Notes
Article history
The research reported in this issue of the journal was funded by the PHR programme as project number 10/3002/07. The contractual start date was in October 2011. The final report began editorial review in September 2013 and was accepted for publication in June 2014. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PHR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Professor Eileen Kaner is a National Institute for Health Research (NIHR) Public Health Research funding board panel member. Professor Elaine McColl is a member of the NIHR Journal Editorial Group. Denise Howel is a NIHR Health Services and Delivery Programme board panel member.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2014. This work was produced by Newbury-Birch et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Structure of the report
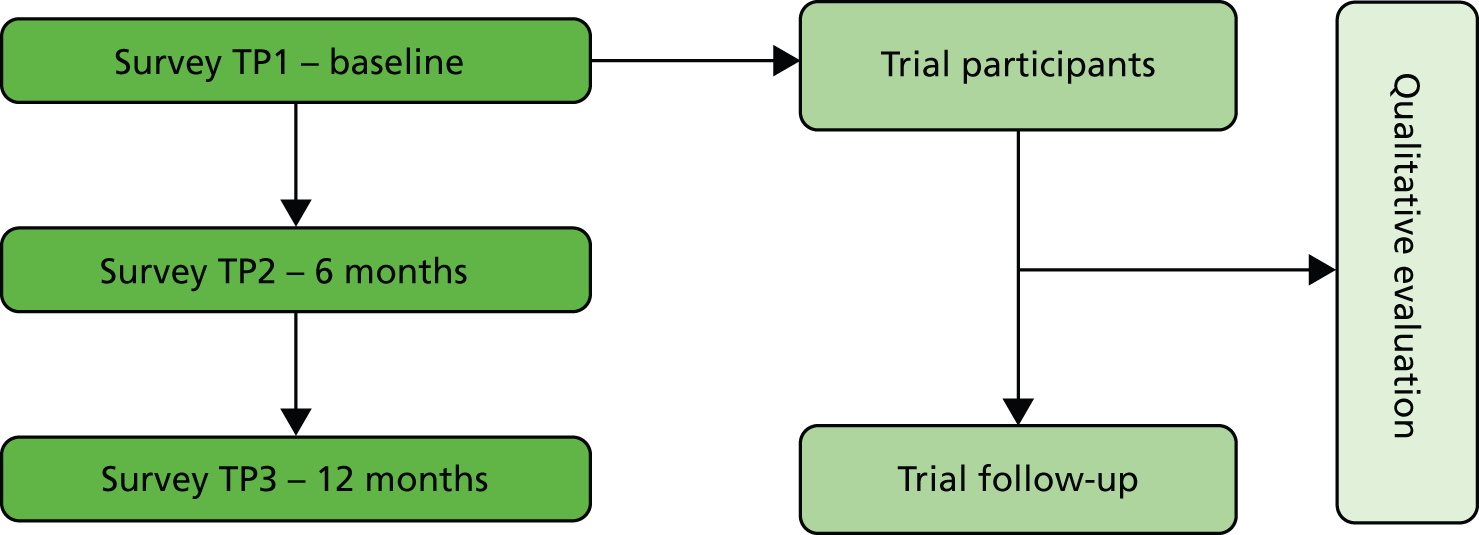
This study assessed the feasibility of a cluster randomised controlled trial (cRCT) of Alcohol Screening and Brief Intervention (ASBI) (in a school setting) to reduce hazardous drinking in adolescents. This was achieved by way of a three-arm parallel group cluster randomised (with randomisation at the level of school) external (rehearsal) pilot feasibility trial in young people aged 14–15 years in Year 10 at seven secondary/high schools across one small local authority area of North East England. The trial ran in parallel with a repeat cross-sectional survey, three times in the same year group and at the same schools, which facilitated screening (case identification for the trial at the first time point). The study included an integrated qualitative process evaluation (Figure 1) with key stakeholders. The three arms were control, intervention 1 and intervention 2. Young people allocated to the control arm received feedback and an alcohol information leaflet only. Young people allocated to intervention 1 took part in a 30-minute one-to-one structured intervention session based on motivational interviewing (MI) principles with a member of trained school staff. Young people allocated to intervention 2 received the same input as intervention 1 plus a subsequent session, facilitated by trained school staff, with parental/family involvement.
FIGURE 1.
Data time points for the study. TP, time point.
Research questions
The Medical Research Council (MRC) has presented a framework for the evaluation of complex interventions. 1 This work represents the development and piloting phases of the framework. Conducting a full-scale cRCT and economic evaluation of ASBI compared with ‘standard care’ in this population is likely to need many schools and to be resource intensive. As there are uncertainties regarding rates of eligibility, consent, participation in the intervention and retention for follow-up and regarding the feasibility and acceptability of the intervention for a range of stakeholders (teachers, learning mentors, young people and parents) this feasibility study was essential to inform the design and conduct of a larger scale definitive study.
The study sought to answer the following research questions: ‘Is it feasible to deliver ASBI in schools in England?’ and ‘What are the likely eligibility, consent, participation and retention rates of young people in a UK-relevant trial of ASBI compared with standard practice?’. Answers to these research questions will inform the development of a definitive multicentre cRCT to evaluate the effectiveness and cost-effectiveness of ASBI in reducing hazardous drinking in adolescents. Our hypothesis for the definitive cRCT will be that ASBI is more effective and cost-effective at reducing hazardous drinking in adolescents than a control condition of usual advice in high/comprehensive schools, as well as feedback on their drinking and an information leaflet.
Research objectives
-
To conduct a three-arm pilot feasibility cRCT (with randomisation at the level of school) to assess the feasibility of a future definitive cRCT of ASBI in a school setting.
-
To explore the feasibility and acceptability of ASBI and trial processes to staff, young people and parents.
-
To explore the fidelity of the interventions as delivered by school-based learning mentors.
-
To estimate the parameters for the design of a definitive cRCT of ASBI, including rates of eligibility, consent, participation and retention at 12 months.
-
To pilot the collection of cost and resource-use data to inform the cost-effectiveness/utility analysis in a definitive trial.
-
To develop the protocol for a definitive cRCT and economic evaluation of the impact of ASBI compared with standard advice to reduce alcohol consumption.
Chapters of the report
The report is structured as a series of eight chapters detailing the design, management and outcomes of the pilot feasibility study. The report begins by providing the background to the research and outlines key literature informing the design and conduct of the study (see Chapter 2). Following this, a chapter is dedicated to each core component of the study. Chapter 3 explores the design of intervention materials as well as the training and support provided to school staff in the delivery of the project. Chapter 4 reports the design, methods and results of the repeated cross-sectional survey. Chapter 5 provides the design, methods and results of the external pilot trial. Chapter 6 details the design, methods and results of the integrated qualitative process evaluation. Chapter 7 details the design, methods and results of the health-economic evaluation of the study. Finally, Chapter 8 provides a synthesis of the main findings from the pilot feasibility study, together with an assessment of whether the study met its aims and objectives, before detailing any recommendations for a future definitive cRCT.
Research ethics
The research study was granted ethical approval in November 2011 by Newcastle University, which acted as a sponsor for the research (reference 0508), and the trial is registered with the ISRCTN register as ISRCTN07073105. Approval was also granted by the local education authority in the study catchment area. Ethical approval was extended to accommodate a change in study protocol in October 2012, which related to measures completed at the 12-month follow-up of trial participants.
Changes to the original study protocol
The study protocol was published in 2012. 2
-
The published protocol indicates 6- and 12-month follow-ups for the trial group; however, it is not clear on the protocol that the full year group was followed up at 6 months and 12 months, as no identifiable data were taken at the year group level or the trial participant level at 6 months, therefore we have identifiable data for only the trial group at baseline and 12-month follow-up. The reason for this was that having a one-on-one interaction with the learning mentor could have acted as a ‘top-up’ to the intervention. We do not intend to include a 6-month follow-up in the proposed definitive study.
-
Objective 5 of the study – ‘to pilot the collection of cost and resource-use data to inform the cost-effectiveness/utility analysis in a definitive trial’ – was not included in the original study protocol.
-
The original protocol reported the control group as Personal, Social, Health and Economic Education (PSHE) only; however, the control condition was PSHE and also included the young person receiving feedback that he/she was drinking in a way that may be harmful and being provided with an advice leaflet. The reason that we added feedback and the leaflet (and therefore a change to the protocol) was that the research team and the University Ethics Committee believed that this was the minimally acceptable thing we could ethically do should a young person be identified as a risky drinker.
Research management
The Programme Management Group (PMG) was responsible for ensuring the appropriate, effective and timely implementation of the project. The PMG met once per month (more or less frequently dependent on the needs of the project) and comprised the Chief Investigator, Project Manager, co-applicants, named collaborators and researchers working on the project. Professor Eilish Gilvarry chaired this group. A Trial Steering Group (TSG) was also appointed to provide an independent assessment of the data analysis and to help determine if a future definitive trial is merited. This group met biannually and their remit was the progress of the study against projected rates of recruitment and retention, adherence to the protocol, participant safety and the consideration of new information of relevance to the research question. Professor Mark Bellis chaired this group. Written terms of reference were agreed and used by the PMG and TSG (see Appendix 1).
Research governance
The project complied with the requirements of the Data Protection Act 1998 and the Freedom of Information Act 2000, and other UK and European legislation relevant to the conduct of clinical research. The project was managed and conducted in accordance with the MRC’s guidelines on good clinical practice in clinical trials (www.mrc.ac.uk), which includes compliance with national and international regulations on the ethical involvement of patients in clinical research (including the Declaration of Helsinki, sixth revision 2008). All data were held in a secure environment with participants’ information identified by a unique participant identification number. Master registers containing the link between participant identifiable information and participant identification numbers were stored in a secure area that was separate from the majority of data. All staff working on the project were employed by academic organisations and subject to the terms and conditions of service and contracts of employment of the employing organisations. Where relevant, staff were trained in good clinical practice and all staff worked to written codes of confidentiality. The project used standardised research and clinical protocols, and adherence to the protocols was monitored by the PMG and TSC.
Patient and public involvement
Patient and public involvement (PPI) was sought at different time points and at multiple levels, and is reflected upon throughout this report.
Patient and public involvement representatives included local authority employees, parents, young people and members of staff at participating school sites. Their contribution to the development, management and delivery of this research included input into the design and conduct of the feasibility study (the local authority lead for education was a co-applicant for this research) and piloting of study documentation and intervention materials (parents and young people) to ensure readability and understanding (see Chapter 3). Participating schools were also heavily involved in the conduct of the feasibility study (trial and survey) and were regarded as key stakeholders (see Chapters 4 and 6). Finally, Chapter 8 includes modifications recommended for a definitive trial, which include input from PPI representatives.
Chapter 2 Background to the research
Key points for Chapter 2
-
Adolescents in England are among the heaviest drinkers in Europe, with consumption highest in the north-east.
-
Young people are more vulnerable than adults to the adverse effects of alcohol owing to a range of physical and psychosocial factors that often interact.
-
Literature shows that the ASBI for young people has been successful for selected individuals in certain settings.
-
There is currently insufficient evidence to be confident about the use of ASBI to reduce risky drinking and alcohol-related harm in younger adolescents in a school setting.
-
Despite well-documented parental influences over adolescent alcohol use, the evidence for interventions to reduce young people’s drinking that include family members is equivocal.
Prevalence
Adolescents in England are among the heaviest drinkers in Europe. 3 The percentage of young people who have ever had an alcoholic drink in England increases with age from 12% of those aged 11 years to 74% of those aged 15 years,4 and the prevalence of drinking in the last week rises from 1% of those aged 11 years to 25% of those aged 15 years. 4 Although the proportion of young people in England aged between 11 and 15 years who report that they have ever drunk alcohol decreased from 54% to 43% between 2007 and 2012, the mean amount of alcohol consumed by this age group has fluctuated between 10.4 units per week in 2011 and 14.6 units per week in 2008, with an increase to 12.5 units per week in 2012. There are, however, age-related differences in patterns of consumption. The amount consumed among those aged 14 years has increased from 13.2 units per week in 2007 to 16.15 units in 2012, whereas for 15-year-olds the mean amount has decreased slightly from 14.2 units per week in 2007 to 12.3 units in 2012. 4 This clearly shows that drinking increases throughout adolescence, but recent data show that this is not immutable with changes in trends between years and age.
In particular, the north-east has been shown to have the highest rates of alcohol misuse by young people in England, with 51% of 11- to 15-year-olds reporting having ever drunk alcohol. 4 This compares with 48% in the south-east, 46% in the north-west and 31% in London. 4 Further, the mean alcohol consumption in the previous week for young people in England in 2011 was highest in the north-east and north-west (15.7 units per week) compared with the south-east (11.0 units) and London (9.4 units). 4 Therefore, the north-east is a key place to study the issue of alcohol risk reduction in young people.
Consequences of drinking
The impact of alcohol on the development and behaviour of young people has been well researched in early,5 middle6 and late adolescence. 7 It is now well known that young people are much more vulnerable than adults to the adverse effects of alcohol due to a range of physical and psychosocial factors that often interact. 8 These adverse effects include physiological factors resulting from a typically lower body mass and less efficient metabolism of alcohol;5,6 neurological factors due to changes that occur in the developing adolescent brain after alcohol exposure;6,9–11 cognitive factors due to psychoactive effects of alcohol that impair judgement and increase the likelihood of accidents and trauma;12 and social factors that arise from a typically high-intensity drinking pattern that leads to intoxication and risk-taking behaviour. 13,14 The social factors are compounded by the fact that young people have less experience of dealing with the effects of alcohol than adults15 and they have fewer financial resources to help buffer the social and environmental risks that result from drinking alcohol. 7
Evidence suggests that hazardous drinking among young people occurs commonly in the context of other forms of ‘disinhibitory behaviour’, such as aggression and risk-taking. 16 Although these behaviours are well known to be linked,16 it is not clear if drinking leads to these behavioural problems or if they all arise due to a common linked trait. 17 A significant positive association between alcohol dose and aggression for both genders has been found. 18 As a result of the above risk factors, the list of negative consequences that result from drinking in young people is extensive and includes physical, psychological and social problems in both the shorter and the longer term. Immediate problems result from accidents and trauma, physical and sexual assault (including rape in young people), criminal behaviour (including driving while intoxicated and riding as a passenger with an intoxicated driver) and early onset of sexual intercourse and sexual risk-taking. 8,14,19 In relation to education, alcohol use can have a negative effect on school performance20 and those who have drunk are also more likely to have truanted from school. 4 Longer-term problems include the development or exacerbation of mental health problems,21 self-harm and/or suicidal behaviour. 22 Moreover, individuals who begin drinking in early life have a significantly increased risk of developing alcohol use disorders, including dependence, later in life. 23,24 Owing to this extensive array of damage, the prevention of excessive drinking in young people is a global public health priority. 25 In 2009, the Chief Medical Officer for England provided recommendations on alcohol consumption in young people,26 based on an evidence review of the risks and harms of alcohol to young people. 8 The recommendations state that children should abstain from alcohol before the age of 15 years and those aged 15–17 years are advised not to drink, but if they do drink it should be no more three to four units and two to three units per week in males and females, respectively, on no more than 1 day per week. 26
Young people’s views on their own health
It is important to note that young people often feel that they want to be empowered to be part of any decision-making in relation to their own health and feel that they have choices (C Sands, Newcastle University, 2013, unpublished data). For young people, confidentiality is a key issue, particularly within the school setting. However, to young people it is really important that they are familiar with the staff working with them, and therefore these issues should be taken into consideration when undertaking research with young people.
Primary and secondary prevention interventions for risky drinking
There is a large volume of evidence on primary prevention in the school setting,27–32 which is directed at all young people, whether they drink alcohol or not, with the aim of delaying the age at which drinking begins, and which uses general health education to prevent underage drinking. This body of work has shown mixed results and been reported to be methodologically weak,33 with only a relatively small number of programmes reporting positive outcomes. 30 One programme that has shown effectiveness is the School Health and Alcohol Harm Reduction Project (SHAHRP) project, a curriculum programme delivered across two consecutive school years in Ireland with 2349 pupils (mean age of 13.84 years at baseline and 16.48 years at final follow-up at 32 months). The programme had an explicit harm-reduction goal that explores knowledge, attitudes, alcohol consumption, and context of use and harms associated with a person’s own, or other people’s, use of alcohol. This showed significant improvements among young people in the intervention group in relation to alcohol knowledge and significant reductions in alcohol consumption. 34 Furthermore, research from the USA found that targeting young people and parents simultaneously but separately was effective in postponing the onset of heavy drinking among adolescents. 35,36 However, the results are equivocal, with some studies showing effectiveness and others not, and questions remain about the applicability to the UK setting. 27 As has been shown, there is limited evidence to support primary prevention programmes to reduce alcohol consumption in young people. Thus secondary prevention, i.e. targeting interventions at young people who are already drinking alcohol, is likely to be a more effective strategy, as the interventions will have more salience for the individuals receiving them.
Various screening measures have been used with young people to identify those who are at risk from their drinking including using measures of total alcohol consumption, levels of binge drinking and alcohol-related injury levels. 37 Research suggests standardised alcohol screening tools, such as the Alcohol Use Disorders Identification Test (AUDIT)38 are a highly sensitive and specific means of identifying current hazardous use of alcohol in adult populations, including college students. 39–41 Among adult drinkers, the AUDIT detects approximately 92% of genuinely excessive drinkers (sensitivity) and excludes approximately 94% of false cases (specificity),42,43 for which a cut-off score of ≥ 8 (out of a possible score of 40) is used to detect hazardous use of alcohol and alcohol-related problems. Broken down further, respondents can be categorised as ‘abstainers’ (0); ‘lower risk’ drinkers (1–7); at ‘increasing risk’ (8–15); at ‘higher risk’ (16–19); or ‘probably dependent’ (≥ 20).
There is some evidence from emergency department settings in the USA to suggest that the AUDIT is an appropriate means of detecting hazardous use of alcohol and alcohol-related problems among adolescents. 44–46 However, evidence remains equivocal whether it is either practical or appropriate for use with adolescents in other settings, including primary care and education. At 10 items, the length and wording of the full AUDIT may make it impractical for use with adolescents. 42,47 Evidence is especially equivocal as to the AUDIT tool’s ability to detect hazardous level drinking (the AUDIT positive score) among this age group or whether the concepts of hazardous or harmful drinking in adults are similarly meaningful in adolescents. Several studies have used AUDIT positive cut-off scores of ‘8’, designed for use with adults, to screen for alcohol use disorders among adolescents. 47,48 In comparison, other evidence supports using lower cut-off points, which generally fall between ‘2’ and ‘4’,43,49,50 when using the AUDIT in adolescent populations. For example, Chung et al. 44 recommend using a cut-off score of ‘4’ with young people aged 13–19 years (sensitivity 0.94; specificity 0.80) and Knight et al. 50 suggest that a score of ‘2’ is optimum for the identification of alcohol problems and disorders among those aged 14–18 years (sensitivity 0.88; specificity 0.81). Santis et al. 49 suggest different scores according to the level of alcohol consumption, with cut-off points of ‘3’ for hazardous, harmful and dependent alcohol use (sensitivity: 96%; specificity: 63.3%), ‘5’ (sensitivity: 75%; specificity: 64.5%) and ‘7’ (sensitivity 64%; specificity 75%), respectively.
Others suggest using a shortened version of the AUDIT tool, such as AUDIT-C (AUDIT-Consumption), which is scaled 0–12, and for which a score of ≥ 5 (among adults) is used to indicate increasing or higher risk drinking. 40,51 No specific score for young people has yet been recommended. It has also been shown that a single question screen based on drinking frequency can adequately identify youths with alcohol-related problems. 52,53 Bailey et al. 53 used the frequency of binge drinking (question three of the AUDIT tool – six or more drinks in one drinking session) to identify risky drinking in young people. 53 Thus, there is no clear consensus on which screening tool should be used, the validity of lower AUDIT or AUDIT-C cut-off points for use with adolescent populations or as to what this score should be, and whether the AUDIT or AUDIT-C or another measure should be the screening measure of choice. It could therefore be argued that in a school setting a shorter screening tool could be useful, and quick, to administer.
In terms of interventions for dealing with people who are drinking at harmful or hazardous levels, ASBI is a secondary preventative activity, aimed at individuals whose consumption level or pattern is likely to be harmful to their health or well-being. 54 They generally consist of screening (to identify relevant recipients) followed by structured advice or counselling of short duration, which is aimed at reducing alcohol consumption or decreasing the number or severity of problems associated with drinking. 55 They are based on social cognitive theory (from health psychology), which is drawn from the concept of social learning. 56 Here, behaviour is regarded to be the result of an interaction between individual, behavioural and environmental factors. It is assumed that each individual has cognitive (thinking) and affective (feeling) attributes that affect not only how they behave, but also how their behaviour is influenced and/or reinforced by aspects of the external world. Thus ASBIs generally focus on individuals’ beliefs and attitudes about a behaviour, their sense of personal confidence (self-efficacy) about changing it and how an individual’s behaviour sits in relation to other people’s actions (normative comparison).
A key feature of ASBI is that it is designed to be delivered by generalist practitioners (not addiction specialists) and targeted at individuals who are generally not experiencing severe problems (such as alcohol dependence) and who may not even be aware that they are experiencing alcohol-related risk or harm. Thus the goal is usually reduced alcohol consumption or a decrease in alcohol-related problems. 57 There is variation in the duration and frequency of ASBI58 but there are two broad types: simple structured advice – based on the FRAMES (Feedback, Responsibility, Advice, Menu, Empathy and Self-efficacy)59 – and behaviour change counselling – based on MI. This is a person-centred approach that aims to resolve conflicts regarding the pros and cons of behaviour change and thus enhance motivation. MI is characterised by empathy and an avoidance of direct confrontation. Elicited statements associated with positive behaviour change are encouraged so as to support self-efficacy and a commitment to take action. Since the time available for delivering BI may not allow for MI in its full form,58 its ethos and techniques have been59 distilled into a more directive format called Behaviour Change Counselling. 60
There is a large amount of high-quality evidence to support the effectiveness of ASBI with adults who have an alcohol use disorder. 58 Most of the evidence for ASBI demonstrates effectiveness for non-treatment-seeking adults in primary health care. 58,61–68 Furthermore, meta-analyses have consistently reported that students aged ≥ 18 years who received ASBI subsequently reduced their drinking behaviour compared with control group participants who typically received assessment only. 69,70 The key elements of the ASBI were personalised feedback on alcohol consumption, typically with a normative component70 and/or MI approaches. Such interventions typically achieved small to medium effect sizes71 across multiple measures of alcohol consumption, including quantity, frequency and intensity of drinking. The effects of BIs on drinking behaviour often peaked in the shorter term (generally 6 months) then diminished over time. 69 However, reductions in alcohol-related problems often took longer to emerge but were found in longer-term follow-up (12–18 months). Hence it is important to have BI outcomes measuring both consumption and alcohol-related problems and to follow-up participants at shorter- and longer-term time points.
Numerous systematic reviews have been published on ASBI in younger adolescents in recent years37,72–79 (details given in Appendix 2). Jackson et al. ’s review37 of ASBI for young people in health settings identified eight controlled trials53,80–85 for young people. The work was part of a larger review of ASBI in adults and young people. The trials were published between 1999 and 2009 and the majority (seven)80–86 were carried out in the USA. Study population sizes ranged from 34 to 655 young people and included young people aged between 12 and 24 years with two of the included studies being for those aged ≥ 18 years only. Five of the trials tested a brief MI, which lasted between 20–45 minutes,81,83–86 whereas one tested an audio programme;80 another involved a more intense programme of MI which included four sessions53 and one comprised an interactive laptop computer-based intervention. 82 The length of follow-up varied between 2 and 12 months. Four of the studies53,83–85 found statistically significant benefits as a result of the intervention. However, one80 of the studies found negative consequences following intervention, with an increase in heavy alcohol use among the intervention group. The authors offer two possible explanations for this. First, adolescents in the control group, unlike adolescents in the intervention groups, reported less bingeing after baseline, suggesting self-report bias in the direction anticipated if the control adolescents were trying to please the researchers. Second, the authors argue that the apparent increase in self-reported alcohol use in the intervention groups relative to the control groups was the result of an educational intervention influence leading adolescents to be more forthright. 80 Wachtel and Staniford77 also reviewed the literature in relation to alcohol misuse and binge drinking in adolescents in the clinical setting (hospital-based emergency departments, college health centres and adolescent healthcare clinics). 77 The review included 14 studies,53,80,82–85,87–94 12 of which were from the USA. 53,80,82–85,87–91,93 Nine of the included studies83,84,87–93 related to young people aged ≥ 18 years and included a heterogeneous range of interventions from very brief MI to four group sessions of 30–40 minutes, which meant that generalisability could not be ascertained. A review of the literature by Yuma-Guerrero et al. 78 around BI in emergency departments in the USA for young people identified seven randomised controlled trials (RCTs). 82–85,95–97 The primary studies included young people aged 12–20 years. Four82–84,98 of the included studies demonstrated a significant intervention effect; however, none reduced both alcohol consumption and alcohol-related consequences.
Mitchell et al. ’s systematic review75 identified 15 studies81,82,85,86,95–105 of alcohol and drug interventions delivered to adolescents in primary care (one study81), emergency departments (seven studies82,85,95–98,103), schools (five studies99,101,104–106) and other settings (one study with homeless young people86 and one in the community100) with young people aged 12–21 years. The authors identify the need for screening instruments to be brief to administer and quick and easy to score and interpret. 75 Because of the heterogeneous populations (ages 12–22 years), inclusion criteria (adolescents who use alcohol and drugs as well as those who reported being in a car with an intoxicated driver but who themselves had not used alcohol or drugs) and differences in outcome measures, the data did not allow for meta-analysis, although some individual studies did show reductions in alcohol consumption at follow-up. The review identified two studies101,102,106 (three articles) carried out in further education colleges in the UK, with older young people aged between 16 and 20 years, in which no differences were found between groups at 12-month follow-up.
Three systematic reviews included meta-analyses of ASBI for young people. 73,74,76 Tripodi et al. 76 carried out a meta-analytic review on interventions for alcohol abuse in a range of settings. Sixteen primary studies were included with young people aged 12–19 years. 81,105,107–120 The studies included various interventions including BI, cognitive–behavioural therapy (CBT) and multidimensional family therapy. The main outcome measures included abstinence and quantity of alcohol use measured between 1 and 12 months post intervention. Pooled effects of standardised mean differences indicate that interventions significantly reduce alcohol consumption [Hedges’ g = −0.61; 95% confidence interval (CI) −0.83 to −0.40]. Stratified analyses revealed larger effects for individual treatment (Hedges’ g = −0.75; 95% CI −1.05 to −0.40) compared with family-based treatments (Hedges’ g = −0.46; 95% CI −0.66 to −0.26). 76
Jensen et al. ’s review74 of the effectiveness of MI for substance-use interventions for adolescents included 21 primary studies, of which 12 had alcohol-related outcomes. 53,81,85,86,99–102,108,121–123 These studies were from a variety of different settings: educational,99,101,102,123 community53,86,100,108 and health. 81,85,121,122 No information was given on the nature of the interventions; however, the number of sessions ranged from one to four. The age range included in the studies was 12–23 years. Included studies that addressed alcohol and other drug use yielded a small, but significant, post-treatment effect size in reduction of substance use [mean d (standard mean difference) = 0.146 (95% CI 0.059 to 0.233), n = 16)].
Carney et al. ’s meta-analysis73 aimed to identify and evaluate early interventions that target adolescent substance use (alcohol and illicit drugs) as a primary outcome, and criminal or delinquent behaviours as a secondary outcome. They identified nine studies53,81,85,86,97,99,109,124,125 in emergency departments, juvenile correctional facilities, alternative high schools and a homeless drop-in centre – eight from the USA81,85,86,97,99,109,124,125 and one from Australia. 53 Study sizes ranged from 18 to 472. The age range was 15–17 years. Results showed that single sessions of BIs significantly reduced the frequency of alcohol use among young people (I2 = 0%; z = 2.13; overall effect, p = 0.03). 73
Conrod et al. 126–128 have carried out a number of trials in London of group-based personality-targeted prevention for young people aged 13–14 years who are risky drinkers or drug users. The interventions consisted of two 90-minute group sessions that incorporated components of motivational enhancement therapy and CBT. The intervention was unique in that it targeted personality traits rather than problems. In fact, alcohol and drug use were a minor focus of the intervention. Young people have been followed up every 6 months for 2 years and long-term effects (at 2 years) have been found for problem drinking (measured using the Rutgers Alcohol Problems Index (RAPI) tool) (p = 0.02) and binge-drinking rates (p = 0.03). Finally, a study of US accident and emergency attendees97,129 who received ASBI showed reductions in aggression, as well as reductions in alcohol misuse following a brief alcohol intervention.
It has been shown that the family is a source of both risk and protective factors for adolescent alcohol use. 8 Parents in particular have been found to have a significant effect upon alcohol initiation and patterns of use. 130 Such parental factors include parental modelling,131–133 supervision and discipline,8 quality of parent–child relationship and communication among others. 134 It is therefore important to identify whether parents can play a role in helping to reduce their children’s drinking.
Parents
The majority of parents are aware that their children are drinking. 135 Parenting ‘style’ and ‘good’ family relationships have been demonstrated to have a positive effect on young people’s drinking behaviour regardless of family structure or whether parents consume alcohol. 8,134,136 Excessively authoritarian and permissive parenting styles are both associated with earlier onset of alcohol use or higher levels of drinking behaviour,137,138 and Foxcroft and Lowe139 identify a possible curvilinear relationship between control and adolescent drinking, where significantly stricter or lax parenting styles appear to increase the frequency of alcohol misuse.
Parents can also be a primary source of the supply of alcohol to young people. 140,141 This may be through the provision of money, by having alcohol available or by purchasing alcohol for young people directly. Easy availability of alcohol is associated with increased adolescent alcohol consumption142 and Elliott et al. 141 found that 65% of drinkers (aged 11–17 years) accessed alcohol via their parents. Further, it is implicitly assumed that if parents purchase alcohol for their children directly, the amount of alcohol consumed can be strictly monitored. In other words, that providing young people with alcohol will stop them from accessing it elsewhere, thus reducing the risk of alcohol-related harm. Again, the evidence for this is equivocal. On the one hand, Bellis et al. 143 found that (in contrast with other ways of obtaining alcohol) young people (aged 15–16 years) whose parents bought alcohol for them were less likely to drink in a public setting, ‘binge’ drink, drink heavily or drink frequently. On the other hand, receiving alcohol from a parent or getting it from home has been demonstrated to be the strongest predictor of increased alcohol use over time. 144 However, Gilligan et al. 145 found that negative outcomes from parental provision of alcohol are dependent on the context of supply. In other words, if parents supplied young people with alcohol, this did not increase the odds of risky drinking (although it also did not have the protective effect that motivated the behaviour). However, if alcohol was supplied for consumption without parental supervision then the odds of risky drinking were four times higher.
Given the well-documented parental influences over adolescent alcohol use, interventions that aim to involve parents who enhance parents’ awareness of the variables and strategies that can delay onset and reduce consumption levels in their child offer an opportunity for limiting the harms of adolescent drinking. 134
Alcohol Screening and Brief Interventions that include parents
Mixed effects have been found for ASBI for reducing young people’s drinking that include family members. 33,54,146,147
A RCT examining the effectiveness of 45–60 minutes of individual motivational interviewing (IMI) compared with IMI and a family check-up session found that both interventions resulted in significant reduction of drinking outcomes at 3-, 6- and 12-month follow-ups. The family check-up consisted of a 1-hour meeting, at which the parent(s) and the young person discussed family beliefs regarding alcohol and other drug use. Results show there was only one significant between-group difference on the number of high-volume drinking days at 3- and 6-month follow-up, with family check-up reporting lower alcohol prevalence compared with IMI. This effect had diminished at 12-month follow-up. 103
A RCT with three arms: (1) two 60-minute individual sessions of BI (young person and interventionist only); (2) two 60-minute individual sessions of BI (young person and interventionist only) and a BI session with the parent(s) [parent(s) and interventionist only]; and (3) control arm of assessment only found that both intervention groups showed significantly better drinking outcomes than the control arm for number of alcohol days and number of binge days with a small sample (n = 78). The intervention arm that included parental involvement reported significantly fewer alcohol days at 6-month follow-up than the intervention group without parental involvement but no difference in number of binge days. 105 This study was repeated with a large sample (n = 315) and, again, both intervention arms were found to be superior to the control condition. Significant between-group differences were reported by this trial in favour of the arm with parental involvement for drug outcomes but not alcohol. Indeed, the intervention arm without parental involvement reported significantly greater alcohol abstinence in the previous 90 days than the arm with parental involvement. 125
Mixed results have been found for intensive BIs for drug and alcohol using adolescents, with parental involvement (see Appendix 2). 112,115,117,148,149 However, significant variation exists between experimental conditions examined with regards to both the intensity and the frequency of the intervention (ranging from a single 1-hour family check-up to 64 hours of family and individual CBT), as well as the theoretical basis of the therapeutic approach. Moreover, the heterogeneity of the adolescent samples, which included dually diagnosed adolescents, risky drinkers, drug and alcohol users, runaways and gang-affiliated young people, made it difficult to compare the findings of the trials. Therefore, the evidence is equivocal.
Rationale for the present research
The literature shows that ASBI for young people has been successful for selected individuals, in certain settings. In particular, the current available evidence relates primarily to white, USA-based subjects, most often in educational settings and at the older end of the youth spectrum (see Appendix 2). However, there is currently insufficient evidence to be confident about the use of ASBI to reduce excessive drinking and/or alcohol-related harm in younger adolescents and in a school setting. Nevertheless, the current evidence base suggests that the most effective forms of BI are those containing personalised feedback about a young person’s drinking behaviour and MI approaches to help reduce levels of alcohol-related risk. Furthermore, there is some evidence to show that involving parents in ASBI may be beneficial. This present work builds on the evidence base by focusing on ASBI to reduce hazardous drinking in younger adolescents (aged 14–15 years). It is highly likely that if a BI was effective at reducing hazardous drinking, it might also result in a range of other positive behavioural outcomes, as has been found in the adult literature as well as work with older adolescents.
Chapter 3 Development of intervention materials and training
Key points for Chapter 3
-
Learning mentors were identified to be best placed within a school setting to deliver an intervention about alcohol. They were trained in study procedures and intervention delivery.
-
The study incorporated control, intervention 1 and intervention 2 conditions, all manualised and designed to be delivered on a one-to-one basis to young people who screened positive for risky drinking and left their name on the questionnaire.
-
Young people who were in control group schools met with the learning mentor who explained the study to them, and provided feedback that they may be drinking at a risky level, along with an alcohol information leaflet to take away and read.
-
In addition to feedback and an alcohol information leaflet, young people allocated to intervention 1 took part in a 30-minute, six-step, interactive intervention led by the learning mentor.
-
In addition to receiving intervention 1, young people who received intervention 2 were invited to attend a subsequent session with parental/family involvement, designed to last approximately 30–60 minutes, led by the learning mentor.
-
Learning mentors were asked to record time spent with participants using open-ended case diaries.
Introduction
The present study incorporated control, intervention 1 and intervention 2 conditions. All three interventions were manualised to ensure consistency of delivery across schools allocated to that arm of the trial and reproducibility by other deliverers (see Appendix 3). Owing to availability of resources, all tools and manuals were provided in the English language only. All young people recruited into the trial, regardless of arm, continued to receive ‘standard alcohol advice’, delivered as part of the school curriculum. The first section of this chapter is concerned with defining what this consisted of in the study catchment area. In addition, young people in schools allocated to the control arm received feedback that they may be drinking at a risky level and an alcohol information leaflet. Young people in schools allocated to the intervention 1 arm took part in a 30-minute one-to-one structured intervention session with a trained learning mentor. In addition to receiving intervention 1, young people in schools allocated to the intervention 2 arm were invited to attend a subsequent session, facilitated by trained school staff, with parental/family involvement, designed to last approximately 30–60 minutes. Young people from schools allocated to intervention 1 and intervention 2 received the same alcohol advice leaflet as those allocated to control. All young people recruited into the trial were followed up 12 months post intervention.
The rest of the chapter describes the design of intervention materials, as well as the training and support provided to learning mentors in the delivery of interventions. The rationale behind, and development of, each intervention condition (control, intervention 1, intervention 2) is detailed, and the outcomes of piloting of materials and consultation with key groups (parents and young people) are outlined with any resultant modifications to intervention materials reported.
Defining ‘standard alcohol advice’
In order to fully understand the control context, it was first important to determine the scope of ‘standard alcohol advice’ received by all young people aged 14–15 years at secondary school (Years 10 and 11). Provision of classroom-based drug and alcohol education continues to be recognised as an important aspect of the secondary school curriculum (for those aged 11–16 years) for England, Scotland and Wales, and is generally tackled within PSHE classes. PSHE is non-statutory yet the provision of high-quality PSHE forms a significant part of the Office for Standards in Education, Children’s Services and Skills (OFSTED) inspections and contributes to the statutory responsibility of schools to ‘promote children and young people’s personal and economic well-being; offer sex and relationships education; prepare pupils for adult life and provide a broad and balanced curriculum’,150 delivered as part of a wider ‘well-being’ remit through the National Healthy Schools Programme151 and the Social and Emotional Aspects of Learning (SEAL) strategy. 151
However, there are no prescriptive guidelines on what PSHE should actually entail, as long as it encompasses these wider statutory responsibilities. As a result, schools have developed their own versions of PSHE, and different ways to deliver it, rather than following standardised frameworks of study. 150 Our observations mirror this and the research team recorded different PSHE arrangements in each of the participating schools. For example, several schools timetabled weekly lessons dedicated to PSHE topics, sometimes described as ‘citizenship’ or ‘extended tutorial’. One participating school had no PSHE provision and instead timetabled a ‘health day’ once per academic year. Schools were also able to elect a key ‘well-being’ focus for the coming academic year. Thus, if they chose to elect alcohol rather than another area (such as self-harm or sexual health) then this could feasibly have an impact on educational provision. Thus, the control context was a highly variable condition, with ‘standard alcohol advice’ defined in this study as the regular provision of classroom-based alcohol education to Year 10 pupils as delivered at each particular school site.
School staff identified to deliver interventions
Learning mentors are specifically trained to provide a service complementary to that of teachers and other school staff, addressing the needs of children who require assistance in overcoming barriers to learning in order to achieve their full potential. All secondary schools have learning mentors working in them. They work with a range of pupils, but give priority to those who need the most help, especially those experiencing multiple disadvantages. Mentoring covers a wide range of issues, from punctuality, absence, bullying, challenging behaviour and abuse to working with able and gifted pupils who are experiencing difficulties. Learning mentors support, motivate and challenge pupils who are underachieving. They help pupils overcome barriers to learning caused by social, emotional and behavioural problems. Learning mentors need good listening skills and an understanding of health and social issues that affect children and young people’s development. The mentors mainly work with children who experience ‘barriers to learning’, including poor literacy/numeracy skills, underperformance against potential, poor attendance, disaffection, danger of exclusion, difficult family circumstances and low self-esteem. Thus, learning mentors were thought to be most well-placed within a school setting to deliver an intervention to young people about alcohol use.
Local areas vary in their essential qualifications for appointment for learning mentors. However, as a minimum, they need to have a good standard of general education, especially literacy and numeracy, as well as experience of working with young people. Within the present study, learning mentors were defined as the members of school staff trained in the delivery of the control condition/interventions to participating students. However, in practice, within each school, titles, roles and responsibilities varied, and this did not constitute a homogeneous professional group. Thus, for consistency, school staff responsible for the delivery of interventions are referred to only as learning mentors throughout the rest of this report.
Patient and public involvement: selecting an alcohol information leaflet (control)
All young people recruited into the trial were provided with an alcohol advice leaflet. It was important that this leaflet was age appropriate (for 14- to 15-year-olds) and suitable for use in a school setting, yet with a presentation style favoured by young people. Owing to time and resource constraints, it was not feasible for the study team to design a new alcohol information leaflet. Instead, we reviewed a large amount of national and regional resources (including materials from the Department of Health, NHS Choices, Home Office, Talk to FRANK, Change4Life, ‘Know Your Limits’ and resources from local youth drug and alcohol services) and liaised with experts in the field. Two appropriate packs or leaflets were sourced, both designed by the Comic Company (www.comiccompany.co.uk/: the ‘Cheers! Your Health’ alcohol leaflet, and ‘snapper’, a quiz question folding game). Both leaflets were discussed with colleagues at Newcastle University, who are experts in working with young people in the school setting and who supported their use. Following this, they were piloted during five focus groups held with young people from years 9–11 (aged 13–16 years) at participating schools.
Young people across all focus groups agreed that the ‘Cheers! Your Health’ alcohol leaflet and ‘snapper’ resources were suitable for young people aged 14–15 years, and these materials were selected as alcohol advice leaflets and provided to young people in all arms of the pilot trial (see Appendix 3). In particular, young people indicated that encouraging them to engage with anything in a non-pictorial way would be challenging. Young people wanted the information presented to them in a fun or humorous way, without too much text, and liked leaflets to include games or puzzles. In particular, positive comments about the ‘Cheers! Your Health’ leaflet included that it was ‘detailed’, ‘interesting’ and ‘interactive’.
Young people who were in the control group schools met with the learning mentor who explained the study to them. The young people were told that they may be drinking alcohol in a way which may be harmful to them. Once consented to the study the young people were given the alcohol leaflets mentioned above to take away and read.
Development of intervention 1
The intervention 1 session was a manualised intervention, which combined simple structured advice and behaviour change counselling techniques commonly used within the extended BI. The tool was a colourful, six-step intervention, intended to be an interactive discussion between the young person and the learning mentor (see Appendix 3). It sought to increase awareness of risks and enable the young person to consider their motivations for changing their alcohol use. The intervention was designed to last approximately 30 minutes and take place in the learning mentor’s office or alternative suitable space. It was expected that young people would be taken out of class to attend appointments with learning mentors. The rest of this section details each step of the intervention tool in turn. Intervention 1 consists of six sections.
Intervention 1
Section one: how many units are in my drink?
This section sought to raise the young person’s awareness of the units of alcohol contained in drinks that are commonly consumed by young people. It was similar to the information commonly provided in simple structured advice. 152 Young people were encouraged to calculate the number of units that they drank during a typical drinking day. This calculation was then used as a basis for discussing the recommended levels for adults and the Chief Medical Officer’s (CMO’s) recommendation that young people aged < 15 years do not drink alcohol at all and to enable personalised feedback about the risks associated with the young person’s drinking. The young person was also asked to consider how common alcohol use is by young people aged 14–15 years. Learning mentors then advised the young people of the actual numbers before asking young people to reflect upon their thoughts about this. This component was informed by social learning theory. 56 This information was delivered in accordance with the elicit–provide–elicit approach to informing within MI.
Section two: typical drinking day
Young people were asked to discuss their typical drinking day in more detail within this section of the intervention. This background description was intended to provide a useful context for the ensuing discussion about the young person’s drinking, associated risk and change. The typical drinking day was informed by the SIPS Brief Lifestyle Counselling (BLC) structure (www.sips.iop.kcl.ac.uk/blc.php). It was developed to provide greater structure and useful prompts about drinking behaviour (with, where, because) for both the young person and the learning mentor. In particular, the additional prompts were intended to provide information that might have been useful in the identification of risk (e.g. when a young person consumes alcohol this may increase or decrease risk), as well as reinforce positive drinking behaviours (e.g. times when young people drink in ways that are not risky) and the behaviours that may become the focus of change.
Section three: are there any risks with my drinking?
