Notes
Article history
The research reported in this issue of the journal was funded by PGfAR as project number RP-PG-0610-10112. The contractual start date was in May 2012. The final report began editorial review in October 2017 and was accepted for publication in February 2019. As the funder, the PGfAR programme agreed the research questions and study designs in advance with the investigators. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PGfAR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Luke Vale was a member of the National Institute for Health Research (NIHR) Programme Grants for Applied Research programme panel from 2008 to 2016, a member of the NIHR Health Technology Assessment programme Clinical Evaluation and Trials panel from 2014 to 2018, and Director of the NIHR Research Design Service North East and North Cumbria from 2012 to 2018.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2019. This work was produced by Colver et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2019 Queen’s Printer and Controller of HMSO
SYNOPSIS
Setting the scene
All young people – defined by the World Health Organization as any person between the ages of 10 and 24 years1 – experience transformations in their lives and their understanding of the world as they grow older. Although it may not be possible for all, young people need to achieve four crucial developmental tasks: (1) consolidate their identity, (2) achieve independence from their parents, (3) establish adult relationships outside their families, and (4) find a vocation. 2 A fundamental principle is that when young people have a need for health care, this care must be provided in a manner that is appropriate to their stage of development. The term used to describe this principle is developmentally appropriate health care (DAH). DAH should underpin all health care for young people and in particular for those with a long-term condition. However, the term has been ill-defined and used inconsistently; in turn, this has made it difficult to assess whether or not it has been implemented in reported studies. 3,4
Furthermore, a young person with a long-term condition has to move from children’s to adults’ services. This process is called ‘transition’ and is defined as the purposeful, planned process that addresses the medical, psychosocial, educational and vocational needs of adolescents and young adults with chronic physical, neurodevelopmental and medical conditions as they move from child-centred to adult-oriented health care systems. 5 ‘Transfer’ is the formal ‘event’ when the medical care of a young person is moved from children’s to adults’ services.
The UK and Australia are the only two high-income countries with national guidance on transition, although academies and specialty groups also make recommendations. 7–9 The need for improved transitional health care is set out in recent policy and recommendations, such as advice from the Department of Health and Social Care in 200610 and 2008,11 recommendation 23 from the 2010 Kennedy Report,12 the 2015 Care Quality Commission report From the Pond to the Sea13 and National Institute for Health and Care Excellence (NICE) guidance on transition in 2016. 14 Commissioners, provider organisations and clinicians have a role to play in such improvements.
The number of young people surviving to adulthood is increasing; many children with long-term conditions that once commonly caused death in childhood now live into adulthood. In a typical NHS Trust serving a population of 270,000, about 100 young people with chronic illness, a complex physical impairment or a neurodevelopmental disorder reach the age of 16 years each year. 15 As transition takes place over about 7 years, the number in transition at any time in a typical trust is approximately 700.
New understanding of adolescent and young adult brain development and its associations with behaviour16 further reinforce the need for transitional health care to be set in a developmental context.
Transition is important because:
-
Many young people with a range of long-term conditions have poor social outcomes, following transition, in areas of social participation, employment or further education. For example, young adults with long-term conditions, such as cancer, congenital bowel anomalies and renal disease,17 congenital heart disease18 and chronic physical disability,19 and those with chronic illness,20,21 have demonstrated delays in autonomy, psychosexual and social development. Furthermore, few young adults with neurodevelopmental disorders, such as autism spectrum disorder (ASD), attain their potential for participation in society. 22
-
Chronic illnesses, such as diabetes mellitus and renal disease,23 are prone to deteriorate during the adolescent years; they need frequent medical monitoring and treatment optimisation. Young people reported finding it difficult to negotiate transition in services for haematology,24 type 1 diabetes mellitus,25 epilepsy,26,27 physical disability28,29 and rheumatology. 30 Conditions such as cerebral palsy give rise to symptoms that interfere with daily living, such as pain, spasticity and seizures. Most mental health disorders of adults develop during adolescence just at the time when the commissioning and provision of services is most likely to move from child- and family-focused to adult symptom-orientated mental health services. There are concerning rejection rates after solid organ transplants. 31
-
Some adults’ services are not routinely provided (e.g. for adults with attention deficit hyperactivity disorder32 or ASD). Other adults’ services, such as physiotherapy and mental health services,33 have different, and usually narrower, entry criteria. Some services that require multidisciplinary co-ordination (e.g. for those with cerebral palsy) are provided in childhood but are rarely provided in adulthood. 34
Central government guidance and direction has sought to improve services for transitional health care but there remains a need to improve services. 13,14 In 2017, a national CQUIN (Commissioning for Quality and Innovation National Goals)35 was introduced around transitions from children to young people’s mental health services.
Developments in health-care transition during the period of the research programme
Since the start of the programme in 2012, there have been developments in the field of transition of which we have taken account.
Results of published evaluative studies remain difficult to generalise from because they are usually about an intervention in one clinical setting, for one condition and using a locally designed intervention. The Cochrane review36 of interventions to improve transition, published in 2016, confirmed the lack of good evidence. Studies with more rigorous protocols have since been conducted. 37–40 A systematic review41 in 2017 reported the limitations of methods used in comparative studies of transition interventions. It found, for example, that most were small, single-condition studies, used unvalidated questionnaires, and did not report the age of transfer or the age at and time of questionnaire completion. In designing our research, we had anticipated such methodological limitations and addressed them in the methods we used for the longitudinal study [work packages (WPs) 2.1, 2.2 and 2.3].
Two Delphi studies proposed a suite of outcomes42 and process measures43 for evaluating transition. Our choice of outcomes in the longitudinal study is in line with these international studies.
A synthesis of qualitative studies of young people’s views about transition44 confirmed that there is much literature about the issues and difficulties encountered, and supported our decision not to undertake further exploratory work with young people.
As anticipated, arrangements for commissioning NHS services have continued to change during the research programme. However, the commissioning focus of our research concerns ‘what’ and ‘how’ to commission. We intended that our findings would be relevant to any commissioning structure, including whether or not commissioning and service provision are brought together in the same organisation.
Aims and objectives of the research programme
The overall aim of the programme was to promote the subjective well-being and health of young people with long-term conditions by generating evidence to enable NHS commissioners and trusts to facilitate the successful transition of young people from children’s to adults’ health care, thereby improving health and social outcomes.
To address this aim, the programme had three objectives:
-
to work with young people with long-term conditions to determine what successful transition means to them and what is important in their transitional health care
-
to identify the features of transitional health care that are effective and efficient
-
to determine how transitional health care should be organised, provided and commissioned.
Three separate WPs addressed each of these objectives. We present a summary of each WP and then bring together the results of all nine strands to inform our conclusions and their implications. As an overview, and to aid orientation, the WPs are summarised in Box 1, followed by Figure 1, which shows how the WPs influenced each other.
-
To form and maintain a young people’s advisory group for the programme.
-
To consult with the young people’s advisory group on all aspects of the programme.
-
To explore the usefulness of a ‘health passport’ through research co-led by the young people’s advisory group.
-
To explore the importance that young people attach to different components of successful transition.
-
To examine whether or not the proposed beneficial features of services predict outcomes for young people with type 1 diabetes mellitus, cerebral palsy or ASD and an associated mental health problem.
-
To determine the resource use and costs of care.
-
To investigate the factors that promote or inhibit the introduction of the proposed beneficial features of services.
-
To assess the relative efficiency of illustrative models of transition.
-
To identify, describe and understand the factors that enable or inhibit the introduction of organisation-wide DAH for young people.
-
To identify the structures, processes and relationships between commissioning entities in the NHS and other agencies relevant to transitional health care.
-
To identify the facilitators of and barriers to commissioning for transitional health care.
-
To identify how transitional health care could be better commissioned.
-
To synthesise learning from the research programme on ‘what’ and ‘how’ to commission.
-
To learn about the most useful way to provide research-based evidence to inform commissioners.
FIGURE 1.
How the WPs influenced each other. DCE, discrete choice experiment; UP, United Progression.
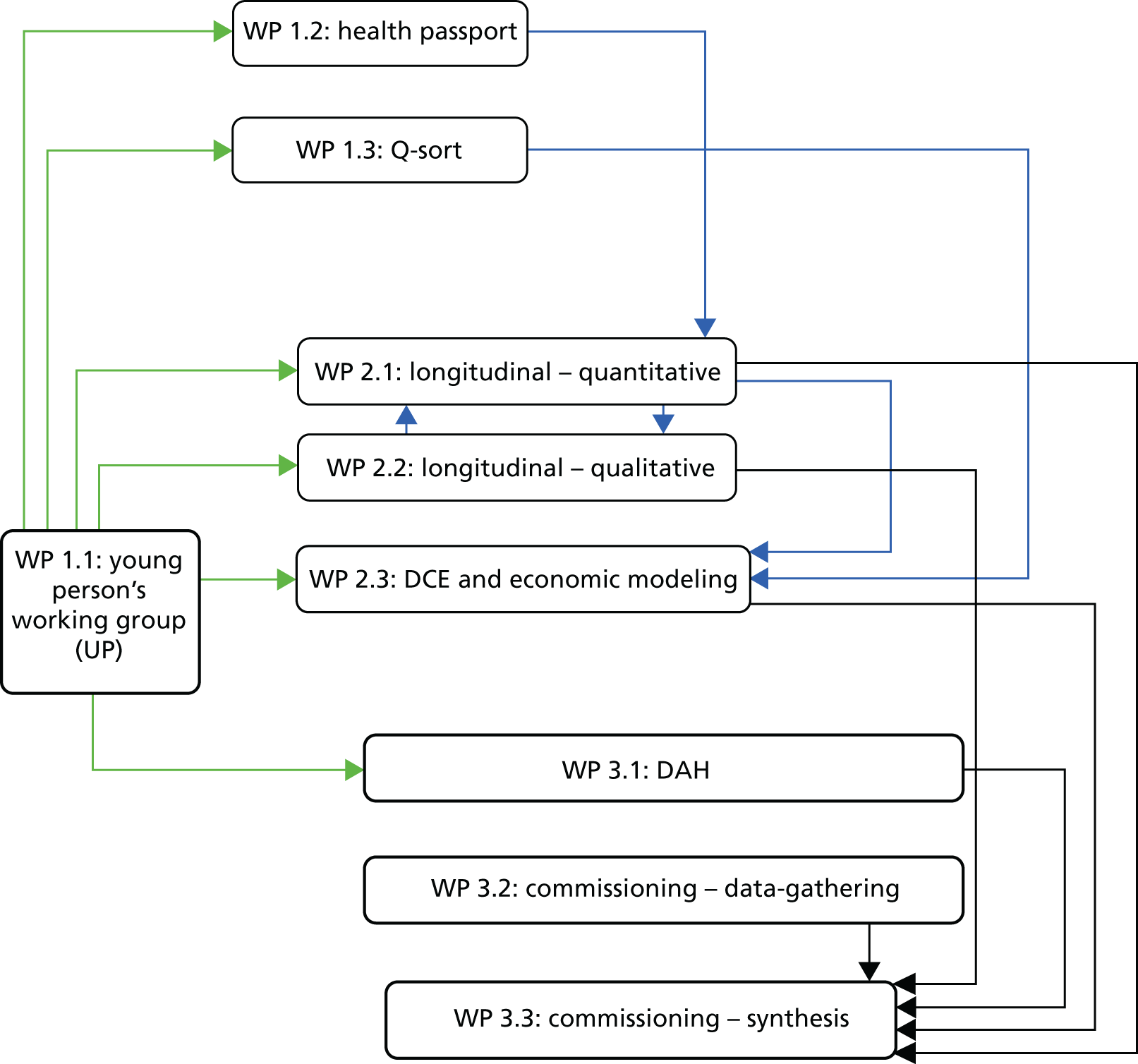
At the end of the account of each WP, we indicate its links to the other WPs and how each WP contributed to the seven main implications of our work.
In Appendix 1 is a summary of work we completed before applying for a Programme Grant.
In Appendix 2 are the management arrangements for the programme and a diagram showing how key groups interacted.
Work package 1.1: work of the United Progression group
Addressing objective 1: to work with young people with long-term conditions to determine what successful transition means to them and what is important in their transitional health care
We ensured that the contributions of the young people were integrated with the research programme in meaningful ways for the young people and the research. Funds from the programme ensured that enough staff time was available to facilitate meaningful involvement of young people throughout the 5-year programme.
The young people called their group United Progression (UP; the term UP will be used in the remainder of this report).
Aims
-
To form and maintain UP.
-
To consult with UP throughout the duration of the programme.
Method
Preliminary work during the development of the grant application
Discussion between a time-limited young person’s group and co-applicants concluded that a ‘partnership’ approach to involvement should be the fundamental value. Development of skills and confidence would be required to enable young people to contribute to a research programme. Peer support workers would be recruited to facilitate the induction and skills development of the advisory group.
Development of and recruitment to UP
Three part-time peer support workers were appointed. Recruitment to UP was undertaken by the programme’s patient and public involvement (PPI) lead.
At the start of the programme, UP members were aged between 15 and 20 years. All had experience of accessing a range of health-care services. Recruitment occurred in a range of ways: via young people’s health services, local schools and local young people’s health action groups. With membership growing steadily in the early months, the group consisted of over 20 members, and active participation fluctuated over time in line with exams, family events and other commitments. Most meetings had around eight members present. UP had 26 members over the 5 years. By the end of the programme, eight of the original members still attended regularly; this was crucial, as they brought their 5-year insights to the final research outputs.
UP met monthly over the 5-year programme. UP members had a hot meal and socialised before meetings began.
UP members were involved in advisory, consultative and dissemination roles – not as research participants.
Maintaining and sustaining the engagement of UP
Induction for UP members included a description of the project, a meeting with members of the management team, a glossary of research terminology, and attending and presenting at the programme’s launch.
Each monthly meeting was planned to be enjoyable for UP, and to ensure that there was enough guidance and support for the tasks that UP had agreed to do. Careful planning was needed for communication between UP and the programme management board to ensure fruitful interaction. The PPI lead was the link between UP and the board. The board set out timely, structured commissioning briefs for the PPI lead, rather than sending direct requests to UP. The PPI lead ensured that tasks were relevant and achievable and that young people had the skills to deliver them.
Impact on the programme
UP provided input to many WPs. For example, UP piloted the Q-sort tool in WP 1.3. UP commented on the ‘proposed beneficial features’ (PBFs) that were central to the longitudinal research described in WP 2.1; subsequently, two features (‘transfer readiness’ and ‘direct payments’) were dropped as they were unclear or not relevant to health-care transition. UP designed recruitment and retention materials for the longitudinal research of WP 2.1. UP responded to the findings of WPs; for example, they made a training DVD (digital versatile disc) on the importance and implementation of DAH for WP 3.1.
UP contributed directly to dissemination activities throughout the programme. They presented at the launch in Newcastle upon Tyne in October 2012, and ran a session at the final dissemination conference in London in October 2017. They wrote blogs for the programme’s website. UP representatives sat on the interview panels for the research associates and contributed to their induction, and sat on the external advisory board.
UP advocated for the programme and offered their skills and expertise to local and national groups. UP helped to develop training materials for doctors in partnership with the Royal College of Paediatrics and Child Health, MindEd and the Association for Young People’s Health. This generated several videos. UP represented the Transition programme at the Department of Health and Social Care’s ‘Takeover Day’ in London in 2015.
Finally, UP worked with the Council for Disabled Children to disseminate their experiences and present early results of the programme to other young people’s groups between autumn 2015 and spring 2017. These meetings also enabled young people involved in research elsewhere to share their experiences with UP. In these meetings, UP disseminated results of the programme relating to the Q-sort study (WP 1.3), health passport work (WP 1.2) and the concept of DAH (WP 3.1). Meetings took place with Child Health Action Team (CHAT) North Tyneside; two Croydon groups; Together for Short Lives young person group; St Oswald’s Hospice, Newcastle upon Tyne; Transition2 group in Derby; and the Chatterboxes youth group in Bournemouth. Three facilitator guides (one example is given in Appendix 10) were developed for other groups to use, especially voluntary organisations.
In Appendix 3 are the certificate UP designed for participants in the longitudinal study (WP 2.1); UP’s Microsoft PowerPoint® (Microsoft Corporation, Redmond, WA, USA) presentation for the programme’s launch; and one of the conference posters prepared by UP.
Key findings
-
UP influenced many of the WPs of the programme, and was involved in a wide range of dissemination and advocacy activities.
-
As the members of UP grew in confidence, their contributions became increasingly useful to the programme. The support and training offered to UP were very important, although they were resource intensive.
-
Members of UP reported that they enjoyed the challenges, the relationships they formed with other young people and their greater understanding of research.
Inter-relationships with other parts of the programme
UP influenced many aspects of the programme through their input to several WPs. The only two WPs they did not influence directly were those (WPs 3.2 and 3.3) on commissioning for transition.
Further analysis and discussion of the role of UP is presented in Involvement of patients, the voluntary sector and the public. This section also summarises the internal evaluation of the work UP undertook and points to our published paper. 45
Although not unique to our programme, when professionals, managers and commissioners attend meetings where young people contribute and have been closely involved in the work presented, such young-person involvement strengthens the assurance that the audience attaches to the work.
UP thoughts and opinions directly influenced implication 2 on DAH and the toolkit we developed to assist with introduction of such care across an organisation. By advising on questionnaire content, wording and feasibility, UP directly influenced both what research participants were asked to complete and the key implications of our work, namely implication 4 concerning joint planning, implication 5 concerning young people’s approaches to transition, implication 6 concerning features associated with better outcomes and implication 7 concerning features likely to optimise service uptake.
Work package 1.2: health passport
Addressing objective 1: to work with young people with long-term conditions to determine what successful transition means to them and what is important in their transitional health care
We determined that engaging UP in a research study co-led by them would help them better understand research processes and generate knowledge important to the programme. UP chose ‘health passports’ as the focus of their work. These are usually a portable means of recording health information. 46,47
Aim
-
To explore the usefulness of health passports in a project co-led by UP.
Methods
UP examined a range of passports designed to help young people navigate health services and concluded that there was no clear definition of what a ‘health passport’ was. As there were many health passports already available, UP decided that it would not be useful to develop another one. However, as no robust analysis of health passport use has been undertaken, UP aimed to examine the use and usefulness of some health passports already used by young people with long-term conditions.
UP contacted health-care professionals from a children’s hospital, a physical disabilities team, an adolescent rheumatology team and a voluntary organisation. UP asked professionals about their experience of health passports and this helped to identify questions and issues to explore with young people, such as:
-
What kind of passports are used and what are their essential components?
-
Who uses health passports and who benefits from them?
-
How are they used and how are young people supported to use them?
UP then worked with the patient satisfaction team in the lead trust to devise a questionnaire to assess the views of young people about health passports. Then the professionals in the above organisations helped UP link to young people who used health passports. However, this proved difficult as ethics and research governance permissions were required; it was impossible to achieve this across several organisations within the available time.
Analysis
Young people from one service returned questionnaires (n = 13) and, although the response rate was low (20%), interesting findings emerged. None of the 13 participants said that they completed the health passport alone; the majority said that they thought passports were ‘useful’, but half of them never took them to health-care appointments. The passports were considered more useful to health professionals than to young people themselves.
Strengths and limitations
This work identified some qualitative findings about health passports. However, the work did not generate, as intended, enough quantitative data from which to draw definitive conclusions. It was difficult to obtain all of the research governance permissions in a timely manner to enable UP to approach as many young people as they had intended. The approaches also depended on the willingness and time of local health professionals to approach young people. For other parts of the programme, all such preliminary contacts and undertakings had been formalised before the programme started. For this work, co-generated by UP, planning could not begin until UP had worked through its ideas, which was at least 1 year into the programme.
Such challenges have been reported before. A Dutch group undertook participatory research with young people with chronic illness48 and concluded that, although the activity benefited the young people, it was an inefficient and unreliable way to gather research data. Similar benefits to young people were reported in a study in Vancouver. 49
Key findings
-
There is a lack of conceptual clarity and no clear definition about what is meant by ‘health passport’.
-
The work raises questions about whether or not a health passport is a tool truly held by young people. Who should complete it and when? Do young people really want it to ‘travel’ with them to appointments and between services?
-
Even studies by enthusiasts for health passports found difficulties. Participants used their document only occasionally and its perceived utility was modest;50 only one-quarter completed a survey, and, of those who then agreed to a telephone discussion, only one-third had used their passport. 46
Inter-relationship with other parts of the programme
This WP contributed directly to the longitudinal study WP 2.1. A health passport was discussed as a candidate PBF of transitional health care. However, the initial work that UP undertook indicated that ‘health passport’ meant different things to different people, and although it was considered useful by some professionals, young people appeared to value it much less. We therefore decided not to include health passport as a PBF. This decision was vindicated by the subsequent survey work that UP undertook.
The confidence that members of UP gained by carrying out their research and their greater appreciation of research methodology enhanced the quality of all of their contributions to the programme, which were set out in the earlier account of WP 1.1. It also increased their self-confidence, and this is discussed in Involvement of patients, the voluntary sector and the public and in our associated published paper. 45
UP presented the health passport work at the Department of Health and Social Care’s ‘Takeover Day’, where interest was expressed in taking the passport work forward nationally.
UP presented their work as a poster at several meetings, including the final dissemination meeting at The King’s Fund, London, in October 2017. UP’s poster presentation is in Appendix 4.
Work package 1.3: Q-sort study
Addressing objective 1: to work with young people with long-term conditions to determine what successful transition means to them and what is important in their transitional health care
Qualitative research undertaken with young people during and after transition has been systematically reviewed. The first review51 identified four main issues: young people’s feelings and concerns, young people’s recommendations about components of transition services, outcomes after transfer and mode of transfer. The second review44 examined the point of transfer and identified four themes: facing changes in significant relationships, moving from a familiar to an unknown ward culture, being prepared for transfer and achieving responsibility.
The work of this WP has been published in Hislop et al. 52 and material in this section is based on that paper. Reprinted from Journal of Adolescent Health, Vol. 59, Hislop J, Mason H, Parr IR, Vale L, Colver A, Views of young people with chronic conditions on transition from pediatric to adult health services, 245–53, Copyright 2016, with permission from Elsevier.
Aims
-
To explore the views of young people about transition.
-
To identify and describe these views using Q-methodology.
Methods
Q-methodology combines quantitative and qualitative methods to investigate the range of possible views on a subject. It involves the rank ordering (Q-sort) by participants of a set of statements (Q-set) about a topic, after which a by-person factor analysis of the Q-sorts is used to reveal shared perspectives on the topic. Further details are in our published paper. 52
The Q-set of statements relevant to young people in transition was generated using quotations from two reviews of qualitative studies44,51 and our own mapping review of service models. 53 These were coded into a set of emergent themes, ‘planning’, ‘staff related’, ‘maturity’, ‘parent-related’ and ‘other’, which were then recategorised into several subthemes. One representative statement from each subtheme was selected. Following consultation with UP, the wording was adjusted and each final statement was prepared for sorting by participants onto a triangular grid. The statements are set out in table 1 of the published article. 52
Q-methodology requires that individuals in the sample are likely to hold different views. Therefore, maximum variation sampling was used, by age, gender, health condition and whether or not the young person had transferred. We sought 45 young people, aged 14–22 years, with a long-term condition that would soon require or had recently required them to transfer from children’s to adults’ services. Those with intellectual disability who could not complete the Q-sort were excluded. The number of participants is usually, but not necessarily, smaller than the Q-set. 54 The aim is to have four or five persons defining each anticipated viewpoint; there are often two to four, and rarely more than six. Accordingly, the breadth and diversity of viewpoints is probably best achieved when a participant group contains between 40 and 60 participants. 55
Clinicians from 10 adults’ and children’s specialties in a NHS Trust with tertiary and secondary care responsibilities invited young people with long-term conditions to participate. Q-sorts were administered face to face by the researcher.
Analysis
The degree to which an individual’s Q-sort corresponds to each factor derived from the factor analysis is given by their ‘factor loading’. This is a correlation coefficient between +1 and –1; the closer to 1, the more similar an individual’s Q-sort is to the factor. Individuals are ‘exemplars’ for a factor if they have a significant factor loading on that factor alone (p ≤ 0.01). We used PQMethod software (version 2.11; Peter Schmolck, University of the Bundeswehr, Munich, Germany) with centroid factor analysis followed by varimax rotation. 56 Outputs include the number of exemplars per factor, eigenvalues and factor variance, which provide information on the proportion of variance for the entire study explained by each factor. These are used alongside the postsort qualitative information to determine the ‘factor solution’: the final number of factors identified.
For each factor, an idealised ‘composite’ Q-sort is computed, illustrating how a person with a factor loading of 1 would have laid out their statement cards. Attention is paid to statements that characterise each factor, for example those placed in the +3 and –3 position on the grid, and those statements that distinguish between factors.
We found that a four-factor solution was optimal from a statistical viewpoint and most meaningful in clinical terms.
Factor 1: young people with a ‘laid back’ approach to transition
These young people were not particularly worried about transition. They did not think that transition would make much difference to them and expected their new health team to provide similar care to that which they had experienced in children’s services. They were happy to be guided by staff on how to manage their condition and wanted continued involvement of their parents in their care. They also wanted to be well informed about their condition.
Factor 2: young people with an anxious approach to transition
For these individuals, transition mattered very much; it worried them, they did not want transfer to happen at a set age, and they wanted a written plan in place for this. They wanted to be able to say goodbye to their current doctors, and they thought that the post-transfer service would provide different care, and that seeing different staff might not help build trust. They thought that their condition was difficult to live with and all areas of their life were affected by it. They did not know what kinds of support would be available to them in future. They wanted their parents involved in their care.
Factor 3: young people with an autonomy-seeking approach to transition
These young people wanted independence and autonomy during transition and were characterised by their wish for the withdrawal of parental involvement in their care. They wanted doctors to speak to them, rather than to their parents. They wanted doctors to offer suggestions and choices but allow them to make decisions. They were more developmentally mature in terms of their responses to statements about leaving home and living independently. They preferred flexible timings for clinics and wanted to leave the paediatric environment. They showed that they wanted to meet adult staff before transfer, and then see the same doctors in order to develop trust.
Factor 4: young people with a socially oriented approach to transition
These young people valued social interaction with family, peers and professionals to assist transition. They thought that it was important to interact with those involved in their care. They wanted to meet others in a similar situation and wanted their parents to remain involved in their care. They were comfortable with other staff being present at consultations and, for example, did not find it difficult if students were present. They felt attached to doctors (wanting a chance to say goodbye before transfer) and wanted a particular person at the clinic to help them plan the practical side of managing their condition.
There is more discussion of these factors in our published paper. 52
Strengths and limitations
Owing to the purposive sampling, claims cannot be made about how many individuals hold each point of view. Nor can inferences be made about subgroup sizes based on gender, age or condition.
We do not know if the four styles are stable over time. The views of some young people might relate to underlying personality characteristics and, therefore, might not change substantially. Alternatively, preferences may change as young people develop or as their health or health care changes.
Key findings
-
Reviews of qualitative studies44,51 of transition have not revealed how individuals approach the dilemmas they face. Our results add a new dimension.
-
Four factors or interaction styles of approaching transition were identified: ‘laid back’, ‘anxious’, ‘autonomy-seeking’ and ‘socially oriented’.
-
These four diverse styles show that there is not one view on transition. Thus, a ‘one size fits all’ approach is inappropriate and tailoring care to each to each young person is crucial.
Inter-relationship with other parts of the programme
The recognition of these four interaction styles for approaching transition is a new finding and yields one of the seven key implications of the programme: implication 5.
The Q-sort study contributed to the design of the discrete choice experiment (DCE) (WP 2.3), which identified aspects of transitional health care that young people are more likely to take up. This in turn informed the economic analyses (WP 2.3).
Work package 2.1: longitudinal study (quantitative)
Addressing objective 2: to identify the features of transitional health care that are effective and efficient
Although there is some preliminary evidence of the benefit of transition programmes in diabetes care,57,58 there has been little research with young people with complex physical impairments. 59 Furthermore, the lack of planned transfer to adult mental health services for young people with neurodevelopmental disorders has been highlighted. 60 Therefore, to be as generalisable as possible across long-term conditions, a cohort of young people with one of three very different conditions was recruited: individuals with type 1 diabetes mellitus as an exemplar of chronic illness; with cerebral palsy as an exemplar of complex physical impairment; and with ASD who continued to access children’s services for an associated mental health problem as an exemplar of neurodevelopmental disorder.
Following examination of published policy documents and research literature, nine proposed PBFs of services were identified and defined for the study. These were age-banded clinic, meet adult team before transfer, promotion of health self-efficacy, written transition plan, appropriate parent involvement, key worker, co-ordinated team, holistic life-skills training, and transition manager for clinical team. The Glossary provides the definitions of the features. Table 2 of the published protocol61 gives the details of the policy documents and tabulation of the research literature justifying their inclusion.
The following papers have been published from this WP:
-
Protocol61
-
Analysis of baseline data62
-
Young people’s experience of the PBFs63
-
Unmet needs of those with cerebral palsy64
-
Clinical course in diabetes mellitus65
-
Longitudinal analysis identifying that only three of the PBFs are associated with better outcomes. 66
Aims
To examine whether or not the PBFs of services are associated with better outcomes for young people with type 1 diabetes mellitus, cerebral palsy, or ASD and an associated mental health problem.
Hypothesis
In combination, and separately for type 1 diabetes mellitus, cerebral palsy and ASD, access to PBFs during the transition from children’s to adults’ health care predicts better health and social outcomes.
Methods
Sampling frame and site selection
In the UK, all young people with type 1 diabetes mellitus aged < 15 years attend secondary hospital care. Between June 2012 and October 2013, young people with type 1 diabetes mellitus were recruited from children’s services in five UK health-care provider NHS Trusts that were at different stages of development of transitional health care. These five NHS Trusts were in Greater London and north, south-west and south-east England. Young people with ASD and an associated mental health problem were recruited from four NHS Trusts, two of which claimed to have a readily available adults’ service to which to transfer young people. Similarly, all young people with ASD and an identified mental health problem attend specialised secondary care services. These four NHS Trusts were in north and south-west England. Young people with cerebral palsy were recruited from one NHS Trust in south-east England and randomly sampled from two regional population registers, the North of England Collaborative Cerebral Palsy Survey67 and the Northern Ireland Cerebral Palsy Register,68 that covered 17 NHS Trusts.
We conducted a survey, before submitting our application, that showed that the trusts varied greatly in the extent to which they provided PBFs; this was confirmed by the formal survey in all the trusts described in the previous paragraph undertaken during the study (see Proposed beneficial features).
All participants were aged 14–18 years 11 months at recruitment and had not transferred to adults’ services. Participants had no significant learning disabilities.
Procedures
Young people and their parent(s) were visited on four occasions, 1 year apart, by a locally based research assistant at home or at a clinic.
Information on date approached, date of birth, gender and postcode was collected. Postcodes were used in England to calculate the Index of Multiple Deprivation,69 and in Northern Ireland to calculate the Multiple Deprivation Measure. 70 The Index of Multiple Deprivation and the Multiple Deprivation Measure are markers of community-level socioeconomic status; higher scores indicate more socioeconomic deprivation.
We defined ‘date of transfer’ as the date of the final appointment with a paediatrician or principal children’s health specialist. This included when a young person saw a paediatrician and adult physician jointly to introduce a member of the adult team. If there was not a letter stating the transfer date, the date when the young person turned 18 years of age was recorded. At the study’s end, the young person’s status was recorded as still in children’s services, transferred to adults’ services, transferred to primary care, or left study.
To maximise the use of data, we carried out longitudinal analyses on the ‘final’ visit, defined as visit 4 unless there was a visit 3 that was not followed by a fourth visit, in which case visit 3 was used as the ‘final’ visit. At the ‘final’ visit, 274 young people (73.3%) had valid follow-up data for analysis (112 with diabetes mellitus, 74 with cerebral palsy and 88 with ASD).
Measures
We captured generic outcome measures about satisfaction with services, participation in life situations and well-being.
Parents and young people completed the Mind the Gap scale71 about their satisfaction with services. Satisfaction is conceptualised as the ‘gap’ between ratings of ‘ideal’ and ‘current’ care: the greater the ‘gap’ score, the lower the satisfaction. It yields an overall score and three subdomain scores.
Young people completed the Rotterdam Transition Profile,72 a nine-domain questionnaire on participation, defined as involvement in life situations. 73 For each domain, participants select the statement that best describes their current situation. Each statement represents one of three phases of transition: phase 1, childhood/dependence on parents; phase 2, experimenting and orienting to the future; and phase 3, adulthood/independence.
A three-item questionnaire captured the young person’s independence in appointments, and had a score range of 3–15 (15 being the most independent). 74
At visits 3 and 4, young people completed a frequency of social participation questionnaire,75 especially developed for adolescents; it has UK general population data available for comparison. Two ‘factors’ are captured: ‘getting on with people’ and ‘community recreation’. 76
Young people completed the Warwick–Edinburgh Mental Wellbeing Scale (WEMWBS), a 14-item questionnaire developed in the UK and valid in the age range 13–21 years. 77 It has UK general population data available for comparison.
No further psychometric analyses were carried out on the Mind the Gap scale and the Rotterdam Transition Profile because they have been validated and used with young people with a variety of long-term conditions. 71,72,78 However, for the WEMWBS, internal consistency was assessed using Cronbach’s alpha with 95% confidence intervals to check that it was an appropriate measure to use in all three groups, particularly the group with ASD and an associated mental health problem.
In addition, the following condition-specific outcomes and process measures were captured.
-
Type 1 diabetes mellitus. Participants were assigned to a ‘satisfactory’ or ‘suboptimal’ clinical course at visits 2, 3 and 4. Following consultation with specialists in adult and paediatric diabetes, participants were deemed to have a satisfactory clinical course if, for each year of the study, HbA1c (glycated haemoglobin) level was < 7% above baseline, there were no hospital admissions for diabetic ketoacidosis, clinic attendance was > 75% and attendance for retinal screening was 100%. 65
-
Cerebral palsy. An unmet-needs questionnaire was developed based on a model widely used in disability research. 79 The questionnaire was completed separately by the young person and the parent. Categorical principal components analysis identified two domains: daily activity health care and medical care. 64
-
ASD and an associated mental health problem. Young people completed the self-report Hospital Anxiety and Depression Scale (HADS), which has subscales for anxiety and depression. 80 The psychometric properties of this scale have been shown to be valid for use with young people with ASD. 81
Proposed beneficial features
A summary checklist about the PBFs was discussed by the research assistant with each young person at the first (baseline) visit. Then, at the second, third and fourth home visits, the checklist of PBFs experienced by the young person over each preceding 12 months was completed by the research assistants, in discussion with the young person (and with parents). This was supported by diary information recorded by the young person about their consultations. The research assistants also consulted health records to extract information about provision of PBFs; this included whether or not there was evidence that the clinic had a staff member with the role of transition manager for the clinical team (which was not directly asked to young people). Each PBF was recorded as received (or not) at least once during the year before the visit. For each PBF, we also established a trajectory of exposure, over the course of the study, deemed optimal or suboptimal according to whether or not:
-
In at least 1 of the 3 years there was exposure to the feature. This applied to the features ‘age-banded clinic’, ‘meet the adult team before transfer’, ‘written transition plan, ‘holistic life-skills training’ and ‘transition manager for clinical team’.
-
In at least 2 of the 3 years there was exposure to the feature. This applied to the features ‘key worker’ and ‘co-ordinated team’.
-
In each of the 3 years there was exposure to the feature. This applied to the features ‘promotion of health self-efficacy’ and ‘young person and/or parent satisfied with level of parent involvement’.
-
When visit(s) had been missed, and the trajectory could not be assessed, the trajectory was recorded as missing.
After the first year of the study, a questionnaire was sent to each of the 35 services attended by the young people recruited to ask whether or not their service aimed to provide each of the PBFs.
