Notes
Article history
The contractual start date for this research was in July 2017. This article began editorial review in February 2023 and was accepted for publication in March 2024. The authors have been wholly responsible for all data collection, analysis and interpretation, as well as for writing up their work. The Global Health Research editors and publisher have tried to ensure the accuracy of the authors’ article and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Permissions
Copyright statement
Copyright © 2024 Banstola et al. This work was produced by Banstola et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Banstola et al.
Background and introduction
Injuries are an important public health problem in Nepal despite being predictable and largely preventable. The Global Burden of Diseases Study 2019 estimated that injuries account for 7.8% of all deaths and 9.6% of Nepal’s total disability-adjusted life-years. 1 Around 50% of road trauma victims with survivable injuries die in the prehospital setting in low- and middle-income countries (LMICs) like Nepal2 because they do not receive timely first aid and transfer to a health facility. 3,4 The World Health Organization (WHO) has advocated improved prehospital care through the Decade of Action for Road Safety 2011–20. 5 The Second Decade of Action for Road Safety 2021–30, recently proclaimed by the UN General Assembly, has also encouraged the strengthening of prehospital care, including emergency medical services (EMS) for trauma care. 6 At the national level, the Government of Nepal, in its Health Sector Implementation Plan (2016–21), prioritised the establishment of EMS to speed up prehospital care. 7 Nepal’s first national conference on prehospital care for emergencies (19–20 July 2018) declared that ‘every citizen should be able to access quality prehospital care’. 8 Furthermore, the 2021 Emergency Care System Assessment joint report by the Ministry of Health and Population and the WHO identified 39 key priorities to enhance Nepal’s emergency care system including prehospital care. 9
Providing high-quality prehospital care to injured persons, followed by good medical treatment, can save lives and prevent or reduce the severity of disability. 10,11 A 2012 study on the impact of prehospital care in LMICs identified that implementing proper prehospital care could reduce the risk of death in injured patients by 25%. 12 Prehospital EMS are well established in most high-income countries, but the provision is limited in LMICs. 13,14 In LMICs, family members, friends, the police, firefighters, taxi drivers and bystanders are often the first to be present at the scene of an injury event and often provide immediate care and transport to the hospital. 15 Where ambulance staff do attend, their ability to provide care will vary depending on the training they have received. Many LMICs have inadequate prehospital trauma care systems. 16 As a result, fewer victims get treatment at the scene of their injury and are simply transported rapidly to a healthcare facility. 17
In Nepal, organised EMS systems started in 2011 with the establishment of the Nepal Ambulance Service (NAS), a non-profit, non-governmental organisation based in Kathmandu. 18–20 Two years later, Dhulikhel EMS started offering ambulance services with medical care by trained paramedics in Kavrepalanchowk District, where Dhulikhel hospital is located. 18 Before these services started in Nepal and still in places where such services do not operate, ambulance services, if available, are provided by the nearest hospital. These ambulances are primarily vehicles (sometimes with a stretcher and an oxygen cylinder) for conveying patients to the hospital. Such paid-for ambulance services do not usually involve emergency medical technicians (EMTs) or drivers trained in first aid. Patients and their families will call for the hospital ambulance to collect them or make their way to the hospital. 20 There is no national telephone number to call to request an ambulance. 9
Through a previous study investigating the status of the first response system in Nepal, we found that there were few organised prehospital emergency care providers. 21 Only a few studies have examined ambulance services in Nepal and have indicated that most are poorly equipped, lacking essential supplies and trained EMTs and paramedics. 22,23 One hospital-based study reported that 31% of patients arrived at the hospital by ambulance, and only 24% of them received medical care from EMTs on the way to the hospital. 24 Studies have also shown that few people called for an ambulance, and most of them received the service with an average waiting time of 34 minutes for the ambulance. 24,25 A recent study, which evaluated the emergency care units in seven tertiary referral centres in Kathmandu using the WHO Hospital Emergency Unit Assessment Tool, revealed that 15–35% of patients in these hospitals arrive by ambulances staffed with formally trained prehospital providers, some of whom follow their own prehospital protocols. 26
No studies have been reported from Nepal that specifically explore the prehospital emergency care provided for trauma victims. There is also little information on prehospital care time intervals, that is the time taken to reach patients and convey them to a suitable health facility. Finally, there is no evidence of the challenges of providing prehospital care for trauma victims in Nepal from the perspective of those directly involved in providing care, such as ambulance drivers, EMTs or service managers.
Aims and objectives
This study aimed to:
-
explore the mechanism and nature of injury of trauma victims managed by an EMS provider in Nepal
-
estimate prehospital time intervals occurring during the care and transport processes and
-
explore the perceptions and experiences of prehospital care service providers in providing care for trauma victims.
Methods
Study design
This case study used mixed methods (secondary data analysis and qualitative semistructured interviews). The use of quantitative and qualitative approaches, in combination, provides a better understanding of the research problem than either approach alone.
Study setting
The NAS was selected for the case study because it is the largest prehospital emergency care provider in the country, providing services in three out of the seven provinces in Nepal – Bagmati Province (Kathmandu Valley and Bharatpur/Chitwan); Gandaki Province (Pokhara); and Lumbini Province (Butwal). The Kathmandu Valley is the most developed and populated (2.5 million population) area of Nepal, which includes the city of Kathmandu (capital), Lalitpur, Bhaktapur, Kirtipur and Madhyapur Thimi. Chitwan (579,984 population) is a lowland plain region, while Pokhara (414,141 population) is a hilly region, and Butwal (118,462 population) is a combination of hills and plains. The NAS provides fully equipped ambulances via a central dispatch facility with radio communication between area hospitals and ambulances, along with medical care by trained EMTs on the way to the hospital. 18–20 In addition, the NAS has established a three-digit emergency phone number (102) which could, in the future, form the basis of a national phone number to summon assistance following acute illness or injury. Therefore, the NAS has the scale of organisation and workload to explore our research questions.
Study participants
For the qualitative component of the study, we interviewed a diverse group of staff employed by the NAS, including ambulance drivers, EMTs, dispatch officers and service managers. The number of participants was based on the concept of information power proposed by Malterud et al. 27 We asked the gatekeepers of NAS to help us identify potential participants and to reassure potential participants that they have permission from NAS to participate in the study. The participants were selected purposively using a sampling frame to ensure participation across the breadth of roles within the organisation.
Data collection
Written permission from NAS was obtained to access its call records and interview the staff.
Quantitative data
Nepal Ambulance Service staff (FS) generated a de-identified data set of all callouts by the service over 1 year (May 2019–May 2020) and provided it to the research team in Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA) format.
Qualitative data
We provided a participant information sheet and a consent form to potential participants and invited them to ask questions about the study before deciding whether to participate. Written consent was taken from participants where it was feasible to complete recruitment face to face. Where it was not possible to meet participants face to face due to restrictions imposed by the COVID-19 pandemic, consent was recorded verbally by phone, and the audio recording was kept as the record of consent. The confidentiality and anonymity of participants were protected by assigning a unique identification number to each participant.
The interviews were conducted to explore the perceptions of prehospital care service providers regarding their experience of providing care for injured persons. Semistructured interview schedules (see Appendix 1) were developed for each group of prehospital care providers based on the available literature, adhering to the guidelines for successful qualitative research,28 and finalised before data collection. All interviews were conducted either online or face to face by the second author (PG) at a location and time convenient to each participant. The interviews were digitally audio-recorded. Participants were offered 1200 Nepali rupees (approximately £8) as a token of appreciation for their time and participation.
Data management
Quantitative data
The data set received from NAS was checked for data field completion, for consistency in the application of categories or codes, and to look for data outliers that may indicate a data entry error. Any data concerns were discussed with the NAS staff (FS) before finalising the data set. The cleaned data were stored securely on a password-protected computer at the University of the West of England (UWE Bristol) and backed up on a UWE cloud-based drive.
Qualitative data
Verbatim transcriptions of interviews recorded in Nepali were translated into English. The transcription and translation were done by experienced transcribers and translators and verified by researchers (AB and PG) by comparing the translated script with the audio file. To ensure anonymity, any personal identifiable information was removed from transcriptions and replaced with a unique identification code. The digital recordings of the interviews were stored securely on a password-protected computer in the Nepal Injury Research Centre (NIRC) office. All paper records were kept in a secure and locked location in the NIRC office, where only authorised persons had access.
