Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its proceeding programmes as project number 10/1008/30. The contractual start date was in May 2011. The final report began editorial review in June 2013 and was accepted for publication in October 2013. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2014. This work was produced by Pryjmachuk et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Background
Self-care, self-care support and the mental health of children and young people
The mental health of children and young people (CYP) is a major public health concern in the UK. Around one in five CYP will have mild to moderate mental health problems;1 around 1 in 10, a diagnosable mental disorder. 2,3 Given that these statistics are far from insignificant, it is entirely reasonable for clinicians, researchers and policy-makers to examine and question the delivery and organisation of mental health services for CYP, or ‘CAMHS’ (an acronym for child and adolescent mental health services) as they are colloquially known in the UK and Australia.
Regarding the delivery and organisation of such services, evidence from the 2008 CAMHS Review in England4 suggests that mental health service provision for CYP is not always as comprehensive, consistent or effective as it could be, nor is it especially responsive, accessible or child centred. Moreover, the CAMHS Review adds that, when accessing these services, CYP and their parents are often faced with unhelpful legal and administrative processes, unacceptable regional and local variations and busy professionals who have little time to understand the evidence base for effective interventions. In Wales, similar concerns were reported by a Wales Audit Office review in 2009. 5
There is, therefore, clear scope for improvement in the delivery and organisation of CAMHS in England and Wales. Indeed, the National Institute for Health Research (NIHR) has already funded delivery and organisational research into alternatives to CAMHS inpatient care6 and the risks associated with such care. 7 Additionally, over the last decade or so, there has been a growing consensus in British health care – reflected most recently in policy documents such as the NHS Constitution8 and, in mental health, No Health Without Mental Health 9 – that health care must be patient centred and underpinned by a partnership between those receiving and those delivering care.
The most explicit form of patient-centred care is, perhaps, self-care. The utility of self-care in the delivery and organisation of health and social care is limited, however, in that, in its truest sense, self-care excludes anyone other than the individual – including health and social care professionals – from the caring equation. Although there are obviously situations in which true self-care is appropriate (taking aspirin for a mild headache or doing some exercise to maintain a healthy weight, for example), many health concerns, especially the more severe, enduring and complex ones, necessitate the intervention of a professional of one kind or another – whether that intervention is merely guidance and support, or something more like ‘treatment’ in the traditional sense of the word. In these circumstances, there is ample scope for health and other care professionals to work with individuals in order to facilitate self-care as an immediate, short-term or long-term goal, especially when a spirit of partnership and patient centredness permeates the practices of those professionals. 10–12 With this in mind, the ways and means by which self-care might be supported and facilitated by others becomes important. The focus of our inquiry is thus not self-care per se but self-care support (or ‘support for self-care’ as it sometimes known).
There is a notable amount of research and literature on self-care support in long-term physical health conditions, both in adult and (to a lesser extent) children’s services. 13–15 There have also been some inroads in adult mental health, where self-care is often referred to as ‘self-help’. For example, the recent growth in self-help for common mental health problems16 has been captured by England’s Improving Access to Psychological Therapies (IAPT) initiative,17 an initiative which has led to the formation of stand-alone primary care mental health services largely operating independently of routine secondary care mental health services. There has also been NIHR-commissioned research work on self-care in adult mental health,12 and the emphasis on ‘recovery’ – which maps well onto a framework of self-care18 – has been promoted by both the previous Labour and current coalition administrations as a key philosophy of adult mental health care.
Regarding services for CYP in general, self-care and self-care support also dovetail well with recent government policy for CYP. The relationship with policy was perhaps more explicit in the previous Labour administration, which wove themes such as supporting parents in their parenting role, early intervention, integrated working and the active participation of CYP into flagship policies such as Every Child Matters19 and the Children’s Plan,20 than in the current coalition administration. Although the coalition has a less specific focus on measurable outcomes,21 there is nothing in current policy that is necessarily at odds with a philosophy of self-care; indeed, the rebadging of ‘every child matters’ as ‘help children achieve more’ implies that support is necessary for CYP to achieve (though there have been some concerns that ‘achieve more’ refers primarily to educational achievement22), and elements of self-care and self-care support are implicit in aspects of the CYP’s IAPT initiative (see below), which was introduced during the lifetime of this study.
Nevertheless, the role that self-care support can play in the mental health of CYP is a largely unexplored area. It is not known, for example, whether or not self-care support interventions and services are being commissioned and provided in England and Wales – the geographical remit of the NIHR Service Delivery and Organisation programme at the time the study was commissioned – nor whether there exists a substantive body of literature in this area. There is no Cochrane Library entry for this area of work, and the only work we know of that is explicitly embedded in a self-care support framework is the work related to attention deficit hyperactivity disorder (ADHD) that some of us (Kirk; Pryjmachuk) carried out as part of a previous NIHR study,15 and a few examples (eating disorders, bed-wetting and behavioural disorders) cited in a Department of Health effectiveness report on self-care. 23 We are aware of some peripheral work where self-care support might be implied, such as a Canadian (non-systematic) review of self-help therapies for childhood disorders24 and a systematic review of self-help technologies for emotional problems in young people25 (undertaken in part by a member of our team, Bower), as well as British research into psychological well-being in CYP in schools,26–28 resilience29 and the generic Social and Emotional Aspects of Learning (‘SEAL’) initiative in schools. 30 However this research has not been systematically explored or co-ordinated within the wider context of self-care support.
The position on self-care support in the mental health of CYP remains opaque despite the launch, shortly after this project commenced, of a CYP’s IAPT initiative in England. 31 Unlike IAPT in adult mental health care, the CYP’s IAPT initiative is not explicitly tied to the notion of self-care (self-help) nor does it operate as a stand-alone service. Instead, the initiative is designed to transform CAMHS through staff (re)training, the use of evidence-based therapies and routine outcome measurements. 31 This is not to say that CYP’s IAPT has no relevance to a project on self-care support in CYP’s mental health (indeed, as we will discuss later, some of our findings have a significant overlap with some of the operating principles of the CYP’s IAPT), just that self-care and self-care support are not explicit in its principles.
Defining self-care and self-care support
Definitions of self-care vary according to who engages in the self-care behaviour (individual, family or community); what the context is (health promotion, illness prevention, limiting the impact of illness or restoration of health); and the degree to which health professionals are involved. 15
A consistent aspect to the various definitions is the conceptualisation of patients/service users as active, knowledgeable individuals rather than passive recipients of health care. The Department of Health32 sees self-care as:
The actions people take for themselves . . . to stay fit and maintain good physical and mental health; meet social and psychological needs; prevent illness or accidents; care for minor ailments and long-term conditions; and maintain health and wellbeing after an acute illness or discharge from hospital[.]
Reproduced from Department of Health. Self-Care – A Real Choice, Self-Care – A Practical Option. Document reference 266332. London: Department of Health; 2005. p. 1. The National Archives is acknowledged as custodian of this document
Self-care has currency in contemporary health-care provision for a number of reasons: a changing pattern of illness from one of acute to one of chronic (long-term) illnesses, together with a change in philosophy from cure to care; dissatisfaction with depersonalised (and, in mental health, often stigmatising) medical care, recently and bleakly crystallised in the Francis Inquiry report into care at Mid-Staffordshire Hospitals;33 consumerism and the desire for personal control in health matters and in interactions with health-care professionals, which is underpinned by the easy availability of health-related information on the internet; an increased awareness of the role lifestyle plays in relation to longevity and quality of life; and, finally, the need to increase access to care while controlling escalating health-care costs. 32,34 Research evidence into the effectiveness of self-care suggests it has many benefits: the development of more effective working relationships with professionals; increases in patient/service user satisfaction; improvements in self-confidence; improved quality of life; increased concordance with interventions; more appropriate use of services; and increased patient knowledge and sense of control. 23,35,36 Moreover, self-care often couples better outcomes with cost savings. 37
As noted earlier, our study focuses on self-care support rather than self-care per se. As the Department of Health notes,14 support for self-care can come in a variety of guises (e.g. information provision, skills training, professional education) and can be delivered through a variety of platforms (e.g. devices and technologies, real and virtual networks). The NHS has a particular role to play in self-care support: through its organisational structures and networks and the appropriate provision of information, interventions and technologies, it can (indeed, it has a responsibility to) create environments that support self-care – though self-care support may, of course, be delivered by other providers in the public, private and third sectors or even spontaneously by service users, as can be the case in real (physical) or virtual (online) support groups and networks.
Within this study, we have defined self-care as:
Any action a child or young person (or their parents) takes to promote their mental health, to prevent mental ill health, or to maintain or enhance their mental health and well-being following recovery from mental ill health.
Self-care support is thus:
Any service, intervention or technology directly or indirectly provided by the public, private or third sectors that aims to enhance the ability of children and young people (or their parents) to self-care in relation to their mental health and well-being.
Our study, therefore, focuses not only on self-care support for specific mental health conditions in CYP, but additionally on self-care support that might promote mental health, prevent mental ill health or help maintain mental health following recovery.
The organisation of child and adolescent mental health services
Throughout this report, we will make reference to two organisational hierarchies that have permeated the organisation of, and the literature on, child and adolescent mental health (CAMH) service provision. The first is very much a British approach; the second is used more internationally, though it is far from irrelevant to UK service provision and there is a degree of overlap between the two.
