Notes
Article history
The research reported in this issue of the journal was funded by PGfAR as project number RP-PG-0611-20013. The contractual start date was in December 2013. The final report began editorial review in November 2019 and was accepted for publication in October 2021. As the funder, the PGfAR programme agreed the research questions and study designs in advance with the investigators. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PGfAR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2022 Sparrow et al. This work was produced by Sparrow et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2022 Sparrow et al.
SYNOPSIS
Background
Cataract surgery is one of the most frequently undertaken surgical procedures, with approximately 450,000 operations undertaken annually by the NHS, at an estimated cost of £450M. 1 The cost-effectiveness of cataract surgery for established cataracts is uncontroversial, and surgery is recommended by the National Institute for Health and Care Excellence (NICE). 3 For individuals affected by a gradual onset and progression of visual difficulty from cataracts, the decision as to when to delay and when to proceed with cataract surgery remains a matter of judgement, with many, sometimes competing, factors requiring consideration.
Although most cataract surgery is highly successful, there is evidence of unmet need and local variation in how referrals for cataract surgery were processed. 2 There are inevitable risks associated with the procedure, and these need to be considered in the context of visual requirements, visual difficulty and potential to benefit. Standard pre-operative assessment for cataract surgery currently relies heavily on measurement of visual acuity (VA),3 a test conducted one eye at a time, in a darkened space, with self-reported visual difficulty all too frequently receiving secondary consideration at best.
Programme structure and interlinkage of work packages
The cataract research programme consisted of four interlinking mixed-methodology work packages (WPs) (Figure 1), with work from each WP feeding forward to contribute to and inform subsequent elements. The overarching theme throughout the programme was the development and assessment of clinical tools intended to support and enhance pre-operative decision-making by patients considering cataract surgery and health-care professionals (HCPs) delivering their care.
FIGURE 1.
Research pathway diagram. Cat-PROM5, Cataract Patient-Reported Outcome Measure, five items; PROM, patient-reported outcome measure.
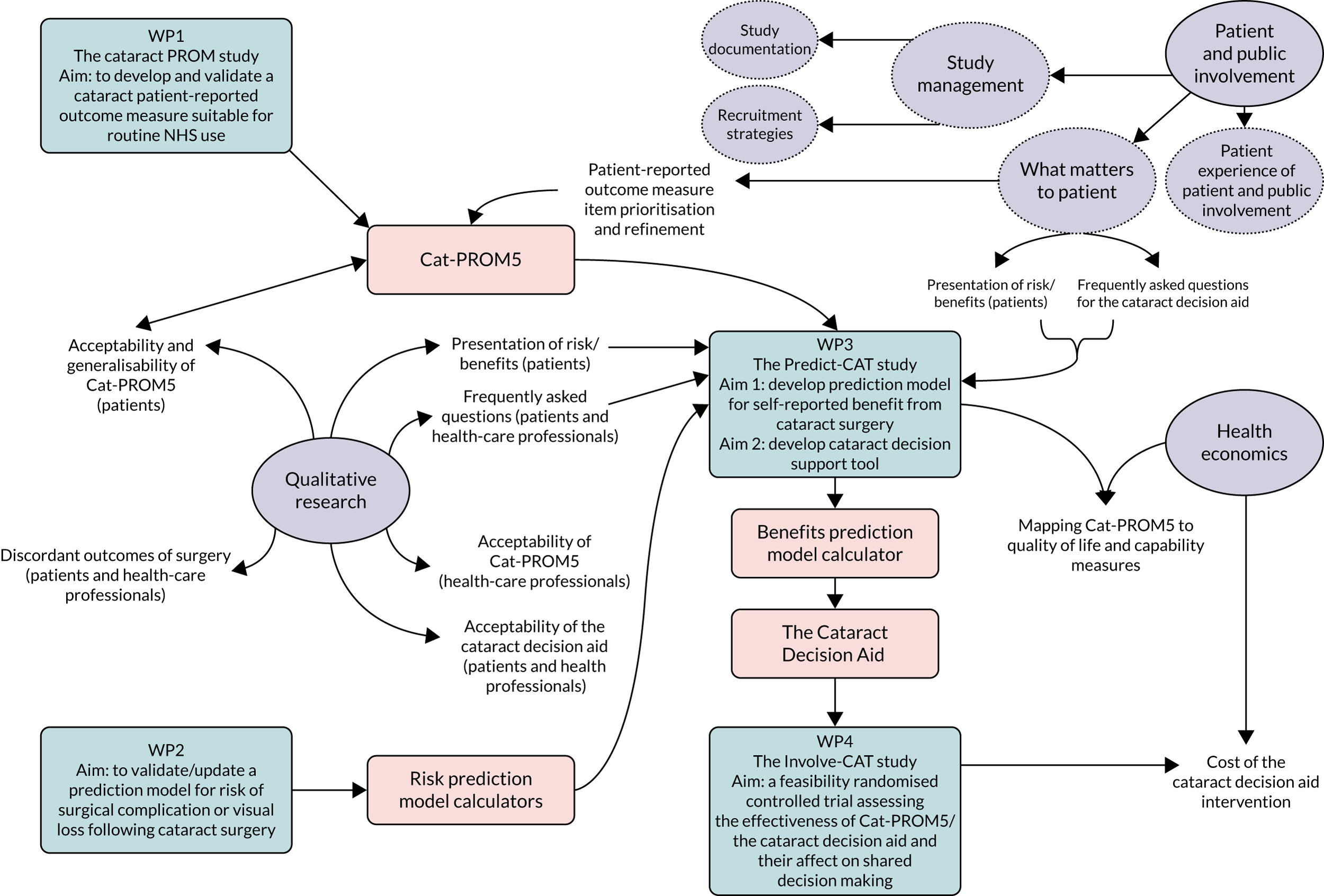
Work package 1 comprised the development, assessment and validation of a psychometrically robust cataract patient-reported outcome measure (PROM) for the measurement of visual difficulty from cataracts and its relief from surgical intervention. The resultant self-reported measure, Cataract Patient-Reported Outcome Measure, five items (Cat-PROM5), was taken forward to WP3, in which prediction models for the Cat-PROM5 outcome were developed to predict the likely patient self-reported post-surgery benefit. Occasionally, surgery can have adverse outcomes that are of importance to patients and HCPs. In WP2, existing prediction models for established adverse outcomes were reassessed on fresh, routinely collected NHS electronic medical record data for two important adverse outcomes: an intraoperative complication [posterior capsule rupture (PCR)] and VA loss affecting the eye that was operated on following surgery.
Using questionnaire data collected in WP3, a parallel health economics mapping exercise was undertaken to translate the Cat-PROM5 scores into established health economic utilities, thus facilitating future health economics research in cataract studies through reducing questionnaire burden on study participants. Qualitative work elements ran through each of the WPs to gain a rounded picture of the preferred formats for the development of clinical tools based on outputs of the prediction models and the information requirements of both patients and HCPs. Through this approach, a cataract decision aid (CDA) was developed, providing patients and HCPs with relevant information on cataracts and cataract surgery, including personalised predictions of both the likely post-operative self-reported visual benefit and possible adverse outcomes. In WP4, we assessed the feasibility of a future fully powered randomised controlled trial (RCT) with the CDA as an intervention.
In addition to the four main WPs, a number of additional studies were opportunistically undertaken and these have provided ‘added value’ to the cataract research programme overall.
Patient and public involvement
The cataract research programme was supported by a Patient and Public Involvement (PPI) Patient Advisory Group (PAG) throughout the programme, from the grant development stage through to programme completion, with group sessions and comments from group members contributing positively and successfully to many aspects of the work.
The lead applicant established the PAG at the pre-application stage. The initial group consisted of five patients who had attended the cataract treatment service at the Bristol Eye Hospital who had received surgery on one or both eyes. Therefore, the patients were experts on their own experience, could meaningfully contribute their personal thoughts and understanding of their visual abilities and difficulties, and were ideally placed to advise the management team on a wide range of themes related to the programme. During the programme, some group members left for personal reasons and were succeeded by new members recruited from the hospital cataract service.
Professor David Evans, who previously led People in Health West of England,4 was the chairperson of the PAG, which met twice a year at the Bristol Eye Hospital (n = 10 meetings in total). At the inaugural meeting, ‘ground rules’ were established, with the aim of fostering a positive and supportive informal environment to encourage open discussion. Meetings were formatted to include a programme overview and progress report, followed by a task, and concluded with feedback on the impact of their contributions to date.
The PAG members who were unable to attend the meetings were invited to contribute remotely if they were able to and, between meetings, contributions were gathered from members by e-mail, over the telephone or by post, depending on their preferences and on the task involved. Where relevant, documents were shared prior to each meeting to allow members to have time to become familiar with the content and the research methodology was explained to the group at a level commensurate with their prior knowledge and the requirements of the task.
The following is a summary of the main themes under which the PAG contributed to the running of the programme:
-
Pre-application stage
-
Prior to submission of the application, patient representatives met to review the main aims of the research and discuss their own experiences and thoughts on patient decision support.
-
-
Prior to ethics approvals
-
The group made suggestions for improvement of the format and content of patient information sheets and informed consent forms to ensure readability. This included changes to the font, layout, length and some of the wording to improve plain English.
-
PAG members suggested improvements to the promotional materials of the cohort study (named Predict-CAT) to promote interest in the study and highlight the potential benefits to participants.
-
They discussed and supported the idea of a ‘self-referral’ system whereby potential participants could be sent study information by post following their hospital appointment and refer themselves to the study team. This improved the recruitment rate of the Predict-CAT study and contributed 15% of the overall participants.
-
-
Questionnaire item reduction
-
During the development cycles of the cataract PROM questionnaire, the PAG were invited to take part in a group exercise to help guide decisions on the relative priority of questions being considered for the final version of the Cat-PROM5 questionnaire (where initial statistical analysis results were supportive). The exercise involved the PAG members commenting on how important they felt the question was to cataract patients and the theme or domain to which they thought the question related.
-
-
Qualitative discussion
-
Members of the PAG were invited by e-mail to make comments on the drafted topic guides for the qualitative Predict-CAT substudy (Predict-CAT-Qual), specifically on whether or not the proposed questions were understandable.
-
The group were invited to discuss the acceptability of the presentation of risk during a face-to-face meeting.
-
Prior to the commencement of focus groups with study participants, and led by Christalla Pithara, PAG members discussed their experiences and thoughts on shared decision-making (SDM) and the use of decision aids. PAG members were also asked to comment on the type of information that is important for patients to receive in advance of their operation to inform the ‘mismatching outcomes’ element of the qualitative work.
-
Led by Natalie Joseph-Williams and Daniella Holland-Hart, the PAG members took part in a focus group that focused on the question of what matters to patients when deciding to have surgery [to inform the development of the frequently asked questions (FAQs) section of the CDA] and also provided feedback on the drafting of the CDA.
-
-
PAG evaluation workshop
-
At the final PAG meeting, Professor David Evans led a group exercise to map the experiences of the group members and management team, and to collectively and individually reflect on their experiences of PAG participation. Using a modified version of the ‘cube’ framework for PPI process evaluations,5 patient members demonstrated their experience across four dimensions related to their perception of their involvement in research. The analysis of this exercise is under way at the time of writing and it is planned to share the findings of this and the group discussion at a later date. The programme team feel that the duration of PAG membership and the number of meetings that were held provided a unique experience and opportunity to elucidate what does and does not work well in PPI within ophthalmology services and, therefore, the team are of the view that our findings may benefit future research.
-
The cataract research programme was also supported by PPI in the following ways:
-
Prior to the commencement of the cataract research programme, developers of the host questionnaires Vision Core Measure 1 (VCM1)6 and Visual Symptoms and Quality of life questionnaire (VSQ),7 which together formed the basis of Cat-PROM5 development, used patient interviews to identify themes and issues relevant to patients (with the VCM1 consulting visually impaired patients and the VSQ consulting cataract patients).
-
A former patient of the Bristol Eye Hospital Cataract Care Service sits on the Programme Steering Committee and provided expert commentary, knowledge and guidance from a user perspective throughout the programme.
-
A patient representative also sat on the User Reference Group (URG), which was established to discuss the developing versions of the CDA.
Work package 1: development of Cat-PROM5, a brief cataract patient-reported outcome measure
Aims
-
To develop a short, psychometrically robust and responsive cataract PROM questionnaire measuring the construct ‘visual difficulty related to cataract’, which is suitable for use in high-volume surgical environments.
-
To compare and contrast the newly developed PROM with the current ‘best-of-class’ instrument that is available for use in routine cataract surgical services using both quantitative and qualitative methodologies.
Approach
From our earlier questionnaire work, candidate questions were harvested from two published questionnaires: the VCM16 and the VSQ7 PROMs. Under the construct ‘visual difficulty due to cataract’, 21 questions were reoperationalised into the first developmental version of the questionnaire. Three iterative cycles of questionnaire administration, analysis and item reduction were used to arrive at the final item set of five questions; the psychometric performance of these five questions was confirmed in the final cycle of independent data collection and analysis. Following confirmation of the psychometric performance of the five-item set, its performance was also compared in a head-to-head study with the existing, longer, ‘best-of-class’ 9-item questionnaire, the Cataract questionnaire 9-item Short Form (Catquest-9SF). 8,9 In a separate qualitative exercise, the final item set was evaluated in a group of patients that included people who had cataracts and other ocular comorbidities.
Data collection
People with age-related cataracts who were awaiting first- or second-eye cataract surgery at four participating centres (Bristol, Torbay, Gloucestershire and Brighton) were potentially eligible for recruitment.
The inclusion criteria were being aged ≥ 50 years, the ability to understand and complete development versions of the Cataract PROM and Catquest-9SF in English, and the willingness to participate and to provide informed consent. The exclusion criterion was visually significant ocular or systemic comorbidity.
Three iterative cycles of data collection and analysis were undertaken. The initial cycle, ‘cycle 0’, or pilot, was restricted to pre-operative questionnaire completions and predominantly took place in Bristol. The development cycle, ‘cycle 1’, and the confirmatory cycle, ‘cycle 2’, each collected both pre- and post-operative data.
Data analysis
Rasch analysis was the primary analytical method used,10–12 supported by supplementary analyses. Among the many advantages of Rasch analysis are that it allows for the selection of unidimensional questions (items) that together measure an underlying latent trait (here, difficulty with vision due to cataracts), it assesses the performance of the individual items (disordering, fit, differential item functioning), it indicates the overall reliability of the item set and it delivers a continuous scale or measurement of the underlying latent trait. Supplementary analyses included principal components analysis and confirmatory factor analysis. 11,13–17
Data were collected by participants completing developmental versions of the new Cataract PROM questionnaire, as well as the established Catquest-9SF for purposes of comparison.
Cataract patient-reported outcome measure development
Analysis of the 200 ‘cycle 0’ completions resulted in the removal of 10 items based on a range of statistical techniques, including sequential Rasch (partial credit model) analyses (items were excluded if they had disordered thresholds, poor fit or category-average disordering, and the worse-performing item of an intentionally included pair of duplicate questions was excluded), principal components analysis and confirmatory factor analysis.
The resulting unidimensional 11-item set was taken forward to a development cycle, ‘cycle 1’, in which 316 patients completed questionnaires at both pre- and post-operative time points. Preliminary analysis revealed that the selection of fewer than five items resulted in a consistent and significant drop in psychometric performance (Rasch reliability) and it was decided to aim for a five-item final set. The two best performing items were selected for inclusion, followed by a systematic search for the next-best three items, based on 84 possible combinations. Through a comprehensive selection process that included assessment of Rasch performance parameters, responsiveness to surgery, patient preferences [as advised by the programme’s PPI PAG] and expert opinion, the remaining three items were chosen.
The final five-item set was checked in a confirmatory cycle, ‘cycle 2’, in which 306 pre- and post-operative completions were made.
Comparison with Cataract questionnaire 9-item Short Form
Psychometric Rasch analysis confirmed that the five-item set performed at least as well or better than the previous, longer and more restrictive ‘best-of-class’ instrument, the Catquest-9SF. 18
Qualitative element
A qualitative study on a separate small group of patients explored the face-validity and acceptability of both the Cat-PROM5 and Catquest-9SF questionnaires. 18,19 In this group, participants included people with visually significant comorbidities. Semistructured face-to-face interviews were guided by an interview schedule or topic guide, with new points added as analysis progressed to enable the exploration of emerging themes. 20 Transcribed data were coded using standard software for the collation, storage, analysis and management of qualitative data (NVivo; QSR International, Warrington, UK), and analysed using techniques of constant comparison derived from grounded theory methodology. 21,22 Emerging themes and codes in transcripts and across the data set were then compared to look for shared or disparate views among participants. 23 Data collection and analysis continued until the point of data saturation.
A total of 16 interviews were conducted with nine men and seven women: 11 of the patients were awaiting their cataract surgery and five had recently undergone surgery. Thirteen participants had other visual comorbidities. Overall, participants found both questionnaires acceptable, although patients with severe visual comorbidities noted that it was difficult to separate how the cataract and their other conditions affected their quality of life. Most participants preferred the large-font format of Cat-PROM5. Some participants preferred questions with more response options, as in Cat-PROM5, whereas others preferred fewer response options, as in the Catquest-9SF. The specific scenarios of the Catquest-9SF created some uncertainty for those whose other health problems affected the issue being addressed and where the issue was not relevant to their lives; respondents were uncertain about how to respond. By contrast, Cat-PROM5 enabled them to determine the individual vision-related factors that they perceived to be important and to respond to the questions easily.