Section three of intervention 1 built upon section two and encouraged the young person to consider the risks associated with their alcohol use. The intention was that, by asking the young person to identify risks relevant to him/her, the young person would begin to identify motivation for change. It was expected that this would lead naturally on to how important it is for the young person to change their drinking. Young people were then advised of the common risks associated with drinking above CMO recommendations before being asked to reflect upon this in relation to their own drinking. As well as acting as a further prompt to identifying risks relating to their drinking, the delivery of this information was again in accordance with the elicit–provide–elicit approach to informing within MI.
Section four: importance/confidence
Section four encouraged the young person to rate the importance of changing his/her drinking and confidence in ability to change using a scaling question. Importance scales are used within behaviour change counselling in order to elicit change talk and assess readiness to change. 153 By prompting the young person to consider what would need to happen in order for this number to increase, ratings may also be positively affected and motivation developed. Confidence scales are useful in identifying barriers to change. Exploration around this can enable the young person to find ways to overcome these barriers and assist in the development of a coping plan in section six.
Section five: what do I think about reducing my drinking?
Section five asked the young person to consider the ‘bad’ and the ‘good’ things about reducing their drinking. This is comparable to the ‘pros and cons of changing your drinking’, which is included in the extended BI tool (www.sips.iop.kcl.ac.uk/blc.php) and discussed by Rollnick et al. 153 The terminology ‘pros and cons’ was changed to ‘bad and good’ to make the language more age appropriate.
Section six: what could I do about my drinking?
The final section of intervention 1 was concerned with developing an action plan and coping plan for change. It was acknowledged that not all young people will want to agree to making such a plan. For those who did, it was expected that the young person would set his/her own goals, facilitated by the learning mentor, based upon the content of the MI. The purpose of this section of the intervention was to elicit commitment talk from the young person,154 as well as identifying existing life skills and developing coping strategies to enable young people to achieve and maintain change. Learning mentors employed a strengths-based approach wherein self-efficacy is promoted.
Development of intervention 2
Although BIs are mostly delivered on a one-to-one basis, intervention 2 sought to build upon the rationale for intervention 1 by involving parents. Young people from schools allocated to intervention 2 received an individual BI (intervention 1), followed by a group family intervention based on MI principles held approximately 1 month after. 155 By involving parents within a family intervention, the approach focused upon the dynamic between the individual, attitudes and the environment. 56 Indeed, the addition of a family intervention has elsewhere been found to improve drinking outcomes in adolescents at follow-up. 103
Intervention 2 was a manualised intervention based upon the principles of MI. It was intended to be a discussion that built upon intervention 1 described above, wherein the young person and the learning mentor explored the young person’s drinking and their motivation for change. Intervention 2 sought to build upon the young person’s motivation by encouraging the parents/family members to share their thoughts about the young person’s drinking. The young person and the parents/family member were then encouraged to consider an action plan for change. The intervention was designed to last approximately 30–60 minutes (see Appendix 3). At the end of the session parents were provided with a parenting information leaflet about young people and alcohol use. It was expected that this session would take place either during or after school hours, either within the school or in a community centre nearby, and would take place only if the young person consented to parental involvement and parents subsequently agreed to take part. Intervention 2 consisted of four sections.
Intervention 2
Section one: review of first session
Similar to techniques used within motivational enhancement therapy, section one provided a review of the first session. It was preferable if this review was led and delivered by the young person in order to promote an empowering child-centred approach to the family intervention. However, if the young person felt unable to do this, the learning mentor would summarise the content of intervention 1. Using the intervention 1 sheet, it was expected that the review of the first session would reinforce the young person’s motivation, by emphasising change talk. 154 It also provided background information for the parents/family members to inform the ensuing discussion about the young person’s drinking, associated risk and change, and the parents’/family members’ concerns about this.
Section two: what concerns you about your child’s drinking?
Section two of intervention 2 built upon section one and encouraged the parents/family members to share any concerns they have about their child’s drinking. It was intended that by asking the parent to share their feelings, the young person would begin to consider their drinking from another person’s perspective, which would build upon their current motivation for change. It was expected that this would lead naturally on to a discussion about how important it was for the young person to change their drinking.
Section three: importance/confidence
Section three encouraged the parents/family members to rate (using a scaling question) the importance of their child changing their drinking and their confidence in their ability to help them to change. Although the importance scale was used in intervention 1 to assess the young person’s readiness to change, within intervention 2 the aim is to develop further the young person’s motivation. By prompting the parents/family members to share why they have rated the importance in a particular way, as well as what would need to happen in order for this number to increase, it was expected that both the parents/family members and the child’s motivation to support and achieve change may be positively affected and motivation developed. Confidence scales are useful in identifying barriers to change. Specifically asking how confident the parents/family members feel in their ability to help the young person encourages a ‘family approach’ to change while also finding ways to overcome barriers and assist in the development of a coping plan in section four.
After identifying barriers and how confident parents/family members may feel about their ability to help the young person overcome these barriers, the learning mentor provided information detailed on the tool regarding the potential influence of parents/family members upon young people and their drinking, as well as the benefit of a supportive relationship. The learning mentors then asked parents/family members and the young person to reflect upon this and share their views. The delivery of this information was in accordance with the elicit–provide–elicit approach to informing within MI. It was also informed by the approach used within the Spirito et al. 103 study on family MI with alcohol-positive teenagers.
Section four: what could I do about my drinking?
The final section of intervention 2 was concerned with developing a family action plan and family coping plan for change. This was informed by the extended BI and the intervention manual for the family intervention used by Spirito. 103 It was acknowledged that not all families would want to agree tomake such a plan. If they did, it was expected that the young person and parents/family members would negotiate these goals, facilitated by the learning mentor and based upon the combined content of interventions 1 and 2. The purpose of this section of the intervention was to elicit commitment talk154 from the young person and parents/family members, enabling them to work together to agree an action plan and develop coping strategies to enable young people to achieve and maintain change.
The young person and parents/family members were encouraged to think of two or three good reasons for change. This was to reinforce motivation. They were then encouraged to set goals for change and, in doing so, evoke ‘commitment talk’. It was expected that the learning mentor would explore the feasibility of these goals with all parties. The later part of the action plan was concerned with developing a coping plan. This was largely informed by the discussion, which developed from the confidence scale. Here the young person was asked about times or situations when change might have been difficult to achieve or maintain before then considering how they might deal with such times or situations. Planning for change in this way is assumed to be the most effective way to achieve and succeed. Through identifying by whom and how the young person may be supported in their efforts, the parents/family members were afforded an opportunity to support and encourage the young person. This also allows families to plan for and celebrate success. 103
Patient and public involvement: piloting of interventions
Interventions 1 and 2 were piloted with one young person and their mother by the research interventionist who had experience in MI techniques (December 2011 and February 2012, respectively). The intervention 1 session lasted approximately 25 minutes, whereas the intervention 2 session lasted approximately 45 minutes. The young person suggested adding information about calories to the intervention 1 tool as a way of making information about alcohol use more memorable and pertinent to young people. In particular, they suggested that they would have found this to be an effective motivator to changing drinking behaviour. A focus group was also held, in February 2012, with a convenience sample of four female parents, to discuss the intervention 2 tool, as well as anticipated methods for contacting parents to take part in the intervention. In particular, this group highlighted that the initial approach of school staff would be very important when introducing the project to parents for the first time over the telephone.
Modifications to the intervention materials as a result of piloting and consultation
As a result of piloting and consultation, the following modifications were made to intervention tools and materials:
-
Provision of information about calories on the intervention 1 tool. The number of calories in popular food items (depicted using pictures) was mapped against alcohol brands and quantities that were popular with young people.
-
A slight change to the guidance that was provided to school staff in relation to contacting parents for the first time about taking part in intervention 2. Specifically, the importance of non-judgemental language was reinforced with the learning mentors.
Training and support
All learning mentors received training prior to commencing the study. The training was split into four sessions, with each session lasting a minimum of 1 hour and a maximum of 3 hours. PowerPoint 2010 slides (Microsoft Corporation, Redmond, WA, USA) were used to guide each training session. An intervention manual relevant to each arm of the trial was provided to supplement the training (see Appendix 3).
Training was conducted in a community venue or school, as outreach training has been found to be the most cost-effective implementation strategy for ASBI delivery in other settings. 156 The training was jointly delivered by an experienced interventions trainer and researcher, using training materials that were customised for the school setting. A total of 27 learning mentors across the seven schools were trained by the research team. The biggest individual school team of learning mentors comprised nine members of staff, whereas the smallest had two members of staff.
The first training session was delivered to learning mentors from all seven schools as a group to raise awareness of the risks associated with young people drinking and to introduce the study. The training included a PowerPoint presentation, group discussion and simulated young-person scenarios. Learning mentors were also trained to issue the participant information leaflet, gather informed consent from the young person, and deliver the alcohol information leaflet (control intervention). This concluded the training for learning mentors from schools allocated to the control intervention arm of the trial who, in order to prevent contamination, received no training on interventions 1 or 2.
Learning mentors at schools randomised to intervention 1 and 2 were then trained to deliver intervention 1. Again, learning mentors were trained together as a group. In addition to a PowerPoint presentation, training consisted of a demonstration of how to deliver the intervention and simulated young-person scenarios. Learning mentors randomised to intervention 2 were asked to return for a further half-day training session. For intervention 2, training sessions were delivered per school site, as a training date could not be identified which accommodated all learning mentors. This session trained learning mentors in how to gather informed consent from parents for the intervention and organise and facilitate intervention 2, as well as how to respond to difficult disclosures.
The final training session focused on delivery of the 12-month follow-up appointment. Training consisted of a PowerPoint presentation and a demonstration of how to deliver each of the measures included in the follow-up assessment. All learning mentors received the same training; however, training sessions were delivered per school site, as a training date could not be identified which accommodated learning mentors from all participating schools. A manual relevant to the 12-month follow-up appointment was provided to supplement the training (see Appendix 3).
Learning mentors were supported in the delivery of interventions and follow-up appointments by the research team, who organised weekly visits throughout the study period to answer questions or concerns, collect materials from completed interventions (such as consent forms and hard copies of intervention tools) and encourage learning mentors to complete outstanding interventions. The research team also provided telephone and e-mail support. Finally, learning mentors were provided with a case diary sheet, on which they were asked to record any interactions with the individual young people in the trial (see Appendix 3). A main resource-use component of the economic evaluation (for the larger definitive trial) will be the cost of learning mentor time required to prepare for and conduct interventions and follow up with the young people during the trial. Thus, time spent for the present study was calculated by observing the average minutes per case, as documented in self-completed case diaries. The appropriateness of the case diary tool for collecting these data was assessed according to rates of missing data (incomplete or wholly unused diaries) and of diaries missing relevant information (see Chapter 7).
Chapter 4 Survey
Key points for Chapter 4
-
Seven schools took part in a set of three cross-sectional surveys administered at baseline (TP1), 6 months (TP2) and 12 months (TP3). Surveys administered at TP1 facilitated screening for the pilot trial.
-
Six per cent (n = 87) of parents indicated that they did not wish their child to take part in the study by completing and returning a tick-box opt-out form.
-
Survey response rates among pupils whose parents allowed them to take part were 92% at baseline (TP1), 90% at 6 months (TP2) and 84% at 12 months (TP3).
-
Levels of missing data were low for all variables.
-
A comparison of the distributions of AUDIT and AUDIT-C scores between subgroups at TP1 demonstrated that gender, smoking and sexual behaviour were significantly associated with young people’s current drinking behaviour.
-
Mean AUDIT scores were higher for young people who did not leave their names on the questionnaire than for those who did.
-
Comparison of scores over three time points suggests there was little or no change in measures of alcohol use, alcohol-related problems and well-being within this age group over the course of a year, except for small but statistically significant shifts upwards in the distributions of AUDIT, AUDIT-C and A-SAQ scores between the first and second surveys.
This chapter reports the methods and results of a set of three cross-sectional school surveys, administered at baseline (TP1), at 6 months (TP2) and at 12 months (TP3).
Methods
Recruitment of school sites
Written approval was obtained from the relevant local education authority, stating that it was willing for the project to go ahead in the study catchment area. All secondary/high schools in the study catchment area governed by the relevant local authority were eligible to take part in the study. Contact details for each school were provided by the local education authority. Contact from the research team with each school site was initially made by telephoning and e-mailing the school office and securing appropriate points of contact, such as the Head or Deputy Head (of Year 10 or the whole school) and pastoral leads. These individuals are described here and throughout this report as ‘lead liaisons’ and are defined as the key member of staff at each school site who made or brokered the decision about participation in the study on behalf of their school.
During an initial meeting between the research team and lead liaisons, the study protocol was explained and lead liaisons were provided with a short written outline of the study in an attempt to secure school participation. A written outline was provided, as it was anticipated that lead liaisons would need to share details of the study with other members of the school management team, such as head teachers (if not already the point of contact) or the board of governors. Final approval to participate in the study was then obtained from the head teacher on behalf of the school and board of governors at each school, and communicated by the school lead liaison to the research team verbally or by e-mail. A second visit was arranged by the research team to all participating schools in order to organise screening of Year 10 pupils and training for school staff who had responsibility for the delivery of interventions. Each school site received a £1000 payment to cover costs associated with the research.
Recruitment of pupils
In advance of the study, all parents/legal guardians of young people in Year 10 at participating schools were informed by letter that the study would be taking place in their child’s school (see Appendix 3). Letters were addressed on site at each participating school and posted directly to parents. Letters included a prepaid return envelope, addressed to the research team at the Newcastle University. Parents were given the option to indicate that they did not wish their child to take part in the study by completing and returning a tick-box opt-out form. Parents were asked to return this form within 2 weeks of the date shown on the letter. Returning this form to the research team resulted in their child not being included in both the survey and the pilot trial. No further parental consent for young people’s participation was sought. An opt-out process, rather than opt-in, was chosen, as sending letters home in order to obtain permission from parents for all young people to fill in a screening survey (and potentially take part in the trial) ran the risk of bias in recruitment and the potential loss of a large number of participants. An opt-out process was supported by the local education authority in the study catchment area, who advised that collection of health and lifestyle data without parental opt-in was a routine approach in school settings. Further, collection of questionnaire data in schools without parental opt-in is a method widely used in various national youth surveys of alcohol consumption and other health behaviours, such as those conducted by the NHS Information Centre annually exploring drinking and drug use by young people aged 11–15 years in England and Wales. 4
All Year 10 pupils at participating schools, except those whose parents had opted out of the research, were asked to complete a health and lifestyle questionnaire administered during a predefined school lesson falling in the week that the survey was due to take place. Pupils were asked to complete the questionnaire at three separate time points: TP1 (between November 2011 and January 2012), TP2 (6 months later: June and July 2012) and TP3 (12 months later: November and December 2012), by which time they were in Year 11. The research team provided support to school staff in implementing the survey tailored to the needs of the school setting. In advance of the survey, packs containing the correct number of survey materials were delivered to each school. The lead liaison in each school was actively involved in setting the survey date. All surveys took place during tutorial or PSHE lessons. However, tutorials or PSHE lessons did not follow exactly the same format at each school and their duration ranged from 30 minutes to 1 hour or an entire day. A minimum of one researcher was present at each school site when surveys took place. At each time point, data collection predominantly took place across one day at each school. However, young people absent on the date of the survey were followed up by school staff to minimise missing data. If young people were opted out by their parents, class teachers provided them with an alternative task while their peers completed questionnaires (e.g. outstanding homework or computer-based research). Young people were informed at every survey that their involvement was voluntary and the survey could be completed anonymously. At TP1 young people were asked to indicate willingness to participate in the pilot trial by including their contact details on the questionnaire. All young people who completed the questionnaire at TP1 were provided with a healthy living leaflet and £5.00 retail gift voucher.
Questionnaire measures
Young people were asked to complete a series of questionnaires including the A-SAQ, a modified version of the M-SASQ (Modified-Single Alcohol Screening Question),157 which aims to identify whether an individual’s drinking is above low risk, with the quantity/frequency measures adjusted to reflect guidelines for an adolescent population of half the adult daily limits (three units). 26 Young people were asked ‘In the last 6 months how often have you drunk more than three units of alcohol?’ with the response options of ‘Never’, ‘Less than four times’, ‘Four or more times but not every month’, ‘At least once a month but not every week’, ‘Every week but not every day’ and ‘Every day’. The A-SAQ contained pictorial references of what constitutes a unit of alcohol. A score of ‘four or more times’, or more frequently, indicated a positive screen and was indicative of being potentially eligible for inclusion in the trial.
The survey also included a general lifestyle questionnaire addressing a number of questions (diet, smoking, sexual behaviour and exercise) that were taken from the European school Survey Project on Alcohol and other Drugs (ESPAD) study3 and the Gateshead Millennium Study. 158 The 14-item WEMWBS was used to assess general psychological health. 159 The tool uses a five-point Likert scale, which gives a score of ‘1–5’ per question, giving a minimum score of ‘14’ and maximum score of ‘70’. A higher WEMWBS score indicates a higher level of mental well-being. 160 It has been shown to be valid and reliable with young people aged ≥ 13 years in England. 161 As well as the A-SAQ, alcohol use frequency, quantity (on a typical occasion) and heavy episodic drinking was also assessed using the 10-question AUDIT,162 with cut-offs recommended for adults (8+)162 and young people (2+),50 as well as a positive score for the AUDIT-C screen of 5+ used for adults (see Chapter 2, Primary and secondary prevention interventions for risky drinking). Alcohol-related problems were assessed using the validated 23-question RAPI tool, which includes measures on aggression. 163 The RAPI has been well validated for use with both clinical and community adolescent samples. 163,164 The EQ-5D-Y, which is a recently developed young-person version of the EQ-5D, was used to assess health-utility scores. 165 It is a quality of life measure used extensively in economic evaluations. The tool divides health status into five dimensions (mobility, self-care, usual activities, pain/discomfort, and anxiety/depression). Each of these dimensions has three possible levels giving 243 possible health states. 165 A modified S-SUQ was used to inform the health and social resource costs for any future economic evaluation. 166 Finally, demographic information (gender and ethnicity) was collected from each pupil who completed a questionnaire. Young people were asked to place their questionnaire in a blank envelope, which they sealed themselves and handed to the teacher. The young person had the option of inserting a completed questionnaire with or without their name or a blank questionnaire into the envelope.
Statistical analysis
For all variables the percentage of missing and implausible values was reported, along with either a five-number summary (minimum, lower quartile, median, upper quartile, maximum) for numeric variables, or percentages in each category for categorical variables. Details of the scoring system for numeric scales are given in Appendix 5.
Descriptive analysis
The survey variables are reported separately at the three time points (TP1, TP2 and TP3). For all of the variables we report the number of observations and percentage of missing and implausible values. In addition, five-number summaries are reported for the numeric variables, and the distributions of categorical variables are reported as percentages.
Comparisons between subgroups of young people at time point 1
For the TP1 survey data, AUDIT and AUDIT-C scores were compared by subgroups of gender, smoking status and sexual behaviour. Smoking status and sexual behaviour were of interest to see if those young people who displayed risky drinking behaviour were also more likely to take risks in other lifestyle choices. Three different cut-off points are used to compare the distribution of AUDIT and AUDIT-C scores (a score of 2+ or 8+ for AUDIT, and a score of 5+ for AUDIT-C). Differences between scores were tested using Mann–Whitney and Kruskal–Wallis analysis of variance tests as appropriate. Correlation coefficients were calculated for AUDIT and AUDIT-C scores with RAPI and WEMWBS to explore the association between drinking, well-being and alcohol-related problems.
Comparisons of results of surveys at different time points
To investigate any change over the 12-month period in drinking behaviour, alcohol-related problems and quality of life, a comparison of the distribution of A-SAQ, AUDIT, AUDIT-C, RAPI and WEMWBS was made at all three time points (TP1, TP2 and TP3). Data from the three time points were regarded as being independent, as the young people did not leave their names in TP2 and TP3, and so measures were analysed using Kruskal–Wallis tests. If significant differences were established across the three time points for a given variable, formal comparisons between the pairs of consecutive time points (TP1 and TP2; TP2 and TP3) were made using Mann–Whitney U-tests.
Comparison of named and anonymous pupils
For each school, the number of young people completing questionnaires was reported and the percentage of those young people who provided their names was calculated. Differences in percentages scoring positive for A-SAQ and differences in mean AUDIT scores were calculated for those who provided their names and those who did not, in order to establish if there was a difference in drinking behaviour between these groups.
Distribution of missing values within questionnaires
If an individual item was missing from within a questionnaire, this meant that the overall questionnaire score was also missing. To investigate whether there were particular items that were more often missing, a breakdown of missing data by question was provided for the AUDIT, RAPI and WEMWBS questionnaires.
Results
Recruitment and retention
The local education authority provided accurate pupil numbers for Year 10 for the seven schools participating in the study. There were 1388 young people across all seven schools that could feasibly complete the survey at TP1. On the days that the surveys were to be completed there were differing numbers of young people absent from school, making the final numbers of completed surveys 1280 at TP1, 1256 at TP2 and 1161 at TP3 (Figure 2).
FIGURE 2.
Completion of surveys at all three time points (TP1, TP2 and TP3).
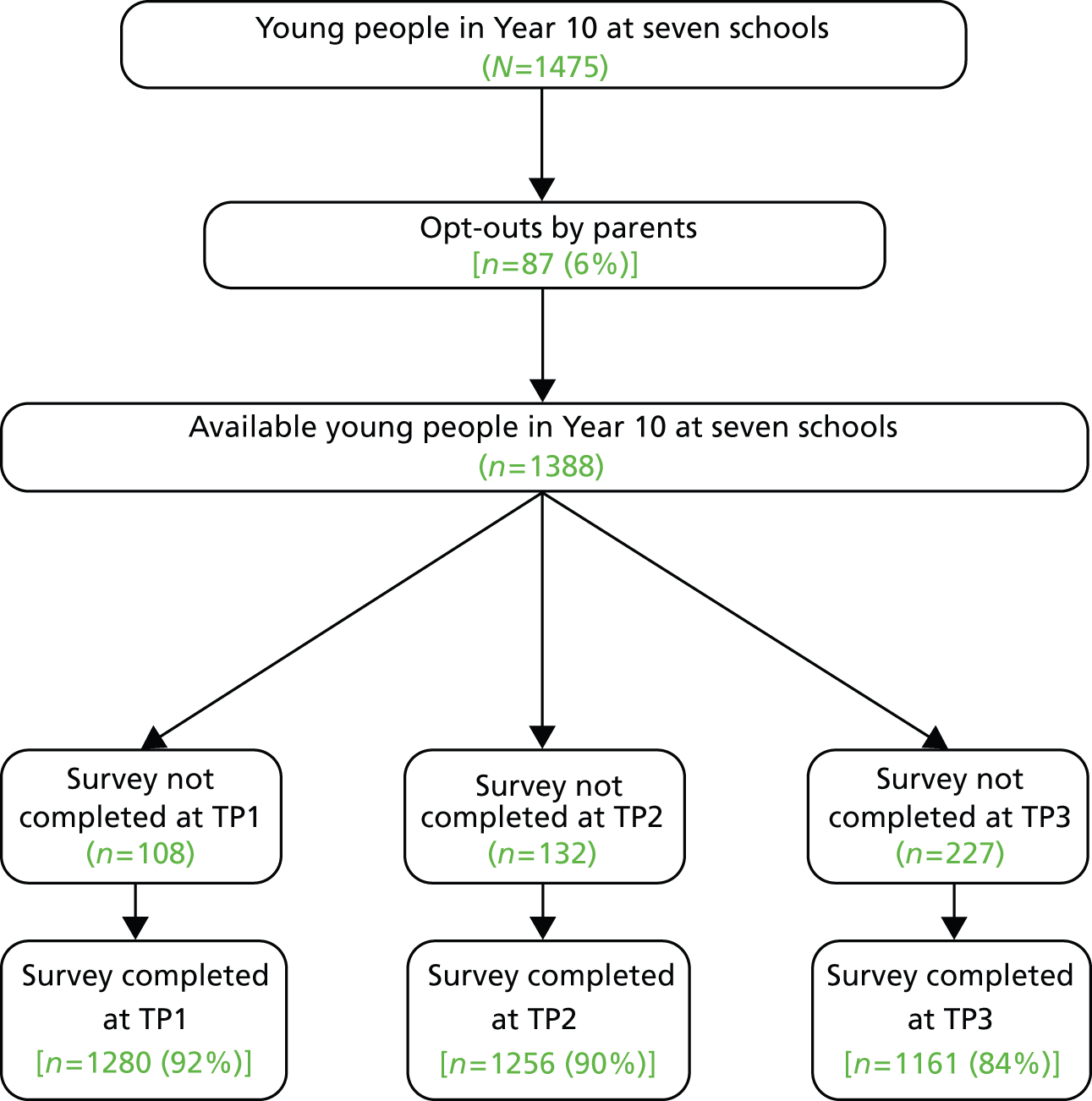
Table 1 shows the number and percentage of young people who completed the questionnaire on the prearranged day and the number and percentage followed up in the days following.
| Time point | Initial survey | Collected after initial surveya | ||
|---|---|---|---|---|
| n | % | n | % | |
| 1 | 1178 | 92.0 | 102 | 8.0 |
| 2 | 1139 | 90.7 | 117 | 9.3 |
| 3 | 1028 | 88.5 | 133 | 11.5 |
Missing data
Descriptive statistics for numeric variables in the survey are reported in Table 2. Levels of completion across all three time points were high. There were 80 missing responses for WEMWBS and only one missing response for AUDIT score at this time point. WEMWBS also had the most missing values at TP1 and TP2. At TP1 and TP2, levels of missing data ranged from 1% and 2% (AUDIT), respectively, and from 12% to 13% (WEMWBS). The WEMWBS scale was the last set of questions in the survey pack, which may explain the higher rate of missing data.
| Measure (potential scale range) | N | Missing (%) | Implausible values (%)a | n available | Minimum | Lower quartile | Median | Upper quartile | Maximum |
|---|---|---|---|---|---|---|---|---|---|
| AUDIT (0–40) | |||||||||
| TP1 | 1280 | 6.0 | – | 1203 | 0 | 0 | 2 | 8 | 40 |
| TP2 | 1256 | 6.4 | – | 1176 | 0 | 1 | 4 | 8 | 40 |
| TP3 | 1161 | 0.1 | – | 1160 | 0 | 1 | 4 | 9 | 40 |
| AUDIT-C (0–12) | |||||||||
| TP1 | 1280 | 5.6 | – | 1208 | 0 | 0 | 2 | 4 | 12 |
| TP2 | 1256 | 5.3 | – | 1189 | 0 | 1 | 3 | 5 | 12 |
| TP3 | 1161 | 3.3 | – | 1123 | 0 | 1 | 3 | 5 | 12 |
| RAPI (0–69) | |||||||||
| TP1 | 1280 | 5.6 | – | 1208 | 0 | 0 | 1 | 6 | 69 |
| TP2 | 1256 | 7.7 | – | 1159 | 0 | 0 | 1 | 6 | 69 |
| TP3 | 1161 | 4.1 | – | 1113 | 0 | 0 | 1 | 6 | 69 |
| WEMWBS (14–70) | |||||||||
| TP1 | 1280 | 11.6 | – | 1132 | 14 | 42 | 48 | 55 | 70 |
| TP2 | 1256 | 13.1 | – | 1091 | 14 | 42 | 49 | 55 | 70 |
| TP3 | 1161 | 6.9 | – | 1081 | 14 | 41 | 49 | 55 | 70 |
| Physical activity last week (0–7) | |||||||||
| TP1 | 1280 | 8.8 | 6.1 | 1089 | 0 | 2 | 4 | 5 | 7 |
| TP2 | 1256 | 5.9 | 6.1 | 1106 | 0 | 2 | 4 | 5 | 7 |
| TP3 | 1161 | 4.7 | 6.5 | 1031 | 0 | 2 | 3 | 5 | 7 |
| Physical activity usual (0–7) | |||||||||
| TP1 | 1280 | 7.0 | 6.2 | 1112 | 0 | 2 | 4 | 5 | 7 |
| TP2 | 1256 | 5.3 | 4.8 | 1130 | 0 | 2 | 4 | 5 | 7 |
| TP3 | 1161 | 3.4 | 4.7 | 1068 | 0 | 2 | 4 | 5 | 7 |
| Fruit (0–14) | |||||||||
| TP1 | 1280 | 3.0 | 0.8 | 1232 | 0 | 1 | 2 | 3 | 12 |
| TP2 | 1256 | 3.4 | 0.9 | 1202 | 0 | 1 | 2 | 3 | 12 |
| TP3 | 1161 | 1.6 | 0.6 | 1136 | 0 | 1 | 2 | 3 | 12 |
| Vegetables (0–22) | |||||||||
| TP1 | 1280 | 5.8 | 0.8 | 1196 | 0 | 1 | 2 | 3 | 15 |
| TP2 | 1256 | 4.5 | 0.5 | 1176 | 0 | 1 | 2 | 3 | 20 |
| TP3 | 1161 | 2.8 | 0.6 | 1121 | 0 | 1 | 2 | 3 | 20 |
There were similar low levels of missing data for the main categorical variables reported in Table 3, ranging from 0.1% for gender at TP3 to 4.5% for the question about sex without a condom at TP2. Again, there were no missing values reported for the questions relating to how free time was spent, as these were tick boxes for positive answers, and a blank could indicate either that that they did not take part in that activity or they had not answered the question. However, there were 42 (3.3%) young people who did not tick any boxes at TP1, 44 (3.5%) at TP2 and 62 (5.3%) at TP3.
| Variable | Distribution over categoriesa by time point (%) | ||
|---|---|---|---|
| TP1 (n = 1280) | TP2 (n = 1256) | TP3 (n = 1161) | |
| AUDIT: above suggested cut-off points | |||
| % participants scoring ≥ 2 (adolescents)b | 58.1 | 66.1 | 68.8 |
| % participants scoring ≥ 8 (adults)c | 26.0 | 29.3 | 31.8 |
| AUDIT-C: above suggested cut-off points | |||
| % participants scoring ≥ 5 (adults)c | 20.7 | 29.1 | 32.6 |
| A-SAQ (over last 6 months) | |||
| Missing (%) | 14 (1.1) | 24 (1.9) | 4 (0.3) |
| Never | 35.2 | 27.8 | 28.7 |
| Fewer than four times | 25.5 | 25.4 | 24.6 |
| Four or more times but not every month | 11.7 | 14.7 | 15.0 |
| One or more per month but not every week | 13.9 | 16.1 | 16.3 |
| Every week but not every day | 12.6 | 14.0 | 13.6 |
| Every day | 1.0 | 2.0 | 2.0 |
| % with positive scored | 39.3 | 46.8 | 46.7 |
| Sex regretted after alcohol | |||
| Missing (%) | 38 (3.0) | 52 (4.1) | 22 (1.9) |
| Never had sex | 63.7 | 56.9 | 52.7 |
| Yes | 8.1 | 10.3 | 13.6 |
| No | 28.3 | 32.8 | 33.7 |
| Sex without condom after alcohol | |||
| Missing (%) | 40 (3.1) | 56 (4.5) | 21 (1.8) |
| Never had sex | 64.5 | 57.5 | 53.0 |
| Yes | 7.9 | 10.3 | 12.8 |
| No | 27.6 | 32.3 | 34.2 |
| Variable | Distribution over categoriesa by time point (%) | ||
|---|---|---|---|
| TP1 (n = 1280) | TP2 (n = 1256) | TP3 (n = 1161) | |
| Gender | |||
| Missing (%) | 8 (0.6) | 17 (1.4) | 1 (0.1) |
| Male | 49.5 | 48.7 | 47.8 |
| Ethnic group | |||
| Missing (%) | 17 (1.3) | 35 (2.8) | 13 (1.1) |
| White | 94.1 | 93.3 | 93.2 |
| Smoker | |||
| Missing (%) | 44 (3.4) | 38 (3.0) | 33 (2.8) |
| Yes | 19.6 | 24.6 | 23.1 |
| Age when first smoked | |||
| Missing (%) | 33 (2.6) | 25 (2.0) | 14 (1.2) |
| Never | 66.6 | 60.4 | 60.2 |
| ≤ 8 years | 1.6 | 2.2 | 2.4 |
| 9–10 years | 2.8 | 2.4 | 3.1 |
| 11–12 years | 12.0 | 11.5 | 10.6 |
| 13–14 years | 14.9 | 16.7 | 14.7 |
| > 14 years | 2.1 | 6.7 | 9.2 |
| Use of free timeb | |||
| With friends at your house or theirs | 34.8 | 32.4 | 37.8 |
| Go out somewhere with friends | 60.6 | 62.3 | 54.1 |
| Spend time with your family | 17.5 | 13.9 | 17.1 |
| Spend time with siblings | 6.5 | 5.7 | 6.5 |
| Spend time by yourself | 21.8 | 21.3 | 23.8 |
Analysis of time point 1 data
Distribution of AUDIT and AUDIT-C scores
Figure 3 shows the distribution of the AUDIT and AUDIT-C scores for the whole sample. Scores had a positively skewed distribution, with 340 (28.4%) and 341 (28.2%) individuals scoring the minimum on AUDIT and AUDIT-C, respectively. Scores were recorded up to the maximum of the scales, with three (0.3%) young people scoring the maximum on AUDIT and 10 (0.8%) on AUDIT-C. The median AUDIT score was ‘2’ and the mode was ‘0’ (never drink); the median for AUDIT-C was ‘2’ with a mode of ‘0’. The figures also illustrate the differing proportions of young people who would be categorised as ‘positive’ using suggested cut-off values for adults (8+) and young people (2+).
FIGURE 3.
Distribution of the AUDIT score with (a) young person (score of ‘2+’) and adult (score of ‘8+’) cut-offs; and (b) AUDIT-C cut-offs (score of ‘5+’).
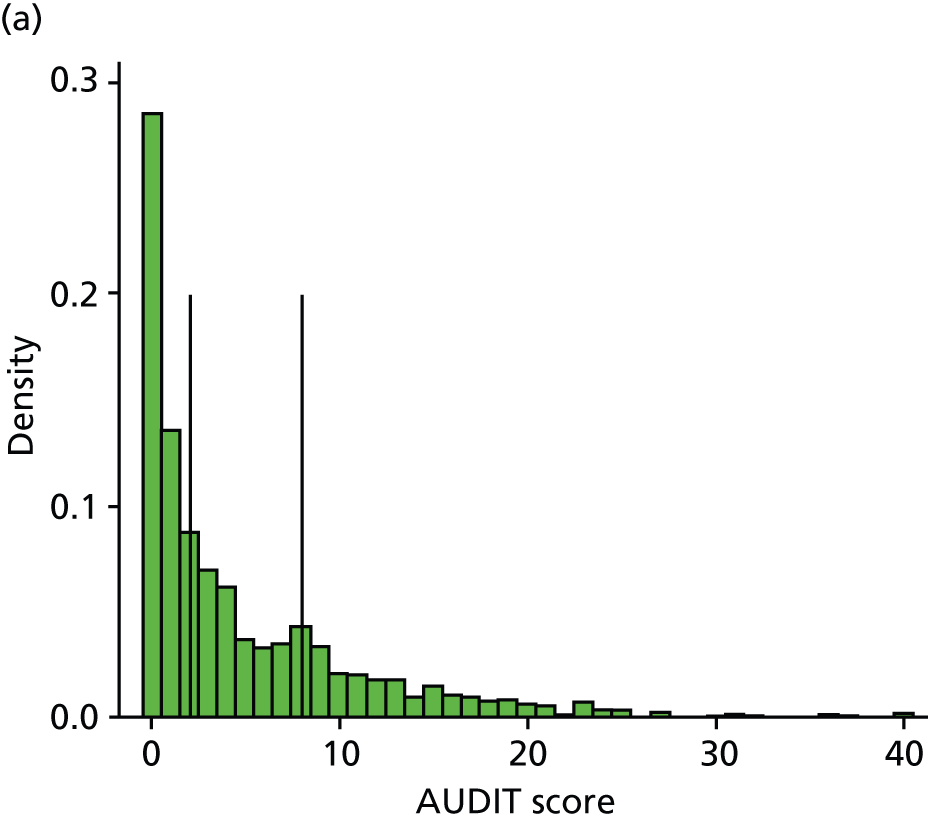
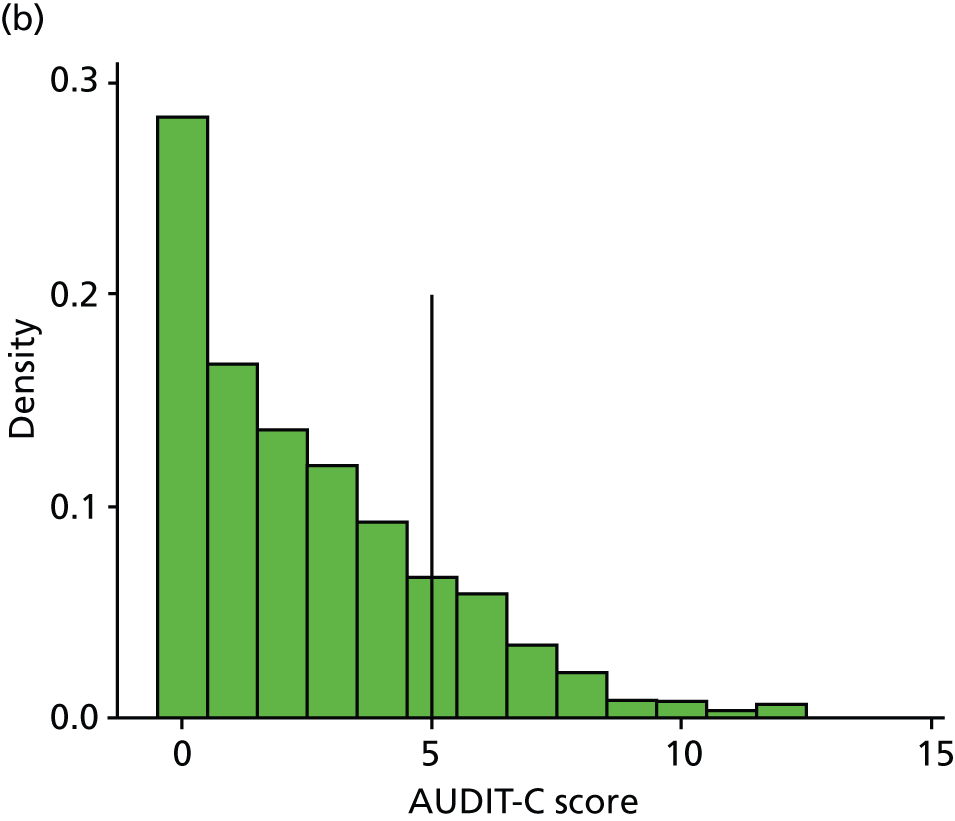
Twenty-six per cent (n = 307) of the sample had an AUDIT score of ≥ 8 (the cut-off used for determining alcohol use disorders in adults)162 and 58% (n = 691) scored ≥ 2 (the modified cut-off suggested for adolescents). 50 In addition, albeit using a breakdown designed for use with adults, 28% scored ‘0’ and could be categorised as ‘abstainers’; 46% ‘lower risk’ (1–7); 18% ‘increasing risk’ (8–15); 4% ‘higher risk’ (16–19); and 4% ‘possible dependence’ (20+) on the full AUDIT. Twenty per cent (n = 245) of the sample screened positive for hazardous or harmful drinking using a cut-off of ‘5’ on AUDIT-C.
Differences in AUDIT and AUDIT-C scores by gender
There was a difference in the distribution of AUDIT scores at TP1 by gender, with girls having a tendency to have higher scores (a median score of ‘3’ in girls as opposed to ‘2’ in boys). A similar shift in distributions was also seen for AUDIT-C scores, for which the median scores were ‘2’ in girls as opposed to ‘1’ in boys. This is illustrated in Figure 4. Mann–Whitney U-tests confirmed that these were statistically significant differences (p < 0.0001 and p = 0.0005, respectively).
FIGURE 4.
Distribution of AUDIT and AUDIT-C scores by gender. Box plots of (a) AUDIT score by gender; and (b) AUDIT-C score by gender.
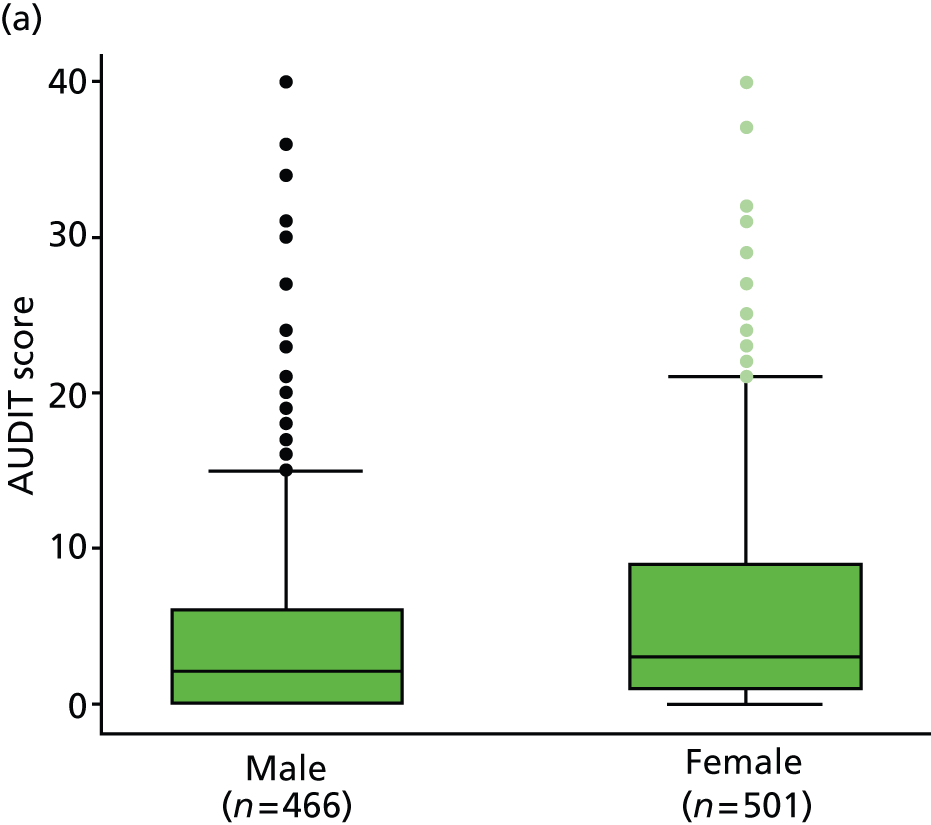
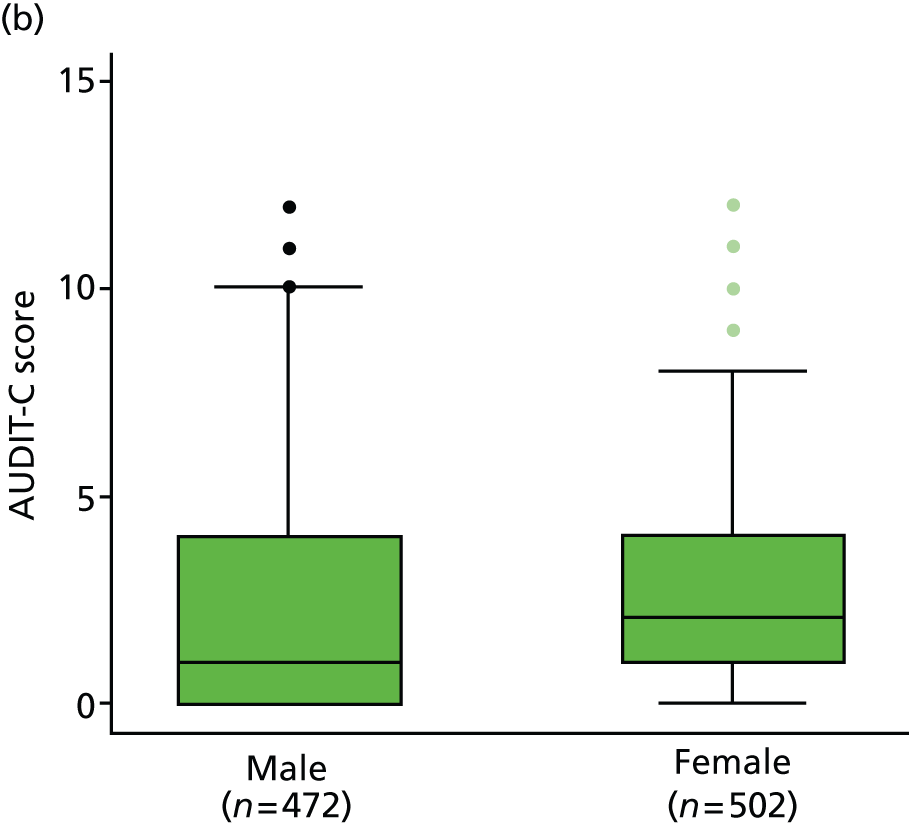
Differences in AUDIT-C score by smoking status
There was a marked difference in the distribution of AUDIT scores by smoking status, with those who smoked having a tendency to have higher scores (a median score of nine in smokers compared with one in non-smokers). A similar shift in distributions was also seen for AUDIT-C scores, for which the median scores were ‘4’ in smokers as opposed to ‘1’ in non-smokers. This is illustrated in Figure 5. Mann–Whitney tests confirmed that these were statistically significant differences (p < 0.0001 for both tests).
