Notes
Article history
The research reported in this issue of the journal was funded by the PHR programme as project number 10/3002/09. The contractual start date was in November 2011. The final report began editorial review in April 2016 and was accepted for publication in September 2016. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PHR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Harry Sumnall reports that his department has previously received funding from the alcohol industry (indirectly via the industry-funded Drinkaware) for unrelated primary research. David Foxcroft reports that his department has previously received funding from the alcohol industry for unrelated prevention programme training work. The sponsor university (Liverpool John Moores University) received and administered a payment from the alcohol industry for the printing of pupil workbooks in the Glasgow trial site.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2017. This work was produced by Sumnall et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
Scientific background and explanation of rationale
Adolescence is a period in which young people experiment with alcohol and establish use behaviours, and, as they age, the amount and frequency of use increases. 1 There is some evidence to suggest that earlier initiation of drinking is associated with later problematic misuse of alcohol (e.g. Bonomo et al. 2 and DeWit et al. 3), although systematic review has highlighted weaknesses in the evidence base for this. 4 The complexity of the relationship between earlier use and later problems is confounded by factors such as parental drinking and problem behaviours and/or behavioural disinhibition (e.g. Donovan et al. 5) and, accordingly, some authors have concluded that earlier initiation is better characterised as a marker of general risk proneness than as a causal influence. 6 However, there is stronger evidence to suggest that earlier age of self-reported drunkenness and the establishment of regular alcohol drinking is associated with a greater risk of adult alcohol-related problems. 4 Other acute and long-term consequences of heavy alcohol use in young people are evident, and these adversely impact on health, educational achievement, societal cohesion, criminality, welfare and well-being. 7,8 There are also clear geographic differences in the burden that alcohol places on the population, and these are closely associated with other major indicators of ill health and health inequalities (e.g. Public Health England9). Indeed, differences in alcohol use and the consequences of alcohol use are thought to be one of the major determinants of health and social inequalities. 10,11
Prevalence of alcohol use in the UK
The consumption of alcohol by those under the age of 18 years remains a public health concern in the UK. Evidence continues to suggest that, although the proportion of adolescents drinking alcohol across the UK has declined in recent years, those who do drink appear to be consuming more on each occasion. 12–18 Although this may be true at a national level, regional variations in drinking patterns also exist. 14,16,19 In comparison with the rest of the UK, drinking prevalence and excessive weekly drinking among adolescents has increased in Northern Ireland (NI) in recent years. 15 The results of the most recent Young Persons’ Behaviour and Attitudes Survey20 show that, of those who had ever drunk a full alcoholic drink (not just had a sip or taste), 56% had done so by the age of 13 years and 84% had done so by the age of 15 years. This is in comparison with 32% of 13-year-olds and 70% of 15-year-olds in Scotland reporting lifetime consumption of a full drink. 21 This does suggest a greater degree of alcohol use overall in NI than in Scotland (period prevalence). However, when comparing lifetime drunkenness in Scotland and NI, figures show that 39.3% of 11- to 16-year-olds in NI report lifetime drunkenness20 compared with 44% of 13-year-olds and 70% of 15-year-olds in Scotland. 21
Consequences of drinking
Adolescents are much more vulnerable than adults to the adverse effects of alcohol because of a range of physical and psychosocial factors that often interact (e.g. Newbury-Birch et al. 7). These adverse effects include (1) neurological factors due to changes that occur in the developing adolescent brain after alcohol exposure (e.g. Windle et al. ,22 Zeigler et al. 23 and Witt24); (2) cognitive factors due to the psychoactive effects of alcohol, which impair judgement and increase the likelihood of accidents and trauma (e.g. Rodham et al. 25); (3) social factors that arise from a typically high-intensity drinking pattern that leads to intoxication and risk-taking behaviour (e.g. Ellickson et al. 8 and MacArthur et al. 26); and (4) physiological factors resulting from a typically lower body mass and less efficient metabolism of alcohol (e.g. Windle et al. 22 and Zucker et al. 27). Physiological factors are compounded by the fact that young people have less experience of dealing with the effects of alcohol than adults, and that have fewer financial resources to help buffer the social and environmental risks that result from drinking alcohol. 28
Parental influence on young people’s drinking
Family factors are important in determining the nature and extent of adolescent alcohol use. These relate not only to the structure of families but also to family cohesion, family communication about issues such as substance use, parental modelling of behaviour (e.g. parental use of substances or rules on substance use), family management, parental monitoring/supervision, parent/peer influences and availability of alcohol in the family home. 16 For example, it has been argued that a trusting relationship between adolescents and their parents with open expression of ideas and feelings is an important factor in the reduction of health risk behaviours (e.g. Bahr et al. 29 and Riesch et al. 30). Moreover, parent–child communication processes have been proposed to mediate the effects of risk factors on problematic behaviour30 and better family communication processes have been shown to be protective against negative alcohol-related outcomes in young people. 31–35
The rapid escalation in the numbers of lifetime users and levels of use throughout adolescence is mirrored by the progressive detachment of adolescents from their parents and an increase in parental tolerance of adolescent drinking behaviour. 36 Although there are significant shifts in attachments of adolescents from parents to peers, there is still evidence that the influence of parents is considerable up to later adolescence and into early adulthood. 37 In a review of current evidence, Gilligan et al. 38 classified the environmental factors that determine adolescents’ propensity to engage in risky drinking as (1) social and (2) peer or family/parental. In the case of the latter, children are exposed to and learn about alcohol from an early age. 38 There has been much debate regarding the extent (if at all) to which parental tolerance of adolescent supervised drinking in the home, and by extension parental supply of alcohol to their children, can reduce heavier drinking and result in greater responsibility in terms of alcohol use. Young people’s drinking behaviours are said to be affected by their parents’ attitudes towards this behaviour and by parental supervision of their drinking (e.g. van der Vorst et al. 36), and parents often supply alcohol to their children, believing that it teaches them responsible drinking. 39 However, the risk arising from parental supply of alcohol is not well understood, and there is little evidence to support this as a harm-reducing practice. 38 In fact, although there is evidence suggesting that parental disapproval of drinking and limiting the supply of alcohol reduce adolescent drinking behaviour,36,40 some have suggested that parental supply of alcohol may reduce barriers to drinking, encouraging more frequent drinking and consumption of greater amounts of alcohol and even promoting a progression to unsupervised drinking. 41
Perceived parental approval of drinking has been linked to heavy drinking among high school and college students (e.g. Abar et al. 42). In support of the argument that permitting drinking at home promotes drinking in other contexts, van der Vorst et al. 43 reported that adolescents who were permitted to drink at home were also more likely to drink outside the home and to report more alcohol-related problems over a 2-year period than those who were not permitted to drink at all. In a survey of around 12,000 15- to 16-year-olds in the UK, Bellis et al. 44 reported that among those identifying any measure of unsupervised consumption, or heavy or frequent drinking, there was a significantly greater likelihood of alcohol-related violence, regretted sex or forgetting things after drinking. Furthermore, those reporting any measure of unsupervised consumption were also more likely to drink frequently and to drink heavily. 44 Livingston et al. ,45 in a 1-year follow-up of young women making the transition from high school to college, reported that those who were allowed to drink at home, either at meals or with friends, reported more frequent heavy episodic drinking (HED) at college, but those allowed to drink with friends reported the heaviest drinking episodes at both time points. However, in one Dutch longitudinal study, van der Vorst et al. 43 reported no differences in progression to problem drinking among young people whose parents provided high or low levels of supervision of alcohol use.
Universal interventions for preventing alcohol-related problems
Reviews of effective school-based universal alcohol prevention programmes for adolescents have failed to consistently identify interventions that are well designed, well implemented and properly evaluated (e.g. Jones et al. ,46 Foxcroft and Tsertsvadze,47–49 Nation et al. ,50 Faggiano et al. 51 and Spoth et al. 52). Foxcroft and Tsertsvadze,47–49 in their reviews of school-based universal interventions, were unable to recommend any single prevention initiative. However, one conclusion, which is consistent in all reviews, is that prevention interventions that effectively develop social skills appear to be superior in their impact to those that seek to enhance only knowledge (e.g. Foxcroft and Tsertsvadze,48,49 Nation et al. 50 and Faggiano et al. 51). In the absence of substantial evidence on particular programmes, guidance issued by the National Institute for Health and Care Excellence (NICE)53 in 2007 called for partnership working between schools and other stakeholders in efforts to prevent misuse. NICE also suggested that school-based interventions should aim to increase knowledge about alcohol, to explore perceptions about alcohol use and to help develop decision-making skills, self-efficacy and self-esteem. In family settings, universal prevention typically takes the form of supporting the development of parenting skills including parental support, nurturing behaviours, establishing clear boundaries or rules and parental monitoring. 47 Social and peer resistance skills, the development of behavioural norms and positive peer affiliations can also be addressed with these types of approaches. Most of the studies included in Foxcroft and Tsertsvadze’s 2011 Cochrane review47 of family-based alcohol prevention activities reported positive effects on behaviour and, although these tended to be small, they were generally consistent and persisted into the medium to longer term.
School-based alcohol education programmes in the UK for those aged < 18 years have predominantly been classified as universal, as they have been typically targeted at all pupils regardless of screened or perceived level of alcohol-related risk. 54 Outcomes assessed in universal prevention programmes have included those related to quantity and frequency of alcohol use (e.g. period prevalence, frequency of drunkenness, HED), as well as harms associated with consumption. 48 With respect to this last set of outcomes, harms can arise both from the actions of the drinker (e.g. accidents, health problems) and from the drinking of others (e.g. drunk driving, violence). Universally targeted alcohol prevention programmes (e.g. McBride et al. ,55 Newton et al. 56 and Vogl et al. 57) that aim to reduce harms associated with alcohol may, therefore, provide messages of harm reduction rather than focus on abstinence. In addition to aiming to reduce alcohol-related harm through reducing consumption, these types of programmes aim to reduce those direct and indirect harms reported by those recipients who continue to drink.
Introduction to the intervention components of STAMPP
The Steps Towards Alcohol Misuse Prevention Programme (STAMPP) combined a school-based alcohol harm reduction curriculum and a brief parental intervention that is designed to support parents in setting family rules around drinking. Chapter 2 (see Intervention) provides further information on the development, delivery and content of the intervention.
The classroom component of STAMPP is the School Health and Alcohol Harm Reduction Project (SHAHRP), which is an example of a universally targeted classroom intervention. It combines a harm reduction philosophy with skills training, education and activities designed to encourage positive behavioural change. 55,58 It is a curriculum-based programme delivered in two phases over a 2-year period, and is described by its developers as having an explicit harm reduction goal. The development of the SHAHRP is described by Farringdon et al. 59 It was originally developed in the 1990s in Western Australia, and the core components of the intervention were based on a systematic literature review of effective substance use education. The curriculum was written by practising teachers (with experience of developing student-centred learning approaches), with the assistance of research academics, and underwent piloting, evaluation and further development processes. Key evidence-based features of the programme include (according to the formative evaluation of the SHAHRP):59
-
social inoculation (phase 1 of the intervention, delivered prior to alcohol initiation)
-
relevance to drinking trajectories of recipients (i.e. phase 2 of the intervention, introducing harm reduction, is implemented after pupils are most likely to have initiated alcohol use)
-
core intervention (phase 1) with booster sessions (phase 2)
-
experientially focused and based on the drinking experiences of young people
-
skills based with normative components
-
incorporation of utility knowledge about alcohol use.
Includes specialist training of programme deliverers (e.g. teachers)
In the original Australian programme evaluation,55 which compared the intervention group with the control group receiving education as normal (EAN), the intervention group reported significantly less alcohol use: a difference in quantity of 31.4%, 31.7% and 9.2% at 8, 17 and 32 months after baseline, respectively; and significant differences in reports of hazardous drinking, defined as consuming more than two (female)/four (male) standard drinks (10 g of alcohol) per occasion, once per month or more often at 8 months (25.7%) and 17 months (33.8%) after baseline but not at the 32-month follow-up (4.2%). Intervention students also reported significantly greater knowledge at the 8-month follow-up, and this was maintained at the 20-month follow-up but not at 32 months. In addition, there was a significant difference between the study groups in the number of self-reported harms they experienced from their own use of alcohol after both phases of the intervention. This was maintained 17 months after the intervention but not at the final follow-up at 32 months. Finally, the intervention group developed significantly better alcohol-related attitudes (attitudes that supported less harmful alcohol-related behaviours) from first follow-up at 8 months, and this was maintained to the 32-month follow-up point.
A previous investigation of the SHAHRP utilising a non-experimental design was conducted in NI by some of the current STAMPP investigators,60 and found that, after appropriate adaptation (e.g. normative epidemiological facts updated, timings of lessons altered), participation in the SHAHRP was associated (across 32 months of follow-up) with benefits for pupils. Between-group comparison showed that intervention pupils reported significantly fewer alcohol-related harms over time, and, when drinking behaviour trajectories were modelled using latent class growth modelling, intervention pupils were significantly more likely than pupils receiving EAN to be members of those latent classes that reported less increase in drinking over time, that had a larger increase in alcohol knowledge and healthy attitudes, and that were more likely to report a smaller increase or no increase at all in alcohol-related harms.
The parental component of STAMPP was developed by the trial team and was based on earlier work by Koutakis et al. ,61 who found that giving advice to parents about setting strict rules around alcohol consumption reduced drunkenness and delinquency in 13- to 16-year-olds in Sweden (the Örebro Prevention Programme). The original Swedish intervention was based on empirical evidence that suggested that lower levels of youth alcohol drinking were associated with stricter parental attitudes against youth alcohol use and involvement in structured, adult-led activities. Similarly, permissive parental attitudes towards children’s alcohol use have been shown to be better predictors of offspring alcohol use than parents’ own use. 62 However, the original Swedish programme was relatively intensive (six 20-minute standardised presentations and discussion given to parents of 13- to 16-year-olds during regular school-based parent–teacher meetings) and so Koning et al. 63,64 adapted this intervention further (a single parents evening) and combined it with a school-based alcohol curriculum (the Dutch Healthy School and Drugs programme). They found that this combined intervention was associated with a significantly reduced rate of frequency of drinking or weekly drinking, and this was partly mediated by changes in parental rules and attitudes towards alcohol (i.e. stricter rules and attitudes were developed).
Explanation of rationale
Given the prevalence of underage drinking in the UK, the reported problems, costs and harms associated with this behaviour and the lack of a robust UK evidence base for universal alcohol prevention interventions, this work aimed to investigate an adapted form of the evidence-based SHAHRP55,60 in a culturally appropriate and curriculum consistent manner in the NI and Glasgow/Inverclyde post-primary school settings. Furthermore, considering the strong links between family behaviours and young people’s substance use, the effect of introducing a parental component to the core SHAHRP curriculum was examined.
Specific objectives
Primary objectives
-
To ascertain the effectiveness and cost-effectiveness of a combined classroom and parental intervention (STAMPP) in reducing alcohol consumption (HED, defined as self-reported consumption of ≥ 6 units for males and ≥ 4.5 units for females in a single episode in the previous 30 days) in school pupils (in school year 9 in NI or in S2 in Scotland in the academic year 2012–13 and aged 12–13 years) at 33 months after the baseline time point (T3).
-
To ascertain the effectiveness of STAMPP in reducing alcohol-related harms, as measured by the number of self-reported harms (harms caused by own drinking) in school pupils (school year 9 or S2 in the academic year 2012–13 and aged 12–13 years) at T3.
Secondary objectives
-
To ascertain the effectiveness and cost-effectiveness of STAMPP in reducing alcohol consumption (HED, defined as self-reported consumption of ≥ 6 units for male students and ≥ 4.5 units for female students in a single episode in the previous 30 days) in school pupils (school year 9 or S2 in the academic year 2012–13) at 12 months after the baseline time point (T1), and 24 months after the baseline time point (T2).
-
To ascertain the effectiveness of STAMPP in reducing alcohol consumption (self-reported alcohol use in lifetime, previous year and previous month; number of drinks in ‘typical’ and last-use episodes; age of alcohol initiation, unsupervised drinking) in school pupils (school year 9 or S2 in the academic year 2012–13), at T1, T2 and T3.
-
To ascertain the effectiveness of STAMPP in reducing alcohol-related harms, as measured by self-reported harms caused by own drinking at T1 and T2 and self-reported harms caused by the drinking of others at T1, T2 and T3, in school pupils (school year 9 or S2 in the academic year 2012–13).
Chapter summary: introduction to the research
Although alcohol use in the general population of young people is falling in the UK, there are regional differences, and those who initiate use early, are regular drinkers or report early drunkenness are more likely to experience adverse outcomes or a greater number of years of ill health. The responses to young people’s alcohol use have traditionally focused on school-based educational approaches, although general population policies, such as restrictions on marketing and pricing increases, are also likely to affect consumption. However, the evidence base for school-based universal alcohol interventions (i.e. those that target a whole population, regardless of level of risk) is weak and, although some skills-based approaches have been shown to produce changes in different indicators of alcohol use, effect sizes are often small and the longevity of the intervention effect is limited. Other research has shown that family factors are an important determinant of young people’s alcohol use. For example, in those families in which there is good communication and authoritative rules on alcohol are in place, young people are less likely to drink. In keeping with the literature on school-based interventions, however, there are few family-based programmes that have found significant reductions in indicators of alcohol use and alcohol harm.
This research sought to determine the effectiveness of a programme, STAMPP, that is a school-based alcohol harm reduction curriculum with a brief parental intervention designed to support parents/carers in setting family rules around drinking. We examined whether or not STAMPP was effective in reducing HED and self-reported harms related to recipients’ own use of alcohol. The programme rationale was that stricter parental/carer rules and attitudes towards alcohol would reinforce learning and skills development in the classroom. The classroom component, SHAHRP, was a universally targeted curriculum that combines a harm reduction philosophy with skills training, education and activities designed to encourage positive behavioural change. It was delivered in two phases over a 2-year period and was adapted from an original Australian programme in an early study,55 with the assistance of education and prevention specialists. The brief intervention delivered to intervention pupils’ parent(s)/carer(s) comprised a short, standardised presentation delivered at specially arranged evenings on school premises. The presentation included an overview of the Chief Medical Officer (CMO)’s guidelines for drinking in childhood,65 information on alcohol prevalence in young people, corrected (under)estimates of youth drinking rates and highlighted the importance of setting strict family rules around alcohol. The presentation was followed by a brief discussion on setting and implementing authoritative family rules on alcohol. All intervention pupils’ parents/carers were followed up by a mailed leaflet, whether or not they attended the parents’ evening, which provided a summary of the key information delivered in the evening and coincided with phase 2 of the classroom intervention.
Chapter 2 Methods
Trial design and setting
A cluster randomised controlled trial (CRCT) in NI and Glasgow/Inverclyde Education Authority areas in the UK, with schools as the unit of randomisation.
Sample and participants
The sampling frame comprised all mainstream post-primary schools in NI (n = 208) and Glasgow/Inverclyde (n = 36). All schools in the sampling frame were initially assessed for satisfaction of the inclusion criteria and willingness to participate in the trial. Schools in the Eastern Health Board of NI, which included the capital city Belfast, were excluded, as the classroom component, SHAHRP, was already being delivered to some schools in that area by a non-governmental organisation independently of the trial.
Male and female students attending mainstream secondary schools in NI and Glasgow/Inverclyde were included. Schools were randomised into the trial and baseline data were collected when pupils were in school year 8 or S1, and the intervention was delivered when pupils were in school year 9 or S2 in the academic year 2012–13 and aged 12–13 years.
Pupils not in the specified school year and age group, and pupils in non-mainstream and vocational education (e.g. pupil referral units, further education colleges) were excluded. Pupils with special educational needs in mainstream classrooms were excluded at the discretion of teachers, as the intervention materials had not been developed for use with this population.
In each participating school, all students in attendance at the time of data collection were asked to complete the project questionnaires. Questionnaires were administered to participants at the baseline time point (T0) in June 2012 and at three follow-up points: T1, T2 and T3.
Intervention
Students in the intervention condition received the SHAHRP,55 as previously adapted and tested for use in NI. 60 The parent(s) or carer(s) of intervention condition students were also invited to receive a brief intervention. All intervention pupil parents/carers, regardless of attendance at the parents’ evenings, were mailed a follow-up information leaflet.
Phase 1 of the NI SHAHRP classroom curriculum consisted of six lessons (with 16 activities) delivered to students in school year 9 or S2 (aged at least 12 years) by trained teachers. Phase 2 consisted of four lessons (with 10 activities) delivered in school year 10 or S3 (aged 13–14 years) by trained teachers.
Training sessions for teachers took place annually in a neutral location and included an introduction to the concepts involved in alcohol harm reduction, rehearsal of delivery of each of the sessions in that phase of delivery and raising of awareness of potentially difficult issues/areas. Teachers were trained by the STAMPP trial manager prior to phase 1, and by the STAMPP trial manager, STAMPP research assistant and an alcohol worker from a local third-sector organisation before phase 2. Phase 1 was delivered between September and December 2012 and phase 2 was delivered between September and December 2013. Curriculum activities incorporated various strategies for interactive dissemination including delivery of utility information, skill rehearsal, individual and small group decision-making, and discussions based on scenarios suggested by students. There was a particular emphasis on identifying alcohol-related harms in specific scenario-based exercises (e.g. a night out) and specific discussions on strategies that might be employed to reduce harms.
Phase 1 lessons broadly examined myths about alcohol, reasons why people drink or do not drink alcohol, alcohol and the body, the relationship between amount consumed and behavioural consequences, alcohol and the media, and real-life situations. Phase 2 lessons focused on more specific adolescent drinking behaviours, real-life scenarios or potential experiences while in an environment in which alcohol is consumed. These lessons specifically examined peer pressure, similarities and differences between males and females in a drinking context, drink spiking, responsibilities towards friends, grading of risk environments or situations and peer advice around alcohol.
Interactive involvement was a key feature of the lessons, and a workbook and compact disc (CD) accompanied both phases of the project, allowing for more active learning. Further details of the SHAHRP curriculum used in this study can be found elsewhere. 60 However, an important difference between the present study and that of McKay et al. 60 is that the pupils in the present study were 1 year younger at both intervention stages. The targeting of younger pupils in the current trial (i.e. ages 12–13 years) was justified on the basis of survey data suggesting that the median age of initiation of alcohol use was < 13 years. 20,21 In addition, the intervention was only delivered by teachers in the current study, whereas in the earlier work, both teachers and external facilitators (youth workers) were used. Pupils in Scotland received the SHAHRP curriculum but, when necessary, the materials were further refined for the cultural context. For example, information that was provided about emergency services related to the Scottish Ambulance Service rather than the Police Service of Northern Ireland.
The classroom component of STAMPP differed from the original Australian SHAHRP curriculum in a number of ways. The Australian programme was targeted at pupils aged ≥ 13 years in phase 1 (as was the original NI adaptation of the SHAHRP described in Chapter 1, Introduction to the intervention components of Steps Towards Alcohol Misuse Prevention Programme), the curriculum was longer (17 activities delivered in 8–10 lessons in phase 1, and 12 activities delivered over 5–7 weeks in phase 2) and Australian reference data were used in the lessons.
The brief intervention delivered to the parent(s)/carer(s) of children in the intervention comprised a short, standardised presentation delivered by a team of trained facilitators (independent of the trial team) at specially arranged parent evenings on school premises. The presentation included an overview of the CMO’s 2009 guidelines for drinking in childhood,65 information on alcohol prevalence in young people and corrected (under)estimates of youth drinking rates, and it highlighted the importance of setting strict family rules around alcohol, with the recognition that children often model their own alcohol use behaviour on that of their parent(s)/carer(s). The presentation was followed by a brief discussion on setting and implementing authoritative family rules on alcohol. All intervention pupils’ parent(s)/carer(s) were followed up by a mailed leaflet (March 2014) that provided a summary of the key information delivered over the course of the evening. The delivery of the parental intervention coincided with phase 2 of the SHAHRP between September and December 2013.
The parental/carer activity was developed by the research team for this trial, and was partly based on the Dutch adaptation of the Swedish Örebro Prevention Programme undertaken by Koning et al. 64 These researchers delivered a brief intervention to parents on setting strict rules around alcohol in combination with a school-based alcohol curriculum (the Dutch Healthy School and Drugs programme). The parental component in STAMPP differed from the Dutch intervention in a number of ways. First, the Dutch activity was delivered at two annual parent evenings as part of general school discussions; second, the intervention was delivered by a member of the Dutch research team; third, the content of the presentations used Dutch data and was orientated towards challenging societal alcohol norms; and, fourth, attendees set their own family alcohol rules through discussion with a classroom learning mentor, whereas in STAMPP rules were based on the CMO’s guidance. 65 Both approaches utilised a follow-up mailed information leaflet.
The control group participants continued with EAN within their school, which would include standard personal, social and health education but would not be uniform across all such schools. Parents/carers of control students received no intervention. Provision of alcohol use education as part of statutory education or usual school activities (and, therefore, not able to be experimentally manipulated) was monitored through information collected as part of an online teacher questionnaire (see Chapter 4, Online survey with teachers).
Please refer to Appendix 1 for the logic models underpinning the intervention.
Outcome measures
Primary outcomes
-
Self-reported alcohol use (HED, defined as self-reported consumption of ≥ 6 units for male students and ≥ 4.5 units for female student in a single episode in the previous 30 days) assessed at T3. This was dichotomised at never/one or more occasions.
-
The number of self-reported harms (harms caused by own drinking) assessed at T3.
Secondary outcomes
-
Self-reported alcohol use (HED; defined as self-reported consumption of ≥ 6 units for male students and ≥ 4.5 units for female students in a single episode in the previous 30 days) assessed at T1 and T2. This was dichotomised at never/one or more occasions.
-
The number of self-reported harms (harms caused by own drinking) assessed at T1 and T2.
-
Self-reported alcohol use (lifetime, previous year and previous month) assessed at T1, T2 and T3.
-
Support service utilisation assessed at T2 and T3.
-
The number of self-reported harms caused by the drinking of others assessed at T1, T2 and T3. This was assessed in all participants.
-
Age of alcohol initiation (age at which a whole alcoholic drink was first consumed, not just a sip or a shared drink) assessed at T1, T2 and T3.
-
Unsupervised alcohol use (prevalence of drinking with peers without the supervision of parents/guardians) assessed at T1, T2 and T3.
-
The number of units of alcohol consumed in a ‘typical’ episode and the last-use episode assessed at T1, T2 and T3.
Description of primary and secondary outcome measures
Alcohol use behaviours (quantity, frequency and period prevalence measures) and definitions of use were taken from two major surveys on alcohol use in young people: the European Survey Project on Alcohol and other Drugs (ESPAD)13 and Smoking, Drinking and Drug Use in Young People (11–15 years) survey. 12 Frequency and age of first drunkenness were derived from the Growing Up Unequal: Gender and Socioeconomic Differences in Young People’s Health and Well-Being. Health Behaviour in School-Aged Children (HBSC) Study: International Report From The 2013/2014 Survey. 66,67
Harms associated with own use of alcohol were measured using a 16-item scale, developed for the Australian SHAHRP trial (internal consistency 0.9)58 (see Appendix 3). Harms associated with other people’s use of alcohol were measured using a six-item scale (internal consistency 0.7). 55 For both harm scales, participants were asked to indicate on a Likert scale how many times in the past 6 months they had experienced each individual harm. For example, participants were asked to report the frequency of having a hangover after drinking (question 4), and of getting into a physical fight when drinking (question 7).
Data on service use by participants were collected using a bespoke instrument that incorporated items taken from the Client Service Receipt Inventory,68 which was specifically adapted for childhood,69 and items relating to the use of judicial services. The instrument included an information page with definitions of some of the public services in case the students were unfamiliar with them. The instrument was designed with input from relevant professionals (e.g. an educational psychologist, social workers, Scottish and Northern Irish teachers), and was reviewed by a social researcher who was experienced in delivering questionnaires to children, and by other health economists. The instrument asked participants to report their use of services in the previous 6 months, and data were linearly interpolated over the study period to fill in gaps in survey periods and allow for total costs to be estimated. 70 Intervention costs were also measured. These included costs associated with staff training, delivery of the intervention, travel and consumables. In the STAMPP trial, intervention schools delivered the classroom component as part of their usual curriculum time, and so additional delivery costs were not incurred. However, this might not necessarily be true for future delivery, hence the inclusion of estimates of these costs in the economic evaluation.
Other self-reported measures
In addition to the primary and secondary outcomes, study questionnaires also included additional measures and scales. These were included to allow future mediation analysis and other exploratory analyses outside of the data analysis plan (DAP).
-
The period prevalence of alcohol use (self-reported alcohol use in lifetime, previous year, previous 6 months and previous month).
-
The frequency of lifetime (self-defined) drunkenness (Likert scale, ‘never’ to ‘more than 10 times’) and age of first drunkenness.
-
The context of alcohol use [e.g. abstention, unsupervised drinking (prevalence of drinking without the supervision of parents/guardians) or supervised drinking].
-
Support service utilisation, for use in the health economic analysis. 69
-
Parental rules on drinking. 36 This was a 10-item scale developed by van der Vorst et al. 36 to measure the degree to which parents permitted their children to consume alcohol in various situations, such as ‘drinking in the absence of parents at home’ or ‘coming home drunk’. Higher scores indicated stricter rules about alcohol consumption. Response categories ranged from 1 (‘completely applicable’) to 5 (‘not applicable at all’). van der Vorst et al. 36 reported an internal consistency of 0.92.
-
Alcohol knowledge and attitudes. Alcohol-related knowledge was measured using a 19-item knowledge index55 (internal consistency of 0.73). Attitudes were measured using a six-item scale (internal consistency of 0.64). 55
-
Brief Sensation Seeking Scale-4. 71 A four-item scale based on the longer Brief Sensation Seeking Scale (internal consistency of 0.66). 72 Participants indicated responses to all items on five-point scales (strongly disagree to strongly agree).
-
Three domains of self-efficacy (academic, social and emotional) were assessed using the Self-Efficacy Questionnaire for Children73 (internal consistency 0.88). This is a 24-item questionnaire assessing (1) social self-efficacy for the perceived capability for peer relationships and assertiveness; (2) academic self-efficacy for the perceived capability to manage one’s own learning behaviour, to master academic subjects and to fulfil academic expectations; and (3) emotional self-efficacy that pertains to the perceived capability of coping with negative emotions. Items are scored on a five-point Likert scale (‘not at all’ to ‘very well’).
Changes to trial outcomes after commencement
The original primary outcome was self-reported frequency of consumption of more than five ‘drinks’ in a single drinking episode. This was originally chosen on the basis of inclusion in young people’s substance use surveys (e.g. ESPAD), other academic research, World Health Organization guidelines on HED and by the original grant tender document and reviewer feedback. However, concerns arose because it became clear that a ‘drink’ could refer to drinks of different alcohol strength and volume.
The current UK CMO’s guideline65 is that children should not drink alcohol at all, but if they do they should be at least 15 years old, never drink more than once a week, be supervised by a parent or carer and never exceed the recommended adult daily limits (3–4 units of alcohol for men and 2–3 units for women). However, equivalent unit guidelines do not exist for children.
In the UK alcohol literature, it is common to refer to ‘standard drinks’, which are interpreted as containing 1 alcohol unit (8 g of alcohol). It should be noted that internationally there are different definitions with respect to grams of alcohol in such a measure.
As the objective of the intervention was to reduce hazardous and harmful drinking, the STAMPP Trial Management Group (TMG) agreed that primary outcome should be defined as ≥ 6 units for males and ≥ 4.5 units for females; both are 1.5 times the CMO’s maximum daily guideline for adults,65 and this was ratified by the Study Steering Committee (SSC). This change was implemented before the final wave of data collection, unblinding and any analysis of trial outcome measures at any data collection point had been undertaken.
In the survey, participants were presented with pictorial prompts of how much alcohol is represented by ≥ 6/≥ 4.5 UK units (see Appendix 3). Pictures presented the most popular drinks consumed in the two study areas and respondents were asked to report the frequency of consuming this amount of alcohol over the previous month.
Parent/carer completed measures
Parents/carers completed a short postal questionnaire that measured family rules on alcohol and parental self-efficacy in implementing rules and controlling adolescent behaviour. Alcohol Rules was a 10-item scale measuring the degree to which parents permit their children to consume alcohol in various situations, such as ‘in the absence of parents at home’ or ‘at a friend’s party’ (α = 0.86–0.90). 62 Parental self-efficacy was measured using a three-item scale assessing the level of confidence that a parent had in their own ability to prevent their child from drinking (α = 0.67). 74 These data were collected to inform future mediation analysis and were not included in the DAP; therefore, analysis of these data is not included in this report.
Definitions/calculations
The questionnaire outcome scores were calculated in accordance with the original coding system outlined in their corresponding publication (see Outcome measures). A data dictionary was prepared and is available from the authors upon request.
To assess the costs of the intervention for the purposes of economic analysis, overall costs of providing the programme were estimated. This included programme set-up costs and the costs of implementing and delivering the programme. The overall cost per participant and cost per school were also estimated. The costs of implementing and delivering the programme included staff time, venue and equipment costs, provision of support facilities and materials utilised.
Data collection
Students
Data collection took place in schools in a location determined by the co-ordinating teacher. The trial manager co-ordinated the data collection diary in accordance with the preference of schools and, as such, was not blinded to intervention status.
Data were collected through self-completed questionnaires. The primary outcome measure and the service use questionnaire were completed individually. Questions were read out loud by field researchers, in accordance with a preprepared script (see Appendix 4), and participants recorded their answers in an answer book, which also included the written question. The field research team included some members of the trial team (trial manager and research assistant) and temporarily employed researchers who had no other involvement in the trial. When possible, data were collected under examination-like conditions. Participants were identified across waves through a research team-allocated code. The test procedure lasted approximately 40 minutes. At the end of the session, answer books were collected by the field researcher and returned to the field office.
Data were optically scanned (Restore plc, London, UK) and delivered to the Northern Ireland Clinical Trials Unit (NICTU) for processing, cleaning and quality assurance. Data sets were securely transferred to the trial statistician (who was blinded) and health economist (who was also blinded) at the beginning of the data analysis period and to the sponsor institution for secure back-up.
Parents
Questionnaires were posted to parents/carers, self-completed and returned directly to the field office in self-addressed envelopes.
Sample size
It was calculated that a sample size of 90 schools (45 per study arm; 80 pupils per school) would be powerful enough [80%, α = 0.05, intracluster correlation coefficient (ICC) = 0.09, based on data from the Belfast Youth Development Study75] to detect a standardised effect size of δ = 0.2 or a 10% absolute reduction in risk (51% vs. 41%) for the primary outcome (HED). Assuming 20% attrition within each cluster (from 100 to 80 pupils), the target sample size was 90 schools and 9000 students at baseline.
Research ethics committee approvals, consent and research governance
The research was approved by Liverpool John Moores University Research Ethics Committee (reference number 11/HEA/097). For data collection from students within schools, the research ethics committee required opt-out consent [i.e. parent(s)/carer(s) were advised about the research requirements and could communicate a refusal for their child to participate]. Students could also refuse to participate at the time of data collection. For data collection from parent(s)/carer(s), consent was provided through the return of a completed questionnaire.
The trial was funded by the National Institute for Health Research (NIHR) Public Health Research programme, sponsored by Liverpool John Moores University, managed by a TMG of study investigators and staff, and overseen by an independent SSC appointed by, and reporting to, the NIHR. The International Standard Randomised Controlled Trial Number is ISRCTN47028486.
Randomisation
Stratified randomisation of clusters (schools) to intervention or control conditions was performed by a NICTU staff member not involved in the trial and blind to the identity of the schools. Schools were stratified by school type (all-boys’ school/all-girls’ school/coeducation school), socioeconomic status (SES) [percentage of pupils entitled to free school meals (FSMs), categorised as a tertile split: low, moderate or high] and school size.
Randomisation was conducted as an electronic ‘card sort’. Within each stratum, each school had a random number attached. The schools were then sorted by ascending random number and this process was repeated several times by holding down the refresh formula function key. This made it impossible to view intermediate allocations, and the final order was taken as the school allocation.
Two schools in NI that were in very close geographical proximity, and as a result shared staff and facilities, and, therefore, they were treated as one unit to avoid contamination. Two schools in NI that shared pastoral care arrangements were also treated as one unit to avoid contamination. Stratified randomisation was used to balance the arms and was performed separately for Glasgow/Inverclyde and for NI. Schools in Glasgow/Inverclyde were stratified based on FSM provision. As a larger number of schools were recruited in NI, two stratification factors were identified: FSM provision and school type.
The trial manager matched the school codes used in the randomisation to school names, and this matching was then independently verified by the NICTU to ensure allocation concealment. Randomisation took place when children were in school year 8 or S1.
Blinding
Schools and participants were not blinded to study condition. Intervention trainers and delivery staff (teachers) were not blinded to study condition. Data collection was undertaken by a team of researchers that included the trial manager and a dedicated research assistant, neither of whom was blinded to study condition, or by temporarily contracted research staff who were blinded to study condition.
Data analysis of primary and secondary outcomes was undertaken by the project statistician and health economist, with a data set that was blinded for study condition.
Statistical methods
General considerations
Data analysis was prespecified in the DAP and approved by the SSC.
Participant population
-
Complete case (CC) population: all randomised pupils with complete follow-up data at T3, including health economic service utilisation data [the intention-to-treat (ITT) population for whom T3 follow-up data were obtainable].
-
ITT population: all subjects who were randomised. Analysis was based on randomisation rather than on receipt of intervention.
Primary and secondary analyses were performed using the CC population. The health economic analysis was also conducted on the CC population. Sensitivity analysis was conducted on the ITT population (employing a range of methods to deal with missing data; see Missing data).
Pupils who joined a trial school after T0 (June 2012) but before phase 1 of the intervention began (September–December 2012) were first captured at T1 (June 2013). These pupils were included in the primary and secondary analyses. Pupils who joined trial schools after the beginning of the intervention were excluded from the primary and secondary analyses, unless they had moved from another participating school.
Missing data
Missing on scale items: when subjects were missing on individual scale items, the coding instruction for the scale was followed. If no guidance was given, those participants with at least 80% of items completed had the remaining 20% pro-rated.
Missing on primary outcome data: a comparison of the baseline characteristics of cases with primary outcome data and cases was undertaken when these were missing.
Depending on the pattern of missingness, one or more of the following sets of analysis were produced as a sensitivity analyses and compared with analysis on the CC population.
Intention-to-treat analysis employing multiple imputation
Information at T1 and T2 was used to impute credible scores for any missing outcome measures at T3, using multiple imputation with 50 imputed data sets.
Intention-to-treat analysis employing a worst-case analysis
All respondents with missing primary outcome data in the intervention arm were assumed to have ‘failed’ (to have consumed ≥ 6/≥ 4.5 units in a single session in the previous month). All respondents with missing primary outcome data in the control arm were assumed to have ‘succeeded’ (not consumed ≥ 6/≥ 4.5 units in a single session in the previous month.
Intention-to-treat analysis employing a ‘missing = success’ analysis
All missing respondents, regardless of trial arm, were assumed not to have consumed ≥ 6/≥ 4.5 units in a single session in the previous month.
Intention-to-treat analysis employing a ‘missing = failure’ analysis
All missing respondents, regardless of trial arm, were assumed to have consumed ≥ 6/≥ 4.5 units in a single session in the previous month.
Missing on baseline covariate data
For time-invariant baseline covariates (sex and SES), missing values at T0 were derived from observed values at follow-up (T1, T2 or T3) when possible. For any remaining missing values in baseline covariates, mean imputation was employed. 76
Outliers
Any unusual measurements were automatically flagged, checked and re-entered when necessary by the trial statistician. Any outlier values that remained after data cleaning and checking were investigated for authenticity. The influence of outlier values on the primary analysis was checked, and any significant influences detected were reported and discussed in Chapter 3.
Analysis time frame
Baseline
The baseline data were collected after randomisation (T0) when pupils were in school year 8 or S1.
Follow-up visits
Adolescent participants were followed up after T1, T2 and T3.
Statistical analyses
Descriptive analysis
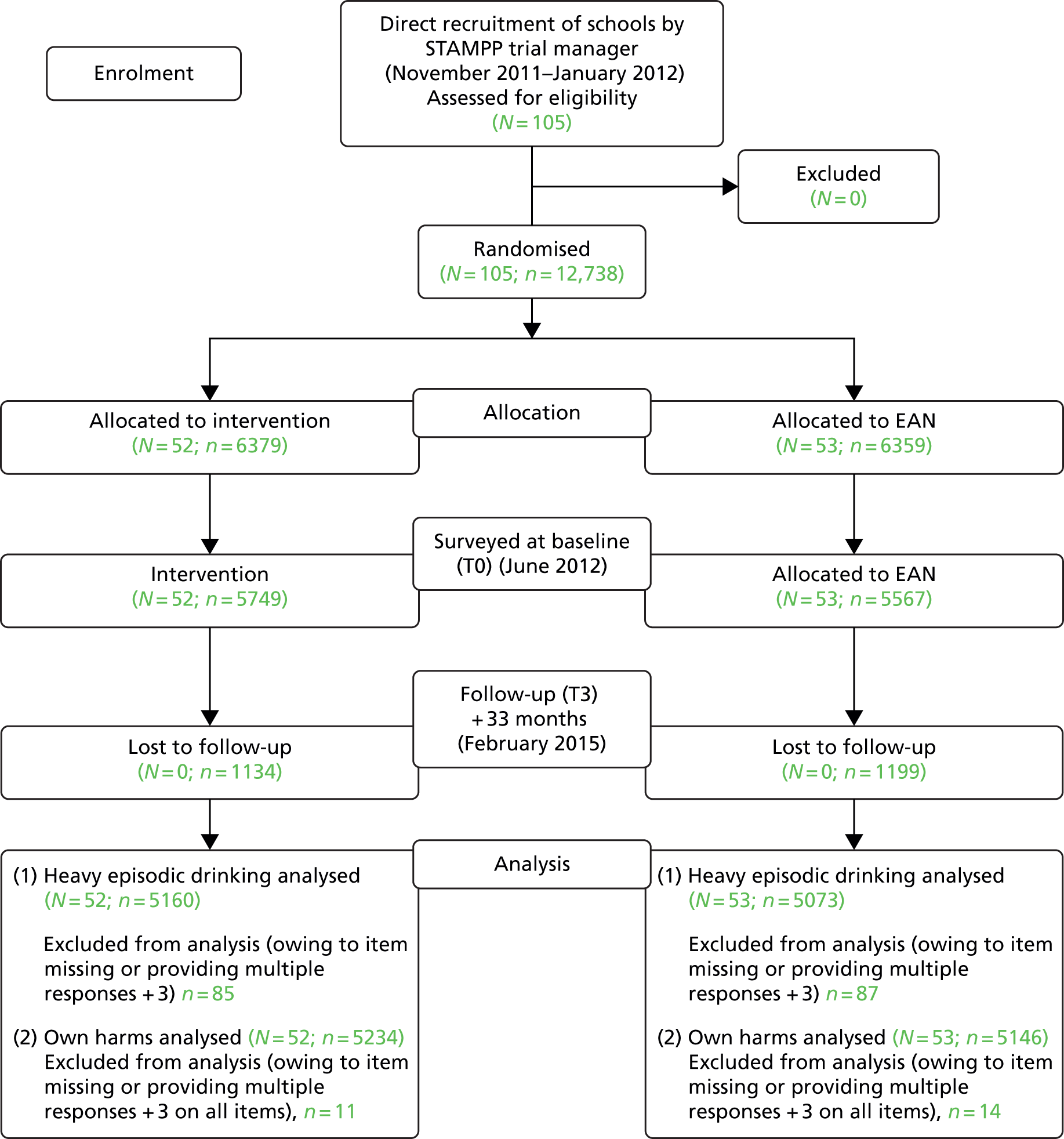
Summary statistics on school and pupil recruitment, withdrawal and dropout were collated for both trial arms and reported as a participant flow diagram for reporting of CRCTs (Figure 1).
FIGURE 1.
School and participant flow diagram: STAMPP. Analysis was conducted at T3 on pupils who had completed each of the primary outcome measures. N, number of schools; n, number of pupils.
Intraclass correlation coefficient
The ICC for the primary outcomes was calculated and is reported in Chapter 3 [see Heavy episodic drinking T3 (binary outcome)]. This was calculated overall and for each arm separately.
Fidelity test
Appropriate descriptive analysis was used to examine the extent to which the necessary conditions required to permit a valid test of the treatment efficacy were met. This included assessment of achieved statistical power, patterns of attrition, and treatment integrity and discriminability (i.e. that STAMPP was sufficiently distinct from EAN) across the trial sites. This work included analysis of both qualitative and quantitative data.
Randomisation check
Descriptive summaries of baseline participant characteristics from the two trial arms were tabulated to assess between-group equivalence across the trial arms (checked on randomisation). The descriptive data were tabulated to compare attendees at the parental session with those who completed the follow-up questionnaire only. Descriptive summaries were produced for baseline data at the school level. These data were used to check comparability between study arms and generalisability of the study population.