Limitations
To develop Cat-PROM5 as an instrument that is specific to cataract-related visual difficulty, the developmental cycles excluded people with visually significant, non-cataract ocular or systemic comorbidities. This approach could have affected the generalisability of the new questionnaire and this issue was addressed by undertaking a separate qualitative study of the final Cat-PROM5 questionnaire to understand the potential impact of this issue. The qualitative findings were reassuring (as were subsequent studies within work package 3 that included people with visually significant comorbidities).
Key findings
A brief, psychometrically robust questionnaire was developed that performed at least as well or better than the previous, longer, ‘best-of-class’ alternative. The Cat-PROM5 questionnaire has excellent reliability (Rasch 0.9, person separation 2.98, low differential item functioning, Cronbach alpha 0.89), is unidimensional (infit–outfit 0.84–1.14, residual eigenvalues ≤ 1.5), is valid (strong correlation with existing longer measure, R = 0.85), is repeatable (Rasch scale intraclass correlation coefficient 0.89) and is responsive to surgery (baseline to follow-up Cohen delta –1.45). The Cat-PROM5 questionnaire is flexible, allowing patients to map their personal visual difficulties to the questions, and it is sufficiently brief to make it feasible to implement it into routine, high-volume cataract surgical services.
The Cat-PROM5 questionnaire is available for download as a supplementary online form at https://static-content.springer.com/esm/art%3A10.1038%2Feye.2018.1/MediaObjects/41433_2018_BFeye20181_MOESM134_ESM.pdf
Relationship with other work packages
Cat-PROM5 was established as the Cataract PROM for the programme and was taken forward to WP3, Predict-CAT (the development of benefits prediction models, presentation of risk information and development of a CDA), and WP4, the feasibility study for a future RCT (named Involve-CAT), as the measure of self-reported benefit.
Work package 2: cataract surgery risk models for posterior capsule rupture and visual acuity loss
Aim
To validate or update existing risk models for PCR and monocular harm using multicentre data from 180,000 electronic medical records (EMRs) for cataract surgery.
Approach
We modelled two key outcomes that are of importance in cataract surgery. These are the two primary safety outcomes used in the National Ophthalmology Database (NOD) audit. 1
Posterior capsular rupture is defined, for the purposes of the National Cataract Audit, as ‘posterior capsule rupture with or without vitreous prolapse or zonule rupture with vitreous prolapse’ and abbreviated as PCR. 24 It should be noted that the definition excludes zonule dehiscence where no vitreous prolapse has occurred. PCR is the most frequently arising intraoperative complication and is reported for 1.1% of operations in the National Audit; the next most frequently reported specific complication is recorded as arising in just 0.3% of operations. 24 When PCR, as defined above, occurs, there is an approximately sixfold-increased risk of vision loss, an approximately 40-fold-increased risk of post-cataract retinal detachment and an approximately eightfold-increased risk of endophthalmitis (serious post-operative infection in the eye). 25 PCR is regarded by NICE as an adverse and harmful event in cataract surgery3 and is a key safety outcome in the National Cataract Audit, and avoidance of PCR has high validity with surgeons. 24
Visual acuity loss in the eye undergoing surgery refers to vision that is significantly worse after the operation than it was before, as measured using the sight test letter reading chart. VA loss arises in 0.5% of operations and is the second key National Cataract Audit safety outcome, in which it is defined as a doubling (or worse) of the visual angle. 24
Data collection
Multicentre data were obtained from the NOD1 through a data-sharing agreement with the data controller, the Health Quality Improvement Partnership (HQIP). The data consisted of the patients’ electronic medical records and covered cataract surgery undertaken by participating centres between 2006 and 2010. The anonymised sample consisted of 180,114 eyes from 127,685 patients (see Report Supplementary Material 1 for further details of outcomes, exposures and distributions).
Data analysis
Known and suspected candidate predictors for PCR and VA loss were evaluated using a logistic regression analysis.
Posterior capsule rupture
Posterior capsule rupture data were complete. In this sample, PCR arose in 3514 out of 180,114 (1.95%) eyes.
Visual acuity loss
There were some missing VA data. Of the 180,114 eyes in the sample, 147,962 had pre-operative VA readings. For 104,437 (70.6%) eyes, these were corrected VA readings; for 43,525 (29.4%) eyes, these were uncorrected readings. A further 1591 eyes had pre-operative pinhole readings only, but these were not used in this analysis. Of the 180,114 eyes in the sample, 116,038 had post-operative VA readings. For 74,887 (64.5%) eyes, these were corrected VA readings; for 28,678 (24.7%) eyes, these were uncorrected VA readings; and for 12,473 (10.8%) eyes, these were pinhole VA readings, which were accepted post operation. Of the 147,962 eyes with pre-operative VA readings, 95,561 (64.6%) had post-operative VA readings. For 60,578 (63.4%) eyes, they were corrected VA readings; for 24,460 (25.6%), they were uncorrected VA readings; and for 10,523 (11.0%), they were pinhole VA readings. In this sample of operations, undertaken between 2006 and 2010, the VA of 1455 out of 95,561 (1.52%) eyes deteriorated after cataract surgery, a proportion which has significantly reduced since these (early) data were collected. 24
Backwards and forwards logistic regression was carried out, taking account of the clustered nature of the data (the fact that left and right eyes from the same patient are unlikely to be independent). Having established the logistic regression model, the model statistics were reported (see Report Supplementary Material 1).
Key findings
Posterior capsule rupture
The following variables entered into/remained in the logistic regression model: age, surgeon grade, pupil size, glaucoma, brunescent/white cataract, no fundal view/vitreous opacities, previous vitrectomy, pseudoexfoliation/phacodonesis and other ocular pathology. The area under the receiver operating characteristic (ROC) curve (C-stat) for this model was 0.64, indicating fair fit.
Visual acuity loss
The following variables entered into/remained in the logistic regression model: PCR, age, axial length, pupil size, gender and the following copathologies; glaucoma, age-related macular degeneration, diabetic retinopathy, corneal pathology, brunescent/white cataract, previous vitrectomy, other macular pathology, other retinal vascular pathology and other ocular pathology. The area under the ROC curve (C-stat) for this model was 0.71, indicating reasonable fit.
Both the PCR and VA loss models were broadly similar to our earlier work carried out on 55,678 cataract operations undertaken before and up to 2006,26 suggesting that the models were reasonably stable prior to 2010.
Limitations
Overall, the main limitation of this work was the fact that the data that was obtained related to surgery undertaken between 2006 and 2010. In addition, some VA data were missing, with only 64.6% of eye operations having both a pre- and a post-operative VA measurement available for calculation of the VA loss measure.
Electronic patient data are recorded by clinical staff, including surgeons, and it is possible that not all adverse outcomes (PCR and VA) were accurately recorded.
To address the limitation of these surgeries being from a relatively early cohort of operations, fresh data were requested from the NOD through an updated data-sharing agreement with the data controller (HQIP). The fresh data allowed analysis of model stability through time to be performed for PCR on data up to 2014.
Relationship with other work packages
Based on these approaches, calculators estimating the risk of PCR and VA loss were taken forward to WP3 for the determination of patients’ preferred mode of presenting risk information and the identification of patients’ concerns for the FAQs and development of the CDA. The CDA was subsequently tested in the WP4 feasibility RCT.
Added value: posterior capsule rupture model stability through time
Aim
To review methodological options for development of the risk prediction model for PCR on extended, more up-to-date data, and to assess PCR model stability through time.
Approach
Available options for logistic regression model building were reviewed and applied to the data. In this methodological exercise we chose to analyse PCR only, as the data for this key surgical outcome were complete.
Data collection
Multicentre data were obtained from NOD1 through a data-sharing agreement with the data controller, HQIP. The data covered cataract surgery undertaken by participating centres between 2000 and 2014. The anonymised sample consisted of 602,459 operations conducted on the eyes of 404,857 patients.
Data analysis
Three approaches to candidate risk predictor selection for model building were used: (1) a clinically sound list of predictors; (2) the χ2 p-value of < 0.10 was used for predictors to exclude those that, from the outset, appeared unlikely to be statistically important; and (3) a univariate effect size (ES) satisfying 0.9 > odds ratio (OR) > 1.20 was used to exclude small, and therefore clinically unimportant, effects.
Following these analyses, stability through time was considered. Early years were excluded, as the sample sizes were smaller and the number of less common risk indicators were too few, which would generate unstable results. The 10-year period from 2005 to 2014 was taken forward to assess logistic regression model stability through time. The models derived from the three options for initial selection of candidate predictors were applied to each year separately, and were assessed for stability across the 10 years.
Key findings
The three candidate predictor selection options resulted in slightly different lists of predictors, indicating that the method of selection of candidate predictors (clinically sound, or χ2 p < 0.1, or 0.9 > OR > 1.20) was important. Model fit was fair to moderate for all of the models, with C-statistics near or slightly above 0.6.
The models, which were derived using the full set of data, were applied to each of the years separately and parameters examined for stability across the years. For a number of variables, statistical significance was not consistently achieved within years. Overall, for all of the initial candidate selection options, the models were stable for the period 2005–11. The year 2012 was an atypical year, not being consistent with earlier or later periods, whereas 2013 and 2014 were comparable.
These results confirm that, although the models are generally temporally stable, there are inconsistencies through time that underline the importance of reviewing risk models from time to time when these models are being used to adjust for outcomes of centres and surgeons.
Limitations
The data used in these analyses are ageing, and these analyses could be brought up to date through analysis of a fresh sample.
Because of the problem of missing VA data, it was not deemed appropriate to extend the analysis to include VA loss.
Relationship with other work packages
This ‘added value’ item in the programme provided key information about the stability of the PCR risk model and the model-based risk calculator used in the CDA (WP4).
The wider implications of these findings include confirmation that the risk model, although stable across certain periods, is prone to shifts; this emphasises the need to review and revise the models that are being used in national audits to adjust for case complexity of centres and surgeons (see Report Supplementary Material 2).
Added value: cataract outcomes in people aged ≥ 90 years
Aim
To report operative complications (PCR) and VA outcomes for cataract surgery in people aged ≥ 90 years.
Approach
We performed an analysis of elderly patients undergoing cataract surgery.
Data collection and analysis
A subgroup analysis of data obtained through a data-sharing agreement with the NOD and HQIP (as noted in Data collection) was undertaken. We analysed the outcomes of 25,856 cataract operations undertaken in 19,166 people aged ≥ 90 years between the years 2000 and 2014. 27
Key findings
A significant operative complication (PCR) occurred in 2.7% of all operations. Although this is higher than the rate found among younger patients, the surgical risk remains relatively low. 24
Post-operative VA was available for 61.8% of eyes, with VA being good enough for the patient to drive (Snellen VA 6/12) in 74.4% overall, and 84.7% reaching this level out of those without a visually significant comorbidity.
Limitations
The main limitation of this study was the reduced proportion of patients with a post-operative VA recording.
Relationship with other work packages
This work was a standalone substudy offering added value to the programme overall.
This ‘added value’ analysis has been published. 27
Added value: refractive outcomes of cataract surgery
Post-operative refraction (spectacle requirement) is determined by the choice of the replacement lens implanted into the eye during a cataract operation. The outcome of the refraction dictates the spectacle correction required following surgery.
Aim
To undertake a proof-of-concept analysis to identify indicators of refractive outcome using complex numbers as a basis for analysis.
Approach
The measurement of refraction consists of three variables (sphere, cylinder and axis), which makes the analysis and reporting of refraction problematic; a variety of simplified measures are used clinically to choose an appropriate lens implant at the time of surgery. A comprehensive measure of refraction can, however, be achieved using complex numbers. 28 This complex-numbers approach has been used in this proof-of-concept analysis to assess its methodological feasibility for use as a comprehensive refractive outcome measure for cataract surgery that, crucially, does not approximate or discard any of the information in the refractive result.
Data collection and analysis
A fresh third set of electronic medical record data was obtained from the NOD through an updated data-sharing agreement with HQIP. Data on 1,070,601 cataract operations were received. The primary refractive outcome of interest was available for 491,414 of these operations. The primary outcome was trivariate and was modelled using a multivariate, normal, multilevel model and four multilevel structures. 29
Key findings
Despite the methodological complexity of the analytical approach, it was feasible to apply the method to refractive outcome data and rigorously model indicators of post-operative refraction. Analysis revealed that ocular comorbidities did not impact refractive outcome to a clinically important extent, but the complex-numbers methodology revealed a greater spread of refractive outcomes than expected. This method will be of interest to surgeons for outcomes assessment and refinement of refractive outcomes.
Limitations
Less than half of the full set of data contained all of the information required for the analysis, potentially reducing the generalisability of the results. However, the purpose of the analysis was to demonstrate feasibility through a proof-of-concept analysis, which was achieved.
Relationship with other work packages
This analysis is a standalone item with regard to the other WPs, but post-operative refraction is highly relevant to patients’ post-operative perception of their surgical outcome. The relationship between refractive outcome and patients’ self-reported opinion has been highlighted in the findings of the WP4 discordant outcomes study (see Work package 4, Qualitative element 2: mismatching outcomes).
Further information
-
Report Supplementary Material 1 provides additional detail on the logistic regression analyses that were undertaken, based on 180,000 cataract procedures.
-
Report Supplementary Material 2 provides ‘added value’ to the programme through an analysis of the stability through time of the risk models, based on 600,000 cataract procedures.
-
Report Supplementary Material 3 provides ‘added value’ to the programme through an analysis of outcomes for people aged ≥ 90 years, based on 25,000 cataract procedures.
-
‘Added value’ is provided to the programme through an analysis of indicators of refractive outcomes, using a novel approach to analysis of refraction data, based on a subgroup of 491,414 operations for which relevant pre- and post-operative refractive data were available.
Work package 3: Predict-CAT and the development of a cataract decision aid and cataract decision quality measure
Quantitative elements: the Predict-CAT cohort study
Aim
To develop a benefits prediction model for personalised prediction of self-reported Cat-PROM5 benefit from cataract surgery.
Approach
We conducted a cohort study of 1500 people undergoing cataract surgery to phenotype the participants, with a view to identify pre-operative indicators of post-operative self-reported benefit from surgery in terms of final post-operative outcome and improvement from pre-operative baseline.
Data collection
The cohort study took place at two sites: Bristol and Gloucestershire. Pre-operative patients approaching cataract surgery were invited to participate. The inclusion criteria were aged ≥ 50 years; approaching either first- or second-eye cataract surgery; willingness to participate and provide informed consent; and the ability to understand and complete the Cat-PROM5, EuroQol-5 Dimensions, three-level version, (EQ-5D-3L), EuroQol-5 Dimensions, three-level version, with vision ‘bolt-on’ domain (EQ-5D-3L+VIS), EuroQol-5 Dimensions, five-level version (EQ-5D-5L) and ICEpop CAPability measure for Older people (ICECAP-O) questionnaire instruments as required. Following recovery, postal questionnaire completions were made between 6 and 8 weeks after surgery. Full recruitment of 1506 participants was achieved, with 1204 patients recruited in Bristol and 302 in Gloucestershire. It is noteworthy that encouragement from our Patient Advisory Group to introduce a self-referral option resulted in 15% of Bristol’s recruitment through this route. Following withdrawals, losses to follow-up and data cleaning, 1181 participants had complete data for analysis (Figure 2).
FIGURE 2.
The Predict-CAT flow diagram. a, Some people gave more than one reason; b, the number analysed varies between reports because of data completeness. BEH, Bristol Eye Hospital; GHNHSFT, Gloucestershire Hospitals NHS Foundation Trust. HE, health economics questionnaire.