British child and adolescent mental health services and the ‘tier’ system
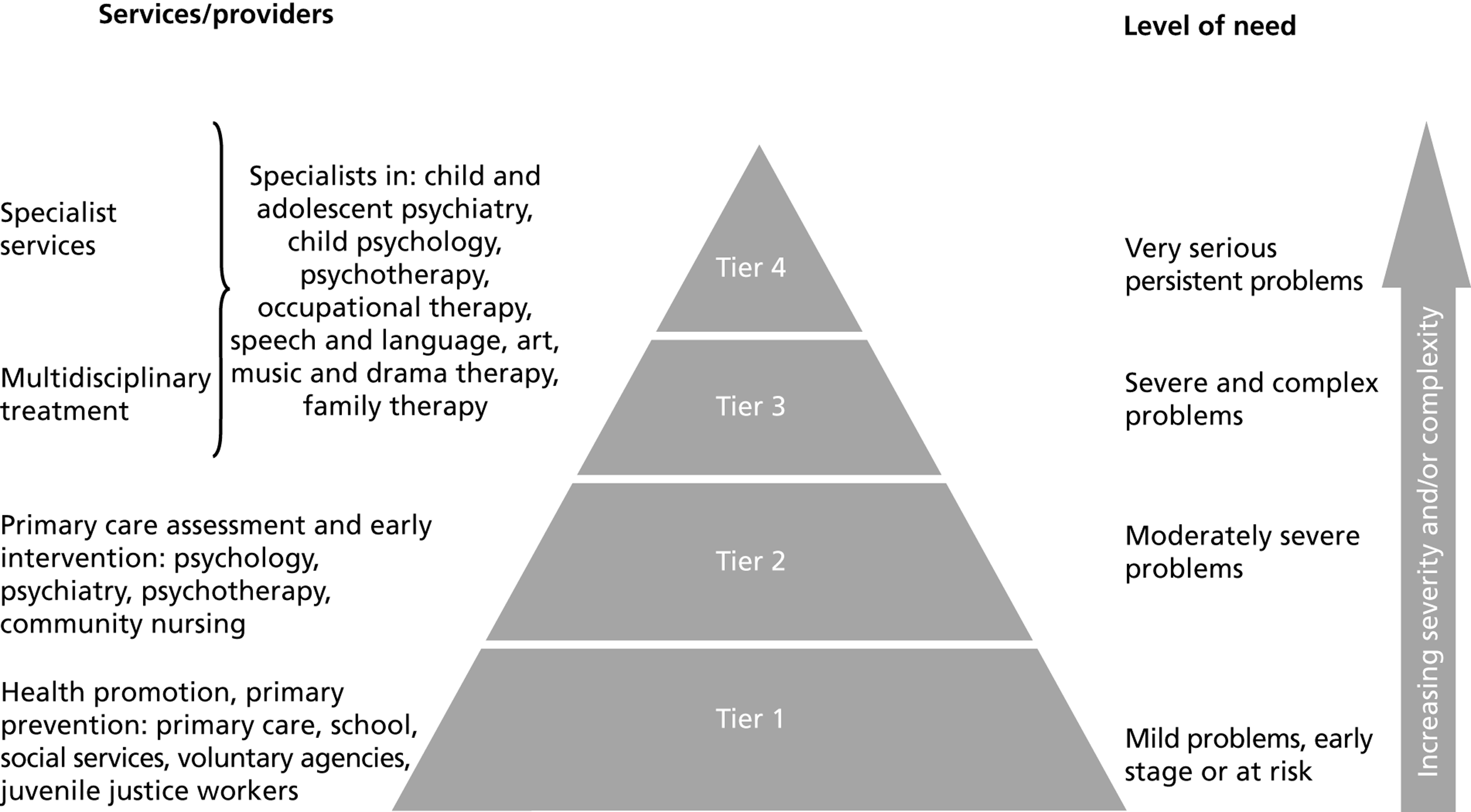
Given that we are interested in self-care support across primary, secondary and even tertiary care, it is worth briefly discussing the organisation of CAMHS in the UK. Since the publication of the seminal NHS Health Advisory Service report Together We Stand in 1995,38 CAMHS have been organised within a hierarchy of four tiers ( Figure 1 ). Tier 4 equates to very specialised, normally inpatient services, including generic as well as specialised inpatient services such as eating disorders units. Tiers 2 and 3 roughly equate to specialised, but less intense, services. Day patient services tend to be Tier 3 services, for example, whereas outpatient and early intervention services would correlate with Tier 2 services. Tiers 2 to 4 are also associated with increasing levels of complexity in the CYP’s mental health experiences and personal circumstances. Tier 1 is the tier embedded within non-specialist, universal children’s services (e.g. in education, child care and primary care) and is concerned with the provision of mental health education and advice, mental health promotion, and prevention and screening in mental health.
Although the scope for improving service delivery and organisation cuts across both specialist (Tiers 2 to 4) and non-specialist (Tier 1) CAMHS provision, the scope for improvement is perhaps more marked in Tier 1 provision because mental health promotion and mental ill health prevention are central to provision at this tier. Moreover, and as a consequence, services at this tier can also help reduce referrals to the potentially stigmatising higher tiers. However, because there seemed to be little knowledge about self-care support at any level of CAMHS provision, we did not limit our investigation to any particular tier(s).
Intervention levels
The British tiers approach offers a service- and needs-focused perspective on the organisation of CAMHS; it is not the only approach, however. An alternative approach – also hierarchical and popular in both the USA and Australia – is to organise by intervention, whereby interventions are categorised according to the specific populations of CYP for whom they are suitable. These populations are determined by the presence or absence of symptoms and the degree to which symptoms, if present, are mild or severe ( Table 1 ). In taking this approach, the lower intervention levels (universal and selective) can be seen broadly as preventative interventions, whereas the higher levels (indicated and treatment) can be seen broadly as interventions designed to manage specific symptoms.
| Group | Level | Details |
|---|---|---|
| Preventative | Universal | Includes all CYP Enhances resilience in all children regardless of risk Screening not required Avoids stigmatisation |
| Selective | Selects CYP at risk Involves screening |
|
| Management | Indicated | Selects CYP displaying mild symptoms Involves screening |
| Treatment | Targets CYP with a diagnosed condition |
Study overview
The need for this study was based on three principal factors: the relative paucity of research on mental health self-care support for CYP; the potential to change and enhance service provision in this area, to the benefit of both the NHS and the service user; and its capacity to build upon and complement existing work on CYP’s mental health, including work carried out by members of the study team. This last point is pertinent as the study was commissioned to follow on from a previous NIHR-funded study that several of us were involved in,15 and it is complemented by a variety of relevant research from all of the study team members, including work with school nurses,40 work on emotional well-being in schools27,28 and work on self-help technologies in CYP’s mental health. 25
In carrying out the study, we were guided, advised and supported by a stakeholder advisory group (SAG), made up of representatives from the health, education and social care professions as well as CYP and parent representatives (for details, see Appendix 1 ).
Aims and objectives
The aims of the study were:
-
to identify and evaluate the types of mental health self-care support used by, and available to, CYP and their parents
-
to establish how such support interfaces with statutory and non-statutory service provision.
These aims were operationalised via a series of specific objectives, namely:
-
the provision of a descriptive overview of mental health self-care support services for CYP in England and Wales, including a categorisation of these services according to a self-care support typology developed in a previous study
-
an examination of the effectiveness of such services
-
an examination of the factors influencing the acceptability of such services to CYP and their parents
-
an exploration of the barriers to the implementation of mental health self-care support services for CYP
-
an exploration of the interface between such self-care support services and the NHS and other statutory and non-statutory service providers, in order to guide future planning in health and social care
-
the identification of future research priorities for the NHS in this area.
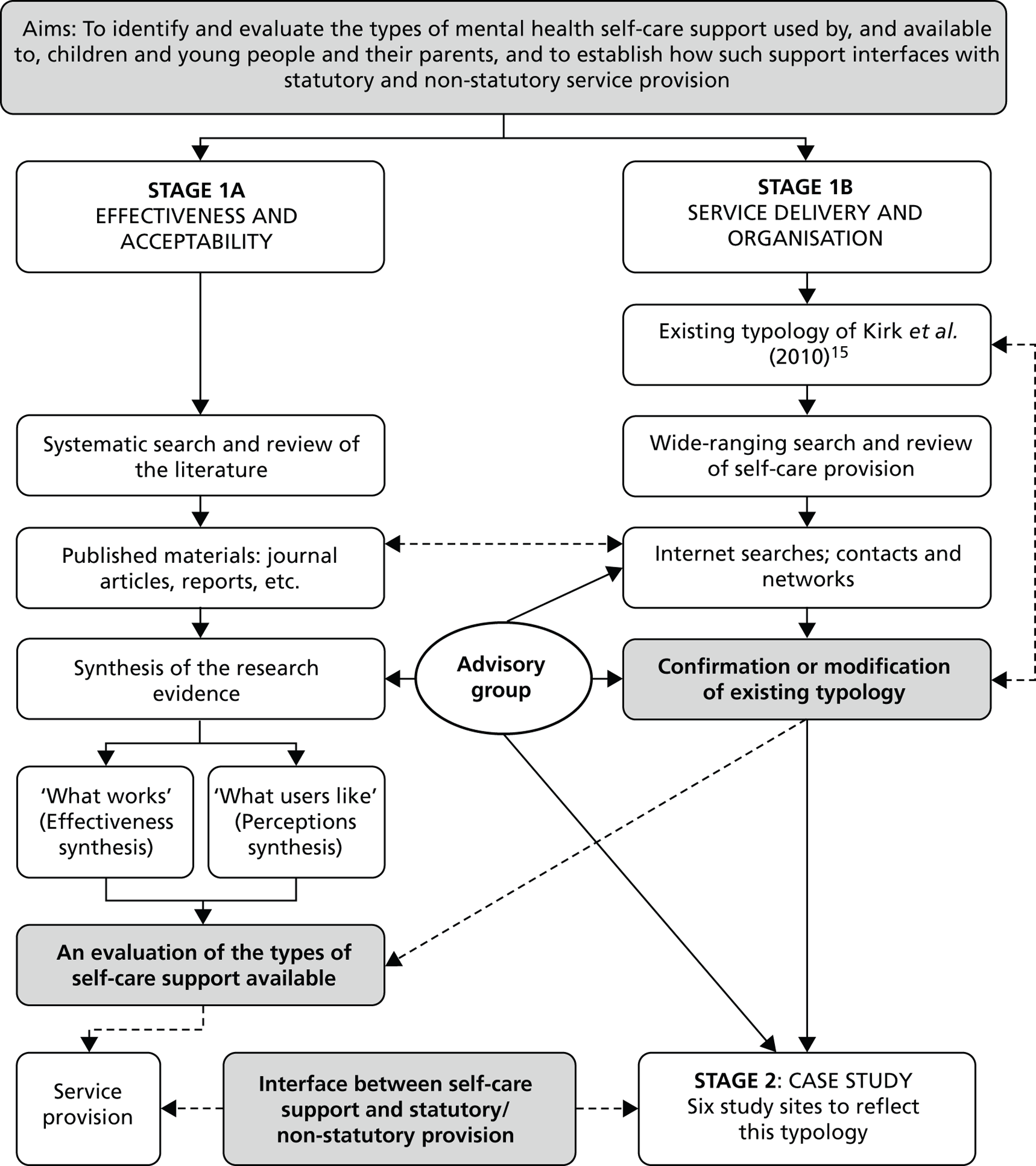
The study comprises an evidence synthesis combined with primary research, conducted as two overlapping stages over a 2-year period. Stage 1 consisted of two inter-related elements that ran concurrently, both of which were designed to help us identify the types of mental health self-care support available to CYP. Stage 1a was designed to address questions about the effectiveness and acceptability of such self-care support, and consisted of a systematic search and two inter-related reviews of the international literature, together with a meta-analysis. Stage 1b was designed to identify service provision relating to mental health self-care support for CYP in England and Wales, and consisted of a wide-ranging and systematic search of relevant resources (the internet, physical and virtual networks, policy documents, etc.) in order to elicit a ‘typology’ of service provision similar to the one we produced for a previous NIHR project. 15
Stage 2 involved a case study of service provision and was undertaken once Stage 1b’s systematic search was complete. In Stage 2, qualitative data were collected from key stakeholders in six sites, chosen to represent the typology emerging from Stage 1b, and in order to further explore issues such as acceptability, barriers to implementation, and the interface between self-care support services and statutory/non-statutory sector provision.
