Notes
Article history
The research reported in this issue of the journal was funded by PGfAR as award number RP-PG-0612-20002. The contractual start date was in December 2014. The draft manuscript began editorial review in September 2021 and was accepted for publication in October 2023. As the funder, the PGfAR programme agreed the research questions and study designs in advance with the investigators. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PGfAR editors and production house have tried to ensure the accuracy of the authors’ manuscript and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Permissions
Copyright statement
Copyright © 2024 Wykes et al. This work was produced by Wykes et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Wykes et al.
Synopsis
Background
The prevalence of schizophrenia is estimated to be 15.2 per 100,000 people. 1 The disorder’s chronicity and morbidity means the economic burden is immense, estimated in 2012 as £19B, and for each patient each year as £60k in societal costs and £36k in public sector costs. 2 Onset typically occurs in late adolescence, a time of transition to adulthood and an increase in educational and career aspirations, interpersonal growth and personal responsibility. Recurrent episodes are common with a gradual worsening of functioning over time. The effects of schizophrenia on life expectancy are substantial,3 with poor employment prospects4 and difficulties achieving satisfying social relationships. Positive symptoms are the core feature of the diagnosis of schizophrenia, but cognitive deficits typically precede onset5 and continue after the remission of hallucinations and delusions and are the main source of continued poor functioning. 6,7 Furthermore, while positive symptoms typically improve with antipsychotic medication, cognitive dysfunction does not substantially change. 8
The need for early intervention to make long-lasting differences in people’s lives is urgent and currently a focus of UK mental health policies, such as No Health without Mental Health. 9 With a high economic burden as well as personal burdens and a poor prognosis, it is essential to explore whether new therapies can improve the recovery trajectory and decrease health and social care costs. Embedding treatments early, such as in Early Intervention Services (EIS), may confer potentially long-lasting benefits. NHS EIS provide care soon after a diagnosis of psychosis to optimise recovery. Designed for those between ages 14 and 65 years,10 they provide Intensive case management for 3 years with a mix of pharmacological, psychological and social support. There was early optimism that EIS would have durable benefits but, despite quick access to multimodal treatments, it has been difficult to demonstrate that short-term improved outcomes are long lasting,11,12 although individual studies show better results. 13 Overall, the results are like those of Fulford and colleagues14 that 60% of service users were neither working nor studying 5 years after psychosis onset irrespective of receiving EIS. Clearly, the current ingredients of recovery-focused treatments are not achieving their full potential for later function. Cognitive impairment is highly predictive of future outcome, so treatments to improve them may provide an added boost to promote recovery and EIS are ideally placed to deliver these.
Cognitive remediation (CR) therapy is a psychological intervention targeting cognitive dysfunction associated with psychosis, with the goal of improving functional outcomes. It aims to improve everyday functioning through increases in (1) metacognitive awareness about one’s own strengths and weaknesses as well as thinking skills and their impact on everyday behaviour and (2) metacognitive regulation of that behaviour. 15 Evidence from the largest meta-analysis to date demonstrates durable effects of CR on global cognition and functioning. 16 Cognitive remediation can improve cognitive and functional recovery such as social relationships and the opportunity to work or take part in further education and is also associated with perceived improvement in cognitive skills. 17 It is also associated with increased confidence and motivation. 18–20
The research programme
The Enhancing Cognition and quality of Life in early PSychosiEs (ECLIPSE) research programme had four work packages (WPs) to investigate the optimal method of implementing CR into EIS in a way that is acceptable to young people. It measured the effects of different implementation models, explored what organisational factors optimise successful introduction, and developed and evaluated a therapist training programme. However, all the separate parts of the programme involved EIS staff and service users in detecting preferences and satisfaction, which provided context for the efficacy measures in our trial. The success of implementation was also evaluated in a cost-effectiveness analysis.
Objectives
These were to:
-
measure service user and staff preferences (WP1);
-
investigate the effect of organisational climate and team challenges (WP1);
-
develop a CR training programme (WP2);
-
evaluate implementation models (WP3);
-
evaluate cost-effectiveness of implementation models (WP3);
-
produce a successful implementation guide (WP4);
-
determine who would benefit from such treatment and at what illness stage (WP4).
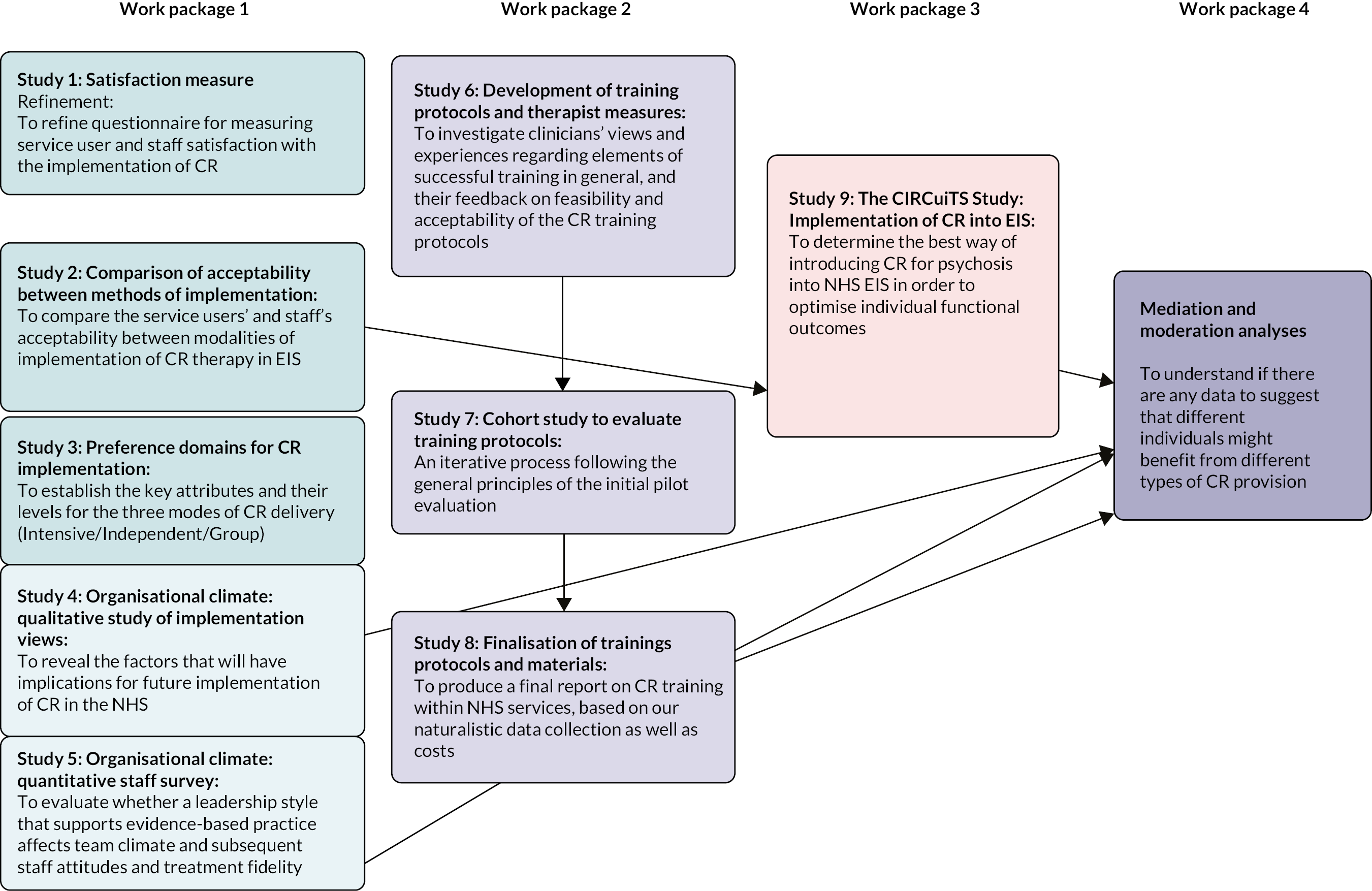
The research pathway for the ECLIPSE programme is outlined in Figure 1.
Computerised Interactive Remediation of Cognition – a Training for Schizophrenia™
The cognitive remediation therapy (CRT) employed in the programme was Computerised Interactive Remediation of Cognition – a Training for Schizophrenia (CIRCuiTS;21 www.circuitstherapyinfo.com/). This is based on a successful paper-and-pencil therapy and was developed with service users and therapists to increase engagement with younger people with psychosis who value computerised therapy. 22,23 CIRCuiTS™ is a feasible mode of delivery, acceptable to service users,24 and shows efficacy in improving cognitive function. 25
FIGURE 1.
The research pathway diagram.
Work package 1 – acceptability, preference and organisational influences for cognitive remediation in first-episode psychosis
Evidence-based treatments can only be successfully implemented if they are acceptable to both service users and the clinical staff providing them. 26 This WP investigated the acceptability and preference domains for methods of treatment implementation and the organisational climate in which this therapy will be delivered.
This was part of the development phase of the programme and provides measures and contexts for the other studies. Using a mixed-methods design, we explored service users and EIS staff perceptions of the key components of satisfaction and produced self-report measures of satisfaction with computerised CR therapy. These measures were then used as outcomes in the implementation trial investigating different methods of CR implementation. This WP also involved service user researchers in collecting and analysing the data.
This WP was designed to address the following:
-
Refine existing measures of service user and staff satisfaction measures for use with computerised CR (Study 1) and validate the measures psychometrically (Study 2a).
-
Compare the acceptability of CR implementation methods in EIS (Study 2b).
-
Explore the preference domains for CR implementation (Study 3).
-
Organisational climate: a qualitative perspective (Study 4) and a quantitative perspective (Study 5).
Work package 1 (i): measuring cognitive remediation acceptability
Study 1 – cognitive remediation satisfaction measure refinement
Background
We know from large meta-analyses that CR interventions are effective. 16 When deciding the best method to implement CR into EIS, it is crucial to investigate acceptability to those who receive the therapy. Acceptability is generally measured by dropout rates and session engagement, although user satisfaction data are increasingly being captured.
Studies have shown overall user satisfaction with CR,27–29 with service users reporting perceived improvements in cognition, although the effects are not always lasting. 20 This in turn has a positive effect on their everyday functioning and improves their sense of well-being. 18–20,24,28–32 In terms of the elements of CR, the number of sessions is generally acceptable20,24,33 and high value is placed on the therapist’s role. 18–20,24,30–32 Group therapy is popular with users and clinicians,28,30,32 although sometimes it had the potential for distraction, insecurity and competitiveness. 18 The experience of using computers in CR therapy has generally been positive;18,19,24 however, a lack of access and skill has been cited as issues. 30 Some areas of dissatisfaction have been highlighted, including performance anxiety19 and intensity of commitment,18,28,31,32 and a lack of progress can make users more aware of their limitations and create frustration. 20,31
Measures of satisfaction with treatment success exist but have traditionally been developed by researchers or clinicians and may not reflect aspects of therapy that are valuable to service users. 34 We use a participatory methodology, developed by Rose and colleagues,35 which involves service users at every stage of the research process.
The aim is to generate two self-report measures of satisfaction with computerised CR, from the perspectives of users and staff. These measures will then be used as outcomes in the trial investigating different methods of CR implementation.
Method
Design
Two focus groups of service users (each of n = 6–8) from EIS each met twice, the second time for the purpose of respondent validation. This was facilitated by service user researchers, digitally recorded and transcribed. The same process was carried out with EIS staff members.
Sample
Purposive sampling was used to recruit EIS participants from a single site, aged 18–35 years, within the first 3 years of their illness. All service users were considered eligible if they could give written consent and communicate in English. All EIS staff were eligible if they gave written consent.
Procedure
Repeated focus groups35 were facilitated by service user researchers, digitally recorded and transcribed for both service users and staff. At the outset, the service user group was shown a live demonstration of CIRCuiTS and the staff group a presentation. A topic guide generated discussion on the content and format of the intended measure. We used an existing service user satisfaction measure, previously designed for a paper-and-pencil evaluation20 and built an interview guide (Report Supplementary Material 1) for assessing satisfaction with CIRCuiTS with that measure. 24 The service user researchers conducted a thematic analysis on the first focus group, and these data were used to develop a new draft measure. This draft measure was taken to the second focus groups for checking. The data were thematically analysed a second time and the final measure amended accordingly.
Data analysis
Thematic analysis was used for data analysis. Constant comparison in initial coding and identification of the main themes and subthemes were carried out.
Results
Participants
All eight service user participants had a diagnosis of psychosis and were from minority ethnic communities; 87% were men with a median age of 28 years. Eleven clinical staff (69%) were women, 10 (63%) were of white ethnic origin and ranged in age from 20 to 40 years. The majority (n = 14; 88%) were care coordinators.
Focus groups – the content of the measures
Using CIRCuiTS
Although CIRCuiTS appealed to many of the service users, some initially felt daunted by its apparent complexity and thought that it would be too hard to complete. Service users felt it was important to capture the levels of initial confidence as it had a bearing on their motivation and ability to undertake the therapy, as well as being a potential indicator of the level of support they were receiving.
You’d be like ‘no, this is too much for me’. Some of it I’d be trying to do but I think to myself ‘you’ve got to be like a rocket genius to actually get it all right’.
A new item was added: ‘I felt confident when I first saw the CIRCuiTS programme’. Support from the therapist was seen as vital. Clear explanations and support would help to address their lack of confidence, and this led to the generation of another new item: ‘I valued the support my therapist gave me during CIRCuiTS’. Support to work on the computer was discussed, leading to the inclusion of: ‘I needed extra computer support during the therapy sessions’.
Measure format
On many occasions, participants mentioned difficulties they had with attention, concentration, memory and planning (the cognitive targets of CR). Their first impressions were that the self-report measure was too complicated. Participants also expressed their difficulties verbalising their thinking and writing responses. They felt frustrated by open-ended questions which took too long to answer and preferred closed questions with set response options.
Some people’s brains work better than others. It just frustrates me knowing that it took me like ten minutes just to think of the reason. I’ve got it in my head but it’s how I’m going to word it.
SU2
Although this was the majority opinion, one participant found forced choice responses frustrating. A decision was made to keep the closed questions, but to add a comments box at the end of the questionnaire so that participants could answer more fully if they wished to.
It’s a bit of an ultimatum. I just think the English language qualitatively can reflect a plethora of emotions and ideas and limiting a person to two answers that you want to hear is sort of not conducive to a scientific study.
SU5
During the second wave of focus groups, there was consensus amongst service user participants that the measure was comprehensive and of an appropriate length and wording.
Measures
The resulting self-report measures contained 31 items each. The majority (n = 23) were brief statements with a six-point Likert response scale; six were categorical items and two open-ended items. Optional free-text space was provided for each question. The measure was grouped into four domains: (1) Therapy Sessions: eight items on the understanding and use of different components of the CIRCuiTS therapy. (2) The Therapist: five items about understanding the role of the therapist and about levels of engagement and support. (3) The Effects of Therapy: 12 items about the ability to apply skills learnt from CIRCuiTS into everyday life and the personal impact of undertaking and ending the therapy. (4) Using the Computer: four items asking about the ease of use of the computer or tablet and the CIRCuiTS programme. The final two items concern satisfaction with the delivery method and overall satisfaction. The staff survey followed the same format but with items asking about the client rather than themselves. There was consensus that the measures were comprehensive and of an appropriate length and wording. A higher total score indicated better satisfaction.
Discussion
Using participatory methods, we developed measures of satisfaction with computerised CR, which were used in our ECLIPSE trial. The measure encompasses the issues that focus group participants consider most important and is reflective of users’ and staff perceptions and satisfaction of CR, as found in the literature.
Service users and staff alike prioritised the cognitive, functional and psychological effects of CR, echoing the existing literature. 18–20,28–32 This resulted in a large bank of items, many of which included an additional impact statement ‘this made me/my client feel …’. Participants also wanted several items on the components of therapy included in the measures, focusing particularly on the length and number of sessions and perceptions of the tasks, strategies and ratings process. It is hoped that the new item on the delivery mode will help to illuminate whether social interaction has a bearing on outcomes, as identified in previous research. 18,28,30,32 Both measures include five items on the role of the therapist, reflecting the high value placed on the therapist by both service users and staff in our study. Personal and professional skills of therapists and a strong working alliance are consistently cited as important influences on therapy outcomes. 18–20,24,30–32 Previous research has shown general acceptability of computerised therapy, although lack of access and skills can hinder progress. 18,19,24,30 This was an important issue, particularly for our service user participants. Their resulting measure asks about difficulties using computers or tablets, the computerised CIRCuiTS programme and whether any support is needed.
