Notes
Article history
The research reported in this issue of the journal was funded by the PHR programme as award number 17/92/39. The contractual start date was in March 2019. The draft manuscript began editorial review in November 2022 and was accepted for publication in October 2023. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PHR editors and production house have tried to ensure the accuracy of the authors’ manuscript and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Permissions
Copyright statement
Copyright © 2024 Pallan et al. This work was produced by Pallan et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Pallan et al.
Chapter 1 Introduction/background
Nutrition in adolescents
Adolescence is a key period of growth and development, during which young people undergo dramatic physical and psychosocial changes. 1 Good nutrition is essential to support these changes, while poor nutrition can lead to a variety of health consequences, including obesity, which is increasing in prevalence worldwide,2 compromised growth and higher non-communicable disease risk in later life. 3 Adolescence is one of the major risk periods for obesity development. In England, over one-third of children have excess weight, and nearly one-quarter have obesity by the age of 15 years,4 putting them at risk of short- and long-term morbidity. 5,6
Overall, evidence from the UK National Diet and Nutrition Survey (NDNS) indicates that dietary intake in adolescents in the UK is suboptimal. Consumption of free sugars (defined as all sugars added to foods by the manufacturer, cook or consumer, and natural sugars found in honey, syrups and unsweetened fruit juices7) is high, contributing to 12.5% of the daily energy intake of 11- to 18-year-olds,8 which substantially exceeds the recommended 5% of daily energy intake from free sugars. 9 Sugar-sweetened beverage (SSB) consumption is one of the key contributors to this high sugar intake, with those aged 11–18 years consuming more than any other age group. 8
In addition to contributing to energy density and the development of obesity,10–12 high intake of free sugars and SSBs are major risk factors for dental caries. 13 Almost half of UK adolescents aged 15 years have some caries experience,14 which, as well as causing pain and distress, can impact on school attendance, academic performance and psychosocial well-being. 15,16
Other aspects of dietary intake are also of concern in the adolescent age-group, including higher than recommended intakes of saturated fatty acids and lower than recommended intakes of fibre and fruit and vegetables (F&V). Only 12% of the 11–18 years age group meet the recommendation of five daily portions of F&V. 8,17 Again, these patterns of dietary intake can lead to higher risk of obesity and later non-communicable diseases such as cancers and cardiovascular disease. 18–20 Poor dietary intake, dental health and obesity in adolescence all demonstrate a socioeconomic gradient, with the most disadvantaged being at greatest risk. 21–24
Adolescence is a key period for establishing dietary patterns, with rapid biological development and increased nutrient needs, greater autonomy over dietary decisions, and more interaction with peers and the wider environment. 25 Dietary patterns established in adolescence often track into adulthood,26,27 and thus adolescence represents an important period in the life course for intervention to influence food and drink choices and encourage the development of healthy dietary patterns.
The role of schools in supporting healthy nutrition
Among the many influences on adolescent dietary intake and eating behaviours, schools play a significant role. 28 Younger adolescents spend a substantial portion of their time at school, and it is widely recognised that supporting health and well-being is an integral part of the overall educational remit of schools. 29,30 Adolescents attending secondary schools in the UK typically consume at least one meal per day at school, so the school setting offers an opportunity for intervention to improve the nutritional intake of their pupils.
The provision of school meals as a public health measure has a long history, predominantly to address undernutrition. 31 School feeding programmes are in place in many countries,32 and there is evidence to suggest that they have educational and health benefits in disadvantaged communities and low income settings. 33 In the UK, some provision of school meals for poorly nourished children was introduced in the late 19th century, and in 1941 a national school meal policy was launched that enabled the provision of school meals to all children who wanted them. 34 Since the late 20th century, when large increases in obesity prevalence among children started to be seen, the focus of school meals in the UK and other high-income countries has shifted from addressing undernutrition to providing high-quality, nutritionally balanced foods and drinks with lower energy density. 31,34 In terms of the influence on dietary intake of interventions to improve the nutritional quality of school meals and other school food provision, some positive effects have been seen. For example, F&V schemes in schools and the introduction of nutritional standards and guidelines for school food have been shown to have a beneficial impact on nutritional intake in the short term. 35,36
The influence of schools on healthy eating and nutritional intake not only involves food provision, but also encompasses the physical, social and cultural environmental aspects of schools and school communities. 28,37 This is reflected in a wide range of school-based approaches to improving healthy eating, which include alterations to the food and dining environment, educational and behavioural approaches, and whole-school approaches involving peers, parents and communities. 38 Overall, the evidence for school-based intervention to improve nutrition, through either school food provision or a wider environmental approach, is mixed. In particular, there is an evidence gap in relation to the effects of these interventions on secondary-school-aged pupils, with few studies of high quality and no clear messages about the most effective approaches for improving dietary intake. 38,39
National school food policy in England
Nutritional standards for school food as a strategy for improving children’s dietary intake were first introduced in the UK in 1941 along with the introduction of the national school meals policy, and various revisions to these standards were introduced over the following three decades. The nutritional standards were removed in the 1980s as part of a wider move to reduce the welfare state. 34 In 1992, in response to the poor quality of school meals, the Caroline Walker Trust convened a working group to develop nutritional guidelines for school lunches, and although these were accepted as the standards that school meals should ideally meet, they were not compulsory for schools. 40 In an attempt to address the increasing levels of obesity and poor nutritional intake in children, some regulation of school food was reintroduced in England in 2001 to ensure that school caterers provided healthy school food options, but there was little evidence of any impact on children’s nutritional intake in school. 34,41 From 2006, following a national review of school meals prompted by a campaign led by Jamie Oliver to improve the quality of school food,41 comprehensive food- and nutrient-based school food standards (SFS) legislation was introduced in England and applied to state-funded schools. 42 Alongside the SFS, the government established the School Food Trust as a non-governmental public body between 2006 and 2011 to work to improve the quality of school food (and ensure that schools met the SFS) and promote the education and health of children. 41
In 2012, the government commissioned a further independent review, undertaken by Henry Dimbleby and John Vincent, and the following year they published the School Food Plan (SFP; see The School Food Plan). 43 Actions for the government that were outlined in the SFP included the introduction of a revised set of SFS, designed to be operationally easier for school food providers to implement, and legislation for these revised standards came into force in January 2015. 44
Exemptions to national school food standards legislation
The way in which the SFS legislation in England has been applied means that a group of state-funded schools are exempt from the statutory requirement to comply with the SFS. Academies and free schools (state-funded schools that are independent of local authorities) that were established between 2010 and 2014 are not required by law to comply with the SFS. 45 However, as part of the SFP, and following the introduction of the revised SFS in 2015, these exempt schools were encouraged to voluntarily sign up to the SFS. 46,47 By March 2016, only around one-third of the exempt schools had done so. 48 Although the legislation has not been changed to address this exemption of schools, in the last 18 months of this study there has been a shift in the expectation of the government, whose position is now that all schools, regardless of their exemption status, should be complying with the SFS. 49
The current national school food standards
The SFS currently in place are food-based (rather than nutrient based) but underpinned by a nutrient framework. Before their introduction, the standards were pilot tested to ensure that they led to the same or improved nutrient content of school meals compared with the 2006 SFS. 50
The SFS specify six groups of foods and drinks: (1) starchy foods; (2) F&V; (3) milk and dairy; (4) meat, fish, eggs, beans and other non-dairy sources of protein; (5) foods high in fat, sugar and salt (HFSS); and (6) healthier drinks. There are rules for portion, variety and frequency of provision for each group. The standards are divided into three groups: those applying to school lunch, those applying to foods provided in school other than at lunchtime, and standards that apply across the whole school day. 51 Standardised checklists are available to assist schools and caterers in checking their compliance with the SFS. 51
Despite their legislative status, there are no formal national arrangements for monitoring schools’ compliance with the SFS. 52 Responsibility for ensuring the SFS are met is placed with the governing bodies of schools, but in England there is no requirement for school governors to report on their school’s SFS compliance. 49 As part of their inspection visits to schools, Office for Standards in Education,Children’s Services and Skills (Ofsted, the English schools inspection body) observe the school canteen food and environment and the effect of this on pupils’ behaviour, but they do not review SFS compliance. 53
The School Food Plan
The SFP established a set of wide-ranging recommendations for actions by the government, schools and headteachers to promote a ‘whole-school’ approach to a healthy-eating culture and ethos in schools. 43 One of the central aims of the SFP was to increase school meal uptake, both for economic reasons (higher demand drives better-quality food provision at lower cost) and because there is evidence to suggest that packed lunches are of poorer nutritional quality than school meals. 54,55 The other key aim was to provide practical support, advice and information for headteachers and others involved in school leadership in the form of a set of non-statutory recommendations for action to help improve the quality and uptake of school food and incorporate healthy eating into all aspects of school life and the wider school community. 43
Broadly, the recommendations in the SFP for schools include actions relating to leadership, vision and a whole-school approach; school food monitoring and accountability; school food provision and affordability; the physical and social eating environment; food education encompassing healthy-eating knowledge and skills; linking healthy eating to wider health and well-being; and involving school children and the wider school community in school food and healthy eating.
A checklist of actions for headteachers and guidance for school leadership teams and governors were developed to assist schools in implementing the SFP recommendations and a whole-school approach to creating a healthy-eating culture and ethos. 56–58 The Department for Education (DfE) continues to encourage the implementation of SFP recommendations and the use of these checklists and guidance in schools. 59
Evaluation of English national school food policy to date
Evaluation of the impact of the SFS on nutritional intake following the introduction of the 2006 food- and nutrient-based standards has been conducted among younger children in primary and middle schools. Repeated cross-sectional studies were conducted pre and post introduction of the SFS, collecting nutritional intake data from children aged 4–7 years in primary schools (n = 12)60,61 and children aged 11–12 years in middle schools (n = 6)62 to determine the effect of the SFS on lunchtime and total dietary intake. Following the introduction of the SFS, improvements were seen in the overall nutritional intake of children aged 4–7 years, with the greatest improvements seen in those receiving a school-provided lunch (vs. having a packed lunch). 60,61 By contrast, in the 11–12 years age group, there was limited evidence of a positive impact on the nutritional intake of children following introduction of the SFS, and levels of free sugar intake remained well above the recommended guidelines. 62 Another study examined how food provision and food choices had changed following the introduction of the 2006 standards in a sample of 136 primary schools across England, and reported that lunchtime food provision was healthier, with more fruit, vegetable and salad provision, and less starchy foods cooked in oil, desserts, crisps and confectionery. In line with this, improvements were seen in children’s F&V consumption. 63
Evidence of impact of the SFS on the dietary intake of secondary school pupils is more limited. One study in 80 secondary schools compared school food provision and consumption of foods and drinks by pupils aged 11–18 years at lunchtime in 2011 with that in 2004. 64 They reported an improvement in the nutritional content of school food, with the greatest impact on the availability of confectionery. Small improvements were observed in pupils’ lunchtime food consumption, such as decreased consumption of starchy foods cooked in oil and slight increases in F&V intake. Total dietary intake was not examined.
Since the introduction of the revised SFS in 2015, there have been no large-scale evaluations of their impact on nutritional intake52 and no comprehensive evaluations of the implementation of the SFP actions in secondary schools. In 2017, the Jamie Oliver Food Foundation published A Report on the Food Education Learning Landscape. 65 This reported findings from surveys, interviews and focus groups with school leaders, governors, teachers, children and parents, and focused on food education and the food culture in schools. Key findings relating to secondary schools were cheap and unhealthy (SFS non-compliant) foods on offer throughout the school day; noisy dining environments, often with long queues; inconsistent messaging with unhealthy foods used for fundraising and as rewards; and patchy provision of food education. More recently, in 2020, Guy’s and St Thomas’ Charity (Impact on Urban Health) published a report66 that outlined the findings of a study of primary and secondary schools across London, in which the food on offer, pupils’ food choices and the wider dining and food environments were observed. Only a small number of secondary schools participated, but the key findings in these schools were poor awareness and implementation of school food policies, food offers that were non-compliant with the SFS (particularly at breakfast and breaktimes), and pupils often choosing less healthy options, such as ‘grab and go’ food, even when a more nutritionally balanced meal was on offer. Both reports highlighted the lack of monitoring and enforcement of the SFS in secondary schools. In addition, similar issues were highlighted in the 2019 State of the Nation: Children’s Food in England report by Food for Life, Soil Association. Through consultation with 30 caterers, they estimated that around 60% of secondary schools may not be compliant with the SFS and recommended better monitoring of SFS compliance. 67 The need for robust and independent monitoring of food standards compliance in schools was also identified by Dame Sally Davies in the report she published as outgoing Chief Medical Officer for England in 2019, Time to Solve Childhood Obesity. 68
Two papers, one published in 201369 and one published in 2022,52 provide a comprehensive summary of the introduction and changes to the SFS over the last 20 years across all UK nations, including England. The first reported that in England, since the introduction of compulsory SFS in 2006, school lunch uptake had increased, and there was some evidence to suggest nutritional benefit from the standards, particularly in younger children. 69 However, the 2022 paper identified that no studies had examined the impact of the updated food-based SFS on children’s nutritional intakes, and highlighted that this lack of studies, together with the lack of monitoring of compliance of the SFS, made it difficult to determine the impact of the SFS policy on children’s nutritional intake. 52
School food policy in the context of wider government strategy
The SFS legislation remains an important national strategy for tackling childhood obesity and is a key component of the government’s report Childhood Obesity: A Plan for Action. 70,71 In this, the government states plans to update the SFS, with a particular focus on reducing the sugar content of foods. 71 However, this was put on hold during the COVID-19 pandemic, and the focus has moved to ensuring compliance with the current SFS. 72 Also as part of the their childhood obesity action plan, the government’s DfE introduced the healthy schools rating scheme in 2019. 73 This is a school self-assessment scheme to achieve bronze, silver or gold awards based on a number of factors related to healthy eating and physical activity, which include compliance with the national SFS and food education provision.
More recently, in 2021, Henry Dimbleby led the development of an independent national food strategy report74 in which he makes broad-ranging recommendations for the food system in England. In this are a suite of recommendations relating to food education and a recommendation to extend free school meal (FSM) eligibility. Following this independent report, the government launched two White Papers in 2022: Levelling Up the United Kingdom and the Government Food Strategy. 75,76 While not all of Dimbleby’s recommendations were taken up, in these White Papers the government set out plans to provide training to school governors on a whole-school approach to food, and to invest up to £5M in the food curriculum with the aim of children leaving secondary school with the knowledge of how to cook six basic recipes to support healthy eating. It also set out the intention to test approaches to ensuring transparency of school food arrangements and compliance with the SFS.
Rationale for evaluation of school food standards and School Food Plan in secondary schools
There is a clear gap in the research relating to the implementation of the most recent iteration of the SFS in secondary schools and their impact on school pupils’ nutritional intake, and no studies evaluating the SFS have explored their impact on dental health, even though sugar consumption is high in adolescents and is targeted within the SFS. Similarly, although there have been some attempts to characterise the secondary school food environment and culture, there have been no full evaluations of the implementation of SFP recommendations since it was launched in 2013. Furthermore, there has been no economic evaluation of the SFS or the SFP.
All previous studies evaluating the impact of the national SFS on pupils’ nutritional intake have reported pre- and post-implementation data, with no contemporaneous comparator group. The exemption from the SFS of academies and free schools established between 2010 and 2014 provided us with an opportunity to compare the implementation of the SFS and SFP and to compare pupil nutritional intake in schools mandated and schools not mandated to comply with the SFS during the same time period, albeit this latter group have been encouraged to voluntarily comply with the standards. As we have outlined in Exemptions to national school food standards legislation, since the start of this study, the national landscape has changed and there has been a shift in the government’s approach to the national SFS, the current expectation being that all schools should comply with the standards. 49 In this report we present and interpret our findings considering these changing expectations.
Chapter 2 Study aims and objectives
We conducted the Food provision, cUlture and Environment in secondary schooLs (FUEL) study,77 in which we aimed to compare the implementation (including economic considerations) of the SFS and the SFP, and the nutritional intake and dental health of pupils in two groups of secondary school academies and free schools: those mandated and those not mandated to comply with the SFS. We also set out to explore the variation in implementation of the SFS and SFP and the food culture and environment across both school groups, and whether this variation is associated with nutritional intake and dental health. In relation to nutritional intake, we were interested in a range of key nutrients and food groups, but we focused on free sugar intake as our main outcome of interest, given the high consumption of free sugars in the adolescent age group8 and the focus of several of the school standards on reducing the intake of foods and drinks high in free sugars. 51
Research objectives
-
In secondary schools either mandated or not mandated to comply with the national SFS legislation, compare:
-
school food provision and compliance with the SFS
-
the school food environment/culture and the food curriculum, and implementation of the SFP actions
-
the nutritional intake and dental health of school pupils, focusing on free sugar intake as the primary outcome
-
the costs of food provision, food curriculum delivery, and other measures to influence the school food culture and environment.
-
-
Explore the variation in compliance with the SFS and implementation of SFP actions in secondary schools and use this to develop a typology of schools.
-
Use the developed school typology to explore associations between the school types and pupil dietary and dental outcomes.
Research questions
-
In secondary schools mandated or not mandated to comply with the national SFS, are there differences in:
-
provision of school food?
-
sales of different food types?
-
uptake of school-provided food?
-
the school food environment, culture and curriculum?
-
-
How does implementation of the SFS and SFP vary across secondary schools, and how does the school context influence this?
-
What are the different school types in relation to SFS and SFP implementation?
-
What is the economic impact of the SFS and SFP?
-
In pupils attending secondary schools mandated or not mandated to comply with the national SFS, are there differences in:
-
nutritional intake (including free sugar intake) at school lunchtime, in school time and overall?
-
dental caries experience?
-
-
Do any differences in pupil dietary and dental outcomes across the SFS-mandated and SFS-non-mandated schools vary by:
-
year group?
-
lunch source (school-provided vs. brought from elsewhere)?
-
socioeconomic status?
-
-
Is there an association between the identified school types and dietary and dental outcomes in school pupils?
Chapter 3 Methods
Study design
The study design was an observational, multiple-methods study comprising two phases. The first phase involved collecting a variety of data on SFS/SFP implementation, and school and pupil outcomes in the SFS-mandated and SFS-non-mandated schools. These data were used to compare outcomes across the two groups and develop a typology of schools based on SFS and SFP implementation. The second phase was a qualitative case study in which a small number of schools were identified to understand the experiences of schools in implementing and embedding the SFS and SFP, and the influence of the wider school context on this implementation. In addition, we undertook an economic evaluation to assess how the costs and outcomes compare across SFS-mandated and SFS-non-mandated schools.
Setting and population
The sampling frame for the study comprised secondary-phase academies and free schools located in 14 local authority areas in the West Midlands (Birmingham, Coventry, Dudley, Herefordshire, Sandwell, Shropshire, Solihull, Staffordshire, Stoke-on-Trent, Telford and Wrekin, Walsall, Warwickshire, Wolverhampton and Worcestershire) and 8 local authority areas in the East Midlands (Derby, Derbyshire, Leicester, Leicestershire, Northamptonshire, Nottingham City, Nottinghamshire and Rutland). The West and East Midlands include urban and rural areas and have populations of around 6 million and 5 million, respectively. Compared with other regions in England, the West Midlands has a young age structure, with 18% of the population under 15 years of age. 78 Both regions have relatively high ethnic diversity, with 24% of the West Midlands and 18% of the East Midlands populations of ethnicities other than White British,79 and contain a number of local authority areas with high deprivation (e.g. Birmingham, Walsall, Wolverhampton, Nottingham). 80
Sampling and sample size calculation
Schools
To generate our sampling frame, we identified all state-funded secondary school academies and free schools in the 22 local authority areas outlined above using DfE routine data. As we were comparing two groups of schools, those mandated and those not mandated to comply with the SFS, we restricted the sampling frame to include only academies and free schools. The reason for this was that these are the only types of state-funded secondary schools that can potentially have exemption from the SFS (i.e. if they were established between 2010 and 2014). We excluded other secondary school types as they are all legally required to comply with the SFS and so could only be recruited to the SFS-mandated group, and we wanted to enable comparability in terms of other school characteristics across the two school groups. The excluded school types significantly differ from academies and free schools in their governance structures (local authority-maintained schools) or because they are specialist/alternative educational providers, and therefore their inclusion in the SFS-mandated group would reduce comparability across the two school groups. In 2019, at the start of this study, academies and free schools were providing education to 72% of secondary school pupils in England,81 and by the end of the study this figure had risen to 80%. 82
We used stratified sampling, based on propensity score methods,83 to increase the comparability of schools and reduce the influence of confounding. Propensity scores were generated using the following school characteristics:
-
local authority area
-
establishment type (academy sponsor-led, academy convertor or free school)
-
rural or urban categorisation
-
number of pupils
-
percentage of female pupils
-
proportion of pupils from ethnic minorities groups
-
proportion of pupils with English as an additional language (EAL)
-
proportion of pupils with special educational needs (SEN)
-
proportion of pupils eligible for FSM
-
Income Deprivation Affecting Children Index [IDACI, a component of the Index of Multiple Deprivation (IMD) representing the proportion of children aged 0–15 years living in income-deprived families, measured for the lower-layer super output area in which the school is situated]
-
presence or absence of a sixth form (education provision for 16- to 18-year-olds)
-
selective or non-selective admission policy
-
religious status: faith school or secular.
The propensity score was derived from a logistic regression model, fitted using these variables to predict whether SFS compliance was mandated. The schools were split into four strata using the propensity score quartile cut-offs, and within each strata schools were divided into SFS-mandated and SFS-non-mandated schools, generating eight sampling groups within the sampling frame. Schools in each group were randomly ordered and invited sequentially, the intention being to recruit schools from across all eight groups and achieve an even split of SFS-mandated and SFS-non-mandated schools.
Pupils
We sampled pupils attending participating schools. We identified form groups or other class groupings [such as personal, social, health and economic education (PSHE) classes], attempting to select class groupings that were representative of the general year group and avoiding groupings that were streamed according to academic ability or related to a non-core, selected subject. From these class groupings, one class from each of years 7 (age 11–12 years), 9 (age 13–14 years) and 10 (age 14–15 years) were selected to ensure that a range of ages was included in the sample. Pupils in these three selected classes were invited to take part in data collection.
School staff and governors
We invited a selection of staff and governors from participating schools to take part in the study, aiming for at least four representatives from each school (see School-level data capture for details of the staff groups recruited).
Sample size
We conducted a power analysis to estimate the required sample size, based on the comparison of free sugar intake in pupils attending SFS-mandated and SFS-non-mandated schools. We used data on free sugar intake pre and post implementation of the 2006 legislation from a study conducted in English middle schools84 to inform the analysis. The study reported a reduction in free sugar intake at school lunch of 6 g [standard deviation (SD) 11 g] in pupils consuming school-provided food, and 2 g (SD 13 g) in those consuming packed lunches; therefore, for this study we based our power analysis on the ability to detect a 4-g difference between groups. Assuming a SD of 11 g, an intracluster correlation coefficient (ICC) of 0.1 (a conservative estimate85) and balanced cluster sizes, we estimated that to detect this difference with at least 90% power and at 5% significance, we would require 990 evaluable participants and 22 clusters (schools) in each group (total schools, n = 44; total participants, n = 1980). Within each year group cluster, we anticipated that there would be a minimum of 15 students, with a total of at least 45 students for each school (average cluster size, n = 45).
An additional power analysis was conducted in November 2021, as it became apparent that we were unlikely to achieve the original target school sample size (n = 44) due to ongoing interruptions resulting from the COVID-19 pandemic. At this point, based on data collected until that time, we calculated that the average number of students participating from each school was 68, and we took note that it was unlikely that we would be able to recruit equal numbers of schools to the SFS-mandated and SFS-non-mandated groups (due to a lower number of SFS-mandated schools in the sampling frame). We therefore used a cluster size of 68 and accounted for a likely imbalance across the school groups in this additional power analysis. With all the other parameters kept the same, we estimated that 14 schools in the SFS-mandated and 20 schools in the SFS-non-mandated groups would give 87% power, and 17 schools in the SFS-mandated and 23 schools in the SFS-non-mandated groups would give 92% power.
Recruitment and consent
Recruitment materials, including school, school staff and participant invitation letters, and school staff, pupil and parent information sheets and consent forms, were reviewed by the study public advisory groups (see Public involvement methods) and revised according to their feedback.
School and pupil recruitment commenced in October and November 2019, respectively, and was due to be completed in the 2019–20 academic year. However, because of restrictions in place in England during the COVID-19 pandemic, recruitment and data collection were suspended in March 2020 but recommenced in May 2021 and ran until April 2022.
Schools
Postal and e-mail invitations, including a study information leaflet, were sent to the headteachers of schools in a staggered manner, inviting several schools from each of the eight sampling groups at a time. Invitations were followed by telephone calls to schools, with additional e-mails sent as required. For schools expressing an interest, we arranged face-to-face or remote (telephone call or video) meetings to discuss the study and explain what taking part would involve, and to provide an opportunity for the school to ask questions. Once a school agreed to participate, they were asked to complete and sign a school agreement outlining the expectations of the school and the research team. Schools received a £300 payment for participating in phase I and a tailored report detailing the school’s compliance with the SFS and implementation of SFP actions. Schools were asked to provide the study team with a specific study liaison member of staff.
Staff/governors
Relevant staff and governors were identified by the liaison person and invited to take part by e-mail, which included a participant information leaflet. Written consent was obtained. Invited staff were those identified within the school to have roles relating to food provision, the eating environment, the food curriculum or SFS/SFP implementation (including headteachers, catering staff, PSHE leads, teachers with responsibility for the food/cooking curriculum and relevant representatives from the governing body).
Pupils
All pupils in selected classes were invited to participate. Parents were given written detailed information about the study at least 1 week prior to the first data collection session. Schools assisted in the distribution of this information to parents in different formats (e.g. e-mail, post, website). Parents were not asked for active consent but were given the opportunity to complete and return a form to opt their child out of participating in the study. This approach to parental consent was used to ensure that there was no socioeconomic bias in our sample, as previous research has shown that active consent letters distributed by schools are less likely to be returned by more socioeconomically disadvantaged parents. 86 Participant information leaflets were distributed to pupils at least 1 week prior to data collection. Researchers also gave a verbal overview of the study on the day of the first data collection session and pupils were invited to ask questions. Written assent was be obtained from pupils whose parents had not opted them out of participating. Based on the advice we received from our youth public advisory group (see Public involvement methods), pupils were given a £5 shopping voucher as a thank-you for taking part.
Data collection
Theoretical considerations guiding data collection
We developed a logic model to outline the processes by which the SFS and SFP are assumed to produce health gains (Figure 1). Through this model we articulated that health gain is generated:
FIGURE 1.
Logic model for the influence of SFS and SFP actions on children’s dietary intake and health outcomes.
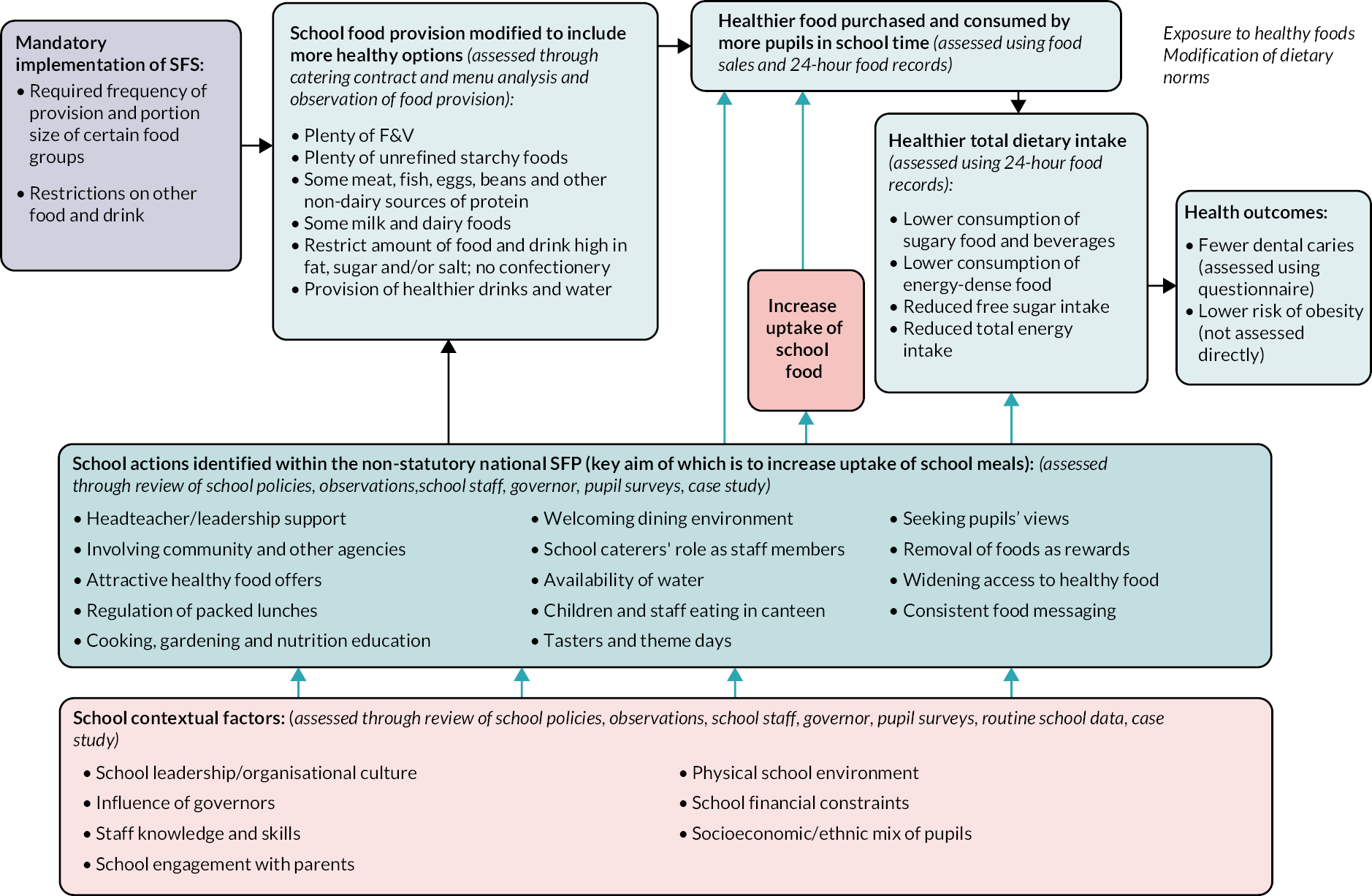
-
directly via a change in school food consumption
-
indirectly through healthy food environments, and curricular and other activities that are designed to change pupils’ dietary knowledge, attitudes and beliefs, which impact on their food and drink consumption in and out of school.
The logic model also outlines that the extent to which the SFS and SFP positively impact on dietary intake and health depends on their implementation within a school, which is influenced by contextual factors (e.g. school leadership, the wider school culture, the physical environment).
The logic model, along with the principles outlined in the UK Medical Research Council framework for process evaluation,87 guided our data collection strategy. We planned to capture data aligned with each of the boxes in the logic model, enabling us to assess schools’ compliance with the SFS and implementation of the SFP actions. We also planned to assess the wider school context and the extent to which the two national school food policies (SFS and SFP) were adopted by and embedded within schools. Broadly, we structured our data collection to encompass:
-
food provision
-
the school food culture and environment
-
costs relating to school food provision, culture and environment
-
school contextual data
-
embedding of school food policy within schools
-
school meal uptake
-
school food sales
-
pupil outcomes (nutritional intake and dental caries experience; see Pupil outcomes).
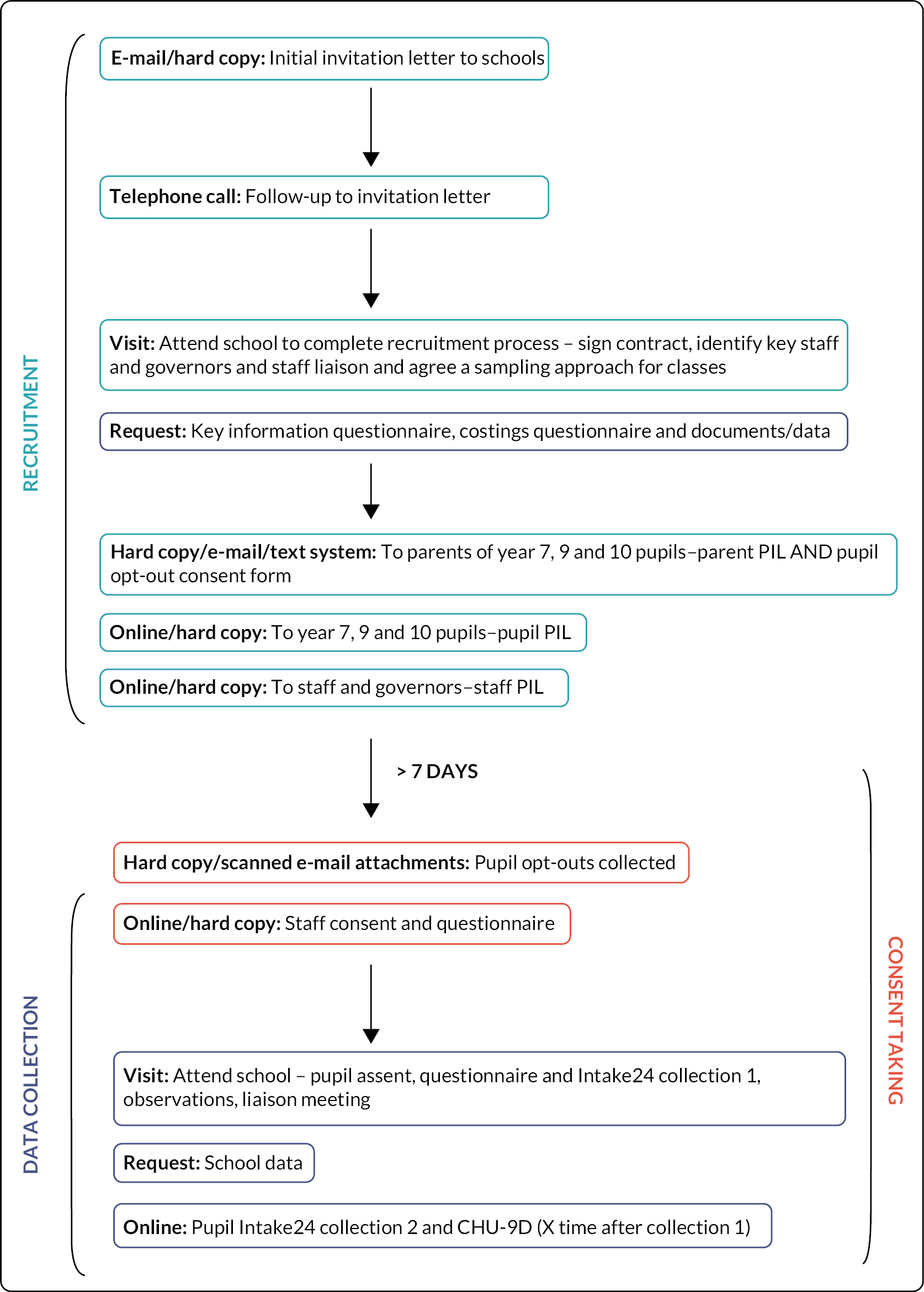
Data collection was undertaken at the school and the individual pupil levels and is outlined below. Recruitment and data collection processes are presented in Figure 2.
FIGURE 2.
Recruitment and data collection flow chart. CHU-9D, Child Health Utility 9-Dimensions; PIL, participant information leaflet.
School-level data capture
School surveys and document collection
Schools were asked to complete two paper-based surveys (available on the study web page at www.fundingawards.nihr.ac.uk/award/17/92/39). The first was a survey to collect information on catering and dining arrangements, school meal uptake and features in place to support healthy eating (key information survey). In this survey, schools were also asked to nominate relevant staff/governors to be invited to complete the staff/governor survey. The second was a survey to collect information on costs relating to food provision, food/healthy-eating education and other support for healthy eating (costing survey). The two school surveys were reviewed by our public advisors (senior school leaders) and were edited based on feedback on the wording and ease of completion. Because of the initially low response rates for the costing survey, it was shortened and converted to an online format in November 2021, which was again reviewed by a public advisor.
We also collected key documents relating to food provision and food/healthy-eating education, including catering contracts (where external catering providers were in place), school food and other relevant policies (e.g. behaviour policy), information on the school curriculum relating to food and diet, minutes of meetings relating to school food (e.g. Board of Governors meetings, School Council/Student Voice meetings), school development plans or school self-evaluation forms, and other documents identified by the school relating to food provision or food/healthy-eating education, for example school-administered pupil surveys and school food reviews.
Current school menus were obtained for each food outlet and mealtime, where available, to enable assessment of menus against the SFS.
Staff and governor surveys
Questionnaires were sent to key staff and governors who had been identified within the school to have roles relating to the school food provision, environment, curriculum and/or SFS/SFP implementation. These were available in online or paper formats (including a stamped addressed return envelope). Four separate questionnaires (available on the study web page at www.fundingawards.nihr.ac.uk/award/17/92/39) were developed for the key staff/governor groups: (1) catering survey, (2) senior leadership survey, (3) teaching survey and (4) governor survey. The purpose of these surveys was to:
-
assess implementation of SFP recommendations
-
gather their views on the school food culture and environment
-
assess the extent to which the two national policies were embedded within their school.
Questions relating to SFP implementation were informed by the SFP headteacher, governor and school checklists. 56–58 Questions relating to the embedding of the SFS and SFP were adapted from the Normalisation Measure Development (NoMAD) survey [underpinned by normalization process theory (NPT) and designed to assess how a way of working becomes embedded as normal practice88,89]. Staff/governor surveys were reviewed by relevant public advisors and were edited based on feedback on the wording and ease of completion.
Observation of school canteens and food outlets
Researchers visited all participating schools to undertake a 1-day observation of the school food provision and eating areas (including dining and communal facilities), the food on offer and the wider environment in the school. An observation tool (available on the study web page at www.fundingawards.nihr.ac.uk/award/17/92/39) was developed to enable assessment of the food provision against the SFS and assessment of implementation of SFP actions and to gather data on the eating and wider school environment, including where food and drink is available and where pupils go to consume foods. The observation tool captured all foods and drinks available in food outlets, including main meals, snacks, drinks and condiments. Items in the observation tool relating to the implementation of SFP actions were informed by the headteachers, school governors and school healthy-eating culture and ethos checklists. 56–58 The observation tool was piloted by two researchers in one secondary school (not within the sampling frame) prior to data collection and edited for ease of completion.
All school food provision occasions over the course of a single day were observed, which typically included breakfast, mid-morning break and lunch provision, and occasionally afternoon-break/after-school provision. For each occasion researchers completed an observation tool for each food outlet and dining area in the school.
Members of the core research team and sessional researchers were employed to undertake school observations. Sessional researchers received a half-day training session prior to data collection visits and were supported during their first observation by a member of the core research team. Observation tools were checked by a member of the research team following data collection visits so that any queries could be resolved.
School food sales data
To assess sales of food in schools, we requested aggregated itemised data on food sales from participating schools’ online payment management systems for two designated months in the current/previous academic year (June and November). For schools recruited in 2021–2, we also requested food sales data from June to November 2019 to enable a comparison of pre-pandemic sales with current sales. Sales data were converted to Microsoft Excel files where required, with the conversion checked for accuracy.
Pupil outcomes
We aimed to compare dietary intake and indicators of dental caries in pupils in the SFS-mandated and SFS-non-mandated secondary school groups. As one of the main outcomes of interest was free sugar intake, and for the purposes of our sample size calculation, we defined our primary outcome as intake of free sugars (in grams). We assessed free sugar intake during school day lunch, while present at school, and during the full 24-hour period of the same school day.
Secondary nutritional outcomes were:
-
percentage of dietary energy intake from free sugars
-
total energy intake (TEI; kcal)
-
total fat intake (g)
-
fibre intake (g)
-
fruit and vegetable portions consumed
-
number of SSBs consumed
-
number of sugar and chocolate confectionery items consumed
-
number of HFSS foods consumed (defined according to the Nutrient Profiling model90)
-
free sugar intake providing ˃ 5% of 24-hour TEI
-
consumption of five or more portions of F&V during a 24-hour period
-
number of eating/drinking occasions (excluding plain water) during a 24-hour period.
As with the primary outcome, the secondary nutritional outcomes numbered 1–8 above were assessed during school day lunch, while present at school, and during the full 24-hour period of the same school day.
Dental outcomes were:
-
the presence of any symptoms indicating dental caries in the past 3 months
-
the number of dental caries symptoms in the past 3 months
-
past dental caries treatment.
Pupil data capture
Pupils were invited to two computer-based sessions, completed during timetabled lessons, and asked to complete (1) an online survey (using REDCap software;91 available on the study web page at www.fundingawards.nihr.ac.uk/award/17/92/39) hosted at the University of Birmingham and (2) an online 24-hour dietary recall. For the first session, at least one researcher was present to facilitate the session. This included providing a verbal overview of the participant information leaflet, answering any questions related to participation and providing assistance throughout the session to pupils who required it. The second session was facilitated by the class teacher approximately 2–4 weeks later. Paper copies of the surveys were available if there were any issues with computer/internet access. In some situations, pupils were asked to complete the survey or 24-hour dietary recall at home, for example if a pupil was late to the session, if a pupil had issues with computer/internet access or if the school could not find a timetabled session to complete the second data collection session.
Dietary intake
Dietary intake data were collected using Intake24, an online self-completion 24-hour recall tool that is based on the multiple pass method (shown to be the most accurate for assessing dietary intake in older children and adolescents92) and has been used successfully to collect data from secondary-school-aged children. 93 A comparison of Intake24 with interviewer-led recall in participants aged 11–24 years reported that Intake24 underestimated energy intake by just 1% and differences in mean macronutrient/micronutrient intakes between the two methods were within 4%. 93 Photographs are used for portion size estimation, a method that has shown good agreement with 4-day weighed intakes in adolescents. 94,95 Intake24 matches foods and drinks to the NDNS food database containing over 2300 foods, and links to nutrient composition data from the UK Nutrient Databank codes. 96
While Intake24 contains several culturally diverse food items, it does not include some traditional foods that would be commonly consumed by some cultural groups in the Midlands population (particularly South Asian traditional foods). To improve the applicability of the tool to the study population, the research team adapted Intake24 for a more culturally diverse population. Adaptation methods included piloting Intake24 with members of minority ethnic communities, community nutritionist consultation and literature review to identify food/drinks commonly consumed by minority ethnic groups but not included in the Intake24 database. Identified foods (n = 63) were added to Intake24. Nutrient composition data for these items were obtained by matching to existing items in Intake24 or from other existing food composition sources. 97,98
We collected dietary intake data from pupils for a minimum of one complete 24-hour school day period and a maximum of two complete, non-consecutive school days. In Intake24, pupils entered all foods and drinks consumed at named mealtimes and outside mealtimes as appropriate. Pupils were asked to provide information of the source of the food/drink consumed (school café/canteen/shop; school vending machine; shop café/restaurant/fast food place/take away/vending machine outside school; from home) and location of consumption (in school; at home; on the journey to/from school; another location) for each eating occasion. Source of foods/drinks consumed was used to generate the explanatory variable ‘lunch source’. This variable was further coded into two categories: 100% school-provided (school café/canteen/shop or school vending machine) or other (shop café/restaurant/fast food place/take away/vending machine outside school, home, or multiple sources including school and elsewhere).
Dental health
Data on dental health were gathered in the session 1 survey. We used validated self-report measures from the national Child Dental Health Survey14,99 to assess dental symptoms in the previous 3 months (toothache, a sensitive tooth, bleeding or swollen gums, a broken tooth, mouth ulcers, bad breath, a filling or a decayed tooth taken out) and treatment received in the past (filling of a permanent or milk tooth, permanent or milk tooth taken out due to decay, a general anaesthetic before dental treatment or sedation before dental treatment) to indicate caries experience. The survey also included questions on frequency of tooth-brushing and self-rated dental health.
Sociodemographic and other data
The online surveys included questions relating to sociodemographic characteristics of pupils, including age, gender, ethnicity (using the 2011 Census classification) and postcode data. Postcodes were mapped to IMD 2019 scores100 and used to obtain water fluoridation levels at participants’ homes (obtained from the websites of local water companies). Participants were also asked if they were receiving FSM.
In the first survey, we also asked questions relating to SFP recommendations, for example availability of water and awareness of school food policies, and gathered participants’ views on the school food culture and environment, for example the eating experience, facilities and school support for healthy eating. In the second survey, we asked questions relating to pupil expenditure on food and included the Child Health Utility 9-Dimensions (CHU-9D),101–103 a preference-based paediatric health-related quality of life (HRQoL) measure.
Data matching and cleaning
Data from the online (REDCap) surveys were matched to dietary data (Intake24) using a one-time unique username for each pupil, which pupils entered into their online survey and Intake24 record. Where different usernames were required (e.g. the username failed on one of the systems), an alternative username was provided and a note was made so that the records could be matched. Some REDCap survey records could not be matched with Intake24 records due to errors in pupil data entry (e.g. wrong username entered), in which case the dietary data for these pupils could not be included. Some pupils completed the online survey but did not finish their 24-dietary recall within the allocated time slot.
Session 1 and session 2 data were matched on personally identifiable characteristics recorded in the online surveys, that is name, date of birth, postcode and school. Some participants completed only session 1 or session 2 of the data collection due to absence from school, or pupil non-assent for one of the two sessions. As a result, some participants had only one Intake24 record and had missing survey data collected at only one of the two time points; for example, dental outcome data were collected in session 1 only and CHU-9D data were collected in session 2 only. Data on receipt of a FSM were originally collected in the session 2 survey only. This question was subsequently added to the session 1 survey to reduce the number of missing data due to non-completion of session 2. In some schools (n = 5), we were unable to complete the second session of data collection with pupils due to prolonged school closures put in place as part of the COVID-19 pandemic response.
Other cleaning steps applied to the sociodemographic data were as follows: adjusting year of birth when respondents had entered implausible values; reassigning school year group where appropriate (based on date/time stamp of survey completion and age); converting addresses to postcodes; and assigning free-text descriptions of ethnicity to existing defined categories where appropriate (only when these matched defined categories, e.g. White British).
A series of steps were required for cleaning nutritional intake data generated from Intake24 records. These are provided in Appendix 1, Table 31.
Nutritional outcomes were generated from the cleaned data, and the distribution of values for each outcome was checked in Stata version 17 (StataCorp LP, College Station, TX, USA) to identify outliers, defined as values above or below 3 SDs from the mean. The Intake24 data underlying identified outliers were visually inspected for potential errors (e.g. portion sizes, duplication of items), and a judgement was made about whether these records were plausible, taking an inclusive approach. Where records were deemed to be implausible due to excessive portion sizes, these were edited by taking the Wrieden average portion values,104 where available, or alternatively the most common portion size for that item from the Intake24 data set. If more detail was provided by the participant regarding portion size, for example three packets of crisps, we used this information to calculate the revised portion size. Items deemed to be duplications of foods/drinks already entered by a participant were removed. Full records considered to be implausible were removed (these are detailed in the results below).
Public involvement methods
Aim
Through our public involvement activities, we aimed to consult with young people, parents and school staff/governors on the design and conduct of the study, including recruitment, data collection, data presentation and dissemination.
Recruitment and membership
Throughout the study, we had a teacher in a school senior leadership role as part of our research team (SW; see Acknowledgements), who provided advice on a range of aspects of the study, including engaging schools and pupils, access to school-owned food sales data, considerations around school management and governance systems, and planning data collection as part of timetabled school sessions.
We convened three public advisory groups: (1) young people, (2) parents and (3) school staff and governors. Members of the young people’s group were originally recruited through two schools with whom we had established relationships. In each school we met face to face with two groups of six pupils (year 7, age 11–12 years; and year 10, age 14–15 years), with a total of 24 pupils involved. As the study progressed, we linked with the established Young People’s Advisory Group for the National Institute for Health and Care Research (NIHR) West Midlands Clinical Research Network. We met with this group via video call on two occasions, with 7–9 young people in attendance.
We initially recruited a group of four parents of secondary school pupils via personal contacts and networks within the University of Birmingham. This group met face to face on one occasion, with further interaction over e-mail due to the national lockdown in response to the COVID-19 pandemic (March 2020). A new parent group was established towards the end of the study (July 2022) using social media and participating school contacts. This group comprised eight members and met remotely on one occasion to advise on study dissemination.
The school staff/governor group members were recruited through personal contacts and networks within the University of Birmingham. This group met on four occasions, both face to face and remotely, with additional interaction over e-mail during the national lockdown. Membership of this group fluctuated between three and six members and included teachers, senior leadership team (SLT) representatives and governors. Members of all public advisory groups received reimbursement for time and expenses.
We also had three public representatives on our Study Steering Committee (SSC): SB (teacher with a senior leadership role in a multi-academy trust; SSC member March 2019–January 2020), AH (SSC member January 2020–September 2022) and CM (retired headteacher and chief executive officer of multi-academy trust; SSC member March–September 2022). These public representatives provided advice and oversight throughout the study.
Methods of engagement
We developed terms of reference for the parent and staff advisory groups. In the initial meetings with all the public advisory groups, we presented a summary of the study and outlined the role of the group. During group meetings, we used an interactive approach to engaging with our public advisors. This involved working in small groups to review study materials with questions to prompt discussion, and using voting buttons, emoticons, the chat function (if online) and audio–visual materials to engage group members. We took structured notes and presented the thoughts and views expressed in the meetings to the Study Management Team and the SSC for consideration.
Data analyses
Assessment of school food standards adherence
We assessed compliance with the SFS based on (1) observation of mealtimes across a full school day and (2) review of weekly menus. The purpose of completing an assessment of SFS compliance on the 1-day observational data was to capture the off-menu foods on offer in secondary schools such as breakfast and breaktime offers, drinks, condiments, snacks and sandwiches. The observational data also enabled us to gain further information on menu items, as menus often lacked detail such as the types of fruit/vegetables or cakes/biscuits offered. The menu review was required in addition to the 1-day observational data to enable assessment of standards that apply to schools on a weekly (e.g. starchy foods cooked in fat or oil) or 3-weekly (e.g. oily fish) basis.