FIGURE 5.
Distribution of AUDIT and AUDIT-C scores by smoking status. Box plots of (a) AUDIT score by smoking status; and (b) AUDIT-C score by smoking status.
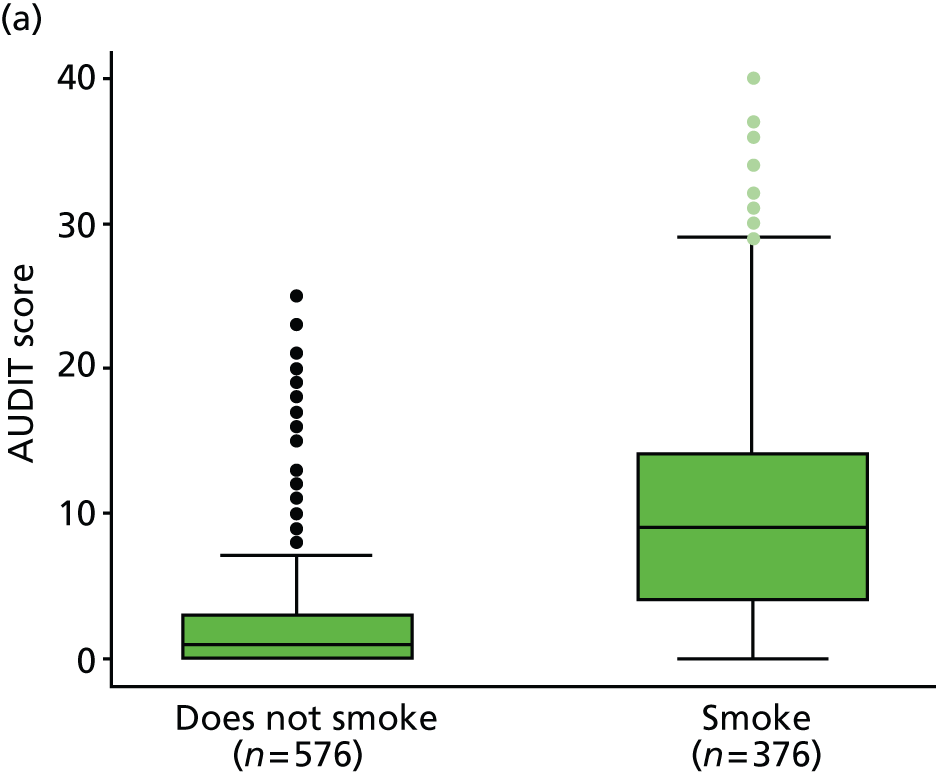
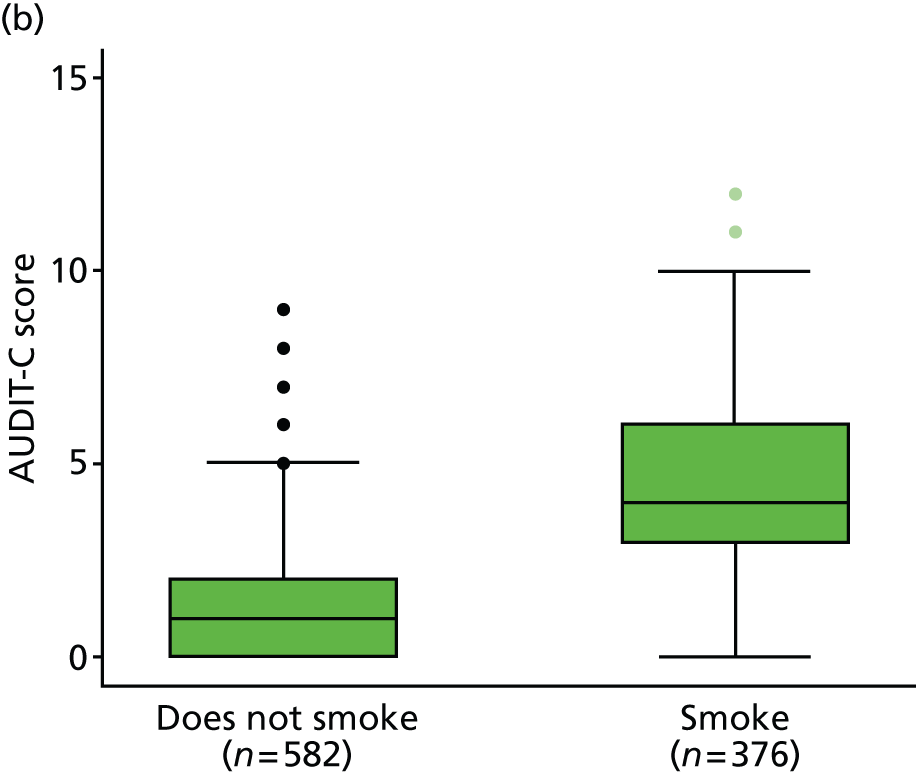
Differences in AUDIT score by sexual behaviour
There was a marked difference in the distribution of AUDIT scores by sexual behaviour (measured here by use of condoms), with a tendency to have higher scores as the sexual behaviour was more risky. Young people were asked if they had ever engaged in sex without a condom after drinking alcohol, and the median score was ‘16’ in those who had not used a condom after alcohol; ‘5’ in those who had engaged in sex with a condom; and ‘1’ in those who had never had sex at all. Note that those who had never had sex will include some young people who had not ever drunk alcohol. A similar shift in distributions was also seen for AUDIT-C scores, for which the median scores were ‘6’ in those who had not used a condom, ‘3’ in those who had engaged in sex with a condom, and ‘1’ in those who never had sex. This is illustrated in Figure 6. Kruskal–Wallis tests confirmed that these were statistically significant differences (p = 0.0001 for both tests).
FIGURE 6.
AUDIT and AUDIT-C scores by condom use. Box plots of (a) AUDIT score by condom use; and (b) AUDIT-C score by condom use.
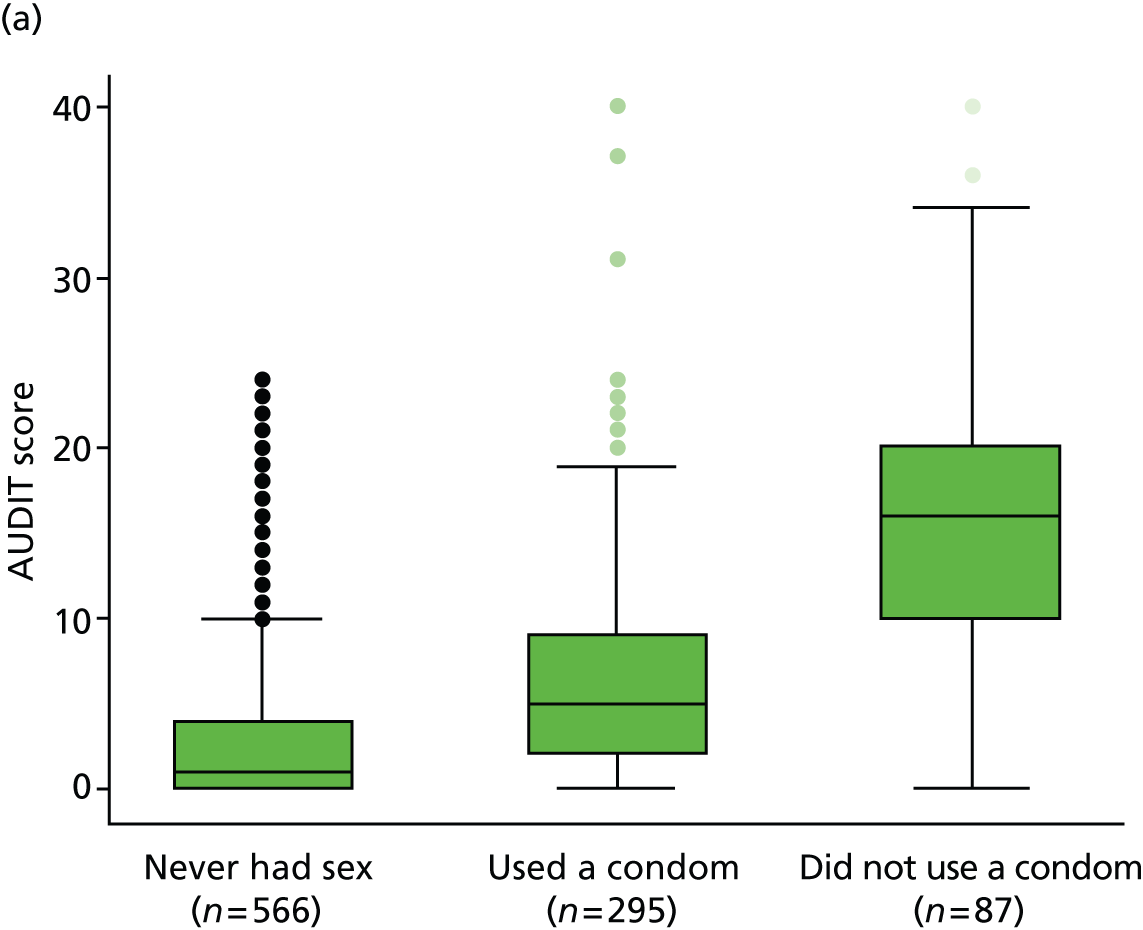
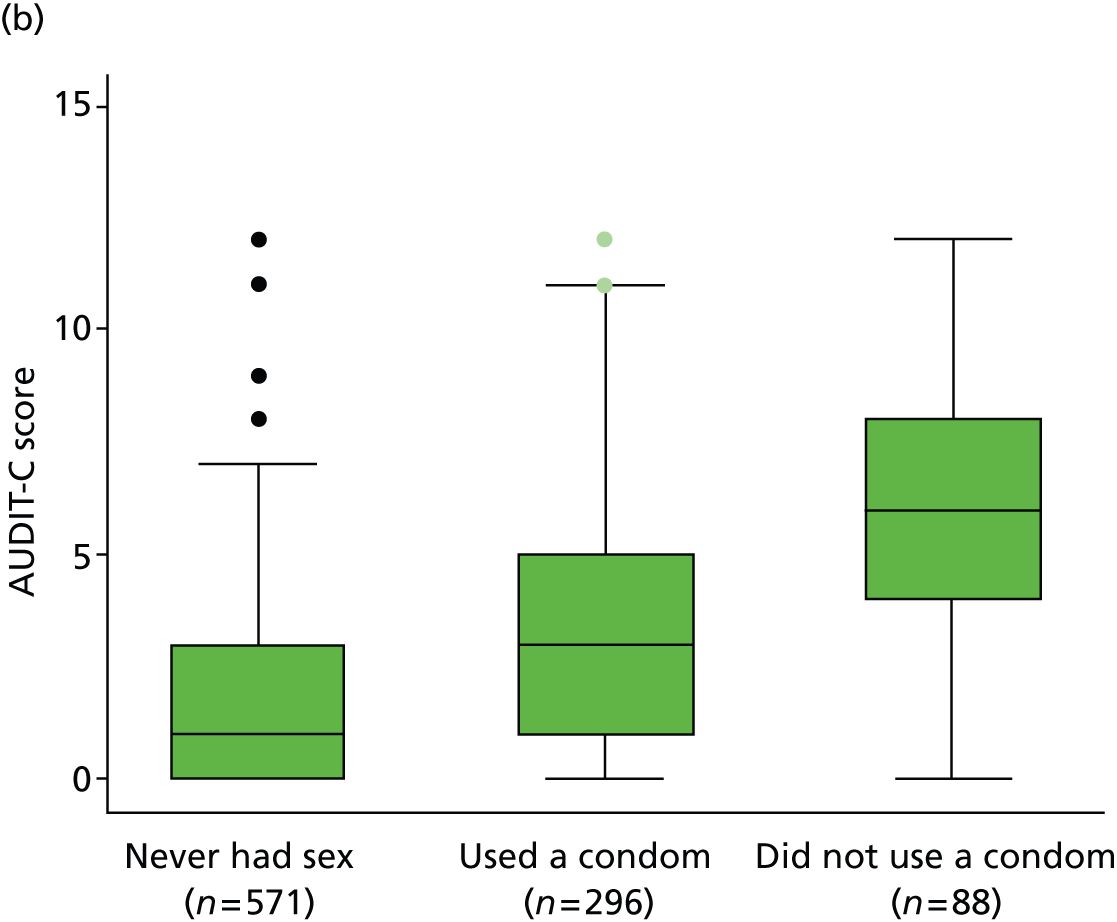
Distribution of Rutgers Alcohol Problems Inventory and Warwick–Edinburgh Mental Well-being Scale scores
The RAPI score was calculated on only those who had drunk alcohol and had a positively skewed distribution with a median of ‘2’ (n = 877). Six hundred and two (50%) individuals scored ‘0’ and three (0.3%) scored the maximum of ‘69’. The WEMWBS score was calculated for all young people who completed the measure and had a median of ‘48’ (n = 1123). This is comparative to other studies with young people aged 13–16 years (median ‘49’). 161 Twelve young people scored the minimum of ‘14’ (1.1%) and 21 (1.9%) the maximum of ‘70’. The distributions of these two variables are shown in Figure 7.
FIGURE 7.
Distribution of RAPI and WEMWBS scores. Histograms of the distribution of (a) the RAPI score excluding those who never drink alcohol; and (b) the WEMWBS.
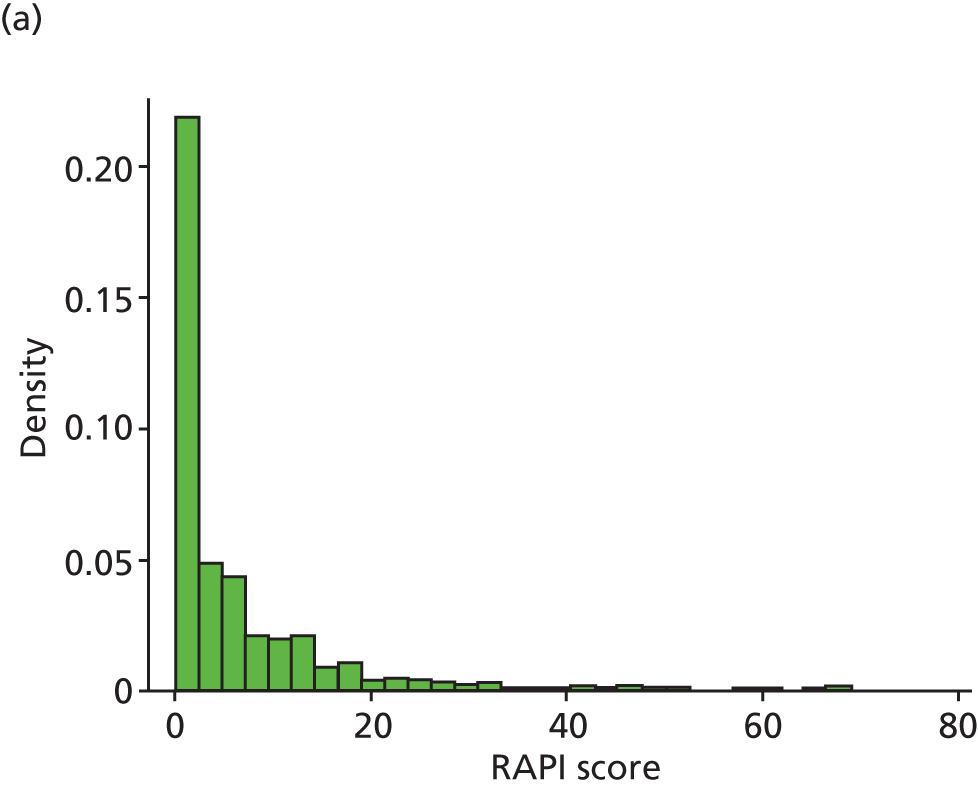
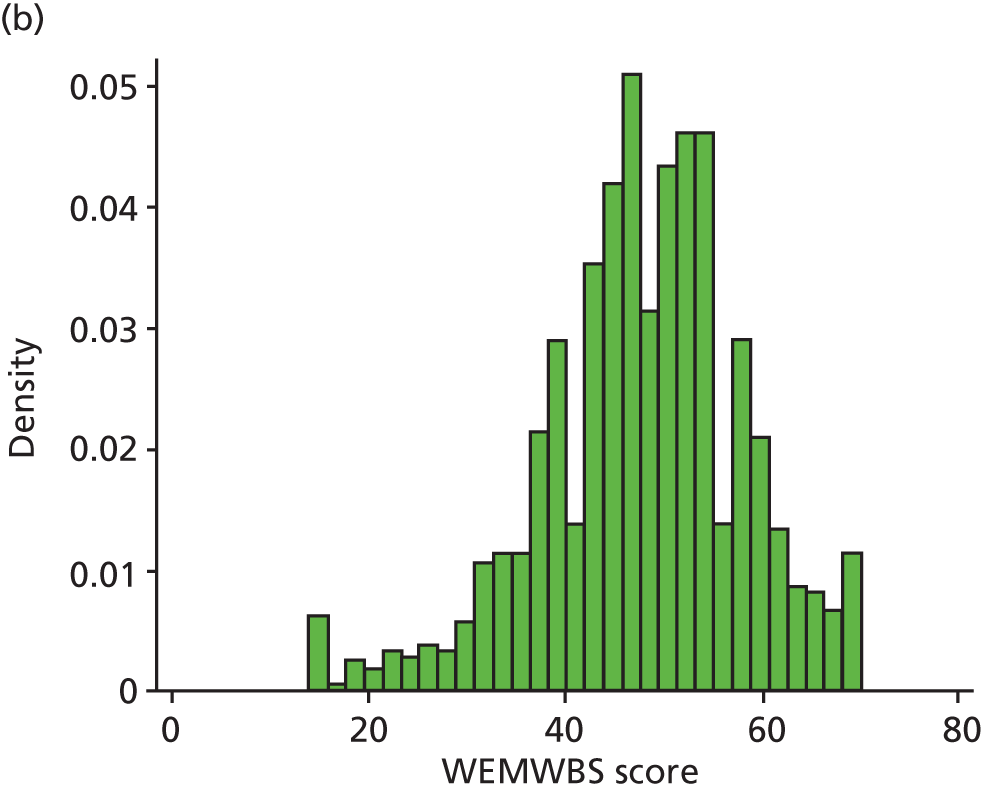
Associations between measures at time point 1
The strength of association between AUDIT, AUDIT-C, RAPI and WEMWBS was assessed using Spearman’s correlation coefficients and is shown in Table 4 and Figure 8. Unsurprisingly, there was a strong correlation between AUDIT and AUDIT-C scores. The RAPI score showed a moderate association with both AUDIT and AUDIT-C score: this is illustrated in Figure 8. However, the WEMWBS score showed very weak correlations with all of the other measures.
FIGURE 8.
Associations between AUDIT and AUDIT-C and RAPI.
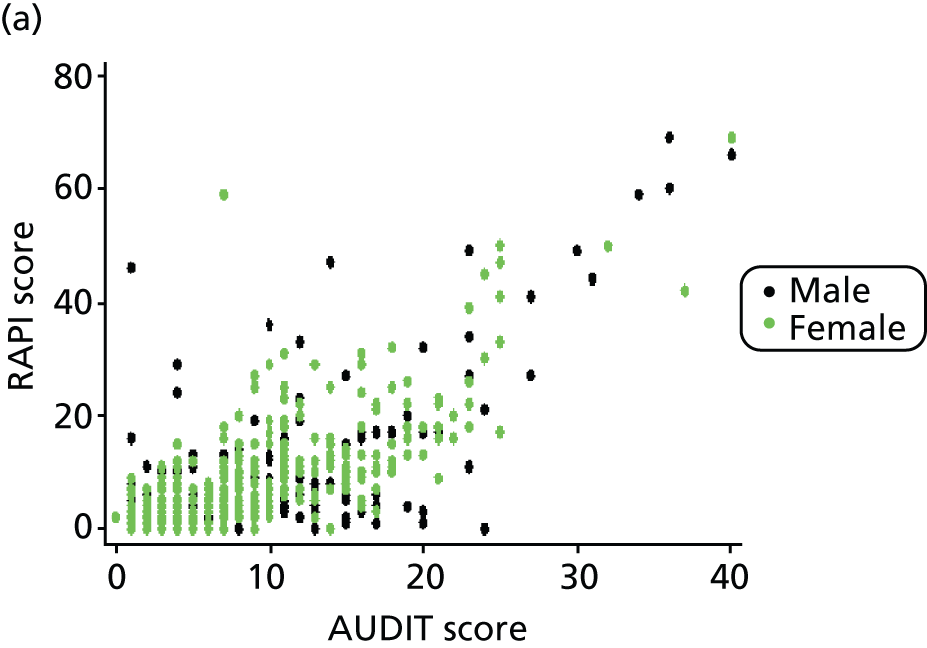
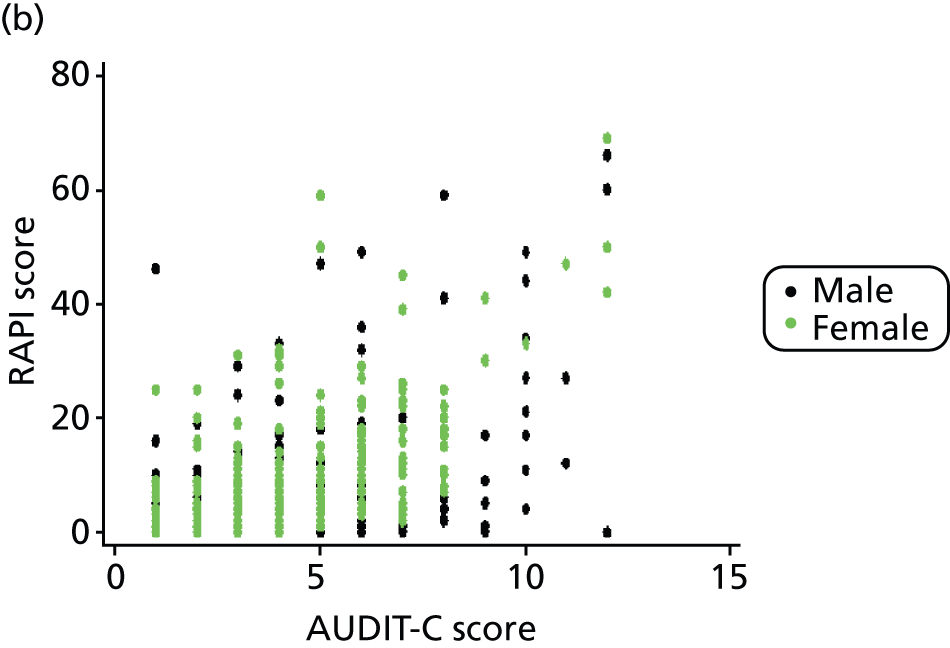
| AUDIT | AUDIT-C | RAPI | |
|---|---|---|---|
| AUDIT-C | 0.96 | ||
| RAPI | 0.76 | 0.65 | |
| WEMWBS | –0.13 | –0.08 | –0.22 |
Results of comparison of surveys at different time points
The distributions of the numeric variables across the three time points were summarised in Table 1. There appeared to be a slight shift upwards in some variables, as seen in changes to medians or quartiles. However, the distributions of AUDIT, AUDIT-C, RAPI and WEMWBS scores were formally compared across the three time points using the Kruskal–Wallis test. There was no significant difference between RAPI scores and WEMWBS scores over time (p> 0.05). However, there were significant differences over time for both AUDIT and AUDIT-C scores, with both following the same pattern when data at pairs of time points were compared using Mann–Whitney U-tests. The median AUDIT scores were ‘2’, ‘4’ and ‘4’ at the three time points, and the consecutive median AUDIT-C scores were ‘2’, ‘3’ and ‘3’. The differences between TP1 and TP2 were statistically significant; however, there were no significant differences between TP2 and TP3. These results show a small shift upwards in the distributions of AUDIT and AUDIT-C over the 12-month period. UK guidelines recommend at least 1 hour per day of exercise for young people aged 5 to 25 years. 167 The median number of days in the previous week in the present study in which there was at least an hour of physical activity was four days at TP1 and TP2, and three days at TP3. The median number of days including physical exercise that were reported in a typical week was four days at all time points. The recommended daily intake of fruit and vegetables per day is five (www.nhs.uk/Livewell/5ADAY/Pages/5ADAYhome.aspx). The median number of daily portions of fruit consumed by young people in the present study was two at all time points, and the median daily portions of vegetables was also two at all time points.
The distributions of the categorical variables across the three time points were summarised in Table 3. For the alcohol-related categorical variables reported in Table 3a, the percentage of participants scoring ‘2’ or above (the cut-off suggested for adolescents) increased from 58% at TP1 to 66% (TP2) and 69% at TP3. The percentage of participants who scored ≥ 8 (the adult cut-off) was 26% at TP1, 29% at TP2 and 32% at TP3. For AUDIT-C, 21% of participants scored ≥ 5 (the adult cut-off) at TP1, 29% at TP2 and 32.6% at TP3.
The distribution of alcohol frequency categories measured by the A-SAQ appears to have shifted slightly upwards over time. Thirty-nine per cent of participants reported drinking at least four times but not every month (i.e. scored positive) with 47% at TP2 and TP3. As A-SAQ is an ordered categorical variable, the distribution over time was also compared using Kruskal–Wallis and Mann–Whitney tests. As with the pattern seen in AUDIT and AUDIT-C, the differences between TP1 and TP2 were statistically significant, as were the differences between TP1 and TP3; however, there were no significant differences between TP2 and TP3.
There was a slight decline in the number of young people who had never had sex over time and there was an increase over time of young people regretting sex after consuming alcohol and having sex without using a condom after consuming alcohol.
For the non-alcohol-related categorical variables reported in Table 3b, there was a slight increase in the number of smokers over the year. The majority of young people spent their free time going out with friends, although this reduced from 61% and 62% at TP1 and TP2, respectively, to 54% at TP3. After this, the next most popular answer was to spend time with friends in their own home or their friends’ homes. Spending time with brothers and sisters or with family were the least popular options.
Comparison of named and anonymous participants
The percentage of participants leaving their name on the TP1 questionnaire varied considerably between schools, from as few as 37% up to 74%. The percentage of participants who left their names and scored positive on the A-SAQ varied from 11% to 34% across schools (as a percentage of the total participants completing the survey). A further 21.3% of participants scored positive on the A-SAQ but did not leave their names, so were potentially eligible but not willing to participate. Combining results across the participating schools, the mean AUDIT score of those young people who left their names was lower than those who did not. Using a Mann–Whitney U-test on combined data across schools, there was a statistically significant difference between the distributions of AUDIT scores in those young people who did and did not (p = 0.0002), with a tendency towards higher scores in those who did not leave their name (means of 5.7 vs. 4.4). The results are summarised in Table 5.
| School | No. of participants completing survey at TP1 | % participants leaving name | % participants scoring positive on A-SAQ and leaving name | % participants scoring positive on A-SAQ and not leaving name | Mean AUDIT score of participants who left name | Mean AUDIT score of participants who did not leave name |
|---|---|---|---|---|---|---|
| A | 167 | 72.5 | 23.3 | 13.2 | 3.9 | 6.8 |
| B | 115 | 52.2 | 20.9 | 18.3 | 4.5 | 5.5 |
| C | 81 | 74.1 | 34.6 | 14.8 | 6.7 | 9.9 |
| D | 307 | 36.5 | 11.1 | 24.8 | 3.6 | 4.8 |
| E | 240 | 47.5 | 16.3 | 27.1 | 4.1 | 6.7 |
| F | 215 | 39.5 | 13.5 | 22.8 | 4.8 | 5.2 |
| G | 155 | 50.3 | 20.0 | 18.1 | 4.5 | 5.4 |
| Total | 1280 | 49.2 | 17.5 | 21.3 | 4.4 | 5.7 |
Missing data within measures
Table 6 shows a breakdown of missing data for the items making up a questionnaire score. When an item was missing from a measure, an overall score was not computed for that measure. With the exception of the second item on the AUDIT scale, there seems little sign that items are problematic in terms of being missing more often. For the AUDIT score, the second item had a high number of missing values, because there was no tick box for young people who do not drink. This was accounted for when calculating the overall AUDIT score by automatically giving these young people an AUDIT score of ‘0’ if they had responded that they had not drunk alcohol in the last 6 months using the first question in the AUDIT scale (the lowest category). For the other AUDIT questions, missing data values ranged from 0.3% to 3.5%. There were slightly more missing data for RAPI questions, with the percentage of missing values ranging from 1.4% to 4.6%. WEMWBS has the most missing data of all of the measures, ranging from 2.8% to 9%. Overall, there were fewer missing data at TP3 and the most missing data at TP2. The response rate to the whole survey was lower at TP3, so the lower percentage missing on individual items at TP3 may reflect the fact that pupils present on the day of the survey were more likely to complete more items.
| Measure | Question | % missing | ||
|---|---|---|---|---|
| TP1 (n = 1280) | TP2 (n = 1256) | TP3 (n = 1161) | ||
| AUDIT | How often do you have a drink containing alcohol? | 1.3 | 1.8 | 0.5 |
| How many standard drinks containing alcohol do you drink on a typical day when you are drinking? | 21.1 | 17.4 | 2.0 | |
| How often have you had six or more standard drinks if female, or eight or more if male, on a single occasion in the last 6 months? | 3.5 | 3.4 | 1.3 | |
| How often during the last 6 months have you found that you were not able to stop drinking once you had started? | 1.2 | 2.5 | 0.3 | |
| How often in the last 6 months have you failed to do what was normally expected of you because of your drinking? | 1.5 | 2.8 | 0.5 | |
| How often in the last 6 months have you needed an alcoholic drink in the morning to get you going? | 1.0 | 2.5 | 0.5 | |
| How often in the last 6 months have you had a feeling of guilt or regret after drinking? | 1.3 | 2.9 | 0.7 | |
| How often in the last 6 months have you not been able to remember what happened when drinking the night before? | 1.6 | 2.9 | 0.6 | |
| Have you or someone else been injured as a result of your drinking? | 1.6 | 3.3 | 0.9 | |
| Has a relative/friend/doctor/health worker been concerned about your drinking or advised you to cut down? | 2.0 | 3.1 | 0.8 | |
| RAPI (how many times in the last 6 months) | Not able to do your homework or study for a test | 2.2 | 3.7 | 1.4 |
| Got into fights with other people | 1.8 | 3.7 | 1.4 | |
| Missed out on other things because you spent too much money on alcohol | 1.9 | 3.9 | 1.5 | |
| Went to work or school high or drunk | 2.2 | 3.7 | 1.5 | |
| Caused shame or embarrassment to someone | 2.2 | 3.9 | 1.8 | |
| Neglected your responsibilities | 2.3 | 4.3 | 1.6 | |
| Relatives avoided you | 2.1 | 4.1 | 1.6 | |
| Felt you needed more alcohol than you used to in order to get the same effect | 2.0 | 3.8 | 1.6 | |
| Tried to control your drinking | 2.3 | 4.2 | 2.0 | |
| Had withdrawal symptoms | 2.3 | 4.0 | 1.7 | |
| Noticed a change in your personality | 2.3 | 4.2 | 1.7 | |
| Felt you had a problem with alcohol | 2.4 | 4.6 | 1.8 | |
| Missed a day (or part of a day) of school or work | 2.5 | 4.1 | 1.8 | |
| Wanted to stop drinking but could not | 2.3 | 4.3 | 2.0 | |
| Suddenly found yourself in a place that you could not remember getting to | 2.5 | 4.3 | 1.7 | |
| Passed out or fainted suddenly | 2.7 | 4.1 | 2.0 | |
| Had a fight, argument or bad feeling with a friend | 3.0 | 4.4 | 1.9 | |
| Had a fight, argument or bad feeling with a family member | 3.2 | 4.5 | 1.8 | |
| Kept drinking when you promised yourself not to | 3.0 | 4.3 | 2.0 | |
| Felt you were going crazy | 3.0 | 4.4 | 2.0 | |
| Had a bad time | 2.9 | 4.3 | 1.9 | |
| Felt physically or psychologically dependent on alcohol | 3.0 | 4.2 | 1.7 | |
| Was told by a friend, neighbour or relative to stop or cut down drinking | 2.9 | 4.2 | 1.8 | |
| WEMWBS (how often) | I’ve been feeling optimistic about the future | 5.9 | 8.3 | 2.8 |
| I’ve been feeling useful | 5.6 | 8.6 | 3.2 | |
| I’ve been feeling relaxed | 5.9 | 8.7 | 3.7 | |
| I’ve been feeling interested in other people | 6.3 | 9.0 | 3.5 | |
| I’ve had energy to spare | 5.8 | 8.5 | 3.1 | |
| I’ve been dealing with problems well | 5.7 | 8.3 | 3.2 | |
| I’ve been thinking clearly | 6.0 | 8.6 | 3.4 | |
| I’ve been feeling good about myself | 5.8 | 8.2 | 3.4 | |
| I’ve been feeling close to other people | 6.3 | 8.3 | 3.8 | |
| I’ve been feeling confident | 5.7 | 8.4 | 3.5 | |
| I’ve been able to make up my own mind about things | 5.6 | 8.5 | 3.6 | |
| I’ve been feeling loved | 6.2 | 8.9 | 3.8 | |
| I’ve been interested in new things | 5.8 | 8.4 | 3.4 | |
| I’ve been feeling cheerful | 5.5 | 8.4 | 3.3 | |
Summary
The survey response rates among pupils whose parents allowed them to take part were 92% at baseline (TP1), 90% at 6 months (TP2) and 84% at 12 months (TP3). Levels of missing data were low for all variables. The highest rate of missing data was seen for WEMWBS, which was the last set of questions in the survey pack. A comparison of the distributions of AUDIT and AUDIT-C scores between subgroups at TP1 demonstrated that gender, smoking and sexual behaviour were significantly associated with young people’s current drinking behaviour. The comparisons of scores over three time points suggests that there was little or no change in measures of alcohol use, alcohol-related problems and well-being within this age group over the course of a year, except for small but statistically significant shifts upwards in the distributions of AUDIT, AUDIT-C and A-SAQ between the first and second surveys. In every school, mean AUDIT scores were higher for young people who did not leave their names on the questionnaire than for those who did.
Chapter 5 External pilot trial
Key points for Chapter 5
-
Seven schools were randomised to the three trial arms – control (n = two), intervention 1 (n = two), intervention 2 (n = three) – and retained at 12-month follow-up.
-
Sixteen per cent of young people who completed the survey at TP1 met eligibility criteria for the trial; 80% of those eligible were recruited into the trial.
-
Eighty per cent of those recruited into the trial completed the 12-month follow-up.
-
Of the 75 young people recruited to intervention 2, only eight (10%) received both the individual and family-centred interventions: the remainder received only the individual-level intervention (intervention 1).
-
There were very low levels of missing data at both baseline and 12-month follow-up.
-
The TLFB was completed with all young people who attended at 12-month follow-up. There was some evidence that results on AUDIT, AUDIT-C and A-SAQ scales showed a slight shift to less alcohol consumption or risk behaviours at 12 months compared with baseline.
The external pilot trial was a parallel-group, three-arm cRCT with randomisation at the level of schools. A cluster randomised design was chosen to reduce the potential for bias due to contamination between young people allocated to different arms within the same school. The three arms were control, intervention 1 and intervention 2 (details of interventions are given in Chapter 3). The primary aim of the pilot trial was to assess feasibility and acceptability to plan a future definitive trial, including estimating rates of eligibility, consent, participation and retention at 12 months.
Process and measures: baseline
The questionnaire distributed at TP1 provided young people with the opportunity to volunteer their contact information or to complete the questionnaire anonymously. This TP1 questionnaire facilitated screening for the trial, and young people who screened positive for risky alcohol use using the A-SAQ and who provided their name at TP1 were invited to attend an appointment with a learning mentor to assess eligibility and provide consent. Young people were excluded from participation if they were already seeking help for an alcohol use disorder (AUD), receiving support from child and adolescent mental health services or had not been given consent by parents to take part.
Process and measures: 12-month follow-up
Twelve-month follow-up appointments with trial participants took place when young people had begun the next school year (Year 11). Collection of follow-up data began in January 2013 and was completed in April 2013. Trial participants who had moved schools during this time and were unable to be contacted for this appointment were lost to the trial. No trial participants had language or literacy problems that required additional support with reading the documentation. The session involved completion of three separate questionnaires: A-SAQ, AUDIT and 28-day TLFB, chosen to measure different aspects of drinking behaviour and anticipated to be primary or secondary outcome measures in a future definitive trial. All three measures were completed during a single one-to-one appointment with a learning mentor, which took place during school time. The order of presentation of A-SAQ and AUDIT were randomised and completed by the young person alone, with the TLFB being the last tool completed with the learning mentor. Wherever possible, the same learning mentor conducted both intervention and follow-up sessions. However, owing to staffing changes at participating schools, on some occasions a different learning mentor conducted the follow-up appointment. If this learning mentor was a newly recruited member of school staff then he/she was provided with a condensed training session, focusing on the intervention delivery phase of the study, in addition to training in how to deliver the 12-month follow-up appointment. The planned primary outcome for a future definitive trial is the 28-day TLFB questionnaire, completed by trial participants at 12-month follow-up. The TLFB has been validated for use in this population168–170 and involves a retrospective interview administered by the learning mentor to ascertain actual alcohol consumed over the 28-day period prior to the interview. Four alcohol consumption measures were derived from the 28-day TLFB: total alcohol units consumed in a 28-day period, percentage of days abstinent, mean number of drinks per drinking day, and number of days on which alcohol consumption was more than two units. The questionnaire invites participants to recall their daily alcohol consumption over the 28-day period and can examine total alcohol consumption as well as patterns of alcohol consumption (see Appendix 3). It is important that sufficient information is recorded to calculate accurately the units of alcohol consumed, including the type (and brand) of alcohol and the volume (or size of container) of alcohol consumed. To facilitate collection of data, learning mentors were provided with prepared copies of the 28-day TLFB questionnaire. Tools were marked with dates (such as Christmas, examination periods and local football games) in order to provide prompts and aid form completion. Other memorable dates specific to the young person were identified and used to aid recollection.
Design
Pilot trial sample size
As this was a pilot trial, a formal power calculation was not required. However, providing data to design a future definitive trial is an important function of a pilot study. A minimum number of 30 participants per intervention group at follow-up has been recommended to estimate key parameters for this purpose. 171 We used data from previous studies to estimate the proportions of young people who would be eligible, consent to enter the study and provide data at 12-month follow-up. 97,127 Our estimates suggest that the minimum number of 30 per arm providing follow-up data would be achieved if all pupils in Year 10 across seven schools were invited to take part (Figure 9). Note that we estimated that recruitment would be much lower for the intervention 2 arm, so two schools were randomised to each of the control and intervention 1 arms, but three schools were randomised to the intervention 2 arm.
FIGURE 9.
Estimates of eligibility, recruitment and retention used to plan the sample size of the pilot trial. The estimates are based on previous studies: a, 22% follow-up;127 b, 79% follow-up;126 c, 88% conservative estimate of take-up rate taken from Walton et al. 97 and Conrod et al. ;127 d, 65% follow-up rate. 172
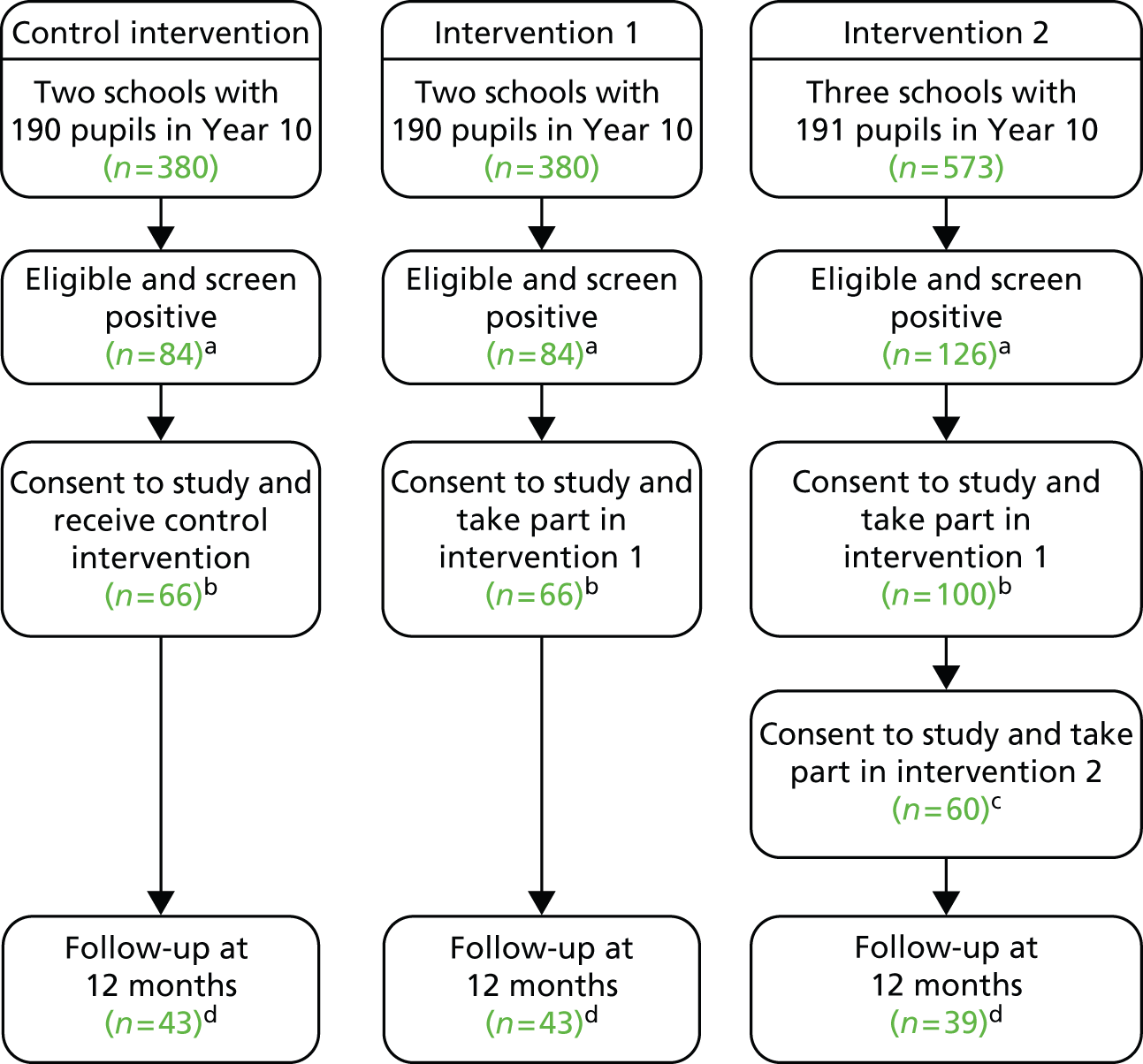
Pilot trial outcomes
-
Percentage of those who did not meet exclusion criteria, completed the TP1 survey and were positive on A-SAQ, and provided their name and contact details (% eligible).