Analysis
Recruitment
Eight hundred and seventy-eight young people were approached and 374 were recruited to the study; 118 with ASD, 106 with cerebral palsy and 150 with diabetes mellitus. Further details and a flow diagram are in figure 1 of our published paper on baseline characteristics. 62 Whereas recruitment rates were reasonably good for the ASD group (50.9% of those approached) and diabetes mellitus group (64.7%), the rate of recruitment of those with cerebral palsy was lower (25.6%). This may be due to the method of recruitment, which was to send letters of invitation rather than for their clinician to approach young people and their families directly.
As described in our baseline characteristics paper,62 participants with diabetes mellitus or cerebral palsy were comparable, in terms of condition severity, with larger population samples. However, for those with ASD this was more difficult to assess because we recruited individuals who also had an associated mental health problem.
The target of 150 in each group was achieved for young people with diabetes mellitus but not for those with ASD who were in contact with mental health services (n = 118) or for those with cerebral palsy (n = 106) (see Appendix 5, Figure 12). For each young person, a parent or carer was invited to participate; 369 agreed (367 parents, one grandparent and one foster parent). Thus, data from a parent or carer were available for 98.6% of the young people.
Participants did not differ significantly from non-participants by age or gender, as shown in table 1 of our published paper on baseline characteristics. 62 Overall, participants had significantly (p < 0.001) lower scores on the Index of Multiple Deprivation (i.e. they were less deprived) than non-participants; however, the difference in overall Index of Multiple Deprivation score, on a continuous scale ranging from 0.5 to 87.8, was only 6.1.
Retention
Most of this analysis is reported in our published paper on the longitudinal analysis. 66 A total of 304 (81.3%) young people remained in the study by visit 2, with 259 (69.3%) by visit 3 and 243 (65%) by visit 4 (see Appendix 5, Figure 13). Forty young people became uncontactable (see Appendix 6, Figure 13). Among the 71 who told us that they wanted to leave the study, the main reason (n = 22) was ‘no longer being interested’. Another 19 had other commitments that came with being older, such as sitting exams, university work, or part- or full-time jobs. Furthermore, some young people’s mental health was too poor to allow visits. This highlights the natural challenges of undertaking longitudinal research during a life stage when so much change is happening.
A total of 274 (73%) young people had data for the ‘final’ visit (defined in Methods as visit 4 unless there was a visit 3 that was not followed by a fourth visit, in which case visit 3 was used). Of these 274 young people, 58% were male, and 112 had diabetes mellitus, 74 had cerebral palsy and 88 had ASD.
Text in the following paragraph is from our published paper. 66 This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
The mean time between the baseline and final visits was 2.9 years [standard deviation (SD) 0.4 years, range 1.8–3.9 years]. There were no significant differences between those remaining in the study and those not remaining with respect to sex (p = 0.6), age (p = 0.6), condition (p = 0.6), diabetes sites (p = 0.4) or ASD sites (p = 0.6) or condition severity (diabetes mellitus, p = 0.7; cerebral palsy, p = 0.9; ASD, p = 0.7). However, in Northern Ireland, those with cerebral palsy who were lost to follow-up came from areas with, on average, greater socioeconomic deprivation (p = 0.03) than did those remaining in the study. On examining socioeconomic factors, based on actual circumstances rather than on area of residence, there was more loss to follow-up in families with single parents.
To where did young people transfer?
For the 274 young people with a ‘final’ visit, Table 1 shows whether they remained in children’s services or transferred to adults’ services or primary care, by condition.
| Status | Total, N (%)a | Condition, n (%) | ||
|---|---|---|---|---|
| Diabetes mellitusa | Cerebral palsy | ASD | ||
| Remained in children’s service | 49 (18) | 19 (17) | 10 (14) | 20 (23) |
| Transferred to adults’ service | 148 (54) | 89 (80) | 35 (47) | 24 (27) |
| Transferred to primary care | 76 (28) | 3 (3) | 29 (39) | 44 (50) |
Of those with diabetes mellitus, almost all transferred to an adults’ service, whereas the proportion of those with cerebral palsy who transferred to primary care was substantial, and this was even greater for those with ASD.
Baseline and subsequent changes in the outcome measures
A total of 304 (81.3%) of the young people took part in the second visit (diabetes mellitus, n = 128; cerebral palsy, n = 85; ASD, n = 91); 259 took part in the third visit and 243 took part in the fourth visit.
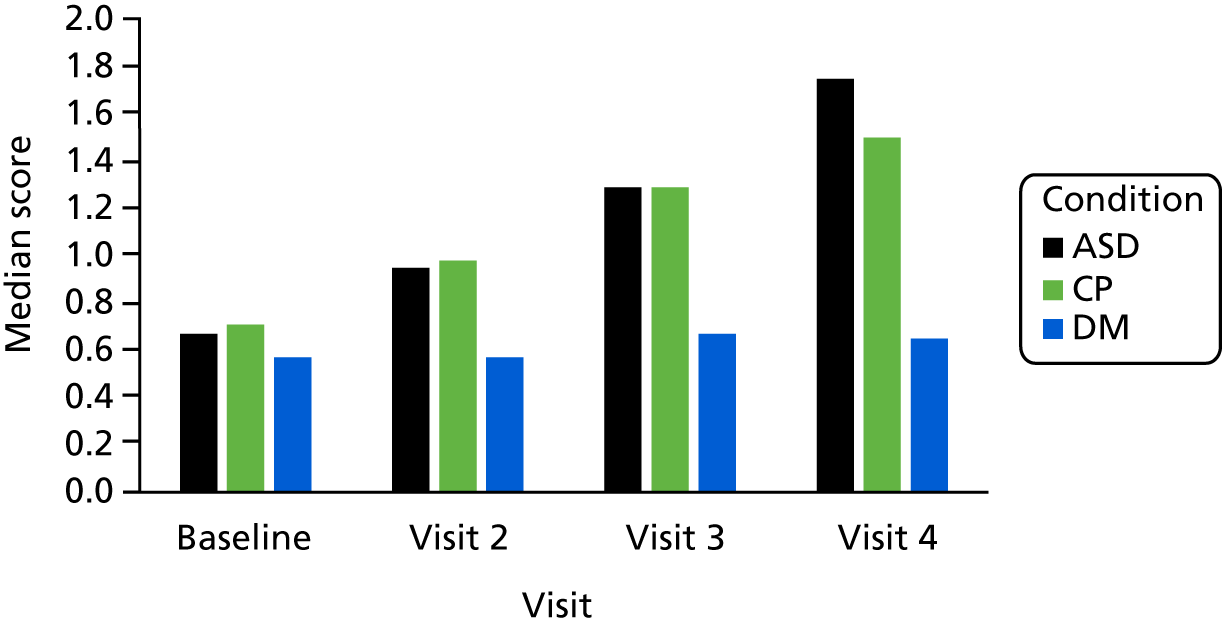
Satisfaction with services
Satisfaction with services was generally good, as the ‘gap’ scores (the difference between the respondent’s ideal and current care) were small. Parents’ satisfaction was significantly lower than their children’s. Over the four visits, satisfaction with services did not change for those with diabetes mellitus, but for those with cerebral palsy or ASD it steadily worsened (Figure 2).
FIGURE 2.
Mind the Gap median score, young person reported: change over time by condition. CP, cerebral palsy; DM, diabetes mellitus.
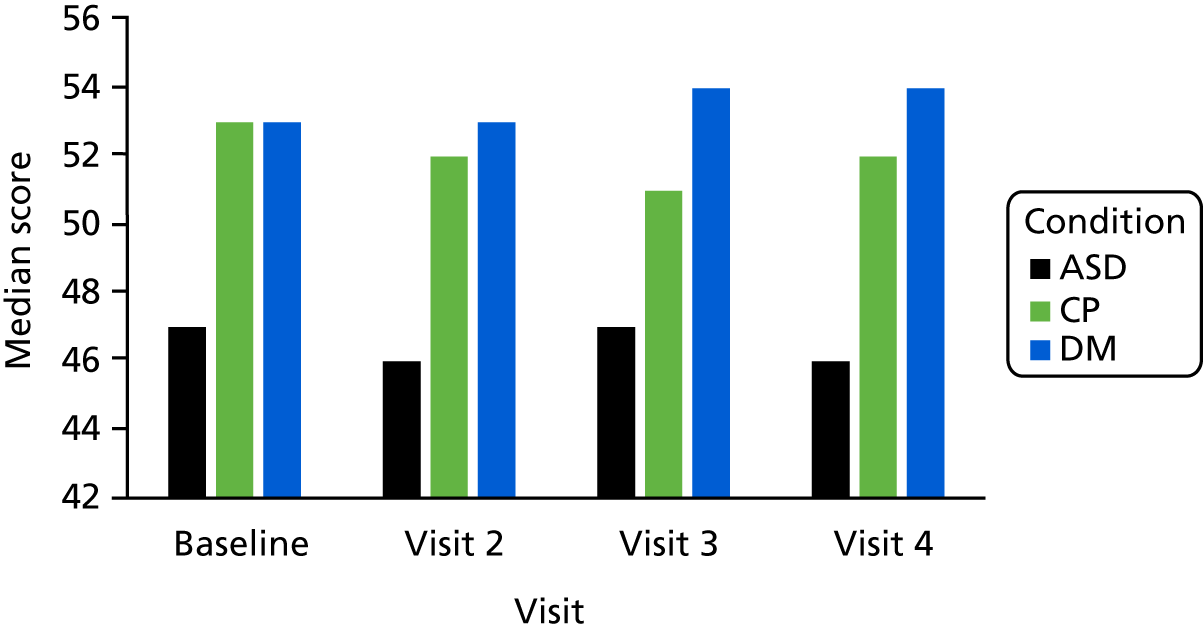
Well-being
The median baseline well-being scores of those with diabetes mellitus or cerebral palsy were similar to each other and to those in the general population, and significantly higher (p < 0.001) than the scores of those with ASD. In the general population of 13- to 16-year-olds, the median score on the WEMWBS was 48.8. 77 In those aged > 16 years in the general population in England, the median was 50.7. 82
Over the four visits, the well-being scores of those with diabetes mellitus, cerebral palsy or ASD were steady. Those with ASD continued to have significantly lower well-being scores (p < 0.001) (Figure 3).
FIGURE 3.
The WEMWBS: change over time by condition group. CP, cerebral palsy; DM, diabetes mellitus.
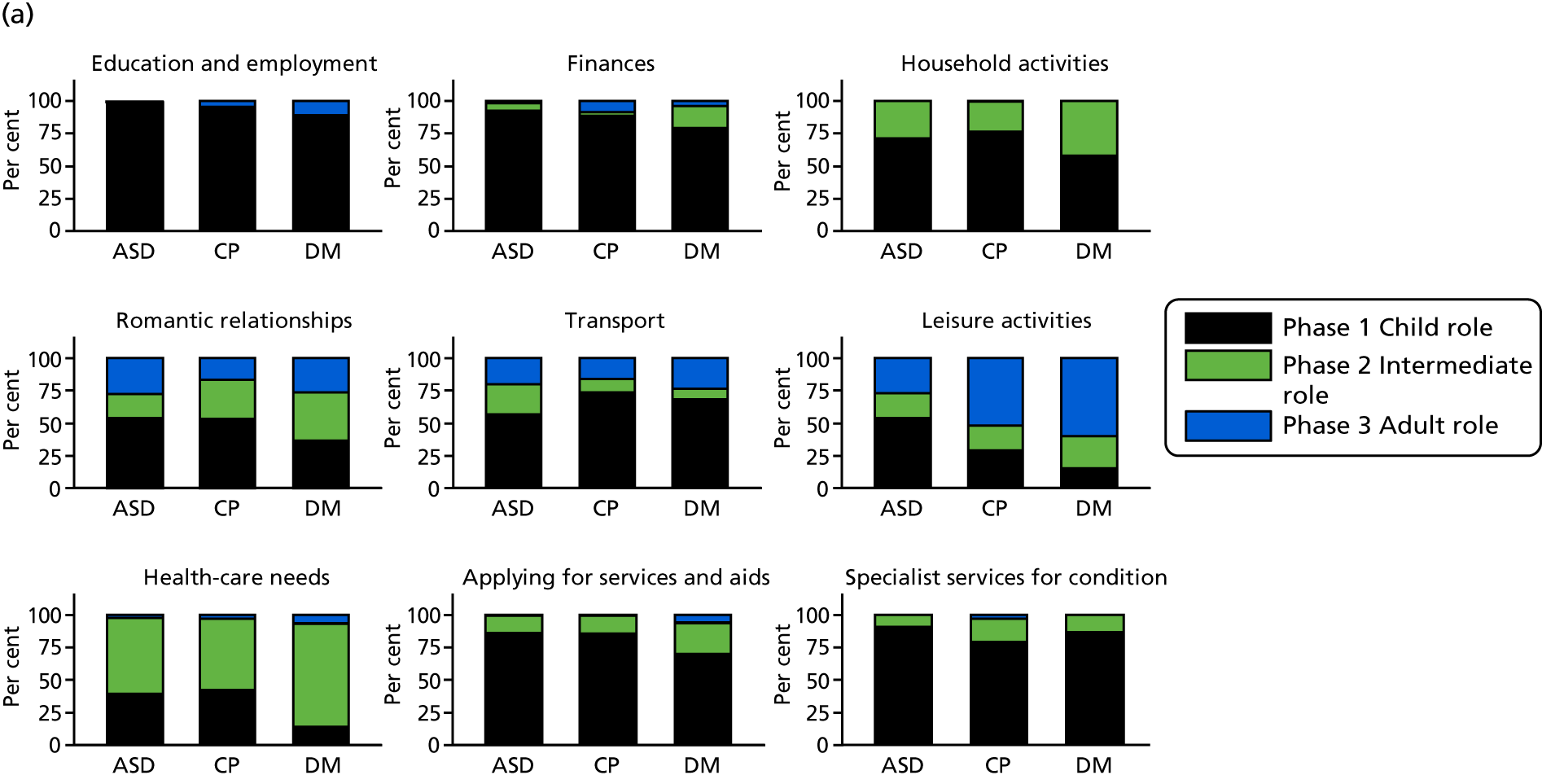
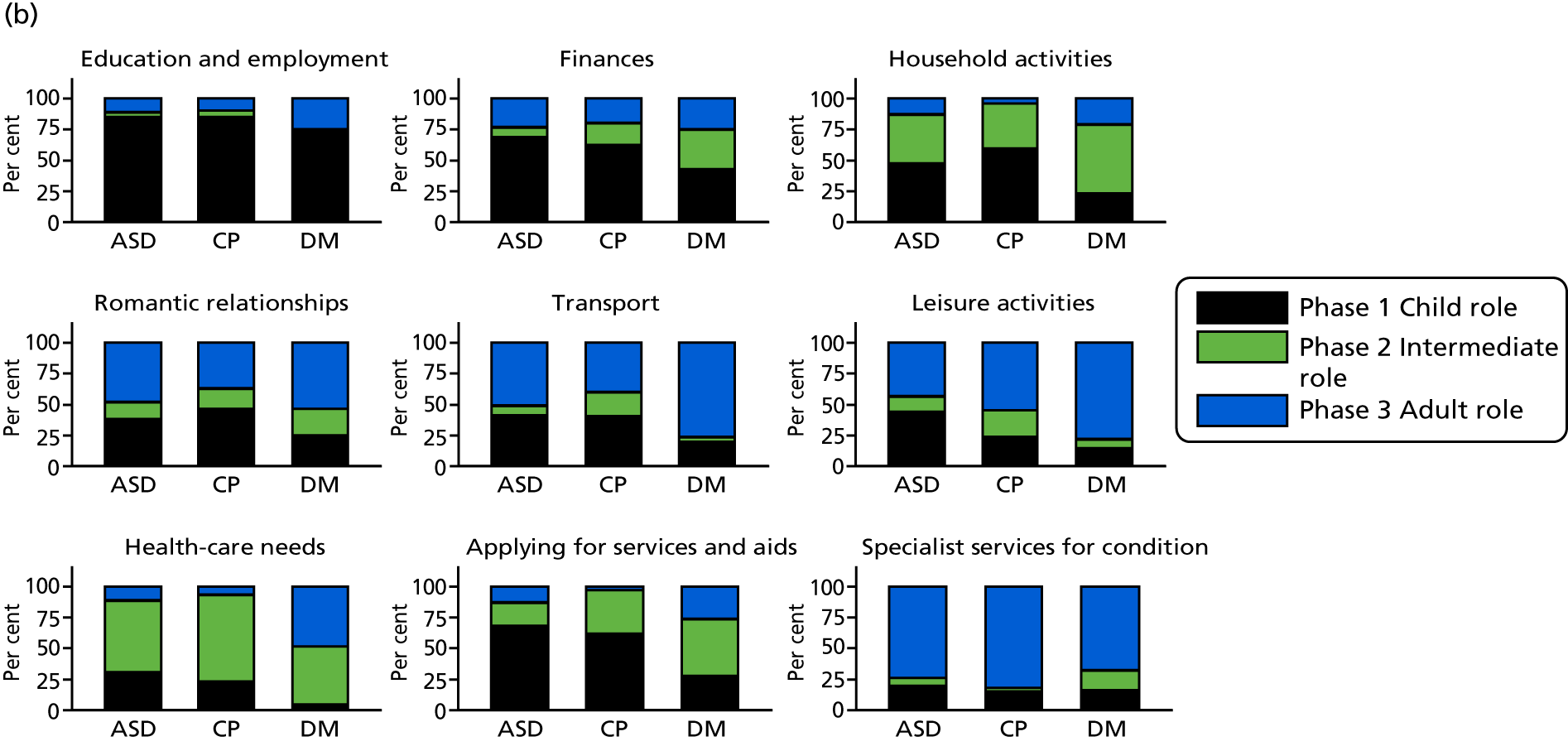
Rotterdam Transition Profile
On every domain of the Rotterdam Transition Profile, except ‘education and employment’, significant differences were found between the three conditions (most p-values were < 0.01). A larger proportion of young people with diabetes mellitus were in a more independent phase of participation than those with ASD or cerebral palsy. Over the four visits, young people steadily moved to a more independent phase of transition on every domain. Those with diabetes mellitus remained further ahead than those with ASD or cerebral palsy (Figure 4). As the phase for the domain ‘using specialist services for condition’ was determined entirely by the structure of the services and could not be influenced by the young person, we dropped it from this and further analysis.
FIGURE 4.
Rotterdam Transition Profile. Percentages of participants per phase at (a) baseline and (b) visit 4, by condition. CP, cerebral palsy; DM, diabetes mellitus.
Social participation
The mean score for the ‘getting on with people’ domain was significantly lower (p < 0.001) for participants than in the general population, whereas the score for the ‘community recreation’ domain was similar (Table 2). Those with diabetes mellitus had higher mean scores than those with ASD or cerebral palsy for ‘getting on with people’, and higher scores than those with ASD for ‘community recreation’. Scores for ‘getting on with people’ improved by visit 4 for all three conditions but remained lower than in the general population.
| Domain | General population | Study population | ||
|---|---|---|---|---|
| Number | Mean (SD) | Number | Mean (SD) | |
| Getting on with people | 478 | 0.004 (1.37) | 253 | –1.09 (1.79) |
| Community recreation | 479 | 0.27 (0.15) | 253 | 0.26 (0.17) |
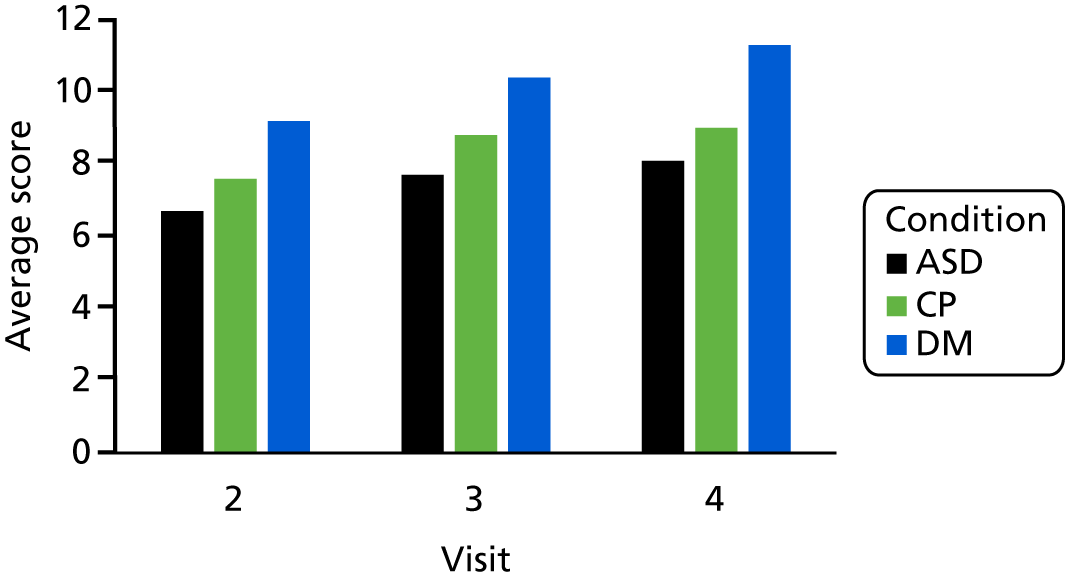
Independence in Appointments
The Independence in Appointments questionnaire was added from visit 2 onwards. At visit 2, the average score was 8. Those with diabetes mellitus had higher scores than those with ASD or cerebral palsy, and these differences persisted even though all scores increased, indicating more independence (Figure 5).
FIGURE 5.
Independence in Appointments scale: change over time, by condition. CP, cerebral palsy; DM, diabetes mellitus.
Time from final paediatric appointment to first appointment in adults’ service
We could examine this only for young people with diabetes mellitus. For those with cerebral palsy, it was usually unclear with which professional the first appointment should be. For example, sometimes a young person had transferred to an adult physiotherapist but was still seeing a paediatrician.
For those with diabetes mellitus who had transferred, the mean time to adult appointment was 5.2 months (SD 4.9 months). The median time was 3.7 months [interquartile range (IQR) 3–6 months]. The proportion seen by adults’ services within 6 months of final paediatric appointment was 75%.
Diabetes mellitus condition-specific measure of clinical course
The proportion of young people with diabetes mellitus with satisfactory clinical course reduced over the study period (clinical course was determined from a composite score from HbA1c value, eye screening, clinic attendance and no diabetic ketoacidosis):65
-
by visit 2, 65 out of 128 (51%) had a satisfactory clinical course
-
by visit 3, 49 out of 112 (43%) had a satisfactory clinical course
-
by visit 4, 32 out of 108 (29%) had a satisfactory clinical course.
These results, and further reporting in our published paper65 (in which we report only on the 108 who had full data to visit 4), indicate that the well-being of young people with diabetes mellitus and their satisfaction with transition services were not closely related to the condition’s clinical course.
Cerebral palsy condition-specific measure of unmet need
As reported by parents, the proportion of young people with cerebral palsy with some unmet needs increased during the follow-up on the ‘daily living health care’ and ‘medical care’ domains. 64 As reported by the young person, an increase in unmet needs was seen only in the ‘daily living health care’ domain (Figure 6). When considering only those with some unmet needs, mean scores decreased slightly for the ‘daily living health care’ domain and remained the same for the ‘medical care’ domain, as reported by both young people and parents. These results were for the 64 young people who provided data at every visit. The results were similar when we examined data from each visit, whether or not data were available from other visits.
FIGURE 6.
Needs reported by (a) young person; and (b) parent.
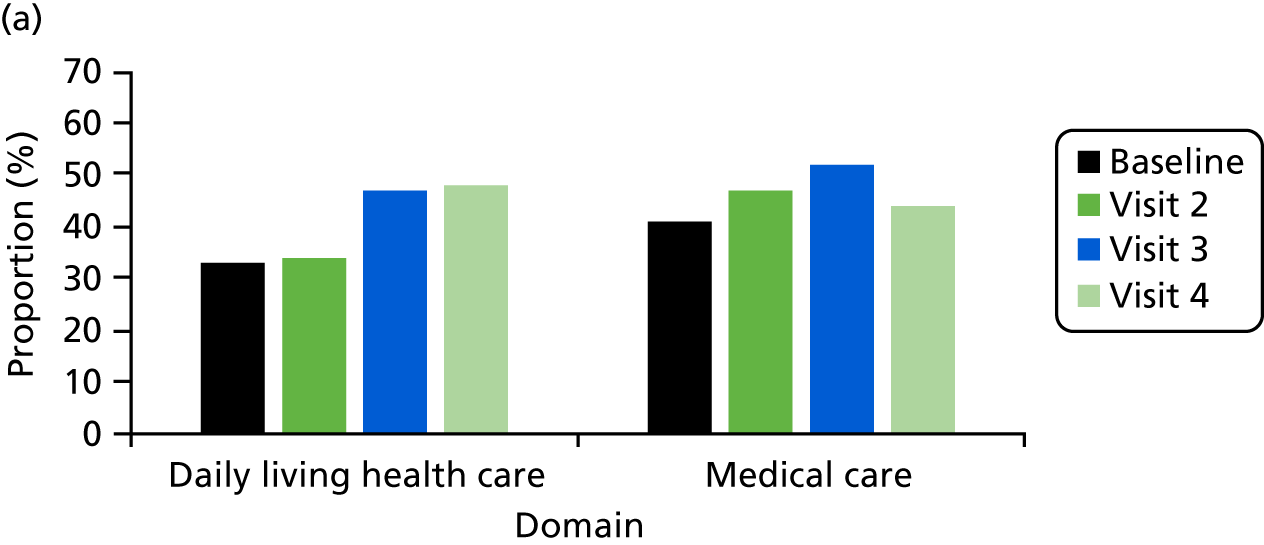
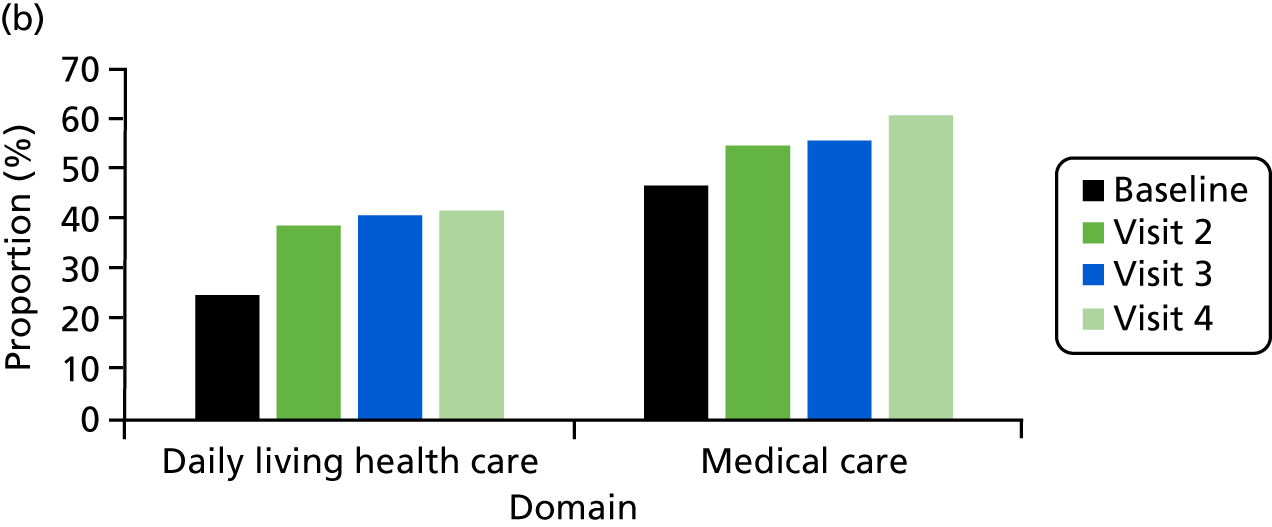
These results draw attention to the need for more co-ordinated care in adults’ services for those with cerebral palsy. We discuss this further in our published paper64 and compare UK practice with that of other countries.
Autism spectrum disorder condition-specific measure of anxiety and depression
The proportion of young people with ASD and an associated mental health problem with an ‘abnormal’ score on the ‘anxiety’ and ‘depression’ domains (as measured by the HADS) remained similar between baseline and visit 4 (‘abnormal’ means above the recommended threshold score for a likely disorder) (Figure 7). The results were similar if analysed for the participants with data at baseline or visit 4, or if analysed for only those participants with data at baseline and visit 4.
FIGURE 7.
Proportions of normal, borderline and abnormal scores from the HADS at baseline and visit 4.

Further analysis of those with ASD is provided in Appendix 5. Having an additional diagnosis of attention deficit hyperactivity disorder or taking medication were predictors of a transfer to adult mental health services. Overall, the young people in our sample appeared to be doing reasonably well, with 67.5% in full-time education (either school or college) at the end of the study. Under one-third were in neither education nor employment. Analysis of HADS trajectories found that some young people were doing well, managing their mental health and able to engage successfully with services. However, the majority were experiencing episodes or continued levels of high anxiety. Qualitative data revealed that many young people struggled when faced with more challenging academic and social environments.
Proposed beneficial features
Some material in this section is from Colver et al. 63 This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
The proposed beneficial features that services reported that they provided over the first year (i.e. before visit 2)
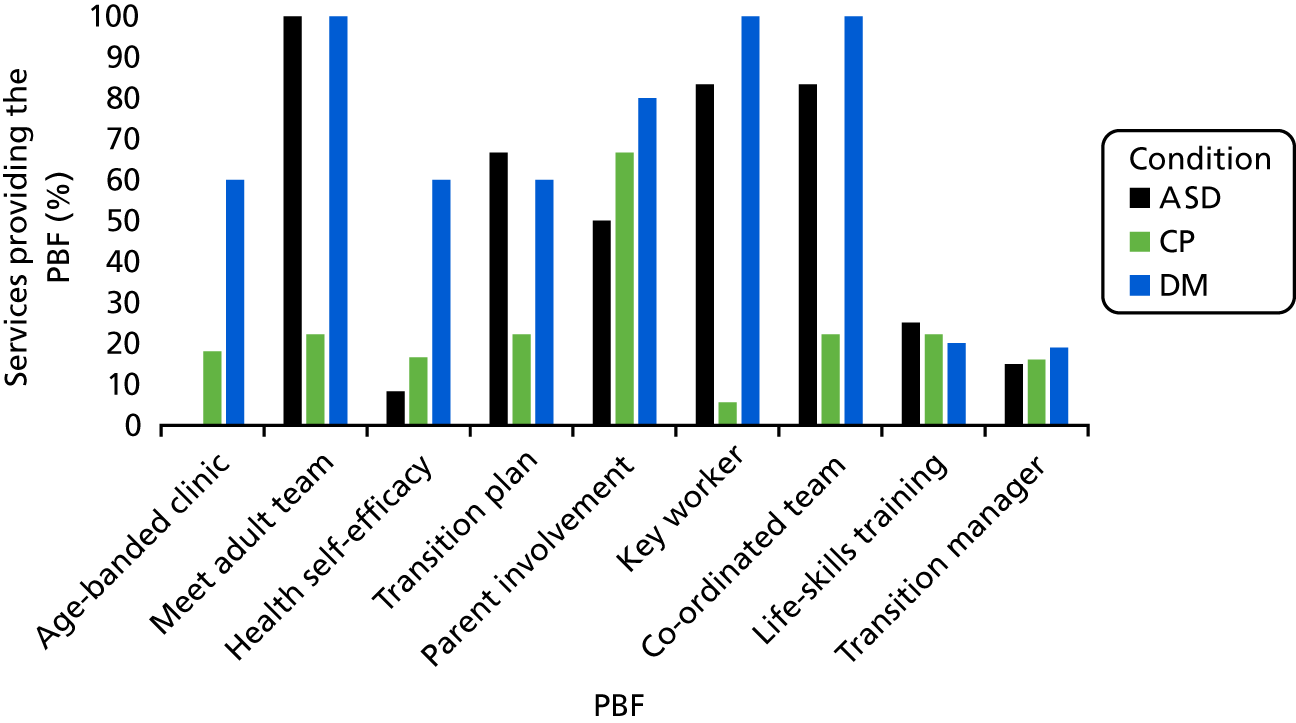
The following paragraph is covered in more detail in our published paper. 63 Overall, the nine PBFs of services for transitional health care were often not offered to young people in our study by NHS services. Fewer than half of the 35 services stated that they provided an ‘age-banded clinic’, ‘written transition plan’, ‘transition manager for clinical team’, ‘protocol for promotion of health self-efficacy’ or ‘holistic life-skills training’. Features were offered by services most often for young people with diabetes mellitus and least often for those with cerebral palsy (Figure 8).
FIGURE 8.
Percentage of ‘yes’ responses from each service by condition, stating whether or not the PBF was offered. CP, cerebral palsy; DM, diabetes mellitus.
The proposed beneficial features that young people reported that they experienced over the first year (i.e. before visit 2)
The content of the following paragraph is covered in more detail in our published paper,63 which integrates the findings from this WP and the qualitative work of WP 2.2. At visit 2, young people often reported that they had not experienced the features that services said they provided. Agreement between the young person’s report and what the service said it offered was 30% for ‘written transition plan’, 43% for ‘holistic life-skills training’ and 49% for ‘key worker’. Agreement was better for ‘appropriate parent involvement’, at 77%; for ’age-banded clinic’, at 77%; for ‘promotion of health self-efficacy‘, at 80%; and for ‘co-ordinated team’, at 69%.
Associations of proposed beneficial features with outcomes
Two approaches were adopted to assessing the associations of PBFs with outcomes. In both, we used the young person’s account of whether or not they had experienced a PBF, rather than what the service reported that it provided or aspired to provide.
In the first approach, it was established at each research visit whether or not the young person had experienced each PBF at least once in the previous year, and this was recorded as yes or no. A separate analysis was then conducted for each PBF (as the independent variable) against the outcomes. This was undertaken for each annual period. Thus, this approach is a series of analyses that examine associations over 1 year, directly related to what the young person is experiencing at the time.
In the second approach, a consolidated indicator was compiled for each PBF for the duration of the study. The criteria for being optimal or suboptimal varied by PBF and was calculated as outlined in Methods. The proportions of young people experiencing optimal or suboptimal consolidated indicators are shown in Table 3. In the analyses, the independent variable was whether the consolidated indicator was optimal or suboptimal for each PBF; the dependent variables were the outcomes captured at the ‘final’ visit.
| PBF | Consolidated indicator | All, n (%) | Diabetes, n (%) | Cerebral palsy, n (%) | ASD, n (%) | p-value |
|---|---|---|---|---|---|---|
| Age-banded clinic | Optimal | 145 (53) | 109 (97) | 16 (22) | 20 (23) | < 0.001 |
| Suboptimal | 111 (40) | 2 (2) | 54 (73) | 55 (62) | ||
| Missing | 18 (7) | 1 (1) | 4 (5) | 13 (15) | ||
| Meet adult team before transfer | Optimal | 111 (40) | 73 (65) | 16 (22) | 22 (25) | < 0.001 |
| Suboptimal | 133 (49) | 31 (28) | 54 (73) | 48 (55) | ||
| Missing | 30 (11) | 8 (7) | 4 (5) | 18 (20) | ||
| Promotion of health self-efficacy | Optimal | 116 (42) | 76 (68) | 18 (24) | 22 (25) | < 0.001 |
| Suboptimal | 151 (55) | 29 (26) | 56 (76) | 66 (75) | ||
| Missing | 7 (3) | 7 (6) | ||||
| Written transition plan | Optimal | 48 (17) | 32 (29) | 11 (15) | 5 (6) | < 0.001 |
| Suboptimal | 185 (68) | 62 (55) | 59 (80) | 64 (73) | ||
| Missing | 41 (15) | 18 (16) | 4 (5) | 19 (21) | ||
| N/A | 2 (1) | 1 (1) | 1 (1) | |||
| Both young person and parent happy with parent involvement | Optimal | 93 (34) | 36 (32) | 28 (38) | 29 (33) | 0.444 |
| Suboptimal | 141 (51) | 55 (49) | 33 (45) | 53 (60) | ||
| Missing | 38 (14) | 21 (19) | 12 (16) | 5 (6) | ||
| N/A | 2 (1) | 1 (1) | 1 (1) | |||
| Key worker | Optimal | 79 (29) | 56 (50) | 3 (4) | 20 (23) | < 0.001 |
| Suboptimal | 170 (62) | 47 (42) | 68 (92) | 55 (62) | ||
| Missing | 25 (9) | 9 (8) | 3 (4) | 13 (15) | ||
| Co-ordinated team | Optimal | 167 (61) | 104 (93) | 25 (34) | 38 (43) | < 0.001 |
| Suboptimal | 66 (24) | 2 (2) | 40 (54) | 24 (27) | ||
| Missing | 25 (9) | 6 (5) | 4 (5) | 15 (17) | ||
| N/A | 16 (6) | 5 (7) | 11 (13) | |||
| Holistic life-skills training | Optimal | 132 (48) | 74 (66) | 18 (24) | 40 (45) | < 0.001 |
| Suboptimal | 117 (43) | 28 (25) | 52 (70) | 37 (42) | ||
| Missing | 25 (9) | 10 (9) | 4 (6) | 11 (13) | ||
| Transition manager for clinical team | Optimal | 60 (22) | 27 (24) | 14 (19) | 19 (21) | 0.947 |
| Suboptimal | 143 (52) | 67 (60) | 34 (46) | 42 (48) | ||
| Missing | 71 (26) | 18 (16) | 26 (35) | 27 (31) | ||
| Total (n) | 274 | 112 | 74 | 88 |
All models were adjusted for age, sex, condition and potential for clustering by site. Significant associations (p < 0.05) from these models were further adjusted for transfer status, time since transfer to final visit (if applicable) and time to first adult appointment (if applicable).