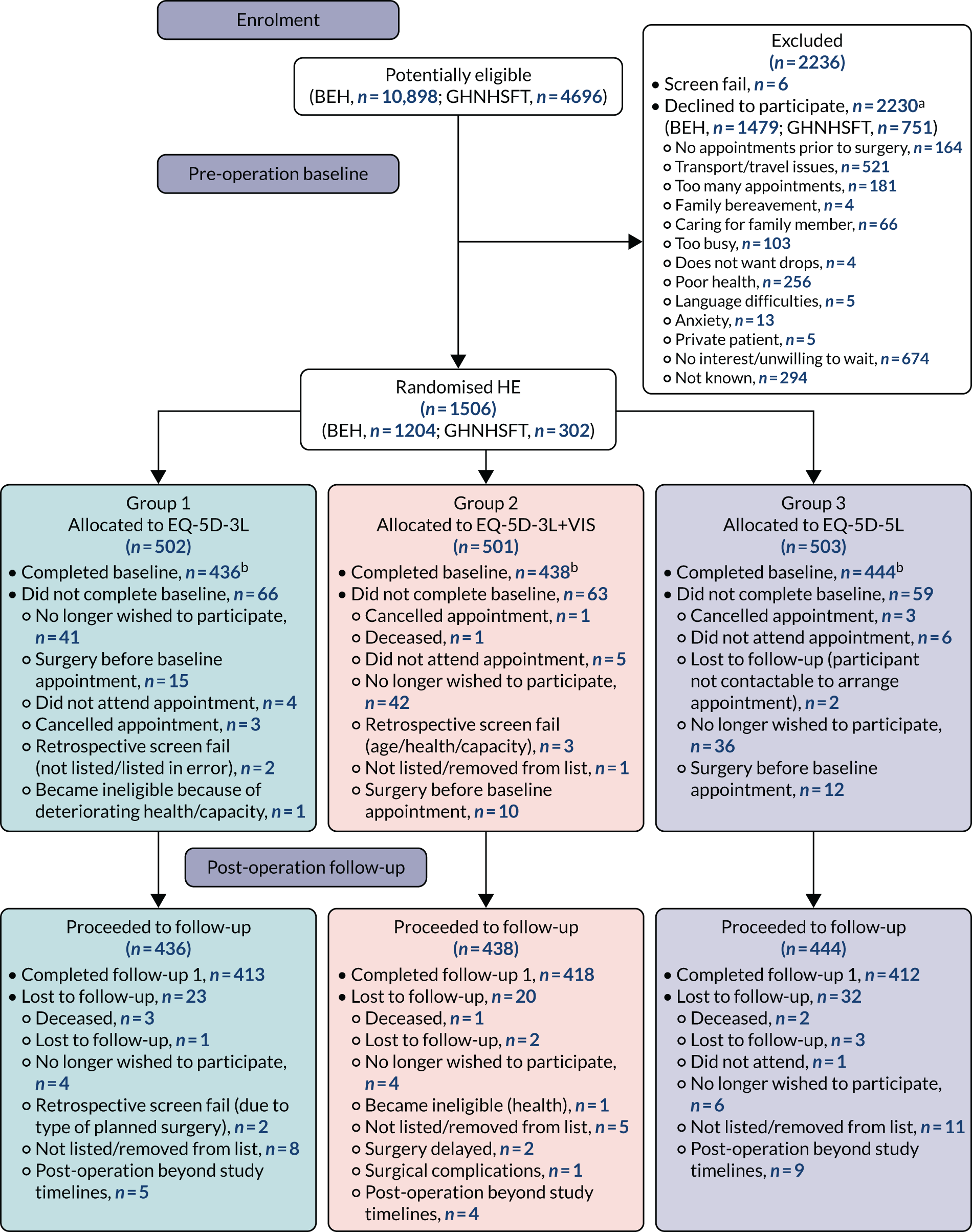
Data analysis
Among the 1181 participants with valid data, scattered missing data items remained. To preserve the sample from further attrition, these missing data items were imputed using multivariate imputation by chained equations (MICE) in which 20 data sets were created with missing data replaced by imputed values, each entailing 10 cycles of regression switching. This method relies on the missing at random (MAR) assumption. In parallel with the multiple imputation analyses, complete-case analyses were also undertaken (with missing values ignored). The complete-case analyses were based on 1089 complete cases.
Initial descriptive analyses of candidate predictor and outcome variables were undertaken, followed by linear regression modelling of two Cat-PROM5 Rasch-calibrated outcome variables. The final outcome was modelled in two forms: first, as the post-operative score and, second, as the improvement from baseline (the difference between the pre- and post-operative scores = delta approach). Potential predictors were categorised into blocks according to timeline order, from earlier to later, and from the most general diseases to the most specific. All models included age, gender and the baseline Cat-PROM5 status as predictors, regardless of their observed ‘statistical importance’. Skewed distributions were transformed if necessary, variables were entered into the model in ordered blocks and an F-test was performed for each block as a whole. If the p-value for the block was > 0.05 then the whole block was rejected. If the p-value of the test for the block was < 0.05, the specific predictors were examined and those with small effects were iteratively removed. After each stage, all of the predictors were reviewed by an experienced ophthalmologist for whether the list and the model made clinical sense, and predictors without plausible clinical meaning were removed. Following model construction, the model diagnostics were checked and acted on if necessary. (See Report Supplementary Material 4 for further details.)
Results
The results from both approaches (ignoring missing values and applying multiple imputation) produced very similar results. The models based on analysis of the multiply imputed sets of data for the Cat-PROM5 post-operative final outcome achieved an R2 of 29.1%; for improvement in Cat-PROM5 from pre to post operation, the models achieved an R2 of 31.2%. The final models with and without imputation, together with model diagnostics, are available in Report Supplementary Material 4.
Key findings
Full recruitment to the cohort study was achieved. The losses to follow-up were below the level of 20% for which we had planned. Some further losses arose because of missing key variables, but the resulting sample of just under 1200 was sufficiently powerful for the intended analyses with and without multiple imputation.
Models with and without imputation produced similar results.
The benefit indicators required for the model comprise data items that are readily accessible in the context of patient care. The only indicator that is not routinely collected in pre-operative clinics is reading vision, but this is easily tested and its requirement should not present a significant barrier to implementation.
Limitations
The main limitation of this element of the work was the moderate fit of the prediction models, each with an R2 ≈ 0.30.
Although the two chosen analytical approaches produced very similar models, it is possible that data were not missing at random, which may have introduced bias in the results based on multiple imputation.
The performance of these models was further assessed using fresh data in WP4.
Relationship with other work packages
The self-reported benefits prediction models were set alongside the models predicting adverse outcome risk from WP2, with all of these models taken forward into the CDA developed in WP3, qualitative element 2. The CDA was, in turn, taken forward to the WP4 feasibility RCT.
Qualitative element 1: Predict-CAT-Qual – presentation, content and perceptions of usefulness of information for cataract patients
Aims
-
To identify the most acceptable way of presenting risk and benefit probability information to patients as part of a CDA.
-
To identify cataract surgery-specific FAQs from patients and HCPs to inform the development of a CDA.
-
To explore the acceptability of Cat-PROM5 to health-care providers.
-
To explore the perceived issues of shared and informed decision-making during cataract surgery patient counselling with patients and HCPs to inform the development and implementation of a CDA in routine practice.
Approach
The qualitative research elements ran alongside the quantitative research. The purpose of this work was to gather views and insights that could be used to inform the development of the decision support tools being developed in the programme. Recruitment was from patients attending the cataract services, with stratification where feasible, for example for gender. Interviews were guided by an interview schedule or topic guide, and were audio-recorded, transcribed verbatim and analysed using NVivo software. 20,22,23 Focus groups similarly followed a standard approach to methodology, data collection and analysis. 30,31
This work included conducting:
-
Focus groups and interviews with patients to inform
-
The presentation format of risk information for the development of a risk and benefit probability calculator.
-
The presentation, issues of concern, supporting information and FAQs for the development of a CDA.
-
-
Interviews with HCPs to
-
Explore the acceptability of Cat-PROM5.
-
Inform content development and explore the usefulness of decision aids in clinical practice.
-
Consider the attitudes towards and practice of shared decision-making.
-
Data collection
Patients
Two focus groups and 15 one-to-one semistructured interviews were conducted with 33 individuals attending the Bristol clinics and two attending the Gloucestershire clinics. The mean age of patient participants was 77 years, with the youngest participant aged 55 years and the oldest aged 86 years. Of the 33 patient participants, 14 were women, all but one was white British, and English was the first language of all patient participants. The majority of patient participants were from more affluent geographical areas, and most were suffering from other eye comorbidities. In addition to the formal qualitative approach, the interpretation of the findings was supported by the programme PPI PAG.
Health-care professional interviews
Eight interviews with clinicians based in Bristol and three with clinicians based in Gloucestershire were conducted between March 2017 and February 2018 (total interviews, n = 11). Eight of the HCP participants were female. Four HCP participants were ophthalmologists, three were nurses and four were optometrists.
Results
Risk–benefit information
Patients participating in the study were shown four numerical ways of presenting risk and benefit information, each accompanied by a pictogram visually representing that probability: a percentage (%), n out of 100 individuals, the number of people treated for one person to experience a benefit/complication, and the probability as a decimal. Patient participants preferred ‘n out of 100 individuals’ as it was the most easily understood format for presenting both risks and benefits, which corresponded with the preferred option of the PAG.
Information for frequently asked questions for a cataract decision aid: patients
Frequently asked questions were identified through patient participants’ narratives discussing the information they found useful at the time, questions they would have asked now but did not ask then, and emerging gaps in knowledge of surgery-specific issues. The items that were of specific concern to patients included:
-
What the surgery will entail (dispelling myths and alleviating anxiety).
-
The potential risks in relation to the potential benefits from the surgery.
-
Post-surgery complications and self-care.
-
Information about the intraocular lens options and refractive implications post surgery.
-
How long is it safe to wait to have the surgery before risks overtake benefits?
-
The impact of comorbidities on the risks and benefits.
-
Other people’s experiences.
Information for frequently asked questions for a cataract decision aid: health-care professionals
Information that HCPs highlighted as being of perceived importance included:
-
Risks and benefits.
-
Providing information about refractive outcomes.
-
About the surgery and surgery aftercare.
-
Whether or not surgery is needed.
-
Waiting times.
Cataract decision aid: health-care professionals views on Cat-PROM5
Overall participants thought that Cat-PROM5 captured how vision-related quality of life might be affected by cataracts. The majority thought that the outcome measure was short, simple and easy for patients to complete on their own. Participants thought that it captured information that was of importance to HCPs, but a few commented on the usefulness of knowing the specific areas affected by cataracts, something that was not directly captured by Cat-PROM5. Several believed Cat-PROM5 captured information that was already used to inform decision-making. Participants thought that having a structured way of capturing vision-related quality of life (VRQoL) information would make the discussions taking place during consultations more consistent, introduce the patient perspective in decision-making, standardise and formalise the way that VRQoL information is collected and recorded, and facilitate post-surgery assessment of surgery outcome.
Shared decision-making: health-care professionals
Shared decision-making appears to be inconsistently practised by HCPs. The majority of HCP participants thought there was variability in practice and inconsistencies in the kind of information discussed with patients, the way that this information is discussed and explained, and how decisions are made by individual clinicians. Some HCPs thought that this variability resulted in inequities regarding who was offered surgery. All HCP participants agreed that the introduction of standardised and structured ways to support the information exchange process would enhance practice; for example, the introduction of Cat-PROM5 would ensure that the VRQoL of each patient is taken into consideration and also formally reported in patients’ health records, and the use of FAQs and decision support tools would enhance the information exchange process and support informed and shared decision-making.
Health-care professionals were open to the use of decision support tools in clinical practice, but several challenges to implementation were discussed, mainly the time needed to implement these in routine practice and how well the decision support tool and its aims fit with current care pathways.
Key findings
Patients preferred ‘n out of 100’, as it was the most easily understood format for risk presentation.
Issues of perceived interest, concern or importance for cataract surgery were elicited from patients and HCPs. This knowledge informed the development of the FAQs section of the CDA (WP3, qualitative element 2).
Cat-PROM5, as part of a CDA, was seen as worthwhile by HCPs in terms of standardising the assessment of self-reported difficulty suffered by patients with cataracts.
A CDA and shared decision-making in cataract surgery were mostly seen as relevant and necessary by HCPs, with risk information considered to be an important aspect of a shared discussion.
Limitations
Moderate sample sizes from a small number of centres may limit the generalisability of these findings, although recruitment continued until saturation was achieved, which will ameliorate this potential risk.
Relationship with other work packages
The format for the presentation of the personalised risk/benefit information and the information content for the FAQs were taken forward to the CDA in WP3, qualitative element 2, the Predict-CAT instrument development stage.
Cat-PROM5’s acceptability to HCPs and views on shared decision-making informed the approach to engagement with this service-critical group with regard to the set-up of the WP4 feasibility RCT.
Qualitative element 2: development of a cataract decision aid and a cataract decision quality measure
Aims
-
To develop a CDA in a FAQ format in which the likelihood of the Cat-PROM5 self-reported benefit is set alongside risks of harm (surgical complications/VA loss) to provide an integrated decision support tool with personalised prediction of outcomes.
-
To develop a cataract decision quality measure (CDQM) for the cataract surgery decision.
-
To conduct qualitative user testing of the personalised CDA with patients and clinicians to assess usability, acceptability, utility and expected impact.
-
To refine the personalised CDA and CDQM for use in WP4 (the feasibility trial).
Approach
The International Patient Decision Aid Standards (IPDAS) Collaboration Checklist32 for the development and quality assessment of patient decision aids was used to guide the development of the CDA. We used a collaborative, multistage development process involving key stakeholders, and we conducted qualitative user testing interviews with patients and clinicians. Recruitment was from the cataract services, with purposive stratification where feasible [e.g. gender and professional group (surgeon, nurse, optometrist)]. Interviews were guided by an interview schedule or topic guide, and were audio-recorded, transcribed verbatim and analysed. 20,22,23 The focus group followed the standard approach to methodology, data collection and analysis. 30,31
Development of the prototype cataract decision aid
The multistage, iterative process used to develop and refine the CDA included a number of key activities and data sources:
-
A CDA User Reference Group (URG) of HCPs and patient representatives was convened. The role of the URG was to act as an editorial team to oversee the development of the CDA (including agreeing the clinical evidence content and patients’ FAQs) and the associated CDQM.
-
A total of 16 individuals were recruited to the URG, including two patient representatives, six members of the study team and eight clinicians (working within cataract services of the four NHS trusts participating in the cataract research programme).
-
-
A focus group was conducted with the cataract research programme PPI PAG members.
-
Five members of the PAG attended the focus group session. The audio-recorded focus group was transcribed and feedback gathered.
-
-
To further inform the evidence-based content of the CDA, several sources of data/evidence were consulted:
-
Focus groups and patient interviews that were previously conducted as part of WP3, qualitative element 1.
-
The scoping review of published guidelines and literature.
-
Expert opinion.
-
Predicted harm models (WP2).
-
A prototype CDA was developed in agreement with the URG using the data gathered, as outlined above.
The prototype CDA comprised the following elements:
-
Introduction page.
-
Section A: FAQs.
-
Section B: What matters to you? What questions do you have?
-
Section C: personalised information about your likely outcomes.
This version of the CDA was used for the user testing interviews.
User testing of the prototype cataract decision aid
User testing of the CDA was conducted with patients and clinicians to assess usability, acceptability, utility and expected impact. The four NHS cataract surgical centres involved in the cataract research programme (Bristol, Gloucestershire, Torbay and Brighton) were used to identify and recruit patients and clinicians for the user testing interviews.
Patients were eligible to participate if they were post-operative patients who had undergone cataract surgery at least 6 weeks previously. User testing interviews were conducted with a total of 26 participants: 20 patient participants (10 male and 10 female) and six clinician participants (four ophthalmologists, one nurse and one optometrist). Clinician input was supplemented by the URG and the study management team.
Semistructured interview questions for the patient participants covered the following topics: views on the usefulness of the CDA; understanding of the content (including terminology, presentation of risks, etc.); views on the FAQs included, and the ranking of the candidate FAQs (to discover if any excluded FAQs should be included); and views on the different parts of the CDA (the personalised risk section, space for questions, etc.), the layout/design, readability, when/how they would like to receive the CDA and potential improvements.
Semistructured interview questions for the clinician participants covered the following topics: views on the usefulness of the CDA (for themselves and patients), the accuracy/comprehensiveness of the content, views on the different parts of the CDA (the personalised risk section, space for questions, etc.), fit within local clinical systems, potential influence on their behaviour, perceived barriers to and facilitators of use, and contextual factors that might impact future implementation.
Patient and clinician participants were sent a copy of the prototype CDA prior to the telephone interview. All patient and clinician audio-recordings were transcribed verbatim for qualitative analysis and were imported into NVivo. A framework analysis approach was used to analyse the data, based on the key topic areas covered by the interview guide (usefulness, use in clinical practice, etc.) and the different components of the CDA (FAQs, personalised information section, etc.). New emerging themes that had not been captured by the initial framework were added.
Framework analysis was conducted on 26 user testing interview transcripts. Patient and clinician data were analysed together, but any key differences in perspective were noted. The initial framework was guided by the interview schedule and consisted of five categories: (1) initial thoughts on the CDA and the purpose of the CDA, (2) perceived usefulness of the CDA, (3) CDA content, (4) CDA design/format and (5) implementation in a clinical setting. Two new categories were added to the framework during analysis: (6) information provision and preferences and (7) decision-making role and experiences. Data were summarised into a matrix for each category in the analytical framework. Verbatim quotes were extracted and entered.
Refining the prototype cataract decision aid
The results from the user testing interviews with patients and clinicians were used to refine the prototype CDA. The key sections included in the prototype CDA remained the same, but the pages in the booklet increased from seven to nine. Additional questions were added to section A (FAQs), and further clarification and details were added. Presentation changes were made to section C (personalised information about your likely outcomes), technical terms were replaced with plain English terms and an additional page for notes was added.
Cataract decision quality measure
Decision quality measures (DQMs) are condition-specific instruments that have been developed to assess patients’ understanding of available treatment options, their personal preferences, their perceived readiness to make a decision and the alignment between their preferences and preferred option. DQMs are made up of four key sections: (1) knowing your options (knowledge questions), (2) what is important to you? (preference questions), (3) thinking about the decision you face (readiness to decide, standard items that are not condition specific) and (4) choice of treatment (which assesses current treatment preference). We drew on our experience of developing DQMs for other clinical areas (breast cancer, tonsillectomy, etc.) as part of a SDM implementation programme.
We aimed to develop a CDQM, which would subsequently be used in the WP4 randomised feasibility trial. The content of the CDA was used to inform the knowledge questions used in the CDQM (section A). The candidate FAQs included in the CDA and the feedback received from patients during the user testing interviews and from the PAG focus group (about what mattered most to them) informed the preference questions (section B). The readiness-to-decide questions (section C) were standardised generic questions that have been used in other previously developed DQMs. Section D (choice of treatment) was guided by the available options.
