Notes
Article history
The contractual start date for this research was in July 2017. This article began editorial review in February 2023 and was accepted for publication in January 2024. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The Global Health Research editors and publisher have tried to ensure the accuracy of the authors’ article and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Permissions
Copyright statement
Copyright © 2024 Pandey et al. This work was produced by Pandey et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Pandey et al.
Background and introduction
Globally, injuries are a serious public health problem. Around the world, injuries cause more than 5 million deaths each year and account for 9% of all deaths. 1 Low- and middle-income countries (LMICs) such as Nepal suffer an especially high burden of injury morbidity and mortality. This results from many factors, including greater exposure to injury risks, less effective prevention strategies and poorly developed emergency and trauma care services. 2 In Nepal, most people access the healthcare system via their local health post or subhealth post, which is staffed by healthcare workers and nurses. If their need is greater, they would use their nearest primary healthcare centre where they would be able to see a doctor, and if necessary they would travel to their nearest public hospital. In addition, there are a large number of private hospitals and medical colleges which contribute to the healthcare system. The public have to pay for care at every type of health facility, which will influence their choices and access to care.
Sources of data in Nepal are limited, with few surveys using population-representative samples. Data derived from the Nepal census in 2001 showed an injury-related mortality rate of 42/100,000 for men and 19/100,000 for women. 3 The majority of injury-related deaths were among people aged 15–64 years (67%), followed by 21% for those aged below 15 years and 12% for those aged 65 and above. These data were collected during survey interviews with family members and therefore may be at risk of recall bias. 3 A systematic review showed that most studies reporting the epidemiology of injuries in Nepal are based on small hospital case series and are therefore prone to bias. 4 A recent study, using Global Burden of Disease (GBD) estimates, reports that in Nepal in 2017, the death rate from all types of injuries was 56/100,000 people. 5 The GBD estimates rely on modelling as the data sources used for the study are often incomplete. 6 Some of the routinely used sources of injury data such as vital registration, police records and hospital facility records are collected by different agencies but are not routinely collated. 7 In Nepal there is currently no formal surveillance system to monitor injury morbidity or mortality, and death registration, though mandatory, is incomplete.
The Department of Health Services (DoHS) within the Ministry of Health and Population in Nepal uses Health Management Information System (HMIS) data to report annual healthcare service use. Healthcare settings across all districts of Nepal collect data on inpatient and outpatient attendance, and submit data electronically to central government every month. 8 Each year a report will be published which summarises data on child health, family health and infectious disease management, but has not to date compiled a review of injury data. 8
Aims and objectives
The HMIS is a potential source of data that could be used to explore the epidemiology of hospitalised injuries in Nepal. The aim of this study was to assess the utility of HMIS data to describe burden of injuries in Nepal and to explore inequalities in injury admissions by age and sex, and trends over time.
Methods
Study design
We analysed routinely collected HMIS data reporting admissions to hospitals and healthcare facilities, published by the DoHS over 8 years between 2009/10 and 2016/17 through its annual reports. These reports are in the public domain, downloadable as pdf files. The DoHS was not able to provide access to the raw data at the time of the study. During the study period, the HMIS collected data from health posts (first point of contact for basic health services in the community), primary healthcare centres, district hospitals zonal, subregional and regional hospitals and some private hospitals. 8 The data published in the data annex of each annual report vary in format and detail by year. However, the reports consistently publish data annexes of all inpatient morbidity by International Classification of Disease (ICD-10) codes, split by age and sex. Therefore, we downloaded data files from each annual report between 2009/10 and 2016/178–15 and used an online pdf converter to extract data into MS Excel® (Microsoft Corporation, Redmond, WA, USA) data files for analysis. The annual report consisted of outpatients and inpatients data. We used the data which were published as inpatient admissions for injuries in this study. However, it is not clear whether ‘inpatient admission’ means the patient stayed overnight or were discharged the same day. We were unable to analyse data relating to outpatient attendance for injuries because the frequency counts of these presentations were available only at district level and not disaggregated to report outpatient attendance by age and sex.
Data coding
The data in the MS Excel files were cleaned to identify any errors introduced by the conversion process, such as missing values or duplicate entries. Files were combined to generate a final dataset for analysis. ICD-10 injury codes were then used to identify which admissions were considered to be ‘injury admissions’ for our analyses. A complete set of ICD-10 injury codes was not published in each data annex. Therefore, to combine data across years, ICD-10 injury codes were collated into higher-level categories describing different types of injuries. These categories replicate injury types published in GBD 2017 studies. 16 Hence, the results of analysis could be compared with the GBD estimates. ICD-10 codes relating to exposure to inanimate mechanical forces were included in the ‘Other unintentional injuries’ category, while data coded as exposure to animate mechanical forces were included in the ‘Animal contact’ category if the codes described animal-related injuries (e.g. bites). Codes relating to adverse effects of medical treatment were included in the poisoning category, unless they were specific to self-harm. Globally, self-harm data are widely recognised as underestimated due to poor data collection, difficulty determining intent or methods and perceptions of criminalisation and stigma. 17–19 Therefore, we combined ICD-10 codes that specifically described ‘intentional’ harm with similar types of injuries where intent was ‘undetermined’. We excluded ‘Injury by body parts’ from our analysis to avoid the risk of double-counting, limiting our analyses to T, V, W, X and Y codes. Coding was conducted by the lead author, with queries discussed with the research team. A summary of injury-type categories and their associated ICD-10 codes is shown in Appendix 1, Table 4. The injury classification, codes and subcodes with their frequency by year are shown in Report Supplementary Material 1; these data were used for analysis.