School food standards compliance criteria were guided by the UK statutory instrument The Requirements for School Food Regulations 201444 and School Food Standards Practical Guidance. 51 A SFS question-and-answer document was also used to check the interpretation and definitions of food categories. 105
Some additional definitions of food categories beyond those given in the SFS documentation were required to categorise all foods and drinks offered, for example desserts, confectionery and snacks (available on the study web page at www.fundingawards.nihr.ac.uk/award/17/92/39). We did not collect recipes, so we developed and applied rules for some of the food types described in the SFS; for example, for ‘fruit-based desserts’ (with a content of at least 50% fruit measured by volume of raw ingredients), we included desserts such as fruit pie, fruit crumble, fruit cobbler and jelly made with fruit. For other dessert items, the research team searched the internet and reviewed a standard recipe (e.g. British Broadcasting Corporation Good Food) for the dessert or a similar item to make a judgement on whether it met the criteria for a fruit-based dessert. Drinks and prepackaged snacks, biscuits and cakes were reviewed for compliance using the ingredients lists detailed on brand or shopping websites.
All foods and drinks recorded in the observation tool and menus were extracted into Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA) spreadsheets and coded based on the food/drink type. One researcher carried out data extraction, and two researchers familiar with the SFS independently coded foods and drinks and judged SFS compliance for the two sets of data (observation and menu), entering their judgements into a data entry form. The judgements of the two researchers were compared, and, where discrepancies arose, the research team met to agree on a final judgement. The 1-day observation data judgements and menu judgements were combined into an overall SFS compliance judgement for each standard. Details on the standards assessed and how judgements were combined across 1-day and menu assessments are available on the study web page (www.fundingawards.nihr.ac.uk/award/17/92/39).
As a final quality check, the coded food/drink data were back-checked against menus and observations for any missing foods/drinks or errors in data entry, and final SFS judgements for all schools were checked for consistency in application (MM). Any judgements that were deemed inaccurate were reviewed and corrected by two researchers (MM and AD). Final judgement options were yes (meets standard), no (does not meet standard), can’t tell (it was not possible to assess compliance due to lack of information) or not applicable (standard did not apply). Not applicable (N/A) was used for standards relating to drinks, condiments, dried fruit and crackers/breadsticks when these items were not sold/not available in the school. We calculated the proportion of standards met for each school using the number of assessable standards as the denominator (i.e. excluding ‘can’t tell’ judgements).
Assessment of School Food Plan actions
Actions included in the SFP were identified following a comprehensive review of relevant SFP resources: the checklist for headteachers, the creating a culture and ethos of healthy-eating guidance, and the guidance for school governors. 56–58 Some actions were unique to each document, whereas others were repeated or similar across documents. Those that were repeated or similar were merged to form single actions, retaining as much of the original wording as possible. We identified a total of 69 actions, which we grouped into 9 ‘themes’ based on the headings used in the SFP resources. More detail about the specific actions within each theme is provided in Appendix 2, Table 32.
We assessed the implementation of SFP actions using a variety of data sources, including researcher observation, survey responses from schools, staff and pupils, and the review of school documents, for example curriculum documents, catering contract and meeting minutes. Further detail on the source of data for specific actions and data points/questions used for assessment is provided in Appendix 2, Tables 32 and 33.
A judgement of red, amber or green (RAG) was made on each action for each data source, with red indicating that the action had not been implemented, amber indicating that it had been partially implemented and green indicating full implementation. If data were missing (e.g. incomplete survey responses or documents not provided by schools), a judgement could not be made, indicated by a ‘no judgement’ rating. A final judgement of high, medium or low implementation was made for each action point based on RAG ratings across all data sources, with rules for combining these judgements agreed in advance by the research team (available in Appendix 2, Table 34). The assessment was conducted by one researcher. Uncertainties were discussed with the research team, who then agreed on a final judgement.
The proportion of actions judged as ‘high’, ‘medium’ or ‘low’ was calculated using the number of assessable standards as the denominator (i.e. excluding those actions for which a judgement could not be made).
Assessment of the embedding of national school food policy within schools
Questions were developed to assess the embedding of the SFS and SFP within schools. These were adapted from the NoMAD instrument88,89 (based on NPT106) with statements mapping onto the relevant NoMAD constructs and their constituent components in relation to coherence (individual and collective sense-making), cognitive participation (relational work, building a community of practice), collective action (operational work, enacting a new set of practices) and reflexive monitoring (appraisal, understanding how a new set of practices affects individuals and others). Details of relevant questions and their relation to NPT constructs are available on the study web page (www.fundingawards.nihr.ac.uk/award/17/92/39). Data from these questions were extracted from the staff and governor survey data sets and responses presented in tables and graphs to explore variation in responses across the SFS-mandated and SFS-non-mandated school groups and across staff/governor groupings [see Embedding of the school food standards and School Food Plan national school food policies within schools (research objectives 1a and 1b)].
Development of typology schools in relation to school food provision and support for healthy eating
School-level data were used to identify different school ‘types’ in a two-stage process. In the first stage, we used SFS compliance data to generate school types. In the second stage, we inspected SFP implementation data to identify subtypes within the types generated in stage 1.
Stage 1
Among the 32 SFS, we focused on two subsets of standards. These were selected based on their relation to obesity or dental health (i.e. food/drinks that are energy-dense and/or high in fat or sugar; n = 12 standards) or their relation to achieving a wide range of foods across the week (variety; n = 15 standards). The rationale for selecting these standards were as follows: (1) reducing obesity and improving dental health are public health priorities in this age group, and the pupil outcomes explored in this study relate to these priorities; and (2) one of the aims of the SFS is to ensure that children have access to a healthy, balanced diet with a wide range/variety of foods. The selected standards and those which were excluded are detailed in Appendix 3, Table 35.
The extent of compliance with the two sets of standards was rated as ‘low’, ‘medium’ or ‘high’ based on the proportion of standards met, with ≤ 33% indicating low compliance, 34–66% indicating medium compliance and ≥ 67% indicating high compliance. Any actions that could not be assessed were removed from the denominator. The schools were then grouped into types according to the two ratings that they received for the two sets of SFS (those relating to obesity and dental health and those relating to dietary variety).
Stage 2
We selected ‘indicator’ SFP actions (n = 17 out of 69) and classified schools as having ‘low’, ‘medium’ or ‘high’ levels of implementation for each of these actions based on the overall judgements described in Assessment of School Food Plan actions. We selected actions where there was a wide variation in implementation across schools and we excluded actions were there was a low response rate (i.e. where there were a large number of schools where no judgement could be made) to enable better comparison of implementation across schools. The selected actions are detailed in Appendix 3, Table 36.
The selected actions represent eight of the nine themes that we identified within the SFP actions. No indicator actions were selected within the theme of ‘School Food Policy’ because there was little variation in implementation of actions across schools and a high proportion of schools where no judgement could be made.
The school types identified in stage 1 (based on compliance with two sets of SFS standards) were divided into SFP subtypes A and B based on the proportion of selected SFP actions receiving a ‘high’ rating, with type A indicting a lower level of SFP implementation (≤ 50% SFP actions implemented to a high level) and type B indicating a higher level of SFP implementation (> 50% SFP actions implemented to a high level).
We presented school contextual data for the identified school types to explore any differences in the wider school context between the types.
School food uptake and sales data analysis
School food uptake
Data on uptake of school lunches at the school level were self-reported through the school key information survey. As these data were missing for some schools, we also used individual pupil participant data on the source of their lunch consumed during the school day from Intake24 records to give an estimate of the proportion of uptake of school lunches in each school. For each of these data sources we calculated the mean percentage uptake across all schools and across SFS-mandated and SFS-non-mandated schools.
School food sales
Owing to differences in how schools label foods within their payment systems and variation in the level of detail captured in food sales records, we were unable to explore all food/drink items sold in the schools. Instead, we focused on ‘indicator items’ from within the broader categories of foods detailed in the SFS (i.e. those prohibited, such as confectionery; restricted, such as pastry items; or encouraged, such as fruit), which appeared to be consistently recorded in the sales data across different schools. The indicator items included in our analyses are:
-
starchy foods cooked in fat/oil
-
pastry items
-
desserts, cakes, biscuits, puddings
-
confectionery, chocolate or chocolate-coated products
-
non-compliant snacks
-
fruit
-
vegetable sides and salads
-
non-compliant drinks
-
compliant drinks
-
plain water
-
other drinks.
Further details on the rationale for their inclusion, examples and exclusions are available on the study web page (www.fundingawards.nihr.ac.uk/award/17/92/39).
We calculated the number of each indicator item sold over the month as a proportion of total sales for the month. Some items were removed from the ‘total sales’ calculation, for example condiments, non-food/non-drink items and staff sales (where indicated). All schools had some items coded as miscellaneous, but the extent to which this code was used by schools varied. We calculated the proportion of the total sales that were coded as miscellaneous for each school to explore this variation (details are available on the study web page at www.fundingawards.nihr.ac.uk/award/17/92/39), as this presents a potential limitation when comparing sales of indicator items across schools (i.e. indicator items may be coded as miscellaneous in some schools but not in others).
We compared total sales across SFS-mandated schools and SFS-non-mandated schools for pre-COVID-19 pandemic time periods (June 2019, November 2019) and mid-/post-pandemic time periods (June 2020, November 2020, November 2021). We also estimated sales per pupil using the number of pupils on roll for the period of overall data collection to account for variation in school sizes.
We compared mean sales of indicator items as a proportion of the total sales for the month of data provided to give an overall summary of sales of indicator items for all schools. We also compared the monthly mean sales for indicator items as a proportion of the total sales in SFS-mandated and SFS-non-mandated schools.
Analyses of pupil nutritional intake and dental health data
The study statistical analysis plan is available on the study web page (www.fundingawards.nihr.ac.uk/award/17/92/39).
Generation of pupil nutritional intake outcomes
Nutritional outcomes were generated from raw Intake24 data in Microsoft Excel using pivot tables for the three time points, as follows:
-
During school day lunch, which incorporated all foods and drinks participants indicated as ‘lunch’ using the Intake24 predefined meal names.
-
While present at school (school day), which incorporated any foods and drinks eaten between 9.00 a.m. and 2.00 p.m. inclusive, representing a typical school day but accounting for later start times and earlier finish times in some schools (based on information from participating schools about their school hours); and any foods or drinks consumed outside this period but on school premises, based on meal location provided by the participant (to account for earlier/later start/finish times in some schools, and the availability of breakfast, afternoon break or after-school food provision in some schools).
-
During the full 24-hour period of the same school day.
The process of generating the nutritional outcomes is presented in Appendix 4, Table 37.
Generation of pupil dental outcomes
Three dental outcomes were generated from the survey data relating to dental health:
-
Presence of dental caries (binary outcome) was indicated by self-report of the presence of at least one of the following conditions in the previous 3 months: toothache, sensitive tooth, bleeding or swollen gums, a broken tooth, mouth ulcers, bad breath, a filling, or a decayed tooth taken out.
-
Number of dental caries symptoms (count variable), indicated by the number of conditions listed above that were self-reported as present.
-
Treatment for dental caries (binary variable) was indicated by self-report of at least one of the following: a filling of a permanent or milk tooth or a permanent or milk tooth taken out due to decay.
Descriptive statistics
Descriptive statistics were used to summarise the primary and secondary outcomes for the study sample overall and by SFS group (SFS-mandated and SFS-non-mandated). Where participants had two 24-hour dietary intake (Intake24) records, the mean outcomes were presented.
Primary analysis
The primary outcome of free sugar intake (measured in grams) at lunch, during the school day and during the whole day (24 hours) was compared for pupils who attended SFS-mandated schools and pupils who attended SFS-non-mandated schools. The primary outcome was recorded in Intake24 for a minimum of 1 day and a maximum of 2 days for each participant. Each available observation was used in our analyses. For the comparisons of free sugar intake and other secondary nutritional outcomes at lunch and across the school day, participants with zero TEI at these time points were excluded. Linear multilevel models were used, with random effects allowing for repeated 24-hour dietary recall information for students, and clustering of students within classes and schools. However, we looked to simplify the models where appropriate when analysing the data. Following assessment of the random effects, we retained allowance for repeated assessment for individuals and clustering within schools but included year group as a fixed effect, rather than a random effect. The model was used to evaluate differences in outcomes between SFS status (mandated/non-mandated) adjusted for school-level and pupil-level variables (see adjustment variables: Adjustment).
Secondary analyses
There were 11 additional nutritional outcomes, 8 of which were explored at each of the 3 time points: school lunch, school day and over 24 hours. The analyses of these outcomes used multilevel linear models or multilevel Poisson models depending on the variable type (continuous or integer counts) and were constructed in the same way as described for the primary outcomes.
There were three dental outcomes, collected at one time point. Models for these outcomes used multilevel logistic or Poisson models (depending on binary or integer count outcome data) to evaluate differences between SFS status with adjustment for confounders, again with random effects allowing for the clustering of students within schools.
Adjustment
School- and pupil-level covariates were included as adjustment variables. School-level variables initially included those used for generating propensity scores (listed in Schools) as well as model of catering provision (in-house or external catering) and academic year of data collection (2019–20, 2020–1, 2021–2) to account for the potential influence of COVID-19 restrictions on school food provision and uptake and pupil dietary behaviours. Pupil-level variables included year group, age (generated from date of birth), gender (male, female, other/not stated), ethnicity (using 2011 Census high-level categories: Asian/Asian British, Black/African/Caribbean/Black British, White, and other/mixed/multiple/not stated), IMD (2019) quintiles (based on home postcode) and lunch source (100% school-provided or not; obtained from Intake24 records). Home and school water fluoridation levels (based on postcodes) and tooth-brushing frequency (from the pupil survey) were added as adjustment variables to the dental outcome models.
We simplified the models by reducing the number of school-level variables included as covariates. We conducted a backwards elimination process on the model with the outcome of free sugar intake at lunch. The school-level variables of in-house/external school food provision, percentage of pupils eligible for FSM and time of data collection were included as model covariates because of their relevance to the research question, and a backwards elimination process was conducted on all other school-level variables using an alpha value of 0.1. Following this process, establishment type, urban/rural location, number of pupils, percentage of male pupils, percentage of ethnic minorities pupils, percentage of pupils with EAL and selective/non-selective admissions policy variables were excluded from this and all other models with nutritional intake outcomes.
We undertook a similar process for the model with the outcome of number of dental caries symptoms. Following a backwards elimination process for school-level variables, establishment type, urban/rural location, number of pupils, percentage of male pupils, percentage of pupils with EAL, school religious status and selective/non-selective admissions policy variables were excluded from this and all other models with dental outcomes.
Missing data
Pupils with no dietary intake record or dental outcome data were excluded from descriptive tables and analyses. Pupils with missing nutritional or dental outcomes data were excluded from analyses focused on that outcome. For demographic variables, if more than 5% of the data were missing, we imputed data where appropriate for use in a sensitivity analysis. The main analyses used complete-case data.
Alpha value and confidence intervals
The alpha level used for our analyses was 0.05. For the primary analysis the alpha value used for determining statistical significance was 0.05, as demonstrated by the sample size calculation. All secondary analyses and subgroup analyses were not formally powered. The 95% confidence intervals (CIs) for the coefficients in the models were presented. For all models, goodness-of-fit statistics (Akaike information criterion, Bayesian information criterion, log-likelihood) were calculated.
Subgroup analysis and interaction effects
Two-way interactions between SFS-mandated/non-mandated status and lunch source, year group and IMD quintile group were included in the models to explore whether there were subgroup differences in the associations between school SFS status and nutritional outcomes in relation to these characteristics. Each interaction effect was introduced separately into each of the nutritional outcome models.
Exploratory comparison of outcome across identified school types
To explore differences in outcomes across the school types (see Development of typology schools in relation to school food provision and support for healthy eating for school typology development), we constructed models for our primary and secondary outcomes as described in Primary analysis and Secondary analyses, but with school type as covariate instead of SFS status. Adjustment variables (as previously described) were included in the models.
Sensitivity analyses
We performed sensitivity analyses using imputed data where missingness was ≥ 5%. Additionally, a sensitivity analysis was also investigated where missing age data were replaced by mean age of year group. To explore the impact of implausible dietary intake reporting on the study analyses, we also conducted a sensitivity analysis for all primary and secondary outcomes from which we excluded all participants who reported a total 24-hour energy intake of < 400 kcal or > 4000 kcal, which were the cut-off values used to examine implausible reporting in the NDNS. 107
Health economic evaluation
The aim of the economic evaluation was to assess the economic impact of implementing the national SFS and the wider SFP in secondary schools in the Midlands. The objectives of the economic evaluation were:
-
to estimate the costs of implementing SFS, the SFP, and of food provision and food education in schools
-
to summarise the costs and consequences of the SFS and SFP in the secondary schools mandated to comply with the SFS (SFS-mandated schools) and in the schools not mandated to comply with the SFS (SFS-non-mandated schools).
Approach to the economic evaluation
The study health economic analysis plan is available on the study web page (www.fundingawards.nihr.ac.uk/award/17/92/39).
The economic analyses took the form of a micro-costing analysis and a cost–consequences analysis. For the micro-costing analysis, the costs of implementing and delivering the SFS and SFP plus the costs of school food provision were calculated for each school using data provided by the school-reported costing survey. For the cost–consequences analysis, the costs of implementing and delivering the SFS and the SFP, the costs of school food provision, and selected consequences (i.e. pupil outcomes) were summarised in the form of a balance sheet for the two groups of schools being compared (SFS-mandated and SFS-non-mandated). A societal sector perspective was adopted for the cost–consequences analysis, meaning that the distribution of costs and consequences borne by schools, catering companies, volunteers, and families and pupils were considered and highlighted. The time horizon for the analyses was 1 year. No discount rate was applied as the data covered a period of < 1 year. All costs were converted to Great British pounds 2021 based on the UK Consumer Price Index as published by Office for National Statistics. 108 Statistical analyses were conducted using Stata.
Costs
All schools were asked for data to capture any one-off or occasional costs associated with the implementation and delivery of the SFS and the SFP, ongoing annual costs associated with food provision and costs associated with other activities to support healthy eating, for example staff training (in addition to those outlined in the SFP). The survey was initially developed by the FUEL study team as a paper-based questionnaire and tailored to individual schools based on the observed school characteristics. The questions reflected each of the elements of the SFS and the SFP. However, after a low response rate and poor completion, the FUEL study team adapted the survey by shortening it to focus on what was deemed the most important resource use items and converted it to an online format using REDCap. The survey was sent to liaison persons at each participating school. The schools were offered help with completing the survey. The paper-based and online versions of the survey are available on the study web page (www.fundingawards.nihr.ac.uk/award/17/92/39).
Unfortunately, the school resource-use data (from both paper-based and online surveys) had large numbers of missing data, so these were supplemented with secondary data on catering expenditure by schools. 109 Legally, all schools in England are required to report expenditure data under predetermined budget headings, and this information is publicly available on an annual basis for both catering staff and catering supplies (including the costs of providing FSM and milk). However, it does not include expenditures associated with mealtime assistance and midday supervisors, any training for catering staff or costs related to maintenance and improvement to the canteen. Further detail on what is included in this data capture is provided on the study web page (www.fundingawards.nihr.ac.uk/award/17/92/39). For all schools, the catering expenditure for the year 2018–9 was used to reflect catering before the COVID-19 pandemic, apart from four schools for which all other study data were collected during the pandemic (2020–1 academic year), and therefore the same year was used for the catering expenditure to reflect spending during the pandemic.
The costs for pupils and families were collected in the pupil survey (see Sociodemographic and other data and the study web page at www.fundingawards.nihr.ac.uk/award/17/92/39). The pupils were asked to indicate how much they typically spent on food per day during the school day, purchased both at school and at food outlets outside school. The answer options were given in ranges (e.g. £1–2.99). The average spending per pupil per day was calculated by using the mid-point value for each category and summed to calculate the total spending per pupil.
All resource use was valued in monetary terms using appropriate UK unit costs (see Appendix 5, Table 38) or participant valuations estimated at the time of data collection.
Outcomes
The outcome measures for the health economic analysis included:
-
dietary intake
-
dental health outcomes
-
educational outcomes
-
quality-adjusted life-years (QALYs) derived from the CHU-9D utility scores.
The data were collected using the study-specific questionnaires for the pupils as described in Sociodemographic and other data. QALYs were measured using the CHU-9D instrument, which was included in the second pupil survey. The CHU-9D has previously been used to measure QALYs in general population samples of children and adolescents and has been shown to have good psychometric performance. 110 Utility scores were derived from responses to the CHU-9D using preference weights obtained from a sample of the UK adult general population. 103
The dietary intake outcomes, detailed in Generation of pupil nutritional intake outcomes, were included in the cost–consequences analysis. The outcomes corresponding to the dietary intake during the school day were selected. These outcomes were calculated only for the pupils whose TEI during school day was above zero. Additional outcomes related to dietary intake during 24 hours and included in the cost–consequences analysis were:
-
> 5% of 24-hour TEI from free sugar
-
consumption of five or more portions of F&V per day
-
number of eating/drinking occasions (excluding plain water).
All dental health outcomes, detailed in Generation of pupil dental outcomes, were included in the cost–consequences analysis.
Educational outcomes data were collected from publicly available school performance tables111 for the year 2019 to reflect school performance before the COVID-19 pandemic. Relevant indicators were identified by the FUEL study team in consultation with the SSC and school public advisors. The following indicators were included in the cost–consequences analysis:
-
absenteeism –
-
overall rate of absence
-
persistent absence.
-
secondary performance –
-
progress 8 score (a measure of the progress children make between the end of primary school and the end of secondary school relative to the national average, based on attainment 8 scores)
-
attainment 8 score (a measure of the average academic performance of a secondary school in eight defined subjects)
-
staying in education or entering employment
-
grade 5 or above in English and Maths General Certificate of Secondary Education (GCSEs; a subject-specific academic qualification taken in England, Wales and Northern Ireland).
Micro-costing
All schools that completed the costing survey were included in the micro-costing analyses. The resource use was summarised for each school separately, multiplied by the relevant unit costs, and summed to calculate the total ongoing costs of implementing and delivering the SFS and SFP. The wider costs of food provision and creating a healthy food culture, including the costs for schools, catering providers and volunteer time, were included. To calculate the per-pupil costs of food provision/creating a healthy-food culture, these total costs were divided by the number of pupils in the relevant school for the year when the cost data were collected. Given that the main costs related to food provision, we accounted for school meal uptake by also calculating the costs per pupil based on the number of pupils reported to have school meals. Where data from the schools on the number of pupils having school meals were not available, school meal uptake was estimated from pupil participant data (Intake24). As there was variation in how well the schools completed the survey, the percentage of missing cost data was calculated for each school.
Several assumptions had to be made beyond those outlined in Appendix 5, Table 38. These assumptions were validated internally by the FUEL study team. To calculate the resource use associated with mealtime supervision, we assumed that breakfast time lasted 15 minutes, breaktime lasted 15 minutes and lunchtime lasted 1 hour, in the absence of other data to support this. For some schools, data on the duration of mealtimes were available, and these were used instead. To calculate the cost of classroom cover during staff training, it was assumed that one training session lasted 2 hours and corresponded to the unit cost of teaching staff time (i.e. £20 per hour). The school gardening club sessions were assumed to last 1 hour with one staff member leading the session.
Cost–consequences analysis
All schools participating in the FUEL study were included in the cost–consequences analysis, where costs and consequences were listed for each school in the form of a balance sheet. Furthermore, the average values were calculated for the SFS-mandated and SFS-non-mandated schools. The following costs were included in the cost–consequences analysis: the costs of food provision calculated from the micro-costing analysis (both from a school and a public sector perspective); catering expenditure; and the costs for pupils/families, including the cost of buying food during the school day and the cost of buying the ingredients for the cooking lessons. The total costs, the costs per pupil based on the total number of pupils in each school, and the costs per pupil based on the school meal uptake are presented. The following outcomes were included as described in Outcomes: QALYs, educational outcomes, dietary intake outcomes and dental health outcomes.
Qualitative case study
In phase 2 of the study, we conducted in-depth qualitative research with a subsample of schools using a case study approach. In establishing the focus of the case study enquiry, we have drawn on Maguire’s explorations of policy ‘enactment’ in English schools, with an intention to capture how school food policy was read alongside/against contextual factors by different school stakeholders. 112
An initial aim was to use data generated from this qualitative phase to further refine the school typology developed from the high-level school data collected from all schools, sampling schools from each identified type. However, COVID-19 restrictions meant that we were unable to run the qualitative phase sequentially to the main study and were instead required to carry out data collection for both phases concurrently. The sampling approach was modified, and the qualitative case study was therefore used as a means of exploring policy enactment across different contexts, rather than to further develop our school typology.
A case study approach was selected for this qualitative exploration, as it offers ‘an intensive, holistic description and analysis of a bounded phenomenon’113 and is suited to exploring the contextual basis of phenomena. 114 This approach is being increasingly utilised in health research. 115,116
In this project, we used a collective case study design116 comprising multiple parallel case sites (schools). The use of multiple case sites allowed us to select a range of schools that were broadly representative of schools in the main sample in order to enable a comparison of school food policy enactment across schools and the contextual influences at play.
Aim and objectives
The central aim was to explore with school staff and governors in more depth the way in which the SFS, SFP and local school food policy or initiatives were introduced, embedded and sustained in the schools, and their perceived influence on the dietary intake of pupils.
In relation to pupils, we sought to explore:
-
views on school food and the school food environment and contextual factors influencing these views
-
how pupils interact with the school food environment and the wider outside school environment in terms of their eating behaviour
-
perceived negative impacts of SFS or SFP and regulation of foods provided.
Sampling approach
In our modified school sampling approach, we aimed to ensure representation of schools with a high proportion of pupils eligible for FSM and a mix of schools based on SFS status and catering provision (external and in-house). We aimed to recruit four case sites from the 36 participating schools.
Our participant sampling approach was to identify key school management, teaching and catering staff, along with governors, in each of the case sites. We invited these identified staff/governors to participate in an interview. Interviews were planned with flexibility of setting – either face to face or via video/telephone call – to reflect that research was conducted during the COVID-19 pandemic. It was anticipated that, depending on the size of the school, four to six staff/governor participants per school would be interviewed. Our sampling approach in relation to pupils was to sample pupils from year groups 7, 9 and 10, aligning with the main study. It was anticipated that two or three focus groups would be conducted in each of the case sites, involving approximately 16–24 pupils in each school.
Recruitment and consent
Schools
Participating schools were stratified into two groups by SFS status initially, and then each list was ordered from highest to lowest by proportion of pupils eligible for FSM. Schools were invited from each list in descending order. Once two schools had been recruited, we reviewed the model of catering provision of these schools and prioritised recruitment of schools using the alternative provision from each SFS group as required. Schools had been informed at the start of the main study that they might be invited to take part in the case study phase. At the time of case site recruitment, an invitation was sent to the existing liaison person for the school. Schools received a further £150 for their participation in the case study phase.
Staff
In each case site, researchers liaised with the named school liaison person to identify staff with a particular involvement in school food. Key individuals, including catering staff, teachers, governors and senior leaders, were invited for interview. Staff/governor participants were given detailed written information about the study, what their participation would involve and how their data would be processed. They were asked to complete a consent form (online or paper).
Pupils
Schools were asked to select students who were representative of the school’s student population in relation to demographic characteristics, including sex, ethnicity and FSM eligibility. Researchers asked for approximately 10–12 pupils to be invited to each year-group-specific focus group, with the aim of having 8 pupils in each group (given anticipated absences on the day of fieldwork and an expectation that not all pupils would consent). In one school, whole tutor groups of 30 pupils were invited due to a miscommunication between the research team and the school.
Parents of eligible students were given written detailed information about the study, what their child’s participation would involve and how their child’s data would be processed. Schools were asked to assist in the distribution of this information to parents. As with the main study, parents were not asked for active consent but given the opportunity to complete and return a form to opt their child out of taking part in the study. Prior to data collection pupils received detailed study information, including what we were requesting of them and how their data would be processed. Written assent was also obtained from pupils whose parents did not opt them out of participating. Each pupil received a £5 shopping voucher as a thank-you for participating in a focus group.
Data collection
Data collection was conducted during the 2021–2 academic year. Each school was visited on one occasion by different members of the research team (MM, RD, AD, LM, RA) who conducted interviews and focus groups. On one occasion, our public representative on the SSC (CM) also attended to observe.
Focus groups were conducted face to face in a quiet space and during the timetabled school day. Interviews with staff were individual and face to face, with the option of remote administration if required, and were also conducted in a quiet space during the timetabled school day. Semi-structured topic guides were used to guide the discussion (see the study web page at www.fundingawards.nihr.ac.uk/award/17/92/39).
During the fieldwork, two to four researchers typically visited each case site, with one to two researchers per interview/focus group. In the focus groups, the ‘lead’ researcher focused on facilitating the focus group, while the second researcher’s role oriented around recording observational notes, operating the audio-recorder and collecting demographic data from pupils and staff.
All interviews and focus groups were recorded using a digital audio-recorder. Verbal permission was sought before recording, in addition to the written consent/assent provided by participants.
Demographic data were also collected from participants via a paper/online questionnaire. For pupils, this included questions about their ethnicity, home postcode and FSM take-up and whether they bought food from school. For staff, questions related to their specific role in the school and the number of years they had been in post.
Participants were assigned participant IDs and their demographic records were pseudonymised. Audio-recordings were transcribed by an external transcription service, which was asked to remove identifiable data such as names, organisational names and geographical areas. Researchers could refer to the original audio file during the analysis phase if required. For staff interviews, transcripts were labelled using the participant ID number. For focus groups, the transcript was treated as one unit, and excerpts were not assigned to individual participants.
Topic guide development
Prior to conducting data collection, the research team developed semi-structured topic guides (available on the study web page at www.fundingawards.nihr.ac.uk/award/17/92/39). Piloting of the focus group topic guides took place with the youth public advisory group during a remote 1-hour meeting (see Public involvement methods). Participants were asked if they found any questions difficult to understand and whether anything should be changed. Staff topic guides were checked by the school advisory group and adaptations were made based on their feedback.
In the focus groups, questions explored pupils’ views of the school food environment and contextual factors influencing this, and how they interact with this and the wider outside school environment in terms of their eating behaviour (the questions are available on the study web page at www.fundingawards.nihr.ac.uk/award/17/92/39). We also explored their views and experiences of any negative impact of SFS or SFP and regulation of foods provided. Interviews with school staff were designed to be broad initially to encourage interviewees to tell their ‘story’ relating to their experiences of the SFS and SFP, and how the provision of food, eating environments and the food/cooking curriculum have been shaped within their schools. This narrative style was a means of enabling participants to influence the content of the interview by introducing topics and issues they felt to be most relevant.
In addition, May’s NPT106 was used to frame prompts within the topic guide, so that, if it was not volunteered by the interviewees, we could surface information to help us guide our thinking about how key informants made sense of the SFS/SFP.
Slightly different topic guides were developed according to the interviewee’s role in the school (catering, teaching, senior leadership or governor). The topic guides used are available on the study web page (www.fundingawards.nihr.ac.uk/award/17/92/39).
Analysis
A thematic analysis of data gathered from the case study was conducted and was informed by the Framework analytical approach. 117
Audio-recordings from both interviews and focus groups were transcribed verbatim by an external transcription service (stage 1) and underwent quality checking by members of the research team (stage 2) to enable early familiarisation with this textual data. With the aid of NVivo v11 (QSR International, Warrington, UK), five members of the research team (MM, RA, CR, MP, PA) were involved in the initial exploratory coding (stage 3) of a small number of transcripts selected from researchers’ memory as being particularly interesting. Here, an inductive approach was utilised to generate codes and group them into categories.
Following initial coding, a working analytical framework (codebook) was developed (stage 4) (the codebook is available on the study web page at www.fundingawards.nihr.ac.uk/award/17/92/39). This consisted of seven parent codes (categories) and a large number of subcodes, each of which had positive and negative values that corresponded to whether or not that particular aspect of school food was present. We also used two a priori codes relating to views on the SFS and implementation, and awareness and implementation of the SFP. Subsequently, three members of the team (MM, RA, CR) were each allocated a single case site, with a fourth case site split between two researchers (RA, CR), and the framework was applied to the coding of all transcripts related to each site (stage 5). After generating framework matrices in NVivo (stage 6), with interviewees/focus groups in rows and codes in columns, each member of the analysis team wrote coding summaries for their allocated sites. Summaries were reviewed collaboratively (MM, RA, CR, MP, PA) to support identification and discussion of interpreted themes. Thematic summaries were initially compiled for each individual case site and then combined by comparing sites and exploring common and contrasting themes across sites, (stage 7), in line with other health services research using Framework analysis in a case study approach. 116 The thematic overview was sense-checked by the wider team.
Chapter 4 Results
School sample
There were 482 schools included within our sampling frame across the 22 local authorities in the Midlands: 193 (40%) mandated to comply and 289 (60%) not mandated to comply with the SFS. Thirty-six schools completed data collection in the main study, representing 7.5% of eligible/invited schools. Thirteen schools in the sample (36%) were mandated and 23 schools (64%) were not mandated to comply with the SFS, which broadly reflects the proportion of schools in each group in the sampling frame. Of the remaining 446 schools that did not participate, 6 withdrew (in 3 of these cases this was related to delays caused by the COVID-19 pandemic), 39 expressed an interest in participating but subsequently did not complete data collection, 106 declined to participate and 295 did not respond.
Table 1 presents the characteristics of schools in the study sample, and characteristics of schools in the SFS-mandated and SFS-non-mandated groups.
| Characteristic | All schools (N = 36), mean (SD) (range) or n (%) | SFS-mandated schools (N = 13), mean (SD) (range) or n (%) | SFS-non-mandated schools (N = 23), mean (SD) (range) or n (%) |
|---|---|---|---|
| Number of pupils | 1084.36 (287.77) (612–1774) | 1013.77 (197.70) (690–1312) | 1124.26 (325.30) (612–1774) |
| % female | 54.95 (15.55) (43.81–100.00) | 50.09 (2.02) (46.36–53.81) | 57.69 (18.99) (43.81–100.00) |
| % ethnic minorities | 29.33 (23.30) (4.10–98.20) | 23.90 (17.90) (7.50–63.10) | 32.40 (25.72) (4.10–98.20) |
| % EAL | 13.85 (16.28) (0.70–66.10) | 10.47 (12.43) (1.50–45.10) | 15.77 (18.08) (0.70–66.10) |
| % FSM | 19.77 (12.67) (2.80–61.80) | 22.68 (7.65) (13.60–43.60) | 18.13 (14.69) (2.80–61.80) |
| % SEN | 11.62 (4.11) (4.15–20.44) | 11.16 (3.55) (7.16 –19.91) | 11.88 (4.44) (4.15–20.44) |
| IDACI | 0.15 (0.11) (0.02–0.58) | 0.18 (0.09) (0.06–0.35) | 0.13 (0.12) (0.02–0.58) |
| Establishment type | |||
| Academy converter | 23 (63.89) | 4 (30.77) | 19 (82.61) |
| Academy sponsor-led | 13 (36.11) | 9 (69.23) | 4 (17.39) |
| Presence of sixth form | 26 (72.22) | 10 (76.92) | 16 (69.57) |
| Religious status | |||
| Faith school | 3 (8.33) | 1 (7.69) | 2 (8.70) |
| Secular | 33 (91.67) | 12 (92.31) | 21 (91.30) |
| Location | |||
| Rural | 6 (16.67) | 1 (7.69) | 5 (21.74) |
| Urban | 30 (83.33) | 12 (92.31) | 18 (78.26) |
| Catering provision | |||
| External | 21 (58.33) | 8 (61.54) | 13 (56.52) |
| In-house | 15 (41.67) | 5 (38.46) | 10 (43.48) |
| School water fluoridation levela (mg/l) | 0.51 (0.30) (0.08–0.99) | 0.57 (0.37) (0.08–0.99) | 0.48 (0.25) (0.08–0.92) |
| Academic year of data collection | |||
| 2019–20 | 12 (33.33) | 5 (38.46) | 7 (30.43) |
| 2020–1 | 4 (11.11) | 1 (7.69) | 3 (13.04) |
| 2021–2 | 20 (55.56) | 7 (53.85) | 13 (56.52) |
We asked schools in the SFS-non-mandated group whether they had voluntarily signed up to the SFS. Of the 23 schools in this group, 11 had voluntarily signed up (48%), 6 had not signed up (26%) and three did not know (13%). Data were missing for two schools.
Compliance with school food standards (research objective 1a)
Table 2 shows the mean level of compliance with the SFS for all schools and by SFS-mandated/SFS-non-mandated status. No schools in the sample were fully compliant with the SFS. The average overall compliance was 64%, with similar levels of compliance in SFS-mandated and SFS-non-mandated schools. There was variation in the extent to which each of the three sets of standards were met (lunchtime standards; standards that apply across the whole school day; and standards that apply only to foods served outside lunch). Lunchtime standards had the highest level of compliance, with an average of 81% of standards being met, ranging from 44% to 94%. Standards that apply across the whole school day had low levels of compliance (these are separate standards from the lunchtime standards but incorporate foods/drinks served at lunch as well as at other times of the day), at an average of 43% compliance across all schools, ranging from 25% to 67%. Standards for foods served outside lunch (e.g. at breakfast and breaktime) had an average of 64% compliance across schools, ranging from 25% to 100%, with slightly higher compliance in SFS-mandated schools (66% vs. 62% in SFS-non-mandated). Full judgements on compliance with the SFS for each school are available on the study web page (www.fundingawards.nihr.ac.uk/award/17/92/39).
| Percentage of standardsa met | |||
|---|---|---|---|
| All schools, mean % (range) | SFS-mandated, mean % (range) | SFS-non-mandated, mean % (range) | |
| All standards | 64.2 (53.1–77.4) | 63.5 (53.1–77.4) | 64.6 (53.1–75.0) |
| Lunchtime standards | 80.6 (43.9–93.8) | 80.6 (43.8–92.9) | 80.6 (62.5–93.8) |
| Standards that apply across the whole school day | 43.3 (25.0–66.7) | 41.3 (25.0–58.3) | 44.4 (25.0–66.7) |
| Standards for foods served outside lunch | 63.7 (25.0–100.0) | 66.0 (25.0–100.0) | 62.3 (25.0–100.0) |
Table 3 shows the proportion of schools meeting each standard (based on our 1-day school food observations and review of weekly menus). In general, standards related to ensuring a balance of food groups during lunch, and a range of options from food groups across the week, had high levels of compliance. There was 100% compliance across all 36 schools for some standards, for example one or more portions of starchy foods every day at lunch, one or more portions of fruit every day and at least three different types of vegetables each week.
| Standards | Schools providing data | Schools meeting the standard, N (%) | ||
|---|---|---|---|---|
| All schools | SFS-mandated | SFS-non-mandated | ||
| Lunchtime standards | ||||
| One or more portions of starchy foods every day | 36 | 36 (100.0) | 13 (100.0) | 23 (100.0) |
| Bread with no added fat or oil available every day | 35 | 10 (28.6) | 4 (33.3) | 6 (26.1) |
| Three or more different starchy foods each week | 36 | 35 (97.2) | 12 (92.3) | 23 (100.0) |
| One or more wholegrain varieties of starchy food each week | 36 | 29 (80.5) | 10 (76.9) | 19 (82.6) |
| One or more portions of vegetables/salad as an accompaniment every day | 36 | 36 (100.0) | 13 (100.0) | 23 (100.0) |
| One or more portions of fruit every day | 36 | 36 (100.0) | 13 (100.0) | 23 (100.0) |
| A dessert containing at least 50% fruit two or more times per week | 18 | 5 (27.8) | 1 (25.0) | 4 (28.6) |
| At least three different types of vegetables each week | 36 | 36 (100.0) | 13 (100.0) | 23 (100.0) |
| At least three different types of fruit each week | 36 | 32 (88.9) | 11 (84.6) | 21 (91.3) |
| A portion of meat, fish, eggs, beans and other non-dairy sources of protein food every day | 36 | 35 (97.2) | 12 (92.3) | 23 (100.0) |
| A portion of meat or poultry on 3 or more days per week | 36 | 36 (100.0) | 13 (100.0) | 23 (100.0) |
| Oily fish once or more every 3 weeks | 27 | 10 (37.0) | 4 (50.0) | 6 (31.6) |
| For vegetarians, a portion of non-dairy protein on 3 or more days each week | 35 | 33 (94.3) | 12 (92.3) | 21 (95.4) |
| A portion of milk or dairy foods every day | 36 | 35 (97.2) | 12 (92.3) | 23 (100.0) |
| Desserts, cakes and biscuits are allowed at lunchtime. They must not contain any confectionery | 35 | 3 (8.6) | 0 (0.0) | 3 (13.6) |
| Savoury crackers or breadsticks can be served at lunch with fruit or vegetables or dairy fooda | 36 | 32 (88.9) | 12 (92.3) | 20 (86.9) |
| Standards that apply across the whole school day | ||||
| Starchy foods cooked in fat or oil no more than 2 days a week | 36 | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| A meat or poultry product no more than twice a week | 36 | 7 (19.4) | 2 (15.4) | 5 (21.7) |
| Lower fat milk and lactose reduced milk must be available for drinking at least once a day during school hours | 36 | 28 (77.7) | 9 (69.2) | 19 (82.6) |
| No more than two portions of food that have been deep-fried, batter-coated or breadcrumb-coated, each week | 36 | 4 (11.1) | 0 (0.0) | 4 (17.4) |
| No more than two portions of food which include pastry each week | 35 | 5 (14.3) | 3 (23.1) | 2 (9.1) |
| No snacks, except nuts, seeds, vegetables and fruit with no added salt, sugar or fat | 36 | 18 (50.0) | 7 (53.8) | 11 (47.8) |
| No confectionery, chocolate or chocolate-coated products | 36 | 2 (5.5) | 0 (0.0) | 2 (8.7) |
| Where dried fruit is provided it must have no more than 0.5% vegetable oil as a glazing agenta | 32 | 31 (96.9) | 11 (100.00) | 20 (95.2) |
| Salt must not be available to add to food after it has been cooked | 35 | 32 (91.4) | 12 (92.3) | 20 (90.9) |
| Any condiments must be limited to sachets or portions of no more than 10 g or one teaspoonful | 34 | 17 (50.0) | 5 (41.6) | 12 (54.5) |
| Compliant drinks only | 36 | 5 (13.9) | 2 (15.4) | 3 (13.0) |
| Free fresh drinking water at all times | 35 | 34 (97.1) | 12 (92.3) | 22 (100.0) |
| Food provided outside lunch | ||||
| Fruit and/or vegetables available at every outlet | 36 | 29 (80.5) | 9 (69.2) | 20 (86.9) |
| No savoury crackers or breadsticksa | 36 | 33 (91.6) | 13 (100.0) | 20 (86.9) |
| No cakes or biscuits | 36 | 6 (16.6) | 4 (30.7) | 2 (8.7) |
| No desserts other than yoghurt or fruit-based desserts | 31 | 21 (67.7) | 8 (66.6) | 13 (68.4) |
The standards that we found to have low compliance mostly related to the restriction of foods and drinks high in fat, sugar or salt, for example starchy foods cooked in fat/oil on more than 2 days a week, no confectionery, chocolate or chocolate-coated products (only 6% met this standard), no cakes and biscuits outside lunch time (17% met this standard), and no more than two portions of deep-fried, batter-coated or breadcrumb-coated foods each week (11% met this standard). Only 14% of schools met the compliant drinks standard.
Overall, compliance with individual standards was similar in SFS-mandated and SFS-non-mandated schools, but there were some differences. A higher proportion of SFS-mandated schools complied with some standards (e.g. restriction of pastry items, and no cakes and biscuits sold outside lunch), but for other standards the SFS-non-mandated schools had higher compliance (e.g. no desserts, cakes or biscuits containing confectionery, restricted provision of fried or batter-/breadcrumb-coated foods, and availability of fruit/vegetables at every outlet).
Implementation of the School Food Plan actions (research objective 1b)
The mean proportion of identified SFP actions that were implemented to a high level in participating schools was 41%, ranging from 25% to 63%. The proportion of highly implemented standards was similar in SFS-mandated and SFS-non-mandated schools [42% (range 25–56%) for SFS-mandated, and 41% (range 29–63%) for SFS-non-mandated]. The percentage of schools receiving a judgement of ‘high’, ‘medium’ and ‘low’ for each action is provided in Appendix 6, Table 39, for all schools and by SFS group. For some actions, for example school food policies, there was a large number of missing data, so most schools have not had a judgement made for this action. Levels of implementation for all actions and all schools are available on the study web page (www.fundingawards.nihr.ac.uk/award/17/92/39).
Table 4 shows the SFP actions that were rated as being implemented to a ‘high’ level in > 50% of participating schools. Actions with many missing judgements were excluded from these tables (details are available on the study web page at www.fundingawards.nihr.ac.uk/award/17/92/39). Of the nine identified SFP themes, six had at least one action that was implemented to a high level in the majority of schools. These themes were a whole-school approach, school policies, catering provision and standards, the lunchtime experience, food education and increasing school meal access and take-up.
| SFP action | Schools providing data | Schools with ‘high’ implementationa N (%) | ||
|---|---|---|---|---|
| All schools | SFS-mandated | SFS-non-mandated | ||
| Whole-school approach | ||||
| Drinking water freely and easily available | 36 | 29 (80.6) | 11 (84.6) | 18 (78.3) |
| Demonstrate a culture/ethos of healthy eating to Ofsted | 32 | 20 (62.5) | 7 (70.0) | 13 (59.1) |
| Healthy-eating messages consistent across subjects and at lunchtime | 35 | 18 (51.4) | 8 (66.7) | 10 (43.5) |
| Policies | ||||
| Stay-on-site rule for break and lunchtime | 32 | 31 (96.9) | 10 (100.0) | 21 (95.5) |
| Catering provision and standards | ||||
| Catering staff supported to develop and learn | 26 | 19 (73.1) | 6 (66.7) | 13 (76.5) |
| The lunchtime experience | ||||
| Pupils having packed lunches and school meals sit together | 33 | 33 (100.0) | 12 (100.0) | 21 (100.0) |
| Catering staff happy/engaged | 36 | 32 (88.9) | 12 (92.3) | 20 (87) |
| Multiple service points | 36 | 29 (80.6) | 12 (92.3) | 17 (73.9) |
| Strategies to reduce queuing times | 35 | 27 (77.1) | 10 (83.3) | 17 (73.9) |
| Catering provider offers themed days | 24 | 17 (70.8) | 4 (44.4) | 13 (86.7) |
| Pupils have enough time to eat their lunch | 36 | 22 (61.1) | 8 (61.5) | 14 (60.9) |
| Food education | ||||
| Healthy eating as part of mandatory teaching | 32 | 30 (93.8) | 11 (100.0) | 19 (90.5) |
| Healthy eating taught across a range of subjects | 33 | 30 (90.9) | 11 (100.0) | 19 (86.4) |
| Cooking in curriculum for all pupils | 36 | 32 (88.9) | 11 (84.6) | 21 (91.3) |
| Qualified food education specialist | 33 | 26 (78.8) | 8 (72.7) | 18 (81.8) |
| Enough timetabling/resources for teaching cooking | 33 | 24 (72.7) | 8 (72.7) | 16 (72.7) |
| Increasing school meal access and take-up | ||||
| Cashless payment system | 31 | 28 (90.3) | 9 (90.0) | 19 (90.5) |
| School meal take-up is reported/monitored | 30 | 23 (76.7) | 7 (77.8) | 16 (76.2) |
| Food is available to pupils at breakfast time | 32 | 22 (68.8) | 7 (70.0) | 15 (68.2) |
There was some variation in the proportion of schools implementing these SFP actions to a high level across the SFS-mandated and SFS-non-mandated school groups (e.g. more SFS-mandated schools had multiple service points in the canteen and taught healthy eating across a range of subjects, whereas more SFS-non-mandated schools offered themed days as part of their catering provision).
We also explored the SFP actions that were rated as having ‘low’ implementation in > 50% of the participating schools, which are presented in Table 5. There were actions across all nine identified SFP themes that were not well implemented by the majority of schools.
| SFP action | Schools providing data | Schools with ‘low’ implementation,a N (%) | ||
|---|---|---|---|---|
| All schools | SFS-mandated | SFS-non-mandated | ||
| Whole school approach | ||||
| Sweets are not given as rewards | 36 | 25 (69.4) | 10 (76.9) | 15 (65.2) |
| Healthy-eating messages are promoted across the school | 36 | 21 (58.3) | 7 (53.8) | 14 (60.9) |
| Leadership and oversight on school food | ||||
| Governors lead on and engage with school food | 28 | 18 (64.3) | 6 (66.7) | 12 (63.2) |
| Policies | ||||
| Whole school food policy | 36 | 32 (88.9) | 13 (100.0) | 19 (82.6) |
| Engagement | ||||
| Pupils have the opportunity to assist catering staff | 36 | 34 (94.4) | 12 (92.3) | 22 (95.7) |
| School makes menus available in advance | 35 | 23 (65.7) | 8 (61.5) | 15 (68.2) |
| Catering provision and standards | ||||
| Compliance with the SFS checked | 29 | 23 (79.3) | 7 (70.0) | 16 (84.2) |
| School food award/quality assured scheme | 32 | 25 (78.1) | 8 (80.0) | 17 (77.3) |
| Catering team using the professional standards | 26 | 18 (69.2) | 6 (66.7) | 12 (70.6) |
| Catering staff integrated into school life | 26 | 14 (53.8) | 5 (55.6) | 9 (52.9) |
| Catering practices | ||||
| Prizes/incentives for a healthy packed lunch | 35 | 35 (100.0) | 12 (100.0) | 23 (100.0) |
| Catering staff encourage pupils to try new foods | 36 | 34 (94.4) | 12 (92.3) | 22 (95.7) |
| Cheaper ‘set menu’ meal offered to encourage a balanced meal | 30 | 17 (56.7) | 4 (36.4) | 13 (68.4) |
| The lunchtime experience | ||||
| Catering provider offers samples of the food | 36 | 34 (94.4) | 12 (92.3) | 22 (95.7) |
| Pupils don’t feel rushed to purchase foods from school | 36 | 26 (72.2) | 9 (69.2) | 17 (73.9) |
| School asks for feedback on the lunchtime experience | 19 | 11 (57.9) | 3 (60.0) | 8 (57.1) |
| Food education | ||||
| Growing/gardening is in the curriculum for all pupils | 35 | 35 (100.0) | 13 (100.0) | 22 (100.0) |
| Growing is taught outside the curriculum | 36 | 32 (88.9) | 12 (92.3) | 20 (87) |
| Cooking is taught outside the curriculum | 36 | 24 (66.7) | 9 (69.2) | 15 (65.2) |
| Increasing school meal access and take-up | ||||
| Governors obtain and review take-up data each term | 23 | 17 (73.9) | 7 (87.5) | 10 (66.7) |
Again, there was some variation between SFS-mandated and SFS-non-mandated schools in terms of the proportion of schools implementing standards to a low level (e.g. SFS-mandated schools were more likely to be rated as low on having a whole school food policy and on governors who obtain and review take-up data each term, whereas SFS-non-mandated schools were more likely to be rated as low on making menus available in advance, offering a cheaper ‘set menu’ to encourage a balanced meal and having an independent check of compliance with the SFS, either from governors or an external service).
