for the management of Achilles tendinopathy. A pilot trial. J Bodyw Mov Ther 2013;17:309-15.
- Dingemanse R, Randsdorp M, Koes BW, Huisstede BMA. Evidence for the effectiveness of electrophysical modalities for treatment of medial and lateral epicondylitis: a systematic review. Br J Sports Med 2014;48:957-65. https://doi.org/10.1136/bjsports-2012-091513.
- Dogan SK, Ay S, Evcik D. The effectiveness of low laser therapy in subacromial impingement syndrome: a randomized placebo controlled double-blind prospective study. Clinics (Sao Paulo, Brazil) 2010;65:1019-22.
- Doiron-Cadrin P, Lafrance S, Saulnier M, Cournoyer É, Roy J-S, Dyer J-O, et al. Shoulder rotator cuff disorders: a systematic review of clinical practice guidelines and semantic analyses of recommendations. Arch Phys Med Rehabil 2020. https://doi.org/10.1016/j.apmr.2019.12.017.
- Dorrestijn O, Stevens M, Winters JC, van der Meer K, Diercks RL. Conservative or surgical treatment for subacromial impingement syndrome? A systematic review. J Shoulder Elbow Surg 2009;18:652-60. https://doi.org/10.1016/j.jse.2009.01.010.
- Dragoo JL, Wasterlain AS, Braun HJ, Nead KT. Platelet-rich plasma as a treatment for patellar tendinopathy: a double-blind, randomized controlled trial. Am J Sports Med 2014;42. https://doi.org/10.1177/0363546513518416.
- Drew B, Smith T, Littlewood C, Sturrock B. Do structural changes explain the response to exercise in tendinopathy? A systematic review. Br J Sports Med 2014;48:966-72. https://doi.org/10.1111/iep.12034.
- Dumont TL, MacIntyre DL, Harris SR. Effects of a six-week eccentric exercise program on patients with patellar tendinopathy: single-subject research study. Physiother Can 2006;58:130-47.
- Dupuis F, Barrett E, Dubé M-O, McCreesh KM, Lewis JS, Roy J-S. Cryotherapy or gradual reloading exercises in acute presentations of rotator cuff tendinopathy: a randomised controlled trial. BMJ Open Sport Exerc Med 2018;4.
- Efstratiadis A, Koinis A, Stasinopoulos D, Soursos G. The effectiveness of exercise versus arthroscopic surgery subacromial impingement syndrome of the shoulder. Interscientific Health Care 2016;8:1-8.
- Eken Gedik D, Dost Surucu G, Yildirim A, Karabiber M. Effectiveness of autologous blood injection in the treatment of lateral epicondylitis: randomized clinical study. Duzce Med J 2016;18:1-7.
- Ellegaard K, Christensen R, Rosager S, Bartholdy C, Torp-Pedersen S, Bandholm T, et al. Exercise therapy after ultrasound-guided corticosteroid injections in patients with subacromial pain syndrome: a randomized controlled trial. Arthritis Res Ther 2016;18. https://doi.org/10.1186/s13075-016-1002-5.
- Elsodany AM, Alayat MSM, Ali MME, Khaprani HM. Long-term effect of pulsed nd: yag laser in the treatment of patients with rotator cuff tendinopathy: a randomized controlled trial. Photomed Laser Surg 2018;36:506-13. https://doi.org/10.1089/pho.2018.4476.
- Engebretsen K, Grotle M, Bautz-Holter E, Sandvik L, Juel NG, Ekeberg OM, et al. Radial extracorporeal shockwave treatment compared with supervised exercises in patients with subacromial pain syndrome: single blind randomised study. BMJ (Clin Res Ed) 2009;339. https://doi.org/10.1136/bmj.b3360.
- Engebretsen K, Grotle M, Bautz-Holter E, Ekeberg OM, Juel NG, Brox JI. Supervised exercises compared with radial extracorporeal shock-wave therapy for subacromial shoulder pain: 1-year results of a single-blind randomized controlled trial. Phys Ther 2011;91:37-4. https://doi.org/10.2522/ptj.20090338.
- Entrellardat Tortillol E. Effectiveness of percutaneus needle electrolysis and eccentric exercise in chronic patellar tendinopathy. J Invasive Tech Phys Ther 2019;02. https://doi.org/10.1055/s-0039-3401858.
- Eraslan L, Yuce D, Erbilici A, Baltaci G. Does Kinesiotaping improve pain and functionality in patients with newly diagnosed lateral epicondylitis?. Knee Surg Sports Traumatol Arthrosc 2018;26:938-45.
- Eraslan L, Baltaci G, Yuce D, Erbilici A. Effects of physiotherapy approaches on pain and strength in lateral epicondylitis: a randomized clinical trial2303 board# 50 May 29, 930 AM-1100 AM. Med Sci Sports Exerc 2015;47.
- Evangelos NPT, Anorthosis PT, Dimitrios S. Treatment of chronic patellar tendinopathy using an exercise program consisting of eccentric training and static stretching exercises combined with high intensity light therapy. A pilot study. MOJ Orthop Rheumatol 2018;10:157-61.
- Everhart JS, Cole D, Sojka JH, Higgins JD, Magnussen RA, Schmitt LC, et al. Treatment options for patellar tendinopathy: a systematic review. Arthrosc J Arthrosc Related Surg Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc 2017;33:861-72. https://doi.org/10.1016/j.arthro.2016.11.007.
- Faber E, Kuiper JI, Burdorf A, Miedema HS, Verhaar JAN. Treatment of impingement syndrome: a systematic review of the effects on functional limitations and return to work. J Occup Rehabil 2006;16:7-25.
- Fahlström M, Jonsson P, Lorentzon R, Alfredson Hå. Chronic Achilles tendon pain treated with eccentric calf-muscle training. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 2003;11:327-33.
- Farfaras S, Sernert N, Hallström E, Kartus Jü. Comparison of open acromioplasty, arthroscopic acromioplasty and physiotherapy in patients with subacromial impingement syndrome: a prospective randomised study. Knee Surg Sports Traumatol Arthrosc 2016;24:2181-91.
- Faria APGS, Martinho KO, Silva EB, Dantas EHM. The effects of different resources fotottherapeutic on the pain in individuals bearers of syndrome of the impact of the shoulder. Fitness Perform J (Online Ed) 2006;5:54-61.
- Färnqvist K, Pearson S, Malliaras P. Adaptation of tendon structure and function in tendinopathy with exercise and its relationship to clinical outcome. J Sport Rehabil 2020;29:107-15.
- French HP, Woodley SJ, Fearon A, O’Connor L, Grimaldi A. Physiotherapy management of greater trochanteric pain syndrome (GTPS): an international survey of current physiotherapy practice. Physiotherapy (UK) 2020;109:111-20. https://doi.org/10.1016/j.physio.2019.05.002.
- Frizziero A, Trainito S, Oliva F, Nicoli Aldini N, Masiero S, Maffulli N. The role of eccentric exercise in sport injuries rehabilitation. Br Med Bull 2014;110.
- Frizziero A, Vittadini F, Pignataro A, Gasparre G, Biz C, Ruggieri P, et al. Conservative management of tendinopathies around hip. Muscles Ligaments Tendons J 2016;6:281-92. https://doi.org/10.11138/mltj/2016.6.3.281.
- Frohm A, Saartok Tö, Halvorsen K, Renström P. Eccentric treatment for patellar tendinopathy: a prospective randomised short-term pilot study of two rehabilitation protocols. Br J Sports Med 2007;41.
- Furia JP, Rompe J-D, Maffulli N, Cacchio A, Schmitz C. Radial extracorporeal shock wave therapy is effective and safe in chronic distal biceps tendinopathy. Clin J Sport Med 2017;27:430-7. https://doi.org/10.1097/JSM.0000000000000399.
- Ganderton C, Semciw A, Cook J, Pizzari T. Does menopausal hormone therapy (MHT), exercise or a combination of both, improve pain and function in post-menopausal women with greater trochanteric pain syndrome (GTPS)? A randomised controlled trial. BMC Women Health 2016;16.
- García I, Lobo C, López E, Serván JL, Tenías JM. Comparative effectiveness of ultrasonophoresis and iontophoresis in impingement syndrome: a double-blind, randomized, placebo controlled trial. Clin Rehabil 2016;30:347-58. https://doi.org/10.1177/0269215515578293.
- Gärdin A, Movin T, Svensson L, Shalabi A. The long-term clinical and MRI results following eccentric calf muscle training in chronic Achilles tendinosis. Skelet Radiol 2010;39:435-42.
- Gatz M, Betsch M, Tingart M, Michalik R, Migliorini F, Dirrichs T, et al. Effect of a 12-week eccentric and isometric training in achilles tendinopathy on the gastrocnemius muscle: an ultrasound shear wave elastography study. Muscles Ligaments Tendons J 2020;10:92-9. https://doi.org/10.32098/mltj.01.2020.12.
- Gatz M, Betsch M, Dirrichs T, Schrading S, Tingart M, Michalik R, et al. Eccentric and isometric exercises in achilles tendinopathy evaluated by the VISA-A score and shear wave elastography. Sports Health 2020. https://doi.org/10.1177/1941738119893996.
- Gebremariam L, Hay EM, van der Sande R, Rinkel WD, Koes BW, Huisstede BMA. Subacromial impingement syndrome – effectiveness of physiotherapy and manual therapy. Br J Sports Med 2014;48:1202-8. https://doi.org/10.1136/bjsports-2012-091802.
- Giombini A, Di Cesare A, Safran MR, Ciatti R, Maffulli N. Short-term effectiveness of hyperthermia for supraspinatus tendinopathy in athletes: a short-term randomized controlled study. Am J Sports Med 2006;34. https://doi.org/10.1177/0363546506287827.
- Giray E, Karali-Bingul D, Akyuz G. The effectiveness of kinesiotaping, sham taping or exercises only in lateral epicondylitis treatment: a randomized controlled study. PM R 2019;11:681-93.
- Goldgrub R, Cote P, Sutton D, Wong JJ, Yu H, Randhawa K, et al. The effectiveness of multimodal care for the management of soft tissue injuries of the shoulder: a systematic review by the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration [with consumer summary]. J Manipulative Physiol Ther 2016;39:121-39.
- Gonsalves J, Kuyer E, McKay T, Moffat A, Palmer S. The Effectiveness of Exercise Therapy in Reducing Pain and Improving Clinical Outcomes in Rotator Cuff Tendinopathy: A Systematic Review. University of British Columbia; 2012.
- GonzÁLez PP, Brahim MBEN. Treatment of shoulder impingement syndrome in adolescent tennis players. / Tractament de la síndrome subacromial en tennistes adolescents. Apunts Educ Fís Esports 2018:32-47.
- Gonzalez-Iglesias J, Cleland JA, del Rosario Gutierrez-Vega M, Fernandez-de-las-Penas C. Multimodal management of lateral epicondylalgia in rock climbers: a prospective case series. J Manipulative Physiol Ther 2011;34:635-42.
- Gornoski LE, Coronado RA, George SZ. Clinical outcomes of electro-therapeutic point stimulation in conjunction with exercise for the treatment of patients with chronic knee pain: a case series. Orthop Phys Ther Pract 2014;26:182-7.
- Granviken F, Vasseljen O. Home exercises and supervised exercises are similarly effective for people with subacromial impingement: a randomised trial. J Physiother 2015;61:135-41.
- GrymelKulesza E, Polak A, Kubacki J, SkrzepPoloczek B, Krol P. The effect of a multi-modality therapy including active exercises, classic massage, cryotherapy and a combination of ultrasound and electrical stimulation on rotator cuff injuries. Fizjoterapia Polska 2007;7:107-23.
- Gunay Ucurum S, Kaya DO, Kayali Y, Askin A, Tekindal MA. Comparison of different electrotherapy methods and exercise therapy in shoulder impingement syndrome: a prospective randomized controlled trial. Acta Orthop Traumatol Turc 2018;52:249-55. https://doi.org/10.1016/j.aott.2018.03.005.
- Gürsel YK, Ulus Y, Bilgiç A, Dinçer G, van der Heijden GJM. Adding ultrasound in the management of soft tissue disorders of the shoulder: a randomized placebo-controlled trial. Phys Ther 2004;84:336-43.
- Gutiérrez-Espinoza H, Araya-Quintanilla F, Cereceda-Muriel C, Álvarez-Bueno C, Martínez-Vizcaíno V, Cavero-Redondo I. Effect of supervised physiotherapy versus home exercise program in patients with subacromial impingement syndrome: a systematic review and meta-analysis. Phys Ther Sport 2020;41:34-42. https://doi.org/10.1016/j.ptsp.2019.11.003.
- Haahr JP, Andersen JH. Prognostic factors in lateral epicondylitis: a randomized trial with one-year follow-up in 266 new cases treated with minimal occupational intervention of the usual approach in general practice. Rheumatology 2003;42:1216-25. https://doi.org/10.1093/rheumatology/keg360.
- Haahr JP, Østergaard S, Dalsgaard J, Norup K, Frost P, Lausen S, et al. Exercises versus arthroscopic decompression in patients with subacromial impingement: a randomised, controlled study in 90 cases with a one year follow up. Ann Rheum Dis 2005;64:760-4.
- Habets B, Van Cingel REH. Eccentric exercise training in chronic mid-portion A chilles tendinopathy: a systematic review on different protocols. Scand J Med Sci Sports 2015;25:3-15.
- Hakguder A, Tastekin N, Birtane M, Uzunca K, Zateri C, Sut N. Comparison of the short-term efficacy of physical therapy in subacromial impingement syndrome patients with stage I and II magnetic resonance imaging findings. Turk J Rheumatol 2011;26:127-34. https://doi.org/10.5606/tjr.2011.019.
- Hallgren HC, Holmgren T, Oberg B, Johansson K, Adolfsson LE. A specific exercise strategy reduced the need for surgery in subacromial pain patients. Br J Sports Med 2014.
- Hanratty CE, McVeigh JG, Kerr DP, Basford JR, Finch MB, Pendleton A, et al. The effectiveness of physiotherapy exercises in subacromial impingement syndrome: a systematic review and meta-analysis. Semin Arthritis Rheum 2012;42:297-316. https://doi.org/10.1016/j.semarthrit.2012.03.015.
- Hawk C, Minkalis AL, Khorsan R, Daniels CJ, Homack D, Gliedt JA, et al. Systematic review of nondrug, nonsurgical treatment of shoulder conditions. J Manipulative Physiol Ther 2017;40:293-319. https://doi.org/10.1016/j.jmpt.2017.04.001.
- Hazar Z, Baltacı G. Effects of ‘‘throwers ten’ exercise program on pain and function in shoulder impingement syndrome: a pilot study. Orthop J Sports Med 2014;2. https://doi.org/10.1177/2325967114S00153.
- Head J, Mallows A, Debenham J, Travers MJ, Allen L. The efficacy of loading programmes for improving patient-reported outcomes in chronic midportion Achilles tendinopathy: a systematic review. Musculoskelet Care 2019;17:283-99. https://doi.org/10.1002/msc.1428.
- Heitkamp HSJ, Kapitza C. The management of mid-portion achilles tendinopathy from a physiotherapeutic point of view: a systematic review. Sportverletz Sportschaden Organ Der Gesellschaft Fur Orthopadisch-Traumatologische Sportmedizin 2019. https://doi.org/10.1055/a-0877-3407.
- Hernandez Herrero D, Berjillos Donamayor A, de la Corte Rodriguez H, Diaz Garcia F, Tena Davila C, Moraleda Perez S, et al. Elbow tendinosis treated by several electrotherapy techniques: a prospective randomized study. Patologia Del Aparato Locomotor 2006;4:131-8.
- Heron SR, Woby SR, Thompson DP. Comparison of three types of exercise in the treatment of rotator cuff tendinopathy/shoulder impingement syndrome: a randomised control trial assessing. Physiotherapy 2017;103:167-73.
- Herrington L, McCulloch R. The role of eccentric training in the management of Achilles tendinopathy: a pilot study. Phys Ther Sport 2007;8:191-6.
- Ho LOL, Kwong WL, Cheing GLY. Effectiveness of microcurrent therapy in the management of lateral epicondylitis: a pilot study. Hong Kong Physiother J 2007;25:14-20. https://doi.org/10.1016/S1013-7025%2808%2970004-6.
- Holmgren T, Hallgren HB, Öberg B, Adolfsson L, Johansson K. Effect of specific exercise strategy on need for surgery in patients with subacromial impingement syndrome: randomised controlled study. BMJ 2012;344.
- Hong QN, Durand M, Loisel P. Physiotherapists’ management of patients with lateral epicondylitis (extensor tendinosis): results of a provincial survey. including commentary by MacDermid J. Physiother Can 2004;56:215-28.
- Hong QN, Durand MJ, Loisel P. Exploring the evidence for occupational therapists’ interventions with clients with lateral epicondylitis. Br J Occup Ther 2004;67:274-81.
- Hoogvliet P, Randsdorp MS, Dingemanse R, Koes BW, Huisstede BMA. Does effectiveness of exercise therapy and mobilisation techniques offer guidance for the treatment of lateral and medial epicondylitis? A systematic review. Br J Sports Med 2013;47:1112-9.
- Houck J, Neville C, Tome J, Flemister A. Randomized controlled trial comparing orthosis augmented by either stretching or stretching and strengthening for stage II tibialis posterior tendon dysfunction. Foot Ankle Int 2015.
- Hutchison A-M, Beard D, Pallister I, Topliss CJ, Williams P. Is physiotherapy effective for patients with a chronic mid-body Achilles tendinopathy? A systematic review of non-surgical and non-pharmacological interventions. Int Musculoskelet Med 2011;33:152-60. https://doi.org/10.1179/1753615411Y.0000000010.
- Iglesias JG, de Lara Osacar AR, Gonzalez CF, López JT, Llopis MM, Lado SI. C0088 ultrasound-guided intratissue percutaneous electrolysis, dry-needling, diathermy and eccentric exercise in achilles tendinopathy in runners. A case series. Br J Sports Med 2018;52.
- Innocenti T, Ristori D, Miele S, Testa M. The management of shoulder impingement and related disorders: a systematic review on diagnostic accuracy of physical tests and manual therapy efficacy. J Bodyw Mov Ther 2019;23:604-18. https://doi.org/10.1016/j.jbmt.2018.08.002.
- Jasnauskaitė-Gedrimė D, Gedrimas D, Karpavičienė A, Skurvydas A. Effect of visual and auditory feedback exercises on shoulder function in rotator cuff tendonitis patients. Baltic J Sport Health Sci 2018;109:20-6.
- Jayaseelan DJ, Moats N, Ricardo CR. Rehabilitation of proximal hamstring tendinopathy utilizing eccentric training, lumbopelvic stabilization, and trigger point dry needling: 2 case reports. J Orthop Sports Phys Ther 2014;44:198-205. https://doi.org/10.2519/jospt.2014.4905.
- Jayaseelan DJ, Kecman M, Alcorn D, Sault JD. Manual therapy and eccentric exercise in the management of Achilles tendinopathy. J Man Manipulative Ther 2017;25:106-14.
- Jerosch J, Wustner P. The effect of a sensorimotor exercise program in patients with subacromial pain syndrome. Unfallchirurg 2002;105:36-43. https://doi.org/10.1007/s113-002-8163-3.
- Johansson KM, Adolfsson LE, Foldevi MOM. Effects of acupuncture versus ultrasound in patients with impingement syndrome: randomized clinical trial. Phys Ther 2005;85:490-501.
- Johansson K, Bergström A, Schröder K, Foldevi M. Subacromial corticosteroid injection or acupuncture with home exercises when treating patients with subacromial impingement in primary care – a randomized clinical trial. Fam Pract 2011;28:355-65. https://doi.org/10.1093/fampra/cmq119.
- Johnson MD, Alvarez RG. Nonoperative management of retrocalcaneal pain with AFO and stretching regimen. Foot Ankle Int 2012;33:571-81.
- Jonsson P. Eccentric Training in the Treatment of Tendinopathy. Sweden: Umea University; 2009.
- Jonsson P, Wahlström P, Öhberg L, Alfredson Hå. Eccentric training in chronic painful impingement syndrome of the shoulder: results of a pilot study. Knee Surg Sports Traumatol Arthrosc 2006;14:76-81.
- Jonsson P, Alfredson H, Sunding K, Fahlström M, Cook J. New regimen for eccentric calf-muscle training in patients with chronic insertional Achilles tendinopathy: results of a pilot study. Br J Sports Med 2008;42:746-9.
- Jowett S, Crawshaw DP, Helliwell PS, Hensor EMA, Hay EM, Conaghan PG. Cost-effectiveness of exercise therapy after corticosteroid injection for moderate to severe shoulder pain due to subacromial impingement syndrome: a trial-based analysis. Rheumatology (Oxford, England) 2013;52:1485-91. https://doi.org/10.1093/rheumatology/ket149.
- Juul-Kristensen B, Larsen CM, Eshoj H, Clemmensen T, Hansen A, Bo Jensen P, et al. Positive effects of neuromuscular shoulder exercises with or without EMG-biofeedback, on pain and function in participants with subacromial pain syndrome - a randomised controlled trial. J Electromyogr Kinesiol Off J Int Soc Electrophysiol Kinesiol 2019;48:161-8. https://doi.org/10.1016/j.jelekin.2019.07.009.
- Kachanathu SJ, Alenazi AM, Hafez AR, Algarni AD, Alsubiheen AM. Comparison of the effects of short-duration wrist joint splinting combined with physical therapy and physical therapy alone on the management of patients with lateral epicondylitis. Eur J Phys Rehabil Med 2019;55:488-93. https://doi.org/10.23736/S1973-9087.19.05280-8.
- Kachanathu SJ, Zedan AME, Hafez AR, Alodaibi FA, Alenazi AM, Nuhmani S. Effect of shoulder stability exercises on hand grip strength in patients with shoulder impingement syndrome. Somatosens Mot Res 2019;36:97-101. https://doi.org/10.1080/08990220.2019.1604335.
- Kachingwe AF, Phillips B, Sletten E, Plunkett SW. Comparison of manual therapy techniques with therapeutic exercise in the treatment of shoulder impingement: a randomized controlled pilot clinical trial. J Man Manipulative Ther 2008;16:238-47.
- Kang F-J, Chiu Y-C, Wu S-C, Wang T-G, Yang J-l, Lin J-J. Kinesiology taping with exercise does not provide additional improvement in round shoulder subjects with impingement syndrome: a single-blinded randomized controlled trial. Phys Ther Sport 2019;40:99-106.
- Kaux J-F, Forthomme Bé, Namurois M-H, Bauvir P, Defawe N, Delvaux F, et al. Description of a standardized rehabilitation program based on sub-maximal eccentric following a platelet-rich plasma infiltration for jumper’s knee. Muscles Ligaments Tendons J 2014;4:85-9.
- Kaux JF, Croisier JL, Bruyere O, Rodriguez De La Cruz C, Forthomme B, Brabant G, et al. One injection of platelet-rich plasma associated to a submaximal eccentric protocol to treat chronic jumper’s knee. J Sports Med Phys Fitness 2015;55:953-61.
- Kaux J-F, Bruyere O, Croisier J-L, Forthomme Bé, Le Goff C, Crielaard J-M. One-year follow-up of platelet-rich plasma infiltration to treat chronic proximal patellar tendinopathies. Acta Orthop Belg 2015;81:251-6.
- Kaya E, Zinnuroglu M, Tugcu I. Kinesio taping compared to physical therapy modalities for the treatment of shoulder impingement syndrome. Clin Rheumatol 2011;30:201-7. https://doi.org/10.1007/s10067-010-1475-6.
- Kaya DO, Baltaci G, Toprak U, Atay AO. The clinical and sonographic effects of klnesiotaping and exercise in comparison with manual therapy and exercise for patients with subacromial impingement syndrome: a preliminary trial. J Manipulative Physiol Ther 2014;37:422-32. https://doi.org/10.1016/j.jmpt.2014.03.004.
- Kearney RS, Parsons N, Costa ML. Achilles tendinopathy management: a pilot randomised controlled trial comparing platelet-rich plasma injection with an eccentric loading programme [with consumer summary]. Bone Joint Res 2013;2:227-32.
- Kearney R, Costa ML. Insertional achilles tendinopathy management: a systematic review. Foot Ankle Int 2010;31:689-94. https://doi.org/10.3113/FAI.2010.0689.
- Kedia M, Williams M, Jain L, Barron M, Bird N, Blackwell B, et al. The effects of conventional physical therapy and eccentric strengthening for insertional Achilles tendinopathy. Int J Sports Phys Ther 2014;9.
- Kesikburun S, Tan AK, Yilmaz B, Yaşar E, Yazicioğlu K. Platelet-rich plasma injections in the treatment of chronic rotator cuff tendinopathy: a randomized controlled trial with 1-year follow-up. Am J Sports Med 2013;41. https://doi.org/10.1177/0363546513496542.
- Ketola S, Lehtinen J, Arnala I, Nissinen M, Westenius H, Sintonen H, et al. Does arthroscopic acromioplasty provide any additional value in the treatment of shoulder impingement syndrome?: a two-year randomised controlled trial. J Bone Joint Surg Br Vol 2009;91:1326-34. https://doi.org/10.1302/0301-620X.91B10.22094.
- Ketola S, Lehtinen JT, Arnala I. Arthroscopic decompression not recommended in the treatment of rotator cuff tendinopathy: a final review of a randomised controlled trial at a minimum follow-up of ten years. Bone Joint J 2017;99‐B:799-805. https://doi.org/10.1302/0301-620X.99B6.BJJ-2016-0569.R1.
- Ketola S, Lehtinen J, Rousi T, Nissinen M, Huhtala H, Arnala I. Which patients do not recover from shoulder impingement syndrome, either with operative treatment or with nonoperative treatment?. Acta Orthop 2015;86:641-6. https://doi.org/10.3109/17453674.2015.1033309.
- Ketola S, Lehtinen J, Elo P, Kortelainen S, Huhtala H, Arnala I. No difference in long-term development of rotator cuff rupture and muscle volumes in impingement patients with or without decompression: a randomized MRI study of 140 patients. Acta Orthop 2016;87:351-5. https://doi.org/10.1080/17453674.2016.1177780.
- Kim S, Kwon O, Weon J, Oh J. The effect of the Neurac training on shoulder isokinetic performance in patients with acute-phase subacromial impingement syndrome. Man Ther 2016;25.
- Kim J, Shin D, Song C. Visual feedback to improve the effects of scapular stabilization exercises on pain intensity, range of motion, strength, and disability in patients with shoulder impingement syndrome. Med Sci Technol 2017;58:42-8. https://doi.org/10.12659/MST.904039.
- Kim SJ, Yeo SM, Noh SJ, Ha C-W, Lee BC, Lee HS, et al. Effect of platelet-rich plasma on the degenerative rotator cuff tendinopathy according to the compositions. J Orthop Surg Res 2019;14. https://doi.org/10.1186/s13018-019-1406-4.
- Kim SY, Dvir Z, Oh JS. The application of the Neurac technique vs. manual therapy in patients during the acute phase of subacromial impingement syndrome: a randomized single-blinded controlled trial. J Back Musculoskelet Rehabil 2020;33:645-53. https://doi.org/10.3233/BMR-170884.
- Kim J, Lee SC, Chun Y, Jun HP, Seegmiller JG, Kim KM, et al. Effects of a 4-week short-foot exercise program on gait characteristics in patients with stage II posterior tibial tendon dysfunction. J Sport Rehabil 2020;30:120-8. https://doi.org/10.1123/jsr.2019-0211.
- Kingma JJ, de Knikker R, Wittink HM, Takken T. Eccentric overload training in patients with chronic Achilles tendinopathy: a systematic review. Br J Sports Med 2007;41.
- Knobloch K, Schreibmueller L, Longo UG, Vogt PM. Eccentric exercises for the management of tendinopathy of the main body of the Achilles tendon with or without the AirHeel™ Brace. A randomized controlled trial. A: effects on pain and microcirculation. Disabil Rehabil 2008;30:1685-91.
- Knobloch K, Schreibmueller L, Longo UG, Vogt PM. Eccentric exercises for the management of tendinopathy of the main body of the Achilles tendon with or without an AirHeel Brace. A randomized controlled trial. B: effects of compliance. Disabil Rehabil 2008;30. https://doi.org/10.1080/09638280701785676.
- Kongsgaard M, Qvortrup K, Larsen J, Aagaard P, Doessing S, Hansen P, et al. Fibril morphology and tendon mechanical properties in patellar tendinopathy: effects of heavy slow resistance training. Am J Sports Med 2010;38:749-56.
- Korakakis V, Whiteley R, Tzavara A, Malliaropoulos N. The effectiveness of extracorporeal shockwave therapy in common lower limb conditions: a systematic review including quantification of patient-rated pain reduction. Br J Sports Med 2018;52:387-40. https://doi.org/10.1136/bjsports-2016-097347.
- Koszalinski A, Flynn T, Hellman M, Cleland JA. Trigger point dry needling, manual therapy and exercise versus manual therapy and exercise for the management of Achilles tendinopathy: a feasibility study. J Man Manipulative Ther 2020:1-10.
- Krämer R, Lorenzen J, Vogt PM, Knobloch K. Systematic review about eccentric training in chronic achilles tendinopathy. Sportverletz Sportschaden Organ Der Gesellschaft Fur Orthopadisch-Traumatologische Sportmedizin 2010;24:204-11. https://doi.org/10.1055/s-0029-1245820.
- Kristensen J, Franklyn-Miller A. Resistance training in musculoskeletal rehabilitation: a systematic review. Br J Sports Med 2012;46:719-26. https://doi.org/10.1136/bjsm.2010.079376.
- Kromer TO, de Bie RA, Bastiaenen CHG. Physiotherapy in patients with clinical signs of shoulder impingement syndrome: a randomized controlled trial. J Rehabil Med 2013;45:488-97. https://doi.org/10.2340/16501977-1142.
- Kromer TO, Tautenhahn UG, de Bie RA, Staal JB, Bastiaenen CHG. Effects of physiotherapy in patients with shoulder impingement syndrome: a systematic review of the literature. J Rehabil Med 2009;41:870-80. https://doi.org/10.2340/16501977-0453.
- Kromer TO, de Bie RA, Bastiaenen CHG. Effectiveness of physiotherapy and costs in patients with clinical signs of shoulder impingement syndrome: one-year follow-up of a randomized controlled trial. J Rehabil Med 2014;46:1029-36. https://doi.org/10.2340/16501977-1867.
- Kuhn JE. Exercise in the treatment of rotator cuff impingement: a systematic review and a synthesized evidence-based rehabilitation protocol. J Shoulder Elbow Surg 2009;18:138-60.
- Kulig K, Lederhaus ES, Reischl S, Arya S, Bashford G. Effect of eccentric exercise program for early tibialis posterior tendinopathy. Foot Ankle Int 2009;30:877-85.
- Kulig K, Reischl SF, Pomrantz AB, Burnfield JM, Mais-Requejo S, Thordarson DB, et al. Nonsurgical management of posterior tibial tendon dysfunction with orthoses and resistive exercise: a randomized controlled trial. Phys Ther 2009;89:26-37.
- Kvalvaag E, Brox JI, Engebretsen KB, Soberg HL, Juel NG, Bautz-Holter E, et al. Effectiveness of radial extracorporeal shock wave therapy (rESWT) when combined with supervised exercises in patients with subacromial shoulder pain. Am J Sports Med 2017;45:2547-54.
- Kvalvaag E, Roe C, Engebretsen KB, Soberg HL, Juel NG, Bautz-Holter E, et al. One year results of a randomized controlled trial on radial Extracorporeal Shock Wave Treatment, with predictors of pain, disability and return to work in patients with subacromial pain syndrome. Eur J Phys Rehabil Med 2018;54:341-50. https://doi.org/10.23736/S1973-9087.17.04748-7.
- Laitinen S, Toivanen M. Patella-, akilles-ja hamstring-tendinopatioiden harjoitusterapia: Systemaattinen kirjallisuuskatsaus. Kaakkois-Suomen ammattikorkeakoulu; 2017.
- Land H, Gordon S, Watt K. Effect of manual physiotherapy in homogeneous individuals with subacromial shoulder impingement: a randomized controlled trial. Physiother Res Int J Res Clin Phys Ther 2019;24. https://doi.org/10.1002/pri.1768.
- Larsson MEH, Käll I, Nilsson-Helander K. Treatment of patellar tendinopathy – a systematic review of randomized controlled trials. Knee Surg Sports Traumatol Arthrosc 2012;20:1632-46.
- Larsson R, Bernhardsson S, Nordeman L. Effects of eccentric exercise in patients with subacromial impingement syndrome: a systematic review and meta-analysis. BMC Musculoskelet Disord 2019;20.
- Leduc BE, Caya J, Tremblay S, Bureau NJ, Dumont M. Treatment of calcifying tendinitis of the shoulder by acetic acid iontophoresis: a double-blind randomized controlled trial. Arch Phys Med Rehabil 2003;84:1523-7.
- Lee S, Ko Y, Lee W. Changes in pain, dysfunction, and grip strength of patients with acute lateral epicondylitis caused by frequency of physical therapy: a randomized controlled trial. J Phys Ther Sci 2014;26:1037-40.
- Lee WC, Ng GYF, Zhang ZJ, Malliaras P, Masci L, Fu SN. Changes on tendon stiffness and clinical outcomes in athletes are associated with patellar tendinopathy after eccentric exercise. Clin J Sport Med Off J Can Acad Sport Med 2020;30:25-32. https://doi.org/10.1097/JSM.0000000000000562.
- Lee D-R, Kim LJ. Internal- and external-rotation peak toque in little league baseball players with subacromial impingement syndrome: improved by closed kinetic chain shoulder training. J Sport Rehabil 2016;25:263-5. https://doi.org/10-1123/jsr.2014-0333.
- Lee WC. The Mechanical, Physiological and Therapeutic Effects of Eccentric Exercise Combined with Extracorporeal Shockwave Therapy in Athletes with Patellar Tendinopathy. Hong Kong: The Hong Kong Polytechnic University; 2017.
- Littlewood C, Malliaras P, Mawson S, May S, Walters SJ. Self-managed loaded exercise versus usual physiotherapy treatment for rotator cuff tendinopathy: a pilot randomised controlled trial. Physiotherapy 2014;100:54-60.
- Long L, Briscoe S, Cooper C, Hyde C, Crathorne L. What is the clinical effectiveness and cost-effectiveness of conservative interventions for tendinopathy? An overview of systematic reviews of clinical effectiveness and systematic review of economic evaluations. Health Technol Assess 2015;19:5-73. https://doi.org/10.3310/hta19080.
- LopezdeCelis C, BarraLopez ME, GonzalezRueda V, BuenoGracia E, RodriguezRubio PR, TricasMoreno JM. Effectiveness of diacutaneous fibrolysis for the treatment of chronic lateral epicondylalgia: a randomized clinical trial. Clin Rehabil 2018;32:644-53. https://doi.org/10.1177/0269215517738114.
- Ludewig PM, Borstad JD. Effects of a home exercise programme on shoulder pain and functional status in construction workers. Occup Environ Med 2003;60:841-9.
- Maenhout AG, Mahieu NN, De Muynck M, De Wilde LF, Cools AM. Does adding heavy load eccentric training to rehabilitation of patients with unilateral subacromial impingement result in better outcome? A randomized, clinical trial. Knee Surg Sports Traumatol Arthrosc 2013;21:1158-67.
- Maffulli N, Walley G, Sayana MK, Longo UG, Denaro V. Eccentric calf muscle training in athletic patients with Achilles tendinopathy. Disabil Rehabil 2008;30:1677-84.
- Maffulli N, Papalia R, D’Adamio S, Diaz Balzani L, Denaro V. Pharmacological interventions for the treatment of Achilles tendinopathy: a systematic review of randomized controlled trials. Br Med Bull 2015;113:101-15. https://doi.org/10.1093/bmb/ldu040.
- Mafi N, Lorentzon R, Alfredson H. Superior short-term results with eccentric calf muscle training compared to concentric training in a randomized prospective multicenter study on patients with chronic Achilles tendinosis. Knee Surg Sports Traumatol Arthrosc 2001;9:42-7. https://doi.org/10.1007/s001670000148.
- Magnussen RA, Dunn WR, Thomson AB. Nonoperative treatment of midportion Achilles tendinopathy: a systematic review. Clin J Sport Med 2009;19:54-6.
- Manias P, Stasinopoulos D. A controlled clinical pilot trial to study the effectiveness of ice as a supplement to the exercise programme for the management of lateral elbow tendinopathy. Br J Sports Med 2006;40:81-5. https://doi.org/10.1136/bjsm.2005.020909.
- Marik TL, Roll SC. Effectiveness of occupational therapy interventions for musculoskeletal shoulder conditions: a systematic review. Am J Occup Ther Off Publ Am Occup Ther Assoc 2017;71:7101180020p1-p11. https://doi.org/10.5014/ajot.2017.023127.
- Martinez-Silvestrini J, Newcomer KL, Gay RE, Schaefer MP, Kortebein P, Arendt KW. Chronic lateral epicondylitis: comparative effectiveness of a home exercise program including stretching alone versus stretching supplemented with eccentric or concentric strengthening. J Hand Ther 2005;18:411-20.
- Marzetti E, Rabini A, Piccinini G, Piazzini DB, Vulpiani MC, Vetrano M, et al. Neurocognitive therapeutic exercise improves pain and function in patients with shoulder impingement syndrome: a single-blind randomized controlled clinical trial. Eur J Phys Rehabil Med 2014;50:255-64.
- Mathew A, Afsaneh A. A combination approach using manual therapy and exercise in the treatment of shoulder impingement syndrome. Indian J Physiother Occup Ther 2013;7:87-9.
- Mayer F, Hirschmüller A, Müller S, Schuberth M, Baur H. Effects of short-term treatment strategies over 4 weeks in Achilles tendinopathy. Br J Sports Med 2007;41.
- McAleenan M, McVeigh JG, Cullen M, Sayers F, McCrea K, Baxter D. The effectiveness of night splints in Achilles tendinopathy: a pilot study. Physiother Ireland 2010;31:28-33.
- Mc Auliffe S, Korakakis V, Hilfiker R, Whiteley R, O’Sullivan K. Participant characteristics are poorly reported in exercise trials in tendinopathy: a systematic review. Phys Ther Sport 2021;48:43-5. https://doi.org/10.1016/j.ptsp.2020.12.012.
- McClure PW, Bialker J, Neff N, Williams G, Karduna A. Shoulder function and 3-dimensional kinematics in people with shoulder impingement syndrome before and after a 6-week exercise program. Phys Ther 2004;84:832-48.
- McCormack JR, Underwood FB, Slaven EJ, Cappaert TA. Eccentric exercise versus eccentric exercise and soft tissue treatment (Astym) in the management of insertional achilles tendinopathy. Sports Health 2016.
- McDevitt AW, Snodgrass SJ, Cleland JA, Leibold MBR, Krause LA, Mintken PE. Treatment of individuals with chronic bicipital tendinopathy using dry needling, eccentric-concentric exercise and stretching; a case series. Physiother Theory Pract 2020;36:397-40. https://doi.org/10.1080/09593985.2018.1488023.
- Melegati G, Tornese D, Bandi M. Effectiveness of extracorporeal shock wave therapy associated with kinesitherapy in the treatment of subacromial impingement: a randomised, controlled study [Efficacia della terapia con onde d’urto ex̀tracorporee associata a chinesiterapia nel trattamento della sindrome da conflitto subacromiale: Studio randomizzato controllato]. J Sports Traumatol Related Res 2000;22:58-64.
- Mendonça LD, Leite HR, Zwerver J, Henschke N, Branco G, Oliveira VC. How strong is the evidence that conservative treatment reduces pain and improves function in individuals with patellar tendinopathy? A systematic review of randomised controlled trials including GRADE recommendations. Br J Sports Med 2020;54:87-93.
- Menek B, Algun C, Tarakci D. Effectiveness of Mulligan Mobilization on Range of Motion and Function in Individuals with Subacromial Impingement Syndrome 2018. https://doi.org/10.1007/s00198-018-4465-1.
- Menta R, Randhawa K, Côté P, Wong JJ, Yu H, Sutton D, et al. The effectiveness of exercise for the management of musculoskeletal disorders and injuries of the elbow, forearm, wrist, and hand: a systematic review by the Ontario Protocol for Traffic Injury Management (OPTIMa) collaboration. J Manipulative Physiol Ther 2015;38:507-20.
- Miccinilli S, Bravi M, Morrone M, Santacaterina F, Stellato L, Bressi F, et al. A triple application of kinesio taping supports rehabilitation program for rotator cuff tendinopathy: a randomized controlled trial. Ortop Traumatol Rehabil 2018;20:499-505.
- Michener LA, Walsworth MK, Burnet EN. Effectiveness of rehabilitation for patients with subacromial impingement syndrome: a systematic review. J Hand Ther Off J Am Soc Hand Ther 2004;17:152-64.
- Morgan BC, Deyle GD, Petersen EJ, Allen CS, Koppenhaver SL. Dry needling in the management of patients meeting clinical diagnostic criteria for subacromial pain syndrome: a case series. Int J Sports Phys Ther 2019;14:637-54. https://doi.org/10.26603/ijspt20190637.
- Morton S, Chan O, King J, Perry D, Crisp T, Maffulli N, et al. High volume image-guided injections for patellar tendinopathy: a combined retrospective and prospective case series. Muscles Ligaments Tendons J 2014;4:214-9.
- Morton S, Chan O, Price J, Pritchard M, Crisp T, Perry JD, et al. High volume image-guided injections and structured rehabilitation improve greater trochanter pain syndrome in the short and medium term: a combined retrospective and prospective case series. Muscles Ligaments Tendons J 2015;5:73-87.
- Mulligan EP, Huang M, Dickson T, Khazzam M. The effect of axioscapular and rotator cuff exercise training sequence in patients with subacromial impingement syndrome: a randomized crossover trial. Int J Sports Phys Ther 2016;11:94-107.
- Munteanu SE, Scott LA, Bonanno DR, Landorf KB, Pizzari T, Cook JL, et al. Effectiveness of customised foot orthoses for Achilles tendinopathy: a randomised controlled trial. Br J Sports Med 2015;49. https://doi.org/10.1136/bjsports-2014-093845.
- Murphy M, Travers M, Gibson W, Chivers P, Debenham J, Docking S, et al. Rate of improvement of pain and function in mid-portion achilles tendinopathy with loading protocols: a systematic review and longitudinal meta-analysis. Sports Med 2018;48:1875-91. https://doi.org/10.1007/s40279-018-0932-2.
- Murphy MC, Travers MJ, Chivers P, Debenham JR, Docking SI, Rio EK, et al. Efficacy of heavy eccentric calf training for treating mid-portion Achilles tendinopathy: a systematic review and meta-analysis. Br J Sports Med 2019;53:1070-7.
- Nazligul T, Akpinar P, Aktas I, Unlu Ozkan F, Cagliyan Hartevioglu H. The effect of interferential current therapy on patients with subacromial impingement syndrome: a randomized, double-blind, sham-controlled study. Eur J Phys Rehabil Med 2018;54:351-7. https://doi.org/10.23736/S1973-9087.17.04743-8.
- Newcomer KL, Laskowski ER, Idank DM, McLean TJ, Egan KS. Corticosteroid injection in early treatment of lateral epicondylitis. Clin J Sport Med 2001;11:214-22.
- Nha Hong Q, Durand MJ, Loisel P. Physiotherapists’ management of patients with lateral epicondylitis (extensor tendinosis): results of a provincial survey. Physiother Can 2004;56:215-25.
- Nilsson P, Thom E, Baigi A, Marklund B, Mansson J. A prospective pilot study of a multidisciplinary home training programme for lateral epicondylitis. Musculoskelet Care 2007;5:36-50. https://doi.org/10.1002/msc.97.
- Nimgade A, Sullivan M, Goldman R. Physiotherapy, steroid injections, or rest for lateral epicondylosis? What the evidence suggests. Pain Pract 2005;5:203-15. https://doi.org/10.1111/j.1533-2500.2005.05307.x.
- Nishizuka T, Iwatsuki K, Kurimoto S, Yamamoto M, Hirata H. Efficacy of a forearm band in addition to exercises compared with exercises alone for lateral epicondylitis: a multicenter, randomized, controlled trial. J Orthop Sci 2017;22:289-94. https://doi.org/10.1016/j.jos.2016.11.011.
- Nørregaard J, Larsen CC, Bieler T, Langberg H. Eccentric exercise in treatment of Achilles tendinopathy. Scand J Med Sci Sports 2007;17:133-8.
- Notarnicola A, Maccagnano G, Tafuri S, Forcignanò MI, Panella A, Moretti B. CHELT therapy in the treatment of chronic insertional Achilles tendinopathy. Lasers Med Sci 2014;29:1217-25. https://doi.org/10.1007/s10103-013-1510-3.
- Nowotny J, El-Zayat B, Goronzy J, Biewener A, Bausenhart F, Greiner S, et al. Prospective randomized controlled trial in the treatment of lateral epicondylitis with a new dynamic wrist orthosis. Eur J Med Res 2018;23. https://doi.org/10.1186/s40001-018-0342-9.
- Nyberg A, Jonsson P, Sundelin G. Limited scientific evidence supports the use of conservative treatment interventions for pain and function in patients with subacromial impingement syndrome: randomized control trials. Phys Ther Rev 2010;15:436-52. https://doi.org/10.1179/1743288X10Y.0000000016.
- Ohberg L, Alfredson H. Effects on neovascularisation behind the good results with eccentric training in chronic mid-portion Achilles tendinosis?. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 2004;12:465-70.
- Ohberg L, Lorentzon R, Alfredson H. Eccentric training in patients with chronic Achilles tendinosis: normalised tendon structure and decreased thickness at follow up. Br J Sports Med 2004;38:8-11.
- Oken O, Kahraman Y, Ayhan F, Canpolat S, Yorgancioglu ZR, Oken OF. The short-term efficacy of laser, brace, and ultrasound treatment in lateral epicondylitis: a prospective, randomized, controlled trial. J Hand Ther 2008;21:63-8. https://doi.org/10.1197/j.jht.2007.09.003.
- Olaussen M, Holmedal Ø, Mdala I, Brage S, Lindbæk M. Corticosteroid or placebo injection combined with deep transverse friction massage, Mills manipulation, stretching and eccentric exercise for acute lateral epicondylitis: a randomised, controlled trial. BMC Musculoskelet Disord 2015;16.
- Olaussen M, Holmedal O, Lindbaek M, Brage S, Solvang H. Treating lateral epicondylitis with corticosteroid injections or non-electrotherapeutical physiotherapy: a systematic review. BMJ Open 2013;3. https://doi.org/10.1136/bmjopen-2013-003564.
- O’Neill S, Watson P, Barry S. Eccentric Rehabilitation for Runners with Achilles Tendinopathy Improves Endurance Capacity of the Plantarflexors n.d.:401-3. https://doi.org/10.1016/j.physio.2015.03.2052.
- Örsçelik A, Seven MM, Yıldız Y. Kronik lateral epikondilit tedavisinde proloterapi uygulamaları./Prolotherapy interventions in treatment of chronic lateral epicondylitis. Spor Hekimligi Dergisi Turk J Sports Med 2016;51:111-16.
- Ortega-Castillo M, Medina-Porqueres I. Effectiveness of the eccentric exercise therapy in physically active adults with symptomatic shoulder impingement or lateral epicondylar tendinopathy: a systematic review. J Sci Med Sport 2016;19:438-53.
- Østerås H, Torstensen TA, Arntzen G, Østerås BS. A comparison of work absence periods and the associated costs for two different modes of exercise therapies for patients with longstanding subacromial pain. J Med Econ 2008;11:371-81. https://doi.org/10.3111/13696990802191564.
- Østerås H, Torstensen TA, Haugerud L, Østerås BS. Dose-response effects of graded therapeutic exercises in patients with long-standing subacromial pain. Adv Physiother 2009;11:199-20. https://doi.org/10.3109/14038190802239729.
- Østerås H, Myhr G, Haugerud L, Torstensen TA. Clinical and MRI findings after high dosage medical exercise therapy in patients with long lasting subacromial pain syndrome: a case series on six patients. J Bodyw Mov Ther 2010;14:352-60. https://doi.org/10.1016/j.jbmt.2009.06.004.
- Østerås H, Torstensen TA, Østerås B. High-dosage medical exercise therapy in patients with long-term subacromial shoulder pain: a randomized controlled trial. Physiother Res Int J Res Clin Phys Ther 2010;15:232-42. https://doi.org/10.1002/pri.468.
- Ozgen M, Fırat S, Sarsan A, Topuz O, Ardıç F, Baydemir C. Short- and long-term results of clinical effectiveness of sodium hyaluronate injection in supraspinatus tendinitis. Rheumatol Int 2012;32. https://doi.org/10.1007/s00296-010-1577-0.
- Paavola M, Malmivaara A, Taimela S, Kanto K, Inkinen J, Kalske J, et al. Subacromial decompression versus diagnostic arthroscopy for shoulder impingement: randomised, placebo surgery controlled clinical trial. BMJ (Clin Res Ed) 2018;362. https://doi.org/10.1136/bmj.k2860.
- Page MJ, Green S, McBain B, Surace SJ, Deitch J, Lyttle N, et al. Manual therapy and exercise for rotator cuff disease. Cochrane Database Syst Rev 2016;2016. https://doi.org/10.1002/14651858.CD012224.
- Page MJ, Green S, Mrocki MA, Surace SJ, Deitch J, McBain B, et al. Electrotherapy modalities for rotator cuff disease (Cochrane review) [with consumer summary]. Cochrane Database Syst Rev 2016.
- Panni AS, Tartarone M, Maffulli N. Patellar tendinopathy in athletes: outcome of nonoperative and operative management. / Tendinite rotulienne chez des athletes: resultats d’une therapie operatoire et non operatoire. Am J Sports Med 2000;28:392-7.
- Paoloni JA, Appleyard RC, Nelson J, Murrell GAC. Topical glyceryl trinitrate treatment of chronic noninsertional achilles tendinopathy: a randomized, double-blind, placebo-controlled trial. JBJS 2004;86.
- Park JY, Park HK, Choi JH, Moon ES, Kim BS, Kim WS, et al. Prospective evaluation of the effectiveness of a home-based program of isometric strengthening exercises: 12-month follow-up. Clin Orthop Surg 2010;2:173-8.
- Parle PJ, Riddiford-Harland D, Howitt CD, Lewis JS. Acute rotator cuff tendinopathy: does ice, low load isometric exercise, or a combination of the two produce an analgaesic effect?. Br J Sports Med 2017;51:208-9.
- Pasin T, Ataoglu S, Pasin O, Ankarali H. Comparison of the effectiveness of platelet-rich plasma, corticosteroid, and physical therapy in subacromial impingement syndrome. Arch Rheumatol 2019;34:308-16. https://doi.org/10.5606/ArchRheumatol.2019.7225.
- Payne C. Clinical Applications of Shear Wave Elastography to Achilles Tendon Imaging and the Monitoring of a Rehabilitation Protocol for Achilles Tendinopathy 2018.
- Pearson J, Rowlands D, Highet R. Autologous blood injection to treat achilles tendinopathy? A randomized controlled trial. J Sport Rehabil 2012;21. https://doi.org/10.1123/jsr.21.3.218.
- Pearson SJ, Stadler S, Menz H, Morrissey D, Scott I, Munteanu S, et al. Immediate and short-term effects of short- and long-duration isometric contractions in patellar tendinopathy. Clin J Sport Med Off J Can Acad Sport Med 2018.
- Pekyavas NO, Baltaci G. Short-term effects of high-intensity laser therapy, manual therapy, and Kinesio taping in patients with subacromial impingement syndrome. Lasers Med Sci 2016;31:1133-41. https://doi.org/10.1007/s10103-016-1963-2.
- Penderghest CE, Kimura IF, Gulick DT. Double-blind clinical efficacy study of pulsed phonophoresis on perceived pain associated with symptomatic tendinitis. J Sport Rehabil 1998;7:9-19.
- Pérez-Merino L, Casajuana MC, Bernal G, Faba J, Astilleros AE, González R, et al. Evaluation of the effectiveness of three physiotherapeutic treatments for subacromial impingement syndrome: a randomised clinical trial. Physiotherapy 2016;102:57-63. https://doi.org/10.1016/j.physio.2015.01.010.
- Petersen W, Welp R, Rosenbaum D. Chronic Achilles tendinopathy: a prospective randomized study comparing the therapeutic effect of eccentric training, the AirHeel brace, and a combination of both. Am J Sports Med 2007;35:1659-67.
- Peterson M, Butler S, Eriksson M, Svärdsudd K. A randomized controlled trial of exercise versus wait-list in chronic tennis elbow (lateral epicondylosis). Ups J Med Sci 2011;116:269-79.
- Peterson M, Elmfeldt D, Svärdsudd K. Treatment practice in chronic epicondylitis: a survey among general practitioners and physiotherapists in Uppsala County, Sweden. Scand J Prim Health Care 2005;23:239-41.
- Pienimaki T, Karinen P, Kemila T, Koivukangas P, Vanharanta H. Long-term follow-up of conservatively treated chronic tennis elbow patients. A prospective and retrospective analysis. Scand J Rehabil Med 1998;30:159-66.
- Pieters L, Lewis J, Kuppens K, Jochems J, Bruijstens T, Joossens L, et al. An update of systematic reviews examining the effectiveness of conservative physical therapy interventions for subacromial shoulder pain. J Orthop Sports Phys Ther 2020;50:131-41. https://doi.org/10.2519/jospt.2020.8498.
- Praet SF, Purdam C, Welvaert M, Vlahovich N, Lovell G, Burke LM, et al. Oral supplementation of specific collagen peptides combined with calf-strengthening exercises enhances function and reduces pain in achilles tendinopathy patients. Nutrients 2019;11. https://doi.org/10.3390/nu11010076.
- Prat PI, Cibrowski D, Zuliani A, Stecco A. Efficacy of fascial manipulation and eccentric exercise for lateral elbow pain. J Bodyw Mov Ther 2018;22. https://doi.org/10.1016/j.jbmt.2018.09.028.
- Pribicevic M, Pollard H. A multi-modal treatment approach for the shoulder: a 4 patient case series. Chiropr Osteopat 2005;13:1-9.
- Punnoose A, Norrish A, Wellwood I, Pak K. The Effectiveness of Shockwave Therapy on Achilles and Patellar Tendinopathy: A Systematic Review and Meta-analysis n.d. https://doi.org/10.1016/j.physio.2015.03.1139.
- Purdam CR, Jonsson P, Alfredson H, Lorentzon R, Cook JL, Khan KM. A pilot study of the eccentric decline squat in the management of painful chronic patellar tendinopathy. Br J Sports Med 2004;38:395-7.
- Queiros Da Silva C, Cotte T, Vicard L, Chantelot L, Ferret JM. Contribution of excentric isokinetic work in the treatment of calcaneal tendinopathy and thigh muscle injury: results of a prospective study. J Traumatol Sport 2005;22:219-25. https://doi.org/10.1016/S0762-915X%2805%2983222-X.
- Araya-Quintanilla F, Espinoza HG, Eguía RA, Cornejo NP, Fuenzalida JV. Ejercicio excéntrico declinado en la tendinopatía patelar crónica: revisión sistemática. Revista Andaluza De Medicina Del Deporte 2012;5:75-82.
- Araya-Quintanilla F, Moyano Galvez V. Exercise therapy for lateral epicondylalgia: systematic review. Revista De La Sociedad Espanola Del Dolor 2015;22:253-70.
- Rabello LM, van den Akker-Scheek I, Brink MS, Maas M, Diercks RL, Zwerver J. Association between clinical and imaging outcomes after therapeutic loading exercise in patients diagnosed with achilles or patellar tendinopathy at short- and long-term follow-up: a systematic review. Clin J Sport Med Off J Can Acad Sport Med 2018. https://doi.org/10.1097/JSM.0000000000000624.
- Radovanovic G, Wolfarth B, Legerlotz K. Interleukin-6 levels drop after a 12 week long physiotherapeutic intervention in patients with Achilles tendinopathy – a pilot study. Transl Sports Med 2019;2:227-33. https://doi.org/10.1002/tsm2.95.
- Radpasand M, Owens E. Combined multimodal therapies for chronic tennis elbow: pilot study to test protocols for a randomized clinical trial. J Manipulative Physiol Ther 2009;32:571-85. https://doi.org/10.1016/j.jmpt.2009.08.010.
- Ram R, Meeuwisse W, Patel C, Wiseman DA, Wiley JP. The limited effectiveness of a home-based eccentric training for treatment of Achilles tendinopathy. Clin Invest Med n.d.;2013:E197-E206.
- Razavi M, Jansen GB. Effects of acupuncture and placebo TENS in addition to exercise in treatment of rotator cuff tendinitis. Clin Rehabil 2004;18. https://doi.org/10.1191/0269215504cr849oa.
- Resteghini P, Khanbhai T, Mughal S, Zivardeen Z. Double blind randomised controlled trial: injection of autologous blood for chronic patella tendinopathy. Clin J Sport Med Off J Can Acad Sport Med n.d. https://doi.org/10.1097/JSM.0000000000000099.
- Reyhan AC, Sindel D, Dereli EE. The effects of Mulligan’s mobilization with movement technique in patients with lateral epicondylitis. J Back Musculoskelet Rehabil 2020;33:99-107. https://doi.org/10.3233/BMR-181135.
- Riley SP, Cote MP, Leger RR, Swanson BT, Tafuto V, Sizer PS, et al. Short-term effects of thoracic spinal manipulations and message conveyed by clinicians to patients with musculoskeletal shoulder symptoms: a randomized clinical trial. J Man Manipulative Ther 2015;23:3-11. https://doi.org/10.1179/2042618613Y.0000000066.
- Rio E, Kidgell D, Purdam C, Gaida J, Moseley GL, Pearce AJ, et al. Isometric exercise induces analgesia and reduces inhibition in patellar tendinopathy. Br J Sports Med 2015;49:1277-83.
- Røe C, Brox JI, Bøhmer AS, Vøllestad NK. Muscle activation after supervised exercises in patients with rotator tendinosis. Arch Phys Med Rehabil 2000;81:67-72.
- Røe C, Ødegaard TT, Hilde F, Maehlum S, Halvorsen T. No effect of supplement of essential fatty acids on lateral epicondylitis. Tidsskrift for Den Norske Laegeforening: Tidsskrift for Praktisk Medicin, Ny Raekke 2005;125:2615-8.
- Romero-Morales C, Martín-Llantino PJ, Calvo-Lobo C, Beltran-Alacreu H, López-López D, Sánchez-Gómez R, et al. Effectiveness of eccentric exercise and a vibration or cryotherapy program in enhancing rectus abdominis muscle thickness and inter-rectus distance in patients with chronic mid-portion achilles tendinopathy: a randomized clinical trial. Int J Med Sci 2018;15:1764-70. https://doi.org/10.7150/ijms.28656.
- Romero-Morales C, Javier Martín-Llantino P, Calvo-Lobo C, Palomo-López P, López-López D, Fernández-Carnero J, et al. Ultrasonography effectiveness of the vibration vs cryotherapy added to an eccentric exercise protocol in patients with chronic mid-portion Achilles tendinopathy: a randomised clinical trial. Int Wound J 2019;16:542-9.
- Romero-Rodriguez D, Gual G, Tesch PA. Efficacy of an inertial resistance training paradigm in the treatment of patellar tendinopathy in athletes: a case-series study. Phys Ther Sport 2011;12:43-8.
- Rompe JD, Segal NA, Cacchio A, Furia JP, Morral A, Maffulli N. Home training, local corticosteroid injection, or radial shock wave therapy for greater trochanter pain syndrome. Am J Sports Med 2009;37:1981-90. https://doi.org/10.1177/0363546509334374.
- Rompe JD, Nafe B, Furia JP, Maffulli N. Eccentric loading, shock-wave treatment, or a wait-and-see policy for tendinopathy of the main body of tendo Achillis: a randomized controlled trial. Am J Sports Med 2007;35:374-83.
- Rompe JD, Furia J, Maffulli N. Eccentric loading versus eccentric loading plus shock-wave treatment for midportion achilles tendinopathy: a randomized controlled trial. Am J Sports Med 2009;37:463-70.
- Rosety-Rodriguez M, Ordonez-Munoz F, Huesa-Jimenez F, Rosety Rodriquez J, Gomez-Rodriguez F, Rosety-Plaza M. Eccentric training programs for infrapatellar tendinopathy: new strategies for an old problem. Patologia Del Aparato Locomotor 2006;4:105-7.
- Ross MH, Smith MD, Mellor R, Vicenzino B. Exercise for posterior tibial tendon dysfunction: a systematic review of randomised clinical trials and clinical guidelines [with consumer summary]. BMJ Open Sport Exerc Med 2018;4.
- Roy J-S, Moffet Hé, Hébert LJ, Lirette R. Effect of motor control and strengthening exercises on shoulder function in persons with impingement syndrome: a single-subject study design. Man Ther 2009;14:180-8. https://doi.org/10.1016/j.math.2008.01.010.
- Roy JS, Moffet H, McFadyen BJ. The effects of unsupervised movement training with visual feedback on upper limb kinematic in persons with shoulder impingement syndrome. J Electromyogr Kinesiol 2010;20:939-46. https://doi.org/10.1016/j.jelekin.2009.10.005.
- Saggini R, Di Stefano A, Galati V, Panelli E, Valeri M, Di Pancrazio L, et al. Long-term effectiveness of combined mechanotransduction treatment in jumper’s knee. Eur J Inflamm 2012;10:515-24. https://doi.org/10.1177/1721727X1201000327.
- Saithna A, Gogna R, Baraza N, Modi C, Spencer S. Eccentric exercise protocols for patella tendinopathy: should we really be withdrawing athletes from sport? A systematic review. Open Orthop J 2012;6:553-7. https://doi.org/10.2174/1874325001206010553.
- Sosa C, Lorenzo Calvo A, Jiménez Sáiz SL, Bonfanti N. Eccentric Exercise in Treatment of Patellar Tendinopathy in High Level Basketball Players: A Randomized Clinical Trial n.d. https://doi.org/10.1519/JSC.0000000000000721.
- Saltychev M, Äärimaa V, Virolainen P, Laimi K. Conservative treatment or surgery for shoulder impingement: systematic review and meta-analysis. Disabil Rehabil 2015;37:1-8. https://doi.org/10.3109/09638288.2014.907364.
- Sanderson LM, Bryant A. Effectiveness and safety of prolotherapy injections for management of lower limb tendinopathy and fasciopathy: a systematic review. J Foot Ankle Res 2015;8. https://doi.org/10.1186/s13047-015-0114-5.
- Sandford FM, Sanders TA, Wilson H, Lewis JS. A randomised controlled trial of long-chain omega-3 polyunsaturated fatty acids in the management of rotator cuff related shoulder pain. BMJ Open Sport Exerc Med 2018;4. https://doi.org/10.1136/bmjsem-2018-000414.
- Santamato A, Panza F, Notarnicola A, Cassatella G, Fortunato F, De SJL, et al. Is extracorporeal shockwave therapy combined with isokinetic exercise more effective than extracorporeal shockwave therapy alone for subacromial impingement syndrome? A randomized clinical trial. J Orthop Sports Phys Ther 2016;46:714-25. https://doi.org/10.2519/jospt.2016.4629.
- Saracoglu I, Emuk Y, Taspinar F. Does taping in addition to physiotherapy improve the outcomes in subacromial impingement syndrome? A systematic review. Physiother Theory Pract 2018;34:251-63. https://doi.org/10.1080/09593985.2017.1400138.
- Satyendra L, Byl N. Effectiveness of physical therapy for Achilles tendinopathy: an evidence based review of eccentric exercises. Isokinet Exerc Sci 2006;14:71-80.
- Savoie A, Mercier C, Desmeules F, Frémont P, Roy J-S. Effects of a movement training oriented rehabilitation program on symptoms, functional limitations and acromiohumeral distance in individuals with subacromial pain syndrome. Man Ther 2015;20:703-8. https://doi.org/10.1016/j.math.2015.04.004.
- Say F, Gurler D, Bulbul M. Platelet-rich plasma versus steroid injection for subacromial impingement syndrome. J Orthop Surg (Hong Kong) 2016;24:62-6.
- Sayana MK, Maffulli N. Eccentric calf muscle training in non-athletic patients with Achilles tendinopathy. J Sci Med Sport 2007;10:52-8.
- Saylor-Pavkovich E. Strength exercises combined with dry needling with electrical stimulation improve pain and function in patients with chronic rotator cuff tendinopathy: a retrospective case series. Int J Sports Phys Ther 2016;11:409-22.
- Scott A, LaPrade RF, Harmon KG, Filardo G, Kon E, Della Villa S, et al. Platelet-rich plasma for patellar tendinopathy: a randomized controlled trial of leukocyte-rich PRP or leukocyte-poor PRP versus saline. Am J Sports Med 2019;47:1654-61.
- Scott LA, Munteanu SE, Menz HB. Effectiveness of orthotic devices in the treatment of Achilles tendinopathy: a systematic review. Sports Med (Auckland, NZ) 2015;45:95-110. https://doi.org/10.1007/s40279-014-0237-z.
- Selvanetti A, Barrucci A, Antonaci A, Martinez P, Marra S, Necozione S. L’esercizio eccentrico nella rieducazione funzionale dell’ epicondilite: studio randomizzato controllato (Role of the eccentric exercise in the functional reeducation of lateral epicondylitis: a randomised controlled clinical trial) [Italian]. Medicina Dello Sport 2003;56:103-13.
- Sen U, Karagülle M, Erkorkmaz Ü. The efficacy of balneotherapy in the patients with subacromial impingement syndrome. Turkiye Klinikleri J Med Sci 2010;30:906-13.
- Senbursa G, Baltaci G, Atay A. Comparison of conservative treatment with and without manual physical therapy for patients with shoulder impingement syndrome: a prospective, randomized clinical trial. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 2007;15:915-21.
- Şenbursa G, Baltaci G, Atay ÖA. The effectiveness of manual therapy in supraspinatus tendinopathy. Acta Orthop Traumatol Turc 2011;45:162-7.
- Seven MM, Ersen O, Akpancar S, Ozkan H, Turkkan S, Yildiz Y, et al. Effectiveness of prolotherapy in the treatment of chronic rotator cuff lesions. Orthop Traumatol Surg Res 2017;103:427-33. https://doi.org/10.1016/j.otsr.2017.01.003.
- Sevier TL, Stegink-Jansen C. Astym treatment vs. eccentric exercise for lateral elbow tendinopathy: a randomized controlled clinical trial. PeerJ 2015;3. https://doi.org/10.7717/peerj.967.
- Shalabi A, Kristoffersen-Wilberg M, Svensson L, Aspelin P, Movin T. Eccentric training of the gastrocnemius-soleus complex in chronic Achilles tendinopathy results in decreased tendon volume and intratendinous signal as evaluated by MRI. Am J Sports Med 2004;32:1286-96.
- Shire AR, Stæhr TAB, Overby JB, Bastholm Dahl M, Sandell Jacobsen J, Høyrup Christiansen D. Specific or general exercise strategy for subacromial impingement syndrome – does it matter? A systematic literature review and meta analysis. BMC Musculoskelet Disord 2017;18. https://doi.org/10.1186/s12891-017-1518-0.
- Silbernagel KG, Thomeé R, Thomeé P, Karlsson J. Eccentric overload training for patients with chronic Achilles tendon pain – a randomised controlled study with reliability testing of the evaluation methods. Scand J Med Sci Sports 2001;11:197-206.
- Silbernagel KG, Thomeé R, Eriksson BI, Karlsson J. Full symptomatic recovery does not ensure full recovery of muscle-tendon function in patients with Achilles tendinopathy. Br J Sports Med 2007;41:276-80.
- Silbernagel KGv, Brorsson A, Lundberg M. The majority of patients with Achilles tendinopathy recover fully when treated with exercise alone: a 5-year follow-up. Am J Sports Med 2011;39:607-13.
- Simpson M, Smith TO. Quadriceps tendinopathy – a forgotten pathology for physiotherapists? A systematic review of the current evidence-base. Phys Ther Rev 2011;16:455-61.
- Şimşek HH, Balki S, Keklik SS, Öztürk H, Elden H. Does Kinesio taping in addition to exercise therapy improve the outcomes in subacromial impingement syndrome? A randomized, double-blind, controlled clinical trial. Acta Orthop Traumatol Turc 2013;47:104-10.
- Smidt N, van der Windt DAWM, Assendelft WJJ, Devillé WLJM, Korthals-de Bos IBC, Bouter LM. Corticosteroid injections, physiotherapy, or a wait-and-see policy for lateral epicondylitis: a randomised controlled trial. Lancet 2002;359:657-62. https://doi.org/10.1016/S0140-6736(02)07811-X.
- Smidt N, Assendelft WJJ, Arola H, Malmivaara A, Green S, Buchbinder R, et al. Effectiveness of physiotherapy, for lateral epicondylitis: a systematic review. Ann Med 2003;35:51-62. https://doi.org/10.1080/07853890310004138.
- Söderberg J, Grooten WJ, Äng BO. Effects of eccentric training on hand strength in subjects with lateral epicondylalgia: a randomized-controlled trial. Scand J Med Sci Sports 2012;22:797-803.
- Solomons L, Lee JJY, Bruce M, White LD, Scott A. Intramuscular stimulation vs sham needling for the treatment of chronic midportion Achilles tendinopathy: a randomized controlled clinical trial. PLOS One 2020;15. https://doi.org/10.1371/journal.pone.0238579.
- Stasinopoulos D. Cyriax physiotherapy, a supervised exercise programme and Bioptron light for the treatment of lateral epicondylitis. Clin Rehabil 2005;20:12-23. https://doi.org/10.1191/0269215506cr921oa.
- Stasinopoulos D, Stasinopoulos I. Comparison of effects of eccentric training, eccentric-concentric training, and eccentric-concentric training combined with isometric contraction in the treatment of lateral elbow tendinopathy. J Hand Ther 2017;30:13-9.
- Stasinopoulos D, Stasinopoulos I. Comparison of effects of exercise programme, pulsed ultrasound and transverse friction in the treatment of chronic patellar tendinopathy [with consumer summary]. Clin Rehabil 2004;18:347-52.
- Stasinopoulos D, Stasinopoulos I. Comparison of effects of Cyriax physiotherapy, a supervised exercise programme and polarized polychromatic non-coherent light (Bioptron light) for the treatment of lateral epicondylitis. Clin Rehabil 2006;20:12-23.
- Stasinopoulos D, Stasinopoulos I, Pantelis M, Stasinopoulou K. Comparing the effects of exercise program and low-level laser therapy with exercise program and polarized polychromatic non-coherent light (bioptron light) on the treatment of lateral elbow tendinopathy. Photomed Laser Surg 2009;27:513-20.
- Stasinopoulos D, Stasinopoulos I, Pantelis M, Stasinopoulou K. Comparison of effects of a home exercise programme and a supervised exercise programme for the management of lateral elbow tendinopathy. Br J Sports Med 2010;44:579-83.
- Dimitrios S, Ioannis S, Kalliopi S. A pilot trial to study the effectiveness of an exercise programme in the treatment of rotator cuff tendinopathy. Biol Exerc 2014;10.
- Stergioulas A. Effects of low-level laser and plyometric exercises in the treatment of lateral epicondylitis. Photomed Laser Surg 2007;25:205-13. https://doi.org/10.1089/pho.2007.2041.
- Stergioulas A, Stergioula M, Aarskog R, Lopes-Martins R, Bjordal JM. Effects of low-level laser therapy and eccentric exercises in the treatment of recreational athletes with chronic achilles tendinopathy. Am J Sports Med 2008;36:881-7.