Where our study differs is in its design, specifically, the involvement of people with psychosis and clinical staff to generate two measures of satisfaction of CR. Although there was consensus on many of the items, there were some differences in content and changes in language which reflected the priorities of the two different groups. For the service users, it was important to ensure that the measure could be completed by people who might be experiencing symptoms and cognitive difficulties associated with psychosis.
The main aim of the trial is to investigate the optimal mode of CR delivery. In addition to measuring goal attainment, symptoms, functioning and well-being, the data from this study can highlight which elements of CR are most acceptable to staff and service users and provide valuable insight into improving CR in the future.
Study 2 – psychometric validation of the cognitive remediation satisfaction measures
Aim
This study tested the psychometric properties of the measures developed in Study 1.
Method
Design
Using the cognitive remediation satisfaction (CRS) created in Study 1, an online survey was conducted at the end of therapy (WP3, Study 9 – the cognitive remediation trial) to ensure independence from the therapist so that researchers would not know who had received therapy. To test reliability, participants completed the CRS twice with at least a 1-week gap. Data from these repeat ratings are reported to assess reliability and validity. Satisfaction data for the different methods of CR implementation are provided together with the trial data for context.
Recruitment
Potential participants were those recruited to take part in the main trial (see WP3) where they had consented to be randomised to one of the four groups: Intensive CR, Independent CR, Group CR or Treatment as Usual (TAU). They were included if they were aged 16 to 45 years, attending EIS for at least 3 months, had a diagnosis of non-affective psychosis and were able to give informed consent. Exclusion criteria were an inability to communicate in English, an underlying organic or neurological condition or a comorbid diagnosis of learning disability.
Staff participants were NHS healthcare staff working in EIS where the CR trial took take place. Participants were required to give informed consent. Due to involvement in other non-ECLIPSE studies, only three trial sites were able to take part in Study 2a.
Sample size calculation for the differences between treatment arms
For a comparison of two arms with n = 60 participants, there is an estimated 60% power to detect a (standardised) effect size of 0.4 (or larger), which reduces to 39% for a comparison between an arm with n = 60 (Intensive and Group arms) and an arm with n = 25 (Independent therapy) (using Stata sampsi procedure). This revised calculation resulted from lower-than-expected recruitment that was even lower for the staff, and so we decided not to carry out any formal testing of staff satisfaction between arms. Recruitment issues are discussed in WP3.
Procedures
All those receiving CR treatment were asked to complete the satisfaction measure at the end of the 12-week CR intervention in addition to the Working Alliance Inventory (WAI). 33 Staff were asked to complete the satisfaction measure by trial therapists who were in contact with the teams.
Measures
Cognitive remediation satisfaction: The 31-item measure had 23 items, scored on a 1–6 Likert scale with 1 being ‘Strongly disagree’ to 6 being ‘Strongly agree’; 6 categorical items; and 2 open-ended questions. There was also space for participants to comment.
Working Alliance Inventory. 36 The WAI is a 36-item validated measure of the relationship between client and therapist. Items are rated on a 1–7 Likert scale. As the WAI measures therapy engagement, it was used to establish convergent validity for the measure under development. We assumed that there would be a correlation between the two measures as they both measure different aspects of satisfaction with therapy. For these analyses, we removed the therapist items from the overall satisfaction total score to prevent direct overlap.
Psychometric analysis
Total satisfaction scores were calculated after reverse scoring some items so that higher scores indicated higher satisfaction. The overall score was prorated if fewer than 20% of the items scores were missing.
We also used a 19-item satisfaction scale that excluded satisfaction with the therapist, open-ended and categorical items and the overall satisfaction’item. Frequencies were reported for the categorical items not included in the scale.
Reliability: Cronbach’s alpha was calculated for the total satisfaction score to assess internal consistency. Test–retest reliability was explored for each item from the repeated assessments using a weighted κ-statistic and an intraclass correlation calculated for the overall scale. Items were dropped from the scale where they had either low test–retest reliability, low internal consistency or considered to have low face validity.
Concurrent validity: Assessed by correlating CRS and WAI scores.
Results
Service users
One hundred and fifty participants completed the CRS once and 60 (40%) twice. Their mean age was 26.5 years [standard deviation (SD) = 5.99], 38 (25%) were women and 81 (54%) were from minority ethnic communities. The repeat assessment sample was broadly similar with a mean age of 26.6 years, 25% female and 36% white people, 32% black people, 15% Asian and 17% other.
After pro-rating, 144 of 150 participants had a total satisfaction score with a mean of 85.43 (SD 9.04), and a median of 86.00 and a range of 55.00–108.00.
Overall, Cronbach’s alpha was 0.703 (range item alpha: 0.673–0.736), suggesting reasonable reliability. Item Q10 (I learnt how to use a computer/tablet during therapy) and Q12 (I needed extra computer support during the therapy sessions) were dropped as they had negative item-rest correlations. They were also about the use of computers rather than CR and so were judged to have low face validity. This left a 17-item measure and alpha increased to 0.755. With this change, the mean was 77.91 (SD 8.83), median was 79 (72–83) and the range was 48–100.
Q4 (I found some of the tasks or exercises too difficult) also had a negative item-rest correlation but was not judged to have low face validity and was not removed from the scale.
The single overall satisfaction item (separate to the scale) did not have a high correlation with the whole scale score (Pearson’s r = 0.55).
Test–retest analyses
Sixty participants completed the measure twice with an average gap of 9.23 days (SD 6.21). Intraclass correlation (a measure of overall inter-rater agreement) for the satisfaction scale was estimated as 0.77 [95% confidence interval (CI) 0.65 to 0.86] within participants.
Non-scale items
Most participants thought the sessions were the right length (121; 90%) and there were the right number of sessions (129, 89%). Most (99%) reported that they got on well with their therapist and valued their support, thought their therapist was a good teacher, and that they were able to provide feedback to each other during the therapy.
Concurrent validity
One hundred and twenty-nine participants completed both CRS and WAI (214.88; SD = 26.06). Pearson’s correlation between the WAI and CRS scores was estimated as 0.51 (95% CI 0.38 to 0.63).
Staff
Thirty-nine staff completed the CRS staff version. The survey was anonymous; therefore, no demographic information was collected. Scores were prorated if more than 80% items were completed, leaving n = 28. Mean staff scores were 70.51 (SD = 12.83) with a median of 73.72, a range of 42.29–88.00.
Overall Cronbach’s alpha for the satisfaction score was 0.900, indicating very high reliability. There are negative item-rest correlations for Q29 and Q30, but face validity would not suggest dropping them from the scale.
The correlation between the scale score and the overall item score was 0.860.
Half the staff reported that they believed the clients found the length of sessions about right (n = 18, 50%), 17 (47%) did not know and one thought it was too long. Sixteen (43%) staff thought their client found the frequency of sessions about right, 18 (4%) did not know and 3 (3%) thought there were too many sessions per week.
Thirty-three (87%) staff reported that their client seemed to engage well with the therapist, 30 (87%) agreed that the client felt the therapist was a good teacher, 33 (92%) reported their client was able to communicate openly with their therapist and 31 (87%) felt the client was able to value the support the therapist gave.
Discussion
Both scales had reasonable–good reliability and, for the service user scale, good validity. The items dropped from the CRS were important to service users and so will be retained in the measure but not included in the total scale score. They are items that need to be considered in the introduction of a computerised CR as this may affect the outcomes.
Study 3 – preference domains for implementation of cognitive remediation
Background
To incorporate service user and staff views of implementation, we need to understand their preferences. We will build on previous work to develop a more extensive instrument including specific CR activities and implementation methods in a self-report format.
Method
Design
Focus groups with EIS users (three groups) and EIS staff (two groups) were convened and met twice to discuss the domains of interventions most important to individuals. Each focus group lasted up to 2 hours and was facilitated by two trained researchers. The focus groups were recorded digitally and transcribed.
Participants
We aimed to recruit approximately 18–24 service users (6–8 per group) and 12–16 (6–8 per group) staff to take part in the focus groups. The study was carried out in EIS which were not taking part in the trial (Study 9).
Service users
Service users taking part in the focus groups were using EIS, had a diagnosis of non-affective psychosis and aged 18–35 years. They were excluded if they were not able to give written informed consent or unable to communicate in English.
Staff
All staff participants were working in EIS. There were no exclusion criteria.
Focus groups
We collected information about what they would value in a therapy session. Example questions were the amount of therapist involvement, the importance of the context in which therapy is provided (e.g. individual/group). Through probing, the focus group members teased out the range of key attributes for the modes of CR delivery (Intensive/Independent/Group) employed in the trial (WP3 Study 9). See Report Supplementary Material 2 for the topic guide.
Data analysis
Thematic analysis was used with constant comparison in initial coding and identification of the main themes and subthemes.
Results
Sample characteristics
Twenty-three participants took part in the study: 10 service users and 13 staff members. The majority of service user participants were from ethnic minority groups (80%), half were men and the mean age was 27 years (range 20–35 years). In the staff groups, just over half were male (54%), the majority were white people (85%) and the mean age was 44 years (range 32–55 years).
Thematic analysis
Thematic analysis was used with constant comparison in initial coding and identification of the main themes and subthemes. This was based on Braun and Clarke’s (2006)37 widely used methodology of six steps: (1) becoming familiar with the data, (2) generating initial codes, (3) searching for themes, (4) revising themes, (5) defining themes and (6) writing up.
Both groups preferred intensive, one-to-one sessions. Group delivery was seen by service users as a valuable opportunity for interaction and support. There was consensus that independent delivery would be unlikely to provide sufficient support. Service users made a strong case for a flexible, staged approach in delivery, moving towards independence. Staff and service users showed a preference for regular, hourly sessions, once a week that continued for as long as needed. The consensus across participants was that the venue should be local, for ease of access, in a confidential environment such as a community mental health team. Service users and staff valued the provision of verbal and written information on the CIRCuiTS therapy and its benefits. Both staff and service users wanted a flexible and personalised therapy, with choice and collaboration over the delivery method and therapist, but also emphasised strong engagement, personal and professional therapist skills.
There were both staff and user perception that the level of commitment expected from CR was too onerous. Staff worried that there would be little time left for normal care and were particularly concerned about the impact on risk monitoring. The accessibility of CR was raised as a concern, particularly for those with limited access to computers.
Discussion
In terms of delivery, one-to-one sessions were valued most, primarily due to their higher level of therapeutic support. These were followed closely by group sessions, which were seen as a valuable opportunity for connection with peers. These results confirm the importance of a strong therapeutic alliance and social interaction evidenced in previous studies. 28 Independent delivery was seen as unlikely to provide sufficient support, and concerns were raised regarding the accessibility of computerised therapy. This echoes previous studies and suggests that assessment of skills and provision of computer support are critical. 30 Regular, locally held, hourly sessions were preferred, and both groups saw the benefits of flexible and personalised therapy, lasting for as long as needed. Although research indicates that the optimal duration of CR is 3 months,38,39 our participants felt that additional, drop-in sessions would be helpful. There were concerns from service users that the level of commitment might be burdensome, corroborating Bryce et al.’s28 previous study. Overall, however, CR was seen as providing a valuable opportunity for interaction, as well as improving cognitive deficits and associated everyday functioning.
This study has evidenced a strong preference for client-centred, flexible CR, providing support for a hybrid model of delivery as outlined by Medalia et al. 30 and Palumbo. 27 Both service users and staff value methods of delivery which include higher levels of therapist support and opportunities for interaction.
Work package 1 (ii): organisational climate
Study 4 – organisational climate: a qualitative perspective
Background
Without clear implementation guidelines and a clear understanding of the service contexts themselves, CR treatments will not become widely available. To bridge this gap, we need to understand the organisational context in which implementation is to occur. One factor likely to affect both implementation and clinical outcomes is organisational climate, the culture in which services operate. It can facilitate or hinder the implementation of new interventions within healthcare systems. 40–42
Method
This study explored the organisational climate of teams involved in ECLIPSE, prior to the start of the trial. The semistructured interview schedule covered the following: (1) team working and culture; (2) team attributes and attitudes towards change; (3) individual attributes and attitudes towards change; (4) views on the implementation of the proposed intervention (CR) and (5) views on their NHS Trust as an organisation. These themes were compared across the teams to understand shared or unique barriers and facilitators to implementation. See Report Supplementary Material 3 for the interview schedule.
Participants
Participants were staff working in EIS at ECLIPSE sites. Inclusion criteria were the ability to communicate in English and give informed consent.
Analysis
Preliminary coding and categorisation into primary and secondary themes were undertaken independently by two raters using NVivo 12 (QSR International, Warrington, UK). The researchers then reinterrogated and discussed their individual analysis to derive further themes and categories to produce a final framework using inductive themes. 43 This process was carried out for each team separately.
Results
Participants
Forty-two interviews across four teams were carried out pre trial. The teams were labelled A–D and consisted of a mix of nurses, psychiatrists, psychologists, occupational therapists and support workers. Team A (N = 11) was in an urban/suburban location and team participants had an average of 6.7 years in the service. Team B (N = 10) participants were in a suburban location and had an average length of service of 4.8 years. Team C (N = 11), an urban/inner city team, had an average of 3.2 years of service. Team D (N = 11), an urban service, had an average of 4.6 years of service.
Main themes and analysis
The pre-trial data suggest that teams were interested in research and innovation. One driver for the successful implementation of CR was a recognition of the need and potential benefit to service users. Staff consistently acknowledged the clinical need for the treatment of cognitive difficulties in psychosis. These themes were universal across all participating teams.
Democratic decision-making allowed staff to be able to work effectively and was seen as key to successful implementation.
The culture of this team is, I’d say it’s more of a flattened hierarchy than a lot of other teams, as in when they have the clinical meeting everyone attends, you know, regardless of your band and everyone’s input is just as valid.
Teams who felt supported by senior staff and had shared experiences in decision-making were most willing to take on extra responsibility. Staff who felt involved in individual care plans reported a more positive attitude to incorporating new therapies to routine care. On a practical level, teams with a wide variety of professional skills and experience were seen as an advantage when bringing in new therapeutic activities. A new intervention that has an evidence base to back it was also seen as an activity worth trying.
I’m up for that. Yes, I’m always happy to try things. I mean if there’s an evidence to it and it works, then yes, why not, you know, I don’t see anything wrong with that
Absolutely, yes, and everyone’s keen to sort of, you know, add another arrow to the bow in terms of their own professional development.
Staff members who had few opportunities for open communication and who felt less involved in decision-making within their team had more negative attitudes and were more resistant when discussing CR implementation. High staff turnover was also an inhibiting factor in addition to limited resources.
And because there have been so many changes within the team in terms of the way that we work and the people that we work with, I think it might be that that could continue and that the ball would keep on rolling or it might mean I guess that people get fatigued and overwhelmed with too much change happening at one time and get a bit exhausted …
Discussion
Clinical need and potential benefit to service users were the drivers identified for successful CR adoption. All teams emphasised the importance of the evidence base, as well as anecdotal first-hand experience of the effectiveness of new interventions. This is supported by the literature in that people embrace change more readily if they believe the outcome to be successful and beneficial. 44–46 Clear communication from team leaders of the rationale and efficacy of CR was cited as vital for implementation to be successful.
A perceived flattened hierarchy and shared decision-making were much valued. Most team leaders adopted a facilitative, consultative management style and encouraged active participation in discussions which seemed effective in planning for, and reflecting on, proposed changes. Individuals in key leadership roles had a large influence on keeping their teams feeling empowered and working towards common goals.
Overstretched resources were often cited as a hindrance to adopting new working practices which has been noted consistently in other mental healthcare settings. 47–49 In this study, CR was characterised by many as time intensive and resource heavy since service users are recommended to receive two-to-three CR sessions per week.
Engaging all team members in the implementation process through cooperative and consultative decision-making can stimulate a flattened hierarchical structure, empowering staff to overcome existing and new NHS pressures and effectively deliver evidence-based care. The consideration of local conditions and organisational microclimates mediate the successful implementation of new interventions and is needed in addition to generic, context-free variables such as resources before new interventions can be introduced.
