Notes
Article history
The research reported in this issue of the journal was funded by the PHR programme as project number 15/55/44. The contractual start date was in September 2016. The final report began editorial review in October 2020 and was accepted for publication in April 2021. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PHR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Disclaimer
This report contains transcripts of interviews conducted in the course of the research and contains language that may offend some readers.
Permissions
Copyright statement
Copyright © 2022 Hunt et al. This work was produced by Hunt et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2022 Hunt et al.
Chapter 1 Introduction and aims
Context
This report describes a study evaluating the process and outcomes of developing and implementing a smoke-free policy in 2018 throughout Scotland’s prison estate. We first outline the legislative and policy context for the study when it was originally designed (see Legislative and policy context prior to commencement of the Tobacco in Prisons study), and then indicate changes to our study protocol that were necessitated by the announcement, in July 2017, of a date (November 2018) to implement a smoke-free prison policy across Scotland’s prisons (see The announcement of new prison rules on smoking, July 2017), in part precipitated by early findings from the study. We then provide a brief overview of relevant literature.
Legislative and policy context prior to commencement of the Tobacco in Prisons study
When we first applied to the National Institute for Health Research’s (NIHR’s) Public Health Research (PHR) board for funding for the Tobacco in Prisons (TIPs) study in 2015, discussions were under way within the Scottish Prison Service (SPS), NHS Health Scotland and Scottish Government about whether or not (and, if so, when and how) changes in prison smoking rules should be formulated and implemented in Scotland. One outcome from these discussions was the publication of a specification for national smoking cessation services in prisons in Scotland,1 because provision across prisons and health boards was known to vary. The specification reinforced the need for ‘equitable’ and ‘consistent’ support for all people in custody who wish to stop smoking,1 which is reportedly up to three in five people in custody (PiC). 2 These discussions, including through a multidisciplinary National Tobacco Strategy Workstream convened by SPS, also informed a document entitled Continuing Scotland’s Journey Towards Smoke-free Prisons,3 which was published on SPS’s website on 13 September 2016 and laid out potential future policy options. This document’s purpose was to obtain agreement to strengthen smoking rules in Scottish prisons. 4 It presented the case for reconsidering current prison rules on smoking in Scotland’s prisons and three potential options for policy-makers to consider. Two members of the TIPs research team (KH and HS) took an active part in regular meetings convened by SPS’s Tobacco Strategy Group at SPS headquarters during the period 2014/15. Their review of existing literature5 informed the policy options paper, and the proposed TIPs study design (a three-phase multimethods study following a natural experimental methodology, as submitted to NIHR in 2015) to evaluate any policy change was included in section 4.7 of the document. 3
The need to reconsider smoking rules in Scotland’s prisons in 2014/15 was informed by many factors. First, legislation [Smoking, Health and Social Care Act (Scotland) 2005]6 enacted in March 2006 banned smoking in indoor public places; however, prisons did not ‘fall within the scope of a “no smoking” place as defined by the Act,’3 although ministers pledged that prisons would operate within the ‘principles’ of the legislation. 3 Second, in 2013, the Scottish Government announced its aspirations to make Scotland ‘tobacco free’ by 2034;7 high rates of smoking among PiC (SPS’s biennial Prisoner Survey suggested that 74% were smokers in 2013,2 and 72% were smokers in 20158 – around three times the national average) presented a challenge to this vision. Indeed, the Scottish Government’s Tobacco Strategy Group noted that ‘[C]reating a smoke-free prison service should be seen as a key step on our journey to creating a smoke-free Scotland’ (contains public sector information licensed under the Open Government Licence v3.0.). 7 Third, the need to find ways to support a reduction in smoking among PiC was consistent with the Scottish Government’s public health and inequalities strategy. 9 A joint action plan concerning smoking in prisons was submitted to ministers in early 2016. Although the nature and exact timing of any policy change in Scotland was yet to be decided when the TIPs study began, some people who were concerned about second-hand smoke (SHS) exposures were pressing for a short timescale. However, others thought that progress should first be made in reducing levels of smoking among PiC to make any changes towards greater restrictions on smoking in prison achievable, supported and enforceable, or thought that smoke-free prisons were unachievable.
In view of growing concern that high levels of smoking among PiC may damage both their health and that of prison staff and non-smoking PiC through exposure to SHS, alongside the lack of clarity about if, when and how Scotland may change its rules on smoking in prisons,3 we proposed a three-phase multimethods study to evaluate any changes in policy, designed in consultation with key stakeholders in the prison and health services in Scotland and in the Scottish Government. At that time (2015), PiC in Scotland’s prisons were permitted to smoke in their own cells and during outdoor recreation only; staff were not permitted to smoke anywhere on prison grounds3 and e-cigarettes were not available in prisons.
Phase 1 (which commenced in September 2016) proposed multiple components to understand SHS and smoking levels across all of Scotland’s 15 prisons, and the attitudes and experiences of staff and PiC in relation to smoking among PiC, smoking restrictions in prisons and a potential smoking ban. 10 Phase 2 was designed to examine the process of preparing for any change in prison smoking rules (assuming a decision to change the rules was announced) and phase 3 was designed to evaluate the impacts of any such changes. Funding for the later phases of the study was contingent on any substantial change in policy being announced within 2 years. 10 Phase 1 of TIPs included a more comprehensive baseline measurement of levels of SHS across a prison system than had been undertaken in any country to date (see Chapter 2, Interviews with representatives of other jurisdictions, and Chapter 4). 11
The announcement of new prison rules on smoking, July 2017
Phase 1 assessments of SHS exposures in 2016 demonstrated high, although variable, levels of SHS in Scottish prisons, particularly in residential halls11 (see Chapter 4), and partially influenced the decision to introduce a comprehensive smoke-free policy across Scotland’s prison estate. 4 At a press conference, on the day of publication (17 July 2017) of the phase 1 SHS results, Colin McConnell, then SPS Chief Executive, described the findings as ‘a call to action’. He said ‘[I]t is not acceptable that those in our care and those who work in our prisons should be exposed to second hand smoke’ and announced that all of Scotland’s prisons (including the open prison, Castle Huntly) would become smoke free in November 2018. 4 This necessitated revisions to the protocol for the TIPs study12 to take account of the newly announced policy and implementation date (30 November 2018); changes to the protocol also took account of our experience of conducting phase 1 data collection. The timings for the three-phase multimethods TIPs study were thus set as: phase 1 (September 2016–July 2017, baseline assessment before the policy was formulated; ‘pre-announcement phase’), phase 2 (August 2017–November 2018 in anticipation of policy implementation; ‘preparatory phase’) and phase 3 (December 2018–May 2020; ‘post-implementation phase’). 12
Overview of the existing literature (see also Hunt et al.5,12)
Smoking bans in public places decrease exposure to SHS,13 with direct health benefits. 14 Smoking rates have fallen in the general population, except among those in the most deprived areas,7,15 but a review16 in 2008 found that, across Europe, 64–88% of PiC smoked, and another17 in 2018 reported similarly high rates among PiC in low- and middle-income countries in Europe, but substantially lower rates in Africa. An international review18 based on 85 articles published from 2012 to 2016 showed that, in all but one of 36 countries, smoking rates for those incarcerated exceeded rates in the community and concluded that ‘because smoking prevalence is heightened in prisons, offering evidence-based interventions to nearly 15 million smokers passing through [prisons] yearly would improve global health’. 18
High levels of smoking among PiC have resulted in high SHS levels in prisons, even with some restrictions on smoking in these settings. Smoking among PiC thus poses a health risk not just to those who smoke but also to non-smoking PiC and staff, particularly staff opening up or entering cells. Internationally, smoking among prison staff is thought to be high, but evidence is sparse (only one study19 was identified in a recent review).
As the TIPs study was being designed, some countries (e.g. New Zealand, Canada, USA, Australia) had implemented total (i.e. all indoor and outdoor areas) or partial smoke-free policies within their prison estate (see Chapter 3, Interviews with representatives of other jurisdictions) and comprehensive smoke-free policies had been adopted by Broadmoor Secure Hospital in 2007 and Scotland’s State (high-secure psychiatric) Hospital in 2011. Introducing smoke-free legislation in the prison setting presents considerable challenges, underpinned by the social and cultural meanings of tobacco products and smoking in day-to-day prison life, the complexities of managing addiction (including nicotine addiction and associated problems, e.g. poor mental health), and the regulation and delivery of nicotine replacement, and other medications, within the prison environment. 5,20–22 Smoking has been described as ‘integral’ to prison life, serving as ‘a surrogate currency, a means of social control, as a symbol of freedom in a group with few rights and privileges, a stress reliever and social lubricant,’20 and a means of dealing with boredom and the need to ‘kill time’. Use of tobacco by PiC for ‘self-protection, insulating against physical attacks or acts of violence’ and ‘to alleviate immediate danger’ has been described. 23 Given this context, it is perhaps unsurprising that much of the discourse around removing tobacco from prisons has focused on the risk of unrest, at the expense of discussion of potential public health gains. 24
Relatively little research has been published on the process or outcomes of prison smoking ‘bans’. The best evidence available in 2015/16, following New Zealand’s experience of implementing a comprehensive ban,25,26 suggested that at least 1 year is needed to prepare for a smoke-free policy in prisons. Measures of SHS in 32 residential locations in the first four prisons in England to go smoke-free in 2016 showed a reduction of SHS by around two-thirds 3 months after implementation. 27 An analysis of smoking bans in prisons in the US suggested that they can reduce the risk of death among PiC (particularly where more comprehensive indoor and outdoor bans are in place), reduce initiation of smoking in prison, improve health of staff and reduce costs. 28 However, research in Australia suggests very high levels of relapse to smoking after release from smoke-free prisons. 29,30
The introduction of smoke-free prisons therefore has the potential to protect and improve the health of prison staff and PiC,12 but many questions remain about the process and outcomes of introducing a smoke-free policy in prisons. If PiC can be supported to become lifelong non-smokers, these benefits may extend into the community after their release, potentially magnifying their impact on reducing health inequalities and on families of those who are, or have been, in custody in smoke-free prisons. However, there could be risks to the safety and well-being of staff and PiC (as well as potentially costly risks of damage to the fabric of prison buildings and facilities) if prison smoking ‘bans’ do not attract sufficient acceptance from staff and PiC to be enforceable, or if increased tobacco control measures threaten safety and security at the institutional or individual level.
Research objectives
Overall aims
-
To evaluate the process of implementing a smoke-free policy in Scottish prisons to (1) strengthen the evidence base on what is likely to facilitate successful implementation of smoke-free prison policies for other jurisdictions, and (2) inform planning and communication strategies in Scotland and elsewhere.
-
To evaluate the impact of implementing a smoke-free policy in Scottish prisons on (1) changes in smoking status and exposure to SHS, (2) changes in related health indicators among PiC and staff and (3) organisational/cultural impacts.
Objectives
-
To understand barriers to and facilitators of the implementation of smoke-free policies in prisons through a scoping of evidence and experiences internationally within other jurisdictions [work package (WP) 1 (WP1)].
-
To evaluate changes in smoking and exposures to SHS following the implementation of a smoke-free policy in Scotland’s prisons, associated health-related indicators and costs, and other intended and unintended consequences (WP2).
-
To understand staff attitudes to and experiences of smoking-related issues in the prison context, including access to/restriction on tobacco and tobacco-related products (including e-cigarettes) in the prison environment, if/how these vary between prisons and how these changed leading up to and following the implementation of the smoke-free policy (WP3).
-
To understand PiC’s attitudes and experiences of smoking-related issues in the prison context, including access to/restrictions on tobacco/tobacco-related products (including e-cigarettes) in the prison environment, if/how these vary between prisons and how these changed leading up to and following the implementation of the smoke-free policy (WP4).
-
To evaluate the provision and impact of smoking cessation services across Scottish prisons; experiences of providers, users and potential users of these services in the lead-up to implementation of smoke-free prisons; and efforts to harmonise smoking cessation services from 2016 (WP5).
-
To share emerging findings in a timely and ongoing way so that they can inform the development of services, strategies and decision-making in the health and prison services about how best to implement the smoke-free policy, taking account of the views and experiences of PiC and prison staff (WP6).
Patient and public involvement
From the earliest design stages and throughout the conduct of the study, the TIPs study was designed to ensure that the voices of PiC and prison staff were heard and fed back in anonymised form to those within the SPS and NHS overseeing the processes and procedures involved in considering, preparing for and implementing the smoke-free prison policy in Scotland.
We participated in nine SPS Tobacco Strategy Group meetings in 2015 and in further discussions with policy-makers within the Scottish Government, the SPS, NHS Health Scotland and staff trade unions. A research advisory group (RAG) was constituted by the SPS in 2016 (membership included the head of SPS Health and Wellbeing and representatives of staff health and safety, trade unions and people leading tobacco control in NHS Health Scotland and the Scottish Government). RAG members gave extensive feedback on all aspects of the design, including study materials and approaches, and commented on all early findings from phase 1 through face-to-face meetings at SPS headquarters (Edinburgh, UK). Chapter 9 describes our partnership working from phase 2 onwards in more detail.
Prior to starting any fieldwork, Kate Hunt (or, on occasion, HS) visited every prison with Sarah Corbett (SPS Health and Wellbeing team and, from 2016, Smoke Free Prisons Project Policy Manager) or Ruth Parker (then SPS Head, Health and Wellbeing team). During these visits, we met the Governor-in-Charge or their appointed deputy and any members of staff with whom they wanted us to discuss the proposed research design and procedures. Opportunities to meet with those residing in prisons prior to commencement of the study were limited, but allowing them a voice as PiC or as users of smoking cessation services in prisons was fundamental to all phases of the study.
Chapter 2 Methodology
Project overview
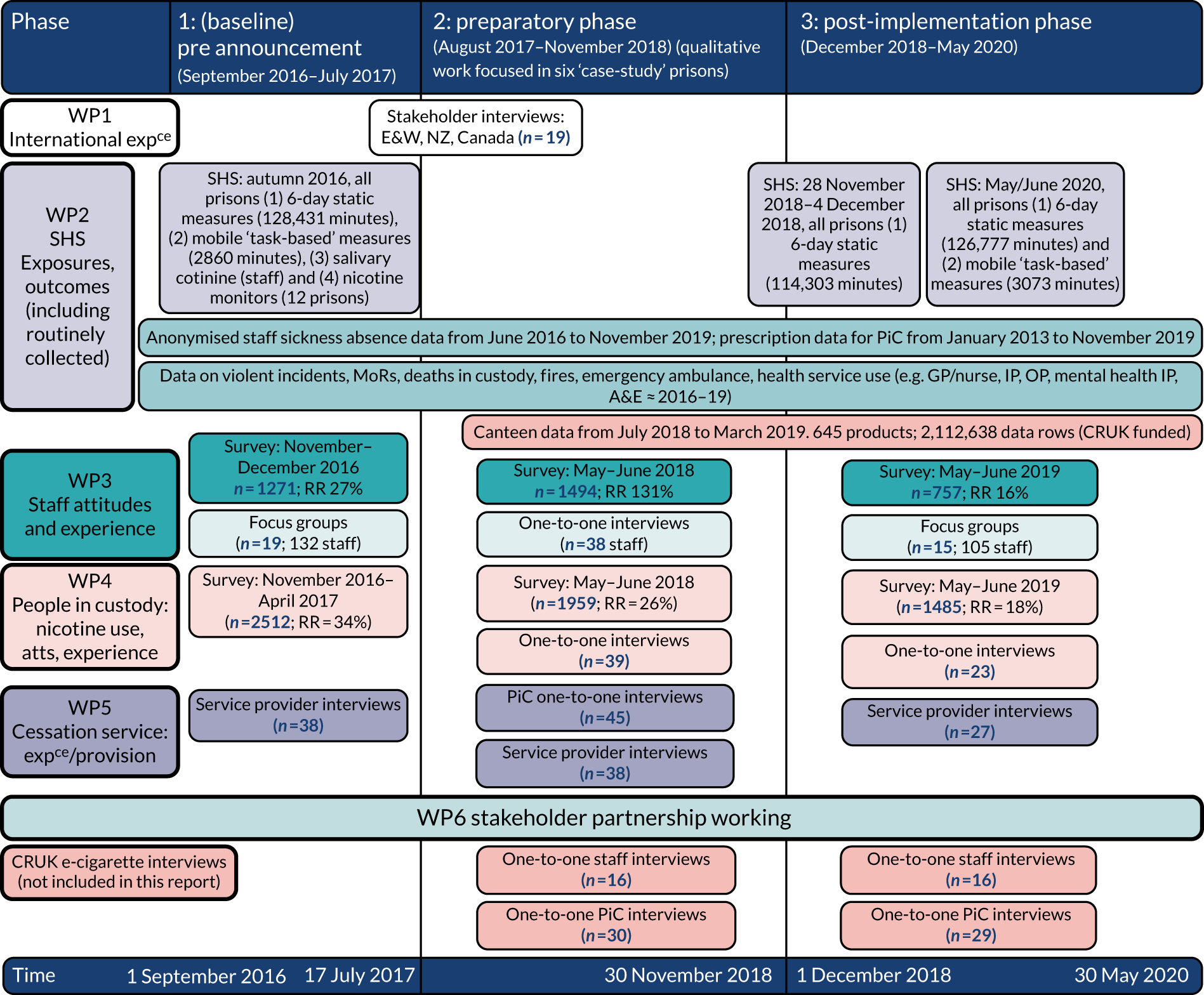
The TIPs study was a three-phase, multimethods study using a natural experimental methodology to assess the development and impact of the implementation of the smoke-free prison policy across Scotland’s prison estate on 30 November 2018. As indicated in Chapter 1, Context, the SPS announced in July 2017 that its prisons would become smoke free from November 2018, informed by the measurement of SHS exposures conducted as part of phase 1 of TIPs;11 the study protocol (V2.5)12 describes the revised timeline. Figure 1 depicts the study’s six integrated WPs, conducted across three phases;12 in summarising information about sample sizes and timings of different elements of TIPs, it gives an indication of the breadth and depth of the data collected and analysed. It also notes additional primary data collected for a complementary study, funded by Cancer Research UK (CRUK; London, UK), of the introduction of rechargeable e-cigarettes (hereafter ‘e-cigarettes’, unless otherwise stated) for information; these data do not contribute to this report. As detailed below, most of the research involved the collection and analysis of data relating to all 15 of Scotland’s prisons; some more detailed data collection was conducted in six of the (closed) prisons. We refer to these as ‘case study’ prisons in this report and they were selected in consultation with the SPS to represent a range of prisons and of PiC. However, although they were the sites for our more intensive qualitative research, they are not traditional case studies (e.g. we did not conduct observation research within these prisons). Furthermore, to respect assurances about anonymity and confidentiality given to participating prisons, staff and PiC, we do not provide extensive detail about the sites or local policies.
FIGURE 1.
Overview of the TIPs study methods and data by study phase. A&E, accident and emergency; atts, attitudes; E&W, England and Wales; expce, experience; GP, general practitioner; IP, inpatient; MoR, management of offenders at risk owing to any substance; NZ, New Zealand; OP, outpatient; RR, return rate.
All aspects of the study obtained ethics approval from both the SPS Research Access and Ethics Committee and from the University of Glasgow College of Social Sciences Ethics Committee.
Interviews with representatives of other jurisdictions (work package 1)
To understand the barriers to and facilitators of the implementation of smoke-free prison policies within other jurisdictions, we conducted telephone interviews with personnel (including health staff) in prisons that had introduced smoking bans to elicit views and advice on key challenges, successes and pitfalls. Originally, we aimed to include personnel from New Zealand, the Isle of Man, Canada, the USA and Australia. 12 However, consultation with SPS staff and focus group data from phase 1 of TIPs [see Focus groups and interviews with prison staff (work package 3) and people in custody (work package 4)] indicated their greater interest in recent experience in prisons that had become smoke free in England and Wales (E&W) from 2016 onwards. Hence, we weighted sampling to include more prisons in E&W than elsewhere. Additional ethics permission for interviews in E&W was obtained from the HM Prison and Probation Service National Research Committee (REF 2017–140).
In-depth interviews were conducted with 19 people (17 one-to-one interviews and one paired interview, at the request of the participants) (see Appendix 1 for topic guide). In-depth interviews were selected as the most appropriate method, balancing pragmatic considerations in conducting the interviews in recognition of both distance and pressures on participants’ time and the utility of in-depth interviews in allowing people to discuss their views and experiences in confidence. The sample included 13 participants in prison-based roles and six non-operational staff. Almost all had been directly involved in the implementation of a smoke-free prison policy at a national, regional or local level. Participants were encouraged to speak freely and raise any relevant issues. After obtaining informed consent, interviews lasting 28–58 minutes (mean 43 minutes) were audio-recorded with participants’ permission. All data were transcribed by an external transcribing agency which, as for all transcription for the TIPs study, had signed a confidentiality agreement. To preserve participants’ anonymity, data were de-identified prior to analysis. Analysis followed the principles described in Approach to qualitative analysis for focus groups and interviews with staff, people in custody and representatives from other jurisdictions and Appendix 2.
Measuring exposures to second-hand smoke (work package 2)
When the TIPs study was originally funded, we had planned to be the first study internationally to undertake comprehensive measures of SHS across a whole national prison estate prior to any decision about when and how to change prison smoking rules, and after implementation of any changes, measuring markers of SHS in all Scotland’s prisons in phases 1 and 3. 10 As described in the updated TIPs protocol,12 we extended these plans to include additional measurements in the week of implementation. Here we describe the methods used at each time point, that is 2016 (pre announcement), November/December 2018 (in the week that the ban was introduced) and May 2019 (6 months post implementation).
Over the course of the TIPs study, we used four methods of assessment: fixed-site monitoring of airborne concentrations of fine particular matter (PM2.5; particulate matter ≤ 2.5 μm in diameter), mobile-task monitoring of PM2.5; fixed-site air nicotine concentrations and cross-shift changes in cotinine concentrations in saliva of non-smoking staff. Data on outdoor ambient air PM2.5 concentrations were also obtained to provide reference levels. These measures are described below, in TIPs publications11,31,32 and a report provided to the SPS in July 2017. 33
Staff training and engagement
In preparation for the phase 1 assessments of air quality, representatives from Scotland’s 15 prisons were invited to a half-day training session (29 September 2016) at the SPS College. This provided the opportunity to train attendees as ‘citizen scientists’ through an overview of the TIPS study, training in the air quality measurement and the specific measuring devices used in the study (see Fixed-site monitoring and Alternative Scottish Prison Service exposure measures – fixed-site nicotine concentrations and cotinine concentrations in saliva of non-smoking staff), and the rationale for taking saliva samples from non-smoking staff in phase 1. A half-day training session was also provided for prison staff on 8 November 2018 in preparation for air quality measurements in the week of policy implementation and in phase 3. On completion of these sessions, at least one designated trained staff member from each prison took responsibility for a box containing the instrumentation and associated forms.
Fixed-site monitoring
Following earlier validation studies,34 Dylos DC1700 air quality monitors (Dylos Corporation, Riverside, CA, USA) were used to measure concentrations of PM2.5 to estimate SHS levels via fixed-site and mobile-task monitoring methods. These devices measure particle concentrations every second and log an average measurement result for each minute of use. Details of the method of converting particle number concentration to PM2.5 mass concentration, together with calibration of the Dylos monitors against AM510 SidePak Personal Aerosol Monitors (TSI Incorporated, Shoreview, MN, USA) are provided elsewhere. 31 Fixed-site monitoring over a 6-day period was undertaken within the same location, in one residential hall, at the three time points, overseen by the trained designated staff member(s), in each prison: in phase 1 (during 1 week in the period 30 September–22 November 2016),11,33 in the week of implementation (09.00 on 28 November 2018 to 09.00 on 4 December 2018),32 and in phase 3, 6 months after the smoke-free policy was implemented (09.00 on 22 May 2019 to 09.00 on 28 May 2019). 31 During phase-1 training, the designated prison staff had discussed their choice of location for the 6-day fixed-site continuous monitoring in a residential area within their prison with members of the TIPs study WP2 team. On occasion, the TIPs study researchers (KH, HS, ED) also went to the prison site to discuss the exact location of the instruments in more detail with the designated prison staff. The location needed to be secure (e.g. at the staff desk) to prevent accidental or malicious interference, within reach of an electrical plug and within the atrium/landing of one residential hall. The designated prison staff were responsible for ensuring that the location and daily equipment checks were recorded on the forms provided, together with relevant contextual information.
After each 6-day period, the designated prison staff securely packed the device and forms, and returned them either directly to a research team member for immediate download or by secure courier. Data were downloaded using Dylos Logger software (v3.1.0.0) (Dylos Corporation), and typical daily PM2.5 exposure profiles were constructed for each prison, as described in detail elsewhere. 11,31–33
Mobile-task monitoring
Mobile-task monitoring was undertaken in phases 1 and 3 only; it was not feasible to conduct these measures in the week of implementation because of operational considerations. After the 6-day fixed-site monitoring data were downloaded, the Dylos DC1700 monitors were returned to the designated staff. In 2016, staff were asked to choose four to eight tasks to assess SHS concentrations in various locations (e.g. gyms, workshops) and during specific activities (e.g. cell searches, maintenance, meal service), based on their knowledge and perceptions of areas with potential SHS exposures;11 in 2019, they were asked to include the same monitoring locations/activities assessed in 2016. 31 The monitoring period for each ‘task-based’ measurement lasted ≈ 30 minutes, and staff recorded time, location and associated activity for each measurement. Data from the mobile-task monitoring were downloaded after the instruments had been returned to research staff in person or by secure courier. Time-weighted average exposure concentrations were estimated for the typical shift patterns of residential staff pre and post smoke-free policy implementation (see Demou et al. 31 for full details).
Alternative second-hand smoke exposure measures: fixed-site nicotine concentrations and cotinine concentrations in saliva of non-smoking staff
In phase 1 only, estimates of SHS exposure calculated using the Dylos DC1700 monitors were compared with (1) measures of nicotine concentration from a sodium bisulfate-treated filter in passive diffuse monitors (‘nicotine monitors’) placed next to each Dylos monitor during the fixed-site 6-day measurements; and (2) salivary cotinine measures (a biomarker of recent SHS exposure) obtained from samples collected during fieldwork across all 15 prisons, between 7 November 2016 and 16 January 2017, to enable an estimation of the amount of nicotine inhaled over a work shift. As the main measure of change in SHS exposures over time in this report (see Chapter 4), and in the models reported in Chapter 8, are derived from the fixed- and mobile-task Dylos measurements, here the methods and findings of the nicotine monitor and salivary cotinine measures are summarised only. Full details are published elsewhere,11 but we note that measures from the nicotine monitors demonstrated a high association with the Dylos-derived estimate (R2 = 0.91). 11
For the salivary cotinine measures, non-smoking prison staff were invited to provide pre- and post-shift samples of saliva on entry to and exit from the secure area of the prison. Eligible staff were non-smokers not using any nicotine product (e.g. gums, patches, e-cigarettes) who neither lived with a smoker nor travelled to work in a vehicle in which anyone had smoked. Written consent was obtained from all volunteers (n = 422). Saliva samples were collected by TIPs research staff, who had been trained using similar methods developed for other occupational groups. 13 They recorded the exact time of sample collection pre and post shift so that exposure time over the shift could be calculated. The storage, shipping and analysis of samples are described elsewhere. 11 Our revised study protocol12 details the rationale for not repeating saliva measures in phase 3; the principal reasons were high correlations between measures of SHS exposures,11 the burden imposed by the measurement procedures on staff as they entered/left the prison and on the prison regime, and minimising costs to maximise value for money of funding.
Outside air pollution
Fine particulate matter is not specific to SHS and also occurs in outdoor and indoor air from traffic and industrial pollution sources. Most previous studies measuring PM2.5 in prisons have not accounted for concentrations of PM2.5 in outdoor air. To identify whether or not ambient/outside air pollution was likely to have contributed significantly to the PM2.5 concentrations measured in prisons, we acquired data from the nearest local authority PM2.5 static environmental measuring device. Hourly outdoor PM2.5 concentration data were downloaded from www.scottishairquality.scot (accessed 30 September 2021) for each monitoring period. 11,31,32 Data for the appropriate measurement periods from the outdoor monitor closest to each prison were used. 11,31,32 The median distance between each prison and the nearest PM2.5 measuring station was 16 km (range 3–133 km), with all but one within 50 km.
Statistical analysis: second-hand smoke data
Statistical analysis was conducted in Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA), R version 3.6.1 (The R Foundation for Statistical Computing, Vienna, Austria), and IBM SPSS Statistics v23 (IBM Corporation, Armonk, NY, USA). Analysis of objective measures of SHS followed previously published methods. 34 To test the significance of change between different measurement periods, mean PM2.5 concentrations were log-transformed and a paired t-test conducted across mean concentrations from all prisons for each comparison (see Demou et al. 31).
Our PM2.5 data provided time-resolved information on SHS concentrations over the course of each day, with lower levels at night-time and peaks evident during the day and evening periods. These unique data, gathered for 6-day periods from all prisons, enabled the reconstruction of exposures of residential staff during different shift patterns. 35–37 Using information on shifts provided by the SPS, time-weighted average shift exposures were estimated for a ‘typical’ residential officer in a Scottish prison, taking into account the average levels of exposure in an area and the time spent in each area. The four (overlapping) shifts were an ‘early shift’ (modelled as a 6-hour shift; staff on this shift have the responsibility of unlocking cells first thing in the morning), a ‘day shift’ (modelled as 8 hours), a ‘back shift’ (modelled as a 9-hour shift) and the ‘night shift’ (modelled as 10 hours).
Surveys of prison staff and people in custody (work packages 3 and 4)
Online surveys of prison staff and paper-based surveys of PiC were conducted in each phase. Participation was entirely voluntary for both groups and we offered no incentives to either group for completion. Methods of data collection are summarised below; further details are provided elsewhere. 38–40 As noted in our protocol, we consulted widely within the prison service on whether staff should be asked to enter their unique SPS employee identifier (ID), so that we could send reminders to those who had not returned a questionnaire and remove duplicate responses, with assurances that staff IDs would be immediately removed, or whether the survey should be completely anonymous. The most widely expressed view was that staff would not wish to divulge their staff ID or other potentially identifying information; hence, all staff questionnaires were entirely anonymous and could not be traced back to individual staff members. Union representatives of prison staff indicated that we should anticipate a high response rate from both smoking and non-smoking staff, at least in phase 1, given the concern expressed by some prison staff about exposure to SHS during the course of their work. Similarly, for PiC, we have no data that enable us to link responses to individuals. Hence, we are unable to link survey responses over the three different time points; for both groups they were repeat cross-sectional surveys.
Survey circulation/distribution
In each phase, an invitation with information on the TIPs study and a link to the staff survey were circulated to an appointed contact (‘staff contact’) in each prison, with a request to forward these to all prison (but not NHS/visiting) staff. The online survey was housed by information technology (IT) staff at the University of Glasgow, to ensure the highest standards of security. As the TIPs research team, SPS management and union representatives believed that it was very important that the research was clearly seen to be independent of SPS management, the questionnaire link was forwarded directly by the research team to the nominated staff contact in each prison for them to forward to all staff in their prison. 12 Staff were informed that the survey would take 10–15 minutes to complete. Staff surveys were open November–December 2016 (phase 1), May–July 2018 (phase 2) and May–July 2019 (phase 3). One reminder was sent (via the staff contacts) in phase 1, two in phase 2 and three in phase 3. The staff contacts were provided with current response rates when reminders were sent, and this information was sometimes included in the e-mail to staff.
Surveys with PiC were undertaken from November 2016 to April 2017 (phase 1), June to July 2018 (phase 2) and June to July 2019 (phase 3). We wanted to ensure that PiC were provided with information about the questionnaire to enable them to make an informed decision about whether or not they wished to take part. In our original planning,12 we thus wanted to offer the opportunity for PiC to discuss any questions they might have about the study directly with a member of the research team, before deciding whether or not to participate. We also wanted to ensure that people were able to complete their questionnaires without disturbance from other prisoners, given the role of smoking and tobacco products in prison life, including in relation to bullying and intimidation.
We discussed ways to maximise inclusion of any potential participants with literacy or other learning difficulties, including carefully considering the content, wording and layout of the questionnaire. When the SPS conducts its biannual prisoner survey, PiC with literacy/learning difficulties are offered help with questionnaire completion by other PiC. We wanted to avoid this for our surveys (to allow PiC to express their views without concerns about reprisals from any other PiC), and so planned for provision of impartial (research team) assistance if required. This involved offering to make trained fieldworkers available to any PiC who required help.
We anticipated that the administration of questionnaires to PiC would be completed over a short time period in each prison (≈ 1–3 days, depending on operational considerations and prison size), with sufficient fieldworkers available to support administration of the survey. We agreed to liaise closely with the prison governor/their appointed representative(s) about the best way to achieve our aims in respect of prisoner questionnaire administration in their prison (e.g. numbers of fieldworkers required), recognising that operational considerations would determine the preferred means of administration of the survey with PiC in each prison. 12 In our original planning for the phase 1 survey of PiC and our funding application, we anticipated that questionnaires would be distributed to a proportion of PiC by TIPs fieldwork/research staff (who would be available to help with confidential completion), aiming for returns from around 20% of PiC.
In phase 1, in two prisons, TIPs staff were escorted around residential areas and distributed questionnaires to all PiC who said they were willing to complete one, answered queries and helped with completion if necessary. In a third prison, TIPs staff were asked to distribute the questionnaires during an evening meal. 12 However, in the remaining 12 prisons, the staff contacts expressed a strong preference for us to use similar methods to those used in the SPS’s own biennial Prisoner Survey,2,8,41 because the escorting of several research staff in prison residential facilities can prove very onerous to the prison regime. Sufficient questionnaires were therefore supplied to each prison so that prison staff could distribute one to every PiC. To allow PiC the opportunity to complete their questionnaire in private, questionnaires were generally distributed immediately prior to an overnight lock-up. To reassure PiC that no-one in the prison (staff or other PiC) would be able to see their responses, PiC were asked to return the completed questionnaire in a sealed envelope (provided with the questionnaire). Although the method that we were required to use for most prisons in phase 1 (and all prisons subsequently) inhibited confidential support in questionnaire completion for those with literacy or learning difficulties, return rates from the three prisons where TIPs staff distributed questionnaires were below the overall 34% return rate. Because prison staff distribution was preferred by prisons and resulted in higher return rates, this method was used in all prisons in phases 2 and 3.
Survey content
The surveys were designed to take approximately 10–15 minutes to complete (although time to complete was longer for some PiC) and to cover relevant predictors, effect modifiers and mediators, and outcomes. Wherever possible, the questionnaires included identical items for the two participant groups (staff/PiC) and across all phases to maximise opportunities for comparison and to use validated/existing measures. Report Supplementary Materials 1 and 2 detail the survey questions and basic frequencies for surveys for all phases and both groups. Items were based on previous surveys of health;42–44 smoking;42,45–47 experiences of PiC;41 and smoking bans in public places, prisons or secure hospitals,19,43,48–51 and comprised the following:
-
basic sociodemographic items (sex, age, education; for staff – work role, band, number of prison-based working hours per week, number of years worked in prisons in total and in their current prison; and for PiC – whether convicted or on remand, with length of sentence and time until release if convicted, and length of time in current prison)
-
current smoking, smoking history, e-cigarette use and vaping history, past year smoking cessation attempts and support
-
health, including general health, sickness absence (staff), medication use and asthma diagnosis; International Union Against Tuberculosis and Lung Disease self-reported past month respiratory (wheezing/whistling, shortness of breath, morning cough, other cough, phlegm) and sensory symptoms (red/irritated eyes, runny nose/sneezing, sore/scratchy throat);52 and a standardised measure of health status,53 for which we received permission to amend the ‘usual activity’ examples for the survey of PiC
-
estimated exposure to SHS and e-cigarette vapour within the prison
-
opinions on smoking among PiC, prison smoking bans (adapted from surveys of US prison staff19 and Scottish bar workers’ attitudes to smoke-free places51), e-cigarettes and, in phase 3, the introduction of the Scottish prison smoking ban.
Survey feedback to prisons and participants
In addition to feeding back results to the study’s SPS RAG and at regular meetings of the SPS stakeholder advisory group (SAG) for the implementation of smoke-free prisons, phase 1 and phase 2 survey results (basic frequency distributions) were formatted into easy-to-read documents that were posted on the SPS SharePoint (SPS intranet system, accessible to all staff) and e-mailed to the staff contacts in each prison (phase 1 reports were tailored to include overall and each prison’s individual results). Phase 1 main results were also compiled into summary infographics that were distributed as hard copies (and so were available to PiC) and electronically.
Focus groups and interviews with prison staff (work package 3) and people in custody (work package 4)
Recruitment and data collection
Staff
To investigate the opinions and experiences of staff in more depth, we aimed to conduct focus groups with staff in all 15 Scottish prisons in phases 1 and 3, and interviews with staff in six ‘case-study’ prisons in phase 2 (see Figure 1).
Focus groups in phases 1 and 3 were chosen to ensure a wide range of staff across the prison service (i.e. in every prison) to express their views on smoking in prisons, smoking regulations and management of nicotine addiction (including e-cigarettes) and smoking bans,54 with minimal disruption to the prison regime. Focus groups can also be used to explore areas of agreement and disagreement within the group. Furthermore, prison staff were judged to be able to respect the confidentiality of views expressed by their colleagues in the context of the focus group.
A point of contact within each prison was asked to arrange a group in their prison, ideally inviting up to eight staff, including smokers and non-smokers and staff in residential and other roles. In phase 1, a total of 132 staff from 14 prisons took part in 17 focus groups (range of participants 5–12) and two paired interviews (conducted from November 2016 to April 2017) (see also Brown et al. 54,55).
In phase 2, our strategy was to elicit more detailed data from the six ‘case study’ prisons, rather than collecting some data from all prisons. This made it practical to conduct one-to-one interviews with staff and 38 staff (32 men and 6 women) across the six prisons were interviewed [range 10–62 minutes (mean 36 minutes)]. Again, the point of contact within the prison was asked to approach a mixture of smoking and non-smoking staff in a range of roles who might be interested. Most (n = 24) were non-smokers and often worked in residential areas within the prison (n = 18) (data on smoking status and/or work role were missing for five participants).
In our original protocol10 we did not plan to include further qualitative work with prison staff in phase 3. However, when the protocol was amended following the announcement of a specific timetable for the implementation of smoke-free prisons,12 we sought permission from NIHR to include focus groups in phase 3 to explore in depth the views of staff on the success (or otherwise) of the (process of) implementation (see also Brown et al. 56). These groups included a total of 105 staff from across all prisons, in 15 focus groups (range of participants 3–14), conducted from May to August 2019. Four SPS staff members who had taken a leading role in the implementation of the smoke-free policy at the local (prison) level were also interviewed to capture their perspectives on the transition. Most of the staff participating were male (n = 83), prison officers (n = 71) and never- or ex-smokers (n = 91); around one-quarter (n = 28) reported ever using e-cigarettes.
Topic guides for the focus groups (summary versions provided in Appendix 1, together with those for one-to-one staff interviews) covered such issues as participant background, opinions of smoke-free policy, perspectives on working in a smoke-free prison (including successes/challenges and positive/negative consequences), compliance and enforcement of the smoking ban, and lessons learned.
People in custody
Interviews with PiC were conducted in phases 2 and 3 in the six ‘case-study’ prisons (see also Brown et al. 56), selected in consultation with the SPS to represent a range in terms of size and population as noted earlier (see Project overview). Data collection took place between October 2017 and February 2018 in phase 2, and between May and August 2019 in phase 3, 6–8 months after implementation. Abbreviated topic guides are provided in Appendix 1. The point of contact in each prison was asked to approach participants [aiming to interest a range of people with respect to their smoking (vaping in phase 3) status, length of sentence, and (if appropriate for their prison) gender] (Table 1). We chose to conduct one-to-one interviews with PiC, rather than focus groups, to ensure that each person could express their views in confidence, without fear of reprisals for voicing opinions that they perceived not to be shared or popular with other people in the group, or within the prison community more broadly, and concerns that other people in a group context may not fully respect the need for confidentiality after a group had concluded. Designated points of contact (nominated staff who liaised with the research team in each of these prisons) provided information to potential participants; these staff contacts were well briefed in our aim to recruit people with a wide range of views, whether supportive of or opposed to the smoke-free prison policy, and to include smokers, ex-smokers and non-smokers.
| Characteristic | Phase 2 (n) | Phase 3 (n) |
|---|---|---|
| Sex (n) | ||
| Male | 32 | 18 |
| Female | 6 | 5 |
| Remanded/convicted status (n) | ||
| Convicted | 35 | 23 |
| Remanded | 3 | 0 |
| Sentence length (n) | ||
| Short term | 15 | 13 |
| Long term | 20 | 10 |
| Smoking status (n) | ||
| Smoker | 26 | – |
| Ex-smoker | 7 | – |
| Never smoker | 5 | – |
| Vaping status (n) | ||
| Vaper | – | 17 |
| Ex-vaper | – | 6 |
| Never vaper | – | 0 |
| Interview length (minutes) | ||
| Minimum | 21 | 22 |
| Maximum | 59 | 68 |
| Average | 33 | 38 |
Topic guides for the phase 3 interviews with 23 PiC in the six ‘case study’ prisons largely covered similar topics to those covered in the phase 3 focus groups with staff (see Appendix 1): participant background, opinions of the smoke-free prison policy, perspectives on living/working in a smoke-free prison (including successes/challenges and positive/negative consequences), compliance and enforcement of smoke-free prison policy, and lessons learnt.
Approach to qualitative analysis for focus group and interviews with staff, people in custody and representatives from other jurisdictions
All focus groups and interviews were audio-recorded, with permission from all participants involved, and transcribed by an external transcribing service that had signed a confidentiality agreement. To preserve participants’ anonymity, data were de-identified prior to analysis.
De-identified transcripts were thematically analysed, supported by the framework approach, following a process described in Appendix 2 and in publications based on the qualitative data. 38,54,55 In brief, data were organised under themes and summarised and displayed in a grid format (row = focus group/interview; column = theme) in NVivo 12 (QSR International, Warrington, UK). For pragmatic reasons, for two of the data sets, transcripts were summarised against themes in Microsoft Word (Microsoft Corporation, Redmond, WA, USA) [WP1 interviews with representatives from other jurisdictions and WP3 (phase 2) interviews with prison staff]. Detailed thematic analysis entailed comprehensively and systematically searching framework grids and reviewing data excerpts to identify and compare perspectives and experiences. Using an iterative process, different dimensions of the data were organised into themes and subthemes. Extracts from interviews have been selected to evidence and illustrate key findings. In the staff and PiC interviews/focus groups, quotations are attributed to participants (staff/PiC) using a serial number (a letter randomly allocated to each prison specifically for this report and a participant number) and an indication of smoking/vaping status [smoker (S), ex-smoker (ExS), never-smoker (NS), vaper (V), ex-vaper (ExV) and never-vaper (NV)].
Interviews with users and providers of smoking cessation support in prison (work package 5)
Interviews with health-care and prison staff providing smoking cessation support
Qualitative interviews were conducted with staff responsible for managing and delivering cessation support across Scotland’s prison estate. Participants were from three main areas: topic specialists working in health board Stop Smoking Services (SSSs), practitioners working in prison health-care and addiction services who were trained to provide cessation support, and SPS officers who had volunteered or been nominated by prison management to support cessation delivery in the lead-up to implementation (see Appendix 3, Table 27). To maximise efficiency, and particularly to reduce burden on participants, the majority of interviews were conducted as one-to-one interviews either face-to-face or by telephone using a semistructured topic guide (see Appendix 1) at participants’ convenience. Interviews lasted 40–60 minutes and were audio-recorded with participants’ consent, fully transcribed and analysed using NVivo software to aid data management.
Phase 1 fieldwork was conducted from February to June 2017, phase 2 from May to August 2018, and phase 3 from May to September 2019. Interviews in phases 1 and 3 were conducted with participants from across the entire Scottish prison estate and the health board cessation services where the prisons were located. Interviews in phase 2 were conducted with participants from the six ‘case study’ prisons and the local health board cessation services supporting these prisons. To preserve anonymity, quotations are attributed to speakers using designation and study phase.
Interviews with about smoking cessation support
During phase 2, one-to-one qualitative interviews were conducted face-to-face with 45 PiC in five of the six ‘case study’ prisons in May and June 2018 using a semistructured topic guide (see Appendix 1). Participants all had recent experiences of using local prison cessation support and were at various stages in their journey to becoming smoke free (see Appendix 3, Table 28). They included PiC who were currently attending a 12-week cessation programme, had relapsed and had successfully completed the programme. All interviews (duration 30–60 minutes) were conducted face-to-face and audio-recorded, with participants’ consent, then fully transcribed, anonymised and analysed using NVivo software to aid data management. Analysis followed similar principles to those outlined above.
Analyses of routine data (work package 2)
Medications
Analyses of medications prescribed for PiC were designed to investigate any associations between the smoke-free prison policy and the dispensing of medications for smoking cessation, nicotine replacement and specific smoking-related health conditions, and potential unintended consequences among people in prisons in Scotland. Data (number of items dispensed in prison) were provided by National Procurement, NHS National Services Scotland (NSS) from January 2014 (3.5 years prior to the announcement of the smoke-free policy in July 2017) to the end of November 2019 (1 year post implementation). The data series’ were analysed using autoregressive integrated moving average (ARIMA) time series methods, incorporating two prespecified breakpoints (date of announcement to 17 July 2017, and date of implementation to 30 November 2018). Two analytical approaches were tested for the presence of structural breaks and outliers using (1) a Wald test applied to the white noise residuals of the seasonal autoregressive integrated moving average (SARIMA) errors model, and (2) an indicator saturation applied to the white noise residuals of the SARIMA errors model. In each approach, the estimated breakpoints were then incorporated into the final intervention model ensuring efficient effect estimates and standard errors. Measures of overcrowding were included in all models as potential confounding factors. Interpretation was informed by the TIPs qualitative workstreams. The primary analysis included the 14 closed prisons only, as the nature, implementation and effectiveness of the smoke-free policy is likely to differ substantially in open versus closed establishments. Secondary analyses included all Scottish prisons. Analyses were delayed by reallocation of staff who were leading the analyses to service public health roles during the COVID-19 outbreak and are reported in detail in a paper published57 after the reporting period for this grant; see Acknowledgements, Publications.
Staff sickness absence
Analyses of staff sickness absence data were designed to explore any changes in staff sickness absence rates before and after the introduction of the smoke-free policy across the SPS. Weekly days lost were provided in anonymised form by the SPS for the 13 publicly managed prisons. Data were requested from June 2016 (1 year prior to the announcement of the smoke-free policy) to the end of November 2019 (1 year post implementation). The data series were analysed using the Box–Jenkins ARIMA time series methodology. For the SPS sickness absence time series, we adopted an input series to allow the change in policy on smoking (intervention) to be modelled. Specifically, the intervention was modelled as a 0 up to 30 November 2018 (date of prisons going smoke free) and then coded as a 1 after that date. The announcement of the date for a change of the smoking policy in Scottish prisons (July 2017) was also taken into account in the model, as this involved designing and implementing the changes necessary for the smoke-free policy to come into effect and, although there was no intervention per se at this point (i.e. policy change), other changes may have occurred (e.g. raised awareness of SHS levels leading to decreased smoking among PiC outwith permitted areas, information on SHS levels affecting strictness in enforcing current rules). We used a dummy variable to account for the announcement (value of 0 from June 2016 to July 2017, value of 1 from July 2017 to November 2018, and value of 0 from November 2018 onwards). As all prisons implemented smoke-free rules on the same date and the policy was the same across Scotland, there was no ‘control/comparator’ population. However, we examined differences by sickness absence causes (self-reported in the data), by job (operational vs. non-operational) and across ‘baseline SHS exposure prison types’. Other sensitivity analyses (SAs) (e.g. placebo intervention dates) were explored. Final analyses were delayed (because the COVID-19 outbreak led to a delay in obtaining all data from the SPS) and will be reported separately.
Health economic evaluation (work package 2)
Overview and overall aims
The aim of the health economic evaluation was to estimate the change in health-related costs and outcomes following the implementation of Scotland’s smoke-free prison policy. The cost-effectiveness of the policy was evaluated over two time periods: first, within the time period of the study (within-study analysis) and, second, over a lifetime (long-term analysis), for both operational staff and PiC, from the perspective of the NHS and including nicotine-related products. The within-study and long-term analyses are reported in line with current best practice. 58 Further detail is provided in Report Supplementary Material 3.
Within-study analysis
Cohort and time frame
The time period of the within-study analysis was 1 June 2016 (1 year prior to policy announcement) to 30 November 2019 (1 year after implementation). Costs and outcomes are compared over the three phases of the TIPs study (‘pre announcement’, ‘preparatory’ and ‘post implementation’; see Figure 1).
Data from Scotland’s 14 closed prisons were included in all analyses. Data from PiC in Scotland’s only open prison were excluded from base-case analyses where possible, as the PiC spend some time in the wider community (e.g. at work, with family) and have access to tobacco while away from the prison, but were included in SAs. Report Supplementary Material 3, Table 4, illustrates, for each category of cost and outcome, whether or not open prison data could be identified and excluded. Staff at the open prison were included in all analyses for prison staff.
Non-operational staff were excluded from the analyses given that they are less likely to be exposed to SHS at work and so less likely to be affected by the smoke-free policy.
Data measurement and valuation
Resource use included two categories: health service use (staff and PiC), and tobacco and e-cigarettes spend (staff and PiC). Resource use data were obtained from several sources: TIPs staff and PiC surveys (Surveys of staff and people in custody); summary data on spend by PiC in the prison shop (‘canteen’), sourced from the SPS for an allied complementary study funded by Cancer Research UK (see Figure 1) (Cath Best, University of Stirling, 2021, personal communication); and NHS NSS data. Different resource categories were available for different time periods, collected at different frequencies and in different formats; details of resource use data are provided in full in Report Supplementary Material 3, Table 1. In brief, health service resource use categories comprised general practitioner (GP) and nurse visits for staff and PiC, and for PiC only; outpatient attendances; inpatient and mental health stays; accident and emergency (A&E) visits; ambulance incidents; and summary measures of medication dispensing. Nicotine product resources comprised tobacco for staff and PiC, and e-cigarettes for PiC only.