Outcome measure scores from the questionnaires were summarised and tabulated for the trial arms. Descriptive statistics, with confidence intervals (CIs) when appropriate, were used for the tabulation of outcomes in the trial arms. CIs presented were adjusted to allow for clustering effects.
Analysis of primary outcomes
The initial outcome analysis was an ITT using the CC population such that all cases were assessed regardless of intervention and intervention dosage. However, as the study design was clustered (i.e. randomisation occurred at the school level) the lack of independency between individual cluster members was taken into account to avoid underestimated standard errors (SEs) (which would otherwise inflate statistical significance). For each primary outcome, a two-level regression model was fitted, with pupils nested within schools, to assess the impact of STAMPP on the outcome measures. For self-reported consumption of ≥ 6/≥ 4.5 units, the model used was logistic regression. For the number of self-reported harms, a negative binomial model was used.
The primary outcome model was adjusted for the impact of covariates on intervention outcome. Covariates included in the models were those used within the randomisation process (sex and SES), baseline outcome measures (consumption of ≥ 6/≥ 4.5 units and number of self-reported harms depending on outcome) and location (NI or Glasgow/Inverclyde). For each primary outcome, a statistically significant result was concluded if the p-value for the trial arm explanatory variable was < 0.025.
Analysis of secondary outcomes
Differences in self-reported alcohol use (HED, defined as self-reported consumption of ≥ 6 units in a single episode in the previous 30 days for males and ≥ 4.5 units for females, which was dichotomised at never/one or more occasions) at T1 and T2 were assessed using two-level logistic regression models with covariates (baseline alcohol use, sex, SES and location). Similar models were constructed for self-reported alcohol use in lifetime, previous year and previous month (all dichotomised) and for unsupervised alcohol use (drinking without the supervision of parents/carers, which was dichotomised) at T1, T2 and T3.
A negative binomial model with covariates (baseline harms, sex, SES and location) was estimated for the number of self-reported harms (harms caused by own drinking) at T1 and T2. Similar models were estimated for the number of self-reported harms caused by the drinking of others and the number of drinks consumed in ‘typical’ and last-use episodes at T1, T2 and T3.
Time to alcohol initiation (age at which a whole alcoholic drink was first consumed, and not just a sip or a shared drink) at T1, T2 and T3 was compared between trial arms by estimating a two-level Cox proportional hazards model in those who had not already initiated alcohol consumption at baseline (T0). The model controlled for sex, SES and location.
Subgroup analyses
To explore differential treatment effects on the primary and secondary outcome measures, prespecified interaction terms were fitted between trial arm and baseline measures thought to predict the effect of treatment.
These were:
-
age, in months, of the pupil at baseline
-
gender
-
SES (using the proportion of FSM provision)
-
alcohol use behaviour at baseline: age of initiation, use of alcohol in the year prior to baseline, context of use (abstainer/supervised/unsupervised)
-
grammar/secondary school analysis (only in NI).
Sensitivity analyses or model testing
Analyses were undertaken to assess the robustness of the outcome analysis. These included the repetition of the analysis on alternative specification of outcomes measures, using the ITT population and with different missing data models.
Health economic evaluation
A within-trial cost-effectiveness analysis (CEA) was undertaken to assess the cost-effectiveness of STAMPP compared with EAN in reducing HED (defined as self-reported consumption of ≥ 6 units for males and ≥ 4.5 units for females in a single episode in the previous 30 days, and which was dichotomised at never/one or more occasions) in year 9 or S2 pupils (aged ≥ 13 years on the 1 September 2012) at T2 and T3. The methodology adhered to the NICE’s Guide to the Methods of Technology Appraisal. 77
A societal perspective was adopted for the analysis in order to capture resource use related to each child’s contact with the NHS, Personal Social Services and criminal justice services. Data on service use by all participants from T0 to T3 were collected using the tool described in Description of primary and secondary outcome measures.
Pupil service use and intervention-related resource use from T0 to T3 were quantified as outlined in the paragraphs above, and unit costs were applied from national sources such as the NHS reference costs, the Personal Social Services Research Unit’s unit costs of health and social care and the unit costs of criminal justice. When national costs were not available, unit costs were identified in consultation with the appropriate finance departments of the resource provider.
Consistent with the primary outcome of the study, the primary economic effectiveness measure was the number of pupils who reported HED at T3. The secondary economic effectiveness measure was the number of heavy drinking episodes at T3. The latter was calculated using data on the frequency of heavy drinking episodes in the previous 30 days collected at the four survey time points. Data were linearly interpolated over the study period to fill in gaps in survey periods and to obtain an estimate of the number of heavy drinking episodes over the study period.
As the time horizon of STAMPP extended beyond a 12-month period, a 3.5% discounting rate was applied, as recommended by NICE. 77
Incremental cost-effectiveness ratios (ICERs) were calculated. The primary CEA estimated the incremental cost per young person experiencing HED avoided due to STAMPP at T2 and T3. The secondary analysis estimated the incremental cost per episode of heavy drinking avoided due to STAMPP at T2 and T3. Multiple regression models were used to predict costs and effects, adjusted for covariates and taking into account the clustered nature of the data. CRCTs raise analytical issues for CEA; costs in particular may be more similar within, rather than between, clusters. CEA should recognise both that costs and effects are correlated and that individuals are clustered within settings. Thus, appropriate models were used that recognised the clustered nature of the data. 78
Uncertainty in the cost-effectiveness measures was investigated using non-parametric bootstrapping with 1000 replications of the ICERs. The resulting replicates were plotted on the cost-effectiveness plane and used to construct cost-effectiveness acceptability curves (CEACs).
Software used
Data cleaning, data management and preliminary analysis were undertaken using IBM SPSS, version 21 (IBM Corporation, Armonk, NY, USA). Mplus, version 7.11 (Muthén & Muthén, Los Angeles, CA, USA), was used for the multivariate regression models. Stata/IC, version 12.0 (StataCorp LP, College Station, TX, USA), was used for the health economic analysis and to verify Mplus models and generate odds ratios (ORs). NVivo, version 10 (QSR International, Warrington, UK), was used for the qualitative analysis.
Public and patient involvement
In addition to participation in the intervention, data collection activities and process evaluation, target group and stakeholder involvement had already been built into the development of the classroom intervention. During the development process, a working group was established, which consulted teachers, local service co-ordinators and voluntary/community sector colleagues on curriculum adaptation. Adapted materials were piloted with pupils in school years 10 and 11 in NI. During the trial, the primary outcome measures were also piloted with a sample of pupils not taking part in the research and their feedback was received. Refinements were made to the questionnaire materials on the basis of this.
A number of public-orientated dissemination activities also took place across the life of the trial, including seminars aimed at academics, school staff and other stakeholders; informational presentations; and the preparation of summary documents for schools describing emerging findings across the trial. Two summary seminars for representatives of schools and stakeholder organisations are also planned for the school year 2016–17 after trial completion.
Changes to protocol
The final version of the protocol was version 7. Significant changes (i.e. those not related to simple language and terminology) to the protocol are detailed below (signed off by the SSC and accepted by the funder):
-
Version 4, 14 June 2013, in accordance with guidance from the SSC:
-
The primary research question was specified: ‘What is the (cost) effectiveness of STAMPP in reducing alcohol consumption (frequency of consuming > 5 drinks in a single episode in the previous 30 days) in year 9 pupils at + 18 months after intervention?’
-
Assessments at other time points were specified as secondary research questions.
-
-
Version 5, 21 November 2013, in accordance with discussions at the TMG held in October 2013:
-
The primary and secondary research questions were restated as objectives to match the DAP and timed as months from baseline and not post intervention.
-
The primary and secondary measures (as defined within the DAP) were added to the protocol, in addition to the general description of the measures used within the study.
-
The immediate post-intervention follow-up was removed to match the DAP.
-
Parent/carer measures were described.
-
-
Version 6, 15 January 2014, in accordance with discussions at the TMG held in December 2013:
-
A second primary outcome was added to reflect the harm reduction basis of the intervention: ‘To ascertain the effectiveness of STAMPP in reducing alcohol-related harms as measured by the number of self-reported harms (harms caused by own drinking) in second-form pupils (school year 9 or S2 in the academic year 2012/2013) at + 33 months (T3) from baseline’.
-
-
Version 7, 8 April 2014, in accordance with discussions at the TMG held in March 2014:
-
Clarified the primary outcome measure: ‘To ascertain the effectiveness and cost-effectiveness of STAMPP in reducing alcohol consumption (defined as self-reported consumption of ≥ 6 units in a single episode in the previous 30 days for males and ≥ 4.5 units for females) in school pupils (school year 9 or S2 in the academic year 2012/2013) at + 33 months (T3) from baseline. This will be dichotomised at never/one or more occasions’.
-
Summary of methods
This was a CRCT conducted in NI and Glasgow/Inverclyde Education Authority areas, with schools as the unit of randomisation. The participants were male and female school students (school year 9 or S2 in the academic year 2012–13 and aged 12–13 years) attending mainstream secondary schools in the study areas. In each participating school, all students in attendance at the time of data collection were asked to complete the project questionnaires. Schools were randomised into the trial and baseline data were collected when pupils were in school year 8 or S1.
The study was powered to detect a standardised effect size of δ = 0.2, or a 10% absolute reduction in risk (51% vs. 41%) for the primary outcome of HED (80%, α = 0.05, ICC 0.09) and the target sample size was 90 schools and 9000 students at baseline. Following recruitment, schools (n = 105) were randomised into intervention (schools, n = 52; pupils, n = 6379) or control (schools, n = 53; pupils, n = 6359) groups.
The primary outcomes were (1) self-reported alcohol use (HED, defined as the self-reported number of occasions of consumption of ≥ 6 units for males and ≥ 4.5 units for females in a single episode in the previous 30 days, which was dichotomised at never and one or more occasion); and (2) the number of self-reported harms (harms caused by own drinking). The primary economic effectiveness measures were in line with the primary outcome measures. Primary outcomes were assessed at T3 using a self-completed questionnaire.
A number of secondary outcomes were also assessed and included the primary outcomes assessed at T1 and T2, self-reported alcohol use (lifetime, previous year and previous month), support service utilisation, the number of self-reported harms caused by the drinking of others, age of alcohol initiation, unsupervised alcohol use and the number of units of alcohol consumed in ‘typical’ and last-use episodes.
Primary and secondary analyses and the health economic analysis were performed using the CC population. For each primary outcome, a two-level regression model was fitted, with pupils nested within schools. For self-reported consumption of ≥ 6/≥ 4.5 units, the model used was logistic regression. For the number of self-reported harms, a negative binomial model was used. For each primary outcome, significance was set at p < 0.025.
The cost-effectiveness of STAMPP was estimated using conventional decision rules and reported as ICERs when appropriate. Uncertainty in the cost-effectiveness measures was investigated by bootstrapping multilevel models relating to public service costs and outcomes and using the incremental costs and outcomes to generate 1000 replications of the ICERs. The resulting replicates were plotted on the cost-effectiveness plane and used to construct CEACs.
Process outcomes were assessed across eight prespecified domains using nine data sources. Assessments included focus group with pupils, an online survey with teachers, interviews with senior school staff and stakeholders. Fidelity and completeness of delivery were assessed using bespoke tools and calculation of participation rates at the parent/carer evening.
Chapter 3 Results
Participant flow
Figure 1 shows the participant flow through the trial. Recruitment began in November 2011 and ended in January 2012. Our original sample size calculation indicated that a total of 90 schools (with a mean of 80 pupils) were needed to ensure sufficient statistical power. However, we oversampled (105 schools) and, as no schools dropped out over the course of the trial, all schools were retained. As this was a CRCT of an intervention taking place over several weeks, pupil numbers refer to those who completed the questionnaire at each data collection period. No participant or parent/carer requested that data be retrospectively removed from analysis. Multiple data collection ‘mop-up’ visits were undertaken with schools; therefore, attrition represents pupils who were absent on data collection days rather than formal dropout.
Baseline characteristics of participants
A total of 11,316 pupils across 105 school participated in the T0 data sweep. Tables 1 and 2 provide descriptive statistics of the pupils at T0 across the study arms.
| Indicator | Trial arm, n (%) | Total (N = 11,316), n (%) | |
|---|---|---|---|
| Control (N = 5567) | Intervention (N = 5749) | ||
| Gender | |||
| Male | 2787 (51.1) | 2834 (50.0) | 5621 (50.5) |
| Female | 2670 (48.9) | 2829 (50.0) | 5499 (49.5) |
| Missing | 110 | 86 | 196 |
| FSM provision | |||
| No | 4289 (77.3) | 4436 (77.5) | 8725 (77.4) |
| Yes | 1258 (22.7) | 1290 (22.5) | 2548 (22.6) |
| Missing | 20 | 23 | 43 |
| Location | |||
| NI | 2196 (38.2) | 3553 (61.8) | 7022 (62.1) |
| Scotland | 2098 (37.7) | 2198 (38.2) | 4294 (37.9) |
| Missing | 0 | 0 | 0 |
| HED | |||
| No | 5082 (92.2) | 5261 (92.4) | 10,343 (92.3) |
| Yes | 432 (7.8) | 431 (7.6) | 863 (7.7) |
| Missing | 53 | 57 | 110 |
| Ethnicity | |||
| White | 4492 (95.3) | 4495 (94.5) | 8987 (94.9) |
| Non-white | 248 (4.7) | 293 (5.5) | 541 (5.1) |
| Missing | 827 | 961 | 1788 |
| Indicator | Trial arm, n (mean, SD) | Total (N = 11,316), n (mean, SD) | |
|---|---|---|---|
| Control (N = 5567) | Intervention (N = 5749) | ||
| Harms | 5561 (0.8, 1.9) | 5725 (0.8, 2.1) | 11,286 (0.8, 2.0) |
| Missing | 6 | 24 | 30 |
| Agea | 5432 (12.5 years, 0.4 years) | 5601 (12.5 years, 0.4 years) | 11,033 (12.5 years, 0.4 years) |
| Missing | 135 | 148 | 283 |
Just under two-thirds (62%) of study participants were located in NI, with the remainder sampled from schools in Glasgow/Inverclyde. There was an equal split of girls and boys in the total baseline sample and across the study arms. Around one-quarter (23%) of the participants reported being in receipt of FSMs, and fewer than 1 in 10 (8%) reported any HED (primary outcome measures) at baseline (T0). The sample was predominantly from a white ethnic background.
Table 2 provides a summary of the baseline characteristics for two continuous indicators; respondents’ age and self-reported alcohol-related harms experienced as a result of own drinking (primary outcome measure). The mean age of the sample at baseline (T0) was 12.5 years [standard deviation (SD) 0.4 years] and the mean reported number of harms was 0.8 (SD 2.0).
In addition to the primary alcohol outcomes (HED and alcohol-related harms), the study also assessed a range of basic alcohol consumption indicators at baseline (T0) (Table 3). Although one-quarter of the pupils had consumed at least one full drink at some stage in their lives, 1 in 5 had drunk alcohol in the previous year, over 1 in 10 had drunk alcohol in the previous 6 months and 1 in 20 had consumed alcohol within the previous month.
| Alcohol indicator | Trial arm, n (%) | Total (N = 12,738), n (%) | |
|---|---|---|---|
| Control (N = 6359) | Intervention (N = 6379) | ||
| Lifetime use | |||
| Yes | 1359 (24.6) | 1367 (23.9) | 2726 (24.2) |
| No | 4170 (75.4) | 4350 (76.1) | 8520 (75.8) |
| Missing | 830 | 662 | 1492 |
| Previous year’s use | |||
| Yes | 1086 (19.7) | 1119 (19.6) | 2205 (19.7) |
| No | 4424 (80.3) | 4583 (80.4) | 9007 (80.3) |
| Missing | 849 | 677 | 1526 |
| Previous 6 months’ use | |||
| Yes | 673 (12.2) | 711 (12.5) | 1384 (12.3) |
| No | 4835 (87.8) | 4990 (87.5) | 9825 (87.7) |
| Missing | 851 | 678 | 1529 |
| Previous month’s use | |||
| Yes | 254 (4.6) | 261 (4.6) | 515 (4.6) |
| No | 5440 (95.4) | 5433 (95.4) | 10,673 (95.4) |
| Missing | 665 | 685 | 1550 |
In addition to those pupils attending participating schools at T0, pupils who were absent at T0 but present at T1 data collection (i.e. missing on the day of the T0 data collection) and pupils who joined participating schools before the delivery of phase 1 of the intervention in the autumn term of 2012 (between T0 and T1) were included in the study population. Table 4 provides the characteristics of the full combined baseline sample (i.e. pupils present at T0 and/or at T1).
| Baseline characteristic | Trial arm, n (%) | Total (N = 12,738), n (%) | |
|---|---|---|---|
| Control (N = 6359) | Intervention (N = 6379) | ||
| Gender | |||
| Male | 3222 (51.4) | 3167 (50.1) | 6389 (50.7) |
| Female | 3052 (48.6) | 3151 (49.9) | 6203 (49.3) |
| Missing | 85 | 61 | 146 |
| FSM provision | |||
| No | 4865 (77.1) | 4874 (77.0) | 9739 (77.1) |
| Yes | 1447 (22.9) | 1452 (23.0) | 2899 (22.9) |
| Missing | 47 | 53 | 100 |
| Location | |||
| NI | 3893 (61.2) | 3849 (60.3) | 7742 (60.8) |
| Scotland | 2466 (38.8) | 2530 (39.7) | 4996 (39.2) |
| Missing | 0 | 0 | 0 |
Randomisation check
A formal test of the randomisation process was performed on the baseline assessments of the original primary outcomes and key individual pupils’ characteristics [gender, SES (recipient of FSMs), consuming five or more drinks in the previous month, number of self-reported harms] to assess between-group equivalence across the trial arms (Table 5). Consuming five or more drinks in the previous month was the original primary outcome in the trial, but this was amended after commencement (see Chapter 2, Changes to protocol). The trial arms were equivalent across all of the variables assessed at T0.
| Randomisation variable | Trial arm, n (%) | Estimate | SE | p-valuea | |
|---|---|---|---|---|---|
| Control | Intervention | ||||
| Gender (female) | 2670 (48.9) | 2829 (50.0) | 0.041 | 0.195 | 0.833 |
| FSM provision | 1258 (22.7) | 1290 (22.5) | –0.009 | 0.149 | 0.954 |
| Five or more drinks | 432 (7.8) | 431 (7.6) | –0.037 | 0.172 | 0.835 |
| Number of self-harms, mean (SE)b | 0.8 (0.039) | 0.8 (0.043) | 0.053 | 0.136 | 0.695 |
Response rates
Of the full sample (those who completed a questionnaire at either T0 or T1, N = 12,738), 10,405 also completed the questionnaire at T3 (81.7%). Table 6 presents the dropout rate by sample characteristic. Dropout rates were higher among male pupils (19%), those who were in receipt of FSMs (25.8%) and those who had used alcohol at baseline (25.4%). There was little difference in dropout between the control and intervention arms of the trial (around 1 percentage point difference). Dropout also varied by location, with a higher rate in Scotland (24%) than in NI (15%), and by school; across schools, dropout rates varied from 1.5% to 32% (see Table 35, Appendix 5).
| Baseline characteristic | Trial arm, n (%) | Total (N = 2333, 18.3%), n (%) | |
|---|---|---|---|
| Control (N = 1199, 18.9%) | Intervention (N = 1134, 17.8%) | ||
| Gender | |||
| Male | 638 (19.8) | 591 (18.7) | 1229 (19.2) |
| Female | 537 (17.6) | 517 (16.4) | 1054 (17.0) |
| Missingb (gender) | 24 | 26 | 50 |
| FSM provision | |||
| No | 808 (16.6) | 756 (15.3) | 1564 (16.0) |
| Yes | 375 (25.9) | 357 (25.7) | 732 (25.8) |
| Missing (FSM) | 16 | 21 | 37 |
| Location | |||
| NI | 623 (16.0) | 520 (13.5) | 1143 (14.8) |
| Scotland | 576 (23.4) | 614 (24.3) | 1190 (23.8) |
| Missing (location) | 0 | 0 | 0 |
| Lifetime use of alcohol | |||
| No | 755 (16.1) | 730 (15.4) | 1485 (15.8) |
| Yes | 426 (26.3) | 382 (24.3) | 808 (25.4) |
| Missing (lifetime use) | 18 | 22 | 40 |
| Arm | |||
| Control | – | – | 1199 (18.9) |
| Intervention | – | – | 1134 (17.8) |
| Missing (arm) | – | – | 0 |
Description of primary outcomes
The primary outcome analysis employed two primary outcome measures. The first related to self-reported episodes of single-session HED and the second to self-reported experiences of harms related to own drinking.
HED (T3): self-reported alcohol use defined as self-reported consumption of ≥ 6 units for males and ≥ 14.5 units for females in a single episode in the previous 30 days, assessed at T3. This was dichotomised at none/one or more occasions.
Drinking harms (T3): the number of self-reported harms (harms caused by own drinking) assessed at T3. Items included harms such as getting into physical fight or being sick after drinking. The outcome was a count of the number of discrete harms reported (0–16). Therefore, for example, a score of 3 represented a report of three separate harms experienced. The individual harms were not weighted in any way. Pupils who provided a valid response to at least 1 of the 16 items were included in the count. Only pupils who failed to answer any of the 16 items were set to item missing.
Table 7 provides the basic count and percentages of respondents reporting HED at T3 by study arm. Around one in five participants reported at least one episode of HED in the previous 30 days. The prevalence of HED was 9 percentage points higher in the control group (26%) than in the intervention group (17%). It was also possible to examine HED prevalence calculated on a base of those pupils reporting lifetime alcohol use at baseline. This gives an indication of the progression from drinking onset to heavier drinking patterns (Table 8). Among drinkers at baseline, around half had engaged in HED at T3 within the control schools, compared with just over one-third in intervention schools.
| Number of HED occasions | Trial arm, n (% valid) | Total (N = 12,738), n (% valid) | |
|---|---|---|---|
| Control (N = 6359) | Intervention (N = 6379) | ||
| None | 3773 (74.4) | 4281 (83.0) | 8054 (78.7) |
| One or more occasion | 1300 (25.6) | 879 (17.0) | 2179 (21.3) |
| Missing at T3 | 1286 | 1219 | 2505 |
| Number of HED occasions | Trial arm, n (% valid) | Total (N = 2011), n (%) | |
|---|---|---|---|
| Control (N = 987) | Intervention (N = 1024) | ||
| None | 498 (50.5) | 660 (64.5) | 1158 (57.6) |
| One or more occasion | 489 (49.5) | 364 (35.5) | 853 (42.4) |
Table 9 provides the basic count and percentages of respondents reporting alcohol-related harms (due to own drinking) at T3 by study arm. This variable was heavily skewed with a preponderance of zeros (no harms reported). Around two-thirds of pupils (63%) reported no alcohol-related harms at T3. The median number of harms was equivalent in each study arm (0), although the interquartile range was smaller in the intervention arm than in the control arm (2 and 3, respectively).
| Number of reported harms | Trial arm, n (% valid) | Total (N = 12,738), n (% valid) | |
|---|---|---|---|
| Control (N = 6359) | Intervention (N = 6379) | ||
| 0 | 3126 (60.7) | 3408 (65.1) | 6534 (62.9) |
| 1 | 434 (8.4) | 385 (7.4) | 819 (7.9) |
| 2 | 282 (5.5) | 251 (4.8) | 533 (5.1) |
| 3 | 235 (4.6) | 218 (4.2) | 453 (4.4) |
| 4 | 242 (4.7) | 187 (3.6) | 429 (4.1) |
| 5 | 200 (3.9) | 160 (3.1) | 360 (3.5) |
| 6 | 142 (2.8) | 153 (2.9) | 295 (2.8) |
| 7 | 142 (1.9) | 125 (2.4) | 267,2.6) |
| 8 | 96 (1.4) | 106 (2.0) | 202 (1.9) |
| 9 | 71 (1.2) | 77 (1.5) | 148 (1.4) |
| 10 | 61 (1.2) | 60 (1.1) | 121 (1.2) |
| 11 | 43 (0.8) | 33 (0.6) | 76 (0.7) |
| 12 | 29 (0.6) | 39 (0.7) | 68 (0.7) |
| 13 | 16 (0.3) | 12 (0.2) | 28 (0.3) |
| 14 | 8 (0.2) | 11 (0.2) | 19 (0.2) |
| 15 | 7 (0.1) | 3 (0.1) | 10 (0.1) |
| 16 | 12 (0.2) | 6 (0.1) | 18 (0.2) |
| Missing at T3 | 1213 | 1145 | 2358 |
As with the HED outcome, the distribution of harms among those pupils who were drinking at the outset of the intervention (here defined as those who reported ever drinking at T0) was examined. In control schools, around 68% of existing drinkers reported experiencing one or more harms at T3, compared with around 62% of pupils in intervention schools (Table 10).
| Number of reported harms | Trial arm, n (% valid) | Total (N = 2053), n (% valid) | |
|---|---|---|---|
| Control (N = 1012) | Intervention (N = 1041) | ||
| 0 | 327 (32.3) | 391 (37.6) | 718 (35.0) |
| 1 | 108 (10.7) | 114 (11.0) | 222 (10.8) |
| 2 | 84 (8.3) | 70 (6.7) | 154 (7.5) |
| 3 | 70 (6.9) | 81 (7.8) | 151 (7.4) |
| 4 | 81 (8.0) | 67 (6.4) | 148 (7.4) |
| 5 | 78 (7.7) | 51 (4.9) | 129 (6.3) |
| 6 | 58 (5.7) | 56 (5.4) | 114 (5.6) |
| 7 | 58 (5.7) | 55 (5.3) | 113 (5.5) |
| 8 | 41 (4.1) | 44 (4.2) | 85 (4.1) |
| 9 | 29 (2.9) | 34 (3.3) | 63 (3.1) |
| 10 | 24 (2.4) | 29 (2.8) | 53 (2.6) |
| 11 | 25 (2.5) | 18 (1.7) | 43 (2.1) |
| 12 | 12 (1.2) | 15 (1.4) | 27 (1.3) |
| 13 | 8 (0.8) | 7 (0.7) | 15 (0.7) |
| 14 | 2 (0.2) | 8 (0.8) | 10 (0.5) |
| 15 | 4 (0.4) | 1 (0.1) | 5 (0.2) |
| 16 | 3 (0.3) | 0 (0.0) | 3 (0.1) |
Primary outcome analysis
The primary outcome analysis consisted of a series of multilevel regression models, adjusted for the clustering of pupils within schools (two-level regression models with a random intercept) using the CC population (those pupils who provided alcohol data at T3). School was the clustering variable. Models with random slopes and intercepts were also estimated (slopes and intercepts as outcomes). However, as none of the slope parameters was significant, the random intercept models were used. The slope and intercepts as outcomes models can be found in Appendix 5 (see Tables 36 and 37).
In addition to the primary outcomes, the regression models also included covariates at both level 1 (within/pupil level) and level 2 (between/school level).
Within-level (pupil) covariates
Baseline HED (T0): self-reported HED (defined as self-reported consumption of more than five drinks in a single episode in the previous 30 days) assessed at T0. This was dichotomised at never/one or more occasions. Mean imputation76 was used to impute values for those respondents who were missing on this variable.
Baseline drinking harms (T0): the number of self-reported harms in the previous 6 months reported at T0 (0–16). Mean imputation was used to impute values for those respondents who were missing on this variable. 76
Between-level (school) covariates
Intervention arm: this was a binary covariate in which schools in the control arm were coded 0 and schools in the intervention arm were coded 1.
Free school meal provision (randomisation stratification factor): schools were classified into three groups based on FSM provision. The allocation was based on a tertile split using information provided by head teachers on the proportion of pupils in receipt of FSMs: low FSM provision (0–15.4%), moderate FSM provision (15.5–30.4%) and high FSM provision (≥ 30.5%). This covariate was treated as a continuous indicator.
School type (randomisation stratification factor): given the larger number of schools in NI, an additional stratification factor was used in the randomisation. This was school type (all-boys’ school/all-girls’ school/coeducation school). Schools in Glasgow/Inverclyde were all assigned to the coeducation type. This covariate was represented by two dummy variables (coeducation was the comparison category).
Location: a binary variable was generated to indicate the location of the schools (NI/Scotland). This variable was used to adjust for clustering at the Education Authority level.
The path diagram of the regression model is presented in Figure 2. For the HED outcome, a two-level logistic model was estimated. For the harm outcome, a two-level negative binomial regression was estimated. All models were estimated in Mplus.
FIGURE 2.
Path diagram for the multilevel model.
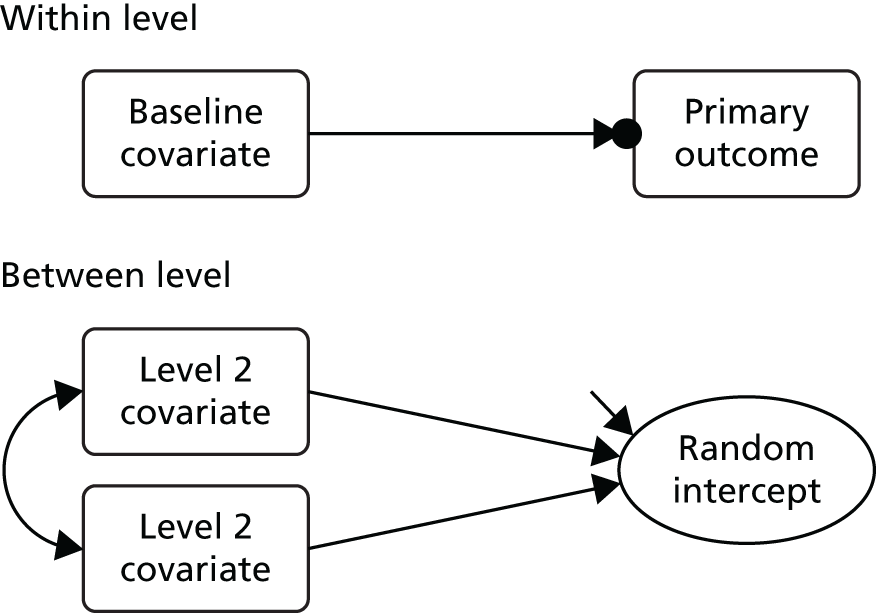
Heavy episodic drinking T3 (binary outcome)
Mplus employs a latent response variable and a threshold to incorporate a binary outcome within its general modelling framework (see Heck and Thomas79 for further details). The threshold can be considered the cut-off point in the latent response variable that predicts the transition from 0 to 1 in the dichotomous outcome. It is equivalent to an intercept, but with an opposite sign.
As the between-level random intercept was specified as a latent continuous variable, the between-level parameters were linear regression coefficients rather than log-odds coefficients. The within-group (pupil-level) residual variance was not estimated (as the latent response variable was not observed), but was fixed (at 3.29 as the standard logistic distribution has a mean of 0 and a variance of π2/3, or approximately 3.29) (see Heck and Thomas79).
Taking the within-level (pupil) variance (fixed at 3.29) and the between-level (school) variance, estimated using a null two-level model (i.e. no predictor variables at either level), it was possible to calculate an ICC for HED [ICC = between-level variance/(between-level variance + 3.29)]. The between-level variance for the full sample was 0.454. The corresponding ICC for the full sample was 0.121.
Table 11 provides the parameter estimates from a two-level random intercept model. Models with random intercept and slope were also estimated; however, none of the level two predictor variables was significant when regressed on the slope. Therefore, a random intercept model was selected for the primary outcome analysis. Given the use of two primary outcomes, a significance level of 0.025 was employed.
| ITT CC analysis | Estimate | SE | OR | p-value |
|---|---|---|---|---|
| Within level | ||||
| Baseline HED | 1.395 | 0.093 | 4.036 | < 0.001 |
| Between level | ||||
| Intervention arm | –0.516 | 0.102 | < 0.001 | |
| FSM provision (tertile) | 0.239 | 0.073 | 0.001 | |
| School type | ||||
| Boys’ school – dummy | –0.186 | 0.200 | 0.351 | |
| Girls’ school – dummy | –0.546 | 0.266 | 0.040 | |
| Location (NI) | 0.422 | 0.109 | < 0.001 | |
| School-level residual variance | 0.176 | 0.035 | < 0.001 | |
| Threshold (HEDT3$1) | 1.574 | 0.124 | < 0.001 | |
Heavy episodic drinking (T0) was a significant predictor of HED at T3. This can be thought of as a cluster-specific effect of HED at baseline on the log-odds of HED at T3 for a given school. It represents the increase in the logit of HED at T3 (1.4) between two individuals in the same school, of whom one was a non-heavy episodic drinker (i.e. they did not report an episode of HED in the questionnaire, regardless of whether they were already drinking alcohol or abstaining) at baseline and the other was a heavy episodic drinker at baseline. At the school level, the parameter estimates were significant for the intervention arm, the proportion of children eligible for FSMs and location. This represents a significant intervention effect. Schools in the intervention arm had lower levels of HED (their intercepts) than those in the control arm. Likewise, schools in NI and schools with smaller proportion of children receiving FSMs also had lower intercepts.
The OR for the treatment effect was 0.596 (SE 0.0596). The corresponding 95% CI for the OR ranged from 0.490 to 0.725.
Sensitivity analysis on heavy episodic drinking outcome
To test the sensitivity of the HED outcome, a range of alternative models were estimated, each applying a different assumption about those pupils missing at the study end point (T3) (Table 12). These included:
-
ITT analysis employing multiple imputation using the Markov chain Monte Carlo method (n = 50 imputed data sets) to estimate plausible primary outcome values for those pupils missing at T3 based on their demographic characteristics (pupil gender and location) and previous alcohol consumption (HED and harms self-reported at T2).
-
ITT analysis with a ‘worst case’ assumption that all missing respondents consumed ≥ 6/≥ 4.5 units in a single session in the previous month, regardless of trial arm.
-
ITT analysis with a ‘best case’ assumption that all missing respondents did not consume ≥ 6/≥ 4.5 units in a single session in the previous month, regardless of trial arm.
-
ITT analysis with a ‘conservative case’ assumption that all respondents with missing primary outcome data in the intervention arm consumed ≥ 6/≥ 4.5 units in a single session in the previous month, and that all respondents with missing primary outcome data in the control arm did not consume ≥ 6/≥ 4.5 units in a single session in the previous month.
| Analysis | Estimate | SE | OR | p-value |
|---|---|---|---|---|
| ITT multiple imputation analysis | ||||
| Within level | ||||
| Baseline HED | 1.145 | 0.088 | 3.142 | < 0.001 |
| Between level | ||||
| Intervention arm | –0.402 | 0.088 | < 0.001 | |
| FSM provision (tertile) | 0.229 | 0.063 | < 0.001 | |
| School type | ||||
| Boys’ school – dummy | –0.193 | 0.184 | 0.293 | |
| Girls’ school – dummy | –0.427 | 0.212 | 0.044 | |
| Location | 0.477 | 0.096 | < 0.001 | |
| Residual variances | 0.124 | 0.027 | 0.106 | |
| Threshold (HEDT3$1) | 1.562 | 0.112 | 0.053 | |
| ITT worst case analysis | ||||
| Within level | ||||
| Baseline HED | 1.287 | 0.084 | 3.623 | < 0.001 |
| Between level | ||||
| Intervention arm | –0.320 | 0.076 | < 0.001 | |
| FSM provision (tertile) | 0.294 | 0.057 | < 0.001 | |
| School type | ||||
| Boys’ school – dummy | –0.282 | 0.156 | 0.070 | |
| Girls’ school – dummy | –0.160 | 0.107 | 0.135 | |
| Location | 0.419 | 0.088 | < 0.001 | |
| Residual variance | 0.101 | 0.020 | < 0.001 | |
| Threshold (HEDT3worst$1) | 0.922 | 0.090 | < 0.001 | |
| ITT best case analysis | ||||
| Within level | ||||
| Baseline HED | 0.940 | 0.080 | 2.559 | < 0.001 |
| Between level | ||||
| Intervention arm | –0.482 | 0.098 | < 0.001 | |
| FSM provision (tertile) | 0.160 | 0.068 | 0.019 | |
| School type | ||||
| Boys’ school – dummy | –0.162 | 0.192 | 0.400 | |
| Girls’ school – dummy | –0.564 | 0.260 | 0.030 | |
| Location | 0.299 | 0.104 | 0.004 | |
| Residual variance | 0.160 | 0.032 | < 0.001 | |
| Threshold (HEDT3best$1) | 1.729 | 0.117 | < 0.001 | |
| ITT conservative case analysis | ||||
| Within level | ||||
| Baseline HED | 1.098 | 0.083 | 2.999 | < 0.001 |
| Between level | ||||
| Intervention arm | 0.712 | 0.089 | < 0.001 | |
| FSM provision (tertile) | 0.257 | 0.066 | < 0.001 | |
| School type | ||||
| Boys’ school – dummy | –0.288 | 0.187 | 0.122 | |
| Girls’ school – dummy | –0.484 | 0.207 | 0.019 | |
| Location | 0.348 | 0.096 | < 0.001 | |
| Residual variances | 0.144 | 0.030 | < 0.001 | |
| Threshold (HEDT3con1$1) | 1.858 | 0.114 | < 0.001 | |
| ITT single-level model with robust SEs | ||||
| Baseline HED | 1.447 | 0.100 | 4.249 | < 0.001 |
| Intervention arm | –0.515 | 0.102 | 0.598 | < 0.001 |
| FSM provision (tertile) | 0.193 | 0.075 | 1.213 | 0.010 |
| School type | ||||
| Boys’ school – dummy | –0.142 | 0.204 | 0.868 | 0.486 |
| Girls’ school – dummy | –0.490 | 0.221 | 0.613 | 0.026 |
| Location | 0.426 | 0.111 | 1.531 | < 0.001 |
| Threshold (HEDT3$1) | 1.501 | 0.134 | < 0.001 | |
As an additional sensitivity analysis, a single-level model, was also estimated, in which the SEs for the predictor variables were adjusted to account for the level of clustering (using the type = complex option in Mplus). 80–82
For all of the sensitivity analysis models (with the exception of the conservative case model), the intervention arm coefficient remained significant and retained the same sign (i.e. being a school in the intervention arm is associated with having a lower intercept). However, in the conservative case model (in which missing cases in the intervention arm were assumed to have all engaged in HED and missing cases in the control arm were set to non-drinking) the sign of the intervention coefficient changed but remained significant.
Drinking harms (T3)
The number of self–reported drinking harms was modelled as a count variable. Given the preponderance of zeros (no reported harms), both Poisson and negative binomial two-level regression models were estimated. The negative binomial model was selected because of a lower Akaike information criterion and a significant dispersion parameter. In this model (Table 13), the intervention indicator was non-significant, suggesting no difference between the intervention and control schools in relation to pupils’ self-reported harms (incident rate ratio 0.916, 95% CI 0.780 to 1.052).
| Analysis | Estimate | SE | p-value |
|---|---|---|---|
| CC analysis | |||
| Within level | |||
| Baseline harms | 0.211 | 0.011 | < 0.001 |
| Between level | |||
| Intervention arm | –0.101 | 0.083 | 0.222 |
| FSM provision (tertile) | 0.168 | 0.061 | 0.006 |
| School type | |||
| Boys’ school – dummy | –0.083 | 0.204 | 0.685 |
| Girls’ school – dummy | –0.380 | 0.236 | 0.107 |
| Location | 0.433 | 0.082 | < 0.001 |
| Residual variances | 0.115 | 0.026 | < 0.001 |
| Intercept (HarmsT3) | –0.042 | 0.093 | 0.649 |
| Dispersion (HarmsT3) | 3.563 | 0.207 | < 0.001 |
| ITT (multiple imputation) analysis | |||
| Within level | |||
| Baseline harms | 0.171 | 0.009 | < 0.001 |
| Between level | |||
| Intervention arm | –0.075 | 0.073 | 0.307 |
| FSM provision (tertile) | 0.170 | 0.053 | 0.001 |
| School type (coeducation) | |||
| Boys’ school – dummy | –0.085 | 0.189 | 0.652 |
| Girls’ school – dummy | –0.287 | 0.176 | 0.104 |
| Location | 0.499 | 0.075 | < 0.001 |
| Residual variances | 0.081 | 0.021 | < 0.001 |
| Intercept (HarmsT3) | 0.010 | 0.086 | 0.912 |
| Dispersion (HarmsT3) | 3.557 | 0.187 | < 0.001 |
| ITT single-level model with robust SEs | |||
| Baseline harms | 0.211 | 0.011 | < 0.001 |
| Intervention arm | –0.087 | 0.076 | 0.253 |
| FSM provision (tertile) | 0.162 | 0.054 | 0.003 |
| School type (coeducation) | |||
| Boys’ school – dummy | 0.039 | 0.180 | 0.830 |
| Girls’ school – dummy | –0.266 | 0.159 | 0.093 |
| Location | 0.420 | 0.076 | < 0.001 |
| Residual variances | |||
| Intercept (HarmsT3) | 0.005 | 0.093 | 0.960 |
| Dispersion (HarmsT3) | 3.761 | 0.219 | < 0.001 |
Significant predictors within the model included baseline harms (pupil level) and location, and the proportion of pupils receiving FSMs (school level). An identical model was estimated on the imputed data sets, yielding similar results.
Secondary outcomes
A range of secondary outcomes was also examined within the study. These included the primary outcomes assessed at T2:
-
HED (T2): self-reported alcohol use defined as self-reported consumption of more than five drinks, assessed at T2. This was dichotomised at none/one or more occasions. This outcome was assessed via a two-level logistic regression model. Around 12.4% of respondents reported HED at T2 using this measure. In the intervention arm, HED was reported by 10.9% (n = 573) and in the control arm by 13.9% (n = 722) of participants.
-
Drinking harms to self (T2): the number of self-reported harms (harms caused by own drinking) assessed at T2. The outcome was a count of the number of discrete harms reported (0–16) and was assessed by a two-level negative binomial model. In the intervention arm, 74.3% of participants reported no drinking harms and in the control arm 71.5% of participants reported no harms.
In addition, a number of secondary outcomes at T3 and T2 were also examined, including:
-
Lifetime drinking (T3): whether or not the pupils had ever consumed a full drink of alcohol at T3 (two-level logistic regression model).
-
Previous year’s drinking (T3): whether or not the pupils had consumed a full drink of alcohol in the previous year, assessed at T3 (two-level logistic regression model).
-
Previous month’s drinking (T3): whether or not the pupils had consumed a full drink of alcohol in the previous month, assessed at T3 (two-level logistic regression model).
-
Harm from others (T3 and T2): the number of self-reported harms experienced that were the result of other people’s drinking, assessed at both T2 and T3 (two-level negative binomial models).
-
Age at onset (T2 and T3): self-reported age at which respondent first consumed a full drink, assessed at both T2 and T3 (two-level Cox regression model).
-
Unsupervised drinking (T2 and T3): whether or not the pupils were permitted, by their parent(s)/carer(s), to consume alcohol (with small group of friends or at parties) with no adult present, assessed at both T2 and T3 (two-level logistic regression model).
-
Number of drinks consumed (T3 and T2): pupils were asked whether or not they usually drank from a range of different alcoholic drinks [beer, alcopops, spirits cider, wine, [brand name] (a popular brand of fortified wine, with caffeine), others] and, if so, how much they usually drank. The values for each drink were summed together to give a total. As the underlying items continued decimals, the total value was multiplied by 10 to create whole numbers.
The secondary outcome analysis also included covariates at level 1 (individual) and level 2 (school) when appropriate.
Level 1 covariates
Relevant drinking variable (T0): for each outcome, the corresponding baseline characteristic was included in the model. Mean imputation was used to impute values for those respondents who were missing on this variable. The only model not to include a baseline covariate was age at onset.
Level 2 covariates
Treatment arm: this was a binary covariate in which schools in the control arm were coded 0 and schools in the intervention arm were coded 1.
Free school meal provision (randomisation stratification factor): schools were classified into three groups based on FSM provision. The allocation was based on a tertile split based on information provided by head teachers on the proportion of pupils in receipt of FSMs: low FSM provision (0–15.4%), moderate FSM provision (15.5–30.4%), high FSM provision (≥ 30.5%).
School type (randomisation stratification factor): given the larger number of schools in NI, an additional stratification factor was used in the randomisation. This was school type (all-boys’ school/all-girls’ school/coeducation school). Schools in Glasgow/Inverclyde were all assigned to the coeducation type. This indicator was used represented by two dummy variables (coeducation was the comparison category).
Location: a dummy variable was generated to indicate the location of the schools (NI/Scotland).