Data analysis
Quantitative data
First, we separated the trauma calls from non-trauma calls. For this study, trauma callouts were defined as those where one of the following injuries were recorded in the NAS patient registry: transport injuries (road injuries and other transport injuries), falls, drowning, burns, poisonings, animal-related injuries, and injuries arising from natural hazards, self-harm, interpersonal violence, conflict and terrorism. To identify the mechanism and nature of injury, free-text information in the ‘chief complaint/group’ field that described the reason for the callout was extracted and coded. AB prepared the initial coding and discussed it with GS and JM to develop a data dictionary (see Appendices 2 and 3, Tables 5 and 6) that was applied consistently to all data. Prehospital was defined as care or EMS provided by NAS staff for injured patients (described earlier) before they reach a hospital. Missing data were not imputed due to their non-random nature, which would introduce bias if imputed. Therefore, data from only complete cases were analysed using descriptive statistics to describe trauma victims’ characteristics and estimate prehospital time intervals during the care process using Microsoft Excel Version 16.0. Analysis was led by AB.
Qualitative data
The interview data were analysed using inductive thematic analysis to identify patterns of meanings or themes. 28 NVivo (March 2020 release) (QSR International, Warrington, UK) was used to apply codes consistently and organise the data related to each code. Two researchers (AB and PG) did the initial coding. They discussed their coding with two additional researchers (GS and JM) to develop a coding framework that was then applied consistently to all transcripts. After coding all transcripts, similar codes were clustered in groups to make candidate themes. Final themes were developed through discussion and agreement with the research team.
Patient and public involvement
The study was supported by a prehospital care stakeholder advisory group. The group did not involve patients or members of the public.
Results
Quantitative findings
A total of 9182 callouts were handled between May 2019 and May 2020. Of these, 1408 (15.3%) were trauma calls (including calls to transport trauma victims between hospitals). Of the 1408 trauma calls, 682 (48.4%) were trauma callouts for which prehospital care or EMS were provided for injured patients before they reached a hospital. Of the total 682 prehospital trauma cases, 60.7% were male and 39.3% were female, with a median age of 43 (interquartile range; 27–65 years). People aged over 60 years old were the largest group of service users (32.0%), followed by those aged between 18 and 29 years old (24.2%) (Tables 1 and 2).
| Mechanism of injury | Asphyxia | Assault | Bites and stings | Burns | Cut | Fall | Road traffic crash | Self-harm | Unspecified | Total, n (%) |
|---|---|---|---|---|---|---|---|---|---|---|
| Sex | ||||||||||
| Female | 1 | 1 | 2 | 9 | 8 | 117 | 32 | 17 | 81 | 268 (39.3) |
| Male | 3 | 8 | 7 | 13 | 14 | 127 | 98 | 11 | 133 | 414 (60.7) |
| Total, n (%) | 4 (0.6) | 9 (1.3) | 9 (1.3) | 22 (3.2) | 22 (3.2) | 244 (35.8) | 130 (19.1) | 28 (4.1) | 214 (31.4) | 682 (100.0) |
| Age category (in years) of injury victims | ||||||||||
| 0–4 | 1 | 0 | 0 | 2 | 0 | 3 | 1 | 0 | 2 | 9 (1.3) |
| 5–9 | 0 | 0 | 0 | 1 | 1 | 5 | 0 | 0 | 5 | 12 (1.8) |
| 10–14 | 0 | 0 | 0 | 1 | 1 | 5 | 1 | 0 | 3 | 11 (1.6) |
| 15–17 | 0 | 0 | 0 | 0 | 1 | 4 | 5 | 1 | 4 | 15 (2.2) |
| 18–29 | 0 | 3 | 2 | 6 | 11 | 33 | 52 | 15 | 43 | 165 (24.2) |
| 30–44 | 1 | 6 | 4 | 2 | 4 | 39 | 33 | 8 | 40 | 137 (20.1) |
| 45–59 | 0 | 0 | 2 | 3 | 1 | 46 | 22 | 1 | 40 | 115 (16.9) |
| ≥ 60 | 2 | 0 | 1 | 7 | 3 | 109 | 16 | 3 | 77 | 218 (32.0) |
| Total, n (%) | 4 (0.6) | 9 (1.3) | 9 (1.3) | 22 (3.2) | 22 (3.2) | 244 (35.8) | 130 (19.1) | 28 (4.1) | 214 (31.4) | 682 (100.0) |
| Nature of injury | Burn | Choking | Fracture | Head injury | Musculoskeletal injuries | Poisoning | Spinal injury | Wound | Unspecified | Total, n (%) |
|---|---|---|---|---|---|---|---|---|---|---|
| Sex | ||||||||||
| Female | 9 | 1 | 86 | 14 | 17 | 15 | 31 | 14 | 81 | 268 (39.3) |
| Male | 13 | 3 | 140 | 46 | 24 | 11 | 38 | 32 | 107 | 414 (60.7) |
| Total, n (%) | 22 (3.2) | 4 (0.6) | 226 (33.1) | 60 (8.8) | 41 (6.0) | 26 (3.8) | 69 (10.1) | 46 (6.7) | 188 (27.6) | 682 (100.0) |
| Age group (in years) | ||||||||||
| 0–4 | 2 | 1 | 2 | 0 | 0 | 0 | 0 | 0 | 4 | 9 (1.3) |
| 5–9 | 1 | 0 | 7 | 0 | 1 | 0 | 0 | 1 | 2 | 12 (1.8) |
| 10–14 | 1 | 0 | 3 | 1 | 0 | 0 | 1 | 2 | 3 | 11 (1.6) |
| 15–17 | 0 | 0 | 6 | 2 | 0 | 1 | 0 | 1 | 5 | 15 (2.2) |
| 18–29 | 6 | 0 | 43 | 14 | 13 | 13 | 9 | 18 | 49 | 165 (24.2) |
| 30–44 | 2 | 1 | 41 | 16 | 11 | 8 | 10 | 11 | 37 | 137 (20.1) |
| 45–59 | 3 | 0 | 30 | 11 | 9 | 1 | 22 | 8 | 31 | 115 (16.9) |
| ≥ 60 | 7 | 2 | 94 | 16 | 7 | 3 | 27 | 5 | 57 | 218 (32.0) |
| Total, n (%) | 22 (3.2) | 4 (0.6) | 226 (33.1) | 60 (8.8) | 41 (6.0) | 26 (3.8) | 69 (10.1) | 46 (6.7) | 188 (27.6) | 682 (100.0) |
Falls were the most common injury mechanism (35.8%), followed by road traffic crashes (19.1%). The mechanism of injury was unspecified in 31.4% of cases (see Table 1).
Fractures accounted for 33.1% of cases, followed by suspected spinal injury (10.1%). The type of injury was not specified in 27.6% of cases (see Table 2).
Table 3 shows the mean values of different time intervals in handling trauma cases by the prehospital care providers. On average, ambulances were dispatched within 2 minutes of the call being received, and the ambulance arrived at the scene in an average of 15 minutes (range 3–68 minutes). EMTs spent an average of 10 minutes at the scene providing care before taking an average of 17 minutes to transport the patient to the hospital (range 2–285 minutes). The total mean prehospital time interval from receiving a call to arrival at the hospital was 48 minutes.
| Time intervals (in minutes) | Mean (SD) | Median | Mode | Minimum | Maximum | 95% CI | |
|---|---|---|---|---|---|---|---|
| 1. | Activation time (call received to ambulance dispatch) | 1.56 (0.32) | 2 | 2 | 1 | 12 | 1.53 to 1.58 |
| 2. | Response time (ambulance dispatch to arrival at scene) | 15.09 (6.13) | 14 | 13 | 3 | 68 | 14.41 to 15.37 |
| 3. | On-scene time (arrival at scene to departure from scene) | 10.16 (6.44) | 10 | 10 | 3 | 100 | 9.46 to 10.47 |
| 4. | Transport time (departure from scene to arrival at hospital) | 20.30 (19.38) | 17 | 15 | 2 | 285 | 19.02 to 21.59 |
| 5. | Total prehospital time (1–4) | 47.52 (24.17) | 43 | 45 | 20 | 368 | 46.03 to 49.42 |
Qualitative findings
We invited 18 staff employed in the NAS to participate in the qualitative study. Seventeen participants agreed to participate and were interviewed in February and March 2021; eight worked as EMTs, five worked as ambulance drivers, two as dispatch officers and two worked in managerial positions. One staff member declined to participate because he was unavailable during the data collection period. Participants ranged in age between 24 and 62 years. All EMTs had a mandatory vocational degree as either a community medicine assistant or an auxiliary nurse midwife. Participants in the managerial positions had a master’s degree, while the dispatch officers had bachelor’s degrees in management. Four out of five ambulance drivers had not completed their secondary education. Further demographic information of the participants is presented in Table 4. Interviews lasted an average of 42 minutes.