Embedding of the school food standards and School Food Plan national school food policies within schools (research objectives 1a and 1b)
A total of 181 staff members and governors responded to the staff/governor survey, a response rate of 52% (n = 347 were invited). Table 6 shows the respondent characteristics. The majority of respondents were female (72%), and the most common age group was 30–49 years of age (52%). The largest number of respondents across the staff groups were the catering staff group (32%), followed by SLT representatives (25%), teachers (23%) and governors (21%). Forty-three staff from SFS-mandated schools and 138 staff from SFS-non-mandated schools answered the questionnaire.
| Characteristic | All schools, n (%) (n = 181) | SFS-mandated schools, n (%) (n = 43) | SFS-non-mandated schools, n (%) (n = 138) |
|---|---|---|---|
| Staff group (n = 181) | |||
| Catering | 57 (31.5) | 11 (25.6) | 46 (33.3) |
| SLT | 45 (24.9) | 13 (30.2) | 32 (23.2) |
| Teacher | 41 (22.7) | 9 (20.9) | 32 (23.2) |
| Governor | 38 (21.0) | 10 (23.3) | 28 (20.3) |
| Gender (n = 179) | |||
| Male | 51 (28.5) | 16 (37.2) | 35 (25.5) |
| Female | 124 (71.5) | 27 (62.8) | 101 (73.7) |
| Age (years; n = 180) | |||
| 18–29 | 11 (6.1) | 1 (2.3) | 10 (7.3) |
| 30–49 | 94 (52.2) | 24 (55.8) | 71 (51.8) |
| 50–64 | 65 (36.1) | 15 (34.9) | 49 (35.8) |
| ≥65 | 10 (5.6) | 3 (7.0) | 7 (5.1) |
| Years worked at school (n = 175) | |||
| < 2 | 42 (23.5) | 7 (16.7) | 36 (26.3) |
| 3–5 | 40 (22.3) | 7 (16.7) | 33 (24.1) |
| 6–10 | 38 (21.2) | 14 (33.3) | 24 (17.5) |
| > 10 | 59 (33.0) | 14 (33.3) | 44 (32.1) |
Awareness of the school food standards and School Food Plan
Table 7 presents the awareness and perceived implementation of, and familiarity with, the SFS and SFP by staff group and by SFS-mandated/SFS-non-mandated school groups. Nearly 80% of all staff were aware of the SFS, and this was similar across school groups (SFS-mandated, 80%; SFS-non-mandated, 75%). Catering staff reported highest awareness of (78.9% aware) and familiarity with (median familiarity score = 7.5/10) the SFS. Among staff reporting that they were aware of the SFS, the perception that the SFS were being implemented in the respondent’s school ranged from 48% to 80% across the different staff groups, with the highest proportion seen in the SLT group. This was similar across SFS-mandated (69%) and SFS-non-mandated (67%) schools.
| All school respondents (n = 181) | Catering staff (n = 57) | SLT members (n = 45) | Teachers (n = 41) | Governors (n = 38) | SFS-mandated school respondents (n = 43) | SFS-non-mandated school respondents (n = 138) | |
|---|---|---|---|---|---|---|---|
| SFS | |||||||
| Aware of SFS, n (%) | 133 (79.2) (n = 168) | 45 (78.9) | 35 (77.8) | 27 (65.9) | 26 (68.4) | 32 (80.0) | 102 (74.5) |
| Perceived implementation in school,a n (%) | 89 (67.9) (n = 131) | 33 (73.3) (n = 45) | 28 (80.0) (n = 35) | 13 (48.1) (n = 27) | 15 (57.7) (n = 26) | 22 (68.8) (n = 32) | 68 (66.7) (n = 102) |
| Involved in implementation/oversight of SFS, n (%) | 45 (39.5) (n = 115) | 29 (64.4) (n = 45) | 11 (31.4) (n = 35) | 4 (14.8) (n = 27) | 0 (0.0) (n = 26) | 10 (31.3) (n = 32) | 35 (35.0) (n = 101) |
| Familiarity score,b median (IQR) | 5 (4) (n = 117) | 7.5 (3.3) (n = 40) | 5 (3) (n = 31) | 4 (2) (n = 22) | 3.5 (4) (n = 24) | 5 (4) (n = 27) | 5 (4) (n = 90) |
| SFP | |||||||
| Aware of SFP, n (%) | 66 (41.8) (n = 158) | 27 (47.4) | 13 (28.9) | 12 (29.3) | 12 (31.6) | 16 (44.4) (n = 36) | 50 (36.2) |
| Perceived implementation in school,a n (%) | 39 (59.1) (n = 65) | 20 (74.1) (n = 27) | 7 (53.8) (n = 13) | 4 (33.3) (n = 12) | 8 (66.7) (n = 12) | 11 (68.8) (n = 15) | 28 (56.0) (n = 50) |
| Involved in implementation/oversight of SFP, n (%) | 23 (42.6) (n = 54) | 16 (59.2) (n = 27) | 5 (38.5) (n = 13) | 1 (8.3) (n = 12) | 0 (0.0) (n = 12) | 5 (31.3) (n = 15) | 18 (36.0) (n = 50) |
| Familiarity score,b median (IQR) | 5 (4.3) (n = 54) | 7 (4.5) (n = 23) | 4 (3.3) (n = 11) | 3 (3.3) (n = 9) | 5 (4.8) (n = 11) | 7 (3) (n = 13) | 4.5 (4.3) (n = 42) |
| Extent to which SFP is embedded in day-to-day work,c median (IQR) | 5 (4.5) (n = 52) | 8 (4) (n = 23) | 4 (3.5) (n = 11) | 3 (4.3) (n = 9) | 4 (5.6) (n = 9) | 7 (6) (n = 12) | 5 (5) (n = 41) |
Around 40% of all staff were involved in the SFS implementation and/or oversight in their schools. The catering staff group had the highest proportion reporting that they were involved (64%). No school governor respondents and only 31% of SLT respondents reported being involved in the implementation or oversight of the SFS. School governors also reported being the least familiar with the SFS (median familiarity score = 3.5/10). Similar proportions of staff were involved in SFS implementation across SFS-mandated (31%) and SFS-non-mandated (35%) schools. Familiarity with the SFS was similar across mandated and non-mandated school groups.
Awareness of the SFP was much lower, with around 42% of all staff reporting that they were aware of the SFP. The group with lowest awareness were SLT members, and those with highest awareness were caterers. Awareness of the SFP was slightly higher in SFS-mandated (44%) than in SFS-non-mandated schools (36%), as was the perception that SFP actions were being implemented. Of those aware of the SFP, 69% and 56% reported that SFP actions were implemented in their schools in SFS-mandated and SFS-non-mandated schools, respectively. The perception that SFP actions were being implemented in their school was highest in the catering staff group (74% of those aware of the SFP).
Around 43% of all staff who were aware of the SFP said they were involved in implementing the SFP recommendations, with the highest proportion seen in catering staff (59%). Again, no school governors reported involvement in the implementation or oversight of the SFP. A slightly higher proportion of staff in SFS-non-mandated schools (36%) reported involvement in SFP implementation than those in mandated schools (31%). Overall familiarity median score was 5 for all staff, ranging from 3 to 7 within staff groups. Familiarity with the SFP was higher for SFS-mandated than for SFS-non-mandated schools, and, regarding staff groups, highest in the catering and lowest in the teacher groups. The extent to which the SFP was perceived to be embedded into daily work was highest for catering and lowest for teaching staff, and higher for SFS-mandated than for SFS-non-mandated schools.
Implementation of the school food standards: normalization process theory constructs
Responses to the questions on implementation of the SFS, relating to the four NPT constructs, are presented in Figure 3.
FIGURE 3.
Staff responses to questions relating to NPT implementation constructs for the SFS. Note: number of respondents for each statement ranges from 112 to 119; x-axis indicates the percentage of respondents within each agreement category.
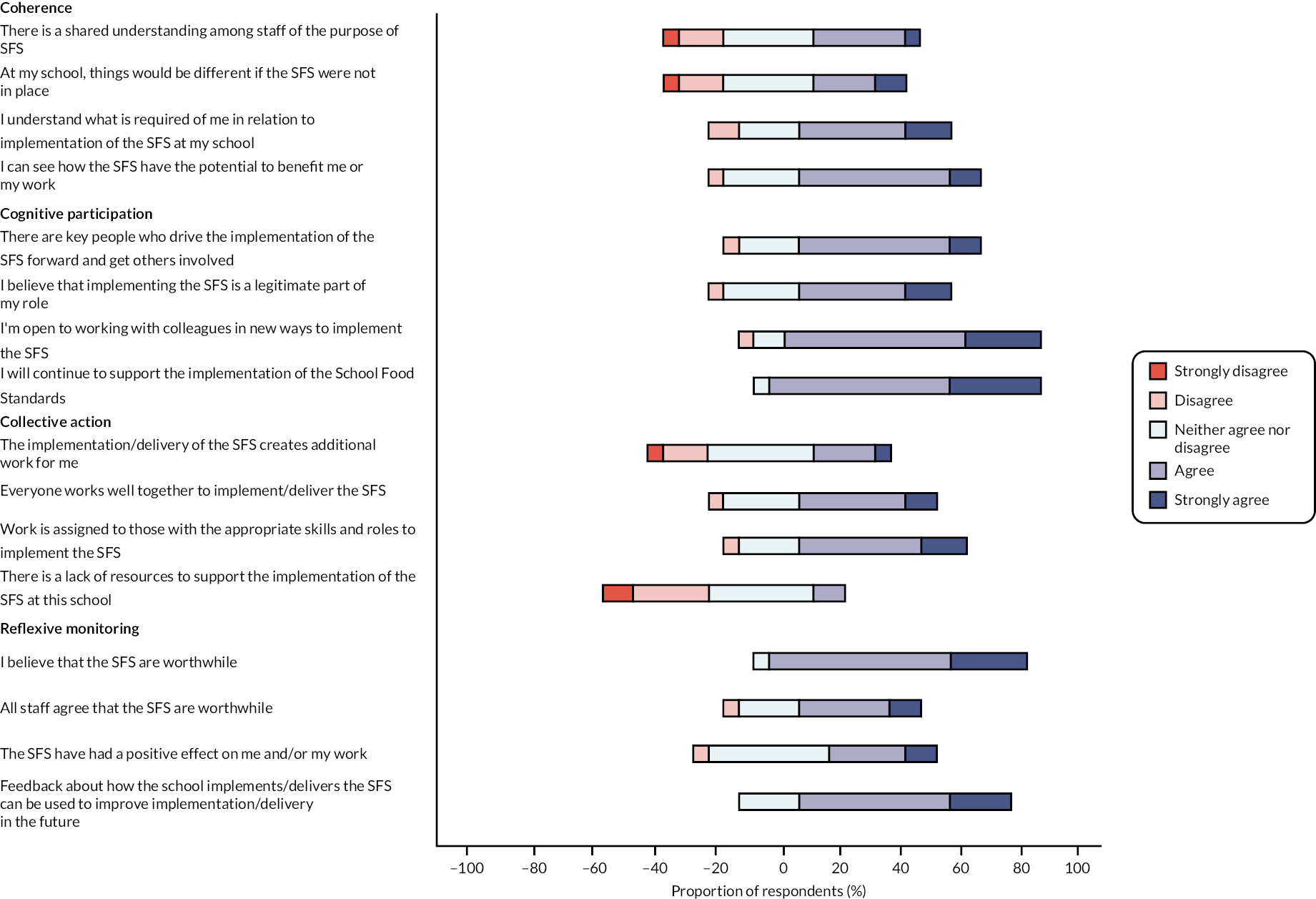
Coherence (sense-making)
Just over one-third of all staff (36%) agreed that there was a shared understanding among staff in their school about the purpose of the SFS, and just 29% believed that things would be different if the SFS were not in place. Around half of respondents (52%) understood what is required of them in relation to the SFS, and 60% said they could see how the SFS had the potential to benefit them and their work. Table 1 in Report Supplementary Material 1 provides additional detail by SFS group. Compared with SFS-non-mandated schools, more staff in SFS-mandated schools believed that things would be different if the SFS were not in place (44% vs. 24%), understood what is required of them (59% vs. 49%) and could see the potential benefits of the SFS (70% vs. 56%).
Cognitive participation (engagement)
Around 62% of all staff felt that there were key people in their school who drove the implementation of the SFS: 56% in SFS-mandated and 64% in SFS-non-mandated schools. Among those answering the question, 52% in SFS-mandated schools and 54% of staff in SFS-non-mandated schools agreed that implementing the SFS was a legitimate part of their role. Staff were open to working with colleagues in new ways to implement the SFS (77% in SFS-mandated and 85% in SFS-non-mandated) and 85% and 90% would continue to support the implementation of the SFS in SFS-mandated and SFS-non-mandated schools, respectively.
Collective action (implementation)
Generally, only a minority of respondents involved in implementation of the SFS perceived that it created extra work for them (26%), and this was lower in SFS-mandated schools (24%) than in SFS-non-mandated schools (27%). Overall, 49% felt that everyone worked well together to implement the SFS, but the agreement was higher in SFS-mandated schools (62%) than in SFS-non-mandated schools (46%). Over half of all staff felt that work was assigned to the correct staff (56%; 63% in SFS-mandated and 55% in SFS-non-mandated schools). Staff overall felt that there were enough resources, with only 4% in SFS-mandated schools and 12% in SFS-non-mandated schools reporting a lack of resources.
Reflexive monitoring (informal and formal appraisal)
Ninety-six per cent of staff in SFS-mandated and 85% of staff in SFS-non-mandated schools believed that the SFS were worthwhile; however, when staff were asked to consider general staff opinion across the school, 34% in SFS-non-mandated and 75% in SFS-mandated schools agreed that all staff believed the SFS were worthwhile. Thirty-eight per cent of those in SFS-mandated schools and 34% of staff in SFS-non-mandated schools believed that the SFS had a positive effect on their work, and 69%, compared with 71%, felt that feedback about how their school implements/delivers the SFS could be used to improve their implementation in the future in SFS-non-mandated and SFS-mandated schools, respectively.
Implementation of the School Food Plan: normalization process theory constructs
Responses to the questions on implementation of the SFP actions, relating to the four NPT constructs, are presented in Figure 4. A detailed table of responses is provided in Report Supplementary Material 1, Table 2.
FIGURE 4.
Staff responses to questions relating to NPT implementation constructs for the SFP. Note: number of respondents for each statement ranges from 54 to 56; x-axis indicates the percentage of respondents within each agreement category.
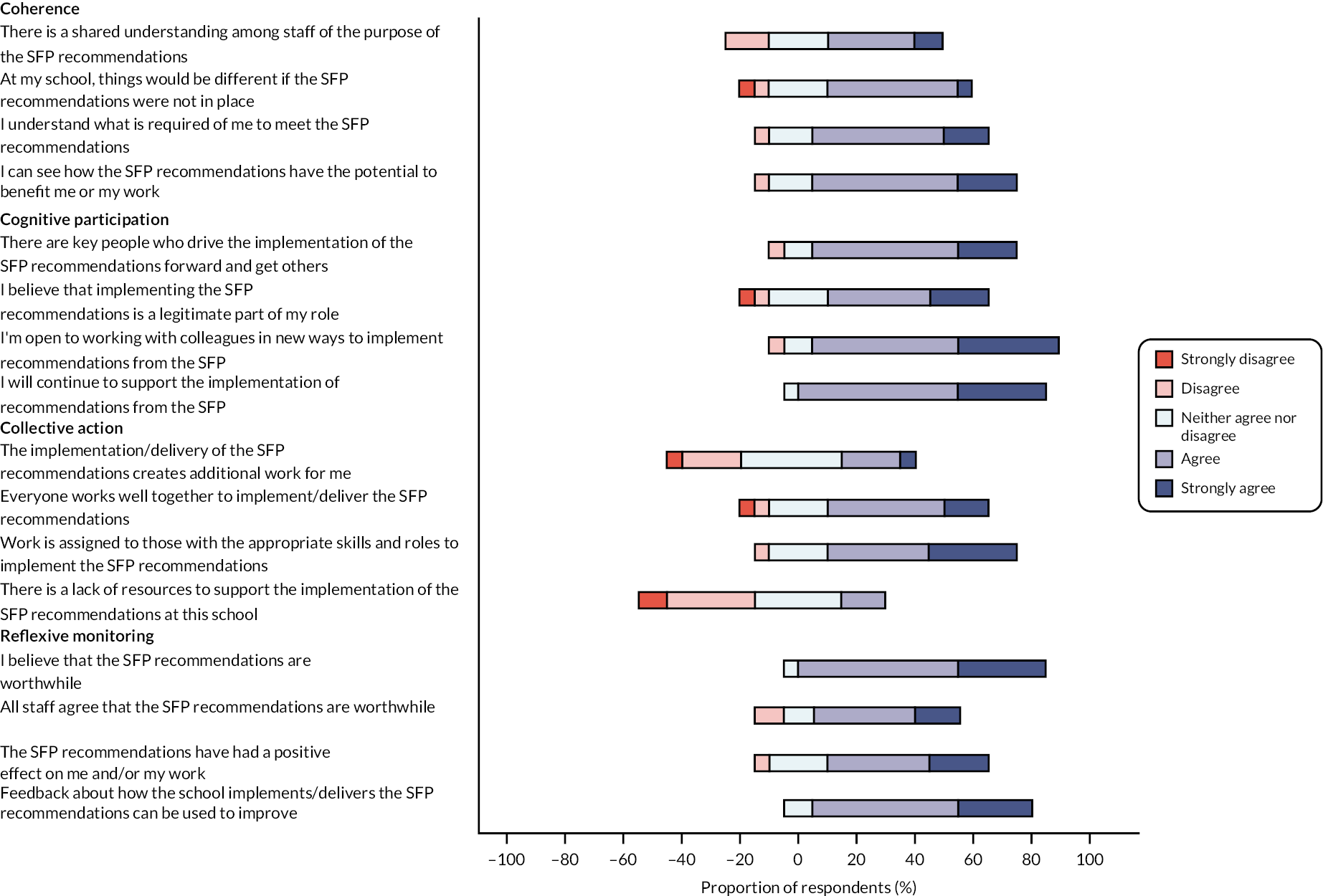
Coherence (sense-making)
Overall, of the respondents who were aware of the SFP, 41% reported that there was a shared understanding of the SFP. This differed across SFS-mandated (36%) and SFS-non-mandated schools (43%). Fifty per cent of staff in SFS-non-mandated schools, compared with 71% of staff in SFS-mandated schools, felt that things would be different in their school if the SFP actions were not in place. An understanding of what was required of them was lower for staff in SFS-mandated schools (57% vs. 66% in SFS-non-mandated schools). In the SFS-mandated schools, 86% of respondents felt that they could see how the SFP actions benefitted them, compared with 62% in SFS-non-mandated schools.
Cognitive participation (engagement)
Across all staff who were aware of the SFP, 71% (79% in SFS-mandated and 68% in SFS-non-mandated schools) felt that there were key people to drive implementation the SFP actions in their school. Just over half of all staff (55%) believed that implementing the SFP actions was part of their role. Seventy-nine per cent of staff in SFS-mandated and 83% in SFS-non-mandated schools were open to working with colleagues in new ways to implement the SFP actions, and most staff (93% in SFS-mandated vs. 81% in SFS-non-mandated) supported the continued implementation of the actions.
Collective action (implementation)
Generally, a small proportion of respondents felt that the implementation of the SFP actions created extra work for them (8% in SFS-mandated and 27% in SFS-non-mandated schools). Only 39% of staff in the SFS-mandated schools felt that everyone worked well together to implement and deliver the SFP actions, compared with 56% in SFS-non-mandated schools. Sixty-one per cent and 64% agreed that work was assigned to the correct individuals in SFS-non-mandated and SFS-mandated schools, respectively. As with the SFS, most staff felt that there were appropriate resources for implementing the SFP actions.
Reflexive monitoring (informal and formal appraisal)
A higher percentage of staff in the SFS-mandated schools (93%) than in the SFS-non-mandated schools (83%) believed the SFP actions were worthwhile, but, as with the SFS, perceptions of all staff across the school on the SFP being worthwhile were lower (46% in SFS-non-mandated vs. 71% in SFS-mandated). More staff in SFS-mandated schools felt that the SFP had a positive effect on their work (71% vs. 49% in SFS-non-mandated schools). Overall, staff felt that feedback about the SFP implementation would be useful (70% in SFS-non-mandated schools vs. 93% in SFS-mandated schools).
Detailed tables of staff responses to NPT-based questions by staff group are provided in Report Supplementary Material 1, Tables 3 and 4.
School food typology (research objective 2)
Initially, four school types were identified (types 1–4) based on levels of implementation of the two sets of SFS (standards relating to obesity and dental health and standards relating to variety). Types 1 and 3 were then divided into A and B subtypes based on their implementation of the indicator SFP actions. Table 8 shows the types and the number of schools in each type.
| Type (based on SFS) | Compliance with obesity/dental-health-related SFS | Compliance with dietary variety-related SFS | Subtype (based on SFP) | Level of SFP Implementation | N (%) schools |
|---|---|---|---|---|---|
| 1 | Low | High | 1A | Low | 15 (42) |
| 1B | High | 6 (17) | |||
| 2 | Medium | Medium | 2B | High | 1 (3) |
| 3 | Medium | High | 3A | Low | 5 (14) |
| 3B | High | 8 (22) | |||
| 4 | High | High | 4A | Low | 1 (3) |
The largest proportion of the schools in the sample were type 1A (42%), while the smallest groups were types 2 and 4, which included only one school each. These types could therefore not be subdivided; however, the type 2 school had high levels of SFP implementation (> 50% of the selected SFP indicator actions implemented to a high level; subtype B) and type 4 had lower levels of SFP action (< 50% of the selected SFP indicator actions implemented to a high level; subtype A). Table 9 shows which SFP actions were rated as having been implemented to a high or low/medium level for the different subtypes.
| Subtype | Implementation level rated ‘high’a | Implementation level rated ‘low’ or ‘medium’ |
|---|---|---|
| 1A |
|
|
| 1B |
|
|
| 2B |
|
|
| 3A |
|
|
| 3B |
|
|
| 4A |
|
|
|
Each subtype varied in the actions rated as being implemented to a high or low/medium level, but, in general, schools in types 1A and 3A (low SFP implementers) had low levels of parental engagement with school food, did not have strategies in place for promoting school meal take-up, did not offer a cheaper ‘set menu’ to encourage a balanced meal, did not integrate catering staff into school life and did not consider the environment when choosing their suppliers. On the other hand, schools in types 1B and 3B performed well on considering the environment when choosing their suppliers, demonstrating a culture and ethos of healthy eating to Ofsted and having an attractive dining environment. Type 2B performed well on encouraging a sit-down meal and having senior leaders that lead on and engage with school food, and types 2B and 4A had food available to pupils at breakfast time and made efforts to promote school meal take-up, but both were similar to 1A–3A in actions that they implemented to a low/medium level (e.g. low levels of parental engagement with school food, did not offer a cheaper ‘set menu’ to encourage a balanced meal, did not integrate catering staff into school life and did not consider the environment when choosing their suppliers).
Table 10 shows the contextual data for the school types. Type 1 schools (low compliance with SFS related to obesity/dental health; high compliance with SFS related to variety) were more likely to have a sixth form and a higher proportion of pupils receiving FSM than type 3 schools (medium compliance with SFS related to obesity/dental health; high compliance with SFS related to variety). The higher-performing schools in terms of SFS (types 3 and 4) were more likely to have in-house catering. Type 3 schools had the lowest uptake of school food at lunchtime from the participants in our pupil sample, while the type 2 school had the highest uptake as a result of a policy prohibiting packed lunches except in exceptional circumstances.
| Type | N in urban area (%) | Mean pupils, n (range) | % with sixth form | Mean % FSM (range) | Mean % ethnic minorities (range) | % with external caterers | Mean % pupils having school- luncha (range) |
|---|---|---|---|---|---|---|---|
| 1A (n = 15) | 13 (86.6) | 1192 (612–1774) | 14 (93.3) | 19.5 (2.8–61.8) | 26.1 (5.2–98.2) | 10 (66.6) | 54.9 (36.6–71.3) |
| 1B (n = 6) | 6 (100.0) | 990 (857–1181) | 5 (83.3) | 26.7 (18.2–43.6) | 33.5 (8.6–82.1) | 5 (83.3) | 59.0 (41.9–76.4) |
| 2B (n = 1) | 1 (100.0) | 1110 | 1 (100.0) | 21.4 | 63.1 | 1 (100.0) | 94.0b |
| 3A (n = 5) | 4 (80.0) | 895 (690–1162) | 2 (40.0) | 12 (6–15.9) | 20.7 (8–47) | 1 (20.0) | 44.0 (26.2–67.2) |
| 3B (n = 8) | 5 (62.5) | 1096 (820–1692) | 3 (37.5) | 18.2 (7.2–34.9) | 27.1 (4.1–58.5) | 4 (50.0) | 53.4 (28.8–70.5) |
| 4A (n = 1) | 1 (100.0) | 867 | 1 (100.0) | 32.2 | 79.4 | 0 (0) | 63.9 |
School food uptake and sales (research objective 1a)
Uptake of school lunches
School lunch uptake data were reported by 20 schools (56% of sample), but there was a large difference in the proportion of SFS-mandated and SFS-non-mandated schools providing this information (23% of SFS-mandated schools vs. 74% of SFS-non-mandated schools). On average, schools reported that 54% of pupils purchased school lunch, with a similar range of values for SFS-mandated and SFS-non-mandated schools. The SFS-mandated group includes one school that had a policy of no packed lunches, so it includes a school with 100% school meal uptake (reported by the school). We also calculated the proportion of pupil participants having school-provided food for lunch in each participating school from Intake24 data. We observed similar levels of school lunch uptake using this pupil-reported data (Table 11).
| Schools providing data, n (%) | Mean school-reported % school lunch uptake (range) | Mean pupil-reporteda % school lunch uptake (range) | |
|---|---|---|---|
| Mandated | 3 (23.1) | 57.0 (31.0–100.0) | 55.5 (26.2–94) |
| Not mandated | 17 (73.9) | 52.9 (35.0–75.0) | 54.8 (28.8–76.4) |
| Total | 20 (55.5) | 53.5 (31.0–100.0) | 55.1 (26.2–94) |
School food sales
Thirteen of 36 schools (36%) provided monthly itemised food sales data. Eleven of these schools provided data for more than one time period. The number of food and drink items sold in 1 month ranged from 8821 (ID6 – a small school that reported 54% school meal uptake) to 62,592 (ID17 – a large school reporting 70% school meal uptake). The average number of food/drink items sold per pupil attending the school for each month ranged from 12 (ID39 and ID45, June 2020) to 36 (ID14, November 2019). Sales data were not requested for June 2020 due to restricted school openings during the first national lockdown in response to the COVID-19 pandemic.
For schools providing data for both June and November of any year (n = 9), sales per pupil were higher in November than in June. For schools providing data before the COVID-19 pandemic and during the pandemic (n = 4), total sales were substantially lower during the pandemic (i.e. November 2019 vs. November 2020–November 2021). Comparisons between SFS-mandated and SFS-non-mandated schools were limited due to the small number of SFS-mandated schools providing data, with only one school providing data over multiple time points. However, when the mean for all schools and all time points was taken for the SFS-mandated and SFS-non-mandated groups, sales per pupil were similar (Table 12).
| Mean number of sales per pupil (range) | ||||||
|---|---|---|---|---|---|---|
| June 2019 | November 2019 | November 2020a | June 2021a | November 2021a | Mean for all time points | |
| SFS-mandated, n = 3 | 20b | 19b | 20b | 28 (25–31) | 23 (19–31) | |
| SFS-non-mandated, n = 10 | 22 (15–29) | 28 (20–36) | 20 (14–24) | 13 (12–15) | 15 (13–16) | 21 (12–36) |
| All schools, n = 13 | 22 (15–29) | 27 (20–36) | 20 (14–24) | 14 (12–15) | 21 (13–31) | 21 (12–36) |
Sales of indicator items
Foods and drinks identified as indicator items comprised 26–77% of total sales for schools. The remaining items are those that were not indicator items (e.g. pizza, sandwich, yoghurt, crumpet, meals) or those that were ambiguous (e.g. 75 pence bag, ‘grab and go’, drink, lite bite, extra, miscellaneous). Table 13 presents the sales of the indicator items per month, expressed as a percentage of the total items sold.
| Indicator item | Mean percentage of total sales per month (range) | |||||
|---|---|---|---|---|---|---|
| June 2019 | November 2019 | November 2020 | June 2021 | November 2021 | All time periods | |
| Confectionery/chocolate | 1.2 (0–3.7) | 1 (0–3.4) | 1.2 (0–3.1) | 1.2 (0–2.9) | 1.9 (0–7.7) | 1.2 (0–7.7) |
| Starchy foods in fat or oil | 2.6 (1.3–4.8) | 2.7 (0.6–4.7) | 3 (0–4.9) | 1.7 (0–3.8) | 2 (0–4.1) | 2.4 (0–4.9) |
| Pastry items | 7.7 (5.3–9.6) | 6.3 (1.4–16.9) | 6.8 (3.6–11.7) | 4 (0.4–9.0) | 3.3 (0.1–7.9) | 5.6 (0.1–16.9) |
| Dessert, cakes, biscuits | 16.8 (8.3–25.3) | 16.8 (7.4–27.1) | 14.7 (5.0–23.4) | 16.8 (8.6–26.4) | 19.8 (10.0–33.1) | 16.8 (5.0–33.1) |
| Other non-compliant snacks | 0.6 (0–1.5) | 1.4 (0–5.7) | 2.3 (0–5.8) | 1.8 (0–7.9) | 1.9 (0–7.3) | 1.7 (0–7.9) |
| Fruit | 0.9 (0.2–1.9) | 0.9 (0.2–1.7) | 0.9 (0.5–1.4) | 0.9 (0.1–1.9) | 1.3 (0.4–2.4) | 1.0 (0.1–2.4) |
| Vegetable | 0 (0–0.1) | 0.2 (0–1.0) | 0.3 (0–1.1) | 0.4 (0–1.6) | 1.3 (0.4–5.2) | 0.4 (0–5.2) |
| Compliant drink | 8.4 (4.3–13.8) | 12.5 (6.3–19.0) | 10.2 (6.6–13.9) | 7.2 (1.0–13.2) | 8.8 (0.7–14.9) | 9.8 (0.7–19.0) |
| Plain water | 5.1 (0.9–8.6) | 4.8 (1.0–9.9) | 5 (2.9–8.0) | 7.2 (3.1–14.6) | 3.5 (3.2–4.8) | 5.2 (0.9–14.6) |
| Non-compliant drink | 9.2 (0–21.4) | 5 (0.9–13.9) | 6.2 (1.2–11.1) | 6.7 (0.4–12.7) | 6.4 (3.0–10.7) | 6.3 (0–21.4) |
| Other drink | 0.2 (0–0.5) | 1.1 (0–3.9) | 0.7 (0–2.9) | 5.6 (0–12.2) | 4.1 (0–12.5) | 2.4 (0–12.5) |
| Indicator items as % of total sales | 52.7 (30.0–76.9) | 52.5 (25.8–74.0) | 51.2 (42.6–62.0) | 53.6 (43.0–61.0) | 54.3 (49.0–61.5) | 52.8 (25.8–76.9) |
Of the indicator items, desserts, cakes and biscuits had the highest mean percentage of total sales, ranging from 5% to 33% across the included schools. Desserts, cakes and biscuits are permitted within the SFS at lunchtime only, as long as they do not contain confectionery. It was not possible to tell the extent to which the desserts, cakes and biscuits offered were compliant (i.e. did not contain confectionery) or non-compliant (i.e. contained confectionery) from the sales data, and we were not able to consistently determine the proportion of desserts, cakes and biscuits that were sold outside lunchtime (also indicative of non-compliance).
Drinks made up a large proportion of total sales in some schools, accounting for 11–34% of total sales, with sales of known non-compliant drinks accounting for 0–21% of total sales. Sales of plain water ranged from 1% to 15% of total sales, while compliant drinks ranged from 1% to 19% of total sales.
Confectionery/chocolate items (not permitted within the SFS) and other SFS-non-compliant snacks (e.g. crisps) also constituted a substantial proportion of sales in some schools, ranging from 1% to 7% of total sales and from 0% to 8% of total sales, respectively. Pastry items and starchy foods cooked in fat/oil are permitted twice a week within the SFS. These items constituted 0–17% and 0–5% of total sales, respectively.
In general, F&V made up a low proportion of sales (ranging from 0.1% to 2% and 0.4% to 5% of total sales, respectively). It is important to note that vegetable dishes in particular were difficult to identify within the data; sometimes these would be incorporated into a main meal and so would not be identifiable in the food sales records. Only items clearly marked as salad, vegetable sides or baked beans were included in this category. These values are therefore likely to be an under-representation of the sales of vegetables.
The proportion of items classed as miscellaneous also provides some insight into the quality of the food sales data, giving an indication of the proportion of items that could not be identified as indicator foods or otherwise by the descriptive labels provided (details of miscellaneous items are available on the study web page at www.fundingawards.nihr.ac.uk/award/17/92/39). The proportion of miscellaneous items ranged from 0% to 9%, suggesting that most items could be identified; however, it remains likely that some items have been missed from our classification of indicator foods and the degree of missing data varies by school.
Sales of indicator foods by school food standards-mandated/school food standards-non-mandated status
Of the three SFS-mandated schools providing food sales data, two provided November data only, and one included pre-pandemic data (2019). Of the 10 SFS-non-mandated schools, 2 provided November data only, and 6 included pre-pandemic data.
Figure 5 provides details of sales of indicator items as a percentage of total sales per month by SFS group. Sales of confectionery/chocolate items (which are not permitted within the SFS) and pastry items were higher in SFS-non-mandated schools than in SFS-mandated schools (1.5% vs. 0% and 6% vs. 4% of total sales, respectively). Sales of desserts, cakes and biscuits were slightly higher in SFS-non-mandated schools (17% vs. 15.5%). Sales of starchy foods cooked in fat/oil and other non-compliant snacks were slightly higher in SFS-mandated schools (4% vs. 2% and 4% vs. 1% of total sales, respectively). Sales of fruit were the same across both groups, while sales of vegetables and salads were higher in SFS-non-mandated schools (0.5% vs. 0.1%). Sales of non-SFS-compliant drinks were higher in SFS-mandated schools than in SFS-non-mandated schools (10% vs. 6%), but sales of SFS-compliant drinks were also higher (12% vs. 9%), while sales of plain water were lower (3% vs. 6%).
FIGURE 5.
Sales of indicator items as a percentage of total sales per school per month, by SFS-mandated and SFS-non-mandated schools.
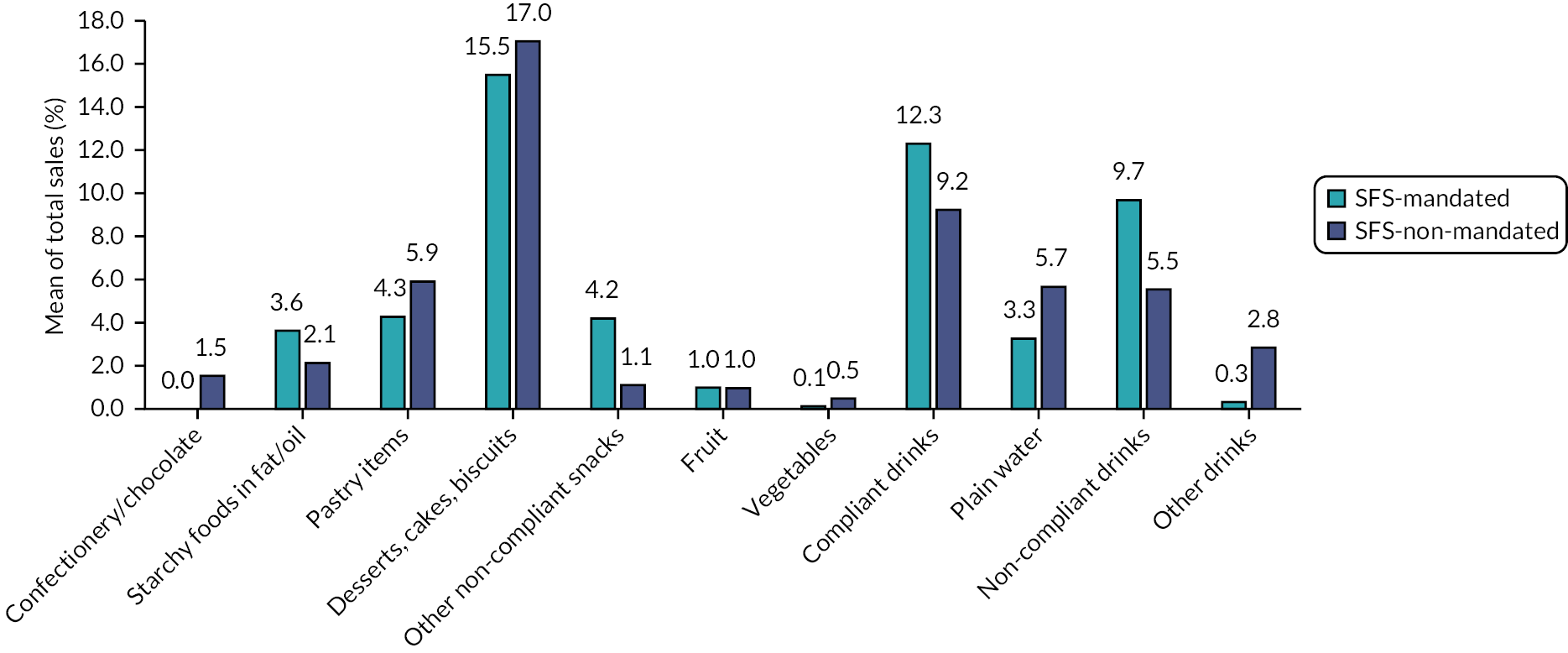
There are key limitations to note with these data. Only three SFS-mandated schools provided data, so outliers (e.g. high values in single schools) are likely to have a larger impact on the mean values for this group, and only one-third of the school sample provided sales data overall, which limits the representativeness of the data and the usefulness of comparisons across the two groups.
Full details of mean monthly sales of indicator items by school are provided in Report Supplementary Material 2, Table 1.
Pupil sample
Across the 36 participating schools, 2543 pupils (of approximately 2575 invited) consented to participate in the study and provided some valid data (99%). Note that an approximate figure is given for number of pupils invited because of difficulties in obtaining absolute numbers from schools (e.g. pupils absent on the day that paper invitations were sent, or non-response of teaching staff to requests for figures, in which case average class size for the school was used). Thirty-two parental opt-out forms were received. Among the participating pupils, 90 provided no outcome data and were excluded from the pupil outcome analysis. Of the 2453 pupil participants providing some outcome data, 2273 provided nutritional and 2268 provided dental outcome data. Participant recruitment and reasons for missing outcome data are presented in Figure 6.
FIGURE 6.
Recruitment of pupil participants.
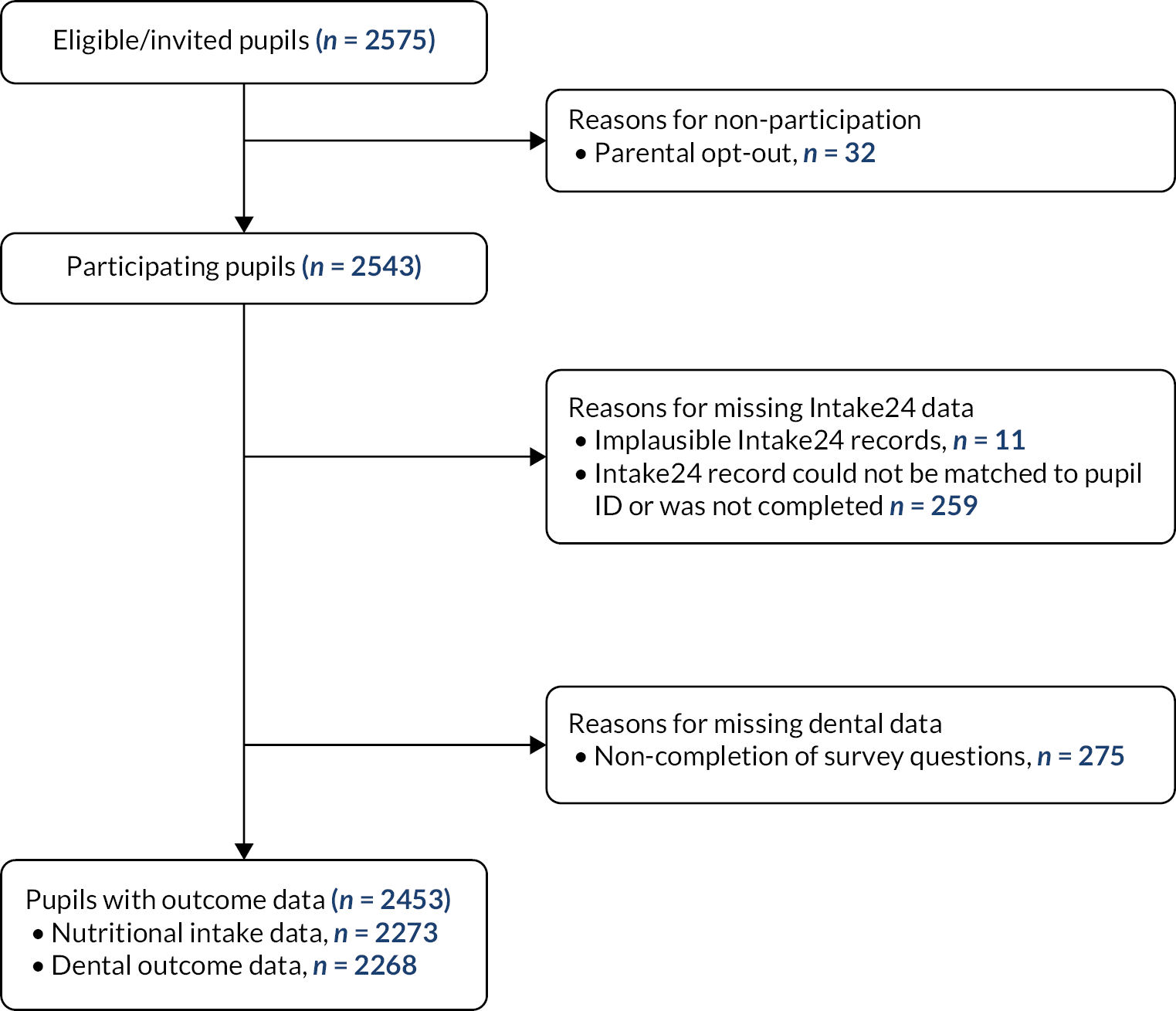
We compared characteristics of those with and those without outcome data, and those with and those without nutritional intake (primary outcome) data (see Report Supplementary Material 3, Tables 1 and 2). Pupils with missing primary and other outcome data were more likely to be in the youngest year group and male.
Pupil participant characteristics are presented in Table 14. Of 2453 participants, 836 were in the SFS-mandated and 1617 were in the SFS-non-mandated school group. The SFS-mandated school group had a higher proportion of participants from more deprived areas, in receipt of FSM and of white ethnicity, and a lower proportion of female participants.
| Characteristic | Total (N = 2453), n (%) | Attending SFS-mandated schools (N = 836), n (%) | Attending SFS-non-mandated schools (N = 1617), n (%) |
|---|---|---|---|
| Year group | |||
| 7 | 826 (33.67) | 292 (34.93) | 534 (33.02) |
| 9 | 826 (33.67) | 274 (32.78) | 552 (34.14) |
| 10 | 801 (32.65) | 270 (32.30) | 531 (32.84) |
| Age (years), mean (SD) | 13.63 (1.29) | 13.64 (1.33) | 13.63 (1.27) |
| Missing | 60 | 24 | 36 |
| IMD quintile group | |||
| 1 (highest deprivation) | 574 (25.74) | 253 (34.10) | 321 (21.57) |
| 2 | 375 (16.82) | 157 (21.16) | 218 (14.65) |
| 3 | 442 (19.82) | 161 (21.70) | 281 (18.88) |
| 4 | 412 (18.48) | 89 (11.99) | 323 (21.71) |
| 5 (lowest deprivation) | 427 (19.15) | 82 (11.05) | 345 (23.19) |
| Missing | 223 | 94 | 129 |
| Sex | |||
| Female | 1348 (54.95) | 417 (49.88) | 931 (57.58) |
| Male | 1018 (41.50) | 385 (46.05) | 633 (39.15) |
| Other/unknown | 87 (3.55) | 34 (4.07) | 53 (3.28) |
| Ethnicity | |||
| White | 1709 (69.67) | 619 (74.04) | 1090 (67.41) |
| Asian/Asian British | 375 (15.29) | 92 (11.00) | 283 (17.50) |
| Black/African/Caribbean/Black British | 137 (5.58) | 40 (4.78) | 97 (6.00) |
| Mixed/multiple | 134 (5.46) | 53 (6.34) | 81 (5.01) |
| Other ethnic group/unknown | 98 (4.00) | 32 (3.83) | 66 (4.08) |
| FSM | |||
| Yes | 290 (15.38) | 117 (19.80) | 173 (13.37) |
| No | 1491 (79.10) | 437 (73.94) | 1,054 (81.45) |
| Pupil did not know | 104 (5.52) | 37 (6.26) | 67 (5.18) |
| Missing | 568 | 245 | 323 |
| Consuming a school-provided lunch | |||
| Never | 395 (26.64) | 104 (26.67) | 291 (26.62) |
| Less than once a week | 146 (9.84) | 26 (6.67) | 120 (10.98) |
| 1–2 times a week | 219 (14.77) | 51 (13.08) | 168 (15.37) |
| 3–4 times a week | 180 (12.14) | 50 (12.82) | 130 (11.89) |
| Every school day | 543 (36.61) | 159 (40.77) | 384 (35.13) |
| Missing | 970 | 446 | 524 |
Comparison of pupil outcomes across school food standards-mandated and school food standards-non-mandated school groups (research objective 1c)
Nutritional intake
Of the 2273 participants providing nutritional intake data, 1046 (46%) had two 24-hour dietary records, with the remaining 54% having one record. The proportion of participants with two 24-hour dietary intake records was lower in the SFS-mandated school group than in the SFS-non-mandated group (37% vs. 51%).
Pupils’ mean nutrient intakes at lunch, across the school day and over 24 hours are shown by SFS-mandated and SFS-non-mandated schools in Table 15. There was some variation across SFS-mandated and non-SFS mandated schools, with pupils from SFS-mandated schools reporting less free sugar intake at lunch, but more during the school day and over 24 hours, and a higher percentage TEI from free sugar across the whole day (24 hours). Pupils in the SFS-mandated schools had lower energy, fat, fibre and F&V intake across all time periods, and a lower proportion of pupils in the SFS-mandated schools consumed five or more F&V portions in 24 hours.
| Nutrient/food item | Luncha | School dayb | 24 hours | |||
|---|---|---|---|---|---|---|
| SFS-mandated (n = 715), mean (SD) | SFS-non-mandated (n = 1373), mean (SD) | SFS-mandated (n = 734), mean (SD) | SFS-non-mandated (n = 1414), mean (SD) | SFS-mandated (n = 773), mean (SD) | SFS-non-mandated (n = 1500), mean (SD) | |
| Free sugar (g) | 15.58 (18.40) | 16.89 (19.83) | 27.98 (33.81) | 26.17 (29.30) | 75.36 (61.88) | 72.33 (63.01) |
| % TEI from free sugar | 12.03 (13.68) | 12.26 (13.40) | 14.09 (12.68) | 13.84 (12.82) | 15.77 (9.54) | 14.77 (9.24) |
| TEI (kcal) | 503.12 (317.90) | 540.57 (352.05) | 701.27 (482.81) | 714.59 (484.98) | 1736.38 (876.57) | 1785.23 (880.46) |
| Fat intake (g) | 20.34 (15.02) | 21.72 (17.16) | 28.13 (21.09) | 29.01 (23.55) | 67.19 (38.83) | 68.81 (40.25) |
| Fibre intake (g) | 4.57 (3.26) | 4.81 (3.29) | 6.00 (4.36) | 6.14 (4.24) | 14.87 (8.18) | 15.81 (8.28) |
| F&V portions | 0.61 (0.84) | 0.86 (1.06) | 0.83 (1.10) | 1.06 (1.30) | 2.30 (2.10) | 2.74 (2.21) |
| Number of SSB items | 0.12 (0.31) | 0.09 (0.26) | 0.18 (0.44) | 0.14 (0.37) | 0.48 (0.77) | 0.37 (0.69) |
| Number of HFSS items | 0.89 (0.92) | 0.93 (0.92) | 1.39 (1.22) | 1.44 (1.17) | 2.94 (1.93) | 3.01 (1.89) |
| Number of sugar/chocolate confectionery items | 0.13 (0.32) | 0.13 (0.34) | 0.25 (0.46) | 0.23 (0.44) | 0.42 (0.61) | 0.43 (0.66) |
| >5% of 24-hour TEI from free sugar, n (%) | 693 (89.65) | 1323 (88.20) | ||||
| ≥5 portions F&V/24 hours, n (%) | 65 (8.41) | 194 (12.93) | ||||
| Number of eating/drinking occasions/24 hours | 4.14 (1.22) | 4.23 (1.17) | ||||
Nutritional intake: adjusted analyses using multilevel models
Intracluster correlation coefficient estimation
School-level ICCs were estimated for the nutritional intake outcomes from null models. The school-level ICCs for free sugar intake at school lunch, across the school day and over 24 hours were 0.03, 0.02 and 0.02, respectively. The ICCs for the continuous nutritional outcome models are available in Report Supplementary Material 4, Tables 1 and 2.