Table 14 presents the random-intercept models for the primary outcomes at T2. The results were similar to those found at T3. The baseline measures were significant, as was location. For the HED outcomes, both FSM provision (tertile split) and school type were significant. The intervention arm was significant at the 0.05 level (β = –0.241; p = 0.041). The 2.5% CIs for this parameter ranged from –0.010 to –0.473. However, it failed to reach the much stricter threshold used in the primary analysis (p = 0.025). It should be noted that the HED indicator used at T3 and, as specified in the DAP, was different from that used at T2. In particular, this measure did not use gender-specific splits, referred to drinks rather than units and did not provide any visual guides to help with the estimation of the amount consumed. This suggests that the significant intervention effect may have been partly dependent on the precision of the measurement instrument used to collect the primary outcome data. The age at which differences in HED were assessed may have been important when assessing intervention outcomes.
| Analysis | Estimate | SE | OR | p-value |
|---|---|---|---|---|
| HED T2 (ITT CC population logistic model) | ||||
| Within level | ||||
| Baseline HED | 1.891 | 0.101 | 6.623 | < 0.001 |
| Between level | ||||
| Treatment arm | –0.241 | 0.118 | 0.041 | |
| FSM provision (tertile) | 0.308 | 0.079 | < 0.001 | |
| School type | ||||
| Boys’ school – dummy | –0.708 | 0.297 | 0.017 | |
| Girls’ school – dummy | –0.608 | 0.186 | 0.001 | |
| Location | 0.732 | 0.134 | < 0.001 | |
| Residual variance | 0.214 | 0.047 | < 0.001 | |
| Threshold (HEDT2$1) | 2.698 | 0.144 | < 0.001 | |
| Harms to self T2 (ITT CC population negative binomial model) | ||||
| Within level | ||||
| Baseline harms drinking | 0.297 | 0.016 | < 0.001 | |
| Between level | ||||
| Treatment arm | –0.144 | 0.118 | 0.222 | |
| FSM provision (tertile) | 0.162 | 0.086 | 0.059 | |
| School type | ||||
| Boys’ school – dummy | –0.247 | 0.302 | 0.415 | |
| Girls’ school – dummy | –0.246 | 0.200 | 0.217 | |
| Location | 0.716 | 0.132 | < 0.001 | |
| Residual variance | 0.267 | 0.054 | < 0.001 | |
| Intercepts (SHarmsT2) | –0.779 | 0.133 | < 0.001 | |
| Dispersion | 4.478 | 0.304 | < 0.001 | |
Table 15 presents the outcome models for the secondary outcomes assessed at T3. None of the intervention parameter estimates was significant in these models.
| Analysis | Estimate | SE | OR | p-value |
|---|---|---|---|---|
| Lifetime drinking T3 (ITT CC population logistic model) | ||||
| Within level | ||||
| Baseline HED | 2.070 | 0.081 | 7.922 | < 0.001 |
| Between level | ||||
| Treatment arm | –0.125 | 0.102 | 0.221 | |
| FSM provision (tertile) | 0.040 | 0.070 | 0.566 | |
| School type | ||||
| Boys’ school – dummy | –0.182 | 0.209 | 0.384 | |
| Girls’ school – dummy | –0.501 | 0.233 | 0.031 | |
| Location | 0.597 | 0.113 | < 0.001 | |
| Residual variance | 0.209 | 0.035 | < 0.001 | |
| Threshold (LifeT3$1) | 0.419 | 0.114 | < 0.001 | |
| Previous year’s drinking T3 (ITT CC population logistic model) | ||||
| Within level | ||||
| Baseline previous year’s drinking | 1.822 | 0.086 | 6.187 | < 0.001 |
| Between level | ||||
| Treatment arm | –0.126 | 0.096 | 0.190 | |
| FSM provision (tertile) | 0.011 | 0.065 | 0.867 | |
| School type | ||||
| Boys’ school – dummy | –0.176 | 0.211 | 0.404 | |
| Girls’ school – dummy | –0.401 | 0.229 | 0.080 | |
| Location | 0.615 | 0.105 | < 0.001 | |
| Residual variances | 0.177 | 0.032 | < 0.001 | |
| Threshold (LYearT3$1) | 0.485 | 0.103 | < 0.001 | |
| Previous month’s drinking T3 (ITT CC population logistic model) | ||||
| Within level | ||||
| Baseline previous month’s drinking | 1.329 | 0.114 | 3.779 | < 0.001 |
| Between level | ||||
| Treatment arm | –0.149 | 0.094 | 0.113 | |
| FSM provision (tertile) | 0.114 | 0.069 | 0.100 | |
| School type | ||||
| Boys’ school – dummy | –0.333 | 0.213 | 0.117 | |
| Girls’ school – dummy | –0.330 | 0.237 | 0.163 | |
| Location | 0.381 | 0.104 | < 0.001 | |
| Residual variances | 0.148 | 0.028 | < 0.001 | |
| Threshold (LMonthT3$1) | 1.459 | 0.102 | < 0.001 | |
| Harms from others drinking T3 (ITT CC population negative binomial model) | ||||
| Within level | ||||
| Baseline harms (others) | 0.330 | 0.016 | < 0.001 | |
| Between level | ||||
| Treatment arm | 0.000 | 0.057 | 0.994 | |
| FSM provision (tertile) | 0.077 | 0.042 | 0.066 | |
| School type | ||||
| Boys’ school – dummy | 0.117 | 0.116 | 0.313 | |
| Girls’ school – dummy | –0.070 | 0.172 | 0.683 | |
| Location | 0.167 | 0.063 | 0.008 | |
| Residual variance | 0.050 | 0.014 | < 0.001 | |
| Dispersion | 1.301 | 0.071 | < 0.001 | |
| Intercept | –0.733 | 0.061 | < 0.001 | |
| Age at onset T3 (ITT CC population Cox regression model) | ||||
| Between level | ||||
| Treatment arm | –0.095 | 0.067 | 0.156 | |
| FSM provision (tertile) | 0.054 | 0.047 | 0.251 | |
| School type | ||||
| Boys’ school – dummy | –0.299 | 0.146 | 0.041 | |
| Girls’ school – dummy | –0.407 | 0.145 | 0.005 | |
| Location | 0.344 | 0.075 | < 0.001 | |
| Residual variance | 0.097 | 0.017 | < 0.001 | |
| Unsupervised drinking T3 (ITT CC population logistic model) | ||||
| Within level | ||||
| Baseline unsupervised drinking | 1.782 | 0.091 | < 0.001 | |
| Between level | ||||
| Treatment arm | –0.142 | 0.092 | 0.123 | |
| FSM provision (tertile) | 0.128 | 0.067 | 0.058 | |
| School type | ||||
| Boys’ school – dummy | 0.002 | 0.207 | 0.992 | |
| Girls’ school – dummy | –0.236 | 0.236 | 0.318 | |
| Location | 0.564 | 0.102 | < 0.001 | |
| Residual variance | 0.148 | 0.029 | < 0.001 | |
| Threshold (Unsuper$1) | 0.148 | 0.029 | < 0.001 | |
| Number of drinks T3 (ITT CC population negative binomial model) | ||||
| Within level | ||||
| Baseline number of drinks | 0.126 | 0.009 | < 0.001 | |
| Between level | ||||
| Treatment arm | –0.078 | 0.075 | 0.297 | |
| FSM provision (tertile) | 0.123 | 0.048 | 0.011 | |
| School type | ||||
| Boys’ school – dummy | –0.277 | 0.181 | 0.127 | |
| Girls’ school – dummy | –0.167 | 0.177 | 0.346 | |
| Location | 0.363 | 0.075 | < 0.001 | |
| Residual variances | 0.073 | 0.020 | < 0.001 | |
| Intercept (NumDrkT3) | 3.521 | 0.082 | < 0.001 | |
| Dispersion (NumDrkT3) | 5.371 | 0.306 | < 0.001 | |
Table 16 presents the models for the secondary outcomes assessed at T2. Again, none of the intervention parameter estimates was significant in these models.
| Analysis | Estimate | SE | OR | p-value |
|---|---|---|---|---|
| Harms from others drinking T2 (ITT CC population negative binomial model) | ||||
| Within level | ||||
| Baseline harms (others) | 0.421 | 0.017 | < 0.001 | |
| Between level | ||||
| Treatment arm | –0.058 | 0.060 | 0.331 | |
| FSM provision (tertile) | 0.132 | 0.044 | 0.003 | |
| School type | ||||
| Boys’ school – dummy | 0.144 | 0.108 | 0.182 | |
| Girls’ school – dummy | 0.075 | 0.119 | 0.528 | |
| Location | 0.255 | 0.071 | < 0.001 | |
| Residual variance | 0.058 | 0.011 | < 0.001 | |
| Dispersion | 1.032 | 0.078 | < 0.001 | |
| Intercept | –1.079 | 0.069 | < 0.001 | |
| Age at onset T2 (ITT CC population Cox regression model) | ||||
| Between level | ||||
| Treatment arm | –0.055 | 0.074 | 0.461 | |
| FSM provision (tertile) | 0.084 | 0.048 | 0.078 | |
| School type | ||||
| Boys’ school – dummy | –0.528 | 0.197 | 0.007 | |
| Girls’ school – dummy | –0.453 | 0.169 | 0.007 | |
| Location | 0.408 | 0.083 | < 0.001 | |
| Residual variance | 0.176 | 0.028 | < 0.01 | |
| Unsupervised drinking T2 (ITT CC population logistic model) | ||||
| Within level | ||||
| Baseline unsupervised drinking | 2.114 | 0.097 | < 0.001 | |
| Between level | ||||
| Treatment arm | –0.087 | 0.100 | 0.387 | |
| FSM provision (tertile) | 0.166 | 0.066 | 0.012 | |
| School type | ||||
| Boys’ school – dummy | –0.306 | 0.217 | 0.159 | |
| Girls’ school – dummy | –0.207 | 0.135 | 0.124 | |
| Location | 0.669 | 0.112 | < 0.001 | |
| Residual variance | 0.170 | 0.038 | < 0.001 | |
| Threshold (Unsuper$1) | 1.883 | 0.118 | < 0.001 | |
| Number of drinks T2 (ITT CC population negative binomial model) | ||||
| Within level | ||||
| Baseline unsupervised | 0.170 | 0.013 | < 0.001 | |
| Between level | ||||
| Treatment arm | –0.088 | 0.096 | 0.360 | |
| FSM provision (tertile) | 0.125 | 0.068 | 0.067 | |
| School type | ||||
| Boys’ school – dummy | –0.574 | 0.259 | 0.026 | |
| Girls’ school – dummy | –0.181 | 0.147 | 0.220 | |
| Location | 0.583 | 0.105 | < 0.001 | |
| Residual variances | 0.153 | 0.035 | < 0.001 | |
| Intercept (NumDrkT2) | 2.836 | 0.106 | < 0.001 | |
| Dispersion (NumDrkT2) | 5.671 | 0.340 | < 0.001 | |
Subgroup analyses on primary outcomes
To explore differential treatment effects on the primary measures, interaction terms were fitted between trial arm and baseline measures thought to predict the effect of treatment. Initial prespecified subgroup analysis examined baseline alcohol consumption (lifetime use, previous year’s use, age at onset and unsupervised drinking). Given the high correlations of lifetime use, previous year’s use and the two primary outcomes assessed at baseline (HED and alcohol-related harms) (Table 17), subgroup models were estimated on a base of just baseline drinkers (lifetime and previous year’s use) to examine the possibility of the intervention having a differential impact on drinkers compared with non-drinkers at baseline.
| Outcome | Lifetime use (T0) | Previous year’s use (T0) |
|---|---|---|
| HED | 0.426 | 0.434 |
| Alcohol-related harms | 0.506 | 0.515 |
For HED, the treatment arm was significant in both the drinker-only models (both previous year and ever use) and the corresponding non-drinker-only models (Table 18). This means that no differential intervention effect on HED, dependent on baseline drinking, was detected. However, for alcohol-related harms as a result of own drinking, although the intervention was associated with a significant reduction in the number of self-reported harms among drinkers (either defined as lifetime or previous year’s use at baseline), it did not reduce self-reported harms among the non-drinkers at baseline. When the lifetime use and previous year’s use subgroup effects were examined via interaction terms (on the full CC population) the interaction terms for harms were non-significant, as were the interaction terms for age at onset and unsupervised drinking.
| Outcome | n | Estimate | SE | p-value |
|---|---|---|---|---|
| HED primary outcome models | ||||
| Treatment arm | ||||
| Limited to pupils reporting that they had ever used alcohol at T0 | 2011 | –0.504 | 0.127 | < 0.001 |
| Limited to pupils reporting that they had never used alcohol at T0 | 7145 | –0.570 | 0.123 | < 0.001 |
| Limited to pupils reporting that they had used in previous year at T0 | 1617 | –0.484 | 0.141 | 0.001 |
| Limited to pupils reporting that they had not used in previous year at T0 | 7512 | –0.582 | 0.118 | < 0.001 |
| Harms primary outcomes models | ||||
| Treatment arm | ||||
| Limited to pupils reporting that they had ever used alcohol at T0 | 2053 | –0.145 | 0.054 | 0.008 |
| Limited to pupils reporting that they had never used alcohol at T0 | 7233 | –0.094 | 0.097 | 0.330 |
| Limited to pupils reporting that they had used in previous year at T0 | 1644 | –0.127 | 0.058 | 0.028 |
| Limited to pupils reporting that they had not used in previous year at T0 | 7615 | –0.069 | 0.096 | 0.314 |
In the additional prespecified subgroup analysis model that was estimated (age, gender), the corresponding interaction terms were all non-significant.
Adverse events
No adverse events were reported throughout the duration of the trial related to receipt of the intervention or to participation in the STAMPP research process.
Summary of results
Overall retention was high (81.7%). No schools withdrew from the trial and no pupils or parents/carers withdrew consent. The intervention was effective in reducing HED, but not in reducing harms resulting from own drinking. The prevalence of HED was 9 percentage points higher in the control group (26%) than in the intervention group (17%) at T3. This represented a significant intervention effect (estimate –0.516, SE 0.102; p < 0.001). The OR for the intervention effect was 0.596 (SE 0.0596). The corresponding 95% CI for the OR ranged from 0.490 to 0.725. Around two-thirds of pupils (63%) reported no alcohol-related harms at T3 (control, 60.7%; intervention, 65.1%). The median number of harms was equivalent in each study arm (n = 0), although the interquartile range was smaller in the intervention arm than in the control arm (2 and 3, respectively). The negative binomial model used showed that the intervention arm was not a significant predictor of harms (estimate –0.101, SE 0.083; p = 0.222; incident rate ratio 0.916, 95% CI 0.780 to 1.052). Examining secondary outcomes, no parameter estimates were significant for the intervention arm, indicating no effects of the intervention. Similarly, no significant interactions were identified in the prespecified subgroup analyses.
Chapter 4 Process evaluation: methods and results
Process measures
The overall process evaluation was informed by the framework developed by Grant et al. ,83 for CRCTs, and ran alongside the assessment of outcomes. Process measure data were collected across a number of different studies with a view to obtaining information in the following domains (Figure 3 shows a summary).
FIGURE 3.
Summary of data used to assess process outcomes.
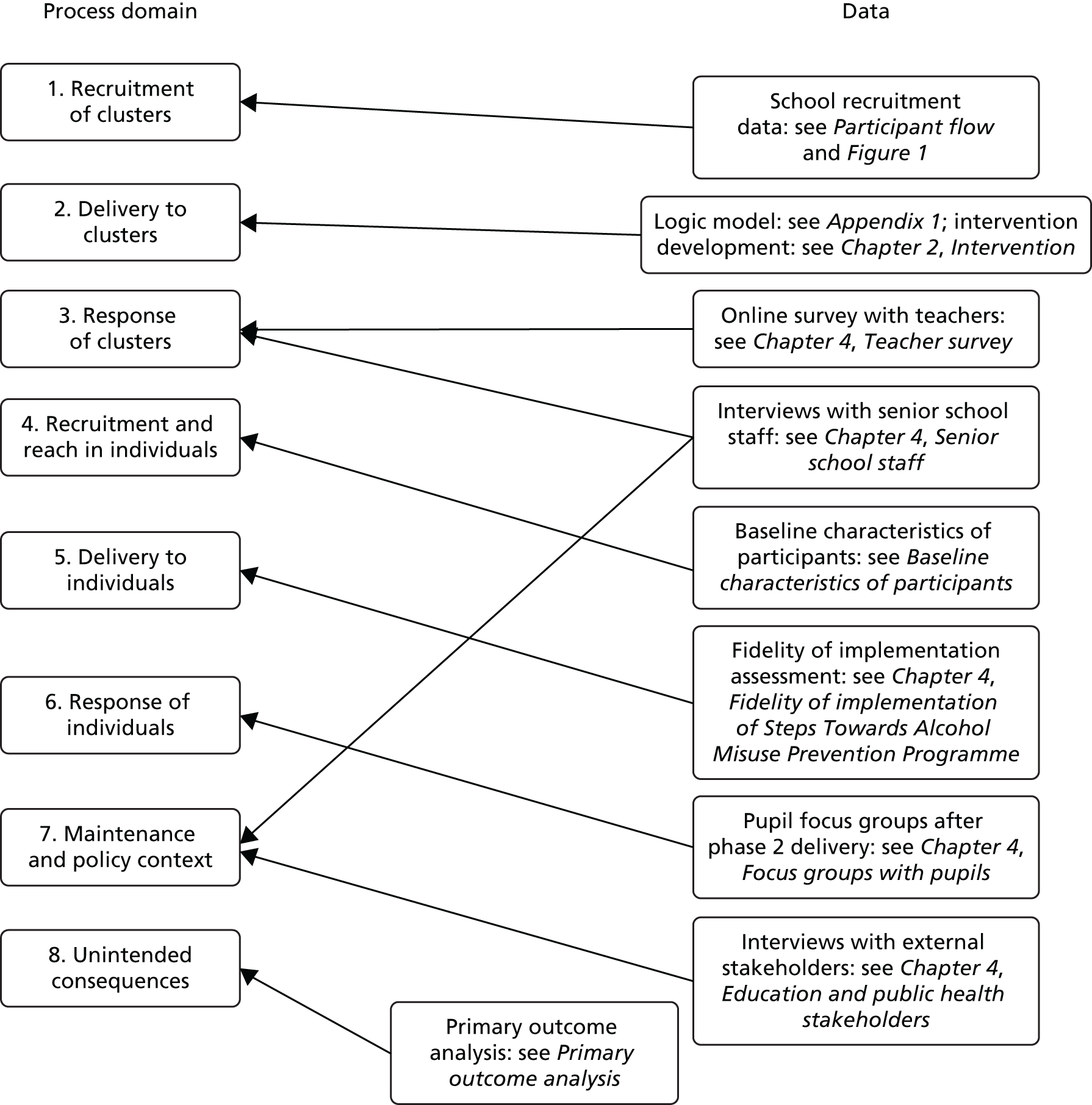
-
Recruitment of clusters: the number of schools agreeing or refusing to participate was documented. Consideration was given to the differences between schools that agreed to participate and those that did not.
-
Delivery to clusters: the interventions delivered to pupils and parents were described, including intervention development and the intervention logic model.
-
Response of clusters: teacher experiences of the classroom component (or EAN for the control group), such as participation in delivery, perceptions of the effectiveness of the classroom component and perceptions of the engagement of recipients, were assessed.
-
Recruitment and reach in individuals: statistical comparison of subject demographics (age, sex) and baseline alcohol use behaviours was undertaken in order to identify differences between control and intervention conditions, to compare representativeness against general population data and to test for randomisation failure.
-
Delivery to individuals: this component assessed implementation fidelity, that is, the intervention that was delivered to recipients and whether or not this was delivered as intended. Assessment of implementation fidelity in STAMPP provided data on the adherence, dose and quality of delivery, participant responsiveness and programme differentiation.
-
Response of individuals: this component assessed the target population’s experience of, and response to, the intervention, and analysed experiences of the intervention in the classroom, the implementation of lessons to alcohol use/opportunities outside of school (to probe experiences of the rule-setting component of the intervention) and understanding of alcohol-related risks (as presented in the SHAHRP curriculum).
-
Maintenance and policy context: this component assessed intervention implementation and maintenance with regard to stakeholder support, staff, resources, setting and support organisations required in order to maintain the reach of target populations, provision of future intervention services and to achieve wider (local) policy objectives.
-
Unintended consequences: the analysis of primary and secondary outcomes was the main source of information about unintended consequences of the intervention. The trial was considered to have produced unintended consequences if a significantly greater number of students reported an episode of consuming ≥ 6/≥ 4.5 units in the previous 30 days at T3. A trial risk register was also maintained throughout the research and adverse events were recorded.
Data were collected through a mixture of monitoring exercises, and through surveys and qualitative work with pupils, teachers and other stakeholders. Information on other alcohol-related activities delivered concurrently in schools was collected as part of an online teacher questionnaire (see Chapter 4, Online survey with teachers). Although a rich data set was obtained from the qualitative work, only key findings and specific discussions for each component are presented here, and the general discussion/conclusions are synthesised in the discussion (see Chapter 6) and conclusions (see Chapter 7) chapters.
Qualitative process evaluation methods
Pupil focus groups
Focus groups were conducted both with pupils who had received the SHAHRP classroom component of STAMPP and with pupils who received EAN. Focus groups were conducted with two research aims in mind: first, to determine the degree to which participants in the classroom curriculum engaged with, enjoyed and perceived that they benefited from participation; and, second, to ascertain to what extent control participants who received EAN engaged with, enjoyed and perceived that they benefited from participation.
Focus groups were chosen for several reasons: they provided a quick and convenient way to collect data from several participants concurrently;84 participants prompted each other to consider the issue to a greater extent and subsequently responded to other opinions, leading to greater discussion;85 they provided an opportunity for participants to feel more comfortable discussing an issue in a group setting than in one-to-one interviews;84,86 and, finally, they did not discriminate against participants who had difficulties with reading or writing. 84
Purposive sampling was used to ensure that both participating study geographies were represented, and that there was an equal representation of sex, intervention and control participants and those attending different school types (grammar vs. secondary). All schools approached agreed to participate. A total of 16 schools in NI and Scotland participated: eight intervention and eight control schools (representing 15% of the schools involved in the trial).
A contact teacher in each school selected what they considered to be a representative sample of their school year 10 or S3 pupils (aged 13–14 years) for participation. A total of 129 pupils participated in the focus groups [male, n = 62 (48%); female, n = 67 (52%)], with a mean of eight participants per group. Group size ranged from 6 to 12 pupils. Participants did not receive any compensation for their involvement.
The focus groups were completed in May/June 2014 when intervention students had completed both phases of the SHAHRP. They took place in a quiet classroom during school time, and the mean duration was 34 minutes. As per the questionnaire surveys, informed parental consent was obtained through each school prior to participation in the focus groups. Participants were also asked to sign an informed consent form on the day of the focus group.
A series of open-ended questions was developed in order to stimulate discussion, to minimise any bias87 and to ensure consistency between the focus groups. An introductory question was used to set the pupils at ease and to build rapport between the researcher and the participants (‘When you hear the word alcohol, what do you think of?’). Intervention participants were then asked to respond to prompts about phases 1 and 2 of the SHAHRP curriculum. A sample question would be ‘What was your overall impression of part 2?’. Control participants were asked to comment on EAN in their schools. Both intervention and control participants were asked to answer questions in relation to learning about alcohol in school more generally, for example: ‘Did you find it easy or difficult to discuss these issues with your teacher?’ The researchers used prompts throughout the focus group discussions in order to clarify answers or to explore and obtain details about a specific issue that may have arisen. This helped to ensure that detailed responses giving the participants’ true opinions were collected. For the discussion schedule, refer to Appendix 6. The discussions were digitally recorded and transcribed verbatim by a professional stenographer.
The transcribed focus groups were analysed using thematic analysis as defined by Braun and Clarke. 88 This procedure involved six steps: (1) familiarisation, (2) generating initial codes, (3) searching for themes, (4) reviewing themes, (5) defining and naming themes and (6) producing the report. The analysis was conducted by the same researchers who conducted the focus groups using both the software package NVivo version 10 and manual coding. Meetings were held between the researchers over a 4-week period to discuss areas of consensus and discrepancy, and to review and revise emerging themes.
Online survey of teachers
Online self-report questionnaires were completed by teachers who had facilitated the classroom intervention and by teachers who had facilitated EAN. The questionnaires were designed to ascertain the intervention teachers’ perceptions of the SHAHRP intervention. The questionnaires were also designed to gather information about both the intervention and control teachers’ experience of alcohol and health education delivery in general.
Two different online self-report questionnaires were developed for intervention and control teachers. All included items were bespoke and designed by the investigators. The questionnaires for both intervention and control teachers contained the following items:
-
Demographic information: this included the participants’ name, location (i.e. NI or Glasgow/Inverclyde), school name, sex, age, teaching experience and subject specialisation.
-
Questions on experience of delivering general health and alcohol education in school: the participants were asked whether or not they had ever delivered or organised general health or alcohol education or talks in school. They were also asked to indicate whether or not they had ever attended external training about alcohol. The teachers could choose from two response options: yes or no.
-
Questions on who was best placed to provide alcohol advice: the participants were asked to indicate who they believed was best placed to provide advice to students about alcohol. A range of options was provided [i.e. ‘you, as a teacher’, ‘a doctor/GP (general practitioner)’, etc.]. Each option was answered on a six-point Likert scale from ‘strongly disagree’ to ‘strongly agree’.
-
Open-text response: respondents were asked about their views on alcohol, health and other prevention activities in school.
A series of additional statements was included in order to gather information about the intervention teachers’ perceptions of SHAHRP. The participants were asked to indicate if SHAHRP engaged, and was enjoyed by, pupils; whether or not SHAHRP was suitable for the age of the pupils; whether or not the activities were easy to follow and if the resources supported its delivery; and whether or not SHAHRP was easy to accommodate in the curriculum and if it fitted in with school strategy. A sample statement was: ‘SHAHRP engaged the interest of pupils’. All statements had a four-point Likert response option, from ‘strongly disagree’ to ‘strongly agree’. High scores on these statements indicated that participants had provided a positive evaluation of SHAHRP. The participants were also given the opportunity to provide open-text statements on their personal evaluation of both phases of SHAHRP.
Statements were also included to gather information about the intervention teachers’ thoughts on the future delivery of SHAHRP. The statements ranged from whether or not they would continue to deliver SHAHRP if it was proven to be effective to whether or not it was likely that there would be senior management support delivery of SHAHRP in the future. A sample statement was: ‘There is likely to be curriculum time to deliver SHAHRP in the future’. Statements were answered on a four-point Likert scale from ‘strongly disagree’ to ‘strongly agree’. High scores on these statements indicated a more positive outlook on the future delivery of SHAHRP. Participants were again invited to provide open-text statements on the challenges and opportunities facing delivery of SHAHRP in the future.
Teachers were invited to participate via an announcement on the school’s noticeboard or by e-mail. The notice provided information about the study survey and included a web link to the survey (intervention or control). E-mails with equivalent text were also sent to the contact teacher in each school (intervention or control), and it was requested that they circulate the e-mail to all teachers who had delivered alcohol education within their school. The questionnaire took between 5 and 7 minutes to complete. The data were collected between February 2015 and July 2015. The data were exported to IBM SPSS version 21.0 and analysed using a variety of descriptive techniques.
Please note that, because of space constraints, only data pertaining to the delivery of the SHAHRP, additional exposure to alcohol interventions and EAN are reported here. Additional information collected will be reported in follow-up publications.
Interviews with senior school staff
Head teachers and/or senior school staff (hereafter senior staff) in intervention and control schools participated in individual interviews. The purpose of this work was to obtain a better understanding of how STAMPP complemented (or otherwise) the school’s existing response to alcohol and to identify some of the challenges facing future delivery.
Purposive sampling was used to ensure that senior staff from both participating study sites (NI and Scotland) and trial arms (intervention and control) were represented. The participation of a representative sample ensured that data saturation was achieved and that a variety of perspectives was accounted for.
The interviews were conducted either face to face or by telephone, and were conducted between September and October 2015. Interviews were recorded and then transcribed by a professional stenographer. Ethics approval was obtained separately from the main trial from Liverpool John Moores University (reference number 14/EHC/015).
Semistructured interview guides based on a series of open-ended questions were developed in order to stimulate discussion, minimise any biases87 and ensure consistency between the interviews. Different interview guides were developed for senior staff in intervention and control schools (see Appendix 6).
The interviews in intervention and control schools included questions about their experience of alcohol use and alcohol education within their schools, the future dissemination of the STAMPP trial results and the potential future delivery of STAMPP in their schools. The interviews in intervention schools also included questions about their motivation to participate in, and their experience of, STAMPP delivery and the STAMPP trial. The interviews in control schools included questions about their motivation to participate in and their experience of the trial. The interviews were analysed using the procedures recommended by Braun and Clark,88 and involved six steps: (1) familiarisation, (2) generating initial codes, (3) searching for themes, (4) reviewing themes, (5) defining and naming themes and (6) producing the report.
Interviews with external stakeholders
Stakeholders in NI and Scotland also participated in individual interviews. Stakeholders included employees of the Department of Health, Social Services and Public Safety Northern Ireland (DHSSPSNI) and the Public Health Agency (PHA) in NI, and included employees of Glasgow Psychological Services, Inverclyde Psychological Services and Glasgow Education Services in Scotland. The purpose was to attain a better understanding of how STAMPP fits in with local current and planned intervention and service delivery strategies and priorities, how STAMPP might complement current approaches and what the most important considerations are when thinking about opportunities for future implementation.
Purposive sampling was used to ensure that stakeholders from both participating study sites (NI and Scotland) and trial arms (intervention and control) were represented. The interviews were conducted either face to face or by telephone, and were conducted between September and October 2015. Interviews were recorded and then transcribed by a professional stenographer. Ethics approval was obtained from Liverpool John Moores University.
The interviews with stakeholders included questions about alcohol education in general and how STAMPP compared with other approaches to alcohol use and how it fitted in with their organisations’ alcohol or health policy and strategic priorities. The support that these agencies would or would not provide for future delivery was also addressed. The interviews were analysed using the procedures recommended by Braun and Clark. 88
Findings
Focus groups with pupils
The results are presented across four themes, namely learning outcomes, materials, mode of delivery and delivery style. These themes were defined prior to the analysis of the data and were used to analyse the intervention and control participants’ views on their alcohol education. A full description of the analysis and coding methodology applied to the interviews is available from the authors on request.
Learning outcomes
The intervention participants were positive in tone about the education they had received and felt that participation in the programme was beneficial. They identified a number of alcohol-specific topics that they learned about as a result of taking part in the intervention, and analysis of responses revealed that elements from all 10 lessons in the programme were commented on and discussed. The topics discussed included ‘units of alcohol’, the related alcohol content of drinks and ‘drinking guidelines’, the ‘effects’ and ‘consequences’ of alcohol use, media portrayal of alcohol and ‘real-life situations’ in which alcohol consumption occurs. In contrast, the participants in the control group held negative views about EAN. They felt that not only was EAN rarely delivered, but any education that they did receive was about things that they already knew. The education was subsequently described as lacking structure, not engaging, boring and repetitive:
It’s really repetitive. We get it a lot every year, and it’s basically just the same information every single year, and it’s all negative views.
Female, control group, Scotland
It, sort of, gave you an insight into the units of alcohol, like, in each drink and shows how they can vary and affect your system differently.
Female, intervention group, NI
During the focus groups, intervention participants engaged in in-depth discussions on learning about topics, such as the consequences and effects of alcohol use, which were strong themes in the intervention curriculum. They indicated that this information would help them in making decisions about alcohol consumption both at the present time and in the future. For some, the realisation that the information presented could affect future decision-making offset the possible criticism of participating in a scenario-based project on a topic that they (or some of their friends) were not currently engaged in (i.e. alcohol use). In contrast, although those in the control group indicated that topics, such as the consequences and effects of alcohol use, were addressed during EAN, their discussions were not in-depth and they did not address how the possession of this information might be beneficial either at the present time or in the future:
Plus, like, for later in life, it’s giving them information of alcohol and they can decide, because they know the facts about it. So they’re able to decide, knowing the facts, whether they want to drink or not, they know the facts and the consequences it’s going to have on them.
Male, intervention group, NI
. . . they basically teach us don’t do it at this age because it will have consequences, extreme consequences that will come back at you in the future . . .
Female, control group, Scotland
The intervention participants also engaged in in-depth discussions on learning about ‘units of alcohol’. They identified the resulting benefits from learning about this issue, such as knowing about how amount consumed broadly relates to behavioural outcomes. They also appreciated learning about real-life situations involving alcohol. They could relate to this information from their own experiences and/or from stories that they had heard from others. The project taught them about how to deal with certain situations and ensure their own and other people’s safety in a drinking context. The workbook for phase 2 in particular was commended for providing this information and in the opinion of many this made the project more relevant:
I quite liked the bit about the real-life situations because then you could, like, put it into real-life context. And then if you were ever put in a situation like that, you could know how to deal with it, and all.
Male, intervention group, NI
However, a small number of criticisms emerged concerning the ‘real-life’ situations that were presented. One participant felt that the information was repetitive; another felt that the real-life situations presented were too extreme and unrealistic; and another felt that the situations were not age-appropriate and instead were focused on the drinking experiences of older people. These same criticisms were evident among those in the control group, but to a much greater degree. These participants felt that younger drinkers’ social behaviour and consumption levels were portrayed negatively and inaccurately and that the education received was not age appropriate:
I know they cover when you drink when you’re older, but underage drinking, they could, kind of, cover in that, because there’s not much about that.
Male, intervention group, Scotland
It was well extreme. Like, no one our age is going to drink to that extent, like. The one on the video, like, had probably about a litre of vodka.
Male, control group, NI
The intervention participants mentioned some alcohol-specific topics that they felt should have been contained in the programme but were not. These topics included information on alcoholism, the effects of alcohol on elderly people and more examples of ‘real-life’ situations that were relevant to people their own age. In relation to the real-world relevance, there was some criticism that the specific scenarios presented might be more relevant for those already engaged in drinking. It should be noted that each of these recommendations were made on only a single occasion.
Materials
The intervention materials discussed were the workbooks and CDs for phases 1 and 2; the EAN materials discussed, which differed from school to school, were workbooks, other written materials such as handouts and/or videos.
The intervention participants held a positive attitude towards the NI-adapted SHAHRP workbooks. They felt that completing these helped them to learn about alcohol and to remember the facts they had learned. Although mentioned less frequently, the design of the workbooks, the inclusion of activities and challenges and the relatively small amount of writing required were also discussed positively. In contrast, EAN workbooks and other materials were negatively appraised and failed to engage the participants:
I think it’s better when you’re, like, writing out in a book because you take it in more, as opposed to sitting there and, like, reading it.
Female, intervention group, Scotland
We’re so used to books, you, kind of, just ignore them now.
Female, control group, NI
Despite the positive appraisal, there was some criticism of the intervention workbooks. Some participants indicated that they disliked having to do any writing and would have preferred more discussion and activities. In some cases, it was felt that having to write made the project seem similar to just another lesson. Similarly, during the control focus groups, and to a much greater degree, the participants called for less reliance on written materials and for greater utilisation of interactive materials such as videos and games:
Well, in a way, you know, there could have been, like, more physical activities instead of, like, always doing it in the book.
Male, intervention group, NI
It’s more books and, like, what we already know, rather than stuff we can ask about and, like, videos and stuff.
Female, control group, NI
The intervention participants discussed the similarities and differences between the phase 1 and 2 workbooks. It was broadly agreed that alcohol-specific topics such as ‘units of alcohol’ and ‘consequences of alcohol use’ were addressed in both. However, it was also widely accepted that differences between the workbooks exist. Participants thought that the first workbook contained basic information and facts about alcohol; in comparison, the second workbook was more advanced and contained greater detail and examination of specific drinking contexts and experiences. The second workbook addressed real-life situations and was regarded as more relevant to the participants’ drinking behaviour and experiences:
Yeah, because in the first book, it was all about units and stuff, and the second one, it was more about the dangers and what could happen to you if you were drinking, the scenarios that you could be in . . .
Male, intervention group, Scotland
The participants believed that the workbooks were delivered in the appropriate order. The workbook for phase 1 provided the information and facts about alcohol that could then be used when dealing with the real-life situations presented in the workbook for phase 2. The material contained within the workbooks was also generally regarded as age appropriate. In fact, on a number of occasions, participants suggested that beginning the project 1 year later in school year 10 or S3 (as opposed to school year 9 or S2) would have been inappropriate. The materials for phase 1 would have seemed too immature, as the participants would have already possessed knowledge of the information presented:
Because this one [workbook for phase 1] was more like a teaching one, like this one explained it and, kind of, like, gave you answers and your teacher went through with you and, kind of, explained the facts and everything on you. So when that book came along [workbook for phase 2], you were able to think of the stuff you had learned, like, beforehand and you could put that, like, to the test and make sure you knew everything.
Male, intervention group, NI
I think if it was done maybe end of year 10, we would already have known most, well, quite a lot of the stuff that was already in the book, which would have made it, kind of, pointless, most of that section.
Male, intervention group, NI
Some participants felt that it was important to deliver all the material in both workbooks and in the order presented; the first workbook provided a good introduction to the subject area before dealing with the more in-depth detail provided in the second workbook:
I would say you should do the two of them because you’ll learn in general and then it’s, like, more real-life situations.
Female, intervention group, Scotland
On the other hand, a smaller number of participants believed that just the second workbook was sufficient to convey the core messages of the intervention because of the greater information and detail provided and the real-life situations examined:
I kind of feel like the first one isn’t needed as much as the second one. Because the second one has more to do with, like, experiences and things you may see. Whereas the first one is just, sort of, straight up knowledge and everything.
Female, intervention group, NI
Finally, the use of the CD to accompany lessons appears to have been sporadic. Full and continued use of the CD was evident in very few groups, with partial use (at specific stages, for example to show media adverts) more common. Two specific factors in its use appear to have been school resources (the availability of information technology equipment) and the motivation of the individual teacher:
. . . we didn’t have the whiteboard.
Female, intervention group, NI
We only used the CD to watch videos.
Female, intervention group, Scotland
Participants indicated that the CDs, when used, were an enjoyable and helpful resource. In comparison to continuously reading and writing about the topic in workbooks or hearing about it from teachers, they found that the videos and interactive games were preferable and more interesting:
I think it’s not as, like, I don’t want to say boring but, you know, you’re not constantly looking at the book and listening to the teacher, you can do it for yourself on the computer.
Male, intervention group, NI
In control schools, videos also appear to have been preferable and more engaging than written materials, and were widely used. These included educational videos produced by the NHS and the police. A number of participants believed that the videos effectively delivered a message that promoted abstinence. However, the majority indicated that some videos were out of date, were repetitive, delivered a negative message about alcohol and presented unrealistic and inaccurate information about alcohol use and antisocial behaviour and violence among teenagers. Furthermore, a number of participants in three of the focus groups indicated that the message was not age appropriate (targeted at older people, e.g. young adults going to nightclubs):
Yeah, they’re all pretty old, so, you know, the messages back then would have been, kind of, different because obviously people can learn different things, so the curricular could change or something. And they could base it on different facts that have been discovered since then, like, this amount of alcohol won’t hurt you if you’re this old.
Female, control group, Scotland
Mode of delivery
In general, intervention participants indicated that they found it easy to discuss the subject of alcohol with their teachers; however, control participants were quite negative in this regard. These differing views may be related to the intervention participants’ positive views and experiences of the programme in comparison with the control participants’ negative views and experiences of EAN. The intervention teachers may also have been more capable of facilitating alcohol education because of the pre-programme training they received.
Intervention participants found it easy to discuss the subject of alcohol with their teachers, particularly if the discussions focused on facts and information. Discussions that focused on their own drinking experiences (or the drinking of their peer group), however, were likely to be meaningful only if the specific teacher in question had a ‘good’ personality, was younger, understood the complexity of adolescent drinking and/or would be empathetic to the pressures facing young people; these points were also alluded to during the control focus group discussions, but to a lesser extent. Moreover, some intervention participants had stated that undertaking programmes, such as the SHAHRP, with school teachers (as opposed to external speakers) meant that it was not just a one-off event in the school year:
. . . quite easy to discuss it with our form teacher, like, because he’s quite laid back . . .
Male, intervention group, NI
It, kind of, depends on the teacher . . . the younger ones are, kind of, more understanding about it . . .
Female, control group, NI
The converse was also often stated, particularly among those in the control groups, namely that it would be difficult if the specific teacher in question was believed to have an ‘unattractive’ personality, was older and/or less likely to understand the complexity of adolescent drinking and lacked empathy. In the control groups, there was a widely held belief that teachers only presented a negative view of alcohol, they made a ‘big deal’ out of it, they made the topic boring and they were judgemental:
But if you had someone who was just stubborn in the mornings and wouldn’t talk to youse, it would make it far harder.
Male, intervention group, NI
You’d be dreading to go to a class because teachers are nosey and they’ll probably ask you if you’ve drunk alcohol and all that type of stuff.
Male, control group, NI
Intervention participants stated that it was desirable for the teacher in question to be knowledgeable about and have had experience of alcohol use, as they could utilise their knowledge and experience during the lessons. For example, one focus group indicated that their teacher had been proficient in first aid and had integrated that knowledge with the programme content. Those in the control group were more likely to focus on the lack of knowledge that some teachers would have in comparison with external specialist drug and alcohol workers and described how this could undermine a teacher’s credibility to teach the subject:
I think it is important what kind of teacher you have, because with our teacher she, kind of, told us all about experiences that she had with alcohol and people who did drink alcohol, and the consequences of their choice to drink alcohol.
Male, intervention group, NI
. . . they [external facilitators] study it, they know what they’re talking about . . .
Male, control group, Scotland
Knowing the teacher, having a good relationship with them, trusting them and believing that they would maintain confidentiality were also regarded as important factors that could help both intervention and control participants to discuss the issue of alcohol with their teachers. If this relationship and trust did not exist, they would be less likely to do so. In such a case, participants, particularly those in the control group, discussed the perceived risks of being open and honest with teachers about this issue, such as a fear that they would regret discussing the issue with a teacher that they saw every day, a fear that teachers would develop a negative opinion of them if they expressed certain views on alcohol, a fear that teachers would disclose information provided by the participants and a fear that by even discussing the issue teachers would presume that the participants were already drinking alcohol. In contrast, they would not see an external facilitator every day and there would be a greater level of anonymity if opinions or personal experiences were disclosed:
The teachers can be, kind of, judgemental and, say, like, you said something about drinking, they can, kind of, like, make a name for you and, like, they could go around . . . like, they could tell other people, they can go to the staff room, like, did you hear about this student. They can do things like that and just not really trustworthy.
Male, control group, NI
I think it’s like the projects probably better with the teacher because, like, you see them every day and obviously you get to, like, to know the teacher. Whereas if it was just someone come in for 1 day, you might feel a bit more uncomfortable with answering questions and stuff like that.
Male, intervention group, Scotland
Delivery style
The discussion of delivery style was focused less on the role of the teacher and more on the interactive nature (or lack thereof) of alcohol education. In general, the intervention participants were satisfied with the programme delivery style. The opportunity to discuss the issue of alcohol with their classmates was appreciated, as it allowed people to share their opinions and experiences and listen to others’ opinions and experiences. Overall, there was a desire for more of that delivery style. In contrast, participants in the control group indicated that they would find it difficult to discuss the issue of alcohol in the presence of their classmates. The different views on this issue may be because of the positive experience of alcohol education that intervention participants had, in contrast with that of participants in the control group, who may not have had the opportunity to experience such a situation and learn about its benefits:
Well, firstly, we used to do, like, our whole class did a class discussion of it. So it was helpful that everyone got to share their opinions and views, and everyone gets to see where they’re coming from. So that kind of learns you another aspect of other people’s views of the book.
Male, intervention group, NI
With specific reference to the interactive and discussion-focused approach, there were some issues that made this less or more difficult for both intervention and control participants. These issues included an individual’s own drinking behaviour and the friendship networks or peer dynamics within the classroom. Participants indicated that some pupils might not discuss alcohol use and disclose their own drinking behaviour because they fear judgement from others and becoming the subject of gossip. This was true of drinkers and non-drinkers alike (and depended on the general perceived drinking norms within the group) and was particularly prevalent among control participants. It was broadly suggested that those who consume alcohol might be less likely to disclose and discuss this behaviour, as they would probably be in the minority at this age. Furthermore, control participants indicated that if they did decide to discuss the issue, their expressed opinions and thoughts might be influenced by the presence of classmates and may not accurately represent their true opinions and thoughts. ‘Peer pressure’ was also mentioned in some groups, and this was related to a perceived pressure to impress classmates either by saying that you were or were not a drinker (depending on the overall norms established in the room):
I think there always is, like, that fear that you’re going to be judged in the group discussions when you know all the people and you see them every day. If you say something like if you did drink, you think some people might be really scared to actually say that because they could get really badly judged for it and they could be teased about it.
Female, intervention group, NI
And just like you said, yeah, I was drinking and it can kind of just also be judgemental, like . . . or even not even your friends, like, just general people in the group, like, they hear you’ve been drinking and they can go pass it on to someone else and just, kind of, you know, it makes a name for you.