Data analysis
Data analysis was carried out using Microsoft Excel. To explore changes in injury rates over time, we used total population values published in each DoHS annual report to calculate crude rates of total unintentional injuries and self-harm by year and repeated this for specific injury types. 8–15 It was not possible to calculate age-standardised rates, as the published population data were not given in consistent age categories across the years studied (age-specific population projections based on the 2011 census were available for the years 2011/12–2016/17, but these do not match the total population size published in the DoHS annual reports, so were not considered reliable enough for the purposes of comparing crude and age-standardised rates). We calculated rates with 95% confidence intervals for all injury types used in this study. We present trends over time in crude rates of total unintentional injuries and self-harm in a line graph. We present a table of crude rates by year for each type of unintentional injury, with correlation coefficients to describe any trends over time. As a primary aim of this study was to explore inequalities in injury occurrence, to explore potential inequality by age and sex, and changes over time, we ranked causes of injuries by age and sex, over two time periods, 2011/12 – 2013/14 and 2014/15 – 2016/17. Findings are formatted in ranking tables as used by the World Health Organization (WHO). 1 We used medium variant age- and sex-specific population projections from the 2011 census to generate these rates. 20 Age- and gender-specific population projections were not available for the years 2009/10 or 2010/11, so they were excluded from this analysis. The data available did not enable an analysis by level of deprivation.
Equation for calculating the 95% confidence interval of the injury rate:
Results
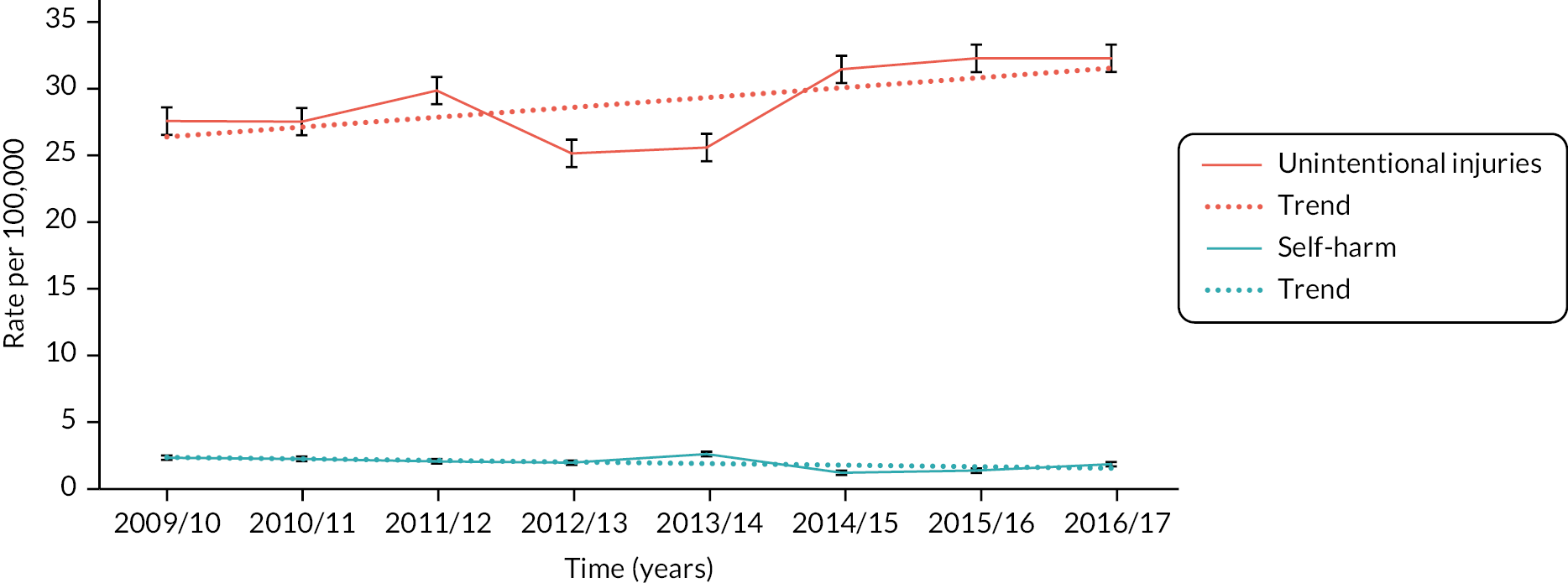
The crude rate of total unintentional injuries requiring hospital admission appears to increase between 2009/10 and 2016/17 from 27.53/100,000 (95% CI 26.91 to 28.15) to 32.23/100,000 (95% CI 31.57 to 32.88) (r = 0.62), while that for self-harm was more stable, but reduced from 2.34/100,000 (95% CI 2.16 to 2.52) in 2009/10 to 1.85/100,000 (95% CI 1.69 to 2.01) in 2016/17 (r = –0.60) (Figure 1) (see Appendix 2, Table 5).
FIGURE 1.
Crude rates per 100,000 population of total unintentional injury and self-harm requiring hospitalisation between 2009/10 and 2016/17. Note: Error bars have been included for self-harm injuries but are too narrow to appear on the figure.
Over time, the rates of some types of injuries have changed. Transport-related injuries have become the most common cause of injury admissions at a rate of 10.55/100,000 (95% CI 10.17 to 10.92), followed by animal contact (8.29/100,000, 95% CI 7.96 to 8.63) (Table 1). Over the same period, reported rates of admissions for poisoning have halved from 7.52/100,000 to 3.62/100,000, and admissions following a fall are reported to have dropped from 4.26/100,000 to 0.41/100,000. Admissions following burns and scalds have remained relatively constant.