Key findings
By involving key stakeholders in the development of the CDA, we were able to ensure that input from patients and clinicians was considered in terms of the content, format and planned use, and that the CDA best reflects the needs of the end users. Initial input from the cataract PAG highlighted the issues that matter the most to patients when making the decision about cataract surgery (including likelihood of success/benefits, pain, what happens during the surgery, side effects/risks, eyesight changes and post-surgery recovery), and these were incorporated into the CDA. Evidence syntheses ensured that the information provided in the CDA was evidence-based, for example the FAQs in section A. Incorporating the risk calculator element that was developed as part of WP2 (section C) ensured that individualised risk-information could be provided to patients, and further input from clinicians helped to ratify the accuracy of the CDA content.
The qualitative user-testing interviews found that patients and clinicians were generally positive about the CDA. Both patients and clinicians felt that the CDA would provide a trustworthy source of information, including adequate and accurate information. Clinicians felt that it would act as a framework and a reminder to cover certain information that they might otherwise not cover, and patients felt that the CDA provided them with answers to the questions that they would want answered before making a decision. Patients and clinicians felt that the CDA would reinforce the idea that a ‘choice’ exists with regard to cataract surgery, would encourage better patient involvement in cataract surgery decisions, was easy to understand and could feasibly be integrated into clinical care pathways. Some concerns were expressed by clinicians regarding the time needed to complete the personalised risk element of the CDA in the consultation and they had some reservations over how much information patients would want about their individualised risks. However, there was a disparity between what clinicians’ felt that their patients might want in terms of risk information and what patients said they wanted after reflecting on previous experiences in which they had not received this information. Overall, it was felt that the CDA would be feasible to use in routine clinical settings.
Limitations
Despite significant efforts to recruit clinicians from all four collaborating sites, it was not possible to recruit from one site. However, the clinical input was strong from the URG and the research programme team.
Relationship with other work packages
The Predict-CAT qualitative work (FAQs, etc.) fed directly into the development of the CDA. Both the CDA and the CDQM were taken forward as key instruments in the WP4 feasibility RCT.
Health economics: performance of health utilities and calibration of Cat-PROM5
Standard health economic indices of utility are known to be insensitive to mild to moderate vision loss. 33 In this health economic section, their performance in people with cataracts was evaluated and calibrated against Cat-PROM5 in accordance with International Society for Pharmacoeconomics and Outcomes Research (ISPOR) guidance. 34
Aims
-
To evaluate the performance of existing and emerging health economic indices (the preference-based measures EQ-5D-3L, EQ-5D-3L+VIS, EQ-5D-5L and ICECAP-O) in people undergoing cataract surgery.
-
To investigate how cataract-related visual disability measured using Cat-PROM5 can be calibrated or mapped against existing and emerging health economic indices of utility.
Data collection
Data for these health economic elements of the programme were collected as part of the WP3 Predict-CAT cohort study at two sites in England. The questionnaires were completed both pre and post operation for all participants, with questionnaire data available for 1315 participants. The Cat-PROM5 and ICECAP-O data were collected from all participants, with collection of the other health economic utilities (the EQ-5D-3L, EQ-5D-3L+VIS and EQ-5D-5L) undertaken on a 1 : 1 : 1 random allocation basis.
Data analysis
Performance
Descriptive statistics for each of the instruments were considered in terms of floor and ceiling effects, convergent validity, known groups and responsiveness to surgery. Currently, there are two algorithms for generating EQ-5D-5L preference-based utilities for a UK sample: the Euro-Qol-5 Dimensions, five-level version, value set for England (EQ-5D-5L-VSE) and the EuroQol-5 Dimensions Crosswalk (EQ-5D-5L-CW). 35–37 Both algorithms were used here.
Calibration
Linear models and adjusted limited dependent variable mixture models were estimated. Full data were available for 1181 patients undergoing cataract surgery. Cat-PROM5 was mapped to two quality-of-life measures (the EQ-5D-3L and EQ-5D-5L) and one capability measure (the ICECAP-O). We did not map to the EQ-5D-3L+VIS questionnaire because of the infrequent use of the questionnaire and its unclear relevance to the calculation of quality-adjusted life-years. Separate models were estimated for pre- and post-operative outcomes. Model performance was assessed using likelihood statistics, graphical inspections of model fit and error measurements, including mean square error.
Results
Key findings
Performance
The EQ-5D-3L and EQ-5D-5L did not perform well across almost every measure of validity and responsiveness and they had the largest ceiling effects (Table 1); the EQ-5D-3L+VIS had a lower ceiling effect and better convergent validity with Cat-PROM5. The EQ-5D-3L+VIS was able to differentiate between patient groups who did and did not report benefit from surgery and improved quality of life after surgery; however, it also identified small positive ESs in patients who reported no benefit or improved quality of life after surgery. The ICECAP-O also had a low ceiling effect and there was some evidence of convergent validity with Cat-PROM5; it performed best on many measures of responsiveness. 38
| Criterion | Preference-based measure | ||||
|---|---|---|---|---|---|
| EQ-5D-3L+VIS | EQ-5D-3L | EQ-5D-5L-VSE | EQ-5D-5L-CW | ICECAP-O | |
| Ceiling effect | ✓ | ✗ | ✗ | ✗ | ✓ |
| Floor effect | ✓ | ✓ | ✓ | ✓ | ✓ |
| Convergent validity | |||||
| Cat-PROM5 correlation | ✓ | ✗ | ✓ | ✗ | ?a |
| VA correlation | ✗ | ✗ | ✗ | ✗ | ✗ |
| Known groups validity | |||||
| First-eye or second-eye surgery | ✗ | ✗ | ✗ | ✗ | ✗ |
| Habitual near VA in the operated eye (logMAR) | ✓ | ✗ | ✗ | ✗ | ?b |
| Ocular comorbidities | ✗ | ✗ | ✗ | ✗ | ✗ |
| Responsiveness | |||||
| Change scores and ESs | |||||
| Visual quality of life | ✗ | ✗ | ✗ | ✗ | ✓ |
| Patient-perceived benefit of surgery | ✗ | ✗ | ✗ | ✗ | ?c |
| Change in near VA in operated-on eye | ✗ | ✗ | ✗ | ✗ | ✗ |
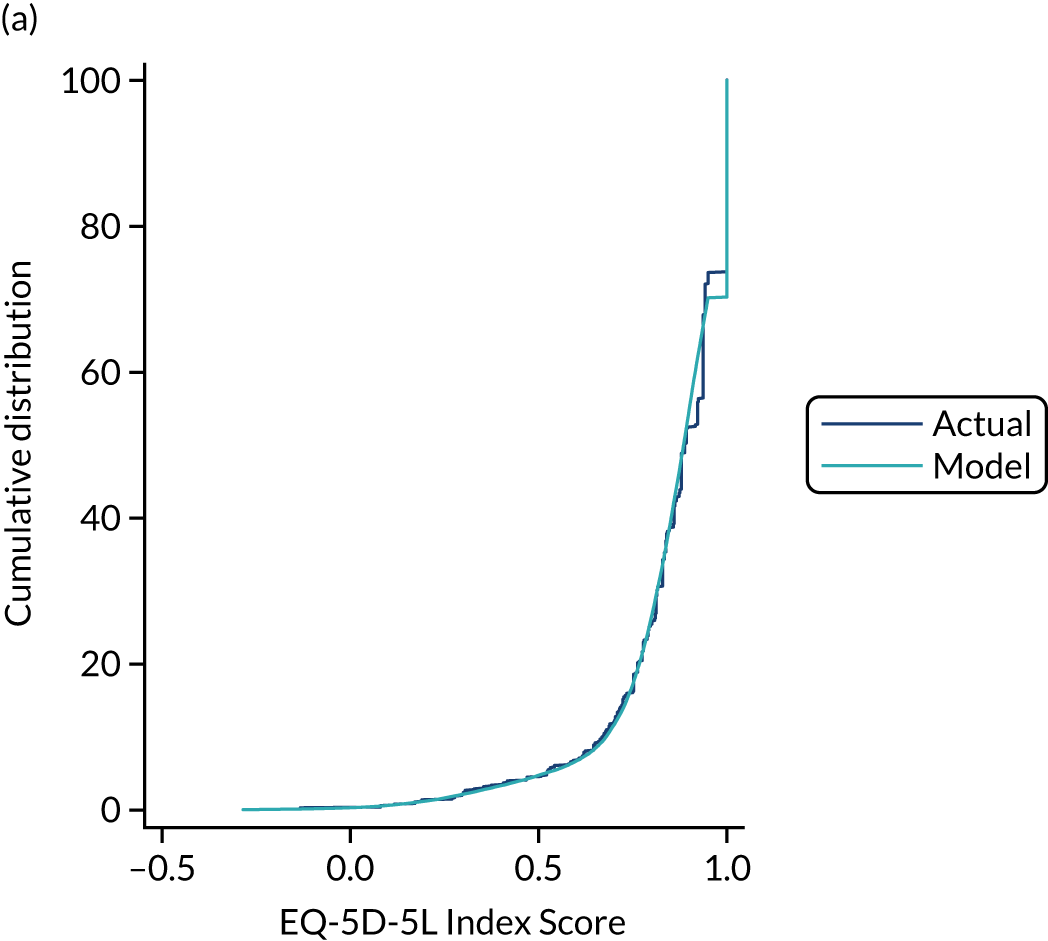
Calibration/mapping
The adjusted limited dependent variable mixture models dominated linear models on all performance criteria. The mixture models offered good to excellent fit. Three-component models that allowed component membership to be a function of covariates (sex, age and diabetic status) that conditioned on some or all of these covariates (depending on the target measure and pre- and post-operative status) performed better than models with fewer components that did not condition on covariates (Figure 3). The models for EQ-5D-3L did not converge post surgery under any mixture model, possibly because of the large number of participants reporting perfect (EQ-5D-3L index score = 1) quality of life. 39
FIGURE 3.
Calibration/mapping: comparison of actual and predicted follow-up distributions. (a) EQ-5D-5L; and (b) ICECAP-O.
Limitations
A limitation of the study was that the three versions of the EuroQol-5 Dimensions (EQ-5D) questionnaire were completed by different patient cohorts. If participants were to have completed every questionnaire, the response burden would have been excessive.
Relationship with other work packages
In addition to the links and dependencies within the Predict-CAT WP3 cohort study noted here, these health economic elements of the programme link Cat-PROM5, developed in WP1, to established and emerging health economic utilities that are preference-based measures. This work is indirectly linked to the WP4 feasibility RCT as it would inform the choice of a preference-based measure to be included in any future fully powered RCT. Furthermore, the calibration or mapping exercise would allow health economic analyses to be undertaken based on the Cat-PROM5 data without the need to increase questionnaire completion burden through adding a health economics preference-based measure to the trial protocol.
Further information
-
Report Supplementary Material 4 provides further information on the Predict-CAT cohort study and the development of the self-reported outcomes and benefits models.
-
Report Supplementary Material 5 provides further information on the qualitative elements of WP3 relating to the format and content of information for patients based on input from patients and HCPs.
-
Report Supplementary Material 6 provides further information on the development of the CDA.
-
Report Supplementary Material 7 provides further information on the performance of existing and emerging health economic indices when used for cataract surgery. 38
-
Report Supplementary Material 8 provides further information on calibration or mapping of Cat-PROM5 to emerging health economic indices. 39
Work package 4: feasibility study of the cataract decision aid trial and qualitative study of mismatching outcomes
Quantitative elements: feasibility of a cataract decision aid randomised controlled trial and validation of benefits prediction models
Aims
-
To undertake a feasibility study for a possible future fully powered RCT of the use of a CDA, incorporating personalised risk and benefit information, to improve shared decision-making in cataract surgery.
-
To estimate the sample size for a possible future fully powered RCT.
-
To assess the accuracy of the self-reported outcomes and benefits prediction model developed in the programme.
Approach
This feasibility study, named ‘Involve-CAT’, took the form of a two-arm RCT with the CDA as an intervention. The intervention group was defined as the group of patients in whom the CDA was used, while patients in the standard-care control group underwent standard NHS care. The allocation of patients to groups was conducted through a 1 : 1 block randomisation process by centre. It was assumed that, within each centre, five or six participants should be allocated within each arm (receiving the CDA intervention vs. not receiving the intervention). The research process was multistage, starting with pre-screening and proceeding through assessment of patient eligibility for the study, recruitment, obtaining consent, randomisation, baseline clinical and self-reported pre-operative vision assessment with Cat-PROM5, randomisation to either the CDA intervention or defaulting to standard care, making a shared decision about surgery, and finally documenting the outcome of the operation, including a post-operative self-reported vision difficulty assessment with Cat-PROM5.
The CDQM developed as a part of WP3 was used to assess patients’ decision quality. The CDQM is a measure intended to capture patients’ knowledge about options, preferences and readiness to make a decision about the treatment. It was treated as a primary outcome in this study. The CDQM questionnaire was completed twice, first before the consultation at the baseline visit and then immediately following the consultation. A secondary quantitative outcome was Cat-PROM5, a self-reported measure of vision quality developed and validated in WP1 of the grant programme. The Cat-PROM5 questionnaire was completed by patients twice, initially at the baseline pre-operative time point and then at the post-operative follow-up visit.
Pre-operative parameters were used to predict the expected post-operative Cat-PROM5 responses based on the two ‘benefits prediction’ models developed in WP3. The predicted responses were then compared against the actual self-reported outcomes following surgery to assess the validity of the predictions.
Sample size calculations were undertaken to assess the size of a possible future fully powered RCT.
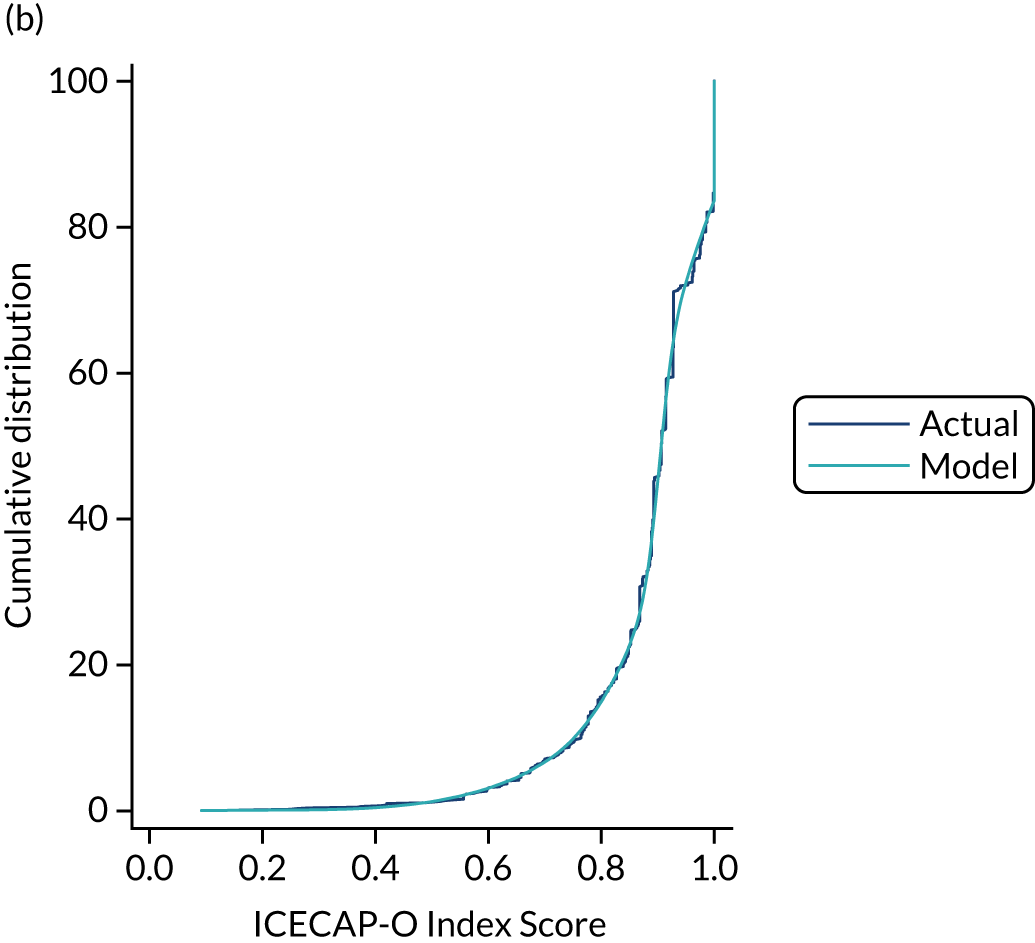
Data collection
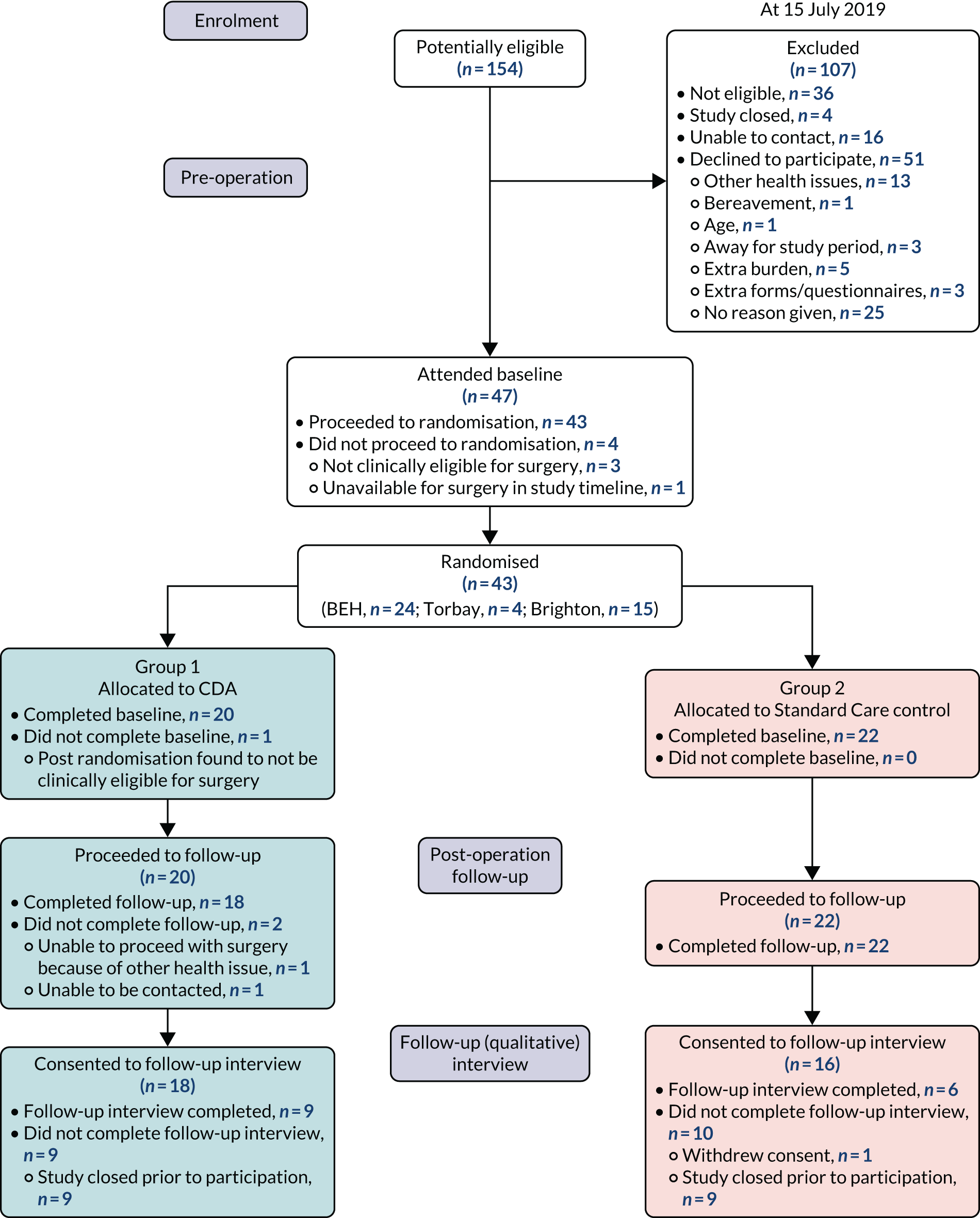
The study assumed recruitment of 40 participants from four cataract research centres (Bristol, Torbay, Brighton and Gloucestershire), that is 10 patients per centre. During the study, however, it became clear that Gloucestershire would be unable to join the study owing to local capacity issues and Torbay would be able to join the study only later, owing to staff illness. This required over-recruitment by Bristol and Brighton; nonetheless, full recruitment of 42 completing patients was achieved (Figure 4).