- Steunebrink M, Zwerver J, Brandsema R, Groenenboom P, van den Akker-Scheek I, Weir A. Topical glyceryl trinitrate treatment of chronic patellar tendinopathy: a randomised, double-blind, placebo-controlled clinical trial. Br J Sports Med 2013;47:34-9.
- Steuri R, Sattelmayer M, Elsig S, Kolly C, Tal A, Taeymans J, et al. Effectiveness of conservative interventions including exercise, manual therapy and medical management in adults with shoulder impingement: a systematic review and meta-analysis of RCTs. Br J Sports Med 2017;51:1340-7.
- Struijs PAA, Damen P, Bakker EWP, Blankevoort L, Assendelft WJJ, van Dijk CN. Manipulation of the wrist for management of lateral epicondylitis: a randomized pilot study. Phys Ther 2003;83:608-16.
- Struijs PAA, Kerkhoffs GMMJ, Assendelft WJJ, van Dijk CN. Conservative treatment of lateral epicondylitis: brace versus physical therapy or a combination of both—a randomized clinical trial. Am J Sports Med 2004;32:462-9. https://doi.org/10.1177/0095399703258714.
- Struijs PA, Korthals-de Bos IB, van Tulder MW, van Dijk CN, Bouter LM, Assendelft WJ. Cost effectiveness of brace, physiotherapy, or both for treatment of tennis elbow. Br J Sports Med 2006;40:637-43.
- Struyf F, Nijs J, Mollekens S, Jeurissen I, Truijen S, Mottram S, et al. Scapular-focused treatment in patients with shoulder impingement syndrome: a randomized clinical trial. Clin Rheumatol 2013;32:73-85. https://doi.org/10.1007/s10067-012-2093-2.
- Subaşi V, Toktaş H, Seçil Demirdal Ü, Türel A, Çkir T, Kavuncu V. Water-based versus land-based exercise program for the management of shoulder impingement syndrome. / Omuz Subakromiyal Sıkışma Sendromunun Tedavisinde Su İçi Egzersizler ile Kara Egzersizlerinin Karşılaştırılması. Turk J Phys Med Rehabil Turkiye Fiziksel Tip Ve Rehabilitasyon Dergisi 2012;58:79-84.
- Subaşı V, Çakır T, Arıca Z, Sarıer RN, Filiz MB, Doğan ŞK, et al. Comparison of efficacy of kinesiological taping and subacromial injection therapy in subacromial impingement syndrome. Clin Rheumatol 2016;35:741-6. https://doi.org/10.1007/s10067-014-2824-7.
- Sussmilch-Leitch S, Collins NJ, Bialocerkowski AE, Warden SJ, Crossley KM. Physical therapies for Achilles tendinopathy: systematic review and meta-analysis. J Foot Ankle Res 2012;5.
- Svernlov B, Adolfsson L. Non-operative treatment regime including eccentric training for lateral humeral epicondylalgia. Scand J Med Sci Sports 2001;11:328-34.
- Sweeting KR, Whitty JA, Scuffham PA, Yelland MJ. Patient preferences for treatment of achilles tendon pain: results from a discrete-choice experiment. Patient 2011;4:45-54. https://doi.org/10.2165/11532830-000000000-00000.
- Syvertson P, Dietz E, Matocha M, McMurray J, Baker R, Nasypany A, et al. A treatment-based classification algorithm to treat achilles tendinopathy: an exploratory case series. J Sport Rehabil 2017;26:260-8. https://doi.org/10.1123/jsr.2016-0033.
- Szczurko O, Cooley K, Mills EJ, Zhou Q, Perri D, Seely D. Naturopathic treatment of rotator cuff tendinitis among Canadian postal workers: a randomized controlled trial. Arthritis Rheum 2009;61. https://doi.org/10.1002/art.24675.
- Tahran Ö, Yeşilyaprak SS. Effects of modified posterior shoulder stretching exercises on shoulder mobility, pain, and dysfunction in patients with subacromial impingement syndrome. Sports Health 2020;12:139-48. https://doi.org/10.1177/1941738119900532.
- Taskaynatan MA, Ozgul A, Ozdemir A, Tan AK, Kalyon TA. Effects of steroid iontophoresis and electrotherapy on bicipital tendonitis. J Musculoskelet Pain 2007;15. https://doi.org/10.1300/J094v15n04_06.
- Taunton JE, Ryan MB, Wong T. Eccentric-only heel drop training: examining a dose response in patients with achilles tendinosis. (Abstract). Clin J Sport Med 2004;14:382-3.
- Thijs KM, Zwerver J, Backx FJG, Steeneken V, Rayer S, Groenenboom P, et al. Effectiveness of shockwave treatment combined with eccentric training for patellar tendinopathy: a double-blinded randomized study. Clin J Sport Med 2017;27:89-96.
- Thompson G, Pearson JF. No attributable effects of PRP on greater trochanteric pain syndrome. N Z Med J 2019;132.
- Tonks JH. Evaluation of Short-term Conservative Treatment in Patients with Tennis Elbow (Lateral Epicondylitis): A Prospective Randomised, Assessor-Blinded Trial. University of Central Lancashire; 2012.
- Tonks JH, Pai SK, Murali SR. Steroid injection therapy is the best conservative treatment for lateral epicondylitis: a prospective randomised controlled trial. Int J Clin Pract 2007;61:240-6. https://doi.org/10.1111/j.1742-1241.2006.01140.x.
- Townsend C, Von Rickenbach KJ, Bailowitz Z, Gellhorn AC. Post-procedure protocols following platelet-rich plasma injections for tendinopathy: a systematic review. PM R J Injury Function Rehabil 2020. https://doi.org/10.1002/pmrj.12347.
- Trampas A, Kitsios A. Exercise and manual therapy for the treatment of impingement syndrome of the shoulder: a systematic review. Phys Ther Rev 2006;11:125-42.
- Trudel D, Duley J, Zastrow I, Kerr EW, Davidson R, MacDermid JC. Rehabilitation for patients with lateral epicondylitis: a systematic review. J Hand Ther 2004;17:243-66. https://doi.org/10.1197/j.jht.2004.02.011.
- Tsehaie J, Poot DHJ, Oei EHG, Verhaar JAN, de Vos R-J. Value of quantitative MRI parameters in predicting and evaluating clinical outcome in conservatively treated patients with chronic midportion Achilles tendinopathy: a prospective study. J Sci Med Sport 2017;20:633-7.
- Tumilty S, Munn J, Abbott JH, McDonough S, Hurley DA, Baxter GD. Laser therapy in the treatment of achilles tendinopathy: a pilot study. Photomed Laser Surg 2008;26:25-30. https://doi.org/10.1089/pho.2007.2126.
- Tumilty S, McDonough S, Hurley DA, Baxter GD. Clinical effectiveness of low-level laser therapy as an adjunct to eccentric exercise for the treatment of Achilles’ tendinopathy: a randomized controlled trial. Arch Phys Med Rehabil 2012;93:733-9.
- Tumilty S, Baxter GD. Heavy load eccentric exercise for Achilles tendinopathy; too much of a good thing?. Physiotherapy 2015;101:e1546-e7.
- Tumilty S, Mani R, Baxter GD. Photobiomodulation and eccentric exercise for Achilles tendinopathy: a randomized controlled trial. Lasers Med Sci 2016;31:127-35. https://doi.org/10.1007/s10103-015-1840-4.
- Turgut E, Duzgun I, Baltaci G. Effects of scapular stabilization exercise training on scapular kinematics, disability, and pain in subacromial impingement: a randomized controlled trial. Arch Phys Med Rehabil 2017;98. https://doi.org/10.1016/j.apmr.2017.05.023.
- Turgut E, Duzgun I, Baltaci G. Stretching exercises for subacromial impingement syndrome: effects of 6-week program on shoulder tightness, pain, and disability status. J Sport Rehabil 2018;27:132-7. https://doi.org/10.1123/jsr.2016-0182.
- Turgut E, Duzgun I. Two-year follow-up of the therapeutic exercise program for patients with rotator cuff tendinopathy: a single group study to investigate the effects on pain and disability. Ann Rheum Dis n.d.
- Tyler TF, Thomas GC, Nicholas SJ, McHugh MP. Addition of isolated wrist extensor eccentric exercise to standard treatment for chronic lateral epicondylosis: a prospective randomized trial. J Shoulder Elbow Surg 2010;19:917-22.
- Valera-Garrido F, Minaya-Munoz F, Medina-Mirapeix F. Ultrasound-guided percutaneous needle electroysis in chronic lateral epicondylitis: short-term and long-term results. Acupunct Med 2014;32:446-54.
- Valles-Carrascosa E, Gallego-Izquierdo T, Jimenez-Rejano J, Plaza-Manzano G, Pecos-Martin D, Hita-Contreras F, et al. Pain, motion and function comparison of two exercise protocols for the rotator cuff and scapular stabilizers in patients with subacromial syndrome [with consumer summary]. J Hand Ther 2018;31:227-37.
- Vander Doelen T, Jelley W. Non-surgical treatment of patellar tendinopathy: a systematic review of randomized controlled trials. J Sci Med Sport 2020;23:118-24.
- van der Worp H, Zwerver J, Hamstra M, van den Akker-Scheek I, Diercks RL. No difference in effectiveness between focused and radial shockwave therapy for treating patellar tendinopathy: a randomized controlled trial. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 2014;22:2026-32. https://doi.org/10.1007/s00167-013-2522-z.
- Vinuesa-Montoya S, Aguilar-Ferrándiz ME, Matarán-Peñarrocha GA, Fernández-Sánchez M, Fernández-Espinar EM, Castro-Sánchez AM. A preliminary randomized clinical trial on the effect of cervicothoracic manipulation plus supervised exercises vs a home exercise program for the treatment of shoulder impingement. J Chiropr Med 2017;16:85-93. https://doi.org/10.1016/j.jcm.2016.10.002.
- Virta L, Mortensen M, Eriksson R, Möller M. How many patients with subacromial impingement syndrome recover with physiotherapy? A follow-up study of a supervised exercise programme. Adv Physiother 2009;11:166-73.
- von Wehren L, Pokorny K, Blanke F, Sailer J, Majewski M. Injection with autologous conditioned serum has better clinical results than eccentric training for chronic Achilles tendinopathy. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 2019;27:2744-53. https://doi.org/10.1007/s00167-019-05465-8.
- van Ark M, Cook JL, Docking SI, Zwerver J, Gaida JE, Van Den Akker-Scheek I, et al. Do isometric and isotonic exercise programs reduce pain in athletes with patellar tendinopathy in-season? A randomised clinical trial. J Sci Med Sport 2016;19:702-6.
- van Ark M, Rio E, Cook J, van den Akker-Scheek I, Gaida JE, Zwerver J, et al. Clinical improvements are not explained by changes in tendon structure on UTC following an exercise program for patellar tendinopathy. Am J Phys Med 2018;97:708-14.
- Van Der Vlist AC, Van Oosterom RF, Van Veldhoven PLJ, BiermaZeinstra SMA, Waarsing JH, Verhaar JAN, et al. Effectiveness of a high volume injection as treatment for chronic Achilles tendinopathy: randomised controlled trial. BMJ 2020;370.
- van Rijn D, van den Akker-Scheek I, Steunebrink M, Diercks RL, Zwerver J, van der Worp H. Comparison of the effect of 5 different treatment options for managing patellar tendinopathy: a secondary analysis. Clin J Sport Med 2019;29:181-7.
- van Usen C, Pumberger B. Effectiveness of eccentric exercises in the management of chronic Achilles tendinosis. Internet J Allied Health Sci Pract 2007;5:1-14.
- Walsh N, Phelan M. An Investigation of an Exercise Class Versus Individual Exercise Sessions in the Management of Rotator Cuff Impingement Syndrome 2015. https://doi.org/10.1136/annrheumdis-2015-eular.1025.
- Wang CJ, Ko JY, Chan YS, Weng LH, Hsu SL. Extracorporeal shockwave for chronic patellar tendinopathy. Am J Sports Med 2007;35. https://doi.org/10.1177/0363546506298109.
- Wang TL, Fu BM, Ngai G, Yung P. Effect of isokinetic training on shoulder impingement. Genet Mol Res 2014;13:744-57. https://doi.org/10.4238/2014.January.31.1.
- Warden SJ, Metcalf BR, Kiss ZS, Cook JL, Purdam CR, Bennell KL, et al. Low-intensity pulsed ultrasound for chronic patellar tendinopathy: a randomized, double-blind, placebo-controlled trial. Rheumatology (Oxford, England) 2008;47. https://doi.org/10.1093/rheumatology/kem384.
- Wasielewski NJ, Kotsko KM. Does eccentric exercise reduce pain and improve strength in physically active adults with symptomatic lower extremity tendinosis: a systematic review. Database Abstracts Rev Effects (DARE) 2008.
- Wegener RL, Brown T, O’Brien L. The use of elastic therapeutic tape and eccentric exercises for lateral elbow tendinosis: a case series. Hand Ther 2015;20:56-63. https://doi.org/10.1177/1758998315580823.
- Wegener RL, Brown T, O’Brien L. A randomized controlled trial of comparative effectiveness of elastic therapeutic tape, sham tape or eccentric exercises alone for lateral elbow tendinosis. Hand Ther 2016;21. https://doi.org/10.1177/1758998316656660.
- Weir A, Jansen J, Van de Port IGL, Van de Sande HBA, Tol JL, Backx FJG. Manual or exercise therapy for long-standing adductor-related groin pain: a randomised controlled clinical trial. Man Ther 2011;16:148-54.
- Wen DY, Schultz BJ, Schaal B, Graham ST, Kim BS. Eccentric strengthening for chronic lateral epicondylosis: a prospective randomized study. Sports Health 2011;3:500-3. https://doi.org/10.1177/1941738111409690.
- Werner A, Walther M, Ilg A, Stahlschmidt T, Gohlke F. Self-training versus conventional physiotherapy in subacromial impingement syndrome. Zeitschrift Fur Orthopadie Und Ihre Grenzgebiete 2002;140:375-80.
- Wesner M, Defreitas T, Bredy H, Pothier L, Qin Z, McKillop AB, et al. A pilot study evaluating the effectiveness of platelet-rich plasma therapy for treating degenerative tendinopathies: a randomized control trial with synchronous observational cohort. PLOS ONE 2016;11. https://doi.org/10.1371/journal.pone.0147842.
- Wetke E, Johannsen F, Langberg H. Achilles tendinopathy: a prospective study on the effect of active rehabilitation and steroid injections in a clinical setting. Scand J Med Sci Sports 2015;25:e392-e9.
- Whalley RL, McQueen K, Powell R. A Self-Management Program for Lateral Epicondyle Tendinopathy 2019:570-1. https://doi.org/10.1016/j.jht.2019.09.032.
- Wheeler PC. Extracorporeal shock wave therapy plus rehabilitation for insertionaland noninsertional achilles tendinopathy shows good results across a range of domains of function. J Foot Ankle Surg Off Publ Am Coll Foot Ankle Surg 2019;58:617-22. https://doi.org/10.1053/j.jfas.2018.11.005.
- Wheeler PC. Novel interventions for recalcitrant patella tendinopathy: results may favour autologous blood injection (ABI) over radial-extra-corporeal shockwave therapy (r-ESWT) – a prospective cohort study. J Clin Orthop Trauma 2022;26. https://doi.org/10.1016/j.jcot.2022.101781.
- Wiedmann M, Mauch F, Huth J, Burkhardt P, Drews BH. Treatment of mid-portion Achilles tendinopathy with eccentric training and its effect on neovascularization. Sports Orthop Traumatol 2017;33:278-85. https://doi.org/10.1016/j.orthtr.2017.06.004.
- Wiegerinck JI, Kerkhoffs GM, van Sterkenburg MN, Sierevelt IN, van Dijk CN. Treatment for insertional Achilles tendinopathy: a systematic review. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 2013;21:1345-55. https://doi.org/10.1007/s00167-012-2219-8.
- Wiener M, Mayer F. Auswirkungen von physiotherapie auf die maximale drehmomententwicklung und schmerzempfindung bei supraspinatustendinose (Effects of physiotherapy on peak torque and pain in patients with tendinitis of the supraspinatus muscle) [German]. Deutsche Zeitschrift Fur Sportmedizin 2005;56:383-7.
- Wilson JK, Sevier TL, Helfst R, Honing EW, Thomann A. Comparison of rehabilitation methods in the treatment of patellar tendinitis. J Sport Rehabil 2000;9:304-14.
- Wilson F, Walshe M, O’Dwyer T, Bennett K, Mockler D, Bleakley C. Exercise, orthoses and splinting for treating Achilles tendinopathy: a systematic review with meta-analysis [with consumer summary]. Br J Sports Med 2018;52:1564-74.
- Woodley BL, Newsham-West R, Baxter GD. Chronic tendinopathy: effectiveness of eccentric exercise [with consumer summary]. Br J Sports Med 2007;41:188-98.
- Wright AA, Donaldson M, Wassinger CA, Emerson-Kavchak A. Subacute effects of cervicothoracic spinal thrust/non-thrust in addition to shoulder manual therapy plus exercise intervention in individuals with subacromial impingement syndrome: a prospective, randomized controlled clinical trial pilot study. J Man Manipulative Ther (Maney Publishing) 2017;25:190-20. https://doi.org/10.1080/10669817.2016.1251377.
- Yazmalar L, Sarıyıldız MA, Batmaz İ, Alpaycı M, Burkan YK, Özkan Y, et al. Efficiency of therapeutic ultrasound on pain, disability, anxiety, depression, sleep and quality of life in patients with subacromial impingement syndrome: a randomized controlled study. J Back Musculoskelet Rehabil 2016;29:801-7.
- Yeldan I, Cetin E, Ozdincler AR. The effectiveness of low-level laser therapy on shoulder function in subacromial impingement syndrome. Disabil Rehabil 2009;31:935-40. https://doi.org/10.1080/09638280802377985.
- Yelland M, Rabago D, Ryan M, Ng S-K, Vithanachchi D, Manickaraj N, et al. Prolotherapy injections and physiotherapy used singly and in combination for lateral epicondylalgia: a single-blinded randomised clinical trial. BMC Musculoskelet Disord 2019;20. https://doi.org/10.1186/s12891-019-2905-5.
- Yelland MJ, Sweeting KR, Lyftogt JA, Ng SK, Scuffham PA, Evans KA. Prolotherapy injections and eccentric loading exercises for painful Achilles tendinosis: a randomised trial. Br J Sports Med 2011;45:421-8. https://doi.org/10.1136/bjsm.2009.057968.
- Yerlikaya M, Talay Çaliş H, Tomruk Sütbeyaz S, Sayan H, Ibiş N, Koç A, et al. Comparison of effects of leukocyte-rich and leukocyte-poor platelet-rich plasma on pain and functionality in patients with lateral epicondylitis. Arch Rheumatol 2017;33:73-9. https://doi.org/10.5606/ArchRheumatol.2018.6336.
- Yildirim MA, Ones K, Celik EC. Comparision of ultrasound therapy of various durations in the treatment of subacromial impingement syndrome. J Phys Ther Sci 2013;25:1151-4.
- Yilmaz M, Eroglu S, Dundar U, Toktas H. The effectiveness of high-intensity laser therapy on pain, range of motion, functional capacity, quality of life, and muscle strength in subacromial impingement syndrome: a 3-month follow-up, double-blinded, randomized, placebo-controlled trial. Lasers Med Sci 2022;37:241-50. https://doi.org/10.1007/s10103-020-03224-7.
- Young M, Cook J, Purdam C, Kiss S, Alfredson H. Conservative treatment of patellar tendinopathy: a randomised trial comparing two treatment regimes – abstract. J Sci Med Sport 2002;5.
- Young JL, Rhon DI, de Zoete RMJ, Cleland JA, Snodgrass SJ. The influence of dosing on effect size of exercise therapy for musculoskeletal foot and ankle disorders: a systematic review. Braz J Phys Ther 2017;22:20-32. https://doi.org/10.1016/j.bjpt.2017.10.001.
- Yu J, Park D, Lee G. Effect of eccentric strengthening on pain, muscle strength, endurance, and functional fitness factors in male patients with achilles tendinopathy. Am J Phys Med Rehabil 2013;92:68-76.
- Yu H, Randhawa K, Cote P, Collaboration O. The effectiveness of physical agents for lower-limb soft tissue injuries: a systematic review [with consumer summary]. J Orthop Sports Phys Ther 2016;46:523-54.
- Yuksel E, Yesilyaprak SS. The Effectiveness of Scapular Stabilization Exercises in Patients with Subacromial Impingement Syndrome and Scapular Dyskinesis 2015. https://doi.org/10.1136/annrheumdis-2015-eular.5594.
- Yuruk ZO, Kirdi N. The Effects of Radial Extracorporeal Shock Wave Therapy on Subjective Pain and Functionality in Patients with Lateral Epicondylitis n.d.
- Knobloch K, Schreibmueller L, Kraemer R, Jagodzinski M, Richter M, Zeichen J, et al. Eccentric training and an Achilles wrap reduce Achilles tendon capillary blood flow and capillary venous filling pressures and increase tendon oxygen saturation in insertional and midportion tendinopathy: a randomized trial. Am J Sports Med 2007;35:189-96. https://doi.org/10.1177/0363546506295700.
- Romero-Morales C, MartinLlantino PJ, CalvoLobo C, San AntolinGil M, LopezLopez D, Pedro MBD, et al. Vibration increases multifidus cross-sectional area versus cryotherapy added to chronic non-insertional Achilles tendinopathy eccentric exercise. Phys Ther Sport 2020;42:61-7.
- Rabusin CL, Menz HB, McClelland JA, Evans AM, Malliaras P, Docking SI, et al. Efficacy of heel lifts versus calf muscle eccentric exercise for mid-portion Achilles tendinopathy (HEALTHY): a randomised trial. Br J Sports Med 2020.
- Rompe JD, Furia J, Maffulli N. Eccentric loading compared with shock wave treatment for chronic insertional achilles tendinopathy: a randomized, controlled trial. J Bone Joint Surg Series A 2008;90:52-61. https://doi.org/10.2106/JBJS.F.01494.
- Genc E, Duymaz T. Effectiveness of kinesio taping in bicipital tendinitis treatment: a randomized controlled trial kinesio taping in bicipital tendinitis. Ann Clin Anal Med 2020;11:498-503.
- Ramon S, Russo S, Santoboni F, Lucenteforte G, Di Luise C, de Unzurrunzaga R, et al. Focused shockwave treatment for greater trochanteric pain syndrome: a multicenter, randomized, controlled clinical trial. J Bone Joint Surg Am Vol 2020;102:1305-11.
- Silder A, Sherry MA, Sanfilippo J, Tuite MJ, Hetzel SJ, Heiderscheit BC. Clinical and morphological changes following 2 rehabilitation programs for acute hamstring strain injuries: a randomized clinical trial. J Orthop Sports Phys Ther 2013;43:284-99. https://doi.org/10.2519/jospt.2013.4452.
- Schroven W, Vles G, Verhaegen J, Roussot M, Bellemans J, Konan S. Operative management of isolated posterior cruciate ligament injuries improves stability and reduces the incidence of secondary osteoarthritis: a systematic review. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 2021. https://doi.org/10.1007/s00167-021-06723-4.
- Stasinopoulos D, Manias P. Comparing two exercise programmes for the management of lateral elbow tendinopathy (tennis elbow/lateral epicondylitis) – A controlled clinical trial. Open Access J Sci Technol 2013;1.
- Rodriguez-Huguet M, Gongora-Rodriguez J, Lomas-Vega R, Martin-Valero R, Diaz-Fernandez A, Obrero-Gaitan E, et al. Percutaneous electrolysis in the treatment of lateral epicondylalgia: a single-blind randomized controlled trial. J Clin Med 2020;9:1-11. https://doi.org/10.3390/jcm9072068.
- McQueen KS, Powell RK, Keener T, Whalley R, Calfee RP. Role of strengthening during nonoperative treatment of lateral epicondyle tendinopathy. J Hand Ther 2021;34:619-26. https://doi.org/10.1016/j.jht.2020.10.009.
- Ilhanli I, Guder N, Gul M. Platelet-rich plasma treatment with physical therapy in chronic partial supraspinatus tears. Iran Red Crescent Med J 2015;17. https://doi.org/10.5812/ircmj.23732.
- Breda SJ, Oei EHG, Zwerver J, Visser E, Waarsing E, Krestin GP, et al. Effectiveness of progressive tendon-loading exercise therapy in patients with patellar tendinopathy: a randomised clinical trial. Br J Sports Med 2020.
- Lee W-C, Ng GY-F, Zhang Z-J, Malliaras P, Masci L, Fu S-N. Changes on tendon stiffness and clinical outcomes in athletes are associated with patellar tendinopathy after eccentric exercise. Clin J Sport Med Off J Can Acad Sport Med 2017. https://doi.org/10.1097/JSM.0000000000000562.
- Polimeni V, Panuccio A, Furfari P, Crupi D, Barreca G, Forgione C, et al. Preliminary study on the efficacy of various rehabilitation therapies for shoulder pain. Eura Medicophys 2003;39:59-63.
- Blume C, Wang-Price S, Trudelle-Jackson E, Ortiz A. Comparison of eccentric and concentric exercise interventions in adults with subacromial impingement syndrome. Int J Sports Phys Ther 2015;10:441-55.
- Rhon DI, Boyles RB, Cleland JA. One-year outcome of subacromial corticosteroid injection compared with manual physical therapy for the management of the unilateral shoulder impingement syndrome: a pragmatic randomized trial. Ann Intern Med 2014;161:161-9. https://doi.org/10.7326/M13-2199.
- McGee C, Kersting E, Palmer-McLean K, Davies GJ. Standard rehabilitation vs standard plus closed kinetic chain rehabilitation for patients with shoulder impingement: a rehabilitation outcomes study. Phys Ther 1999;79.
- Cha J-Y, Kim J-H, Hong J, Choi Y-T, Kim M-H, Cho J-H, et al. A 12-week rehabilitation program improves body composition, pain sensation, and internal/external torques of baseball pitchers with shoulder impingement symptom. J Exerc Rehabil 2014;10:35-44. https://doi.org/10.12965/jer.140087.
- de Oliveira FCL, Pairot de Fontenay B, Bouyer LJ, Desmeules F, Roy JS. Kinesiotaping for the rehabilitation of rotator cuff-related shoulder pain: a randomized clinical trial. Sports Health 2020.
- Buyuksireci DE, Turk AC. Evaluation of the effectiveness of dexamethasone iontophoresis in patients with subacromial impingement syndrome. J Orthop Sci 2021;26:786-91. https://doi.org/10.1016/j.jos.2020.09.007.
- Beaudreuil J, Lasbleiz S, Yelnik A, Bardin T, Orcel P. Effect of dynamic humeral centering on painful active elevation of the arm in subacromial impingement syndrome: a randomized trial. Ann Phys Rehabil Med 2012;55:e158-61.
- Ketola S, Lehtinen J, Rousi T, Nissinen M, Huhtala H, Konttinen YT, et al. No evidence of long-term benefits of arthroscopic acromioplasty in the treatment of shoulder impingement syndrome. Bone Joint Res 2013;2:132-9. https://doi.org/10.1302/2046-3758.27.2000163.
- Pekgoz F, TaAkiran H, Mutlu EK, Atalay A, Celiker R. Comparison of mobilization with supervised exercise for patients with subacromial impingement syndrome. Turk J Phys Med Rehabil 2020;66:184-92.
- Koç C, Kurt EE, Koçak FA, Erdem HR, Konar NM. Does balneotherapy provide additive effects to physical therapy in patients with subacute supraspinatus tendinopathy? A randomized, controlled, single-blind study. Int J Biometeorol 2021;65:301-10. https://doi.org/10.1007/s00484-020-02032-6.
- Hotta GH, Gomes de Assis Couto A, Cools AM, McQuade KJ, Siriani de Oliveira A. Effects of adding scapular stabilization exercises to a periscapular strengthening exercise program in patients with subacromial pain syndrome: a randomized controlled trial. Musculoskelet Sci Pract 2020;49. https://doi.org/10.1016/j.msksp.2020.102171.
- Chaconas EJ, Kolber MJ, Hanney WJ, Daugherty ML, Wilson SH, Sheets C. Shoulder external roator eccentric training versus general shoulder exercise for subacromial pain syndrome: a randomized controlled trial. Int J Sports Phys Ther 2017;12:1121-33. https://doi.org/10.26603/ijspt20171121.
- Jeong TH, Oh J, Lee HJ, Yang YJ, Nha K, Suh J. The effect of the combined stretching and strengthening exercise on the clinical symptoms in posterior tibial tendon dysfunction patient. J Korean Foot Ankle Soc 2008;12:47-54.
- Oliveira L. It is not always what it appears. Clin J Sport Med 2022;32:e204-e5. https://doi.org/10.1097/JSM.0000000000001017.
- Rodriguez-Huguet M, Gongora-Rodriguez J, Rodriguez-Huguet P, Ibanez-Vera AJ, Rodriguez-Almagro D, Martin-Valero R, et al. Effectiveness of percutaneous electrolysis in supraspinatus tendinopathy: a single-blinded randomized controlled trial. J Clin Med 2020;9:1-13. https://doi.org/10.3390/jcm9061837.
- Sawada T, Okawara H, Nakashima D, Iwabuchi S, Matsumoto M, Nakamura M, et al. Effects of alternating heat and cold stimulation using a wearable thermo-device on subjective and objective shoulder stiffness. J Physiol Anthropol 2022;41. https://doi.org/10.1186/s40101-021-00275-9.
- Malliaris P, Cridland K, Hopmans R, Littlewood S, Page R, Harris I, et al. Internet and telerehabilitation-delivered management of rotator cuff-related shoulder pain (INTEL trial): randomized controlled pilot and feasibility trial. JMIR MHealth UHealth 2020;8. https://doi.org/10.2196/24311.
- Morrissey D, Roskilly A, Twycross-Lewis R, Isinkaye T, Screen H, Woledge R, et al. The effect of eccentric and concentric calf muscle training on Achilles tendon stiffness. Clin Rehabil 2011;25:238-42.
- MacDonald K, Day J, Dionne C. Effect of eccentric exercises at the knee with hip muscle strengthening to treat patellar tendinopathy in active duty military personnel: a randomized pilot. Orthop Phys Ther Pract 2019;31:8-16.
- Sprague AL, Couppe C, Pohlig RT, Snyder–Mackler L, Silbernagel KG. Pain-guided activity modification during treatment for patellar tendinopathy: a feasibility and pilot randomized clinical trial. Pilot Feasibility Stud 2021;7. https://doi.org/10.1186/s40814-021-00792-5.
Appendix 1 Detailed search strategies
Search strategy scoping review
Search last updated 28 April 2020
| Embase (Ovid) | (exercise OR exercise*.mp OR “isometric exercise” OR kinesiotherapy OR Eccentric.mp OR concentric.mp OR “heavy slow resistance”.mp OR “isokinetic exercise” OR plyometrics OR “muscle stretching” OR “muscle training”) AND (tendinitis OR Tendinopathy.mp OR “tendon injury” OR “shoulder injury” OR “rotator cuff injury” OR “tennis elbow” OR tendin.mp OR tendon.mp OR bursitis OR “shoulder impingement syndrome” OR 2posterior tibial tendon dysfunction” OR “Greater trochanteric pain syndrome”.mp) |
| CINAHL (EBSCO-host) | (MH Exercise OR AB exercise* OR MH “muscle strengthening” OR MH “rehabilitation” OR MH “eccentric contraction” OR TX “heavy slow resistance exercis*” OR AB eccentric OR AB concentric OR AB isokinetic OR MH “therapeutic exercise”) AND (MH tendinopathy OR MH “arm injuries” OR “tendon injuries” OR MH tendons OR TX tendin* OR TX tendon* OR AB bursitis OR MH Bursitis OR MH “Posterior tibial tendon dysfunction” OR MH “shoulder impingement syndrome” OR AB “Greater trochanteric pain syndrome”) |
| MEDLINE (EBSCO-host) | (MH exercise OR AB exercise* OR MH “isometric contraction” OR MH rehabilitation OR TX eccentric OR TX concentric OR TX “heavy slow resistance” OR TX isokinetic) AND (MH tendinopathy OR MH “shoulder injuries” OR MH tendons OR MH “tendon injuries OR TX tendin* OR tendon* OR MH bursitis OR AB bursitis OR MH “posterior tibial tendon dysfunction” OR MH “shoulder impingement syndrome” OR AB “greater trochanteric pain syndrome”) |
| SPORTDiscus (EBSCO-host) | (DE exercise OR DE “exercise therapy” OR AB exercise* OR TX eccentric OR TX concentric OR TX “heavy slow resistance” OR DE “isokinetic exercise” OR DE plyometrics OR DE “strength training” OR DE “stretch (physiology)” OR DE “isometric exercise” OR DE rehabilitation) AND (DE tendinitis OR DE tendinosis OR AB tendinopathy OR DE “tendon injuries” OR “shoulder injuries” OR DE “tennis elbow” OR AB tendin* OR AB tendon* OR DE bursitis OR AB “shoulder impingement syndrome” OR AB “posterior tibial tendon dysfunction” OR AB “greater trochanteric pain syndrome”) |
| Amed (EBSCO-host) | (ZU exercise OR ZU “exercise therapy” OR AB exercise OR ZU “muscle stretching exercises” OR ZU “isometric contraction” OR ZU rehabilitation OR TZ eccentric OR TZ concentric OR TX “heavy slow resistance” OR TX isokinetic OR AB plyometric) AND (ZU tendinopathy OR ZU “tendon injuries” OR ZU tendons OR ZU “shoulder injuries” OR ZU “tennis elbow” OR TX tendin* OR TX tendon* OR ZU bursitis OR AB bursitis OR ZU “shoulder impingement syndrome” OR ZU “posterior tibial tendon dysfunction” OR AB “greater trochanteric pain syndrome”) |
| Open Grey | Tendinopathy AND exercise Tendin* AND exercise Tendon AND exercise |
| Mednar | Tendinopathy AND exercise Tendin* AND exercise Tendon AND exercise |
| New York Academy Grey Literature Report | Tendinopathy AND exercise Tendin* AND exercise Tendon AND exercise |
| EThOS | Tendinopathy AND exercise Tendin* AND exercise Tendon AND exercise |
| Google Scholar | Tendinopathy AND exercise Tendin* AND exercise Tendon AND exercise |
| JBI Evidence Synthesis | Tendinopathy AND exercise |
| Cochrane Library | Tendinopathy AND exercise Tendin* AND exercise Tendon AND exercise |
| PEDro | Tendinopathy AND exercise Tendin* AND exercise Tendon AND exercise |
| Epistemonikos | (tendinopathy OR tendon* OR tendin*) AND exercise |
| CORE | Tendinopathy AND exercise Tendin* AND exercise Tendon AND exercise |
| Clinicialtrials.gov | Tendinopathy AND exercise Tendin* AND exercise Tendon AND exercise |
| ISRCTN | Tendinopathy AND exercise Tendin* AND exercise Tendon AND exercise |
| EU CTR | Tendinopathy AND exercise Tendin* AND exercise Tendon AND exercise |
| ANZCTR | Tendinopathy AND exercise Tendin* AND exercise Tendon AND exercise |
Search strategy efficacy reviews
Search last updated 19 January 2021
| Embase (Ovid) | (exercise OR exercise*.mp OR “isometric exercise” OR kinesiotherapy OR Eccentric.mp OR concentric.mp OR “heavy slow resistance”.mp OR “isokinetic exercise” OR plyometrics OR “muscle stretching” OR “muscle training”) AND (tendinitis OR Tendinopathy.mp OR “tendon injury” OR “shoulder injury” OR “rotator cuff injury” OR “tennis elbow” OR tendin.mp OR tendon.mp OR bursitis OR “shoulder impingement syndrome” OR 2posterior tibial tendon dysfunction” OR “Greater trochanteric pain syndrome”.mp) |
| CINAHL (EBSCO-host) | (MH Exercise OR AB exercise* OR MH “muscle strengthening” OR MH “rehabilitation” OR MH “eccentric contraction” OR TX “heavy slow resistance exercis*” OR AB eccentric OR AB concentric OR AB isokinetic OR MH “therapeutic exercise”) AND (MH tendinopathy OR MH “arm injuries” OR “tendon injuries” OR MH tendons OR TX tendin* OR TX tendon* OR AB bursitis OR MH Bursitis OR MH “Posterior tibial tendon dysfunction” OR MH “shoulder impingement syndrome” OR AB “Greater trochanteric pain syndrome”) |
| MEDLINE (EBSCO-host) | (MH exercise OR AB exercise* OR MH “isometric contraction” OR MH rehabilitation OR TX eccentric OR TX concentric OR TX “heavy slow resistance” OR TX isokinetic) AND (MH tendinopathy OR MH “shoulder injuries” OR MH tendons OR MH “tendon injuries OR TX tendin* OR tendon* OR MH bursitis OR AB bursitis OR MH “posterior tibial tendon dysfunction” OR MH “shoulder impingement syndrome” OR AB “greater trochanteric pain syndrome”) |
| SPORTDiscus (EBSCO-host) | (DE exercise OR DE “exercise therapy” OR AB exercise* OR TX eccentric OR TX concentric OR TX “heavy slow resistance” OR DE “isokinetic exercise” OR DE plyometrics OR DE “strength training” OR DE “stretch (physiology)” OR DE “isometric exercise” OR DE rehabilitation) AND (DE tendinitis OR DE tendinosis OR AB tendinopathy OR DE “tendon injuries” OR “shoulder injuries” OR DE “tennis elbow” OR AB tendin* OR AB tendon* OR DE bursitis OR AB “shoulder impingement syndrome” OR AB “posterior tibial tendon dysfunction” OR AB “greater trochanteric pain syndrome”) |
| Amed (EBSCO-host) | (ZU exercise OR ZU “exercise therapy” OR AB exercise OR ZU “muscle stretching exercises” OR ZU “isometric contraction” OR ZU rehabilitation OR TZ eccentric OR TZ concentric OR TX “heavy slow resistance” OR TX isokinetic OR AB plyometric) AND (ZU tendinopathy OR ZU “tendon injuries” OR ZU tendons OR ZU “shoulder injuries” OR ZU “tennis elbow” OR TX tendin* OR TX tendon* OR ZU bursitis OR AB bursitis OR ZU “shoulder impingement syndrome” OR ZU “posterior tibial tendon dysfunction” OR AB “greater trochanteric pain syndrome”) |
| Open Grey | Tendinopathy AND exercise Tendin* AND exercise Tendon AND exercise |
| Mednar | Tendinopathy AND exercise Tendin* AND exercise Tendon AND exercise |
| New York Academy Grey Literature Report | Tendinopathy AND exercise Tendin* AND exercise Tendon AND exercise |
| EThOS | Tendinopathy AND exercise Tendin* AND exercise Tendon AND exercise |
| Google Scholar | Tendinopathy AND exercise Tendin* AND exercise Tendon AND exercise |
| JBI Evidence Synthesis | Tendinopathy AND exercise |
| Cochrane Library | Tendinopathy AND exercise Tendin* AND exercise Tendon AND exercise |
| PEDro | Tendinopathy AND exercise Tendin* AND exercise Tendon AND exercise |
| Epistemonikos | (tendinopathy OR tendon* OR tendin*) AND exercise |
| CORE | Tendinopathy AND exercise Tendin* AND exercise Tendon AND exercise |
| Clinicialtrials.gov | Tendinopathy AND exercise Tendin* AND exercise Tendon AND exercise |
| ISRCTN | Tendinopathy AND exercise Tendin* AND exercise Tendon AND exercise |
| EU CTR | Tendinopathy AND exercise Tendin* AND exercise Tendon AND exercise |
| ANZCTR | Tendinopathy AND exercise Tendin* AND exercise Tendon AND exercise |
Search strategy mixed method review
MEDLINE – 29 March 2021
-
MH exercise
-
AB exercis*
-
MM rehabilitation
-
AB rehabilitation
-
MH physical therapy modalities
-
AB “physical therap*”
-
AB physiotherapy*
-
#1 OR … #8 = 503,671
-
MH tendinopathy
-
MH shoulder injuries
-
MH “tendon injuries”
-
TX tendin*
-
TX tendon*
-
MH bursitis
-
AB bursitis
-
MH posterior tibial tendon dysfunction
-
MH shoulder impingement syndrome
-
AB “greater trochanteric pain syndrome”
-
#9 OR … #18 = 103,386
-
AB fidelity
-
AB acceptability
-
AB adherence
-
AB feasibility
-
AB perception*
-
AB qualitative
-
AB barrier*
-
AB facilitat*
-
AB satisfact*
-
#20 OR … #28 = 1,736,478
-
#8 AND #19 AND #29 = 1,057
-
#30 (Limiter – Date of publication: 1998–2021) = 925
CINAHL – 29 March 2021
-
MH exercise
-
AB exercis*
-
MM rehabilitation
-
AB rehabilitation
-
AB “physical therapy modalities”
-
AB “physical therap*”
-
AB physiotherapy*
-
#1 OR … #8 = 224,836
-
MH tendinopathy
-
MH shoulder injuries
-
MH “tendon injuries”
-
TX tendin*
-
TX tendon*
-
MH bursitis
-
AB bursitis
-
MH posterior tibial tendon dysfunction
-
MH shoulder impingement syndrome
-
AB “greater trochanteric pain syndrome”
-
#9 OR … #18 = 43,916
-
AB fidelity
-
AB acceptability
-
AB adherence
-
AB feasibility
-
AB perception*
-
AB qualitative
-
AB barrier*
-
AB facilitat*
-
AB satisfact*
-
#20 OR … #28 = 504,314
-
#8 AND #19 AND #29 = 621
-
#30 (Limiter – Date of publication: 1998–2021) = 598
AMED – 29 March 2021
-
SU exercise
-
AB exercis*
-
SU rehabilitation
-
AB rehabilitation
-
SU physical therapy modalities
-
AB “physical therap*”
-
AB physiotherapy*
-
#1 OR … #8 = 92,869
-
SU tendinopathy
-
SU shoulder injuries
-
SU “tendon injuries”
-
TX tendin*
-
TX tendon*
-
SU bursitis
-
AB bursitis
-
SU posterior tibial tendon dysfunction
-
SU shoulder impingement syndrome
-
AB “greater trochanteric pain syndrome”
-
#9 OR … #18 = 4,967
-
AB fidelity
-
AB acceptability
-
AB adherence
-
AB feasibility
-
AB perception*
-
AB qualitative
-
AB barrier*
-
AB facilitat*
-
AB satisfact*
-
#20 OR … #28 = 25,279
-
#8 AND #19 AND #28 = 176
-
#29 (with Date Limiter: 1998 – 2021) = 171
EMBase – 29 March 2021
-
SU exercise
-
AB exercis*
-
SU rehabilitation
-
AB rehabilitation
-
AB “physical therapy modalities”
-
AB “physical therap*”
-
AB physiotherapy*
-
#1 OR… #7 = 730,391
-
SU tendinopathy
-
SU “shoulder injuries”
-
SU “tendon injuries”
-
TW tendin*
-
TW tendon*
-
SU bursitis
-
AB bursitis
-
SU posterior tibial tendon dysfunction
-
SU “shoulder impingement syndrome”
-
AB “greater trochanteric pain syndrome”
-
#9 OR … #18 = 100,563
-
AB fidelity
-
AB acceptability
-
AB adherence
-
AB feasibility
-
AB perception*
-
AB qualitative
-
AB barrier*
-
AB facilitat*
-
AB satisfact*
-
#21 OR … #29 = 2,263,117
-
#8 AND #20 AND #30 = 1276
-
#31 (Limiters – Date of Publication: 1998 – 2021) = 114
SPORTDiscus – 29 March 2021
-
SU exercise
-
AB exercis*
-
SU rehabilitation
-
AB rehabilitation
-
AB “physical therapy modalities”
-
AB “physical therap*”
-
AB physiotherapy*
-
#1 OR … #7 = 243,194
-
SU tendinopathy
-
SU shoulder injuries
-
SU “tendon injuries”
-
TX tendin*
-
TX tendon*
-
SU bursitis
-
AB bursitis
-
AB “posterior tibial tendon dysfunction”
-
AB “shoulder impingement syndrome”
-
AB “greater trochanteric pain syndrome”
-
#9 OR … #18 = 46,413
-
AB fidelity
-
AB acceptability
-
AB adherence
-
AB feasibility
-
AB perception*
-
AB qualitative
-
AB barrier*
-
AB facilitat*
-
AB satisfact*
-
#20 OR … #28 = 81,169
-
#8 OR #19 OR #29 = 764
-
#30 (Limiters – Date of Publication: 1998 – 2021) = 723
PEDro – 29 March 2021
-
tendin* AND exercise = 145 (title and abstract)
-
tendon* AND exercise = 118 (title and abstract)
Appendix 2
| Study details (first author, year, country) | Study type | Tendinopathy type | Exercise type | Primary ICON domain | Secondary ICON domain | Summary |
|---|---|---|---|---|---|---|
| Di Lorenzo, 2006, Italy208 | RCT – cross-over | Rotator cuff | Strengthening, flexibility | Pain without further specification, disability | NA | Suprascapular nerve blocks can only provide temporary pain relief, and so must be part of a total pain management programme if they are to avoid chronic pain conditions. Combining suprascapular nerve block with standard rehabilitative therapy may improve the outcome of painful rotator cuff tendinopathy. |
| Güler, 2009, Turkey209 | RCT | Rotator cuff | Flexibility, strengthening | Pain on loading/activity, ROM, disability | NA | Ketoprofen and lidocaine prilocaine phonophoresis were more effective on pain and ROM than ketoprofen phonophoresis alone in the 3rd month after treatment in patients with SIS. |
| Abat, 2014, Spain210 | QE – without control | Patellar | Strengthening | Disability | NA | EPI combined with an eccentric-based rehab programme showed excellent clinical and functional improvements in the patellar tendon compared to eccentric only exercise. |
| Abat, 2014, Spain211 |
QE – without control | Patellar | Strengthening | Participant/atient rating overall condition, disability | NA | Treatment with the US-guided EPI® technique and eccentric exercises in patellar tendinopathy resulted in a great improvement in knee function and a rapid return to the previous level of activity after few sessions. The procedure has proven to be safe with no recurrences on a long-term basis. |
| Abat, 2015, Spain212 |
QE – without control | Patellar | Strengthening | Disability | Participation, disability | Treatment with US-guided EPI technique and eccentric exercises resulted in improved knee function and rapid return to previous activity in patellar tendinopathy patients. |
| Abat, 2016, Spain213 | RCT | Patellar | Strengthening | Disability | NA | Combining USGET and eccentric exercise resulted in better outcomes for patellar tendinopathy patients than using conventional electro-physiotherapy techniques. |
| Abdulla, 2015, Canada214 | Systematic reviews/secondary analysis | Rotator cuff | NA | NA | NA | Evidence suggests that supervised and home-based progressive shoulder strengthening and stretching are effective for the management of subacromial impingement syndrome. |
| Aceituno-Gomez, 2019, Spain215 | QE – with control (with pre-test) | Rotator cuff | Flexibility, strengthening | Pain without further specification, disability, sensory modality | Medication use | High-intensity laser therapy plus exercise did not give greater improvements in pain and functionality in patients with subacromial syndrome than exercise alone. |
| Ager, 2019, Canada215 | Pilot – randomised | Rotator cuff | Flexibility | Disability | Disability, pain on loading/activity, PFC | Both rehabilitation approaches, grounded in active exercises, were not statistically different from each other, and derived similar benefits over time for a military population. This suggests that a group intervention for a RC tendinopathy has potential to be just as effective as a one-on-one approach for a military population. |
| Akgun, 2004, Turkey216 | RCT | Rotator cuff | Strengthening, flexibility | Pain on loading/activity, disability, pain over a specified time | NA | Subacromial corticosteroid injections in the acute or subacute phase of SIS provided additional short-term benefit without any complication when used together with NSAIDs and exercise. |
| Akin, 2013, Turkey217 | Observational – cohort | Rotator cuff | Flexibility, strengthening | Pain on loading/activity, pain over a specified time, disability | NA | Ultrasound with exercise and paracetamol had superior benefits for patients compared to exercise and paracetamol alone. |
| Akkaya, 2017, Turkey218 | RCT | Rotator cuff | Flexibility | Pain over a specified time, pain on loading/activity, ROM, disability structure | NA | Weighted and un-weighted solo pendulum exercises achieved significant clinical improvements but showed no differences in ultrasonographic acrohumeral distance measurements between groups. |
| Akkurt, 2018, Turkey219 | RCT | Lateral elbow | Flexibility | function capacity, pain on loading/activity, pain over a specified time | NA | Both epicondylitis bandage and hand-wrist resting orthosis are effective treatment options for lateral epicondylitis-induced pain, functional status, muscle strength, and QoL. Neither treatment option was superior to the other. |
| Aktas, 2007, Turkey220 | RCT | Rotator cuff | Flexibility | Pain on loading/activity, disability | NA | Electromagnetic therapy did not provide additional benefit in acute-phase rehabilitation programme f SIS. |
| Akyol, 2012, Turkey221 | RCT | Rotator cuff | Flexibility, strengthening | Pain without further specification, ROM, disability, physical function | NA | No statistically significant difference was found between the groups. As it is effective, superficial heat and exercise programme may be a preferable treatment for SIS. |
| Al Dajah, 2014, Saudi Arabia222 | RCT | Rotator cuff | Flexibility | Pain without further specification, ROM | NA | A single session of a combination of soft-tissue mobilisation, contract-relax PNF and facilitated abduction and external rotation was effective in reducing glenohumeral pain and improving external rotation and overhead reach. |
| Al-Abbad, 2013, Saudi Arabia223 | Systematic reviews/secondary analysis | Achilles | NA | NA | NA | There is satisfactory and consistent evidence for the effectiveness of low-energy ESWT in the treatment of chronic insertional and noninsertional Achilles tendinopathies. |
| Alfredson, 1999, Sweden224 | QE – without control | Achilles | Strengthening | PFC | NA | Heavy-loaded, eccentric calf-muscle training seems to be a good treatment mode for chronic Achilles tendinosis. |
| Alfredson, 1998, Sweden17 | QE – with control (with pre-test) | Achilles | Strengthening | PFC, pain on loading/activity | NA | Our treatment model with heavy-load eccentric calf-muscle training has a very good short-term effect on athletes in their early forties. |
| Alfredson, 2003, Sweden225 | QE – without control | Achilles | Strengthening | Pain on loading/activity, structure | NA | Eccentric training was not associated with lowered intratendinous glutamate levels. |
| Alvarez, 2006, United States226 | Observational – cohort | Tibialis posterior | Strengthening | PFC, pain on loading/activity, pain over a specified time | NA | Patients with stage I or II PTTD can be effectively treated non-operatively with an orthosis and structured exercises. |
| Andriolo, 2019, Italy227 | Systematic reviews/secondary analysis | Patellar | NA | NA | NA | Several nonsurgical approaches for the treatment of chronic patellar tendinopathy were documented with overall positive outcomes. Limitations and differences were highlighted. |
| Apostolos, 2004, NR228 | Pilot – randomised | Lateral elbow | Strengthening | Pain without further specification, physical function | NA | Active laser therapy in combination with plyometric exercise is more effective than plyometric exercises alone in the treatment of lateral epicondylitis. |
| Arias-Buria, 2017, Spain229 | RCT | Rotator cuff | Strengthening | Disability | Pain over a specified time, participant/patient rating overall condition, adverse effects/events | The addition of trigger-point dry needling with an exercise programme was effective for improving disability in subacromial pain syndrome. |
| Arias-Buria, 2015, Spain230 | RCT | Rotator cuff | Strengthening | Pain over a specified time | Disability | US-guided percutaneous electrolysis combined with eccentric exercises resulted in better short-term outcomes compared to eccentric exercises alone. |
| Arnal-Gomez, 2020, Spain231 | Systematic reviews/secondary analysis | Achilles | NA | NA | NA | Eccentric exercises performed over 6–12 weeks were effective for AT alone or in combination with vibration, nutritional supplements, soft-tissue treatment, laser, or shockwave. |
| Askling, 2014, Sweden232 | RCT | Hamstring | Flexibility, strengthening, aerobic | Participation, adverse effects/events | NA | A rehabilitation protocol emphasising lengthening type of exercises is more effective than a protocol containing conventional exercises in promoting time to return in Swedish elite sprinters and jumpers. |
| Aytar, 2015, Turkey233 | RCT | Rotator cuff | Other, flexibility | Disability, pain on loading/activity, pain over a specified time | ROM, participant/patient rating overall condition | No significant benefit in shoulder function, pain, ROM or satisfaction was observed in scapular mobilisation compared with sham or supervised exercise groups in patients with SAIS. |
| Bae, 2011, Korea (Republic of)234 | Control (with pre-test) | Rotator cuff | Other, strengthening | ROM, PFC | NA | The motor control and strengthening programme improved pain, function, strength and ROM. |
| Bagcier, 2019, Turkey235 | QE – with control (with pre-test) | Lateral elbow | Flexibility, strengthening | Pain without further specification, physical function | NA | ESWT and DN combination therapy in lateral epicondylitis provide better clinical outcomes than ESWT treatment alone. |
| Bahr, 2006, Norway131 | RCT | Patellar | Strengthening | Disability | Participant/patient rating overall condition, PFC | No added benefit was observed for surgical treatment to eccentric strength training. Eccentric training should be offered for 12 weeks before tenotomy is considered for the treatment of patellar tendinopathy. |
| Bakkegaard, 2015, Denmark236 | Observational – cohort | Achilles | Flexibility, strengthening | Physical activity, pain – clinician applied stress/examination, pain over a specified time, structure | NA | Heterogeneity is a prognostic marker in AT. Tendon thickness, hypoechogenicity and increased Doppler activity can be used as objective outcome parameters for the treatment effect of AT. |
| Bal, 2009, Turkey237 | RCT | Rotator cuff | Flexibility, strengthening, other | Pain over a specified time, disability, participant/patient rating overall condition | NA | There was no distinct advantage of low-level laser therapy over exercise alone for shoulder impingement. |
| Balius, 2016, Spain238 | RCT | Achilles | Strengthening | Disability | Pain on loading/activity, structure, adverse effects/events | Taking dietary supplements (mucopolisaccharides, type I collagen, vitamin C) seems to be therapeutically useful for management of tendinopathies, providing some additional benefit to physical therapy especially in early stages of the disease, when the tendon does not present severe matrix and vascular changes. |
| Bang, 2000, United States239 | RCT | Rotator cuff | Flexibility, strengthening | Disability, pain on loading/activity, PFC | NA | Manual physical therapy applied by experienced physical therapists combined with supervised exercise in a brief clinical trial is better than exercise alone for increasing strength, decreasing pain and improving function in patients with shoulder impingement syndrome. |
| Barr, 2009, United Kingdom240 | Systematic reviews/secondary analysis | Lateral elbow | NA | NA | NA | Large effect sizes were demonstrated in favour of corticosteroid injections at short-term follow-up, and physiotherapeutic interventions are effective at intermediate- and long-term follow-up. |
| Barra-Lopez, 2013, Spain241 | RCT | Rotator cuff | NR | Pain without further specification | Disability, ROM | Both intervention and placebo groups showed statistically significant improvement. |
| Barratt, 2017, United Kingdom242 | Systematic reviews/secondary analysis | Gluteal (including GTPS) | NA | NA | NA | Based on pain, CI demonstrated superior outcomes for up to 3 months compared with home training, radial shockwave therapy (RSWT) and usual care. RSWT and home training had limited evidence. |
| Barratt, 2018, United Kingdom243 | Other | Lateral elbow | Strengthening | NA | NA | Insufficient loading could have resulted in reduced treatment effectiveness whereas exercising into pain resulted in a higher number of responders. |
| Barrett, 2018, United Kingdom154 | Qualitative | Rotator cuff | Flexibility, strengthening, other | NA | NA | Exercise class was positively evaluated by all participants – seen as a conducive environment to develop relationships, friendships, humour and fun, gaining mastery of their exercises, and encourage the transition toward self-management. It was also evaluated as the preferred mode of physiotherapy delivery for those who had previous one-to-one physiotherapy experience. |
| Basas, 2018, Spain244 | Observational – cohort | Patellar | Strengthening, flexibility | Pain on loading/activity | NA | In a small group of high-level jumping athletes with chronic painful JK, a strength protocol combined with electrical stimulation showed promising clinical results with significant pain reduction during tendon loading activity. |
| Baskurt, 2003, Turkey245 | QE – without control | Lateral elbow | Flexibility, strengthening | Pain on loading/activity, pain over a specified time, physical function | NA | Iontophoresis and phonophoresis of naproxen are equally effective electro-therapy methods in the treatment of lateral epicondylitis. |
| Baskurt, 2011, Turkey246 | QE – without control | Rotator cuff | Flexibility, strengthening, other | Pain without further specification, ROM, physical function | NA | Scapular stabilisation combine with stretching and strengthening exercises can be more effective in the short term for SIS. |
| Bastia, 2019, Italy247 | Systematic reviews/secondary analysis | Other – adductor related groin pain | NA | NA | NA | Surgery allows shorter return to sport time than conservative treatment but heterogeneity of available studies and lack of dedicated RCTs make it impossible to draw definitive conclusions. |
| Bateman, 2014, United Kingdom248 | Pilot – feasibility | Rotator cuff | Strengthening | Disability, pain without further specification, other | NA | Although the results of this small study did not show statistically significant differences in outcome measures, two patients in the eccentric exercise group did improve sufficiently such that they cancelled their planned arthroscopic shoulder surgery. |
| Baumer, 2016, United States249 | RCT | Rotator cuff | Strengthening, other, flexibility | PFC, pain over a specified time, | NA | Physical therapy demonstrated a positive impact on clinical measures (VAS, WORC, ROM) in symptomatic individuals but not observed in the asymptomatic group. |
| Bek, 2012, Turkey250 | QE – without control | Posterior tibial tendon | Strengthening | Pain without further specification, disability, PFC | NA | While supervised, patient-selective programme ay provide better improvement in tibialis posterior strength than home-based rehabilitation, both programmes seem to be effective in relieving pain and improving functional outcome in patients with Grade 1–3 PTTD. |
| Bell, 2013, New Zealand251 | RCT | Achilles | Strengthening | Disability | Participant/patient rating overall condition, participation | The addition of two peritendinous autologous blood injections administered one month apart to a standardised eccentric training programme provides no added benefit in the treatment of mid-portion AT. |
| Bennell, 2010, Australia188 | RCT | Rotator cuff | Other, strengthening, flexibility | Pain on loading/activity, participant/patient rating overall condition | PFC, participation, QoL, adverse effects/events | Immediately after the intervention, active treatment produced similar benefits on shoulder pain and function compared with a realistic placebo. However, significant improvements in pain and function were found in favour of active treatment at follow-up. |
| Bernhardsson, 2011, Sweden252 | QE – without control | Rotator cuff | Other, strengthening, Flexmibility | Pain without further specification, function | Disability, Participant/patient rating overall condition | A 12-week eccentric strengthening programme targeting the rotator cuff and incorporating scapular control and correct movement pattern can be effective in decreasing pain and increasing function in patients with subacromial impingement syndrome. |
| Beyer, 2015, Denmark18 | RCT | Achilles | Strengthening | Disability | Pain on loading/activity, participation, participant/patient rating overall | Both traditional eccentric exercise and HSR yield positive, equally good and lasting clinical results in patients with AT. HSR is associated with greater patient satisfaction after 12 weeks but not after 52 weeks. |
| Bianco, 2019, United States253 | Observational – case series/reports | Patellar | Strengthening | applied stress/examination, disability, function, ROM, physical function | NA | Improvements in outcome measures were observed even in a short time. |
| Bisset, 2006, Australia254 | RCT | Lateral elbow | Strengthening, flexibility | function capacity, participant/patient rating overall condition, clinical | Pain over a specified time, disability | Physiotherapy combining elbow manipulation and exercise has a superior benefit to wait-and-see and to corticosteroid injections in the short term (6 weeks), providing a reasonable alternative to injections in the mid to long term. |
| Bisset, 2005, Australia255 | Reviews/secondary analysis | Lateral elbow | NA | NA | NA | Few conclusions can be drawn from the limited number of studies with contradicting findings. |
| Bisset, 2009, Australia256 | RCT | Lateral elbow | NR | PFC | NA | Sensorimotor deficits were not improved by either intervention – physiotherapy, injection, and wait-and-see. |
| Bjordal, 2008, Norway257 | Systematic reviews/secondary analysis | Lateral elbow | NA | NA | NA | In contradiction to previous reviews, this review identifies optimal doses at which low-level laser therapy offers short-term pain relief and less disability in LE, both alone and in conjunction with exercise. |
| Bjornsson Hallgren, 2017, Sweden258 | RCT | Rotator cuff | Strengthening, flexibility | Disability, pain over a specified time, pain on loading/activity, QoL, other | NA | More patients in the specific exercise group managed to avoid surgery compared to the unspecific exercise group at 5-year follow-up supporting its prescription as an initial treatment for patients with subacromial pain. |
| Blackwood, 2012, United Kingdom259 | Pilot – randomised | Patellar | Strengthening, other | Pain without further specification, disability | NA | This study demonstrated that the design was feasible, with both groups significantly improving pain/function but with significantly greater improvement in the group that received transverse friction massage prior to exercise. |
| Blume, 2015, United States260 | RCT | Rotator cuff | Strengthening | Pain without further specification, disability, ROM, physical function | NA | Both submaximal eccentric and concentric PREs resulted in improved function, AROM and strength in patients with SAIS. No difference found between the two exercise modes. |
| Boesen, 2017, Denmark162 | RCT | Achilles | Strengthening, aerobic | Disability | Pain on loading/activity, structure, PFC, participant/patient rating overall condition, participation | Treatment with HVI or PRP in combination with eccentric training in chronic AT seems more effective in reducing pain, improving activity level, and reducing tendon thickness and intratendinous vascularity than eccentric training alone. HVI may be more effective in improving outcomes of chronic AT than PRP in the short term. |
| Boesen, 2019, Denmark163 | RCT | Achilles | Strengthening | Disability | Pain over a specified time, structure, participant/patient rating overall condition | HVI with or without corticosteroid in combination with eccentric training seems effective in AT. HVI with corticosteroid showed a better short-term improvement than HVI without corticosteroid, indicating a short-term effect of corticosteroid in the treatment of AT. |
| Bostrom, 2019, Norway261 | RCT | Lateral elbow | Strengthening | Other | Pain over a specified time, disability, Medication use, participation, participant/patient rating | The acceptable level of compliance observed in the treatment groups confirms the feasibility of a larger-scale trial with minor adjustments to improve attrition rates. While both treatments were effective in significantly reducing pain, exercise alone provided inferior results. |
| Boudreau, 2019, Canada262 | RCT | Rotator cuff | Strengthening | Disability | Disability, pain on loading/activity, structure | No additional benefit was found to adding coactivation to regular rotator cuff strengthening exercises at 6 weeks. |
| Bowring, 2010, United Kingdom263 | Reviews/secondary analysis | Tibialis posterior | NA | NA | NA | Further research required with the limited and poor-quality evidence in the treatment of TPTD. |
| Boyles, 2009, United States264 | Observational – cohort | Rotator cuff | Flexibility | Pain on loading/activity, pain over a specified time, disability, participant/patient rating overall condition | NA | Manipulation demonstrated short-term relief of pain and function. |
| Branson, 2017, Australia265 | RCT | Lateral elbow | Strengthening | Participant/patient rating overall condition | Pain on loading/activity, disability, structure | Corticosteroid injection demonstrated superior outcomes on the Patient Rated Tennis Elbow Evaluation than other intervention measures; however, its long-term efficacy and recurrence rate was unclear. |
| Braun, 2010, United Kingdom266 | Systematic reviews/secondary analysis | Rotator cuff | NA | NA | NA | MT and exercise seem effective for subacute and chronic shoulder impingement with short- to medium-term effectiveness, but varying methodological quality and risk of bias in reviews and trials warrant caution in the interpretation of the results. |
| Braun, 2013, United Kingdom267 | Systematic reviews/secondary analysis | Rotator cuff | NA | NA | NA | Nine RCTs were included and synthesised narratively. This review update provides some further evidence supporting the effectiveness of MT and exercises for shoulder impingement, but methodological deficits/risk of bias warrant cautious interpretation. |
| Brown, 2006, Australia268 | RCT | Achilles | Strengthening | Disability, adverse effects/events | NA | Using a functional grade of severity and a functional outcome measure in a double-blind placebo-controlled trial we failed to confirm the benefit of aprotinin in tendinopathy. |
| Brox, 1999, Norway269 | RCT | Rotator cuff | Flexibility, other | Disability | Pain on loading/activity, pain over a specified time, function, psychological factors, medication use, PFC | At 2.5 years follow-up, both arthroscopic surgery and supervised exercises are better treatments than placebo with no significant difference between the 2 active treatments. |
| Bury, 2016, United Kingdom270 | Systematic reviews/secondary analysis | Rotator cuff | NA | NA | NA | SFA for RCSP confers benefit (pain and functional improvement) over generalised approaches up to six weeks but this benefit is not apparent by 3 months. Early changes in pain are not clinically significant. With regard to scapula position/movement, the evidence is conflicting. |
| Cacchio, 2011, Italy271 | RCT | Hamstring | Aerobic, Strengthening | Pain without further specification, disability | specified time, participant/patient rating overall condition | SWT is a more effective treatment to conservative treatment for proximal hamstring tendinopathy. |
| Cairns, 2018, United Kingdom272 | Systematic reviews/secondary analysis | Patellar | NA | NA | NA | There is a lack of studies assessing the effectiveness of interventions for patellar tendon-related pain in children and adolescents. Based on the available studies, there is weak evidence to support the use of dextrose injection with local anaesthetic and no evidence to support the use of specific types of exercises. |
| Calis, 2011, Turkey273 | RCT | Rotator cuff | Flexibility, strengthening | Pain on loading/activity, pain over a specified time, ROM, disability | NA | Ultrasound and laser treatments were not superior to each other in the treatment of SIS |
| Campbell, 2019, United Kingdom151 | Qualitative | Tibialis posterior | NA | NA | NA | Treatment burden is an important factor in the management of PTTD |
| Canbulat, 2013, Turkey274 | RCT | Rotator cuff | Flexibility, strengthening, other | Disability | NA | The addition of core stabilisation exercises to standard comprehensive physiotherapy applied in the rehabilitation of patients with subacromial impingement syndrome significantly improves treatment effectiveness. |
| Cannell, 2001, Canada275 | RCT | Patellar | Aerobic, strengthening | Pain without further specification, PFC | NA | Progressive drop squats and leg extension/curl exercises can reduce the pain of jumper’s knee in a 12-week period and resulted in a high proportion of patients returning to sport. |
| Carlisi, 2018, Italy276 | Pilot – non-randomised | Rotator cuff | Strengthening, flexibility | F-ESWT is equally effective as eccentric exercises using elastic resistance in reducing shoulder pain. | ||
| Celik, 2019, Turkey277 | RCT | Lateral elbow | Flexibility, strengthening | Pain onloading/activity, QoL, participant/patient rating overall condition, | NA | Both photo-biomodulation and ESWT are useful and can be used in the treatment of LE based on improvements in handgrip strength. Improvements for elbow extension and shoulder flexion strength and VAS were mainly observed in the photo-biomodulation group. |
| Celik, 2009, Turkey278 | Control (with pre-test) | Rotator cuff | Flexibility, strengthening | NA | NA | Despite initial short-term pain relief from injection, both groups demonstrated improvements at 3 and 6 weeks. |
| Celik, 2009, Turkey279 | QE – without control | Rotator cuff | Flexibility, strengthening | Pain without further specification, psychological factors | NA | Both groups had significant improvements in pain and disability measures; however, exercise programme within pain-free ROM showed additional improvements in VAS and face scores in SIS. |
| Cerdan Fabregat, 2019, Spain280 | Observational – case series/reports | Achilles | Strengthening | Pain without further specification, disability, structure | NA | A combined programme of PNE with eccentric exercises was effective at improving outcomes for chronic tendinopathy of the Achilles tendon body. |
| Challoumas, 2019, United Kingdom281 | Systematic reviews/secondary analysis | Rotator cuff, lateral elbow, patellar, Achilles | NA | NA | NA | Surgery is not superior to exercise and therefore recommend only after a long course (at least 12 months) of evidence-based loading exercise has failed. |
| Chan, 2000, Hong Kong, China (SAR)282 | Pilot – feasibility | Lateral elbow | Flexibility, strengthening | Pain without further specification, PFC, function, participant/patient | NA | The programme improved patients’ work capacities and satisfaction while maintaining pain symptoms at a low level. |
| Chary-Valckenae re, 2018, France283 | RCT | Rotator cuff | Flexibility | Disability | QoL | Spa therapy consisting of mineral water baths and mud applications together with supervised self-mobilisation in a thermal pool provided significant benefit in pain, function and QoL in patients with chronic shoulder pain compared to usual care. |
| Chen, 2017, Taiwan284 | QE – without control | Other – subscapularis tendinopathy | Flexibility, strengthening | Pain without further specification, ROM, physical function | NA | Combined treatment (eccentric, ESWT, and conventional) improved patients with noncalcific subscapular tendinosis. |
| Chen, 2020, Singapore285 | Reviews/secondary analysis | Lateral elbow | NA | NA | NA | There is evidence that eccentric exercise can reduce pain and improve function in lateral elbow tendinopathy. |
| Cheng, 2007, China286 | RCT | Rotator cuff | Strengthening | Disability, participation | NA | Workplace-based rehabilitation programme appeared to be more effective in facilitating the return to work process of the injured worker following intervention. |
| Cherry, 2012, United States287 | RCT | Lateral elbow | Flexibility | PFC, pain on loading/activity, disability | NA | Exercise and cryotherapy used in isolation or in combination reduce the symptoms of lateral epicondylitis. Cryo-MAX® was preferred over conventional cold packs but it did not have any additional therapeutic benefit. |
| Chester, 2008, United Kingdom288 | Pilot – randomised | Achilles | Strengthening | Pain on loading/activity, disability, QoL | NA | Both interventions were equally effective and acceptable to patients with no adverse effects. |
| Cho, 2017, Korea (Republic of)289 | QE – with control (with pre-test) | Patellar | Strengthening, flexibility, aerobic | Pain without further specification, disability, PFC, pain | NA | A rehabilitation exercise programme was more effective at improving pain, strength and function in patellar tendinopathy than injection therapy alone. |
| Chung, 2004, Canada290 | RCT | Lateral elbow | Flexibility | Pain over a specified time, pain on loading/activity | QoL, PFC | ESWT combined with stretching were no more effective than stretching alone in the treatment of lateral epicondylitis. |
| Chung, 2005, Canada291 | RCT | Lateral elbow | Flexibility | Pain over a specified time | PFC, QoL | ESWT does not appear to be an effective treatment for individuals with previously untreated lateral epicondylitis. |
| Cioni, 2017, Italy292 | Systematic reviews/secondary analysis | Rotator cuff | NA | NA | NA | The reviewed literature confirms the effectiveness of exercise for tendinopathies; however, it was not found to be superior to other existing methods. |
| Citaker, 2005, Turkey293 | RCT | Rotator cuff | Flexibility, strengthening | Pain without further specification, ROM | NA | Mobilisation and PNF methods were both effective, but mobilisation is a painless technique and therefore was better tolerated than PNF. |
| Clarke, 2010, United Kingdom294 | Observational – cohort | Lateral elbow | Flexibility, strengthening | Disability, structure | NA | This study shows that the presence of an LCL tear and the size of the largest intrasubstance tears are predictors of poor outcome. No correlation with tendon thickness or neovascularity was seen. |
| Clarke, 2011, United Kingdom295 | RCT | Patellar | Aerobic, flexibility, strengthening | Disability | Structure | Ultrasound-guided injection of autologous skin-derived tendon-like cells can be safely used in the short term alongside exercise to treat patellar tendinopathy, with faster response of treatment and significantly greater improvement in pain and function than with plasma alone. |
| Cleland, 2004, United States296 | Observational – cohort | Lateral elbow | Strengthening, flexibility | Function, other | NA | Local management plus cervical MT may be more efficient for managing patients with LE. |
| Clifford, 2019, United Kingdom179 | Pilot – randomised | Gluteal (including GTPS) | Strengthening | Disability | Pain without further specification, participant/patient rating overall condition, psychological factors, disability, QoL, physical activity | Isometric and isotonic exercise programmes appear to be effective for individuals with GTPS. |
| Coghlan, 2008, Australia297 | Reviews/secondary analysis | Rotator cuff | NA | NA | NA | Three trials reported no difference between surgery and physiotherapy alone or with education. |
| Conroy, 1998, United States298 | QE – with control (with pre-test) | Rotator cuff | Flexibility, strengthening | Loading/activity, pain over a specified time, clinical examination findings, ROM, function | NA | Both groups improve mobility and function in shoulder impingement syndrome but only joint mobilisation relieves pain over a 24-hour period. |
| Cook, 2014, United States172 | RCT | Rotator cuff | Strengthening, flexibility | Disability | Pain without further specification, participant/patient rating overall condition, other | A standardised cervical mobilisation on a tender cervical segmental level combined with a comprehensive shoulder treatment protocol did not result in any added improvement on pain and DASH scores in the treatment of SIS. |
| Coombes, 2016, Australia299 | RCT | Lateral elbow | NA | QoL | NA | Findings are in agreement with a large body of evidence that does not support corticosteroid injection as a first-line intervention for lateral epicondyitits. Physiotherapy is less costly and appears to provide greater QoL outcomes over the long term, supporting its use as an intervention. |
| Coombes, 2013, Australia176 | RCT | Lateral elbow | Other, strengthening | Participant/patient rating overall condition, other | Patient rating overall condition, pain over a specified time, disability, QoL, medication | Multimodal physiotherapy provided no beneficial long-term effect on complete recovery, recurrence, pain, disability or QoL. However, in the absence of a corticosteroid injection, physiotherapy may provide a short-term benefit across all outcomes. Corticosteroid injections generally result in a poorer clinical outcome. |
| Crawshaw, 2010, United Kingdom300 | RCT | Rotator cuff | Flexibility, strengthening, other | Disability | Use, participant/patient rating overall condition, adverse effects/events | At 12 weeks, steroid injection combined with exercise showed similar effectiveness to exercise alone. However, earlier improvement in pain and function was observed with corticosteroid injection combined with exercise and MT. |
| Crill, 2014, United States301 | Observational – case series/reports | Achilles | Strengthening | Structure | Function | Medial gastrocnemius muscle fascicles increase in length as a result of training, which could lead to a rightward shift in the length–tension curve and possibly prevent future muscular injuries. |
| Croisier, 2001, Belgium302 | QE – without control | Achilles, lateral elbow, patellar | Strengthening | Specified time, PFC, participation, structure | NA | Eccentric training is effective in reducing pain, improving strength, return to activities, and tendon recovery. |
| Croisier, 2002, Belgium303 | QE – without control | Achilles, patellar, other – epicondylian | Strengthening | Pain without further specification, PFC, disability | NA | Eccentric exercise appears to be an effective treatment modality for various chronic tendinopathies. |
| Croisier, 2007, Belgium304 | QE – with control (with pre-test) | Lateral elbow | Strengthening, flexibility | Pain on loading/activity, PFC, disability, structure | NA | Isokinetic adapted eccentric training significantly reduced pain intensity, improved tendon structure, strength, disability, and participation compared to the non- strengthening control group in the management of chronic lateral epicondylar tendinopathy. |
| Cullinane, 2014, New Zealand305 | Systematic reviews/secondary analysis | Lateral elbow | NA | NA | NA | There is support for the inclusion of eccentric exercise as part of a multimodal therapy programme for improved outcomes in patients with lateral epicondylitis. |
| Cumpston, 2009, Australia306 | Systematic reviews/secondary analysis | Rotator cuff | NA | NA | NA | There is insufficient evidence to assess if glyceryl trinitrate patches are effective in treating rotator cuff disease. Three small studies, one at moderate risk of bias and two at high risk of bias, assessed the effectiveness of glyceryl trinitrate but each report ed different treatment regimens and different outcome measures. They also included participants with differing duration of symptoms (acute/chronic). Heterogeneity limited the pooled analysis of the available data. |
| Dale, 2016, United States173 | Pilot – randomised | Lateral elbow | Other, strengthening | Pain over a specified time, physical function | NA | Compared to a standard intervention the pilates-based intervention only resulted in greater improvement in the PRTEE outcome. |
| Dan, 2019, Australia307 | Systematic reviews/secondary analysis | Patellar | NA | NA | NA | Uncertainty remains over the benefits of surgery over therapeutic interventions such as eccentric exercises or sclerosing injections for treating patellar tendinopathy. |
| de Jonge, 2011, Netherlands60 | RCT | Achilles | Flexibility, strengthening | Disability | Participant/patient rating overall condition, participation | This RCT showed no clinical (VISA-A) and ultrasonographic superiority of PRP injection over a placebo injection in chronic AT at 1 year combined with an eccentric training programme. |
| de Jonge, 2015, Netherlands308 | Observational – cohort | Achilles | strengthening, flexibility | Disability, structure | NA | While tendinous structures appear to improve following a conservative approach, there were no differences in VISA-A scores between groups. |
| de Jonge, 2010, Netherlands309 | RCT | Achilles | Strengthening | Patient rating overall condition, structure, disability | NA | Eccentric exercises with or without a night splint improved functional outcome at one year follow-up. There was no added benefit to clinical outcome with the addition of night splint. |
