Notes
Article history
The research reported in this issue of the journal was funded by the PHR programme as project number 09/3005/04. The contractual start date was in April 2011. The final report began editorial review in June 2015 and was accepted for publication in November 2015. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PHR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Professor Rona Campbell is the Director of DECIPHer Impact, a not-for-profit company that is wholly owned by the Universities of Bristol and Cardiff, and whose purpose is to license and support the implementation of evidence-based health promotion interventions. Professor Tim J Peters was a member of the National Institute for Heath Research (NIHR) Clinical Trials Unit standing advisory committee during the conduct of this study, but is no longer a member. Professor Russell Jago has been a member of the Research Funding Board for the NIHR Public Health Research Board since October 2014. Dr Laura Howe reports grants from the Medical Research Council during the conduct of the study. Outside the submitted work Dr Laura Howe reports grants from Wyeth Nutrition; the US National Institutes of Health (National Institute on Aging); the Economic and Social Research Council; the Economic and Social Research Council and Biotechnology and Biological Sciences Research Council (cofunding); the Medical Research Council; and the British Heart Foundation. The AFLY5 RCT is funded by the UK National Institute for Health Research (NIHR) Public Health Research programme (09/3005/04), which also paid the salary of Emma L Anderson and Sian L Wells. Debbie A Lawlor and Laura D Howe work in a unit that receives funds from UK Medical Research Council (MC_UU_12013/5). Ruth R Kipping and Rona Campbell work in the Centre for the Development and Evaluation of Complex Interventions for Public Health Improvement (DECIPHer), a UK Cross Research Council Public Health Research Centre of Excellence; joint funding (MR/KO232331/1) from the British Heart Foundation, Cancer Research UK, Economic and Social Research Council, Medical Research Council, the Welsh Government and the Wellcome Trust, under the auspices of the UK Clinical Research Collaboration, is gratefully acknowledged. LDH is supported by a UK Medical Research Council Population Health Scientist fellowship (G1002375). Debbie A Lawlor (NF-SI-0611–10196) and Tim J Peters (NF-SI-0512–10026) are NIHR senior investigators. This study was undertaken in collaboration with the Bristol Randomised Trials Collaboration (BRTC), a UKCRC-registered clinical trials unit (CTU) in receipt of NIHR CTU support funding. None of the funders had involvement in the TSC, the data analysis, data interpretation, data collection, or writing of the paper.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2016. This work was produced by Lawlor et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
Scientific background
Low levels of physical activity and of fruit and vegetable consumption in childhood track into adulthood1–3 and are associated with adverse health outcomes, including greater adiposity and associated adverse cardiometabolic risk factors, poorer bone mineralisation, behavioural problems, low mood and poorer academic attainment. 4–10
School-based interventions have the potential to reach the vast majority of children, and systematic reviews of school-based interventions aimed at increasing physical activity, decreasing sedentary behaviour and improving fruit and vegetable consumption suggest some beneficial effect. 11–16 However, they also highlight the general poor quality of included studies and caution that the pooled results might exaggerate the effectiveness of the interventions. 11–16
Evidence for the effectiveness of school-based interventions to improve diet and physical activity
A systematic review that included 44 school-based randomised controlled trials (RCTs) found beneficial effects on moderate or vigorous physical activity (MVPA) during school hours, but the authors noted that benefits might have been exaggerated as a result of the outcome assessment being self-/parent-reported and not blind to school allocation in most trials, and also that the marked loss to follow-up in several trials might have led to biased findings. 11 Furthermore, it could be argued that it is not surprising, given that the interventions largely included extra compulsory physical activity lessons, that greater time spent in MVPA during school hours was found. Evidence from observational epidemiological studies suggests that compulsory physical activity lessons in school are associated with more school-based activity, but not with more total activity17,18 and that, long term, those who attended schools with more compulsory physical activity have similar levels of physical activity, physical fitness and body mass index (BMI) as young adults. 18 A second systematic review included only studies in which physical activity had been assessed objectively by accelerometers and did not restrict the outcome to activity during school hours; the review included school-based studies, as well as those of interventions in other settings. 12 It reported beneficial effects of interventions, with no evidence that this differed between school-based or family/other setting interventions. The authors commented that the magnitude of the effect was small and unlikely to be of health benefit,12 although modest shifts in risk factors can produce important public health benefit. One systematic review identified five RCTs of school-based intervention to reduce sedentary behaviour and reported that all of them were effective. 15 Results were not pooled formally and the outcome in all of the studies was based on self-/parent-reporting. 15 In a more recent systematic review and meta-analysis, evidence from 34 RCTs suggested that both school-based interventions and interventions in other settings were effective in reducing time spent in sedentary behaviour and, consequently, in reducing mean BMI. 16 Only nine of these studies reported that random allocation was adequately concealed, and only eight reported blinding of the outcome assessment; sedentary behaviour was assessed by self-/parent-report in all studies. 16 Two recent systematic reviews of school-based interventions to increase fruit and vegetable consumption identified 19 RCTs and 27 RCTs or non-randomised trials, respectively. 13,14 One review, which focused solely on primary school interventions, concluded that computer-based interventions were effective (based on pooling of two RCTs), but pooling of other trials did not suggest interventions were effective. 13 The authors noted that the majority of studies did not describe the randomisation method and it was not possible to ascertain if allocation was concealed for most of the 19 RCTs reviewed. The authors also noted that most did not take account of clustering (non-independence between children from the same school) in their analyses, despite all being cluster RCTs. 13 The second review also focused on children in the primary school age range (5–12 years), but they concluded on the basis of pooled results from 21 (out of 27) controlled trials that school-based interventions were effective at increasing fruit but not vegetable consumption. 14 Again, the poor quality of the majority of the trials was noted by the authors.
Rationale for the Active for Life Year 5 intervention
We began work to design, pilot and then fully evaluate a school-based intervention to improve levels of activity and diet and other health outcomes in children in 2006. Consistent with recommendations of the UK Medical Research Council and others for the evaluation of complex interventions, our aim was to develop an intervention that was theory based and built on evidence from appropriate reviews of the literature, and then to test its feasibility and complete pilot work prior to seeking funds for a full-scale RCT. 19,20 Among national and international policy-makers and researchers there has been a strong belief for some decades that simple interventions in schools can change unhealthy behaviours to healthy ones. 21,22 We wanted to test this and, therefore, sought an intervention that would be possible to deliver in schools with minimal disruption to the main aim of educating children and moreover that would be relatively inexpensive. Lastly, we wanted an intervention that focused on children under the age of 11 years because of evidence that persistent overweight/obesity23 and the association of greater adiposity with future coronary heart disease is established by this age. 24
Our original literature search identified a cluster RCT in 11- to 12-year-olds25 and a quasi-randomised trial of 8- to 9-year-olds,26 both completed by the same group of researchers and of a similar intervention that fit with the type of intervention we wanted to develop for use in the UK. The intervention, based on social cognitive theory27 with a particular emphasis on improving child self-efficacy to make behavioural change,28 aimed to reduce childhood obesity and improve health via changes in physical activity, diet and screen viewing. These studies found beneficial effects, including on overweight/obesity in girls in the older age group; in the study of the younger age group, BMI was not assessed.
Between 2006 and 2008 we worked with primary school teachers, the local primary care trust (public health commissioners) and local council (government) in South Gloucestershire, in the south-west of England, to determine whether or not this intervention could be adapted for use in the UK, whether or not it was feasible to deliver the adapted intervention within the national curriculum and whether or not there was evidence of promise for the intervention from a pilot RCT sufficient to justify a full-scale RCT. This work showed that, with minor adaptations, the intervention could be delivered within the UK national curriculum for year 5 children (aged 9–10 years) and the pilot RCT suggested that it might be effective. 29 We had a limited budget for the pilot and so within it were not able to test the use of accelerometers. The process evaluation within the pilot RCT found that the teachers thought the intervention should be extended to include parents if it was to be maximally effective. 29,30 We therefore obtained a further small budget and undertook qualitative work with parents and teachers to develop the intervention in such a way that it involved parents; this showed that parent-interactive homework assignments would be feasible and acceptable to them. 30 We then completed a feasibility study (examining before-and-after intervention changes in the same children) of adding parent-interactive homework assignments to Active for Life Year 5 (AFLY5) and of collecting accelerometer data. 30,31 Results from that work provided further support for going ahead with a full-scale RCT of the AFLY5 intervention that then included parent-interactive homework assignments, as well as lessons. None of the schools or teachers who were involved in the feasibility and pilot work has been included in the main RCT, which is presented in this monograph.
Rationale for our study design
Given the importance of establishing healthy behaviours in relation to physical activity and diet, the potential for effectively doing this via schools, but the lack of high-quality trials to date in this area, the rationale for undertaking the AFLY5 RCT was to address the weaknesses that existed in school-based RCTs to promote healthy diet and levels of physical activity at the time that we began the study. Specifically, in our study design we aimed to ensure that (i) random allocation was concealed; (ii) an objective assessment of time spent in MVPA and sedentary behaviour were collected using accelerometers; (iii) the fieldworkers collecting outcome data from children were blind to school allocation; and (iv) the intervention did not focus solely or primarily on increasing physical activity through physical education (PE) classes in school. 32 The intervention was designed to change the child’s behaviours in a non-compulsory way, and so measurements were concerned with the whole day and both weekdays and weekends, not just during school hours. We also aimed to (v) undertake one of the largest RCTs in this area; (vi) take account of the clustered nature of the design in the sample size calculation and analysis; (vii) work with the schools to ensure loss to follow-up was minimised; and (viii) examine the effect of the intervention both immediately after its completion and again 12 months later in order to determine whether or not any effects were sustained. 32,33
Aims and objectives
The aim of our study was to test the effect of a primary school-based intervention, which we had shown in pilot and feasibility work could be readily incorporated to the UK national school curriculum, to improve levels of physical activity and diet in 9- to 10-year-olds. Our specific objectives were:
-
to investigate the effectiveness of the AFLY5 school-based intervention to:
-
increase physical activity, reduce sedentary behaviour and increase fruit and vegetable consumption in children
-
affect pre-specified secondary outcomes [child-reported time spent screen viewing at the weekend and on weekdays, consumption of snacks, high-fat food and high-energy drinks, BMI, waist circumference (WC), general overweight/obesity and central overweight/obesity]
-
influence pre-specified potential mediators
-
-
to test the cost-effectiveness of the intervention
-
to determine whether or not the intervention was delivered with a high level of fidelity and identify any barriers to its implementation.
Chapter 2 Trial design and methods
Study design
Active for Life Year 5 is a school-based, cluster RCT. The trial protocol was published in 2011, prior to any recruitment or data collection, and a more detailed statistical analysis plan was subsequently published before any analysts had access to data. 32,33 The trial was registered at the controlled trials register prior to recruitment of schools or data collection (www.controlled-trials.com/ISRCTN50133740).
Ethics approval and research governance
We obtained ethics approval from the University of Bristol’s Faculty of Medicine and Dentistry Committee for Ethics (reference number 101115). Once schools agreed to participate in the study, parents/guardians of children in year 4 were sent a letter and information sheet about the study with an opt-out consent form for their child for each of the measurements. They were given the opportunity to contact the research team to discuss the study and also information about being able to withdraw at any stage. An information sheet for the child was sent with the letter that was sent to the parents. The children were given a second copy of this information sheet at the time that measurements were undertaken and they were asked to give signed assent to each of the measurements. Any child whose parents had refused consent for all measurements was not included in the study, although they may have received the AFLY5 lessons and homework assignments, as these were delivered at the school level as part of the school curriculum. Any child whose parents refused consent for one or more (but not all) measurements did not have those measurements undertaken but were included in the study. Any child refusing assent for a measurement at any time did not have that measurement taken (irrespective of whether or not the parent had not refused consent).
Eligibility and recruitment
State primary or junior schools with years 4–6 pupils in the Bristol City and North Somerset administrative areas were eligible for inclusion. Between March and July 2011 all state primary and junior schools with children in years 4–6 (aged 8–11 years) in the areas covered by Bristol City Council (93 schools) and North Somerset Council (55 schools) were invited to participate. Both of these areas are in the south-west of England and include a range of levels of deprivation, as well as urban and rural areas. Special schools (for children whose additional needs cannot be met in a mainstream setting) were excluded because they were unlikely to be teaching the standard UK national curriculum and the children may not have been able to take part in all the measurements. One hundred and forty-eight schools were invited and 63 expressed an interest in taking part, with three schools subsequently withdrawing their interest. Sixty schools were recruited (46 in Bristol City and 14 in North Somerset). Participants were children in year 4 (aged 8–9 years) at the time of recruitment.
Randomisation
Prior to randomisation school heads were asked to complete a brief questionnaire about the school. This included three questions that asked them to list all activities the school was engaged in that related to (1) increasing physical activity, (2) decreasing sedentary behaviour and (3) promoting a healthy diet in pupils. Responses were free text and, on the basis of these responses, each school was classified as either high (one or more initiatives) or low (no initiatives) involvement in health-promoting initiatives relevant to the outcomes of this trial. When heads (or teachers they delegated the task to) reported initiatives that were part of the UK national curriculum or that they had been awarded ‘healthy schools’ or ‘healthy schools plus’ status these were not included as involvement in an initiative, as these are widespread in the south-west of England and we were looking for additional initiatives that varied between schools. Schools were also defined as being in an area of high, medium or low deprivation by splitting them into thirds based on their score on the English Index of Multiple Deprivation (IMD) 2010. 34 Schools were grouped into six mutually exclusive strata by these two characteristics and randomly allocated to control or intervention within these strata. 32,33 Randomisation was undertaken by DAL who was unaware of any characteristics of the schools (school identifications were used to relate them to the two stratifying variables and DAL had no knowledge of which schools these identifications linked to); it was concealed by using the Bristol Randomised Trials Collaboration’s automated (remote) system. After randomisation, one school refused to undertake the intervention; the head reported that they had hoped they would be randomised to control and did not have the time or capacity to accommodate the intervention. The school did agree to participate in all pupil measurement sweeps. This school is included in the randomised group (intervention) for the main intention-to-treat (ITT) analysis and is excluded from the per-protocol analysis.
Intervention
Full details of the intervention have been published in the trial protocol and pilot study. 29,32 It comprised:
-
Training for year 5 classroom teachers and learning support assistants (LSAs), provided by the trial manager, a nutritionist and a PE specialist. The training took place over a whole day (8–9 hours) in a location away from any of the schools and where the teachers/LSAs and those delivering the training would not be interrupted. Teachers/LSAs were given a choice of days to attend the training and schools were financially compensated for the cost of replacement teachers while their staff attended training. At the training days the rationale for the intervention was explained and each lesson and homework assignment were discussed and then taught in interactive ways. Time was provided for questions and discussion. Teachers were instructed to deliver 16 lessons, 10 of which had associated homework assignments to be handed out by the teachers. They were told that they could adapt the teaching plans and materials, as they would with other lessons (e.g., to suit their own style and the range of abilities in their class), but that the aims and knowledge/skills to be imparted should remain the same.
-
Provision of 16 lesson plans and teaching materials, including pictures, compact discs (CDs) and journals for year 5 teachers or LSAs to deliver over two out of the three school terms in year 5 (6–7 months). The 16 lessons included nine lessons that were primarily related to how to be more active and less sedentary and why this was important, six related to healthy nutrition and how to achieve this and one about reducing screen viewing. Each lesson did, however, combine different aspects of healthy behaviour. For example, in the physical activity lessons the children played games based on the food groups using photographs of food, which reinforced the content of the nutrition lessons. Similarly, in the lesson (and associated homework assignment) for reducing screen viewing [called ‘Freeze my TV’ (television)] children were taught how to replace regular TV watching with active play on some days.
-
Provision of 10 parent–child interaction homework activities. The homework assignments were designed to involve parents and other family members in the behaviour change process by reinforcing the messages delivered during lessons. The homework assignments included activities such as ‘Freeze my TV’, in which time normally spent watching TV would be replaced with physically active play, involving the parents and other family members, that the child would write a log about; cooking simple healthy food at home; thinking of different ways to add an extra serving of fruit or vegetables to their diet every day for a week on the ‘5-a-day planner’; and measuring the sugar content of drinks that the family have at home or include in school/work lunch packs.
-
Information was provided for schools to insert (as they wished) in the school newsletters about the importance of increasing physical activity, reducing sedentary behaviour and improving diet. This information was available on the CDs given to all schools with their training packs. Schools were free to edit this information and insert none, all or some of it.
-
Written information for parents on how to encourage their children to eat healthily and be active was delivered via the school children at the start of the intervention in the form of the Change 4 Life: Top Tips for Kids leaflet produced by the Department of Health. 35
The intervention took place when the children were in school year 5 (aged 9–10 years) after baseline assessment. Our previous feasibility work showed that the AFLY5 intervention was aligned to the UK national curriculum for key stage 2 (which is used for all children aged 7–11 years). 29 Schools randomised to the control group continued standard education provision for the school year, including any involvement in additional health-promoting activities, but had no access to the intervention teacher training and no known access to the teaching materials, which have not been published and were not made available by the research team beyond the intervention schools.
Sample size calculation
The sample size calculation was based on the intracluster correlation coefficients for different outcomes and other information collected during pilot/feasibility work. 29,32,33 For each of the three primary outcomes we determined the number of schools required (assuming 25 pupils per school) to detect at least a 0.25- to 0.30-standard deviation (SD) difference between pupils in intervention and control schools with 80–90% power, a two-sided alpha of 0.05 and allowing for 15% loss to follow-up or missing data. 32 For secondary outcomes we took account of multiple testing and aimed to have at least 80% power at an alpha of 0.01 for all of these, including the ability to detect a relative minimum difference of 30% in general or central overweight/obesity. 32 These calculations showed that we needed to recruit 60 schools with a total of at least 1500 children, with 1275 (after allowing for loss to follow-up/missing data) available for the primary analyses.
Outcome measures
All primary and secondary outcome measurements are listed in Box 1.
-
Accelerometer-assessed mean time per day spent doing MVPA.
-
Accelerometer-assessed mean time per day spent in sedentary activity.
-
Self-reported (validated questionnaire) servings of fruit and vegetables consumed per day.
-
Self-reported (validated questionnaire) mean time spent screen viewing on a typical weekday.
-
Self-reported (validated questionnaire) mean time spent screen viewing on a typical weekend day.
-
Self-reported (validated questionnaire) servings of snacks consumed per day.
-
Self-reported (validated questionnaire) servings of high-fat foods consumed per day.
-
Self-reported (validated questionnaire) servings of high-energy drinks consumed per day.
-
Body mass index determined from weight and height measured in classrooms by two study fieldworkers.
-
Waist circumference measured in classrooms by two study fieldworkers.
-
General overweight/obesity, determined by the International Obesity Task Force thresholds of BMI for children (taking account of their age and sex). 36
-
Central overweight/obesity determined by thresholds of UK age- and sex-specific reference charts for WC and defined by the International Diabetes Federation. 37
Participant assessments
Baseline assessments (prior to intervention) were undertaken when the children were in the final term of year 4 or early in the first term of year 5. Outcomes assessment was completed immediately post intervention (end of year 5 and start of year 6), and again at 1 year post intervention (end of year 6). Identical protocols and procedures were used at all three assessments. They were undertaken by trained fieldworkers who had completed enhanced Criminal Records Bureau (CRB)/Disclosure and Barring Service checks. The fieldworkers were blinded to the allocation of schools to the arms of the trial. This was achieved by a clear separation within the research team, whereby only the study project manager and one administrator (neither of whom was involved in data collection or analyses) knew which schools had been allocated to intervention and which to control. These people were told of the importance of not discussing school allocations with anyone. Furthermore, we made every effort for the intervention to be built into normal school lessons in such a way that it did not alert children to the fact that they were in an intervention school. We assumed this would prevent the children from saying things to the fieldworkers that would indicate whether they were in an intervention or control school. Teachers were reminded at the training session not to discuss the intervention with the fieldworkers who collected data on children in schools and these fieldworkers were sent to schools in an order that had no relationship to which arm of the trial the schools were in.
Accelerometer measurements
We used ActiGraph GT3X+ accelerometers (ActiGraph, Pensacola, FL, USA) to assess physical activity and sedentary time. Accelerometers were distributed at the school visit and collected 6 days later from the schools to allow 5 days of data collection (3 weekdays and 2 weekend days). The children were asked to wear them during the day (except when bathing or swimming or participating in contact sports such as karate). Time spent in MVPA was defined as any time spent in activities that generated ≥ 2296 counts per minute and in sedentary behaviour was defined as time spent in activities generating between 0 and 100 counts per minute. 33 Children were included in the analyses of accelerometer-based outcomes if they had at least 3 days with at least 8 hours of valid accelerometer data on each of those days. 33 In these analyses any period of ≥ 60 minutes of continued counts of zero activity were defined as the child not wearing their accelerometer and such periods were removed from analyses. Children (and their parents via written guidance) were told to take the accelerometer off when they went to bed and put it back on as soon as they got out of bed. Our analyses of the raw data suggested that none of the children wore their accelerometer while in bed.
Anthropometric measurements
All anthropometric measurements were completed with children in a private room with two CRB-checked, trained fieldworkers present. Weight was measured without shoes in light clothing to the nearest 0.1 kg using a Seca digital scale (Seca UK, Birmingham, UK). Height was measured, to the nearest 1 mm, without shoes using a portable Harpenden stadiometer (Holtain Anthropometric Instruments Ltd, Wales). Fieldworkers were trained to ensure the correct position for height assessment. WC was measured to the nearest 1 mm at the mid-point between the lower ribs and the pelvic bone with a flexible tape and repeated three times. 38 When BMI and WC were treated as continuous outcome variables, standardised z-scores (also known as SD scores) were derived internally by subtracting the mean BMI/WC for a given sex and age category (in 6-monthly categories) from the observed measure and dividing by the SD for the sex and age category. For binary outcomes, the International Obesity Task Force age (in 6-monthly categories) and sex-specific thresholds for overweight were used to define whether a child was overweight/obese based on BMI. 36 For WC any child above the 90th percentile for age- and sex-specific values derived from UK-relevant centiles37 was defined as having central overweight/obesity, as suggested by the International Diabetes Federation. 39 We did not test inter-rater reliability for these measurements, but given the ways in which we tried to ensure that the fieldworkers were blinded to which arm the schools were randomised we doubt that any measurement error would differ between the randomised arms.
Diet and screen viewing questionnaire data
Servings of fruit and vegetables consumed and other dietary outcomes were assessed using the ‘Day in the Life Questionnaire’, which has been previously validated for use in children of the same age as those in this study. 40,41 The method we used for determining servings of different food types from the text responses to this questionnaire, including reliability and validity checks have been previously published. 33,40 Servings of daily fruit and vegetable consumption and other dietary outcomes were assessed using an established and validated scoring scheme. 40,42,43 An abbreviated and updated version of a previously validated screen viewing questionnaire was used to assess self-report sedentary behaviour,44 with details of how we derived variables from this questionnaire previously reported. 29,33
Potential mediators
Potential mediators are listed in Box 2.
-
Self-reported (validated questionnaire) physical activity self-efficacy.
-
Self-reported (validated questionnaire) fruit and vegetable consumption self-efficacy.
-
Child-reported (validated questionnaire) perceived maternal logistic support for physical activity.
-
Child-reported (validated questionnaire) perceived paternal logistic support for physical activity.
-
Child-reported (validated questionnaire) perceived maternal modelling of physical activity.
-
Child-reported (validated questionnaire) perceived paternal modelling of physical activity.
-
Child-reported (validated questionnaire) perceived maternal limitation of sedentary behaviour. a
-
Child-reported (validated questionnaire) perceived paternal limitation of sedentary behaviour. a
-
Child-reported (validated questionnaire) perceived parental modelling for healthy fruit and vegetable consumption. b
-
Child’s knowledge test (unvalidated questionnaire) related to intervention.
For sedentary behaviour we could not identify any validated questionnaire assessing parental modelling of healthy sedentary behaviour for use in children, and so have only collected information regarding maternal and paternal limiting of sedentary behaviour for which we were able to identify validated questionnaires.
For fruit and vegetable consumption we could not identify any validated questionnaires that provided relevant information for mothers and fathers separately or for logistical support of healthy fruit and vegetable consumption for use in children.
Physical activity self-efficacy was assessed using a validated questionnaire that consists of 26 items, each of which was answered by the child indicating their level of agreement on a 5-point scale (scored 1 to 5), where lower scores on this scale indicated lower self-efficacy. 45,46 Fruit and vegetable self-efficacy was assessed using a validated questionnaire consisting of 21 items, each of which was answered by the child indicating their level of agreement on a 5-point scale (scored 1 to 5), where lower scores indicate lower self-efficacy. 47 Parental support for physical activity and reducing sedentary behaviour was assessed using a validated 24-item scale, which provides information on modelling of parental physical activity behaviours (five items for each parent separately), logistical support (three items for each parent separately) and parental support for reduction of screen viewing (four items for each parent separately). 48,49 Each question is scored between 1 and 4, with lower scores indicating low levels of modelling or support for physical activity and low levels of limiting sedentary behaviour. Parental modelling of fruit and vegetable consumption was tested using a 12-item validated questionnaire that asked questions about mothers and fathers (or caregivers) together. 50 We were unable to identify a validated questionnaire for parental logistic support of fruit and vegetable consumption at the time of starting the study. We developed a test to specifically test the knowledge that children in the intervention schools should have gained via the intervention. We piloted the test on children of the same age as participants in AFLY5, but who had no involvement with the study or the participants who were in it, in order to make sure that it was understandable to the age of children in AFLY5. The knowledge test is shown in Appendix 1. It included nine questions each with a three-level multiple-choice response, where just one of the answers was correct and, therefore, the children could score between 0 and 9 on this test.
All potential mediators were assessed by questionnaires that were combined together into one document, together with the diet and screen viewing outcome measurements, and administered in the classroom for the children to complete in the presence of at least one of the trained study fieldworkers who answered any queries and assisted the children with reading and writing according to the study protocol. This instructed them to help with reading and spelling specific words, or understanding the meaning of a particular question, but not to suggest any answers.
Statistical analysis
Full details of the statistical analyses have been published and they include details of how all of the accelerometer variables were determined and how measurements used in this study were quality control checked. 32,33
Comparison of baseline characteristics
We compared relevant summary statistics of baseline characteristics between participants who were allocated to an intervention school and those allocated to a control school in order to determine whether or not any potentially influential imbalance had occurred (by chance) between these two groups. These comparisons also included accelerometer characteristics, including wear time, time with consecutive zero levels of activity, etc., to test our assumption that the characteristics that are used in criteria for deriving the accelerometer variables do not vary by randomised group. For all continuous and score variables we checked distributions using histograms and normal plots to examine how close to normality these were before deciding which summary statistics to present; mean (SD) or median [interquartile range (IQR)].
We did not compare baseline characteristics between the two groups with a statistical test (p-value) as any low values would simply represent a type 1 error under the assumption that we adequately randomly allocated participants. 51 As described in the general study protocol paper our procedures for randomly allocating schools to control or intervention were adequate. 32
Testing the effect of Active for Life Year 5 on outcomes immediately after the intervention
For all continuously measured primary and secondary outcomes at the immediate follow-up we used multilevel linear regression models to account for the clustering (non-independence) of children within schools; multilevel logistic regression was used for the two binary secondary outcomes (general and central overweight/obesity). The main analyses were ITT, with missing dates dealt with as described below. 33 All analyses included adjustment for the following baseline variables: age, sex, the baseline measure of the outcome being analysed, and the two pre-randomisation stratifying variables (involvement in other healthy behaviour-promoting activities and school-level deprivation). 33
We also did a secondary, per-protocol analysis, in which classes in the intervention arm were included in the analysis only if teachers had taught at least 70% (11/16) of the AFLY5 lessons. 33 As our unit of randomisation was schools and all pupils in any class will have been taught the same number of lessons, this means that whole classes (rather than selected children within intervention classes of schools) for which the teacher did not teach at least 70% of lessons were excluded from the per-protocol analyses. Some of the intervention schools had more than one year 5 class (the maximum was three classes per school). In the main per-protocol analyses presented here, exclusions were made on the basis of classes (i.e., if one out of three classes did not reach the threshold of 70% of lessons taught, only children from that class, and not the whole school, were excluded); repeating the analyses on the basis of whole schools did not materially alter the results (data are available from the authors on request). We assessed the number of lessons taught by reviewing the teacher-completed log, where possible, or by confirming these details with the teacher in person or by telephone. We had information on lessons taught for 29 of the 30 schools allocated to the intervention, including the school noted earlier that refused to do any part of the intervention. For the one school for which we were completely ignorant of how many lessons had been taught, we carried out analyses first assuming that they had taught at least 11 lessons and then repeated assuming that they had taught fewer than 11. The results were identical for these two alternatives.