| EMT | Ambulance driver | Dispatch officer | Senior manager | |
|---|---|---|---|---|
| Stations | ||||
| Kathmandu | 6 | 3 | 2 | 2 |
| Pokhara | 1 | 1 | 0 | 0 |
| Chitwan | 1 | 1 | 0 | 0 |
| Sex | ||||
| Male | 4 | 5 | 0 | 2 |
| Female | 4 | 0 | 2 | 0 |
| Average period of employment at NAS | 7.7 years | 6.2 years | 5.5 years | 7 years |
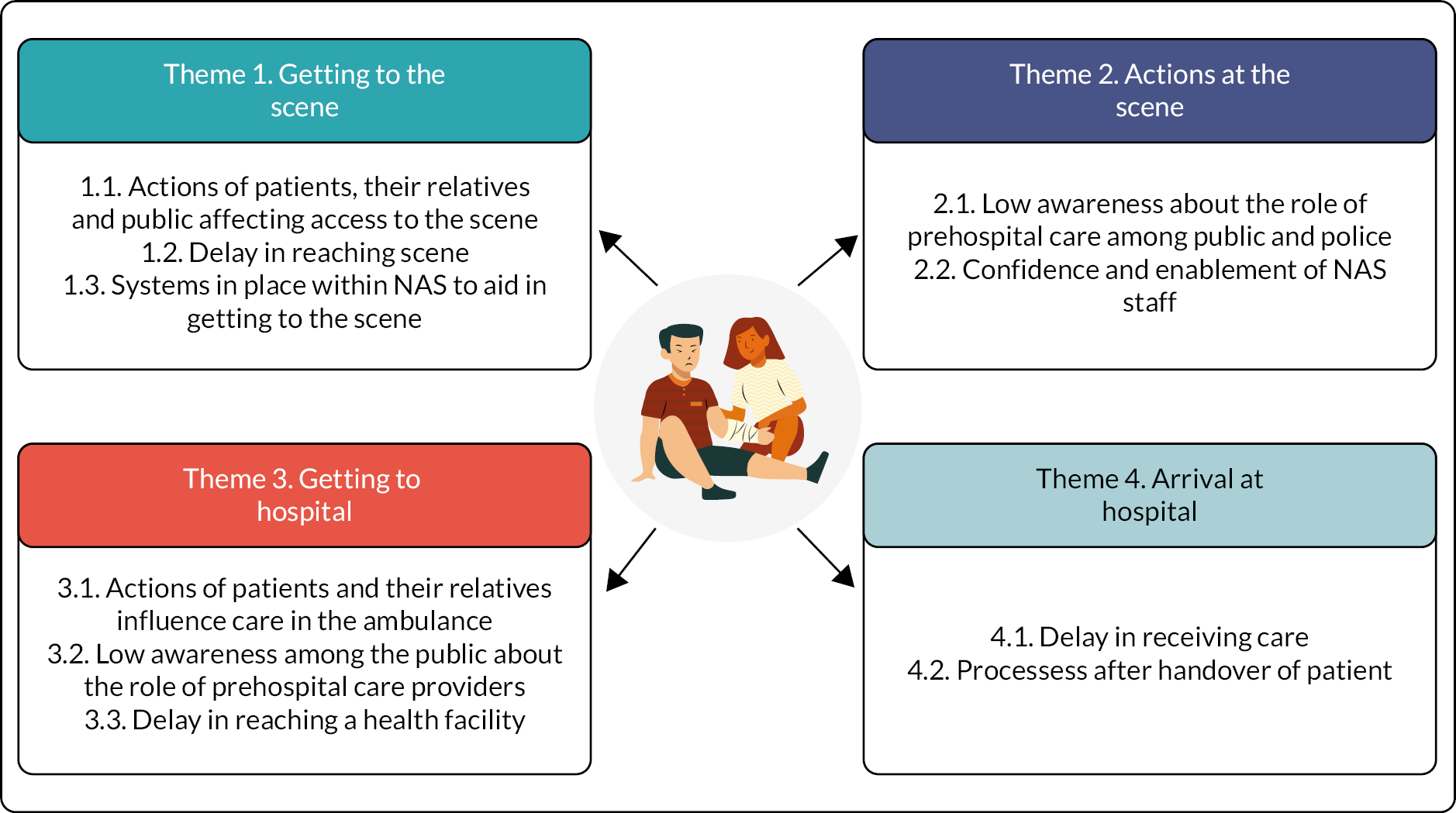
Thematic analysis of the transcript data led to the identification of a framework through which to describe factors affecting prehospital care. Participants’ narratives identified issues during four key periods of provision of care which were presented as themes: (1) Getting to the scene, (2) Action at the scene, (3) Getting to hospital and (4) Arrival at hospital. Within each of these themes, two or three subthemes were identified (Figure 1).
FIGURE 1.
A diagrammatic representation of themes and subthemes.
The term ‘accident’ is no longer used in injury prevention research. 29 However, the study participants used the word ‘accident’ to describe road traffic crashes and injuries. Hence, the word appears in participants’ quotes.
Getting to the scene
Actions of patients, their relatives and public affecting access to the scene
The dispatch officers in the head office of NAS receive calls from the public. They take details of the patient, such as name, age, location and chief complaint. They then forward the details to EMTs through a walkie-talkie, and the EMTs follow up on the patient’s call to get more detailed information. Most EMTs and dispatchers reported that the callers were sometimes anxious about their relatives and did not provide detailed patient information. Some EMTs reported that people at the scene would call several ambulance providers and use whichever one arrived first. Such actions sometimes meant that when they arrived on scene, the patient had already left and hence they were not required to provide treatment or transportation.
We call them before we leave, and they [the public] instruct us to come, but upon reaching the specified location, people tell us they went in another ambulance.
P4 – EMT
Emergency medical technicians and dispatch officers expressed concern about the hoax calls they received. They reported that hoax calls blocked telephone lines from people who needed an ambulance. In addition, the EMTs complained that when they arrived at the given location and found nothing, the original caller had their phone turned off or the line was busy. One dispatch officer described how threatened she felt when she received hoax calls or heard unacceptable language from the caller.
These fake calls make things very difficult for us. Some people say whatever they want, they use unacceptable language that gives us goosebumps, and yet we still have to respond to the call. We have previously discussed this matter with senior managers, but nothing has been done. Even the police acknowledge that such cases occur everywhere and it cannot be resolved.
P13 – Dispatch officer
Delay in reaching scene
The EMTs and the drivers reported several factors, such as heavy traffic, poor road conditions and public protests, which led to delays in reaching the scene. Ambulance drivers said they use the siren to help navigate through the traffic and are supported by the traffic police in normal circumstances. However, some EMTs and ambulance drivers felt that when there are protests or delays due to traffic being held back to allow very important persons (VIPs) to travel, the police do not prioritise the ambulance getting through. Three of the EMTs suggested that there should be a separate lane designated for ambulances, with one participant suggesting a separate lane could allow all emergency vehicles to travel, including ambulances, fire engines, police vans or hearses. Other EMTs suggested having a single national emergency number so that the traffic police can promptly get the message and manage traffic before the arrival of an emergency vehicle. One EMT said that road users should show empathy towards the victim by allowing ambulances to move through a traffic jam.
Regarding traffic control, it would be beneficial to have a single hotline number for all emergency services, similar to those used abroad.
P1 – EMT
In addition to congestion, most of the EMTs and the drivers reported that the poor road conditions, including potholes, meant that ambulances needed to drive slowly, hence creating a delay in reaching the scene. One of the EMTs complained that most of the time, information about road blockages due to construction was poorly communicated, causing them to have to look for alternative routes when trying to reach the patient. Because of the delays in reaching the patients, many EMTs and drivers found that the patient’s family or relatives had found alternative means to get to the hospital such as taxis as they are readily available. Some EMTs shared incidences where these delays led to the patient’s death, to which they expressed feeling helpless for not being able to save the patient.