Primary outcome: free sugar intake
Multilevel models to compare free sugar intake at lunch, during the school day and during the whole day (24 hours) between SFS-mandated and SFS-non-mandated school groups are presented in Table 16. Pupils’ mean free sugar intake at lunch was lower in the SFS-mandated schools than in the SFS-non-mandated schools by 2.78 g (95% CI –4.66 to –0.9 g), but this difference was not found for school day or 24-hour free sugar intake. We also found other variables that were significantly associated with free sugar intake. At the individual level, pupils who solely consumed school-provided food at lunch had a lower free sugar intake at lunch than those obtaining at least some of their lunch from home or outside school, when controlling for other variables (–3.55 g, 95% CI –5.18 to –1.91 g). The same trend was seen for free sugar intake during the school day, but not for 24-hour free sugar intake. At the school level, higher IDACI deprivation scores and secular status were significantly associated with higher free sugar intake at lunch and across the school day. A similar trend was seen with 24-hour intake, but the differences were non-significant. The presence of a sixth form was significantly associated with lower free sugar intake at lunch. Pupils who participated in data collection in the 2020–1 academic school year (n = 4 schools) had significantly lower free sugar intake at lunch than those who provided data in the 2019–20 year. This may reflect changes to school food provision in relation to the COVID-19 pandemic measures that were in place in schools at the time. By the 2021–2 academic year, school food provision had largely returned to normal.
| Coefficient | Lunch free sugar intake (g) (n = 1878) | School day free sugar intake (g) (n = 1934) | 24-hour free sugar intake (g) (n = 2045) | ||||
|---|---|---|---|---|---|---|---|
| MD (95% CI) | p-value | MD (95% CI) | p-value | MD (95% CI) | p-value | ||
| School SFS statusa | SFS-mandated | –2.78 (–4.66 to 0.90) | 0.004 | 0.22 (–3.02 to 3.47) | 0.89 | 1.15 (–5.30 to 7.61) | 0.73 |
| Sexb | Male | –0.21 (–2.00 to 1.59) | 0.82 | 0.39 (–2.38 to 3.17) | 0.78 | 4.17 (–1.24 to 9.59) | 0.13 |
| Other/unknown | 0.36 (–4.63 to 5.36) | 0.89 | –0.49 (–8.16 to 7.17) | 0.90 | –12.91 (–27.51 to 1.69) | 0.08 | |
| Age (years) | –1.13 (–3.67 to 1.42) | 0.39 | 0.44 (–3.51 to 4.38) | 0.83 | 0.83 (–6.83 to 8.49) | 0.83 | |
| Ethnicityc | Asian/Asian British | –1.69 (–4.12 to 0.74) | 0.17 | –3.92 (–7.72 to –0.11) | 0.04 | –11.48 (–18.94 to –4.02) | 0.003 |
| Black/African/Caribbean/Black British | 1.71 (–2.31 to 5.73) | 0.40 | 7.30 (1.07 to 13.53) | 0.02 | 4.53 (–7.48 to 16.55) | 0.46 | |
| Mixed/multiple | –3.04 (–6.80 to 0.73) | 0.11 | –4.16 (–9.96 to 1.63) | 0.16 | –11.38 (–22.73 to –0.03) | 0.049 | |
| Other/unknown | 2.57 (–2.35 to 7.49) | 0.31 | 5.45 (–1.98 to 12.89) | 0.15 | 4.44 (–9.80 to 18.68) | 0.54 | |
| IMD quintile groupd | 2 | 2.29 (–0.53 to 5.11) | 0.11 | 2.53 (–1.82 to 6.88) | 0.25 | 3.38 (–5.06 to 11.81) | 0.43 |
| 3 | 1.41 (–1.47 to 4.30) | 0.34 | 1.76 (–2.74 to 6.25) | 0.44 | 1.81 (–6.92 to 10.54) | 0.68 | |
| 4 | 0.87 (–2.19 to 3.92) | 0.58 | –0.12 (–4.88 to 4.63) | 0.96 | 2.33 (–6.95 to 11.61) | 0.62 | |
| 5 (least deprived) | 0.32 (–2.73 to 3.37) | 0.84 | 0.87 (–3.91 to 5.65) | 0.72 | 1.75 (–7.62 to 11.11) | 0.72 | |
| Lunch sourcee | 100% school-provided | –3.55 (–5.18 to –1.91) | < 0.001 | –2.06 (–4.57 to 0.45) | 0.11 | 3.80 (–0.92 to 8.52) | 0.12 |
| School % FSM | 0.07 (–0.04 to 0.18) | 0.21 | –0.009 (–0.19 to 0.17) | 0.92 | 0.15 (–0.21 to 0.51) | 0.41 | |
| School IDACI | 0.12 (0.02 to 0.23) | 0.03 | 0.27 (0.08 to 0.45) | 0.005 | 0.34 (–0.02 to 0.71) | 0.07 | |
| School sixth formf | Yes | –3.18 (–5.14 to –1.21) | 0.002 | –1.69 (–5.11 to 1.73) | 0.33 | –2.08 (–8.91 to 4.75) | 0.55 |
| School catering provisiong | External | 1.12 (–0.67 to 2.91) | 0.22 | 1.54 (–1.56 to 4.64) | 0.33 | 3.84 (–2.31 to 9.99) | 0.22 |
| School religious statush | Secular | 5.01 (1.88 to 8.14) | 0.002 | 5.81 (0.28 to 11.34) | 0.04 | 3.32 (–7.81 to 14.44) | 0.56 |
| Data collection yeari | 2020–1 | –3.51 (–6.77 to –0.25) | 0.04 | –1.07 (–6.72 to 4.59) | 0.71 | –3.08 (–14.31 to 8.16) | 0.59 |
| 2021–2 | 0.49 (–1.52 to 2.51) | 0.63 | 1.27 (–2.20 to 4.75) | 0.47 | –0.13 (–7.01 to 6.75) | 0.97 | |
| Year groupj | Year 9 | 0.88 (–4.61 to 6.37) | 0.75 | –3.76 (–12.23 to 4.70) | 0.38 | –2.90 (–19.40 to 13.60) | 0.73 |
| Year 10 | 0.94 (–6.97 to 8.86) | 0.82 | –6.13 (–18.38 to 6.12) | 0.33 | –5.72 (–29.49 to 18.06) | 0.64 | |
Some differences were seen in pupils’ 24-hour free sugar intake across ethnic groups, with the Asian and mixed ethnic groups having lower free sugar intake than the white ethnic group. The Asian group also had a significantly lower free sugar intake across the school day, but not at school lunch. The black ethnic group had significantly higher free sugar intake across the school day, but the difference for this group was non-significant in the other models.
Secondary nutritional outcomes
The regression coefficients for SFS-mandated schools compared with SFS-non-mandated schools for the secondary nutritional outcome models are presented in Table 17. Full models are provided in Report Supplementary Material 5, Tables 1–9.
| Nutritional outcome | MD, IRR or OR for SFS-mandated schools compared with SFS-non-mandated schools | |||||
|---|---|---|---|---|---|---|
| Lunch (n = 1878) | School day (n = 1934) | 24 hours (n = 2045) | ||||
| MD/IRR (95% CI) | p-value | MD/IRR (95% CI) | p-value | MD/IRR/OR (95% CI) | p-value | |
| Free sugar (g); MD | –2.78 (–4.66 to –0.90) | 0.004 | 0.22 (–3.02 to 3.47) | 0.89 | 1.15 (–5.30 to 7.61) | 0.73 |
| % TEI from free sugar; MD | –0.90 (–2.76 to 0.95) | 0.34 | –0.31 (–2.04 to 1.42) | 0.72 | 0.77 (–0.53 to 2.07) | 0.25 |
| TEI (kcal); MD | –54.97 (–88.87 to –21.07) | 0.001 | –31.95 (–75.88 to 11.99) | 0.15 | –78.71 (–175.43 to 18.01) | 0.11 |
| Fat (g); MD | –2.19 (–3.79 to –0.58) | 0.01 | –1.39 (–3.48 to 0.69) | 0.19 | –2.98 (–7.10 to 1.14) | 0.16 |
| Fibre (g); MD | –0.25 (–0.69 to 0.18) | 0.26 | –0.17 (–0.65 to 0.31) | 0.48 | –0.96 (–2.11 to 0.19) | 0.10 |
| F&V portions; MD | –0.24 (–0.36 to –0.11) | < 0.001 | –0.21 (–0.34 to –0.08) | 0.002 | –0.35 (–0.64 to –0.06) | 0.02 |
| SSB items; IRR | 1.11 (0.85 to 1.46) | 0.45 | 1.16 (0.85 to 1.58) | 0.36 | 1.29 (1.00 to 1.65) | 0.047 |
| HFSS items; IRR | 0.92 (0.83 to 1.01) | 0.09 | 0.97 (0.89 to 1.05) | 0.43 | 0.99 (0.92 to 1.06) | 0.72 |
| Sugar/chocolate confectionery items; IRR | 0.97 (0.75 to 1.25) | 0.81 | 1.21 (1.01 to 1.46) | 0.04 | 1.04 (0.91 to 1.20) | 0.56 |
| > 5% of 24-hour TEI from free sugar; OR | 1.28 (0.94 to 1.75) | 0.12 | ||||
| ≥5 portions F&V/24 hours; OR | 0.70 (0.49 to 1.02) | 0.06 | ||||
| Eating and drinking occasions/24 hours; IRR | 0.99 (0.95 to 1.04) | 0.81 | ||||
Despite the lower free sugar intake at lunch in pupils from SFS-mandated schools (the primary outcome), there was no significant difference in the percentage of TEI from free sugar at lunch or other time points. Compared with those in SFS-non-mandated schools, pupils in SFS-mandated schools had significantly lower lunch TEI (–54.97 kcal, 95% CI –88.87 to –21.07 kcal) and fat intake (–2.19 g, 95% CI –3.79 to –0.58 g), and this trend remained across the school day and 24 hours, although the difference was not significant at these two time points. Pupils in SFS-mandated schools had significantly lower F&V intake at lunch (–0.24 portions, 95% CI –0.36 to –0.11 portions), across the school day and during 24 hours. This group also had lower odds of consuming at least five F&V portions in 24 hours, but this was non-significant.
In terms of model covariates, of note in these models were the associations between lunch source and nutritional outcomes. Participants who had a 100% school-provided lunch had lower TEI, fat, fibre and F&V intake both at lunch and across the school day. These participants also had lower consumption of HFSS and confectionery items during lunch, across the school day and over 24 hours (see Report Supplementary Material 5).
To explore whether the lower nutrient and food intakes observed for the SFS-mandated school group could be explained by the lower TEI intake in this group, we re-ran the nutritional outcome models with TEI as an additional adjustment variable. The regression coefficients for these models are presented in Table 18 (full models are available in Report Supplementary Material 6, Tables 1–7). When TEI was adjusted for, there was no longer a significant difference in free sugar or fat intake at lunch between the SFS-mandated and the SFS-non-mandated school groups, but the significantly lower F&V consumption in the SFS-mandated school group was still present in all three models, with a difference in intake of 0.20, 0.19 and 0.29 portions at lunch, across the school day and over 24 hours, respectively. In these TEI adjusted models, there was also significantly higher consumption of sugar and chocolate confectionery items across the school day, and SSBs over 24 hours in the SFS-mandated than in the SFS-non-mandated school group.
| Nutritional outcome | MD or IRR for SFS-mandated schools compared with SFS-non-mandated schools | |||||
|---|---|---|---|---|---|---|
| Lunch (n = 1878) | School day (n = 1934) | 24 hours (n = 2045) | ||||
| MD/IRR (95% CI) | p-value | MD/IRR (95% CI) | p-value | MD/IRR (95% CI) | p-value | |
| Free sugar (g); MD | –1.13 (–2.89 to 0.64) | 0.21 | 1.55 (–1.4 to 4.51) | 0.31 | 4.78 (–1.31 to 10.87) | 0.12 |
| Fat (g); MD | 0.31 (–0.30 to 0.92) | 0.32 | –0.01 (–0.80 to 0.77) | 0.98 | 0.25 (–1.13 to 1.63) | 0.72 |
| Fibre (g); MD | 0.15 (–0.10 to 0.41) | 0.24 | 0.04 (–0.29 to 0.38) | 0.79 | –0.38 (–1.12 to 0.36) | 0.31 |
| F&V portions; MD | –0.20 (–0.32 to –0.08) | 0.001 | –0.19 (–0.31 to –0.06) | 0.005 | –0.29 (–0.56 to –0.02) | 0.03 |
| SSB items; IRR | 1.15 (0.87 to 1.52) | 0.32 | 1.16 (0.85 to 1.59) | 0.35 | 1.32 (1.03 to 1.69) | 0.03 |
| HFSS items; IRR | 0.99 (0.89 to 1.10) | 0.82 | 0.99 (0.91 to 1.07) | 0.73 | 1.02 (0.94 to 1.10) | 0.69 |
| Sugar/chocolate confectionery items; IRR | 1.08 (0.84 to 1.38) | 0.56 | 1.25 (1.04 to 1.50) | 0.02 | 1.08 (0.95 to 1.23) | 0.24 |
Dental outcomes
Dental outcomes and other factors related to dental health are presented for participants in the SFS-mandated and SFS-non-mandated school groups in Table 19. Some marginal variations were present across the two school groups, with a lower proportion of pupils in the SFS-mandated group having dental caries symptoms, and a slightly higher proportion in this group receiving dental caries treatment in the past. Home fluoridation levels were higher, but the proportion of pupils brushing their teeth at least twice a day was lower in the SFS-mandated school group.
| Characteristic | Total (N = 2453), n (%) | Attending SFS-mandated schools (N = 836), n (%) | Attending SFS-non-mandated schools (N = 1617), n (%) |
|---|---|---|---|
| Presence of dental caries symptoms | 1469 (64.77) | 496 (63.84) | 973 (65.26) |
| Missing | 185 | 59 | 126 |
| Number of dental caries symptoms; mean (SD) | 1.27 (1.29) | 1.21 (1.25) | 1.29 (1.31) |
| Missing | 185 | 59 | 126 |
| Received dental caries treatment | 1033 (45.55) | 360 (46.33) | 673 (45.14) |
| Missing | 185 | 59 | 126 |
| Toothbrushing frequency | |||
| Less than once a day | 31 (1.38) | 15 (1.95) | 16 (1.08) |
| Once a day | 279 (12.41) | 124 (16.10) | 155 (10.49) |
| Twice a day or more | 1938 (86.21) | 631 (81.95) | 1307 (88.43) |
| Missing | 205 | 66 | 139 |
| Home water fluoridation level (mg/l); mean (SD) | 0.49 (0.30) | 0.57 (0.35) | 0.45 (0.26) |
| Missing | 202 | 74 | 128 |
Dental outcomes: adjusted analyses using multilevel models
Multilevel models to compare the presence and number of dental caries symptoms in the previous 3 months and the past receipt of treatment for dental caries between SFS-mandated and SFS-non-mandated schools are presented in Table 20. There were no significant differences in the presence or the number of dental caries symptoms or in the likelihood of dental caries treatment between the SFS-mandated and SFS-non-mandated school groups. Male participants had lower odds of caries [odds ratio (OR) 0.76, 95% CI 0.62 to 0.94], less extensive symptoms and lower odds of dental caries treatment, when adjusting for other variables. There were no significant differences across the individual and school-level deprivation indicators (IMD quintile group, school % FSM, school IDACI) in the odds of having any dental caries symptoms, but there were differences in the number of symptoms experienced in the previous 3 months and receipt of caries treatment. Compared with the most deprived IMD quintile group, other groups had less caries symptoms and lower odds of caries treatment, although there was no gradient present across the groups, and the rate/ORs were only significant for IMD quintile groups 2 and 3. At the school level, a higher percentage of pupils with FSM eligibility was marginally associated with more caries symptoms but a higher school IDACI score (indicating higher income deprivation in families with children in the area surrounding the school) was associated with marginally lower caries symptoms. Toothbrushing at least twice a day was associated with lower odds of dental caries symptoms and treatment and a smaller number of caries symptoms.
| Coefficient | Presence of dental caries symptoms in the last 3 months | Number of dental caries symptoms in the last 3 months | Past dental caries treatment | ||||
|---|---|---|---|---|---|---|---|
| OR (95% CI) | p-value | IRR (95% CI) | p-value | OR (95% CI) | p-value | ||
| School SFS statusa | SFS-mandated | 0.90 (0.70 to 1.16) | 0.42 | 0.92 (0.83 to 1.02) | 0.10 | 1.07 (0.85 to 1.33) | 0.57 |
| Sexb | Male | 0.76 (0.62 to 0.94) | 0.01 | 0.80 (0.73 to 0.88) | < 0.001 | 0.80 (0.66 to 0.98) | 0.03 |
| Other/unknown | 0.99 (0.55 to 1.77) | 0.97 | 1.00 (0.80 to 1.25) | 0.99 | 0.63 (0.36 to 1.09) | 0.10 | |
| Age (years) | 1.04 (0.77 to 1.41) | 0.79 | 0.90 (0.79 to 1.02) | 0.10 | 0.71 (0.54 to 0.95) | 0.02 | |
| Ethnicityc | Asian/Asian British | 0.92 (0.67 to 1.25) | 0.58 | 1.05 (0.92 to 1.19) | 0.51 | 1.05 (0.78 to 1.41) | 0.77 |
| Black/African/Caribbean/Black British | 0.65 (0.41 to 1.04) | 0.07 | 0.84 (0.68 to 1.05) | 0.12 | 0.55 (0.34 to 0.89) | 0.02 | |
| Mixed/multiple | 0.70 (0.45 to 1.08) | 0.11 | 0.90 (0.74 to 1.10) | 0.30 | 0.94 (0.61 to 1.44) | 0.77 | |
| Other/unknown | 1.00 (0.56 to 1.77) | 0.99 | 1.10 (0.88 to 1.39) | 0.40 | 0.89 (0.52 to 1.53) | 0.70 | |
| IMD quintile groupd | 2 | 1.07 (0.77 to 1.48) | 0.69 | 0.82 (0.71 to 0.94) | 0.005 | 0.74 (0.54 to 1.00) | 0.05 |
| 3 | 0.99 (0.70 to 1.39) | 0.95 | 0.85 (0.74 to 0.99) | 0.03 | 0.65 (0.47 to 0.90) | 0.01 | |
| 4 | 0.86 (0.60 to 1.23) | 0.41 | 0.91 (0.78 to 1.06) | 0.22 | 0.81 (0.57 to 1.14) | 0.23 | |
| 5 (least deprived) | 1.06 (0.73 to 1.53) | 0.75 | 0.95 (0.82 to 1.11) | 0.54 | 0.84 (0.60 to 1.19) | 0.34 | |
| School % ethnic minorities | 1.00 (0.99 to 1.00) | 0.55 | 1.00 (0.99 to 1.00) | 0.01 | 1.00 (0.99 to 1.00) | 0.75 | |
| School % FSM | 1.00 (0.99 to 1.01) | 0.95 | 1.01 (1.00 to 1.01) | 0.04 | 1.01 (0.99 to 1.02) | 0.36 | |
| School IDACI | 0.99 (0.98 to 1.00) | 0.18 | 0.99 (0.99 to 1.00) | 0.002 | 0.99 (0.98 to 1.00) | 0.11 | |
| School sixth forme | Yes | 1.41 (1.10 to 1.80) | 0.006 | 1.19 (1.07 to 1.33) | 0.001 | 1.04 (0.83 to 1.30) | 0.73 |
| School catering provisionf | External | 1.35 (1.06 to 1.72) | 0.02 | 1.18 (1.06 to 1.30) | 0.002 | 0.95 (0.76 to 1.18) | 0.64 |
| Data collection yearg | 2020–1 | 0.73 (0.49 to 1.10) | 0.14 | 0.97 (0.81 to 1.15) | 0.71 | 1.07 (0.74 to 1.54) | 0.72 |
| 2021–2 | 0.94 (0.73 to 1.22) | 0.67 | 0.98 (0.88 to 1.09) | 0.72 | 0.71 (0.57 to 0.90) | 0.004 | |
| Year grouph | Year 9 | 0.81 (0.43 to 1.55) | 0.53 | 1.06 (0.81 to 1.40) | 0.65 | 2.01 (1.09 to 3.70) | 0.03 |
| Year 10 | 0.81 (0.32 to 2.05) | 0.66 | 1.27 (0.86 to 1.88) | 0.24 | 3.25 (1.35 to 7.83) | 0.009 | |
| Toothbrushing frequencyi | At least twice a day | 0.69 (0.51 to 0.94) | 0.02 | 0.79 (0.70 to 0.89) | < 0.001 | 0.74 (0.56 to 0.97) | 0.03 |
| Home fluoridation level (mg/l) | 1.25 (0.51 to 3.08) | 0.63 | 1.06 (0.75 to 1.51) | 0.74 | 0.65 (0.28 to 1.49) | 0.31 | |
| School fluoridation level (mg/l) | 0.67 (0.26 to 1.77) | 0.42 | 0.88 (0.60 to 1.29) | 0.51 | 1.17 (0.48 to 2.82) | 0.73 | |
Exploration of interaction effects between schools’ school food standards-mandated status and pupils’ characteristics
We explored potential subgroup differences in the association between school SFS-mandated/SFS-non-mandated status and nutritional outcomes by adding interaction terms to the adjusted nutritional outcome models. We tested interactions with SFS-mandated/SFS-non-mandated status for the following characteristics:
-
pupil’s lunch source (100% school-provided food consumed vs. some/all food consumed is not school-provided)
-
IMD quintile group
-
year group.
For all nutritional outcome models at lunch, across the school day and over 24 hours, there were few significant interaction terms, indicating that there were no clear subgroup differences in the association between school SFS-mandated/SFS-non-mandated status and pupil nutritional intake for lunch source, IMD group or year group. The coefficients for the interaction terms in the models are given in Appendix 7, Tables 40–42, and the full models are provided in Report Supplementary Material 7.
Sensitivity analyses
Missing deprivation (Index of Multiple Deprivation) data and age data
The percentage of pupils with primary outcome data, but missing data for IMD were 11% and 8% for participants in the school SFS-mandated and SFS-non-mandated groups, respectively. Therefore, we re-ran our primary analysis to include imputed IMD values. Where a pupil had missing IMD data, we used the median IMD rank for pupils in their school and assigned them to the appropriate IMD quintile group. The coefficients in the complete-case and the IMD-imputed models were similar, with no changes in their significance or direction (see Report Supplementary Material 8, Table 1). The significant difference in free sugar intake at lunch between SFS-mandated and SFS-non-mandated school groups remained in the IMD-imputed model [mean difference (MD) –2.03 g, 95% CI –3.76 to –0.30 g; p = 0.02].
Although data on age were missing for only 2.6% of the sample with primary outcome data, we also explored the impact of missing age data on this primary analysis by re-running our model to include imputed age values. Where pupils had missing age data, we used the average age for their year group in their school. The coefficients for the complete-case and the age-imputed models were again similar (see Report Supplementary Material 8, Table 2), with the significant difference in free sugar intake at lunch remaining between school SFS-mandated and SFS-non-mandated groups (–2.88 g, 95% CI –4.75 to –1.02 g; p = 0.003).
Exclusion of participants reporting 24-hour total energy intake of > 4000 or < 400 kcal
To explore the impact of implausible dietary intake reporting, we re-ran our primary analysis excluding participants who reported a 24-hour TEI of < 400 or > 4000 kcal. The adjusted model coefficients were similar for the outcome of free sugar intake at lunch (see Report Supplementary Material 8, Table 3), with a significant difference between SFS-mandated and SFS-non-mandated school groups remaining (MD –2.29 g, 95% CI –4.07 to –0.50 g; p = 0.01). The significance and direction of other coefficients in the model remained the same.
Exploratory comparison of pupil outcomes across school types (research objective 3)
Comparison of pupil nutritional outcomes across the four-group school typology based on school food standards compliance
We explored differences in pupil outcomes across the four identified school types based on levels of implementation of (1) standards relating to obesity and dental health; and (2) standards relating to dietary variety, adjusting for individual-level and school-level factors, as in the primary analyses. The nutritional outcome model regression coefficients for the school types are presented in Table 21. The full models are provided in Report Supplementary Material 9, Tables 1–9.
| Nutrient/food outcome | School typea | MD or IRR | |||||
|---|---|---|---|---|---|---|---|
| Lunch (n = 1878) | School day (n = 1934) | 24 hours (n = 2045) | |||||
| MD/RR (95% CI) | p-value | MD/IRR (95% CI) | p-value | MD/IRR (95% CI) | p-value | ||
| Free sugar (g); MD | 2 | –4.83 (–11.85 to 2.18) | 0.18 | 2.08 (–9.92 to 14.07) | 0.73 | 17.75 (–6.16 to 41.67) | 0.15 |
| 3 | 1.50 (–1.12 to 4.11) | 0.26 | 2.23 (–2.19 to 6.65) | 0.32 | 1.72 (–6.96 to 10.40) | 0.70 | |
| 4 | 1.52 (–3.61 to 6.64) | 0.56 | 0.17 (–8.53 to 8.87) | 0.97 | 2.26 (–14.79 to 19.30) | 0.80 | |
| % TEI from free sugar; MD | 2 | –8.12 (–14.48 to –1.76) | 0.01 | –5.21 (–11.45 to 1.03) | 0.10 | 1.25 (–3.97 to 6.47) | 0.64 |
| 3 | 1.18 (–1.12 to 3.49) | 0.32 | 1.35 (–0.91 to 3.60) | 0.24 | 0.30 (–1.54 to 2.14) | 0.75 | |
| 4 | –3.50 (–8.19 to 1.18) | 0.14 | –2.56 (–7.13 to 2.02) | 0.27 | –0.68 (–4.48 to 3.13) | 0.73 | |
| TEI (kcal); MD | 2 | 20.51 (–124.90 to 165.92) | 0.78 | –4.87 (–170.30 to 160.57) | 0.95 | 192.14 (–184.12 to 568.40) | 0.32 |
| 3 | –0.52 (–53.35 to 52.31) | 0.99 | 22.33 (–39.27 to 83.94) | 0.48 | –6.92 (–142.42 to 128.58) | 0.92 | |
| 4 | 55.30 (–51.70 to 162.30) | 0.31 | 75.77 (–43.62 to 195.16) | 0.21 | 106.70 (–163.52 to 376.91) | 0.44 | |
| Fat (g); MD | 2 | 2.79 (–3.71 to 9.30) | 0.40 | 0.62 (–7.23 to 8.47) | 0.88 | 9.00 (–6.72 to 24.71) | 0.26 |
| 3 | –0.32 (–2.71 to 2.07) | 0.79 | 0.31 (–2.61 to 3.23) | 0.83 | –1.78 (–7.49 to 3.92) | 0.54 | |
| 4 | 1.83 (–2.96 to 6.61) | 0.45 | 3.70 (–1.98 to 9.37) | 0.20 | 3.74 (–7.51 to 15.00) | 0.52 | |
| Fibre (g); MD | 2 | 1.43 (–0.22 to 3.07) | 0.09 | 0.78 (–1.03 to 2.59) | 0.40 | 1.62 (–3.07 to 6.30) | 0.50 |
| 3 | 0.07 (–0.52 to 0.66) | 0.81 | 0.31 (–0.35 to 0.97) | 0.36 | –0.13 (–1.78 to 1.52) | 0.88 | |
| 4 | 0.41 (–0.81 to 1.62) | 0.51 | 0.43 (–0.89 to 1.76) | 0.52 | –0.43 (–3.85 to 2.99) | 0.80 | |
| F&V portions; MD | 2 | –0.39 (–0.93 to 0.15) | 0.15 | –0.30 (–0.81 to 0.21) | 0.25 | –0.33 (–1.54 to 0.88) | 0.59 |
| 3 | 0.10 (–0.09 to 0.29) | 0.30 | 0.18 (–0.004 to 0.37) | 0.06 | 0.28 (–0.15 to 0.71) | 0.20 | |
| 4 | 0.008 (–0.39 to 0.41) | 0.97 | 0.06 (–0.31 to 0.43) | 0.76 | –0.14 (–1.03 to 0.74) | 0.75 | |
| SSB items; IRR | 2 | 0.55 (0.14 to 2.13) | 0.39 | 0.68 (0.16 to 2.86) | 0.60 | 1.36 (0.48 to 3.85) | 0.56 |
| 3 | 0.91 (0.63 to 1.33) | 0.64 | 0.72 (0.46 to 1.13) | 0.15 | 0.78 (0.54 to 1.13) | 0.20 | |
| 4 | 0.82 (0.37 to 1.82) | 0.62 | 0.97 (0.41 to 2.28) | 0.95 | 0.77 (0.36 to 1.64) | 0.50 | |
| HFSS items; IRR | 2 | 0.86 (0.56 to 1.34) | 0.51 | 0.96 (0.71 to 1.31) | 0.82 | 1.12 (0.86 to 1.44) | 0.40 |
| 3 | 1.05 (0.91 to 1.20) | 0.49 | 1.08 (0.97 to 1.20) | 0.17 | 1.06 (0.96 to 1.16) | 0.25 | |
| 4 | 1.18 (0.88 to 1.58) | 0.27 | 1.09 (0.87 to 1.35) | 0.47 | 1.11 (0.92 to 1.34) | 0.26 | |
| Sugar/chocolate confectionery items; IRR | 2 | 0.44 (0.05 to 3.61) | 0.45 | 2.70 (1.30 to 5.59) | 0.008 | 1.45 (0.84 to 2.49) | 0.18 |
| 3 | 0.92 (0.66 to 1.30) | 0.65 | 1.07 (0.83 to 1.37) | 0.62 | 1.09 (0.90 to 1.33) | 0.38 | |
| 4 | 2.15 (1.16 to 3.98) | 0.02 | 1.41 (0.86 to 2.30) | 0.17 | 1.46 (1.02 to 2.10) | 0.04 | |
Compared with the type 1 schools (low implementation of obesity/dental health-related SFS and high implementation of dietary variety-related SFS), pupils in the type 2 school (medium implementation of both sets of SFS) had a lower percentage of TEI from free sugar at lunch (–8.12%, 95% CI –14.48% to –1.76%). The same trend was seen for the school day, but the difference was non-significant, and there was little difference over 24 hours.
Compared with type 1 schools, there were some differences in consumption of sugar and chocolate confectionery items in the types 2 and 4 schools. The type 2 school (medium implementation of obesity/dental health-related SFS and dietary variety-related SFS) had a higher consumption of confectionery items during the school day (IRR 2.70, 95% CI 1.30 to 5.59), but a lower consumption of these items at lunch (non-significant). Of note here is that the type 2 school had a very high percentage (94%) of pupils consuming a school-provided lunch. Pupils in the type 4 school (high implementation of obesity/dental health-related SFS and dietary variety-related SFS) had a higher consumption of confectionery items at lunch (IRR 2.15, 95% CI 1.16 to 3.98) and over 24 hours (IRR 1.46, 95% CI 1.02 to 2.10) than those in type 1 schools.
Level of school compliance with school food standards related to obesity/dental health and dietary variety and pupil nutritional outcomes
Due to the limitations of only having one school each in types 2 and 4, we constructed additional models to explore the relationship between school SFS compliance and pupil nutritional outcomes. We developed two variables based on the data used to inform the development of the four school types: (1) the percentage of the 12 standards related to obesity and dental health met by the school and (2) the percentage of the 15 standards related to dietary variety met by the school. We ran models, including both SFS-related variables and individual and school-level covariates, to explore the association between these variables and pupil nutritional outcomes. The nutritional outcome model regression coefficients for these two SFS-related variables are presented in Table 22. The full models are provided in Report Supplementary Material 10, Tables 1–9.
| Nutrient/food outcome | % SFS-met variablea | Regression coefficient or IRR | |||||
|---|---|---|---|---|---|---|---|
| Lunch (n = 1878) | School day (n = 1934) | 24 hours (n = 2045) | |||||
| Coefficient/IRR (95% CI) | p-value | Coefficient/IRR (95% CI) | p-value | Coefficient/IRR (95% CI) | p-value | ||
| Free sugar (g) | Obesity/dental health | 0.06 (–0.03 to 0.14) | 0.18 | 0.11 (–0.02 to 0.25) | 0.11 | 0.29 (0.03 to 0.56) | 0.03 |
| Dietary variety | 0.04 (–0.05 to 0.14) | 0.39 | 0.04 (–0.11 to 0.20) | 0.58 | 0.14 (–0.17 to 0.44) | 0.37 | |
| % TEI from free sugar | Obesity/dental health | 0.02 (–0.05 to 0.09) | 0.52 | 0.03 (–0.03 to 0.10) | 0.32 | 0.03 (–0.03 to 0.09) | 0.30 |
| Dietary variety | 0.14 (0.07 to 0.22) | < 0.001 | 0.12 (0.05 to 0.20) | 0.001 | 0.05 (–0.01 to 0.12) | 0.11 | |
| TEI (kcal) | Obesity/dental health | 0.18 (–1.33 to 1.68) | 0.82 | 1.26 (–0.62 to 3.14) | 0.19 | 3.59 (–0.49 to 7.68) | 0.09 |
| Dietary variety | –2.14 (–3.88 to –0.41) | 0.02 | –1.10 (–3.28 to 1.07) | 0.32 | –1.07 (–5.78 to 3.64) | 0.66 | |
| Fat (g) | Obesity/dental health | –0.006 (–0.07 to 0.06) | 0.86 | 0.04 (–0.05 to 0.13) | 0.40 | 0.07 (–0.10 to 0.24) | 0.42 |
| Dietary variety | –0.12 (–0.19 to –0.04) | 0.003 | –0.06 (–0.16 to 0.04) | 0.24 | –0.13 (–0.34 to 0.07) | 0.19 | |
| Fibre (g) | Obesity/dental health | 0.004 (–0.01 to 0.02) | 0.613 | 0.01 (–0.009 to 0.03) | 0.30 | 0.03 (–0.03 to 0.08) | 0.34 |
| Dietary variety | –0.03 (–0.05 to –0.01) | 0.001 | –0.02 (–0.05 to –0.002) | 0.03 | –0.01 (–0.07 to 0.05) | 0.68 | |
| F&V portions | Obesity/dental health | 0.0000 (–0.006 to 0.006) | 0.99 | 0.003 (–0.003 to 0.009) | 0.39 | 0.004 (–0.01 to 0.02) | 0.60 |
| Dietary variety | 0.0002 (–0.007 to 0.007) | 0.96 | 0.0003 (–0.007 to 0.007) | 0.94 | –0.0006 (–0.02 to 0.02) | 0.94 | |
| SSB items; IRR | Obesity/dental health | 0.99 (0.98 to 1.01) | 0.33 | 1.00 (0.98 to 1.01) | 0.51 | 1.00 (0.99 to 1.01) | 0.78 |
| Dietary variety | 1.00 (0.98 to 1.01) | 0.87 | 1.00 (0.98 to 1.02) | 0.94 | 1.00 (0.99 to 1.01) | 0.95 | |
| HFSS items; IRR | Obesity/dental health | 1.00 (1.00 to 1.01) | 0.44 | 1.00 (1.00 to 1.01) | 0.09 | 1.00 (1.00 to 1.01) | 0.06 |
| Dietary variety | 1.00 (0.99 to 1.01) | 0.96 | 1.00 (1.00 to 1.01) | 0.37 | 1.00 (1.00 to 1.00) | 0.82 | |
| Sugar/chocolate confectionery items; IRR | Obesity/dental health | 1.01 (1.00 to 1.02) | 0.19 | 1.01 (1.00 to 1.02) | 0.02 | 1.01 (1.00 to 1.01) | 0.01 |
| Dietary variety | 1.00 (0.99 to 1.02) | 0.79 | 1.00 (0.99 to 1.01) | 0.78 | 1.00 (0.99 to 1.01) | 0.61 | |
There were some associations between nutritional intake and the percentage of dietary variety standards met by the school. This variable was positively associated with the percentage of TEI from free sugar at lunch (0.14%, 95% CI 0.07% to 0.22%), with the same positive association across the school day. There were small but significant inverse associations between the percentage of dietary variety standards met, and lunch TEI (–2.14 kcal, 95% CI –3.88 to –0.41 kcal) and lunch fat intake (–0.12 g, 95% CI –0.19 to –0.04 g). The direction of association was the same for the school day and 24-hour models, but the coefficients were not significant. There was also a small negative association between the percentage of dietary variety standards met and fibre intake at lunch (–0.03 g, 95% CI –0.05 to –0.01 g) and across the school day, but no association between this variable and F&V intake.
There was a very small positive association with the percentage of obesity/dental health-related standards met and free sugar intake, but only in the 24-hour intake model (0.29 g, 95% CI 0.03 to 0.56 g). Consistent with this was an association between the percentage of these standards met and consumption of sugar and chocolate confectionery items in the school day and 24-hour models, with a higher percentage of standards met associated with a higher consumption (school day model IRR 1.01, 95% CI 1.00 to 1.02). The same direction of association was seen in the lunch model, but it was not significant. This finding is, to an extent, consistent with the finding of higher confectionery consumption in the types 2 and 4 schools (see models presented in Comparison of pupil nutritional outcomes across the four-group school typology based on school food standards compliance), as these schools had medium and high compliance with the obesity/dental-health-related standards, respectively, and higher consumption of confectionery items during the school day/at lunch, compared with type 1 schools, which had low compliance with the obesity/dental-health-related standards.
Comparison of pupil nutritional outcomes across the six-group school typology based on school food standards compliance and School Food Plan implementation
We also explored pupil nutritional outcomes across the six school types that we identified by subdividing the initial SFS-compliance-based types according to their level of implementation of SFP actions (described in Development of typology schools in relation to school food provision and support for healthy eating). The nutritional outcome model regression coefficients for these school types are presented in Appendix 8, Table 43, and the full models are provided in Report Supplementary Material 11, Tables 1–9. Overall, there were few additional differences across the six school types. There were significant differences in consumption of HFSS items, with a marginally higher consumption of these items across the school day and over 24 hours in school types 1B and 3B (i.e. types with higher implementation of SFP actions than the reference type 1A). A similar, but non-significant, association was seen for school lunch consumption.
Comparison of pupil dental outcomes across school types
We constructed adjusted models to explore differences in dental outcomes, using the SFS-based four-group school typology and the SFS- and SFP-based six-group school typology. There were no significant differences in the presence or number of caries symptoms in the previous 3 months, or in caries treatment received in the past across either the four- or six-group typologies. The full models are provided in Report Supplementary Material 12, Tables 1 and 2.
Results of the economic evaluation (research objective 1d)
Micro-costing
Twenty-two schools completed the costing survey and were included in the micro-costing analysis. The condensed summary of micro-costing is presented in Table 23. The micro-costing is available on the study web page (www.fundingawards.nihr.ac.uk/award/17/92/39). The results are presented separately for the schools that completed the paper-based version (n = 8) and the online version (n = 14). Of these 22 schools, 6 were mandated and 16 were not mandated to comply with the SFS. Thirteen schools had external caterers and nine schools had in-house catering.
| School ID | Catering provision | % of pupils receiving FSM | Annual ongoing school costs (£2021)a | School cost per student (£2021)a | Cost per student based on school meal uptake (£2021)a | Annual ongoing societal costs (£2021)a | Societal cost per student (£2021)a | Societal cost per student based on school meal uptake (£2021)a | Average annual spending on cooking ingredients per pupil (£2021)a | % of missing data – ongoing costs |
|---|---|---|---|---|---|---|---|---|---|---|
| SFS-mandated | ||||||||||
| ID11 | In-house | 15.0 | 67,851 | 86 | 209 | 67,851 | 86 | 209 | 107 | 10 |
| ID27 | In-house | 19.7 | 256,744 | 221 | 535 | 256,744 | 221 | 535 | 38 | 23 |
| ID26 | External | 21.4 | 191,100 | 172 | 172 | 191,100 | 172 | 172 | ND | 0 |
| ID32 | External | 21.9 | 122,400 | 104 | 199 | 220,680 | 187 | 359 | ND | 50 |
| ID36 | External | 31.1 | – | – | – | 191,100 | 166 | 256 | ND | 50 |
| ID44 | External | 18.2 | 64,400 | 80 | 167 | 135,380 | 169 | 352 | ND | 29 |
| SFS-non-mandated | ||||||||||
| ID17 | In-house | 6.4 | 222,709 | 126 | 187 | 222,709 | 126 | 187 | 15 | 11 |
| ID24 | In-house | 15.9 | 176,312 | 152 | 303 | 176,363 | 152 | 304 | 23 | 18 |
| ID13 | In-house | 6.0 | 212,850 | 242 | 520 | 212,850 | 242 | 520 | ND | 0 |
| ID31 | In-house | 14.8 | 434,460 | 355 | 844 | 434,460 | 355 | 844 | ND | 60 |
| ID33 | In-house | 9.5 | 186,359 | 195 | 553 | 186,359 | 195 | 553 | ND | 0 |
| ID42 | In-house | 32.3 | 8500 | 10 | 16 | 8500 | 10 | 16 | ND | 67 |
| ID45 | In-house | 14.1 | 105,740 | 68 | 169 | 105,740 | 68 | 169 | ND | 80 |
| ID01 | External | 18.2 | 231,628 | 239 | 328 | 233,422 | 241 | 331 | M | 67 |
| ID07 | External | 2.8 | 91,394 | 149 | 408 | 92,522 | 151 | 413 | N/A | 0 |
| ID22 | External | 9.0 | 115,105 | 142 | 237 | 142,403 | 176 | 293 | 39 | 14 |
| ID30 | External | 19.4 | 151,389 | 120 | 410 | 151,389 | 120 | 410 | 38 | 23 |
| ID25 | External | 12.6 | M | M | M | M | M | M | ND | 89 |
| ID29 | External | 12.8 | 70,600 | 48 | 63 | 193,450 | 131 | 173 | ND | 50 |
| ID38 | External | 49.4 | 861,950 | 867 | 2311 | 974,563 | 982 | 2613 | ND | 0 |
| ID39 | External | 3.4 | 28,700 | 19 | 30 | 28,700 | 19 | 30 | ND | 30 |
| ID43 | External | 28.5 | 54,440 | 55 | 97 | 122,690 | 125 | 218 | ND | 38 |
The annual ongoing costs associated with implementing and delivering the SFS and the SFP, and of food provision for schools ranged from £8500 to £861,950, with a mean of £182,732. The equivalent per-pupil cost ranged from £10 to £869, with a mean of £173 (based on the total number of pupils), and from £16 to £2311, with a mean £388 (based on the school meal uptake rate).
Annual ongoing societal costs of food provision included costs to schools, catering providers and volunteer time and ranged from £8500 to £974,563 with a mean of £207,094. Annual ongoing societal costs per pupil ranged from £9 to £982, with a mean of £195 (based on the total number of pupils), and from £16 to £2613, with a mean of £426 (based on school meal uptake rate). Eleven schools did not report any societal costs in addition to the school costs, and hence for these schools the total estimate from the societal perspective was the same as from the school perspective.
Staff costs, including catering staff, teaching staff involved in meal supervision, and teaching staff involved in delivering cooking lessons, were the three largest cost categories; they were also in the top five of the best completed categories with the smallest number of missing data. The costs associated with the employment of catering staff ranged from £37,166 to £191,100, with a mean of £108,719. The costs associated with teaching staff supervising meals ranged from £13,974 to £191,100 with a mean of £72,488. The costs of providing cooking lessons varied across the schools, and for all schools that completed the paper-based version, these costs were consistently lower than the costs for the schools that completed the online version. For the paper-based version, the costs ranged from £2400 to £9640 (mean £5733), and for the online version, the costs ranged from £23,400 to £102,960 (mean £106,519).
Six schools with external caterers reported the cost of their catering contract. Four schools reported having zero cost contracts, potentially indicating a profit-sharing arrangement with the caterers. One school reported a cost of £9003 and one school reported a cost of £200,000.
All schools provided data on the availability of vending machines. Five out of 22 schools reported having vending machines and the costs of their maintenance ranged from £1794 to £7176 per year depending on the number of vending machines available in each school. All schools that completed the paper-based survey reported the number of water fountains. The annual maintenance costs for these ranged from £34 to £102 (mean £55). Fifty per cent of the schools that completed the online survey reported the cost of providing water to pupils; these costs ranged from £200 to £4000 per year (mean £1700).
The schools that completed the paper-based survey were asked to indicate the costs associated with setting up and maintaining the school food payment system. One school reported a one-off cost of £15,000 associated with setting up the system and three schools reported annual ongoing costs ranging from £2000 to £2648.
Five schools reported spending between £0 and £3000 per year on maintaining the dining environment. One school reported spending £60,000 per year on ‘other’ maintenance. Six schools reported spending £682 on average per year, ranging between £250 and £2199, on food rewards for the pupils. Seven schools reported spending between £200 and £5000 per year on school food (e.g. breakfast) clubs.
Four schools reported having a food growing area and spending between £600 and £8200 on its maintenance per year. This is the only food-related activity for which the involvement of volunteers (e.g. parents) was mentioned by any of the schools. Three schools reported organising gardening clubs with annual costs ranging from £600 to £1400. Three schools reported having school cooking clubs with annual cost ranging from £1200 to £2002. Six schools reported costs associated with staff well-being training that ranged from £100 to £1500 per year. Only one school reported the use of independent food monitoring by third parties, at an annual cost of £2000. Two schools reported spending £500 and £1000 per year, respectively, on promoting healthy eating by, for example, organising healthy-eating events. Two schools reported the costs of providing subsidies to the staff associated with food provision: one reported an annual cost of £81,900 and the other reported an annual cost of £10,000.
Six schools provided information on the costs of purchasing ingredients for cooking lessons incurred by pupils and/or families. These costs ranged from £1913 to £35,827 per year for all pupils or from £15 to £107 per year per pupil. This question was only asked in the paper-based version of the survey.
In general, the surveys were not well completed. The percentage of missing data varied from 0% to 89%, with an average of 21% missing in the schools that completed the paper-based version, and 39% in the online version. The cost categories with the highest percentage of missing data were other ongoing maintenance costs (86% of missing data), annual costs of subsidies for the staff (71% of missing data) and staff well-being training (59% of missing data).