| de la Fuente, 2019, Spain310 | Systematic reviews/secondary analysis | Patellar | NA | NA | NA | Active exercise in general, and particularly eccentric exercise, is the most effective treatment for patellar tendinopathy. Ultrasound-guided electrolysis, hyperthermia and taping are also useful. |
| De Mey, 2012, Belgium311 | QE – without control | Rotator cuff | Other | PFC | NA | Six-week scapular exercise improved pain, symptoms and activation levels in overhead athletes with mild SIS. |
| de Miguel Valtierra, 2018, Spain312 | RCT | Rotator cuff | Other, strengthening | Disability | Pain over a specified time, disability, sensory modality specific pain, participant/patient rating overall condition | Inclusion of US-guided percutaneous electrolysis in a treatment approach including MT and exercise resulted in no significant differences in shoulder-related disability and pressure pain sensitivity in subjects with subacromial p ain syndrome. |
| De Reu, 2018, Belgium313 | RCT | Rotator cuff | Strengthening | Modality-specific pain, structure | NA | There were no significant differences between groups to determine which, if any, exercise programme was superior. |
| de Vos, 2010, Netherlands314 | RCT | Achilles | Strengthening, flexibility | Disability | Participant/patient rating overall condition, participation | Among patients with chronic midportion AT treated with an eccentric exercise programme, a PRP injection compared with a saline injection did not result in greater improvement in pain and activity. |
| de Vos, 2012, Netherlands315 | Observational – cohort | Achilles | Strengthening | Disability, structure | NA | While VISA-A score improved after 24 weeks, there is no short-term increase in organised tendon structure after eccentric exercise. Tendon structure is unrelated to clinical severity of symptoms. |
| de Vos, 2007, Netherlands59 | RCT | Achilles | Strengthening | Disability, participant/patient rating overall condition | NA | A night splint has no added benefit to eccentric exercises in the treatment of chronic midportion AT. There was no significant difference between the two groups in VISA-A score and patient satisfaction. |
| de Vos, 2007, Netherlands316 | Observational – cohort | Achilles | Strengthening | Disability, pain on loading/activity | NA | There were no correlations between neovascularisation and VIS-A or VAS scores at baseline. Therefore, performing ultrasound to characterise tissues at baseline has no prognostic value. |
| de Vos, 2011, Netherlands317 | RCT | Achilles | Flexibility, strengthening | Structure | Other, PFC | No significant differences in tendon structure within a 24-week time period were observed when PRP injections were used with exercise compared to placebo. |
| Deans, 2012, United Kingdom318 | Observational – case series/reports | Achilles | Strengthening | Disability | NA | Autologous-conditioned plasma can provide a potential treatment solution for chronic AT. |
| Dejaco, 2017, Netherlands319 | RCT | Rotator cuff | Strengthening, flexibility | Disability | Pain on loading/activity, ROM, PFC | 12-week-isolated eccentric training programme of the RC is beneficial for shoulder function and pain after 26 weeks in patients with RC tendinopathy. However, it is no more beneficial than a conventional exercise programme for the RC and scapular muscles. |
| Desjardins-Charbonneau, 2015, Canada319 | Systematic reviews/secondary analysis | Rotator cuff | NA | NA | NA | For patients with RC tendinopathy, based on low- to moderate-quality evidence, MT may decrease pain; however, it is unclear whether it can improve function. |
| Desjardins-Charbonneau, 2015, Canada320 | Systematic reviews/secondary analysis | Rotator cuff | NA | NA | NR | Kinesiology taping significantly improved pain-free ROM; however, there is insufficient evidence on the effectiveness of kinesiology taping or non-elastic taping used alone or in conjunction with other interventions in patients with RC tendinopathy. |
| Desmeules, 2004, Canada321 | QE – with control (with pre-test) | Rotator cuff | Flexibility, other, Stmrengthening | Disability | ROM, PFC, pain on loading/activity | A reduction of acromio-humeral distance narrowing is strongly associated with functional improvement following rehabilitation. Ultrasound measurement of acromio-humeral distance might help identify SIS patients who will benefit from rehabilitation. |
| Desmeules, 2003, Canada322 | Reviews/secondary analysis | Rotator cuff | NA | NA | NA | There is limited evidence to support the efficacy of therapeutic exercise and MT to treat impingement syndrome. |
| Desmeules, 2015, Canada323 | Systematic reviews/secondary analysis | Rotator cuff | NA | NA | NA | US therapy is not superior to placebo and is of no added benefit when used in conjunction with exercise in terms of pain reduction and self-reported function based on low-level evidence. |
| Desmeules, 2016, Canada324 | Systematic reviews/secondary analysis | Rotator cuff, other – bicipital, subdeltoid bursitis | NA | NA | NA | Due to the limited number of studies (six studies) and the overall high risk of bias of the studies included in this review, no conclusions can be drawn on the efficacy of TENS for the treatment of rotator cuff tendinopathy. |
| Desmeules, 2016, Canada325 | Systematic reviews/secondary analysis | Rotator cuff | NA | NA | NA | Three RCTs of moderate methodological quality provided low- to moderate-grade evidence that therapeutic exercises provided in a clinical setting are an effective modality to treat workers suffering from rotator cuff tendinopathy and to promote return-to-work. |
| Devereaux, 2016, Canada326 | RCT | Rotator cuff | Flexibility, strengthening, other | applied stress/examination, pain without further specification, | NA | The improvements in pain and function observed with an NSAID or precut kinesiology tape as adjuvant treatments were no greater than with rehabilitation exercise alone. |
| Diaz, 2016, Spain327 | Systematic reviews/secondary analysis | Patellar | NA | NA | NA | Eccentric exercises are effective in treating patellar tendinopathy; however, no evidence has shown that they are better than other currently applied treatments (such as shockwaves, stretches, night splints, etc.). On the other hand, no specific protocol for applying these exercises has been established. |
| Dickens, 2005, United Kingdom328 | QE – with control (no pre-test) | Rotator cuff | Other, strengthening | Disability | NA | All patients in this study improved their Constant score with physiotherapy. |
| Dilek, 2016, Turkey329 | RCT | Rotator cuff | Flexibility, strengthening, other | Clinical examination findings | specified time, pain on loading/activity, pain without further specification, disability, ROM, physical function | Although proprioceptive exercises may provide better proprioceptive acuity, no additional positive effect on other clinical parameters was observed. |
| Dimitrios, 2012, Greece330 | QE – with control (with pre-test) | Patellar | Strengthening, flexibility | Disability, drop-out or discontinued treatment | NA | Eccentric training and static stretching exercises are superior to eccentric training alone to reduce pain and improve function in patients with patellar tendinopathy at the end of the treatment and at follow-up. |
| Dimitrios, 2013, Cyprus331 | QE – with control (with pre-test) | Lateral elbow | Strengthening, flexibility | Pain over a specified time, function, PFC, drop out or discontinued | NA | A specific supervised exercise programme is superior to a specific HEP in reducing pain and improving function in patients with LET at the end of the treatment and at the 3-month follow-up. |
| Dingemanse, 2014, Netherlands332 | Systematic reviews/secondary analysis | Medial elbow, golfer’s elbow, lateral elbow | NA | NA | NA | Potential effectiveness of ultrasound for the management of LE was found on mid-term follow-up. Moderate evidence was also found in favour of laser therapy over plyometric exercises on short-term follow-up. For all other modalities only limited, conflicting or evidence of no difference in effect was found. |
| Dogan, 2010, Turkey333 | RCT | Rotator cuff | Flexibility | Pain on further specification, ROM, | NA | Laser therapy was no more effective than placebo laser. |
| Doiron-Cadrin, 2020, Canada334 | Systematic reviews/secondary analysis | Rotator cuff | NA | NA | NA | Only three CPGs were of high quality, while six were low. All CPGs recommended active treatment modalities, such as an exercise programme in the management of rotator cuff disorders. Acetaminophen or nonsteroidal anti-inflammatory drug prescriptions and corticosteroid injections were presented as modalities that may be recommended to decrease pain. Recommendations related to medical imagery and surgical opinion varied among the guidelines. The most commonly recommended return-to-work strategies included intervening early, use of a multidisciplinary approach, and adaptation of work organisation. |
| Dorrestijn, 2009, Netherlands335 | Systematic reviews/secondary analysis | Rotator cuff | NA | NA | NR | No high-quality RCTs were available. According to the best-evidence synthesis, there is no evidence for differences in pain and shoulder function between conservatively and surgically treated patients with SIS. |
| Dragoo, 2014, United States336 | RCT | Patellar | Strengthening | Disability | Disability, pain without further specification, QoL | A regimen of standardised eccentric exercise and ultrasound-guided leukocyte-rich PRP injection with DN accelerates the recovery from patellar tendinopathy relative to exercise and ultrasound-guided DN alone, but the apparent benefit of PRP is short-term. |
| Drew, 2014, United Kingdom337 | Systematic reviews/secondary analysis | Rotator cuff, tibialis posterior, lateral elbow, medial elbow/golfer’s | NA | NA | NA | The literature does not support observable structural change as an explanation for the response of therapeutic exercise, except for some support from heavy-slow resistance training. |
| Dumont, 2006, Canada338 | Observational – case series/reports | Patellar | strengthening, flexibility | Pain on loading/ activity, function | PFC | The eccentric exercise programme showed mixed clinical benefits for four patients with patellar tendinopathy but none of the patients achieved full recovery within the suggested six-week treatment period. |
| Dupuis, 2018, Canada339 | RCT | Rotator cuff | Strengthening, flexibility | Disability | Pain over a specified time, structure, physical function | Both groups showed statistically significant improvements on symptoms and function at 2 weeks and 6 weeks but there was no difference between the short-term effect of cryotherapy and a gradual reloading exercise programme. |
| Efstratiadis, 2016, Greece340 | Reviews/secondary analysis | Rotator cuff | NA | NA | NA | Exercise equally effective as surgery for pain and function. |
| Eken Gedik, 2016, Turkey341 | QE – with control (with pre-test) | Lateral elbow | Flexibility, strengthening | modality specific pain, PFC, disability, participant/patient | NA | Autologous blood injection is effective in patients with LE and this effectiveness has continued at 6 months. Therefore, autologous blood injection, which has relatively fewer side effects, might be included among long-term treatment options for LE. |
| Ellegaard, 2016, Denmark342 | RCT | Rotator cuff | Strengthening, other | Pain over a specified time, pain on loading/activity | Pain on loading/activity, pain over a specified time, clinical examination findings, structure, disability, PFC | 10 weeks of unilateral exercise as an adjunct to subacromial steroid injections did not im prove the primary outcome of shoulder pain due to SAPS and enlarged subacromial bursa, compared to exercise. |
| Elsodany, 2018, Saudi Arabia343 | RCT | Rotator cuff | Flexibility, other, strengthening | Pain without further specification, ROM, disability | NA | Pulsed Nd:YAG laser combined with an exercise programme seems to be more effective in the treatment of patients with rotator cuff tendinopathy than a sham laser with exercises. |
| Engebretsen, 2009, Norway344 | RCT | Rotator cuff | Other, strengthening | Disability | Loading/activity, pain over a specified time, function, ROM, | Supervised exercises are superior to ESWT in terms of shoulder pain, disability and some work-related outcomes. |
| Engebretsen, 2011, Norway345 | RCT | Rotator cuff | Other, strengthening | Disability | Loading/activity, pain over a specified time, function, participation, medication use, psychological | Both radial ESWT and the supervised exercise regime devised by Bohmer (1998) provided similar benefits in pain and function-related outcomes. However, exercise may be superior for work-related outcomes. |
| Entrellardat Tortillo, 2019, Spain346 | QE – without control | Patellar | Strengthening | Disability, pain without further specification, structure | NA | Percutaneous needle electrolysis combined with eccentric overload exercise represent a treatment which may be effective for most cases of chronic patellar tendinopathy. |
| Eraslan, 2018, Turkey347 | RCT | Lateral elbow | Strengthening, flexibility | Loading/activity pain over a specified time, PFC | NA | Kinesiotaping effectively decreased pain intensity, recovered grip strength, and improved function in patients with lateral epicondylitis undergoing rehabilitation. |
| Eraslan, 2015, Turkey348 | RCT | Lateral elbow | Flexibility, strengthening | Pain over a specified time, pain on loading/activity, physical function | NA | Kinesiotape is effective in reducing pain associated with lateral epicondylitis, recovering grip strength and may be considered an effective method of treatment. |
| Evangelos, 2018, Cyprus349 | Pilot – non-randomised | Patellar | Strengthening, flexibility | Disability, drop-out or discontinued treatment | NA | Eccentric and static stretching exercise programme combined with HILT is an effective treatment approach for patients with chronic PT. |
| Everhart, 2017, United States350 | Systematic reviews/secondary analysis | Patellar | NA | NA | NA | A total of 15 studies were included. Reporting quality was high, and there was no systematic evidence of reporting bias. Initial treatment of PT can consist of eccentric squat-based therapy, shockwave, or PRP as monotherapy or an adjunct to accelerate recovery. Surgery or shockwave can be considered for patients who fail to improve after 6 months of conservative treatment. Corticosteroid therapy should not be used in the treatment of PT. |
| Faber, 2006, Netherlands351 | Systematic reviews/secondary analysis | Rotator cuff | NA | NA | NA | 19 articles were included in this review. For functional limitations, there is strong evidence that ESWT is not effective, moderate evidence that exercise combined with MT is more effective than exercise alone, that ultrasound is not effective, and that open and arthroscopic acromioplasty are equally effective in the long ter m. Most studies used ROM and pain as outcome measures whereas functional limitations were less often used. |
| Fahlström, 2003, Sweden352 | QE – with control (with pre-test) | Achilles | Strengthening | Pain on loading/activity, participation, participant/patient rating overall | NA | Treatment with eccentric calf-muscle training produced good clinical results in patients with chronic painful mid-portion Achilles tendinosis, but not in patients with chronic insertional Achilles tendon pain. |
| Farfaras, 2016, Sweden353 | RCT | Rotator cuff | Other, flexibility, strengthening | Disability, QoL | NA | Outcomes did not demonstrate significant differences between the three groups 2–3 years after intervention. |
| Faria, 2006, Portugal354 | QE – with control (with pre-test) | Rotator cuff | Flexibility, strengthening | Pain without further specification | NA | All treatment groups effectively reduced pain. However, it is not clear whether the significant differences observed between groups could be due to factors other than the primary intervention in the absence of randomisation. |
| Farnqvist, 2020, Sweden355 | Systematic reviews/secondary analysis | Achilles | NA | NA | NA | There was strong evidence that Achilles tendon thickness does not decrease in parallel with improved clinical outcomes. It remains unknown whether a longer time to follow-up is more important than the intervention for a change in tendon thickness. |
| Fournier Belley, 2018, Canada164 | RCT | Rotator cuff | Other, flexibility, strengthening | Disability | Structure, PFC | Results do not demonstrate any improved treatment outcomes from the addition of a tDCS during a rehabilitation programme for individuals with rotator cuff tendinopathy. |
| French, 2019, Ireland356 | Survey | Gluteal (including GTPS) | NA | NA | NA | This international survey found that education used in conjunction with exercise for the management of GTPS is in line with current evidence. Some clinicians use adjunct treatments without clear rationale or supporting evidence. |
| Frizziero, 2014, Italy357 | Systematic reviews/secondary analysis | Patellar, rotator cuff, Lateral elbow, other – adductor-related groin | NA | NA | NA | Evidence for eccentric exercise in Achilles and patellar tendinopathies may be useful in other tendinopathies. Review highlights large variability and lack of high-quality evidence. |
| Frizziero, 2016, Italy 358 | Systematic reviews/secondary analysis | Greater trochanteric, calcific, iliopsoas, adductor, proximal hamstring | NA | NA | NA | Conservative treatment is effective in the treatment of hip tendinopathies. Exercise should be considered first line of treatment. |
| Frohm, 2007, Sweden359 | RCT | Patellar | Aerobic, strengthening, flexibility | Disability | PFC, pain on loading/activity | In patients with patellar tendinopathy pain, two-legged eccentric overload training twice per week, using the new device (Bromsman), was as efficient and safe as the present standard daily eccentric one-legged rehabilitation-training regimen using a decline board. |
| Furia, 2016, United States360 | Observational – case control | Other – distal biceps | Strengthening | Pain without further specification, disability | NA | Both rESWT and the control treatment effectively improve pain and disability for distal biceps tendinopathy. |
| Ganderton, 2018, Australia189 | RCT | Gluteal (including GTPS) | Strengthening, flexibility | Disability | Disability, participant/patient rating overall condition, pain without further specification | Lack of treatment effect was found with the addition of an exercise programme to a comprehensive education on GTPS management. The improved outcomes of the responders in the GLoBE group indicate that there may be a subgroup of patients with a GTPS diagnosis that benefit from a GLoBE intervention programme. |
| Ganderton, 2016, Australia361 | RCT | Gluteal (including GTPS) | Strengthening | Disability | Disability, participant/patient rating overall condition, QoL, NR | GLoBE intervention did not demonstrate additional benefit to comprehensive education in GTPS management. |
| Garcia, 2016, Spain362 | RCT | Rotator cuff | Flexibility, strengthening, other | Disability | QoL, disability | In patients with impingement syndrome, a combination of ultrasonophoresis and an exercise programme is better than a combination of iontophoresis and the same exercise programme or the exercise programme alone. |
| Gardin, 2010, Sweden363 | QE – without control | Achilles | Strengthening | Structure, disability | NA | Eccentric training provided improved pain and performance that was sustained over 4.2 years for Achilles tendinosis. |
| Gatz, 2020, Germany364 | QE – with control (with pre-test) | Achilles | Strengthening | Structure | NA | No measurable effect using shear wave elastography was observed for either eccentric or eccentric and isometric groups on gastrocnemius medialis and lateralis over a 12-week intervention. |
| Gatz, 2020, Germany365 | RCT | Achilles | Strengthening | Disability | Structure, disability, participant/patient rating overall condition | No additional clinical benefits of adding ISOs to a basic EE programme could be found in this preliminary RCT study over a period of 3 months. SWE was able to differentiate between insertional and midportion tendon tissue and localise reported symptoms to sublocations but this did not correlate with better clinical scores (VISA-A) over a 3-month follow-up period. |
| Gebremariam, 2014, Netherlands366 | Systematic reviews/secondary analysis | Rotator cuff | NA | NA | NA | Given the lack of detail surrounding exercise protocols within the included studies, it was concluded that a large degree of ambiguity still exists around particular exercise protocols and modalities. Despite this, exercise is still a favourable treatment option. |
| Ferrer, 2018, United States177 | Observational – cohort | Rotator cuff | Strengthening | Structure | PFC, disability | Exercise therapy improved measures of strength and patient-reported outcomes but did not have a significant impact on glenohumeral kinematics. |
| Giombini, 2006, Italy367 | RCT | Rotator cuff | Flexibility | Pain over a specified time, pain on loading/activity, clinical examination findings, | NA | Patients who received hyperthermia experienced significantly better pain relief than patients receiving ultrasound or exercises, making it an effective management for supraspinatus tendinopathy. |
| Giray, 2019 Turkey368 | RCT | Lateral elbow | Strengthening, flexibility | Disability | PFC, pain over a specified time, pain on loading/activity, disability | Kinesiotaping in addition to exercises is more effective than sham taping and exercises alone in improving pain in daily activities and arm disability due to lateral epicondylitis. |
| Goldgrub, 2016, Canada369 | Systematic reviews/secondary analysis | Rotator cuff | NA | NA | NA | The current evidence suggests that combining multiple interventions into one programme of care does not lead to superior outcomes for patients with subacromial impingement syndrome or nonspecific shoulder pain. |
| Gonsalves, 2012, Canada370 | Systematic reviews/secondary analysis | Rotator cuff | NA | NA | NA | Exercise is an effective modality for treating rotator cuff tendinopathies with specific high-intensity regimes likely to be more beneficial than more general and low-intensity exercise regimes. |
| Gonzalez, 2018, Saudi Arabia371 | QE – without control | Rotator cuff | Flexibility, other, strengthening | Participation, clinical examination findings | NA | The design of the intervention used was proven effective in treating shoulder impingement syndrome. It considered the need to increase the subacromial space, foster shoulder stability and avoid the interruption of the practice of physical activity. |
| González-Iglesias, 2011, Spain372 | Observational – case series/reports | Lateral elbow | Flexibility | Disability | Sensory modality-specific pain | Hypoalgesia and function improved for rock climbers with treatment. |
| Gornoski, 2014, United States373 | Observational – case series/reports | Patellar, Quadriceps, other – pesanserine | Flexibility, strengthening | Pain over a specified time, disability | NA | There is added benefit to electro-therapeutic point stimulation as an adjunct to standard stretching and strengthening exercise. |
| Granviken, 2015, Norway374 | RCT | Rotator cuff | Other, flexibility, strengthening | Disability | Pain over a specified time, clinical examination findings, psychological factors, ROM, participation, participant/patient rating overall | No significant differences in pain and disability were found between home exercises and supervised exercises of more than the first session of a 6-week exercise regime for people with subacromial impingement. |
| Grymel-Kulesza, 2007, Poland375 | RCT | Rotator cuff | NR | Pain over a specified time, clinical examination findings, PFC, ROM | NA | A multi-modal physiotherapy regime which combined ultrasound, TENS, massage and exercise therapy may be more beneficial for treating rotator cuff tendinopathy than modalities using a comparable treatment regime composed of cryotherapy. |
| Gunay Ucurum, 2018, Turkey376 | RCT | Rotator cuff | Strengthening, flexibility | Pain on loading/activity, QoL, disability | NA | Application of ultrasound, interferential current and TENS in addition to exercise therapy in shoulder impingement syndrome treatment had similar improvements in terms of pain, function and physical component of QoL. However, interferential current treatment showed significantly better outcomes for the mental component of QoL. |
| Gürsel, 2004, Turkey377 | RCT | Rotator cuff | Flexibility, strengthening | Pain on loading/activity, ROM, disability | NA | There is no added benefit to the use of 1-MHz US in combination with other interventions in the management of painful shoulder conditions to merit its wide use. |
| Gutierrez-Espinoza, 2020, Chile378 | Systematic reviews/secondary analysis | Rotator cuff | NA | NA | NA | There was no demonstrable clinical benefit of direct physiotherapist supervision to the early rehabilitation of SIS. |
| Haahr, 2003, Denmark379 | RCT | Lateral elbow | Flexibility | Participant/patient rating overall condition | Other, participation, economic impact costs | Poor prognosis at 1 year of follow-up for lateral epicondylitis was related to manual work and high baseline pain, whilst no relation was found between the type of medical treatment given/chosen and prognosis. |
| Haahr, 2006, Denmark43 | RCT | Rotator cuff | NA | impact costs, participation, participant/patient rating overall | NA | The results of surgical decompression were equal to those of conservative treatment, and the surgery group had more income transferrals during the first year of follow-up. |
| Haahr, 2005, Denmark380 | RCT | Rotator cuff | Other | Disability, pain over a specified time | NA | Surgical treatment of rotator cuff syndrome with subacromial impingement was not superior to physiotherapy with training. |
| Habets, 2015, Netherlands381 | Systematic reviews/secondary analysis | Achilles | NA | NA | NA | Strong evidence was found for both the Alfredson protocol and gradual onset of exercises during the first week with no definitive conclusion regarding the most effective training parameters. |
| Hakguder, 2011, Turkey382 | QE – with control (with pre-test) | Rotator cuff | Flexibility, strengthening | Disability, pain on loading/activity, pain over a specified time | NA | Patients with SIS who have partial rupture of supraspinatus tendon benefit from physical therapy consisting of US, TENS, superficial heat and exercise, with a decrease in pain, limitation of motion, and increase in functional status in the short term. |
| Hallgren, 2014, Sweden383 | RCT | Rotator cuff | Strengthening | Disability, other | Disability, pain on loading/activity, pain over a specified time, QoL | Specific exercises produced positive short-term improvements at 1-year follow-up and reduced the need for surgery. Full-thickness tear and a low CMS score appear to be predictors of poor outcome. |
| Hanratty, 2016, United Kingdom155 | Qualitative | Rotator cuff | NA | NA | NA | Experienced musculoskeletal physical therapists believe that exercise is central in treating patients with SIS and that gaining patient buy-in to its importance, patient education, promoting self-management and postural advice are central to the successful treatment of people with SIS. |
| Hanratty, 2012, United Kingdom384 | Systematic reviews/secondary analysis | Rotator cuff | NA | NA | NA | 16 studies were included. Physiotherapy exercises are effective in the management of SAIS. However, heterogeneity of the exercise interventions, coupled with poor reporting of exercise protocols, prevented conclusions being drawn about which specific components of the exercise protocols (i.e. type, intensity, frequency and duration) are associated with best outcomes. |
| Haslerud, 2015, Norway28 | Systematic reviews/secondary analysis | Rotator cuff | NA | NA | NA | Optimal LLLT can offer clinically relevant pain relief and initiate a more rapid course of improvement, both alone and in combination with physiotherapy interventions. |
| Hawk, 2017, United states385 | Systematic reviews/secondary analysis | Rotator cuff | NA | NA | NA | Low-moderate evidence exists in support of the use of MT as an efficacious treatment modality for SIS. In addition it was found that exercise, particularly when delivered as part of broader physical therapy treatment, was beneficial for SIS. Evidence is more limited for calcific tendonitis. |
| Hazar, 2014, Turkey386 | Pilot – randomised | Rotator cuff | Strengthening | Pain without further specification, disability | NA | Throwers Ten exercise positively affected pain alleviation and functional recovery in shoulder impingement patients. |
| Head, 2019, United Kingdom387 | Systematic reviews/secondary analysis | Achilles | NA | NA | NA | There is conflicting evidence regarding the superiority of eccentric loading over other types. Do-as-tolerated repetition volumes may be more effective at improving short-term function compared to the standardised Alfredson protocol. |
| Heitkamp, 2019, Germany388 | Systematic reviews/secondary analysis | Achilles | NA | NA | NA | The Alfredson protocol and heavy slow resistance training may be the most recommendable types of calf muscle training. |
| Hernandez, 2006, Spain389 | RCT | Lateral elbow | Flexibility, strengthening | Pain without further specification, function | NA | Combination of physical therapies with stretching and strengthening exercises effective for epicondylitis patients. |
| Heron, 2017, United Kingdom390 | RCT | Rotator cuff | Flexibility, strengthening | Disability | NA | Open chain, closed chain and range of movement exercises all seem to be effective in bringing about short-term changes in pain and disability in patients with rotator cuff tendinopathy. |
| Herrington, 2007, United Kingdom391 | Pilot – randomised | Achilles | Strengthening, flexibility | Disability | NA | The addition of a 12-week eccentric exercise programme to conventional treatment of ultrasound and deep transverse frictions is more effective in treating AT than conventional treatment alone. |
| Ho, 2007, China (SAR)392 | Pilot – randomised | Lateral elbow | Strengthening, flexibility | PFC, sensory modality-specific pain, | NA | Exercise alone is already effective for the management of lateral epicondylitis. The addition of microcurrent therapy to exercise does not enhance the treatment effect. |
| Holmgren, 2012, Sweden393 | RCT | Rotator cuff | Strengthening, flexibility | Disability | Pain on loading/activity, pain over a specified time, QoL, participant/patient rating overall condition, disability, other | Specific exercise strategy focussing on strengthening eccentric exercises for the rotator cuff and concentric/eccentric exercises for the scapula stabilisers is effective in reducing pain and improving shoulder function in patients with persistent subacromial impingement syndrome. By extension, this exercise strategy reduces the need for arthroscopic subacromial decompression at 3 months. |
| Hong, 2004, Canada394 | Survey | Lateral elbow | NA | NA | NA | More than 30 different treatments used tor acute, subacute, and chronic lateral epicondylitis were identified. Treatments most commonly used by physiotherapists were stretching exercises, ice and ultrasound therapy. |
| Hong, 2004, Canada395 | Survey | Lateral elbow | NA | NA | NA | Occupational therapists used a variety of interventions, including education, activities/exercises, assistive devices, environment and pain management modalities that differed according to the phases of their clients’ condition. |
| Hoogvliet, 2013, Netherlands396 | Systematic reviews/secondary analysis | Lateral elbow | NA | NA | NA | Short-term analgesic effects of manipulation techniques may allow for more vigorous stretching and strengthening exercises, which were found to be affective for recovery in lateral epicondylitis. |
| Horstmann, 2013, Germany16 | RCT | Achilles | Other, flexibility | examination findings, participant/patient rating overall condition, pain on loading/activity, other | NA | Vibration training may be an alternative or a complementary treatment in patients who do not respond well to eccentric training, especially in those with insertional pain. |
| Houck, 2015, United States397 | RCT | Tibialis posterior | Strengthening, flexibility | Disability, function, PFC | NA | A moderate-intensity, home-based exercise programme minimally improves outcomes over orthosis wear alone in participants with stage II TPTD. The improvements observed were smaller than those reported in some previous controlled and uncontrolled clinical trials, suggesting that positive effects on function and pain in response to exercise may require higher intensity than this home-based programme for participants with TPTD. |
| Hutchison, 2011, United Kingdom398 | Systematic reviews/secondary analysis | Achilles | NA | NA | NA | Methodological quality was adequate for all 9 studies; however, blinding was a limitation for most. Different interventions for AT with varying efficacy were reported. Therefore, there is insufficient evidence to determine which method of physiotherapy is most appropriate for a chronic mid-body AT. |
| Iglesias, 2018, Spain399 | Observational – case series/reports | Achilles | Strengthening | Disability, structure | NA | US-guided intra-tissue percutaneous electrolysis, dry-needling, diathermy and eccentric exercise are safe and clinically cost-effective treatment options in the management of mid-substance AT when delivered in conjunction with an eccentric exercise programme. |
| Ingwersen, 2017, Denmark191 | RCT | Rotator cuff | Flexibility, other, strengthening | Disability | Pain over a specified time, pain on loading/activity, PFC, ROM, | No superior benefit of PHLE was seen when compared with LLE in primary or secondary outcomes. |
| Innocenti, 2019, Italy400 | Systematic reviews/secondary analysis | Rotator cuff | NA | NA | NA | Six RCTs and 2 cross-sectional studies were appraised. Studies presented low to moderate risk of bias. Musculoskeletal physiotherapy seems to be an effective treatment for patients with shoulder pain although it is still based on weak diagnostic clinical instruments. The adoption of more functional and prognostic assessment strategies is advisable to improve coherence between evaluation and treatment. |
| Jasnauskaitė-Gedrimė, 2018, Lithuania401 | RCT | Rotator cuff | Other, flexibility, strengthening | ROM, PFC, QoL | NA | Visual feedback exercises had greater effect on shoulder functions and the QoL compared to auditory feedback exercises. |
| Jayaseelan, 2014, United States402 | Observational – case series/reports | Hamstring | Strengthening, other | Pain without further specification, function, palpation, participant/patient rating | NA | In both runners, eccentric loading of the hamstrings, lumbopelvic stabilisation exercises, and trigger-point dry needling provided short- and long-term pain reduction and functional benefits. |
| Jayaseelan, 2017, United States403 | Observational – case series/reports | Achilles | Strengthening, flexibility | Pain without further specification, sensory modality specific pain, participant/patient rating | NA | Joint mobilisation and manipulation in addition to eccentric exercise showed immediate improvements in symptoms and function which were maintained at 12 weeks and at 9 months. |
| Jayaseelan, 2019, United States148 | Observational – case series/reports | Achilles, patellar | Aerobic, flexibility | Pain without further specification, sensory modality specific pain, disability, other | NA | Tendinopathy, while often described as local pain and dysfunction, may be associated with dysfunction of the nervous system. Identifying and treating pain mechanisms in addition to relevant impairments may be an appropriate intervention approach for individuals with tendinopathy. |
| Jerosch, 2002, Germany404 | QE – without control | Rotator cuff | Other | Disability, PFC | NA | The present study shows that patients with subacromial pathology suffer from a proprioceptive deficit which can be improved by a special rehabilitation programme within 4 weeks. |
| Johansson, 2005, Sweden405 | RCT | Rotator cuff | Flexibility, strengthening | Examination findings, disability | NA | Acupuncture was more effective than ultrasound when applied in addition to home exercises. |
| Johansson, 2011, Sweden406 | RCT | Rotator cuff | Flexibility, strengthening | Disability | QoL, participant/patient rating overall condition | Acupuncture treatments combined with home exercises and subacromial corticosteroid injection both decreased pain and improved function in SIS patients. Neither was superior to the other. |
| Jonsson, 2005, Sweden186 | RCT | Patellar | Strengthening | Pain on loading/activity, disability, participant/patient rating overall condition | NA | Eccentric, but not concentric, quadriceps training on a decline board seems to reduce pain in jumper’s knee |
| Johnson, 2012, United States407 | Observational – case series/reports | Achilles | Flexibility | Disability | NA | The use of an AFO and stretching regimen improved FFI scores in patients suffering from retrocalcaneal heel pain. |
| Johnston, 1999, Canada168 | Observational – case series/reports | Other – iliopsoas syndrome | Flexibility, strengthening, other | Participant/patient rating overall condition | NA | Hip rotation strengthening and stretching programme appears to improve function with iliopsoas syndrome. |
| Jonsson (a), 2009, Sweden408 | QE – without control | Achilles | Strengthening | Pain on loading/activity, participant/patient rating overall condition, disability | NA | Treatment with painful eccentric calf-muscle training showed good clinical results based on VAS scores, patient satisfaction and return to pre-injury activity levels in patients with chronic painful mid-portion Achilles tendinosis, but not in patients with chronic insertional Achilles tendon pain. |
| Jonsson (b), 2009, Sweden408 | Pilot – non-randomised | Achilles | Strengthening | loading/activity, participant/patient rating overall | NA | The short-term pilot study demonstrated promise of a new eccentric exercise model for tendinopathy. |
| Jonsson (c), 2010, Sweden408 | Pilot – non-randomised | Patellar | Strengthening | loading/activity, participant/patient rating overall | A | Eccentric strengthening exercise performed on a decline board had better pain relief and treatment satisfaction compared to a similar programme completed on a flat surface. |
| Jonsson, 2006, Sweden409 | Pilot – non-randomised | Rotator cuff | Strengthening | Pain onloading/activity, participant/patient rating | NA | Painful eccentric supraspinatus and deltoideus training might be effective at decreasing pain and improving function in SIS patients with a long duration of disabling pain symptoms. |
| Jonsson, 2008, Sweden410 | Pilot – non-randomised | Achilles | Strengthening | loading/activity, participant/patient rating overall | NA | This new model of painful eccentric calf-muscle training showed promising clinical results in the majority of patients. |
| Jowett, 2013, United Kingdom411 | RCT | Rotator cuff | NA | Economic impact costs | NA | Corticosteroid injection plus exercise delivered by therapists may be a cost-effective use of resources compared with exercise alone and lead to lower healthcare costs and less time off work. |
| Juul-Kristensen, 2019, Denmark412 | RCT | Rotator cuff | Other, flexibility, strengthening | Pain over a specified time | PFC, pain over a specified time | BIONEX and NEX were both effective in reducing pain to a clinically relevant level, while EMG biofeedback did not make a difference. The current neuromuscular shoulder exercise protocol is recommended. |
| Kachanathu, 2019, Saudi Arabia413 | RCT | Lateral elbow | Flexibility | Pain without further specification | ROM, PFC | Wrist joint splinting in addition to physical therapy for a short duration was effective at improving pain intensity in patients with lateral epicondylitis. |
| Kachanatu, 2019, Saudi Arabia414 | QE – without control | Rotator cuff | Flexibility, other | PFC | NA | SSE’s significantly improved isometric hand grip strength of SIS patients. |
| Kachingwe, 2008, United States415 | Pilot – randomised | Rotator cuff | Flexibility, other, strengthening | Pain over a specified time, disability, ROM | NA | Performing glenohumeral mobilisations and mobilisation-with-movement in combination with a supervised exercise programme may result in a greater decrease in pain and improved function for patients. |
| Kang, 2019, Taiwan416 | RCT | Rotator cuff | Other, strengthening | Structure, disability, pain without further specification | NA | Four weeks of strengthening and stretching exercises with or without kinesiology taping improved functional performance in subjects with SIS and RSP. Kinesiology taping did not demonstrate an additional effect on RSP. |
| Kaux, 2014, Belgium417 | QE – without control | Patellar | Flexibility, strengthening, aerobic, other | Pain without further specification, disability | NA | This re-educative protocol based on sub-maximal eccentric exercises added to PRP infiltrations decreased pain and improved function in patellar tendinopathy. |
| Kaux, 2015, Belgium418 | Observational – case series/reports | Patellar | Strengthening | Pain without further specification, disability, participation | NA | Local injection of PRP coupled with a programme of eccentric rehabilitation improves pain and functional symptoms of patients with chronic jumper’s knee up to 1 year after injection. |
| Kaux, 2015, Belgium419 | Observational – cohort | Patellar | Strengthening, flexibility | Loading/activity, sensory modality specific pain, disability, PFC | NA | Local infiltration of PRP combined with a submaximal |
| Kaya, 2011, Turkey420 | QE – with control (with pre-test) | Rotator cuff | Strengthening, flexibility | Disability, pain over a specified time, pain without further specification, pain on loading/activity | NA | kinesiotaping was more effective than the local modalities at the first week and the positive effect maintained at the second week of the treatment. Therefore, it may be an alternative treatment option for shoulder impingement syndrome. |
| Kaya, 2014, Turkey421 | Pilot – randomised | Rotator cuff | Flexibility, Strengthening | Pain on loading/activity, pain over a specified time, disability, structure | NA | There were no differences in pain reduction and disability between kinesiotaping with exercise and MT with exercise in patients with subacromial impingement. |
| Kearney, 2013, United Kingdom422 | Pilot – randomised | Achilles | Strengthening | Disability | QoL | This pilot study provided key data to inform a larger study and shows that the methodology is feasible. |
| Kearney, 2010, United Kingdom423 | Systematic reviews/secondary analysis | Achilles | NA | NA | NA | 11 articles met the eligibility criteria. There is a consensus that conservative methods should be used before operative interventions. Current evidence for conservative treatment favours eccentric loading and shockwave therapy, although there is limited evidence by which to judge their effectiveness. |
| Kedia, 2014, United States424 | RCT – cluster | Achilles | Strengthening | QoL, disability, pain without further specification | NA | Conventional physical therapy consisting of gastrocnemius, soleus and hamstring stretches, ice massage on the Achilles tendon, and use of heel lifts and night splints with or without eccentric training is effective for treating insertional AT. |
| Kelly, 2010, United Kingdom424 | Systematic reviews/secondary analysis | Rotator cuff | NA | NA | NA | Exercise is shown to be effective to some degree in the management of subacromial impingement syndrome, although methodological quality must be taken into account. |
| Kesikburun, 2013, Turkey425 | RCT | Rotator cuff | Flexibility, strengthening | Disability | Examination findings, ROM, adverse effects/even ts, disability | At 1-year follow-up, a PRP injection was found to be no more effective in improving QoL, pain, disability, and shoulder ROM than placebo in patients with chronic RCT who were treated with an exercise programme. |
| Ketola, 2009, Finland426 | RCT | Rotator cuff | Other, strengthening | Pain without further specification | Pain over a specified time, disability, participation | Arthroscopic acromioplasty provides no clinically important effects over a structured and supervised exercise programme alone in terms of subjective outcome or cost-effectiveness when measured at 24 months. |
| Ketola, 2017, Finland427 | RCT | Rotator cuff | Other, strengthening | Pain without further specification | Participation, disability, pain over a specified time | The natural history of rotator cuff tendinopathy probably plays a significant role in the results in the long term. Even though the patients who underwent operative treatment had a stronger belief in re covery from surgery, the exercise group obtained similar results. Both intention-to-treat and per protocol analysis showed no significant differences between the two groups. |
| Ketola, 2015, Finland428 | RCT | Rotator cuff | Strengthening | Pain without further specification | Pain over a specified time, disability, participation | Both treatment groups had less pain at 2 and5 years. Duration of symptoms, marital status (single), long periods of sick leave, and lack of professional education appeared to increase the risk of persistent pain despite the treatment. Patients with impingement with radiological acromioclavicular (AC) joint degeneration also had more pain. Based on our findings, it is difficult to recommend arthroscopic acromioplasty for any specific subgroup. Patients in the exercise group who later went on with surgical option did not get better after the operation, which further challenges the development of a treatment algorithm as it suggests those who do not respond to non-operative treat ment should not be operated on either. |
| Ketola, 2016, Finland429 | RCT | Rotator cuff | Other | Structure | NA | Arthroscopic acromioplasty does not have any long-term benefit based on radiological findings of muscle volumes. Also, the frequency of perforating supraspinatus rupture was similar irrespective of whether or not surgery was performed. Acromioplasty is not justified as a treatment for dynamic shoulder impingement syndrome. |
| Kim, 2016, Korea (Republic of)430 | RCT | Rotator cuff | Strengthening | Pain without further specification, disability, ROM, physical function | NA | Neurac training is a more effective treatment for acute SIS when improvements in muscular strength are also desired. |
| Kim, 2017, Korea (Republic of)431 | RCT | Rotator cuff | Other | Pain without further specification, ROM, physical function | NA | The use of visual feedback and 3D motion images can improve pain and function in SIS. |
| Kim 2019, Korea (Republic of)432 | control (with pre-test) | Rotator cuff | Other, strengthening | Disability, structure | NA | Exp group (PRP) had better clinical outcomes than exercise. |
| Kim, 2020, Korea (Republic of) 433 | RCT | Rotator cuff | Other, strengthening | Function capacity, pain without further specification, Disability, ROM | NA | Both the Neurac modality and MT induced pain relief, improved function, and increased ROM. The Neurac intervention also resulted in a significant enhancement of shoulder muscle strength, indicating its superiority as an effective therapeutic modality for this particular patient group. |
| Kim, 2020, Korea (Republic of)434 | QE – without control | Posterior tibial tendon | Strengthening | PFC | NA | A 4-week SFE programme may have positive effects on changing muscle activation patterns for tibialis anterior and fibularis longus muscles. Although it could not influence their structural deformity and ankle joint movement, it could produce a potential benefit of decreased tibialis posterior activation. |
| Kingma, 2007, Netherlands435 | Systematic reviews/secondary analysis | Achilles | NA | NA | NA | The effects of eccentric exercise training in patients with chronic AT on pain are promising; however, the magnitude of the effects cannot be determined. |
| Knobloch, 2008, Germany436 | RCT | Achilles | Strengthening | Pain without further specification, structure | NA | No microcirculatory changes are evident in non-compliant and compliant patients with AT undergoing 12 weeks of eccentric training. |
| Knobloch, 2007, Germany192 | QE – without control | Achilles | Strengthening | Disability, structure | NA | 12-week eccentric training is not harmful to microcirculatory Achilles tendon level. It is beneficial, easy to apply and should be promoted broadly among patients with mid-portion as well as insertional tendinopathy without bony abnormalities as the microcirculatory changes and the pain-level reduction indicate that both groups may benefit from painful eccentric training. |
| Knobloch, 2008, Italy437 | RCT | Achilles | Strengthening | Pain without further specification, disability, structure | NA | Patients with tendinopathy of the main body of the AT experienced improved clinical outcome with both management options. Although tendon microcirculation was optimised in the combined group of eccentric training and AirHeel Brace, these micro-vascular advantages do not translate into superior clinical performance when compared with eccentric training alone. |
| Knobloch, 2010, Germany182 | Observational – cohort | Achilles | Strengthening | Pain on loading/activity, disability | NA | Symptomatic females suffering AT do not benefit as much as symptomatic males from 12 weeks of eccentric training as far as pain reduction and improvement of VISA-A scores are concerned. |
| Kongsgaard, 2009, Denmark21 | RCT | Patellar | Strengthening | Disability | Pain on loading/activity, participant/patient rating overall condition, structure | Corticosteroid injection has good short-term but poor long-term clinical effects, in patellar tendinopathy. Heavy-slow resistance exercise has good short- and long-term clinical effects accompanied by pathology improvement and increased collagen turnover. |
| Kongsgaard, 2010, Denmark438 | Observational – cohort | Patellar | Strengthening | Disability, pain on loading/activity, structure | NA | Positive clinical effect of heavy resistance training was accompanied by changes in fibril morphology, perhaps indicative of more new fibrils. |
| Korakakis, 2018, Qatar439 | Systematic reviews/secondary analysis | Gluteal (including GTPS), hamstring, | NA | NA | NA | Low level of evidence suggests that ESWT may be effective for some lower-limb conditions in the short, mid and long-term management of PHT. |
| Koszalinski, 2020, United States440 | Pilot – feasibility | Achilles | Strengthening, flexibility | Function | Modality specific pain, participant/patient rating overall condition, pain without further specification, PFC | Significant differences reported for within-group analysis for FAAM, NPRS, pain pressure threshold and strength in both groups at 4 weeks and 3 months. |
| Kramer, 2010, Germany441 | Systematic reviews/secondary analysis | Achilles | NA | NA | NA | Although no recommendations can yet be made regarding dosage and duration, the effects of eccentric training in conservative treatment of chronic mid-portion-AT are promising. |
| Kristensen, 2012, United Kingdom442 | Systematic reviews/secondary analysis | Achilles, patellar | NA | NA | NA | Resistance training is a valuable method of conservative treatment for chronic musculoskeletal conditions irrespective of age or gender. Higher-intensity approaches were more efficacious than those of lower intensities. Furthermore high-intensity RT did not increase the likelihood of injury provided that regimes introduce loads progressively. |
| Kromer, 2013, Germany443 | RCT – cluster | Rotator cuff | Strengthening, flexibility, other | Disability, participant/patient rating overall condition | Pain over a specified time, participant/patient rating overall condition | Individually adapted exercises were effective in the treatment of patients with shoulder impingement syndrome. Individualised manual physi otherapy contributed only a minor amount to the improvement in pain intensity. |
| Kromer, 2009, Germany444 | Systematic reviews/secondary analysis | Rotator cuff | NA | NA | NA | This review shows an equal effectiveness of physiotherapist-led exercises compared with surgery in the long term and of home-based exercises compared with combined physiotherapy interventions in patients with shoulder impingement syndrome. |
| Kromer, 2014, Germany445 | RCT | Rotator cuff | Strengthening, flexibility, other | Disability, participant/patient rating overall condition | Disability, psychological factors, economic impact costs | The use of MT including physiotherapy provides no additional benefits and is more expensive in comparison to exercise-only interventions. |
| Kuhn, 2009, United States446 | Systematic reviews/secondary analysis | Rotator cuff | NA | NA | NA | Exercise is effective as a treatment for the reduction of pain and improving function but fewer statistical and clinical significant effects are seen on the ROM or strength. Supervised exercise was not different than HEPs. |
| Kulig, 2009, United States447 | Observational – case series/reports | Posterior tibial tendon | Flexibility, strengthening | PFC, participant/patient rating overall condition, disability, pain on loading/activity, physical activity | NA | A 10-week tendon-specific eccentric programme resulted in improvements in symptoms and function without changes in tendon morphology or neovascularisation. |
| Kulig, 2009, United States448 | RCT | Posterior tibial tendon | Strengthening | Disability, PFC, Pain on loading/activity | NA | People with early stage tibialis posterior tendinopathy benefited from a programme of orthoses wear and stretching. Eccentric and concentric progressive resistive exercises further reduced pain and improved perceptions of function. |
| Kvalvaag, 2017, Norway449 | RCT | Rotator cuff | Strengthening, other | Disability | Pain on loading/activity, function, medication use | Radial ESWT offered no additional benefit to supervised exercises in the treatment of subacromial shoulder pain after 24 weeks, except in the subgroup of patients with calcification in the rotator cuff. |
| Kvalvaag, 2018, Norway450 | RCT | Rotator cuff | Flexibility, strengthening | Disability | Pain on loading/activity, pain over a specified time, function, QoL, participation | Radial ESWT was not superior to sham rESWT in addition to supervised exercises in the long term for patients with subacromial pain syndrome. Marital status (single), frequent use of pain medication, not working at baseline, negative outcome expectations, low self-reported general health status and few supervised exercise sessions predicted a poor outcome on SPADI after one year. |
| Laitinen, 2017, Finland451 | Systematic reviews/secondary analysis | Hamstring, patellar, Achilles | NA | NA | NA | For both patellar and AT, eccentric exercise was effective in relieving pain, but less consistent evidence for tendinopathic changes. HSR exercise was equally as effective as eccentric training for pain relief and appears superior for patient satisfaction. Combining stretching and eccentric training appeared to enhance effects of pain relief. In general, there are beneficial effects for at least one outcome across all the modalities studied. |
| Land, 2019, Australia452 | RCT | Rotator cuff | Flexibility | ROM | Pain without further specification, disability | Upper thoracic and posterior shoulder interventions with a targeted home exercise that addresses thoracic spine or posterior shoulder tightness improves the signs and symptoms of SIS. |
| Langberg, 2007, Denmark133 | QE – with control (with pre-test) | Achilles | Strengthening | Structure, pain on loading/activity | NA | 12 weeks of eccentric training stimulates collagen type I synthesis in chronically injured human Achilles tendon. This increased synthesis is accompanied by a significant reduction in pain in the tendon during loading. |
| Larsson, 2012, Sweden453 | Systematic reviews/secondary analysis | Patellar | NA | NA | NA | Eccentric exercise should be considered as an effective treatment modality for patellar tendinopathy. |
| Larsson, 2019, Sweden454 | Systematic reviews/secondary analysis | Rotator cuff | NA | NA | NA | Seven studies (eight articles) were included, six were meta-analysed. Included studies were of moderate quality. Evidence of low certainty suggests that eccentric exercise may provide a small but likely not clinically important reduction in pain compared with other types of exercise in patients with subacromial impingement syndrome. It is uncertain whether eccentric exercise improves function more than other types of exercise (very low certainty of evidence).Methodological limitations of existing studies make these findings susceptible to change in the future. |
| Leduc, 2003, Canada455 | RCT | Rotator cuff | Flexibility | Disability, ROM, structure | NA | Treatment of calcifying tendinitis of the shoulder with acetic acid iontophoresis and physiotherapy did not result in better clinical or radiological effects than those observed in subjects treated with physiotherapy alone. SPADI score and shoulder ROM improved significantly in both groups. |
| Lee, 2014, Korea (Republic of)456 | RCT | Lateral elbow | Flexibility, strengthening | Further specification, disability, physical function | NA | Three days per week for 3 weeks of physical therapy improves pain and function in patients with acute lateral epicondylitis. After 3 weeks, 6 days per week is the most effective treatment frequency. |
| Lee, 2017, Hong Kong, China (SAR)457 | RCT | Patellar | Strengthening | On loading/activity, pain over a specified time, disability | NA | Eccentric exercise-induced modulation on tendon mechanical properties and clinical symptoms i associated in athletes with patellar tendinopathy. |
| Lee, 2016, Korea (Republic of)458 | QE – without control | Rotator cuff | Strengthening | PFC | NA | Closed kinetic chain shoulder exercise was effective in increasing shoulder-IR and -ER peak torque, which is related to improved throwing velocity in baseball players. |
| Lee, 2017, China459 | QE – with control (with pre-test) | Patellar | Strengthening | Over a specified time, pain on loading/activity, disability | NA | Eccentric exercise alone was effective in increasing tendon strain and reducing pain. The addition of ESWT did not provide any further benefits. |
| Levy, 2009, United Kingdom150 | Qualitative | Achilles, patellar, rotator cuff | NA | NA | NA | Five themes – motivation, confidence, coping, social support, and pain emerged from the thematic analysis. Specifically, a lack of motivation and confidence was perceived to have a negative effect upon home-based rehabilitation adherence while ineffective coping strategies, over support and pain, appeared to have an adverse influence on rehabilitation adherence in a clinic setting. The use of effective coping strategies and varied types of social support aided reha bilitation adherence. |
| Lim, 2018, Australia12 | Systematic reviews/secondary analysis | Patellar | NA | NA | NA | Fifteen studies (3 isometric, 2 HSR, and 10 eccentric) were included for this review. It is recommended that the findings from isometric exercises (Grade A) can be trusted to guide clinical practice, whereas eccentric exercises (Grade B) can be trusted to guide clinical practice in most clinical situations. It is recommended that HSR exercises (Grade C) should be applied carefully to individual clinical circumstances and interpreted with care. |
| Littlewood, 2012, United Kingdom35 | Systematic reviews/secondary analysis | Rotator cuff | NA | NA | NA | Home and supervised exercise programmes might be more effective than no intervention or placebo and as effective as minimal or active comparators (brace, physiotherapy, surgery). |
| Littlewood, 2013, United Kingdom7 | Systematic reviews/secondary analysis | Rotator cuff | NA | NA | NA | 26 reviews were retrieved. Exercise and multimodal physiotherapy appear to be effective interventions for rotator cuff tendinopathy, although the clinical significance of this effect is unclear. Combining MT with exercise is not currently supported, neither is the use of corticosteroid injections or acupuncture. This interpretation is drawn from systematic reviews comprising mainly small RCTs that frequently measure outcome in a heterogeneous manner, limiting the strength of any conclusions. |
| Littlewood, 2014, United Kingdom460 | Pilot – randomised | Rotator cuff | Strengthening | Disability | QoL, Other | Greater improvements in SPADI score were observed in the self-management exercise group. |
| Littlewood, 2016, United Kingdom34 | RCT | Rotator cuff | Strengthening | Disability | Disability | Self-management programmes based on a single exercise were comparable to usual physiotherapy in the short, medium and long term. |
| Littlewood, 2014, United Kingdom156 | Qualitative | Rotator cuff | NA | NA | NA | With certain caveats including the need to recognise and respond to individual characteristics, implement effective knowledge translation strategies and the need to engage with appropriately timed pro-active follow-up, the potential to implement programmes of self-managed loaded exercise for patients with rotator cuff tendinopathy in the real world and in further research studies appears feasible but challenging. |
| Littlewood, 2015, United Kingdom23 | Systematic reviews/secondary analysis | Rotator cuff | NA | NA | NA | Contextual factors related to the therapist and the patient, for example, geographical location and setting, do not appear to significantly influence treatment outcomes. Resistance training is an important element in the rehabilitation process; however, the optimal level of resistance and other dosage factors remains unclear. Programmes should generally be conducted for 12 weeks to display good results. |
| Littlewood, 2015, United Kingdom107 | Qualitative | Rotator cuff | NA | NA | NA | Some physiotherapist-related barriers and facilitators concerning implementation of research findings identified included the apparent differences between the preferred therapeutic approach of the physiotherapists and the self-managed exercise inter vention. The physiotherapists recognised their role as knowledge translators but certain attributes of the intervention appeared to serve as both a barrier and facilitator, particularly the simplicity. Opinion regarding the optimal symptom response during exercise prescription also differed. These factors need to be recognised and considered. |
| Long, 2015, United Kingdom461 | Systematic reviews/secondary analysis | Lateral elbow | NA | NA | NA | Clinical effectiveness evidence from the high-quality systematic reviews identified in this overview continues to suggest uncertainty as to the effectiveness of many conservative interventions for the treatment of LET. Although new RCT evidence has been identified with either placebo or active controls, there is uncertainty as to the size of effects reported within them because of the small sample size. Conclusions regarding cost-effectiveness are also unclear. |
| Lopez-de-Celis, 2018, Spain462 | RCT | Lateral elbow | Flexibility | Pain over a specified time | Sensory modality specific pain, PFC, disability, participant/patient rating overall condition | Diacutaneous fibrolysis added to physical therapy provides better results (including pain-free grip strength) in the treatment of chronic lateral epicondylalgia, with greater clinical satisfaction among patients. |
| Ludewig, 2003, United States463 | RCT | Rotator cuff | Flexibility, strengthening | Disability | NA | HEPs are more effective in reducing symptoms and improving function (Shoulder Rating Questionnaire, shoulder satisfaction score) than the control group in construction workers with shoulder pain. |
| Luginbuhl, 2008, Switzerland174 | RCT | Lateral elbow | Strengthening | function capacity, ROM, disability | NA | No beneficial effect of either the forearm support band or the strengthening exercises could be found. |
| Maenhout, 2013, Belgium464 | RCT | Rotator cuff | Strengthening | Disability, participant/patient rating overall condition, PFC | NA | Adding heavy-load eccentric training resulted in a higher gain in isometric strength at 90 degrees of scapular abduction, but was not superior for decreasing pain and improving shoulder function. The addition of a limited number of physiotherapy sessions combined with a daily HEP is highly effective in patients with impingement. |
| Maffulli, 2008, United Kingdom465 | QE – without control | Achilles | Strengthening, flexibility | Disability | NA | Eccentric exercises in athletic patients provide comparable clinical outcome compared to our previous results in non-athletic patients. |
| Maffulli, 2015, United Kingdom466 | Systematic reviews/secondary analysis | Achilles | NA | NA | NA | There was no significant evidence to advise any particular pharmacological treatment as the best advisable non-operative option for AT. |
| Mafi, 2001, Sweden467 | RCT | Achilles | Strengthening | loading/activity, participant/patient rating overall | NA | Eccentric calf muscle training showed superior results to concentric training in the treatment of chronic Achilles tendinosis based on patient satisfaction and return to activity level. |
| Magnussen, 2009, United States468 | Systematic reviews/secondary analysis | Achilles | NA | NA | NA | There was more evidence in support of eccentric exercise in comparison to the other conservative treatment methods assessed (e.g. ESWT, injections, sclerosing agents). |
| Malliaras, 2013, United Kingdom61 | Systematic reviews/secondary analysis | Achilles, patellar | NA | NA | NA | Lack of high-quality evidence. Findings do not support eccentric-only exercise. Clinicians recommended to consider eccentric-concentric exercise with or without eccentric-only exercise for Achilles and patellar tendinopathy. More high-quality research required. |
| Manias, 2006, Greece469 | RCT | Lateral elbow | Flexibility, strengthening | Pain over a specified time, other | NA | Supplementing exercise with ice offers no added benefit to patients with LET. |
| Mani-Babu, 2014, United Kingdom27 | Systematic reviews/secondary analysis | Gluteal (including GTPS), patellar, Achilles | NA | NA | NA | Moderate evidence indicates that (1) ESWT is more effective than home training and corticosteroid injection in the short and long term for GTPS, (2) ESWT is more effective than eccentric loading for insertional AT and equal to eccentric loading for midportion AT in the short term, and (3) combining ESWT and eccentric loading in midportion AT may produce superior outcomes to eccentric loading alone. Therefore, ESWT is an effective intervention and should be considered for GTPS, PT and AT particularly when other nonoperative treatments have failed. |
| Marik, 2017, United States470 | Systematic reviews/secondary analysis | Rotator cuff | NA | NA | NA | There is strong evidence that ROM, strengthening exercises and joint mobilisations can improve function and decrease pain in people with SIS. |
| Martinez-Silvestrini, 2005, United States471 | QE – with control (with pre-test) | Lateral elbow | Flexibility, strengthening | function capacity, disability, QoL, pain without further specification, participant/patient rating | NA | No significant differences in outcome among the groups. |
| Marzetti, 2014, Italy472 | RCT | Rotator cuff | Other | Disability | Participant/patient rating overall condition, pain on loading/activity, pain over a specified time | Neurocognitive rehabilitation is effective in reducing pain and improving function in patients with shoulder impingement syndrome, with benefits maintained for at least 24 weeks. |
| Masood, 2014, Finland166 | QE – without control | Achilles | Strengthening | PFC, structure, disability, pain without further specification | NA | Eccentric rehabilitation was effective in improving leg strength in AT. It also resulted in redistribution of relative electrical activity, but not metabolic activity, within the triceps surae muscle. |
| Matthew, 2013, United Arab Emirates473 | Observational – case series/reports | Rotator cuff | Other, strengthening, flexibility | Pain without further specification, ROM, disability | NA | Glenohumeral mobilisations with movement combined with a supervised exercise programmemay result in a greater decrease in pain and improved function. |
| Mayer, 2007, Germany474 | RCT | Achilles | Strengthening, other | Disability, pain on loading/activity, PFC | NA | A 4-week treatment of deep friction and ultrasound in combination with sensorimotor and eccentric training, as well as insoles with longitudinal arch support, might reduce pain (at rest and in activity) in most patients with AT. |
| McAleenan, 2010, United Kingdom475 | Pilot – randomised | Achilles | Strengthening | Disability | Function, participant/patient rating overall condition | Eccentric exercise combined with a night splint appears to improve outcomes in AT over the control group. |
| Mc Auliffe, 2017, Ireland476 | Qualitative | Achilles | NA | NA | NA | Persistent AT is associated with a significant psychosocial impact, particularly in terms of participation in daily life and valued activities. |
| McClure, 2004, United States477 | Observational – cohort | Rotator cuff | Strengthening, flexibility, other | function capacity, disability, QoL | NA | Findings suggest a relatively simple exercise programme combined with patient education may be effective. |
| McCormack, 2016, United States478 | RCT | Achilles | Strengthening | Disability | specified time, participant/patient rating overall condition | Soft tissue treatment (Astym) plus eccentric exercise was more effective than eccentric exercise alone at improving function during both short- (26 weeks) and long-term (52 weeks) follow-up periods. |
| McDevitt, 2020, United States479 | Observational – case series/reports | Other – bicipital tendinopathy | Strengthening, flexibility | Specified time, clinical examination findings, participant/patient rating overall | NA | Findings from this case series suggest that DN and eccentric-concentric exercise may be beneficial for the management of patients with chronic BT tendinopathy. |
| Melegati, 2000, Italy480 | RCT | Rotator cuff | Flexibility, strengthening | Disability | NA | Groups A (kinesitherapy) and B (ESWT + kinesitherapy) achieved a significant constant score improvement, whereas the increase in group C (control) was not significant. |
| Mellor, 2018, Australia30 | RCT | Gluteal (including GTPS) | Strengthening, other | Participant/patient rating overall condition, pain over a specified time | Disability, function, PFC, psychological factors, physical activity, QoL | EDX is an effective management approach for gluteal tendinopathy. Education plus exercise and corticosteroid injection use resulted in higher rates of patient-reported global improvement and lower pain intensity than no treatment at 8 weeks. In the long term (52-weeks), education plus exercise led to better global improvement than corticosteroid injection use, but no difference in pain intensity. |
| Mendonça, 2020, Netherlands481 | Systematic reviews/secondary analysis | Patellar | NA | NA | NA | Compared to minimal intervention, conservative treatment did not improve pain and function in patients with patellar tendinopathy. |
| Menek, 2019, Turkey482 | RCT | Rotator cuff | Flexibility, strengthening | Pain without further specification, ROM, disability, QoL | NA | Mulligan mobilisation was more effective than general treatment methods for pain as well as normal joint motion, DASH scoring and some parameters of SF-36 compared with general treatment methods. |
| Menta, 2015, Canada483 | Systematic reviews/secondary analysis | Lateral elbow | NA | NA | NA | Based on the findings of this review, the relative effectiveness of stretching vs. strengthening for the wrist extensors remains unclear for the management of persistent lateral epicondylitis. |
| Meyer, 2009, New Zealand24 | Systematic reviews/secondary analysis | Achilles | NA | NA | NA | Owing to insufficient reported compliance data, a conclusion on the relative effectiveness of various compliances was not feasible. According to our review, the relative effectiveness of various dosages of eccentric exercises for AT is still unclear |
| Miccinilli, 2018, Italy484 | RCT | Rotator cuff | Flexibility, strengthening | loading/activity, disability, ROM, PFC | NA | Our findings are not strong enough to recommend the application of kinesio-taping during RC tendinopathy rehabilitative treatment. |
| Michener, 2004, United States485 | Systematic reviews/secondary analysis | Rotator cuff | NA | NA | NA | The low to mediocre methodologic quality, small sample sizes and general lack of long-term follow-up limit these findings for the development of useful clinical practice guidelines. The limited evidence currently available suggests that exercise and joint mobilisations are efficacious for patients with SAIS. Laser therapy appears to be of benefit only when used in isolation, not in combination with therapeutic exercise. Ultrasound is of no benefit, and acupuncture trials present equivocal evidence. |
| Morgan, 2019, United States486 | Observational – case series/reports | Rotator cuff | Strengthening, flexibility | Disability | Pain over a specified time, ROM, participant/patient rating overall condition | This case series provides insight to the observed short- and intermediate-term effects of dry needling combined with exercise for subacromial pain syndrome. The results are encouraging for dry needling as an adjunct to exercise for treating patients with subacromial pain syndrome. |
| Morton, 2014, United Kingdom487 | Observational – case series/reports | Patellar | Aerobic, strengthening | Participant/patient rating overall condition, adverse effects/events, | NA | High-volume image-guided injections should be considered in the management of recalcitrant PT as the majority of subjects showed improvement in their VISA-P score. |
| Morton, 2015, United Kingdom488 | Observational – case series/reports | Gluteal (including GTPS) | Aerobic, strengthening | Pain without further specification, disability | NA | Both the retrospective and prospective groups showed a statistically significant reduction in pain following a high-volume guided injection and structured rehabilitation in patients with GTPS. |
| Mulligan, 2016, United States489 | RCT – cross-over | Rotator cuff | Other, strengthening, flexibility | Loading/activity, disability, function, participant/patient rating overall | NA | Patients with SAIS demonstrate improvement in pain and function with a standardised programme of physical therapy regardless of group exercise sequencing. |
| Munteanu, 2015, Australia490 | RCT | Achilles | Strengthening | Disability, participation | QoL, physical activity, participant/patient rating overall condition, other | Customised foot orthoses, prescribed according to the protocol in this study, are no more effective than sham foot orthoses for reducing symptoms and improving function in people with mid-portion AT undergoing an eccentric calf-muscle exercise programme. |
| Murphy, 2018, Australia491 | Systematic reviews/secondary analysis | Achilles | NA | NA | NA | A total of 31 separate cohorts (24 studies) were eligible, with follow-up ranging from 2 weeks to 6 months. An improvement in pain and function as early as 2 weeks that appeared to peak at 12 weeks was demonstrated. |