Study 5 – organisational climate: a quantitative perspective
Background
Effective leaders can foster change and innovation in teams and organisations36,50–53 and improve attitudes towards adopting evidence-based practices (EBPs). 54 In mental health services, leadership is associated with better staff attitudes and organisational commitment,55 improved working alliance,56 employee attitudes towards EBP57 and client-level outcomes including satisfaction with services and quality of life. 58 Effective leadership can also improve organisational climate54 and moderate negative effects of service system change, resulting in better staff retention. 59 Leadership focused on a specific strategic imperative can create a context for effective services, implementation and maintenance.
Team managers are responsible for their staff implementing interventions, engaging service users and meeting administrative requirements and can be considered as organisational change agents with potential to inspire and motivate staff to implement change. 60,61 The effects of leadership on implementation outcomes are held to be mediated by organisational climate for implementation. 62 An effective ‘implementation climate’ captures the extent to which employees perceive implementation as valued, supported and rewarded by their organisation. Thus, leadership and management theory suggest that the effects of leadership on implementation outcomes such as staff attitudes are likely to be mediated through organisational implementation climate.
The aim of this component of the ECLIPSE study is to evaluate whether a leadership style that supports EBP affects team climate, subsequent staff attitudes and treatment fidelity. We propose the following hypotheses:
-
Implementation leadership will be significantly positively associated with implementation climate.
-
Implementation climate will be significantly positively associated with attitudes towards CR.
-
Implementation leadership will be significantly positively associated with attitudes towards CR.
-
The effect of implementation leadership on attitudes towards CR will be mediated through implementation climate.
Method
Design
An online survey was conducted with staff involved in the wider trial at the start of recruitment. The survey contained validated measures of implementation leadership and climate, attitudes to EBP and implementation citizenship that have been used in other studies of mental health services in the USA and Europe.
Participants
Staff members from EIS across 6 UK sites (10 teams) were recruited through opportunity sampling. Teams were selected based on their participation in the ECLIPSE trial. All staff members were eligible to participate if they gave informed consent.
Procedure
Website links were sent to participants and team leaders, and after following the URL link, participants provided electronic consent. The survey included questions about an individual’s demographic characteristics (e.g. age) and was followed by four measures that took 15 minutes to complete. This was completed both before the start of the CR interventions (wave 1) and afterwards (wave 2).
Measures
Implementation Leadership:63 The Implementation Leadership Scale (ILS) was developed by the investigative team and has excellent reliability and convergent and discriminant validity and predicts climate. The ILS is a brief 12-item measure with four subscales: proactive leadership (α = 0.95), knowledgeable leadership (α = 0.96), supportive leadership (α = 0.95), perseverant leadership (α = 0.96) and a total score (α = 0.98). All items referred to CR as the EBP of interest.
Implementation Climate Assessment64 assesses individual, team and organisational support for implementation and is assessed by the 18-item Implementation Climate Assessment Scale (ICS) adapted for motivational enhancement therapy (MET) andcognitive–behavioural therapy (CBT). The ICS assesses the degree to which EBPs are expected, supported and rewarded and has excellent internal consistency (Cronbach’s alpha = 0.91) and predicts behavioural health staff outcomes. The six subscales are as follows: focus on EBP (α = 0.91), educational support for EBP (α = 0.84), recognition for EBP (α = 0.88), rewards for EBP (α = 0.81), selection for EBP (α = 0.89) and selection for openness (α = 0.91). All items referred to CR as the EBP of interest.
Evidence-Based Practice Attitude Scale-50 (EBPAS-5065) was adapted for mental health providers. For these analyses, we used subscales from the original 15-item measure with four subscales to assess attitudes towards EBP as a function of perceived appeal of EBP, requirements to use EBP, provider openness and perceived divergence between EBP and usual care. EBPAS total scores (α = 0.76) represent global attitudes towards adopting EBP and subscale alphas range from 0.66 to 0.91. Responses are scored on a 5-point scale (0 = not at all, 4 = to a very great extent); scores are associated with individual provider attributes and organisational characteristics. All items referred to CR as the EBP of interest.
Analyses
Measures were scored according to recommendations by the measure developers. Bivariate correlations were used to examine hypotheses 1–3, and multilevel path analyses accounting for the nested data structure were used to assess hypothesis 4.
We tested whether a leadership style that supports EBP affects implementation climate and subsequent staff attitudes towards CR. Path analyses controlled for the nested data structure (i.e. clinicians nested in teams) and the model tested were whether the effects of leadership on implementation outcomes (i.e. attitudes towards EBP, fidelity) are partially or fully mediated through implementation climate. We used maximum likelihood estimation with robust standard errors (SEs) to account for the nested design. We used the Sobel test for mediation. 66,67
Results
We had data from 47 individuals in 8 clusters (teams), pre intervention and 22 individuals in 4 clusters post intervention. Pre-intervention hypotheses 1 and 3 were supported. ILS scores were positively correlated with ICS scale scores (r = 0.46, p < 0.01), but not EBPAS scale scores (r = 0.27, p = 0.07), and hypothesis 2 was supported as ICS scale scores were significantly positively correlated with EBPAS scale scores (r = 0.32, p < 0.05) (Table 1).
| Mean (SD) | ILS | ICS | EBPAS | |
|---|---|---|---|---|
| ILS | 1.60 (1.24) | 1.00 | ||
| ICS | 1.32 (0.80) | 0.46** | 1.00 | |
| EBPAS | 2.20 (0.75) | 0.27 | 0.32* | 1.00 |
Post intervention, hypothesis 1 was supported; however, hypotheses 2 and 3 were not supported. ILS scale scores were positively correlated with ICS scale scores (r = 0.47, p < 0.05) but not with EBPAS scale scores (0.09, p > 0.05). While all correlations were in the expected directions, ILS and ICS scale scores were positively, but not significantly, correlated with EBPAS scale scores (Table 2).
| Mean (SD) | ILS | ICS | EBPAS | |
|---|---|---|---|---|
| ILS | 1.01 (0.81) | 1.00 | ||
| ICS | 1.37 (0.53) | 0.47* | 1.0 | |
| EBPAS | 2.57 (0.54) | 0.09 | 0.14 | 1.0 |
The first path analysis utilised pre-intervention data and the second used data from the post-intervention time point. Figure 2 shows the standardised regression coefficients. The Sobel test demonstrated that the association of ILS with EBPAS was significantly mediated through ICS scale scores (S = 2.21, SE = 0.032, p = 0.03), and the direct path from ILS to EBPAS scale scores was then not statistically significant so indicates full mediation.
FIGURE 2.
Pre-intervention path analysis.
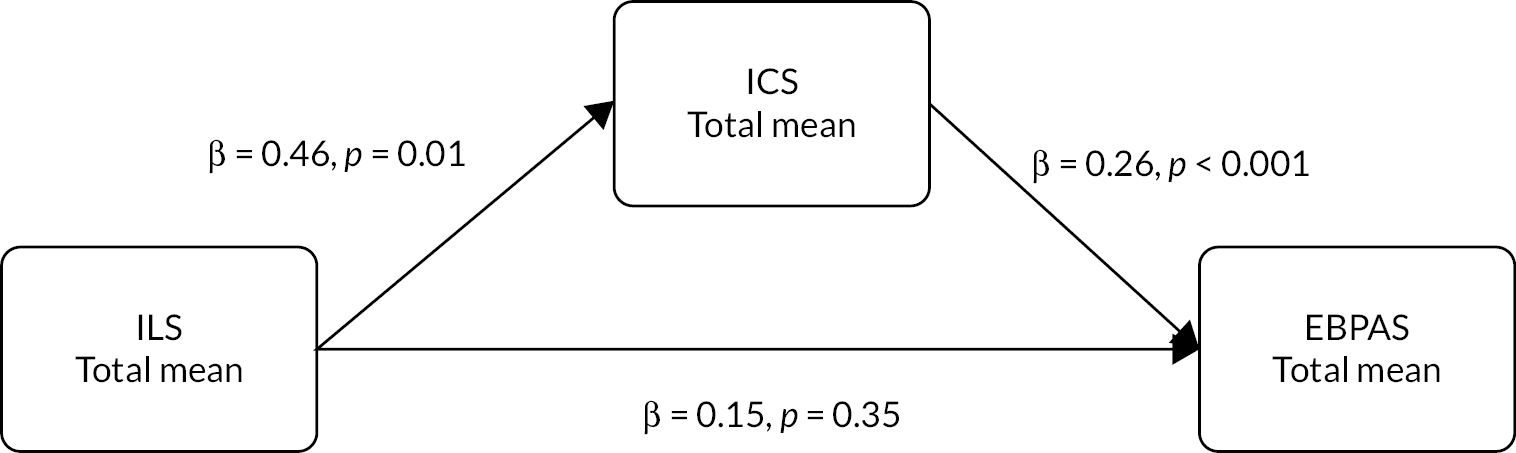
Figure 3 shows the same model for post-intervention data. The Sobel test demonstrated that the association of ILS with EBPAS was not significantly mediated through ICS scale scores (S = 0.64, SE = 0.058, p = 0.52), and these results indicate no significant direct or partial mediation effects for the post-intervention data.
FIGURE 3.
Post-intervention path analysis.
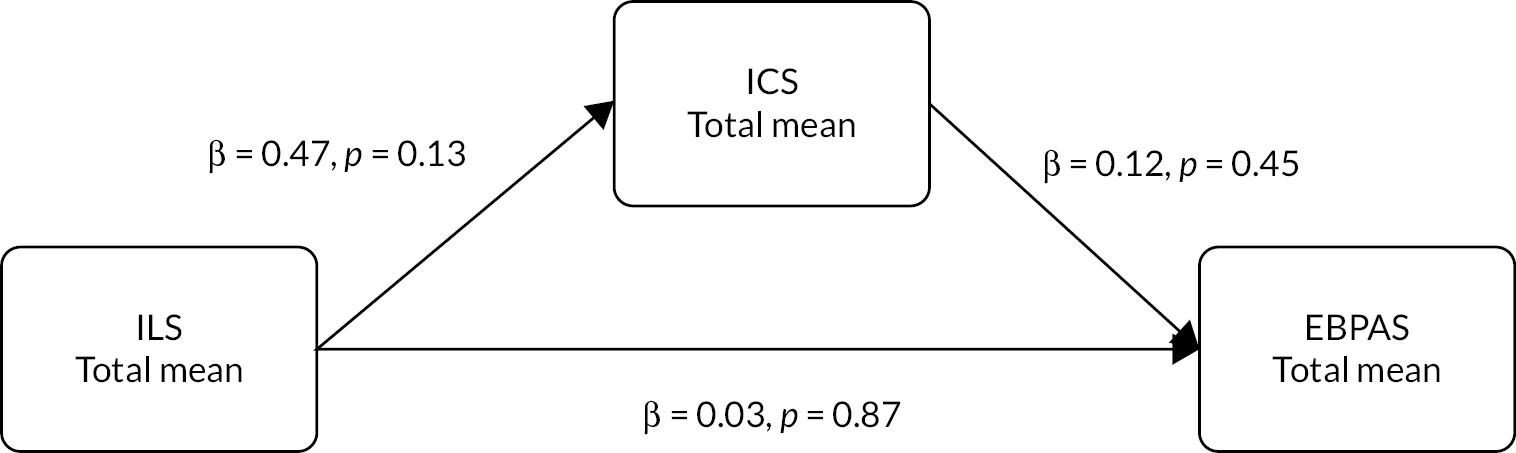
As the pre- and post-intervention models have different sample sizes and number of clusters, it is not possible to directly compare pre- and post-intervention models.
Discussion
Attitudes towards adoption of new innovations in behavioural health may be affected by a number of factors including leadership and organisational climate and culture. 57,68 However, leaders set the tone and climate for the use of new innovations. We hypothesised that the effect of team leadership on team members’ attitudes towards CR would be mediated through implementation climate. We first examined bivariate correlations between the three variables. Although for the pre-intervention period we hypothesised a bivariate association between ILS and EBPAS, it was not statistically significant; the effect was marginal (i.e. p = 0.07) and in the expected direction. Pre intervention, we found full mediation of the effect of leadership on attitudes through implementation climate, but for post intervention, only the bivariate correlation of leadership and climate was statistically significant. While this could be due to the small sample size, the magnitude of the correlations and path coefficients was smaller than for the pre-intervention data and seems to indicate a shift in these associations over time. However, caution is warranted as we did not have a sufficient sample size to assess effects across the two time points. Future studies should examine specific approaches and strategies to develop strong leadership and climate that supports EBP implementation. The leadership and organizational change for implementation strategy was designed to support first-level leaders (e.g. team leaders) and align activities in their organisations to develop an ‘implementation climate’ that communicates to staff that the use of EBP is expected, supported and rewarded in their organisation. 64,69,70 Such deliberate strategies that focus on improving the work lives of mental health providers and the quality of behavioural health interventions hold promise to improve quality of care and better patient outcomes.
Work package 2: developing cognitive remediation training
Cognitive remediation addresses cognitive impairments via learning, practice and feedback. Although therapy is computerised and can be completed independently, therapist involvement is highly valued and important for therapy outcomes16 and is emphasised in the recent White Paper on good clinical practice in CR. 71 However, access to qualified therapists remains patchy.
A priority for the more widespread adoption of CR is dissemination of service delivery expertise, particularly with treatment guidelines. 72–75 CR is carried out only in a few specialist NHS teams and so the development of efficient and cost-effective training for a large-scale roll-out is essential. Online training increases availability, flexibility, geographical reach and potentially reduces teaching and learning time. Repeating sessions if needed and practice can also aid learning on an individual basis, which is not available for in-person teaching. It is effective, acceptable and feasible for other psychological therapies,76,77 for example, CBT.
Our research group has delivered CR training courses to multidisciplinary clinicians for the past 15 years. We used this experience, including substantial clinician feedback on training quality, to develop an online course to train clinicians to deliver CR and a training supervisor’s course.
This WP was designed to address the following:
-
develop a training programme for therapists (Study 6)
-
test the feasibility and acceptability of the developed training (Study 7)
-
recommend modifications for the developed training package (Study 8).
Study 6 – developing training protocols
Background
Training programmes need to build on clinicians’ views and experiences both about elements of successful training in general and what they consider the feasibility and acceptability of the CR training protocols.
Method
Design
We carried out four focus groups with targeted clinicians from mental health services. We aimed for four to nine participants in each group, which was facilitated by two researchers, digitally recorded and transcribed. Each focus group lasted up to 2 hours.
Procedures
We ran two focus groups with CR trainees and with senior clinicians familiar with CR. To facilitate discussion, both groups were shown the training slides and materials used in face-to-face training.
Topic guide
Following the presentation (1), CR trainee participants were asked to give feedback on the following:
-
Will this training be:
-
Effective in achieving the learning aims, objectives and outcomes?
-
Feasible for clinicians (or clinical researchers) working within the NHS or in services abroad to complete?
-
Acceptable to the trainees and their managers?
-
Following the presentation (2) Training for Trainers, participants were asked to give feedback regarding the following questions:
-
Will this model of training be feasible to deliver within the NHS and abroad?
-
Will it be:
-
Effective in achieving the learning aims, objectives and outcomes?
-
Feasible for clinical psychologists working within the NHS or in services abroad to complete?
-
Acceptable to the trainees and their managers?
-
-
Can you foresee any potential barriers or challenges?
Participants
Training to deliver CR: Participants were mental health nurses, occupational therapists, assistant psychologists, nursing assistants or other mental health professionals who were experienced in working with people with a diagnosis of schizophrenia. They were identified by NHS managers or members of the research team.
Training for Trainers groups: Participants were clinical or counselling psychologists who were experienced in working with people with a diagnosis of schizophrenia. They were identified by NHS managers or members of the research team.
All participants were provided with written information consent forms for the study. The consent was taken by researchers, who also facilitated the focus groups.
Analysis
Feedback was noted and used in amending planned training programmes. Formal analyses were not necessary.
Trainee focus group
Focus group attendees found it very helpful to have an overview of CIRCuiTS before starting the training itself. An accompanying manual glossary and training slides were recommended and contact details of a trainer in case of questions. They felt that 5 weeks might be too short to complete training and suggested 6–8 weeks instead. Some were worried that if the training was too quick, then they would forget the information. A recap and introduction at the start of each module were felt to be helpful. Trainees also preferred intuitive software so that they could maximise their time on the CR training rather than learning new software.