| Types of unintentional injuries | 2009/10 | 2010/11 | 2011/12 | 2012/13 | 2013/14 | 2014/15 | 2015/16 | 2016/17 | (r) |
|---|---|---|---|---|---|---|---|---|---|
| Transport injuries (95% CI) |
4.28 (4.03 to 4.52) |
4.03 (3.79 to 4.26) |
5.38 (5.11 to 5.65) |
5.89 (5.60 to 6.18) |
5.38 (5.11 to 5.66) |
9.71 (9.35 to 10.08) |
10.33 (9.95 to 10.70) |
10.55 (10.17 to 10.92) |
0.93 |
| Animal contact (95% CI) |
2.68 (2.48 to 2.87) |
3.21 (3.00 to 3.42) |
3.88 (3.65 to 4.11) |
4.03 (3.79 to 4.27) |
3.63 (3.40 to 3.85) |
5.9 (5.62 to 6.19) |
8.6 (8.26 to 8.94) |
8.29 (7.96 to 8.63) |
0.91 |
| Falls (95% CI) |
4.26 (4.02 to 4.51) |
3.11 (2.90 to 3.11) |
3.18 (2.98 to 3.39) |
2.68 (2.48 to 2.87) |
2.74 (2.54 to 2.93) |
1.84 (1.68 to 2.00) |
0.78 (0.68 to 0.89) |
0.41 (0.34 to 0.49) |
–0.96 |
| Fire, heat and hot substances (95% CI) |
6.03 (5.74 to 6.32) |
5.81 (5.53 to 6.09) |
5.5 (5.23 to 5.77) |
4.36 (4.12 to 4.61) |
5.07 (4.80 to 5.33) |
6.1 (5.81 to 6.39) |
4.73 (4.48 to 4.98) |
6.76 (6.46 to 7.06) |
0.08 |
| Poisoning (95% CI) |
7.52 (7.19 to 7.84) |
7.89 (7.56 to 8.21) |
7.42 (7.10 to 7.73) |
4.77 (4.51 to 5.03) |
4.69 (4.44 to 4.95) |
4.66 (4.41 to 4.91) |
5.34 (5.07 to 5.61) |
3.62 (3.40 to 3.84) |
–0.87 |
| Environmental heat or cold exposure (95% CI) |
0.10 (0.06 to 0.14) |
0.17 (0.12 to 0.22) |
0.34 (0.27 to 0.41) |
0.14 (0.10 to 0.18) |
0.11 (0.07 to 0.15) |
0.11 (0.07 to 0.15) |
0.15 (0.11 to 0.20) |
0.14 (0.09 to 0.18) |
–0.20 |
| Other unintentional injuries (95% CI) |
2.16 (1.99 to 2.33) |
2.86 (2.66 to 3.06) |
3.6 (3.38 to 3.82) |
2.68 (2.48 to 2.87) |
3.28 (3.07 to 3.28) |
1.25 (1.12 to 1.38) |
1.22 (1.09 to 1.35) |
1.58 (1.44 to 1.73) |
–0.59 |
| Drowning (95% CI) |
0.01 (0.00 to 0.02) |
0.02 (0.00 to 0.04) |
0.04 (0.02 to 0.07) |
0.02 (0.00 to 0.03) |
0.02 (0.00 to 0.04) |
0.02 (0.00 to 0.03) |
0.00 (0.00 to 0.01) |
0.02 (0.01 to 0.04) |
–0.23 |
| Foreign body (95% CI) |
0.49 (0.41 to 0.58) |
0.4 (0.33 to 0.47) |
0.46 (0.38 to 0.53) |
0.55 (0.46 to 0.63) |
0.63 (0.53 to 0.72) |
0.37 (0.30 to 0.44) |
0.5 (0.41 to 0.58) |
0.55 (0.46 to 0.63) |
0.25 |
| Exposure to forces of nature (95% CI) |
0.00 (0.00 to 0.01) |
0.00 (0.00 to 0.01) |
0.00 (0.00 to 0.01) |
0.00 (0.00 to 0.01) |
0.00 (0.00 to 0.01) |
1.4 (1.26 to 1.54) |
0.57 (0.48 to 0.65) |
0.31 (0.25 to 0.38) |
0.54 |
The types of unintentional injuries leading to hospital admission differ for males and females and this difference appears to have changed over time (Table 2). Unintentional poisoning was the leading cause of admissions for women during the period 2011/12–2013/14, falling to the fourth most common cause of injury admissions during 2014/15–2016/17. Crude rates of poisoning fell for both sexes over time. Animal contact injuries and transport-related injuries were ranked at third and fourth in 2011/12–2013/14, rising to first and second in 2014/15–2016/17. Both showed significant increases in crude rates for each sex, greater than were likely to have occurred by chance. In contrast, for men in Nepal, transport-related injuries have remained the leading cause of unintentional injury admissions across this 6-year period. Even though crude rates of fire, heat and hot substances injuries increased over the two time periods, this group of injuries, which was the second most common cause of admissions for both men and women during 2011/12–2013/14, fell to the third most common cause for both sexes during 2014/15–2016/17.