Female, control group, NI
However, to a lesser extent, and among those in the control group, some participants indicated that because alcohol use is recognised as a relatively normalised behaviour, they would be willing to discuss the issue and to disclose their behaviour and experiences without fear of judgement by others.
Intervention and control participants indicated that they would be more willing to discuss alcohol use and their own drinking behaviour if a spirit of friendship and trust existed between classmates. On a few occasions, and when prompted to do so, participants also thought that the success of the programme would be dependent on what type of class group it was conducted in (i.e. a year or form class, in which people would know each other better and would be together as a class more often, vs. a split class, which is the basis for specialist subjects, with pupils joining from different form classes):
No, it’s not difficult to speak with your friends around you, because they’re people you can trust, even if the form teacher’s in the room, you still have friends who you’d hang around with just in the school.
Male, intervention group, NI
Yeah, because, like, you’ve been with them for 3 years, you can be a lot more open with them. Like, in first year, you might not know your class that well and I suppose, like, you couldn’t really talk that much in them.
Female, control group, NI
The interactive nature of SHAHRP requires small group discussion and, in this regard, it was suggested that allowing participants to choose their own discussion groups within classes might facilitate more meaningful discussion and interaction:
I don’t think so because you’re in groups and you can, like, choose your groups, so you can have discussions in your groups. It’s not like the whole class have to be listening, like, and if you don’t want to share with the whole class, you don’t have to.
Female, intervention group, NI
Intervention participants also briefly mentioned other techniques that teachers could utilise to promote discussion among classmates. For example, teachers could set boundaries for the discussion beforehand, and, if teachers set an example by disclosing their own experiences, participants might feel comfortable to follow suit.
Teacher survey
The total number of respondents who completed the online survey was 111: 70 intervention (63%) teachers and 41 (37%) control teachers. Table 19 provides a breakdown of participants within the intervention and control arms of the trial, respectively. Overall, 25 schools (16 schools in NI and nine schools in Scotland) were represented by the 68 responses received from intervention teachers, and 14 schools (10 schools in NI and four schools in Scotland) were represented by the 40 responses received from control teachers.
| Characteristic | Trial arm, n (%) | |
|---|---|---|
| Intervention | Control | |
| Location | ||
| NI | 49 (72) | 24 (60) |
| Scotland | 19 (28) | 16 (40) |
| % male | 38 (54) | 12 (30) |
| Age group (years) | ||
| 20–30 | 7 (10) | 1 (3) |
| 31–40 | 25 (37) | 16 (40) |
| 41–50 | 19 (28) | 11 (28) |
| 51–60 | 16 (24) | 7 (18) |
| > 60 | 1 (2) | 5 (13) |
| Years’ teaching experience | ||
| 1–5 | 6 (9) | 1 (3) |
| 6–15 | 26 (38) | 18 (4) |
| > 15 | 36 (53) | 21 (52) |
| Teaching or having the responsibility for the delivery of citizenship and personal, social and health education or school’s equivalent subject | 46 (70) | 21 (52) |
Evaluation of Northern Ireland-adapted SHAHRP (intervention participants)
Table 20 provides data on teachers’ opinions of the NI-adapted SHAHRP curriculum. All teachers agreed or strongly agreed that SHAHRP fitted in with the school’s health and well-being strategy, that it engaged the interest of pupils and was enjoyed by them, and that lessons were easy to follow. There was also a high level of agreement (> 90%) with respect to accommodating SHAHRP in the curriculum, usefulness of supporting resources and age/experientially appropriate content.
| Indicator | Mean ranking (SD) | Opinion (%) | |||
|---|---|---|---|---|---|
| 1: strongly disagree | 2: disagree | 3: agree | 4: strongly agree | ||
| SHAHRP engaged the interest of pupils | 3.36 (0.49) | 0 | 0 | 64 | 36 |
| The pupils enjoyed SHAHRP | 3.30 (0.46) | 0 | 0 | 70 | 30 |
| SHAHRP was easy to accommodate in the curriculum | 3.32 (0.56) | 0 | 4 | 36 | 60 |
| The content of the lessons and activities was right for the age and experience of pupils | 3.38 (0.62) | 0 | 6 | 50 | 44 |
| The activities were clear and easy to follow | 3.46 (0.50) | 0 | 0 | 54 | 46 |
| SHAHRP resources supported delivery of the lessons and activities | 3.42 (0.58) | 0 | 4 | 50 | 46 |
| SHAHRP fits in well with our school’s health and well-being strategy | 3.46 (0.50) | 0 | 0 | 54 | 46 |
Teachers were asked to provide an overall assessment of their opinion of SHAHRP: 92% responded positively or very positively, but 8% viewed the intervention negatively. These negative views seemed to be related to the age-appropriateness and ‘user friendliness’ of some of the supporting material:
Seemed a bit advanced for some of the pupils in my class who could not relate to some of the activities. The video for example on the Night Out featured people in their 20s.
The disc could be better re navigation – need to go through the whole lesson – if you stop mid way – need to click through all the slides.
. . . I did feel my class were maybe a bit young to fully grasp all the aims we were trying to achieve.
Positively evaluated free-text responses received included:
Particularly liked the lesson on the impact of the media.
I liked the overall approach. I feel that it is a very planned approach to alcohol education. I think that there is a great deal of depth in the materials, without giving the pupils information overload.
It was easy to access. Pitched at the correct level and the pupils engaged with the materials.
Like the noticeable difference in maturity and stretches the pupils understanding of consequences further than the previous year.
Very good [phase 2 materials], I like that it takes a different approach. It is less factual than the [phase 1] book. Which is important, as it could easily get very repetitive. I like the way that the book focuses on the consequences, but without being preaching to the pupils about alcohol.
Future delivery of SHAHRP (intervention participants)
Teachers were also asked about the future delivery of SHAHRP. Overall, 96.2% of participants agreed or strongly agreed with the statement ‘I would like to continue delivering SHAHRP if the research shows that it is effective’. Even if SHAHRP was not shown to be effective, 47.1% agreed that they would like to continue delivering SHAHRP and 15.7% strongly agreed. On the other hand, 29.4% of participants disagreed and 7.8% strongly disagreed.
Overall, 92% of participants agreed or strongly agreed that they felt confident in their skills and abilities to deliver SHAHRP in the future. With respect to confidence in their ability to support and train colleagues in their school to deliver SHAHRP in the future, 72% agreed or strongly agreed that they could, 22% disagreed and 6% strongly disagreed.
With respect to probable curriculum time in the future to deliver SHAHRP, 88.3% of participants agreed or strongly agreed; senior management support in this regard was viewed to be important and 94% agreed or strongly agreed that it would likely be present. Finally, participants responded to the statement ‘SHAHRP helps my school achieve its emotional health and well-being priorities’. Overall, 98.1% of participants indicated that they agreed or strongly agreed.
Finally, participants were asked to provide free-text responses concerning the challenges and opportunities for delivery of SHAHRP in the future. Respondents suggested that resources and materials would need to be updated and that there may be time constraints:
Resources may require to be updated.
I have really enjoyed the materials. My school are currently using the materials with the current S2 and S3 pupils. Having a large supply of booklets, would be very useful. Even having the booklets on an electronic version, as if we run out of booklets, we can just print of as many as we need.
Time constraints can be an issues – [we only have] 1 period per week [for personal development (PD) classes] and we have other core modules to cover.
Some final positive summative responses were also received:
Alcohol education can only be a good influence for young people.
It is [in my opinion] a very worthwhile insert to the PSE [personal and social education] programme.
Who should deliver alcohol education?
The intervention and control participants were also asked to indicate who they believed was best placed to provide education or advice to students about alcohol. Relative rankings are shown in Table 21. Interestingly, both intervention and control teachers ranked the same roles as the highest, with specialist providers favoured by both groups, followed by someone who had personally overcome alcohol-related problems. Teachers were ranked sixth by the intervention group and ninth by the control group. With respect to the parental component of STAMPP, both groups ranked parents/carers, delivered in the family home, relatively low; however, both groups ranked support teachers or classroom assistants as deliverers as the lowest.
| Intervention | Mean ranking (SD) | Control | Mean ranking (SD) |
|---|---|---|---|
| A specialist external youth or alcohol service provider | 5.38 (0.83) | A specialist external youth or alcohol service provider | 5.40 (1.03) |
| Someone who has overcome alcohol problems | 4.92 (1.07) | Someone who has overcome alcohol problems | 5.13 (1.31) |
| Police | 4.84 (1.28) | Police | 5.13 (0.99) |
| An A&E doctor/nurse | 4.75 (1.51) | An A&E doctor/nurse | 5 (1.26) |
| A doctor/GP | 4.58 (1.46) | A doctor/GP | 4.72 (1.23) |
| You, as a teacher | 4.40 (1.18) | A school nurse | 4.36 (1.06) |
| A school nurse | 4.32 (1.23) | Parents/carers, delivered in family home | 4.21 (1.67) |
| A school psychologist | 4.19 (1.39) | A school psychologist | 3.93 (1.27) |
| Parents/carers, delivered in family home | 3.89 (1.43) | You, as a teacher | 3.65 (1.41) |
| A teacher of other classes | 3.88 (1.24) | School friends/peers | 3.45 (1.60) |
| Parents/carers, delivered in school | 3.23 (1.38) | A teacher of other classes | 3.40 (0.96) |
| School friends/peers | 3.14 (1.49) | Parents/carers, delivered in school | 3.08 (1.44) |
| A support teacher or classroom assistant | 2.73 (1.45) | A support teacher or classroom assistant | 2.43 (1.26) |
Senior school staff
In total, 19 senior staff were interviewed: eight in control schools in NI, six in intervention schools in NI, two in control schools in Scotland and three in intervention schools in Scotland. The results of interviews with senior school staff are presented in four sections: (1) alcohol and schools; (2) experience of STAMPP delivery and the trial; (3) future delivery of STAMPP; and (4) dissemination of the trial results.
Alcohol and schools
Alcohol has previously principally been delivered through subjects such as science, PD and PSE. Schools have tried to educate pupils about the biological consequences of alcohol use and/or the impact that use has on families and social situations. The majority of participants indicated that their schools had developed their own educational resources, drawing on materials from a variety of external sources, but that these were usually assembled in an unstructured manner from a variety of different sources. Many participants were negative about their experiences of EAN, citing the dated and limited resources that were available, its repetitive nature and limitations on time available for delivery. Some participants believed that staff lacked confidence in their ability to deliver this education, primarily because of a lack of training and expertise. They indicated that schools would welcome new resources and training that improved on previous alcohol education provision:
It would have been just resources that you would have obtained out of various books that you’d have put together, to create a unit of work for teachers to deliver in the PD class.
Intervention school, NI
The majority of participants reported that their schools also used outside speakers, such as the police or recovering alcoholics. Some believed this to be more effective because they thought that external speakers generally have greater expertise and, accordingly, students would pay more attention to them. On the other hand, some participants were sceptical about the value of outside speakers, given that some may be poor public speakers or unable to engage with children, and could potentially deliver an inappropriate message.
Experience of STAMPP delivery and trial
Intervention group participants were pleased to have been randomised to that trial arm, as this allowed them access to novel resources and the associated teacher training. Those in the control group were generally disappointed, as they did not gain this access. However, both groups were aware of the methodological importance of a control group, and that after the trial they would be able to access project materials if they wished. Both control and intervention participants recognised the value of the research and associated benefits in terms of pupil learning.
Control participants reported no concerns about participating either before or during the trial. This was because they believed that the research was well organised, regular updates were provided and participation would have no major impact on school time or resources. Furthermore, those in the intervention group had no concerns about these issues or, for example, on safeguarding issues or the possible reputational damage to the school if parents and community members thought that STAMPP was being delivered in response to specific alcohol concerns in the school.
Intervention participants broadly believed that delivery of STAMPP had a positive impact on their students. In their view, it enhanced students’ knowledge of alcohol use and its associated risks. They believed that the experience of the SHAHRP would help students to make informed choices and lead healthier and safer lives. Furthermore, the harm reduction approach of the SHAHRP was praised, as other programmes that they had experience of that promoted abstinence were believed to have failed to engage recipients:
We now have a cohort of young people who . . . have a good baseline level of knowledge of alcohol and its use, its misuse, the science behind alcohol, units of alcohol . . . so they have the tools in order to make positive . . . informed choices.
Intervention school, Scotland
The two-phase nature of the programme was praised for its consistency (the second part building on the learning of the first) and was thought to result in students both gaining more information and being better able to retain the learning. Moreover, the interactive nature of the SHAHRP and the discussions it promoted were praised and regarded by pupils as enjoyable.
The classroom resources were well regarded. The teacher manuals, student workbooks and CDs were all praised for their user-friendliness, their attractive layout and the manner in which they made it easier to facilitate the lessons because they contained all the necessary information, meaning that not a lot of preparation was required from teachers.
Selecting teachers to deliver the SHAHRP did not present any difficulties for school management, as it was quite often delivered as part of the health and well-being curriculum. Schools would generally have staff already delivering this curriculum and it was these teachers who were chosen to deliver the SHAHRP. In many cases, teachers deliver the health and well-being curriculum to the same year group throughout their time in school, and some of these teachers were often also head of year or were a form teacher, and so their regular contact with pupils aided the development of trust and rapport. Participants were confident in the ability of these staff to deliver the programme, although the provision of a training day and the user-friendly materials were considered to be helpful:
I had all the knowledge at my fingertips, so that was really good. And I also attended the training, which I found very helpful as well. So I felt well-equipped to go into the class to speak to them . . .
Intervention school, NI
However, a practical issue was that of the time demands of the SHAHRP. Some participants had difficulty implementing the programme in full. The participants highlighted that they had to ensure that other health and well-being issues, such as drug education, were also covered. Some control participants also reported that data collection initially presented organisational difficulties in terms of arranging a suitable location and time, but with experience this concern was resolved.
Future delivery of STAMPP
Future delivery of STAMPP if it was shown to be effective
In general, participants indicated that their schools would be willing to continue or begin delivery of SHAHRP if STAMPP was shown to be effective. Those in intervention schools indicated that continued delivery would be supported because they valued SHAHRP. The content, the message delivered and the programme delivery style were all praised:
I will continue to use it because I view it . . . as a very valuable resource . . . These kids didn’t know prior to this what a unit or two units of alcohol was, and it’s not really in . . . any of the resources that we have to deliver at the minute.
Intervention school, NI
Senior staff in control schools indicated support for the future delivery of SHAHRP if STAMPP was found to be effective. However, a small number indicated that the decision to begin delivery, even if effective, would also depend on a number of other factors, including their own evaluation of the usefulness and cost of the resources, and whether or not there was curriculum time available.
The participants were asked to indicate if their school would also attempt to deliver the parental intervention. Despite concerns in a number of schools about poor attendance, the general response was positive. Some indicated that parents would be appreciative of receiving information and guidance. Only two control participants indicated that they would not hold a specific parents’ event because of poor attendance at previous events, although one of them suggested that some of the content could be delivered at a standard parents’ night instead. A number of initiatives that schools could employ to boost attendance were highlighted. These included reminding parents about events by text message, e-mail and letter.
One participant reported that they would not deliver the parental component because of a perceived lack of confidence in dealing with this subject with parents. An external facilitator would be welcomed in this case.
Future delivery of STAMPP if it was shown to be no more effective than education as normal
The participants were asked to discuss the potential future delivery of SHAHRP if it was found that STAMPP was not more effective than EAN for the overall sample but was more effective for some subgroups (e.g. unsupervised drinkers, children from lower SES backgrounds). The majority indicated that their schools would support delivery in these circumstances, with a small number reporting that such a decision would depend on feasibility and the number of students who would benefit. The general view was that it would be worth delivering if the analysis showed a positive impact, particularly on those who were most vulnerable. Some participants reported that their school was obliged to work with targeted groups and would specifically work with those from lower SES backgrounds:
. . . we’re always looking at initiatives for the lower socioeconomic groups . . . And even when you look at Extended Schools funding and projects that can be implemented that will affect the [FSM provision] children, you’re going to get even more support than you would do maybe to other groups.
Control school, NI
The majority of participants indicated that universal delivery would continue. Reasons cited for this included a belief that everybody was entitled to the same high-quality education; that even if a only a group of students benefited, there would be no negative impact if the other students also received the curriculum; and that within any school class there would be students with different experiences of alcohol. Targeting students was regarded as something that would be difficult to do and could potentially stigmatise children. However, a small number of participants indicated that delivery could take place in a targeted manner. It was reported that some students were already ‘targeted’ to receive initiatives (such as counselling) and that they were identified through, for example, social services, self-referral and/or deterioration in school work.
The participants were also asked to discuss the potential future delivery of SHAHRP if it was found to be no more effective than EAN but if teachers liked the approach, curriculum and materials. Intervention participants were unanimous in their belief that schools would continue delivery in this situation, primarily because of their positive evaluation and experience of the programme. Control participants also, in general, indicated that their schools would begin delivery in this situation. A number of factors influenced their view. For example, if teachers and students liked the programme (in terms of delivery style), this would be considered as a form of ‘effectiveness’; if teachers liked the systematic approach and materials of SHAHRP, they are also likely to be confident in their ability to deliver it; and schools welcome all up-to-date new resources. However, it was noteworthy that a number of participants from control schools indicated that cost and logistical issues (such as teacher training and the time required to deliver SHAHRP) would need to be considered before a decision would be made about delivery in such a situation.
Practicalities of future delivery
Two issues were prominent during this discussion, namely the training of teachers and the acquisition of resources. Teachers are not experts in the subject area and, in order for them to feel confident in their ability to deliver SHAHRP and to be engaged in delivery, they require training:
. . . we’re supposed to be so-called experts in all the different fields, but I know from personal experience . . . that a lot of teachers will kind of stick to what they’re confident in, and if they’re not confident, they’ll avoid it or they’ll just skim through it.
Control school, NI
The participants indicated that the cost of resources might present a challenge to future delivery. It was highlighted that printing costs could be reduced if the resources were presented in an electronic format, which schools were already regularly doing, and which was regarded positively by teachers and students. The participants noted that resources would need to be updated when required.
A small number indicated that integrating SHAHRP into their curriculum might be challenging. One participant indicated that the intervention was relatively lengthy and that their school might adapt this as a condensed version and integrate it with other programmes such as drugs education.
Dissemination of the STAMPP trial results
Participants indicated that they wished to learn about the results of the trial and the effectiveness of STAMPP, including its effects on, for example, alcohol-related harm, drinking behaviour and/or changes in knowledge and attitudes. Two participants elaborated upon why this information would be useful to them. First, those who were delivering STAMPP would want to know if it was supported by research. Second, teachers or those who favoured the intervention would be able to use the research in their attempts to persuade senior management to support it in the school.
It was advised that the reported data should be school specific and should reflect the intricacies of school type (e.g. Catholic vs. state school), the location of the school (e.g. rural vs. urban, NI vs. Scotland) and participant differences (e.g. gender).
. . . I would question . . . for example, attitudes or maybe the age at which maybe boys are beginning to drink, what’s happening maybe with our boys here, would that completely or accurately reflect . . . what’s happening across all of NI . . .
Control school, NI
The participants indicated that the findings should be disseminated to a range of people, including governors and senior management, the school principal, staff, parents and students. The reporting of findings should be tailored to each group’s needs. For example, parents would only require a summary. The favoured method of dissemination was electronic publication, including through e-mail, on school websites and via social media.
Education and public health stakeholders
There were eight stakeholders interviewed: four in NI and four in Scotland. Results of interviews with education and public health stakeholders are presented in three sections: (1) alcohol education in NI and Scotland, (2) evaluation of STAMPP and the STAMPP trial and (3) future delivery of STAMPP.
Alcohol education in Northern Ireland and Scotland
With respect to addressing alcohol-related issues, there were mixed views among stakeholders in NI on the relative contribution of education approaches (such as STAMPP) compared with other initiatives (such as the licensing, regulation and taxation). Two participants in NI believed that approaches addressing pricing, marketing and availability of alcohol would have a greater impact on drinking behaviour, with one questioning the effectiveness of educational approaches as a whole and citing a lack of supporting evidence. However, three of the four stakeholders in NI and all of those in Scotland believed that a combined approach that included education was required. Among a number of participants, there was a belief that education could influence cultural and social alcohol-related attitudes and norms, which consequentially would impact drinking behaviour:
. . . there’s no single way of combating alcohol misuse or drug misuse, and that actually you need to take a broad package approach . . . while education in and of itself might not show great impacts, I think it helps set cultural and social norms which could, down the line, change behaviours.
Stakeholder, NI
Evaluation of STAMPP and the STAMPP trial
The stakeholders generally agreed that the SHAHRP classroom component corresponded with their overall alcohol and health policies or strategic priorities for young people. In parts of NI (not the trial geographies), the SHAHRP had already been commissioned under the New Strategic Direction for Alcohol and Drugs Phase 2 (2011–16),89 although, in general, the PHA funds targeted rather than universal programmes. According to one PHA stakeholder, SHAHRP is regarded as the most evidence-based programme implemented in the region. Education and prevention is a key aim of the PHA alcohol and drug strategy, and the harm reduction approach also reflected the priorities of stakeholders in the DHSSPSNI. In Glasgow and Inverclyde, SHAHRP was viewed as a key component of the approach to adolescent alcohol use. The objectives of SHAHRP were consistent with Glasgow Psychological Service’s strategy to reduce alcohol and drug use by young people, and the harm reduction approach of SHAHRP was also supported. It was believed that the content of SHAHRP, although similar to parts of the existing Scottish education curriculum, had a clearer structure, and the materials were viewed as attractive and user-friendly.
The parental intervention was regarded as complementing the classroom intervention as, in the view of one of the PHA stakeholders, it was similar to a currently funded parental intervention (Talking to Children About Tough Issues). The stakeholder from the DHSSPSNI also reported that they had recently begun to recognise the potential benefit of working with parents.
. . . the classroom element had been commissioned under that strategy and we did recognise the need to reach outside schools as well and talk to parents. So I do think it fits in within the overall policy and strategy.
Stakeholder, NI
There was agreement among all stakeholders that the inclusion of both a parental and a classroom component made STAMPP distinct. Furthermore, in NI, the utilisation of an educational and skill development harm reduction approach with the targeted age group rather than an educational abstinence approach was another distinctive characteristic. However, it was not clear from respondents if STAMPP was distinct in Scotland, with disagreement evident among those from Glasgow and Inverclyde Psychological Services.
Future delivery of STAMPP
Future delivery of STAMPP if it was shown to be effective
The majority of stakeholders indicated that, if STAMPP was shown to be effective, colleagues and other stakeholders, policy actions, money and material resources would support future implementation. Evidence-based practice was valued, particularly if delivered by teachers, and some participants indicated that their organisations would experience pressure from their partners to support implementation if intervention effectiveness was demonstrated.
However, support would be contingent on a number of factors. For example, a stakeholder from the PHA emphasised that support would be contingent on how effective STAMPP is in comparison to other programmes that are already delivered. If the intervention were only equally effective, it would be unlikely that the programmes currently delivered would be replaced because of retraining and commissioning costs. This participant was also cognisant of the possibility that current funding for training and resources may be withdrawn because of budget cuts, a point also made by those from the Glasgow and Inverclyde Psychological Services. The participants also indicated that support for the parental intervention may require further consideration, as it could be a challenge to persuade schools to deliver and parents to attend, and there are also potential difficulties with regard to the provision of funding and resources:
. . . if it was shown to be effective, the first thing that would strike me would be how effective, and how effective relative to the services and programmes that we already fund. If we were looking at STAMPP showing this was effective but other research showing what we’re already funding was equally effective, there’d be no real reason to swap them. But if it was stronger, if it was showing, you know, more effects what we’re doing, certainly we would be led by the evidence. Now money and resources is a different question. At the minute, we’re facing cuts.
Stakeholder, NI
Future delivery of STAMPP if it was shown to be no more effective than education as normal
The participants were asked to discuss the potential future delivery of STAMPP if it was not shown to be more effective than EAN for the overall sample, but was effective for some subgroups. All stakeholders indicated that it would be delivered in this circumstance. In Scotland, there is a focus on helping adolescents who are regarded as vulnerable. For example, a Glasgow Psychological Services stakeholder reported that under the Scottish Attainment Challenge (https://education.gov.scot/improvement/Pages/sac1tosac11scottishattainmentchallenge.aspx), their organisation has been provided with funding to effect positive change among vulnerable adolescents:
. . . if it wasn’t that successful overall but it hit the most vulnerable pupils, they would go for it. Because at the moment, there’s a thing called the Attainment Challenge in Scotland, which seven authorities have got money and have to effect change for the most vulnerable.
Stakeholder, Scotland
The stakeholders in NI also indicated that their organisations would be supportive of future delivery if STAMPP were shown to be effective for subgroups. However, there was disagreement on how future delivery would take place. One stakeholder from the PHA indicated that because it would difficult to identify individuals in need of targeted help, because they are unlikely to all be in the same setting, and because of the risk of stigmatisation, it would continue to be delivered universally. However, the majority indicated that targeted delivery would take place for reasons of ‘cost-effectiveness’. It was even suggested that if the intervention was found to be effective overall, but was significantly more effective for subgroups, it might only be delivered to these pupils in order to attain the greatest return for resources invested. Two participants also suggested proceeding in accordance with the principle of proportionate universalism, whereby STAMPP would still be delivered universally, but for example, if the findings indicated that STAMPP was more effective for those in disadvantaged areas, implementation would be prioritised in schools in those areas.
The participants were asked to discuss potential support if STAMPP was shown not to be more effective than EAN, but teachers still liked the systematic approach and materials. The majority indicated that future delivery would not receive support in this scenario. The cost of delivery of a programme that is not better than that which is currently delivered could not be justified just because teachers liked it. It was also recognised that if an ineffective intervention was implemented, it would be utilising school time that could be assigned to an effective programme.
Practicalities of future delivery
The practicalities that future delivery would entail were discussed. The majority indicated that their primary concern would be poor implementation fidelity. Particular attention is paid to fidelity during a randomised controlled trial (RCT), but in the real world facilitators are likely to adapt programmes informally. For example, a programme may be condensed by teachers to facilitate competing curriculum demands, or if an intervention was delivered to a targeted subgroup it may be informally tailored by teachers to suit (perceived) pupil need.
Stakeholders in Scotland highlighted the need for an implementation model. A Glasgow Psychological Service’s stakeholder indicated that the STAMPP CRCT was adaptable to local needs, and that they would look to the CRCT for guidance. Another stakeholder from the same organisation warned that attention was rarely paid to the ‘science behind implementation’. If an intervention was introduced to a new location or school, local or school-related factors would need to be taken into consideration:
. . . that’s why lots of . . . interventions crash and burn . . . there’s not enough attention given to the implementation . . . in the real world . . . they try and transplant that on to a place like the east end of Glasgow . . . And there’s not enough time given to looking at what’s the workforce . . . what’s the sort of client group . . . in terms of kids . . . what are the outcomes we’re looking for . . . it can’t just be thrown in and expect results in one place that you got in another . . .
Stakeholder, Scotland
Additional process measures
Usual alcohol-related activities in both intervention and control schools over the course of the study
As part of the online teacher survey (see Online survey with teachers), intervention and control teachers were asked to provide details of all prevention and health education that had been delivered in the school (i.e. not limited to year groups receiving STAMPP) in addition to regular PD curricula. The assessment took the form of a self-completed monthly ‘diary’, and teachers were asked to include any activities that they thought were relevant. These were retrospectively classified by the research team. This was undertaken in order to assess the provision of competing or additional alcohol education in the trial sites.
The SHAHRP intervention was delivered in most schools as part of their personal, social, health and economic (PSHE) (or local equivalent) provision, and did not replace statutory activities. Overall, 88.5% of intervention schools self-reported at least one activity that they thought was relevant, resulting in a total of 58 discrete monthly activities. However, of these, very few were classed as relevant to alcohol prevention. Two intervention schools reported provision of eight separate 1-hour-long alcohol information sessions delivered by a local, non-governmental organisation across the time period, and one of these sessions was delivered to pupils who would have also received the SHAHRP. One respondent reported a single 1-hour information session on alcohol delivered by the local police force, but this was to pupils who were older than those in the trial sample. One school reported two presentations of a theatre-based alcohol intervention but did not specify the target age group. Finally, one school reported a generic 1-hour session on harms in the family home, which included a discussion of alcohol.
In 93.3% of control schools, participants reported at least one activity that they thought was relevant, resulting in a total of 47 discrete monthly activities. Of these activities, two respondents reported generic alcohol awareness sessions across different year groups, including pupils in the target years, and one respondent reported a single 1-hour information session on alcohol delivered by the local police force.
Based on these reported data, it was concluded that provision of additional alcohol education/prevention activities in control and intervention sites was minimal (see also Chapter 6, Self-assessment of risk of bias).
Fidelity of implementation of STAMPP
Methodology
Intervention teachers were asked to complete two self-report surveys concerning fidelity and completeness of delivery of the two phases of SHAHRP. Although a method such as independent observation may produce more reliable and valid data,90–92 it was not possible to utilise this method because of time and resource limitations. Self-report surveys were therefore considered the most efficient form of data collection because a large number of teachers were involved in delivery of the programme.
The surveys used to self-assess fidelity are included in Appendix 7. The respondents were required to indicate the extent to which they delivered the activities within each phase. They could choose from three response options: 0, ‘not at all’; 1, ‘partially’; and 2, ‘fully’. The participants were also asked to indicate how many lessons in total they needed to complete the activities. To be delivered as intended, phase 1 should have been completed in six lessons and phase 2 in four. Finally, the participants were asked to indicate the degree to which they used the accompanying CD to support project delivery (a CD accompanied both phases 1 and 2). They could provide their answer using a 10-point Likert response option: 1, ‘I never used it’, to 10, ‘I used it at all times’.
After delivery of each phase, the intervention teachers were sent an e-mail that contained the relevant self-report survey and an invitation to complete it. If more than one teacher within a school delivered SHAHRP, the aforementioned e-mail was sent to the contact teacher of the school, who was asked to distribute the questionnaire to the teachers who had delivered the programme. Each questionnaire took 2–3 minutes to complete. The data collected were exported to IBM SPSS version 21.0 for analysis.
Phases 1 and 2 contained 17 and 12 activities, respectively. If participants indicated that they did not complete an activity at all, this activity was assigned a score of zero. If they indicated that they partly or fully completed an activity, this activity was assigned a score of one. The scores from each activity were summed.
The activities in phases 1 and 2 should be completed in six and four lessons, respectively. In order to reflect this requirement, the summed activity score was divided by the number of lessons that the teacher indicated was needed to complete the material.
However, it was also possible that the activities were completed in a fewer lessons than required (suggesting that not all material had been covered adequately). The summed activity score could not be divided by the number of lessons in this case, as it would produce an inflated score. In this scenario, the number of lessons needed to complete the material was recoded to reflect the distance from the ideal number. For example, if a teacher indicated that the activities were completed in five lessons, one below the ideal number in phase 1, the number of lessons was recoded as 7, one above the ideal number. The summed activity score was then divided by this recoded number.
The use of the CD to support project delivery accounted for the final 10% of fidelity of implementation of each phase. The Likert response 1, ‘I never used it’, was recoded to 0 in order to represent 0% fidelity in terms of the use. The other ratings remained the same. For example, a score of 5 accounted for 5% of overall fidelity of the phase.
The two scores were added to provide a composite indicator of fidelity of implementation for the classroom intervention for each phase.
Owing to resource constraints, less information was collected on the delivery of the parental intervention. Data are presented on attendance at the parental evenings and the number of questionnaires returned, which were used as an indicator of acknowledgement of reading the mailed information.
Results
School intervention
Overall, across all intervention schools that returned data (47; 87%), phase 1 was assessed to have been implemented with 72.69% fidelity and phase 2 was implemented with 68.76% fidelity (Table 22).
| Phase of delivery | Score (%) | ||
|---|---|---|---|
| Mean (SD) | Minimum | Maximum | |
| Phase 1 | 72.69 (17.98) | 28.23 | 94.35 |
| Phase 2 | 68.76 (20.60) | 34.71 | 100 |
There was variation between schools with respect to the number of lessons in which content was delivered. The mean number of lessons needed to complete all the activities in phase 1 was 8.09 (SD 2.61), whereas activities should have been completed in six lessons (Table 23). The mean number of lessons needed to complete the activities in phase 2 (Table 24) was 6.65 (SD 3.02), whereas activities should have been completed in four lessons. The CD of supporting materials was used with 74.8% fidelity in phase 1 and 69.8% fidelity in phase 2.
| Component | Score (%) | ||||
|---|---|---|---|---|---|
| Mean (SD) | Minimum possible | Maximum possible | Minimum recoded | Maximum recoded | |
| Summation of activities | 15.92 (2.18) | 0 | 17 | 0 | 17 |
| Mean number of lessons | 8.09 (2.61) | 0 | N/A | 3 | 20 |
| Recoded lessons | 8.32 (2.40) | 6 | N/A | 6 | 20 |
| Activities/lessons | 2.06 (0.54) | 0 | 2.83 | 0 | 2.83 |
| CD | 7.48 (2.76) | 0 | 10 | 0 | 10 |
| Component | Score (%) | ||||
|---|---|---|---|---|---|
| Mean (SD) | Minimum possible | Maximum possible | Minimum recoded | Maximum recoded | |
| Summation of activities | 12 (0.00) | 0 | 12 | 12 | 12 |
| Mean number of lessons | 6.65 (3.02) | 0 | N/A | 3 | 20 |
| Recoded lessons | 6.72 (2.97) | 4 | N/A | 4 | 20 |
| Activities/lessons | 2.06 (0.70) | 0 | 3 | 0.60 | 3 |
| CD | 6.98 (2.65) | 0 | 10 | 0 | 10 |
Table 38 (see Appendix 8) presents fidelity scores for each school that returned data. These scores ranged from 28.23% to 94.35% in phase 1 and from 34.71% to 100% in phase 2.
Parental intervention
Overall, parental/carer participation was low. In total, 319 parents/carers attended the intervention nights in NI (9% of those eligible), and 63 parents attended in Scotland (2.5% of those eligible).
With respect to the mailed intervention, 1074 returns were received from parents/carers in NI (31% return rate) and 440 were received in Scotland (18% return rate).
Summary of process evaluation
With regard to process evaluation components, clusters were successfully recruited into STAMPP, randomisation was successful and schools were comparable across intervention arms at baseline. No adverse events were reported.
The classroom component of STAMPP was delivered largely as intended, although there was some variation in fidelity of implementation scores between schools, namely through the number of lessons required to deliver the content. Our survey did not provide the reasons why the recommended number of lessons was not adhered to; however, considering the busy school curriculum, this may have been a result of competing demands or extension of some of the lessons and themes. For example, we became aware that one class had produced a short play based on their discussions and learning about the curriculum, so these type of activities may have been included. The curriculum was enjoyed by pupils, who reported that they found it interesting, informative and relevant to their own experiences or how they believed they might use alcohol in future. This contrasted with the largely negative perceptions of alcohol education reported by pupils in the EAN condition. However, it may be possible that bias in pupil interviews was non-equivalent. As they generally reported positive engagement with SHAHRP, this may have led to discounting or under-reporting of other negative aspects. Similarly, although alcohol EAN tended to be viewed negatively overall, this may have led to under-reporting of positive aspects. On the whole, the classroom materials were perceived as useful and were used as intended by the majority of teachers and pupils. Teacher evaluations of the classroom component were also largely positive, and it was viewed as complementing the schools’ wider health and well-being strategies. Teachers and school management believed that it was possible to accommodate the programme in the curriculum, supporting resources were useful and content was both experientially and age-appropriate.
Stakeholders in both trial geographies reported that STAMPP corresponded to their current policy and strategic aims, and that, if it was shown to be effective, it may form part of their future delivery of support for young people. In keeping with the views of some teachers, stakeholders emphasised the importance of assessing the impact of SHAHRP as a targeted intervention, as this was in line with many of their priorities. This would require further investigation.
In contrast, there was very low uptake of the parental/carer component, and postal returns of the parent/carer survey, which were used as an indicator of implementation of mailed intervention materials, were also relatively low. It should therefore be concluded that this component of the intervention was not successfully delivered.
Chapter 5 Economic evaluation: methods and results
Aim and perspective
The overall aim of the economic evaluation was to assess the cost-effectiveness of STAMPP compared with EAN in reducing HED in year 9 or S2 pupils. The study was a CEA alongside the main trial. The primary CEA estimated the incremental cost per young person experiencing HED avoided because of STAMPP at T2 and T3. The secondary CEA estimated the incremental cost per episode of heavy drinking avoided because of STAMPP at T2 and T3. A public sector perspective was adopted for the analysis that encompassed the costs to local authorities, NHS, personal social services and criminal justice services. Within the economic evaluation, we undertook and reported on the following:
-
analysis of intervention resource use and costs
-
analysis of public sector resource use and costs at each time point using all data that were available
-
analysis of total costs at T2 and T3 using data from pupils with complete cost data only
-
analysis of outcomes at T2 and T3 using data from pupils with complete cost data only
-
CEA at T2 and T3 using data from pupils with complete cost and outcome data.
Intervention resource use and costs
We calculated the economic cost of STAMPP according to the principle of opportunity cost, that is, we attempted to place a value on the benefits that were forgone by STAMPP being delivered instead of something else. We therefore included the full value of all the resources it used, regardless of whether or not the resources were directly purchased for the study.
The content of EAN within schools was assessed as part of the process evaluation (see Chapter 4, Usual alcohol-related activities in both intervention and control schools over the course of the study), and this supported the assumption that a similar level of resources were used, thus the costs were not included in the analysis.
The identification of appropriate intervention resource use was guided by a number of sources. These included the practical guide by Ritzwoller et al. 93 to costing behavioural interventions and methods used in other behavioural interventions such as the Diabetes Education and Self-Management for Ongoing and Newly Diagnosed (DESMOND) programme,94 A Stop Smoking In Schools Trial (ASSIST)95 and the First-aid Advice and Safety Training (FAST) parent programme. 96 In keeping with both Hollingworth et al. 95 and Mytton et al. ,96 resources were categorised according to the stage at which they were used in the research process: planning and preparation for delivery (stage 1) or delivery itself (stage 2).
Pre-startup resources associated with the development of STAMPP were not included in the analyses, as they would not be incurred should the intervention be mainstreamed in the future. These included the development of the teacher manual and pupil workbook content, the planning of the lessons and the design of the materials.
Stage 1 resources in STAMPP covered the recurring costs that were associated with printing/copying the intervention materials (teacher manual, pupil workbook, parent/guardian information sheets and CDs) and the delivery of teacher training (trainer fees, venue, catering and teacher cover). No cost associated with the purchasing and licensing of STAMPP intervention is foreseen, and so it is not included here. Stage 2 resources covered the recurring costs that were associated with teacher time input for delivery of phases 1 and 2 of the programme. The cost of teaching time was included even though the intervention was delivered within normal working hours and so would not have incurred an extra cost to the public sector. In doing so, we captured the opportunity cost of the benefits to pupils that were forgone by STAMPP being delivered instead of other lessons.
Resources used during stages 1 and 2 were recorded retrospectively by the project team, and costs were obtained from invoices when available. The costs associated with printing the intervention materials were not available, as these resources were present at the start of the trial. We therefore obtained printing quotations and deflated it to the appropriate price year using the Consumer Price Index. 97 The local authority in Glasgow/Inverclyde covered all of the costs associated with the training of the teachers including teacher cover, venue and catering, and so these were also not available. We therefore used the costs that were available for NI and applied them to Scotland. The majority of teachers delivering the intervention were at a junior level, thus we used point 3 on the main pay scale,98 including 24% for employers’ costs.
Pupils’ service use and costs
Data on service use by all pupils from baseline to T3 were collected using an instrument administered at T0, T1, T2 and T3. The instrument incorporated some items taken from the Client Service Receipt Inventory68 specifically adapted for childhood69 and items relating to the use of judicial services (see Appendix 9). The instrument included an information page with definitions of some of the public services in case the students were unfamiliar with them. The instrument was designed with input from relevant professionals (e.g. educational psychologist, social workers, Scottish and Northern Irish teachers) and reviewed by a social researcher who was experienced in delivering questionnaires to children, and other health economists. The instrument asked pupils to report their use of services in the previous 6 months, thus providing service use data for the 6 months before baseline, 7–12 months, 19–24 months and 28–33 months.
Individual-level service use was combined with unit costs (Table 25) to estimate a cost for each pupil for each of the four survey time periods. Unit costs were obtained from publicly available sources99–101 and set at 2013–14. For school counsellors/guidance teachers we assumed a mid-point, point 2, on the upper pay scale98 and included 24% for employers’ costs. As there were gaps in the survey period in which no cost data were collected (baseline to 6 months, 12–18 months and 24–27 months), we used interpolation of the available cost data to fill in these gaps. This was done separately for each participant to obtain an estimate of their total service use costs at T2 and T3. Total costs could not be calculated for those pupils who had any missing cost data points, as these were required for the interpolation.
| Service | Unit cost | Source |
|---|---|---|
| Education | ||
| School nurse | 50.00 | Unit Costs of Health and Social Care 2014,100 p. 85 |
| School counsellor/guidance teacher | 35.02 | Department of Education NI (per 1 hour of teacher time, point 2 of upper scale)98 |
| Intervention teacher | 25.89 | Department of Education NI (per 1 hour of teacher time, point 3 of the main pay scale)98 |
| Educational psychologist | 41.00 | Unit Costs of Health and Social Care 2014,100 p. 156 |
| Education welfare officer/home-school liaison officer | 27.00 | Unit Costs of Health and Social Care 2014,100 p. 155 |
| Health | ||
| GP surgery visit | 46.00 | Unit Costs of Health and Social Care 2014,100 p. 195 |
| GP out-of-hours | 115.00 | Unit Costs of Health and Social Care 2014,100 p. 191 (home visit unit cost assumed as above) |
| Nurse (other than school nurse) | 13.70 | Unit Costs of Health and Social Care 2014,100 p. 192 (per 15.5-minute surgery consultation) |
| Hospital appointment | 109.00 | Unit Costs of Health and Social Care 2014,100 p. 111 |
| A&E | 233.00 | Unit Costs of Health and Social Care 2014,100 p. 111 (see and treat and convey) |
| Overnight hospital stay | 658.33 | NHS Reference Costs 2013–1499 (weighted average length of stay and cost of paediatric non-elective long stays) |
| Psychologist | 50.00 | Unit Costs of Health and Social Care 2014,100 p. 51 |
| Counsellor (other than at school) | 50.00 | Unit Costs of Health and Social Care 2014,100 p. 51 |
| Social worker | 79.00 | Unit Costs of Health and Social Care 2014,100 p. 206 (per 1 hour including travel) |
| Telephone helpline | 3.99 | National Society for the Prevention of Cruelty to Children Annual Report and Account 2014/2015101 cost per call to Childline deflated to 2013–14 |
| Criminal justice | ||
| Youth justice service | 84.00 | Unit Costs of Health and Social Care 2014,100 p. 224 (face-to-face contact) |
| Police service | 325.00 | Unit Costs of Health and Social Care 2014,100 p. 149 |
Analysis of intervention resource use and costs
Stage 1 costs were added together to get a total cost. Stage 2 costs relating to the delivery of the intervention at a class level were multiplied by the total number of classes that received the intervention to get a total cost. This was estimated by dividing the number of pupils receiving the intervention at baseline (n = 5749) by 30, which was used as an estimate of the maximum number of pupils per class. Stage 2 costs relating to the delivery of the parental component were calculated by multiplying the number of schools by the costs of delivering one session. The stage 1 and stage 2 costs were totalled and divided by the number of pupils receiving the intervention at baseline to obtain the mean cost per pupil.
Analysis of pupils’ public sector service use and costs
The analysis of service use included the pupils present at each survey time point. If there were any missing fields within the service use questionnaire, it was assumed that the relevant service had not been used. Descriptive statistics were used to summarise service use and costs at each time point for the different categories of the public sector (education, health and criminal justice).
As interpolation was used to calculate total costs, only pupils with complete cost data up to T2 or T3 could be included in the analysis of total costs. The costs of service use in the 6 months before T0 were not included in the total costs but were used in the interpolation. The total costs were analysed using a multilevel mixed-effects regression model controlling for pupils’ baseline costs, school location (NI/Scotland), school level of FSM provision (low, 0–15.4%; moderate, 15.5–30.4%; high, ≥ 30.5%), school type (all-boys’ school/all-girls’ school/coeducation school) and clustering. With the exception of baseline costs, the same covariates were used in the analysis of the primary outcome data and prespecified in the data management plan. The incremental costs associated with STAMPP were estimated using the margins command in Stata. This command first calculates the marginal (treatment) effect for each individual with their observed levels of covariates and then averages these values across all individuals to obtain the average marginal effect.