| Murphy, 2019, Australia492 | Systematic reviews/secondary analysis | Achilles | NA | NA | NA | Seven studies met the inclusion criteria. Current evidence suggests that HECT may be superior to natural history and traditional physiotherapy while HECT may be inferior to other exercise interventions. However, due to methodological limitations, small sample size and a lack of data we are unable to be confident in the results of the estimate of the effect, as the true effect is likely to be substantially different. |
| Nazligul, 2018, Turkey493 | RCT | Rotator cuff | Flexibility | specified time, pain on loading/activity, disability | NA | IFC therapy had no additional benefit over NSAID, cryotherapy and exercise programme in the treatment of SIS. |
| Newcomer, 2001, United States494 | RCT | Lateral elbow | Flexibility, strengthening | further specification, disability, physical | NA | A corticosteroid injection does not provide a clinically significant improvement in the outcome of LE. |
| Nha Hong, 2004, Canada495 | Survey | Lateral elbow | NA | NA | NA | More than 30 different treatments used for acute, subacute and chronic lateral epicondylitis were identified. Treatments most commonly used by physiotherapists were stretching exercises, ice an d ultrasound therapy. The results serve as a baseline to guide future research. |
| Nilsson, 2007, Sweden496 | Pilot – non-randomised | Lateral elbow | Strengthening, flexibility | Disability, PFC, participation | NA | A 4-week structured home training programme can improve function and reduce sick leave in patients with lateral epicondylitis. Positive effects were sustained over 16 weeks. |
| Nimgade, 2005, United States497 | Systematic reviews/secondary analysis | Lateral elbow | NA | NA | NA | Steroid injections appear the most successful short-term intervention for pain relief. Active physiotherapy appears efficacious regardless of time frame. |
| Nishizuka, 2017, Japan498 | RCT | Lateral elbow | Flexibility | Disability | Pain without further specification, participant/patient rating overall condition, clinical examination findings | A forearm band may have no more than a placebo effect and is not recommended based on its effectiveness. |
| Norregaard, 2007, Denmark499 | RCT | Achilles | Strengthening | Palpation, participant/patient rating overall condition, disability | NA | Symptoms gradually improved during the 1-year follow-up period and were significantly better assessed by pain and symptoms after 3 weeks and all later visits. However, no significant differences could be observed between the two groups. |
| Notarnicola, 2014, Italy500 | QE – with control (with pre-test) | Achilles | Flexibility, strengthening | Pain without further specification, disability | NA | Cryo high-energy laser therapy (CHELT) gave quicker and more effective pain relief compared to ESWT at 2-month and 6-month follow-up. |
| Nowotny, 2018, Germany501 | RCT | Lateral elbow | Strengthening | further specification, PFC, ROM, disability | NA | The use of an elbow orthosis appears to reduce pain and improve other subjective outcome measures. However, the long-term results do not appear to be any greater than those received through physiotherapy alone. |
| Nyberg, 2010, Sweden502 | Systematic reviews/secondary analysis | Rotator cuff | NA | NA | NA | Exercise may be as effective as surgery in SIS patients, particularly high-dose exercise and exercise in combination with MT. |
| Ohberg, 2004, Sweden503 | QE – without control | Achilles | Strengthening | Structure, participation, participant/patient rating overall condition | NA | A good clinical result after eccentric training seems to be associated with a more normal tendon structure and no remaining neovascularisation. Action on the area with neovessels during the eccentric training regimen might possibly be responsible for the good clinical results. |
| Ohberg, 2004, Sweden504 | QE – without control | Achilles | Strengthening | Structure, participant/patient rating overall condition | NA | Eccentric calf-muscle training in patients with painful mid-portion chronic Achilles tendinosis has good short- and mid-term clinical results. At ultrasonographic follow-up, in most patients, tendon thickness is decreased and the structure is normalised. Structural abnormalities that remain at follow-up seem to be associated with residual pain in the tendon |
| Oken, 2008, Turkey505 | RCT | Lateral elbow | Strengthening, flexibility | function capacity, pain over a specified time, participant/patient rating | NA | A brace has a shorter beneficial effect than US and laser therapy in reducing pain in lateral epicondylitis. Laser therapy is more effective than the brace and US treatment in improving grip strength. |
| Olaussen, 2015, Norway506 | RCT | Lateral elbow | Flexibility, strengthening | Participant/patient rating overall condition | further specification, function, PFC, pain – clinician applied stress/examination, disability, adverse effects/events | Placebo injection with physiotherapy consisting of deep transverse friction massage, Mills manipulation, stretching and eccentric exercises showed no clear beneficial effect on acute lateral epicondylitis. CI with physiotherapy had a large positive effect on success of treatment at 6 weeks, no difference at 12 weeks, worsening at 26 weeks but no significant negative effect at 52 weeks compared to control. No significant differences in primary and secondary measures between CI and placebo injection suggest no added effect to steroid injection. |
| Olaussen, 2013, Norway507 | Systematic reviews/secondary analysis | Lateral elbow | NA | NA | NA | Manipulation with exercise and exercise with stretching have a short-term effect on lateral elbow tendinopathy outcomes, with the latter also having a long-term effect. |
| O’Neill, 2015, United Kingdom508 | Control (with pre-test) | Achilles | Strengthening | PFC | NA | Eccentric rehabilitation significantly increases endurance capacity of the symptomatic and non-symptomatic leg. |
| Orscelik, 2016, Turkey509 | Observational – cohort | Lateral elbow | flexibility, strengthening | further specification, disability | NA | Prolotherapy is a safe and effective treatment for chronic LE. |
| Ortega-Castillo, 2016, Spain510 | Systematic reviews/secondary analysis | Rotator cuff, lateral elbow | NA | NA | NA | 12 studies were selected. Eccentric exercise may reduce pain and improve strength in upper-limb tendinopathies, but whether its effectiveness is much better than other forms of treatment remains questionable. |
| Osteras, 2008, Norway511 | RCT | Rotator cuff | Aerobic, strengthening | Participation, economic impact costs | NA | In patients with chronic subacromial pain, high-dose exercise therapy might be an efficient treatment approach. |
| Osteras, 2009, Norway512 | RCT | Rotator cuff | Aerobic, strengthening, flexibility | Pain without further specification | Disability, PFC | There is a dose–response effect when using active graded exercises to treat patients with long-standing subacromial pain. |
| Osteras, 2010, Norway513 | Observational – case series/reports | Rotator cuff | Aerobic, strengthening | loading/activity, PFC, | NA | In patients with uncomplicated subacromial pain syndrome, high-dosage medical exercise therapy might be an efficient treatment approach. |
| Osteras, 2010, Norway514 | RCT | Rotator cuff | Strengthening, aerobic | Pain on loading/activity | NA | In long-term subacromial pain syndrome, high-dosage medical exercise therapy is superior to a conventional low-dosage exercise programme. |
| Ozgen, 2012, Turkey515 | RCT | Rotator cuff | Flexibility, strengthening | Loading/activity, Pamin over a specified time, disability, participant/patient rating overall condition, Medication | NA | Physical therapy modalities and sodium hyaluronate application supplemented by HEP had similar effects in short and long term for ST. Sodium hyaluronate application may be a better alternative with regard to effectiveness and side effects for other treatment methods applied intra-articulary. |
| Paavola, 2018, Finland516 | RCT | Rotator cuff | Flexibility, strengthening, other | Pain on loading/activity | QoL, participant/patient rating overall condition | Arthroscopic subacromial decompression provided no benefit over diagnostic arthroscopy in patients with shoulder impingement syndrome. |
| Page, 2016, Australia517 | Systematic reviews/secondary analysis | Rotator cuff | NA | NA | NA | Effects of MT and exercise may be similar to those of glucocorticoid injection and arthroscopic subacromial decompression, but this is based on low-quality evidence. Adverse events associated with MT and exercise are relatively more frequent than placebo but mild in nature. |
| Page, 2016, Australia518 | Systematic reviews/secondary analysis | Rotator cuff | NA | NA | NA | 47 trials, with exercise included as adjunct. PEMF may not provide clinically relevant benefits over placebo, and therapeutic ultrasound, LLLT and PEMF may not provide additional benefits when combined with other physical therapy interventions. There is low-quality evidence for ultrasound being more beneficial than placebo for calcific tendinitis. LLLT may have short-term benefits over placebo in rotator cuff disease. |
| Panni, 2000, Italy519 | Observational – cohort | Patellar | Strengthening, flexibility | Palpation, pain on loading/activity, participant/patient rating overall condition | NA | After 6 months, 33 patients showed symptomatic improvement and were able to resume their sports. Nonoperative measures failed in 9 patients with stage 3 tendinopathy and surgery was performed. In the group treated nonoperatively, results were better in the patients who had stage 2 tendinopathy than in those with stage 3. Adequate nonoperative management should be attempted before deciding to undertake surgery. |
| Paoloni, 2004, Australia520 | RCT | Achilles | Flexibility, strengthening | loading/activity, pain over a specified time, palpation, PFC, adverse effects/events, | NA | Topical glyceryl trinitrate significantly reduced pain with activity and at night, improved functional measures, and improved outcomes in patients with AT. |
| Park, 2010, Korea (Republic of)521 | RCT | Lateral elbow | Strengthening | Pain without further specification, disability | NA | Isometric strengthening exercises done early in the course of LE (within 4 weeks) provide a clinically significant improvement. |
| Parle, 2017, Australia522 | Pilot – randomised | Rotator cuff | Strengthening | further specification, disability, physical function | NA | This pilot cohort study showed preliminary results in favour of the effectiveness of both ice and isometric ER exercise in pain relief and better function. |
| Pasin, 2019, Turkey523 | QE – with control (with pre-test) | Rotator cuff | Flexibility, strengthening | Pain on loading/activity, disability, QoL | NA | All three treatment modalities improved Quick DASH, UCLA shoulder rating scale, VAS at rest and during activity, and SF-36 pain subgroup scores in the treatment of SIS. |
| Payne (a), 2018, United Kingdom524 | QE – with control (with pre-test) | Achilles | Strengthening | function capacity, ROM, structure, disability, pain without further specification | NA | After a 12-week eccentric exercise programme, measured variables in the pathological Achilles tendon did not reach parity with those in the non-affected tendon. VISA-A score, max AP diameter and Doppler score remained significantly different between the two tendon sides. |
| Payne (b), 2018, United Kingdom524 | Observational – cohort | Achilles | NA | Pain without further specification, disability, structure | NA | The removal of the mechanical loading elicited by a 12-week eccentric exercise programme results in regression of both subjective and objective measures (VISA-A, SWE) within a symptomatic pathological Achilles tendon. |
| Pearson, 2012, New Zealand525 | RCT | Achilles | Strengthening | Disability | Other | There is some evidence for small short-term symptomatic improvements with the addition of autologous blood injection to standard treatment for AT. |
| Pearson, 2018, Australia526 | RCT – cluster | Patellar | Strengthening | Pain on loading/activity, Structure | NA | Pain was significantly reduced after isometric loading on both SLDS and hop tests. Pain and quadriceps function improved over the 4 weeks. Short-duration isometric contractions are found to be as effective as longer-duration contractions for relieving patellar tendon pain when total time under tension is equalised. |
| Pekyavas, 2016, Turkey527 | RCT | Rotator cuff | Flexibility, strengthening | loading/activity, ROM, disability | NA | HILT and MT were found to be more effective in reducing pain and disability and improving ROM in patients with SAIS. |
| Penderghest, 1998, United States528 | RCT | Rotator cuff, other – biceps and triceps, patellar | Strengthening, Flexibility | Pain without further specification, sensory modality specific pain | NA | Stretching, strengthening and cryothrerapy significantly decreased the levels of perceived pain associated with symptomatic tendinitis regardless of whether the subjects received phonophoresis. |
| Perez-Merino, 2016, Spain529 | RCT | Rotator cuff | Strengthening, flexibility | Pain without further specification, disability | NA | Ultrasound, iontophoresis with dexketoprofen and phonophoresis with dexketoprofen can improve pain, shoulder function and physical functioning and symptoms in the upper limb in patients with SIS without a complete tear of the rotator cuff. |
| Petersen, 2007, Germany530 | RCT | Achilles | Strengthening | Pain on loading/activity, disability, QoL, adverse effects/events | NA | The AirHeel brace is as effective as eccentric training in the treatment of chronic AT. There is no added benefit to combining both treatments. |
| Peterson, 2011, Sweden531 | RCT | Lateral elbow | Strengthening | Pain on loading/activity | function capacity, disability, QoL | Exercise appears to be superior to the control group in reducing pain in chronic lateral epicondylosis. |
| Peterson, 2005, Sweden532 | Survey | Lateral elbow | NA | NA | NA | A large number of treatment methods including ergonomic counselling, stretching, orthotic devices, TENS, acupuncture and dynamic exercises were reported in chronic epicondylitis, none of which is properly evidence-based and some of which are even known to be ineffective. |
| Peterson, 2014, Sweden185 | RCT | Lateral elbow | Strengthening | Pain on loading/activity | PFC, disability, QoL | Eccentric graded exercise reduced pain and increased muscle strength in chronic tennis elbow more effectively than concentric graded exercise at follow-up. However, there were no significant differences in function or qua lity of life measures between the two groups. |
| Pienimaki, 1998, Finland533 | RCT | Lateral elbow | Strengthening, flexibility | Participation, pain on loading/activity, other, disability | NA | Progressive exercise showed beneficial long-term effects at the 36-month follow-up compared to ultrasound treatment in terms of pain alleviation, working ability and the functional overall condition. |
| Pieters, 2020, Belgium534 | Systematic reviews/secondary analysis | Rotator cuff | NA | NA | NA | There is a growing body of evidence to support exercise therapy as an intervention for subacromial shoulder pain. |
| Praet, 2019, Australia535 | RCT – cross-over | Achilles | Strengthening, aerobic | Disability, structure, other, adverse effects/events | NA | Oral supplementation of specific collagen peptides may accelerate the clinical benefits of a well-structured calf-strengthening and return-to-running programme in patients with chronic AT. |
| Praet, 2018, Australia130 | Pilot – randomised | Achilles | Strengthening, aerobic | Structure, participant/patient rating overall condition, participation, adverse | NA | Oral supplementation of specific collagen peptides may accelerate the clinical benefits of a well-structured calf-strengthening and return-to-running programme in AT patients. |
| Prat, 2018, Italy536 | RCT | Lateral elbow | Strengthening | PFC, participation, disability | NA | Eccentric exercise in combination with fascial manipulation appears to be more effective than exercise alone for reducing pain and enhancing function in lateral elbow pain. |
| Pribicevic, 2005, Australia537 | Observational – case series/reports | Rotator cuff | Strengthening | Pain without further specification, participation, ROM | NA | Case series demonstrate the potential benefit of a multimodal chiropractic protocol in resolving symptoms associated with a suspected clinical diagnosis of shoulder impingement syndrome. |
| Punnoose, 2015, United Kingdom538 | Reviews/secondary analysis | Achilles, patellar | NA | NA | NA | ESWT did not show significant improvements in symptoms or pain compared to other treatments or control. |
| Purdam, 2004, Australia539 | Pilot – non-randomised | Patellar | Strengthening | Pain on loading/activity, participation | NA | This pilot study indicates that an eccentric exercise programme using the decline squat is a potential treatment for subjects with chronically painful patellar tendinopathy. |
| Queiros da Silva, 2005, France540 | Observational – cohort | Hamstring, quadriceps, achilles | Aerobic, strengthening, other, flexibility | PFC, participation | NA | This work enabled us to optimise the rehabilitation protocol for subacute muscle and tendon injuries of the lower limb using eccentric isokinetic work with a dynometer to improve healing. |
| Araya Quintanilla, 2012, Chile541 | Systematic reviews/secondary analysis | Patellar | NA | NA | NA | Four studies were found. There is conflicting evidence that eccentric declined exercise is more effective than standard eccentric exercise in pain management and improved functionality in the short, medium and long term in patients with patellar tendinopathy. |
| Araya Quintanilla, 2015, Chile542 | Systematic reviews/secondary analysis | Lateral elbow | NA | NA | NA | Exercise can be used either alone or alongside other therapeutic interventions to enhance strength and reduce pain in LE patients. |
| Rabello, 2018, Netherlands543 | Systematic reviews/secondary analysis | Achilles, patellar | NA | NA | NA | Improvements in clinical outcomes in tendinopathy seem to be associated with improved imaging outcomes, which supports the use of imaging as a complementary examination. |
| Radovanovic, 2019, Germany544 | Pilot – non-randomised | Achilles | Strengthening | Disability, other | NA | VISA-A scores increased while plasma IL-6 levels decreased significantly after treatment. Patients with insertional did not significantly differ from patients with mid-portion AT. There were no differences between different types of intervention |
| Radpasand, 2009, United States545 | Pilot – randomised | Lateral elbow | Strengthening | Disability, PFC, pain over a specified time | NA | Both multimodal programmes demonstrated changes in all of the outcomes. However, there was no information on feasibility and effect size to inform future RCT. |
| Ram, 2013, Canada546 | QE – without control | Achilles | Strengthening | Participant/patient rating overall condition | Pain on loading/activity, disability, structure | Although patient-reported symptoms improved over time, eccentric training did not satisfy patient expectations following treatment despite compliance with home-based programmes. |
| Razavi, 2004, Sweden547 | QE – with control (with pre-test) | Rotator cuff | Strengthening | Loading/activity, ROM, function, participant/patient rating overall condition, medication | NA | Both groups increased range of movement; no difference was found between the effect of additional acupuncture treatment and placebo TENS in the treatment of rotator cuff tendinitis. |
| Resteghini, 2014, United Kingdom548 | Pilot – randomised | Patellar | Strengthening | Pain without further specification, disability | NA | Both autologous blood injections and saline injections (plus eccentric exercise) had similar efficacy in those with recalcitrant PT. |
| Reyhan, 2020, Turkey549 | RCT | Lateral elbow | Flexibility, strengthening | Loading/activity, pain over a specified time, disability, PFC, participant/patient rating | NA | MWM plus exercise and cold therapy is safe and effective at improving elbow pain, functional capacity and grip strength. |
| Riley, 2015, United States550 | RCT | Rotator cuff | Strengthening | Disability | Loading/activity, pain over a specified time | Immediate and short-term improvements were observed from manipulation, irrespective of type. |
| Rio, 2015, Australia551 | RCT – cross-over | Patellar | Strengthening | Pain on loading/activity, PFC | NA | Resistance training with isometric contractions reduced tendon pain immediately for at least 45 min post-intervention and increased maximal voluntary isometric contraction, whereby reduction in pain was paralleled by a reduction in cortical inhibition. |
| Rio, 2017, Australia167 | RCT | Patellar | Strengthening | Pain on loading/activity | Disability | Both isometric and isotonic contraction protocols appear efficacious for in-season athletes to reduce pain; however, isometric contractions demonstrated significantly greater immediate analgesia throughout the 4-week trial. |
| Rio, 2019, Australia167 | Observational – case series/reports | Patellar | Strengthening | Pain on loading/activity, disability | NA | A simple double-leg isometric squat exercise using a portable rigid belt significantly reduced patellar tendon pain in a real-world sporting environment across different sports. |
| Roe, 2000, Norway552 | QE – without control | Rotator cuff | Other, flexibility, strengthening | PFC, pain on loading/activity | NA | Pain reduction after supervised exercises was associated with an improved maximal voluntary isometric contraction force, but the difference in maximal voluntary contraction force between the two sides was maintained. Muscle activity measured by EMG during maximal contraction increased in both the afflicted and unafflicted sides. |
| Roe, 2005, Norway553 | RCT | Lateral elbow | Strengthening | PFC, pain over a specified time | NA | Supplementation with essential fatty acids appears to have no additional benefit in comparison to eccentric training alone. |
| Romero Morales, 2018, Spain554 | RCT | Achilles | Strengthening | Structure | NA | The present study showed a RA thickness increase in both groups in favour of the EE vibration programme with respect to cryotherapy added to EE in short and mid term in maximal isometric contraction and at rest in subjects with chronic mid-portion AT. IRD was decreased in both groups without between-group differences. |
| Romero Morales, 2019, Spain555 | RCT | Achilles | Strengthening | Structure | NA | Both an eccentric exercise vibration training programme and cryotherapy with eccentric exercise produced a thickness and cross-sectional area increase at 0, 2, 4 and 6 cm in maximal isometric contraction and at rest in subjects with chronic mid-portion AT. However, eccentric exercise vibration training showed a statistically greater cross-sectional area increase than the cryotherapy group. |
| Romero-Rodriguez, 2011, Spain556 | Observational – case series/reports | Patellar | Strengthening, aerobic, flexibility | Function capacity, pain without further specification | NA | Short-term training using inertial eccentric overload resulted in improved muscle function and reduced subjective pain in long-lasting patellar tendinopathy. |
| Rompe, 2009, Germany557 | QE – without control | Gluteal (including GTPS) | Flexibility, strengthening | Specified time, participant/patient rating overall condition | Adverse effects/even ts, medication use | The role of corticosteroid injection for greater trochanter pain syndrome needs to be reconsidered following positive results with radial shockwave therapy at 4 months. |
| Rompe, 2007, Germany558 | RCT | Achilles | Strengthening | Participant/patient rating overall condition, pain over a specified time, sensory modality specific pain | NA | At 4-month follow-up, eccentric loading and low-energy SWT showed comparable results. The wait-and-see strategy was ineffective for the management of chronic recalcitrant AT. |
| Rompe, 2009, Germany559 | RCT | Achilles | Strengthening | Participant/patient rating overall condition, pain over a specified time, medication | NA | The likelihood of recovery after 4 months was higher after a combined approach of both eccentric loading and SWT compared to eccentric loading alone. |
| Roos, 2004, Sweden193 | RCT | Achilles | Strengthening | Disability, physical activity | NA | Eccentric exercises reduce pain and improve function in patients with AT. |
| Rosety-Rodriguez, 2006, Spain560 | Control (with pre-test) | Patellar | Strengthening | Pain without further specification, participation | NA | Conservative treatment based on decline eccentric programmeshowed better results than standard squat programme. |
| Ross, 2018, Australia561 | Systematic reviews/secondary analysis | Posterior tibial tendon | NA | NA | NA | Local strengthening exercises provide some benefit in PTTD. Eccentric exercises maybe be superior to concentric in improving pain, disability and foot function outcomes. |
| Rowe (b), 2012, United Kingdom11 | Qualitative | Achilles | NA | NA | NA | A number of themes were identified, including general perceptions of AT, and found strong evidence (eccentric exercise training, ESWT), moderate evidence (orthoses, low-level laser therapy, concentric exercises, splinting/bracing, active rest), conflicting/inconclusive evidence/no RCTs (TGTN, therapeutic ultrasound, taping, joint/soft tissue mobilisations, calf stretches). |
| Rowe (a), 2012, United Kingdom11 | Systematic reviews/secondary analysis | Achilles | NA | NA | NA | Eccentric loading exercises have the strongest supporting evidence of all the conservative treatment modalities, with strong evidence for ESWT. |
| Roy, 2009, Canada562 | Observational – case series/reports | Rotator cuff | Other, strengthening | Disability | Examination findings, PFC, pain on loading/activity | There is evidence to support the use of shoulder control exercises to reduce pain and improve function based on the SPADI in people with shoulder impingement. |
| Roy, 2010, Canada563 | Observational – cohort | Rotator cuff | Other | further specification, physical function | NA | Unsupervised training appears to be a good complement to supervised training to normalise the kinematic impairments of people with SIS. |
| Saggini, 2012, Italy564 | QE – without control | Patellar | Strengthening | further specification, disability, structure, participant/patient rating | NA | The addition of ESWT to classic vibration and eccentric training yielded significantly greater improvement in function and reduction in drug consumption than those without ESWT. |
| Saithna, 2012, United Kingdom565 | Reviews/secondary analysis | Patellar | NA | NA | NA | There is no high-quality evidence to support the withdrawal from sport in the management of patellar tendinopathy. |
| Sosa, 2014, Spain566 | RCT | Patellar | Strengthening | Disability | NA | No significant differences after 4 weeks in either group. |
| Saltychev, 2015, Finland567 | Systematic reviews/secondary analysis | Rotator cuff | NA | NA | NA | Moderate evidence suggests that surgical treatment is not more effective than active exercises on reducing pain intensity caused by shoulder impingement. However, evidence on the effectiveness of surgical or conservative treatment of shoulder impingement was found to be limited. |
| Sancho, 2019, Australia178 | Observational – cohort | Achilles | Strengthening, aerobic | Other, adverse effects/events | Pain onloading/activity, psychological factors, participant/patient rating overall condition, PFC | Addition of a pain-guided progressive hopping intervention to recommended education and exercise is feasible for recreational runners with AT. |
| Sanderson, 2015, Australia568 | Systematic reviews/secondary analysis | Achilles | NA | NA | NA | There is limited evidence that prolotherapy injections are a safe and effective treatment for AT. |
| Sandford, 2018, United Kingdom569 | RCT | Rotator cuff | Strengthening, other | Without further specification, QoL, function, participant/patient rating overall condition, ROM, physical | NA | The effect of omega−3 polyunsaturated fatty acid supplementation on disability and pain outcomes in people with rotator cuff-related shoulder pain is no greater than placebo. |
| Sandford, 2017, United Kingdom157 | Qualitative | Rotator cuff | Other | NA | NA | The main enablers to exercise were highlighted as equipment, the perceived benefit from the actual exercises, incorporating exercise into an established routine, the longer follow-up, and more intensive monitoring and feedback received in the trial. Barriers included the lack of motivation, lack of suitable equipment, and pain, whether it was improving or worsening. Incorporating these enablers and addressing barriers may provide potential benefits. |
| Santamato, 2016, Italy570 | RCT | Rotator cuff | Strengthening | Pain on loading/activity, disability | PFC | In subjects with SAIS, combined administration of focussed ESWT and IE for the rotator cuff resulted in greater reduction of pain, as well as superior functional recovery and muscle endurance in the short to medium term, compared with ESWT alone. |
| Saracoglu, 2018, Turkey571 | Systematic reviews/secondary analysis | Rotator cuff | NA | NA | NA | Clinical taping in addition to physiotherapy interventions (e.g. exercise, electro-therapy and MT) might be an optional modality for managing patients with shoulder impingement syndrome, especially for the initial stage of the treatment. |
| Satyendra, 2006, United States572 | Systematic reviews/secondary analysis | Achilles | NA | NA | NA | Eccentric exercise is an effective non-invasive treatment for patients suffering with AT. |
| Savoie, 2015, Canada573 | QE – without control | Rotator cuff | Other, flexibility, strengthening | Disability | NA | The rehabilitation programme yielded improvements in symptoms (WORC) and functional limitations (DASH) in participants with SPS. Moreover, it led to an increase of the AHD, thus, potentially decreasing subacromial compression, particularly in participants with a smaller baseline AHD. |
| Say, 2016, Turkey574 | Observational – cohort | Rotator cuff | Flexibility, strengthening | Without further specification, ROM | NA | Steroid injection was more effective than PRP injection for treatment of SIS in terms of the Constant score and VAS for pain at 6 weeks and 6 months. |
| Sayana, 2007, United Kingdom575 | QE – without control | Achilles | Strengthening, flexibility | Disability | NA | Eccentric exercises, though effective in the majority of patients, may not benefit sedentary patients to the same extent reported in athletes. |
| Saylor-Pavkovich, 2016, United States576 | Observational – case series/reports | Rotator cuff | Strengthening | Disability, pain without further specification | NA | There is novel evidence to support the efficacy of combining both strength and dry needling as conservative treatment modalities. |
| Scott, 2019, Canada577 | RCT | Patellar | Strengthening | Disability | Specified time, participant/patient rating overall condition, medication use, other, adverse | Combined with an exercise-based rehabilitation programme, a single injection of leukocyte-rich PRP or leukocyte-poor PRP was no more effective than saline for the improvement of patellar tendinopathy symptoms. |
| Scott, 2015, Australia578 | Systematic reviews/secondary analysis | Achilles | NA | NA | NA | Weak evidence showed that an ankle joint dorsiflexion night splint was equally effective as a calf muscle eccentric exercise programme but strong evidence suggests that night splint was not beneficial when added to a calf muscle eccentric exercise programme. Similarly, moderate evidence showed that the AirHeel brace was as effective as a calf muscle eccentric exercise but this intervention was not beneficial when added to eccentric exercise. Findings suggest that calf muscle eccentric exercise, a relatively inexpensive intervention, should be used first in the management of mid-portion AT. These findings may also aid clinical decision-making in the context of AT, where an individualised treatment regime is required. |
| Seitz, 2019, United States165 | Observational – case-control | Rotator cuff | Other, strengthening | PFC, disability | NA | A single exercise of prone horizontal abduction may be a viable treatment option in the short term in individuals with mild pain and functional loss due to rotator cuff-related shoulder pain, precipitating neuromuscular adaptations that carry over into a functional overhead lifting task. |
| Selvanetti, 2003, Italy579 | RCT | Lateral elbow | Flexibility, strengthening | loading/activity, medication use, clinical examination findings, participant/patient rating overall | NA | Eccentric exercise was more effective than placebo in reducing pain and improving function for lateral epicondylitis in the short term. |
| Sen, 2010, Turkey580 | QE – with control (with pre-test) | Rotator cuff | Flexibility | On loading/activity, pain over a specified time | NA | Balneotherapy can be safely applied for patients with SIS because it provides satisfactory results and improved QoL. |
| Şenbursa, 2007, Turkey581 | RCT | Rotator cuff | Flexibility, strengthening | Pain without further specification, ROM, sensory modality specific pain, function | NA | The patients treated with manual physical therapy applied by experienced physical therapists combined with super vised exercise in a brief clinical trial showed improvement of symptoms including improved strength, pain and function earlier than with exercise programme. |
| Şenbursa, 2011, Turkey582 | RCT | Rotator cuff | Other, flexibility, strengthening | Loading/activity, pain over a specified time, ROM, PFC, clinical examination | NA | Supervised exercise, supervised and MT, and home-based exercise are all effective and promising treatments for patients with subacromial impingement syndrome. The addition of an initial MT may improve outcomes with exercise. |
| Seven, 2017, Turkey583 | RCT | Rotator cuff | Other, flexibility | Pain on loading/activity, disability, ROM, adverse effects/events | NA | Prolotherapy is an easily applicable treatment which may be superior in enhancing pain and function outcomes in comparison to exercise alone. |
| Sevier, 2015, United States584 | RCT | Lateral elbow | Flexibility, strengthening | Disability | Pain on loading/activity, function, PFC | Astym therapy is an effective treatment option for patients with LE tendinopathy, as an initial treatment, and after an eccentric exercise programme has failed. |
| Shalabi, 2004, Sweden585 | Observational – cohort | Achilles | Strengthening | Structure, disability | NA | The tendon volume and intratendinous signal decreased after 3 months of eccentric calf-muscle strength training. The reduced intratendinous signal correlated to diminished pain. |
| Shire, 2017, Denmark586 | Systematic reviews/secondary analysis | Rotator cuff | NA | NA | NA | There is insufficient evidence to support or refute the effectiveness of specific resistive exercise strategies in the rehabilitation of subacromial impingement syndrome. |
| Silbernagel, 2001, Sweden587 | RCT | Achilles | Flexibility, strengthening | Activity, participation, medication use, other, participant/patient rating overall condition, ROM, pain on loading/activity, palpation, | NA | The eccentric overload protocol used in the present study can be recommended for patients with chronic pain from the Achilles tendon. More patients achieved full recovery, improved pain and ROM in the Exp group compared to the control group. |
| Silbernagel, 2007, Sweden588 | QE – without control | Achilles | Strengthening | PFC | NA | Full symptomatic recovery in patients with AT does not ensure full recovery of muscle-tendon function |
| Silbernagel, 2007, Sweden138 | RCT | Achilles | Strengthening | Disability, pain on loading/activity | ROM, PFC | Our treatment protocol, which gradually increases the load on the Achilles tendon and calf muscle, demonstrated significant improvements. Continuing tendon loading activity such as running and jumping with the use of a pain-monitoring model did not have any adverse effect. |
| Silbernagel, 2011, United States589 | Observational – case series/reports | Achilles | NA | Disability, physical activity, psychological factors, PFC | NA | No significant differences in VISA-S scores were found between 1-year and 5-year follow-up for participants with continuous symptoms. Patients with new symptoms experienced a significant increase in VISA-S scores at 5-year follow-up compared to 1-year follow-up. Majority of participants recovered fully with exercise. |
| Simpson, 2011, United Kingdom590 | Systematic reviews/secondary analysis | Quadriceps | NA | NA | NA | There were no clear recommendations on how to specifically treat quadriceps tendinopathy, perhaps as it is less common. |
| Şimşek, 2013, Turkey591 | RCT | Rotator cuff | Other | further specification, disability, ROM, physical function | NA | Findings were inconclusive and require further research. |
| Skovlund, 2020, Denmark169 | Observational – case series/reports | Patellar | Aerobic, strengthening | specified time, pain on loading/activity, structure, PFC, adverse effects/events, participant/patient | NA | Clinical and structural improvements in patellar tendon function were obtained after short-term (3 weeks), low-volume (9 sessions) low-load blood flow restriction training. |
| Smidt, 2002, Netherlands592 | RCT | Lateral elbow | Flexibility, strengthening | Participant/patient rating overall condition, pain over a specified time, disability | PFC, sensory modality specific pain, participant/patient rating overall condition | Injection showed better outcomes at 6 weeks. In the long term, physiotherapy had better results than the wait-and-see policy although differences were not significant. |
| Smidt, 2003, Netherlands593 | Systematic reviews/secondary analysis | Lateral elbow | NA | NA | NA | Insufficient evidence for exercises and mobilisation techniques, due to low power, poor validity and large heterogeneity. |
| Soderberg, 2012, Sweden594 | RCT | Lateral elbow | Strengthening | PFC | Other, pain mover a specified time | Daily home eccentric exercise regimen is effective in increasing functional pain-free grip strength and reducing cases suffering from lateral epicondylalgia. |
| Solomons, 2020, Canada595 | RCT | Achilles | Strengthening | Disability | Participant/patient rating overall condition, ROM, Structure | The addition of intramuscular stimulation to standard rehabilitation for AT did not result in any improvement over the expected clinical benefit achieved with exercise-based rehabilitation alone. |
| Stasinopoulos (a) Chapter 3, 2005, United Kingdom596 | Systematic reviews/secondary analysis | Lateral elbow | NA | NA | NA | There was strong evidence to suggest that physiotherapy, ultrasound, shockwave therapy and electromagnetic field therapy were ineffective for the treatment of lateral epicondylitis. A lack of evidence existed for the effectiveness of other modalities, exercise in particular. |
| Stasinopoulos (b) Chapter 5, 2005, United Kingdom596 | Survey | Lateral elbow | NA | NA | NA | Clinicians appear to believe that Cyriax, supervised exercises and Bioptron treatments have the same treatment goals, but that exercise may be the least time-consuming and more logistically and financially feasible due to the ability to complete the sessions in a home environment. |
| Stasinopoulos, 2017, Cyprus597 | RCT | Lateral elbow | Strengthening, flexibility | Pain over a specified time, function, PFC, drop-out or discontinued treatment | NA | Eccentric training, eccentric-concentric training and eccentric-concentric training combined with isometric contraction reduced pain and improved function at the end of the treatment and follow-up. The eccentric-concentric training combined with isometric contraction produced the largest effect at the end of the treatment and follow-up. |
| Stasinopoulos, 2004, Greece598 | RCT | Patellar | Flexibility, strengthening | Participant/patient rating overall condition | NA | Exercise programme was a more effective treatment than ultrasound and transverse friction at the end of the treatment and at the follow-ups. |
| Stasinopoulos, 2006, Greece599 | QE – with control (with pre-test) | Lateral elbow | Flexibility, strengthening | Pain over a specified time, function, PFC | NA | Cyriax physiotherapy, a supervised exercise programme, and polarised polychromatic non-coherent light reduced pain and improved function at the end of the treatment and at any of the follow-up time points. The supervised exercise programme produced the largest effect in the short, intermediate and long term. |
| Stasinopoulos, 2009, Greece600 | QE – with control (with pre-test) | Lateral elbow | Flexibility, strengthening | specified time, PFC, drop-out or discontinued | NA | An exercise programme onsisting of eccentric and static stretching exercises, and LLLT or polarised polychromatic non-coherent light are both adequate treatme nt modalities for patients with LET. |
| Stasinopoulos, 2010, Greece601 | QE – with control (with pre-test) | Lateral elbow | Flexibility, strengthening | Specified time, function, PFC | NA | Supervised exercise programme is superior to HEP to reduce pain and improve function in patients with LET at the end of the treatment and at the follow-up. |
| Stasinopoulos, 2013, Greece331 | QE – with control (with pre-test) | Achilles | Strengthening, flexibility | Disability, drop-out or discontinued treatment | NA | Alfredson exercise protocol was superior to that of the Stanish model in improving pain and function in patients with AT. |
| Stasinopoulos, 2014, Cyprus602 | Pilot – non-randomised | Rotator cuff | Flexibility, strengthening | Pain over a specified time, drop-out or discontinued treatment | NA | Exercise programme, consisting of isotonic strengthening, including eccentric, and static stretching exercises, reduced the pain in patients with rotator cuff tend inopathy at the end of the treatment and 3 months after the end of treatment. |
| Stefansson, 2019, Iceland184 | RCT | Achilles | Strengthening | Disability, sensory modality specific pain, ROM, structure | NA | Pressure massage is a useful treatment for AT. Compared with eccentric exercise treatment, pressure massage similarly improved VISA-A scores and ankle ROM. Combining the treatments did not further improve the outcome. |
| Stephens, 2019, United Kingdom158 | Survey | Gluteal (including GTPS) | Flexibility, strengthening, other | NA | NA | This large survey highlights that physiotherapists in the UK most commonly use education on load management and self-management strategies, alongside strengthening exercises targeting the hip abductors for patients with GTPS. |
| Stergioulas, 2007, Greece603 | RCT | Lateral elbow | Strengthening, flexibility | loading/activity, pain – clinician-applied stress/examination, ROM | NA | Combination of laser along with plyometric exercises and stretching is more effective than placebo laser and exercise in the treatment of patients with LE |
| Stergioulas, 2008, Norway604 | RCT | Achilles | Strengthening, flexibility | Pain on loading/activity | Other, ROM, palpation | Low-level laser therapy with the parameters used in this trial seems to be a safe and effective method for more rapid recovery when combined with an eccentric exercise regimen. It is emphasised that using power densities below 100 mW/cm2 seem to be important for good outcomes. |
| Steunebrink, 2013, Netherlands605 | RCT | Patellar | Strengthening | Disability | Patient rating overall condition, pain on loading/activity, adverse effects/even ts, medication use, | Continuous topical GTN treatment in addition to an eccentric exercise programme does not improve clinical outcome compared to placebo patches and an eccentric exercise programme in patients with chronic patellar tendinopathy. |
| Steuri, 2017, Switzerland606 | Systematic reviews/secondary analysis | Rotator cuff | NA | NA | NA | Although there was only very low-quality evidence, exercise should be considered for patients with shoulder impingement symptoms and tape, ECSWT, laser or MT might be added. NSAIDS and corticosteroids are superior to placebo, but it is unclear how th ese treatments compare to exercise. |
| Stevens, 2014, United Kingdom175 | RCT | Achilles | Strengthening | Disability | Pain without further specification, adverse effects/events | Performing a 6-week do-as-tolerated programme of eccentric heel-drop exercises compared to the recommended 180 repetitions per day did not lead to lesser improvement for individuals with midportion AT, based on VISA-A and VAS scores. |
| Struijs, 2003, Netherlands607 | Pilot – Randomised | Lateral elbow | Flexibility, strengthening | Participant/patient rating overall condition | Clinician applied stress/examination, pain over a specified time, disability, physical | The cohort study provided preliminary results in favour of manipulation of the wrist over ultrasound, friction massage, stretching, and strengthening exercises for the management of lateral epicondylitis in short follow-up. |
| Struijs, 2004, Netherlands608 | RCT | Lateral elbow | Flexibility, strengthening | Participant/patient rating overall condition, other, pain without further specification, disability | patient rating overall condition, PFC, Pain – clinician-applied stress/examination | Conflicting results were found. Brace treatment might be useful as initial therapy. Combination therapy has no additional advantage compared to physical therapy but is superior to brace only for the short term (6 weeks). |
| Struijs, 2006, Netherlands609 | RCT | Lateral elbow | NA | Economic impact costs | NA | No clinically relevant or statistically significant differences in costs were identified between the three strategies. |
| Struyf, 2013, Belgium610 | RCT | Rotator cuff | Other, flexibility | Disability | Examination findings, Pain on loading/activity, ROM, PFC | A rehabilitation programme that included motor control exercises, scapular mobilisations and stretching is effective for reducing pain and disability for patients with shoulder impingement syndrome. |
| Subasi, 2012, Turkey611 | RCT | Rotator cuff | Strengthening, flexibility | Pain without further specification, ROM, disability | NA | Both groups of exercise combined with conservative physical therapy modalities produce favourable results for pain and function. However, water-based activities may confer superior benefits. |
| Subasi, 2016, Turkey612 | QE – with control (with pre-test) | Rotator cuff | Flexibility, strengthening | Pain on loading/activity, ROM, disability | NA | Both kinesiological taping and steroid injection in conjunction with an exercise programme can be beneficial in the rehabilitation of SIS. Kinesiological taping can be considered a safe and inexpensive alternative for SIS especially for patients who have anxiety problems about injections or for whom steroid injections are contraindicated. |
| Sussmilch-Leitch, 2012, Australia613 | Systematic reviews/secondary analysis | Achilles | NA | NA | NA | Practitioners can consider eccentric exercise as an initial intervention for AT, with the addition of laser therapy as appropriate. Shockwave therapy may represent an effective alternative. |
| Svernlov (a), 2001, Sweden614 | Pilot – randomised | Lateral elbow | Flexibility | Applied stress/examination, pain without further specification, participation, physical | NA | Significant improvements observed for VAS and grip strength warrants clinical use of this regime. |
| Svernlov (b), 2001, Sweden614 | QE – with control (with pre-test) | Lateral elbow | Strengthening, flexibility | Applied stress/examination, pain without further specification, participation, physical | NA | Significant improvements seen in pain and grip strength following eccentric training regime in a majority of patients with lateral humeral epicondylagia, regardless of duration, and it is possibly superior to conventional stretching. |
| Sweeting, 2011, Australia615 | Survey | Achilles | NA | NA | NA | Exercise is preferred as the primary mode of treatment in patients with AT as patients preferred exercise treatment as a standalone option which cost less, had a greater chance of success and allowed for an earlier return to pain-free activity. |
| Syvertson, 2017, United States616 | Observational – case series/reports | Achilles | Strengthening | Specified time, disability, participant/patient rating overall condition | NA | This exploratory case series showed promising short-term clinical results with a small group of participants diagnosed with AT. |
| Szczurko, 2009, Canada617 | RCT | Rotator cuff | Flexibility, strengthening | Disability | QoL, pain without further specification, other, ROM | Both naturopathic and standardised physical exercise groups provided significant improvements in shoulder function, with greater improvement in favour of the naturopathic group. Statistically significant improvements in QoL measures were also observed in the naturopathic group compared to the physical exercise group. |
| Tahran, 2020, Turkey618 | RCT | Rotator cuff | Other, flexibility, strengthening | Pain on loading/activity, disability, ROM | NA | All treatments improved pain, shoulder mobility, function and disability in patients with SIS. However, modified posterior shoulder stretching exercises in addition to a treatment programme was superior to the treatment programme alone in improving pain with activity, internal rotation ROM and dysfunction. Moreover, stretching provided clinically significant improvements. |
| Taskaynatan, 2007, Turkey619 | QE – with control (with pre-test) | Other – bicipital tendonitis | Flexibility, strengthening | Loading/activity, disability, ROM, participant/patient rating overall | NA | Treatment modalities targeting biceps tendon pathologies; isolated or accompanying other shoulder pathologies, may increase the improvement. |
| Taunton, 2004, Canada620 | RCT | Achilles | Strengthening | Function capacity, disability, structure, participant/patient rating | NA | Significant improvements on pain levels, function and return to activity were observed in the Exp group despite no improvement in calf muscle strength. |
| Thanasas, 2011, Greece62 | RCT | Lateral elbow | Flexibility, strengthening | Pain without further specification, function | NA | PRP treatment seems to effectively reduce pain in chronic lateral elbow epicondylitis and is superior to autologous blood in the short term. |
| Thijs, 2017, Netherlands621 | RCT | Patellar | Strengthening | Disability | Loading/activity, participant/patient rating overall condition, adverse effects/even | There was no additional effect of 3 sessions ESWT in participants with PT treated with eccentric exercises as no significant differences for primary and secondary outcomes were found. |
| Thompson, 2019, New Zealand622 | RCT | Gluteal (including GTPS) | Strengthening | further specification, disability | Other, medication use | A single injection of PRP resulted in no significant improvement for GTPS compared with a placebo injection. |
| Tonks, 2012, United Kingdom623 | RCT | Lateral elbow | Strengthening, flexibility | Other | Loading/activity, disability, PFC, | In the short term, the injection group showed superior effectiveness, whereas exercise is more effective for long-term management of tennis elbow. |
| Tonks, 2007, United Kingdom624 | RCT | Lateral elbow | Flexibility, strengthening | PFC | Disability, adverse effects/even ts, PFC | Steroid injection alone is advocated as the first-line of treatment for patients presenting with tennis elbow following significant improvements when compared to physiotherapy. |
| Townsend, 2020, United States625 | Systematic reviews/secondary analysis | Achilles, rotator cuff, lateral elbow | NA | NA | NA | The clinical effectiveness of PRP remains controversial and there is limited evidence on the effect of post-PRP protocols with substantial heterogeneity in protocols. |
| Trampas, 2006, Greece626 | Systematic reviews/secondary analysis | Rotator cuff | NA | NA | NA | Limited data suggest that manual and exercise therapy may be more effective than other interventions for managing shoulder impingement syndrome, although methodological quality is low. |
| Trudel, 2004, Canada627 | Systematic reviews/secondary analysis | Lateral elbow | NA | NA | NA | This review has determined, with at least level 2b evidence, that a number of treatments, including acupuncture, exercise therapy, manipulations and mobilisations, ultrasound, phonophoresis, Rebox, and ionisation with diclofenac all show positive effects in the reduction of pain or improvement in function for patients with lateral epicondylitis. There is also at least level 2b evidence showing laser therapy and pulsed electromag netic field therapy to be ineffective. |
| Tsehaie, 2017, Netherlands628 | Observational – cohort | Achilles | Strengthening | Disability | Structure | Tendon volume and CSA decreased significantly after 24 weeks of conservative treatment. As these differences were within the MDC limits, they could be a result of a measurement error. Furthermore, MRI parameters at baseline did not predict the change in symptoms, and therefore have no added value in providing a prognosis in daily clinical practice. |
| Tumilty, 2008, New Zealand629 | Pilot – feasibility | Achilles | Strengthening | Disability | Specified time, PFC | This pilot study demonstrated the feasibility of a RCT to assess the effect of LLLT in AT. |
| Tumilty, 2012, New Zealand630 | RCT | Achilles | Strengthening | Disability | Pain over a specified time | No evidence for clinical effectiveness of adding LLLT to eccentric exercises for the treatment of AT. |
| Tumilty, 2015, New Zealand631 | RCT – cross-over | Achilles | Strengthening | Disability | NA | The Alfredson protocol of heavy-load eccentric exercise for AT provide no extra benefit over exercises performed twice per week for 12 weeks. Four weeks of low-level laser th erapy as an adjunct to an eccentric exercise regime of two sessions per week provide superior results compared to exercise alone. |
| Tumilty, 2016, New Zealand632 | RCT | Achilles | Strengthening | Disability | Pain without further specification, structure | The group receiving laser as an adjunct to exercise regime 2 improved significantly more than all other groups. |
| Turgut, 2017, Turkey633 | RCT | Rotator cuff | Flexibility, strengthening, other | ROM, disability, pain on loading/activity, pain over a specified time | NA | Progressive exercise training independent from specific scapular stabilisation exercises provides decreased disability and pain severity in impingement syndrome. All groups showed improvement; however, there were no significant differences between the groups. |
| Turgut, 2018, Turkey634 | Observational – cohort | Rotator cuff | Flexibility | Examination findings, pain on loading/activity, pain over a specified time, | NA | Six-week stretching programme resulted in increased flexibility and decreased pain and disability in participants with SI. |
| Turgut, 2018, Turkey635 | QE – without control | Rotator cuff | Flexibility, other | Disability | NA | Pain and disability gains can be achieved with 6-week progressive exercise training for participants with rotator cuff tendinopathy. |
| Tyler, 2010, United States636 | RCT | Lateral elbow | Flexibility, strengthening | On loading/activity, PFC, sensory | NA | All outcome measures for chronic lateral epicondylosis were markedly improved with the addition of an eccentric wrist extensor exercise to standard physical therapy through the novel use of an inexpensive rubber bar. |
| Valera-Garrido, 2014, Spain637 | QE – without control | Lateral elbow | Flexibility, strengthening | Loading/activity, sensory modality specific pain, pain – clinician-applied stress/examination | NA | Symptoms and degenerative structural changes of chronic lateral epicondylitis are reduced after US-guided PNE associated with eccentric exercises and stretching, |
| Valles-Carrascosa, 2018, Spain638 | RCT | Rotator cuff | Strengthening, other, flexibility | Pain on loading/activity, ROM | Disability | Both rotator cuff eccentric exercise protocols with scapular stabilising and stretching of upper trapezius were equally effective in improving pain, function and active ROM in the short term in patients with subacromial syndrome. |
| Vander Doelen, 2020, Canada639 | Systematic reviews/secondary analysis | Patellar | NA | NA | NA | Nine RCTs fitted the inclusion criteria. Isometric exercise, patellar strapping, sports taping, eccentric exercise, injections with PRP, ABI and saline and DN demonstrated a short-term pain relieving and functional improvement effect in subjects with patellar tendinopathy. Longer-term follow-up on interventions involving eccentric exercise, DN and injections with PRP, ABI and saline showed sustained pain reduction and improvement in knee function. |
| van der Worp, 2014, Netherlands640 | RCT | Patellar | Strengthening | Disability | Pain on loading/activity, participant/patient rating overall condition | There is no difference between focused and radial shockwave therapy for chronic patellar tendinopathy in addition to eccentric training. Both treatment groups showed a slight improvement after treatment and it is impossible to recommend one ESWT treatment over the other in terms of effectiveness. |
| Verrall, 2011, Australia149 | Observational – case-control | Achilles | Flexibility | Pain on loading/activity | NA | A modified 6-week eccentric heel-drop training regimen as the only treatment for chronic AT resulted in a high degree of patient satisfaction, reduced pain and a successful return to pre-morbid activity levels. These results were best for mid-substance rather than insertional tendinopathy. |
| Vinuesa-Montoya, 2017, Spain641 | RCT | Rotator cuff | Flexibility, strengthening | Further specification, disability, clinical examination | NA | Cervicothoracic manipulative treatment with mobilisation plus exercise therapy may improve intensity of pain and ROM compared with home exercise alone. |
| Virta, 2009, Sweden642 | Observational – cohort | Rotator cuff | Strengthening, other | Disability | NA | Supervised exercise should be the first treatment option for patients with SIS. |
| Visnes, 2005, Norway129 | RCT | Patellar, quadriceps | Strengthening | Disability | Participant/patient rating overall condition, PFC | There was no effect on knee function (VISA) from a 12-week programme with eccentric training among a group of volleyball players with patellar tendinopathy who continued to train and compete during the treatment period. Whether the training would be effective if the patients did not participate in sports activity is not known. |
| von Wehren, 2019, Switzerland643 | Observational – cohort | Achilles | Strengthening | Disability, structure | NA | Both therapies led to improvement of MRI findings, including reduction of tendon thickness and tendon quality. Autologous conditioned serum injections show greater clinical long-term benefit as compared to eccentric training and, therefore, offer a good alternative to eccentric training. |
| van Ark, 2013, Netherlands170 | Observational – case series/reports | Patellar | Strengthening, aerobic, flexibility | Disability | Loading/activity, PFC, adverse effects/events, medication | The combination treatment which includes a physical programme after PRP injection reported in this study is feasible and seems to be promising for patients in the late/degenerative phase of patellar tendinopathy. |
| van Ark, 2016, Australia644 | RCT | Patellar | Strengthening | Pain on loading/activity | Disability, participant/patient rating overall condition | This study found favourable results for athletes with patellar tendinopathy without modification of the training. Both isometric and isotonic exercise programmes reduced pain and improved function in athletes with patellar tendinopathy during a season. |
| van Ark, 2018, Netherlands645 | RCT | Patellar | Strengthening | Structure, pain on loading/activity, pain over a specified time, disability | NA | Structural properties and dimensions of the patellar tendon on UTC did not change after a 4-wk isometric or isotonic exercise programme for athletes with patellar tendinopathy, despite an improvement in symptoms. It seems that structural improvements are not required for a positive clinical outcome. |
| van der Plas, 2012, Netherlands105 | RCT | Achilles | Strengthening | Disability | Participant/patient rating overall condition, pain without further specification, other | At 5-year follow-up, a significant increase of VISA-A score can be expected. After the 3-month Alfredson’s heel-drop exercise programme, almost half of the patients had received other therapies. Although improvement of symptoms can be expected at long term, mild pain may remain. |
| Vlist, 2020, Netherlands646 | Control (with pre-test) | Achilles | Strengthening | Pain on loading/activity | PFC | Isometric and isotonic exercises do not result in immediate pain relief in patients with mid-portion AT. |
| van der Vlist, 2020, Netherlands141 | Systematic reviews/secondary analysis | Achilles | NA | NA | NA | NMA of 29 RCTs concluded that active treatments (exercise therapy, acupuncture, exercise + shockwave, mucopolysaccharides + exercise therapy, exercise + injection and exercise + night splint) are superior to wait-and-see. However, there was no clear difference between active treatment modalities at either 3- or 12-month follow-up. |
| Van Rijn, 2019, Netherlands647 | Systematic reviews/secondary analysis | Patellar | NA | NA | NA | Exercise, eccentric training in particular, is important in the management of PT. The role of ESWT remains uncertain. |
| van Usen, 2007, Australia648 | Systematic reviews/secondary analysis | Achilles | NA | NA | NA | 12 studies were included. The best options for managing Achilles tendinosis were medication and eccentric exercises. Eccentric exercises are simple to perform and provide a cost-effective, safe and efficient treatment option. They should be considered first for all patients, before invasive interventions such as surgery and drug therapy. |
| Vuvan, 2020, Australia187 | RCT | Lateral elbow | Strengthening | Disability, participant/patient rating overall condition, PFC | Pain over a specified time, sensory modality specific pain | Unsupervised isometric exercise was effective in improving pain and disability, but not perceived rating of change and pain-free grip strength when compared with wait-and-see at 8 wk. With only one of the three primary outcomes being significantly improved, it is doubtful if isometric exercises can be an efficacious standalone treatment. |
| Walsh, 2015, Ireland649 | NR | Rotator cuff | Strengthening | Disability | NA | Exercise classes produced similar or better outcomes in terms of pain, physical measurement and function compared to individual instruction. The implications for time management and efficiency make the class model an attractive and effective method for the management of rotator cuff impingement syndrome. |
| Wang, 2007, Taiwan650 | RCT | Patellar | Strengthening | Loading/activity, palpation, disability, medication use, other, structure | NA | ESWT appeared to be more effective and safer with lower symptom recurrence than traditional conservative treatments in the management of patients with chronic patellar tendinopathy. |
| Wang, 2014, Hong Kong, China (SAR)651 | Systematic reviews/secondary analysis | Rotator cuff | NA | NA | NA | There is currently not enough evidence available to support or refute the effectiveness of isokinetic training for SIS. This does not reflect a true lack of effect, but rather a lack of RCTs in this area. |
| Warden, 2008, United States652 | RCT | Patellar | Strengthening | Pain on loading/activity | Disability, participant/patient rating overall condition, adverse effects/events, other | Low-intensity pulsed ultrasound does not provide any additional benefit over and beyond placebo in the management of patellar tendinopathy. |
| Wasielewski, 2007, United States653 | Systematic reviews/secondary analysis | Achilles, patellar | NA | NA | NA | Eccentric exercise is an effective form of treatment for tendinopathies of the lower limb; however, limited evidence exists to support its superiority over other forms of therapeutic treatment. |
| Dragoo, 2014, United States336 | RCT | Patellar | Strengthening, flexibility, aerobic | Disability | Pain without further specification, disability, QoL | The addition of a US-guided leukocyte-rich PRP injection improved significantly more than dry needling group in VISA at 12 weeks, but differences were not significant at 26 weeks. |
| Wegener, 2015, Australia654 | Observational – case series/reports | Lateral elbow | Strengthening | further specification, physical function | NA | The use of elastic therapeutic tape in conjunction with eccentric exercises may be clinically beneficial in the treatment of lateral elbow tendinosis. |
| Wegener, 2016, Australia655 | RCT | Lateral elbow | Flexibility, strengthening | Disability, PFC | QoL, participation | Whilst all groups improved on key outcomes, it is possible that exercise alone and/or natural recovery were responsible for improvements. |
| Weir, 2011, Netherlands656 | RCT | Other – adductor-related groin pain | Strengthening, other | ROM, pain – clinician-applied stress/examination | NA | The multi-modal programme resulted in a significantly quicker return to sports than exercise therapy plus return to running but neither treatment was very effective. |
| Wen, 2011, United States657 | RCT | Lateral elbow | Strengthening | Pain without further specification | Pain without further specification | The authors were unable to show any statistical advantage to eccentric exercises for lateral epicondylosis compared with local modalities and stretching exercises. |
| Werner, 2002, Germany658 | RCT | Rotator cuff | Flexibility, strengthening | Participant/patient rating overall condition, disability | NA | Strengthening of the centering muscles around the humeral head led to positive outcomes for subacromial impingement. Self training after instruction showed no difference from physiotherapist-supervised exercises. |
| Wesner (a), 2016, Canada659 | Pilot – feasibility | Rotator cuff | NR | Pain without further specification, disability, participation | NA | Preliminary results indicate intratendinous, ultrasound-guided PRP injection may lead to improvements in pain, function and MRI-documented tendon pathology. |
| Wesner(b), 2016, Canada659 | Observational – cohort | Achilles, patellar, lateral elbow, rotator cuff | NR | Pain without further specification, participation | NA | Preliminary results indicate intratendinous, ultrasound-guided PRP injection may lead to improvements in pain, function and MRI-documented tendon pathology. |
| Wetke, 2015, Denmark660 | QE – without control | Achilles | Strengthening, flexibility, aerobic | Pain on loading/activity, participant/patient rating overall condition | Pain over a specified time, other, pain – clinician-applied stress/examination | We evaluated the effectiveness of a training protocol and found that only a minority succeeded with exercises alone. |
| Whalley, 2019, United States661 | Observational – cohort | Lateral elbow | NR | Disability, pain without further specification | NA | Education-based self-management improved pain, function, and helped individuals with LET return to work sports and daily activities |
| Wheeler, 2019, United Kingdom662 | Observational – case series/reports | Achilles | Flexibility, strengthening, other | Pain without further specification | Function, QoL, psychological factors, physical | Improvements in multiple outcomes were observed in patients with insertional and non-insertional AT following a combination of ESWT and home rehabilitation. |
| Wheeler, 2020, United Kingdom663 | Observational – cohort | Achilles | Flexibility, strengthening | further specification, other, | NA | ESWT and HVIGI are both effective treatments for recalcitrant AT. |
| Wiedmann, 2017, Germany664 | RCT | Achilles | Strengthening | Structure, pain without further specification, physical | NA | Eccentric training improved the VISA-A and VAS scores after 12 weeks more than physiotherapy treatment. |
| Wiegerinck, 2013, Netherlands665 | Systematic reviews/secondary analysis | Achilles | NA | NA | NA | ESWT seems effective in patients with non-calcified insertional AT. There was mixed support for eccentric exercises and not possible to draw conclusions regarding surgical treatments. |
| Wiener, 2005, Germany666 | RCT | Rotator cuff | Flexibility, strengthening | Further specification, PFC | NA | Although physiotherapy helps to build up the muscular strength of the rotator cuff, the influence on pain remains essential to improve weakness in painful movements and hence should be given more attention. |
| Wilson, 2000, United States667 | RCT | Patellar | Flexibility, strengthening | disability, other | NA | Findings suggest that ASTM advantage resulted in improved clinical outcomes in treating patellar tendinitis. |
| Wilson, 2018, Ireland668 | Systematic reviews/secondary analysis | Achilles | NA | NA | NA | Exercise can be recommended for AT to reduce pain and improved function and QoL compared to non-exercise, placebo or advice to rest. However, the optimal mode of exercise remains unclear. |
| Woodley, 2007, New Zealand669 | Systematic reviews/secondary analysis | Achilles, lateral elbow, patellar | NA | NA | NA | There is a lack of high-quality research to support the clinical effectiveness of eccentric exercise over other treatments in the management of tendi nopathies. |
| Worsley, 2013, United Kingdom26 | Observational – case series/reports | Rotator cuff | Other | Disability | Pain without further specification, PFC, | The 10-week motor control intervention for shoulder impingement increased function and reduced pain. Recovery mechanisms were indicated by changes in muscle recruitment and scapular kinematics. |
| Wright, 2017, United Kingdom670 | Pilot – randomised | Rotator cuff | Flexibility, other, strengthening | Disability, pain over a specified time | Psychological factors, ROM, PFC | The addition of cervicothoracic spinal thrust/non-thrust to the shoulder treatment only group did not significantly alter improvement in pain or function in patients with subacromial pathology. Both approaches appeared to provide an equally notable benefit on all outcomes and met the criteria for clinical relevance for both pain and function. |
| Yazmalar, 2016, Turkey671 | RCT | Rotator cuff | Flexibility, strengthening | Disability, psychological factors, other, QoL | NA | TENS and exercise are effective on pain, disability, and sleep disturbance but may not be effective on other psychosocial measures like anxiety, depression and fatigue in patients with SIS. |
| Yeldan, 2009, Turkey672 | QE – with control (with pre-test) | Rotator cuff | Flexibility, strengthening | Loading/activity, pain over a specified time, disability, PFC, ROM | NA | No significant difference between LLLT and placebo LLLT when they are supplementing an exercise programme for treatment of shoulder impingement syndrome. |
| Yelland, 2019, Australia673 | RCT | Lateral elbow | Other, strengthening | Disability, participant/patient rating overall condition | Loading/activity, pain over a specified time, QoL, PFC | No significant differences amongst the physiotherapy, prolotherapy and combined groups in PRTEE and global impression of change measures over a year. |
| Yelland, 2011, Australia674 | RCT | Achilles | Strengthening | Disability | Participant/patient rating overall condition, pain over a specified time | Prolotherapy and particularly eccentric loading exercises combined with prolotherapy gave more rapid improvements in Achilles tendinosis symptoms than eccentric loading exercises alone. Long-term VISA-A scores were similar. |
| Yerlikaya, 2018, Turkey675 | QE – with control (with pre-test) | Lateral elbow | Flexibility, strengthening | Further specification, PFC, structure, adverse | NA | Lateral epicondylitis does not seem to be affected by either leukocyte-rich PRP or leukocyte-poor PRP on pain and function in the short term. |
| Yildirim, 2013, Turkey676 | RCT | Rotator cuff | Flexibility, strengthening | On loading/activity, pain over a specified time, psychological factors | NA | Nine minutes of ultrasound administration was more effective than 4 minutes at relieving pain and improving functionality. |
| Yilmaz, 2015, Turkey677 | Observational – cohort | Rotator cuff | Strengthening | patient rating overall condition, pain on loading/activity, pain over a specified time, disability, | NA | A specific conservative treatment programme is highly effective in improving pain, disability and hand grip strength in shoulder subacromial pain problems. |
| Young, 2002, Australia678 | RCT | Patellar | Strengthening | On loading/activity, physical function | NA | Both exercise programmes positively affected pain, function and strength. |
| Young, 2005, Australia132 | RCT | Patellar | Strengthening | Disability | Clinician-applied stress/exami nation, pain over a specified time | Both exercise protocols improved pain and sporting function in volleyball players over 12 months. The decline squat protocol offers greater clinical gains during a rehabilitation programme for patellar tendinopathy in athletes who continue to train and play with pain. |
| Young, 2017, United States679 | Systematic reviews/secondary analysis | Achilles | NA | NA | NA | Session duration, frequency, total number of visits, and overall length of care may all be dosing variables with limited value for determining effective exercise prescription. However, the limited number of studies prevents any definitive conclusions. |
| Young, 2018, United States22 | Reviews/secondary analysis | Patellar | NA | NA | NA | Optimal dosing is still unclear for patellar tendinopathy as no trends were observed with exercise dosing. |
| Yu, 2013, Korea (Republic of)680 | QE – with control (with pre-test) | Achilles | Strengthening, aerobic | Further specification, physical function | NA | Eccentric strengthening was more effective than concentric strengthening in reducing pain and improving function in patients with AT. |
| Yu, 2016, Canada681 | Systematic reviews/secondary analysis | Achilles | NA | NA | NA | Evidence suggests that patients with persistent midportion AT may benefit from shockwave therapy. However, the current evidence does not support the use of splints. There was high risk of bias in the RCTs included in this study. |
| Yuksel, 2015, Turkey682 | RCT | Rotator cuff | Other, strengthening, flexibility | Pain without further specification, PFC, clinical examination findings, disability | NA | The addition of scapular stability exercises had added benefit to traditional treatment modalities and is recommended for patients with scapular dyskinesis. |
| Yuruk, 2016, Turkey683 | RCT | Lateral elbow | Flexibility, strengthening | Pain on loading/activity, physical function | NA | The addition of shockwave to exercise is more effective than placebo shockwave with exercise. |
Appendix 3 Citation analysis
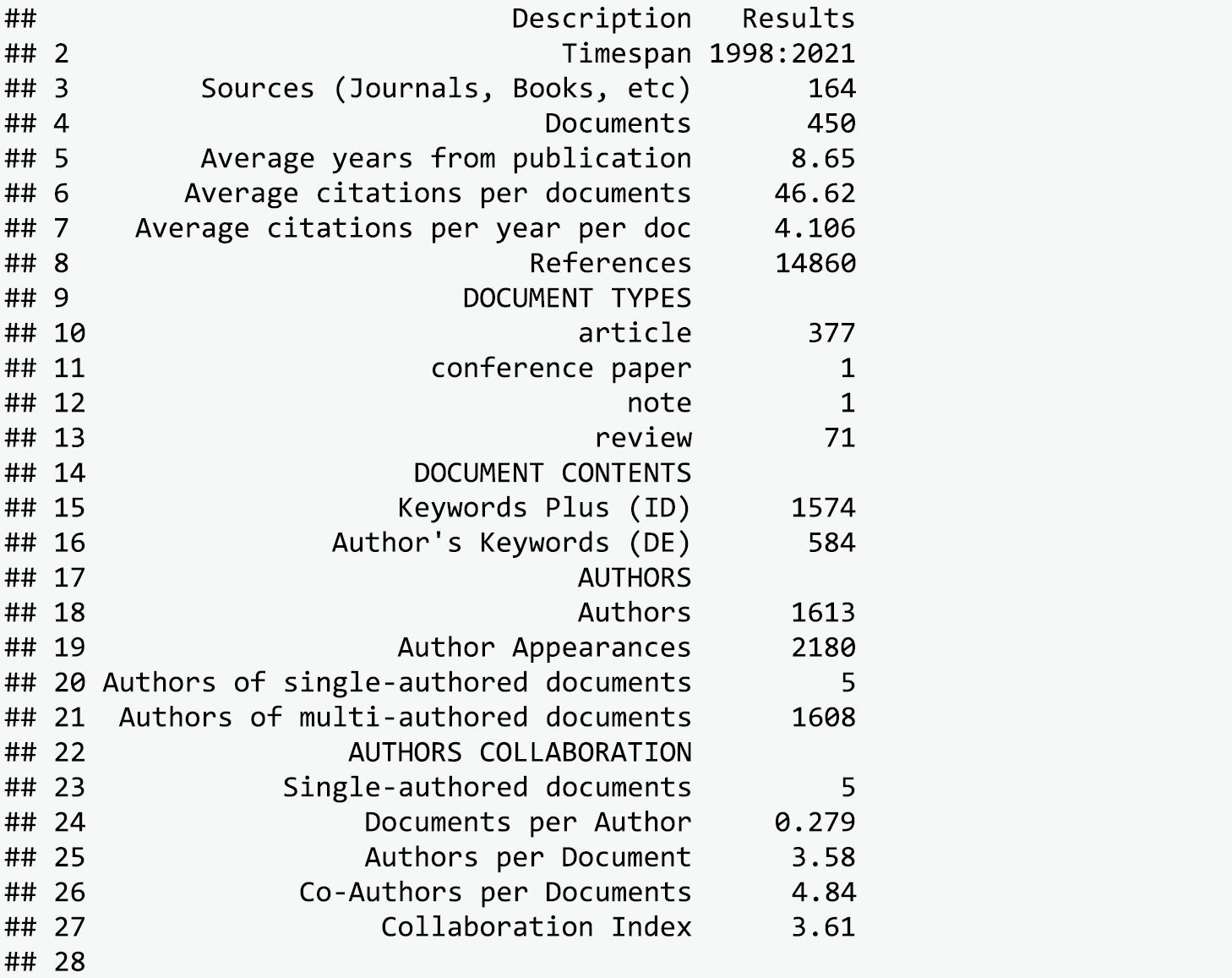

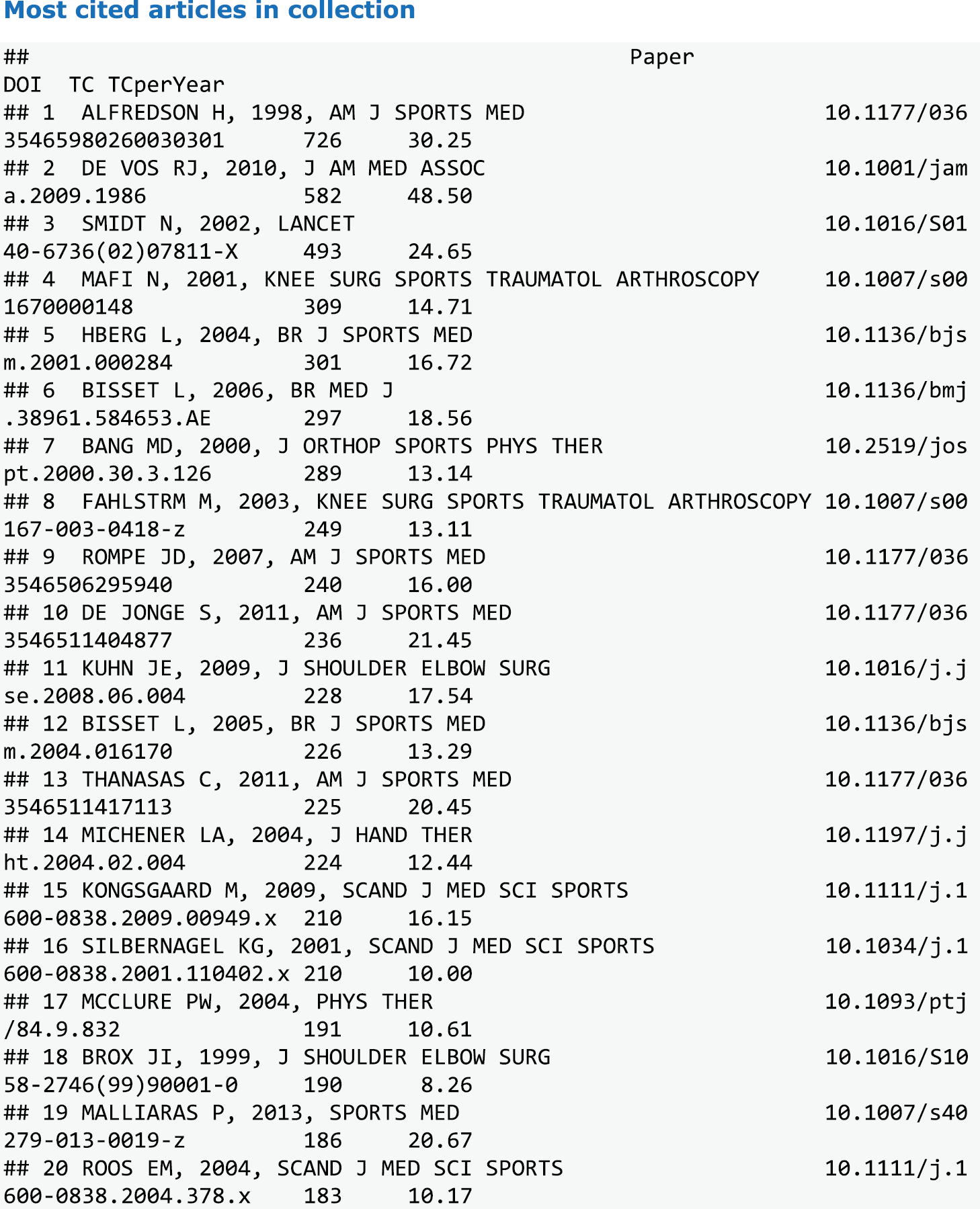
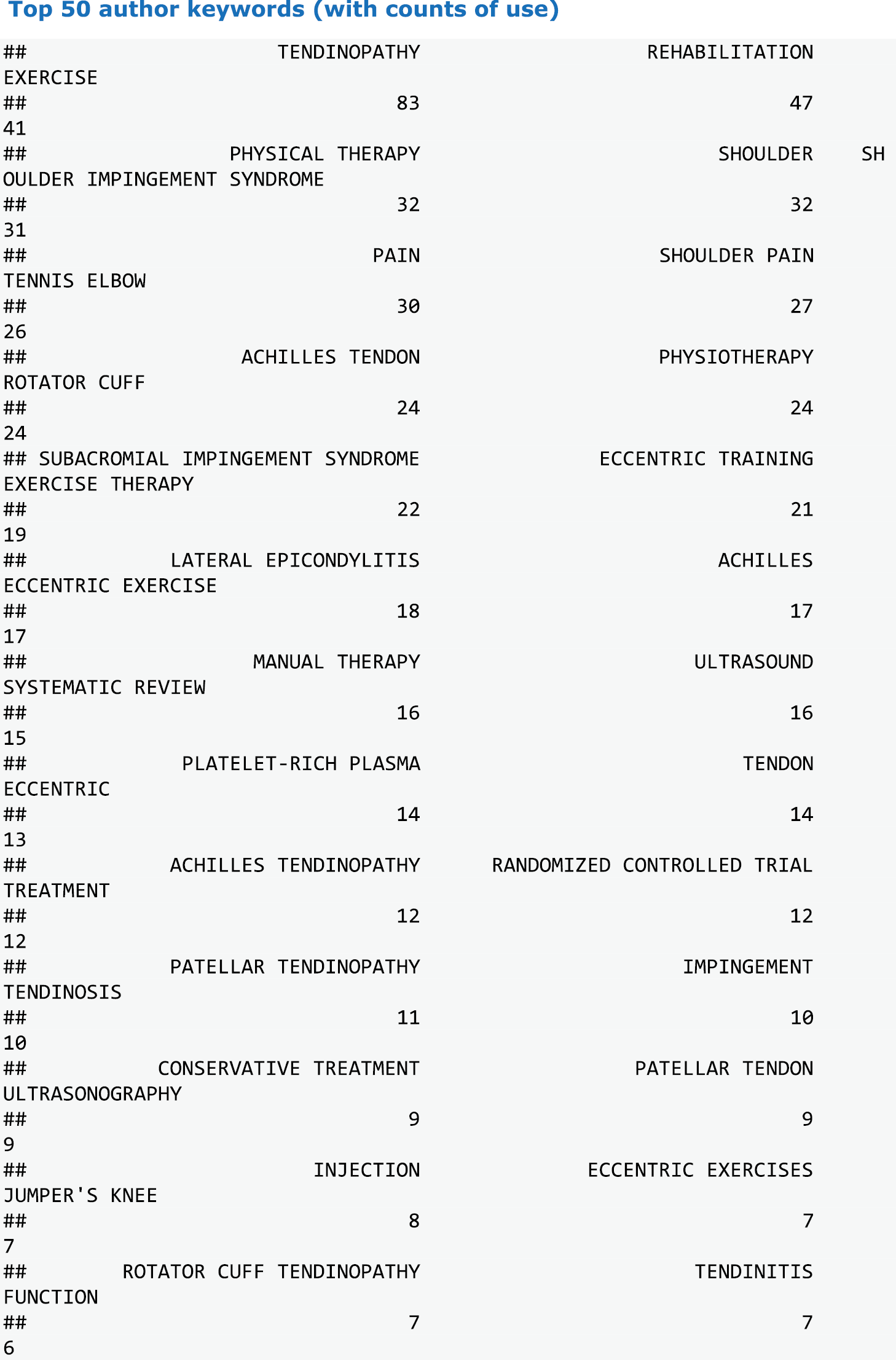
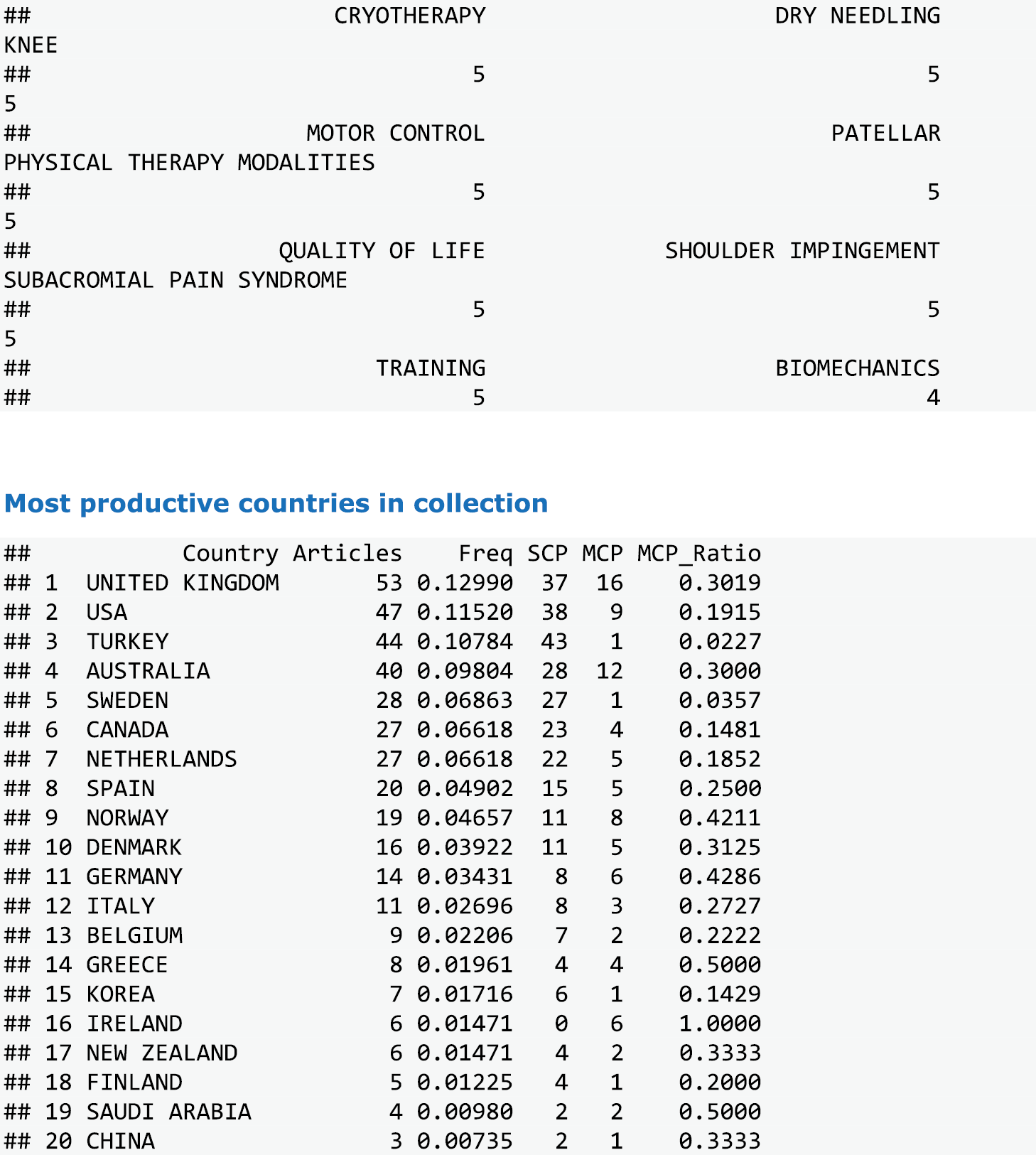
FIGURE 23.