Examining the Rotterdam Transition Profile, we performed the logistic regression by comparing phases 1 and 2 with phase 3.
Table 4 sets out the effect sizes for all associations that reached significance of p ≤ 0.05.
| PBF | PBFs by ‘year-by-year’ visits | Consolidated PBF indicator at final visit | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Period | Outcome | Whether regression b-coefficient or odds ratio | 95% confidence interval | p-value | Outcome | Whether regression b-coefficient or odds ratio | 95% confidence interval | p-value | |
| Appropriate parent involvement | 1 | MTG: total | −0.48 | −0.76 to −0.19 | 0.001 | MTG: total | −0.67 | −0.97 to −0.37 | < 0.001 |
| 1 | MTG: environment | −0.57 | −0.92 to −0.21 | 0.001 | MTG: environment | −0.71 | −1.17 to −0.26 | 0.006 | |
| 1 | MTG: provider | −0.52 | −0.82 to −0.22 | 0.001 | MTG: provider | −0.75 | −0.99 to −0.52 | < 0.001 | |
| 1 | RTP: domestic | [0.14a] | 0.03 to 0.67 | 0.01 | RTP: finances | [0.6a] | 0.92 to 0.39 | 0.02 | |
| 1 | RTP: health care | [0.35a] | 0.17 to 0.72 | 0.004 | WEMWBS | 2.18 | 0.21 to 4.15 | 0.03 | |
| 1 | RTP: services and aids | [0.42a] | 0.18 to 0.97 | 0.04 | |||||
| 2 | MTG: total | −0.60 | −1.00 to −0.21 | 0.003 | |||||
| 2 | MTG: environment | −0.65 | −1.08 to −0.21 | 0.004 | |||||
| 2 | MTG: provider | −0.48 | −0.90 to −0.06 | 0.03 | |||||
| 2 | MTG: process | −0.82 | −1.32 to −0.31 | 0.002 | |||||
| 3 | WEMWBS | 4.47 | 1.96 to 6.97 | 0.001 | |||||
| 3 | MTG: total | −0.87 | 0.45 to 1.29 | 0.001 | |||||
| 3 | MTG: environment | −0.91 | −1.44 to −0.37 | < 0.001 | |||||
| 3 | MTG: provider | −0.95 | −1.37 to −0.52 | < 0.001 | |||||
| 3 | MTG: process | −0.63 | −1.18 to −0.07 | 0.03 | |||||
| 3 | WEMWBS | 3.45 | 0.92 to 5.99 | 0.008 | |||||
| Promotion of health self-efficacy | 1 | MTG: total | −0.51 | −0.87 to −0.15 | 0.006 | MTG: total | −0.32 | −0.62 to −0.03 | 0.04 |
| 1 | MTG: environment | −0.63 | −1.06 to −0.18 | 0.005 | MTG: environment | −0.57 | −1.03 to −0.11 | 0.02 | |
| 1 | MTG: provider | −0.47 | −0.85 to −0.09 | 0.02 | MTG: process | −0.37 | −0.70 to −0.04 | 0.03 | |
| 1 | MTG: process | −0.46 | −0.91 to −0.01 | 0.04 | |||||
| 1 | RTP: finances | [0.26a] | 0.07 to 0.93 | 0.04 | |||||
| 1 | RTP: domestic | [0.04a] | 0.01 to 0.21 | 0.001 | |||||
| 2 | MTG: total | −0.51 | −0.91 to −0.11 | 0.01 | |||||
| 2 | MTG: provider | −0.49 | −0.90 to −0.08 | 0.02 | |||||
| 2 | MTG: process | −0.70 | −1.21 to −0.19 | 0.007 | |||||
| 2 | MTG: total | −0.60 | −1.01 to −0.20 | 0.004 | |||||
| 3 | MTG: environment | −0.90 | −1.40 to −0.40 | < 0.001 | |||||
| 3 | MTG: provider | −0.52 | −0.95 to −0.11 | 0.01 | |||||
| Meet adult team before transfer | 1 | RTP: domestic | 6.29a | 1.60 to 24.80 | 0.009 | RTP: education/employment | 2.33a | 1.21 to 4.55 | 0.01 |
| 1 | RTP: health care | 2.71a | 1.24 to 5.90 | 0.01 | RTP: finances | 2.78a | 1.10 to 7.14 | 0.03 | |
| 1 | RTP: services and aids | 5.15a | 2.08 to 12.78 | < 0.001 | RTP: services and aids | 2.50a | 1.06 to 5.88 | 0.04 | |
| 1 | RTP: transport | 2.01a | 1.06 to 3.79 | 0.03 | Autonomy in appointments | 1.60 | 0.32 to 2.87 | 0.02 | |
| 1 | RTP: education/employment | 3.24a | 1.09 to 9.65 | 0.04 | |||||
| Meet adult team before transfer (continued) | 1 | Autonomy in appointments | 1.69 | 0.80 to 2.58 | < 0.001 | ||||
| 2 | RTP: finances | 2.64a | 0.92 to 6.62 | 0.02 | |||||
| 2 | RTP: transport | 2.08a | 1.11 to 3.90 | 0.02 | |||||
| 2 | Autonomy in appointments | 1.00 | 0.01 to 2.0 | 0.05 | |||||
| 3 | RTP: health care | 2.11a | 1.03 to 4.34 | 0.004 | |||||
| 3 | Autonomy in appointments | 1.46 | 0.34 to 2.59 | 0.01 | |||||
| Key worker | 1 | RTP: leisure | [0.56a] | 0.32 to 0.96 | 0.04 | ||||
| 2 | MTG: provider | −0.66 | −1.04 to −0.28 | 0.001 | |||||
| 2 | MTG: process | −0.69 | −1.17 to −0.21 | 0.005 | |||||
| 3 | RTP: education/employment | [0.40a] | 0.20 to 0.95 | 0.02 | |||||
| Holistic life-skills training | 1 | RTP: domestic | [0.19a] | 0.04 to 0.93 | 0.04 | ||||
| 1 | RTP: services and aids | [0.34a] | 0.12 to 0.94 | 0.04 | |||||
| 2 | MTG: provider | [0.43] | 0.03 to 0.84 | 0.04 | |||||
| 3 | MTG: total | −0.46 | −0.87 to −0.05 | 0.03 | |||||
| 3 | MTG: provider | −0.57 | −0.99 to −0.14 | 0.009 | |||||
| 3 | RTP: domestic | 2.47a | 1.10 to 5.58 | 0.003 | |||||
| 3 | RTP: romantic relationships | [0.52a] | 0.26 to 0.98 | 0.04 | |||||
| Written transition plan | 1 | RTP: romantic relationships | [0.43a] | 0.19 to 0.96 | 0.04 | ||||
| 2 | MTG: total | −0.72 | −1.39 to −0.04 | 0.04 | |||||
| 2 | MTG: process | −1.19 | −1.39 to −0.04 | 0.007 | |||||
| Co-ordinated team | 1 | RTP: domestic | [0.19a] | 0.04 to 0.93 | 0.04 | MTG: provider | −0.67 | −1.25 to −0.09 | 0.03 |
| 3 | RTP: health care | [0.17a] | 0.04 to 0.82 | 0.03 | RTP: education/employment | [0.31a] | 0.11 to 0.82 | 0.02 | |
| 3 | RTP: services and aids | [0.22a] | 0.06 to 0.81 | 0.02 | RTP: domestic | [0.41a] | 0.19 to 0.91 | 0.03 | |
| Transition manager for clinical team | No associations | RTP: domestic | 2.63a | 1.16 to 5.88 | 0.02 | ||||
| RTP: services and aids | [0.41a] | 0.20 to 0.86 | 0.02 | ||||||
| RTP: romantic relationships | [0.52a] | 0.31 to 0.89 | 0.02 | ||||||
| Age-banded clinic | 1 | WEMWBS | 3.08 | 0.18 to 5.98 | 0.04 | ||||
| 1 | Autonomy in appointments | 1.44 | 0.48 to 2.4 | 0.003 | |||||
| 2 | RTP: education/employment | 5.22a | 1.21 to 22.53 | 0.03 | |||||
Interpretation of the associations of proposed beneficial features with outcomes
This is presented in more detail in our published paper. 66 This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
Three PBFs of transitional health care had significant (p ≤ 0.01) positive associations with better outcomes, namely ‘appropriate parent involvement’, ‘promotion of health self-efficacy’ and ‘meeting the adult team before transfer’. The b-coefficients indicated changes of approximately 0.5 SDs with respect to the satisfaction with services scale (SD 1.5 in our population), well-being (SD 7.0 in our population) and autonomy in appointments (SD 3.0 in our population). The odds ratios indicated increased likelihoods of being in a more independent phase of transition.
The other six PBFs had few statistically significant positive associations (p ≤ 0.01) with better outcomes in the year-by-year analysis, had a number of negative associations and had no positive associations with the consolidated indicator of exposure to PBFs.
‘Appropriate parent involvement’ and ‘promotion of health self-efficacy’ were reported to have been experienced satisfactorily by fewer than half of participants across transition across the three conditions. However, they were experienced by more young people with diabetes mellitus than those with cerebral palsy or ASD. For ‘meeting the adult team before transfer’, around two-thirds of young people with diabetes mellitus reported that they had met a member of the adult team, but fewer than one-quarter of those with cerebral palsy or ASD had done so. Thus, we found a different quality of experience of transitional health care between young people with a long-term illness (diabetes mellitus) and those with a long-term disability.
Strengths and limitations
Looking first at the strengths, our study drew 374 young people from across the UK and from many NHS Trusts. This is the largest sample for research in the UK in terms of examining transition longitudinally and collecting hypothesis-driven data from young people at home visits (compared with data-linkage studies from administrative data sets). Although we cannot be certain of representativeness and, therefore, generalisability across UK regions and NHS Trusts, we studied individuals from Greater London; north, south-east and south-west England; and Northern Ireland. Furthermore, we drew individuals from 27 NHS Trusts, and the trusts varied greatly in the number and variety of the PBFs they offered (see Figure 8).
We recruited from all young people with cerebral palsy in two population registers and all young people with diabetes mellitus or ASD and an associated mental health problem in nine NHS Trusts widely distributed across England (all such young people are seen in secondary care). Thus, complete populations of individuals with one of the three conditions were sampled from (e.g. rather than those attending particular schools, specialised tertiary health-care services or voluntary support groups).
The three conditions chosen were exemplars of chronic illness (diabetes mellitus), complex physical impairment (cerebral palsy) and neurodevelopmental impairment (ASD); they were deliberately chosen because they varied in terms of health needs, psychosocial complexity and availability of adults’ services. Thus, we consider that generalisability to other conditions is likely.
The 374 participants did not differ significantly from those declining to take part, other than for a small effect of deprivation. The distribution of severity of the three conditions was similar to that in national samples. 62 Those with the conditions had a wide range of severity; for example, the young people with cerebral palsy ranged from wheelchair users to those with independent ambulation. Attrition did not appear to create bias, as there were no significant differences between those remaining and those not remaining in the study with respect to sex, age, condition, diabetes site or ASD site. In Northern Ireland, there was a small effect of deprivation on the attrition of those with cerebral palsy. Thus, we think that, after non-participation and attrition, our study group continued to be representative of those we aimed to recruit.
Turning to the limitations, our study did not include young people with a learning disability because in the UK there is already a lifespan service for such individuals, and we would not have been able to base our quantitative studies on self-completed questionnaires, nor our qualitative work on interviews with young people. However, the exclusion of such individuals means that our results cannot be generalised to them.
Recruitment, especially of those with cerebral palsy, was more difficult than we expected. A possible explanation may be the method of recruitment, which was letters of invitation, rather than the young people’s clinician approaching them directly, as was undertaken for those with diabetes mellitus or ASD. Overall retention at 70% was acceptable in comparison with other longitudinal studies of adolescent populations. 32
It might be desirable to follow up young people for longer in adults’ services to assess later outcomes of transitional health care, but this is unlikely to be feasible. The fact that some young people were still in children’s services does not invalidate analyses; our study was about transition, not specifically health-care transfer. Table 1 shows the number still in children’s services.
Because of their personal circumstances, there was variability in precisely when the young people were seen by researchers. This is one reason why we chose the ‘final visit’ to be visit 4 or visit 3 (if the young person did not have a visit 4). Some of the visit 3s were considerably delayed and too close to a fourth visit to justify further data collection during the study. We examined the association of exposure to a PBF over the previous year in relation to outcomes. However, what constitutes optimal exposure over 3 years when, for instance, exposure occurs in one year but not the others? We made a clinical judgement about this for each feature for the consolidated longitudinal analysis. The decisions were agreed among our group, but others might have made different judgements.
Some PBFs, such as ‘written transition plan’, were infrequently provided and therefore we had less statistical power to detect associations with outcomes.
Key findings
-
There were striking mismatches between the PBFs of transitional health care that a service said it provided and the features that young people reported to have experienced.
-
PBFs were both provided and experienced less often in services for those with cerebral palsy and ASD than for those with type 1 diabetes mellitus.
-
Average satisfaction with services was reasonable at baseline (rating of ideal service only slightly higher than rating of actual service). It remained steady for those with type 1 diabetes mellitus but worsened significantly over the study period for those with ASD or cerebral palsy.
-
The well-being scores for each group remained similar over time. Those with type 1 diabetes mellitus or cerebral palsy had an average subjective well-being at baseline similar to that of the general population. Those with ASD and an associated mental health problem reported significantly lower well-being than those in the other two groups, and this difference persisted over the course of the study.
-
For participation in life activities, there were significant differences between the three conditions, with young people with type 1 diabetes mellitus in more independent phases of transition than those with ASD or cerebral palsy. All made progress over time, but those with type 1 diabetes mellitus remained more independent.
-
Condition-specific outcomes worsened during the study for those with type 1 diabetes mellitus or cerebral palsy. The proportion of young people with ASD with so-called ‘abnormal’ anxiety and depression scores remained the same from baseline to visit 4, with over one-third having abnormal levels of anxiety.
-
The features of services for transitional health care associated with better outcomes were ‘appropriate parent involvement’, ‘promotion of health self-efficacy’ and ‘meeting the adult team before transfer’.
Inter-relationship with other parts of the programme
We were guided by advice from UP (WPs 1.1 and 1.2) in determining the wording of some questionnaires, which PBFs to include, how to approach young people and how to interpret the differences between what PBFs services said they provided and what young people experienced.
A subsample of the cohort in this WP were recruited to the qualitative longitudinal sample for WP 2.2.
Work package 2.3 constructed the DCE that was administered at visit 3.
This WP addressed the main hypothesis of the programme. In drawing conclusions about the clinical significance and validity of the findings (see Conclusions), we were further influenced by discussions with UP (WPs 1.1 and 1.2); we triangulated the findings with the results of the qualitative work in WP 2.2 and the health economic analysis in WP 2.3.
The findings of this WP informed the content of the DAH toolkit in WP 3.1b.
The findings of this WP contributed directly to implication 6 of the programme.
Work package 2.2: longitudinal study (qualitative)
Addressing objective 2: to identify the features of transitional health care that are effective and efficient
Recent reviews have explored different aspects of transitional health care, focusing on the experiences of young people44,51 and parents. 83 This work shows how transitional health care disrupts the lives of young people and their families. That by Lugasi et al. 51 shows how young people describe children’s services as ‘a familiar and comfortable environment, and reported feelings of trust toward their health care providers’. A young person’s feeling of certainty in children’s services and uncertainty about what to expect in adults’ services was confounded by direct or second-hand experiences of suboptimal care from adults’ services. 44,51 Transfer can be experienced as an ‘abrupt event’ by young people as a result of lack of knowledge and information about what to expect. 44,51 Reviews of models and strategies of the delivery of transitional health care53,84 have offered ideas about how specific practices might minimise this disruption.
Aim
The aim was to investigate how young people with long-term conditions experience services for transitional health care.
Methods
More information about methods is in Appendix 6, which includes the interview guide.
A longitudinal multimethod qualitative study was conducted with young people recruited from the longitudinal quantitative study (WP 2.1). Young people were initially approached by a member of the WP 2.1 study team and, if they wanted more information, they were contacted by telephone or e-mail by WP 2.2 researchers previously unknown to them.
Data collection took place between June 2013 and June 2016. Recruitment was driven by criterion sampling (i.e. diagnosis, age, service) and theoretical sampling (i.e. experience of service, comorbidities, social network). 85 Young people were aged between 14 and 18 years at the first interview. Each young person identified a ‘significant other’ person in their life and a health professional significant to their health care whom they wanted to include in this qualitative study, and to nominate one consultation that the researcher could observe. Thirteen young people took part in this study. Family members who took part were 10 mothers, three fathers or stepfathers and one brother. Nineteen health professionals were also identified: seven paediatric consultants, five paediatric nurses/allied health professionals, three adult consultants and four adult nurses/allied health professionals. We interviewed 13 of these: nine from children’s services and four from adults’ services.
Thirteen young people received a first interview, of whom four were interviewed again at least 18 months later. They were interviewed on their own or with a relative, if they wished, at their home or at a clinic. Fourteen family members received a first interview, of whom eight were interviewed again at least 18 months later. In total, we undertook 40 first interviews (Table 5). In 30 of these, the young person was pre transfer to adults’ services and in 12 they were post transfer.
| Participants | Diabetes mellitus | Cerebral palsy | ASD | Total |
|---|---|---|---|---|
| Took part in first interview | ||||
| Young person | 4 | 5 | 4 | 13 |
| Family member | 4 | 6 | 4 | 14 |
| Health professional | 4 | 4 | 5 | 13 |
| Total | 12 | 15 | 13 | 40 |
| Participants observed in consultations | ||||
| Young person | 3 | 2 | 2 | 7 |
| Family member | 3 | 3 | 2 | 8 |
| Health professional | 6 | 3 | 2 | 11 |
| Total | 12 | 8 | 6 | 26 |
Observations were recorded in contemporaneous field notes. Formal interviews (face to face or by telephone) lasting between 30 and 120 minutes were audio-recorded, transcribed and edited to ensure respondents’ anonymity and then analysed alongside anonymised field notes. All analysis was conducted according to the standard procedures of qualitative analysis. 86 We used procedures from first-generation grounded theory (coding, constant comparison, memoing87), and from analytic induction (deviant case analysis88). Data collection and analysis occurred concurrently, so that issues raised in earlier phases of fieldwork were explored in subsequent ones, including in follow-up interviews. We undertook independent coding and cross-checking, team data sessions and data triangulation (different times and persons) and between-method triangulation (interview, observation).
Analysis
The full report is in Appendix 6. The report focuses on the observational data and interviews, with accompanying commentary and quotations in relation to the nine PBFs. The work is summarised below under three headings:
-
disrupting relationships of trust
-
supporting successful transfer
-
enabling in(ter)dependence.
Disrupting relationships of trust
As one parent outlined, the actual process of transfer from children’s to adults’ services ‘takes 5 minutes’. However, crossing this organisational boundary was reported to take practical, cognitive and emotional work, often over a long time.
The family, especially the mother, had usually developed good understanding of how to support the management of the young person’s health condition, and how to navigate the children’s health service. The children’s health professionals often had significant knowledge of the young person and their wider psychosocial context. In most cases, young people had a long relationship with a particular service, and so they had built up trust over time with health professionals they saw regularly.
The organisational process of transfer ended those relationships of trust with known children’s health professionals and so called into question the expectations, knowledge and practices of the young people and their families. Transfer is a disruption or, following Garfinkel,89 a breach in taken-for-granted experiences, knowledge and expectations. It involves young people and parents having to adapt to a new set of circumstances.
Supporting successful transfer
All professionals were aware of the implications of ‘unsuccessful’ transition and how people could ‘drop off the system’ or ‘disengage’. All children’s health-care professionals had implemented formal or informal plans for transfer that sought to prepare the young person and their family (Table 6, which relates to evidence of implementation of PBFs). Children’s health-care professionals stated that they sought to introduce the idea of transition and transfer within consultations over time. Plans about transition were, generally, ‘something we talked about, there wasn’t really anything written down’ and, ideally, ‘tailored to the young person’s needs’. Such plans might also be ‘weaved into clinic letters’.
| PBF | Evidence of implementation | Determinants of implementationa |
|---|---|---|
| Age-banded clinic | Limited: seen only in diabetes services | Often not feasible because of the logistics of managing appointments, space restrictions or small numbers of young people. In practice, situated alongside other adult clinics, with parents and professionals alarmed by visibility of ill adults. Young people report ‘not being fussed’ |
| Meet adult team before transfer | Variable: some services offer a single joint meeting or shared appointments | Dependent on relations with adult team(s). In services that provide it, meetings do not always happen. Problematic when low frequency of meetings, young person has moved away (e.g. to university), adult practitioner is not the person who will provide care, or general practitioner is not known to young person (i.e. transfer to primary care) |
| Promotion of health self-efficacy | Variable: some services provided but in an informal, ad hoc way | Can occur in context of long-term, trust-based relationships with a specific health professional. Minimal health promotion if lack of continuity of personnel or low frequency of visits, or when not part of service culture |
| Written transition plan | Very limited: one service offered formal plan | One service had implemented, but withdrew because of lack of resources and motivation. Some professionals resisted written plans, saying that these get forgotten or lost, and that personal interaction is far more important. However, informal practices can lead to lack of awareness, knowledge and understanding of transfer process |
| Parents engaged appropriately | Extensive: all services report engaging parents | Service norm for some practitioners. Some see interdependence as demonstrating problematic attachment, and so seek to minimise parental involvement, often referring to legal issues around patient confidentiality |
| Key worker | Variable: services may report key worker, but young people and parents often unaware | In practice, most young people and families name ‘their’ de facto key worker as someone whom they trust and see consistently, and is supportive and accessible. Often, a parent – usually the mother – takes this role |
| Co-ordinated team | Variable: some services demonstrated some aspects | Largely dependent on service structures. Collaboration and co-ordination between team members can occur formally and informally |
| Holistic life-skills training | Very limited: some services provided elements albeit in an informal, ad hoc way | Some services had not considered this, whereas others had but thought that it was not their responsibility. Education, social services, charities and family often provided this; if not, young people, parents and services thought that they should. All thought that young people should be signposted to relevant services outside the NHS |
| Transition manager for clinical team | Very limited: one service reported recent introduction | One service saw this as a need, but was still developing a remit for the role. Many services would like to implement this, but it is dependent on resources and competing demands |
Meeting members of the adult team before transfer was crucial for the young people and parents who experienced it; this generally happened at a single face-to-face meeting. Such meetings, however fleeting, offered symbolic and practical benefits and initiated relationships. The meetings helped young people and their parents to manage potential anxiety and offered more certainty about the health-care transfer process.
For young people and families, developing an adequate awareness of the transfer process itself and learning about the people and expectations of adults’ services was important. Some young people and family members said that they had not received any support or information about the process. This was most marked when young people’s appointments were infrequent or where services were in flux. Faced with such uncertainty, some young people and families felt abandoned, and unsure about many aspects of the new service they were about to transfer to.
Enabling in(ter)dependence
At the heart of transition is the aim to shift responsibility for managing health and health services from parents to the young person. This WP highlighted that the support of family, especially mothers, was central to enabling this ‘independence’. Family members play a significant role and often contribute much effort to the negotiation of the multitude of transitions that the young person experiences, especially the health-care transition.
Within the children’s health context, family members may act as ‘key worker’ in the clinic and home, providing the young person with some continuity of care, a point of reference and a source of emotional support. They can also act as advocates, offer practical support in managing health-care needs, facilitate access to services, prompt or ask questions, research available evidence, gather information and check a young person’s understanding. For the most part, health professionals in adults’ and children’s contexts are aware of the work of young people’s families in supporting and enabling them. New routines, norms and expectations evolve so that health professionals, families and young people in adults’ and children’s contexts can experiment with new ways of being interdependent.
Immediately leading up to and after transfer, young people may experience tensions; for example, ‘legal’ independence is thrust on them, but they still prefer interdependence. Some services or health professionals can compound this tension, especially in adult contexts, where parental involvement is considered an example of ‘overattachment’ or ‘overdependence’ and is therefore seen as problematic and to be discouraged. Working with the ‘parent team’ can support a shift towards more ‘partnership’, ‘shared care’ or ‘consulting’ roles.
Strengths and limitations
Conducting serial and triangulated interviews enabled us to confirm stories and capture evolving perspectives. Observing consultations enabled us to compare what people do against what they said they did in these contexts. Although both the form and the content of health care received may differ among the three exemplar groups, the organisation and experiences of the transition and transfer process showed many more similarities than differences.
The findings have face validity, as they relate well to the findings in other WPs and other studies in the literature, especially how transition and transfer can be disorientating for young people and their families. 44,51,83 This study strongly echoes work on how young people build relations of trust with health professionals and services,44,51 especially where those relations are consistent and supportive,58 as well as work on how the family, especially the mother, have built relations of trust with health professionals and services. 83
In its nature, qualitative work is in-depth but small-scale, a consequent strength being the richness of data and a weakness being the small number of case examples. We aimed to recruit 15 families and achieved 13. We had difficulties in recruiting young people, with many seeing the breadth and depth of data collection as an additional burden while they were already taking part in WP 2.1. The retention of young people for follow-up and/or post-transfer interviews was poor, so learning about the adult context was limited. We were unable to contact some young people, and some of those we did contact declined follow-up interviews; they either withdrew or suggested that we speak to their parents or health professionals. Thus, our findings are valid in relation to the data we collected; however, it is possible that we did not identify key messages that would have been relevant after the transfer to adults’ services.
Key findings
-
Transition and transfer are disorientating for young people and their families. They have practical, cognitive and emotional impacts. Importantly, they disrupt often hard-earned knowledge of how best to navigate the children’s health-care system effectively.
-
Health professionals need to help young people and their families adjust to and mitigate these disruptions. The key practices that minimise this disruption are being clear in discussions and documents about processes, discussing how adults’ and children’s practices differ, undertaking joint clinics and meetings with members of the adult team that the young person will actually be seeing and including family members in the process.
-
Transition is about enabling young people to become responsible for their own health care. However, family members remain crucial. Such involvement is normal, not dysfunctional, and for people in other age groups is largely accepted. Family members can be helped to adjust their roles to have more partnership and sharing of care and consultation with their son or daughter.
Inter-relationship with other parts of the programme
This WP, 2.2, was informed by WP 1.1 in which the UP group commented on the draft interview schedule and the practicalities of the planned visits to young people and clinic consultations.
The sample for WP 2.2 was a subsample of that in WP 2.1 and so the two WPs worked closely together.
Our published article,63 on intended provision of PBFs and whether or not they are experienced by young people, integrated quantitative findings from WP 2.1 with qualitative findings from this WP 2.2. Our article directly influenced our decision to use the young person’s experience of each PBF as the exposure in our regression analyses, rather than what the service said it aimed to provide.
The findings of this WP influenced interpretation of the three PBFs associated with improved outcomes in the conclusions section. This discussion informed one of the seven key implications of the programme, implication 6.
Work package 2.3: discrete choice experiment and economic analysis
Addressing objective 2: to identify the features of transitional health care that are effective and efficient
This WP examines the economic aspects of transition. It has two parts:
-
discrete choice experiment
-
economic modelling.
Discrete choice experiment
Discrete choice experiments are regularly used in health economics to elicit preferences for health-care products and programmes, and in the valuation of preferences for health states. 90–92 Further details are in Appendix 7.
Aim
The aim was to quantify the strength of young people’s preferences for aspects of health services for transition using a DCE.
Methods
A DCE describes a service in terms of a number of characteristics, or ‘attributes’ (e.g. the flexibility of appointments, parental involvement). The extent to which an individual values an intervention is expected to depend on the ‘level’ these attributes take (e.g. can appointments be made outside office hours or not?). Thus, a DCE explores relative preferences about how services can be organised, by choosing between services with differing levels of their attributes. 93
The design and conduct of the DCE involved four steps.
Step 1: identifying attributes and levels
Attributes and levels were informed by the Q-sort (WP 1.3). Other information was drawn from previous research about important features of transition. 94 The design and presentation of the DCE were undertaken with the members of the transition research programme’s Collaborative Group and with UP. The chosen attributes and levels are shown in Table 7.
| Attribute | Number of levels | Description |
|---|---|---|
| Flexibility | 2 |
0 = does not offer appointments outside office hours 1 = offers appointments outside office hours |
| Staff at appointments | 4 |
0 = do not see the same staff at my appointments and do not have a key worker 1 = do not see the same staff at my appointments but have a key worker 2 = see the same staff at my appointments but do not have a key worker 3 = see the same staff at my appointments and have a key worker |
| Staff communication | 2 |
0 = yes 1 = no |
| Parental involvement | 2 |
0 = discouraged 1 = welcomed ‘if I want it’ |
| Decisions about care | 2 |
0 = staff discuss my care with me but they make the decisions 1 = staff give me choices but expect me to make the decisions |
| Extra support | 2 |
0 = no 1 = yes |
Step 2: experimental design
The number of attributes and levels described in Table 7 give 128 possible combinations. Statistical manipulation, using Ngene software (2017; ChoiceMetrics, Sydney, NSW. Australia), reduced the number of scenarios. The resulting D-efficient design had 24 questions, which were further reduced by ‘blocking’ them into three groups, so that each respondent needed to complete only eight questions. Young people also answered questions about their current care, defined by the same attributes and levels used in the DCE. For each question, respondents chose between two hypothetical ways in which a service might be organised (see Appendix 7 for specimen questions).
Step 3: data collection
The DCE was completed at visit 3 of the longitudinal study (WP 2.1). Several decision aids were piloted and then used to assist young people who had difficulty completing the DCE (see Appendix 7).
Step 4: data analysis and interpretation
Data were analysed within a random utility model framework using logistic regression techniques. The analysis estimated the predicted uptake of the service: the more an attribute is preferred, the higher the predicted uptake.
Analysis
In total, 247 participants completed at least one DCE question (fully completed, n = 223; partially completed, n = 24); 101 participants did not complete the DCE as they had withdrawn or were lost to follow-up. Young people with ASD were significantly less likely to respond than those with diabetes mellitus [16/87 vs. 7/112 (χ2 = 10.50, degrees of freedom = 2; p ≤ 0.001)].
Appendix 7 presents detailed results. In summary, 43 respondents always chose current care and 60 never chose current care. Those not currently receiving any service were significantly less likely to choose current care (p < 0.001). Each attribute and level was often preferred by many young people, as was current care. Table 8 shows that in a service where none of the attributes was present, the uptake of the service would be 78%. Adding a new service attribute, such as flexible appointments, predicted an uptake of 81%.
| Attribute | Probability of uptake (95% confidence interval) |
|---|---|
| Current service (none of the attributes) | 0.78 (0.75 to 0.81) |
| New service with flexible appointments | 0.81 (0.78 to 0.84) |
| New service with a key worker | 0.79 (0.74 to 0.85) |
| New service seeing the same staff at each appointment | 0.90 (0.85 to 0.94) |
| New service seeing the same staff and having a key worker | 0.88 (0.84 to 0.92) |
| New service with good staff communication | 0.93 (0.91 to 0.95) |
| New service with parental involvement | 0.93 (0.90 to 0.95) |
| New service offering young people decisions about treatment | 0.91 (0.88 to 0.93) |
| New service offering extra support to young people for their future | 0.86 (0.83 to 0.89) |
When demographic characteristics (gender, age at data collection and condition) were taken into account, all attributes, except flexibility of appointments, were preferred to a service with none of the attributes (see Appendix 7, Table 23).
Preference for current care was stronger among young men than among young women. Preference for current care was also stronger among those who had not transferred from children’s to adults’ services than among those who had. Young men had a stronger preference for out-of-hours clinics than young women did, and a weaker preference for making their own decisions about treatment. Young people with ASD had weaker preferences for parental involvement, and for being the ones to make decisions about their treatment, than those with cerebral palsy.
Strengths and limitations
A DCE can be demanding to complete. Although most young people were able to respond, proportionately fewer with ASD did so. It is possible that these young people have different preferences from those who did complete the DCE. Furthermore, it is possible that the DCE failed to accurately capture the preferences of those young people who completed it. On this latter issue, some reassurance was provided by the broad similarities between the DCE findings and the ranking exercise. The advantage of the DCE over the ranking exercise was that the DCE provided an indication of the relative importance of each attribute.
Discrete choice experiments are widely accepted as a methodological approach preferred by many organisations. For example, they form the basis of eliciting EQ-5D-5L (EuroQol-5 Dimensions, five-level version) population tariffs throughout the world95 and the Center for Devices and Radiological Health has stated that DCEs are a suitable method of eliciting patient preferences. 96 The approach we adopted was consistent with best practice. The aids to completion of the DCE might have infringed strict DCE methodology, but they enabled young people, with a wide range of confidence, intellectual ability and flexibility of thinking, to complete it. Indeed, the use of aids to completion has been advocated. 97–99
A fixed-effects modelling assumed that respondents were consistent in their choices over time. Although such an approach was not incorrect, more sophisticated econometric modelling could be used to explore heterogeneity and whether or not participants considered only a subset of attributes when choosing among alternatives. This might help explain why an appreciable proportion of respondents always chose current care.
Key findings
-
Young people with long-term conditions, including those with ASD, could complete a DCE.
-
In total, attributes were preferred to them not being present, except for flexibility of appointments.
-
Preference for current care was strong and more pronounced among young men than among young women. This preference was stronger among those who had not transferred.
-
Most young people (and especially women) least valued being able to have appointments outside office hours.
-
Young people valued services in which information was passed to the right person, parental involvement was welcomed, staff offered choice and allowed young people to make decisions about their care, the same staff were seen at each clinic appointment and extra support was available for preparation for everyday life. Young people valued seeing the same staff at each clinic appointment more than having a key worker.
Inter-relationship with other parts of the programme
From WP 1.1, UP contributed much to the design of the DCE questionnaire. DCEs have not been undertaken often with young people. The understanding of the choice options was therefore discussed and piloted with UP.
The content of the DCE was, in part, informed by the Q-sort study of WP 1.3.
The DCE was administered at visit 3 in the longitudinal study WP 2.1.
This WP, 2.3.1, informed WP 2.3.2 on economic analysis.
The results of this WP led directly to one of the implications of the programme, implication 7, concerning elements of service that would make it more likely that transition services were taken up by young people.