The costs occurring in years 2 and 3 of the study were discounted at 3.5%, in keeping with NICE (2013) guidance. 77
Outcomes
Consistent with the primary outcome of the study, the primary economic effectiveness measure was the number of pupils who reported any HED in the previous 30 days at T3. This was based on responses to the question ‘How often in the past month have you drank [sic] 4.5 (female)/6 (male) or more units of alcohol?’. As we were also interested in outcomes at T2, we dichotomised responses to the question ‘How often in the past month would you have drank [sic] more than five full drinks in the one drinking session?’, and thus the outcome at T2 was slightly different from the primary outcome at T3.
The secondary economic effectiveness measure was the number of heavy drinking episodes at T3. This was calculated using the survey data on the frequency of heavy drinking episodes in the previous 30 days collected at the four survey time points. As pupils reported only on the number of heavy drinking episodes they had experienced in the previous 30 days at each of the time point, linear interpolation was used to complete gaps in the survey periods separately for each participant in order to obtain an estimate of their total number of heavy drinking episodes at T2 and T3.
Analysis of outcomes
The analysis of the primary economic effectiveness measure included all pupils responding to the relevant outcome variable at T2 and T3. Descriptive statistics were used to summarise the proportion of pupils in each arm reporting a heavy drinking episode in the previous 30 days at T2 and T3. These effects were analysed using a multilevel mixed-effects logistic regression model controlling for pupils’ baseline drinking, school location, school level of FSM provision, school type and clustering. The incremental effects associated with STAMPP were estimated using the margins command in Stata.
As interpolation was used to calculate the total number of heavy drinking episodes, the analysis of the secondary effectiveness measure included only pupils who had complete heavy drinking episode data to T2 or T3. Descriptive statistics were used to summarise heavy drinking episodes at T2 and T3. These effects were analysed using a multilevel mixed-effects regression model controlling for pupils’ baseline drinking, school location, school level of entitlement to FSMs and clustering. It was not appropriate to discount the primary outcome, as it was dichotomous and measured at a single time point. Non-parametric bootstrapping was used to calculate 95% bootstrap CIs of mean incremental effects drawing 1000 samples of the same size as the original sample separately for each group with replacement. Significance (p < 0.05) was judged when the CIs excluded zero. The number of heavy drinking episodes occurring in T2 and T3 of the study were discounted at 3.5%, in keeping with the NICE (2013) guidance. 77
Cost-effectiveness analysis
For pupils to be included in the CEA they needed to have complete cost and outcome data. Therefore, the population differed from that used in the separate analyses of total costs and outcomes. For the primary analysis at T3, this meant pupils with cost data from baseline to T3 and a response to the primary outcome variable at T3. For the primary CEA at T2, this meant pupils with cost data from baseline to T2 and a response to the outcome variable at T2. For pupils to be included in the secondary CEAs at T3, they needed complete cost data from baseline to T3 and complete heavy drinking episodes data from baseline to T3. For inclusion in the secondary CEA at T2, pupils needed complete cost data from baseline to T2 and complete heavy drinking episodes data from baseline to T2.
The cost-effectiveness of STAMPP was estimated using conventional decision rules102 and reported as an ICER if appropriate. The ICER is a measure of the additional cost per additional unit of effect produced by one intervention compared with another. For an intervention to be considered cost-effective, the ICER must be less than the maximum amount of money that a decision-maker would be willing to pay per unit of effect, that is, their willingness-to-pay (WTP) threshold. Uncertainty in the cost-effectiveness measures was investigated by bootstrapping the multilevel models and using the incremental costs and effects to generate 1000 replications of the ICERs. The resulting replicates were plotted on the cost-effectiveness plane and used to construct CEACs. Construction of these curves involved a series of lines being placed on the plane representing the different WTP thresholds that a decision-maker may have. The proportion of ICER replicates falling below each WTP threshold equated to the probability of STAMPP being cost-effective at that threshold. The curves for the primary CEA specifically showed the probability of STAMPP being cost-effective compared with EAN at different threshold levels of WTP to avoid a pupil experiencing an episode of heavy drinking in the previous 30 days at (1) T3 and (2) T2. The curves for the secondary CEA showed the probability of STAMPP being cost-effective at different threshold levels of WTP to avoid an episode of heavy drinking at (1) T3 and (2) T2. There is no generally accepted threshold value for cost per pupil experiencing any HED avoided or cost per heavy drinking episode avoided. We looked at range of thresholds, including the cost of the intervention per pupil, and compared our findings with those of other economic evaluations that have been performed in this research area.
All analyses were performed using Stata/IC version 12.
Sensitivity analysis
The robustness of the results from the CEA was explored via the following one-way sensitivity analyses.
-
Missing total costs and the primary outcome at T3 were filled simultaneously using multiple imputation by chained equations. In the multiple imputation model we included all of the variables that were to be included in the subsequent multilevel models, that is, the treatment variable, baseline costs, baseline drinking, school location, school level of entitlement to FSMs and clustering. We also included 6- to 12-month costs and 6- to 12-month drinking. We used predictive mean matching for costs and a logit model for the primary outcome. Five imputed data sets were generated and the results were combined.
-
Total costs and total heavy drinking episodes at T3 were discounted at a rate of 1.5%, as suggested by NICE103 for public health interventions. The multilevel models were re-estimated without adjusting for baseline covariates but still adjusting for clustering.
-
As a linear time trend was assumed between data time points, this might have led to total costs and total heavy drinking episodes being under-/overestimated if said trend was not appropriate. The impact of increasing and decreasing total costs and total heavy drinking episodes at T3 by 5% were, therefore, explored.
Results
There were 11,316 pupils present at the baseline assessment: 5749 in the intervention group and 5567 in usual education. A total number of 12,738 pupils took part in the study, with 6379 in the intervention group and 6359 in the control group.
Intervention resource use and costs
The resources and costs used in the planning, preparation and delivery of the intervention are presented in Table 26. The total costs are presented in Table 27. The mean cost per school was £818 and the mean cost per pupil was £15. The largest proportion of the costs was associated with the training of the teachers, as this involved teaching cover, location costs and facilitator costs. The second largest cost was associated with the delivery of the intervention in the classroom setting. In the light of the low uptake of the parental component of STAMPP, we also present the cost of delivering the STAMPP classroom component only. This reduced costs to £692 per school and £13 per pupil.
| Resource use | Unit cost (£) | Number of units | Total cost (£) | Cost details |
|---|---|---|---|---|
| Stage 1 planning and preparation for delivery | ||||
| Intervention materials | ||||
| Phase 1 teacher manual | N/A | 145 | 240 | 16 pages |
| Phase 2 teacher manual | N/A | 145 | 293 | 22 pages |
| Phase 1 pupil workbook | N/A | 5749 | 2623 | 20 pages |
| Phase 2 pupil workbook | N/A | 5749 | 2623 | 20 pages |
| Parent and guardian information sheet | N/A | 5749 | 255 | Single-sided page |
| Parent and guardian information sheet (follow-up) | N/A | 5749 | 255 | Single-sided page |
| Phase 1 CD | 1.40 | 145 | 203 | Cost of duplication |
| Phase 2 CD | 1.40 | 145 | 203 | Cost of duplication |
| Training of the teachers (phase 1) | ||||
| NI | ||||
| Training | 500.00 | 3 | 1500 | Training delivered by a non-government organisation facilitator (£500 per day) |
| Teachers | 161.79 | 107 | 17,312 | Based on 1-day (6.5 hours) teaching cover for a junior teacher at £24.89/hour |
| Location and associated cost (e.g. room hire) | 25.00 | 107 | 2675 | Local hotel costs including food and refreshments (£25/head) |
| Scotland | ||||
| Training | 500.00 | 2 | 1000 | Training delivered by a non-government organisation facilitator (£500 per day) |
| Teachers | 161.79 | 38 | 6148 | Based on 1-day (6.5 hours) teaching cover for a junior teacher at £24.89/hour |
| Location and associated cost (e.g. room hire) | 25.00 | 38 | 950 | Local hotel costs including food and refreshments (£25/head) |
| Training of the teachers (phase 2) | ||||
| NI | ||||
| Training sessions | 500.00 | 3 | 1500 | Training delivered by a non-government organisation facilitator (£500 per day) |
| Teachers | 24.89 | 83 | 2066 | Based on 1-day (6.5 hours) teaching cover for a junior teacher |
| Location and associated cost (e.g. room hire) | 28.78 | 83 | 2389 | Local hotel costs including food and refreshments (£28.78/head) |
| Scotland | ||||
| Trainer | 500.00 | 1 | 500 | Training delivered by a non-government organisation facilitator (£500 per day) |
| Teachers | 24.89 | 38 | 946 | Based on 1-day (6.5 hours) teaching cover for a junior teacher |
| Location and associated cost (e.g. room hire) | 28.78 | 38 | 1094 | Local hotel costs including food and refreshments (£28.78/head) |
| Stage 2 delivery | ||||
| Phase 1 teacher time input | 14.52 | 6 | 87 | Based on 35-minute lessons |
| Phase 2 teacher time input | 14.52 | 4 | 58 | Based on 35-minute lessons |
| Parental component delivery | 250.00 | 53 | 13,250 | Delivered by a non-government organisation facilitator (£500 per day) |
| Resource use | Total cost (£) |
|---|---|
| Stage 1 planning and preparation for delivery | |
| Materials | 6694 |
| Training | 38,079 |
| Stage 1 subtotal | 44,773 |
| Stage 2 delivery | |
| Teaching | 27,877 |
| Facilitator | 13,250 |
| Stage 2 subtotal | 41,127 |
| Cost for the STAMPP classroom componenta | 72,650 |
| Mean cost/school for classroom componentb | 692 |
| Mean cost/pupil for classroom componentc | 13 |
| STAMPP total cost | 85,900 |
| Mean cost/schoola | 818 |
| Mean cost/pupilb | 15 |
Public sector service use by pupils and associated costs
Pupils’ use of public sector services in the 6 months before baseline, from 6 to 12 months, from 18 to 24 months and from 27 to 33 months is in Appendix 10 (see Tables 39–42, respectively). The public service costs over the study period are shown in Figure 4. The public service costs (£) over the study period by group and by category are shown in Table 43, Appendix 10. As stated in Analysis of pupils’ public sector service use and costs, the analysis of service use included the pupils present at each survey time point.
FIGURE 4.
Public service costs (£) over the study period by group and by category.
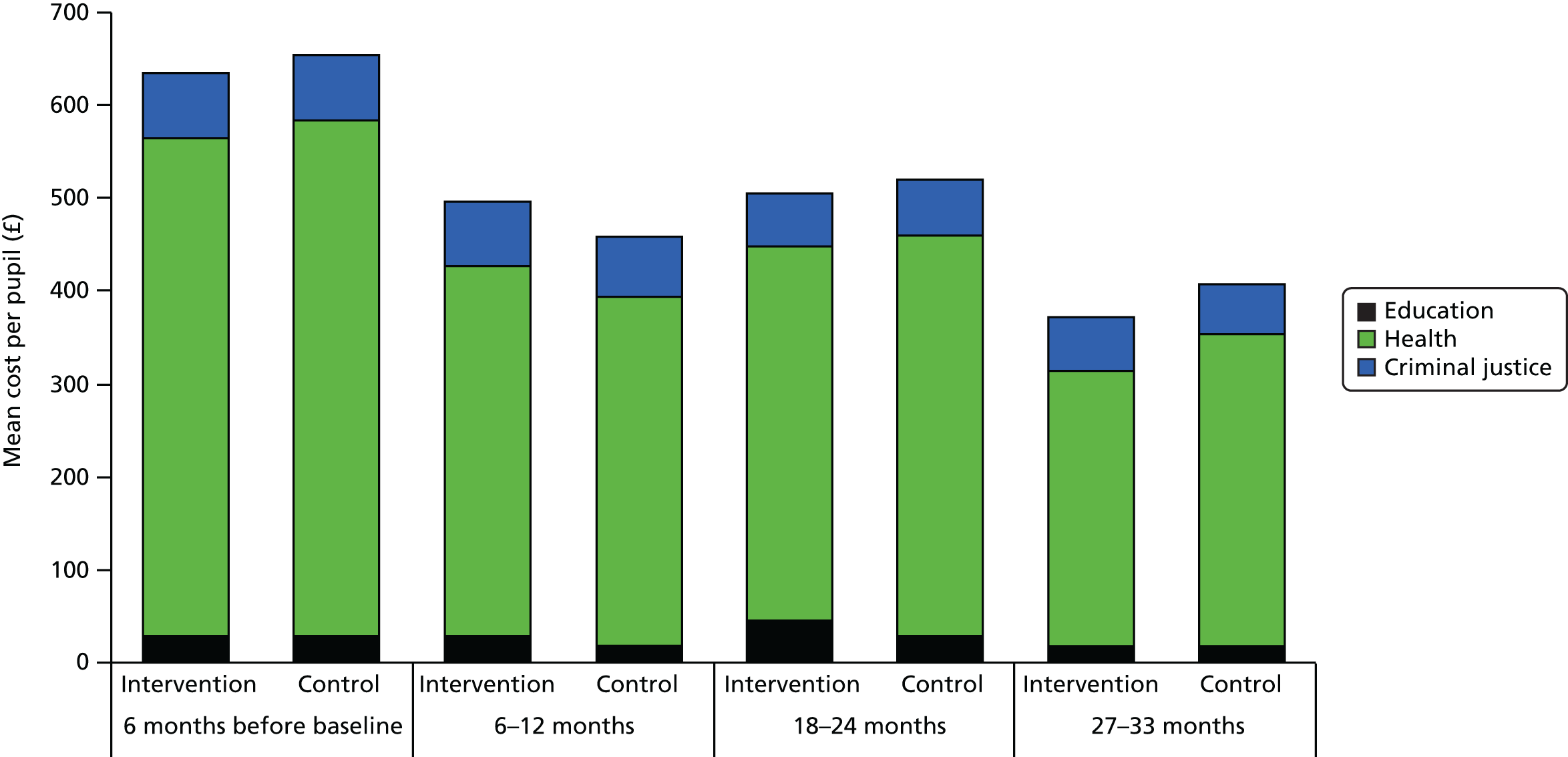
The total costs of pupils’ use of public services over the study period following interpolation of costs and adjustment for baseline covariates and clustering are shown in Figure 5 (see also Table 44, Appendix 10). As detailed in Analysis of pupils’ public sector service use and costs, only pupils with complete cost data were included in the analysis of total costs. The numbers were similar across groups for the analysis of total costs at T2 and T3. At T2, the mean cost was £2006 for intervention pupils and £1916 for control pupils. At T3, the mean cost was £2307 for intervention pupils and £2292 for control pupils. Thus, differences were small and not statistically significant. The total costs did not include the cost per pupil to deliver the intervention.
FIGURE 5.
Total public service costs (£) by group and by category at T2 and T3.
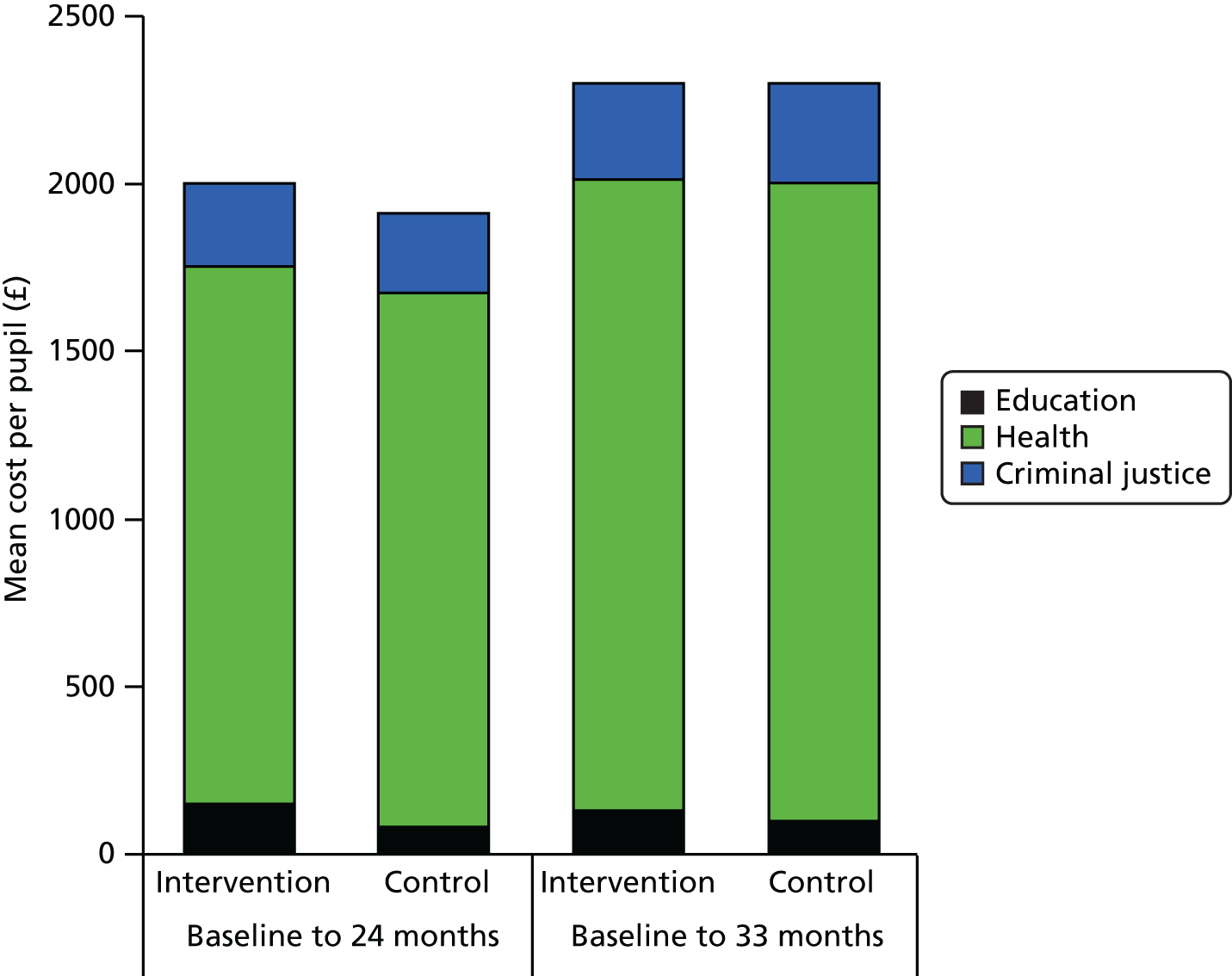
Outcomes
The proportion of pupils reporting a heavy drinking episode in the previous 30 days is shown in Table 28. The response rates to the outcome variables were similar across groups at each time point. At T2, fewer pupils in the intervention arm than in the control arm reported drinking heavily in the previous 30 days (11% vs. 13%). At T3, the percentage of pupils reporting a heavy drinking episode had increased in both groups: to 17% of pupils in the intervention group and to 25% in the control group (note that the figures reported in Chapter 3, Description of primary outcomes are based on unadjusted data and, therefore, differ slightly to the figures presented here). The difference of 8% was statistically significant. It is important to highlight that the outcome variable at T2 and T3 differed slightly, as detailed in Outcomes. Pupils’ heavy drinking episodes over the study period are presented in Table 29. Pupils in the intervention group reported statistically significantly fewer heavy drinking episodes at both T2 and T3 than those in the control arm.
| Time point | Trial arm | Difference (95% CI) | |||
|---|---|---|---|---|---|
| Intervention | Control | ||||
| Number analysed (% total) | Proportion (95% CI) | Number analysed (% total) | Proportion (95% CI) | ||
| T2 | 5250 (82.3) | 0.11 (0.09 to 0.12) | 5176 (81.4) | 0.13 (0.11 to 0.16) | –0.02 (–0.04 to –0.00) |
| T3 | 5160 (80.9) | 0.17 (0.15 to 0.19) | 5073 (79.8) | 0.25 (0.22 to 0.27) | –0.08 (–0.11 to –0.05) |
| Time point | Trial arm | Difference (95% CI) | |||
|---|---|---|---|---|---|
| Intervention | Control | ||||
| Number analysed (% total) | Mean (95% CI) | Number analysed (% total) | Mean (95% CI) | ||
| T2 | 4683 (73.4) | 3.38 (2.94 to 3.82) | 4578 (72.0) | 4.11 (3.78 to 4.42) | –0.72 (–1.35 to –0.10) |
| T3 | 4128 (64.7) | 4.68 (4.11 to 5.25) | 3945 (62.0) | 5.40 (4.98 to 5.83) | –0.73 (–1.54 to –0.08) |
Cost-effectiveness analysis
For the purposes of the CEA, outcomes are reported in terms of cases avoided; thus, a positive difference reflects a smaller number of pupils in the intervention arm experiencing a heavy drinking episode in the previous 30 days or a smaller number of heavy drinking episodes being experienced in the intervention arm. Negative costs reflect a cost saving in favour of the intervention. The cost per pupil for the intervention (£15) was added to each pupil in the intervention arm.
At T3 the number of pupils that had complete cost and outcome data and could therefore be included in the CEA was similar across groups (approximately two-thirds of all pupils). At T2 the number of pupils included in the analysis was again similar across groups, but higher than at T3 (approximately three-quarters of all pupils).
The results from the primary CEA at T2 and T3 are shown in Table 30. At T3 there was small cost saving associated with STAMPP (–£17.19) and a significantly greater proportion of pupils experiencing a heavy drinking episode avoided (0.07 or 7%). In other words, the STAMPP intervention is cost-saving and is beneficial in reducing HED. In this situation, the negative ICER is not calculated, as its magnitude does not convey any meaning. 104 STAMPP can be said to dominate EAN; however, as the difference in costs was not statistically different, only weak dominance can be claimed. 105
| Analysis | Intervention, number analysed (% total) | Control, number analysed (% total) | Difference in total health service costs (£) (95% CI) | Difference in effect (proportion of pupils who reported a heavy drinking episode in previous 30 days avoided) (95% CI) | Cost per pupil who reported a heavy drinking episode in previous 30 days avoided (95% CI) |
|---|---|---|---|---|---|
| T2 | 4757 (74.8) | 4653 (73.2) | 62.88 (–262.56 to 388.32) | 0.02 (0.01 to 0.03) | 3162.09 (–19,921.24 to 26,245.43) |
| T3 | 4189 (65.7) | 4037 (63.5) | –17.19 (–402.84 to 368.46) | 0.07 (0.06 to 0.09) | Dominant |
| Sensitivity analyses for primary CEA at T3 | |||||
| Multiple imputation for missing cost and outcome data at T3 | 6379 (100) | 6359 (100) | 34.10 (–299.44 to 367.44) | 0.08 (0.07 to 0.09) | 404.88 (3625.58 to 4435.35) |
| Discounting costs and outcome at 1.5% at T3 | – | – | –17.63 (–410.62 to 375.36) | 0.07 (0.06 to 0.09) | Dominant |
| Adjustment of costs and outcome data for cluster only | – | – | –49.23 (–419.52 to 321.07) | 0.08 (0.06 to 0.10) | Dominant |
| 5% increase in costs | – | – | –18.05 (–422.98 to 386.88) | 0.07 (0.06 to 0.09) | Dominant |
| 5% decrease in costs | – | – | –16.33 (–382.70 to 350.04) | 0.07 (0.06 to 0.09) | Dominant |
Uncertainty surrounding the estimates of total costs and outcomes is represented by the bootstrapped ICERs on the cost-effectiveness plane for the primary analysis at T3 (Figure 6). The majority of points straddle the north-east and south-east quadrants, indicating that, although STAMPP is likely to be more effective than EAN, there is considerable variability about the cost estimates.
FIGURE 6.
Cost-effectiveness plane for the primary CEA at T3 showing bootstrapped replications of mean incremental costs and pupils who avoided a heavy drinking episode.
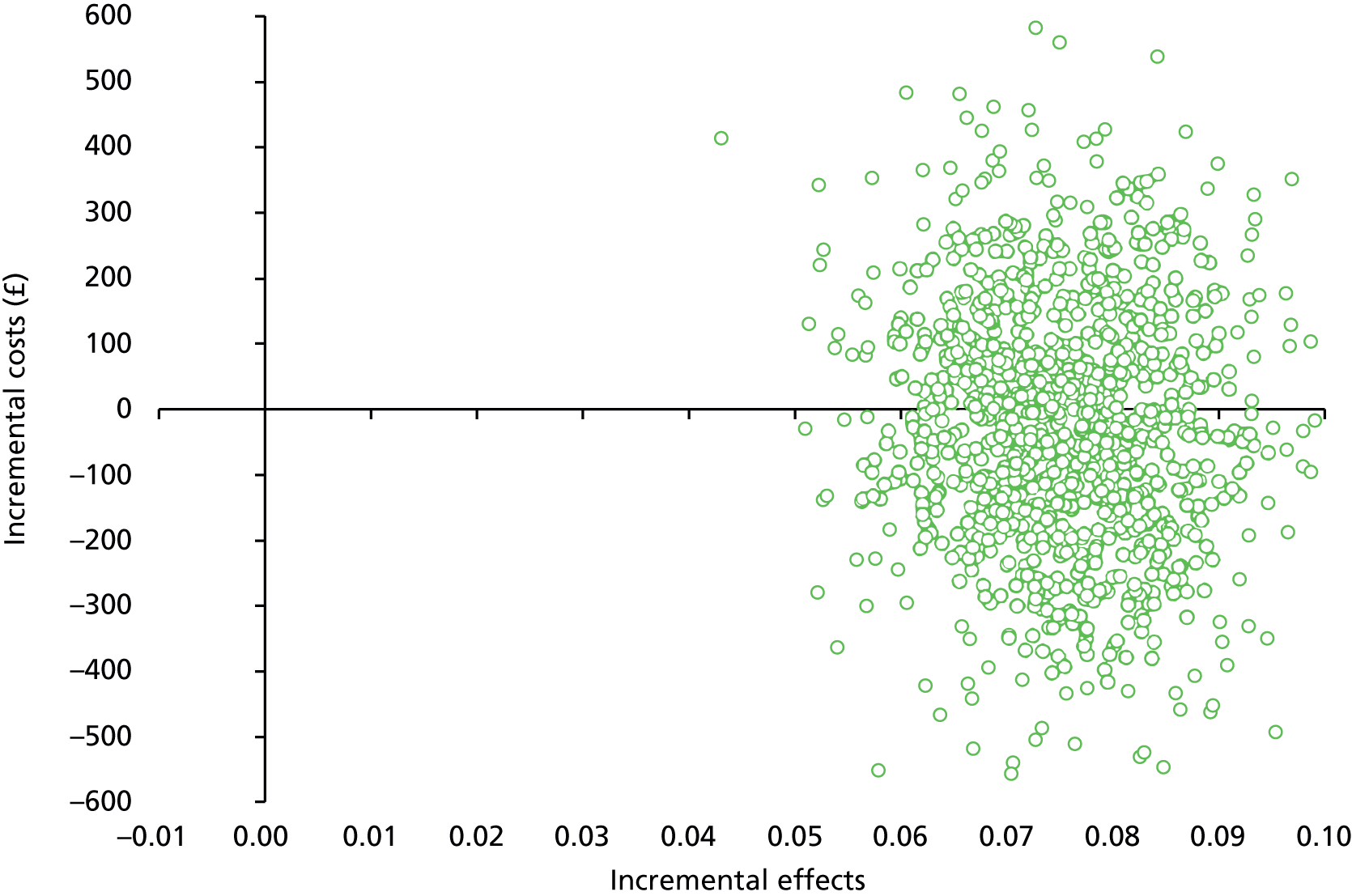
At T2, the intervention arm had marginally higher costs and again a significantly greater proportion of pupils who avoided a heavy drinking episode (0.02), equating to a cost per pupil who avoided a heavy drinking episode of £3162. The cost-effectiveness plane for the analysis (Figure 7) shows a similar pattern to the T3 analysis but with a slightly greater proportion of points in the north-east quadrant, indicating that the intervention is associated with slightly higher costs than the analysis at T3.
FIGURE 7.
Cost-effectiveness plane for the primary CEA at T2 showing bootstrapped replications of mean incremental costs and pupils who avoided a heavy drinking episode.
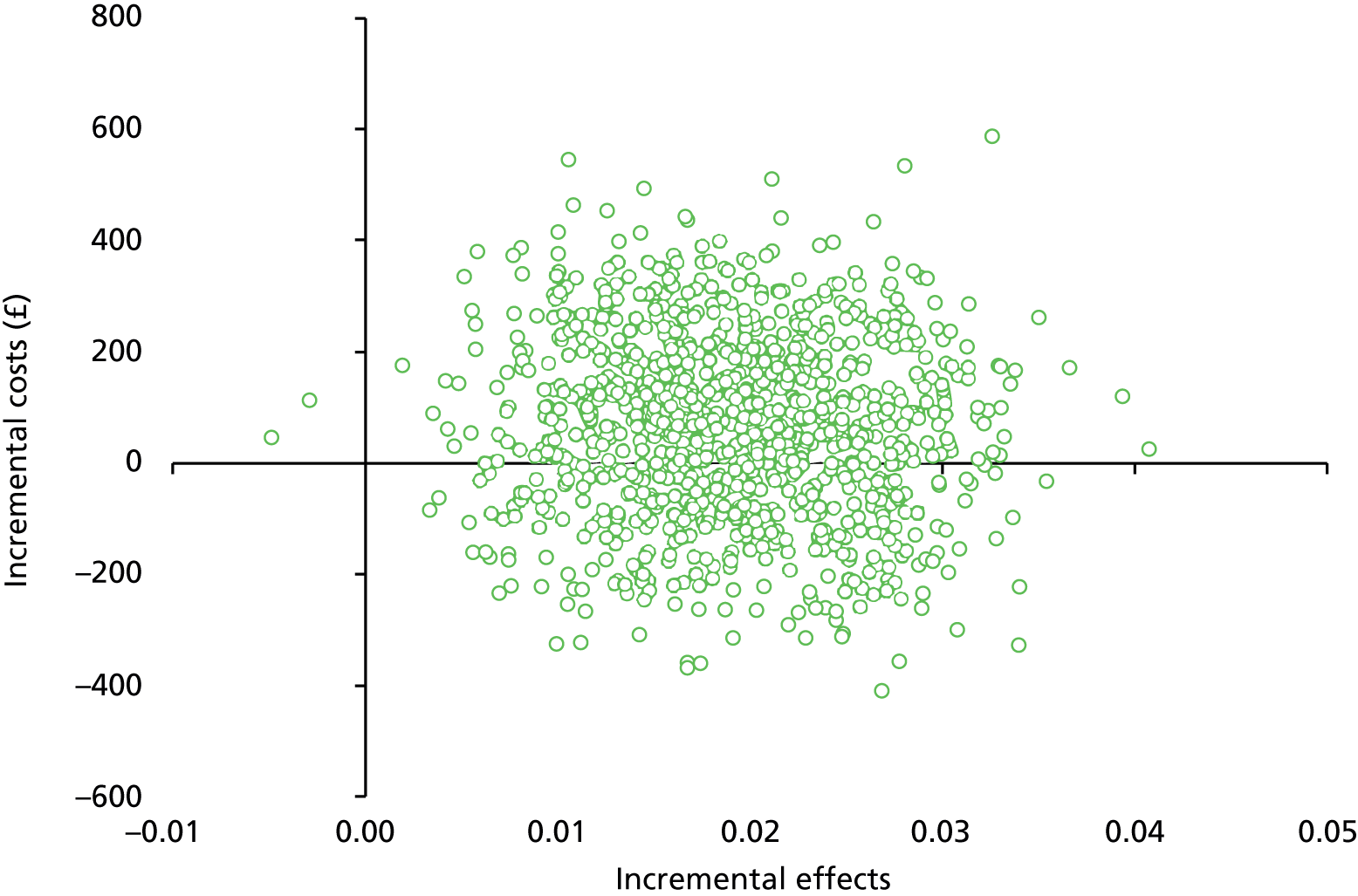
The CEACs for the primary CEA are presented in Figure 8. When WTP thresholds ranging from £0 to £800 are considered, it can be seen that at T3 the probability of STAMPP being cost-effective compared with EAN ranges from 55% to 67%. Uncertainty in the cost-effectiveness of the intervention remains substantial until much higher WTP values, with an 80% probability being displayed at a WTP of £2000. At T2, the probability of cost-effectiveness is consistently lower at each WTP threshold, with values ranging from 35% to 38%. The implication is that, in the short term, STAMPP is not likely to be cost-effective. However, taking a longer-term view, STAMPP is likely to be cost-effective. If decision-makers were only willing to pay the £15 (the cost of STAMPP per pupil), the probability would be 56% at T3 and 35% at T2.
FIGURE 8.
Cost-effectiveness acceptability curves showing the probability of STAMPP being cost-effective compared with EAN for the primary CEA at T2 and T3.

The results of the sensitivity analyses for the primary CEA are presented in Table 30 and the corresponding CEACs are in Figure 9. After the multiple imputation of missing data, the probability of STAMPP being cost-effective was lower at each WTP threshold, ranging from 40% to 55%. The outputs from the models including the Monte Carlo error are presented in Appendix 8, Tables 45 and 46. In contrast, when the multilevel models were re-estimated adjusting only for baseline covariates, the probability of cost-effectiveness was consistently higher, ranging from 65% to 76%. Reducing the discount rate to 1.5% and increasing/decreasing costs by 5% had little effect on the cost-effectiveness of STAMPP.
FIGURE 9.
Cost-effectiveness acceptability curves showing the probability of STAMPP being cost-effective compared with EAN for the sensitivity analyses for primary CEA.
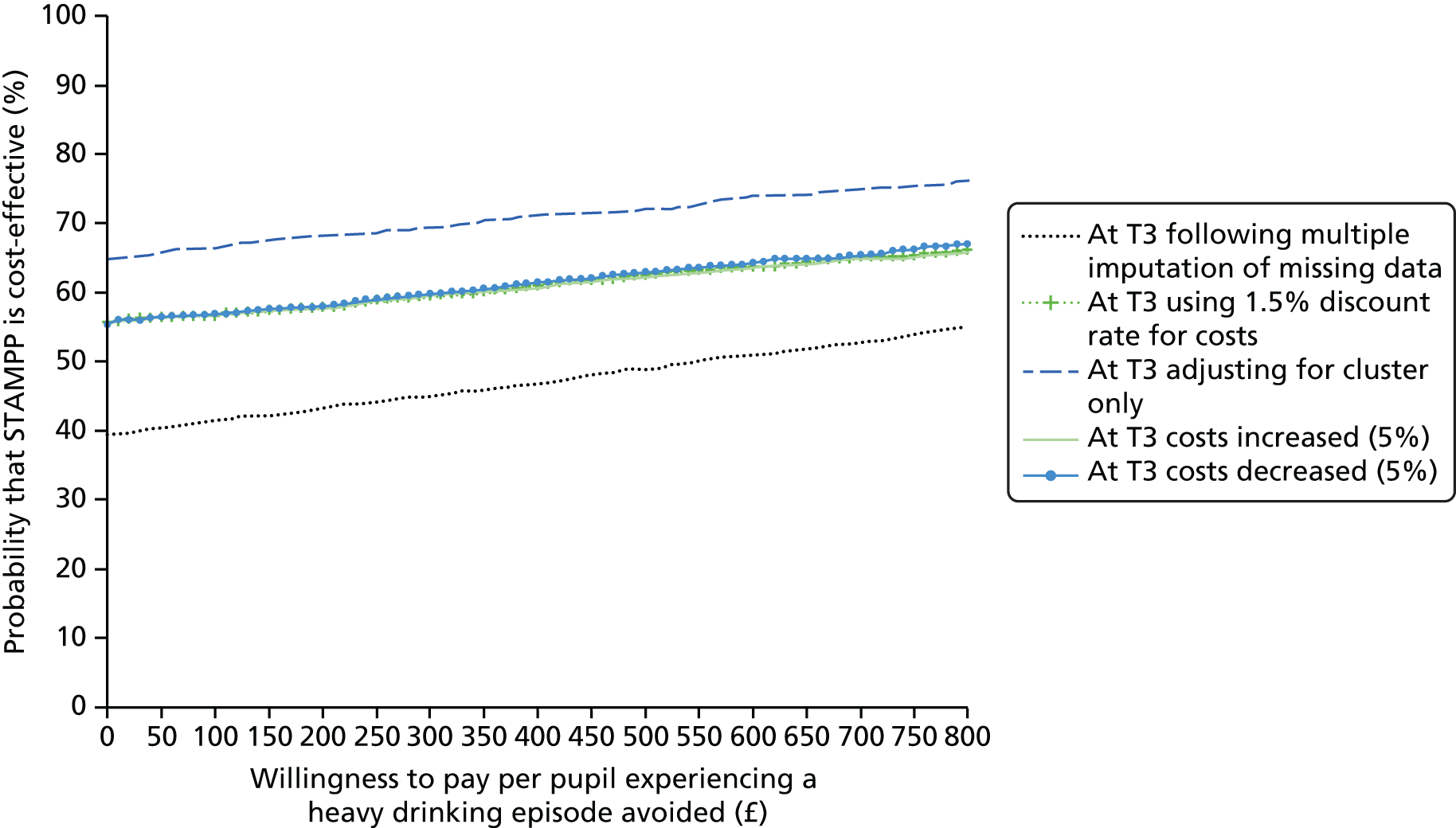
The results from the secondary CEAs are presented in Table 31. For the secondary CEAs at T3, STAMPP was associated with higher costs (£31) and more episodes of heavy drinking avoided (0.73), equating to a cost per heavy drinking episode avoided of £42. Neither difference was statistically significant. The cost-effectiveness plane for this analysis is presented in Figure 10. The majority of points lie in the north-east and south-east quadrants, indicating that STAMPP is likely to be more effective but that there is considerable variability in the cost estimates. For the secondary CEA at T2, STAMPP was again associated with higher costs (£84) and more heavy drinking episodes avoided (0.72), equating to £116.34 per heavy drinking episode avoided. Again, the differences were not statistically significant. The cost-effectiveness plane for the analysis (Figure 11) shows a similar pattern to the T3 analysis but with a slightly greater proportion of points in the north-east quadrant, indicating that the intervention is associated with slightly higher costs than the analysis at T3. The CEACs for the secondary CEAs are presented in Figure 12. When WTP thresholds ranging from £0 to £800 are considered, it can be seen that, at T3, the probability of STAMPP being cost-effective compared with EAN ranges from 43% to 96%. At T2, this probability is lower for lower WTP thresholds, ranging from 30% to 98%. If decision-makers were willing to pay only £15 (the cost of STAMPP per pupil), the probability would be 45% at T3 and 32% at T2.
| Analysis | Intervention, number analysed | Control, number analysed | Difference in total health service costs (£) (95% CI) | Difference in effect (cases of heavy drinking episodes avoided) (95% CI) | Cost per heavy drinking episode avoided (95% CI) |
|---|---|---|---|---|---|
| T2 | 4683 | 4578 | 83.98 (–234.26 to 402.22) | 0.72 (0.29 to 1.16) | 116.34 (–1426.35 to 1659.03) |
| T3 | 4128 | 3945 | 31.27 (–351.67 to 414.21) | 0.73 (0.15 to 1.30) | 42.93 (–2530.65 to 2616.51) |
| Sensitivity analyses for secondary analysis | |||||
| Discounting costs and outcome at 1.5% at T3 | 4128 | 3945 | 30.42 (–360.24 to 421.08) | 0.74 (0.16 to 1.33) | 40.85 (–2616.84 to 2698.53) |
| Adjustment of costs and outcome data for cluster only | 4128 | 3945 | –8.47 (–383.42 to 366.47) | 1.00 (0.34 to 1.65) | Dominant |
| 5% increase in costs | 4128 | 3945 | 29.71 (–334.09 to 393.50) | 0.73 (0.15 to 1.30) | 40.78 (–2404.11 to 2485.68) |
| 5% decrease in costs | 4128 | 3945 | 32.83 (–369.25 to 434.92) | 0.73 (0.15 to 1.30) | 45.08 (–2657.18 to 2747.33) |
| 5% increase in cases of heavy drinking | 4128 | 3945 | 31.27 (–351.67 to 414.21) | 0.77 (0.16 to 1.37) | 40.89 (–2410.14 to 2491.91) |
| 5% decrease in cases of heavy drinking | 4128 | 3945 | 31.27 (–351.67 to 414.21) | 0.69 (0.15 to 1.24) | 45.19 (–2663.84 to 2754.22) |
FIGURE 10.
Cost-effectiveness plane for the secondary CEA at T3 showing bootstrapped replications of mean incremental costs and heavy drinking episodes avoided.
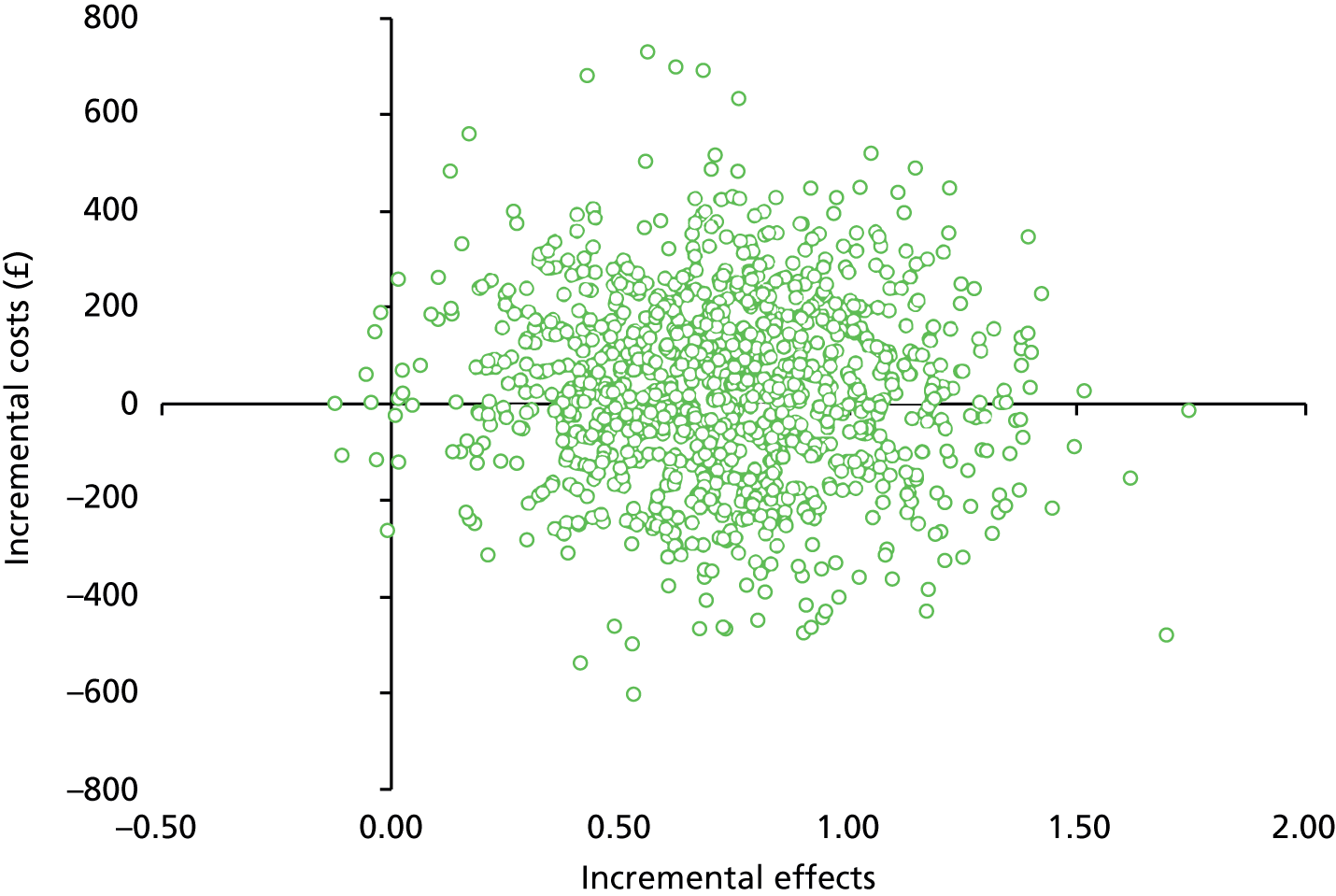
FIGURE 11.
Cost-effectiveness plane for the secondary CEA at T2 showing bootstrapped replications of mean incremental costs and heavy drinking episodes avoided.