| Rank | 2011/12–2013/14 | 2014/15–2016/17 | ||
|---|---|---|---|---|
| Female | Male | Female | Male | |
| 1 | Poisoning 6.76 (6.15 to 7.01) |
Transport injuries 7.77 (7.49 to 8.05) |
Animal contact 8.47 (8.20 to 8.75) |
Transport injuries 13.63 (13.27 to 13.99) |
| 2 | Fire, heat and hot substances 5.07 (4.85 to 5.29) |
Fire, heat and hot substances 5.20 (4.97 to 5.43) |
Transport injuries 7.18 (6.92 to 7.43) |
Animal contact 6.87 (6.61 to 7.12) |
| 3 | Animal contact 4.19 (4.00 to 4.39) |
Poisoning 4.82 (4.61 to 5.04) |
Fire, heat and hot substances 6.08 (5.85 to 6.31) |
Fire, heat and hot substances 5.75 (5.52 to 5.98) |
| 4 | Transport injuries 3.78 (3.59 to 3.96) |
Animal contact 3.72 (3.53 to 3.91) |
Poisoning 5.39 (5.17 to 5.61) |
Poisoning 3.73 (3.54 to 3.91) |
| 5 | Other unintentional injuries 3.33 (3.15 to 3.51) |
Other unintentional injuries 3.25 (3.07 to 3.43) |
Other unintentional injuries 1.30 (1.20 to 1.41) |
Other unintentional injuries 1.43 (1.32 to 1.55) |
| 6 | Falls 2.80 (2.63 to 2.96) |
Falls 3.13 (2.95 to 3.30) |
Falls 0.88 (0.79 to 0.97) |
Falls 1.16 (1.05 to 1.26) |
| 7 | Foreign body 0.44 (0.37 to 0.50) |
Foreign body 0.69 (0.60 to 0.77) |
Exposure to forces of nature 0.72 (0.64 to 0.80) |
Exposure to forces of nature 0.83 (0.74 to 0.91) |
| 8 | Environmental heat or cold exposure 0.17 (0.13 to 0.21) |
Environmental heat or cold exposure 0.25 (0.20 to 0.29) |
Foreign body 0.44 (0.38 to 0.51) |
Foreign body 0.51 (0.44 to 0.58) |
| 9 | Drowning 0.02 (0.01 to 0.04) |
Drowning 0.04 (0.02 to 0.05) |
Environmental heat or cold exposure 0.13 (0.10 to 0.17) |
Environmental heat or cold exposure 0.13 (0.10 to 0.17) |
| 10 | Exposure to forces of nature 0.00 (0.00 to 0.01) |
Exposure to forces of nature 0.00 (0.00 to 0.01) |
Drowning 0.02 (0.00 to 0.03) |
Drowning 0.01 (0.00 to 0.03) |
Considering variation in admissions by age, burns and scalds are consistently the leading cause of unintentional injury admissions for children and young people aged 0–14 years over time (Table 3). Over the same period, transport injuries and animal contact injuries increased in both rate and ranking, moving from fourth and fifth rankings during the period 2011/12–2013/14 to third and second rankings, respectively, during 2014/15–2016/17. Transport injuries were the leading cause of unintentional injury admissions for people aged 15–59 years and over 60 years for both time periods, though for both age groups, the crude rates increased significantly over time. Poisoning and animal contact were the second and third most common causes of admission for people aged 15–59 years in 2011/12–2013/14, changing to third and second rankings over time. For those aged over 60 years, animal-related injury increased in rate over time but remained the second most common cause of injury-related admission for this age group.
| Rank | 2011/12–2013/14 | 2014/15–2016/17 | ||||
|---|---|---|---|---|---|---|
| 0–14 years | 15–59 years | 60 + years | 0–14 years | 15–59 years | 60 + years | |
| 1 | Fire, heat and hot substances 7.80 (7.47 to 8.13) |
Transport injuries 7.81 (7.56 to 8.06) |
Transport injuries 5.51 (4.94 to 6.07) |
Fire, heat and hot substances 8.47 (8.12 to 8.83) |
Transport injuries 13.82 (13.50 to 14.14) |
Transport injuries 10.02 (9.28 to 10.76) |
| 2 | Poisoning 3.22 (3.00 to 3.43) |
Poisoning 7.76 (7.51 to 8.01) |
Animal contact 5.14 (4.60 to 5.69) |
Animal contact 3.64 (3.41 to 3.87) |
Animal contact 9.57 (9.30 to 9.84) |
Animal contact 9.28 (8.57 to 9.99) |
| 3 | Falls 2.59 (2.40 to 2.78) |
Animal contact 4.94 (4.74 to 5.14) |
Falls 4.42 (3.91 to 4.92) |
Transport injuries 3.58 (3.35 to 3.81) |
Poisoning 5.93 (5.72 to 6.14) |
Fire, heat and hot substances 5.58 (5.02 to 6.13) |
| 4 | Transport injuries 2.13 (1.95 to 2.30) |
Other unintentional injuries 4.17 (3.98 to 4.35) |
Fire, heat and hot substances 4.37 (3.87 to 4.88) |
Poisoning 2.26 (2.08 to 2.44) |
Fire, heat and hot substances 4.65 (4.46 to 4.83) |
Poisoning 3.53 (3.09 to 3.97) |
| 5 | Animal contact 1.98 (1.81 to 2.15) |
Fire, heat and hot substances 3.71 (3.53 to 3.88) |
Other unintentional injuries 3.04 (2.62 to 3.46) |
Falls 0.90 (0.78 to 1.01) |
Other unintentional injuries 1.57 (1.47 to 1.68) |
Other unintentional injuries 1.93 (1.61 to 2.25) |
| 6 | Other unintentional injuries 1.84 (1.68 to 2.00) |
Falls 2.96 (2.80 to 3.12) |
Poisoning 2.72 (2.33 to 3.12) |
Other unintentional injuries 0.81 (0.70 to 0.92) |
Exposure to forces of nature 1.08 (0.99 to 1.17) |
Falls 1.49 (1.20 to 1.77) |
| 7 | Foreign body 0.77 (0.66 to 0.87) |
Foreign body 0.40 (0.34 to 0.46) |
Foreign body 0.83 (0.61 to 1.05) | Foreign body 0.59 (0.50 to 0.69) |
Falls 1.01 (0.92 to 1.10) |
Foreign body 0.96 (0.74 to 1.19) |
| 8 | Environmental heat or cold exposure 0.43 (0.35 to 0.51) |
Environmental heat or cold exposure 0.10 (0.07 to 0.12) |
Environmental heat or cold exposure 0.05 (0.00 to 0.10) |
Exposure to forces of nature 0.12 (0.08 to 0.16) |
Foreign body 0.35 (0.30 to 0.40) |
Exposure to forces of nature 0.96 (0.74 to 1.19) |
| 9 | Drowning 0.06 (0.03 to 0.09) |
Drowning 0.01 (0.00 to 0.02) |
Drowning 0.00 |
Environmental heat or cold exposure 0.11 (0.07 to 0.15) |
Environmental heat or cold exposure 0.16 (0.12 to 0.19) |
Environmental heat or cold exposure 0.07 (0.01 to 0.13) |
| 10 | Exposure to forces of nature 0.00 |
Exposure to forces of nature 0.00 (0.00 to 0.01) |
Exposure to forces of nature 0.00 |
Drowning 0.02 (0.00 to 0.04) |
Drowning 0.01 (0.002 to 0.02) |
Drowning 0.01 (0.00 to 0.04) |
Discussion
We have explored the utility of routine HMIS data to illustrate the burden of injuries requiring hospitalisation over time in Nepal and inequalities in incidence by age and sex. We found that crude rates of injury admissions rose over the 8-year period between 2009/10 and 2016/17, and this trend could help us understand likely trends in the future. Increases in injury admissions were largely explained by increases in transport-related injuries and animal injuries. Over the same period, crude rates of admissions for falls, poisonings and self-harm declined. Inequalities exist in admission to hospital for injury by age and sex. Males have more admissions than females overall, and people of different ages are admitted at varying rates for different types of injury. The observed trends over time are to be treated with caution as the rates are not age-standardised, because the population data published alongside the event frequencies were not given in consistent age categories across the years studied. However, a comparison of crude rates and age-adjusted rates using population projections by age group (not presented here) suggest there is minimal difference in the trends observed over time.