Focus group attendees believed it was important to incorporate service user views about what is important to them and what topics they would like addressed. Over the years, our team developed and refined this approach and trainees agreed it was important.
Training for Trainers: focus groups feedback
Overall feedback from the Training for Trainers focus group indicated that the model of training is acceptable. To maximise success, they recommended that at least three people from each trust should be included to provide each other with support, as well as gain opportunities for professional development. Participants proposed that training be expanded to include a variety of staff, such as occupational therapists. They also suggested that trainees should not be spoon-fed and that some input from them is required for ownership of the training, such as giving them some flexibility (e.g. a list of exercises to choose from to present/teach). It was also important to think about their own clinical examples. Interaction between trainees was recommended to maintain motivation, perhaps via some assessment and presentations in front of colleagues, which sets a level of expectation. It was recommended that accreditation should require trainees to have a test of specific trainer skills at the end of the course. To maintain momentum and establish CR services, it was suggested that an online discussion forum should continue after the end of the training for support and networking.
Package production
The e-learning consultancy, make sense design, provided a project proposal, a demo of the Elucidat module-building software and presentations and tutorials on the principles of designing high-quality e-learning material. A draft module was created by the CIRCuiTS team which was refined through approximately 7 iterations into a working draft, which was used as the template for the remaining 10 training modules. Films and other media content for the training were produced by Nice Media. The team chose Docebo as the learning management system (LMS) to host the online training and provided advice on structuring an effective e-learning environment and on the data that could be generated for the planned ECLIPSE study. In early 2017, a group of clinicians in Australia agreed to informally pilot the module drafts and provided structured feedback which was used for the final refinements. Working versions of all modules and other training content were uploaded to the Docebo LMS.
Study 7 – acceptability and feasibility of training for cognitive remediation therapists
Background
The training package developed in Study 6 was tested for acceptability and feasibility.
Method
Study design
All recruited participants had access to the training and completed measures to evaluate the feasibility, acceptability and potential benefits of the programme.
Measures
-
sociodemographic information;
-
feasibility:
-
training dates and times were used to calculate the total time required to complete each module;
-
participants who completed the training within 6 weeks were classified as having completed the programme in the recommended time window;
-
-
potential benefits;
Participants were required to complete a knowledge questionnaire (minimum of 80% to pass) to show competencies.
-
acceptability.
Participants completed a satisfaction questionnaire.
Lastly, those who had completed the training were offered a face-to-face (which later moved to online because of the COVID-19 pandemic) clinical workshop.
Data analysis
We used descriptive statistics for sample characteristics and to understand training completion times. We carried out logistic regression to investigate whether professional role, education or experience affected the ability to pass the knowledge questionnaire. The potential predictors were as follows: (1) psychologist versus other professional groups, (2) university degree, (3) years practicing since qualification and (4) years working with psychosis.
Thematic analysis of free-text feedback was carried out by two researchers independently who adhered to Braun and Clarke’s (2006) six steps. 37,78 This informed how the programme could be further modified and improved.
Results
Participants
A total of 135 participants from 8 NHS trusts consented to take part in the study. Of these, 70 (67.3 %) completed the training. Out of the 70 completers, 60 (85.7%) also successfully passed the knowledge questionnaire at the end of the training (full completers), leaving 10 (14.3 %) who completed the training but failed the knowledge questionnaire (partial completers), giving some indication of the potential benefits of the training.
Sociodemographic characteristics
See Report Supplementary Material 4.
The majority completing the course had an undergraduate degree, worked in outpatient settings and qualified < 10 years ago with around 7 years’ experience of working with psychosis.
Full completers tended to be younger. The mean average years since qualifying, time in the current NHS Trust and working in psychosis was shortest among full completers who were mainly psychologists and nurses.
Training completion time
The median to complete training for full and partial completers was 34 days, but there was a wide range. Although the median time was 5 weeks (the expected training time), partial completers often took much longer.
Time to complete the knowledge questionnaire was predicted by years since qualifying and years working with psychosis with significantly fewer years on average in the group that passed the knowledge questionnaire. Participants’ profession or education did not significantly affect the ability to pass the knowledge questionnaire (Report Supplementary Material 5).
Training satisfaction
Fifty-six per cent (N = 34) of full completers and 50% (N = 5) of partial completers felt they had made a lot of progress, but more full completers felt they would make a lot of further progress in implementing what they had learnt during training (partial: N = 3; 30%; full: N = 45; 75%). Most full and partial completers reported understanding the programme well (N = 40; 57%). The majority (80%) of partial and full completers said they would recommend the training programme to others.
Thematic analysis
Two researchers conducted a thematic analysis on the free-text responses in the satisfaction questionnaire to examine the different perspectives and identify common themes.
Emerging themes and exemplar quotes.
Question 1: What did you like about the training programme?
Bringing cognitive remediation to life
Participants valued applying their learning to real-life experiences. Living with cognitive difficulties from a service user’s perspective was understood more empathically through the three course examples of service user journeys.
It was helpful following the three case studies throughout the course and seeing videos of therapy sessions – this brought CR to life.
Psychologist, inpatient service
Course design and content
The course and modules were considered well designed and easy to follow, having a bite-sized structure, logical flow and clear focus.
Interactive, split into discrete modules, learning clarified at the beginning of each module.
Occupational therapist, specialist service
Question 2: What could be improved?
Technical issues
Difficulties related to using technology fell into two categories: (1) software issues and (2) local technology limitations causing barriers to learning:
… [the] programme is very frustrating to use if internet is slow because you have to load so many pages.
Allied health professional, Early Intervention Service
Course content
Course content emerged as a suggested area for improvement, particularly the final knowledge quiz.
The multiple answers … was a bit demoralising. You might have had all but one point correct, but the answer was marked as wrong. Some of the answers were open to interpretation.
Psychologist, inpatient service
Online versus in-person
Practical challenges of online delivery of the training included difficulty reading or remembering on-screen text, with a preference for more audio, video or hard-copy presentation of information.
I do find online learning more challenging than face-to-face learning because when I read things on a screen, I don’t tend to retain them as easily … I find it easier to watch videos or to have the information narrated as I go along.
Student, community mental health team
Could be supplemented with a face-to-face training session to give the opportunity to ask a qualified therapist any questions around delivering the program.
Allied health professional, community mental health team
Appreciation
This theme conveyed a strong sense of gratitude for the online training.
I am extremely grateful for the opportunity to complete this training … this was a great alternative under the circumstances – COVID-19, cost and practical difficulties of travelling away from home … I think CIRCuiTS is an amazing tool!
Psychologist, inpatient service
Discussion
The training was feasible, although completion time was not consistently in line with our expected 6 weeks. The large range of completion times can be partly explained by the COVID-19 pandemic which resulted in services coming under immense pressure, staff redeployment and a reprioritisation of training. Qualitative feedback also highlighted other barriers such as technical difficulties and having to fit in the training around work. Modules that covered an introduction to CR, theory and research were particularly long to complete. A study inclusion criterion was protected time each week to dedicate to the training; however, anecdotal feedback revealed this was rarely supported.
When completers who had passed or failed the knowledge questionnaire were compared, unsuccessful participants had longer training completion times with gaps suggesting that training momentum is important. Fewer years since qualifying and working in psychosis predicted those who were successful at passing the knowledge questionnaire, and this was statistically significant. Newly qualified participants were more familiar with completing a training course alongside a clinical role and/or their roles could be less demanding. It is also unsurprising that more participants who passed the questionnaire reported feeling satisfied with the training programme.
Most training completers felt they had made a lot of progress and said they would recommend the training to others. Qualitative feedback highlighted the importance of including case studies, practice, well-designed and easy-to-follow modules that were interactive; kept participants engaged and included multimedia presentations. Learners also benefitted from the independence and freedom of online learning, but some expressed a desire for interaction, knowledge sharing and support from fellow learners. These feelings might have been exacerbated by the isolation many people suffered as a context of the COVID-19 pandemic.
Study 8 – modifications to training package
A growing literature suggests online psychological therapy teaching can make a positive difference to competency and reach those with limited access to formal training. Our online CR training was feasible to complete, acceptable to participants and appeared to have benefits on clinicians’ competencies. Despite our positive findings and verbatim feedback, we are making the following recommendations to improve the programme’s feasibility and acceptability:
-
Remove more in-depth theory and research from early modules and include this information in extra learning modules.
-
Provide individual module manuals ready to download at the end of each module.
-
Set up an online training forum including a forum for qualified therapists to support interaction, knowledge sharing, peer supervision and support from fellow therapists.
-
Review the knowledge questionnaire to ensure that questions are not ambiguous or subjective, and consider the length, difficulty and the provision of correct answer clarification.
-
At the start of the training programme, provide clear recommendations about using the fastest internet speed possible, the latest device, browser and operating system versions and completing each module in one sitting.
-
Encourage trainees to gain support from their manager to complete the training in terms of having protected time, the opportunity to implement CIRCuiTS post training and ongoing clinical supervision. Emphasise frequent, regular training sessions, as momentum is key to success.
Supervisors in training programme
Alongside the training for therapists, we also developed a template for training supervisors. This programme was developed after we had a pool of trained clinicians with sufficient clinical experience and interest to take on the role of supervisor. Many services felt that developing their own supervisors would be beneficial and useful to the long-term sustainability of CIRCuiTS implementation. A template for supervisor training was developed based on meeting a set of competencies and skills. The programme provides a template for demonstrating sufficient knowledge and capabilities relevant to providing safe, high-quality supervision of CIRCuiTS therapists. It also encourages leadership skills to promote CR in the service and support the needs to the programme implementation.
To apply for the Supervisors in Training programme prospective, supervisors will have to:
-
have completed the CIRCuiTS online training;
-
have practised as a CIRCuiTS therapist and received supervision for 12 months;
-
have completed therapy with at least two service users.
In addition, they must aim to meet competencies in the following areas:
-
demonstrate knowledge relevant to providing supervision to CIRCuiTS therapists;
-
demonstrate advanced therapist knowledge and skills;
-
demonstrate ability to apply knowledge and own therapy practice skills to deliver safe, high-quality supervision;
-
demonstrate practice leadership skills and capabilities.
Currently, our ECLIPSE therapy lead, Matteo Cella, supports the first three therapists undertaking this training as a pilot scheme. We will review the training template and adapt it to include trainees’ feedback, and the resulting training portfolio template will also be hosted online to facilitate record keeping, commenting and editing.
Work package 3: evaluating cognitive remediation implementation methods
Study 9
Background
Common to all CR studies is whether learnt skills generalise to cognitive functions, for example, memory and executive function. CR can be delivered in different modalities including individual (1 : 1) therapist supervision; group supervision with one therapist and independent working with self-determined, infrequent access to therapist supervision. All three implementation methods have been used with different CR software programmes but there has been no direct test of them using the same software programme. WP3 was designed to assess these different modalities and the effect of differing background services on outcomes in NHS EIS for psychosis using CIRCuiTS CR.
The primary difference between these treatment methods is the level of therapist support and hence a difference in costs. Previous studies have shown that therapist support has tangible effects79 and service users have positive views about therapists being present. 18,20 Therefore, the cost of the service should be balanced against the impact of therapist support.
Aim
To determine the optimal method of introducing CR for psychosis into NHS EIS considering improvement in self-determined social function, improvement in cognitive function and cost-effectiveness.
Primary objective
To determine the best CR implementation method as assessed by the participant’s stated goals using the Goal Attainment Scale (GAS).
Secondary objectives
To determine the best implementation method to improve cognitive function, social function, self-esteem and negative symptoms.
To determine which CR implementation method is most cost-effective.
Method
Design
This was a multiarm multisite (MAMS) randomised controlled trial with outcome assessors blind to group allocation. Participants were recruited from EIS in 12 mental health trusts, linked to 6 universities, serving urban/rural diverse populations. In each trust, CR was delivered in Independent, Intensive and Group formats. A fourth group, TAU, was included. An interim analysis was planned based on health economic outcomes, with the possibility of arms being closed that showed higher costs and worse clinical outcomes compared with other arms. Full details can be found in Wykes et al. 80
Participants
Members of the clinical team obtained permission from participants to be approached for consent.
Inclusion criteria: (1) attending an EIS and at least 3 months from the onset of the first episode of psychosis with clinical stability as judged by the clinical team; (2) aged between 16 and 45 years; (3) research diagnosis of non-affective psychosis, that is, schizophrenia, schizoaffective or schizophreniform disorder according to the Mini-International Neuropsychiatric Interview 5.0.0;81 (4) ability to give informed consent.
Exclusion criteria were as follows: (1) not able to communicate in English sufficiently to participate in cognitive testing; (2) suffering from an underlying organic condition affecting cognition; (3) have a comorbid diagnosis of intellectual disability.
Allocation and blinding
Participants were randomised by the King’s Clinical Trials Unit using block randomisation with randomly varying block sizes and stratified by site. Participants were initially randomised in blocks with proportion 4 : 4 : 3 : 4 (Group, Independent, Intensive and TAU). Later, pre-generated randomisation lists were used for alternative proportions for blocks of < 15 participants. This was changed later to 1 : 1: 1 : 1 and 1 : 1 after the interim analysis using the independent web-based randomisation service. Only therapists and the trial statistician were unblinded to group allocation.
Assessments
These were collected within 4 weeks of randomisation (baseline), 15–19 weeks post randomisation (post treatment) and 39 ± 2 weeks post randomisation (follow-up).
Primary outcome
The GAS82 measures the extent of achieving a participant’s goals, identified at baseline, following CR. Participants chose their own goals that were scored in a standardised way and weighted on importance and difficulty. Post therapy, research workers scored goal attainment in conjunction with each participant and an overall standardised score calculated.
Secondary outcomes
Cognitive function
At each assessment, we collected The Cambridge Neuropsychological Test Automated Battery (CANTAB83) subtests of Single and 5-Choice Reaction Time; Paired Associated Learning; Spatial Working Memory; One-touch Stockings of Cambridge; Emotion Recognition Task; Rapid Visual Information Processing; Attention Switching Task, the Computerised Wisconsin Card Sorting Task,84 the Rey Auditory Verbal Learning Test85 and the Rey Osterrieth Complex Figure. 86
Symptoms
Clinical Assessment Interview for Negative Symptoms (CAINS). 87
Self-esteem
The Rosenberg Self-Esteem Scale (RSE). 89
Context measures
Sociodemographic and clinical information, age, sex, ethnicity, employment, education, living situation, medical history, The Wechsler Test of Adult Reading92 and Wechsler Abbreviated Scale of Intelligence II™,93 was only collected at baseline. Positive and Negative Symptom Scale (PANSS)94 and current medications and dose were collected at each assessment.
Intervention
CIRCuiTS: All participants were offered a maximum of 42 hours. Therapy was delivered by a trained assistant psychologist and had weekly supervision from the centre (www.circuitstherapyinfo.com).
-
Intensive CR. 10.5 weeks, 2 weekly sessions of 60–180 minutes with a CR therapist.
-
Group CR. 14 weeks, 3 weekly sessions of 90 minutes in a group of 4 with a CR therapist. Groups were comprised of a maximum of four participants with a therapist.
-
Independent CR. 1 : 1 orientation with a therapist followed by 41 sessions to complete in their own time. Telephone support and drop-in sessions with a therapist were available (maximum 1 hour/fortnight).
-
Treatment as Usual. Standard care and clinical contact routinely offered by EIS.
Analyses
The main analyses estimate the following treatment effect contrasts for the primary and secondary outcomes:
-
Group versus Intensive;
-
Independent versus TAU;
-
Group + Intensive versus TAU.
All analysis approaches used the intention-to-treat (ITT) population and follow the ECLIPSE Statistical Analysis Plan v1.0 270720, which is outlined in Report Supplementary Material 6. For the primary outcome (GAS T-score), a linear mixed model was used but with the inclusion of a dummy indicator for baseline missingness of the GAS score (as per White and Thompson95).
The same model was used for secondary outcomes. The number of hours of structured activity outcome was first log-transformed as the initial analysis showed the residuals to be non-normally distributed.
No formal adjustment of p-values for multiple testing for multiple comparisons across arms or measures was made.
Sensitivity analyses were carried out for the primary outcome as outlined in the Statistical Analysis Plan with further clarification detailed in Report Supplementary Material 7.
Results
Recruitment (randomisation) over time
Recruitment fell below target resulting in (1) changes to randomisation from group to single participant to avoid long waits for therapy and (2) the interim analysis being undertaken before reaching the intended sample size.