Country collaboration network diagram.
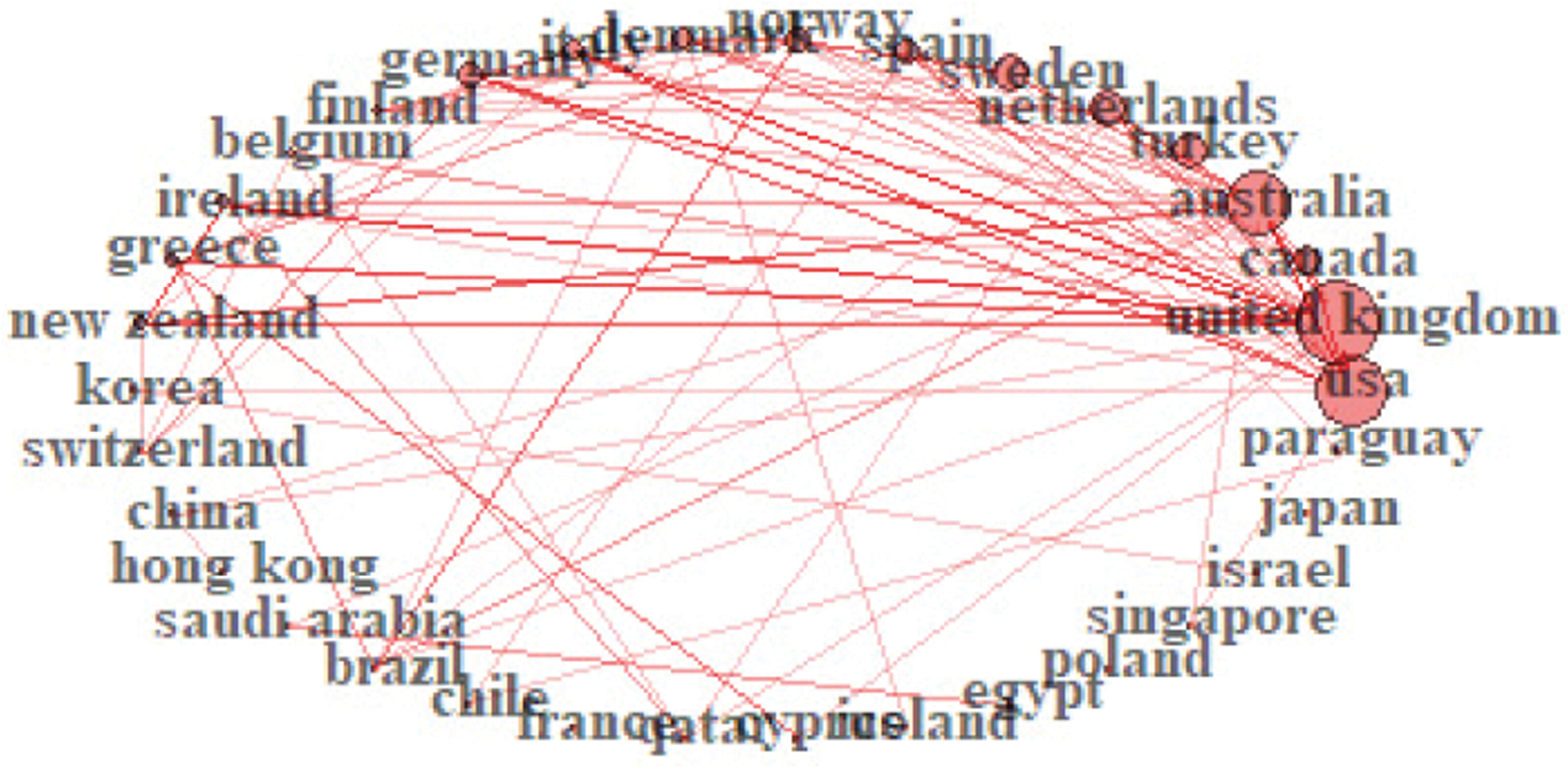
FIGURE 24.
Reference distribution over time.
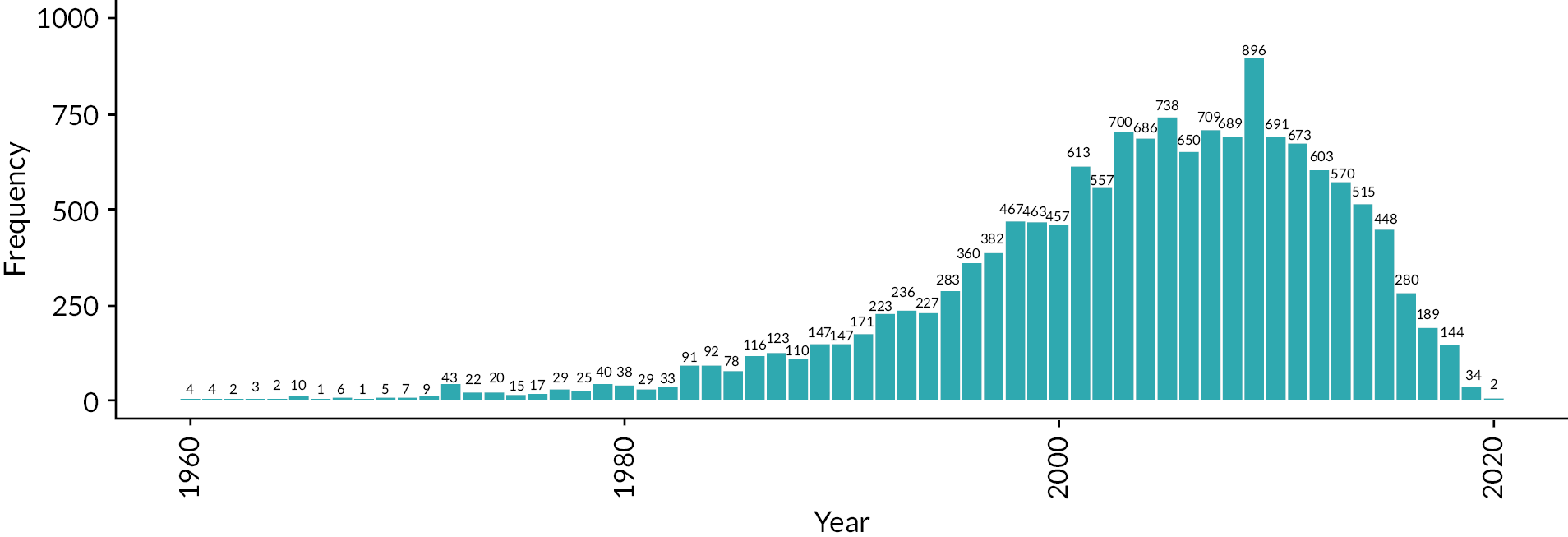


Appendix 4 Effectiveness review table of definitions
| Therapy class | Definition | Therapy treatment | Definition |
|---|---|---|---|
| Resistance | Exercise designed primarily to increase strength of muscles by causing them to produce substantive force against an applied resistance, which can take several forms, including the mass of the body or its segments, isoinertial resistance, elastic resistance, or strength training equipment such as isokinetic devices. In tendinopathy, the stimulus may also be intended to provoke tendon remodelling, reduce pain and improve function. | Concentric only | Includes movements where force produced overcomes the resistance such that muscle shortening occurs. |
| Eccentric only | Includes movements where force produced is less than the resistance such that controlled muscle lengthening occurs. | ||
| Concentric and eccentric | Includes movements where force produced exceeds the resistance in one phase and is less than the resistance in another such that controlled muscle lengthening and shortening occurs. | ||
| Isokinetic | Uses specialised exercise equipment such that the resistance is adjusted in real time to ensure joint angular velocity remains constant. | ||
| Isometric | Includes muscular actions against a resistance such that joint angle remains constant. | ||
| Flexibility | Exercise designed to increase joint ROM and extensibility of muscles and/or associated tissues. Also referred to as range-of-motion exercises or stretching. | Static | Joint range-of-motion actions where the movement is held at or near the end ROM. |
| Dynamic | Joint range-of-motion actions where the movement is performed continuously into and out of the end ROM. | ||
| PNF | Proprioceptive neuromuscular facilitation is a technique combining passive stretching and isometric action to achieve maximum ROM. | ||
| Ballistic | Uses the momentum of a moving body or a limb to increase joint ROM, bouncing into (or out of) a stretched position. | ||
| Proprioception | Exercise designed to enhance the sensation of the joint relative to body position and movement, sense of force, and to encourage muscular stabilisation of the joint in the absence of external stabilising devices, e.g. ankle brace. | Sense of joint position and force | Exercise aimed at enhancing the ability to perceive joint position and force with minimal external cues. |
| Balance | Includes exercise that requires the person to keep or return the displacement of centre of gravity over the base of support through various environmental conditions and changes in body position. | ||
| Movement pattern retraining | Exercise aimed at re-education of motor control and movement patterns that may involve specific retraining of under- or over-active muscles and alteration of kinematic rotation + translation timing between body segments. May also be termed motor control or stabilisation. | ||
| Plyometric | Exercise where a resistance is overcome by a muscle rapidly stretching then shortening. | Plyometric | Exercise where a resistance is overcome by a muscle rapidly stretching then shortening. |
| Vibration | Exercise where body segments are held stationary or actively displaced as per definitions for other treatment classes whilst applying a rapid oscillating resistance | Vibration | Exercise where body segments are held stationary or actively displaced as per definitions for other treatment classes whilst applying a rapid oscillating resistance |
| Broad therapy class | Definition | Specific therapy class | Definition |
|---|---|---|---|
| Non-active (placebo, sham, wait and see) | Includes any appropriate inactive treatment such as waiting list control, sham shockwave, sham laser, sham taping or true placebo. | Non-active (placebo, sham, wait and see) | Includes any appropriate inactive treatment such as waiting list control, sham shockwave, sham laser, sham taping or true placebo. |
| Electro-therapy | Modality that delivers therapeutic levels of physical energy to a biological system, e.g. soft tissue. | Shockwave | ESWT (radial or focussed). |
| Laser | Low level laser therapy. | ||
| Other | Other less common electro-therapies such as ultrasound, radar and diadynamic current. | ||
| Kinetics | Treatment using external devices that alters the kinematics/kinetics of the limb. | Immobilisation | Any intervention that prevents specific features of joint movement, e.g. splinting. |
| Altered loading | Any intervention aimed at altering tendon loading, e.g. taping, tennis elbow clasp/brace and orthotics. | ||
| MT | MT is the skilled application of ‘hands-on’ techniques to treat soft tissues and joint structures for the purpose of improving pain, increasing ROM, stimulating tissue repair response, and/or improving function. | MT | MT is the skilled application of ‘hands-on’ techniques to treat soft tissues and joint structures for the purpose of improving pain, increasing ROM, stimulating tissue repair response, and/or improving function. |
| Injection therapy | Injection therapy for tendinopathy typically involves direct administration of a pharmacologically active drug or combination of drugs using a syringe and needle or equivalent. It may or may not be image-guided. | Autologous | An autologous injection is an injection of a substance drawn from the patient to whom it is then given, usually at the tendinopathy site after content manipulation with the purpose of stimulating tissue healing. |
| Drug | An injection of a classified drug, often mixed with another drug (e.g. corticosteroid with local anaesthetic), for the purpose of reducing pain and stimulating tissue healing. | ||
| Volumetric | An injection deliberately constructed to administer a large volume of fluid to exert a mechanical, as well as pharmacological, effect on the tissues to reduce pain, promote tissue healing and mobilise adherent tissue. | ||
| Surgery | Any relevant surgical intervention for tendinopathy | Minimally invasive peritendinous | Minimally invasive procedure with small portals and insertion of surgical tools in the peritendinous area. |
| Open intra-tendinous | A more traditional open approach where the tendon is exposed and the peri-tendinous and intra-tendinous areas are surgically treated. |
| Domain | ICON definition | Example tools |
|---|---|---|
| Disability | Composite scores of a mix of patient-rated pain and disability due to the pain, usually relating to tendon-specific activities/tasks. | VISA scales; DASH; quick DASH; SPADI; patient-rated tennis-elbow evaluation questionnaire; Constant Murley Score; WORC (Western Ontario Rotator Cuff Index); AOFAS (American Orthopaedic Foot & Ankle Society); Roles and Maudsley score; ASES (American Shoulder & Elbow Surgeons Index); Tegner activity score; Lysholm knee scale; Pain-free function questionnaire; Ankle activity score; Subjective elbow value (SEV); Placzek score; Shoulder disability questionnaire; International Knee Documentation Committee form (IKDC); Penn Shoulder score (University of Pennsylvania shoulder score) (PSS); Brief pain inventory (BPI); UCLA Shoulder Rating Scale; FILLA – functional index of leg and lower limb; Neer Shoulder Score; Nirschl phase rating scale; American Shoulder and Elbow Surgeon’s (MASES) questionnaire; Mayo Elbow Performance Score (MEPS); Shoulder rating questionnaire (SRQ) |
| Pain on loading/activity | Patient-reported intensity of pain performing a task that loads the tendon | VAS; NRS; Pain experience scale |
| Pain over a specified time | Patient-reported pain intensity over period of time, e.g. morning/night/24 hours/1 week | VAS; NRS Painful days in 3 months |
| Pain without further specification | Patient asked about pain levels without reference to activity or timeframe | VAS; NRS; Borg CR10 Scale; Pain status |
| PFC | Quantitative measures of physical tasks (e.g. hops, times walk, single leg squat); includes muscle strength | Counter movement jump; one-leg triple hop; single-leg decline squat; muscle strength measured by dynamometry (hand-held, isokinetic); repetition maximum; manual muscle testing. |
| Participation | Patient rating of the level of participation/engagement across areas of their life | Sport participation; return to sport; work ability; return to work; sick leave |
| Patient rating overall condition | Single-assessment numerical evaluation of symptom status | Global impression/rating of change; patient-acceptable symptom status/state |
| QoL | General well-being | EQ5D; EQ3D; SF-36 or SF-12; Assessment of QoL (AQoL); Nottingham Health Profile; Gothenburg QoL Instrument |
| Adverse effects/events | Unwanted unintended effects of treatments | Adverse event reporting |
| ROM (shoulder only) | Active or passive ROM in specified plane, measured in degrees. | Hand-held goniometer; inclinometer |
Appendix 5 Table of included studies in effectiveness review
| Study | Design | Participants (number (n); sex (% female); mean (sd) age; mean (sd) symptom duration in months) |
TAs | Treatment classes | Findings | Review included |
|---|---|---|---|---|---|---|
| Achilles | ||||||
| Balius 2016 Spain238 |
RCT | N = 37 % female 20.4 Age 41.4 (11.7) Symptoms NR Training status Other |
6 | 6× ‘Exercise only’ | Findings confirmed the therapeutic potential of eccentric exercise at reactive and degenerative stages of tendinopathy. MCVC supplementation decreased pain more than eccentric exercise alone (reactive tendinopathy) Personalised stretching regime supplemented with MCVC may be appropriate for some patients. |
1a, 1c, 2, 3 |
| Tumilty 2016 New Zealand632 |
RCT | N = 80 % female 58.8 Age 47.4 (9.7) Symptoms NR Training status Other |
4 | 2× ‘Exercise, Non-Active’; 2× ‘Exercise, Electro-Therapy’ | Two exercise sessions per week equivalent to twice-daily sessions, with added benefit using laser as an adjunct to exercise. | 3 |
| Stefansson 2019 Iceland184 |
RCT | N = 58 % female 20.0 Age NR Symptoms NR Training status Other |
3 | 1× ‘Exercise only’; 1× ‘Non-Exercise only’; 1× ’Exercise, Manual-Therapy’ | Similar results for pressure massage and eccentric exercise. Combining pressure massage and eccentric exercise did not improve outcomes. | 1a, 1c, 3 |
| Horstmann 2013 Germany16 |
RCT | N = 58 % female 44.8 Age 45.3 (7.7) Symptoms NR Training status Recreational |
3 | 2× ‘Exercise only’; 1× ‘Non-Active’ | Vibration training may be an alternative or a complementary treatment in patients who do not respond well to eccentric training, especially in those with insertional pain. | 3 |
| Rompe 2007 Germany558 |
RCT | N = 75 % female 61.3 Age 48.5 (10.6) Symptoms 10.8 (8.5) Training status Other |
3 | 1× ‘Exercise only’; 1× ‘Non-Exercise only’; 1× ‘Non-Active’ | At 4-month follow-up, eccentric loading and low-energy shockwave therapy showed comparable results. The wait-and-see strategy was ineffective for the management of chronic recalcitrant AT. | 1a, 1b, 1c, 3 |
| Yelland 2011 Australia673 |
RCT | N = 43 % female NR Age 46.7 (NR) Symptoms 17 (NR) Training status Other |
3 | 1× ‘Exercise only’; 1× ‘Non-Exercise only’; 1× ‘Exercise, Injection’ | Prolotherapy and particularly eccentric loading exercises combined with prolotherapy gave more rapid improvements in Achilles tendinosis symptoms than eccentric loading exercises alone. Long term VISA-A scores were similar. | 1a, 1b, 1c, 3 |
| Mayer 2007 Germany474 |
RCT | N = 28 % female 0.0 Age 38.2 (6.2) Symptoms 13.5 (15.4) Training status Recreational |
3 | 1× ‘Exercise, Electro-Therapy, Manual-Therapy’; 1× ‘Non-Exercise only’; 1× ‘Non-Active’ | A 4-week treatment of deep friction and ultrasound in combination with sensory motor and eccentric training, as well as insoles with longitudinal arch support, might reduce pain (at rest and in activity) in most patients with AT. | 3 |
| Roos 2004 Sweden193 |
RCT | N = 44 % female 52.3 Age 45 (26–60)** Symptoms 5.5 (1–180)* Training status Recreational |
1× ‘Exercise only’; 1× ‘Exercise, Kinetics’; 1× ‘Non-Exercise only’ | Eccentric exercises reduce pain and improve function in patients with AT. | 1a, 1b, 1c, 3 | |
| Petersen 2007 Germany530 |
RCT | N = 86 % female 40.0 Age 42.5 (11.1) Symptoms 7.4 (2.3) Training status Recreational |
3 | 1× ‘Exercise only’; 1× ‘Non-Exercise only’; 1× ‘Exercise, Kinetics’ | The AirHeel brace is as effective as eccentric training in the treatment of chronic AT. There is no added benefit to combining both treatments. | 1a, 1c, 3 |
| Boesen 2017 Denmark162 |
RCT | N = 44 % female 52.3 Age 45 (26–60)** Symptoms 5.5 (1–180)** Training status Recreational |
3 | 2× ‘Exercise, Injection’; 1× ‘Exercise, Non-Active’ | Treatment with HVI or PRP in combination with eccentric training in chronic AT seems more effective in reducing pain, improving activity level, and reducing tendon thickness and intratendinous vascularity than eccentric training alone. HVI may be more effective in improving outcomes of chronic AT than PRP in the short term. | 3 |
| Praet 2019 Australia130 |
RCT | N = 20 % female 35.0 Age 43.7 (7.9) Symptoms 54 (90) Training status Recreational |
2 | 1× ‘Exercise only’; 1× ‘Exercise, Non-Active’ | Oral supplementation of specific collagen peptides may accelerate the clinical benefits of a well-structured calf-strengthening and return-to-running programme in patients with chronic AT. | 1a, 1c, 3 |
| Kedia 2014 United States424 |
RCT | N = 36 % female 72.2 Age 53.6 (9.2) Symptoms NR Training status Other |
2 | 2× ‘Exercise, Kinetics’ | Conventional physical therapy consisting of gastrocnemius, soleus and hamstring stretches, ice massage on the Achilles tendon, and use of heel lifts and night splints with or without eccentric training is effective for treating insertional AT. | 3 |
| Bell 2013 New Zealand251 |
RCT | N = 53 % female 47.0 Age 49 (10.1) Symptoms 30.9 (60.3) Training status Recreational |
2 | 1× ‘Exercise, Injection’; 1× ‘Exercise, Non-Active’ | The addition of two peritendinous autologous blood injections administered 1 month apart, to a standardised eccentric training programme provides no added benefit in the treatment of mid-portion AT. | 3 |
| Boesen 2019 Denmark163 |
RCT | N = 28 % female 0.0 Age 43.0 (6.0) Symptoms 10.1 (4.8) Training status Other |
2 | 2× ‘Exercise, Injection’ | HVI with or without corticosteroid in combination with eccentric training seems effective in AT. HVI with corticosteroid showed a better short‐term improvement than HVI without corticosteroid, indicating a short‐term effect of corticosteroid in the treatment of AT. | 3 |
| Beyer 2015 Denmark18 |
RCT | N = 58 % female 31.9 Age 48.0 (2.0) Symptoms 18.1 (4.3) Training status Other |
2 | 2× ‘Exercise only’ | Both traditional eccentric exercise and HSR yield positive, equally good and lasting clinical results in patients with AT. HSR is associated with greater patient satisfaction after 12 weeks but not after 52 weeks. | 1a, 1b, 1c, 2, 3 |
| Stergioulas 2008 Norway604 |
RCT | N = 52 % female 37.5 Age 29.5 (4.8) Symptoms 9.9 (3) Training status Other |
2 | 1× ‘Exercise, Electro-Therapy’; 1× ‘Exercise, Non-Active’ | Low-level laser therapy, with the parameters used in this study, accelerates clinical recovery from chronic AT when added to an eccentric exercise regimen. For the LLLT group, the results at 4 weeks were similar to the placebo LLLT group results after 12 weeks. |
3 |
| de Vos 2010 Netherlands314 |
RCT | N = 54 % female 52.0 Age 49.5 (8.7) Symptoms 7.1 (4.6–20.9)* Training status Other |
2 | 1× ‘Exercise, Injection’; 1× ‘Exercise, Non-Active’ | Among patients with chronic AT who were treated with eccentric exercises, a PRP injection compared with a saline injection did not result in greater improvement in pain and activity. | 3 |
| de Vos 2007 Netherlands59 |
RCT | N = 63 % female 41.3 Age 44.6 (8) Symptoms 30.6 (50.6) Training status Recreational |
2 | 1× ‘Exercise only’; 1× ‘Exercise, Kinetics’ | A night splint has no added benefit to eccentric exercises in the treatment of chronic midportion AT. There was no significant difference between the two groups in VISA-A score and patient satisfaction. | 1a, 1b, 1c, 3 |
| Stevens 2014 United Kingdom175 |
RCT | N = 28 % female 60.7 Age 48.7 (10.8) Symptoms 7.4 (4.0) Training status Other |
2 | 2× ‘Exercise only’ | Performing a 6-week do-as-tolerated programme of eccentric heel-drop exercises compared to the recommended 180 repetitions per day, did not lead to lesser improvement for individuals with midportion AT, based on VISA-A and VAS scores. | 1a, 1b, 1c, 3 |
| Mafi 2001 Sweden467 |
RCT | N = 44 % female 45.5 Age 48.3 (8.8) Symptoms 20.5 (3–120)** Training status Other |
2 | 2× ‘Exercise only’ | Eccentric calf-muscle training showed superior results to concentric training in the treatment of chronic Achilles tendinosis based on patient satisfaction and return to activity level. | 1a, 1c, 2, 3 |
| Nørregaard 2007 Denmark499 |
RCT | N = 35 % female 49.0 Age 42.0 (2.0)*** Symptoms 28.4 (8.8)*** Training status Other |
2 | 2× ‘Exercise only’ | Symptoms gradually improved during the 1-year follow-up period and were significantly better assessed by pain and symptoms after 3 weeks and all later visits. However, no significant differences could be observed between the two groups. | 1a, 1b, 1c, 2, 3 |
| Silbernagel 2007 Sweden138 |
RCT | N = 38 % female 47.4 Age 46.0 (8.0) Symptoms 36.2 (66.5) Training status Other |
2 | 2× ‘Exercise only’ | Our treatment protocol, which gradually increases the load on the Achilles tendon and calf muscle, demonstrated significant improvements. Continuing tendon loading activity such as running and jumping with the use of a pain-monitoring model did not have any adverse effect. | 1a, 1c, 3 |
| Alfredson 1998 Sweden17 |
Quasi-experimental | N = 30 % female 20.0 Age 44.0 (7.0) Symptoms 25.9 (3–100)** Training status Recreational |
2 | 1× ‘Exercise only’; 1× ‘Non-Exercise only’ | Our treatment model with heavy-load eccentric calf-muscle training has a very good short-term effect on athletes in their early forties. | 1a, 1c, 3 |
| Rompe 2009 Germany559 |
RCT | N = 68 % female 55.9 Age 49.7 (9.9) Symptoms 14.5 (6.0) Training status Other |
2 | 1× ‘Exercise only’; 1× ‘Exercise, Electro-Therapy’ | The likelihood of recovery after 4 months was higher after a combined approach of both eccentric loading and shockwave therapy compared to eccentric loading alone. | 1a, 1c, 3 |
| Silbernagel 2001 Sweden587 |
RCT | N = 47 % female 22.5 Age 44.0 (12.5) Symptoms 30.5 (40.7) Training status Recreational |
2 | 2× ‘Exercise only’ | The eccentric overload protocol used in the present study can be recommended for patients with chronic pain from the Achilles tendon. More patients achieved full recovery, improved pain and ROM in the Exp group compared to the control group. | 1a, 1b, 1c, 2, 3 |
| Knobloch 2008 Italy437 |
RCT | N = 92 % female 35.0 Age 47.5 (11.0) Symptoms NR Training status Recreational |
2 | 1× ‘Exercise, Kinetics’; 1× ‘Exercise only’ | Patients with tendinopathy of the main body of the AT experienced improved clinical outcome with both management options. Although tendon microcirculation was optimised in the combined group of eccentric training and AirHeel Brace, these micro-vascular advantages do not translate into superior clinical performance when compared with eccentric training alone. | 1b, 3 |
| Tumilty 2012 New Zealand630 |
RCT | N = 33 % female 55.0 Age 46.1 (7.8) Symptoms NR Training status Other |
2 | 1× ‘Exercise, Electro-Therapy’; 1× ‘Exercise, Non-Active’ | No evidence for clinical effectiveness of adding LLLT to eccentric exercises for the treatment of AT. | 3 |
| Notarnicola 2014 Italy500 |
Quasi-experimental | N = 60 % female 56.8 Age 58.5 (13.3) Symptoms NR Training status Other |
2 | 2× ‘Exercise, Electro-Therapy’ | Cryo high-energy laser therapy (CHELT) gave quicker and more effective pain relief compared to ESWT at 2-month and 6-month follow-up. | 3 |
| Wiedmann 2017 Germany664 |
RCT | N = 20 % female 65.0 Age 43.0 (6.0) Symptoms NR Training status Other |
2 | 1× ‘Exercise only’; 1× ‘Non-Exercise only’ | Eccentric training improved the VISA-A and VAS scores after 12 weeks more than physiotherapy treatment. | 1a, 1c, 3 |
| Yu 2013 Korea (Republic of)680 |
Quasi-experimental | N = 32 % female 0.0 Age 30.3 (1.6) Symptoms 11.7 (2.1) Training status Other |
2 | 2× ‘Exercise only’ | Eccentric strengthening was more effective than concentric strengthening in reducing pain and improving function in patients with AT. | 1a, 1c, 2, 3 |
| Alfredson 1999 Sweden224 |
Quasi-experimental | N = 24 % female 14.3 Age 42.6 (9.0) Symptoms 23.7 (3–100)** Training status Recreational |
2 | 1× ‘Exercise only’; 1× ‘Non-Exercise only’ | Heavy-loaded, eccentric calf-muscle training seems to be a good treatment mode for chronic Achilles tendinosis. | 1a, 1c, 3 |
| Pearson 2012 New Zealand525 |
RCT | N = 40 % female 62.5 Age 50.0 (8.2) Symptoms 11.0 (10.0) Training status Other |
2 | 1× ‘Exercise, Injection’; 1× ‘Exercise only’ | There is some evidence for small short-term symptomatic improvements with the addition of autologous blood injection to standard treatment for AT. | 1a, 1c, 3 |
| McCormack 2016 United States478 |
RCT | N = 15 % female 68.8 Age 53.6 (38–69)** Symptoms 9.9 (NR) Training status Other |
2 | 1× ‘Exercise only’; 1× ‘Exercise, Manual-Therapy’ | Soft tissue treatment (Astym) plus eccentric exercise was more effective than eccentric exercise alone at improving function during both short- (26 weeks) and long-term (52 weeks) follow-up periods. | 1b, 3 |
| Gatz 2020 Germany365 |
RCT | N = 42 % female 35.7 Age 50.0 (12.0) Symptoms 27.5 (23.8) Training status Other |
2 | 2× ‘Exercise only’ | No additional clinical benefits of adding ISOs to a basic EE programme could be found in this preliminary RCT study over a period of 3 months. SWE was able to differentiate between insertional and midportion tendon tissue and localise reported symptoms to sublocations but this did not correlate with better clinical scores (VISA-A) over a 3-month follow-up period. | 1a, 1b, 1c, 2, 3 |
| Jonsson 2009 Sweden408 |
Quasi-experimental | N = 15 % female 13.3 Age 25.0 (NR) Symptoms 17.5 (13.2) Training status Other |
2 | 2× ‘Exercise only’ | Treatment with painful eccentric calf-muscle training showed good clinical results based on VAS scores, patient satisfaction, and return to pre-injury activity levels in patients with chronic painful mid-portion Achilles tendinosis, but not in patients with chronic insertional Achilles tendon pain. | 1a, 1b, 1c, 2, 3 |
| van Der Vlist 2020 Netherlands646 |
RCT | N = 79 % female 51.0 Age 47.9 (9.0) Symptoms 14.3 (NR) Training status Other |
2 | 1× ‘Exercise, Injection’; 1× ‘Exercise only’ | High-volume injection without corticosteroids in addition to usual care is not effective for symptom reduction in patients with chronic midportion AT. | 3 |
| Knobloch 2007 Germany684 |
RCT | N = 20 % female 45.0 Age 32.5 (11.0) Symptoms NR Training status |
2 | 1× ‘Exercise only’; 1× ‘Non-Active’ | An eccentric-training programme performed daily over 12 weeks reduced the increased paratendinous capillary blood flow in AT by as much as 45% and decreased pain level based on a VAS. Local paratendon oxygenation was preserved while paratendinous postcapillary venous filling pressures were reduced after 12 weeks of eccentric training, which appears to be beneficial from the perspective of microcirculation. | 1a, 1c, 3 |
| Romero-Morales 2020 Spain685 |
RCT | N = 61 % female 26 Age 41.6 (8.7) Symptoms 4.25 (3.5) Training status Other |
2 | 2× ‘Exercise only’ | Authors encourage the use of vibration with respect to cryotherapy added to eccentric exercise programmes in order to enhance multifidus cross-sectional area in addition to lower-limb functionality in individuals who suffer from chronic non-insertional AT. | 1a, 1c, 2, 3 |
| Knobloch 2007 Germany192 |
RCT | N = 118 % female 40 Age 48.5 (12) Symptoms NR Training status Other |
2 | 1× ‘Exercise, Kinetics’; 1× ‘Exercise only’ | Achilles tendon oxygen saturation is increased and capillary venous clearance facilitated using an Achilles wrap in addition to daily 12-week eccentric training. | 1a, 1b, 1c, 3 |
| Rabusin 2020 Australia686 |
RCT | N = 100 % female 52.0 Age 45.85 (9.4) Symptoms 20.25 (NR) Training status Other |
2 | 1× ‘Non-Exercise only’; 1× ‘Exercise only’ | In adults with mid-portion AT, heel lifts were more effective than calf muscle eccentric exercise in reducing pain and improving function at 12 weeks. | 1a, 1b, 1c, 3 |
| Rompe 2008 Germany687 |
RCT | N = 50 % female 60.0 Age 39.8 (11) Symptoms 25.55 (9.45) Training status Other |
2 | 1× ‘Exercise only’; 1× ‘Non-Exercise only’ | Eccentric loading as applied in the present study showed inferior results to low-energy shockwave therapy as applied in patients with chronic recalcitrant tendinopathy of the insertion of the Achilles tendon at 4-month follow-up. | 1a, 1b, 1c, 3 |
| de Jonge 2008 Netherlands309 |
RCT | N = 70 % female NR Age 44.6 (26–59) ** Symptoms 30.7 (2–204) ** Training status Other |
2 | 1× ‘Exercise only’; 1× ‘Non-Exercise only’ | Eccentric exercises with or without a night splint improved functional outcome at 1-year follow-up. At follow-up there was no significant difference in clinical outcome when a night splint was used in addition to an eccentric exercise. | 1a, 1b, 1c, 3 |
| Biceps | ||||||
| Genc 2020 Turkey688 |
RCT | N = 80 % female 62.5 Age 45.8 (8.5) Symptoms 5.2 (4.6) Training status Other |
2 | 1× ‘Exercise, Kinetics’; 1× ‘Exercise only’ | Kinesiotaping application decreases pain and increases the functional capacity level and can also play a role in improving the general QoL in biceps tendinitis treatment. | 3 |
| Gluteal (including GTPS) | ||||||
| Rompe 2009 Germany557 |
RCT | N = 68 % female 55.9 Age 49.7 (9.9) Symptoms 14.5 (6) Training status Other |
3 | 1× ‘Exercise only’; 2× ‘Non-Exercise only’ | Both corticosteroid injection and home training were significantly less successful than was shockwave therapy at 4-month follow-up. Corticosteroid injection was significantly less successful than was home training or shockwave therapy at 15-month follow-up. | 1b, 3 |
| Ganderton 2018 Australia189 |
RCT | N = 90 % female 100 Age 61.83 (7.81) Symptoms NR Training status Other |
2 | 2× ‘Exercise only’ | Lack of treatment effect was found with the addition of an exercise programme to a comprehensive education on GTPS management. The improved outcomes of the responders in the GLoBE group indicate that there may be a subgroup of patients with a GTPS diagnosis that benefit from a GLoBE intervention programme. | 1b, 3 |
| Ramon 2020689 |
RCT | N = 102 % female 71.5 Age 56.35 (11.95) Symptoms NR Training status Other |
2 | 1× ‘Exercise, Electro-Therapy’; 1× ‘Exercise, Non-Active’ | F-ESWT in association with a specific exercise programme is safe and effective for GTPS, with a success rate of 86.8% at 2 months after treatment, which was maintained until the end of follow-up. | 3 |
| Slider 2013 United States690 |
RCT | N = 24 % female 79.2 Age 24.0 (9.0) Symptoms NR Training status Recreational |
2 | 2× ‘Exercise only’ | In general, subjects with an acute hamstring strain injury treated with either the PATS or PRES rehabilitation programme demonstrated a similar degree of muscle recovery at the time of return to sport. Despite this, there were no subjects who exhibited complete resolution of injury on MRI, and 2 of the 4 subjects who reinjured themselves did so within the first 2 weeks after return to sport. | 2, 3 |
| Hamstring | ||||||
| Cacchio 2011 Italy271 |
RCT | N = 40 % female 32.5 Age 23.95 (2.09) Symptoms 20.3 (6.3) Training status Performance |
2 | 1× ‘Non-Exercise only’; 1× ‘Exercise, Manual-Therapy’ | SWT is a more effective treatment to conservative treatment for proximal hamstring tendinopathy. | 3 |
| Askling 2014 Sweden232 |
RCT | N = 56 % female 32 Age 20 (3.6) Symptoms NR Training status Performance |
2 | 2× ‘Exercise only’ | A rehabilitation protocol emphasising lengthening type of exercises is more effective than a protocol containing conventional exercises in promoting time to return in Swedish elite sprinters and jumpers. | 3 |
| Lateral elbow/tennis elbow | ||||||
| Coombes 2013 Australia176 |
RCT | N = 165 % female 38 Age 49.7 (8.1) Symptoms 16.0 (10–26)* Training status Other |
4 | 1× ‘Non-Exercise only’; 1× ‘Exercise, Injection, Manual-Therapy’; 1× ‘Non-Active’;1×× ’Exercise, Manual-Therapy, Non-Active’ | Multimodal physiotherapy provided no beneficial long-term effect on complete recovery, recurrence, pain, disability or QoL. However, in the absence of a corticosteroid injection, physiotherapy may provide a short-term benefit across all outcomes. Corticosteroid injections generally results in a poorer clinical outcome. | 3 |
| Tonks 2007 United Kingdom624 |
RCT | N = 34 % female NR Age 44.3 (7.1) Symptoms NR Training status Other |
4 | 2× ‘Non-Exercise only’; × ’Exercise only’ | Patients who received steroid injection were statistically significantly better for all outcome measures at follow up. No statistically significant effect of physiotherapy nor interaction between physiotherapy and injection was found. | 1a, 1b, 1c, 3 |
| Tonks 2012 United Kingdom623 |
RCT | N = % female 54.6 Age 45.46 (8.2) Symptoms 3.8 (0.5–24)** Training status Other |
3 | 1× ‘Non-Active’; 1× ‘Non-Exercise only’; 1× ‘Exercise, Electro-Therapy, Manual-Therapy’ | In the short term, the injection group showed superior effectiveness, whereas exercise is more effective for long-term management of tennis elbow. | 3 |
| Smidt 2002 Netherlands592 |
RCT | N = 185 % female 50.27 Age 47 (41–54)* Symptoms 11 (8–16)* Training status Other |
3 | 1× ‘Non-Exercise only’; 1× ‘Exercise only’; 1× ‘Exercise, Injection, Kinetics’ | Injection showed better outcomes at 6 weeks. In the long term, physiotherapy had better results than the wait-and-see policy although differences were not significant. | 3 |
| Luginbuhl 2008 Switzerland174 |
RCT | N = 30 % female 72.7 Age 47 (9) Symptoms 10 (11) Training status Other |
3 | 1× ‘Exercise, Kinetics’; 1× ‘Exercise, Non- Active’; 1× ‘Exercise only’ | No beneficial effect of either the forearm support band or the strengthening exercises could be found. | 1a, 1c, 3 |
| Wegener 2016 Australia655 |
RCT | N = 40 % female 70 Age 49.52 (8.09) Symptoms NR Training status NR |
3 | 2× ‘Non-Exercise only’; 1× ‘Exercise only’ | Whilst all groups improved on key outcomes, it is possible that exercise alone and/or natural recovery were responsible for improvements. | 1a, 1c, 3 |
| Stasinopoulos 2006 Greece599 |
Quasi-experimental | N = 75 % female 38.6% Age 40.3 (5.8) Symptoms 5 (NR) Training status Other |
3 | 3× ‘Exercise, Electro-Therapy’ | Cyriax physiotherapy, a supervised exercise programme and polarised polychromatic non-coherent light reduced pain and improved function at the end of the treatment and at any of the follow-up time points. The supervised exercise programme produced the largest effect in the short, intermediate and long term. | 1a, 1c, 3 |
| Lee 2014 Korea (Republic of)456 |
RCT | N = 40 % female 57.5 Age 44.26 (9.5) Symptoms NR Training status Other |
3 | 1× ‘Exercise, Injection, Manual-Therapy’; 1× ‘Exercise, Manual-Therapy, Non-Active’; 1× ’Non-Active’ | 3 days per week for 3 weeks of physical therapy improves pain and function in patients with acute lateral epicondylitis. After 3 weeks, 6 days per week is the most effective treatment frequency. | 3 |
| Olaussen 2015 Norway506 |
RCT | N = 177 % female 40 Age 46.9 (9.7) Symptoms 1.8 (0.9–2.3)* Training status Other |
3 | 3× ‘Exercise only’, ‘Exercise only’, ‘Exercise only’ | Placebo injection with physiotherapy consisting of deep transverse friction massage, Mills manipulation, stretching and eccentric exercises showed no clear beneficial effect on acute lateral epicondylitis. CI with physiotherapy had a large positive effect on success of treatment at 6 weeks, no difference at 12 weeks, worsening at 26 weeks but no significant negative effect at 52 weeks compared to control. No significant differences in primary and secondary measures between CI and placebo injection suggest no added effect to steroid injection. |
3 |
| Stasinopoulos 2017 Cyprus597 |
RCT | N = 34 % female 55.8 Age 43.7 (4.6) Symptoms 6 (NR) Training status Recreational |
3 | 1× ‘Exercise only’; 2× ‘Exercise, Injection’ | Eccentric training, eccentric-concentric training and eccentric-concentric training combined with isometric contraction reduced pain and improved function at the end of the treatment and follow-up. The eccentric-concentric training combined with isometric contraction produced the largest effect at the end of the treatment and follow-up. | 1a, 1c, 2, 3 |
| Yerlikaya 2018 Turkey675 |
Quasi-experimental | N = 90 % female 71.1 Age 48.6 (8.8) Symptoms NR Training status Other |
3 | 3× ‘Exercise only’ | Lateral epicondylitis does not seem to be affected by either leukocyte-rich PRP or leukocyte-poor PRP on pain and function in the short term. | 1a, 3 |
| Martinez-Silvestrini 2005 United States471 |
Quasi-experimental | N = 81 % female 46.8 Age 45.5 (7.7) Symptoms NR Training status Other |
3 | 1× ‘Exercise, Electro-Therapy’; 1× ‘Exercise, Electro-Therapy, Kinetics’; 1× ‘Exercise, Electro-Therapy’ | Eccentric strengthening for the wrist extensors in subjects with lateral epicondylitis demonstrated improvement at 6x weeks but was not statistically different from that achieved with a conservative programme with stretching or a concentric strengthening programme. | 1a, 1c, 2, 3 |
| Eraslan 2018 Turkey347 |
RCT | N = 45 % female 24.4 Age 47.9 (6.6) Symptoms NR Training status Other |
3 | 1× ‘Exercise, Kinetics’; 1× ‘Exercise, Non-Active’; 1× ‘Exercise only’ | Kinesiotaping effectively decreased pain intensity, recovered grip strength, and improved function in patients with lateral epicondylitis undergoing rehabilitation. | 3 |
| Giray 2019 Turkey368 |
RCT | N = 30 % female 86.7 Age 44.46 (9.92) Symptoms 1.69 (NR) Training status Other |
3 | 1× ‘Exercise, Electro-Therapy, Manual-Therapy’; 1× ‘Non-Exercise only’; 1× ‘Exercise, Electro-Therapy, Kinetics, Manual-Therapy’ | Kinesiotaping in addition to exercises is more effective than sham taping and exercises alone in improving pain in daily activities and arm disability due to lateral epicondylitis. | 1a, 1c, 3 |
| Struijs 2004 Netherlands608 |
RCT | N = 180 % female 55.7 Age 45.33 (9.33) Symptoms 20 (27.7) Training status Other |
3 | 1× ‘Exercise, Electro-Therapy’; 1× ‘Exercise, Non-Active’ | Conflicting results were found. Brace treatment might be useful as initial therapy. Combination therapy has no additional advantage compared to physical therapy but is superior to brace only for the short term (6 weeks). | 3 |
| Yuruk 2014 Turkey683 |
RCT | N = 30 % female 76.6 Age 47.17 (8.02) Symptoms 22.13 (21.29) Training status Other |
2 | 1× ‘Exercise only’; 1× ‘Exercise, Kinetics’ | The addition of shockwave to exercise is more effective than placebo shockwave with exercise. | 3 |
| Nowotny 2018 Germany501 |
RCT | N = 31 % female 57 Age 46 (NR) Symptoms NR Training status Other |
2 | 1× ‘Exercise, Manual-Therapy, Non-Active’; 1× ‘Exercise, Manual-Therapy’ | The use of an elbow orthosis appears to reduce pain and improve other subjective outcome measures. However, the long-term results do not appear to be any greater than those received through physiotherapy alone. | 1a, 1c, 3 |
| Røe 2005 Norway691 |
RCT | N = 55 % female 54.55 Age 42.45 (8.89) Symptoms 13.09 (16.6) Training status Other |
2 | 1× ‘Exercise, Non-Active’; 1× ‘Exercise, Electro-Therapy’ | Supplementation with essential fatty acids appears to have no additional benefit in comparison to eccentric training alone. | 3 |
| Chung 2004 Canada290 |
RCT | N = 60 % female 38.3 Age 46.17 (8.01 Symptoms 4.7 (3.3) Training status Other |
2 | 2× ‘Exercise, Electro-Therapy’ | ESWT combined with stretching were no more effective than stretching alone in the treatment of lateral epicondylitis. | 3 |
| Celik 2019 Turkey277 |
RCT | N = 24 % female 74 Age 48.1 (19.3) Symptoms 8.2 (6–10)* Training status Other |
2 | 1× ‘Exercise, Kinetics’; 1× ‘Exercise only’ | Both photobiomodulation and ESWT are useful and can be used in the treatment of LE based-on improvements in handgrip strength. Improvements for elbow extension and shoulder flexion strength and VAS were mainly observed in the photobiomodulation group. | 3 |
| Nishizuka 2017 Japan498 |
RCT | N = 110 % female 39.1 Age 53.6 (11.8) Symptoms 2.04 (1.77) Training status Other |
2 | 2× ‘Exercise, Kinetics’ | A forearm band may have no more than a placebo effect and is not recommended based on its effectiveness. | 1a, 1b, 3 |
| Söderberg 2012 Sweden594 |
RCT | N = 37 % female 57.1 Age 49 (11.5) Symptoms NR Training status Other |
2 | 1× ‘Exercise, Electro-Therapy’; 1× ‘Exercise, Electro-Therapy, Kinetics, Manual-Therapy’ | Daily home eccentric exercise regimen is effective in increasing functional pain-free grip strength and reducing cases suffering from lateral epicondylalgia. | 3 |
| Kachanathu 2019 Saudi Arabia413 |
RCT | N = 40 % female 45 Age 37.9 (0.27) Symptoms NR Training status Other |
2 | 1× ‘Exercise, Manual-Therapy’; 1× ‘Exercise only’ | Wrist joint splinting in addition to physical therapy for a short duration was effective at improving pain intensity in patients with lateral epicondylitis. | 3 |
| Reyhan 2020 Turkey549 |
RCT | N = 40 % female 82.5 Age 42.4 (9.9) Symptoms 4 (0.78) Training status Other |
2 | 2× ‘Exercise, Electro-Therapy’ | MWM plus exercise and cold therapy is safe and effective at improving elbow pain, functional capacity, and grip strength. | 1a, 1b, 3 |
| Stasinopoulos 2009 Greece600 |
Quasi-experimental | N = 50 % female 54.0 Age 45.9 (6.7) Symptoms NR Training status Other |
2 | 1× ‘Exercise, Electro-Therapy’; 1× ‘Exercise, Non-Active’ | An exercise programme consisting of eccentric and static stretching exercises, and LLLT or polarised polychromatic non-coherent light are both adequate treatment modalities for patients with LET | 3 |
| Stergioulas 2007 Greece603 |
RCT | N = % female Age Symptoms Training status |
2 | 2× ‘Exercise only’ | Combination of laser along with plyometric exercises and stretching is more effective than placebo laser and exercise in the treatment of patients with LE. | 3 |
| Stasinopoulos 2010 Greece601 |
Quasi-experimental | N = % female Age Symptoms Training status |
2 | 1× ‘Exercise only’; 1× ‘Exercise, Electro-Therapy’ | Supervised exercise programme is superior to HEP to reduce pain and improve function in patients with LET at the end of the treatment and at the follow-up. | 1a, 1c, 3 |
| Wen 2011 United States657 |
RCT | N = 28 % female 46.4 Age 46 (7.3) Symptoms 3.3 (2.2) Training status Other |
2 | 1× ‘Exercise, Electro-Therapy’; 1× ‘Exercise, Electro-Therapy, Manual-Therapy’ | The authors were unable to show any statistical advantage to eccentric exercises for lateral epicondylosis compared with local modalities and stretching exercises. | 1a, 1c, 3 |
| Bagcier 2019 Turkey235 |
Quasi-experimental | N = 40 % female NR Age 41.25 (13.53) Symptoms 4.55 (1.89) Training status Oth er |
2 | 2× ‘Exercise, Electro-Therapy, Manual-Therapy’ | ESWT and DN combination therapy in lateral epicondylitis provide better clinical outcomes than ESWT treatment alone. | 3 |
| Croisier 2007 Belgium304 |
Quasi-experimental | N = 92 % female 60.9 Age 39 (8) Symptoms 8 (3.5) Training status Other |
2 | 2× ‘Exercise, Electro-Therapy, Manual-Therapy’ | Isokinetic adapted eccentric training significantly reduced pain intensity, improved tendon structure, strength, disability and participation compared to the non-strengthening control group in the management of chronic lateral epicondylar tendinopathy. | 3 |
| Tyler 2010 United States636 |
RCT | N = 21 % female 55 Age 48.9 (3.7) Symptoms 1.59 (0.61) Training status Other |
2 | 1× ‘Exercise only’; 1× ‘Non-Active’ | All outcome measures for chronic lateral epicondylosis were markedly improved with the addition of an eccentric wrist extensor exercise to standard physical therapy through the novel use of an inexpensive rubber bar. | 3 |
| Peterson 2011 Sweden531 |
RCT | N = 81 % female 42 Age 48.25 (8.35) Symptoms 23.3 (35.9) Training status Other |
2 | 2× ‘Exercise only’ | Exercise appears to be superior to the control group in reducing pain in chronic lateral epicondylosis. | 1a, 1c, 3 |
| Dimitrios 2013 Cyprus692 |
Quasi-experimental | N = 60 % female 36.7 Age 47.57 (5.9) Symptoms 4.5 (NR) Training status Other |
2 | 1× ‘Exercise, Kinetics’; 1× ‘Exercise, Injection, Kinetics’ | A specific supervised exercise programme is superior to a specific HEP in reducing pain and improving function in patients with LET at the end of the treatment and at the 3-month follow-up. | 1a, 1b, 2, 3 |
| Gedik 2016 Turkey341 |
Quasi-experimental | N = 45 % female 74.2 Age 52.33 (8.93) Symptoms 24.4 (21.5) Training status Other |
2 | 1× ‘Exercise only’; 1× ‘Non-Active’ | Autologous blood injection is effective in patients with LE and this effectiveness has continued at 6 months. Therefore, autologous blood injection is effective and has relatively few side effects. | 3 |
| Vuvan 2019 Australia187 |
RCT | N = 39 % female 28 Age 48.5 (9) Symptoms 4 (NR) Training status Other |
2 | 1× ‘Exercise only’; 1× ‘Exercise, Manual-Therapy’ | Unsupervised isometric exercise was effective in improving pain and disability, but not perceived rating of change and pain-free grip strength when compared with wait-and-see at 8 weeks. With only one of the three primary outcomes being significantly improved, it is doubtful if isometric exercises can be an efficacious standalone treatment. | 1a, 1b, 1c, 3 |
| Sevier 2015 United States584 |
RCT | N = 90 % female 57.9 Age 46.95 (6.55) Symptoms NR Training status Other |
2 | 1× ‘Exercise only’; 1× ‘Exercise, Non-Active’ | Astym therapy is an effective treatment option for patients with LE tendinopathy, as an initial treatment, and after an eccentric exercise programme has failed. | 1a, 1b, 1c, 3 |
| Park 2010 Korea (Republic of)521 |
RCT | N = % female Age Symptoms Training status |
2 | 1× ‘Exercise, Kinetics’; 1× ‘Exercise only’ | Isometric strengthening exercises done early in the course of LE (within 4 weeks) provide a clinically significant improvement. | 1a, 1c, 3 |
| Svernlov 2001 Sweden614 |
Quasi-experimental | N = 57 % female 61.3 Age 50.15 (NR) Symptoms 6.3 (NR) Training status Other |
2 | 2× ‘Exercise only’ | Significant improvements observed for VAS and grip strength warrant clinical use of this regime. | 1a, 1c, 3 |
| Peterson 2014 Sweden185 |
RCT | N = 120 % female 47.5 Age 47.9 (8.1) Symptoms NR Training status Other |
2 | 1× ‘Exercise, Manual-Therapy’; 1× ‘Exercise, Electro-Therapy’ | Eccentric graded exercise reduced pain and increased muscle strength in chronic tennis elbow more effectively than concentric graded exercise at follow-up. However, there were no significant differences in function or QoL measures between the two groups. | 1a, 1c, 2, 3 |
| Rodríguez-Huguet 2020 Spain693 |
RCT | N = 36 % female 25 Age 40.04 (9.88) Symptoms NR Training status Other |
2 | 2× ‘Exercise, Kinetics’ | This study provides evidence that percutaneous electrolysis could be more effective than trigger-point dry needling for short- and medium-term improvement of pain and pressure pain thresholds in lateral epicondylalgia when added to an eccentric exercise programme. | 3 |
| McQueen 2020 United States694 |
RCT | N = 59 % female 63 Age NR Symptoms NR Training status Other |
2 | 2× ‘Exercise only’ | This study demonstrates that a therapy programme consisting of a low number of visits spaced out over 12 weeks based on education, stretches, activity modification and pain management techniques is effective at reducing pain and increasing function in patients with lateral epicondyle tendinopathy. The addition of strengthening to this programme did not improve outcomes. | 3 |
| Manias 2006 United Kingdom469 |
RCT | N = 40 % female 67.5 Age 42.86 (6.23) Symptoms NR Training status Other |
2 | 2× ‘Exercise only’ | An exercise programme consisting of eccentric and static stretching exercises had reduced the pain in patients with lateral epicondyle tendinopathy at the end of the treatment and at the follow-up whether or not ice was included. | 1a, 1c, 3 |
| Stasinopoulos 2013 Greece331 |
RCT | N = 60 % female 36.7 Age 48.0 (5.9) Symptoms 4.5 (NR) Training status Other |
2 | 1× ‘Non-Exercise only’; 1× ‘Exercise, Injection, Manual-Therapy’; 1× ‘Non-Active’;1× ’Exercise, Manual-Therapy, Non-Active’ | A specific supervised exercise programme is superior to a specific HEP in reducing pain and improving function in patients with lateral epicondyle tendinopathy at the end of the treatment and at the 3-month follow-up. | 1a, 1c, 2, 3 |
| Other | ||||||
| Chen 2017 Taiwan284 |
RCT | N = 120 % female NR Age NR Symptoms NR Training status Other |
4 | 4× ‘Exercise, Electro-Therapy, Manual-Therapy’ | Combined treatment (eccentric, ESWT and conventional) improved patients with noncalcific subscapular tendinosis. | 3 |
| Ilhanli 2015695 |
RCT | N = 62 % female 72.6 Age 59.4 (10.2) Symptoms 7.2 (3.8) Training status Other |
2 | 1× ‘Non-Exercise only’; 1× ‘Exercise, Electro-Therapy’ | When we compared with physical therapy, PRP seemed to be a well-tolerated application which showed promising results in patients with chronic partial supraspinatus tears. | 3 |
| Turgut 2017 Turkey633 |
RCT | N = 30 % female 46.7 Age 36.45 (17.5) Symptoms 6.28 (5.4) Training status Other |
2 | 2× ‘Exercise only’ | Progressive exercise training independent from specific scapular stabilisation exercises provides decreased disability and pain severity in impingement syndrome. All groups showed improvement; however, there were no significant differences between the groups. | 1a, 1c, 2, 3 |
| Patellar | ||||||
| Scott 2019 Canada577 |
RCT | N = 57 % female 15 Age 32 (8.3) Symptoms 24.7 (22.3) Training status Recreational |
3 | 2× ‘Exercise, Injection’; 1× ‘Exercise, Non-Active’ | Combined with an exercise-based rehabilitation programme, a single injection of leukocyte-rich PRP or leukocyte-poor PRP was no more effective than saline for the improvement of patellar tendinopathy symptoms. | 3 |
| Cho 2017 Korea (Republic of)289 |
Quasi-experimental | N = 30 % female 46.7 Age 33.1 (29.1) Symptoms 15.1 (16.1) Training status Other |
3 | 1× ‘Exercise, Injection’; 1× ‘Exercise only; 1× ’Non-Exercise only’ | A rehabilitation exercise programme was more effective at improving pain, strength and function in patellar tendinopathy than injection therapy alone. | 1a, 1c, 3 |
| Kongsgaard 2009 Denmark21 |
RCT | N = 37 % female 0 Age 32.4 (8.8) Symptoms 18.7 (12.3) Training status Recreational |
3 | 1× ‘Non-Exercise only’; 2× ‘Exercise only’, ‘Exercise only’ | Corticosteroid injection has good short-term but poor long-term clinical effects, in patellar tendinopathy. Heavy-slow resistance exercise has good short- and long-term clinical effects accompanied by pathology improvement and increased collagen turnover. | 1a, 1b, 1c, 2, 3 |
| van Ark 2016 Australia644 |
RCT | N = 19 % female 6.9 Age 23 (4.7) Symptoms 35.8 (33.8) Training status Recreational |
2 | 2× ‘Exercise only’ | This study found favourable results for athletes with patellar tendinopathy without modification of the training. Both isometric and isotonic exercise programmes reduced pain and improved function in athletes with patellar tendinopathy during a season. | 1a, 1b, 1c, 2, 3 |
| Bahr 2006 Norway131 |
RCT | N = 40 % female 12.5 Age 30.5 (7.9) Symptoms 34 (28.7) Training status Other |
2 | 1× ‘Exercise only’; 1× ‘Exercise, Surgery’ | No added benefit was observed for surgical treatment to eccentric strength training. Eccentric training should be offered for 12 weeks before tenotomy is considered for the treatment of patellar tendinopathy. | 1a, 1b, 1c, 3 |
| Warden 2008 United States652 |
RCT | N = 37 % female 18 Age 27 (7) Symptoms 44.4 (43.2) Training status Other |
2 | 1× ‘Exercise, Electro-Therapy’; 1× ‘Exercise, Non-Active’ | Low-intensity pulsed ultrasound does not provide any additional benefit over and beyond placebo in the management of patellar tendinopathy. | 3 |
| Clarke 2010 United Kingdom294 |
RCT | N = 60 % female 10.9 Age 36 (20–51)** Symptoms 11.1 (6–39)** Training status Other |
2 | 2× ‘Exercise, Injection’ | Ultrasound-guided injection of autologous skin-derived tendon-like cells can be safely used in the short term alongside exercise to treat patellar tendinopathy, with faster response of treatment and significantly greater improvement in pain and function than with plasma alone. | 3 |
| Steunebrink 2013 Netherlands605 |
RCT | N = 33 % female 24.2 Age 32.9 (10) Symptoms 11 (8) Training status Recreational |
2 | 1× ‘Exercise only’; 1× ‘Exercise, Non-Active’ | Continuous topical GTN treatment in addition to an eccentric exercise programme does not improve clinical outcome compared to placebo patches and an eccentric exercise programme in patients with chronic patellar tendinopathy. | 1a, 1b, 1c, 3 |
| Pearson 2018 Australia526 |
RCT | N = 16 % female 0 Age 28 (4.25) Symptoms 34.17 (1.95) Training status Performance |
2 | 2× ‘Exercise only’ | Pain was significantly reduced after isometric loading on both SLDS and hop tests. Pain and quadriceps function improved over the 4 weeks. Short-duration isometric contractions are found to be as effective as longer duration contractions for relieving patellar tendon pain when total time under tension is equalised. | 1a, 1c, 3 |
| Visnes 2005 Norway129 |
RCT | N = 29 % female 38.5 Age 26.58 (NR) Symptoms 73.6 (62.3) Training status Performance |
2 | 1× ‘Exercise only’; 1× ‘Non-Active’ | There was no effect on knee function (VISA) from a 12-week programme with eccentric training among a group of volleyball players with patellar tendinopathy who continued to train and compete during the treatment period. Whether the training would be effective if the patients did not participate in sports activity is not known. | 1a, 1c, 3 |
| Thijs 2017 Netherlands621 |
RCT | N = 52 % female 29 Age 28.6 (6.7) Symptoms 19.5 (24.7) Training status Recreational |
2 | 1× ‘Exercise, Electro-Therapy’; 1× ‘Exercise, Non-Active’ | There was no additional effect of 3 sessions of ESWT in participants with PT treated with eccentric exercises as no significant differences for primary and secondary outcomes were found. | 3 |
| Young 2005 Australia132 |
RCT | N = 17 % female 23.5 Age 27.3 (1.8) Symptoms NR Training status Performance |
2 | 2× ‘Exercise only’ | Both exercise protocols improved pain and sporting function in volleyball players over 12 months. The decline squat protocol offers greater clinical gains during a rehabilitation programme for patellar tendinopathy in athletes who continue to train and play with pain. | 1a, 1c, 2, 3 |
| Abat 2016 Spain213 |
RCT | N = 60 % female 21.7 Age 31.0 (6.2) Symptoms 29.2 (32.0) Training status Recreational |
2 | 2× ‘Exercise, Electro-Therapy’ | Combining USGET and eccentric exercise resulted in better outcomes for patellar tendinopathy patients than using conventional electrophysiotherapy techniques. | 3 |
| Rosety-Rodriguez 2006 Spain560 |
Quasi-experimental | N = 46 % female 0.0 Age NR Symptoms NR Training status Other |
2 | 2× ‘Exercise, Electro-Therapy, Manual-Therapy’ | Conservative treatment based on decline eccentric programme showed better results than standard squat programme. | 3 |
| Lee 2017 Hong Kong, China (SAR)459 |
RCT | N = 28 % female 0.0 Age 22.6 (3.4) Symptoms 33.5 (26.2) Training status Recreational |
2 | 1× ‘Exercise, Electro-Therapy’; 1× ‘Exercise, Non-Active’ | Eccentric exercise-induced modulation on tendon mechanical properties and clinical symptoms is associated in athletes with patellar tendinopathy. | 3 |
| Rio 2017 Australia167 |
RCT | N = 20 % female 10.0 Age 22.5 (4.7) Symptoms NR Training status Performance |
2 | 2× ‘Exercise only’ | Both isometric and isotonic contraction protocols appear efficacious for in-season athletes to reduce pain; however, isometric contractions demonstrated significantly greater immediate analgesia throughout the 4-week trial. | 1a, 1c, 3 |
| Jonsson 2005 Sweden186 |
RCT | N = 15 % female 13.3 Age 24.9 (8.2) Symptoms 17.5 (13.2) Training status Performance |
2 | 2× ‘Exercise only’ | Eccentric, but not concentric, quadriceps training on a decline board seems to reduce pain in jumper’s knee. | 1a, 1b, 1c, 2, 3 |
| Dimitrios 2012 Greece330 |
Quasi-experimental | N = 60 % female 36.7 Age 47.6 (5.9) Symptoms 4.5 (NR) Training status Other |
2 | 2× ‘Exercise only’ | Eccentric training and static stretching exercises are superior to eccentric training alone to reduce pain and improve function in patients with patellar tendinopathy at the end of the treatment and at follow-up. | 1a, 1b, 1c, 2, 3 |
| Breda 2020 Netherlands696 |
RCT | N = 76 % female 23.7 Age 24 (3.9) Symptoms 98.5 (NR) Training status Performance |
2 | 2× ‘Exercise only’ | In patients with patellar tendinopathy, progressive tendon-loading exercises resulted in a significantly better clinical outcome after 24 weeks than eccentric exercise therapy. Progressive tendon-loading exercises are superior to eccentric exercise therapy and are therefore recommended as initial conservative treatment for patellar tendinopathy. | 1a, 1b, 1c, 2, 3 |
| Lee 2017 Hong Kong, China (SAR)697 |
RCT | N = 34 % female 0.0 Age 22.6 (3.4) Symptoms 33.6 (26.2) Training status Performance |
2 | 1× ‘Exercise, Electro-Therapy’; 1× ‘Exercise, Non-Active’ | Eccentric exercise alone was effective in increasing tendon strain and reducing pain. The addition of ESWT did not provide any further benefits. | 3 |
| Rotator cuff | ||||||
| Hallgren 2014 Sweden383 |
RCT | N = 50 % female 37.0 Age 52 (30–65)** Symptoms 18 (6–186)* Training status Other |
4 | 2× ‘Exercise only’;2× ‘Exercise, Surgery’ | Specific exercises produced positive short-term improvements at 1-year follow-up and reduced the need for surgery. Full-thickness tear and a low CMS score appear to be predictors of poor outcome. | 1a, 1c, 2, 3 |
| Pekyavas 2016 Turkey527 |
RCT | N = 70 % female NR Age 47.1 (13.8) Symptoms NR Training status Other |
4 | 1× ‘Exercise only’;1× ‘Exercise, Kinetics’;1× ‘Exercise, Kinetics, Manual-Therapy’; 1× ‘Exercise, Electro-Therapy, Kinetics, Manual-Therapy’ | HILT and MT were found to be more effective in reducing pain and disability and improving ROM in patients with SAIS. | 1a, 1c, 3 |
| Hallgren 2017 Sweden258 |
RCT | N = 108 % female 34.1 Age 58 (NR) Symptoms NR Training status Other |
4 | 2× Exercise only’; 2× ‘Exercise, Surgery’ | More patients in the specific exercise group managed to avoid surgery compared to the unspecific exercise group at 5-year follow-up, supporting its prescription as an initial treatment for patients with subacromial pain. | 1a, 1c, 2, 3 |
| Polimeni 2003 Italy698 |
RCT | N = 50 % female 72.0 Age 56 (16) Symptoms NR Training status Other |
4 | 1× ‘Exercise only’; 3× ‘Exercise, Electro-Therapy’ | All patients experienced improvement with treatment, but the association of physical therapy and functional rehabilitation did not seem to lead to added benefit for the patient. | 1a, 3 |
| Faria 2006 Portugal354 |
Quasi-experimental | N = 103 % female NR Age 52.5 (NR) Symptoms NR Training status Other |
3 | 1× ‘Exercise, Manual-Therapy’; 2× Exercise, Electro-Therapy, Manual-Therapy’ | All treatment groups effectively reduced pain. However, it is not clear whether the significant differences observed between groups could be due to factors other than the primary intervention in the absence of randomisation. | 3 |
| Brox 1999 Norway269 |
RCT | N = 125 % female 44.0 Age 47.6 (23–66)** Symptoms NR Training status Other |
3 | 1× ‘Exercise, Surgery’; 1× ‘Non-Active’; 1× Exercise only’ | At 2.5 years follow-up, both arthroscopic surgery and supervised exercises are better treatments than placebo with no significant difference between the two active treatments. | 1a, 1b, 3 |
| Pérez-Merino 2016 Spain529 |
RCT | N = 99 % female 56.3 Age 54.4 (9.4) Symptoms 7.4 (7.7) Training status Other |
3 | 3× ‘Exercise, Electro-Therapy’ | Ultrasound, iontophoresis with dexketoprofen and phonophoresis with dexketoprofen can improve pain, shoulder function and physical functioning and symptoms in the upper limb in patients with SIS without a complete tear of the rotator cuff. | 3 |
| Ludewig 2003 United States463 |
RCT | N = 85 % female 0.0 Age 48.8 (2.1) Symptoms NR Training status Other |
3 | 1× ‘Exercise only’; 2× ‘Non-Active’ | HEPs are more effective in reducing symptoms and improving function (Shoulder Rating Questionnaire, shoulder satisfaction score) compared to the control group in construction workers with shoulder pain. | 1a, 1b, 3 |
| Paavola 2018 Finland516 |
RCT | N = 186 % female 69.8 Age 50.6 (5.0) Symptoms 19.5 (18.9) Training status N R |
3 | 1× ‘Exercise only’; 2× ‘Non-Exercise only’ | Arthroscopic subacromial decompression provided no benefit over diagnostic arthroscopy in patients with shoulder impingement syndrome. | 1a, 1b, 3 |
| Calis 2011 Turkey273 |
RCT | N = 52 % female 67.3 Age 49.2 (12.6) Symptoms 3.0 (1–24)** Training status Other |
3 | 2× ‘Exercise, Electro-Therapy’; 1× ‘Exercise only’ | Ultrasound and laser treatments were not superior to each other in the treatment of SIS. | 1a, 3 |
| Melegati 2000 Italy480 |
RCT | N = 90 % female 65.5 Age 54.4 (3.0) Symptoms NR Training status Other |
3 | 1× ‘Exercise only’; 1× ‘Exercise, Electro-Therapy’; 1× ‘Non-Active’ | Groups A (kinesitherapy) and B (ESWT + kinesitherapy) achieved a significant constant score improvement, whereas the increase in group C (control) was not significant. | 1a, 3 |
| Tahran 2020 Turkey618 |
RCT | N = 67 % female 30.5 Age 52.9 (11.0) Symptoms NR Training status Other |
3 | 2× ‘Exercise only’; 1× ‘Exercise, Electro-Therapy’ | All treatments improved pain, shoulder mobility, function and disability in patients with SIS. However, modified posterior shoulder stretching exercises in addition to a treatment programme was superior to the treatment programme alone in improving pain with activity, internal rotation ROM and dysfunction. Moreover, stretching provided clinically significant improvements. | 1a, 3 |
| Land 2019 Australia452 |
RCT | N = 60 % female 50.0 Age 51.0 (5.3) Symptoms 8.5 (4.0) Training status Other |
3 | 2× ‘Exercise, Manual-Therapy’; 1× ‘Non-Exercise only’ | Upper thoracic and posterior shoulder interventions with a targeted home exercise that addresses thoracic spine or posterior shoulder tightness improves the signs and symptoms of SIS. | 3 |
| García 2016 Spain362 |
RCT | N = 78 % female 60.1 Age 58.8 (14.2) Symptoms NR Training status Other |
3 | 1× ‘Exercise, Non-Active’; 2× ‘Exercise, Electro-Therapy, Non-Active’ | In patients with impingement syndrome, a combination of ultrasonophoresis and an exercise programme is better than a combination of iontophoresis and the same exercise programme or the exercise programme alone. | 3 |
| Devereaux 2016 Canada326 |
RCT | N = 100 % female 37.9 Age 48.0 (11.9) Symptoms NR Training status Other |
3 | 1× ‘Exercise, Kinetics’; 2× ‘Exercise only’ | The improvements in pain and function observed with an NSAID or precut kinesiology tape as adjuvant treatments were no greater than with rehabilitation exercise alone. | 1a, 1b, 3 |
| Heron 2017 United Kingdom390 |
RCT | N = 120 % female 41.0 Age 49.9 (NR) Symptoms NR Training status Other |
3 | 3× ‘Exercise only’ | Open chain, closed chain, and range of movement exercises all seem to be effective in bringing about short-term changes in pain and disability in patients with rotator cuff tendinopathy. | 1a, 1c, 2, 3 |
| Walther 2004 Germany161 |
RCT | N = 60 % female 43.3 Age 50.7 (NR) Symptoms 27.3 (NR) Training status Other |
3 | 2× ‘Exercise only’; 1× ‘Non-Exercise only’ | There were no statistically significant differences among the groups. Guided self-training can lead to results similar to those of conventional physiotherapy. | 1a, 1c, 2, 3 |
| Maenhout 2013 Belgium464 |
RCT | N = 61 % female 59.0 Age 39.8 (13.0) Symptoms NR Training status Other |
2 | 2× ‘Exercise only’ | Adding heavy-load eccentric training resulted in a higher gain in isometric strength at 90 degrees of scapular abduction, but was not superior for decreasing pain and improving shoulder function. The addition of a limited number of physiotherapy sessions combined with a daily HEP is highly effective in patients with impingement. | 1a, 1c, 2, 3 |
| Nazligul 2018 Turkey493 |
RCT | N = 65 % female 56.6 Age 50.0 (9.1) Symptoms 4.7 (25.1) Training status Other |
2 | 1× ‘Exercise, Electro-Therapy’; 1× ‘Exercise, Non-Active’ | IFC therapy had no additional benefit over NSAID, cryotherapy and exercise programme in the treatment of SIS. | 3 |
| Ellegaard 2016 Denmark342 |
RCT | N = 99 % female 59.0 Age 48.5 (13.1) Symptoms NR Training status Other |
2 | 2× ‘Exercise, Injection’ | 10 weeks of unilateral exercise as an adjunct to subacromial steroid injections did not improve the primary outcome of shoulder pain due to SAPS and enlarged subacromial bursa, compared to exercise. | 3 |
| Dogan 2010 Turkey333 |
RCT | N = 52 % female 63.5 Age 53.6 (11.3) Symptoms 13.2 (21.2) Training status Other |
2 | 1× ‘Exercise, Electro-Therapy’; 1× ‘Exercise, Non-Active’ | Laser therapy was no more effective than placebo laser. | 3 |
| Engebretsen 2009 Norway344 |
RCT | N = 104 % female 50.0 Age 48.0 (10.6) Symptoms 12.5 (NR) Training status Other |
2 | 1× ‘Exercise only’; 1× ‘Non-Exercise only’ | Supervised exercises are superior to ESWT in terms of shoulder pain, disability and some work-related outcomes. | 1a, 1b, 3 |
| Kromer 2014 Germany445 |
RCT | N = 90 % female 51.1 Age 51.8 (11.2) Symptoms 24.1 (35.1) Training status Other |
2 | 1× ‘Exercise, Manual-Therapy’; 1× ‘Exercise only’ | The use of MT including physiotherapy provides no additional benefits and is more expensive in comparison to exercise only interventions. | 1a, 1c, 3 |
| Seven 2017 Turkey583 |
RCT | N = 101 % female 45.5 Age 48.5 (11.6) Symptoms 19.5 (12.4) Training status Other |
2 | 1× ‘Exercise, Injection’; 1× ‘Exercise only’ | Prolotherapy is an easily applicable treatment which may be superior in enhancing pain and function outcomes in comparison to exercise alone. | 1a, 1b, 3 |
| Engebretsen 2011 Norway345 |
RCT | N = 104 % female 50.0 Age 48.0 (10.6) Symptoms 12.5 (NR) Training status Other |
2 | 1× ‘Exercise only’; 1× ‘Non-Exercise only’ | Both radial ESWT and the supervised exercise regime devised by Bohmer (1998) provided similar benefits in pain and function-related outcomes. However, exercise may be superior for work-related outcomes. | 1a, 1b, 3 |
| Conroy 1998 United States298 |
RCT | N = 14 % female 71.4 Age 52.8 (13.4) Symptoms NR Training status Other |
2 | 2× ‘Exercise, Manual-Therapy’ | Both groups improve mobility and function in shoulder impingement syndrome but only joint mobilisation relieves pain over a 24-hour period. | 3 |
| Celik 2009 Turkey278 |
Quasi-experimental | N = 56 % female 71.4 Age 50.0 (NR) Symptoms NR Training status Other |
2 | 1× ‘Exercise, Electro-Therapy, Injection, Manual-Therapy’; 1× ‘Exercise, Electro-Therapy, Manual-Therapy’ | Despite initial short-term pain relief from injection, both groups demonstrated improvements at 3 and 6 weeks. | 3 |
| Başkurt 2011 Turkey246 |
Quasi-experimental | N = 40 % female 67.5 Age 51.4 (10.0) Symptoms NR Training status Other |
2 | 2× ‘Exercise only’ | Scapular stabilisation combined with stretching and strengthening exercises can be more effective in the short term for SIS. | 1a, 2, 3 |
| Celik 2009 Turkey279 |
Quasi-experimental | N = 30 % female 76.0 Age 52.0 (34–70)** Symptoms NR Training status Other |