Stage 1a addressed research objectives 1, 2 and 3; Stage 1b, research objectives 1 and 5. Stage 2 addressed research objectives 3, 4 and 5. All of the stages of the study contributed to research objective 6. A schematic overview of the study can be found in Figure 2 .
FIGURE 2.
Schematic overview of the study.
The report
This report is organised such that Chapter 2 outlines the methods underpinning Stage 1a – the systematic literature reviews and meta-analysis – while the findings from these reviews and the meta-analysis are reported in Chapter 3 . Chapter 4 provides an overview of the methods and findings from the mapping exercise (Stage 1b), and Chapter 5 an overview of the methods and findings from the case study research (Stage 2). Chapter 6 , the discussion chapter, synthesises the data from the various strands of the study, concluding with some comments on the implications of the study for commissioners and managers of services, as well as for the practice and research communities.
A note on terminology
Throughout this report, we use ‘parent’ in preference to other terms such as ‘guardian’ or the more widespread ‘carer’ merely to avoid inelegant terms such as ‘parent/carer’ or ‘parent/guardian’. We have done this purely because our experience of working with parents is that they prefer this term. In opting for this preference, however, we fully acknowledge that some of those successfully parenting children are not necessarily biological parents.
Chapter 2 Systematic reviews and meta-analysis: methods
This chapter focuses on Stage 1a of the study, presenting the methods for the two inter-related systematic literature reviews that we carried out. We conducted these reviews in order to address research objectives 2 and 3, which were concerned with the effectiveness and the acceptability of mental health self-care support interventions and services for CYP, respectively. The findings from the two systematic reviews are reported in the next chapter.
The effectiveness review was undertaken as a systematic review with meta-analysis, whereas the acceptability review was premised on service user and service provider views of the interventions and services provided. We have termed the former our ‘effectiveness’ review and the latter our ‘perceptions’ review. The protocol for the effectiveness review is registered with the PROSPERO database, number CRD42012001981.
The literature reviews: methods
Review question
The systematic reviews were driven by two related questions:
-
What empirical studies have been undertaken on mental health self-care support for CYP?
-
What is the evidence for the effectiveness and acceptability of such support?
Inclusion criteria
Inclusion criteria for both the effectiveness and perceptions reviews were determined through an appropriate Population, Interventions, Comparators, Outcomes and Study (PICOS) designs formulation. 41
Population
Our population was ‘children and young people’, defined as those under the age of 18 years. This reflects the definition of the United Nations Convention on the Rights of the Child,42 of which the UK is a signatory. Because of differing international views of the age range for a ‘young person’, there is often ambiguity at the top of the childhood range (17+ years), thus we also considered studies with populations that included young people up to 25 years of age, so long as we had evidence that the mean age of participants was, or the majority of participants were, under the age of 18 years.
Interventions
Using our definition of self-care (see Chapter 1 ), we included any health, social care or educational intervention or service designed to support or facilitate CYP (or their parents) to take action to promote their mental health, prevent mental ill health, or maintain or enhance their mental health and well-being following recovery from mental ill health. We therefore included self-care support interventions and services which targeted CYP with specific mental health problems as well as those designed to improve the general mental health of CYP. As we were interested in self-care support rather than self-care per se, a support ‘agent’ (e.g. a health, social care or education professional, peer or lay person) who worked with the CYP and/or their parents needed to be present for the intervention or service to qualify.
Comparators
For the effectiveness review, we were unsure whether or not we would find sufficient trials with a control or other such comparison group (see Study design below), and so did not specify a comparator at the outset. As the perceptions review was concerned with absolute, rather than relative, service user views of specific self-care support interventions and services, this aspect of the PICOS framework was disregarded for the perceptions review.
Outcomes
For the effectiveness review, we were interested in whether or not self-care support interventions brought about a demonstrable positive change in mental health. Included studies, therefore, needed to contain a valid standardised mental health measure. We also considered, where available, a range of relevant secondary outcomes (measures of general functioning, general well-being and self-esteem, for example). For the perceptions review, we were not interested in outcomes per se, but in qualitative and quantitative data that captured service user or service provider views.
Study design
For the effectiveness review, we were initially interested in studies containing trials, with ‘trial’ being defined as any study in which there was, at minimum, a relevant pre- and postintervention outcome measure. This meant that, initially, uncontrolled pre/post designs, non-randomised controlled trials and randomised controlled trials (RCTs) were all included. We did, however, add a caveat that should there be sufficient RCTs, we would restrict the effectiveness review solely to RCTs. For the perceptions review, we included any empirical study (qualitative or quantitative) in which service user and/or service provider views about any element of the self-care support intervention or service were available.
Search strategy
To estimate the size and scope of the literature, we first conducted a brief scoping review. 43 Our experience with literature searching in a previous NIHR project exploring self-care support in CYP’s physical health15 led us to believe that using ‘child/young person’, ‘mental health’, ‘self-care’ and associated medical subject heading (MeSH) synonyms in combination might be an appropriate baseline strategy for a scoping search. We consequently searched the MEDLINE, Cumulative Index to Nursing and Allied Health Literature (CINAHL) and PsycINFO databases using this strategy, only to find that the search produced very few relevant returns.
Although we had little idea of the size of the literature on mental health self-care support for CYP, there was sufficient expertise in the team to know that there was more material in the literature than our scoping search suggested. Thus, to prepare for a more comprehensive search, the team subsequently identified additional synonyms for our three search categories (child/young person, mental health and self-care). We gave particular emphasis to synonyms for ‘self-care’ as, unlike in CYP’s physical health, it seemed that self-care was not generally a part of the professional language of CYP’s mental health and was unlikely to be indexed as such. Members of the SAG were also particularly helpful in helping us understand how self-care might be conceptualised in this context and in developing a wider range of search terms.
As our review question demanded that we focus on empirical studies, we included a fourth category – empirical research – in our search strategy. The final search terms used in the review are presented in Box 1 .
-
Child/young person = child* OR p#ediatric OR teen* OR adolesc* OR young person OR young people OR youth OR school
-
Mental health = a OR b OR c
-
[mental health synonyms] mental health OR emotional health OR psychological health OR psychological well*being OR emotional health OR emotional* litera* OR emotional well*being OR emotional* competen* OR aspects of learning OR self esteem OR self efficacy OR CAMHS OR resilien* OR feelings
-
[mental disorder synonyms] mental disorder OR psychiatr* OR mental illness OR mentally ill OR mental* distress* OR emotional problem* OR emotional difficult* OR emotional* distress*
-
[conditions] ADHD OR attention deficit OR conduct disorder OR behavio*r problem* OR anger OR angry OR aggress* OR affective disorder OR anxi* OR worr* OR depress* OR obsessive compulsive OR OCD OR traumatic stress OR PTSD OR suicid* OR self harm* or self injur* OR psychos*s OR schizophren* OR eating disorder OR anorexi* OR bulimi* OR mood disorder OR phobi* OR school refusal OR panic OR enuresis OR bedwetting OR encopresis OR soiling
-
-
Self-care = a OR b OR C OR d OR e OR f
-
[self-care synonyms] self manag* OR self car* OR self help* OR self report* OR self monitor* OR self medicat* OR self administer* OR self treat* OR self control* OR collaborat* OR expert patient OR patient involve* OR patient participat*
-
[models] parenting OR parent training OR cognitive therapy OR CBT OR behavio#r* therapy OR behavio#r* modification OR solution focus#ed OR mindfulness OR promot* OR exercise OR mutual support OR peer support OR buddy OR buddies OR friend OR partnership OR mentor* OR empower*
-
[generic intervention synonyms] intervention OR prevention OR training OR program* OR coach* OR behavio#r* management OR toolkit
-
[psychoeducation synonyms] psychoeducation OR group education OR patient education OR patient information OR information giving OR educational material* OR bibliotherapy OR manual *OR leaflet OR booklet OR pamphlet
-
[skills synonyms] communication skills OR decision making OR goal setting OR action plan* OR problem solving OR coping skills OR assertiveness OR conflict resolution
-
[telemedicine synonyms] tele* OR virtual communit* OR ehealth OR messaging OR multimedia OR Internet OR computer* OR online OR web based OR web site OR world wide web OR technolog* OR email OR social networking OR interactive OR cyber* OR chat room OR forum OR electronic OR web 2
-
-
Empirical research = study OR design OR review OR synthes* OR pilot OR case OR mixed method OR quantitative OR experiment* OR trial OR RCT OR questionnaire OR survey OR follow up OR qualitative OR interview* OR focus group OR experience OR observation* OR descripti* OR evaluat* OR ethnograph* OR view OR perception
Aggregate search = 1 AND 2 AND 3 AND 4
* = truncation; # = wildcard.