Cost–consequences analysis
Thirty-six schools (SFS-mandated, n = 13; SFS-non-mandated, n = 23) and 2543 pupils were included in the cost–consequences analysis (2273 providing nutritional outcome data, 2268 providing dental outcome data and 1495 providing HRQoL data). The summary of the analysis is presented in Table 24 and the full analysis is available on the study web page (www.fundingawards.nihr.ac.uk/award/17/92/39). Compared with the schools that were not mandated, SFS-mandated schools had a higher IDACI, a higher proportion of pupils eligible for FSM (23% vs. 18%), a lower proportion of pupils from black and ethnic minority groups (24% vs. 32%) and a lower proportion of pupils whose first language is other than English (11% vs. 16%).
| School information | Costs | HRQoL | Educational outcomes | Nutritional intake (during school day) | Dental outcomes | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| School | Catering provision | School IDACI | % FSM | School spending on catering (£, 2021)a | School spending on catering per pupil (£, 2021)a | School spending on catering per number of pupils having school meals (£, 2021)a | Average daily spending on food while at school (£, 2021)a | QALY | Overall absence (%) | Persistent absence (%) | Progress 8 score | Attainment 8 score | Grade 5 or above in English and maths GCSEs (%) | Staying in education or entering employment (%) | Free sugar (g) | % TEI from free sugar | TEI (kcal) | Fat (g) | F&V portions | Fibre (g) | Average number of caries symptoms |
| SFS-mandated schools | |||||||||||||||||||||
| ID03 | In-house | 0.12 | 20 | 190,486 | 148 | 222 | 3.26 | 0.8311 | 5 | 14 | –0.05 | 46 | 31 | 98 | 22.0 | 9.9 | 744 | 28.7 | 0.8 | 7.2 | 2.1 |
| ID08 | External | 0.12 | 25 | 67,291 | 79 | 190 | NA | NA | 7 | 16 | –0.46 | 39 | 26 | NA | 32.1 | 17.9 | 721 | 30.5 | 0.9 | 5.9 | 2.3 |
| ID11 | In-house | 0.07 | 15 | 56,939 | 70 | 175 | 3.13 | 0.8438 | 6 | 13 | –0.43 | 42 | 32 | 90 | 29.6 | 14.1 | 738 | 29.0 | 0.8 | 6.0 | 1.8 |
| ID12 | External | 0.12 | 14 | 24,846 | 43 | 95 | 2.45 | 0.7654 | 5 | 12 | 0.57 | 46 | 39 | 95 | 17.2 | 10.6 | 691 | 27.2 | 1.2 | 7.1 | 1.6 |
| ID16 | External | 0.20 | 44 | 243,136 | 315 | 494 | NA | NA | 5 | 11 | –0.06 | 46 | 45 | 96 | 36.3 | 14.6 | 777 | 31.2 | 0.6 | 5.6 | 2.4 |
| ID18 | In-house | 0.22 | 22 | 140,794 | 117 | 229 | NA | NA | 5 | 13 | 0.23 | 48 | 39 | 95 | 22.6 | 12.2 | 643 | 26.6 | 0.5 | 5.3 | 2.0 |
| ID26 | External | 0.23 | 21 | 401,000 | 361 | 361 | 2.60 | 0.8562 | 2 | 2 | NA | NA | NA | NA | 20.6 | 9.3 | 583 | 23.9 | 0.7 | 6.1 | 1.5 |
| ID27 | In-house | 0.25 | 20 | 115,948 | 104 | 242 | 3.60 | 0.8340 | 6 | 20 | –0.23 | 46 | 45 | 92 | 41.8 | 19.1 | 753 | 28.8 | 0.7 | 5.6 | 2.1 |
| ID32 | External | 0.09 | 22 | 104,560 | 93 | 170 | 4.42 | 0.8321 | 6 | 16 | NA | NA | NA | NA | 23.8 | 15.6 | 634 | 25.8 | 1.0 | 5.1 | 1.8 |
| ID36 | External | 0.35 | 31 | 54,868 | 48 | 74 | 2.93 | 0.8314 | 8 | 25 | –0.45 | 33 | 22 | NA | 37.7 | 17.5 | 781 | 29.0 | 1.1 | 6.5 | 1.8 |
| ID41 | In-house | 0.06 | 23 | 236,037 | 245 | 387 | 3.48 | 0.8297 | 7 | 17 | –0.01 | 45 | 41 | NA | 25.4 | 13.9 | 633 | 26.8 | 0.9 | 5.3 | 1.7 |
| ID44 | External | 0.18 | 18 | – | – | – | 3.99 | 0.7971 | 7 | 20 | –0.39 | 40 | 23 | NA | 30.4 | 17.5 | 677 | 28.2 | 0.7 | 5.1 | 1.7 |
| ID46 | External | 0.26 | 20 | 35,199 | 42 | 74 | NA | NA | 6 | 15 | 0.47 | 48 | 56 | 92 | 32.0 | 13.9 | 805 | 32.7 | 0.8 | 7.2 | 2.1 |
| Mean for SFS-mandated schools | 128,547 | 128 | 209 | 3.32 | 0.8302 | 6 | 15 | –0.07 | 43 | 36 | 94 | 28.0 | 14.1 | 701 | 28.1 | 0.8 | 6.0 | 1.9 | |||
| SFS-non-mandated schools | |||||||||||||||||||||
| ID01 | External | 0.03 | 18 | 133,547 | 145 | 189 | 3.90 | 0.7998 | 4 | 8 | 0.74 | 53 | 49 | 100 | 26.4 | 11.9 | 795 | 33.0 | 0.8 | 7.0 | 2.1 |
| ID02 | External | 0.29 | 20 | 314,716 | 284 | 580 | 3.37 | 0.8565 | 7 | 17 | –0.63 | 41 | 34 | 94 | 43.1 | 18.6 | 849 | 34.6 | 1.4 | 7.1 | 1.6 |
| ID05 | In-house | 0.21 | 20 | 77,644 | 92 | 318 | NA | NA | 7 | 23 | –0.44 | 43 | 30 | 91 | 37.1 | 17.1 | 936 | 39.3 | 1.1 | 7.1 | 1.8 |
| ID06 | In-house | 0.58 | 62 | 181,169 | 237 | 440 | 2.56 | 0.8480 | 5 | 15 | –0.08 | 43 | 37 | 91 | 28.3 | 16.0 | 672 | 27.4 | 0.7 | 5.4 | 1.9 |
| ID07 | External | 0.01 | 3 | 12,000 | 20 | 54 | 2.87 | 0.7891 | 3 | 6 | 0.74 | 78 | 100 | 100 | 23.3 | 10.8 | 781 | 33.4 | 1.6 | 8.1 | 2.0 |
| ID10 | External | 0.17 | 35 | 130,442 | 144 | 279 | 3.24 | 0.7980 | 6 | 17 | 0 | 46 | 42 | 88 | 30.4 | 16.0 | 742 | 30.3 | 0.7 | 5.7 | 2.1 |
| ID13 | In-house | 0.10 | 6 | 237,072 | 273 | 580 | 2.97 | 0.8356 | 4 | 8 | 0.61 | 73 | 98 | 98 | 22.5 | 12.3 | 641 | 24.1 | 1.6 | 6.8 | 2.0 |
| ID14 | External | 0.05 | 7 | 43,481 | 48 | 92 | 2.50 | 0.8833 | 6 | 15 | –0.1 | 47 | 40 | 95 | 24.0 | 12.6 | 745 | 30.7 | 1.2 | 6.7 | 2.0 |
| ID17 | In-house | 0.02 | 6 | 28,987 | 17 | 24 | 3.43 | 0.8284 | 4 | 7 | 0.45 | 59 | 67 | 97 | 22.6 | 10.8 | 685 | 27.3 | 1.2 | 6.3 | 2.1 |
| ID22 | External | 0.08 | 9 | 4000 | 5 | 8 | 4.14 | 0.8341 | 4 | 8 | 0.23 | 50 | 47 | 94 | 24.0 | 14.5 | 709 | 29.1 | 1.0 | 6.3 | 2.2 |
| ID24 | In-house | 0.13 | 16 | 235,000 | 202 | 404 | 4.04 | 0.8545 | 6 | 15 | –0.13 | 45 | 31 | 96 | 26.5 | 17.4 | 679 | 28.7 | 0.7 | 5.3 | 2.0 |
| ID25 | External | 0.13 | 13 | 55,904 | 37 | 106 | 3.59 | 0.8476 | 5 | 11 | –0.1 | 47 | 40 | 97 | 26.9 | 13.1 | 680 | 28.6 | 1.1 | 5.5 | 1.9 |
| ID29 | External | 0.06 | 13 | – | – | – | 4.14 | 0.8324 | 5 | 8 | 0.2 | 51 | 49 | 97 | 17.6 | 12.1 | 522 | 21.7 | 0.6 | 4.2 | 1.9 |
| ID30 | External | 0.13 | 19 | 46,586 | 48 | 126 | 3.48 | 0.8292 | 6 | 15 | 0.07 | 49 | 49 | 89 | 28.9 | 15.3 | 769 | 31.0 | 0.9 | 6.3 | 2.0 |
| ID31 | In-house | 0.06 | 15 | 97,314 | 95 | 189 | 3.45 | 0.8458 | 5 | 11 | 0.27 | 52 | 56 | 94 | 28.2 | 11.3 | 846 | 35.1 | 1.0 | 6.4 | 1.9 |
| ID33 | In-house | 0.23 | 10 | 153,217 | 159 | 455 | 3.23 | 0.7963 | 5 | 9 | 0.27 | 52 | 65 | NA | 22.7 | 14.3 | 715 | 28.6 | 1.2 | 6.2 | 1.9 |
| ID35 | In-house | 0.03 | 9 | 386,148 | 257 | 389 | 3.54 | 0.8429 | 5 | 10 | –0.13 | 47 | 44 | 94 | 22.8 | 14.3 | 585 | 23.4 | 0.9 | 5.2 | 1.8 |
| ID37 | External | 0.08 | 9 | 311,610 | 387 | 840 | 4.74 | 0.8383 | 5 | 8 | 0.12 | 54 | 61 | 99 | 31.0 | 15.5 | 764 | 30.3 | 1.4 | 6.6 | 1.9 |
| ID38 | External | 0.14 | 49 | 179,098 | 192 | 480 | 3.90 | 0.8167 | 6 | 16 | 0.51 | 44 | 28 | 93 | 26.3 | 17.2 | 659 | 24.3 | 1.1 | 5.2 | 2.2 |
| ID39 | External | 0.16 | 3 | – | – | – | 3.12 | 0.8381 | 4 | 6 | 0.56 | 61 | 74 | 98 | 17.7 | 9.7 | 647 | 25.9 | 1.2 | 5.8 | 1.8 |
| ID42 | In-house | 0.18 | 32 | 159,429 | 212 | 302 | 3.65 | 0.7988 | 4 | 5 | 0.4 | 45 | 31 | 87 | 28.5 | 14.0 | 714 | 29.2 | 0.8 | 5.7 | 1.9 |
| ID43 | External | 0.06 | 29 | 45,551 | 61 | 81 | 2.42 | 0.8343 | 6 | 15 | 0.16 | 45 | 36 | 99 | 21.1 | 12.2 | 685 | 2.2 | 1.2 | 6.6 | 2.2 |
| ID45 | In-house | 0.07 | 14 | 243,284 | 155 | 388 | 3.99 | 0.7999 | 5 | 14 | –0.35 | 44 | 37 | 94 | 21.2 | 13.1 | 571 | 2.2 | 0.8 | 4.9 | 2.2 |
| Mean for SFS-non-mandated schools | 133,748 | 133 | 275 | 3.47 | 0.8274 | 5 | 12 | 0.15 | 51 | 50 | 95 | 26.2 | 13.9 | 715 | 29.0 | 1.1 | 6.1 | 2.0 | |||
Costs
The average annual school costs of implementing and delivering the SFS and the SFP and of food provision in the SFS-mandated schools were £140,499 compared with £196,809 in the SFS-non-mandated schools. The average annual school costs of food provision per pupil (based on the total number of pupils) were £133 in the SFS-mandated schools and £186 in the SFS-non-mandated schools. The average annual school costs of food provision per pupil (based on the school meal uptake) were £256 in the SFS-mandated schools and £432 in the SFS-non-mandated schools.
The average annual ongoing societal costs of implementing and delivering the SFS and the SFP and of food provision were £177,142 in the SFS-mandated schools and £219,075 in the SFS-non-mandated schools. The average annual societal costs per pupil based on the total number of pupils were £167 in the SFS-mandated schools and £206 in the SFS-non-mandated schools, and based on the school meal uptake rate were £314 in the SFS-mandated schools and £471 in the SFS-non-mandated schools. The percentage of missing data in the SFS-mandated schools was lower than in the SFS-non-mandated schools (27% vs. 34%).
The cost differences were corroborated with the public data on catering expenditure: the SFS-mandated schools spent less on catering than the SFS-non-mandated schools. Using the publicly available data, the average annual total spending on catering was £128,546 in the SFS-mandated schools and £133,748 in the SFS-non-mandated schools. The average spending on catering per pupil based on the total number of pupils was £128 in the SFS-mandated schools and £133 in the SFS-non-mandated schools, and based on the school meal uptake rate was £209 in the SFS-mandated schools and £275 in the SFS-non-mandated schools.
Pupils in the SFS-mandated schools reported spending slightly less on food while at school than did the pupils in the SFS-non-mandated schools: £3.32 versus £3.47. Pupils’ annual spending on ingredients for the cooking lessons was higher in the SFS-mandated schools than in the SFS-non-mandated schools (£64 vs. £39).
Outcomes
Pupils in the SFS-mandated schools reported slightly higher HRQoL than the pupils in the SFS-non-mandated schools: 0.8302 compared with 0.8274. SFS-mandated schools had a higher percentage of missing HRQoL data, with no data available for 4 out of 13 schools (n = 390 pupils). In the SFS-non-mandated group, the HRQoL data were available for 22 out of 23 schools (n = 1105 pupils). HRQoL data are further summarised for the pupil sample in Appendix 9, Table 44.
The SFS-non-mandated schools consistently performed better than the SFS-mandated schools according to all selected educational outcomes. Both overall absenteeism and persistent absenteeism were lower in the SFS-non-mandated schools. The progress eight and attainment eight scores were higher in the SFS-non-mandated schools and there was a higher proportion of pupils with grade 5 or above in English and Maths GCSEs and a higher proportion of pupils staying in education or entering employment in these schools than in the SFS-mandated schools.
Pupils in the SFS-mandated schools had higher free sugar in their diet during the school day than did the pupils in the SFS-non-mandated schools. On average, pupils in the SFS-mandated schools consumed 27.98g of sugar during the school day compared with 26.17 g mong pupils in the SFS-non-mandated schools. Pupils in the SFS-mandated schools consumed a larger percentage of TEI from sugar during the school day, and a higher proportion of pupils in the SFS-mandated schools consumed over 5% of TEI from free sugar during the whole day (24 hours). Pupils in the SFS-mandated schools consumed slightly more SSB and sugar and chocolate confectionery items during the school day, and slightly fewer HFSS items during the school day. Pupils in the SFS-non-mandated schools had a slightly higher TEI, fat intake and fibre intake, and a larger number of F&V portions during school day than pupils in the SFS-mandated schools. Furthermore, the pupils in the SFS-non-mandated schools had a higher number of eating and drinking occasions, and a higher proportion of pupils in the SFS-non-mandated schools consumed five or more portions of F&V during the whole day (24 hours) than did the pupils in the SFS-mandated schools.
However, pupils in the SFS-mandated schools had a lower presence of dental caries and a slightly lower mean number of caries symptoms than the pupils in the SFS-non-mandated schools. A higher proportion of pupils in the SFS-mandated schools reported having caries treatment in the past.
Results of the qualitative case study (research objective 2)
Sample description
In total, 16 out of 36 schools were invited to take part, and 4 progressed to data collection (25% response rate). Table 25 provides details of the characteristics of case sites using 2021–2 school census data.
| SFS status | % FSM | IDACI decile | Provision | % ethnic minorities | |
|---|---|---|---|---|---|
| School 1 | Mandated | High | 3 | External | High |
| School 2 | Not mandated | Low | 3 | In-house | Low |
| School 3 | Not mandated | High | 5 | External | High |
| School 4 | Mandated | High | 8 | In-house | Low |
In total, 21 staff members and governors participated across the 4 case sites and represented members of school leadership (38%), catering (19%), teaching (29%) and the governing bodies (14%) (Table 26).
| Staff group | School 1 | School 2 | School 3 | School 4 | Total |
|---|---|---|---|---|---|
| Senior leadership team | 3 | 3 | 1 | 1 | 8 |
| Teacher | 1 | 1 | 1 | 2 | 6 |
| Catering manager | 1 | 1 | 1 | 1 | 4 |
| School governor | 1 | 1 | 1 | 0 | 3 |
| Total | 6 | 6 | 4 | 4 | 21 |
In total, 137 (male, n = 67; female, n = 68) pupils participated across the 4 school sites, with roughly equal proportions of year 7 (39%), year 9 (28%) and year 10 (33%) pupils. There was wide variation across case sites in terms of other participant characteristics, with FSM eligibility ranging from 9% to 53% and the proportion of ethnic minorities participants ranging from 25% to 97% (Table 27).
| Characteristics | School 1, n (%) | School 2, n (%) | School 3, n (%) | School 4, n (%) | Total, n (%) |
|---|---|---|---|---|---|
| Year 7 | 27 (46) | 6 (30) | 12 (38) | 9 (33) | 54 (39) |
| Year 9 | 15 (26) | 6 (30) | 8 (25) | 9 (33) | 38 (28) |
| Year 10 | 16 (28) | 8 (40) | 12 (37) | 9 (33) | 45 (33) |
| Ethnic minoritya | 28 (66) | 5 (25) | 31 (97) | 15 (56) | 89 (65) |
| FSMb | 5 (9) | 3 (15) | 17 (53) | 9 (33) | 34 (25) |
| Femalec | 24 (41) | 12 (60) | 17 (53) | 15 (56) | 68 (50) |
| Total | 58 | 20 | 32 | 27 | 137 |
Between three and seven interviews were conducted with school staff at each of the four case sites. The average duration of interviews was 35 minutes, with a range of 16–80 minutes. Three pupil focus groups were conducted at each school, with an average length of 34 minutes, ranging from 15 to 46 minutes.
Description of case sites
Table 28 provides further details about the characteristics of case site obtained from researcher observations, the key information survey and pupil data from the main study (phase I).
| School 1 | School 2 | School 3 | School 4 | |
|---|---|---|---|---|
| Breakfast provision | Free | Free for pupils with SEN | Free | Paid |
| Break provision | No | Yes | Yes | Yes |
| Number of food outlets | 1 | 1 | 1 | 1 |
| School meal take-upa | 94% | 44% | 66% | 63% |
| Notes | Spacious dining room | Small dining room | Spacious dining room | Spacious dining room |
| Family dining service | High breakfast uptake | Long queues | ||
| SFS % met | 53 | 70 | 65 | 65 |
| SFP % rated as high | 40 | 41 | 43 | 53 |
| SFS type/SFP subtype | 2B | 3A | 1A | 1B |
All schools offered breakfast, with half offering this for free to all pupils (both of these schools had a high proportion of pupils eligible for FSM). School 1 did not offer breaktime food provision. This site had the highest proportion of pupils having school food, as the school had a ‘family dining service’ and did not allow packed lunches except in exceptional cases. In the remaining schools, school meal take-up ranged from 44% to 66%. Schools ranged in their compliance with the SFS from 53% to 70% and in their implementation of the SFP from 40% to 53%. Schools from three out of the four SFS types (1–3) and four of six SFP subtypes were represented in the sample.
Summary of themes interpreted from the data
Table 29 provides an overview of six themes interpreted from the data. These were mainly derived from site-specific subthemes; however, some did not appear in all schools (e.g. perception of the importance of food in school; wider context of school food). We also identified three interwoven themes that appeared to underlie the narratives described in some of the themes, which are summarised in Interwoven themes. Descriptions on individual site-specific subthemes are provided in Appendix 10, Table 45. Each theme is described below with supporting quotations provided. Similarities and differences across case sites are discussed within each theme.
| Theme | Site-specific subthemes | Interwoven themesa | |||||
|---|---|---|---|---|---|---|---|
| School 1 | School 2 | School 3 | School 4 | ||||
| Perception of the importance of food in school |
|
||||||
| Eating experience |
|
|
|
|
Conflicting priorities | Mixed messages | Misunderstandings |
| Difficulties in school catering |
|
|
|
|
|||
| Delivering food education |
|
|
|
|
|||
| Healthy eating at school |
|
|
|
||||
| Wider context of school food |
|
|
|
||||
Perception of the importance of food in school
This theme arose only in school 1. Pupils and staff felt that food had an important role in the school, and this was largely due to the presence of a ‘family breakfast’ and ‘family lunch’, which were core parts of the day. Because staff ate with pupils, conversations about food between staff, pupils and parents were routine, and included opportunities to give feedback on the menu:
The thing is what people eat in this building and therefore how we do food in this building directly influences the conversations that every adult has with every adult in this building, because there isn’t one child who hasn’t talked to their teacher about food in this building, be that positively or negatively, over lunch, in tutor time, with a parent, like parents’ evening.
Teacher
Discussions with pupils at family lunch were seen as an opportunity to reinforce some ideas around nutrition and healthy eating. The presence of staff at lunchtime also offered the opportunity to monitor pupils’ eating behaviours:
We know what every child is eating, we can also monitor when you think about the challenges adolescents face, particularly eating disorders with children.
SLT
As the school did not offer breaktime food provision, a policy was in place for snacks and drinks brought from home, namely that large bags of crisps and sweets or SSBs were not permitted. Staff and pupils had a good awareness of this policy and staff played a part in monitoring and enforcing it through routine ‘equipment checks’. This further reinforced a sense that food was important in the school, as well as reinforcing healthy-eating messages. Staff also encouraged healthy eating by giving ‘points’ for bringing in a healthy snack.
Eating experience
One strong theme across all case sites was the eating experience. There were different views from staff and pupils about whether lunchtime was a positive experience. The social aspect of eating was highlighted as important by staff and pupils:
It’s a time for learning social interactions … They will know who they are going to sit with … A lot of social things are done, friends are made.
Governor
In school 1, the school’s decision to have family lunch was about having a sit-down meal, eating well, building confidence in communicating with others, providing a sense of responsibility and teamwork, developing dining etiquette/table manners, developing life skills and enhancing well-being. This was valued by both staff and pupils:
I think health in its entirety, it’s not just about what you put in your body, it’s about the interactions you have with people, and so the very nature of sitting down and asking someone how their maths lesson was, and doing that with maybe an adult on the table, maybe not with an adult at the table, but having that sense of community while you’re eating is actually a really wholesome experience, and I think it’s really healthy for both body and mind.
Teacher
I think if you’re up and out of your seat all the time you’re not actually eating food, so I think it helps for people to actually sit down and eat their food instead of eating out of their seat all the time.
Year 9
Because the teachers also eat with the students as well, so it encourages them that they can have a nice little chat to the teachers as well.
Year 9
In other schools, some pupils described negative lunchtime experiences. Lunchtime was viewed as a time-pressured event, and it was typically a fraught, unpleasant experience, with pupils spending considerable time in queues with ensuing behavioural issues. A number of pupils, particularly those who attended lunchtime clubs, spoke of having very little time to make choices or to eat their food. Pupils described rushing to get in the queue due to anxiety about food running out or having limited choice if they did not get to the queue early enough. This rush was misconstrued by staff as indicative of enthusiasm about and satisfaction with the service:
When we do inter-house, they give you 2 minutes to eat lunch, and it’s quite annoying because I remember missing 10 minutes of my lesson because I had to eat, because they gave me 1 minute to eat.
Year 7
There’s a bit less choice but also the thing with looking at the ingredients if you want to look at them you have no time, because if they’re shooing you along… Hurry, hurry.
Year 9
You just have to queue for ages and then all the hot food is gone.
Year 10
Pupils perceived some school dining spaces as offering an unpleasant physical environment. Lack of space and noise in dining rooms were consistently talked about in focus groups. There was a strong sense from pupils of wanting more flexible dining. Pupils talked about being outside as a means of getting away from noisy and cramped dining rooms, even if it meant being exposed to poor weather and sitting on the ground. Pupils wanted food that was quick to purchase and convenient to eat, partly due to a desire to take food away (‘grab and go’), minimise the time spent in the dining hall and maximise their time to socialise:
All the tables are really close together so you’re basically leaning on people.
Year 10
I have the sound of these chairs just engrained in my memory now, when everyone stands up and it clatters, it’s just chaotic.
Year 9
I prefer taking it out.
Prefer to eat outside.
It’s much less cramped than inside.
Year 10
For many, the potential social aspect of lunch was disrupted by queuing. While on the one hand many pupils looked forward to lunch, on the other it was an unsatisfactory experience for many.
Difficulties in school catering
This theme takes into account the drivers around the food offer (from a school perspective) and the drivers around food choices (from a pupil perspective).
Pupils’ priorities appeared to be a desire for meals that were filling, value for money, tasty, convenient and easy to consume. Many pupils thought that the ‘healthier’ meals on offer did not fit these criteria.
For schools, serving healthy and nutritious food was only one consideration when they were designing menus. The need to ensure pupils ate something rather than nothing was a consideration for at least one school. A key concern was keeping catering costs low. As a result, the popularity of items (‘what sells’) was a key driver of provision; this was perceived as being driven by a profit motive when schools employed external companies, but by ‘breaking even’ in schools with in-house catering.
So it’s a balance of keeping the kids happy but also sticking to being healthy … It’s a balance of getting your sales, but also trying to stick to being a healthy school.
Catering
I think it’s very clear that they [the catering provider] are trying to get as much profit as possible from what they do, and I don’t think that’s always in the benefit of the children.
Teacher
This was linked to a feeling that the school and the pupils were not always getting ‘value for money’, sometimes because of small portion sizes. While some pupils were happy with the canteen prices, others felt that the school food pricing was a ‘scam’, and there was a lack of trust in catering provision from pupils as a result:
I would say they scam you.
Because you can go to a shop and buy five cookies for £1, but they sell one for 85p.
Year 9
At one school (school 4) there appeared to be a lack of understanding among pupils that unhealthy foods may have been priced higher partly to discourage pupils from purchasing them.
Pupils also expressed mixed views about the quality of the food. Some found it adequate, good and/or healthy, but there were also many negative comments relating to food hygiene, flavour, texture and lack of choice, particularly relating to the range of cuisines on offer.
In all four case sites, there appeared to mechanisms in place for pupils to offer feedback on school food, varying from informal spontaneous feedback to catering staff to structured methods such as consultation with the school council, surveys (including student-led surveys) and taster sessions. However, these opportunities tended to be reported by staff, and the pupils in our sample described a different experience. For example, some students felt there were no opportunities for feedback while others felt that the mechanisms in place for feedback were ineffective. There was a sense that feedback opportunities in some schools were infrequent and did not reach all pupils:
I think there is a suggestion box over there but that’s not advertised.
I have never noticed it.
I literally just looked around now looking for any way and there it’s hidden because there’s usually a bunch of pupils standing there, it’s not very well advertised.
I bet they don’t check it either.
No.
Year 9
Where feedback opportunities were available, some pupils felt that the feedback was not acted on. This was echoed in staff comments that pupil feedback was largely unrealistic and at odds with healthy-eating efforts:
They are taking our opinions, but sometimes it doesn’t get back.
Year 9
We have a suggestion box, but 75% of it will be full of ridiculous ideas that aren’t possible.
Catering
It was clear that, in working within tight budgets, some catering managers used a range of practices to ease these tensions and conflicts around school food. Minimising wastage, that is, leftovers at the end of service, was an essential component of budget management, alongside decisions around the quality of produce purchased and how ingredients were used/combined:
So they have still got veg, I know it’s frozen, but to buy in the amounts that we use fresh already prepared doesn’t fit the budget for a school meal.
Catering
This theme suggests that school food is an almost impossible balancing act; concerns about (rising) costs, wastage, school meal uptake, customer satisfaction and nutritional quality created pressures for caterers and school leaders that were often difficult to resolve in practice without adversely affecting the quality of food. In one school, there was clear tension between school management and the catering provider as a result.
Delivering food education
There were varied attitudes towards the relative importance of various aspects of food education. For example, cooking was seen as an important ‘life skill’, and part of developing pupils' independence. However, some pupils reported that food lessons were often spent creating sweet dishes rather than a substantial main meal, although one teacher explained how the inclusion of sweet dishes was part of an effort to teach pupils healthier alternatives to typical recipes:
I would say [food lessons are] quite fun but you only really learn how to make desserts. There are a few main courses, but it would have been a lot more useful, especially in the future or when you’re first starting out living on your own if you learnt more about how to prepare cheap meals for yourself.
Year 9
We teach them meals that they can use after they leave school … we cook sweet things, but with fruit and less sugar, so giving them a few recipes that are a healthier alternative to the high sugar stuff as well.
Teacher
On the other hand, there was a sense that the subject of food preparation and nutrition was not given the same status as more traditional subjects such as history and geography.
Healthy-eating education was also seen as important, and schools indicated that this was incorporated across the curriculum and in extracurricular activities, including citizenship, physical education, PSHE, science and assemblies, sometimes in a systematic way. Whereas staff might see this as ‘embedding’ food/healthy-eating education in the wider curriculum, pupils perceived this delivery as piecemeal and patchy:
It’s like once or twice a year you get to really hear about it, but it’s not really brought up much after you have done food tech.
It’s once in a blue moon in an assembly.
I feel like since Year 10 I haven’t learnt anything about healthy eating or food or anything.
Year 10
Particularly with regard to citizenship and PSHE, there seemed a strong sense that healthy eating was vying with many other important issues, some of which schools are legally compelled to deliver lessons on:
I don’t think food education would be high up on the agenda in terms of what people perceive are the needs of children, particularly from an SMSC RSHE [Spiritual, Moral, Social and Cultural; Relationships and Sex Education and Health Education] perspective, and I think that if you ask most people what needs to be on the agenda most people talk about online safety, would be talking about the whole spectrum of sexual health, mental health, these things are really high up, and even within the media really high up there, I don’t think anyone really would suggest that healthy eating would be up there.
Teacher
Healthy eating at school
This theme related to perceptions of the importance of healthy eating at school, if/how the school supports healthy eating, and the barriers to healthy eating.
Pupils and staff felt it was important that schools supported healthy eating. They understood that healthy eating prevented ill health later in life. Some staff and pupils also linked healthy eating to learning:
I think it’s important because if you haven’t eaten your brain won’t work and you go to sleep in lessons and you’re not prepared to learn.
Year 7
Pupils knew the importance of eating healthily but perceived that the healthy options offered at school were not filling and/or tasty and/or value for money. Healthy eating was not generally at the forefront when pupils were making decisions about what to eat:
I don’t think the pot with the fruit is really that healthy.
You get a tiny amount of that for a very high price.
Year 10
We don’t go there and think I am eating something really healthy, it’s just that it tastes nice when we’re eating it.
Year 7
Pupils’ opinions were mixed about whether school food was healthy. In some schools (school 3 and 4), the use of Fridays as a ‘treat’ day reinforced the idea that the majority of school food was healthy and enhanced the desirability of the ‘Friday foods’:
The food is mainly healthy, because on Friday is the end of the week we can have a treat like pizza or burgers […] but mainly throughout the week it’s mainly healthy.
Year 7
At some sites, thought had been invested into how to make healthy food affordable and appealing, for example adding cheaper fruit or waste fruit to fruit salads and cooking vegetables in more interesting ways:
If they like corn on the cob, roasted veg, squash, sweet potato, which they would never normally have, but if we roast it with garlic then they will see it and they will choose it. But if it’s just a general carrots on the menu [they won’t eat it].
Catering
Pupils and staff spoke about the lack of consistent messaging around healthy eating, in that healthy-eating teaching is not reinforced in the school food provision and not encouraged by staff, and this also applied to foods and drinks brought in from outside:
There’s no point telling us to eat healthy, then in the canteen they are not serving healthy meals.
Year 10
Even if you’re buying loads of bad stuff they won’t say anything to you. To be honest they probably don’t really care.
Year 9
However, there were occasions where staff tried to redirect pupils to healthier choices. For example, staff at one school did monitor food choices at the point of payment and would intervene if they felt unhealthy choices had been made (although this was largely targeted at pupils having FSM):
The canteen staff are really good, because when it comes to the free school meal, youngsters they will say to them if they come with all biscuits they are like ‘no’, or they will call me on the radio and I am like, ‘No you can’t have two waffles’. We will have conversations with them and make them get something healthy.
SLT
Pupils also reported policies aimed at promoting healthy eating. In particular, in school 1, pupils’ awareness of the schools’ policy on drinks and snacks brought into school suggested that it was indeed strictly monitored:
You’re only allowed water, only water.
So you’re not allowed to bring in other drinks?
No fizzy drinks, no juice, no squash.
No fizzy drinks or energy drinks, no canned drinks, nothing, just water, or flavoured.
Year 10
In some schools, the pricing of ‘healthy’ foods also gave the appearance to pupils that healthy eating messages were not supported in practice:
You get about six grapes and it costs you about 80p … When I go outside and buy the grapes from there it’s £1 but they are really big and stuff, so they have more quantity, but in school it’s really small and expensive.
Year 9
Other factors that were seen to contrast with the idea that schools were supportive of healthy eating in some case study sites included the lack of choice at the end of service, the negativity of the lunchtime experience, the perception of poor quality of food, a lack of operational water fountains and poor provision for special diets, for example vegetarian, vegan and those with food allergies.
There was a staff perception that pupils had strong preferences for unhealthy food:
I know that if given the choice children tend to choose the unhealthy, the quick option.
SLT
To some extent, this contrasted with the pupil perspectives described in the ‘Difficulties in school catering’ theme: healthy eating was just one of a number of factors that pupils considered when making their choices. However, some pupils also acknowledged a preference for unhealthy food such as waffles and chips.
This theme highlights a mismatch between staff and pupil experiences and perceptions related to healthy eating. From the staff perspective, the pupils were making poor/unhealthy choices, which might signal the need for increased regulation. However, from a pupil perspective, the healthy food offer did not align with what they wanted from school food, and in some cases they sensed contradictions in the messaging around healthy eating.
Wider context of school food
Particularly for schools 1, 3 and 4, views expressed in relation to school food and food education were often countered with acknowledgement of the constraints of broader contextual issues, largely related to the demographic characteristics of the schools’ pupil populations.
This included a consideration of ethnic diversity, and it was important to these schools that this be reflected in the food provision, including meeting cultural requirements such as providing Halal meals. In some schools, this provision was considered inadequate by pupils and staff:
If they do have something that I can have that day I will be able to get it, but then sometimes they just won’t have anything Halal so I will just have to get a drink but you do get a bit hungry.
Year 7
There were also high levels of deprivation within these schools, and so it was critical to staff that pupils, particularly those entitled to FSM, were able to get a hot main meal while at school. In some schools, this drove the pricing of hot main meals, which was set at the FSM price.
In some cases, voicing concerns around pupil hunger elicited emotional reactions during interviews, and it was clear that staff felt strongly that school meal provision was an essential part of their pastoral role. This was reinforced by a focus of some staff/governors on prioritising energy consumption and filling up, in addition to the nutritional content of the meals:
I think the school is very aware that we live in a very deprived area, always has been, and as such we’re also well aware that oddly enough that very important is quantity, and equally we are aware that many kids don’t get much quality at home, so we have an emphasis on that.
Governor
We never refuse a child a meal … if a child comes and said they have had nothing to eat we feed them, we don’t charge them we just feed them, and I think that’s pastoral care.
Catering
However, this did not fully match the experience of pupils. We heard from at least one pupil receiving FSM who experienced having to go without, and from one pupil not eligible for FSM who had not been able to purchase food due to a lack of credit on their account:
I think that the free school meal thing is good for people who need it, but so my mum also struggles with money though but she still works, but we’re not allowed the free school meals, so she’s constantly having to put on money, and that’s why I have my £3 budget for a day. So it has to last me for a week or so, she might put on £15 and that’s to last me for a while, because she has to keep putting it on, and when I don’t have enough and they won’t let me have anything.
Year 7
There was a narrative of school food as a lever for achieving equity (in nutrition and attainment) and addressing food insecurity throughout these three case studies. There was also a desire to minimise any stigma associated with receiving a FSM:
We have our family lunch in terms of what the students are actually eating from a food point of view, and that’s all built really around the disadvantaged child and the pupil premium child to make sure that everybody gets the same meal, they all get a hot meal a day. There’s no stigma attached to students who get a certain meal because they are pupil premium, and others can bring in packed lunch from home, everybody has a school dinner.
SLT
The SLT felt that the primary problem with food outside school was the lack of access to affordable food, with some families having to juggle the constraints of time and money:
If you removed any social barriers I don’t think a child at this school would decide to eat unhealthily because they were ignorant of it [it’s] socioeconomic factors … outside of school a lot of time, ironically enough, it’s not the food they are bringing in that’s the problem it’s the lack of food.
SLT
In response to the socioeconomic situations of pupils, two schools offered free breakfast to all pupils. Uptake was high and there was a sense that this contributed to improved attendance (case study 3). However, the costs to the school were substantial:
Free breakfast is a significant cost, because it requires two staff to supervise, it requires a woman on the counter, so it needs three staff in total, and then we have to pay a membership fee to FareShare [a network of charitable food redistributors], and so there’s an annual membership as well. Then if our minibus driver is collecting there’s his cost as well. So providing free breakfast comes with a cost.
SLT
There was also a sense from staff that the local food environment did not support healthy eating:
But if they have got pocket money to spend at the shop that parents aren’t in control of that money, we’re not in control of that, what’s the cheapest and easiest thing for them to buy, it’s chocolate, it’s crisps, it’s sweets, and that’s a relentless battle isn’t it really? As I say it’s those everyday conversations, and we’re not going to win every single one of those, we can’t control what the students are eating on their way to and from the academy.
SLT
Interwoven themes
These interwoven themes underpin many of the narratives brought out in the descriptions above.
Conflicting priorities
There was a sense of varying priorities and agendas between multiple stakeholders. This included between (1) the school and its pupils, for example pupil drivers behind food choice compared with what is made available; (2) different school staff groups, for example caterers and senior leadership/governors relating to expectations of school food and the reality of what is achievable; and (3) teaching staff, curriculum demands and broader education policy in relation to the position/status of healthy-eating education. This interwoven theme was apparent in the themes ‘eating experience’, ‘difficulties in school catering’, ‘delivering food education’, ‘healthy eating at school’ and ‘wider context of school food’.
Mixed messages
Messaging around healthy eating was often seen as inconsistent across the school. For example, teaching around healthy eating was not reinforced in the school food offer or in monitoring of foods brought from outside, and the healthiest foods did not meet the needs/expectations of pupils (e.g. in relation to pricing, quality, flavour and convenience). Likewise, the teaching of cakes and dessert recipes in food preparation and nutrition lessons contrasted with healthy-eating messages. There were also contrasting interpretations around what is or is not healthy from both staff and pupils (see Appendix 10, Table 45). Although schools saw themselves as supporting healthy eating and creating positive eating experiences, factors such as negative lunchtime experiences, lack of choice at the end of service or for those with dietary needs, and a sense that feedback on school food was not acted on gave pupils a very different perception. This interwoven theme was apparent in the themes ‘eating experience’, ‘difficulties in school catering’, ‘school’s influence upon healthy eating’ and ‘delivering food education’.
Misunderstandings
School staff and pupils sometimes had contrasting perspectives that suggested misunderstandings about school food. For example, staff assumed that the rush of pupils to leave the canteen was related to pupils’ desire to socialise, whereas in some cases this was the result of wanting to get away from the negative indoor experience. Likewise, staff assumed that the rush to the canteen meant that pupils were satisfied with the service, whereas this rush appeared to be driven by other factors such as not wanting to spend too long in the queue or anxiety about a lack of choice at the end of service. Pupils also misinterpreted the motives of school catering provision; for example, the high cost of school food was seen as a ‘scam’, and pupils were sometimes disparaging about the quality of food and choice of offer, yet unaware of the high demands on catering provision relating to staff costs, rising costs of produce, the practicalities of school kitchens and high levels of waste. These misunderstandings also related to opportunities for pupils and staff to engage with one another on school food. For example, staff felt that students had ample opportunity to input into school food decisions such as menu options, while some pupils felt that there were few opportunities or that their ideas were dismissed. In relation to food education, pupils were not aware that the sweet recipes being taught were healthier versions. This interwoven theme was apparent in the themes ‘eating experience’, ‘difficulties in school catering’, ‘delivering food education’ and ‘healthy eating at school’.
Implementation of the school food standards and School Food Plan
Data were also examined to understand implementation of the SFS and SFP, which naturally focuses on the staff perspective.
The school food standards
Staff had a high awareness of the SFS and that there was a legal mandate to comply with these. This was apparent across all case study schools and not only in SFS-mandated schools. There were also high levels of support for the standards, which were seen largely as helpful and impactful on day-to-day practice. Implementation of the SFS was sometimes underpinned by external training of catering teams, use of online resources and internal meetings between catering staff and SLT.
For catering staff from external catering providers, compliance with the SFS was seen as embedded in the provision, as menus were centrally planned and there was a high level of control about items that could be purchased from suppliers:
Just the company that we work for, because obviously they stick to the food standards, so we’re limited to what we can order with our suppliers, so we’re blocked in, so we can’t order anything that we’re not allowed to, that doesn’t stick with the food standards and stuff like that.
Catering
However, it was apparent from the data that the SFS were viewed as just one factor among several that informed the design of menus and food provision:
You adjust [the food offer] a little bit to what they want, but also the guidelines.
Catering
Given that many other factors were involved in school food provision, this sometimes resulted in the de-prioritisation of the SFS in practice. Staff in three case study schools acknowledged that they did not fully comply with the SFS, and this was largely because the standards were incompatible with the style of service (in the case of family dining from the need to provide a limited number of choices for the service to be practicable) or with a provision that was appealing to pupils (and therefore ensured high uptake):
Not everything is approved [by the] government, because that doesn’t fit with the school’s family service, so.
Catering
I think it’s a combination of trying to meet what they should have, so the food standards, but also you have to also give them something they’re actually going to want to eat as well. So I think it’s a really hard balance for the canteen to offer things that are ... have those key nutrients in, have what they need, are giving them a good diet, particularly for the students where that might be their only hot meal of the day, but equally if the canteen serves up things that is not appealing to them they are not going to have anything to eat.
Teacher
Sometimes efforts to engage the pupil body in designing menus was felt to be counterproductive, and pupil preference was seen to be at odds with implementation of the SFS:
School food standards, so we work by that, but it’s very difficult to stick to it when we have got the school council trying to get involved and trying to make decisions with our menus and stuff.
Catering
There was variability in the extent to which particular standards could be easily implemented. For example, schools talked about ensuring that SFS-compliant drinks were available and having high levels of compliance with lunchtime standards. This was supported by stocking items sold as ‘compliant’ or using ‘compliant’ suppliers:
We only ever buy school compliant drinks, and they are very popular actually, sales of them.
SLT
We stick to it to a degree at lunchtimes, in fact at lunchtimes I think we are quite we are compliant … but it’s at breaktimes that maybe we’re not as compliant.
SLT
However, one interviewee was sceptical of suppliers labelling items as ‘compliant’:
For example the recommendation to have low sugar compliant, there’s this thing about compliant drinks, companies saying that they are compliant, but when you look at them, look at the label they are not really in comparison with the size of the drink, the amount of sugar.
Governor
The ease with which standards could be applied appear to relate to pupil satisfaction. For example, SFS-compliant drinks were seen as popular, so this standard was easy to implement, whereas prohibiting the sales of processed meat products, pastries and cakes/biscuits was seen as both unpopular from a pupil perspective and financially damaging because of the resulting reduced sales/canteen use:
We don’t follow [the standards] wholeheartedly at breaktime, because we need to keep a balance between breaking even with our costs as well as providing the nutritional standards.
SLT
Non-compliance with particular standards also related to ways in which pupils purchase food. For example, pupils were seen to purchase/eat their lunch at breaktime, so it was felt that having unhealthy foods available at lunchtime only would be unfair on the pupils. The selling of ‘healthier’ items was also seen as an expenditure that was not cost-effective if pupil uptake was poor. Some catering staff felt that pupils ‘wouldn’t eat’ if the less healthy items (e.g. pastry) were not made available:
I wouldn’t say we are fully compliant because I am not supposed to, I know I am only supposed to serve cakes at lunch, but because of some of our students only use us for break then how can I deny them cakes and biscuits? So some of it is I think 95% is alright, but sometimes it’s not common sense, because some of the children will come at break because they don’t want to come at lunchtime, so how can I not serve cakes at break?
Catering
It’s like I put salmon fishcakes on every week but I probably only sell two. If I did 20 or 30 they would go in the bin, so I do provide what they say, well, they say provide a salmon product every third week, don’t they? We have got them available but whether I sell them, it’s very difficult.
Catering
These competing demands between meeting SFS and providing an appealing offer also applied to breakfast provision, but this appeared to be primarily an issue for the school offering a paid-for-breakfast only. In the schools offering a universal free breakfast (n = 2) or a targeted free breakfast (n = 1), there was a limited breakfast offer, comprising combinations of toast and cereal, fruit and fruit juice, eggs and/or packaged breakfast goods. By contrast, the school with a paid-for breakfast offered a wide range of items including bacon, eggs, tomato, hashbrowns, bacon/sausage baps, pain au chocolat, chocolate chip cookies, yoghurt and fruit. Given these items were available every day, this contributed to the school’s non-compliance with some standards. For all schools, the motive for providing breakfast was to ensure that children were not going hungry in the morning. However, in the school with a paid-for breakfast, the catering manager felt a need to offer ‘desirable’ options to encourage pupils to eat breakfast, whereas this concern about preference was not present at schools offering a free breakfast:
You are going to have to use bacon, you are going to have to use sausage more than perhaps they [the school food standards] like you to, but what other things would you put on the menu? And believe me I have tried everything. I have even tried making my own blueberry pancakes for breakfast, I have tried all sorts of things. I have tried breakfast wraps, I have tried all different things, but what I have done now is just stuck really with the things that are selling.
Catering manager, school 4
Pain au chocolat isn’t healthy but if that’s all someone is having for breakfast isn’t that better than nothing?
Catering manager, school 4
There was also evidence from two schools that a lack of understanding or alternative interpretations of standards (e.g. what snacks are compliant) may have been contributing to non-compliance, and another school felt overloaded with the number of standards:
Because it’s quite hard sometimes to rack your brains on, there’s so many criteria as to what I can get in that pot.
Catering
Catering teams reported having good support from the school in implementing the SFS. However, there was variability in the extent to which SLT were involved or knowledgeable about the SFS. In one school, the SLT reported having a lack of detailed knowledge, as this was viewed as the responsibility of the external catering provider:
So I don’t [use the school food standards], because it’s an external provider, so that all sits with them. They have a contract, it’s their responsibility to do that.
SLT
Although two out of the three governors interviewed appeared to be aware of the SFS, monitoring of the SFS did not appear to be seen as part of their role. In two schools there was an apparent disconnect between the catering team’s acknowledgement of non-compliance with the SFS and the governors’ expectations that the school was fully compliant:
We pay [catering provider name] contractually at a level which gives us the assurance, hopefully, that they provide what is appropriate and that which conforms to government guidelines in terms of school provision in the UK.
Governor
The School Food Plan
There was variation in awareness of the SFP. Some staff/governors had not heard of it, or they had heard of it but had little knowledge of what it was, but there was a feeling that they ‘should’ know about it:
Full disclaimer no [I’m not aware of the SFP]. I will be honest no. So I wouldn’t even know where to start with that, if that’s something I should know about that would be really helpful [laughs].
Teacher
Some school staff/governors had an awareness of the SFP but did not directly take steps to implement it. However, there was a sense that the school activities were underpinned by heathy eating generally, and so many of the ideas within the SFP would already be in action even though the SFP was not referenced specifically.
Due to a lack of awareness of the SFP or a lack of knowledge about its purpose, those interviewed felt that it would come under the remit of the catering team. However, one catering manager who was aware of the SFP felt that it was ‘on the education side’.
One school had a high awareness of the SFP as they had been involved in a programme to support its implementation (School Food Champions). In this school, the process of attempting to implement the SFP had been driven by a previous food preparation and nutrition teacher. From her perspective, she had felt able to implement the SFP because of engagement with the external programme and because the ‘whole school’ was supportive.
Processes that were put in place to support implementation in this school (via engagement with the School Food Champions programme) included goal-setting, sharing examples of success from other schools and providing virtual support. It was also supported informally via the teachers’ own networks, for example a ‘food teachers’ Facebook group.
There were webinars, which in that time, it wasn’t that long ago really, but it was really exciting to be having a webinar, and now we’re doing it all the time. So they gave help, and there were teachers from the rest of the country that were on-board, and sharing ideas and experiences.
Governor, ex-food preparation and nutrition teacher
In this school, implementation was supported via staff meetings, including a meeting with the catering manager. Motivations for implementing the SFP related to increasing the uptake of school meals and improving student behaviour through improvements in nutrition. It was also felt to be worthwhile because the person leading on this work had seen marked increases in school meal uptake among those pupils eligible for pupil premium funding, and it had ‘energised’ the student body.
There appeared to be some legacy of the school’s involvement in the programme, although it was apparent that newer staff were not aware of the school’s engagement with the SFP, and there was a sense that it needed to be revisited:
I think there needs to be a real drive quite consistently, it has to be quite consistent.
Governor, ex-food preparation and nutrition teacher
Public involvement: results
The outcomes of our engagement with our public advisory groups are outlined in Table 30.
| Group | Group details | Outcomes |
|---|---|---|
| Young people | Six meetings |
|
| Parents | Two meetings and e-mail communication |
|
| School staff/governors | Four meetings and e-mail communication |
|
Chapter 5 Discussion
Summary of the key findings
Implementation of the school food standards
A key finding of this study is that no schools fully complied with the SFS. On average, schools met 64% of the standards. Standards applying to school lunchtime had the highest compliance (average 81% met), followed by standards for food other than lunch (average 64% met), and finally standards that apply across the whole day (average 43% met). Most secondary schools have extensive provision of food that includes breakfast and breaktime offers (30 and 34 schools in this study provided breakfast and breaktime food, respectively), and so the low compliance of standards across the whole day and for food other than lunch is a concern when considering the overall food offer of secondary schools.
There was large variation in compliance across the 36 schools. However, there was only a marginal difference in average levels of compliance when comparing SFS-mandated and SFS-non-mandated schools. Some larger variations were seen across the two groups for individual standards. Given that during the period of this study there has been increasing government encouragement and expectation of schools that are exempt from SFS-legislation to comply with it,49 this is an unsurprising finding. In our SFS-non-mandated school sample, 48% reported that they had voluntarily signed up to the SFS.
On further examination of compliance with the individual standards across all schools, the lunchtime standards relating to ensuring a good balance of food and nutrition daily and throughout the week were generally well complied with, but standards relating to the restriction of unhealthy food items (mostly standards relating to foods other than lunch and the whole day) were much less well met. For example, standards relating to the restriction of cakes, biscuits, confectionery, pastry, fried foods, processed meat products and SSBs were not complied with in the majority of participating schools. Although we had limited data from schools on food sales, and there were issues with comparisons across schools, the data we obtained provided further evidence of low compliance with these standards, as a substantial proportion of food sales comprised these restricted or prohibited items. We found that, overall, sales of desserts, cakes, biscuits, confectionery, chocolate, pastries, starchy foods cooked in fat or oil and SFS-non-compliant drinks/snacks accounted for 34% of all sales.
Our case study data help with further interpretation of these findings. There was a sense from both school leadership and catering staff that there needs to be flexibility around meeting the SFS, and an acknowledgement by some that the standards were not always adhered to, especially at breakfast and breaktimes. The driving factors in this appeared to be related to staff perceptions of what the pupils wanted (based on items that appeared to sell well), thus ensuring uptake of school food, which is important for catering service viability and profit. There was a perception among staff and caterers that healthier alternatives to the more traditional breakfast and breaktime foods (bacon, sausages, pastry products, etc.) were not purchased by pupils, but they also acknowledged that some pupils buy their lunch at breaktime, and so low compliance with the SFS at breaktime is an issue for this reason.
Other factors influencing compliance with certain standards that we identified in our case study data related to ease of implementation. Some were perceived as easier to implement (e.g. compliant drinks) and others much more difficult, for example providing oily fish, which resulted in concerns about low uptake and wastage, which in turn has an impact on profit. Overall, levels of compliance with the SFS, together with the understanding we have gained from the case study phase, provide some evidence that even though the updated standards introduced in 2015 were simplified to make it easier for schools to comply, many implementation challenges remain in the secondary school context.
In addition to assessing compliance with the SFS, we explored how well the SFS had been embedded as a policy in participating schools through surveys with school leaders, teachers with responsibility for/interest in food and nutrition, caterers and governors, informed by NPT. 106 The majority of participants were aware of the SFS and perceived that the policy had been implemented in their schools, with minimal difference between schools mandated and schools not mandated to comply with the SFS. Of note is that no school governors who reported implementation of the SFS in their schools perceived that they had a role in the SFS policy implementation, despite the government expectation that it the school governing body is responsible for ensuring that the SFS are met. 49 Overall, the majority of participants who were aware of the SFS were engaged with the policy and perceived that there was collective action in their schools to implement it. However, only one-third of respondents felt that there was a shared understanding of the purpose of the SFS policy across their schools. There were some differences across respondents from SFS-mandated and SFS-non-mandated schools, with a higher proportion from mandated schools having an understanding of the benefits of the SFS and what is required to deliver them (coherence), a perception that everyone worked well together to implement the SFS (collective action) and a belief that the SFS were worthwhile (reflexive monitoring). It is possible that these differences were due to the differences in statutory obligation to comply with the SFS across the two groups.
In line with our staff survey findings, the case study phase suggested generally high levels of support for the SFS from staff and governor interviewees, but the governors did not recognise oversight and monitoring of the SFS as part of their role. There was a sense among school senior leaders and governors in schools with external catering companies that the responsibility of SFS implementation rested with the catering company, implying that the SFS as a policy was not centrally embedded in the schools. There was also a perception that use of specific ‘approved’ suppliers (e.g. those designated by the catering company) provided assurance that pre-packaged items such as drinks and snacks were SFS-compliant; however, we found that in many schools some of these drinks and snacks were not compliant.
In the case study data, there was a disconnect between the school leadership perceptions and the catering provider perceptions in terms of the extent to which the schools were compliant with the SFS, with examples of those in leadership positions assuming full school compliance as part of the contractual obligations of their external catering company. By contrast, school caterers (both external and in-house) had developed a more pragmatic and flexible approach to the implementation of the SFS, balancing conflicting priorities. These included cost/profit, customer (pupil) preferences (driven by a number of factors, including convenience, taste and cost) and competition from outside (i.e. pupils can choose to buy preferred foods/drinks from food outlets before or after school or bring them from home if schools are not offering these products).