We did additional analyses to assess whether or not the effect of the intervention on accelerometer-assessed outcomes differed by weekday or weekend day and whether or not the results were affected by implausible values. 33
We undertook a number of sensitivity analyses to examine whether or not our results were robust to any biases caused by missing data (see below).
Dealing with missing data
For the main analyses we used ITT. ITT requires all participants in a clinical trial to be included in the main analyses in the groups to which they were randomised. 51,52 This is straightforward if there is no loss to follow-up or missing data on some outcomes at follow-up among those who have been randomised, but is less straightforward where there is loss to follow-up/missing data. 52,53 A 4-point framework for dealing with missing outcome data has been proposed to deal with this issue and we were guided by that framework. 52,53 It emphasises the fact that all approaches [including complete case analysis (CCA), that is, including only those with observed outcome data] rely on assumptions that in any given situation may be more or less plausible but are always untestable. 52,53
Assumptions of missing data methods
Complete case analyses and several of the common methods for imputing/dealing with missing data assume that missing data are missing at random (MAR). The assumption underlying MAR is that having taken account of observed data in analyses, effects in those with missing data do not differ from those with no missing data. Another way of thinking about this is that the effect of a randomised intervention is the same in those with missing data as in those without missing data. Having similar proportions of participants with missing data in each arm of a trial is reassuring with respect to the MAR assumption being correct, but is not a guarantee, as the plausible reasons for missing data in each arm could be different but result in similar proportions with missing data.
In AFLY5, we minimised the extent of missing data through catch-up data collection, whereby for each participating school at each phase of data collection there was a day for main data collection, but some children may be absent from school on that day; therefore, for each school we had ‘catch-up’ days to obtain data on these children. As a result, the likely reasons for a child having missing follow-up data for all outcomes at one or both of the follow-up assessments are that the child moved school between data collection phases or the child was absent from school for a prolonged period or missed school frequently, such that they missed the main and catch-up data collection days. Missing one or more (but not all) of the specific measurements at follow-up could occur if the child did not give assent or, for the accelerometer-based outcomes, the child did not return the accelerometer or did not wear it for the required period of time. In the case of the AFLY5 RCT, MAR is plausible as randomisation was at the level of the schools, parental opt-out consent was ascertained at the start of the study and relevant for all data collection times, and it was implausible that the delivery of the intervention lessons and homework assignments in the intervention schools, or lack of these in the control groups, would affect the likelihood of a child being absent on days of data collection, declining assent for a particular measure or not returning the accelerometer or wearing it for the required time. Information from the local councils suggested that movement between schools was relatively low, but it is possible that children who moved may differ from those who did not on the basis of unobserved characteristics. Children who moved school might be from families who are relatively unorganised with children often moving school or they could be from families who move their child from state to private school in year 6 in order to attend private secondary school (in Bristol the proportion of children in private secondary school education is higher than than the average for the UK). The possibility that these types of missing data would bias our findings was assessed in sensitivity analyses.
Methods of dealing with missing data and sensitivity analyses
Baseline measurements
Any child who was registered at one of the recruited schools at the time of randomisation and whose parents did not refuse consent to participate was classed as a recruited study participant. The numbers of participants with valid data for each of the baseline measurements varied. For example, numbers of participants with accelerometer data are lower than for other measurements because some participants did not wear their accelerometer for sufficient time for data to be valid and some did not return their accelerometer. Numbers of participants with BMI and WC measurements are lower than for the dietary outcomes because some children did not provide assent for these measures. We checked whether or not missing data for any particular measure were similar in the two randomised groups. In order to include all children with the follow-up outcome measure (including those with a missing baseline value) and also be able to take account of the baseline value, we used the method suggested by White and Thompson53 for dealing with missing baseline values; this method includes an indicator variable for any missing values. 53
Outcome measurements
In the main analyses we used multilevel linear regression models accounting for the clustered nature of the data in AFLY5. For the main approach to all analyses any child with the measured outcome at follow-up was included; we carried out these analyses for each outcome separately so the numbers included in the analyses between each outcome vary. An indicator variable was used for missing baseline data as described above. This approach assumes that data are MAR. In addition to the main analyses, a number of sensitivity analyses were undertaken to test the robustness of our missing data assumption (Table 1).
| Analysis | Dealing with missing data | Assumptions | Implications/rationale |
|---|---|---|---|
| Maina | All participants were included if they have the particular outcome being assessed measured at the follow-up An indicator variable (indicating whether or not baseline data are missing for each outcome), together with allocation of a ‘temporary’ value to those with missing baseline data, was used to deal with missing baseline data53 |
Data are MAR | The number included in these main analyses differs for each outcome |
| S1 | Similar to above, but for each measurement participants were included only if both baseline and follow-up data were observed for each outcome | As above | Numbers differ for each outcome Allows assessment of whether or not those with missing baseline data differ in terms of the trial effect compared with those who do not have missing baseline data |
| S2 | Similar to above, but participants were included only if both baseline and follow-up data were recorded for all three primary outcomes | As above | Numbers are the same for each of the three primary outcomes but differ for each secondary outcome Allows assessment of whether or not any apparent differences in effect for the three primary outcomes were due to differences between these outcomes in missing data mechanisms |
| S3 | Similar to the main analyses, but for any child with a missing follow-up measure the child was allocated a value that is 10% ‘healthier’ for a given outcome than all participants with observed data (irrespective of randomised group). This was done by calculating the 10% value of the mean or median follow-up measure for each outcome and then adding this value to or subtracting this value from (depending on whether healthier levels are higher or lower for the particular outcome) the outcome mean or median; this final value was then imputed to the outcome value for every child with missing follow-up data | Those with missing outcome data, on average, behave in a relatively healthy way | Numbers are the same for all outcomes Allows assessment of the possibility that missing data are more likely to occur in families from a higher socioeconomic position as a result of moving from state to private education This will also test whether or not selection bias occurred as a result of limiting analyses to those with the required wear time for the accelerometer-based outcomes (data are more likely to be missing for this outcome than for other outcomes), as these analyses include all recruited participants |
| S4 | Similar to the main analyses, but in the case of a missing follow-up measure the child was allocated a value that is 10% ‘less healthy’ for a given outcome than all participants with observed data (irrespective of randomised group). This was done by calculating the 10% value of the mean or median follow-up measure for each outcome and then adding this value to or subtracting this value from (depending on whether less healthy levels are higher or lower for the particular outcome) the outcome mean or median; this final value was then imputed to the outcome value for every child with missing follow-up data | Those participants with missing data, on average, behave in less healthy ways than those who do not have missing data through mechanisms that are not captured by observed data | Numbers are the same for all outcomes Allows assessment of the possibility that missing data may be more likely in families from a lower socioeconomic position and missing data can be explained by the family being more dysfunctional or, perhaps, because the child has to care for a relative at home or has a high rate of truancy, and whether or not this form of missing data biases our assessment of the trial effect This will also test whether or not selection bias occurred as a result of limiting analyses to those with the required wear time for the accelerometer-based outcomes (data are more likely to be missing for this outcome than for other outcomes), as these analyses include all recruited participants |
Examining potential mediation effects
Although we did aim to examine some mediators when we first submitted our proposal, these were unspecified and, therefore, we did not take them into account in our sample size calculation. The justification for undertaking these analyses was that we felt that exploring whether the intervention had an effect on mediators that are relevant to the intervention was important for fully understanding the process by which the intervention worked, or why it did not work. For example, we may have found that the intervention was effective and that this was in part mediated by the child’s knowledge, but not by self-efficacy. Or we may have found that the intervention did not work and also that it had no effect on any of the mediators, which would suggest either that it was poorly delivered or that it did not effectively work on the proximal characteristics that it was expected to work on. To balance the importance of looking at mediation with the fact that our original sample size calculation did not take account of this mediation analysis we considered these analyses to be exploratory.
These analyses were largely undertaken in accordance with the published analytical plan that had been approved by the Trial Steering Committee (TSC). 32,33 The analysis plan in relation to mediation was discussed with the TSC (meeting on 1 March 2015) and two changes to the plan for the mediation analyses were agreed. In the original analysis plan we specified that we would explore mediation in relation only to the primary outcomes. Following further discussion, the TSC felt that exploring mediation in relation to secondary outcomes was equally informative and that we should explore whether or not the mediators influenced any of the effects on the three secondary outcomes that were affected by the intervention. In the original analysis plan we indicated that we would take account of multiple testing when exploring the effect of the intervention on mediators and explore whether or not they mediated effects on secondary outcomes only if they passed this ‘multiplicity-corrected’ test. On further reflection, the TSC felt that this was inappropriate because for potential mediation the magnitude of the effect is more important than the p-value.
Mediation was assessed for the effect of the intervention on both primary and secondary outcomes. Mediation analysis assumes that the intervention influences the mediator(s) and through this influence the mediator produces its effect on the outcome(s). Therefore, the first stage in the mediation analyses was to examine the effect of the intervention on the mediators (hence in these analyses mediators are treated as outcomes in the regression analyses).
-
First, we determined the effect of the intervention on each of the 10 measured mediators (see Box 2).
-
Each of these mediators was treated as a continuously measured variable, and in the first stage we explored the differences in mean scores of each mediator using the same ITT, as used in the analyses of outcomes secondary and sensitivity analyses.
-
In these analyses we included the following baseline and stratified covariables: age, sex, the baseline measure of each mediator, whether or not the school was involved in other health-promoting activities and school-level deprivation. (Note that knowledge was not assessed at baseline so there was no corresponding measure of this.)
-
-
Second, we explored whether or not mediators explained the effect of the intervention on outcomes. This second stage was conducted only if (1) the intervention had been shown to affect one or more of the outcomes; and (2) the intervention had been shown to affect one or more of the mediators relevant to an outcome that the intervention had affected (first stage of mediation analyses described above).
-
If the two criteria above were fulfilled we used multilevel multivariable linear regression to test the effect of the intervention on outcomes. We then repeated that analysis with any relevant mediator added and compared the effect of the intervention on the outcome before and after adjustment for the mediator.
-
A relative reduction (change towards the null) of ≥ 10% of the initial effect of the intervention on outcome was considered to indicate some evidence of mediation. In other words, if the effect estimate with adjustment for baseline and stratifying variables moved towards the null by ≥ 10% with the addition of one or more mediating variables, we considered that mediation had occurred as a result of those variables.
Testing differences of effect by sex and by area deprivation
As noted in our detailed statistical analysis plan, this trial had good statistical power for determining main effects, but did not include sufficient participants to examine whether effects differed by participant or school characteristics. 33 However, it was agreed with the TSC that, given the interest in whether or not girls and boys differ in their response to school-based health promotion interventions and also whether or not the effect of such interventions is greater in schools from more affluent areas (where resources to effectively add to the curriculum are greater than in schools in poorer areas), we would present stratified results by these characteristics. The analytical approaches for these stratified analyses were similar to the main ITT analyses but:
-
We examined effects separately in girls and boys and present effect estimates and 95% confidence intervals (CIs) within each of these strata. We also tested for evidence that effects differed by sex by including an interaction term of intervention × sex
-
We examined effects separately in thirds of the IMD34 and present effect estimates and 95% CIs within each of these three strata. We also tested for evidence that effects differed by IMD thirds by including an interaction term of intervention × IMD.
Testing the effect of the Active for Life Year 5 intervention on outcomes 1 year after the end of the intervention
In our published analysis plan, we described examining trajectories of change with time from baseline through to the immediate and the later 12-month follow-up. To do that we planned to use a multilevel model that estimates a trajectory of the three repeat measurements within each individual, with random effects quantifying the estimated person-specific deviation from the study mean in terms of the intercept (baseline measurement) and rate of change (slope between baseline and the 12-month follow-up). We planned to fit an interaction term between the intervention and time since baseline so that we could explore whether or not there were differences between the two randomised groups in the change in outcome between baseline and immediate follow-up and the change in outcome between immediate follow-up and 12-month follow-up. However, when we attempted to run these models, they did not converge. This is likely to be because there were only three measurement occasions, meaning that the model did not have sufficient degrees of freedom. Models converged when only a random effect for the intercept (not the slope) was included, but we did not feel that this was an appropriate way of modelling the data. Therefore, we conducted analyses at a single time point for the immediate follow-up (i.e. we assessed the effect of the intervention on outcomes at the 12-month follow-up) and plotted a graph showing the effect of the intervention at immediate follow-up and again (using the same analysis method) 12 months later (following 12 months with no intervention), so that we could compare effects at the two time points. We used the same ITT multilevel (to account for clustering within schools) analysis approach for the 12-month follow-up as was used for the main analyses with the outcomes assessed immediately after the intervention.
For these later follow-up analyses we focused only on main effects with primary and secondary outcomes. We did not complete secondary per-protocol, mediation or stratified (by sex and school-based deprivation) analyses. This decision was made on the basis of the large number of analyses that were undertaken for the first effectiveness analyses (immediately after intervention) and the importance of not ‘overanalysing’ data. The aim of the analyses of 12-month outcomes was to determine whether or not any immediate effects were sustained and/or any new effects emerged.
Economic evaluation
The objectives of the economic evaluation were to evaluate, through cost–consequences analyses, the difference in costs and the difference in effectiveness between the two arms of the trial. The primary analysis took a combined provider and school perspective, with a teacher perspective reported separately. The secondary analysis included a parental and NHS perspective.
Resource use collection and valuation
Intervention-related resource use was collected contemporaneously with the trial. Electronic spreadsheets were used by researchers to record how much time (in minutes) they spent performing intervention-related tasks that would be applied equally to all schools, for example the organisation of the training days (hereafter these are referred to as global tasks), and tasks that would be school specific, for example telephone calls between trial staff and the individual schools (referred to as school-specific tasks). This included time spent on organising and attending the teacher training days, organising the distribution of AFLY5 teaching and homework materials and any intervention-related time spent on telephone calls and e-mails. Additional intervention-related expenses including printing costs, trainers’ fees, supply teachers’ expenses, refreshments and venue hire were also recorded. Trial-related resource use, for example those used for data collection, was not collected.
Teachers completed a questionnaire that provided information on their direct costs, such as travel to the training day and cost of a replacement teacher while they attended training. Throughout the intervention they completed a log detailing when they delivered each lesson and homework assignment, how much time it took them to prepare for the lesson and deliver it and whether or not this was more than, the same as or less than the time they would spend on non-AFLY5 lessons. The log also asked teachers to record any extra resources, such as printing, that they had needed in order to deliver any of the lessons. In order to assess opportunity costs (i.e. the value of forgone benefit that could be obtained from a resource in its next-best alternative use) teachers were also asked to record for each lesson who had delivered it and who would normally have taught the lesson that the AFLY5 lesson had displaced, where it was felt that a lesson had been displaced.
A postal self-completed questionnaire was sent (via the schools) to the parents of the children in both intervention and control schools. The questionnaires were sent at the end of the intervention period in two rounds (March and May 2012), depending on whether the baseline for the child occurred at the end of year 4 or early in year 5. The questionnaire (see Appendix 2) related to the previous 6 months, covering approximately the second 6 months of the intervention period (1 school year ≈10.5 months). The questionnaire was designed to enable the calculation of how much parental time was spent (1) helping children with homework related to exercise, health and well-being; (2) taking children to out-of-school activities; and (3) absent from work owing to exercise-related injuries in their children. Parents were also asked about the health-care services their children may have used as a result of exercise-related injuries and to record their expenditure on out-of-school activities and food. At the beginning of the intervention, parents were given a ‘parent log’ and asked to prospectively record any trial-related resource use. The log was designed to act as an ‘aide-memoire’ to help parents complete the follow-up questionnaire and to potentially reduce the amount of recall bias. We did not collect the logs or data from them.
Resources used were valued using unit costs obtained from different relevant sources (Table 2). Administrative time used in the intervention was valued using University of Bristol salary scales. Where appropriate, intervention-related expenses were valued as the prices on submitted invoices. Primary school claims for replacement teachers were used to value attendance at the training days for the school teachers. Teachers’ time in relation to additional travel to the training meetings and in the calculation of opportunity cost were valued using the ‘School Teachers’ Review Body’ Report. 54 The UK Office for National Statistics (ONS) survey of hours and earnings55 was used to value parental time. Health service use was valued using either Curtis’ unit costs of health and social care56 or the Department of Health reference costs. 57,58 Costs were valued in 2012/13 prices.
| Resource | Unit cost (£) | Source of cost (2012/13) |
|---|---|---|
| Research staff time (£/minute) | 0.39a | University of Bristol salary scales |
| Administrative staff time (£/minute) | 0.21b | University of Bristol salary scales |
| Primary school teachers time (£/minute) | Varies | School Teachers’ Review Body: 22nd report (2013)54 |
| Teaching assistant time (£/minute) | 0.21 | Web-based resourcesc |
| Parental time (£/hour) | 15.15d | ONS 2013 survey of hours and earnings55 |
| Telephone call connection charge (£/call) | 0.15 | BT Telecommunications Group |
| Telephone call (£/minute) | 0.09 | BT Telecommunications Group |
| Printing costs | 6693.90 | University of Bristol print services |
| Other lesson materials (e.g. CDs) | 320.90 | Invoices |
| Consumables used during lesson delivery | Varies | As reported in teachers’ logs |
| Training venue hire costs | 110.00 | Invoices |
| Trainers’ fees for training days | 2165.80 | Invoices |
| Teachers’ attendance at training days | 5095.00 | Primary school claims |
| Refreshments (food and drinks) | 723.60 | Invoices |
| Other teacher-incurred training day costs | 6.50 | Invoices |
| Car mileage (£/mile) | 0.45 | University of Bristol travel reimbursement policy |
| Car park fee | 10.00 | Fees charged at local car park |
| Return fare (train) | 4.00 | First transport |
| Return fare (bus) | 1.20 | First transport |
| GP visit | 45.00 | Lesley Curtis (2013)56 |
| Practice nurse visit | 13.43 | Lesley Curtis (2013)56 |
| Physiotherapist at GP practice | 17.00 | Lesley Curtis (2013)56 |
| Minor injury unit visit | 73.14e | NHS Reference Costs 2010–1157 |
| Walk-in centre | 50.15e | NHS Reference Costs 2010–1157 |
| Accident and emergency department visit | 115.00 | NHS Reference Costs 2012–1358 |
| Physiotherapist outpatient appointment | 42.00 | NHS Reference Costs 2012–1358 |
| Fracture clinic appointment | 131.00 | NHS Reference Costs 2012–1358 |
| Other secondary care services | Varies | NHS Reference Costs 2012–1358 |
Cost–consequences analyses
A cost–consequences approach was used for the economic evaluation. This is when the differences in costs and consequences between the two arms of the trial are given in tabular form, and there is no attempt to estimate a summary score to encapsulate all the costs and benefits [for example, the incremental cost-effectiveness ratio (ICER)]. Decision-makers are left to attribute their own weights to the relative importance of these costs. This approach was chosen because of the number of primary and secondary outcomes assessed in this trial and because it is not known what society would be willing to pay for a unit decrease or increase in the outcomes, such as children’s time spent in MVPA and sedentary behaviour and consumption of fruit and vegetables, that were studied in the AFLY5 intervention. It would therefore have been difficult to produce and interpret ICERs and cost-effectiveness acceptability curves showing the probability of the intervention being cost-effective given society’s willingness to pay for a unit decrease or increase in each of the outcomes evaluated. In addition, this approach is recommended by the UK National Institute for Health and Care Excellence when undertaking public health evaluations. 59 Costs were not discounted as they occurred within a 1-year period.
Primary analysis
The analyses from the combined provider and school perspective and the separate teacher perspective assumed that costs in the control schools would be zero. This is justified on the basis that the control schools neither received teacher training nor delivered the intervention and, therefore, no costs of the intervention can be attributable to these schools. Control schools may have had pre-existing activities that were in addition to the ‘legal’ school requirements and/or introduced new activities during the study period that would have costs and potentially affect our outcomes. However, the randomisation process stratified on pre-existing activities (so these would be equal between the schools) and, as this was adequately concealed, as with all RCTs, it is reasonable to assume that there are no differences between the randomised groups other than the intervention under study. Resources used for global tasks and school-specific tasks were divided by the number of students in the intervention (n = 1064) to obtain a per-pupil amount of resource use. The costs per pupil were estimated by multiplying the units of the resource use for each category by their unit costs. Where only a cost had been given, such as for the trainers’ fee, this was divided by the number of pupils to obtain the cost per pupil. The total cost per pupil was calculated as the sum of the cost of the resource use items. Similarly, the overall cost of the intervention was calculated by summing the intervention costs within each category that had been calculated by multiplying the total resource use by its unit cost. In addition, a total cost of the intervention per school was calculated by multiplying the costs per pupil by the number of pupils in each school (for global resources) and adding this to the specific costs for each school. The opportunity cost of implementing AFLY5 in schools was calculated as the cost difference between AFLY5 and the usual lesson that would be taught in that school, with the cost for the AFLY5 lesson estimated as the time spent delivering the lesson multiplied by the salary of the teacher who taught the AFLY5 lesson; similarly, for the usual lesson but using information from the logs as to who would have taught each lesson. Delivery times were assumed to be the same for both lessons.
Secondary analysis
Resources were grouped into three categories: parental time, household expenditure on intervention-related costs and NHS resource use. Costs were estimated by multiplying the units of resource use by their respective unit costs. The total cost for each subject for each category was calculated as the sum of the costs of the resource use items. The mean resource use and cost was calculated by arm of trial.
Ordinary least squares regression, adjusted for the same baseline variables that were used in the effectiveness analyses (described above), was used to estimate the mean incremental costs of parental time, household expenditure on food and children’s out-of-school activities and NHS resource use. Additionally, the first two groups were combined to estimate the total incremental costs from a parental perspective and further adjustment for the number of household members was undertaken when estimating the costs related to the expenditure on food. Non-parametric bootstrapping was employed to obtain bias-corrected 95% CIs. 60
Missing data and sensitivity analyses
Primary analysis
There were important levels of missing data for three of the variables used in the primary analyses: car mileage, opportunity cost and other teachers’ costs to attend the training day. We assumed that these data were MAR (i.e. we assumed, by taking account of observed data, that teachers who did not provide these data did not differ from those who did). We therefore assumed that the cost per pupil calculated using data from teachers in schools who provided complete information was an appropriate average and then multiplied this by the number of pupils in the intervention arm to obtain the total resource use for each of these categories.
After making this assumption our main analyses from the combined provider and school perspective and separate teacher perspective were CCAs.
A series of sensitivity analyses were used to test the robustness of the results:61
-
Teachers’ attendance at the training days was costed on the basis of their salary and the duration of the training, rather than the expense claim made by the school for a replacement teacher.
-
The cost of hiring a venue for training was set at £110.00 for all three training days (i.e. total cost for venue hire £330.00). This was the actual cost of hiring an external venue for one of the three training days. The other two training days took place in a University of Bristol venue that was free to us. Thus, in the main analyses the actual cost of venue hire for the training was £110.00.
-
In estimating the opportunity cost of delivering the lesson, the name of the teacher delivering the usual lesson was assumed to be the same as the named teacher who delivered the AFLY5 lesson to account for the missing information in relation to this ‘usual teacher’ variable.
Secondary analysis
Only 626 (28%) parental questionnaires [278 (13%) in the intervention and 348 (16%) in the control arm] were returned. There were also large numbers of missing item responses (up to 50% for some variables). Thus, there were considerable numbers of missing data for the analyses from the parental/household and NHS perspective. Given this level of missing data, any form of analysis is potentially biased. Taking this together with the fact that these are secondary analyses, we have undertaken CCAs here using maximum numbers for each item.
Chapter 3 Results of the effect and cost–consequences of Active for Life Year 5
Results of immediate effect of the intervention
Participant numbers
Figure 1 shows the trial profile. The number of pupils in each class/school year was larger than we had anticipated and, therefore, having recruited 60 schools, the number of pupils included was greater than the required 1500. Of the 2242 potentially eligible students in the 60 participating schools, 10 left the school prior to randomisation and baseline data collection and the parents or carers of 11 pupils did not consent to their child’s participation in any aspect of the study. All other children (n = 2221; 1064 in the schools that were randomised to intervention and 1157 in the control schools), irrespective of whether or not they had all measurements recorded, were included in the trial and used as denominators for baseline comparisons between the two randomised groups.
FIGURE 1.
Trial profile. N refers to number of schools; n is the number of participants (school pupils). None of the schools withdrew from the study and so all of the randomised units are present at baseline and follow-up. The percentage given in brackets for the proportion of children with data at both baseline and follow-up is of the total number of children who were pupils in the randomised schools at baseline. Not all of the pupils with a follow-up measure necessarily have a baseline measure (or vice versa), because of different pupils being absent at both main and catch-up assessments at each time point and because of pupils leaving or moving between schools. In all analyses those who were randomised were analysed in the group (intervention or control) to which they were randomised.
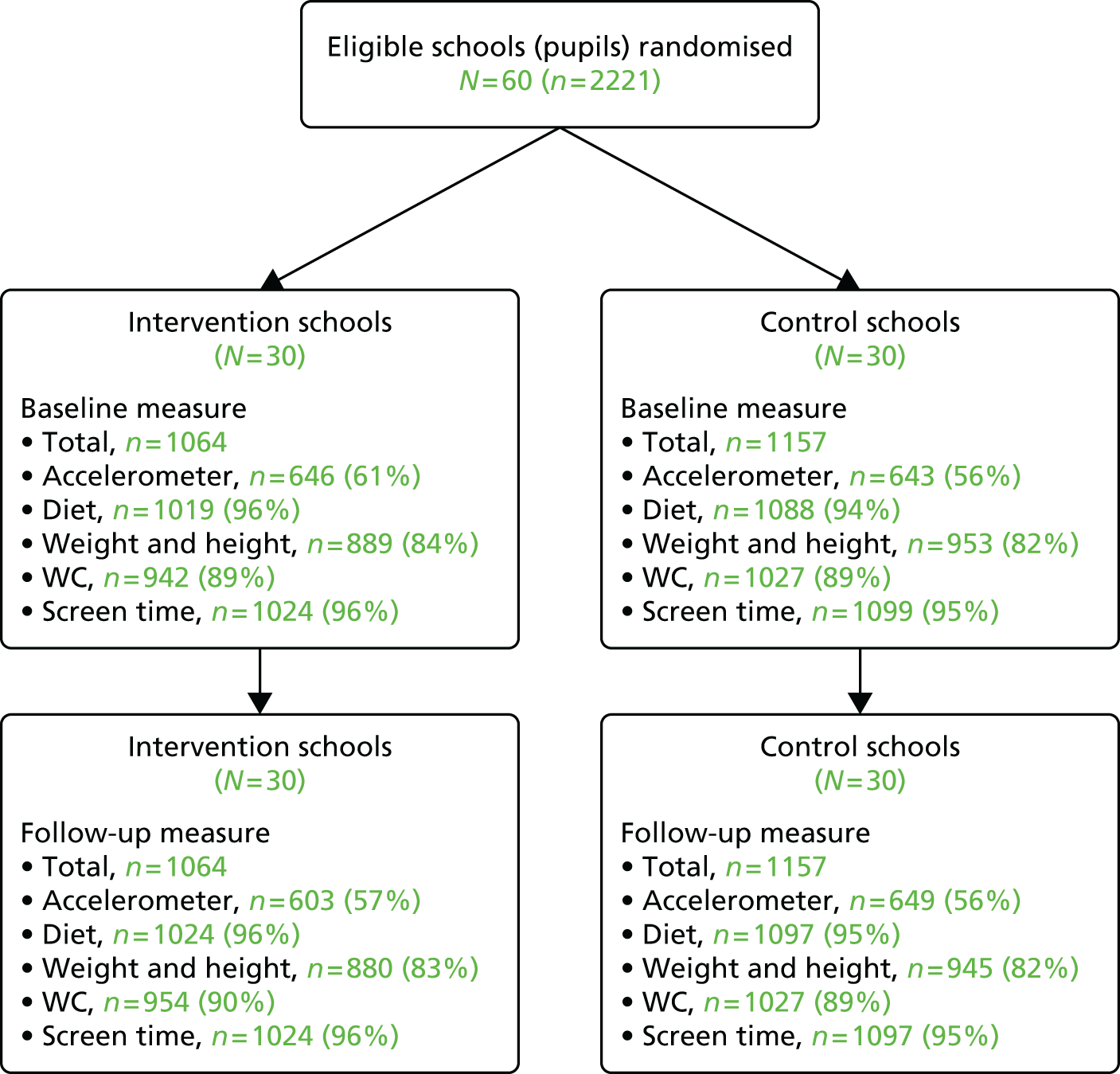
These numbers include a small number of participants (n = 65) whose parent/caregiver refused consent for one or more measurements (most commonly weight and occasionally waist). Up to two catch-up visits were made to schools to obtain data on any pupils who were absent on the day of data collection for their school, but inevitably some pupils will have been absent on the day of both the main and catch-up visits to their school at either baseline or follow-up. No child refused assent to complete the questionnaires, but in a small number of cases it was not possible to code the dietary data because we could not read what was written or identify a food from a brand name. A small number of pupils did not assent to waist or weight measurements, and the proportion of pupils with valid accelerometer data was influenced by the requirement that they had 3 days, each with at least 8 hours of valid wear time. 33 In total, at both baseline and follow-up, between 82% and 96% of participants had data on diet outcomes, BMI and WC, and approximately 60% had valid accelerometer data (see Figure 1). With the exception of valid accelerometer data the number of children included in the main analyses (1825 to 2121) was greater than the 1275 that our sample size calculations showed were required for the main analyses. For accelerometer-based measurements, data were available for 1252 children for the main analyses, 23 (0.02%) fewer than the estimated requirement. 33 Proportions with valid data for each measure were similar at both baseline and follow-up, and in intervention and control schools (see Figure 1).