Searches were conducted in the following databases: MEDLINE (medicine); CINAHL (nursing and allied health); PsycINFO (psychology); Applied Social Sciences Index and Abstracts (ASSIA) (applied social care); Education Resources Information Center (ERIC) (education); and All Evidence-Based Medicine (EBM) Reviews. All EBM Reviews is a multifile database, accessible via the OvidSP interface, that incorporates the seven EBM Reviews databases, namely ACP Journal Club, Database of Abstracts of Reviews of Effects (DARE), Cochrane Central Register of Controlled Trials (CCRCT), Health Technology Assessment (HTA), Cochrane Database of Systematic Reviews (CDSR), NHS Economic Evaluation Database (NHS EED) and Cochrane Methodology Register (CMR).
We limited our search to studies published from 1 January 1995 onwards as 1995 can be considered a watershed in British CAMH practice, being the year in which the seminal report Together We Stand 38 was published (see Chapter 1 ). No other limiters were applied. The searches were conducted in July 2011.
Search results and study selection
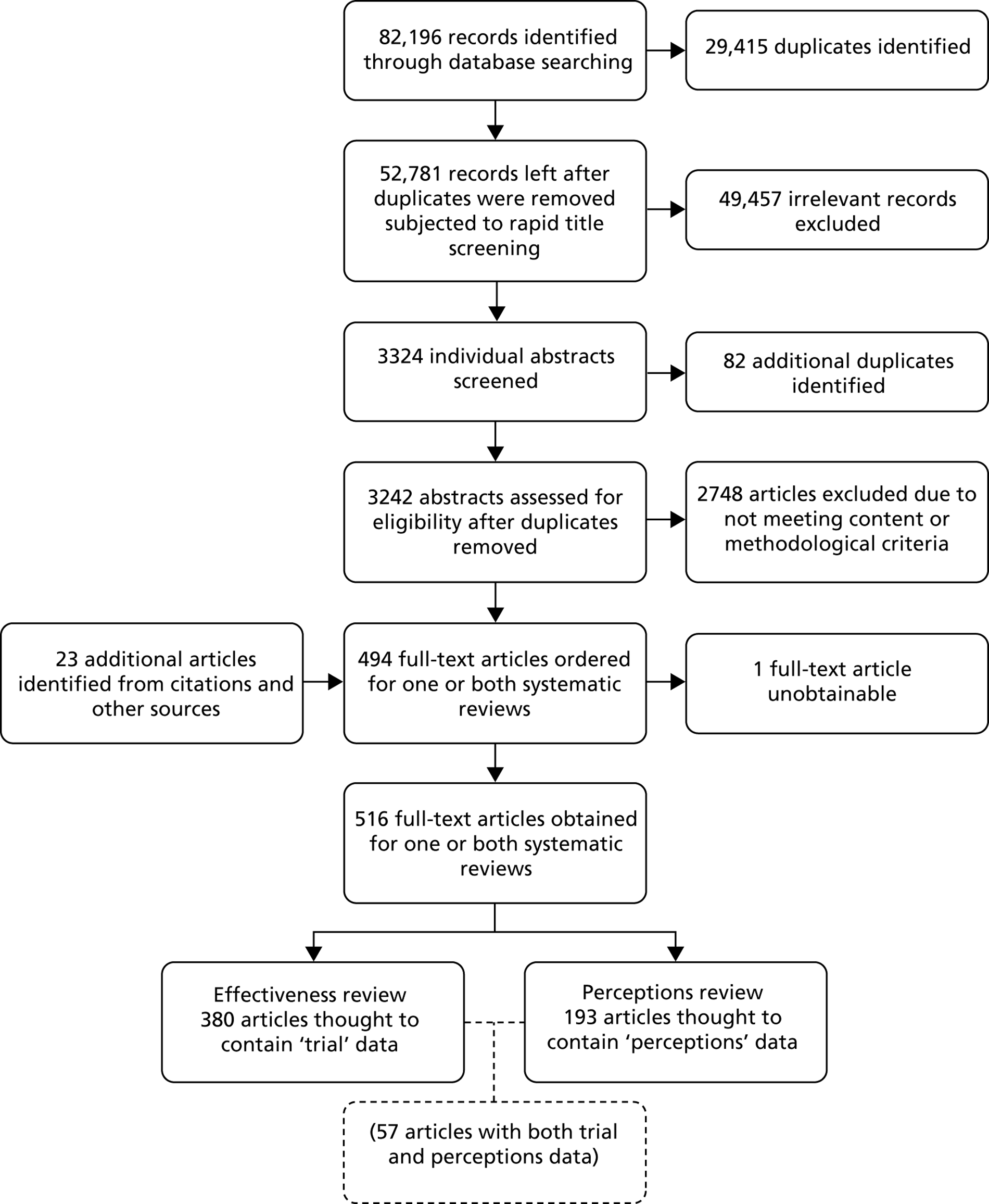
The aggregate search results from each of the six databases searched were exported into Reference Manager Version 11 (Thomson ResearchSoft, San Francisco, CA, USA). The titles were screened by one team member (Elvey) and duplicates were removed. The remaining records were then screened for relevance by reading titles and abstracts; owing to a high number of extraneous records about physical conditions (including psychological well-being in these conditions), relevant terms (e.g. cancer, asthma) were entered into the Reference Manager search function and the results were removed. Non-empirical books, general review articles, letters, commentaries, etc. were screened out in a similar manner. As Figure 3 illustrates, these processes reduced the number of records to 3324.
FIGURE 3.
Flow diagram for the initial pool of articles.
The data on the remaining 3324 articles were exported from Reference Manager to a Microsoft Access 2010 database (Microsoft Corporation, Redmond, WA, USA). Using Access enabled us to enhance our records management by the creation of additional fields (see Appendix 2 ). A further 82 duplicates were identified within the Access database, leaving a pool of 3242 abstracts for consideration. This was a substantial number of abstracts to deal with in the time available, so one team member (Elvey) used the search function in Access to speed the process of finding terms which would allow us to remove articles on the basis of irrelevance to the study. These included articles that focused primarily on issues that we considered peripheral to mental health and mental disorder – articles focusing, in particular, on resilience, bullying, aggression and general, rather than serious or ‘diagnosed’, behaviour problems – unless there was explicit reference to CYP’s mental health symptomatology, for example anxiety, depression or externalising symptoms.
The abstracts of the remaining 494 articles were independently screened by two team members (Elvey and Pryjmachuk), who categorised the source according to its study design [using an adaptation of the National Institute for Health and Care Excellence (NICE) algorithm44 for classifying study designs] and also assessed whether or not it met our inclusion criteria and, if so, for which review – effectiveness, perceptions or both. Where there was agreement on inclusion, a full copy of the source was obtained. Where there was insufficient information in the abstract to enable a judgement to be made on its inclusion, or where there was disagreement between the two team members, the abstract was put into abeyance while a full copy of the source was obtained. If, after a full copy of the source had been obtained, there was still disagreement on inclusion, a third member of the team (Kirk or Kendal) was asked to arbitrate.
In all, 494 full-text articles were initially identified as potentially relevant for one or both of the reviews. One article (a paper from China) proved impossible to obtain via the University of Manchester interlibrary loans and document supply service, despite making international requests, and a further 23 articles were identified through the reference lists and bibliographies of retrieved articles, making a grand total of 516 full-text articles in our initial pool.
Most of the full-text articles were obtained in portable document format (PDF). Consequently, where there was insufficient information in an abstract to determine an article’s eligibility for one or both reviews, rather than read the entire article, we were able to rapidly search the respective PDF, using the ‘full search’ function in Adobe Reader X (Adobe Systems Incorporated, San Jose, CA, USA). This arose when the abstract was vague about whether a RCT was being reported or not (in which case the PDF was searched using the term ‘random’) or, most often, to determine eligibility for the perceptions review, in which case the PDF was searched using the full search outlined in Box 2 .
Acceptability: accepta (acceptable, acceptability); uptake; adher (adhere, adhered, adherence); engage (engage(s), engaged, engagement); evalua (evaluate(s), evaluation).
Perceptions: perce (perception(s), perceived); perspect (perspective(s)); view (view(s)); feedback; experience (experience(s)).
Satisfaction: satisf (satisfied, satisfaction); prefer (prefer(s), preferred, preference).
Access: access (access, accessible); choice; barrier (barrier(s)).
Adobe Reader full search: match any of “accepta uptake adher engage evalua perce perspect view feedback experience satisf prefer access choice barrier”.
In total, 323 of the initial pool of 516 articles were allocated to the effectiveness review, 136 to the perceptions review and 57 to both reviews, giving a pool of 380 full-text articles for the effectiveness review and a pool of 193 for the perceptions review.
Effectiveness review
Study selection
Of the 380 full-text articles in the initial pool for the effectiveness review, a further two were identified as duplicates, leaving 378 articles for consideration. These 378 articles represented 335 separate studies (some studies generated more than one paper) and two members of the study team (Elvey and Pryjmachuk) independently considered each study against the inclusion criteria. Eighty-six studies were excluded on content grounds – including a few studies concerned with enuresis and encopresis, which the study team and stakeholder group felt did not really fit in with our conceptualisation of mental health problems in CYP – and one on the grounds that it was published before 1995, leaving some 248 content-eligible studies ( Figure 4 ).
FIGURE 4.
Flow diagram of eligible studies for the effectiveness review.