Unit costs: valuing resource use
Unit costs were for the year 2017/18 in Great British pounds (GBPs) and are presented in Report Supplementary Material 3, Table 2.
The GP and nurse costs were taken from the Unit Costs of Health and Social Care 2017 report published by the Personal Social Services Research Unit. 59 For PiC, the mean cost of a GP or nurse visit was calculated, as there was no way of ascertaining which visits were made by a GP and which were made by a nurse. Outpatient attendance, inpatient and mental health stays, ambulance incident and A&E attendance unit costs were taken from the Information Services Division Scotland cost book. 60
The cost of medications was included in the National Procurement data set as ‘gross value’. The average cost of a cigarette for staff was obtained from the Office for National Statistics. 61 PiC’s canteen spend was included in the SPS canteen data set (Best et al. , personal communication).
We applied unit costs to the relevant resource use to calculate total costs for each resource use.
Outcomes
Several health and organisational outcomes were included in the analyses, sourced from TIPs study data and the SPS. Outcomes comprised: SHS levels, health related quality-of-life, violence-related incidents, deaths in custody, fires and the management of offenders at risk owing to any substances (MoR).
Analysis
Base-case analysis
Three analyses were conducted for the within-study base-case analysis and are described in the following sections. For each of these analyses, where possible, data on PiC incarcerated in the open prison were excluded. To account for an increased number of PiC within the Scottish prison system, the effects of overcrowding were adjusted for using a ratio of prison population to contracted available places; this was feasible in the cost–consequences interrupted time series analysis only.
The cost–consequences analysis (CCA) analysis presented disaggregated costs and outcomes of interest to stakeholders in a balance sheet format, with no attempt to aggregate costs and outcomes into a single measure. 62 Disaggregated costs and outcomes were presented for all three phases of the within-study time period as a monthly mean per person per phase. The change in costs and outcomes between phases was estimated using two techniques, depending on the format of the data: (1) where data were available monthly at an aggregate level, interrupted time series methods were used to estimate the changes and predict the monthly means; and (2) where data were available at an individual level in each phase (but with no linkage between phases), a regression framework was used.
The cost-effectiveness analysis (CEA) analysis result is presented as an incremental cost per additional 10 µg/m3 change in SHS, comparing pre-announcement and post-implementation costs and SHS outcome (Measuring exposures to second-hand smoke and Chapter 4, Changes in indicators of second-hand smoke concentration between phases 1 and 3). We compared costs for 12-month periods in the pre-announcement (June 2016–May 2017) and post-implementation (December 2018–November 2019) phases of the smoke-free policy, and SHS measures from November 2016 (pre announcement) and May 2019 (post implementation). The change in costs and SHS were estimated using a simple decision tree model with two arms.
The cost–utility analysis (CUA) analysis result is presented as an incremental cost per quality-adjusted life-year (QALY), comparing pre-announcement and post-implementation costs and QALYs. QALYs were a combination of quality of life and length of life; the quality of life was the utility extracted from the staff and PiC surveys and the length of life was 1 year. Costs covered the same time period as in the CEA. The CUA result is presented as an incremental cost per QALY. The change in costs and SHS was estimated using a simple decision tree model with two arms.
Uncertainty
Uncertainty was explored in two SAs:
-
Sensitivity analysis 1 (SA1). The base-case analysis excluded PiC’s costs and outcomes for the open prison, where possible; a SA was conducted where these data were included. A summary of where it was possible to include and exclude the open prison for resource use and outcomes is presented in Report Supplementary Material 3, Table 4.
-
Sensitivity analysis 2 (SA2). In the base-case analysis, medications that were indicators of treatment for nicotine dependence and for smoking-related illnesses or associated symptoms were included only; a SA was conducted where all medications were included.
Long-term analysis
Overview
The aim of the long-term analysis was to conduct a CUA to estimate the incremental lifetime costs and QALYs for operational staff and PiC, with and without the smoke-free prison policy in place. Sources informing model parameters included literature, TIPs study outcomes, SPS reports and information, and expert opinion. Unit costs were for the year 2017/18 in GBP and the model perspective took a broader approach than NHS only, including personal spend on tobacco and e-cigarette products and NHS health-care costs. The outcome measure was the QALY. Costs and outcomes incurred beyond the first cycle were discounted at 3.5%, as recommended by NICE. 63,64 Cycle length was 1 year and the model was run for a total of 70 cycles.
The model populations were operational staff and PiC. Comparators were ‘with smoke-free policy’ and ‘without smoke-free policy’ and results were compared to estimate a lifetime incremental cost-effectiveness ratio (ICER) of mean cost per QALY. Uncertainty was measured using a probabilistic sensitivity analysis (PSA) to estimate confidence intervals around the ICER; the effect on the ICER of different scenarios was explored in SAs.
Model structure
A Markov model was used, in which a notional cohort of people travelled through model states accumulating costs, quality of life and life expectancy, depending on their smoking status and SHS exposure.
The model structure diagram is presented in Figure 2. Cohorts of staff and PiC entered the model at the start of their SPS employment (staff) or first incarceration (PiC), and both cohorts were closed, that is no additional staff or PiC were added during the time period of the model. The states in the model were not health states, but mainly related to smoking statuses, which were assigned different morbidity and mortality transitions; this is typical of other cost-effectiveness smoking cessation models. Four states were included: ‘tobacco smoker’, ‘quit/tobacco abstinent’, ‘non-tobacco smoker’ and ‘death’. A ‘tobacco smoker’ was defined as someone who smokes tobacco and did not include e-cigarette users. A person who had/was ‘quit/tobacco abstinent’ was someone who was a smoker on entry to the model and who had stopped smoking (voluntarily or otherwise) during their prison work/custodial sentence or after leaving the prison environment. A ‘non-tobacco smoker’ was someone who did not smoke tobacco prior to working/having a custodial sentence in prison and did not take up tobacco smoking while in prison or post prison.
FIGURE 2.
Long-term model diagram.
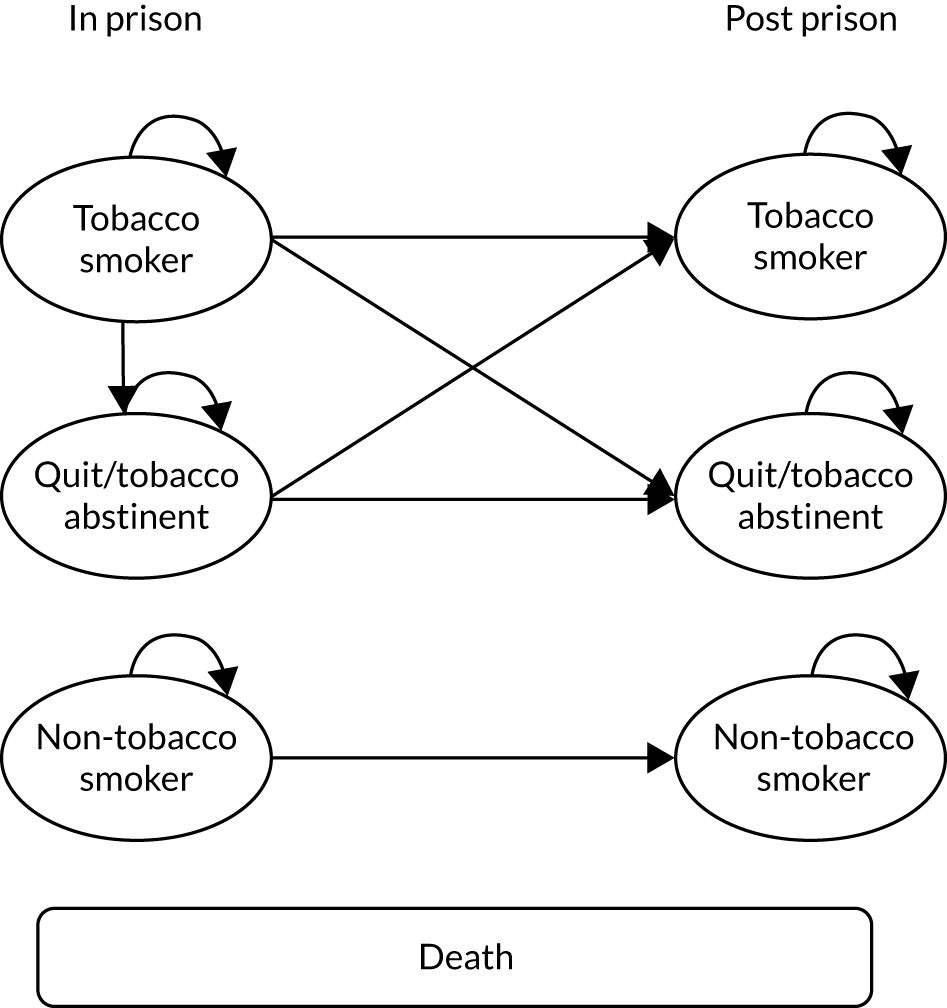
The structure was split into two time periods: ‘in prison’ and ‘post prison’. For staff, ‘in prison’ represented the time employed by the SPS and ‘post prison’ represented the time after working for the SPS (assumed to be retirement). For PiC, ‘in prison’ represented the time in custody and ‘post prison’ represented the time after release.
The cohorts entered the model in the ‘in-prison’ section as ‘tobacco smoker’, ‘quit/tobacco abstinent’ or ‘non-tobacco smoker’. After the implementation of the smoke-free policy, all ‘tobacco smokers’ in the PiC cohort immediately become ‘quit/tobacco abstinent’ on entering the ‘in-prison’ section of the model.
In the ‘post-prison’ section, ‘tobacco smokers’ from the ‘in-prison’ section remained ‘tobacco smokers’ (except PiC who were ‘quit/tobacco abstinent’ ‘in prison’ as a result of the smoke-free policy; 100% of these reverted to ‘tobacco smokers’ ‘post prison’). Those in the ‘quit/tobacco abstinent’ state in the ‘in-prison’ section could remain ‘quit/tobacco abstinent’ or resume tobacco smoking on entering the ‘post-prison’ section.
‘Non-tobacco smokers’ in the ‘in-prison’ period remained non-smokers in the ‘post-prison’ period. We assumed that ‘non-tobacco smokers’ ‘in prison’ were exposed to SHS in the ‘without smoke-free policy’ comparator and were not exposed to SHS ‘with smoke-free policy’.
Anyone in the model could transition to the ‘death’ state at any time and from any state.
Assumptions
Several structural assumptions were made for the Markov model:
-
A ‘non-tobacco smoker’ in the ‘post-prison’ period was not exposed to SHS because of the lack of evidence to support alternative assumptions.
-
People who did not smoke on entering the model (non-smokers reported in the SPS’s 16th Prisoner Survey 201741) were assumed to be never smokers, as there was no information on whether they were never or former smokers (recent or otherwise); they were thus assigned ‘never-smoker’ utilities mortality and morbidity.
-
‘Tobacco smokers’ immediately became ‘quit/tobacco abstinent’ on entry to the model in the ‘with smoke-free policy’ comparator, and were allocated former smoker utilities, risk of morbidity and mortality, in line with other economic smoking cessation models. 65
-
‘Non-tobacco smokers’ did not take up smoking in the model; this assumption was mitigated by applying the prevalence of PiC smoking in prisons41 to model seeding.
Model transitions and parameters
Full details of the model transitions and parameters are described in Report Supplementary Material 3; parameters are provided in Report Supplementary Material 3, Table 5.
In summary, model transitions comprised smoking status and prevalence; smoking status and sex-specific morbidity; and smoking status, age and sex-specific mortality. Model parameters comprised intervention costs; smoking-related, disease-related health-care costs; nicotine product costs; QALY outcome; age of the cohorts entering the model; length of time both cohorts spend in the ‘in-prison’ time period of the model and the total population numbers in each cohort.
Analysis
The Markov model was constructed in Microsoft Excel for Office 365 (Microsoft Corporation). Male and female staff and PiC were modelled using different parameters; the results were combined by applying a ratio of male to female. For the operational staff male/female split, 73% were male and 27% were female (based on the position on 31 March 2020); this information was provided by the SPS (Emma Christie, Scottish Prison Service, 2020, personal communication). For PiC, the male/female split reported in the Scottish Prison Service Prisoner Survey 201741 (95% male, 5% female) was used. Results were presented for mean costs and QALYs per staff and PiC, and an ICER was calculated for each cohort. The cost-effectiveness of these results was assessed using the £20,000 willingness-to-pay threshold. 64
Uncertainty
To reflect the uncertainty of input parameter estimates, we carried out a PSA using established methods66 to estimate the confidence intervals (CIs) around the difference in costs and QALYs and the ICER. Appropriate distributions were fitted to means as follows: relative risks characterised by log-normal distribution, costs characterised by gamma distribution, and utility values characterised by beta distribution. Random picks were taken from these distributions. Guidance67 on model convergence was followed and 1000 iterations were undertaken. Results were displayed as estimates on a cost-effectiveness plane.
Scenario analyses
Ten scenarios were explored to assess uncertainty in the model assumptions; full descriptions are available in Report Supplementary Material 3, Table 6. The scenarios explored included varying the levels of resuming tobacco smoking for PiC on release from prison, varying the length of sentence for PiC, using health utilities from the TIPs surveys for PiC, an alternative to PiC mortality-standardised mortality ratios, varying nicotine product spend for PiC, and using a different discount rate.
Overall impact of policy
The overall impact of implementing the smoke-free policy was assessed by estimating the prison population total costs and QALYs for all PiC and operational staff over a lifetime. The overall implementation cost to the SPS included in this analysis was the total amount that the SPS expected to spend on the vaping kits (£150,000). 68
Chapter 3 International landscape
Interviews with representatives from other jurisdictions
We analysed data from our interviews with staff representatives from three other jurisdictions that had already implemented smoke-free policies in prisons (New Zealand,25 parts of Australia69 and E&W) to identify factors that may aid implementation of a smoke-free prison policy elsewhere. Most of the representatives interviewed (15/19) were from E&W.
In 2011, New Zealand was the first of these jurisdictions to go smoke free in prisons, and its comprehensive approach to implementation appears to have guided other jurisdictions. The themes identified through analyses of our participant interviews in relation to implementation strategies were substantively similar across jurisdictions, although there were some notable variations in practice. One important difference was in relation to e-cigarettes. We note that New Zealand prisons (2011) and those in parts of Australia (2013) went smoke free before e-cigarettes became more widely available internationally; in contrast, e-cigarettes were made available in prisons in E&W when smoke-free policies were rolled out across the estate in 2016–18, and participants from these jurisdictions reflected on their place in implementing a smoke-free policy in prisons (see Smoking cessation support).
Managing policy implementation
Several dimensions of project management in relation to removing tobacco from prisons were discussed by participants. First, allowing good time – as far as possible – was regarded as helpful, as it gave prisons the opportunity to prepare for the implementation of smoke-free policies and for PiC (and staff) to adjust to changes and prepare to abstain or quit tobacco (‘You can’t start too early I don’t think,’ interview 11). There were some suggestions that it is helpful to set a ‘clear date’ for implementation to generate the impetus to drive forward preparatory work:
. . . we started to prep for going smoke-free [several years] before we actually did. Because we kept getting told it’s going to be introduced, it’s going to be introduced. But it never did. But rather than stand down our preparation . . . we just ran the meeting quarterly to keep it . . . everybody’s agenda . . . as soon as we had a clear date we just cranked things up.
WP1, interview 16
Second, participants articulated the importance of appropriate governance arrangements. This included an adequately resourced implementation team to guide and support prisons, and local implementation groups within prisons, involving local personnel with sufficient capacity and credibility/seniority, to take forward the smoke-free policy. Other examples that participants discussed related to the use of a ‘readiness assessment’ tool to drive and monitor progress (ensuring that associated documents were not too onerous to complete), and processes for foreseeing and responding promptly to potential risks associated with removing tobacco from prisons. Regular and open communication at all levels about progress, successes and challenges in preparing to go smoke free was described as important, as were opportunities for peer-to-peer support and sharing of good practice across the prison estate and from other jurisdictions that had implemented a smoke-free prison policy:
. . . rather than . . . [saying] ‘Right, governors! This is what you’ve got to do, crack on!’, we really did try to go in and support them . . . We would do our reports and we would have a look at their report that they’d submit each month and . . . we would go in and say, ‘Well, we were concerned about this’ or actually, ‘Yes, we’re really happy with your progress’ . . . It was . . . colleagues trying to help other colleagues . . .
WP1, interview 13
Third, participants highlighted that good partnership working, including with external partners, was likely to be beneficial, including prison and health services having shared responsibility for implementation, supporting one another in their respective roles and communicating regularly to monitor progress and identify issues. Support from all functions in prisons (a ‘whole-prison approach’) in preparing for smoke-free rules was also considered beneficial:
I think it can feel for the health providers that this is kind of their project and they’re on their own and it’s just about delivering smoking cessation with as many [PiC] as you can as quickly as you can, but that really isn’t actually the biggest issue. The biggest issue is the whole-prison approach to this and what everybody’s doing to chip in.
WP1, interview 6
Finally, our interview data highlighted the need for ongoing management of smoke-free policies post implementation to support continued success (e.g. strategies for effective management of nicotine dependence among new arrivals) and to support efforts to reduce any unintended adverse consequences of smoke-free policies (e.g. addressing contraband tobacco black markets and supporting PiC who find smoking abstinence challenging).
Communication and engagement
Participants also described how extensive communication and engagement with PiC, staff and other stakeholders about the forthcoming changes to smoking rules could aid successful implementation:
Communication was absolutely crucial and vital in everything that we did . . . we just made sure that it was always communicated where we were at with the project, what the next steps were.
WP1, interview 19
Ideas about ways to build awareness, support and acceptance for smoke-free prison policies included using multiple communication channels to publicise the policy (e.g. posters, leaflets, prison television screens, prisoner radio, announcements over a loudspeaker system, displays in the prison library, publicising smoke-free rules in the visitor centre); cascading information via peer mentors/PiC representatives to enhance message credibility and reduce misinformation and rumours; repeating communications over time to maintain visibility, dispel beliefs that smoke-free rules would not be implemented as intended and ensure that new arrivals were well informed of the impending changes:
It was about the continued promotion of [smoke-free policy]. . . . [C]hanging the posters every time, so that it doesn’t become another piece of paper stuck on the wall. They changed design, they’d change the patterns on it, just to make it more eye-catching, to raise the awareness. . . . Lots of leaflets . . . articles on the prison radio . . . we couldn’t over publicise it, we couldn’t overcommunicate it, there’s no such thing as overcommunication. We just had to keep communicating in different formats for it.
WP1, interview 7
Given that smoke-free rules can be met with negativity or concern from some PiC and staff, participants suggested that it was important to explain the rationale for the policy in positive terms and highlight benefits of eliminating active/passive smoking for the health of everyone working and living in prison, although acknowledging potential short-term problems that might arise:
It’s always key to get the majority of [PiC] to see that we’re doing this for the right reasons and for them not to buy in into any potential trouble . . . [many] influential prisoners would actually buy into this, because they are . . . into their fitness a lot of them.
WP1, interview 4
Strategies to communicate the underlying rationale included using testimonials/quotations from PiC who had successfully quit smoking, debunking myths (e.g. ‘smoking has a calming effect on the body’, ‘smoke-free prisons cause riots’), developing written communications and having briefings for staff (e.g. on contingency planning), and linking smoke-free policies to aspirations among many PiC to live healthier lives. Likewise, some participants thought it was important to acknowledge and mitigate concerns about potential risks of a smoke-free prison policy in written and oral communications with frontline staff and during planning:
The other thing we needed to combat was a lot of naysayers saying that prisoners are going to go extremely violent, they’re going to act out, they’re going to do all these things, they’re going to find other fire equipment and burn down your prisons, I mean, you know, scaremongering going on. And of course we didn’t just dismiss it, clearly we took it very seriously.
WP1, interview 1
Participants suggested that consulting and involving PiC and staff in preparations for the implementation of smoke-free policies and, crucially, acting on feedback were potentially beneficial [‘Straightaway, get them (PiC) involved. They come up with innovation, of ways of how they can cope (without tobacco). And use their ideas on that,’ WP1, interview 7]. Good engagement with the family and friends of PiC, courts and relevant community groups was also mentioned.
Smoking cessation support
Participants stressed that the availability of evidence-based support to help PiC abstain or quit smoking was crucial to the successful implementation and the ongoing management of a smoke-free policy. Although types of smoking abstinence/cessation support and delivery arrangements varied within and across jurisdictions, some potentially transferable ideas were discussed. It was suggested that service capacity could be increased by training prison and/or health-care/drug treatment staff to deliver brief advice or enhanced support on quitting or abstaining to PiC, with appropriate support for financial or logistical issues. Some participants also suggested that involvement of PiC in delivering smoking abstinence or cessation advice may potentially help to ensure that support was available during evenings and weekends and reached those who respond more effectively to peer support.
Participants described various ways to try to address potential barriers to the uptake of smoking abstinence/cessation, for example through actively promoting services and encouraging PiC to seek help, ideally pre implementation. These included posters around the prison, leaflets for PiC and visits to halls by staff/peer mentors to publicise SSSs and carry out carbon monoxide (CO) monitoring (to increase motivation to change smoking behaviours):
We used to visit the wings . . . put a little bit of a display, I’d have the carbon monoxide monitor as well. So, we’d test a few lads and, obviously, a lot of them were quite shocked at how high they were. That worried them, and that was quite a good incentive tool as well, the carbon monoxide monitor, they all wanted to have a go on that, so that was good. Then, obviously, that made them see, obviously, ‘We have got smoking cessation here . . . if you need any support’.
WP1, interview 15
Participants also described organisational strategies that could encourage PiC to cut down or stop smoking. These included ceasing or reducing tobacco sales several weeks prior to the implementation date and creating smoke-free wings (e.g. as part of a phased approach). Some noted that engaging PiC in smoking cessation programmes may present opportunities for other health promotion (e.g. nutrition).
Interview participants from E&W generally believed that e-cigarettes had played an important role in the management of nicotine addiction in prisons and the successful implementation of the smoke-free prison policy:
We really pushed to have supplies of that in the prison before we went smoke-free. And I think that that is one of the crucial factors that made it successful.
WP1, interview 8
Participants suggested that e-cigarettes (or other smoking cessation aids) should be introduced in good time prior to smoke-free rules, together with information on proper use of e-cigarettes, so that PiC could switch from smoking to vaping if they wished and to minimise incorrect/ineffective product use. However, some worries were expressed about the potential misuse of e-cigarettes by PiC and the potential, as yet unknown, health effects of vaping.
Other measures to support policy implementation
Other measures that participants said could support the successful implementation of a smoke-free policy included increasing access to a range of activities to help PiC to achieve and sustain smoking abstinence (e.g. opportunities for physical exercise; prisoner reading groups; diversions such as puzzles, crosswords, colouring and knitting) and improving facilities (e.g. by painting cells or common areas to remove nicotine stains). Participants spoke about the potential need for additional support measures for PiC who are vulnerable to reduce harms and alleviate anxiety:
. . . the key ones . . . in preparation for prisons going live, is about making sure that there is support available to those men and women who are struggling . . . whether they are hard to reach, have mental health issues [at risk of self-harm or suicide]. But equally, we have to watch for prisoners who are of a significant age, and may have smoked for 60 or 70 years.
WP1, interview 5
With respect to prison staff, participants suggested that it may be helpful to offer access to health clinics and cessation support to reduce opposition to new smoke-free rules, particularly if these have an impact on staff smoking behaviour.
Summary
Interviews were conducted with 19 people working in other countries that had implemented smoke-free policies in prison. The majority were working in prisons in E&W because people in the Scottish prison service were most interested in the experience of their counterparts in E&W, as their experience of implementing a smoke-free policy was most recent. The themes identified through analyses of our participant interviews in relation to implementation strategies were substantively similar across jurisdictions, with the exception of the use of e-cigarettes (made available to PiC in E&W only, in preparation for the removal of tobacco). Several factors were identified as important in preparation: allowing prisons, PiC and staff sufficient time to prepare for implementation of smoke-free policies, with some suggestions that a ‘clear date’ for implementation could generate the impetus for preparatory work; appropriate governance arrangements, such as the use of a ‘readiness assessment’ tool, to drive and monitor progress and identify any support needed; good partnership working with external partners and within prisons (a ‘whole-prison’ approach); and the development of ongoing management policies (e.g. strategies for effective management of nicotine dependence among new arrivals). Good, continuing and credible communication (with PiC and prison staff) and appropriate provision of smoking cessation support were also identified as being of crucial importance, and people also identified the need for a range of alternative activities for PiC and the specific support that may be needed for particularly vulnerable prisoners.
Chapter 4 Evaluating exposures to second-hand smoke
The important findings from this study related to measurements of exposures to SHS are reported in brief only, as they are reported in considerable detail in three peer-reviewed scientific papers11,31,32 published during the TIPs project, and our 2017 report to the SPS33 published on its website. Details on the methods used are also summarised in section 2.3 of that report. 33 We note in Chapter 1 that the results influenced SPS’s decision to go smoke free. Measurements of air quality using Dylos DC1700 were undertaken in phase 1 (between 30 September and 22 November 2016),11,33 the week of implementation of the smoke-free policy (28 November to 3 December 2018),32 and in phase 3, 6 months post implementation (22–28 May 2019). 31
Data integrity
The integrity of the residential hall fixed-site 6-day monitoring data was generally high. In total, 128,431 minutes of 6-day fixed-site data were recorded in residential halls of prisons in phase 1 (baseline), 114,303 minutes in the week of implementation and 126,777 minutes in phase 3. In addition, a total of 2860 minutes of mobile ‘task-based’ measurements (from a total of 86 different scenarios) were recorded at baseline and 3073 minutes (from a total of 77 scenarios) in phase 3.
At baseline, median airborne concentrations of nicotine measured in the same fixed residential sites over the same period correlated strongly (R2 value of 0.91). Analysis of changes in cotinine concentrations measured in saliva samples from non-smoking staff (n = 422 non-smoking volunteers across the 15 prisons) collected at the beginning and end of a shift suggested that prison staff were exposed to an average concentration of SHS PM2.5 of 24.8 μm/m3. 11 We focus here on reporting the results of SHS exposure measurements provided in terms of PM2.5 concentrations from the Dylos DC1700 instruments, as these allow comparison across the TIPs study period.
Changes in indicators of second-hand smoke concentration between phases 1 and 3
Fixed-site measures
Phase 1 measures of PM2.5 concentrations demonstrated high levels of SHS in residential halls in Scottish prisons, although considerable variation existed between prisons (Figure 3, Table 2, and see Semple et al. 11) and partially informed the decision to introduce the smoke-free policy across Scotland’s 15 prisons. 4 Measures in the week of implementation of the smoke-free policy demonstrated a substantial fall in every prison (overall median reduction 81%) in PM2.5 concentrations compared with concentrations in 2016. 32 This was sustained or further improved 6 months after implementation (p < 0.001 overall); median PM2.5 concentrations of the May 2019 6-day fixed-site measurements were reduced by > 91% compared with 2016 concentrations. 31
FIGURE 3.
Area monitoring results from 2016, 2018 (immediately pre and post ban) and 2019. Dashed horizontal line represents the World Health Organization’s (WHO) annual guidance value for PM2.5 (10 µg/m3). 70 At the time this work was carried out we used the 2005 WHO Air quality guidelines. The WHO have subsequently (September 2021) released new guidelines71 with an annual average PM2.5 guideline of 5 µg/m3.
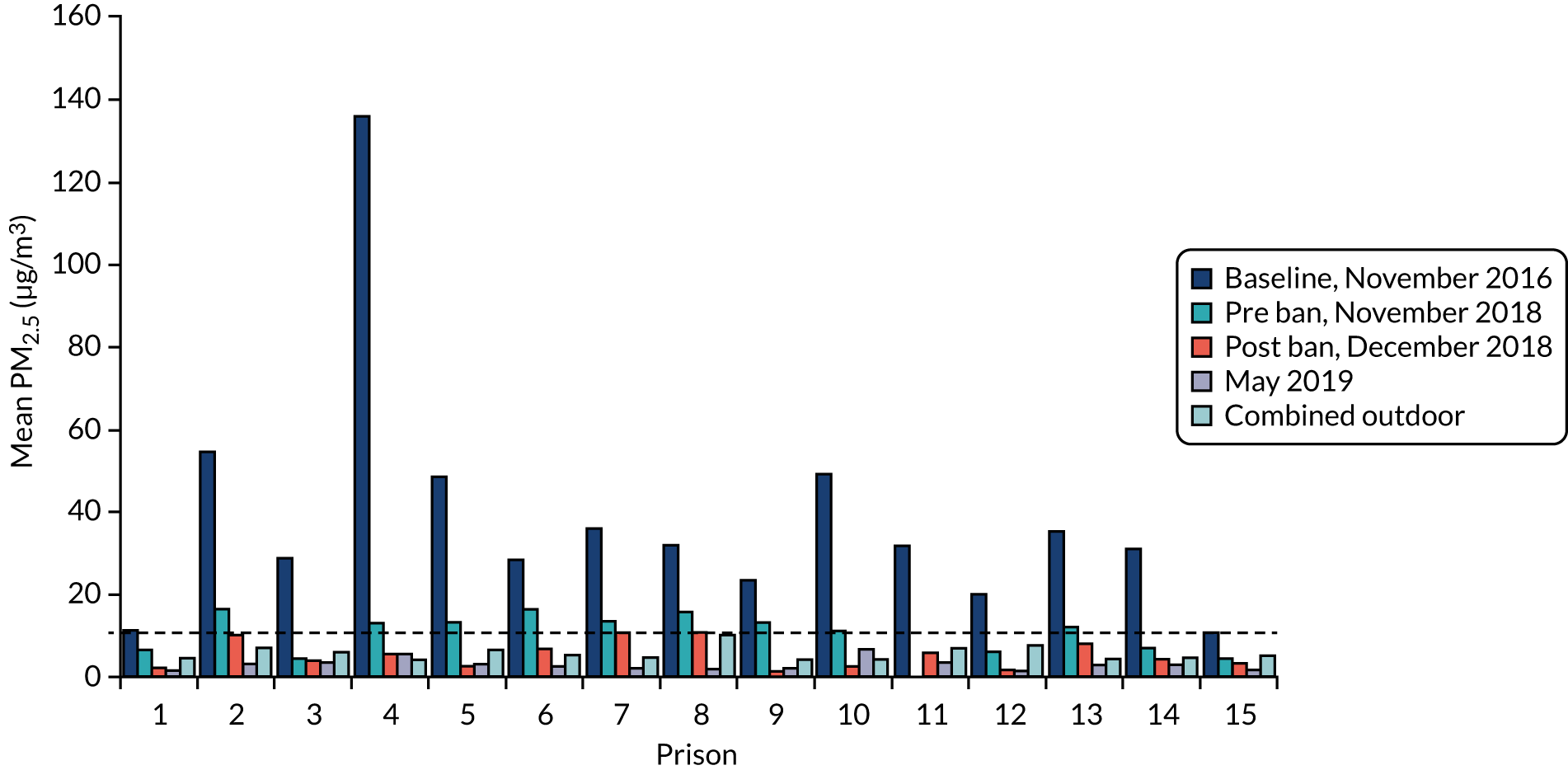
| Prison ID | PM2.5 (µg/m3) | |||||
|---|---|---|---|---|---|---|
| 2016 | 2018 | 2019 | ||||
| Indoor (SD) | Outdoora | Indoor (SD) | Outdoora | Indoor (SD) | Outdoora | |
| 1 | 11.2 (9.4) | 6.6 | 3.5 (3.5) | 4.3 | 1.7 (1) | 3.5 |
| 2 | 54.6 (37.5) | 11.4 | 14.6 (5.2) | 6.9 | 3.3 (2.4) | 3.5 |
| 3 | 28.8 (16.7) | 10.5 | 3.9 (2.0) | 5.0 | 3.6 (1.8) | 2.9 |
| 4 | 135.9 (189.4) | 5.2 | 10.5 (21.4) | 4.9 | 5.9 (15.6) | 3.0 |
| 5 | 48.6 (62.4) | 9.4 | 4.9 (5.2) | 6.7 | 3.4 (2) | 3.8 |
| 6 | 28.5 (15.8) | 5.9 | 12.1 (6.7) | 6.4 | 2.8 (2) | 4.0 |
| 7 | 36 (15.1) | 6.4 | 11.3 (4.8) | 5.8 | 2.3 (1.7) | 2.4 |
| 8 | 31.7 (16.2) | 22.8 | 9.4 (6.2) | 3.9 | 2.1 (6.7) | 4.5 |
| 9 | 23.4 (13.5) | 5.3 | 4.8 (4.8) | 4.9 | 2.1 (1.5) | 3.1 |
| 10 | 49.2 (48.6) | 5.7 | 6.4 (4.6) | 4.7 | 6.8 (4.9) | 2.8 |
| 11 | 32 (20.8) | 11.5 | 5.1 (3.6) | 5.3 | 3.6 (4.4) | 4.3 |
| 12 | 19.8 (12.1) | 12.6 | 3.8 (2.7) | 6.9 | 1.5 (0.9) | 3.5 |
| 13 | 35.3 (21) | 5.3 | 10.7 (4.8) | 5.0 | 3 (4) | 2.9 |
| 14 | 31.1 (18.8) | 6.5 | 5.8 (3.9) | 5.8 | 3.3 (2.7) | 2.4 |
| 15 | 10.5 (8.7) | 7.7 | 4 (4.8) | 4.3 | 1.7 (2.4) | 3.5 |
| Median | 31.7 | 6.6 | 5.8 | 5.0 | 3.0 | 3.5 |
Mobile ‘task-based’ measures
Analyses of phase 1 data showed that exposures were likely to be highest for operational/residential staff. Analyses of the post-ban (phase 3) task-based measurements showed that all were low in 2019 (the only task with a median > 10 µg/m3 was cell searches), and all were lower in 2019 than in 2016, with an average reduction of 70%. Reductions were marked in areas/for tasks that had high levels in 2016 (e.g. a reduction for morning cell unlocking of 89%) and were lowest for cell searches (median concentrations reduced by 74%). Estimates of time-weighted average exposures for staff working in residential areas of the prisons in 2019 no longer showed the marked diurnal variation that was evident in phase 1, nor the high peak exposures first thing in the morning during cell unlocking (see figure 1 in Semple et al. 11). Indeed, the time-weighted average exposures in 2019 demonstrated reductions of > 90% across all shifts, and all time-weighted average exposure concentrations were lower than PM2.5 concentrations measured in outdoor air at the nearest measurement centre (see Demou et al. 31 for more details).
Summary
Measurements of SHS-derived fine particulate matter (PM2.5) were undertaken using Dylos DC1700 devices in each prison in 2016, before any change in policy had been formulated, in the week of implementation of the smoke-free policy and again at 6 months post implementation. In total, 128,431 minutes of air quality data were gathered over approximately 6-day continuous periods from fixed positions in residential halls of prisons in phase 1, 114,303 minutes in the week of implementation and 126,777 minutes in phase 3. An additional 2860 and 3073 minutes of short (approximately 30-minute) mobile ‘task-based’ measures were recorded in phase 1 and phase 3, respectively. Phase 1 measures of PM2.5 concentrations demonstrated high levels of SHS in the residential halls, although with considerable variation during the day and between prisons. Phase 1 mobile ‘task-based’ measurements showed that exposures were likely to be highest for operational/residential staff. These data partially informed the decision to introduce the smoke-free prison policy in Scotland.
Measures in the week of implementation of the smoke-free policy showed a substantial fall in PM2.5 concentrations in all prisons (overall median reduction of 81%), which was sustained or further improved 6 months after implementation, when median PM2.5 concentrations of the 6-day fixed-site measurements were reduced by > 91%, compared with 2016 concentrations. Phase 3 task-based measurements showed that all concentrations were lower in 2019 than in 2016, with an average reduction of 70%. Reductions were marked in areas/for tasks that had high levels in 2016. Time-weighted average PM2.5 exposures estimated for prison staff for 2019 demonstrated reductions of > 90% across all shifts when compared with 2016 results.
Chapter 5 Staff perspectives, opinions and experiences
Introduction
Work package 3 of the TIPs study was designed to elicit the attitudes and experiences of staff working within the prison service in Scotland in relation to smoking, current and potential changes to rules on smoking (and e-cigarettes), and SHS. It comprised (1) cross-sectional fully anonymised online surveys open to staff in all 15 prisons in phase 1 (pre announcement), phase 2 (preparatory phase) and phase 3 (post implementation); and (2) focus groups with prison staff across Scotland in phase 1 (n = 19, 132 staff in total) and phase 3 (n = 15, 95 staff in total) and one-to-one interviews with 38 staff in ‘case study’ prisons in phase 2 (see Figure 1). Further details are available in publications from the study. 40,54,55,72
Online surveys of prison staff: phases 1, 2 and 3
Return rates, sociodemographic and work-based characteristics
The tables in Report Supplementary Material 1 show the basic frequency distributions of all staff survey items at each phase (numbers and percentages rounded to integers for simplicity of presentation; similar documents were provided to prison staff as feedback). These show the questions as asked in the surveys, but not in the order in which they appeared. The results below are based on these distributions, with most tables showing collapsed categories and between-phase differences tested via chi-squared tests (categorical variables) or F-tests (continuous variables).
Surveys were returned by 1271 (27%) prison-based staff in phase 1, 1494 (31%) in phase 2 and 757 (16%) in phase 3. There was considerable between-prison variation in return rates at each phase (Table 3), despite repeated reminders about the online survey for staff. The variation is likely to reflect staff access to appropriate facilities to complete the questionnaire and pressures on staff time in their daily work, as well as their interest in completing the questionnaire. In each prison, we relied on our designated staff contact to forward the link to the survey and the reminders. Given the levels of response overall, and variation in response by prison and phase, all figures presented below should be interpreted with caution. For published papers relating to results on opinions,39,72 simple weights were derived to adjust for this variation; unweighted and weighted results were virtually identical.
| Prison | Return rate (%) | |||||
|---|---|---|---|---|---|---|
| Staff | PiC | |||||
| Phase 1 | Phase 2 | Phase 3 | Phase 1 | Phase 2 | Phase 3 | |
| Addiewell | 10 | 14 | 5 | 32 | 11 | 11 |
| Barlinnie | 33 | 30 | 9 | 34 | 25 | 15 |
| Castle Huntly | 38 | 55 | 24 | 10 | 35 | 13 |
| Cornton Vale | 21 | 38 | 25 | 57 | 40 | 50 |
| Dumfries | 38 | 61 | 28 | 45 | 40 | 46 |
| Edinburgh | 30 | 22 | 21 | 38 | 21 | 11 |
| Glenochil | 26 | 17 | 7 | 41 | 19 | 19 |
| Grampian | 34 | 25 | 43 | 26 | 23 | 11 |
| Greenock | 28 | 57 | 13 | 32 | 29 | 35 |
| Inverness | 34 | 45 | 29 | 60 | 34 | 26 |
| Kilmarnock | 11 | 19 | 18 | 35 | 8 | 4 |
| Low Moss | 20 | 33 | 15 | 19 | 60 | 46 |
| Perth | 26 | 42 | 15 | 49 | 29 | 16 |
| Polmont | 26 | 29 | 11 | 26 | 21 | 11 |
| Shotts | 29 | 26 | 9 | 33 | 19 | 13 |
| Overall | 27 | 31 | 16 | 34 | 25 | 18 |
| Total, n | 1271 | 1494 | 757 | 2512 | 1959 | 1485 |
Apart from slightly smaller proportions of males and operational staff in phases 2 and 3, sociodemographic and work-based characteristics were very similar across phases (see Report Supplementary Material 1, Tables 128–132). The proportion of males reflects that of the SPS as a whole (69% in March 201974) and the age breakdown was broadly similar, although there were fewer in the younger and older age bands among TIPs study respondents than in the SPS as a whole (in the SPS as a whole, 28% were aged ≤ 34 years, 49% were aged 35–54 years and 23% were aged ≥ 55; equivalent figures for the TIPs study were 24%, 60% and 16%, respectively, in phase 1; 25%, 56% and 19%, respectively, in phase 2; and 22%, 57% and 20%, respectively, in phase 3).
Self-report exposure to second-hand smoke/second-hand vapour at work
The mean reported average exposure to other people’s cigarette smoke in a prison reduced from 16.3 hours per week in phase 1 to 12.7 hours per week in phase 2, and then markedly (to 3.6 hours per week) in phase 3 (p < 0.001), and the proportion of staff reporting no exposure rose from 19% (phase 1) to 27% (phase 2) to 74% (phase 3) (p < 0.001). Despite very careful question wording, it is possible that, in phase 3, some staff interpreted this question as referring to e-cigarette vapour.
In phases 2 and 3, staff were asked roughly how often (never, sometimes, often, always) they were exposed to ‘other people’s smoke’ and ‘vapour or smells from other people’s electronic cigarettes’ in a range of locations. Figure 4 highlights the marked drop in any (sometimes, often, always) ‘smoke’ and increase in ‘vapour’ exposure between phases 2 and 3. As smoking/vaping was/is permitted in cells with closed doors and during outdoor exercise only, it also suggests that some staff were identifying illicit activity.
FIGURE 4.
Staff (%) reporting any exposure to cigarette smoke/e-cigarette vapour in various location: phases 2 and 3 (with significance of difference, p-value).

Opinions on (rules about) smoking and tobacco in prisons
The proportion of staff reporting that the current rules about tobacco smoking among PiC were not strict enough (vs. too strict/about right) dropped from 67% in phase 1, when smoking was permitted in cells within residential areas and outdoors only, to 51% in phase 2 and 23% in phase 3 (p < 0.001). Over time, the proportion reporting the rules were not well followed by PiC (vs. very/quite well followed) dropped from 43% (phase 1) to 33% (phase 2) to 16% (phase 3) (p < 0.001) (see Report Supplementary Material 1, Tables 20 and 21). Similar questions on e-cigarette use were asked in phase 3 only, when 29% of staff said the rules were not strict enough and 24% said that they were not well followed.
In all phases, staff (and PiC) were asked a series of opinion questions around prison smoking bans, comprising seven items with five answer options, and a single item on agreement with increased smoking restrictions in Scottish prisons (see Report Supplementary Material 1). We have published analyses of phase 1 data40 reporting the structure of opinions in respect of prison smoking bans (whether or not more than one dimension), and correlates of that/those dimension(s). Exploratory factor analyses (principal components analysis, varimax rotation) distinguished two identical factors for both groups, which explained 16% more total variance than an analysis constrained to a single factor. The two factors, the first representing ‘positive about bans’ opinions and the other representing beliefs that ‘bans will be difficult’, were saved and formed the dependent variables in analyses of association.
Staff scores were significantly (p < 0.001) higher than those of PiC for ‘positive about bans’, but lower on ‘bans will be difficult’. In multivariable analyses, staff ‘positive about bans’ factor scores were significantly associated with not smoking, better general health, more respiratory symptoms and working in an operational role, whereas reporting fewer sensory symptoms and lower measured prison SHS levels (see Chapter 2, Fixed-site monitoring), but not own smoking, were independently associated with ‘bans will be difficult’. 40
Further published analyses72 compared opinions of both staff and PiC in respect to prison smoking bans (as above) and the use of e-cigarettes among those in custody across all three phases. Response categories were collapsed (if necessary) so that all were binary outcomes and differences were tested using logistic regression analyses, adjusting for sociodemographic variables associated with both phase and opinions. Table 4 shows these results, along with those of identical analyses relating to more general opinions on smoking in prisons. Staff opinions shifted over time, with differences between phases 1 and 3 and, for several items, between phases 1 and 2 and/or 2 and 3. Support for prison smoking bans increased in anticipation of/following the ban, whereas there were large decreases in the proportions agreeing that prison smoking bans ‘cause a lot of trouble’ and ‘are hard to enforce’, particularly between phases 2 and 3 (note that concerns that bans ‘cause a lot of trouble’ had increased in staff between phases 1 and 2). Staff support for e-cigarette use by PiC increased in anticipation of the ban, remaining stable following its implementation. Agreement that ‘staff should be protected from cigarette smoke at work’ was almost universal at each phase; agreement that ‘prisoners who don’t smoke should be protected from cigarette smoke’ was also very high throughout. Agreement that smoking should not be allowed in any indoor or outdoor prison areas was highest in phase 3, when agreement with both ‘there should be more NHS support for prisoners who want to stop smoking’ and ‘prisoners should not be forced to stop smoking’ was lowest.
| Opinion item | Phase (%) | Significant differencesa | ||
|---|---|---|---|---|
| 1 | 2 | 3 | ||
| Prison smoking bans (agree/strongly agree) | ||||
| Prison smoking bans are a good idea | 74 | 69 | 86 | 1 < 3, 2 < 3 |
| Prison smoking bans cause a lot of trouble | 58 | 69 | 33 | 1 < 2, 1 > 3, 2 > 3 |
| Prison smoking bans help prisoners stop smoking long term | 50 | 39 | 42 | 1 > 2, 1 > 3 |
| Prison smoking bans are hard to enforce | 62 | 60 | 35 | 1 > 3, 2 > 3 |
| Most staff want prison smoking bans | 62 | 58 | 73 | 1 < 3, 2 < 3 |
| Prison smoking bans are OK if enough stop-smoking support is available | 67 | 68 | 75 | 1 < 3, 2 < 3 |
| Prison smoking bans are OK if prisoners allowed e-cigarettes | 35 | 43 | 58 | 1 < 2, 1 < 3, 2 < 3 |
| Smoking restrictions in Scottish prisons | ||||
| In favour of (hypothetical/impending/actual) increased smoking restrictions in Scottish prisons | 79 | 70 | 84 | 1 > 2, 1 < 3, 2 < 3 |
| Prisoners’ access to e-cigarettes (agree) | ||||
| Should e-cigarettes be available to prisoners to buy from the canteen? | 53 | 73 | 79 | 1 < 2, 1 < 3, 2 < 3 |
| Should e-cigarettes be given to prisoners temporarily to help with tobacco withdrawal when admitted to prison? | 47 | 68 | 68 | 1 < 2, 1 < 3 |
| Should e-cigarettes be available to help prisoners stop smoking/manage without tobacco? | 54 | 75 | 73 | 1 < 2, 1 < 3 |
| Smoking in prisons (agree/strongly agree) | ||||
| Staff should be protected from cigarette smoke at work | 96 | 95 | 96 | – |
| Prisoners who do not smoke should be protected from cigarette smoke | 95 | 94 | 91 | 1 > 3 |
| There should be more NHS support for prisoners who want to stop smoking | 69 | 71 | 60 | 1 > 3, 2 > 3 |
| Prisoners should not be forced to stop smoking | 39 | 39 | 27 | 1 > 3, 2 > 3 |
| Prisoners who smoke are unlikely to ever stop long term | 42 | 43 | 38 | – |
| Smoking should not be allowed in any indoor prison areas | 79 | 76 | 83 | 2 < 3 |
| Smoking should not be allowed in any outdoor prison areas | 38 | 41 | 50 | 1 < 3, 2 < 3 |
Opinions about e-cigarettes generally
In phases 2 and 3, staff were asked a standard question about the relative harms of e-cigarettes and ‘regular cigarettes’. Although the proportion who thought e-cigarettes were (a lot) less harmful or completely harmless remained stable (37% in phase 2 and 40% in phase 3), an increased proportion (from 20% to 27%, respectively) thought that they were equally or (a lot) more harmful and a decreased proportion (from 43% to 33%, respectively) reported that they ‘did not know’. As Table 5 shows, other opinions about e-cigarettes also became more negative among respondents over this period. Differences between phases 2 and 3 were greater in respect of increased agreement that e-cigarettes are ‘addictive’ and ‘raise safety issues’, and increased disagreement that they are ‘as good as other nicotine replacement therapies to help people stop smoking’ and ‘should be allowed in public places where tobacco cigarettes are not allowed’.
| How much do you agree e-cigarettes . . . | Phase | Agreement (%) | Significance of chi-squared test | ||
|---|---|---|---|---|---|
| (Strongly) agree | No opinion | (Strongly) disagree | |||
| . . . can stop people smoking? | 2 | 61 | 26 | 13 | |
| 3 | 63 | 20 | 18 | 0.002 | |
| . . . are addictive? | 2 | 54 | 43 | 3 | |
| 3 | 68 | 29 | 3 | < 0.001 | |
| . . . are as good as other nicotine replacement therapies to help people stop smoking? | 2 | 31 | 56 | 12 | |
| 3 | 36 | 43 | 21 | < 0.001 | |
| . . . should be allowed in public places where tobacco cigarettes are not allowed? | 2 | 16 | 16 | 68 | |
| 3 | 11 | 10 | 79 | < 0.001 | |
| . . . raise safety issues? | 2 | 52 | 39 | 9 | |
| 3 | 62 | 30 | 8 | < 0.001 | |
Only phase 3 included a series of questions about staff experience of e-cigarette vapour during their daily work (see Report Supplementary Material 1, Tables 41–45). Around 50% of responding staff indicated that they thought that e-cigarette vapour was ‘bad for [their] health’, and 40% that it ‘has an unpleasant smell’; one-quarter to one-third indicated that it made them cough, irritated their eyes or affected their breathing.