-
Percentage of eligible young people who were recruited to trial (% recruited).
-
Percentage of those recruited who provided data at 12-month follow-up (% retained).
A key aim of the feasibility study was to investigate whether the primary and secondary outcomes and baseline characteristics in a definitive trial could be measured on all participants.
Methods
Randomisation
Schools agreed to take part in the study prior to randomisation, and were subsequently informed of their allocated intervention. Allocation to trial arm was conducted by the study statistician with randomisation at the school level. The study catchment area enabled broad population coverage and the randomisation achieved balance on two school-level variables (numbers of pupils in school year and proportion receiving free school meals) (Table 7). Neither school staff and pupils nor researchers were blind to the intervention allocated.
| School site and study condition | No. of pupils in Year 10 | % of free school meals |
|---|---|---|
| School F (control) | 250 | 12 |
| School G (control) | 176 | 6 |
| School E (intervention 1) | 268 | 8 |
| School A (intervention 1) | 194 | 15 |
| School C (intervention 2) | 98 | 33 |
| School B (intervention 2) | 138 | 13 |
| School D (intervention 2) | 351 | 2 |
It is common in cRCTs that participants are not blind to the intervention they receive. 173 In this pilot trial, schools were not aware of to which trial arm they had been assigned at the time they agreed to take part. In addition, the pupils were screened before the random allocation of their school to trial arms was known. They were told that they might be chosen to receive advice on their drinking in one of three ways, and were not aware of which this might be at the time they were invited to take part in the study. This approach should have avoided any potential bias at the recruitment stage. 174
It was necessary for the learning mentors to be aware of the trial allocation. There is potential for ‘resentful demoralisation’ of those delivering the intervention if they have not been allocated to the trial arm that they prefer. 175 However, in this study, the head teachers and learning mentors were very keen to receive any training about dealing with alcohol issues (and those in all arms received general advice) and there did not appear to be any disappointment with the allocations.
Statistical analysis
The eligibility, recruitment and retention rates for the schools and young people have been summarised in a Consolidated Standards of Reporting Trials (CONSORT) diagram (Figure 10). The data collected for trial participants at TP1 and TP3 were summarised with descriptive statistics by trial arm, and combined across trial arms. This was to investigate suitability of scales and variables for a future definitive study, to establish baseline characteristics, and to summarise the outcomes. The percentage of missing and implausible values was reported for all variables, along with either a five-number summary (minimum, lower quartile, median, upper quartile, maximum) for numeric variables, or numbers and percentages in each category for categorical variables. In addition, at TP3, the variables derived from the 28-day TLFB and the AUDIT and AUDIT-C measures were summarised by their mean and standard deviation (SD): these were used to inform a sample size calculation for a definitive trial, and the comparison of mean and median values allowed consideration of the shape of each distribution. All analyses used the intention-to-treat populations.
FIGURE 10.
Trial CONSORT diagram. LM, learning mentor.
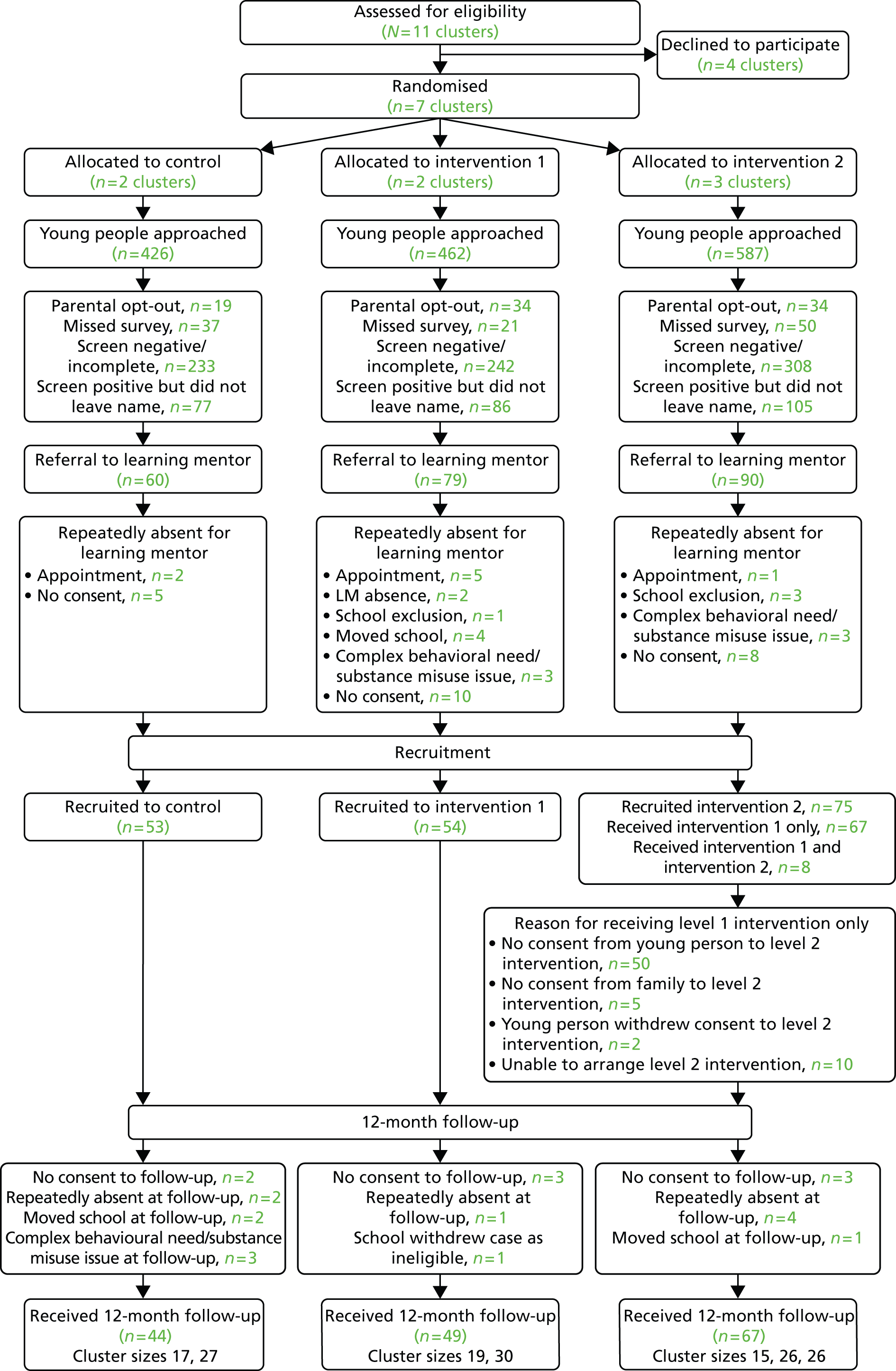
Results
Recruitment and retention
Eleven schools were assessed as eligible to participate in the trial (Figure 10). Four of the eleven schools did not respond to our contact/declined to participate, and seven schools agreed to meet with the research team to discuss the project. One school said no to participating in the study, based on current workload and staff commitments. Three schools did not return telephone and e-mail messages. Once the required number of schools were recruited (seven) the research team did not continue to contact the three schools from which we had received no response. All schools who met with a researcher subsequently agreed to take part in the study. Therefore seven schools were randomised to the three trial arms – two to the control arm, two to intervention 1 and three to intervention 2. There were 1475 young people aged 14 and 15 years in Year 10 across the seven schools. Of those, 195 (13.2%) were either opted out by parents or not at school when the survey took place. A further 1051 (71.3%) scored negative on the A-SAQ (783, 53.1%). Of the total, 498 scored positive on the A-SAQ (38.9%). There were 268 who scored positive but did not leave their names (268, 18.2%). This left 229 young people (15.5% of combined year groups) who were potentially eligible for the trial and were referred to a learning mentor to discuss their possible enrolment in the trial. This number was lower than expected (i.e. 22%), probably because not all young people left their names, to allow them to be contacted about the trial. At this stage, a further 47 young people were not recruited to the pilot trial for a number of reasons including repeatedly not turning up for their appointment with the learning mentor (8, 3.5%), not consenting (23, 10.0%), moving school (4, 1.7%) or behavioural issues (10, 4.4%). This left 182 (79.5% who were eligible) young people who were recruited to the trial. This recruitment rate is close to that expected when planning the study. There were 53 in the Control arm, 54 in the Intervention 1 arm who received Intervention 1 and 75 in Intervention 2 arm.
All young people allocated to the control and intervention 1 arms received their intervention as planned. In the intervention 2 arm, all 75 received intervention 1 but 57 young people and/or their families did not consent to the family meeting (intervention 2), and a family meeting could not be arranged for a further 10, leaving just eight young people who received both Interventions 1 and 2 (10.7% of those allocated to the intervention 2 arm) (see Figure 10).
Across all arms, eight young people did not consent to follow-up at 12 months (TP3). In addition, seven were repeatedly absent at follow up, three had moved school, three had behavioural issues and one was withdrawn by the school. This meant that 160 (88%) young people completed the 12-month follow-up: 44 (83%) in the control arm, 49 (90.1%) in intervention 1 and 67 (89.3%) in intervention 2. These retention rates were higher than those that were expected when planning the trial. So, overall, of the initial 1475 young people approached, 15.5% were eligible for the trial (14.2% of self-reported drinkers); 79.5% of the 229 eligible young people were recruited; and 88% of the 182 recruited provided follow-up data.
Characteristics of trial participants at baseline (time point 1)
Categorical data
The categorical baseline characteristics for the trial participants are summarised in Table 8.
| Variable | TP1 baseline data: distribution over categoriesa by trial arm (%) | |||
|---|---|---|---|---|
| Control, n = 53 | Intervention 1, n = 54 | Intervention 2, n = 75 | Overall, n = 182 | |
| Gender | ||||
| Missing | 0 | 0 | 0 | 0 |
| Male | 43.4 | 37.0 | 50.7 | 44.5 |
| Ethnic group | ||||
| Missing (%) | 0 | 1 (1.9) | 0 | 1 (0.5) |
| White | 96.2 | 100.0 | 98.7 | 98.3 |
| A-SAQ (per last 6 months) | ||||
| Missing | 0 | 0 | 0 | 0 |
| Four or more times but not every month | 34.0 | 31.5 | 29.3 | 31.3 |
| Once or more per month but not every week | 30.2 | 35.2 | 37.3 | 34.6 |
| Every week but not every day | 35.9 | 31.5 | 33.3 | 33.5 |
| Every day | 0 | 1.9 | 0 | 0.6 |
| Sex regretted after alcohol | ||||
| Missing (%) | 0 | 0 | 4 (5.3) | 4 (2.2) |
| Never had sex at all | 58.5 | 42.6 | 47.9 | 49.4 |
| Yes | 15.1 | 22.2 | 22.5 | 20.2 |
| No | 26.4 | 35.2 | 29.6 | 30.3 |
| Sex without condom after alcohol | ||||
| Missing (%) | 0 | 0 | 4 (5.3) | 4 (2.2) |
| Never had sex at all | 58.5 | 42.6 | 49.3 | 50.0 |
| Yes | 13.2 | 20.4 | 18.3 | 17.4 |
| No | 28.3 | 37.0 | 32.4 | 32.6 |
| Smoker | ||||
| Missing (%) | 1 (1.9) | 1 (1.9) | 4 (5.3) | 6 (3.3) |
| Yes | 44.2 | 35.9 | 40.9 | 40.3 |
| Age when first smoked | ||||
| Missing (%) | 0 | 1 (1.9) | 1 (1.3) | 2 (1.1) |
| Never smoked | 34.0 | 37.7 | 33.8 | 35.0 |
| ≤ 8 years | 0.0 | 1.9 | 4.1 | 2.2 |
| 9–10 years | 5.7 | 1.9 | 8.1 | 5.6 |
| 11–12 years | 30.2 | 28.3 | 21.6 | 26.1 |
| 13–14 years | 28.3 | 26.4 | 29.7 | 28.3 |
| > 14 years | 1.9 | 3.8 | 2.7 | 2.8 |
| Use of free timeb | ||||
| With friends at your house or theirs | 32.1 | 33.3 | 48.0 | 39.0 |
| Go out somewhere with friends | 79.2 | 66.7 | 72.0 | 73.1 |
| Spend time with your family | 11.3 | 7.4 | 13.3 | 11.0 |
| Spend time with siblings | 1.9 | 0.0 | 8.0 | 3.8 |
| Spend time by yourself | 17.0 | 18.5 | 18.7 | 17.6 |
Gender was not evenly distributed across the trial groups. The intervention 1 arm comprised 37% males, with control and intervention 2 having 43% and 51% males, respectively. Ethnic group was fairly evenly distributed, with very few non-white participants in each arm, reflecting the ethnic mix of the local authority. 175
The eligibility criterion for the trial was a minimum A-SAQ score (reporting drinking more than three units at least four or more times in the last 6 months), so at TP1 all reported at least this frequency. There are similar percentages of participants across the trial arms reporting consumption in the three highest categories possible at this time point. Just one participant in the intervention 1 arm reported daily drinking.
Overall, 40% of participants reported that they were smokers, although the intervention 1 arm had a slightly lower percentage than the other two groups (36%). This compares with 29% of young people aged 14 years and 45% aged 15 years in the general population. 4 The age when participants first smoked was fairly evenly distributed across the three trial arms. Few began smoking before the age of 10 years, with a majority of current smokers beginning to smoke between the ages of 11 and 14 years. Forty-nine per cent of participants said they had never had sex (control, 59%; intervention 1, 43%; intervention 2 48%). Of those who had engaged in sex, 40% had regretted sex after drinking alcohol and 35% had sex without a condom after drinking alcohol. There were slightly fewer young people answering ‘yes’ to those questions in the control arm than in the other two arms.
The use of free time questions seemed to be similarly distributed across the trial arms. The most popular way to spend free time was going out with friends, with 73% of participants ticking this box. The next most popular use of free time was meeting friends at the friend’s or the participant’s home, with 39% of participants responding positively. However, there were substantially more answering positively in the intervention 2 group (48%). Spending time with brothers and sisters, with family or on their own were the least popular options (3.8%, 11% and 17.6% respectively).
We looked to see whether there were any problems with either missing data or implausible values for some scales, to help decide which variables should be included in a future trial. Missing values for the categorical baseline characteristics (see Table 9) were very low, with the maximum being four respondents to the questions about smoking status and sex in the intervention 2 arm. No missing values were recorded for the questions about free time, as these were tick-box questions for positive answers. However, there was one (1.0%) young person in the control arm, two (3.7%) young people in the intervention 1 group and two (2.7%) young people in the intervention 2 group who did not tick any boxes about the way they spent their free time, which may indicate that none of these activities was one in which they took part and also that they did not answer these questions.
| Measure (potential scale range) | Variable by trial arm | TP1: baseline data for trial participants | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | Missing (%) | Implausible values (%)a | n available | Minimum | Lower quartile | Median | Upper quartile | Maximum | ||
| AUDIT (0–40) | Control | 53 | 5.7 | – | 50 | 1 | 3 | 8 | 13 | 25 |
| Intervention 1 | 54 | 1.9 | – | 53 | 1 | 5 | 9 | 13 | 36 | |
| Intervention 2 | 75 | 6.7 | – | 70 | 0 | 4 | 8 | 13 | 31 | |
| Overall | 182 | 4.9 | – | 173 | 0 | 4 | 8 | 13 | 36 | |
| AUDIT-C (0–12) | Control | 53 | 5.7 | – | 50 | 1 | 2 | 4 | 6 | 10 |
| Intervention 1 | 54 | 1.9 | – | 53 | 1 | 3 | 5 | 6 | 12 | |
| Intervention 2 | 75 | 6.7 | – | 70 | 0 | 3 | 4 | 6 | 10 | |
| Overall | 182 | 4.9 | – | 173 | 0 | 3 | 4 | 6 | 12 | |
| RAPI (0–69) | Control | 53 | 0.0 | – | 53 | 0 | 0 | 5 | 12 | 59 |
| Intervention 1 | 54 | 1.9 | – | 53 | 0 | 3 | 7 | 12 | 60 | |
| Intervention 2 | 75 | 8.0 | – | 69 | 0 | 1 | 5 | 12 | 49 | |
| Overall | 182 | 3.8 | – | 175 | 0 | 2 | 6 | 12 | 60 | |
| WEMWBS (14–70) | Control | 53 | 3.8 | – | 51 | 18 | 40 | 45 | 53 | 64 |
| Intervention 1 | 54 | 5.6 | – | 51 | 14 | 39 | 45 | 54 | 69 | |
| Intervention 2 | 75 | 18.7 | – | 61 | 23 | 44 | 47 | 55 | 70 | |
| Overall | 182 | 10.4 | – | 163 | 14 | 39 | 46 | 54 | 70 | |
| Physical activity last week – days (0–7) | Control | 53 | 7.5 | 7.5 | 45 | 0 | 2 | 4 | 5 | 7 |
| Intervention 1 | 54 | 7.4 | 7.4 | 46 | 0 | 2 | 4 | 5 | 7 | |
| Intervention 2 | 75 | 9.3 | 8.0 | 62 | 0 | 3 | 4 | 6 | 7 | |
| Overall | 182 | 8.2 | 7.7 | 153 | 0 | 2 | 4 | 5 | 7 | |
| Physical activity typical week days (0–7) | Control | 53 | 3.8 | 7.5 | 47 | 0 | 2 | 4 | 5 | 7 |
| Intervention 1 | 54 | 7.4 | 5.5 | 47 | 0 | 2 | 4 | 5 | 7 | |
| Intervention 2 | 75 | 6.7 | 12.0 | 61 | 0 | 2 | 4 | 5 | 7 | |
| Overall | 182 | 6.0 | 8.8 | 155 | 0 | 2 | 4 | 5 | 7 | |
| No. of pieces of fruit on a typical day (0–14) | Control | 53 | 1.9 | 0.0 | 52 | 0 | 1 | 2 | 3 | 6 |
| Intervention 1 | 54 | 0.0 | 0.0 | 54 | 0 | 1 | 2 | 2 | 10 | |
| Intervention 2 | 75 | 1.3 | 0.0 | 74 | 0 | 1 | 2.5 | 3 | 10 | |
| Overall | 182 | 1.1 | 0.0 | 180 | 0 | 1 | 2 | 3 | 10 | |
| Portions of vegetables on a typical day (0–22) | Control | 53 | 3.8 | 0.0 | 51 | 0 | 1 | 2 | 3 | 6 |
| Intervention 1 | 54 | 1.9 | 0.0 | 53 | 0 | 1 | 2 | 3 | 7 | |
| Intervention 2 | 75 | 6.7 | 0.0 | 70 | 0 | 1 | 2 | 3 | 10 | |
| Overall | 182 | 4.4 | 0.0 | 175 | 0 | 1 | 2 | 3 | 10 | |
Numeric data
The distribution of numeric baseline (TP1) variables for the trial participants is summarised in Table 9.
The AUDIT scores were similarly distributed across the trial arms, with median scores per arm of 8 to 9. There was a wide range of scores reported. AUDIT-C scores were similarly distributed across the trial arms, with median scores of 4 or 5, and a wide range of scores reported. The RAPI score measured alcohol problems, with higher scores indicating more risky drinking. Median scores were comparatively low and similar between trial arms (medians of 5 or 7).
The WEMWBS scale assessed general psychological health, with higher scores indicating greater well-being. Extremes at both ends of the scale were occasionally reported. Typical values were similarly distributed across the trial arms, with median scores of 45 or 47.
For the measures of physical activity and daily consumption of portions of fruit and vegetables there was little difference between distributions across the trial arms. The median numbers of days on which participants exercised in the last or a typical week was two. Fruit and vegetable consumption was low, with two being the median number of items consumed on a typical day.
We looked to see whether there were any problems with either missing data or implausible values for some scales to help decide which variables should be included in a future trial. For AUDIT and AUDIT-C there were three missing values in the control group, one in the intervention 1 arm and five in the intervention 2 arm. For the RAPI, there were no missing scores in the control group, one missing score in intervention 1, and six missing scores in intervention 2. For WEMWBS, the numbers of missing scores were two, three and 14, respectively, across the arms. For the measures of physical activity and the amount of fruit and vegetables consumed, up to seven young people failed to answer. There were no implausible values for portions of fruit and vegetables consumed, but for the measures of physical activity there were between four and nine implausible values in each arm (reporting activity on > 7 days per week).
Results of outcome measures at 12-month follow-up (time point 3)
The four outcome measures derived from 28-day TLFB plus the results of A-SAQ, AUDIT and AUDIT-C collected at 12-month follow-up (TP3) are reported in Table 10. The five-number summaries show that there is a lot of variation within the groups. Across all the trial participants the range for the units of alcohol consumed in the 28-day period was 0–235 units, with a median of 10.3, a mean of 22.7, and a large SD of 36.3. There were occasional participants who reported consuming very high total amounts of alcohol; however, staff were trained in how to use the TLFB to maximise the validity of the answers. Typical levels are less well balanced between trial arms, with median levels of around eight in the control and intervention 2 arm and 14 in the intervention 1 arm.
| Measure (potential scale range) | Trial arm | TP3: 12-month follow-up trial outcomes | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Missing (%) | Minimum | Lower quartile | Medium | Upper quartile | Maximum | Mean | SD | |||
| Units of alcohol consumed in 28-day period | Control | 44 | 0 | 0 | 0.8 | 8.4 | 31.8 | 234.7 | 27.6 | 47.9 | |
| Intervention 1 | 49 | 0 | 0 | 1.3 | 14.1 | 33.6 | 93.4 | 22.6 | 25.4 | ||
| Intervention 2 | 67 | 8 (11.9) | 0 | 0 | 8 | 21.4 | 189.9 | 19.1 | 34.1 | ||
| Overall | 160 | 8 (5.0) | 0 | 0.7 | 10.3 | 30.0 | 234.7 | 22.7 | 36.3 | ||
| Percentage days’ abstinence | Control | 44 | 0 | 68 | 86 | 93 | 96 | 100 | 90.8 | 8.7 | |
| Intervention 1 | 49 | 0 | 75 | 86 | 93 | 96 | 100 | 91.5 | 6.8 | ||
| Intervention 2 | 67 | 4 (6.0) | 50 | 86 | 93 | 100 | 100 | 91.2 | 10.4 | ||
| Overall | 160 | 4 (2.5) | 50 | 86 | 93 | 96 | 100 | 91.2 | 8.8 | ||
| Drinks per drinking day | Control | 44 | 10 (22.7) | 0.5 | 3.1 | 7.8 | 12.2 | 28.3 | 9.3 | 8.1 | |
| Intervention 1 | 49 | 8 (16.3) | 0.6 | 2.9 | 7.6 | 11.7 | 21.3 | 8.1 | 5.7 | ||
| Intervention 2 | 67 | 26 (38.8) | 0.8 | 4 | 5.6 | 10.7 | 28 | 7.9 | 6.2 | ||
| Overall | 160 | 44 (27.5) | 0.5 | 3.3 | 7.3 | 11.0 | 28.3 | 8.4 | 6.6 | ||
| Days, more than two units | Control | 44 | 0 | 0 | 0 | 1 | 3 | 9 | 2.1 | 2.3 | |
| Intervention 1 | 49 | 0 | 0 | 0 | 2 | 3 | 6 | 1.9 | 1.9 | ||
| Intervention 2 | 67 | 8 (11.9) | 0 | 0 | 1 | 3 | 14 | 1.8 | 2.4 | ||
| Overall | 160 | 8 (5.0) | 0 | 0 | 1 | 3 | 14 | 1.9 | 2.2 | ||
| AUDIT (0–40) | Control | 44 | 0 | 0 | 3 | 6 | 10 | 28 | 7.1 | 5.6 | |
| Intervention 1 | 49 | 0 | 0 | 4 | 6 | 11 | 24 | 7.5 | 5.6 | ||
| Intervention 2 | 67 | 4 (6.0) | 0 | 3 | 5 | 9 | 21 | 6.1 | 4.4 | ||
| Overall | 160 | 4 (2.5) | 0 | 3 | 5 | 9.5 | 28 | 6.8 | 5.2 | ||
| AUDIT-C (0–12) | Control | 44 | 0 | 0 | 3 | 4 | 6 | 10 | 4.4 | 2.4 | |
| Intervention 1 | 49 | 0 | 0 | 3 | 5 | 6 | 9 | 4.4 | 2.4 | ||
| Intervention 2 | 67 | 1 (1.5) | 0 | 2 | 4 | 5 | 9 | 3.9 | 2.0 | ||
| Overall | 160 | 1 (0.6) | 0 | 3 | 4 | 6 | 10 | 4.2 | 2.2 | ||
| A-SAQ | Distribution across categories (%): frequency in last 6 months | ||||||||||
| Never | Fewer than four times | Four or more times but not every month | More than once per month but not every week | Every week but not every day | Every day | ||||||
| Control | 44 | 1 (2.3) | 6.9 | 18.6 | 25.6 | 32.6 | 16.3 | 0 | |||
| Intervention 1 | 49 | 0 | 8.2 | 14.3 | 32.7 | 28.6 | 16.3 | 0 | |||
| Intervention 2 | 67 | 0 | 6.0 | 28.4 | 26.9 | 23.9 | 14.9 | 0 | |||
| Overall | 160 | 1 (0.6) | 6.9 | 21.4 | 28.3 | 27.7 | 15.7 | 0 | |||
Percentage days abstinent (from TLFB) had similar distributions across the trial arms (median per arm = 93%), as did days consuming more than two units (median per arm = 1 or 2). For drinks per drinking day, there was also some variability between the trial arms (medians 7.8, 7.6 and 5.8). Note that this variable cannot be calculated for those participants who do not consume any alcohol in the 28-day period.
There was a wide range observed in AUDIT scores at TP3 (0–28), but little variation between trial arms (medians 5–6). A similar pattern was seen in AUDIT-C scores, for which the trial arm median scores were ‘4–5’. For AUDIT and AUDIT-C we have data at TP1 and TP3. The median AUDIT score across all arms was lower at TP3 (‘5’) than at TP1 (‘8’), although there is no change in medians for AUDIT-C (‘4’) between TP1 and TP3. No formal comparisons were carried out, so any changes must be interpreted with caution. Some young people were lost to follow-up because of complex behavioural problems, repeated absence, moving school, or deciding that they no longer wished to participate in the trial. The median AUDIT score at TP1 of the 22 participants who dropped out by TP3 was ‘14.5’ and their median AUDIT-C score was ‘5.5’. Given some of the reasons for loss to follow-up, it is perhaps not surprising that typical AUDIT scores for young people retained at TP3 were lower than at baseline for all of those entering the trial. However, when only those participants who provided AUDIT scores at both TP1 and TP3 are included in the analysis, there does appear to be a slight tendency towards a reduction in AUDIT scores (although this was not seen for AUDIT-C scores). This is illustrated in Figure 11 where the distribution of individual changes in AUDIT scores is shown across trial arms. There was considerable variation in the change scores (AUDIT score at TP1 – AUDIT score at TP3) indicating both increases and decreases over the year. However, although the median change is zero for the control and intervention 2 trial arms, it can be seen that, in all arms, the positive changes (indicating lower AUDIT score at TP3) tend to be larger than the negative ones. However, any difference between trial arms must be interpreted with caution, as they are based on data from only two or three clusters.
FIGURE 11.
Distribution of individual change in AUDIT scores between TP1 and TP3 by trial arm.
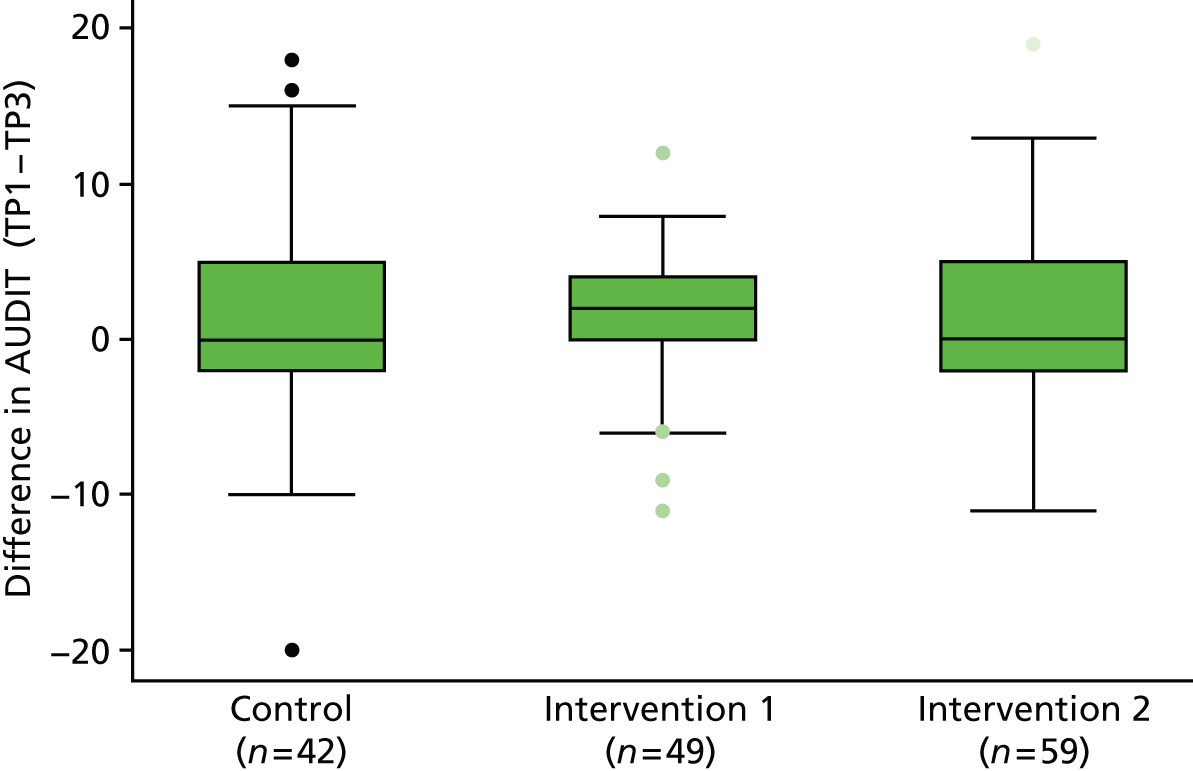
We also had the distribution of the A-SAQ question available at TP1 and TP3. The summary statistics in Table 10 show that the distribution was shifted towards less frequent consumption at TP3 than at TP1. All had reported drinking four or more times in the last 6 months at TP1, but by TP3, 28% across all arms reported less frequent drinking than this. The percentage of young people reporting drinking every week had also approximately halved in all arms.
The reduction in alcohol use over 12 months in the AUDIT and A-SAQ measure was observed in all trial arms. This may have reflected a general change in drinking behaviour or socially desirable responses due to taking part in the trial, rather than a response to a particular intervention.
At TP3, levels of missing data were very low. For the TLFB measures (units of alcohol consumed in a 28-day period, percentage of days when abstinent, and days consuming more than two units), only the intervention 2 arm had any missing data. This amounted to 12% of missing data for units of alcohol consumed and days consuming more than two units, and 6% for percentage days abstinent. The higher numbers of missing values for drinks per drinking day is due to some of the young people not drinking at all during the 28-day period, and therefore not having a value for this. This applied to 10 young people in the control group (23%), eight in intervention 1 (16%) and 26 in intervention 2 (39%). For the other outcome measures at TP3, there were missing data again only for AUDIT and AUDIT-C in the intervention 2 arm – 6% and 1.5%, respectively. One young person failed to complete the A-SAQ in the control group.
Fidelity of the interventions
Fidelity of an intervention within research refers to the extent to which the intervention is true to the therapeutic principles on which it is based. 176 It requires the manualisation of the intervention wherein the philosophy, principles and procedures of the intervention are clearly described. This manual can then be used by the individuals delivering the intervention in order to deliver a standardised approach. 177 Moreover, a manualised intervention with verified fidelity enables the research to be replicated or the intervention to be implemented in practice.
Learning mentors were asked to record at least one session each; however, only six recordings of intervention delivery were made. In this study the BECCI was used to measure fidelity. BECCI is a tool developed specifically to measure the microskills of behaviour change counselling and MI. 178 The instrument focuses upon the practitioner’s consulting behaviour and attitude rather than the patient’s response. A qualified member of the team (RM) rated intervention 1 and intervention 2 audio-recordings. Rating was completed in line with the BECCI Manual for Coding Behaviour Change. 179 The mean BECCI score for the six recorded interventions was ‘2.5’, which suggested that the learning mentors were all found to be delivering behaviour change counselling to ‘some extent’ or to ‘a good deal’ as assessed with the BECCI. The median BECCI score was ‘2.55’, with the range 1.9–3.0 (individual scores were 1.9, 2.1, 2.3, 2.8, 2.9 and 3.0). Learning mentors typically performed well when discussing the risks associated with the young person’s alcohol use. Lower scores were assessed when measuring microskills relating to discussing and exploring behaviour change. Future training of mentors in intervention delivery should focus upon discussing behaviour change with young people.
The small number of interventions that were recorded is a weakness that would need addressing in a full trial. In the feasibility study, learning mentors, randomised to either group other than the control, were approached and asked to record a minimum of one recording. A more formal approach to fidelity measurement is required. In a definitive study, learning mentors will be asked to record a simulated intervention with an actor immediately following training but before commencing the trial. Further training can then be provided on areas of practice weakness. A specific date will then be agreed for a further recording of intervention delivery with a trial participant.
Summary
The required number of schools (seven) were recruited into the feasibility pilot trial and retained at 12-month follow-up. Ninety-two per cent of young people in Year 10 (aged 14–15 years) across the seven schools completed the survey used to screen for inclusion into the trial. Sixteen per cent of those completing the survey met eligibility criteria and 80% of those eligible were recruited into the trial. Eighty-eight per cent of those recruited into the trial completed the 12-month follow-up. However, of the 75 recruited into the intervention 2 arm, only eight (10%) received both individual and family-centred interventions: the remainder received only the individual-level intervention (intervention 1). The trial arms were not well balanced on all variables at baseline, but this is not surprising for a cluster randomised trial with very few clusters and heterogeneity between clusters. There were very low levels of missing data on each score or variable at both baseline and 12-month follow-up. Furthermore the interview held to complete the 28-day TLFB was successfully achieved in all who attended the 12-month follow-up meeting with a learning mentor. Finally, there was some evidence that results on AUDIT, AUDIT-C and A-SAQ scales showed a slight shift to less alcohol consumption or risk behaviours at 12 months compared with baseline.
Chapter 6 Interviews with staff, young people and parents
Key points for Chapter 6
-
Semistructured interviews were conducted with six lead liaisons, 13 learning mentors, 27 young people and seven parents (n = 53).
-
Overall, the school was considered to be a feasible and acceptable environment to intervene with young people who are risky drinkers.
-
Learning mentors were seen as being best placed to discuss alcohol with young people owing to their role within the school, their existing supportive relationships with young people and the trust that young people placed in them.
-
The screening survey was found to be feasible, although in future work some consideration may need to be given to means of enhancing young people’s privacy in order to increase acceptability.
-
Intervention 1 was found to be feasible and mostly acceptable. Some learning mentors expressed hesitation at informing young people for whom their drinking placed them at risk of harm and the calorie-focused content resulted in mixed views from both learning mentors and young people.
-
Intervention 2 did not appear to be feasible. Learning mentors, parents and young people questioned the utility of an intervention that they believed was not engaging the ‘right’ people. Although parents who did engage in intervention 2 found the intervention to be acceptable, most young people and their parents who were offered did not express a desire to take part in this intervention or a benefit from doing so, and some young people who were interviewed told us that they did not want their parents involved.
For the integrated qualitative evaluation of the study, semistructured interviews were conducted with four key groups of participants: school lead liaisons; learning mentors; young people; and parents. This chapter begins with a description of the methods used in the conduct and analysis of these interviews, continues with a summary of the key findings, and concludes with a discussion of the overarching emergent themes from the qualitative phase of the study, alongside the limitations of the work.
Methods
Semistructured interviews were selected as the primary mode of qualitative data collection in order to inform a more in-depth understanding of the overarching research questions for the study. The aims for all sets of interviews were to explore the feasibility and acceptability of screening and BI approaches in the school setting, and to elicit participants’ views on the study measures and processes used in delivering the project. Key topics for interviews with young people and their parents included consent procedures; parental involvement in interventions; the comprehensibility and burden of study measures and follow-up procedures; and the appropriateness of school-led health promotion work across the school–home interface. All interviews were conducted between May and August 2012. Each participant was interviewed once and interviews were timed to take place as soon as possible after their involvement in study procedures had ended. Interviews with lead liaisons, learning mentors and young people were performed and analysed by KL. Interviews with parents were performed and analysed by SS.
Sampling strategy
As this was a qualitative study, the aim of sampling was to achieve data saturation and maximum variation of perspectives. School lead liaisons were defined as the seven key individuals who made or brokered the decision about participation in the study on behalf of their school. As there were only seven lead liaisons involved, all were approached for interview. Purposive sampling was undertaken within the remaining three participant groups to ensure maximum variation within the study population. For learning mentor interviews, defined as the members of school staff trained in the delivery of the control condition/interventions to participating students, sampling criteria were according to socioeconomic positioning of the school in which the learning mentor was used, and study condition.
For young people, sampling criteria were gender, socioeconomic status (SES) of school and the level of intervention received. SES and gender were considered important for this group because these factors are known to be related to drinking behaviour in this age group. 180 In addition, young people within the intervention 2 arm of the study were purposively sampled to include both those who agreed to family involvement and those who refused. This sampling frame resulted in 16 subgroups of young people to represent in interview.
For parent interviews, sampling criteria were SES of school and whether or not intervention 2 had successfully taken place. The latter criterion was included for two main reasons. First, there were a number of parents whom learning mentors had been unable to contact, using a range of different methods, to take part in a family intervention despite numerous attempts. Second, there were occasions when the parent agreed to take part in the intervention but the intervention did not take place, because either the parents or the young person changed their mind at a later date. It was felt that both of these groups of parents could give a useful insight into the complexities and dynamics of parental involvement in this form of intervention.
Recruitment and consent
A range of approaches was used in order to recruit interview participants into the study. Lead liaisons were approached directly by the researcher (KL) and learning mentors were, in turn, approached by their line manager (when not the school lead liaison) to ask if they would agree to be interviewed. Learning mentors acted as gatekeepers for interviews with young people, making the initial contact with the young person concerned, and setting up interview appointments on behalf of the researcher (KL). At each approach it was stressed that participation was entirely voluntary.
Learning mentors also helped facilitate access to parents for interview purposes. First, they contacted parents directly to confirm whether it was acceptable for a researcher (SS) to contact them about participation in an interview. If a parent had declined the family intervention (or learning mentors had struggled to contact them to arrange it), school staff attempted to contact them again (by phone, text message, e-mail and letter) to explain the purpose of interviews and to ask if their contact details could be given to the researcher. Parents were reassured that if they declined they would not be contacted about the study again.
Alternatively, if parents could not be contacted using these channels, learning mentors asked young people to invite parents for an interview and sent a message home with the young person, who was asked to provide contact information after checking with their parents that it was acceptable to pass this information on. It must be stressed that if young people withdrew their own consent for approaching parents then parents were not contacted to participate in an interview. Following an initial positive approach by the young person concerned, the researcher (SS) subsequently contacted parents, using a variety of methods (telephone, text message, e-mail and/or letter) to arrange interviews.
Interviews with lead liaisons, learning mentors and young people were all performed within their respective school setting. Interviews with parents took place at a time and place most convenient to the participant concerned. In practice, interviews were generally community based, comprising a mix of home interviews and interviews that took place in public locations, such as local coffee shops. One interview took place in the interviewee’s place of work.
Informed consent was taken at the beginning of interviews, after ensuring that the interviewee had read the Participant Information Sheet and been given an opportunity to discuss any questions or concerns with the interviewer. Interviews lasted between 20 and 90 minutes and were all digitally recorded, with the resultant data transcribed verbatim by professional transcribers. All interviewees were allocated a participant reference code to ensure anonymity and confidentiality, and an anonymisation log was maintained.
Interviews with participants
Table 11 summarises the number of interviews by interview group, according to school and study condition. Six of the seven lead liaisons were interviewed as part of the qualitative evaluation of the study. The remaining lead liaison was on maternity leave during this period and could not be interviewed during the study time frame. Thirteen participating learning mentors were interviewed. The majority of participating learning mentors were female and this dynamic is reflected in interview participants (male = 2, female = 11).
| School (condition) | No. of participants | N | ||
|---|---|---|---|---|
| Learning mentors | Young people | Parents | ||
| G (control) | 1 | 4 | n/a | 5 |
| F (control) | 2 | 4 | n/a | 6 |
| E (level one) | 2 | 4 | n/a | 6 |
| A (level one) | 1 | 3 | n/a | 4 |
| D (level two) | 3 | 4 | 3 | 10 |
| C (level two) | 2 | 4 | 1 | 7 |
| B (level two) | 2 | 4 | 3 | 9 |
| N | 13 | 27 | 7 | 47 |
In total, 27 young people were interviewed as part of this research (male = 12, female = 15). Every attempt was made to ensure that the sampling frame was saturated (i.e. at least one respondent arising from each cell). However, it should be acknowledged that the potential pool of young people who had agreed to intervention 2 was extremely limited, thus, in reality, all participants were approached for interview. In particular, there were no high SES males who agreed to intervention 2 and so it was not possible to interview a young person from within this category.
Finally, semistructured interviews were conducted with seven parents, all of whom were mothers. Three (of seven) schools were randomised to the intervention 2 arm of the study, with family members from these three schools invited to take part in an interview. Although it was initially anticipated that a mix of mothers, fathers and other nominated family members such as grandparents would participate in the intervention 2 family intervention, in practice, with the exception of one family intervention with a father, only mothers took part. One father (who said no to the family intervention) agreed to take part in an interview but later changed his mind upon the researcher’s arrival. This parent appeared to be very uncomfortable with the prospect of taking part in an interview, stating to the researcher several times that his child did not drink and did not have a problem with alcohol. Six interviewees had taken part in a family intervention; one interviewee had not. This was because the young person did not want to give up their free time to take part and changed his/her mind – not because the parent said no. Although we set out to interview parents who did not participate in an intervention, owing to the small number of parents recruited to the parental component of intervention 2, interviews with parents proved the most challenging to arrange and there were clear barriers to participation. Nevertheless, despite interviewing only one non-participating parent, this account provided a rich and comprehensive insight into the complexities and dynamics of parental involvement. Further, the accounts of lead liaisons, learning mentors and young people were also instrumental in developing our understanding of parental involvement.
On completion of the 53 interviews it was deemed by the research team that data saturation had been reached: this was determined as the point at which no new themes were emerging from the interviews.