The interim analysis used end-point data from 100 participants: TAU (n = 20), Group (n = 33), Independent (n = 22) and Intensive (n = 25). The Data Monitoring Committee recommended closing the Independent arm based on these data and [together with the National Institute of Health and Care Research (NIHR) panel] closing the TAU arm based on the logistical need to maximise expected future recruitment to the Intensive and Group arms. Revised power calculations for the subsequent feasible target participant numbers used a sample size of 438 participants giving an expected total of 158 and 141 participants to the Group and Intensive arms at the end of the trial. For the contrast of Group versus Intensive, assuming 80% with end-point and follow-up data, with a plausible correlation structure, making no allowance for clustering and retaining the effect size of 0.3 for a comparison of active arms gave 79% power (two-tailed alpha = 0.05). The final analysis plan included assessment of the impact of the interim analysis on treatment effect estimates.
The first participant was consented on 1 June 2016 and randomised on 14 September 2016 and the last on 2 December 2019 and randomised on the 9 January 2020.
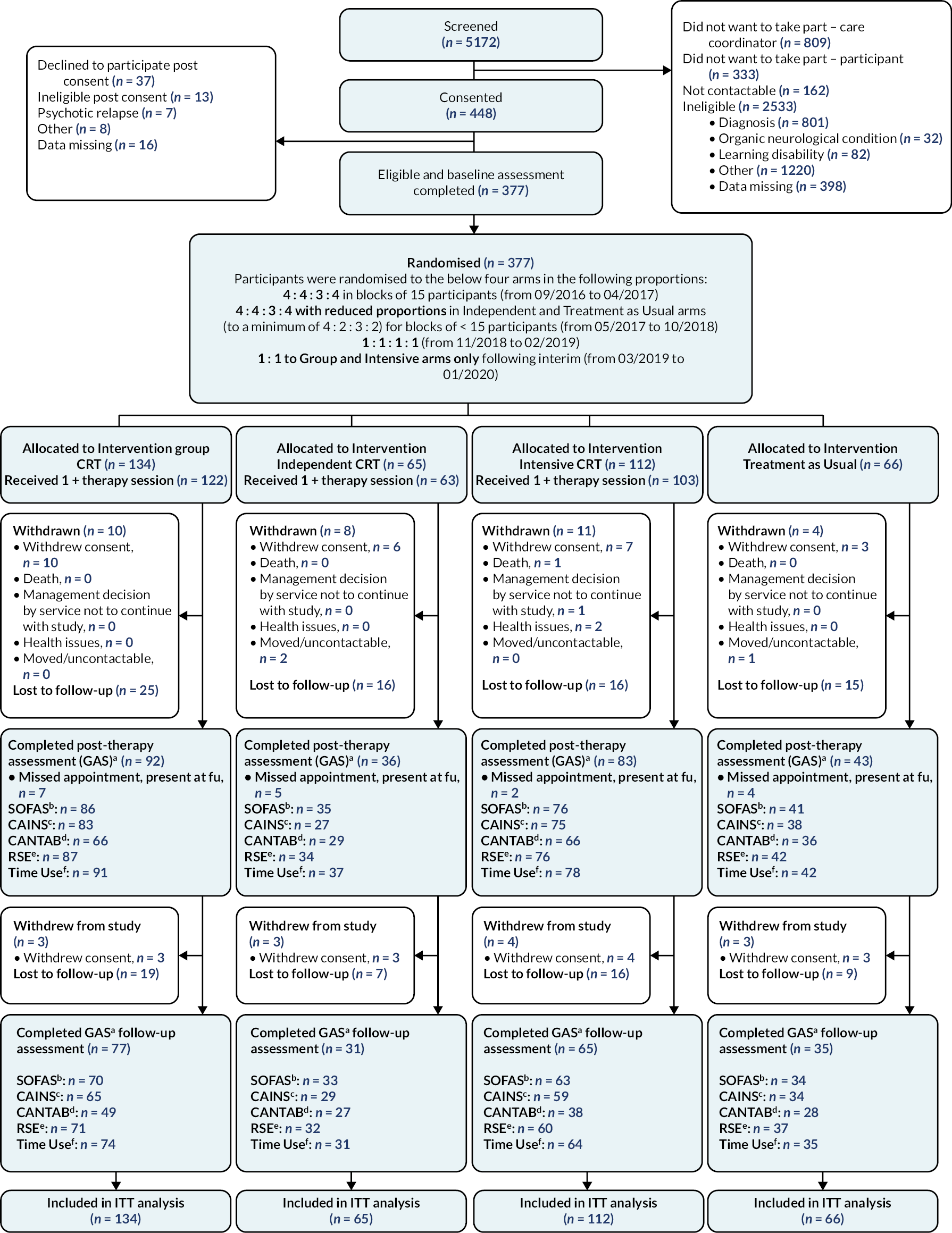
Consolidated Standards of Reporting Trials diagram
Figure 4 shows the Consolidated Standards of Reporting Trials (CONSORT) diagram for the trial. Three hundred and seventy-seven participants were randomised and all randomised participants were included in the ITT analyses.
FIGURE 4.
Consolidated Standards of Reporting Trials diagram. Present at FU, present at follow-up; a, GAS; b, SOFAS; c, CAINS total score; d, Composite cognitive score as measured using the CANTAB; Wisconsin Card Sorting Task (WCST); Digit span task and the Rey Auditory Verbal Learning Test; e, Rosenberg Self Esteem Scale; f, The Time Use Survey – total hours in structured activity.
Recruitment
Recruitment by trial arm and site
Women comprised 27.1% (n = 102) of participants and the mean age of the entire sample was 25.7 years (SD = 6.05). Forty-nine per cent (n = 185) of participants were white, 105 (27.9%) and the remaining were black, Asian or of mixed heritage (Report Supplementary Material 8). Two hundred and fifty (66.3%) were unemployed, 52 (13.8%) in full-time education and 35 (9.3%) in full-time employment. Living arrangements consisted of 116 (54.4%) at home with parents, 116 (30.8%) in their own home and the remaining 55 (14.5%) lived in hostels, group homes or temporary accommodation. The mean duration of untreated psychosis was 8.64 months (SD = 18.5).
Hours of therapy attended were as follows: Group arm 14.6 hours (SD = 12.72), Independent arm 8.8 hours (SD = 9.9) and Intensive arm 19.4 hours (SD = 12.8).
Results for primary outcome (Goal Attainment Scale)
There was no evidence of a difference in GAS (weighted T-score) scores between the Group and Intensive arms, or in the Independent arm compared with TAU. There was a statistically significant difference between Group and Intensive arms combined versus TAU at post therapy. All the sensitivity analyses gave results consistent with the primary analysis.
At post therapy, the GAS mean difference between Group versus Intensive was 0.737 (SE = 1.652; p = 0.655; lower CI = –2.50 to upper CI = 3.975); Independent versus TAU was 0.695 (SE = 2.448; p = 0.777; lower CI = –4.104 to upper CI = 5.493); Group + Intensive versus TAU was 5.734 (SE = 1.958; p = 0.003; lower CI = 1.898 to upper CI = 9.571).
At 6 months post therapy, the mean difference between Group versus Intensive was 1.975 (SE = 1.984; p = 0.319; lower CI = –1.913 to upper CI = 5.863); Independent versus TAU was –1.353 (SE = 2.938; p = 0.645; lower CI = –7.112 to upper CI = 4.407); Group + Intensive versus TAU was 2.665 (SE = 2.374; p = 0.262; lower CI = –1.988 to upper CI = 7.319).
Results for secondary outcomes
Please see Report Supplementary Material 9 for a list of outcome measures. For all outcomes, higher scores are interpreted as better except for the CAINS where lower scores are better. These results show no strong evidence of a difference in outcomes for any of the contrasts, except for the global cognition scores shown in bold, for which there appears to be a difference in the Group + Intensive versus TAU contrast of 1.479 (95% CI 0.395 to 2.564; p = 0.008) at post therapy but not at the 6-month follow-up. At post therapy, the mean difference between Group versus Intensive was 0.192 (SE = 0.499; p = 0.699; lower CI = –0.785 to upper CI = 1.170); Independent versus TAU was 1.348 (SE = 0.701; p = 0.054; lower CI = –0.026 to upper CI = 2.722); Group + Intensive versus TAU was 1.479 (SE = 0.553; p = 0.008; lower CI = –0.395 to upper CI = 2.564).
Satisfaction by trial arm
Mean differences in satisfaction score were in favour of Group CR over Intensive CR and Independent CR and in favour of Intensive CR over Independent CR. However, there was no evidence (using a p < 0.05 threshold) that these differences were statistically significant. The mean satisfaction score for the Group CR was 78.43 (SD = 9.09), Independent CR 75.95 (SD = 8.61) and Intensive CR 78.15 (SD = 8.71). The mean difference estimate between Group and Intensive CR was 2.33 (p = 0.314), Group and Independent 2.04 (p = 0.367) and Intensive and Independent 0.29 (p = 0.856).
Adverse events
Ninety-five adverse events (AEs) and 59 serious adverse events (SAEs) were reported. Two AEs were related to the intervention (hearing voices from the CR computer; sending abusive texts to the therapist about compensation), but no SAE was related to the trial. Most SAEs were mental state deteriorations requiring urgent assessment (N55) or medical hospital admissions (N2). There were two deaths both in the Intensive arm, but neither were judged as trial related.
Primary aim of the health economic analysis
To assess if Group or Intensive CRT is cost-effective in terms of health and social care costs and quality-adjusted life-years (QALYs) compared with TAU.
Methods
The primary outcome measure for the cost-effectiveness analysis was the QALY gained from baseline to 6 months post intervention, calculated from the EQ-5D measure. The secondary outcome was the GAS at 15 weeks post randomisation.
Service use was measured by an adapted version of the self-complete CSRI, collected at each assessment. Costs for service user and the intervention were calculated by combining service use data with appropriate unit cost information. The intervention cost also included a one-off average per patient cost for therapist training, supervision and online access to CIRCuiTS for those receiving therapy. No additional intervention costs were allocated to the TAU group.
Analyses
We performed two cost-effectiveness analyses (Group CR vs. TAU; Intensive CR vs. TAU) from the perspective of the NHS and Personal Social Services (PSS) perspective (preferred by NICE). We compared costs from each perspective and combined them with QALYs and GAS scores.
For the primary analysis, NHS/PSS costs and QALYs were adjusted for baseline costs/baseline EuroQol-5 Dimensions, three-level version scores, trial arm, site and period. For secondary analyses (which included employment and criminal justice costs), NHS/PSS costs and GAS scores were adjusted for baseline costs/baseline GAS-T-score, trial arm, site, period and a dummy indicator for baseline missingness.
An incremental cost-effectiveness ratio was calculated to identify the extra cost incurred per QALY gain or unit increase in GAS score. Cost-effectiveness planes and their corresponding cost-effectiveness acceptability curves (CEACs) were produced from bootstrapped regression models.
Sensitivity analysis
Deterministic sensitivity analysis was conducted by varying the intervention costs upwards and downwards by 10%, 25% and 50%.
Key findings
For the primary cost-effectiveness analysis, there were no significant differences in costs (Group CR vs. Intensive CR, £26,383 per QALY; Group CR vs. TAU, £4306 per QALY; Intensive CR and TAU, £3170 per QALY). However, there were varying levels of uncertainty around the results (i.e. the probability of cost-effectiveness at £20,000 per QALY (NICE, 201596), represented by the CEAC. Group CR versus TAU and Intensive CR versus TAU had significantly higher QALYs than TAU, suggesting that Group CR and Intensive CR provided more benefit compared with TAU.
Discussion
The trial found a benefit in achieving personal recovery goals if the CR therapy was provided in either the Group or Intensive format. We found no statistically significant differences in almost all the secondary outcomes, although we did find a difference in our cognitive outcome but only at post therapy, so this effect waned over time.
Both the Group and Intensive methods included a therapist, and this is now recommended in the Good Practice for Cognitive Remediation White Paper,71 and benefits have since been found for including a trained therapist in two recent meta-analyses. 16,97 However, we found it difficult to find any evidence of differences between these two therapy options which differed in the amount of personal one-to-one contact. This contrasts with the results from the Kambeitz-Ilankovic et al. 98 meta-analysis which suggested an increasing cognitive benefit with more human support. It may be that Group treatment, although providing less personal contact, might benefit participants from the continued presence of the therapist to provide help if needed, and the support of group peers. Peer support was mentioned by service users in the development of the satisfaction measure as just as important as individual support from a clinician. The Group treatment also had slightly higher satisfaction scores but the differences between arms were very small and not statistically significant.
The health economic analyses, despite finding no significant differences in costs, suggest that the cost per QALY is below the NICE cost-effectiveness threshold for the Group and the Intensive arms and so both are considered cost-effective.
Challenges
This study included several challenges. The first was to acquire the resources to employ therapists at the different sites from Excess Treatment Costs. The process for accessing these resources has now changed making it somewhat easier to employ therapists in psychological treatment trials. Our second challenge was our decision to maximise the therapist’s time (reducing costs) through block randomisation. This involves recruiting until you reach the block size and then randomising all participants at the same time. Problems arose when the NHS service was too small or geographically spread out, so that attaining a block of people to randomise was very difficult. In response to these difficulties, we changed the randomisation process twice to make sure that individuals were not waiting too long for treatment. Our study was designed as a multiarm multistage trial which is a novel format in mental health studies and has mostly been used in medical treatments. We used a continuous measure to identify any benefits of the treatment; again, this is novel as most previous MAMS studies use binary variables or at least categorical data. MAMS trials are thought to be more efficient as they include an interim analysis which can indicate whether to drop an arm to maximise recruitment and usefulness of the study outcomes. Due to recruitment difficulties, we had fewer people in the study than previously envisaged, but it still allowed us to make decisions on the cost-effectiveness data supplemented with acceptability information (dropout, sessions attended and satisfaction) and so our interim was also helped by using service user information.
Work package 4: implementation
This WP was designed to understand if there are any data to suggest that certain individuals might benefit from different types of CR provision. Here, we have tried to identify any variables that affect the outcome, where moderating variables are those identified before therapy that could influence outcomes and mediating variables are those that change with therapy and affect benefits. The examination of mediation and moderation in ECLIPSE is potentially made more complex due to having multiple trial arms. However, if we can assume that variation in the ITT estimates across arms derives principally from the variation in the time-on-task achieved in each arm, this allows for a more powerful and focused assessment of mediation and moderation.
Using an analysis of covariance model, we investigated whether the differences in benefit from the treatment arms could be reduced to differences in time-on-task and found a significant effect of time-on-task increasing the GAS outcome by 0.187 (95% CI 0.062 to 0.312; p = 0.003) for each hour of therapy. Wald’s tests of interaction terms found no significant differences in the effects of time-on-task between the Group and Intensive therapy arms (1df p = 0.753) and no difference between these pooled therapist-assisted and independently undertaken treatment effects (1df p = 0.630). Once accounting for the common time-on-task effect across active treatment arms, no differences by treatment arm remained (3df Wald2 = 4.47, p = 0.215).
Mediation
Mediation analysis tries to identify how therapy affects the outcome to both understand and subsequently enhance the benefits. Following a literature review, an overall cognitive composite appeared as a likely mediator between time-on-task and the functional GAS outcome. 98 We have shown this potential effect in Figure 5.
FIGURE 5.
A potential model of the effects of cognition on Goal Attainment.