If the patient’s family does not inform us about the condition of the road and only provides us with the location, instructing us to reach there, then we have to find an alternative way to reach the location, which takes time.
P7 – EMT
Some EMTs and one driver reported they sometimes have difficulty identifying the location of the emergency. They think that this is due to the caller being unsure of their location, putting this down to the high influx of people into Kathmandu valley from other districts. In addition, one EMT advised that the situation worsened when there was poor phone network coverage, as they could not communicate with the patient’s family or relatives over the phone. Hence, he suggested that the availability of global positioning system (GPS) devices inside an ambulance would make it easier to identify the location of the call, especially at night when there are fewer people on the streets who can direct the ambulance to the patient’s house.
We can identify the area from the place’s name, but it is challenging to identify the home. Most of our patients are from outside the valley, and some live in huts or tin sheet houses, which can make it difficult for us [to locate them]. Nevertheless, they can identify us, so we ask people to come to the road and wave to us when they see our vehicle.
P5 – Driver
Systems in place within Nepal Ambulance Service to aid in getting to the scene
One of the dispatch officers talked about the systems used by the NAS that eased work. She said that using a walkie-talkie had enabled her to communicate easily with the ambulance drivers and EMTs at different stations. She added that the availability of a navigation system (e.g. GPS tracker) at the central office helps understand where the ambulances are heading and provides real-time information on their location. The system allowed the dispatch officers to assign a new case to the ambulance staff on that particular route.
A GPS tracker allows us to monitor the real-time location of our ambulances and the direction they are heading. In case of an emergency call, we use GPS to track all the ambulances and assign the case to the ambulance on that particular route.
P11 – Dispatch officer
The same dispatch officer also highlighted the need to use criteria-based dispatch when prioritising ambulance calls. Patients can request an ambulance to take them to the hospital for a follow-up appointment. She reported the practice of prioritising ambulance services to emergency cases when the service is receiving multiple calls.
We determine whether a case is an emergency or a regular follow-up. Sometimes, regular follow-up cases may coincide with an emergency case, so we ask those who are going for a follow-up visit to wait.
P11 – Dispatch officer
Actions at the scene
Low awareness about the role of prehospital care among public and police
The EMTs and the drivers perceived that many of the public and police were unaware of NAS’s prehospital care service, believing that the role of NAS was just limited to transporting patients. Most EMTs and a few drivers reported that when attending road traffic crashes, patients’ families, the general public and police rush to transport the victims without appropriate stabilisation or first aid. One driver reported that the public and police transfer road crash victims in a way that people pack their things in a sack. The study participants (EMTs and drivers) claimed the public lacked awareness of the importance of carefully handling the patient at the scene. The EMTs provided numerous incidents where the victims could have died had they not been provided with prehospital care.
Patients may experience internal bleeding, bleeding from head injuries, or any other wound. These patients require bleeding control and fluids, which may cause a slight delay, but it is better for their long-term health. However, sometimes the public transfers patients in vehicles without controlling bleeding or providing fluids. By the time the patient reaches the hospital, they may have died due to blood loss.
P1 – EMT
In most accident cases, things happen too fast. Victims are taken [to hospital] in a taxi or any available vehicle, by bystanders. For the public, saving a life means taking victims to hospital quickly. However, that is wrong because they do not transfer the patient in a stable position and take them in a hurry. Due to this, they may cause more harm, including bleeding.
P6 – Driver
Confidence and enablement of Nepal Ambulance Service staff
Apart from the dispatch officers, most of the staff (EMTs and drivers) reported receiving regular training, every 6 or 12 months for at least 3–7 days. One of the participants shared his experience of receiving training opportunities in Switzerland. He expressed how the international training exposure boosted his confidence in his current EMT role.
The EMTs reported several trauma-related incidents and the care they provided to trauma victims. One of the senior managers in the study emphasised that all the EMTs and the dispatch officers are required to follow specific protocols when providing prehospital care. He described how the EMTs needed to call senior doctors working with NAS if they wanted to use medicines that were not mentioned in the protocol.
We have a protocol for all staff or dispatch officers who work for our ambulance service. After the patient is placed inside the ambulance, the EMTs should follow a specific protocol.
P12 – Senior manager
One EMT explained how they handle mass casualties in road traffic crashes. She explained the triage system, which involved a colour-coding scheme using black, yellow, green and red. Red tags require immediate treatment and hence are the first priority.
The EMTs and drivers reported working as a team. All drivers described how they support EMTs to deliver prehospital care. The drivers reported how they felt respected in their roles.
We have only one EMT, and our driver supports us in measuring the [blood] pressure, setting up the saline [drip] lifting the patient, and using the C-collar. They also help us with bandaging and opening the bandage. They are familiar with the location of all the equipment, including the type of board used for backbone fractured patients, wheelchairs for asthma patients, and the position to keep them in. They assist us with everything.
P4 – EMT
I have experience driving other vehicles, but I prefer driving this one. Unlike other vehicles, we are not insulted while driving the ambulance.
P3 – Driver
Having supplies of appropriate equipment and medicines enabled the staff to provide effective care. One EMT described a cupboard inside the ambulance where equipment and medicines were stored, while a ‘red bag’ or ‘Go-bag’ was packed with essential medicines and equipment for immediate use. After handling an emergency case, each EMT replaces the equipment and medicines they have used from the red bag with supplies from the cupboard. All the EMTs perceived that they were provided with adequate medicines and equipment.
The equipment will be stored in that cupboard. The equipment I used from the red bag will be replaced from the cupboard into the red bag.
P14 – EMT
Getting to the hospital
Actions of patients and their relatives influence care in the ambulance
Some EMTs and drivers described how the behaviour of some patient’s families and relatives affected their ability to provide optimal care. For example, they described occasions where they were scolded by relatives while performing first aid as it was perceived to be wasting time. They described how some families were reluctant to answer questions asked by EMTs on their route to hospital, and in anger, they ask for them to be just rushed to hospital.
The patient’s family instructs us to move quickly and not ask any questions.
P1 – EMT
The patient is experiencing excessive bleeding, and our EMT is working to control it. They do everything possible to help the patient, even if it takes 5–7 minutes. However, the patient’s family may ask ‘why we are delaying in reaching the hospital?’.
P10 – Driver
All the EMTs described the challenges of deciding which hospital to take the patient to. They emphasised that most of the time, it was negotiated between the patient’s representatives and the EMTs. However, a few EMTs reflected that sometimes the victim’s family insist on visiting a particular hospital without understanding the availability of services and beds. The EMTs expressed their frustration when the patient was not able to be accepted, and they then had to search for another hospital for the same patient.
If the patient requires immediate medical attention, we will take them to the nearest health centre. We will explain to the patient’s family or friends that we are taking the patient to this health facility due to their condition, and they should not worry. After stabilizing the patient, we will take them to any hospital of their choice.
P14 – EMT
Sometimes, the patient’s families disagree with us on the hospital we select, which can be challenging and stressful for us. Although we advise the patient’s family or friends to confirm the availability of an ICU bed in a government hospital [before travelling], they believe they know best and do not listen to us. When we reach the hospital, we find that the ICUs are packed, and we have to move to another hospital.
P4 – EMT
None of the EMTs had been accused of wrongful treatment by a victim’s family. However, news reports of families blaming doctors for the death of their relatives led two of the EMTs to observe that they feared receiving such allegations in the future. All the EMTs expressed a need for a law to protect themselves from such prosecution.
When something happens to the patient, what if they attack us inside the vehicle? Who will be responsible for it? For instance, if the patient dies, the patient’s family may become angry and attack us. Who would take responsibility? Therefore, there should be a law to protect us.
P15 – EMT
Low awareness among the public about the role of prehospital care providers
Both the EMTs and the drivers perceived that the public and police had limited awareness of the role of prehospital care providers. The participants described examples where the victim’s family were surprised to see the EMTs providing treatment inside the ambulance or at the scene. Many of the public they engaged with assumed that the ambulance services only transferred patients to hospital. Many EMTs and drivers suggested that awareness campaigns, such as demonstrations and mock scenarios, could help make people aware of their services and how to contact them. They recommended such campaigns in schools, businesses and community groups.
We have heard patients say, ‘Wow, this type of treatment is available in this ambulance.’ We provide the best possible care to our patients.
P5 – Driver
A ‘video’ should be made for the public, showing how patients are received and treated when a road accident has occurred. Awareness should be spread through small groups such as mothers and loan-saving groups, as well as in offices and schools.