Baseline characteristics
Baseline characteristics, including for accelerometer return and wear time, were similar in intervention and control schools with the exception of reported screen viewing time on Saturdays, which was 15 minutes greater per day in participants from the control schools than in the intervention schools (Table 3).
| Characteristic | Unit and type of summary measure | Intervention schools (N = 1064)a | Control schools (N = 1157)a | ||
|---|---|---|---|---|---|
| n | Distribution | n | Distribution | ||
| Age | Mean (SD) years | 1024 | 9.5 (0.3) | 1099 | 9.5 (0.3) |
| MVPAb | Mean (SD) minutes | 912 | 59 (23) | 928 | 56 (21) |
| Sedentary behaviourb | Mean (SD) minutes | 912 | 422 (72) | 928 | 416 (68) |
| Servings of fruit and vegetables | Median (IQR) number/day | 1019 | 1 (0–2) | 1088 | 1 (0–2) |
| Servings of snacks | Median (IQR) number/day | 1019 | 2 (1–3) | 1088 | 2 (1–3) |
| Servings of high-fat foods | Median (IQR) number/day | 1019 | 0 (0–1) | 1088 | 1 (0–1) |
| Servings of high-energy drinks | Median (IQR) number/day | 1019 | 2 (1–3) | 1088 | 2 (1–3) |
| BMI | Mean (SD) z-score | 889 | –0.06 (0.94) | 953 | 0.05 (1.04) |
| WC | Mean (SD) z-score | 942 | –0.03 (0.97) | 1027 | 0.03 (1.02) |
| Screen viewing on a weekday | Median (IQR) minutes | 1024 | 105 (45–240) | 1099 | 105 (45–225) |
| Screen viewing on a Saturday | Median (IQR) minutes | 1024 | 90 (30–240) | 1099 | 105 (30–240) |
| Total number of valid days of wearing accelerometerc | Median (IQR) days | 912 | 3 (2–5) | 928 | 3 (2–4) |
| Total number of valid weekdays of wearing accelerometerc | Median (IQR) days | 979 | 2 (2–3) | 1025 | 2 (1–3) |
| Total hours of wearing accelerometer on valid daysb | Mean (SD) hours/day | 912 | 11.6 (1.5) | 928 | 11.5 (1.4) |
| Hours of wearing accelerometer on valid weekdaysc | Mean (SD) hours/day | 896 | 11.8 (1.6) | 919 | 11.7 (1.5) |
| Categorical variables | |||||
| Sex | n (%) female | 520 | 49% | 608 | 52% |
| n (%) male | 544 | 51% | 549 | 48% | |
| General overweight/obesity | n (%) no | 717 | 81% | 743 | 78% |
| n (%) yes | 172 | 19% | 210 | 22% | |
| Central overweight/obesity | n (%) no | 601 | 64% | 631 | 61% |
| n (%) yes | 341 | 36% | 396 | 39% | |
| Returned accelerometer | n (%) no | 85 | 8% | 132 | 11% |
| n (%) yes | 979 | 92% | 1025 | 89% | |
| Wore accelerometer for requested amount of time | n (%) no | 820 | 77% | 953 | 82% |
| n (%) yes | 244 | 23% | 204 | 18% | |
| Wore accelerometer for required amount of time | n (%) no | 418 | 39% | 514 | 44% |
| n (%) yes | 646 | 61% | 643 | 56% | |
| School involved in other health-promoting activities | n (%) no | 264 | 25% | 446 | 39% |
| n (%) yes | 800 | 75% | 711 | 61% | |
| School deprivation score | n (%) low | 315 | 30% | 460 | 40% |
| n (%) medium | 368 | 35% | 345 | 30% | |
| n (%) high | 381 | 36% | 352 | 30% | |
Main intention-to-treat analyses
In the main ITT analysis with adjustment for baseline variables, none of the three primary outcomes differed between children in schools allocated to the AFLY5 intervention and those allocated to control schools (Table 4). The intervention was effective on three out of nine of the secondary outcomes after taking account of multiple testing in these analyses: pupils’ self-reported time spent on screen viewing at the weekend (Saturday) and self-reported consumption of snacks and of high-energy drinks were lower in intervention schools than in control schools (see Table 4). There was no strong evidence that the intervention affected the other secondary outcomes in these analyses, especially after taking into account multiple testing.
| Outcome (primary/secondary) | Control group (reference group) | Intervention group | Main comparison between the two groups (intervention vs. control) | ||||
|---|---|---|---|---|---|---|---|
| n a | Mean (SD) or number (%) | n a | Mean (SD) or number (%) | n a | Difference in means or odds ratio (95% CI) | p-value | |
| Continuous outcomes (differences in means) | |||||||
| Time spent in MVPA (minutes per day) | 649 | 56.65 (23.42) | 603 | 55.25 (22.33) | 1252 | –1.35 (–5.29 to 2.59) | 0.50 |
| Time spent in sedentary behaviour (minutes per day) | 649 | 451.84 (65.40) | 603 | 454.08 (66.78) | 1252 | –0.11 (–9.71 to 9.49) | 0.98 |
| Servings of fruit and vegetables (number per day) | 1097 | 1.81 (1.55) | 1024 | 1.89 (1.70) | 2121 | 0.08 (–0.12 to 0.28) | 0.42 |
| Time spent screen viewing (minutes per day, weekday) | 1097 | 145.45 (133.95) | 1024 | 132.52 (125.37) | 2121 | –15.56 (–33.56 to 2.45) | 0.09 |
| Time spent screen viewing (minutes per day, Saturday) | 1097 | 175.64 (171.79) | 1024 | 155.33 (154.43) | 2121 | –20.86 (–37.30 to –4.42) | 0.01 |
| BMI (z-score)b | 945 | 0.05 (1.03) | 880 | –0.05 (0.95) | 1825 | –0.02 (–0.08 to 0.03) | 0.41 |
| WC (z-score)b | 1027 | 0.08 (1.04) | 954 | –0.08 (0.94) | 1981 | –0.12 (–0.23 to –0.01) | 0.03 |
| Servings of snacks (number per day) | 1097 | 2.46 (1.59) | 1024 | 2.24 (1.49) | 2121 | –0.22 (–0.38 to –0.05) | 0.01 |
| Servings of high-fat foods (number per day) | 1097 | 0.88 (0.96) | 1024 | 0.79 (0.97) | 2121 | –0.10 (–0.24 to 0.03) | 0.13 |
| Servings of high-energy drinks (number per day) | 1097 | 2.45 (1.61) | 1024 | 2.21 (1.44) | 2121 | –0.26 (–0.43 to –0.10) | 0.002 |
| Binary outcomes (odds ratios) | |||||||
| Generally overweight/obese | 945 | 198 (20.95%) | 880 | 166 (18.86%) | 1825 | 0.89 (0.61 to 1.31) | 0.56 |
| Centrally overweight/obese | 1027 | 510 (49.66%) | 954 | 416 (43.61%) | 1981 | 0.72 (0.50 to 1.04) | 0.08 |
Per-protocol analyses
Table 5 shows the results of the per-protocol analyses for primary and secondary outcomes. In these analyses children from 16 classes in 12 out of the 30 intervention schools were excluded because their teacher had delivered fewer than 70% of the lessons. The results of the per-protocol analyses were broadly consistent with the ITT analyses results, with no evidence of effect on the three primary outcomes or most of the secondary outcomes. As with the ITT analyses, there was evidence of beneficial effect on self-reported screen viewing on Saturdays and consumption of high-energy drinks. The point estimate for the reduction in self-reported consumption of snacks was similar to that seen in the ITT analysis but the strength of evidence was marginal, particularly after multiple testing was taken into account.
| Outcome (primary/secondary) | Control group (reference group) | Intervention group | Main comparison between the two groups (intervention vs. control) | ||||
|---|---|---|---|---|---|---|---|
| n a | Mean (SD) or number (%) | n a | Mean (SD) or number (%) | n a | Difference in means or odds ratio (95% CI) | p-value | |
| Continuous outcomes (differences in means) | |||||||
| Time spent in MVPA (minutes per day) | 649 | 56.65 (23.42) | 424 | 54.39 (21.55) | 1073 | –2.12 (–6.70 to 2.47) | 0.37 |
| Time spent in sedentary behaviour (minutes per day) | 649 | 451.84 (65.40) | 424 | 453.68 (67.42) | 1073 | 0.44 (–10.32 to 11.21) | 0.94 |
| Servings of fruit and vegetables (number per day) | 1097 | 1.81 (1.55) | 722 | 1.99 (1.77) | 1819 | 0.18 (–0.05 to 0.41) | 0.12 |
| Time spent screen viewing (minutes per day, weekday) | 1097 | 145.45 (133.95) | 722 | 124.20 (118.88) | 1819 | –19.11 (–39.59 to 1.37) | 0.07 |
| Time spent screen viewing (minutes per day, Saturday) | 1097 | 175.64 (171.79) | 722 | 146.99 (147.15) | 1819 | –24.61 (–42.06 to –7.17) | 0.006 |
| BMI (z-score)b | 945 | 0.05 (1.03) | 613 | –0.05 (0.96) | 1558 | –0.01 (–0.07 to 0.05) | 0.82 |
| WC (z-score)b | 1027 | 0.08 (1.04) | 665 | –0.06 (0.94) | 1692 | –0.09 (–0.21 to 0.04) | 0.17 |
| Servings of snacks (number per day) | 1097 | 2.46 (1.59) | 722 | 2.29 (1.54) | 1819 | –0.18 (–0.38 to 0.02) | 0.07 |
| Servings of high-fat foods (number per day) | 1097 | 0.88 (0.96) | 722 | 0.86 (0.99) | 1819 | –0.04 (–0.19 to 0.11) | 0.62 |
| Servings of high-energy drinks (number per day) | 1097 | 2.45 (1.61) | 722 | 2.18 (1.44) | 1819 | –0.29 (–0.48 to –0.09) | 0.005 |
| Binary outcomes (odds ratios) | |||||||
| Generally overweight/obese | 945 | 198 (20.95%) | 613 | 111 (18.11%) | 1558 | 0.96 (0.62 to 1.48) | 0.84 |
| Centrally overweight/obese | 1027 | 510 (49.66%) | 665 | 295 (44.36%) | 1692 | 0.87 (0.58 to 1.32) | 0.52 |
Sensitivity analyses
The sensitivity analyses that we undertook to explore assumptions about missing data produced results that were consistent with the main analyses (Tables 6–9). When we looked separately at time spent in MVPA and time spent in sedentary behaviour by weekday and weekend, the results were consistent with each other and with the main results (both values for the difference between the two estimates p > 0.2; Table 10).
| Outcome (primary/secondary) | Main comparison between the two groups (intervention vs. control) | ||
|---|---|---|---|
| n a | Difference in means or odds ratio (95% CI) | p-value | |
| Continuous outcomes (differences in means) | |||
| Time spent in MVPA (minutes per day) | 1200 | –1.56 (–5.42 to 2.30) | 0.43 |
| Time spent in sedentary behaviour (minutes per day) | 1200 | –0.25 (–10.12 to 9.63) | 0.96 |
| Servings of fruit and vegetables (number per day) | 2025 | 0.11 (–0.09 to 0.30) | 0.27 |
| Time spent screen viewing (minutes per day, weekday) | 2038 | –15.53 (–33.28 to 2.22) | 0.09 |
| Time spent screen viewing (minutes per day, Saturday) | 2038 | –21.92 (–38.26 to –5.57) | 0.009 |
| BMI (z-score)b | 1640 | –0.03 (–0.07 to 0.02) | 0.23 |
| WC (z-score)b | 1816 | –0.11 (–0.22 to –0.01) | 0.03 |
| Servings of snacks (number per day) | 2025 | –0.21 (–0.37 to –0.05) | 0.01 |
| Servings of high-fat foods (number per day) | 2025 | –0.10 (–0.24 to 0.03) | 0.13 |
| Servings of high-energy drinks (number per day) | 2025 | –0.26 (–0.42 to –0.09) | 0.003 |
| Binary outcomes (odds ratios) | |||
| Generally overweight/obese | 1640 | 0.80 (0.49 to 1.30) | 0.37 |
| Centrally overweight/obese | 1816 | 0.68 (0.46 to 1.01) | 0.05 |
| Outcome | Main comparison between the two groups (intervention vs. control) | ||
|---|---|---|---|
| n a | Difference in means or odds ratio (95% CI) | p-value | |
| Continuous outcomes (differences in means) | |||
| Time spent in MVPA (minutes per day) | 901 | –2.98 (–7.56 to 1.61) | 0.20 |
| Time spent in sedentary behaviour (minutes per day) | 901 | 0.28 (–10.29 to 10.85) | 0.96 |
| Servings of fruit and vegetables (number per day) | 901 | 0.04 (–0.20 to 0.28) | 0.77 |
| Time spent screen viewing (minutes per day, weekday) | 901 | –7.51 (–26.40 to 11.39) | 0.44 |
| Time spent screen viewing (minutes per day, Saturday) | 901 | –21.61 (–46.75 to 3.54) | 0.09 |
| BMI (z-score)b | 809 | 0.01 (–0.06 to 0.08) | 0.83 |
| WC (z-score)b | 863 | –0.06 (–0.18 to 0.05) | 0.30 |
| Servings of snacks (number per day) | 901 | –0.17 (–0.38 to 0.04) | 0.11 |
| Servings of high-fat foods (number per day) | 901 | –0.19 (–0.36 to –0.02) | 0.03 |
| Servings of high-energy drinks (number per day) | 901 | –0.22 (–0.43 to –0.02) | 0.04 |
| Binary outcomes (odds ratios) | |||
| Generally overweight/obese | 809 | 0.84 (0.44 to 1.60) | 0.60 |
| Centrally overweight/obese | 863 | 0.87 (0.51 to 1.46) | 0.59 |
| Outcome | Main comparison between the two groups (intervention vs. control) | ||
|---|---|---|---|
| n a | Difference in means or odds ratio (95% CI) | p-value | |
| Continuous outcomes (differences in means) | |||
| Time spent in MVPA (minutes per day) | 2221 | –1.25 (–4.67 to 2.18) | 0.48 |
| Time spent in sedentary behaviour (minutes per day) | 2221 | –0.11 (–9.27 to 9.05) | 0.98 |
| Servings of fruit and vegetables (number per day) | 2221 | 0.08 (–0.12 to 0.28) | 0.42 |
| Time spent screen viewing (minutes per day, weekday) | 2221 | –15.56 (–33.56 to 2.45) | 0.09 |
| Time spent screen viewing (minutes per day, Saturday) | 2221 | –20.86 (–37.30 to –4.42) | 0.01 |
| BMI (z-score}b | 2221 | –0.01 (–0.06 to 0.04) | 0.61 |
| WC (z-score)b | 2221 | –0.11 (–0.22 to –0.01) | 0.03 |
| Servings of snacks (number per day) | 2221 | –0.22 (–0.38 to –0.05) | 0.01 |
| Servings of high-fat foods (number per day) | 2221 | –0.10 (–0.24 to 0.03) | 0.13 |
| Servings of high-energy drinks (number per day) | 2221 | –0.26 (–0.43 to –0.10) | 0.002 |
| Binary outcomes (odds ratios) | |||
| Generally overweight/obese | 2221 | 0.99 (0.75 to 1.31) | 0.94 |
| Centrally overweight/obese | 2221 | 0.72 (0.50 to 1.04) | 0.08 |
| Outcome | Main comparison between the two groups (intervention vs. control) | ||
|---|---|---|---|
| n a | Difference in means or odds ratio (95% CI) | p-value | |
| Continuous outcomes (differences in means) | |||
| Time spent in MVPA (minutes per day) | 2221 | –1.01 (–4.52 to 2.51) | 0.58 |
| Time spent in sedentary behaviour (minutes per day) | 2221 | –1.83 (–10.18 to 6.52) | 0.67 |
| Servings of fruit and vegetables (number per day) | 2221 | 0.08 (–0.12 to 0.28) | 0.42 |
| Time spent screen viewing (minutes per day, weekday) | 2221 | –15.56 (–33.56 to 2.45) | 0.09 |
| Time spent screen viewing (minutes per day, Saturday) | 2221 | –20.86 (–37.30 to –4.42) | 0.01 |
| BMI (z-score)b | 2221 | –0.01 (–0.06 to 0.04) | 0.61 |
| WC (z-score)b | 2221 | –0.11 (–0.22 to –0.01) | 0.03 |
| Servings of snacks (number per day) | 2221 | –0.22 (–0.38 to –0.05) | 0.01 |
| Servings of high-fat foods (number per day) | 2221 | –0.10 (–0.24 to 0.03) | 0.13 |
| Servings of high-energy drinks (number per day) | 2221 | –0.26 (–0.43 to –0.10) | 0.002 |
| Binary outcomes (odds ratios) | |||
| Generally overweight/obese | 2221 | 0.99 (0.75 to 1.31) | 0.94 |
| Centrally overweight/obese | 2221 | 0.72 (0.50 to 1.04) | 0.08 |
| Outcome | Main comparison between the two groups (intervention vs. control) on week days | Main comparison between the two groups (intervention vs. control) on weekend days | ||||
|---|---|---|---|---|---|---|
| n a | Difference in means or odds ratio (95% CI) | p-value | n a | Difference in means or odds ratio (95% CI) | p-value | |
| Time spent in MVPA (minutes per day) | 1252 | –1.28 (–6.16 to 3.61) | 0.61 | 1053 | 0.28 (–3.73 to 4.29) | 0.89 |
| Time spent in sedentary behaviour (minutes per day) | 1252 | 2.04 (–9.51 to 13.58) | 0.73 | 1053 | –6.11 (–18.73 to 6.51) | 0.34 |
Analyses stratified by sex and school area level of deprivation
Table 11 shows the results presented separately for girls and boys. The effect estimates for the accelerometer-measured primary outcomes looked different in girls and boys, with the effect of the intervention on time spent in MVPA being very close to the null in girls but decreased (opposite to the effect expected) in boys and on time spent in sedentary behaviour decreased in girls but increased in boys (again the opposite of what we expected). However, as noted in the section Testing differences of effect by sex and by area deprivation, these stratified analyses are exploratory and we did not design the study with an aim (or sufficient numbers of participants) to be able to detect sex differences. Furthermore, there was no strong statistical evidence that these effects did differ by sex (both pinteraction = 0.4). For all other outcomes, with the exception of consumption of snacks, the effects were broadly similar in girls and boys. The intervention appeared to have a stronger effect on reducing the consumption of snacks in girls than in boys, with statistical evidence that this difference was unlikely to be caused by chance (pinteraction = 0.006).
| Outcome | Effects in girls | Effects in boys | p interaction b | ||
|---|---|---|---|---|---|
| n a | Difference in means or odds ratio (95% CI) | n a | Difference in means or odds ratio (95% CI) | ||
| Continuous outcomes (differences in means) | |||||
| Time spent in MVPA (minutes per day) | 971 | 0.05 (–3.88 to 3.98) | 857 | –1.69 (–6.34 to 2.97) | 0.4 |
| Time spent in sedentary behaviour (minutes per day) | 971 | –1.97 (–14.66 to 10.73) | 857 | 1.61 (–10.16 to 13.37) | 0.4 |
| Servings of fruit and vegetables (number per day) | 1077 | 0.11 (–0.12 to 0.35) | 1044 | 0.07 (–0.17 to 0.32) | 0.6 |
| Time spent screen viewing (minutes per day, weekday) | 1077 | –12.42 (–27.48 to 2.64) | 1044 | –15.00 (–42.71 to 12.72) | 0.8 |
| Time spent screen viewing (minutes per day, Saturday) | 1077 | –23.24 (–40.40 to –6.07) | 1044 | –16.75 (–41.58 to 8.09) | 0.6 |
| BMI (z-score)c | 915 | –0.01 (–0.08 to 0.06) | 910 | –0.04 (–0.10 to 0.03) | 0.7 |
| WC (z-score)c | 999 | –0.14 (–0.26 to –0.02) | 982 | –0.09 (–0.21 to 0.02) | 0.7 |
| Servings of snacks (number per day) | 1077 | –0.37 (–0.58 to –0.15) | 1044 | –0.05 (–0.27 to 0.17) | 0.006 |
| Servings of high-fat foods (number per day) | 1077 | –0.11 (–0.26 to 0.05) | 1044 | –0.09 (–0.25 to 0.07) | 0.9 |
| Servings of high-energy drinks (number per day) | 1077 | –0.34 (–0.54 to –0.14) | 1044 | –0.17 (–0.39 to 0.04) | 0.1 |
| Binary outcomes (odds ratios) | |||||
| Generally overweight/obese | 915 | 0.91 (0.52 to 1.59) | 910 | 0.80 (0.47 to 1.38) | 0.9 |
| Centrally overweight/obese | 999 | 0.79 (0.51 to 1.21) | 982 | 0.67 (0.42 to 1.06) | 0.6 |
Table 12 shows the results according to school area level of deprivation (divided into thirds). For some outcomes, point estimates did seem to suggest that the intervention had different effects within thirds of school area deprivation, but there was no consistency across the thirds for differences in most outcomes (that is no monotonic difference with each category increase in deprivation) and no statistical support for differences by the IMD. 34 The two possible exceptions were time spent in sedentary behaviour assessed by accelerometer and self-reported screen viewing on weekdays. For time spent in sedentary behaviour assessed by accelerometer the intervention appeared to result in greater time spent in sedentary behaviour (opposite to what was expected) in pupils from schools in the middle deprivation third, with some statistical support for this being different from that seen in the lowest third, but the effect was similar in the two extremes (lowest and highest thirds of deprivation). For self-reported screen viewing on weekdays there did appear to be a monotonic increase in effect (reduced time spent screen viewing) as deprivation category increased, but there was no statistical support for differences between categories and this pattern was not seen for reported screen viewing at weekends.
| Outcome | Lowest third deprivation score | Middle third deprivation score | Highest third deprivation score | p comparing middle third with lowest third | p comparing highest third lowest third | |||
|---|---|---|---|---|---|---|---|---|
| n a | Difference in means or odds ratio (95% CI) | n a | Difference in means or odds ratio (95% CI) | n a | Difference in means or odds ratio (95% CI) | |||
| Time spent in MVPA (minutes per day) | 654 | 1.23 (–5.20 to 7.66) | 602 | –1.50 (–6.84 to 3.84) | 572 | –3.00 (–10.63 to 4.63) | 0.7 | 0.5 |
| Time spent in sedentary behaviour (minutes per day) | 654 | –9.06 (–28.92 to 10.79) | 602 | 13.86 (–0.04 to 27.76) | 572 | –6.91 (–20.39 to 6.58) | 0.05 | 0.8 |
| Servings of fruit and vegetables (number per day) | 741 | 0.09 (–0.43 to 0.60) | 689 | 0.18 (–0.04 to 0.40) | 691 | 0.09 (–0.16 to 0.34) | 0.9 | 0.9 |
| Time spent screen viewing (minutes per day, weekday) | 741 | –1.63 (–36.39 to 33.13) | 689 | –19.20 (–41.07 to 2.68) | 691 | –27.01 (–58.33 to 4.30) | 0.4 | 0.5 |
| Time spent screen viewing (minutes per day, Saturday) | 741 | –33.35 (–56.36 to –10.33) | 689 | –8.26 (–32.26 to 15.73) | 691 | –25.08 (–59.32 to 9.16) | 0.3 | 0.3 |
| BMI (z-score)b | 638 | –0.04 (–0.14 to 0.06) | 593 | –0.01 (–0.11 to 0.09) | 594 | –0.02 (–0.11 to 0.08) | 0.9 | 0.5 |
| WC (z-score)b | 692 | –0.14 (–0.31 to 0.04) | 646 | –0.08 (–0.22 to 0.05) | 643 | –0.14 (–0.36 to 0.07) | 0.7 | 0.9 |
| Servings of snacks (number per day) | 741 | –0.03 (–0.25 to 0.20) | 689 | –0.19 (–0.47 to 0.10) | 691 | –0.45 (–0.74 to –0.16) | 0.9 | 0.2 |
| Servings of high-fat foods (number per day) | 741 | –0.14 (–0.38 to 0.10) | 689 | –0.15 (–0.37 to 0.07) | 691 | –0.05 (–0.28 to 0.19) | 0.9 | 0.7 |
| Servings of high-energy drinks (number per day) | 741 | –0.25 (–0.59 to 0.09) | 689 | –0.13 (–0.39 to 0.14) | 691 | –0.41 (–0.62 to –0.20) | 0.3 | 0.7 |
| Generally overweight/obese | 638 | 0.70 (0.35 to 1.39) | 593 | 1.01 (0.51 to 2.02) | 594 | 1.09 (0.55 to 2.19) | 0.5 | 0.5 |
| Centrally overweight/obese | 692 | 0.55 (0.30 to 1.02) | 646 | 0.88 (0.53 to 1.47) | 643 | 0.78 (0.36 to 1.67) | 0.5 | 0.7 |
Results of mediation analyses
As with the main effect analyses, a total of 2221 children (1064 in the schools that were randomised to intervention and 1157 in the control schools) were potentially included in some of the mediation analyses (see Figure 1). No child refused assent to complete the questionnaires; thus, we have baseline data for each mediator for over 87% of participants and follow-up data for each mediator for over 92%. The proportions with data for each measure were similar at both baseline and follow-up and in intervention and control schools.