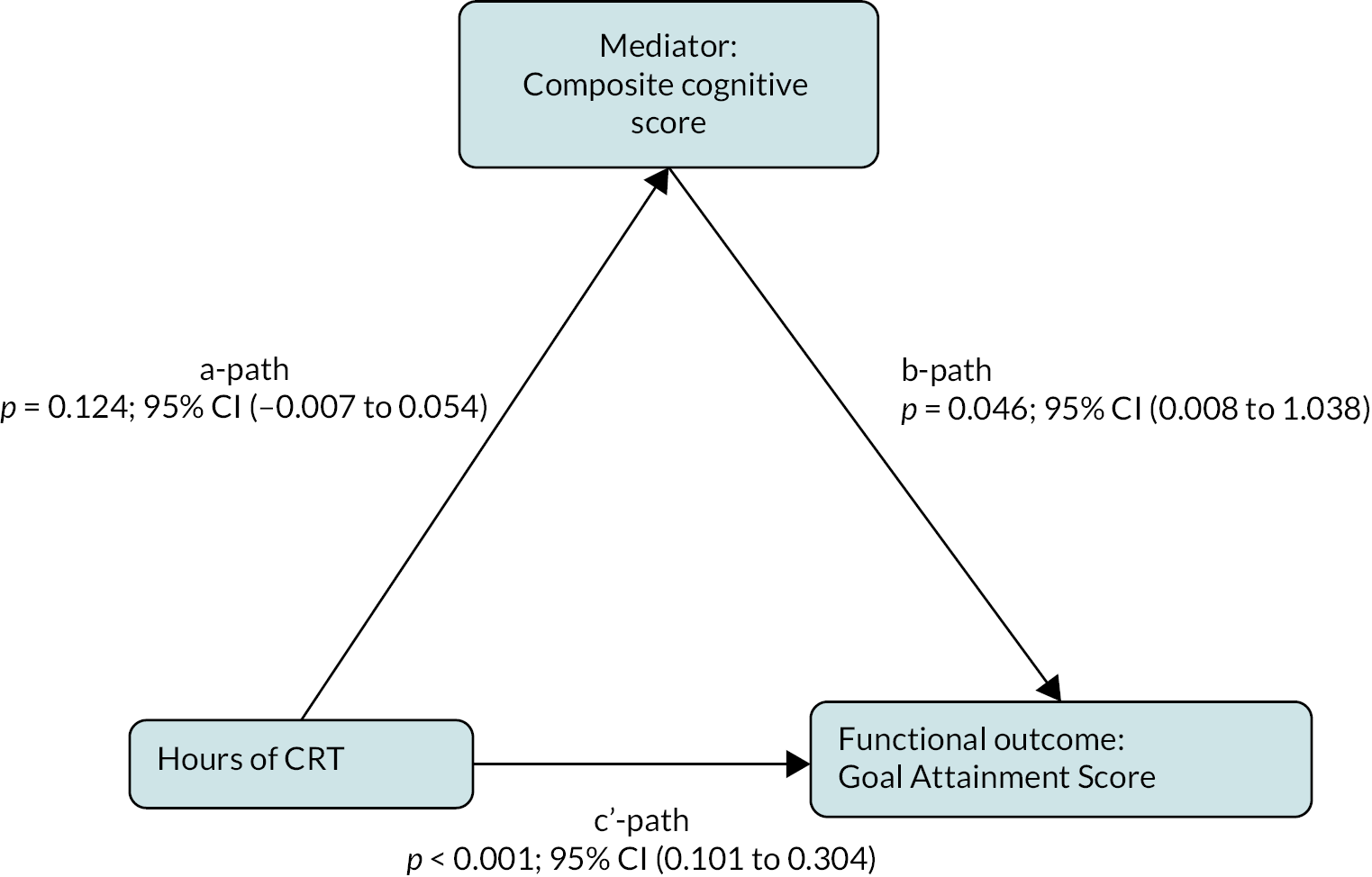
We investigated whether simplifying treatment differences to differences in time-on-task applied to the whole mediation model, including the cognitive mediator and not just the GAS outcome and included baseline variables for both mediator and outcome to minimise confounder bias, as per Landau et al. 99 Although the model fitted well [RMSEA = 0.00; TLI = 1.0122; (27df), p = 0.668], the mediated path from time-on-task to cognition and cognition to functional outcome proved to be small and non-significant (Coeff = 0.014, p = 0.248, 95% CI –0.009 to 0.037).
Moderation
The a and b paths in Figure 5 represent distinct processes and could be affected by different moderators, and it is also possible that potential moderators occurred along the other therapeutic pathway that c’-path represents.
Following a further literature review, we decided that the total PANSS score might moderate the relationship between time-on-task and cognition – the a-path100 – while the CAINS score might moderate the b-path. PANSS moderation was non-significant (p = 0.098) and similarly for the c’-path (p = 0.782). However, moderation of the b-path by the CAINS score was statistically significant (p = 0.016) while along the c’-path was non-significant (p = 0.612).
Participants with high CAINS scores spent on average an hour more on CR tasks than low CAINS scorers. Thus, the mediation effect of change in cognitive score on the change in GAS was estimated for each of the high and low CAINS groups. As we would expect, larger changes in the cognitive composite were associated with larger changes in the GAS score outcome. However, for the high CAINS group, no relationship was seen. This suggests that negative symptoms can interfere with mobilising improvements in general cognition to achieve a desired functional outcome.
Main programme discussion
The programme grant set out to understand the issues for implementing CRT into the NHS using the EIS as an exemplar of where that might be of benefit. Previously, most evaluations of CR have been provided to people with a long history of psychosis. Our choice of EIS was specifically to try to improve the recovery trajectory so that people with a diagnosis of schizophrenia did not lose skills and to support cognition so that the improved cognition following therapy could be transferred to real-world activities. EIS also offer other recovery programmes and so there is also a cost-benefit for providing a boost to cognition which might then benefit recovery as found by Bowie et al. 71
Our results show that leaders can affect the climate for CR use, and that influences staff attitudes about CR at least at pre-assessment. But this was not supported at post assessment which may mean that experience of CR and understanding its benefits have reduced the influence of the leader or organisational climate.
Our new online training for therapists’ programme was acceptable and feasible and at least half the individuals who volunteered to take part completed all the modules. The pilot study for the supervisor training is underway, which will allow us to have a suite of available training.
The trial of benefits provided clear data not only on the two types of therapy that were most beneficial – Group and Intensive – but they were also both cost-effective, and the costs of the improvements lay well within the NICE guidelines cost bands. We were also able to test models of how therapy affects our personalised recovery outcome and demonstrated that cognitive change mediated the benefits of therapy and that the transfer of these cognitive changes was affected by negative symptoms.
Considerations for future research
There are several considerations for researchers embarking on a large programme like ECLIPSE, and we have set out some of those issues here.
Impact of the COVID-19 pandemic
The pandemic occurred before we were able to complete our assessments. This meant that we were not able to see people face to face as easily, but through creative discussions with our patient and public involvement advisers (PPI), we developed both remote and no-contact methods of collecting data while still being supported by a researcher, either online or on the phone. We also moved our supervised training workshops at the end of online therapist training to online. We were also able to help people complete therapy by switching to some online support. These adaptations were agreed by the sponsor NHS Trust and complied with all the guidelines at each stage of the pandemic. So, despite the pandemic, we were able to keep in contact with most participants and complete therapy, assessments and our therapist training. The main negative effect was that we were unable to repeat focus groups with staff at the end of therapy to assess their views of the CR implementation. The pandemic increased staff workloads and so we decided not to increase them even more by asking for participation in this study.
The importance of PPI
Service users were involved at each stage of the project. They helped us to define our primary outcome for the trial and the design of individual studies and were very important in providing suggestions for encouraging recruitment in all studies as well as helping us to consider ways to keep their engagement. For instance, we sent cards at Christmas to remind people about projects and sent newsletters to show our progress to both service users and staff. Although there are often challenges of working with service users and service user researchers, we experienced none in this study and are very grateful to all our PPI advisers. Some members of our Patient Advisory Group (PAG) also agreed to be authors of our papers after critical revisions.
Challenges of National Health Service research
Working in busy NHS services has several challenges which we have mentioned in other chapters, but we will briefly recap. NHS staff have little time, and despite their enthusiasm for different projects, the lack of time does affect their ability to take part in studies, so this did lead to fewer staff completing the satisfaction measure and completing the online survey for assessing organisational climate. This problem also affected the time set aside for our new therapy training. Some trainees took a long time to complete or did not manage to complete all the modules, and we had anecdotal evidence that professional development time that was supposed to be dedicated to this training was often just a pipe dream. These problems were independent of the pandemic. One NHS Trust early in the programme agreed to take part in the trial but only allowed us to collect data from service user participants and not from staff as they felt it would be too much of a burden. We also had some difficulty acquiring Excess Treatment Costs, and although some of those problems have been alleviated by recent changes, some remain. The main difficulty for psychological treatment trials is that a trained therapist is needed, and they will have time when they are not in face-to-face contact with a participant and this time is not currently accounted for in the calculation of Excess Treatment Costs.
Changes to studies
Apart from adaptations required because of the pandemic, we did have recruitment problems in several studies. For the trial, we changed our randomisation process to utilise all consenting participants quickly. For the future, we advise against large block allocation (15 people) and suggest smaller blocks (3 or 4) or individual randomisation. But despite this and the other challenges, including the ambitious design of some studies, it was a success.
Future research
We intend to continue to use our data to understand how we might improve CR benefits. For instance, items in the satisfaction measure at baseline may affect the outcomes and we may be able to tease out the specific cognitive change measures that predict success. CIRCuiTS is built to improve metacognition, and we have some assessments that will allow us to test whether metacognition is also a mediator of treatment outcome. We found that the effects of therapy were related to the number of sessions received, and we know from previous research that therapists can influence that. We want to investigate this therapist effect further with other measures, such as Working Alliance.
Conclusion
Our programme provided data on all parts of the implementation pathway and especially used both staff and service user views to develop and evaluate important factors. All these data provide a clear pathway towards implementation across the NHS, and expand guidance from CR provision to chronic populations, to those at much earlier stages of the schizophrenia diagnosis. We have provided advice, guidance, training and clear evidence of benefit for this large-scale roll-out.
PPI involvement
ECLIPSE has had a strong commitment to PPI throughout all stages of the programme grant. Service user researchers were employed on the grant throughout the life of the programme. They have been involved in all aspects of the research, from study design, data collection to writing up for publication. Below we set out where and how we involved service users in the programme.
Design and changes: We began the programme with a development grant where we discussed with staff and service users how we might introduce concepts of cognitive problems into EIS as well as directly to service users and carers. They helped us to produce three informative leaflets that introduced the potential of a psychological treatment that could help with these cognitive difficulties. We also involved the Young People’s Mental Health Research Advisory Group (www.maudsleybrc.nihr.ac.uk/patients-public/help-shape-our-research/) to help develop the design and information about studies including the Participant Information Sheet, Consent form and other promotional material for the trial. The whole study was also reviewed by the Feasibility and Acceptability Support Team for Researchers (FAST-R) service at the NIHR Maudsley Biomedical Research Centre prior to submitting for ethical review. FAST-R provided advice on language in service user-facing documents so that they were more readable and accessible.
Programme management. Our Steering Committee had two representatives of service users and carers, but we wanted to provide more general support, and so at the start of the programme, we established a PAG with five members, one of whom served as the chairperson. The group met regularly and were invited to comment on all participant-facing documents, such as information sheets and newsletters and advised on the best approaches to recruitment. They were particularly helpful when we were having difficulties with recruitment and suggested ways to encourage participant engagement, which was lengthy for the trial as it was over a 6-month period. The PAG provided advice on our mid-study assessment criteria and what was important to consider before we dropped any arms of the study.
As the COVID-19 pandemic began, we needed to switch to remote assessments and they were able to advise on potential difficulties and how to mitigate them. This included greater attrition, possibly due to lack of motivation and increased stress during the crisis. We also asked them to consider which of our outcomes we should focus on throughout. Although we have given them an overview of the programme outcomes, we will be presenting them with the results of the final analyses with all the study team present, so we can understand their point of view on the data. Our PAG members are also invited to be authors on our papers.
Programme implementation. We have employed expert researchers with a history of using mental health services. This has been particularly important when we ran focus groups as the quality of data improves when the power is reduced between participant and researcher. The service user researchers also carried out the analyses, and for all our focus groups, we involved a member checking or validation process so that participants could comment on the analyses.
Further research. In addition to the research reported in this programme, with the help of the PAG, we are embarking on a novel Multi-Criterion Decision Modelling study to consider how to weigh outcomes in our trial. They advised on the different criteria (cost-effectiveness, cognitive outcome, recovery outcome, satisfaction with treatment, etc.) that we should include in a survey of staff and service users. We are going to use the survey data to inform the weightings for each criterion so we can produce a model example of how to understand the different outcomes in a trial. These data should provide a more informative way of making decisions about what services to provide and goes beyond the current simple calculations made by NICE.
Additional information
Acknowledgements
We would like to acknowledge the therapists and researchers who worked on ECLIPSE: Sweedal Alberts, Ellie Ball, Ravneet Bhogal, Adam Crowther, Conor Deegan, Felix Dransfield, Jo Evans, Rebecca Forsyth, Sam French, Sally Gascoine, Catherine Gray, Markella Grigoriou, Rachel Harrison, Katie High, Manveen Kaur, Orla Kelly, Carl Krynicki, Paris Lalousis, Francis Lammas, Sofia Loizou, Rachel Michel, Rhiannon Murden, Rebecca Nee, Katie Newberry, Abigail Oliver, Aparajita Pandey, Alexandria Philipps, Izabela Pilecka, Samantha Pogue, Thomas Price, Harriet Rankin, Sibella Riccio, Ross Robinson, Charlie Stewart, Leena Subramanian, Jordan Troup, Stacey Underdown, Tjasa Velikonja, Andrew Watson, Lauren Wilcock and Paolo Williams
And the wider team: Geraldine Davis, Ania Szefer, Emily Barnes, our Patient Advisory Group.
Eileen Joyce and Til Wykes are grateful to Cambridge Cognition for the use of CANTAB Connect and Lynis Lewis, Service Director, Noclor who helped with the organisation of Excess Treatment Costs.
Contributions of authors
Til Wykes (https://orcid.org/0000-0002-5881-8003) (Professor of Clinical Psychology and Rehabilitation) is the co-lead applicant; she co-designed the overall research programme, was involved in and supervised all work packages, designed the analyses with the lead statisticians and prepared the results for publication.
Eileen Joyce (https://orcid.org/0000-0003-0469-2844) (Professor of Neuropsychiatry) is the co-lead applicant; she co-designed the overall research programme, was involved in the clinical training and clinical oversight of WP3, designed the analyses with the lead statisticians and prepared the results for publication.
Emese Csipke (https://orcid.org/0000-0003-0911-9262) (Research Fellow, Psychology) is the programme co-ordinator; she supervised work packages, researchers, sites and prepared results for publication.
Dominic Stringer (https://orcid.org/0000-0001-5624-1733) (Research Fellow, Statistics) conducted the statistical analyses and prepared results for publication.
Andrew Pickles (https://orcid.org/0000-0003-1283-0346) (Professor of Biostatistics and Psychological Methods) is a co-applicant, helped with the design of the trial, designed, supervised and conducted the statistical analyses and prepared the results for publication.
Paul McCrone (https://orcid.org/0000-0001-7001-4502) (Professor of Healthcare Economics) is a co-applicant, helped with the design of the trial, designed, supervised and conducted the health economic analyses and prepared results for publication.
Matteo Cella (https://orcid.org/0000-0002-5701-0336) (Reader in Clinical Psychology) is a co-applicant, helped with the design of the trial, supervised the therapy and prepared the results for publication.
Rumina Taylor (https://orcid.org/0000-0003-1208-5569) (Clinical Psychologist) helped develop the training for CR therapists, carried out the feasibility work and prepared the results for publication.
Rose Tinch-Taylor (https://orcid.org/0000-0003-3861-6364) (Research Associate, Statistics) conducted the statistical analyses and prepared the results for publication.
Janet Boadu (https://orcid.org/0000-0001-7012-3514) (Research Associate, Health Economist) conducted the health economic analyses and prepared the results for publication.
Gregory Aarons (https://orcid.org/0000-0001-8969-5002) (Professor of Psychiatry) is a co-applicant, helped with the design of the trial, co-designed the quantitative evaluation of organisational climate, carried out the analyses and prepared the results for publication.
Max Birchwood (https://orcid.org/0000-0002-7476-0171) (Professor of Youth Mental Health) is a co-applicant, helped with the design of the trial and was responsible for oversight of programme study procedures and clinical supervision of local research assistant and therapist.
Sue Dopson (https://orcid.org/0000-0002-3763-9751) (Professor of Organisational Behaviour) is a co-applicant, helped with the design of the trial, designed and supervised the qualitative organisational climate study.
David Fowler (https://orcid.org/0000-0001-5806-2659) (Professor of Psychology) is a co-applicant, helped with the design of the trial and was responsible for oversight of the randomised trial procedures and clinical supervision of local research assistant and therapist.