Transport injuries
Transport injuries have become a major cause of hospital admission for people of all ages and both sexes in Nepal. Most published data on road traffic injuries (RTIs) in Nepal arise from that collected by the police. 4 The findings of this study for transport injuries are consistent with a secondary analysis of Nepal traffic police data, which showed that RTIs had more than doubled between 2001 and 2013 from 4596 to 11,986 reported casualties. 21 Data from the WHO report on the Global Status of Road Safety22 suggest that deaths from RTIs in South-East Asia have been steadily increasing, and estimates are now 20.7/100,000. Over the last decade, Nepal has experienced rapid motorisation. As a landlocked mountainous country, roads are the main method for transporting goods and services. The number of registered vehicles on Nepal’s roads has increased from 1,755,821 to 2,783,428 over the 3 years to 2016/17. 23 Many roads in Nepal are poorly constructed and maintained, and there is a general lack of safety infrastructure such as light-controlled junctions, pavements and designated crossing points for pedestrians. 24 As not all road traffic crashes are reported to the police, data on hospitalisations following an RTI are valuable, as they may provide more accurate records, closer to WHO estimates.
Animal contact
The global burden of injuries arising from animal contact is due mostly to bites from snakes and dogs. We observed that the rate of admission for animal-related injuries increased over threefold between 2009/10 and 2016/17, and that animal injuries requiring admission were more common in women than in men. The rate was similar for 15–59 years and age 60 or above, which were higher than in children. A community survey in eastern Nepal found that snake bite was common in adults, particularly in rural areas with agricultural workers being most at risk. 25 No published studies reporting dog bites were found in a systematic review of injuries in Nepal,4 despite street dogs being very common and rabies being widespread. However, a hospital-based injury surveillance study by our team found that dog bites were a common cause of hospital attendance,26 particularly in children. 27 A community survey done in rural Bangladesh found that 81% of animal contact events did not need hospitalisation. 28 Our analysis found that the codes used to report admission following animal contact varied from year to year with markedly fluctuating frequencies suggesting that coding rules for bites in HMIS may be inconsistently applied.
Fire, heat and hot substances
Although burn injuries are decreasing globally,6 this study observed rates of admissions to hospital following burns and scalds to be relatively constant over time. The rate of admissions was highest for children and was similar for both men and women. These findings differ from those reported by the WHO that globally women are more likely to be affected than men, as many burns and scalds are sustained during food preparation, which is mostly carried out by women. 29 A recent community survey from Nepal showed that burns are in fact a common cause of injury, yet only a small proportion of patients attend hospital after a burn or scald. 30 People in rural areas are thought to be more vulnerable to burn-related morbidity and mortality because of the lack of pre-hospital services. 31
Falls
We found a steady decrease over time in the rate of admissions following a fall. This is in contrast to global data estimates which show that, worldwide, fall injuries are the leading cause of unintentional injury deaths, secondary to transport injuries. 6 The reason for the low rate of admissions for fall injuries in Nepal in this study is unclear, but it is possible that this could be an artefact due to how falls are coded in the HMIS system, with a preference for coding the consequence of the fall (e.g. a fracture), or the body part affected (e.g. hip) rather than the underlying cause of the injury. Failure to capture the mechanism of the injury event significantly limits the utility of such data to inform injury prevention initiatives.
Exposure to forces of nature
In April 2015, a devastating earthquake struck Nepal. The Ministry of Home Affairs reported 8020 deaths and 16,033 injuries following the earthquake. 32 It was therefore surprising to find relatively few cases of admission for injuries reported for the year 2014/15. Reasons for the low reporting may have been due to many patients being cared for by the 131 foreign medical teams who were deployed in field hospitals across Nepal after the earthquake. These field hospitals did not submit data on the casualties treated to the HMIS. In addition, even where people attended Nepalese hospitals, it is understood that the usual HMIS reporting practices in Nepalese hospitals were disrupted following the earthquake. 33 Where cases were reported, they may have been coded only to indicate the body parts injured (e.g. leg fracture) rather than the underlying cause of the injury (e.g. hit by falling object).
Poisoning and self-harm
We found that the majority of self-harm cases were coded as being of undetermined intent. Among 4368 self-harm cases, 176 were recorded as intentional, and 4192 as of undetermined intent. Moreover, among all cases of self-harm, the vast majority of these cases were poisoning. We found the rate of admissions following poisoning and self-harm both gradually decreased over the period from 2009/10 to 2016/17. A systematic review of fatal self-poisoning found that between 2006 and 2015, intentional poisoning comprised 13.7% of all suicidal deaths globally and 38.5% in the South-East Asia region. 18 The GBD study reported decreasing trends in self-harm6 concluding that a decrease in poverty could be the reason for decreasing global cases of self-harm. However, Nepal remains one of the lowest income countries of the world and national sources of data suggest a growing incidence of suicide and self-harm. Self-harm in Nepal particularly affects women and girls, and appears to be fuelled by low empowerment of women and gender-based violence. 34 A systematic review of publications reporting injuries in Nepal4 found 40 publications, mostly hospital case series, reporting poisoning, self-harm or suicide. The cause of self-harm and suicide was frequently through the ingestion of pesticides and in the majority of publications the intentionality of the ingestion was not explored. A study exploring suicide reporting networks found that the cases of self-harm and suicides may not present to health facilities, especially in rural areas because of lack of transportation and fear of police involvement and criminalisation. 19 Cases in hospital records may not be reported as such in the HMIS, being classified as cardiac failure or asphyxiation. Moreover, the same study stated that social stigma and cultural and administrative issues cause under-reporting of self-harm and suicide cases. 19 A recent review paper reported that globally, suicide data are not complete because of inaccurate registration of suicides suggesting that cases recorded as ‘undetermined intent’ may frequently be intentional, and therefore, ‘undetermined intent’ cases should be included when calculating rates of suicide. 17 Poisoning, often through the ingestion of pesticides, is frequently reported as the most common cause of suicide. 17,18 The risk of underestimation of the true burden of suicide suggests that the coding of poisoning and self-harm in routinely reported HMIS data may benefit from further scrutiny.