Opinions about the introduction of the smoking ban in Scottish prisons
In phase 3, staff were asked their opinions about the lead-up to, and implementation of, the smoking ban. As Table 6 shows, around four-fifths thought that the preparation was good, people were kept well informed and introducing e-cigarettes had ‘made the smoking ban easier for both prisoners and staff’. Almost three-quarters agreed that the introduction of the ban had been ‘largely trouble-free for the prison service’, five times the proportion who disagreed with this statement. Three-quarters also believed that the ban had ‘led to improved working conditions for staff’ and ‘made the prison smell better’, and around half believed that it had helped improve staff health, the quality of life and health of PiC and made the prison look better; only about 1 in 10 disagreed with any of these statements. However, almost half agreed that the ban had ‘led to more use of illegal drugs’, between one-quarter and one-third that it had ‘made prisoners more anxious’, led to more physical or verbal assaults or aggression and ‘made prisoner behaviour more difficult to manage’, and very few thought it had led to more purposeful activity or made PiC happier.
| Opinion item | Agreement (%) | ||
|---|---|---|---|
| (Strongly) agree | No opinion | (Strongly) disagree | |
| Lead-up to the smoking ban | |||
| Preparation for the smoking ban was good | 77 | 10 | 12 |
| Staff and prisoners were well informed about the smoking ban | 88 | 5 | 7 |
| Introduction of e-cigarettes/vapes made the smoking ban easier for prisoners and staff | 79 | 12 | 9 |
| Implementation of the smoking ban | |||
| The introduction of the smoking ban has been largely trouble free for the prison service | 71 | 15 | 14 |
| The smoking ban has . . . (ordered greatest to least agreement) | |||
| . . . led to improved working conditions for staff | 74 | 15 | 11 |
| . . . made the prison smell better | 73 | 15 | 11 |
| . . . helped improve staff health | 68 | 24 | 8 |
| . . . helped improve prisoner health | 58 | 31 | 10 |
| . . . helped improve prisoners’ quality of life | 56 | 34 | 10 |
| . . . made the prison look better | 49 | 32 | 19 |
| . . . led to more use of illegal drugs | 45 | 36 | 19 |
| . . . helped prisoners stop smoking for good | 38 | 39 | 24 |
| . . . made prisoners more anxious | 33 | 40 | 27 |
| . . . led to more verbal assaults/aggression by prisoners | 33 | 36 | 31 |
| . . . made prisoner behaviour more difficult to manage | 27 | 36 | 37 |
| . . . led to more physical assaults/physical aggression by prisoners | 23 | 42 | 34 |
| . . . led to more prisoners taking part in purposeful activity | 12 | 55 | 32 |
| . . . made prisoners happier | 7 | 57 | 36 |
| . . . led to more fires in prisons | 6 | 37 | 57 |
Phase 3 also included questions on how much of a problem certain issues were at the time. As Table 7 shows, by far the most serious perceived problems related to PiC adapting e-cigarettes for drugs or adapting their chargers for various purposes. Around half the staff also identified bullying over e-cigarettes among PiC as a moderate/serious problem and one-quarter to two-thirds thought tobacco-related debt, bullying and illicit trade or use were moderate/serious problems.
| Opinion item | Response (%) | ||
|---|---|---|---|
| Not a problem | Minor problem | Moderate/serious problem | |
| Prisoners adapting e-cigarettes/vapes to use for drugs | 5 | 20 | 75 |
| Prisoners adapting chargers for e-cigarettes/vapes | 7 | 26 | 67 |
| Prisoners bullying one another over e-cigarettes/vapes | 7 | 37 | 55 |
| Prisoners getting into debt over tobacco | 20 | 43 | 36 |
| Tobacco coming in from the outside | 18 | 48 | 34 |
| Prisoners bullying one another over tobacco | 22 | 44 | 34 |
| Prisoners trading or buying tobacco | 18 | 50 | 32 |
| Prisoners still smoking tobacco | 18 | 54 | 27 |
Staff smoking
Report Supplementary Material 1, Tables 109–126, report on staff smoking and e-cigarette use. In each phase, around half the staff returning a survey had ever smoked and 1 in 10 currently smoked tobacco cigarettes. Electronic cigarette experimentation increased between phase 1 and phase 2, and current use increased between phase 2 and phase 3.
Among the (relatively small numbers) of current tobacco cigarette smokers, there was a suggestion of reduced craving in phase 3 after implementation of the ban, but no evidence that cigarette consumption or time from waking to first cigarette had reduced, nor of increased efforts to stop smoking. In phase 3, staff who smoked tobacco cigarettes were asked whether not being able to smoke at work had become any easier or harder since implementation of the ban; 29% reported it was (much) easier, 62% about the same and 9% (much) harder.
Staff self-reported health
Frequencies for staff self-reported health are shown in Report Supplementary Material 1, Tables 81–108. Staff ratings of general health remained stable across the study (‘very good’ vs. ‘good’ vs. ‘fair’/’bad’/‘very bad’ reported by 35%, 53% and 12% in phase 1, respectively; 33%, 56% and 11% in phase 2, respectively; and 32%, 54% and 14% in phase 3, respectively). Self-reported doctor-diagnosed asthma also remained stable (20% in phases 1 and 2, 19% in phase 3), as did days off work for health reasons in the past year (50%, 53% and 53% reported none in phases 1–3, respectively; 19%, 19% and 17% reported ≥ 28 days). Past year GP visits reduced slightly (26%, 28% and 31% reported none in phases 1–3, respectively; 31%, 27% and 24% reported three or more, respectively; p = 0.020). GP visits in the past 3 months for a cold, breathing problems or eye irritation (84%, 86% and 88% reported none in phases 1–3, respectively; 7%, 5% and 4% reported two or more, respectively; p = 0.058) changed little, and the number of prescribed medicines for a cold, breathing problems or eye irritation over the past 3 months was stable; over-the-counter purchases reduced between phase 1 and phase 2 (40%, 32% and 32% reported any in phases 1–3, respectively; p < 0.001). As Figure 5 shows, this pattern was evident for eight of the nine International Union Against Tuberculosis and Lung Disease self-reported past month respiratory and sensory symptoms, the only exception being eye irritation, which decreased between phase 2 and phase 3. These patterns may reflect time-of-year effects. The five ‘your health today’ items and visual analogue scale (‘best’ to ‘worst’ health) on the EuroQol-5 Dimensions (EQ-5D) were stable across phases.
FIGURE 5.
Staff (%) reporting past 4 weeks’ experience of each symptom in each phase (with significance of difference, p-value).
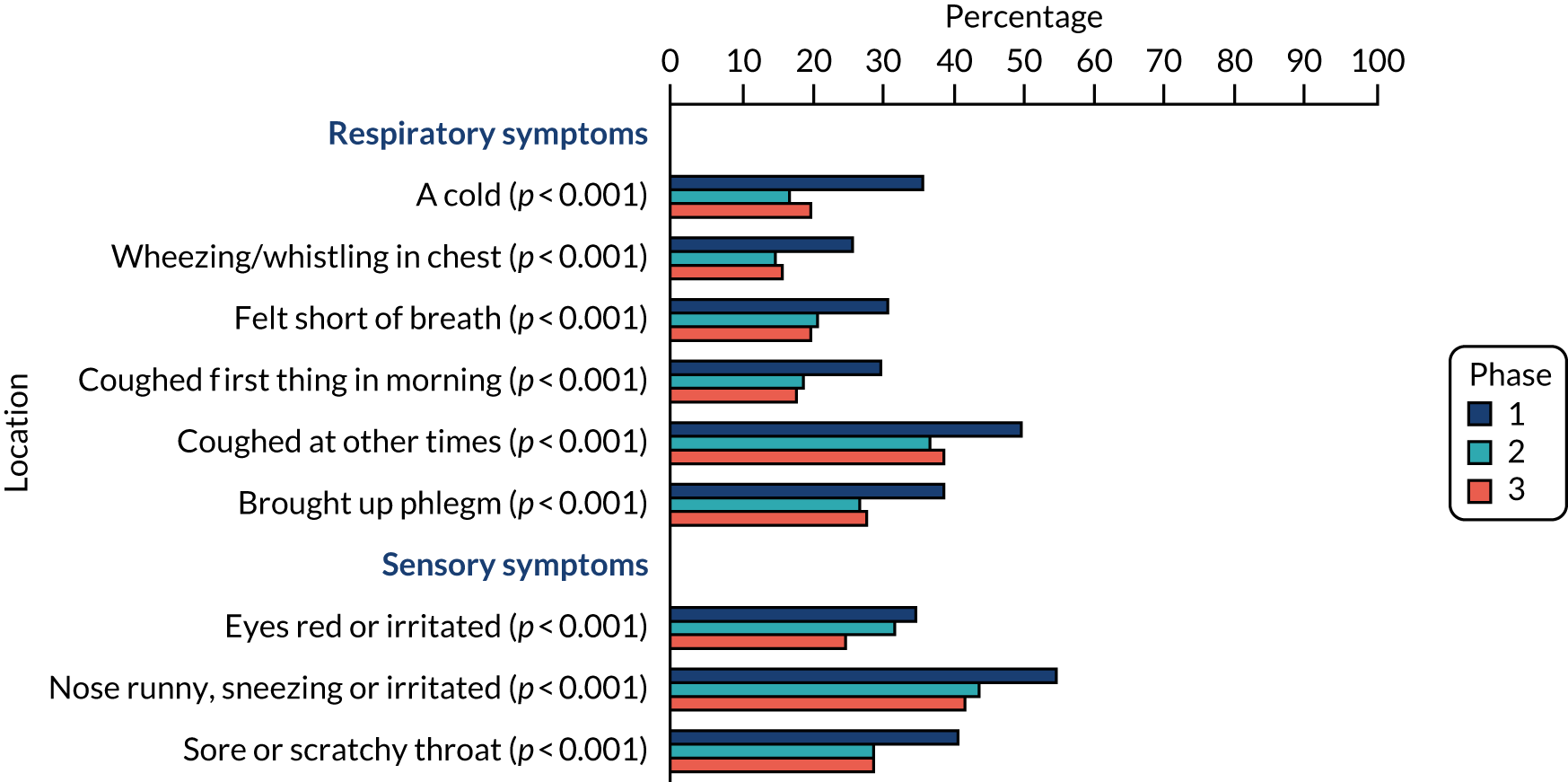
Staff focus groups: phase 1 (pre announcement)
Seventeen focus groups and two paired interviews were conducted with staff in 14 of Scotland’s 15 prisons during TIPs phase 1 to explore perspectives on current smoking rules for PiC and on potential implementation of a smoke-free policy in prisons in the future. Key findings from the focus groups are published elsewhere. 54,55
Perspectives on the (then current) smoking rules for people in custody
At the time data were collected, PiC were permitted to smoke in designated rooms (cells) and certain outdoor spaces (the use of e-cigarettes in prison was prohibited). These smoking rules had come into force in 2006 when restrictions on smoking in public places were introduced in wider society in Scotland. Some participants suggested that the introduction of partial rather than comprehensive smoke-free rules in 2006 was due to concerns about the consequences of totally prohibiting PiC from smoking, for example risks of negative organisational impacts (‘a lot of trouble’), as well as understandings that prisons were homes for PiC. Some staff expressed disappointment that the prison service had not taken the opportunity then to fully protect non-smokers from exposure to SHS at work, favouring the ‘rights’ of PiC over theirs:
It [decision about smoking rules in 2006] was based on human rights, it was based on the prisoner having human rights. The argument’s always been from staff, well, what about our human rights? We don’t have a choice, we have to go into a smoke-filled environment.
ExS, I2
Perspectives on the potential future smoke-free policy
In the focus groups, staff deliberated about issues raised by any future comprehensive smoke-free policy. Part of the discussion centred on the perceived fairness of restricting PiC’s smoking behaviours. One reason smoke-free rules were considered potentially unfair was because they would reduce the choices of PiC and remove something PiC associated with pleasure. It was pointed out that PiC would be one of only a few groups in society subject to potentially prolonged periods of mandated smoking abstinence, as smokers in the general public were free to move between smoking-permitted and smoke-free spaces. In addition, staff commented that it might be an odd situation if controlled medications such as methadone were available in prisons, but tobacco, a legal substance, was not:
And that’s the big contradiction here, if they ban smoking, right. It’s OK for the Prison Service to ensure that somebody can get their methadone, or their valium, or whatever drug they happen to be on. But woe betide, they can’t have a cigarette. The cigarette is legal . . .
NS, L5
However, on balance, staff generally believed that smoking restrictions for PiC were equitable, justifiable and necessary to protect the health of non-smoking staff and PiC (provided support was available in prisons to help with nicotine dependence):
They’ve got a duty to look after those who don’t smoke. Forget staff . . .
NS, G5
Prisoners and that as well, yes.
S, G1
So, see prisoners that don’t smoke, the amount of guys that I’ve had to allocate into a smoking cell when they’ve been a non-smoker because we’re chock-a-block.
NS, G5
Some staff saw involuntary exposure to SHS in prisons as a form of injustice, particularly given that the adverse effects of SHS had been known for some time: ‘the time it’s taking. The facts are out there that passive smoking is harmful to your health. It should be finished in the establishments, end of’ [S, A(2)23].
Discussion about a future smoke-free policy for PiC also focused on practical issues in respect of making the transition from a high rate of tobacco use among PiC to smoking abstinence. Concerns were expressed that smoke-free rules for PiC would be unworkable because of the significance some PiC placed on smoking (e.g. to pass time or alleviate negative emotions) and the role of tobacco in prison culture (e.g. a social activity, form of currency):
I think it’s unworkable up here . . . I think . . . there are certain things that keep the roof on a situation, if you pardon the analogy. And for me, in here anyway, it’s the ability for them to smoke. And the likes of TV and stuff. I think you take that away from them, I think you’re opening another can of worms.
NS, A(1)1
In contrast, others expressed more confidence that a change in smoking rules was achievable because similar policies had been introduced in other institutions caring for high-smoking prevalence populations (e.g. state hospital) and the prison service had succeeded in the past in managing other challenging organisational changes:
. . . there’s plenty of things that we’ve maybe done as a service over the decades where we’ve taken something away and people have gone ‘Oh they’ll never cope with that, and, we’ll get this and we’ll get that’. And maybe we’ve had a . . . you know, a few incidents or a couple of months of unrest, but then it settles down again . . .
NS, N3
A range of potential negative consequences of introducing smoke-free rules for PiC were raised: reduced wellbeing, self-harm and suicide, confrontations, violence, riots, contraband, bullying, use of alternatives (e.g. smoking teabags, substance use) and increased staff stress:
It will distress some people [in custody]. I know, because when I was smoking, if I went into a situation where it’s like, right, OK, you cannot smoke now, it would be torture, it would be absolute torture, especially when they’re already distressed . . . a cigarette can really help them calm down . . .
ExS, C1
I think there’s potential for conflict. I think there’s also . . . it’s now . . . it’s just something else just the same as they get drugs in to jail, it’ll be something else for them to smuggle and abuse.
NS, H3
Potential negative consequences of smoke-free rules were discussed by all groups as significant and important, but not necessarily a reason not to change the smoking policy. There was broad consensus across the groups that staff had the experience to manage any problems associated with banned substances in prisons, and some suggested that possible problems would be short-lived, waning once PiC adjusted to the ‘new normal’:
I think it would be a big issue at first, but then it’s like anything, people get used to it. People never thought the [community] smoking ban would come in, and it did, and then they got used to it. And I think there is, I think what we’re talking about . . .
NS, E6
We’d have to suck it up for the first wee while.
NS, E3
. . . in the population of the prison, I’m going to think, my opinion is . . . in the main, they would get, people would get used, the prisoners would get used to it.
NS, E6
At the same time, staff highlighted the need for measures to mitigate the risks of removing tobacco from prisons. First, there was a need to ensure that PiC and staff were well informed about any planned changes to smoking rules, with adequate time to prepare for the future removal of tobacco: ‘everybody would need to know that it was coming on this date and this is happening. The same as they did in the pubs and clubs’ [NS, A(3)13]. Second, they suggested the importance of involving PiC in planning activities, including identifying people who were willing to champion no smoking rules among their peers:
. . . if you were to get maybe a few prisoners involved who were willing to take this and encourage others as well, rather than it all just coming from . . . it’s . . . you know, it’s something that prison officers are coming out with. If you can get them to participate . . . in this process of how we could bring it in and what would be acceptable in the prisons, that might work a wee bit better.
ExS, A(4)25
Third, some staff identified a need to allocate adequate resources to the smoke-free project, ensuring that frontline staff had full management support. Fourth, participants identified opportunities for learning from other prisons systems that had introduced smoke-free policies and potentially piloting or phasing in smoke-free policies in some residential areas in prisons or parts of the prison estate.
Finally, staff identified the need for PiC to have access to the behavioural support and tools required to move beyond or manage nicotine dependence in prisons:
We [should] ramp things up in custody, get the smoking cessation in place, people on it. If we can get the majority of the population to reduce their smoking prior to the date, your transition is pretty smooth. But if you don’t do any of the leg work . . . we’re gonna be smoke-free, they’ll have big budgets to pay, because there will be big issues.
NS, F14
Although prison staff were generally supportive of nicotine substitutes being available in prisons to help PiC manage without tobacco, divergent views were expressed about whether or not the use of e-cigarettes should be permitted in prisons [alongside nicotine replacement therapy (NRT), as reported in more detail in Brown et al. 55]. Some comments suggested that e-cigarettes could be important for PiC who would want to continue using nicotine or who might not find conventional smoking cessation methods appealing or effective:
I see the benefit in giving prisoners that option, because it’s their choice at the end of the day. Not all of them will want to stop. It’s alright saying ‘give them the help and the benefit to stop smoking’, but most of them might not want to stop.
ExS, E4
Obviously, we can just bring it [smoke-free policy] in and we can say we’re doing it, and that’s the end of it. But to offer them a viable alternative that they might buy into [would be better].
ExS, D10
Some staff thought replacing smoking with vaping in prisons would be a ‘step in the right direction’, because e-cigarette vapour was believed to be markedly less dangerous than SHS to bystanders and might aid a difficult organisational change:
. . . I’ll probably be happier with them having something like that [e-cigarettes] than I would having to deal with second-hand cigarette smoke . . . it might still be a problem down the line and we might need to get rid of them, but if it’s a step in the right direction . . .
NS, H3
In contrast, others expressed anxieties about e-cigarettes being used by PiC because of incomplete evidence on the absolute risks of exposure to e-cigarette vapour:
I don’t think there is [currently] enough evidence to say [whether e-cigarettes should be allowed in prisons]. They are saying that they’re, for argument’s sake, 90 per cent less of a risk than it is with tobacco smoke. But there’s still a risk, and we still don’t know what that risk is, or what that level of risk is.
ExS, O7
There was also a great deal of discussion among staff about distinct potential risks of use of e-cigarettes in the prison context. For instance, staff commonly recognised that the repurposing of items was a part of prison culture and they expected that this would also happen with e-cigarettes (e.g. to conceal contraband, take drugs or charge mobile phones smuggled into prisons). Concerns were also raised about potential harms to staff or PiC from product defects or incorrect use of e-cigarettes:
You see the cynic’s working on me just now, and I’m thinking to myself . . . they’ll end up somehow being able to incorporate whatever drug they wish into the e-cigarette because they’ve got all day to sit and think about these things . . .
ExS, K3
Staff interviews in ‘case study’ prisons: phase 2
Findings from the interviews with 38 prison staff carried out during phase 2 in the 9–12 months prior to introduction of the smoke-free prison policy are presented below. There is a high degree of consistency of results between the staff interviews presented here and the phase 1 focus groups (with a different sample of prison staff) reported in Staff focus groups: phase 1 (pre announcement) and elsewhere. 54,55
Opinions on the impending smoke-free prison policy
Consistent with the views expressed by staff focus group participants in phase 1, several potential benefits and drawbacks of moving to smoke-free rules were reported by staff interviewed in phase 2. On one hand, anticipated benefits of the impending policy change centred on protecting prison staff from SHS exposures, creating a cleaner and more pleasant working environment for staff and health benefits for PiC who quit or abstained from smoking in prison as a result of the change in smoking rules:
It was something that I was pushing quite a bit for anyway especially on the staff side . . . being a non-smoker and never smoked before I was feeling the effects of somebody that smoked and I was thinking about my own health.
NS, A8
Some staff also suggested that the families of PiC might benefit too, as a result of potential financial savings and children growing up in smoke-free homes, if those leaving custody continued not to smoke post liberation. It is notable that some participants reported that they or other prison staff had become more positive or accepting of the smoke-free policy in the preparatory phase, as a result, for example, of work that was under way in prisons to publicise the forthcoming change in rules among PiC (see Perspectives on measures to support implementation of smoke-free policy in prison).
They’ve [PiC] been told well in advance for it to sink in and it’s been what everyone’s speaking about, so I think that’s a great, great, great, help that they’ve had time to think about it and they know that it’s happening. So, aye, I’m a wee bit more positive on it now, but we’ve still got a few months so we’re working on it.
NS, A3
On the other hand, potential drawbacks of the smoke-free policy still centred on concerns about restricting the individual choice of PiC in respect of smoking [‘If they’re going to smoke, they’re going to smoke, so why not let them smoke outside? . . . that’s the Scottish Government for you, wanting a healthier lifestyle’ (NS, A2)] and the potential for unintended adverse consequences following the removal of tobacco from prisons, as described in Perspectives on potential future smoke-free policy. Consistent with the phase 1 staff focus group findings, there remained a belief that prison staff would find a way to manage any problems that might arise following the implementation of the smoke-free prison policy.
Opinions on making e-cigarettes available in prisons
To our knowledge, single use e-cigarettes had not yet gone on sale in the prisons when these phase 2 staff interviews were conducted, although discussions about their introduction were taking place. In the phase 2 interviews, staff expressed similar opinions about the potential benefits and risks of making e-cigarettes available for use in prison by PiC to those expressed by staff in the phase 1 focus groups. 55 Some regarded e-cigarettes as a safer alternative to tobacco smoking for users and bystanders and suggested that e-cigarettes could reduce potential problems associated with smoke-free prisons for PiC, staff and the prison service. Some likened allowing PiC to use e-cigarettes to harm reduction practices for PiC dependent on illegal drugs such as heroin:
. . . I think we have to offer the prisoners something, and that would soften the blow to nothing, and they use them outside, and if they go down the line of the same as we’re doing here [with respect to current smoking rules], they have it in their cell and they have it in the exercise yard, end of . . . but to just go from tobacco to nothing I think would be a huge risk, and if we can bring in the vapes, it would soften up.
NS, B5
In contrast, several potential risks of making e-cigarettes available in prisons were mentioned in the staff interviews, including potential health harms for PiC who use e-cigarettes and for staff exposed to e-cigarette vapour, possible financial burdens for PiC, problems if PiC are unable to make e-cigarettes last until the next delivery from the prison shop (canteen) and continued high rates of nicotine addiction in the prison population:
Have they been proven safe? What are we going to do in another year, 18 months when you’ve done your studies, there’s other people done studies, ‘Ah, those e-cigarettes are not safe! Right, [their name], go and take the e-cigarette off them’? ‘Oh, right, no bother!’
ExS, E2
. . . you can see what’s going to happen in a few years’ time, you’re going to have people who are very addicted to the e-cigarette, understandably, they’re going to be addicted to nicotine . . .
Unknown, C4
There was also some unease that e-cigarettes might create organisational problems, as it was anticipated that some PiC would find alternative uses for e-cigarettes that violated prison rules, for example to charge mobile phones or take illegal drugs. Hence, there was support among some staff for making e-cigarettes available in prisons for a limited period to reduce potential harms:
I think just the fact that they can be used to charge mobile phones . . . it’s just a big no-no unless they can find a way round that. ‘Cause it would just be a security nightmare.
NS, B2
I think it [e-cigarettes] could be used in the run up, but once the ban’s actually in place, I don’t think there should be any sort of, substitutes because we’ve got a whole year [leading up to smoke-free policy], so I think everybody should be aware of the fact that it’s coming.
S, B3
Staff continued to express some confusion about e-cigarettes generally, and there were requests for information on the specific products that would be available to purchase in prisons.
Perspectives on measures to support implementation of smoke-free prison policy
Preparations in prisons for the implementation of the smoke-free policy were at a relatively early stage at the time of these phase 2 staff interviews (9–12 months prior to implementation). Local co-ordinators and implementation teams were planning and starting to deliver a programme of work to aid the transition to smoke-free rules, led by the national team at SPS headquarters. A member of staff with responsibility for local policy implementation anticipated that the governance arrangements for the transition to smoke-free rules would confer benefits, for example consistency in the implementation of smoke-free rules across the estate and an effective means of sharing learning and good practice. One of the key preparations to date, as reported by staff interviewees, was a communications campaign to raise awareness of the forthcoming policy among PiC, including ‘countdown’ posters in all prisons:
There is information [about the smoke-free policy] coming out quite regular, there is a notice every month now, just a countdown basically, there’s 10 months to go, there’s 9 months to go.
NS, B3
There was support among staff for plans to increase and extend communications in subsequent months, because they expected clarity and dialogue with PiC and staff to be key to the successful implementation of smoke-free rules:
. . . I’m aware that some of the feedback from prisoners and staff will be that they’re not really quite sure what’s happening [about specific details of the smoke-free policy] and to some extent that’s because we’ve not had definitive stuff to put out . . . now that things are starting to progress, we will increase our communication, that’s really our main sort of strategy, I think, is letting people know what is happening, ‘Here’s what’s going to happen, here’s the support that’s available and here’s how you access it’.
NS, A1
Some suggested that it would be beneficial for communications to be delivered through multiple channels and include the benefits of stopping smoking, the rationale for the smoke-free policy and how it would be implemented, and the support available to help PiC to quit or abstain from smoking, including information on tobacco substitutes and if/when e-cigarettes might be available. Staff explained that more detail about the smoke-free policy/e-cigarettes and basic information/training in respect of smoking abstinence/cessation would help with answering questions from PiC, encouraging and assisting their quit attempts and avoiding or diffusing potentially challenging situations. Some expressed an interest in learning from the successes and challenges of the recent implementation of a smoke-free prison policy in E&W. In addition to sharing information, staff suggested that it would be beneficial to consult and involve PiC and staff in the transition to smoke-free rules:
I suppose a lot of things in the prison is about good communication, good engagement, early engagement, involving prisoners, as opposed to doing it to them, doing it with them. That’s how we have set up for the local smoke-free team, we’ve had engagement with the prisoners but we’ll be, once we get into the new year, settling down and have a contribution from the prisoners within the forums that we’ve got . . .
S, B4
Analysis of the interview data suggested a good correspondence between the requests and suggestions for communication and engagement strategies for the smoke-free policy made by frontline staff and the plans and ideas discussed by other SPS staff directly involved in and responsible for policy implementation.
Another major focus for staff interviewed in phase 2 was how to support PiC to reduce, abstain or quit smoking, ideally prior to implementation of smoke-free rules. Their requests, ideas and plans for strengthening smoking abstinence/cessation support in prisons related to three main areas. The first was increasing the capacity of the prison smoking cessation service and encouraging uptake among PiC who smoked, for example by training prison officers to provide specialist smoking cessation support or employing additional specialist health-care staff. Second, they suggested expanding support options and tools in prisons to help individuals to stop smoking (e.g. informal encouragement/assistance from prison staff, especially ex-smokers; peer-to-peer support among PiC; and by making e-cigarettes/nicotine substitutes (widely) available in prison):
It’s all about getting the nicotine substitute right for November [implementation], in my opinion, for a nicotine addict . . . it needs to be right, it needs to be available, it should be available a few months before . . .
S, E1
Third, the importance of providing distractions or alternatives to smoking in prison for PiC was highlighted, although some staff recognised that this was likely be challenging owing to factors such as the prison regime, funding and security restrictions in prisons. Examples of potentially feasible ideas mentioned by staff included dissemination of an in-cell fitness plan, giving PiC access to self-help digital versatile discs (DVDs) and increasing access to/encouraging greater use of the prison gym and/or recreation time where possible:
What do they do when they’re not smoking? How do you manage that? That’s a risk. Do we buy more gymnasium stuff? Do we offer more PT? Do we offer more exercise? All that kind of thing . . . so it’s about kind of working with prisoners as I say, focus groups, having that chat with them and see what they didn’t like, what they might like to kind of have in place and see kind of where we go from there.
NS, E4
Staff focus groups in all prisons: phase 3
One focus group was conducted in each prison (n = 15) during phase 3 to explore perspectives of staff on the smoke-free rules and any positive and negative outcomes of the new policy for PiC, staff and the operation of prisons. Key findings are also reported elsewhere (Brown et al. 56).
Perspectives on the smoke-free prison policy
Staff generally expressed support for the smoke-free policy because of the need to eliminate SHS in prisons for the safety and comfort of staff and non-smoking PiC:
What a difference it makes to your life . . . you go home, you feel better, smell better. Particularly in [one] hall, they smoked very heavily, I found, and although I didn’t smell it during the day, but going to the gym and then having a shower and then putting my clothes back on, I could smell it on my clothes. I’m also asthmatic and I found it didn’t help my asthma to any extent at all.
NS NV, K6
Another reason staff favoured the policy was because of the perceived need to reduce smoking rates among PiC and support health improvement in prisons:
I was always supportive of it because the people who live here are in our care . . . should be really going out healthier than when they come in. You can’t be doing that effectively if they’re sitting in a cell for significant periods of time smoking tobacco . . .
ExS ExV, MA1
It was suggested that the total prohibition of smoking in prisons had created greater parity between rules in prisons and in other public spaces and workplaces in Scotland. Shared cultural norms in respect of smoking were felt to be important for individuals moving between prison and the wider community:
. . . it’s reflective of what’s happening outside . . . when they’re outside and they’re in society, they go into a restaurant, they can’t smoke in that restaurant. If they go into a pub, they can’t smoke in a pub . . . That’s life.
ExS-NV, B5
Some groups expressed disappointment about what some felt had been the lengthy timescale for prohibiting smoking in prisons relative to implementing smoke-free laws in wider society. In one group, a staff member suggested evidence from TIPs on SHS exposure levels in prisons had helped to precipitate the smoking policy change in Scottish prisons:
Ten years it took before they actually got around to actually enforcing it to prisoners, and the only reason they got around to doing that is because you [TIPs] got involved, and that’s the truth. If you hadn’t got involved, if you hadn’t done your studies, pointed out the fact that landings [residential areas] were still . . . passive smoking was still high in the areas and all the rest of the things that happened, the Scottish Government, and especially the SPS, would never have pushed it . . . so I would say thanks to you lot for getting involved and . . . saying, actually, there is a high level of passive smoking . . .
NS-NV, I7
Similarly, staff in another prison described the SHS results as a ‘turning point’ in drawing attention to a workplace hazard (SHS) that had become normalised and to some degree tolerated or accepted in prison:
. . . it’s the environment we’ve worked in for years, the culture, and it just shows you it needs experts and all that to come in and go ‘There’s a risk here’ . . .
Yes.
. . . because you just get caught up and that’s the norm. But it’s a far better place to work now.
We always, kind of, minimised it to a degree to ourselves . . . the second-hand smoke, they smoke in their cells, it’s not affecting us, but when you actually start to see how that smoke can go anywhere within that area the figures support it, you go, ‘Wow!’ That was the turning point, I think.
By contrast, in a few instances, staff voiced (strong) opposition to the smoke-free rules for PiC because they believed that PiC should have choice about smoking as a matter of principle and because it was seen to be unfair to prevent someone using a substance (tobacco) in prison that can legally be consumed in wider society:
It’s not as though we’re doing it to reflect what’s happening in society because that’s all about encouraging people to make healthy choices. We’re not getting people to make healthy choices.
ExS-NV, J2
These staff voiced a need for greater government investment in alternative (or additional) measures to improve PiC’s well-being and holistic health, including measures to help them understand and address the causes of substance use.
Some suggested that making tobacco a banned substance in prison might also be viewed unfavourably by some staff because it created another set of rules for them to enforce:
. . . there’s enough rules that we’re trying to enforce on a daily basis without them moving goalposts and moving the ideas. You can’t just tell folk what to do all the time . . .
ExS-NV, B2
Notably, there was broad consensus among participating staff, irrespective of levels of support for the new smoking rules, that the transition to smoke-free prisons had caused substantially less disruption than expected:
I think we were all expecting there to be a major problem when they actually stopped smoking and I think . . . for 2 weeks we sat on . . . you know, with bated breath waiting for it to happen, and it didn’t. . . . it was a very, very smooth transition, considering what we did with the population that I would suspect 80/90 per cent of them did smoke, you know. It’s an amazing difference . . .
SV, E6
The smooth transition was also said to have enhanced the popularity of the policy among staff:
[. . . in the lead-up to the ban some staff were saying] ‘We’re going to lose this jail, we’re going to lose this!’, really negative aspect of the potential problems. Then as it went on and on, we’ve seen that it’s not as big an impact as we thought it was. Then that negativity then moved to more of a positivity in relation to their health as well as the prisoners they’re dealing with . . .
NS-NV, FA
Staff mentioned several measures that they believed had facilitated the implementation of the smoke-free policy in Scotland’s prisons, including effective planning and oversight of smoke-free policy implementation by staff working in SPS headquarters and individual prisons, taking account of learning from other smoke-free prison systems, key stakeholders having good awareness of impending changes to smoke-free rules thanks to effective communication and engagement, contributions and support from prison staff and partner organisations (particularly the NHS), acceptance of new smoke-free rules by PiC, and availability of tools and support to help PiC to manage without tobacco or quit nicotine in prison.
Outcomes of the smoke-free prison policy
Second-hand smoke
Protection against the health risks and discomfort of SHS exposures was reported to be the major benefit of implementing a smoke-free policy in Scottish prisons:
I’m asthmatic . . . I don’t need to use my inhaler half as much . . . since the ban came in, I would probably say, aye. I don’t have chest infections. I mean, when you’re working in that environment, you’re just constantly subjected to it. I think the air quality was pretty poor when they were doing the [TIPs air quality] tests.
SV, O6
Staff reported previously worrying not only about the dangers of SHS for themselves, but also about negative impacts on their families:
Now you can open the door and there’s no smell of it. And it makes a huge difference ‘cause obviously it’s their smell, there has to be fumes and whatever carried through that, so you’re not breathing any of that in. It’s a huge, huge difference now.
ExS-NV, G10
Yeah, there was always that jail smell, wasn’t there, that you used associate with your work, but it’s not there now.
NS-NV, G4
You were taking it home with you. You were looking . . .
ExS-V, G5
. . . your clothes were smelling of the smoke. And if you’ve never smoked, it’s quite hard. But you expected that. That was the normal.
NS-NV, G11
Staff also spoke about how the eradication of SHS in prisons had created ‘safer’ and cleaner living environments for PiC:
. . . it’s a far better and safer environment for not just the staff, but the prisoners. [Name of prison] has just very recently gone back into sharing cells . . . we’re back into double cells and, you know, doing risk assessments [for] prisoners. And it makes it slightly easier for us to do that with more non-smoking prisoners within their setting.
ExS-NV, L4
There were comments not just about how substantially the situation in prisons regarding SHS levels had improved (particularly for residential staff) since the implementation of smoke-free rules, but also about how quickly this happened. For example, one staff member described being struck by the change in air quality about 1 week after smoke-free rules were introduced:
I came back [to work post implementation of the ban] and I was in [residential hall], and it wasn’t after ‘til about a couple of minutes in the flat talking to the staff, I could smell, and I wasn’t smelling tobacco, you actually smelt kind of fresh air, and that’s when it really hit home to me. You don’t realise the environment we work in . . . it wasn’t until I was back and they had a week of non-smoking . . . and I was standing [specific location], and you could virtually smell fresh air. That’s what brought it home to me that it made such [a difference] and in such a small period of time.
NS-NV, K3
Smoking abstinence/cessation
Improvements to the health of PiC who were no longer smoking because of the smoke-free rules were also seen as a positive development, although uncertainty was expressed about how long people might remain tobacco abstinent post release:
. . . some that were smokers said they do feel better, now that they have given it up . . . when you take them back out of this environment, they may just go straight back onto smoking. But it does give them the tool, that they know they can [stop] if they have to.
NS-NV, C5
Another potential benefit of the smoke-free rules mentioned in some groups was the financial benefits for PiC who quit nicotine or were spending less on e-cigarettes than they previously spent on tobacco in prisons.
Disruption in prisons
Despite initial fears, no major incidents (e.g. riots) were known to have occurred:
. . . what about in terms of trouble [in the smoke-free period]?
Minimal, what I’ve heard of. Next to nothing.
And there’s never been any that I know in any other establishment.
No, nobody [PiC] seems to have . . . went out their way to make a point that we’re doing this because it’s smoking. Maybe because they’re not getting a visit, maybe because they’re not getting to see the nurse . . . But tobacco’s never really raised its head in that department.
Coping without tobacco
Staff reported that PiC had widely accepted the smoke-free rules, even if they did not agree with them, and it was suggested that, overall, PiC had adjusted reasonably well to not being able to smoke in prison:
. . . on the whole how well or not do you think the people in custody are coping without tobacco . . .?
I don’t see much difference . . . You have your occasional feeling that [they are] wanting a cigarette and you just explain to them that it’s a smoke-free environment, I can get this [nicotine substitute] for you . . . and that seems to be enough for them, really.
At the same time, it was recognised that smoking abstinence might be more challenging for certain groups, including new admissions to prisons and PiC with no or low motivation to quit or who struggle to manage nicotine dependence using replacement products such as e-cigarettes.
There was little indication in the data that staff thought that the smoke-free rules had resulted in a substantially negative impact on the risk of self-harm, suicide or poor mental health in prisons. However, one group voiced concerns about potential adverse effects and suggested that data on relevant outcomes should be monitored as part of wider TIPs work.
Contraband tobacco and illegal drug use
Contrary to experiences in some other jurisdictions, contraband tobacco was not reported to be a major problem in prisons in Scotland in the smoke-free period:
. . . we were talking, when we first went smoke-free, about having to liaise with the police every time . . . We had the number for the local police station, we had conversations with them about how we were going to do it. It hasn’t really materialised, due to the small numbers. We’re still finding lighters, we found a bag of lighters yesterday, but nowhere near, I don’t think, what they were expecting.
NS-NV, C1
. . . we find lighters in cell searches and stuff like that. But you don’t smell tobacco, and it would be quite obvious if someone was smelling tobacco. It makes it easier to smell what they shouldn’t be smoking, anyway, like . . .
NS-NV, K4
We were expecting tobacco products every day, for weeks.
S-ExV , K6
I know, it was just like, nothing.
ExS-V, K1
Staff suggested that the absence of major issues with contraband tobacco was because of factors such as the availability of e-cigarettes, acceptance of the smoke-free policy and difficulties concealing and smuggling contraband tobacco. Some suggested that illegal drugs might be being used as a substitute for tobacco in smoke-free prisons or that illegal drug use was being aided by the availability of e-cigarettes (see E-cigarettes):
Are they transferring their nicotine habit and replacing it by using other substances as a coping strategy? We don’t know, but I have seen, over the last 6 months to a year, more and more people being placed on ‘at risk’.
S-NV, J3
Issues relating to smoke-free policy in the open prison
Staff reported improvements in air quality in the open prison following the implementation of smoke-free rules (confirmed by objective SHS measures collected as part of the TIPs study). However, there were suggestions that the number of rule violations was larger than in closed prisons. Staff suggested that some clandestine smoking (particularly on prison grounds) was going undetected, partly because of competing pressures on staff time:
I think, from a staffing point of view, with the health and well-being, and the health and safety side of things, I think it’s improved it tremendously, from passive smoke, and the dangers of that. I know they maybe still go out in the fields, and stuff like that, and they’re still not allowed to, it’s their choice to do that. But certainly, in the accommodation, it’s a lot healthier for staff and other prisoners . . .
NS-NV, A9
The reason that the implementation of smoke-free rules had been more challenging in the open prison was because PiC could access (and legally consume) tobacco while on work placement in the community or on home leave. Staff recognised that it was very challenging for some PiC to abstain from smoking when returning to prison after spending time in the community and noted that serious violations of smoke-free rules could come at a personal cost to PiC who are at a critical point in their sentences:
It [smoke-free rules in the open prison] puts individuals, and staff, in a precarious position, whereby they’re out one minute, smoking, and they’re coming back into the establishment, and they’re not allowed to smoke . . . So, you know, we could be setting them up to fail, as such, in a way, as well. I know from stopping for a couple of years at a time . . . the least wee trigger, it doesn’t matter what it is, will pull you back into it.
S-V, A5
In this context, staff noted that the Quit Your Way Prison Programme (NHS Inform, Glasgow, UK) in the open prison was still experiencing a high demand for support from PiC, and staff voiced a need for continued investment to ensure that PiC were adequately helped if they experienced smoking lapses/relapses.
Despite these challenges, staff also spoke about potential benefits for PiC who have succeeded in reducing or stopping smoking following the introduction of smoke-free rules in the open prison:
I think sometimes, we are focusing quite a bit on the negatives, but what about the non-smokers. I’ve seen people that have come out of this, and seem to be doing alright, and doing quite well. I know we’ve got our hardcore guys, but I’ve certainly seen guys, and I’ve had guys, and you must’ve had them, [name], who have done quite well.
NS-NV, A7
There are a few people . . . they’ve maybe been thinking about stopping, and used this as an opportunity. But they’re in the minority. The majority of them are, ‘This has been forced upon us, we don’t want to stop, but if we don’t stop we’re losing our home leaves’, so it’s fighting a losing battle, really.
ExS-V, A1
E-cigarettes
A recurring theme in the focus groups was that making e-cigarettes available in prison had been instrumental in mitigating potential negative effects of the smoke-free prison policy for PiC, staff and the prison service [‘there has to be an alternative (to tobacco in prison) . . . They’ve (e-cigarettes) taken everything away and all the potential problems of violence and stuff like that coming in . . .’ (S-NV, J3)]. [The views of staff and PiC on e-cigarettes have been explored in much more detail in our complementary CRUK-funded study55,73 (see also Acknowledgements, Publications).] However, some staff questioned or expressed doubts about whether or not e-cigarettes would be beneficial overall in prisons, and some suggested they should not have been introduced because they were not without their own challenges. Staff also voiced questions and concerns about the fact that the evidence base on the health risks of e-cigarettes to users and bystanders is still developing. Some staff suggested that it had taken considerable time before the dangers of SHS exposure were understood and that a similar situation might occur with e-cigarette vapour and erode the health gains of prohibiting smoking in prisons:
The long-term effects, again, as somebody who’s worked here for 20 years, we don’t know the effects of second-hand smoke on our lungs, for all those years that it’s caused us. And now we don’t know the effects of a vape, what that’s causing us.
ExS-NV, N6
Unease was expressed by some staff about many PiC continuing to use e-cigarettes 6–8 months into the smoke-free period, for example because of uncertainties about the long-term effects of vaping; beliefs that some e-cigarette users in prisons (and in wider society) were misinformed that e-cigarettes were ‘safe’ to use, rather than less harmful than smoking tobacco; and/or suggestions that e-cigarette use might be at odds with the goals of smoking cessation.
E-cigarettes had reportedly created some problems in prisons similar to those previously caused by tobacco, such as PiC vaping outside designated areas, PiC experiencing difficulties managing e-liquid supplies and borrowing or trading e-cigarettes and potentially getting into debt.
A final problem that staff identified with making e-cigarettes available within prisons was that they could be misused, for example to take illegal drugs such as new psychoactive substances (NPSs). Although NPS use was not new in prisons, staff discussed how e-cigarettes provided some PiC with an easy and discreet means of ingesting NPSs without requiring access to smoking materials:
. . . well, I’d say it’s a big problem, they’d find another way to do it [take NPS] if it wasn’t these vapes. It is a convenient way, I think, for them to do it because we are finding the little broken vapes all over the place all the time.
ExS-NV, G13
I think the handy thing for it is if you were using a lighter and you were trying to smoke that bit of paper, you either need to put it in to a cigarette or just try and inhale the fumes as it burns. Where now they’ve got a device that they can hold and draw it at once . . . It’s like an aid to it.
ExS-NV, G10
However, NPS use in prisons was recognised to be linked to a wider range of factors beyond smoke-free rules and e-cigarettes:
NPS is going to be the drug of choice, anyway. And whether they took it through a vape, or whether they smoked it . . .
That’s the drug of choice.
. . . it’s the drug of choice, just with the change in society. Any mandatory drug testing, it doesn’t show up a lot, because it’s chemicals . . .
Easy to get it into the jails, as well. It’s not like cannabis where you’ve got a lump of it, and you’ve got to try and conceal it somewhere. It can be a bit of paper and you don’t even see it, that’s just . . .
Is it cheaper as well?
Yeah, uh-huh.
Staff voiced concerns about the adverse effects of NPSs in prisons, including risks for bystanders who experience secondary exposures to NPSs and potentially aggressive or violent behaviour by those under the influence of NPSs, as reported and explored in a parallel set of individual interviews with prison staff as part of the CRUK-funded study (Brown et al. 56). There were also a few reports that e-cigarettes had been used as weapons by PiC and that some PiC had tried to adapt e-cigarette chargers to use with illicit mobile telephones (although they questioned how effectively this worked).
Staff voiced support for measures to help to minimise potential unintended adverse consequences of e-cigarette use in prisons (particularly problems in respect of NPS use). Ideas included reviewing e-cigarette products sold in the ‘canteen’ and greater help in prisons for PiC who want to cut down or quit vaping or have co-occurring conditions, such as poor mental health. Arguments for and against a potential outright ban on the sale of e-cigarettes in prisons in the future covered some similar themes to those discussed in earlier phases of the study by staff in respect of tobacco bans, such as whether or not it would be legitimate, fair and practicable to restrict use of a popular, pleasurable product in prisons to protect or improve health.
Summary
Work package 3 explored prison staff’s attitudes to and experiences of PiC smoking, current smoking (and e-cigarette) rules, and potential changes and SHS using (1) online surveys for staff in all prisons in phases 1–3, (2) focus groups with staff across Scotland in phase 1 and phase 3 and (3) one-to-one interviews with staff in ‘case study’ prisons in phase 2. As survey return rates were below one-third and lowest in phase 3 (27% in phase 1, 31% in phase 2, 16% in phase 3), survey findings should be interpreted with caution.
The proportion saying that rules about smoking for PiC were not strict enough and not well followed fell from 67% and 43%, respectively, in phase 1, to 51% and 33% in phase 2, respectively, and 23% and 16% in phase 3, respectively. Staff scores on a composite measure, ‘positive about bans’, were higher than for PiC, but lower for ‘bans will be difficult’. Greater positivity about potential smoking bans was associated with being a NS, being in better health, having more respiratory symptoms and working in an operational role. Those working in prisons with lower measured SHS levels and reporting fewer sensory symptoms were more likely to agree that ‘bans will be difficult’. Support for prison smoking bans increased in anticipation of/following the ban, and there were large decreases in agreement that prison smoking bans ‘cause a lot of trouble’ and ‘are hard to enforce’. Respondents almost universally agreed that ‘staff should be protected from cigarette smoke at work’ at each phase, and agreement that ‘prisoners who don’t smoke should be protected from cigarette smoke’ was also high.
Around three-quarters agreed that the introduction of the ban had been ‘largely trouble-free for the prison service’, had ‘led to improved working conditions for staff’ and ‘made the prison smell better’. Around half believed that it had helped to improve staff health, the quality of life and health of PiC and the appearance of the prison. However, around half thought that it had ‘led to more use of illegal drugs’, and one-quarter to one-third thought that it had ‘made prisoners more anxious’, led to more physical or verbal assaults or aggression and ‘made prisoner behaviour more difficult to manage’. Few thought that it had led to more purposeful activity or made PiC happier. Post-implementation survey responses indicate that the most serious perceived problem related to PiC adapting e-cigarettes devices and chargers.
In the phase 1 focus groups, on balance, staff thought that further restrictions to PiC smoking were equitable, justifiable and necessary to protect the health of non-smoking staff and PiC. Some were disappointed that the prison service had not protected them from SHS exposure at work earlier and regarded this as a form of injustice given the known adverse effects of SHS. However, concerns were expressed that smoke-free prison rules could be unworkable and about unintended consequences (including reduced well-being among PiC, confrontations and violence, riots, contraband, bullying, use of alternatives and increased staff stress). Others expressed more confidence that smoking rules could be changed and there was broad consensus that staff had experience of managing a wide range of problems and the prison service had successfully managed other challenging organisational changes. Some anticipated that any problems would be short-lived, as PiC adjusted to the ‘new normal’. Participants highlighted the need for PiC and staff to be well informed about any rule changes, with adequate time, resources and management support for frontline staff in preparation for the removal of tobacco. They recognised the importance of involving PiC, including peer ‘champions’, and learning from other jurisdictions with smoke-free policies. Staff articulated the need for smoking cessation support and tools, but divergent views were expressed about whether or not e-cigarettes should be permitted. Some thought replacing smoking with vaping would be a ‘step in the right direction’ and might aid a difficult organisational change. Others expressed anxieties about e-cigarettes because of incomplete evidence on the risks of exposure to e-cigarette vapour. There was much discussion about the potential risks of e-cigarettes that were distinct for the prison context.
One-to-one phase 2 staff interviews raised many of the same issues. Anticipated benefits included reducing SHS to protect the health of PiC and staff and creating an improved working environment. Drawbacks continued to focus on concerns about choice for PiC and potential adverse consequences. Views on e-cigarettes also mirrored phase 1 findings; some suggested that introducing them would ‘soften’ the impact of the ban but potential risks of making e-cigarettes available were raised, including potential health harms for e-cigarette users and staff exposed to their vapour, possible financial burdens for PiC and problems if PiC were unable to make e-cigarettes last between deliveries from the prison ‘canteen’. There was some unease that some PiC would find uses for e-cigarettes that violated prison rules. Staff discussed the need to increase the capacity, options for and uptake of prison smoking cessation services and support, ideally prior to the implementation of smoke-free rules.
In the phase 3 focus groups, staff generally expressed support for the smoke-free policy. Protection against the health risks and unpleasantness of SHS exposures was reported to be the major benefit of the policy. Staff noted how substantially SHS levels had improved (particularly for residential staff) and the rapidity of this change. The TIPs SHS results were described as a ‘turning point’ in drawing attention to a workplace hazard that had become normalised and to some degree tolerated in prisons. Staff anticipated improvements to PiC’s health, but expressed uncertainty about how long people would remain tobacco abstinent post release. Some identified potential financial benefits for PiC who quit nicotine or spent less on e-cigarettes than they had previously spent on tobacco. They suggested that more similar cultural norms around smoking were important as individuals moved between prison and the community. A few still voiced opposition to smoke-free rules because they believed that PiC should have a choice about smoking and because they regarded it as unfair to prevent PiC from using tobacco when it can legally be consumed in wider society.