Kathryn Greenwood (https://orcid.org/0000-0001-7899-8980) (Professor of Clinical Psychology) was responsible for oversight of the randomised trial and clinical supervision of local research assistant and therapist.
Sonia Johnson (https://orcid.org/0000-0002-2219-1384) (Professor of Psychiatry) is a co-applicant, helped with the design of the trial and was responsible for oversight of the randomised trial and clinical supervision of local research assistant and therapist.
Jesus Perez (https://orcid.org/0000-0003-0740-190X) (Professor of Psychiatry) is a co-applicant, helped with the design of the trial and was responsible for oversight of the randomised trial and clinical supervision of local research assistant and therapist.
Rosa Ritunnano (https://orcid.org/0000-0002-7967-5830) (Psychiatrist) was responsible for oversight of the randomised trial and clinical supervision of local research assistant and therapist.
Andrew Thompson (https://orcid.org/0000-0002-0567-6013) (Professor of Youth Mental Health) was responsible for oversight of the randomised trial and clinical supervision of local research assistant and therapist.
Rachel Upthegrove (https://orcid.org/0000-0001-8204-5103) (Professor of Psychiatry and Youth Mental Health) is a co-applicant, helped with the design of the trial and was responsible for oversight of the randomised trial and clinical supervision of local research assistant and therapist.
Jon Wilson (https://orcid.org/0000-0002-5279-6237) (Consultant Psychiatrist) was responsible for oversight of the randomised trial and clinical supervision of local research assistant and therapist.
Clare Reeder (https://orcid.org/0000-0001-9151-1946) (Clinical Psychologist) is a co-applicant, helped with the design of the trial, helped develop the training for CR therapist and prepared the results for publication.
Disclosure of interests
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, are available in the toolkit on the NIHR Journals Library report publication page at https://doi.org/10.3310/LMFP9667.
Primary conflicts of interest: Support for the programme of research came from a NIHR Applied Research Programme grant (RP-PG-0612-20002). In addition, vital support was provided by our Patient Advisory Board and the independent Data Monitoring Committee who had input into each stage of the study. Til Wykes and Andrew Pickles were partly funded by the National Institute for Health Research (NIHR) Maudsley Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King’s College London and their NIHR Senior Investigator Awards. Eileen Joyce was partly funded by the NIHR University College London Hospitals Biomedical Research Centre. NIHR Applied Research Collaborations (ARC) supported Max Birchwood (West Midlands), Jesus Perez (East of England) David Fowler (Kent, Surrey and Sussex). The UK Clinical Research Collaboration-registered King’s Clinical Trials Unit at King’s Health Partners, which is partly funded by the NIHR Biomedical Research Centre for Mental Health at South London and Maudsley NHS Foundation Trust and King’s College London and the NIHR Evaluation, Trials and Studies Coordinating Centre supported our randomisation. Til Wykes (with Clare Reeder) developed the cognitive remediation software programme that was used in this programme. They hold, with KCL, the IP for CIRCuiTS™ and the Online Training Course.
Data-sharing statement
Data are available on request from the corresponding author after submission of an analysis plan and following approval from the other ECLIPSE Co-Investigators.
Ethics statement
We obtained ethics approval for the various projects from: King’s College London (LRS15/16-1724) and Camden and Kings Cross NHS Research Ethics Committee (15/ LO/1960), Nottingham NHS Research Ethics Committee East Midlands (16/EM/0410), Surrey Borders NHS Research Ethics Committee (14/LO/1829), London Chelsea NHS REC (15/LO/1816), Gwasanaeth Moesag Ymchwll NHS REC (16/WA/0054, KCL (LRS 14/15-1713).
Information governance statement
King’s College London is committed to handling all personal information in line with the UK Data Protection Act (2018) and the General Data Protection Regulation (EU GDPR) 2016/679. Under the Data Protection legislation, Olenka Colgias is the Data Controller, and you can find out more about how we handle personal data, including how to exercise your individual rights and the contact details for our Data Protection Officer https://www.kcl.ac.uk/terms/privacy.
Department of Health and Social Care disclaimer
This publication presents independent research commissioned by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by interviewees in this publication are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, MRC, NIHR Coordinating Centre, the Programme Grants for Applied Research programme or the Department of Health and Social Care.
This monograph was published based on current knowledge at the time and date of publication. NIHR is committed to being inclusive and will continually monitor best practice and guidance in relation to terminology and language to ensure that we remain relevant to our stakeholders.
Publications
Papers
Wykes T, Joyce E, Velikonja T, Watson A, Aarons G, Birchwood M, et al. The CIRCuiTS study (Implementation of cognitive remediation in early intervention services): protocol for a randomised controlled trial. Trials 2018;19:183. https://doi.org/10.1186/s13063-018-2553-3
Lammas F, Phillips A, Dopson S, Joyce E, Csipke E, Wykes T. The organisational climate of NHS Early Intervention Services (EIS) for psychosis: a qualitative analysis. BMC Health Serv Res. 2022;22:509. https://doi.org/10.1186/s12913-022-07790-0
Wykes T, Stringer D, Boadu J, Tinch-Taylor R, Csipke E, Cella M, et al. Cognitive remediation works but how should we provide it? An adaptive randomized controlled trial of delivery methods using a patient nominated recovery outcome in first-episode participants. Schizophr Bullet 2023;49:614–25. https://doi.org/10.1093/schbul/sbac214
Evans J, Tinch-Taylor R, Csipke E, Cella M, Pickles A, McCrone P, et al. Satisfaction with cognitive remediation therapy: its effects on implementation and outcomes using the cognitive remediation satisfaction scale. Schizophr 2023;9:67. https://doi.org/10.1038/s41537-023-00390-9
Papers in submission
Taylor R, Crowther A, Tinch-Taylor R, Lewin CDC, Cali C, Reeder C, et al. Evaluation of a new inline cognitive remediation therapy (CIRcuiTS) training for mental health professionals [published online ahead of print November 30 2023]. Psychol Psychother 2023. https://doi.org/10.1111/papt.12510
Tinch-Taylor, R. et al. Using Mediation and Moderation to Evaluate Models of How Cognitive Remediation Affects Recovery in People with Early Psychosis. (submitted).
Tinch-Taylor R, Pickles A, Stringer D, Csipke Emese, Cella M, McCrone P, et al. Understanding the mechanisms of cognitive remediation on recovery in people with early psychosis: a mediation and moderation analysis. (submitted)
Conference presentations
Cella M. Development and Evaluation of an Online Cognitive Remediation Therapy Training Programme for Mental Health Professionals. Schizophrenia International Research Society, Florence, May 2022.
Csipke E, Tinch-Taylor R, Evans J, Pickles A, Cella M, Joyce E, et al. A Service User Led Comparison of Acceptability Between Methods of Implementation of Cognitive Remediation. Schizophrenia International Research Society, Florence, May 2022.
Cspike E, Tinch-Taylor R, Evans J, Pickles A, Cella M, Joyce E, et al. Service User Satisfaction with Computerised Cognitive Remediation. European College of Neuropharmacology, Lisbon, October 2021.
Tinch-Taylor R, Csipke E, Pickles A, McCrone P, Reeder C, Birchwood M, et al. Satisfaction with Cognitive Remediation Therapy: Its Effects on Implementation and Outcomes Using the Cognitive Remediation Satisfaction Scale. Schizophrenia International Research Society, Toronto, May 2023.
Wykes T. Delivering Cognitive Remediation Therapy in First Episode Psychosis Health Care Services: An Adaptive Randomised Trial. European Psychiatric Association, Paris, June 2022.
Wykes T, Joyce E, Stringer D, Boadu J, Cella M, Csipke E, et al. Delivering Cognitive Remediation Therapy in First Episode Psychosis Health Care Services: An Adaptive Randomised Trial. Schizophrenia International Research Society, Florence, May 2022.
Disclaimers
This article presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, CCF, PGfAR or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the PGfAR programme or the Department of Health and Social Care.
References
- McGrath J, Saha S, Chant D, Welham J. Schizophrenia: a concise overview of incidence, prevalence, and mortality. Epidemiol Rev 2008;30:67-76. https://doi.org/10.1093/epirev/mxn001.
- Schizophrenia Commission . Effective Interventions in Schizophrenia, the Economic Case (The London School of Economics, Editor) 2012.
- Hjorthøj C, Stürup AE, McGrath JJ, Nordentoft M. Years of potential life lost and life expectancy in schizophrenia: a systematic review and meta-analysis. Lancet Psychiatry 2017;4:295-301. https://doi.org/10.1016/S2215-0366(17)30078-0.
- Doran CM, Kinchin I. A review of the economic impact of mental illness. Aust Health Rev 2017;43:43-8. https://doi.org/10.1071/AH16115.
- Dora E, Murray RM. Meta-analysis of cognitive deficits in ultra-high risk to psychosis and first-episode psychosis: do the cognitive deficits progress over, or after, the onset of psychosis?. Schizophr Bull 2014;40:744-55. https://doi.org/10.1093/schbul/sbt085.
- Leeson VC, Sharma P, Harrison M, Ron MA, Barnes TRE, Joyce EM. IQ trajectory, cognitive reserve, and clinical outcome following a first episode of psychosis: a 3-year longitudinal study. Schizophr Bull 2011;37:768-77. https://doi.org/10.1093/schbul/sbp143.
- Reeder C, Harris V, Pickles A, Patel A, Cella M, Wykes T. Does change in cognitive function predict change in costs of care for people with a schizophrenia diagnosis following cognitive remediation therapy?. Schizophr Bull 2014;40:1472-81. https://doi.org/10.1093/schbul/sbu046.
- Keefe RS, Harvey PD. Implementation considerations for multisite clinical trials with cognitive neuroscience tasks. Schizophr Bull 2008;34:656-63. https://doi.org/10.1093/schbul/sbn042.
- Department of Health and Social Care . No Health Without Mental Health: A Cross-Government Mental Health Outcomes Strategy for People of All Ages 2011. www.gov.uk/government/publications/no-health-without-mental-health-a-cross-government-outcomes-strategy (accessed June 2021).
- National Institute for Health and Care Excellence . Implementing the Early Intervention in Psychosis Access and Waiting Time Standard: Guidance n.d. nice.org.uk (accessed August 2021).
- Rammou A, Fisher HL, Johnson S, Major B, Rahaman N, Chamberlain-Kent N, et al. Negative symptoms in first-episode psychosis: clinical correlates and 1-year follow-up outcomes in London Early Intervention Services. Early Interv Psychiatry 2019;13:443-52. https://doi.org/10.1111/eip.12502.
- Tapfumaneyi A, Johnson S, Joyce J, Major B, Lawrence J, Mann F, et al. MiData Consortium . Predictors of vocational activity over the first year in inner-city early intervention in psychosis services. Early Interv Psychiatry 2015;9:447-58. https://doi.org/10.1111/eip.12125.
- Wunderink L, Sytema S, Nienhuis FJ, Wiersma D. Clinical recovery in first-episode psychosis. Schizophr Bull 2009;35:362-9. https://doi.org/10.1093/schbul/sbn143.
- Fulford D, Piskulic D, Addington J, Kane JM, Schooler NR, Mueser KT. Prospective relationships between motivation and functioning in recovery after a first episode of schizophrenia. Schizophr Bull 2018;44:369-77. https://doi.org/10.1093/schbul/sbx096.
- Wykes T, Reeder C. Cognitive Remediation Therapy for Schizophrenia: Theory and Practice. London: Routledge; 2005.
- Vita A, Barlati S, Ceraso A, Nibbio G, Ariu C, Deste G, et al. Effectiveness, core elements, and moderators of response of cognitive remediation for schizophrenia: a systematic review and meta-analysis of randomized clinical trials. JAMA Psychiatry 2021;78:848-58. https://doi.org/10.1001/jamapsychiatry.2021.0620.
- Barlati S, Deste G, Galluzzo A, Perin AP, Valsecchi P, Turrina C, et al. Factors associated with response and resistance to cognitive remediation in schizophrenia: a critical review. Front Pharmacol 2019;9. https://doi.org/10.3389/fphar.2018.01542.
- Contreras NA, Lee S, Tan EJ, Castle DJ, Rossell SL. How is cognitive remediation training perceived by people with schizophrenia? A qualitative study examining personal experiences. J Ment Health 2016;25:260-6. https://doi.org/10.3109/09638237.2016.1167856.
- Hargreaves A, Daly-Ryan N, Dillon R, Donohoe G. Independent computerized cognitive remediation for psychosis: an investigation of patient experiences. J Nerv Ment Dis 2018;206:606-13. https://doi.org/10.1097/NMD.0000000000000852.
- Rose D, Wykes T, Farrier D, Doran AM, Sporle T, Bogner D. What do clients think of cognitive remediation therapy? a consumer-led investigation of satisfaction and side effects. Am J Psychiatr Rehabil 2008;11:181-204. https://doi.org/10.1080/15487760801963694.
- Reeder C, Wykes T. Computerised Interactive Remediation of Cognition: Interactive Training for Schizophrenia (CIRCUITS). London: Kings College London; 2010.
- Kurtz MM, Seltzer JC, Fujimoto M, Shagan DS, Wexler BE. Predictors of change in life skills in schizophrenia after cognitive remediation. Schizophr Res 2009;107:267-74. https://doi.org/10.1016/j.schres.2008.10.014.
- Newman MG, Szkodny LE, Llera SJ, Przeworski A. A review of technology-assisted self-help and minimal contact therapies for anxiety and depression: is human contact necessary for therapeutic efficacy?. Clin Psychol Rev 2011;31:89-103. https://doi.org/10.1016/j.cpr.2010.09.008.
- Reeder C, Pile V, Crawford P, Cella M, Rose D, Wykes T, et al. The feasibility and acceptability to service users of CIRCuiTS, a computerized cognitive remediation therapy programme for schizophrenia. Behav Cogn Psychother 2016;44:288-305. https://doi.org/10.1017/S1352465815000168.
- Reeder C, Huddy V, Cella M, Taylor R, Greenwood K, Landau S, et al. A new generation computerised metacognitive cognitive remediation programme for schizophrenia (CIRCuiTS): a randomised controlled trial. Psychol Med 2017;47:2720-30. https://doi.org/10.1017/S0033291717001234.
- Proctor E, Silmere H, Raghavan R, Hovmand P, Aarons G, Bunger A, et al. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Adm Policy Ment Health 2011;38:65-76. https://doi.org/10.1007/s10488-010-0319-7.
- Palumbo D, Mucci A, Giordano GM, Piegari G, Aiello C, Pietrafesa D, et al. The efficacy, feasibility and acceptability of a remotely accessible use of CIRCuiTS, a computerized cognitive remediation therapy program for schizophrenia: a pilot study. Neuropsychiatr Dis Treat 2019;15:3103-13. https://doi.org/10.2147/NDT.S221690.
- Bryce S, Warren N, Ponsford J, Rossell S, Lee S. Understanding the lived experience of cognitive remediation in schizophrenia: a qualitative comparison with an active control. Psychiatr Rehabil J 2018;41:302-11. https://doi.org/10.1037/prj0000309.
- Medalia A, Erlich MD, Soumet-Leman C, Saperstein AM. Translating cognitive behavioral interventions from bench to bedside: the feasibility and acceptability of cognitive remediation in research as compared to clinical settings. Schizophr Res 2019;203:49-54. https://doi.org/10.1016/j.schres.2017.07.044.
- Medalia A, Saperstein AM, Stefancic A, Meyler S, Styke S, Qian M, et al. Feasibility and acceptability of remotely accessed cognitive remediation for schizophrenia in public health settings. Psychiatry Res 2021;301. https://doi.org/10.1016/j.psychres.2021.113956.
- O’Reilly K, Donohoe G, O’Sullivan D, Coyle C, Corvin A, O’Flynn P, et al. A randomized controlled trial of cognitive remediation for a national cohort of forensic patients with schizophrenia or schizoaffective disorder. BMC Psychiatry 2019;19. https://doi.org/10.1186/s12888-019-2018-6.
- Cella M, Reeder C, Wykes T. Group cognitive remediation for schizophrenia: exploring the role of therapist support and metacognition. Psychol Psychother 2016;89:1-14. https://doi.org/10.1111/papt.12062.
- Vidarsdottir OG, Roberts DL, Twamley EW, Gudmundsdottir B, Sigurdsson E, Magnusdottir BB. Integrative cognitive remediation for early psychosis: results from a randomized controlled trial. Psychiatry Res 2019;273:690-8. https://doi.org/10.1016/j.psychres.2019.02.007.