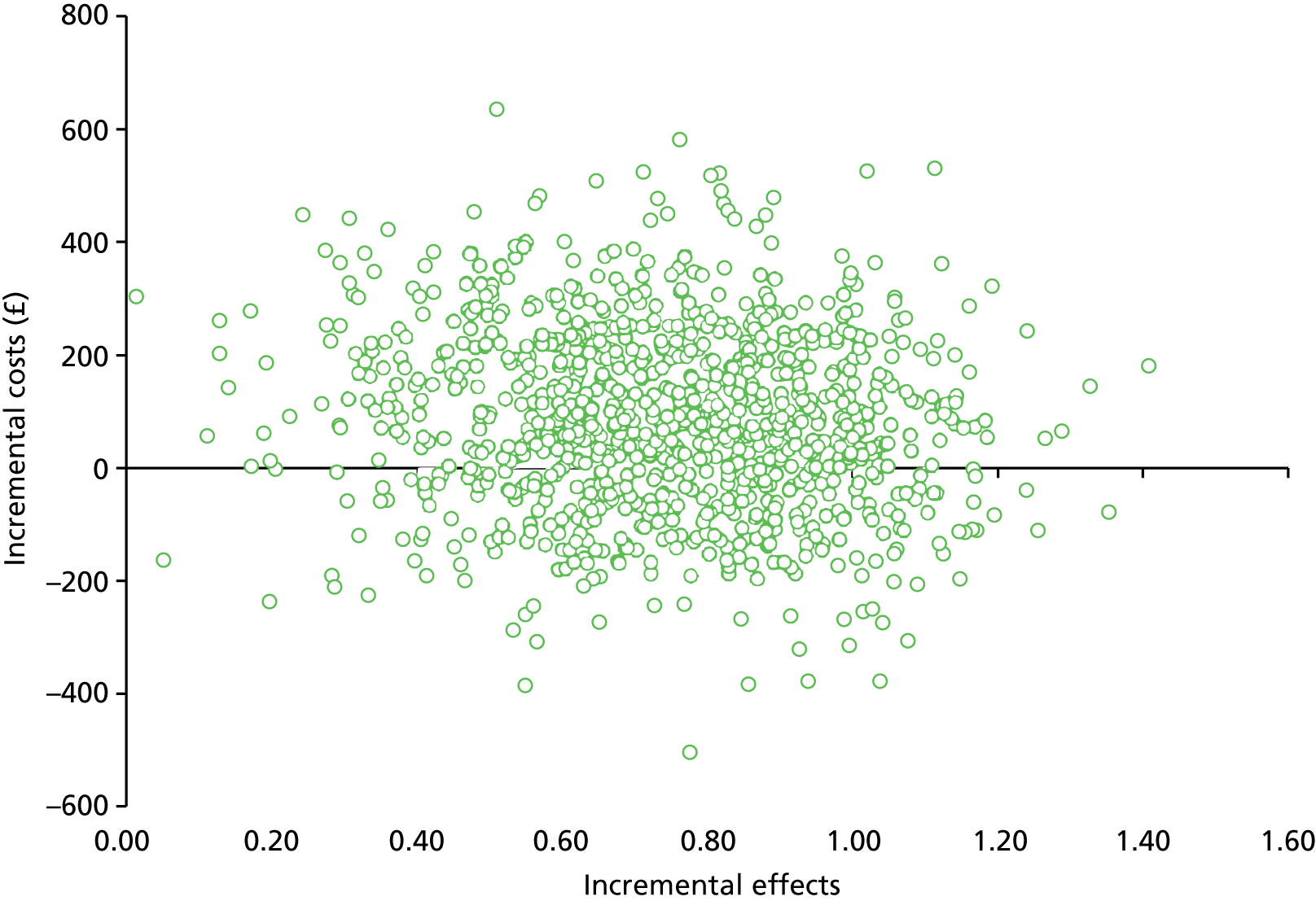
FIGURE 12.
Cost-effectiveness acceptability curves showing the probability of STAMPP being cost-effective compared with EAN for the secondary CEAs at T2 and T3.
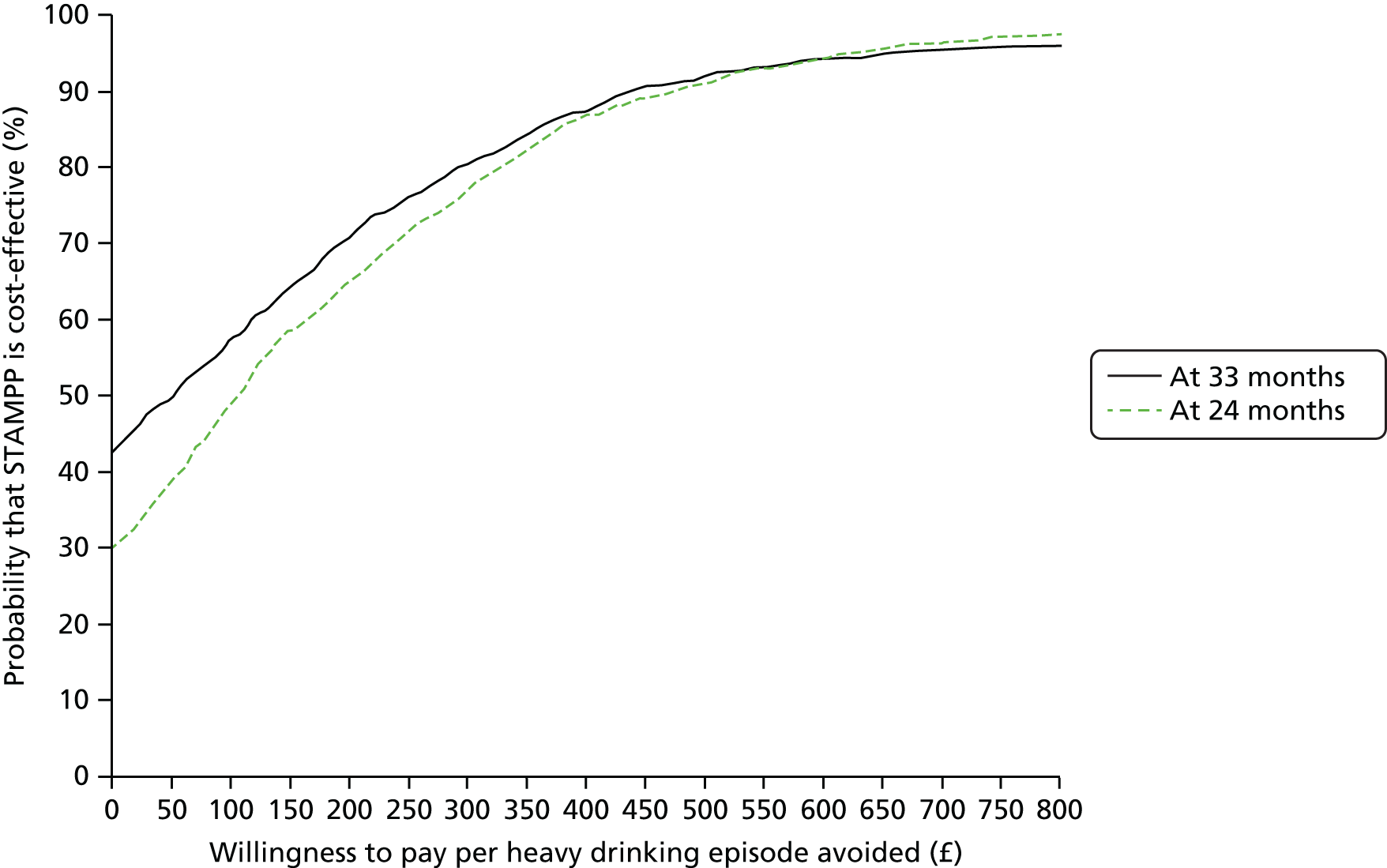
The results of the sensitivity analyses for the secondary CEAs are presented in Table 31, and the corresponding CEACs are presented in Figure 13. When the multilevel models were re-estimated, adjusting only for baseline covariates, the probability of STAMPP being cost-effective was consistently higher, ranging from 52% to 100%. Reducing the discount rate to 1.5% and increasing/decreasing costs and effects by 5% had little effect on the cost-effectiveness of STAMPP.
FIGURE 13.
Cost-effectiveness acceptability curves showing the probability of STAMPP being cost-effective compared with EAN for the sensitivity analyses for the secondary CEAs.
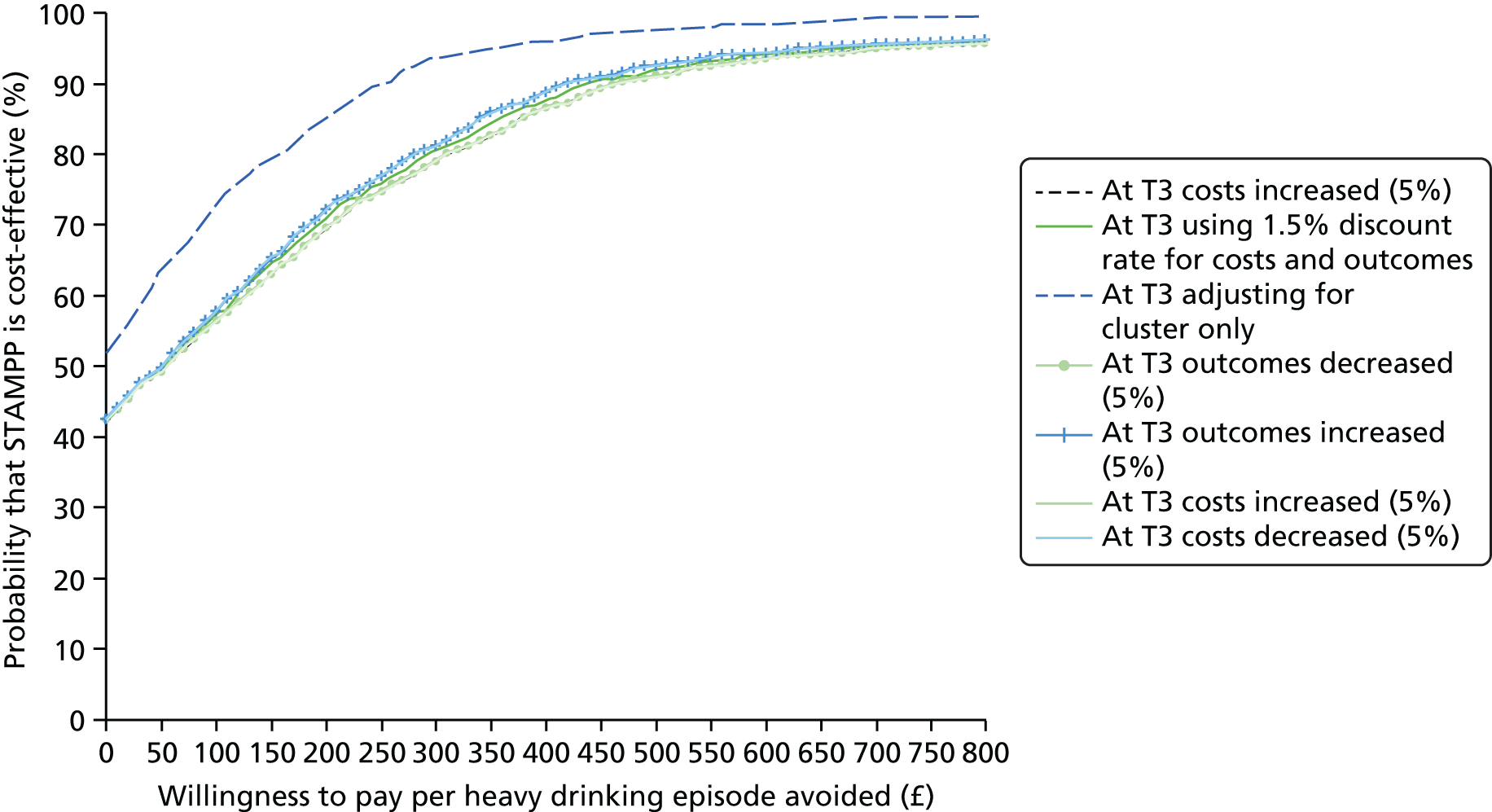
Summary of economic analysis
The Steps Towards Alcohol Misuse Prevention Programme is a relatively low-cost intervention that successfully reduces HED. STAMPP did not bring about clear public sector cost-savings; however, it neither increased them nor lead to any cost-shifting within the public sector categories. STAMPP can therefore be considered to weakly dominate EAN because it is both cost-neutral and more effective. Furthermore, STAMPP appears to be more cost-effective in the longer term, as it has a greater impact on pupils when they are older and more likely to be consuming alcohol. Further research is required to establish whether or not the cost-effectiveness of STAMPP is sustained in the long term.
Chapter 6 Discussion
Introduction
In a large CRCT (STAMPP) combining an adapted version of the SHAHRP with a brief parental information component, we found that the intervention reduced self-reported HED in the past 30 days at T3 follow-up compared with EAN, but that it did not reduce self-reported harms associated with own drinking. Similarly, intervention pupils reported significantly fewer heavy drinking episodes in total at T2 and T3 than control pupils. There were no clear cost savings in terms of service utilisation associated with the intervention. However, from a health economic perspective, STAMPP was considered to weakly dominate EAN, as it was associated with a cost saving and was more effective.
At first glance, it is difficult to reconcile these apparently inconsistent findings. However, one explanation may lie in the manner in which all three outcomes were assessed and/or analysed. HED was assessed using one question written on a detailed and colourful page including pictures of drinks and corresponding unit content, allowing participants to accurately determine drinking in the past month. With regard to harms, it is possible that the specific harms examined were not age-appropriate. Although they are similar to those used in previous Australian and Northern Irish studies, the participants in the present study were approximately 1 year younger than the participants in both of those studies. On reflection, harms examined such as getting sick, getting in trouble with the police or attending a hospital may have been less relevant than the unasked harms of, for example, losing possessions, losing friendships or damaging their reputation that probably accompany early adolescent drinking behaviour. In addition, not taking frequency of harms into account in the primary analyses may have resulted in a loss of information. This suggests that our primary outcome measure of alcohol-related harm, as specified in the DAP, may not have been sensitive enough to detect age-appropriate harms, and thus was not able to identify any other alcohol-related harm (in addition to harm related to alcohol toxicity) that may have occurred and/or been prevented during the trial.
There were no clear or consistent effects identified in planned secondary or subgroup analyses [age, gender, SES, alcohol use at baseline, location (Scotland vs. NI)]. Stronger claims about the preventative impact of the intervention could be made if a clear pattern of consistent effects across a range of related outcome measures had been identified. It is possible that longer-term follow-up might reveal such effects, especially with regard to self-reported harms, which were low in both control and intervention pupils (the median number of harms was 0 in both arms; 68% of existing drinkers in control schools reported experiencing one or more harms at final follow-up compared with around 62% of existing drinkers in intervention schools). One indication of the potential developmental prevention impact of the intervention is that, at T2, HED showed a small reduction associated with the intervention, an impact that was stronger at T3 follow-up, albeit with a different follow-up measure. It is plausible that the final outcome measure for HED used at T3 was a more sensitive measure than the other measure used at earlier follow-ups (more than five drinks in an episode) and we cannot discount this possibility. The use of mediation analysis to assess lagged effects of changes in hypothesised targeted programme constructs may help to better understand these developmental effects.
In the light of the lack of statistically significant subgroup interaction effects and suggestions of multicollinearity between HED at baseline and the main effects in the model, we undertook additional exploratory analyses outside of the DAP. When the primary outcome models were restricted to just drinkers (defined as either lifetime use or previous year’s use at baseline), drinking pupils in the intervention schools reported fewer harms than those drinking pupils in the control schools. However, it must be noted that when the lifetime use and previous year’s use subgroup effects were examined via interaction terms (on the full CC population), the interaction terms for harms were non-significant, as were the interaction terms for age at onset and unsupervised drinking.
A number of sensitivity analyses were conducted to estimate the impact of analytical decisions on the HED primary outcome. These all supported the chosen analysis, with the exception of the conservative case model (for which missing cases in the intervention arm were all assumed to have engaged in HED and missing cases in the control arm were set to non-drinking), in which the sign of the intervention coefficient changed while remaining significant. This indicated that the model results were robust (i.e. a school effect was found in four of the five tests), except when subject to extreme missing data assumptions (i.e. the conservative case model).
At baseline, 7.8% of control and 7.6% of intervention pupils reported HED (defined as drinking more than five drinks in one episode). The prevalence of HED (using the primary outcome definition) was 26% in the control group and 17% in the intervention group at final follow-up. It is difficult to directly compare these figures with other contemporaneous UK surveys of adolescent alcohol use because of the use of different questions, sampled age groups and recall periods,106 but data from the control group seem broadly equivalent to other estimates. For example, 53.3% of 11- to 16-year-old pupils surveyed in the 2013 NI Young Persons Behaviour and Attitudes survey reported being drunk on at least one occasion in the previous month. The 2013 Scottish Schools Adolescent Lifestyle and Substance Use Survey107 reported that 44% of 15-year-olds reported having ever felt ‘really drunk/drunk’ in their lifetime. In England, from the Smoking, Drinking and Drug Use among Young People in England survey,12 12.3% of 13-year-olds (equivalent to our baseline sample mean age) reported being drunk (self-defined) in the previous 4 weeks, and this increased to 53% of 15-year-old lifetime drinkers (comparable with our T3 sample). For comparison, in the 2011 pan-European Union ESPAD, 54% of 15- to 16-year-olds reported consuming more than five drinks in a single episode.
A Cochrane review of the effectiveness of universal school-based alcohol education programmes identified 53 studies for inclusion, including 11 alcohol-specific interventions (the remainder were generic approaches or targeted multiple substances). 47,108 No included studies were conducted in the UK. Of the 11 alcohol-specific interventions, six found beneficial effects of intervention. Outcome measures differed between those studies reporting significant findings, although three reported similar outcome measures to those included here (‘binge drinking’). In the original SHAHRP evaluation conducted in Australia, significant intervention effects were reported at 32 months and, although ORs were not presented, it was estimated that intervention pupils were 4.2% less likely to consume at risky levels [defined as reporting two (female)/four (male) standard drinks (10 g of alcohol) per occasion once per month or more often]. 55 A German skills-based activity delivered over four interactive lessons to a similarly aged sample as STAMPP was associated with an OR of lifetime ‘binge drinking’ of OR 0.56 (95% CI 0.41 to 0.77) at 4 months and an OR of 0.74 (95% CI 0.57 to 0.97) at 12 months. 109 Finally, an Australian online alcohol harm reduction curriculum for 13-year-olds (CLIMATE Alcohol Program) reported significant intervention effects (no OR reported) for ‘binge drinking’ (a single occasion over the previous 3 months) for girls but not for boys 12 months after delivery. 57 Interestingly, and in contrast with STAMPP, self-reported harms were also significantly reduced in girls using the same assessment scale employed in the current study. Finally, for comparison, the earlier NI study of the SHAHRP60 (32 months of follow-up), which employed a non-randomised design and used latent class growth modelling, intervention pupils were more likely to be in trajectories that reported fewer alcohol units consumed in the previous episode and fewer alcohol-related harms (no OR reported). Overall, the OR associated with STAMPP (OR 0.596, 95% CI 0.49 to 0.73) suggests that programme effects are comparable with those reported previously for similar interventions using similar outcome measures. However, caution is warranted when drawing comparisons between STAMPP and earlier studies conducted in Australia and NI. STAMPP used a different research design (CRCT vs. quasi-experimental designs in the Australian and NI SHAHRP studies), a younger age group and a different outcome measure at final follow-up. We also incorporated a parental intervention (albeit with low uptake). Furthermore, the earlier NI study was delivered against a higher population prevalence of drinking.
The total cost to deliver STAMPP was £85,900, equivalent to £818 per school and £15 per pupil. NICE published public health guidance53 for use in primary and secondary schools on sensible alcohol consumption, which revealed the paucity of evidence from economic evaluations in this area. The authors of the review identified three studies that provided sufficient information on resource use to allow a cost per student to be calculated. The costs ranged from £20 to £150 (cost year 2005/6). 55,110,111 Thus, at a cost of £15 per pupil, STAMPP is a relatively low-cost intervention that successfully reduces HED. These costs reflect the cost of introducing and delivering STAMPP on one occasion. In reality, once teachers have been trained they will not need to be retrained on an annual basis, requiring only refresher training. Similarly, if STAMPP was delivered instead of existing alcohol EAN, which would likely be the case based on the findings of our process interviews, the cost per pupil would also fall.
The analysis of public service costs showed that there was an overall reduction in the use of public sector services over the 33-month study period for both groups. There were, however, no differences between groups and no differences in the use of the subcategories of education, health and criminal justice services. Costs were estimated from a public sector perspective, which was justified considering one of the principal objectives of STAMPP was to reduce alcohol-related harms in teenagers. It was hypothesised that this would in turn reduce the use of health and judicial services and the need for additional support within the school setting to address behavioural and emotional problems. The absence of statistically significant difference in public service costs between groups is in keeping with the analysis of the harms data from the trial [see Chapter 3, Drinking harms (T3)]. No differences were observed in the number of self-reported harms by pupils between groups and, indeed, both groups reported low levels of harms overall.
The primary CEA (using the number of pupils experiencing a heavy drinking episode in the previous 30 days) at T3 indicated that STAMPP weakly dominated EAN. At a notional WTP threshold of £15 (reflecting the cost of STAMPP per pupil observed in this study), the probability of STAMPP being cost-effective was 56%. This level of uncertainty reflects the considerable variability in the cost differences between groups. At T2, this probability of cost-effectiveness was considerably lower, at 35%, because of the additional variability in the effectiveness of the intervention. A similar pattern of results was observed in the secondary CEAs (using the number of heavy drinking episodes); the intervention was more cost-effective at T3 than at T2. However, the probability of cost-effectiveness was lower at each time point (45% and 32%, respectively, at a WTP of £15) than in the primary CEA. This was because of greater variability in both costs and outcomes. The greater variability in effectiveness is not surprising considering that the effectiveness measure used in the secondary CEAs was based on a continuous outcome, in contrast to the binary outcome used in the primary analysis. Overall, the implication is that STAMPP is more cost-effective in the longer term, as it has a greater impact on pupils when they are older, more likely to drink and drinking more. In light of the literature, which links heavy drinking in adolescence to alcohol dependence and poor health outcomes in adulthood (e.g. Bonomo et al. 2), it is important to investigate if the (cost) effectiveness of STAMPP is sustained or even increases in the long term.
The sensitivity analyses indicated that the results of the CEA were robust to small changes in the parameters, that is, discounting and small increases in cost and effectiveness. However, when costs and effects were not adjusted for baseline covariates, the probability of STAMPP being cost-effective increased. This suggests that the cost-effectiveness of STAMPP may vary between subgroups and warrants further investigation to identify which pupils and/or schools might benefit the most from the receiving the intervention. Furthermore, when multiple imputation was used to impute missing cost and outcome data, the cost-effectiveness of STAMPP decreased. Considering multiple imputation is based on the assumption that data are missing at random, it is of some concern that the results of this sensitivity analysis differ somewhat from the primary analysis. The proportions of missing data in different groups were similar within all of the health economic analyses; thus, further investigation is warranted into the imputation model used as well as the pattern of missingness.
The process evaluation showed that clusters were successfully recruited into STAMPP, randomisation was successful, and pupils in schools were comparable across intervention arms at baseline. No adverse events were reported. The intervention was delivered with a good degree of fidelity and was enjoyed and/or acceptable to students, teachers, schools and other stakeholders. Overall, pupils thought that the intervention content was age appropriate, although from the comments received in some focus groups (and from the survey data), even within the same year group, pupils will have different drinking histories and there will be differences in rates of initiation and in establishment of more regular drinking patterns. The standard materials provided to pupils, in particular those focusing on the consequences of drinking, may therefore need to be adapted for some target groups if the intervention is delivered in routine practice. Furthermore, although participants valued the workbooks, pupils have changing expectations with regard to modes of delivery of learning materials, particularly with regard to new technologies and platforms, and so intervention materials may need to be adapted to keep pace with changes in learning platforms (e.g. electronic materials delivered through online platforms or tablets).
In contrast, there was very low uptake of the parental/carer component, and postal returns of the parent/carer survey, which were used as an indicator of implementation of mailed intervention materials, were also relatively low. This component was therefore not successfully delivered. We did not have a comprehensive response to the teacher survey assessing EAN practice in control schools, but reports from responders indicated that EAN was rarely delivered (n = 3 reports) and primarily consisted of single sessions of general alcohol awareness activities delivered by external organisations (e.g. police, alcohol charities). Therefore, we concluded that there was a clear differentiation between intervention and control schools.
Strengths and limitations
The key strengths of the trial were the large sample size (schools and pupils), low rates of attrition (no schools dropped out) and relatively high rates of matched data (> 80% depending on outcome) across survey waves. This means that the primary analysis on HED was sufficiently powered. This calculation used estimates of HED derived from the 2011 ESPAD study13 for the same age as the STAMPP pupils, with the estimated ICC derived from the Belfast Youth Development Survey. 75 Unfortunately, neither the Belfast Youth Development Survey nor the ESPAD contained comparable measures of drinking harms. The NI SHAHRP study,60 which did use a self-report harm measure, was undertaken with an older age group of pupils, and so was also not an appropriate base for a sample size calculation. Therefore, as no formal sample size calculation was undertaken for alcohol-related harms, there is the possibility that the null result for this outcome was because of lack of power. However, given the large achieved sample size, the relatively low levels of subject attrition, the use of covariates within the models (providing additional power) and the relatively small observed differences between study arms, we do not suspect that the null finding was because of insufficient sample size. It is more likely that the self-reported harm measures were not sensitive enough to likely harms experienced by the participants and thus any potential benefit was hidden. The classroom component was delivered with acceptable fidelity and was positively received by both pupils and teachers. However, there was a higher dropout rate (i.e. non-matched data across T0 to T3) among pupils who were male (19%), who were in receipt of FSMs (25.8%) or who had used alcohol at baseline (25.4%). Although we controlled for these variables in our analyses, it is uncertain why there was a higher level of missing data in these groups. Sex, SES and previous alcohol use have been shown in other UK studies to be predictors of school non-attendance (e.g. truanting, exclusion),12,112,113 although this would account for only some of the missing data. We were unable to identify previous studies examining predictors of retention or missing data in UK adolescent alcohol prevention interventions, but in the Australian and NI trials of the SHAHRP, there was an overall attrition of 24.1% and 12.8% at 32 months, respectively. 58,60 In the trial of the Dutch Preventing Heavy Alcohol Use in Adolescents (PAS) programme, from which our parental intervention was derived, overall attrition was 12.5%, and dropouts differed from completers in being older, drinking more and having parents with lower levels of education. 64 A systematic review of universal school-based interventions concluded that there was no difference between effective and non-effective interventions on the basis of attrition. 108 It would therefore be important for future work to determine why baseline drinking groups in particular produced more missing data, as this group would potentially benefit most from alcohol interventions, and inclusion in the data set may have adjusted our analyses.
A major limitation of the work was the failure to attract parents/carers to the brief intervention evening (9% in NI and 2.5% in Scotland), despite the support of many of the schools. Relatively low rates of return of the parental questionnaire (31% and 18%, respectively) also suggested that only a minority may have read the mailed information. Although we conducted an ITT analysis, which helped to preserve sample size, and achieved participation rates are likely to reflect family attendance in routine practice,114–116 this meant that we were unable to draw any confident inferences about the combined impact of the school and parental intervention (see Koning et al. 117) or the relative contribution of each component. In practical terms, this means that although the analyses presumed delivery of the combined intervention, discussions with stakeholders about research findings and future delivery are likely to focus on the classroom component (i.e. SHAHRP).
Failure to engage parents/carers in school-based substance use prevention is a consistent finding. 118–122 However, other trials have reported success at engaging family members. For example, in a recent feasibility study of the Welsh family-based alcohol prevention intervention Kids, Adults Together programme,123 50% of pupils (n = 158 intervention pupils in total) reported that at least one family member who was invited to a family event attended (although only 6.5% of eligible parents/carers returned a study questionnaire), suggesting that acceptable participation rates in the UK are achievable. These authors identified two key processes that they believe supported engagement. First, pupils were keen to attend the event with their parents/carers and, second, the family event was not marketed as an alcohol education event and was positioned around parents/carers wanting to attend the event to see their children’s school work and what activities they had been involved in. Similarly, in the Dutch PAS study there was a high level of parental retention in the parent only (75.9%) and combined parent and student (72.4%) intervention arms. 64 In keeping with the Kids, Adults Together programme, PAS parental events were part of regular school parents’ evenings, which a large number would have attended anyway. Future implementers of STAMPP should therefore consider such engagement approaches, which were not feasible in the current trial because of the timing of intervention delivery, the large number of schools involved which made co-ordination difficult, a lack of time within regularly planned parents evenings (which primarily focus on pupil progress) and education policy initiatives in one trial site that necessitated using parental evening time to introduce a new curriculum.
Our primary outcome assessments relied on self-report, which may have led to inaccurate reporting of alcohol use and associated harms through memory, social desirability and other biases. 124 Although adolescent self-reported alcohol questionnaires are generally reliable,125,126 there may be differences in reliability between early and late adolescence63 and studies of recanting in substance use surveys suggest that this may be an understudied bias in prevention research. 127 However, all pupils received the same questionnaire and pictorial prompts, and the recall period for the primary outcome used in this study was the previous 30 days, and so, if bias had existed, this would have been minimal and equivalent across trial arms. Less attention has been paid to the validity of assessments of alcohol-related harms, although similar social desirability and self-representation biases are likely to exist. 128 In this study, alcohol-related harms were measured using a 16-item scale, and previous work has shown the scale to have an internal consistency of α = 0.9. However, we do not know if pupils consistently interpreted the harms in the same way. Although some of the self-reported harms were likely to be interpreted in a straightforward manner (e.g. ‘did you vomit after drinking?’), similarly to differences in young people’s self-perception of drunkenness,129 there may be individual differences in interpretation of the harms assessed in this study and different thresholds applied for an indicator being perceived as being a ‘problem’ (e.g. having a hangover after drinking). As mentioned previously, it is also possible that some of these harms were not age appropriate and thus these were low frequency in our population. Without a method for objectively verifying the level of harm in this population, it is difficult to know whether or not these self-reported data were biased.
The assessment of HED (or ‘binge drinking’) in adolescents, as used in our consumption primary outcome, is complicated by the lack of standardised definitions in both adults and adolescents. 130 We adapted the current CMO’s guidelines for adults65 for this study, but regardless of this problem we were able to show a reduction in our measure of alcohol consumption. The introduction of the improved pictorial response sheet no doubt enhanced the accuracy of responses and reduced any potential bias given the problems with the concept of a ‘drink’ for not only the participants but for the research community as a whole.
There were a number of limitations to the economic evaluation. The study was not specifically powered to detect statistically significant differences in costs or cost-effectiveness. Although CEA does not typically make decisions based on significance rules,131 having a sufficiently powered study will allow decision-makers to be more confident in the value claim. 104 The resources used during the planning, preparation and delivery of the intervention were largely recorded retrospectively, and costs were obtained from invoices when these were available. We endeavoured to use plausible assumptions when actual data were not available, but the consistent and prospective collection of resource use and costs would lead to more robust data. The resource use questionnaire was completed by the pupils without any input from their parents or guardians. This was done because of resource limitations and to preserve confidentiality, and although definitions of the services were provided and the terminology simplified, it could be argued that more accurate costs would have been obtained with parental input. However, it was difficult to engage parents in the intervention, as reflected in the poor attendance to the parental evenings (see Chapter 4, Fidelity of implementation of STAMPP), so it is likely that response rates would have been poor.
We included pupils in the CEA only if they had complete cost and effect data. As a result, only two-thirds of the pupils were included in the T3 CEA and three-quarters in the T2, and the rest we assumed were missing at random. As discussed earlier, further investigation is required to establish whether or not this assumption is flawed.
The curriculum was delivered in most schools as part of their PSHE education (or local equivalent) curriculum and did not replace statutory activities. However, we did not assess spillover effects of STAMPP on other types of related school activity or curriculum, and so this must be considered a limitation of the trial.
Our approach to assessing fidelity of implementation and comparator bias was pragmatic in the context of the resources available and the large number of schools enrolled in the trial. Although our assessment of fidelity was based on an existing framework,132 and provided useful information, ideally, in addition to self-report we would have preferred to have recorded and/or observed some classroom and parent/carer sessions for independent rating of deliverer competencies, quality and completeness of delivery and target group responsiveness. Similarly, although we are confident that we identified other alcohol actions delivered to schools and we are able to conclude that delivery of competing interventions was very low, we were unable to make comparable assessments of exposure to community-based alcohol activities such as mass media campaigns and health promotion with an alcohol component. However, we were unaware of any major initiatives being delivered across the course of the trial, and the successful randomisation would have militated against some effects.
Other weaknesses and limitations of the research are identified in Self-assessment of risk of bias.
Further research
We found that STAMPP was effective in reducing self-reported HED T3, when pupils were aged 15–16 years. It will be important to assess whether or not these reductions are sustained and if effects on harms emerge as pupils get older, alcohol use behaviours become more frequent and patterns of use are established. 12,133,134 Booster interventions (e.g. brief interventions of proven effectiveness in adolescents and young adults) that build upon the skills developed in STAMPP may prove useful in sustaining behavioural change. 135 As the trial team included those who were responsible for the adaptation and development of the intervention, it is also important that any future replications are conducted independently. 136 The use of data linkage techniques to match the study cohort to additional educational, community and statutory service data sets (e.g. examination performance, hospital admissions, GP data, involvement with the criminal justice system) may also help to understand whether or not the changes reported in the current study lead to meaningful changes in health and well-being outcomes. 137 This recommendation also applies to other alcohol prevention research that predominantly uses simple proxy outcomes of use,49 and this practice has been criticised for not providing useful information for commissioners who are tasked with funding interventions on the basis of demonstrable improvements in health and well-being.
In an earlier secondary analysis assessing implementation of the adapted SHAHRP in NI,138 multilevel growth modelling was used to examine differential intervention impact when recipients were retrospectively classed according to alcohol use status (abstainer or existing drinker) and context of use (unsupervised or parental/carer supervised drinker) at baseline. Significant positive behavioural effects in terms of amounts consumed, frequency of drinking and self-reported alcohol-related harms were observed almost exclusively among pupils classed as baseline unsupervised drinkers. This was notable, as although the SHAHRP was delivered as a universal curriculum, it suggested that it might also have utility as a targeted intervention. In the current study, the preplanned subgroup analysis showed that there was no interaction between baseline drinking status and treatment effect. However, when exploratory analyses were undertaken, which examined drinking status groups independently, significant intervention effects emerged (HED and self-reported harms). These findings suggest that STAMPP may have had a differential impact on those pupils who would be considered most at risk from alcohol use (e.g. unsupervised baseline drinkers). 139
With respect to further development of STAMPP intervention, our rich data set means that it will be possible to conduct mediation analysis to further develop programme theory and to test the assumptions of our logic model (see Appendix 1). This may lead to a better understanding of which components of the intervention (e.g. specific lessons) were most successful and which require strengthening. 140 Identifying supportive or inert elements of the programme may lead to the development of a shorter optimised curriculum, which would reduce resource requirements and potentially increase the attractiveness of the intervention to funders. Similarly, analysis of moderation effects might identify local contextual and population factors that exert differential influences on outcomes. 141
Extending this line of work, research examining the fidelity of implementation in more detail may help to refine delivery. Although we reported relatively high completeness of delivery with respect to content, there was variation in the number of lessons required to deliver, and it is uncertain what effect this may have had on programme outcomes. In a secondary analysis of the European Drug Addiction Prevention (EU-Dap) trial substance use prevention curriculum, another skills-based interactive prevention programme, class size, composition (e.g. sex ratio, academic ability) and social connectedness between pupils, were shown to be important predictors of programme implementation. 114 Understanding these factors is important, because in routine practice, outside of the structures of a RCT, the intervention may not be delivered as intended, and formal and informal changes introduced by delivery staff may lead to a loss of programme integrity. 90 Furthermore, although based in the classroom, the adapted SHAHRP curriculum may not necessarily be optimally delivered by teachers,60 and some pupils in the process evaluation suggested that their response to the lessons was dependent on pre-existing relationships with school staff. In future programme development and evaluation, different trial arms should include the assessment of alternative deliverers, such as trained prevention and youth service workers, who have specialist skills to help better engage young people in health programmes.
Considering our failure to recruit into the parental intervention, further research is required to better understand how to engage and retain parents/carers in prevention activities. 91,123 This is also important, as delivery of preventative activities outside of the structures of research trials frequently leads to lower implementation quality. 90 Universal interventions such as STAMPP require a range of recruitment strategies, as there will be different barriers to, and facilitators of, attendance in parental/carer-based actions. Research is therefore needed to assess the relative efficacy of recruitment strategies such as incentives, mass media campaigns, the removal of barriers to attendance (e.g. providing transport and childcare) and the use of key community recruiters (influential individuals and organisations). 91 Furthermore, it is also important to understand if some parent/carer subgroups (e.g. differentiated according to child drinking risk) are more likely to respond to particular recruitment strategies and if this will lead to recruitment biases.
Broadening our research recommendations to the wider prevention field, and drawing upon our stakeholder interviews, it is clear that although universal interventions are valued, they compete for resources and must sit alongside other alcohol-related community actions and policy initiatives, which may moderate observed effects. 92 By-laws and licensing decisions can affect local alcohol environments (e.g. density of alcohol outlets, opening hours and local marketing), and actions such as industry-driven corporate social responsibility initiatives, marketing and packaging regulations and community-based initiatives may complement or disrupt school-based actions. 93–97 There is also increasing interest in schools as environments for health promotion through actions that modify the physical and social environment. 98 Interventions and curricula, such as STAMPP, are therefore not being delivered in isolation, and, although study design characteristics such as randomisation control for internal biases, there is a need to better understand how interventions complement each other, the dynamic interplay between intervention components at different levels (e.g. the interaction between norms correction activities in a prevention curriculum and the placement of alcohol advertisements in the local area), and how interventions can be optimised within such complex health systems. 99 The use of systems mapping exercises and the study of alcohol prevention as a complex system may be one means to maximise effects from combinations of different prevention types. 100
Implications for practice
Our findings suggest that STAMPP is a candidate for inclusion in local strategies to reduce alcohol-related harm where reduction in HED is a stated aim. Although the reported outcomes were relatively modest, STAMPP is one of the few UK school-based alcohol prevention programmes to show effectiveness in reducing HED in adolescents. Although any universal prevention programme on its own is unlikely to lead to sustained changes in population levels of alcohol use,92,101 the harm reduction focus of the classroom component of STAMPP may complement national and local actions targeting price, availability and affordability of alcohol and the licensing of alcohol outlets. Furthermore, although we have not yet conducted such an analysis, previous studies of universal prevention programmes have also shown benefits for participants considered at greater risk of harm, whether as a result of their substance use behaviour or population characteristics (e.g. Vigna-Taglianti et al. 102 and Spoth et al. 103). With appropriate adaptation (e.g. language and comprehensibility, delivery outside mainstream classrooms), STAMPP may be a useful form of alcohol education for higher-risk and vulnerable groups.
The classroom intervention was easily implemented by teachers (conditional on support by school management) after suitable training and support materials were relatively inexpensive (workbooks and supporting CD/electronic material). Schools that have identified alcohol education as a priority would be in a good position to offer the classroom curriculum as part of existing PSHE provision, and teachers in this subject are likely to have the required general professional skills to facilitate delivery. Although we acknowledge curriculum pressures, considering the current poor state of substance use education in the UK,104,105 STAMPP would make a useful contribution to health and social education in schools.
However, in the current trial, uptake of the brief intervention was poor, and although all intervention students parent(s)/carer(s) received the intervention leaflet, the return of materials to indicate reading/acknowledgement was low. It is, therefore, difficult to make any practice recommendations about this component of the programme. If commissioners or providers decide to implement STAMPP in future, then they must decide whether the full programme or only the classroom intervention is delivered. Relying on passive mechanisms (e.g. advertisements and information) is unlikely to encourage attendance and, although some of the techniques to encourage participation discussed in this section are likely to be costly (e.g. providing transport and childcare), others rely more on planning than resources (e.g. scheduling events as part of regular school parents’ evenings).
Generalisability
Although we are mindful of differences in school autonomy, governance and oversight, and we acknowledge regional variability in alcohol use behaviours (e.g. Public Health England9), we believe that the findings of this trial are generalisable to other geographies of the UK. However, as discussed throughout this report, parental/carer engagement was poor, and so generalisability may only be relevant to the classroom curriculum. Schools enrolled in the trial were drawn from urban and more rural areas, and from across the socioeconomic gradient. Furthermore, subgroup analysis showed that there were no differential intervention effects on the basis of school geography (i.e. NI vs. Glasgow/Inverclyde). Interviews with stakeholders, including local commissioners, did not identify any significant barriers to future delivery, beyond those expected relating to funding and local priorities. Similarly, teachers and senior school staff believed that STAMPP would help them to achieve their health and well-being aims in line with wider school policies.
Self-assessment of risk of bias
We conducted a self-assessment of bias in accordance with criteria adapted from the Cochrane Collaboration methodological handbook. 106 For each domain, TMG members assessed the level of bias with respect to three outcomes: unclear risk, which is interpreted as plausible bias that raises some doubt about the results; low risk, which is interpreted as plausible bias that is unlikely to seriously alter the results; medium risk, which is interpreted as plausible bias that moderately weakens confidence in the results; and high risk, which is interpreted as plausible bias that seriously weakens confidence in the results. Final ratings were achieved through consensus. We identified a medium risk of bias in relation to performance bias, as this was not a double-blind study. However, using an EAN comparator, it was not possible to conceal intervention allocation from teachers, who received specialised training and curriculum materials, or from pupils, who would typically receive little or no alcohol education in their usual school year. We self-rated detection bias as having a medium risk. This was because of resource constraints and because some of the data collection was undertaken by members of the trial team. We self-assessed conflict of interest bias as having a medium/high risk for two main reasons. The first reason was that the printing of curriculum workbooks in one intervention site (Glasgow only) was funded through dedicated money awarded by the alcohol industry. However, this funder was not involved in any aspects of research or intervention design and did not have any subsequent involvement in the trial, its management, analysis or write up. The second reason underpinning this rating was related to the involvement of three members of the trial team (including the principal investigator) in the original NI adaptation of the school curriculum, and all members of the TMG contributed to the development of the parental component. Finally, two members of the TMG reported that their university departments had historically received research grants from parts of the alcohol industry for unrelated research. Neither had individually directly benefited from this funding and it is reported here for transparency.
Selection bias: low risk
Randomisation was performed by computer algorithm [Microsoft Excel® 2010 (Microsoft Corporation, Redmond, WA, USA) spreadsheet] via an independent trials unit. Field office personnel were not involved in randomisation. Allocation concealment was maintained via the independent randomisation of pre-recruited schools to trial arms. Fidelity of initial randomisation was verified by independent trials unit staff.
Unit of analysis biases: low risk
Students were the main unit of analysis but allocation was by school. Statistical analyses accounted for the hierarchical nature of the data via mixed models. Loss to follow-up was relatively low at both school and individual level. Differential attrition at school level was not a concern.
Performance bias: medium risk
Teachers and students were not blind to the intervention. Therefore, it is plausible that this could have affected their behaviour and/or responses (see Detection bias: unclear or medium risk) and may have led to either under- or over-reporting of alcohol use because of social desirability biases.
Detection bias: unclear or medium risk
Primary outcomes were self-reported using bespoke questionnaire items that were administered by external (to the school) researchers, including trial team field researchers, and that were developed specifically for this study by the trial team. Primary outcome data were collected through self-completed questionnaires, and these were completed individually. Questions were read out loud by field researchers in accordance with a pre-prepared script. This may have led to either under- or over-reporting of alcohol use because of social desirability biases.
Some of the field researchers were not blind to intervention condition and, therefore, some of the data collection was not blinded. Data coding was undertaken by scanning completed questionnaires (conducted by a commercial document scanning company) and the validity of the scans was checked by the independent Clinical Trials Unit. Statistical analysis of primary outcomes was undertaken blind to intervention condition. Health economic analysis was blind to intervention condition.
Attrition bias: low risk
Loss to follow-up was low at both school and individual levels. Differential attrition at school or individual level was not a concern.
Reporting bias: low risk
All analyses were planned in advance and stated in the trial protocol and DAP. Reporting of outcomes followed this protocol.
Comparator bias: unclear risk
Although data were collected from teachers through an online survey (see Chapter 4, Online survey with teachers), information about additional alcohol-related activities in the control condition (in communities or by parents) that could potentially weaken the comparison between the active intervention and control groups was not comprehensive. However, in both control and intervention conditions, teachers reported few additional alcohol-related activities that were self-assessed to bias the outcomes (see Chapter 4, Usual alcohol-related activities in both intervention and control schools over the course of the study).
Conflict of interest bias: medium/high risk
One trial team member stated that their department had previously received funding from the alcohol industry for unrelated prevention programme training work. Another trial team member stated that their department had previously received funding from the alcohol industry (indirectly via the industry-funded Drinkaware) for unrelated primary research. Three trial team staff had been involved in adapting the original Australian school-based intervention for use in NI and one trial team member was involved in training teachers to deliver the intervention. The sponsor university (Liverpool John Moores University) received and administered a payment from the alcohol industry for printing of pupil workbooks in the Glasgow trial site. All trial team staff contributed to the development of the parental intervention. The impact of these biases cannot be objectively assessed by the research team, although funders had no part in the design, delivery and analysis of the trial. Independent replication would help to answer this question.