Baseline characteristics, including mean values for each of the mediator variables, were similar among pupils randomised to intervention schools and those randomised to control schools (Table 13).
| Characteristic | Intervention schools (N = 1064) | Control schools (N = 1157) | ||
|---|---|---|---|---|
| Number | Mean (SD) or n (%) | Number | Mean (SD) or n (%) | |
| Physical activity self-efficacy | 1017 | 96.0 (15.3) | 1085 | 95.3 (16.0) |
| Fruit and vegetable self-efficacy | 1016 | 87.5 (15.4) | 1079 | 85.7 (17.7) |
| Perceived maternal logistic support for physical activity | 989 | 9.2 (2.4) | 1065 | 9.1 (2.4) |
| Perceived paternal logistic support for physical activity | 931 | 9.0 (2.4) | 1002 | 8.8 (2.6) |
| Perceived maternal modelling of physical activity | 991 | 14.3 (3.8) | 1069 | 14.3 (4.1) |
| Perceived paternal modelling of physical activity | 934 | 15.2 (3.7) | 1010 | 15.0 (3.9) |
| Perceived maternal limitation of sedentary behaviour | 989 | 11.3 (3.5) | 1067 | 11.0 (3.6) |
| Perceived paternal limitation of sedentary behaviour | 930 | 10.8 (3.5) | 1003 | 10.4 (3.6) |
| Perceived parental modelling of fruit and vegetable consumption | 1013 | 33.5 (8.0) | 1078 | 33.0 (8.5) |
Mediation effects on outcomes
Following the intervention, there was evidence that 3 of the 10 potential mediators (fruit and vegetable self-efficacy, maternal limitation of sedentary behaviour and knowledge) were higher in the intervention group than in the control group (Table 14).
| Outcome | Control group (reference group) | Intervention group | Main effect (group difference) | ||||
|---|---|---|---|---|---|---|---|
| n a | Mean (SD) | Number | Mean (SD) | n a | Difference in means (95% CI) | p-value | |
| Physical activity self-efficacy | 1092 | 97.4 (12.2) | 1022 | 97.4 (13.8) | 2114 | –0.2 (–1.4 to 1.0) | 0.74 |
| Fruit and vegetable self-efficacy | 1093 | 87.2 (15.8) | 1020 | 89.7 (14.4) | 2113 | 2.2 (0.7 to 3.8) | 0.005 |
| Perceived maternal logistic support for physical activity | 1077 | 9.5 (2.2) | 1006 | 9.5 (2.3) | 2083 | –0.1 (–0.3 to 0.1) | 0.56 |
| Perceived paternal logistic support for physical activity | 1033 | 9.0 (2.4) | 977 | 9.2 (2.4) | 2010 | 0.1 (–0.1 to 0.3) | 0.45 |
| Perceived maternal modelling of physical activity | 1079 | 14.8 (3.6) | 1006 | 14.8 (3.7) | 2085 | 0.1 (–0.2 to 0.3) | 0.71 |
| Perceived paternal modelling of physical activity | 1033 | 15.3 (3.6) | 975 | 15.5 (3.7) | 2008 | 0.1 (–0.2 to 0.5) | 0.48 |
| Perceived maternal limitation of sedentary behaviour | 1078 | 11.3 (3.5) | 1006 | 11.8 (3.4) | 2084 | 0.5 (0.1 to 0.8) | 0.01 |
| Perceived paternal limitation of sedentary behaviour | 1031 | 10.6 (3.5) | 977 | 10.9 (3.5) | 2008 | 0.4 (–0.1 to 0.8) | 0.09 |
| Perceived parental modelling of fruit and vegetableconsumption | 1089 | 33.9 (7.8) | 1017 | 34.4 (7.9) | 2106 | 0.7 (–0.3 to 1.6) | 0.17 |
| Knowledge | 1092 | 7.1 (1.4) | 1021 | 7.5 (1.5) | 2113 | 0.5 (0.2 to 0.7) | < 0.001 |
Table 15 shows the main effect of the intervention on the three secondary outcomes found to be affected by the intervention, both before and after adjustment for potential mediators. Adjustment for maternal limitation of sedentary behaviour and child knowledge attenuated the effect of the intervention on time spent screen viewing at the weekend by 22%. There was no notable change in the effect of the intervention on consumption of snacks or high-energy drinks following adjustment for mediators.
| Outcome | Main effect of the intervention on the outcomes (group difference)a | Main effect (group difference) of the intervention on the outcomes after adjusting for relevant potential mediators | Reduction in association (%) | ||||
|---|---|---|---|---|---|---|---|
| n b | Difference in means (95% CI) | p-value | n b | Difference in means (95% CI) | p-value | ||
| Time spent screen viewing (minutes/day, Saturday) | 2121 | –20.86 (–37.3 to –4.42) | 0.01 | 2083 | –16.26c (–33.26 to 0.74) | 0.06 | 22.05 |
| Servings of snacks (number/day) | 2121 | –0.22 (–0.38 to –0.05) | 0.01 | 2112 | –0.20d (–0.37 to –0.04) | 0.02 | 9.1 |
| Servings of high-energy drinks (number/day) | 2121 | –0.26 (–0.43 to –0.1) | 0.002 | 2112 | –0.26d (–0.43 to –0.09) | < 0.001 | 0 |
Effect of the Active for Life Year 5 intervention on outcomes at 12-month follow-up
Figure 2 shows the trial profile with numbers followed up at 12 months. Figures are broadly similar to those shown in Figure 1 for the analyses immediately after intervention, showing high levels of retention of study participants.
FIGURE 2.
The 12-month follow-up profile. N, number of schools; n, number of participants (school pupils).

None of the schools withdrew from the study and so all of the randomised units are present at baseline and follow-up. The percentages given in brackets in Figure 2 are based on the total number of children who were pupils in the randomised schools at baseline. Not all of the pupils with a follow-up measure necessarily have a baseline measure (or vice versa), because of different pupils being absent at both main and catch-up assessments at each time point and because of pupils leaving or moving between schools. In all analyses, those who were randomised were analysed in the group (intervention or control) to which they were randomised.
Figures 3 and 4 show differences in means between the control and intervention group, for the three primary (see Figure 3) and nine secondary outcomes (see Figure 4), at baseline, immediate follow-up and 12-month follow-up. These show that mean differences (and odds ratios for general and central overweight/obesity) between children in intervention and control schools were essentially the same at the 12-month follow-up as they were immediately after the intervention.
FIGURE 3.
Difference in means between the control and intervention groups for the three primary outcomes at baseline, immediate follow-up and 12 months post intervention. (a) Difference in mean time spent in MVPA; (b) difference in mean time spent sedentary; and (c) difference in mean number of servings of fruit and vegetables.
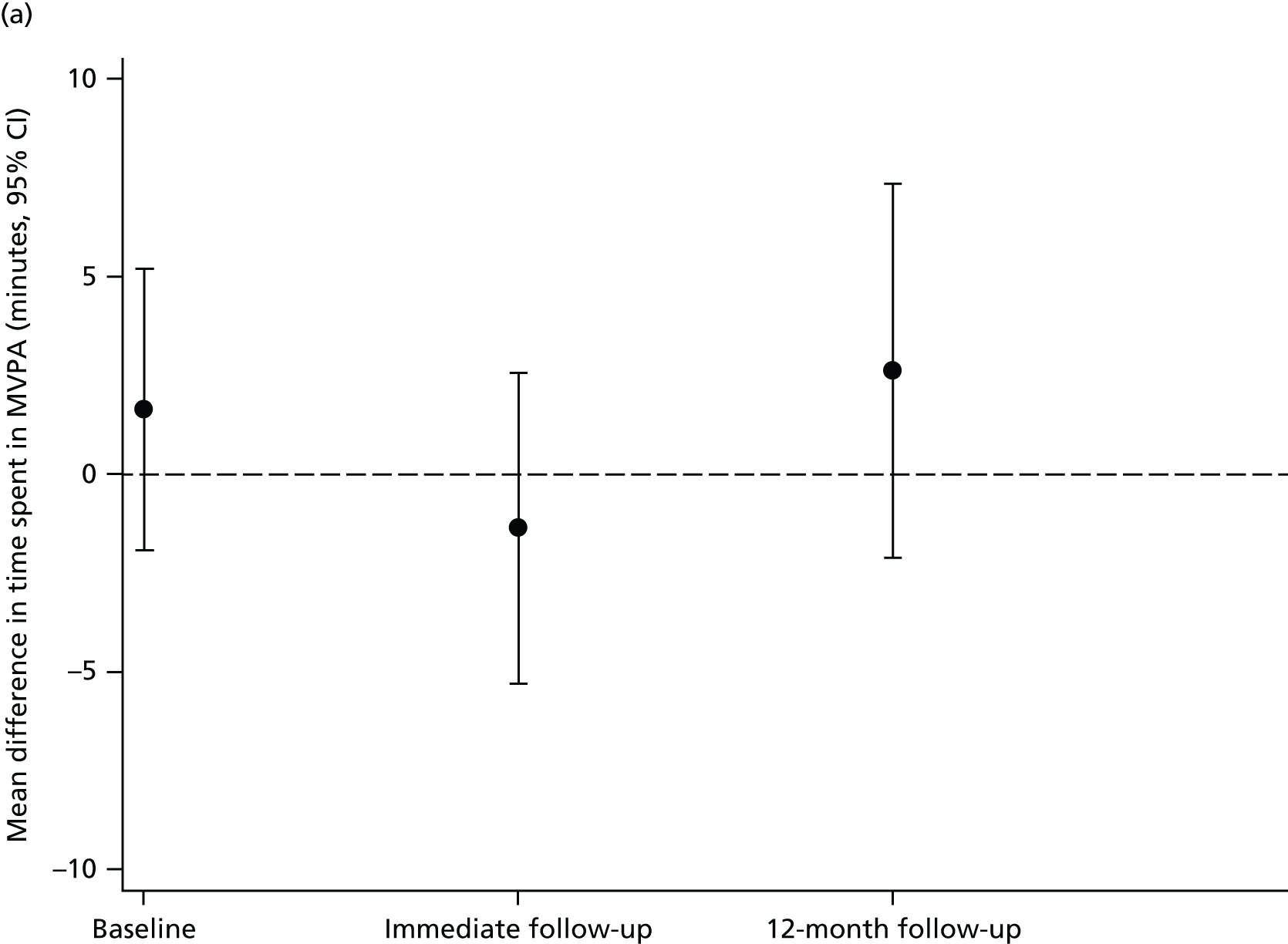
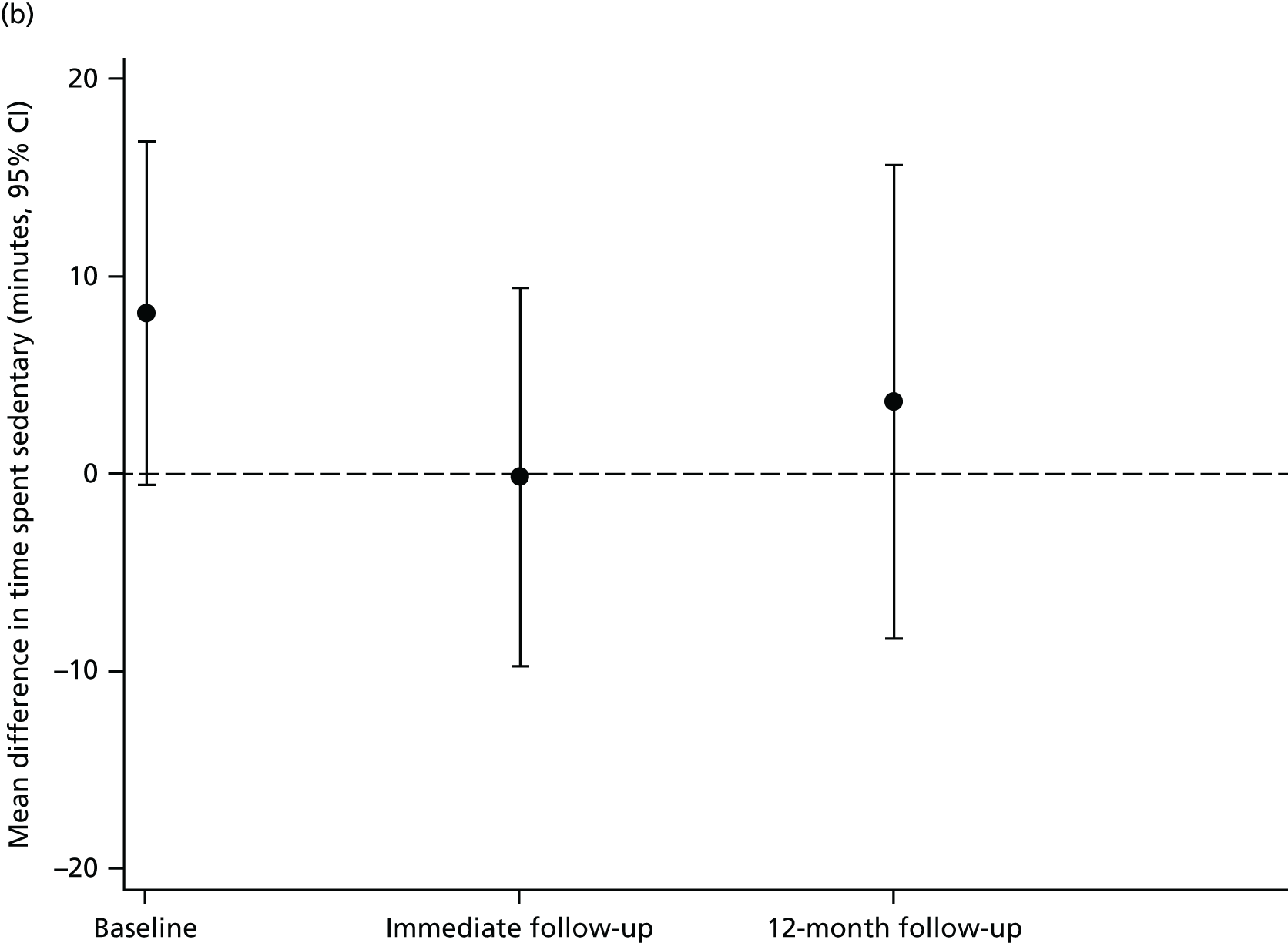
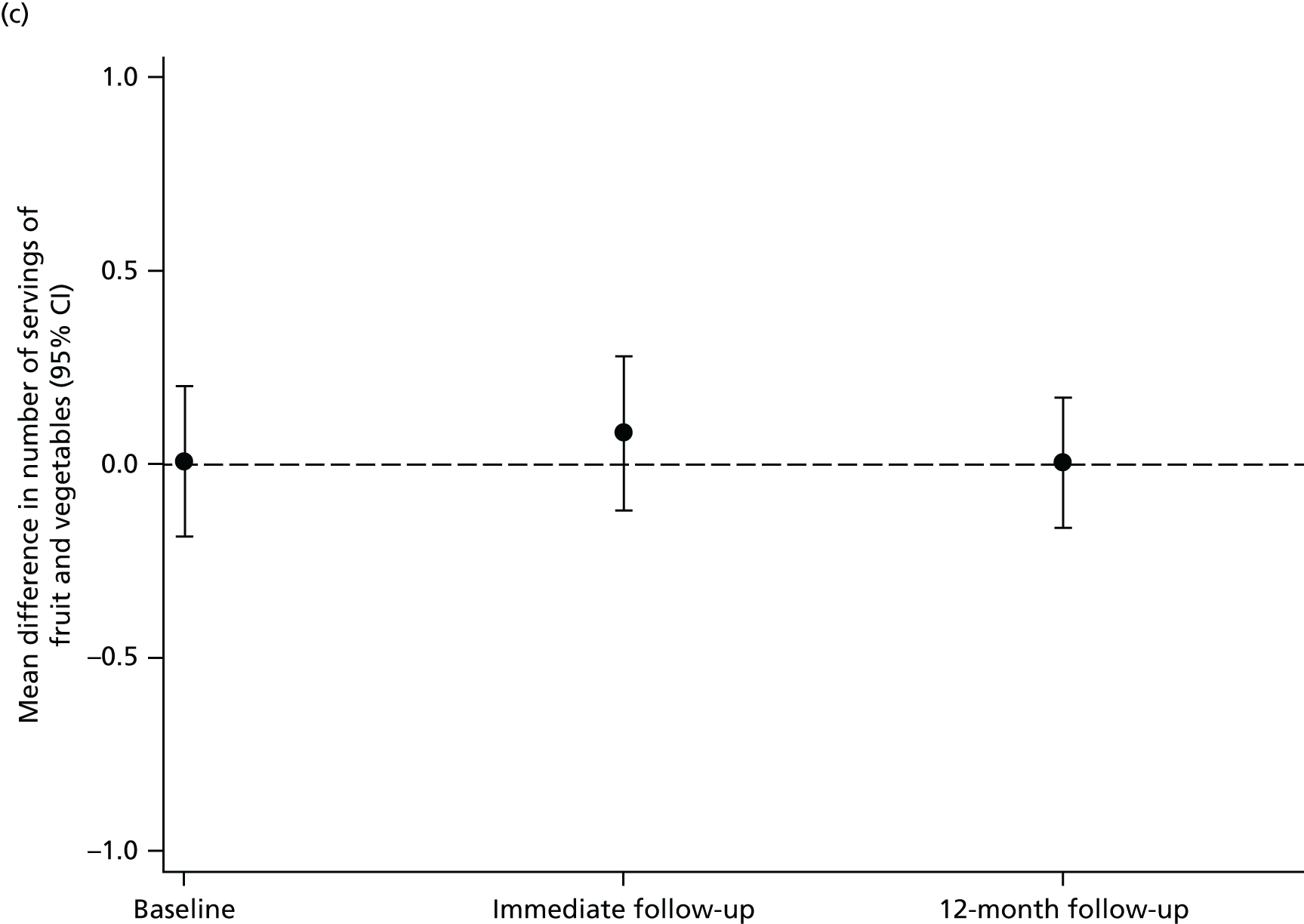
FIGURE 4.
Difference in means between the control and intervention groups for the nine secondary outcomes at baseline, immediate follow-up and 12 months post intervention. (a) Difference in mean weekday screen viewing time; (b) difference in mean Saturday screen viewing time; (c) difference in mean BMI z-score; (d) difference in mean WC z-score; (e) difference in mean number of servings of snacks; (f) difference in mean number of servings of high-fat food; (g) difference in mean number of servings of high-energy drinks; (h) difference in mean odds ratio for being overweight; and (i) difference in mean odds ratio for being centrally overweight.
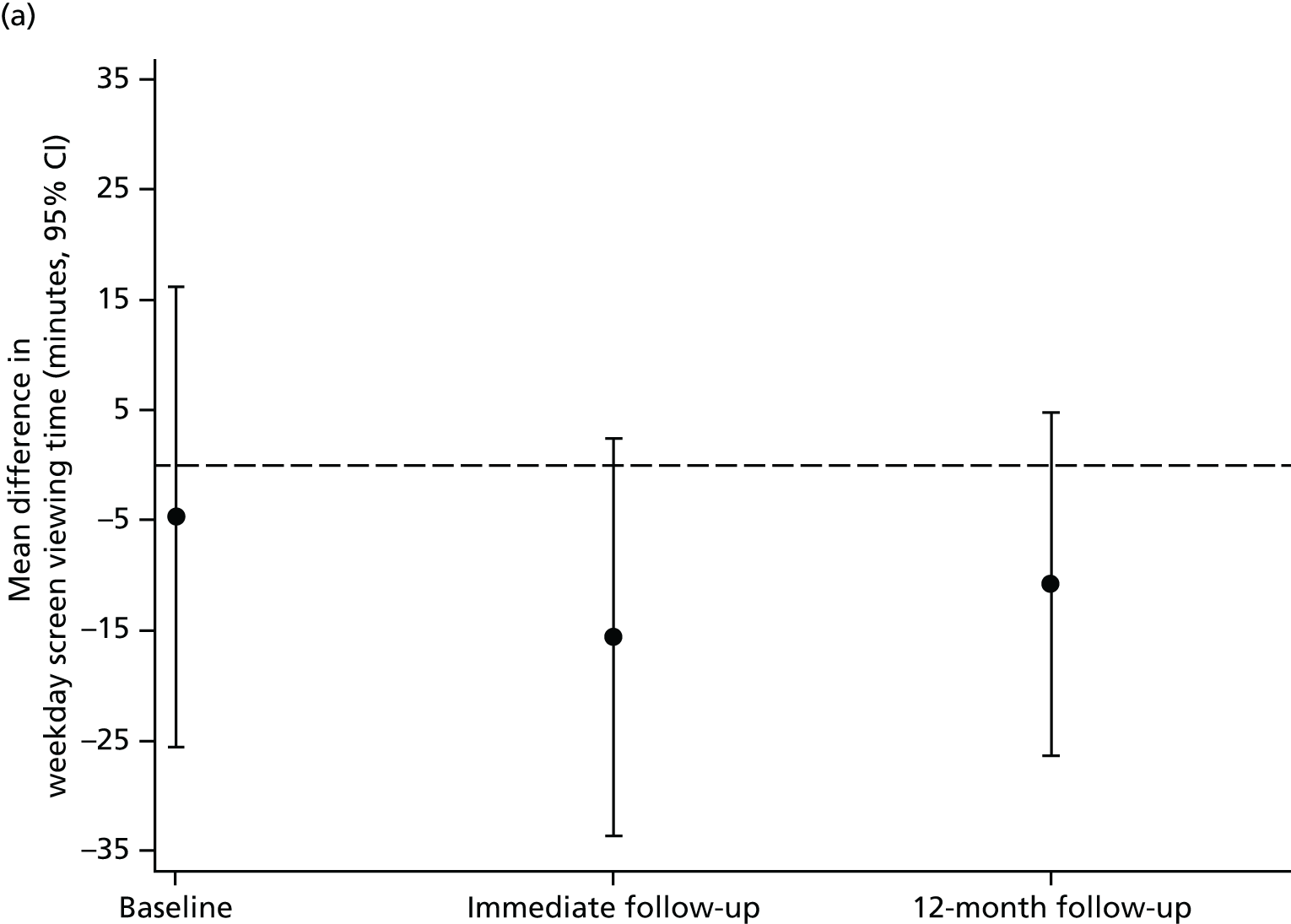
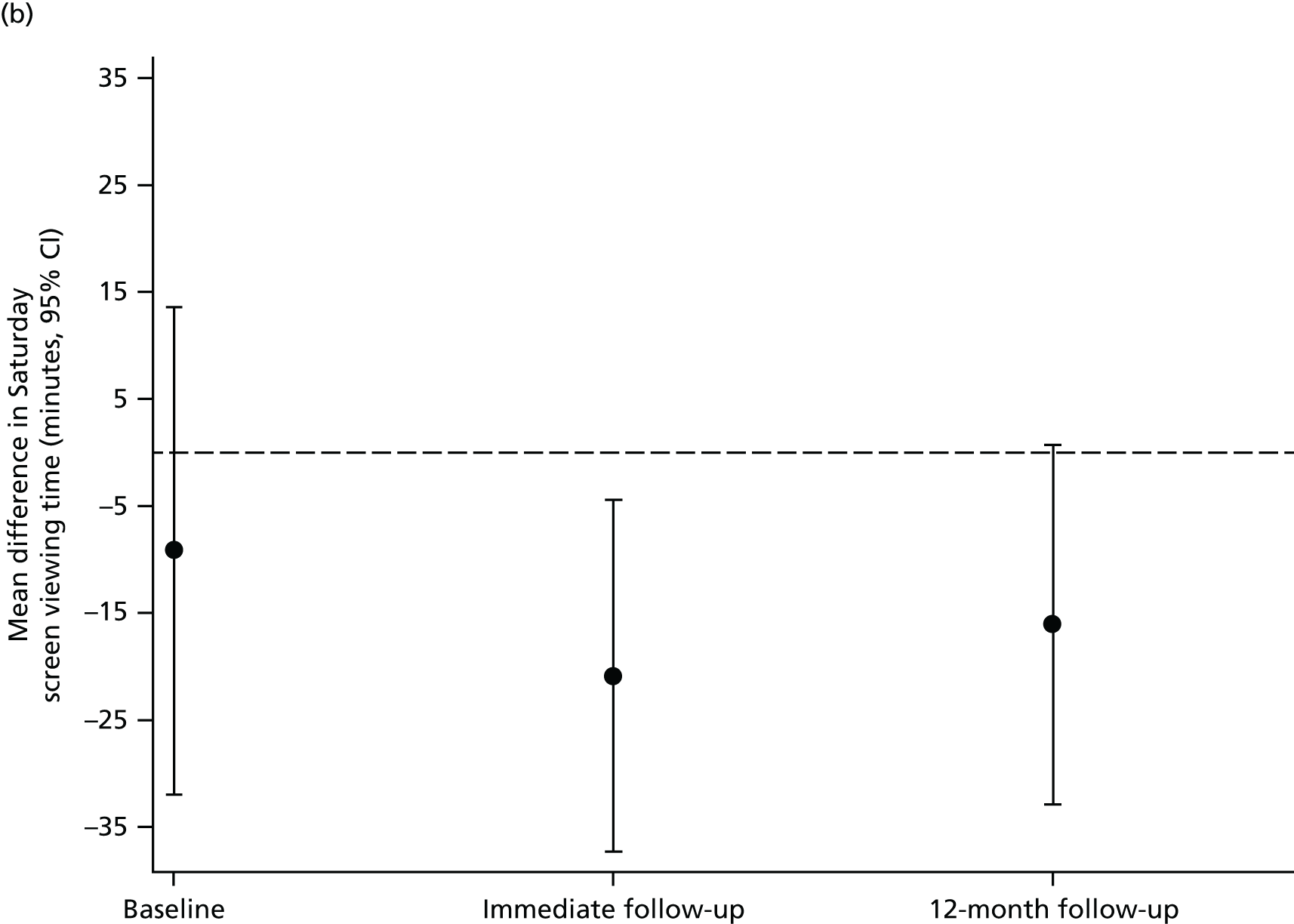
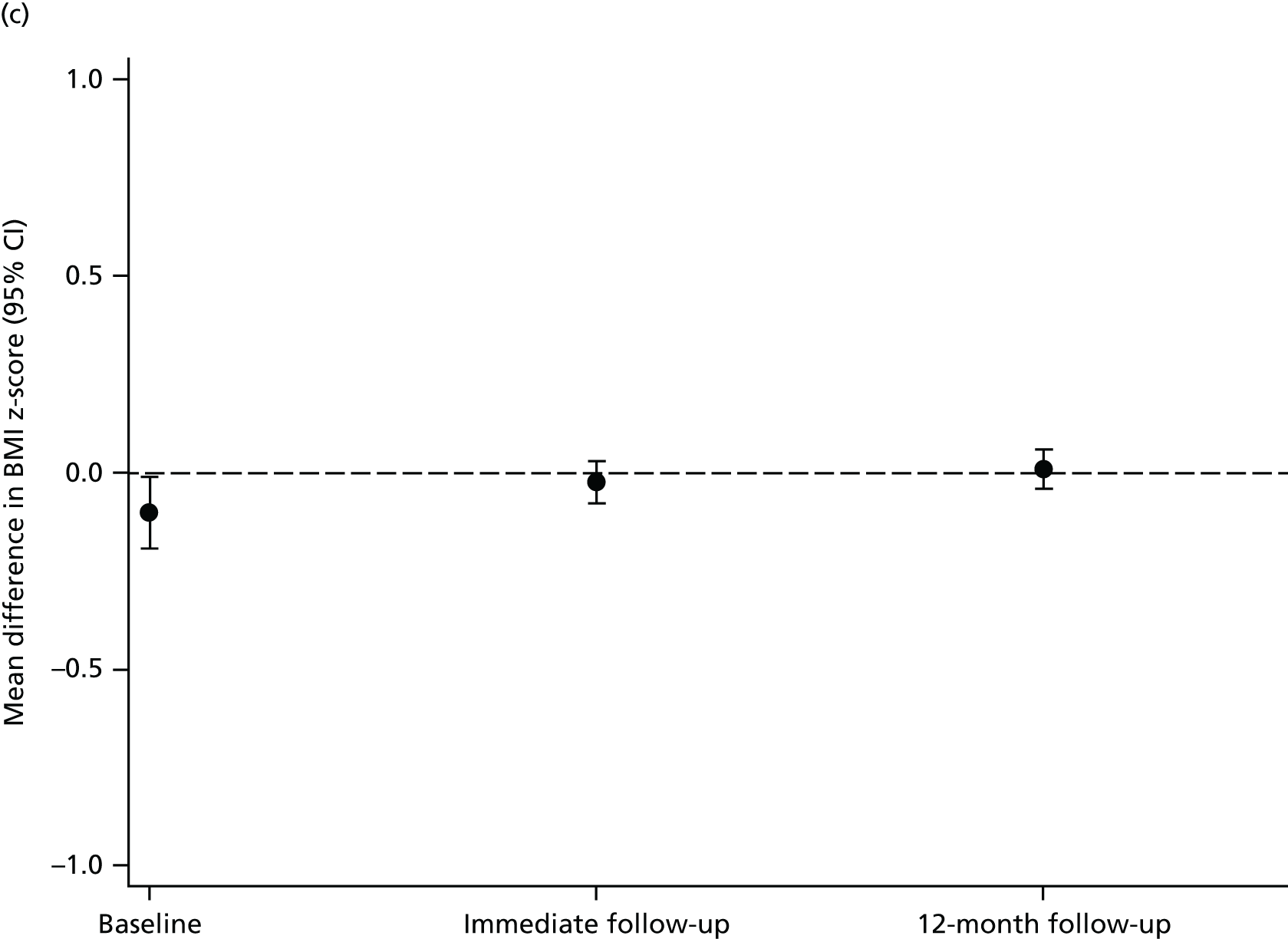

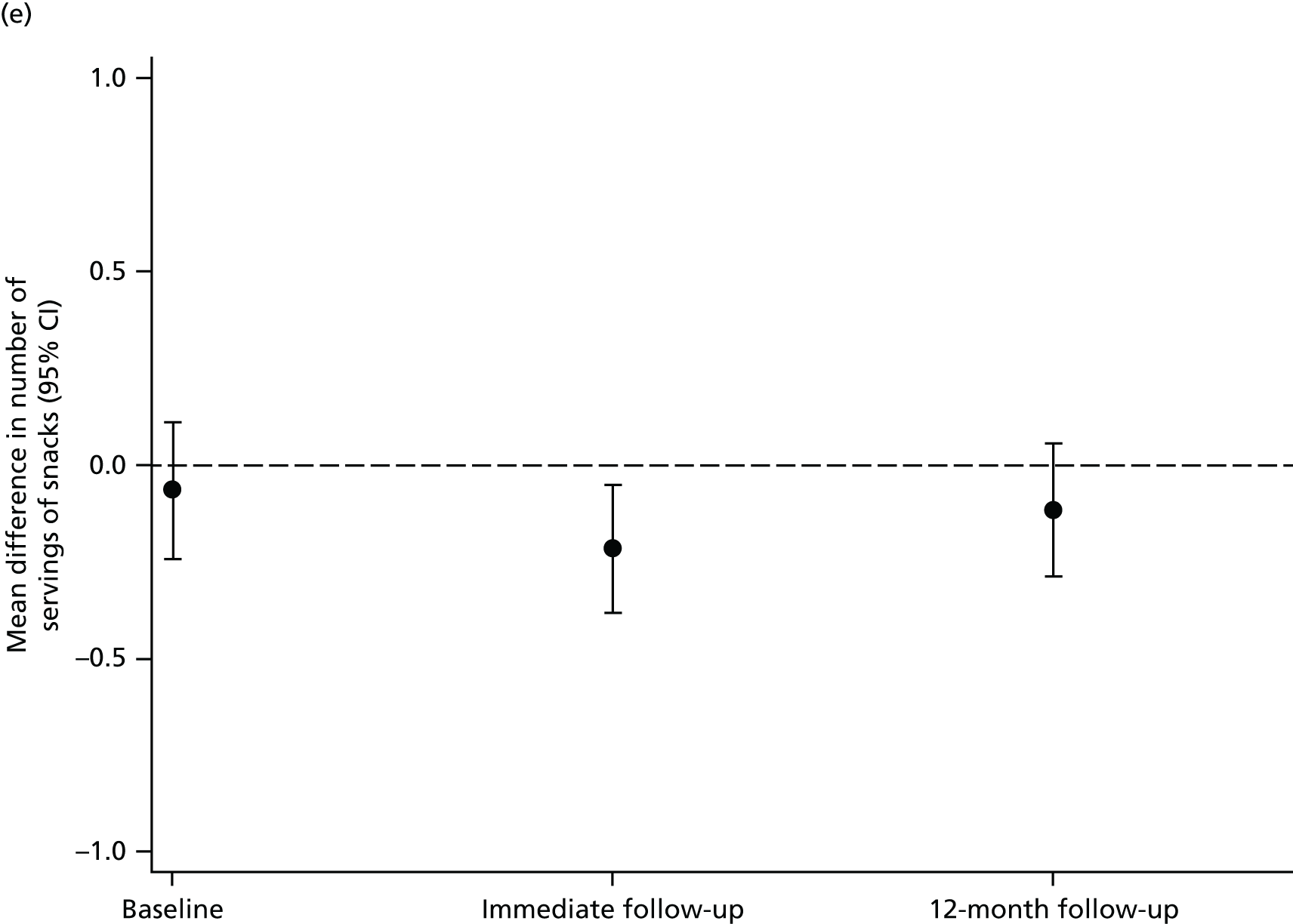
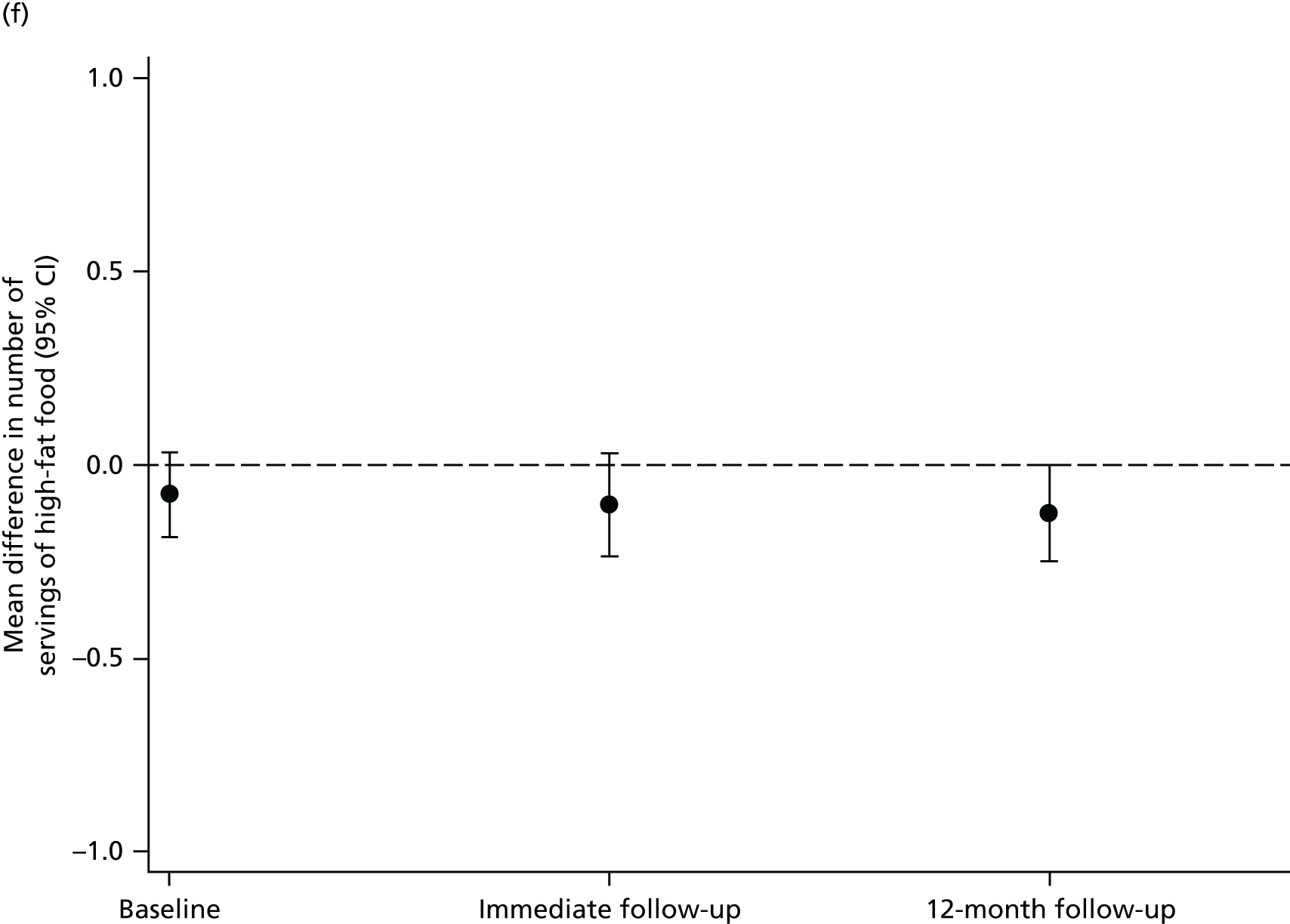
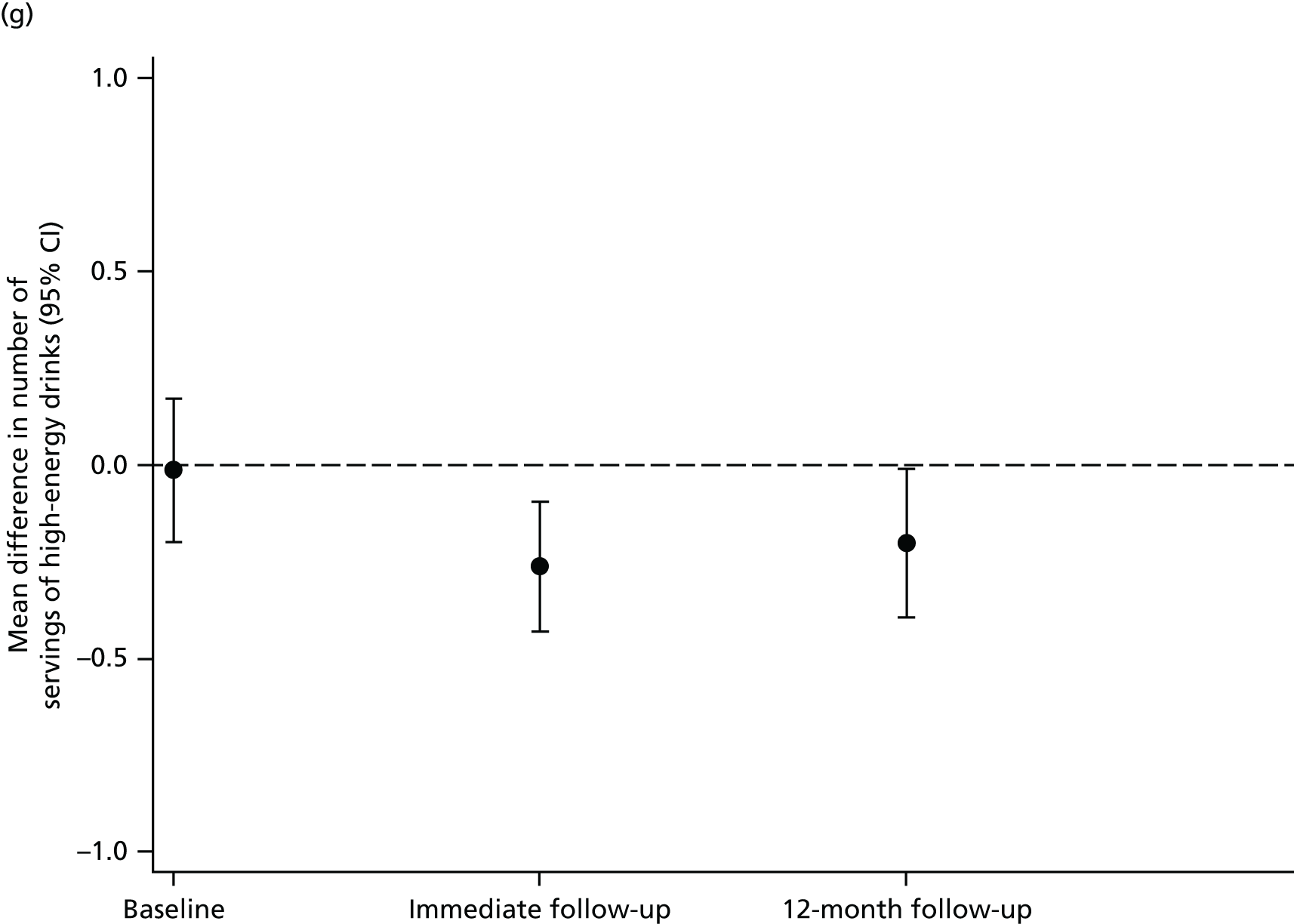
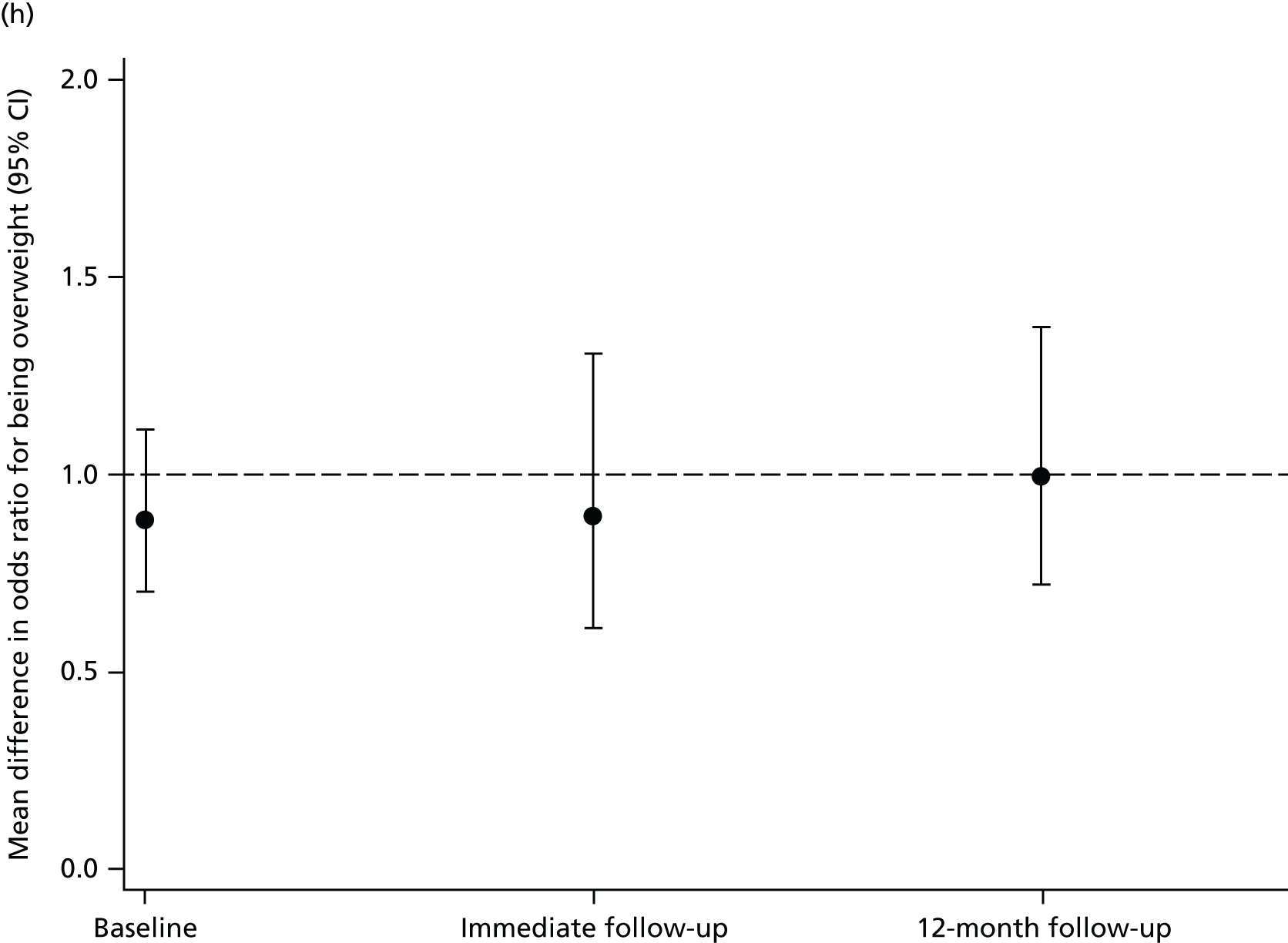

Table 16 shows differences in means for all outcomes at the long-term follow-up from the main ITT analyses. None of the three primary outcomes differed between children in schools allocated to the AFLY5 intervention and those allocated to the control group at the end of the 12-month follow-up. Differences in secondary outcomes were consistent with those seen at the end of the immediate follow-up with no evidence that the previously reported beneficial effects for child-reported screen viewing at weekends, consumption of snacks and consumption of high-energy drinks had notably diminished over time. Consumption of high-fat foods also appeared lower in children from intervention schools. However, none of these reached our predefined level of statistical significance after accounting for multiple testing. There was no evidence of effect of the intervention on other secondary outcomes.
| Outcome | Control group (reference group) | Intervention group | Main comparison between the two groups (intervention vs. control) | ||||
|---|---|---|---|---|---|---|---|
| n a | Mean (SD) or number (%) | n a | Mean (SD) or number (%) | n a | Difference in means or odds ratio (95% CI) | p-value | |
| Continuous outcomes (differences in means) | |||||||
| Time spent in MVPA (minutes per day) | 522 | 52.56 (20.67) | 527 | 54.37 (22.23) | 1049 | 2.48 (–1.80 to 6.77) | 0.26 |
| Time spent in sedentary behaviour (minutes per day) | 522 | 461.78 (66.33) | 527 | 465.46 (70.61) | 1049 | 2.79 (–7.78 to 13.37) | 0.26 |
| Servings of fruit and vegetables (number per day) | 1062 | 1.80 (1.55) | 990 | 1.82 (1.59) | 2051 | 0.01 (–0.16 to 0.17) | 0.94 |
| Time spent screen viewing (minutes per day, weekday) | 1062 | 148.01 (126.39) | 990 | 138.88 (125.00) | 2051 | –10.74 (–26.30 to 4.81) | 0.18 |
| Time spent screen viewing (minutes per day, Saturday) | 1062 | 180.52 (164.82) | 990 | 167.71 (156.28) | 2051 | –16.03 (–32.82 to 0.73) | 0.06 |
| BMI (z-score) | 923 | 0.03 (1.02) | 870 | –0.03 (0.97) | 1793 | 0.01 (–0.04 to 0.06) | 0.72 |
| WC (z-score) | 993 | 0.03 (1.04) | 935 | –0.03 (0.95) | 1928 | –0.04 (–0.13 to 0.05) | 0.36 |
| Servings of snacks (number per day) | 1062 | 2.11 (1.55) | 990 | 1.99 (1.47) | 2051 | –0.11 (–0.29 to 0.06) | 0.19 |
| Servings of high-fat foods (number per day) | 1062 | 0.86 (0.94) | 990 | 0.74 (1.07) | 2051 | –0.12 (–0.25 to 0.00) | 0.05 |
| Servings of high-energy drinks (number per day) | 1062 | 2.38 (1.58) | 990 | 2.19 (1.45) | 2051 | –0.20 (–0.39 to -0.01) | 0.04 |
| Binary outcomes (odds ratios) | |||||||
| Generally overweight/obese | 923 | 194 (21.02) | 870 | 175 (20.11) | 1793 | 1.00 (0.72 to 1.37) | 0.98 |
| Centrally overweight/obese | 993 | 421 (42.40) | 935 | 394 (42.14) | 1928 | 1.08 (0.80 to 1.46) | 0.62 |
Results from the per-protocol analyses were consistent with the results of the ITT analyses (Table 17) and, as with the analyses for immediate outcomes, results did not differ in sensitivity analyses, testing our assumptions regarding missing data.
| Outcome | Control group (reference group) | Intervention group | Main comparison between the two groups (intervention vs. control) | ||||
|---|---|---|---|---|---|---|---|
| n a | Mean (SD) or number (%) | n a | Mean (SD) or number (%) | n a | Difference in means or odds ratio (95% CI) | p-value | |
| Continuous outcomes (differences in means) | |||||||
| Time spent in MVPA (minutes per day) | 523 | 52.46 (20.78) | 356 | 54.15 (22.27) | 879 | 2.65 (–2.12 to 7.42) | 0.28 |
| Time spent in sedentary behaviour (minutes per day) | 523 | 463.53 (77.48) | 356 | 466.17 (70.58) | 879 | 3.86 (–8.80 to 16.51) | 0.55 |
| Servings of fruit and vegetables (number per day) | 1062 | 1.80 (1.55) | 701 | 1.91 (1.66) | 1762 | 0.05 (–0.15 to 0.25) | 0.63 |
| Time spent screen viewing (minutes per day, weekday) | 1062 | 148.01 (126.39) | 701 | 134.98 (120.94) | 1762 | –8.97 (–26.81 to 8.87) | 0.32 |