Data quality
We found that injury data were collected and reported differently from year to year. In some years some injuries were not recorded at all, or were coded differently (see Report Supplementary Material 1). These inconsistencies in coding practice limit the opportunity to use the HMIS data to monitor injury trends and explore inequalities in injury incidence. They may also provide an explanation for the dip in admissions seen between 2012/13 and 2013/14. A standard set of indicators, a well-designed reporting format and trained data entry staff are known to enhance the quality of HMIS data. 35 Thus, good quality routine hospital data requires investment and resources particularly in workforce training and regular feedback. In terms of population data by calendar year and age group, which are needed to calculate age-specific and age-standardised rates, the DoHS annual reports do not use detailed or consistent age categories, so cannot be used for this purpose. Age-specific population projections are available from 2011/12 onwards, based on the 2011 census, but these become inherently less reliable over the 10-year period of projections, and we found these to substantially underestimate the total population compared to the DoHS figures; we therefore concluded that they should not be used for the purposes of presenting age-standardised rates. Future analyses, including the calculation of age-standardised rates, will require reliable age- and gender-specific population estimates by calendar year.
Future research
Further research using raw HMIS data could enable more detailed analyses of inequalities in injury admissions by ethnic group and geographical area and could address the potential issue of double-counting cases. Qualitative research involving data coders would help understand the process of coding and the challenges faced by HMIS coders in healthcare settings. These findings could facilitate training to improve the accuracy and consistency of application of codes. Regular, periodic reviews of routinely collected HMIS injury data could support policy-makers, informing injury prevention strategies and the identification of vulnerable groups for targeted or universal injury prevention interventions.
Lessons learned
These findings illustrate the potential for HMIS data to be of interest to both clinicians caring for patients with injuries and for policy-makers planning and managing health services. The data show the high and increasing burden placed on hospitals by largely preventable injury events. The data-quality issues identified can be addressed through guidance, training and monitoring of data collectors and coders.
Limitations
This is the first time that HMIS data have been used to explore trends and inequalities by age and sex in injury-related admissions in Nepal. HMIS data are routinely collected with an established system for regular reporting, and it has the potential to provide a cost-effective system for the surveillance of hospitalised injuries in LMICs such as Nepal. The data used in this study are from multiple healthcare facilities across all districts in Nepal and therefore not subject to single hospital or locality biases. While the HMIS collates information from many government hospitals in Nepal, they do not include data from all public, private and national non-government health facilities and therefore underestimate the true burden of hospital admissions due to injuries. As we did not have access to the raw data, we were unable to explore inequalities in injury occurrence by ethnicity or deprivation, or determine whether multiple codes were associated with individual admissions. In the absence of sound population data by age, we were unable to estimate age-standardised rates. Moreover, we could not estimate the severity of the injuries as the available data does not represent the number of days in hospital. The HMIS data are not a complete source of injury burden as all injured cases do not access the health service, maybe because of the need to pay, a lack of awareness about the possible complications of injury, lack of access to health care in rural areas and easy availability of specialised private hospitals. This study was conducted as a Master’s dissertation project and reflects the data available at the time the lead author was studying. As the project involved analysing published reports in the public domain, more recent records were not available.
Conclusions
Admissions to hospital for transport and animal-related injuries appear to be increasing in Nepal. Together with burns, scalds and poisoning, these largely preventable injuries are placing a significant and avoidable burden on the healthcare system. Although these data fail to capture injuries cared for at home, in the emergency department or in outpatients, in the absence of a bespoke injury surveillance system, the HMIS has the potential to provide valuable data to inform injury prevention policy and practice. Further assessment to understand factors affecting completeness and accuracy appears warranted.
Key learning points
-
Crude injury rates in hospital admissions are increasing over time, particularly for RTIs.
-
Inequalities in injury admissions exist by both age and sex, and these could be monitored over time using HMIS data.
-
Data-quality issues exist but could be addressed through training and monitoring.
Additional information
Acknowledgements
This study was conducted as a dissertation project by the first author towards the award of an MSc Public Health from the University of the West of England. The authors thank the dissertation module leader Dr Nick De Viggiani, UWE. We also thank Dr Matthew Ellis for reviewing the manuscript and providing constructive comments.
Dissemination
The findings of this study have been shared with the Department of Health Services at the Ministry of Health and Population, in the Government of Nepal.
Patient and public involvement
This study involved a secondary analysis of existing data. The public and patients were not involved in the design or analysis of data in this study.
Equality, diversity and inclusion
This study involved a secondary analysis of existing data, which included exploration of inequalities in injury occurrence by age and sex. No participants were recruited to the study.
CRediT contribution statement
Bidhya Pandey (https://orcid.org/0000-0002-6222-9383): Methodology, Formal analysis, Writing – original draft.
Isabelle Bray (https://orcid.org/0000-0002-5353-3287): Supervision, Validation, Writing – editing and reviewing.
Sunil K Joshi (https://orcid.org/0000-0002-2704-5060): Data curation, Validation, Writing – editing and reviewing.
Julie A Mytton (https://orcid.org/0000-0002-0306-4750): Conceptualisation, Methodology, Writing – editing and reviewing.
All authors qualify for authorship of this manuscript. All authors approved the final version.