FIGURE 4.
The Involve-CAT Consolidated Standards of Reporting Trials flow diagram. BEH, Bristol Eye Hospital.
Data analysis
The effects of the intervention were analysed in two ways. For the summary scores expressed by a single value [i.e. knowledge about cataract (section A), readiness for decision-making (section C) and Cat-PROM5], t-tests were undertaken for both dependent (paired) samples and independent samples. Tests for dependent samples were performed to assess the importance of the intraindividual changes in CDQM scores from before to after the consultation and in the Cat-PROM5 measures from before to after surgery. The t-tests for independent samples were used to assess the differences post consultation and post surgery, respectively, for those two measures between study arms. For the linked sections of the CDQM questionnaire that compared reported preferences with the decisions actually made (sections B and D), Spearman’s rho was calculated as a basic statistic capturing levels of concordance between what was reported as important for patients and what was actually chosen.
A power study was undertaken to inform a sample size estimate, providing calculations of the sample sizes needed for a possible future fully powered RCT to investigate the impact of the CDA on the quality of patient decisions. The magnitudes of the ESs were chosen according to Cohen’s classification of standardised ESs40 [standard deviation (SD) of unity].
Bland and Altman plots were used to compare predicted outcomes with observed outcomes for the two benefits prediction models (prediction of the final post-operative outcome and prediction of the improvement in score from pre to post operation).
Results
The level of data collection completeness was good for the feasibility study primary and secondary variables, both before and after intervention/surgery (range 100–88% complete). The intervention group and standard-care control group were similar across key variables at baseline, indicating successful randomisation. Although it is expected that, in a feasibility study, statistical power would be insufficient to arrive at any conclusions, standard analyses were undertaken on the collected data to confirm feasibility for such analyses and to gain insights into the likely future performance of the outcome measures.
Primary outcome: cataract decision quality measure
The tests (for independent samples) conducted after the consultation/operation showed no important differences between the CDA intervention group and the standard-care control group prior to the consultation (at baseline) or after the consultation (at follow-up) for knowledge (section A) or readiness to decide (section C). In this small sample, using the CDA did not improve the knowledge or readiness to decide about cataracts and their treatment.
Comparisons between baseline and post consultation showed no change for knowledge in either group. However, unexpectedly, readiness to make a decision declined after the consultation in the intervention group, with little change observed for the standard-care control group.
Additional basic psychometric analyses were undertaken for questions in sections A and C using classical test theory (CTT) to detect possibly malfunctioning questions. The properties of the set of questions conceived as a scale of knowledge (section A) revealed that it would benefit from review and further refinement (low Cronbach’s alphas and low item-to-total correlations, including some negative correlations). On the other hand, the basic CTT analyses performed on items deemed as a scale of readiness to make a decision about cataract surgery (section C) showed that it has promising features and the scale could form the subject of further analyses conducted from a modern test theory perspective.
Secondary outcome: Cat-PROM5
No significant differences were observed between the intervention group and the standard-care control group at either pre-operative baseline or post-operative time points for the Cat-PROM5 scores. As expected, significant improvements in the Cat-PROM5 scores were observed between baseline and post-operative completions for both groups (paired t-tests). Despite there being no significant differences in the Cat-PROM5 scores post operation, the score improvement in the CDA intervention group (3.40) was almost half a logit larger than that in the standard-care control group (2.96).
Sample size estimate
In the absence of a clear primary outcome ES emerging from the feasibility study, a standard power calculation approach was adopted for sample size estimation for a possible future RCT. 41 For the t-tests for independent groups, a small ES (0.2 SD) would be detectable with 80% power using a sample size of 800 (1 : 1 allocation, 400 in each group). A medium ES (0.5 SD) would be detectable with > 90% power using a sample size of 200 (1 : 1 allocation, 100 in each group). The secondary outcome, Cat-PROM5, did, however, demonstrate non-significant higher levels of self-reported outcome in the intervention group. Based on this observed secondary-outcome ES and a 1 : 1 group allocation, a total sample size of 250 would be required for the detection of this effect with 80% power, and a sample size of 325 would be needed for 90% power.
Performance of the Cat-PROM5 benefits prediction models
The correlation coefficient between predicted outcome and actual outcome was 0.57 for the final post-operative outcome and 0.21 for the change in score between pre- and post-operative Cat-PROM5 completions.
Key findings
-
It was feasible to achieve timely and full recruitment despite one of the study sites being unable to participate owing to lack of capacity to undertake the research, and the start of recruitment at another site being delayed owing to staff health.
-
Data collection completeness for key variables was good and statistical analysis of the collected data was feasible.
-
Analysis of the CDQM primary outcome revealed psychometric imperfections in the performance of the knowledge section, which would benefit from review and refinement in advance of a fully powered trial.
-
For independent groups, a small ES (0.2 SD) would be detectable with 80% power using a sample size of 800 (1 : 1 allocation, 400 in each group) and a medium ES (0.5 SD) would be detectable with 90% power using a sample size of 200 (1 : 1 allocation, 100 in each group).
-
The performance of the prediction model for the final Cat-PROM5 post-operative outcome was superior to the model for prediction of change in the Cat-PROM5 score from pre- to post-operative time points.
Limitations
One limitation of WP4 was related to the CDQM, the knowledge section of which would benefit from further development work prior to consideration of its use as an outcome in a fully powered RCT.
A further limitation was the fact that the prediction model (developed in the WP3 Predict-CAT cohort study) for a change in the Cat-PROM5 score did not demonstrate high predictive power in the WP4 model validation exercise. This is explained by the fact that a subtraction of two measures (post-operative Cat-PROM5 score – pre-operative Cat-PROM5 score) has greater variance and is, therefore, subject to higher uncertainty. However, the final Cat-PROM5 prediction model was confirmed to have reasonable predictive power.
Relationship with other work packages
WP4 depended on the following outputs from each of the earlier work packages:
-
Cat-PROM5 from WP1.
-
Risk models for PCR and VA loss from WP2.
-
Benefits prediction models, qualitative elements guiding instrument development, the CDA and the CDQM from WP3.
Qualitative element 1: perceptions of the cataract decision aid for shared decision-making
Aims
-
To explore how a CDA incorporating personalised risk and benefit information influences pre-operative SDM for cataract patients and HCPs.
-
To explore how patients and HCPs perceive the CDA in the context of routine care.
Approach
All audio recordings of consultations (CDA group and standard-care control group) in which the surgeon and patient discussed the treatment options for cataract surgery were transcribed verbatim, anonymised and analysed in NVivo. 21,23 This included scoring consultations using the Observer OPTION 5 instrument,42 comparing appointments with the CDA (the intervention group) and without the CDA (the standard-care control group) of the feasibility RCT. 43,44 Sampling was both opportunistic (available HCPs) and purposive (a balance of HCP groups and genders for patients).
Recruitment
Patient consultations
All pre-operative consultations with the surgeon were audio-recorded and included in the qualitative assessment.
Post-consultation follow-up interviews
From among the participants in the main WP4 study, we aimed to recruit 10–12 patients (five or six of whom received the CDA, and five or six of whom did not receive the CDA) as well as one to three surgeons per participating site (who had used the CDA) to take part in audio-recorded follow-up interviews. The Cardiff University team were notified of participants (patients and surgeons) who had agreed to be contacted for a follow-up interview on the main WP4 study consent form.
Data collection and analysis
All audio-recordings of consultations (CDA and control groups) in which the surgeon and patient discussed the treatment options for cataract surgery were transcribed verbatim. Recordings of all 42 RCT appointments were scored in relation to SDM. Audio-recordings of the follow-up interviews were also transcribed verbatim and transcripts were entered into NVivo for analysis. A framework analysis approach45 was used to analyse the data, based on the key topic areas covered by the interview guide (usefulness, use in clinical practice, experiences of the pre-operative decision-making process, etc.) and also the model of SDM in clinical practice. 46 This model outlines three key stages of the SDM process, characterised by different types of ‘talk’: choice, option and decision.
Post-consultation follow-up interviews with patients and surgeons qualitatively analysed their perceptions of the appointments and the CDA. Separate interview schedules (topic guides) were used for surgeon and patient follow-up interviews (see Report Supplementary Material 11).
A total of 15 patient follow-up interviews were undertaken: 10 in the CDA group and five in the standard-care control group (Brighton, n = 5; Bristol, n = 7; Torbay, n = 3).
Six clinician participants who participated in the CDA arm of the study participated in the post-consultation follow-up interviews across three participating sites (Brighton, n = 1; Bristol, n = 4; Torbay, n = 1). The clinician participants were surgeons (ophthalmologists), four of whom were male and two of whom were female.
Key findings
Several key issues arose that would be likely to have an impact on the effectiveness of the CDA, and the extent to which it could be easily integrated into routine care or as part of a possible future full-scale RCT:
-
Overall, the Observer OPTION 5 scores revealed that there was a significant difference in mean total scores between the CDA arm and standard-care control arm, with all five items scoring higher, on average, in the CDA consultations than in the standard-care control consultations. These results indicate that when clinicians use the CDA with patients, a greater number of SDM behaviours are present and they are carried out to a greater extent.
-
Analyses revealed that the key SDM tasks of introducing the choice and eliciting patient’s preferences were not always carried out, regardless of whether or not the CDA was used.
-
Consultants did not consistently perceive the choices of ‘surgery, delay or decline’ as useful or legitimate and, therefore, some did not agree with the presentation of choices in the CDA.
-
Many of the patients had strong prior preferences and had already decided that they wanted the surgery. Thus, it would be difficult to reintroduce the choice talk at the consultation stage. This indicated that the SDM discussion around having or declining cataract surgery might be better placed or at least initiated earlier in the clinical care pathway, before patients had formed strong prior preferences of what they wanted.
-
The CDA was very effective at providing information to patients about their options, including their personalised risk, but it did little in the way of supporting the introduction of choice or the elicitation of patients’ preferences, partly because of the patients’ prior preferences.
-
A number of approaches could help to rebalance the process towards SDM. For example, more work could be undertaken in the consultation to reintroduce the concept of choice, emphasising that surgery is not a foregone conclusion and providing a clear rationale for patient involvement in the decision-making process; or the introduction of choice could be initiated earlier in the care pathway, for example with a community optometrist, an ‘optician’.
-
Overall, surgeons felt that the CDA could be integrated into routine clinical settings and delivered as part of a larger RCT. However, changes would need to be made to the way in which the CDA is delivered, with options including:
-
The CDA could be used as part of a two-stage process. It could be introduced to patients before the consultation, ideally being sent to patients with their appointment letters. In the consultation, the ‘what matters to me’ and ‘personalised risks and benefits’ sections could be elaborated and discussed.
-
The CDA could be introduced at an earlier point in the care pathway, such as prior to referral to the hospital.
-
More consistent and adequate clinician training in SDM could be provided to the wider team of HCPs who would deliver the CDA.
-
The risk calculators could be better integrated into the local clinical systems, with as much of the information pre-populated prior to the consultation as possible.
-
Limitations
Cataract patient pathways vary considerably between centres. This study involved three centres and different implementation considerations may apply in other centres. The sample sizes were not large, but saturation indicated that these were reasonable.
Relationship with other work packages
The earlier WPs all fed into this element of the work, which looks forward to a possible future RCT of the CDA that acknowledges the lessons learnt here.
Qualitative element 2: mismatching outcomes
Aim
To explore background and specific instances of discordance of outcomes where the perception of the health professional was at odds with that of the patient following cataract surgery.
Approach
We sought out patients with discordant or mismatching outcomes among the WP3 Predict-CAT study cohort participants, and consultants at the four collaborating centres were also separately asked to identify and recruit patients in their centre who had discordant outcomes. HCPs from the collaborating centres with experience of this relatively uncommon phenomenon were invited to join the study.
Discordance could be either positive or negative, defined as:
-
Negative mismatching outcomes
-
The patient is unhappy with good surgery and VA outcomes, that is patients who are dissatisfied with the outcome of their surgery or perceive a negative outcome, despite there being no clear clinical explanation for experiencing a poor outcome. Examples might include dysphotopsia, reflections, glare or residual minor refractive error.
-
-
Positive mismatching outcomes
-
The patient is happy with poor surgery or VA outcomes, that is patients who report satisfaction/positive outcomes when the VA or technical elements of the surgery appear to indicate that a normally symptomatic clinical problem exists, of which the patient seems to be unaware. Examples might include reduced VA, intraocular lens subluxed or mild to moderate macular dysfunction.
-
Data collection
Data collection for this substudy was organised in two separate strands.
The first strand included semistructured one-to-one interviews with patients identified as falling within the mismatching outcomes definition, which were carried out face to face or over the telephone. The second strand of the study involved semistructured one-to-one interviews with HCPs who were involved in cataract care delivery and had experience with the phenomenon of discordant outcomes. 20
We interviewed seven patients. Three patient participants were identified through the Predict-CAT study; four patient participants were identified by HCPs in clinics and using the mismatching outcomes definitions disseminated to each centre. Nine HCPs were interviewed, one HCP participant was an optometrist and eight were consultant ophthalmologists.
Data analysis
All interviews were, with participants’ consent, audio-recorded, fully transcribed and anonymised. Anonymised transcripts were analysed in NVivo 10, guided by principles of thematic analysis. 47
Key findings
-
Discordance in most patients’ experience was the result of unexpected changes in visual ability after surgery, for example changed spectacle prescriptions and problems with peripheral vision, but two participants experienced unexpected symptoms, such as floaters and dry eyes, which they felt compromised their quality of life.
-
Patient narratives highlighted the nuanced and multidimensional ‘lived experience’ of vision, whereby patients might be happy with one aspect of vision, for example distance vision, but dissatisfied with another, perhaps more valued, aspect that determined their overall judgement on the outcome of the surgery.
-
The factors raised by HCPs to explain the phenomenon were linked to medical practice, doctor–patient communication and patient-specific attributes. The factors linked to medical practice were primarily the technologies used, for example the choice of lens implant and unintended optical side effects resulting from individual lenses, and the use of measurement and testing devices that are able to capture the visual experiences of the patients.
-
HCPs and patients thought that the quality of the doctor–patient relationship shaped patients’ perceptions of the outcome. Both believed that there was a need for SDM when making decisions on lens choice and refractive aims of the surgery.