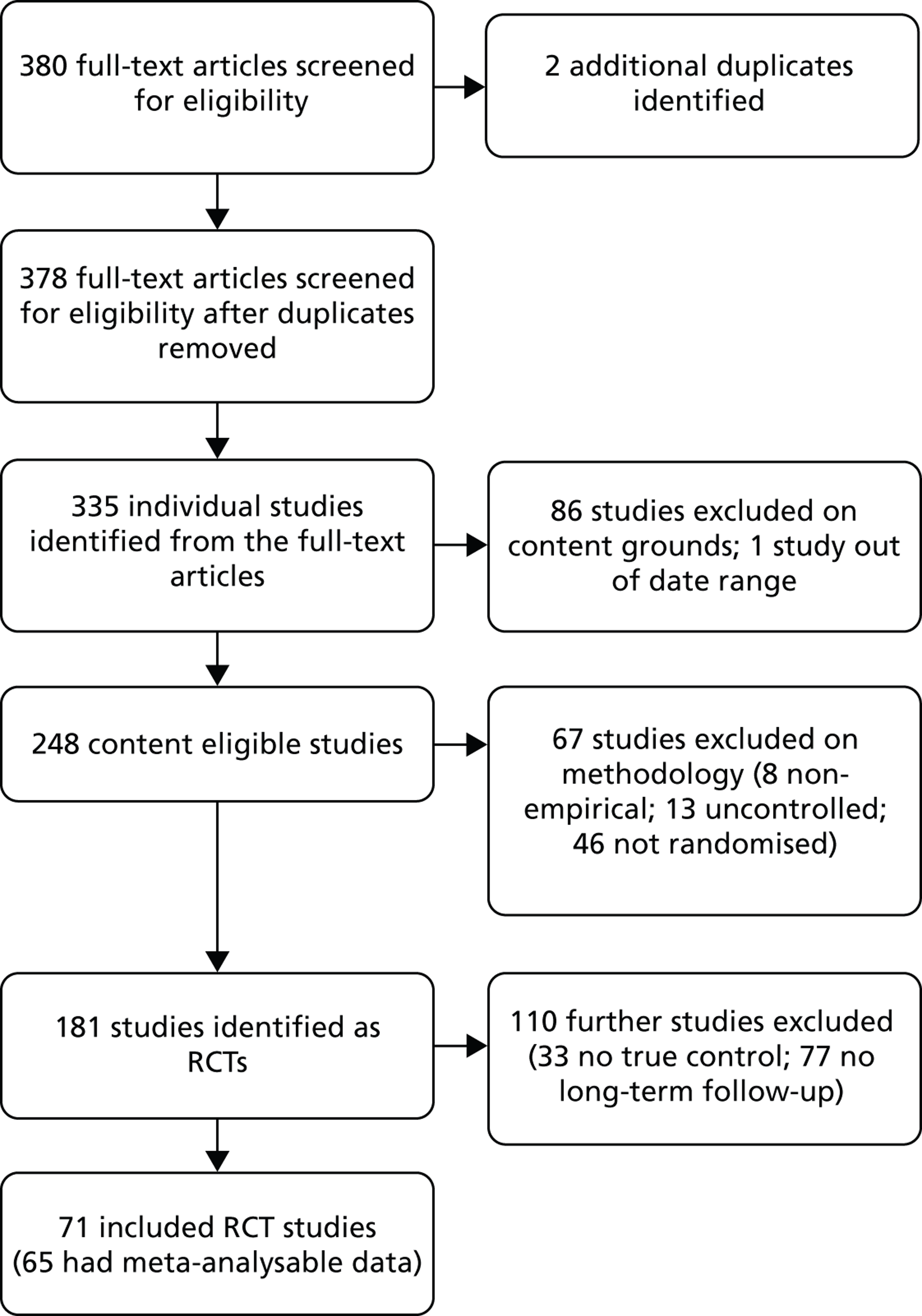
Eight of the content-eligible studies had no empirical data, leaving us with 240 trials (‘trial’ meaning, at minimum, an uncontrolled pre/post design). Given the small proportion of uncontrolled (5.4%) and non-randomised trials (19.2%), we made a post hoc decision to restrict to formal RCTs, leaving us with 181 studies. The very large number of trials meant that it was not possible to extract and analyse data from all of the studies, and we made a second post hoc decision to include only those studies that met the following criteria:
-
RCTs with a ‘control’ comparator (defined as a waiting list, usual care or attention/placebo control, for example), as these provided the best evidence concerning the primary research question (evidence for the effectiveness of mental health self-care support for CYP)
-
RCTs with long-term follow-up (defined as follow-ups longer in duration than the immediate postintervention follow-up, as these provided the best evidence for the effectiveness of mental health self-care support for CYP in providing enduring gains).
This left us with 71 RCT studies focusing on the longer-term effectiveness of mental health self-care support interventions for CYP and their families. A list of these studies can be found in Table 2 .
| Included in the meta-analysis (n = 63, or n = 71 including substudies) | Excluded from the meta-analysis | |
|---|---|---|
| Not meta-analysable (n = 6) | Outliers (n = 2, or n = 3 including substudies) | |
|
||
Data extraction
Non-English-language papers were translated prior to data extraction. For the effectiveness review, descriptive data for all 71 RCTs were extracted onto a study-specific data extraction sheet (see Appendix 3 ) by one team member (Pryjmachuk), with other team members (Elvey, Kendal and Kirk) providing a second, independent extraction. The two independent extractions were subsequently combined into a separate document (see Appendix 4 for an example) with any discrepancies being resolved through discussion, with referral to a third member of the team for arbitration where a consensus could not be reached.
Quality assessment
In reviews published by The Cochrane Library, quality is assessed by the application of the Cochrane Collection risk of bias tool, a tool that explores several factors known to introduce biases into trials, including the way in which participants are allocated (randomised) into groups; the extent to which this allocation is concealed; the blinding of all those involved, including participants and researchers; the way in which incomplete outcome data are dealt with; and the use of selective outcome reporting. 140
For the current analysis, as well as describing the overall quality of the trials in the review, we sought to assess the impact of study quality through formal quantitative assessment of the relationship between quality and outcomes. To conduct these analyses, we chose a dichotomous measure based on allocation concealment, as this is the aspect of quality most consistently associated with outcomes in trials141,142 and is particularly relevant when outcomes are subjective, as is the case with the bulk of mental health assessments in the current review. 143 Other measures in conventional risk of bias assessments, such as blinding, are less relevant in the current context, as the nature of self-care support means that the conditions for blinding are rarely achievable. Allocation concealment was judged as adequate or inadequate according to the relevant section from the Cochrane risk of bias tool. Two members of the team (Pryjmachuk and Bower) independently assessed all of the included studies on this criterion so that each study could be categorised as either a high-quality (adequate) or a low-quality (inadequate or unclear) study. As with other elements of data extraction, any discrepancies here were resolved by discussion between the data extractors.
As sufficient RCTs were available, our primary data synthesis for the effectiveness review was meta-analysis, although it is augmented by a brief descriptive synthesis of the original 71 included RCTs.
Effectiveness data synthesis: the meta-analysis
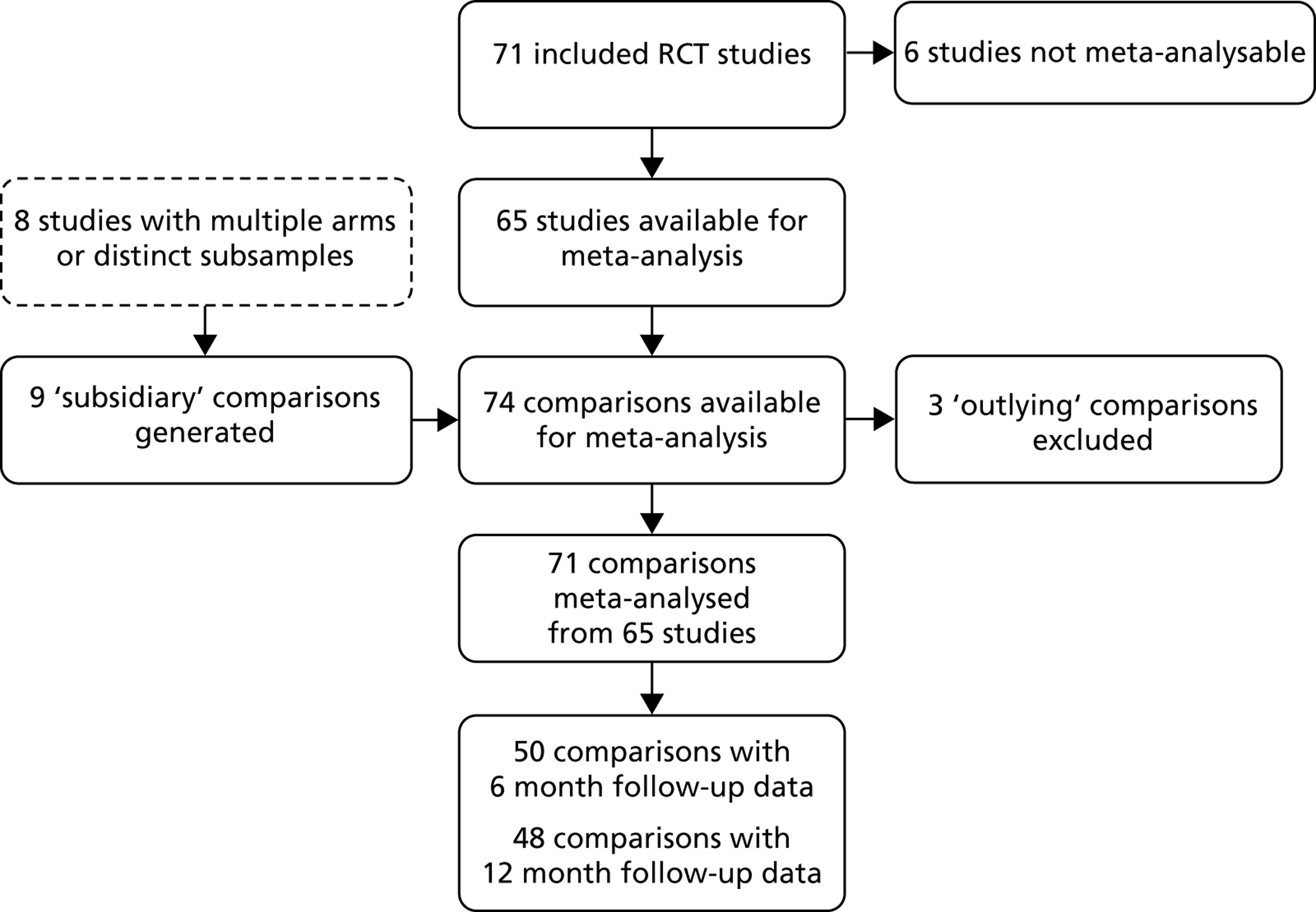
Figure 5 outlines the flow of studies, from the original 71 included studies to those that were ultimately meta-analysed. During the data extraction process (see below), we found that we were unable to obtain useable data from six studies, and eight of the studies had multiple arms or distinct subsamples, which generated nine subsidiary or ‘substudy’ RCTs.
FIGURE 5.
Flow diagram of eligible studies for the meta-analysis.