Economic analysis
We assessed the relative efficiency of illustrative models of transition. WP 2.1 captured information from health records on the PBFs received by young people, their use of health services (and hence cost), and their health-related quality of life (HRQoL). We estimated the relative cost-effectiveness and presented the economic data and other study findings in a balance sheet.
The full account of the methods and analysis are in Appendix 7.
Aims
-
To determine the resource use and costs of the PBFs.
-
To assess the relative efficiency of illustrative models of transition.
Methods
Using the same decision rule as in WP 2.1, a trajectory for each PBF, deemed satisfactory or unsatisfactory, was assigned to each participant based on the data captured from the health notes.
Costs to the NHS covered the costs of consultations, medication and investigations. Data needed for costing were obtained by the research assistants from the health records, with additional information on service use gathered at each annual visit after the baseline visit. To aid recall, young people had kept diaries of contacts with health and personal social services. A unit cost was then applied to each service accessed using routine sources. 100,101 Average pre- and post-transfer costs were then calculated.
Costs were then analysed to estimate the annual cost for a service where there was a PBF and for a service where there was no PBF. These costs were further split according to whether the young person was pre or post transfer, and, if post transfer, whether to primary or secondary care.
Young people completed the EQ-5D-Y at each of the four annual visits. This instrument captures HRQoL for use in economic analyses. 102 Data from the EQ-5D-Y were converted to utility scores using the value set for adults. 103 Utility scores range from 0 to 1, with 1 indicating best health. A simple scoring system was also adopted for the EQ-5D-Y. Each of its five domains was assigned equal weight, and each level of each domain was scored 1, 2 or 3, depending on severity. Thus, each domain scored from 1 to 3, with 3 being worst health. Summing the scores for each domain generated a ‘sumscore’ that ranged from 5 to 15, with 15 being worst health. A similar approach to analysing these data was adopted for cost.
The data on costs and HRQoL were incorporated into a simple Markov model (Figure 9) in which all young people start in children’s services, aged 14 years, and are followed for 10 years, the time over which a young person would be expected to be undergoing transition. The model considers a hypothetical cohort of 1000 young people. Each year, they have a probability of transferring from children’s services to primary care or moving into adults’ services. If, in any year, they do not make the transfer, then they remain in children’s services, indicated by the ellipse connected to the children’s services state. The chance of being in a given state in a given year (the ‘rate of transfer’; see Appendix 7) was calculated by considering the number of people who transferred from children’s services each year, and the ratio of young people transferred to adults’ services to those transferred to primary care.
FIGURE 9.
Structure of the economic model.

Those remaining in a given year in the children’s services state are represented by the ellipse connected to the children’s services state.
For each state in Figure 9, an annual cost, utility and sumscore value was assigned as described above. Cumulative costs, quality-adjusted life-years (QALYs) and sumscores were estimated for the 10-year time horizon, and all costs and effects were discounted at the UK recommended rate of 3.5% per annum.
The results of the model and the DCE were combined with findings from other areas of the research programme in a balance sheet analysis. In this analysis, we present those outcomes that could favour a hypothetical intervention compared with a situation in which there was no support during the transition from children’s to adults’ services.
Analysis
Estimation of use of health services and costs
There were 7755 health-care contacts over the study period. Another 627 scheduled contacts were cancelled in advance or without enough prior notification (classified as ‘did not attend’). The numbers of participants providing data were 286 (76.2%) at visit 2, 249 (66.4%) at visit 3 and 216 (57.6%) at visit 4.
The median number of health-care contacts across all years was 19 (IQR 20). This varied by condition, ranging from 14 (IQR 27.8) for those with cerebral palsy to 16 (IQR 23) for those with ASD and 23 (IQR 13.8) for those with diabetes mellitus. Over time, the median number of visits decreased. Visits for those with cerebral palsy dropped from 7 to 5, for those with diabetes mellitus dropped from 8 to 7, and for those with ASD increased from 5 to 6. Full details are in Appendix 7.
Combining data on use of services with unit cost data allowed an estimation of the cost of care for each young person. Data were available on 301 young people (78.6%). The overall median cost per participant was £4954 (IQR £6103). Diabetes mellitus was the costliest condition, and cerebral palsy the least costly, with considerable variation between individuals. The difference between the cost for those with diabetes mellitus and the cost for those with ASD was statistically significant (p < 0.001). The difference in pre- and post-transfer costs was not statistically significant (p < 0.05), although there was a trend both overall and by condition (Table 9).
| All (IQR) | ASD (IQR) | Cerebral palsy (IQR) | Diabetes mellitus (IQR) | |
|---|---|---|---|---|
| For all | ||||
| Number | 301 | 96 | 77 | 125 |
| Median costs (£) | 4954 (6103) | 2351 (4211) | 2394 (5606) | 7003 (3667) |
| Median costs per annum (£) | 2307 (2705) | 1659 (2573) | 1447 (2725) | 2915 (2422) |
| For those pre transfer | ||||
| Number | 279 | 88 | 67 | 121 |
| Median costs (£) | 2420 (4506) | 1694 (2454) | 1370 (4215) | 4434 (5136) |
| Median costs per annum (£) | 1673 (2242) | 915 (1277) | 949 (1974) | 2410 (1587) |
| For those post transfer | ||||
| Number | 194 | 56 | 48 | 87 |
| Median costs (£) | 2080 (3470) | 1262 (2540) | 1395 (3015) | 3114 (3440) |
| Median costs per annum (£) | 1371 (1862) | 645 (1883) | 707 (1673) | 1849 (1193) |
Estimation of health-related quality of life
Data from the EQ-5D-Y were available for 373 respondents at baseline and for 244 respondents by visit 4. The median sumscore score was 5 for every domain at every time point (i.e. half of the respondents reported ‘no problems’). The mean sumscores increased over time (i.e. health worsened), as did the scores for each domain. During the follow-up period, the proportion of individuals experiencing problems on each domain (a score of 2 or 3) increased significantly (p < 0.001) for each of the five domains (see Appendix 7).
The median sumscore for all participants across all time points was 6 (IQR 2.79), which indicates that at least half of participants experienced a problem on at least one domain. Average sumscores were not associated with gender, and nor were pre- or post-transfer scores. In addition, there were significant differences in sumscores by condition, as participants with diabetes mellitus had significantly lower scores (i.e. better health) (p < 0.001) at all time points (Table 10).
| All (IQR) | ASD (IQR) | Cerebral palsy (IQR) | Diabetes mellitus (IQR) | |
|---|---|---|---|---|
| For all | ||||
| Number | 301 | 96 | 83 | 122 |
| Median sumscore | 6 (2.79) | 7 (2) | 7 (2.98) | 5.20 (1) |
| Median utility score | 0.83 (0.30) | 0.75 (0.26) | 0.70 (0.43) | 0.94 (0.14) |
| For those pre transfer | ||||
| Number | 269 | 86 | 70 | 113 |
| Median sumscore | 6 (2) | 7 (2) | 7 (3) | 5 (1) |
| Median utility score | 0.85 (0.27) | 0.75 (0.26) | 0.72 (0.43) | 0.95 (0.13) |
| For those post transfer | ||||
| Number | 230 | 68 | 66 | 96 |
| Median sumscore | 6 (3) | 7 (2) | 7 (2.75) | 5 (1) |
| Median utility score | 0.82 (0.29) | 0.76 (0.24) | 0.70 (0.33) | 0.95 (0.16) |
The median utility score across all participants was 0.83 (IQR 0.30). Average utility scores were not associated with gender, or pre- or post-transfer scores. However, the scores of those who had transferred were significantly higher for those transferring to adults’ services (median 0.86, IQR 0.37) than for those transferring to primary care (median 0.78, IQR 0.38). As we found for the sumscore, participants with diabetes mellitus had significantly higher utility scores (p < 0.001) at all time points (Table 10).
Experience of proposed beneficial features
Data on experience of the PBFs are reported in Appendix 7, Table 34. These and the economic evaluation used two methods to determine whether or not a PBF had been experienced.
A form was completed each year by the research associate from data in the young person’s health records. It consisted of details of clinic visits, professionals in attendance, medical tests undertaken and whether or not PBFs had been experienced. This was called the ‘final account of consultation’. Following the home visits with further discussion of appointments and PBFs and completion with the young person of a questionnaire, it became clear that the final account was incomplete for some young people. Therefore, analysis was also undertaken with data combined from both sources.
Economic evaluation model
The parameter values used in the economic model are reported in detail in Appendix 7. The analysis considered each PBF separately and, given the limited data available, should be considered exploratory. Given the exploratory nature, a probabilistic sensitivity analysis was not conducted as there was considerable imprecision in the results. The results are best considered as either illustrative of the approach taken or hypothesis-generating about possible PBFs to consider when developing an intervention to improve transition.
Tables 9 and 10 show the estimated costs and effects (sumscore and QALYs). Table 11 shows the incremental cost-effectiveness for a service incorporating each PBF alone compared with a service where no features were present. We could not compare individual PBFs with a situation in which all PBFs were provided, as only one participant had experienced all PBFs. As the presence of PBFs is based on face-to-face discussions and health records, a sensitivity analysis was performed using both data sources.
| PBF | ICER using PBFs captured from final account (£) | ICER using PBFs captured from both sources (£) |
|---|---|---|
| Meet adult team before transfer | Dominateda | 7121 |
| Age-banded clinic | 36,487 | 13,176 |
| Holistic life-skills training | 10,991 | 5618 |
| Key worker | 15,259 | 4811 |
| Transition manager for clinical team | 64,359 | 12,592 |
| Appropriate parent involvement | N/A | 7070 |
| Promotion of health self-efficacy | N/A | 5127 |
| Co-ordinated team | 52,100 | 8596 |
| Transition plan | N/A | 11,259 |
| Cost per 1 unit change in sumscore | ||
| Meet adult team before transfer | 15,092 | 7011 |
| Age-banded clinic | 22,693 | 12,662 |
| Holistic life-skills training | 5692 | 4563 |
| Key worker | 13,363 | 3878 |
| Transition manager for clinical team | 23,364 | 7114 |
| Appropriate parent involvement | N/A | 5345 |
| Promotion of health self-efficacy | N/A | 5341 |
| Co-ordinated team | 12,746 | 7700 |
| Transition plan | N/A | 8947 |
Experience of proposed beneficial features
The data reported in Table 34 (see Appendix 7) and in Table 11 illustrate that the results are sensitive to the methods used to decide whether or not a PBF was experienced. The higher the incremental cost-effectiveness ratio, the less likely it is that an intervention would be considered value for money.
Three PBFs performed better regardless of whether the determination of ‘satisfactory’ PBF exposure was based on the final account or on the data from both sources. These PBFs were ‘provision of holistic care’, ‘having a key worker’ and ‘promotion of health self-efficacy’.
‘Meeting the adult team’ was sensitive to the source of data and was considerably more advantageous when the estimates were based on the data from both sources. ‘Having a written transition plan’ and ‘having a transition manager for clinical team’ performed relatively poorly.
Balance sheet
Using data from the economic analyses and from elsewhere in the programme, a balance sheet was developed to summarise the pros and cons of providing a service with a PBF compared with a service without PBFs (Table 12). The development and implementation of a service containing one or more PBFs would incur a cost of a magnitude determined by how that PBF was delivered.
| Favours service containing the adaptability needed from the findings of the Q-sort, the preferences in the DCE and the PBFs in the prospective study | Favours service not containing the adaptability needed from the findings of the Q-sort, the preferences in the DCE and the PBFs in the prospective study | Source |
|---|---|---|
| Avoided the currently unknown costs of providing beneficial features. Costs of some may be modest (e.g. a ‘written transition plan’) whereas others are substantial (e.g. adoption of a multidisciplinary team) | Costs not estimated | |
| A service should be flexible enough to meet the needs of individuals; one size does not fit all and needs may change over time. A service needs to consider the condition, the stage of development and the young person’s personality | Q-sort (WP 1.3) and DCE (WP 2.3.1) | |
| High predicted uptake of a service with no PBFs (78%, 95% confidence interval 75% to 81%) | DCE (WP 2.3.1) | |
| Predicted uptake of a service is higher when the service includes parent involvement, when the same staff are seen at each clinic appointment and where the young receive good communication and are offered the opportunity to make decisions | From the DCE: a strong preference for current care; no strong preference for a ‘key worker’ or flexibility of appointments | DCE (WP 2.3.1) |
| Increasing engagement may help prevent deterioration of the young person’s condition over time | Anticipated impact not measured in study | |
| ‘Appropriate parent involvement’, ‘promotion of health self-efficacy’ and ‘meeting the adult team’ improved outcomes | Analysis of longitudinal data (WP 2.1) | |
| Estimated additional benefit to health service of adopting any of the above features, except ‘being cared for by a co-ordinated team’ | Estimated additional cost to health services of adopting any of the PBFs | Economic model analysis (WP 2.3.2) |
| Longer-term model cautiously suggests that ‘holistic life-skills training’, ‘having a key worker’ and ‘promotion of health self-efficacy’ might be value for money | Longer-term model cautiously suggests that ‘transition manager for clinical team’, ‘age-banded clinic’ and ‘meeting the adult team before transfer’ might not be value for money’ | Economic model analysis (WP 2.3.2) |
| No evidence of a difference | ||
| Lack of clarity about what was meant by a health passport, something that might be valued but was rarely used | Works conducted by UP (WP 1.2) | |
| During transition, there was no evidence of any effect on outcomes of ‘having a transition plan’, ‘attending an age-banded clinic’, ‘being cared for by a co-ordinated team’, ‘being part of a service with a transition manager for clinical team’ or ‘having access to holistic life-skills training’ | Analysis of longitudinal data (WP 2.1) | |
| Over the duration of the longitudinal study, there was no evidence of any effect on costs or HRQoL of ‘having a transition plan’, ‘attending an age-banded clinic’, ‘being cared for by a co-ordinated team’, ‘being part of a service with a transition manager for clinical team’ or ‘having access to holistic life-skills training’ | Analysis of costs and EQ-5D data in the economic analysis (WP 2.3.2) | |
The limited data available from the economic model suggest that implementation of a new service will increase the use of NHS services at least over a 10-year time horizon for a young person aged 14 years entering a ‘transition’ service. There appear to be no harms to the young person from any of the PBFs.
Strengths and limitations
A concern was whether or not the HRQoL instrument was sufficiently sensitive to capture an influence of PBFs. The study was powered not on the EQ-5D-Y but rather on the outcomes used in WP 2.1. We did have sufficient power to identify clinically significant changes in the EQ-5D-Y but, for analysis by condition, sample size meant that some real effects of difference may not have been detectable. In relation to the PBFs, power was limited if a feature was often absent.
Alternatively, the HRQoL instrument might have been sufficiently sensitive, but follow-up was too short to capture any influence of PBFs.
The DCE suggested that experiencing some of the PBFs might increase young people’s engagement with health services, which, in turn, might alleviate longer-term harms (and costs) due to inadequate health care. The economic evaluation was exploratory and compared only services with individual PBFs with a service with no PBFs. Therefore, no probabilistic sensitivity analysis was conducted, as is normally recommended for health technology assessment economic evaluations; a quantified estimate of the effect associated with various combinations of PBFs was not possible. Therefore, the economic conclusions should be interpreted with care.
It was necessary to annuitise the cost data for participants to allow a comparison with the EQ-5D-Y data. Thus, certain costs for participants for items mentioned occasionally, but likely to apply over the course of the study, were calculated as a daily rate following the aggregation of the visit data. For example, as insulin prescriptions were not consistently reported in the data, these were costed separately according to existing literature and then inflated to the current price year. We think that this made best use of the available data and is unlikely to have distorted the results.
The data collected on outcomes, costs and health service use were complex to interpret because there was loss to follow-up and differing health-care transfer arrangements, and the intervals between the annual visits by the research assistants were not always exactly 1 year. Strict econometric modelling, despite considerable efforts, proved to difficult to undertake. Therefore, a less robust exploratory analysis was adopted, which drew out key implications and generated a balance sheet. Conclusions were not wholly in concordance with some conclusions from other parts of the programme, but the triangulation of findings allowed key consistent conclusions and implications to be identified and reported.
Key findings
-
There were significant differences in both costs and HRQoL between conditions.
-
The average utility and sumscores were similar in those pre and post transfer.
-
The median annual cost (covering the costs of consultations, medication and investigations) was £7003 for an individual with diabetes mellitus, £2934 for an individual with cerebral palsy and £2350 for an individual with ASD.
-
Both costs and HRQoL declined over time for all conditions.
-
A service involving a PBF is unlikely to reduce NHS costs over a 10-year time horizon but might increase them.
-
We have examined the potential consequences of a service with flexible appointments and that encourages ‘appropriate parental involvement’ and ‘promoting health self-efficacy’. A judgement is needed about whether or not such a service would be worth the extra cost, given that it may increase engagement with health services and prevent deterioration in health in the long term.
Inter-relationship with other parts of the programme
Data collected during WP 2.1 (the quantitative longitudinal study) about costs of consultations and exposure to PBFs were essential for the economics analysis.
The results from the DCE (WP 2.3a) contributed to interpretation of the economic analysis.
The results of this WP led directly to one of the implications of the programme, implication 7, concerning value for money.
Work package 3.1: introduction of developmentally appropriate health care
Addressing objective 3: to determine how transitional health care should be organised, provided and commissioned
This WP examined how DAH can be introduced across NHS Trusts. It had two parts:
-
WP 3.1.1: identification and description of factors that enable or inhibit the introduction of trust-wide DAH
-
WP 3.1.2: development of a toolkit for the introduction of DAH.
From our work, there are two published papers. 3,4 The report on the implementation of DAH is in Appendix 8.
Work package 3.1.1
There is a need to provide health care that meets the needs of young people. Youth-friendly health services104,105 is one concept discussed in the literature. However, we need to move from the ad hoc provision of youth-friendly services to youth-responsive health systems106 that respond to young people’s changing developmental needs. 25 DAH recognises the changing biopsychosocial developmental needs of young people and the need to empower young people by embedding health education and health promotion in consultations. In this WP we developed a working definition of DAH:
DAH recognises the changing biopsychosocial developmental needs of young people and the need to empower young people by embedding health education and health promotion in consultations. In operational terms, DAH focuses on health-care professionals’ approach to and engagement with each young person and their carers alongside the structure of the organisations in which care takes place.
DAH offers a foundation for good practice in the health care of young people and so it should underpin transitional health care.
Aim
The aim was to identify, describe and understand the factors that enable or inhibit the introduction of DAH across NHS Trusts.
Methods
We convened a 1-day seminar in Birmingham on DAH. This brought together 29 delegates with expertise and experience from health services research, public health, social policy, clinical practice and the voluntary sector.
A scoping review, using recognised methods,107 was conducted to explore the use and meanings attributed to the concept of DAH. Articles were subjected to manifest and latent content analysis. 108
More detail about methods is in Appendix 8, which also includes the interview guide.
A qualitative, multisite, ethnographic study was then conducted across three hospitals in England: a district general hospital, a paediatric tertiary hospital and an adult tertiary hospital. Health professionals were recruited from six medical and surgical specialties (diabetes, emergency care, general paediatrics, outpatients, rheumatology, and trauma and orthopaedics) chosen to represent the heterogeneous services found in NHS hospitals. In addition, individuals from chaplaincy, psychology, radiology and youth work, as well as those leading training sessions, were recruited to explore a broader range of the staff and contexts with which young people are engaged. Managers were recruited at each site if their roles were relevant to the provision of services for young people in paediatrics and/or adult care.
Data collection took place over three phases between June 2013 and January 2015. Recruitment was initially through gatekeepers, and then through a mix of snowball, criterion and theoretical sampling. A total of 192 participants were recruited. Approximately 1600 hours of non-participant observations were conducted, alongside 65 formal qualitative interviews (Table 13). Observations of interactions between staff, young people and family members and between staff (in departments, wards, clinics, team meetings and training workshops) were recorded in contemporaneous field notes. Interviews were audio-recorded, transcribed, edited to ensure anonymity and then analysed alongside field notes.
| Participants | Site (n) | Total (N) | ||
|---|---|---|---|---|
| District general hospital | Paediatric tertiary hospital | Adult tertiary hospital | ||
| Participants observed | ||||
| Health professional | 65 | 27 | 11 | 103 |
| Manager | 57 | 0 | 15 | 72 |
| Total | 122 | 27 | 26 | 175 |
| Participants interviewed | ||||
| Health professional | 13 | 18 | 10 | 41 |
| Manager | 13 | 6 | 5 | 24 |
| Total | 26 | 24 | 15 | 65 |
| Overall participants | ||||
| Health professional | 78 | 45 | 21 | 144 |
| Manager | 70 | 6 | 20 | 96 |
| Total | 148 | 51 | 41 | 240 |
| Participants who were both interviewed and observed | 39 | 5 | 4 | 48 |
| Total number of participants | 109 | 46 | 37 | 192 |
Analysis used qualitative methods86 from first-generation grounded theory (coding, constant comparison, memoing87) and procedures from analytic induction (deviant case analysis88). Because data collection and analysis occurred concurrently, issues raised in earlier phases of fieldwork could be explored in subsequent ones. We undertook independent coding and cross-checking, team data sessions and member validation with some of the participants in the fieldwork. The analysis was informed by normalization process theory (NPT). 109
Analysis
Our scoping review3 found that there was no agreed definition of DAH. DAH was linked to domains of adolescent medicine, young people, chronic conditions and transitional health care, but there was much diversity in conceptualisation, terminology and age ranges.
The following summary of the implementation of DAH is described in more detail in Appendix 8. This cites many quotations from the interviews and observations and has accompanying commentary.
The core of DAH was that the young person’s developmental stage should be the starting point for appropriate provision of services. We also found a wide variety of understandings of DAH across clinical and managerial staff in all the sites (see Farre et al. 4). Some did not recognise it as a concept, to some it made little sense and others found it difficult to conceptualise: it was ‘a bit amorphous’. Many focused on the need to create a more age-appropriate, youth-friendly environment106 in the physical spaces of waiting room and wards (e.g. having age-appropriate leaflets and computer games). Others, especially those who worked with young people, were more likely to mention interpersonal aspects, such as developmentally appropriate communication, norms around confidentiality and a holistic focus. Using the concepts of NPT, we identified little coherence across sites and staff, the use of a variety of definitions (‘differentiation’), a lack of shared understanding of the purpose of DAH (‘communal specification’) and diverse understanding of the potential impact of DAH on their work (‘individual specification’).
There were also different views on the worth of DAH (‘internalisation’) across sites and staff (see Appendix 8). The numbers of young people accessing health services were often perceived to be small, so in organisational terms they may be ‘just below the radar’. Compared with the elderly, they were considered to be ‘rarely unwell’. This may be compounded by the intermediate status of young people in the UK health-care system: one senior manager said ‘adult services don’t really want them because they are too young and the child services don’t really want them because they are too old’. None of the sites had a senior clinical or management lead for young people. Although young people’s champions were considered important, there were dangers in relying too much on key individuals. It should be ‘about consistency of approach, not a person’. So, in NPT terms, there were key people driving DAH forward (‘initiation’), but these were rarely senior members of staff. At times, we observed that when a young people’s champion left a specific team, there was then a reduction in team members becoming involved in and staying committed (cognitive participation) to the implementation of DAH.
Across the three sites, local networks tailored services to the needs of young people. However, in all of the sites, DAH was unevenly distributed. Some thought that no ‘special arrangements’ were required and that, by implication, DAH was not a legitimate part of their work (legitimation). Informal networks of trust existed at each site, where certain people or teams were understood to have the right skill mix, or mindset, or access to resources, to work effectively with young people. In this way, specific groups of people or teams were willing to work with others to enable DAH (enrolment), were motivated to deliver DAH over time (activation), had the relevant mix of skills (skill set workability) and were able to deliver DAH (relational integration). Young people tended to be directed to such teams. Thus, some of the inequities in skills and experience across the organisations were self-sustaining.
In all sites, service development for young people rested with the informal, organisation-wide group of young people’s champions. Such groups promoted initiatives to raise awareness across the organisation, create change, offer support and learn from each other.
In two of the sites, training took place at an annual study day. At another site, we observed training about DAH being planned and delivered by a group of managers, clinicians and allied health-care professionals who met every few months. At this site, dissemination reached well beyond the special interest group; it was clearly supported by the organisation (‘contextual integration’). The training was linked to the development of a DAH strategy and consisted of ‘delivering key messages’ from various government policy initiatives, such as the You’re Welcome Criteria. 94 This strategy was supported with resources from senior management. The focus of the strategy and training was on:
-
organisational-level factors, such as provision of age-banded clinics and staff appraisal, which included training goals around young people
-
clinic- and consultation-level factors, such as signposting to sexual health, drug and alcohol services, and copying clinic letters to young people
-
training and awareness factors such as adolescent development and confidentiality.
Strengths and limitations
As detailed in-depth work was required, it was realistic to work in a small number of sites: three sites in two UK regions were studied. A limitation was that only three sites in two UK regions were studied. A significant number of staff participated and a wide range of settings were encompassed, including outpatient, inpatient and emergency care. Although the hospitals had a history of championing research and innovative service provision for young people, this did not include a defined service for adolescent medicine. In addition, the clinical specialties at each site were at different stages of understanding of DAH, thereby providing the study with ranges of experience. We think, therefore, that we captured a broad range of relevant views, but it is likely that not all were covered.
Key findings
-
Although there were different understandings of DAH in the literature and across clinical and managerial staff, common themes led us to propose a working definition:
DAH recognises the changing biopsychosocial developmental needs of young people and the need to empower young people by embedding health education and health promotion in consultations. In operational terms, DAH focuses on health-care professionals’ approach to and engagement with each young person and their carers alongside the structure of the organisations in which care takes place.
-
DAH is needed equally in adults’ and children’s services.
-
The organisational barriers to introducing DAH were:
-
No single group was responsible for young people.
-
There was perceived (incorrectly) to be a small number of young people attending hospital; and also a perception that young people were rarely unwell.
-
The mindset and skill set of many staff were not ready.
-
Good practice led by enthusiasts was not sustainable.
-
-
The organisational solutions to introducing DAH were to:
-
move beyond pockets of good practice to buy-in and formal support at NHS Trust board level and from senior managers in both adults’ and children’s services
-
ensure that planning engages adults’ and children’s services from the outset
-
ensure a trust-wide strategy and training about DAH.
-
Inter-relationship with other parts of the programme
The preliminary findings of this WP, together with the video created by UP, were presented at an external seminar held in Birmingham for invited delegates.
The immediate effect of this WP was to influence the content of the toolkit for implementation of DAH (WP 3.1.2). The findings shaped the format of the toolkit in terms of:
-
the emphasis on different domains (e.g. consultation, team and organisation)
-
the content – explicit description of DAH, references to resources used by people at sites, including training
-
the examples of good practice.
Developmentally appropriate health care was an important topic in the discussions we had with commissioners (WP 3.3), and one of the key implications, implication 2, of our research is that the introduction of DAH across a NHS organisation be considered by commissioners and NHS provider organisations.
Work package 3.1.2
Aim
The aim was the development of a toolkit for the introduction of DAH.
Methods
We consulted with the Association of Young Person’s Health, as it had experience in developing similar resources. We supplied it with the content and websites to which the content could be linked. After three revisions, the toolkit was piloted by requesting comments from 10 senior NHS managers, adult and paediatric health-care professionals, the research associates who undertook the ethnographic work, and the Royal College of General Practitioners. The toolkit was revised again and then launched at the dissemination conference of the research programme in October 2017. The toolkit is downloadable from the website of the sponsoring trust, Northumbria Healthcare, which also holds the copyright. Every 3 months we will ensure that the websites linked to the toolkit remain active; and every 12 months revise content if necessary. The URL of the toolkit is http://research.ncl.ac.uk/transition/.
Work package 3.2: commissioning – interviews and case studies
Addressing objective 3: to determine how transitional health care should be organised, provided and commissioned
‘Commissioning’ is the process by which public services are organised and contracted to meet population needs. Health-care commissioners follow a cyclical process of assessment of population needs, setting priorities, developing strategies in line with objective outcomes, procuring services and measuring outcomes. 110 The need for better commissioning for transition was highlighted in recommendation 32 of the Kennedy Report,12 which stated that:
Ensuring a smooth transfer between children’s and adults’ services should be a priority for local commissioners.
Kennedy, p. 110. 12
The first objective of NHS England’s Research and Development Strategy 2013–18111 is:
To identify and prioritise commissioning health services research topics and co-ordinate this work with the Department of Health, NIHR [National Institute for Health Research]. . .
Department of Health and Social Care, NHS England, p. 8. 111
From this work, we have published two papers. 112,113 There is also a report on WP 3.2 in Appendix 9.
Aims
-
To identify the structures, processes and relationships between commissioning entities in the NHS and other agencies relevant to transitional health care.
-
To identify the facilitators of and barriers to commissioning for services for transitional health care.
-
To identify how services for transitional health care could be better commissioned.
Methods
This work was overseen by an invited Steering Group, which met on four occasions.
The work was undertaken sequentially in six stages.
-
Stage 1: literature review. A systematic review was undertaken to identify published peer-reviewed evidence about commissioning for transition.
-
Stage 2: qualitative interviews with stakeholders. Twenty-nine interviews were conducted by telephone (n = 3) or in person (n = 26) with individuals from Clinical Commissioning Groups (CCGs), Health and Well-being Boards, local authorities, general practices and the third sector. Most of the interviews were conducted with people in north-east England. A second site in the Midlands was selected because the local Health and Well-being Board had transition as a priority, and there was a Commissioning Support Unit. Further details of the methods are in Appendix 9, which includes the interview schedule, and in our published paper. 112
-
Stage 3: case studies. Using the findings of the literature review and the interviews, criteria were developed for seeking sites at which transition was being formally addressed. Three sites, covered by three CCGs, were visited in the north-west, the south-west and the West Midlands of England. Across the three sites, 11 semistructured interviews were conducted. The details of the methods are in Appendix 9.
-
Stage 4: seminar in London on commissioning for transition. This brought together additional expertise and experience from public health, social policy, commissioning and research into commissioning. Thirty invited delegates attended.
-
Stage 5: interviews with commissioners for adults’ services. We realised that we had talked with few commissioners for adults’ services. Therefore, we arranged face-to-face interviews (n = 5) with commissioners for adults’ services in two CCGs in north-east England (n = 3), a CCG in south-east England and a regional commissioner for specialised adults’ services for NHS England in the Midlands.
-
Stage 6: synthesis and conclusions.
Analysis
Stage 1: literature review
No published papers on commissioning for transition were identified. Of 66 publications whose full-text was reviewed, 17 were potentially informative for the wider work of the Transition programme, in particular recommendations for providers. The grey literature was then reviewed and revealed nothing of additional significance. The details of the analysis are in Appendix 9 and in our published paper. 112
Stage 2: qualitative interviews
A number of issues related to commissioning were identified, which clustered around four meta-themes: (1) policy and legislation; (2) organisational structures, processes and pathways; (3) professional roles and relationships, service-level co-ordination, signposting and support; and (4) commissioning process and practice, including outcomes planning and delivery, and contract evaluation. From this work, key factors were identified that seemed likely to facilitate commissioning for transitional health care. These were:
-
commissioning within a CQUIN114 framework
-
Commissioning for Transition co-ordinators, within a framework of DAH, to work across all services in an organisation rather than for a particular condition
-
joint commissioning either as cross-sectoral in education, health and social care, or as within-health, including the involvement of general practice
-
commissioners and providers jointly agreeing what should be commissioned.
Another issue raised frequently in the interviews was the need for ‘outcomes-based commissioning’. We found great variability in what this meant and how outcomes might be measured. Furthermore, we could not identify a setting in which outcomes-based commissioning was happening.
Full details of the analysis are in Appendix 9 and in our published paper. 112
Stage 3: case studies with site visits
The full report is in Appendix 9, and some of the implications are reported in our published paper. 113
Case study A
At this site, a CQUIN was considered a necessary first step to quality improvement, as it helped develop a culture, at least within children’s services, of shared purpose and value around transition. The CQUIN was also perceived to be useful for standardising the introduction and use of the ‘Ready, Steady, Go, Hello’ forms,115 a set of documentation supported by NHS England. Participants reported that the implementation of the CQUIN contributed towards raising the profile and visibility of transition among clinicians.
Reported barriers included a lack of engagement of general adults’ services. Sometimes, this was compounded by the lack of a specific adults’ service for children to be transferred to. In other cases, the need for some young people to be transferred to other trusts was reported as difficult to plan. Furthermore, because CQUINs were assessed by numerical targets, rather than by factors shaping quality and innovation, this might negate quality improvement. Finally, concerns were raised that transition extends for many years beyond the time frame of a 1-year CQUIN.
Case study B
At this site, a lead nursing manager, funded by the Strategic Clinical Network, played a central role as a regional champion facilitating the implementation of a region-wide CQUIN. This leader worked across 14 NHS Trusts. All participants reported that this leadership played an important role in raising awareness and best practice about transition among commissioners and providers. At trust level, the CQUIN contributed to the development of a Transition Steering Committee and a trust-wide transition co-ordinator responsible for collaborating with professionals across specialties.
Reported barriers included a lack of engagement of adults’ services in the meetings of the Transition Steering Committee and a lack of clarity about the role and responsibilities of commissioners of adults’ care. Young people’s participation and feedback was limited and fragmented across different services. Finally, echoing the findings of case study A, conceptualising the CQUIN in terms of indicators and targets did not necessarily translate into meaningful conversations about quality and innovation.
Case study C
At this site, there was a partnership whose overall aim was to develop and implement an integrated mental health service for those aged 0–25 years. This involved decommissioning the existing child and adolescent mental health services (CAMHS) and co-producing a new service specification. Participants reported that a key feature of the new service was the enthusiasm about and commitment of commissioners to improving transitional health care. Furthermore, participants emphasised the importance of health, social and third-sector involvement and co-production with service users of the new service specification. It was supported at national level by the National Clinical Director for Children, Young People and Transition to Adulthood, and at regional level by the Collaboration for Leadership in Applied Health Research and Care.
Reported barriers included uncertainty about transition after the age of 25 years and challenges relating to engagement of adults’ services. In addition, negotiating the decommissioning process with the outgoing provider had been challenging. Participants thought that some stakeholders were reluctant to adopt the new service. Finally, inadequate information-sharing procedures were evident following the configuration of the new service.
Stage 4: seminar
Many views and insights were expressed, which are summarised in a report. The main benefit to the programme was how much the co-applicants learned about the NHS Commissioning Framework and how to influence commissioning.
Stage 5: further interviews with commissioners of adults’ services
Further interviews with adults’ services commissioners in CCGs revealed that transition did not get ‘onto their radar’. Transition was acknowledged to be important but, as there was no national imperative, other priorities over-rode it. This is despite the introduction of a national CQUIN on transition in mental health services116 part-way through our research programme. The only meetings at which transition was ever mentioned were those about diabetes. The overarching opinion was that contracts with trusts covered broad strategic approaches to clinical care and were not specified at the level of detail that would include arrangements for transition. Rather, CCGs would assume that a health-care provider would deal with decisions about transition and transfer of health care as it saw fit.
Participants suggested that reasons why transition did not get ‘onto the radar’ included (1) commissioners had no ‘levers’ such as national quality indicators or resources for transitional health care (just talking with a trust does not make better transition happen), (2) commissioners could not show ‘return on investment’ (i.e. improved transition would not convert easily to more activity for the same money or to less activity for less money) and (3) other competing urgent priorities.
Most commissioners were aware of NICE guidance on transition but acknowledged that, like other NICE guidance, new guidance was considered in the context of local priorities. Furthermore, it was suggested that NICE guidance about a particular condition or disease is easier to use than guidance directed towards the operation of a complex intervention.
Commissioners who were also general practitioners made two important points. First, long-term conditions, such as non-severe asthma, allergy and some mental health disorders, are often currently managed entirely by primary care. Although transition occurs, there is no need for the transfer of health care. Second, even for conditions that need secondary care, ‘the role of primary care should start at the time of diagnosis’. The general practitioner commissioners were concerned that, in some instances, children’s health services appear to exclude primary care. This lack of joint working risks creating, for children, young people and their parents, a lack of confidence in their primary care team and an overdependency on secondary paediatric care, which in turn leads to a strong desire for secondary adults’ care.