Implementation of the School Food Plan
All schools in our study were implementing some of the actions recommended in the SFP, even though evidence from our survey of school senior leadership, teachers, caterers and governors showed that fewer than half of respondents were aware of the SFP. Again, there was large variation in implementation across the schools, with the percentage of actions implemented ranging from 25% to 63%. There were no substantial differences in the level of implementation across SFS-mandated and SFS-non-mandated schools, which was expected, as the SFP is non-statutory national guidance that applies to all schools.
We explored implementation of the actions across our nine identified themes within the SFP but were limited in doing so to a certain degree by a large number of missing data from schools on some of the actions. Nevertheless, we were able to identify actions within themes that were either well or poorly implemented. Of note, no actions within the themes of leadership and oversight on school food, engagement (with pupils, parents and the community) and catering practices (catering staff encouraging healthy behaviours and nutritional balance) were implemented to a high level in the majority of schools. Within all other themes, some actions were well implemented and some not well implemented by the majority of schools.
Actions relating to the lunchtime experience presented a very mixed picture in terms of level of implementation, with some contrasting findings. Although over three-quarters of schools had implemented strategies to reduce queuing times and over 60% were assessed (using multiple participant perspectives) as providing pupils with enough time to eat lunch, in the majority of schools pupils reported feeling rushed when purchasing school food. Also of note was that many schools (58%) did not ask for feedback from their pupils on the lunchtime experience. This lack of opportunity for feedback is supported by our finding on the related SFP action of providing opportunities for pupils to contribute views on school food (within the theme of leadership and oversight on school food), which was also not well implemented, with only just over one-quarter of schools rated as having a high level of implementation, and nearly half of schools rated as having a low level of implementation (see Appendix 6). There was also a mixed picture for food education. Curricular education relating to food and healthy eating was assessed to be well implemented in most schools, but education around growing and extracurricular food education was not implemented in most schools.
Particular SFP actions to note that were poorly implemented in the majority of schools included governor leadership and engagement with school food (low implementation in 64% of schools), independent checking of compliance of the school with the SFS by either governors or an external service (low implementation in 79% of schools) and governor review of school food uptake data each school term (low implementation in 74% of schools). These findings are coherent with the governor survey findings, which provided evidence that governors do not identify they have a role in implementation and oversight of the SFS. This perception of governors also surfaced in the case study, but they did perceive that they had a role relating to school food. Governors in schools in socioeconomically deprived areas were concerned about undernutrition and were focused on making sure those in need had adequate energy intake and nutrition rather than being concerned about compliance with the SFS. This was also the case for senior leadership staff in these schools; they were concerned about a lack of food, as well as unhealthy and imbalanced diets in their pupils. Also of note here is that no schools in this study had participated in the government’s healthy schools rating scheme, which includes self-assessment of SFS compliance. 73 This gives a further indication of the minimal oversight on healthy school food and SFS compliance among school SLTs and governors in secondary schools.
Our case study data helped us to further interpret our findings in relation to the implementation of SFP actions. Both staff and pupils in some of the case sites perceived that consistent messages around healthy eating were not present, and some pupils perceived that there was a lack of action from staff when they saw pupils consuming unhealthy foods and drinks. This resonates with our findings that some actions related to a whole-school approach, including the promotion of healthy-eating messages across the school, were not well implemented in most schools. There was also a strong negative perception of the lunchtime experience by pupils from some of the case sites, including a lack of time to purchase and eat their food, queuing, fear of food running out and crowded dining environments. These negative perceptions were not particularly echoed by staff in these case sites, which, in the light of our findings that some strategies to improve the lunchtime experience are well implemented in most schools, may suggest that even though these strategies might be in place, they are not achieving the desired effect. In one case site, the lunchtime experience was perceived positively by both staff and pupils. This school had a policy of all pupils having a school-provided lunch, and family-style dining was in place, with staff and pupils sitting together at tables and eating the same food. This school was the only school in our sample to adopt this method at mealtimes, and the key motivation for doing so related to supporting the social and holistic development of the pupils, rather than aiming to improve nutritional intake per se. In general, the family-style lunch was positively viewed by staff, governors and pupils, and pupils valued the opportunity to sit and eat with staff. This finding was corroborated in our assessment of SFP implementation, as this was the only school in which pupils did not feel rushed to buy their food (information is available on the study web page at www.fundingawards.nihr.ac.uk/award/17/92/39).
Our case study data highlighted differences among school staff and pupils’ perceptions of the opportunities for pupils to feedback about school food and the eating experience. From the staff perspective, there were opportunities for pupils to give their feedback, but often pupils either were not aware of systems of feedback or felt that they were inadequate. Some pupils felt that no action was taken in response to the feedback that they gave.
Our case study also provided some insights around food education in schools, which is a key component of the SFP. Overall, food education was viewed as important by school staff and was perceived as sitting within broader holistic ‘life learning’. However, staff acknowledged that it was difficult to fit it in with other educational priorities, and some staff felt that food and healthy eating were not high on the agenda in their schools. In line with this view, some pupils perceived that food education outside of food preparation and nutrition lessons was scant and ad hoc. There was also a perception among some pupils that practical education on cooking often involved preparing desserts and so was less useful in developing the skills needed for future independent living.
In terms of the survey data on how well the SFP was embedded within schools as a policy, from school senior leadership staff, teachers with responsibility for/interest in food, caterers and governors, among those aware of the SFP (i.e. under half of respondents), around 60% perceived that the SFP was being implemented in their schools, and catering staff reported being most involved in implementation. Fewer than half of the respondents who were aware of the SFP felt that there was a shared understanding of it in their schools (coherence) and that staff worked well together to implement the SFP (collective action), although there were higher levels of engagement (cognitive participation). The SFP was perceived by most as worthwhile. As with the SFS, governors did not feel that they had a role in the implementation of the SFP in their schools.
Within our case study, there was variation in the awareness of the SFP as a national policy, but all four schools had initiatives and actions to support healthy eating, which were in line with some of the SFP actions. There was some tension between school teaching/leadership staff and caterers as to where the responsibility for SFP implementation lay, but this may in part be due to the limited awareness and understanding of the SFP among some participants. In one case site, there had been explicit implementation of the SFP as a policy, and, as a result, the whole school and community were involved in school food and healthy eating. A key driver of implementing the SFP in this school had been to increase school meal uptake, and this had been achieved following implementation of a variety of SFP actions. This SFP implementation had been driven by a particular staff member (a food preparation and nutrition teacher) who had received support through an external programme. However, this person no longer held a teaching post at the school, and the current food preparation and nutrition teacher had little awareness of the SFP.
Another perception among school staff articulated in the case sites was the sense that the school was limited in its influence on pupil food choices, with staff acknowledging the wider socioeconomic, demographic and environmental influences driving these dietary behaviours both in and out of school. They felt that if pupils chose to bring unhealthy foods into school or chose the unhealthier options in school, there was little they could do about it. The case site that used the family dining model was an exception. In this school there was a policy prohibiting certain drinks and snacks, which staff felt was important in reinforcing education around healthy eating.
One of the central aims of the introduction of the SFP was to increase the uptake of school food. However, in our participating schools, on average, only just over half of school pupils were having school lunches. There was no difference across SFS-mandated and SFS-non-mandated school groups, but large variation was seen across schools, with uptake ranging from one-third to three-quarters of pupils (excluding the case site that had a family-style lunch approach and a policy of compulsory school lunches). In the case study, pupils articulated views that may contribute to their decisions to have school-provided food. There were mixed views on the quality of school food, and other issues that arose were the lack of diverse cuisines, lack of catering for special dietary needs, and mistrust over school food pricing and value for money of foods. Crucially, pupils felt they could get more for their money from food outlets outside school. The lunchtime experience was also a factor for pupils when making decisions on purchasing school food, with school food being perceived as a risk because of food running out and limited choice if they were at the back of the queue.
School types
As a way of trying to capture and articulate the variation across schools in relation to school food provision and the food and healthy-eating culture and environment, we attempted to develop a typology of schools in relation to the SFS and the SFP. Using an approach we developed to type schools based on their SFS compliance, we categorised the majority of schools into two types: both had high compliance with SFS relating to increasing dietary variety, but one had low compliance with standards relating to obesity and dental health (type 1) and the other had medium compliance with this latter set of standards (type 3).
There were two schools in our sample that were assigned as different types. The school identified as type 2 had a more restrictive food offer, with lower compliance with standards related to dietary variety than the other three school types and medium compliance with the standards related to obesity and dental health. This school was also the case site (school 1) with a family-style dining approach and limited meal choices both at breakfast and lunch, which may explain a lower compliance with standards relating to dietary variety. However, with the more controlled menu and limited choice available in this school, one might think that there would be opportunity to be highly compliant with the standards related to obesity and dental health, yet this was not the case. In fact, in the qualitative data from this school, catering staff reported that the need to cater according to the family dining approach was one of the factors making it more challenging to comply with the SFS (related to the need to ensure that all pupils were happy with the limited choices on offer).
The school identified as type 4 was different from other schools because it was the only school that had high compliance with the standards relating to obesity and dental health and high compliance with the dietary variety-related standards. Thus, the four identified types provided us with a range of levels of compliance with the SFS targeting different aspects of achieving healthy nutritional intake, which enabled us to explore nutritional intake in pupils across the different school types. Our subtyping based on implementation of the SFP actions was less clear-cut, and we were hampered by a substantial number of missing data from schools. There were no patterns or clusters of actions that were implemented in some schools and not in others. Therefore, we based our subtypes on the proportion of SFP actions implemented.
Pupil nutritional intake and dental health, and school food policy
Comparison of pupil outcomes in SFS-mandated and SFS-non-mandated schools
After adjustment for a variety of school-level and individual-level factors, we detected a small (2.8 g) difference in free sugar intake at lunch between pupils in SFS-mandated and pupils in SFS-non-mandated schools, with those in the SFS-mandated schools having the lower intake. TEI, fat and F&V intake were also lower in pupils from SFS-mandated schools. When we adjusted for TEI in our models, the difference in free sugar and fat intake at lunch was no longer present. However, a consistently lower F&V intake was present in pupils from SFS-mandated schools at lunch, across the school day and over the whole day (24 hours). The difference in F&V intake was one-fifth of a portion at lunch and around one-third of a portion over the whole day. Although this is small difference, it is nutritionally meaningful given the low intake of F&V in the UK adolescent population (mean intake of 2.9 portions per day). 17 In the models adjusted for TEI, there was also higher consumption of confectionery items across the school day and SSB items over 24 hours in the SFS-mandated group.
Although these differences suggest that pupils in the SFS-mandated schools have lower energy intake and lower quality nutritional intake, our data on the implementation of the SFS in the mandated and non-mandated schools do not provide a clear explanation of this difference. Overall, there were no substantial differences in the level of compliance with the SFS, although there was large variation in compliance in both school groups. With standards relating to F&V consumption, we found that they were generally highly complied with across the SFS-mandated and SFS-non-mandated school groups, but with some small differences. Slightly lower proportions of SFS-mandated schools provided at least three different types of fruit each week (85% vs. 91%) and providing fruit or vegetables at every food outlet (69% vs. 87%). The standards relating to high-sugar items were generally poorly complied with across both school groups, but again there were some small differences. The standards relating to the availability of confectionery items were marginally better complied with in the SFS-non-mandated schools; however, standards relating to sales of cakes and biscuits outside of lunchtime had higher compliance in the SFS-mandated group (31% vs. 9%). Similar to SFS compliance, there was variation in the implementation of the wider actions to support healthy eating set out in the SFP across both groups of schools, with no clear-cut differences.
Given these implementation findings, we cannot attribute the differences in pupil nutritional intake across the two school groups to differences in implementation of the SFS or the SFP. Furthermore, our analyses exploring how source of school lunch and school SFS-mandated status interacted suggested that the difference in nutritional intake at lunchtime across the SFS-mandated and SFS-non-mandated school groups was not significantly larger when considering pupils who consumed a school-provided lunch. If SFS compliance, and therefore healthier school food, was mainly responsible for the differences in nutritional intake across the two school groups, we would have expected to see a greater difference in those having a school-provided lunch. Instead, school-provided lunch, regardless of school SFS-mandated status, tended to be a consistent significant predictor of school lunch nutritional outcomes.
We adjusted for a range of factors at the school and individual levels, including measures of deprivation at both levels, to try to account for confounding. However, it is possible that the differences in F&V, confectionery and SSB items across the SFS-mandated and SFS-non-mandated groups are due in part to other factors for which we have not assessed and accounted. For example, the density and nature of food outlets surrounding schools could influence nutritional intake, but we were unable to explore this in the study.
We found no differences in pupil dental health outcomes across the SFS-mandated and SFS-non-mandated schools, which, given the minimal differences in nutritional intake, is unsurprising.
Comparison of nutritional intake across the school typology
We detected some differences in pupil nutritional intake across the school types defined by the level of compliance with two sets of SFS related to obesity/dental health and dietary variety. Pupils in the type 2 school had a lower lunchtime percentage of TEI from free sugar than those in the reference group (type 1). This type had lower compliance with standards related to providing dietary variety than all other types and only medium compliance with the obesity and dental health-related standards. Pupils in the type 4 school had higher consumption of confectionery at lunch than type 1 schools, which is counterintuitive as the type 4 school had high compliance with the obesity/dental health-related standards and was one of only two schools that complied with the standard on prohibiting the sales of confectionery/chocolate products, whereas type 1 schools had low compliance with these standards. Higher confectionery consumption during the school day was also seen in the type 2 school, which is again counterintuitive as it had better compliance with the obesity/dental health-related standards than type 1 schools. Acknowledging the limitations of our school subtyping using our data on implementation of SFP actions, we also explored differences in pupil nutritional intake across these subtypes. We found some suggestion that among pupils from school types with higher implementation of SFP actions (subtype B) there was higher consumption of HFSS items outside school lunch.
Interpretation of these differences across school types was limited by the fact that there was only one school each assigned to types 2 and 4. To overcome this limitation, we explored the association between nutritional outcomes and the percentage of standards met that related to obesity and dental health and to dietary variety. High compliance with dietary variety-related standards was associated with higher percentage of TEI from free sugar at lunch and during the school day, and high compliance with obesity/dental health-related standards was associated with higher free sugar intake and intake of confectionery items outside school lunch. The findings of these analyses are consistent with our school type comparisons. A possible explanation for the association between compliance with the standards related to obesity and dental health and consumption of higher sugar foods is that if the sale of foods that are desirable to this age group (including high-sugar foods) is restricted by the school, it is more likely that pupils will obtain these foods from elsewhere and consume them in school and across the whole day. Our case study data gave some indication that this could be the case. There was a sense from many school staff that the school has little influence over what pupils buy outside school, and a sense from pupils that schools did not monitor/care what was being brought in from outside. On the other hand, pupils appeared amenable to buying healthy items (understanding the value of healthy eating) as long as these met their need for convenience, taste and value for money.
Costs and economic impacts of school food policy
The economic evaluation was designed as a cost–consequences analysis due to the range of outcomes potentially impacted by the SFS and SFP, and the wide range of costs to be included. A comprehensive micro-costing approach was essential for this study to fully estimate the societal-sector cost of the SFS and the SFP. However, encouraging the schools to complete the costings survey was challenging, mainly due to the difficulty of identifying the relevant staff member who had the knowledge to complete the survey. Halfway through the study, this led to the survey being adapted and shortened to an online version to try to boost completion rates, but completion remained a problem. The data that were collected produced a wide range of costs reported, and, in some cost categories, these costs ranged substantially between schools.
The cost–consequences analysis suggests that the costs in the SFS-mandated schools are lower than those in the SFS-non-mandated schools, and this direction of difference remained the same across all the different methods for measuring costs. Given that the costing analysis was fraught with methodological difficulties, we cannot be certain of the exact magnitude of this difference; however, it did appear to show SFS-mandated schools having consistently lower costs for items relevant to the SFS and the SFP. However, the data on the implementation of the SFS and the SFP do not provide an explanation for this. The initial plan for the economic evaluation included an exploratory cost–utility analysis. 77 Due to the lack of baseline data, a large proportion of missing cost data, and the uncertainty in the cost and outcomes data, this analysis was no longer feasible.
Overall, this study has highlighted the methodological challenges of collecting cost data in school settings, and, despite the substantial study resources devoted to the data collection, this remained a challenge. We supplemented our analysis with the publicly available catering expenditure data reported by the schools. It should be noted that these data do not include all costs of food provision incurred by the schools. Therefore, some important differences across the schools and the two main school groups compared in this study might not have been captured when comparing the schools based on their catering expenditure. Furthermore, for the majority of the schools, the actual expenditure for the year 2021–2 would be expected to be higher than in 2018–9, even after adjusting for the Consumer Price Index, due to the increase in the proportion of pupils receiving FSM. 118
It is important to note that the socioeconomic differences across the two school groups might have influenced both the costs and the pupil outcomes. For example, the SFS-mandated schools had on average a higher IDACI score than the SFS-non-mandated schools; this indicates higher deprivation, and it might be associated with poorer educational performance, lower quality of life and poorer dietary intake independently from the food provision in these schools. Furthermore, the SFS-mandated schools had a higher proportion of pupils eligible to receive FSM than did the SFS-non-mandated schools. This might be reflected in the funding that is available to support the eligible pupils.
Comparison with existing evidence
Implementation of the school food standards and School Food Plan
Our findings of incomplete compliance with the national SFS in our study sample is consistent with the 2020 Guy’s and St Thomas’ Charity report Serving Up Children’s Health. 66 This London-based study only included a small number of secondary schools, but also highlighted low compliance with the SFS, especially with foods served for breakfast and at breaktimes. Our study builds on this previous work by identifying the standards with particularly low compliance (i.e. the standards relating to the restriction of unhealthy foods, which often apply to food served across the whole day and outside of lunchtime) and provides additional insight into the reasons why these standards have low compliance (i.e. the need to balance pupil preferences, school food uptake and financial viability with SFS compliance). The low compliance with the SFS concerned with restricting unhealthy foods and drinks is also corroborated by evidence on nutritional intake from school food in UK secondary school children. High consumption of sweet and savoury snacks119 and high levels of ultra-processed foods and drinks120 have been reported in the secondary school age group consuming school food at lunch.
The lack of monitoring and oversight of SFS compliance by school governing bodies that we have found has been previously emphasised. 52,65,66 This study sheds further light on this issue in terms of the misconception around roles and responsibilities in implementing the SFS, with governing bodies and school senior leadership representatives often seeing this as the responsibility of the catering provider, and a lack of recognition from governors of their role in overseeing SFS compliance. However, particularly in schools in areas with high deprivation, we found that school governors, senior leaders and teachers focus on food in the context of food insecurity, with their major concern being school pupils going hungry.
In our exploration of implementation of the SFP, we identified similar issues to those presented by Hart and Page, who examined qualitative data on school food education and culture from pupils attending schools in England, along with survey data from school leaders, food teachers and parents. 121 They found that in secondary schools there was lack of a whole-school approach, with mixed messages around healthy eating and foods high in fat, salt and sugar given as rewards. They also reported views of overcrowding in dining areas, and pupils perceiving that healthier foods were expensive and poor value for money. In line with these findings, we found that the SFP actions around consistent healthy-eating messaging across the school, and sweets not used as rewards, were generally not well implemented in schools. Our case study data highlighted the issue of crowding and poor dining environments and pupils’ perceptions of healthy food being poor value for money.
Another key finding of the Hart and Page study was the variable provision of food education and practical food preparation skills and the low status of food education in secondary schools. 121 Our SFP assessment suggests that curricular food and healthy eating is generally delivered well in schools, but our case study data is more in line with this previous study, with healthy food/eating education being perceived as low priority, patchy and ad hoc from a pupil perspective, and a lack of focus on healthy food when teaching practical cooking skills.
A consistent theme throughout our findings in relation to both the SFS and the SFP was that these were not priorities for most schools’ SLTs and governing bodies, although they did identify that SFS compliance and support for healthy eating were important and part of the school’s role. This resonates with findings of a mixed-methods study with English secondary school headteachers and chairpersons of governing bodies. 122 The authors explored participants’ perspectives on adolescent obesity prevention in school settings and reported that, while headteachers and governors recognised that schools have a role in supporting healthy eating (and other obesity-related behaviours) and saw it as part of holistic adolescent development, they identified a range of factors that prevented them from prioritising actions to support this, including financial pressures and the requirement from national government to focus on academic achievement. Financial issues relating to school food provision and other educational priorities competing with the need to provide food and healthy-eating education also featured in our case study data.
School food and pupil nutritional intake
No existing studies have explored the influence of the current SFS (introduced in 2015) on secondary school pupil nutritional intake, but the limited evidence from two studies examining pupil nutritional intake before and after the introduction of the 2006 SFS in secondary-school-aged pupils suggested only a marginal positive impact on dietary intake at lunch64 and very limited impact on total dietary intake. 62 In our exploratory findings on the level of SFS implementation and pupil nutritional intake, although we did not detect any beneficial associations, our analyses suggest that there may be an undesired association between SFS implementation and pupil nutritional intake. We found that higher compliance with standards related to dietary variety and higher compliance with standards related to obesity and dental health were associated with higher intake of sugar/sugary foods, with these associations mostly seen over the school day or over 24 hours.
Consideration of factors influencing adolescents’ food choices may help to explain this suggestion in our data of an unfavourable association between SFS compliance and sugar intake. Although adolescents have an awareness of the need for and benefits of a healthy diet, the main drivers for their food choices are desirability, value for money and convenience, with peer and social influences also playing a part. 25,123 Our case study data surfaced the issue around school food’s perceived poor value for money, and also the low desirability of the food on offer in some instances. As adolescents have increasing autonomy over their food choices, these drivers may lead them to purchase foods from out of school or obtain foods from home, especially if the foods that are desirable to them are restricted in the school food offer. The perception in our case study of schools and school food having limited influence on pupils’ food choices, outside the canteen offer, is coherent with this potential explanation.
Another factor that may contribute to poorer-quality dietary intake during school time, even when the school food offer is relatively healthy overall (i.e. with relatively high compliance with the SFS), is the way in which secondary school food sales are organised. Pupils are often able to purchase food at multiple times throughout the day from multiple service points, with no requirement to purchase a set meal. As highlighted in Hart and Page’s study,121 this freedom to purchase single items can lead to a pupil making multiple purchases of unhealthier foods (e.g. high in sugar and/or fat) throughout the day, even if there is a range of healthy foods on offer. Again, this resonates with our case study data, in which school staff perceived pupils as opting for the unhealthy options available in schools.
This perceived propensity of pupils to choose less healthy foods and purchase the more convenient ‘grab and go’ options (avoiding the main meal options that are more nutritionally balanced) was also found in a qualitative study with catering staff in three Welsh middle schools (pupils aged 11–14 years). 124 The caterers perceived that a variety of influences led to these pupil choices, including taste preferences (i.e. desirability), pricing and convenience. Consistent with our findings about pupil lunchtime experiences, the caterers commented on the pupils having to queue and being rushed at lunchtime, which prompted them to purchase less nutritionally balanced food options (e.g. sandwiches, pasta pots, pizza slices and cakes) that are portable and more easily consumed without sitting down. Also in line with our qualitative findings, caterers in this study acknowledged that they sold unhealthy foods that were not compliant with the SFS that are in place, but that omission of these items would significantly affect food sales and thus threaten financial viability.
Strengths and limitations
Strengths
A key strength of this study is our use of a multiple-methods approach, incorporating both quantitative and qualitative data collection. This has enabled us to gain a detailed understanding of how the SFS and SFP are implemented in secondary schools. Our school sampling approach enabled us to include schools with a range of different characteristics.
We collected extensive data from schools, achieving a comprehensive understanding of SFS compliance through menu analysis and researcher observation, and SFP implementation through multiple data sources. Our tools for collecting data relating to school food provision and SFP actions were developed using existing online resources and legislative documents, which also supported interpretation of the SFS and SFP actions. Use of multiple data sources for SFP assessment also allowed for different perspectives to be captured and enhanced the credibility of the assessments. Our systematic approach to SFS and SFP assessment, with rules agreed on how multiple data sets were combined, enhanced the transparency and reliability of the assessments.
The study included a large sample of school pupils, which is broadly representative of the national population in terms of ethnicity (with 70% of participants in our sample from white ethnic groups compared to 71% across state secondary schools in England in 2022) and deprivation (26% of our sample were in the most deprived quintile). We had a high response rate (99%) and collected a range of outcome data using validated tools. This included our online dietary assessment tool (Intake24), which we adapted for use in an ethnically diverse population. In our pupil outcome analyses, we used multilevel modelling to account for potential clustering and explored the effect of missing data and misreporting of dietary intake on the findings through our sensitivity analyses.
We conducted a qualitative case study with four school sites, sampled to provide some representation of our main study sample, to better understand the wide variation in SFS and SFP implementation across secondary schools. We used topic guides with broad opening questions to allow participants to guide the discussion and our inductive analysis approach enabled our interpretation to reflect the most relevant issues for participants. A team of five researchers were involved in analysing the qualitative data, allowing for a range of interpretations to be considered and providing an opportunity to challenge assumptions and preconceptions. We used a structured method of data analysis,117 and have presented verbatim quotations from participants in our results, providing transparency in the development of our interpretative themes.
Limitations
There are several limitations within this study. To maximise study power, we aimed to recruit an even number of schools in the SFS-mandated and SFS-non-mandated groups but were unable to do so. However, the proportion of participating schools in each group reflected that of the wider sampling frame (64% and 60% SFS-non-mandated schools in our sample and the sampling frame, respectively). There were some differences in the characteristics of schools and pupil participants between the SFS-mandated and SFS-non-mandated school groups, but we adjusted for school and pupil characteristics in our pupil outcome analyses to account for these.
There were also some differences in our pupil characteristics from those of the secondary school pupil population across England. For example, the proportion of pupils reporting that they had a FSM in our sample was 15.4%. This compares with 20.9% FSM eligibility in secondary-school-aged pupils nationally. 118 This difference may be explained partly by substantial increases in the FSM eligibility in the population over the duration of the study (eligibility was 15.9% in 2020) and partly by a degree of under-reporting in our sample, as pupils were asked to self-report this information. Not all pupils would be aware of their eligibility for FSM, and some may have chosen not to report that they were eligible.
Regarding data collection, there were substantial disruptions in schools recruited in the 2019–20 academic year due to school closures in response to the COVID-19 pandemic. This resulted in lower complete data collection in these schools, for example non-completion of the second pupil data collection session or non-response to school surveys and document requests. This affected a greater number of SFS-mandated schools, since a higher proportion of SFS-mandated schools were undergoing data collection at that time (38% of SFS-mandated schools vs. 30% of SFS-non-mandated). School food provision and the dining arrangements in schools were also temporarily changed to accommodate COVID-19 measures in schools in the summer term of 2021. We collected data in four schools during this school term and so may not have obtained a representation of their typical food provision and environment. This impacted on SFS-non-mandated schools to a greater extent than SFS-mandated schools (13% of SFS-non-mandated schools vs. 8% of SFS-mandated schools). We adjusted for academic year of data collection in our pupil outcome analyses to account for changes that may have occurred in the 2020–1 year in response to the pandemic.
Some schools had low levels of completion of the second pupil data collection session or school surveys for other reasons, for example if they could not find time to run a second pupil session, the school liaison person was absent, or there was a lack of response to requests for school surveys and documents (these issues arose in both school groups). In addition, the costings survey was complex and difficult to complete, despite our attempts to simplify it, and this may have influenced the response from schools. The sales data proved difficult to obtain from schools, resulting in large numbers of missing data. We also had a low overall response rate to surveys from staff, and particularly from governors. This limited our ability to assess the implementation of SFP actions in some schools. It also reduced our ability to make meaningful comparisons between SFS-mandated and SFS-non-mandated school groups in our analysis of SFS and SFP policy implementation, as there were proportionally fewer staff/governor survey responses in SFS-mandated schools than in SFS-non-mandated schools. Overall, the substantial number of missing data prohibited the full assessment of SFP implementation in some schools.
In addition, the large number of missing cost data impacted the economic evaluation. This was somewhat mitigated by supplementing our analysis using publicly available data on schools’ catering expenditure, but it prevented us from conducting an exploratory cost–utility analysis in line with the study protocol. 77 We explored the impact of missing data on pupil characteristics in our pupil outcome analyses through imputation and sensitivity analyses.
Regarding pupil nutritional outcome data, there was some loss of dietary data due to being unable to match pupil demographic data to Intake24 data, but this affected only 4.7% of Intake24 records (165 of 3488). Another limitation of the pupil dietary data is that although we planned to collect two non-consecutive 24-hour dietary recall records per pupil, 54% had one only record. This only provides one ‘snapshot’ of dietary intake, which may not be representative of typical intake. Misreporting is a common limitation of self-reported dietary intake measures such as 24-hour recall, especially in adolescent populations,125 so there is likely to be some measurement error in the nutritional outcomes. This impacts particularly on reported energy intakes, which are likely to be an underestimation of true intakes. However, we would expect this misreporting to be similar in the two SFS comparison groups. We explored the impact of the inclusion of dietary records reporting extreme values of 24-hour energy intake in our pupil outcome sensitivity analyses. The dental outcome data collected from pupil participants were self-reported and not from objective dental examination, and so may not accurately reflect the dental health of the sample. However, the self-report questions were taken from the National Children’s Dental Health Survey and have been previously tested for use in this age group.
In our pupil outcome analyses, we explored multiple nutritional outcomes, each during three different time periods. Therefore, it is possible that some of the findings that reached statistical significance were as a result of multiple testing, rather than a true difference between groups. We did not apply a correction for multiple testing as this analysis was exploratory, and we have interpreted our findings according to patterns seen (e.g. across the three time periods investigated). Regarding the analysis of dental outcomes, while we adjusted for toothbrushing habits and home water fluoridation status, we did not adjust for eating behaviours and habits, which may impact on dental health.
In terms of the qualitative component, we had planned to sample our case sites using our developed school typology. However, we were unable to do this, as we had to conduct the main and qualitative phases of the study concurrently, rather than sequentially, due to study interruptions relating to the COVID-19 pandemic. This meant that we missed an opportunity to explore the experiences of SFS/SFP implementation in SFS type 4 school, which had the highest level of SFS compliance. Another limitation was that the pupil focus groups were larger than planned, due to a variety of reasons, which may have impacted on the data collected. For example, there may have been fewer opportunities for everyone in the group to voice their opinion and more pupils talking over one another, which may have affected the quality of the audio data.
Implications of findings
Implications for policy and practice
In this study we have demonstrated no difference in compliance with the SFS between schools mandated and schools not mandated to follow them, and minimal or no differences among the two school groups in the implementation of actions to support healthy eating (outlined in the SFP), food-related costs, and the nutritional intake and dental health of pupils. This has limited implications for policy for the following reason: since the introduction of the 2015 SFS legislation, exempt schools have been encouraged to voluntarily sign up to the standards, and more recently this has been a firm government expectation. 49 Therefore, in the current context, there is no practical difference between the two school groups that we compared in terms of the expectation for them to comply with the SFS.
Our findings of incomplete implementation of the SFS in secondary schools, regardless of whether they have a statutory requirement to comply, have greater implications for policy and practice. These findings suggest that the standards are challenging to fully implement in a secondary school context. The extensive provision of school food at eating occasions other than school lunch, the sale of single items for purchase (and no obligation for pupils to choose the set menu meals), and the need to provide foods and drinks to meet the pupils’ demands to ensure school food uptake and financial viability, are all factors that contribute to this incomplete compliance. There was also some evidence of difficulty in interpreting and applying the SFS within schools (e.g. in relation to the compliance of pre-packaged snacks). From a policy perspective, this raises a question as to how policy around the provision of healthy school food can be adapted and developed to better suit the secondary school context of food provision, without impacting on the viability of school food catering services. There is also the question of how schools and caterers can better be supported to interpret and apply the standards in the context of a financially viable food provision service. From a school and catering practice perspective, there may be changes to the way in which food is provided and choices are presented to pupils (e.g. nutritionally balanced meals in favour of single items, and portable healthy meal options), which could encourage healthier school food choices. Our finding that schools were not perceived to be offering meaningful opportunities for pupils to feedback on school food is relevant here. Better communication between schools and pupils would enable the multiple drivers of pupils’ decisions relating to school food to be understood in more detail, which would inform the changes needed by schools and caterers to enhance the healthy food offer and increase school meal uptake.
The lack of oversight of healthy nutritionally balanced school food provision and SFS compliance in schools has previously been highlighted and is a prominent finding in this study. The government has started to address the absence of external accountability for school governing bodies in relation to compliance with the SFS through their Levelling Up the United Kingdom White Paper,75 in which they announced a pilot programme involving local authorities assuring school compliance with the SFS. However, given the extensive remit and other priorities of governing bodies and school SLTs, support and training for schools and school governing bodies in terms of negotiating food provision contracts and putting in place internal mechanisms to monitor compliance is likely to be needed alongside a system of external accountability. It is worth noting here that a formal process of external monitoring and inspection of school food is in place in Scotland, which may provide valuable learning for the English context. 52
Overall, the SFP as a policy was not adopted in schools, and although all schools had some curricular and environmental measures in place relating to food and healthy eating, these were, in most cases, not a central priority in the schools. In that sense, the SFP, which was launched nearly a decade ago and set out actions for schools to support them in developing a whole-school approach to create a healthy-eating culture, has not achieved the desired outcomes in the secondary school setting. In line with our findings on food education, in his independent National Food Strategy report,74 Dimbleby reflected that despite the legal requirement to teach cookery and nutrition up to the age of 14 years (introduced following the SFP), food education was still not taken seriously. He set out a recommendation to address this (recommendation 3), which included government actions to reinstate the food A-Level and review other qualifications in food; require schools to work with food and food education accreditation schemes; and include rigorous inspection of food lessons within the national Ofsted inspection framework. Dimbleby also highlighted the need for the government to increase the numbers of specialist food teachers in secondary schools and provide funding for the ingredients used in cookery lessons. He suggested that the implementation of these recommendations be led by a dedicated ‘Eat and Learn’ team situated within the DfE. Dimbleby also reiterated the need for a whole-school approach to food (originally set out in the SFP) and specified that this should be championed at the governmental level. 74 Our findings support the need for this, as we found that some actions related to a whole-school approach, such as the promotion of consistent healthy-eating messaging across the school, were not well implemented in most schools. To date, most of Dimbleby’s recommendations have not been translated into government policy, despite the publication of the Government Food Strategy White Paper in 2022. 76
Finally, acknowledging the limitations of dietary assessment in our study (see Limitations), our findings suggest that even when the SFS are relatively well implemented, this either has no beneficial effect on the nutritional intake of pupils or may even lead to marginally worse nutritional intake. To an extent, addressing the issues of poor SFS implementation and the lack of prioritisation of healthy eating and nutrition should lead to more beneficial effects on pupil dietary intake; however, it is important to recognise that adolescents are interacting in a variety of environments and have increasing autonomy over their food choices. Therefore, schools need to be considered as only one part of the food system that influences adolescents’ dietary intake, and it is important to address other aspects of this system to substantially influence nutritional intake in this age group. 126
To sum up, this study has provided a range of evidence that could inform the future direction of school food policy and practice. Work is now needed to translate this evidence into recommendations for specific actions on school food, and identify which bodies are responsible for their implementation (e.g. national government, local authorities, schools, caterers). We are currently conducting this work, involving multiple stakeholders, in an ongoing NIHR Policy Research Programme-funded study (NIHR204247).
Future research recommendations
Key areas of future research have been identified through this study. At the individual level, there is a need to better understand how school food provision and environments influence the food choices of adolescents. Given our findings, we particularly need to understand how more restrictive food policies and provision in schools may shape adolescent food choices and their decisions on where they obtain the food that they consume in school (i.e. school vs. home vs. external food outlets). Related to this, we need to better understand how healthier food can be provided that matches the preferences of secondary school pupils. For example, healthier school food may be achieved by providing nutritionally balanced ‘sit-down’ meals or offering healthier ‘grab and go’ options. Currently, the SFP has an emphasis on ‘sit-down’ meals and set menus, but a further understanding of whether this is what pupils want would inform future school food provision arrangements.
At the school level, we need to better understand how secondary schools can increase the focus on the school food and healthy-eating agenda so that it is part of the core of daily school business and a whole-school approach to healthy eating is fostered. We particularly need to explore challenges that schools experience in prioritising school food and food education (e.g. managing competing educational priorities) and the support that they require to enable them to overcome these challenges. As part of this, we need to be able to evaluate the economic implications for schools taking actions to improve school food and support healthy eating. In this study, we demonstrated the difficulty of conducting economic evaluations in school settings; therefore, there is an additional need for methodological research to understand how to appropriately capture the economic impact of providing healthy school food and developing a healthy school food culture and environment.
On a societal level, we need to further understand the wider food system influences on adolescent nutritional intake and how these interact with school influences, including how the home and school food environments interact to influence nutritional intake in this age group. Ultimately this will help us to identify a range of interventions, targeting different parts of the food system, that will complement secondary school efforts to positively influence adolescent nutrition. Finally, it is imperative to involve schools, caterers and pupils in the development of further research questions, as this will enhance the relevance of future school food research.
Chapter 6 Conclusions
This is the first study to comprehensively evaluate the implementation of two key national school policies (the SFS, updated in 2015, and the SFP) in secondary schools. We found that no participating schools fully complied with the SFS and that there was wide variation in the level of compliance across schools, regardless of whether they were exempt from the SFS legislation. There has been increasing expectation from the government for exempt schools to comply with the legislation, so this finding is unsurprising. In general, compliance was higher with the standards related to the provision of healthy foods and variety to support a nutritionally balanced diet, and lower with the standards restricting the sale of unhealthy foods and drinks. This was reflected in sales of foods in school items higher in sugar and fat constituting over one-third of all sales. The lowest levels of compliance were with standards related to foods served across the whole school day and outside lunchtime.
Catering staff acknowledged this lack of compliance with the SFS, especially at breakfast and breaktimes, but articulated the multiple issues that need to be balanced when planning school food provision, including pupil preferences and demand, costs and wastage, all of which contribute to financial viability. Related to this we found that school food uptake widely varied across schools, with food quality, diversity of cuisines, value for money and the food purchasing experience being factors that influence pupils’ food choices. Despite the government’s expectation that school governing bodies have responsibility for monitoring and oversight of the SFS, governors themselves did not recognise this as part of their role.
Among school leaders, staff and caterers there was low awareness of the SFP and those who were aware of it did not perceive it to be well implemented in their schools. Nevertheless, all schools were taking some steps to positively influence eating and diet that were in line with the recommended actions within the SFP, but in most schools this was not a central priority for the school senior leadership and governing bodies. In schools with high deprivation, the priority for the school leadership around nutrition was ensuring some energy intake and preventing hunger, as well as ensuring nutritional quality. All schools were delivering some education on food and healthy eating within the curriculum, but our qualitative findings suggest that this was often not a high educational priority in schools.
Our exploration of pupil nutritional intake revealed some differences between those attending schools legally required to comply with the SFS and those attending schools exempt from the SFS legislation. However, our assessment of SFS implementation across the two school groups did not suggest that there were differences in compliance that would explain these observed differences in pupil nutritional intake. Therefore, other, unmeasured factors may be contributing to this finding. We did not find any differences in the dental outcomes that we measured between the two groups of pupils, but we would have expected to find differences only if there were large differences in intake of free sugars and high sugar foods, which was not the case. Similar to our findings on pupil nutritional intake, in our cost–consequences analysis, we found differences in costs across the two school groups and differences in additional outcomes (e.g. HRQoL and educational outcomes), but we could not attribute these to differences in SFS compliance. Poor-quality and missing cost data posed an additional limitation in interpretation of the cost–consequences analysis.
On further investigation of pupil nutritional intake in relation to the level of compliance of schools with the SFS, we found no strong evidence that higher compliance is associated with healthier nutritional intake. In fact, our findings suggest that higher compliance with the standards restricting unhealthier foods may be associated with marginally higher intakes of high-sugar foods. This may be explained to some extent by our case study findings in which some school staff expressed that pupils will choose to obtain and consume unhealthy foods, regardless of actions taken by the school. The pupil perspective in our case study was that the healthy school food options often did not give them what they wanted from school food, such as convenience, taste and value for money.
Overall, our findings highlight the difficulty of implementing the SFS within the secondary school context, the absence of monitoring and oversight of SFS compliance, the limited time and capacity to focus on healthy eating and balanced nutrition in secondary schools (due to multiple competing priorities), and the lack of positive impact of current school food policy on pupils’ dietary intake. Measures need to be taken to ensure that standards for school food can be implemented within the secondary school context and that healthy eating and nutrition is a central priority in schools.
Public involvement: reflections
Public involvement was crucial to the design and delivery of this research and featured at multiple time points from development of the research proposal to planning dissemination of outputs. This engagement was impactful as it led to improvements in the study, for example better accessibility/comprehension of participant information and data collection tools, more effective recruitment approaches, and ensuring that the most relevant and salient messages for each stakeholder group will be disseminated in appropriate and accessible ways. This was enabled through our approach to public advisory meetings, particularly in terms of ensuring that group members knew what was expected of them, and the interactive approaches we used in the meetings. We were flexible when working with the public advisory groups, for example offering meetings at times that suited public advisors. We also adapted our approach in response to COVID-19-related restrictions, moving to online meetings, which have now been established as our main way of working with these groups (giving the additional benefit of removing geographical constraints on participation).
We successfully engaged with three groups of key stakeholders (young people, parents and school staff/governors). However, a limitation was that this engagement was not always maintained throughout the study. For example, none of the parents from the original parent advisory group were retained as advisors following the COVID-19 interruption. This was partly due to these parents no longer feeling engaged (some no longer had school-aged children and we lost contact with others) and partly due to an acknowledgement from the research team that we needed a larger, more engaged and more diverse group of parents. This led to a recruitment drive of parents, with selections made to ensure that a range of parents were included in terms of locality and sociodemographic characteristics (e.g. eligibility for FSM, ethnicity). In addition, we changed our mode of engagement with youth advisors by accessing an established young people’s advisory group, facilitated by the NIHR Clinical Research Network. This enabled us to utilise the existing organisational support of the network and better maintain engagement with our youth advisors. Our school staff group has also fluctuated because of changes in members’ roles and situations (e.g. retirement, parental leave) and recognition that we needed more representatives from some stakeholder groups (e.g. governors). We also acknowledge that although we had initial input from an external catering provider, we have not had any representatives who are currently involved in catering provision at secondary schools, and we have not had any input from teachers involved in food education.
Our public advisors have already advised on some key elements of dissemination, for example key messages and information formats, and will further support this work by their continued engagement in a planned follow-up study to use the findings of this study to develop recommendations to enhance existing national school food policy (funded by the NIHR Policy Research Programme; project reference NIHR204247; timeline: November 2022–February 2024).
Equality, diversity and inclusion
Our research aligns with the NIHR principles of equality, diversity and inclusion (EDI), particularly in our engagement with a diverse range of public contributors and in the methods we employed in our research. Our sampling approach and recruitment methods aimed to achieve to a diverse participant sample. The inclusion of children from low-income families, living in deprived areas and/or from minority ethnic groups was considered crucial in this project as these factors are known to be associated with dietary intake, dental health and obesity in adolescence. 21–23,127
Our research was situated in the West and East Midlands, which comprises areas with high ethnic diversity and a wide range of deprivation levels. We incorporated a range of characteristics into our school sampling approach, including proportions of pupils from ethnic minorities groups, with EAL, eligible for FSM, and with special education needs, as well as level of deprivation. This resulted in a study sample that was broadly representative of the secondary school population in terms of the proportion of pupils from minority ethnic groups and was over-represented by pupils living in areas with high deprivation. In addition, our approach to the sampling of schools in the case study phase incorporated FSM eligibility, and we were able to recruit three schools (out of four in the sample) with higher-than-average levels of FSM eligibility. This resulted in 25% of pupil participants who were receiving FSM, ensuring inclusion of their voices, which are often missing from qualitative research on this topic. 128
We also asked our public advisory groups to review our participant information and participant-facing data collection tools to check that the language was appropriate and acceptable, and made participant information available in accessible formats on our study web pages, so that people with disabilities could access this. We adopted an inclusive approach when designing our survey questions. We used census questions to collect data on demographic characteristics, including sex and ethnic group, and these questions underwent extensive user testing and were developed with stakeholders to enhance their acceptability and clarity. We also included a free-text option for participants to describe their sex or ethnic group in their own words, and an option for those who would ‘prefer not to say’, so that they did not feel excluded from the research. We also demonstrated an inclusive approach in our adaptation of the dietary recall tool Intake24, which was edited to incorporate a wider range of traditional foods consumed by those from minority ethnic groups so that its relevance to a culturally diverse population was enhanced. This was achieved in consultation with members of, and those working with, minority ethnic communities in the West Midlands.
In our analysis of the differences in pupil outcomes between SFS-mandated and SFS-non-mandated schools, we explored the potential influence of socioeconomic deprivation. In our case study, we explored issues including food insecurity, food provision for pupils eligible for FSM, school food pricing and meeting the needs of a diverse range of pupils.
Our public involvement activities also demonstrated our commitment to EDI. Our initial youth engagement was carried out in two schools, one of which was situated in an area in the top decile for deprivation (IMD), with 50% of pupils eligible for FSM. Later in the study, we linked with the regional NIHR Clinical Research Network’s Young People’s Advisory Group, which has an ethnically diverse membership. Most recently, our parent advisory group has been established with equality, diversity and inclusion in mind. We asked interested parents to complete a short screening questionnaire, which included demographic questions and free-text boxes that parents could use to tell us about their reason for applying for the role. We used this information to select parents based on demographic characteristics (sex, location, ethnicity) and other characteristics described, such as having a child eligible for FSM, with special education needs or with dietary restrictions. This has enabled us to create a group of parents with varied perspectives and experiences of school food.
The rich data set produced in this study, which includes key characteristics related to EDI, will provide future opportunities to answer research questions that are specific to understanding health inequalities and are currently underdeveloped in the existing literature, such as how the diets of pupils eligible for FSM differ from those of pupils who are not, and the variation in nutritional intakes across ethnic groups. As a result, this work may contribute towards a broader evidence base on inequalities in nutrition and the role of school food in addressing these.
Additional information
Acknowledgements
We wish to acknowledge funding for this study from the National Institute for Health and Care Research Public Health Research programme (NIHR award ref: 17/92/39). We would like to thank the young people, parents, schools, school staff and governors who participated in the study. We would like to acknowledge all the administrative and research staff who contributed to the study: David Alexander, Katie Youngwood, Frances Mason, Daniel Mensah, Estera Sevel, Florence Edwards, Ankita Gupta, Anisah Ali, Lucy Carver, Natalie Quinn-Walker, James Bhol and Prajakta Gandhi. We would also like to acknowledge the students and sessional staff workers who supported data collection. We would like to thank Maisie Rowland and Ivan Poliakov for their technical support and expertise in relation to Intake24. We would like to thank the young people who served as youth advisors, and members of the parent and school staff advisory groups. We would like to thank Carly Tibbins, Jennifer Thomas and Steven Moore for supporting the youth public engagement activities. We would also like to thank Scott Wheeldon for his advisory role in the study.
Study Steering Committee
We would like to acknowledge members of the external SSC for overseeing the study: Professor Robert West (University of Leeds; chairperson), Professor Christopher Owen (St George’s, University of London), Dr Alexander Turner (Putnam PHMR Ltd), Dr Helen Carter (public health consultant; Public Health England, West Midlands; Steering Committee member until January 2021), Mrs Sheila Birdi (public representative until January 2020), Ms Ann Hughes (public representative, January 2020–September 2021) and Clare Madden (public representative, September 2021–October 2022).
Protocol details and trial registration
The original study protocol was submitted to the NIHR Public Health Research programme for approval on 1 February 2019. Several revisions and additions were made to the protocol during the study, which are available on the study web page (www.fundingawards.nihr.ac.uk/award/17/92/39). The protocol was published as a journal article in 2020. 77 This trial is registered as ISRCTN68757496 (registered 17 October 2019).
Contributions of authors
Miranda Pallan (https://orcid.org/0000-0002-2868-4892) (Professor of Child and Adolescent Public Health) was the co-chief investigator of the study. She led the design and conduct of the study and contributed to the preparation of all chapters in the study report.
Marie Murphy (https://orcid.org/0000-0003-1177-1890) (Research Fellow, Public Health) was the study co-ordinator and was a member of the study management team. She contributed to the study design and delivery and the preparation of all chapters in the study report.
Breanna Morrison (https://orcid.org/0000-0002-7473-2402) (Research Fellow, Biostatistics) undertook all statistical analyses relating to pupil nutritional and dental outcomes and contributed to the preparation of the methods and results tables relating to these analyses.
Irina Pokhilenko (https://orcid.org/0000-0001-6390-2851) (Research Fellow, Health Economics) undertook the economic evaluation and prepared all sections of the report relating to this.
Alice Sitch (https://orcid.org/0000-0001-7727-4497) (Associate Professor in Biostatistics) was a co-investigator and member of the study management team. She contributed to the design and conduct of the study and the interpretation of the study findings relating to pupil outcomes.
Emma Frew (https://orcid.org/0000-0002-5462-1158) (Professor in Health Economics) was a co-investigator and member of the study management team. She contributed to the design, analysis and writing of the health economic components of the study.
Clare Rawdin (https://orcid.org/0000-0002-6169-796X) (Research Associate, Public Health) contributed to the analysis and writing of the qualitative components of the study.
Rachel Adams (https://orcid.org/0000-0002-1798-3854) (Research Fellow, Primary care & Public Health) contributed to the design, conduct, analysis and writing of the qualitative components of the study.
Ashley Adamson (https://orcid.org/0000-0003-3735-2846) (Professor of Public Health Nutrition) was a co-investigator and member of the study management team. She contributed to the study design, adaptation of Intake24 and interpretation of the study findings.
Suzanne Bartington (https://orcid.org/0000-0002-8179-7618) (Clinical Research Fellow in Environmental Health) was a co-investigator and member of the study management team. She contributed to the study design and interpretation of the study findings.
Alexandra Dobell (https://orcid.org/0000-0002-9047-9101) (Research Fellow, Public Health) contributed to the study delivery and prepared the section of the report relating to the embedding of the SFS and SFP policies.
Rhona Duff (https://orcid.org/0000-0003-3214-524X) (Research Associate, Public Health) was the research associate for 34 months of the study and was a member of the study management team. She contributed to the study design and delivery, and adaptation of Intake24.
Tania Griffin (https://orcid.org/0000-0003-0146-4440) (Lecturer in Nutrition and Population Health) was a co-investigator and member of the study management team. She contributed to the study design and interpretation of the study findings.
Kiya Hurley (https://orcid.org/0000-0002-5084-5410) (Research Fellow, Public Health) was a co-investigator and member of the study management team. She contributed to the study design and interpretation of the study findings.