Data extraction
Outcome data for the meta-analysis were independently extracted into a Microsoft Excel 2010 spreadsheet (Microsoft Corporation, Redmond, WA, USA) by two team members (Pryjmachuk and Bower). Data were extracted only for those outcome measures identified as ‘direct mental health’ measures ( Table 3 ; see also Appendix 6 ).
| Meta-analysed | Outliers | Not meta-analysable |
|---|---|---|
|
The data extracted for each outcome measure included, where available:
-
the sample sizes for the intervention and control groups at randomisation
-
whether or not a clustered RCT design had been employed and, if so, the number of ‘units’ (schools, clinics, etc.) in each cluster
-
the numerical data necessary to calculate a standardised effect size at each declared follow-up time point, such as the sample sizes, means and standard deviations for the intervention and control groups, or the sample sizes and an event count (e.g. numbers ‘diagnosed anxious’) for each group.
In two studies (Barrett 200547 and Cowell 2009;57 see Table 2 ), discrete subsamples had been used which necessitated splitting each study into several comparisons. Similarly, in six multi-intervention studies (Kendall 2008,83,84 King 2000,86 Pfiffner 1997,101 Simon 2011,112 Stice 2008118,119 and Sánchez-García 2009b;139 again, see Table 2 ), more than one intervention was identified as a self-care support intervention and so these interventions were separated out into individual comparisons. Where a single study included multiple comparisons, the control group sample was split proportionately between each comparison to avoid double counting.
Some notes need to be made about the data extraction for a few other studies. Bernstein 200549,50 was a multi-intervention study [with both cognitive–behavioural therapy (CBT) and ‘parent training’ as self-care support interventions], but the study combined the data for the two interventions at the longer-term follow-up point, meaning that only the combined CBT/parent training data were useable in our meta-analysis. In Hahlweg 2010,73 only the data from mothers were useable. Both Lowry-Webster 200139,90 and Spence 2003113,114 had ‘high anxiety’ subsamples within their overall samples, so a decision was made in each case to use only the total sample. In the multi-intervention Multimodal Study of Children with ADHD (MTA) 1999 study,95–98 only the ‘intensive behavioural treatment’ arm qualified as a discrete self-care support intervention. Similarly, in Rosa Alcázar 2009,106 only ‘IAFS’ (Intervention for Adolescents with Social Phobia) qualified as such. Sheffield 2006110 was a complex four-arm trial which merged universal and high-risk samples across both a targeted and a universal intervention, so a decision was made to use only data from the full sample (universal intervention).
On completion of the outcome data extraction, the two independently extracted Excel spreadsheets were compared and any discrepancies and errors in the extraction were discussed and resolved by the two data extractors.
Primary outcome measure selection
Table 4 outlines the distribution of the various outcome measures used in the 71 included RCT studies. The distribution of outcome measures will be discussed further in the next chapter, but for now it is worth noting that the most frequent direct measure of mental health symptomatology in CYP was one which was obtained from the CYP rather than any other source.
| Source | Direct MH measure, n (%) | Indirect MH measure, n (%) | General functioning, n (%) | Resilience, n (%) | General well-being, n (%) | Self-esteem, n (%) |
|---|---|---|---|---|---|---|
| Child | 56 (79) | 29 (41) | 11 (15) | 7 (10) | 3 (4) | 10 (14) |
| Parent | 27 (38) | 19 (27) | 10 (14) | 1 (1) | 0 (0) | 1 (1) |
| Teacher | 8 (11) | 5 (7) | 4 (6) | 0 (0) | 0 (0) | 0 (0) |
| Clinician | 36 (51) | 10 (14) | 11 (15) | 1 (1) | 0 (0) | 0 (0) |
| Any source a | 71 (100) | 41 (58) | 28 (39) | 8 (11) | 3 (4) | 10 (14) |
In principle, meta-analysis requires the selection of a single measure from each comparison. As almost 79% of the included studies included CYP self-report data (see Table 4 ), preference was given to a validated CYP self-report measure based on a continuous score directly related to the condition on which the intervention was focused (e.g. a depression outcome measure for an intervention designed to help CYP with depression, an externalising outcome measure for an intervention designed to help CYP with behaviour problems, and so on). If more than one measure qualified on this basis, a global or total symptoms measure was chosen in preference to a specific (subscale) measure, and if more than one global measure was available, we made a judgement about which was the most established.
If no CYP self-report, continuous measures were available, parent-reported measures were selected; for the few studies that had neither child- nor parent-reported measures, clinician-reported measures (usually measures eliciting a diagnosis) were employed. Where a choice needed to be made between intensity/severity scales and frequency/number of problems scales, intensity scales took precedence. The primary outcome measures selected from each study are listed in Table 3 .
Once the primary outcome measures for each study had been determined, a combined Excel spreadsheet was prepared ready for transfer to Comprehensive Meta-Analysis (CMA) (Biostat, Inc., Englewood, NJ, USA), the meta-analysis software we employed. In preparing this spreadsheet, studies were also grouped according to the follow-up time points for which data were available. We were able to categorise the studies into three broad follow-up periods relatively easily: approximately 6 months, approximately 12 months and approximately 24 months post intervention.
Data preparation: missing data, cluster adjustments and effect direction
Where sample sizes were missing at follow-up, they were estimated by assuming an arbitrary 70% follow-up from baseline (such imputation will only influence the weight associated with the comparison in the meta-analysis, not the estimate of effect of that study). Where there were missing standard deviations, these were estimated using included studies that had the same outcome measure. Missing standard deviations for the Center for Epidemiologic Studies-Depression Scale (CES-D) at 6-month and 12-month follow-ups in Compas 200956 were estimated from other studies with 6-month CES-D data (two studies: Clarke 199553 and Garber 200967) and 12-month CES-D data (four studies: Clarke 1995,53 Clarke 2001,54 Clarke 200255 and Sawyer 2010108,109).
Three studies (Evans 2007,65 Compas 200956 and Tol 2008128) reported only a raw effect size which needed to be converted to a standard error in order to be compatible with CMA.
Cluster trials are frequently used in trials of psychological and mental health interventions as a way of avoiding bias associated with contamination. In line with guidance from the Cochrane Handbook for Systematic Reviews of Interventions,140 the sample sizes of approximately one-third of studies using cluster randomisation were adjusted by dividing the original sample by the ‘design effect’, which was calculated using the formula 1 + (M – 1) × ICC, where M is the mean cluster size (total sample size divided by total number of clusters) and ICC is the intracluster correlation coefficient, which we assumed to be 0.02.
The effect direction for each primary outcome was coded in CMA such that effects in favour of the intervention (self-care support) were coded negative. All coded effect directions were compared for consistency with what was reported narratively in the papers describing each study.
Primary and secondary analyses
Analyses were conducted in CMA using a random-effects model in each case. Our primary analysis focused on the long-term effectiveness of self-care support interventions in mental health symptomatology in CYP. We also explored subgroup analyses using a variety of prespecified ‘moderators’ (i.e. variables that were associated with the benefit of self-care support) that were chosen on the basis of theory and practical considerations. These moderators were the intervention level (see Chapter 1 , Table 1 ); the mental health condition and the age group the intervention was designed for; the theoretical model underpinning the intervention; the recipients (child/young person, parent or family); whether the intervention was school-based or not; group versus individual interventions; whether the agent was mental health trained or not; and the length of the intervention. Concealment of allocation was also included as a moderator.
There were relatively limited follow-up data at 24 months, so for all analyses we restricted the data to two follow-up points: around 6 months and around 12 months. In all cases, the meta-analysis results are presented in terms of a standardised mean difference (effect size) with 95% confidence limits, together with the relevant I 2 statistic which is a measure of consistency (heterogeneity) across the included studies. I 2 scores above 75%, 50% and 25% are said to have high, moderate and low heterogeneity (inconsistency) respectively. 144 Interpretation of the pooled outcome in meta-analyses with high I 2 scores should be treated with caution. For the primary analyses only, we have additionally provided forest plots, produced via Stata Version 12.0 (StataCorp LP, College Station, TX, USA).
Perceptions review
The perceptions review centred on the views that the various stakeholders – CYP, their families and staff – had about mental health self-care support interventions and services for CYP. It was concerned with aspects of these interventions and services such as acceptability, satisfaction and accessibility.