Commissioners of adults’ services were well aware of the small number of young people with very complex care needs that required expensive, bespoke clinical and interagency care, but they were often not aware of the much larger numbers of adolescents with long-term conditions who were negotiating transition and attending community and hospital-based services.
Commissioners for specialised services at NHS England suggested that most specifications for children’s services included transition; and for some conditions, such as diabetes and renal services, a broad expectation about transition was also included in contracts for adults’ services. However, they acknowledged that most adults’ service specifications contained little, if any, reference to transition or health-care transfer. Furthermore, there was no monitoring of service delivery by commissioners of either transition more broadly or the transfer of health care from children’s to adults’ services. For some conditions, national audits of practice, which include examination of transition, were undertaken by professional groups.
Stage 6: synthesis
We prepared a first draft of our synthesis and proposals for discussion with commissioners, which was then refined; this is reported in WP 3.3.
Strengths and limitations
Despite increased awareness about transition since the publication of the NICE transition guideline14 and quality standard117 in 2016, commissioning for transition is a new field of enquiry. This means that our research conclusions are primarily based on the evidence generated during the research programme through research interviews, site visits and discussions with commissioning groups.
Given the fast pace of policy change, and with over 200 CCGs across England, one of the challenges of this WP was to capture a wide range of contemporaneous views and perspectives. We think that the combination of the range of methods employed (interview, seminar, site visits), the relatively broad geographical distribution across the UK, and engagement with CCGs and specialised commissioning at NHS England gave us a reasonably comprehensive understanding.
Key findings
-
Commissioners and providers of adults’ services regard transition as the responsibility of commissioners and providers of children’s services to deal with and improve.
-
Whether contract specifications include transition very broadly or in detail, implementation of transition is not usually then monitored by commissioners – partly because there are no nationally agreed outcome and quality indicators to use.
-
Although a CQUIN for transition can raise the awareness of service managers and clinical teams about transition, the short-term requirement for indicators to be documented can make the introduction of a CQUIN a box-ticking exercise, rather than a commitment to organisational change that may in turn lead to quality improvement.
-
A Transition Steering Committee and trust-wide transition co-ordinator in a NHS Trust are effective in discharging an organisation-wide commitment to improving transition.
Inter-relationship with other parts of the programme
Our understanding of commissioning processes developed from this WP allowed us to ensure, as far as possible, that we were well informed when we visited commissioners in WP 3.3. We were able to approach commissioners with specific questions and specific suggestions and then test these out. As will be shown in WP 3.3, we then formulated definitive conclusions with specific implications for commissioners. Our final conclusions are relevant, possible to implement and likely to be adopted by commissioners because of this sequential process of identifying issues and then testing them out with commissioners.
The findings of this WP informed the content of the DAH toolkit in WP 3.1b.
Through their effect on WP 3.3, the results of WP 3.2 directly determined what we included and how we framed implications 1, 2 and 6 of the programme.
Work package 3.3: commissioning – seeking consensus
Addressing objective 3: to determine how transitional health care should be organised, provided and commissioned
Aims
-
To synthesise learning from the programme on what and how to commission.
-
To learn about the most useful way to provide research-based evidence to inform commissioners, through local and national meetings and visits.
Methods
Using results from WP 3.2 on commissioning, from WP 3.1 on DAH and from WPs 2.1 and 2.2 on features of services for transitional health care associated with better outcomes, we developed two brief documents setting out for commissioners the preliminary key research findings and implications of the programme. We wanted to learn from commissioners whether or not we were presenting material that they thought was relevant and useful, and in an appropriate manner. We presented these documents to the following groups and individuals, modifying their contents as we proceeded:
-
an academic at a university in south-west England who had undertaken research into evidence-based commissioning and what influences commissioners’ decision-making
-
a children’s health commissioner (also general practitioner) in a CCG in north-east England
-
chief executives of a CCG consortium in north-east England
-
chief executives of a CCG consortium in south-east England
-
the Clinical Leadership Committee for specialist services at NHS England
-
three telephone interviews with members of the above Clinical Leadership Committee
-
a commissioner of specialist services for mental health in north England
-
a commissioner of specialist services for long-term conditions in adults in the Midlands.
Thus, we talked with seven commissioners individually and with three committees at which 21 commissioners were present.
During the consultation meetings, we presented the key findings about the outcomes and lessons from the programme, focusing on the commissioning pathway and guidance. We encouraged, through discussion with various stakeholders, critical reflection to ensure the relevance of the emergent findings, identify key lessons learned, and explore the implications of these lessons for developing a nationally consistent and comprehensive approach to commissioning for transition. The discussions were central to challenging, modifying and enhancing our guidance for commissioning for transitional health care for young people with long-term conditions.
We kept notes of the content of all the meetings.
Analysis
Below are summaries of our discussions based on the notes of the meetings. We used an iterative process, based on the advice and suggestions we received, to modify and revise the summary documents and the way we presented our proposals to commissioners.
Discussion with academic in south-west England
This person explained that commissioners are likely to be interested in our broader knowledge of transition, not just in the research findings. Commissioners regularly seek advice from colleagues and trusted experts. By showing that we are also keen to learn from them, we may come to be regarded as a trusted source of information.
We should avoid jargon and make sure our messages are demonstrably relevant to patients. We should aim to present three or four key messages that are clear, practical, evidence based and cost neutral or will save money. If we wish to draw the attention of commissioners to a particular problem, especially one that they may not have been aware of, then we also need to propose a solution – preferably one that reduces cost or at least does not cost more.
Discussions with Clinical Commissioning Groups
In general, CCG commissioners said that our proposed summary documents were useful, well written and articulated. Several commissioners were enthusiastic about our work and recognised the implications for their commissioning practice. We were advised to be explicit about how proposals from the research programme would yield improved outcomes.
All commissioners welcomed the concept of DAH, although many had not encountered it before.
Commissioners asked us how they would know that providers were improving transition in their services, or at least that they were doing what they had been commissioned to do.
Discussions with commissioners for specialist services at NHS England, both at regional level and centrally
The research programme should focus on solutions.
Although the key implications of the programme could be implemented within existing service provision, with little or no extra cost, we were advised that senior managers and health-care providers tended to request extra funds whenever change was proposed; we should try to anticipate such arguments.
We were advised to set out the risks of ‘not transitioning well’ as well as highlighting the potential longer-term poor health outcomes.
The toolkit on DAH was considered an excellent idea. Although directed to NHS organisations (managers, teams and individual clinicians), it should also be educational for commissioners.
Those young people for whom there was no equivalent specialist tertiary adults’ service might be transferred to the CCG for secondary care or to primary care. These pathways should be stated explicitly by commissioners through service specifications and contractual arrangements.
Some specifications for specialist adults’ and children’s services do include specific mention of transition. However, commissioners may not then follow it through to hold trusts to account. There is a need for quality standards or indicators for transition.
There was general agreement that transition is currently considered to be the responsibility of children’s commissioners and children’s health-care providers. To achieve change, this underlying premise needs to be challenged so that arrangements for transition include adults’ service commissioners and providers. All agreed the approach to improving transition should be owned at trust board level.
Synthesis
Almost all of the commissioners we visited thought that now was an opportune time to focus on transition, in the context of the publication of the 2016 NICE guidance14 and quality standard for transition. 117
Many commissioners stated that they had been aware of the need to address transition but had not been certain about how best to achieve this; having a relatively small number of specific evidence-based proposals from our research programme was timely and useful.
Participants acknowledged that transition is currently considered the responsibility of children’s commissioners and children’s health-care providers; they thought that this should change, and that commissioners and providers of adults’ health care should be equally responsible.
There was also recognition of the need to achieve an integrated approach to working relationships within health and between health and social care commissioning to support shared responsibility for and ownership of transitional health care of young people. In the light of the recent publication of the NICE guidance on transition, commissioners acknowledged the potential impact of integrated commissioning for transitional health care.
There was a general, but not universal, view that it was easier to be prescriptive in service specifications if there was evidence to support it. However, this depends on what is meant by evidence. Those trained in public health were more likely to use research evidence, but other commissioners were more likely to use local information and local experiences, with research evidence influencing only 20% of them. 118 It was, however, acknowledged that the commissioning proposals from our research programme could support the development of evidence-based commissioning for transitional health care.
Strengths and limitations
This is, as far as we are aware, the first work to study commissioning for transition. We were able to identify some major issues for commissioning, and gain an understanding of the context in which commissioners work and the parameters they use to direct health-care provider organisations in commissioning transition.
As most commissioners we talked with agreed that transition was important and that now was an opportune time to introduce change, it would have been useful to meet with commissioners who were more sceptical about the importance of transition.
Our presentations to commissioners focused on a small number of implications for commissioners; these were refined as discussed above. This inevitably meant that we could not share the detail and complexities of all of the findings of the research programme.
We have published two papers on commissioning112,113 and we are preparing a third.
Key findings
Box 2 shows the final version of the document, after all of its modifications, that we discussed with commissioners. It is also the final version of the document for commissioners that we presented at the dissemination meeting at The King’s Fund in October 2017.
Successful transition is a priority for all children with long-term conditions, not just the small group of young people with very complex needs who require integrated commissioning across CCGs, Health and Well-being Boards, education and social services to fund bespoke multiagency packages of care.
1. Our findings indicate that there is an important role for commissioners of adults’ services to commission transitional health care, in addition to commissioners of children’s services, with whom responsibility for transitional health care currently lies.
Commissioners and providers regarded transition as the responsibility of children’s services. This is inappropriate, given that transition extends to approximately the age of 24 years.
2. ‘Developmentally appropriate health care’ is a crucial aspect of transitional health care. Our findings indicate the importance of health services being commissioned to ensure that providers deliver DAH across all health-care services, and that this will be facilitated by commitment from senior provider and commissioner leaders.
Developmentally appropriate health care is the subject of a toolkit we have developed in which DAH is defined, and that is a resource for education and training (www.northumbria.nhs.uk/?s=dahtoolkit).
One important element of DAH is that young people, in both adults’ and children’s services, need to be seen by themselves for at least some of the consultation. However, our research shows that the involvement of parents in a manner that suits both parties (and this will vary between different young person/parent dyads) leads to better outcomes, in terms of satisfaction with services, disease control, continuity of health care and maturation to adult roles. Currently, adults’ services often exclude parents from consultation on the grounds of confidentiality. This should not happen provided that a young person gives permission for a parent to be present for some of the consultation.
3. Where an adults’ service to which to transfer young people with a long-term condition is not commissioned, our findings indicate an important role for commissioners in setting out explicitly that the transfer arrangements will usually be to primary care, and require appropriate documentation and assistance to the young person to make their first appointment.
4. Our findings indicate the importance of commissioning to ensure that a young person and family meet the adult team before transfer.
Our research shows that meeting the adult team before transfer of health care predicts better adult outcomes. The joint appointment would involve the staff who will be caring for the young person in the adults’ service or primary care.
5. Our findings indicate an important role for commissioners in ensuring that health-care provider organisations establish a Transition Steering Committee with a trust-wide transition co-ordinator.
Our research suggests that this enables an organisation to develop and deliver an organisation-wide approach. We found good practice led by enthusiasts rarely generalised to other specialties or adults’ services.
The text presented in this box is derived from 29 telephone conversations with commissioners (2013/14), three site visits to commissioning organisations (2015/16) and from with 28 NHS commissioners at meetings over the period 2016/17. These commissioners may not have been typical of NHS commissioners, as we have set out in limitations.
Inter-relationship with other parts of the programme
The summary of findings for commissioners in Box 2 includes proposals about DAH that were explored in WP 3.1 and about the PBFs that were explored in the longitudinal study WPs 2.1 and 2.2.
What we learned about the commissioning process in WPs 3.2 and 3.3 has directly informed our conclusions about how commissioning might be improved, and directly informed how best to present this evidence to those responsible for commissioning health care in different NHS settings.
This WP directly determined what we included and how we framed implications 1, 2 and 6 of the programme.
Involvement of patients, the voluntary sector and the public
Work of UP
The research programme worked with a young person’s advisory group that met once per month (named by the young people as UP). It was facilitated by Gail Dovey-Pearce, co-applicant and clinical psychologist, who also provided regular updates to the Programme Management Board. The work of UP is reported under WPs 1.1 and 1.2 and in Appendices 3 and 4.
Voluntary sector
The Council for Disabled Children was a co-applicant to, and received a budget from, the programme. Represented initially by Helen Wheatley as co-applicant and then by Caroline Bennett, the Council attended Programme Management Board meetings quarterly in Newcastle upon Tyne. The Council:
-
Worked closely with Janet McDonagh and Gail Dovey-Pearce to establish UP and to plan the first external seminar on DAH in September 2014.
-
Was a key member of the groups leading WPs 1.1 and 1.2 on young person involvement and WPs 3.2 and 3.3 on commissioning.
-
Assisted UP to disseminate early results of the programme on the Q-sort study, health passports and DAH (WPs 1.3, 1.2 and 3.1, respectively). This dissemination reached 75 young people through discussion groups between autumn 2015 and spring 2017. The discussion groups were preceded by a planning meeting in Newcastle upon Tyne by a steering group of young people including two members of UP. The meetings took place with CHAT in North Tyneside, two Croydon groups, Together for Short Lives, Transition2 group in Derby, and Chatterboxes youth group in Bournemouth. The meetings generated three workbooks (see Appendix 10) for other groups to use, especially voluntary organisations in the health sector. Since 25 September 2017, the resources have been disseminated to 469 young people’s organisations and have been shared with the members of the Council for Disabled Children’s networks.
Association of Young People’s Health: toolkit for introducing developmentally appropriate health care across a NHS Trust
The Association of Young Person’s Health advised on and set the format and style of the toolkit, based on similar work it had undertaken with the Royal College of General Practitioners. The development of the toolkit is reported in WP 3.1 and Appendix 8.
National Institute for Health Research meeting in Exeter on patient and public involvement involving young people, November 2013
Gail Dovey-Pearce represented the programme at this meeting. She jointly led, with Chris Morris, Associate Professor in Child Health at the University of Exeter, a workshop on engagement of young people in PPI. The presentation included a video produced by UP.
Patient and public involvement representation on the External Advisory Board
The membership of the External Advisory Board included representation from one charity, two parents of disabled children, and two young people with long-term conditions. The board met five times during the programme. Meetings were arranged to accommodate the availability of its members and at points when the input of the External Advisory Board would be useful. UP sent a representative to each meeting on a rotational basis. An informal meeting was held on the morning of the External Advisory Board meeting during which only topics of likely interest to the young people and parents were discussed. The afternoon session followed a formal agenda.
Newsletters and circulation list
We distributed a 4-monthly newsletter to all registering interest in the programme. This included the voluntary sector and, in particular, the five organisations that had provided letters of support for the programme. We also circulated seven newsletters written specifically for participants in the longitudinal study WP 2.1 (see Appendix 10 for an example).
Two external seminars funded by The Health Foundation
We applied successfully to The Health Foundation for funding for two external seminars. Their purpose was to help us consider two important aspects of our research programme: DAH and commissioning for transition. We brought together professional experts, the voluntary sector and young people from a much wider range of disciplines and expertise than were in the programme’s team. Each seminar had about 30 invited delegates.
The first seminar, on DAH, was held in Birmingham in October 2014. UP and the Council for Disabled Children contributed a great deal to the planning and presentations of this seminar.
The second seminar, on commissioning for transition, was held in London in June 2016.
The National Institute for Health Research website
Based on the annual reporting of our PPI work to NIHR and the representation of UP on the External Advisory Board, NIHR placed details of the work of UP on the NIHR website in November 2014 as an example of excellent practice.
Plain English summary for the final report
The UP group and lay members of the External Advisory Group reviewed this summary.
Impact of UP
The sponsoring Trust (Northumbria Healthcare NHS Foundation Trust) funded a satellite study, led by Gail Dovey-Pearce, to examine and understand the factors that influenced involvement of young people in the programme and what the perceived impact and benefits were.
There are no pre-defined standards against which to measure PPI work; the field is still working towards defining the processes of involvement and the ‘quality’ of involvement work. In this mixed-methods study, the views of the adult researchers and young people working on the programme were explored. The evaluation drew on existing proposals and theories, including the Medical Research Council’s Public Involvement Impact Assessment Framework. 119 Members of the transition team, with knowledge of most aspects of the programme’s work, carried out the data collection using qualitative methods. Further details are in our published paper. 45
Having witnessed the impacts of young people’s input, the adult researchers said that they attached increasing importance to it; they valued the ‘authentic voice’ that UP provided. The adult researchers noted the evolving process that took the work forward and the importance of not taking an overmechanistic approach, with overdefined, a priori goals.
The young people thought that they had received a structure with overall aims but with the freedom to work within those parameters. They experienced less anxiety than the adult researchers, who had raised questions about how this process would work in practice. The young people considered that they developed personally and professionally, and that they were making a difference to the NHS and to other young people using services.
Recently, there has been a call to move away from studies of ‘what’ involvement achieves to those of ‘how’ good involvement happens. 120 The findings of this satellite study suggest that cycles of active work allow involvement, thinking and practice to progress during a project. Every research study has its own opportunities and challenges to achieve active and meaningful involvement.
Conclusion to the patient and public involvement section
Overall, we consider that young people were involved throughout the programme, with defined input to most of the WPs. They received support and developed skills to be able to take active roles in partnership with the adult researchers. A ladder of young person engagement, proposed by Hart,121 is shown in Figure 10. Our research programme moved flexibly between the rungs of meaningful and active involvement (rungs 4–8), while avoiding the levels that are closer to tokenism and decoration (rungs 1–3).
FIGURE 10.
Hart’s ladder of young people’s participation. Reproduced with permission from Adam Fletcher, Common Action Consulting, 23 August 2017. 122
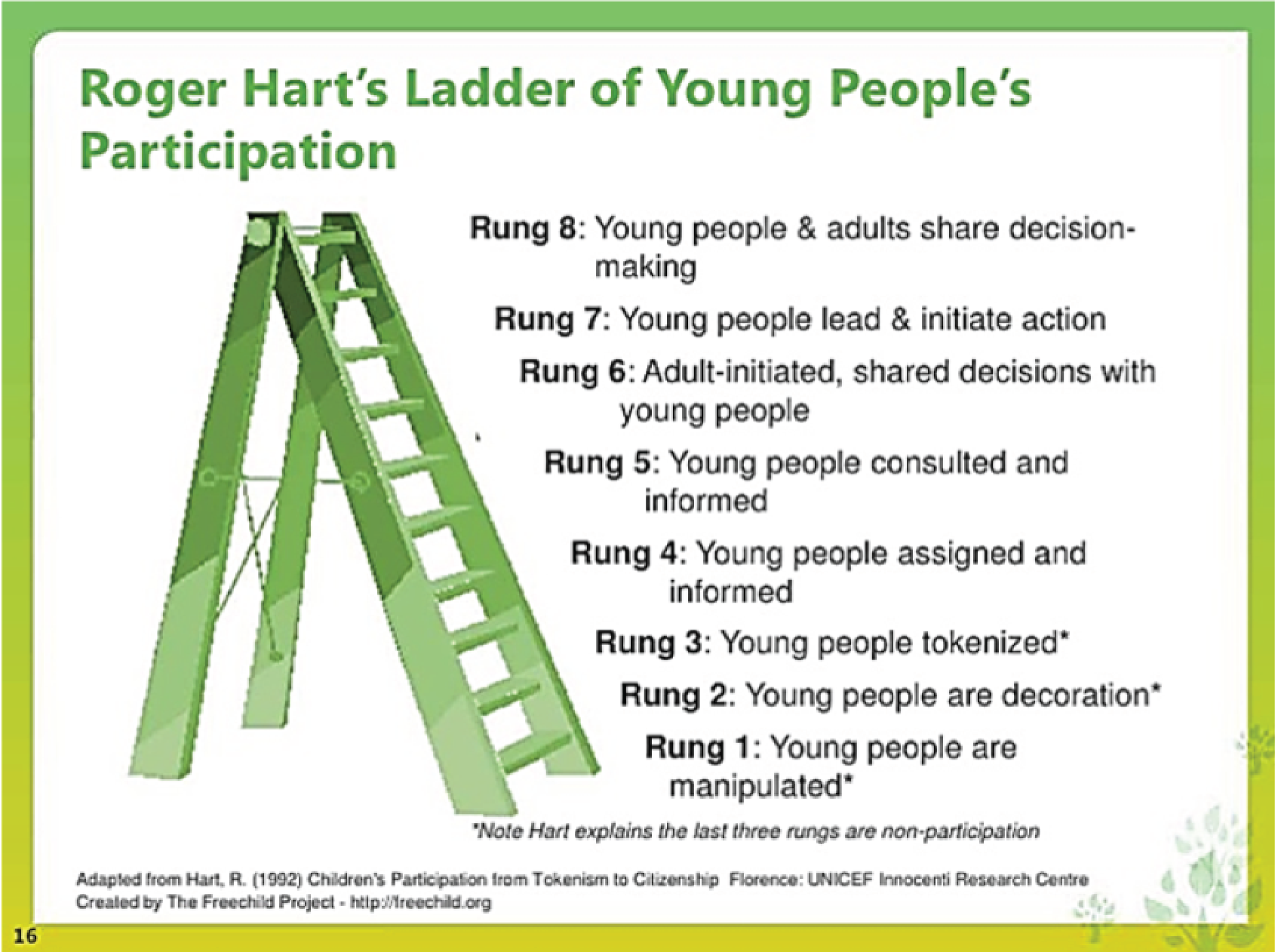
There are no agreed methods for involving young people in a long-term health research programme. We were fortunate to have well-funded involvement resources to support young people, and this was key to carrying out a detailed analysis of our involvement work. We could have adopted a less time-consuming and less costly approach, which could have drawn on expertise from established young people’s special interest groups. We do not know whether or not such an approach would have been as successful.
What was and was not successful?
What was successful?
Integration of work packages
We achieved our aim to have a set of nine WPs that were closely integrated. Our conclusions and their implications were informed by the input of young people, the longitudinal study and the work on implementation in trusts and with commissioners.
Patient and public involvement
Our PPI was of high quality. We formed this view based on the interest NIHR showed in highlighting the work of UP on its website, the invitation from the Department of Health and Social Care to UP to attend the ‘take over’ day, the views of the External Advisory Board and the internal evaluation undertaken by Gail Dovey-Pearce (reported in Involvement of patients, the voluntary sector and the public and in our published paper45).
Small number of feasible implications
We succeeded in our intention to conclude with a small number of feasible implications that will have utility for NHS commissioners and for those responsible for the delivery of clinical services. During consultations, we were advised that documents containing large numbers of recommendations and aspirational statements are difficult for commissioners and chief executives to use.
What was not successful?
Administrative challenges
Research and development permissions
Obtaining NHS ethics permissions for the various WPs was relatively straightforward. However, obtaining research and development permissions from individual NHS Trusts was time-consuming and frustrating, not least because every trust had different procedures and expected different amounts of detail. Especially time-consuming was obtaining ‘research passports’ and ‘letters of access’ for staff who worked across universities and trusts.
Human resource issues
We experienced many staff changes over the 5 years at the levels of co-applicant, local principal investigator and research assistant. The reasons included career break, maternity leave, change of job, physical illness, mental illness and merging of NHS organisations. Despite our best efforts (which included new research assistants receiving detailed training at each change), these workforce disruptions led to some loss of continuity of contact with some young people. This may have had some adverse impact on retention rates in the longitudinal study.
Recruitment and retention of young people as research participants
Although recruitment rates were reasonably good for the ASD (50.9%) and diabetes mellitus (64.7%) groups, the rate for those with cerebral palsy was lower (25.6%).
The overall retention rate, at 70%, was in keeping with other studies.
Working with principal investigators at each site
The principal investigators had a genuine interest in research and in the Transition programme, but some had not appreciated how much time was needed to spend with their research assistant for high-quality supervision. Some of this, therefore, had to be done from Newcastle, which was sometimes challenging – not least because we could not directly influence human resource issues in each trust.
Conclusions
Introduction
Our research has taken a comprehensive approach to transition in the UK: we have involved young people, we have investigated key components of transitional health care rather than specific models and have identified components associated with better outcomes, we have examined how transition is commissioned (or, frequently, not commissioned) and we have examined how improving transitional health care in NHS Trusts could be managed.
A key theme in the qualitative research literature is that young people look forward to growing up, and look forward (albeit with some anxiety at times) to further education or training, having a job and leaving children’s health services. Most studies that include young adults a year or so after transfer find that young adults say that they are pleased to have transferred to adults’ health care and that most of their earlier anxieties have gone away. 123
Poor outcomes after transition cannot all be attributable to poor transitional health care. Young people may demonstrate poor outcomes and worrying health-related behaviour before their transition starts, which may then amplify during transition. For example, young people with poor adherence to medication for liver transplant after transfer had had poor adherence before transfer,124 and young people with cerebral palsy have poor participation when aged 8–12 years. 125 In our research programme, we found in our baseline assessment of those joining the study that the participation of those with cerebral palsy or ASD was already lower than that of those with diabetes mellitus, and that the mental well-being of those with ASD was already lower than that of those with diabetes mellitus or cerebral palsy. Furthermore, young people’s lives may be disrupted for mental health reasons or because of family or social circumstances. These young people need specialist care; however, the potential for poor outcomes should not be attributed solely to poor transitional health care but rather should take into account the problems that the young people pose for health services, regardless of their age or whether or not they are in transition.
Strengths
External evaluation of real world rather than internal evaluation of a locally developed intervention
Most groups undertaking research into transition evaluate their own interventions; essentially, they undertake an audit or clinical evaluation of their service. However, we have successfully completed a hypothesis-driven, longitudinal, observational study of features being provided, or not, across 27 NHS Trusts (35 services). We had a large cohort, and this was the first study of its kind.
Prospective data collection during transition
We captured data from young people while they were in transition and across their point of transfer. Therefore, we have information about young people’s experiences and outcomes at the time they were receiving services, rather than on what they thought afterwards about what they had or should have received. This has rarely been done before and gives us confidence that our conclusions will be helpful to young people who are in the midst of transition.
Seeking findings relevant to a broad range of long-term conditions
We sought to identify the features of good transitional health care that were appropriate to those with any long-term condition. Although we selected specific conditions for the longitudinal study, they were deliberately chosen as conditions that give rise to a wide range of different health needs, psychosocial complexity and availability of adults’ services.
Engagement with commissioners
Our examination of commissioning is a novel aspect of the research programme. Arrangements for commissioning NHS services have continued to change over the period of the research programme and will continue to do so. However, the commissioning focus of our research concerns ‘what’ and ‘how’ to commission. Thus, our findings should be relevant to any commissioning structure, including whether or not commissioning and service provision are brought together in the same organisation.
Outcomes and processes measures (indicators) of transition
The range of outcomes we chose was informed by the International Classification of Functioning, Disability and Health: Children and Youth Version73 and, after discussion with international transition researchers, conformed to many of the recommendations of later international Delphi surveys,42,43 as set out in Table 14.
| Framework | Outcome or process measure | Captured by research programme | Instrument |
|---|---|---|---|
| NHS Outcomes Framework126 | Preventing premature death | No | |
| Enhancing quality of life for those with long-term conditions | Yes |
WEMWBS Rotterdam Transition Profile Social participation questionnaire EQ-5D-Y |
|
| Helping people to recover from episodes of ill health | Yes | Condition-specific outcomes | |
| Ensuring that people have a positive experience of care | Yes | Mind the Gap questionnaire | |
| Treating and caring for people in a safe environment | No | ||
| US Triple Aim127 | Experience of care | Yes | Mind the Gap questionnaire |
| Health of the specific population | Yes | Condition-specific outcomes | |
| Cost of care | Yes |
EQ-5D-Y Capturing health-care provider contacts (and, thus, costs) Economic modelling |
|
| Delphi North America42 | Quality of life | Yes |
WEMWBS Rotterdam Transition Profile Social participation questionnaire EQ-5D-Y |
| Understanding one’s condition, knowledge of medication, self-management, adherence to medication, understanding health insurance | No | ||
| Attending health-care appointments | Yes | We captured first appointments in adults’ services | |
| Avoiding hospitalisation | Yes | Diabetic ketoacidosis in diabetes | |
| Social participation | Yes | Social participation questionnaire | |
| Delphi International Indicators43 | Patient not lost to follow-up | Yes | We captured appointments in adults’ services |
| Attending scheduled visits in adults’ care | Yes | We captured appointments in adults’ services | |
| Patient building a trusting relationship with adult provider | Yes | Mind the Gap questionnaire | |
| Continuing attention for self-management | Yes | One PBF was ‘promotion of health self-efficacy’ | |
| Patient’s first visit in adults’ care within 3–6 months of transfer | Yes | We captured date of first appointment in adults’ service | |
| Number of accident and emergency visits for regular care in the past year | No | ||
| Patient and family satisfaction with transfer of care | Yes | Mind the Gap questionnaire | |
| Maintain/improve standard of disease control evaluation | Yes | Condition-specific outcomes | |
| NICE Quality Standard117 | Planning for transition should start by age of 13 years | No | |
| Young people should have an annual transition review meeting | No | ||
| Young people should have a ‘named worker’ | Yes | One PBF was ‘having a key worker’ | |
| Young people should meet adult team before transfer | Yes | One PBF was ‘meeting adult team before transfer’ | |
| Young people who miss their first appointment in adults’ services should be contacted and given further opportunities to engage | No |
Subjective well-being and participation in life (e.g. social, educational, workplace) are generic outcomes (i.e. they are not specific to a particular condition). Well-being has been emphasised as an important and often neglected outcome in the evaluation of transitional health care. 128
Few studies have addressed such generic, distal outcomes. Assessing such outcomes brings some attendant difficulties:
-
Poor adult outcomes are not necessarily due to a failure of transition. For example, in complex physical problems such as cerebral palsy, participation outcomes for adults are particularly poor for those with more severe impairment,129 yet participation is already much reduced in 8- to 12-year-old children with cerebral palsy. 125
-
Many chronic illnesses such as diabetes mellitus, renal failure and cystic fibrosis generate more medical complications the longer the individual has the condition. Thus, even when process measures of optimal care may be satisfactory, health outcomes may worsen.
Process measures of transitional health care usually assume that providing services that young people like and maintaining a young person’s contact with health services will yield better outcomes. However, although Betz and Smith130 recognised that such measures may be relatively easy to collect, we do not know if they lead to an improvement in more distal outcomes.
Non-attendance at appointments might seem an easily captured and interpretable process measure, but we found that it is not. Many of the reasons for non-attendance are logical and valid, rather than indicating disengagement with services. In addition, rating by number or percentage of missed appointments is difficult to interpret. The number of expected appointments per year varies by condition (individuals with diabetes mellitus may expect at least four per year) and by disease activity (e.g. is the appointment for a routine follow-up or because of a worrying deterioration of disease control?).
In investigating relationships between process measures and outcomes, Cramm et al. 131 found that satisfaction with transitional care was associated with better social and emotional quality of life 1 year later in those with diabetes mellitus or neuromuscular disorders. Sattoe et al. 132 found that process measures such as ‘patient not lost to follow-up’, ‘attending scheduled visits’ and ‘satisfaction with care’ were not related to social participation. In their study, ‘continuing attention to self-management’ was the only process measure associated with better HRQoL.
Limitations
Quality of delivery of proposed beneficial features
The nine PBFs that we studied were carefully defined and captured but we could not assess the quality with which each feature was delivered. For example, ‘meeting the adult team before transfer’ might have been tokenistic in some trusts and carefully planned in others. However, we examined exposure to each PBF across many trusts and on three occasions, and we think that much of any variation in quality will have been ironed out by the statistical method we adopted.
Longitudinal representation of proposed beneficial features
It was relatively straightforward to examine the association of exposure to each PBF over the previous year with generic and condition-specific outcomes. However, it was more difficult to decide how to represent each PBF over the duration of the longitudinal study. What constitutes optimal exposure over 3 years when, for instance, exposure occurs in one year but not in the others? We made a pragmatic, clinically informed judgement about this for each feature. The decision tree (WP 2.1) was agreed by the team of the Transition programme, but others might have come to different judgements.
Social participation
After 1 year, we realised that the Rotterdam Transition profile was not sufficient to capture some aspects of social participation. We added a social participation questionnaire, but this could be administered only at the third and fourth visits, thereby limiting our longitudinal analysis of this outcome.
Self-reported questionnaires
Most outcome data are from self-reported questionnaires. We recognise that this may be influenced by individual reporting styles, which make valid comparisons more difficult. However, we used questionnaires that were well validated; we had a large sample size, which tends to minimise the impact of variation due to reporting style; the questionnaire completion was manualised and repeated each year so that any reporting styles would be consistent for each participant; we used a number of different instruments with score ranges suitable for group statistical analysis; and, finally, the constructs about which we were largely concerned were about young people’s perceptions of their health, well-being and social participation.
Statistical power
In line with our original calculations, we had sufficient power to identify clinically significant changes in the outcomes. However, for analysis by condition, the sample size meant that some real effects of difference might not have been detectable. In relation to the PBFs, power was limited if a feature was often absent.
Economic modelling
The data collected on outcomes, costs and health service use were complex to interpret because there was loss to follow-up and differing health-care transfer arrangements, and the interval between the annual visits by the research assistants was not always 1 year (young people have a lot going on in their lives and visits often had to be rescheduled). Strict econometric modelling, despite considerable efforts, proved more difficult to undertake as a result of the nature of the data. A less robust exploratory analysis was adopted. This was able to draw out some key implications and generated a balance sheet. This was not wholly in concordance with some conclusions from other parts of the programme, but the triangulation of findings allowed key consistent conclusions and implications to be identified and reported.
Generalisability of the findings
With respect to young person involvement
Our work represents the views of young people because we consulted over 5 years with the UP group; UP disseminated findings to young-person groups across the UK; in the longitudinal study, young people with long-term conditions completed the questionnaires; and in the qualitative research work, young people were interviewed.
With respect to the longitudinal study
This is the largest sample for research in the UK in terms of examining transition longitudinally and collecting hypothesis-driven data from young people at home visits (compared with data-linkage studies from administrative data sets). Although we cannot be certain of representativeness and, therefore, generalisability across UK regions and NHS Trusts, we studied individuals from Greater London, north, south-east and south-west England, and Northern Ireland. Furthermore, we drew individuals from 27 NHS Trusts, and these trusts varied greatly in the number and variety of the PBFs they offered.
We recruited from all young people with cerebral palsy in two population registers and all young people with diabetes mellitus or ASD and an associated mental health problem in nine NHS Trusts widely distributed across England (all such young people are seen in secondary care). Thus, complete populations of individuals with one of the three conditions were sampled from (e.g. rather than those attending particular schools, specialised tertiary health-care services or voluntary support groups).
The three conditions chosen were exemplars of chronic illness (diabetes mellitus), complex physical impairment (cerebral palsy) and neurodevelopmental impairment (ASD); these were chosen deliberately to provide variation in health needs, psychosocial complexity and availability of adults’ services. Thus, we consider that generalisability to other conditions is likely. This is supported by the fact that studies of young people with specific conditions usually conclude that the important issues are generic rather than about the specific disease (e.g. diabetes mellitus,133 inflammatory bowel disease,134 cystic fibrosis,135 attention deficit hyperactivity disorder,136 urology137 and disabilities138).
However, as intended in our protocol, we did not include individuals with a significant learning disability, and our findings cannot generalise to this group. Nor did we include those with degenerative conditions. If progression is slow, as for instance with cystic fibrosis, transition is similar to that in other conditions and a formal transfer of health-care needs to take place. If progression is rapid, as for instance with some brain tumours, then the wider social and educational aspects of transition take place very differently. Furthermore, it may not be appropriate for transfer of health care to occur because it would be unnecessarily disruptive, with the young person likely to become incapacitated and/or die fairly soon after transfer; rather, advance care planning should be in place, as recommended by Together for Short Lives. 139
The 374 participants did not differ significantly from those declining to take part, other than for a small effect of deprivation. The distribution of severity of the three conditions was similar to that in national samples. 62 Those with the conditions had a wide range of severity; for example, the young people with cerebral palsy ranged from wheelchair users to those with independent ambulation. Attrition did not appear to create a bias, as there were no significant differences between those remaining and those not remaining in the study with respect to sex, age, condition, diabetes site or ASD site. In Northern Ireland, there was a small effect of deprivation on the attrition of those with cerebral palsy. Thus, we think that, after non-participation and attrition, our study group continued to be representative of those we aimed to recruit.