There was widespread agreement, irrespective of levels of support for the new rules, that the transition to smoke-free prisons was much less disruptive than expected. Despite initial fears, no major incidents were known to have occurred. Several measures were believed to have facilitated implementation, including effective planning and oversight by staff working in SPS headquarters and individual prisons, drawing on learning from other prison systems; widespread awareness of impending changes as a result of effective communication and engagement; support from prison staff and partner organisations (particularly the NHS); acceptance of the new smoke-free rules by PiC; and availability of support to help PiC quit or manage without tobacco. It was thought that PiC had mainly accepted smoke-free rules, even if they did not agree with them, and that, overall, PiC had adjusted reasonably well to not being able to smoke in prison, although smoking abstinence was recognised to be more challenging for certain groups, such as new admissions or people with low motivation to quit. Contrary to experiences elsewhere, contraband tobacco was not seen as a major problem. The availability of e-cigarettes was seen as one instrumental factor in mitigating potential negative effects of the smoke-free prison policy for PiC and staff. However, some staff questioned whether or not e-cigarettes would prove beneficial overall in prisons long term and some suggested that they should not have been introduced. Questions and concerns were voiced about the evidence base on the health risks of e-cigarettes to users and bystanders. E-cigarettes were reported to create some problems, such as PiC vaping outside designated areas, experiencing difficulties managing e-liquid supplies, borrowing or trading e-cigarettes and potentially getting into debt. A final problem identified was misuse, for example staff discussed how e-cigarettes provided some PiC with an easy and discreet means of ingesting NPSs. Staff suggested measures to minimise potential adverse consequences of e-cigarette use, including reviewing the e-cigarette products sold on the ‘canteen’ and greater help for PiC who want to cut down or quit vaping.
Chapter 6 Perspectives, opinions and experiences of people in custody
Introduction
Work package 4 of the TIPs study was designed to elicit the attitudes and experiences of those in custody within the prison service in Scotland with respect to smoking and its place within prison cultures, smoking rules and the (impending) smoking ban, and e-cigarettes. It comprised (1) cross-sectional fully anonymised surveys open to PiC in all 15 prisons in phase 1 (pre announcement), phase 2 (preparatory phase) and phase 3 (post implementation); and (2) one-to-one interviews with 38 PiC in ‘case study’ prisons in phase 2 and 23 PiC in phase 3 (see Figure 1). Further details are available in publications from the study40,54,72 and Appendix 2.
Surveys of people in custody
Tables in Report Supplementary Material 2 show the basic frequency distributions of all survey items for PiC at each phase (numbers and percentages rounded to integers for simplicity of presentation).
Return rates, sociodemographic and prison-based characteristics
Surveys were returned by 2512 (34%) PiC in phase 1, 1959 (25%) in phase 2 and 1485 (18%) in phase 3, with considerable between-prison variation in return rates (as for staff, see Chapter 5, Return rates, sociodemographic and work-based characteristics, and Table 3). Return rates tended to be lower in the two privately run prisons, and the notably lower return rate in the post-implementation phase is despite following identical procedures for each phase (with the exception of three prisons in phase 1 described above, see Chapter 2, Survey circulation/distribution). As noted for prison staff (see Chapter 5, Return rates, sociodemographic and work-based characteristics), given the levels of response overall and the variation in response by prison and by phase, all figures presented below should be interpreted with caution. Analyses using simple weights derived to adjust for this variation for published papers relating to results on opinions39,72 produced virtually identical results to those based on unweighted data.
Sociodemographic and prison-based characteristics (see Report Supplementary Material 2, Tables 146–153) were very similar across all phases. The proportion of males returning questionnaires at each phase (91–93%) was slightly lower than the proportion of males across Scottish prisons as a whole (95% in 2018–1974), but the proportion convicted (82–83%) was similar (80% in 2018–1974). Around 50% were aged 31–50 years, and one-fifth or less were aged ≥ 51 years.
Self-reported exposure to second-hand smoke/vapour
In phases 2 and 3, PiC, like staff, were asked how often (never, sometimes, often, always) they were exposed to ‘other people’s smoke’ and ‘vapour or smells from other people’s electronic cigarettes’ in various locations. Figure 6 shows a marked drop in any (sometimes, often, always) reported ‘smoke’ exposure in cells, the halls and during outdoor exercise, paralleled by increases in ‘vapour’ exposure between phases. It also suggests that PiC perceived that illicit tobacco smoking continued at some level, and that there was some e-cigarette use in locations (work-sheds, gyms, education centres) where it was not permitted under prison rules, in phase 3.
FIGURE 6.
Reporting by PiC of any exposure to cigarette smoke/e-cigarette vapour in various locations.

Opinions on (rules about) smoking and tobacco in prisons
The proportion reporting that the current rules about tobacco smoking among PiC were not well followed (vs. very/quite well followed) was stable between phase 1 (24%) and phase 2 (26%), but dropped in phase 3 (18%) (p < 0.001). In phase 3 only, around one-quarter (23%) of PiC reported that rules about e-cigarettes were not well followed.
People in custody were asked the same prison smoking ban opinion questions as staff in each phase,40,72 and factor analyses of phase 1 data identified the same factors in both groups: ‘positive about bans’ (lower scores among PiC than staff) and ‘bans will be difficult’ (higher scores among PiC) (see Chapter 5 and Sweeting et al. 40). In multivariable analyses among PiC, ‘positive about bans’ factor scores were very strongly associated with not smoking, and with reporting no asthma, more sensory symptoms, higher educational level and prisoner status [unconvicted vs. convicted (with different release dates)]. Only current smoking was significantly associated with ‘bans will be difficult’ among PiC (Sweeting et al. 40). Further multivariable analyses restricted to PiC who smoked found the number of cigarettes per day was inversely associated with ‘positive about bans’, and having craved cigarettes and a past year quit attempt were associated with both factors. As described (see Chapter 5, Online surveys of prison staff: phases 1, 2 and 3), further published analyses72 compared opinions of staff and PiC in respect of prison smoking bans and e-cigarette use by PiC across phases.
As shown for staff [see Chapter 5, Opinions on (rules about) smoking and tobacco in prisons], the opinions among the PiC who responded appeared to shift over time (Table 8). Although generally much less positive than staff, support among PiC for prison smoking bans increased somewhat in anticipation of/following the ban, whereas there were substantial decreases between phase 2 and phase 3 in the proportions agreeing that prison smoking bans ‘cause a lot of trouble’ and ‘are hard to enforce’. This was not paralleled by a change in the proportion in favour of increased smoking restrictions in Scottish prisons; just 35% of respondents in phase 3 agreed that prison smoking bans were ‘a good idea’. Nor was there change in agreement that prison smoking bans ‘are OK if prisoners are allowed e-cigs’ or that e-cigarettes should ‘be available to help prisoners stop smoking/manage without tobacco’. Although agreement that smoking should not be allowed in any indoor or outdoor areas was highest in phase 3, as for staff, agreement by PiC that ‘prisoners who don’t smoke should be protected from cigarette smoke’ and that ‘there should be more NHS support for prisoners who want to stop smoking’ was lowest at this point.
| Opinion item | Phase (%) | Significant differencesa | ||
|---|---|---|---|---|
| 1 | 2 | 3 | ||
| Prison smoking bans (agree/strongly agree) | ||||
| Prison smoking bans are a good idea | 22.4 | 25.3 | 35.4 | 1 < 3, 2 < 3 |
| Prison smoking bans cause a lot of trouble | 81.2 | 79.9 | 58.2 | 1 > 3, 2 > 3 |
| Prison smoking bans help prisoners stop smoking long term | 20.7 | 23.3 | 24.4 | – |
| Prison smoking bans are hard to enforce | 64.5 | 58.6 | 35.7 | 1 > 2, 1 > 3, 2 > 3 |
| Most staff want prison smoking bans | 32.7 | 41.8 | 44.6 | 1 < 2, 1 < 3 |
| Prison smoking bans are OK if enough stop-smoking support is available | 36.6 | 42.6 | 43.9 | 1 < 2, 1 < 3 |
| Prison smoking bans are OK if prisoners allowed e-cigarettes | 48.4 | 44.9 | 48.5 | – |
| Smoking restrictions in Scottish prisons | ||||
| In favour of (hypothetical/impending/actual) increased smoking restrictions in Scottish prisons | 23.5 | 25.0 | 27.3 | – |
| Prisoners’ access to e-cigarettes (agree) | ||||
| Should e-cigarettes be available to prisoners to buy from the canteen? | Not asked of PiC in all phases | |||
| Should e-cigarettes be given to prisoners temporarily to help with tobacco withdrawal when admitted to prison? | Not asked of PiC in all phases | |||
| Should e-cigarettes be available to help prisoners stop smoking/manage without tobacco? | 90.1 | 90.2 | 88.8 | – |
| Smoking in prisons (agree/strongly agree) | ||||
| Staff should be protected from cigarette smoke at work | 55.4 | 58.3 | 57.4 | – |
| Prisoners who do not smoke should be protected from cigarette smoke | 68.2 | 70.6 | 57.1 | 1 > 3, 2 > 3 |
| There should be more NHS support for prisoners who want to stop smoking | 76.4 | 76.2 | 70.6 | 1 > 3, 2 > 3 |
| Prisoners should not be forced to stop smoking | 78.5 | 78.2 | 74.5 | 2 > 3 |
| Prisoners who smoke are unlikely to ever stop long term | 43.1 | 53.3 | 56.6 | 1 < 2, 1 < 3 |
| Smoking should not be allowed in any indoor prison areas | 44.3 | 52.1 | 50.9 | 1 < 2, 1 < 3 |
| Smoking should not be allowed in any outdoor prison areas | 17.9 | 20.8 | 22.9 | 1 < 3 |
Opinions about e-cigarettes generally
In phases 2 and 3, PiC were asked a standard question about the relative harms of e-cigarettes and ‘regular cigarettes’. As with staff, the proportion who thought e-cigarettes were (a lot) more harmful increased (26% in phase 2, 43% in phase 3), whereas the proportion who thought they were (a lot) less harmful dropped (from 37% to 26%), as did the proportion reporting that they did not know (37% to 31%) (p < 0.001).
As Table 9 shows, again, like staff (see Chapter 5, Opinions about e-cigarettes generally), PiC expressed more negative views about e-cigarettes in phase 3 than phase 2, with increased agreement that e-cigarettes are ‘addictive’ and ‘raise safety issues’, and decreased agreement that they ‘can stop people smoking’ and ‘are as good as other nicotine replacement therapies to help people stop smoking’.
| How much do you agree e-cigarettes . . . | Phase | Agreement (%) | Significance of chi-squared test | ||
|---|---|---|---|---|---|
| (Strongly) agree | No opinion | (Strongly) disagree | |||
| Can stop people smoking? | 2 | 70 | 19 | 11 | |
| 3 | 58 | 16 | 26 | < 0.001 | |
| Are addictive? | 2 | 48 | 40 | 11 | |
| 3 | 74 | 18 | 8 | < 0.001 | |
| Are as good as other nicotine replacement therapies to help people stop smoking? | 2 | 46 | 37 | 17 | |
| 3 | 40 | 31 | 29 | < 0.001 | |
| Should be allowed in public places where tobacco cigarettes are not allowed? | 2 | 48 | 23 | 28 | |
| 3 | 47 | 20 | 33 | 0.005 | |
| Raise safety issues? | 2 | 36 | 44 | 21 | |
| 3 | 49 | 34 | 17 | < 0.001 | |
Opinions about the introduction of the smoking ban in Scottish prisons
The phase 3 survey included the same questions for PiC as for staff on opinions about the lead-up to and implementation of the smoking ban. In general, PiC were less positive than staff: only around one-third thought that preparation had been good and that implementation had been largely trouble free. However, almost two-thirds thought that people were kept well-informed and the introduction of e-cigarettes had made things easier for both PiC and staff (Table 10). Two-thirds also indicated that the ban had ‘made prisoners more anxious’, around half indicated that it had led to ‘more physical/verbal assaults’ and ‘more use of illegal drugs’ and only 1 in 10 indicated that it had ‘made prisoners happier’. However, around half thought the ban had ‘helped improve prisoner health’ and staff health and had ‘made the prison smell better’, and around one-quarter to one-third thought that it had ‘made the prison look better’, ‘improved prisoners’ quality of life’, led to ‘more purposeful activity’ and ‘helped prisoners stop smoking for good’.
| Asked in phase 3 only | Agreement (%) | ||
|---|---|---|---|
| (Strongly) agree | No opinion | (Strongly) disagree | |
| Lead-up to the smoking ban | |||
| Preparation for the smoking ban was good | 33 | 27 | 40 |
| Staff and prisoners were well informed about the smoking ban | 61 | 23 | 15 |
| Introduction of e-cigarettes/vapes made the smoking ban easier for prisoners and staff | 59 | 21 | 20 |
| Implementation of the smoking ban | |||
| The introduction of the smoking ban has been largely trouble free for the prison service | 33 | 31 | 36 |
| The smoking ban has . . . (ordered greatest to least agreement) | |||
| . . . made prisoners more anxious | 64 | 23 | 11 |
| . . . led to more verbal assaults/aggression by prisoners | 54 | 28 | 18 |
| . . . led to more use of illegal drugs | 53 | 29 | 17 |
| . . . helped improve prisoner health | 52 | 24 | 24 |
| . . . made the prison smell better | 50 | 21 | 28 |
| . . . led to more physical assaults/physical aggression by prisoners | 49 | 31 | 19 |
| . . . helped improve staff health | 46 | 35 | 19 |
| . . . led to improved working conditions for staff | 42 | 36 | 22 |
| . . . helped improve prisoners’ quality of life | 39 | 28 | 33 |
| . . . led to more prisoners taking part in purposeful activity | 30 | 40 | 29 |
| . . . made the prison look better | 29 | 28 | 42 |
| . . . helped prisoners stop smoking for good | 27 | 28 | 45 |
| . . . made prisoners happier | 12 | 31 | 56 |
| . . . led to more fires in prisons | 12 | 42 | 46 |
The phase 3 surveys also included questions on how much of a problem certain issues currently were. PiC generally identified problems as less serious than staff did. However, both groups identified PiC adapting e-cigarettes to use for drugs as the most serious problem (Table 11). Around one-third of PiC identified bullying over e-cigarettes and debt over tobacco as moderate/serious problems and one-quarter thought that bullying over tobacco, trading/buying tobacco and tobacco coming into the prison from outside and being smoked were moderate/serious problems. Although around two-thirds of staff identified the adaptation of e-cigarette chargers as a moderate/serious problem (see Table 7), less than one-quarter of PiC did.
| Asked in phase 3 onlya | How much of a problem . . . (%) | ||
|---|---|---|---|
| Not | Minor | Moderate/serious | |
| Prisoners adapting e-cigarettes/vapes to use for drugs | 41 | 18 | 41 |
| Prisoners bullying one another over e-cigarettes/vapes | 43 | 23 | 34 |
| Prisoners getting into debt over tobacco | 50 | 17 | 33 |
| Prisoners bullying one another over tobacco | 54 | 19 | 28 |
| Prisoners trading or buying tobacco | 51 | 20 | 28 |
| Tobacco coming in from the outside | 51 | 22 | 26 |
| Prisoners adapting chargers for e-cigarettes/vapes in any way | 59 | 16 | 24 |
| Prisoners still smoking tobacco | 52 | 24 | 23 |
In phase 3, PiC who had ever smoked were asked an additional series of question about the smoking ban. Over two-thirds indicated that it was hard not being allowed to smoke and wanted to smoke, and over half felt angry, more bored and reported weight gain as a result of not being allowed to smoke (Table 12). Only around one-quarter indicated that they were not smoking by choice rather than because of the ban. However, approaching half also agreed with three more positive items (the ban ‘is a good opportunity to stop smoking’, not smoking ‘is easier when no-one else smokes’ and feeling ‘healthier’).
| Asked in phase 3 onlya | Agreement (%) | ||
|---|---|---|---|
| (Strongly) agree | No opinion | (Strongly) disagree | |
| It is hard not being allowed to smoke in prison | 69 | 10 | 21 |
| I would like to smoke in prison | 69 | 10 | 20 |
| I feel angry about not being allowed to smoke in prison | 61 | 16 | 23 |
| I feel more bored because I am not allowed to smoke in prison | 57 | 17 | 26 |
| I have gained weight because I am not allowed to smoke in prison | 56 | 20 | 25 |
| The smoking ban is a good opportunity to stop smoking | 51 | 15 | 34 |
| It is easier not smoking in prison when nobody else smokes | 47 | 16 | 36 |
| I feel healthier because I am not allowed to smoke in prison | 43 | 23 | 34 |
| I do not smoke in prison by choice, not just because of the smoking ban | 28 | 18 | 54 |
Smoking among people in custody
At each phase, almost 9 in 10 of those in custody who returned a survey had ever smoked tobacco cigarettes (Table 13); the average age when a cigarette was first tried (asked in phase 1 only) was 12 years. Almost three-quarters currently smoked in phases 1 and 2, and although rates were significantly lower in phase 2, smokers’ average number of cigarettes smoked (19 per day) and past week cigarette expenditure (£13.33) were identical. In phases 1 and 2, almost every smoker smoked in their cell, and, although around half reported having felt like they wanted to stop smoking during their current prison stay, three-quarters had not stopped at all.
| Variable | Phase | Significance of chi-squared test/F-statistic | ||
|---|---|---|---|---|
| 1 | 2 | 3 | ||
| Among all PiC (%) | ||||
| Ever smoked tobacco cigarettes | ||||
| Yes (vs. no) | 88 | 85 | 85 | 0.022 |
| Currently smoke tobacco cigarettes | ||||
| Yes (vs. no) | 74 | 70 | — | 0.002 |
| Smoked tobacco cigarettes when last lived outside prison | ||||
| Yes (vs. no) | 77 | — | 78 | 0.773 |
| Ever tried e-cigarette or vaping device | ||||
| Yes (vs. no) | 47 | 54 | 76 | < 0.001 |
| Currently use e-cigarette or vaping device | ||||
| Daily | — | 7 | 62 | |
| Use less than daily | — | 18 | 6 | |
| Do not use | — | 75 | 32 | < 0.001 |
| Among current (phases 1 and 2) tobacco smokers (%) | ||||
| Do you smoke in your cell? | ||||
| Yes (vs. no) | 98 | 98 | — | 0.705 |
| During your current prison stay have you felt like you wanted to stop smoking? | ||||
| Yes (vs. no) | 53 | 48 | — | 0.007 |
| During your current prison stay, what is the longest that you have stopped smoking for? | ||||
| Not stopped at all | 68 | 67 | — | |
| Stopped for up to 1 week | 14 | 15 | — | |
| Stopped for ≥ 1 week | 19 | 18 | — | 0.297 |
| Among current (phases 1 and 2)/ever (phase 3) tobacco smokers | ||||
| How much have you craved cigarettes today? (%) | ||||
| Not at all | 8 | 8 | 27 | |
| Hardly at all/a little | 31 | 29 | 26 | |
| Somewhat/quite a bit/a great deal | 62 | 62 | 47 | < 0.001 |
| Do you think you will smoke after you are released? (%) | ||||
| Think I will | 74 | 65 | 48 | |
| Do not know | 17 | 24 | 25 | |
| Think I will not | 9 | 11 | 27 | < 0.001 |
| Among current (phases 1 and 2) tobacco smokers | ||||
| Cigarettes (including roll-ups) usually smoked each day (mean, n) | 19.3 | 19.3 | — | 0.871 |
| Past week expenditure on cigarettes/tobacco (mean, £) | 13.33 | 13.35 | — | 0.954 |
| Among current (phases 2 and 3) e-cigarette users (mean, £) | ||||
| Past week expenditure on e-cigarettes | — | 1.98 | 10.46 | < 0.001 |
Table 13 also compares current (phases 1 and 2) and ever (phase 3) smokers in respect of current craving and anticipated smoking post release. In phase 3, half of ever-smokers (some of whom would have been smoke free for a significant length of time) reported craving a cigarette ‘somewhat’, ‘quite a bit’ or ‘a great deal’, although only around half thought they would smoke post release (a substantial proportion answered ‘do not know’ to this question).
Finally, Table 13 shows that the proportion of PiC who had ever tried an e-cigarette rose from around half to three-quarters between phases 1 and 3, and highlights the large increase in daily use (from 7% to 62% of all those in custody) and expenditure (from £1.98 to £10.46 per week among e-cigarette users) between phases 2 and 3.
Opinions about support for quitting smoking
In phases 1 and 2, current smokers were asked how much help they thought they would receive from different sources if they wanted to stop or cut down their smoking. Most support was anticipated from family members (Table 14). Only 1 in 10 anticipated a lot of help from prison staff and other PiC, and only one-quarter (phase 2 only) anticipated a lot of help from prison health-care staff, with one-third thinking they that would provide no help at all.
| Variable | Phase (%) | Significance of chi-squared test | |
|---|---|---|---|
| 1 | 2 | ||
| Prison health-care staff (phase 2 only) | |||
| A lot | 23 | ||
| A little | 43 | ||
| No help at all | 34 | ||
| The prison staff (phase 1)/the other prison staff (phase 2) | |||
| A lot | 11 | 9 | |
| A little | 30 | 29 | |
| No help at all | 59 | 62 | 0.075 |
| Other prisoners | |||
| A lot | 7 | 10 | |
| A little | 35 | 31 | |
| No help at all | 58 | 59 | 0.003 |
| Your family | |||
| A lot | 33 | 29 | |
| A little | 31 | 31 | |
| No help at all | 36 | 40 | 0.016 |
| Your friends outside prison | |||
| A lot | 17 | 17 | |
| A little | 32 | 28 | |
| No help at all | 51 | 55 | 0.047 |
When ever smokers were asked in phase 3 when they stopped smoking, 15% indicated that this was in/before 2017, 10% that this was in January–October 2018, 43% that this was in November–December 2018 (i.e. immediately after the ban) and 32% that this was in January–June 2019. Assuming that the last group predominantly represents those admitted to prison since the introduction of the smoking ban, it seems that the vast majority of PiC continued to smoke right up to the ban’s introduction.
Finally, at each phase, the surveys asked PiC about potential strategies to help stop smoking or manage without tobacco. In phase 1 and phase 2, these were asked of current smokers in respect of the past year; in phase 3, they were asked of PiC, as appropriate, in respect of (1) the year before introduction of the ban and (2) since living in a smoke-free prison. In phases 1 and 2, around one in three had tried to get a place on a prison stop-smoking programme and used nicotine therapy, around one in five had attended a group programme and 1 in 10 had attended a one-to-one programme or used prescribed medication (Table 15). Rates of almost every activity were similar in respect of the year before the introduction of the ban and since living in a smoke-free prison; the exception was use of NRT, which was higher since living in a smoke-free prison. However, the most striking figures relate to the use of e-cigarettes, used to help stop smoking or manage without tobacco by 40% of phase 2 current smokers, 51% in the year before the introduction of the ban and 89% of those who stopped smoking in 2018–19.
| Asked of different group of PiC in different phases | Phase (%) | Significance of chi-squared test | ||
|---|---|---|---|---|
| 1 | 2 | 3 | ||
| Phases 1 and 2, current smokers: in the past year have you . . . | ||||
| tried to get a place on a prison stop smoking programme? | 29 | 32 | – | 0.160 |
| tried going to a group stop smoking programme? | 16 | 22 | – | 0.001 |
| tried a one-to-one stop smoking programme? | 9 | 11 | – | 0.143 |
| tried using NRT? | 29 | 30 | – | 0.707 |
| tried taking prescribed medication? | 9 | 14 | – | < 0.001 |
| tried using e-cigarettes? | – | 40 | – | |
| Phase 3, PiC who stopped smoking in 2018/19 and were in prison in year prior to ban: in the year before the introduction of the smoking ban did you . . . | ||||
| try to get a place on a prison stop smoking programme? | – | – | 32 | |
| go to a group stop smoking programme? | – | – | 27 | |
| go to a one-to-one stop smoking programme? | – | – | 11 | |
| use NRT? | – | – | 34 | |
| take prescribed medication? | – | – | 14 | |
| use e-cigarettes? | – | – | 51 | |
| Phase 3, those who stopped smoking in 2018 or 2019: since living in a smoke–free prison have you . . . | ||||
| tried to get a place on a prison stop smoking programme? | – | – | 39 | |
| been to a group stop smoking programme? | – | – | 29 | |
| been to a one-to-one stop smoking programme? | – | – | 13 | |
| used NRT? | – | – | 45 | |
| taken prescribed medication? | – | – | 11 | |
| used e-cigarettes? | – | – | 89 | |
At every phase, the surveys for staff and PiC asked how good they thought their local NHS prison smoking cessation support was. Staff results suggested a perceived improvement over time (from 45% rating as ‘very’ or ‘quite good’ in phase 1 to 61% in phase 3); however, for PiC, the percentage saying ‘very’ or ‘quite good’ remained stable (40% in phase 1, 42% in phase 2, 43% in phase 3).
Health of people in custody
Ratings of general health among PiC were much lower than for staff. They were lowest in phase 3 (‘very good’ vs. ‘good’ vs. ‘fair’, ‘bad’ or ‘very bad’ reported by 19%, 41% and 40% in phase 1, respectively; 22%, 39% and 39% in phase 2, respectively; and 16%, 41% and 43% in phase 3, respectively) (p < 0.001). Self-reported doctor-diagnosed asthma remained stable (25% in all phases), as did any contact with medical staff in the past 3 months (reported by 20–22%, depending on phase), prescribed medicines (15–17%) and purchase of over-the-counter medicines (6–8%) for a cold, breathing problems or eye irritation.
Self-reported experience in the past month of the nine International Union Against Tuberculosis and Lung Disease respiratory and sensory symptoms40 varied across phases (Figure 7). Three (coughed first thing in the morning, coughed at other times of day, phlegm) reduced between phases and one (eyes red or irritated) increased; three others (cold, nose runny/sneezing, sore/scratchy throat) reduced between phases 1 and 2, increasing again in phase 3. In contrast to patterns observed among staff, these patterns do not appear to reflect time-of-year effects.
FIGURE 7.
People in custody (%) reporting past 4 weeks’ experience of each symptom in each phase.
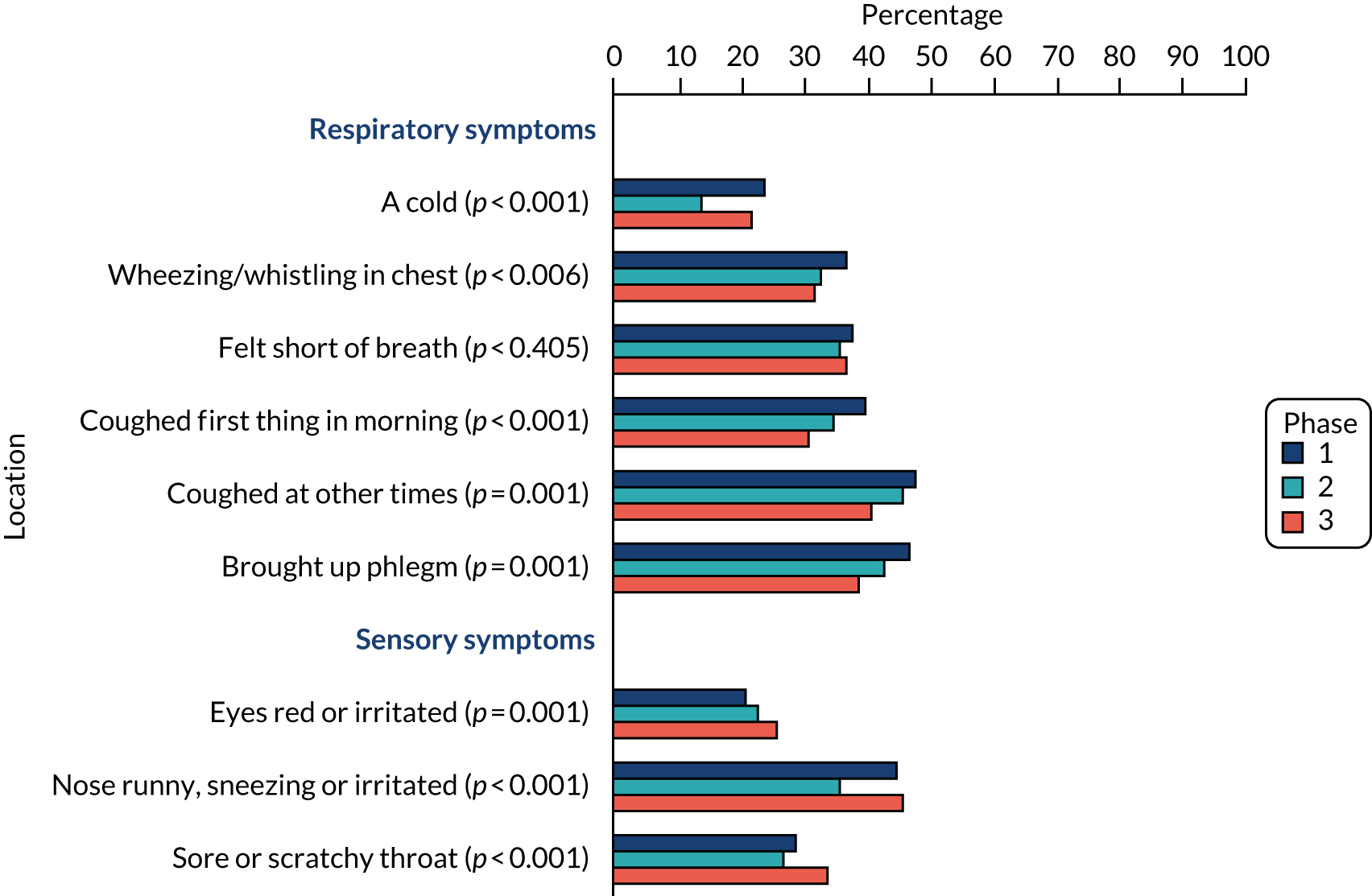
Three of the five ‘your health today’ items (self-care issues, pain/discomfort, anxiety/depression) included in the EQ-5D-5L increased between phase 2 and phase 3 (see Report Supplementary Material 2, Tables 72–76). There was a small decrease in ratings on the visual analogue scale (where 100 represents ‘the best’ health you can imagine).
Preparatory phase (phase 2) interviews with people in custody in ‘case study’ prisons
Here, we summarise and, where relevant, expand on key findings from the interviews with 38 PiC in the preparatory phase, which are reported in detail elsewhere. 75
Facilitators of and barriers to smoking abstinence or cessation in prison
Participants suggested several potential facilitators of smoking abstinence or cessation in prison that may support implementation of smoke-free rules. First, some discussed motivations to stop smoking in the future, including general concerns about the health effects of smoking or specific health problems, wanting to make positive lifestyle changes while in prison (e.g. quitting drugs and tobacco, losing weight and/or improving physical fitness), the high price of tobacco in prison, dislike of the smell of smoke, growing ‘sick’ of feeling dependent on tobacco and a family member (e.g. child) asking them to stop.
Second, as reported by a separate sample of users of smoking cessation services in prison (see Chapter 7), participants in the WP4 sample with experience of the service were also generally positive about its work:
So I went down . . . and I spoke to the lady [smoking cessation advisor], the lady was really, really nice, so open, we could sit and talk about things, and things like that.
S, F2
Third, certain features of the prison environment appeared to have the potential to help with smoking abstinence or cessation, such as lack of access to drugs and alcohol, which was reported to be a potential relapse trigger in wider society. Purposeful activity (e.g. involvement in work parties/education or going to the prison gym) was seen as potentially helpful to smoking reduction or cessation, because smoking was prohibited in these spaces and PiC were able to occupy their time and reduce boredom.
In contrast, potential barriers to smoking abstinence or cessation in prison, and consequently to the implementation of smoke-free rules, centred on three main themes. First, smoking tobacco was considered an important part of many PiC’s daily routines and a social activity that brought PiC together. Participants reported that smoking could provide an ‘escape’ from prison life and a way of managing recurring and sometimes acute feelings of boredom, stress and anxiety, particularly during evenings and weekends. There was a perception that smoking had a calming influence and helped to avert ‘trouble’ in prisons:
So, to me, smoking’s an escape. When I think about bad things, sometimes I have a smoke and it will take my mind off things . . . there’s people in here that need that, they need that escape . . .
S, E2
Second, some participants reported attitudes and beliefs about smoking that may inhibit abstinence/cessation, such as beliefs that smoking is effective for managing stress, misunderstandings or minimisation of the health risks of smoking, and perceptions that willpower alone is the best way to quit smoking and so those lacking willpower to quit will inevitably fail:
And what about in terms of some gyms offer one-to-one help or group help for people who want to give up. Did you ever think about that?
No, because what can they do? They can talk about it, everyone can talk about what you’re going to do, but it’s willpower inside of you, if you haven’t got the willpower to quit smoking, then you’re never going to stop.
Third, several potential barriers linked to smoking cessation services in prison were discussed, including waiting times, a desire for staff to take greater account of individual need and circumstances in the delivery of support, delays receiving NRT from the prison pharmacy and disruption to smoking cessation treatment when PiC transfer between prisons.
Opinions of the impending smoke-free prison policy
Opinions of the impending smoke-free policy varied. Arguments against the introduction of total restrictions on PiC smoking centred on two main themes. First, some expressed strong beliefs that the policy was unfair, as it would remove individual freedom (sometimes referred to as a ‘right’) to smoke and take away a pleasurable activity and a potential tool for managing stress and boredom in prisons, particularly as tobacco is a legal substance to purchase outside prisons:
They’re just taking another thing away from us, they’re just taking another thing . . . which I can understand, the health benefits of it. But if it’s people’s choice, do you know what I mean? So where is it going to end.
S, C1
I don’t understand why they’re doing it [banning smoking] in a jail though because they’re not going to stop smoking out there, so I don’t see why they should stop it in here.
S, B1
Second, some suggested that current restrictions on PiC smoking (e.g. only allowing indoor smoking in designated cells) should provide staff with adequate protection from SHS exposure. Some PiC advocated for alternative measures in prisons to reduce SHS exposure, such as stricter enforcement of existing smoking rules, implementation of indoor-only smoke-free policies or creating voluntary smoke-free wings.
On the other hand, arguments in favour of the smoke-free prison policy related to two main sets of issues. It was acknowledged that the smoke-free rules may improve the health of PiC and might enable them to spend more of their income on other items they valued, such as telephone calls to friends and family. Protecting non-smoking staff and PiC from SHS exposure was seen as another important potential benefit, and it was acknowledged that the smoking ban may also improve the living and working environment in prison (e.g. by removing the smell of stale smoke):
. . . it is becoming a healthier country, so I reckon it’s just inevitable and a good idea to do it in the prisons, because even if a certain percentage of the people that come into prison stop smoking or they’ve stopped smoking before they come in, and they come in, and if there’s an environment there to keep it going, that’s a good thing. Even if there’s people come in and don’t smoke for whatever length of time they’re in prison and they go out, it’s still a healthier thing. If they’re going out with other people that don’t smoke it could stick . . .
S, D5
Participants also identified a number of potential negative unintended consequences of a smoke-free policy for PiC, including increased feelings of stress, anxiety and anger; increases in unhealthy behaviours such as the consumption of sugary drinks or snacks or illegal drugs; increases in prisoner-to-prisoner and/or prisoner-to-staff conflict or violence; and negative effects of sanctions on those unable or unwilling to comply with the smoke-free policy.
People in custody were asked to identify specific groups who might face particular challenges in respect of the smoke-free rules. The examples they provided included PiC with high levels of smoking dependence and/or low motivation or ability to quit, older people who had smoked habitually for many years and PiC with mental health problems. Some identified unique challenges relating to the length and stage of custodial sentences. For instance, it was suggested that people on longer sentences might feel anxious or angry about the prospect of a very long period of smoking abstinence or worry about having to change their established routines, as continuity is often valued by those serving long sentences in prison. By contrast, there were perceptions that, although not without its challenges, smoke-free rules could be less challenging for PiC serving shorter sentences. Participants suggested new arrivals into prison might struggle with lack of access to tobacco while adjusting to a new and challenging environment; many said that the early days and weeks of life in smoke-free prisons would be especially hard for people with complex needs, such as dependency on illegal drugs and/or alcohol:
. . . I know myself if I was coming in, getting detoxed off the drugs and I get my Valium and then they detox me off of smoking as well, I think that’d be a bit much.
You think that might tip people over the edge?
I think I’d be a bit mouthy. Right. I would be banging my door. And wouldn’t be . . . want to be mouthy. It would just be the situation, know what I mean, stop smoking plus stop the drugs. Getting detox, detox off two of them. I think that’d be a bit much.
As contraband was acknowledged to be part of prison culture, some believed that the prison service would be unable to prevent tobacco from being smuggled into smoke-free prisons and sold at inflated prices, contributing to (ongoing) problems of debt and bullying for some PiC:
I read in that prison paper that like a pouch of good tobacco is £100 or something it was going for in England. It could end up getting people that havnae [haven’t] got money into a lot of debt.
And other things like bullying around that maybe?
That’s what I mean; there always ends up bullying with debt because if people cannae [can’t] pay their debt – I’ve seen it loads of times, and that’s just in the 7 months I’ve been in.
The potential for smoke-free rules to lead to disturbances or ‘riots’ in prisons was frequently discussed. Participants often regarded the idea of getting involved in disturbances or riots as foolish and likely to be ineffective. However, some believed that other PiC, such as those who felt angry about the smoke-free rules or with ‘nothing to lose’, might try to cause problems.
Measures to support the implementation of the smoke-free prison policy
Support was expressed for a range of measures to aid the implementation of smoke-free prison policies. It is important to note first that many PiC found it challenging initially to consider any measures that may aid implementation of the smoke-free policy without verbal prompting (from the researcher) to stimulate the discussion where necessary.
There was good awareness of plans to implement smoke-free prison policies among the PiC interviewed in phase 2. Even so, participants supported a continued focus on and expansion of communication in the lead-up to their implementation:
I think giving more information on it and let guys know a wee bit more about it, rather than stick a note up on the wall saying ‘come November next year there’ll be no smoking in the prison’. That’s it . . . What’s coming? What’s going to replace it, you know what I mean? Are we going to get . . . can we get an e-cigarette even if we’ve got [to] purchase it ourselves? Or whatever. If you are supplying it, what’s it going to be? So that we know. And we can get ourselves prepared for it.
S, D6
Some suggested that it would be useful for communications to cover issues such as the rationale for smoke-free rules and how these will be implemented (e.g. when tobacco sales would end), the health effects of smoking and benefits of smoking cessation, and options to help PiC to abstain from or quit smoking. There was support for greater consultation with PiC about how smoke-free rules are introduced and opportunities for dialogue about smoking rule changes between PiC and staff.
Although it was not yet known at the time of these phase 2 interviews whether or not e-cigarettes would be allowed, there were expectations that an enhanced package of stop smoking aids and support would be available to support people to abstain or quit smoking, similar to the help available for PiC who are dependent on illegal drugs or alcohol:
I mean, when you come in here, if you’re on alcohol, instantly you can get Librium or whatever and you can detox that way. Or if you’re on heroin you can get meth [methadone] or whatever. They do that instantly and they’re going to have to do exactly the same thing with smoking, the exact same process as that. That would work . . .
S, D2
People in custody felt that it was important that waiting times for specialist services were reduced and that additional strategies could be tried to increase awareness and engagement with services (e.g. drop-in sessions in residential areas for PiC who wanted to reduce or stop smoking). It was suggested that incentives might be provided to PiC who successfully became smoke free prior to smoking rule changes. One participant suggested that PiC who managed to give up smoking should have the opportunity to sample different foods (as smoking cessation can lead to an improvement in sense of taste); another suggested offering more gym sessions. Although PiC did not always feel that they would benefit from peer support, they recognised this might help others, particularly during periods when cessation advisors were unavailable.
High (but not universal) support was expressed about making e-cigarettes available to PiC to support cessation or as an alternative to tobacco. However, some uncertainties or concerns were raised, for example about what e-cigarettes contain, the health benefits and risks of vaping, and whether or not e-cigarettes would be affordable:
I’d bring them [e-cigarettes] in as soon as because, you know, all you’re going to do is if you wait is you’ll get a changeover but people are going to . . . people that are going to smoke up to the date are going to smoke but a lot of guys . . . you’ll maybe get . . . even if you were to get a quarter or a third of the people going, . . . ‘I’m going to switch just now, so it’s easier’, it just means that you’ve got a quarter less people to worry about when the time comes . . .
S, C2
The analysis also suggested that engagement in purposeful activity, particularly during evenings and weekends, might enhance well-being and support smoking abstinence or cessation. Examples of potentially valuable activities identified by PiC included opportunities to participate in new work parties or courses, going to the prison gym and playing sport. Suggestions for in-cell activities included chess/drafts, arts and crafts and colouring books.
Post-implementation (phase 3) people in custody interviews
Findings from interviews with 23 PiC conducted 6–8 months after implementation of the smoke-free policy are presented below (see also Brown et al. 56).
Opinions on the smoke-free prison policy
Consistent with the phase 2 interviews, there was substantial variation in opinions about the smoke-free policy. Some PiC expressed either predominantly negative or, in a few cases, very positive views of the smoke-free rules. Others voiced mixed opinions, reflecting tensions between autonomy and health protection/improvement. Smoke-free prison rules created internal conflict for some PiC:
Personally it [smoke-free rules] didn’t bother me, I, it was actually probably better for me, saves me money. I’m getting healthier, you know it is probably going to save years of my life but it is just one of those things again about, well it is my choice really about where does it stop, you know, really? Now you can’t drink, you can’t smoke, you can’t have sex, you know. What else is there to be at? Smoking was the last thing you could really do, you know?
ExV, B3
People in custody also recognised potential tensions between their own needs and the needs of others living (or working) in prison:
What’s your views on the smoking ban now?
. . . I don’t think I can speak for everybody . . . I think it’s been good for me because I’ve came so far now that I don’t think, there’ll not be any turning back. So yeah, I’ve made that change in my life and I’m going to stick to it.
And what if other [countries were considering smoke-free prison rules?] Do you have thoughts on whether it’s the right direction for a prison system to go?
I don’t know, because it, in another sense it’s like taking people’s, that, a lot of girls [women in custody] that’s the only thing they maybe had was smoking . . .
There were several suggestions that an alternative measure (e.g. indoor smoking ban) would have allowed PiC to retain some control over smoking and protect non-smokers from SHS:
. . . people should be allowed to smoke, it’s like your human right, isn’t it? Even if it was an outdoor thing or something, when you go out for exercise you can smoke or something, but I do think you should be allowed to smoke . . . but at the same time I understand why as a non-smoking staff member I wouldn’t want to be in a wing that smelled of smoke, I understand why for the health benefits . . .
ExV, B2
Arguments against the smoke-free policy
As illustrated above, a key argument voiced against the smoke-free prison policy by PiC was the undermining of individual freedom (‘rights’) and removal of a substance that provided pleasure and reportedly helped some to cope with poor mental health and environmental stressors:
If I’ve got a fag in my hand, I’m alright. Doesn’t need to be lit. I’m fine because it’s there. I know it’s there. When I’ve not got that, you’re constantly . . . you’re coming in to a high stress situation, you’re already at your most vulnerable you could be and then you’re just off everything . . . ’cause let’s face it, if we didn’t have mental health problems, we wouldn’t be in here in the first place. But just taking away that one wee . . . I think it’s like a form of torture . . .
V, E4
In this context, some PiC saw the removal of tobacco in prison as a punishment:
I didn’t think they would do it, to be quite truthful . . . Because it’s taking a right off us, it’s our right. Like I say, we’re here as punishment, not for punishment. That’s them taking something else off us. We’ve had our freedom taken off us as it is, and now they’re taking that off us. What’s next?
V, D1
The introduction of comprehensive restrictions on smoking in prisons but not wider society heightened feelings that smoke-free prison policies were unfair:
. . . you can’t ban prisoners and the staff from smoking on the outside, in public, yet, we’re using these as, technically, our homes for a short period of time.
V, E3
Other arguments against the smoke-free prison policy were beliefs that prohibitions on smoking were a greater hardship for some PiC and that mandatory smoking abstinence was ineffective in facilitating behaviour change.
Arguments for the smoke-free policy
Key arguments in favour of the policy centred on the benefits of (enforced) smoking abstinence for PiC. In some instances, PiC spoke enthusiastically about how the smoke-free rules had made it possible or necessary for them to be smoking abstinent in prison:
. . . when the smoking ban came in, I was over the moon, I really was . . . because I’ve tried so many times to stop and I’ve never been able to. I knew the fact that I was in prison and I wasn’t going to be able to get tobacco so I had no option, I had to stop.
V, F4
A participant also spoke positively about smoke-free rules removing easy access to materials (e.g. lighters) that could be used to take illegal drugs. Another positive of the smoke-free rules related to benefits for non-smokers of eliminating SHS in prisons:
[Pre implementation] you could smell [SHS] . . . And then it just disappeared, totally disappeared [post implementation]. So, aye, what a difference, what a difference in smell. See for the officers . . . here and that on the hall every day, so I can see why they brought it in, I really do.
ExV, F3
Some PiC said that they felt more positive about the policy now they were able to see benefits for themselves and others:
. . . the smoking ban is the best thing they could’ve done to be honest. Definitely. I feel as if . . . in hindsight, you know, smoking . . . you’re getting told you can’t smoke anywhere. You feel angry. You see it as a right almost, a right that has been . . . taken away from you . . . But in terms of the long run . . . the health benefits, they outweigh the negatives of it. Definitely . . . Aye. At the time, I would say I couldn’t understand. But when you look back on it, like, it’s beneficial for everybody. Because you say, ‘Oh the people that smoke have the right to smoking’. But what about everybody that doesn’t smoke? . . . they’re getting second-hand smoke . . . through . . . no fault of their own . . .
ExV, C1
Outcomes of the smoke-free policy
Smoking cessation
Although a few reported no improvements, PiC generally acknowledged health benefits from abstaining from smoking in prison. Examples included cleaner hands, reduced coughing, improved senses of taste and smell, more energy, increased levels of physical activity and greater stamina when exercising:
. . . before the smoking ban came in, I wouldn’t even think about the gym. But now I’m a bit healthier, I’ve been eating right, and doing more things and I find it a lot better to go to the gym. Because I’m not out of breath as much, I can last without it, I can go two, three, four times a week.
V, A3
Another suggested that interventions that help individuals to avoid relapse to smoking after release from prison would be potentially acceptable (for those motivated to achieve long-term abstinence) and necessary for long-term benefit from smoke-free prison policies:
. . . would it be valuable to offer . . . some kind of support or help [when leaving prison]?
. . . definitely. Because I think the time that’s going to be the most critical for someone, is that first hour, when they really go out . . . what [do] they do first? I know mine, just now, would be to go to the shop and to get some tobacco . . . But it shouldn’t be that, because that’s . . . there’s more to life than smoking tobacco . . . but that’s the main way it is, just now. And I think that’s what a lot of people are thinking, is getting out to have a cigarette.
In contrast, unwanted weight gain was mentioned as a potential downside of abstaining from smoking in prison.
Second-hand smoke exposures
Improvements in respect of the appearance, cleanliness and smell of the prison environment were raised in some interviews:
The smell is a lot better. You don’t see that haze of smoke over the place any more . . . there’s no way the place will ever be spotless, but it’s a lot cleaner than it was.
V, A2
Improved air quality in prisons was generally recognised as significant for the health of non-smokers (although a few PiC were unconvinced that SHS exposures posed a substantial problem for staff or suggested that they were an accepted and inevitable hazard of working in prisons).
Coping with the smoke-free rules
Despite different views on the smoke-free policy, there was broad consensus that, on the whole, PiC were managing well without tobacco after a period of adjustment:
It’s not really much of an issue.
V, B4
. . . I wouldn’t have voted for it in the first place but it, kind of, is what it is now and that’s just the way it is. And it’s actually not as bad, like, as what you think it’s going to be.
V, C5
However, the first few days or weeks after arriving in prison were recognised to be difficult for previous smokers, particularly those arriving with no funds to purchase e-cigarettes (which became available for use and purchase very shortly before the smoking ban) from the canteen.
Many said that abstaining from smoking had been less difficult than expected because of the availability of NRT and/or e-cigarettes:
I didn’t think I was going to be able to cope with [going from smoking to] the vape. Thought I was going to be . . . raging.
Is that what happened?
No. No, it was actually alright.
It was also suggested that there were benefits in accepting the smoke-free rules and recognising that the situation would not change.
How did you feel when you didn’t have the option of buying [tobacco]?
Alright . . . If it’s not there, you’re not going to think about it. Kind of, you know, you can’t get it so . . . there’s no use moaning about it . . . may as well just get on with it. It doesn’t matter what you do, how much trouble you make . . . or how many times you complain . . . it’s gone.
A few PiC complained that nicotine substitutes provided insufficient satisfaction or craving relief, or reported increases in stress or anxiety following the implementation of the smoke-free rules. Older PiC, people serving long sentences and PiC with poor mental health were seen as more likely to experience difficulties.
Disruption in prison
People in custody discussed concerns prior to the policy change about the risks of significant disorder (e.g. ‘riots’) within prisons. However, a recurring theme was that the transition to smoke-free rules had caused substantially less disruption (for PiC, staff and the prison service) than PiC had expected:
. . . a lot of people that I spoke to were very nervous about it . . . back of people’s minds was that people were going to start fighting and rioting and things . . . but . . . there’s been nothing. I’m really surprised.
V, A2
I think a lot believed . . . there would be a lot of trouble in the jails. And I think, they actually believed that they would stop it, and just let us smoke. Because there was talk about . . . there would be riots, and silly things, and that people wouldn’t accept it . . . But it was just, aye, it went by without.
V, F5
Some suggested that enforced smoking abstinence was a cause of increased irritability among PiC and may have been a contributing factor in some incidences of PiC behaving aggressively or assaulting other PiC:
How much trouble, if any, actually, was there?
Hardly any. Moaning, that’s it. Maybe a couple of fights with people who were frustrated. That’s about it.
Because tobacco is not around . . . people are always on edge . . . lot of more fights now, than what there used to be, and more arguments.
Other possible factors acknowledged were personality differences, drug use (e.g. NPSs) and disputes about e-cigarettes (see Opinions on the smoke-free prison policy).