Emma Lancashire (https://orcid.org/0000-0001-8601-4400) (Senior Research Fellow, Public Health) was study co-ordinator for 36 months of the study, as well as a co-investigator and member of the study management team. She contributed to the study design and delivery and interpretation of the study findings.
Louise McLeman (https://orcid.org/0000-0003-0329-246X) (Research Associate, Public Health) was the research associate for 9 months of the study and contributed to the study design, delivery and school-level data analysis.
Sandra Passmore (https://orcid.org/0000-0002-7476-7242) (Senior Adviser for Services for Education, Birmingham) was a co-investigator and member of the study management team. She contributed to the study design and interpretation of the study findings.
Vahid Ravaghi (https://orcid.org/0000-0003-3056-3704) (Lecturer in Dental Public Health) was a co-investigator and member of the study management team. He contributed to the study design and interpretation of the study findings.
Suzanne Spence (https://orcid.org/0000-0002-7089-7197) (Research Fellow, Public Health Nutrition) was a member of the study management team. She contributed to the study design and interpretation of the study findings.
Peymane Adab (https://orcid.org/0000-0001-9087-3945) (Professor of Chronic Disease Epidemiology and Public Health) was co-chief investigator and a member of the study management team. She provided support to Miranda Pallan, who led the study, and contributed to the study conception, design, conduct and interpretation of the study findings.
All authors read and approved the final version of the report.
Disclosure of interests
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, are available in the toolkit on the NIHR Journals Library report publication page at https://doi.org/10.3310/TTPL8570.
Primary conflicts of interest: Additional research grants related to the research topic were received by Miranda Pallan, Marie Murphy, Emma Frew, Ashley Adamson, Suzanne Spence and Peymane Adab. Miranda Pallan has received National Institute for Health and Care Research (NIHR) grants (127551, NIHR131396, NIHR204247) and funding from Public Health England and The Office of Health Improvement and Disparities. Marie Murphy has received a NIHR grant (NIHR204247) and research funding from the UK Prevention Research Partnership Initiative (UKPRP). Emma Frew has received NIHR grants (NIHR152858, NIHR204247, NIHR300773, NIHR133099, NIHR203012, NIHR 13/164/51, RP-PG-0618-20008) and a UK Research and Innovation (UKRI) grant. Ashley Adamson has received a NIHR grant (NIHR127745) and research funding from the UK Prevention Research Partnership. Suzanne Spence has received research funding from NIHR (NIHR204247, NIHR School of Public Health Research), the Medical Research Council (MRC) Public Health Intervention Development (PHIND) programme and UKPRP. Peymane Adab has received NIHR grants (NIHR132630, 16/137/95, 17/128/04, 17/42/42, NIHR129593, NIHR135211, NIHR131396, NIHR204247), and research funding from the MRC and the Colt Foundation. Miranda Pallan served as a board member (unpaid) of Birmingham Food Council (Community Interest Company) from September 2019 to September 2022, and is a member of the oversight committees of two NIHR-funded studies (NIHR131572, NIHR135081) and a MRC-funded study (Chair). Alice Sitch receives funding from the NIHR Birmingham Biomedical Research Centre (BRC-1215-20009). Emma Frew holds a NIHR Professorship (NIHR300773), is a member of the NIHR Public Health Research Programme Funding Committee, is an elected board member of the International Health Economics Association and has received funding to support travel to the UK Association for the Study of Obesity (ASO) conference (funding from ASO). Ashley Adamson is Director of the NIHR School of Public Health Research. Suzanne Spence is chairperson of the Nutrition Society School Food Systems Special Interest Group, a member of the School Food Plan Alliance, and was co-chairperson of the UK Society for Behavioural Medicine Child Health Special Interest Group until 2022. Peymane Adab is chairperson of the NIHR Public Health Research Programme Funding Committee, Deputy Director of the NIHR School for Public Health Research, a member of the NIHR Public Health Research Programme Prioritisation Committee, a member of the Wellcome Trust Early Career Advisory Group in Population and Public Health, chairperson of two NIHR-funded study oversight committees (NIHR135081, NIHR127745), a member of a MRC-funded study oversight group, an assessor for Panel A, subpanel 2 in the 2021 Research Excellence Framework and a former member of the Obesity Health Alliance Independent Obesity Strategy Working Group (2019–21). Peymane Adab was also a member of the NIHR Palliative and End of Life Care Research Partnerships call panel and the NIHR/UKRI ‘Long COVID’ (Research into the longer-term effects of COVID-19 in non-hospitalised individuals) funding call panel in 2021, and a member of the NIHR COVID-19 Recovery and Learning Funding Committee in 2020.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Ethics statement
Ethical approval was obtained from the University of Birmingham Ethical Review Committee on the 20 August 2019 (ERN_18-1738).
Information governance statement
The University of Birmingham organisation/institution is committed to handling all personal information in line with the UK Data Protection Act (2018) and the General Data Protection Regulation (EU GDPR) 2016/679. Under the Data Protection legislation, the University of Birmingham is the Data Controller, and you can find out more about how we handle personal data, including how to exercise your individual rights and the contact details for our Data Protection Officer here: www.birmingham.ac.uk/privacy
Publication
Murphy M, Pallan M, Lancashire E, Duff R, Adamson AJ, Bartington S, et al. The Food provision, cUlture and Environment in secondary schooLs (FUEL) study: protocol of a mixed methods evaluation of national School Food Standards implementation in secondary schools and their impact on pupils’ dietary intake and dental health. BMJ Open 2020;10:e042931.
Pallan M, Murphy M, Morrison, B, Sitch A, Adamson A, Bartington S, et al. National school food standards in England: a cross-sectional study to explore compliance in secondary schools and impact on pupil nutritional intake. Int J Behav Nutr Phys Act 2024;21:123. https://doi.org/10.1186/s12966-024-01672-w
Disclaimers
This article presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the PHR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the PHR programme or the Department of Health and Social Care.
References
- Viner RM, Ross D, Hardy R, Kuh D, Power C, Johnson A, et al. Life course epidemiology: recognising the importance of adolescence. J Epidemiol Community Health 2015;69:719-20.
- NCD Risk Factor Collaboration . Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet 2017;390:2627-42.
- Norris SA, Frongillo EA, Black MM, Dong Y, Fall C, Lampl M, et al. Nutrition in adolescent growth and development. Lancet 2021;399:172-84.
- Conolly A, Craig S, Gebert S. Health Survey for England 2018 Overweight and Obesity in Adults and Children 2019. https://files.digital.nhs.uk/52/FD7E18/HSE18-Adult-Child-Obesity-rep.pdf (accessed 15 June 2024).
- Dietz WH. Health consequences of obesity in youth: childhood predictors of adult disease. Pediatrics 1998;101:518-25.
- Han JC, Lawlor DA, Kimm SYS. Childhood obesity. Lancet 2010;375:1737-48.
- Scientific Advisory Committee on Nutrition . Carbohydrates and Health 2015. www.gov.uk/government/uploads/system/uploads/attachment_data/file/445503/SACN_Carbohydrates_and_Health.pdf (accessed 14 July 2023).
- Bates B, Collins C, Jones K, Page P, Roberts C, Steer T, et al. National Diet and Nutrition Survey Rolling Programme Years 9 to 11 (2016 2017 to 2018 2019): A Survey Carried Out on Behalf of Public Health England and the Food Standards Agency 2020. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/943114/NDNS_UK_Y9-11_report.pdf (accessed 14 July 2023).
- Butriss J. Why 5%? An Explanation of the Scientific Advisory Committee on Nutrition’s Recommendations about Sugars and Health, in the Context of Current Intakes of Free Sugars, Other Dietary Recommendations and the Changes in Dietary Habits Needed to Reduce Consumption of Free Sugars to 5% of Dietary Energy 2015. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/489906/Why_5__-_The_Science_Behind_SACN.pdf (accessed 14 July 2023).
- Keller A, Bucher Della Torre S. Sugar-sweetened beverages and obesity among children and adolescents: a review of systematic literature reviews. Child Obes 2015;11:338-46.
- Ambrosini GL, Johns DJ, Northstone K, Emmett PM, Jebb SA. Free sugars and total fat are important characteristics of a dietary pattern associated with adiposity across childhood and adolescence. J Nutr 2015;146:778-84.
- Malik VS, Pan A, Willett WC, Hu FB. Sugar-sweetened beverages and weight gain in children and adults: a systematic review and meta-analysis. Am J Clin Nutr 2013;98:1084-102.
- Sheiham A, James WPT. Diet and dental caries: the pivotal role of free sugars reemphasized. J Dent Res 2015;94:1341-7.
- Holmes R, Porter J, Vernazza C, Tsakos G, Ryan R, Dennes M. Children’s Dental Health Survey 2013. Country Specific Report: England 2015. https://files.digital.nhs.uk/publicationimport/pub17xxx/pub17137/cdhs2013-england-report.pdf (accessed 14 July 2023).
- Guarnizo-Herreño CC, Wehby GL. Children’s dental health, school performance, and psychosocial well-being. J Pediatr 2012;161:1153-9.
- Seirawan H, Faust S, Mulligan R. The impact of oral health on the academic performance of disadvantaged children. Am J Public Health 2012;102:1729-34.
- Public Health England . NDNS: Results from Years 9 to 11 (Combined) – Statistical Summary 2020. www.gov.uk/government/statistics/ndns-results-from-years-9-to-11-2016-to-2017-and-2018-to-2019/ndns-results-from-years-9-to-11-combined-statistical-summary (accessed 7 November 2022).
- Maynard M, Gunnell D, Emmett P, Frankel S, Smith GD. Fruit, vegetables, and antioxidants in childhood and risk of adult cancer: the Boyd Orr cohort. J Epidemiol Community Health 2003;57:218-25.
- Bradlee ML, Singer MR, Qureshi MM, Moore LL. Food group intake and central obesity among children and adolescents in the Third National Health and Nutrition Examination Survey (NHANES III). Public Health Nutr 2010;13:797-805.
- Mellendick K, Shanahan L, Wideman L, Calkins S, Keane S, Lovelady C. Diets rich in fruits and vegetables are associated with lower cardiovascular disease risk in adolescents. Nutrients 2018;10.
- Noonan RJ. Poverty, weight status, and dietary intake among UK adolescents. Int J Environ Res Public Health 2018;15.
- Desbouys L, Méjean C, De Henauw S, Castetbon K. Socio-economic and cultural disparities in diet among adolescents and young adults: a systematic review. Public Health Nutr 2020;23:843-60.
- Rouxel P, Chandola T. Socioeconomic and ethnic inequalities in oral health among children and adolescents living in England, Wales and Northern Ireland. Community Dent Oral Epidemiol 2018;46:426-34.
- Public Health England . National Child Measurement Programme (NCMP): Trends in Child BMI 2020. https://www.gov.uk/government/statistics/national-child-measurement-programme-ncmp-trends-in-child-bmi-between-2006-to-2007-and-2018-to-2019/national-child-measurement-programme-ncmp-trends-in-child-bmi (accessed 15 June 2024).
- Neufeld LM, Andrade EB, Suleiman AB, Barker M, Beal T, Blum LS, et al. Food choice in transition: adolescent autonomy, agency, and the food environment. Lancet 2022;399:185-97.
- Cruz F, Ramos E, Lopes C, Araújo J. Tracking of food and nutrient intake from adolescence into early adulthood. Nutrition 2018;55–56:84-90.
- Appannah G, Murray K, Trapp G, Dymock M, Oddy WH, Ambrosini GL. Dietary pattern trajectories across adolescence and early adulthood and their associations with childhood and parental factors. Am J Clin Nutr 2021;113:36-4.
- Townsend N, Foster C. Developing and applying a socio-ecological model to the promotion of healthy eating in the school. Public Health Nutr 2013;16:1101-8.
- World Health Organization . Health Promoting Schools 2022. www.who.int/health-topics/health-promoting-schools (accessed 18 September 2022).
- Jourdan D, Gray NJ, Barry MM, Caffe S, Cornu C, Diagne F, et al. Supporting every school to become a foundation for healthy lives. Lancet Child Adolesc Health 2021;5:295-303.
- Oostindjer M, Aschemann-Witzel J, Wang Q, Skuland SE, Egelandsdal B, Amdam GV, et al. Are school meals a viable and sustainable tool to improve the healthiness and sustainability of children’s diet and food consumption? A cross-national comparative perspective. Crit Rev Food Sci Nutr 2017;57:3942-58.
- World Food Programme . State of School Feeding Worldwide 2020 2020. www.wfp.org/publications/state-school-feeding-worldwide-2020 (accessed 14 July 2023).
- Kristjansson B, Petticrew M, MacDonald B, Krasevec J, Janzen L, Greenhalgh T, et al. School feeding for improving the physical and psychosocial health of disadvantaged students. Cochrane Database Syst Rev 2007;1.
- Evans CEL, Harper CE. A history and review of school meal standards in the UK. J Hum Nutr Diet 2009;22:89-9.
- Jaime PC, Lock K. Do school based food and nutrition policies improve diet and reduce obesity?. Prev Med 2009;48:45-53.
- Micha R, Karageorgou D, Bakogianni I, Trichia E, Whitsel LP, Story M, et al. Effectiveness of school food environment policies on children’s dietary behaviors: a systematic review and meta-analysis. PLOS ONE 2018;13.
- Moore L, de Silva-Sanigorski A, Moore SN. A socio-ecological perspective on behavioural interventions to influence food choice in schools: alternative, complementary or synergistic?. Public Health Nutr 2013;1:1000-5.
- O’Brien KM, Barnes C, Yoong S, Campbell E, Wyse R, Delaney T, et al. School-based nutrition interventions in children aged 6 to 18 years: An umbrella review of systematic reviews. Nutrients 2021;13.
- McHugh C, Hurst A, Bethel A, Lloyd J, Logan S, Wyatt K. The impact of the World Health Organization Health Promoting Schools framework approach on diet and physical activity behaviours of adolescents in secondary schools: a systematic review. Public Health 2020;182:116-24.
- Crawley H. Nutrient-Based Standards for School Food: A Summary of the Standards and Recommendations of the Caroline Walker Trust and the National Heart Forum 2005. www.cwt.org.uk/wp-content/uploads/2014/07/eatingwell.pdf (accessed 14 July 2023).
- Nelson M. The school food trust: transforming school lunches in England. Nutr Bullet 2011;36:381-9.
- The Education (Nutritional Standards for School Lunches) (England) Regulations 2006. London: The Stationery Office; 2006.
- Dimbleby H, Vincent J. The School Food Plan 2013. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/936238/The_School_Food_Plan.pdf (accessed 14 July 2023).
- Great Britain . The Requirements for School Food Regulations 2014. www.legislation.gov.uk/uksi/2014/1603/regulation/8/made (accessed 19 September 2022).
- Department for Education . School Food in England: Departmental Advice for Governing Boards 2016. www.egfl.org.uk/sites/default/files/Facilities/Health_safety/School_food_in_England-July2016.pdf (accessed 14 July 2023).
- Department for Education . Revised Standards for Food in Schools: Government Response to the Consultation on Revised School Food Standards 2014. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/320697/Government_Response_-_Revised_Standards_for_School_Food_Consultation_FINAL.pdf (accessed 14 July 2023).
- The School Food Plan . Sign Up to the Standards 2013. https://www.schoolfoodplan.com/report/introduce-food-based-standards-for-all-schools/ (accessed 15 June 2024).
- LocalGov . Nearly 2,500 Academies Not Signed up to Healthy School Meal Standards 2016. www.localgov.co.uk/Nearly-2500-academies-not-signed-up-to-healthy-school-meal-standards/40554 (accessed 24 September 2022).
- Department for Education . School Food in England 2021. www.gov.uk/government/publications/standards-for-school-food-in-england/school-food-in-england#exemptions-to-the-school-food-regulations (accessed 22 September 2022).
- Mucavele P, Nicholas J, Sharp L. Development and Pilot Testing of Revised Food-Based Standards for School Lunches in England 2013. www.schoolfoodplan.com/wp-content/uploads/2014/02/School-Food-Plan-Pilot-study-EVALUATION-REPORT-Final-V3.pdf (accessed 19 September 2022).
- Department for Education . School Food Standards Practical Guide 2015. https://www.gov.uk/government/publications/school-food-standards-resources-for-schools/school-food-standards-practical-guide (accessed 15 June 2024).
- McIntyre RL, Adamson AJ, Nelson M, Woodside J, Beattie S, Spence S. Changes and differences in school food standards (2010–2021) and free school meal provision during COVID‐19 across the UK: potential implications for children’s diets. Nutr Bull 2022;47:230-45.
- Ofsted . Ofsted Inspections of Maintained Schools and Academies 2014. www.gov.uk/government/collections/ofsted-inspections-of-maintained-schools (accessed 14 July 2023).
- Evans CE, Cleghorn CL, Greenwood DC, Cade JE. A comparison of British school meals and packed lunches from 1990 to 2007: meta-analysis by lunch type. Br J Nutr 2010;104:474-87.
- Evans CE, Mandl V, Christian MS, Cade JE. Impact of school lunch type on nutritional quality of English children’s diets. Public Health Nutr 2016;19:36-45.
- Department for Education . A Checklist for Head Teachers 2013. www.gov.uk/government/publications/school-food-standards-resources-for-schools/checklist-for-headteachers (accessed 14 July 2023).
- Department for Education . Guidance: Creating a Culture and Ethos of Healthy Eating 2016. www.gov.uk/government/publications/school-food-standards-resources-for-schools/creating-a-culture-and-ethos-of-healthy-eating (accessed 14 July 2023).
- Department for Education . School Food: Guidance for Governors 2023. https://www.gov.uk/government/publications/school-food-standards-resources-for-schools/school-food-guidance-for-governors (accessed 15 June 2024).
- Department for Education . School Food Standards: Resources for Schools 2019. www.gov.uk/government/publications/school-food-standards-resources-for-schools (accessed 19 September 2022).
- Spence S, Delve J, Stamp E, Matthews JN, White M, Adamson AJ. The impact of food and nutrient-based standards on primary school children’s lunch and total dietary intake: a natural experimental evaluation of government policy in England. PLOS ONE 2013;8.
- Spence S, Matthews JN, White M, Adamson AJ. A repeat cross-sectional study examining the equitable impact of nutritional standards for school lunches in England in 2008 on the diets of 4–7y olds across the socio-economic spectrum. Int J Behav Nutr Phys Activ 2014;11.
- Spence S, Delve J, Stamp E, Matthews JN, White M, Adamson AJ. Did school food and nutrient-based standards in England impact on 11–12Y olds nutrient intake at lunchtime and in total diet? Repeat cross-sectional study. PLOS ONE 2014;9.
- Haroun D, Harper C, Wood L, Nelson M. The impact of the food-based and nutrient-based standards on lunchtime food and drink provision and consumption in primary schools in England. Public Health Nutr 2011;14:209-18.
- Nicholas J, Wood L, Harper C, Nelson M. The impact of the food-based and nutrient-based standards on lunchtime food and drink provision and consumption in secondary schools in England. Public Health Nutr 2013;16:1052-65.
- Page A, Hart CS. Jamie Oliver Food Foundation . A Report on the Food Education Learning Landscape 2017. www.akofoundation.org/wp-content/uploads/2017/11/2_0_fell-report-final.pdf (accessed 14 July 2023).
- Guy’s and St Thomas’ Charity . Serving up Children’s Health: Opportunities and Barriers in the School Food System to Prioritise Nutritious Food for Our Young People 2020. https://urbanhealth.org.uk/wp-content/uploads/2020/12/Serving-up-childrens-health.pdf (accessed 14 July 2023).
- Food for Life . State of the Nation: Children’s Food in England 2019. www.foodforlife.org.uk/~/media/files/sotn/sotn_2019.pdf (accessed 2 July 2023).
- Davies S. Time to Solve Childhood Obesity: An Independent Report by the Chief Medical Officer 2019. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/837907/cmo-special-report-childhood-obesity-october-2019.pdf (accessed 2 July 2023).
- Adamson A, Spence S, Reed L, Conway R, Palmer A, Stewart E, et al. School food standards in the UK: implementation and evaluation. Public Health Nutr 2013;16:968-81.
- HM Government . Childhood Obesity: A Plan for Action 2016. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/546588/Childhood_obesity_2016__2__acc.pdf (accessed 14 July 2023).
- HM Government . Childhood Obesity: A Plan for Action. Chapter 2 2018. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/718903/childhood-obesity-a-plan-for-action-chapter-2.pdf (accessed 14 July 2023).
- Long R, Danechi S, Roberts N. School Meals and Nutritional Standards in England 2022. https://researchbriefings.files.parliament.uk/documents/SN04195/SN04195.pdf (accessed 14 July 2023).
- Department for Education . Healthy Schools Rating Scheme Guidance for Schools 2022. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1112071/Final_Healthy_schools_rating_scheme.pdf (accessed 14 July 2023).
- Dimbleby H. National Food Strategy Independent Review: The Plan 2021. www.nationalfoodstrategy.org/ (accessed 14 July 2023).
- HM Government . Levelling Up the United Kingdom 2022. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1052708/Levelling_up_the_UK_white_paper.pdf (accessed 14 July 2023).
- HM Government . Government Food Strategy 2022. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1082027/government-food-strategy-print-ready.pdf (accessed 14 July 2023).
- Murphy M, Pallan M, Lancashire E, Duff R, Adamson AJ, Bartington S, et al. The Food provision, cUlture and Environment in secondary schooLs (FUEL) study: protocol of a mixed methods evaluation of national School Food Standards implementation in secondary schools and their impact on pupils’ dietary intake and dental health. BMJ Open 2020;10.
- Office for National Statistics . Population and Household Estimates, England and Wales: Census 2021 2022. www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/bulletins/populationandhouseholdestimatesenglandandwales/census2021 (accessed 25 September 2022).
- Office for National Statistics . Population Estimates by Ethnic Group, England and Wales 2021. www.ons.gov.uk/peoplepopulationandcommunity/culturalidentity/ethnicity/datasets/populationestimatesbyethnicgroupenglandandwales (accessed 25 September 2022).
- Office for National Statistics . Mapping Income Deprivation at a Local Authority Level 2021. www.ons.gov.uk/peoplepopulationandcommunity/personalandhouseholdfinances/incomeandwealth/datasets/mappingincomedeprivationatalocalauthoritylevel (accessed 25 September 2022).
- Roberts N, Danechi S. FAQs: Academies and Free Schools 2019. https://researchbriefings.files.parliament.uk/documents/SN07059/SN07059.pdf (accessed 2 July 2023).
- Gov.uk . Schools, Pupils and Their Characteristics: Academic Year 2022 23 2023. https://explore-education-statistics.service.gov.uk/find-statistics/school-pupils-and-their-characteristics (accessed 2 July 2023).
- Rubin DB. Estimating causal effects from large data sets using propensity scores. Ann Intern Med 1997;127:757-63.
- Adamson AJ, White M, Stead M. The Process and Impact of Change in the School Food Policy on Food and Nutrient Intake of Children Aged 4–7 and 11–12 Years Both In and Out of School: A Mixed Methods Approach n.d. www.phrc.online/assets/uploads/files/PHRC_B5_07_Final_Report_1.pdf (accessed 1 May 2022).
- Juras R. Estimates of intraclass correlation coefficients and other design parameters for studies of school-based nutritional interventions. Eval Rev 2016;40:314-33.
- Spence S, White M, Adamson AJ, Matthews JN. Does the use of passive or active consent affect consent or completion rates, or dietary data quality? Repeat cross-sectional survey among school children aged 11–12 years. BMJ Open 2015;5.
- Moore GF, Audrey S, Barker M, Bond L, Bonell C, Hardeman W, et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ 2015;350.
- Rapley T, Girling M, Mair FS, Murray E, Treweek S, McColl E, et al. Improving the normalization of complex interventions: part 1 – development of the NoMAD instrument for assessing implementation work based on normalization process theory (NPT). BMC Med Res Methodol 2018;18:1-17.
- Finch TL, Girling M, May CR, Mair FS, Murray E, Treweek S, et al. Improving the normalization of complex interventions: part 2 – validation of the NoMAD instrument for assessing implementation work based on normalization process theory (NPT). BMC Med Res Methodol 2018;18:1-13.
- Department of Health . Nutrient Profiling Technical Guidance 2011. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/216094/dh_123492.pdf (accessed 14 July 2023).
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap): a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377-81.
- Burrows TL, Martin RJ, Collins CE. A systematic review of the validity of dietary assessment methods in children when compared with the method of doubly labeled water. J Am Diet Assoc 2010;110:1501-10.
- Bradley J, Simpson E, Poliakov I, Matthews JN, Olivier P, Adamson AJ, et al. Comparison of INTAKE24 (an online 24-h dietary recall tool) with interviewer-led 24-h recall in 11–24 year-old. Nutrients 2016;8.
- Foster E, Matthews JN, Lloyd J, Marshall L, Mathers JC, Nelson M, et al. Children’s estimates of food portion size: the development and evaluation of three portion size assessment tools for use with children. Br J Nutr 2008;99:175-84.
- Foster E, Hawkins A, Barton KL, Stamp E, Matthews JN, Adamson AJ. Development of food photographs for use with children aged 18 months to 16 years: Comparison against weighed food diaries: the Young Person’s Food Atlas (UK). PLOS ONE 2017;12.
- Roe M, Pinchen H, Church S, Finglas P. McCance and Widdowson’s the composition of foods seventh summary edition and updated composition of foods integrated dataset. Nutr Bull 2015;40:36-9.
- Stadlmayr B, Charrondiere UR, Enujiugha VN, Bayili RG, Fagbohoun EG, Samb B, et al. West African Food Composition Table 2012. www.fao.org/3/a-i2698b.pdf (accessed 17 July 2020).
- Public Health England . Composition of Foods Integrated Dataset (CoFID) 2019. www.gov.uk/government/publications/composition-of-foods-integrated-dataset-cofid (accessed 26 September 2022).
- Anderson T, Thomas C, Ryan R, Dennes M, Fuller E. Children’s Dental Health Survey 2013: Technical Report England, Wales and Northern Ireland 2015. https://files.digital.nhs.uk/publicationimport/pub17xxx/pub17137/cdhs2013-technical-report.pdf (accessed 3 July 2023).
- Ministries of Housing, Communities and Local Government . English Indices of Deprivation 2019 2020. www.gov.uk/government/statistics/english-indices-of-deprivation-2019 (accessed 25 September 2022).
- Stevens KJ. Working with children to develop dimensions for a preference-based, generic, pediatric, health-related quality-of-life measure. Qual Health Res 2010;20:340-51.
- Stevens K. Assessing the performance of a new generic measure of health-related quality of life for children and refining it for use in health state valuation. Appl Health Econ Health Policy 2011;9:157-69.
- Stevens K. Valuation of the child health utility 9D index. PharmacoEcono 2012;30:729-47.
- Wrieden WL, Longbottom PJ, Adamson AJ, Ogston SA, Payne A, Haleem MA, et al. Estimation of typical food portion sizes for children of different ages in Great Britain. Br J Nutr 2008;99:1344-53.
- The School Food Plan . School Food Standards Regulations: Q&Amp;A for Consultation 2014. www.schoolfoodplan.com/wp-content/uploads/2014/03/Standards-Consultation-QA-6-March-2014.pdf (accessed 24 September 2022).
- May C, Finch T. Implementing, embedding, and integrating practices: an outline of normalization process theory. Sociology 2009;43:535-54.
- Public Health England, National Food Standards Agency . Evaluation of Changes in the Dietary Methodology in the National Diet and Nutrition Survey Rolling Programme from Year 12 (2019 to 2020): Stage 1 2021. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1019257/Stage_1_evaluation_report__1_.pdf (accessed 14 July 2023).
- Office for National Statistics . Consumer Price Inflation Tables 2022. www.ons.gov.uk/economy/inflationandpriceindices/datasets/consumerpriceinflation (accessed 15 October 2022).
- Gov.uk . Schools Financial Benchmarking 2022. https://schools-financial-benchmarking.service.gov.uk/ (accessed 15 October 2022).
- Rowen D, Keetharuth AD, Poku E, Wong R, Pennington B, Wailoo A. A review of the psychometric performance of selected child and adolescent preference-based measures used to produce utilities for child and adolescent health. Value Health 2021;24:443-60.
- Gov.uk . Compare the Performance of Schools and Colleges in England n.d. www.gov.uk/school-performance-tables (accessed 15 June 2024).
- Maguire M, Braun A, Ball S. ‘Where you stand depends on where you sit’: the social construction of policy enactments in the (English) secondary school. Discourse 2015;36:485-99.
- Merriam SB. Case Study Research in Education: A Qualitative Approach. San Francisco, CA: Jossey-Bass Publishers; 1998.
- Priya A. Case study methodology of qualitative research: key attributes and navigating the conundrums in its application. Sociol Bull 2021;70:94-110.
- Boblin SL, Ireland S, Kirkpatrick H, Robertson K. Using Stake’s qualitative case study approach to explore implementation of evidence-based practice. Qual Health Res 2013;23:1267-75.
- Crowe S, Cresswell K, Robertson A, Huby G, Avery A, Sheikh A. The case study approach. BMC Med Res Methodol 2011;11.
- Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol 2013;13.
- Gov.uk . Schools, Pupils and Their Characteristics 2022. https://explore-education-statistics.service.gov.uk/find-statistics/school-pupils-and-their-characteristics (accessed 6 November 2022).
- Haney E, Parnham JC, Chang K, Laverty AA, von Hinke S, Pearson-Stuttard J, et al. Dietary quality of school meals and packed lunches: a national study of primary and secondary school children in the UK. Public Health Nutr 2022;26:425-36.
- Parnham JC, Chang K, Rauber F, Levy RB, Millett C, Laverty AA, et al. The ultra-processed food content of school meals and packed lunches in the United Kingdom. Nutrients 2022;14.
- Hart CS, Page A. The capability approach and school food education and culture in England: ‘gingerbread men ain’t gonna get me very far’. Cambridge J Educ 2020;50:673-93.
- Booth E, Halliday V, Cooper RJ. Headteachers’ and chairs of governors’ perspectives on adolescent obesity and its prevention in English secondary school settings. J Public Health (Oxf) 2021;43:e213-e23.
- Strömmer S, Shaw S, Jenner S, Vogel C, Lawrence W, Woods‐Townsend K, et al. How do we harness adolescent values in designing health behaviour change interventions? A qualitative study. Br J Health Psychol 2021;26:1176-93.
- Gilmour A, Gill S, Loudon G. Perspectives of UK catering staff on adolescents’ food choices at school. J Child Nutr Manag 2021;45.
- Ravelli MN, Schoeller DA. Traditional self-reported dietary instruments are prone to inaccuracies and new approaches are needed. Front Nutr 2020;7.
- Hargreaves D, Mates E, Menon P, Alderman H, Devakumar D, Fawzi W, et al. Strategies and interventions for healthy adolescent growth, nutrition, and development. Lancet 2021;399:198-210.
- El‐Sayed A, Scarborough P, Galea S. Ethnic inequalities in obesity among children and adults in the UK: a systematic review of the literature. Obes Rev 2011;12:e516-34.
- Thomas J, Sutcliffe K, Harden A, Oakley A, Oliver S, Rees R, et al. The barriers to, and the facilitators of, healthy eating among children: findings from a systematic review. Childhood Obesity Contemporary Issues 2005:223-50.
- National Diet and Nutrition Survey . Appendix A Dietary Data Collection and Editing for Year 9 of the NDNS RP 2018. https://s3.eu-west-2.amazonaws.com/fsa-catalogue2/NDNS+Y1-9_Appendix+A_Diary_FINAL.pdf (accessed 14 July 2023).
- HM Revenue and Customs . Check If Your Drink Is Liable for the Soft Drinks Industry Levy 2018. https://www.gov.uk/guidance/check-if-your-drink-is-liable-for-the-soft-drinks-industry-levy (accessed 17 June 2024).
- Department for Education . School Teachers’ Pay and Conditions Document 2021 and Guidance on School Teachers’ Pay and Conditions 2021. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1110811/School_teachers__pay_and_conditions_document_2021_and_guidance_on_school_teachers__pay_and_condi.pdf (accessed 14 July 2023).
- NASUWT: The Teachers’ Union . Briefing: Directed Time and the 32.5-Hour Week 2022. https://www.nasuwt.org.uk/static/909eb3a1-3235-4e28-b02ee66ad3886143/Directed-Time-and-the-32-5-hour-Week-Briefing-England.pdf (accessed 15 June 2024).
- National Education Union . Pay Scales for Support Staff n.d. https://neu.org.uk/advice/member-groups/support-staff/pay-scales-support-staff (accessed June 15 2024).
- School Food Trust . A Fresh Look at Vending in Schools 2007. http://www.schoolfoodtrust.org.uk/schools/resources/a-fresh-look-at-vending-in-schools (accessed accessed 19 January 2024).
- Gov.uk . National Minimum Wage and National Living Wage Rates 2022. www.gov.uk/national-minimum-wage-rates (accessed 6 November 2022).
- Islington Council . Sample Pack Cooking Matters Toolkit: A Comprehensive Toolkit and Guidance for Teaching Cooking and Nutrition in Primary Schools n.d. www.london.gov.uk/what-we-do/health/healthy-schools-london/awards/sites/default/files/cooking%20matters%20toolkit%20sample%20pack_0.pdf (accessed 19 January 2024).
Appendix 1 Data cleaning steps
| Issue | Description of issue | Resolution |
|---|---|---|
| Zero portion sizes | Some rows included food/drink items with a portion size of zero | These were removed as they did not contribute nutritional data |
| Time to complete check | Records completed too quickly (≤ 2 minutes) or too slowly (≥ 60 minutes) were deemed to be inaccurate | Full records were removed for these participants |
| Adding new items where multiple items had been entered per row, for example ‘fish and chips’ | The data were manually searched for incidences where the participant had entered more than one food/drink item on a single row and had not subsequently added these | The missed item(s) were added based on the best matched/most common item in the existing data, using the most common portion size from the existing data |
| Disingenuous items removed | Some pupils entered implausible items, for example non-food/drink items | These rows were excluded, and where necessary full records were removed |
| Unreasonable amounts were adjusted | Intake24 flags any portions sizes deemed to be ‘unreasonable’ | Unreasonable portion sizes were checked and new portion sizes were assigned where necessary using the Wrieden average values104 |
| In the Intake24 database, some nutrient values were missing for specific food items, and some food items were missing | Errors in the Intake24 database meant that some items (typically sandwiches) were missing background nutritional data. In addition, some items consumed by participants were missing from the Intake24 database. Examples included Chinese buns, wontons, and Rubicon (drink) | Missing foods were matched to similar items where appropriate and nutritional data located using existing database. Where a similar item could not be found, the NDNS Nutrient databank96 or a composition database from another country (e.g. for traditional foods originating from other countries) were used where available. Wrieden average portion weights for similar items were used104 |
| Reassigned brandy butter entries | There were an implausible number of records that featured ‘brandy butter’. These were deemed to be an error on the basis that this was the first search term that appeared when a user entered ‘butter’ | All brandy butter records were changed to butter and the nutritional data adjusted accordingly |
| Meal location – re-categorise free-text answers | Meal location featured a free-text option. Some participants entered free text that could be assigned to predefined categories | Free-text options were reassigned to predefined categories where appropriate |
| Meal location – combining responses | Several options for meal location | These were recategorised into a smaller number of categories |
| Eating occasion/meal name – re-categorise non-standard answers | There is an option in Intake24 to enter a new eating occasion that can be named using a free-text option | These were recategorised to predefined eating occasion/meal name categories where appropriate |
| Food source | There were multiple options for where items were purchased, as follows: school café/canteen/shop; school vending machine; shop café/restaurant/fast food place/take away/vending machine outside school; from home. This was a multiple choice question | These were re-categorised into three options:
|
| Duplicate usernames | Some participants mistakenly used the same username | These were identified and new usernames were assigned. As it is not clear which record used the correct username, these records could not be matched to participant online survey records |
Appendix 2 Assessment of School Food Plan actions
| Summary action | Observation | KIS | CS | Documents | Caterersa | Teachersa | Governorsa | SLTa | Pupilsa |
|---|---|---|---|---|---|---|---|---|---|
| Theme 1: whole-school approach | |||||||||
| Does the school have a culture of healthy eating? | Y | Y | Y | Y | Y | ||||
| Does the school demonstrate a culture and ethos of healthy eating to Ofsted? | Y | Y | Y | ||||||
| Do staff eat in the canteen with pupils (headteacher and staff)? | Y | Y | Y | Y | |||||
| Are healthy eating messages promoted across the school? | Y | Y | Y | Y | Y | Y | Y | ||
| Are healthy-eating messages consistent across subjects and at lunchtime? | Y | Y | Y | Y | |||||
| Does the school use sweets as rewards? | Y | Y | Y | Y | Y | Y | |||
| Does the school grow any of the food it provides to pupils? | Y | Y | |||||||
| Are staff supported to improve their knowledge on health and well-being? | Y | Y | Y | Y | Y | Y | |||
| Is drinking water freely and easily available? (During lunch and across the school day) | Y | Y | |||||||
| Theme 2: leadership and oversight on school food | |||||||||
| Do senior leaders lead on and engage with school food, for example observe pupils eating, implement the SFP? | Y | Y | Y | ||||||
| Is healthy eating considered in the school development plan/school evaluation? | Y | Y | |||||||
| Do school governors lead on and engage with school food, for example observe what pupils are eating and drinking? | Y | Y | |||||||
| Are there opportunities for pupils to contribute views on school food, for example school nutrition action group? | Y | Y | Y | Y | Y | Y | |||
| Does the school use external agencies for support, for example drafting catering contract, increasing quality of school meals? | Y | ||||||||
| Theme 3: policies | |||||||||
| Is there a school food policy? | Y | Y | |||||||
| Is there a policy on food brought from home, for example bans on crisps and confectionery? | Y | ||||||||
| Is there a policy on drinks? | Y | ||||||||
| Is there a stay-on-site rule for break and lunch time? | Y | Y | |||||||
| Are staff aware of and implementing the school food policy? | Y | Y | Y | Y | |||||
| Are pupils aware of the school food policy? | Y | ||||||||
| Theme 4: engagement | |||||||||
| Do pupils have the opportunity to assist catering staff, for example preparing, cooking or serving the food served at lunch? | Y | Y | |||||||
| Does the school consult with parents on school food? | Y | Y | Y | Y | Y | ||||
| Does the school make menus available in advance? | Y | ||||||||
| Are there opportunities for parents to sample/try school food, for example parents’ evening, open day? | Y | ||||||||
| Are parents encouraged to participate in cooking or gardening clubs? | Y | ||||||||
| Does the school engage with the community on school food or food education activities? | Y | Y | Y | Y | Y | ||||
| Theme 5: catering provision | |||||||||
| Are catering staff integrated into school life, for example attend staff meetings or parents evenings? | Y | ||||||||
| Are catering staff supported to develop and learn? | Y | ||||||||
| Does the contract specification include the SFS, professional standards, food quality and lunchtime experience? | Y | ||||||||
| Is compliance with the SFS checked, for example by governors, independent assessment? | Y | Y | Y | ||||||
| Is the catering team, including mid-day supervisors, using the professional standards? | Y | ||||||||
| Does the school have a food award or participate in a food quality assured scheme, for example Food for Life Schools Award? | Y | Y | |||||||
| Does the caterer have a clear, written plan for increasing take-up over a set period? | Y | ||||||||
| Do caterers consider the environment when choosing their suppliers? | Y | Y | |||||||
| Theme 6: catering practices | |||||||||
| Do catering staff encourage pupils to experiment with new foods? | Y | ||||||||
| Do catering staff encourage pupils to eat healthily? | Y | Y | |||||||
| Is a cheaper ‘set menu’ meal offered for encourage a balanced meal? | Y | ||||||||
| Are pupils offered prizes and other incentives for bringing in a healthy lunch? | Y | Y | |||||||
| Theme 7: the lunchtime experience | |||||||||
| Does the school ask for feedback on the lunchtime experience? | Y | ||||||||
| Is the dining environment attractive? | Y | Y | Y | Y | Y | Y | |||
| Is the dining environment calm? | Y | Y | |||||||
| Are there strategies to reduce queuing times? | Y | Y | |||||||
| Are lunch breaks staggered? | Y | Y | |||||||
| Are there multiple service points (food service points and till points)? | Y | ||||||||
| Do pupils feel rushed to purchase food from school food outlets? | Y | ||||||||
| Do pupils have enough time to eat their lunch? | Y | Y | Y | Y | Y | ||||
| Is there sufficient time during the lunch break for eating as well as activities or clubs? | Y | Y | |||||||
| Is a sit-down meal encouraged, for example enough space for eating at a table, family-style service? | Y | Y | |||||||
| Does the school provide proper crockery? | Y | ||||||||
| Does the school allow those with packed lunches to sit together with those purchasing a school meal? | Y | ||||||||
| Do catering providers offer samples of the food for children to taste? | Y | ||||||||
| Do catering providers offer themed days? | Y | ||||||||
| Are catering staff (including midday supervisors) happy and engaged with school staff and pupils? | Y | Y | Y | Y | Y | Y | |||
| Theme 8: food education | |||||||||
| Does the curriculum offer the opportunity for all pupils to learn cooking? | Y | Y | Y | ||||||
| Does the curriculum offer the opportunity for all pupils to learn food growing/gardening? | Y | Y | Y | Y | |||||
| Is healthy eating instilled as part of mandatory teaching of food education? | Y | Y | |||||||
| Is healthy eating taught across a range of subjects within the curriculum? | Y | Y | |||||||
| Is cooking taught outside of the curriculum, for example clubs? | Y | Y | Y | ||||||
| Is growing taught outside the curriculum, for example clubs? | Y | Y | Y | ||||||
| Is there enough timetabling, space and practical resources (equipment, ingredients) for teaching cooking? | Y | Y | |||||||
| Does the school ensure all pupils can access ingredients for cooking activities? | Y | ||||||||
| Does the school use a qualified subject specialist to teach food education? | Y | Y | |||||||