With respect to commissioning
Our work is novel. We interviewed, carried out case studies and consulted widely with commissioners and senior managers, CCGs and specialised commissioning, and regional and national specialised commissioning, and in many locations across the UK. Thus, we think that our findings are generalisable to the UK and to other countries with well-developed health-care provision.
With respect to the economic analysis
As we state in our account of WP 2.3, strict econometric modelling, despite considerable efforts, proved too difficult to undertake because of the nature of the data, and a less robust exploratory analysis was adopted. This drew out some key implications and generated a balance sheet. This was not wholly in concordance with some conclusions from other parts of the programme, but the triangulation of findings allowed key consistent conclusions and implications to be identified and reported.
Interpretation of the findings in the light of current policy, practice and research
Policy context
In Setting the scene at the start of the Synopsis, we summarised the policy context that led to our application for a programme of research. Since then, there have been a number of key developments in England. NICE guidance on transition was published in 2016. 14 A national CQUIN for transition of those with mental health problems35 was introduced by NHS England in 2018. Guidance on commissioning for transition for individuals with special educational needs was published by NHS England in 2018. 140 Following the death of an individual with ASD just before the transfer of their care, in July 2018 the Healthcare Safety Investigation Branch published a report that included recommendations for improving the services for young people with mental health problems in transition. 141
In 2018, the Chancellor of the Exchequer indicated that there would be considerable financial investment in the NHS over the following 10 years. We were asked, based on our research findings, to contribute a proposal for improving transitional health-care practice. Proposals about transitional care were subsequently mentioned in five places in the 2019 NHS Forward Plan. 142
Commissioning for transition
Our literature review (see Appendix 9) found no published or grey literature about commissioning for transition. Our discussions with commissioners showed that transition has been regarded as the responsibility of children’s service commissioners and children’s service providers. This is inappropriate as transition extends to approximately the age of 24 years. Commissioners also tend to consider the numbers of young people in transition to be small; this seems to be because commissioners may be actively engaged with only the small number of very complex cases of young people who require bespoke packages of care integrated across health care, social care and education. Commissioners also reported that a lack of evidence made it difficult for them to be prescriptive about transitional health care. We hope that our research programme will help in this respect. Similarly, commissioners found it difficult to be prescriptive because they lacked indicators with which to assess compliance. Development of indicators is needed, and a workshop on indicators for transition was led by NHS England at the meeting in London in October 2017 at which we disseminated our complete findings for the first time.
Developmentally appropriate health care
The concept of DAH is now widely accepted in the UK (e.g. by NICE14 and the Royal College of Physicians143) and internationally (e.g. in Canada144 and the USA128). Good practice in adolescent and young adult health, of which DAH is the foundation, applies particularly to the group of adolescents and young adults in transition. This may suggest that those providing care need an appreciation of DAH, and this will be the case particularly for the care of young people with long-term conditions who may have additional conditions or complications requiring consultations in a range of settings with a number of specialists. Such care is equally important in adults’ and children’s services due to the ongoing development of young people up to the approximate age of 24 years. We have amplified the evidence base for the concept of DAH. We have shown, within England, the key organisational factors that promote and inhibit the implementation of DAH. A consequence of providing DAH across a NHS organisation is that the potential problem of ‘at what age should a young person transfer’ ceases to exist because the young person’s developmental needs are taken into account by both adults’ and children’s services.
In WP 3.1, we identified the barriers to introducing DAH as (1) no single group in provider organisations being responsible for young people, (2) a perception (incorrect) that only small numbers of young people attend hospital and (3) concerns that staff may not have the necessary mindset or skill set. Our findings indicated the importance of health services being commissioned to ensure that providers deliver DAH across all health-care services, and that this could be facilitated by commitment from senior provider and commissioner leaders. Our work on commissioning in WPs 3.2 and 3.3 found that commissioners understood the importance of DAH and the need for it to be commissioned.
Although these organisational barriers and facilitators would apply to many health systems where change was sought, our work is the first to examine them in the context of DAH.
In WP 3.1, we developed a ‘toolkit’ to support the introduction of DAH; this is in Appendix 8 and available at www.northumbria.nhs.uk/?s=dahtoolkit. Training of staff in NHS organisations in DAH will be needed. We hope that the toolkit will be useful both in itself and because it points to other training resources.
Engaging with clinical services: ensuring continuity
Our qualitative work in WP 2.2 found that the point of transfer (whatever the adult provision might be) is intrinsically disruptive for families and young people. Families and young people will have been familiar, often for many years, with how to navigate children’s services, who to talk with if worried, where to get medication from and so on. Transfer disrupts their knowledge and relationships, and thus their confidence and trust, not because the adults’ services are inherently better or worse but because of the change that, at first, families and young people do not fully understand or feel confident to engage with. Thus, there is a need to move away somewhat from asking how young people are helped to mature and adjust, to asking how systems and processes for young people and their families might enable them to regain their knowledge, confidence and trust as quickly as possible. These processes might include ensuring that parents remain closely involved if the young person wants this (as they provide continuity); and meeting with the adult team before transfer (which may remove some uncertainty, especially if this meeting introduces the professional whom the young person will be seeing in future). These are two of the PBFs that were associated with better outcomes in WP 2.1. The above interpretation reinforces the conclusion of a major study by Allen et al. ,58,145 albeit that it focused solely on those with diabetes mellitus.
Improving transition across a NHS organisation
Several of the trusts we visited, or whose managers we talked with in WP 3.2, had a Transition Steering Committee, chaired or convened by a trust-wide transition co-ordinator. These arrangements were effective in bringing about change across adults’ and children’s services and across specialties. They took advantage of the skills and enthusiasm of those already providing good practice and they organised trust-wide training that brought together those from different specialties and from adults’ and children’s services.
Young people’s approach to transition
In WP 1.3, the Q-sort study identified four interaction styles that young people adopted when approaching transition: ‘laid back’, ‘anxious’, ‘autonomy-seeking’ and ‘socially oriented’ (welcoming support from, and frequent discussions with, family, friends and health-care professionals). Discussing and understanding young people’s views and preferences about and during transition would be likely to help clinicians and young people develop personalised planning for transition, and effective engagement with adults’ care.
In the discussions led by UP and the Council for Disabled Children with other young person groups (see Involvement of patients, the voluntary sector and the public), this finding was validated. Young people readily identified with one of the styles. However, some also said that their style had changed; for instance, when they were younger they might have been ‘anxious’ but some years on they were now ‘seeking autonomy and being in control’.
The literature on asking young people about their transition is large (including systematic reviews44,51) and we did not want to repeat such studies. However, ‘Q-sort’ methodology has not been used before in transition and, in identifying these four interaction styles, we have added new findings to the literature.
Changes in outcomes in the longitudinal study (work package 2.1)
Average satisfaction with services was reasonable at baseline (rating of ideal service only slightly higher than rating of actual service). It remained steady for those with diabetes mellitus but worsened significantly for those with ASD or cerebral palsy across the study period. The importance of transition has been recognised by diabetes services for over a decade, and the Diabetes Tariff146 includes transition. It is probable that, in services for ASD and cerebral palsy, the transition process is less streamlined, with consequent reductions in young people’s and parents’ satisfaction with services.
For those with diabetes mellitus or cerebral palsy, their average subjective well-being at baseline was similar to that of the general population and remained so during the study. Those with ASD and an associated mental health problem reported significantly lower well-being than the other two groups and this difference persisted over the course of the study – almost certainly due to the impact of their mental health problem.
For participation in life activities, there were significant differences between the three conditions, with young people with diabetes mellitus in more independent phases of transition than those with ASD or cerebral palsy. All made progress over time but those with diabetes remained more independent.
Condition-specific measures worsened over the course of the study for those with diabetes mellitus or cerebral palsy. The proportions of young people with ASD with ‘abnormal’ anxiety and depression scores remained the same from baseline to the ‘final’ visit.
Proposed beneficial features
We found that the provision of our nine PBFs in 2013/14 was patchy. Fewer than half of the health services stated that they provided ‘age-banded clinics’, ‘transition plans’, ‘transition manager for clinical teams’, ‘protocols for promoting health self-efficacy’ or ‘holistic life-skills training’ (all but ‘transition manager for clinical team’ are recommended by NICE14). Features were provided less often in services for those with cerebral palsy or ASD than for those with diabetes mellitus. Thus, there is much room for improvement across all of the services attended by the young people recruited to this UK-wide study.
Three PBFs were consistently associated with better outcomes in the longitudinal study WP 2.1: ‘appropriate parent involvement’, ‘promotion of health self-efficacy’ and ‘meeting the adult team before transfer’. We advise that strong effort be directed to maintaining or introducing them to a high standard.
In WP 2.1, ‘appropriate parent involvement’ was found to be associated with outcomes concerning satisfaction with services, well-being, some aspects of participation and meeting the health needs of those with cerebral palsy. Interviews in WP 2.2 revealed how important parents were to the process of transition. The involvement of parents as young people think appropriate is a crucial element of DAH. In WP 2.3.1, the DCE showed that ‘appropriate parent involvement’ was the second most highly rated choice. WP 2.3.2 (economic modelling) concluded that ‘appropriate parent involvement’ would be likely to maximise service uptake and may represent good value for money.
Allen et al. ’s147 study of diabetes and transition emphasised the importance of parents during transition. Heath et al. ’s83 systematic review of studies of parents’ perceptions of their role in transition concluded:
Parents can be key facilitators of their child’s healthcare transition, supporting them to become experts in their own condition and care.
Heath et al. 83
Two other recent reports148,149 investigated the parent/young person dyad and reached similar conclusions to ours: that the parent and young person need to share care but that this dynamic will continuously change. NICE14 emphasises ‘appropriate parent involvement’ throughout its report; it was an overarching principle in section 1.1.1, and sections 1.2.19–1.2.22 were devoted to the involvement of parents.
In WP 2.1, ‘promotion of health self-efficacy’ was found to be associated with outcomes concerning satisfaction with services and meeting health needs of those with cerebral palsy. Interviews in WP 2.2 revealed that both parents and young people thought that this was a central element of transition. The interviews also suggested that health self-efficacy may be not only about managing one’s condition but also about how to manage one’s health services. ‘Promotion of health self-efficacy’ is a central component of DAH. WP 2.3.2 (economic modelling) concluded that ‘promotion of self-efficacy’ would be likely to represent good value for money.
Klaasen et al. 150 developed a health self-management scale. Sattoe et al. 151 found that ‘continuing attention to self-management’ was associated with better HRQoL. There is conflicting evidence about whether a structured approach, including motivational techniques for raising health self-efficacy in diabetes mellitus, influences glycaemic control. 152,153 Mackie et al. 154 showed the benefit of a 1-hour, nurse-led intervention to promote knowledge and confidence about one’s condition, in this case congenital heart disease. NICE14 (in section 1.2.17) recommends ‘promotion of health self-efficacy’.
In WP 2.1, ‘meeting the adult team before transfer’ was found to be associated with better outcomes in participation and in diabetes management. There was a negative association between having met with an adult team and one of the Mind the Gap subdomains. We infer that lower satisfaction was due to the young person’s lack of familiarity with the adult team. Interviews in WP 2.2 found ‘meeting the adult team’ to be important, although sometimes the arrangements rendered it ineffective because the young person could not attend if the opportunity was only offered once per year, or the young person met someone who was subsequently not responsible for their care. If undertaken well, the meeting really helped with the potentially disrupting and disorientating consequences of transfer described in WP 2.2. WP 2.3.2 (economic modelling) concluded that evidence of the value for money of ‘meeting the adult team’ was ambiguous.
Our definition of meeting the adult team before transfer included having clinics where adult and paediatric physicians consulted jointly. In other studies, such joint clinics have shown to lead to improvements in process indicators in renal services,155 diabetes services,156 urology services137 and rheumatology services. 157 NICE14 (in sections 1.3.5 and 1.3.6) recommends ‘meeting the adult team before transfer’.
One PBF, ‘having a key worker’, was significantly associated with greater service satisfaction only during the second study period (between visits 2 and 3); it had no associations with longitudinal analysis and some negative associations with participation.
Sloper et al. 158 found strong evidence for the value of key workers for families with children with special educational needs. NICE14 (in sections 1.2.5–1.2.10) calls for a ‘named worker’.
The difficulty with ‘key worker’ may be the practicality of operationalising this rather than the principle of having one. Staff changes as a result of leaving post, restrictions in job plans, service restructuring, or sickness or maternity leave make it difficult to provide a key worker for all young people with long-term conditions, even though it may work well for the few for whom there is continuity.
Five PBFs had few significant associations with better outcomes: ‘holistic life-skills training’, ‘transition plan’, ‘age-banded clinic’, ‘having a transition manager for clinical team’ and ‘co-ordinated team’. WP 2.3.2 (economic modelling) did not find any benefit in terms of costs or HRQoL. Nor were the last three recommended by NICE. 14
Regarding ‘having access to holistic life-skills training’, our qualitative work in WP 2.2 found that all parents and young people thought that signposting to educational and social services and to charities was essential. Some services were more ambivalent, and were not even sure if it was their responsibility to probe these wider areas of a young person’s life.
‘Having a written transition plan’ is recommended by NICE14 (in section 1.3.4) but it does not specifically mention that the plan should be a written document. Qualitative work in WP 2.2 found conflicting views about a ‘written’ plan: such plans take time to draw up, they become out of date and they get lost, and who should hold them? Some professionals said that personal interaction was far more important. On the other hand, the lack of a formal plan left many families disorientated and wondering if the service did not have the resources to provide for care after transfer.
These last six PBFs, for which we did not find evidence of benefit, were included in our programme because there had been a number of small studies, typically internal evaluations of local interventions, that suggested benefit (e.g. benefit of a transition manager for clinical team159). We acknowledge that the absence of evidence is not the same as lack of benefit. However, our study was hypothesis driven and had clear, pre-identified outcomes. Even if these five PBFs should not be rejected, our findings indicate that resources (which include training) would be best directed first to embedding into service provision the three beneficial features for which we found convincing evidence of benefit.
Health economics
The short-term cost of introducing the three key PBFs that we found to be associated with better outcomes will depend on precisely how the feature is delivered. If a NHS organisation intends to adopt a trust-wide approach to transition, including ensuring that services are developmentally appropriate, then it could be advantageous for them to consider allocating sessions to a co-ordinator. Such a role could involve chairing a Transition Steering Committee and assisting directorates and teams of health-care professionals and providing instruction in DAH. The toolkit we have developed could assist this process (see Appendix 8).
Arranging for every young person and their parents to meet an adult team member before transfer will require organisation and clinic time. Where there are already clinics at which adults’ and children’s clinicians consult together, such meetings happen automatically. However, where care is being transferred to primary care, a meeting attended by a member of the children’s services team may enable this feature and support the young person’s confidence to make further appointments.
The DCE (WP 2.3.1) suggested that, over a 10-year time horizon, a service allowing appropriate parental involvement, where the same staff are seen at each clinic, and where young people have the opportunity to make decisions about care, would maximise uptake. A service involving ‘appropriate parent involvement’ and ‘protocol for promotion of young person’s confidence in managing their health condition’ may represent good value for money, but a service involving a ‘transition manager for clinical team’ or ‘age-banded clinic’ might represent less value for money. However, the results are tentative as the economic evaluation was exploratory. The balance sheet highlighted that adoption of the new approaches to transition, outlined above, needs to balance the extra cost against the increased engagement with health services and prevention of deterioration in health in the long term.
Key implications for the practice of commissioners, managers and clinicians
Our findings indicate the following:
-
An important role for commissioners of adults’ services is in commissioning for transitional health care, in addition to the current commissioning that is undertaken almost solely by children’s commissioners.
Commissioners and providers regarded transition as the responsibility of children’s services. This is inappropriate, given that transition extends to approximately the age of 24 years.
Sometimes a specialist secondary care adults’ service does not exist and transfer will occur from a specialist children’s service to primary care. Our findings indicate an important role for commissioners in setting this out explicitly, including the need for appropriate documentation and assistance to the young person to make their first appointment.
-
Developmentally appropriate health care is a crucial aspect of transitional health care. Our findings indicate the importance of health services being commissioned to ensure that providers deliver DAH across all health-care services, and that this will be facilitated by commitment from senior provider and commissioner leaders.
DAH recognises the changing biopsychosocial developmental needs of young people and the need to empower young people by embedding health education and health promotion in consultations. In operational terms, DAH focuses on health-care professionals’ approach to and engagement with each young person and their carers alongside the structure of the organisations in which care takes place.
-
The importance of NHS organisations adopting a trust-wide approach to implementation of better transitional health care.
In many trusts, good practice led by enthusiasts rarely generalised to other specialties or to adults’ services. Where organisations had a Transition Steering Committee, chaired by a trust-wide transition co-ordinator, this took advantage of the skills and enthusiasm of those already providing good practice, and assisted with training and consistent implementation in adults’ and children’s services and across specialties.
-
The importance of joint planning between children’s health-care providers, adults’ health-care providers and primary care; this is likely to improve both the transfer of individual young people and the adoption of ways of working that improve care for this population.
-
The importance of adults’ and children’s health-care providers exploring routinely with a young person how they approach transition, taking account of the young person’s interaction style and personalising the clinical approach thereafter.
-
Young people adopt one of four broad interaction styles when approaching their transition: ‘laid back’, ‘anxious’, ‘autonomy-seeking’ and ‘socially oriented’ (i.e. welcomed support from and frequent discussions with family, friends and all health-care professionals).
-
The features ‘appropriate parent involvement’, ‘promotion of health self-efficacy’ and ‘meeting the adult team before transfer’ were associated with better satisfaction with services, participation, subjective well-being and measures of disease control. These findings provide practical content to be considered in NHS commissioning specifications.
‘Having a key worker’ inconsistently predicted better outcomes; ‘having a transition plan’, ‘co-ordinated team’, ‘attending an age-banded clinic’, ‘having a transition manager for clinical team’ and ‘having access to holistic life-skills training’ were not associated with better outcomes.
-
Maximal service uptake could be achieved by a service that encourages parental involvement, ensures that the same staff are seen at each clinic, emphasises the importance of good communication with young people, and encourages young people to make decisions about their care. A service involving a ‘parental involvement that suited both parent and young person’ and a ‘protocol for promotion of young people’s confidence in managing their health condition’ may offer good value for money, but a service involving a ‘transition manager for clinical team’ or an ‘age-banded clinic’ is less likely to offer value for money.
Finally
Parents and young people often have negative impressions of what care will be like in adults’ services. 160 They may think that adults’ services will be less supportive, more fragmented and not linked sufficiently to children’s service providers. However, our findings indicate that there are benefits and positives of transferring to adults’ health care, advantages that could be planned for and explained to young people and their parents by children’s services. Transitions are a part of all of our lives, although planning for these normal developmentally appropriate changes may be more challenging for those with long-term health conditions.
Recommendations for future research
Recent years have seen an increase in research around transition, but most studies are small-scale and difficult to generalise from. Systematic reviews published during the research programme highlight the difficulties of drawing conclusions from the studies reviewed. The Cochrane review36 and NICE guidance14 recognised that the evidence base was weak. We think that the next 2 years would be too early for a further major literature review.
We suggest, in order of priority, the following areas for further research:
-
How might the findings of the programme be introduced and implemented by commissioners and NHS organisations?
Although no study can be definitive, we think that we have reported sufficient evidence to justify research into observation and evaluation of the implementation of the findings in a range of trusts and long-term conditions. Our conclusions are drawn from triangulation of quantitative, qualitative and health economic studies.
-
The role of primary care. This was also a NICE research priority. 14 What are the most effective and efficient ways for primary health-care services to be involved in improving transition and in following up young people after transfer, whether or not they meet the criteria for adults’ services?
Such a study would also address the needs of young people with conditions such as moderate asthma or eczema, who are usually looked after entirely by primary care.
A systematic review of primary care interventions around transition found only three articles, of which only one was set in general practice, and that was in the USA. 161 The review concluded that there was a need for intervention studies to guide improved integration of primary and secondary care over the period of transition.
-
Managing one’s health. This was also a NICE research priority. 14 What is the best way to support young people to manage their health?
We found that promotion of health self-efficacy during transition was associated with better outcomes. Sattoe and colleagues have completed a body of work investigating how to promote health self-efficacy. 162,163 Further research is needed to understand how self-management training can be best built into transition planning, across a range of health conditions, including mental health. This, therefore, is a research question for clinical and health psychology research to understand the context and mechanisms of behaviour change during health-care transition.
Acknowledgements
Health-care organisations supporting the programme
-
Avon and Wiltshire Mental Health Partnership NHS Trust (formerly North Bristol NHS Trust).
-
Belfast Health and Social Care Trust.
-
University of Birmingham.
-
Birmingham Women’s Children’s Hospital NHS Foundation Trust.
-
Heart of England NHS Foundation Trust.
-
Council for Disabled Children.
-
Frimley Health NHS Foundation Trust (formerly Heatherwood and Wexham Park Hospitals NHS Trust).
-
University of Manchester.
-
Newcastle University.
-
Newcastle upon Tyne Hospitals NHS Foundation Trust.
-
Norfolk and Norwich University Hospitals NHS Foundation Trust.
-
Northern Health and Social Care Trust.
-
Northumberland, Tyne and Wear NHS Foundation Trust.
-
Northumbria Healthcare NHS Foundation Trust.
-
Queen’s University Belfast.
-
Royal United Hospitals Bath NHS Foundation Trust.
-
South Eastern Health and Social Care Trust.
-
Southern Health and Social Care Trust.
-
Tees Esk and Wear Valleys NHS Foundation Trust.
-
University Hospitals Birmingham NHS Foundation Trust.
-
Western Health and Social Care Trust.
We thank the following for their contributions to the programme.
External Advisory Board
Chairperson: Simon Pleydell. Members: Shona Chambers (Cerebra), Lizzie Chambers (Together for Short Lives), Allan Colver (chief investigator), Jim Mackey and Chris Price (sponsoring trust), Carl May (medical sociology), Alison Murray (parent), Marij Roebroeck (international advisor), AnneLoes van Staa (international advisor), Scott Wilkes (academic general practitioner), NIHR advisors, and rotating members from the programme’s young’s person advisory group, UP.
Programme Management Board
Helena Gleeson, Consultant Endocrinologist, who was an advisor to the board. She liaised with the Royal College of Physicians, presented at meetings and contributed constructive criticism at board meetings and to the final report.
Nichola Chater, Consultant in Rehabilitation Medicine, who was an advisor to the board. She presented at meetings and contributed constructive criticism at board meetings and to the final report.
Caroline Potts, Research and Development Manager, who represented the sponsor on the board and facilitated many arrangements with the sponsor.
Work packages 1.1 and 1.2
Amy Jones and Dan Notley, Health Play Specialist/Patient Involvement Leads, who helped with the facilitation of UP.
Tracy Scott, Research Associate, who helped with the facilitation of UP; and also contributed to WP 2.1 through data collection at home visits, maintaining regular communication with the co-ordinating centre and attending training workshops at the co-ordinating centre.
Sophie Fairgrieve, Sophie Walker, Monica Parker and Molly Pledger, who were peer-support workers.
Work package 1.3
Helen Mason, Lecturer in Health Economics, who assisted with the design and analysis of the Q-sort study and contributed to a published academic paper.
All of the young people who took part in this study.
The consultant physicians and surgeons who helped to recruit young people to the study: Alan Anderson, Laura Baines, Steve Ball, Katherine Barlow, William Bliss, Nicola Brown, Su Bunn, Penny Burt, Tim Cheetham, Denise Chisholm, Lucy Craig, Jean Crosier, Anita Devlin, Simon Doe, Peter Dryden, Anna Eden, Rob Forsyth, Helen Foster, Dee Frost, Hany Gabra, Binu George, Helen Hanson, Sally Harding, Yvonne Hart, Karen Heslop, Gareth Hosie, Bernard Higgins, Mark Hudson, Margaret Jackson, Ann Kirk, Jill Kisler, Heather Lambert, Nicki Leech, Lorraine Lentell, Raj Lodh, John Macfarlane, Mike McKean, Debbie McParlin, John Mansfield, Margaret Miller, Jackie O’Sullivan, John O’Sullivan, Leila Qizalbash, Trudy Pederson, Rob Pickard, Ben Reynolds, Mandy Robinson, Wendy Robson, Clare Smith, Jayne Straker, Julian Thomas, Matthew Thomas, Mary Vallely, Ramesh Venkateswaran and Lucy Wirz.
Work packages 2.1, 2.2 and 2.3
The principal investigators at NHS sites who supervised the research assistants and assisted with recruitment at each site: Amanda Billson, Anastasia Bem, Stuart Bennett, Stephen Bruce, Tim Cheetham, Diana Howlett, Zilla Huma, Mark Linden, Maria Lohan, Cara Maiden, Melanie Meek, Jenny Milne, Julie Owens, Jackie Parkes, Fiona Regan and Nandu Thalange.
The research assistants who undertook data collection: Kam Ameen-Ali, Sarah Balne, Shaunak Deshpande, Louise Foster, Charlotte George, Louisa Fear, Kate Hardenberg, Guio Garcia Jalon, Holly Roper, Tracy Scott, Catherine Sheppard, Louise Ting and Hazel Windmill.
Michaela Fay, Research Assistant, for her work collecting qualitative data in a variety of settings and contribution to analysis of these data.
Rose Watson, Research Assistant, for her work collecting quantitative data at home visits; and her work collecting qualitative data in a variety of settings, with analysis of these data under supervision.
Julija Stoniute, Research Assistant, for her work on the analysis of economic data with Jennifer Hislop.
Mark Deverill, Senior Lecturer in Health Economics, for his work in planning some aspects of the research and setting up its early phases.
John Macfarlane, Consultant in Rehabilitation Medicine, for his work in planning some aspects of the research and recruiting study participants.
Susan Gray, Trainee in Paediatrics, for her help in preparing our published paper on those with diabetes.
Christopher King, Trainee in Child and Adolescent Psychiatry, for his help in preparing our draft paper on those with ASD.
The WEMWBS was funded by the Scottish Government National Programme for Improving Mental Health and Well-being, commissioned by NHS Health Scotland, developed by the University of Warwick and the University of Edinburgh, and is jointly owned by NHS Health Scotland, the University of Warwick and the University of Edinburgh.
Work package 3.1
Elizabeth Rankin, who was the principal investigator at one NHS site and supervised a research assistant in the recruitment of participants.
Albert Farre, Research Associate, who undertook a leading role in conducting ethnographic fieldwork across two NHS sites and led on the writing of two published papers.
Victoria Wood, Research Associate, who undertook a leading role in conducting ethnographic fieldwork across one NHS site and contributed to two published papers.
Work packages 3.2 and 3.3
The members of the Steering Group for this WP: Dr Laura Baines, Dr Steve Ball, Dr Belinda Bateman, Ms Beverley Barclay, Professor Bryony Beresford, Dr Tim Cheetham, Dr Helena Gleeson, Ms Helen Hirst, Dr Mark Hudson, Dr David Jones, Dr Nicola Leech, Professor Robert Pickard, Mr Steve Rundle, Dr Gill Turner and Mr Ian Walton.
Angela Bate, Lecturer in Health Economics, for her work in planning the research and setting up its early phases.
Sara McCafferty, Research Associate, for her work conducting interviews and initial elements of analysis in WP 3.2 and contributing to an academic paper.
Niina Kolehmainen, Consultant Occupational Therapist, for her work analysing and reporting data from qualitative interviews in WP 3.2 and contributing to an academic paper.
Overarching
The programme’s young people’s group (UP) and the local CHAT.
Secretarial, financial and administrative staff: Sarah Nolan, Alison Mulvenna, Jaqueline Story and Norman Marillier.
Student helpers: Sarah Longwell, Rachel Pearse and Folasade Solanke for help with preparation of papers; and Vito Puyat, for help with data entry.
Helen Wheatley for her co-ordinating work over the first year of the programme on behalf of the Council for Disabled Children.
We acknowledge the support of the NIHR Clinical Research Network.
We thank the sponsor, Northumbria Healthcare NHS Foundation Trust.
Contributions of authors
Allan Colver is Professor of Community Child Health at Newcastle University and a Consultant Paediatrician. He was the grant holder and led the programme of research. He led WP 3.3 and was directly involved in all other WPs except 2.2 and 2.3. He drafted the final report and is responsible for the final version and submission to NIHR. He is the corresponding author and guarantor of the work.
Tim Rapley was Senior Lecturer in Medical Sociology at Newcastle University and is now Professor of Applied Health Care Research at Northumbria University. He was a co-applicant. He led WP 2.2, co-led WP 3.1 and was directly involved in WP 1.1. In WPs 2.2 and 3.1, this work involved designing the qualitative work, supervising research assistants and analysing the transcripts of qualitative data. He assisted with many aspects of the engagement of young people in the programme’s work. He co-designed the DAH toolkit. He contributed detailed adjustments to the draft report and approved the final version.
Jeremy R Parr is Professor of Paediatric Neurodisability at Newcastle University and a consultant paediatrician. He was a co-applicant. He was directly involved in WPs 1.3, 2.1, 2.2 and 3.1. This work involved co-designing these quantitative and qualitative studies, contributing to supervision of research assistants, lead contacts with clinicians for the Q-sort study, overseeing recruitment of people with diabetes mellitus for the longitudinal study, assisting with design of the DCE, and co-designing the DAH toolkit. He contributed detailed adjustments to the draft report and approved the final version.
Helen McConachie is Professor of Child Clinical Psychology at Newcastle University. She was a co-applicant. She led WP 2.1. This work included involvement in the design of the original programme, co-design of the longitudinal study, arranging training of the research assistants, monitoring data collection and completeness, and advising on data analysis. She contributed detailed adjustments to the draft report and approved the final version.
Gail Dovey-Pearce is a Consultant Clinical Psychologist at Northumbria Healthcare NHS Foundation Trust. She was a co-applicant. She led WPs 1.1 and 1.2 and was directly involved in WPs 2.1 and 3.1. Her work involved leading on the engagement and involvement of young people, including setting up and running UP, supervising the collection of longitudinal data across two sites, and facilitating the qualitative interviews at one site. She contributed detailed adjustments to the draft report and approved the final version.
Ann Le Couteur is Professor of Child and Adolescent Psychiatry at Newcastle University and a consultant child and adolescent psychiatrist. She was a co-applicant. She was directly involved in WPs 2.1, 2.2, 3.2 and 3.3. This work included involvement in the design of the original programme, liaising with sites that recruited those with ASD, interviewing commissioners and critically reviewing qualitative and quantitative data. She contributed detailed adjustments to the draft report and approved the final version.
Janet E McDonagh is a Clinical Senior Lecturer in Paediatric and Adolescent Rheumatology at the University of Manchester. She was a co-applicant. She co-led WP 3.1 and was directly involved in WPs 1.1 and 1.2. This work included involvement in the design of the original programme, being local principal investigator at one of the three participating sites of WP 3.1, interpreting data and writing papers from WP 3.1, providing direct input and support for the health passport work of WP 1.2, and identifying and establishing links with relevant organisations elsewhere in the UK for WPs 1.1 and 1.2 to ensure generalisability of the outputs of the programme. She co-designed the DAH toolkit. She contributed detailed adjustments to the draft report and approved the final version.
Caroline Bennett is Assistant Director of the Council for Disabled Children, London. She was a co-applicant. She was directly involved in WPs 1.1, 1.2 and 3.1. This work involved regular assistance with the engagement of young people in the programme’s work. She facilitated workshops in London and Newcastle that enabled young people from across the country to discuss preliminary results of the programme. She developed facilitator guides for the subsequent rollout of these workshops. She contributed detailed adjustments to the draft report and approved the final version.
Jennifer Hislop was a Research Associate in Health Economics at Newcastle University. She contributed to WPs 1.3 and 2.3. This work involved interviewing young people in the WP 1.3 Q-sort study and analysing the data. She contributed to one published paper. In WP 2.2 she developed a DCE and she modelled the health economic data. She contributed detailed adjustments to the draft report and approved the final version.
Gregory Maniatopoulos is a Senior Research Associate in Medical Sociology at Newcastle University. He led WP 3.2 and was directly involved in WP 3.3. His work involved analysis of qualitative data, three in-depth site visits, and contributions to two submitted papers, one of which he led. He contributed detailed adjustments to the draft report and approved the final version.
Kay D Mann was a Research Assistant in Epidemiology at Newcastle University. She contributed to WP 2.1. This work involved cleaning, coding and analysing data from all collection phases. She contributed detailed adjustments to the draft report and approved the final version.
Hannah Merrick was a Research Assistant at Newcastle University. She contributed to WP 2.1, drafted and distributed newsletters, organised internal seminars and identified relevant new publications in the field. The work in WP 2.1 involved collecting, checking and analysing data. She contributed to two published papers. She contributed detailed adjustments to the draft report and approved the final version.
Mark S Pearce is Professor of Applied Epidemiology at Newcastle University. He was a co-applicant. He was directly involved in WPs 2.1 and 2.3. This work involved supervision of a research assistant and detailed discussions about methods of analysis and interpretation of results. He contributed detailed adjustments to the draft report and approved the final version.
Debbie Reape was Deputy Director of Nursing at Northumbria Healthcare NHS Foundation Trust. She was a co-applicant. She was directly involved in WPs 1.1, 1.2, 3.1 and 3.2. This work involved assistance with many aspects of the engagement of young people in the programme’s work. As senior manager in the sponsoring trust, she facilitated meetings and provided contacts for interviews with commissioners. She participated in data collection in WP 3.2 at meetings with commissioners. She contributed detailed adjustments to the draft report and approved the final version.
Luke Vale is The Health Foundation Professor of Health Economics at Newcastle University. He was a co-applicant. He led WPs 1.3 and 2.3 and was involved in WP 3.2. This work involved planning the economic work and supervising a research assistant in this work. He also supervised a research associate in the WP 3.2 on commissioning. He contributed to three published papers from these WPs. He contributed detailed adjustments to the draft report and approved the final version.
Publications
Watson R, Parr J, Joyce C, May C, Le Couteur A. Models of healthcare transition for young people with complex health needs: a scoping review. Child Care Health Dev 2011;37:780–91. https://doi.org/10.1111/j.1365-2214.2011.01293.x
Colver A, Longwell S. New understanding of adolescent brain development: relevance to transitional healthcare for young people with long term conditions. Arch Dis Child 2013;98:902–7. https://doi.org/10.1136/archdischild-2013-303945
Colver AF, Merrick H, Deverill M, Le Couteur A, Parr J, Pearce MS, et al. Study protocol: Longitudinal study of the transition of young people with complex health needs from child to adult health services. BMC Public Health 2013;13:675. https://doi.org/10.1186/1471-2458-13-675
Farre A, Wood V, Rapley T, Parr JR, Reape D, McDonagh JE. Developmentally appropriate healthcare for young people: a scoping study. Arch Dis Child 2015;100:144–51. https://doi.org/10.1136/archdischild-2014-306749
Merrick H, McConachie H, Le Couteur A, Mann K, Parr JR, Pearce MS, et al. Characteristics of young people with long term conditions close to transfer to adult health services. BMC Health Serv Res 2015;15:435. https://doi.org/10.1186/s12913-015-1095-6
Farre A, Wood V, McDonagh JE, Parr JR, Reape D, Rapley T. Health professionals’ and managers’ definitions of developmentally appropriate healthcare for young people: conceptual dimensions and embedded controversies. Arch Dis Child 2016;101:628–33. https://doi.org/10.1136/archdischild-2015-309473
Hislop J, Mason H, Parr JR, Vale L, Colver A. Views of young people with chronic conditions on transition from pediatric to adult health services. J Adolesc Health 2016;59:345–53.