The relatively smooth transition to smoke-free prisons was attributed both to the co-operation of PiC and to preparations made by SPS to help PiC manage without tobacco (e.g. extensive publicity in prisons around the impending rules and giving PiC the option of switching to e-cigarettes in the absence of tobacco).
Contraband tobacco and illegal drug use
As with staff, PiC reported that contraband tobacco was not a major problem in prisons in Scotland 6–8 months after the implementation of the smoke-free rules. Any current violations of the smoke-free rules were generally suggested to be relatively infrequent or small scale:
I don’t think it’s too bad, to tell you the truth. I mean, I’ve only . . . I’ve seen a handful of lassies [women] with tobacco. That’s it . . .
V, E5
Clandestine smoking was suggested to have occurred in the early weeks after the smoke-free rules were introduced, when stockpiled canteen-bought tobacco was still available. [Despite this, TIPs SHS measurements taken in the week of implementation of smoke-free rules32 suggest substantial and almost immediate reductions in SHS exposures in all 15 prisons (see Chapter 4, Fixed-site measures).]
People in custody commented on the high price of contraband tobacco-related products:
. . . £50 [for] a lighter . . . £20 for a couple of roll-ups, if you could get them. We’re £100 for a half ounce of tobacco. Now, your heroin, your crack cocaine, your hash, none of that costs anywhere near as much as it does for a fag . . .
V, E4
Other reasons for the relative lack of contraband tobacco in prisons included widespread acceptance of smoke-free rules and the difficulty of concealing tobacco or consuming it discretely in smoke-free environments.
Is there much tobacco around, left?
No, not really, no. Because to be honest with you, it’s too bulky, you know what I mean, people would rather just get heroin, or thingy . . . It’s the bulk, the size of it, do you know what I’m talking about?
Some participants suggested that some PiC may be using illegal drugs as a substitute for smoking tobacco.
E-cigarettes
The use of e-cigarettes among PiC in Scotland is explored in detail elsewhere. 38 E-cigarettes were seen as likely to have been crucial in implementing the smoke-free policy without major disorder in prisons.
It was more of a non-event because people weren’t being asked just to stop the habit, do you know what I mean, so people had something else to replace it with, it’s healthier. But, yes, I think it would have been a bigger ask and I think it would have been more difficult to manage if the vaping [had not been allowed] . . .
V, A4
E-cigarettes were reportedly helping many PiC to cope with smoking abstinence in prison, including for nicotine withdrawal and cravings: ‘Yes, it takes the craving away, yes, it does, yes. I thought I’d be gasping again, but, no it’s alright’ (V, E2). They were seen as a replacement for previous psychological and cultural aspects of smoking in prisons; some PiC found e-cigarettes or flavoured e-liquids pleasurable [‘I enjoy it now because of the flavours. I know that sounds mental, but I buy different flavours and a new one comes on, I want to try the new flavour’ (F4-CV)] and e-cigarettes were used to pass time, particularly when PiC reported having few distractions or activities that they considered meaningful, and in response to stressors:
. . . if anything smoking is one of the things that gives you time . . . passes the time. See if you [were] sitting in your cell and you’ve nothing to do, just have a wee fag here and there. Then if you take that away, you’ve . . . I found myself sitting staring at the walls, what am I doing? . . . But when they brought out the vapes, they gave everybody that chance to still have that . . . hand-to-mouth . . . action and stuff.
V, C1
However, PiC also indicated that e-cigarette use in prisons brought challenges. Although e-cigarettes were helping previous smokers to cope with abstaining from smoking in prison, they were not always satisfied with e-cigarettes [‘I’m just struggling, I’m not getting what I need out of it [vaping]’ (V, C4)]. Some were opting, from the relatively small range of products on sale in prisons, for lower-strength e-liquids to avoid compromising on flavour and this may have contributed to problems with nicotine withdrawal and cravings. In addition, PiC were not always comfortable with ‘swapping’ one form of dependence for another and did not necessarily intend to continue using e-cigarettes in the future (for various reasons):
I would have preferred to just stop [using nicotine], and that was it. Because now, I’m addicted to the vape, even though I think it’s rubbish.
V, F5
Some PiC who wanted to cut down or stop vaping in prison expressed a need for behavioural or pharmacological support to help them achieve their goals:
[you said] that long term [you would] prefer not to vape. Is that something that you think you’ll be able to do by yourself? Or would it be useful if there was a service you could go to and get a bit of help . . .?
Uh-huh. That would probably be good, because I think the support that we had, gave each other in the smoking group, was good. Like egging each other. ‘You can do it!’ Or watching somebody that had done it and it gave you that wee push . . .
For some, perspectives on using e-cigarettes in prison were complex. On the one hand, they described a physical or psychological ‘need’ or desire for e-cigarettes to help with smoking abstinence. On the other hand, they expressed annoyance or frustration about some aspects of vaping. Such internal conflict was potentially heightened because PiC were not choosing to use e-cigarettes in the same way as other groups of e-cigarette users in wider society. In our sample, exogenous factors (i.e. smoke-free rules) were a primary driver for the uptake of e-cigarettes in prison.
What can you do, you know what I mean, there’s nothing I can do about it. I can’t say ‘right, you know, I [don’t] want this vape, I don’t want to smoke [vape] these’ . . .
V, D1
Although some PiC mentioned health benefits from switching from smoking to vaping in prison, a recurring theme was that the long-term effects of e-cigarette use were not yet known. This led to some suggestions that PiC were ‘testing’ e-cigarettes. A related issue was reports that some PiC were experiencing health problems that they suggested may be linked to/exacerbated by e-cigarettes (e.g. sore throat, chest tightness/pains, breathlessness):
That’s the problem, we don’t have the research . . . we’ve got a few years of research on vapes, but not the same amount of research as we have on cigarettes . . .
V, B2
People in custody who managed to reduce spending on nicotine by switching to e-cigarettes (or who stopped buying nicotine products altogether post implementation) appreciated the financial gains. Nonetheless, concerns about the affordability/value for money of e-cigarettes recurred in the data, particularly for people without external financial support or on lower prison wages:
You feel it for the people living off maybe a fiver a week, and these things are £3.20, you buy a packet of them then you’ve got £1-odd left to buy . . . food is better than e-cigs [e-cigarettes].
V, E2
They’re [e-cigarettes] dear. They’re, like, £7 for the actual vape and you have to buy the charger and that’s another £4 . . . that’s £11 to start without the capsules to put in them. So even the girls [women in custody] that have got jobs, you only get paid, like, £10.80. In most jobs anyway. So you wouldn’t even be able to afford them, like, to buy them off one canteen, unless you’ve got money sent in.
V, E5
E-cigarettes, like tobacco previously, were a sought-after commodity and participants discussed difficulties that could occur when PiC ran out of e-liquids (e.g. borrowing e-liquids at a potentially inflated cost):
You see people actually running up and down . . . Chasing the capsules [e-liquids] . . . cause the capsules in here are like gold dust. As soon as somebody’s got, ‘Oh can I get a loan of it, can I get a loan of it? I’ll get you two back’. . . anything just to get . . . and I’ve seen me sitting watch people like that, you know, it’s quite ridiculous how . . . for a wee tiny bit of nicotine, you’re offering to buy them two back . . . three back.
V, F2
People in custody described differences between borrowing e-liquids (currently) and tobacco (pre implementation) because tobacco was easily divisible into small quantities whereas pre-filled e-liquids are not:
. . . people just don’t have money, do you know what I mean, but they want to smoke [vape]. Before it wasn’t that bad giving somebody a bit of snout [tobacco] every day but you can’t really give somebody a packet of capsules every day. . . . you can’t give them a bit, you know, it is a capsule or nothing. So, personally, I feel sorry for people.
ExV, B3
A final risk of e-cigarettes in prisons raised by some participants was that e-cigarettes were providing a (discreet) way for some PiC to take illicit drugs such as NPSs: ‘people can adapt them or whatever to their own ends, but they can do that with other stuff that was already there’ (V, A4).
Summary
Work package 4 explored PiC’s attitudes to and experiences of PiC smoking and its place within prison culture, smoking rules and the (impending) smoking ban, and e-cigarettes. It comprised cross-sectional surveys open to PiC in all prisons in phase 1 (return rate 34%), phase 2 (25%) and phase 3 (18%); and one-to-one interviews in ‘case study’ prisons in phases 2 and 3. As for staff, return rates fell over time, with considerable between-prison variation, and survey findings should be interpreted with caution.
At each phase, almost 9 in 10 PiC had ever smoked and almost three-quarters currently smoked in phase 1 and phase 2. The proportion who had ever tried e-cigarettes rose from around half to three-quarters between phase 1 and phase 3, reflecting their common use once they were available for purchase in prison. PiC were less positive than staff about the impending ‘ban’ in all phases. ‘Positive about bans’ factor scores were associated with not smoking, higher educational level, prisoner status and reporting no asthma and more sensory symptoms. Support increased somewhat in anticipation of/following the ban. The proportions agreeing that prison smoking bans ‘cause a lot of trouble’ and ‘are hard to enforce’ decreased after implementation, but, in phase 3, just 35% of respondents agreed that prison smoking bans were ‘a good idea’. Views about advantages and disadvantages were mixed. Two-thirds indicated that the ban had ‘made prisoners more anxious’, around half that it led to ‘more physical/verbal assaults’ and ‘more use of illegal drugs’ and only 1 in 10 that it had ‘made prisoners happier’. However, around half thought that it helped improve prisoner and staff health, and made the prison look or smell better. In phase 3, over two-thirds of ever-smoking PiC indicated not being allowed to smoke was hard; over half felt angry, more bored and reported weight gain. Only around one-quarter indicated that they were not smoking because of the ban, but almost half agreed that the ban ‘is a good opportunity to stop smoking’ and not smoking ‘is easier when no-one else smokes’. Ratings of general health among PiC were much lower than for staff and were lowest in phase 3. In general, PiC were less positive than staff about preparation for implementation, although most thought people were kept well informed and the introduction of e-cigarettes had made things easier for PiC and staff. PiC expressed more negative views about e-cigarettes in phase 3 than in phase 2, with increased agreement that they are ‘addictive’ and ‘raise safety issues’, and decreased agreement that they ‘can stop people smoking’.
Participants in phase 2 interviews raised potential facilitators of smoking abstinence or cessation in prisons, such as particular motivations to stop smoking (including concerns about health, wanting to make positive lifestyle changes while in prison, the price of tobacco and growing ‘sick’ of feeling dependent on tobacco). Certain features of the prison environment appeared to have the potential to help with smoking abstinence or cessation, such as restricted access to drugs and alcohol, purposeful activity (e.g. prison-based work or education, going to the prison gym). Common barriers to smoking abstinence or cessation in prison were the importance of smoking in many PiC’s daily routines and social interactions, beliefs about smoking (e.g. that it is effective for managing stress), misunderstandings or minimisation of the health risks and perceptions that willpower alone is the best way to quit. Barriers linked to the use of smoking cessation services in prison included waiting times, delays receiving NRT from the prison pharmacy and disruption to smoking cessation treatment when PiC transfer between prisons.
Opinions of the impending smoke-free policy varied. Some considered such policy to be unfair, removing the freedom or ‘right’ to smoke (an activity often framed as pleasurable and useful for managing stress and boredom in prisons). Arguments in favour of the policy related to its potential to improve PiC’s health and enable them to spend more on other valued items, such as family telephone calls, to protect non-smoking staff and PiC from SHS exposure and to improve the living and working environment in prison. Anticipated negative consequences for PiC included increased feelings of stress, anxiety and anger, and increases in unhealthy behaviours (e.g. the consumption of sugary drinks/snacks or illegal drugs), and prisoner-to-prisoner or prisoner-to-staff conflict. Participants suggested that new arrivals may struggle without tobacco while adjusting to a new and challenging environment, particularly people with complex needs, such as dependency on drugs or alcohol. Some believed it would be difficult to prevent the sale of contraband tobacco. Potential disturbances or ‘riots’ in prisons in response to the smoke-free policy were frequently discussed, although such actions were often regarded as unlikely to be effective. PiC were aware of plans to implement the smoke-free policy but were keen for more detailed communication, covering issues such as the rationale for the smoke-free rules, the process of implementation (e.g. when tobacco sales would end), the health benefits of smoking cessation and options to support PiC to quit smoking. They expected that enhanced stop smoking aids and support would become available to support PiC, with reduced waiting times and additional strategies to increase awareness and engagement with services. High (but not universal) support was expressed about making e-cigarettes available to PiC to support cessation or as an alternative to tobacco. However, some uncertainties or concerns were raised, such as concerns about the health benefits and risks of vaping, and whether or not e-cigarettes would be affordable. Increased opportunities for purposeful activity, particularly during evenings and weekends, were seen as important for well-being and to support smoking abstinence.
In phase 3, there was substantial variation in opinions about the smoke-free policy. Some PiC expressed predominantly negative or, in a few cases, very positive views, whereas others voiced mixed opinions, reflecting tensions between autonomy and health protection/improvement. Some continued to express the view that the policy undermined individual freedom and removed a substance that provided pleasure and reportedly helped some to cope with poor mental health and environmental stressors. In some instances, PiC spoke about how the smoke-free rules had enabled them to become smoking abstinent in prison and some felt more positive about the policy now that they were able to see benefits for themselves and others. Several acknowledged health benefits from abstaining from smoking, including reduced coughing, improved senses of taste and smell, more energy and greater stamina when exercising. Despite mixed views, there was some consensus that, on the whole, PiC were managing without tobacco after a period of adjustment, although certain groups were recognised as having more difficulties (new arrivals, people who were older, serving long sentences or with poor mental health).
As for staff, PiC reported that the transition to the smoke-free rules had caused substantially less disruption (for PiC, staff and the prison service) than expected. Some suggested that enforced smoking abstinence was causing increased irritability among PiC and was a contributory factor in some instances of aggressive or violent behaviour among PiC. The relatively smooth transition to smoke-free prisons was attributed to PiC’s cooperation, SPS’s preparations to support PiC to manage without tobacco and e-cigarettes being made available in prisons. Like staff, PiC reported that contraband tobacco was not a major problem 6–8 months after the implementation of the smoke-free rules; any violations were generally suggested to be relatively infrequent or small scale. Clandestine smoking was reported to have occurred in the weeks after implementation when stockpiled tobacco was still available. Reasons for the relative lack of contraband tobacco included high price, widespread acceptance of smoke-free rules and the difficulty of concealing or consuming tobacco discretely in smoke-free environments. E-cigarettes were reportedly helping many PiC to cope with smoking abstinence in prison and were seen as a replacement for previous psychological and cultural aspects of smoking in prisons, such as helping to pass time and deal with stressors. However, PiC also indicated that e-cigarettes brought challenges in prisons and some were dissatisfied with e-cigarettes. Some PiC expressed a need for behavioural or pharmacological support to help them cut down or stop vaping while in prison.
For some, perspectives on using e-cigarettes in prison were complex. Although some PiC mentioned health benefits of switching from smoking to vaping in prison, PiC also discussed the lack of evidence on long-term effects of e-cigarette use or reported health problems that they suggested may be linked to/exacerbated by e-cigarettes (e.g. sore throat, chest tightness/pains, breathlessness). PiC who had reduced their nicotine-related spending by switching to e-cigarettes (or stopped buying nicotine products altogether post implementation) appreciated the financial gains. Nonetheless, there were concerns about the affordability or value for money of e-cigarette products and that, like tobacco previously, they had become a sought-after commodity and could cause difficulties when PiC ran out of or could not afford e-liquids.
Chapter 7 Provision and use of smoking cessation services
Interviews with staff responsible for managing and delivering cessation support in Scottish prisons
Expectations and beliefs regarding the smoke-free policy
Before the announcement of the ban, the prospect of prisons going smoke free was a major topic of discussion among SSSs and prison health-care staff responsible for delivering cessation support, with questions raised about how it should be introduced and potential implications for the organisation of cessation support. There was broad support for the move towards smoke free, with many describing it as a positive development for prisoner health and an opportunity to limit smoking uptake on release:
There will be health benefits for everybody. Even for the prisoners who don’t smoke . . . Even for prisoners who are digging their heels in saying ‘You can’t introduce this – my rights’ but there’s going to be health benefits to them as well.
SSS, advisor, phase 1
I think it is an important thing . . . It gives them an ideal opportunity, because one of the things we say to them is ‘Turn a negative by being in the prison into a positive!’ whereby, when you get discharged, at least you are walking out those gates a lot healthier than you were when you came in.
SSS, manager, phase 1
Although the smoke-free policy was widely welcomed on public health grounds, many recognised that its introduction brought significant challenges, reporting that this topic was frequently raised by PiC using health-care and cessation services. Most took the view that a comprehensive indoor and outdoor smoking ban throughout the prison estate was necessary to achieve compliance and maximise health gains. Few involved in delivering cessation services supported the concept of a partial ban or a phased introduction within individual prisons.
There were reports of some PiC actively welcoming the policy, but it was a focus of anxiety for others (particularly smokers serving long sentences):
Maybe it’s their first time in prison. They’ve got a different mind-set. If you’ve got someone who’s been smoking for umpteen years . . . it’s their form of currency, it’s their income, it’s what they use to gamble, it’s what they use for relationships, it’s what they use for comfort and all of a sudden you’re taking that away . . .
Addictions caseworker, trained advisor, phase 1
Such concerns were echoed by some SSS and health-care staff, who feared that the policy could result in clients who were less motivated to quit being compelled to engage with the service, and being hostile to cessation support. There were calls for information regarding how other jurisdictions (particularly E&W) had adapted to similar bans: ‘I think we have to look at successful models down in England and we have to replicate that’ (addictions caseworker, trained advisor, phase 1).
Response to and preparations for the smoking ban
Much of the attention in anticipation of potential changes to smoking rules focused on how services would cope with expected increases in demand for cessation support. Hence, early preparations and a long lead time were considered important, to ensure that capacity was in place to respond in a timely manner as smokers came forward for support and to flatten demand by giving smokers sufficient opportunities to quit:
If there’s a longish lead in time, then it may well not be a huge demand for Stop Smoking Services because people will start preparing for it.
Health improvement senior manager, phase 1
If we get plenty of lead-up time, we are able to say ‘You can come back and we will do it again’ . . . it might take them several attempts. I think that will be helpful rather than just saying to somebody who has come for the first time, ‘Oh God, I am struggling [to help you]’.
Health-care manager, phase 1
At the time of the phase 1 interviews, before the policy announcement was made, interviewees noted no noticeable change in demand for cessation services. However, by phase 2, advisors started to note significant increases, typically from smokers wishing to retain more autonomy and avoid being forced to quit as the ban was implemented:
It tends to be a group where . . . they [PiC] want to do it for them[selves], they don’t want to wait until November [2018] when they take it [smoking] away. So, I think it’s like a kind of power trip that they have got. ‘Oh, I’m going to stop smoking now, not just because you’re telling me to!’
SPS officer, trained advisor, phase 2
Most prisons had also established service planning groups by phase 2, although ensuring the engagement of key stakeholders, particularly senior prison management, could be challenging in the early stages. Interviewees in other prisons reported investing in additional staff resources to reduce waiting times, which exceeded 16 weeks in some cases, and many described making changes to service protocols to help manage waiting times, most significantly a decision to move to a rolling group programme, allowing new users to join groups as existing members dropped out.
Consideration was also given to additional forms of support for PiC, such as drop-in sessions, peer support networks and recruiting peer educators, or PiC who had been through the quit process, as local champions:
. . . what we need to look at is how we build that network of informal support so that when people are trying to stop smoking they are given encouragement and help when things aren’t going so well.
Health improvement senior manager, phase 1
. . . we need to work stronger to get champions, smoking cessation champions within the prisons. Staff and prisoners doing that work for us in the setting of the prison.
SSS manager, phase 1
Similarly, many recognised the importance of engaging prison staff as advocates – promoting the service on residential halls, encouraging referrals and supporting PiC to attend group sessions:
. . . if they are smokers themselves [prison staff], there can often be a barrier there, because a lot of the staff might think the actual same as what the prisoners think. So staff can help, but they need a bit training first.
SSS advisor, phase 2
Although evidence from phase 1 interviews indicated that most prisons were starting to consider how services might be reconfigured to meet increased demand, decision-making was tempered by unknowns, particularly whether or not NRT would be made more widely available and, most significantly, whether or not e-cigarettes would be introduced into prisons.
. . . depends what other options they put in if they put the ban in. If they leave it as it is the now, and the only option people have is to come through our service to get NRT, then yeah, you would need more staff. But, if they offer the e-cig [e-cigarettes] or people the chance to purchase their own NRT, or some other NRT management service away from the Stop Smoking Service then . . .?
Addictions caseworker, trained advisor, phase 1
By the time of the phase 2 interviews, a number of significant changes had been implemented following the announcement that prisons would go smoke free, mostly focused on building capacity. Many were designed to streamline access to support groups and pharmacotherapies and included reducing reliance on prison staff to escort PiC to sessions by arranging meetings in residential areas, using improved access to residential areas to raise awareness of the service and fast-track referrals, enabling smoking advisors to distribute NRT directly to service users and providing additional staff support to reduce administrative burdens (e.g. recording the distribution of NRT). Many interviewees also reported delivering cessation training to prison staff volunteers. In some prisons, these officers were able to co-facilitate cessation groups. However, there was often a lack of clarity about their role, and in many prisons this support did not materialise as a result of other work pressures and lack of confidence in operating in a therapeutic role:
I’m not too keen on the whole idea of being involved in medications and stuff like that . . . don’t feel like the training that I’ve done at the time would be enough for something like that . . . it’s not something I’ve ever known anything about so it’s all brand new to me so I still feel it’s a bit raw for me to be doing something like that.
SPS officer, trained advisor, phase 2
Most frontline workers delivering cessation support found that they had sufficient time to plan for the introduction of the ban. However, the decision by prison authorities to introduce e-cigarettes late in the preparatory phase presented significant challenges, such as services needing to reallocate resources at short notice and delays in the implementation of new pathways for supporting prisoners who smoked:
There was an issue when SPS suddenly announced it’s going to [provide] free vapes, because the NHS had no knowledge . . . nobody had told us this is what is happening. They were writing the guidelines at that point, and suddenly, it’s like, ‘What’s that about, where did that come from?’ . . . We had to rewrite the specification.
SSS co-ordinator, phase 3
It meant we didn’t get the plans for the prisons pathways out until the ban came in. We were meant to be delivering a service post-ban and the pathway didn’t come in until the day [of the ban] . . . It was a massive piece of work.
Senior SSS manager, phase 3
It was suggested that larger prisons, with more diverse populations and greater prisoner turnover, were less able to adapt to increased demand than smaller prisons, and there was some evidence that prisons that relied on existing health-care staff to deliver cessation support were under greater pressure than those that were not, because of other demands on their time:
We really need to change the service. We just couldn’t cope, because there is a lot of other things other than smoking . . . we’ve got a lot of people with alcohol addiction, drug addiction and then all the primary care stuff. And, as I say, we’ve only got two members of staff.
Health-care manager, phase 1
In addition to changes made, participants working in smoking cessation identified areas where the service would need to adapt and develop, the most significant being a need to implement measures for identifying and supporting smokers on entry to prison (e.g. through provision of free NRT):
. . . we’d need to look at the possibility of giving people NRT as they come in the door. ‘Cause it’s not fair to leave somebody if they have a billion other things going on, and to have nicotine withdrawal in there as well. So I think it would be an idea to look at maybe the admissions process, and if they could access something at that point, and then maybe come into our group.
Addictions caseworker, trained advisor, phase 1
Prison reception was recognised as a key pressure point, with significant demands already on admissions staff. Some smoking advisors working on the frontline also saw a need to reconfigure the service to cater for people with limited motivation to quit who would nevertheless require support in managing nicotine withdrawal using NRT and/or e-cigarettes. Although there was wide recognition that prisons had a duty of care to offer symptom relief for those not prepared to make a quit attempt, questions were raised about who would have responsibility for delivering this support and the long-term implications of providing ongoing access to NRT on health and prisoner smoking rates post release:
There’ll be two types of person who come into prison . . . you’ll have some people who will engage with our service and want to address the whole health behaviour change and make the necessary adjustments to their life, and they will require the support that we currently deliver . . . As opposed to the group of people who only want symptomatic relief . . . at the moment we’re focusing everything on providing service for people who want to quit.
Health improvement manager, phase 1
. . . there’ll be a lot of prisoners who are coming in . . . they’ll take the NRT because they have to and they can’t smoke. But the minute they go out the door they haven’t got the slightest intention of staying stopped.
SSS manager and advisor, phase 1
Implicit within these discussions was a belief that many PiC, particularly more vulnerable prisoner groups and those with poor literacy, would struggle to use NRT as an effective cessation aid in the prison environment without structured support, and that it was more likely to be relied on (intentionally or otherwise) as a form of symptom relief or substitute for tobacco.
Attitudes towards introducing e-cigarettes
As noted, a decision to introduce free e-cigarette starter packs in September 2018 was made reportedly without adequate notice or consultation with local cessation services and national planners. Prior to this decision, the introduction of e-cigarettes to support the implementation of smoke-free rules was much discussed, with many frontline workers suggesting that it would prove extremely popular with PiC who smoked. Its potential was seen largely as a direct replacement for smoking. Some questioned whether or not SSS should have an active role in their use by PiC and some suggested that e-cigarettes might undermine existing cessation programmes:
I’m not sure that there would be a role for the NHS to supply them [e-cigarettes], or for there to be a provision. I think if they [PiC] want to use them they should be able to buy that at the canteen, . . . if they want to use their money on that, then so be it.
Health-care manager, phase 1
They need to know that the e-cigarette is maintaining that high nicotine level. We have to say to them of course it’s still a lot safer than smoking a cigarette, but by using the e-cigarette they’re keeping it high, so when it comes to coming off the patches, they will find they probably increase their use of their e-cigarette to maintain the original level, and then by the time they finish the programme, they’re still quite addicted to nicotine.
Health-care nurse, trained advisor, phase 2
This led to calls for lower strength nicotine e-liquids to be available on canteen lists.
Staff in cessation services and prison health care had mixed attitudes towards introducing e-cigarettes. Some (a number of whom described their services as ‘e-cigarette friendly’) expressed support for their introduction. It was argued that e-cigarettes were a more appropriate product than NRT for managing short-term abstinence and so had the potential to make the transition to living in smoke-free prisons more manageable:
. . . it’s much easier when you’re taking away something to be able to give them something. I think they will see it more favourably than NRT.
SSS manager and advisor, phase 1
Others held varying views: they agreed that e-cigarettes could potentially aid the transition process, but were concerned about possible, as yet, unknown dangers of long-term use, and about substituting a smoking culture with a vaping culture and how this would have an impact on nicotine addiction and tobacco use in the longer term:
I can see it both ways. If you could go smoke-free without it [e-cigarettes], I think it would be the best thing but – you are just worried about everyone – a few years down the line, everyone would be using an e-cig in the prison . . . everyone would try it and before you know it the whole prison would be smoking them.
SSS advisor, phase 1
I think that [introducing e-cigarettes] would act as a deterrent on people actually trying to stop smoking. I know the message is, it is safer than actually smoking tobacco. But I don’t think you would get as many people as focused on an actual total quit.
SSS manager, phase 1
These views were partly borne out by experience, with demand for cessation support reported to have fallen significantly immediately after (rechargeable) e-cigarettes were introduced (see below). However, despite reservations, most agreed that, on balance, e-cigarettes were worth serious consideration: ‘I’m not a fan of e-cigarettes, but I’d rather have something as opposed to nothing’ (addictions caseworker, trained advisor, phase 1). Nonetheless, participants were conscious that e-cigarettes raised security issues, reporting concerns that they could be doctored as a delivery device for illicit drugs: ‘because of the nature of what they are, I would be surprised if they would ever be allowed’ (SSS advisor, phase 1).
Following their introduction, many found the rechargeable e-cigarettes a more viable product than single use e-cigarettes, which were frequently described by PiC to be ‘useless’ or ineffective. However, levels of familiarity and understanding of vaping and the specific devices introduced into Scottish prisons was thought to be poor, with some recognising this as an important area of new learning. Cessation services’ response to such gaps varied between prisons and health boards. Some services assumed a proactive role, helping to ensure that PiC and prison staff were properly informed on e-cigarette use and nicotine content; others (at least initially) took the position that, as prison authorities were responsible for the decision to introduce e-cigarettes and to distribute starter packs, it was the responsibility of prison staff to offer support and explain their use:
. . . there’s a real learning need for us there to understand them better. Devices change and things change all the time so we really need to get our heads round about it to support people well because I don’t know that our knowledge is great on it. We go from delivering a service that we know inside out to this whole new ball game.
Health-care worker, trained advisor, phase 2
These differences potentially meant that PiC in some prisons were better supported. Importantly, irrespective of the position assumed within each prison, many smoking advisors on the frontline reported that PiC frequently approached them for advice when they had problems with vaping or their device and that e-cigarettes were a common topic of discussion in cessation groups, particularly leading up to implementation.
Impact of the ban on approaches to delivering cessation support
Inevitably, this was a period of considerable change for those supporting people in managing nicotine addiction or wanting to quit smoking. The 2018 ‘Smoke-free prison pathway’ service specification79 outlines requirements for the delivery of behavioural and pharmacological support for managing nicotine additions in prisons and describes how the NHS Quit Your Way Prison programme is expected to deliver pharmacotherapy and/or behavioural support to PiC wanting to ‘withdraw from nicotine’ while in prison and to PiC with no funds in need of (free) NRT to manage withdrawal symptoms. (Subsequent guidance in 2020 – after TIPs data were collected – provides advice on delivery of pharmacotherapy and/or behavioural support to PiC who want to cut down or stop use of e-cigarettes. 80) Interviews with service providers highlighted some differences in precisely how Quit Your Way Prison programmes were operating in different prisons. Three main approaches were identified.
The first approach was geared to establishing a process of rapid referral and improved availability of free NRT, resulting in a corresponding reduction in provision of behavioural support. Although some specialist group support was retained for specific sections of the prisoner population, the provision of rolling groups (ramped up during the lead-up to implementation) was replaced post implementation with weekly 5-minute one-to-one sessions to provide NRT and brief advice as required. Despite the high numbers receiving support, waiting times were short. Ability to meet high levels of service demand was facilitated by the switch to one-to-one support and changes to processes for dispensing NRT.
The second approach involved delivering a conventional ‘smoking cessation’ programme for smokers entering prison. The programme was intended to follow a conventional 12-week programme, combining free NRT with behavioural support, mirroring support offered to smokers in the wider community. Significant improvements in delivery had been achieved by enabling advisors to meet service users on prison halls, and, more recently, by advisors having the authority to distribute NRT to PiC directly.
The third approach involved delivering a hybrid service to meet the diverse needs of PiC. The conventional 12-week programme was modified to a 6-week programme (or one-to-one sessions on the halls, where required) post implementation in response to increased demand and to match the service’s changing behavioural goals. The provision of free NRT was conditional on group attendance to help users manage their e-cigarette use and nicotine intake, and to limit NRT wastage and stockpiling. Post implementation, programme content changed to meet a range of PiC’s needs, incorporating guidance on the use of e-cigarettes and how to cut down and stop vaping. These changes reflected a belief that it had evolved into an ‘e-cigarette focused service’ with an emphasis on managing nicotine use, a journey that was seen as a process of trial and error. To support the evolution of the service, senior service staff invested time and energy into familiarising themselves with the e-cigarette products sold in prisons, and delivered information sessions for PiC (and SPS staff). Advisors experimented with providing separate support groups to address the divergent and reportedly more pressing needs of new admissions, who were often dealing with continued enforced nicotine withdrawal for the first time. They also responded to existing PiC looking for advice on how to control their vaping, often because of rising expenditure on vapes and emerging health concerns. However, this sometimes proved to be impractical because of logistical challenges and pressures on staff resources. It was also noted that prioritising new admissions could create tensions with PiC who had self-referred and were required to wait for a place. In some prisons, all PiC were eligible to receive support, irrespective of whether someone was classified as a smoker or vaper. However, referral to ongoing support for stopping vaping on liberation was contentious, as some local community services only provided support to smokers wishing to quit. In this sense, advisors saw the programme as a test bed for potential e-cigarette-focused services in the community, providing insight into issues such as how to monitor nicotine intake and titrate using different e-liquid concentrations.
Several potential challenges in delivering in the new context of smoke-free prisons were identified in the provider interviews. Examples included difficulties in respect of rapid identification of needs/wishes of smokers being admitted to prisons and issues with referral pathways on entry and exit from prison, differing interpretations of new service goals and outcomes (e.g. some advisors voiced reluctance to work with e-cigarette users), knowledge deficits (e.g. understandings of e-cigarettes) and challenges in making NRT (widely) available in prison for those requiring symptom relief and minimise potential risks of waste.
Interviews with people in custody with recent experiences of smoking cessation services in Scottish prisons
In the lead-up to the implementation of the smoke-free prison rules, 45 interviews were conducted with PiC who had recent experience of prison smoking cessation services, as part of WP5. Their views on the smoke-free prison policy and facilitators of and barriers to stopping smoking in prison were largely similar to views expressed by a separate sample of PiC who had participated in interviews at a similar time as part of WP4. Analysis of the two complementary data sets is presented elsewhere;75 key findings from WP5 only are reported below.
Views and expectations regarding the smoke-free prison policy
In interviews conducted in the preparatory phase, PiC who had used the service displayed a similar range of views to the wider prison population (see Chapter 6, Surveys of people in custody and Brown et al. 75), although these tended to vary according to where they were in their quit attempt. Those expressing predominantly negative opinions about the policy tended to still be smoking or had relapsed, perhaps reflecting a general anxiety about quitting, even where they acknowledged real personal health benefits:
It’s a bad thing as far as I’m concerned because I’m being pushed to change my ways . . . the last time I gave up I wanted to do it, you know. But, I mean, I should still want to do it because I’ve got bad legs. I could end up getting them chopped off or something because I’ve got diseased arteries in my legs . . . but I think people just hate to get pushed without being asked.
Male, never tried stopping smoking in prison
Others (often PiC who had given up, were non-smokers or making good progress in their quit attempt) held more complex positions on the ban. These participants often recognised tangible benefits for their health and living environment (e.g. removal of the smell of smoke or cues that might trigger relapse), but also understood the challenges for peers who were unable or unprepared to stop smoking, expressing strong solidarity with them. Particular concern was expressed for those seen as most likely to be affected by the ban (i.e. those on longer sentences or who were more vulnerable) who relied on smoking to cope. A few in this group also acknowledged the position of prison staff and their exposure to SHS:
It depends on what way you’re looking at it. For me personally I think, I think it is a good idea for people’s health. But at the same time I think people should be allowed to do what they want to do with respect to smoking, something that’s legal if you’re over 16.
Female, tried stopping smoking in prison
Like other PiC (see Chapter 6, Surveys of people in custody), all believed that there would be some pushback post implementation, ranging from an expectation that some PiC might get ‘a bit grumpy’ or ‘nippy’, to suggestions that groups might coalesce around the issue. These narratives appeared to be fuelled by hearsay about the implementation of smoking bans in E&W, which were believed to have caused trouble or ‘riots’ in some prisons. Key trigger points and areas of tension (beyond the implementation itself) included Christmas, when PiC typically experience greater stress; the removal of tobacco from the canteen (rumours were circulating at the time of the interviews about when this would be); and the inability of certain prisons/prisoner groups to cope with the ban. Some PiC were viewed as less prepared for and less able to cope with the removal of tobacco:
. . . 30 November is a bad time. See with Christmas coming up . . . it’s a particularly bad period, sort of stressful period . . . you’re away from your family . . . So the added of not being allowed to smoke for guys that want to smoke, it’s going to be even harder . . .
Male, tried stopping smoking in prison
I think the guys have got enough warning . . . enough opportunities available. But certainly jails like Barlinnie where it’s shorter-term prisoners, yeah, it will cause problems . . . guys coming in have big drug habits, they’ll be relying on nicotine . . . For them it’s going to be a massive shock and it’s going to come out of the blue . . . So in here I don’t think there will be a problem. In other prisons, yeah.
Male, tried stopping smoking in prison
There was also discussion regarding the ban’s potential impact on the emergence of illicit tobacco, competition for tobacco products and ensuing tensions, such as debt and jealousies about inequitable access:
Not everyone’s going to be able to afford that, that’s crazy money. Obviously, there’s going to start a bit of jealousy, maybe a little bad talking behind people’s backs. Some might lead to fighting. It might lead to people telling officers, like, such-and-such has got such-and-such. People getting themselves searched, things getting taken off them.
Male, tried stopping smoking in prison
It is noteworthy that, within this prisoner group, negative effects rarely manifested in resentment towards prison staff, despite recognition that concerns for staff health had been a driving force behind the policy. Indeed, as noted, some PiC expressed sympathy about staff exposure to SHS, although it was also believed that any failure by staff to comply with the ban post implementation (e.g. ‘fly smoking’ in unoccupied cells) could lead to heightened tensions:
There’s a lot of staff in here that go into cells and have a fly smoke, right? . . . I’ll turn a blind eye to it just now, because they shouldn’t be doing it anyway, even when it’s allowed [for PiC] to smoke. But when the ban comes in . . . I’ll be saying something about it because if we can’t do it then they shouldn’t be doing it.
Female, tried stopping smoking in prison
Finally, although most anticipated some negative reactions, many PiC (whatever their views) felt that any resistance was likely to be relatively short-lived while ‘things settled down’.
Facilitators of and barriers to initiating and maintaining a successful quit attempt
Facilitators
Extraneous facilitators of a successful quit attempt identified by PiC interviewed in the preparatory period included the increase in tobacco pack sizes (and associated cost) in May 2017 in the UK, which acted as a trigger to a quit attempt, and PiC making progress in overcoming another addiction, which could provide the motivation and opportunity to attempt to quit smoking.
Cessation-related facilitators were directly related to the way the support was configured and delivered. The cessation programme as a whole, and the commitment and expertise of specialist staff in particular, were widely praised:
She’s [smoking advisor] been through my journey with me, she’s really nice, I think that makes all the difference . . . she’s been really good when I’ve came. She’s like, she’s gave me great tips, she’s sent me colouring-in stuff and puzzles through the post . . . she’s been very supportive . . . They’re approachable and I think that makes a difference.
Female, tried stopping smoking in prison
Three aspects of support emerged as key facilitators: carbon monoxide monitoring, meeting/speaking with others attempting to stop and impending implementation of the smoke-free policy.
Carbon monoxide monitoring
For some service users, a key element of the cessation programme was the structure it provided, with weekly CO breath tests acting as a reward and tangible evidence and reassurance that their health was improving:
. . . the wee carbon dioxide [sic] machine . . . inspired you to go and see, because when I first blew it I was a 28 which most of them were only blowing 11s and 12s and I blew a 28 so I was rocket, know what I mean? And then recently I’ve been blowing 1s and 2s, which they say a non-smoker still blows . . . It just inspires you to do it, to have a go, because you want to beat that wee machine too.
Male, tried stopping smoking in prison
However, CO monitoring could also be an area of tension and anxiety when readings exceeded the strict cut-off point that some services and advisors appeared to apply that then required users to leave the programme. Others reportedly relaxed these rules if they judged a person remained committed to quitting.
Meeting/speaking with others attempting to stop
Some PiC found the opportunity to meet as a group and speak with (similarly committed) peers going through the same process very helpful in their journey to stopping smoking. Meeting with others on the same flat or hall was said to have added advantages, not least the ability to exchange support with peers outside the context of the group:
. . . hearing everybody’s attempt . . . how they’re doing it, how good they’re doing.
Male, tried stopping smoking in prison
Being in a group, aye. It’s ‘cause it’s all the people from the same hall . . . all trying to stop together . . . it’s a lot easier.
Male, tried stopping smoking in prison
However, some PiC were judged to be less committed to smoking cessation (e.g. those seen smoking on the halls, despite claiming in the group that they had given up), making engagement less purposeful, whereas others were more comfortable in one-to-one than group sessions.
Impending implementation of smoke-free policy
The impending implementation date was an important factor motivating many PiC to make a quit attempt, including some who had never previously tried to stop. This appeared to relate primarily to retaining a sense of control:
I know I’ll be really bitter if they **** stop me from smoking rather than me stopping before that. So I’d rather make myself stop than the prison.
Male, tried stopping smoking in prison
Findings also suggested that more sustained quit attempts tended to be undertaken by people with other/additional reasons for quitting (e.g. a strong desire to leave prison and return to their family smoke free).
Barriers
Prior to implementation of the smoke-free policy, the main barriers to smoking cessation identified by PiC were associated with the wider prison environment and culture. Many smokers described the challenges of quitting in a confined environment where smoking was highly prevalent, particularly if they shared accommodation with a smoker:
If you’re outside . . . you can move away from situations, but in here it’s confined . . . there’s people walking about smoking, there’s people in the cell smoking. So, it’s a little more hard because it’s in your face here. You need a lot more willpower . . .
Male, never tried stopping smoking in prison
Several significant smoking cessation service-related issues were also mentioned by PiC, notably waiting times to access behavioural support and/or pharmacotherapy in prison.
Views and experiences of e-cigarettes and vaping
Similar to the support from staff and PiC for e-cigarettes described in Chapters 5 and 6, PiC interviewed for WP5 generally welcomed e-cigarettes as a potential alternative to tobacco, often viewing them as a means of ameliorating the likelihood of trouble or unrest following implementation of the ban. However, few who were actively seeking to stop smoking expressed a desire to take up any of these products. Although some of those trying to quit had experimented with (single-use) e-cigarettes and bought them as a back-up to deal with cravings and possible relapses, most making a concerted effort to quit expressed a strong desire to ‘beat’ their nicotine addiction, often indicating that this was their primary motivation for attending the cessation programme:
I don’t really want to give up one addiction for another . . . swapping one addiction for another, isn’t it? I don’t see vapes as being a device to help you give up. I see them purely as a replacement.
Male, never tried stopping smoking in prison
Personally, if you’re stopping, then go the whole hog, don’t just do it half measures, kind of thing. Because at the end of the day, they’re still taking nicotine into their system, and they’ll go back to cigarettes . . .
Male, tried stopping smoking in prison
For some, switching to e-cigarettes was perceived to increase PiC’s risk of returning to smoking on release. Indeed, some thought that PiC who wished to take up smoking after they were released regarded vaping as a temporary means of abstaining from smoking while in prison:
. . . until you’ve actually given up all of it, you know, you’re still taking nicotine. You potentially could start smoking tomorrow, you know what I mean . . . the nicotine would still be there like.
Male, tried stopping smoking in prison
They’ll just stop smoking tobacco and start smoking them [vapes] . . . So [if] you don’t want to continue smoking in between November and your exit from prison, they’ll just use e-cigarettes so they can still get their nicotine and then continue smoking when they get out.
Male, tried stopping smoking in prison
There was a general awareness that single-use e-cigarettes had been available from the canteen (these interviews were conducted during the 2 months before the decision to introduce rechargeable vaping devices), but they were viewed predominantly negatively, with numerous reports of poor product reliability and value for money:
. . . these daft [single-use] e-cigarettes . . . they’re garbage . . . bought a couple off the canteen sheet and they’re quite expensive . . . £2.50 for one ‘cigarette’ and you get 250 puffs out of it. You weren’t even getting what it says. No, so they’re shite.
Male, tried stopping smoking in prison
Some PiC who were more knowledgeable about e-cigarettes were strong advocates for the introduction of rechargeable devices, which were believed to be more effective replacements for tobacco:
. . . they’re really good, really, really good but they’re obviously going to be available on the shop with the vapes as well, I think the vapes are coming in. But obviously that is a good thing for people that just don’t want to stop smoking, they’re just going to maybe smoke that until they get released. But I don’t want to move from fags to another thing and then get released and I’m smoking e-cigs and that, I just want to try and cut it off all together.
Female, never tried stopping smoking in prison
However, as reported earlier (see Chapter 6, Surveys of people in custody), PiC’s knowledge of e-cigarettes and vaping was limited and participants identified a need for additional information and education on their use, and a workable mechanism to enable PiC to purchase more expensive rechargeable devices.
Perceived gaps in provision and suggested improvements
Suggested improvements to the cessation service at the time of interview focused predominantly on two areas, reflecting previous findings relating to barriers to service delivery, although other perceived gaps were raised.
Improved access to support
There were numerous requests from PiC for reduced waiting times (where these existed) and access to additional support outside formal sessions, beyond 12 weeks or on release (to deal with additional relapse triggers, such as alcohol or cannabis use):
. . . the smoking cessation thing in here, it is a good thing, because if you’ve got that every week . . . once you get past that 3-month period, the support kind of stops from there. Whereas, I know they can’t prolong it until the person’s out, but it would be better if there was something else there to help you, just in case you relapse . . .
Male, tried stopping smoking in prison
The decision in some prisons to allow advisors greater access to PiC in residential areas appeared to have partially addressed these concerns and highlighted a potential role for trained SPS staff and peer mentors to promote the service and support referrals and delivery in prison:
. . . it could be a good thing because if you’re then in the hallways, it’s more of a support thing because if you’re going to the group every week and that member of staff’s there, you’re kind of building up that rapport . . . you’re maybe having a bad day and you see that member of staff in the hall and you think well they know what was going on for me last week because I saw them at the group.
Male, never tried stopping smoking in prison
There was strong support for the health-care and NHS staff delivering cessation support, especially where a prior relationship existed (e.g. an advisor was also a PiC’s addiction support worker). However, there were mixed feelings about SPS staff being smoking advisors, depending in part on the personality of the staff concerned and their pre-existing relationships with the service user. The independence, expertise and enthusiasm of NHS and addiction staff were seen as key strengths of the existing service:
They know what they’re talking about . . . got a lot of skills and a lot of knowledge around [the] whole non-smoking thing . . . a hub of information. So if you’re going to do anything in life then you’re better off dealing with a person who knows what they’re talking about, rather than someone who hasn’t got a clue.
Male, tried stopping smoking in prison
Consistent pharmacotherapy supplies
Consistent with experiences expressed by some cessation service staff (see Interviews with staff responsible for managing and delivering cessation support in Scottish prisons), some PiC expressed desires for improvements in pharmacotherapy prescribing to resolve supply issues and associated risks of relapse. There were also requests for lower pricing and a full range of nicotine doses of NRT in the canteen:
. . . you used to get two [chances of accessing cessation support]. But because everything is so busy, coming into the ban, I think you just get the one chance now, or you have to buy your own off the canteen, ‘cause you can get it on the canteen sheet now. That’s why I was saying, it would be fine if we got the three stages on the canteen sheet, rather than the highest, step one . . . So, like, we have the chance, if we slip up, we could go back and buy them off the canteen ourselves, rather than coming off the 7-mg patches, and then only being available the 25 ml in the canteen. You don’t really want to be going back to that, from the 7 [-mg patch] or maybe the 14 [-mg patch] would be enough.
Male, never tried stopping smoking in prison
Although issues relating to waiting times and access to pharmacotherapies were within the domain of cessation support, most suggested improvements related to broader aspects of prison management and provision.
Other gaps
The need for more diversionary activities to keep people, and in particular their hands and minds, busy when tobacco is removed was identified as a significant gap. Requests included greater access to computer games, number/word/jigsaw puzzles and craft materials (colouring books, paints, needlework, etc.), physical activities and outdoor games (e.g. bowling), gym time, yoga classes and relaxation therapies. Some suggested that high-value materials (e.g. computer games, personal hygiene products) could be used as rewards for stopping. Those currently available (e.g. air fresheners, mugs, certificates), although not dismissed by service users, were considered of limited value. Smoke-free spaces were thought to remove temptation and make quitting easier. Requests included the guarantee of smoke-free cells, halls and flats for non-smokers and those trying to quit:
It would be a lot better if there was sections, like non-smoking . . . if you were really wanting to stop, you know, you could go into sections, and you could manage.
Male, never tried stopping smoking in prison
There was also extensive criticism of the single-use e-cigarettes in circulation at the time of these interviews and, as noted above, a call by some PiC for rechargeable e-cigarettes with more effective nicotine delivery systems. Participants also discussed compensating for the loss of tobacco products from the canteen with more food products, including a wider range of both healthy and less healthy options. Some PiC also called for the relaxation of prison rules, for example to allow greater access to telephones:
I don’t know if they’re going to put more stuff on [the canteen list] when the ban comes . . . obviously if they’re taking that [tobacco] off us I think we should have a substitute . . . the money I had spent on cigarettes I could be putting into munchies.
Male, never tried stopping smoking in prison
People in custody also identified the importance of cessation support being available at reception, not just at induction, which was where PiC were more likely to be offered a referral to cessation support. Suggestions included free NRT or e-cigarettes for incoming smokers and some form of ongoing behavioural support, although few were able to conceptualise how this might look post implementation. Some noted that CO testing was likely to prove inoperable once smoking was prohibited:
. . . they’d need some nicotine replacement straight away as they come in . . . Because most people that come in are usually alcoholic, drug dependent, so if they’re already coming off them, adding nicotine into the mix as well . . .
Female, tried stopping smoking in prison
There’s still going to be nicotine addiction. You know, you can freely buy nicotine on the canteen after the 30 November . . . It’s not tobacco anymore, it’s vapes, it’s this, it’s that. So guys will be just equally addicted to the vapes, and they’ve got the nicotine mints and the patches, as they will anything else. So it should be still there as a nicotine reduction course.
Male, tried stopping smoking in prison
Finally, although not always widely supported, it was evident that the ‘count-down’ poster campaign had successfully established and confirmed the impending introduction of the smoke-free policy. There were calls, however, for additional materials to promote cessation services, to highlight the benefits of quitting and living in a smoke-free environment, and for additional information on how the policy would be introduced and what support would be available:
. . . there’s a poster that every month they bring it down . . . 9 months to go, 8 months to go, 7 months to go. So, they are giving you plenty warning, like, this is actually happening. So, there’s nobody’s got an excuse now to say, ‘Oh I didn’t know about it’, like, everybody knows about it.
Male, tried stopping smoking in prison
I don’t even think there’s enough information about smoking cessation in the halls. There’s no posters, or anything like that. The only, I don’t know, I think there’s a poster just outside this door. And the only other thing is, the health-care referral forms, they’ve got the smoking cessation bit on them, and I think that’s about it.