| Time spent screen viewing (minutes per day, Saturday) | 1062 | 180.52 (164.82) | 701 | 159.35 (149.97) | 1762 | –21.73 (–41.19 to –2.26) | 0.03 |
| BMI (z-score) | 923 | 0.03 (1.02) | 612 | –0.03 (0.98) | 1535 | 0.01 (–0.05 to 0.07) | 0.69 |
| WC (z-score) | 993 | 0.03 (1.04) | 657 | –0.04 (0.94) | 1650 | –0.03 (–0.13 to 0.06) | 0.52 |
| Servings of snacks (number per day) | 1062 | 2.11 (1.55) | 701 | 2.07 (1.48) | 1762 | –0.03 (–0.23 to 0.16) | 0.72 |
| Servings of high-fat foods (number per day) | 1062 | 0.86 (0.94) | 701 | 0.75 (1.15) | 1762 | –0.11 (–0.26 to 0.04) | 0.14 |
| Servings of high-energy drinks (number per day) | 1062 | 2.38 (1.58) | 701 | 2.22 (1.43) | 1762 | –0.18 (–0.41 to 0.5) | 0.12 |
| Binary outcomes (odds ratios) | |||||||
| Generally overweight/obese | 923 | 194 (21.02) | 612 | 121 (19.77) | 1535 | 0.98 (0.68 to 1.41) | 0.91 |
| Centrally overweight/obese | 993 | 421 (42.40) | 657 | 272 (41.40) | 1650 | 1.06 (0.76 to 1.49) | 0.72 |
Results of the economic evaluation
Primary analyses
Table 18 shows a breakdown of the resource use and costs incurred during the training days and the delivery of the AFLY5 lessons from the combined school and provider perspective. The main cost drivers for the intervention were the claims by the schools for replacement teachers needed to cover the teachers’ attendance at the training days (£5.00 per pupil, £5095.00 in total); the trainers’ fees (£2.00 per pupil, £2166.00 in total); the time spent by the research staff organising and attending the training days (£2.00 per pupil, £2492.00 in total); and the printing costs of the materials for the AFLY5 lessons and the homework (£6.00 per pupil, £6694.00 in total). We estimated the opportunity cost of implementing AFLY5 in schools (i.e. the cost of teaching AFLY5 minus the cost of teaching the usual curriculum based on data from schools in the control arm) to be £0.05 per pupil. The costs varied by school, ranging from approximately £13.00 to £36.00 per pupil. The variations between the schools were driven by the costs of the teachers’ attendance at the training days.
| Resource (intervention arm only) | Resource use per pupil | Unit cost (£) | Cost per pupil (£) | Total cost (£) (n = 1064) |
|---|---|---|---|---|
| Training days | ||||
| Research staff time: organisation of and attendance at training days (£/minute) | 6.00 | 0.39 | 2.34 | 2492.00 |
| Administrative staff time spent organising and attending training days (minutes) | 0.59 | 0.21 | 0.12 | 131.00 |
| Telephone calls: connection charge (£/call) | 0.06 | 0.15 | 0.008 | 8.85 |
| Telephone calls: cost (£/minute) | 0.17 | 0.09 | 0.015 | 15.93 |
| Trainers’ fees (£) | N/A | N/A | 2.04 | 2166.00 |
| Refreshments (£) | N/A | N/A | 0.68 | 724.00 |
| Venue hire (£) | N/A | N/A | 0.10 | 110.00 |
| Primary schools staff time on telephone calls (£/minute) | 0.14 | Varies | 0.04 | 42.90 |
| Teachers’ attendance at training days (£) | N/A | N/A | 4.79 | 5095.00 |
| Car mileage to attend training days (£/mile) | 0.38a | 0.45 | 0.17a | 184.00 |
| Car park fee (£) | N/A | 10.00 | 0.07 | 70.00 |
| Transport fare (bus) to attend training days (£/return) | N/A | 2 | 0.002 | 2 |
| Transport fare (train) to attend training days (£/return) | N/A | 4 | 0.004 | 4 |
| Other teacher-incurred training day costs (£) | N/A | N/A | 0.006b | 6.83 |
| Delivery of intervention | ||||
| Research staff time: production of teaching and homework materials (£/minute) | 1.00 | 0.39 | 0.39 | 417 |
| Administrative staff time: production of teaching and homework materials (£/minute) | 1.66 | 0.21 | 0.35 | 371 |
| Telephone calls: connection charge (£ per call) | 0.005 | 0.15 | 0.001 | 0.75 |
| Telephone call: cost (£ per minute) | 0.01 | 0.09 | 0.001 | 1.35 |
| Consumables used to prepare the intervention: printing (£) | N/A | N/A | 6.29 | 6694.00 |
| Other consumables used to prepare the intervention (CDs, folders, dividers) (£) | N/A | N/A | 0.30 | 321.00 |
| Consumables used during the lessons (£) | N/A | N/A | 0.04 | 40.00 |
| Opportunity cost of delivering AFLY5 | N/A | N/A | 0.05c | 48.00 |
| Total cost of intervention (£) | N/A | N/A | 17.80 | 18,944 |
The cost–consequence analysis showed that, for the three secondary outcomes that were affected by the intervention, it cost £18 per child (£18,944 in total) to reduce self-reported time spent on screen viewing at the weekend by 20.86 minutes, self-reported consumption of snacks by 0.22 snacks per day and self-reported consumption of high-energy drinks by 0.26 servings per day.
From the teachers’ perspective, teachers spent, on average, more time travelling to the training day venue than they usually spent travelling to school; this equated to an additional 0.68 minutes’ travel time per pupil, generating an extra cost of £0.19 per child (£206 in total).
Sensitivity analyses
Table 19 shows the results of sensitivity analyses for the primary (perspective of combined provider and school). These results suggest that the main analyses are robust to our assumptions regarding missing data.
| Analysis | Cost per pupil (£) | Total cost (£) |
|---|---|---|
| Main analyses: total cost of the intervention (£) | 17.80 | 18,944.00 |
| Sensitivity analysis 1: increased venue hire cost | ||
| Total cost of the intervention (£) | 18.01 | 19,164.00 |
| Sensitivity analysis 2: cost of teachers attending training day | ||
| Total cost of the intervention (£) | 17.60 | 18,728.00 |
| Sensitivity analysis 3: opportunity cost of teaching AFLY5 | ||
| Total cost of the intervention (£) | 17.81 | 18,951.00 |
Secondary analyses
Only 626 (28%) parental questionnaires [278 (13%) in the intervention and 348 (16%) in the control arm] were returned. In the returned questionnaires the item non-response varied between 0% and 6%. Table 20 shows the results of the cost differences between the intervention and control arms from the perspective of the parents and the NHS, using a CCA and including maximum numbers for each item. After adjustment for the child’s age, sex, area deprivation level for the school and the engagement of the school in health-promoting activities (over and above AFLY5), all of the parental and NHS costs appeared greater in those from schools randomised to intervention compared with those randomised to control. However, all of these results were imprecisely estimated with wide CIs consistent with no difference. With the exception of the NHS costs, adjustment for covariables produced notable differences in comparison with the unadjusted results (although results were all consistent with the null hypothesis, whether or not adjusted). The IMD34 is the covariable that has most effect, and it contributed to change in all of the results that differed with adjustment. Other covariables that contributed to some of the change in results with adjustment were age (total cost from a parental perspective), child’s sex (costs of parental time) and the level of school involvement in healthy activities (expenditure in out-of-school activities). The greater NHS cost is likely to be exaggerated as it was influenced by one participant who was reported to have had surgery for a condition that is unlikely to have been influenced by the intervention (adrenal surgery); this was despite the question that specifically asked about treatments that were related to physical activity injury. Other variables in the cost–consequence analyses were largely normally distributed with no evidence of effect by ‘outliers’.
| Item | Mean costs (SD) (£) intervention | Mean cost (SD) (£) control | Unadjusted difference in mean costs (95% CI) (£) | Adjusted difference in mean costs (95% CI) (£) |
|---|---|---|---|---|
| Total parental time (n = 557) | 693.00 (898.00) | 759.00 (942.00) | –65.71 (–221.00 to 86.00) | 19.88 (–133.00 to 199.00) |
| Total household expenditure (n = 596) | 2383.00 (851.00) | 2337.00 (805.00) | 45.98 (–80.11 to 176.00) | 127 (–6.65 to 259.00) |
| Total household expenditure adjusted for household members (n = 587) | 74.84 (–65.94 to 200.00) | |||
| Total costs | ||||
| Parental perspective (n = 536) | 3109.00 (1367.00) | 3090.00 (1291.00) | 19.06 (–201.00 to 246.00) | 196.00 (–40.12 to 430.00) |
| Parental perspective adjusted for household members (n = 528) | 134.00 (–84.55 to 387.00) | |||
| NHS perspective (n = 589) | 122.00 (1816.00) | 16.95 (72.99) | 105.50 (–10.75 to 558.40) | 113.96 (–11.76 to 641.22) |
Chapter 4 Process evaluation
Introduction
The purpose of completing a process evaluation of the AFLY5 trial was to contextualise the trial effectiveness and cost-effectiveness results, with respect to how the intervention may or may not have worked and, if it was found to be effective, what might be required for it to be sustained in the real world.
Aims
There were three main aims of the process evaluation:
-
to assess the fidelity of the intervention delivery
-
to assess whether or not the intervention worked in the way that it was expected to, in terms of the intervention logic model (see Figure 5)
-
to consider the sustainability of the intervention and how it could be rolled out if it was shown to be effective.
Research questions
In order to address the aims of the process evaluation, we devised the following research questions (RQs), shown below in relation to the research aims:
-
Aim 1: to assess the fidelity of the intervention delivery.
-
RQ 1. To what extent was the intervention delivered as planned?
-
RQ 2. In what ways, if any, did the teachers adapt the programme and what were the reasons for these adaptations?
-
-
Aim 2: to assess whether or not the intervention worked in the way that it was expected to, in terms of the intervention logic model (see Figure 5).
-
RQ 3. What changes did the children make in response to the intervention?
-
RQ 4. What changes were feasible for them to make?
-
-
Aim 3: to consider the sustainability of the intervention and how it could be rolled out if it was shown to be effective?
-
RQ 5. What could we do to improve AFLY5?
-
RQ 6. What are the implications for future school-based diet and physical activity interventions?
-
Logic model
The logic model for AFLY5 (Figure 5) attempts to visually represent the theoretical underpinnings of the intervention, the content of the intervention, the processes by which the intervention was assumed to work, the context in which the intervention was delivered and the outcomes it was hoped would be achieved. The AFLY5 intervention draws on social cognitive theory. 27,28 Mediators (children’s knowledge and self-efficacy) that, according to social cognitive theory, would be a key method through which the intervention might result in behaviour change, were included in the model and the process evaluation explored evidence of whether or not the intervention influenced these mediators from the perspective of reports by the children in focus groups (Chapter 3 provides the quantitative effects on these mediators).