Kolehmainen N, McCafferty S, Maniatopoulos G, Vale L, Le Couteur A, Colver A; on behalf of the Transition Collaborative Group. What constitutes successful commissioning of transition from children’s to adults’ services for young people with long-term conditions, and what are the challenges? An interview study. BMJ Paediatr Open 2017;1:e000085. https://doi.org/10.1136/bmjpo-2017-000085
Colver A, McConachie H, Le Couteur A, Dovey-Pearce G, Mann KD, McDonagh JE, et al. ; Transition Collaborative Group. A longitudinal, observational study of the features of transitional healthcare associated with better outcomes for young people with long-term conditions. BMC Med 2018;16:111.
Colver A, Pearse R, Watson RM, Fay M, Rapley T, Mann KD, Le Couteur A, Parr JR, McConachie H. on behalf of the Transition Collaborative Group. How well do services for young people with long term conditions deliver features proposed to improve transition? BMC Health Serv Res 2018;18:337.
Gray S, Cheetham T, McConachie H, Mann KD, Parr JR, Pearce MS, Colver A on behalf of the Transition Collaborative Group. A longitudinal, observational study examining the relationships of patient satisfaction with services and mental wellbeing to their clinical course in young people with Type 1 diabetes mellitus during transition from child to adult health services. Diabet Med 2018;35:1216–22.
Maniatopoulos G, Le Couteur A, Vale L, Colver A. Falling through the gaps: exploring the role of integrated commissioning in improving transition from children’s to adults’ services for young people with long-term health conditions in England. J Health Serv Res Policy 2018;23:107–15.
McDonagh JE, Farre A, Gleeson H, Rapley T, Dovey-Pearce G, Reape D, et al. ; Transition Collaborative Group. Making healthcare work for young people. Arch Dis Child 2018;103:623. https://doi.org/10.1136/archdischild-2017-314573
Solanke F, Colver A, McConachie H; Transition collaborative group. Are the health needs of young people with cerebral palsy met during transition from child to adult healthcare? Child Care Health Dev 2018;44:355–63. https://doi.org/10.1111/cch.12549
Uljarević M, Richdale A, Hedley D, Cai R, McConachie H, Merrick H, et al. The Hospital Anxiety and Depression Scale: Factor Structure and Psychometric Properties in older adolescents and young adults with Autism Spectrum Disorder. Autism Res 2018;11:258–69.
Dovey-Pearce G, Walker S, Fairgrieve S, Parker M, Rapley T. The burden of proof: the process of involving young people in research [published online ahead of print February 15 2019]. Health Expect 2019.
Data-sharing statement
Anonymised data will be made available to the scientific community with as few restrictions as feasible. Qualitative data cannot be released due to anonymity and consent concerns. All enquiries and data requests should be submitted to the corresponding author for consideration (using a specific form available on request). Access to data may be granted following review.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, CCF, NETSCC, PGfAR or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the PGfAR programme or the Department of Health and Social Care.
References
- WHO Study Group on Young People and ‘Health for All by the Year 2000’ . Young People’s Health – A Challenge for Society: Report of a WHO Study Group on Young People and ‘Health for All by the Year 2000’ n.d.
- Roisman GI, Masten AS, Coatsworth JD, Tellegen A. Salient and emerging developmental tasks in the transition to adulthood. Child Dev 2004;75:123-33. https://doi.org/10.1111/j.1467-8624.2004.00658.x.
- Farre A, Wood V, Rapley T, Parr JR, Reape D, McDonagh JE. Developmentally appropriate healthcare for young people: a scoping study. Arch Dis Child 2015;100:144-51. https://doi.org/10.1136/archdischild-2014-306749.
- Farre A, Wood V, McDonagh JE, Parr JR, Reape D, Rapley T. Transition Collaborative Group . Health professionals’ and managers’ definitions of developmentally appropriate healthcare for young people: conceptual dimensions and embedded controversies. Arch Dis Child 2016;101:628-33. https://doi.org/10.1136/archdischild-2015-309473.
- Blum RW, Garell D, Hodgman CH, Jorissen TW, Okinow NA, Orr DP, et al. Transition from child-centered to adult health-care systems for adolescents with chronic conditions. A position paper of the Society for Adolescent Medicine. J Adolesc Health 1993;14:570-6. https://doi.org/10.1016/1054-139X(93)90143-D.
- Hepburn CM, Cohen E, Bhawra J, Weiser N, Hayeems RZ, Guttmann A. Health system strategies supporting transition to adult care. Arch Dis Child 2015;100:559-64. https://doi.org/10.1136/archdischild-2014-307320.
- Cooley WC, Sagerman PJ. American Academy of Pediatrics . Supporting the health care transition from adolescence to adulthood in the medical home. Pediatrics 2011;128:182-200. https://doi.org/10.1542/peds.2011-0969.
- Mazur A, Dembinski L, Schrier L, Hadjipanayis A, Michaud PA. European Academy of Paediatric consensus statement on successful transition from paediatric to adult care for adolescents with chronic conditions. Acta Paediatr 2017;106:1354-7. https://doi.org/10.1111/apa.13901.
- Foster HE, Minden K, Clemente D, Leon L, McDonagh JE, Kamphuis S, et al. EULAR/PReS standards and recommendations for the transitional care of young people with juvenile–onset rheumatic diseases. Ann Rheum Dis 2017;76:639-46. https://doi.org/10.1136/annrheumdis-2016-210112.
- Transition: Getting it Right for Young People. Improving the Transition of Young People with Long Term Conditions from Children’s to Adult Health Services. London: Department of Health and Social Care; 2006.
- Transition: Moving on Well. A Good Practice Guide for Health Professionals and their Partners on Transition Planning for Young People with Complex Health Needs or a Disability. London: Department of Health and Social Care; 2008.
- Kennedy I. Getting it Right for Children and Young People. Overcoming Cultural Barriers in the NHS so as to Meet Their Needs. London: Department of Health and Social Care; 2010.
- From the Pond into the Sea. Children’s Transition to Adult Health Services. Newcastle upon Tyne: Care Quality Commission; 2014.
- Transition from Children’s to Adults’ Services for Young People using Health or Social Care Services. London: NICE; 2016.
- Colver A. How Can Health Services Contribute Most Effectively to Facilitating Successful Transition of Young People with Complex Health Needs from Childhood to Adulthood?. NIHR Programme Development Grant, Work Stream 6, Newcastle University; 2011.
- Colver A, Longwell S. New understanding of adolescent brain development: relevance to transitional healthcare for young people with long term conditions. Arch Dis Child 2013;98:902-7. https://doi.org/10.1136/archdischild-2013-303945.
- Stam H, Hartman EE, Deurloo JA, Groothoff J, Grootenhuis MA. Young adult patients with a history of pediatric disease: impact on course of life and transition into adulthood. J Adolesc Health 2006;39:4-13. https://doi.org/10.1016/j.jadohealth.2005.03.011.
- Lyon ME, Kuehl K, McCarter R. Transition to adulthood in congenital heart disease: missed adolescent milestones. J Adolesc Health 2006;39:121-4. https://doi.org/10.1016/j.jadohealth.2005.09.008.
- Queirós FC, Wehby GL, Halpern CT. Developmental disabilities and socioeconomic outcomes in young adulthood. Public Health Rep 2015;130:213-21. https://doi.org/10.1177/003335491513000308.
- Pinquart M. Achievement of developmental milestones in emerging and young adults with and without pediatric chronic illness – a meta-analysis. J Pediatr Psychol 2014;39:577-87. https://doi.org/10.1093/jpepsy/jsu017.
- Maslow GR, Haydon A, McRee AL, Ford CA, Halpern CT. Growing up with a chronic illness: social success, educational/vocational distress. J Adolesc Health 2011;49:206-12. https://doi.org/10.1016/j.jadohealth.2010.12.001.
- Smith N. Research Study on Age Appropriate Services for Young People with Neurodevelopmental Disorders. Birmingham: ECOTEC; 2010.
- Ardissino G, Testa S, Daccò V, Paglialonga F, Viganò S, Felice-Civitillo C, et al. Puberty is associated with increased deterioration of renal function in patients with CKD: data from the ItalKid Project. Arch Dis Child 2012;97:885-8. https://doi.org/10.1136/archdischild-2011-300685.
- Bolton-Maggs PH. Transition of care from paediatric to adult services in haematology. Arch Dis Child 2007;92:797-801. https://doi.org/10.1136/adc.2006.103804.
- Dovey-Pearce G, Hurrell R, May C, Walker C, Doherty Y. Young adults’ (16–25 years) suggestions for providing developmentally appropriate diabetes services: a qualitative study. Health Soc Care Community 2005;13:409-19. https://doi.org/10.1111/j.1365-2524.2005.00577.x.
- Iyer A, Appleton R. Transitional services for adolescents with epilepsy in the U.K.: a survey. Seizure 2013;22:433-7. https://doi.org/10.1016/j.seizure.2013.02.014.
- Lewis SA, Noyes J. Effective process or dangerous precipice: qualitative comparative embedded case study with young people with epilepsy and their parents during transition from children’s to adult services. BMC Pediatr 2013;13. https://doi.org/10.1186/1471-2431-13-169.
- Ko B, McEnery G. The needs of physically disabled young people during transition to adult services. Child Care Health Dev 2004;30:317-23. https://doi.org/10.1111/j.1365-2214.2004.00422.x.
- Lindsay S. Spaces of well-being among young adults with physical disabilities transitioning from pediatric to adult healthcare. Disabil Health J 2018;11:149-54. https://doi.org/10.1016/j.dhjo.2017.03.018.
- Jordan A, McDonagh JE. Recognition of emerging adulthood in UK rheumatology: the case for young adult rheumatology service developments. Rheumatology 2007;46:188-91. https://doi.org/10.1093/rheumatology/kel368.
- Harmon WE, McDonald RA, Reyes JD, Bridges ND, Sweet SC, Sommers CM, et al. Pediatric transplantation, 1994–2003. Am J Transplant 2005;5:887-903. https://doi.org/10.1111/j.1600-6135.2005.00834.x.
- Eklund H, Cadman T, Findon J, Hayward H, Howley D, Beecham J, et al. Clinical service use as people with attention deficit hyperactivity disorder transition into adolescence and adulthood: a prospective longitudinal study. BMC Health Serv Res 2016;16. https://doi.org/10.1186/s12913-016-1509-0.
- Belling R, McLaren S, Paul M, Ford T, Kramer T, Weaver T, et al. The effect of organisational resources and eligibility issues on transition from child and adolescent to adult mental health services. J Health Serv Res Policy 2014;19:169-76. https://doi.org/10.1177/1355819614527439.
- Cerebral Palsy in Under 25s: Assessment and Management. London: NICE; 2017.
- Brief Guide: Transitions out of Children and Young People’s Mental Health Services CQUIN. Newcastle upon Tyne: Care Quality Commission; 2018.
- Campbell F, Biggs K, Aldiss SK, O’Neill PM, Clowes M, McDonagh J, et al. Transition of care for adolescents from paediatric services to adult health services. Cochrane Database Syst Rev 2016;29. https://doi.org/10.1002/14651858.CD009794.pub2.
- Tsybina I, Kingsnorth S, Maxwell J, Bayley M, Lindsay S, McKeever P, et al. Longitudinal Evaluation of Transition Services (‘LETS Study’): protocol for outcome evaluation. BMC Pediatr 2012;12. https://doi.org/10.1186/1471-2431-12-51.
- Kreuzer M, Prüfe J, Bethe D, Vogel C, Großhennig A, Koch A, et al. The TRANSNephro-study examining a new transition model for post-kidney transplant adolescents and an analysis of the present health care: study protocol for a randomized controlled trial. Trials 2014;15. https://doi.org/10.1186/1745-6215-15-505.
- Sattoe JN, Peeters MA, Hilberink SR, Ista E, van Staa A. Evaluating outpatient transition clinics: a mixed-methods study protocol. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2016-011926.
- Acuña Mora M, Sparud-Lundin C, Bratt EL, Moons P. Person-centred transition programme to empower adolescents with congenital heart disease in the transition to adulthood: a study protocol for a hybrid randomised controlled trial (STEPSTONES project). BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2016-014593.
- Le Roux E, Mellerio H, Guilmin-Crépon S, Gottot S, Jacquin P, Boulkedid R, et al. Methodology used in comparative studies assessing programmes of transition from paediatrics to adult care programmes: a systematic review. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2016-012338.
- Fair C, Cuttance J, Sharma N, Maslow G, Wiener L, Betz C, et al. International and interdisciplinary identification of health care transition outcomes. JAMA Pediatr 2016;170:205-11. https://doi.org/10.1001/jamapediatrics.2015.3168.
- Suris JC, Akre C. Key elements for, and indicators of, a successful transition: an international Delphi study. J Adolesc Health 2015;56:612-18. https://doi.org/10.1016/j.jadohealth.2015.02.007.
- Fegran L, Hall EO, Uhrenfeldt L, Aagaard H, Ludvigsen MS. Adolescents’ and young adults’ transition experiences when transferring from paediatric to adult care: a qualitative metasynthesis. Int J Nurs Stud 2014;51:123-35. https://doi.org/10.1016/j.ijnurstu.2013.02.001.
- Dovey-Pearce G, Walker S, Fairgrieve S, Parker M, Rapley T. The burden of proof: the process of involving young people in research [published online ahead of print February 15 2019]. Health Expect 2019. https://doi.org/10.1111/hex.12870.
- Wolfstadt J, Kaufman A, Levitin J, Kaufman M. The use and usefulness of MyHealth passport: an online tool for the creation of a portable health summary. Int J Child Adolesc Health 2011;3:499-506.
- Freeman M, Stewart D, Shimmell L, Missiuna C, Burke-Gaffney J, Jaffer S, et al. Development and evaluation of The KIT: Keeping It Together™ for Youth (the ‘Youth KIT’) to assist youth with disabilities in managing information. Child Care Health Dev 2015;41:222-9. https://doi.org/10.1111/cch.12199.
- van Staa A, Jedeloo S, Latour JM, Trappenburg MJ. Exciting but exhausting: experiences with participatory research with chronically ill adolescents. Health Expect 2010;13:95-107. https://doi.org/10.1111/j.1369-7625.2009.00574.x.
- Coser LR, Tozer K, Van Borek N, Tzemis D, Taylor D, Saewyc E, et al. Finding a voice: participatory research with street–involved youth in the youth injection prevention project. Health Promot Pract 2014;15:732-8. https://doi.org/10.1177/1524839914527294.
- Gorter JW, Stewart D, Cohen E, Hlyva O, Morrison A, Galuppi B, et al. Are two youth-focused interventions sufficient to empower youth with chronic health conditions in their transition to adult healthcare: a mixed-methods longitudinal prospective cohort study. BMJ Open 2015;5. https://doi.org/10.1136/bmjopen-2014-007553.
- Lugasi T, Achille M, Stevenson M. Patients’ perspective on factors that facilitate transition from child-centered to adult-centered health care: a theory integrated metasummary of quantitative and qualitative studies. J Adolesc Health 2011;48:429-40. https://doi.org/10.1016/j.jadohealth.2010.10.016.
- Hislop J, Mason H, Parr JR, Vale L, Colver A. Views of young people with chronic conditions on transition from pediatric to adult health services. J Adolesc Health 2016;59:345-53. https://doi.org/10.1016/j.jadohealth.2016.04.004.
- Watson R, Parr JR, Joyce C, May C, Le Couteur AS. Models of transitional care for young people with complex health needs: a scoping review. Child Care Health Dev 2011;37:780-91. https://doi.org/10.1111/j.1365-2214.2011.01293.x.
- Brouwer M. Q is accounting for tastes. J Advertising Res 1999;39:35-9.
- Stainton Rogers R, Smith JA, Harré R, Van Langenhofe L. Rethinking Methods in Psychology. Thousand Oaks, CA: Sage; 1995.
- Watts S, Stenner P. Doing Q Methodological Research. Theory, Method and Interpretation. London: Sage Publications Ltd; 2012.
- Price CS, Corbett S, Lewis-Barned N, Morgan J, Oliver LE, Dovey-Pearce G. Implementing a transition pathway in diabetes: a qualitative study of the experiences and suggestions of young people with diabetes. Child Care Health Dev 2011;37:852-60. https://doi.org/10.1111/j.1365-2214.2011.01241.x.
- Allen D, Cohen D, Hood K, Robling M, Atwell C, Lane C, et al. Continuity of care in the transition from child to adult diabetes services: a realistic evaluation study. J Health Serv Res Policy 2012;17:140-8. https://doi.org/10.1258/jhsrp.2011.011044.
- Kirk S. Transitions in the lives of young people with complex healthcare needs. Child Care Health Dev 2008;34:567-75. https://doi.org/10.1111/j.1365-2214.2008.00862.x.
- Paul M, Street C, Wheeler N, Singh SP. Transition to adult services for young people with mental health needs: a systematic review. Clin Child Psychol Psychiatry 2015;20:436-57. https://doi.org/10.1177/1359104514526603.
- Colver AF, Merrick H, Deverill M, Le Couteur A, Parr J, Pearce MS, et al. Study protocol: longitudinal study of the transition of young people with complex health needs from child to adult health services. BMC Public Health 2013;13. https://doi.org/10.1186/1471-2458-13-675.
- Merrick H, McConachie H, Le Couteur A, Mann K, Parr JR, Pearce MS, et al. Characteristics of young people with long term conditions close to transfer to adult health services. BMC Health Serv Res 2015;15. https://doi.org/10.1186/s12913-015-1095-6.
- Colver A, Pearse R, Watson RM, Fay M, Rapley T, Mann KD, et al. How well do services for young people with long term conditions deliver features proposed to improve transition?. BMC Health Serv Res 2018;18. https://doi.org/10.1186/s12913-018-3168-9.
- Solanke F, Colver A, McConachie H. Transition collaborative group . Are the health needs of young people with cerebral palsy met during transition from child to adult health care?. Child Care Health Dev 2018;44:355-63. https://doi.org/10.1111/cch.12549.
- Gray S, Cheetham T, McConachie H, Mann KD, Parr JR, Pearce MS, et al. A longitudinal, observational study examining the relationships of patient satisfaction with services and mental well-being to their clinical course in young people with Type 1 diabetes mellitus during transition from child to adult health services. Diabet Med 2018;35:1216-22. https://doi.org/10.1111/dme.13698.
- Colver A, McConachie H, Le Couteur A, Dovey-Pearce G, Mann KD, McDonagh JE, et al. A longitudinal, observational study of the features of transitional healthcare associated with better outcomes for young people with long-term conditions. BMC Med 2018;16. https://doi.org/10.1186/s12916-018-1102-y.
- Colver AF, Gibson M, Hey EN, Jarvis SN, Mackie PC, Richmond S. Increasing rates of cerebral palsy across the severity spectrum in North-East England 1964–1993. The North of England Collaborative Cerebral Palsy Survey. Arch Dis Child Fetal Neonatal Ed 2000;83:F7-12. https://doi.org/10.1136/fn.83.1.F7.
- Dolk H, Parkes J, Hill N. Trends in the prevalence of cerebral palsy in Northern Ireland, 1981–1997. Dev Med Child Neurol 2006;48:406-12. https://doi.org/10.1017/S0012162206000909.
- Department of Health and Social Care . English IMD 2010 Data 2011. www.communities.gov.uk/publications/corporate/statistics/indices2010 (accessed 22 March 2017).
- Northern Ireland Multiple Deprivation Measure 2010. Belfast: Northern Ireland Statistics and Research Agency; n.d.
- Shaw KL, Southwood TR, McDonagh JE. British Society of Paediatric and Adolescent Rheumatology . Development and preliminary validation of the ‘Mind the Gap’ scale to assess satisfaction with transitional health care among adolescents with juvenile idiopathic arthritis. Child Care Health Dev 2007;33:380-8. https://doi.org/10.1111/j.1365-2214.2006.00699.x.
- Donkervoort M, Wiegerink DJ, van Meeteren J, Stam HJ, Roebroeck ME. Transition Research Group South West Netherlands . Transition to adulthood: validation of the Rotterdam Transition Profile for young adults with cerebral palsy and normal intelligence. Dev Med Child Neurol 2009;51:53-62. https://doi.org/10.1111/j.1469-8749.2008.03115.x.
- International Classification of Functioning, Disability and Health: Children and Youth Version: ICF-CY. Geneva: World Health Organization; 2007.
- van Staa A. On Your Own Feet Research Group . Unravelling traidic communication in hospital consultations with adolescents with chronic conditions: the added value of mixed methods research. Patient Educ Couns 2011;82:455-64. https://doi.org/10.1016/j.pec.2010.12.001.
- Tuffrey C, Bateman BJ, Colver AC. The Questionnaire of Young People’s Participation (QYPP): a new measure of participation frequency for disabled young people. Child Care Health Dev 2013;39:500-11. https://doi.org/10.1111/cch.12060.
- Michelsen SI, Flachs EM, Damsgaard MT, Parkes J, Parkinson K, Rapp M, et al. European study of frequency of participation of adolescents with and without cerebral palsy. Eur J Paediatr Neurol 2014;18:282-94. https://doi.org/10.1016/j.ejpn.2013.12.003.
- Clarke A, Friede T, Putz R, Ashdown J, Martin S, Blake A, et al. Warwick–Edinburgh Mental Well–being Scale (WEMWBS): validated for teenage school students in England and Scotland. A mixed methods assessment. BMC Public Health 2011;11. https://doi.org/10.1186/1471-2458-11-487.
- Sonneveld HM, Strating MM, van Staa AL, Nieboer AP. Gaps in transitional care: what are the perceptions of adolescents, parents and providers?. Child Care Health Dev 2013;39:69-80. https://doi.org/10.1111/j.1365-2214.2011.01354.x.
- Quine L, Pahl J. Stress and Coping in Families Caring for a Child with Severe Mental Handicap: A Longitudinal Study. Canterbury: Institute of Social and Applied Psychology and Centre for Health Services, University of Kent; 1989.
- Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand 1983;67:361-70. https://doi.org/10.1111/j.1600-0447.1983.tb09716.x.
- Uljarević M, Richdale A, Hedley D, Cai R, McConachie H, Merrick H, et al. The Hospital Anxiety and Depression Scale: factor structure and psychometric properties in older adolescents and young adults with autism spectrum disorder. Autism Res 2018;11:258-69. https://doi.org/10.1002/aur.1872.
- Taggart F, Stewart-Brown S, Parkinson J. Warwick–Edinburgh Mental Well-Being Scale (WEMWBS) User Guide – Version 2. Edinburgh: NHS Health Scotland; 2016.
- Heath G, Farre A, Shaw K. Parenting a child with chronic illness as they transition into adulthood: a systematic review and thematic synthesis of parents’ experiences. Patient Educ Couns 2017;100:76-92. https://doi.org/10.1016/j.pec.2016.08.011.
- Crowley R, Wolfe I, Lock K, McKee M. Improving the transition between paediatric and adult healthcare: a systematic review. Arch Dis Child 2011;96:548-53. https://doi.org/10.1136/adc.2010.202473.
- Rapley T, Flick U. The SAGE Handbook of Qualitative Data Analysis. London: Sage; 2013.
- Rapley T, Silverman D. Qualitative Research. London: Sage; 2016.
- Glaser B. The constant comparative method of qualitative analysis. Soc Probl 1965;12:436-45. https://doi.org/10.2307/798843.
- Seale C. The Quality of Qualitative Research. London: Sage; 1999.
- Garfinkel H. Studies in Ethnomethodology. Englewood, NJ: Prentice-Hall; 1997.
- Flynn TN, Louviere JJ, Marley AA, Coast J, Peters TJ. Rescaling quality of life values from discrete choice experiments for use as QALYs: a cautionary tale. Popul Health Metr 2008;6. https://doi.org/10.1186/1478-7954-6-6.
- Ryan M, Netten A, Skåtun D, Smith P. Using discrete choice experiments to estimate a preference-based measure of outcome – an application to social care for older people. J Health Econ 2006;25:927-44. https://doi.org/10.1016/j.jhealeco.2006.01.001.
- Coast J, Al-Janabi H, Sutton EJ, Horrocks SA, Vosper AJ, Swancutt DR, et al. Using qualitative methods for attribute development for discrete choice experiments: issues and recommendations. Health Econ 2012;21:730-41. https://doi.org/10.1002/hec.1739.
- Lancsar E, Louviere J. Conducting discrete choice experiments to inform healthcare decision making: a user’s guide. PharmacoEconomics 2008;26:661-77. https://doi.org/10.2165/00019053-200826080-00004.
- You’re Welcome Quality Criteria: Making Health Services Young Person Friendly. London: Department of Health and Social Care; 2011.
- EuroQol . EQ-5D-5L User Guide n.d. https://euroqol.org/wp-content/uploads/2016/09/EQ-5D-5L_UserGuide_2015.pdf (accessed 27 March 2019).
- Patient Preference Information – Voluntary Submission Review in Premarket Approval Applications, Humanitarian Device Exemption Applications, De Novo Requests and Inclusion in Decision Summaries and Device Labelling: Guidance for Industry, Food and Drug Administration Staff and Other Stakeholders. Silver Spring, MD: US Food and Drug Administration; 2016.
- McCaffery KJ, Dixon A, Hayen A, Jansen J, Smith S, Simpson JM. The influence of graphic display format on the interpretations of quantitative risk information among adults with lower education and literacy: a randomized experimental study. Med Decis Making 2012;32:532-44. https://doi.org/10.1177/0272989X11424926.
- Tait AR, Voepel-Lewis T, Zikmund-Fisher BJ, Fagerlin A. The effect of format on parents’ understanding of the risks and benefits of clinical research: a comparison between text, tables, and graphics. J Health Commun 2010;15:487-501. https://doi.org/10.1080/10810730.2010.492560.
- Tait AR, Voepel-Lewis T, Zikmund-Fisher BJ, Fagerlin A. Presenting research risks and benefits to parents: does format matter?. Anesth Analg 2010;111:718-23. https://doi.org/10.1213/ANE.0b013e3181e8570a.
- Curtis L, Burns A. Unit Costs of Health and Social Care 2016. Canterbury: Personal Social Services Research Unit, University of Kent; 2016.
- British National Formulary. London: BMJ Group and Pharmaceutical Press; 2017.
- Wille N, Badia X, Bonsel G, Burström K, Cavrini G, Devlin N, et al. Development of the EQ-5D-Y: a child-friendly version of the EQ-5D. Qual Life Res 2010;19:875-86. https://doi.org/10.1007/s11136-010-9648-y.
- Dolan P, Kahneman D. Interpretations of utility and their implications for the valuation of health. Econ J 2008;118:215-34. https://doi.org/10.1111/j.1468-0297.2007.02110.x.
- Ambresin AE, Bennett K, Patton GC, Sanci LA, Sawyer SM. Assessment of youth-friendly health care: a systematic review of indicators drawn from young people’s perspectives. J Adolesc Health 2013;52:670-81. https://doi.org/10.1016/j.jadohealth.2012.12.014.
- Sawyer SM, Ambresin AE, Bennett KE, Patton GC. A measurement framework for quality health care for adolescents in hospital. J Adolesc Health 2014;55:484-90. https://doi.org/10.1016/j.jadohealth.2014.01.023.
- Towards Adolescent–Responsive Health Systems: Steering the Transition from Adolescent-Friendly Projects to Adolescent–Responsive Health Systems. Geneva: World Health Organization; 2014.
- Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol 2005;8:19-32. https://doi.org/10.1080/1364557032000119616.
- Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res 2005;15:1277-88. https://doi.org/10.1177/1049732305276687.
- May C, Finch T. Implementing, embedding and integrating practices: an outline of normalization process theory. Sociology 2009;43:535-54. https://doi.org/10.1177/0038038509103208.
- Ovretveit J. Purchasing for Health: A Multi-disciplinary Introduction to the Theory and Practice of Purchasing. Buckingham: Open University Press; 1995.
- Research and Development Strategy 2013–2018. Research is Everybody’s Business. London: Department of Health and Social Care; 2013.
- Kolehmainen N, McCafferty S, Maniatopoulos G, Vale L, Le-Couteur AS, Colver A. What constitutes successful commissioning of transition from children’s to adults’ services for young people with long-term conditions and what are the challenges? An interview study. BMJ Paediatr Open 2017;1. https://doi.org/10.1136/bmjpo-2017-000085.
- Maniatopoulos G, Le Couteur A, Vale L, Colver A. Falling through the gaps: exploring the role of integrated commissioning in improving transition from children’s to adults’ services for young people with long-term health conditions in England. J Health Serv Res Policy 2018;23:107-15. https://doi.org/10.1177/1355819617752744.
- The Incentives Team Commissioning Strategy. Commissioning for Quality and Innovation (CQUIN) Guidance for 2016/17. London: NHS England; 2016.
- Nagra A, McGinnity PM, Davis N, Salmon AP. Implementing transition: ready steady go. Arch Dis Child Educ Pract Ed 2015;100:313-20. https://doi.org/10.1136/archdischild-2014-307423.
- Commissioning for Quality and Innovation (CQUIN) Guidance for 2017–2019. London: NHS England; 2016.
- Transition from Children’s to Adults’ Services. London: NICE; 2016.
- Clarke A, Taylor-Phillips S, Swan J, Gkeredakis E, Mills P, Powell J, et al. Evidence-based commissioning in the English NHS: who uses which sources of evidence? A survey 2010/2011. BMJ Open 2013;3. https://doi.org/10.1136/bmjopen-2013-002714.
- Popay J, Collins M. The Public Involvement Impact Assessment Framework Guidance. Universities of Lancaster, Liverpool and Exeter; 2014.
- Staley K, Buckland SA, Hayes H, Tarpey M. ‘The missing links’: understanding how context and mechanism influence the impact of public involvement in research. Health Expect 2014;17:755-64. https://doi.org/10.1111/hex.12017.
- Hart R. Children’s Participation from Tokenism to Citizenship. Florence: UNICEF International Child Development Centre; 1992.
- Common Action Consulting . Roger Hart’s Ladder of Young People’s Participation 2017. https://commonaction.org (accessed 23 August 2017).
- Tuchman LK, Slap GB, Britto MT. Transition to adult care: experiences and expectations of adolescents with a chronic illness. Child Care Health Dev 2008;34:557-63. https://doi.org/10.1111/j.1365-2214.2008.00844.x.
- Annunziato RA, Emre S, Shneider B, Barton C, Dugan CA, Shemesh E. Adherence and medical outcomes in pediatric liver transplant recipients who transition to adult services. Pediatr Transplant 2007;11:608-14. https://doi.org/10.1111/j.1399-3046.2007.00689.x.
- Fauconnier J, Dickinson HO, Beckung E, Marcelli M, McManus V, Michelsen SI, et al. Participation in life situations of 8–12 year old children with cerebral palsy: cross sectional European study. BMJ 2009;338. https://doi.org/10.1136/bmj.b1458.
- NHS Outcomes Framework 2016 to 2017 At-A-Glance. London: Department of Health and Social Care; 2017.
- Prior M, McManus M, White P, Davidson L. Measuring the ‘triple aim’ in transition care: a systematic review. Pediatrics 2014;134:e1648-61. https://doi.org/10.1542/peds.2014-1704.
- Scal P. Improving health care transition services: just grow up, will you please. JAMA Pediatr 2016;170:197-9. https://doi.org/10.1001/jamapediatrics.2015.3268.
- Michelsen SI, Uldall P, Hansen T, Madsen M. Social integration of adults with cerebral palsy. Dev Med Child Neurol 2006;48:643-9. https://doi.org/10.1017/S0012162206001368.
- Betz CL, Smith K. Measuring health care transition planning outcomes: challenges and issues. Int J Child Adolesc Health 2011;3:463-72.
- Cramm JM, Strating MM, Sonneveld HM, Nieboer AP. The longitudinal relationship between satisfaction with transitional care and social and emotional quality of life among chronically ill adolescents. Appl Res Qual Life 2013;8:481-91. https://doi.org/10.1007/s11482-012-9209-3.
- Sattoe JNT, Hilberink SR, van Staa A. How to define successful transition? An exploration of consensus indicators and outcomes in young adults with chronic conditions. Child Care Health Dev 2017;43:768-73. https://doi.org/10.1111/cch.12436.
- Diabetes Transition and Young Adult Service Specification and Guidance Document. Leeds: NHS England; 2016.
- Askew K, Bamford J, Hudson N, Moratelli J, Miller R, Anderson A, et al. Current characteristics, challenges and coping strategies of young people with cystic fibrosis as they transition to adulthood. Clin Med 2017;17:121-5. https://doi.org/10.7861/clinmedicine.17-2-121.
- Gray J. Inflammatory Bowel Disease Transition to Adult Health Care Guidance for Young People. Brighton: Oyster Healthcare Communications; 2008.
- Young S, Adamou M, Asherson P, Coghill D, Colley B, Gudjonsson G, et al. Recommendations for the transition of patients with ADHD from child to adult healthcare services: a consensus statement from the UK adult ADHD network. BMC Psychiatry 2016;16. https://doi.org/10.1186/s12888-016-1013-4.
- Shalaby MS, Gibson A, Granitsiotis P, Conn G, Cascio S. Assessment of the introduction of an adolescent transition urology clinic using a validated questionnaire. J Pediatr Urol 2015;11:89.e1-5. https://doi.org/10.1016/j.jpurol.2014.11.024.
- Chamberlain MA, Kent RM. The needs of young people with disabilities in transition from paediatric to adult services. Eura Medicophys 2005;41:111-23.
- Together for Short Lives . Care Planning in Advance n.d. www.togetherforshortlives.org.uk/wp-content/uploads/2018/01/FamRes-Care-Planning-in-Advance-Factsheet.pdf (accessed 10 August 2018).
- Commissioning for Transition to Adult Services for Young People with Special Educational Needs and Disability (SEND). London: NHS England; 2018.
- Investigation into the Transition from Child and Adolescent Mental Health Services to Adult Mental Health Services. Farnborough: Healthcare Safety Investigation Branch; 2018.
- NHS Forward Plan. London: NHS England; n.d.
- Goddard A. On the Margins of Medical Care. Why Young Adults and Adolescents Need Better Healthcare. London: Royal College of Physicians; 2015.
- Grant C, Pan J. A comparison of five transition programmes for youth with chronic illness in Canada. Child Care Health Dev 2011;37:815-20. https://doi.org/10.1111/j.1365-2214.2011.01322.x.
- Allen D, Cohen D, Robling K, Hood K, Atwell C, Lane C, et al. The Transition from Paediatric to Adult Diabetes Services: What Works, For Whom and in What Circumstances? Final Report. London: NIHR Service Delivery and Organisation programme; 2010.
- Randell T. Developing a best practice tariff in paediatric diabetes. Pract Diabetes 2012;29:176-7. https://doi.org/10.1002/pdi.1685.
- Allen D, Channon S, Lowes L, Atwell C, Lane C. Behind the scenes: the changing roles of parents in the transition from child to adult diabetes service. Diabet Med 2011;28:994-1000. https://doi.org/10.1111/j.1464-5491.2011.03310.x.
- Hanna KM, Dashiff CJ, Stump TE, Weaver MT. Parent–adolescent dyads: association of parental autonomy support and parent–adolescent shared diabetes care responsibility. Child Care Health Dev 2013;39:695-702. https://doi.org/10.1111/j.1365-2214.2012.01373.x.
- Nguyen T, Henderson D, Stewart D, Hlyva O, Punthakee Z, Gorter JW. You never transition alone! Exploring the experiences of youth with chronic health conditions, parents and healthcare providers on self-management. Child Care Health Dev 2016;42:464-72. https://doi.org/10.1111/cch.12334.
- Klassen AF, Grant C, Barr R, Brill H, Kraus de Camargo O, Ronen GM, et al. Development and validation of a generic scale for use in transition programmes to measure self-management skills in adolescents with chronic health conditions: the TRANSITION-Q. Child Care Health Dev 2015;41:547-58. https://doi.org/10.1111/cch.12207.