Male, tried stopping smoking in prison
Summary
Interviews with cessation service providers were conducted in phases 1, 2 and 3. Before the announcement of the ban, the prospect of prisons going smoke free was a major topic of discussion among SSSs and prison health-care staff responsible for delivering cessation support; many expressed similar views to those raised by prison staff and PiC (e.g. questions about how it should be introduced and implications for the organisation of cessation support). There was broad support for the move towards the smoke-free policy, with many describing it as a positive development for prisoner health and an opportunity to limit smoking uptake on release, but the challenges were, again, recognised. Few of those delivering cessation services supported partial bans or a phased introduction. A suitable lead-in time was favoured to support increased capacity, flatten demand and allow for more than one quit attempt. Some services made changes to their protocols to manage waiting times and the importance of engaging prison staff as advocates was noted. In the lead-up to implementation, changes to the services were made to streamline access to support groups and pharmacotherapy. The decision taken to introduce e-cigarettes into the prisons soon before implementation presented some challenges, such as the reallocation of services. Larger prisons and those that relied on health-care staff to deliver cessation support were reported to be under greater pressure in responding to demand. Providing for smokers as they came into prison also presented challenges, especially given the many pressures on admissions staff, as did supporting people who did not wish to give up smoking to manage without tobacco.
The advantages and disadvantages of e-cigarettes were discussed by cessation providers before they were introduced; many frontline workers recognised that they might be popular with PiC who smoked, but some suggested that they may undermine existing cessation programmes and substitute a smoking culture with a vaping culture. Demand for cessation support was reported to have decreased immediately after e-cigarettes became available. Many frontline workers reported that they were frequently approached by PiC for advice on e-cigarette use and they noted a learning need to service providers on evidence on e-cigarettes and specific products available. The service providers interviewed noted different modifications needed to the cessation support, depending on the different approaches in different prisons. (Subsequently, new guidance on supporting PiC to cut down or quit vaping was developed. 80) Several potential challenges to service delivery in the new context of smoke-free prisons were identified in the provider interviews. Examples included difficulties in rapid identification of needs/wishes of smokers being admitted to prisons and with referral pathways on entry and exit from prison, differing interpretations of new service goals and outcomes (e.g. some advisors voiced a reluctance to work with e-cigarette users), knowledge deficits (e.g. about e-cigarettes) and challenges in making NRT available for those requiring symptom relief and minimising risks of waste.
Interviews were conducted with PiC with recent experience of prison smoking cessation services in phase 2. Their views on the impending smoke-free prison policy and facilitators of and barriers to stopping smoking in prison were largely similar to the views expressed by the separate sample of PiC who had participated in phase 2 interviews as part of WP4. Smoking cessation service users who expressed predominantly negative opinions about the policy tended to still be smoking or had relapsed, perhaps reflecting a general anxiety about quitting, even where they acknowledged real personal health benefits. There was also discussion regarding the potential impact on the emergence of illicit tobacco, competition for tobacco products and ensuing tensions, and the potential inability of certain prisons/prisoner groups to cope with the ban. Although most anticipated some negative reactions to the smoke-free policy, many of these service users (whatever their views) felt any resistance was likely to be relatively short-lived.
The cessation programme as a whole, and the commitment and expertise of specialist staff in particular, were widely praised. The independence, expertise and enthusiasm of NHS and addiction staff were seen as key strengths of the existing service. Key aspects of smoking cessation support that were highlighted as helpful were CO monitoring and the chance to meet and speak with other PiC who were attempting to quit, in addition to the impending implementation of the smoke-free policy. Barriers to cessation included the wider prison environment and (smoking) culture. Suggested areas for improvement in the lead-up to the smoke-free policy implementation included reductions in waiting times and access to additional support outside formal sessions or in preparation for release. Some expressed desires for improvements in pharmacotherapy prescribing to resolve supply issues and associated risks of relapse. There were also requests for lower pricing, a full range of nicotine doses of NRT in the canteen and more diversionary activities to keep people’s hands and minds occupied.
As with PiC interviewed in WP4, e-cigarettes were discussed as a potential alternative to tobacco, and a means of ameliorating the likelihood of trouble or unrest following the implementation of the ban. However, few who were actively seeking to stop smoking in phase 2 expressed a desire to take up any of these products and switching to e-cigarettes was perceived to increase the risk of returning to smoking on release. PiC’s knowledge of e-cigarettes and vaping was limited and participants identified a need for additional information and education on their use.
As with the PiC interviewed in WP4, these service users talked about how the ‘count-down’ poster campaign had successfully established and confirmed the impending introduction of the smoke-free policy. They too highlighted the opportunity for additional materials to promote cessation services and the benefits of quitting and living in a smoke-free environment, and requested additional information on how the policy would be introduced and what support would be available.
Chapter 8 Modelling of health and economic outcomes
This chapter reports the results from the various health economic analyses. The objective of the health economics evaluation was to estimate the change in outcomes and costs after the implementation of the smoke-free policy.
Within study
Results are presented for the base case previously described in Chapter 2, Health economic evaluation (work package 2), Within study analysis.
Cost–consequences analysis
The regression framework analysis compares costs and outcomes across all three phases. Results demonstrate no statistically significant change between phases (Table 16). For staff, there was a trend for GP costs to decrease each phase, and there was a small increase in tobacco spend between the pre-announcement and preparatory phases, and a decrease between the preparatory and post-implementation phases: an overall decrease across the study period. For PiC, both SAs and base-case analyses demonstrated a trend for GP/nurse costs to increase over the three phases.
| Costs | Phase, observed monthly mean cost (£) (SD); n | Change between phases | |||||
|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 1 vs. 2 | 2 vs. 3 | |||
| Coefficient (95% CI) | p-value | Coefficient (95% CI) | p-value | ||||
| Base-case analysis | |||||||
| Operational staff GP visits | 3.03 (8.26); 991 | 2.67 (7.88); 1001 | 1.99 (5.89); 513 | –0.364 (–1.07 to 0.345) | 0.32 | –0.675 (–1.45 to 0.099) | 0.09 |
| PiC GP/nurse visits | 3.64 (10.84); 2354 | 4.32 (23.54); 1783 | 4.77 (26.65); 1336 | 0.677 (–0.399 to 1.75) | 0.22 | 0.447 (–1.32 to 2.22) | 0.62 |
| Operational staff tobacco | 16.91 (64.28); 993 | 16.96 (58.54); 1008 | 15.98 (58.08); 514 | 0.049 (–5.34 to 5.44) | 0.99 | –0.979 (–7.19 to 5.23) | 0.76 |
| PiC tobacco | 24.93 | 24.93 | N/A | N/A | N/A | ||
The interrupted time series analysis compared costs and outcomes across the three phases and adjusted for overcrowding. Time series graphs for costs and outcomes with statistically significant results are included in Figure 8; the remaining graphs are available from the corresponding author.
FIGURE 8.
Interrupted time series results (statistically significant costs and outcomes). (a) Outpatient attendances; (b) cost of inpatient length of stay; (c) cost of mental health length of stay; (d) cost of A&E attendances; (e) cost of ambulance incidents; (f) cost of smoking-related illness medications; (g) cost of e-cigarettes; (h) number of fires; and (i) number of people managed on MoRs policy. MoRs, management of offenders at risk due to any substance.
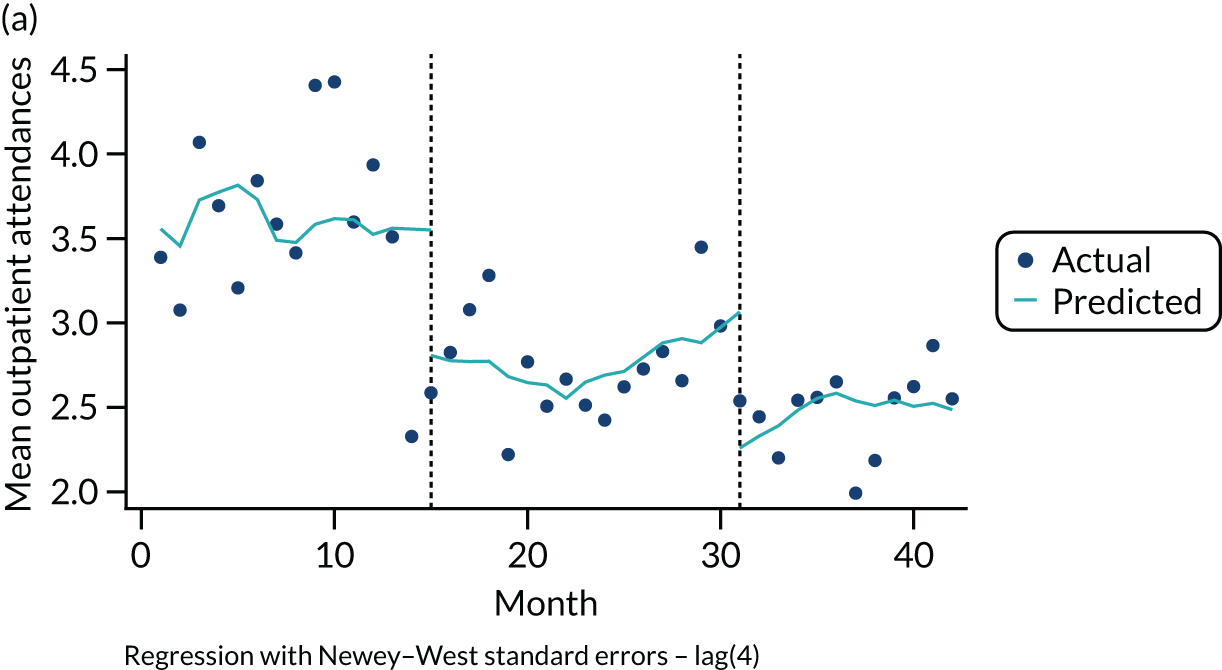
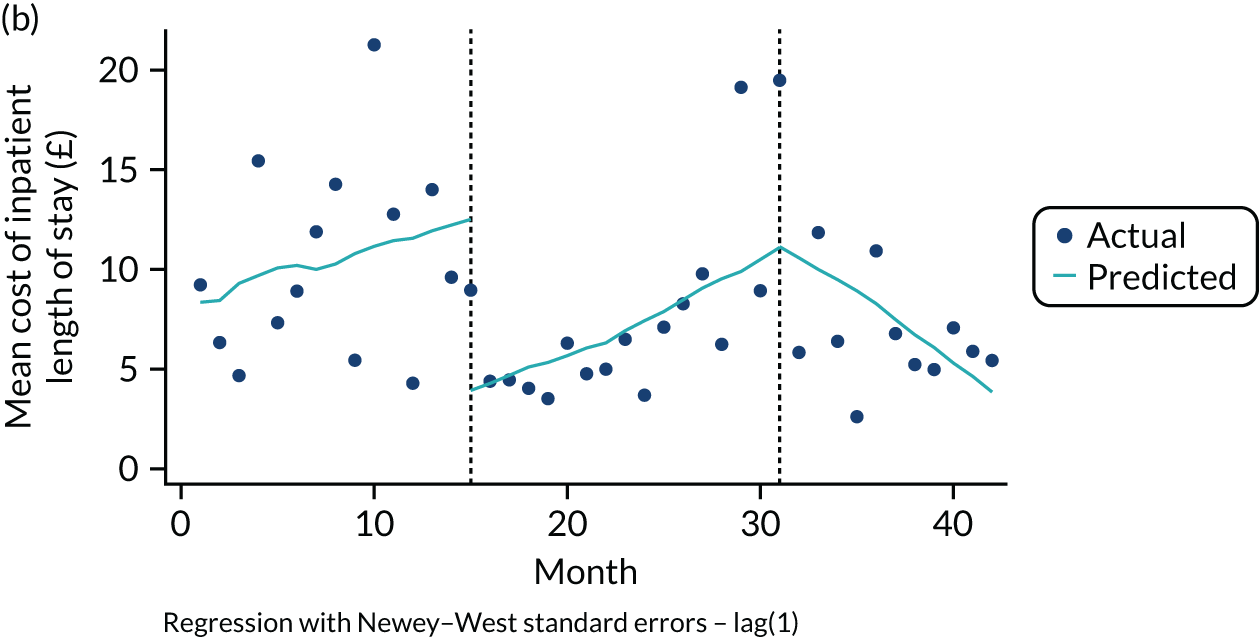
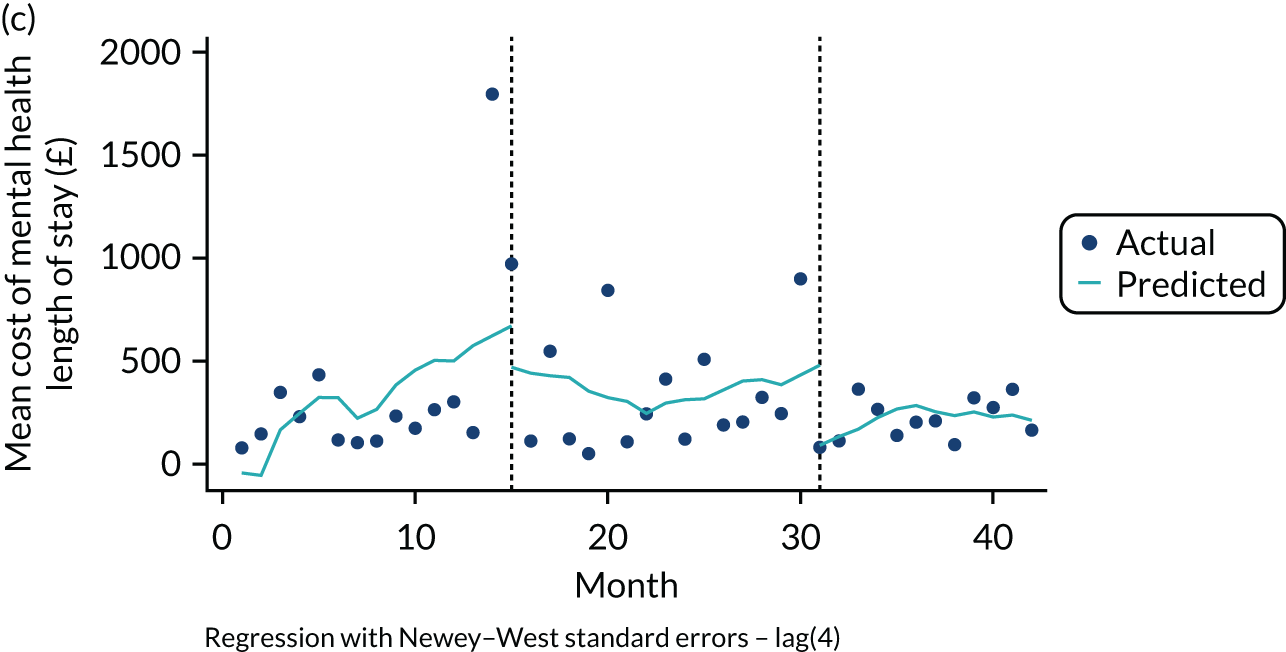

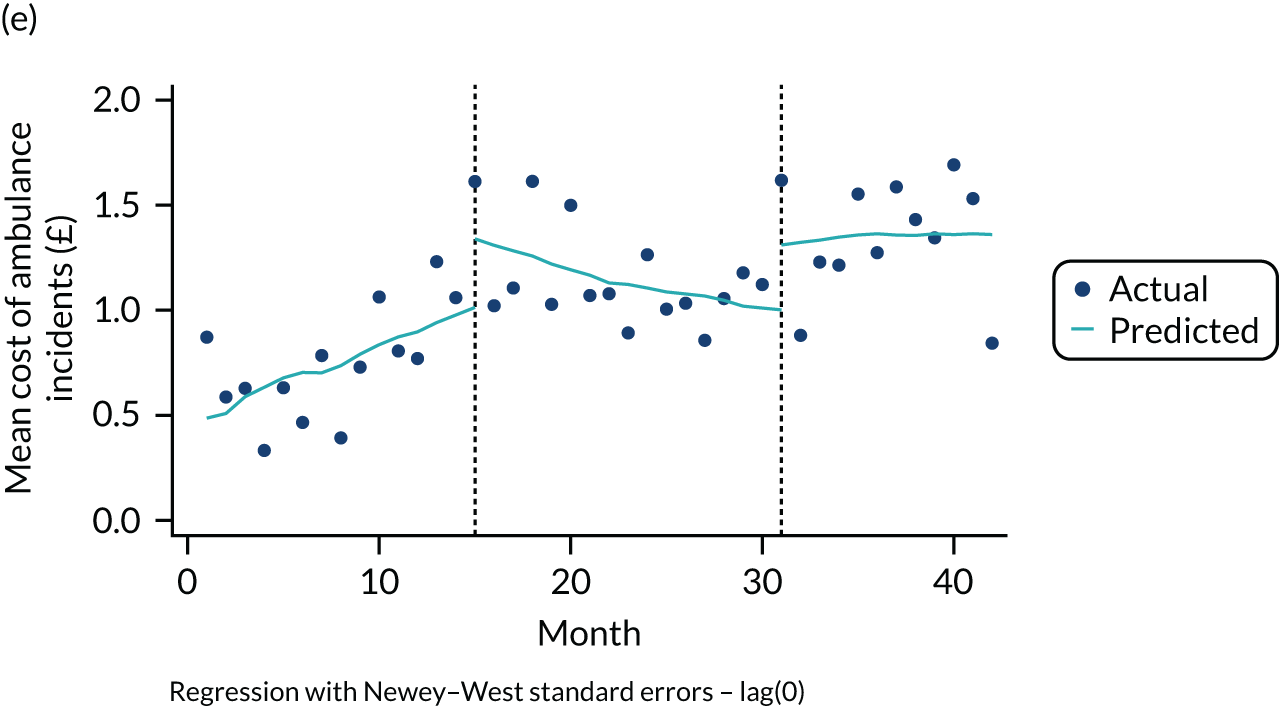
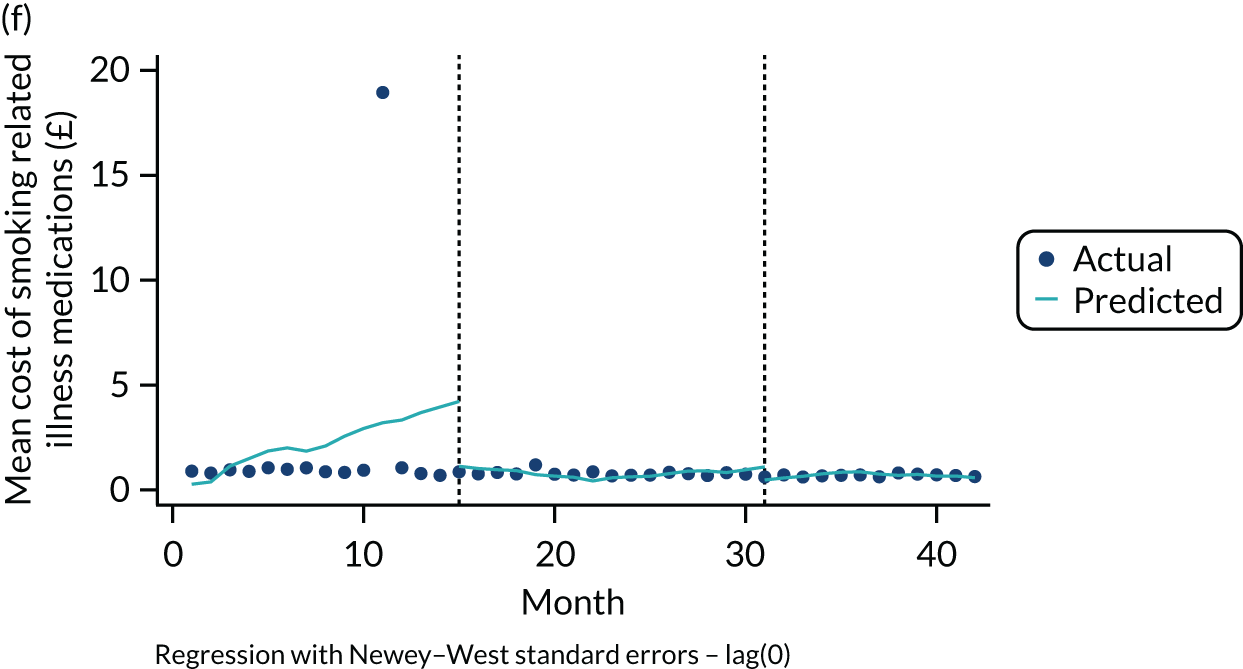
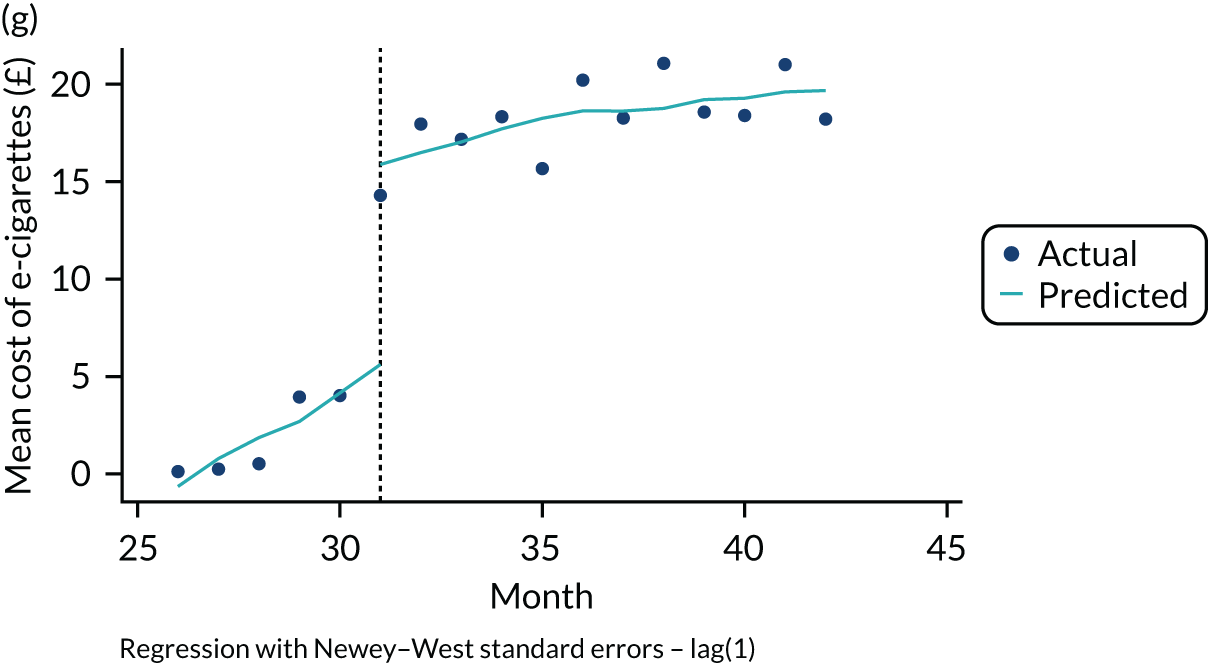
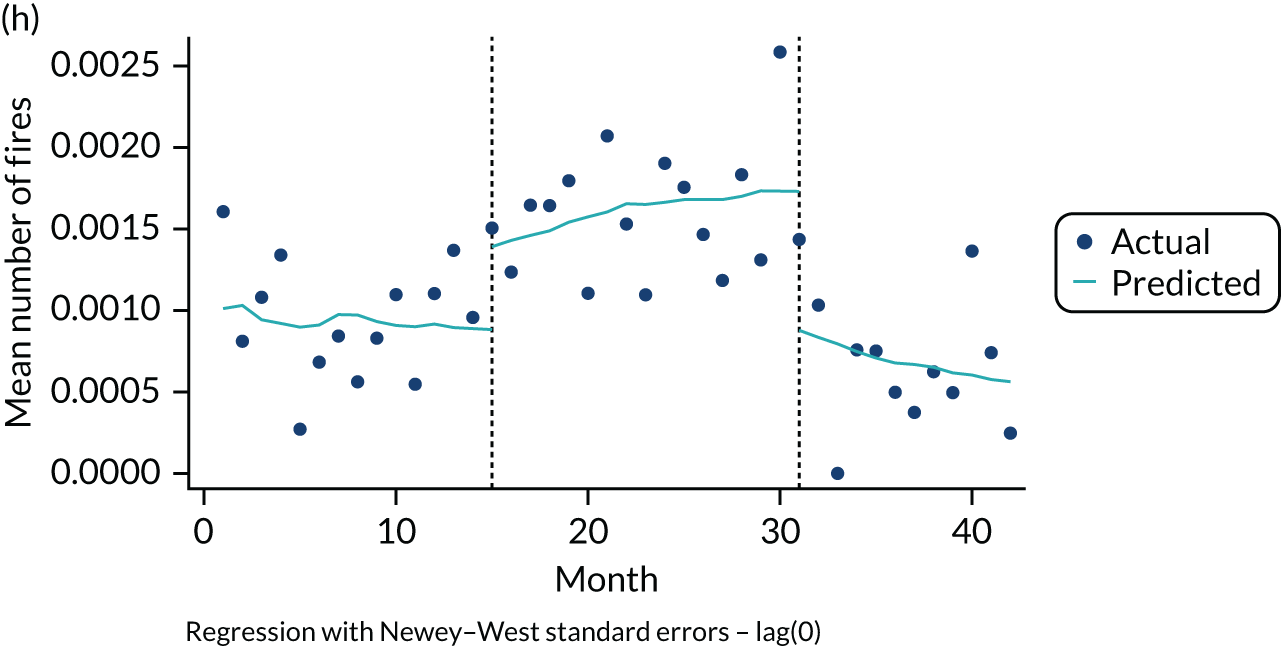
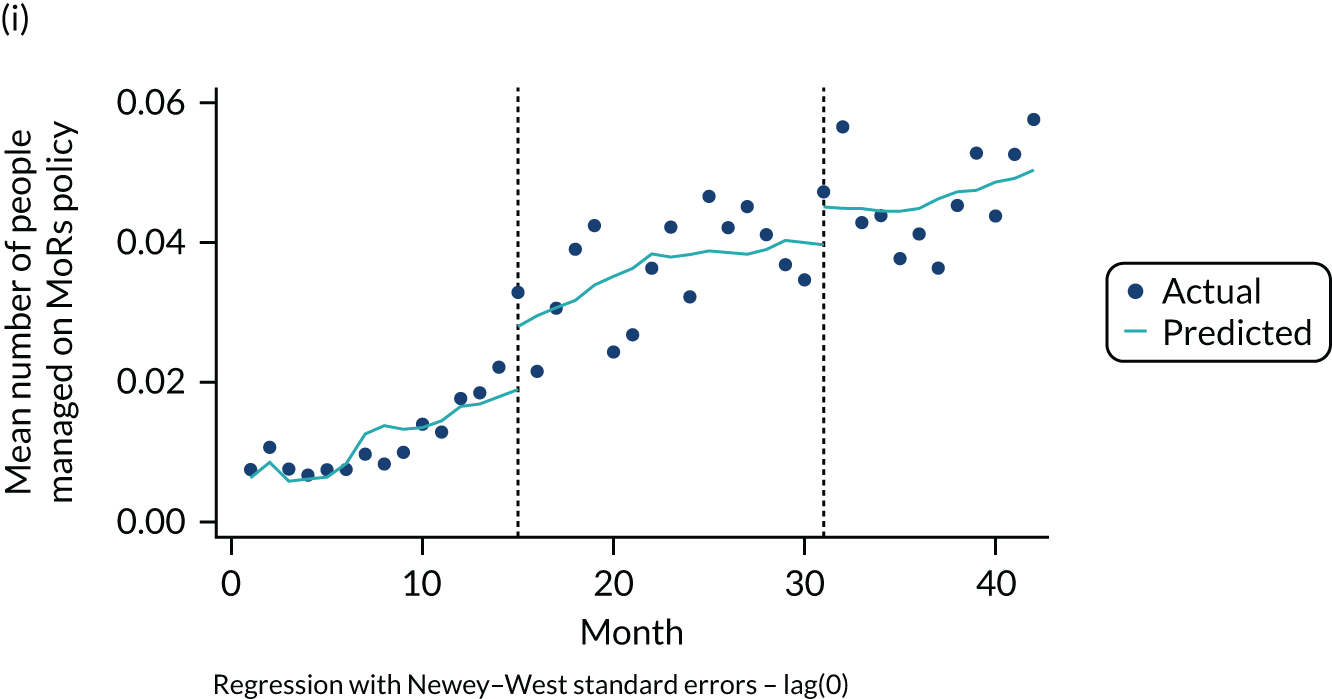
There was no consistent pattern in the results in terms of changes between specific phases (Table 17). However, all resource categories showed a trend towards decreasing costs over the study period, except ambulance incidents, medication for nicotine-dependence and e-cigarettes. Outpatient attendances and smoking-related illness medication costs saw a decrease each phase, ambulance incidents and medication for nicotine-dependence saw an increase each phase, and inpatient, mental health, and A&E costs decreased from the pre-announcement to the post-implementation phase.
| Cost | Phase, predicted means (£) | Change in phases | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 1 vs. 2 | 2 vs. 3 | |||||||
| Step change | Slope change | Step change | Slope change | ||||||||
| Coefficient (95% CI) | p-value | Coefficient (95% CI) | p-value | Coefficient (95% CI) | p-value | Coefficient (95% CI) | p-value | ||||
| Base case | |||||||||||
| Outpatient | 3.61 | 2.76 | 2.48 | –0.731 (–1.64 to 0.173) | 0.11 | –0.003 (–0.093 to 0.086) | 0.94 | –0.609 (–0.875 to –0.343) | 0.00a | –0.004 (–0.056 to 0.048) | 0.87 |
| Inpatient | 10.4 | 6.94 | 7.71 | –8.56 (–14.9 to –2.23) | 0.01a | 0.110 (–0.498 to 0.719) | 0.72 | 0.443 (–6.93 to 7.81) | 0.90 | –1.13 (–1.85 to –0.409) | 0.00a |
| Mental health stays | 321 | 370 | 217 | –193 (–729 to 342) | 0.47 | –62.7 (–140 to 15.0) | 0.11 | –266 (–497 to –35.3) | 0.03a | 4.96 (–25.4 to 35.3) | 0.33 |
| A&E visits | 1.53 | 1.71 | 1.46 | 0.045 (–0.146 to 0.236) | 0.64 | –0.037 (–0.065 to –0.010) | 0.01a | –0.061 (–0.206 to 0.083) | 0.40 | –0.047 (–0.080 to –0.013) | 0.01a |
| Ambulance | 0.739 | 1.15 | 1.35 | 0.330 (–0.081 to 0.740) | 0.11 | –0.061 (–0.108 to –0.014) | 0.01a | 0.340 (–0.084 to 0.764) | 0.11 | 0.025 (–0.045 to 0.094) | 0.48 |
| Medication (nicotine dependence) | 1.83 | 2.39 | 2.73 | –0.210 (–0.622 to 0.203) | 0.31 | 0.051 (–0.014 to 0.116) | 0.12 | –0.621 (–1.78 to 0.541) | 0.29 | –0.041 (–0.208 to 0.126) | 0.62 |
| Medication (smoking-related illness) | 2.20 | 0.793 | 0.688 | –3.05 (–9.77 to 3.66) | 0.36 | –0.312 (–0.975 to 0.351) | 0.35 | –0.279 (–0.794 to 0.236) | 0.28 | 0.001 (–0.039 to 0.041) | 0.98 |
| E-cigarettes | N/A | 1.77 | 18.26 | N/A | N/A | 11.3 (9.33 to 13.3) | 0.00a | –0.741 (–1.33 to –0.155) | 0.02a | ||
| Medication (all) | 91.1 | 115 | 138 | 13.1 (–7.81 to 34.1) | 0.21 | –1.38 (–3.76 to 0.994) | 0.25 | 1.98 (–18.2 to 22.1) | 0.84 | –0.219 (–3.52 to 3.08) | 0.89 |
Statistically significant changes between phases comprised the following: outpatient attendance costs decreased between the preparatory and post-implementation phases, inpatient length of stay costs decreased between the pre-announcement and preparatory phases and costs increased between the preparatory and post-implementation phases with a decrease in slope. The cost of mental health stays decreased between the preparatory and post-implementation phases. For A&E costs, the slope showed a decrease between all phases. The ambulance cost decreased from the pre-announcement to the preparatory phase. E-cigarette costs increased between the preparatory and post-implementation phases, a statistically significant step and slope change; however, this was expected as e-cigarettes became available to purchase in the preparatory phase and sales increased once tobacco was removed from the canteen list at the end of the preparatory phase.
None of the medication categories in sensitivity or base-case analyses shows a statistically significant change between phases, although it is worth highlighting an outlier in smoking-related illness medications in month 11 skewing results, because of single special line prescription; this resulted in an inflation of the predicted mean in the pre-announcement phase and so should be interpreted with caution. Analysis of the medication dispensed for PiC over the study period is also described in more detail elsewhere (see Acknowledgements, Publications).
Table 18 presents CCA outcomes from the regression framework analysis. The mean PM2.5 level decreased in each phase, from 38.44 µg/m3 in phase 1 to 11.15 µg/m3 in phase 2 and to 3.14 µg/m3 in phase 3, a statistically significant result. 11,31,32 There was a trend for staff health utilities to increase each phase, but this was not statistically significant. Health utilities for PiC decreased between phases; the decrease between the preparatory and post-implementation phases was statistically significant. Further analysis on the PiC health utility decreases showed that this was largely because of responses to the anxiety/depression domain of the EQ-5D (see Report Supplementary Material 2, Table 76).
| Outcome | Phase, observed mean (SD); n | Change in phases | |||||
|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 1 vs. 2 | 2 vs. 3 | |||
| 95% CI | p-value | 95% CI | p-value | ||||
| Levels of second-hand smoke, PM2.5 (µg/m3) | 38.44 (55.54) | 11.15 (4.93) | 3.14 (5.06) | –27.3 (–43.8 to –10.8) | 0.00a | –8.01 (–10.5 to –5.6) | 0.00a |
| Utilities (staff) | 0.859 (0.121); 1002 | 0.862 (0.127); 925 | 0.863 (0.135); 455 | 0.003 (–0.008 to 0.014) | 0.59 | 0.001 (–0.014 to 0.015) | 0.90 |
| Utilities (PiC) | 0.736 (0.248); 2268 | 0.725 (0.246); 1729 | 0.682 (0.270); 1298 | –0.010 (–0.026 to 0.005) | 0.18 | –0.043 (–0.062 to –0.025) | 0.00a |
Similarly to the costs analysis, there was no consistent pattern in terms of changes in outcomes between phases (Table 19). Overall numbers of ‘prisoner on staff’ assaults and deaths in custody remained constant, and numbers of ‘prisoner on prisoner’ assaults, fires and MoRs increased. The predicted monthly mean remained constant for ‘prisoner on staff’ assaults and showed changes between phases, and all-cause deaths in custody remained constant across the phases. Statistically significant results comprised a small increase for ‘prisoner on prisoner’ assaults between the preparatory and post-implementation phases, a small increase in fires between the pre-announcement and preparatory phases and a slighter larger decrease in the number of fires between the preparatory and post-implementation phases, and an increase in the number of PiC managed under MoRs policy between the pre-announcement and preparatory phases (see Figure 8). All SAs confirm these results (see Report Supplementary Material 3).
| Outcome | Phase, predicted means | Change in phases | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 vs. 2 | 2 vs. 3 | ||||||||||
| 1 | 2 | 3 | Step change | Slope change | Step change | Slope change | |||||
| Coefficient (95% CI) | p-value | Coefficient (95% CI) | p-value | Coefficient (95% CI) | p-value | Coefficient (95% CI) | p-value | ||||
| Prisoner-on-staff assaults | N/A | 0.004 | 0.004 | N/A | N/A | –0.001 (–0.003 to 0.001) | 0.31 | –0.0001 (–0.0004 to 0.0002) | 0.37 | ||
| Prisoner-on-prisoner assaults | N/A | 0.029 | 0.040 | N/A | N/A | 0.004 (–0.001 to 0.009) | 0.15 | –0.0008 (–0.002 to 0.0001) | 0.09 | ||
| All-cause deaths in custody | 0.0003 | 0.0003 | 0.0004 | –0.00003 (–0.0003 to 0.0003) | 0.87 | 0.00002 (–0.00002 to 0.00005) | 0.42 | 0.0002 (–0.0001 to 0.0005) | 0.30 | 0.000002 (–0.00005 to 0.00004) | 0.92 |
| Fires | 0.0009 | 0.0016 | 0.0007 | 0.0005 (0.00002 to 0.001) | 0.04a | 0.00004 (–0.00004 to 0.0001) | 0.32 | –0.0009 (–0.002 to –0.00002) | 0.045a | –0.00005 (–0.0001 to 0.00005) | 0.34 |
| MoRs | 0.012 | 0.036 | 0.046 | 0.009 (0.0006 to 0.017) | 0.04a | 0.00005 (–0.0008 to 0.0009) | 0.91 | 0.003 (–0.007 to 0.013) | 0.57 | –0.0002 (–0.001 to 0.001) | 0.80 |
Cost-effectiveness analysis
Annual costs used in the CEA analysis were broken down into components for the pre-announcement and post-implementation phases of the smoke-free policy (Table 20). Total staff costs were higher in the pre-announcement phase (£33 more) than in the post-implementation phase; this is mirrored by the PiC results (£65 more). The PiC difference in costs was largely driven by inpatient costs, medication for smoking-related illnesses and spending on e-cigarettes when compared with tobacco; however, for smoking-related illness medication this was largely due to the outlier described in Cost-consequences analysis. Cost categories that were more costly post implementation, compared with pre announcement for PiC, include GP/nurse visits, mental health stays, ambulance incidents and medication for nicotine dependence. The largest component cost was mental health stays. In SAs where all medications were added (i.e. SA1), costs were higher post implementation than with pre announcement; when data for the open prison were added (i.e. SA2) results mirrored base-case results (see Report Supplementary Material 3, Table 9).
| Resource | Cost (£) | |
|---|---|---|
| Pre announcement | Post implementation | |
| Operational staff | ||
| GP visits | 36 | 24 |
| Tobacco | 194 | 173 |
| Total for staff | 230 | 197 |
| PiC | ||
| Health services resources | ||
| GP/nurse visits | 44 | 57 |
| Inpatient | 122 | 92 |
| Outpatient | 45 | 30 |
| Mental health stays | 2548 | 2599 |
| A&E visits | 18 | 18 |
| Ambulance | 8 | 16 |
| Medication: smoking-related illness | 29 | 8 |
| Medication: nicotine dependence | 21 | 33 |
| Personal | ||
| Tobacco | 302 | – |
| E-cigarettes | – | 219 |
| Total for PiC | 3137 | 3072 |
Table 21 presents the cost-effectiveness results, described as a cost per additional 10 µg/m3 reduction in PM2.5. Base-case results were similar for staff and PiC. The post-implementation phase dominated the pre-announcement phase; this means that the post-implementation phase was less costly and there were lower levels of SHS than in the pre-announcement phase. This result was mirrored in SA2. In SA1, the cost per additional 10 µg/m3 reduction in PM2.5 was £149; the post-implementation phase was more costly and had lower levels of SHS than the pre-announcement phase.
| Analysis | Time point | Difference | ICER | |
|---|---|---|---|---|
| Pre announcement | Post implementation | |||
| Base case | ||||
| Operational staff | ||||
| Mean cost (£) | 230 | 197 | –33 | |
| Mean PM2.5 (10 µg/m3) | 3.84 | 0.31 | 3.53 | |
| Cost per additional 10 µg/m3 reduction in PM2.5 | –£10.00 (post dominates pre) | |||
| PiC | ||||
| Mean cost (£) | 3137 | 3072 | –65 | |
| Mean PM2.5 (10 µg/m3) | 3.84 | 0.31 | 3.53 | |
| Cost per additional 10 µg/m3 reduction in PM2.5 | –£18.00 (post dominates pre) | |||
| SA1: all medication | ||||
| PiC | ||||
| Mean cost (£) | 4195 | 4720 | 525 | |
| Mean PM2.5 (10 µg/m3) | 3.84 | 0.31 | 3.53 | |
| Cost per additional 10 µg/m3 reduction in PM2.5 | £149.00 | |||
| SA2: including open prison | ||||
| Mean cost (£) | 3134 | 3069 | –65 | |
| Mean PM2.5 (10 µg/m3) | 3.84 | 0.31 | 3.53 | |
| Cost per additional 10 µg/m3 reduction in PM2.5 | –£18 (post dominates pre) | |||
Cost–utility analysis
Costs are the same as those in the CEA. Table 22 presents the CUA results using a cost-per-QALY measure. For the staff base-case analysis, the post-implementation phase dominated the pre-announcement phase; this means that the post-implementation phase was less costly and had lower levels of SHS than the pre-announcement phase. For the PiC base-case analysis, the cost-per-QALY change was £1200; the post-implementation phase was less costly and less effective than the pre-announcement phase, and the resulting ICER was positive, with negative incremental costs and QALYs. In SA1, the pre-announcement phase dominated the post-implementation phase, being less costly and more effective. In SA2, results mirrored the base-case results.
| Analysis | Time point | Difference | ICER | |
|---|---|---|---|---|
| Pre announcement | Post implementation | |||
| Base case | ||||
| Operational staff | ||||
| Mean cost (£) | 230 | 197 | –33 | |
| Mean QALY gained/(lost) | 0.859 | 0.863 | 0.004 | |
| Cost per QALY (£) | –8460 (post dominates pre) | |||
| PiC | ||||
| Mean cost (£) | 3137 | 3072 | –65 | |
| Mean QALY gained/(lost) | 0.736 | 0.682 | –0.054 | |
| Cost per QALY (£) | 1204 | |||
| SA1: all medication | ||||
| PiC | ||||
| Mean cost (£) | 4195 | 4720 | 525 | |
| Mean QALY gained/(lost) | 0.736 | 0.682 | –0.054 | |
| Cost per QALY (£) | –9723 (post is dominated by pre) | |||
| SA2: including open prison | ||||
| PiC | ||||
| Mean cost (£) | 3134 | 3069 | –65 | |
| Mean QALY gained/(lost) | 0.736 | 0.685 | –0.051 | |
| Cost per QALY (£) | 1272 | |||
Long-term analysis
Base-case results
A breakdown of costs for the base-case results is presented in Table 23. Total costs were lower with the smoke-free policy (post implementation) than without it for both PiC (£32,848 vs. £33,749) and staff (£10,462 vs. £11,183). For both PiC and staff, the largest portion of total costs related to personal costs of tobacco and e-cigarette products (89% and ≈ 60%, respectively); implementation costs (here, costs of providing e-cigarette starter packs) were minimal.
| Cohort | Comparator: with or without smoke-free policy | Mean costs (£) | |||
|---|---|---|---|---|---|
| Implementation | Morbidity | Personal | Total | ||
| PiC | Without | 0 | 3626 | 30,122 | 33,749 |
| With | 14 | 3608 | 29,226 | 32,848 | |
| Operational staff | Without | 0 | 4169 | 7013 | 11,183 |
| With | 0 | 4160 | 6302 | 10,462 | |
Base-case analysis results are presented in Table 24. As well as costs being lower with the smoke-free policy than without, QALYs were higher in the smoke-free comparator for PiC and staff, suggesting that both cohorts benefit from an increase in quality of life with a smoke-free policy. PiC benefit from a greater increase in QALYs than staff (0.126 vs. 0.094).
| Cohort | Comparator: with or without smoke–free policy | Mean total costs (£) | Mean total QALYs | Incremental costs (mean) (95% CI) (£) | Incremental QALYs (mean) (95% CI) | ICER estimate (95% CI) (£) |
|---|---|---|---|---|---|---|
| PiC | Without | 33,749 | 16.456 | |||
| With | 32,848 | 16.582 | –900 (–1562 to –222) | 0.126 (0.076 to 0.172) | –7133 (–14,940 to –1937) | |
| Operational staff | Without | 11,183 | 20.015 | |||
| With | 10,462 | 20.109 | –720 (–874 to –568) | 0.094 (0.054 to 0.144) | –7689 (–13,836 to –4889) | |
For both PiC and staff, ‘with the smoke-free’ policy dominates the ‘without smoke-free’ policy comparator, meaning that mean lifetime costs were lower and quality of life was higher with the smoke-free policy than without it. For completeness, the resulting negative ICERs are presented. No 95% CIs cross zero, indicating that there was little uncertainty in the dominance of the ‘with smoke-free’ comparator.
The cost-effectiveness plane is presented in Figure 9. Plots represent the 1000 bootstrap iterations in each cohort; the triangles represent the respective PSA mean point estimates and the red line represents the £20,000 cost-effectiveness threshold; all estimates below this line are considered cost-effective compared with the £20,000 willingness-to-pay threshold.
FIGURE 9.
Cost-effectiveness plane.
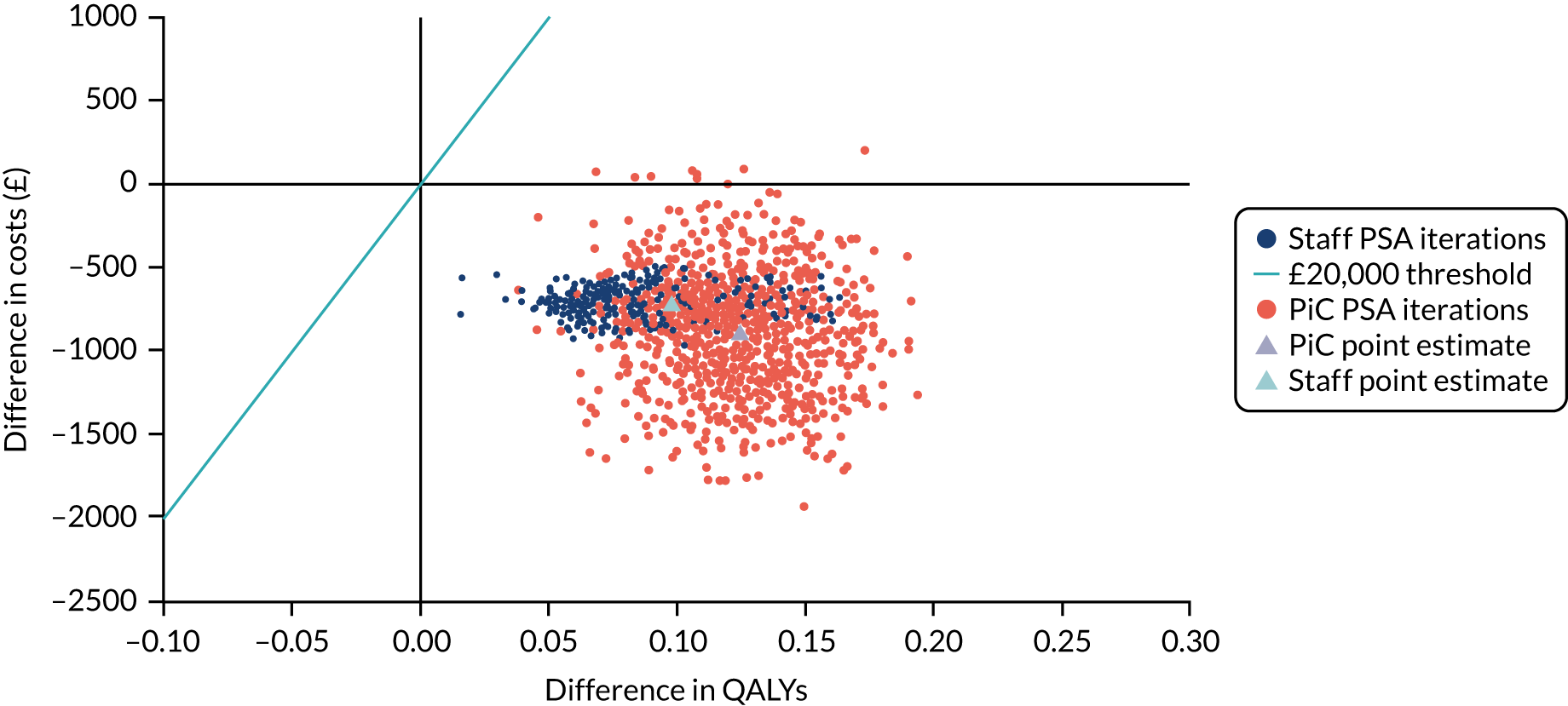
Nearly all estimates were in the south-east quadrant of the cost-effectiveness plane, where the ‘with smoke-free policy’ is less costly and more effective than without, for both PiC and staff. At the £20,000 willingness-to-pay threshold, the smoke-free policy for both cohorts would be considered cost-effective compared with not having the smoke-free policy.