Chapter 7 Conclusions
The results of this large CRCT provide support for the effectiveness and cost-effectiveness of a combined and adapted SHAHRP intervention and brief parental intervention for reducing HED, but not alcohol-related harms, in young people over a 33-month follow-up period. One possible interpretation of these findings is that reducing HED without impacting the self-reported harms assessed in this study is not a desirable outcome for a prevention or harm reduction programme. This requires more detailed consideration in further research. One reason for this outcome might be a lack of age-appropriateness of the alcohol-related harms assessed. It is also plausible that effects on harms would manifest later; again, further research would clarify this possibility. As there was low uptake of the parental component, it is uncertain if the intervention effect was accounted for by the classroom component alone.
Acknowledgements
We are grateful to all participants who took part in the research, including students, teachers, school managers and support staff, parents and carers and other stakeholders. We would also like to express our thanks to Professor Laurence Moore and the members of our SSC and the NIHR Public Health Research programme project management team, which helped to guide the research through all phases. We are extremely grateful for the generous support offered by the PHA of NI and the Educational Boards and Psychological Services of Glasgow and Inverclyde, in particular to Gerry Bleakney, Séamus Mullin and Owen O’Neill (NI), and to Maura Kearney and Kate Watson (Scotland) for their support in the initial stages of design and recruitment of schools. We also wish to thank colleagues in the NICTU for data management and quality assurance.
Finally, we wish to acknowledge and thank Dr Nyanda McBride (Curtin University), who was part of the original SHAHRP development and research team, for helpful discussions in the development of this research.
Contributions of authors
Harry Sumnall (Professor, Substance Use, Liverpool John Moores University) was the project lead; he contributed to the conception and overall design of the study, and to the writing and editing of the final report.
Ashley Agus (Health Economist, NICTU) conducted the health economic evaluation and write-up.
Jon Cole (Professor, Tactical Decision-Making, University of Liverpool) contributed to the conception and overall design of the study, and to the writing and editing of the final report.
Paul Doherty (Data Manager, NICTU) was responsible for data management, including quality assurance and data governance.
David Foxcroft (Professor, Community Psychology and Public Health, Oxford Brookes University) contributed to the conception and overall design of the study, and to the writing and editing of the final report.
Séamus Harvey (Researcher, Liverpool John Moores University) was the trial researcher; he contributed to all aspects of the work and was responsible for analysing and writing the process evaluation chapter and contributing to the final report.
Michael McKay (STAMPP Trial Manager, Liverpool John Moores University) was the trial manager; he oversaw teacher training, was the liaison lead with schools and stakeholders, led the field research and contributed to the conception and overall design of the study, as well as to the writing and editing of the final report.
Lynn Murphy (Manager, NICTU) contributed to the conception and overall design of the study, and managed the contribution of the NICTU.
Andrew Percy (Senior Lecturer, Queen’s University Belfast) contributed to the conception and overall design of the study, undertook the statistical analysis and contributed to the writing and editing of the results chapter and the final report.
Publications
McBride N, Mckay M, Sumnall HR. SHAHRP: School Health and Alcohol Harm Reduction Project – developments in Australia and the UK. Educ Health 2013;31:79-83.
McKay MT, Cole JC, Percy A, Worrell F, Mello ZR. Reliability and factorial validity of Adolescent Time Inventory-Time Attitude (ATI-TA) scores in Scottish and Northern Irish adolescents. Pers Individual Diff 2015;86:412–16.
Morgan GB, Wells KE, Andretta JR, McKay MT. Temporal attitudes profile transition among adolescents: a longitudinal examination using mover-stayer latent transition analysis [published online ahead of print 5 September 2016]. Psychol Assess 2016.
Harvey SA, McKay MT, Sumnall HR. Adolescents’ reflections on school-based alcohol education in the UK: education as usual compared with a structured harm reduction intervention. J Subst Use 2016;21:640–5.
McKay MT, Percy A, Cole JC, Worrell FC, Andretta JR. The relationship between time attitudes profiles and self-efficacy, sensation seeking, and alcohol use: an exploratory study. Pers Individual Diff 2016;97:203–9.
Protocol
Available from www.nets.nihr.ac.uk/projects/phr/10300209 (last accessed 6 April 2016).
Data sharing statement
Anonymised data from this study can be obtained from the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health.
References
- Fillmore KM, Golding JM, Graves KL, Kniep S, Leino EV, Romelsjö A, et al. Alcohol consumption and mortality. I. Characteristics of drinking groups. Addiction 1998;93:183-20. https://doi.org/10.1046/j.1360-0443.1998.9321834.x.
- Bonomo YA, Bowes G, Coffey C, Carlin JB, Patton GC. Teenage drinking and the onset of alcohol dependence: a cohort study over seven years. Addiction 2004;99:1520-8. http://dx.doi.org/10.1111/j.1360-0443.2004.00846.x.
- DeWit DJ, Adlaf EM, Offord DR, Ogborne AC. Age at first alcohol use: a risk factor for the development of alcohol disorders. Am J Psychiatry 2000;157:745-50. http://dx.doi.org/10.1176/appi.ajp.157.5.745.
- Maimaris W, McCambridge J. Age of first drinking and adult alcohol problems: systematic review of prospective cohort studies. J Epidemiol Community Health 2014;68:268-74. http://dx.doi.org/10.1136/jech-2013-203402.
- Donovan JE, Molina BS. Childhood risk factors for early-onset drinking. J Stud Alcohol Drugs 2011;72:741-51. https://doi.org/10.15288/jsad.2011.72.741.
- Buchmann AF, Schmid B, Blomeyer D, Becker K, Treutlein J, Zimmermann US, et al. Impact of age at first drink on vulnerability to alcohol-related problems: testing the marker hypothesis in a prospective study of young adults. J Psychiatr Res 2009;43:1205-12. https://doi.org/10.1016/j.jpsychires.2009.02.006.
- Newbury-Birch D, Gilvarru E, McArdle P, Ramesh V, Stewart S, Walker JB, et al. Impact of Alcohol Consumption on Young People: A Review of Reviews. London: Department for Children, Schools and Families; 2008.
- Ellickson PL, Tucker JS, Klein DJ. Ten-year prospective study of public health problems associated with early drinking. Pediatrics 2003;111:949-55. https://doi.org/10.1542/peds.111.5.949.
- Local Alcohol Profiles for England. London: Public Health England; 2015.
- Jones L, McCoy E, Bates G, Bellis MA, Sumnall HR. Understanding the Alcohol Harm Paradox. London: Alcohol Research UK; 2015.
- Marmot M. Social determinants of health inequalities. Lancet 2005;365:1099-104. http://dx.doi.org/10.1016/S0140-6736(05)71146-6.
- Fuller E. Smoking, Drinking and Drug Use Among Young People in England in 2014. London: Health and Social Care Information Centre, Lifestyles Statistics; 2015.
- Hibell B, Guttormsson U, Ahlström S, Balakireva O, Bjarnason T, Kokkevi A, et al. The 2011 ESPAD Report. Substance Use Among Students in 36 European Countries. Stockholm: Swedish Council for Information on Alcohol and Other Drugs (CAN); 2012.
- McInnes A, Blackwell D. Self-reported drinking behaviour of school age children in Sunderland over a fourteen-year period. Education and Health 2013;31:67-76.
- Smith LA, Foxcroft DR. The effect of alcohol advertising, marketing and portrayal on drinking behaviour in young people: systematic review of prospective cohort studies. BMC Public Health 2009;9. http://dx.doi.org/10.1186/1471-2458-9-51.
- Velleman R. Children, Young People and Alcohol: How They Learn and How to Prevent Excessive Use. York: Joseph Rowntree Foundation; 2009.
- Westlake S, Yar M, Bajeka M, Osborne M, Yar M, Meltzer H. Focus on Health: 2006 Edition. London: Office for National Statistics; 2006.
- Martinic M, Measham F. Swimming with Crocodiles: Extreme Drinking and Young People. New York: NY: Routledge; 2008.
- Miller PM, Plant M. Drinking, smoking, and illicit drug use among 15 and 16 year olds in the United Kingdom. BMJ 1996;313:394-7. https://doi.org/10.1136/bmj.313.7054.394.
- Young Persons’ Behaviour and Attitudes Survey. Belfast: Northern Ireland Statistics and Research Agency; 2014.
- Scottish Schools Adolescent Lifestyle and Substance Use Survey 2013. Edinburgh: Information Services Division; 2013.
- Windle M, Spear LP, Fuligni AJ, Angold A, Brown JD, Pine D, et al. Transitions into underage and problem drinking: summary of developmental processes and mechanisms: ages 10–15. Alcohol Res Health 2009;32:30-4.
- Zeigler DW, Wang CC, Yoast RA, Dickinson BD, McCaffree MA, Robinowitz CB, et al. American Medical Association . The neurocognitive effects of alcohol on adolescents and college students. Prev Med 2005;40:23-32. http://dx.doi.org/10.1016/j.ypmed.2004.04.044.
- Witt ED. Research on alcohol and adolescent brain development: opportunities and future directions. Alcohol 2010;44:119-24. http://dx.doi.org/10.1016/j.alcohol.2009.08.011.
- Rodham K, Brewer H, Mistral W, Stallard P. Adolescents’ perception of risk and challenge: a qualitative study. J Adolesc 2006;29:261-72. http://dx.doi.org/10.1016/j.adolescence.2005.05.012.
- MacArthur GJ, Smith MC, Melotti R, Heron J, Macleod J, Hickman M, et al. Patterns of alcohol use and multiple risk behaviour by gender during early and late adolescence: the ALSPAC cohort. J Public Health 2012;34:i20-30. http://dx.doi.org/10.1093/pubmed/fds006.
- Zucker RA, Donovan JE, Masten AS, Mattson ME, Moss HB. Early developmental processes and the continuity of risk for underage drinking and problem drinking. Pediatrics 2008;121:252-72. http://dx.doi.org/10.1542/peds.2007-2243B.
- Brown SA, McGue M, Maggs J, Schulenberg J, Hingson R, Swartzwelder S, et al. Underage alcohol use: summary of developmental processes and mechanisms: ages 16–20. Alcohol Res Health 2009;32:41-52.
- Bahr SJ, Marcos AC, Maughan SL. Family, educational and peer influences on the alcohol use of female and male adolescents. J Stud Alcohol 1995;56:457-69. https://doi.org/10.15288/jsa.1995.56.457.
- Riesch SK, Anderson LS, Krueger HA. Parent–child communication processes: preventing children’s health-risk behavior. J Spec Pediatr Nurs 2006;11:41-56. http://dx.doi.org/10.1111/j.1744-6155.2006.00042.x.
- Barnes HL, Olson DH. Parent–adolescent communication and the circumplex model. Child Dev 1985;56:438-47. https://doi.org/10.2307/1129732.
- Nash SG, McQueen A, Bray JH. Pathways to adolescent alcohol use: family environment, peer influence, and parental expectations. J Adolesc Health 2005;37:19-28. http://dx.doi.org/10.1016/j.jadohealth.2004.06.004.
- Resnick MD, Bearman PS, Blum RW, Bauman KE, Harris KM, Jones J, et al. Protecting adolescents from harm. Findings from the National Longitudinal Study on Adolescent Health. JAMA 1997;278:823-32. https://doi.org/10.1001/jama.1997.03550100049038.
- Steinberg L. We know some things: adolescent–parent relationships in retrospect and prospect. J Res Adolesc 2001;11:1-20. https://doi.org/10.1111/1532-7795.00001.
- Wills TA, Cleary SD. How are social support effects mediated? A test with parental support and adolescent substance use. J Pers Soc Psychol 1996;71:937-52. https://doi.org/10.1037/0022-3514.71.5.937.
- van der Vorst H, Engels RC, Meeus W, Deković M, Van Leeuwe J. The role of alcohol-specific socialization in adolescents’ drinking behaviour. Addiction 2005;100:1464-76. http://dx.doi.org/10.1111/j.1360-0443.2005.01193.x.
- Turrisi R, Ray AE. Sustained parenting and college drinking in first-year students. Dev Psychobiol 2010;52:286-94. http://dx.doi.org/10.1002/dev.20434.
- Gilligan C, Kypri K, Lubman D. Changing parental behaviour to reduce risky drinking among adolescents: current evidence and future directions. Alcohol Alcohol 2012;47:349-54. http://dx.doi.org/10.1093/alcalc/ags022.
- Roberts R, Beckwith M, Watts D. Mothers’ intentions to introduce their adolescent to alcohol use: does mothers’ alcohol use effect intentions?. Aust N Z J Public Health 2010;34:281-7. http://dx.doi.org/10.1111/j.1753-6405.2010.00527.x.
- Ryan SM, Jorm AF, Lubman DI. Parenting factors associated with reduced adolescent alcohol use: a systematic review of longitudinal studies. Aust N Z J Psychiatry 2010;44:774-83. http://dx.doi.org/10.1080/00048674.2010.501759.
- Kypri K, Dean JI, Stojanovski E. Parent attitudes on the supply of alcohol to minors. Drug Alcohol Rev 2007;26:41-7. http://dx.doi.org/10.1080/09595230601037018.
- Abar C, Abar B, Turrisi R. The impact of parental modeling and permissibility on alcohol use and experienced negative drinking consequences in college. Addict Behav 2009;34:542-7. http://dx.doi.org/10.1016/j.addbeh.2009.03.019.
- van der Vorst H, Engels RC, Burk WJ. Do parents and best friends influence the normative increase in adolescents’ alcohol use at home and outside the home?. J Stud Alcohol Drugs 2010;71:105-14. https://doi.org/10.15288/jsad.2010.71.105.
- Bellis MA, Morleo M, Hughes K, Downing J, Wood S, Smallthwaite L, et al. A cross-sectional survey of compliance with national guidance for alcohol consumption by children: measuring risk factors, protective factors and social norms for excessive and unsupervised drinking. BMC Public Health 2010;10. http://dx.doi.org/10.1186/1471-2458-10-547.
- Livingston JA, Testa M, Hoffman JH, Windle M. Can parents prevent heavy episodic drinking by allowing teens to drink at home?. Addict Behav 2010;35:1105-12. http://dx.doi.org/10.1016/j.addbeh.2010.08.005.
- Jones L, James M, Jefferson T, Lushey C, Morleo M, Stokes E, et al. A Review of Effectiveness and Cost Effectiveness of Interventions Delivered in Primary and Secondary Schools to Prevent and/or Reduce Alcohol Use by Young People Under 18 Years Old. London: NICE; 2007.
- Foxcroft DR, Tsertsvadze A. Universal family-based prevention programs for alcohol misuse in young people. Cochrane Database Syst Rev 2011;9. http://dx.doi.org/10.1002/14651858.CD009308.
- Foxcroft DR, Tsertsvadze A. Universal multi-component prevention programs for alcohol misuse in young people. Cochrane Database Syst Rev 2011;9. http://dx.doi.org/10.1002/14651858.CD009307.
- Foxcroft DR, Tsertsvadze A. Universal school-based prevention programs for alcohol misuse in young people. Cochrane Database Syst Rev 2011;5. http://dx.doi.org/10.1002/14651858.CD009113.
- Nation M, Crusto C, Wandersman A, Kumpfer KL, Seybolt D, Morrissey-Kane E, et al. What works in prevention: principles of effective prevention programs. Am Psychol 2003;58:449-56. https://doi.org/10.1037/0003-066X.58.6-7.449.
- Faggiano F, Vigna-Taglianti FD, Versino E, Zambon A, Borraccino A, Lemma P. School-based prevention for illicit drugs use: a systematic review. Prev Med 2008;46:385-96. http://dx.doi.org/10.1016/j.ypmed.2007.11.012.
- Spoth R, Greenberg M, Turrisi R. Preventive interventions addressing underage drinking: state of the evidence and steps toward public health impact. Pediatrics 2008;121:311-36. https://doi.org/10.1542/peds.2007-2243E.
- Alcohol: School-Based Interventions. London: NICE; 2007.
- Parker H, Egginton R. Adolescent recreational alcohol and drugs careers gone wrong: developing a strategy for reducing risks and harms. Int J Drug Policy 2002;13:419-32. https://doi.org/10.1016/S0955-3959(02)00154-8.
- McBride N, Farringdon F, Midford R, Meuleners L, Phillips M. Harm minimization in school drug education: final results of the School Health and Alcohol Harm Reduction Project (SHAHRP). Addiction 2004;99:278-91. http://dx.doi.org/10.1111/j.1360-0443.2003.00620.x.
- Newton NC, Andrews G, Teesson M, Vogl LE. Delivering prevention for alcohol and cannabis using the internet: a cluster randomised controlled trial. Prev Med 2009;48:579-84. https://doi.org/10.1016/j.ypmed.2009.04.009.
- Vogl L, Teesson M, Andrews G, Bird K, Steadman B, Dillon P. A computerized harm minimization prevention program for alcohol misuse and related harms: randomized controlled trial. Addiction 2009;104:564-75. http://dx.doi.org/10.1111/j.1360-0443.2009.02510.x.
- McBride N, Midford R, Farringdon F, Phillips M. Early results from a school alcohol harm minimization study: the School Health and Alcohol Harm Reduction Project. Addiction 2000;95:1021-42. https://doi.org/10.1046/j.1360-0443.2000.95710215.x.
- Farringdon F, McBride N, Midford R. School health and alcohol harm reduction project: formative development of intervention materials and processes. Int J Health Promot Educ 1999;37:137-43. https://doi.org/10.1080/14635240.1999.10806116.
- McKay MT, McBride NT, Sumnall HR, Cole JC. Reducing the harm from adolescent alcohol consumption: results from an adapted version of SHAHRP in Northern Ireland. J Subst Use 2012;17:98-121. https://doi.org/10.3109/14659891.2011.615884.
- Koutakis N, Stattin H, Kerr M. Reducing youth alcohol drinking through a parent-targeted intervention: the Orebro Prevention Program. Addiction 2008;103:1629-37. http://dx.doi.org/10.1111/j.1360-0443.2008.02326.x.
- van der Vorst H, Engels RC, Meeus W, Deković M. The impact of alcohol-specific rules, parental norms about early drinking and parental alcohol use on adolescents’ drinking behavior. J Child Psychol Psychiatry 2006;47:1299-306. http://dx.doi.org/10.1111/j.1469-7610.2006.01680.x.
- Koning IM, Engels RC, Verdurmen JE, Vollebergh WA. Alcohol-specific socialization practices and alcohol use in Dutch early adolescents. J Adolesc 2010;33:93-100. http://dx.doi.org/10.1016/j.adolescence.2009.05.003.
- Koning IM, Vollebergh WA, Smit F, Verdurmen JE, Van Den Eijnden RJ, Ter Bogt TF, et al. Preventing heavy alcohol use in adolescents (PAS): cluster randomized trial of a parent and student intervention offered separately and simultaneously. Addiction 2009;104:1669-78. http://dx.doi.org/10.1111/j.1360-0443.2009.02677.x.
- Donaldson L. Guidance on the Consumption of Alcohol by Children and Young People. London: Department of Health; 2009.
- Inchley J, Currie D, Young T, Samdal O, Torsheim T, Augustson L, et al. Growing Up Unequal: Gender and Socioeconomic Differences in Young People’s Health and Well-Being. Health Behaviour in School-Aged Children (HBSC) Study: International Report From The 2013/2014 Survey. Geneva: World Health Organization; 2016.
- Elgar FJ, Roberts C, Parry-Langdon N, Boyce W. Income inequality and alcohol use: a multilevel analysis of drinking and drunkenness in adolescents in 34 countries. Eur J Public Health 2005;15:245-50. http://dx.doi.org/10.1093/eurpub/cki093.
- Beecham J, Knapp M, Thornicroft G, Brewin CR, Wing J. Measuring Mental Health Needs. London: Gaskell; 1992.
- Knapp M, Scott S, Davies J. The cost of antisocial behaviour in younger children. Clin Child Psychol Psychiatry 1999;4:457-73. https://doi.org/10.1177/1359104599004004003.
- Seidl H, Meisinger C, Wende R, Holle R. Empirical analysis shows reduced cost data collection may be an efficient method in economic clinical trials. BMC Health Serv Res 2012;12. http://dx.doi.org/10.1186/1472-6963-12-318.
- Stephenson MT, Hoyle RH, Palmgreen P, Slater MD. Brief measures of sensation seeking for screening and large-scale surveys. Drug Alcohol Depend 2003;72:279-86. https://doi.org/10.1016/j.drugalcdep.2003.08.003.
- Hoyle RH, Stephenson MT, Palmgreen P, Lorch EP, Donohew RL. Reliability and validity of a brief measure of sensation seeking. Pers Individ Differ 2002;32:401-14. https://doi.org/10.1016/S0191-8869(01)00032-0.
- Muris P. A brief questionnaire for measuring self-efficacy in youths. J Psychopathol Behav Assess 2001;23:145-9. https://doi.org/10.1023/A:1010961119608.
- Koning IM, Van den Eijnden RJ, Glatz T, Vollebergh WA. Don’t worry! Parental worries, alcohol-specific parenting and adolescents’ drinking. Cognit Ther Res 2013;37:1079-88. https://doi.org/10.1007/s10608-013-9545-0.
- McCrystal P, Higgins K, Percy A. The Belfast Youth Development Study 2004: Technical Report to the Research and Development Office. Belfast: Institute of Child Care Research, Queen’s University Belfast; 2004.
- White IR, Thompson SG. Adjusting for partially missing baseline measurements in randomized trials. Stat Med 2005;24:993-1007. https://doi.org/10.1002/sim.1981.
- Guide to the Methods of Technology Appraisal. London: NICE; 2013.
- Grieve R, Nixon R, Thompson SG. Bayesian hierarchical models for cost-effectiveness analyses that use data from cluster randomized trials. Med Decis Making 2010;30:163-75. http://dx.doi.org/10.1177/0272989X09341752.
- Heck RH, Thomas SL. An Introduction to Multilevel Modeling Techniques: MLM and SEM Approaches Using Mplus. New York, NY: Routledge; 2015.
- Koning IM, van den Eijnden RJ, Verdurmen JE, Engels RC, Vollebergh WA. Long-term effects of a parent and student intervention on alcohol use in adolescents: a cluster randomized controlled trial. Am J Prev Med 2011;40:541-7. http://dx.doi.org/10.1016/j.amepre.2010.12.030.
- Malmberg M, Overbeek G, Kleinjan M, Vermulst A, Monshouwer K, Lammers J, et al. Effectiveness of the universal prevention program ‘Healthy School and Drugs’: study protocol of a randomized clustered trial. BMC Public Health 2010;10. http://dx.doi.org/10.1186/1471-2458-10-541.
- Malmberg M, Kleinjan M, Overbeek G, Vermulst A, Monshouwer K, Lammers J, et al. Effectiveness of the ‘Healthy School and Drugs’ prevention programme on adolescents’ substance use: a randomized clustered trial. Addiction 2014;109:1031-40. http://dx.doi.org/10.1111/add.12526.
- Grant A, Treweek S, Dreischulte T, Foy R, Guthrie B. Process evaluations for cluster-randomised trials of complex interventions: a proposed framework for design and reporting. Trials 2013;14. http://dx.doi.org/10.1186/1745-6215-14-15.
- Kitzinger J. Qualitative research: introducing focus groups. BMJ 1995;311:299-302. https://doi.org/10.1136/bmj.311.7000.299.
- van Teijlingen E, Pitchforth E. Focus group research in family planning and reproductive health care. J Fam Plann Reprod Health Care 2006;32:30-2. https://doi.org/10.1783/147118906775275299.
- Williams A, Lavender T, Richmond DH, Tincello DG. Women’s experiences after a third-degree obstetric anal sphincter tear: a qualitative study. Birth 2005;32:129-36. http://dx.doi.org/10.1111/j.0730-7659.2005.00356.x.
- Patton M. Qualitative Research and Evaluation Methods. Thousand Oaks, CA: Sage; 2002.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Research Psychol 2006;3:77-101. https://doi.org/10.1191/1478088706qp063oa.
- New Strategic Direction for Alcohol and Drugs Phase 2 (2011–16). Belfast: Northern Ireland DHSSPSNI; 2011.
- Dane AV, Schneider BH. Program integrity in primary and early secondary prevention: are implementation effects out of control?. Clin Psychol Rev 1998;18:23-45. https://doi.org/10.1016/S0272-7358(97)00043-3.
- Dusenbury L, Brannigan R, Hansen WB, Walsh J, Falco M. Quality of implementation: developing measures crucial to understanding the diffusion of preventive interventions. Health Educ Res 2005;20:308-13. https://doi.org/10.1093/her/cyg134.
- Durlak JA, DuPre EP. Implementation matters: a review of research on the influence of implementation on program outcomes and the factors affecting implementation. Am J Community Psychol 2008;41:327-50. http://dx.doi.org/10.1007/s10464-008-9165-0.
- Ritzwoller DP, Sukhanova A, Gaglio B, Glasgow RE. Costing behavioral interventions: a practical guide to enhance translation. Ann Behav Med 2009;37:218-27. http://dx.doi.org/10.1007/s12160-009-9088-5.
- Gillett M, Dallosso HM, Dixon S, Brennan A, Carey ME, Campbell MJ, et al. Delivering the diabetes education and self management for ongoing and newly diagnosed (DESMOND) programme for people with newly diagnosed type 2 diabetes: cost effectiveness analysis. BMJ 2010;341. http://dx.doi.org/10.1136/bmj.c4093.
- Hollingworth W, Cohen D, Hawkins J, Hughes RA, Moore LA, Holliday JC, et al. Reducing smoking in adolescents: cost-effectiveness results from the cluster randomized ASSIST (A Stop Smoking In Schools Trial). Nicotine Tob Res 2012;14:161-8. http://dx.doi.org/10.1093/ntr/ntr155.
- Mytton J, Ingram J, Manns S, Stevens T, Mulvaney C, Blair P, et al. The feasibility of using a parenting programme for the prevention of unintentional home injuries in the under-fives: a cluster randomised controlled trial. Health Technol Assess 2014;18. http://dx.doi.org/10.3310/hta18030.
- CPI Annual Percentage Change: 1989 to 2015. London: Office for National Statistics; 2015.
- Department of Education Northern Ireland . Circular 2013 14 – Teacher’s Pay and Allowances from 1st September 2013 2014. www.education-ni.gov.uk/publications/circular-201413-teachers-pay-and-allowances-1-september-2013 (accessed December 2016).
- Reference Costs 2013–14. London: Department of Health; 2014.
- Curtis L. Unit Costs of Health and Social Care 2014. Canterbury: Personal Social Services Research Unit, University of Kent; 2014.
- Piece by Piece. Annual Report and Account 2014/15. London: National Society for the Prevention of Cruelty to Children; 2015.
- Johannesson M, Weinstein MC. On the decision rules of cost-effectiveness analysis. J Health Econ 1993;12:459-67. https://doi.org/10.1016/0167-6296(93)90005-Y.
- Methods for the Development of NICE Public Health Guidance. London: NICE; 2012.
- Glick HA, Doshi JA, Sonnad SS, Polsky D. Economic Evaluation in Clinical Trials. Oxford: Oxford University Press; 2007.
- Drummond M, Schulper M, Torrance G, O’Brien B, Stoddart G. Methods for the Economic Evaluation of Health Care Programmes. Oxford: Oxford University Press; 2005.
- Healey C, Rahman A, Faizal M, Kinderman P. Underage drinking in the UK: changing trends, impact and interventions. A rapid evidence synthesis. Int J Drug Policy 2014;25:124-32. http://dx.doi.org/10.1016/j.drugpo.2013.07.008.
- Scottish Schools Adolescent Lifestyle and Substance Use Survey (SALSUS) National Overview 2013. Edinburgh: NHS National Services Scotland; 2014.
- Foxcroft DR, Tsertsvadze A. Universal alcohol misuse prevention programmes for children and adolescents: Cochrane systematic reviews. Perspect Public Health 2012;132:128-34. http://dx.doi.org/10.1177/1757913912443487.
- Morgenstern M, Wiborg G, Isensee B, Hanewinkel R. School-based alcohol education: results of a cluster-randomized controlled trial. Addiction 2009;104:402-12. http://dx.doi.org/10.1111/j.1360-0443.2008.02471.x.
- Eisen M, Zellman GL, Murray DM. Evaluating the Lions-Quest ‘Skills for Adolescence’ drug education program. Second-year behavior outcomes. Addict Behav 2003;28:883-97. https://doi.org/10.1016/S0306-4603(01)00292-1.
- Werch CE, Pappas DM, Carlson JM, Edgemon P, Sinder JA, DiClemente CC. Evaluation of a brief alcohol prevention program for urban school youth. Am J Health Behav 2000;24:120-31. https://doi.org/10.5993/AJHB.24.2.5.
- Green R, Ross A. Young People’s Alcohol Consumption and its Relationship to Other Outcomes and Behaviour. London: Department for Education; 2010.
- Permanent and Fixed Period Exclusions in England: 2013 to 2014. London: Department for Education; 2015.
- Caria MP, Faggiano F, Bellocco R, Galanti MR. EU-Dap Study Group . Classroom characteristics and implementation of a substance use prevention curriculum in European countries. Eur J Public Health 2013;23:1088-93. http://dx.doi.org/10.1093/eurpub/cks191.
- Prinz RJ, Smith EP, Dumas JE, Laughlin JE, White DW, Barrón R. Recruitment and retention of participants in prevention trials involving family-based interventions. Am J Prev Med 2001;20:31-7. https://doi.org/10.1016/S0749-3797(00)00271-3.
- Bauman KE, Ennett ST, Foshee VA, Pemberton M, Hicks K. Correlates of participation in a family-directed tobacco and alcohol prevention program for adolescents. Health Educ Behav 2001;28:440-61. https://doi.org/10.1177/109019810102800406.
- Koning IM, van den Eijnden RJ, Engels RC, Verdurmen JE, Vollebergh WA. Why target early adolescents and parents in alcohol prevention? The mediating effects of self-control, rules and attitudes about alcohol use. Addiction 2011;106:538-46. http://dx.doi.org/10.1111/j.1360-0443.2010.03198.x.
- Stead M, Stradling B, MacKintosh AM, MacNeil M, Minty S, Eadie D. Delivery of the Blueprint Programme. Full Report of the Evaluation of the Implementation of Blueprint. Stirling: Institute of Social Marketing, University of Stirling; 2007.
- Stead M, Stradling R, MacNeil M, MacKintosh AM, Minty S. Implementation evaluation of the Blueprint multi-component drug prevention programme: fidelity of school component delivery. Drug Alcohol Rev 2007;26:653-64. http://dx.doi.org/10.1080/09595230701613809.
- Faggiano F, Vigna-Taglianti F, Burkhart G, Bohrn K, Cuomo L, Gregori D, et al. The effectiveness of a school-based substance abuse prevention program: 18-month follow-up of the EU-Dap cluster randomized controlled trial. Drug Alcohol Depend 2010;108:56-64. http://dx.doi.org/10.1016/j.drugalcdep.2009.11.018.
- Kreeft PVD, Wiborg G, Galanti MR, Siliquini R, Bohrn K, Scatigna M, et al. ‘Unplugged’: a new European school programme against substance abuse. Drugs (Abingdon Engl) 2009;16:167-81. https://doi.org/10.1080/09687630701731189.
- Rothwell H, Segrott J. Preventing alcohol misuse in young people aged 9-11 years through promoting family communication: an exploratory evaluation of the Kids, Adults Together (KAT) Programme. BMC Public Health 2011;11. http://dx.doi.org/10.1186/1471-2458-11-810.
- Segrott J, Rothwell H, Hewitt G, Playle R, Huang C, Murphy S, et al. Preventing alcohol misuse in young people: an exploratory cluster randomised controlled trial of the Kids, Adults Together (KAT) programme. Public Health Res 2015;3.
- Leigh BC, Gillmore MR, Morrison DM. Comparison of diary and retrospective measures for recording alcohol consumption and sexual activity. J Clin Epidemiol 1998;51:119-27. https://doi.org/10.1016/S0895-4356(97)00262-X.
- Lintonen T, Ahlström S, Metso L. The reliability of self-reported drinking in adolescence. Alcohol Alcohol 2004;39:362-8. http://dx.doi.org/10.1093/alcalc/agh071.
- Walton MA, Chermack ST, Shope JT, Bingham CR, Zimmerman MA, Blow FC, et al. Effects of a brief intervention for reducing violence and alcohol misuse among adolescents: a randomized controlled trial. JAMA 2010;304:527-35. http://dx.doi.org/10.1001/jama.2010.1066.
- Percy A, McAlister S, Higgins K, McCrystal P, Thornton M. Response consistency in young adolescents’ drug use self-reports: a recanting rate analysis. Addiction 2005;100:189-96. http://dx.doi.org/10.1111/j.1360-0443.2004.00943.x.
- Davis CG, Thake J, Vilhena N. Social desirability biases in self-reported alcohol consumption and harms. Addict Behav 2010;35:302-11. http://dx.doi.org/10.1016/j.addbeh.2009.11.001.
- Müller S, Piontek D, Pabst A, Kraus L. The relationship between alcohol consumption and perceived drunkenness: a multilevel cross-national comparison in samples of adolescents. Alcohol Alcohol 2011;46:399-406. http://dx.doi.org/10.1093/alcalc/agr032.
- Courtney KE, Polich J. Binge drinking in young adults: data, definitions, and determinants. Psychol Bull 2009;135:142-56. http://dx.doi.org/10.1037/a0014414.
- Claxton K. The irrelevance of inference: a decision-making approach to the stochastic evaluation of health care technologies. J Health Econ 1999;18:341-64. https://doi.org/10.1016/S0167-6296(98)00039-3.
- Carroll C, Patterson M, Wood S, Booth A, Rick J, Balain S. A conceptual framework for implementation fidelity. Implement Sci 2007;2. http://dx.doi.org/10.1186/1748-5908-2-40.
- Meng Y, Holmes J, Hill-McManus D, Brennan A, Meier PS. Trend analysis and modelling of gender-specific age, period and birth cohort effects on alcohol abstention and consumption level for drinkers in Great Britain using the General Lifestyle Survey 1984–2009. Addiction 2014;109:206-15. http://dx.doi.org/10.1111/add.12330.
- Patton R, Deluca P, Kaner E, Newbury-Birch D, Phillips T, Drummond C. Alcohol screening and brief intervention for adolescents: the how, what and where of reducing alcohol consumption and related harm among young people. Alcohol Alcohol 2014;49:207-12. http://dx.doi.org/10.1093/alcalc/agt165.
- Tanner-Smith EE, Lipsey MW. Brief alcohol interventions for adolescents and young adults: a systematic review and meta-analysis. J Subst Abuse Treat 2015;51:1-18. http://dx.doi.org/10.1016/j.jsat.2014.09.001.
- Gorman DM, Conde E. Conflict of interest in the evaluation and dissemination of ‘model’ school-based drug and violence prevention programs. Eval Program Plann 2007;30:422-9. http://dx.doi.org/10.1016/j.evalprogplan.2007.06.004.
- Fernandez-Hermida JR, Calafat A, Becoña E, Tsertsvadze A, Foxcroft DR. Assessment of generalizability, applicability and predictability (GAP) for evaluating external validity in studies of universal family-based prevention of alcohol misuse in young people: systematic methodological review of randomized controlled trials. Addiction 2012;107:1570-9. http://dx.doi.org/10.1111/j.1360-0443.2012.03867.x.
- McKay M, Sumnall H, McBride N, Harvey S. The differential impact of a classroom-based, alcohol harm reduction intervention, on adolescents with different alcohol use experiences: a multi-level growth modelling analysis. J Adolesc 2014;37:1057-67. http://dx.doi.org/10.1016/j.adolescence.2014.07.014.
- Bellis MA, Hughes K, Morleo M, Tocque K, Hughes S, Allen T, et al. Predictors of risky alcohol consumption in schoolchildren and their implications for preventing alcohol-related harm. Subst Abuse Treat Prev Policy 2007;2. http://dx.doi.org/10.1186/1747-597X-2-15.
- Fairchild AJ, MacKinnon DP, Sloboda Z, Petras H. Defining Prevention Science. Boston, MA: Springer; 2014.
- MacKinnon DP, Luecken LJ. How and for whom? Mediation and moderation in health psychology. Health Psychol 2008;27:99-100. http://dx.doi.org/10.1037/0278-6133.27.2(Suppl.).S99.
Appendix 1 The STAMPP logic model and intervention content
The STAMPP logic models were developed during the application and early phases of the trial, and were based on the process evaluation of the Australian delivery of the classroom component, SHAHRP,59,107 and learning arising from the implementation of the NI adaptation of the curriculum. 60 The logic model for the parental component was based on the mediation analysis of Koning et al. ,117 who developed the original activities that our parental brief intervention was based upon (the Dutch PAS programme).
The logic model provided hypothesised causal pathways between intervention receipt and primary and secondary outcomes at final follow-up. The model was extended to include long-term behavioural impacts of the programmes, although assessments of these are beyond the timelines of the current project. The model provided a framework upon which the process evaluation methodology was partly based (see Chapter 2, Definitions/calculations).
Table 32 provides the overall logic model of STAMPP and describes, in general terms, how the classroom and parental activities are hypothesised to lead to long-term changes in alcohol use and alcohol-related harms.
| Programme processes | Impacts | ||
|---|---|---|---|
| Immediate | Short-term | Behavioural | |
| → | |||
| Pupils attending the classroom component of STAMPP and receiving the programme as intended will . . . | . . . gain greater alcohol knowledge, develop healthier attitudes towards alcohol, understand the role that alcohol plays in young people’s lives, be better able to identify situations in which alcohol use may increase risk, and be better able to understand how drinking alcohol affects their behaviour and that of their friends, which will . . . | . . . lead to a delay in the initiation of alcohol use and in the establishment of regular drinking, a reduction in the frequency of HED and avoidance of risky drinking situations, which will . . . | . . . lead to a sustained reduction in harmful and hazardous drinking and a reduction in alcohol-related harm (caused by own drinking or drinking of others), which will lead to a reduction in alcohol-related mortality and morbidity |
| Parents receiving the parental component of STAMPP and receiving the programme as intended will . . . | . . . be better able to set and implement family rules on alcohol use, communicate these more effectively with children, which will . . . | . . . modify children’s attitudes towards alcohol and limit opportunities for alcohol use in the family home, which will . . . | . . . support long-term positive outcomes in their children |
One-day training events were held in each study site before both phases of delivery of the classroom component. Training for the following academic year (from September onwards) took place in the preceding June. Training included sessions on alcohol knowledge (e.g. effects of alcohol use, prevalence rates, risk and protective factors for alcohol use), sharing experiences of the programme when delivered elsewhere and skills and lesson delivery rehearsal for each of the SHAHRP lessons.
Training involved examination of each of the SHAHRP lessons, which were entitled: ‘Myths about alcohol’; ‘Units of alcohol’; ‘Reasons why people do/don’t drink’; ‘Alcohol and the body’; ’consequences of “levels” of drinking’; ‘Blood alcohol concentration’; ‘Social and personal harms’; ‘Alcohol policy’; ‘Alcohol and the media’; ‘Advice for teenagers’; ‘A “night out”’; ‘Pressures faced by young drinkers’; and ‘Scenario-based discussion’. The six phase 1 lessons primarily encouraged knowledge development in pupils, and this was built on in phase 2, in which the lessons focused on more specific adolescent drinking behaviours, real-life scenarios or potential experiences while in an environment where alcohol is consumed. Phase 2 activities encouraged reflection, discussion and rehearsal of skills relating to alcohol-related peer pressure, similarities or differences for males and females in a drinking context, drink spiking, responsibilities towards friends, risk perception and assessing hazards related to alcohol in different environments or situations and peer advice around alcohol.
Teachers were also provided with a collection of electronic support materials to help them deliver the lessons. These included structured lesson plans and suggested techniques for information dissemination, group activities, role-plays and discussion points. Sample questions, to help facilitate discussion, and coaching points to aid in the management of the activities were included for each lesson. Teachers were also provided with videos [digital versatile disc (DVD)] that supported delivery of the lessons and student discussions. These included examples of alcohol marketing techniques and regional close circuit television footage of alcohol-related disorder in the night-time economy. Pupils were issued with separate workbooks for each phase of delivery that were designed to engage their interest. The workbooks provided information necessary for the students to perform practical activities and encouraged them to further explore each activity. In addition, the workbooks provided space for the students to record what they had learned as a way of consolidating the activity. Materials from the version of SHAHRP used in the STAMPP trial are available from the authors on request.
The classroom component of STAMPP, SHAHRP, was not based on a specific theory but on the original programme, which researchers described as an evidence-based programme based on literature review (Table 33). 59 In developing STAMPP, we have drawn upon two main theories in order to understand how the programme might work: social norms theory108 and social cognitive theory. 109 Briefly, social norms theory suggests that behaviour is influenced by incorrect perceptions of how other members of a social group (e.g. classmates, friendship groups) think and behave. Misperceptions between perceived and actual norms lead to an overestimation of behaviours such as alcohol use, healthy behaviours being underestimated and individuals changing their behaviour to approximate the misperceived norm. By establishing healthier or more accurate reference norms, individuals may modify their behaviour towards more healthy activities. Similarly, social cognitive theory is derived from earlier social learning theories, and suggests that alcohol use behaviour is learned through modelling, imitation and responding to the emotions of others, and that this is influenced by individual cognitions, attitudes and beliefs. It is related to social norms theory in that it considers how individual behaviour relates to that of others. The classroom component of STAMPP aims to develop relevant skills in students to help them recognise these influences on alcohol use and to develop counterstrategies to avoid harm.
| Evidence-based approach | SHAHRP strategy |
|---|---|
| Timing and programming | |
| Inoculation approach (intervening with the target audience prior to behaviour) | Phase 1 of the SHAHRP intervention is conducted prior to onset of alcohol use for most of the study population |
| Relevancy approach (intervening with the target audience on initiation of behaviour; developmentally appropriate programme) | Phase 2 of the SHAHRP intervention is conducted when prevalence data indicate that most of the study population have initiated use |
| In the context of developmentally appropriate school health curriculum | The SHAHRP intervention complements, and does not replace, each school’s health education curriculum |
| Content and teaching methodology | |
| Based on the experiences of young people (is student centred) | Findings from focus groups and student feedback of earlier testing of SHAHRP provided the basis for intervention and research instruments |
| Students are involved in the planning of interventions | As above |
| Provides accurate normative information | Up-to-date normative information is incorporated into the SHAHRP intervention materials |
| Includes a harm minimisation approach rather than being based solely on goals of non-use or delayed use | SHAHRP focused on providing strategies to reduce alcohol misuse and harm experienced by the students’ own and others’ use of alcohol |
| Programmes should include social resistance skills training that is relevant to students | Each phase of the SHAHRP intervention provides social resistance skills training |
| Programmes should be interactive. Programmes should be skills/activity based | The SHAHRP intervention primarily comprises skills and activity-based elements |
| Programmes should incorporate utility knowledge (knowledge that is of practical use to the target audience) | The SHAHRP intervention incorporated positive-action oriented utility information gathered during the formative stage of development |
The School Health and Alcohol Harm Reduction Project is an example of a resistance skills training programme and includes elements of alcohol-specific personal and social skills training. 59,110–112 In accordance with the underpinning theory, it includes three main strategies: (1) teaching students to recognise high-risk situations, (2) increasing the awareness of external influences on behaviour and (3) combining self-control (i.e. the ability to control responses, to interrupt undesired behavioural tendencies and refrain from acting upon them) with refusal skills training (i.e. in order to improve self-efficacy in avoiding unhealthy behaviours but not with the consequence of social disadvantage for the young person with their peers). The knowledge delivered through SHAHRP (e.g. lessons on the effects of alcohol, description of alcohol units) does not have direct preventative effects, but is used to shape alcohol attitudes and to support situation specific decision-making. Accordingly, using the prevention taxonomy of Foxcroft,113 we classify the SHAHRP as a universal developmental programme.
Our parental intervention was based on the parental component of the Dutch PAS programme,64 which was based on research indicating that restrictive parenting practices (e.g. monitoring of children’s alcohol use, healthy attitudes towards alcohol, alcohol rule-setting) was associated with reduced prevalence of children’s alcohol use. In subsequent mediation analyses, it was shown that the PAS programme effect was mediated through children’s perceptions of parental rules, child self-efficacy and child self-control. 117 There was an interaction between children’s attitudes towards alcohol and perceived parental rules on intervention outcomes, suggesting that perception of the rules set by parents shaped the attitudes of their children towards alcohol. 114 Parental rule-setting on alcohol led to an increase in child self-control, which led to reduced weekly drinking at final assessment. Furthermore, parental rule-setting had direct effects on children’s alcohol use. No reciprocal sequential mediation was found (i.e. child self-control did not predict later parental rules), suggesting that the mediated relationship was robust. We hypothesise that the parental component of STAMPP works in a similar manner; parental rule-setting and monitoring reinforces the lessons received in the classroom through shaping healthier attitudes towards alcohol, and has direct effects on child drinking by reducing opportunities for use in the family home and by providing positive behavioural models around drinking.