P7 – EMT
Delay in reaching a health facility
Participants described how they were often delayed when transferring the patient to the hospital. They explained that vehicles bounced up and down on the bumpy road, and the EMTs described having to pull the ambulance to the side of the road due to the poor road conditions to provide treatment to the patient.
Some EMTs were more concerned about traffic congestion, especially on long journeys that led to delays reaching the hospital. They described how the delay due to traffic congestion could lead to running out of oxygen en route to the hospital. On such occasions, they would call another ambulance with oxygen and transfer the patient to the new vehicle.
Sometimes, if the oxygen supply runs out or the vehicle breaks down … and there is a shortage of oxygen …, we will contact 102 ambulances from Kathmandu’s central office to transfer the patient.
P15 – EMT
Arrival at hospital
Delay in receiving care
Two EMTs and a dispatch officer complained that the hospital sometimes refused to treat unidentified patients, which delayed receipt of care. In a road traffic crash, the victim’s identity is often unknown, and the hospital prefers not to receive road traffic victims without their families or relatives, as it does not want to take financial responsibility for those patients. Most participants acknowledged the support provided by the traffic police to hospitalise unidentified road crash victims.
If we are taking a patient to a government hospital, if we do not have police with us, the hospital will ask us who will look after the patient and who will be responsible if the patient dies?
P14 – EMT
Two EMTs and a driver described how they had more equipment (such as trollies, wheelchairs or spine boards) than the hospital. This led to difficulties when trying to handover patients in the emergency department.
We carefully transport patients to hospital on spine boards, and using C-collars. However, government hospitals do not have spine boards.
P1 – EMT
Three EMTs and a driver described the challenge of finding vacant beds, particularly intensive care unit (ICU) beds in government hospitals. They offered examples of where they had to support patients for several hours while searching for a hospital. Therefore, one EMT suggested there should be a system that provides updates on beds, ventilators and ICU availability so that they could make informed decisions about where to take the patient and patients could receive timely treatment.
After arriving at hospital, we discovered that there were no available beds or ICU beds, and they [the patient] could not afford a private hospital. We tried moving from one government hospital to another, but the beds were all occupied. At that moment, we felt helpless and unsure of where to take the patient. We have encountered situations where ambulances have been on the move for 3–4 hours searching for a hospital.
P1 – EMT
Processes after handover of patient
The participants described their actions to ensure that a good service was provided to trauma patients. For example, one EMT described how they used a checklist at the end of their shift to indicate the equipment and medicines they had used during their duty. This system ensured that the ambulance was always fully stocked.
I have to fill up out a request form [checklist] and list the equipment that I have used from the drawer [present inside the ambulance]. Then, I need to replace the equipment and submit the form to the main office. The office will immediately provide replacements.
P8 – EMT
Both the dispatchers in the study explained the patient surveys they undertook to understand better the service they provided. The survey was conducted with every third case admitted to hospital.
We follow up on cases by asking patients about their experience with our EMTs, our ambulance service, our charges, and whether they would be interested in using our service again. We conduct surveys either a day later or 2–3 days after the patient has been admitted to hospital.
P11 – Dispatch officer
Discussion
This is the first study that used mixed methods to explore time intervals at all stages of care, from ambulance dispatch, arrival at scene, time spent at the scene and time spent travelling from the scene to handover at a hospital in Nepal. The qualitative findings helped to explain the factors that affected delays during those different stages of care. We found that falls and road traffic crashes were the commonest causes of trauma requiring an ambulance and that the most common type of injury dealt with was fractures. The mean interval from a call being received to arriving with the patient at a hospital was approximately 48 minutes, though this period was, on occasion, much longer. Multiple issues were identified that influenced the service provider’s ability to give high-quality and timely care.
The high proportion of missing data limits the ability to evaluate the prehospital trauma care system and illustrates the need to invest in and develop the system. Incorporating the mechanism of injury and the nature of the injury in routine data collection systems may benefit the design and delivery of prehospital care provision in Nepal.
A case study that described the establishment of NAS reported the average time to arrival at the scene of 26 minutes during the first 2 years of delivery. 20 However, the response time was an average for all kinds of emergencies, including trauma, which in that study only accounted for 10% of callouts. There was no analysis of the time intervals occurring during the prehospital care process and no information on the proportion of complete data in that study. Another study also from Nepal showed that patients had waited for over half an hour for an ambulance. 24 However, it was not clear in that study if the time included the activation time (call received to ambulance dispatch) or the reason for the callout. Both these studies used data from 2013, so neither reflects the current context in which prehospital care is provided. Since 2013, contextual changes have included greater recognition of the need for an effective prehospital care system and significant increases in the volume of traffic on Nepal roads.
Most high-income countries collect and report prehospital time intervals. In LMICs, the evidence is comparatively limited. 30 Different countries will have different prehospital time periods because of the different contexts in which they operate, including the resources within an EMS system, a trained workforce, and public awareness and engagement with the system. In Qatar, on-scene and total prehospital time were 21 and 72 minutes, respectively. 31 The longer duration at the scene in Qatar may reflect its ability to provide emergency care prior to transfer, while in our study, EMTs were often hindered from doing so by families. In Iran, the response, on-scene, transport and total prehospital time were much shorter than in our study which may reflect differences in service provision, topography or road quality between Nepal and Iran. 32
The time taken to reach a health facility is crucial in reducing mortality in trauma patients. Receiving definitive care in a hospital within 60 minutes is described as the ‘golden hour’ and is associated with better patient outcomes. 33 A hospital-based cross-sectional study in Ethiopia reported several factors, such as the availability of nearby facilities, transport infrastructure and community awareness of where and when to go, that influenced how quickly patients arrived at the hospital. 34 Similar to the study by G/Ananya et al.,34 our study found poor road conditions and heavy traffic as one of the major causes of delays in reaching the scene and, after that, getting to the hospital. Poor road conditions and heavy traffic were also cited as barriers to prehospital care by other studies from LMICs. 35,36 Our participants suggested having a single designated lane for emergency vehicles so that their services would not be slowed by heavy traffic. However, as the cities of Nepal were not planned with road infrastructure suitable for designated lanes, this solution would be challenging to deliver.
Lack of integration of multiple systems was one of the commonly cited barriers to improving and expanding EMS coverage in a study of 13 LMICs across Africa, Asia and Latin America. 15 The participants in this study and the study conducted by Chokotho et al. 3 suggested having a national emergency telephone number that works for all communication with service providers. In the absence of this, the participants in the Chokothos’ study reported several instances where the public or the traffic police were the first to arrive at the scene and transported the trauma victims to the hospital without providing any first aid.
Inadequate knowledge and skills among staff have been identified as barriers to providing effective prehospital trauma care in some LMICs. 17,37 While our study did not attempt to measure the knowledge and skills among the prehospital care providers, the participants reported how the refresher training they received boosted their confidence to deliver their roles and responsibilities. Lack of protocols, inadequate training plans for prehospital trauma care providers, shortages of medicines (e.g. painkillers) and equipment (e.g. defibrillator and monitoring equipment), absence of GPS and an inadequate number of radio channels were reported to be barriers to providing effective prehospital trauma care for trauma victims in Iran. 17 In contrast, participants in our study reported that the availability of protocols for providing prehospital care, adequate medicines and equipment, availability of a GPS and adequate walkie-talkie (radio) were factors that facilitated prehospital care. In addition to the availability of resources and training that facilitated prehospital care in our study, it was found that there was good teamwork between ambulance drivers and EMTs in the delivery of prehospital care.
Equality, diversity and inclusion
Injuries are known to be socially patterned, with males sustaining more injuries than females, and with injuries being more prevalent in communities experiencing greater disadvantage. Children, the elderly and those living with a disability are at increased risk of injury overall, and may be at risk of specific types of injury. In a country such as Nepal where the patient needs to pay at the point of care, household income influences health-seeking behaviour following an injury. Considering these inequalities, we analysed the callout data by age and sex, but we were unable to conduct analyses by other indicators of inequality because of the data available. In the qualitative component of our study, we purposively sought male and female participants from all four roles; however, due to the predominance of men in such roles, the number of female participants was lower than that of men.