Scenario analyses results
The results for the scenario analyses are presented in Table 25; the results for scenarios 1–9 apply to PiC only. ICERs varied from –£25,215, when applying the resumption of smoking on release rate reported in the TIPs PiC questionnaire (scenario 1), to –£2089, when canteen tobacco spend while in prison was applied to tobacco smokers after release (scenario 9). None of the scenario analyses resulted in a positive ICER.
| Comparator: with or without smoke-free policy | Mean total costs (£) | Mean total QALYs | Incremental costs (£) | Incremental QALYs | ICER (£) |
|---|---|---|---|---|---|
| Base-case PiC results | |||||
| Without | 33,749 | 16.456 | |||
| With | 32,848 | 16.582 | –900 | 0.126 | –7133 |
| 1. PiC smoking resumption on release: TIPs questionnaire | |||||
| Without | 33,749 | 16.456 | |||
| With | 24,869 | 16.808 | –8880 | 0.352 | –25,215 |
| 2. PiC smoking resumption on release: 90% | |||||
| Without | 33,749 | 16.456 | |||
| With | 29,657 | 16.672 | –4092 | 0.217 | –18,893 |
| 3. PiC time in prison: 1 year | |||||
| Without | 37,478 | 16.393 | |||
| With | 36,693 | 16.449 | –784 | 0.056 | –13,904 |
| 4. PiC time in prison: 10 years | |||||
| Without | 23,841 | 16.737 | |||
| With | 22,443 | 17.075 | –1398 | 0.338 | –4134 |
| 5. PiC time in prison: 17 years | |||||
| Without | 17,504 | 17.039 | |||
| With | 15,674 | 17.541 | –1830 | 0.503 | 3640 |
| 6. Utilities TIPs PiC questionnaire | |||||
| Without | 33,749 | 15.256 | |||
| With | 32,848 | 15.385 | –900 | 0.129 | –6997 |
| 7. PiC mortality: aSpaulding et al.18 | |||||
| Without | 36,967 | 17.598 | |||
| With | 36,043 | 17.732 | –923 | 0.134 | –6884 |
| 8. ‘In-prison’ tobacco and NVP spend: TIPs questionnaire | |||||
| Without | 34,281 | 16.456 | |||
| With | 33,317 | 16.582 | –964 | 0.126 | –7635 |
| 9. ‘Post-prison’ tobacco spend: canteen ‘in-prison’ data | |||||
| Without | 7772 | 16.456 | |||
| With | 7508 | 16.582 | –264 | 0.126 | –2089 |
| 10. 1.5% D | |||||
| PiC without | 47,107 | 22.635 | |||
| PiC with | 45,946 | 22.776 | –1160 | 0.141 | –8224 |
| Operational staff without | 18,322 | 29.352 | |||
| Operational staff with | 17,369 | 29.460 | –953 | 0.109 | –8776 |
Two scenarios resulted in lower incremental costs than the base-case analysis: scenario 3 (PiC time in prison: 1 year) and scenario 9 ‘post-prison’ tobacco spend: canteen ‘in-prison’ data. Scenario 3 resulted in lower incremental cost for personal spend as a result of less time in prison with lower tobacco costs applied, and scenario 9 resulted in lower incremental costs as a result of similar tobacco costs in both the ‘in-prison’ and ‘post-prison’ periods. The remaining scenarios had higher or similar incremental costs to the base-case scenario. The two scenarios with the largest incremental costs were the ones exploring the effects of varying assumptions about the resumption of tobacco smoking following release; these showed greater savings because of lower personal spending on tobacco following release.
One scenario, scenario 3 (PiC time in prison: 1 year) resulted in lower incremental QALYs than the base-case scenario (0.056 vs. 0.126, respectively).
In two scenarios, only costs were affected: scenarios 8 and 9 had the same incremental QALYs as the base-case, and the remaining scenarios estimated an increase in incremental QALYs. The scenarios with the greatest increase in QALYs were scenario 1 [PiC smoking resumption on release: TIPs questionnaire (0.352)], scenario 4 [PiC time in prison: 10 years (0.338)] and scenario 5 [PiC time in prison: 17 years (0.503)].
Overall impact of policy
Total cohort costs and QALYs are presented in Table 26 for PiC, staff, and PiC and staff combined. Cost reductions related to morbidity costs and personal tobacco costs with the smoke-free policy equated to approximately £6.7M in the PiC cohort, £2.3M in the staff cohort and £9.0M overall. The number of QALYs gained with the smoke-free policy equate to 947 in the PiC cohort, 304 in the staff cohort and 1251 overall.
| Cohort | Comparator: with or without smoke-free policy | Mean total costs (£) | Mean total QALYs | Incremental costs (£) | Incremental QALYs |
|---|---|---|---|---|---|
| PiC (n = 7500) | With | 253,115,277 | 123,418 | ||
| Without | 246,408,195 | 124,365 | –6,707,082 | 947 | |
| Operational staff (n = 3244) | With | 36,276,065 | 64,929 | ||
| Without | 33,939,310 | 65,233 | –2,336,755 | 304 | |
| Combined | With | 289,391,342 | 188,347 | ||
| Without | 280,347,504 | 189,597 | –9,043,838 | 1251 | |
Summary
The objective of the health economics evaluation was to estimate the change in outcomes and costs after the implementation of the smoke-free policy.
The within-study CCA compared costs and outcomes across the three phases. In the interrupted time series analysis, all resource categories showed a trend towards decreasing costs over the study period, except ambulance incidents, medication for nicotine dependence and e-cigarettes. Changes were seen between phases for costs of outpatient attendance, inpatient stays, metal health stays, A&E visits, ambulance callouts and e-cigarettes. Similar to the costs analysis, there was no consistent pattern in terms of changes in outcomes between phases. Overall numbers of ‘prisoner-on-staff’ assaults and deaths in custody remained constant, and numbers of ‘prisoner-on-prisoner’ assaults, fires and MoRs increased. The within-study CEA showed that total staff costs were higher in pre-announcement phase than they were in the post-implementation phase; this is mirrored by PiC results.
In the long-term health economic modelling, total costs were lower with the smoke-free policy than without it for both PiC and staff. For both PiC and staff, ‘with the smoke-free’ policy dominates the ‘without smoke-free’ policy comparator, meaning that mean lifetime costs were lower and quality of life was higher with the smoke-free policy than without it. At the £20,000 willingness-to-pay threshold, the smoke-free policy for both cohorts would be considered cost-effective, compared with not having the smoke-free policy. Several scenarios were modelled to estimate the impact of varying assumptions about various parameters in the models. The scenarios with the biggest impact on results were two scenarios exploring the effects of varying assumptions about the resumption of tobacco smoking following release; these showed greater savings because of lower personal spend on tobacco following release. Population-level cost reductions related to morbidity costs and personal nicotine costs, with the smoke-free policy equating to approximately £6.7M in the PiC cohort, £2.3M in the staff cohort and £9.0M overall.
Chapter 9 Partnership working and stakeholder engagement (work package 6)
As indicated in Chapter 1, Legislative and policy context prior to commencement of the Tobacco in Prisons study, and Chapter 1, Patient and public involvement, we worked closely with key stakeholders in the original design of the study. We participated in SPS Tobacco Strategy Group meetings in 2015 and in further discussions with policy-makers within the Scottish Government, SPS, NHS Health Scotland and staff trade unions. The TIPs RAG constituted by SPS in 2016 included the head of SPS Health and Wellbeing; representatives of staff health and safety, and trade unions; and people leading tobacco control in NHS Health Scotland and the Scottish Government. RAG members provided extensive feedback on all aspects of the design, including study materials and approaches. Prior to starting any fieldwork, during visits to every prison with a member of the SPS Health and Wellbeing team, we met the Governor-in-Charge or their appointed deputy and any members of staff with whom they wanted us to discuss the proposed research design and procedures. RAG members commented on early findings from phase 1 through face-to-face meetings at SPS headquarters, and we presented preliminary findings related to the SHS results to Governors-in-Charge and other key stakeholders within prison, health services and government, preceding and during external peer review.
During phase 2, the preparatory phase after the date of implementation of the smoke-free rules had been announced, we attended the monthly meetings of the SPS’s SAG supporting those charged with detailed planning in the lead-up to implementation. Under a standing agenda item, we provided written and/or verbal updates on emerging findings from all aspects of the TIPs study, ensuring that any relevant information was disseminated to key stakeholders in as timely a manner as possible to inform ongoing strategies. Pre and post implementation, we have presented emerging findings to colleagues in the Scottish Government and tobacco control agencies [e.g. Action on Smoking and Health (ASH) Scotland (Edinburgh, UK)] at one-to-one meetings and presentations to the Research and Evaluation Sub-Group of the Scottish Ministerial Working Group on Tobacco Control, in addition to many presentations at public health and tobacco- or addiction-related conferences nationally and internationally.
We have interviewed several key stakeholders to understand whether or not and how TIPs findings and our approach to partnership working were useful; these interviews have also been used to support impact case studies for the UK’s Research Excellence Framework 2021. The value of our partnership working approach is illustrated by an extract from an interview with Linda Dorward, the SPS lead for the smoke-free prisons project, for a ‘vlog’ for WEPHREN’s (Worldwide Prison Health Research and Engagement Network) coverage on World No Tobacco Day 2019, which highlighted Scotland’s success in implementing smoke-free rules and reducing SHS in prisons:
[it’s been] a tremendous success . . . within 18 months, we went from every prison in Scotland allowing people [in custody] to smoke to smoke-free . . . A big part was partnership working . . . [including] initial bit of research onto the second-hand smoke levels in prisons. That made us sit up and take notice of the issues we had . . . Also that backing from [TIPs] pre-, during and post- has . . . allowed us to measure how good or badly we’ve been doing in embedding the project . . . it’s worked really, really well . . . The fact that you guys were doing some very informed and robust focus groups and questionnaires allowed us to check whether our message was getting home. So having you as part of our SAG meetings was really important. And you feeding back on some of the research . . . was really helpful for us.
She described the SHS results as ‘an absolute game changer . . . finding out that very broadly speaking . . . working in a residential area of a prison was like living with a smoker. It was shocking and unacceptable . . . so that effectively moved things’. A representative from Scottish Government agreed, saying:
What TIPs brought us was the catalyst . . . without TIPs, I think we probably still wouldn’t have smoke-free prisons [in Scotland] . . . and the transition certainly would not have been as smooth. It gave us some credible evidence which was very persuasive politically for the decision makers, but also for the people who’d have to implement it. So, the timing for implementation became suddenly very accelerated . . . without TIPs that wouldn’t have happened . . . I think the phase 2 was as important as the phase 1. The phase 1 gets us to an evidence base for making decisions. The phase 2 is much more focused on how the actual policy change would be made . . . it’s one of the rare brilliant times where you can see the research smoothing the way for the policy.
A lead on public health in Health Scotland agreed, describing the TIPs study as ‘a great example of how Health Scotland and, you know, third sector and then academia can work together’.
Another success of partnership working was our innovative ‘citizen science’ approach to the collection of data on air quality (see Chapter 2, Staff training and engagement, and Chapter 2, Mobile-task monitoring), working directly with staff working within the prisons. The SPS Head of Health and Safety, who helped to facilitate the SHS data collection, valued the way these staff were involved in the research process and the positive impact on continuing professional development:
It’s been fantastic that we’ve went through the stages [of the research] and provided [staff and the unions] a baseline [SHS exposure] to what it is now, through a proper process that they understand . . . how it was monitored and measured . . . [T]hat’s all in all perfect for me . . . it’s been a benefit, a massive benefit, to transfer information to the people on the shop floor.
As well as presenting a model of partnership working for the prison smoke-free policy, stakeholders also described TIPs as a model of ‘best practice’ for partnership working in the development and implementation of challenging policy, from SPS, government and health service perspectives. The SPS lead for implementation of the smoke-free prison project stated:
[E]verybody involved in the project, I think, deems it a success and an absolute best-practice model of working in partnership with yourselves and the TIPs project, but also with the NHS, with our own trade union side, and with those across the prison service. It’s worked really, really well and made a tremendous difference to people’s lives . . . Because the research was so influential in developing these successful working partnerships, it had a direct influence on shifting the culture of practice in the SPS for the benefits of prisoners and staff alike.
A Scottish Government representative said this partnership approach had:
. . . engendered a real enthusiasm for further change in other fields . . . the partnership aspect of TIPs and the enthusiasm with all parties to it, the enthusiasm people had for it, has been very helpful in a lot of wider policies as well. So things you wouldn’t necessarily get credit for.
In addition, the SPS lead for smoke-free prisons suggested that:
. . . the smoke-free prisons partnership working has . . . raised the profile of what we can do working together, where that wasn’t there before.
Chapter 10 Overall synthesis of findings
Overview of findings from work packages 1–6
This study is the first, to our knowledge, to undertake a detailed evaluation across a national prison system of a major organisational change, that is the development of, announcement of, preparation for and implementation of a comprehensive smoke-free policy. It included analysis of data collected on SHS exposures, a wide range of other outcomes, and the opinions and experiences of PiC, prison staff, and users and providers of smoking-cessation support services (through surveys and in-depth one-to-one interviews or focus groups) prior to formulating the policy change, in the period between its announcement and implementation, and after the new policy became part of the organisation’s status quo. It also included the analysis of routinely collected data (e.g. outpatient/inpatient visits, medications dispensed for PiC, staff sickness absence), which contributed to a health economic analysis that assessed cost-effectiveness in the short and long term. The study involved close but independent partnership working with staff within the SPS, within individual prisons and within SPS headquarters, and rapid feedback of emerging findings on an ongoing basis throughout the first two phases of the study to inform strategies and provide feedback on their reception and impact in preparation for implementation.
Interviews with people from other jurisdictions with experience in implementing a smoke-free prison policy (WP1) highlighted a number of factors that were seen to be beneficial, adding to previous reports:25 adequate time to prepare to allow for increased access and reduced barriers to smoking cessation support and for good and widespread communication and engagement with staff and PiC, and increased provision of alternative (diversionary) activities. Participants also pointed to the need for adequate governance structures at the local and national level to support implementation and post-implementation management of smoke-free rules, and the benefit of good partnership working with relevant external agencies. Those who had worked in prisons in E&W also stressed the potential benefits of making e-cigarettes available as an alternative to tobacco.
The measurements of SHS exposures (as part of WP2) demonstrated average levels of exposure at baseline in 2016 in the range of 20–30 µg/m3, that is levels that were similar to reports from a small number of prisons in E&W27,76 and to those expected for a non-smoker living with a smoker. Some tasks (e.g. cell searches) could lead to exposures that were more similar to those experienced in a bar13 prior to the smoke-free laws introduced in the community in 2006/7 in the UK. 11 The publication of these results partially influenced SPS’s decision to introduce a comprehensive smoke-free prison policy from November 2018. 4 Data on SHS concentrations collected in the week of implementation showed a substantial fall in levels of PM2.5 across all prisons. 32 Data collected 6 months post implementation suggested that this reduction was maintained or enhanced; on average, the median reduction in PM2.5 concentrations was 91%, resulting in levels that were as low as or lower than concentrations measured in outdoor air at the closest measuring station to each prison. In addition, analyses of the 2019 measurements showed that the higher levels of exposure seen in 2016 for staff working on particular shifts (‘early’ shift) or undertaking certain tasks (e.g. cell searches, opening cells in the morning) had been effectively eliminated by 2019.
Surveys (repeat cross-sections) of prison staff, conducted alongside in-depth qualitative research with staff as part of WP3, were returned by 27% of prison-based staff in phase 1, 31% in phase 2 and 16% in phase 3. These relatively low return rates, and the variation in return rates by prison and phase reported earlier, mean that survey results should be interpreted with caution, and in the context of other findings from the TIPs study. However, sociodemographic and work-based characteristics were similar across phases, and the sex and age distributions were similar to those within the SPS as a whole. The survey results highlighted some concerns among staff about both SHS exposures and the challenges of introducing smoke-free rules in the prison context. Phase 1 data showed staff (particularly non-smokers) were more positive about smoking bans than PiC. A number of individual variables and the objectively measured prison SHS levels in phase 1 were associated with staff opinions on prison smoking bans. 40 Survey findings suggested that staff support for prison smoking bans increased in anticipation of and, more so, following the ban. However, staff opinions on e-cigarettes were more negative following the ban. Views on preparation in the lead-up to the ban and on the results of the ban were largely (very) positive, although staff highlighted particular issues with illegal drugs and the adaptation of e-cigarette devices following implementation, consistent with their reports of some challenges encountered (described in more detail elsewhere, O’Donnell/Brown, personal communication; see Acknowledgements, Publications). Reported exposure to tobacco smoke decreased across phases, markedly so between phase 2 and phase 3, reflecting the results from our objective measurements of SHS exposures, but reported exposure to e-cigarette vapour increased between phase 2 and phase 3.
The findings from qualitative research conducted with prison staff over the course of the study were largely consistent with the survey results but illustrated (the complexity of) some of these perceived issues, benefits and concerns in more depth. For example, analysis of focus groups with staff across the prison service in phase 1 revealed considerable concern (and some anger and frustration) about exposures to SHS,54 and mixed views about whether or not e-cigarettes had a place within prisons. 55 Staff debated the fairness or otherwise of ongoing SHS exposures at work on the one hand, and the imposition of a ban on smoking for PiC on the other, recognising the central place of tobacco for many people in their care. 5,20–22,38,54,55,75,77 On balance, they recognised a need to protect the health and welfare of both staff and PiC. They also expressed concerns about the challenges of introducing stricter rules on smoking, and about whether or not a comprehensive ban on tobacco would be ‘workable’ and enforceable, although several remarked on the prison service’s track record in ‘getting a difficult job done’ when needed. The perceived challenges included protecting the well-being of PiC; the risk of increases in confrontations, violent incidents, bullying and the use of alternative substances; and the resultant increased stresses inherent in their roles at work. They also suggested strategies to mitigate these challenges. Some reflected media coverage of prison bans elsewhere24 in expressing worries that a ban may precipitate serious unrest or riots.
In-depth interviews with staff in the six ‘case-study’ prisons in the early part of the preparatory phase showed that many of these concerns and issues remained as preparations for going smoke-free were under way. Many staff were pleased about the prospect of eliminating or reducing SHS exposures, but still worried about the potential challenges. There was continuing discussion about whether or not e-cigarettes would be allowed in Scottish prisons and, if so, whether they would be an essential part of a smooth transition or bring their own potential risks and organisational problems. Staff also expressed continuing concerns about how best to support PiC in the lead-up to implementation.
Focus groups with staff in all prisons around 6 months post implementation supported the survey data in showing, in general, strong staff support for the smoking ban, although a minority still suggested that it was unfair to ban a substance that could be legally bought outside prison (a fact also true of alcohol, which none suggested should be sold in prisons). Participants described the TIPs study SHS exposure data as a ‘turning point’, and there was broad consensus about the relatively smooth nature of the transition to smoke-free rules, and that staff and PiC now accepted these as the ‘new normal’. There was widespread, if sometimes reluctant, recognition that the implementation had been well managed at all levels. Contrary to expectations and to experiences elsewhere, contraband tobacco was viewed as a less serious issue than anticipated. Many thought that e-cigarettes were instrumental in the smooth transition, a ‘game changer’, but concerns were also raised about the perceived limited evidence base on long-term effects of vaping and exposure to second-hand vapour, and about use of rechargeable vaping devices for the consumption of illegal drugs.
As highlighted above for the staff surveys, results from surveys of PiC should be interpreted with caution, particularly for the post-implementation period (return rates: phase 1, 34% of PiC; phase 2, 25%; phase 3, 18%). Nonetheless, sociodemographic and prison-based characteristics were similar across phases, and similar to those reported across the SPS as a whole. The phase 1 survey confirmed that, prior to the implementation of the ban, smoking rates among PiC were very high2,8,16,18,41,78 and most continued to smoke during the lead-up to its introduction, following which levels of e-cigarette use increased very substantially. This was by far the most commonly reported strategy for managing without tobacco within smoke-free prisons. With the exception of reduced coughing and phlegm, the self-reported health of PiC remained stable or slightly worsened across phases, but reported SHS exposure decreased, particularly between phase 2 and phase 3, when reported exposure to e-cigarette vapour increased. Phase 1 data indicated that PiC (and particularly smokers) were much less positive about smoking bans than staff. Like staff, support for prison smoking bans among PiC increased in anticipation of and following the ban. However, again as with staff, their opinions on e-cigarettes were more negative post ban. Views on preparation in the lead-up to implementation and on the outcomes of the ban were also less positive than those of staff, although around half indicated that it had helped improve their health. Like staff, survey responses from PiC were most likely to identify issues with illegal drugs as being the most problematic following implementation.
In general, the views (both positive and negative) expressed in the surveys triangulated well with those from in-depth, one-to-one interviews with PiC, where the complexity and multidimensionality of people’s views could be more fully explored. Qualitative interviews with PiC in the six ‘case-study’ prisons in the preparatory phase suggested (potential) facilitators of implementation, including increased provision of stop-smoking support and the introduction of e-cigarettes (which were not yet permitted within Scottish prisons at the time of these interviews). The central place of tobacco in prison culture, its major role in helping many manage negative emotions such as stress and boredom, and the high prevalence of smoking and the ‘normality’ of smoking were seen as major barriers. Opinions about the impending ban varied, with arguments in favour relating to both potential financial and health gains.
In-depth interviews with PiC in the post-implementation phase confirmed staff views (and, in many cases, surprise) about the lack of ‘trouble’ associated with the transition to smoke-free rules and the speed with which they were accepted. Even when participants continued to disagree with the policy, some advantages were identified, although some continued to hold negative or complex, mixed views. The PiC interviews supported the consensus among staff that contraband tobacco was not a big issue. The introduction of (rechargeable) e-cigarettes was seen as important in this, and in helping many to cope without tobacco. Again, as with staff, PiC recognised that introducing e-cigarettes had also brought challenges: some found them less satisfying than smoking cigarettes, worried about swapping one form of dependence for another or expressed a desire to cut down or quit vaping altogether. Feedback of these views informed the development of new guidance from NHS Health Scotland on how health professionals might support PiC wishing to cut down or quit within prisons. 80 E-cigarette use and its implications (both positive and potentially negative) are explored in more detail in a complementary CRUK-funded study (see Brown et al. 38,73 and Acknowledgements, Publications), but views expressed in the different samples interviewed in the two studies corroborated findings from each other.
These was also a high degree of corroboration of these findings from the interviews with separate samples of providers and potential users of smoking cessation services, conducted as part of WP5. Pre ban, most prison cessation services adopted a fairly uniform approach, typically combining NRT with 12 weeks of group-based behavioural support delivered by trained health-care and addiction staff based within the prison, smoking advisors from local community SSSs, or in a few cases by both groups in combination. It was noted that for some PiC groups (e.g. protected prisoners), one-to-one support was more appropriate and necessary. Most providers of prison cessation services considered the ≈ 16-month notification period for the ban sufficient to prepare, although the lack of advanced warning for the provision of ‘starter packs’ in September 2018, and the subsequent sale of rechargeable e-cigarette products, presented some challenges for some prisons, particularly those that identified vapers as a new client group. Those providing services in most prisons sought to use the preparatory phase to increase their capacity to deliver cessation support – to deal with increased demand and reduce waiting times. Many prisons reported a significant jump in demand following the announcement of the ban, which increased further as the implementation date approached, then decreased after the introduction of e-cigarettes.
Increased staff levels and numbers of sessions were common means of addressing capacity issues. However, in many cases it was the negotiation of procedural changes with other prison authorities that was key to improving service efficiency. One that proved particularly effective was negotiating access to PiC on residential halls to minimise the burden on prison officers of escorting PiC to/from groups; another was authorising smoking advisors to distribute NRT directly to those attending groups to reduce pressures on pharmacies and GPs. In addition, many services switched from a closed to a rolling group model, whereby PiC who dropped out could be immediately replaced by someone on the waiting list.
Although these changes to practice and procedure proved particularly useful to facilitating a greater throughput, other changes were less successful, most notably the decision in many prisons to train prison officers to co-facilitate support groups. The reasons for this were not always immediately apparent, but pressures on prison officer time, staff sick leave and a lack of confidence in adopting a therapeutic role were common themes. In addition, PiC reported mixed views about prison staff co-facilitating groups, with pre-existing relationships with and trust in individual prison staff being key factors.
Post implementation, there was strong evidence of diversification in the ways in which cessation services in different prisons adapted to the new smoke-free regime. Factors that may help explain this divergence include differences in prison populations (e.g. different rates of prisoner ‘churn’ explaining the emphasis on supporting new admissions in large admitting prisons), concerns about prisoner unrest (which, in some prisons, may explain the development of systems for ensuring wide availability of free NRT), the attitudes of different services to the provision of e-cigarettes and vapes (which, in some services, appeared to explain a lack of innovation and engagement with the new challenges posed by the introduction of these new technologies for PiC, and in others a desire to respond to and meet these needs) and delays in the launch of the new national specification for pathways of support (in part attributed to late notification of the decision to introduce e-cigarette starter packs into Scottish prisons).
The introduction of the ban also led to the emergence of some new barriers to delivering support, most notably challenges in monitoring nicotine intake, establishing new service goals and outcomes, and identifying and accessing PiC seeking support on admission. There was also some significant new learning and areas of potential development, most significantly the emergence of new services to support PiC who wished to cut down or quit vaping, as mentioned above; analysis of the WP5 interviews with PiC supported the WP4 interviews in highlighting a need for an enhanced specification to address the needs posed by vaping in Scottish prisons. 80 Finally, support for the introduction of e-cigarettes among those working in smoking cessation was mixed. Although many saw this as a means of easing the transition to the new smoke-free prison environment and a safer alternative to smoking, some concerns were voiced about the effect on longer-term health gains and, in particular, smoking rates for ‘ex-smokers’ released back into the community. It was noteworthy that links between cessation services in prisons and the community were often poor. This was identified as a key area for future service development and is likely to be a critical area for future study.
There was strong consistency in findings from the WP5 interviews with service providers and service users in the pre-implementation phase. The prospect and, in particular, the announcement of the ban was an important trigger for some PiC who smoked to engage with and take up cessation support, using this period as an opportunity to quit smoking and retain control (i.e. not allowing events outside their control to force them to stop). Most service-user feedback about the cessation services was positive. Key features highlighted were the expertise and active engagement of smoking advisors, the provision of regular CO monitoring as a means of assessing progress and having opportunities to meet and speak with other like-minded PiC trying to quit. Criticisms of the service from PiC largely mirrored those expressed by service providers (long waiting times, disruption in accessing group sessions, inconsistencies in NRT supplies). Other issues and areas of potential improvement highlighted pre implementation included a need for diversionary activities to keep people’s hands and minds occupied, provision of smoke-free spaces and cells to remove or reduce the temptation to smoke and to make quitting easier, and enhanced communication about smoke-free services and how the ban would be introduced. Like service providers, some PiC also anticipated prison reception and admission procedures would be key areas post implementation, with (free) provision of NRT and/or e-cigarettes seen as likely to be helpful in assisting PiC who smoked to deal with nicotine cravings on admission. Perhaps not surprisingly, there was less certainty about how the cessation service might evolve post implementation and what kind of support would be required.
As highlighted by many frontline staff delivering cessation support, the (potential) introduction of e-cigarettes was a major topic of discussion among PiC prior to implementation. Although most PiC actively trying to quit smoking believed that the introduction of vapes would be extremely popular among the wider prison population, some were reluctant to engage with these products themselves, as they saw their use as undermining their desire to ‘beat’ their nicotine addiction. Many also saw the single-use e-cigarettes, which were available from prison canteens at the time of interviews, to be of poor quality and an inadequate substitute for cigarettes. Consequently, these products were widely rejected by PiC in favour of more advanced devices.
An additional element of WP2 was the analysis of health-related and other outcomes, both those collected specifically for the study and the routinely collected data provided by the prison or health services; analysis of these outcomes underpins the health economic analysis. More detailed reports of the analyses of medications prescribed for PiC and staff sickness absence are available elsewhere,57 delayed in both cases as a result of the outbreak of COVID-19. The health economic analyses point to the cost-effectiveness of the smoke-free policy. Base-case CEA results for both staff and PiC demonstrated that post-implementation costs and SHS levels were lower than those pre announcement. Base-case CUA results for staff demonstrated that the post-implementation period was less costly and associated with higher quality of life than in the pre announcement period; however, for PiC, although costs were also less, quality of life was lower post-implementation than pre announcement. SAs generally supported the base-case results, demonstrating that over a short time horizon, implementing the smoke-free policy was cost-effective.
The base-case results of the lifetime model demonstrated that in the period ‘with smoke-free policy’ costs were lower and QALYs were greater than without the policy, for both PiC and staff, and confirmed cost-effectiveness as judged against a £20,000 willingness-to-pay threshold. Several scenario analyses confirmed the robustness of the base-case results, but the scenarios with the greatest effect on the ICER were varying smoking resumption rates on release from prison (decreasing rates associated with improved quality of life and decreased costs for PiC) and changing assumptions about the length of sentence (increasing length resulted in increased quality of life and lower personal costs for PiC).
As far as we are able to ascertain, this is the first health economic evaluation of implementing a smoke-free policy in a national prison service, and so we are unable to compare our results with existing evidence from other prison services. The individual QALY gains are 0.126 and 0.094 for PiC and staff, respectively; the accepted minimally important QALY difference is 0.074 (95% CI –0.011 to 0.140),81 small compared with the model results, but the CI includes the model results so we can assume that model results would be considered important by decision-makers. Previous research on quality of life for hospital employees, comparing an inside smoking ban with an inside and outside ban (a quit rate of 34% compared with 2%), found a lifetime benefit of 0.355 QALYs. 82 SAs exploring a 25% quit rate for PiC on release from prison demonstrated a 0.352 QALY gain. A study evaluating the cost-effectiveness of a complex intervention to reduce SHS exposure in children83 used the same cost-effectiveness analysis outcome as used here; the authors estimated an ICER of £131 per additional 10 µg/m3 reduction in PM2.5, compared with £18 in the present study.
Strengths and limitations
The TiPs study has a number of major strengths. A notable strength is its breadth, depth and multidisciplinary approach. Furthermore, we collected and analysed comprehensive baseline primary and secondary (routinely collected) data before the formulation and subsequent announcement of a major policy change (and associated organisational changes), and up to 1 year after policy implementation, across a whole prison system, including objective measurements of SHS exposures, data from prison staff and PiC (i.e. those working and living in the prisons) on their health, smoking histories, opinions and experiences of smoking (restrictions) within prisons, and from providers of smoking cessation support, and on health service use by PiC, and other outcomes (e.g. incidents of violence or incidents of fires). Our close but independent partnership working with the Scottish prison and health services was an additional strength that facilitated access to a wide range of routinely collected data and ensured rapid feedback of emergent findings to inform implementation strategies. Furthermore, we incorporated comprehensive follow-up post implementation to evaluate health and other outcomes, including possible unintended negative outcomes. The ability to compare and triangulate findings from inter-related work packages is a major strength, adding weight to the findings from individual study components.
A strength of the health economic analysis was that both operational staff and PiC were included, providing a full picture of the effects of reducing SHS exposures and the direct effects of tobacco use on PiC. The within-study analysis used data from TIPs staff and PiC surveys, providing unique insight into costs and health effects. Although there were limitations in the way data on health-care use were identified for PiC, this research adds valuable evidence. Data provided by SPS added to the robustness of the results and allowed evaluation of a wider range of outcomes. Other strengths of the analysis include the use of a Markov model structure, as in other recent economic evaluations of smoking cessation,65,84–86 a conservative approach to parameter estimation, and SAs where evidence was scarce. This health economic analysis thus provides a foundation for further research and demonstrates consistent results for an initial benchmark in cost-effectiveness and economic evidence for jurisdictions contemplating a smoke-free prison policy.
The main limitation with respect to the surveys of PiC and staff was the low (but not now untypical) return rates, particularly in the post-implementation period when the smoke-free policy was widely accepted as the ‘new normal’ and ‘here to stay’, possibly affecting people’s motivations to take time to complete the survey. Thus, findings (e.g. changes over time) need to be interpreted with caution. Furthermore, the surveys of staff and PiC were repeat cross sections, not longitudinal, posing further limitations on interpretation of changes over time. However, the characteristics of those who responded changed little across the phases (for both staff and PiC), and mirrored those of the wider populations of staff and PiC as far as could be ascertained. In addition, many of the survey findings mirrored those from our extensive qualitative data collected over the study period.
Inevitably, within the restricted environments of the prisons, we were limited in the extent to which we were able to consult PiC about the proposed research in the design phases. In the visits that we made to every prison in Scotland prior to the commencement of the research, we were able to speak to only a relatively small number of PiC in advance of our formal fieldwork. However, the surveys and large number of one-to-one interviews with PiC did allow them to freely express their views during the course of the study. We relied on gatekeepers to facilitate access to those participating in the qualitative components of the study, and there may be differences in the opinions and experiences of those who elected to take part compared with the wider body of prison staff or residents. In all research, the use of gatekeepers has a potential, often unquantifiable, impact on the sample; in research in the prison context, it is inevitable that gatekeepers will play a role in the selection of the sample for the protection of both PiC and researchers. We made considerable efforts to ensure that participants were well informed in advance of the study and willing to take part, particularly for PiC, and that gatekeepers understood the range of participants that we sought to include in the qualitative samples to adequately represent a breadth of views. During the course of the interviews and focus groups, prison staff and PiC spoke in what appeared to be frank (and on occasions, very frank) terms, and a wide range of views were articulated.
There were more opportunities for prison staff to have input into the design, focus and conduct of different aspects of the study, through a variety of channels. These included through their union representatives prior to formal fieldwork at RAG meetings, during training for and discussion of the proposed measurements of SHS and during our visits to all prisons in Scotland to discuss the proposed research in the summer of 2016, prior to the commencement of the study that September. During this process, some staff members sought clarification and reassurance about the purpose of the research, the independence of the research team, the proposed methods for measuring SHS levels and assurances that all views expressed would be completely anonymised. An example of the way in which our plans were modified as a result of this PPI was our decision to ensure that the surveys of staff included no means of identification (e.g. staff number).
The main limitations to the health economic analyses include the difficulty in identifying and integrating different formats of data from multiple sources. There are no validated methods for identifying PiC resource use in NHS NSS data. The within-study data from NHS NSS relied on unconventional methods to identify health-care use by PiC, which led to potentially excluding people on remand or with a short prison sentence; this was also the case for A&E data identified using the ‘postcode of residence’. The main limitation in the lifetime model was scarcity of evidence for input parameters. Intervention costs were based solely on SPS spend on ‘starter’ vaping kits for PiC, and this is undoubtedly an underestimate as there will have been staff training costs, costs for communicating about the smoke-free policy and increased provision of smoking cessation services and NRT, and, potentially, costs associated with any contingency preparations for potential unrest in one or more prisons. No costs were included for monitoring SHS in prisons when assessing the need for the policy, although this is likely to be an important factor for other jurisdictions when considering introducing comprehensive smoke-free prison policies.
As in all models, assumptions that we have made may under- or over-estimate cost-effectiveness. Assumptions that under-estimate cost-effectiveness include the base-case assumption of 100% resumption of smoking on release, quit attempts over and above the background quit rate of 2% and Office for National Statistics costs being applied to reported number of cigarettes smoked as reported in the TIPS PiC questionnaire. The fact that e-cigarette product costs were assigned to all ‘quit/tobacco abstinent’ in the ‘with the smoke-free policy comparator’ ‘in-prison’ period will offset the effect of omitting NRT and smoking cessation service use. Assumptions that may over-estimate cost-effectiveness include personal staff spend being restricted to tobacco spend; lack of evidence on the time-lag between SHS exposure and disease onset (hence no time-lag was accounted for); staff and PiC who enter the model as ‘non-tobacco smokers’ being allocated utilities, morbidity and mortality rates of never-smokers; and the assumption that non-smoking staff and PiC are not exposed to SHS outside prison. Furthermore, the use of e-cigarettes was included in the model as a personal cost to PiC who are former smokers only, not in the model in relation to harms or benefits, because it is likely to be some time before there is concrete evidence on health-related outcomes, particularly those associated with long-term use. In addition, our qualitative data suggested that some PiC may use e-cigarettes differently to the general population, so any harms or benefits may also prove to be different in this population.
The lifetime model of costs at a population level estimates lifetime cost savings of around £9M. Although we were unable to include full intervention, SHS monitoring or smoking cessation costs, this figure illustrates the level of additional spend that was viable when implementing the smoke-free policy in Scottish prisons to keep the policy cost neutral. In addition, it is important to reiterate that the implementation of the smoke-free policy across the Scottish prison estate was achieved with no major unrest or damage to property, nor increases in reports of assaults and fires. Had any of these events occurred, the costs to the SPS and the public purse could have been extremely high, as well as having caused difficulties, hardships and adverse physical and mental health consequences for PiC if facilities within the prisons had been significantly compromised.
Implications for prison services
This report contains a number of specific recommendations that may facilitate a successful transition to smoke-free prisons. Practical recommendations include (1) having independent measures of indicators of probable exposures to SHS, before and after implementation, of a smoke-free policy to provide concrete evidence to people living and working in prisons of the extent of the need for a smoke-free policy in the first place and quantification of change brought about by the policy; (2) finding mechanisms for the prison service to engage and communicate with staff and PiC, and understand and be seen to respond to their views, at the earliest possible stage; and (3) providing clear detailed information for PiC, and for prison and other staff involved in their care, about the process and timing of introducing the policy change. One highly important factor for consideration for jurisdictions in the future will be whether, and if so for how long, they provide or allow access to e-cigarettes as a substitute for smoking. For some jurisdictions, where the sale or e-cigarette products is restricted or limited in wider society, e-cigarette use among PiC is unlikely to be considered an option. In countries where e-cigarette use is permitted and widespread in wider society, there is likely to be considerable debate until further and unequivocal evidence emerges on whether typical vaping practices and cultures within prisons hinder or help any aspiration to encourage people to become nicotine free in prison, or to remain smoke-free on release from prison.
Although the findings from the study have added substantially to what was previously a sparse evidence base, they do suggest important areas for future research including on:
-
the number of people who remain tobacco abstinent, with and without the use of e-cigarettes, on release from smoke-free prisons, and ways to maximise pre- and post-release support for tobacco and/or nicotine cessation
-
the experience and likely effectiveness of new guidance for those wanting support to cut down/quit vaping in prison, to inform pre-release support and transferability to other settings
-
long-term use of e-cigarettes in prison, and (cost) effectiveness of support for people wishing to be nicotine-free [alongside (or not) aspirations to overcome former addictive behaviours]
-
the impact for those leaving prison of returning to a smoking household/social network (for people who have become tobacco abstinent while in custody, with or without e-cigarettes), and any positive or negative impacts on family members
-
updated estimates of outcomes and impacts of the smoke-free prison policy in Scotland, utilising any new evidence worldwide on smoking relapse post release, on e-cigarettes, or changes in e-cigarette use in prisons (where permitted)
-
the impact of COVID-19 and associated restrictions on experiences of living in a smoke-free environment, and coping mechanisms in the face of additional stresses and restrictions (e.g. diminished visitor contact), including the use of e-cigarettes.
Acknowledgements
We would like to thank all of the PiC who took part in the surveys and face-to-face interviews for their participation and candour. We are also grateful to all the staff working in Scotland’s 15 prisons, who so helpfully facilitated fieldwork throughout all phases in the study; participated in surveys, interviews or focus groups; and escorted PiC and research staff to suitable rooms for interviews or fieldwork. We are particularly grateful to the staff points of contacts and to the Governors-in-Charge and their deputies for granting access and making arrangements locally for our many visits to their prisons for orientation and consultation and to undertake fieldwork. We appreciate their help amid the many pressures they have on their time and resources.
We are extremely grateful for the ongoing support for the project from staff at SPS headquarters. In particular, we would like to thank Sarah Corbett (formerly SPS Health and Wellbeing team and, from 2016 to 2019, Smoke Free Prisons Programme Policy Manager), Ruth Parker (formerly Head of the Health and Wellbeing team), Linda Dorward (formerly Smoke Free Prisons Programme Lead), Emma Christie, Lesley McDowell, Leucine Teymoortian (formerly Smoke Free Prison Administrator), Scott Sidwell (Head of Health and Safety), Jim Carnie, and Stuart Brown and colleagues. We are also grateful to all members of the SAG, including SPS headquarters staff named above; representatives from the operations, communications, human resources and legal departments; representatives from NHS Health Scotland (and NHS Forth Valley, NHS Greater Glasgow and Clyde, and NHS Lothian); Scottish Government Tobacco Control; staff trade unions (Prison Officers’ Association and Public and Commercial Services, and Trades Union Side); and ASH Scotland. All provided helpful feedback on detailed plans for fieldwork and on monthly updates of ongoing findings. Many also participated in the RAG for TIPs, which was constituted by SPS. The views expressed are those of the authors and not necessarily those of the SPS.
We would also like to thank the members of our Study Steering Group: Dr Andrew Fraser (chairperson), Professor Amanda Amos, Dr Nancy Loucks and Professor Carol Tannahill.
We would like to thank Professor Olivia Wu for her detailed comments on the write up of the health economic methods, and for her critical review of the conduct, interpretation and write-up of the health economic analyses; and Danny Mackay for invaluable advice on the ongoing analyses of interrupted time series in relation to prescribed medications and staff sickness absence. We would also like to thank Dr Andrea Mohan for her input on the WP5 data management and analysis, and colleagues at the MRC/CSO Social and Public Health Sciences Unit at the University of Glasgow for assisting with data collection in phase 1 and data management and analysis of the survey data, including Marcela Gavigan, Elaine Hindle, Matt Tolen, David Walker, Julie Watson, Kate Campbell [PHR Facility, Social and Public Health Sciences Unit (SPHSU)], Greig Logan and Abita Bhaksar.
We would like to thank NIHR for funding the TIPs project (15/55/44). We would like to thank Dr Catherine Best for providing these summary variables.
Contributions of authors
Kate Hunt (https://orcid.org/0000-0002-5873-3632) (Professor of Behavioural Sciences and Health and Principal Investigator for TIPs) led the original and amended design of the study following the announcement of the comprehensive smoke-free prisons policy, and secured funding. She contributed to the collection, analysis, interpretation and write up of SHS exposure measures in phases 1–3; the qualitative data collection, analysis, interpretation and write up in phases 1–3; and the design, data collection and interpretation for the surveys in phases 1–3. She wrote the first draft of the full report [revising sections contributed by section authors (AB, DE, NM, HS. SS)] and revised the draft after critical contributions from co-authors and reviewers. She regularly attended meetings of the RAG and SAG at SPS headquarters, maintained communication with senior SPS colleagues, and provided ongoing feedback of results to SPS and Health Scotland on all aspects of the study during phases 1–3.
Ashley Brown (https://orcid.org/0000-0002-2307-5916) (Research Fellow) contributed to the amended design of TIPs and securing funding. She led the data collection, analysis and write up for all phases 2 and 3 qualitative data collection for WP3 and WP4 (face-to-face interviews/focus groups with prison staff and PiC) and led the analysis and write up of the phase 1 staff focus groups. She undertook the interviews, analysis and write up of WP1 interviews with people from other jurisdictions. She contributed in detail to the interpretation of data across the project and provided critical comments on all sections of the report. She regularly attended meetings of the RAG and SAG at SPS headquarters, maintained communication with senior SPS colleagues, and provided ongoing feedback of results to SPS and Health Scotland on qualitative findings during phases 2 and 3.
Douglas Eadie (https://orcid.org/0000-0001-9969-9162) (Research Fellow and Co-investigator) contributed to the original and amended design of TIPs and securing funding. He led the data collection, analysis and write up for all qualitative data collection for WP5 (qualitative interviews with providers and users of smoking cessation services in Scotland’s prisons); fed back results to SPS on WP5 findings during phases 1–3; contributed to the interpretation of the data across the project; and provided critical comments on sections of the report.
Nicola McMeekin (https://orcid.org/0000-0003-2918-8820) (Research Assistant and Co-investigator) led the analysis, interpretation and write up of the health economic analyses; provided critical input into the design, analysis and interpretation of other routinely collected data; provided ongoing feedback of analysis plans and results of the health economic analyses to SPS and Health Scotland; and provided critical comments on sections of the report.
Kathleen Boyd (https://orcid.org/0000-0002-9764-0113) (Reader and Co-investigator) contributed to the original and amended design of TIPs and securing funding. She oversaw the design and analysis of the health economic analyses, and provided critical input into the design, analysis and interpretation of other routinely collected data.
Linda Bauld (https://orcid.org/0000-0001-7411-4260) (Bruce and John Usher Chair of Public Health and Co-investigator) contributed to the original and amended design of TIPs and securing funding. She contributed to the analysis, interpretation and write up of qualitative data collection for WP5 (qualitative interviews with providers and users of smoking cessation services in Scotland’s prisons), and analysis and interpretation of data related to e-cigarettes. She provided expert advice to SPS on e-cigarettes during phases 1 and 2, contributed to the interpretation of the data across the project and provided critical comments on sections of the report.
Philip Conaglen (https://orcid.org/0000-0002-8605-7045) (Consultant in Public Health and Co-investigator) contributed to the original and amended design of TIPs and securing funding. He contributed to the design of the analysis of routinely collected data included within the health economic analysis, and contributed to the interpretation of data across the project.
Peter Craig (https://orcid.org/0000-0002-7653-5832) (Professor of Public Health Evaluation and Co-investigator) contributed to the original and amended design of TIPs and securing funding. He contributed to the design, interpretation and write up of the analysis of routinely collected data included within the health economic analysis; contributed to the interpretation of data across the project; and provided critical comments on the report.
Evangelia Demou (https://orcid.org/0000-0001-8616-525X) (Research Fellow and Co-investigator) contributed to the original and amended design of TIPs and securing funding. She led the analysis, interpretation and write up of data on staff sickness absence; provided critical input into the design, analysis and interpretation of other routinely collected data; contributed to the collection, analysis, interpretation and write up of SHS exposure measures in phases 1–3 and focus groups in phase 1; and provided critical comments on the report.
Alastair Leyland (https://orcid.org/0000-0003-3741-7099) (Professor of Public Health Statistics and Co-investigator) contributed to the original and amended design of TIPs and securing funding. He contributed to the design, interpretation and write up of the analysis of routinely collected data included within the health economic analysis; contributed to the interpretation of data across the project; and provided critical comments on the report.
Jill Pell (https://orcid.org/0000-0002-8898-7035) (Henry Mechan Professor of Public Health) contributed to the original and amended design of TIPs and securing funding. She contributed to the design, interpretation and write up of the analysis of routinely collected data included within the health economic analysis, and contributed to the interpretation of data across the project.
Richard Purves (https://orcid.org/0000-0002-6527-0218) (Research Fellow and Co-investigator) contributed to the original and amended design of TIPs and securing funding. He contributed to the data collection, analysis, interpretation and write up of qualitative data collection for WP5.
Emily Tweed (https://orcid.org/0000-0001-6659-812X) (Clinical Lecturer in Public Health and Co-investigator) contributed to the amended design of TIPs and securing funding. She led the analysis, interpretation and write up of data on medication prescribed to PiC; provided critical input into the design, analysis and interpretation of other routinely-collected data; and provided critical comments on the report.
Tom Byrne (National Prisons Pharmacy Advisor, Health Improvement Scotland) contributed to the analysis and interpretation of routinely collected data, in particular data on medication prescribed to PiC.
Ruaraidh Dobson (https://orcid.org/0000-0001-8136-8373) (Research Fellow) contributed to the collection, analysis, interpretation and write up of SHS exposure measures in phases 1–3 and provided critical comments on sections of the report.
Lesley Graham (https://orcid.org/0000-0002-5654-2330) (previously Clinical Lead for Alcohol, Drugs and Health in Justice Settings, Information Services Division) contributed to the analysis and interpretation of routinely collected data, contributed to the interpretation of the data across the project and provided critical comments on the report.
Danielle Mitchell (https://orcid.org/0000-0001-8692-5407) (Research Assistant) contributed to the data management and analysis of qualitative data and provided critical comments on sections of the report.
Rachel O’Donnell (https://orcid.org/0000-0003-2713-1847) (Research Fellow) contributed to the collection, analysis, interpretation and write up of SHS exposure measures in phases 1–3 and provided critical comments on the report.
Helen Sweeting (https://orcid.org/0000-0002-3321-5732) (Reader and Co-investigator) contributed to the original and amended design of TIPs and securing funding. She led the design, analysis, write up and interpretation of the surveys of PiC and prison staff in phases 1–3, including contact with points of contacts in all prisons, and wrote up the first draft of findings from all surveys; contributed to the collection, analysis, interpretation and write up of SHS exposure measures in phases 1–3 and the focus groups in phases 1 and 3; contributed to the interpretation of data across the project; provided ongoing feedback on the survey findings to SPS and Health Scotland; and provided critical comments on the report.
Sean Semple (https://orcid.org/0000-0002-0462-7295) (Associate Professor and Co-investigator) contributed to the original and amended design of TIPs and securing funding. He led the training of SPS staff in SHS exposure; the collection, analysis, interpretation and write up of SHS exposure measures in phases 1–3; contributed to the interpretation of data across the project; provided ongoing feedback and expert advice on the measurement of SHS exposure to SPS, Health Scotland and the Scottish Government; and provided critical comments on the report.
Publications
Phase 1
Semple S, Sweeting H, Demou E, Logan G, O’Donnell R, Hunt K, on behalf of the Tobacco in Prisons (TIPs) Research Team (2017). Characterising the exposure of prison staff to second-hand tobacco smoke. Ann Work Expo Health 2017;61:809–21.
Semple S, Sweeting H, Demou E, Logan G, O’Donnell R, Hunt K, on behalf of the Tobacco in Prisons (TIPs) Research Team) (2017). Staff Exposure to Second-hand Tobacco Smoke in Scotland’s Prisons. Edinburgh: Scottish Prison Service; 2017.
Brown A, Sweeting H, Logan G, Demou E, Hunt K. Prison staff and prisoner views on a prison smoking ban: evidence from the Tobacco in Prisons study. Nicotine Tob Res 2019;21:1027–35.
Brown A, Sweeting H, Semple S, Bauld L, Logan G, Hunt K. Views of prison staff in Scotland on the potential benefits and risks of e-cigarettes in smoke-free prisons: a qualitative focus group study. BMJ Open 2019;9:e027799.
Sweeting H, Semple S, Demou E, Brown A, Hunt K. Predictors of opinions on prison smoking bans: analyses of survey data from Scottish staff and prisoners. Tob Induc Dis 2019;17:47.
Phase 2
Brown A, Eadie D, Purves R, Mohan A, Hunt K. Perspectives on smokefree prison policy among people in custody in Scotland. Int J Prison Health 2020;16:389–402.
Semple S, Dobson R, Sweeting H, Brown A, Hunt K, on behalf of the Tobacco in Prisons (TIPs) research team. The impact of implementation of a national smoke-free prisons policy on indoor air quality: results from the Tobacco in Prisons study. Tob Control 2020;29:234–6.
Phase 3
Demou E, Dobson R, Sweeting H, Brown A, Sidwell S, O’Donnell R, et al. From smoking-permitted to smokefree prisons: a 3-year evaluation of the changes in occupational exposure to second-hand smoke across a national prison system. Ann Work Expo Health 2020;64:959–69.
Sweeting H, Brown A, Demou E, Hunt K. Prisoners and prison staff express increased support for prison smoking bans following implementation across Scotland: results from the Tobacco in Prisons Study (letter). Tobacco Control 2020.