FIGURE 5.
Logic model. Ofsted, Office for Standards in Education, Children’s Services and Skills.
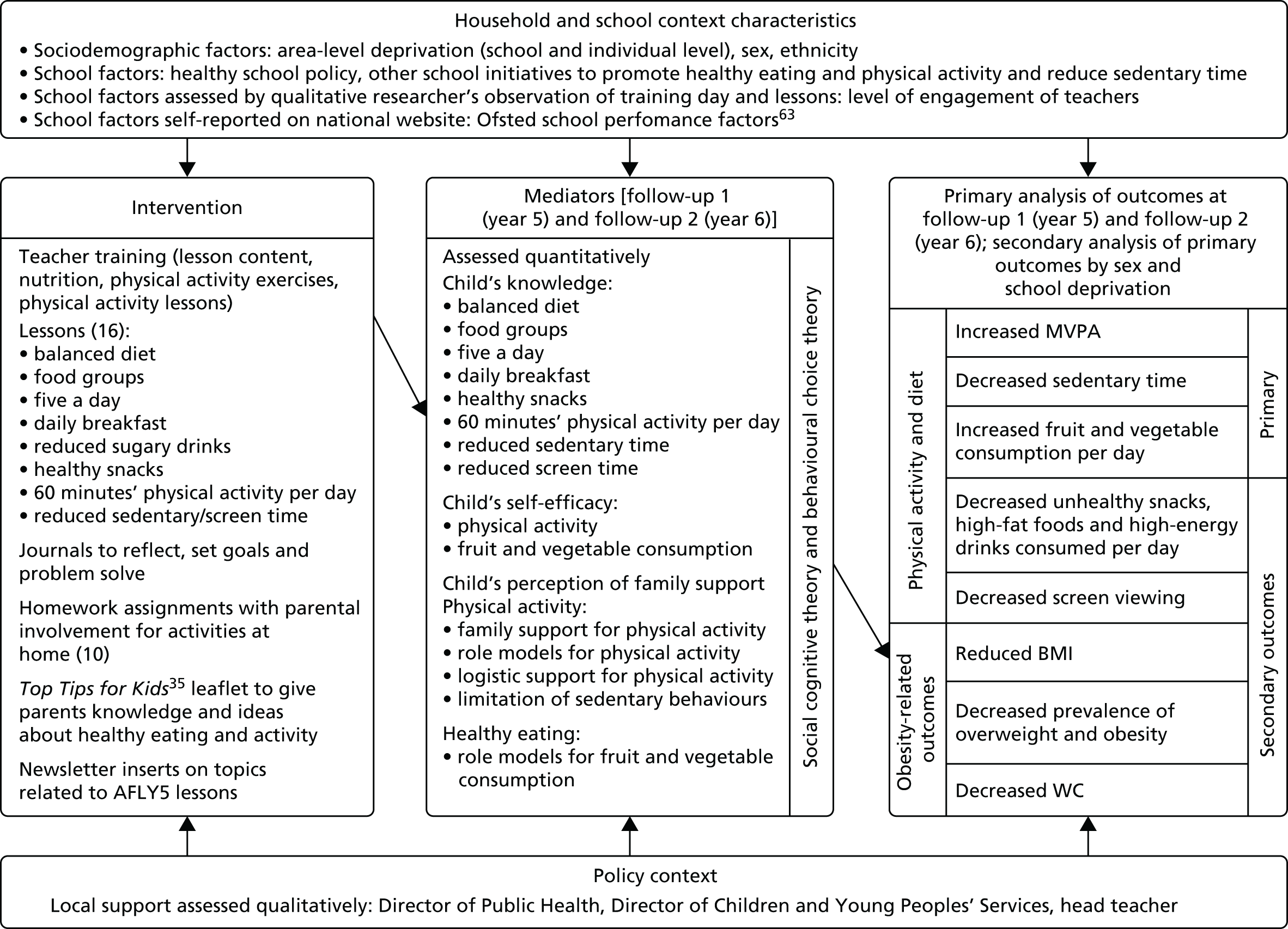
Contextual factors, such as household characteristics or school and policy contexts, that could impact on the intervention and might be relevant to how effectively it might be disseminated if it were shown to be cost-effective were also included in the model and explored in the process evaluation.
Methods
The methods of data collection used in this process evaluation, from whom the data were collected, when they were collected and which RQs the data contributed to are summarised in Table 21. With the exception of two teacher training observation sessions, all observation sessions, interviews and focus groups were carried out by the same trained qualitative researcher. A second trained qualitative researcher carried out the first two teacher training sessions, and the two researchers discussed and shared observation notes and research techniques prior to the handover.
| Type of data collection required | Whom it will be collected from? | Time frame for collection | Research aimsa |
|---|---|---|---|
| School audits | |||
| Baseline | Teachers/head teachers | June 2011–October 2011 | A2 RQ4 A2 RQ6 |
| Follow-up 1 | Teachers | April 2012–September 2012 | |
| Follow-up 2 | Teachers | February 2013–July 2013 | |
| Teacher training observations | Teachers | September 2011–January 2012 | A1 RQ1 A1 RQ2 A1 RQ3 A2 RQ5 A2 RQ6 |
| Teacher training evaluation forms | Teachers | September 2011–January 2012 | A1 RQ2 A1 RQ2 A1 RQ3 A2 RQ4 A2 RQ5 |
| Lesson observations | Teachers, children | November 2011–April 2012 | A1 RQ1 A1 RQ2 A1 RQ3 A2 RQ3 A2 RQ4 A2 RQ5 A2 RQ6 |
| Teacher logs | Teachers | September 2011–June 2012 | A1 RQ1 A1 RQ2 A1 RQ3 A2 RQ5 A2 RQ6 |
| Interviews | |||
| Teachers | Teachers | October 2012–May 2013 | A1 RQ1 A1 RQ2 A1 RQ3 A2 RQ3 A2 RQ4 A2 RQ5 A2 RQ6 |
| Head teachers | Head teachers | October 2012–May 2013 | A1 RQ1 A1 RQ2 A1 RQ3 A2 RQ3 A2 RQ4 A2 RQ5 A2 RQ6 |
| Parents | Parents | November 2012–May 2013 | A1 RQ1 A1 RQ2 A1 RQ3 A2 RQ3 A2 RQ4 A2 RQ5 A2 RQ6 |
Additional interviews were planned at the outset of AFLY564 but did not take place. We had intended to interview teachers a second time at the same time as the 12-month follow-up to see whether or not they had a lasting impression of the follow-up. However, it became apparent that these interviews were unlikely to add substantial new information to the large number of data that had been collected (see Table 21), and we were concerned that conducting these interviews would reduce the time the researcher had available for coding and analysing the existing data. We had also intended to interview Directors of Public Health. However, those interviews became infeasible because of significant structural changes in public health in England occurring at the time that work would have been conducted. Lastly, we did not intensively chase head teachers who did not respond to our requests for an interview.
Sampling and recruitment
The process evaluation for AFLY5 involved collecting data from five groups, with participants in these groups being selected from both intervention and control schools:
-
year 5 teaching staff
-
head teachers
-
parents of year 5 pupils
-
year 5 pupils (aged 9–10 years): as the topics covered in the focus groups with these pupils did not relate to key intervention issues these data will be reported separately from this report.
The intervention teaching staff were chosen to provide direct feedback on experiences of delivering the intervention, intervention fidelity and how it could be improved. The other four groups included participants from intervention and control schools to obtain an overview of how both AFLY5 and normal diet, physical activity and healthy living education lessons were delivered and received within the school setting.
Selection of intervention and control schools for the process evaluation
All intervention arm AFLY5 year 5 teaching staff were invited to participate in a one-to-one in-depth interview with the aim that we would continue to interview all who agreed to participate until we had clearly reached saturation in the analysis. For data collection from control arm year 5 teachers, control and intervention arm head teachers, pupils and parents, we planned to sample from 12 purposively selected schools on a first come, first served basis until saturation was reached. These schools were selected to represent different levels of area deprivation (high, medium and low) and different Ofsted (Office for Standards in Education, Children’s Services and Skills) scores at the time of entry into the study (July 2011) (high vs. low). 63 Of these, six would be intervention and six would be control schools. Participation in the process evaluation was not compulsory and, if a school declined, this did not affect its participation in the main part of the study. Initially, if a school declined, a school with a similar profile was approached to replace it. In practice, we were unable to reach our recruitment target this way and eventually opened up the invitation to all AFLY5 schools in order to recruit 12 schools to the process evaluation.
For all types of data collection the final number recruited was guided by the point at which saturation was reached (i.e. the point at which no new data were emerging). If this had clearly been reached before the anticipated number of participants had been interviewed, or focus groups conducted, then the number would be lower. If it had not been reached by the end of the anticipated numbers we would have attempted to recruit more participants. The anticipated numbers are based on our previous experience with similar research and from published research in similar areas. 31,65–67
The numbers of actual schools/participants that participated in interviews/focus groups, along with the anticipated numbers, are indicated in Table 22.
| Group | Participants | Data collection method | Number of schools | Number of participants | ||
|---|---|---|---|---|---|---|
| Anticipated | Actual | Anticipated | Actual | |||
| Intervention | Year 5 teachers | Interview | 30 | 15 | 30–48 | 20 |
| Head teachers | Interview | 6 | 4 | 6 | 4 | |
| Parents of year 5 pupils | Interview | 6 | 6 | 12–18 | 14 | |
| Year 5 pupils | Focus group | 6 | 6 | 36–48 | 36 | |
| Control | Year 5 teachers | Interview | 6 | 6 | 6–18 | 8 |
| Head teachers | Interview | 6 | 6 | 6 | 6 | |
| Parents of year 5 pupils | Interview | 6 | 6 | 12–18 | 15 | |
| Year 5 pupils | Focus group | 6 | 6 | 36–48 | 34 | |
Recruitment of teaching staff
We aimed to recruit as many as possible of the teaching staff who delivered the intervention to allow us to obtain very detailed information about their delivery of the AFLY5 lessons. This included whether they talked about the AFLY5 lessons when asked general questions about teaching health promotion or about the study in general, and also their responses to prompts about the AFLY5 teaching materials, training days, etc. They were invited by e-mail to take part in an interview, with the aim of interviewing one teacher per school. The information sheet and consent form were attached to the e-mail. If they had not replied after 2 weeks, a follow-up call was made or e-mail sent.
We also recruited eight control arm AFLY5 teaching staff members, which included at least one from each of the six process evaluation control schools (selected as described above). We anticipated that with teachers from just these six control arm AFLY5 schools we would obtain sufficient information to understand if the current syllabus (without AFLY5) covered some or a substantial part of the topics covered in the AFLY5 lessons.
Recruitment of head teachers
Intervention and control arm head teachers were invited from the 12 schools (six intervention and six control) as listed above. They were contacted via telephone or e-mail, with a follow-up telephone call around 2 weeks later. Once the head teacher indicated that he or she was willing for the school to participate, a convenient time was arranged for the interview to take place.
Recruitment of parents or guardians and children
All parents or guardians of year 5 children in the 12 selected schools (six intervention and six control) were sent a letter informing them of the parental interviews and child focus groups. In the case of the parental interviews, an information sheet and reply form were included informing the parents about the interviews and asking if they wanted to take part. Parents who replied to say they were interested in participating were contacted by telephone to arrange a convenient time for either a telephone or a face-to-face interview. If they opted for a telephone interview, parents were sent a consent form through the post. If they opted for a face-to-face interview, a consent form was completed in person before the interview started. Consent for parent interviews was on an opt-in basis.
In the same information pack parents were also sent an information sheet relating to the children’s focus group. Parental consent for the children’s participation in the focus group was on an opt-out basis, meaning any child could potentially be approached to participate in the focus group unless their parent had opted them out. Pupils from the selected 12 schools whose parents had not opted their child out of the focus group research were purposively sampled and invited to participate in the focus groups. Pupils were purposively sampled to ensure a balance of sexes, those with high and low levels of reported self-efficacy for physical activity and high and low levels of parental support for physical activity. Information on these characteristics was collected from all pupils participating in AFLY5 as part of the baseline questionnaire. The children were given an information sheet before deciding whether or not to take part in the focus groups. The children were then asked to give written assent to participate in the focus group on the day prior to starting.
Data collection
The data were anonymised and any comments or observations relating to specific individuals or schools in a way that could allow them to be recognised were removed.
School audits, baseline and follow-up
Audits were attempted in all schools (both intervention and control) once per academic year during baseline, intervention and follow-up periods of the study (June 2011–July 2013). They were used to assess physical activity provision, including the number of scheduled PE lessons per week and time allocated for unsupervised outdoor play, school physical activity and nutrition policy (active travel, break-time play, packed lunch policy, etc.) and number and type of school clubs provided. In 2011, these audits were carried out over the telephone by a member of the AFLY5 team using a pro forma. In 2012 and 2013, the audits were filled out by teachers in schools during the measurement process.
Teacher training observation
Observations took place during the teacher training days for the group of teachers randomised to AFLY5. The aim was to observe how effectively the messages of the training day were conveyed by the trainers, and how these messages were received by the teachers. Observations included noting any questions and issues raised by the teachers. Consent to observe the training day was sought from the trainers and the teachers. A copy of the observation guide is in Appendix 3.
Teacher training evaluation forms
The AFLY5 training day was assessed using an evaluation form, which was completed by the teachers who had received the training. A copy of the evaluation form is in Appendix 4. The aim was to ask teachers about their engagement with, and understanding of, the training provided and if they felt they knew enough or required more information.
Lesson observations
We asked teachers for permission to observe the teaching of the AFLY5′ lessons. There are 16 lessons in the syllabus and we wanted to observe each of these lessons twice, which would have allowed us to observe in each school at least once. There were also two pilot observations. The observations did not assess the general teaching ability of staff and no feedback was provided to anyone at the school other than the teacher, and only when specifically requested. This was made very clear to the school (both in the information letter and in person). No recording equipment was used (visual or audio) during the observations, only hand-written notes were taken. Observations took place only in the intervention schools. A copy of the observation guide is in Appendix 5.
Teacher log
We asked all year 5 teachers in intervention schools to complete a log of session delivery during the intervention period (September 2011–June 2012) (n = 48). The log asked teachers to report the date that the sessions were delivered, whether homework assignments were set and returned and any problems or positive comments about the lesson. A copy of the teacher log is given in Appendix 6.
Interviews
Intervention and control arm AFLY5 teaching staff were interviewed to obtain information about their views on what contributes to healthy lifestyles in general and for children specifically, on teaching health promotion, whether they believe school- or education-based health promotion is effective in changing children’s behaviours and what teaching activities they are involved in that are concerned with health promotion (and specifically promoting healthy diet and physical activity). They were also asked how they felt about delivering these lessons and their likely effectiveness. Information was sought on the teachers’ views of the children wearing the accelerometers and any barriers they perceived to them doing this for the required time and returning the accelerometers. There were also some questions about the intervention for the teaching staff in intervention schools, mainly related to how they found the experience. A copy of the topic guide is provided in Appendix 7. The interviews were held post intervention either at school or at a location chosen by the participant, at a time convenient for them. The interviews took up to 60 minutes.
Intervention and control arm AFLY5 head teachers were interviewed to obtain information about their views on healthy lifestyles in general and for children specifically, on teaching health promotion in schools and if they believe school- or education-based health promotion is effective in changing children’s behaviours. Information on what health-promoting activities (in any area of health promotion) were taking place in their school at the time and their views on schools participating in research were also sought. The head teachers from schools that had taken part in AFLY5 were also asked about their views of the school taking part in this study. A copy of the topic guide is provided in Appendix 8. The interviews were held post intervention at school, during the school day, and took up to 60 minutes.
Intervention and control arm AFLY5 parents were interviewed to obtain information about their knowledge of healthy lifestyles, whether they are aware of their children learning about healthy lifestyles in school, their involvement in any homework assignments concerned with healthy lifestyles or health promotion and what they remembered about their children being measured in school. The topic guide can be seen in Appendix 9. The interviews were held post intervention either face to face, at their child’s school or the university, or over the telephone, between 8 a.m. and 9 p.m. The interviews took up to 60 minutes.
Focus groups
Focus groups with intervention and control arm AFLY5 pupils were conducted to obtain information about their views on what things make them healthy, how easy or hard they find it to do things that make/keep them healthy. The topic guide is presented in Appendix 10. These questions were asked to provide broader contextual data on the children’s understanding of issues related to diet and physical activity and the teaching of these subjects in schools, irrespective of whether students were in the intervention or control arm. These focus groups do not provide information in relation to the three research aims of the process evaluation and are therefore not reported in this monograph. Data from them may be used in separate future publications.
Analysis
Qualitative and quantitative process data were initially analysed separately and the different data sources were then combined for each aim and RQs to address each RQ. How the data were analysed and synthesised together is described in the sections below.
Types of data
Structured data
Both quantitative and more open qualitative responses from questionnaires or other structured data collection instruments (e.g. school audit forms, teacher training evaluation forms and teacher logs) were entered into a Microsoft Access® (2013 version, Microsoft Corporation, Redmond, WA, USA) database. These data were then exported into Microsoft Excel® (2013 version, Microsoft Corporation, Redmond, WA, USA) and from there imported into NVivo (version 10, QSR International, Warrington, UK) or Stata (version 11, StataCorp LP, College Station, TX, USA).
Observation data
The hand-written notes taken during the observation sessions were typed up, using forms specific to the type of data collection. Any comments that could identify people or schools were anonymised before the transcripts were imported into NVivo. Codes were agreed by at least two members of the team. The observation notes were coded and analysed thematically, with attention paid to the five different types of data present:
-
verbatim quotes
-
non-verbatim quotes
-
actual observations
-
reflections ‘in the moment’
-
reflections after the event.
A framework was drawn up with examples relating to thematic analysis. This does not preclude the use of data relating to individual cases (teachers, lessons or schools). This analysis focused on how the teachers related to the training and any suggestions on how to improve the training. Quantitative aspects of the lesson observations were aggregated and descriptive statistics produced.
Teachers’ logs
The quantitative data from the teachers’ logs were used to calculate descriptive statistics such as the number of children attending per session, length of session, etc. The qualitative open responses were analysed thematically, with particular attention paid to school context characteristics, as well as how individual lessons worked in reality. In turn, the analysis helped us to understand how the intervention functioned as a whole, with particular attention paid to the reasons for any changes or amendments to the protocol/syllabus and whether or not they were successful, any unintended consequences of the intervention that could be incorporated or avoided in the future, engagement of participants (pupils, teachers and parents) and the acceptability of the intervention overall.
Interviews
Interviews were digitally recorded and verbatim transcripts prepared from the sound files. The transcripts were checked for accuracy against the sound files and corrections were made if required. Any comments that could identify people or schools were anonymised before the transcripts were imported into NVivo. All of the transcripts were read and re-read in order to gain an overall understanding of participants’ views and experiences. A framework analysis approach was then used in which initial codes were assigned to the text. These codes were discussed by three authors, refined and amended via an iterative process. The codes were then organised to identify overarching themes that were further discussed by the team. Illustrative quotes that captured each theme were then derived.
The quotes collected as part of these themes were analysed further with particular focus on participants’ views of the intervention, school and community context characteristics, knowledge, self-efficacy, parental support and behaviour change. Particular attention was paid to the reasons for any changes or amendments to the protocol/syllabus, any unintended consequences of the intervention that could be incorporated or avoided in the future, engagement of participants, acceptability of the intervention, perceptions of self-efficacy, or other contextual issues relating to the school or household environments.
Quality implementation indicators
When carrying out the analysis, particular attention was paid to elements that we felt were essential for the successful delivery of the intervention (following the style of the quality assurance framework developed for the ASSIST smoking cessation intervention). 68 These ‘essential elements’ drew on both quantitative and qualitative findings from the process evaluation. The qualitative data provided important details that ensured that, if the intervention was effective in quantitative terms, we could be sure that it was also ‘successful’ in qualitative terms, according to the children, parents, teachers and head teachers who were involved.
This allowed us to create a more realistic picture of the intervention using a combination of all the methods used in the process evaluation, providing a view of the intervention ‘in the round’. This involved looking at fidelity in a less mechanical way (although the more quantitative data will still be used), in particular considering key aspects of intervention implementation such as:
-
Whether or not teachers attended training.
-
If it was a positive learning environment.
-
The dose: including children only receiving part of the intervention.
-
Children’s behaviour.
-
Ethos: how the intervention material is handled and delivered.
-
Adaptations of material: this could include ‘personal embellishment’ that aids delivery or adaptations that are made in order to make the teaching culturally sensitive issues, which are likely to be ‘in the spirit’ of the intervention and not changing the content, or it could include changes such as removing some of the lessons or homeworks such that some of the key messages were lost.
This required consideration of, for example, whether or not the adaptations, etc., were ‘in the spirit’ of what we were trying to do.
As we considered fidelity to be more than just delivering the intervention lessons we needed to pay attention to these other elements because, if the AFLY5 intervention was shown to be effective, it would have been these observations that would have enabled us to provide useful guidance on what makes for successful intervention implementation.
Results of the process evaluation
The six intervention schools used for the process evaluation are listed in Table 23, according to their IMD and Ofsted score. 34,63
| IMD score34 | High level of teaching (Ofsted score outstanding or good)63 | Low level of teaching (Ofsted score satisfactory or inadequate)63 |
|---|---|---|
| Low | School 24 School 56 |
|
| Medium | School 58 | School 50 |
| High | School 36 School 3 |
It was not possible to recruit a school for each of the six options generated using this method; however, the spread of schools reveals an equal number of schools with high and low levels of teaching quality (three in each group), while the spread across the IMD scores34 also shows two schools per IMD group (low, medium and high).
The qualitative data, from interviews with 20 teachers (from all intervention schools) and 14 parents (from the six intervention schools in the process evaluation), presented below provide a more nuanced picture to contextualise the quantitative data. Quantitative and qualitative data on the modernising amendments made to the lessons in terms of length, differentiation for pupil ability and increased engagement are presented before the final section which focuses on the teachers’ views of the intervention.
Training and preparation
A total of 44 teachers from 29 schools delivered the intervention. Overall, 43 participants attended the training; 42 of these were teachers and one was a LSA. Data from the teacher training evaluation questionnaires indicated that 42 of the 43 (98%) teachers/teaching assistants who attended training agreed or strongly agreed with the statements ‘I feel confident that I can teach the nutrition sessions as per the lesson plans’ and ‘I feel confident that I can teach the physical activity sessions as per the lesson plans’. Teacher interview data indicated that, on the whole, they appreciated having the opportunity to work through the programme during the training and, in particular, the opportunity to receive instruction on the physical activity component:
I think the training we got when we came for the Active for Life was really, really helpful ‘cause it certainly pointed out a few things to us . . . about like how easy it was to run different activities.
School 15, teacher 2 interview
. . . I really liked the physical exercise training. And the activities that were supplied. Thought that was really good and gave me lots of ideas. I still use them, even though I’ve moved on to a different class . . . I thought the lady who ran the course was quite inspirational.
School 50, teacher 3 interview
Using data reported by the 39 teachers who noted at least one lesson preparation time in the teacher log, the median length of lesson preparation time calculated across lessons delivered was 10 minutes (IQR 10–20 minutes). Also from the teacher logs, 38 teachers noted at least once whether the lesson preparation time was more than, less than, or the same as usual (n = 450 lessons with data for this question). More preparation than usual was required for 46% of lessons, less time than usual for 15% and the same preparation as usual for 38% of lessons. During the interviews several teachers indicated negative feelings about the extra preparation time required and noted that it was often required for the physical activity sessions:
I mean once the resources were made it was fine . . . I don’t spend a lot of time preparing PE lessons. So I mean it might have been 15 minutes of reading through notes whilst it would have taken me 5 minutes normally so we are not talking a lot of time but . . . if it takes you 15 minutes and you are teaching it for 45 minutes how much, how long does each lesson take to prepare?
School 10, teacher 2 interview
Dose
Of the 44 teacher logs, 41 were completed and returned to the study team. The remaining three teachers were contacted by telephone and asked to provide only the number of lessons delivered and (if possible) the dates of delivery. Data from these 44 teachers showed that the mean number of lessons delivered was 12.3 out of all 16 lessons (SD 3.7 lessons, median 13.5 lessons, range 1–16 lessons) which equates to 77% of the intervention. Of the 41 teachers that returned teacher logs and indicated that they had delivered some of the intervention, all of them delivered lesson 1, but delivery declined over the intervention period such that only 46% delivered lesson 16. Seven teachers out of 41 (17%) delivered all 16 of the lessons. The data from the teacher logs and interviews revealed that by far the most commonly mentioned reason for not delivering all the lessons was lack of time to fit all the lessons into an already full curriculum. This is explored further using data from the teacher interviews (see Chapter 4, Amendments).
The mean number of homework assignments delivered, calculated from data given in the teacher logs, was 6.2 out of a total of 10 (SD 2.6, range 2–10) equating to 62%. Teachers who did not hand out the homework assignments stated in both the teacher logs and interviews that they had to prioritise core skills homework above those from the intervention:
All our homework is literacy + numeracy at the moment, building up to end of year tests.
School 51, teacher 1, lesson 11 – written extract from teacher’s log
In interviews with the parents, 5 out of 13 stated with certainty that their children had received AFLY5 lessons, and could remember homework items that were definitely part of the AFLY5 programme. Other parents were unsure about whether or not their children had received the lessons and homework assignments.
Reach
The reach, or percentage of children receiving all the lessons taught, calculated from teacher log data, was 95%. The time frame over which the lessons were delivered was a median of 17.7 weeks (IQR 9.1–23.3 weeks). The teacher logs indicated that there were two main patterns of delivery: (1) a regular dose, fairly evenly spread out; and (2) a varied dose that changed in response to lack of time, curriculum or engagement issues. As one teacher explained during an interview, they delivered AFLY5 in a variable dose because of the length of time required to deliver the AFLY5 programme and the potential for diminishing engagement over time:
. . . it went over a term or well over one term, normally every term’s like a fresh start, something completely different . . . so they need that chopping and changing ‘cause otherwise . . . they’d hate it and that’s with anything, that’s not just with Active for Life.
School 56, teacher 2 interview
Teaching staff
Based on the information reported in the teacher logs, among the 44 classes, all AFLY5 lessons over the full period were delivered by the same teacher in 51%, by two teachers in 20%, by three teachers in 22% and by four or more teachers in the remaining 7%. Out of the 80 teachers or teaching assistants listed as delivering at least one AFLY5 lesson, 49% had received the training. Of the 494 lessons for which data on who delivered the lesson were available, 386 (78%) were delivered by someone who had received the training. Of the 108 sessions recorded as taken by staff not trained in the intervention, 25 (23%) were covered by a main class teacher, 20 (19%) were taken by Preparation, Planning and Assessment (PPA) cover staff, who enabled teachers to work away from the classroom, 13 (12%) were delivered by supply teachers, nine (8%) by student teachers, nine (8%) by teachers whose status was not recorded, one (1%) by a LSA and the remaining 31 sessions (29%) were taken by people whose status was not recorded. AFLY5 lessons were considered suitable for handing over, since the lesson plan, worksheets and homework assignments were prepared. As data from the teacher logs and interviews revealed, the lessons that were handed over to these staff members, who were not trained in the use of AFLY5, were often the physical activity or PE lessons:
I only taught a few lessons my PPA cover took the majority . . . He did more the physical the activities, because he was taking PE.
School 45, teacher 1, interview
Amendments
The written materials provided no guidance about amending or adapting the lessons, but teachers were told at the teacher training sessions that they should teach the lessons in the order that they were listed and that they could amend content as long as the message and learning outcomes remained the same. Observations of the teacher training sessions indicated that teachers were already considering, at that stage, how the lessons could be adapted.
As they sit back down the teachers discuss how they might need to adapt a lesson for their own classes. One teacher is heard to say: ‘My kids can’t read so those work cards won’t work’.
Observation notes, teacher training session on ‘Physical Activity games’ held on 27/09/2011
The participants (teachers) engage well with trainer 4, making comments or asking questions throughout the session about how particular activities might work in their classes or how they might adapt the games.
Observation notes, teacher training session on ‘A Safe Workout’ held on 03/10/2011
Data from 39 teacher logs, when cross-referenced with 30 lesson observations, revealed that whether or not the lesson was amended was recorded for a total of 468 sessions, and that 28% were amended. A majority (89%) of the teachers amended the resources or lesson content on at least one occasion, and each of the 16 lessons was amended by at least one of the teachers. Comparisons between lesson observations and teacher intervention delivery logs revealed that some teachers did not record amendments that were noted during the lesson observation. On 20 occasions the teacher stated that they had not amended the session, but in nine (45%) of these sessions the observer indicated that amendments had been made, suggesting that teachers may have under-reported amending the lessons or had a different understanding of what constituted an amendment.