| Do food education schemes of work focus on savoury cooking? | Y | Y | Y | ||||||
| Theme 9: increasing school meal access and take-up | |||||||||
| Is food available to pupils at breakfast time? | Y | Y | |||||||
| If so, is it affordable and accessible for all pupils, for example subsidised? | Y | ||||||||
| Is school meal take-up is reported/monitored? | Y | ||||||||
| Do school governors obtain and review take-up data each term? | Y | Y | Y | ||||||
| Are efforts made by school leadership to promote school meal take-up, for example subsidising meals (other than FSM)? | Y | Y | Y | ||||||
| Are efforts made to ensure those eligible for FSM are using their entitlement? | Y | ||||||||
| Are pupils with allergies able to access a school meal? | Y | Y | Y | ||||||
| Does the school use a cashless payment system? | Y | Y | |||||||
| Summary action | Data points to assess SFP action |
|---|---|
| Theme 1: Whole-school approach | |
| Does the school have a culture of healthy eating? |
|
| Does the school demonstrate a culture and ethos of healthy eating to Ofsted? |
|
| Do staff eat in the canteen with pupils (headteacher and staff)? |
|
| Are healthy-eating messages promoted across the school? |
|
| Are healthy-eating messages consistent (across subjects and at lunchtime)? |
|
| Does the school use sweets as rewards? |
|
| Does the school grow any of the food it provides to pupils? |
|
| Are staff supported to improve their knowledge on health and well-being? |
|
| Is drinking water freely and easily available (during lunch and across the school day)? |
|
| Theme 2: leadership and oversight on school food | |
| Do senior leaders lead on and engage with school food, for example observe pupils eating, implement the SFP? |
|
| Is healthy eating considered in the school development plan/school evaluation? |
|
| Do school governors lead on and engage with school food? For example, do they observe what pupils are eating and drinking? |
|
| Are there opportunities for pupils to contribute views on school food, for example school nutrition action group? |
|
| Does the school use external agencies for support, for example drafting catering contract, increasing quality of school meals? |
|
| Theme 3: policies | |
| Is there a school food policy? |
|
| Is there a policy on food brought from home, for example bans on sugary drinks, crisps and confectionery? |
|
| Is there a policy on drinks? |
|
| Is there a stay-on-site rule for break and lunch time? |
|
| Are staff aware of and implementing the school food policy? |
|
| Are pupils aware of the school food policy? |
|
| Theme 4: engagement | |
| Do pupils have the opportunity to assist catering staff, for example preparing, cooking or serving the food served at lunch? |
|
| Does the school consult with parents on school food? |
|
| Does the school make menus available in advance? |
|
| Are there opportunities for parents to sample/try school food, for example parents’ evening, open day? |
|
| Are parents encouraged to participate in cooking or gardening clubs? |
|
| Does the school engage with the community on school food or food education activities? |
|
| Theme 5: catering provision | |
| Are catering staff integrated into school life, for example attend staff meetings or parents evenings? |
|
| Are catering staff supported to develop and learn? |
|
| Does the contract specification include the SFS, professional standards, food quality and lunchtime experience? |
|
| Is compliance with the SFS checked, for example by governors, independent assessment? |
|
| Are the catering team, including mid-day supervisors, using the professional standards? |
|
| Does the school have a food award or participate in a food quality assured scheme, for example Food for Life Schools Award |
|
| Does the caterer have a clear, written plan for increasing take-up over a set period? |
|
| Do caterers consider the environment when choosing their suppliers? |
|
| Theme 6: catering practices | |
| Do catering staff encourage pupils to experiment with new foods? |
|
| Do catering staff encourage pupils to eat healthily? |
|
| Is a cheaper ‘set menu’ meal offered for encourage a balanced meal? |
|
| Are pupils offered prizes and other incentives for bringing in a healthy lunch? |
|
| Theme 7: the lunchtime experience | |
| Does the school ask for feedback on the lunchtime experience? |
|
| Is the dining environment attractive? |
|
| Is the dining environment calm? |
|
| Are there strategies to reduce queuing times? |
|
| Are lunch breaks staggered? |
|
| Are there multiple service points (food service points and till points)? |
|
| Do pupils feel rushed to purchase food from school food outlets? |
|
| Do pupils have enough time to eat their lunch? |
|
| Is there sufficient time during the lunch break for eating as well as activities or clubs? |
|
| Is a sit-down meal encouraged, for example enough space for eating at a table, family-style service? |
|
| Does the school provide proper crockery? |
|
| Does the school allow those with packed lunches to sit together with those purchasing a school meal? |
|
| Do catering providers offer samples of the food for children to taste? |
|
| Do catering providers offer themed days? |
|
| Are catering staff (including midday supervisors) happy and engaged with school staff and pupils? |
|
| Theme 8: food education | |
| Does the curriculum offer the opportunity for all pupils to learn cooking? |
|
| Does the curriculum offer the opportunity for all pupils to learn food growing/gardening? |
|
| Is healthy eating instilled as part of mandatory teaching of food education? |
|
| Is healthy eating taught across a range of subjects within the curriculum? |
|
| Is cooking taught outside the curriculum, for example clubs? |
|
| Is growing taught outside of the curriculum, for example clubs? |
|
| Is there enough timetabling, space and practical resources (equipment, ingredients) for teaching cooking? |
|
| Does the school ensure all pupils can access ingredients for cooking activities? |
|
| Does the school use a qualified subject specialist to teach food education? |
|
| Do food education schemes of work focus on savoury cooking? |
|
| Theme 9: increasing school meal access and take-up | |
| Is food available to pupils at breakfast time? |
|
| If so, is it affordable and accessible for all pupils, for example subsidised? |
|
| Is school meal take-up is reported/monitored? |
|
| Do school governors obtain and review take-up data each term? |
|
| Are efforts made by school leadership to promote school meal take-up, for example subsidising meals (other than FSM)? |
|
| Are efforts made to ensure those eligible for FSM are using their entitlement? |
|
| Are pupils with allergies able to access a school meal? |
|
| Does the school use a cashless payment system? |
|
| Type of assessment | Guiding principles |
|---|---|
| Agreement/disagreement assessments (mainly survey responses or researcher observation responses) | If combined agree/strongly agree is:
|
Notes:
|
|
| Where there are multiple data sources the following rules should be applied to make a summary judgement either (1) for a summary action or (2) across different items of information from one data collection tool |
|
|
|
Notes: for summary judgements including WHITE, the following rules should be applied:
|
Appendix 3 Selected school food standards and School Food Plans actions for typology assessment
| Standards grouping | Selected standards |
|---|---|
|
|
|
|
|
|
| Theme | Actions included |
|---|---|
| Whole-school approach |
|
| Leadership on and oversight of school food |
|
| Engagement |
|
| Catering provision and standards |
|
| Catering practices |
|
| The lunchtime experience |
|
| Food education |
|
| Increasing school meal access and take-up |
|
Appendix 4 Generating nutritional outcomes from Intake24 data
| Outcome | Generation of outcome |
|---|---|
| Free sugar | Total free sugar was a pregenerated variable in Intake24 raw data |
| Percentage of dietary energy intake from free sugar | Total free sugar and energy (kcal) were pregenerated variables in Intake24 raw data. Calculated total free sugar as a percentage of total energy for the specified time period |
| TEI (kcal) | Energy (kcal) was a pregenerated variable in Intake24 raw data |
| Total fat intake (g) | Total fat was a pregenerated variable in Intake24 raw data |
| Fibre intake (g) | AOAC fibre was a pregenerated variable in Intake24 raw data |
| Number of F&V portions consumed | Defined using ‘five-a-day’ portion guidance, as outlined in the NDNS.129 Weight values were extracted for the following pregenerated variables for all foods and drinks including composite dishes: fruit, dried fruit, fruit juice, smoothie fruit, tomatoes, tomato puree, brassicaceae, yellow red green, beans, other vegetables. Cereal bars and fruit bars that were < 100% fruit were excluded from the calculation. Fruit/vegetables in predefined categories were also excluded (soft drinks, confectionery, cakes and biscuits, sugar, preserves and sweet spreads, savoury snacks and ice cream). Weight values for dried fruit were multiplied by three to account for effects of drying, and tomato puree was multiplied by five to account for effects of concentration. With the exception of fruit juices/smoothies and beans, the total weight of all F&V variables was calculated and divided by 80g to provide the number of portions. A portion of fruit juices and smoothies combined was defined as 150g and was capped at one portion per day.129 For beans, a portion (80g) was capped at one portion per day |
| Number of SSBs consumed | This outcome incorporates drinks liable for the UK Soft Drinks Industry Levy130 within the following food categories and codes: carbonated drinks, ready-to-drink fruit drinks, cordials and squashes, water, alcohol. The number of drink items (regardless of portion size) within each category was summed to provide the outcome variable |
| Number of sugar and chocolate confectionery items consumed | The number of items within the chocolate and sweets Intake24 food categories was summed (regardless of portion size) |
| Number of HFSS foods consumed | Defined according to the nutrient profiling model.90 The following food categories were excluded by the research team as they are typically eaten in small quantities in association with another item recorded in Intake24, and not as standalone items, so application of the nutrient profiling model to these items would be inappropriate: plain milk (including soya and goat’s milk), butter, fat spreads and oils, table sugar and preserves/syrups, cordials and squashes, ketchup and other sauces (condiments), salt, herbs and spices and dressings |
| Free sugar intake providing ˃ 5% of 24-hour TEI | Binary outcome indicating whether the value calculated for percentage of dietary energy intake from free sugars is > 5% for the 24-hour period. |
| Consumption of five or more portions of F&V during a 24-hour period | Binary outcome indicating whether the number of F&V portions for the 24-hour period is > 5 |
| Number of eating/drinking occasions (excluding plain water) during 24-hour period | Count of the number of unique eating and drinking occasions entered by a participant, except for occasions when plain water was the only item consumed |
Appendix 5 Details of unit costs for valuation of resource use in the economic evaluation
| Item | Unit of measurement | Unit cost | Description | Calculation | Source |
|---|---|---|---|---|---|
| Teaching staff time | Per hour | £20 | Gross average annual salary for other teachers in England (excluding the London area) divided by 39 weeks, 5 working days and 8 working hours | £31,338 (range £25,714–36,961)/39 weeks/5 days/8 hours | Teachers’ salary: DfE131 Teachers’ working weeks: NASUWT Teacher’s Union132 |
| Catering staff time | Per hour | £11.47 (catering assistants); £19.47 (catering manager, chef) | Local government pay scale for support staff, hourly pay mid-scale of the lower and the higher portions of the scale | National Education Union133 | |
| Vending machine maintenance | Per week | £46 | Weekly average rental | School Food Trust:134 | |
| Water fountain maintenance | Per year | £17 | Average cost of maintaining a water fountain | School data: one FUEL school reported spending £50 per year on maintaining three water fountains | |
| Volunteer time | Per hour | £8.91 | National Living Wage (for those aged ≥23 years) | UK government,135 based on the unit cost of an hour of unpaid work | |
| Ingredients for cooking classes | Average cost per pupil spent every fourth lesson | £5, unless a different estimate was reported by the school | Islington Council136 |
Appendix 6 Levels of implementation of School Food Plan actions across schools
| SFP themes and actions | Number of schools providing data | Schools rated high,a n (%) | Schools rated medium,a n (%) | Schools rated low,a n (%) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All | SFS | non-SFS | All | SFS | non-SFS | All | SFS | non-SFS | All | SFS | non-SFS | |
| Whole-school approach | ||||||||||||
| Culture of healthy eating | 36 | 13 | 23 | 12 (33.3) | 3 (23.1) | 9 (39.1) | 14 (38.9) | 7 (53.8) | 7 (30.4) | 10 (27.8) | 3 (23.1) | 7 (30.4) |
| Demonstrate a culture and ethos of healthy eating to Ofsted | 32 | 10 | 22 | 20 (62.5) | 7 (70) | 13 (59.1) | 8 (25) | 2 (20) | 6 (27.3) | 4 (12.5) | 1 (10) | 3 (13.6) |
| Staff eat in the canteen with pupils | 35 | 13 | 22 | 11 (31.4) | 4 (30.8) | 7 (31.8) | 8 (22.9) | 4 (30.8) | 4 (18.2) | 16 (45.7) | 5 (38.5) | 11 (50) |
| Healthy-eating messages promoted across the school | 36 | 13 | 23 | 4 (11.1) | 0 (0) | 4 (17.4) | 11 (30.6) | 6 (46.2) | 5 (21.7) | 21 (58.3) | 7 (53.8) | 14 (60.9) |
| Healthy-eating messages consistent | 35 | 12 | 23 | 18 (51.4) | 8 (66.7) | 10 (43.5) | 9 (25.7) | 1 (8.3) | 8 (34.8) | 8 (22.9) | 3 (25) | 5 (21.7) |
| Sweets are not given as rewards | 36 | 13 | 23 | 2 (5.6) | 1 (7.7) | 1 (4.3) | 9 (25) | 2 (15.4) | 7 (30.4) | 25 (69.4) | 10 (76.9) | 15 (65.2) |
| Grow food to provide to pupils | 10 | 1 | 9 | 2 (20) | 1 (100) | 1 (11.1) | 0 (0) | 0 (0) | 0 (0) | 8 (80) | 0 (0) | 8 (88.9) |
| Staff training on health and well being | 32 | 10 | 22 | 10 (31.3) | 3 (30) | 7 (31.8) | 11 (34.4) | 5 (50) | 6 (27.3) | 11 (34.4) | 2 (20) | 9 (40.9) |
| Drinking water freely and easily available | 36 | 13 | 23 | 29 (80.6) | 11 (84.6) | 18 (78.3) | 5 (13.9) | 1 (7.7) | 4 (17.4) | 2 (5.6) | 1 (7.7) | 1 (4.3) |
| Leadership and oversight on school food | ||||||||||||
| Senior leaders lead on and engage with school food | 36 | 13 | 23 | 16 (44.4) | 7 (53.8) | 9 (39.1) | 15 (41.7) | 4 (30.8) | 11 (47.8) | 5 (13.9) | 2 (15.4) | 3 (13) |
| Healthy eating considered in the school development plan/school evaluation | 28 | 9 | 19 | 9 (32.1) | 4 (44.4) | 5 (26.3) | 5 (17.9) | 1 (11.1) | 4 (21.1) | 14 (50) | 4 (44.4) | 10 (52.6) |
| Governors lead on and engage with school food | 28 | 9 | 19 | 3 (10.7) | 0 (0) | 3 (15.8) | 7 (25) | 3 (33.3) | 4 (21.1) | 18 (64.3) | 6 (66.7) | 12 (63.2) |
| Opportunities for pupils to contribute views | 36 | 13 | 23 | 10 (27.8) | 4 (30.8) | 6 (26.1) | 9 (25) | 4 (30.8) | 5 (21.7) | 17 (47.2) | 5 (38.5) | 12 (52.2) |
| School use external agencies for support | 10 | 3 | 7 | 1 (10) | 0 (0) | 1 (14.3) | 0 (0) | 0 (0) | 0 (0) | 9 (90) | 3 (100) | 6 (85.7) |
| Policies | ||||||||||||
| School food policy | 36 | 13 | 23 | 4 (11.1) | 0 (0) | 4 (17.4) | 0 (0) | 0 (0) | 0 (0) | 32 (88.9) | 13 (100) | 19 (82.6) |
| Policy on food brought from home | 12 | 7 | 5 | 12 (100) | 7 (100) | 5 (100) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Policy on drinks | 11 | 5 | 6 | 11 (100) | 5 (100) | 6 (100) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Stay-on-site rule for break and lunch time | 32 | 10 | 22 | 31 (96.9) | 10 (100) | 21 (95.5) | 1 (3.1) | 0 (0) | 1 (4.5) | 0 (0) | 0 (0) | 0 (0) |
| Staff aware of and implementing the school food policy | 4 | 0 | 4 | 3 (75) | 0 (0) | 3 (75) | 1 (25) | 0 (0) | 1 (25) | 0 (0) | 0 (0) | 0 (0) |
| Pupils and parents aware of the school food policy | 2 | 1 | 1 | 0 (0) | 0 (0) | 0 (0) | 2 (100) | 1 (100) | 1 (100) | 0 (0) | 0 (0) | 0 (0) |
| Engagement | ||||||||||||
| Pupils have the opportunity to assist catering staff | 36 | 13 | 23 | 0 (0) | 0 (0) | 0 (0) | 2 (5.6) | 1 (7.7) | 1 (4.3) | 34 (94.4) | 12 (92.3) | 22 (95.7) |
| School consults with parents on school food | 32 | 10 | 22 | 13 (40.6) | 5 (50) | 8 (36.4) | 9 (28.1) | 2 (20) | 7 (31.8) | 10 (31.3) | 3 (30) | 7 (31.8) |
| School makes menus available in advance | 35 | 13 | 22 | 2 (5.7) | 1 (7.7) | 1 (4.5) | 10 (28.6) | 4 (30.8) | 6 (27.3) | 23 (65.7) | 8 (61.5) | 15 (68.2) |
| Opportunities for parents to sample/try school food | 26 | 9 | 17 | 10 (38.5) | 5 (55.6) | 5 (29.4) | 3 (11.5) | 0 (0) | 3 (17.6) | 13 (50) | 4 (44.4) | 9 (52.9) |
| Parents encouraged to participate in cooking or gardening clubs | 17 | 3 | 14 | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 17 (100) | 3 (100) | 14 (100) |
| School engages with the community on school food or food education activities | 32 | 10 | 22 | 9 (28.1) | 4 (40) | 5 (22.7) | 12 (37.5) | 3 (30) | 9 (40.9) | 11 (34.4) | 3 (30) | 8 (36.4) |
| Catering provision and standards | ||||||||||||
| Catering staff integrated into school life | 26 | 9 | 17 | 9 (34.6) | 4 (44.4) | 5 (29.4) | 3 (11.5) | 0 (0) | 3 (17.6) | 14 (53.8) | 5 (55.6) | 9 (52.9) |
| Catering staff supported to develop and learn | 26 | 9 | 17 | 19 (73.1) | 6 (66.7) | 13 (76.5) | 1 (3.8) | 0 (0) | 1 (5.9) | 6 (23.1) | 3 (33.3) | 3 (17.6) |
| Contract specification includes the SFS, professional standards, food quality and lunchtime experience | 8 | 2 | 6 | 4 (50) | 0 (0) | 4 (66.7) | 0 (0) | 0 (0) | 0 (0) | 4 (50) | 2 (100) | 2 (33.3) |
| Compliance with the SFS checked | 29 | 10 | 19 | 1 (3.4) | 1 (10) | 0 (0) | 5 (17.2) | 2 (20) | 3 (15.8) | 23 (79.3) | 7 (70) | 16 (84.2) |
| Catering team using the professional standards | 26 | 9 | 17 | 5 (19.2) | 3 (33.3) | 2 (11.8) | 3 (11.5) | 0 (0) | 3 (17.6) | 18 (69.2) | 6 (66.7) | 12 (70.6) |
| School food award/quality assured scheme | 32 | 10 | 22 | 7 (21.9) | 2 (20) | 5 (22.7) | 0 (0) | 0 (0) | 0 (0) | 25 (78.1) | 8 (80) | 17 (77.3) |
| Caterer has a clear, written plan for increasing take-up | 7 | 2 | 5 | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 7 (100) | 2 (100) | 5 (100) |
| Caterers consider the environment when choosing their suppliers | 28 | 9 | 19 | 12 (42.9) | 5 (55.6) | 7 (36.8) | 4 (14.3) | 1 (11.1) | 3 (15.8) | 12 (42.9) | 3 (33.3) | 9 (47.4) |
| Catering practices | ||||||||||||
| Catering staff encourage pupils to experiment with new foods | 36 | 13 | 23 | 0 (0) | 0 (0) | 0 (0) | 2 (5.6) | 1 (7.7) | 1 (4.3) | 34 (94.4) | 12 (92.3) | 22 (95.7) |
| Catering staff encourage pupils to eat healthily | 35 | 13 | 22 | 1 (2.9) | 0 (0) | 1 (4.5) | 21 (60) | 7 (53.8) | 14 (63.6) | 13 (37.1) | 6 (46.2) | 7 (31.8) |
| Cheaper ‘set menu’ meal offered to encourage a balanced meal | 30 | 11 | 19 | 13 (43.3) | 7 (63.6) | 6 (31.6) | 0 (0) | 0 (0) | 0 (0) | 17 (56.7) | 4 (36.4) | 13 (68.4) |
| Prizes and other incentives for bringing in a healthy lunch | 35 | 12 | 23 | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 35 (100) | 12 (100) | 23 (100) |
| The lunchtime experience | ||||||||||||
| School asks for feedback on the lunchtime experience | 19 | 5 | 14 | 8 (42.1) | 2 (40) | 6 (42.9) | 0 (0) | 0 (0) | 0 (0) | 11 (57.9) | 3 (60) | 8 (57.1) |
| Dining environment is attractive | 36 | 13 | 23 | 18 (50) | 9 (69.2) | 9 (39.1) | 12 (33.3) | 3 (23.1) | 9 (39.1) | 6 (16.7) | 1 (7.7) | 5 (21.7) |
| Dining environment calm | 36 | 13 | 23 | 3 (8.3) | 1 (7.7) | 2 (8.7) | 21 (58.3) | 7 (53.8) | 14 (60.9) | 12 (33.3) | 5 (38.5) | 7 (30.4) |
| Strategies to reduce queuing times | 35 | 12 | 23 | 27 (77.1) | 10 (83.3) | 17 (73.9) | 5 (14.3) | 1 (8.3) | 4 (17.4) | 3 (8.6) | 1 (8.3) | 2 (8.7) |
| Lunch breaks staggered | 36 | 13 | 23 | 18 (50) | 7 (53.8) | 11 (47.8) | 3 (8.3) | 0 (0) | 3 (13) | 15 (41.7) | 6 (46.2) | 9 (39.1) |
| Multiple service points | 36 | 13 | 23 | 29 (80.6) | 12 (92.3) | 17 (73.9) | 4 (11.1) | 1 (7.7) | 3 (13) | 3 (8.3) | 0 (0) | 3 (13) |
| Pupils do not feel rushed to purchase foods from school food outlets | 36 | 13 | 23 | 1 (2.8) | 1 (7.7) | 0 (0) | 9 (25) | 3 (23.1) | 6 (26.1) | 26 (72.2) | 9 (69.2) | 17 (73.9) |
| Pupils have enough time to eat their lunch | 36 | 13 | 23 | 22 (61.1) | 8 (61.5) | 14 (60.9) | 9 (25) | 5 (38.5) | 4 (17.4) | 5 (13.9) | 0 (0) | 5 (21.7) |
| Sufficient time during the lunch break for eating as well as activities or clubs | 36 | 13 | 23 | 9 (25) | 1 (7.7) | 8 (34.8) | 19 (52.8) | 8 (61.5) | 11 (47.8) | 8 (22.2) | 4 (30.8) | 4 (17.4) |
| Sit-down meal encouraged | 36 | 13 | 23 | 16 (44.4) | 4 (30.8) | 12 (52.2) | 11 (30.6) | 5 (38.5) | 6 (26.1) | 9 (25) | 4 (30.8) | 5 (21.7) |
| Proper crockery | 35 | 12 | 23 | 14 (40) | 2 (16.7) | 12 (52.2) | 4 (11.4) | 2 (16.7) | 2 (8.7) | 17 (48.6) | 8 (66.7) | 9 (39.1) |
| Packed lunches and school meals sit together | 33 | 12 | 21 | 33 (100) | 12 (100) | 21 (100) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Catering providers offer samples of the food | 36 | 13 | 23 | 0 (0) | 0 (0) | 0 (0) | 2 (5.6) | 1 (7.7) | 1 (4.3) | 34 (94.4) | 12 (92.3) | 22 (95.7) |
| Catering providers offer themed days | 24 | 9 | 15 | 17 (70.8) | 4 (44.4) | 13 (86.7) | 2 (8.3) | 0 (0) | 2 (13.3) | 5 (20.8) | 5 (55.6) | 0 (0) |
| Catering staff happy and engaged with school staff and pupils | 36 | 13 | 23 | 32 (88.9) | 12 (92.3) | 20 (87) | 3 (8.3) | 1 (7.7) | 2 (8.7) | 1 (2.8) | 0 (0) | 1 (4.3) |
| Food education | ||||||||||||
| Curriculum offers the opportunity for all pupils to learn cooking | 36 | 13 | 23 | 32 (88.9) | 11 (84.6) | 21 (91.3) | 0 (0) | 0 (0) | 0 (0) | 4 (11.1) | 2 (15.4) | 2 (8.7) |
| Curriculum offers the opportunity for all pupils to learn food growing/gardening | 35 | 13 | 22 | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 35 (100) | 13 (100) | 22 (100) |
| Healthy eating instilled as part of mandatory teaching of food education | 32 | 11 | 21 | 30 (93.8) | 11 (100) | 19 (90.5) | 1 (3.1) | 0 (0) | 1 (4.8) | 1 (3.1) | 0 (0) | 1 (4.8) |
| Healthy eating taught across a range of subjects within the curriculum | 33 | 11 | 22 | 30 (90.9) | 11 (100) | 19 (86.4) | 1 (3) | 0 (0) | 1 (4.5) | 2 (6.1) | 0 (0) | 2 (9.1) |
| Cooking taught outside of the curriculum, for example clubs | 36 | 13 | 23 | 3 (8.3) | 1 (7.7) | 2 (8.7) | 9 (25) | 3 (23.1) | 6 (26.1) | 24 (66.7) | 9 (69.2) | 15 (65.2) |
| Growing taught outside of the curriculum, for example clubs | 36 | 13 | 23 | 2 (5.6) | 1 (7.7) | 1 (4.3) | 2 (5.6) | 0 (0) | 2 (8.7) | 32 (88.9) | 12 (92.3) | 20 (87) |
| Enough timetabling, space and practical resources (equipment, ingredients) for teaching cooking | 33 | 11 | 22 | 24 (72.7) | 8 (72.7) | 16 (72.7) | 5 (15.2) | 0 (0) | 5 (22.7) | 4 (12.1) | 3 (27.3) | 1 (4.5) |
| All pupils can access ingredients for cooking activities | 15 | 4 | 11 | 14 (93.3) | 3 (75) | 11 (100) | 0 (0) | 0 (0) | 0 (0) | 1 (6.7) | 1 (25) | 0 (0) |
| Qualified subject specialist to teach food education | 33 | 11 | 22 | 26 (78.8) | 8 (72.7) | 18 (81.8) | 1 (3) | 0 (0) | 1 (4.5) | 6 (18.2) | 3 (27.3) | 3 (13.6) |
| Focus on savoury cooking | 36 | 13 | 23 | 14 (38.9) | 6 (46.2) | 8 (34.8) | 17 (47.2) | 5 (38.5) | 12 (52.2) | 5 (13.9) | 2 (15.4) | 3 (13) |
| Increasing school meal access and take-up | ||||||||||||
| Food available to pupils at breakfast time | 32 | 10 | 22 | 22 (68.8) | 7 (70) | 15 (68.2) | 5 (15.6) | 2 (20) | 2 (9.1) | 6 (18.8) | 1 (10) | 5 (22.7) |
| Breakfast is affordable and accessible for all pupils | 6 | 2 | 4 | 5 (83.3) | 2 (100) | 3 (75) | 0 (0) | 0 (0) | 0 (0) | 1 (20) | 0 (0) | 1 (25) |
| School meal take-up is reported/monitored | 30 | 9 | 21 | 23 (76.7) | 7 (77.8) | 16 (76.2) | 3 (10) | 0 (0) | 3 (14.3) | 4 (13.3) | 2 (22.2) | 2 (9.5) |
| Governors obtain and review take-up data each term | 23 | 8 | 15 | 4 (17.4) | 1 (12.5) | 3 (20) | 2 (8.7) | 0 (0) | 2 (13.3) | 17 (73.9) | 7 (87.5) | 10 (66.7) |
| Efforts made to promote school meal take-up | 31 | 9 | 22 | 12 (38.7) | 5 (33.3) | 7 (31.8) | 9 (29) | 1 (11.1) | 8 (36.4) | 10 (32.2) | 3 (33.3) | 7 (31.8) |
| Efforts made to ensure those eligible for FSM are using their entitlement | 18 | 7 | 11 | 8 (44.4) | 3 (42.8) | 5 (45.5) | 2 (11.8) | 1 (16.7) | 1 (9.1) | 8 (47.1) | 3 (50) | 5 (45.5) |
| Pupils with allergies able to access a school meal | 35 | 13 | 22 | 14 (40) | 5 (38.5) | 9 (40.9) | 14 (40) | 6 (46.2) | 8 (36.4) | 7 (20) | 2 (15.4) | 5 (22.7) |
| Cashless payment system | 31 | 10 | 21 | 28 (90.3) | 9 (90) | 19 (90.5) | 0 (0) | 0 (0) | 0 (0) | 3 (9.7) | 1 (10) | 2 (9.5) |
Appendix 7 Interaction effects in the pupil nutritional outcome models
| Outcome | Lunch, coefficient (95% CI), p-value | School day, coefficient (95% CI), p-value | 24-hour day, coefficient (95% CI), p-value |
|---|---|---|---|
| Free sugar | 0.007 (–3.52 to 3.53), p = 0.997 | –1.35 (–6.75 to 4.06), p = 0.63 | –4.06 (–14.23 to 6.11), p = 0.43 |
| % TEI from free sugar | –1.86 (–4.44 to 0.72), p = 0.16 | –2.16 (–4.55 to 0.22), p = 0.08 | –1.34 (–2.96 to 0.27), p = 0.104 |
| TEI | 52.13 (–7.00 to 111.25), p = 0.08 | 38.33 (–42.05 to 118.71), p = 0.35 | 3.25 (–146.06 to 152.56), p = 0.97 |
| Fat intake | 2.62 (–0.32 to 5.56), p = 0.08 | 1.67 (–2.17 to 5.50), p = 0.39 | –0.62 (–7.46 to 6.22), p = 0.86 |
| Fibre intake | 0.46 (–0.14 to 1.05), p = 0.13 | 0.56 (–0.17 to 1.30), p = 0.13 | 0.57 (–0.86 to 2.00), p = 0.43 |
| F&V portions | 0.15 (–0.04 to 0.34), p = 0.124 | 0.15 (–0.08 to 0.37), p = 0.20 | 0.28 (–0.11 to 0.66), p = 0.16 |
| Number of SSBs | 0.72 (0.43 to 1.22), p = 0.22 | 0.92 (0.57 to 1.48), p = 0.74 | 0.81 (0.59 to 1.10), p = 0.18 |
| Number of HFSS items | 1.05 (0.87 to 1.28), p = 0.59 | 0.98 (0.84 to 1.15), p = 0.83 | 0.97 (0.86 to 1.09), p = 0.58 |
| Number of confectionery items | 1.25 (0.60 to 2.59), p = 0.55 | 1.03 (0.68 to 1.57), p = 0.88 | 0.88 (0.66 to 1.17), p = 0.37 |
| Outcome | Interaction term | Lunch, coefficient (95% CI), p-value | School day, coefficient (95% CI), p-value | 24-hour day, coefficient (95% CI), p-value |
|---|---|---|---|---|
| Free sugar | SFS-IMD quintile 2 | –2.70 (–8.28 to 2.88), p = 0.34 | –2.32 (–10.92 to 6.28), p = 0.60 | –5.56 (–22.18 to 11.06), p = 0.51 |
| SFS-IMD quintile 3 | –2.46 (–8.03 to 3.12), p = 0.39 | –3.38 (–12.11 to 5.34), p = 0.45 | –11.96 (–28.70 to 4.77), p = 0.16 | |
| SFS-IMD quintile 4 | –1.80 (–8.04 to 4.44), p = 0.57 | –1.55 (–11.27 to 8.16), p = 0.75 | –1.64 (–20.50 to 17.23), p = 0.87 | |
| SFS-IMD quintile 5 | –0.98 (–7.25 to 5.29), p = 0.76 | 0.53 (–9.29 to 10.34), p = 0.92 | 17.14 (–1.88 to 36.16), p = 0.08 | |
| % TEI from free sugar | SFS-IMD quintile 2 | –1.89 (–5.92 to 2.14), p = 0.36 | –1.63 (–5.36 to 2.11), p = 0.39 | 0.89 (–1.71 to 3.50), p = 0.50 |
| SFS-IMD quintile 3 | –3.21 (–7.34 to 0.93), p = 0.13 | –2.76 (–6.61 to 1.10), p = 0.16 | –0.74 (–3.43 to 1.95), p = 0.59 | |
| SFS-IMD quintile 4 | –1.35 (–5.94 to 3.24), p = 0.56 | –1.33 (–5.59 to 2.94), p = 0.54 | 0.31 (–2.70 to 3.32), p = 0.84 | |
| SFS-IMD quintile 5 | 1.67 (–2.98 to 6.32), p = 0.48 | 1.80 (–2.54 to 6.13), p = 0.42 | 3.57 (0.51 to 6.63), p = 0.02 | |
| TEI | SFS-IMD quintile 2 | –5.80 (–98.98 to 87.38), p = 0.903 | –20.98 (–149.23 to 107.27), p = 0.75 | –92.40 (–334.90 to 150.10), p = 0.46 |
| SFS-IMD quintile 3 | 42.30 (–51.57 to 136.17), p = 0.38 | –0.24 (–129.37 to 128.89), p = 0.997 | –93.83 (–340.17 to 152.51), p = 0.46 | |
| SFS-IMD quintile 4 | 32.72 (–72.11 to 137.55), p = 0.54 | 11.39 (–132.70 to 155.49), p = 0.88 | –90.92 (–367.84 to 185.99), p = 0.52 | |
| SFS-IMD quintile 5 | –66.67 (–172.25 to 38.91), p = 0.22 | –67.97 (–213.02 to 77.09), p = 0.36 | –28.12 (–308.31 to 252.06), p = 0.84 | |
| Fat intake | SFS-IMD quintile 2 | –0.78 (–5.37 to 3.81), p = 0.74 | –0.005 (–6.06 to 6.05), p = 0.999 | –6.10 (–16.92 to 4.71), p = 0.27 |
| SFS-IMD quintile 3 | 1.80 (–2.82 to 6.41), p = 0.45 | 0.47 (–5.64 to 6.57), p = 0.88 | –2.47 (–13.42 to 8.49), p = 0.66 | |
| SFS-IMD quintile 4 | 2.96 (–2.20 to 8.11), p = 0.26 | 2.36 (–4.44 to 9.17), p = 0.50 | –5.25 (–17.55 to 7.05), p = 0.40 | |
| SFS-IMD quintile 5 | –1.57 (–6.75 to 3.61), p = 0.55 | –1.38 (–8.23 to 5.48), p = 0.69 | –4.55 (–16.97 to 7.88), p = 0.47 | |
| Fibre intake | SFS-IMD quintile 2 | 0.07 (–0.86 to 1.00), p = 0.88 | –0.03 (–1.19 to 1.13), p = 0.96 | 0.30 (–2.01 to 2.61), p = 0.80 |
| SFS-IMD quintile 3 | 0.29 (–0.67 to 1.24), p = 0.56 | –0.24 (–1.43 to 0.95), p = 0.69 | –0.93 (–3.32 to 1.46), p = 0.45 | |
| SFS-IMD quintile 4 | –0.12 (–1.18 to 0.95), p = 0.83 | –0.44 (–1.76 to 0.88), p = 0.51 | –1.13 (–3.81 to 1.54), p = 0.42 | |
| SFS-IMD quintile 5 | –0.61 (–1.68 to 0.47), p = 0.27 | –0.80 (–2.14 to 0.53), p = 0.24 | –0.19 (–2.91 to 2.54), p = 0.89 | |
| F&V portions | SFS-IMD quintile 2 | –0.03 (–0.33 to 0.27), p = 0.85 | –0.01 (–0.37 to 0.34), p = 0.93 | 0.12 (–0.50 to 0.73), p = 0.71 |
| SFS-IMD quintile 3 | –0.06 (–0.37 to 0.24), p = 0.68 | –0.20 (–0.55 to 0.16), p = 0.28 | –0.10 (–0.73 to 0.54), p = 0.76 | |
| SFS-IMD quintile 4 | –0.10 (–0.44 to 0.24), p = 0.56 | –0.11 (–0.51 to 0.28), p = 0.57 | 0.17 (–0.54 to 0.88), p = 0.64 | |
| SFS-IMD quintile 5 | –0.09 (–0.43 to 0.25), p = 0.61 | –0.06 (–0.46 to 0.35), p = 0.79 | 0.17 (–0.56 to 0.89), p = 0.65 | |
| Number of SSBs | SFS-IMD quintile 2 | 1.04 (0.50 to 2.17), p = 0.92 | 1.39 (0.68 to 2.86), p = 0.37 | 1.15 (0.70 to 1.90), p = 0.57 |
| SFS-IMD quintile 3 | 0.86 (0.40 to 1.88), p = 0.71 | 1.30 (0.61 to 2.75), p = 0.50 | 0.83 (0.49 to 1.39), p = 0.48 | |
| SFS-IMD quintile 4 | 0.87 (0.36 to 2.11) p = 0.76 | 1.05 (0.44 to 2.50), p = 0.92 | 0.94 (0.52 to 1.68), p = 0.83 | |
| SFS-IMD quintile 5 | 1.62 (0.67 to 3.95), p = 0.29 | 2.01 (0.86 to 4.68), p = 0.11 | 1.82 (1.00 to 3.29), p = 0.048 | |
| Number of HFSS items | SFS-IMD quintile 2 | 1.12 (0.84 to 1.48), p = 0.44 | 1.12 (0.89 to 1.41), p = 0.35 | 1.12 (0.93 to 1.33), p = 0.23 |
| SFS-IMD quintile 3 | 1.08 (0.82 to 1.43), p = 0.58 | 1.05 (0.83 to 1.33), p = 0.67 | 0.98 (0.82 to 1.18), p = 0.83 | |
| SFS-IMD quintile 4 | 1.10 (0.82 to 1.49), p = 0.52 | 1.06 (0.82 to 1.36), p = 0.66 | 1.04 (0.85 to 1.28), p = 0.67 | |
| SFS-IMD quintile 5 | 1.02 (0.75 to 1.40), p = 0.90 | 1.11 (0.86 to 1.44), p = 0.43 | 1.09 (0.89 to 1.34), p = 0.42 | |
| Number of confectionery items | SFS-IMD quintile 2 | 0.96 (0.44 to 2.09), p = 0.91 | 1.15 (0.66 to 2.01), p = 0.63 | 1.35 (0.88 to 2.06), p = 0.17 |
| SFS-IMD quintile 3 | 0.70 (0.32 to 1.50), p = 0.36 | 0.81 (0.47 to 1.42), p = 0.47 | 1.01 (0.66 to 1.54), p = 0.97 | |
| SFS-IMD quintile 4 | 0.78 (0.35 to 1.75), p = 0.55 | 0.95 (0.52 to 1.73), p = 0.86 | 1.32 (0.82 to 2.10), p = 0.25 | |
| SFS-IMD quintile 5 | 0.87 (0.38 to 1.99), p = 0.75 | 0.90 (0.49 to 1.65), p = 0.73 | 1.25 (0.79 to 1.97), p = 0.33 |
| Outcome | Interaction term | Lunch, coefficient (95% CI), p-value | School day, coefficient (95% CI), p-value | 24-hour day, coefficient (95% CI), p-value |
|---|---|---|---|---|
| Free sugar | SFS-Year 9 | 0.56 (–3.87 to 4.99), p = 0.81 | –1.25 (–8.07 to 5.57), p = 0.72 | 3.66 (–9.71 to 17.03), p = 0.59 |
| SFS-Year 10 | 1.02 (–3.42 to 5.45), p = 0.65 | –2.85 (–9.70 to 3.99), p = 0.41 | –4.13 (–17.50 to 9.24), p = 0.55 | |
| % TEI from free sugar | SFS-Year 9 | 1.95 (–1.20 to 5.09), p = 0.23 | 0.08 (–2.84 to 3.01), p = 0.96 | –0.54 (–2.60 to 1.52), p = 0.61 |
| SFS-Year 10 | 1.92 (–1.23 to 5.07), p = 0.23 | 0.23 (–2.71 to 3.17), p = 0.88 | –0.75 (–2.81 to 1.32), p = 0.48 | |
| TEI | SFS-Year 9 | –25.12 (–98.78 to 48.54), p = 0.50 | –20.14 (–122.27 to 81.99), p = 0.70 | 108.36 (–85.13 to 301.86), p = 0.27 |
| SFS-Year 10 | –12.49 (–86.22 to 61.23), p = 0.74 | –78.92 (–181.41 to 23.58), p = 0.13 | –54.26 (–247.77 to 139.24), p = 0.58 | |
| Fat intake | SFS-Year 9 | –0.97 (–4.60 to 2.66), p = 0.60 | –0.34 (–5.16 to 4.48), p = 0.89 | 7.27 (–1.37 to 15.92), p = 0.10 |
| SFS-Year 10 | –0.56 (–4.20 to 3.07), p = 0.76 | –3.31 (–8.14 to 1.53), p = 0.18 | –2.34 (–10.98 to 6.31), p = 0.60 | |
| Fibre intake | SFS-Year 9 | –0.71 (–1.43 to 0.02), p = 0.06 | –0.42 (–1.33 to 0.50), p = 0.37 | 0.44 (–1.38 to 2.27), p = 0.63 |
| SFS-Year 10 | –0.29 (–1.01 to 0.44), p = 0.44 | –0.66 (–1.58 to 0.26), p = 0.16 | –0.88 (–2.70 to 0.95), p = 0.35 | |
| F&V portions | SFS-Year 9 | –0.17 (–0.40 to 0.07), p = 0.16 | –0.11 (–0.39 to 0.17), p = 0.45 | 0.03 (–0.45 to 0.52), p = 0.90 |
| SFS-Year 10 | 0.09 (–0.14 to 0.33), p = 0.43 | 0.07 (–0.21 to 0.35), p = 0.63 | –0.13 (–0.61 to 0.36), p = 0.61 | |
| Number of SSBs | SFS-Year 9 | 1.09 (0.60 to 2.00), p = 0.78 | 1.32 (0.75 to 2.33), p = 0.34 | 1.27 (0.86 to 1.87), p = 0.23 |
| SFS-Year 10 | 1.34 (0.72 to 2.50), p = 0.35 | 1.22 (0.67 to 2.22), p = 0.51 | 1.30 (0.87 to 1.95), p = 0.21 | |
| Number of HFSS items | SFS-Year 9 | 0.92 (0.74 to 1.14), p = 0.46 | 0.90 (0.75 to 1.08), p = 0.25 | 0.96 (0.84 to 1.11), p = 0.59 |
| SFS-Year 10 | 1.01 (0.82 to 1.25), p = 0.92 | 0.96 (0.80 to 1.15), p = 0.67 | 0.99 (0.86 to 1.14), p = 0.92 | |
| Number of confectionery items | SFS-Year 9 | 0.79 (0.44 to 1.43), p = 0.43 | 0.75 (0.49 to 1.16), p = 0.20 | 0.89 (0.64 to 1.24), p = 0.48 |
| SFS-Year 10 | 1.03 (0.57 to 1.84), p = 0.92 | 0.96 (0.63 to 1.47), p = 0.84 | 0.80 (0.57 to 1.12), p = 0.19 |
Appendix 8 Nutritional outcomes by school food standard/School Food Plan school type (six-group typology)
| Nutrient/food outcome | School typea | MD or IRR | |||||
|---|---|---|---|---|---|---|---|
| Lunch (n = 1878) | School day (n = 1934) | 24 hours (n = 2045) | |||||
| MD/IRR (95% CI) | p-value | MD/IRR (95% CI) | p-value | MD/IRR (95% CI) | p-value | ||
| Free sugar (g); MD | 1B | –0.80 (–4.05 to 2.46) | 0.63 | 2.46 (–2.77 to 7.69) | 0.36 | 2.60 (–7.82 to 13.01) | 0.63 |
| 2B | –4.91 (–11.98 to 2.16) | 0.17 | 0.91 (–10.74 to 12.57) | 0.88 | 16.12 (–7.62 to 39.86) | 0.18 | |
| 3A | –1.19 (–4.50 to 2.12) | 0.48 | –0.06 (–5.48 to 5.35) | 0.98 | –2.41 (–13.23 to 8.42) | 0.66 | |
| 3B | 2.76 (–0.31 to 5.82) | 0.08 | 4.77 (–0.23 to 9.77) | 0.06 | 5.41 (–4.62 to 15.45) | 0.29 | |
| 4A | 0.89 (–4.40 to 6.17) | 0.74 | 0.84 (–7.79 to 9.46) | 0.85 | 2.76 (–14.48 to 20.01) | 0.75 | |
| % TEI from free sugar; MD | 1B | 0.44 (–2.30 to 3.17) | 0.75 | 0.16 (–2.56 to 2.89) | 0.91 | –0.26 (–2.46 to 1.94) | 0.82 |
| 2B | –8.46 (–14.62 to –2.31) | 0.007 | –5.39 (–11.65 to 0.88) | 0.09 | 1.19 (–4.02 to 6.41) | 0.65 | |
| 3A | –0.26 (–3.09 to 2.58) | 0.859 | 0.56 (–2.31 to 3.42) | 0.70 | –0.41 (–2.74 to 1.92) | 0.73 | |
| 3B | 2.20 (–0.39 to 4.79) | 0.10 | 1.87 (–0.73 to 4.48) | 0.16 | 0.59 (–1.54 to 2.71) | 0.59 | |
| 4A | –3.45 (–8.08 to 1.17) | 0.14 | –2.57 (–7.24 to 2.10) | 0.28 | –0.83 (–4.69 to 3.04) | 0.68 | |
| TEI (kcal); MD | 1B | –34.74 (–96.63 to 27.14) | 0.27 | 31.80 (–42.31 to 105.90) | 0.40 | 105.12 (–51.63 to 261.87) | 0.19 |
| 2B | 24.78 (–113.60 to 163.15) | 0.73 | –19.55 (–182.81 to 143.71) | 0.81 | 149.65 (–209.46 to 508.75) | 0.41 | |
| 3A | –38.61 (–102.52 to 25.30) | 0.24 | –4.33 (–80.68 to 72.02) | 0.91 | –48.76 (–212.12 to 114.60) | 0.56 | |
| 3B | 7.22 (–51.31 to 65.75) | 0.81 | 53.76 (–17.04 to 124.57) | 0.14 | 64.89 (–86.11 to 215.88) | 0.40 | |
| 4A | 37.76 (–65.91 to 141.43) | 0.48 | 84.15 (–36.32 to 204.62) | 0.17 | 140.00 (–121.92 to 401.91) | 0.30 | |
| Fat (g); MD | 1B | –0.62 (–3.41 to 2.16) | 0.66 | 2.37 (–1.12 to 5.87) | 0.18 | 5.10 (–1.26 to 11.45) | 0.12 |
| 2B | 2.71 (–3.37 to 8.79) | 0.38 | –0.33 (–8.03 to 7.36) | 0.93 | 6.81 (–7.48 to 21.10) | 0.35 | |
| 3A | –2.16 (–5.00 to 0.68) | 0.14 | –0.91 (–4.51 to 2.70) | 0.62 | –4.18 (–10.74 to 2.39) | 0.21 | |
| 3B | 0.57 (–2.05 to 3.19) | 0.67 | 2.19 (–1.15 to 5.52) | 0.20 | 1.97 (–4.14 to 8.07) | 0.53 | |
| 4A | 1.32 (–3.24 to 5.89) | 0.57 | 4.43 (–1.26 to 10.12) | 0.13 | 5.30 (–5.08 to 15.68) | 0.32 | |
| Fibre (g); MD | 1B | –0.05 (–0.77 to 0.67) | 0.89 | 0.36 (–0.42 to 1.15) | 0.36 | 1.22 (–0.73 to 3.17) | 0.22 |
| 2B | 1.43 (–0.23 to 3.08) | 0.09 | 0.66 (–1.12 to 2.44) | 0.47 | 1.29 (–3.33 to 5.91) | 0.59 | |
| 3A | –0.03 (–0.78 to 0.73) | 0.94 | 0.33 (–0.49 to 1.15) | 0.43 | 0.15 (–1.92 to 2.21) | 0.89 | |
| 3B | 0.11 (–0.58 to 0.79) | 0.76 | 0.46 (–0.29 to 1.21) | 0.23 | 0.25 (–1.63 to 2.13) | 0.79 | |
| 4A | 0.38 (–0.86 to 1.62) | 0.55 | 0.56 (–0.76 to 1.89) | 0.41 | 0.02 (–3.40 to 3.45) | 0.99 | |
| F&V portions; MD | 1B | –0.05 (–0.28 to 0.18) | 0.65 | –0.03 (–0.26 to 0.19) | 0.77 | 0.39 (–0.11 to 0.89) | 0.13 |
| 2B | –0.37 (–0.90 to 0.17) | 0.18 | –0.28 (–0.79 to 0.23) | 0.28 | –0.43 (–1.61 to 0.76) | 0.48 | |
| 3A | 0.16 (–0.08 to 0.40) | 0.19 | 0.23 (–0.004 to 0.47) | 0.05 | 0.41 (–0.12 to 0.94) | 0.13 | |
| 3B | 0.05 (–0.17 to 0.26) | 0.69 | 0.14 (–0.08 to 0.36) | 0.21 | 0.37 (–0.11 to 0.86) | 0.13 | |
| 4A | –0.007 (–0.41 to 0.39) | 0.97 | 0.05 (–0.33 to 0.43) | 0.80 | 0.007 (–0.87 to 0.89) | 0.99 | |
| SSB items; IRR | 1B | 0.96 (0.60 to 1.55) | 0.87 | 1.22 (0.71 to 2.07) | 0.47 | 1.04 (0.67 to 1.62) | 0.85 |
| 2B | 0.55 (0.14 to 2.13) | 0.39 | 0.64 (0.15 to 2.65) | 0.53 | 1.34 (0.47 to 3.83) | 0.58 | |
| 3A | 0.69 (0.41 to 1.13) | 0.14 | 0.60 (0.34 to 1.07) | 0.08 | 0.77 (0.48 to 1.25) | 0.29 | |
| 3B | 1.05 (0.69 to 1.61) | 0.81 | 0.85 (0.52 to 1.40) | 0.53 | 0.80 (0.52 to 1.22) | 0.30 | |
| 4A | 0.78 (0.34 to 1.77) | 0.55 | 1.04 (0.44 to 2.48) | 0.93 | 0.78 (0.36 to 1.70) | 0.54 | |
| HFSS items; IRR | 1B | 1.13 (0.95 to 1.35) | 0.18 | 1.26 (1.10 to 1.44) | 0.001 | 1.22 (1.10 to 1.35) | < 0.001 |
| 2B | 0.83 (0.54 to 1.28) | 0.40 | 0.91 (0.67 to 1.23) | 0.52 | 1.06 (0.84 to 1.33) | 0.62 | |
| 3A | 1.02 (0.86 to 1.21) | 0.81 | 1.11 (0.98 to 1.27) | 0.11 | 1.08 (0.98 to 1.20) | 0.13 | |
| 3B | 1.13 (0.96 to 1.31) | 0.13 | 1.17 (1.04 to 1.32) | 0.01 | 1.14 (1.03 to 1.25) | 0.008 | |
| 4A | 1.23 (0.92 to 1.65) | 0.16 | 1.20 (0.96 to 1.50) | 0.11 | 1.21 (1.02 to 1.42) | 0.03 | |
| Sugar/chocolate confectionery items; IRR | 1B | 1.07 (0.67 to 1.72) | 0.78 | 1.37 (0.98 to 1.91) | 0.06 | 1.19 (0.93 to 1.52) | 0.16 |
| 2B | 0.44 (0.05 to 3.63) | 0.45 | 2.47 (1.19 to 5.15) | 0.02 | 1.37 (0.80 to 2.37) | 0.25 | |
| 3A | 0.82 (0.53 to 1.26) | 0.37 | 1.09 (0.79 to 1.50) | 0.59 | 1.10 (0.86 to 1.41) | 0.45 | |
| 3B | 1.01 (0.69 to 1.49) | 0.94 | 1.21 (0.90 to 1.62) | 0.21 | 1.18 (0.94 to 1.48) | 0.16 | |
| 4A | 2.19 (1.14 to 4.20) | 0.02 | 1.62 (0.97 to 2.72) | 0.06 | 1.58 (1.08 to 2.30) | 0.02 | |
Appendix 9 Sample of pupils with health-related quality-of-life data
| Characteristic | Total, mean QALY (SD); n (%) | Attending SFS-mandated schools, mean QALY (SD); n (%) | Attending SFS-non-mandated schools, mean QALY (SD); n (%) |
|---|---|---|---|
| All pupils | 0.8281 (0.1231); 1495 (100%) | 0.8302 (0.1254); 390 (100%) | 0.8274 (0.1224); 1105 |
| Year group | |||
| 7 | 0.8464 (0.1137); 474 (31.71) | 0.8365 (0.1243); 144 (36.92) | 0.8507 (0.1086); 330 (29.86) |
| 9 | 0.8262 (0.1162); 521 (34.85) | 0.8246 (0.1247); 121 (31.03) | 0.8267 (0.1136); 400 (36.2) |
| 10 | 0.8127 (0.1361); 500 (33.44) | 0.8283 (0.1279); 125 (32.05) | 0.8075 (0.1385); 375 (33.94) |
| Age (years); mean (SD) | 13.68 (1.27) | 13.59 (1.36) | 13.71 (1.24) |
| Missing | 37 | 13 | 24 |
| IMD quintile | |||
| 1 (highest deprivation) | 0.8261 (0.1289); 295 (21.52) | 0.8260 (0.1305); 98 (27.61) | 0.8261 (0.1284); 197 (19.39) |
| 2 | 0.8366 (0.1193); 202 (14.73) | 0.8538 (0.1035); 76 (21.41) | 0.8263 (0.1272); 126 (12.4) |
| 3 | 0.8216 (0.1224); 267 (19.47) | 0.8163 (0.1268); 72 (20.28) | 0.8236 (0.1210); 195 (19.19) |
| 4 | 0.8252 (0.1217); 305 (22.25) | 0.8382 (0.1111); 58 (16.34) | 0.8222 (0.1240); 247 (24.31) |
| 5 (lowest deprivation) | 0.8344 (0.1176); 302 (22.03) | 0.8179 (0.1406); 51 (14.37) | 0.8378 (0.1124); 251 (24.7) |
| Missing | 124 | 35 | 89 |
| Sex | |||
| Female | 0.8146 (0.1227); 833 (57.61) | 0.8083 (0.1383); 204 (54.26) | 0.8167 (0.1172); 629 (58.79) |
| Male | 0.8553 (0.1127); 613 (42.39) | 0.8632 (0.0934); 172 (45.74) | 0.8522 (0.1193); 441 (41.21) |
| Other/unknown | 49 | 14 | 33 |
| Ethnicity | |||
| White | 0.8248 (0.1248); 1,044 (71.31) | 0.8195 (0.1339); 275 (71.99) | 0.8267 (0.1214); 769 (71.07) |
| Asian/Asian British | 0.8409 (0.1176); 235 (16.05) | 0.8656 (0.0909); 57 (14.92) | 0.8330 (0.1242); 178 (16.45) |
| Black/African/Caribbean/Black British | 0.8521 (0.1081); 93 (6.35) | 0.8662 (0.0897); 24 (6.28) | 0.8472 (0.1140); 69 (6.38) |
| Mixed/multiple | 0.8105 (0.1244); 73 (4.99) | 0.8008 (0.1212); 20 (5.24) | 0.8142 (0.1265); 53 (4.9) |
| Other ethnic group/unknown | 0.8579 (0.1306); 19 (1.3) | 0.9094 (0.0418); 6 (1.57) | 0.8342 (0.1514); 13 (1.2) |
| Missing | 31 | 8 | 23 |
| FSM | |||
| Yes | 0.7834 (0.1380); 91 (9.59) | 0.7938 (0.1347); 29 (13) | 0.7785 (0.1404); 62 (8.54) |
| No | 0.8339 (0.1173); 817 (86.09) | 0.8396 (0.1150); 182 (81.61) | 0.8322 (0.1179); 635 (87.47) |
| Pupil did not know | 0.8428 (0.1125); 41 (4.32) | 0.8101 (0.1726); 12 (5.38) | 0.8563 (0.0758); 29 (3.99) |
| Missing | 546 | 167 | 379 |
Appendix 10 Description of subthemes in the case study qualitative analysis phase
| Subtheme | Key points (staff or pupil perspective indicated in parentheses) |
|---|---|
| School 1 | |
| Importance/value placed on school food |
|
| Rationale for family lunch |
|
|
|
|
|
| Compromises related to family lunch |
|
|
|
| Tensions related to family lunch |
|
| Devaluation of food education |
|
| Limited influence of school upon health behaviours |
|
| School 2 | |
| Need for flexible dining |
|
| ‘Grab and go’ at lunch |
|
| School food as a balancing act |
|
| School food lacking diversity |
|
| Losing the battle over healthy eating |
|
| Challenges within food education |
|
| School 3 | |
| Lunchtime experience |
|
| Food quality |
|
| Support/lack of support for healthy eating |
|
| Demographic drivers |
|
| Financial drivers and their effects |
|
| School 4 | |
| Lunchtime experience |
|
| Food quality |
|
|
|
| Cost to caterer and pupil |
|
| Healthy eating |
|
| Socioeconomics |
|
List of abbreviations
- CHU-9D
- Child Health Utility 9-Dimensions
- DfE
- Department for Education
- EAL
- English as an additional language
- FSM
- free school meals
- FUEL
- Food provision, cUlture and Environment in secondary schooLs
- F&V
- fruit and vegetable
- GCSE
- General Certificate of Secondary Education
- HFSS
- high fat, sugar and salt
- HRQoL
- health-related quality of life
- ICC
- intracluster correlation coefficient
- IDACI
- Income Deprivation Affecting Children Index
- IMD
- Index of Multiple Deprivation
- NDNS
- National Diet and Nutrition Survey
- NIHR
- National Institute for Health and Care Research
- NoMAD
- Normalisation Measure Development Questionnaire
- NPT
- normalization process theory
- Ofsted
- Office for Standards in Education, Children’s Services and Skills
- PSHE
- personal, social, health and economic education
- QALY
- quality-adjusted life year
- RAG
- red, amber and green
- SEN
- special educational needs
- SFP
- School Food Plan
- SFS
- school food standards
- SLT
- senior leadership team
- SSB
- sugar-sweetened beverage
- SSC
- Study Steering Committee
- TEI
- total energy intake
Notes
-
Staff responses to questions relating to NPT implementation constructs for the SFS and SFP
-
Sales of food and drink indicator items for all schools and all time periods
-
Individual and school characteristics of participants with and without outcome data
-
Intracluster correlation coefficients for pupil nutritional outcome models
-
Full models for nutritional outcomes with interaction effects
-
Full models for nutritional outcomes by SFS type – four-group typology
-
Full models for nutritional outcomes by level of SFS implementation
-
Full models for nutritional outcomes by SFS and SFP type – six-group typology
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/TTPL8570).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