Data analysis
The interview data were analysed thematically,181 with the Framework approach, devised by Ritchie and Lewis,182,183 utilised to organise the analysis. The Framework approach, which is a structured organisation of themes, ensured that the analysis could be easily viewed and assessed by others in the research team. 184 Coding of transcripts was performed by the researchers who had conducted the interviews (KL for lead liaison, learning mentor and young person interviews; SS for parent interviews). A computer software program, such as NVivo, was not used during data analysis, as the research team felt that use of a program that ‘cuts’ the data into smaller chunks would inhibit us from looking at the data in its totality, risk information being taken out of its original context and potentially lead to ‘over coding’, through which a deeper level of interpretation is lost. 185 Instead, coding was performed by hand, using paper copies of transcripts. Later, resulting frameworks of codes were recorded in table format in a spreadsheet document. Each participant was listed as a column, and each code, and related subcode, listed as a row. When a participant discussed a code, the page and line number reference was placed in the relevant cell of the table. This enabled effective organisation, storage and retrieval of coded data. Each group of interviews was analysed separately from each other. Regular meetings were held with members of the research team with expertise in qualitative techniques to discuss and challenge emergent themes and exchange analytical thoughts. This is referred to as pragmatic double coding by Barbour. 186 The aim of these meetings was not to value one point of view over another, rather they aimed to ‘maximise the analytic potential of exceptions or potential alternative explanations’ (p. 1026). 186
Findings
Feasibility and acceptability within the school setting
For many of the schools, being involved in research was a familiar activity and something with which they felt comfortable. A strong finding was that it was highly important that contact about SIPS JR-HIGH came from a local university. Participants felt that they had existing relationships with Newcastle University, and they felt that they could trust this university to ensure a collaborative approach to the research. Whereas other non-local universities might just have been seen to ‘use’ the school and the pupils (often this was from prior experience), Newcastle University could be trusted to feed back results to the school. Further, involvement with local universities was important in terms of raising aspiration for the pupils.
I feel we’ve got very strong relationship with Newcastle University, we’ve worked with you in the past doing research projects and I just always think I reserve my yes’s for research, cause we can only do so much . . . Em, but no I just think I mean we’ve done, we’ve done, we’ve done a number of things over the years em, with Newcastle em, I just think it’s always done well it’s always done well its always done with a lot of thought the planning’s always been excellent its always worked in the execution you get the impression there is a lot of kind of clout behind what’s happening em, so no I, I don’t know, I think partly it is the University em, and our relationship with them that kind of drives it a little bit.
Lead liaison, female
I think working with a local university you know we kind of feel like, I don’t want to say simpatico but you know we feel like, we feel like there is that kind of, that relationship where you know you’re very supportive of what, of what we’re doing in schools and, and, and likewise we want to you know support, support you.
Lead liaison, female
The school was generally considered to be an appropriate setting for addressing alcohol use in young people. Parents acknowledged that schools offered great opportunity for positive influence upon young people as well as access to adults they could trust and talk to outside the home environment. Learning mentors and lead liaisons also viewed addressing alcohol use by young people as a legitimate function of the school. Indeed, a number of the learning mentors and lead liaisons highlighted that alcohol is part of a wider range of issues faced by young people, that are considered within personal, social and health education.
I’m not sure that things like risk-taking and behaviour can stand alone, they’re actually more about self-esteem, personal development, resilience, identifying change, triggers, response, knowing that you’ll have some dips and you’ll have some dips, what can you draw upon motivationally yourself or with others to get back out. So I don’t think and that’s what happens quite a lot in education, you know the PSHE programmes like you know spring term year eight, week seven, road safety. I mean it’s more around personal skills and personal development I think.
Lead liaison, female
Learning mentors in particular highlighted the opportunity that the school environment offered to intervene with young people regarding alcohol. However, a number of learning mentors questioned whether young people would feel able to discuss their alcohol use within a school setting, highlighting the fear of ramifications. Some young people commented on this issue also, questioning whether the school would share information with parents. Trust, therefore, was considered by learning mentors and young people to be important to the feasibility and acceptability of ASBI within a school setting.
Although it was suggested that a school should be responsive to its pupils’ needs and both educate and care for the young people, members of staff cannot and should not fulfil all roles. There was a firm view that ‘teachers should just teach’, with both parents and young people reflecting that the authority that teachers hold within their role may be conflicted if they were privy to sensitive information relating to young people’s alcohol consumption. The pastoral focus typically involved within the learning mentor role resulted in a sense that addressing adolescent drinking was compatible with their responsibilities. Parents in particular identified learning mentors as being the ‘right’ member of staff to deliver the intervention. Most of the learning mentors reported feeling comfortable discussing alcohol with young people, feeling that they had legitimacy and adequacy within their role. Importantly, young people felt that they could talk to learning mentors about alcohol, with some commenting upon the existing relationship they have with learning mentors as well as the trust in sharing ‘private’ matters.
Because the mentors I know, he’s really canny so we had a good talk about it. So he made us get all my questions out so it was fine after . . . Every time he sees me he just asks me how I’m doing and that, so it’s fine, really. I’m not worried about what. Because he said it would be private so I’m fine with him knowing.
Young person, male
Almost half of the learning mentors reported that they had found it challenging to incorporate organising and delivering the intervention into their working week. For some, this difficulty related to restrictions being placed on when they could see the young people due to the academic curriculum. Contacting parents and children in order to organise the interventions was highlighted as being time-consuming. Others discussed unforeseen difficulties, such as a staff member being on sick leave. However, one learning mentor acknowledged that delivering intervention 1 to young people who had screened positive had been time-consuming, although she felt able to ‘make time’ for this within her role, owing to the importance she ascribed to the activity.
I mean that’s just one of those things, [it was] much more than I thought it was going to be but I’d still do it again because I believe in it, if I believe in something then I’ll make time for it.
Learning mentor, female
Although it was acknowledged that there was an additional burden of time, most learning mentors felt that they could feasibly include delivering ASBI within their role. One learning mentor reported ease at including the intervention in her working week:
I make my own timetable if you like. So I am not stuck to – I need to be here, here and here at certain times; so I can fit it in there. I can just go ‘Right I will just clear my diary for two days and just see – and fit all them in’.
Learning mentor, female
Indeed, some learning mentors commented that they regularly address emotional and behavioural issues with young people within their current role and as such did not perceive addressing alcohol with young people to be an additional task.
A lot of the things we talk about at the moment aren’t education related they’re to do with could be self-esteem or stress or we’ve had chats with people about eating disorders things like that you know we’ve had deep, I’m saying we as in I’m talking about the mentors because we do a similar job you know what I mean, we have spoken about lots of different things so again its necessary in our job role it’s not something that we sort of feel forced to do.
Learning mentor, male
Acceptability of the organisation and management of the study
Lead liaisons discussed their views of the initial approach by researchers regarding their potential involvement in the research project. This approach was viewed positively, with lead liaisons feeling that they were given enough information to enable them to make the decision regarding study participation. Further to this, lead liaisons talked favourably about the timing of the initial approach within the school timetable as well as the period of planning that had been incorporated into the study design:
I think it was fairly you know we’d had enough time to plan it, it wasn’t as if ‘oh can you do this next week?’ There was plenty of time to sort of plan ahead.
Lead liaison, male
It just hit at the time. I think when [researcher] got in touch it was when I was thinking of the next year’s curriculum and the next year’s planning and I had time to sit and listen to what she was saying.
Lead liaison, female
Moreover, lead liaisons were also very positive about the continued support offered by the research team to the involved schools as the study progressed:
. . . er I mean there were things I came back to which is I say more like the nitty gritty you know how’s it gonna happen you know, how are we going to do it type thing. Er and that was fine and that’s where [researcher] came in and we worked with [researcher] on the best way of making sure that we reached the maximum number of young people.
Lead liaison, male
Acceptability of training
Lead liaisons and learning mentors spoke very positively about the training that they received as part of the study. Indeed, lead liaisons viewed the training, skill development and the potential benefit this would have upon the pupils to be an incentive to participate in the study:
So from my point of view I think the real driver was em, you know if students are identified with issues or problems or maybe just beginnings of that I knew that em, those students would be offered intervention with our learning mentors but the university very kindly had trained so they felt even more skilled up talking to students. And I just thought that has to be a positive end result for us.
Lead liaison, female
Learning mentors were trained as a group together, at a time and place that was most convenient to them. This provided valuable opportunities to learn from each other and discuss the issues raised by the training in a group of peers:
I think the training was perfect, going . . . getting out the mix of going out of school for training and in school was good, going out for me because it meant that it was a break from in here and going somewhere else and em speaking with other people about it, like other learning mentors and seeing what other schools are involved. I thought that was really good. Em, and then the fact that you were able to come to us, that makes a huge difference. I don’t think you would have had the response that you have had if it was constantly that we need to go over there.
Learning mentor, female
Further, the learning mentors felt that the training and associated documents, such as the manual, prepared them fully for the study:
No I thought, we were all trained very well and we had loads of paperwork, loads of information and loads of prompts which were excellent, you know, you could read through a stage one, two, three, four, step one, two, three right through erm, lots of ideas here that we could ask, and I thought, you know, we were very well prepared.
Learning mentor, female
In addition, the learning mentors and lead liaisons reported that they felt the after-training support was very important:
[Researcher] came in quite a lot as well and we managed, we had quite a lot of time to talk to her you know and get advice from her and information . . . it was really handy to have her there to bounce questions off her and things like that so I felt that worked really well
Learning mentor, female
Importantly, study training and involvement was perceived to have a lasting benefit for the school. Learning mentors positively discussed benefits to their professional development, while one lead liaison reported intention to use the intervention tools within PSHE:
I thought they [intervention materials] were really good actually, no they were really really good. And I’m hoping that we might be able to use them actually. I’ve sort of shared them with the person, I hope its alright, with the person in PSHE who does that and there were certainly a lot of interesting ideas that we could develop from that sheet.
Lead liaison, male
Feasibility and acceptability of screening
Although most young people felt fully informed about the research project before taking part, some young people told us that teachers who were supervising did not always fully explain why the screening survey was taking place in their class. In particular, they were often unclear about the implications of including their name on the survey rather than anonymously, i.e. that they would be invited to an appointment with a learning mentor if they screened positive using a measure of hazardous and harmful alcohol consumption. This confusion is illustrated in the following quotes from young people:
I’m always used to doing tests and obviously you put your name down, and I thought it was a bit like a test really. I just put my name down, then when Miss called us I was like ‘Damn it’.
Young person, male
. . . teacher just says, ‘There’s a questionnaire on your desk. Whoever fills it like in gets a £5 cinema voucher.’ That’s all he said.
Young person, male
In general, young people told us that they chose to participate in the research project ‘to be helpful’ rather than because they felt that they were in need of advice about alcohol.
Although lead liaisons reported that they were highly satisfied with the organisation of the screening survey with particular reference to the minimal impact it had upon teaching, a number of learning mentors questioned the feasibility and acceptability of this method. Learning mentors expressed some concern about confidentiality and the impact this may have upon accuracy of reporting, highlighting the potential for young people either to exaggerate or under-report their alcohol use. Indeed, a number of young people did comment that they were concerned that teachers or fellow pupils may read their answers over their shoulder. There were some young people who reported that ‘there were quite a few people taking the mick with it, saying they were out every weekend drinking three bottles of vodka . . .’ (Young person, female). However, most young people who were interviewed stated that they did give honest and accurate responses about their drinking behaviour.
. . . if you’re doing something that’s about your well-being . . . your like habits and stuff like that you’ve got to be mature about it; you’ve got to be serious. You can’t be writing stuff like that on a survey. Like somebody’s going to use for you know however long it is like feeding the results for and stuff like that. I just think it’s a bit silly to be honest.
Young person, male
Nevertheless consideration must be given to young people giving social desirable answers, either to ‘look good’ to their friends or to give answers they think teachers want to hear:
What was really, erm, stood out that we look at, and I pointed, I pointed out to [researcher] is that they, we did ours in tutor groups, right, and you could actually see there was like between five and six people all out of the same tutor group, all the same peer group, I know they’re all the same peer group, all in the same sort of sets, top sets, and they all came out as a band. One whole bunch, and you had to ask yourself, they would have been sitting next to each other when they did the survey, the original survey, and you, they probably asked each other, well, didn’t we go such and such, didn’t we do this, they’d have talked to each other about it.
Learning mentor, female
Feasibility and acceptability of intervention 1
Learning mentors praised the attractive design of the intervention 1 tool, the fact it enabled a logical yet flexible flow to the process of intervention delivery and, crucially, that it was engaging and interactive in style. Young people generally found the intervention acceptable, with some young people commenting that they found the advice given to be informative.
It contained the information that I needed and things that I wasn’t sure about, it explained a lot. What alcohol does and how it can affect us. I think you need more things like that in school, talking about it more, because kids when I was thirteen you don’t understand it.
Young person, male
There were, however, mixed views on the calorie-focused element of the intervention. Most learning mentors felt that discussing calorie content was a particularly effective way to engage with the young people. However it became apparent that a minority of learning mentors had avoided talking in any depth with young people about the calorie content of alcoholic drinks because of concerns that this could potentially exacerbate existing anxieties about weight. Young people expressed similar conflicting views with some reporting interest at this information, whereas for other young people who were concerned about weight, the calorie focus of the intervention did have unexpected consequences. They discussed ensuring they did not eat on the day of a drinking episode or going for a run the day after a drinking occasion to counteract the excess calories.
Intervention 1 is based upon the principles of MI. As discussed at length elsewhere, personalised feedback to help young people realise the risks associated with their specific drinking patterns is fundamental to the approach. Most learning mentors reported that they felt able to advise young people who had screened positive that their drinking placed them at risk of harm. Importantly, learning mentors reported that the intervention enabled young people to assess for themselves the amount of alcohol they were consuming. Moreover, young people commented that the act of writing down their drinking patterns and calculating the units made them see their drinking in a different way.
. . . because putting it on paper how many units I was taking in was quite bad. So with my exams coming through, I’m taking them now, it was like cut down.
Young person, male
Some learning mentors reported that they had avoided providing personalised feedback to young people on the risks associated with their alcohol consumption. In one school, learning mentors advised young people whom they had chosen at random, which is contradictory to the MI approach.
Feasibility and acceptability of intervention 2 (parental involvement)
Parental involvement was considered to be valuable to the intervention, as well as relationships between the school and the family (by some learning mentors and lead liaisons). A number of learning mentors described communicating with and involving parents as a standard part of their role. However, others anticipated major barriers to parental involvement, and were concerned that it crossed an ‘unspoken boundary’ in relation to the school–home divide. Indeed many learning mentors involved in delivering intervention 2 reported that it had been difficult to contact parents to discuss participation, with parents not responding to telephone and written contact about the study. Others advised that some parents did not attend appointments arranged. Furthermore, there was a concern that only those young people and parents in lesser need of support around alcohol use would take part (‘lower’ level drinkers with positive parental relationships). This was contrasted with the parents and young people most in need of an alcohol intervention who were seen as unlikely to participate (‘higher’ level drinkers with more problematic family dynamics):
. . . the parents of the kids you really need to see tend not to turn up . . . You know so I don’t feel as though we got the ones, and the ones that were on the list didn’t want their parents involved, they were probably ones that you know, were the park drinkers or the you know that did it behind somebody’s back.
Learning mentor, female
Young people who agreed to their parent(s) being involved in the intervention reinforced this belief, reporting that their parents had existing knowledge about their drinking and this was the primary factor influencing their participation in intervention 2. In contrast, if their parent did not know about their drinking then young people were far less inclined to consent to a family intervention session.
If my mum had no idea about my drinking and she came in and we had to discuss it. I don’t know how I would’ve dealt with that.
Young person, female
. . . it is just a private part, which is why I didn’t want to bring her in.
Young person, female
Further, participating parents often questioned the relevance of intervention 2 to their individual situation. In particular, parents interviewed felt they already benefited from an open and trusting relationship between themselves and their child and as such, were ‘not the right type’ of people to be involved: intervention 2 did not teach them anything that they did not already know.
I mean it’s not really something that affects us a great deal, we’re possibly not the right people for you to be talking to, because it doesn’t have much of an impact on our lives . . . for what you’re trying to gain from this we might not be the right people to talk to because we’re open, we talk about everything and it’s not an issue in our house.
Parent, female
Rather than consider the involvement of parents in intervention 2, the learning mentors, young people and parents shared the view that the intervention was not effective in engaging the parents and young people who may benefit from this intervention. Parental motivation for participation was based upon assisting the school in research and was not considered to be beneficial in addressing risky drinking by young people. Importantly, parents and young people did not express a desire to engage in intervention 2 or a benefit from doing so.
Summary
It would seem that the school is both a feasible and an acceptable environment to intervene with young people who are risky drinkers. Learning mentors in particular are well placed to discuss alcohol with young people owing to their role within the school, their existing supportive relationships with young people and the trust that the young people place in them. Although it is acknowledged that the delivery of the interventions can be time-consuming, there was the sense that the activity remains feasible. The training provided to learning mentors was considered to fully prepare them for their role within the study. Importantly, acceptability of intervention delivery was high; intervening with young drinkers was often seen as important and necessary aspects of the learning mentors’ work.
Overall, the screening survey was found to be feasible, although in future work some consideration may need to be given to means of enhancing the young people’s privacy in order to increase acceptability. Teachers were often present, overseeing the class while the young people completed the screening survey. These teachers had not been trained in best-practice approaches to this research method, however, and had received only minimal information regarding the purpose of the survey. Delivering training to teachers regarding informed consent and the importance of enhancing and maintaining confidentiality is likely to improve the overall acceptability of the screening survey.
Intervention 1 was found to be feasible and mostly acceptable. Some learning mentors expressed hesitation at informing young people for whom their drinking placed them at risk of harm, choosing instead to advise the young people who had been selected at random. This is suggestive of an outstanding training need for the learning mentors. As such, future work should ensure that the training programme emphasises the importance of personalised feedback within the delivery of interventions. The calorie-focused content also resulted in mixed views from both young people and learning mentors. As this information is not central to the information, it is recommended that this is not included in an intervention within a definitive trial.
It would appear that intervention 2 is not feasible. Parents and young people did not express a desire to engage in this intervention or a benefit from doing so. Moreover, learning mentors, parents and young people questioned the utility of an intervention which they believed was not engaging the ‘right’ people. Although the parents who did engage in intervention 2 found the intervention to be acceptable, it should be noted that most young people and their parents who were offered did not participate in this intervention. Some young people interviewed told us that they did not want their parents involved. Although we did not interview any parents who chose not to participate in intervention 2, quantitative data presented elsewhere in this report reinforce the findings of the qualitative study that intervention 2 is not feasible, as well as suggesting that it is not acceptable to a large group of young people and parents. Furthermore, by not including an intervention that involves parents in future work, the time-consuming task of contacting parents, arranging appointments and rearranging appointments that are not attended would be alleviated, thus enabling learning mentors to use their time more efficiently.
Chapter 7 Health economics
Key points for Chapter 7
-
The collection of data using the open-ended case diary tool highlighted a number of problems. A structured case diary tool would both be more precise and provide more reliable data while also reducing the data collection burden on the learning mentors in a definitive trial.
-
Percentages of missing data for service use questions from the three survey time points do not seem to be problematic, suggesting that the tool is acceptable for use with young people in a definitive trial.
-
However, some thought should be given to how we measure service use, especially in relation to certain categories (i.e. GP visits).
-
It appears that the EQ-5D is an appropriate tool to use with young people. The majority of young people indicated that they had no problems on the first three dimensions of the EQ-5D-Y (mobility 93%; looking after self 99%; doing usual activities 94%).
-
Higher levels of problems were found in the dimensions of pain or discomfort (19% having some level of problems) and being worried, sad or unhappy (24% having some level of problem). This indicates that there is some opportunity for the definitive trial to improve health, at least in terms of the final two dimensions.
This chapter presents findings from the health economics component of the study that aimed to rehearse the methods of data collection to inform the development of the economic evaluation in a definitive study. The definitive health-economic analyses will show how the costs of introducing and running the BI compare with the current practice; the reason for this is that a full economic evaluation should include current practice as a comparator, as it seeks to inform decisions about whether we should move from current practice to something else. 187 The analyses reported in this section will be used to produce the protocol for a definitive trial and attendant economic evaluation of the impact of brief alcohol intervention compared with standard practice (PSHE) in a school setting to reduce alcohol-related risk or harm.
This chapter focuses on examining what resource-use data we should collect and how these will be analysed. The focus is on the key elements of an economic evaluation, which are costs and consequences, which will be discussed below. The level of completeness of the data has been analysed and the suitability of tools is commented on accordingly. In each of the following sections the results of our analysis are presented with associated discussion and recommendations.
Sections of analysis
Costs Resources and costs required to provide the intervention.
Outcomes/consequences Health-economic outcomes of the intervention including NHS and public services resource-use and health-related quality of life (as measured by EQ-5D-Y).
The health-economic outcomes are based on the participant-completed questionnaires, specifically questions 14 (Resource Use) and 15 (EQ-5D-Y), administered as part of the non-randomised repeat cross-sectional survey. These data were collected at the three survey time points: TP1, TP2 and TP3. Questions 14 and 15 were not separately identifiable for the subgroup of survey participants at TP2 or TP3 when they were followed up within the trial. This pilot trial intended to test only the alcohol-related outcomes at 12 months for the trial participants. Therefore, the data we have available is for the entire survey cohort at these three time points, which is appropriate from a health-economic perspective, as our objectives were met and no economic evaluation was planned in this feasibility study.
Costs
Analysis of resources use and costs associated with both intervention (intervention 1 and intervention 2) and control groups relate to two specific areas: the resources required to provide the intervention; and the resources used subsequently after the intervention (or control). The details of such costs and resources are discussed below.
Intervention cost
Staff cost of intervention
A main resource-use component of the economic evaluation (for a definitive trial) will be the cost of learning mentor time required to prepare for and deliver the BI to young people (and, for intervention 2 only, the session with parents) and to conduct the necessary follow-up with the young people thereafter. Time spent for the feasibility study was calculated by observing the average minutes per case (i.e. young person) as documented in a self-completed case diary. The appropriateness of the case diary tool is assessed according to rates of completely missing data (i.e. unused diaries) and of diaries missing relevant information. The rate of salary (plus employer on costs, such as superannuation and national insurance) will be, in a definitive trial analysis, applied to average learning mentor time, as discussed further below. In this subsection, the case diary result tables are analysed and discussed.
To pilot the case diary tool, we used an open-format diary (shown in Appendix 6). The reason for this decision was twofold; first, having the tool in an open-ended format gave the learning mentors the opportunity to describe the categories of activity to which they were devoting their time, and, secondly, it provided information on how long it took to complete these activities. The original intention was to use the open-ended version of the tool used in the feasibility study in the definitive trial; however, a lesson learned was that it was possible (using the data collected with the original tool) to develop a simpler revised tool that would collect the same level of information but be quicker and easier to complete as well as simplifying data entry and analysis.
Overall, in practice, the open format is appropriate for a pilot but is not ideal in a definitive trial owing to its limitations, which are discussed and explored below and further in the discussion. Although a categorically structured, close-ended format is a preferred choice, we could not have designed an appropriate time diary tool without piloting an open-ended case diary first. For the definitive trial, the new tool should be piloted with learning mentors before being confirmed.
Results
As the primary objective of these data is to inform the design of a more appropriate time diary tool, Tables 12–14 describe the intention-to-treat analysis results, in which groups are compared in terms of how young people were randomised. Solely using an intention-to treat-analysis within clinical trials has its limitations,188 but, as our objective was to assess how appropriately the case diary tool was used for resource-use collection, it is acceptable in this case.
| Intention to treat | Control (in minutes) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | n | % total missinga (n) | % category missingb (n) | % withdrawn/session did not take place (n) | Minimum | Lower quartile | Median | Upper quartile | Maximum | |
| Control arm with young person | ||||||||||
| Prep (case diary) | 53 | 2 | 1.9 (1) | 94.3 (50) | – | 5.0 | 5.0 | 5.0 | 5.0 | 5.0 |
| Delivery (case diary) | 53 | 52 | 1.9 (1) | – | – | 7.0 | 10.0 | 13.75 | 15.0 | 15 |
| Intervention total | 53 | 52 | – | 1.9 (1) | – | 7.0 | 10.0 | 13.75 | 15.0 | 20.0 |
| Follow–upc | ||||||||||
| Prep | 53 | 1 | 26.4 (14) | 54.7 (29) | 17 (9) | 1.0 | 0.50 | 1.0 | 0.50 | 1.0 |
| Delivery (case diary)d | 53 | 30 | 26.4 (14) | – | 17 (9) | 5.0 | 7.5 | 10.0 | 15.0 | 20.0 |
| Delivery (TLFB form)d | 53 | 36 | 15.1 (8) | – | 17 (9) | 1.0 | 2.0 | 7.5 | 10.0 | 20.0 |
| Follow-up total | 53 | 34 | 5.7 (3) | 13.2 (7) | 17 (9) | 5.0 | 7.5 | 10.0 | 15.0 | 20.0 |
| Control total | 53 | 53 | – | – | – | 10.0 | 15.0 | 20.0 | 25.0 | 35.0 |
| Intention to treat | Intervention 1 (in minutes) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | n | % total missinga (n) | % category missingb (n) | % withdrawn/session did not take place (n) | Minimum | Lower quartile | Median | Upper quartile | Maximum | |
| Intervention 1 with young person | ||||||||||
| Prep (case diary) | 54 | 23 | – | 57.4 (31) | – | 3.0 | 5.0 | 15.0 | 20.0 | 70.0 |
| Delivery (case diary) | 54 | 54 | – | – | – | 15.0 | 25.0 | 30.0 | 32.0 | 50.0 |
| Time (intervention sheet) | 54 | 53 | 1.9 (1) | – | – | 5.0 | 20.0 | 25.0 | 30.0 | 90.0 |
| Intervention total | 54 | 54 | – | – | – | 15.0 | 30.0 | 30.0 | 41.25 | 90.0 |
| Follow-upc | ||||||||||
| Prep | 54 | 21 | – | 53.7 (29) | 7.4 (4) | 5.0 | 5.0 | 5.0 | 10.0 | 30.0 |
| Delivery (case diary)d | 54 | 49 | – | 1.9 (1) | 7.4 (4) | 3.0 | 10.0 | 18.0 | 20.0 | 40.0 |
| Delivery (TLFB form)d | 54 | 39 | 22.2 (12) | – | 5.6 (3) | 3.0 | 10.0 | 11.0 | 20.0 | 55.0 |
| Follow-up total | 54 | 50 | – | – | 7.4 (4) | 3.0 | 15.0 | 20.0 | 25.0 | 60.0 |
| Intervention 1 total | 54 | 54 | – | – | – | 18.0 | 40.0 | 54.0 | 65.0 | 120.0 |
| Intention to treat | Intervention 2 (in minutes) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | n | % total missinga (n) | % category missingb (n) | % withdrawn/session did not take placec (n) | Minimum | Lower quartile | Median | Upper quartile | Maximum | |
| Intervention 2 with young person | ||||||||||
| Prep (case diary) | 75 | 46 | 9.3 (7) | 29.3 (22) | – | 1.0 | 5.0 | 10.0 | 12.75 | 220.0 |
| Delivery (case diary) | 75 | 69 | 8.0 (6) | – | – | 5.0 | 20.0 | 30.0 | 30.0 | 99.0 |
| Time (intervention sheet) | 75 | 69 | 8.0 (6) | – | – | 10.0 | 20.0 | 30.0 | 30.0 | 60.0 |
| Intervention total | 75 | 74 | – | 1.3 (1) | – | 6.0 | 25.0 | 31.0 | 45.0 | 255.0 |
| Family meeting | ||||||||||
| Prep (case diary) | 75 | 69 | – | 8.0 (6) | – | 0.0 | 0.0 | 0.0 | 0.0 | 47.0 |
| Delivery (case diary) | 75 | 70 | – | 6.7 (5) | – | 0.0 | 0.0 | 0.0 | 0.0 | 40.0 |
| Time (intervention sheet) | 75 | 75 | – | – | – | 0.0 | 0.0 | 0.0 | 0.0 | 40.0 |
| Family meeting total | 75 | 75 | – | – | – | 0.0 | 0.0 | 0.0 | 0.0 | 85.0 |
| Follow-upc | ||||||||||
| Prep | 75 | 47 | 16 (12) | 12 (9) | 9.3 (7) | 1.0 | 1.0 | 5.0 | 8.0 | 45.0 |
| Delivery (case diary)d | 75 | 56 | 12 (12) | – | 9.3 (7) | 0.0 | 10.0 | 11.0 | 15.0 | 25.0 |
| Delivery (TLFB form)d | 75 | 48 | 28 (21) | – | 8 (6) | 0.0 | 13.50 | 20.0 | 20.0 | 30.0 |
| Follow-up total | 75 | 64 | 5.3 (4) | – | 9.3 (7) | 1.0 | 15.0 | 20.0 | 25.0 | 57.0 |
| Intervention 2 total | 75 | 75 | – | – | – | 12.0 | 34.0 | 52.0 | 68.0 | 270.0 |
Tables 12–14 display the results in two categories within each table, the first category (shown in shaded columns) being how often and how appropriately the case diaries were used as assessed by rates of missing case diaries, rates of partially completed case diaries, and rates of students withdrawn from the study. The second category shows what the results of the completed case diaries were in minutes, as reported in the five-number summary statistics. The summary statistics are shown by the categories created by the decision rules of the research staff (i.e. ‘Prep’, delivery).
The purpose of the first category is to show how the open-ended format case diaries were actually used by the learning mentors to inform what categories need to be included in the definitive time diary. ‘Total missing’ was concluded when a learning mentor did not use his/her case diary at all, whereas ‘Category missing’ was concluded by decision rules set by the research staff. For example, in the first line of Table 12, out of ‘N’ diaries (53), two learning mentors reported preparation (‘Prep’) time before performing the intervention, therefore ‘n’ is two for the ‘Prep’ category.
The purpose of the second category (five-number summary statistics for n) within Tables 12–14 was to observe the range of minutes, as recorded by the learning mentors, so that an appropriate choice of times could be presented on a structured time diary for the definitive trial. To ensure that accurate time ranges were presented, the follow-up time was taken from an additional source (TLFB), with the research staff making the decision rule that the longer of the two times would be recorded. In the definitive trial, the TLFB form will not be used to record the intervention time to reduce administrative burden on the learning mentors. To simplify the process, the learning mentors will be instructed that the only place to record time spent on the intervention is the time diary.
In summary, the collection of data using the open-ended case diary tool highlighted a number of areas in which a more detailed case diary tool would be both more precise and provide more reliable data, while also reducing the data collection burden on the learning mentors. For example, ‘Category missing’ was consistently higher than ‘Total missing’ across study arms, which shows that the learning mentors were using the diaries but were not as likely to list categories specifically. In a full economic evaluation it is important to be able to collect resource use for the different aspects of the intervention, and this will more likely be achieved with a more structured time diary (such as the template in Appendix 6) in a definitive study.
Collection of data relating to learning mentor time via the open-format case diary (see Appendix 3) had a number of limitations:
-
Use of open-format diaries meant that differing levels of data were reported by learning mentors, especially in relation to preparation time. Open-format diaries were used in the study, as learning mentors were asked to record every time they attempted to contact, or successfully made contact with, the young person on this document. This enabled the research team to look at how long was spent arranging and carrying out the interventions.
-
Learning mentors changed mid-case, as shown in Table 15. It was not possible to conclude if such changes affected the completion of diaries. In addition, potential factors, such as training differences or staff changes, are not possible to examine.
-
Missing data cannot be accurately assessed. Learning mentors were given new case diaries at the different stages of the intervention. For example, a blank case diary was given to the learning mentor before the intervention and again before follow-up. Although case diaries were coded to the trial participant, and could be linked at both stages in the intervention, the diary may have been completed differently at different time points. For example, differences in staff workload or time pressure (i.e. how busy the learning mentor was) could have affected the level of data recorded, as could whether the learning mentor conducting each stage of the intervention had changed (i.e. differences in conduct between learning mentors).
-
‘Category missing’ was used in data coding as an indicator of when learning mentors did not, in the open-format case diary (see Appendix 3), provide all of the time data for each of the aspects of the intervention. This is not surprising, as one role of the case diary used in this feasibility study was to identify what aspects of the intervention might be provided. It should be noted that, although the research team made the decision rule regarding what was an incomplete or ‘Category missing’ section of the case diary, directions to include certain categories were not included anywhere on the case diary form to direct learning mentors to do so (see Appendix 3).
-
Times for the delivery of the intervention were taken from both case diaries and intervention materials in which learning mentors were asked to report the start and finish time in both places. The intervention times from both tools were not always the same. When coding the data, a decision rule was adopted to choose the longer of the two intervention times to inform the total.
| Condition | Learning mentor stayed the same, n (%) | Change in learning mentor, n (%) | Total with learning mentor name known at follow-up,a n (%) |
|---|---|---|---|
| Control | 9 (20.5) | 35 (79.5) | 44 (100.0) |
| Intervention 1 | 50 (100.0) | 0 (0.0) | 50 (100.0) |
| Intervention 2 | 27 (42.2) | 37 (57.8) | 64 (100.0) |
| Total | 86 (54.4) | 72 (45.6) | 158 (100.0) |
Learning mentor training time
Training for learning mentors will be provided by SIPS JR-HIGH research staff on site at all locations. The time to deliver the training, per location, will be documented by the SIPS JR-HIGH research staff in hours and minutes (i.e. 2 hours 15 minutes). A list of learning mentors in attendance will be recorded so that the training time (cost) per learning mentor can be incorporated into the cost of running the intervention. The learning mentors are not to record this training time in the intervention time diaries under the ‘Prep’ category, as that category is referring to intervention casework, not the training time. The SIPS JR-HIGH research staff delivering the training will record their time and pay grade so that the cost data can be incorporated into the analysis. In the definitive trial, the SIPS JR-HIGH research staff will keep a record of all time spent on training follow-up which is specifically related to the training of learning mentors. The methods to calculate these costs are discussed in the next section.
Resource-use and unit-cost information
To assess the full cost of the intervention to inform the definitive economic evaluation, both resource-use and unit-cost data will be collected and reported in tables similar to Tables 16 and 17. These tables illustrate an example for a single area of resource use and its associated unit cost. For the definitive trial, full tables will be populated with all applicable measures of intervention resource use and unit costs will be reported. For this feasibility study, the resource-use data and unit-cost sources are not reported as the definitive trial will go beyond the local authority school district.
| Resource category | Unit-cost sourcea |
|---|---|
| Example: learning mentor training time | Example: average learning mentor salary cost to a local authority area – around £21,482 per annum Assuming 46 contracted weeks per year and 37 hours per week at Grade 6, Point 22–24: £20,800–22,165 Of above average amount, approximately: £4296.00 are estimated to be on-costsb |
| Average annual salary | Plus on-costs (i.e. employer’s contribution to national insurance, pension/superannuation) | = No. of working weeks per yeara (divide by 46) | = No. of work hours per weekb (divide by 37) | Divide by 60 minutes = per-minute cost of learning mentor time |
|---|---|---|---|---|
| £17,185.00+ | £4296.00 | = £467.00 | = £12.62 | £0.21 |
In the definitive trial, once the tables have been populated with all relevant resource-use categories and corresponding unit costs, the two tables will be used together to calculate the total cost of running the intervention. All cost outputs will be reported in UK pounds sterling for the final financial year of the definitive study. For example resource-use data (i.e. 45 minutes of learning mentor time) is multiplied by the unit-cost data from Table 17 (i.e. cost per minute of a learning mentor) to calculate the monetary cost of that particular resource use. The data are an estimation of salary and on-costs (based on local authority data) to show the process that will be taken for the costing portion of a future full economic evaluation. For a definitive trial, these data will be sourced by school district centrally through their learning platforms. Cost per minute of staff time will be derived using the formula illustrated in Table 17, which shows that the average resource use for the learning mentor training portion of the intervention would cost £9.45 per learning mentor (45 minutes × £0.21).
Outcomes
Resource use subsequent to the intervention
Questions 14.1–14.6 in the questionnaire completed by young people at TP1, TP2 and TP3 are self-completed resource-use questions relating to use of NHS, criminal and social services (see Appendix 3). Survey participants reported how often in the last 6 months they used a particular health-care or public service. A decision was made regarding whether the evaluation should include data that are attributable only to alcohol use or to all services. It was decided to focus on all service use for two main reasons. First, it was deemed appropriate that all service use was to be captured because attributing use to alcohol would increase the burden on respondents and add in a possible extra element of recall bias. The second, and more important, explanation is that there may be subtle reasons why the use of services differs even when not directly attributable to alcohol use (e.g. use of services is higher because of poorer health caused by higher rates of alcohol use).
In a definitive trial, all service use will be associated with a monetary cost, which will inform portions of the economic evaluation. For this feasibility study no monetary costs were calculated from these data; rather, the data have been reported as a set of descriptive statistics that illustrate the appropriateness of the tools used in the pilot study. The collection of these data within the definitive RCT setting will use recognised and robust methods that should ensure that the data collected is equally accurate in both trial arms and hence the difference in costs is sufficiently robust to inform policy decisions.
Descriptive statistics
Table 18 shows survey data at the following survey time points. For all TP1, TP2 and TP3 variables the percentage of missing and implausible values are reported, along with the five-number summary statistics. The percentage of implausible values and missing data was reported as a percentage of the total cohort groups (N) then removed from the total when calculating the remaining summary statistics (n). Therefore, percentages are based on available data. For n, the five different summary statistics are produced (minimum, lower quartile, median, upper quartile, maximum).
| Variable name | N | % (n) missing | % (n) implausible valuesa | n | Minimum | Lower quartile | Median | Upper quartile | Maximum |
|---|---|---|---|---|---|---|---|---|---|
| TP1: baseline | |||||||||
| School nurse visits | 1280 | 4.2 (54) | 0.9 (12) | 1214 | 0 | 0.0 | 0.0 | 0.0 | 6 |
| Accident and Emergency visits | 1280 | 4.2 (54) | 1.6 (21) | 1205 | 0 | 0.0 | 0.0 | 0.0 | 6 |
| Admitted to hospital | 1280 | 4.5 (58) | 0.9 (12) | 1210 | 0 | 0.0 | 0.0 | 0.0 | 6 |
| Visited GP | 1280 | 4.8 (61) | 3.7 (47) | 1172 | 0 | 0.0 | 0.0 | 2.0 | 6 |
| Visited by social worker | 1280 | 4.5 (57) | 0.7 (9) | 1214 | 0 | 0.0 | 0.0 | 0.0 | 6 |
| Times arrested | 1280 | 4.2 (54) | 0.9 (12) | 1214 | 0 | 0.0 | 0.0 | 0.0 | 6 |
| TP2: 6-month follow-up | |||||||||
| School nurse visits | 1256 | 6.2 (78) | 1.75 (22) | 1156 | 0 | 0.0 | 0.0 | 0.0 | 6 |
| Accident and Emergency visits | 1256 | 6.4 (81) | 2.8 (35) | 1140 | 0 | 0.0 | 0.0 | 0.0 | 6 |
| Admitted to hospital | 1256 | 6.7 (84) | 2.1 (26) | 1146 | 0 | 0.0 | 0.0 | 0.0 | 6 |
| Visited GP | 1256 | 6.6 (83) | 4.4 (55) | 1118 | 0 | 0.0 | 0.0 | 2.0 | 6 |
| Visited by social worker | 1256 | 6.6 (83) | 1.0 (12) | 1161 | 0 | 0.0 | 0.0 | 0.0 | 5 |
| Times arrested | 1256 | 7.0 (88) | 1.8 (22) | 1146 | 0 | 0.0 | 0.0 | 0.0 | 6 |
| TP3: 12-month follow-up | |||||||||
| School nurse visits | 1161 | 4.0 (47) | 2.4 (28) | 1086 | 0 | 0.0 | 0.0 | 0.0 | 6 |
| Accident and Emergency visits | 1161 | 4.0 (46) | 2.8 (32) | 1083 | 0 | 0.0 | 0.0 | 0.0 | 6 |
| Admitted to hospital | 1161 | 4.3 (50) | 1.6 (18) | 1093 | 0 | 0.0 | 0.0 | 0.0 | 6 |
| Visited GP | 1161 | 4.0 (47) | 5.0 (58) | 1056 | 0 | 0.0 | 0.0 | 2.0 | 6 |
| Visited by social worker | 1161 | 4.3 (50) | 1.0 (12) | 1099 | 0 | 0.0 | 0.0 | 0.0 | 6 |
| Times arrested | 1161 | 4.6 (53) | 1.6 (19) | 1089 | 0 | 0.0 | 0.0 | 0.0 | 5 |
The appropriateness of the self-completed questionnaire has been assessed by completion rates, missing data and implausible values. Use of services was generally very low. The majority of participants reported no use of services, although for all services a small number reported some use. The only possible exception to this is visits to the GP which, as might be expected, were more frequent, although still uncommon.
Implausible values were based on the distribution of the data; there was an observable ‘drop off’ with scores of > 6. We therefore defined the data at seven or over as an ‘implausible value’. For the definitive trial, the data will not be observed before analysis, but in this feasibility study we used the data collected to inform decision rules that may also be most appropriate for the definitive trial.
As a result of the analysis the following can be concluded:
-
Although no guidance exists as to what level of missing data is likely to be important, we have calculated the percentages of missing data from the three time points and they do not seem to be problematic, suggesting that the tool is acceptable for use with young people.
-
The level of implausible values at ≥ 7% may be problematic for certain categories (i.e. GP visits). For the rest of the resource-use questions, the percentages of implausible values did not appear to be problematic, based on the summaries in Table 19.
European Quality of Life-5 Dimensions (Youth version)
The EQ-5D-Y was developed as a child-friendly version of the EQ-5D, which is a quality-of-life measure used extensively in economic evaluations. For this pilot, the EQ-5D-Y was chosen as it is especially designed for young people; the main difference relates to the wording of the most severe level for activities of daily living. Using the EQ-5D is in line with NICEs Public Health Methods Guidance and may well be a benchmark for methods by which this intervention will be assessed. The tool divides health status into five dimensions (mobility, self-care, usual activities, pain/discomfort and anxiety/depression). Each of these dimensions has three possible levels giving 243 possible health states. The EQ-5D-Y does not currently have a utility value set to assign to responses, which was not an issue in this case for the following reasons. First, in the feasibility study, the objective was to look at the completion rates of the health-economic tools, therefore the EQ-5D-Y algorithm-derived health-utility scores are not to be reported; rather the five-number summary statistics are reported for the ordinal responses (1–3) to each of the five questions contained within the EQ-5D-Y. Second, since the time of the pilot we have received clarification from the Euroqol group that EQ-5D (the standard version) is valid for use in participants aged ≥ 12 years. We will therefore use the EQ-5D in place of the EQ-5D-Y. Nevertheless, owing to the similarity of the two tools the findings from the feasibility study are still informative.
Within the definitive study, responses to the EQ-5D questionnaire will be transformed using a standard algorithm189 to produce a health-state utility at each time point for each patient. From these data, quality-adjusted life-years (QALYs) for each participant will be calculated using the area-under-the-curve approach. From these data, the mean QALY score for each group can be calculated. There are concerns that the EQ-5D may not capture all relevant outcomes but, as discussed in the subsection below, considerable variation in young people’s responses to the EQ-5D-Y were observed and it is therefore plausible that it will capture important differences.