2 | 2× ‘Exercise, Electro-Therapy’ | Both groups had significant improvements in pain and disability measures; however, exercise programme within pain-free ROM showed additional improvements in VAS and face scores in SIS. | 3 |
| Yeldan 2009 Turkey672 |
Quasi-experimental | N = 60 % female 78.0 Age 55.2 (8.7) Symptoms 6.5 (4.6) Training status Other |
2 | 1× ‘Exercise, Electro-Therapy’; 1× ‘Exercise, Non-Active’ | No significant difference between LLLT and placebo LLLT when they are supplementing an exercise programme for treatment of shoulder impingement syndrome. | 3 |
| Ingwersen 2017 Denmark191 |
RCT | N = 100 % female 46.0 Age 46.1 (10.3) Symptoms 12 (NR) Training status Other |
2 | 2× ‘Exercise, Injection’ | No superior benefit of PHLE was seen when compared with LLE in primary or secondary outcomes. | 3 |
| Arias-Buría 2015 Spain230 |
RCT | N = 36 % female 75.0 Age 57.5 (6.4) Symptoms 10.9 (2.6) Training status Other |
2 | 1× ‘Exercise, Electro-Therapy’; 1× ‘Exercise only’ | Ultrasound-guided percutaneous electrolysis combined with eccentric exercises resulted in better short-term outcomes compared to eccentric exercises alone. | 1a, 1c, 3 |
| Blume 2015 United States699 |
RCT | N = 34 % female 58.0 Age 49.4 (15.6) Symptoms 22.7 (24.3) Training status Other |
2 | 2× ‘Exercise only’ | Both eccentric and concentric PRE programmes resulted in improved function, AROM and strength in patients with SAIS. However, no difference was found between the two exercise modes, suggesting that therapists may use exercises that utilise either exercise mode in their treatment of SAIS. | 1a, 1c, 2, 3 |
| Chary-Valckenaere 2018 France283 |
RCT | N = 185 % female 52.0 Age 54.0 (10.6) Symptoms 76.4 (79.8) Training status Other |
2 | 1× ‘Exercise, Manual-Therapy’; 1× ‘Non-Active’ | Spa therapy consisting of mineral water baths and mud applications together with supervised self-mobilisation in a thermal pool provided significant benefit in pain, function and QoL in patients with chronic shoulder pain compared to usual care. | 3 |
| Boudreau 2019 Canada262 |
RCT | N = 42 % female 52.4 Age 42.9 (12.0) Symptoms 43.0 (46.6) Training status Other |
2 | 2× ‘Exercise only’ | No additional benefit was found to adding coactivation to regular rotator cuff strengthening exercises at 6 weeks. | 1a, 1c, 3 |
| Kim 2017 Korea (Republic of)431 |
RCT | N = 40 % female 72.5 Age 51.1 (10.6) Symptoms NR Training status Other |
2 | 2× ‘Exercise only’ | The use of visual feedback and 3D motion images can improve pain and function in SIS. | 1a, 3 |
| Şimşek, 2013 Turkey591 |
RCT | N = 38 % female 65.8 Age 51.0 (18–69)** Symptoms NR Training status Other |
2 | 1× ‘Exercise, Kinetics’; 1× ‘Exercise only’ | Findings were inconclusive and require further research. | 1a, 1c, 3 |
| Vinuesa-Montoya 2017 Spain641 |
RCT | N = 40 % female 26.8 Age 47.0 (9.0) Symptoms 6.2 (3.8) Training status Other |
2 | 1× ‘Exercise only’; 1× ‘Exercise, Manual-Therapy’ | Cervicothoracic manipulative treatment with mobilisation plus exercise therapy may improve intensity of pain and ROM compared with home exercise alone. | 1a, 1c, 3 |
| Kromer 2013 Germany443 |
RCT | N = 90 % female 51.1 Age 51.8 (11.2) Symptoms 7.8 (9.8) Training status Other |
2 | 1× ‘Exercise, Manual-Therapy’; 1× ‘Exercise only’ | Individually adapted exercises were effective in the treatment of patients with shoulder impingement syndrome. Individualised manual physiotherapy contributed only a minor amount to the improvement in pain intensity. | 1a, 1b, 1c, 3 |
| Şenbursa 2011 Turkey582 |
RCT | N = 47 % female NR Age 49.0 (9.3) Symptoms NR Training status Other |
2 | 1× ‘Exercise only’; 1× ‘Exercise, Manual-Therapy’ | Supervised exercise, supervised and MT, and home-based exercise are all effective and promising treatments for patients with subacromial impingement syndrome. The addition of an initial MT may improve outcomes with exercise. | 1a, 1c, 3 |
| Marzetti 2014 Italy472 |
RCT | N = 48 % female 61.4 Age 62.1 (12.5) Symptoms NR Training status Other |
2 | 2× ‘Exercise only’ | Neurocognitive rehabilitation is effective in reducing pain and improving function in patients with shoulder impingement syndrome, with benefits maintained for at least 24 weeks. | 1a, 1b, 1c, 2, 3 |
| Østerås 2008 Norway511 |
RCT | N = 61 % female 20.0 Age 44.0 (13.9) Symptoms 40.0 (8.1) Training status Other |
2 | 2× ‘Exercise only’ | In patients with longstanding subacromial pain, high-dose medical exercise therapy had better outcomes than low-dose. | 3 |
| Arias-Buría 2017 Spain229 |
RCT | N = 50 % female 26.0 Age 48.5 (5.5) Symptoms 71.9 (21.6) Training status Other |
2 | 1× ‘Exercise only’; 1× ‘Exercise, Manual-Therapy’ | This study found that the inclusion of two sessions of TrP-DN in an exercise programme was effective for improving shoulder pain-related disability at short, medium and long term; however, no greater improvement in shoulder pain was observed. | 1a, 1b, 1c, 3 |
| Vallés-Carrascosa 2018 Spain638 |
RCT | N = 22 % female 54 Age 59.0 (58.5–70.0)* Symptoms Training status Other |
2 | 2× ‘Exercise only’ | Both rotator cuff eccentric exercise protocols with scapular stabilising and stretching of upper trapezius were equally effective in improving pain, function, and active ROM in the short term in patients with subacromial syndrome. | 1a, 1c, 3 |
| Østerås 2010 Norway514 |
RCT | N = 61 % female 20.5 Age 43.9 (13) Symptoms 40.2 (56.3) Training status Other |
2 | 2× ‘Exercise only’ | In long-term subacromial pain syndrome, high-dosage medical exercise therapy is superior to a conventional low-dosage exercise programme. | 1a, 1c, 3 |
| Mulligan 2016 United States489 |
RCT | N = 50 % female 65 Age 50.1 (10.7) Symptoms 7.9 (7.4) Training status Other |
2 | 1× ‘Exercise only’; 1× ‘Exercise, Manual-Therapy’ | Patients with SAIS demonstrate improvement in pain and function with a standardised programme of physical therapy regardless of group exercise sequencing. | 1a, 1b, 1c, 3 |
| Yazmalar 2016 Turkey671 |
RCT | N = 50 % female 44 Age 51.9 (21.5) Symptoms 12.9 (13) Training status Other |
2 | 1× ‘Exercise, Electro-Therapy’;1× ‘Exercise, Non-Active’ | Transcutaneous electrical nerve stimulation and exercise are effective on pain, disability and sleep disturbance but may not be effective on other psychosocial measures like anxiety, depression and fatigue in patients with SIS. | 3 |
| Bennell 2010 Australia188 |
RCT | N = 120 % female 46.7 Age 60.1 (11.3) Symptoms 19 Training status Other |
2 | 1× ‘Exercise, Kinetics, Manual-Therapy’; 1× ‘Non-Active’ | Immediately after the intervention, active treatment produced similar benefits on shoulder pain and function compared with a realistic placebo. However, significant improvements in pain and function were found in favour of active treatment at follow-up. | 3 |
| Kang 2019 Taiwan416 |
RCT | N = 34 % female 70.6 Age 47.6 (11.4) Symptoms Training status Other |
2 | 1× ‘Exercise, Kinetics’; 1× ‘Exercise only’ | Four weeks of strengthening and stretching exercises with or without kinesiology taping improved functional performance in subjects with SIS and RSP. Kinesiology taping did not demonstrate an additional effect on RSP. | 3 |
| Dupuis 2018 Canada339 |
RCT | N = 43 % female 55.8 Age 33.3 (11.7) Symptoms 0.9 (0.3) Training status Other |
2 | 2× ‘Exercise only’ | Both groups showed statistically significant improvements on symptoms and function at 2 weeks and 6 weeks but there was no difference between the short-term effect of cryotherapy and a gradual reloading exercise programme. | 1a, 1b, 1c, 2, 3 |
| Santamato 2016 Italy570 |
RCT | N = 30 % female 53.3 Age 40.2 (5) Symptoms 7.5 (3.9) Training status Other |
2 | 1× ‘Non-Exercise only’; 1× ‘Exercise, Electro-Therapy’ | In subjects with SAIS, combined administration of focussed ESWT and IE for the rotator cuff resulted in greater reduction of pain, as well as superior functional recovery and muscle endurance in the short to medium term, compared with ESWT alone. | 3 |
| Holmgren 2012 Sweden393 |
RCT | N = 97 % female 37.1 Age 52 (8.5) Symptoms 18 Training status Other |
2 | 1× ‘Exercise, Injection, Manual-Therapy’; 1× ‘Exercise, Injection’ | Specific exercise strategy focussing on strengthening eccentric exercises for the rotator cuff and concentric/eccentric exercises for the scapula stabilisers is effective in reducing pain and improving shoulder function in patients with persistent subacromial impingement syndrome. By extension, this exercise strategy reduces the need for arthroscopic subacromial decompression at 3 months. | 3 |
| Menek 2019 Turkey482 |
RCT | N = 30 % female 40 Age 51 (5.5) Symptoms Training status Other |
2 | 2× ‘Exercise, Electro-Therapy’ | Mulligan mobilisation was more effective than general treatment methods for pain as well as normal joint motion, DASH scoring and some parameters of SF-36 compared with general treatment methods. | 3 |
| Juul-Kristensen 2019 Denmark412 |
RCT | N = 58 % female 51 Age 42.9 (12.4) Symptoms NR Training status Other |
2 | 2× ‘Exercise only’ | Electromyography-biofeedback neuromuscular shoulder exercises and neuromuscular shoulder exercises were both effective in reducing pain to a clinically relevant level, while electromyography biofeedback did not make a difference. The current neuromuscular shoulder exercise protocol is recommended. | 1a, 2, 3 |
| Aktas 2007 Turkey220 |
RCT | N = 40 % female 75 Age 51.3 (10.4) Symptoms 4.8 (3.6) Training status Other |
2 | 1× ‘Exercise, Electro-Therapy’; 1× ‘Exercise, Non-Active’ | Electromagnetic therapy did not provide additional benefit in acute phase rehabilitation programme of SIS. | 3 |
| Akkaya 2016 Turkey218 |
RCT | N = 34 % female 67.6 Age 41.7 (8.9) Symptoms 6.9 (4.1) Training status Other |
2 | 2× ‘Exercise only’ | Weighted and unweighted solo pendulum exercises achieved significant clinical improvements but showed no differences in ultrasonographic acrohumeral distance measurements between groups. | 1a, 3 |
| Jasnauskaitė-Gedrimė 2018 Lithuania401 |
RCT | N = 30 % female 43.3 Age 43.4 (12.6) Symptoms Training status Other |
2 | 2× ‘Exercise, Manual-Therapy’ | Visual feedback exercises had greater effect on shoulder functions and the QoL compared to auditory feedback exercises. | 3 |
| Belley 2018 Canada164 |
RCT | N = 40 % female 45 Age 45.5 (10) Symptoms 9.0 (NR) Training status Other |
2 | 1× ‘Exercise, Electro-Therapy, Manual-Therapy’; 1× ‘Exercise, Manual-Therapy, Non-Active’ | Results do not demonstrate any improved treatment outcomes from the addition of anodal transcranial direct-current stimulation during a rehabilitation programme for individuals with rotator cuff tendinopathy. | 3 |
| Johansson 2005 Sweden405 |
RCT | N = 85 % female 69.4 Age 49 (7.5) Symptoms NR Training status Other |
2 | 1× ‘Exercise only’; 1× ‘Exercise, Electro-Therapy’ | Acupuncture was more effective than ultrasound when applied in addition to home exercises. | 1a, 1c, 3 |
| Aceituno-Gómez 2019 Spain215 |
Quasi-experimental | N = 43 % female 60.9 Age 59 (8.9) Symptoms NR Training status Other |
2 | 1× ‘Exercise, Electro-Therapy’; 1× ‘Exercise only’ | High-intensity laser therapy plus exercise did not give greater improvements in pain and functionality in patients with subacromial syndrome than exercise alone. | 1a, 1b, 3 |
| Kim 2020 Korea (Republic of)433 |
RCT | N = 40 % female 100 Age 46.2 (4.6) Symptoms NR Training status Other |
2 | 1× ‘Exercise only’; 1× ’Non-Exercise only’ | Both the Neurac modality and MT induced pain relief, improved function and increased ROM. The Neurac intervention also resulted in a significant enhancement of shoulder muscle strength, indicating its superiority as an effective therapeutic modality for this particular patient group. | 1a, 1b, 3 |
| Dejaco 2017 Netherlands44 |
RCT | N = 36 % female 47.3 Age 49.5 (11.3) Symptoms 19.7 (20.1) Training status Other |
2 | 2× ‘Exercise only’ | 12-week-isolated eccentric training programme of the RC is beneficial for shoulder function and pain after 26 weeks in patients with RC tendinopathy. However, it is no more beneficial than a conventional exercise programme for the RC and scapular muscles. | 1a, 1c, 2, 3 |
| Akyol 2012 Turkey221 |
RCT | N = 40 % female 75.0 Age 59.2 (10.4) Symptoms 12.3 (13.5) Training status Other |
2 | 1× ‘Exercise, Electro-Therapy’; 1× ‘Exercise, Non-Active’ | No statistically significant difference was found between the groups. As it is effective, superficial heat and exercise programme may be a preferable treatment for SIS. | 3 |
| Bang 2000 United States239 |
RCT | N = 50 % female 42.3 Age 43 (9.1) Symptoms 5 (3.3) Training status Other |
2 | 1× ‘Exercise, Manual-Therapy’; 1× ‘Exercise only’ | Manual physical therapy applied by experienced physical therapists combined with supervised exercise in a brief clinical trial is better than exercise alone for increasing strength, decreasing pain and improving function in patients with shoulder impingement syndrome. | 1a, 3 |
| Bae 2011 Korea (Republic of)234 |
Quasi-experimental | N = 35 % female 65.7 Age 49.1 (4.9) Symptoms Training status Other |
2 | 1× ‘Exercise only’; 1× ’Non-Exercise only’ | The motor control and strengthening programme improved pain, function, strength and ROM. | 1a, 3 |
| Gürsel 2004 Turkey377 |
RCT | N = 33 % female 39.5 Age 54.1 (8.9) Symptoms 8.4 (9.7) Training status Other |
2 | 1× ‘Exercise, Electro-Therapy’; 1× ‘Exercise, Electro-Therapy, Non-Active’ | There is no added benefit to the use of 1-MHz ultrasound in combination with other interventions in the management of painful shoulder conditions to merit its wide use. | 3 |
| Østerås 2009 Norway512 |
RCT | N = 56 % female 70.6 Age 44 (13) Symptoms 40.2 (56.3) Training status Other |
2 | 2× ‘Exercise only’ | There is a dose–response effect when using active graded exercises to treat patients with long-standing subacromial pain. | 1b, 3 |
| Ketola 2009 Finland426 |
RCT | N = 134 % female 62.9 Age 47.1(23.3–60.0)** Symptoms 2.6 (NR) Training status Other |
2 | 1× ‘Exercise only’; 1× ‘Exercise, Surgery’ | Arthroscopic acromioplasty provides no clinically important effects over a structured and supervised exercise programme alone in terms of subjective outcome or cost-effectiveness when measured at 24 months. | 1a, 1c, 3 |
| de Miguel Valtierra 2018 Spain312 |
RCT | N = 48 % female 54 Age 54 (7) Symptoms 11.9 (12.5) Training status Other |
2 | 1× ‘Exercise, Manual-Therapy’; 1× ‘Exercise, Electro-Therapy, Manual-Therapy’ | Inclusion of ultrasound-guided percutaneous electrolysis in a treatment approach including MT and exercise resulted in no significant differences in shoulder-related disability and pressure pain sensitivity in subjects with subacromial pain syndrome. | 3 |
| Granviken 2015 Norway374 |
RCT | N = 44 % female 48 Age 47.9 (9.9) Symptoms 14.5 Training status Other |
2 | 2× ‘Exercise only’ | No significant differences in pain and disability were found between home exercises and supervised exercises of more than the first session of a 6-week exercise regime for people with subacromial impingement. | 1a, 1b, 3 |
| Rhon 2014 United States700 |
RCT | N = 98 % female 32 Age 41.0 (12.0) Symptoms 5.7 (9.15) Training status Other |
2 | 1× Exercise, Manual-Therapy’; 1× ‘Exercise, Injection’ | Both groups experienced significant improvement. The manual physical therapy group used less 1-year SIS-related health care resources than the corticosteroid injections group | 3 |
| McGee 1999 United States701 |
RCT | N = 15 % female 7.1 Age 36.4 (12.9) Symptoms NR Training status Other |
2 | 2× ‘Exercise, Electro-Therapy’ | In conclusion, following 6 weeks of physical therapy treatment, patients with shoulder impingement are stronger, less limited in their activities of daily living, and appear to require less medication. Addition of closed kinetic chain exercise to physical therapy treatments does not appear to affect patient outcomes. | 3 |
| Cha 2014 Korea (Republic of)702 |
RCT | N = 30 % female 0.0 Age 21.9 (1.8) Symptoms 5.6 (1.3) Training status Performance |
2 | 1× ‘Exercise, Electro-Therapy’; 1× ‘Non-Active’ | A12-week rehabilitation programme reduced the shoulder pain, improved the body composition and enhanced the isokinetic shoulder internal/external rotators in EG with impingement symptoms. | 3 |
| Littlewood 2016 United Kingdom34 |
RCT | N = 60 % female 50.3 Age 54.7 (NR) Symptoms 14.6 (NR) Training status Other |
2 | 1× ‘Exercise only’; 1× ‘Exercise, Manual-Therapy’ | Self-management programmes based on a single exercise were comparable to usual physiotherapy in the short, mid and long term. | 1a, 1c, 3 |
| Rodríguez-Huguet 2020 Spain693 |
RCT | N = 102 % female 37.5 Age 40.0 (9.9) Symptoms NR Training status Other |
2 | 1× ‘Exercise, Manual-Therapy’; 1× ‘Exercise, Electro-Therapy’ | Percutaneous electrolysis seems to be more effective than trigger-point dry needling in relieving pain and improving ROM and pressure pain threshold supraspinatus values in patients with supraspinatus tendinopathy, both right after treatment and at 1-year follow-up. | 3 |
| de Oliveira 2020 Canada703 |
RCT | N = 52 % female 42.3 Age 30.2 (8.3) Symptoms 22.6 (26.7) Training status Other |
2 | 1× ‘Exercise, Kinetics’; 1× ‘Exercise only’ | Whereas symptoms, functional limitations, ROM and AHD improved in both groups, the addition of KT did not lead to superior outcomes compared with exercise-based treatment alone, in the mid and long term, for individuals with RCRSP. | 1a, 1b, 3 |
| Buyuksireci 2020 Turkey704 |
RCT | N = 46 % female 65 Age 34.6 (8.5) Symptoms 5.0 (NR) Training status Other |
2 | 2× ‘Exercise, Electro-Therapy’ | Adding dexamethasone iontophoresis to physiotherapy for patients with subacromial impingement syndrome seems to provide a better clinical and functional improvement. | 3 |
| Beaudreuil 2012 France705 |
RCT | N = 62 % female 68 Age 58.7 (10.4) Symptoms 28.3 (54.6) Training status Other |
2 | 2× ‘Exercise, Manual-Therapy’ | At 3 months, pain-free ROM, both flexion and abduction, was greater in the DHC group than in the mobilisation group. The number of patients with painful arc during flexion was decreased in the dynamic humeral centring group. | 3 |
| Ketola 2013 Finland706 |
RCT | N = 140 % female 62.9 Age 41.7 Symptoms Training status Other |
2 | 1× ‘Exercise only’; 1× ‘Exercise, Surgery’ | Differences in the patient-centred primary and secondary parameters between the two treatment groups were not statistically significant, suggesting that acromioplasty is not cost-effective. | 1a, 3 |
| Pekgöz 2020 Turkey707 |
RCT | N = 40 % female 55 Age 43.6 (7.8) Symptoms Training status Other |
2 | 1× ‘Non-Exercise only’; 1× ‘Exercise, Electro-Therapy’ | Mobilisation and supervised exercise yield comparable outcomes in patients with SAIS. Patient satisfaction was similar in both groups. | 3 |
| Koç 2020 Turkey708 |
RCT | N = 90 % female 58.9 Age 48.1 (8.8) Symptoms 1.8 (0.6) Training status Other |
2 | 2× ‘Exercise, Electro-Therapy’ | The addition of balneotherapy to physical therapy for subacute supraspinatus tendinopathy can make additional contributions to shoulder ROM, pain, handgrip strength, functional status and QoL. | 3 |
| Hotta 2020 Brazil709 |
RCT | N = 60 % female 70 Age 49 (9) Symptoms 28.5 (24) Training status Other |
2 | 2× ‘Exercise only’ | The inclusion of the isolated scapular stabilisation exercises, emphasising retraction and depression of the scapula, to a progressive general periscapular strengthening protocol did not add benefits to self-reported shoulder pain and disability, muscle strength and ROM in patients with subacromial pain syndrome. | 1a, 1b, 1c, 2, 3 |
| Chaconas 2017 United States710 |
RCT | N = 46 % female 41.7 Age 45.9 (17.4) Symptoms 49.1 (80) Training status Other |
2 | 2× ‘Exercise only’ | An eccentric programme targeting the external rotators was superior to a general exercise programme for strength, pain and function after 6 months. The findings suggest eccentric training may be efficacious to improve self-report function and strength for those with SAPS. | 1a, 1b, 1c, 2, 3 |
| Werner 2002 Germany658 |
RCT | N = 20 % female 50 Age 51.75 (NR) Symptoms 27.5 Training status Other |
2 | 2× ‘Exercise only’ | Strengthening of the centring muscles around the humeral head led to positive outcomes for subacromial impingement. Self-training after instruction showed no difference to physiotherapist-supervised exercises. | 1a, 1b, 1c, 2, 3 |
| Cheng 2007 Hong Kong, China (SAR)286 |
RCT | N = 94 % female Age 32.4 (10.2) Symptoms 23.4 Training status Other |
2 | 2× ‘Exercise only’ | An eccentric programme targeting the external rotators was superior to a general exercise programme for strength, pain and function after 6 months. The findings suggest eccentric training may be efficacious to improve self-report function and strength for those with subacromial pain syndrome. | 1a, 1c, 3 |
| Tibialis posterior | ||||||
| Kulig 2009 United States448 |
RCT | N = 36 % female 77.8 Age 52 (15.4) Symptoms 30.6 (52) Training status Other |
3 | 3× ‘Exercise, Kinetics’ | People with early-stage tibialis posterior tendinopathy benefited from a programme of orthosis wear and stretching. Eccentric and concentric progressive resistive exercises further reduced pain and improved perceptions of function. | 3 |
| Bek 2012 Turkey250 |
Quasi-experimental | N = 49 % female Age 30.7 (16) Symptoms Training status Other |
2 | 1× ‘Exercise, Kinetics’; 1× ‘Exercise, Electro-Therapy, Kinetics, Manual-Therapy’ | While supervised, patient-selective programme may provide better improvement in tibialis posterior strength than home-based rehabilitation, both programmes seem to be effective in relieving pain and improving functional outcome in patients with Grade 1–3 PTTD. | 3 |
| Houck 2015 United States397 |
RCT | N = 38 % female 77.8 Age 57.5 (10.6) Symptoms Training status Other |
2 | 2× Exercise, Kinetics’ | A moderate-intensity, home-based exercise programme minimally improves outcomes over orthosis wear alone in participants with stage II tibialis posterior tendon dysfunction. The improvements observed were smaller than those reported in some previous controlled and uncontrolled clinical trials, suggesting that positive effects on function and pain in response to exercise may require higher intensity than this home-based programme for participants with tibialis posterior tendon dysfunction. | 3 |
| Jeong 2008 Korea (Republic of)711 |
RCT | N = 12 % female 100 Age 52.9 (14.4) Symptoms Training status Other |
2 | 1× ‘Exercise only’; 1× ‘Non-Active’ | A 6-week stretching and strengthening exercise programme significantly reduced pain compared to the control group and only the dorsiflexion was significantly increased in the exercise group in the analysis of ROM. | 3 |
Appendix 6 Effectiveness review strength of evidence and risk of bias assessments
This appendix provides a summary of the risk of bias results for each review, the distribution of data across the outcomes and tendinopathy locations in the featured analyses, and the associated strength of evidence assessment.
Effectiveness review 1A
| Author, year | Random sequence generation | Allocation concealment | Blinding of participants/personnel | Blinding of outcome assessment | Incomplete outcome bias | Selective reporting | Other bias |
|---|---|---|---|---|---|---|---|
| Aceituno-Gómez et al. 2019215 | Low risk | Unclear | Low risk | Low risk | Low risk | Low risk | High risk |
| Akkaya et al. 2016218 | Low risk | Unclear | High risk | High risk | Low risk | Unclear | Low risk |
| Alfredson et al. 199817 | High risk | Unclear | High risk | Unclear | Low risk | Unclear | High risk |
| Alfredson et al. 1999224 | Not applicable (quasi) | Not applicable (quasi) | Not applicable (quasi) | Not applicable (quasi) | Low risk | Unclear | High risk |
| Arias-Buría et al. 2015230 | Low risk | Low risk | High risk | Low risk | Low risk | Unclear | Low risk |
| Arias-Buría et al. 2017229 | Low risk | Low risk | Unclear | Low risk | Unclear | Low risk | High risk |
| Bae et al. 2011234 | Not applicable (quasi) | Not applicable (quasi) | Unclear | Unclear | Unclear | Unclear | High risk |
| Bahr et al. 2006131 | Low risk | Low risk | High risk | Low risk | Low risk | Unclear | Low risk |
| Balius et al. 2016238 | Low risk | Low risk | Unclear | Low risk | Low risk | Unclear | Low risk |
| Bang et al. 2000239 | Low risk | Unclear | Unclear | Low risk | Low risk | Unclear | Low risk |
| Başkurt et al. 2011246 | Low risk | Unclear | High risk | Unclear | Low risk | Unclear | Low risk |
| Beyer et al. 201518 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | High risk |
| Blume et al. 2015699 | Unclear | Low risk | Low risk | Low risk | Low risk | Unclear | Low risk |
| Boudreau et al. 2019262 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Breda et al. 2020696 | Low risk | Low risk | High risk | Low risk | Low risk | High risk | High risk |
| Brox et al. 1999269 | High risk | High risk | High risk | High risk | No data | No data | No data |
| Calis et al. 2011273 | Low risk | Low risk | Unclear | Unclear | Low risk | Unclear | Unclear |
| Chaconas et al. 2017710 | Low risk | Unclear | Unclear | Low risk | High risk | Unclear | High risk |
| Cheng et al. 2007286 | High risk | High risk | Unclear | Unclear | Unclear | Unclear | High risk |
| Cho et al. 2017289 | High risk | High risk | Unclear | Unclear | Low risk | Low risk | Unclear |
| de Vos et al. 200759 | Low risk | Unclear | Low risk | Low risk | Unclear | Low risk | High risk |
| Dejaco et al. 201744 | Low risk | Low risk | Low risk | Low risk | Low risk | High risk | Low risk |
| Devereaux et al. 2016326 | Low risk | High risk | High risk | High risk | High risk | Unclear | Low risk |
| Dimitrios et al. 2012330 | Not applicable (quasi) | Not applicable (quasi) | Low risk | Low risk | Low risk | Unclear | High risk |
| Dimitrios et al. 2013331 | Not applicable (quasi) | Not applicable (quasi) | Low risk | Low risk | Low risk | Unclear | High risk |
| Dupuis et al.339 | Low risk | Low risk | High risk | Low risk | Low risk | Low risk | High risk |
| Engebretsen et al. 2009344 | Low risk | Low risk | High risk | Low risk | Low risk | Unclear | Low risk |
| Engebretsen et al. 2011345 | Low risk | Low risk | High risk | Low risk | Low risk | Unclear | Low risk |
| Gatz et al. 2020365 | Low risk | Low risk | Low risk | Low risk | Unclear | Unclear | High risk |
| Giray et al. 2019368 | Low risk | Low risk | High risk | Low risk | Low risk | Low risk | High risk |
| Granviken et al. 2015374 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Hallgren et al. 2014383 | High risk | Low risk | High risk | Low risk | Unclear | Low risk | Low risk |
| Heron et al. 2017390 | Low risk | Low risk | Low risk | Low risk | High risk | High risk | Low risk |
| Hotta et al. 2020709 | Low risk | Low risk | High risk | Low risk | Low risk | Low risk | High risk |
| Johansson et al. 2005405 | Low risk | Unclear | Unclear | Low risk | Low risk | Unclear | High risk |
| Jonsson et al. 2005186 | Unclear | Unclear | Low risk | Unclear | High risk | Unclear | High risk |
| Jonsson 2009408 | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear |
| Juul-Kristensen et al. 2019412 | Low risk | Low risk | Low risk | Low risk | Low risk | Unclear | Low risk |
| Ketola et al. 2009426 | Low risk | Low risk | Unclear | Low risk | Low risk | Unclear | High risk |
| Ketola et al. 2013706 | Low risk | Low risk | High risk | Low risk | Low risk | Unclear | Low risk |
| Kim et al. 2017431 | Low risk | Unclear | Unclear | Low risk | Unclear | Low risk | Low risk |
| Kim et al. 2020433 | Low risk | Low risk | High risk | High risk | Low risk | Unclear | High risk |
| Knobloch et al. 2007684 | Low risk | Low risk | Unclear | Unclear | High risk | Unclear | High risk |
| Knobloch et al. 2007192 | Unclear | Unclear | High risk | Low risk | Unclear | Unclear | High risk |
| Knobloch et al. 2008437 | Unclear | Low risk | Unclear | Unclear | Unclear | Unclear | High risk |
| Kongsgaard et al. 200921 | Low risk | Low risk | High risk | Low risk | Low risk | Unclear | Low risk |
| Kromer et al. 2014445 | Low risk | Low risk | High risk | High risk | Low risk | Low risk | Low risk |
| Kromer et al. 2013443 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Littlewood et al. 201634 | Low risk | Low risk | High risk | High risk | Unclear | Unclear | High risk |
| Ludewig et al. 2003463 | Low risk | Unclear | High risk | Unclear | Low risk | Unclear | Low risk |
| Luginbuhl et al. 2008174 | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | High risk |
| Maenhout et al. 2013464 | Unclear | High risk | High risk | High risk | Low risk | Unclear | Low risk |
| Mafi et al. 2001467 | Low risk | Unclear | Unclear | Unclear | Unclear | Unclear | High risk |
| Manias et al. 2006469 | High risk | High risk | High risk | High risk | Low risk | Unclear | Unclear |
| Martinez-Silvestrini et al. 2005471 | Unclear | Unclear | Unclear | Unclear | Low risk | Unclear | High risk |
| Marzetti et al. 2014472 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| McCormack et al. 2016478 | Low risk | Low risk | Unclear | Unclear | Low risk | Low risk | Low risk |
| Melegati et al. 2000480 | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | High risk |
| Mulligan et al. 2016489 | Low risk | Low risk | Low risk | Low risk | Low risk | Unclear | High risk |
| Nishizuka et al. 2017498 | Low risk | Low risk | High risk | Unclear | Low risk | Unclear | High risk |
| Nørregaard et al. 2007499 | Low risk | Low risk | Unclear | Unclear | Unclear | Unclear | High risk |
| Nowotny et al. 2018501 | Low risk | Unclear | Low risk | Low risk | High risk | Unclear | High risk |
| Paavola et al. 2018516 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Park et al. 2010521 | Low risk | Unclear | Unclear | Unclear | Unclear | Unclear | High risk |
| Pearson et al. 2012525 | Unclear | Unclear | High risk | Unclear | Low risk | Unclear | High risk |
| Pearson et al. 2018526 | Low risk | Low risk | High risk | Low risk | Low risk | Low risk | High risk |
| Pekyavas et al. 2016527 | Low risk | Low risk | High risk | Low risk | Unclear | Unclear | Low risk |
| Petersen et al. 2007530 | Low risk | Unclear | Unclear | Unclear | Unclear | Unclear | High risk |
| Peterson et al. 2011531 | Low risk | Low risk | Unclear | High risk | Low risk | Low risk | Low risk |
| Peterson et al. 2014185 | Low risk | Unclear | Low risk | High risk | Low risk | Low risk | Low risk |
| Polimeni et al. 2003698 | Unclear | Unclear | High risk | Low risk | Unclear | Unclear | Unclear |
| Praet et al. 2019535 | Low risk | Low risk | Low risk | Low risk | Low risk | Unclear | Low risk |
| Rabusin et al. 2020686 | Low risk | Low risk | High risk | High risk | Low risk | Low risk | High risk |
| Reyhan et al. 2020549 | Low risk | Low risk | Unclear | Unclear | Low risk | Unclear | High risk |
| Rio et al. 2017167 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | High risk |
| Romero-Morales et al. 2020685 | Unclear | Unclear | Unclear | Unclear | Low risk | Low risk | High risk |
| Rompe et al. 2007558 | Low risk | Low risk | Unclear | Low risk | Low risk | Unclear | Low risk |
| Rompe et al. 2008687 | Low risk | Low risk | Unclear | Low risk | Low risk | Unclear | Unclear |
| Rompe et al. 2009557 | Unclear | Low risk | High risk | High risk | Low risk | Unclear | Low risk |
| Rompe et al. 2009559 | Low risk | Low risk | High risk | Low risk | Low risk | Unclear | Low risk |
| Roos et al. 2004193 | Low risk | Unclear | Unclear | Low risk | Low risk | Unclear | Low risk |
| Şenbursa et al. 2011582 | Low risk | Unclear | Unclear | Unclear | Low risk | Unclear | Low risk |
| Seven et al. 2017583 | Low risk | Low risk | High risk | Low risk | High risk | Unclear | Low risk |
| Sevier et al. 2015584 | Low risk | Unclear | High risk | High risk | High risk | Unclear | High risk |
| Stasinopoulos and Manias 2013692 | High risk | High risk | High risk | Low risk | Low risk | Unclear | High risk |
| Stasinopoulos et al. 2006599 | Not applicable (quasi) | Not applicable (quasi) | Unclear | Low risk | Low risk | Unclear | High risk |
| Stasinopoulos et al. 2010601 | Not applicable (quasi) | Not applicable (quasi) | Low risk | Low risk | Low risk | Unclear | High risk |
| Stasinopoulos et al. 2017597 | Low risk | Unclear | Low risk | Low risk | Low risk | Unclear | High risk |
| Stefansson et al. 2019184 | Low risk | Unclear | High risk | Low risk | High risk | Unclear | Low risk |
| Steunebrink et al. 2013605 | Low risk | Low risk | Low risk | Low risk | Low risk | Unclear | Low risk |
| Stevens et al. 2014175 | Unclear | Unclear | High risk | High risk | Unclear | Unclear | High risk |
| Svernlov and Adolfsson 2001614 | Not applicable (quasi) | Not applicable (quasi) | Unclear | Unclear | Unclear | Unclear | High risk |
| Tahran et al. 2020618 | Low risk | Unclear | Low risk | Low risk | Low risk | Unclear | Low risk |
| Tonks et al. 2007624 | Low risk | Low risk | Low risk | High risk | High risk | Low risk | Low risk |
| Turgut et al. 2017633 | Low risk | Unclear | Unclear | Unclear | High risk | Unclear | Low risk |
| Vallés-Carrascosa et al. 2018638 | Low risk | Low risk | Low risk | High risk | Low risk | Low risk | High risk |
| van Ark et al. 2016644 | Low risk | Low risk | Low risk | Unclear | Unclear | Low risk | Low risk |
| Vinuesa-Montoya et al. 2017641 | Low risk | Low risk | High risk | Low risk | Low risk | Low risk | Low risk |
| Visnes et al. 2005129 | Low risk | Low risk | High risk | Low risk | Unclear | Unclear | Unclear |
| Vuvan et al. 2019187 | Low risk | Low risk | High risk | High risk | Low risk | Low risk | Low risk |
| Walther et al. 2004161 | Unclear | Unclear | Unclear | Unclear | Low risk | Unclear | Unclear |
| Wegener et al. 2016655 | Low risk | Low risk | High risk | Low risk | Low risk | Unclear | High risk |
| Wen et al. 2011657 | Unclear | Unclear | Low risk | Unclear | High risk | Unclear | High risk |
| Werner et al. 2002658 | Low risk | Unclear | Unclear | Unclear | Unclear | Unclear | High risk |
| Wiedmann et al. 2017664 | Low risk | Low risk | Unclear | Unclear | Unclear | Unclear | High risk |
| Yelland et al. 2011674 | Low risk | Low risk | High risk | Low risk | Low risk | Unclear | Low risk |
| Yerlikaya et al. 2018675 | Low risk | Unclear | Low risk | Low risk | Unclear | Unclear | High risk |
| Young et al. 2005132 | Unclear | Unclear | High risk | Low risk | High risk | Unclear | High risk |
| Yu et al. 2013680 | Low risk | Low risk | Low risk | Unclear | Low risk | Unclear | Unclear |
| Moderator | Level | Number of studies | Number of TAs | Number of outcomes tendinopathy location | Number of outcomes outcome domain |
|---|---|---|---|---|---|
| Assessment duration | Short (≤12 weeks) | 95 | 146 | RCSP: 565; Achilles: 200; elbow: 100; patellar 61 | Disability: 282; pain: 257; PFC: 197; ROM: 136; function: 44; QoL: 10 |
| Assessment duration | Medium (13–52 weeks) | 18 | 23 | RCSP: 201; Achilles: 110; elbow: 107; patellar 27 | Disability: 138; pain: 118; PFC: 104; ROM: 18; function: 28; QoL: 39 |
| Assessment duration | Long (>52 weeks) | 2 | 2 | Achilles: 200; patellar 61 | Disability: 21; pain: 21; ROM: 4; QoL: 5 |
| Symptom duration | One year or less | 34 | 46 | RCSP: 141; Achilles: 82; elbow: 82; patellar 9 | Disability: 88; pain: 108; PFC: 49; ROM: 29; function: 36; QoL: 4 |
| Symptom duration | Two years or less | 21 | 33 | RCSP: 168; Achilles: 53; elbow: 13; patellar 24 | Disability: 82; pain: 76; PFC: 30; ROM: 37; function: 15; QoL: 18 |
| Symptom duration | Over two years | 21 | 30 | RCSP: 212; Achilles: 132; patellar 37 | Disability: 119; pain: 64; PFC: 142; ROM: 48; function: 8 |
| Supervision | Supervised | 22 | 36 | RCSP: 326; Achilles: 200; elbow: 100; patellar 61 | Disability:69; pain: 83; PFC: 91; ROM: 88; function: 24; QoL: 1 |
| Supervision | Unsupervised | 82 | 113 | RCSP: 421; Achilles: 6; elbow: 24 | Disability: 326; pain: 276; PFC: 151; ROM: 68; function: 48; QoL: 49 |
| Comparison | Outcome | Overall risk of bias | Inconsistency | Imprecision | Indirectness | Small-study effects | Strength of evidence |
|---|---|---|---|---|---|---|---|
| Assessment duration | Short (≤12 weeks) | Low risk | Low risk | Low risk | Low risk | High risk | Moderate |
| Assessment duration | Medium (13–52 weeks) | Low risk | Low risk | Low risk | Low risk | High risk | Moderate |
| Assessment duration | Long (>52 weeks) | Low risk | Low risk | High risk | Low risk | High risk | Low |
| Symptom duration | One year or less | Low risk | Low risk | High risk | Low risk | High risk | Low |
| Symptom duration | Two years or less | Low risk | Low risk | High risk | Low risk | High risk | Low |
| Symptom duration | Over two years | Low risk | Low risk | High risk | Low risk | High risk | Low |
| Supervision | Supervised | Low risk | Low risk | High risk | Low risk | High risk | Low |
| Supervision | Unsupervised | Low risk | Low risk | Low risk | Low risk | High risk | Moderate |
Effectiveness review 1B
| Author, year | Random sequence generation | Allocation concealment | Blinding of participants/personnel | Blinding of outcome assessment | Incomplete outcome bias | Selective reporting | Other bias |
|---|---|---|---|---|---|---|---|
| Aceituno-Gómez et al. 2019215 | Low risk | Unclear | Low risk | Low risk | Low risk | Low risk | High risk |
| Arias-Buría et al. 2017229 | Low risk | Low risk | Unclear | Low risk | Unclear | Low risk | High risk |
| Bahr et al. 2006131 | Low risk | Low risk | High risk | Low risk | Low risk | Unclear | Low risk |
| Beyer et al. 201518 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | High risk |
| Breda et al. 2020696 | Low risk | Low risk | High risk | Low risk | Low risk | High risk | High risk |
| Brox et al. 1999269 | High risk | High risk | High risk | High risk | No data | No data | No data |
| Chaconas et al. 2017710 | Low risk | Unclear | Unclear | Low risk | High risk | Unclear | High risk |
| de Vos et al. 200759 | Low risk | Unclear | Low risk | Low risk | Unclear | Low risk | High risk |
| Devereaux et al. 2016326 | Low risk | High risk | High risk | High risk | High risk | Unclear | Low risk |
| Dimitrios et al. 2012330 | Not applicable (quasi) | Not applicable (quasi) | Low risk | Low risk | Low risk | Unclear | High risk |
| Dupuis et al.339 | Low risk | Low risk | High risk | Low risk | Low risk | Low risk | High risk |
| Engebretsen et al. 2009344 | Low risk | Low risk | High risk | Low risk | Low risk | Unclear | Low risk |
| Engebretsen et al. 2011345 | Low risk | Low risk | High risk | Low risk | Low risk | Unclear | Low risk |
| Ganderton et al. 2018189 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | High risk |
| Gatz et al. 2020365 | Low risk | Low risk | Low risk | Low risk | Unclear | Unclear | High risk |
| Granviken et al. 2015374 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Hotta et al. 2020709 | Low risk | Low risk | High risk | Low risk | Low risk | Low risk | High risk |
| Jonsson 2009408 | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear |
| Kim et al. 2020433 | Low risk | Low risk | High risk | High risk | Low risk | Unclear | High risk |
| Knobloch et al. 2007684 | Low risk | Low risk | Unclear | Unclear | High risk | Unclear | High risk |
| Knobloch et al. 2007192 | Unclear | Unclear | High risk | Low risk | Unclear | Unclear | High risk |
| Knobloch et al. 2008437 | Unclear | Low risk | Unclear | Unclear | Unclear | Unclear | High risk |
| Kongsgaard et al.21 | Low risk | Low risk | High risk | Low risk | Low risk | Unclear | Low risk |
| Kromer et al. 2014445 | Low risk | Low risk | High risk | High risk | Low risk | Low risk | Low risk |
| Kromer et al. 2013443 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Ludewig et al. 2003463 | Low risk | Unclear | High risk | Unclear | Low risk | Unclear | Low risk |
| Marzetti et al. 2014472 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| McCormack et al. 2016478 | Low risk | Low risk | Unclear | Unclear | Low risk | Low risk | Low risk |
| Mulligan et al. 2016489 | Low risk | Low risk | Low risk | Low risk | Low risk | Unclear | High risk |
| Nishizuka et al. 2017498 | Low risk | Low risk | High risk | Unclear | Low risk | Unclear | High risk |
| Nørregaard et al. 2007499 | Low risk | Low risk | Unclear | Unclear | Unclear | Unclear | High risk |
| Østerås et al. 2009512 | Low risk | Low risk | Unclear | High risk | Low risk | Unclear | Low risk |
| Paavola et al. 2018516 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Rabusin et al. 2020648 | Low risk | Low risk | High risk | High risk | Low risk | Low risk | High risk |
| Reyhan et al. 2020686 | Low risk | Low risk | Unclear | Unclear | Low risk | Unclear | High risk |
| Rompe et al. 2007558 | Low risk | Low risk | Unclear | Low risk | Low risk | Unclear | Low risk |
| Rompe et al. 2008687 | Low risk | Low risk | Unclear | Low risk | Low risk | Unclear | Unclear |
| Rompe et al. 2009557 | Unclear | Low risk | High risk | High risk | Low risk | Unclear | Low risk |
| Rompe et al. 2009559 | Low risk | Low risk | High risk | Low risk | Low risk | Unclear | Low risk |
| Roos et al. 2004193 | Low risk | Unclear | Unclear | Low risk | Low risk | Unclear | Low risk |
| Seven et al. 2017583 | Low risk | Low risk | High risk | Low risk | High risk | Unclear | Low risk |
| Sevier et al. 2015584 | Low risk | Unclear | High risk | High risk | High risk | Unclear | High risk |
| Silbernagel et al. 2001587 | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | High risk |
| Steunebrink et al. 2013605 | Low risk | Low risk | Low risk | Low risk | Low risk | Unclear | Low risk |
| Stevens et al. 2014175 | Unclear | Unclear | High risk | High risk | Unclear | Unclear | High risk |
| Tonks et al. 2007624 | Low risk | Low risk | Low risk | High risk | High risk | Low risk | Low risk |
| van Ark et al. 2016644 | Low risk | Low risk | Low risk | Unclear | Unclear | Low risk | Low risk |
| Vuvan et al. 2019187 | Low risk | Low risk | High risk | High risk | Low risk | Low risk | Low risk |
| Werner et al. 2002658 | Low risk | Unclear | Unclear | Unclear | Unclear | Unclear | High risk |
| Yelland et al. 2011674 | Low risk | Low risk | High risk | Low risk | Low risk | Unclear | Low risk |
| Overall risk of bias | Inconsistency | Imprecision | Indirectness | Small-study effects | Strength of evidence |
|---|---|---|---|---|---|
| Low risk | Low risk | Low risk | Low risk | Low risk | High |
| Overall risk of bias | Inconsistency | Imprecision | Indirectness | Small-study effects | Strength of evidence |
|---|---|---|---|---|---|
| Low risk | Low risk | Low risk | Low risk | Low risk | High |
| Overall risk of bias | Inconsistency | Imprecision | Indirectness | Small-study effects | Strength of evidence |
|---|---|---|---|---|---|
| Low risk | Low risk | Low risk | Low risk | Low risk | High |
Effectiveness review 1C
| Author, year | Random sequence generation | Allocation concealment | Blinding of participants/personnel | Blinding of outcome assessment | Incomplete outcome bias | Selective reporting | Other bias |
|---|---|---|---|---|---|---|---|
| Alfredson et al. 199817 | High risk | Unclear | High risk | Unclear | Low risk | Unclear | High risk |
| Alfredson et al. 1999224 | Not applicable (quasi) | Not applicable (quasi) | Not applicable (quasi) | Not applicable (quasi) | Low risk | Unclear | High risk |
| Arias-Buría et al. 2015230 | Low risk | Low risk | High risk | Low risk | Low risk | Unclear | Low risk |
| Arias-Buría et al. 2017229 | Low risk | Low risk | Unclear | Low risk | Unclear | Low risk | High risk |
| Bahr et al. 2006131 | Low risk | Low risk | High risk | Low risk | Low risk | Unclear | Low risk |
| Balius et al. 2016238 | Low risk | Low risk | Unclear | Low risk | Low risk | Unclear | Low risk |
| Beyer et al. 201518 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | High risk |
| Blume et al. 2015699 | Unclear | Low risk | Low risk | Low risk | Low risk | Unclear | Low risk |
| Boudreau et al. 2019262 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Breda et al. 2020696 | Low risk | Low risk | High risk | Low risk | Low risk | High risk | High risk |
| Chaconas et al. 2017710 | Low risk | Unclear | Unclear | Low risk | High risk | Unclear | High risk |
| Cheng et al. 2007286 | High risk | High risk | Unclear | Unclear | Unclear | Unclear | High risk |
| Cho et al. 2017289 | High risk | High risk | Unclear | Unclear | Low risk | Low risk | Unclear |
| de Vos et al. 200759 | Low risk | Unclear | Low risk | Low risk | Unclear | Low risk | High risk |
| Dejaco et al. 201744 | Low risk | Low risk | Low risk | Low risk | Low risk | High risk | Low risk |
| Dimitrios et al. 2012330 | Not applicable (quasi) | Not applicable (quasi) | Low risk | Low risk | Low risk | Unclear | High risk |
| Dimitrios et al. 2013692 | Not applicable (quasi) | Not applicable (quasi) | Low risk | Low risk | Low risk | Unclear | High risk |
| Dupuis et al.339 | Low risk | Low risk | High risk | Low risk | Low risk | Low risk | High risk |
| Ganderton et al. 2018189 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | High risk |
| Gatz et al. 2020365 | Low risk | Low risk | Low risk | Low risk | Unclear | Unclear | High risk |
| Giray et al. 2019368 | Low risk | Low risk | High risk | Low risk | Low risk | Low risk | High risk |
| Hallgren et al. 2014383 | High risk | Low risk | High risk | Low risk | Unclear | Low risk | Low risk |
| Heron et al. 2017390 | Low risk | Low risk | Low risk | Low risk | High risk | High risk | Low risk |
| Hotta et al. 2020709 | Low risk | Low risk | High risk | Low risk | Low risk | Low risk | High risk |
| Johansson et al. 2005405 | Low risk | Unclear | Unclear | Low risk | Low risk | Unclear | High risk |
| Jonsson 2009408 | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear |
| Ketola et al. 2009426 | Low risk | Low risk | Unclear | Low risk | Low risk | Unclear | High risk |
| Knobloch et al. 2007684 | Low risk | Low risk | Unclear | Unclear | High risk | Unclear | High risk |
| Knobloch et al. 2007192 | Unclear | Unclear | High risk | Low risk | Unclear | Unclear | High risk |
| Knobloch et al. 2008437 | Unclear | Low risk | Unclear | Unclear | Unclear | Unclear | High risk |
| Kongsgaard et al.21 | Low risk | Low risk | High risk | Low risk | Low risk | Unclear | Low risk |
| Kromer et al. 2014445 | Low risk | Low risk | High risk | High risk | Low risk | Low risk | Low risk |
| Kromer et al. 2013443 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Littlewood et al. 201634 | Low risk | Low risk | High risk | High risk | Unclear | Unclear | High risk |
| Luginbuhl et al. 2008174 | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | High risk |
| Maenhout et al. 2013464 | Unclear | High risk | High risk | High risk | Low risk | Unclear | Low risk |
| Mafi et al. 2001467 | Low risk | Unclear | Unclear | Unclear | Unclear | Unclear | High risk |
| Manias et al. 2006469 | High risk | High risk | High risk | High risk | Low risk | Unclear | Unclear |
| Martinez-Silvestrini et al. 2005471 | Unclear | Unclear | Unclear | Unclear | Low risk | Unclear | High risk |
| Marzetti et al. 2014472 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| McCormack et al. 2016478 | Low risk | Low risk | Unclear | Unclear | Low risk | Low risk | Low risk |
| Mulligan et al. 2016489 | Low risk | Low risk | Low risk | Low risk | Low risk | Unclear | High risk |
| Nørregaard et al. 2007499 | Low risk | Low risk | Unclear | Unclear | Unclear | Unclear | High risk |
| Nowotny et al. 2018501 | Low risk | Unclear | Low risk | Low risk | High risk | Unclear | High risk |
| Østerås et al. 2009512 | Low risk | Low risk | High risk | High risk | Low risk | Unclear | High risk |
| Park et al. 2010521 | Low risk | Unclear | Unclear | Unclear | Unclear | Unclear | High risk |
| Pearson et al. 2012525 | Unclear | Unclear | High risk | Unclear | Low risk | Unclear | High risk |
| Pearson et al. 2018526 | Low risk | Low risk | High risk | Low risk | Low risk | Low risk | High risk |
| Pekyavas et al. 2016527 | Low risk | Low risk | High risk | Low risk | Unclear | Unclear | Low risk |
| Petersen et al. 2007530 | Low risk | Unclear | Unclear | Unclear | Unclear | Unclear | High risk |
| Peterson et al. 2011531 | Low risk | Low risk | Unclear | High risk | Low risk | Low risk | Low risk |
| Peterson et al. 2014185 | Low risk | Unclear | Low risk | High risk | Low risk | Low risk | Low risk |
| Praet et al. 2019535 | Low risk | Low risk | Low risk | Low risk | Low risk | Unclear | Low risk |
| Rabusin et al. 2020686 | Low risk | Low risk | High risk | High risk | Low risk | Low risk | High risk |
| Rio et al. 2017167 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | High risk |
| Romero-Morales et al. 2020685 | Unclear | Unclear | Unclear | Unclear | Low risk | Low risk | High risk |
| Rompe et al. 2007558 | Low risk | Low risk | Unclear | Low risk | Low risk | Unclear | Low risk |
| Rompe et al. 2008687 | Low risk | Low risk | Unclear | Low risk | Low risk | Unclear | Unclear |
| Rompe et al. 2009557 | Unclear | Low risk | High risk | High risk | Low risk | Unclear | Low risk |
| Rompe et al. 2009559 | Low risk | Low risk | High risk | Low risk | Low risk | Unclear | Low risk |
| Roos et al. 2004193 | Low risk | Unclear | Unclear | Low risk | Low risk | Unclear | Low risk |
| Şenbursa et al. 2011582 | Low risk | Unclear | Unclear | Unclear | Low risk | Unclear | Low risk |
| Sevier et al. 2015584 | Low risk | Unclear | High risk | High risk | High risk | Unclear | High risk |
| Silbernagel et al. 2001587 | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | High risk |
| Silbernagel et al. 2007138 | Low risk | Low risk | High risk | High risk | Low risk | Unclear | Low risk |
| Slider et al. 2013690 | Low risk | Unclear | Low risk | Low risk | Low risk | Unclear | Unclear |
| Stasinopoulos and Manias 2013692 | High risk | High risk | High risk | Low risk | Low risk | Unclear | High risk |
| Stasinopoulos et al. 2006599 | Not applicable (quasi) | Not applicable (quasi) | Unclear | Low risk | Low risk | Unclear | High risk |
| Stasinopoulos et al. 2010601 | Not applicable (quasi) | Not applicable (quasi) | Low risk | Low risk | Low risk | Unclear | High risk |
| Stasinopoulos et al. 2017597 | Low risk | Unclear | Low risk | Low risk | Low risk | Unclear | High risk |
| Stefansson et al. 2019184 | Low risk | Unclear | High risk | Low risk | High risk | Unclear | Low risk |
| Steunebrink et al. 2013605 | Low risk | Low risk | Low risk | Low risk | Low risk | Unclear | Low risk |
| Stevens et al. 2014175 | Unclear | Unclear | High risk | High risk | Unclear | Unclear | High risk |
| Svernlov and Adolfsson 2001614 | Not applicable (quasi) | Not applicable (quasi) | Unclear | Unclear | Unclear | Unclear | High risk |
| Tonks et al. 2007624 | Low risk | Low risk | Low risk | High risk | High risk | Low risk | Low risk |
| Turgut et al. 2017633 | Low risk | Unclear | Unclear | Unclear | High risk | Unclear | Low risk |
| Vallés-Carrascosa et al. 2018638 | Low risk | Low risk | Low risk | High risk | Low risk | Low risk | High risk |
| van Ark et al. 2016644 | Low risk | Low risk | Low risk | Unclear | Unclear | Low risk | Low risk |
| Vinuesa-Montoya et al. 2017641 | Low risk | Low risk | High risk | Low risk | Low risk | Low risk | Low risk |
| Visnes et al. 2005129 | Low risk | Low risk | High risk | Low risk | Unclear | Unclear | Unclear |
| Vuvan et al. 2019187 | Low risk | Low risk | High risk | High risk | Low risk | Low risk | Low risk |
| Walther et al. 2004161 | Unclear | Unclear | Unclear | Unclear | Low risk | Unclear | Unclear |
| Wegener et al. 2016655 | Low risk | Low risk | High risk | Low risk | Low risk | Unclear | High risk |
| Wen et al. 2011657 | Unclear | Unclear | Low risk | Unclear | High risk | Unclear | High risk |
| Werner et al. 2002658 | Low risk | Unclear | Unclear | Unclear | Unclear | Unclear | High risk |
| Wiedmann et al. 2017664 | Low risk | Low risk | Unclear | Unclear | Unclear | Unclear | High risk |
| Yelland et al. 2011674 | Low risk | Low risk | High risk | Low risk | Low risk | Unclear | Low risk |
| Young et al. 2005132 | Unclear | Unclear | High risk | Low risk | High risk | Unclear | High risk |
| Yu et al. 2013680 | Low risk | Low risk | Low risk | Unclear | Low risk | Unclear | Unclear |
| Moderator | Model | Tendinopathy number TAs | Tendinopathy number outcomes | Outcome domain number TAs | Outcome domain number outcomes |
|---|---|---|---|---|---|
| Intensity: body mass | Large effects/upper body | RCSP: 7 Elbow: 4 |
RCSP: 60 Elbow: 8 |
Disability: 8 Pain: 7 Function: 2 |
Disability: 35 Pain: 29 Function: 4 |
| Intensity: additional | Large effects/upper body | RCSP: 27 Elbow: 19 |
RCSP: 184 Elbow: 115 |
Disability: 38 Pain: 32 Function: 18 |
Disability: 121 Pain: 134 Function: 44 |
| Intensity: body mass | Large effects/lower body | Achilles: 20 Patellar: 3 Gluteal: 1 |
Achilles: 112 Patellar: 10 Gluteal: 3 |
Disability: 18 Pain: 19 Function: 4 |
Disability:56 Pain: 61 Function: 8 |
| Intensity: additional | Large effects/lower body | Achilles: 17 Patellar: 16 Gluteal: 1 |
Achilles: 63 Patellar: 56 Gluteal: 14 |
Disability: 30 Pain: 22 Function: 3 |
Disability: 77 Pain: 47 Function: 9 |
| Intensity: body mass | Small effects/upper body | RCSP: 4 Elbow: 1 |
RCSP: 14 Elbow: 1 |
QoL: 0 PFC: 3 ROM: 4 |
QoL: 0 PFC: 7 ROM: 8 |
| Intensity: additional | Small effects/upper body | RCSP: 15 Elbow: 12 |
RCSP: 151 Elbow: 54 |
QoL: 5 PFC: 21 ROM: 10 |
QoL: 31 PFC: 105 ROM: 69 |
| Intensity: body mass | Small effects/lower body | Achilles: 6 Patellar: 1 Gluteal: 1 |
Achilles: 71 Patellar: 6 Gluteal: 6 |
QoL: 2 PFC: 6 |
QoL: 5 PFC: 78 |
| Intensity: additional | Small effects/lower body | Achilles: 5 Patellar: 2 Gluteal: 2 |
Achilles: 43 Patellar: 10 Gluteal: 8 |
QoL: 2 PFC: 8 |
QoL: 10 PFC: 51 |
| Moderator | Model | Overall RoB | Inconsistency | Imprecision | Indirectness | Small-study effects | Strength of evidence |
|---|---|---|---|---|---|---|---|
| Intensity: body mass | All tendinopathies/large-effects | Low risk | Low risk | High risk | Low risk | High risk | Low |
| Intensity: additional | All tendinopathies/large effects | Low risk | Low risk | Low risk | Low risk | High risk | Moderate |
| Intensity: body mass | Upper body/large effects | Low risk | Low risk | High risk | Low risk | High risk | Low |
| Intensity: additional | Upper body/ large effects | Low risk | Low risk | High risk | Low risk | High risk | Low |
| Intensity: body mass | Lower body/ large effects | Low risk | Low risk | Low risk | Low risk | Low risk | High |
| Intensity: additional | Lower body/large effects | Low risk | Low risk | Low risk | Low risk | High risk | Moderate |
| Intensity: body mass | All tendinopathies/small effects | Low risk | Low risk | Low risk | Low risk | Low risk | High |
| Intensity: additional | All tendinopathies/small effects | Low risk | Low risk | Low risk | Low risk | High risk | Moderate |
| Intensity: body mass | Upper body/Small effects | Low risk | Low risk | High risk | Low risk | Low risk | Moderate |
| Intensity: additional | Upper body/small effects | Low risk | Low risk | High risk | Low risk | High risk | Low |
| Intensity: additional | Lower body/small effects | Low risk | Low risk | High risk | Low risk | High risk | Low |
| Intensity: body mass | Lower body/small effects | Low risk | Low risk | High risk | Low risk | Low risk | Moderate |
| Moderator | Model | Tendinopathy number treatment arms | Tendinopathy number outcomes | Outcome domain number treatment arms | Outcome domain number outcomes |
|---|---|---|---|---|---|
| Volume: low volume | Large effects/upper body | RCSP: 26 Elbow: 14 |
RCSP: 164 Elbow: 53 |
Disability: 32 Pain: 27 Function: 13 |
Disability: 95 Pain: 96 Function: 26 |
| Volume: high volume | Large effects/upper body | RCSP: 9 Elbow: 7 |
RCSP: 75 Elbow: 71 |
Disability: 13 Pain: 13 Function: 6 |
Disability: 53 Pain: 72 Function: 21 |
| Volume: low volume | Large effects/lower body | Achilles: 3 Patellar: 7 Gluteal: 1 |
Achilles: 29 Patellar: 22 Gluteal: 3 |
Disability: 8 Pain: 8 Function: 1 |
Disability: 30 Pain: 23 Function: 1 |
| Volume: high volume | Large effects/lower body | Achilles: 33 Patellar: 10 Gluteal: 0 |
Achilles: 133 Patellar: 43 Gluteal: 0 |
Disability: 36 Pain: 31 Function: 5 |
Disability: 87 Pain: 77 Function: 12 |
| Volume: low volume | Small effects/upper body | RCSP: 14 Elbow: 7 |
RCSP: 136 Elbow: 12 |
QoL: 0 PFC: 17 ROM: 12 |
QoL: 0 PFC: 80 ROM: 68 |
| Volume: high volume | Small effects/upper body | RCSP: 3 Elbow: 5 |
RCSP: 20 Elbow: 39 |
QoL: 5 PFC: 6 ROM: 0 |
QoL: 31 PFC: 28 ROM: 0 |
| Volume: low volume | Small effects/lower body | Achilles: 1 Patellar: 0 Gluteal: 2 |
Achilles: 9 Patellar: 0 Gluteal: 12 |
QoL: 0 PFC: 3 |
QoL: 0 PFC: 21 |
| Volume: high volume | Small effects/lower body | Achilles: 11 Patellar: 2 Gluteal: 0 |
Achilles: 106 Patellar: 8 Gluteal: 0 |
QoL: 4 PFC: 10 |
QoL: 12 PFC: 102 |
| Moderator | Model | Overall RoB | Inconsistency | Imprecision | Indirectness | Small-study effects | Strength of evidence |
|---|---|---|---|---|---|---|---|
| Volume: low volume | All tendinopathies/large effects | Low risk | Low risk | Low risk | Low risk | High risk | Moderate |
| Volume: high volume | All tendinopathies/large effects | Low risk | Low risk | Low risk | Low risk | High risk | Moderate |
| Volume: low volume | Upper body/large effects | Low risk | Low risk | High risk | Low risk | High risk | Low |
| Volume: high volume | Upper body/large effects | Low risk | Low risk | High risk | Low risk | High risk | Low |
| Volume: low volume | Lower body/large effects | Low risk | Low risk | High risk | Low risk | High risk | Low |
| Volume: high volume | Lower body/large effects | Low risk | Low risk | Low risk | Low risk | Low risk | High |
| Volume: low volume | All tendinopathies/Smmall effects | Low risk | Low risk | Low risk | Low risk | Low risk | High |
| Volume: high volume | All tendinopathies/small effects | Low risk | High risk | Low risk | Low risk | High risk | Low |
| Volume: low volume | Upper body/small effects | Low risk | Low risk | Low risk | Low risk | Low risk | High |
| Volume: high volume | Upper body/small effects | Low risk | High risk | High risk | Low risk | High risk | Low |
| Volume: low volume | Lower body/small effects | Low risk | High risk | High risk | Low risk | Low risk | Low |
| Volume: high volume | Lower-body/small effects | Low risk | Low risk | High risk | Low risk | High risk | Low |
| Moderator | Model | Tendinopathy number TAs | Tendinopathy number outcomes | Outcome domain number TAs | Outcome domain number outcomes |
|---|---|---|---|---|---|
| Volume: low volume | Large effects/upper body | RCSP: 5 Elbow: 18 |
RCSP: 37 Elbow: 89 |
Disability: 14 Pain: 16 Function: 11 |
Disability: 43 Pain: 61 Function: 22 |
| Volume: high volume | Large effects/upper body | RCSP: 30 Elbow: 5 |
RCSP: 207 Elbow: 36 |
Disability: 33 Pain: 25 Function: 8 |
Disability: 110 Pain: 109 Function: 24 |
| Volume: low volume | Large effects/lower body | Achilles: 33 Patellar: 17 Gluteal: 0 |
Achilles: 143 Patellar: 63 Gluteal: 0 |
Disability: 42 Pain: 34 Function: 6 |
Disability: 108 Pain: 85 Function: 13 |
| Volume: high volume | Large effects/lower body | Achilles: 4 Patellar: 2 Gluteal: 2 |
Achilles: 23 Patellar: 10 Gluteal: 17 |
Disability: 6 Pain: 7 Function: 1 |
Disability: 24 Pain: 22 Function: 4 |
| Volume: low volume | Small effects/upper body | RCSP: 4 Elbow: 9 |
RCSP: 43 Elbow: 45 |
QoL: 3 PFC: 13 ROM: 3 |
QoL: 21 PFC: 48 ROM: 19 |
| Volume: high volume | Small effects/upper body | RCSP: 14 Elbow: 3 |
RCSP: 116 Elbow: 8 |
QoL: 2 PFC: 10 ROM: 10 |
QoL: 10 PFC: 62 ROM: 52 |
| Volume: low volume | Small effects/lower body | Achilles: 9 Patellar: 2 Gluteal: 1 |
Achilles: 58 Patellar: 8 Gluteal: 6 |
QoL: 9 PFC: 4 |
QoL: 12 PFC: 60 |
| Volume: high volume | Small effects/lower body | Achilles: 3 Patellar: 1 Gluteal: 2 |
Achilles: 57 Patellar: 6 Gluteal: 10 |
QoL: 1 PFC: 5 |
QoL: 4 PFC: 69 |
| Moderator | Model | Overall RoB | Inconsistency | Imprecision | Indirectness | Small study-effects | Strength of evidence |
|---|---|---|---|---|---|---|---|
| Volume: low volume | All tendinopathies/large effects | Low risk | Low risk | Low risk | Low risk | High risk | Moderate |
| Volume: high volume | All tendinopathies/large effects | Low risk | Low risk | Low risk | Low risk | High risk | Moderate |
| Volume: low volume | Upper body/large effects | Low risk | Low risk | High risk | Low risk | High risk | Low |
| Volume: high volume | Upper body/large effects | Low risk | Low risk | High risk | Low risk | High risk | Low |
| Volume: low volume | Lower body/large effects | Low risk | Low risk | Low risk | Low risk | High risk | Moderate |
| Volume: high volume | Lower body/large effects | Low risk | Low risk | High risk | Low risk | Low risk | Moderate |
| Volume: low volume | All tendinopathies/small effects | Low risk | High risk | Low risk | Low risk | High risk | Low |
| Volume: high volume | All tendinopathies/small effects | Low risk | Low risk | Low risk | Low risk | Low risk | High |
| Volume: low volume | Upper body/small effects | Low risk | High risk | Low risk | Low risk | High risk | Low |
| Volume: high volume | Upper body/small effects | Low risk | Low risk | Low risk | Low risk | Low risk | High |
| Volume: low volume | Lower body/small effects | Low risk | Low risk | High risk | Low risk | High risk | Low |
| Volume: high volume | Lower body/small effects | Low risk | High risk | High risk | Low risk | Low risk | Low |
| Moderator | Model | Tendinopathy number TAs | Tendinopathy number outcomes | Outcome domain number TAs | Outcome domain number outcomes |
|---|---|---|---|---|---|
| Frequency: low (less than once per day) | Large effects/upper body | RCSP: 14 Elbow: 11 |
RCSP: 105 Elbow: 51 |
Disability: 15 Pain: 18 Function: 12 |
Disability: 57 Pain: 64 Function: 35 |
| Frequency: mid (once per day) | Large effects/upper body | RCSP: 11 Elbow: 8 |
RCSP: 72 Elbow: 55 |
Disability: 19 Pain: 15 Function: 4 |
Disability: 67 Pain: 56 Function: 4 |
| Frequency: high (more than once per day) | Large effects/upper body | RCSP: 10 Elbow: 2 |
RCSP: 64 Elbow: 8 |
Disability: 12 Pain: 6 Function: 1 |
Disability: 39 Pain: 30 Function: 3 |
| Frequency: low (less than once per day) | Large effects/lower body | Achilles: 3 Patellar: 9 Gluteal: 0 |
Achilles: 8 Patellar: 30 Gluteal: 0 |
Disability: 8 Pain: 11 Function: 0 |
Disability: 12 Pain: 26 Function: 0 |
| Frequency: mid (once per day) | Large effects/lower body | Achilles: 9 Patellar: 1 Gluteal: 0 |
Achilles: 31 Patellar: 2 Gluteal: 0 |
Disability: 9 Pain: 5 Function: 1 |
Disability: 18 Pain: 14 Function: 1 |
| Frequency: high (more than once per day) | Large effects/lower body | Achilles: 25 Patellar: 9 Gluteal: 2 |
Achilles: 129 Patellar: 41 Gluteal: 17 |
Disability: 31 Pain: 26 Function: 6 |
Disability: 102 Pain: 69 Function: 16 |
| Frequency: low (less than once per day) | Small effects/upper body | RCSP: 9 Elbow: 1 |
RCSP: 87 Elbow: 3 |
QoL: 0 PFC: 6 ROM: 8 |
QoL: 0 PFC: 44 ROM: 46 |
| Frequency: mid (once per day) | Small effects/upper body | RCSP: 8 Elbow: 5 |
RCSP: 46 Elbow: 41 |
QoL: 3 PFC: 12 ROM: 4 |
QoL: 21 PFC: 45 ROM: 21 |
| Frequency: high (more than once per day) | Small effects/upper body | RCSP: 5 Elbow: 2 |
RCSP: 32 Elbow: 5 |
QoL: 2 PFC: 4 ROM: 2 |
QoL: 10 PFC: 17 ROM: 10 |
| Frequency: low (less than once per day) | Small effects/lower body | Achilles: 2 Patellar: 1 Gluteal: 2 |
Achilles: 26 Patellar: 6 Gluteal: 12 |
QoL: 0 PFC: 5 |
QoL: 0 PFC: 44 |
| Frequency: mid (once per day) | Small effects/lower body | Achilles: 4 Patellar: 0 Gluteal: 0 |