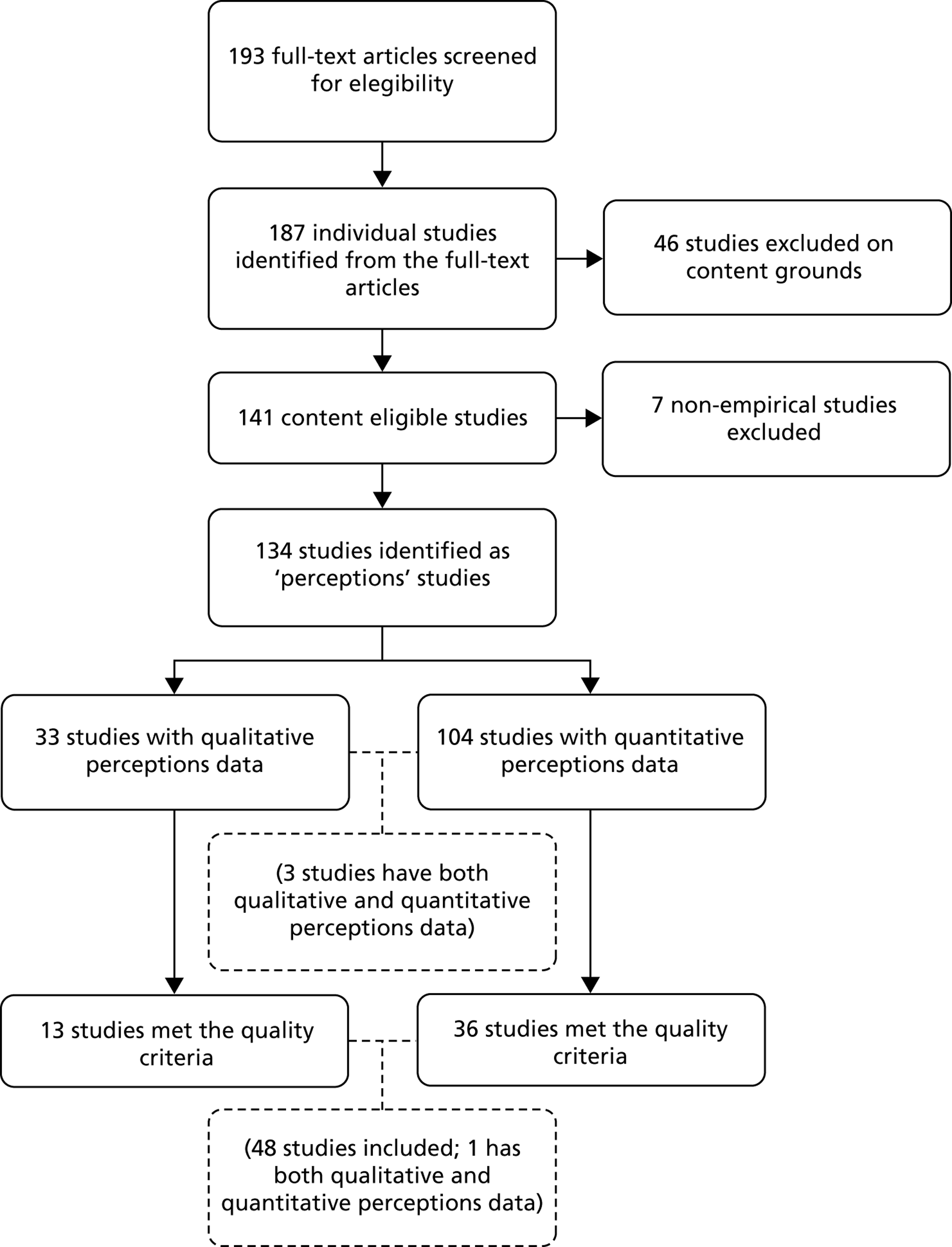
Study selection
For the perceptions review, 187 individual studies were identified from the pool of 193 full-text articles. Forty-six of these studies were excluded on content grounds and seven were identified as non-empirical. This left 134 studies with perceptions data for consideration and quality appraisal: 30 studies with qualitative perceptions data, 101 studies with quantitative perceptions data and 3 studies with both ( Figure 6 ). The application of quality criteria (discussed shortly) ultimately reduced the number of studies to 12 with qualitative perceptions data, 35 with quantitative perceptions data and one with both, making a total of 48 included studies.
FIGURE 6.
Flow diagram of eligible studies for the perceptions review.
Data extraction
As with the effectiveness review, non-English-language papers were translated prior to data extraction. Descriptive data for the 33 qualitative perceptions studies (of which 30 were solely qualitative studies and three were mixed methods studies) were extracted onto a study-specific data extraction sheet (see Appendix 5 ) by one team member (Pryjmachuk), with other team members (Elvey, Kendal and Kirk) providing a second, independent extraction. As with the effectiveness review, the two independent extractions were subsequently combined into a separate document, with any discrepancies being resolved through extractor discussion with referral to a third member of the team for arbitration where a consensus could not be reached. For pragmatic reasons, the 104 quantitative studies (101 solely quantitative and three mixed-methods studies) were filtered for quality prior to data extraction (see below), with data from the 36 quantitative perceptions studies eligible at this point being extracted directly into a Microsoft Excel spreadsheet by one team member (Pryjmachuk) and subsequently verified by a second (Elvey).
Quality assessment
For the qualitative perceptions studies, study quality for all 33 studies was assessed during the overall data extraction by one team member (Pryjmachuk) and independently by the second person extracting (Elvey, Kirk or Kendal). Quality was assessed using a modified version of the quality assessment tool used in our previous NIHR study on self-care support,15 which in turn was adapted from tools developed by Dixon-Woods et al. 145 and the Evidence for Policy and Practice Information and Co-ordinating Centre (EPPI-Centre). 146 A copy of the quality assessment tool can be found in Appendix 5 , embedded into the perceptions review data extraction sheet. Again, any quality assessment discrepancies were resolved by discussion between the extractors and, where necessary, through arbitration by a third member of the team. The tool comprised seven criteria, and for the purpose of this review we decided that a paper had to meet four criteria for inclusion.
We identified 104 studies as containing quantitative perceptions data. This was a substantial number of studies to consider for data extraction so, in contrast to the qualitative studies, we made a pragmatic decision to apply quality criteria prior to, rather than during or after, data extraction. During the process of scanning papers for perceptions data (see Search results and study selection and Box 2 earlier in this chapter), it became evident that trials were the sole source of quantitative perceptions data, i.e. all of the 104 studies containing quantitative perceptions data were controlled or uncontrolled trials. In the main, the quantitative perceptions data came from satisfaction surveys nested within these trials or from statistics concerning intervention uptake or adherence, though we did not consider the latter to be perceptions data. Thus, to manage the number of quantitative perceptions studies, we applied our PICOS criteria (see Inclusion criteria earlier in this chapter), selecting only randomised trials with a true control. Accordingly, only 36 trials with quantitative perceptions data (one of which was a mixed-methods study that also contained qualitative data) were eligible for the perceptions review.
Details of the included studies for the perceptions review can be found in Table 5 .
| Qualitative studies (n = 12) | Quantitative studies (n = 35) | Mixed-methods studies (n = 1) |
|---|---|---|
|
Synthesis of the literature reviews data
The synthesis for the literature reviews data is based on the ‘mixed-methods synthesis’ of the EPPI-Centre,178 an approach to synthesis whereby different data sources (effectiveness, qualitative views and quantitative satisfaction data, for example) are analysed separately but subsequently compared and contrasted. Figure 7 outlines this process schematically.
FIGURE 7.
Schematic diagram of the literature review evidence synthesis.
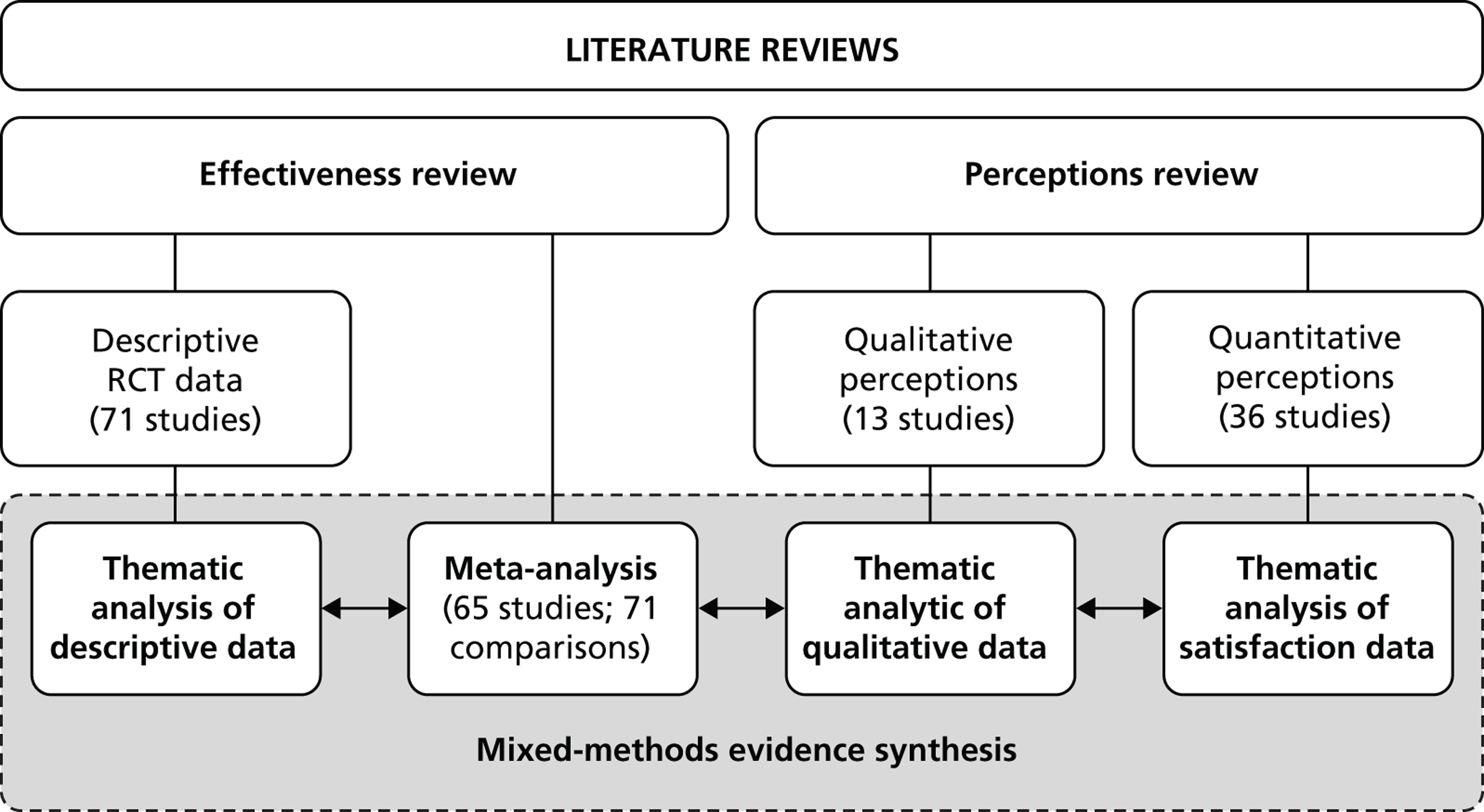
The methods we used for the literature reviews elicited four sets of data: two for the effectiveness review and two for the perceptions review. A meta-analysis can stand on its own as an evidence synthesis as it essentially distils effectiveness data from many studies into a single meaningful statistic. It is, however, useful to triangulate the meta-analysis results with results from other sources in order to gain a more complete understanding of the evidence for self-care support in CYP’s mental health. In order to do this, summary data from the three remaining data sets – the descriptive RCT data, the qualitative perceptions data and the quantitative perceptions data – were individually tabulated and the three summary tables (see Appendices 7–9 ) were distributed around the study team for independent review. For these summary tables, we organised the descriptive data around the specific dimensions of self-care support ‘typology’ derived from our previous NIHR study on self-care support. 15 Further details of the typology are provided in the service mapping chapter (see Chapter 4 ) but, for now, it is sufficient to report that the typology dimensions included the health conditions for which the self-care support intervention or service is designed; the theoretical basis of the intervention or service; its aims (i.e. what makes it a self-care intervention or service); the recipient (child/young person, parent or family); the delivery medium and the degree to which it is individualised; where it is delivered; and who leads it (i.e. the self-care support agent). Key findings from each study, in narrative form, were also included.