During interviews with 20 teachers from intervention schools (nine of whom were from schools included in the process evaluation), those who reported amending lessons said that they did so because they felt that the lessons or resource materials did not fully meet their needs. The reasons for their adaptations fell into four main categories: adjusting length of lessons to suit the overall ability level of a particular class; a need to differentiate for differing pupil ability; conversion for use with new technology; and making the lessons more appealing to pupils to ensure their engagement.
Length of the lessons
The restrictions of fitting the lessons into the curriculum meant that lessons had to be altered according to the needs of children. However, the teachers’ perception of the children’s ability or interest in the lessons themselves also led to amendments to lesson length. As a teacher explained, it was a case of assessing their pupils’ needs almost on a lesson-by-lesson basis rather than applying the lessons as laid out in the plan:
Just because when we looked at them, we go, there’s no way it’s going to take that long, I guess it’s knowing your children, knowing what to do . . .
And we realised that it wouldn’t, you know, what was a 50-minute lesson, you probably run that in half an hour.
School 56, teacher 3
Differentiation to take account of pupil ability
Amendments to the lessons and resource materials were also needed to account for children with lower levels of ability, special education needs or for those who had English as an additional language (EAL). These amendments varied from class to class, although a large number of reported changes related to the mathematical content, such as calculating the time spent on certain activities or the amount of sugar in certain drinks, as well as to the literacy content, as some of the vocabulary was deemed to be too complicated. As this teacher explained:
I did like what the ‘Active for Life’ was trying to do, it didn’t quite fit our curriculum really, and the materials were far too complicated . . . because of the EAL issues.
School 55, teacher 1 interview
Conversion of materials for use with new technologies
Amendments as a result of teaching style most often consisted of new slides that were compatible with interactive whiteboards. As one teacher explained when asked if they had made any amendments to the AFLY5 materials:
We used Active Inspire [interactive whiteboard] . . . when we were teaching the lessons just to get it in a kind of format that we can use, just to make it a bit more user-friendly.
School 28, teacher 2 interview
Engagement
Several of the amendments under the category of engagement could also be seen as ‘user-friendly’ changes, as they were primarily to make the lessons or resource materials more interesting, for either the teachers, the pupils or both. Amendments in this category included altering activities to include new aspects such as writing poems, making-up raps, creating posters or doing role play. As one teacher explained, in relation to the nutrition lessons:
I just changed them, made them more fun. They were really boring.
School 50, teacher 3 interview
The idea that these lessons or materials needed to be made more ‘fun’ was mentioned in both the interviews and teacher logs and was part of a theme identified in the qualitative data that indicated that teachers were unenthusiastic about the teaching materials in their original format because they felt that they were old fashioned.
Teachers’ views of the intervention
Although the quantitative fidelity of implementation data indicate that the AFLY5 intervention was well implemented, the interviews and teacher logs revealed a mixed view of the intervention. Teachers often noted the lack of time that they had to fit the lessons into an already full curriculum. This reasoning allowed teachers to present an acceptable ‘public’ explanation for not always implementing the intervention in full, which pointed to a structural constraint and, thus, did not involve them in overt criticism of the intervention programme. There was a sense, however, both during the interviews and in the analysis of the transcripts, that sometimes lack of time really meant lack of enthusiasm to make time or that lessons were to be fitted in only when there was extra time. Teachers were not wholly negative or positive about the intervention; the vast majority of responses were mixed:
So if anything this year we sort of almost missed it in a way because it was quite good at sort of, you know, filling, when we had little bits of time, pockets of time, we could, we could squeeze it in.
School 50, teacher 1a interview
This did not mean, however, that teachers disliked the overall purpose of AFLY5; on the contrary, they often mentioned how the messages behind the lessons were laudable, but that there were presentational issues. As these teachers explained:
It’s an amazing initiative, I think it was really, really important but it was just a huge amount to get through.
School 56, teacher 2 interview
So we did, a lot of the ideas were very good. But I just felt that the whole programme needs updating.
School 51, teacher 2 interview
Problems or concerns with the resources provided as part of AFLY5 were mentioned by many of the teachers, either for not being suited to their class, as this teacher explains:
Yeah I didn’t use any of your worksheets, I think I adapted every one of your worksheets.
School 10, teacher 1 interview
or for being rather old-fashioned when compared with other available resources:
I would suggest a DVD [digital versatile disc] or website resource to support the learning . . . Although good, the resource does seem unambitious and rather old-fashioned.
School 46, teacher 1, written extract from teacher’s log
The fact that teachers felt they had to alter the materials and that guidance and training on differentiation for ability was not provided as part of AFLY5 meant that there was a good deal of preparation for some teachers and this could also have contributed to the narrative regarding their lack of time. The results presented earlier revealed that 46% of teachers felt that, on average, they needed more time to prepare the AFLY5 lessons than regular lessons. This is perhaps not surprising given that these were completely new lessons. One limitation of this evaluation was that we did not determine how the preparation time for these lessons compared with that for any other completely new lesson. The trend towards more preparation time for PE lessons than nutrition lessons, for some of the teachers, could also reflect a general lack of enthusiasm for PE among some of the teachers. As this teacher reveals, this meant that, when they were running out of time, PE components were often dropped:
And I have to admit if there are any bits that I skipped it was the PE bits because we were doing PE anyway, but those required more preparation for me than a normal PE lesson.
School 10, teacher 1 interview
This could be seen as part of a wider issue relating to the lack of training and lack of confidence in delivering PE experienced by some primary school teachers. As this teacher explains when describing why the AFLY5 training was so helpful:
I am fairly keen on sport and PE in general but perhaps not the most confident in being able to teach it to children and stuff. So sort of taking it on board and being positive about it and seeing a sequence of lessons come about from it was actually very, very good.
School 36, teacher 1 interview
Some schools have found that one way to address this problem was to employ dedicated staff responsible for delivering PE lessons across the school years. Teachers in some schools handed over all their PE lessons to these staff and AFLY5 PE lessons were no exception. Again there was a tendency among some teachers to hand over the PE lessons in particular:
I mean the handbook is quite straightforward and he is a bit of a sports, more of a sports expert so he brought his sports expertise to it and what he tended to do was, he’d do the Active for Life lesson and then he’d finish it up with a game or something so they actually had sort of like extra PE.
School 15, teacher 2 interview
Chapter 5 Discussion
Principal findings of the randomised controlled trial
In this school-based cluster RCT, which is one of the largest to date and which takes account of the limitations of previous RCTs, we found no evidence of effect on our three primary outcomes: accelerometer-assessed time spent in MVPA; accelerometer-assessed time spent in sedentary behaviour; and consumption of fruit and vegetables. This was the case at the follow-up conducted immediately after the intervention and at the follow-up 1 year post intervention (that is, with no further lessons or teaching aimed at promoting healthy activity and dietary levels during that year). At both the immediate and long-term follow-up assessments, we did find that the intervention was effective in reducing child-reported time spent screen viewing at weekends and self-reported consumption of snacks and of high-energy drinks after taking account of multiple testing, but there was no effect on six other secondary outcomes and the effects observed for these secondary outcomes at the long-term follow-up may have been caused by chance. The discrepancy between no effect on accelerometer-assessed total sedentary behaviour and a reduction in reported screen viewing at weekends might reflect some systematic reporting bias (i.e. children from intervention schools remembering some of their lessons and homework assignments, such as ‘Freeze my TV’ and systematically under-reporting screen viewing to please their teachers or the fieldworkers). It is also possible that the intervention was effective specifically on screen viewing activities but that these were replaced with other sedentary behaviours, such as reading, rather than physical activities.
When we assessed potential mediators of the effect of the intervention on the outcomes, we found that the intervention increased children’s perception of maternal efforts to limit the time they spent screen viewing at the weekend and their knowledge related to the key messages of increasing physical activity, reducing sedentary behaviour and healthy eating that the intervention targeted. These two mediators explained approximately one-quarter of the effect of the intervention on screen viewing at the weekend. At the time of undertaking the trial we were unable to identify any validated tools for assessing child self-efficacy for reducing sedentary behaviour and so the parental efforts to limit this behaviour are the only specific mediators that we assessed for it. It is possible that, had we been able to assess child self-efficacy for reducing sedentary behaviour, the intervention might have increased it and that may further explain some of the effect of the intervention on this outcome. That said, we did not find any effect of the intervention on child self-efficacy for physical activity. Despite increasing the children’s perception of the effort that mothers put into limiting their screen viewing and increasing the children’s knowledge, the intervention did not affect accelerometer-assessed sedentary behaviour. It is possible that there is some reporting error by the children in the intervention schools in relation to their self-reported screen viewing at weekends and maternal limiting of this behaviour, as the intervention raised awareness of the need to modify this behaviour. If reporting bias explained these findings we might have expected to see similar results for other child-reported outcomes, which would be similarly biased. However, we do not see effects with other reported outcomes, including one of the primary outcomes, report of fruit and vegetable consumption. 62
In addition to an effect on the children’s report on maternal limiting of sedentary behaviour and on children’s knowledge, the intervention increased child self-efficacy for fruit and vegetable consumption, although in our main analyses the intervention did not affect self-reported levels of fruit and vegetable consumption. The disparity between this effect on self-efficacy and outcome suggests that for children increasing self-efficacy is insufficient to change their behaviour in relation to fruit and vegetable consumption. Although children of this age have some control over what they eat, parents will be responsible for buying food. We were unable to identify any validated tools for assessing the child’s perception of parental support and role modelling of fruit and vegetable consumption. Furthermore, a sense of having self-efficacy to change behaviour is not the same as the child wanting to change that behaviour; both the self-efficacy and desire to change will be needed. Self-efficacy for fruit and vegetable consumption was the only validated dietary self-efficacy questionnaire for children of this age that we could identify at the time of this study but, together with knowledge, it did not mediate the effect of the intervention on either consumption of snacks or high-energy drinks. So increasing children’s self-efficacy for fruit and vegetable consumption does not appear to be an effective means of altering other dietary changes.
The intervention did not have an impact on self-efficacy for being able to complete healthy levels of physical activity or the child’s perception of maternal or paternal logistic support or role modelling of physical activity. It is therefore perhaps not surprising that the intervention did not impact on accelerometer-assessed time spent in MVPA. 62 Physical activity in particular might require more intensive or different interventions than the AFLY5 intervention, to increase self-efficacy and provide supportive environments to enable both children and their parents to increase their physical activity. In recent decades there has been a notable decline in children actively travelling to school (on foot or by bike), as opposed to being driven. 69 The children of today also spend considerably less time in physically active play, both in school and outside school, than earlier generations, with reductions in the length of school break time, smaller school playgrounds and less curriculum time dedicated to physical activity lessons contributing to this. 70–72 Thus, interventions that provide a supportive environment both inside and outside of school might be essential to improve childhood levels of physical activity. This would be consistent with the World Health Organization’s concept of health-promoting schools (HPSs),73 where not only do children learn about healthy behaviours but the school environment is also supportive of healthy behaviours, by, for example, providing secure cycle racks, safe routes (car-limited or car-free) to and from school and healthy foods in canteens. A recent systematic review of the effect of schools adopting the HPS framework identified some positive effects but also noted the need for more robust, high-quality evaluation research in this area. 74
Economic evaluation
Results of the economic analysis showed that the cost per child from a school and provider perspective of implementing the intervention was £18 per pupil (£18,944 in total). Overall, the actual cost per pupil of the intervention is modest and, if the intervention had proved effective, it is unlikely that this cost would have been a barrier to its implementation.
In relation to the secondary analyses, AFLY5 appeared to be more costly than no intervention (control arm) in terms of total household expenditure, costs from a parental perspective and costs from an NHS perspective. However, these differences were imprecisely estimated with wide CIs that included the null value.
Process evaluation
The data recorded in the teacher logs and observations of lessons show that AFLY5 was implemented with a substantial degree of fidelity. Reach was high as 95% of children in intervention schools received lessons, 77% of all the lessons were taught and 62% of the homework assignments were delivered. Teachers did, however, record having to amend and adapt 28% of the lessons. Although teachers voiced support for the aims of AFLY5, their views of the programme itself were more mixed. After their training in AFLY5, teachers recorded feeling confident that they could deliver the lessons, but, when interviewed at the end of the intervention, some reported reticence about delivering the lessons on physical activity and a tendency to delegate this teaching to a colleague. These factors may have affected the quality of the delivery of the intervention and could therefore have influenced the null result.
The findings of the process evaluation have a number of implications for the development and evaluation of public health improvement interventions for use in educational settings. First, the main reason for the omission of lessons or homework assignments given by teachers in AFLY5 was a lack of time and pressure to focus on core literacy and numeracy skills. Finding the time to adapt the AFLY5 lessons for their children was also problematic for teachers. Educational policy in England and elsewhere increasingly emphasises academic attainment, and support for personal, social and health education has been downgraded since the feasibility study. 75 Evidence shows, however, that health and education are inextricably linked, with the more educated enjoying better health and well-being, and students in good health having higher academic attainment. 76 Nevertheless, the primary purpose of schools is to educate, and those seeking to improve students’ health need to work closely with teachers to ensure that interventions are understood to be addressing both educational and health goals so that the time spent on health improvement interventions is not perceived as doing so at the expense of educational attainment.
Second, although most teachers endorsed the need to improve children’s diets and increase levels of physical activity, some also expressed frustration with the lesson materials, which they felt were out of date and too generic. Teachers were particularly frustrated by the work needed to adapt the lesson plans to make them suitable for children with different levels of ability and more interactive so that they could be taught using new technologies such as interactive whiteboards. This probably reflects the rapid change in use of teaching information technology relative to the considerable time period currently required to develop an intervention and rigorously evaluate its effectiveness. Materials used in AFLY5 were originally developed in the USA in the late 1990s,25 then in 2006 adapted for the AFLY5 pilot and feasibility study, which was undertaken during 2006–9. 40 Following an application for funding and further development work,31 the full-scale RCT began in 2011. This timescale highlights the need for a more flexible approach to designing and evaluating interventions and also the challenge in deciding how much to change an intervention that has been used successfully elsewhere. As suggested by Craig and colleagues,77 pilot work should examine developmental uncertainties rather than simply being a small-scale version of the definitive trial. There are already good examples of best practice when it comes to the recruitment and randomisation of schools in trials so that, in the future, smaller-scale piloting of the acceptability of intervention materials, perhaps integrated as an internal pilot stage of the main trial,78 would avoid intervention materials becoming out-dated and speed up the quest for effective public health improvement interventions.
Third, our findings, like those of others,79 draw attention to the concerns that generalist school teachers have about teaching physical activity lessons. In our study some teachers said they valued the training AFLY5 provided on this; however, these lessons were more likely to be delegated to other staff who had not been trained in the AFLY5 intervention. Acknowledging this issue when designing physical activity lessons and ensuring that all those likely to get involved in the delivery of such an intervention are trained in it would help to ensure that fidelity is maintained.
Strengths and limitations of the Active for Life Year 5 study
Main trial design
The study design was carefully developed to take account of known sources of bias in other RCTs in this area. A protocol was published before recruitment started and a detailed analysis plan (to which we have adhered) was written prior to any access to the study data. We developed an intervention according to guidelines for complex interventions (see Rationale for the Active For Life Year 5 intervention)19,20 and we have shown that it was both feasible to deliver and promising in our pilot RCT. 29 Our sample size calculation, which took account of the likely degree of clustering from our pilot and feasibility studies and the number of outcomes that we planned to assess, indicated that we required a total of 1500 participants from 60 schools to be randomised and 1275 included in the primary analyses. 32,33 For all outcomes, except those related to accelerometer data, we achieved considerably higher numbers than this. The number included in the main analyses for accelerometer-based data was very slightly lower than this at both follow-up assessments (n = 1252 at immediate follow-up and n = 1066 at long-term follow-up). Sample size calculations are an approximation of the numbers required, and we doubt that such a small difference will have had a major impact on our conclusions. Participants were instructed to remove the accelerometer during swimming and contact sports; waist-worn accelerometers provide poor assessments of cycling and, as such, it may be the case that some activity in which the participants engaged was not captured. These issues would, however, apply equally to both intervention and control arms and thus should not have affected any assessment of intervention effectiveness. Consistent with widely adopted procedures, we applied an 8 hour per day minimum wear time criterion for our accelerometer data. 33 This may have meant that some participants who were active but wore the monitor for < 8 hours were excluded. We have previously shown that girls, children reporting that their parents restricted their sedentary behaviour and those from schools with larger year group sizes were more likely to wear accelerometers for the required time. 80 Those from more deprived schools and who reported more weekday activity were less likely to meet these requirements. However, the same criteria for how to wear the accelerometers were applied to both intervention arms. Furthermore, wear time was similar in children in intervention and control schools, and in sensitivity analyses at both the immediate and long-term follow-up assessments, using different approaches to deal with missing data, the results were essentially the same as in the main analysis. One school refused to deliver any of the intervention and others did not deliver all of the lessons. However, the per-protocol analyses, which do not differ from the main ITT analysis for either the immediate or the long-term follow-up, show that this does not explain the results.
At the time of applying for funding for the study we did not anticipate assessing effects of the intervention on number of potential mediators that we ultimately assessed. However, these are plausible mediators for our intervention and all have been assessed using questionnaires that have been developed and validated for use in children of the age of those in our trial. 45–50 Given that the original study design did not anticipate all of these analyses, we did not take account of these mediators in our sample size calculation. However, our effect estimates are precisely estimated with narrow 95% CIs, suggesting that we have reasonable power to detect effects if they were present. All of the mediators were reported by the children; thus, in relation to parental mediators, our analyses represent the effect of the intervention on the children’s perception of these. Such perceptions might differ from what the parents actually did, but we would argue that, for both the extent to which the parents provided logistic support and the role modelling of healthy behaviours, the child’s perception is important. For example, parents might undertake most of their physical activity during the day when the child is at school but that is not likely a useful model for the child.
We do not have information on schools that were invited to participate but declined, and this study was undertaken in the south-west of England. Although the participating schools included a range of levels of socioeconomic deprivation, class sizes and both rural and urban settings, we cannot assume that these results are generalisable to all primary school settings.
One of the reviewers of this report expressed concerns that the BMI and WC variables were skewed, both in their original units and when presented as z-scores, and suggested that we should have used lambda-mu-sigma (LMS) or other appropriate methods to deal with the skew of these variables. We can confirm that the residuals in the regression models for all analyses were normally distributed and our conclusions would not be changed by using LMS or other transformations, which might make the results less easy to interpret.
Economic evaluation
One of the main limitations was the incompleteness of data. It is a challenge when conducting economic evaluations alongside public health interventions to motivate teachers and research staff to provide the information needed to cost the intervention, a task often perceived as burdensome. Although the electronic timesheets aided the research staff, teachers found the completion of the logs onerous, and many were incomplete. The response to the parental questionnaire was low, and we are limited in what we can infer about the costs of the intervention from the perspective of the household and the NHS. Additionally, measures of uncertainty could not be calculated for the costs in the primary analysis (from the perspective of the provider and schools) because of the global nature of many of the resource use variables. The cost per quality-adjusted life-year, which would have allowed comparison of AFLY5 with other health-care and public health interventions, was not used in this evaluation because, at the time of designing the trial the EQ-5D-Y (European Quality of Life-5 Dimensions, Youth Version), the child and adolescent version of the EQ-5D questionnaire, had not been developed. Finally, although the residuals of the regression models for the cost–consequence analysis (and primary and secondary outcomes) were largely normally distributed, there was one exception: the NHS costs (one of the cost–consequence secondary outcomes) were not normally distributed and the results for this outcome may have been overestimated by one particular outcome for treatment in a child in the intervention arm that is unlikely to have been related to the intervention.
Process evaluation
The major strength of the process evaluation was the use of multiple sources of data, which has allowed us to cross-check information reported on the same issue. This detailed information has enabled us to build a more complete picture of how the intervention was delivered and received. This nuanced account of how and why the teachers adapted the intervention materials would have been difficult to achieve from the data recorded in the teacher logs alone or by using questionnaires. Another key strength is that the analyses of data were conducted with no knowledge of the effectiveness of the intervention itself. This means that our conclusions regarding fidelity of the intervention’s implementation were not influenced by knowing whether or not the intervention actually worked or vice versa.
One limitation of the process evaluation is that the proportion of teachers who provided data and the number of data provided by them varied considerably across schools. In the case of teacher logs, none was fully completed; therefore, the logs provided only a partial picture of what happened during the AFLY5 lessons. This has implications for the design of future trials in schools, as comprehensive data collection also adds to the time teaching staff have to spend on something that may not be perceived as central to their job. There was potential for bias if only those who felt particularly strongly about either the intervention or the research process itself agreed to take part in interviews. However, as the majority of data considered in the process evaluation came from all of the intervention schools in the trial and a range of views were offered by teachers and parents, it seems unlikely that such a bias has influenced our conclusions markedly.
Recruitment targets for parent interviews were based on previous research31 and were met in all but one of the intervention schools in the process evaluation. The recruitment process itself, however, was lengthy and both the parent and teacher interviews were carried out after the intervention finished, with a median of 288 days between the end of the intervention and the interviews. This could account for the lack of detail and recall in parental accounts and in some teacher accounts.
Comparisons with other studies
Our study builds on previous RCTs in this area by addressing the identified and important weaknesses of previous studies. 11–16 It is one of the few RCTs to have used accelerometers (rather than self-/parental-report) to assess the effect of an intervention in children on MVPA11,12 and the only one that we are aware of to use accelerometers to assess sedentary behaviours. 15,16 Previous trials that have used self-report for these outcomes have also been criticised for the lack of blinding in relation to the intervention and the likelihood that results might have been exaggerated by children or their parents knowing that they were in the intervention arm of the study. Thus, the lack of effect of the AFLY5 intervention on MVPA and sedentary behaviour might reflect a true assessment of school-based interventions that in pilot and feasibility work have been shown to fit within the main school curriculum and are relatively inexpensive. Previous trials that suggested benefit from such interventions, including the ones that our intervention is based on,23,24 were potentially biased by the use of self-/parental-report, lack of blinding of outcome assessments and other limitations.
Meaning of our study findings
There are several reasons why our intervention, and other similar interventions, might not have been effective at improving the primary (and most of the secondary) outcomes. First, the intervention itself might be inadequate. As described in the section for the rationale for this study, we began developing it, in line with guidance for complex interventions, in 2006, some 5 years prior to the start of the main RCT reported here. This time difference reflects the requirements for developing, testing feasibility and piloting the intervention, as well as then obtaining funds for the full RCT. It is possible that over these years the promise shown in earlier feasibility and pilot work had diminished as other local and national interventions aimed at promoting healthy levels of physical activity and diet were implemented in schools or through other settings or forms aimed at children.
Second, and related to our first point, it is possible that, to have an effect on contemporary children, more intensive behavioural change interventions are necessary and/or interventions that target the school environment as well as self-efficacy and knowledge in the children. However, our process evaluation suggested that any more intensive intervention (on top of how busy schools and teaching staff are) might not be acceptable to schools. Our review of the literature does not support greater effect of more intensive interventions. For example, a systematic review and meta-analysis of RCTs and clinical trials of any intervention aimed at increasing objectively assessed physical activity in children found a small increase in levels of activity in those receiving interventions but described the magnitude of this as being of small to negligible clinical importance. 12 There was heterogeneity between studies, with, on average, over half of the variability of time spent in MVPA being the result of between-study differences (I2-statistic = 52%). However, in detailed subgroup and metaregression analyses intervention characteristics, including type and intensity, did not explain this heterogeneity. 12 We are aware of only one further trial that has been published since that review. A recent RCT conducted in Australia in which the intervention consisted of altering school playgrounds and adding ‘loose materials’ that promoted creative free play without an emphasis on sport or activity per se, together with work with parents and teachers to address their concerns about children being allowed to play freely, resulted in a small increase in time spent in MVPA81 of a similar magnitude to that seen in the earlier meta-analysis and was likely to be driven by activity in the school setting that was ‘semi-compulsory’; it is unclear that any effects would last. 12 For our other primary outcomes, sedentary behaviour and fruit and vegetable consumption, we are not aware of any evidence from well-conducted RCTs that more intensive interventions aimed at individual children produce important effects.
Third, in current environments, where car transport is increasingly the norm and access to energy-dense cheap food is widespread, a more upstream societal and environmental approach, together with interventions targeted at schools and individual children, may be necessary to increase children’s physical activity and fruit and vegetable consumption. 82–84 Twin-based studies suggest that fidgeting (one form of activity that might have health benefits) and enjoyment of physical activity in children is strongly genetically heritable but that objectively assessed time spent in MVPA or parental report of time spent in activity is largely determined by shared environment. 85,86 In such studies ‘environment’ would include the school environment and what was taught there, as well as familial and broader social environments, but the difference between enjoyment of physical activity (largely genetic) and actual participation (largely environmental) suggests an important role for supportive physical environments that do not require children to consciously think of the activity as something they are enjoying or not. 85–87
We found beneficial effects of the intervention on three of the secondary outcomes – self-reported screen viewing and consumption of high-energy drinks and snacks – even after taking account of multiple testing. These could be the result of reporting bias by the children. However, we made every effort for the intervention to be built into normal school lessons in such a way that it did not alert children to the fact that they were in an intervention school, and the fieldworkers who collected data from the children were all blinded to school allocation. The beneficial effect for screen viewing might have been influenced by the slight imbalance at baseline for this characteristic, but this difference was adjusted for in all analyses. The effect was specific for just these three outcomes and not for other self-reported outcomes (screen viewing on weekdays, consumption of fruit and vegetables and consumption of high-fat foods). It may be that children feel more able to modify these behaviours than others that we have assessed, although we have no direct evidence to support this. Furthermore, although the effects of the intervention on the secondary outcomes at the long-term follow-up assessment were consistent in magnitude with those seen at the immediate follow-up, they did not reach our predefined level of statistical significance. Thus, our results suggest that the AFLY5 intervention may have some beneficial effect on childhood diet that is sustained for at least 12 months, although we cannot rule out the possibility that the long-term effect is the result of chance. It is unknown whether or not the relatively modest reductions in consumption of snacks (0.22 fewer per day) and high-energy drinks (0.26 fewer servings per day) seen in children from intervention schools, if sustained, would have long-term advantageous effects on levels of adiposity and associated cardiometabolic health, although we saw no effect of the intervention on BMI, WC or general or central overweight/obesity at the immediate or 1-year follow-up in our trial. A 20-minute reduction in screen viewing per weekend day might be important, but if this is not replaced by physical activity (as our accelerometer-based results suggested it was not) may not have real public health benefit. Furthermore, recent evidence suggests that (accelerometer-assessed) sedentary behaviour in children is not associated with future adiposity or cardiometabolic outcomes. 88
Recommendations for future research
Given the general null results of our well-conducted study, together with the findings of our process evaluation, we would suggest that a belief that school-based interventions that include changes to the school curriculum and/or environment are a cost-effective means of improving child health are misplaced. Our results show that such interventions are unlikely to have important magnitudes of effect on children’s health behaviours.
Effective health promotion in primary schools might require more substantial resources and more intensive interventions. However, our process work with parents and teachers show that these would require considerable additional resources so that they can be delivered alongside the demands necessary for the school curriculum. Before further resources are committed to RCTs in schools aimed at modifying children’s behaviours, research into the extent to which schools are able to take on this work in addition to their primary and important aim of educating children needs to be considered.
More generally, with respect to school-based interventions, our process evaluation results suggest that with rapidly changing teaching technologies, it may be necessary for funders and academics to consider how the time from feasibility and primary work through to full trial implementation can be shortened.
It is likely that broader interventions that include schools, but also go beyond these to include families and whole communities, may be required to have important public health effects on these outcomes in children. However, further work, starting with appropriate systematic reviews, intervention development, feasibility testing (as appropriate) and ultimately full RCTs, is required to make such conclusions. Of importance are broader changes that might be required. For example, a detailed review on the effect of sugar on childhood obesity has made important recommendations, including adding taxes to high-sugar foods and controlling the way that such foods are advertised and promoted by retailers. 89
Conclusions
In this school-based cluster RCT, which is one of the largest to date and which takes account of the limitations of previous RCTs, we found no evidence of effect on our three primary outcomes (accelerometer-assessed time spent in MVPA; accelerometer-assessed time spent in sedentary behaviour; and consumption of fruit and vegetables), both immediately and 1 year after the intervention. After taking account of multiple testing, there was evidence that the intervention might be effective in reducing screen viewing at weekends and reducing consumption of snacks and high-energy drinks immediately after the intervention and some suggestion that these effects persist up until 12 months post intervention. However, these lasting effects on the secondary outcomes may be the result of chance.