Disclosure of interests
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, are available in the toolkit on the NIHR Journals Library report publication page at https://doi.org/10.3310/ATAE3098.
Primary conflicts of interest: None of the authors have any conflicts of interest, apart from Julie A Mytton, who was a member of the NIHR HTA Programme MNCH Panel between 2008 and 2015.
Data-sharing statement
Health Management Information System data on injuries were published in the annual reports of the Government of Nepal Department of Health Services and are available from https://dohs.gov.np/. Any other queries should be addressed to the corresponding author for consideration.
Ethics statement
We received ethical approval for this study from the Faculty of Health and Applied Sciences Research Ethics Committee, University of the West of England, Bristol, UK, on 6 June 2019. The reference no. is HAS.19.05.191.
Information governance statement
NIRC is committed to handling all personal information in line with the UK Data Protection Act (2018) and the General Data Protection Regulation (EU GDPR) 2016/679. All data used in this study were published and in the public domain. Data collected through the Health Management Information System are anonymised at source, at the time of data collection. Therefore, no additional actions were required to protect personal identifiable information or to ensure good data governance for this study.
Department of Health and Social Care disclaimer
This publication presents independent research commissioned by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, MRC, NIHR Coordinating Centre, the GHR programme or the Department of Health and Social Care.
This article was published based on current knowledge at the time and date of publication. NIHR is committed to being inclusive and will continually monitor best practice and guidance in relation to terminology and language to ensure that we remain relevant to our stakeholders.
Funding
This article presents independent research funded by the National Institute for Health and Care Research (NIHR) Global Health Research programme as award number 16/137/49 using UK aid from the UK Government to support global health research. The views expressed in this publication are those of the authors and not necessarily those of the NIHR or the UK government. Research is published in the NIHR Global Health Research Journal. See the NIHR Funding and Awards website for further award information.
About this article
The contractual start date for this research was in July 2017. This article began editorial review in February 2023 and was accepted for publication in January 2024. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The Global Health Research editors and publisher have tried to ensure the accuracy of the authors’ article and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Copyright
Copyright © 2024 Pandey et al. This work was produced by Pandey et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
This article reports on one component of the research award Utility of routine data reporting injuries requiring hospitalisation in Nepal: a secondary data analysis. For more information about this research please view the award page [https://www.fundingawards.nihr.ac.uk/award/16/137/49]
List of abbreviations
- DoHS
- Department of Health Services
- GBD
- Global Burden of Disease
- HMIS
- Health Management Information System
- ICD
- International Classification of Disease
- LMICs
- low- and middle-income countries
- RTI
- road traffic injury
- WHO
- World Health Organization
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/ATAE3098).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
References
- Injuries and Violence: The Facts. Geneva: World Health Organization; 2014.
- Gosselin RA, Spiegel DA, Coughlin R, Zirkle LG. Injuries: the neglected burden in developing countries. Bull World Health Organ 2009;87. https://doi.org/10.2471/blt.08.052290.
- Sharma GK. Leading causes of mortality from diseases and injury in Nepal: a report from national census sample survey. J Inst Med 2006;28:7-11. https://doi.org/10.3126/JOIM.V28I1.427.
- Mytton JA, Bhatta S, Thorne M, Pant PR. Understanding the burden of injuries in Nepal: a systematic review of published studies. Cogent Med 2019;6. https://doi.org/10.1080/2331205X.2019.1673654.
- Global Health Data Exchange | GHDx 2017. http://ghdx.healthdata.org/gbd-results-tool (accessed 6 October 2019).
- Roth GA, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories.1980–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1736-88. https://doi.org/10.1016/S0140-6736(18)32203-7.
- Jagnoor J, Ponnaiah M, Varghese M, Ivers R, Kumar R, Prinja S, et al. Potential for establishing an injury surveillance system in India: a review of data sources and reporting systems. BMC Publ Health. 2020;20. https://doi.org/10.1186/s12889-020-09992-9.
- Department of Health Services: Annual Report 2073/74 (2016/17). Kathmandu, Nepal: Department of Health and Population, Ministry of Health and Population; 2018.
- Department of Health Services: Annual Report 2066/67 (2009/10. Kathmandu, Nepal: Department of Health and Population, Ministry of Health and Population; 2011.
- Department of Health Services: Annual Report 2067/68 (2010/11). Kathmandu, Nepal: Department of Health and Population, Ministry of Health and Population; 2012.
- Department of Health Services: Annual Report 2068/69 (2011/12). Kathmandu, Nepal: Department of Health and Population, Ministry of Health and Population; 2013.
- Department of Health Services: Annual Report 2069/70 (2012/13). Kathmandu, Nepal: Department of Health and Population, Ministry of Health and Population; 2014.
- Department of Health Services: Annual Report (2070/71). Kathmandu, Nepal: Department of Health and Population, Ministry of Health and Population; 2015.
- Department of Health Services. Annual Report (2071/72). Kathmandu, Nepal: Department of Health and Population, Ministry of Health and Population; 2016.
- Department of Health Services: Annual Report (2072/73). Kathmandu, Nepal: Department of Health and Population, Ministry of Health and Population; 2017.
- James SL, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet. 2018;392:1789-858. https://doi.org/10.1016/S0140-6736(18)32279-7.
- Snowdon J, Namkee CG. Undercounting of suicides: where suicide data lie hidden. Glob Publ Health. 2020;15:1894-901. https://doi.org/10.1080/17441692.2020.1801789.
- Mew EJ, Padmanathan P, Konradsen F, Eddleston M, Chang SS, Phillips MR, et al. The global burden of fatal self-poisoning with pesticides 2006–15: systematic review. J Affect Disord 2017;219:93-104. https://doi.org/10.1016/j.jad.2017.05.002.
- Hagaman AK, Maharjan U, Kohrt BA. Suicide surveillance and health systems in Nepal: a qualitative and social network analysis. Int J Ment Health Syst. 2016;10. https://doi.org/10.1186/s13033-016-0073-7.