Descriptive statistics
The descriptive statistics from the EQ-5D-Y ordinal values (1–3) are reported and the suitability of the EQ-5D for the definitive trial will be assessed from the perspective of completion rates and missing data. For TP1, TP2 and TP3 the percentage of missing variables is reported. For the EQ-5D-Y, given the phrasing of questions, it was assumed that any response from the three categories for each question (no problems, some problems or a lot of problems) would be valid (Table 20).
| EQ-5D-Y | N | Missing, % (n) | n | No problems, % (n) | Some problems, % (n) | A lot of problems, % (n) |
|---|---|---|---|---|---|---|
| TP1: baseline | ||||||
| Mobility | 1280 | 3.4 (43) | 1237 | 93.3 (1155) | 5.9 (73) | 0.7 (9) |
| Looking after self | 1280 | 3.4 (43) | 1237 | 98.7 (1222) | 0.6 (7) | 0.6 (8) |
| Doing usual activities | 1280 | 3.4 (43) | 1237 | 94.1 (1164) | 5.1 (63) | 0.8 (10) |
| Pain or discomfort | 1280 | 3.5 (45) | 1235 | 81.0 (1000) | 17.2 (213) | 1.8 (22) |
| Worried, sad or unhappy | 1280 | 3.9 (50) | 1230 | 75.5 (929) | 20.7 (255) | 3.7 (46) |
| TP2: 6-month follow-up | ||||||
| Mobility | 1256 | 5.9 (74) | 1182 | 92.8 (1097) | 5.6 (66) | 1.6 (19) |
| Looking after self | 1256 | 6.0 (75) | 1181 | 98.1 (1158) | 1.0 (12) | 0.9 (11) |
| Doing usual activities | 1256 | 6.1 (77) | 1179 | 92.7 (1093) | 6.0 (71) | 1.3 (15) |
| Pain or discomfort | 1256 | 6.2 (78) | 1178 | 77.7 (915) | 20.0 (236) | 2.3 (27) |
| Worried, sad or unhappy | 1256 | 6.2 (78) | 1178 | 70.1 (826) | 25.0 (294) | 4.9 (58) |
| TP3: 12-month follow-up | ||||||
| Mobility | 1161 | 1.5 (17) | 1144 | 92.4 (1057) | 5.9 (67) | 1.7 (20) |
| Looking after self | 1161 | 1.6 (18) | 1143 | 97.1 (1110) | 1.2 (14) | 1.7 (19) |
| Doing usual activities | 1161 | 1.6 (18) | 1143 | 93.4 (1068) | 4.7 (54) | 1.8 (21) |
| Pain or discomfort | 1161 | 1.6 (19) | 1142 | 77.8 (888) | 19.0 (217) | 3.2 (37) |
| Worried, sad or unhappy | 1161 | 1.7 (20) | 1141 | 71.2 (812) | 23.5 (268) | 5.3 (61) |
The rates of missing data are not problematic, as they appear to be consistent across dimensions at each time point. Overall, it appears that the EQ-5D is an appropriate tool to use with young people. Not surprisingly, most young people answered that they had ‘no problems’ on the first three dimensions: mobility, looking after self and doing usual activities, although there was a larger percentage of students reporting having ‘Some’ or ‘A lot’ of problems in the last two dimensions: ‘Pain and discomfort’ and ‘Worried, sad or unhappy’. This suggests that there is some opportunity for the trial interventions to improve health at least in terms of the last two dimensions of the EQ-5D. It is unlikely, however, that a definitive trial could demonstrate any improvement in the first three dimensions unless it were very large.
Cost–consequence analysis
In the definitive trial, if there is not a significant change in health-state utility attributable to the intervention, the trial analysis can also include a cost–consequence analysis. The cost–consequence analysis will allow a focus on a wider range of outcomes than just health and will seek to consider costs and outcomes beyond the trial end point. The results of the analysis will be presented as a balance sheet. 190 The principle underpinning a balance sheet is that the analyst should seek to capture all costs and benefits no matter on whom they may fall – the same principles underpinning a cost–benefit analysis. 191 Although not included in the feasibility trial, data on the use of ‘educational services’ will be elicited via the questionnaire. We will confirm with an expert group what sort of services might be relevant to ensure that data collection is as parsimonious as possible, resulting in the addition of questions in the form of days missed from school/truancy. The use of these services may have resource-use implications that can be factored into the analysis and modelling. Engagement with criminal and social services was measured in the questionnaire in the pilot study and will be collected in the definitive study.
Summary
In relation to collecting case diary data of the time spent by learning mentors on working on interventions, the open-ended format of the case diary proved to have many limitations; however, in order to identify the categories needed in a definitive trial this was important and has enabled us to identify the categories needed for the definitive trial tool (see Appendix 6). The revised tool should be piloted with a few learning mentors prior to beginning the definitive trial to ascertain whether it is ‘user-friendly’.
The majority of young people indicated that they had no problems on the first three dimensions of the EQ-5D-Y (mobility 93%, looking after self 99%, doing usual activities 94%). Higher levels of problems were found in the dimensions of pain or discomfort (19% having some level of problems) and being worried, sad or unhappy (24% having some level of problem). This indicates that there is some opportunity for the definitive trial to improve health, at least in terms of the final two dimensions. Results of this study show that the questions needed for health-economic analysis are acceptable for use with young people; however, some thought should be given to how we measure service use, especially in relation to certain categories (i.e. GP visits).
Chapter 8 Summary and conclusions
This study has successfully tested the feasibility of conducting a trial of ASBI in the school setting with young people aged 14–15 years. As there had been little research carried out in the school setting, examining a single session of one on one ASBI for young people who are drinking at a risky level, this feasibility study was imperative to trial the processes, tools and interventions, as well as the conduct of the study, including recruitment and design, and, finally, the delivery of the interventions. The previous chapters have discussed the results fully. This chapter presents the main findings relating to the study objectives and suggests modifications to the proposed definitive study (shown in italic text).
Objective 1
-
The study succeeded in recruiting seven schools as planned. Part of this success was due to gaining the support and active involvement of the local authority in the study catchment area from the outset. The local authority provided the research team with written confirmation it was happy for the study to proceed in its geographical area, and schools were informed that the project was supported by the local authority.
-
A range of factors influenced school participation in the study: the project presented direct benefits to participating schools in terms of boosting alcohol education provision through additional staff training and the provision of enhanced support for participating students in need.
-
The screening and consent procedure produced sufficient young people to rehearse the trial procedures.
Objective 2
-
Interviews were carried out with six school lead liaisons; 13 learning mentors; 27 young people and seven parents (total n = 53).
-
School setting Qualitative interviews were specifically focused on feasibility and acceptability of the intervention and not on the wider engagement of parents in a school setting. Views from school staff were mixed regarding engagement of parents in the school setting, and appeared to reflect the focus of the school. Therefore, schools that were part of the ‘Extended Schools Agenda’ were more likely to describe school as a ‘hub’ of the local community (and felt that they regularly engaged with parents) than traditional academically focused schools. Although parents felt that school was the correct environment for an intervention aimed at young people’s alcohol use, they were unsure about their own involvement in school-based alcohol education, and suggested that they did not know whether their children would take them seriously if they were involved regularly in formal alcohol education, or whether other young people would always be open and honest in front of their parents. It would seem that the school is both a feasible and an acceptable environment to intervene with young people who are risky drinkers.
-
Learning mentors Learning mentors in particular are well placed to discuss alcohol with young people due to their role within the school, their existing supportive relationships with young people and the trust that the young people place in them. Learning mentors were seen as appropriate members of staff to carry out the interventions by staff, parents and young people.
-
Training The study showed that it was possible to train learning mentors in the research requirements (consent/intervention delivery); the length and content of training was seen as appropriate by learning mentors; learning mentors particularly liked the training manuals with which they were provided.
-
Screening Overall, the screening survey was found to be feasible as has been found in the literature (see Chapter 2). Teachers were often present, overseeing the class while the young people completed the screening survey. These teachers had not been trained in best-practice approaches to this research method, however, and had received only minimal information regarding the purpose of the survey. Delivering training to teachers regarding informed consent and the importance of enhancing and maintaining confidentiality is likely to improve the overall acceptability of the screening survey. In the definitive study, consideration should be given to means of enhancing the young people’s privacy in order to increase acceptability. Study instructions for the young people should be made clearer on the front of the questionnaire at baseline. A standardised set of instructions should be provided for each class, perhaps as a video clip produced by the research team. We believe that these changes would improve the numbers of young people leaving their names on the questionnaires.
-
Intervention 1 was found to be feasible and mostly acceptable. There was some hesitation among learning mentors around informing young people whose drinking placed them at risk. The calorie-focused content also resulted in mixed views from both young people and learning mentors. In the definitive study further emphasis will be placed upon the importance of personalised feedback within the delivery of interventions. All learning mentors randomised to the intervention arm will be audio-recorded while delivering the intervention within a simulated session with an actor (see Objective 3, Fidelity) and further training will be provided to learning mentors who continue to find this aspect of the intervention challenging. As learning mentors (and young people) expressed mixed views about the calorie-focused content of the intervention, this will be removed from the intervention in the definitive trial.
-
Intervention 2 was not feasible to deliver within this study. Parents and young people did not express a desire to engage in this intervention or a benefit doing so, which has been shown in previous studies (see Chapter 2). Findings demonstrated that existing knowledge about young people’s drinking was the primary factor influencing parent participation in intervention 2. Thus, if parents did not know about their drinking, young people were far less inclined to consent to a family intervention. Although parents are a source of both risk and protective factors for adolescent alcohol use, as highlighted in our rapid review, evidence that interventions for alcohol involving parents are viable is equivocal.
-
Moreover, learning mentors, parents and young people questioned the utility of an intervention, which they believed was not engaging the ‘right’ people. Although the parents who did engage in intervention 2 found the intervention to be acceptable, it should be noted that most invited young people and their parents did not participate in this intervention. Some young people interviewed told us that they did not want their parents involved. Furthermore, as shown in Chapter 2 and Appendix 2, the literature around parental involvement is equivocal, with no clear indication that involving parents in interventions to reduce their children’s drinking is effective. This suggests that the definitive trial should focus on working with young people rather than involving parents. 83
Objective 3
-
Fidelity In this study the BECCI index was used to measure the fidelity of the delivery of interventions by the learning mentors. 178 This tool is used to measure the microskills of behaviour change counselling. As such, it focuses upon the practitioner. It is not able to measure the young people’s responses to the intervention or consider characteristics or compositions of the groups receiving the interventions. Six interventions were assessed. The mean score was ‘2.5’, with a range of 1.9–3.0, which suggested that the learning mentors were all found to be delivering the behaviour change counselling aspect of the intervention to ‘some extent’ or to ‘a good deal’, as assessed with the BECCI. The rate of recorded interventions was lower than was anticipated. We acknowledge the lack of detail regarding fidelity assessment and the low number of interventions assessed. Sessions that were assessed showed that learning mentors performed well when discussing the risks associated with young people drinking alcohol. Learning mentors performed less well when discussing motivation for behaviour change and strategies for behaviour change. The suggestion for a definitive trial is to include a minimum of one simulated intervention with an actor immediately after training for all learning mentors who are randomised to the intervention arm. A specific date to be agreed with each learning mentor for a further recording of intervention delivery with a trial participant.
Objective 4
-
Six per cent (n = 87) of parents opted their child out of participating in the study. Discussions with young people and parents on the days of the survey indicate that many of these parents thought they were opting their children into the study, which implies that the letter was confusing. Ninety-two per cent (1280/1388) of Year 10 year groups completed the baseline survey, and of these students 18% met the eligibility criteria of reporting drinking at least four times in the last 6 months on the A-SAQ and left their name on the questionnaire, which showed willingness to be contacted later. This eligibility rate of 18% was slightly lower than we anticipated (presumed to be approximately 22%). At baseline, 40% screened positive on the study screening tool (A-SAQ), but only slightly over half of these young people left their name and so were contactable regarding participation in the pilot trial. Although young people who did not leave their names were drinking more, it is important to note that there was a considerable number who were drinking at risky levels who did leave their names. In the definitive study, instructions should be made simpler and clearer on the letter that goes to parents, with one tick box indicating opt-out with a clear instruction that the young person will be opted out only if the box is ticked and the letter signed. The A-SAQ should be used as the screen for coming into the definitive trial, as it is short and quick to answer, with the AUDIT being asked at both baseline and 12-month follow-up.
-
Survey We found very low rates of missing data for virtually all variables. The highest rate of incomplete data (10%) was on the WEMWBS well-being questionnaire. This was the last set of questions in the survey pack, and it is possible that lack of time or fatigue led to more missing values. There was little evidence of implausible values being recorded, except for a few young people saying that they exercised on more than 7 days per week. There were a few very high values reported for alcohol use and problems but these could not be regarded as implausible. For the definitive study, consideration should be given to reducing the number of questions in the survey instrument.
-
Survey At TP1, 50% of the sample were male and 94% were white. The prevalence of smoking rose from 20% at TP1 to 25% at TP2 and reduced to 23% at TP3. The median number of days that young people reported physical exercise was four at all three time points. The median number of daily portions of fruit and vegetables was two each per day at all three time points.
-
Survey The proportion of young people who reported drinking alcohol fewer than four times in the last 6 months (A-SAQ) was 39% at TP1, 47% at TP2 and 47% at TP3. The proportion of young people who scored positive for an alcohol-use disorder using the AUDIT adult cut-off of 8+ rose from 26% at TP1 to 29% at TP2 to 32% at TP3. Using a cut-off of 2+, recommended for young people, this rate rose from 58% at TP1 to 66% at TP2 to 69% at TP3. The differences in all measures between TP1 and TP2 was significantly different but not between TP2 and TP3. Between the first two surveys, the median scores for AUDIT increased by two points, whereas AUDIT-C increased by one point, but there was no change in median scores between the second and third surveys. This highlights the differences in using different tools and cut-offs for identifying young people who are risky drinkers; however, all measurements show high levels of risky drinking at all three time points. The TLFB is a more robust measurement of alcohol consumption; however, it is more time-consuming to administer therefore for the definitive study the 28-day TLFB should be used as the primary outcome measure at 12-month follow-up.
-
Survey The WEMWBS measures general psychological health, with a scoring range of 14–70, with a higher score indicating higher levels of mental well-being. At TP1 the median score for the WEMWBS was ‘48’, which is comparative to other studies with young people (median 49). 161 The RAPI was calculated only for those who reported drinking. At TP1 the median score was ‘2’. RAPI showed a moderate association with alcohol (using AUDIT 0.76 and AUDIT-C 0.65), whereas WEMWBS showed a very weak correlation (using AUDIT –0.13 and AUDIT-C –0.08).
-
Trial The comparison between subgroups at baseline demonstrated that gender, smoking and sexual behaviour were significantly associated with young people’s current drinking behaviour, using the AUDIT and AUDIT-C.
-
Trial Learning mentors recruited 80% of those young people who were eligible for the pilot trial. This recruitment rate matched that which we had anticipated (approximately 79%). Very few young people did not consent to the study (10%). However, 10% failed to meet with the learning mentor to discuss the trial for a number of reasons, including repeated absence, school exclusion and the existence of complex behavioural needs. This could be seen as a form of voluntary or involuntary withdrawal from the study and would need to be taken account of in a future study.
-
Control Of the 60 young people eligible for the trial, three did not meet with the learning mentor (5%) and five did not give consent (8%). In total, 52 out of 60 were recruited to the trial (87%).
-
Intervention 1 Of the 79 young people eligible for the trial, 15 did not meet with the learning mentor (19%) and 10 did not give consent (13%). In total, 54 out of 79 were recruited to the trial (68%). Therefore, both the control and condition 1 arms were found to be feasible.
-
Intervention 2 Recruitment of young people to the intervention 2 arm was higher than expected. Of the 90 young people eligible for the trial, seven did not meet with the learning mentor (8%) and eight did not give consent to intervention 1 (9%). In total, 75 out of 90 were recruited to the trial and received intervention 1 (83%). However, having agreed to enter the trial, many of the young people in the intervention 2 arm did not receive the full intervention as planned. Of the 75 students recruited into this arm, 25 of these students agreed to their parents being contacted (33%); however, only eight (11% of the 75 and 32% of the 25) received both the individual intervention (intervention 1) and family intervention (intervention 2). There is more work needed to engage with parents in interventions in the school setting. Despite the input of lots of time and resources from the school and research staff, it was not, however, possible to engage parents in the third arm of the trial, reflecting experiences in other studies. 192
-
12-month follow-up Once enrolled in the trial, 88% of trial participants provided data at the 12-month follow-up meeting with the learning mentor (control, 83%; intervention 1, 91%; intervention 2, 89%). This was a higher rate than we had anticipated (65%) and it reflects well on the efforts of the trial team, learning mentors and school processes. The pilot trial has achieved the goal of demonstrating that outcome measures could successfully be collected on a high proportion of participants.
Objective 5
-
There were very low levels of missing data in the baseline survey or the EQ-5D-Y (3.4–3.9%), with the tool being seen as appropriate. The majority of young people indicated that they had no problems on the first three dimensions (mobility 93%, looking after self 99%, doing usual activities 94%). Higher levels of problems were found in the dimensions of pain or discomfort (19% having some level of problems) and being worried, sad or unhappy (24% having some level of problem). This indicates that there is some opportunity for the definitive trial to improve health, at least in terms of the final two dimensions. For the definitive study the EQ-5D-Y and service use should be assessed at baseline and 12-month follow-up. Implausible values, in relation to service use, should be reassessed, especially in the case of visits to the GP, which showed a higher-than-average percentage of ‘implausible’ values, and different implausible levels could be given for different service use.
-
In relation to service use, there was between 4.2% and 4.8% of answers missing at baseline. The majority of young people reported no use of services. The only possible exception was ‘GP visit’. Implausible data (values of seven or more) were found in 3% of all answers at baseline.
-
The use of open-format diaries meant that differing levels of data were reported by learning mentors, especially in relation to preparation time. In the definitive study, case diaries should be made more concise and time categories should be provided. Time should be reported by ticking boxes of preselected times, informed by the summary statistics regarding the times reported in the feasibility study. Different forms will be needed for each arm of the trial. This will enable accurate data to inform an economic evaluation. These forms should be piloted with a small group of learning mentors to establish face validity.
Objective 6
For the definitive trial, we propose a four-region, two-arm, cRCT (randomisation at school level), with integrated economic and process evaluations. This would enable generalisable results and take into account geographical, ethnic and socioeconomic differences, as well as reflecting differences in organisation of education services. The literature shows that ASBI with young people is effective and the results of this present study show that it is feasible and acceptable to intervene with young people aged 14–15 years in the school setting. The intervention with parental involvement was found not to be feasible or acceptable. The hypothesis for the definitive trial would be that ASBI is more effective and cost-effective at reducing hazardous drinking in young people (aged 14–15 years) than a control condition of screening, feedback that the young person may be drinking at a risky level and an information leaflet, as well as usual advice in Year 10 of high/comprehensive schools in England. This research will have a broader impact on both the target community (young people) and wider society in reducing health and social harms and inequalities. Primary and secondary outcome measures will be the same measures used in the pilot feasibility trial.
-
Screening tool A lifestyle survey, as used in the present study, which includes questions relating to risky drinking.
-
Regions North East England, North West England, Kent and South London.
-
Primary outcome measure Reduction in alcohol use using the 28-day TLFB questionnaire193 at 12-month follow up.
-
Secondary outcomes Risky drinking using the A-SAQ2 and AUDIT;162 smoking behaviour; alcohol-related problems using the RAPI;163 emotional well-being using the WEMWBS;159 and quality of life and health utility will be measured using the EQ-5D-Y. 165 A modified S-SUQ will capture health and social resource costs for the integrated economic evaluation. 166 Learning mentor time will be assessed using a revised case diary sheet (see Appendix 6).
-
Proposed design The multicentre, two-armed cRCT, incorporates a control and intervention condition. Schools will be paid £1000 for taking part in the research study for the time involved. Young people will not be given a £5.00 gift voucher, as in the pilot study, for two reasons: (1) it would be very costly and (2) this would not happen if the study was mainstreamed.
-
Screening All pupils in Year 10 (aged 14–15 years) in each of the schools, whose parents have not opted them out of the study, will be asked to complete a voluntary questionnaire that will contain a number of tools including the primary and secondary outcome measure tools. All young people who screen positive and leave their name will be asked to consent to the trial by the learning mentor.
-
Control condition Standard alcohol advice delivered in PSHE lessons delivered by class teachers, feedback to the young person that they are drinking in a way that may be harmful, and provision of an advice leaflet by the learning mentor.
-
Intervention 1 In addition to PSHE, the young people who are eligible (risky drinkers) and consent to participate will be given feedback that they are drinking in a way that may be harmful and provided with an advice leaflet. They will then take part in a 30-minute personalised interactive worksheet-based session, developed during the pilot feasibility trial. This will be delivered by the learning mentor (at school) and consist of structured feedback about their drinking behaviour and advice about the health and social consequences of continued hazardous alcohol consumption. The intervention encompasses the elements of the FRAMES approach for eliciting behaviour change (Feedback, Responsibility, Advice, Menu, Empathy and Self-efficacy). 59
-
12-month follow-up All young people who come into the trial will be invited to meet with the learning mentor 12 months post intervention, during which they will be asked to complete the same battery of questionnaires used at baseline, as well as the 28-day TLFB.
-
Training All learning mentors will receive school-based training in the study procedures and the intervention that is relevant to their school. Learning mentors will be brought together at one of the schools in each geographical area for this training. Such outreach training was found to be the most cost-effective implementation strategy for ASBI delivery in the pilot2 and in other settings. 156 Intervention training for learning mentors will be carried out by an experienced trainer. Learning mentors will be provided with support materials and will be assessed as competent by the trainer prior to embarking on the study. Changes to the training and manual will take into account learning from the pilot feasibility trial. Ongoing support and supervision will be provided by clinical staff working on the project.
-
Fidelity We will carry out a minimum of one audio-recorded intervention delivered per learning mentor within the intervention arm of the trial.
-
Setting High/comprehensive schools are governed by the local authorities in England. Screening will take place in the PSHE or registration class on a classroom basis. Interventions will take place in the learning mentor’s classroom or office space. This will be the anticipated setting for roll-out if the project is implemented.
-
Patient and public involvement participation PPI has been imperative to the success of the pilot feasibility trial and this will be continued in the main trial with involvement from young people and parents; however, we acknowledge that more in-depth PPI work is needed in the definitive trial. We intend to set up a management group to steer the research in each of the schools that take part in the study, which will include teaching staff/learning mentors and young people. Views from these groups will feed into the PMG on a regular basis.
-
Qualitative work Semistructured in-depth interviews will be carried out in each of the schools with staff and young people. The interviews will further explore factors that potentially hinder or enhance the use of ASBI approaches in the school setting and with the target age group, with the aim of exploring future roll-out of such work.
-
Sample size As a two-arm trial, 100 responses would be needed per arm with individual randomisation and a significance level of 5%. We intend to use minimisation to balance out both school size and percentage free school meals. Using other trial parameters as above, this would equate to 220 young people per arm, and a total of 18 schools (nine per arm) when clustering is taken into account.
Acknowledgements
The research team would like to thank all the school staff, young people and parents who took part in the research. We would like to acknowledge the help of Jennifer Birch; Hannah Kaner and Josh Kaner, who were responsible for inputting all of the survey data; Dr Mark Deverill and Professor Luke Vale, who oversaw the health economics section of the research; Chris Speed, Julie Doughty, Pauline Potts and Anna Basu, Newcastle Clinical Trials Unit, for all of their help; and Dr Graeme Wilson, Rachel Tyrell, Jessica Reilly and Janice Armstrong, from the alcohol team at the Institute of Health and Society at Newcastle University, for their help throughout the project. Finally we would like to thank the members of the TSG for their involvement throughout the research.
Study governance references
| Study full title | A pilot feasibility trial of screening and brief alcohol intervention to prevent hazardous drinking in young people aged 14–15 years in a high school setting (SIPS JR-HIGH) | |
| Study short title | SIPS JR-HIGH | |
| Trial sponsor | Newcastle University | |
| Trial funder | NIHR Public Health Research programme | 10/3002/07 |
| Trial registration | International Standard Randomised Controlled Trials Register | ISRCTN07073105 |
| Ethical approval | Newcastle University | 00508/2011 |
Contributions of authors
All authors read and agreed the final draft report.
Dorothy Newbury-Birch (Lecturer in Public Health Research, project management) was the Chief Investigator on the study and took overall responsibility for the study and the writing of the report.
Stephanie Scott (née O’Neil) (Research Associate and SIPS JR-HIGH Project Manager) project managed the study and co-drafted the report.
Amy O’Donnell (Research Assistant, qualitative research) co-analysed and co-drafted the qualitative chapter of the final report.
Simon Coulton (Professor of Health Services Research, health services research) contributed to the design of the study, conduct of the trial and the PMG.
Denise Howel (Senior Lecturer, statistics) contributed to the design of the study, conduct of the trial and PMG, supervised the statistical component of the research, carried out statistical analysis, and co-drafted the survey and trial chapters.
Elaine McColl (Professor of Health Services Research and Director of the Newcastle Clinical Trials Unit, methodology) contributed to the design of the study, conduct of the trial and PMG.
Elaine Stamp (Research Associate, statistics) carried out the statistical analysis of the study and co-drafted the survey and trial chapters.
Erin Graybill, (Research Assistant, health economics) conducted the health-economic analysis and drafted the health-economic chapter.
Eilish Gilvarry (Honorary Professor of Addictions Psychiatry, Consultant Psychiatrist in Addictions, BIs and addictions) contributed to the study design, co-developed the interventions, co-drafted the intervention chapter of the report and chaired the PMG.
Kirsty Laing (Research Assistant, qualitative research) carried out the interviews with school staff and young people and analysed the data.
Ruth McGovern, (Senior Research Interventionist, interventionist and qualitative researcher) co-developed the interventions, assessed intervention fidelity and co-drafted the intervention and qualitative chapters of the report.
Paolo Deluca (Senior Research Fellow, trial management) contributed to the design of the study, conduct of the trial and the PMG.
Colin Drummond (Professor of Addiction Psychiatry, addictions) contributed to the design of the study, the conduct of the trial and the PMG.
Christine Harle (Trial Manager, Newcastle Clinical Trials Unit, trial management) contributed to the design of the study, the conduct of the trial and the PMG.
Paul McArdle (Consultant Child and Adolescent Psychiatrist) contributed to the design of the study, conduct of the trial and PMG, co-developed the interventions and co-drafted the intervention chapter of the report.
Les Tate (Strategy and Commissioning Manager, education) contributed to the design of the study, conduct of the trial and PMG and co-ordinated school involvement in the study.
Eileen Kaner (Professor of Public Health Research and Institute Director, BIs, trial management) contributed to the design of the study, the conduct of the trial and the PMG.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health.
Publication
O’Neil S, Coulton S, Deluca P, Deverill M, Drummond C, Gilvarry E, et al. Brief intervention to prevent hazardous drinking in young people aged 14–15 in a high school setting (SIPS JR-HIGH): study protocol for a randomized controlled trial. Trials 2012;13:166. http://dx.doi.org/10.1186/1745-6215-13-166.
References
- Developing and Evaluating Complex Interventions: New Guidance. London: MRC; 2008.
- O’Neil S, Coulton S, Deluca P, Deverill M, Drummond C, Gilvarry E, et al. Brief intervention to prevent hazardous drinking in young people aged 14–15 in a high school setting (SIPS JR-HIGH): study protocol for a randomized controlled trial. Trials 2012;13. http://dx.doi.org/10.1186/1745-6215-13-166.
- Hibbell B, Guttormsson U, Ahlström S, Balakireva O, Bjarnason T, Kokkevi A, et al. The 2011 ESPAD Report: Substance Use Among Students in 36 European Countries. Stockholm: The Swedish Council for Information on Alcohol and Other Drugs; 2012.
- Fuller E, Henderson H, Nass L, Payne C, Phelps A, Ryley A. Smoking, Drinking and Drug Use Among Young People in England in 2012. London: NatCen Social Research; 2013.
- Zucker R, Donovan J, Masten A, Mattison M, Moss H. Developmental perspective on underage alcohol use. Developmental processes and mechanisms 0–10. Alcohol Res Health 2009;32:16-29.
- Windle M, Spear L, Fuligni A, Angold A, Brown J, Pine D, et al. Transitions into underage and problem drinking summary of developmental processes and mechanisms: ages 10–15. Alcohol Res Health 2009;32:30-4.
- Brown S, McGue M, Maggs J, Schulenberg J, Hingson R, Swartzwelder S, et al. Underage alcohol use: summary of developmental processes and mechanisms: ages 16–20. Alcohol Res Health 2009;32:41-52.
- Newbury-Birch D, Gilvarry E, McArdle P, Stewart S, Walker J, Lock C, et al. The Impact of Alcohol Consumption on Young People: A Review of Reviews. London: Department for Children, Schools and Families; 2009.
- Zeigler D, Wang C, Yoast R, Dickinson B, McCaffree M, Robinowitz C, et al. The neurocognitive effects of alcohol on adolescents and college students. Prev Med 2005;40:23-32. http://dx.doi.org/10.1016/j.ypmed.2004.04.044.
- Witt E. Research on alcohol and adolescent brain development: opportunities and future directions. Alcohol Alcohol 2010;44:119-24. http://dx.doi.org/10.1016/j.alcohol.2009.08.011.
- Squeglia LM, Pulido C, Wetherill RR, Jacobus J, Brown GG, Tapert SF. Brain response to working memory over three years of adolescence: influence of initiating heavy drinking. J Stud Alcohol Drugs 2012;73.
- Rodham K, Brewer H, Mistral W, Stallard P. Adolescents’ perception of risk and challenge: a qualitative study. J Adolesc 2006;29:261-72. http://dx.doi.org/10.1016/j.adolescence.2005.05.012.
- MacArthur G, Smith M, Melotti R, Heron J, Macleod J, Hickman M, et al. Patterns of alcohol use and multiple risk behaviour by gender during early and late adolescence: the ALSPAC cohort. J Public Health 2012;34:i20-30. http://dx.doi.org/10.1093/pubmed/fds006.
- Ellickson P, Tucker J, Klein D. Ten-year prospective study of public health problems associated with early drinking. Pediatrics 2003;111:949-55. http://dx.doi.org/10.1542/peds.111.5.949.
- Murgraff V, Parrott A, Bennett P. Risky single-occasion drinking amongst young people – definition, correlates, policy, and intervention: a board overview of research findings. Alcohol Alcohol 1999;34:3-14. http://dx.doi.org/10.1093/alcalc/34.1.3.
- McGue M, Iacono WG, Legrand LN, Malone S, Elkins I. Origins and consequences of age at first drink. associations with substance-use disorders, disinhibitory behavior and psychopathology, and p3 amplitude. Alcohol Clin Exp Res 2001;25:1156-65. http://dx.doi.org/10.1111/j.1530-0277.2001.tb02330.x.
- Bjork JM, Smith AR, Chen G, Hommer DW. Adolescents, adults and rewards: comparing motivational neurocircuitry recruitment using fMRI. PLOS ONE 2010;5. http://dx.doi.org/10.1371/journal.pone.0011440.
- Duke AA, Giancola PR, Morris DH, Holt JC, Gunn RL. Alcohol dose and aggression: another reason why drinking more is a bad idea. J Stud Alcohol Drugs 2011;72:34-43.
- Perkins W. Surveying the damage: a review of research on consequences of alcohol misuse in college populations. J Stud Alcohol Suppl 2002;14:91-100.
- Miller P, Plant M. Truancy and perceived school performance: an alcohol and drug study of UK teenagers. Alcohol Alcohol 1999;34:886-93. http://dx.doi.org/10.1093/alcalc/34.6.886.
- Barnes G, Mitic W, Leadbeater B, Dhami M. Risk and protective factors for adolescent substance use and mental health symptoms. Can J Commun Ment Health 2009;28:1-15.
- Carpenter C. Heavy alcohol use and suicide: evidence from tougher drunk driving laws. J Policy Anal Manage 2004;23:831-42. http://dx.doi.org/10.1002/pam.20049.
- DeWit DJ, Adlaf EM, Offord DR, Ogborne AC. Age at first alcohol use: a risk factor for the development of alcohol disorders. Am J Psychiatry 2000;157:745-50. http://dx.doi.org/10.1176/appi.ajp.157.5.745.
- Dawson D, Goldstein R, Chou P, Ruan W, Grant B. Age at first drink and the first incidence of adult-onset DSM-IV alcohol use disorders. Alcohol Clin Exp Res 2008;32:1-12. http://dx.doi.org/10.1111/j.1530-0277.2008.00806.x.
- Jernigan D. Global Status Report: Alcohol and Young People. Geneva: WHO; 2001.
- Donaldson L. Guidance on the Consumption of Alcohol by Children and Young People. London: Department of Health; 2009.
- Interventions in Schools to Prevent and Reduce Alcohol Use Among Children and Young People. London: NICE; 2007.
- Spoth R, Greenberg M, Turrisi R. Preventive interventions addressing underage drinking: state of the evidence and steps towards public health impact. Pediatrics 2008;121:S311-36. http://dx.doi.org/10.1542/peds.2007-2243E.
- Foxcroft DR, Ireland D, Lister-Sharp DJ, Lowe G, Breen R. Longer-term primary prevention for alcohol misuse in young people: a systematic review. Addiction 2003;98:397-411. http://dx.doi.org/10.1046/j.1360-0443.2003.00355.x.
- Foxcroft D, Tsertsvadze A. Universal school-based prevention programs for alcohol misuse in young people. Cochrane Database Syst Rev 2011;5. http://dx.doi.org/10.1002/14651858.CD009113.
- Jones L, James M, Jefferson T, Lushey C, Morleo, Stokes E, et al. A Review of the Effectiveness and Cost-effectiveness of Interventions Delivered in Primary and Secondary Schools to Prevent and/or Reduce Alcohol Use by Young People Under 18 Years Old. Liverpool: John Moores University and National Collaborating Centre – Drug Prevention; 2007.
- Jefferson T, Jones L, Bellis M. Interventions Delivered in Primary and Secondary Schools to Prevent and/or Reduce Alcohol Use by Young People Under 18 Years Old: Epidemiology Review and Development of an Epidemiological Model. Liverpool: John Moores University; 2007.
- Alcohol in the European Union. Consumption, Harm and Policy Approaches. Copenhagen: WHO Regional Office for Europe; 2012.
- McKay M, McBride N, Sumnall H, Cole J. Reducing the harm from adolescent alcohol consumption: results from an adapted version of SHAHRP in Northern Ireland. J Subst Use 2012;17:98-121. http://dx.doi.org/10.3109/14659891.2011.615884.
- Koning IM, Van den Eijnden RJ, Verdurmen JE, Engels RC, Vollebergh WA. Long-term effects of a parent and student intervention on alcohol use in adolescents: a cluster randomized controlled trial. Am J Prev Med 2011;40:541-7. http://dx.doi.org/10.1016/j.amepre.2010.12.030.
- Koning IM, van den Eijnden RJJM, Verdurmen JEE, Engels RCME, Vollebergh WAM. A cluster randomized trial on the effects of a parent and student intervention on alcohol use in adolescents four years after baseline; no evidence of catching-up behaviour. Addict Behav 2012;38:2032-9. http://dx.doi.org/10.1016/j.addbeh.2012.12.013.
- Jackson R, Johnson M, Campbell F, Messina J, Guillaume L, Purshouse R, et al. Screening and Brief Interventions: Effectiveness Review to the National Institute for Health and Clinical Excellence. Sheffield: The University of Sheffield, School of Health and Related Research (ScHARR); 2009.
- Babor RF, Grant M. Project on Identification and Management of Alcohol Related Problems. Report on Phase II: A Randomised Clinical Trial of Brief Interventions in Primary Health Care. Geneva: WHO; 1992.
- Aertgeerts B, Buntinx F, Ansoms S, Fevery J. Screening properties of questionnaires and laboratory tests for the detection of alcohol abuse in a general practice population. Br J Gen Pract 2001;51:206-17.
- Miles H, Winstock A, Strang J. Identifying young people who drink too much: the clinical utility of the five-item Alcohol Use Disorders Identification Test (AUDIT). Drug Alcohol Rev 2001;20:9-18. http://dx.doi.org/10.1080/09595230020029347.
- Reinert DF, Allen JP. The Alcohol Use Disorders Identification Test (AUDIT): a review of recent research. Alcohol Clin Exp Res 2002;26:272-9. http://dx.doi.org/10.1111/j.1530-0277.2002.tb02534.x.
- O’Donnell A, Kaner E, Boyle P, Boffetta P, Zatonski W, Lowenfels AB, et al. Alcohol, Science, Policy and Public Health. Oxford: Oxford University Press; 2013.
- Reinert D, Allen J. The Alcohol Use Disorders Identification Test: an update of research findings. Alcohol Clin Exp Res 2007;31:185-99. http://dx.doi.org/10.1111/j.1530-0277.2006.00295.x.
- Chung T, Colby S, Barnett N, Rohsenow D, Spirito A, Monti P. Screening adolescents for problem drinking: performance of brief screens against DSM-IV alcohol diagnoses. Centre for Alcohol and Addiction Studies. J Stud Alcohol 2000;61:579-87.
- Kelly T, Donovan J, Kinnane J, Taylor D. A comparison of alcohol screening instruments among under-aged drinkers treated in emergency departments. Alcohol Alcohol 2002;37:444-50. http://dx.doi.org/10.1093/alcalc/37.5.444.
- Foster AI, Blondell RD, Looney SW. The practicality of using the SMAST and AUDIT to screen for alcoholism among adolescents in an urban private family practice. J Ky Med Assoc 1997;95:105-7.
- Cook RL, Chung T, Kelly TM, Clark DB. Alcohol screening in young persons attending a sexually transmitted disease clinic. J Gen Intern Med 2005;20:1-6. http://dx.doi.org/10.1111/j.1525-1497.2005.40052.x.
- Heron J, Macleod J, Munafò MR, Melotti R, Lewis G, Tilling K, et al. Patterns of alcohol use in early adolescence predict problem use at age 16. Alcohol Alcohol 2012;47:169-77. http://dx.doi.org/10.1093/alcalc/agr156.
- Santis R, Garmendia M, Acuna G, Alvarado ME, Arteaga O. The Alcohol Use Disorders Identification Test (AUDIT) as a screening instrument for adolescents. Drug Alcohol Depend 2009;103:155-8. http://dx.doi.org/10.1016/j.drugalcdep.2009.01.017.
- Knight J, Sherritt L, Harris S, Gates E, Chang G. Validity of brief alcohol screening tests among adolescents: a comparison of the AUDIT, POSIT, CAGE and CRAFFT. Alcohol Clin Exp Res 2003;27:67-73. http://dx.doi.org/10.1111/j.1530-0277.2003.tb02723.x.
- Kriston L, Holzel L, Weiser A-K, Berner MM, Harter M. Meta-analysis: are three questions enough to detect unhealthy alcohol use?. Ann Intern Med 2008;149:879-88. http://dx.doi.org/10.7326/0003-4819-149-12-200812160-00007.
- Chung T, Smith G, Donovan J, Windle M, Faden V, Chen C, et al. Drinking frequency as a brief screen for adolescent alcohol problems. Pediatrics 2012;129:205-12. http://dx.doi.org/10.1542/peds.2011-1828.
- Bailey K, Baker A, Webster R, Lewin T. Pilot randomized controlled trial of a brief alcohol intervention group for adolescents. Drug Alcohol Rev 2004;23:157-66. http://dx.doi.org/10.1080/09595230410001704136.
- Kaner E, Newbury-Birch D, Heather N, Miller P. Evidence-based Addiction Treatment. San Diego, CA: Elsevier; 2009.
- Kaner E, Dickinson H, Beyer F, Pienaar E, Schlesinger C, Campbell F, et al. The effectiveness of brief alcohol interventions in primary care settings: a comprehensive review. Drug Alcohol Rev 2009;28:301-23. http://dx.doi.org/10.1111/j.1465-3362.2009.00071.x.
- Bandura A. Social Learning Theory. Englewood Cliffs, NJ: Prentice Hall; 1997.
- Bien TH, Miller WR, Tonigan JS. Brief interventions for alcohol problems: a review. Addiction 1993;88:315-35. http://dx.doi.org/10.1186/1471-2458-9-380.
- Kaner E, Beyer F, Dickinson H, Pienaar E, Campbell F, Schlesinger C, et al. Effectiveness of brief alcohol interventions in primary care populations. Cochrane Database Syst Rev 2007;2.
- Miller W, Sanchez V. Motivating Young Adults for Treatment and Lifestyle Change. Notre Dame, IN: University of Notre Dame Press; 1993.
- Rollnick S, Mason P, Butler C. Health Behaviour Change: A Guide for Practitioners. Edinburgh: Churchill Livingstone; 1999.
- Ballesteros J, Duffy JC, Querejeta I, Ariño J, González Pinto A. Efficacy of brief interventions for hazardous drinkers in primary care: systematic review and meta-analyses. Alcohol Clin Exp Res 2004;28:608-18. http://dx.doi.org/10.1097/01.ALC.0000122106.84718.67.
- Bertholet N, Daeppen J-B, Wietlisbach V, Fleming M, Burnand B. Brief alcohol intervention in primary care: systematic review and meta-analysis. Arch Intern Med 2005;165:986-95. http://dx.doi.org/10.1001/archinte.165.9.986.
- Whitlock E, Polen M, Green C, Orleans T, Klein J. Behavioral counseling interventions in primary care to reduce risky/harmful alcohol use by adults: a summary of the evidence for the US Preventive Services Task Force. Ann Intern Med 2004;140:557-68. http://dx.doi.org/10.7326/0003-4819-140-7-200404060-00017.
- Littlejohn C. Does socio-economic status influence the acceptability of, attendance for, and outcome of, screening and brief interventions for alcohol misuse: a review. Alcohol Alcohol 2006;41:540-5. http://dx.doi.org/10.1093/alcalc/agl053.
- Saitz R. Alcohol screening and brief intervention in primary care: absence of evidence for efficacy in people with dependence or very heavy drinking. Drug Alcohol Rev 2010;29:631-40. http://dx.doi.org/10.1111/j.1465-3362.2010.00217.x.
- Ockene JK, Adams A, Hurley TG, Wheeler EV, Hebert JR. Brief physician-and nurse practitioner-delivered counseling for high-risk drinkers: does it work?. Arch Intern Med 1999;159. http://dx.doi.org/10.1001/archinte.159.18.2198.
- Ockene JK, Reed GW, Reiff-Hekking S. Brief patient-centered clinician-delivered counseling for high-risk drinking: 4-year results. Ann Behav Med 2009;37:335-42. http://dx.doi.org/10.1007/s12160-009-9108-5.
- Kaner E, Bland M, Cassidy P, Coulton S, Dale V, Deluca P, et al. Effectiveness of screening and brief alcohol intervention in primary care (SIPS trial): pragmatic cluster randomised controlled trial. BMJ 2013;346:1-14. http://dx.doi.org/10.1136/bmj.e8501.
- Carey K, Scott-Sheldon L, Carey M, DeMartini K. Individual-level interventions to reduce college student drinking: a meta-analytic review. Addict Behav 2007;32:2469-94. http://dx.doi.org/10.1016/j.addbeh.2007.05.004.
- Larimer M, Cronce J. Identification, prevention, and treatment revisited: Individual-focused college drinking prevention strategies 1999–2006. Addict Behav 2007;32:2439-68. http://dx.doi.org/10.1016/j.addbeh.2007.05.006.
- Cohen J. Statistical Power of Analysis for the Behavioural Sciences. New York, NY: Academic Press; 1969.
- Calabria B, Shakeshaft A, Havard A. A systematic and methodological review for interventions for young people experiencing alcohol-related harm. Addiction 2011;106:1406-18. http://dx.doi.org/10.1111/j.1360-0443.2011.03418.x.
- Carney T, Myers B. Effectiveness of early interventions for substance-using adolescents: findings from a systematic review and meta-analysis. Subst Abuse Treat Prev Policy 2012;7. http://dx.doi.org/10.1186/1747-597X-7-25.
- Jensen CD, Cushing CC, Aylward BS, Craig JT, Sorell DM, Steele RG. Effectiveness of motivational interviewing interventions for adolescent substance use behavior change: a meta-analytic review. J Consult Clin Psychol 2011;79. http://dx.doi.org/10.1037/a0023992.