Achilles: 50 Patellar: 0 Gluteal: 0 |
QoL: 2 PFC: 2 |
QoL: 2 PFC: 48 |
| Frequency: high (more than once per day) | Small effects/lower body | Achilles: 6 Patellar: 2 Gluteal: 1 |
Achilles: 39 Patellar: 8 Gluteal: 4 |
QoL: 3 PFC: 7 |
QoL: 14 PFC: 37 |
| Moderator | Model | Overall RoB | Inconsistency | Imprecision | Indirectness | Small-study effects | Strength of evidence |
|---|---|---|---|---|---|---|---|
| Frequency: low (less than once per day) | All tendinopathies/large effects | Low risk | Low risk | Low risk | Low risk | High risk | Moderate |
| Frequency: mid (once per day) | All tendinopathies/large effects | Low risk | Low risk | Low risk | Low risk | High risk | Moderate |
| Frequency: high (more than once per day) | All tendinopathies/large effects | Low risk | Low risk | Low risk | Low risk | High risk | Moderate |
| Frequency: low (less than once per day) | Upper body/large effects | Low risk | Low risk | High risk | Low risk | High risk | Low |
| Frequency: mid (once per day) | Upper body/large effects | Low risk | Low risk | High risk | Low risk | High risk | Low |
| Frequency: high (more than once per day) | Upper body/large effects | Low risk | Low risk | High risk | Low risk | High risk | Low |
| Frequency: low (less than once per day) | Lower body/large effects | Low risk | Low risk | High risk | Low risk | High risk | Low |
| Frequency: mid (once per day) | Lower body/large effects | Low risk | Low risk | High risk | Low risk | High risk | Low |
| Frequency: high (more than once per day) | Lower body/large effects | Low risk | Low risk | Low risk | Low risk | High risk | Moderate |
| Frequency: low (less than once per day) | All tendinopathies/small effects | Low risk | Low risk | Low risk | Low risk | High risk | Moderate |
| Frequency: mid (once per day) | All tendinopathies/small effects | Low risk | High risk | Low risk | Low risk | High risk | Low |
| Frequency: high (more than once per day) | All tendinopathies/small effects | Low risk | Low risk | Low risk | Low risk | High risk | Moderate |
| Frequency: low (less than once per day) | Upper body/small effects | Low risk | Low risk | Low risk | Low risk | High risk | Moderate |
| Frequency: mid (once per day) | Upper body/small effects | Low risk | High risk | Low risk | Low risk | High risk | Low |
| Frequency: high (more than once per day) | Upper body/small -effects | Low risk | Low risk | Low risk | Low risk | Low risk | High |
| Frequency: low (less than once per day) | Lower body/small effects | Low risk | High risk | High risk | Low risk | High risk | Very low |
| Frequency: mid (once per day) | Lower body/small effects | Low risk | High risk | High risk | Low risk | Low risk | Low |
| Frequency: high (more than once per day) | Lower body/small effects | High risk | Low risk | High risk | Low risk | High risk | Very low |
Effectiveness review 2
| Author, year | Random sequence generation | Allocation concealment | Blinding of participants/personnel | Blinding of outcome assessment | Incomplete outcome bias | Selective reporting | Other bias |
|---|---|---|---|---|---|---|---|
| Balius et al. 2016238 | Low risk | Low risk | Unclear | Low risk | Low risk | Unclear | Low risk |
| Başkurt et al. 2011246 | Low risk | Unclear | High risk | Unclear | Low risk | Unclear | Low risk |
| Beyer et al. 201518 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | High risk |
| Blume et al. 2015699 | Unclear | Low risk | Low risk | Low risk | Low risk | Unclear | Low risk |
| Breda et al. 2020696 | Low risk | Low risk | High risk | Low risk | Low risk | High risk | High risk |
| Chaconas et al. 2017710 | Low risk | Unclear | Unclear | Low risk | High risk | Unclear | High risk |
| Dejaco et al. 201744 | Low risk | Low risk | Low risk | Low risk | Low risk | High risk | Low risk |
| Dimitrios et al. 2012330 | Not applicable (quasi) | Not applicable (quasi) | Low risk | Low risk | Low risk | Unclear | High risk |
| Dimitrios et al. 2013692 | Not applicable (quasi) | Not applicable (quasi) | Low risk | Low risk | Low risk | Unclear | High risk |
| Dupuis et al.339 | Low risk | Low risk | High risk | Low risk | Low risk | Low risk | High risk |
| Gatz et al. 2020365 | Low risk | Low risk | Low risk | Low risk | Unclear | Unclear | High risk |
| Hallgren et al. 2014383 | High risk | Low risk | High risk | Low risk | Unclear | Low risk | Low risk |
| Heron et al. 2017390 | Low risk | Low risk | Low risk | Low risk | High risk | High risk | Low risk |
| Hotta et al. 2020709 | Low risk | Low risk | High risk | Low risk | Low risk | Low risk | High risk |
| Jonsson 2009408 | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear |
| Juul-Kristensen et al. 2019412 | Low risk | Low risk | Low risk | Low risk | Low risk | Unclear | Low risk |
| Kongsgaard et al.21 | Low risk | Low risk | High risk | Low risk | Low risk | Unclear | Low risk |
| Maenhout et al. 2013464 | Unclear | High risk | High risk | High risk | Low risk | Unclear | Low risk |
| Mafi et al. 2001467 | Low risk | Unclear | Unclear | Unclear | Unclear | Unclear | High risk |
| Martinez-Silvestrini et al. 2005471 | Unclear | Unclear | Unclear | Unclear | Low risk | Unclear | High risk |
| Marzetti et al. 2014472 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Nørregaard et al. 2007499 | Low risk | Low risk | Unclear | Unclear | Unclear | Unclear | High risk |
| Peterson et al 2014185 | Low risk | Unclear | Low risk | High risk | Low risk | Low risk | Low risk |
| Rio et al. 2017167 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | High risk |
| Romero-Morales et al. 2020685 | Unclear | Unclear | Unclear | Unclear | Low risk | Low risk | High risk |
| Silbernagel et al. 2001587 | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | High risk |
| Slider et al. 2013690 | Low risk | Unclear | Low risk | Low risk | Low risk | Unclear | Unclear |
| Stasinopoulos et al. 2017597 | Low risk | Unclear | Low risk | Low risk | Low risk | Unclear | High risk |
| Steunebrink et al. 2013605 | Low risk | Low risk | Low risk | Low risk | Low risk | Unclear | Low risk |
| Turgut et al. 2017633 | Low risk | Unclear | Unclear | Unclear | High risk | Unclear | Low risk |
| van Ark et al. 2016644 | Low risk | Low risk | Low risk | Unclear | Unclear | Low risk | Low risk |
| Walther et al. 2004161 | Unclear | Unclear | Unclear | Unclear | Low risk | Unclear | Unclear |
| Werner et al. 2002658 | Low risk | Unclear | Unclear | Unclear | Unclear | Unclear | High risk |
| Young et al. 2005132 | Unclear | Unclear | High risk | Low risk | High risk | Unclear | High risk |
| Yu et al. 2013680 | Low risk | Low risk | Low risk | Unclear | Low risk | Unclear | Unclear |
| Tendinopathy location | Outcome domain | Resistance vs. flexibility | Resistance vs. proprioception |
|---|---|---|---|
| All | All | 9 studies, 18 comparisons, 152 outcomes | 4 studies, 4 comparisons, 68 outcomes |
| All | Disability | 9 studies, 18 comparisons, 56 outcomes | 4 studies, 4 comparisons, 18 outcomes |
| All | Pain | 5 studies, 13 comparisons, 55 outcomes | 3 studies, 3 comparisons, 15 outcomes |
| All | Function | 1 study, 2 comparisons, 2 outcomes | No data |
| All | PFC | 3 studies, 4 comparisons, 13 outcomes | 2 studies, 2 comparisons, 23 outcomes |
| All | QoL | 2 studies, 2 comparisons, 10 outcomes | No data |
| RCSP | All | 5 studies, 6 comparisons, 79 outcomes | 4 studies, 4 comparisons, 68 outcomes |
| RCSP | Disability | 5 studies, 6 comparisons, 21 outcomes | 4 studies, 4 comparisons, 18 outcomes |
| RCSP | Pain | 3 studies, 3 comparisons, 21 outcomes | 3 studies, 3 comparisons, 15 outcomes |
| RCSP | Function | No data | No data |
| RCSP | PFC | 2 studies, 2 comparisons, 11 outcomes | 2 studies, 2 comparisons, 23 outcomes |
| RCSP | QoL | 2 studies, 2 comparisons, 9 outcomes | No data |
| RCSP | ROM | 2 studies, 2 comparisons, 16 outcomes | 1 study, 1 comparison, 12 outcomes |
| Achilles | All | 2 studies, 9 comparisons, 63 outcomes | No data |
| Achilles | Disability | 2 studies, 9 comparisons, 31 outcomes | No data |
| Achilles | Pain | 1 study, 8 comparisons, 32 outcomes | No data |
| Achilles | Function | No data | No data |
| Achilles | PFC | No data | No data |
| Achilles | QoL | No data | No data |
| Elbow | All | 1 study, 2 comparisons, 8 outcomes | No data |
| Elbow | Disability | 1 study, 2 comparisons, 2 outcomes | No data |
| Elbow | Pain | 1 study, 2 comparisons, 2 outcomes | No data |
| Elbow | Function | 1 study, 2 comparisons, 2 outcomes | No data |
| Elbow | PFC | 1 study, 2 comparisons, 2 outcomes | No data |
| Elbow | QoL | No data | No data |
| Patellar | All | 1 study, 1 comparison, 2 outcomes | No data |
| Patellar | Disability | 1 study, 2 comparisons, 2 outcomes | No data |
| Patellar | Pain | No data | No data |
| Patellar | Function | No data | No data |
| Patellar | PFC | No data | No data |
| Patellar | QoL | No data | No data |
| Gluteal | All | No data | No data |
| Gluteal | Disability | No data | No data |
| Gluteal | Pain | No data | No data |
| Gluteal | Function | No data | No data |
| Gluteal | PFC | No data | No data |
| Gluteal | QoL | No data | No data |
| Comparison | Outcome | Overall RoB | Inconsistency | Imprecision | Indirectness | Small-study effects | Strength of evidence |
|---|---|---|---|---|---|---|---|
| Resistance vs. flexibility | All tendinopathies/all outcomes | Low risk | High risk | Low risk | Low risk | Low risk | Moderate |
| Resistance vs. flexibility | All tendinopathies/disability | Low risk | High risk | High risk | Low risk | Low risk | Low |
| Resistance vs. flexibility | All tendinopathies/pain | Low risk | Low risk | Low risk | Low risk | Low risk | High |
| Resistance vs. flexibility | All tendinopathies/PFC | Unclear | High risk | High risk | Low risk | High risk | Very low |
| Resistance vs. flexibility | All tendinopathies/QoL | Low risk | High risk | High risk | Low risk | Low risk | Low |
| Resistance vs. flexibility | RCSP/All outcomes | Low risk | High risk | High risk | Low risk | High risk | Very low |
| Resistance vs. flexibility | RCSP/disability | Low risk | High risk | High risk | Low risk | High risk | Very low |
| Resistance vs. flexibility | RCSP/pain | Low risk | High risk | High risk | Low risk | Low risk | Low |
| Resistance vs. flexibility | RCSP/PFC | Low risk | High risk | High risk | Low risk | High risk | Very low |
| Resistance vs. flexibility | RCSP/ROM | Unclear | High risk | High risk | Low risk | Low risk | Very low |
| Resistance vs. flexibility | Achilles/all outcomes | Low risk | High risk | Low risk | Low risk | Low risk | Moderate |
| Resistance vs. flexibility | Achilles/disability | Low risk | High risk | High risk | Low risk | Low risk | Low |
| Resistance vs. proprioception | All tendinopathies/all outcomes | Low risk | High risk | High risk | Low risk | High risk | Very low |
| Resistance vs. proprioception | All tendinopathies/disability | Low risk | High risk | High risk | Low risk | Low risk | Low |
| Resistance vs. proprioception | All tendinopathies/pain | Low risk | High risk | High risk | Low risk | High risk | Very low |
| Resistance vs. proprioception | All tendinopathies/PFC | Low risk | High risk | High risk | Low risk | Low risk | Low |
| Resistance vs. proprioception | RCSP/all outcomes | Low risk | High risk | High risk | Low risk | High risk | Very low |
| Resistance vs. flexibility | RCSP/disability | Low risk | High risk | High risk | Low risk | Low risk | Low |
| Resistance vs. flexibility | RCSP/pain | Low risk | High risk | High risk | Low risk | High risk | Very low |
| Resistance vs. flexibility | RCSP/PFC | Low risk | High risk | High risk | Low risk | Low risk | Low |
| Tendinopathy | Outcome domain | Resistance-only vs. flexibility-only | Resistance-only vs. resistance + flexibility |
|---|---|---|---|
| All | All | 3 studies, 10 comparisons, 77 outcomes | 3 studies, 4 comparisons, 26 outcomes |
| All | Disability | 3 studies, 10 comparisons, 35 outcomes | 1 study, 1 comparison, 2 outcomes |
| All | Pain | 2 studies, 9 comparisons, 38 outcomes | 2 studies, 3 comparisons, 5 outcomes |
| All | Function | No data | 1 study, 2 comparisons, 4 outcomes |
| All | PFC | No data | 2 studies, 2 comparisons, 15 outcomes |
| All | QoL | 1 study, 1 comparison, 4 outcomes | No data |
| RCSP | All | 1 study, 1 comparison, 14 outcomes | No data |
| RCSP | Disability | 1 study, 1 comparison, 4 outcomes | No data |
| RCSP | Pain | 1 study, 1 comparison, 6 outcomes | No data |
| RCSP | Function | No data | No data |
| RCSP | PFC | No data | No data |
| RCSP | QoL | 1 study, 1 comparison, 4 outcomes | No data |
| RCSP | ROM | No data | No data |
| Achilles | All | 2 studies, 9 comparisons, 63 outcomes | 1 study, 1 comparison, 14 outcomes |
| Achilles | Disability | 2 studies, 9 comparisons, 31 outcomes | No data |
| Achilles | Pain | 1 study, 8 comparisons, 32 outcomes | 1 study, 1 comparison, 1 outcome |
| Achilles | Function | No data | No data |
| Achilles | PFC | No data | 1 study, 1 comparison, 13 outcomes |
| Achilles | QoL | No data | No data |
| Elbow | All | No data | 1 study, 2 comparisons, 10 outcomes |
| Elbow | Disability | No data | No data |
| Elbow | Pain | No data | 1 study, 2 comparisons, 4 outcomes |
| Elbow | Function | No data | 1 study, 2 comparisons, 4 outcomes |
| Elbow | PFC | No data | 1 study, 2 comparisons, 2 outcomes |
| Elbow | QoL | No data | No data |
| Patellar | All | No data | 1 study, 1 comparison, 2 outcomes |
| Patellar | Disability | No data | 1 study, 1 comparison, 2 outcomes |
| Patellar | Pain | No data | No data |
| Patellar | Function | No data | No data |
| Patellar | PFC | No data | No data |
| Patellar | QoL | No data | No data |
| Gluteal | All | No data | No data |
| Gluteal | Disability | No data | No data |
| Gluteal | Pain | No data | No data |
| Gluteal | Function | No data | No data |
| Gluteal | PFC | No data | No data |
| Gluteal | QoL | No data | No data |
| Comparison | Outcome | Overall RoB | Inconsistency | Imprecision | Indirectness | Small-study effects | Strength of evidence |
|---|---|---|---|---|---|---|---|
| Resistance-only vs. flexibility-only | All tendinopathies/all outcomes | Low risk | High risk | Low risk | Low risk | Low risk | Moderate |
| Resistance-only vs. flexibility-only | All tendinopathies/disability | Low risk | High risk | High risk | Low risk | Low risk | Low |
| Resistance-only vs. flexibility-only | All tendinopathies/pain | Low risk | High risk | Low risk | Low risk | Low risk | Moderate |
| Resistance-only vs. flexibility-only | Achilles/all outcomes | Low risk | High risk | Low risk | Low risk | Low risk | Moderate |
| Resistance-only vs. flexibility-only | Achilles/disability | Low risk | High risk | High risk | Low risk | Low risk | Low |
| Resistance-only vs. resistance + flexibility | All tendinopathies/all outcomes | Low risk | High risk | High risk | Low risk | High risk | Very low |
| Resistance-only vs. resistance + Flexibility | All tendinopathies/PFC | Low risk | High risk | High risk | Low risk | High risk | Very low |
| Tendinopathy | Outcome domain | Eccentric-only vs concentric and eccentric | Eccentric-only vs concentric-only | Eccentric only vs isometric |
|---|---|---|---|---|
| All | All | 6 studies, 7 comparisons, 56 outcomes | 7 studies, 7 comparisons, 57 outcomes | 4 studies, 4 comparisons, 16 outcomes |
| All | Disability | 5 studies, 5 comparisons, 14 outcomes | 5 studies, 5 comparisons, 8 outcomes | 2 studies, 2 comparisons, 7 outcomes |
| All | Pain | 5 studies, 6 comparisons, 18 outcomes | 6 studies, 6 comparisons, 15 outcomes | 2 studies, 2 comparisons, 4 outcomes |
| All | Function | 1 study, 2 comparisons, 4 outcomes | 1 study, 1 comparison, 1 outcome | 3 studies, 3 comparisons, 5 outcomes |
| All | PFC | 3 studies, 4 comparisons, 17 outcomes | 4 studies, 4 comparisons, 23 outcomes | No data |
| All | QoL | No data | 1 study, 1 comparison, 9 outcomes | No data |
| RCSP | All | 2 studies, 2 comparisons, 30 outcomes | 1 study, 1 comparison, 7 outcomes | No data |
| RCSP | Disability | 2 studies, 2 comparisons, 8 outcomes | 1 study, 1 comparison, 2 outcomes | No data |
| RCSP | Pain | 1 study, 1 comparison, 6 outcomes | No data | No data |
| RCSP | Function | No data | No data | No data |
| RCSP | PFC | 2 studies, 2 comparisons, 13 outcomes | 1 study, 1 comparison, 4 outcomes | No data |
| RCSP | QoL | No data | No data | No data |
| RCSP | ROM | 1 study, 1 comparison, 3 outcomes | 1 study, 1 comparison, 1 outcome | No data |
| Achilles | All | 1 study, 1 comparison, 6 outcomes | 3 studies, 3 comparisons, 17 outcomes | 1 study, 1 comparison, 6 outcomes |
| Achilles | Disability | 1 study, 1 comparison, 4 outcomes | 1 study, 1 comparison, 1 outcome | 1 study, 1 comparison, 5 outcomes |
| Achilles | Pain | 1 study, 1 comparison, 2 outcomes | 3 studies, 3 comparisons, 3 outcomes | No data |
| Achilles | Function | No data | No data | 1 study, 1 comparison, 1 outcome2 |
| Achilles | PFC | No data | 1 study, 1 comparison, 13 outcomes | No data |
| Achilles | QoL | No data | No data | No data |
| Elbow | All | 1 study, 2 comparisons, 12 outcomes | 2 studies, 2 comparisons, 31 outcomes | 2 studies, 2 comparisons, 8 outcomes |
| Elbow | Disability | No data | 2 studies, 2 comparisons, 4 outcomes | No data |
| Elbow | Pain | 1 study, 2 comparisons, 4 outcomes | 2 studies, 2 comparisons, 11 outcomes | 2 studies, 2 comparisons, 4 outcomes |
| Elbow | Function | 1 study, 2 comparisons, 4 outcomes | 1 study, 1 comparison, 1 outcome | 2 studies, 2 comparisons, 4 outcomes |
| Elbow | PFC | 1 study, 2 comparisons, 4 outcomes | 2 studies, 2 comparisons, 6 outcomes | No data |
| Elbow | QoL | No data | 1 study, 1 comparison, 9 outcomes | No data |
| Patellar | All | 2 studies, 2 comparisons, 8 outcomes | 1 study, 1 comparison, 2 outcomes | 1 study, 1 comparison, 2 outcomes |
| Patellar | Disability | 2 studies, 2 comparisons, 4 outcomes | 1 study, 1 comparison, 1 outcome | 1 study, 1 comparison, 2 outcomes |
| Patellar | Pain | 2 studies, 2 comparisons, 4 outcomes | 1 study, 1 comparison, 1 outcome | No data |
| Patellar | Function | No data | No data | No data |
| Patellar | PFC | No data | No data | No data |
| Patellar | QoL | No data | No data | No data |
| Gluteal | All | No data | No data | No data |
| Gluteal | Disability | No data | No data | No data |
| Gluteal | Pain | No data | No data | No data |
| Gluteal | Function | No data | No data | No data |
| Gluteal | PFC | No data | No data | No data |
| Gluteal | QoL | No data | No data | No data |
| Comparison | Outcome | Overall RoB | Inconsistency | Imprecision | Indirectness | Small-study effects | Strength of evidence |
|---|---|---|---|---|---|---|---|
| Eccentric-only vs. concentric-only | All tendinopathies/all outcomes | Low risk | High risk | High risk | Low risk | High risk | Very low |
| Eccentric-only vs. concentric-only | All tendinopathies/pain | Low risk | High risk | High risk | Low risk | High risk | Very low |
| Eccentric-only vs. concentric-only | All tendinopathies/PFC | Low risk | High risk | High risk | Low risk | High risk | Very low |
| Eccentric-only vs. concentric-only | Achilles/all outcomes | Low risk | High risk | High risk | Low risk | Low risk | Low |
| Eccentric-only vs. concentric-only | Elbow/all outcomes | Low risk | High risk | High risk | Low risk | Low risk | Low |
| Eccentric-only vs. concentric-only | Elbow/pain | Low risk | High risk | High risk | Low risk | Low risk | Low |
| Eccentric-only vs. concentric and eccentric | All tendinopathies/all outcomes | Low risk | High risk | High risk | Low risk | Low risk | Low |
| Eccentric-only vs. concentric and eccentric | All tendinopathies/disability | Low risk | High risk | High risk | Low risk | Low risk | Low |
| Eccentric-only vs. concentric and eccentric | All tendinopathies/pain | Low risk | High risk | High risk | Low risk | Low risk | Low |
| Eccentric-only vs. concentric and eccentric | All tendinopathies/PFC | Low risk | High risk | High risk | Low risk | High risk | Very low |
| Eccentric-only vs. concentric and eccentric | RCSP/all outcomes | Low risk | High risk | High risk | Low risk | Low risk | Low |
| Eccentric-only vs. concentric and eccentric | RCSP/PFC | Low risk | High risk | High risk | Low risk | Low risk | Low |
| Eccentric-only vs. isometric | All tendinopathies/all outcomes | Low risk | High risk | High risk | Low risk | High risk | Very low |
Effectiveness review 3
| Author, year | Random sequence generation | Allocation concealment | Blinding of participants/personnel | Blinding of outcome assessment | Incomplete outcome bias | Selective reporting | Other bias |
|---|---|---|---|---|---|---|---|
| Abat et al. 2016213 | Not applicable (quasi) | Not applicable (quasi) | Unclear | Unclear | Low risk | Unclear | High risk |
| Aceituno-Gómez et al. 2019215 | Low risk | Unclear | Low risk | Low risk | Low risk | Low risk | High risk |
| Akkaya et al. 2016218 | Low risk | Unclear | High risk | High risk | Low risk | Unclear | Low risk |
| Aktas et al. 2007220 | Low risk | Unclear | Low risk | Low risk | Low risk | Unclear | Low risk |
| Akyol et al. 2012221 | Low risk | Low risk | Low risk | Low risk | Low risk | Unclear | High risk |
| Alfredson et al. 199817 | High risk | Unclear | High risk | Unclear | Low risk | Unclear | High risk |
| Alfredson et al. 1999224 | Not applicable (quasi) | Not applicable (quasi) | High risk | High risk | Low risk | Unclear | High risk |
| Arias-Buría et al. 2015230 | Low risk | Low risk | High risk | Low risk | Low risk | Unclear | Low risk |
| Arias-Buría et al. 2017229 | Low risk | Low risk | Unclear | Low risk | Unclear | Low risk | High risk |
| Bae et al. 2011234 | Not applicable (quasi) | Not applicable (quasi) | Unclear | Unclear | Unclear | Unclear | High risk |
| Bagcier et al. 2019235 | Not applicable (quasi) | Not applicable (quasi) | Unclear | Low risk | Unclear | Unclear | High risk |
| Bahr et al. 2006131 | Low risk | Low risk | High risk | Low risk | Low risk | Unclear | Low risk |
| Balius et al. 2016238 | Low risk | Low risk | Unclear | Low risk | Low risk | Unclear | Low risk |
| Bang et al. 2000239 | Low risk | Unclear | Unclear | Low risk | Low risk | Unclear | Low risk |
| Başkurt et al. 2011246 | Low risk | Unclear | High risk | Unclear | Low risk | Unclear | Low risk |
| Beaudreuil et al. 2012705 | Unclear | Low risk | Low risk | Low risk | Low risk | Unclear | Low risk |
| Bek et al. 2012250 | Low risk | Unclear | High risk | High risk | Low risk | Low risk | Low risk |
| Bell et al. 2013251 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Bennell et al. 2010188 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Beyer et al. 201518 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | High risk |
| Blume et al. 2015699 | Unclear | Low risk | Low risk | Low risk | Low risk | Unclear | Low risk |
| Boesen et al. 2017162 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Boesen et al. 2019163 | Low risk | Low risk | Low risk | Low risk | Low risk | Unclear | Low risk |
| Boudreau et al. 2019262 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Breda et al. 2020696 | Low risk | Low risk | High risk | Low risk | Low risk | High risk | High risk |
| Brox et al. 1999269 | High risk | High risk | High risk | High risk | No data | No data | No data |
| Buyuksireci et al. 2020704 | Low risk | Unclear | High risk | Unclear | Low risk | Unclear | High risk |
| Cacchio et al. 2011271 | Low risk | Low risk | High risk | Low risk | Unclear | Unclear | Low risk |
| Calis et al. 2011273 | Low risk | Low risk | Unclear | Unclear | Low risk | Unclear | Unclear |
| Celik et al. 2009279 | Unclear | Unclear | Low risk | Low risk | Low risk | Low risk | Low risk |
| Celik et al. 2009278 | Unclear | Unclear | Unclear | Unclear | Low risk | Low risk | High risk |
| Celik et al. 2019277 | Low risk | Low risk | Unclear | Unclear | Low risk | Unclear | Unclear |
| Cha et al. 2014702 | Unclear | Unclear | Unclear | Unclear | Low risk | Unclear | Unclear |
| Chaconas et al. 2017710 | Low risk | Unclear | Unclear | Low risk | High risk | Unclear | High risk |
| Chary-Valckenaere et al. 2018283 | Low risk | Low risk | Unclear | Low risk | High risk | Low risk | Low risk |
| Chen et al. 2017284 | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | High risk |
| Cheng et al. 2007286 | High risk | High risk | Unclear | Unclear | Unclear | Unclear | High risk |
| Cho et al. 2017289 | High risk | High risk | Unclear | Unclear | Low risk | Low risk | Unclear |
| Chung et al. 2004290 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Clarke et al. 2010294 | Low risk | Low risk | Low risk | Low risk | Low risk | Unclear | Low risk |
| Conroy et al. 1998298 | Unclear | Unclear | Unclear | Low risk | Low risk | Unclear | Low risk |
| Coombes et al. 2013176 | Low risk | Low risk | High risk | Low risk | Low risk | Low risk | Low risk |
| Croisier et al. 2007304 | Not applicable (quasi) | Not applicable (quasi) | Unclear | Low risk | Unclear | Unclear | High risk |
| de Jonge et al. 2008309 | Unclear | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| de Miguel Valtierra et al. 2018312 | Low risk | Low risk | High risk | Low risk | Low risk | Low risk | High risk |
| De Oliveira et al. 2020712 | Low risk | Low risk | Low risk | Low risk | Low risk | High risk | High risk |
| de Vos et al. 200759 | Low risk | Unclear | Low risk | Low risk | Unclear | Low risk | High risk |
| de Vos et al. 2010314 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Dejaco et al. 201744 | Low risk | Low risk | Low risk | Low risk | Low risk | High risk | Low risk |
| Devereaux et al. 2016326 | Low risk | High risk | High risk | High risk | High risk | Unclear | Low risk |
| Dimitrios et al. 2012330 | Not applicable (quasi) | Not applicable (quasi) | Low risk | Low risk | Low risk | Unclear | High risk |
| Dimitrios et al. 2013331 | Not applicable (quasi) | Not applicable (quasi) | Low risk | Low risk | Low risk | Unclear | High risk |
| Dogan et al. 2010333 | Low risk | Low risk | Low risk | Low risk | Low risk | Unclear | Low risk |
| Dupuis et al.339 | Low risk | Low risk | High risk | Low risk | Low risk | Low risk | High risk |
| Eken Gedik et al. 2016341 | Low risk | Low risk | Unclear | Low risk | Unclear | Unclear | High risk |
| Ellegaard et al. 2016342 | Low risk | Low risk | High risk | Low risk | Low risk | Unclear | Low risk |
| Engebretsen et al. 2009344 | Low risk | Low risk | High risk | Low risk | Low risk | Unclear | Low risk |
| Engebretsen et al. 2011345 | Low risk | Low risk | High risk | Low risk | Low risk | Unclear | Low risk |
| Eraslan et al. 2018342 | Low risk | Low risk | Unclear | Unclear | Unclear | Low risk | Unclear |
| Faria et al. 2006354 | High risk | High risk | Unclear | Unclear | Unclear | Unclear | Unclear |
| Fournier Belley et al. 2018164 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Ganderton et al. 2018189 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | High risk |
| García et al. 2016362 | Low risk | Low risk | Low risk | Low risk | Low risk | Unclear | High risk |
| Gatz et al. 2020365 | Low risk | Low risk | Low risk | Low risk | Unclear | Unclear | High risk |
| Genc et al. 2020688 | Low risk | Low risk | High risk | High risk | Unclear | Unclear | High risk |
| Giray et al. 2019368 | Low risk | Low risk | High risk | Low risk | Low risk | Low risk | High risk |
| Granviken et al. 2015374 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Gürsel et al. 2004377 | Low risk | Low risk | Low risk | Unclear | Unclear | Unclear | High risk |
| Hallgren et al. 2017258 | Unclear | Unclear | Low risk | Low risk | Low risk | Low risk | Low risk |
| Hallgren et al. 2014383 | High risk | Low risk | High risk | Low risk | Unclear | Low risk | Low risk |
| Heron et al. 2017390 | Low risk | Low risk | Low risk | Low risk | High risk | High risk | Low risk |
| Holmgren et al. 2012393 | Low risk | Low risk | Low risk | Low risk | Unclear | Low risk | High risk |
| Hotta et al. 2020709 | Low risk | Low risk | High risk | Low risk | Low risk | Low risk | High risk |
| Houck et al. 2015397 | Low risk | Unclear | Unclear | High risk | Low risk | Low risk | Low risk |
| Ilhanli et al. 2015695 | Low risk | Low risk | Unclear | Low risk | Unclear | Unclear | Low risk |
| Ingwersen et al. 2017191 | Low risk | Low risk | Low risk | Low risk | Low risk | High risk | Low risk |
| Jasnauskaitė-Gedrimė et al. 2018401 | Unclear | Unclear | Unclear | Unclear | Low risk | Unclear | High risk |
| Jeong et al. 2008711 | Unclear | Unclear | Unclear | Unclear | Low risk | Unclear | Unclear |
| Johansson et al. 2005405 | Low risk | Unclear | Unclear | Low risk | Low risk | Unclear | High risk |
| Jonsson et al. 2005186 | Unclear | Unclear | Low risk | Unclear | High risk | Unclear | High risk |
| Jonsson 2009408 | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear |
| Juul-Kristensen et al. 2019412 | Low risk | Low risk | Low risk | Low risk | Low risk | Unclear | Low risk |
| Kachanathu et al. 2019413 | Low risk | Low risk | Unclear | Low risk | Low risk | Unclear | High risk |
| Kang et al. 2019416 | Low risk | Low risk | High risk | Low risk | High risk | High risk | High risk |
| Kedia et al. 2014424 | Low risk | Low risk | Low risk | Low risk | Low risk | Unclear | Low risk |
| Ketola et al. 2009426 | Low risk | Low risk | Unclear | Low risk | Low risk | Unclear | High risk |
| Ketola et al. 2013706 | Low risk | Low risk | High risk | Low risk | Low risk | Unclear | Low risk |
| Kim et al. 2017431 | Low risk | Unclear | Unclear | Low risk | Unclear | Low risk | Low risk |
| Kim et al. 2020433 | Low risk | Low risk | High risk | High risk | Low risk | Unclear | High risk |
| Knobloch et al. 2007684 | Low risk | Low risk | Unclear | Unclear | High risk | Unclear | High risk |
| Knobloch et al. 2007192 | Unclear | Unclear | High risk | Low risk | Unclear | Unclear | High risk |
| Knobloch et al. 2008437 | Unclear | Low risk | Unclear | Unclear | Unclear | Unclear | High risk |
| Koç et al. 2020708 | Low risk | Unclear | High risk | Low risk | Low risk | Unclear | Low risk |
| Kongsgaard et al. 200921 | Low risk | Low risk | High risk | Low risk | Low risk | Unclear | Low risk |
| Kromer et al. 2014445 | Low risk | Low risk | High risk | High risk | Low risk | Low risk | Low risk |
| Kromer et al. 2013443 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Kulig et al. 2009448 | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | High risk |
| Land et al. 2019452 | Low risk | Low risk | Low risk | Low risk | High risk | Unclear | Low risk |
| Lee et al. 2017697 | Low risk | Unclear | Unclear | Unclear | Low risk | Unclear | High risk |
| Lee et al. 2014456 | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | High risk |
| Lee et al. 2017459 | No data | No data | No data | No data | No data | No data | No data |
| Littlewood et al. 201634 | Low risk | Low risk | High risk | High risk | Unclear | Unclear | High risk |
| Ludewig et al. 2003463 | Low risk | Unclear | High risk | Unclear | Low risk | Unclear | Low risk |
| Luginbuhl et al. 2008174 | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | High risk |
| Maenhout et al. 2013464 | Unclear | High risk | High risk | High risk | Low risk | Unclear | Low risk |
| Mafi et al. 2001467 | Low risk | Unclear | Unclear | Unclear | Unclear | Unclear | High risk |
| Manias et al. 2006469 | High risk | High risk | High risk | High risk | Low risk | Unclear | Unclear |
| Martinez-Silvestrini et al. 2005471 | Unclear | Unclear | Unclear | Unclear | Low risk | Unclear | High risk |
| Marzetti et al. 2014472 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Mayer et al. 2007474 | Unclear | Unclear | High risk | High risk | Unclear | Unclear | High risk |
| McCormack et al. 2016478 | Low risk | Low risk | Unclear | Unclear | Low risk | Low risk | Low risk |
| McGee et al. 1999701 | Unclear | Unclear | Unclear | Unclear | High risk | Unclear | High risk |
| McQueen et al. 2020694 | High risk | Unclear | Unclear | Unclear | High risk | Unclear | High risk |
| Melegati et al. 2000480 | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | High risk |
| Menek et al. 2019482 | Low risk | Low risk | Unclear | Unclear | Low risk | Unclear | Unclear |
| Mulligan et al. 2016489 | Low risk | Low risk | Low risk | Low risk | Low risk | Unclear | High risk |
| Nazligul et al. 2018493 | Low risk | Low risk | Low risk | Unclear | Low risk | Unclear | Low risk |
| Nishizuka et al. 2017498 | Low risk | Low risk | High risk | Unclear | Low risk | Unclear | High risk |
| Nørregaard et al. 2007499 | Low risk | Low risk | Unclear | Unclear | Unclear | Unclear | High risk |
| Notarnicola et al. 2014500 | Not applicable (quasi) | Not applicable (quasi) | High risk | Unclear | Unclear | Unclear | High risk |
| Nowotny et al. 2018501 | Low risk | Unclear | Low risk | Low risk | High risk | Unclear | High risk |
| Olaussen et al. 2015506 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Østerås et al. 2009512 | Low risk | Low risk | Unclear | High risk | Low risk | Unclear | Low risk |
| Østerås et al. 2010514 | Low risk | Low risk | High risk | High risk | Low risk | Unclear | High risk |
| Paavola et al. 2018516 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Park et al. 2010521 | Low risk | Unclear | Unclear | Unclear | Unclear | Unclear | High risk |
| Pearson et al. 2012525 | Unclear | Unclear | High risk | Unclear | Low risk | Unclear | High risk |
| Pearson et al. 2018526 | Low risk | Low risk | High risk | Low risk | Low risk | Low risk | High risk |
| Pekgöz et al. 2020707 | Low risk | Low risk | Low risk | Low risk | Low risk | Unclear | Low risk |
| Pekyavas et al. 2016527 | Low risk | Low risk | High risk | Low risk | Unclear | Unclear | Low risk |
| Pérez-Merino et al. 2016529 | Low risk | Unclear | Low risk | Low risk | Unclear | Low risk | Low risk |
| Petersen et al. 2007530 | Low risk | Unclear | Unclear | Unclear | Unclear | Unclear | High risk |
| Peterson et al. 2011531 | Low risk | Low risk | Unclear | High risk | Low risk | Low risk | Low risk |
| Peterson et al. 2014185 | Low risk | Unclear | Low risk | High risk | Low risk | Low risk | Low risk |
| Polimeni et al. 2003698 | Unclear | Unclear | High risk | Low risk | Unclear | Unclear | Unclear |
| Praet et al. 2019535 | Low risk | Low risk | Low risk | Low risk | Low risk | Unclear | Low risk |
| Rabusin et al. 2020686 | Low risk | Low risk | High risk | High risk | Low risk | Low risk | High risk |
| Ramon et al. 2020689 | Unclear | Unclear | Low risk | Low risk | Low risk | Unclear | High risk |
| Reyhan et al. 2020549 | Low risk | Low risk | Unclear | Unclear | Low risk | Unclear | High risk |
| Rhon et al. 2014700 | Low risk | Low risk | High risk | Low risk | Low risk | Low risk | Low risk |
| Rio et al. 2017167 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | High risk |
| Rodríguez-Huguet et al. 2020693 | Low risk | Low risk | Unclear | Low risk | Low risk | Low risk | Low risk |
| Rodríguez-Huguet et al. 2020713 | Low risk | Low risk | Unclear | Low risk | Low risk | Low risk | Low risk |
| Røe et al. 2005553 | No data | No data | No data | No data | No data | No data | No data |
| Romero-Morales et al. 2020685 | Unclear | Unclear | Unclear | Unclear | Low risk | Low risk | High risk |
| Rompe et al. 2007558 | Low risk | Low risk | Unclear | Low risk | Low risk | Unclear | Low risk |
| Rompe et al. 2008687 | Low risk | Low risk | Unclear | Low risk | Low risk | Unclear | Unclear |
| Rompe et al. 2009557 | Unclear | Low risk | High risk | High risk | Low risk | Unclear | Low risk |
| Rompe et al. 2009559 | Low risk | Low risk | High risk | Low risk | Low risk | Unclear | Low risk |
| Roos et al. 2004193 | Low risk | Unclear | Unclear | Low risk | Low risk | Unclear | Low risk |
| Rosety-Rodriguez et al. 2006560 | Low risk | Unclear | Unclear | Unclear | Unclear | Unclear | High risk |
| Santamato et al. 2016570 | Low risk | Low risk | High risk | Low risk | Low risk | Unclear | High risk |
| Scott et al. 2019714 | Low risk | Low risk | High risk | Low risk | Low risk | Low risk | Low risk |
| Şenbursa et al. 2011582 | Low risk | Unclear | Unclear | Unclear | Low risk | Unclear | Low risk |
| Seven et al. 2017583 | Low risk | Low risk | High risk | Low risk | High risk | Unclear | Low risk |
| Sevier et al. 2015584 | Low risk | Unclear | High risk | High risk | High risk | Unclear | High risk |
| Silbernagel et al. 2001587 | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | High risk |
| Silbernagel et al. 2007138 | Low risk | Low risk | High risk | High risk | Low risk | Unclear | Low risk |
| Şimşek et al. 2013591 | Unclear | Unclear | Unclear | Low risk | Unclear | Unclear | Unclear |
| Slider et al. 2013690 | Low risk | Unclear | Low risk | Low risk | Low risk | Unclear | Unclear |
| Smidt et al. 2002592 | Low risk | Low risk | High risk | High risk | Low risk | Unclear | Low risk |
| Söderberg et al. 2012594 | Unclear | Low risk | Low risk | Low risk | Low risk | Unclear | Low risk |
| Stasinopoulos and Manias 2013692 | High risk | High risk | High risk | Low risk | Low risk | Unclear | High risk |
| Stasinopoulos et al. 2006599 | Not applicable (quasi) | Not applicable (quasi) | Unclear | Low risk | Low risk | Unclear | High risk |
| Stasinopoulos et al. 2009600 | Not applicable (quasi) | Low risk | High risk | Low risk | Unclear | Unclear | High risk |
| Stasinopoulos et al. 2010601 | Not applicable (quasi) | Not applicable (quasi) | Low risk | Low risk | Low risk | Unclear | High risk |
| Stasinopoulos et al. 2017597 | Low risk | Unclear | Low risk | Low risk | Low risk | Unclear | High risk |
| Stefansson et al. 2019184 | Low risk | Unclear | High risk | Low risk | High risk | Unclear | Low risk |
| Stergioulas et al. 2007603 | Low risk | Low risk | High risk | Low risk | Unclear | Unclear | Unclear |
| Stergioulas et al. 2008604 | Low risk | Low risk | Low risk | Low risk | Low risk | Unclear | Low risk |
| Steunebrink et al. 2013605 | Low risk | Low risk | Low risk | Low risk | Low risk | Unclear | Low risk |
| Stevens et al. 2014175 | Unclear | Unclear | High risk | High risk | Unclear | Unclear | High risk |
| Struijs et al. 2004608 | Low risk | Low risk | High risk | Low risk | Low risk | Unclear | High risk |
| Svernlov and Adolfsson 2001614 | Not applicable (quasi) | Not applicable (quasi) | Unclear | Unclear | Unclear | Unclear | High risk |
| Tahran et al. 2020618 | Low risk | Unclear | Low risk | Low risk | Low risk | Unclear | Low risk |
| Thijs et al. 2017621 | Low risk | Low risk | Low risk | Low risk | Low risk | Unclear | Low risk |
| Tonks 2012623 | No data | No data | No data | No data | No data | No data | No data |
| Tonks et al. 2007624 | Low risk | Low risk | Low risk | High risk | High risk | Low risk | Low risk |
| Tumilty et al. 2012630 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Tumilty et al. 2016632 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Turgut et al. 2017633 | Low risk | Unclear | Unclear | Unclear | High risk | Unclear | Low risk |
| Tyler et al. 2010636 | Unclear | Unclear | Unclear | Low risk | Unclear | Unclear | High risk |
| Vallés-Carrascosa et al. 2018638 | Low risk | Low risk | Low risk | High risk | Low risk | Low risk | High risk |
| van Der Vlist 2020646 | Low risk | Low risk | High risk | Low risk | Low risk | Low risk | Low risk |
| van Ark et al. 2016644 | Low risk | Low risk | Low risk | Unclear | Unclear | Low risk | Low risk |
| Vinuesa-Montoya et al. 2017641 | Low risk | Low risk | High risk | Low risk | Low risk | Low risk | Low risk |
| Visnes et al. 2005129 | Low risk | Low risk | High risk | Low risk | Unclear | Unclear | Unclear |
| Vuvan et al. 2019187 | Low risk | Low risk | High risk | High risk | Low risk | Low risk | Low risk |
| Walther et al. 2004161 | Unclear | Unclear | Unclear | Unclear | Low risk | Unclear | Unclear |
| Warden et al. 2008652 | Low risk | Low risk | Low risk | Low risk | Low risk | Unclear | Low risk |
| Wegener et al. 2016655 | Low risk | Low risk | High risk | Low risk | Low risk | Unclear | High risk |
| Wen et al. 2011657 | Unclear | Unclear | Low risk | Unclear | High risk | Unclear | High risk |
| Werner et al. 2002658 | Low risk | Unclear | Unclear | Unclear | Unclear | Unclear | High risk |
| Wiedmann et al. 2017664 | Low risk | Low risk | Unclear | Unclear | Unclear | Unclear | High risk |
| Yazmalar et al. 2016671 | Low risk | Unclear | Unclear | Unclear | Unclear | Unclear | High risk |
| Yeldan et al. 2009672 | Low risk | Unclear | Unclear | Unclear | Unclear | Low risk | Low risk |
| Yelland et al. 2011674 | Low risk | Low risk | High risk | Low risk | Low risk | Unclear | Low risk |
| Yerlikaya et al. 2018675 | Low risk | Unclear | Low risk | Low risk | Unclear | Unclear | High risk |
| Young et al. 2005132 | Unclear | Unclear | High risk | Low risk | High risk | Unclear | High risk |
| Yu et al. 2013680 | Low risk | Low risk | Low risk | Unclear | Low risk | Unclear | Unclear |
| Yuruk et al. 2014683 | Low risk | Low risk | Unclear | Unclear | Low risk | Unclear | Unclear |
| Tendinopathy | Outcome domain | Exercise plus non-exercise | Exercise-only | Non-exercise-only | Non-active |
|---|---|---|---|---|---|
| All | All | 103 trials, 909 outcomes | 100 trials, 1035 outcomes | 50 trials, 450 outcomes | 27 trials, 314 outcomes |
| All | Disability | 91 trials, 311 outcomes | 90 trials, 319 outcomes | 42 trials, 111 outcomes | 23 trials, 99 outcomes |
| All | Pain | 69 trials, 282 outcomes | 69 trials, 295 outcomes | 36 trials, 132 outcomes | 20 trials, 69 outcomes |
| All | Function | 69 trials, 282 outcomes | 69 trials, 295 outcomes | 36 trials, 132 outcomes | 20 trials, 69 outcomes |
| All | PFC | 24 trials, 68 outcomes | 24 trials, 83 outcomes | 13 trials, 57 outcomes | 9 trials, 42 outcomes |
| All | QoL | 18 trials, 71 outcomes | 18 trials, 71 outcomes | 8 trials, 25 outcomes | 6 trials, 17 outcomes |
| Outcome | Overall RoB | Inconsistency | Imprecision | Indirectness | Small-study effects | Strength of evidence |
|---|---|---|---|---|---|---|
| All tendinopathies/all outcomes | Low risk | High risk | High risk | Low risk | Low risk | Low |
| All tendinopathies/disability | Low risk | High risk | High risk | Low risk | Low risk | Low |
| All tendinopathies/pain | Low risk | High risk | High risk | Low risk | Low risk | Low |
| All tendinopathies/PFC | Low risk | High risk | High risk | Low risk | Low risk | Low |
| All tendinopathies/QoL | Low risk | High risk | High risk | Low risk | High risk | Very low |
| All tendinopathies/function | Low risk | High risk | High risk | Low risk | Low risk | Low |
| Exercise + electro-therapy [95% CrI] |
Exercise + injection [95%CrI] | Exercise + kinetics [95% CrI] |
Exercise + surgery [95% CrI] |
Exercise + MT [95% CrI] |
Exercise + non-active [95% CrI] |
Outcome domains | Tendinopathy |
|---|---|---|---|---|---|---|---|
| 12 trials, 69 outcomes | 7 trials, 67 outcomes | 16 trials, 156 outcomes | 12 trials, 189 outcomes | 13 trials, 110 outcomes | 5 trials, 37 outcomes | All | All |
| 12 trials, 32 outcomes | 5 trials, 19 outcomes | 14 trials, 48 outcomes | 12 trials, 63 outcomes | 10 trials, 38 outcomes | 5 trials, 16 outcomes | Disability | All |
| 7 trials, 20 outcomes | 5 trials, 20 outcomes | 16 trials, 156 outcomes | 11 trials, 80 outcomes | 9 trials, 33 outcomes | 3 trials, 13 outcomes | Pain | All |
| 3 trials, 5 outcomes | 2 trials, 8 outcomes | 5 trials, 23 outcomes | 1 trial 6 outcomes | 3 trials, 12 outcomes | 2 trials, 6 outcomes | PFC | All |
| 0 trials, 0 outcomes | 1 trial 4 outcomes | 5 trials, 10 outcomes | 0 trials, 0 outcomes | 5 trials, 18 outcomes | 1 trial 2 outcomes | Function | All |
| Therapy class | Outcome | Overall RoB | Inconsistency | Imprecision | Indirectness | Small-study effects | Strength of evidence |
|---|---|---|---|---|---|---|---|
| Exercise + electrotherapy | All tendinopathies/all outcomes | Low risk | High Risk | High risk | Low risk | Low risk | Low |
| Exercise + injection | All tendinopathies/all outcomes | Low risk | Low risk | High risk | Low risk | Low risk | Moderate |
| Exercise + kinetics | All tendinopathies/all outcomes | High risk | Low risk | Low risk | Low risk | Low risk | Moderate |
| Exercise + surgery | All tendinopathies/all outcomes | Low risk | High risk | High risk | Low risk | Low risk | Low |
| Exercise + MT | All tendinopathies/all outcomes | Low risk | High risk | High risk | Low risk | Low risk | Low |
| Exercise + non-active | All tendinopathies/all outcomes | Low risk | High risk | High risk | Low risk | Low risk | Low |
| Exercise + electrotherapy | All tendinopathies/disability | Low risk | High risk | High risk | Low risk | High risk | Very low |
| Exercise + injection | All tendinopathies/disability | Low risk | Low risk | High risk | Low risk | Low risk | Moderate |
| Exercise + kinetics | All tendinopathies/disability | Low risk | Low risk | Low risk | Low risk | Low risk | High |
| Exercise + surgery | All tendinopathies/disability | Low risk | High risk | High risk | Low risk | Low risk | Low |
| Exercise + MT | All tendinopathies/disability | Low risk | Low risk | High risk | Low risk | Low risk | Moderate |
| Exercise + non-active | All tendinopathies/disability | Low risk | High risk | High risk | Low risk | High risk | Very low |
| Exercise + electrotherapy | All tendinopathies/pain | Low risk | High risk | High risk | Low risk | High risk | Very low |
| Exercise + injection | All tendinopathies/pain | Low risk | Low risk | High risk | Low risk | Low risk | Moderate |
| Exercise + kinetics | All tendinopathies/pain | High risk | High risk | High risk | Low risk | Low risk | Very low |
| Exercise + surgery | All tendinopathies/pain | Low risk | High risk | High risk | Low risk | High risk | Very low |
| Exercise + MT | All tendinopathies/pain | Low risk | High risk | High risk | Low risk | Low risk | Low |
| Exercise + non-active | All tendinopathies/pain | Low risk | High risk | High risk | Low risk | Low risk | Low |
| Exercise + kinetics | All tendinopathies/PFC | High risk | High risk | High risk | Low risk | Low risk | Very low |
| Exercise + MT | All tendinopathies/PFC | Low risk | High risk | High risk | Low risk | Low risk | Low |
| Exercise + kinetics | All tendinopathies/function | High risk | High risk | High risk | Low risk | Low risk | Very low |
| Exercise + MT | All tendinopathies/Funmction | Low risk | High risk | High risk | Low risk | Low risk | Low |
Appendix 7 Studies included in mixed-methods review
| First author year |
Methodology design | Setting | Participants (number (n); sex (n); mean age; mean symptom duration) | Intervention (quantitative) Intervention or focus of study (qualitative) |
Feasibility (types; measures/tools) |
Acceptability (types; measures/tools) | Results |
|---|---|---|---|---|---|---|---|
| Rotator cuff | |||||||
| Barrett 2018154 |
Qualitative Qualitative descriptive |
Hospital outpatient physiotherapy (Ireland) |
n = 23 patients 8 males Age 62.5 Symptoms 25.3 months |
6-week group exercise class + HEP | Experiences and perceptions of group-based exercise Semi-structured telephone interviews |
Themes: (i) support, motivation and learning from peers; (ii) preference for exercise class compared to individual physiotherapy; (iii) the physiotherapist as an educator and facilitator; (iv) beliefs about pain and exercise | |
| Bateman 2014248 |
Quantitative RCT (feasibility) |
HEP (UK) |
n = 11 patients 6 males Age 53.5 Symptoms NR |
8-week eccentric rotator cuff exercises vs. concentric strengthening vs. no exercises | Adherence Diary |
NA | Mean Adherence = 86% (of five patients who returned diaries) |
| Bennell 2010188 |
Quantitative RCT |
Clinic and HEP (Australia) |
n = 120 patients 64 males Age 60 Symptoms (median) 19 months |
12-week HEP + MT vs. placebo | Adherence and attendance Log book (adherence), number of physiotherapy session (attendance) |
Tolerability Reporting of events |
Adherence (HEP overall): 82% during intervention period vs. 70% during follow-up; attendance: 91% attended in active group vs. 93% in placebo; tolerability: 10-weeks physiotherapy + HEP (12/55, 22%) reported increased pain with home exercise); 12-week HEP period (7/49 (14%) reported short-term pain with home exercise |
| Boudreau 2019262 |
Quantitative RCT |
HEP (Canada) |
n = 42 patients 20 males Age 49.9 Symptoms 43 months |
6-week HEP of scapular strengthening + rotator cuff muscles vs. rotator cuff strengthening + coactivation | Adherence Log book |
NA | Adherence rate = 85.7% (overall) |
| Conroy and Hayes 1998298 |
Quantitative RCT (pre/post control) |
Physiotherapy clinic and HEP (USA) |
n = 14 patients 8 males Age 52.9 Symptoms NR |
3-week joint mobilisation + comprehensive treatment (hot pack, active ROM, stretching, strengthening, mobilisation, education) vs. comprehensive treatment only | Adherence and Attendance Log (Adherence), Number of attended physiotherapy sessions (Attendance) |
NA | Adherence: 82% for both groups; attendance: 96% for both groups |
| Cook 2014172 |
Quantitative RCT |
Outpatient clinic and academic centres (USA) |
n = 68 patients 37 males Age 52.6 Symptoms 2.7 months |
Duration NR. Shoulder treatment (MT, stretching, isotonic strengthening) + neck mobilisations vs. should treatment only | Adherence Score at discharge |
Satisfaction Patient Acceptable Symptom Scale (PASS) |
Adherence: high (51% overall; 49% shoulder/neck; 55% shoulder), compliant (41% overall; 43% shoulder/neck, 39% shoulder), not (3% overall; 0% shoulder/neck; 6% shoulder), extremely not (4% overall, 8% shoulder/neck; 0% shoulder); satisfaction: all = 56 acceptable vs. 10 unacceptable; shoulder and neck group = 27 acceptable vs. 3 unacceptable |
| Dejaco 201644 |
Quantitative RCT |
Sports medical centre and HEP (Netherlands) |
n = 36 patients 19 males Age 49.5 Symptoms 19.7 months |
Duration NR. Participants allocated to eccentric exercise vs. conventional exercise | Adherence Journal |
NA | Adherence eccentric group 92% vs. 91% in conventional |
| Dupuis 2018339 |
Quantitative RCT |
HEP (Canada) |
n = 43 patients Sex NR Age 38.3 Symptoms < 1 month |
6-week intervention consisting of gradual loading + strengthening (resisted isotonic) vs. rest + cryotherapy + strengthening | Adherence Diary |
NA | Week 2: 33.6/42 sessions cryotherapy group vs. 31.9/42 gradual reloading exercises; week 6: 19.5/28 days cryotherapy group vs. 11.4/28 for exercise group |
| Flores 2017183 |
Quantitative RCT |
Physiotherapy centre (Spain) |
n = 84 patients 44 males Age 40.2 Symptoms NR |
Duration NR. Physiotherapy (stretching and strengthening) + subacromial HA injections vs. physiotherapy only | NA | Tolerability Self-report |
Patients’ perception of tolerability: day 7 = >2.5 (same as injection group); day 15 = 3.0 (same as injection group); day 30 = >3.0 (injection group higher); Day 90 = >3.0 (injection group higher) |
| Ferrer 2018177 |
Quantitative Cohort |
Supervised (NR), HEP (USA) |
n = 5 patients 1 male Age 60.2 Symptoms NR |
12-week exercise intervention (first 6 weeks supervised, last HEP including isometric, active range of movement, progressive resistance) | Adherence Log |
NA | 100% completed programme. One patient showed poor compliance with the HEP protocol and did not give maximal effort during supervised exercise therapy sessions as determined by supervising physical therapist |
| Fournier Belley 2018164 |
Quantitative RCT |
Treatment session NR and HEP (Canada) |
n = 40 patients 22 males Age 45.5 Symptoms 10.2 months |
6-week rehabilitation programme (sensorimotor training, education, strengthening) + a-tDCS vs. rehabilitation programme + sham a-tDCS | Adherence and attendance Log book (Adherence), NR (Attendance) |
NA | Adherence = 86% (between weeks 6 and 12 for HEP overall); attendance: mean attendance rate = 98.75% (4 physical therapy sessions missed, 3 by participant who dropped out) |
| Granviken 2015374 |
Quantitative RCT |
Physiotherapy outpatient clinic and HEP (Norway) |
n = 46 patients 24 males Age 47.9 Symptoms (median) 20.5 months |
6-week HEP (scapular stabilisation, rotator cuff exercises, pain-free ROM) + 1 supervised session vs. 10 supervised sessions + HEP | Adherence and attendance Diary (adherence), number of supervised sessions attended (attendance) |
NA | Adherence: 88% for HEP vs 80% for supervised group + HEP; attendance: 8/10 treatments (median) |
| Hanratty 2016155 |
Qualitative Qualitative descriptive |
NHS and private practice musculoskeletal outpatient departments and orthopaedics, rheumatology and sports medicine clinics (Northern Ireland and Republic of Ireland) |
n = 20 physical therapists 2 males All ≥ 5-y postgraduate experience and formal postgraduate training MT |
Exercise for SIS | Perceptions of the use and types of exercises commonly used in SIS Focus groups |
Exercise was key in SIS management. Overarching theme: the need to ‘gain buy-in to exercise’ at an early stage; main subtheme; patient education | |
| Heron 2017390 |
Quantitative RCT |
Outpatient physiotherapy department and HEP (UK) |
n = 120 patients 71 males Age 49.9 Symptoms 3 months–1 year (n = 78), > 1 year (n = 42) |
6-week three dynamic rotator cuff loading programmes (open chain, closed chain, range of movement) | Adherence Diary |
NA | % of prescribed exercise completed Range of movement (14 returned diaries): 12 (86%) completed 76–100%; 2 (14%) completed 51–75%; open chain (12 returned diaries) 10 (83%) completed 76–100%, 2 (17%) completed 51–75%); closed chain (13 returned diaries) 11 (85%) completed 76–100%, 1 (8%) completed 51–75%, 1 (8%) completed 26–50% |
| Holmgren 2012393 |
Quantitative RCT |
Hospital orthopaedics department and HEP (Sweden) |
n = 97 patients 61 males Age 52 Symptoms 18.5 months |
12-week HEP (eccentric strengthening for rotator cuff, concentric/eccentric for scapular, manual mobilisation) vs. unspecific movement exercises (control) | Adherence and attendance Diary (adherence), session schedule (attendance) |
NA | Adherence: specific exercise group 44 patients missed < 15 days vs. 40 in control group; attendance: in specific exercise and control (non-specific exercise) groups, 80% attended target number of visits |
| Ingwersen 2017191 |
Quantitative RCT |
Clinic and HEP (Denmark) |
n = 100 patients 52 males Age 46.1 Symptoms 12.0 months |
12-week exercise programme PHLE vs. LLE (initial instruction, supervised, and HEP) + concomitant corticosteroid injection | Adherence Diary |
Tolerability Increased pain, decreased strength |
Adherence: 57% compliance in PHLE group vs. 61% in LLE; tolerability (pain): 13/49 (27%) of patients in the PHLE group and 18/51 (35%) in LLE |
| Juul-Kristensen 2019412 |
Quantitative RCT |
Supervised exercises NR and HEP (Denmark) |
n = 49 patients 24 males Age 42.9 Symptoms > 1 month |
8-week BIONEX exercises (scapular focussed) vs. scapular exercises without EMG-biofeedback | Adherence and attendance Diary (adherence), attendance to sessions (attendance) |
NA | Adherence = 86% for BIONEX vs. 88% for exercises without feedback; attendance: 86% attendance for BIONEX vs. 88% for exercises without feedback |
| Kim 2019432 |
Quantitative RCT (prospective non-randomised) |
HEP (South Korea) |
n = 30 patients 33 males Age 54.65 Symptoms NR |
Duration NR. PRP vs. rotator cuff strengthening exercises | Adherence Self-report |
NA | Adherence in exercise group at 6 weeks 90.8% vs. 94.2% at 12 weeks vs. 87.4% at 24 weeks |
| Kromer 2013443 |
Quantitative RCT |
Outpatient physiotherapy clinic and HEP (Germany) |
n = 90 patients 64 males Age 51.8 Symptoms > 24 months |
12-week exercise intervention with individually adapted exercises +examination-based physiotherapy vs. exercises only | Adherence Log book |
NA | Mean exercise frequency per week = 5.5 and during HEP period 3.8 for the intervention and 3.9 for the control group (98.9% returned complete log book after 5 weeks, 94.4% after 12 weeks) |
| Kvalvaag 2018450 |
Quantitative RCT |
NR (Norway) |
n = 143 patients 65 males Age 46.8 Symptoms 3–6 months (n = 29), 6–12 months (n = 37), 12–24months (n = 27), 24 + months (n = 50) |
10-week intervention consisting of RSWT + supervised exercises (scapular positioning + guided movements) vs. sham + supervised exercises | Attendance Measurement NR |
NA | RSWT attendance = 14/20 (70%) (median) treatments (range 2–21) vs. 13/20 (65%) for sham (range 2–20) |
| Littlewood 2014156,* |
Qualitative Qualitative descriptive Mixed-methods |
One private physiotherapy clinic (UK) |
Patients: n = 6 3 males Age 64.7 Physiotherapists: n = 2 0 males Age NR >20-y postgraduate experience |
Self-managed single loaded exercise programme for rotator cuff tendinopathy | Perceived barriers to loaded exercise for rotator cuff tendinopathy Semi-structured interviews |
Themes: (i) expectations and preferences, (ii) characteristics of an unsuccessful outcome, (iii) characteristics of a successful outcome | |
| Littlewood 2015107,** |
Qualitative Qualitative descriptive |
NHS physiotherapy departments (UK) |
n = 13 physiotherapists 7 males 1–32 y postgraduate experience |
Self-managed single loaded exercise programme for rotator cuff tendinopathy | Perceptions of potential implementation barriers and facilitators to self-managed loaded exercise in the context of the UK NHS Semi-structured interviews |
Themes: (i) the physiotherapists preferred therapeutic option; (ii) the role of the physiotherapist; (iii) attributes of the intervention; (iv) attitude to symptom response; (v) response to therapy; (vi) continuing professional development | |
| Littlewood 2014460,* |
Quantitative RCT (pilot) |
Clinic and HEP (UK) |
n = 24 patients 12 males Age 63.2 Symptoms 38.6 months |
12-week programme of self-managed loaded exercise (exercises against gravity, band or hand weight) vs. usual physiotherapy treatment | Adherence Diary |
NA | Overall adherence = 90%. Adherence = 89% for 7/11 who returned complete data vs. 93% of those who returned partial |
| Littlewood 201634,** |
Quantitative RCT |
NR (UK) |
n = 86 patients 43 males Age 54.7 Symptoms (range) 3–120 months |
12-week self-managed loaded exercises | Adherence Diary |
NA | Overall adherence = 78% |
| Malliaris 2020715 |
Quantitative RCT (pilot and feasibility trial) |
Online intervention and HEP (Australia) |
n = 36 patients 4 males Age 53.9 Symptoms 34.6 months |
12-week exercise intervention (shoulder elevation; external rotation) delivered online vs. advice only vs. recommended care vs. recommended care + exercises | Adherence Questionnaire |
NA | 92% adherence in recommended care group vs. 67% in without-telerehabilitation group. 33% of people in recommended care without telerehabilitation performed no exercise at all |
| de Oliveira 2020703 |
Quantitative RCT |
Physical therapy session NR and HEP (Canada) |
n = 52 patients 30 males Age 30.15 Symptoms 22.6 months |
6-week rehabilitation (physical therapy sessions – sensorimotor training) + kinesiotherapy vs. rehabilitation | Adherence and attendance Log book (adherence), attendance at sessions (attendance) |
NA | Adherence: 90.4% for HEP overall; attendance: 92.5% to physical therapy sessions overall |
| Roddy 2021109 |
Quantitative RCT |
HEP (UK) |
n = 256 patients 123 males Age 53.8 Symptoms NR |
12–16-week intervention with following groups: ultrasound-guided corticosteroid injection + physiotherapist-led exercise vs. ultrasound-guided corticosteroid injection + exercise leaflet vs. unguided corticosteroid injection + physiotherapist-led exercise vs. unguided corticosteroid injection + exercise leaflet |
Adherence and attendance Postal questionnaire (adherence), nr (attendance) |
Satisfaction and tolerability Postal questionnaire (satisfaction and tolerability) |
Adherence: greater in physiotherapist-led exercise group than the leaflet group at 6 weeks (85.6% vs. 64.1%) and 6 months (63.2% vs. 50.8%) but not at 12 months (48.9% vs. 53.2%); attendance: 12/128 attended no physiotherapy appointments, 42/128 attended 1–5 sessions, 71/128 6–8 sessions as per protocol + 3/128 9–10 session; satisfaction: confidence and satisfaction greater in supervised exercise group compared to unsupervised; tolerability: exacerbation of shoulder pain after performing exercises 59 (60%) supervised and 60 (59%) unsupervised exercise. Improved within a couple of hours in 22 (37%) supervised and 21 (36%) unsupervised |
| Sandford 2017157 |
Qualitative Qualitative descriptive |
NHS and Home (UK) |
n = 12 patients 6 males Age 54.8 Symptoms 9.8 months |
8-weeks class-based exercise programme with complementary HEP | Factors affecting adherence Semi-structured interviews |
Main enablers: equipment, perceived benefit, longer/more intensive monitoring Main barriers: lack of motivation and equipment, pain |
|
| Seitz 2019165 |
Quantitative Prospective case–control pilot study |
HEP (USA) |
n = 25 patients and healthy controls 10 males Age 30 Symptoms NR |
Duration NR. All participants completed prone horizontal abduction exercise | Adherence | NA | Adherence painful group = 83.1% vs. 79.1% in control group |
| Turgut 2017633 |
Quantitative RCT |
NR (Turkey) |
n = 30 patients 16 males Age 36.5 Symptoms 6.3 months |
12-week exercises intervention of shoulder girdle stretching + strengthening + scapular stabilisation (intervention) vs. shoulder girdle stretching + strengthening only (control) | Adherence Diary |
NA | Adherence of 91% for intervention group vs. 93.5% for control |
| Turgut 2018634 |
Quantitative Quasi-RCT (pre/post single group) |
HEP (Turkey) |
n = 18 patients Sex NR Age 34 Symptoms 5.8 months |
6-week exercise intervention (stretching) | Adherence Diary |
NA | Adherence (mean) = 93.5% (overall) |
| Walther 2004161 |
Quantitative RCT |
Physiotherapy NR and HEP (Germany) |
n = 60 patients 34 males Age 50.7 Symptoms 27 months |
12-weeks self-training centring and stretching exercises vs. conventional physiotherapy vs. functional brace | NA | Tolerability Drop-outs and adverse events |
No drop-outs from exercise |
| White 2020159 |
Qualitative Qualitative descriptive |
Sports medicine surgery and physical therapy (Australia) |
n = 80 expert clinicians Sex NR Age NR ≥ 10 yr postgraduate experience Published on shoulder tendinopathy past 5-years |
Management of rotator cuff tendinopathy | Expert shoulder clinician-researchers’ experiences with managing rotator cuff tendinopathy including practice beliefs towards providing education In-depth semi-structured interviews |
Themes: (i) the need for early, focussed education; (ii) developing therapeutic alliance; (iii) what is required moving forward in current day rotator cuff tendinopathy management | |
| Achilles | |||||||
| Bell 2013251 |
Quantitative RCT |
Sports medicine clinic and HEP (New Zealand) |
n = 53 patients 29 males Age 49 Symptoms NR |
12-week eccentric calf-training programme + blood injection (treatment) or needling only (control) | Adherence Diary |
NA | Adherence treatment group = 65% vs. 62% control |
| Beyer 201518 |
Quantitative RCT |
Fitness centre and HEP (Denmark) |
n = 57 patients 32 males Age 48 Symptoms 18 months |
12-week eccentric exercise training vs. heavy slow resistance training | Adherence Diary |
NA | Reported adherence 78% in eccentric group vs. 92% in heavy slow group |
| Boesen 2017162 |
Quantitative RCT |
HEP (Denmark) |
n = 60 patients 60 males Age 41.96 Symptoms NR |
12-week eccentric exercise programme + high volume injection or platelet rich plasma injection or placebo | Adherence Diary |
NA | 70% of the patients performed more than 75% of the recommended reps; remaining 30% performed between 50% and 75% of the recommended reps |