- Rose D. Partnership, co-ordination of care and the place of user involvement. J Ment Health 2003;12:59-70. https://doi.org/10.1080/09638230021000058300.
- Rose D, Evans J, Sweeney A, Wykes T. A model for developing outcome measures from the perspectives of mental health service users. Int Rev Psychiatry 2011;23:41-6. https://doi.org/10.3109/09540261.2010.545990.
- Jung DI, Chow C, Wu A. The role of transformational leadership in enhancing organizational innovation: hypotheses and some preliminary findings. Leadersh Q 2003;14:525-44. https://doi.org/10.1016/S1048-9843(03)00050-X.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. https://doi.org/10.1191/1478088706qp063oa.
- Buonocore M, Bosia M, Bechi M, Spangaro M, Cavedoni S, Cocchi F, et al. Is longer treatment better? A comparison study of 3 versus 6 months cognitive remediation in schizophrenia. Neuropsychology 2017;31:467-73. https://doi.org/10.1037/neu0000347.
- Kluwe-Schiavon B, Sanvicente-Vieira B, Kristensen CH, Grassi-Oliveira R. Executive functions rehabilitation for schizophrenia: a critical systematic review. J Psychiatr Res 2013;47:91-104. https://doi.org/10.1016/j.jpsychires.2012.10.001.
- Carlfjord S, Andersson A, Nilsen P, Bendtsen P, Lindberg M. The importance of organizational climate and implementation strategy at the introduction of a new working tool in primary health care. J Eval Clin Pract 2010;16:1326-32. https://doi.org/10.1111/j.1365-2753.2009.01336.x.
- Hemmelgarn AL, Glisson C, James LR. Organizational culture and climate: implications for services and interventions research. Clin Psychol: Sci Pract 2006;13:73-89. https://doi.org/10.1111/j.1468-2850.2006.00008.x.
- Glisson C, Durick M. Predictors of job satisfaction and organizational commitment in Human Service Organizations. Adm Sci Q 1988;33:61-8. https://doi.org/10.2307/2392855.
- Corbin J, Strauss A. Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory. Thousand Oaks, CA: SAGE Publications Ltd; 2008.
- Andreasen AR. Social marketing: its definition and domain. J Public Policy Mark 1994;13:108-14. https://doi.org/10.1177/074391569401300109.
- Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process 1991;50:179-211. https://doi.org/10.1016/0749-5978(91)90020-T.
- Rosenstock IM, Strecher VJ, Becker MH. Social learning theory and the health belief model. Health Educ Q 1988;15:175-83. https://doi.org/10.1177/109019818801500203.
- Cleary M, Horsfall J, Happell B. Developing practice in mental health settings. Int J Ment Health Nurs 2010;19:45-52. https://doi.org/10.1111/j.1447-0349.2009.00632.x.
- Thompson DA, O’Leary K, Jensen E, Scott-Findlay S, O’Brien-Pallas L, Estabrooks CS. The relationship between busyness and research utilization: it is about time. J Clin Nurs 2008;17:539-48. https://doi.org/10.1111/j.1365-2702.2007.01981.x.
- Yadav BL, Fealy G. Irish psychiatric nurses’ self-reported barriers, facilitators and skills for developing evidence-based practice. J Psychiatr Ment Health Nurs 2012;19:116-22. https://doi.org/10.1111/j.1365-2850.2011.01763.x.
- Aarons GA, Ehrhart MG, Farahnak LR, Hurlburt MS. Leadership and organizational change for implementation (LOCI): a randomized mixed method pilot study of a leadership and organization development intervention for evidence-based practice implementation. Implement Sci 2015;10. https://doi.org/10.1186/s13012-014-0192-y.
- Damanpour F, Schneider M. Phases of the adoption of innovation in organizations: effects of environment, organization and top managers. Br J Manag 2006;17:215-36. https://doi.org/10.1111/j.1467-8551.2006.00498.x.
- Gumusluoglu L, Ilsev A. Transformational leadership and organizational innovation: the roles of internal and external support for innovation. J Prod Innov Manage 2009;26:264-77. https://doi.org/10.1111/j.1540-5885.2009.00657.x.
- Scott SG, Bruce RA. Determinants of innovative behavior: a path model of individual innovation in the workplace. Acad Manage J 1994;37:580-607. https://doi.org/10.2307/256701.
- Aarons GA, Sommerfeld DH. Leadership, innovation climate, and attitudes toward evidence-based practice during a statewide implementation. J Am Acad Child Adolesc Psychiatry 2012;51:423-31. https://doi.org/10.1016/j.jaac.2012.01.018.
- De Hoogh AHB, Den Hartog DN, Koopman PL, Thierry H, Van den Berg PT, Van der Weide JG, et al. Leader motives, charismatic leadership, and subordinates’ work attitude in the profit and voluntary sector. Leadersh Q 2005;16:17-38. https://doi.org/10.1016/j.leaqua.2004.10.001.
- Aarons GA, Woodbridge M, Carmazzi A. Examining Leadership, Organizational Climate and Service Quality in a Children’s System of Care 2003.
- Aarons GA, Sawitzky AC. Organizational culture and climate and mental health provider attitudes toward evidence-based practice. Psychol Serv 2006;3:61-72. https://doi.org/10.1037/1541-1559.3.1.61.
- Corrigan PW, Lickey SE, Campion J, Rashid F. Mental health team leadership and consumers satisfaction and quality of life. Psychiatr Serv 2000;51:781-5. https://doi.org/10.1176/appi.ps.51.6.781.
- Aarons GA, Sommerfeld DH, Willging CE. The soft underbelly of system change: the role of leadership and organizational climate in turnover during statewide behavioral health reform. Psychol Serv 2011;8:269-81. https://doi.org/10.1037/a0026196.
- Aarons GA, Ehrhart MG, Moullin JC, Torres EM, Green AE. Testing the leadership and organizational change for implementation (LOCI) intervention in substance abuse treatment: a cluster randomized trial study protocol. Implement Sci 2017;12. https://doi.org/10.1186/s13012-017-0562-3.
- Aarons GA, Sommerfeld DH, Walrath-Greene CM. Evidence-based practice implementation: the impact of public versus private sector organization type on organizational support, provider attitudes, and adoption of evidence-based practice. Implement Sci 2009;4. https://doi.org/10.1186/1748-5908-4-83.
- Brimhall KC, Fenwick K, Farahnak LR, Hurlburt MS, Roesch SC, Aarons GA. Leadership, organizational climate, and perceived burden of evidence-based practice in mental health services. Adm Policy Ment Health 2016;43:629-39. https://doi.org/10.1007/s10488-015-0670-9.
- Aarons GA, Ehrhart MG, Farahnak LR. The implementation leadership scale (ILS): development of a brief measure of unit level implementation leadership. Implement Sci 2014;9:45-5. https://doi.org/10.1186/1748-5908-9-45.
- Ehrhart MG, Aarons GA, Farahnak LR. Going above and beyond for implementation: the development and validity testing of the Implementation Citizenship Behavior Scale (ICBS). Implement Sci 2015;10. https://doi.org/10.1186/s13012-015-0255-8.
- Aarons GA, Cafri G, Lugo L, Sawitzky A. Expanding the domains of attitudes towards evidence-based practice: the evidence-based practice attitude scale-50. Adm Policy Ment Health 2012;39:331-40. https://doi.org/10.1007/s10488-010-0302-3.
- Abu-Bader S, Jones TV. Statistical mediation analysis using the Sobel test and Hayes SPSS process macro. Int J Quan Qual Res Meth 2021;9:42-61.
- Hayes AF. Beyond Baron and Kenny: statistical mediation analysis in the new millennium. Commun Monogr 2009;76:408-20. https://doi.org/10.1080/03637750903310360.
- Aarons GA. Transformational and transactional leadership: association with attitudes toward evidence-based practice. Psychiatr Serv 2006;57:1162-9. https://doi.org/10.1176/ps.2006.57.8.1162.
- Klein KJ, Conn AB, Sorra JS. Implementing computerized technology: an organizational analysis. J Appl Psychol 2001;86:811-24. https://doi.org/10.1037/0021-9010.86.5.811.
- Egeland KM, Skar AS, Endsjø M, Laukvik EH, Bækkelund H, Babaii A, et al. Testing the leadership and organizational change for implementation (LOCI) intervention in Norwegian mental health clinics: a stepped-wedge cluster randomized design study protocol. Implement Sci 2019;14. https://doi.org/10.1186/s13012-019-0873-7.
- Bowie CR, Bell MD, Fiszdon JM, Johannesen JK, Lindenmayer JP, McGurk SR, et al. Cognitive remediation for schizophrenia: an expert working group white paper on core techniques. Schizophr Res 2020;215:49-53. https://doi.org/10.1016/j.schres.2019.10.047.
- SIGN . SIGN 131 • Management of Schizophrenia 2013. www.sign.ac.uk/assets/sign131.pdf (accessed 1 November 2022).
- American Psychiatric Association . The American Psychiatric Association Practice Guideline for the Treatment of Patients With Schizophrenia 2020. .psychiatry.org/psychiatrists/practice/clinical-practice-guidelines (accessed 1 November 2022).
- Deutsches Ärzteblatt. Schizophrenia: Clinical Practice Guideline 2020. www.aerzteblatt.de/int/archive/article/214278 (accessed 1 November 2022).
- National Institute for Health and Care Excellence . Rehabilitation for Adults With Complex Psychosis 2020. www.nice.org.uk/guidance/ng181 (accessed 1 November 2022).
- Fairburn CG, Allen E, Bailey-Straebler S, O’Connor ME, Cooper Z. Scaling up psychological treatments: a countrywide test of the online training of therapists. J Med Internet Res 2017;19. https://doi.org/10.2196/jmir.7864.
- Hamilton-Westa K, Batesb A, Hothamc S, Wilsond P. Development of a training programme for primary care mental health staff to support management of depression and anxiety in long-term conditions. Prim Health Care Res Dev 2019;20. https://doi.org/10.1017/S1463423618000658.
- Nowell LS, Norris JM, White DE, Moules NJ. Thematic analysis: striving to meet the trustworthiness criteria. Int J Qual Methods 2017;16. https://doi.org/10.1177/1609406917733847.
- Cella M, Wykes T. The nuts and bolts of cognitive remediation: exploring how different training components relate to cognitive and functional gains. Schizophr Res 2019;203:12-6. https://doi.org/10.1016/j.schres.2017.09.012.
- Wykes T, Joyce E, Velikonja T, Watson A, Aarons G, Birchwood M, et al. The CIRCuiTS study (implementation of cognitive remediation in early intervention services): protocol for a randomised controlled trial. Trials 2018;19. https://doi.org/10.1186/s13063-018-2553-3.
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry 1998;59:22-33.
- Kiresuk TJ, Smith A, Cardillo JE. Goal Attainment Scaling: Applications, Theory, and Measurement. Hillsdale, NJ: Lawrence Erlbaum Associates; 1994.
- Barnett JH, Robbins TW, Leeson VC, Sahakian BJ, Joyce EM, Blackwell AD. Neurosci Biobehav Rev. 2010.
- Heaton RK, Chelune GJ, Talley JL, Kay GG, Curtiss G. Wisconsin Card Sorting Test Manual: Revised and Expanded. Odessa, TX: Psychological Assessment Resources; 1993.
- Lezak MD. Neuropsychological Assessment. New York: Oxford University Press; 1995.
- Rey A, Osterrieth PA. Translations of excerpts from Andre Rey’s Psychological examination of traumatic encephalopathy and P.A. Osterrieth’s The Complex Figure Copy Test. Clin Neuropsychol 1993;7:4-21.
- Forbes C, Blanchard JJ, Bennett M, Horan WP, Kring A, Gur R. Initial development and preliminary validation of a new negative symptom measure: the Clinical Assessment Interview for Negative Symptoms (CAINS). Schizophr Res 2010;124:36-42. https://doi.org/10.1016/j.schres.2010.08.039.
- Lader D, Short S, Gershuny J. The Time Use Survey 2005: How We Spend Our Time. London: Office for National Statistics; 2006.
- Rosenberg M. Society and the Adolescent Self-Image. Middletown, CT: Wesleyan University Press; 1989.
- The EuroQol Group . EuroQol – a new facility for the measurement of health-related quality of life. Health Policy 1990;16:199-208. https://doi.org/10.1016/0168-8510(90)90421-9.
- Beecham J, Knapp M. Measuring Mental Health Needs. London: Gaskell; 2001.
- Wechsler D. Wechsler Test of Adult Reading (WTAR). San Antonio, TX: The Psychological Corporation; 2001.
- Wechsler D. Wechsler Adult Intelligence Scale. San Antonio, TX: The Psychological Corporation; 1997.
- Kay SR, Fiszbein A, Opler LA. The Positive and Negative Syndrome Scale (PANSS) for schizophrenia. Schizophr Bull 1987;13:261-76. https://doi.org/10.1093/schbul/13.2.261.
- White IR, Thompson SG. Adjusting for partially missing baseline measurements in randomized trials. Stat Med 2005;24:993-1007. https://doi.org/10.1002/sim.1981.
- National Institute for Health and Care Excellence . How NICE Measures Value for Money in Relation to Public Health Interventions n.d. www.nice.org.uk/Media/Default/guidance/LGB10-Briefing-20150126.pdf (accessed 27 July 2021).
- Ventura J, Hellemann GS, Thames AD, Koellner V, Nuechterlein KH. Symptoms as mediators of the relationship between neurocognition and functional outcome in schizophrenia: a meta-analysis. Schizophr Res 2009;113:189-99. https://doi.org/10.1016/j.schres.2009.03.035.
- Kambeitz-Ilankovic L, Betz LT, Dominke C, Haas SS, Subramaniam K, Fisher M, et al. Multi-outcome meta-analysis (MOMA) of cognitive remediation in schizophrenia: revisiting the relevance of human coaching and elucidating interplay between multiple outcomes. Neurosci Biobehav Rev 2019;107:828-45. https://doi.org/10.1016/j.neubiorev.2019.09.031.
- Landau S, Emsley R, Dunn G. Beyond total treatment effects in randomised controlled trials: baseline measurement of intermediate outcomes needed to reduce confounding in mediation investigations. Clin Trials 2018;15:247-56. https://doi.org/10.1177/1740774518760300.
- Wykes T, Reeder C, Landau S, Everitt B, Knapp M, Patel A, et al. Cognitive remediation therapy in schizophrenia: randomised controlled trial. Br J Psychiatry 2007;190:421-7. https://doi.org/10.1192/bjp.bp.106.026575.
List of abbreviations
- AE
- adverse event
- CAINS
- Clinical Assessment Interview for Negative Symptoms
- CANTAB
- Cambridge Neuropsychological Test Automated Battery
- CBT
- cognitive–behavioural therapy
- CEAC
- cost-effectiveness acceptability curve
- CIRCuiTS
- Computerised Interactive Remediation of Cognition – a Training for Schizophrenia
- CR
- cognitive remediation
- CRS
- cognitive remediation satisfaction
- CRT
- cognitive remediation therapy
- CSRI
- Client Service Receipt Inventory
- EBP
- evidence-based practice
- EBPAS
- Evidence-Based Practice Attitude Scale
- ECLIPSE
- Enhancing Cognition and quality of Life in early PSychosiEs
- EIS
- Early Intervention Services
- EQ-5D
- EuroQol-5 Dimensions
- FAST-R
- Feasibility and Acceptability Support Team for Researchers
- GAS
- Goal Attainment Scale
- ICS
- Implementation Climate Scale
- ILS
- Implementation Leadership Scale
- ITT
- intention to treat
- LMS
- learning management system
- MAMS
- multiarm multisite
- NICE
- National Institute for Health and Care Excellence
- PAG
- Patient Advisory Group
- PANSS
- Positive and Negative Symptom Scale
- PPI
- patient and public involvement
- PSS
- Personal Social Services
- QALY
- quality-adjusted life-year
- RSE
- Rosenberg Self-Esteem Scale
- SOFAS
- Social and Occupational Functioning Assessment Scale
- TAU
- Treatment as Usual
- WAI
- Working Alliance Inventory
- WP
- work package
Notes
-
Study 9 Additional explanation of statistical methods for sensitivity analyses
-
Study 9 Primary and secondary outcomes by time of assessment
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/LMFP9667).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