-
Participants discussed the need for a more personalised approach to patient counselling to address discordances that were thought to exist between patients’ and HCPs’ understanding of what ‘good vision’ means; address patient preferences and expectations and realign these with a more realistic understanding of the potential outcome; and provide accurate and individualised information on what the patient should expect of their visual abilities after surgery, including use of spectacles for near and distance vision and any potential compromises in aspects of vision other than VA.
-
For patients, trust in the HCPs was also important, and this trust was found to be compromised through breakdowns in the process of care delivery, for example continuity of care, ease of access to post-operative follow-up, and trust in the providers’ abilities to carry out ophthalmological examinations and procedures.
-
HCPs thought that it was important to understand the ‘discordant outcomes’ case profile to identify determinants of discordance and to target patients who might be more prone to dissatisfaction with their outcome so that they could receive more intensive patient counselling.
-
HCPs thought that the presence of comorbidities and a more complex clinical profile, the patients’ visual abilities before the surgery, and the patients’ personality and social characteristics explained discordant outcomes.
-
The participant recruited to the study who had the only positive mismatching outcome also appeared to suffer the most significant visual disability before the surgery.
-
For patients, the quality of cataract surgery counselling received prior to their surgery (trust in HCPs, the quality of their relationship with the HCPs and being engaged in informed and shared decision making) shaped their post-operative experiences.
-
However, several barriers to changing practice were identified, often linked to the challenges of changing current ways of working and the time HCPs had available to engage in such in-depth personalised conversations with patients.
Limitations
As this is a relatively uncommon phenomenon, it was difficult to identify patients who had experienced a discordant outcome following their cataract surgery. There was, however, a consistency between the perceptions of affected patients and HCPs with experience of the phenomenon.
Relationship with other work packages
The WP3 Predict-CAT cohort study was used as a source of patients with discordant outcomes; HCPs from the collaborating centres who had knowledge of the programme and its aims assisted in finding the patients and undertaking interviews. This aspect of the work was, however, relatively self-standing, although it did relate to the key programme themes of patient-focused care and improved SDM.
Health economic elements: implementation costs of a cataract decision aid
Aim
To estimate the implementation costs and potential savings of the use of a CDA.
Approach
This study compared the additional resources incurred as a result of implementing the CDA with those of standard care in the Involve-CAT pilot RCT study. The additional resource was the time taken to collect the data needed for the CDA and administer the CDA during the SDM discussion, and the subsequent impact on discussions in the remaining appointment. There is also potential for the CDA to impact the number of patients choosing to have surgery and, if it affects the risk profile of patients having surgery, the health-care use following surgery (accident and emergency visits, etc.).
Data collection and analysis
The start and end time of each stage of the pilot RCT study appointment were recorded by the clinicians undertaking the research assessment and clinical assessment appointments. Costs were obtained from the Personal Social Services Research Unit (PSSRU). 48 The cost per minute of the clinician’s time was calculated and used to estimate the total resource use for each participant’s clinic appointment. The clinical assessment and CDA were predominantly led by consultant ophthalmologists. The CDA required an additional assessment of near vision. Secondary analysis included the cost of this additional near-vision assessment. The cost differences between study arms were assessed using two-sample t-tests.
Key findings
-
The mean and median durations were longer in the CDA arm than in the standard-care control arm for all intervals reported.
-
Two optometrists recorded how long the assessment of near vision took for a subset of patients in the CDA arm. The mean duration of the assessments for the two assessors was 2.6 minutes.
-
The mean total cost associated with NHS resource use in the primary analysis was £52.20 for the CDA arm and £37.80 for the standard-care control arm (difference £14.40; p = 0.06; n = 40).
-
Inclusion of the additional test for near vision in the secondary analysis increased this difference to £16.87; p = 0.03.
-
As all patients in both arms progressed to surgery, only a small difference was observed for subsequent health-care resource use (single centre, n = 23).
-
The use of a CDA was likely to moderately increase the pre-operative clinic cost as a result of a longer SDM consultation and the need for a near-vision test for the benefits calculator tool.
-
To derive the quality-adjusted life-year data in a future fully powered RCT, the post-operative Cat-PROM5 scores could be mapped to health economic utilities for the CDA intervention and standard-care control groups using the mapping algorithms developed in this research programme.
Limitations
Despite the relatively small sample size in this feasibility RCT, it does appear that the introduction of a CDA would incur modest additional cost.
Relationship with other work packages
All previous elements of the programme, WPs 1–3, fed into this cost analysis.
Added value: ethics perspectives of immediately sequential bilateral cataract surgery
The practice of immediately sequential bilateral cataract surgery is controversial in the UK. On the one hand, there is a low but unquantifiable risk of bilateral vision loss in the event of an adverse event (infection, contamination, etc.) arising that affects more than one operation on an operating list. On the other hand, there are potential efficiency savings and convenience for patients, who require only a single trip to the operating theatre when they have cataracts affecting both eyes.
Aim
To undertake a thematic analysis of a stakeholder meeting exploring the ethics perspectives of immediately sequential bilateral cataract surgery.
Approach
A semistructured independent stakeholder meeting was held at the Royal College of Ophthalmologists London headquarters in June 2018. This event was convened separately from the research programme by one of the programme co-applicants (CL), who approached the chief investigator with a proposal to undertake transcription and qualitative analysis of the discussion that took place at the meeting.
Data collection and analysis
In total, 29 stakeholders attended the meeting; they were invited through purposive sampling. The professions of the stakeholders included but were not limited to ophthalmologists (n = 9), patients (n = 5), religious leaders (n = 4), ophthalmic nurses (n = 3), ethicists (n = 2), lawyers (n = 2) and commissioners (n = 1). Thematic qualitative analysis47 was conducted on the resultant transcript of the discussion.
Key findings
Three overarching themes were identified, which were subdivided into eight subthemes. The themes included (1) beneficence and non-maleficence (patient benefits, patient risks, the uncertainties of risk and patient interpretation of the risk–benefit analysis), (2) autonomy (patient and surgeon choice, informed consent and the barriers to effective communication) and (3) distributive justice (the allocation of resources: the individual vs. the collective).
The stakeholders concluded that the procedure was an ethical undertaking, provided patient autonomy was appropriately considered. This requires an individual interpretation of the risk–benefit balance, which must include an understanding of the low but unquantifiable risk of severe complications, including bilateral blindness. Consequent cost savings to health care that may occur following the implementation of immediately sequential bilateral cataract surgery may be considered a secondary benefit; the primary benefit should be centred on potential (although not yet well defined) patient convenience factors.
Limitations
Although key ethics issues were identified and analysed, the 29 stakeholders who attended could not have included all of the relevant views. This analysis does, however, provide a reference point for the issues and ethics factors surrounding the practice of immediately sequential bilateral cataract surgery.
The true benefits to patients are, as of yet, ill-defined, as are the potential health-care savings. Similarly, the risks of severe bilateral complications and loss of vision remain unquantified and unquantifiable in the light of their rarity.
Further information
-
Report Supplementary Material 9 provides further information on the feasibility study for a possible future fully powered RCT.
-
Report Supplementary Material 10 provides further information on validation of the Cat-PROM5 outcome and benefit prediction models.
-
Report Supplementary Material 11 provides further information on patients’ and HCPs’ views and practice of SDM, and the potential role of the CDA.
-
Report Supplementary Material 12 provides further information on mismatching or discordant outcomes following cataract surgery.
-
Report Supplementary Material 13 provides further information on implementation costs of use of a CDA.
-
Report Supplementary Material 14 provides ‘added value’ to the programme through an analysis of ethics perspectives of immediately sequential bilateral cataract surgery.
Summary of changes to the programme
Changes to work package 3
Operational limitations at the lead site caused a delayed start to recruitment to Predict-CAT as the local trust was not able to provide a clinical examination room for the study in a timely manner. Combined with an initial slower than expected recruitment rate, this prompted the study team to take the following actions after consulting the Programme Steering Committee:
-
An additional recruiting site was opened in Gloucestershire and it recruited 302 Predict-CAT cohort study participants.
-
PAG members were consulted for their opinion and advice on improvement to study advertising material and implementation of a ‘self-referral’ mechanism for recruitment.
-
We sought a 6-month no-cost extension to the programme, which was helpfully granted by the National Institute for Health and Care Research (NIHR).
Changes to work package 4
The feasibility RCT that constituted the WP4 had been planned to take place cross four collaborating sites. One site (Gloucestershire) did not have the capacity to join the study and another (Torbay) had a delayed start owing to staff illness. The recruitment target of 40 participants was, nonetheless, achieved as a result of over-recruitment at two of the sites.
Option Grid
At the time of the grant application, the intention was to develop a patient decision support tool in the format of an Option Grid© (EBSCO Health, Ipswich, MA, USA), in collaboration with co-applicant Professor Glyn Elwyn (previously of Cardiff University, Cardiff, UK). Following Professor Glyn’s departure from Cardiff University and the commercialisation of the Option Grid©, the decision was taken with co-applicant Natalie Joseph-Williams of Cardiff University (who replaced Glyn Elwyn) to continue with the development of a CDA separately from the commercialised Option Grid© collaborative, using similar methodology and the knowledge of staff at Cardiff University (with the exception of the risk–benefit indicator models developed in WP3, which were developed at Bristol as intended). The resulting CDA, developed during WP3 and tested during WP4, remains the property of Cardiff University and will be made available for free use under a Creative Commons Licence.
Work package 1, added value
Additional qualitative work was undertaken to analyse the acceptability of the Cat-PROM5 questionnaire and the coverage of patient concerns (the language/accuracy/relevance of the questionnaire), and to understand the generalisability of the questionnaire to patients with ocular comorbidities.
Work package 2, added value
(See Report Supplementary Material 1–3 and Hughes et al. 49 for further details.)
Additional analyses were undertaken to understand the:
-
Stability of the risk model for the surgical complication of PCR.
-
Cataract surgery outcomes in people aged ≥ 90 years.
-
Indicators of refractive outcomes, using a novel analysis method.
Work package 4, added value
(See Report Supplementary Material 4 for further details.)
A supplementary qualitative analysis of a stakeholder meeting was undertaken to analyse the ethics implications of immediately sequential bilateral cataract surgery.
Reflections on the programme: successes, impacts and issues
Cat-PROM5
Cat-PROM5 has attracted wide interest since its first presentation at the National PROMs Summit (London, UK) in 2016, as well as further interest from the international community since two development papers were published in the Eye journal. 18,19
Cat-PROM5 has been prioritised for implementation by the NHS Wales PROMs, PREMs and Effectiveness Programme. 50 The programme has developed its own software platform for data collection, and Cat-PROM5 has also been translated into Welsh. Utilisation of the questionnaire has begun in cataract surgical centres in Wales, with a view to becoming part of routine cataract care for around 20,000 Welsh cataract patients annually.
The Health Quality Improvement Partnership commissioned the Royal College of Ophthalmologists to undertake a feasibility pilot study of the use of Cat-PROM5 in the National Cataract Audit between 2017 and 2019. 51
The Royal College of Ophthalmologists has prioritised development of the use of Cat-PROM5 as a patient-centred outcome in the National Cataract Audit. 1
A web-based EMR data collection portal has been developed by the providers of the most widely used ophthalmology EMR system in the NHS. The portal allows for flexible data entry either in the hospital setting or by patients in their own home via a secure link e-mailed to them (which can be automated to arrive 2–3 months post operation if desired). The portal transfers data directly into the patient’s EMR.
The providers of the second most widely used ophthalmology EMR system have likewise developed their software to include the functionality to collect Cat-PROM5 data.
The National Institute for Health and Care Excellence recently recommended that referral for cataract surgery should not be based on visual acuity alone, and went on to suggest Cat-PROM5 as a suitable self-reported outcome measure in their quality standards for serious eye disorders. 52
Cat-PROM5 has been used as a quality-of-vision outcome measure in a recently published study comparing conventional cataract surgery with femtosecond laser-assisted surgery. 53
Patients benefit from empowerment through an ability to formally document the visual difficulties they experience as a result of their cataracts.
Health-care providers and surgeons benefit through use of Cat-PROM5 to:
-
Better understand a patient’s visual burden from cataracts.
-
Better support them in SDM pre operation.
-
Demonstrate to patients, commissioners and the public the benefits provided to patients post operation through cataract surgery.
Health utilities mapping tool
In this programme, we have confirmed that standard preference-based quality-of-life and capability measures, as used by NICE for cost-effectiveness analyses, perform relatively poorly in the context of mild to moderate vision loss from cataracts. 38 The mapping tool developed to convert the Cat-PROM5 data to more traditional preference-based quality-of-life and capability measures (the EQ-5D-3L, EQ-5D-5L and ICECAP-O) will enable vision-specific outcome data to be utilised in cost-effectiveness analysis of cataract care. 39
Researchers and research patients benefit from the reduced need for completion of multiple quality-of-life questionnaires, many of which are not responsive to changes in vision.
Risk factor analysis
The statistical modelling approach for the construction of calculators for pre-operative assessment of the risk of surgical complications and loss of vision (validated here during the assessment of 180,000 cataract operations and updated since then) has been integrated in the most widely used ophthalmology EMR system.
Easy access to this risk information allows for better informed consenting of patients approaching cataract surgery and allows services to ensure that complex patients who are at an increased risk of surgical complications are exclusively operated on by highly experienced surgeons.
Pre-operative risk assessment facilitates appropriate case selection for training surgeons so that they perform only straightforward operations while they are gaining experience.
The National Cataract Audit has adopted the approach to adjust provider and individual surgeon outcomes based on case complexity. 24 Since first presenting surgeon’s results back to them on a website in 2010, the PCR rate has declined by over 50% and VA loss rate by almost 40%:
-
Without giving surgeons credit for the complexity of their work through adjustment for case complexity, participation in the audit (currently covering > 100 centres) would have been difficult to achieve. This approach has immeasurably enhanced the quality and surgeons’ acceptance of the National Cataract Audit.
-
Risk adjustment discourages risk-averse behaviours by surgeons who might otherwise wish to ‘improve their statistics’ by operating on the most straightforward cases only.
-
The cost saving to the NHS from avoiding additional treatments that would have been necessary to deal with complications has been estimated at £2M annually.
Specific analysis of the risks and outcomes associated with operating on people aged ≥ 90 years were explored and published in the journal Eye,27 and this work was previously awarded a prize at the European Society of Cataract and Refractive Surgery (ESCRS) conference (Lisbon, Portugal) in 2017.
Documenting acceptably low rates of both adverse surgical events and adverse visual outcomes in this elderly group, which is of increasing demographic importance, will guard against older people not being offered surgery when they would be very likely to benefit from it.
Benefit model
The Cat-PROM5 self-reported outcome prediction tool has not yet been published and, thus, has not attracted attention. However, it can be anticipated that this will be used for personalised prediction of benefits for individual patients in a similar way to how the risk prediction models are currently being used. Making a calculator tool available to clinicians that allows them to predict the likely benefits for patients pre operation could further improve informed consent in future.
Cataract decision aid
The CDA was well received by patients and HCPs; the main perceived concern for the latter was the time required to use the CDA. The feasibility trial used the CDQM as a primary outcome, which produced confusing results. The review and refinement of this as the primary outcome measure would be required in preparation for a fully powered CDA RCT. Furthermore, use of the CDA earlier in the patient’s pathway would enhance its ability to function as intended, as, by the time patients reach a pre-operative assessment, most have the expectation that surgery will be going ahead.
Staff development
It is worthwhile to note the various personal achievements of research staff associated with the programme. Since the commencement of the programme, all administrative programme staff at the sponsor site have received promotions in the NHS and two researchers have gained prestigious academic promotions. We wish to give special thanks to NIHR for its financial support for continuing professional development and for facilitating the advancement of research capacity across the local region (South West England).
Conclusions
In this mixed-methodology cataract research programme, the brief NHS-implementable psychometrically robust cataract PROM, Cat-PROM5, was developed to capture visual difficulty owing to cataract and its relief through surgery, thus bringing the patient’s view of their vision and their voice to the heart of cataract care. Indicators of risks and self-reported benefits related to cataract surgery were identified, and statistically modelled and validated, allowing for the estimation of the risks and potential self-reported benefits for individual cataract patients who are considering surgery. Health economic work evaluated the performance of established and emerging utilities in cataract surgery and these have been mapped to the Cat-PROM5 instrument. Qualitative investigation of discordant or mismatching outcomes highlighted themes relating to patient expectations of surgery and the lack of available clinician time for full explanations of the visual changes and anticipated spectacle requirements following surgery. A CDA incorporating personalised risk and potential benefit information was qualitatively developed and iteratively refined. A feasibility RCT of the CDA as an intervention was undertaken to inform a possible future fully powered trial. Based on quantitative and qualitative evaluations, a future medium-sized trial would be feasible with minor refinements of instrumentation and use of the CDA intervention at an earlier stage in the patient pathway.
Several ‘added value’ projects were undertaken within the programme; these included assessment of the temporal stability of the risk models for adverse outcomes over 1 decade, analysis of the clinical outcomes of cataract surgery for people aged ≥ 90 years, analysis of the impact of ocular comorbidities on refractive outcome using complex numbers, and ethics considerations of cataract surgery on ‘both eyes at the same sitting’.
This programme has added to the body of knowledge through the:
-
Delivery of the brief psychometrically robust NHS-implementable cataract PROM, Cat-PROM5.