Future research
This study has indicated a number of issues that could be researched to further develop the prehospital care system in Nepal. Further qualitative research to understand the perceptions and experiences of trauma victims, road users, emergency department staff, police officers, members of other organisations involved in prehospital care, firefighters and health policy-makers would complement the findings from this study and may identify ways forward. A range of specific barriers to care needs further exploration, for example, factors affecting the handover of trauma patients between ambulance and emergency department staff.
Lessons learnt
This study has indicated ways in which the NAS can strengthen its routine data collection, including the need to minimise missing data and the advantages of collecting and classifying data on the circumstances of an injury event. Both would enable the provider to continually monitor and develop their service. The study shows how a lack of public understanding of the need to stabilise injuries prior to transfer to a hospital can lead to conflict between service providers and service users. Only a proportion of EMS providers currently employ staff trained in prehospital care; therefore, there needs to be a co-ordinated roll-out of training of EMTs alongside public awareness raising of the need for first aid prior to transfer to hospital. Training greater numbers of the public in first aid would enable bystanders to both support victims and enable prehospital care providers to utilise their skills without reproach.
Implications for practice and policy
The findings from this study provide policy-makers with examples of how the existing EMS system could be improved through policy and legislation. The study illustrated how, for example, the current EMS system with multiple providers and lack of co-ordination results in inefficiencies in care provision. Bystanders and relatives call multiple ambulances to identify one that is readily available to take the injured person to the hospital. Poor road conditions and congested traffic that do not give way to the ambulance lead to delays in arriving at the scene and transferring to the hospital. EMTs describe receiving verbal abuse from the public who do not understand the importance of stabilising injuries prior to, or during, transfer. Importantly, they fear physical abuse and prosecution from the relatives of injured patients, should the patient’s injuries prove fatal. Promulgation of a ‘good Samaritan law’, as exists in many countries, would protect service providers seeking to save lives.
Strengths and limitations of the study
The main strength of this study was the use of a mixed-methods design with the qualitative interviews providing insights into the factors influencing the patient and time interval data analysed. We analysed data from one of Nepal’s largest and most established prehospital care providers. A further strength is that we interviewed a diverse group of prehospital care provider staff (ambulance drivers, EMTs, dispatch officers and service managers), which enabled the collection of broader perspectives and a more rounded overview.
In the analysis of callout data, we chose a 1-year period to provide a focused and comprehensive examination within a manageable and funded time frame. We found that for some data fields more than a quarter of the data were missing, limiting the ability to accurately determine the patient needs and response times. We managed this by having a member of NAS staff as part of the study team to maximise the utility of the available records and we introduced ‘unspecified’ categories for both the mechanism and nature of injury to present the findings in a clear and organised manner. Table 5 (see Appendix 2) details the components included within the unspecified category for the mechanism of injury and Table 6 (see Appendix 3) for the nature of injury. Interpretation of the findings of the study therefore needs to take the degree of missing data into consideration. Some data fields that would have been particularly helpful to further understand patients’ needs, such as the part of the body injured, injury severity scores or the care provided, were not routinely captured. Studies from other countries have shown that prehospital care times vary between urban and rural areas, with increased delays in response in rural areas. 31,32,38–40 Our study was not able to conduct such an analysis due to the data available. The qualitative component of this study may have been subject to responder bias if the participants felt uncomfortable reporting something that may have reflected badly on their employer. We managed this risk by making participants aware of the agreement of their managers to their participation in the study and by emphasising that their responses would not be identifiable in any outputs from the study. The participants’ managers were not present during the interviews.
Conclusion
A mixed-methods study was used to explore and better understand prehospital care for trauma victims in Nepal. We identified the delivery of prehospital care to a wide range of trauma patients within a call-to-hospital time of less than an hour. Various factors were identified through the interviews that explain the experience of providing prehospital care, and these had effects across the whole care pathway: from getting to the scene, actions at the scene, getting to the hospital and on arrival at the hospital. The study illustrated the need for improved public awareness about the importance of prehospital care and the role of EMTs. Further action across the EMS system appears warranted and would be supported by changes to policy and legislation to enable and protect prehospital care providers.
Key learning points
-
Falls and road traffic crashes were the commonest causes of trauma requiring an ambulance, with fractures and suspected spinal injuries being the commonest types of injury.
-
The mean interval from a call being received to arriving with the patient at a hospital was 48 minutes, although this could be much longer.
-
High standards of prehospital care were facilitated by the availability of care protocols, regular refresher training, good stocks of medicines and equipment, availability of GPS software, radio contact between the base and crews and good teamwork between ambulance drivers and EMTs.
-
Traffic congestion and poor road maintenance, the expectations of patients, relatives and bystanders and lack of awareness of EMT’s knowledge and skills were barriers to providing prehospital care.
Additional information
Acknowledgements
We acknowledge the support of the NAS for providing access to its data sets and for allowing interviews with its staff. We are thankful to all the participants of our study who consented to participate and share their experiences. We want to acknowledge the support of researchers at the NIHR Global Health Research Group on Nepal Injury Research and the administrative support of Kathmandu Medical College.
CRediT contribution statement
Amrit Banstola (https://orcid.org/0000-0003-3185-9638): Conceptualisation (equal), Formal analysis (equal), Investigation (equal), Methodology (equal), Project administration (lead), Visualisation (equal), Writing – Original draft (lead), Writing – reviewing and editing (lead).
Preeti Gautam (https://orcid.org/0000-0002-2040-5000): Conceptualisation (equal), Formal analysis (equal), Investigation (equal), Methodology (equal), Project administration (supporting), Visualisation (equal), Writing – Original draft (supporting), Writing – reviewing and editing (supporting).
Gary Smart (https://orcid.org/0000-0002-8578-0661): Conceptualisation (equal), Formal analysis (equal), Methodology (equal), Supervision (co-lead), Writing – reviewing and editing (supporting).
Sunil K Joshi (https://orcid.org/0000-0002-2704-5060): Conceptualisation (equal), Formal analysis (equal), Funding acquisition (co-lead), Methodology (equal), Supervision (co-lead), Writing – reviewing and editing (supporting).
Julie Mytton (https://orcid.org/0000-0002-0306-4750): Conceptualisation (equal), Formal analysis (equal), Funding acquisition (co-lead), Methodology (equal), Supervision (co-lead), Writing – reviewing and editing (supporting).
Furba Sherpa: Conceptualisation (equal), Formal analysis (equal), Methodology (equal), Resources, Writing – reviewing and editing (supporting).
Disclosure of interests
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, are available in the toolkit on the NIHR Journals Library report publication page at https://doi.org/10.3310/TMTG2437.
Primary conflicts of interest: Amrit Banstola, Preeti Gautam and Gary Smart have no conflicts of interest to declare. Julie Mytton was a member of HTA MNCH Panel from 2008 to 2015. Sunil K Joshi is an Editorial Board Member of BMJ Injury Prevention.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Ethics statement
Ethical approval was obtained from the Nepal Health Research Council on 13 January 2021 (Reference number 769/2020) and the UWE Bristol, Faculty of Health and Applied Sciences Research Ethics Committee on 26 January 2021 (Reference number HAS.21.01.089).
Information governance statement
The University of the West of England, Bristol (UWE Bristol), as sponsor for this study, is committed to ensuring that all personal information is handled in line with the UK Data Protection Act (2018) and the General Data Protection Regulation (EU GDPR) 2016/679. Under Data Protection legislation, UWE Bristol is the Data Controller and the Nepal Injury Research Centre is the Data Processor, who process personal data in accordance with their instructions. The data governance strategy applied in this study used the ‘five safes’ framework. This is a systematic approach to good data governance, commonly used in government data management systems. The framework breaks data management and governance into five broad issues which need to be addressed: (1) Safe projects, (2) Safe people, (3) Safe settings (which are all amenable to managerial controls), (4) Safe data and (5) Safe outputs (which are amenable to statistical controls). More information on the data governance strategy used in this study is available from the authors on request.
Department of Health and Social Care disclaimer
This publication presents independent research commissioned by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by the interviewees in this publication are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, MRC, NIHR Coordinating Centre, the Global Health Research programme or the Department of Health and Social Care.
Funding
This article presents independent research funded by the National Institute for Health and Care Research (NIHR) Global Health Research programme as award number 16/137/49 using UK aid from the UK Government to support global health research. The views expressed in this publication are those of the author(s) and not necessarily those of the NIHR or the UK government. Research is published in the NIHR Global Health Research Journal. See the NIHR Funding and Awards website for further award information.