| Boesen 2019163 |
Quantitative RCT |
HEP (Denmark) |
n = 28 patients 28 males Age 43 Symptoms 10.1 months |
24-week eccentric exercise programme + high-volume guided injection with corticosteroid or high-volume guided injection without corticosteroid | Adherence Follow-up |
NA | 79% (22/28) performed > 75% of recommended reps |
| Hasani 2021152 |
Qualitative Interpretive description |
Community (gym-based), with 1 of 3 weekly sessions supervised by physiotherapist using videoconference software (Australia) |
n = 8 patients males NR Age 46.1 Symptoms NR n = 7 physiotherapists male = 5 Age = 34.1 |
12-weeks gym-based exercise programme of standing and sitting calf-raises using Smith machine | Experiences, barriers and enablers Semi-structured interviews (patients) Focus groups (physiotherapists) |
Overall satisfaction and acceptability of telehealth monitoring Key themes: acceptability of telehealth; enablers to telehealth adherence; barriers to telehealth adherence; enablers to gym-based exercise adherence; barriers to gym-based exercise adherence |
|
| Herrington and McCulloch 2007391 |
Quantitative RCT (pilot) |
HEP (UK) |
n = 25 patients Sex NR Age 36.8 Symptoms 24.3 months |
12-week eccentric loading programme + deep friction massage, MT + stretches vs. deep friction massage, MT, deep friction (only) | Adherence Diary |
NA | 100% adherence to exercise in all groups |
| Horstmann 201316 |
Quantitative RCT |
NR (Germany) |
n = 58 patients 32 males Age 46 Symptoms NR |
12-week whole body vibration vs. eccentric training vs. wait-and-see | Adherence Diary |
NA | Adherence (whole body vibration) = 2.2/3 per week vs. 3/3 for eccentric |
| de Jonge 2015308 |
Quantitative Cohort |
HEP (Netherlands) |
n = 80 patients 44 males Age 50.3 Symptoms 7.4 months |
12-week stretching and eccentric exercise programme + PRP injection or placebo | Adherence Measurement NR |
NA | Mean adherence 72.8% (overall) |
| Jonsson and Alfredson 2005186 |
Quantitative RCT (prospective randomised study) |
HEP (Sweden) |
n = 15 patients 13 males Age 26 Symptoms NR |
12-week eccentric quadriceps training vs. concentric quadriceps training | NA | Tolerability Drop out |
3/9 (33%) in concentric group dropped out of concentric group due to severe tendon pain during and after training |
| Knobloch 2007192 |
Quantitative RCT |
HEP (Germany) |
n = 20 patients 11 males Age 32.5 Symptoms NR |
12-week eccentric training vs. conventional repetitive cryotherapy | NA | Acceptability Follow-up telephone calls |
Participants reported that the daily programme of about 5-minutes was easy to implement into their daily activities (no data reported) |
| Knobloch 2010182 |
Quantitative Cohort |
HEP (Germany) |
n = 75 patients 38 males Age NR Symptoms 7 months |
12-week eccentric exercise programme | Adherence Telephone call, log book, follow-up examination |
Willingness Self-report |
Adherence: 80% over 12 weeks; willingness: 20% non-compliant (n = 12), 25% (4/12) reported drop-off due to overwhelming pain |
| Mantovani 2020181 |
Quantitative Single-cohort feasibility study |
Private physiotherapy clinic (Italy) |
n = 19 patients 12 males Age 39.2 Symptom duration 22.7 months |
Duration NR. Heavy isometric exercise sequence | NA | Tolerability, willingness and satisfaction with intervention Self-report |
Tolerability: mean tolerability 6.3 ± 2.2; Willingness:100% (17 participants) answered yes; satisfaction: no adverse events, discomfort, or inconveniences reported |
| Masood 2014166 |
Quantitative Longitudinal cohort |
HEP (Finland) |
n = 20 (patients and healthy controls) 14 males Age 27.75 Symptoms 10.4 months |
12-week eccentric exercise group vs. control (no exercise) | Adherence Diary |
NA | Adherence = 90% required days completed, 81% overall training sessions |
| Mc Aulife 2017153 |
Qualitative Interpretive description |
Running clubs and local community (Ireland) |
n = 8 patients 5 males Age 40 Symptoms 20.5 months |
Recruited as part of RCT investigating 12-week exercise intervention | Experience in managing AT Semi-structured telephone interviews |
Contrasting views on expected role of exercise and confidence in proposed exercise intervention | |
| Morrissey 2011716 |
Quantitative RCT |
HEP (UK) |
n = 38 patients 14 males Age 21.4 Symptoms NR |
6-week eccentric or concentric training protocol | Adherence Diary |
NA | Adherence = 45.74% for eccentric group vs. 48.46% for concentric |
| Munteanu 2014490 |
Quantitative RCT |
HEP (Australia) |
n = 140 patients 78 males Age 43.6 Symptoms 31.6 months |
12-week eccentric calf-muscle exercise + customised foot orthosis or sham | Adherence Diary |
NA | Both groups adhered to approximately 57% of exercise |
| Rabusin 2020686 |
Quantitative RCT |
HEP (Australia) |
n = 100 patients 48 males Age 45.9 Symptoms NR |
12-week exercise intervention of heel lifts or eccentric exercise | Adherence Questionnaires |
NA | Adherence weeks 1–2 = 79%; weeks 3–6 = 67%; weeks 7–12 = 60% (overall) |
| Ram 2013546 |
Quantitative Quasi-RCT (longitudinal cohort study) |
HEP (Canada) |
n = 48 patients 19 males Age 39.4 Symptoms > 3 months |
12-week training programme based on Alfredson protocol | Adherence Log book |
NA | 17/20 participants completed > 80% of exercise programme; 3 participant non-compliant due to extreme pain caused by the exercises |
| Rompe 2008687 |
Quantitative RCT |
HEP (Germany) |
n = 50 patients 20 males Age 39.8 Symptoms 25.5 months |
12-week eccentric loading programme vs. repetitive low-energy shockwave therapy | Adherence Measurement NR |
NA | 21/25 completed exercises daily (in exercise group), twice per day |
| Roos 2004193 |
Quantitative RCT |
HEP (Sweden) |
n = 44 patients 21 males Age 45 Symptoms (median) 5.5 months |
12-week eccentric exercises vs. night splint vs. eccentric exercises + night splint | Adherence Diary |
Tolerability Reported side-effects |
Feasibility: adherence good (> 75%) for first 7 weeks in eccentric group, at 12 weeks only 50% good compliance; tolerability: 33% reported muscle soreness with eccentric exercise in first week; no difference between exercise and exercise + splint groups. None reported muscle soreness by 6 weeks but 1/16 (6.3%) reported calf stiffness during the day |
| Sancho 2019178 |
Quantitative Single-cohort feasibility study |
Private physiotherapy clinic and HEP (Australia) |
n = 15 patients 15 males Age 37.9 Symptoms ≥1 month |
12-weeks education + pain-guided progressive exercise (isometrics, isotonics, hopping, running) | Adherence and fidelity Exercise diary |
Satisfaction with intervention Questionnaire |
Adherence 70% Fidelity 50% Barriers: time Enablers: education, perceived benefit, feedback frequency |
| Solomons 2020595 |
Quantitative RCT |
Clinic and HEP (Canada) |
n = 52 patients 24 males Age NR Symptoms 18 months |
12-week standardised exercise programme (progressive isometric, concentric, eccentric, kinetic chain) only (group 1) + intramuscular dry needling (group 2) or sham needling (group 3) | Adherence Diary |
NA | Adherence (> 75% of sessions) = 100% group 1, 92% group 2, 83% group 3 |
| Stefansson 2019184 |
Quantitative RCT |
Clinic and HEP (Iceland) |
n = 60 patients 12 males Age NR Symptoms NR |
12-week eccentric exercise protocol (group 1) vs. pressure massage (group 2) vs. pressure massage + eccentric exercise (group 3) | NA | Tolerability Drop out |
2/19 (11%) dropped out of eccentric group due to exercises aggravating symptoms; 1/21 (4.8%) dropped out of pressure massage and 2/20 (10%) dropped out of combination but no reason provided |
| Stevens 2014175 |
Quantitative RCT |
NR (UK) |
n = 28 patients 11 males Age 48.7 Symptoms 7.4 months |
6-week do-as-tolerated exercise protocol (eccentric) vs. standard | Adherence Completed exercises as planned |
NA | Standard (180 reps) adherence: 92% target reps; do-as-tolerated: 62% target reps, with similar clinical outcomes |
| Tumilty 2012630 |
Quantitative RCT |
Clinic and HEP (New Zealand) |
n = 40 patients 18 males Age 45.05 Symptoms NR |
12-week eccentric exercise programme + active or placebo (low-level laser therapy) | Adherence Log |
NA | Mean sessions completed = 81/168 for laser group vs. 106/168 for placebo |
| Tumilty 2016632 |
Quantitative RCT |
HEP (New Zealand) |
n = 80 patients 33 males Age 47.5 Symptoms NR |
12-week exercise intervention with two regimes (unilateral heavy-load eccentric plantar flexion) + placebo (+ exercise regime 1 (group 1) or 2 (group 3)) or laser (+ exercise regime 1 (group 2) or 2 (group 4)) | Adherence Training log |
NA | Training logs returned: 7 in group 1, 13 in group 2, 14 in group 3, 12 in group 4; reduced exercise regime adherence = 100% vs. Alfredson protocol 70% |
| Verrall 2011149 |
Quantitative RCT |
HEP (Australia) |
n = 190 patients 108 males Age 39 Symptoms ≥ 3 months |
6-week progressive eccentric heel-drop programme followed by return to sport/main activity + continued exercise | Adherence Direct question on whether they completed exercise regime |
NA | 86% completed programme, 8% ceased due to perceived programme failure, 6% ceased due to perceiving it to have been successful before 6-week period over |
| van der Vlist 2020646 |
Quantitative RCT |
General hospital (Sports medicine department) (Netherlands) |
n = 80 39 male patients Age 47.9 Symptom > 14 months |
24-week exercise programme (isometric, concentric, eccentric) + high-volume injection of saline and lidocaine or placebo injection | Adherence Daily log |
NA | The median percentage of performed exercises was 76% in the high-volume injection group vs. 72% in placebo |
| de Vos 200759 |
Quantitative RCT |
HEP (Netherlands) |
n = 63 patients 37 males Age 44.6 Symptoms 30.7 months |
12-week heavy-load eccentric training programme vs. exercise + night-splint | Adherence Diary |
NA | Adherence exercise only group = 72% (excellent/good) and 28% moderate/poor vs. 74% (excellent/good) and 26% moderate/poor for combined |
| de Vos 2010314 |
Quantitative RCT |
HEP (Netherlands) |
n = 54 patients 26 males Age 49.5 Symptoms (median) 16 months |
12-week eccentric exercise programme (usual care) + PRP injection or saline | Adherence Log |
NA | Adherence in PRP = 70.9% vs. 74.6% in placebo |
| Wetke 2015660 |
Quantitative Quasi-RCT (prospective trial) |
HEP (Denmark) |
n = 93 patients 50 males Age 48.8 Symptoms 13 months |
12-week rehabilitation regime (eccentric/concentric exercises – group 0) + ultrasound-guided injections | Adherence Self-report |
NA | 65% of patients answered yes at all four visits (100% compliance) – of these 75% in group 0 (no GCS injections) and 61% in the remainder; 88% answered yes at three visits (75% compliance) 92% in group 0, 87% in the remainder |
| Yelland (Yellend et al., 2009) 2009 |
Quantitative RCT |
Primary care centre and HEP (Australia) |
n = 43 patients Sex NR Age (median) 46 Symptoms (median) 6 months |
12-week eccentric loading exercises vs. prolotherapy vs. loading exercises + prolotherapy | Adherence Diary |
NA | Eccentric group: moderate (25% to 50%) n = 1, good (50% to 75%) n = 2 and excellent (>75%) n = 4; combined: moderate n = 1, good n = 3, excellent n = 5 |
| Patellar | |||||||
| Agergaard 2021180 |
Quantitative RCT |
Commercial fitness centre (Denmark) |
n = 44 patients 44 males Age 30.5 Symptoms 25.15 months |
12-week moderate slow resistance programme vs. heavy slow resistance | Adherence, attendance and fidelity Training diary |
NA | Adherence: heavy slow group = 78% vs. 86% for moderate; attendance: heavy slow group = 81% vs. 86% for moderate; fidelity: 76.8% (heavy slow) vs. 84.5% (moderate) for leg press exercises and time under tension 79.0% (heavy) vs. 85.3% (moderate); 72.9% (heavy slow) vs. 80.3% (moderate) for knee extension and time under tension 77.1% (heavy) vs. 83.4% (moderate); both exercises performed > 90% of load prescribed |
| van Ark 2013170 |
Quantitative Case-series |
University sports medicine centre + HEP (Netherlands) |
n = 5 patients 2 males Age 27 Symptoms 38.4 months |
PRP injection + 12-week 5-phase graded exercise programme guided by correct execution and pain <5/10 VAS | Adherence Self-report single question on 1–10 scale |
NA | Mean compliance 7/10 (overall); non-compliance was due to lack of time, motivation or holidays, other injuries |
| Bahr 2006131 |
Quantitative RCT |
Olympic training centre and HEP (Norway) |
n = 35 patients 35 males Age 30.5 Symptoms 25.15 |
12-week eccentric training (squats) programme vs. surgical treatment + eccentric programme | Adherence Measurement NR |
NA | Adherence eccentric training group: 66% of prescribed dose vs. 72% of prescribed dose in surgery group |
| Breda 2020696 |
Quantitative RCT |
University medical centre and HEP (Netherlands) |
n = 76 patients 58 males Age 24 Symptoms 24 months |
24-week intervention for eccentric exercise vs. progressive tendon-loading exercises | Adherence Online questionnaire |
NA | Adherence tendon-specific exercises 47% for progressive vs. 53.1% after 12 weeks and 40.2% vs. 48.6% after 24 weeks; adherence exercises targeting risk factors 27.5% for progressive vs. 28.2% for eccentric at 12 weeks and 21.4% vs. 21.6% after 24 weeks. Reasons for non-adherence to tendon-specific/targeting risk -factor exercises included: lack of time, pain, preferring sports activities, rest day, lack of motivation |
| Gual 2016190 |
Quantitative RCT |
Volleyball/basketball training practice (Spain) |
n = 53 patients 27 males Age 23.5 Symptoms NR |
24-week intervention (eccentric overload) + usual training vs. usual training only (control group) | NA | Type NR Drop-out |
Seven participants experienced injuries (2 ankle, 5 knee joint) related to exercises |
| MacDonald 2019717 |
Quantitative RCT (pilot) |
HEP (USA) |
n = 31 patients 29 males Age 29.3 Symptoms 10.4 months |
12-week training programme of eccentric squats (standard care) vs. eccentric squats + concentric hip strengthening (treatment) | Adherence Exercise log |
NA | Adherence standard care group = 42.5% vs. 50% for eccentric + 62% for hip muscle strengthening in treatment group |
| Praet 2018130 |
Quantitative RCT (cross-over) |
Outpatient sports medicine clinic (Australia) |
n = 20 patients 13 males Age 44 Symptoms 54 months |
24-week calf-strengthening programme + placebo or specific collagen peptide | Adherence Exercise diary |
NA | Adherence group 1 (specific collagen peptide + exercise) = 84% vs. 78% (placebo) |
| Rio 2017167 |
Quantitative Case-series |
HEP (Australia) |
n = 25 patients 19 males |
4-week programme of isometric double-leg squat using rigid belt | Adherence Self-report |
NA | Median adherence 5 × week (23/25 reported data) |
| Skovlund 2020169 |
Quantitative Case-series |
Department of physical and occupational therapy and institute of sports medicine (Denmark) |
n = 7 patients 7 males Age 29 Symptoms 12 months |
3-week supervised training session (unilateral leg press, knee extension) | Attendance Sessions attended |
NA | Training adherence of 98% |
| Sprague 2021718 |
Quantitative RCT (feasibility pilot) |
University health sciences complex (USA) |
n = 15 patients 10 males Age 26.6 Symptoms 32.2 months |
12-weeks pain-guided vs. pain-free modified heavy slow resistance protocol | Adherence Training diary |
NA | Exercises completed per day: pain-free group 67.1%, pain-guided group 86.1%; days training diary completed: pain-free group 81.3%, pain-guided group 98.4% |
| Thijs 2017621 |
Quantitative RCT |
Sports medicine department and general hospital (Netherlands) |
n = 52 patients 38 male Age 28.6 Symptoms 19.5 months |
12-week eccentric exercise programme for all participants + ESWT or sham | Adherence Measurement NR |
NA | Mean eccentric exercise sessions completed per week: 10.1/14 at 6 weeks and 8.7/14 at 12 weeks for extracorporeal shockwave + exercise group vs. 9.8/14 for sham at 6 weeks and 6.1/14 at 12 weeks |
| Visnes 2005129 |
Quantitative RCT |
HEP (Norway) |
n = 29 patients 19 males Age 26.5 Symptoms 73.6 months |
12-week squat HEP (eccentric) vs. training as usual | Adherence Report |
NA | Mean adherence = 8.2 sessions per week out of 14 target sessions (2 × day, overall); mean adherence 63% (overall) |
| Warden 2008652 |
Quantitative RCT |
HEP (Australia) |
n = 37 patients 30 males Age 27 Symptoms 44 months |
12-week daily eccentric exercise programme (active LIPUS + exercise vs. inactive – LIPUS + exercise) | Adherence Log book |
NA | Adherence = 60% in active group vs. 65% in inactive |
| van der Worp 2014640 |
Quantitative RCT |
Centre for sports medicine and university medical centre (Netherlands) |
n = 43 patients 32 males Age 31.1 Symptoms 35.2 months |
Duration NR. FSWT + eccentric training vs. RSWT + eccentric training | Adherence Online log book |
NA | Mean adherence to exercise programme = 3.2/5 for FSWT vs. 3.8/5 for RSWT |
| Young 2005132 |
Quantitative RCT |
HEP (Australia) |
n = 17 patients 13 males Age 27.3 Symptoms NR |
12-week intervention – decline group vs. step group | Adherence Diary |
NA | Mean adherence of 72% of total possible sessions (overall, no difference between groups) |
| Elbow | |||||||
| Coombes 2013176 |
Quantitative RCT |
Clinic and HEP (Australia) |
n = 165 patients 102 males Age 49.7 Symptoms 3.7 months |
Corticosteroid injection vs. injection + physiotherapy vs. placebo injection vs. placebo injection + physiotherapy for 8 weeks. physiotherapy = 8 sessions + HEP (sensorimotor retraining, concentric, eccentric exercises). Duration NR. | Adherence and attendance Measurement NR (adherence), attendance numbers |
NA | 70% of patients in the physiotherapy groups were compliant with HEP during at least 5 of 7 weeks; mean physiotherapy sessions attended = 7.5/8, 9% (7 patients) completed < 4 sessions |
| Dale 2015173 |
Quantitative RCT |
HEP (USA) |
n = 17 patients 8 males Age 46.5 Symptoms NR |
5-week standard intervention (eccentric + stretch + orthosis) vs. standard + Pilates | Adherence Exercise diary |
NA | Most completed HEP 5–6 × week: always (11% standard; 38% standard + Pilates), mostly (73% standard, 50% standard + Pilates), sometimes (11% standard; 0% standard + Pilates), rarely (0% standard; 12% standard + Pilates) |
| Luginbuhl 2008174 |
Quantitative RCT |
HEP (Switzerland) |
n = 29 patients 13 male Age 47 Symptoms 10 months |
12 weeks forearm support band vs. strengthening exercises (isometric) vs. strengthening + forearm support | Adherence Self-report at follow-up |
Tolerability Drop-out reasons |
Adherence (strengthening): 67% compliant 3-months, 11% 3 × week only, 11% 2 months only, 11% stopped after 3-weeks due to pain; adherence (strengthening + firearm band): 90% compliant, 10% stopped one of the exercises; tolerability: 1/9 (11%) stopped after 3-weeks due to increased pain (strengthening programme group); 1/9 (11%) stopped exercise with ball reporting ball to be too hard (forearm support + strengthening group) |
| Park 2010521 |
Quantitative RCT |
HEP (Korea) |
n = 31 patients Sex NR Age 50.15 Symptoms 6.3 months |
Immediate physiotherapy vs. delayed physiotherapy (after 4 weeks medication); physiotherapy = isometric resistance exercises. Duration NR. | Adherence Exercise diary (ratio) |
NA | 3-month compliance = 0.56 (group 1) and 0.75 (group 2); 6 months = 0.43 (group 1) and 0.38 (group 2); 12 months = 52% of participants did not perform the exercises |
| Peterson 2014185 |
Quantitative RCT |
HEP (Sweden) |
n = 120 patients 63 males Age 47.9 Symptoms 23.5 months |
12-week HEP consisting of eccentric or concentric exercise (with weights) | NA | Tolerability and willingness Drop-out reasons |
Tolerability: 1/60 (1.7%) dropped out at 1-month as could not perform intervention; willingness: drop-outs due to lack of time at various intervals (n = 5) |
| Söderberg 2012594 |
Quantitative RCT |
HEP (Sweden) |
n = 42 patients 18 males Age 49 Duration of symptoms > 6 months = 26; Duration > 1 year = 20; Duration > 2 years = 11 |
6-week HEP with eccentric exercises at pain-free intervals | Adherence Self-report |
Helpfulness Proportion of patients with tennis elbow |
Feasibility: Over 70% compliance for exercise regime and wearing forearm band; Acceptability: proportion of LE cases decreased from 100% to 44% |
| Vuvan 2020187 |
Quantitative RCT |
Clinic and HEP (Australia) | n = 40 patients 29 males Age 48.5 Symptoms 4 months |
8-week progressive isometric HEP programme and single physiotherapy session vs. wait-and-see | Adherence Exercise diary |
Tolerability Pain intensity on NRS; time measure |
Feasibility: mean adherence = 87% to exercise programme (diaries obtained from 20/21 in exercise group); acceptability: mean 1.9 (NRS), median 0–60 seconds (length of time for pain to settle after exercise) |
| Gluteal/greater trochanteric pain syndrome | |||||||
| Clifford 2019179 |
Quantitative RCT (pilot) |
Physiotherapy clinic and HEP (UK) |
n = 30 patients 3 male Age 59.3 Symptoms 23 months |
12-week daily progressive HEP – isometric vs. isotonic + 8 individual physiotherapy sessions | Attendance, fidelity and adherence NR (attendance), diary (fidelity, adherence) |
NA | Attendance: 100% attendance for 8 physiotherapy appointments; fidelity: All but one participant able to progress with loading (isometric group); adherence: 70% completed at least 80% of exercise sessions in isometric group vs. 58% of isotonic |
| Ganderton 2018189 |
Quantitative RCT |
HEP (Australia) |
n = 94 patients 94 Female Age 61.8 Symptoms NR |
12-week exercise programme (GLoBE – isometric loading, kinetic chain, strengthening) vs. sham | Adherence Diary |
Tolerability Adverse events |
Feasibility: 75.8% (mean) adherence for GLoBE vs. 75.99% sham; acceptability: 1/94 (1.1%) participants reported increased pain attributed to exercises; completed intervention and follow-up outcomes |
| Mellor 201830 |
Quantitative RCT |
Clinic and HEP (Australia) |
n = 204 participants 37 males Age 54.8 Symptoms 24 months |
8-week programme education + HEP (strengthening) vs. corticosteroid injection vs. wait-and-see | Adherence Exercise diary |
NA | Overall programme adherence mean of 88% of prescribed exercises completed |
| Stephens 2020160 |
Qualitative Qualitative descriptive |
NHS elective orthopaedic hospital (UK) |
n = 10 patients 1 male Age 62.4 Symptoms 23.6 months |
To understand experiences of GTPS | Experiences and perceptions of individuals with a primary complaint of GTPS Semi-structured telephone interviews |
Themes: (i) living with persistent pain; (ii) understanding the problem and pain; (iii) experiences of previous treatment; (iv) beliefs about activity and exercise; (v) the future | |
| Hamstring | |||||||
| Silder 2013690 |
Quantitative RCT |
HEP (USA) |
n = 24 patients 19 males Age 24 Symptoms NR |
Duration NR. Progressive running and eccentric training vs. progressive agility + trunk stabilisation. Both 5 days per week | Adherence Exercise log |
NA | Adherence = 88% in progressive running group vs. 80% in progressive agility group |
| Iliopsoas syndrome | |||||||
| Johnston 1999168 |
Quantitative Retrospective case series |
HEP (Canada) |
n = 9 patients Age 35.6 1 male Symptoms 12.6 months |
Duration NR. Hip rotation rehabilitation programme | Adherence Telephone interview |
Helpfulness and tolerability Telephone interview |
Feasibility: mean compliance = 2 (moderately compliant); acceptability (tolerability): all exercises caused hip pain, especially quadricep stretch; acceptability (helpfulness): 3/9 (33%) stated exercises with band most beneficial; 2/9 (22%) stated stretching and strengthening most effective in combination; 2/9 (22%) stated stretches most useful; 1/9 (11%) reported the exercises caused pain |
| PTTD | |||||||
| Campbell 2019151 |
Qualitative Interpretative phenomenological analysis |
Private podiatry clinic (USA) |
n = 5 patients 2 males Age 60.2 Symptoms 12.4 months |
Treatment for PTTD | Lived experience of undergoing treatment for PTTD Semi-structured interviews |
Superordinate themes: (i) adverse experience during the patient journey; (ii) treatment burden, (iii) negative self-concept | |
| Mixed tendinopathy | |||||||
| Jayaseelan 2019148 |
Quantitative Case report |
HEP (USA) |
n = 3 patients 2 males Age 35.6 Symptom duration 29.3 |
8-week tailored exercise programme (joint mobilisation, self-stretching, PNE, aerobic exercise) | Adherence Exercise log |
NA | 100% adherence |
| Levy 2009150 |
Qualitative Interpretative phenomenological analysis |
Private physiotherapy clinic (UK) |
n = 6 patients 4 males Age (range) 24–38 Symptoms NR |
Sport injury rehabilitation | Recreational athletes’ experiences and perceptions of adhering to a sport injury rehabilitation programme Semi-structured interviews |
Themes: (i) motivation; (ii) confidence; (iii) coping; (iv) social support; (v) pain | |
Appendix 8 Quality appraisal results mixed-method review
| Question: | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | Score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Author (Year) |
||||||||||||||
| Agergaard et al. (2021)180 |
Y | U | Y | N | N | Y | Y | Y | Y | Y | Y | Y | Y | 10 |
| Bahr et al. (2006)131 |
Y | Y | Y | N | N | N | Y | U | Y | Y | Y | Y | Y | 9 |
| Bateman and Adams (2014)248 |
Y | N | Y | N | N | N | Y | Y | Y | Y | Y | Y | Y | 9 |
| Bell et al. (2013)251 |
Y | Y | N | Y | N | Y | Y | Y | Y | Y | Y | Y | Y | 11 |
| Bennell et al. (2010)188 |
Y | Y | N | Y | N | Y | Y | Y | Y | Y | Y | Y | Y | 11 |
| Beyer et al. (2015)18 |
Y | U | Y | N | N | Y | Y | Y | Y | Y | Y | Y | Y | 10 |
| Boesen et al. (2017)162 |
Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 13 |
| Boesen et al. (2019)163 |
Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 13 |
| Boudreau et al. (2019)262 |
Y | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | Y | Y | 12 |
| Breda et al. (2020)696 |
Y | Y | Y | N | Y | Y | Y | Y | Y | Y | Y | Y | Y | 12 |
| Clifford et al. (2019)179 |
Y | Y | Y | N | N | N | Y | Y | N | Y | Y | Y | Y | 9 |
| Conroy and Hayes (1998)298 |
U | U | Y | Y | N | Y | Y | Y | Y | Y | Y | Y | Y | 10 |
| Cook et al. (2014)172 |
Y | U | Y | N | N | Y | Y | Y | Y | Y | Y | Y | Y | 10 |
| Coombes et al. (2013)176 |
Y | Y | Y | N | N | Y | Y | Y | Y | Y | Y | Y | Y | 11 |
| Dale et al. (2015)173 |
U | U | Y | N | N | U | Y | Y | Y | Y | Y | Y | Y | 8 |
| de Oliveira et al. (2020)703 |
Y | Y | Y | N | N | Y | Y | Y | Y | Y | Y | Y | Y | 11 |
| de Vos et al. (2007)59 |
Y | Y | Y | N | N | Y | Y | Y | Y | Y | Y | Y | Y | 11 |
| de Vos et al. (2010)314 |
Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 13 |
| Dejaco et al. (2017)44 |
Y | Y | Y | Y | N | N | Y | Y | Y | Y | Y | Y | Y | 11 |
| Dupuis et al. (2018)339 |
Y | Y | N | N | N | Y | Y | Y | Y | Y | Y | Y | Y | 10 |
| Flores et al. (2017)183 |
Y | U | Y | N | N | N | Y | Y | Y | Y | Y | Y | Y | 10 |
| Fournier Belley et al. (2018)164 |
Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 13 |
| Ganderton et al. (2018)189 |
Y | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | Y | Y | 12 |
| Granviken and Vasseljen (2015)374 |
Y | Y | Y | N | N | Y | Y | Y | Y | Y | Y | Y | Y | 11 |
| Gual et al. (2016)190 |
Y | U | Y | N | N | U | Y | Y | Y | Y | Y | Y | Y | 9 |
| Heron et al. (2017)390 |
Y | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | Y | Y | 12 |
| Herrington and McCulloch (2007)391 |
U | U | Y | N | N | Y | Y | Y | y | Y | Y | Y | Y | 9 |
| Holmgren et al. (2012)393 |
Y | Y | N | Y | N | Y | Y | Y | U | Y | Y | Y | Y | 10 |
| Horstmann et al. (2013)16 |
Y | Y | Y | N | N | Y | Y | Y | Y | Y | Y | Y | Y | 11 |
| Ingwersen et al. (2017)191 |
Y | Y | N | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 12 |
| Jonsson and Alfredson (2005)186 |
U | U | Y | U | U | U | Y | Y | Y | Y | Y | Y | Y | 8 |
| Juul-Kristensen et al. (2019)412 |
Y | Y | Y | N | N | Y | Y | Y | Y | Y | Y | Y | Y | 11 |
| Knobloch et al. (2007)192 |
U | U | N | N | N | Y | Y | U | U | Y | Y | Y | Y | 6 |
| Kromer et al. (2013)443 |
Y | Y | Y | N | N | Y | Y | Y | Y | Y | Y | Y | Y | 11 |
| Kvalvaag et al. (2018)450 |
Y | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | Y | Y | 12 |
| Littlewood et al. (2014)460 |
Y | Y | N | N | N | N | Y | Y | Y | Y | Y | Y | Y | 9 |
| Littlewood et al. (2016)34 |
Y | Y | Y | N | N | N | Y | Y | Y | Y | Y | Y | Y | 10 |
| Luginbuhl et al. (2008)174 |
Y | U | U | N | N | U | Y | U | U | Y | Y | Y | Y | 6 |
| MacDonald et al. (2019)717 |
Y | Y | Y | N | N | U | Y | Y | U | Y | Y | Y | Y | 9 |
| Malliaras et al. (2020)715 |
Y | Y | N | N | N | Y | Y | Y | Y | Y | Y | Y | Y | 10 |
| Mellor et al. (2018)30 |
Y | Y | Y | N | N | Y | Y | Y | Y | Y | Y | Y | Y | 11 |
| Morrissey et al. (2011)716 |
Y | Y | N | N | N | U | Y | Y | U | Y | Y | Y | Y | 8 |
| Munteanu et al. (2015)490 |
Y | Y | Y | Y | N | U | Y | Y | Y | Y | Y | Y | Y | 11 |
| Park et al. (2010)521 |
Y | U | Y | N | N | U | Y | Y | U | Y | Y | Y | Y | 8 |
| Peterson et al. (2014)185 |
Y | U | N | N | N | N | Y | Y | Y | Y | Y | Y | Y | 8 |
| Praet et al. (2018)130 |
Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 13 |
| Rabusin et al. (2020)686 |
Y | Y | Y | N | N | N | Y | Y | Y | Y | Y | Y | Y | 11 |
| Roddy et al. (2021)109 |
Y | N | N | N | N | Y | Y | Y | Y | Y | Y | Y | Y | 11 |
| Rompe et al. (2008)687 |
Y | Y | Y | N | N | Y | Y | Y | Y | Y | Y | Y | Y | 11 |
| Roos et al. (2004)193 |
Y | Y | Y | N | N | Y | Y | Y | Y | Y | Y | Y | Y | 11 |
| Söderberg et al. (2012)594 |
Y | N | Y | Y | N | N | Y | Y | Y | Y | Y | Y | Y | 10 |
| Silder et al. (2013)690 |
Y | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | Y | Y | 12 |
| Solomons et al. (2020)595 |
Y | Y | N | Y | N | Y | Y | Y | Y | Y | Y | Y | Y | 11 |
| Sprague et al. (2021)718 |
y | N | N | N | N | N | Y | Y | Y | Y | Y | Y | Y | 8 |
| Stefansson et al. (2021)184 |
Y | U | Y | N | N | Y | Y | Y | Y | Y | Y | Y | Y | 10 |
| Stevens and Tan (2014)175 |
Y | Y | Y | N | N | Y | Y | Y | Y | Y | Y | Y | Y | 11 |
| Thijs et al. (2017)621 |
Y | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | Y | Y | 12 |
| Tumilty et al. (2012)630 |
Y | Y | Y | N | Y | Y | Y | Y | Y | Y | Y | Y | Y | 12 |
| Tumilty et al. (2016)632 |
Y | Y | Y | Y | U | Y | Y | Y | Y | Y | Y | Y | Y | 12 |
| Turgut et al. (2017)633 |
Y | U | Y | N | N | U | Y | Y | Y | Y | Y | Y | Y | 9 |
| van der Vlist et al. (2020)646 |
Y | U | Y | Y | N | Y | Y | Y | Y | Y | Y | Y | Y | 11 |
| van der Worp et al. (2014)640 |
Y | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | Y | Y | 12 |
| Visnes et al. (2005)129 |
Y | U | Y | N | N | U | Y | Y | Y | Y | Y | Y | Y | 9 |
| Vuvan et al. (2020)187 |
Y | Y | Y | N | N | Y | Y | Y | Y | Y | Y | Y | Y | 11 |
| Walther et al. (2004)161 |
U | U | Y | N | N | U | Y | U | U | Y | Y | U | Y | 5 |
| Warden et al. (2008)652 |
Y | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | Y | Y | 12 |
| Yelland et al. (2011)674 |
Y | U | N | N | N | Y | Y | Y | Y | Y | Y | Y | Y | 9 |
| Young et al. (2005)132 |
Y | Y | N | N | N | Y | Y | Y | Y | Y | Y | Y | Y | 10 |
| Question: Author (Year) |
1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Score |
|---|---|---|---|---|---|---|---|---|---|---|
| Ferrer et al. (2018)177 |
Y | Y | Y | N | Y | Y | Y | Y | Y | 8 |
| de Jonge et al. (2015)308 |
Y | Y | Y | Y | Y | Y | Y | Y | Y | 9 |
| Knobloch et al. (2010)182 |
Y | Y | Y | N | Y | Y | Y | Y | Y | 8 |
| Mantovani et al. (2020)181 |
Y | NA | NA | N | Y | Y | NA | Y | Y | 5/6 |
| Ram et al. (2013)546 |
Y | NA | NA | N | Y | Y | NA | Y | Y | 5/6 |
| Sancho et al. (2019)178 |
Y | Y | Y | N | Y | Y | Y | Y | Y | 8 |
| Kim et al. (2019)432 |
Y | N | Y | Y | Y | Y | Y | Y | Y | 8 |
| Turgut et al. (2018)634 |
Y | NA | NA | N | Y | Y | NA | Y | Y | 5/6 |
| Verrall et al. (2011)149 |
Y | Y | Y | N | Y | Y | Y | Y | Y | 8 |
| Wetke et al. (2015)660 |
Y | NA | NA | N | Y | U | Y | Y | Y | 5/6 |
| Question: Author (Year) |
1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | Score |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Masood et al. (2014)166 | Y | Y | Y | Y | Y | NA | NA | Y | Y | Y | 8/8 |
| Seitz et al. (2019)165 |
Y | N | Y | Y | Y | NA | NA | Y | Y | Y | 7/8 |
| Question: Author (Year) |
1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | Score |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Johnston et al. (1999)168 |
Y | Y | Y | U | N | Y | Y | Y | Y | Y | 8 |
| Rio et al. (2019) |
Y | Y | Y | U | U | N | Y | Y | N | Y | 6 |
| Skovlund et al. (2020)169 |
Y | Y | Y | U | U | Y | Y | Y | Y | Y | 8 |
| van Ark et al. (2013)170 |
Y | Y | Y | U | U | Y | Y | Y | Y | Y | 8 |
| Question: Author (Year) |
1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | Score |
|---|---|---|---|---|---|---|---|---|---|
| Jayaseelan et al. (2019)148 |
Y | Y | Y | Y | Y | Y | N | Y | 7 |
| Question: Author (year) |
1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | Score |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Barrett et al. (2018)154 |
U | U | U | U | U | N | Y | Y | Y | U | 3 |
| Campbell et al. (2019)151 |
Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 10 |
| Hanratty et al. (2016)155 |
U | U | U | U | U | Y | Y | Y | Y | Y | 5 |
| Hasani et al. (2021)152 |
U | Y | Y | Y | Y | N | Y | Y | Y | Y | 8 |
| Levy et al. (2009)150 |
Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 10 |
| Littlewood et al. (2014)156 |
U | U | U | U | U | U | Y | Y | Y | Y | 4 |
| Littlewood et al. (2015)107 |
Y | Y | Y | Y | Y | Y | U | Y | Y | Y | 9 |
| Mc Aulife et al. (2017)153 |
Y | Y | Y | Y | Y | U | N | Y | Y | Y | 8 |
| Sandford et al. (2017)157 |
Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 10 |
| Stephens et al. (2020)160 |
U | U | U | U | U | Y | Y | Y | Y | Y | 5 |
| White et al. (2020)159 |
U | U | U | U | U | N | N | Y | Y | Y | 3 |
Appendix 9 Findings and illustrations extracted from qualitative studies
| Study: Barrett et al . 2018 154 | |
| Finding | Support, motivation, and learning from peers (U) |
| Illustration | You’re better off to do it in a group … you’d be more determined to do it … you don’t put the whole 100% effort in at home. (Ben) (p. 467) |
| Finding | Preference for exercise class compared to individual shoulder physiotherapy (U) |
| Illustration | The repetitiousness of the class does stay in your mind rather than just going once a month to physio and you’re supposed to be doing all these exercises and so on you know. (Sandra) (p. 467) |
| Finding | The physiotherapist as an educator and facilitator (U) |
| Illustration | In the earlier part they really babysat me and nursed me along and when I got to the point when I was doing the exercises myself … they just observed what was going on … they encouraged me to start swimming. (Mark) (p. 468) |
| Finding | Beliefs about pain and exercise (C) |
| Illustration | Still every day I do my exercises and I find that when I feel the pain coming on in my arm I have a walking stick and I just do exercises with that, I haven’t taken pain killers in I don’t know how long, I am good with pain now. (Margaret) (p. 468) |
| Study: Mc Aulife et al . 2017 153 | |
| Finding | However, in contrast participants also discussed their disbelief and lack of confidence in relation to a proposed exercise intervention (C) |
| Illustration | But i know there are some exercises you should be doing and things like but that. I probably haven’t done as much strength work. I don’t go to the gym. I don’t do any strength work or anything like that. (Participant 1) (p. 110) |
| Finding | Participants also highlighted the expected role of exercise interventions in the management of their AT (C) |
| Illustration | There was a therapy that was recommended to me maybe at the start of the year, it was called heel drops or painful heel drops? They’re on the edge of the steps and you basically flex, you basically flex down and flex up …. Was it 10 minutes a night every night for 12 weeks but in my head that was crazy. (Participant 5) (p. 111) |
| Study: Campbell et al . 2019 151 | |
| Finding | Most of the participants in this cohort experienced some form of treatment burden/fatigue with respect to the prescribed exercises and orthoses. This had psychological consequences when the orthoses or exercises were not having a positive effect in reducing pain or improving function (U) |
| Illustration | I felt awful, yeah I mean I was doing them (exercises) it was painful, and I was quite regimented, I was like I’ve got to do the physio because I’ve got to make it better … it had been going on a really long time it was just getting worse. (Mila) (p. 6) |
| Study: Levy et al . 2009 150 | |
| Finding | Motivation (U) |
| Illustration | Knowing I would be out of action for three to four months was enough motivation to make me want to stick to my rehabilitation programme. My motivation was born out of the fact that I was terribly frustrated with not only being unable to compete, but also missing out on the social side. Simple things like having a drink after the game and partaking in organised social events were things I really enjoyed. (Max) (p. 218) |
| Finding | Confidence (U) |
| Illustration | Although all the prescribed exercises were new to me, I felt confident performing them in the rehabilitation centre because I knew I was being monitored by the physio; however, I felt much less confident performing exercises at home by myself. … I wasn’t entirely sure I was doing the exercises correctly and, as such, I didn’t want to further injure myself, having this concern made it difficult for me to comply with home-based exercises. (Carol) (p. 218) |
| Finding | Coping (U) |
| Illustration | Performing the rehab exercises can be demanding physically and emotionally. … So to have found a physio who was very supportive was very comforting and reassuring. The physio provided good guidance and frequent feedback about how well I was doing; he seemed to have a lot of time for me in the clinic and had taken a keen interest …. This made me feel valued. He wanted me to get better and this came across well. It is because of this that I didn’t want to let him [the physio] down. (Carol) (p. 220) |
| Finding | Social support (U) |
| Illustration | Oh, the support I got from my family and friends was great. My husband has been fantastic watching over me making sure I don’t do anything I shouldn’t. My best friend sometimes came to the rehab centre with me which I really appreciated. (Carol) (p. 221) |
| Finding | Pain (U) |
| Illustration | Pain was something I was concerned about during rehab, because sometimes doing the prescribed exercises was painful, which put doubt in my mind if I should be doing them or not. I suppose some pain is normal in order to get better but I think it is difficult to know the difference between pain that is acceptable and pain that is bad. (p. 222) |
| Study: Stephens et al . 2020 160 | |
| Finding | Lack of success with physiotherapy was attributed to many reasons, including lack of belief about the effectiveness, lack of compliance with treatment and the pain caused by exercise (U) |
| Illustration | I think I had about three different ones (physiotherapists) … and they were also the ones who did the hydrotherapy and acupuncture as well … but the exercises were just putting me in pain, so it didn’t help. (P10) (p.4) |
| Finding | Most participants remained positive about the potential of exercise therapy to improve their condition and were even happy to tolerate discomfort during it (8/10). This was often caveated with the associated desire to understand when symptoms indicated that exercise was detrimental. (U) |
| Illustration | Oh, good Lord yeah. Anything that would help I’d go for … If they told me that it would help [exercise with discomfort], I would do it. [When asked what information would be useful] Would it be detrimental if I pushed myself that little bit further?’ (P8) (p. 5) |
| Finding | However, not all participants (2/10) would find some discomfort with exercise acceptable, as pain elicited during exercise lingered significantly in some cases. (U) |
| Illustration | I wouldn’t do it (put up with discomfort during exercise). And that is purely because if it affects my day to day living … it’s just not worth it. (P6) (p. 5) |
| Study: Hasani et al . 152 | |
| Finding | All participants (8/8) expressed satisfaction with the quality of service they received via telehealth mainly because it was perceived to be efficient. (C) |
| Illustration | I did not have to go and wait in an office or whatever. I could just go to the gym and just get started and if he was not ready or whatever then I could just get into my workout and he [physiotherapist] would join me halfway through sometimes. There was no waiting around.’ (P4) (p. 4) |
| Finding | All participants (8/8) found progressive loading exercises to be an effective form of treatment compared to their experience of previous treatment approaches. (U) |
| Illustration | The idea that it is more about of putting it [Achilles tendon] under load for longer has been a lot more effective than all the stretching, warming and icing and everything else that I have tried before. (P8) (p. 4) |
| Finding | Usability of the software: nearly all participants (7/8) reported that the telehealth software was easy to use. (U) |
| Illustration | The physio would send me a link; I would click on the link on my phone and away [we] go. It was pretty effortless. (P5) (p. 4) |
| Finding | Flexibility in arranging an appointment time. The flexibility and convenience of telehealth allowed participants to schedule treatment/exercise within convenient times that avoided peak gym-use times. (U) |
| Illustration | Because I am a shift worker and I had really odd hours, it made access to the gym at times pretty good because there was nobody else there. (P1) (p. 4) |
| Finding | Therapeutic alliance: all participants (8/8) acknowledged that despite not being face-to-face with their physiotherapist, they still felt reassured by the telehealth contact with their physiotherapist, especially in the early stages when they were gaining familiarity and confidence with the treatment process. (U) |
| Illustration | She [physiotherapist] was patient and did not treat me like an idiot when I did not know what I was doing in the beginning and things like that …. She talked me through it [exercise set-up] well and all that, made it easy to understand. She let me know what I was doing at every stage. (P2) (p. 4) |
| Finding | All participants (8/8) reported that telehealth was motivating and promoted commitment to their exercise programme. (U) |
| Illustration | The audio feedback and them [physiotherapists] telling you to go longer, faster, shorter, harder, whatever their instruction happens to be, that is sort of invaluable. (P3) (p. 5) |
| Finding | Several participants (4/8) complained about poor or no Wi-Fi at their gym. There were reservations about having to use their personal phone internet data for the videoconference call. On several occasions, participants reported they were running out of phone battery, which impacted the length of the session. (U) |
| Illustration | It was the longer regimen that I was on [low-intensity group]. A couple of times my battery went out and I was using up all my data because it was an hour and a half session. (P8) (p. 6) |
| Finding | For a few participants (2/8), assistance was needed to set up the correct camera angle of their phone while they were training on the Smith machine. (U) |
| Illustration | ‘It was more the Smith machine’s limitations in regard to getting the right height for the phone. (P7) (p. 5) |
| Finding | Regular contact: participants appreciated the ability to have regular contact with a physiotherapist for support and obtain immediate feedback to allow them to progress their exercises. (U) |
| Illustration | I think if you did not have to talk to anybody, you might get lazy some days and not bother. Whereas that sort of kept you committed and making sure you will not forget your exercises. (P6) (p. 7) |
| Finding | The nature of the exercise: several participants (5/8) appreciated the simplicity (i.e. two calf-raise exercises) and how clearly they were explained as part of the trial intervention. (U) |
| Illustration | ‘It was simple and easy to do and straight forward. (P4) (p. 7) |
| Finding | Accessibility to the gym: several participants (5/8) accessed a 24-h gym in a convenient location which reportedly assisted with adherence and motivation. (U) |
| Illustration | Access to the 24-hour gym was handy for me, because I work in different hours and have got family and young kids, so it’s quite good that I could go at any time I wanted … and having the various gyms and having access to those around the place definitely helped me, because like I said, I travel a fair bit for work, so that was very handy. (P7) (p. 7) |
| Finding | Self-management education: all participants (8/8) noted that the one-to-one self-management education they received at the start of the rehabilitation programme was helpful and changed the way they perceive their Achilles symptoms. Specifically, the education improved their self-efficacy and ability to understand acceptable pain limits during activity. (U) |
| Illustration | Having a little bit of pain does not mean to say that you should not be doing the exercises. So as long as it is not getting really bad, that guidance on how to manage the pain aspect of it, now that I am thinking about it, was very handy because it gives you framework to decide well is this normal aches and pains or is it something a bit more serious. (P5) (p. 7) |
| Finding | Ability to see progress: all participants (8/8) described the care provided as effective in terms of improvement in symptoms and function. Being able to observe progress and experience less pain was reportedly a key motivator. (U) |
| Illustration | I do not have the pain that I used to. I was getting to the stage at times I was quite immobile at work. But I have not had that ever since the programme inished … which is great. (P1) (p. 7) |
| Finding | Time: making time to commit to regular exercise was reported as a barrier by several participants (6/8). This was commonly because of competing commitments e.g. employment or caregiving. (U) |
| Illustration | It was so time-consuming … I did not have much time to do anything else in the gym. (P5) (p. 7) |
| Finding | Exercise: several participants (5/8) expressed a feeling of leg discomfort from the pressure of the Smith bar on their thigh during their seated calf-raises. (U) |
| Illustration | It was suggested that I use like a foam mat or something, but I was up to about 100 odd kilos, it was quite painful to have the bar on. (P5) (p. 7) |
| Finding | Physiotherapists reflected on the accessibility and convenience of telehealth. Further, physiotherapists felt telehealth enabled more regular contact with participants. (U) |
| Illustration | I found that close contact especially with quite anxious type [participants], just being able to reassure them that where their early stages were absolutely fine and appropriate and to be expected, I think that helped them stick to the course. (PT 4) (p. 8) |
| Finding | Physiotherapists proposed that more encouragement and motivation was needed for participants requiring longer time to complete their sessions (i.e. participants in low-intensity groups who completed 18 repetitions per set rather than six). One of the proposed strategies was a follow-up email post-session. (U) |
| Illustration | I think other people who got irritated around time at the gym they definitely did longer session … I liked the follow-up emails after the session, sort of template kind of idea of what you could send them [to participants] at some point positive things from their session encouraging them for the next week. (PT3) (p. 8) |
| Finding | Technology-related: physiotherapists noted multiple technology-related issues during the telehealth sessions, including poor videoconference quality or loss of video conference connection, insufficient participant phone battery life and inability to operate the videoconference video function. Some sessions had to be discontinued due to technology-related issues. (U) |
| Illustration | Sometimes technical issues and connectivity sort of problems … a couple of times participants have forgot to recharge their phone properly and phone might have sort of drained out. (PT5) (p. 8) |
| Finding | A few physiotherapists discussed the limitations of only having one camera angle to view participants and assist with providing feedback related to calf-exercise fidelity. In some cases, physiotherapists experimented with camera angles to improve visualisation. (U) |
| Illustration | I am not entirely sure of how easy that is [telehealth] to correct technique rather than being there in person to observe that in more detail we see from different angles and adjust things as you are going so. (PT1) (p. 9) |
| Finding | Therapeutic alliance: although physiotherapists reported that the use of telehealth was an effective method for therapeutic interactions, they also reported some barriers to developing a therapeutic alliance. (U) |
| Illustration | I was probably a little slower to develop the relationship, so I found a couple of sessions to sort of warm up and get a bit more hold over messages. (PT1) (p. 9) |
| Finding | Gym-based exercise: physiotherapists reported some challenges accessing the Smith machine for some of their participants especially when the local gym had limited equipment (e.g. only one Smith machine). In some cases sessions had to be rescheduled due to long waiting times. (U) |
| Illustration | I think most people have that gym etiquette that someone is using [the machine] then leave them alone and then just keep the workout or do something else, but couple of times I have had to cancel a session because patients could not access the Smith machine for like half an hour or 40 minutes. (PT5) (p.9) |
| Study: Sandford et al . 2017 157 | |
| Finding | The importance placed on being able to manage their own condition through improved knowledge and a feeling of increased control was highlighted as a recurrent theme within the participants’ transcripts. (U) |
| Illustration | I’ve been through a series of classes and I’ve seen the benefits. I’ve just come to the realisation that it is something that I just have to manage and by doing the exercises I feel I can manage it. Exercise is key for me. (P75) (p. 196) |
| Finding | This illustrates and emphasises the need to find strategies to educate patients regarding expected rehabilitation and recovery times to ensure that their expectations are realistic. (U) |
| Illustration | At first I expected to see an improvement within a few weeks but it was so small. They tried to encourage me saying it was a long haul and by the end they said it would be six to nine months. I think it might have helped to know the six-to-nine-month time frame at the beginning. (P62) (p. 196) |
| Finding | The exercise group was cited as being good fun and helpful by several participants. (U) |
| Illustration | The group aspect was good; it was really fun. I enjoyed doing the exercises every Thursday morning, it was one hour’s really fun and that really helped me a lot. (P56) (p. 196) |
| Study: Hanratty et al . 2016 155 | |
| Finding | Need for patient education (C) |
| Illustration | So, you’re putting the onus back on them [the patient] to be proactive … to allow the patient to self-manage, that exercise is the key. (PT05) (p. 1358) |
| Finding | Achieving patient education (U) |
| Illustration | I started videoing exercises that patients are doing on their phone …. It’s a lot quicker than writing down and using PhysioTools [a computer programme that produces exercise diagrams]. (PT06) (p. 1359) |
| Study: Littlewood et al . 2015 107 | |
| Finding | Prescription of the self-managed loaded exercise programme was a challenge in terms of what might be regarded as the simplistic and restricted nature of the intervention. (C) |
| Illustration | If it was self-management I always wanted to do extra things that I could identify there and then and that was quite hard for me to take a step back. (P8) (p. 281) |
| Finding | For others with greater experience it was apparent that their existing belief system served to facilitate for some, but challenge for most, the rationale underpinning the self managed loaded exercise programme. (U) |
| Illustration | To give one exercise … it was more I had a bit of an issue with that more than the patient did to start with. (P11) (p. 281) |
| Finding | The physiotherapists recognised the importance of knowledge translation and the need to ‘sell’ the self-managed exercise intervention; both of which were underpinned by the need to develop a therapeutic relationship. (U) |
| Illustration | It’s that trust thing … if you give it confidently enough they believe you. (P1) (p. 281) |
| Finding | Most of the physiotherapists appreciated the simplicity, particularly from the perspective of the patient, in terms of improving communication and exercise adherence. (U) |
| Illustration | It’s been a lot simpler treating the self-management group; keeping the exercise regime simpler, the patients have understood it more, erm the conversation between therapist and patient has been clearer. (P11) (p. 282) |
| Finding | This simplicity was not appreciated by all and the physiotherapists considered this from their own perspective and that of the patient. (U) |
| Illustration | For my patients, they certainly found it slightly different, especially those that had experienced private physio before, erm they said oh, is that it? They were, well are you not doing anything else? Is it just one exercise? Is that it? (P8) (p. 282) |
| Finding | Discussion around this factor generated a broad range of responses from those who were very comfortable with the notion, those who were very uncomfortable and those who might be regarded as taking more of a middle ground. (U) |
| Illustration | In terms of the training it was always saying, taught that you don’t want to push in to pain that you don’t, you might get associated inhibition and sort of, of the muscles alongside it so, so different from that point of view. But then, like you said, if you have a look at it from the eccentric loading perspective then we do ask people to, to go in to pain when they’re exercising so erm I could see how it might fit. (P7) (p. 282) |
| Finding | The physiotherapists felt that most of the patients took longer to achieve a worthwhile clinical outcome than might be expected using other means of treatment. (U) |
| Illustration | The only slight barrier was more of the slightly slow progress. (P13) (p. 283) |
| Study: Littlewood et al . 2014 156 | |
| Finding | Additionally, the patients described the role of the physiotherapist, which, in some situations, seemed to compound the negative nature of their prior beliefs. (C) |
| Illustration | Well I think [physiotherapist] felt more or less straight away that it was unfortunate that I’d drawn the short straw in terms of that. (ID37) (p. 82) |
| Finding | This narrative from the patient perspective was in concordance with opinion expressed by one of the physiotherapists, where it can be seen that prior beliefs might impact upon their role in this environment. (C) |
| Illustration | I think there are some clients who from interviewing them, doing the examination, that you get an idea of whether they would be compliant and appropriate, and others you just think it’s totally inappropriate and a waste of time. (T1) (p. 82) |
| Finding | A key barrier to ongoing engagement appeared to be a lack of an early and appreciable response to the therapy. (U) |
| Illustration | I think that when you find that they’re not making a great deal of improvement, you’re less inclined to erm continue it. (ID37) (p. 82) |
| Finding | When the symptoms improved to a certain point, although not resolved, the impetus to continue was also challenged. (C) |
| Illustration | I would continue if it was still badly hurting. (ID13) (p. 82) |
| Finding | Following some early reported benefit from the exercise programme, one patient indicated subsequent difficulty as the symptoms failed to respond as the programme progressed. Despite this, they did not consider regressing the programme or seeking advice, indicating an external locus of control as a potential barrier. (C) |
| Illustration | I just followed whatever the next one was … I just kept thinking I’ll be glad when I go back and I might have something to do a bit easier or something. (ID17) (p. 82) |
| Finding | Some patients still expressed concern about attributes of the intervention. (C) |
| Illustration | At first it seemed like a big task to do, because it was an additional thing to do through the day. (ID18) (p. 82) |
| Finding | Disquiet was expressed about the simplicity of the intervention and hence its lack of potential effectiveness. (U) |
| Illustration | To cap it all it’s such a simple exercise … I just came out thinking waste of time. (ID29) (p. 82) |
| Finding | The influence of the physiotherapist was framed in a more positive way (U) |
| Illustration | She explained it very well and said what the aim was and that if it did hurt what to do … I could ring her if I had problems, and she was very responsive, she rang me back the same day and said what to do … I felt very comfortable, very confident. (ID18) (p. 83) |
| Finding | One patient recognised the role of their partner in providing feedback and stimulating further engagement with the self-managed exercise programme during times when progress was slow. (C) |
| Illustration | My (partner) erm kept saying to me that (they) thought that I was complaining a lot less as time went on. I didn’t feel that but she assured me that I was. (ID15) (p. 83) |
| Finding | Patients also described personal traits that indicated self-efficacious individuals who took control of the programme. (U) |
| Illustration | I kept my diary and I always wrote why I’d not done it so that I could think to myself well how can I fit that in then? (ID18) (p. 83) |
| Finding | Other personal attributes were also described. (U) |
| Illustration | I was driven to get rid of this pain really, so I thought I’m going to give this a really good go and do it properly. (ID18) (p. 83) |
| Finding | Physiotherapists felt able to identify patients who they expected would successfully engage with the self-managed exercise programme. (U) |
| Illustration | I think it’s a certain type of person where you’re going to be able to have success with a regime of exercises and no hands-on, I would say …. People who were very positive about life … they were usually quite outgoing, quite confident in themselves and quite determined. (T1) (p. 83) |
| Finding | One patient reflected upon a previous episode of physiotherapy when engagement with a prescribed exercise programme was limited. (C) |
| Illustration | I didn’t do them … I don’t know – because I thought they were doing it for me. So I came back with the booklet but I didn’t do them. I thought oh well, I’m going back next week. (ID18) (p. 83) |
| Finding | Whereas some patients had found aspects of the intervention difficult to implement, those patients who reported a successful outcome detailed different experiences. (U) |
| Illustration | With it being such an easy exercise it … became part of a routine … I would do, it was short, short and sweet. So it wasn’t a case of having to find time to do it, it just naturally fell into a little sort of routine that I have. (ID29) (p. 83) |
| Finding | With reference to the exercise diary which is used as a key component of the programme as a means of self-monitoring, one patient reflected: (C) |
| Illustration | I stuck the sheet that I was given on the fridge so it was there in the kitchen to remind me every day. (ID29) (p. 83) |
| Finding | Additionally, with regard to the proactive follow-up by the physiotherapist, another patient recognised: (U) |
| Illustration | I knew I was seeing (physiotherapist) on those regular appointments; it was every four weeks wasn’t it? So because I knew I was seeing her, I didn’t want to go to her and say I’ve not done it. So that was a motivator to me. (ID18) (p. 83) |
| Finding | Patients experienced a favourable therapeutic response that persuaded them of the potential value of the programme to them. (U) |
| Illustration | When I started seeing the results … I was so pleased with it that that motivated me on more and more to keep going. (ID18) (p. 83) |
| Study: White et al . 2020 159 | |
| Finding | The need for early, focussed education: ‘some beliefs can be detrimental to rehabilitation options’. (U) |
| Illustration | It’s about trying to reduce anxiety through education or reassurance and to reduce any hypervigilance, which actually may affect their outcome … and ultimately affect their adherence to any exercise intervention. (P1, PT) (p. 3) |
| Finding | Patient-centred care promotes development of a therapeutic alliance: ‘If a patient trusts you then you are generally going to get much better results. (U) |
| Illustration | Some patients might need five minutes of education, another patient may need two or three sessions where it is quite intensive, or they might need to cover different areas, so I think it depends on the patient that you have in front of you similar to what exercise you prescribe. (P1, PT) (p. 3) |
| Finding | What challenges and enablers should be considered in RT education delivery? ‘Maybe we can get better?’ (U) |
| Illustration | Work together in a positive pathway with me describing the exercises and illustrating how to do them and motivate patients and have the patients adhere to the programme. Because adherence is the key to the success. If they come back and they say, well, I forgot your exercises. I did them once a week instead of every day, then we are not moving forward … so it is a shared responsibility. (P2, PT) (p. 3) |
List of abbreviations
- ACTIVE
- Authors and Consumers Together Impacting on Evidence
- ANZCTR
- Australia and New Zealand Clinical Trials Registry
- AT
- Achilles tendinopathy
- CrI
- credible interval
- DASH
- Disabilities of the Arm, Shoulder and Hand
- ESWT
- extracorporeal shockwave therapy
- EU-CTR
- European Union Clinical Trials Registry
- GRADE
- Grading of Recommendations Assessment, Development and Evaluation
- GRIPP2
- Guidance for Reporting Involvement of Patients and the Public 2
- GTPS
- greater trochanteric pain syndrome
- HDI
- Human Development Index
- HEP
- home exercise programme
- ICON
- International Scientific Tendinopathy Symposium Consensus
- JBI
- Joanna Briggs Institute
- MT
- manual therapy
- NMA
- network meta-analysis
- NSAID
- a nonsteroidal anti-inflammatory drug
- NPRS
- numerical pain rating scale
- NRS
- numerical rating scale
- OMERACT
- Outcome Measures in Rheumatoid Arthritis Clinical Trials
- PFC
- physical function capacity
- PRISMA
- Preferred Reporting Items for Systematic reviews and Meta-Analyses
- PRISMA-ScR
- Preferred Reporting Items for Systematic reviews and Meta-Analyses – Extension for Scoping Reviews
- PRP
- platelet-rich plasma
- PTTD
- posterior tibial tendon dysfunction
- QoL
- quality of life
- RC
- rotator cuff
- RCRSP
- rotator cuff-related shoulder pain
- RCT
- randomised controlled trial
- ROM
- range of motion
- SPADI
- Shoulder Pain and Disability Index
- SUCRA
- surface under the cumulative ranking curve
- TA
- treatment arm
- TIDieR
- Template for Intervention Development and Replication
- VAS
- visual analogue scale
- VISA-A
- Victorian Institute of Sports Assessment – Achilles
- VISA-P
- Victorian Institute of Sports Assessment – Patella
- VPC
- variance partition coefficient
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/TFWS2748).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