The AFLY5 intervention had no effect on the majority of potential mediators, particularly those relating to physical activity. AFLY5 did increase child self-efficacy for fruit and vegetable consumption, their knowledge in relation to healthy activity and diet and the extent to which the child believed their mother limited their sedentary behaviour. These effects were found to mediate the association between the intervention and only one of the secondary outcomes (i.e. time spent screen viewing at the weekend) and, even for this outcome, they explained less than one-quarter of the effect. Although the cost of the intervention was relatively low, it is unlikely that this intervention would be implemented within UK primary schools given that the intervention was only shown to improve three secondary outcomes. Although the quantity of lessons and homework assignments delivered was high, the difficulties of incorporating some of the AFLY5 materials into more technologically advanced and interactive current teaching practice, coupled with pressure on teachers’ time and a need to adapt the materials to suit students’ differing abilities and ensure their engagement, resulted in mixed enthusiasm for AFLY5. This, together with a tendency to delegate teaching of physical activity lessons to those not trained in the intervention, may have meant that the intervention messages were not as successfully delivered as anticipated and may explain why the intervention was found not to be effective. It is also possible that more intensive and up-to-date interventions, and those that focus on providing environments that are supportive of healthy behaviours within schools and the broader community, are required to produce beneficial effects on the ability of children to achieve healthy levels of physical activity and a healthy diet, although such an approach would require political commitment and necessary resources.
Overall, our study suggests that relatively simple school-based interventions that are designed to minimise costs to schools and teachers are unlikely to have a major impact on promoting healthy levels of physical activity and healthy diets in primary school children.
Acknowledgements
We thank all the students and teaching staff who took part in AFLY5. We thank all of the AFLY5 staff, including fieldworkers, administrative staff, computing and data management staff, and the trainers who provided teacher training. We thank Dr Julie Mytton (Consultant in Child Public Health, NHS Bristol and Bristol City Council), Dr Hugh Annett (retired Director of Public Health, NHS Bristol and Bristol City Council), Annie Hudson (former Strategic Director for Children, Young People and Skills, Bristol City Council) and Sheila Smith (Strategic Director for Children, Young People and Skills, North Somerset City Council) for their support of the AFLY5 study. NHS Bristol paid for the intervention costs. We also thank the Chair and members of the Trial Steering Committee for their advice and support throughout the project: Professor Janet Cade (University of Leeds), Professor Toby Prevost (Kings College London), Professor Naveed Sattar (University of Glasgow) and Professor Chris Bonell (Institute of Education, London).
Trial registration and ethics approval
The trial was registered with the International Standard Randomised Controlled Trial Number 50133740.
Ethics approval for the study was given by the University of Bristol Faculty of Medicine and Dentistry Committee for Ethics (reference number 101115) in January 2011.
Funding
The AFLY5 RCT is funded by the UK National Institute for Health Research (NIHR) Public Health Research programme (09/3005/04), which also paid the salary of Emma L Anderson and Sian L Wells.
Debbie A Lawlor and Laura D Howe work in a unit that receives funds from UK Medical Research Council (MC_UU_12013/5).
Ruth R Kipping and Rona Campbell work in the Centre for the Development and Evaluation of Complex Interventions for Public Health Improvement (DECIPHer), a UK Cross Research Council Public Health Research Centre of Excellence; joint funding (MR/KO232331/1) from the British Heart Foundation, Cancer Research UK, Economic and Social Research Council, Medical Research Council, the Welsh Government and the Wellcome Trust, under the auspices of the UK Clinical Research Collaboration, is gratefully acknowledged.
Laura D Howe is supported by a UK Medical Research Council Population Health Scientist fellowship (G1002375).
Debbie A Lawlor (NF-SI-0611–10196) and Tim J Peters (NF-SI-0512–10026) are NIHR senior investigators.
This study was undertaken in collaboration with the Bristol Randomised Trials Collaboration (BRTC), a UKCRC-registered clinical trials unit (CTU) in receipt of NIHR CTU support funding.
None of the funders had involvement in the TSC, the data analysis, data interpretation, data collection, or writing of the paper.
Contributions of authors
Debbie A Lawlor led the project, designed the study, wrote the effectiveness and mediation analysis plan, contributed to all effectiveness and mediation analyses, co-wrote the first draft of this monograph and coordinated responses from other authors, and obtained funds to complete the project.
Ruth R Kipping co-led the project, provided input into the creation of the effectiveness analysis plan and obtained funds to complete the project.
Emma L Anderson conducted effectiveness and mediation analyses and co-wrote the first draft of this monograph.
Laura D Howe contributed to all effectiveness and mediation analyses.
Catherine R Chittleborough obtained funds to complete the project.
Aida Moure-Fernandez conducted the economic evaluation and provided input into the writing first draft of the monograph (economic evaluation).
Sian M Noble co-led the project, conducted the economic evaluation, provided input into the writing first draft of the monograph (economic evaluation) and obtained funds to complete the project.
Emma Rawlins contributed to writing the process evaluation plan, collected qualitative data and analysed these and additional data for the process evaluation and provided input into the writing first draft of the monograph (process evaluation).
Sian L Wells was the project manager and worked with the project leaders to recruit schools and organise data collection and contributed to writing the process evaluation plan.
Tim J Peters co-led the project, provided input into the creation of the effectiveness analysis plan and obtained funds to complete the project.
Russell Jago co-led the project, wrote the process evaluation plan, provided input into the creation of the effectiveness analysis plan, provided input into the writing first draft of the monograph (process evaluation) and obtained funds to complete the project.
Rona Campbell co-led the project, wrote the process evaluation plan, provided input into the writing first draft of the monograph (process evaluation) and obtained funds to complete the project.
All authors made critical revisions to the monograph.
Data sharing statement
We are keen for these data to be used widely by the scientific community. Details of the study can be found on the website (www.bris.ac.uk/social-community-medicine/projects/afl/) and anyone interested in using these data should contact the corresponding author in the first instance. We do not have funds for data extraction and putting data files together for collaborators and may have to charge for providing this service.
Publications
The following peer-reviewed AFLY5 journal publications have been published to date (June 2016). Additional publications are planned and the study publication list will be kept up-to-date on the study website (www.bris.ac.uk/social-community-medicine/projects/afl/research/publications.html).
Lawlor DA, Jago R, Noble SM, Chitteborough CR, Campbell R, Mytton J, et al. The Active for Life Year 5 (AFLY5) school based cluster randomised controlled trial: study protocol for a randomised controlled trial. Trials 2011;12:181.
Lawlor DA, Peters TJ, Howe LD, Kipping RR, Noble SM, Jago R. The Active for Life Year 5 (AFLY5) school-based cluster randomised controlled trial: detailed statistical analysis plan. Trials 2013;14:234.
Wells SL, Kipping RR, Jago R, Brown J, Hucker D, Blackett A, et al. Characteristics associated with requested and required accelerometer wear in children. BMJ Open 2013;3:e003402.
Kipping RR, Howe LD, Jago R, Campbell R, Wells S, Chittleborough CR, et al. Effect of intervention aimed at increasing physical activity, reducing sedentary behaviour, and increasing fruit and vegetable consumption in children: Active for Life Year 5 (AFLY5) school based cluster randomised controlled trial. BMJ 2014;348:g3256.
Campbell R, Rawlins E, Wells S, Kipping RR, Chittleborough CR, Peters TJ, et al. Intervention fidelity in a school-based diet and physical activity intervention in the UK: Active for Life Year 5. Int J Behav Nutr Phys Act 2015;12:141.
Jago R, Rawlins E, Kipping RR, Wells S, Chittleborough CR, Peters TJ, et al. Lessons learned from the AFLY5 RCT process evaluation: implications for the design of physical activity and nutrition interventions in schools. BMC Public Health 2015;15:946.
Lawlor DA, Howe LD, Anderson EL, Kipping RR, Campbell R, Wells S, et al. The Active for Life Year 5 (AFLY5) school-based cluster randomised controlled trial: effect on potential mediators. BMC Public Health 2016;6:68.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health.
References
- Lock K, Pomerleau J, Causer L, Altamann DR, McKee M. The global burden of disease attributable to low consumption of fruit and vegetables: implications for the global strategy on diet. Bull World Health Organ 2005;83:100-8.
- Maynard M, Gunnell D, Emmett P, Frankel S, Davey Smith G. Fruit, vegetables, and antioxidants in childhood and risk of adult cancer: the Boyd Orr cohort. J Epid Comm Health 2003;57:218-25. http://dx.doi.org/10.1136/jech.57.3.218.
- Ness AR, Maynard M, Frankel S, Davey Smith G, Frobisher C, Leary SD, et al. Diet in childhood and adult cardiovascular and all cause mortality: the Boyd Orr cohort. Heart 2005;91:894-8. http://dx.doi.org/10.1136/hrt.2004.043489.
- Boreham C, Riddoch C. The physical activity, fitness and health of children. J Sports Sci 2001;19:915-29. http://dx.doi.org/10.1080/026404101317108426.
- Janssen I, Leblanc AG. Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. Int J Behav Nutr Phys Act 2010;7. http://dx.doi.org/10.1186/1479-5868-7-40.
- Ness AR, Leary SD, Mattocks C, Blair SN, Reilly JJ, Wells J, et al. Objectively measured physical activity and fat mass in a large cohort of children. PLOS Med 2007;4. http://dx.doi.org/10.1371/journal.pmed.0040097.
- Ekelund U, Luan J, Sherar LB, Eslinger DW, Griew P, Cooper A, et al. Moderate to vigorous physical activity and sedentary time and cardiometabolic risk factors in children and adolescents. JAMA 2012;307:704-12. http://dx.doi.org/10.1001/jama.2012.156.
- Telama R. Tracking of physical activity from childhood to adulthood: a review. Obes Facts 2009;2:187-95. http://dx.doi.org/10.1159/000222244.
- Maynard M, Gunnell D, Ness AR, Abraham L, Bates C, Blane D. What influences diet in early old age? Prospective and cross-sectional analyses of the Boyd Orr cohort. Eur J Public Health 2006;16:316-24. http://dx.doi.org/10.1093/eurpub/cki167.
- Janz KF, Burns TL, Levy SM. Tracking of activity and sedentary behaviours in childhood: the Iowa Bone Development Study. Am J Prev Med 2005;29:171-8. http://dx.doi.org/10.1016/j.amepre.2005.06.001.
- Dobbins M, Husson H, DeCorby K, LaRocca RL. School-based physical activity programs for promoting physical activity and fitness in children and adolescents aged 6 to 18. Cochrane Database Syst Rev 2013;2. http://dx.doi.org/10.1002/14651858.cd007651.pub2.
- Metcalf B, Henley W, Wilkin T. Effectiveness of intervention on physical activity of children: systematic review and meta-analysis of controlled trials with objectively measured outcomes (EarlyBird 54). BMJ 2012;345. http://dx.doi.org/10.1136/bmj.e5888.
- Delgado-Noguera M, Tort S, Martínez-Zapata MJ, Bonfill X. Primary school interventions to promote fruit and vegetable consumption: a systematic review and meta-analysis. Prev Med 2011;53:3-9. http://dx.doi.org/10.1016/j.ypmed.2011.04.016.
- Evans CE, Christian MS, Cleghorn CL, Greenwood DC, Cade JE. Systematic review and meta-analysis of school-based interventions to improve daily fruit and vegetable intake in children aged 5 to 12 y. Am J Clin Nutr 2012;96:889-901. http://dx.doi.org/10.3945/ajcn.111.030270.
- DeMattia L, Lemont L, Meurer L. Do interventions to limit sedentary behaviours change behaviour and reduce childhood obesity? A critical review of the literature. Obes Rev 2007;8:69-81. http://dx.doi.org/10.1111/j.1467-789X.2006.00259.x.
- van Grieken A, Ezendam NP, Paulis WD, van der Wouden JC, Raat H. Primary prevention of overweight in children and adolescents: a meta-analysis of the effectiveness of interventions aiming to decrease sedentary behaviour. Int J Behav Nutr Phys Act 2012;9. http://dx.doi.org/10.1186/1479-5868-9-61.
- Mallam KM, Metcalf BS, Kirkby J, Voss LD, Wilkin TJ. Contribution of timetabled physical education to total physical activity in primary school children: cross sectional study. BMJ 2003;327:592-3. http://dx.doi.org/10.1136/bmj.327.7415.592.
- Cleland V, Dwyer T, Blizzard L, Venn A. The provision of compulsory school physical activity: associations with physical activity, fitness and overweight in childhood and twenty years later. Int J Behav Nutr Phys Act 2008;5. http://dx.doi.org/10.1186/1479-5868-5-14.
- Developing and Evaluating Complex Interventions: New Guidance. London: Medical Research Council; 2008.
- Baranowski T, Cerin E, Baranowski E. Steps in the design, development and formative evaluation of obesity prevention-related behaviour change trials. Int J Behav Nutr Phys Act 2009;6. http://dx.doi.org/10.1186/1479-5868-6-6.
- Promoting Physical Activity for Children and Young People: NICE Public Health Guidance. London: NICE; 2009.
- US Health Policy Gateway . Recommendations on Physical Activity and Fitness. Secondary Recommendations on Physical Activity and Fitness n.d. http://ushealthpolicygateway.com/payer-trade-groups/health-promotion-disease-prevention/physical-activity-and-fitness/ (accessed August 2015).
- Wardle J, Henning Brodenson N, Cole TJ, Jarvis MJ, Boniface DR. Development of adiposity in adolescence: five year longitudinal study of an ethnically and socioeconomically diverse sample of young people in Britain. BMJ 2006;332:1130-5. http://dx.doi.org/10.1136/bmj.38807.594792.AE.
- Baker JL, Olsen LW, Sorensen TI. Childhood body-mass index and the risk of coronary heart disease in adulthood. N Engl J Med 2007;357:2329-37. http://dx.doi.org/10.1056/NEJMoa072515.
- Gortmaker SL, Peterson K, Wiecha J, Sobol AM, Dixit S, Fox MK, et al. Reducing obesity via a school-based interdisciplinary intervention among youth: Planet Health. Arch Pediatr Adolesc Med 1999;153:409-18. http://dx.doi.org/10.1001/archpedi.153.4.409.
- Gortmaker SL, Cheung LW, Peterson KE, Chomitz G, Cradle JH, Dart H, et al. Impact of a school-based interdisciplinary intervention on diet and physical activity among urban primary school children: eat well and keep moving. Arch Pediatr Adolesc Med 1999;153:975-83. http://dx.doi.org/10.1001/archpedi.153.9.975.
- Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice Hall; 1986.
- Bandura A. Self-Efficacy: The Exercise of Control. New York, NY: Freeman; 1997.
- Kipping RR, Payne C, Lawlor DA. Randomised controlled trial adapting US school obesity prevention to England. Arch Dis Child 2008;93:469-73. http://dx.doi.org/10.1136/adc.2007.116970.
- Kipping RR. Preventing Childhood Obesity 2010.
- Kipping RR, Jago R, Lawlor DA. Developing parent involvement in a school-based child obesity prevention intervention: a qualitative study and process evaluation. J Public Health 2012;34:236-44. http://dx.doi.org/10.1093/pubmed/fdr076.
- Lawlor DA, Jago R, Noble SM, Chittleborough CR, Campbell R, Mytton J, et al. The Active for Life Year 5 (AFLY5) school based cluster randomised controlled trial: study protocol for a randomised controlled trial. Trials 2011;12. http://dx.doi.org/10.1186/1745-6215-12-181.
- Lawlor DA, Peters TJ, Howe LD, Kipping RR, Noble SM, Jago R. The Active for Life Year 5 (AFLY5) school-based cluster randomised controlled trial protocol detailed statistical analysis plan. Trials 2013;14. http://dx.doi.org/10.1186/1745-6215-14-234.
- The English Indices of Deprivation 2010. London: Department for Communities and Local Government; 2011.
- Change 4 Life: Top Tips for Kids. London: Department of Health; 2009.
- Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ 2000;320:1240-3. http://dx.doi.org/10.1136/bmj.320.7244.1240.
- McCarthy HD, Jarrett KV, Crawley HF. The development of waist circumference percentiles in British children aged 5.0–16.9 y. Eur J Clin Nutr 2001;55:902-7. http://dx.doi.org/10.1038/sj.ejcn.1601240.
- Johnson ST, Kuk JL, Mackenzie KA, Huang TT, Rosychuk RJ, Ball GD. Metabolic risk varies according to waist circumference measurement site in overweight boys and girls. J Pediatr 2010;156:247-52. http://dx.doi.org/10.1016/j.jpeds.2009.08.010.
- Zimmet P, Alberti G, Kaufman F, Tajima N, Silink M, Arslanian S, et al. The metabolic syndrome in children and adolescents. Lancet 2007;369:2059-61. http://dx.doi.org/10.1016/S0140-6736(07)60958-1.
- Kipping RR, Jago R, Lawlor DA. Diet outcomes of a pilot school-based randomised controlled obesity prevention study with 9–10 year olds in England. Prev Med 2010;51:56-62. http://dx.doi.org/10.1016/j.ypmed.2010.04.011.
- Edmunds LD, Ziebland S. Development and validation of the Day in the Life Questionnaire (DILQ) as a measure of fruit and vegetable questionnaire for 7–9 year olds. Health Educ Res 2002;17:211-20. http://dx.doi.org/10.1093/her/17.2.211.
- Moore GF, Tapper K, Murphy S, Clark R, Lynch R, Moore L. Validation of a self-completion measure of breakfast foods, snacks and fruits and vegetables consumed by 9- to 11-year-old school children. Eur J Clin Nutr 2007;6:420-30. http://dx.doi.org/10.1038/sj.ejcn.1602531.
- Campbell KJ, Crawford DA, Salmon J, Carver A, Garnett SP, Baur LA. Associations between the home food environment and obesity-promoting eating behaviours in adolescence. Obesity 2007;15:719-30. http://dx.doi.org/10.1038/oby.2007.553.
- Robinson TN. Reducing children’s television viewing to prevent obesity: a randomised controlled trial. JAMA 1999;282:1561-7. http://dx.doi.org/10.1001/jama.282.16.1561.
- Sherwood NE, Taylor WC, Treuth M, Klesges LM, Baranowski T, Zhou A, et al. Measurement characteristics of activity-related psychosocial measures in 8- to 10-year-old African-American girls in the Girls Health Enrichment Multisite Study (GEMS). Prev Med 2004;38:60-8. http://dx.doi.org/10.1016/j.ypmed.2003.12.030.
- Saunders RP, Pate RR, Felton G, Dowda M, Weinrich MC, Ward DS, et al. Development of questionnaires to measure psychosocial influences on children’s physical activity. Prev Med 1997;26:241-7. http://dx.doi.org/10.1006/pmed.1996.0134.
- Domel SB, Baranowski T, Davis HC, Thompson WO, Leonard SB, Baranowski J. A measure of stages of change in fruit and vegetable consumption among fourth- and fifth-grade school children: reliability and validity. J Am Coll Nutr 1996;15:56-64. http://dx.doi.org/10.1080/07315724.1996.10718565.
- Davison KK, Cutting TM, Birch LL. Parents’ activity-related parenting practices predict girls’ physical activity. Med Sci Sports Exerc 2003;35:1589-95.
- Davison KK, Li K, Baskin ML, Cox T, Affuso O. Measuring parental support for children’s physical activity in white and African American parents: the Activity Support Scale for Multiple Groups (ACTS-MG). Prev Med 2011;52:39-43. http://dx.doi.org/10.1016/j.ypmed.2010.11.008.
- Cullen KW, Baranowski T, Rittenberry L, Cosart C, Hebert D, de Moor C. Child-reported family and peer influences on fruit, juice and vegetable consumption: reliability and validity of measures. Health Educ Res 2001;16:187-200. http://dx.doi.org/10.1093/her/16.2.187.
- White IR, Horton NJ, Carpenter J, Pocock SJ. Strategy for intention to treat analysis in randomised trials with missing outcome data. BMJ 2011;342. http://dx.doi.org/10.1136/bmj.d40.
- White IR, Carpenter J, Horton NJ. Including all individuals is not enough: lessons for intention-to-treat analysis. Clin Trials 2012;9:396-407. http://dx.doi.org/10.1177/1740774512450098.
- White IR, Thompson SG. Adjusting for partially missing baseline measurements in randomised trial. Stat Med 2005;24:993-1007. http://dx.doi.org/10.1002/sim.1981.
- School Teachers’ Review Body: 22nd Report. London: Department of Education; 2013.
- Annual Survey of Hours and Earnings. Secondary Annual Survey of Hours and Earnings. London: Office for National Statistics; 2013.
- Curtis L. Unit Costs of Health and Social Care 2013. Canterbury: Personal Social Services Research Unit (PSSRU); 2013.
- National Schedule of NHS Reference Costs. Secondary National Schedule of NHS Reference Costs 2010–2011. London: Department of Health; 2012.
- National Schedule of NHS Reference Costs. Secondary National Schedule of NHS Reference Costs 2012–2013. London: Department of Health; 2014.
- Methods for the Development of NICE Public Health Guidance. London: NICE; 2012.
- Barber JA, Thompson SG. Analysis of cost data in randomised trials: an application of the non-parametric bootstrap. Stat Med 2000;19:3219-36. http://dx.doi.org/10.1002/1097-0258(20001215)19:23%3C3219::AID-SIM623%3E3.0.CO;2-P.
- Gomes M, Ng ES, Grieve R, Nixon R, Carpenter J, Thompson SG. Developing appropriate methods for cost effectiveness analysis of cluster randomised trials. Med Decis Mak 2012;32:350-61. http://dx.doi.org/10.1177/0272989X11418372.
- Kipping RR, Howe LD, Jago R, Campbell R, Wells S, Chittleborough CR, et al. Effect of intervention aimed at increasing physical activity, reducing sedentary behaviour, and increasing fruit and vegetable consumption in children: Active for Life Year 5 (AFLY5) school based cluster randomised controlled trial. BMJ 2014;348. http://dx.doi.org/10.1136/bmj.g3256.
- Ofsted . Ofsted Report 2011. http://reports.ofsted.gov.uk (accessed June 2011).
- Rawlins E, Campbell R, Kipping R, Jago R, Wells SL, Lawlor DA. The Active for Life Year 5 (AFLY5) School-Based Cluster Randomised Controlled Trial Protocol: Process Evaluation Plan v1.3 2014. www.bristol.ac.uk/social-community-medicine/projects/afl/pdf/processevaluationplan.pdf (accessed August 2015).
- Audrey S, Holliday J, Campbell R. It’s good to talk: adolescent perspectives of an informal, peer-led intervention to reduce smoking. Soc Sci Med 2006;63:320-34. http://dx.doi.org/10.1016/j.socscimed.2005.12.010.
- Audrey S, Holliday J, Campbell R. Teachers’ perspectives on the implementation of an effective school-based, peer-led smoking intervention. Health Educ J 2008;67:74-90. http://dx.doi.org/10.1177/0017896908089387.
- Chittleborough CR, Nicolson AL, Basker E, Bell S, Campbell R. Factors influencing handwashing behaviour in primary schools: process evaluation within a randomised control trial. Health Educ Res 2012;27:1055-68. http://dx.doi.org/10.1093/her/cys061.
- Quality Assessment Framework. Cardiff: DECIPHer Impact; 2013.
- National Travel Survey: England 2013. London: Office for National Statistics; 2014.
- Parsad B, Lewis L. Calories In, Calories Out: Food and Exercise in Public Elementary Schools 2005 (NCES 2006–057). Washington, DC: National Centre for Education Statistics; 2006.
- Karsten L. It all used to be better? Different generations on continuity and change in urban children’s daily use of space. Child Geogr 2005;3:275-90. http://dx.doi.org/10.1080/14733280500352912.
- Blatchford P, Bains E. A Follow Up National Survey of Breaktimes in Primary and Secondary Schools. London: University of London; 2006.
- Health Promoting Schools. Geneva: WHO; 2016.
- Langford R, Bonell C, Jones H, Pouliou T, Murphy S, Waters E, et al. The WHO Health Promoting School framework for improving the health and well-being of students and their academic achievement. Cochrane Database Syst Rev 2014;4. http://dx.doi.org/10.1002/14651858.CD008958.
- Bonell C, Humphrey N, Fletcher A, Moore L, Anderson R, Campbell R. Why schools should promote students’ health and wellbeing. BMJ 2014;348. http://dx.doi.org/10.1136/bmj.g3078.
- Suhrcke M, de Paz Nieves C. The Impact of Health and Health Behaviours on Educational Outcomes in High-Income Countries: A Review of the Evidence. Geneva: World Health Organization; 2011.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew P, et al. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337.
- Wittes J, Brittain E. The role of internal pilot studies in increasing the efficiency of clinical trials. Stat Med 1990;9:65-72. http://dx.doi.org/10.1002/sim.4780090113.
- Morgan PJ, Hansen V. Classroom teachers’ perceptions of the impact of barriers to teaching physical education on the quality of physical education programs. Res Q Exerc Sport 2008;79:506-16. http://dx.doi.org/10.1080/02701367.2008.10599517.
- Wells SL, Kipping RR, Jago R, Brown J, Hucker D, Blackett A, et al. Characteristics associated with requested and required accelerometer wear in children. BMJ Open 2013;3. http://dx.doi.org/10.1136/bmjopen-2013-003402.
- Engelen L, Bundy AC, Naughton G, Simpson JM, Bauman A, Ragen J, et al. Increasing physical activity in young primary school children – it’s child’s play: a cluster randomised controlled trial. Prev Med 2013;56:319-25. http://dx.doi.org/10.1016/j.ypmed.2013.02.007.
- Lawlor DA, Pearce N. The Vienna declaration on nutrition and non-communicable diseases. BMJ 2013;347. http://dx.doi.org/10.1136/bmj.f4417.
- Lobstein T, Jackson-Leach R, Moodie ML, Hall KD, Gortmaker SL, Swinburn BA, et al. Child and adolescent obesity: part of a bigger picture. Lancet 2015;385:2510-20. http://dx.doi.org/10.1016/S0140-6736(14)61746-3.
- Roberto CA, Swinburn B, Hawkes C, Haung TT-K, Costa SA, Ashe M, et al. Patchy progress on obesity prevention: emerging examples, entrenched barriers, and new thinking. Lancet 2015;385:2400-9. http://dx.doi.org/10.1016/S0140-6736(14)61744-X.
- Fisher A, van Jaarsveld CHM, Llewellyn CH, Wardle J. Environmental influences on children’s physical activity: quantitative estimates using a twin design. PLOS ONE 2011;5. http://dx.doi.org/10.1371/journal.pone.0010110.
- Huppertz C, Bertel M, van Beijsterveldt CEM, Boomsma DI, Hudziah JJ, de Geus EJC. The impact of shared environmental factors on exercise behaviour from age 7 to 12. Med Sci Sports Exc 2012;44:2025-32. http://dx.doi.org/10.1249/MSS.0b013e31825d358e.
- Hammer M, Fisher A. Are interventions to promote physical activity in children a waste of time? No, finding an intervention that works is essential. BMJ 2012;345. http://dx.doi.org/10.1136/bmj.e6320.
- Stamatakis E, Coombs N, Tilling K, Mattocks C, Cooper A, Hardy LL, et al. Sedentary time in late childhood and cardiometabolic health in adolescence. Pediatrics 2015;135:e1432-41. http://dx.doi.org/10.1542/peds.2014-3750.
- Tedstone A, Targett V, Allen R. Sugar Reduction: The Evidence for Action. London: Public Health England; 2015.
Appendix 1 Knowledge assessment devised by study team
Appendix 2 Parental economic evaluation questionnaire
Appendix 3 Teacher training day observation guide
Appendix 4 Teacher training day evaluation form
Appendix 5 Lesson observation guide
Appendix 6 Teacher log
Appendix 7 Year 5 teacher interviews topic guide
Appendix 8 Head teacher interviews topic guide
Appendix 9 Parents’ interviews topic guide
Appendix 10 Children’s focus groups topic guide
List of abbreviations
- AFLY5
- Active for Life Year 5
- BMI
- body mass index
- CCA
- complete case analysis
- CD
- compact disc
- CI
- confidence interval
- CRB
- criminal records bureau
- EAL
- English as an additional language
- EQ-5D
- European Quality of Life-5 Dimensions
- HPS
- health-promoting school
- ICER
- incremental cost-effectiveness ratio
- IMD
- Index of Multiple Deprivation
- IQR
- interquartile range
- ITT
- intention to treat
- LMS
- lambda-mu-sigma
- LSA
- learning support assistant
- MAR
- missing at random
- MVPA
- moderate or vigorous physical activity
- Ofsted
- Office for Standards in Education, Children’s Services and Skills
- ONS
- Office for National Statistics
- PE
- physical education
- PPA
- preparation, planning and assessment
- RCT
- randomised controlled trial
- RQ
- research question
- SD
- standard deviation
- TSC
- Trial Steering Committee
- TV
- television
- WC
- waist circumference