This article reports on one component of the research award Prehospital emergency care for trauma victims in Nepal: a mixed-methods study. For more information about this research please view the award page (https://fundingawards.nihr.ac.uk/award/16/137/49)
About this article
The contractual start date for this research was in July 2017. This article began editorial review in February 2023 and was accepted for publication in March 2024. The authors have been wholly responsible for all data collection, analysis and interpretation, as well as for writing up their work. The Global Health Research editors and publisher have tried to ensure the accuracy of the authors’ article and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
This article was published based on current knowledge at the time and date of publication. NIHR is committed to being inclusive and will continually monitor best practice and guidance in relation to terminology and language to ensure that we remain relevant to our stakeholders.
Copyright
Copyright © 2024 Banstola et al. This work was produced by Banstola et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
List of abbreviations
- EMSs
- emergency medical services
- EMTs
- emergency medical technicians
- GPS
- global positioning system
- ICUs
- intensive care units
- LMICs
- low- and middle-income countries
- NAS
- Nepal Ambulance Service
- NIRC
- Nepal Injury Research Centre
- UWE
- University of the West of England
References
- Global Burden of Disease Collaborative Network . Global Burden of Disease Study 2019 (GBD 2019) Results 2020. http://ghdx.healthdata.org/gbd-results-tool (accessed 19 October 2022).
- World Health Organization . Save LIVES: A Road Safety Technical Package 2017.
- Chokotho L, Mulwafu W, Singini I, Njalale Y, Maliwichi-Senganimalunje L, Jacobsen KH. First responders and prehospital care for road traffic injuries in Malawi. Prehosp Disaster Med 2017;32:14-9. https://doi.org/10.1017/S1049023X16001175.
- Peden M, Scurfield R, Sleet D, Mathers C, Jarawan E, Hyder AA, et al. World Report on Road Traffic Injury Prevention. Geneva: World Health Organization; 2004.
- World Health Organization . Saving Millions of Lives: Decade of Action for Road Safety 2011–2020 2011.
- United Nations General Assembly . Improving Global Road Safety (Seventy-Fourth Session, Agenda Item 12) 2020. www.un.org/pga/74/wp-content/uploads/sites/99/2020/08/Draft-Resolution-Road-Safety.pdf (accessed 20 October 2022).
- Ministry of Health . Nepal Health Sector Strategy Implementation Plan 2016–2021 2017.
- Ministry of Health and Population . First National Conference on Pre-Hospital Care for Emergencies in Nepal (19–20 July 2018) 2018. https://heoc.mohp.gov.np/health-emergency/pre-hospital (accessed 20 October 2022).
- Ministry of Health and Population . Report on Emergency Care System Assessment and Consensus Based Action Priorities: Nepal 2021. https://cdn.who.int/media/docs/default-source/nepal-documents/whe_nepal/03-final-ecsa-report-2021-min.pdf (accessed 26 January 2024).
- Reynolds TA, Stewart B, Drewett I, Salerno S, Sawe HR, Toroyan T, et al. The impact of trauma care systems in low- and middle-income countries. Annu Rev Public Health 2017;38:507-32. https://doi.org/10.1146/annurev-publhealth-032315-021412.
- Sasser S, Varghese M, Kellermann A, Lormand J. Prehospital Trauma Care Systems. Geneva: World Health Organization; 2005.
- Henry JA, Reingold AL. Prehospital trauma systems reduce mortality in developing countries: a systematic review and meta-analysis. J Trauma Acute Care Surg 2012;73:261-8. https://doi.org/10.1097/TA.0b013e31824bde1e.
- Waseem H, Naseer R, Razzak JA. Establishing a successful pre-hospital emergency service in a developing country: experience from Rescue 1122 service in Pakistan. Emerg Med J 2011;28:513-5. https://doi.org/10.1136/emj.2010.096271.
- Mould-Millman NK, Dixon JM, Sefa N, Yancey A, Hollong BG, Hagahmed M, et al. The state of emergency medical services (EMS) systems in Africa. Prehosp Disaster Med 2017;32:273-83. https://doi.org/10.1017/S1049023X17000061.
- Nielsen K, Mock C, Joshipura M, Rubiano AM, Zakariah A, Rivara F. Assessment of the status of prehospital care in 13 low- and middle-income countries. Prehosp Emerg Care 2012;16:381-9. https://doi.org/10.3109/10903127.2012.664245.
- Mehmood A, Rowther AA, Kobusingye O, Hyder AA. Assessment of pre-hospital emergency medical services in low-income settings using a health systems approach. Int J Emerg Med 2018;11. https://doi.org/10.1186/s12245-018-0207-6.
- Haghparast-Bidgoli H, Hasselberg M, Khankeh H, Khorasani-Zavareh D, Johansson E. Barriers and facilitators to provide effective pre-hospital trauma care for road traffic injury victims in Iran: a grounded theory approach. BMC Emerg Med 2010;10. https://doi.org/10.1186/1471-227X-10-20.
- Shrestha SK, Jacobson C, Dahal S, Shrestha R, Weiner Y, Sheridan A. Reasons for summoning ambulance services in the hilly region of Nepal. Kathmandu Univ Med J 2019;17:141-4.
- Gongal R, Vaidya P. Responding to the need of the society: Nepal Ambulance Service. J Inst Med Nepal 2013;34. https://doi.org/10.3126/jiom.v34i1.9114.
- Walker R, Auerbach PS, Kelley BV, Gongal R, Amsalem D, Mahadevan S. Implementing an emergency medical services system in Kathmandu, Nepal: a model for ‘white coat diplomacy’. Wilderness Environ Med 2014;25:311-8. https://doi.org/10.1016/j.wem.2014.04.006.
- Banstola A, Smart G, Raut R, Ghimire KP, Pant PR, Joshi P, et al. State of post-injury first response systems in Nepal – a nationwide survey. Front Public Health 2021;9. https://doi.org/10.3389/fpubh.2021.607127.
- Pandey NR. Emergency medicine in Nepal: present practice and direction for future. Int J Emerg Med 2016;9. https://doi.org/10.1186/s12245-016-0118-3.
- Acharya R, Badhu A, Shah T, Shrestha S. Availability of life support equipment and its utilization by ambulance drivers. J Nepal Health Res Counc 2017;15:182-6. https://doi.org/10.3126/jnhrc.v15i2.18197.
- Shrestha SK, Koirala K, Amatya B. Patient’s mode of transportation presented in the emergency department of a tertiary care centre, Kavre, Nepal. Kathmandu Univ Med J 2018;16:39-42.
- Gongal R, Dhungana B, Regmi S, Nakarmi M, Yadav B. Need of improvement in emergency medical service in urban cities. J Nepal Med Assoc 2009;48:139-43.
- Kharel R, Thapa GB, Voor T, Pant SR, Adhikari SK, Bist BS, et al. Emergency unit assessment of seven tertiary hospitals in Nepal using the WHO tool: a cross-sectional study. Int J Emerg Med 2023;16:1-11. https://doi.org/10.1186/s12245-023-00484-2.
- Malterud K, Siersma VD, Guassora AD. Sample size in qualitative interview studies: guided by information power. Qual Health Res 2016;26:1753-60. https://doi.org/10.1177/1049732315617444.
- Braun V, Clarke V. Successful Qualitative Research: A Practical Guide for Beginners. Los Angeles, CA: SAGE Publications Ltd; 2013.
- Davis RM, Pless B. BMJ bans ‘accidents’. BMJ 2001;322:1320-1. https://doi.org/10.1136/bmj.322.7298.1320.
- Roudsari BS, Nathens AB, Arreola-Risa C, Cameron P, Civil I, Grigoriou G, et al. Emergency medical service (EMS) systems in developed and developing countries. Injury 2007;38:1001-13. https://doi.org/10.1016/j.injury.2007.04.008.
- Al-Thani H, Mekkodathil A, Hertelendy AJ, Howland I, Frazier T, El-Menyar A. Emergency medical services (EMS) transportation of trauma patients by geographic locations and in-hospital outcomes: experience from Qatar. Int J Environ Res Public Health 2021;18. https://doi.org/10.3390/ijerph18084016.
- Bigdeli M, Khorasani-Zavareh D, Mohammadi R. Pre-hospital care time intervals among victims of road traffic injuries in Iran. A cross-sectional study. BMC Public Health 2010;10. https://doi.org/10.1186/1471-2458-10-406.