- Mitchell S, Gryczynski J, O’Grady K, Schwartz R. SBIRT for adolescent drug and alcohol use: current status and future directions. J Subst Abuse Treat 2013;44:463-72. http://dx.doi.org/10.1016/j.jsat.2012.11.005.
- Tripodi S, Bender K, Litschge C, Vaughn M. Interventions for reducing adolescent alcohol abuse. A meta-analytic review. Arch Pediatr Adolesc Med 2010;164:85-91. http://dx.doi.org/10.1001/archpediatrics.2009.235.
- Wachtel T, Staniford M. The effectiveness of brief interventions in the clinical setting in reducing alcohol misuse and binge drinking in adolescents: a critical review of the literature. J Clin Nurs 2010;19:605-20. http://dx.doi.org/10.1111/j.1365-2702.2009.03060.x.
- Yuma-Guerrero P, Lawson J, Velasquez M, von Sternberg K, Maxson T, Garcia N. Screening, brief intervention, and referral for alcohol use in adolescents: a systematic review. Pediatrics 2012;130:115-22. http://dx.doi.org/10.1542/peds.2011-1589.
- Toumbourou J, Stockwell T, Neighbors C, Marlatt G, Sturge J, Rehm J. Interventions to reduce harm associated with adolescent substance use. Lancet 2007;369:1391-401. http://dx.doi.org/10.1016/S0140-6736(07)60369-9.
- Boekeloo B, Jerry J, Lee-Ougo W, Worrell K, Hamberger E, Russek-Cohen E, et al. Randomized trial of brief office-based interventions to reduce adolescent alcohol use. Arch Pediatr Adolesc Med 2004;158:635-42. http://dx.doi.org/10.1001/archpedi.158.7.635.
- D’Amico EJ, Miles JNV, Stern SA, Meredith LS. Brief motivational interviewing for teens at risk of substance use consequences: a randomized pilot study in a primary care clinic. J Subst Abuse Treat 2008;35:53-61. http://dx.doi.org/10.1016/j.jsat.2007.08.008.
- Maio R, Shope J, Blow F, Gregor M, Zakrajsek J, Weber J, et al. A randomized controlled trial of an emergency department-based interactive computer program to prevent alcohol misuse among injured adolescents. Ann Emerg Med 2005;45:420-9. http://dx.doi.org/10.1016/j.annemergmed.2004.10.013.
- Monti P, Barnett N, Colby S, Gwaltney CJ, Spirito A, Rohsenow DJ, et al. Motivational interviewing versus feedback only in emergency care for young adult problem drinking. Addiction 2007;102:1234-43. http://dx.doi.org/10.1111/j.1360-0443.2007.01878.x.
- Monti P, Colby S, Barnett N, Spirito A, Rohsenow DJ, Myers M, et al. Brief intervention for harm reduction with alcohol positive older adolescents in a hospital emergency department. J Consult Clin Psychol 1999;6:989-94. http://dx.doi.org/10.1037/0022-006X.67.6.989.
- Spirito A, Monti PM, Barnett NP, Colby SM, Sindelar H, Rohsenow DJ, et al. A randomized clinical trial of a brief motivational intervention for alcohol-positive adolescents treated in an emergency department. J Pediatr 2004;145:396-402. http://dx.doi.org/10.1016/j.jpeds.2004.04.057.
- Peterson PL, Baer JS, Wells EA, Ginzler JA, Garrett SB. Short-term effects of a brief motivational intervention to reduce alcohol and drug risk among homeless adolescents. Psychol Addict Behav 2006;20. http://dx.doi.org/10.1037/0893-164X.20.3.254.
- Baer J, Kiviahan D, Blume A, McKnight P, Marlatt A. Brief intervention for heavy-drinking college students: 4-year follow-up and natural history. Am J Public Health 2001;91:1310-16. http://dx.doi.org/10.2105/AJPH.91.8.1310.
- Borsari B, Carey K. Effects of a brief motivational intervention with college student drinkers. J Consult Clin Psychol 2000;68:728-33. http://dx.doi.org/10.1037/0022-006X.68.4.728.
- Borsari B, Carey K. Two brief alcohol interventions for mandated college students. Psychol Addict Behav 2005;19:296-302. http://dx.doi.org/10.1037/0893-164X.19.3.296.
- Carey KB, Carey MP, Maisto SA, Henson JM. Brief motivational interventions for heavy college drinkers: a randomized controlled trial. J Consult Clin Psychol 2006;74:943-54. http://dx.doi.org/10.1037/0022-006X.74.5.943.
- Feldstein S, Forcehimes A. Motivational interviewing with underage college drinkers: a preliminary look at the role of empathy and alliance. Am J Drug Alcohol Abuse 2007;33:737-46. http://dx.doi.org/10.1080/00952990701522690.
- Marlatt G, Baer J, Kivlahan D, Dimeff L, Larimer M, Quigley L, et al. Screening and brief intervention for high-risk college student drinkers: results from a 2-year follow-up assessment. J Consult Clin Psychol 1998;66:604-15. http://dx.doi.org/10.1037/0022-006X.66.4.604.
- Murphy J, Duchnick J, Vuchinich R, Davison J, Karg R, Olson A, et al. Relative efficacy of a brief motivational intervention for college student drinkers. Psychol Addict Behav 2001;15:373-9. http://dx.doi.org/10.1037/0893-164X.15.4.373.
- Thush C, Wiers R, Thiunissen N, Van den Bosch J, Opdenacker J, van Empelen P, et al. A randomized clinical trial of a targeted intervention to moderate alcohol-related problems in at-risk adolescents. Pharmacol Biochem Addict Behav 2007;86:368-76. http://dx.doi.org/10.1016/j.pbb.2006.07.023.
- Bernstein E, Edwards E, Dorfman D, Heeren T, Bliss CB, Bernstein J. Screening and brief intervention to reduce marijuana use among youth and young adults in a pediatric emergency department. Acad Emerg Med 2009;16:1174-85. http://dx.doi.org/10.1111/j.1553-2712.2009.00490.x.
- Johnston BD, Rivara F, Droesch RM, Dunn C, Copass M. Behavior change counseling in the emergency department to reduce injury risk: a randomized, controlled trial. Pediatrics 2002;110:267-74. http://dx.doi.org/10.1542/peds.110.2.267.
- Walton MA, Chermack ST, Shope JT, Bingham CR, Zimmerman MA, Blow FC, et al. Effects of a brief intervention for reducing violence and alcohol misuse among adolescents: a randomized controlled trial. JAMA 2010;304:527-35. http://dx.doi.org/10.1001/jama.2010.1066.
- Bernstein J, Heeren T, Edward E, Dorfman D, Bliss C, Winter M, et al. A brief motivational interview in a pediatric emergency department, plus 10-day telephone follow-up, increases attempts to quit drinking among youth and young adults who screen positive for problematic drinking. Acad Emerg Med 2010;17:890-902. http://dx.doi.org/10.1111/j.1553-2712.2010.00818.x.
- Grenard JL, Ames SL, Wiers RW, Thush C, Stacy AW, Sussman S. Brief intervention for substance use among at-risk adolescents: a pilot study. J Adolesc Health 2007;40:188-91. http://dx.doi.org/10.1016/j.jadohealth.2006.08.008.
- Marsden J, Stillwell G, Barlow H, Boys A, Taylor C, Hunt N, et al. An evaluation of a brief motivational intervention among young ecstasy and cocaine users: no effect on substance and alcohol use outcomes. Addiction 2006;101:1014-26. http://dx.doi.org/10.1111/j.1360-0443.2006.01290.x.
- McCambridge J, Slym RL, Strang J. Randomized controlled trial of motivational interviewing compared with drug information and advice for early intervention among young cannabis users. Addiction 2008;103:1809-18. http://dx.doi.org/10.1111/j.1360-0443.2008.02331.x.
- McCambridge J, Strang J. Deterioration over time in effect of Motivational Interviewing in reducing drug consumption and related risk among young people. Addiction 2005;100:470-8. http://dx.doi.org/10.1111/j.1360-0443.2005.01013.x.
- Spirito A, Sindelar-Manning H, Colby S, Barnett N, Lewander W, Rohsenow D, et al. Individual and family motivational interventions for alcohol positive adolescents treated in an emergency department. Arch Pediatr Adolesc Med 2011;165:269-74. http://dx.doi.org/10.1001/archpediatrics.2010.296.
- Walker D, Roffman R, Stephens R, Berghuis J, Kim W. Motivational enhancement therapy for adolescent marijuana users: a preliminary randomized controlled trial. J Consult Clin Psychol 2006;74:628-32. http://dx.doi.org/10.1037/0022-006X.74.3.628.
- Winters K, Leitten W. Brief intervention for drug-abusing adolescents in a school setting. Psychol Addict Behav 2007;21:249-54. http://dx.doi.org/10.1037/0893-164X.21.2.249.
- McCambridge J, Strang J. The efficacy of a single-session motivational interviewing in reducing drug consumption and perceptions of drug-related risk and harm among young people: Results from a multisite cluster randomized trial. Addiction 2004;99:39-52. http://dx.doi.org/10.1111/j.1360-0443.2004.00564.x.
- Azrin N, McMahon P, Donohue B, Besalel V, Lapinski K, Kogan E, et al. Behavior therapy for drug abuse: a controlled treatment outcome study. Behav Res Ther 1994;32:857-66. http://dx.doi.org/10.1016/0005-7967(94)90166-X.
- Baer J, Garrett S, Beadnell B, Wells E, Peterson P. Brief motivational intervention with homeless adolescents: evaluating effects on substance use and service utilization. Psychol Addict Behav 2007;21:582-6. http://dx.doi.org/10.1037/0893-164X.21.4.582.
- Friedman A, Terras A, Glassman K. Multimodel substance use intervention program for male delinquents. J Child Adolesc Subst Abuse 2002;11:43-65. http://dx.doi.org/10.1300/J029v11n04_03.
- Godley M, Godley S, Dennis M, Funk R, Passetti L. Preliminary outcomes from the assertive continuing care experiment for adolescents discharged from residential treatment. J Subst Abuse Treat 2002;23:21-32. http://dx.doi.org/10.1016/S0740-5472(02)00230-1.
- Godley M, Godley S, Dennis M, Funk R, Passetti L. The effect of assertive continuing care on continuing care linkage, adherence and abstinence following residential treatment for adolescents with substance use disorders. Addiction 2007;102:81-93. http://dx.doi.org/10.1111/j.1360-0443.2006.01648.x.
- Henggeler S, Pickrel S, Bondino M. Multisystemic treatment of substance abusing and dependent delinquents: outcomes, treatment fidelity, and transportability. Ment Health Serv Res 1999;1:171-84. http://dx.doi.org/10.1023/A:1022373813261.
- Kaminer Y, Burleson J. Psychotherapies for adolescent substance abusers: 15-month follow-up of a pilot study. Am J Addict 1999;8:114-19. http://dx.doi.org/10.1080/105504999305910.
- Kaminer Y, Burleson J, Burke R. Efficacy of outpatient aftercare for adolescents with alcohol use disorders: a randomized controlled study. J Am Acad Child Adolesc Psychiatry 2008;47:1405-12. http://dx.doi.org/10.1097/CHI.0b013e318189147c.
- Latimer W, Winters K, D’Zurilla T, Nichols M. Integrated family and cognitive behavioral therapy for adolescent substance abusers: a stage I efficacy study. Drug Alcohol Depend 2003;71:303-17. http://dx.doi.org/10.1016/S0376-8716(03)00171-6.
- Liddle H, Dakof G, Parker K, Diamond G, Barrett K, Tejeda M. Multidimensional family therapy for adolescent drug abuse: results of a randomized clinical trial. Am J Drug Alcohol Abuse 2001;27:651-88. http://dx.doi.org/10.1081/ADA-100107661.
- Liddle H, Dakof G, Turner R, Henderson C, Greenbaum P. Treating adolescent drug abuse: a randomized trial comparing multidimensional family therapy and cognitive behavior therapy. Addiction 2008;103:1660-70. http://dx.doi.org/10.1111/j.1360-0443.2008.02274.x.
- McGillicuddy N, Rychtarik R, Duquette J, Morsheimer E. Development of a skill training program for parents of substance-abusing adolescents. J Subst Abuse Treat 2001;20:59-68. http://dx.doi.org/10.1016/S0740-5472(00)00149-5.
- Santisteban D, Coatsworth J, Perez-Vidal A, Kurtines WM, Schwartz SJ, LaPerriere A, et al. Efficacy of brief strategic family therapy in modifying Hispanic adolescent behavior problems and substance use. J Fam Psychol 2003;17:121-33. http://dx.doi.org/10.1037/0893-3200.17.1.121.
- Tomlinson K, Brown S, Abrantes A. Psychiatric comorbidity and substance use treatment outcomes of adolescents. Psychol Addict Behav 2004;18:160-9. http://dx.doi.org/10.1037/0893-164X.18.2.160.
- Battjes R, Gordon M, O’Grady K, Kinlock T, Katz E, Sears E. Evaluation of a group-based substance abuse treatment program for adolescents. J Subst Abuse Treat 2004;27:123-34. http://dx.doi.org/10.1016/j.jsat.2004.06.002.
- Mason MJ, Posner MA. Brief substance abuse treatment with urban adolescents: a translational research study. J Child Adolesc Subst Abuse 2009;18:193-206. http://dx.doi.org/10.1080/10678280902724184.
- Thush C, Wiers R, Moerbeek M, Ames S, Grenard J, Sussman S, et al. Influence of motivational interviewing on explicit and implicit alcohol-related cognition and alcohol use in at-risk adolescents. Psychol Addict Behav 2009;23:146-51. http://dx.doi.org/10.1037/a0013789.
- Stein L, Colby S, Barnett N, Monti P, Golembeske C, Lebeau-Craven R. Effects of motivational interviewing for incarcerated adolescents on driving under the influence after release. Am J Addict 2006;15:50-7. http://dx.doi.org/10.1080/10550490601003680.
- Winters K, Fahnhorst T, Botzet A, Lee S, Lalone B. Brief intervention for drug-abusing adolescents in a school setting: outcomes and mediating factors. J Subst Abuse Treat 2012;42:279-88. http://dx.doi.org/10.1016/j.jsat.2011.08.005.
- Conrod P, Castellanos N, Mackie C. Personality-targeted interventions delay the growth of adolescent drinking and binge drinking. J Child Psychol Psychiatry 2008;49:181-90.
- Conrod PJ, Castellanos-Ryan N, Strang J. Brief, personality-targeted coping skills interventions and survival as a non-drug user over a 2-year period during adolescence. Arch Gen Psychiatr 2010;67. http://dx.doi.org/10.1001/archgenpsychiatry.2009.173.
- Conrod PJ, O’Leary-Barrett M, Newton N, Topper L, Castellanos-Ryan N, Mackie C, et al. Effectiveness of a selective, personality-targeted prevention program for adolescent alcohol use and misuse: a cluster randomized controlled trial. JAMA Psychiatry 2013;70:334-42. http://dx.doi.org/10.1001/jamapsychiatry.2013.651.
- Cunningham R, Chermack S, Zimmerman M, Shope J, Bingham R, Blow F, et al. Brief motivational interviewing intervention for peer violence and alcohol use in teens: one-year follow-up. Pediatrics 2012;129:1083-90. http://dx.doi.org/10.1542/peds.2011-3419.
- Borsari B, Murphy J, Barnett N. Predictors of alcohol use during the first year of college: implications for prevention. Addict Behav 2007;32:2062-86. http://dx.doi.org/10.1016/j.addbeh.2007.01.017.
- Spijkerman R, Van den Eijnden R, Overbeek G, Engels R. The impact of peer and parental norms and behavior on adolescent drinking: the role of drinker prototypes. Psychol Health 2007;22:7-29. http://dx.doi.org/10.1080/14768320500537688.
- Shortt A, Hutchinson D, Chapman R, Toumbourou J. Family, school, peer and individual influences on early adolescent alcohol use: first-year impact of the Resilient Families programme. Drug Alcohol Rev 2007;26:625-34. http://dx.doi.org/10.1080/09595230701613817.
- Getz J, Bray J. Predicting heavy alcohol use among adolescents. Am J Orthopsychiatry 2005;75:102-16. http://dx.doi.org/10.1037/0002-9432.75.1.102.
- Ryan S, Jorm A, Lubman D. Parenting factors associated with reduced adolescent alcohol use: a systematic review of longitudinal studies. Aust N Z J Psychiatry 2010;44:774-83. http://dx.doi.org/10.1080/00048674.2010.501759.
- Morleo M, Cook P, Elliott G, Phillips-Howard P. Parental knowledge of alcohol consumption: a cross sectional survey of 11–17 year old schoolchildren and their parents. BMC Publ Health 2013;13:1-10. http://dx.doi.org/10.1186/1471-2458-13-412.
- Urberg K, Goldstein MS, Toro PA. Supportive relationships as a moderator of the effects of parent and peer drinking on adolescent drinking. J Res Adolesc 2005;15:1-19. http://dx.doi.org/10.1111/j.1532-7795.2005.00084.x.
- Baumrind D. Familial antecedents of adolescent drug use: a developmental perspective. NIDA Res Monogr 1985;56:13-44.
- Moore G, Rothwell H, Segrott J. An exploratory study of the relationship between parental attitudes and behaviour and young people’s consumption of alcohol. Subst Abuse Treat Prev Policy 2010;5:1-33. http://dx.doi.org/10.1186/1747-597X-5-6.
- Foxcroft D, Lowe G. Adolescent drinking behaviour and family socialisation factors: a meta-analysis. J Adolesc 1991;14:255-73. http://dx.doi.org/10.1016/0140-1971(91)90020-R.
- Ward B, Snow P. Factors affecting parental supply of alcohol to underage adolescents. Drug Alcohol Rev 2011;30:338-43. http://dx.doi.org/10.1111/j.1465-3362.2010.00228.x.
- Elliott G, Morleo M, Harkins C, Cook P, Phillips-Howard P. Parents’ Perceptions of their Children’s Alcohol Consumption. Liverpool: Centre for Public Health, Liverpool John Moores University; 2011.
- Bremner P, Burnett J, Nunney F, Ravat M, Mistral W. Young People, Alcohol and Influences. A Study of Young People and their Relationship with Alcohol. York: Joseph Rowntree Foundation; 2011.
- Bellis M, Phillips-Howard P, Hughes K, Hughes S, Cook P, Morleo M, et al. Teenage drinking, alcohol availability and pricing: a cross-sectional study of risk and protective factors for alcohol-related harms in school children. BMC Publ Health 2009;9. http://dx.doi.org/10.1186/1471-2458-9-380.
- Komro KA, Maldonado-Molina MM, Tobler AL, Bonds JR, Muller KE. Effects of home access and availability of alcohol on young adolescents’ alcohol use. Addiction 2007;102:1597-608. http://dx.doi.org/10.1111/j.1360-0443.2007.01941.x.
- Gilligan C, Kypri K, Johnson N, Lynagh M, Love S. Parental supply of alcohol and adolescent risky drinking. Drug Alcohol Rev 2012;31:754-62. http://dx.doi.org/10.1111/j.1465-3362.2012.00418.x.
- Foxcroft D, Tsertsvadze A. Universal family-based prevention programs for alcohol misuse in young people. Cochrane Database Syst Rev 2011;5.
- Petrie J, Bunn F, Byrne G. Parenting programmes for preventing tobacco, alcohol and drug misuse in children < 18 years: a systematic review. Health Educ Res 2007;22:177-91. http://dx.doi.org/10.1093/her/cyl061.
- Valdez A, Cepeda A, Parrish D, Horowitz R, Kaplan C. An adapted brief strategic family therapy for gang-affiliated Mexican American adolescents. Res Soc Work Pract 2013;23:383-96. http://dx.doi.org/10.1177/1049731513481389.
- Azrin N, Donohue B, Teichner G, Crum T, Howell J, DeCato L. A controlled evaluation and description of individual-cognitive problem solving and family behavior therapies in dually-diagnosed conduct-disordered and substance-dependent youth. J Child Adolesc Subst Abuse 2001;11:1-43. http://dx.doi.org/10.1300/J029v11n01_01.
- Not Yet Good Enough: Personal, Social Health and Economic Education in English Schools. Manchester: Ofsted; 2013.
- Emotional, Behavioural and Social Skills: Guidance. London: DfES; 2005.
- Alcohol-Use Disorders: Preventing the Development of Hazardous and Harmful Drinking. London: NICE; 2010.
- Rollnick S, Miller WR, Butler C. Motivational Interviewing in Health Care: Helping Patients Change Behavior. New York, NY: Guilford Press; 2008.
- Miller W, Rollnick S. Motivational Interviewing: Preparing People for Change. New York, NY: Guilford; 2002.
- Wagner C, Ingersoll K. Motivational Interviewing in Groups. New York: Guilford Press; 2013.
- Kaner EFS, Lock CA, McAvoy BR, Heather N, Gilvarry E. A RCT of three training and support strategies to encourage implementation of screening and brief alcohol intervention by general practitioners. Br J Gen Pract 1999;49:699-703.
- Canagasaby A, Vinson DC. Screening for hazardous or harmful drinking using one or two quantity-frequency questions. Alcohol Alcohol 2005;40:208-13. http://dx.doi.org/10.1093/alcalc/agh156.
- Parkinson KN, Pearce MS, Dale A, Reilly JJ, Drewett RF, Wright CM, et al. Cohort profile: the Gateshead Millennium Study. Int J Epidemiol 2011;40:308-17. http://dx.doi.org/10.1093/ije/dyq015.
- Warwick–Edinburgh Mental Well-Being Scale (WEMWBS). Edinburgh: NHS Health Scotland; 2006.
- Tennant R, Hiller L, Fishwick R, Platt S, Joseph S, Weich S, et al. The Warwick-Edinburgh Mental Well-being Scale (WEMWBS): development and UK validation. HQLO 2007;5.
- Clarke A, Friede T, Putz J, Martin S, Blake A, Adi Y, et al. Warwick-Edinburgh Mental Well-being Scale (WEMWBS): validated for teenage school students in England and Scotland. A mixed methods assessment. BMC Public Health 2011;11. http://dx.doi.org/10.1186/1471-2458-11-487.
- Babor T, De La Fuente J, Saunders J, Grant M. AUDIT, The Alcohol Use Disorders Identification Test, Guidelines for Use in Primary Health Care. Geneva: WHO; 1989.
- White H, Labouvie H. Towards the assessment of adolescent problem drinking. J Stud Alcohol 1989;50:30-7.
- Wiers R, Luitgaarden E, Smulders F. Challenging implicit and explicit alcohol-related cognitions in young heavy drinkers. Addiction 2005;100:806-19. http://dx.doi.org/10.1111/j.1360-0443.2005.01064.x.
- Willie N, Badia X, Bonsel G, Burstrom K, Cavrini G, Devlin N, et al. Development of the EQ-5D-Y: a child-friendly version of the EQ-5D. Qual Life Res 2010;19:875-86. http://dx.doi.org/10.1007/s11136-010-9648-y.
- UKATT Research Team . Cost effectiveness of treatment for alcohol problems: findings of the randomised UK alcohol treatment trial (UKATT). BMJ 2005;331. http://dx.doi.org/10.1136/bmj.331.7516.544.
- Physical Activity Health Improvement and Protection. Start Active, Stay Active: A Report on Physical Activity from the Four Home Countries’ Chief Medical Officers. London: DoH; 2011.
- Brown S, Tapert S, Tate S, Abrantes A. The role of alcohol in adolescent relapse and outcome. J Psychoactive Drugs 2000;32:107-15. http://dx.doi.org/10.1080/02791072.2000.10400216.
- Donohue B, Azrin N, Strada M, Silver N, Teichner G, Murphy H. Psychometric evaluation of self- and collateral timeline follow-back reports of drug and alcohol use in a sample of drug-abusing and conduct-disordered adolescents and their parents. Psychol Addict Behav 2004;18:184-9. http://dx.doi.org/10.1037/0893-164X.18.2.184.
- Waldron H, Slesnick N, Brody J, Turner C, Peterson T. Treatment outcomes for adolescent substance abuse at 4- and 7-month assessments. J Consult Clin Psychol 2001;69:802-13. http://dx.doi.org/10.1037/0022-006X.69.5.802.
- Lancaster G, Dodd S, Williamson P. Design and analysis of pilot studies: recommendations for good practice. J Eval Clin Pract 2004;10:307-12. http://dx.doi.org/10.1111/j. 2002.384.doc.x.
- Schaus J, Sole M, McCoy T, Mullett N, O’Brien M. Alcohol Screening and Brief Intervention in a college student health center: a randomized controlled trial. J Stud Alcohol Drugs 2009;16:131-41.
- Eldridge S, Kerry S. A Practical Guide to Cluster Randomised Trials in Health Services Research. Chichester: Wiley; 2012.
- Hahn S, Puffer S, Torgerson D, Watson J. Methodological bias in cluster randomised trials. BMC Med Res Methodol 2005;5. http://dx.doi.org/10.1186/1471-2288-5-10.
- 2011 Census: Key Statistics for England and Wales, March 2011. London: ONS; 2012.
- Teague G, Bond G, Drake R. Program fidelity in assertive community treatment: development and use of a measure. Am J Orthopsychiatry 1998;68:216-32. http://dx.doi.org/10.1037/h0080331.
- Moncher FJ, Prinz RJ. Treatment fidelity in outcome studies. Clin Psychol Rev 1991;11:247-66. http://dx.doi.org/10.1016/0272-7358(91)90103-2.
- Lane C, Huws-Thomas M, Rollnick S, Hood K, Edwards K, Robling M. Measuring adaptations of motivational interviewing: the development and validation of the Behaviour Change Counselling Index (BECCI). Patient Educ Couns 2005;56:166-73. http://dx.doi.org/10.1016/j.pec.2004.01.003.
- Lane C. The Behaviour Change Counselling Index (BECCI): Manual for Coding Behaviour Change Counselling. Cardiff: University of Wales College of Medicine; 2002.
- Talbot S, Crabbe T. Binge drinking: young people’s attitude and behaviour. London: Crime Concern; 2008.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. http://dx.doi.org/10.1191/1478088706qp063oa.
- Spencer L, Ritchie J, O’Connor W, Ritchie J, Lewis J. Qualitative Research Practice: A Guide for Social Science Students and Researchers. London: SAGE; 2003.
- Ritchie J, Spencer L, O’Connor W, Ritchie J, Lewis J. Qualitative Research Practice: A Guide for Social Science Students and Researchers. London: SAGE; 2003.
- Pope C, Ziebland S, Mays N. Analysing qualitative data. BMJ 2000;320:114-16. http://dx.doi.org/10.1136/bmj.320.7227.114.
- Richards L. Qualitative computing: a methods revolution?. Int J Soc Res Med 2002;5:263-76. http://dx.doi.org/10.1080/13645570210146302.
- Barbour RS. The newfound credibility of qualitative research? Tales of technical essentialism and co-option. Qual Health Res 2003;13:1019-27. http://dx.doi.org/10.1177/1049732303253331.
- Drummond M, Stoddart G, Torrance G. Methods for the Economic Evaluation of Health Care Programmes. Oxford: Oxford University Press; 2005.
- Moncur R, Larmer J. Clinical applicability of intention-to-treat analyses. Evid Base Med 2009;6:39-41.
- Kind P, Hardman G, Macran S. UK Population Norms for EQ-5D. University of York: Centre for Health Economics; 1999.
- Mishan E, Quah E. Cost–Benefit Analysis. Abingdon: Routledge; 2007.
- McIntosh E, Thorson T, Makela M. Changing Professional Practice: Theory and Practice of Clinical Guidelines Implementation. Copenhagen: Danish Institute for Health Services; 1999.
- Heinrichs N, Bertram H, Kuschel A, Hahlweg K. Parent recruitment and retention in a universal prevention program for child behavior and emotional problems: barrier to research and program participation. Prev Sci 2005;6:275-86. http://dx.doi.org/10.1007/s11121-005-0006-1.
- Sobell L, Sobell M. Alcohol Timeline Followback Users’ Manual. Toronto, Canada: Addiction Research Foundation; 1995.
- Dawes MA, Johnson B, Ait-Daoud N, Ma JZ, Cornelius J. A prospective, open-label trial of ondansetron in adolescents with alcohol dependence. Addict Behav 2005;30:1077-85. http://dx.doi.org/10.1016/j.addbeh.2004.10.011.
- Esposito-Smythers C, Spirito A, Uth R, Lachance H. Cognitive behavioral treatment for suicidal alcohol abusing adolescents: development and pilot testing. Am J Addict 2006;15:126-30. http://dx.doi.org/10.1080/10550490601006188.
- Kemp R, Harris A, Vurel E, Sitharthan T. Stop using stuff: trial of a drug and alcohol intervention for young people with comorbid mental illness and drug and alcohol problems. Australas Psychiatry 2007;15:490-3. http://dx.doi.org/10.1080/10398560701439665.
- Liddle H, Rowe C, Dakof G, Henderson C, Greenbaum P. Multidimensional family therapy for young adolescent substance abuse: twelve-month outcomes of a randomized controlled trial. J Consult Clin Psychol 2009;77:12-25. http://dx.doi.org/10.1037/a0014160.
- Slesnick N, Bartle-Haring S, Glebova T, Glade A. Primary alcohol versus primary drug use among adolescents: an examination of differences. Addict Behav 2006;31:2080-93. http://dx.doi.org/10.1016/j.addbeh.2006.02.006.
- Slesnick N, Prestopnik J, Meyers R, Glassman M. Treatment outcome for street-living, homeless youth. Addict Behav 2007;32:1237-51. http://dx.doi.org/10.1016/j.addbeh.2006.08.010.
Appendix 1 Terms of reference for Programme Management Group and Trial Steering Group
A feasibility trial of screening and brief alcohol interventions to prevent hazardous drinking in young people aged 14–15 in a high school setting (SIPS JR-HIGH)
Terms of reference for the Programme Management Group
These terms of reference will guide the scientific, administrative and operational direction of the SIPS JR-HIGH feasibility trial.
Chief Investigator Dr Dorothy Newbury-Birch, Institute of Health & Society, Newcastle University
Aims and objectives
The PMG has the primary aim of ensuring appropriate, effective and timely implementation of the SIPS JR-HIGH trial.
The PMG will strive to achieve this aim by fulfilling the following objectives:
-
identify appropriate sites for conducting the SIPS JR-HIGH trial
-
participate in the development and compilation of data collection instruments and other relevant research and intervention manuals
-
determine tasks, schedules and deliverables of the SIPS JR-HIGH trial
-
determine the appropriateness of trial interventions
-
produce a working protocol for the trial and ensure adherence to the protocol
-
develop a publication protocol
-
facilitate and support the preparation of the ethics application
-
facilitate and support data analysis
-
determine tasks, schedules and deliverables for report writing and publication of findings
-
develop incentives for schools and young people to take part in the trial
-
develop a definitive trial application
-
ensure that adequate supervision/support occurs for research staff.
Membership Eilish Gilvarry (Chair); Dorothy Newbury-Birch (Chief Investigator); Eileen Kaner; Simon Coulton; Elaine McColl; Chris Speed; Denise Howel; Elaine Stamp; Mark Deverill; Erin Graybill; Les Tate; Colin Drummond; Paolo Deluca; Paul McArdle; Stephanie Scott.
Membership of the group will be reviewed as appropriate and as required.
Meeting The PMG will meet once a month or more often if needed. Members are able to join the meeting by teleconferencing. A meeting will be considered quorate when at least three members are in attendance.
Reporting The group will report to the TSG, chaired by Professor Mark Bellis.
Duration The group will function for the entire duration of the SIPS JR-HIGH trial.
A feasibility trial of screening and brief alcohol interventions to prevent hazardous drinking in young people aged 14–15 in a high school setting (SIPS JR-HIGH)
Terms of reference for the Trial Steering Group
These terms of reference will guide the scientific, administrative and operational direction of the SIPS JR-HIGH feasibility trial.
Chief Investigator: Dr Dorothy Newbury-Birch, Institute of Health & Society, Newcastle University
Aims and objectives
The TSG has the primary aims of monitoring implementation of the SIPS JR-HIGH feasibility trial, providing an independent assessment of the data analysis and determining if a future trial is merited.
The TSG has the following objectives:
-
provide overall supervision of the trial on behalf of the trial sponsor and funder and ensure it is conducted to rigorous standards
-
comment on the progress of the trial and adherence to protocol
-
consider new information of relevance to the research question
-
provide advice, through the Chair, to the Chief Investigator and trial funder on all appropriate aspects of the trial
-
provide evidence to support any requests for extensions.
Meeting The TSG will meet biannually. Members are able to join the meeting by teleconferencing. A meeting will be considered quorate when at least three members are in attendance. Dorothy Newbury-Birch and Stephanie Scott will be responsible for calling, organising and minuting the meeting.
Duration The group will function for the entire duration of the SIPS JR-HIGH feasibility trial.
Membership:
| Name | Position |
|---|---|
| Professor Mark Bellis (Chair) | Director, Centre for Public Health and North West Public Health Observatory |
| Ms Catherine Gillespie | Vice Principal |
| Miss Rebecca Leighton – Year One | Young Mayor |
| Mr Isaac Sidney – Year Two | |
| Ms Anne Taylor | Young Mayors’ support worker and mother of adolescents |
| Georgia Hall and Louise Burn | Young person and her mother |
| Dr Gillian Lancaster | Director of the Postgraduate Statistics Centre |
| Membership of the PMG: Dorothy Newbury-Birch (Chief Investigator); Stephanie Scott (Research Associate and Project Manager); Denise Howel (Statistician). Other members of the PMG as necessary | |
Membership of the group will be reviewed as appropriate and as required.