Tweed E, Mackay DF, Boyd K, Brown A, Byrne T, Conaglen P, et al. Evaluation of a national smoke-free prisons policy using medication dispensing: an interrupted time-series analysis. Lancet Public Health 2021;6:E795–804.
Brown A. Understanding the Perspectives of People in Custody and Prison Staff through the Process of a Major Policy Change: The Introduction of Smokefree Prisons in Scotland. PhD thesis. Stirling: University of Stirling; 2021.
Related publications to which the authors of this report contributed
Sweeting H, Hunt K. Evidence on Smoking and Smoking Restrictions in Prisons: A Scoping Review for the Scottish Prison Service’s Tobacco Strategy Group. MRC/CSO Social and Public Health Sciences Unit occasional paper 25 Glasgow: MRC CSO Social and Public Health Sciences Unit; 2015.
Robinson A, Sweeting H, Hunt K. UK news media representations of smoking, smoking policies and tobacco bans in prisons. Tob Cont 2018;27:622–30.
Brown A, O’Donnell R, Eadie D, Purves R, Sweeting H, Ford A, et al. Initial views and experiences of vaping in prison: a qualitative study with people in custody preparing for the imminent implementation of Scotland’s prison smokefree policy. Nicotine Tob Res 2021;23:543–9.
Brown A, O’Donnell R, Eadie D, Ford A, Mitchell D, Hackett A, et al. E-cigarette use in prisons with recently established smokefree policies: a qualitative interview study with people in custody in Scotland. Nicotine Tob Res 2021;23:939–46.
Brown A, Mitchell D, Hunt K. Post-implementation perspectives on smokefree prison policy: a qualitative study with staff and people in custody [published online ahead of print August 27 2021]. Eur J Public Health 2021.
Future publications related to this work can be expected.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data are vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out how patient data are used https://twitter.com/hashtag/datasaveslives. You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the PHR programme or the Department of Health and Social Care.
References
- NHS Health Scotland . Specification for National Prison Smoking Cessation Service in Scotland 2015.
- Carnie J, Broderick R, McCoard S. Scottish Prison Service Prisoner Survey 2013 2013. www.sps.gov.uk/Corporate/PrisonerSurvey2013MainBulletin.aspx (accessed 19 March 2021).
- Scottish Prison Service . Continuing Scotland’s Journey Towards Smoke-Free Prisons 2016.
- Scottish Prison Service . Creating a Smoke Free Prison Environment n.d. www.sps.gov.uk/Corporate/News/Creating_a_Smoke_Free_Prison_Environment.aspx (accessed 19 March 2021).
- Sweeting H, Hunt K. Evidence on Smoking and Smoking Restrictions in Prisons. A Scoping Review for the Scottish Prison Services’ Tobacco Strategy Group. Glasgow: University of Glasgow and MRC/CSO Social and Public Health Science Unit; 2015.
- Great Britain . Smoking, Health and Social Care (Scotland) Act 2005 2005.
- Scottish Government . Creating a Tobacco-Free Generation. A Tobacco Control Strategy for Scotland 2013.
- Carnie J, Broderick R. Scottish Prison Service Prisoner Survey 2015. Edinburgh: Scottish Prison Service; 2016.
- Scottish Government . Equally Well: Report of the Ministerial Task Force on Health Inequalities 2008. www.gov.scot/binaries/content/documents/govscot/publications/corporate-report/2008/06/equally-well-report-ministerial-task-force-health-inequalities/documents/0062206-pdf/0062206-pdf/govscot%3Adocument/0062206.pdf (accessed 28 July 2020).
- Hunt K, Sweeting H, Semple S. on behalf of the TIPs research team . Evaluating Graduated Progress Towards, and Impacts Of, the Implementation of Indoor Smoke Free Prison Facilities in Scotland. Protocol for the Tobacco in Prisons (TIPs) Study 2017. https://fundingawards.nihr.ac.uk/award/15/55/44.
- Semple S, Sweeting H, Demou E, Logan G, O’Donnell R, Hunt K. on behalf of the Tobacco in Prisons (TIPs) Research Team . Characterising the exposure of prison staff to second-hand tobacco smoke. Ann Work Expo Health 2017;61:809-21. https://doi.org/10.1093/annweh/wxx058.
- Hunt K, Sweeting H, Brown A, . Evaluating Graduated Progress Towards, and Impacts Of, the Implementation of Indoor Smoke Free Prison Facilities in Scotland. Protocol for the Tobacco in Prisons (TIPs) Study 2019. https://fundingawards.nihr.ac.uk/award/15/55/44.
- Semple S, Maccalman L, Naji AA, Dempsey S, Hilton S, Miller BG, et al. Bar workers’ exposure to second-hand smoke: the effect of Scottish smoke-free legislation on occupational exposure. Ann Occup Hyg 2007;51:571-80.
- Pell JP, Haw S, Cobbe S, Newby DE, Pell AC, Fischbacher C, et al. Smoke-free legislation and hospitalizations for acute coronary syndrome. N Engl J Med 2008;359:482-91. https://doi.org/10.1056/NEJMsa0706740.
- Hiscock R, Bauld L, Amos A, Platt S. Smoking and socioeconomic status in England: the rise of the never smoker and the disadvantaged smoker. J Public Health 2012;34:390-6. https://doi.org/10.1093/pubmed/fds012.
- Hartwig C, Stover H, Weilandt C. Report on Tobacco Smoking in Prison 2008.
- Mundt AP, Baranyi G, Gabrysch C, Fazel S. Substance use during imprisonment in low- and middle-income countries. Epidemiol Rev 2018;40:70-81. https://doi.org/10.1093/epirev/mxx016.
- Spaulding AC, Eldridge GD, Chico CE, Morisseau N, Drobeniuc A, Fils-Aime R, et al. Smoking in correctional settings worldwide: prevalence, bans, and interventions. Epidemiol Rev 2018;40:82-95. https://doi.org/10.1093/epirev/mxy005.
- Carpenter MJ, Hughes JR, Solomon LJ, Powell TA. Smoking in correctional facilities: a survey of employees. Tob Control 2001;10:38-42. https://doi.org/10.1136/tc.10.1.38.
- Butler T, Richmond R, Belcher J, Wilhelm K, Wodak A. Should smoking be banned in prisons?. Tob Control 2007;16:291-3. https://doi.org/10.1136/tc.2007.021600.
- de Viggiani N. Unhealthy prisons: exploring structural determinants of prison health. Sociol Health Illn 2007;29:115-35. https://doi.org/10.1111/j.1467-9566.2007.00474.x.
- Richmond R, Butler T, Wilhelm K, Wodak A, Cunningham M, Anderson I. Tobacco in prisons: a focus group study. Tob Control 2009;18:176-82. https://doi.org/10.1136/tc.2008.026393.
- Ireland JL. ‘Bullying’ among prisoners: a review of research. Aggress Violent Behav 2000;5:201-15. https://doi.org/10.1016/S1359-1789(98)00031-7.
- Robinson A, Sweeting H, Hunt K. UK news media representations of smoking, smoking policies and tobacco bans in prisons. Tob Control 2018;27:622-30. https://doi.org/10.1136/tobaccocontrol-2017-053868.
- Gautam J, Glover M, Scott A, Welch D. Smoke-free prisons in New Zealand: maximising the health gain. N Z Med J 2011;124:100-6.
- Collinson L, Wilson N, Edwards R, Thomson G, Thornley S. New Zealand’s smokefree prison policy appears to be working well: one year on. N Z Med J 2012;125:164-8.
- Jayes LR, Murray RL, Opazo Breton M, Hill C, Ratschen E, Britton J. Smoke-free prisons in England: indoor air quality before and after implementation of a comprehensive smoke-free policy. BMJ Open 2019;9. https://doi.org/10.1136/bmjopen-2018-025782.
- Binswanger IA, Carson EA, Krueger PM, Mueller SR, Steiner JF, Sabol WJ. Prison tobacco control policies and deaths from smoking in United States prisons: population based retrospective analysis. BMJ 2014;349. https://doi.org/10.1136/bmj.g4542.
- Puljević C, de Andrade D, Coomber R, Kinner SA. Relapse to smoking following release from smoke-free correctional facilities in Queensland, Australia. Drug Alcohol Depend 2018;187:127-33. https://doi.org/10.1016/j.drugalcdep.2018.02.028.
- Puljević C, Segan CJ. Systematic review of factors influencing smoking following release from smoke-free prisons. Nicotine Tob Res 2019;21:1011-20. https://doi.org/10.1093/ntr/nty088.
- Demou E, Dobson R, Sweeting H, Brown A, Sidwell S, O’Donnell R, et al. From smoking-permitted to smokefree prisons: a 3-year evaluation of the changes in occupational exposure to second-hand smoke across a national prison service. Ann Work Expo Health 2020;64:959-69. https://doi.org/10.1093/annweh/wxaa073.
- Semple S, Dobson R, Sweeting H, Brown A, Hunt K. on behalf of the Tobacco in Prisons (TIPs) Research Team . The impact of implementation of a national smoke-free prisons policy on indoor air quality: results from the Tobacco in Prisons study. Tob Control 2020;29:234-6. https://doi.org/10.1136/tobaccocontrol-2018-054895.
- Semple S, Sweeting H, Demou E, Logan G, O’Donnell R, Hunt K. Staff Exposure to Second-hand Tobacco Smoke in Scotland’s Prisons. Edinburgh: Scottish Prison Service; 2017.
- Semple S, Ibrahim AE, Apsley A, Steiner M, Turner S. Using a new, low-cost air quality sensor to quantify second-hand smoke (SHS) levels in homes. Tob Control 2015;24:153-8. https://doi.org/10.1136/tobaccocontrol-2013-051188.
- Jaakkola MS, Jaakkola JJ. Assessment of exposure to environmental tobacco smoke. Eur Respir J 1997;10:2384-97. https://doi.org/10.1183/09031936.97.10102384.
- Jenkins RA, Palausky MA, Counts RW, Guerin MR, Dindal AB, Bayne CK. Determination of personal exposure of non-smokers to environmental tobacco smoke in the United States. Lung Cancer 1996;14:195-213. https://doi.org/10.1016/S0169-5002(96)90223-8.
- Klepeis NE, Ott WR, Switzer P. A multiple-smoker model for predicting indoor air quality in public lounges. Environ Sci Technol 1996;30:2813-20. https://doi.org/10.1021/es960067f.
- Brown A, O’Donnell R, Eadie D, Purves R, Sweeting H, Ford A, et al. Initial views and experiences of vaping in prison: a qualitative study with people in custody preparing for the imminent implementation of Scotland’s prison smokefree policy. Nicotine Tob Res 2021;23:543-9. https://doi.org/10.1093/ntr/ntaa088.
- Sweeting H, Demou E, Brown A, Hunt K. Prisoners and prison staff express increased support for prison smoking bans following a largely trouble-free implementation across Scotland: results from the Tobacco in Prisons Study. Tob Control 2021. https://doi.org/10.1136/tobaccocontrol-2020-055683.
- Sweeting H, Semple S, Demou E, Brown A, Hunt K. Predictors of opinions on prison smoking bans: analyses of survey data from Scottish staff and prisoners. Tob Induc Dis 2019;17. https://doi.org/10.18332/tid/109559.
- Carnie J, Broderick R, Cameron J, Downie D, Williams G. Scottish Prison Service Prisoner Survey 2017 n.d. www.sps.gov.uk/Corporate/Publications/Publication-6101.aspx (accessed 19 March 2021).
- Dean L, McLean J. Scottish Health Survey 2018 Edition, Volume 2, Technical Report 2019.
- Eisner MD, Smith AK, Blanc PD. Bartenders’ respiratory health after establishment of smoke-free bars and taverns. JAMA 1998;280:1909-14. https://doi.org/10.1001/jama.280.22.1909.
- EuroQol Group . EuroQol-a new facility for the measurement of health-related quality of life. Health Policy 1990;16:199-208. https://doi.org/10.1016/0168-8510(90)90421-9.
- Etter JF. Impact of educational outreach visits on smoking cessation activities performed by specialist physicians: a randomized trial. Educ Health 2006;19:155-65. https://doi.org/10.1080/13576280600742386.
- Kraemer S, Gately N, Kessell J. HoPE (Health of Prisoner Evaluation): Pilot Study of Prisoner Physical Health and Psychological Wellbeing. Joondalup, WA: Edith Cowan University; 2009.
- West R, Ussher M. Is the ten-item Questionnaire of Smoking Urges (QSU-brief) more sensitive to abstinence than shorter craving measures?. Psychopharmacology 2010;208:427-32. https://doi.org/10.1007/s00213-009-1742-x.
- Cropsey KL, Kristeller JL. Motivational factors related to quitting smoking among prisoners during a smoking ban. Addict Behav 2003;28:1081-93. https://doi.org/10.1016/S0306-4603(02)00230-7.
- Dickens G, Stubbs J, Popham R, Haw C. Smoking in a forensic psychiatric service: a survey of inpatients’ views. J Psychiatr Ment Health Nurs 2005;12:672-8. https://doi.org/10.1111/j.1365-2850.2005.00892.x.
- Hehir AM, Indig D, Prosser S, Archer VA. Implementation of a smoke-free policy in a high secure mental health inpatient facility: staff survey to describe experience and attitudes. BMC Public Health 2013;13. https://doi.org/10.1186/1471-2458-13-315.
- Hilton S, Semple S, Miller BG, MacCalman L, Petticrew M, Dempsey S, et al. Expectations and changing attitudes of bar workers before and after the implementation of smoke-free legislation in Scotland. BMC Public Health 2007;7. https://doi.org/10.1186/1471-2458-7-206.
- Burney PGJ, Laitinen LA, Perdrizet S, Huckauf H, Tatterstield AE, Chinn S, et al. Validity and repeatability of the IUATLD (1984) Bronchial Symptoms Questionnaire: an international comparison. Eur Respir J 1989;2:940-5.
- EuroQol . EQ-5D-5L 2018. https://euroqol.org/eq-5d-instruments/eq-5d-5l-about/ (accessed 28 August 2020).
- Brown A, Sweeting H, Logan G, Demou E, Hunt K. Prison staff and prisoner views on a prison smoking ban: evidence from the Tobacco in Prisons study. Nicotine Tob Res 2019;21:1027-35. https://doi.org/10.1093/ntr/nty092.
- Brown A, Sweeting H, Semple S, Bauld L, Demou E, Logan G, et al. Views of prison staff in Scotland on the potential benefits and risks of e-cigarettes in smoke-free prisons: a qualitative focus group study. BMJ Open 2019;9. https://doi.org/10.1136/bmjopen-2018-027799.
- Brown A, Mitchell D, Hunt K. Post-implementation perspectives on smokefree prison policy: a qualitative study with staff and people in custody. Eur J Public Health 2021. https://doi.org/10.1093/eurpub/ckab075.
- Tweed E, Mackay DF, Boyd K, Brown A, Byrne T, Conaglen P, et al. Evaluation of a national smoke-free prisons policy using medication dispensing: an interrupted time-series analysis. Lancet Public Health 2021. https://doi.org/10.1016/S2468-2667(21)00163-8.
- Husereau D, Drummond M, Petrou S, Carswell C, Moher D, Greenberg D, et al. Consolidated Health Economic Evaluation Reporting Standards (CHEERS) statement. Clin Ther 2013;35:356-63. https://doi.org/10.1016/j.clinthera.2013.03.003.
- Curtis L, Burns A. Unit Costs of Health and Social Care 2017. Canterbury: PSSRU, University of Kent; 2017.
- Information Services Division Scotland . Finance: Costs; Health Topics 2017 n.d. www.isdscotland.org/Health-Topics/Finance/Costs/File-Listings-2017.asp (accessed 28 August 2020).
- Office for National Statistics . RPI: Ave Price – Cigarettes 20 King Size Filter 2020. www.ons.gov.uk/economy/inflationandpriceindices/timeseries/czmp (accessed 28 August 2020).
- Fenwick E, Macdonald C, Thomson H. Economic analysis of the health impacts of housing improvement studies: a systematic review. J Epidemiol Community Health 2013;67:835-45. https://doi.org/10.1136/jech-2012-202124.
- Attema A, Brouwer W, Claxton K. Discounting in economic evaluations. PharmacoEconomics 2018;36:745-58. https://doi.org/10.1007/s40273-018-0672-z.
- National Institute for Health and Care Excellence . Guide to the Methods of Technology Appraisal: 2013 2013. www.nice.org.uk/article/pmg9/chapter/foreword (accessed 28 August 2020).
- Jones M, Smith M, Lewis S, Parrott S, Coleman T. A dynamic, modifiable model for estimating cost-effectiveness of smoking cessation interventions in pregnancy: application to an RCT of self-help delivered by text message. Addiction 2019;114:353-65. https://doi.org/10.1111/add.14476.
- Briggs AH, Claxton K, Sculpher MJ. Decision Modelling for Health Economic Evaluation. Oxford: Oxford University Press; 2006.
- Hatswell AJ, Bullement A, Briggs A, Paulden M, Stevenson MD. Probabilistic sensitivity analysis in cost-effectiveness models: determining model convergence in cohort models. PharmacoEconomics 2018;36:1421-6. https://doi.org/10.1007/s40273-018-0697-3.
- Foote C. Vaping Kits for Prisoners to Cost £150,000 2019. www.bbc.co.uk/news/uk-scotland-46653366 (accessed 1 July 2021).
- Hefler M, Hopkins R, Thomas DP. Successes and unintended consequences of the Northern Territory’s smoke-free prisons policy: results from a process evaluation. Public Health Res Pract 2016;26. https://doi.org/10.17061/phrp2621619.
- World Health Organization (WHO) Regional Office for Europe . Air Quality Guidelines: Global Update 2005 – Particulate Matter, Ozone, Nitrogen Dioxide and Sulfur Dioxide 2006.
- World Health Organization (WHO) . WHO Global Air Quality Guidelines: Particulate Matter (PM2.5 and PM10), Ozone, Nitrogen Dioxide, Sulfur Dioxide and Carbon Monoxide 2021.
- Sweeting H, Demou E, Brown A, Hunt K. Prisoners and prison staff express increased support for prison smoking bans following implementation across Scotland: results from the Tobacco In Prisons study. Tob Control 2021;30:597-8. https://doi.org/10.1136/tobaccocontrol-2020-055683.
- Brown A, O’Donnell R, Eadie D, Ford A, Mitchell D, Hackett A, et al. E-cigarette use in prisons with recently established smokefree policies: a qualitative interview study with people in custody in Scotland. Nicotine Tob Res 2021;23:939-46. https://doi.org/10.1093/ntr/ntaa271.
- Scottish Prison Service . Scottish Prison Service Annual Report and Accounts 2018–2019 2019.
- Brown A, Eadie D, Purves R, Mohan A, Hunt K. Perspectives on smokefree prison policy among people in custody in Scotland. Int J Prison Health 2020;16:389-402. https://doi.org/10.1108/IJPH-12-2019-0065.
- Semple S, Galea K, Walsh P, Tuckett-Jones B. Report on Second-Hand Smoke in Prisons: Final Report 2015.
- Richmond RL, Butler TG, Indig D, Wilhelm KA, Archer VA, Wodak AD. The challenges of reducing tobacco use among prisoners. Drug Alcohol Rev 2012;31:625-30. https://doi.org/10.1111/j.1465-3362.2012.00435.x.
- Carnie J, Broderick R. Scottish Prison Server Prison Survey 2019. Edinburgh: Scottish Prison Service; 2020.
- NHS Health Scotland . Smoke-Free Prisons Pathway: A Service Specification Supporting People in Our Care 2018.
- Taylor L, Sigerson D, Rennick L, King A. Supporting Individuals to Cut Down and Quit Vaping. Guidance for NHS Quit Your Way Advisers Based in Prisons. Edinburgh: NHS Health Scotland; 2020.
- Walters SJ, Brazier JE. Comparison of the minimally important difference for two health state utility measures: EQ-5D and SF-6D. Qual Life Res 2005;14:1523-32. https://doi.org/10.1007/s11136-004-7713-0.
- Mallender J, Bertranou E, Bacelar M, Roberts S. National Institute for Health and Clinical Excellence – Economic Analysis of Smoking Cessation in Secondary Care 2013. www.nice.org.uk/guidance/ph48/evidence/economic-analysis-of-smoking-cessation-in-secondary-care-pdf-430362685 (accessed 28 August 2020).
- Renwick C, Wu Q, Breton MO, Thorley R, Britton J, Lewis S, et al. Cost-effectiveness of a complex intervention to reduce children’s exposure to second-hand smoke in the home. BMC Public Health 2018;18. https://doi.org/10.1186/s12889-018-6140-z.
- Filby A, Taylor M. Smoking Cessation Interventions and Services. York: York Health Economics Consortium; 2018.
- Li J, Hajek P, Pesola F, Wu Q, Phillips-Waller A, Przulj D, et al. Cost-effectiveness of e-cigarettes compared with nicotine replacement therapy in stop smoking services in England (TEC study): a randomized controlled trial. Addiction 2020;115:507-17. https://doi.org/10.1111/add.14829.
- Pennington B, Filby A, Owen L, Taylor M. Smoking cessation: a comparison of two model structures. PharmacoEconomics 2018;36:1101-12. https://doi.org/10.1007/s40273-018-0657-y.
- Spencer L, Ritchie J, Ormston R, O’Connor W, Barnard M, Ritchie J, et al. Qualitative Research Practice. London: SAGE Publications Ltd; 2014.
- Braun V, Clarke V, Cooper H, Camic PM, Long DL, Panter AT, et al. APA Handbook of Research Methods in Psychology, Vol. 2: Research Designs: Quantitative, Qualitative, Neuropsychological, and Biological. Washington, DC: American Psychological Association; 2012.
Appendix 1 Abbreviated topic guides for qualitative data collection
Work package 1: scoping interview topic guide
Introduction and background
Overview of participant roles and responsibilities: (in general and in relation to smoke-free prisons), time in role/organisation and smoking status. Description of their prison/wider estate: function/category, public/private, prisoner population, and successes and challenges facing the prison – staffing, disruption, time out of cells, etc.
Current and historic smoking restrictions
Current smoking arrangements for PiC and staff: when introduced, where smoking can take place for PiC and staff, whether/what circumstances e-cigarettes can be used for PiC and staff, type/model(s) permitted and how smoking restrictions vary across the prison estate. Process for admission of incoming PiC who smoke: whether or not they are aware they are entering a prison with a smoking ban and views on adequacy of process. Description of pre-ban policies in prison: smoking arrangements for PiC and staff.
Pre-implementation (lead-up to smoking ban)
Trigger(s)/rationale for ban (including drivers at national and local level). Process for communicating ban to prisons/staff/PiC: how prisons were selected to become smoke free; whether voluntary/mandated, piloted/staged; when/how ban was communicated to prisons, staff and PiC; (adequacy of) time to prepare for implementation; initial support for ban from PiC and staff and changes over time; expectations of PiC and staff; and key anticipated risks and benefits. Key measures at national/local level to prepare: who was involved and measures/actions (e.g. communication/engagement with staff, PiC, families, communities; staff training, guidance and support; staffing levels; PiC transfers; provision of ‘smoke-free champions’/peer support, purposeful/other activities (including in-cell activities), and smoking cessation services and support). Key services offered: NRT, whether services available for staff, who delivers cessation service/support, scale of provision, funding, care pathways, whether or not steps taken to harmonise provision across estate, specific measures/support for PiC in vulnerable circumstances and other. Views on effectiveness/success of measures taken in the lead-up: whether or not prison service/staff/PiC felt well prepared for ban (and reasons); what worked well/less well; factors influencing success (including contextual/environmental factors – staffing levels, regime stability); and what, if anything, they would do differently.
Implementation and impacts of smoke-free prisons
Views and experiences of implementation: what it was like in headquarters/prison in days/weeks/months after the ban was introduced; prison staff role in implementing the ban and how well arrangements are working (enforcement, cessation support/interventions, informal guidance/support); what worked well/less well and whether or not this has changed over time; (whether PiC tried to manipulate allocations/transfers to enter/exit smoke-free prisons, what proportion sought NHS support, use of e-cigarettes – how any risks managed; support for most vulnerable/difficult to manage, role of smoke-free champions/peer supporters); factors influencing success; what, if anything, they would do differently. ‘Impacts’ of ban: what ‘success’ means to staff/PiC/prison service; whether/why ban has achieved intended outcomes; variation among prisons, staff, PiC and over time; whether or not there have been any intended consequences of smoking ban; change over time (prevalence of tobacco smoking e-cigarette use before and after ban; use of alternative smoking items; longer-term cessation rates: health for PiC and staff, SHS exposure; physical health; organisational/cultural implications for staff: workload, remit/responsibilities, job satisfaction; incidents of violence/disruption, fires, self-harm and drug use; social/cultural value of tobacco; tobacco/illegal substance black markets; litigation/arguments re rights; economic impacts).
Concluding comments/summary
What measures/actions are most important for successful implementation and what, if anything, they would do differently (any unnecessary measures, any measures that would have been helpful).
Work package 3: phase 1 staff focus group topic guide
Background
How long (each participant) working in this prison, whether or not worked in other prisons, and general atmosphere and relationship in the prison.
Smoking
Smoking status/history of participants: whether or not smoking patterns changed since starting work at this prison and what is it like being a non-smoker working in this prison. Prison context and smoking: how common/’normal’ smoking is in this prison with PiC and staff here; how smoking fits into day-to-day life of this prison; whether or not smoking is more common in this prison than others; extent of ‘trade’ in tobacco between PiC in this prison; when/where PiC usually smoke; exactly where and when are they allowed to smoke; what PiC and staff colleagues think about the current rules around smoking in this prison; when/where do smoking staff smoke usually; how well are smoking rules adhered by staff and PiC; in what ways, if any, are the rules broken; and how colleagues view smoking and PiC who smoke in the prison. Smoking cessation: what might make PiC want to stop smoking while in prison, what might make them not want to stop smoking, what sort of help/support do they (and smoking staff) need to stop smoking, who is best placed to give this support, are different kinds of support needed to give up smoking compared with outside prison, any past experience of smoking cessation services, and what do you think of the support that is available for PiC (and prison staff) who want to stop smoking while in prison.
E-cigarettes
Have you/others you know people used e-cigarettes, what do you think about e-cigarettes, should PiC/staff be allowed to use e-cigarettes in prisons (in what ways would it be a good/bad thing) and what issues could be raised by allowing use of e-cigarettes in prisons?
Experience or threats of violence
Since coming to this prison, any experience of threats of violence or bullying that were so serious that you became afraid, or violence in the past year in this/another prison; were any of these related to tobacco or smoking?
Smoking bans
What did you think when the smoking ban was introduced in Scotland in 2006 (in what ways was it a good/bad thing) and the decision to exempt prisons from the legislation; have you heard about some prisons in Wales and in England going smoke free (what do you think about how this has happened); do people talk about increased smoking restrictions (in prisons) in other countries; what do you/PiC/other prison staff think about introducing smoking bans in prisons; what should Scotland do; how might introducing more smoke-free areas in prisons in Scotland be a good/bad thing and change prison life (for PiC/staff who smoke/do not smoke); what would make it easier/harder to extend smoke-free areas in prisons; and what would make it easier/harder to ban smoking altogether.
Work package 3: phase 2 staff interview topic guide
Background
Roles and responsibilities: in general and in relation to implementation of the ban, time in current role and experience of working in other prisons in Scotland/UK. Prison context: size, prisoner population, regime, accommodation, strengths and any limitations; what it is like to work in the prison on a typical week/weekend day (atmosphere, prisoner–staff and management–staff relationships). Smoking history: their current and past status and what it is like to work in the prison as a smoker/non-smoker.
Awareness and opinions about impending introduction of smoke-free policies in November 2018: level of awareness that Scottish prisons will become smoke free; whether (why) they agree with plans to make prisons smoke free; what might be good/bad about prisons being smoke-free and whether/why their views on smoke-free prisons have changed over time. Views on smoke-free prison policies in England and Wales (and wider society): extent of knowledge; what they think about prisons in Wales and England going smoke-free; and what, if anything, they have heard about how successful they think the policy has been.
Life in prison in anticipation of going smoke free
Experience of working in the prison in the lead-up to the introduction the ban: smoking culture and prisoner/staff smoking habits – how smoking fits into the day-to-day life of the prison (‘normality’ of smoking among PiC and staff); importance and role of tobacco in prisons, including trade; how PiC who smoke are seen by other PiC and staff; how interested PiC are in quitting; how much tobacco PiC buy from canteen; how much PiC usually smoke; how well rules around smoking are followed by PiC and staff; consequences of breaking smoking rules; and any changes in smoking within prisons since July/August 2017 (and if so whether or not related to impending ban from November 2018/introduction of the minimum pack size for cigarettes/other factors). Communication and engagement: whether/when/how plans to make prisons smoke free were communicated to staff, PiC and families – what worked well/less well; whether/what staff and PiC have been talking about in relation to the smoke-free policy; and whether or not staff/PiC have been involved in getting the prison ready to become smoke free (what works well/less well). Stop-smoking support: how easy/difficult for PiC to quit in prison and why; what they think about the help currently available to PiC; what works well/less well; whether or not stop-smoking support is good enough for the prison to become smoke-free; whether/how it has changed since July/August 2017; and what, if anything, could be done to make prisoner stop-smoking support better. E-cigarettes: how much do they know about e-cigarettes and different types of devices/e-flavours/levels of nicotine; whether they have used e-cigarettes outside/inside prison; whether/why PiC should be allowed to use e-cigarettes in prisons in the lead-up to and/or after prisons become smoke free; and any problems related to introducing e-cigarettes in prisons, and ways to resolve any issues. Other aspects of prison life in the lead-up to ban: any other changes in the prison in the lead-up to ban (how well rules are followed by PiC, prison day/regime, atmosphere, how staff/PiC are feeling/behaving, prisoner–prisoner and prisoner–staff relationships).
Implementing the smoke-free policy
What could facilitate a smoke-free environment for staff/PiC from November 2018: how easy/difficult will staff/PiC find it when prisons become smoke free; which groups of staff/PiC might find smoke free easier/harder; what actions could make it easier for staff/PiC; what actions should be taken in the lead-up; and what actions should be taken after the prison has become smoke free. What actions are being taken to implement a smoke-free policy in this prison: before/planned for after the policy is introduced; what is working well/less well; what could be improved; and what actions will be taken in the post-implementation phase to help ensure continued success. Successes, challenges and lessons learned to date in respect of the implementation of smoke-free prisons.
Work package 4: phase 2 people in custody interview topic guide
Background
What it is like in the prison on a typical week/weekend day: how they spend their time; what, if anything, is good/bad about the prison; how well prisoners and staff get along; and what the atmosphere is like. How long they have been in prison and when they expect to get out; whether or not they have been in prison before – roughly how many times and for how long.
Smoking history
For smokers: whether or not they smoked before they came to prison and whether and how their smoking habits have changed since coming to prison, and whether or not they are interested in giving up smoking while in prison. For ex-smokers: when did they quit smoking and what it was like, and what it is like to be an ex-smoker in a prison. For never smoker: what it is like being a non-smoker in a prison.
Awareness of and opinions on prison smoke-free policies
Explore opinions about the introduction of smoke-free policies in Scottish prisons from late November 2018: whether or not they have heard that Scottish prisons will become smoke-free, whether or not they agree with plans to make prisons smoke free, what might be good and bad about prisons being smoke free, and have their views on smoke-free prisons changed over time and reasons for this. Explore views on smoke-free prison policies in England and Wales: what they think about prisons in Wales and England going smoke-free; and what, if anything, they have heard about what life is like in these prisons since they became smoke-free.
Life in prison in anticipation of going smoke free
Explore what it is like to live in the prison in the lead-up to the introduction of a smoke-free policy: how does smoking fit into the day-to-day life of the prison/what is the importance and role of tobacco in prisons; and whether or not there have been any changes in smoking within prisons in the last few months. For current smokers: whether or not they expect to be in the prison when it becomes smoke free in November 2018, and whether and how plans to make prisons smoke free are influencing their own smoking habits. Stop-smoking support: how easy or difficult is it for prisoners to give up smoking while in prison; what they think about the help that is currently available to prisoners who want to stop smoking; what works well and less well; whether or not stop-smoking support is good enough for the prison to become smoke free; whether/how there have been any changes in stop-smoking support in the last few months (e.g. since July/August 2017); and what, if anything, could be done to make prisoner stop-smoking support better. E-cigarettes (vapes): how much, if anything, they have heard about e-cigarettes; whether they have used e-cigarettes outside or inside of prison; whether or not they think that prisoners should be allowed to use e-cigs in prisons in the lead-up to and/or after prisons become smoke free. Communication and engagement with staff and prisoners: whether, when and how plans to make the prison smoke free were communicated to prisoners and their families – what worked well and less well and lessons learned; whether or not prisoners have been involved in getting the prison ready to become smoke-free – what worked well and less well and lessons learned. Whether or not they have noticed any other changes in the prison in the lead-up to the ban.
Implementing a smoke-free policy
[If not already covered] What, if anything, would make it easier for prisoners to live and work in a smoke-free environment from November 2018: how easy or difficult will prisoners find it when the prison becomes smoke free from November 2018, and which groups of staff/prisoners might find smoke-free living easier and which groups might find it harder. What, if anything, they have heard about actions being taken to implement a smoke-free policy in this prison: what is working well and less well about implementation of a smoke-free policy and reasons for this and what could be better about how this prison is implementing a smoke-free policy.
Concluding comments
What the one or two most important issues relating to prison smoke-free policies are; whether there is anything else the participant would like to discuss.
Work package 4: phase 3 people in custody interviews
Background
Age, when (month/year) they entered prison (did they enter prison on their current sentence before or after 30 November 2018), sentence type, sentence length and whether or not this is the first time they have been in prison.
Smoking and vaping status and history pre ban or arrival in custody
Smoking history pre ban or arrival in custody. For previous smokers: when did they start smoking; how many cigarettes/roll ups did they smoke per week at that time; how did they feel about smoking at that time; before entering prison (for this sentence)/before smoke-free rules came in did they try to cut down or stop smoking; what were their reasons for doing so; what support did they use to try to help them to cut down or stop smoking, if anything; did they manage to cut down or stop and for how long; how easy or difficult they found it to try to stop smoking and the reasons for this; before entering prison/before smoke-free rules were they considering or planning to try to cut down or stop smoking? For those who were non-smokers before the introduction of smoke-free rules/before entering prisons: have they ever smoked and if so when and why they decided to quit and how they did it. E-cigarette use history: before entering prison/before introduction of the smokefree policy did they ever use e-cigarettes (when did they start using e-cigarettes and why; did the use e-cigarettes regularly at that time; what, if anything, did they like or dislike about using e-cigarettes at that time; did they use e-cigarettes only or did they also smoke tobacco).
Overall experiences, benefits, and challenges of living in a smoke-free prison
Overall, what it is like living in a smoke-free prison: what is good/bad about living in a smoke-free prison; benefits/issues/challenges; impacts on different groups, for example PiC (including new arrivals and vulnerable prisoner groups), staff, prison service and families. Has the introduction of smoke-free rules been like they imagined (if relevant): how does their experience now compare to the first few days/weeks of living in a smoke-free prison. Explore views on other positive/negative consequences of smoke-free prison policy: ‘trouble’ in prisons; working conditions for staff/living conditions for prisoners; physical and/or mental health and well-being of PiC, families and staff; smoking behaviour; and impacts on prison service/life in prison. What things have influenced the level of success of smoke-free rules in this prison: to what extent was preparation good in this prison for the smoking ban, what helped/did not help and why; and what things are helping/not helping with the ongoing operation of smoke-free rules.
Communication of smoke-free prison rules
How did they hear about the introduction of smoke-free rules in Scottish prisons from 30 November: what were they told, by whom and when; and were there any issues/challenges in respect of the information they were given about smoke-free prison rules.
Smoking abstinence/cessation in smoke-free prison
Overall, how easy or difficult are they finding it not to smoke: what kinds of things they do instead of smoking; how/in what way has the ease/difficulty of not smoking in prison changed over time? Reasons for this; how well are other prisoners managing without tobacco? Are some prisoner groups finding it harder than others? Which groups and why? What kind of support in respect of not smoking/quitting nicotine, if any, have they used or tried to access in (smoke-free) prison since the ban: why did they decide to access or try to access support not to smoke; how easy did they find it to access support/how long did they have to wait; what did they do in the interim; what worked well and less well about the support; and how do they think the support available in this prison to help prisoners not to smoke or quit nicotine long term could be improved. If they entered prison from 30 November 2018, explore what it was like as a smoker to enter a smoke-free prison.
Compliance and enforcement of smoke-free prison rules
How well do prisoners in this prison stick to no-smoking rule: how common is smoking in this prison; how easy or difficult would it be for someone to buy tobacco, lighters/matches. How likely it is that smoking will be detected by staff?
E-cigarettes in a smoke-free prison
What are their views on e-cigarettes generally. What is it like to live in an environment in which prisoners are using e-cigarettes. What do they think about the availability of e-cigarettes in smoke-free prison: what, if anything, has been good/bad about the availability of e-cigarettes in smoke-free prison; and how do other staff/prisoners feel about the sale of e-cigarettes in smoke-free prison. How common is it for prisoners to use e-cigarettes in this prison: has the popularity of e-cigarettes among prisoners changed over time, and do e-cigarettes have more value to some groups of prisoners than other. Have they used e-cigarettes while in smoke-free prison? If yes, explore: what are/were their reasons for using e-cigarettes in (smoke-free) prison; what plans, if any, did they have initially in respect of using e-cigarettes in prison and have they ended up using e-cigarettes in this way; how often do/did they use e-cigarettes; what products have they tried and what are their opinions of them. Have they considered reducing/stopping their intake of nicotine? If yes: reasons for this, what stage they are at, what support, if any, did they get to stop vaping and who from, what worked well and less about the support? What made it easier/more difficult to stop using e-cigarettes in prison? Do they intend to continue using e-cigarettes in the future?
Smoking and vaping behaviour during work placement/home leave or after liberation
What plans, if any, do they have regarding smoking after they leave prison/during work placement/home leave: how do they feel about the idea of not smoking after they leave prison/during work placement/home leave, and how easy or difficult do they think it will be to not to smoke after they leave prison/during work placement/home leave. Reasons for this.
What, if anything, they think could be done to help prisoners avoid returning to smoking after liberation/during work placement/home leave?
Lessons learnt and concluding remarks
What lessons do they think could be learnt from Scotland in relation to how to have a smoke-free prison?
Appendix 2 Approach to qualitative data analysis
With recorded permission, in-depth interviews and focus groups were audio-recorded and transcribed to facilitate analysis.
For focus groups and interviews with staff, PiC and representatives from other jurisdictions, de-identified transcripts were thematically analysed, supported by the framework approach developed at the NatCen87 (which shares similarities with the approach to thematic analysis developed by Braun and Clarke88).
For each data set, the following three steps were broadly followed by TIPs researchers (focus groups in phase 1: AB, HS, ED, GL, SS, LB and KH; PiC interviews in phase 2: AB, DE, RP, AM and KH; staff interviews in phase 2: AB, ED, HS and KH; staff focus groups in phase 3: AB, DM and KH):
-
A thematic framework was developed, informed by a combination of inductive and deductive techniques, such as close reading of transcripts, and taking account of study objectives and wider literature.
-
A framework grid was constructed in NVivo 12 software. Each interview or focus group was given a row in the framework grid and each subtheme in the thematic framework was given its own column. For every interview or focus group, TIPs researchers wrote summaries for each subtheme in the framework grid and included hyperlinks between summaries and raw data. The primary objective of the summarisation process was to support subsequent systematic and transparent thematic analysis of what might otherwise be a large and unwieldy data set. 87 For pragmatic reasons, two data sets, [interviews with representatives from other jurisdictions (WP1) and interviews with prison staff (WP3, phase 2)] transcripts were summarised against themes in Microsoft Word.
-
Thematic analysis was conducted by examining data summaries and transcripts to identify the range and diversity of views, experiences and meanings in the interviews/focus groups. Development of the final themes was iterative; responses were grouped together into categories to form themes and subthemes, which were then structured to provide a coherent narrative for the data. Ongoing refinements were made based on critical reflection, further examination of data summaries and transcripts, and discussion among the research team to reach an agreed interpretation.
For interviews with users and providers of smoking cessation support in prison in phases 1–3 (involving researchers DE, RP, AM and LB), data were also thematically analysed. However, de-identified transcripts were indexed (but not summarised) against a coding scheme. The coded extracts and transcripts were used to develop final themes and subthemes, using a similar process as described above under point three.
Thematic frameworks for interviews with personnel in other jurisdictions (work package 1) and interviews/focus groups with staff (work package 3) and people in custody (work package 4)
-
Interviews with personnel in other jurisdictions (WP1): thematic framework:
-
Background information on participant, prison and prison smoking policies.
-
Preparing to go smoke free –
-
– Governance.
-
– Communication and engagement.
-
– Smoking cessation services.
-
– E-cigarettes.
-
– Other.
-
-
Approach to implementation of the smoke-free prison policy.
-
Experiences of living and working in a smoke-free prison.
-
Perceived positive/negative consequences of the smoke-free prison policy –
-
– Contraband tobacco.
-
– Indiscipline.
-
– Staff health.
-
– PiC health.
-
– Compliance and enforcement.
-
– Other.
-
-
-
Staff focus groups (WP3) in phase 1: thematic framework (‘smoke-free policies’):
-
Overall views on the smoke-free prison policy.
-
Views on the principle of the smoke-free prison policy.
-
Views on the feasibility of the smoke-free prison policy.
-
Views on anticipated negative consequences of the smoke-free prison policy.
-
Views on impacts on different ‘prisoner’ groups.
-
Views on the balance of benefits and risks of the smoke-free prison policy.
-
Views on total versus partial smoke-free prison policy.
-
Views on the simultaneous versus phased introduction of the smoke-free prison policy.
-
Views on timescales for the introduction of the smoke-free prison policy.
-
Views on preparing for the introduction of the smoke-free prison policy.
-
Views on the current rules on smoking in prisons.
-
Views on e-cigarettes (for PiC).
-
-
Staff focus groups (WP3) in phase 1: thematic framework (‘e-cigarettes’):
-
Knowledge about e-cigarettes.
-
Sources of information about e-cigarettes.
-
Perceived harm to users and bystanders.
-
Perceived effectiveness as smoking cessation aid.
-
Perceived potential security risks.
-
Perceived safety of e-cigarettes.
-
Perceived costs of e-cigarettes.
-
Understanding e-cigarette regulation.
-
Views on the role of e-cigarettes in the implementation of the smoke-free prison policy.
-
Language (terminology).
-
Other.
-
-
Staff interviews (WP3) in phase 2: thematic framework:
-
Background.
-
Prison smoking culture.
-
Prison smoking cessation services.
-
Facilitators of and barriers to smoking cessation for in PiC.
-
E-cigarettes in prison.
-
Opinions on the smoke-free prison policy.
-
Potential unintended consequences of the smoke-free prison policy.
-
Potential challenges of the smoke-free policy for different prisoner groups.
-
Experiences of working in prisons in the lead-up to the implementation of the smoke-free policy.
-
Views on factors that might support/hinder the implementation of the smoke-free prison policy.
-
Other.
-
-
Staff focus groups (WP3) in phase 3: thematic framework:
-
Background –
-
– Participant characteristics.
-
– Background information about the prison.
-
– Other.
-
-
The Scottish prison smoking ban (from 30 November 2018) –
-
– Smoking history and attitudes, interest in smoking abstinence or cessation.
-
– Levels of acceptance, support for the prison smoking ban.
-
– Compliance/enforcement of the smoking ban in prison.
-
– Successes/challenges in relation to the ongoing operation management of the ban.
-
– Perspectives on the implementation of the smoking ban in prisons in E&W.
-
-
Other.
-
E-cigarettes in prison –
-
– Levels of support for current rules on e-cigarette use in Scottish prisons.
-
– Compliance/enforcement of rules on e-cigarette use in prisons.
-
– Prevalence of e-cigarette use in prison and among different ‘prisoner’ groups.
-
– Uptake and use of e-cigarettes in prisons.
-
– Choice of e-cigarette products on sale in prison.
-
– Purchasing and managing supplies of e-cigarette products in prison.
-
– Potential risks of addiction to e-cigarettes and long-term use of e-cigarettes.
-
– E-cigarette safety.
-
– Misuse of e-cigarettes in prison.
-
– Other.
-
-
Factors supporting or hindering the implementation of the prison smoking ban and lessons learnt –
-
– Perceptions of the ease or difficulty of the implementation of the smoke-free policy.
-
– Lead-in time, countdown, communication and engagement.
-
– E-cigarettes.
-
– NHS smoking cessation nicotine management products and services and partnership working between the NHS and SPS.
-
– Distraction and alternative activities.
-
– Management of the implementation of the ban at national or local level.
-
– Strategies in relation to the removal of tobacco from prisons.
-
– Factors related to frontline staff and PiC.
-
– Wider trends in smoking, vaping and health behaviours.
-
– Factors related to the implementation of the smoking ban in the open prison.
-
– Other.
-
-
Perceived (positive or negative) consequences of the prison smoking ban and availability of e-cigarettes in prisons –
-
– Working environment in prison and health of staff and visitors.
-
– Smoking or vaping behaviour of staff and visitors.
-
– ‘Trouble in prisons’.
-
– Living environment in prison and health and well-being of PiC.
-
– Financial benefits or problems for PiC.
-
– Contraband tobacco and lighters in prison.
-
– Drug use or displacement use of other substances.
-
– Fires in prisons.
-
– Other organisational impacts.
-
– Use of nicotine and tobacco products after liberation from a smoke-free prison.
-
– Recommendations, suggestions and key areas for improvement in the future in relation to the smoking ban or availability of e-cigarettes in prisons.
-
– Other.
-
-
People in custody interviews (WP4) in phase 2: thematic framework.
-
Background –
-
– Background information on the prison.
-
– Background information on the participant.
-
– Other.
-
-
Opinions on the smoke-free policy –
-
– Opinions on the introduction of the smoke-free policy in Scottish prisons.
-
– Awareness and opinions on the implementation of the smoke-free policy in prisons in E&W.
-
– Other.
-
-
Views and experiences of smoking-related issues leading up to the implementation of the smoke-free policy –
-
– Experiences of living or working in a prison as a smoker or non-smoker.
-
– Prisoner smoking culture and habits (including own smoking habits/history).
-
– Compliance/enforcement of prisoner smoking rules.
-
– Staff smoking habits (while at work).
-
– Smoking cessation in prison.
-
– Understanding and use of e-cigarettes.
-
– Perceived changes in smoking-related issues leading up to the implementation of the smoke-free policy.
-
– Other.
-
-
Views and experiences of early preparations for the implementation of the smoke-free policy –
-
– Awareness and understanding of the smoke-free policy.
-
– Local and national governance of the smoke-free policy.
-
– Planning for the implementation of the smoke-free policy.
-
– Other.
-
-
Views on how to implement a smoke-free policy –
-
– Project management and leadership.
-
– Resources and training.
-
– Communication and engagement with prisoners and staff.
-
– Smoking cessation support.
-
– E-cigarettes.
-
– Staff, peer and family support to quit.
-
– Activities to substitute for smoking or to prevent relapse.
-
– Health and well-being initiatives.
-
– Different measures for different prisoner groups or prison categories.
-
– Enforcement of a smoke-free policy.
-
– Other measures.
-
-
-
People in custody interviews (WP4) in phase 3: thematic framework.
See thematic framework above for ‘staff focus groups (WP3) in phase 3’ (point 5).
Appendix 3 Characteristics of users and providers of smoking cessation services who were interviewed
| Staff designation categories | Phase (n) | ||
|---|---|---|---|
| 1 | 2 | 3 | |
| SSS | |||
| Senior managers | 3 | – | 4 |
| Managers/co-ordinators | 9 | 1 | 4 |
| Smoking cessation facilitators | 8 | 4 | 6 |
| Prison health-care/addiction services | |||
| Health-care managers | 8 | 1 | 4 |
| Trained facilitators | 10 | 11 | 15 |
| Health-care nurse (admissions) | – | – | 1 |
| SPS staff | |||
| Senior managers | – | – | 1 |
| Trained facilitatorsa | – | 10 | 3 |
| Totalb | 38 | 27 | 38 |
| Status | Number of PiC |
|---|---|
| Expected status on 30 November 2018 | |
| In custody | 31 |
| In the community | 8 |
| Uncertain | 6 |
| Previous experience of trying to quit | |
| Never tried before | 8 |
| Never tried in prison before | 4 |
| Tried in prison before | 31 |
| Unknown | 2 |
| Sex | |
| Female | 12 |
| Male | 33 |
List of abbreviations
- A&E
- accident and emergency
- ARIMA
- autoregressive integrated moving average
- ASH
- Action on Smoking and Health
- CCA
- cost–consequences analysis
- CEA
- cost-effectiveness analysis
- CI
- confidence interval
- CO
- carbon monoxide
- CRUK
- Cancer Research UK
- CUA
- cost–utility analysis
- DVD
- digital versatile disc
- E&W
- England and Wales
- EQ-5D
- EuroQol-5 Dimensions
- GBP
- Great British pounds
- GP
- general practitioner
- ICER
- incremental cost-effectiveness ratio
- ID
- identifier
- MoR
- management of offenders at risk owing to any substance
- NIHR
- National Institute for Health Research
- NPS
- new psychoactive substance
- NRT
- nicotine replacement therapy
- NSS
- National Services Scotland
- PHR
- Public Health Research
- PiC
- people in custody
- PM2.5
- fine particulate matter
- PSA
- probabilistic sensitivity analysis
- QALY
- quality-adjusted life-year
- RAG
- research advisory group
- SA
- sensitivity analysis
- SAG
- Stakeholder Advisory Group
- SARIMA
- seasonal autoregressive integrated moving average
- SHS
- second-hand smoke
- SPS
- Scottish Prison Service
- SSS
- Stop Smoking Service
- TIPs
- Tobacco in Prisons
- WP
- work package
Notes
-
Tobacco in Prisons surveys of prison staff: survey questions and frequencies
-
Tobacco in Prisons surveys of people in custody: survey questions and frequencies
-
Health economic analysis: supplementary tables and technical details
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/WGLF1204).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