-
Qualitative assessment of patients’ and HCPs’ perceptions of the potential value of Cat-PROM5 in routine clinical services.
-
Mapping of Cat-PROM5 to established and emerging health economic indices to reduce questionnaire burden on participants in future cataract clinical trials evaluating the cost-effectiveness of novel interventions.
-
Quantification of risk indicators for adverse clinical outcomes in cataract surgery and assessment of risk indicator stability through time.
-
Documentation of the acceptably low rates of both adverse surgical events and adverse visual outcomes in very elderly patients aged ≥ 90 years.
-
Assessment of refractive outcomes based on a comprehensive complex-numbers metric that includes all of the information contained in a refractive measurement.
-
Exploration of the ethics issues surrounding the practice of bilateral simultaneous cataract surgery (operating on both eyes together) as opposed to the current practice of sequential surgery (operations on both eyes, separated in time).
-
Quantification of pre-operative indicators of self-reported Cat-PROM5 benefit from surgery.
-
Development of a CDA incorporating personalised predictions of benefit and risk (based on statistical models) for favourable and adverse outcomes.
-
Qualitative assessment of patients’ and HCPs’ perceptions of the potential value of a CDA with personalised benefit and risk predictions in routine clinical services, and the perceived barriers to its implementation.
-
Assessment of the feasibility of a possible future fully powered RCT of a CDA with personalised benefit and risk predictions.
Limitations
The limitations of each of the substudies have been described in the relevant sections of the Synopsis.
Research recommendations
-
A fully powered RCT of the CDA with personalised risk and potential benefit estimates would clarify its potential role in routine care (subject to further refinements of the outcome measure and use of the intervention earlier in the patient pathway).
-
We recommend regular review and update of the risk models for adverse outcomes to ensure currency, as these models are used to adjust centre and surgeon results for case complexity in the National Cataract Audit.
-
The Cat-PROM5 prediction models would benefit from further validation to better understand their performance.
-
The technical precision of complex-numbers analysis of the refractive outcome invites opportunities to investigate causes of the spread of refractive outcomes, with improvements in the achievement of post-operative spectacle-free vision in mind.
-
Further research is needed to clarify the role of surgery on ‘both eyes at a single sitting’ in terms of safety and the very small risk of bilateral blindness in the event of a common cause issue resulting in damage to the vision of or even blindness in both eyes.
Implications for health care
Implications for health care relate to opportunities to implement structured measurement of the patient’s view of their visual difficulty to improve SDM for cataract surgery, tools for individualised estimates of likely self-reported benefits and adverse outcomes, and better communication between clinical staff and patients to facilitate patients having more realistic expectations of the outcome. The Royal College of Ophthalmologists has piloted the use of Cat-PROM5 as a patient-focused outcome in the National Cataract Audit51 and has prioritised Cat-PROM5 for its future inclusion as a primary effectiveness outcome, thus imbedding the patient’s voice in national audit outcomes assessment. Acceptably low rates of both adverse surgical events and adverse visual outcomes were found in the very elderly. The question of operating on both eyes at a single sitting has taken on fresh relevance where there are surgical backlogs, and we understand that a number of services are using Cat-PROM5 to prioritise early surgery for those whose self-reported vision is the worst affected.
Acknowledgements
The programme team would like to thank all the supporters, past and present, who collectively helped the programme team, both professionally and personally.
Professor John Sparrow was supported and advised by co-applicants Jenny Donovan, Jonathan Sterne, Alan Tennant, Andrew Frost, William Hollingworth, Hazel Taylor, Glyn Elwin, Katherine Brain and Claire Gilbert, who provided specialist professional advice for the planning of particular elements of the programme. We are appreciative of their support at this formative phase.
We are particularly grateful to our Patient Advisory Group (PAG) members: Clarence Nesbitt, Gemma Kennedy, Keith Price, Ilse Temple, Jonathan Kelly, Mary Davies, Robert Finnie, Sheila Tucker, Thomas Radford and David Malster.
We are exceptionally grateful for the tremendously generous support given to us by our PAG members, our Programme Steering Committee patient member and our URG patient member. We are appreciative of the fact that they donated their time and shared their experiences, contributing in an open and honest way, with significant positive impact on the successes of the programme. We take this opportunity to thank them all once again.
We would like to extend our gratitude to our study participants across all four centres for kindly donating their time and experiences to the programme.
To our Programme Steering Committee – Larry Benjamin, Catey Bunce, Nick Strong, Myra Higgins, Steve Hyde, Clara Eaglen and Matthew Winyard – thank you for your guidance and professional support and advice throughout the programme.
We are grateful to our sponsor, University Hospitals Bristol Research and Innovation Department, for its extensive support and guidance throughout the programme, in particular to staff members Mary Perkins, Diana Benton, Elinor Griffiths, Katherine Wale and Eleanor Hiscott. Thank you to Liz Wilkinson (University Hospitals Bristol and Weston NHS Foundation Trust research accountant) for their enduring patience over the years. In addition, lead applicant John Sparrow is grateful for the grant development protected time he received from University Hospitals Bristol Research and Innovation Department.
We are thankful to the Clinical Trials Evaluation Unit (University of Bristol) for its support in the design and maintenance of the study databases used in the cataract PROM, Predict-CAT and Involve-CAT.
Thank you to our NIHR programme managers Vasilis Kontogiannis, Elisabeth Aitkenhead and Michelle Edye.
We are grateful to our nursing teams at University Hospitals Bristol and Weston NHS Foundation Trust for welcoming us into their departments and allowing us to become part of the patient pathway, and to our bookings teams for training, advice and flexibility.
To Robert Elvin, Zameen Brar, Claire Buckland, Steve Chaffey, Lucinda Inman and Desiree Alabanza-Behard, we are incredibly grateful for all of your tremendous efforts in participant recruitment, data entry and administrative support at University Hospitals Bristol and Weston NHS Foundation Trust.
Thank you to our outstanding programme managers Lara Edwards, Pippa Craggs, Abi Loose, Andrew Turner and Frances Paget for their hard work and devotion to the programme.
Thank you to our programme statistician, Mariusz Grzeda, whose hard work and extensive knowledge of statistics formed the basis of most of the qualitative work achieved in the programme (WPs 1–4).
Thank you to our qualitative research collaborators Daisy Elliott, Christalla Pithara and Fiona Fox, led by Jenny Donovan in Bristol, and Daniella Holland-Hart, led by Natalie Joseph-Williams in Cardiff.
Thank you to our health economics collaborators Padraig Dixon, Katie Breheny and Rebecca Kandiyali, led by William Hollingworth.
Thank you to optometrists Ketan Kapoor and Jason Searle, who clinically assessed 1200 patient participants in the Predict-CAT study; to ophthalmologists Venkata Avadhanam, Colin Chu, Samantha Hunt and Sofia Theodoropoulou, for their clinical support during the Involve-CAT study; and to Derek Tole and Sofia Theodoropoulou for their ideas and help with the analyses of patients aged ≥ 90 years.
Thank you to the clinical and administrative teams at our collaborating centres, led by co-applicant and principal investigator Andrew Frost in Torbay and co-applicant and principal investigator Christopher Liu in Brighton, for their substantial efforts in helping us to achieve our goals.
It is with deep regret that we note the loss of our friend, colleague, co-applicant and principal investigator Robert Johnston, who died in September 2016. Rob was instrumental in obtaining EMR data for the cataract surgery risk factor analyses.
We thank Peter Scanlon for his support and local leadership in the Predict-CAT study and for taking over Robert Johnston’s roles as co-applicant and principal investigator in Gloucestershire. Thanks also to the optometric research team in Gloucestershire, led by Sue Carter, who clinically assessed 300 patient participants.
Contributions of authors
John Sparrow (https://orcid.org/0000-0003-3704-0105) (Consultant Ophthalmic Surgeon, with a specialist interest in Cataract Surgery and Glaucoma; Honorary Professor of Ophthalmic Health Services Research and Applied Epidemiology, University of Bristol; Clinical Lead for the National Ophthalmology Database Cataract Audit) was the lead applicant and chief investigator. He was directly responsible for the conception, planning and delivery of all four WPs, and oversight of their analysis and interpretation. He provided leadership and support to study staff and researchers. Previously, he was co-developer of the VSQ and VCM1 questionnaires, which laid the groundwork for development of Cat-PROM5. He undertook statistical (Rasch) analysis during the pilot phase of the Cat-PROM5’s development (WP1). He drafted the final report of the programme and authorised the final version for submission to NIHR. He is the corresponding author and guarantor of the work.
Mariusz Grzeda (https://orcid.org/0000-0003-2777-8763) (Research Programme Statistician) was the programme statistician. His substantial contribution was the analysis and interpretation of data across all four WPs. His specialist area is Rasch analysis, which provided the basis of item reduction for the development of Cat-PROM5 (WP1). In addition, he re-evaluated the statistical risk model for surgical complications (PCR) and assessed the stability of the model through time (WP2, added value). He developed the benefits prediction models for self-reported benefit from cataract surgery using Cat-PROM5 as the outcome measure (WP3). He undertook the quantitative analyses for the feasibility RCT of the CDA and CDQMs and performed the preliminary validation of the Cat-PROM5 benefits prediction model (WP4).
Andrew Frost (https://orcid.org/0000-0002-3665-7878) (Consultant Ophthalmologist and Centre Principal Investigator) was a co-applicant, principal investigator and ophthalmologist centre lead for Torbay. He was closely involved in the item reduction and final development of Cat-PROM5 (WP1), qualitative elements (WPs 3–4) and direct care of Involve-CAT participants (WP4). Previously, Andrew was the lead developer of the VCM1 questionnaire, which (with the VSQ) formed the basis of the Cat-PROM5 item set.
Christopher Liu (https://orcid.org/0000-0002-1045-196X) (Professor of Ophthalmology and Centre Principal Investigator) was a co-applicant, principal investigator and ophthalmologist centre lead for Brighton. He was involved in the development of Cat-PROM5 (WP1), the qualitative elements (WPs 3 and 4), the strategic planning of the discordant outcome qualitative aims and direct care of Involve-CAT participants (WP4). Christopher initiated the project that undertook qualitative analysis of the stakeholder meeting on the ethics perspectives of immediately sequential bilateral cataract surgery.
Robert Johnston [Consultant Ophthalmology and Centre Principal Investigator (deceased)] was a co-applicant, principal investigator and ophthalmologist centre lead for Gloucestershire. He was involved in the development of Cat-PROM5 (WP1), and the data aggregation and data-sharing arrangements required for risk modelling (WP2). He was also involved in the strategic planning for the addition of Gloucestershire Hospitals NHS Foundation Trust (GHNHSFT) as a recruiting site for WP3. It is with deep regret that we note the passing of Robert, our good friend and colleague, in September 2016. Following his death, Robert’s role was taken over by Peter Scanlon.
Peter Scanlon (https://orcid.org/0000-0001-8513-710X) (Professor of Ophthalmology and Centre Principal Investigator) was a co-applicant, principal investigator and ophthalmologist centre lead following the death of Robert Johnston. He facilitated and set up arrangements for the inclusion of GHNHSFT as a second recruitment site for WP3 with Pippa Craggs (https://orcid.org/0000-0001-5705-741X) as programme manager.
Christalla Pithara (https://orcid.org/0000-0003-2958-5201) (Senior Research Associate in Health Services Research) conducted qualitative research across WPs 3 and 4 on the presentation of risk and benefits, perceptions of Cat-PROM5 and the CDA, and discordant outcomes. She was involved in data collection, qualitative data analysis and preparation of the Predict-CAT qualitative study final reports.
Daisy Elliott (https://orcid.org/0000-0001-8143-9549) (Qualitative Medical Research Fellow) conducted the qualitative research on the acceptability and generalisability (to patients with visual comorbidities) of Cat-PROM5 in WP1, and provided planning, supervision and oversight of qualitative work in WP3.
Jenny Donovan (https://orcid.org/0000-0002-6488-5472) (Professor of Social Medicine) was a co-applicant, was responsible for qualitative research design and oversight (WPs 1 and 3–4) and was co-developer of the VCM1 and VSQ questionnaires that formed the basis of Cat-PROM5 development. She also contributed to the strategic planning of the feasibility RCT (WP4).
Natalie Joseph-Williams (https://orcid.org/0000-0002-8944-2969) (Lecturer, with specialist interest in SDM and improving patient care, Cardiff University School of Medicine) was a co-applicant and principal investigator for Involve-CAT (taking over from Glyn Elwyn, who emigrated to the USA and commercialised the Option Grid collaborative). Natalie led the development and user testing of the CDA and CDQMs used in the feasibility RCT (WPs 3–4).
Daniella Holland-Hart (https://orcid.org/0000-0002-1127-5152) (Research Associate) was responsible for co-ordinating the development and user testing of the CDA and CDQMs, and conducting the interviews and qualitative analyses of the feasibility RCT (WPs 3 and 4).
Paul HJ Donachie (https://orcid.org/0000-0002-2989-8972) (Medical Statistician, Royal College of Ophthalmologists National Ophthalmology Database) is a collaborator on the programme. He provided extracted cataract surgery data through the data-sharing agreements (WP2).
Padraig Dixon (https://orcid.org/0000-0001-5285-409X) (Health Economist) produced the calibration-mapping tool to crosswalk to health economic utilities (capability and quality-of-life preference-based measures) from Cat-PROM5 (WP3).
Rebecca Kandiyali (https://orcid.org/0000-0001-8566-9536) (Health Economics Research Fellow) participated in and guided analysis of the performance of health economic utilities (capability and quality-of-life scores) in cataract patients (WP3).
Hazel Taylor (https://orcid.org/0000-0003-3430-5278) (Medical Research Statistician) was a co-applicant and responsible for the strategic planning of the risk-indicator analyses (WP2). She undertook the initial WP2 analyses to review and refine the risk models for PCR and VA loss.
Katie Breheny (https://orcid.org/0000-0001-6886-4049) (Health Economist) analysed the performance of health economic utilities (capability and quality-of-life scores) in cataract patients (WP3) and undertook the health economics elements of the Involve-CAT feasibility study (WP4).
Jonathan Sterne (https://orcid.org/0000-0001-8496-6053) (Professor of Medical Statistics and Epidemiology) was a co-applicant and oversaw the planning of statistical work across all WPs.
William Hollingworth (https://orcid.org/0000-0002-0840-6254) (Professor of Health Economics) was a co-applicant and the health economics lead, responsible for the strategic planning of the health economics elements (WPs 3 and 4).
David Evans (https://orcid.org/0000-0001-6961-7031) (Professor in Health Services Research; previously led People in Health West of England, a collaborative initiative on public involvement in research) was a co-applicant, was chairperson of the PAG throughout the programme and will author a collaborative paper with the PAG members to jointly describe the experiences of the group.
Fiona Fox (https://orcid.org/0000-0001-7313-8105) (Senior Qualitative Research Associate) conducted and analysed the qualitative interviews of patients and HCPs in relation to the discordant outcomes aim (WPs 3 and 4).
Sofia Theodoropoulou (https://orcid.org/0000-0003-3038-5354) (Academic Clinical Lecturer in Ophthalmology) reported on the risk factors and clinical outcomes in the aged ≥ 90 years population (WP2). She was also involved in the direct care of Involve-CAT participants.
Rachael Hughes (https://orcid.org/0000-0003-0766-1410) (Statistician) performed analysis and interpretation of the refractive outcomes of records from the NOD (WP2).
Matthew Quinn (https://orcid.org/0000-0002-8877-5024) (Medical Student) undertook the transcription, coding, qualitative analysis and interpretation of a stakeholder meeting around the ethics implications of immediately sequential bilateral cataract surgery.
Daniel Gray (https://orcid.org/0000-0003-0233-113X) (Doctor of Philosophy Research Student in Sociology) oversaw the qualitative analysis and interpretation of the stakeholder meeting regarding the ethics implications of immediately sequential bilateral cataract surgery.
Larry Benjamin (https://orcid.org/0000-0003-3748-649X) (Consultant Ophthalmologist) provided oversight throughout the programme as chairperson of the Programme Steering Committee and made recommendations for final revisions prior to submission of the final report.
Abi Loose (https://orcid.org/0000-0002-9178-102X) (Research Programme Manager) was a senior trial co-ordinator, latterly the programme manager; and drafted the PPI, impact and limitations sections of the report. She assisted in the operational design of WPs 1 and 3–4, and provided management support at the conclusion of the programme. Alongside David Evans, she will co-author a collaborative paper with the PAG.
Lara Edwards (https://orcid.org/0000-0003-3018-5459) (Research Programme Manager) was the first research programme manager, was responsible for the operational design of WPs 1 and 3 and provided management and leadership during the first 2 years of the programme.
Pippa Craggs (https://orcid.org/0000-0001-5705-741X) (Research Programme Manager) was research programme manager from 2016 to 2018, and provided leadership, management and the operational design of WP4 and the qualitative studies in WP3. She also set up the second recruiting site for WP3 to expand recruitment.
Frances Paget (https://orcid.org/0000-0002-2423-2629) (Research Programme Manager) was a senior trial co-ordinator and interim programme manager, assisted in the operational planning for WP4 and provided management support during the programme’s final year.
Ketan Kapoor (https://orcid.org/0000-0003-3135-7320) (Optometrist) assisted in the operational design and clinician training for the Predict-CAT study and completed clinical examinations of Predict-CAT participants at the lead site.