Appendix 2 Literature review table
| Author (year) | Country (setting) | Methodology | Participants | Control | Intervention (n) | Measures | Outcomes | Referenced in systematic review |
|---|---|---|---|---|---|---|---|---|
| Azrin et al. (1994)107 | USA (counselling centre) | RCT | Illegal drug users; mean age 27.5 years; 68% male; n = 82 | Non-behavioural treatment (n = 36) | Behavioural treatment (n = 46) | 12-month drug use data, including urinalysis | Subjects using drugs in the non-behavioural group decreased to 80% in first month and remained at that general level for remaining 11 months In the behavioural treatment group, subject users decreased progressively to 35% at 12 months. Chi-squared tests at each month showed that the difference between the two treatments was statistically significant for each month after the second month (p < 0.05); 12th month, χ2 = 13.097 (1, n = 82) (p < 0.001) |
77 |
| aAzrin et al. (2001)149 | USA (Youth Justice) | RCT | Dually diagnosed drug and alcohol users; mean age 15.4 years; n = 56; 82% male | No control | Individual cognitive problem-solving therapy 15 sessions (60–90 minutes) or family behavioural therapy × 15 sessions (60–90 minutes) | TLFB | An analysis of alcohol use results indicated no within-subject or between-intervention group differences (p > 0.05), indicating that both interventions had no significant effects on the no. of days these young people used alcohol. Both interventions were found to reduce illicit drugs and conduct disorder (no between-group differences) | None |
| Baer et al. (2001)87 | USA (university) | RCT | High-risk drinkers, 45% male Normative comparison sample, 46% male Age – students < 19 years in autumn of 1990 |
No intervention | Individualised feedback | Baseline interview and questionnaires then yearly follow-up questionnaires for 4 years | Findings suggest that much heavy drinking among college students is transitory. Compared with the high-risk control sample, participants receiving brief individual preventative intervention had significantly greater reductions in negative consequences over the 4-year period | 78 |
| Baer et al. (2007)108 | USA (homeless young people) | RCT | Mild to moderate substance abusers; mean age 17.9 years; 56% male | Usual care (n = 52) | Brief MI (≤ 4 sessions of 60 minutes) (n = 75) | 30-day TLFB | Per-protocol analysis showed there were significant reductions in alcohol use at 3- but not 1-month follow-up assessments (Cohen’s d = 0.20) | 75, 77 |
| Bailey et al. (2004)53 | Australia (youth centre) | RCT | Not restricted to substance users; mean age 15.4 years; 50% male | Usual care but they had fortnightly access to an alcohol or drug counsellor (n = 17) | Brief MI and cognitive/behavioural-based group programme [four sessions (≤ 10 people) of 30 minutes] | AUDIT | Participants in the intervention group reduced their frequency of drinking at the first follow-up assessment, whereas the control group reported increases at the second follow-up assessment (p< 0.005). The control group also increased their hazardous drinking (p < 0.005) and frequency of binge drinking compared with the intervention group (p < 0.005) | 38, 74, 75, 78 |
| Battjes et al. (2004)121 | USA (outpatient substance abuse treatment programme) | Group evaluation (no control) | Mild to moderate substance abusers; mean age 15.9 years; 85% male | No control | Group-based treatment for adolescent substance abuse (19 weekly group sessions of 75 minutes with limited individual and family therapy) (n = 194) | Days of alcohol intoxication in previous 90 days | No statistically significant differences were found with regard to days of alcohol intoxication in past 90 days | 75 |
| Bernstein et al. (2009)95 | USA (emergency department) | Prospective three-group RCT (preliminary) | Marijuana users (excluded if high-risk alcohol use); 71% ≥ 18 years; 37% male | Standard assessed control (n = 71) and non-assessed control (feasibility) | Screening and BI by trained peer educators, including CRAFFT test (n = 68) | TLFB calendar | Small pilot study. There was increased marijuana abstinence and reduced consumption in patients aged 14–21 years. Strongest effects seen at 12-month follow-up (OR 2.89). No differences in risk behaviours or health consequences from baseline to follow-up | 76 |
| Bernstein et al. (2010)98 | USA (emergency department) | Three-group randomised assignment trial | Patients aged 14–21 years giving positive AUDIT test or positive for binge drinking/high-risk behaviours; 87% ≥ 18 years; 45% male | Assessed control (n = 284) and minimally assessed control (n = 286) | Peer-conducted MI, referral to community resources and treatment if indicated and 10-day booster in addition to assessment (n = 283) | 30-day TLFB | No effects were found for between-group consumption or high-risk behaviours. Intervention compared with AC resulted in significant efforts to change behaviour (p < 0.05) | 76, 79 |
| Boekeloo et al. (2004)80 | USA (primary care) | RCT | 12- to 17-year-old adolescents receiving general health examination; 40% male | Usual care (n = 150) | Intervention 1: 15-minute audio programme (n = 150) Intervention 2: 15-minute audio programme and prompts from primary care provider (n = 147) |
Adolescent alcohol beliefs at exit interview and self-reported behaviours at follow-ups | No evidence to suggest BI reduces alcohol intake. At 1-year follow-up, both intervention groups reported more bingeing in the last 3 months than the control group (OR 3.44 and 2.86). Intervention 1 reported more drinking in the last 30 days (OR 2.31) and in the last 3 months (OR 1.76) than the control group | 38, 78 |
| Borsari and Carey (2000)88 | USA (college) | RCT | Student binge drinkers; mean age 18 years; 43% male | No treatment (n = 31) | One session of motivational intervention (n = 29) | Drinks consumed per week, number of times consuming in past month, frequency of binge drinking in last month and RAPI scores | At 6-week follow-up, the BI group showed significant reductions on number of drinks consumed per week, number of times drinking alcohol in past month and frequency of binge drinking in past month | 78 |
| Borsari and Carey (2005)89 | USA (college) | RCT (two groups) | Students referred for alcohol violation with score of ≥ 10 on AUDIT and 2+ binge-drinking episodes in past 30 days; mean age 19 years; 83% male | Intervention 1: Brief MI (no info.) (n = 34) Intervention 2: Advice given but not personalised (no info.) (n = 30) |
AUDIT and typical blood alcohol content | Both intervention groups decreased their alcohol use following the intervention; however, brief MI students reduced alcohol-related problems to a greater extent | 78 | |
| Carey et al. (2006)90 | USA (university) | RCT | Heavy drinking students; mean age 19 years; 35% male | No intervention | Intervention 1: Basic MI – advice (one session of 65 minutes) Intervention 2: Enhanced MI including a decisional balance exercise (one session of 70 minutes) |
Drinks per typical week and drinks per drinking day: Daily Drinking Questionnaire | TLFB reduced consumption but not problems at 1 month relative to control subjects. Basic MI improved all drinking outcomes beyond the effects of the TLFB at 1 month, whereas the enhanced MI did not | 78 |
| Dawes et al. (2005)194 | USA (community treatment centre) | Prospective, open-label trial | Adolescents with DSM-IV alcohol dependence; mean age 18 years; 58% male | No control | Eight-week, prospective, open-label ondansetron (Zofran, GlaxoSmithKline) (4 µg/kg b.i.d) treatment and weekly CBT (n = 12) | Safety and tolerability of drug. Self-reported alcohol consumption | Six out of 12 participants completed 8-week study. Adverse events were mild and of short duration. Very small sample but intention-to-treat analysis showed significant within-group decreases (improvement) for drinks/drinking day (p = 0.01) | 73 |
| D’Amico et al. (2008)81 | USA (primary care clinic) | RCT | High-risk drug and alcohol users; age 12–18 years; male 48% | Usual care (n = 24) | Project CHAT: MI (one session of 15–20 minutes; 5–10 minute booster call) (n = 36) | CRAFFT | No statistically significant differences were found with regard to alcohol consumption | 38, 74–77 |
| Esposito-Smythers et al. (2006)195 | USA (adolescent psychiatric inpatient unit) | Pilot study | Adolescents with co-occurring alcohol use disorder and suicide ideation; mean age 15 years. five females; one male | No control | Six-month acute treatment phase, 3-month maintenance phase and 3-month booster phase administered by study therapists (n = 6) | Treatment feasibility/acceptability. Changes in suicidality, alcohol and marijuana use | Pilot suggests that outpatient CBT is feasible and acceptable to families. Retention was good: five out of six families completed 12-month treatment. Few obstacles were reported. All five participants reported reductions in suicidal ideation. However, two of five made a suicide attempt and were referred back to the treatment. All participants reported a reduction in number of drinking days, heavy drinking days and days of cannabis use | 73 |
| Feldstein and Forcenhimes (2007)91 | USA (university) | RCT | Included participants need to report drinking at least once in the past month and have either a RAPI score of at least ‘3’ or at least one bingeing episode in past 2 weeks; mean age 18.6 years; 21.8% male | No treatment (n = 19) | One-session MI (n = 36) | Binge-drinking question and RAPI | Multivariate tests reveal no significant interaction effects | 78 |
| Friedman et al. (2002)109 | USA (residential facility for court-adjudicated males) | RCT | New court-adjudicated admissions to residential treatment centre who were not ineligible; mean age 15.5 years; 100% male | Control subjects (no treatment) (n = 91) | Botvin LifeSkills Training (20 sessions), PSAV (20 sessions), Values Clarification procedure (20 sessions) – all 55 minutes each (n = 110) | ADAD scores at follow-up | The Botvin LifeSkills Training programme was effective in reducing substance use/abuse and the selling of drugs. Participants who participated more positively in the PSAV programme reduced their violent behaviour at follow-up to a significantly greater degree | 74, 77 |
| Godley et al. (2002)110 | USA (residential treatment system for alcohol or other substance-use disorders) | RCT | Adolescents with alcohol and/or marijuana dependence; age range 12–18 years; 76.3% male | UCC (n = 51) | UCC plus an ACC protocol (n = 63) | Baseline and follow-up interviews using GAIN and Form 90 version of TLFB | ACC participants were significantly more likely to initiate and receive more continuing care services, to be abstinent from marijuana at 3 months post discharge, and to reduce their 3-month post-discharge days of alcohol use Preliminary findings suggest that ACC can increase linkage and retention in continuing care and improve short-term substance-use outcomes |
77 |
| Godley et al. (2007)111 | USA (residential treatment facility) | RCT | Current alcohol and/or other drug dependence (DSM-IV); mean age 16.2 years; 71% male | UCC (n = 81) | ACC (UCC plus 90-day case manager assigned) (n = 102) | GAIN instrument, service contact logs and General Continuing Care Adherence scale | At follow-up up, ACC participants were more likely to link to continuing care services (94% vs. 54%; p < 0.001) ACC group had significantly longer-term abstinence from marijuana. Superior early abstinence outcomes for both conditions predicted longer-term abstinence |
77 |
| Grenard et al. (2007)99 | USA (alternative high schools) | RCT | Mean age 16.1 years; male 67% | Usual care (n = 7) | MI session (one session of 25 minutes ) (n = 11) | Prevalence of alcohol use in past 30 days and lifetime | Small numbers to follow up therefore no statistical difference between groups | 74–76 |
| aHenggeler et al. (1999)112 | USA (Youth Justice) | RCT | Drug and alcohol users; mean age 15.7 years; 79% male | Usual services (referral to probation officer for substance abuse services) | Multisystemic therapy within the home (n = 58) (mean no. of 130 days with a mean of 40 hours’ direct contact and 26 indirect contacts of a mean of 15 minutes each). Control group, usual services (n = 60) | Personal experiences inventory | The multisystemic therapy group showed significantly less alcohol and marijuana use than usual services shortly after treatment [F (1, 112) = 5.40; p < 0.022]; however, this effect was not evident at 6-month follow-up | 77 |
| Johnston (2002)96 | USA (emergency department) | RCT | Adolescents in emergency department undergoing treatment for injury; mean age 16.4 years; 65.2% male | Routine emergency department care (n = 312) | Brief session of behavioural change counselling (n = 317) | Prevalence of positive behaviour change and interim occurrence of medically treated injuries | The intervention was associated with a greater likelihood of positive behaviour change in seatbelt and bicycle helmet use. Behaviour change counselling was not associated with changes in other risk behaviours and could not be shown to significantly reduce the risk of reinjury | 76, 79 |
| Kaminer and Burleson (1999)113 | USA (outpatient aftercare following inpatient treatment) | Pilot | Met DSM-III-R criteria for psychoactive substance use disorders; age range 13–18 years; 62.5% males | No control | Intervention 1: CBT (n = 17) Intervention 2: Interactional treatment (n = 15) |
Teen-addiction severity index, teen treatment services review and SCQ | Small sample size. No effects at 3-month follow-up. At 15 months there was no differential improvement as a function of therapy type | 77 |
| Kaminer et al. (2008)114 | USA (outpatient setting) | RCT | Current DSM-IV diagnosis of AUD, n = 144; mean age 16 years, range 13–18 years; 80% male | NA | Intervention 1: Five-session in-person aftercare Intervention 2: Five-session brief telephone aftercare |
Diagnostic Interview Scale for Children (DISC-IV) at baseline. Urinalysis for marijuana status. Alcohol use, ACQ questionnaire | The likelihood of relapse increased significantly at end of aftercare compared with end-of-treatment outcomes. Likelihood of relapse in young people in ‘No active aftercare’ (NA); however, increased significantly more for young people in combined active aftercare (in-person and brief telephone aftercare) conditions (p = 0.008). ‘Active aftercare’ also showed significantly fewer drinking days (p = 0.044) and fewer heavy drinking days (p = 0.035) per month relative to NA | 77 |
| Kemp et al. (2007)196 | Australia (Community) | RCT | Young people with primary diagnosis of psychotic illness and substance abuse; age range 17–25 years; n = 17; 81% male | TAU (n = 6) | SUS intervention comprising four to six brief MI-/CBT- based sessions | PANSS, DAST-10, AUDIT, Depression Anxiety Subscale (DASS), SES, WHO Quality of Life Scale | Both the SUS and TAU participants showed improvements in alcohol use [F (1, 14) = 4.718; p < 0.05] and substance use [F (1, 14) = 7.0; p > 0.05] The SUS group exhibited a greater reduction in substance and alcohol use than the TAU group |
73 |
| aLatimer (2003),115 USA | USA (drug dependence assessment clinic) | RCT | Drug and alcohol users; mean age 16 years; 77% male | NA | Drugs Harm Psychoeducation Curriculum 16 × 90-minute group sessions (n = 22) Integrated Family and CBT 16 × 60 minutes family therapy sessions and 32 × 90 minutes CBT group sessions (n = 22) |
Diagnostic interview | Drugs Harm Psychoeducation Curriculum group used alcohol 6.06 days (SD 7.15) significantly more than Integrated Family and CBT= 2.03 days (SD = 2.49) (effect size 0.56) at 6-month follow-up | 77 |
| aLiddle et al. (2008),117 USA | USA (community drug treatment clinic) | RCT | Drug and alcohol users; mean age 15 years; 81% male; 72% African American | NA | Individual CBT weekly session for 4–6 months (n = 112) Multidimensional Family Therapy weekly session for 4–6 months (n = 112) |
TLFB | Although there were significant results favouring Multidimensional Family Therapy for drug use and severity, this was not found for alcohol use. Both treatment groups showed reduction in alcohol use however, this was not significant and no significant between group differences were found (12-month follow-up) | 77 |
| Liddle et al. (2001)116 | USA (clinical outpatients) | RCT | Marijuana and alcohol abusing adolescents; mean age 15.9 years, range 13–18 years; n = 182; 80% male | No control | Three interventions: Multidimensional Family Therapy n = 47), Adolescent Group Therapy (n = 53), and Multifamily Educational Intervention (n = 52). 14–16 weekly sessions | Adolescent Drug Use Scale, Acting Out Behaviours Scale | All three interventions showed improvements in drug use and acting out behaviours across time, with the greatest improvements seen in the Multidimensional Family Therapy group | 77 |
| Liddle et al. (2009)197 | USA (community drug abuse treatment agency) | RCT | Referred for outpatient treatment of substance abuse problem; mean age 13.7 years, range 11–15 years; 74% male | No control | Two interventions: Multidimensional Family Therapy (n = 40), Peer Group Therapy (n = 43). Both had 2 × sessions per week, 90 minutes’ duration for 12–16 weeks | GAIN, POSIT, National Youth Survey SRD | Both interventions were effective in reducing substance use. Latent growth curve modelling analyses demonstrated superior effectiveness of Multidimensional Family Therapy over the 12-month follow-up in reducing substance use (effect size: substance use frequency, d = 0.77; substance use problems, d =0.74). Multidimensional Family Therapy also had improved delinquency, family, and school outcomes whereas the peer group therapy did not | 73 |
| Maio et al. (2005)82 | USA (emergency department) | RCT | Young people attending the emergency department with minor injury; mean age 15.9 years, range 14–18 years; n = 580; 66% male | No intervention (n = 285) | Laptop-based interactive programme based on social learning theory completed in the emergency department setting (n = 295). Average completion time = 25 minutes | Alcohol misuse index, binge-drinking episodes | The emergency department-based interactive computer program to limit adolescent alcohol misuse had no significant effect at 3- or 12-month follow-up. Subgroup analysis suggested that there may be a benefit among those participants admitting to drinking and driving at baseline | 38, 76, 78, 79 |
| Marlatt et al. (1998)92 | USA (university) | RCT | High-risk sample selected from screening pool (n = 348) | Normative sample from screening pool (n = 115) and assessment only, control (n = 174) | Individualised MI (n = 174) | Frequency of alcohol consumption, daily drinking questionnaire, RAPI, alcohol dependence scale | All high-risk participants drank less and reported fewer drinking-related problems over a 2-year follow-up period. Participants who received the BI showed significantly greater deceleration of drinking rates and problems over time than the control group | 78 |
| Marsden et al. (2006)100 | UK (community agency) | RCT | Self-report users of MDMA (ecstasy), cocaine powder or crack cocaine; age range 16–22 years; n = 342 | Control – standard written heath risk information (n = 176, 154 analysed) | Stimulant- and alcohol-based brief MI. One session, 45–60 minutes plus standard written heath risk information (n = 166, 145 analysed) | MAP; AUDIT | There were no significant differences in abstinence for ecstasy, cocaine powder or crack cocaine use between the experimental and control groups. Contrasting follow-up with baseline self-reports, there were no between-group effects for changes in the frequency or amount of stimulant or alcohol use | 75, 76 |
| Mason and Posner (2009)122 | USA (medical centres) | Matched group | Cannabis and alcohol users; mean age 16 years; male 81% | NA | Individual motivational enhancement therapy (two sessions of 60 minutes ) then group CBT (three sessions 60–75 minutes) | Global appraisal of individual needs | A significant reduction in number of days of alcohol use in treatment group in past 30 days at 3 months (p = 0.001) and 6 months (p = 0.02) | 75 |
| McCambridge et al. (2004, 2005)102,106 | UK (further educational colleges) | Cluster RCT | Drug use in previous 3 months; age 16–20 years; male 75% | Usual care (n = 105) | Brief MI (one session of 60 minutes) (n = 105) | Severity of Dependence scale | At baseline both groups were drinking a mean of 12.7 units per week. A reduction of 5.71 units was found in the intervention group at 3-month follow-up (p = 0.0002). For drinkers only at baseline, there was a reduction of 6.89 units in the intervention group at 3 months | 75, 76 |
| McCambridge et al. (2008)101 | UK (further education colleges) | RCT | Cannabis users; age 16–20 years | Usual care (n = 164) | Brief MI (one session of 60 minutes) (n = 162) | AUDIT | No statistical differences were found for any of the alcohol outcomes at 3 or 6 months post intervention | 75, 76 |
| aMcGillicuddy et al. (2001), USA118 | USA (community sample) | RCT | Alcohol and drug users; mean age 16.3 years; 73% male | Waiting list (n = 8) | Skill training programme for parents (8 × weekly 2-hour sessions) (n = 14) | TLFB (parent report) | No effects detected for alcohol | 77 |
| Monti (1999)84 USA | USA (emergency department) | RCT | Emergency department users following alcohol-related incident; age range 18–19 years; n = 94 | Standard care (n = 42) | Brief MI (one session of 35–40 minutes) (n = 52) | Alcohol Drinking Index, Young Adult Drinking and Driving Questionnaire, Health Behaviour Questionnaire | Patients who received MI had significantly lower incidence of drinking and driving, traffic violations, alcohol-related injuries and alcohol-related problems than patients who received standard care, 6 months following intervention | 38, 78, 79 |
| Monti et al. (2007)83 | USA (emergency department) | RCT | Alcohol users; age range 18–24 years; n = 198; 68% male | Personalised feedback only, booster sessions at 1 and 3 months (n = 100, 86 analysed) | Brief MI with personalised feedback (one session of 30–45 minutes), telephone booster sessions at 1 month (20 minutes) and 3 months (25–30 minutes) (n = 98, 79 analysed) | BAC, AUDIT, RAPI | Six months after the intervention MI participants drank on fewer days, had fewer heavy drinking days and drank fewer drinks per week in the past month than did feedback-only patients. These effects were maintained at 12 months. Clinical significance evaluation indicated that twice as many MI participants as feedback-only participants reliably reduced their volume of alcohol consumption from baseline to 12 months | 38, 78, 79 |
| Murphy et al. (2001)93 | USA (university) | RCT | Alcohol users, upper 33% of screening sample; n = 84; 54% female | (n = 25) | Two intervention groups: BASICS 50-minute MI session (n = 30), or an educational intervention, 50-minute session with 30 minutes for video and general discussion (n = 29) | Alcohol Dependence Scale, Daily Drinking Questionnaire, RAPI | No overall significant group differences were seen at 3- or 9-month follow-up | 78 |
| Peterson et al. (2006)86 | USA (homeless drop-in centres and street intercept) | RCT | One binge-drinking episode in past 30 days; mean age 17.4 years, range 14–19 years; n = 285; 55% male | Two control groups – assessment only (n = 99) and assessment at follow-up (n = 94) | Brief Motivational Enhancement (1 session of 30 minutes) (n = 92) | Self-report alcohol and drug use frequency – past 30 days | No treatment effects were found with respect to alcohol | 38, 73–76 |
| Santisteban et al. (2003)119 | USA (Hispanic families) | RCT | 126 Hispanic families with adolescent exhibiting externalising behaviour problems (substance use not required); mean age 15.6 years, range 12–18 years; 75% male | Group treatment – adolescents received 6–16 weekly sessions, of 90 minutes’ duration (n = 46) | Brief strategic family therapy – families received 4–20 1-hour sessions depending on clinical severity of presenting problems (n = 80) | Revised Behaviour Problem Checklist, Addiction Severity Index, Family Environment Scale, Structural Family Systems Rating | Substance use (alcohol and marijuana) change scores between intake and termination were statistically significant [Wilks’ λ = 0.89, F (2, 68) = 4.33; p < 0.02, η2 = 0.11] A significant univariate effect emerged for marijuana use, but not for alcohol use |
77 |
| aSlesnick et al. (2006) USA198 | USA (runaway shelter) | Analysis data from two RCTs | Primary alcohol users, n = 123 primary drug users; mean age 15.0 years; 56% female | TAU, n = 101 | Ecological-based family therapy-mean of 10 sessions (SD = 6) (n = 101) | CDISC Form 90 |
Primary alcohol users showed clinically and statistically significant reductions in frequency of alcohol use (from 28% days to 1% days of use = 97% reduction) when assigned to ecological-based family therapy compared with TAU (from 25% of days to 6% days = 76% reductions) at 15-month follow-up. However, alcohol use increased by 32% for primary drug users receiving family therapy (from 3.3% of days to 4.8%) | 73 |
| Slesnick et al. (2007)199 | USA (homeless) | RCT | Homeless young people engaged with drop-in centre; met DSM-IV criteria for substance use disorder; mean age 19.1 years, range 14–22 years; n = 180; 66% male | TAU through a drop-in centre (n = 84). Case management sessions available at young people’s request – mean 3.4 sessions attended | Community reinforcement approach (n = 96); 12 sessions – mean attendance 6.8 sessions | Form 90, POSIT, NYSDS, YSR, CISS, BDI-II, Health Risk Questionnaire | Overall, both the community reinforcement approach and the TAU groups showed improvements over time. Young people assigned to community reinforcement approach compared with TAU reported significantly reduced substance use (37% vs. 17% reduction), depression (40% vs. 23%) and increased social stability (58% vs. 13%) | 73 |
| Spirito et al. (2004)85 | USA (emergency department) | RCT | Treated in emergency department and had evidence of alcohol use (blood/breath/saliva) or self-report consumption within 6 hours of admittance; mean age 15.7 years; n = 152; 64% male | Standard care – 5 minutes’ brief advice and handout (n = 74) | Brief MI (one session of 35–45 minutes) (n = 78) | Adolescent drinking questionnaire, adolescent drinking inventory, young adult drinking and driving questionnaire, adolescent injury checklist, adolescent health behaviour questionnaire | Both MI and standard care conditions resulted in reduced quantity of drinking during the 12-month follow-up. Adolescents who screened positive for problematic alcohol use at baseline reported significantly more improvement on two out of three alcohol-use outcomes (average number of drinking days per month and frequency of high-volume drinking) if they received MI compared with standard care | 38, 74–76, 78, 79 |
| aSpirito et al. (2011)103 USA | USA (emergency department) | RCT | Drug and alcohol users; 54% female; mean age = 15.45 years | IMI session for 45–60 minutes and 5-monthly parenting booster brochures (n = 63) As above with the addition of family check-up (n = 62) |
Adolescent drinking questionnaire | Both conditions resulted in a reduction in all drinking outcomes at 3-, 6- and 12-month follow-up (p = 0.001). Across groups any drinking in previous month decreased from 100% to 39.3% at 3 month, 55.2% at 6 months and 67.9% at 12 months. High-volume drinking occurrence dropped from 84% at baseline to 24% at 3-month follow-up, 35.3% at 6 months and 53.3% at 12 months; all were significantly less than baseline (p < 0.001). There was one significant between-group difference on high-volume drinking days at 3 months with family check-up reporting lower prevalence (14.6%; 95% CI 3.8% to 25.5%) compared with individual IM (32.1%, 95% CI 19.9% to 44.4%), at 6 months. Family check-up was lower (27%; 95% CI 12.7% to 41.3%) than IMI (43.6%, 95% CI 30.5–56.8%). No difference was shown at 12 months. There were no effects on number of drinking days or quantity per drinking occasion. | 76 | |
| Stein et al. (2006)124 | USA (juvenile correctional facility) | RCT | Alcohol and/or marijuana users; mean age 17.1 years, range 14–19 years; n = 105; 90% male | NA | 1 × MI session of 60 minutes; booster of 90 minutes) (n = 59) or relaxation training (n = 45) | DSM-IV, Centre for Epidemiological Studies – depression scale, Risky Behaviours Questionnaire – driving under influence and passenger with driver under influence | Lower rates of those in the ‘Driving under the influence’ and ‘Passenger with driver under the influence’ groups’ risky behaviours were seen with the MI intervention compared with the relaxation training intervention. Effects were moderated by depression; those with low levels of depression receiving MI had the lowest rate of risky behaviours | 73, 74 |
| Thush et al. (2007)94 | Netherlands (school) | RCT | Mean age 15.5 years; range 14–18 years; n = 107; 57% male | Information-only control (n = 54) | ‘Learning to Drink’; 7 × weekly session (6 × 90-minute group sessions, 1 × MI) plus 1 × parent session | Alcohol use questionnaires, RAPI | The intervention was effective in changing several of the targeted cognitive determinants: there was a significant increase in the perception of risk factors for developing alcohol-related problems and a significant decrease in positive alcohol expectancies for a high dose of alcohol in the experimental group compared with the control group. However, no long-term effects of the intervention on drinking behaviour were found (measured at 1 month, 6 months and 12 months) | 78 |
| Thush (2009)123 | Netherlands (low-level vocational schools) | RCT | Mean age 17.1 years, range 15–23 years; n = 125 (n = 110 in analysis); 54% female | Information-only control – received 5 × information leaflets (n = 64, 55 analysis) | 1 × MI session lasting 30 minutes; 5 × information leaflets (n = 61, 55 analysis) | Alcohol use questionnaire, RAPI | There were no differential effects of the MI intervention on drinking behaviour or readiness to change at 1- and 6-month follow-up | 75 |
| Tomlinson et al. (2004)120 | USA (outpatient aftercare following inpatient treatment) | RCT | Adolescents with comorbid substance use disorders and Axis I psychiatric disorder; age range 13–17 years; n = 126 | Substance use disorders only, control group; n = 81 | Subjects admitted to one of five inpatient adolescent treatment programmes: all were abstinence focused, offered individual and group CBT and used 12-step model of treatment | Structured clinical interview of adolescents’ substance abuse history, DSM-IV | Results indicated that comorbid young people received more treatment during the outcome period. However, more comorbid SUD-Axis I disordered adolescents used substances following treatment than substance-use disorders only young people. Among comorbid young people, internalising disordered adolescents were less likely to use substances during the follow-up period, and externalising disordered young people returned to substance use most rapidly after discharge from treatment | 77 |
| aValdez et al. (2013)148 | USA (gang-affiliated Mexican American adolescents) | RCT | Range of risk behaviours exhibited; mean age 15.25 years; 59% male | Referral to social and behavioural services and substance abuse counselling (n = 104) | Brief strategic family therapy × 16 sessions plus four additional educational sessions (n = 96) | 30-day calendar-based tool | Significant differences were found between control and brief strategic family therapy groups re. alcohol at 6 months’ follow-up showing a steady and significant decline over time. Brief strategic family therapy group reported significantly fewer days of alcohol use (m = 1.23, SD.79) number of days compared with control (m = 4.05, SD.74) number of days during last 30 days at 6 months (p = 0.05) | None |
| Walker et al. (2006)104 | USA (school) | RCT | Marijuana users; mean age 15.8 years, range 14–19 years; n = 97 | Delayed feedback control | Motivational enhancement therapy (2× session with health educator, 30–60 minutes) | GAIN-I | Both the motivational enhancement therapy and delayed feedback control groups significantly reduced marijuana use at the 3-month follow-up (p < 0.001); no between-group differences were observed | 76 |
| Walton et al. (2010)97 | USA (emergency department) | RCT | Eligible if reported past-year alcohol use and aggression; mean age 16.8 years, range 14–18 years; n = 726, 56% female | Control group received brochure post screening (n = 235) | SafERteens therapist (n = 254) vs. computer BI (one session of 35 minutes ) (n = 237) | AUDIT, AUDIT-C, POSIT, frequency of aggression towards peers | At 3 months, the therapist intervention showed reductions in the occurrence of peer aggression (therapist −34.3%; control −16.4%; relative risk 0.74; 95% CI 0.61–0.90); experience of peer violence (therapist −10.4%; control −4.7%; relative risk 0.70; 95% CI 0.52 to 0.95); and violence consequences (therapist −30.4%; control −13.0%; relative risk 0.76; 95% CI 0.64 to 0.90). At 6 months, both the therapist intervention and computer intervention showed reductions in alcohol consequences compared with controls (therapist −32.2%; control −17.7%; OR 0.56; 95% CI 0.34 to 0.91; computer −29.1%; control −17.7%; OR 0.57; 95% CI 0.34 to 0.95) | 74, 76, 79 |
| aWinters and Leitten (2007)105 | USA (school) | RCT | Alcohol and drug users; mean age 15.6 years; 62% male | Assessment only (control) (n = 27) | Two sessions of adolescent BI × 60 minutes (n = 26) Two sessions of 60 minutes BI-adolescent plus BI-parent session (n = 126) |
Adolescent Diagnostic Interview and TLFB | There was a significant group by time effect at 6-month follow-up, BI with parent showing significantly lower no. of alcohol use days and no. of binge days than the control, the BI-adolescent group had significantly lower scores on the no. of alcohol use days than the control, whereas the BI-parent had significantly lower no. of alcohol days than the BI-adolescent group | 76, 77 |
| aWinters et al. (2012)125 | USA (school) | RCT | Adolescents with alcohol/drug use disorder; mean age 16 years, range 12–18 years; n = 315; 52% male | Assessment only (control) (n = 56) | Two sessions of BI-adolescent × 60 minutes (n = 135) Two sessions × 60 minutes BI-adolescent plus BI-parent session (n = 123) |
Adolescent Diagnostic Interview and TLFB | Both intervention groups (BI-adolescent and BI-parent) showed significantly better outcomes than control (p < 0.05) for no. of alcohol use days, no. of alcohol abuse symptoms and no. of alcohol dependency symptoms. BI-adolescent was found to be significantly better than BI-parent for no. of days abstinent from alcohol in past 90 days | 74 |
Appendix 3 Study documentation and manual
Parent opt-out letter
Study information leaflet
Screening questionnaire
Health and well-being leaflet
Study manual
Full intervention manual
Participant consent form (control and intervention 1)
Participant consent form (Intervention 2)
Control condition
Intervention 1 tool
Appendix 4 Qualitative study
Information sheet for interviews
| School lead liaisons | ||
|---|---|---|
| Big research question | Mini research question | Ways to approach this question |
| How do they view alcohol use by young people and existing alcohol education within their school? | What are the participant’s thoughts or concerns about alcohol use by young people? | What are your views about alcohol use by young people in general? What is your experience and what are your views about alcohol use by young people in your school? How does alcohol have an impact on the school environment? (Probes: direct impact, i.e. intoxication on school premises, and indirect impact, i.e. health impact on young people affecting educational attainment) |
| What are the participants’ thoughts on existing alcohol education within their school? | Is alcohol use by young people addressed in your school? How? By whom? (Probe on external initiatives)
|
|
| How did the study impact on the school? | Why did they decide to participate in the study? | Can you remember how the research project was initially discussed with you? Was the approach by researchers suitable? Whose decision was it to participate in the study? Why was the decision made? (Probes: what influenced the decision, concerns about alcohol use, did they find any aspect of the study particularly attractive, did they have any prior experience of research in the school, etc.) |
| What did they think of how the study was performed within their school? | Can you describe the process of randomisation? Did you have concerns about the treatment condition to which your school was randomised? How did you find recruiting learning mentors to help with the study? Do you have any thoughts on the fact that the study focused on only Year 10 pupils? (Probes: whether this was the most suitable age group in terms of school practicalities and in terms of alcohol use by young people at this age) A survey was conducted in your school in December as part of the study: how did you find the completion of this survey in your school? Did you have any thoughts on providing the young people with gift vouchers? Did you have any thoughts on providing an opt-out letter to parents for involvement in the survey? (Probes: appropriate? Best way to go about it?) |
|
| For intervention 1 and intervention 2 schools: What do you understand about what learning mentors are doing with young people who are found to be drinking in a way that might be harmful to them? What do you think about this? How did you find the process of enabling these interventions within the school environment? (Probes: learning mentor time, getting agreement from teachers for pupils to be taken out of class, etc.) |
||
| Did the study have an effect on the staff and students involved? | Did any staff come to talk to you about the study? If so, who (learning mentors, teachers, governors) and why? Did any students talk to you about the study? If so, why? Did any parents talk to you about the study? If so, why? Do they think the study has had any wider effects on the school? (Probes: raising awareness of alcohol in school, positive effects, negative effects) How did young people find being taken out of class for the interventions? (Probe: any negative effects) |
|
| What lessons could be learned for future research? | Could anything have been done differently to make the research easier to perform in the school? | If you were approached again to take part in the research would you agree? Why? What worked well? Why? What didn’t work well? Could anything have been done to overcome this? Do they think that alternative ways of performing the study would be helpful? (e.g. a video clip of a researcher informing students how to fill out the survey) |
| How could study findings be effectively disseminated? | Are they interested in dissemination of study findings? To whom? Governors? Staff? Students? Parents? How do they think dissemination would be most effectively performed? |
|
| Learning mentors | ||
| Big research question | Mini research question | Ways to approach this question |
| What are the feelings regarding alcohol use by young people and existing alcohol education within their school? | Does the participant have any thoughts or concerns about alcohol use by young people? | What are your views about alcohol use by young people in general? What are your views about alcohol use by young people in your school? What impact, if any, do you think alcohol use has within the school environment? (Probes: intoxication on school premises and indirect, e.g. health/educational attainment) |
| Does the participant have any thoughts on existing alcohol education within their school? | Is alcohol use by young people addressed in your school? How? By whom? (Probe: external initiatives)
|
|
| What were their experiences of being part of this project? | How did you feel about participation in the research project? | How did you become involved in the research? (Probe: were they involved in the decision) How did you feel about being involved in the research? (Probes: concerns about alcohol use among young people, the form of intervention, concerns over their workload, the nature of their involvement, etc.) Do you have any thoughts on the fact that the study focused on only Year 10 pupils? (Probes: whether this was the most suitable age group in terms of school practicalities and in terms of alcohol use by young people at this age) |
| How did you find the training? | Control group and intervention 1: What do you remember about the training you undertook? Did you have any thoughts on the training session about alcohol use? (Probes: usefulness, manner of delivery, etc.) Did you have any thoughts on the training session about the control and level one interventions? (Probes: usefulness, manner of delivery, etc.) Do you think the training adequately prepared you for taking part in the study?
|
|
| Intervention 2: What do you remember about the training you undertook? Did you have any thoughts on the training session about alcohol use? (Probes on usefulness, manner of delivery, etc.) Did you have any thoughts on the training session about the control and intervention 1? (Probes on usefulness, manner of delivery, etc.) Did you have any thoughts on the training session about intervention 2? (Probes on usefulness, manner of delivery, etc.) Do you think the training adequately prepared you for taking part in the study?
|
||
| What were their experiences of delivering the intervention? | Control group: Did you have any thoughts on the consent procedures? (Probes: opt-out letter for the survey, did they think young people really understood why they left their names on the survey) How did you find delivering the leaflet? (Probe: Was it difficult to identify a child as having screened positive and then not to do anything about it?) Is it possible for you to describe for me how you would go about this conversation with the young person? (Probe: Did they find themselves giving advice anyway?) |
|
| Intervention 1: Did you have any thoughts on the consent procedures? (Probes: opt-out letter for the survey, did they think young people really understood why they left their names on the survey) How did you find delivering the one-to-one intervention within the school environment? (Probes on time and resource issues) Did you have any thoughts on the tool you were given to provide the intervention with? Is it possible for you to describe for me how you would go about delivering an intervention with a young person? Did you find the way that you delivered the intervention differed with different young people? (Probe: personality issues, etc.) Did you find the way that you delivered the intervention differed over time? Was there anything you found particularly enjoyable or easy about delivering the intervention? Was there anything you found particularly difficult about delivering the intervention? Would you change anything about the intervention? Did you think that taking the young person out of class had any negative impact on them? |
||
| Intervention 2: Did you have any thoughts on the consent procedures? (Probes: opt-out letter for the survey, did they think young people really understood why they left their names on the survey) How did you find delivering the one-to-one intervention within the school environment? (Probe: time and resource issues) Questions regarding intervention 1: Did you have any thoughts on the tool that you were given to provide the intervention? Is it possible for you to describe for me how you would go about delivering an intervention with a young person? Did you find the way that you delivered the intervention differed with different young people? Did you find the way that you delivered the intervention differed over time? Was there anything you found particularly enjoyable or easy about delivering the intervention? Was there anything you found particularly difficult about delivering the intervention? Would you change anything about the intervention? Did you think that taking the young person out of class had any negative impact on them? Questions regarding intervention 2: At what point did you discuss the idea of parental involvement with the young person? Did you have any thoughts on the tool that you were given to provide the intervention? How did you find discussing parental involvement with young people? How did young people tend to respond to the idea of parental involvement? Did they talk to you about their reasoning for wanting or not wanting their parents involved? How did you go about the initial approach to parents? How did you find discussing the family intervention with the parent? Was there anything that you found that made this conversation easier/harder for you? Is it possible for you to describe for me how you would go about delivering an intervention with a young person and their parents? Did you find the way that you delivered the intervention differed with different young people and parents? If so, how? Did you find the way that you delivered the intervention differed over time? If so, how? Was there anything you found particularly enjoyable or easy about delivering the intervention? If so, what? Was there anything you found particularly difficult about delivering the intervention? If so, what? Would you change anything about the intervention? How did you find trying to engage young people and their parents in conversation about alcohol use in this way? How appropriate did you find a one-off intervention for this type of work? |
||
| What lessons could be learned for future research? | Could anything have been done differently to make the research easier to perform in the school? | If you were approached again to take part in the research would you agree? Why? What worked well? Why? What didn’t work well? Could anything have been done to overcome this? Do they think that alternative ways of performing the intervention would be helpful? |
| How could study findings be effectively disseminated? | Are they interested in dissemination of study findings? To whom? Staff? Students? Parents? How do they think dissemination would be most effectively performed? |
|
| Young people | ||
| Big research question | Mini research question | Ways to approach this question |
| What role does alcohol play in the participants’ lives? | What does the participant consider to be ‘normal’ alcohol use behaviour for them? | Can you remember when you first started to drink? (Probe: why first started) How often would you say that you drink alcohol? Could you describe to me a typical drinking occasion for you? What do you think are the positive things about drinking for you? Does drinking have any downsides for you? Do you think that you drink about the same as your friends? As the other kids in school? Why is this? |
| What are the major influences on their alcohol behaviour? | Since you started drinking, have there been any times that you have drunk more than is usual for you? Why? Since you started drinking, have there been any times that you have drunk less than is usual for you? Why? Who would you usually drink with? |
|
| What were their experiences of being part of this project? | What did they think of the screening process? | What do you remember about how the study was first mentioned to you? Who talked about it? Can you tell me why you decided to write your name down on the survey? Did you feel that you understood what you were being asked to do and why? Can you tell me what the survey questions asked? How clear were they? Anything confusing? (use questionnaire as aide-memoire) How did you feel answering the questions on the survey?
|
| What was the personal impact of finding out that they had screened positive? | Can you remember being told you had been found to be drinking in a way that might be harmful to you? What did you think this really meant? Can you tell me a little about what that experience was like for you? (Probes: Was it a surprise? Did it upset you?) How did you find having this conversation with the learning mentor? |
|
| What influenced them to consent to take part in the study? | How was the study explained to you? Did you feel that you properly understood what taking part in the study would mean from this conversation? What made you decide that you wanted to take part (Probe: felt they had to, concerns over alcohol use) How did you feel deciding to take part in the study? If you had any questions, how did the learning mentor answer them? |
|
| What were their experiences of receiving the intervention? | Control group: Can you remember what the learning mentor said to you after they told you that you had screened positive? Did you feel that that was enough information to help you? Did you have any thoughts on the leaflets you were given? (Probes: Did they read them? Useful?) |
|
| Intervention 1: Is it possible for you to go through with me what happened during the meeting with the learning mentor? Was there anything you found particularly positive about the intervention? Was there anything you found particularly negative about the intervention? (Probe: being taken out of class) Did you have any thoughts on the leaflets you were given? (Probes: Did they read them? Useful?) |
||
| Intervention 2 – did not agree to parent contact: Can you remember at what point the learning mentor asked you about contacting your parents? What do you think about involving your parent/s in a meeting? (Probe: Do you think it was appropriate to try and involve parents in this kind of intervention or is this something that should be handled by young people alone) Could you tell me a little more about why you didn’t want your parents to be contacted? (Probes: feelings of embarrassment, thinking parents couldn’t help, etc.) |
||
| Intervention 2 – did agree to parent contact: Can you remember at what point the learning mentor asked you about contacting your parents? Could you tell me a little more about why you were happy for your parents to be contacted? How did your parents react to being contacted about the study? Is it possible for you to go through with me what happened during the intervention with your parents? Was there anything you found particularly difficult about the intervention? Was there anything you found particularly positive about the intervention? Do you think it was useful to you to have your parents involved in the intervention? |
||
| Has the intervention had any impact on perceived drinking behaviours? | Do you feel different about drinking now, compared with before you received the intervention?
Has there been anything that you have found that helps you change the way you drink? Has there been anything that has made it particularly difficult to change the way you drink? |
|
| What do they perceive to be the appropriateness of school-led health promotion work across the school–home interface | Where does the participant perceive to be the most appropriate place to have alcohol education? | What do you think of school as a place to have this kind of alcohol education?
|
| What lessons could be learned for future research? | Could anything have been done differently to make the research easier to be part of? | If you were approached again to take part in the research would you agree? Why? What worked well? Why? What didn’t work well? Could anything have been done to overcome this? Do they think that alternative ways of performing the intervention would be helpful? |
| How could study findings be effectively disseminated? | Are they interested in dissemination of study findings? To whom? Staff? Students? Parents? How do they think dissemination would be most effectively performed? |
|
| Parents | ||
| Big research question | Mini research question | Ways to approach this question |
| Sampling Information | SES status of school area and gender | What school does the participant’s child attend? |
| What role does alcohol play in the participant’s lives? | What does the participant consider to be ‘normal’ alcohol use behaviour for them? | How often would you say that you drink alcohol? Could you describe to me a normal drinking occasion for you? What do you like to drink? Have there been any times that you have drunk more than is normal for you? Why? Have there been any times that you have drunk less than is normal for you? Why? What do you think are the positive things about drinking for you? Does drinking have any downsides for you? |
| In what ways have the participants considered their child’s alcohol use? | Have you ever had concerns about your child drinking alcohol? Is alcohol something that you have ever discussed with your child?
|
|
| What were their experiences of being part of this project? | What was the personal impact of finding out that their child had screened positive? | Can you remember receiving the original letter about the study with the opt-out slip?
What did you think that ‘drinking in a way that was possibly harmful’ really meant? Can you remember the initial conversation you had with the learning mentor about taking part in the intervention with your child? Could you go through what was said at this conversation with me? Can you tell me a little about what this conversation was like for you? |
| What were their experiences of receiving the intervention? | Is it possible for you to go through with me what happened during the intervention? Was there anything you found particularly difficult about the intervention? Was there anything you found particularly good about the intervention? Did you have any thoughts on the booklet you were given? (Probes: Did they read it? Was it useful?) What changes would you make to the way the meeting was arranged/conducted? |
|
| Has the intervention had any impact on how they feel about and respond to their child’s drinking behaviour? | Has the intervention made you feel differently about your child’s drinking now? Do you think that having the intervention has had an impact on the way you discuss drinking with your child? |
|
| What do they perceive to be the appropriateness of school-led health promotion work across the school–home interface | Where does the participant perceive to be the most appropriate place to have alcohol education? | What do you think of school as a place to have this kind of alcohol education? Why? If not ideal, where would be more suitable? |
| Does the participant think that parental involvement in this kind of alcohol intervention is appropriate? | How did you feel about being informed that your child had been found to be drinking in a way that might be harmful to them? Was this appropriate? How did you feel about being asked to be involved in the meeting with your child? Was this appropriate? Not all children, found to be drinking in a potentially harmful way and having met with a learning mentor to discuss this, have had an intervention with parental involvement. Do you have any thoughts on this? |
|
| What lessons could be learned for future research? | Could anything have been done differently to make the research easier to be part of? | If you were approached again to take part in the research would you agree? Why? What worked well? Why? What didn’t work well? Could anything have been done to overcome this? Do they think that alternative ways of performing the intervention would be helpful? |
| How could study findings be effectively disseminated? | Are they interested in dissemination of study findings? To whom? Staff? Students? Parents? How do they think dissemination would be most effectively performed? |
|
Appendix 5 Scoring system for numeric scales
| Questionnaire | Scale/subscale details | Question scoring | Overall score | Notes |
|---|---|---|---|---|
| A-SAQ | Single question with a choice of six responses to indicate levels of harmful drinking | 1. never 2. < 4 times 3. ≥ 4 times but not every month 4. ≥ 1 per month but not every week 5. Every week but not every day 6. Every day |
1–6 | A score of ≥ 3 is considered a positive score for possible hazardous or harmful drinking |
| AUDIT | Ten questions about drinking behaviour with five possible responses for q1–8, or three responses for q9 and q10 | Score of 0–4 for q1–8, and 0, 2 or 4 for q9 and q10 | 0–40, for which scores from each question are added | An AUDIT score of ≥ 8 is considered to indicate possible hazardous or harmful drinking in adults. There is currently no agreed score to indicate hazardous or harmful drinking in adolescents |
| AUDIT-C | First three questions of the AUDIT | All questions are scored 0–4 | 0–12, for which scores from each question are added | An AUDIT-C score of ≥ 5 is considered to indicate possible hazardous or harmful drinking in adults. There is currently no agreed score to indicate hazardous or harmful drinking in adolescents |
| RAPI | Twenty-three questions about drinking behaviour, each with four possible responses | All questions are scored 0–3 | 0–69, for which scores from each question are added | Higher RAPI scores indicate more problematic drinking behaviour |
| WEMWBS | Fourteen questions to assess level of happiness and life satisfaction | Each question is scored 1–5 | 14–70, for which scores from each question are added | WEMWBS provides robust results for populations and groups with higher scores indicating higher levels of well-being. It has not yet been validated for monitoring mental well-being in individuals |
| TLFB-28 | Quantitative estimations of daily alcohol consumption | Provides a variety of different estimations of individual consumption levels | The TLFB is a method for assessing recent drinking behaviour. Administered by a learning mentor, it involves asking young people to retrospectively estimate their daily alcohol consumption over a 28-day time period prior to the interview. We will specifically derive total alcohol consumed in a 28-day period, percentage of days abstinent, drinks per drinking day, and number of days drinking more than two units |
Appendix 6 Proposed case diary for definitive study
Glossary
- Alcohol Screening and Brief Intervention
- Alcohol Screening and Brief Intervention is a secondary preventative activity, aimed at individuals whose consumption level or pattern is likely to be harmful to their health or well-being. They generally consist of screening (to identify relevant recipients) followed by structured advice or counselling of short duration, which is aimed at reducing alcohol consumption or decreasing the number or severity of problems associated with drinking.
- Control
- The control condition consisted of feedback that the young person was drinking in a way that may be harmful and provision of an advice leaflet delivered by the school learning mentor.
- Intervention 1
- The intervention 1 condition consisted of feedback that the young person was drinking in a way that may be harmful and provision of an advice leaflet – a 30-minute brief interactive session that combines structured advice and motivational interviewing techniques delivered by the school learning mentor.
- Intervention 2
- The intervention 2 condition consisted of feedback that the young person was drinking in a way that may be harmful and provision of an advice leaflet – a 30-minute brief interactive session that combines structured advice and motivational interviewing techniques, delivered by the school learning mentor, plus a 60-minute session involving family members, also delivered by the school learning mentor.
- Learning mentor
- Learning mentors are specifically trained to provide a service complementary to that of teachers and other school staff, addressing the needs of children who require assistance in overcoming barriers to learning in order to achieve their full potential. Learning mentors support, motivate and challenge pupils who are underachieving. They help pupils overcome barriers to learning caused by social, emotional and behavioural problems.
- Participants to the trial
- Participants to the trial were young people who screened positively on a single alcohol screening question, left their name on the questionnaire and gave consent.
List of abbreviations
- A-SAQ
- Adolescent Single Alcohol Question
- AC
- assessed control
- ADAD
- Alcohol and Drug Abuse Division
- ASBI
- Alcohol Screening and Brief Intervention
- AUD
- alcohol use disorder
- AUDIT
- Alcohol Use Disorders Identification Test
- AUDIT-C
- AUDIT-Consumption (first three questions of full AUDIT)
- BAC
- blood alcohol concentration
- BASICS
- Brief Alcohol Screening and Intervention for College Students
- BDI-II
- Beck Depression Inventory version II
- BECCI
- Behaviour Change Counselling Index
- BI
- brief intervention
- BLC
- Brief Lifestyle Counselling
- CBT
- cognitive–behavioural therapy
- CDISC
- Clinical Diagnostic Interview Schedule for Children
- CI
- confidence interval
- CISS
- Coping Inventory for Stressful Situations
- CMO
- Chief Medical Officer
- CONSORT
- Consolidated Standards of Reporting Trials
- cRCT
- cluster randomised controlled trial
- DAST
- Drug Abuse Screening Test
- DSM-III-R
- Diagnostic Statistical Manual version III, Revised
- DSM-IV
- Diagnostic Statistical Manual version IV
- EQ-5D
- European Quality of Life-5 Dimensions
- EQ-5D-Y
- European Quality of Life-5 Dimensions (Youth version)
- FRAMES
- Feedback, Responsibility, Advice, Menu, Empathy and Self-efficacy
- GAIN
- Global Appraisal of Individual Needs
- GAIN-I
- Global Appraisal of Individual Needs – Initial version
- GP
- general practitioner
- IMI
- Individual Motivational Interviewing
- M-SASQ
- Modified-Single Alcohol Screening Question
- MAP
- Maudsley Addiction Profile
- MDMA
- 3,4-methylenedioxy-N-methylamphetamine
- MI
- motivational interviewing
- MRC
- Medical Research Council
- NIHR
- National Institute for Health Research
- NYSDS
- National Youth Survey Delinquency Scale
- OR
- odds ratio
- PANSS
- Positive and Negative Symptom Scale
- PMG
- Programme Management Group
- POSIT
- Problem Orientated Screening Instrument for Teenagers
- PPI
- patient and public involvement
- PSHE
- Personal, Social, Health and Economic Education
- QALY
- quality-adjusted life-year
- RAPI
- Rutgers Alcohol Problems Index
- RCT
- randomised controlled trial
- S-SUQ
- Short Service Use Questionnaire
- SD
- standard deviation
- SES
- socioeconomic status
- SHAHRP
- School Health and Alcohol Harm Reduction Project
- SRD
- Self-Report Delinquency Scale
- SUD
- substance use disorder
- SUS
- ‘Stop Using Stuff’
- TAU
- treatment as usual
- TLFB
- Timeline Followback
- TP1
- time point 1
- TP2
- time point 2
- TP3
- time point 3
- TSG
- Trial Steering Group
- UCC
- usual continuing care
- WEMWBS
- Warwick–Edinburgh Mental Well-being Scale
- WHO
- World Health Organization
- YSR
- youth self-report