Building on this, the second logic model (Table 34) describes how the STAMPP components (separated into parent and child activities below, although there is an interaction as shown in Figure 1) are hypothesised to produce their expected effects on specific determinants of alcohol use behaviours. Some activities are delivered in phase 1 of the intervention and some in phase 2, and phase 2 activities are designed to build on skills and learning developed in phase 1. This is important, as, during the period between the two intervention phases, the natural trajectory of alcohol use means that some pupils will have initiated alcohol use, and baseline initiates may have begun to develop more regular patterns of use.
| Component | Impacts | ||
|---|---|---|---|
| Immediate | Short-term | Long-term | |
| → | |||
| Classroom processes | |||
| Norms setting: participants better understand sources of pressure to drink and gain a more accurate understanding of alcohol use prevalence in peers and wider society, leading to . . . | . . . a reduction in misperceptions of norms and susceptibility to pro-alcohol influences, leading to . . . | . . . increased time to alcohol initiation in baseline abstainers, reduction in recent alcohol use frequency in initiates and a reduction in the frequency of heavy episodic alcohol drinking in more established drinkers. This will result in . . . | . . . a reduction in alcohol-related mortality and morbidity and fewer (inter)personal social harms experienced |
| Skills training: participants are better able to identify and understand social situations in which alcohol use and harm might arise and to understand the individual and external pressures to drink alcohol, leading to . . . | . . . an increase in self-control and refusal of alcohol use, leading to . . . | ||
| Alcohol knowledge and attitudes: participants gain knowledge and develop healthier attitudes towards health and social effects of alcohol and laws around purchase, leading to . . . | . . . an increase in understanding of how alcohol affects young people’s lives, in order to . . . | . . . reinforce alcohol-related skills developed throughout the curriculum, supporting . . . | . . . young people to make informed decisions about alcohol use |
| Parental processes | |||
| Family rules on alcohol: parents set and enforce rules on alcohol use in the family home and in children’s socialising activities, which will lead to . . . | . . . an increase in children’s perception of parental attitudes and rules towards alcohol, leading to . . . | . . . a reduction in opportunities for alcohol use and development of more healthy attitudes towards alcohol in children, supporting . . . | . . . alcohol-related refusal skills and self-control and causing direct effects on alcohol-use behaviours |
| Parental skills training: parents are better able to understand the role that alcohol plays in young people’s lives so that they are able to respond to alcohol in an authoritative manner, so that . . . | . . . family rules on alcohol are clear and enforced, which will lead to . . . | . . . an increase in confidence in parenting self-efficacy, supporting . . . | . . . long-term increase in children’s awareness of rules and parental attitudes towards alcohol |
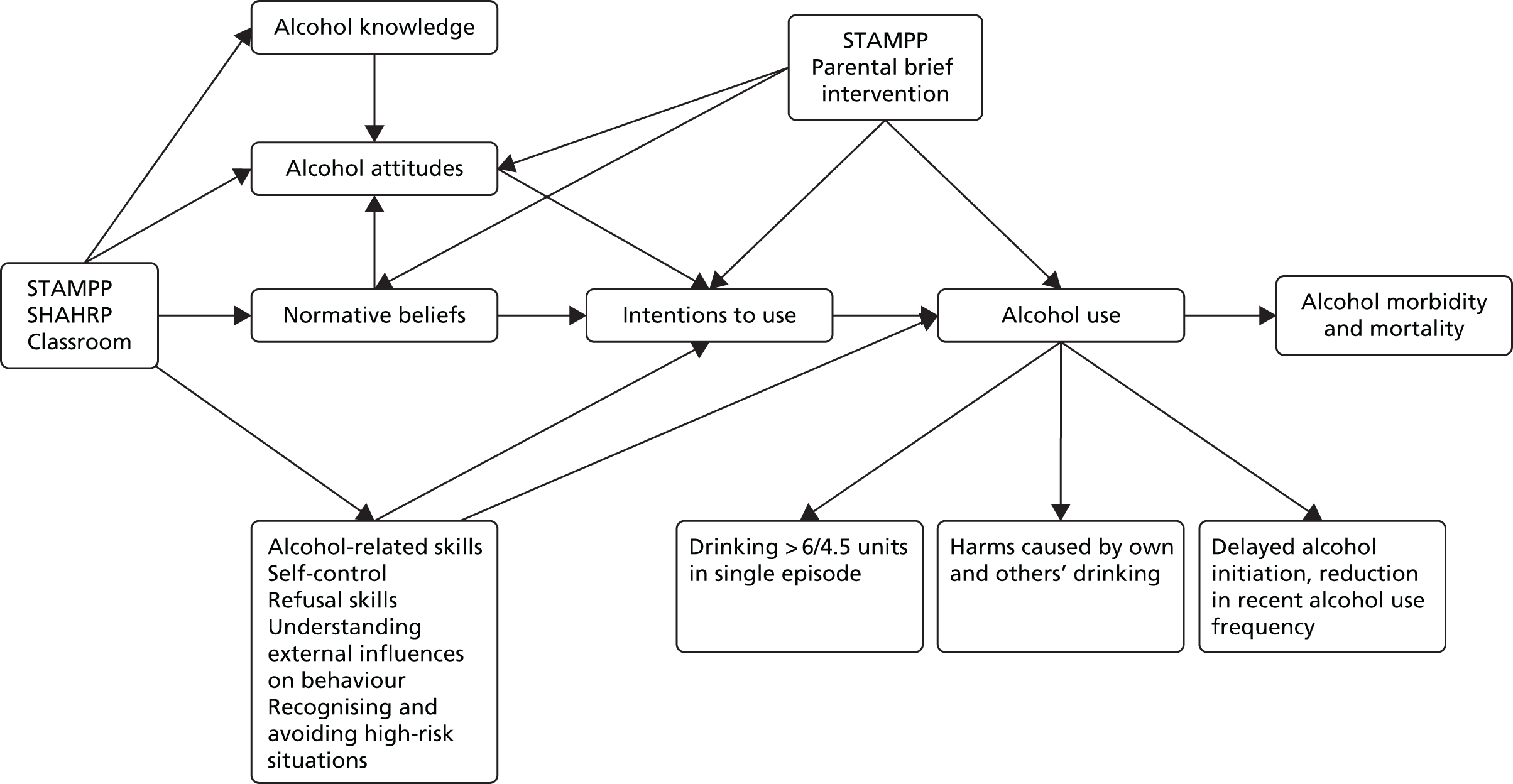
Appendix 2 Consent forms for participation in STAMPP
Parental permission for child participation in STAMPP
Student consent to participate in STAMPP
Appendix 3 Primary outcome 1: answer sheet (and pictorial prompts) for assessing consumption of > 6/4.5 units at 33 months after baseline
Note that as a result of intellectual property considerations, we have had to conceal alcohol brand names and images in this report.
Primary outcome 2: questions assessing harms resulting from own use of alcohol at 33 months after baseline
| In the past 6 months . . . | Never | Once | Twice | 3 or 4 times | 5–11 times | ≥ 12 times |
|---|---|---|---|---|---|---|
| Have you planned to get drunk? | ||||||
| Did you drink more than planned to? | ||||||
| Were you sick after you had been drinking? | ||||||
| Did you have a hangover after you had been drinking? | ||||||
| Were you unable to remember things that had happened when you had been drinking? | ||||||
| Did you verbally abuse someone when you had been drinking? | ||||||
| Did you get into a physical fight when you had been drinking? | ||||||
| Did you damage property when you had been drinking? | ||||||
| Were you sexually harassed when you had been drinking? | ||||||
| Was your school performance affected (e.g. day off) because you had been drinking? | ||||||
| Did you get in trouble with friends because of your drinking? | ||||||
| Did you get in trouble with a boyfriend/girlfriend because of your drinking? | ||||||
| Did you get in trouble with your parents because of your drinking? | ||||||
| Did you get in trouble at school because of your drinking? | ||||||
| Did you get in trouble with the police because of drinking? | ||||||
| Did you have to attend a doctor or hospital because of your own drinking? |
Appendix 4 Example of fieldworker data collection script (alcohol-related questions only)
Appendix 5 Additional analysis tables
| School code | n (%) |
|---|---|
| NI | |
| 1.00 | 25 (19.7) |
| 2.00 | 14 (13.0) |
| 3.00 | 8 (20.5) |
| 5.00 | 14 (25.5) |
| 6.00 | 20 (10.6) |
| 7.00 | 26 (15.1) |
| 8.00 | 15 (8.5) |
| 9.00 | 19 (10.2) |
| 10.00 | 14 (15.6) |
| 11.00 | 2 (1.7) |
| 12.00 | 18 (13.1) |
| 13.00 | 8 (19.5) |
| 14.00 | 9 (8.6) |
| 15.00 | 9 (7.0) |
| 16.00 | 1 (1.5) |
| 17.00 | 19 (15.0) |
| 18.00 | 36 (23.4) |
| 19.00 | 1 (4.5) |
| 20.00 | 21 (17.9) |
| 22.00 | 10 (16.1) |
| 23.00 | 8 (12.1) |
| 24.00 | 17 (13.8) |
| 25.00 | 10 (52.6) |
| 26.00 | 21 (21.2) |
| 27.00 | 18 (19.8) |
| 28.00 | 15 (8.2) |
| 29.00 | 18 (19.4) |
| 30.00 | 7 (5.6) |
| 31.00 | 17 (17.5) |
| 32.00 | 9 (9.9) |
| 33.00 | 2 (2.2) |
| 34.00 | 12 (19.0) |
| 35.00 | 28 (21.7) |
| 36.00 | 11 (11.3) |
| 37.00 | 11 (22.0) |
| 38.00 | 16 (13.3) |
| 39.00 | 40 (28.8) |
| 40.00 | 11 (14.7) |
| 41.00 | 21 (15.2) |
| 42.00 | 19 (15.6) |
| 43.00 | 12 (18.2) |
| 44.00 | 38 (46.9) |
| 45.00 | 6 (14.3) |
| 46.00 | 18 (10.4) |
| 47.00 | 25 (18.8) |
| 48.00 | 26 (18.4) |
| 49.00 | 21 (16.8) |
| 50.00 | 3 (8.8) |
| 51.00 | 46 (19.8) |
| 52.00 | 9 (14.3) |
| 53.00 | 27 (18.1) |
| 54.00 | 17 (26.6) |
| 55.00 | 17 (28.3) |
| 56.00 | 8 (7.9) |
| 57.00 | 12 (8.6) |
| 58.00 | 9 (10.5) |
| 59.00 | 13 (8.8) |
| 60.00 | 5 (23.8) |
| 61.00 | 19 (14.5) |
| 62.00 | 20 (21.5) |
| 63.00 | 5 (4.7) |
| 64.00 | 30 (14.6) |
| 65.00 | 23 (20.2) |
| 66.00 | 7 (5.6) |
| 67.00 | 25 (18.5) |
| 68.00 | 34 (16.3) |
| 69.00 | 16 (11.0) |
| 70.00 | 27 (26.0) |
| 71.00 | 10 (5.0) |
| 72.00 | 15 (16.1) |
| Scotland | |
| 73.00 | 44 (27.3) |
| 74.00 | 6 (21.4) |
| 75.00 | 42 (20.8) |
| 76.00 | 37 (25.7) |
| 77.00 | 16 (23.9) |
| 78.00 | 35 (28.7) |
| 79.00 | 23 (26.1) |
| 80.00 | 46 (27.7) |
| 81.00 | 23 (31.1) |
| 82.00 | 34 (25.6) |
| 83.00 | 34 (20.4) |
| 84.00 | 70 (21.3) |
| 85.00 | 27 (15.4) |
| 86.00 | 38 (25.3) |
| 87.00 | 63 (42.9) |
| 88.00 | 72 (29.0) |
| 89.00 | 30 (33.3) |
| 90.00 | 33 (18.3) |
| 91.00 | 13 (11.3) |
| 92.00 | 40 (19.3) |
| 93.00 | 52 (25.5) |
| 94.00 | 18 (18.4) |
| 95.00 | 44 (29.3) |
| 96.00 | 79 (27.0) |
| 97.00 | 14 (20.6) |
| 98.00 | 44 (31.0) |
| 99.00 | 39 (23.9) |
| 100.00 | 16 (20.0) |
| 101.00 | 37 (22.0) |
| 102.00 | 27 (32.1) |
| 103.00 | 29 (19.3) |
| 104.00 | 24 (18.9) |
| 105.00 | 16 (18.4) |
| 106.00 | 13 (14.6) |
| 107.00 | 12 (11.9) |
| Parameter | Estimate | SE | p-value |
|---|---|---|---|
| ITT CC analysis | |||
| Between level (intercept) | |||
| Intervention arm | –0.518 | 0.106 | < 0.001 |
| FSM provision (tertile) | 0.250 | 0.074 | < 0.001 |
| School type | |||
| Boys’ school – dummy | –0.174 | 0.204 | 0.393 |
| Girls’ school – dummy | –0.554 | 0.270 | 0.040 |
| Location (NI) | 0.443 | 0.115 | < 0.001 |
| Between level (slope) | |||
| Intervention arm | –0.097 | 0.183 | 0.596 |
| FSM provision (tertile) | –0.195 | 0.129 | 0.130 |
| School type | |||
| Boys’ school – dummy | 0.030 | 0.349 | 0.932 |
| Girls’ school – dummy | 0.337 | 0.493 | 0.494 |
| Location (NI) | –0.103 | 0.209 | 0.621 |
| HEDT3 with slope | –0.079 | 0.047 | 0.097 |
| Slope intercept | 1.727 | 0.205 | < 0.001 |
| Residual variance | |||
| HEDT3 | 0.187 | 0.035 | < 0.001 |
| Slope | 0.036 | 0.038 | 0.347 |
| Threshold (HEDT3$1) | 1.597 | 0.125 | < 0.001 |
| Parameter | Estimate | SE | p-value |
|---|---|---|---|
| ITT CC analysis | |||
| Between level (intercept) | |||
| Intervention arm | –0.089 | 0.085 | 0.295 |
| FSM provision (tertile) | 0.174 | 0.061 | 0.004 |
| School type | |||
| Boys’ school – dummy | –0.093 | 0.215 | 0.665 |
| Girls’ school – dummy | –0.329 | 0.234 | 0.159 |
| Location (NI) | 0.526 | 0.085 | < 0.001 |
| Between level (slope) | |||
| Intervention arm | 0.028 | 0.105 | 0.787 |
| FSM provision (tertile) | –0.040 | 0.071 | 0.568 |
| School type | |||
| Boys’ school – dummy | –0.055 | 0.365 | 0.881 |
| Girls’ school – dummy | –0.152 | 0.278 | 0.586 |
| Location (NI) | –0.213 | 0.109 | 0.051 |
| HarmsT3 with slope | –0.048 | 0.015 | 0.001 |
| HarmsT3 intercept | 0.031 | 0.089 | 0.728 |
| Slope intercept | 1.069 | 0.113 | < 0.001 |
| Residual variance | |||
| HarmsT3 | 0.117 | 0.028 | < 0.001 |
| Slope | 0.020 | 0.011 | 0.061 |
Appendix 6 Focus group and interview topic guides
Pupils
All participants
-
Introductory question: when I say the word ‘alcohol’ what do you think of?
SHAHRP recipients
Core questions/prompts
-
Can you remember taking part in an alcohol project using these books (show books)?
-
What were the main things that you learned about alcohol using these books?
-
What was your overall impression of part 1 (purple book)?
Participants are then taken through lessons and asked to give brief feedback
-
What were the things that you liked most about taking part in part 1?
-
Was there anything that you did not like about taking part in part 1?
-
What was your overall impression of part 2 (blue book)?
Participants are then taken through each lesson and asked to give brief feedback
-
What were the things that you liked most about taking part in part 2?
-
Was there anything that you did not like about taking part in part 2?
If not already mentioned by participants
-
Can you remember the CD – did your teacher use it, what did you think of it?
Education as normal recipients (control schools)
Core questions/prompts
-
Do you receive alcohol education in school and, if so, what do you think of it?
-
Do you think that young people generally consider the consequences of alcohol drinking behaviour?
-
What do you think is meant by the ‘immediate’ consequences of alcohol use? (Prompt: examples – health, getting into trouble, falling out with friends).
-
What do you think is meant by the ‘long-term’ consequences of alcohol use? {Prompt: not just long-term health problems but also how immediate behaviours [e.g. Facebook photos (Facebook, Inc., Menlo Park, CA, USA), getting in trouble] might also have long-term consequences}.
-
Do you think that people your age think about the difference between immediate and long-term consequences?
-
Do you think that parents can do anything to prevent alcohol use by people your age? (Prompt: family rules).
-
What do you think about how alcohol or health education is delivered in schools? Where do young people learn about the effects of alcohol – in school or elsewhere? (Prompt: friends, family, doctor, media, etc.).
Optional questions if sufficient time and not already discussed by participants
-
Did you find it easy or difficult to discuss these issues with your teacher (and why)?
-
Did you find it easy or difficult to discuss these issues in the presence of your classmates (and why)?
-
Did you think that the lessons were directly relevant to your understanding of, or experience of alcohol and alcohol use?
-
Would you recommend these resources to other schools for people your age? (Prompt: Would the messages be more suitable for younger or older people? Are the materials age appropriate? Should the content and design be changed?)
Head teachers/principals
Teachers in schools delivering SHAHRP
-
Do they consider alcohol to be an issue of concern in their school?
-
In what way?
-
Prompts: for example specific incidents, general child safeguarding, impact on health, impact on education, special interest of staff, local policy drivers.
-
What has been their experience of alcohol education in the past (not including STAMPP/SHAHRP)?
Prompts: has it responded to children’s alcohol education/needs? Has it been age and experience appropriate? Do they perceive it to be effective? Have they found it easy/difficult to find suitable providers? Has it previously been developed and delivered ‘in-house’?
-
How did delivery of STAMPP/SHAHRP impact on the school?
-
What do they think was the main purpose of STAMPP/SHAHRP and what outcomes were targeted?
-
Why did they decide to participate in the study/intervention delivery?
-
Prompts: for example, concerns about alcohol use in the school, concerns about alcohol use in general, want to contribute to research, interested in alcohol health curriculum and interventions.
-
Did they have any concerns about being chosen to deliver the intervention?
Prompts: if it would raise any safeguarding issues, whether parents might think that participation indicated that the school had an alcohol problem, don’t think alcohol education makes a difference, time and extra resource required for delivery, concerns that the intervention may have been ineffective or led to increased alcohol use.
-
How were the teachers chosen to deliver STAMPP/SHAHRP?
-
How did they find the process of implementing STAMPP/SHAHRP within the school environment? (e.g. finding the right staff, finding the curriculum time, balancing against competing priorities).
-
How do they compare STAMPP/SHAHRP with other health-based interventions they have run in the school?
-
Did any staff, parents or pupils talk to them about alcohol as a result of their school taking part in the study? (Note: these are conversations in addition to any SHAHRP implementation or participation questions.)
-
Future activity
If STAMPP/SHAHRP is shown to be effective, do they think their school would be in a position to continue delivery?
-
If they answered yes to question 4, why? And what support do they think they’d need to continue delivery?
Prompts: for example, training of teachers (or could this be done by existing SHAHRP teachers?), workbook printing costs, research support to understand if it made a difference, etc.
-
STAMPP comprises a classroom and a parental component. If it were to be shown to be effective, would the school also try to deliver the special parents evening to complement the classroom activities? If not, why not?
-
If they answered no to question 4, why not?
Prompts: lack of curriculum time, lack of interest in alcohol education/more pressing priorities, lack of resources, (perceived) lack of support from education/health authorities, etc.
-
STAMPP has been delivered as part of a research trial (RCT). How do you think implementation in the ‘real world’ would differ from this?
-
Dissemination
-
Are they interested in dissemination of study findings (alcohol use and intervention effectiveness)?
-
Prompts: what if the programme is found to be ineffective? What sort of information would they want in this case? Would they still implement an ineffective programme if the teachers and pupils liked it?
-
To whom should study findings be disseminated? Governors? Staff? Students? Parents?
-
How do they think dissemination would be most effectively performed?
Prompts: for example printed materials, electronic publications, short article for school newsletter, etc.
Teachers in control schools
-
Do they consider alcohol to be an issue of concern in their school?
-
In what way?
-
Prompts: for example, specific incidents, general child safeguarding, impact on health, impact on education, special interest of staff, local policy drivers.
-
What has been their experience of alcohol education in the past (not including STAMPP/SHAHRP)?
Prompts: Has it responded to children’s alcohol education/needs? Has it been age and experience appropriate? Do they perceive it to be effective? Have they found it easy/difficult to find suitable providers? Has it previously been developed and delivered ‘in-house’?
-
How did participation in the research trial impact on the school?
-
Why did they decide to participate in the study?
-
Prompts: for example, concerns about alcohol use in the school; concerns about alcohol use in general; want to contribute to research; interested in alcohol health curriculum and interventions.
-
Did they have any concerns about being randomised as a control school?
Prompts: missing out on receiving the intervention, surveys being disruptive, perception not getting anything in return for taking part.
-
Did any staff, parents or pupils talk to them about alcohol as a result of their school taking part in the study? (Note that these are conversations not related to STAMPP/SHAHRP implementation or participation questions.)
-
Did they, or did their staff members (to the best of their knowledge) try to find out more about the SHAHRP independently? What did they learn?
-
Future activity
If STAMPP/SHAHRP is shown to be effective, do they think their school would be in a position to start delivering it in future?
-
If they answered yes to question 4, why? And what support do they think they’d need to deliver it?
Prompts: for example, training of teachers, workbook printing costs, research support to understand if it made a difference etc.
-
STAMPP comprises a classroom and parental component. If it were to be shown to be effective, would the school also try to deliver the special parents evening to complement the classroom activities? If not, why not?
-
If they answered no to question 4, why not?
Prompts: lack of curriculum time, lack of interest in alcohol education/more pressing priorities, lack of resources, (perceived) lack of support from education/health authorities, etc.
-
Dissemination
-
Are they interested in dissemination of study findings (alcohol use)?
-
Prompts: what if the programme is found to be ineffective? What sort of information would they want in this case? Would they still implement an ineffective programme if the teachers and pupils liked it?
-
To whom should study findings be disseminated? Governors? Staff? Students? Parents?
-
How do they think dissemination would be most effectively performed?
Prompts: for example, printed materials, electronic publications, short article for school newsletter, etc.
Public health, education and other stakeholders in trial geographies
-
Is STAMPP similar to or distinct from other approaches to alcohol use in young people in the region/city?
-
What do you know about the aims, objectives and expected outcomes of STAMPP?
-
How does STAMPP fit in with your alcohol/health policy or strategic priorities for young people?
-
In your role, do you have commissioning responsibility for interventions such as STAMPP?
-
With respect to addressing alcohol-related issues, what’s your opinion on the relative contribution, impact and complementarity of alcohol education activities compared with other types of responses? (prompt: e.g. licensing, regulation, taxation, etc.)
The next questions assume that the SHAHRP/STAMPP is shown to be effective:
-
If shown to be effective, do you think it is likely that future implementation of STAMPP/SHAHRP would be supported by colleagues and other stakeholders, policy actions, money and material resources?
-
If yes, are there any additional considerations that need to be taken into account before your organisation might support STAMPP/SHAHRP? [prompt: identifying providers, ensuring self-sustainability (e.g. teachers training colleagues in school on how to deliver), monitoring outcomes, etc.]
-
In your organisation/department, are there key individuals who you think would be able to promote the intervention as part of their role?
-
If no, why not? (prompt: ask them to think about topics such as policy priorities, money and other resources, priority of alcohol education vs. other alcohol actions, autonomy of schools, health and social well-being promotion in general vs. specific alcohol actions)
-
-
STAMPP has been delivered as part of a research trial (RCT). How do you think, if at all, implementation in the ‘real world’ would differ from delivery as part of a RCT?
-
If shown to be effective, do you think schools will want to deliver an intervention such as STAMPP/SHAHRP? Please explain the reasons for your answer.
-
Is there a role for other types of professionals/services in school alcohol education? How might these different roles work together? Do you think it is possible to develop a ‘whole-school’ approach to alcohol that might include interventions, curriculums, screening, and referral and school policies?
Appendix 7 Self-reported classroom fidelity measures
Appendix 8 Fidelity of implementation scores across intervention schools
| School code (randomisation) | Phase, implementation score | |
|---|---|---|
| 1 | 2 | |
| 3 | – | – |
| 5 | – | – |
| 9 | 87.14 | 79.00 |
| 10 | – | 35.00 |
| 11 | – | 90.00 |
| 12 | 83.14 | 96.00 |
| 14 | – | 45.00 |
| 15 | – | 95.00 |
| 16 | 87.14 | 54.00 |
| 18 | 89.44 | – |
| 22 | 65.47 | – |
| 23 | 80.61 | – |
| 24 | 58.50 | – |
| 25 | – | – |
| 28 | 74.18 | 60.24 |
| 31 | 84.71 | 60.00 |
| 33 | – | – |
| 37 | 46.29 | – |
| 40 | 41.00 | 96.00 |
| 42 | 74.04 | 70.00 |
| 44 | 70.68 | – |
| 45 | 28.23 | – |
| 46 | 69.53 | 48.00 |
| 47 | 60.82 | 97.00 |
| 54 | 74.50 | 51.00 |
| 56 | 43.75 | 100.00 |
| 57 | 77.48 | 93.00 |
| 59 | 94.35 | 64.25 |
| 60 | 73.53 | – |
| 64 | 49.74 | 58.70 |
| 65 | 73.53 | – |
| 66 | 75.50 | 39.50 |
| 69 | 78.35 | 96.00 |
| 70 | 77.50 | 55.00 |
| 71 | 74.94 | 53.00 |
| 72 | – | 54.00 |
| 75 | – | 78.00 |
| 77 | – | – |
| 78 | 56.47 | – |
| 81 | 71.53 | – |
| 82 | 74.50 | – |
| 83 | 91.71 | 82.00 |
| 84 | 73.53 | 54.00 |
| 88 | – | – |
| 90 | – | 98.00 |
| 93 | 87.35 | 93.75 |
| 95 | 66.00 | 78.00 |
| 98 | 77.50 | 45.00 |
| 99 | 61.94 | – |
| 100 | 60.26 | 90.00 |
| 102 | 79.61 | 82.00 |
| 103 | – | – |
| 104 | 36.00 | 34.71 |
| 106 | 85.14 | – |
Appendix 9 Questionnaire capturing pupils’ use of resources (health economic analysis)
Appendix 10 Additional economic evaluation tables
| Service | Trial arm | p-value | |||
|---|---|---|---|---|---|
| Intervention (n = 5749) | Control (n = 5567) | ||||
| Number of pupils using the service (%) | Mean use (SD) | Number of pupils using the service (%) | Mean use (SD) | ||
| School nurse | 2047 (35.61) | 0.83 (3.24) | 1886 (33.88) | 0.79 (3.55) | 0.531 |
| School counsellor/guidance teacher | 1070 (18.61) | 0.71 (5.06) | 1085 (19.49) | 0.75 (5.09) | 0.617 |
| Educational psychologist | 143 (2.49) | 0.06 (1.63) | 174 (3.13) | 0.08 (1.5) | 0.477 |
| Education welfare officer/home–school liaison officer | 128 (2.23) | 0.04 (0.42) | 176 (3.16) | 0.07 (0.68) | 0.007 |
| GP surgery visit | 2737 (47.61) | 1.01 (2.14) | 2808 (50.44) | 1.05 (2.03) | 0.266 |
| GP out of hours | 718 (12.49) | 0.2 (0.79) | 712 (12.79) | 0.2 (0.74) | 0.782 |
| Nurse (other than school nurse) | 1284 (22.33) | 0.37 (1.25) | 1316 (23.64) | 0.42 (2.14) | 0.119 |
| Hospital appointment | 2206 (38.37) | 0.8 (3.45) | 2140 (38.44) | 0.74 (2.09) | 0.260 |
| Accident and emergency | 1239 (21.55) | 0.32 (0.83) | 1292 (23.21) | 0.35 (0.93) | 0.152 |
| Overnight hospital stay | 605 (10.52) | 0.42 (5.53) | 676 (12.14) | 0.44 (5.46) | 0.910 |
| Psychologist | 166 (2.89) | 0.05 (0.46) | 154 (2.77) | 0.07 (1.41) | 0.183 |
| Counsellor (other than at school) | 137 (2.38) | 0.07 (1.11) | 156 (2.8) | 0.11 (1.74) | 0.147 |
| Social worker | 263 (4.57) | 0.15 (1.85) | 322 (5.78) | 0.21 (2.46) | 0.174 |
| Telephone helpline | 71 (1.23) | 0.04 (0.97) | 101 (1.81) | 0.03 (0.26) | 0.519 |
| Youth justice service | 64 (1.11) | 0.03 (0.9) | 82 (1.47) | 0.03 (0.53) | 0.887 |
| Police service | 276 (4.8) | 0.09 (0.98) | 304 (5.46) | 0.09 (0.75) | 0.776 |
| Teaching assistant | 619 (10.77) | – | 743 (13.35) | – | – |
| Service | Trial arm | p-value | |||
|---|---|---|---|---|---|
| Intervention (n = 5576) | Control (n = 5564) | ||||
| Number of pupils using the service (%) | Mean use (SD) | Number of pupils using the service (%) | Mean use (SD) | ||
| School nurse | 2325 (41.7) | 0.94 (3.29) | 2053 (36.9) | 0.83 (3.26) | 0.064 |
| School counsellor/guidance teacher | 919 (16.48) | 0.55 (3.92) | 1000 (17.97) | 0.56 (3.35) | 0.906 |
| Educational psychologist | 118 (2.12) | 0.04 (0.71) | 149 (2.68) | 0.08 (1.9) | 0.155 |
| Education welfare officer/ home–school liaison officer | 121 (2.17) | 0.05 (1.36) | 170 (3.06) | 0.05 (0.37) | 0.959 |
| GP surgery visit | 2704 (48.49) | 1.03 (4.38) | 2496 (44.86) | 0.89 (1.82) | 0.023 |
| GP out of hours | 707 (12.68) | 0.2 (0.88) | 607 (10.91) | 0.17 (0.75) | 0.070 |
| Nurse (other than school nurse) | 1143 (20.5) | 0.32 (0.9) | 1017 (18.28) | 0.29 (1.12) | 0.089 |
| Hospital appointment | 1831 (32.84) | 0.61 (1.82) | 1714 (30.81) | 0.57 (1.91) | 0.204 |
| Accident and emergency | 1138 (20.41) | 0.29 (0.77) | 1059 (19.03) | 0.29 (1.04) | 0.963 |
| Overnight hospital stay | 405 (7.26) | 0.26 (2.53) | 400 (7.19) | 0.25 (3.17) | 0.822 |
| Psychologist | 125 (2.24) | 0.06 (0.83) | 149 (2.68) | 0.06 (0.75) | 0.776 |
| Counsellor (other than at school) | 127 (2.28) | 0.07 (0.87) | 135 (2.43) | 0.08 (1.33) | 0.415 |
| Social worker | 236 (4.23) | 0.14 (2.14) | 222 (3.99) | 0.11 (1.58) | 0.508 |
| Telephone helpline | 55 (0.99) | 0.02 (0.4) | 80 (1.44) | 0.03 (0.41) | 0.689 |
| Youth justice service | 58 (1.04) | 0.03 (0.61) | 66 (1.19) | 0.02 (0.29) | 0.084 |
| Police service | 211 (3.78) | 0.08 (1.63) | 230 (4.13) | 0.06 (0.45) | 0.223 |
| Teaching assistant | 552 (9.9) | – | 501 (9) | – | – |
| Service | Trial arm | p-value | |||
|---|---|---|---|---|---|
| Intervention (n = 5290) | Control (n = 5244) | ||||
| Number of pupils using the service (%) | Mean use (SD) | Number of pupils using the service (%) | Mean use (SD) | ||
| School nurse | 1760 (33.27) | 0.66 (2.13) | 1750 (33.37) | 0.73 (3.35) | 0.203 |
| School counsellor/guidance teacher | 812 (15.35) | 0.54 (3.71) | 883 (16.84) | 0.58 (3.43) | 0.639 |
| Educational psychologist | 94 (1.78) | 0.07 (1.69) | 70 (1.33) | 0.05 (1.48) | 0.721 |
| Education welfare officer/ home–school liaison officer | 130 (2.46) | 0.06 (1.2) | 99 (1.89) | 0.04 (0.52) | 0.366 |
| GP surgery visit | 2567 (48.53) | 0.95 (2.09) | 2593 (49.45) | 1.01 (2.53) | 0.169 |
| GP out of hours | 639 (12.08) | 0.21 (1.99) | 639 (12.19) | 0.2 (1.47) | 0.610 |
| Nurse (other than school nurse) | 999 (18.88) | 0.37 (2.58) | 1026 (19.57) | 0.34 (1.74) | 0.536 |
| Hospital appointment | 1622 (30.66) | 0.61 (2.61) | 1690 (32.23) | 0.64 (2.48) | 0.578 |
| Accident and emergency | 999 (18.88) | 0.31 (2.49) | 1079 (20.58) | 0.33 (1.65) | 0.676 |
| Overnight hospital stay | 331 (6.26) | 0.25 (3.2) | 362 (6.9) | 0.29 (6.48) | 0.711 |
| Psychologist | 140 (2.65) | 0.11 (2.33) | 125 (2.38) | 0.08 (0.88) | 0.396 |
| Counsellor (other than at school) | 161 (3.04) | 0.13 (2.52) | 159 (3.03) | 0.12 (1.17) | 0.870 |
| Social worker | 210 (3.97) | 0.16 (3.02) | 224 (4.27) | 0.15 (1.59) | 0.850 |
| Telephone helpline | 72 (1.36) | 0.08 (2.82) | 62 (1.18) | 0.03 (0.77) | 0.233 |
| Youth justice service | 51 (0.96) | 0.08 (3.06) | 43 (0.82) | 0.04 (0.89) | 0.283 |
| Police service | 232 (4.39) | 0.13 (3.17) | 207 (3.95) | 0.08 (1.42) | 0.369 |
| Teaching assistant | 568 (10.74) | – | 461 (8.79) | – | – |
| Service | Trial arm | p-value | |||
|---|---|---|---|---|---|
| Intervention (n = 5245) | Control (n = 5160) | ||||
| Number of pupils using the service (%) | Mean use (SD) | Number of pupils using the service (%) | Mean use (SD) | ||
| School nurse | 1482 (28.26) | 0.63 (2.57) | 1393 (27) | 0.54 (1.96) | 0.036 |
| School counsellor/guidance teacher | 761 (14.51) | 0.62 (3.8) | 777 (15.06) | 0.65 (3.83) | 0.686 |
| Educational psychologist | 51 (0.97) | 0.02 (0.38) | 60 (1.16) | 0.03 (0.5) | 0.284 |
| Education welfare officer/home–school liaison officer | 98 (1.87) | 0.1 (4.07) | 91 (1.76) | 0.06 (1.46) | 0.566 |
| GP surgery visit | 2439 (46.5) | 1.07 (1.87) | 2315 (44.86) | 1.04 (2.21) | 0.474 |
| GP out of hours | 510 (9.72) | 0.16 (0.69) | 465 (9.01) | 0.16 (0.94) | 0.726 |
| Nurse (other than school nurse) | 805 (15.35) | 0.29 (0.97) | 776 (15.04) | 0.28 (0.99) | 0.728 |
| Hospital appointment | 1333 (25.41) | 0.57 (1.67) | 1242 (24.07) | 0.56 (2.00) | 0.828 |
| Accident and emergency | 814 (15.52) | 0.23 (0.67) | 829 (16.07) | 0.26 (0.99) | 0.082 |
| Overnight hospital stay | 226 (4.31) | 0.13 (1.01) | 242 (4.69) | 0.18 (1.88) | 0.100 |
| Psychologist | 118 (2.25) | 0.13 (1.61) | 109 (2.11) | 0.09 (0.92) | 0.068 |
| Counsellor (other than at school) | 127 (2.42) | 0.18 (2.1) | 153 (2.97) | 0.20 (2.04) | 0.670 |
| Social worker | 117 (2.23) | 0.10 (1.3) | 168 (3.26) | 0.14 (1.32) | 0.113 |
| Telephone helpline | 57 (1.09) | 0.04 (0.57) | 52 (1.01) | 0.03 (0.49) | 0.503 |
| Youth justice service | 15 (0.29) | 0.01 (0.29) | 25 (0.48) | 0.02 (0.32) | 0.212 |
| Police service | 144 (2.75) | 0.06 (0.55) | 164 (3.18) | 0.06 (0.60) | 0.908 |
| Teaching assistant | 643 (12.26) | – | 615 (11.92) | – | – |
| Cost domain | Study period | |||||||
|---|---|---|---|---|---|---|---|---|
| 6 months before baseline | 6–12 months | 18–24 months | 27–33 months | |||||
| Intervention | Control | Intervention | Control | Intervention | Control | Intervention | Control | |
| Number analysed (% of total) | 5749 (90.1) | 5567 (87.6) | 5576 (87.4) | 5564 (87.5) | 5290 (82.9) | 5244 (82.5) | 5245 (82.2) | 5160 (81.1) |
| Education, mean (95% CI) | 69.62 (62.20 to 77.04) | 70.92 (63.97 to 77.87) | 69.51 (63.57 to 75.44) | 65.61 (59.83 to 71.39) | 55.97 (50.04 to 61.90) | 59.70 (53.35 to 66.05) | 56.85 (50.93 to 62.77) | 52.64 (47.80 to 57.48) |
| Health, mean (95% CI) | 534.45 (438.49 to 630.41) | 550.96 (454.95 to 646.97) | 397.33 (350.24 to 444.42) | 373.47 (315.71 to 431.23) | 401.26 (311.78 to 490.73) | 430.38 (310.10 to 550.67) | 295.92 (272.03 to 319.81) | 334.72 (294.81 to 374.63) |
| Criminal justice, mean (95% CI) | 31.62 (21.83 to 41.40) | 32.98 (26.40 to 39.57) | 31.37 (17.21 to 45.52) | 21.06 (17.13 to 24.98) | 48.38 (14.65 to 82.10) | 30.40 (17.61 to 43.20) | 20.80 (15.72 to 25.87) | 21.00 (15.47 to 26.53) |
| Total, mean (95% CI) | 635.69 (538.29 to 733.08) | 654.86 (558.06 to 751.65) | 498.20 (447.88 to 548.53) | 460.14 (401.40 to 518.87) | 505.61 (384.45 to 626.76) | 520.49 (396.30 to 644.68) | 373.57 (347.14 to 400.00) | 408.36 (366.45 to 450.28) |
| Cost domain | Trial arm | Difference (95% CI) | |
|---|---|---|---|
| Intervention | EAN | ||
| Baseline to T2 | |||
| Number analysed (% of total) | 4794 (75.2) | 4715 (74.1) | |
| Education, mean (95% CI) | 245.51 (210.59 to 280.42) | 239.20 (203.93 to 274.47) | 6.309 (–43.20 to 55.81) |
| Health, mean (95% CI) | 1610.59 (1382.87 to 1838.31) | 1591.65 (1362.08 to 1821.22) | 18.94 (–305.52 to 343.40) |
| Criminal, mean (95% CI) | 148.75 (101.01 to 196.48) | 85.68 (37.54 to 133.82) | 63.07 (–5.00 to 131.14) |
| Total, mean (95% CI) | 2006.33 (1748.67 to 2263.99) | 1916.37 (1656.62 to 2176.12) | 89.96 (–277.12 to 457.03) |
| Baseline to T3 | |||
| Number analysed (% of total) | 4256 (66.7) | 4103 (64.5) | |
| Education, mean (95% CI) | 286.51 (246.56 to 326.47) | 283.83 (243.40 to 324.26) | 2.68 (–54.02 to 59.38) |
| Health, mean (95% CI) | 1887.02 (1603.01 to 2171.03) | 1904.33 (1615.63 to 2193.04) | –17.31 (–423.82 to 389.19) |
| Criminal, mean (95% CI) | 128.48 (77.76 to 179.20) | 103.42 (51.75 to 155.08) | 25.06 (–47.66 to 97.78) |
| Total, mean (95% CI) | 2307.06 (1989.24 to 2624.88) | 2292.11 (1969.06 to 2615.15) | 14.96 (–439.90 to 469.81) |
| Parameter | Coefficient | SE | t | p-value |
|---|---|---|---|---|
| Treatment arm | 22.50 | 206.14 | 0.11 | 0.91 |
| 5.59 | 2.03 | 0.03 | 0.02 | |
| Baseline drinking | 0.65 | 0.02 | 27.15 | 0.00 |
| 0.00 | 0.00 | 0.09 | 0.00 | |
| School location | 175.95 | 249.15 | 0.71 | 0.48 |
| 6.96 | 2.55 | 0.03 | 0.02 | |
| School type | ||||
| 2 | –299.52 | 345.20 | –0.87 | 0.39 |
| 4.92 | 1.37 | 0.02 | 0.01 | |
| 3 | 625.89 | 372.20 | 1.68 | 0.09 |
| 6.33 | 2.24 | 0.02 | 0.00 | |
| FSM provision | ||||
| 2 | –20.37 | 245.51 | –0.08 | 0.93 |
| 5.16 | 1.54 | 0.02 | 0.02 | |
| 3 | 105.12 | 290.09 | 0.36 | 0.72 |
| 6.82 | 1.95 | 0.02 | 0.02 | |
| Constant | 1713.23 | 372.53 | 4.60 | 0.00 |
| 8.70 | 2.09 | 0.04 | 0.00 | |
| Random-effects parameters | Estimate | SE | ||
| SchoolCode: Identity | ||||
| sd(_cons) | 387.32 | 167.30 | ||
| sd(Residual) | 9140.36 | 269.06 | ||
| Parameter | Coefficient | SE | t | p-value |
|---|---|---|---|---|
| Treatment arm | 0.53 | 0.09 | 5.65 | 0.00 |
| 0.00 | 0.00 | 0.03 | 0.00 | |
| Baseline drinking | 1.41 | 0.09 | 15.66 | 0.00 |
| 0.00 | 0.00 | 0.21 | 0.00 | |
| School location | 0.46 | 0.11 | 4.16 | 0.00 |
| 0.00 | 0.00 | 0.03 | 0.00 | |
| School type | ||||
| 2 | –0.14 | 0.17 | –0.85 | 0.40 |
| 0.00 | 0.00 | 0.02 | 0.01 | |
| 3 | –0.44 | 0.19 | –2.30 | 0.02 |
| 0.01 | 0.00 | 0.03 | 0.00 | |
| FSM provision | ||||
| 2 | 0.41 | 0.12 | 3.54 | 0.00 |
| 0.00 | 0.00 | 0.02 | 0.00 | |
| 3 | 0.49 | 0.13 | 3.73 | 0.00 |
| 0.00 | 0.00 | 0.02 | 0.00 | |
| Constant | –3.14 | 0.22 | –14.45 | 0.00 |
| 0.00 | 0.00 | 0.05 | 0.00 | |
| Random-effects parameters | Estimate | SE | ||
| SchoolCode: Identity | ||||
| sd(_cons) | 0.38 | 0.04 | ||
List of abbreviations
- CC
- complete case
- CD
- compact disc
- CEA
- cost-effectiveness analysis
- CEAC
- cost-effectiveness acceptability curve
- CI
- confidence interval
- CMO
- Chief Medical Officer
- CRCT
- cluster randomised controlled trial
- DAP
- data analysis plan
- DHSSPSNI
- Department of Health, Social Services and Public Safety Northern Ireland
- DVD
- digital versatile disc
- EAN
- education as normal
- ESPAD
- European Survey Project on Alcohol and other Drugs
- FSM
- free school meal
- HED
- heavy episodic drinking
- ICC
- intracluster correlation coefficient
- ICER
- incremental cost-effectiveness ratio
- ITT
- intention to treat
- NI
- Northern Ireland
- NICE
- National Institute for Health and Care Excellence
- NICTU
- Northern Ireland Clinical Trials Unit
- NIHR
- National Institute for Health Research
- OR
- odds ratio
- PAS
- Preventing Heavy Alcohol Use in Adolescents
- PD
- personal development
- PHA
- Public Health Agency
- PSE
- personal and social education
- PSHE
- personal, social, health and economic
- RCT
- randomised controlled trial
- SD
- standard deviation
- SE
- standard error
- SES
- socioeconomic status
- SHAHRP
- School Health and Alcohol Harm Reduction Project
- SSC
- Study Steering Committee
- STAMPP
- Steps Towards Alcohol Misuse Prevention Programme
- T0
- baseline time point
- T1
- 12 months after the baseline time point
- T2
- 24 months after the baseline time point
- T3
- 33 months after the baseline time point
- TMG
- Trial Management Group
- WTP
- willingness to pay