- National Population and Housing Census 2011 (Population Projection 2011 – 2031). Kathmandu, Nepal: Central Bureau of Statistics; 2012.
- Karkee R, Lee AH. Epidemiology of road traffic injuries in Nepal, 2001–2013: systematic review and secondary data analysis. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2015-010757.
- Global Status on Road Safety 2018. Geneva: World Health Organization; 2018.
- Economic Survey 2017/18. Kathmandu, Nepal: Ministry of Finance; 2018.
- Pant PR, Banstola A, Bhatta S, Mytton JA, Acharya D, Bhattari S, et al. Burden of injuries in Nepal, 1990–2017: findings from the Global Burden of Disease Study 2017. Inj Prev 2020;26:i57-66. https://doi.org/10.1136/injuryprev-2019-043309.
- Sharma SK, Chappuis F, Jha N, Bovier PA, Loutan L, Koirala S. Impact of snake bites and determinants of fatal outcomes in south-eastern Nepal. Am J Trop Med Hyg 2004;71:234-8. https://doi.org/10.4269/ajtmh.12-0750.
- Bhatta S, Magnus D, Mytton J, Joshi E, Bhatta S, Adhikari D, et al. The epidemiology of injuries in adults in Nepal: findings from a hospital-based injury surveillance study. Int J Environ Res Publ Health 2021;18. https://doi.org/10.3390/ijerph182312701.
- Magnus D, Bhatta S, Mytton J, Joshi E, Bhatta S, Manandhar S, et al. Epidemiology of paediatric injuries in Nepal: evidence from emergency department injury surveillance. Arch Dis Child 2021;106:1050-5. https://doi.org/10.1136/archdischild-2020-321198.
- Bhuiyan MA, Agrawal P, Wadhwaniya S, Li Q, Alonge O, Rahman AKMF, et al. Animal-related injuries and fatalities: evidence from a large-scale population-based cross-sectional survey in rural Bangladesh. BMJ Open 2019;9. https://doi.org/10.1136/bmjopen-2019-030039.
- Mock C, Peck M, Peden M, Krug E, Ahuja R, Albertyn H, et al. A WHO Plan for Burn Prevention and Care. Geneva: World Health Organization; 2008.
- Phuyal K, Ogada EA, Bendell R, Price PE, Potokar T. Burns in Nepal: a participatory, community survey of burn cases and knowledge, attitudes and practices to burn care and prevention in three rural municipalities. BMJ Open 2020;10. https://doi.org/10.1136/bmjopen-2019-033071.
- Peden M, Oyegbite K, Ozanne-Smith J, Hyder AA, Branche C., Rahman AKMF, et al. World Report on Child Injury Prevention. Geneva: World Health Organization; 2008.
- Nepal Earthquake 2072. Kathmandu, Nepal: Ministry of Home Affairs; 2015.
- WHO . Nepal Earthquake 2015 2015. https://iris.who.int/handle/10665/252737.
- Marahatta K, Samuel R, Sharma P, Dixit L, Shrestha BR. Suicide burden and prevention in Nepal: the need for a national strategy. WHO South-East Asia J Public Health 2017;6:45-9. https://doi.org/10.4103/2224-3151.206164.
- Teklegiorgis K, Tadesse K, Mirutse G, Terefe W. Level of data quality from health management information systems in a resources limited setting and its associated factors, eastern Ethiopia. South Afr J Inf Manag 2016;18. https://doi.org/10.4102/sajim.v18i1.612.
Appendix 1
| Injury category | ICD codes used in the analysis |
|---|---|
| Transport injuries | V01, V02, V04, V05, V09, V12, V16, V18-V20, V22, V23, V29-V31, V35, V37, V39, V43, V47, V50, V52, V56, V57, V59, V64, V69, V79, V80, V84-V90, V93, V97-V99, Y85 |
| Animal contact | T63, W54-W59, X20, X21, X23 |
| Falls | W00, W01, W05, W06, W10, W13, W14, W16-W19 |
| Fire heat and hot substances | T20-T26, T28-T32, W39, X03, X04, X09, X11, X16, X17, X19 |
| Poisoning | T36-T57, T59, T61, T62, T64, T65, T96, X40, X41, X44, X47 |
| Environmental heat or cold exposure | T33-T35, T66, T67 |
| Other unintentional injuries | T70-T75, T78, T79, T95, T98, W26, W27, W31-W34, W40, W49, W51, W52, W78-W80, W83, W85-W87, W89, W92, X59, Y89 |
| Drowning | T75.1, W69, W70, W74 |
| Foreign body | T15-T19, W45 |
| Exposure to forces of nature | T70, W77, X33-X36 |
| Self-harm | T60, X60, X61, X64, X66, X68-X70, X76, X78, X84, Y11, Y14-Y20, Y23, Y24, Y28, Y31, Y34 |
Appendix 2
| Year | Population denominator | Unintentional injuries Rate per 100,000 with 95% CI |
Self-harm Rate per 100,000 with 95% CI |
|---|---|---|---|
| 2009/10 | 27,498,585 | 27.53 (26.91 to 28.15) | 2.34 (2.16 to 2.52) |
| 2010/11 | 27,999,405 | 27.49 (26.88 to 28.11) | 2.25 (2.07 to 2.42) |
| 2011/12 | 28,480,814 | 29.81 (29.17 to 30.44) | 2.07 (1.90 to 2.24) |
| 2012/13 | 27,248,574 | 25.11 (24.52 to 25.71) | 1.96 (1.79 to 2.12) |
| 2013/14 | 27,311,978 | 25.55 (24.95 to 26.15) | 2.61 (2.42 to 2.80) |
| 2014/15 | 27,723,373 | 31.40 (30.74 to 32.06) | 1.21 (1.80 to 1.34) |
| 2015/16 | 28,624,299 | 32.22 (31.56 to 32.87) | 1.37 (1.24 to 1.51) |
| 2016/17 | 28,621,764 | 32.23 (31.57 to 32.88) | 1.85 (1.69 to 2.01) |
| (r) | – | 0.62 | –0.60 |