- Sattoe JN, Bal MI, Roelofs PD, Bal R, Miedema HS, van Staa A. Self-management interventions for young people with chronic conditions: a systematic overview. Patient Educ Couns 2015;98:704-15. https://doi.org/10.1016/j.pec.2015.03.004.
- Channon SJ, Huws-Thomas MV, Rollnick S, Hood K, Cannings-John RL, Rogers C, et al. A multicenter randomized controlled trial of motivational interviewing in teenagers with diabetes. Diabetes Care 2007;30:1390-5. https://doi.org/10.2337/dc06-2260.
- Christie D, Thompson R, Sawtell M, Allen E, Cairns J, Smith F, et al. Structured, intensive education maximising engagement, motivation and long-term change for children and young people with diabetes: a cluster randomised controlled trial with integral process and economic evaluation – the CASCADE study. Health Technol Assess 2014;18. https://doi.org/10.3310/hta18200.
- Mackie AS, Islam S, Magill-Evans J, Rankin KN, Robert C, Schuh M, et al. Healthcare transition for youth with heart disease: a clinical trial. Heart 2014;100:1113-18. https://doi.org/10.1136/heartjnl-2014-305748.
- Harden PN, Walsh G, Bandler N, Bradley S, Lonsdale D, Taylor J, et al. Bridging the gap: an integrated paediatric to adult clinical service for young adults with kidney failure. BMJ 2012;344. https://doi.org/10.1136/bmj.e3718.
- Nakhla M, Daneman D, To T, Paradis G, Guttmann A. Transition to adult care for youths with diabetes mellitus: findings from a universal health care system. Pediatrics 2009;124:e1134-41. https://doi.org/10.1542/peds.2009-0041.
- Stringer E, Scott R, Mosher D, MacNeill I, Huber AM, Ramsey S, et al. Evaluation of a rheumatology transition clinic. Pediatr Rheumatol Online J 2015;13. https://doi.org/10.1186/s12969-015-0016-x.
- Sloper T, Beecham J, Clarke S, Franklin A, Moran N, Cusworth L. Models of Multi-Agency Services for Transition to Adult Services for Disabled Young People and those with Complex Health Needs: Impact and Costs. Progress Report. York: Social Policy Research Unit, University of York; 2009.
- Annunziato RA, Baisley MC, Arrato N, Barton C, Henderling F, Arnon R, et al. Strangers headed to a strange land? A pilot study of using a transition coordinator to improve transfer from pediatric to adult services. J Pediatr 2013;163:1628-33. https://doi.org/10.1016/j.jpeds.2013.07.031.
- Reiss JG, Gibson RW, Walker LR. Health care transition: youth, family, and provider perspectives. Pediatrics 2005;115:112-20. https://doi.org/10.1542/peds.2004-1321.
- Bhawra J, Toulany A, Cohen E, Moore Hepburn C, Guttmann A. Primary care interventions to improve transition of youth with chronic health conditions from paediatric to adult healthcare: a systematic review. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2016-011871.
- Bal MI, Sattoe JN, Roelofs PD, Bal R, van Staa A, Miedema HS. Exploring effectiveness and effective components of self-management interventions for young people with chronic physical conditions: a systematic review. Patient Educ Couns 2016;99:1293-309. https://doi.org/10.1016/j.pec.2016.02.012.
- Sattoe J. Growing Up with a Chronic Condition: Challenges for Self-Management and Self-Management Support. Rotterdam: Erasmus University; 2015.
- McDonagh JE, Viner RM. Lost in transition? Between paediatric and adult services. BMJ 2006;332:435-6. https://doi.org/10.1136/bmj.332.7539.435.
- Hendricks DR, Wehman P. Transition from school to adulthood for youth with autism spectrum disorders . Focus Autism Other Dev Disabil 2009;24:77-88.
- Shattuck PT, Narendorf SC, Cooper B, Sterzing PR, Wagner M, Taylor JL. Postsecondary education and employment among youth with an autism spectrum disorder. Pediatrics 2012;129:1042-9. https://doi.org/10.1542/peds.2011-2864.
- Lounds Taylor J, Adams RE, Bishop SL. Social participation and its relation to internalizing symptoms among youth with autism spectrum disorder as they transition from high school. Autism Res 2017;10:663-72. https://doi.org/10.1002/aur.1709.
- Cappadocia MC, Weiss JA, Pepler D. Bullying experiences among children and youth with autism spectrum disorders. J Autism Dev Disord 2012;42:266-77. https://doi.org/10.1007/s10803-011-1241-x.
- Lake JK, Perry A, Lunsky Y. Mental health services for individuals with high functioning autism spectrum disorder. Autism Res Treat 2014;2014. https://doi.org/10.1155/2014/502420.
- Howlin P, Moss P. Adults with autism spectrum disorders. Can J Psychiatry 2012;57:275-83. https://doi.org/10.1177/070674371205700502.
- Seltzer MM, Shattuck P, Abbeduto L, Greenberg JS. Trajectory of development in adolescents and adults with autism. Ment Retard Dev Disabil Res Rev 2004;10:234-47. https://doi.org/10.1002/mrdd.20038.
- Simonoff E, Pickles A, Charman T, Chandler S, Loucas T, Baird G. Psychiatric disorders in children with autism spectrum disorders: prevalence, comorbidity, and associated factors in a population–derived sample. J Am Acad Child Adolesc Psychiatry 2008;47:921-9. https://doi.org/10.1097/CHI.0b013e318179964f.
- Billstedt E, Gillberg IC, Gillberg C, Gillberg C. Autism after adolescence: population-based 13- to 22-year follow-up study of 120 individuals with autism diagnosed in childhood. J Autism Dev Disord 2005;35:351-60. https://doi.org/10.1007/s10803-005-3302-5.
- Simonoff E, Jones CR, Baird G, Pickles A, Happé F, Charman T. The persistence and stability of psychiatric problems in adolescents with autism spectrum disorders. J Child Psychol Psychiatry 2013;54:186-94. https://doi.org/10.1111/j.1469-7610.2012.02606.x.
- Kuhlthau KA, Warfield ME, Hurson J, Delahaye J, Crossman MK. Pediatric provider’s perspectives on the transition to adult health care for youth with autism spectrum disorder: current strategies and promising new directions. Autism 2015;19:262-71. https://doi.org/10.1177/1362361313518125.
- Cheak-Zamora NC, Teti M, First J. ‘Transitions are scary for our kids, and they’re scary for us’: family member and youth perspectives on the challenges of transitioning to adulthood with autism. J Appl Res Intellect Disabil 2015;28:548-60. https://doi.org/10.1111/jar.12150.
- Beresford B, Moran N, Sloper T, Cusworth L, Mitchell W, Spiers G, et al. Transition to Adult Services and Adulthood for Young People with Autism Spectrum Condition. York: University of York; 2013.
- Taylor JL, Seltzer MM. Employment and post-secondary educational activities for young adults with autism spectrum disorders during the transition to adulthood. J Autism Dev Disord 2011;41:566-74. https://doi.org/10.1007/s10803-010-1070-3.
- Singh SP, Paul M, Ford T, Kramer T, Weaver T, McLaren S, et al. Process, outcome and experience of transition from child to adult mental healthcare: multiperspective study. Br J Psychiatry 2010;197:305-12. https://doi.org/10.1192/bjp.bp.109.075135.
- Islam Z, Ford T, Kramer T, Paul M, Parsons H, Harley K, et al. Mind how you cross the gap! Outcomes for young people who failed to make the transition from child to adult services: the TRACK study. B J Psych Bull 2016;40:142-8. https://doi.org/10.1192/pb.bp.115.050690.
- Paul M, Ford T, Kramer T, Islam Z, Harley K, Singh SP. Transfers and transitions between child and adult mental health services. Br J Psychiatry Suppl 2013;54:s36-40. https://doi.org/10.1192/bjp.bp.112.119198.
- Saqr Y, Braun E, Porter K, Barnette D, Hanks C. Addressing medical needs of adolescents and adults with autism spectrum disorders in a primary care setting. Autism 2018;22:51-6. https://doi.org/10.1177/1362361317709970.
- Crane L, Adams F, Harper G, Welch J, Pellicano E. ‘Something needs to change’: mental health experiences of young autistic adults in England. Autism 2019;23:477-93. https://doi.org/10.1177/1362361318757048.
- Attention Deficit Hyperactivity Disorder. Diagnosis and Management of ADHD in Children, Young People and Adults. London: NICE; 2008.
- Farley MA, McMahon WM, Fombonne E, Jenson WR, Miller J, Gardner M, et al. Twenty-year outcome for individuals with autism and average or near-average cognitive abilities. Autism Res 2009;2:109-18. https://doi.org/10.1002/aur.69.
- Kirby AV, Baranek GT, Fox L. Longitudinal predictors of outcomes for adults with autism spectrum disorder: systematic review. OTJR 2016;36:55-64. https://doi.org/10.1177/1539449216650182.
- Sosnowy C, Silverman C, Shattuck P. Parents’ and young adults’ perspectives on transition outcomes for young adults with autism. Autism 2018;22:29-3. https://doi.org/10.1177/1362361317699585.
- Goodman R. The strengths and difficulties questionnaire: a research note. J Child Psychol Psychiatry 1997;38:581-6. https://doi.org/10.1111/j.1469-7610.1997.tb01545.x.
- Goodman R, Meltzer H, Bailey V. The strengths and difficulties questionnaire: a pilot study on the validity of the self-report version. Eur Child Adolesc Psychiatry 1998;7:125-30. https://doi.org/10.1007/s007870050057.
- Constantino J, Gruber C. Social Responsiveness Scale. Los Angeles, CA: Western Psychological Services; 2005.
- Ritchie J, Spencer L, Bryman A, Burgess RG. Analyzing Qualitative Data. London: Routledge; 1994.
- Stewart-Brown S, Janmohamed K. Warwick–Edinburgh Mental Well-Being Scale User Guide 2008. www.mentalhealthpromotion.net/resources/user-guide.pdf (accessed 1 August 2018).
- Baldwin S, Costley D. The experiences and needs of female adults with high-functioning autism spectrum disorder. Autism 2016;20:483-95. https://doi.org/10.1177/1362361315590805.
- Kirkovski M, Enticott PG, Fitzgerald PB. A review of the role of female gender in autism spectrum disorders. J Autism Dev Disord 2013;43:2584-603. https://doi.org/10.1007/s10803-013-1811-1.
- Southby K, Robinson O. Information, Advocacy and signposting as a low-level support for adults with high-functioning autism spectrum disorder: an example from the UK. J Autism Dev Disord 2018;48:511-19. https://doi.org/10.1007/s10803-017-3331-x.
- Malbrunot-Wagner AC, Bonnemains C, Troussier F, Darviot E, Chiffoleau M, Person C, et al. Transition from pediatric to adult care: experience of a cystic fibrosis care center. Arch Pediatr 2009;16:235-42. https://doi.org/10.1016/j.arcped.2008.12.021.
- Schumacher KL, Meleis AI. Transitions: a central concept in nursing. Image J Nurs Sch 1994;26:119-27. https://doi.org/10.1111/j.1547-5069.1994.tb00929.x.
- Al-Yateem N, Docherty C. Transition: a concept of significance to nursing and healthcare professionals. J Nurs Educ Prac 2015;5:35-40. https://doi.org/10.5430/jnep.v5n5p35.
- Sparacino PS, Tong EM, Messias DK, Foote D, Chesla CA, Gilliss CL. The dilemmas of parents of adolescents and young adults with congenital heart disease. Heart Lung 1997;26:187-95. https://doi.org/10.1016/S0147-9563(97)90055-8.
- Forbes A, While A, Ullman R, Lewis S, Mathes L, Griffiths P. A Multimethod Review to Identify Components of Practice Which May Promote Continuity in the Transition from Child to Adult Care for Young People with Chronic Illness or Disability. London: National Coordinating Centre for NHS Service Delivery and Organisation; 2001.
- Struhkamp RM. Patient autonomy: a view from the kitchen. Med Health Care Philos 2005;8:105-14. https://doi.org/10.1007/s11019-004-1134-2.
- Keller J. Autonomy, relationality, and feminist ethics. Hypatia 1997;12:152-64. https://doi.org/10.1111/j.1527-2001.1997.tb00024.x.
- May C, Montori VM, Mair FS. We need minimally disruptive medicine. BMJ 2009;339. https://doi.org/10.1136/bmj.b2803.
- Arnett J. Young people’s conceptions of the transition to adulthood. Youth Soc 1997;29:3-23. https://doi.org/10.1177/0044118X97029001001.
- McConachie H, Jaffa T, Kurtz Z, Hopkins A. Services for Young People with Chronic Disorders in their Transition from Childhood to Adult Life. London: Royal College of Physicians; 1996.
- Support and Aspiration: A New Approach to Special Educational Needs and Disability. London: HMSO; 2011.
- Bridges JF, Hauber AB, Marshall D, Lloyd A, Prosser LA, Regier DA, et al. Conjoint analysis applications in health – a checklist: a report of the ISPOR Good Research Practices for Conjoint Analysis Task Force. Value Health 2011;14:403-13. https://doi.org/10.1016/j.jval.2010.11.013.
- Transition . The Young People’s Working Group – UP 2017. http://research.ncl.ac.uk/transition/youngpeoplepage/theyoungpeoplesworkinggroup-up/ (accessed 15 July 2017).
- Cummins E, Royle P, Snaith A, Greene A, Robertson L, McIntyre L, et al. Clinical effectiveness and cost-effectiveness of continuous subcutaneous insulin infusion for diabetes: systematic review and economic evaluation. Health Technol Assess 2010;14. https://doi.org/10.3310/hta14110.
- Pratoomsoot C, Smith HT, Kalsekar A, Boye KS, Arellano J, Valentine WJ. An estimation of the long-term clinical and economic benefits of insulin lispro in type 1 diabetes in the UK. Diabet Med 2009;26:803-14. https://doi.org/10.1111/j.1464-5491.2009.02775.x.
- Mokdad AH, Forouzanfar MH, Daoud F, Mokdad AA, El Bcheraoui C, Moradi-Lakeh M, et al. Global burden of diseases, injuries, and risk factors for young people’s health during 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2016;387:2383-401. https://doi.org/10.1016/S0140-6736(16)00648-6.
- Patton GC, Sawyer SM, Santelli JS, Ross DA, Afifi R, Allen NB, et al. Our future: a Lancet commission on adolescent health and wellbeing. Lancet 2016;387:2423-78. https://doi.org/10.1016/S0140-6736(16)00579-1.
- Hargreaves DS, McDonagh JE, Viner RM. Validation of You’re Welcome quality criteria for adolescent health services using data from national inpatient surveys in England. J Adolesc Health 2013;52:50-7.e1. https://doi.org/10.1016/j.jadohealth.2012.04.005.
- Sawyer SM. Developmentally appropriate healthcare for young people with chronic illness: questions of philosophy, policy, and practice. Pediatr Pulmonol 2003;36:363-5. https://doi.org/10.1002/ppul.10369.
- Sawyer SM, Afifi RA, Bearinger LH, Blakemore SJ, Dick B, Ezeh AC, et al. Adolescence: a foundation for future health. Lancet 2012;379:1630-40. https://doi.org/10.1016/S0140-6736(12)60072-5.
- Jones S, Mertyn E, Alhucema P, Monagle P, Newall F. HEEADSSS assessment for adolescents requiring anticoagulation therapy. Arch Dis Child 2012;97:430-3. https://doi.org/10.1136/adc.2011.300085.
- Equity and Excellence: Liberating the NHS. London: Department of Health and Social Care; 2010.
- Turner TP. NHS Commissioning Before April 2013. London: House of Commons Library; 2013.
- Gleeson H, Turner G. Transition to adult services. Arch Dis Child Educ Pract Educ 2012;97:86-92. https://doi.org/10.1136/archdischild-2011-300261.
- West C, Brodie L, Dicker J, Steinbeck K. Development of health support services for adults with spina bifida. Disabil Rehabil 2011;33:2381-8. https://doi.org/10.3109/09638288.2011.568664.
- Dellon ES, Jones PD, Martin NB, Kelly M, Kim SC, Freeman KL, et al. Health-care transition from pediatric to adult-focused gastroenterology in patients with eosinophilic esophagitis. Dis Esophagus 2013;26:7-13. https://doi.org/10.1111/j.1442-2050.2011.01315.x.
- Hall CL, Newell K, Taylor J, Sayal K, Swift KD, Hollis C. ‘Mind the gap’ – mapping services for young people with ADHD transitioning from child to adult mental health services. BMC Psychiatry 2013;13. https://doi.org/10.1186/1471-244X-13-186.
- Freyer DR, Brugieres L. Adolescent and young adult oncology: transition of care. Pediatr Blood Cancer 2008;50:1116-19. https://doi.org/10.1002/pbc.21455.
- Sharma N, O’Hare K, Antonelli RC, Sawicki GS. Transition care: future directions in education, health policy, and outcomes research. Acad Pediatr 2014;14:120-7. https://doi.org/10.1016/j.acap.2013.11.007.
- Appleton R. Resource for Health and Social Care Mental Health Commissioners. ‘Planning Mental Health Services for Young Adults – Improving Transition’ 2011. www.scie-socialcareonline.org.uk/planning-mental-health-services-for-young-adults-improving-transition-a-resource-for-health-and-social-care-commissioners/r/a11G00000017wuUIAQ (accessed 27 March 2019).
- Valuing People Now: The Delivery Plan 2010–2011 ‘Making it Happen for Everyone’. London: Department of Health and Social Care; 2010.
- Better Care: Better Lives: Improving Outcomes and Experiences for Children, Young People and Their Families Living with Life-Limiting and Life-Threatening Conditions. London: Department of Health and Social Care; 2008.
- Making Integration a Reality. Part 1 – Joining Up the Commissioning Across Young People’s Services Across Health, Social Care, Housing and Youth Services. Youth Access/The Young People’s Health Partnership; 2014.
- Improving the Health and Wellbeing of People with Learning Disabilities: An Evidence-Based Commissioning Guide for Clinical Commissioning Groups (CCGs). Improving Health and Lives, Learning Disabilities Observatory; 2012.
- National Autistic Society . Improving Commissioning Standards in Services for Children and Adults With Autism Spectrum Disorders 2006. http://library.autism.org.uk/Portal/Default/en-GB/RecordView/Index/22066 (accessed 27 March 2019).
- Commissioning for Smooth Transitions and Age-appropriate Care for Young People with Life-limiting Conditions in England. A Guide for Clinical Commissioning Groups. Bristol: Together for Short Lives; 2015.
- Valuing People Now: A New Three-Year Strategy for People with Learning Disabilities. ‘Making It Happen For Everyone’. London: Department of Health and Social Care; 2009.
- Lincoln Y, Guba E. Naturalistic Inquiry. Newbury Park, CA: Sage; 1985.
- Kvale S. Doing Interviews. Thousand Oaks, CA: Sage; 2007.
- Rubin H, Rubin I. Qualitative Interviewing: The Art of Hearing Data. Newbury Park, CA: Sage; 2005.
- Patton M. Qualitative Research and Evaluation Methods. Newbury Park, CA: Sage; 2002.
- Yin RK. Case Study Research, Design and Methods. Newbury Park, CA: Sage; 1994.
- Robson C. Real World Research. Oxford: Blackwell; 1993.
- Boyatzis RE. Transforming Qualitative Information: Thematic Analysis and Code Development. Thousand Oaks, CA: Sage; 1998.
Appendix 1 National Institute for Health Research Programme Development Grant
In 2010, we were awarded a Programme Development Grant (RP-DG-1108-10015).
In summary:
-
We learnt from a young person’s group how to develop and run a young person’s advisory group for a programme.
-
We found widespread interest in the research from voluntary organisations; the Council for Disabled Children joined the application.
-
We identified 10 NHS Trusts that would recruit participants to the programme.
-
Meetings with trust chief executives led to modifications to the content of the proposal for a programme.
-
A literature review found that few studies that evaluated transitional health care assessed whether or not the services were sustainable or what helped transition in the long term.
-
We estimated the number of young people our work could benefit in the UK as 25,000 per year group.
-
We piloted questionnaires. We researched different methods for approaching, recruiting and retaining young people in a programme.
Appendix 2 Management and governance of the research programme
An External Advisory Board met once a year, chaired by the chief executive of a NHS Trust (see Acknowledgements).
The programme was managed by the Programme Management Board. This was chaired by the chief investigator and consisted of the programme’s co-applicants and two adult physician advisors. It met every 3 months.
A senior management team, consisting of the chief investigator and the leads for the qualitative, quantitative and health economic work, met every 2 weeks.
The programme’s young people’s advisory group (see WP 1.1) met every month.
Each year a report was submitted to NIHR and subsequently approved.
All studies received positive ethics opinions from either the NHS or Newcastle University.
Figure 11.
Management structure.

Appendix 3 Work of UP
In this appendix and Appendix 4 we present some examples of the work of UP.
Appendix 4 Health passport
Appendix 5 Longitudinal study (quantitative)
In this appendix we present some additional tables/figures mentioned in the synopsis and the draft of a paper submitted for publication.
Age-banded clinic. An intermediate clinic setting, such as a young person’s clinic or a young adult team. In children’s health services, it would mean that children younger than about 14 years would not be at the clinic. In adults’ services it would mean that adults older than about 24 years would not be at the clinic.
Meet adult team before transfer. This could be in a joint clinic where senior paediatric and adult clinicians consult together, or the adult clinician might visit the children’s clinic to be introduced, or the young person might be taken to the adult clinic by a member of the child team to meet the adult team.
Promotion of health self-efficacy. The young person is asked ‘Have you received enough help to increase your confidence in managing your condition?’ The clinic has a written policy about how they will encourage the young person to take responsibility for their health and give them information about their condition.
Written transition plan. This should be created some time before transfer. It should include plans for wider transition, not just the transfer to adult health services. The young person should have a copy of it and it should be updated.
Appropriate parent involvement in their child’s care, but with changing responsibilities. Parent and young person are asked separately if they think that the level of involvement is appropriate. Involvement concerns what happens in the clinic (parent being present or not and who does the talking) and also discussions at home about the young person’s health and how to manage it.
Key worker. This is a single person known to the young person whom they could easily contact or go to if there were any problems with co-ordination or misunderstandings that needed to be sorted out. The role could cross into education and social services. Although a clinic may have a policy to ‘appoint’ a key worker, the young person may report that it is someone else with whom they feel most comfortable.
Co-ordinated team. Some young people need to see a team of people. Those with diabetes mellitus may need to see a doctor, nurse, dietitian and psychologist. Those with cerebral palsy may need to see a doctor, physiotherapist and orthopaedic surgeon. The members of these teams need to work together and communicate well together, and demonstrate to the young person that this is happening. Co-ordination of appointments on the same day demonstrates this.
Holistic life-skills training for education, relationships, finances, employment, housing, social relationships, etc., as well as health maintenance. The young person is asked whether or not they have had any formal life-skills training offered because of their condition. The health service may not provide such training but staff in consultations inquire about such matters and referrals are made to other agencies as needed.
Transition manager for clinical team. The individual who co-ordinates transition in a clinical team may not be known to the young person. The manager will facilitate good working relationships between adults’ and children’s services, ensure that there are appropriate materials available for things such as health education or the transition plan and monitor whether the young person has a suitable appointment in adults’ services and whether or not the appointment is kept.
FIGURE 12.
Recruitment of participants to WP 2.1. CP, cerebral palsy; DM, diabetes mellitus.

FIGURE 13.
Retention to visit 4.
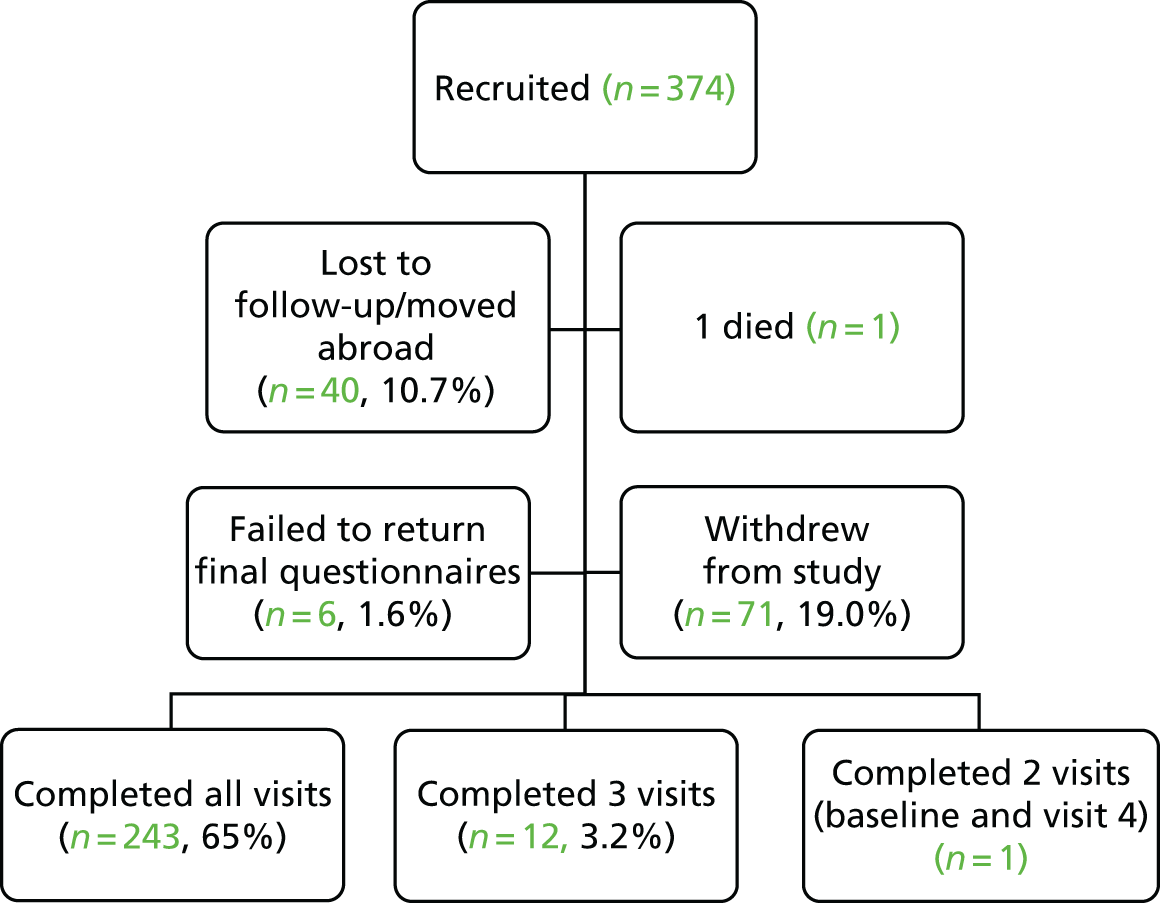
Work package 2.1: longitudinal study
| Reason | Number of dropouts (n = 71) | Example |
|---|---|---|
| Not interested in taking part | 22 | |
| Other commitments | 19 | School, work, university |
| Personal issues | 11 | Young person was too ill, had recent surgery, was a victim of a crime |
| Family issues | 8 | Other family member having health issues |
| Questionnaires too difficult | 4 | |
| No reason given/recorded | 4 | |
| Do not like talking about condition | 2 | Young people were coping well with condition and just wanted to ‘get on with their life’ and not talk about their condition |
| Problems with health service | 1 | One family withdrew from the study because of problems they were experiencing with the service they attended |
Appendix 6 Longitudinal study (qualitative)
In this appendix we set out the report of the qualitative work in WP 2.2, in which 13 young people purposefully sampled from the cohort in the longitudinal study (WP 2.1) are interviewed, along with family member(s) and health professional(s) involved in their care. At the end of the appendix is the interview schedule.
Appendix 7 Discrete choice experiment and economic analysis
This appendix contains the questionnaire used in the DCE, followed by a draft paper that provides further details about the DCE questionnaire. Then there follows Report 2.3.2 Economic analysis.
Questionnaire
Draft paper
Appendix 8 Introduction of developmentally appropriate health care
In this appendix we present a draft of a paper submitted for publication.
Appendix 9 Commissioning
Appendix 10 Patient and public involvement
In this appendix we present an example of a newsletter for participants and an example of a facilitator guide (reproduced with permission) developed with the Council for Disabled Children for dissemination of our results to young people.
Glossary
We use the World Health Organization’s definition of a young person as any person between the ages of 10 and 24 years, and of an adolescent as any person between the ages of 10 and 19 years.
- A long-term condition
- is a condition that cannot currently be cured but can be controlled with medication and/or other therapies. The Chief Medical Officer used this concept in the 2012 report Our Children Deserve Better – Prevention Pays [Department of Health and Social Care. Chief Medical Officer Annual Report 2012: Children And Young People’s Health. London: Department of Health and Social Care; 2013. URL: www.gov.uk/government/publications/chief-medical-officers-annual-report-2012-our-children-deserve-better-prevention-pays (accessed 27 March 2019)], as did the Department of Health and Social Care in its Outcomes Framework for the NHS [Department of Health and Social Care. NHS Outcomes Framework 2016 to 2017 At-A-Glance. London: Department of Health and Social Care; 2017. URL: www.gov.uk/government/publications/nhs-outcomes-framework-2016-to-2017 (accessed August 2017)].In our original submission to the National Institute for Health Research, we used the term ‘complex health needs’ to refer to young people with ‘a physical, mental or health impairment that has the potential for a substantial and long-term adverse effect on their ability to carry out normal day-to-day activities. However, the term ‘complex health needs’ is used increasingly to describe the relatively small number of young people with very complex needs who require a bespoke package of care constructed for each individual, involving multiple agencies including health, educational and social services. These young people are usually known by name to Clinical Commissioning Groups and local authorities. Shortcomings in the co-ordination of care for this group are discussed specifically in the Care Quality Commission’s report From the Pond into the Sea (Care Quality Commission. From the Pond into the Sea. Children’s Transition to Adult Health Services. Newcastle upon Tyne: Care Quality Commission; 2014). The National Institute for Health Research-funded transition research programme was not designed to consider only this very complex group. For this reason, we use the term young people with a ‘long-term condition’ instead of ‘complex health needs’ in the title of the programme and throughout this report to refer to the much larger group of young people who are the focus of the transition research programme.
- Developmentally appropriate health care
- A concept now widely accepted in the UK (e.g. by the National Institute for Health and Care Excellence, the Royal College of Paediatrics and Child Health, and the Royal College of Physicians) and internationally (e.g. in the USA and Canada). It recognises young people’s changing biopsychosocial developmental needs and the need to empower young people by embedding health education and health promotion within consultations. In operational terms, developmentally appropriate health care focuses on the approach of health-care professionals to, and their engagement with, each young person and their carers alongside the structure of the organisations in which care takes place.
- Mental health and well-being
- The World Health Organization states that mental health is not just the absence of mental disorder. It defines mental health as:. . . a state of well-being in which the individual realizes his or her own abilities, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to his or her community.Reprinted with permission from the World Health Organization. Promoting Mental Health: Concepts, Emerging Evidence, Practice. Geneva: World Health Organization; 2005. URL: www.who.int/mental_health/evidence/MH_Promotion_Book.pdf (accessed 3 April 2019). p. 10. Copyright 2005Reproduced with permission from the World Health Organization. Promoting Mental Health: Concepts, Emerging Evidence, Practice. Geneva: World Health Organization; 2005. URL: www.who.int/mental_health/evidence/en/promoting_mhh.pdf (accessed 3 April 2019). p. 10. Copyright 20052005World Health Organization.It is a subjective construct. Participation and mental well-being are important components of quality of life and relate well to the concept of ‘person-centred planning’, which has been strongly supported in the UK by successive governments.
- Participation
- Defined in the International Classification of Functioning, Disability and Health as ‘involvement in a life situation’. (Reprinted with permission from the World Health Organization. International Classification of Functioning, Disability and Health: Children and Youth Version: ICF-CY. Geneva: World Health Organization; 2007. URL: www.who.int/classifications/icf/en/ (accessed April 2019). p. 129. Copyright 2017.) It is an objective construct, even if self-reported.
- Proposed beneficial features
- Defined by us as features of services for transitional health care recommended as good practice and for which there is some evidence of benefit, at least in some conditions (Colver AF, Merrick H, Deverill M, Le Couteur A, Parr J, Pearce MS, et al. Study protocol: longitudinal study of the transition of young people with complex health needs from child to adult health services. BMC Public Health 2013;13:675). At the start of our research, we identified nine features and hypothesised that these ‘proposed beneficial features’ would be associated with better outcomes.
- Age-banded clinic
- An intermediate clinic setting, such as a young person’s clinic or a young adult team. In children’s health services, this means that children younger than about 12 years would not be at the clinic. In adults’ services, it means that adults older than about 24 years would not be at the clinic.
- Appropriate parent involvement
- Parental involvement in their child’s care, but with changing responsibilities. The parent and young person are asked separately if they think that the level of involvement is appropriate. Involvement concerns what happens in the clinic (the parent being present or not and who does the talking) and discussions at home about the young person’s health and how to manage it.
- Co-ordinated team
- Some young people need to see a team of people. Those with diabetes mellitus may need to see a doctor, a nurse, a dietitian and a psychologist. Those with cerebral palsy may need to see a doctor, a physiotherapist and an orthopaedic surgeon. The members of these teams need to work together and communicate well together and demonstrate to the young person that this is happening. Co-ordination of appointments on the same day demonstrates this.
- Holistic life-skills training
- Training for education, relationships, finances, employment, housing, social relationships, etc., as well as health maintenance. The young person is asked whether they have had any formal life-skills training offered because of their condition. The health service may not provide such training but staff in consultations inquire about such matters and referrals are made to other agencies as needed.
- Key worker
- A single person known to the young person whom they could easily contact or go to if there were any problems of co-ordination or misunderstandings that needed to be resolved. The role could cross into education and social services. Although a clinic may have a policy to ‘appoint’ a key worker, the young person may report that their key worker is someone else whom they feel most comfortable with.
- Meet adult team before transfer
- This could be in a joint clinic where senior paediatric and adult clinicians consult together, or the adult clinician might visit the child clinic to be introduced, or the young person might be taken to the adult clinic by a member of the child team to meet the adult team.
- Promotion of health self-efficacy
- The young person is asked ‘Have you received enough help to increase your confidence in managing your condition?’. The clinic has a written policy about how it will encourage the young person to take responsibility for their health and give them information about their condition.
- Transition manager for clinical team
- The individual who co-ordinates transition in a clinical team may not be known to the young person. The manager will facilitate good working relationships between adults’ and children’s services, ensure that there are appropriate materials available for things such as health education or the transition plan and monitor whether or not the young person has a suitable appointment in adults’ services and whether or not the appointment is kept.
- Written transition plan
- This should be created some time before transfer. It should include plans for wider transition, not just the transfer to adults’ health services. The young person should have a copy of it and it should be updated.
- Transfer
- The formal event when medical care of a young person is moved from children’s services to adults’ services.
- Transition
- The purposeful, planned process that addresses the medical, psychosocial, educational and vocational needs of adolescents and young adults with chronic physical, neurodevelopmental and medical conditions as they move from child-centred to adult-oriented health-care systems.
List of abbreviations
- ASD
- autism spectrum disorder
- CCG
- Clinical Commissioning Group
- CHAT
- Child Health Action Team
- CQUIN
- Commissioning for Quality and Innovation National Goals
- DAH
- developmentally appropriate health care
- DCE
- discrete choice experiment
- EQ-5D-Y
- EuroQol 5-Dimensions (Youth)
- HADS
- Hospital Anxiety and Depression Scale
- HbA1c
- glycated haemoglobin
- HRQoL
- health-related quality of life
- IQR
- interquartile range
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- NPT
- normalization process theory
- PBF
- proposed beneficial feature
- PPI
- patient and public involvement
- QALY
- quality-adjusted life-year
- SD
- standard deviation
- UP
- United Progression
- WEMWBS
- Warwick–Edinburgh Mental Wellbeing Scale
- WP
- work package