Jason Searle (https://orcid.org/0000-0002-7133-760X) (Optometrist) conducted clinical examinations of Predict-CAT participants at the lead site.
Publications
Sparrow JM, Grzeda MT, Frost NA, Johnston RL, Liu CSC, Edwards L, et al. Cat-PROM5: a brief psychometrically robust self-report questionnaire instrument for cataract surgery. Eye 2018;32:796–805. https://doi.org/10.1038/eye.2018.1
Sparrow JM, Grzeda MT, Frost NA, Johnston RL, Liu CSC, Edwards L, et al. Cataract surgery patient-reported outcome measures: a head-to-head comparison of the psychometric performance and patient acceptability of the Cat-PROM5 and Catquest-9SF self-report questionnaires. Eye 2018;32:788–95. https://doi.org/10.1038/eye.2017.297
Theodoropoulou S, Grzeda MT, Donachie PHJ, Johnston RL, Sparrow JM, Tole DM. The Royal College of Ophthalmologists’ National Ophthalmology Database Study of cataract surgery. Report 5: clinical outcome and risk factors for posterior capsule rupture and visual acuity loss following cataract surgery in patients aged 90 years and older. Eye 2019;33:1161–70. https://doi.org/10.1038/s41433-019-0389-z
Breheny K, Hollingworth W, Kandiyali R, Dixon P, Loose A, Craggs P, et al. Assessing the construct validity and responsiveness of Preference Based Measures (PBMs) in cataract surgery patients. Qual Life Res 2020;29:1935–46. https://doi.org/10.1007/s11136-020-02443-3
Dixon P, Hollingworth W, Sparrow JM. Mapping to quality of life and capability measures in cataract surgery patients: from Cat-PROM5 to EQ-5D-3L, EQ-5D-5L and ICECAP-O. MDM Policy Pract 2020;5:2381468320915447. https://doi.org/10.1177/2381468320915447
Quinn M, Gray D, Bardan AS, Zarei-Ghanavati M, Sparrow JM, Liu C. A stakeholder meeting exploring the ethical perspectives of immediately sequential bilateral cataract surgery. J Med Ethics 2021;47:e44. https://doi.org/10.1136/medethics-2020-106412
Hughes RA, Aristodemou P, Sparrow JM, Kaye S. Surgeon effects on cataract refractive outcomes are minimal compared with patient comorbidity and gender: an analysis of 490 987 cases [published online ahead of print November 11 2021]. Br J Opthalmol 2021. https://doi.org/10.1136/bjophthalmol-2021-320231
Ethics statement
Ethics approval was obtained for all relevant sections of this report.
Data-sharing statement
Consent for the sharing of individual patient data were not obtained from participants involved in any study under the programme. Consent for sharing of summary-level data may be made on application to Professor John Sparrow.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data is used. #datasaveslives. You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, CCF, PGfAR or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the PGfAR programme or the Department of Health and Social Care.
References
- The Royal College of Ophthalmologists . The National Ophthalmology Database (NOD) Audit n.d. www.nodaudit.org.uk/ (accessed 20 March 2021).
- Iacobucci G. Leading ophthalmologist vows to stamp out 'unjustified' screening for cateract surgery. BMJ 2019;365.
- National Institute for Health and Care Excellence . Cataracts in Adults: Management n.d. www.nice.org.uk/guidance/ng77 (accessed 20 March 2021).
- People in Health West of England . People in Health West of England Home Page n.d. www.phwe.org.uk/ (accessed 20 March 2021).
- Gibson A, Welsman J, Britten N. Evaluating patient and public involvement in health research: from theoretical model to practical workshop. Health Expect 2017;20:826-35. https://doi.org/10.1111/hex.12486.
- Frost NA, Sparrow JM, Durant JS, Donovan JL, Peters TJ, Brookes ST. Development of a questionnaire for measurement of vision-related quality of life. Ophthalmic Epidemiol 1998;5:185-210. https://doi.org/10.1076/opep.5.4.185.4191.
- Donovan JL, Brookes ST, Laidlaw DA, Hopper CD, Sparrow JM, Peters TJ. The development and validation of a questionnaire to assess visual symptoms/dysfunction and impact on quality of life in cataract patients: the Visual Symptoms and Quality of life (VSQ) Questionnaire. Ophthalmic Epidemiol 2003;10:49-65. https://doi.org/10.1076/opep.10.1.49.13775.
- McAlinden C, Gothwal VK, Khadka J, Wright TA, Lamoureux EL, Pesudovs K. A head-to-head comparison of 16 cataract surgery outcome questionnaires. Ophthalmology 2011;118:2374-81. https://doi.org/10.1016/j.ophtha.2011.06.008.
- Lundström M, Pesudovs K. Catquest-9SF patient outcomes questionnaire: nine-item short-form Rasch-scaled revision of the Catquest questionnaire. J Cataract Refract Surg 2009;35:504-13. https://doi.org/10.1016/j.jcrs.2008.11.038.
- Andrich D. Rasch Models for Measurement. Thousand Oaks, CA: SAGE Publications Ltd; 1988.
- Wright BD, Stone MH. Best Test Design. Rasch Measurement. Chicago, IL: MESA; 1979.
- Rasch G. Probabilistic Models for Some Intelligence and Attainment Tests. Copenhagen: The Danish Institute of Education Research; 1960.
- Brown TA. Confirmatory Factor Analysis. New York, NY: The Guilford Press; 2006.
- Wright BD. Local dependency, correlations and principal components. Rasch Meas Trans 1996;1996:509-11.
- Hu L-T, Bentler P, Hoyle RH. Structural Equation Modeling: Concepts, Issues, and Applications. Thousand Oaks, CA: SAGE Publications Ltd; 1995.
- Bentler PM. Comparative fit indexes in structural models. Psychol Bull 1990;107:238-46. https://doi.org/10.1037/0033-2909.107.2.238.
- Kim J-O, Mueller CW. Factor Analysis. Statistical Methods and Practical Issues. London: SAGE Publications Ltd; 1978.
- Sparrow JM, Grzeda MT, Frost NA, Johnston RL, Liu CSC, Edwards L, et al. Cataract surgery patient-reported outcome measures: a head-to-head comparison of the psychometric performance and patient acceptability of the Cat-PROM5 and Catquest-9SF self-report questionnaires. Eye 2018;32:788-95. https://doi.org/10.1038/eye.2017.297.
- Sparrow JM, Grzeda MT, Frost NA, Johnston RL, Liu CSC, Edwards L, et al. Cat-PROM5: a brief psychometrically robust self-report questionnaire instrument for cataract surgery. Eye 2018;32:796-805. https://doi.org/10.1038/eye.2018.1.
- Adamson J, Gooberman-Hill R, Woolhead G, Donovan J. ‘Questerviews’: using questionnaires in qualitative interviews as a method of integrating qualitative and quantitative health services research. J Health Serv Res Policy 2004;9:139-45. https://doi.org/10.1258/1355819041403268.
- Strauss A, Corbin J, Denzin NK, Lincoln YS. Handbook of Qualitative Research. London: SAGE Publications Ltd; 1994.
- Glaser BG, Strauss AL. The Discovery of Grounded Theory. New Brunswick, NJ: Aldine Transaction; 1967.
- Miles MB, Huberman AM. Qualitative Data Analysis. London: SAGE Publications Ltd; 1994.
- Donachie PHJ, Sparrow JM. National Ophthalmology Database (NOD) Audit. Year 5 Annual Report – The Fourth Prospective Report of the National Ophthalmology Database Audit 2020. www.nodaudit.org.uk/u/docs/20/hqsrgmurnv/NOD%20Audit%20Full%20Annual%20Report%202020.pdf (accessed 20 March 2021).
- Day AC, Donachie PH, Sparrow JM, Johnston RL. The Royal College of Ophthalmologists’ National Ophthalmology Database study of cataract surgery: report 1, visual outcomes and complications. Eye 2015;29:552-60. https://doi.org/10.1038/eye.2015.3.
- Narendran N, Jaycock P, Johnston RL, Taylor H, Adams M, Tole DM, et al. The Cataract National Dataset electronic multicentre audit of 55,567 operations: risk stratification for posterior capsule rupture and vitreous loss. Eye 2009;23:31-7. https://doi.org/10.1038/sj.eye.6703049.
- Theodoropoulou S, Grzeda MT, Donachie PHJ, Johnston RL, Sparrow JM, Tole DM. The Royal College of Ophthalmologists’ National Ophthalmology Database Study of cataract surgery . Report 5: clinical outcome and risk factors for posterior capsule rupture and visual acuity loss following cataract surgery in patients aged 90 years and older. Eye 2019;33:1161-70. https://doi.org/10.1038/s41433-019-0389-z.
- Kaye SB, Harris WF. Analyzing refractive data. J Cataract Refract Surg 2002;28:2109-16. https://doi.org/10.1016/S0886-3350(02)01639-5.
- Hughes R, Aristodemou P, Sparrow JM, Kaye S. Surgeon effects on cataract refractive outcomes are minimal compared with patient comorbidity and gender: an analysis of 490 987 cases. Br J Ophthalmol 2021. https://doi.org/10.1136/bjophthalmol-2021-320231.
- Massey OT. A proposed model for the analysis and interpretation of focus groups in evaluation research. Eval Program Plann 2011;34:21-8. https://doi.org/10.1016/j.evalprogplan.2010.06.003.
- Onwuegbuzie AJ, Dickinson WB, Leech NL, Zoran AG. A qualitative framework for collecting and analyzing data in focus group research. Int J Qual Meth 2009;8:1-21. https://doi.org/10.1177/160940690900800301.
- International Patient Decision Aid Standards (IPDAS) Collaboration . IDPAS 2005: Criteria for Judging the Quality of Patient Decision Aids n.d. http://ipdas.ohri.ca/IPDAS_checklist.pdf (accessed 20 March 2021).
- van Gestel A, Webers CA, Beckers HJ, van Dongen MC, Severens JL, Hendrikse F, et al. The relationship between visual field loss in glaucoma and health-related quality-of-life. Eye 2010;24:1759-69. https://doi.org/10.1038/eye.2010.133.
- Wailoo AJ, Hernandez-Alava M, Manca A, Mejia A, Ray J, Crawford B, et al. Mapping to estimate health-state utility from non-preference-based outcome measures: an ISPOR good practices for outcomes research task force report. Value Health 2017;20:18-27. https://doi.org/10.1016/j.jval.2016.11.006.
- Devlin NJ, Shah KK, Feng Y, Mulhern B, van Hout B. Valuing health-related quality of life: an EQ-5D-5L value set for England. Health Econ 2018;27:7-22. https://doi.org/10.1002/hec.3564.
- van Hout B, Janssen MF, Feng YS, Kohlmann T, Busschbach J, Golicki D, et al. Interim scoring for the EQ-5D-5L: mapping the EQ-5D-5L to EQ-5D-3L value sets. Value Health 2012;15:708-15. https://doi.org/10.1016/j.jval.2012.02.008.
- National Institute for Health and Care Excellence . Position Statement on Use of the EQ-5D-5L Valuation Set for England. n.d. www.nice.org.uk/about/what-we-do/our-programmes/nice-guidance/technology-appraisal-guidance/eq-5d-5l (accessed 20 March 2021).
- Breheny K, Hollingworth W, Kandiyali R, Dixon P, Loose A, Craggs P, et al. Assessing the construct validity and responsiveness of Preference-Based Measures (PBMs) in cataract surgery patients. Qual Life Res 2020;29:1935-46. https://doi.org/10.1007/s11136-020-02443-3.
- Dixon P, Hollingworth W, Sparrow J. Mapping to quality of life and capability measures in cataract surgery patients: from Cat-PROM5 to EQ-5D-3L, EQ-5D-5L, and ICECAP-O using mixture modelling. MDM Policy Pract 2020;5. https://doi.org/10.1177/2381468320915447.
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. Mahawah, NJ: Lawrence Erlbaum Associates; 1988.
- Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods 2007;39:175-91. https://doi.org/10.3758/bf03193146.
- Elwyn G, Grande S, Barr P. The Observer Option5 Manual: Measuring Shared Decision Making by Assessing Recordings or Transcripts of Encounters from Clinical Settings n.d. www.glynelwyn.com/uploads/2/4/0/4/24040341/observeroption5manual_july_13_2016.docx.pdf (accessed 20 March 2021).
- Elwyn G, Lloyd A, May C, van der Weijden T, Stiggelbout A, Edwards A, et al. Collaborative deliberation: a model for patient care. Patient Educ Couns 2014;97:158-64. https://doi.org/10.1016/j.pec.2014.07.027.
- Elwyn G, Hutchings H, Edwards A, Rapport F, Wensing M, Cheung WY, et al. The OPTION scale: measuring the extent that clinicians involve patients in decision-making tasks. Health Expect 2005;8:34-42. https://doi.org/10.1111/j.1369-7625.2004.00311.x.
- Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol 2013;13. https://doi.org/10.1186/1471-2288-13-117.
- Elwyn G, Frosch D, Thomson R, Joseph-Williams N, Lloyd A, Kinnersley P, et al. Shared decision making: a model for clinical practice. J Gen Intern Med 2012;27:1361-7. https://doi.org/10.1007/s11606-012-2077-6.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. https://doi.org/10.1191/1478088706qp063oa.
- Personal Social Services Research Unit (PSSRU) . PSSRU Home Page n.d. www.pssru.ac.uk/ (accessed 20 March 2021).
- Hughes R, Aristodemou P, Sparrow JM, Kaye S. Surgeon effects on cataract refractive outcomes are minimal compared with patient comorbidity and gender: an analysis of 490 987 cases [published online ahead of print November 11 2021]. Br J Ophthalmol 2020. https://bjo.bmj.com/content/early/2021/11/10/bjophthalmol-2021-320231.long (accessed 16 February 2022).
- NHS Wales . PROMS, PREMs and Efficiency Programme n.d. www.wales.nhs.uk/promspremsandefficiencyprogramme (accessed 15 February 2022).
- Sparrow JM. The National Ophthalmology Database (NOD) Audit. Patient Reported Outcomes Measures in Cataract Surgery: The Feasibility of Electronically Auditing Self-Reported Outcomes Using Cat-PROM5 2020. www.nodaudit.org.uk/u/docs/20/hrlzatcbwp/PROMs%20Feasbility%20Study%20Report%202020.pdf (accessed 20 March 2021).
- National Institute for Health and Care Excellence . Serious Eye Disorders. Quality Standard [QS180]. Quality Statement 2: Referral for Cataract Surgery n.d. www.nice.org.uk/guidance/qs180/chapter/Quality-statement-2-Referral-for-cataract-surgery (accessed 20 March 2021).
- Roberts HW, Wagh VK, Sullivan DL, Hidzheva P, Detesan DI, Heemraz BS, et al. A randomized controlled trial comparing femtosecond laser-assisted cataract surgery versus conventional phacoemulsification surgery. J Cataract Refract Surg 2019;45:11-20. https://doi.org/10.1016/j.jcrs.2018.08.033.
List of abbreviations
- Cat-PROM5
- Cataract Patient-Reported Outcome Measure, five items
- Catquest-9SF
- Cataract questionnaire 9-item Short Form
- CDA
- cataract decision aid
- CDQM
- cataract decision quality measure
- CTT
- classical test theory
- DQM
- decision quality measure
- EMR
- Electronic Medical Record
- EQ-5D-3L
- EuroQol-5 Dimensions, three-level version
- EQ-5D-3L+VIS
- EuroQol-5 Dimensions, three-level version, with vision ‘bolt-on’ domain
- EQ-5D-5L
- EuroQol-5 Dimensions, five-level version
- EQ-5D-5L-VSE
- EuroQol-5 Dimensions, five-level version, value set for England
- EQ-5D-CW
- EuroQol-5 Dimensions Crosswalk
- ES
- effect size
- FAQ
- frequently asked question
- GHNHSFT
- Gloucestershire Hospitals NHS Foundation Trust
- HCP
- health-care professional
- HQIP
- Health Quality Improvement Partnership
- ICECAP-O
- ICEpop CAPability measure for Older people
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health and Care Research
- NOD
- National Ophthalmology Database
- OR
- odds ratio
- PAG
- Patient Advisory Group
- PCR
- posterior capsule rupture
- PPI
- patient and public involvement
- PROM
- patient-reported outcome measure
- PSSRU
- Personal Social Services Research Unit
- RCT
- randomised controlled trial
- ROC
- receiver operating characteristic
- SD
- standard deviation
- SDM
- shared decision-making
- URG
- User Reference Group
- VA
- visual acuity
- VCM1
- Vision Core Measure 1
- VRQoL
- vision-related quality of life
- VSQ
- Visual Symptoms and Quality of life questionnaire
- WP
- work package
Notes
-
Risk Models for Posterior Capsule Rupture and Visual Acuity Loss
-
Stability through time of a Statistical Model for indicators of Posterior Capsule Rupture in Cataract Surgery
-
Clinical outcome and risk factors for posterior capsule rupture and visual acuity loss following cataract surgery in patients aged 90 years and older
-
Calibration of Cat-PROM5 to Health Utilities
-
Quantitative Analysis of the Feasibility of a Cataract Decision Aid RCT
-
Validation of Cat-PROM5 Benefits Prediction Models
-
Qualitative Analysis of Perceptions of the Cataract Decision Aid for Shared Decision Making
-
A Stakeholder Meeting Exploring the Ethical Perspectives of Immediately Sequential Bilateral Cataract Surgery
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/BAGA4188).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