- Chen CH, Shin SD, Sun JT, Jamaluddin SF, Tanaka H, Song KJ, et al. Association between prehospital time and outcome of trauma patients in 4 Asian countries: a cross-national, multicenter cohort study. PLOS Med 2020;17. https://doi.org/10.1371/journal.pmed.1003360.
- G/Ananya T, Sultan M, Zemede B, Zewdie A. Pre-hospital care to trauma patients in Addis Ababa, Ethiopia: hospital-based cross-sectional study. Ethiop J Health Sci 2021;31:1019-24. https://doi.org/10.4314/ejhs.v31i5.14.
- Alinia S, Khankeh H, Maddah SS, Negarandeh R. Barriers of pre-hospital services in road traffic injuries in Tehran: the viewpoint of service providers. Int J Community Based Nurs Midwifery 2015;3:272-82.
- Kironji AG, Hodkinson P, de Ramirez SS, Anest T, Wallis L, Razzak J, et al. Identifying barriers for out of hospital emergency care in low and low-middle income countries: a systematic review. BMC Health Serv Res 2018;18. https://doi.org/10.1186/s12913-018-3091-0.
- Jafari M, Hosseini M, Maddah SSB, Khankeh H, Ebadi A. Factors behind moral distress among Iranian emergency medical services staff: a qualitative study into their experiences. Nurs Midwifery Stud 2019;8. https://doi.org/10.4103/NMS.NMS_69_18.
- Alinier G, Wilson P, Reimann T, Morris B. Influential factors on urban and rural response times for emergency ambulances in Qatar. Mediterranean J Emerg Med 2018;26:8-13.
- Aftyka A, Rybojad B, Rudnicka-Drozak E. Are there any differences in medical emergency team interventions between rural and urban areas? A single-centre cohort study. Aust J Rural Health 2014;22:223-8. https://doi.org/10.1111/ajr.12108.
- Fatovich DM, Phillips M, Langford SA, Jacobs IG. A comparison of metropolitan vs rural major trauma in Western Australia. Resuscitation 2011;82:886-90. https://doi.org/10.1016/j.resuscitation.2011.02.040.
Appendix 1
Research study: prehospital emergency care for trauma victims in Nepal
Providing high-quality prehospital care to injured persons followed by good medical treatment can save lives, reduce the severity and prevent disability. We want to know what prehospital care is provided to injured persons by EMS in Nepal and what are the opportunities and challenges of providing care?
Introduction (10 minutes)
-
First, thank the participant for joining the interview.
-
Give a brief introduction of yourself, the purpose of the study.
-
Explain the approximate time required (audio-recording, handwritten notes).
-
Encourage participants to speak clearly.
-
Explain that there will be no right or wrong views.
-
Assure anonymity and confidentiality of participant and their views.
-
Explain how participants will not be identifiable from any record or report arising from the interview.
-
Explain that the participant does not have to talk about anything they feel uncomfortable with and can stop at any time for any reason.
-
Sign the consent form (check that the interviewee has signed and s/he is happy for the interview to be audio-recorded).
Warm-up
Introduction by participant with a brief background.
Definition (for reference if needed)
Injured persons: Injured persons are defined as those who had one of these injuries – transport injuries (road injuries and other transport injuries), falls, drowning, burns, poisonings, animal-related, natural disaster, self-harm, interpersonal violence, conflict and terrorism.
Discussion
Now we shall begin our interview. For this, I will be asking you about your experience of providing prehospital care for injured persons. Particularly, I will be interested in your views on the opportunities and challenges of providing prehospital care for injured persons.
[To organise the interview, use the following questions].
For emergency care providers
-
Please tell us what role you do in NAS. What does that role involve? Can you describe your role? How long have you been in your role?
-
Can you tell me what training you have received? How long was that training? What topics were covered in your training? Have you had any refresher training?
-
What is your experience of providing prehospital emergency care to people with injuries?
-
What is/are the best thing(s) about your role?
-
What do you think is the most difficult or challenging part of your role?
-
What is the most discouraging part of your role?
-
What changes could be made to make your role easier?
-
Are there any changes that could be made at a national level that would improve EMS in Nepal?
-
Do you think there is a need for a law which protects prehospital emergency care providers from being prosecuted?
For service managers
-
Please tell us what role you do in NAS. What does that role involve? How long have you been doing that role? Did you receive any training for your role? How long was the training?
-
Can you tell me about the training you provide to the staff? Have your staff received training to support different types of emergency cases including trauma victims? Is there Continuing Professional Development support for the staff?
-
What is your experience of providing prehospital emergency care service?
-
What is/are the best thing(s) about your role?
-
What do you think is the most difficult or challenging part of your role?
-
What is the most discouraging part of your role?
-
What changes could be made to make your role easier?
-
Are there any changes that could be made at a national level that would improve EMS in Nepal?
-
Do you think there is a need for a law which protects prehospital emergency care providers from being prosecuted?
-
Do you have a way of finding out the disposition (admission, discharge, transfer) of the person you have treated and handed over to the hospital?
Wrap-up (10 minutes)
Ending the discussion by saying: Thank you for your time today. We have been discussing this for about an hour. Do you think we missed anything that needs to be discussed?
Interview recording details
| Date: |
|---|
| Participant number: |
| Location (venue): |
| Job role (ambulance driver, emergency medical technician, dispatch operator, service manager): |
| Length of time in the current role: |
| Age group: |
| Sex: |
| Level of education: |
| Length of session: |
| Interviewer’s name |
| Note taker’s name (if any): |
| Observation (if any): |
| Recorder No.: |
Appendix 2
| S.N. | Mechanism of injury | Includes |
|---|---|---|
| 1 | Asphyxia | Choking; milk choking |
| 2 | Assault | Physical assault; firearm (gunshot injury); fighting/with weapons |
| 3 | Bites and stings | Animal bite; bee sting; snake bite |
| 4 | Burns | Burns; electric burns; electric shock |
| 5 | Cut | Cut injury; suture cut includes abrasion; laceration |
| 6 | Fall | Fall injury |
| 7 | Road traffic crash | Road traffic injury; traffic incident |
| 8 | Self-harm | Overdose (drug, alcohol, chemical); Cases of poisoning where intent is not specified; suicide; suicide attempt |
| 9 | Unspecified trauma | Fracture (fracture, hand fracture, hip fracture, leg fracture, ribs fracture, spinal fracture) without known mechanism of injury; body region injured (head injury, leg injury, spinal injury) without known mechanism of injury; ‘traumatic injury’ |
Appendix 3
| S.N. | Nature of injury | Includes |
|---|---|---|
| 1 | Wound | Cut injury (in leg); gunshot injury; suture cut; bleeding (vaginal, leg, ear, nasal); amputation; open wound; hip wound; dressing; wound infection; bites and stings; leg injury (diabetes mellitus) |
| 2 | Fracture | Fracture with or without body region affected; also, subcategorised as femur fracture, hand fracture, head fracture, hip fracture, leg fracture, knee fracture, pelvic fracture, shoulder fracture, ribs fracture, elbow joint fracture |
| 3 | Burn | Burns including electric shock |
| 4 | Choking | Traumatic injury due to choking |
| 5 | Head injury | Head injury includes skull fracture; unconscious following fall or road traffic crash; coma |
| 6 | Poisoning | Poisoning including unconsciousness following poisoning |
| 7 | Musculoskeletal injuries | Suspected sprain and strain; back pain/injury from fall, road traffic crash; leg pain/injury/swelling from fall, road traffic crash, traumatic injury; hip pain; hand pain/injury from fall, road traffic crash; knee/jaw injury due to road traffic crash; body pain due to fall |
| 8 | Spinal injury | Damage to the spinal cord as a result of fall injury or road traffic crash; spinal fracture; other unspecified cause |
| 9 | Unspecified | Includes trauma cases where associated text did not allow categorisation of the nature of injury, that is ‘bone problem’/‘chest pain’/‘COPD’/‘liver problem’/‘sick person’/‘traumatic injury’/‘fall injury due to fall injury; abdominal pain’/‘eye problem’/‘fall injury’/‘accident’/‘breathing problem’/‘RTI’/‘traffic incident’/‘traumatic injury due to RTI’; ‘fighting’; ‘physical assault’; ‘alcoholism’; ‘unconscious/sick person from suicide/suicide attempt’; eye problem/fever due to traumatic injury’; ‘neurological problem due to RTI’; or unknown |