Following an independent review of the three summary tables, any patterns that individual team members identified in each data set were compared and contrasted with those of other team members so that there was a consensus on any key themes emerging from the data. These thematic analyses were compared with each other and with the effectiveness data from the meta-analysis in order to elicit an overall synthesis of the evidence on self-care support in CYP’s mental health.
Chapter 3 Systematic reviews and meta-analysis: results
This chapter presents the results from the systematic reviews. The effectiveness reviews and perceptions reviews are considered separately before being synthesised according to the principles outlined in the previous chapter. For the effectiveness review, we present first a brief, descriptive overview of the included studies, after which we present the results of a meta-analysis of the effectiveness data. Similarly, for the perceptions review, the two data sets (qualitative perceptions data and quantitative perceptions data) are initially described and then analysed. Finally, the four data sources – the descriptive effectiveness data, the meta-analysis data, the qualitative perceptions data and the quantitative perceptions data – are triangulated to elicit a synthesis of the literature on mental health self-care support for CYP.
Effectiveness review
Description of the included effectiveness studies
Descriptive data for the 71 included RCTs39,45–131 are summarised in Appendix 7 . Most (36/71) of the studies were conducted in North America (primarily the USA),49–51,53–57,62–69,77,83–85,87,91,92,95–98,101–104,111,115–126,132–135,137 around a quarter (17/71) in Australia39,47,48,58,59,75,76,78–82,86,88–90,94,105,108–110,113,114,136 and around 20% in Europe (16/7145,46,52,60,61,70–74,99,100,106,107,112,127,129–131,138,139 including seven in the UK52,70–72,74,99,100,127,129–131). The UK accounted for < 10% of the studies.
Around 60% (42/71) of the studies focused on mood disorders,39,45–50,52–59,61–64,66–69,77,81–85,88–91,93,94,103–106,108–114,118,119,121–126,129–131,138,139 mainly anxiety and depression (there was one on bipolar disorder135), with 12 (17%) focusing on serious behaviour problems65,73,75,76,79,80,87,95–102,104,127,132 such as ADHD, oppositional defiant disorder (ODD) and conduct disorder (CD), and eight (11%) on eating disorders. 60,70,71,92,115–117,120,134,136 There were relatively few studies focusing on post-traumatic stress disorder (PTSD) (n = 2),86,128 self-harm (n = 4)72,74,78,137 and generic mental health problems (i.e. interventions designed for any mental health problem; n = 3). 51,107,133 There were no studies on psychosis. Most (31/71) of the studies concerned interventions that could be classified as treatments (see Chapter 1 , Intervention levels),48–52,55,65,66,70,71,74,77,78,81,83–86,91,94–98,101–104,106,111,112,121–127,129–131,133,135,139 with the remainder focusing equally on indicated (n = 11),53,58,59,61–64,67,68,72,87,116,117,128 selective (n = 15)45,46,54,56,57,69,82,99,100,105,110,115,118–120,132,137,138 and universal (n = 15)39,47,60,73,75,76,79,80,88–90,92,93,107–110,113,114,134,136 interventions. If, along with treatment interventions, indicated interventions are broadly considered to be ‘management’ interventions and selective and universal interventions are broadly considered as ‘prevention’ interventions, then most of the interventions considered were designed to manage rather than prevent mental health conditions in CYP.
Most (47/71) of the interventions operated within a cognitive–behavioural framework,39,47–50,52–56,58–64,66–71,77,81–91,93,94,102–107,110–114,118,119,121–126,128–131,133,138,139 although few were labelled explicitly as CBT. Instead, the interventions tended to be described with vague reference to CBT, or to cognitive and/or cognitive–behavioural principles, or they listed elements commonly assumed to be associated with CBT such as cognitive restructuring (e.g. Dobson 2010;64 Garber 200967), problem-solving (e.g. de Cuyper 2004;61 Gillham 2006;68 Hunt 2009;82 Merry 2004;93 Spence 2003113) and exposure (e.g. Barrington 2005;48 Hayward 2000;77 Hudson 200981). Many of the interventions were what might be called ‘branded’ cognitive–behavioural approaches, often with idiosyncratic names, such as FRIENDS (Barrett 2005;47 Bernstein 2005;49 Hunt 2009;82 Lock 2003;88 Lowry-Webster 200139), Cool Kids (Hudson 2009;81 Mifsud 200594), Timid to Tiger (Cartwright-Hatton 201152) and Problem Solving for Life (Spence 2003113).
Parent training interventions were the second most popular group of interventions with around one-fifth of studies (16/71) employing such an approach. 49,50,52,56,73,75,76,79,80,86,87,94–102,112,127,132 In most cases, the parent training was shaped by a behavioural model, often social learning theory (e.g. Hiscock 2008;79 Thompson 2009;127 Patterson 200299,100). The remainder of the interventions were premised on approaches such as dissonance theory (Stice 2003;115 Stice 2006;116 Stice 2009120), mindfulness (e.g. Biegel 2009;51 Havighurst 200975) or general psychotherapeutic approaches (e.g. Stice 2008118), or they were eclectic (e.g. Arnarson 2009;45 Green 2011;72 Hazell 200978).
All of the interventions were ‘manualised’ in that there was a written manual giving instructions to those providing the intervention on how the intervention should be delivered. This is relatively unsurprising given that cognitive–behavioural and parenting interventions – interventions where manualisation is normally inherent – were in the majority. The degree of instruction in the manuals varied from intervention to intervention, with some having a degree of flexibility, but many were rigid, expecting full fidelity from those delivering the intervention.
The self-care elements of the interventions related predominantly to the acquisition of relevant skills, usually involving a method whereby the CYP or the parents are required to undertake some sort of practical exercise, either as part of the formal aspects of the intervention itself (such as a workbook or classroom exercise) or as a homework task. Despite the almost universal focus on ‘activities’ and the nature of the client group (children), surprisingly few activities seemed to centre on creativity and play. Many could be – indeed some were – described as tasks, a word that can have negative connotations. There were a few exceptions – the explicit use of games in Rooney 2006105 and the use of drama, dance and music in Tol 2008,128 for example – though it is worth noting that a lack of reference to creativity and fun in the descriptions of the interventions may be more to do with the sober writing style demanded of academic journals than with design faults in the interventions.
More than 80% of the studies related to interventions focusing on school-age children (5–16 years), with only four studies (Green 2011;72 Rohde 2004;104 Stice 2003;115 Stice 2006116) including 17-year-olds and only three (Hahlweg 2010;73 Patterson 2002;99,100 Thompson 2009127) targeting the under-fives. More than half (40/71) were targeted solely at the CYP,45,46,51,53–55,60–68,72,77,78,85,88,89,91–93,103–110,113–120,128,130,131,134,136–139 26 at the family (which usually meant parents and a child; rarely were siblings included),39,47–50,56–59,69–71,74,81–84,86,87,90,94–98,101,102,111,112,121–127,132,133,135 and only five focused on parents only. 52,73,75,76,79,80,99,100
All of the interventions were delivered face to face; none made use of technology, even technology as simple and ubiquitous as the telephone. Sixteen of the interventions were individual child/young person or individual family interventions;48,65,69–71,74,83–87,95–98,111,121–127,129–131,133,135 the remainder were group interventions or group interventions with occasional individual sessions. Of those studies where a delivery location was given, most of the interventions (33/71) took place in a school setting,39,45–47,49,50,53,57–60,62,63,65,73,82,90–98,102,103,105–110,113,114,116,117,120,128–132,134,136,137 14 at hospital sites or clinics,48,51,52,54,55,61,68,72,78,81,86,99,100,121–126,135 and only five took place in the home environment. 57,74,87,127,133
Where the professional background of the agent providing the support for self-care was known, psychologists tended to dominate, being the agent in over one-third (26/71) of the studies,45–48,52,53,56,58–60,64,69,73,81,83,84,86,91,101,102,105–107,111,112,115,118,119,138,139 though other professionals (teachers, n = 11;39,65,82,88–90,93,108–110,113,114,132,136,137 nurses, n = 8;57,79,80,87,99,100,103,120,127,137 counsellors, n = 753,62,63,82,94,110,120,137) were involved. The agent was a medical doctor (child psychiatrist) in only one study (Vostanis130,131). The agent’s principal responsibility was to deliver and facilitate the self-care support intervention, usually by running groups and individual sessions, though more extensive responsibilities were expected in some interventions, e.g. running summer camps and liaising with teachers (MTA 199995), or facilitating the child in the home-school environment (Pfiffner 2007102). In three-quarters (53/71) of the studies, the agents were trained specifically for the intervention,39,45–51,53–59,62–68,72–74,77–79,82–90,93,94,99,100,103–106,108–114,116–120,127,128,132,133,135,137–139 and in just over half (38/71) of the studies, the agents received formal supervision as part of the intervention protocol. 39,45–50,52,53,56–59,62,63,65,67–69,72–74,78,83–87,90,95–100,103,105,110–114,116–120,127,132,133,137
Outcome measures
A wide variety of outcome measures were employed in the 71 studies (see Chapter 2 , Table 4 ). As it was a necessary inclusion requirement, all 71 studies included a direct measure of CYP’s mental health symptomatology. There was, however, no specific pattern to the number, range or source of additional (secondary) outcome measures employed. Some studies employed only a single outcome measure [e.g. Conduct Problems Prevention Research Group (CPPRG) 2007132 had a single diagnostic measure of serious behaviour problems and Gillham 200668 a single measure of depression] whereas others (e.g. Biegel 200951 and Kolko 201087) had more than 10 different outcome measures. The range of secondary measures included, in 41 of the 71 studies,39,47,51,52,54–56,58,59,61–63,66,70–74,78–84,86–91,95–100,105,107,110,111,113–126,128–131,133,136,137 indirect measures of mental health symptomology (e.g. Clarke 200154 had a measure of externalising symptoms in an intervention designed for depression), as well as measures of general functioning (in 28 studies),51,53–55,65,66,70–72,74,78,85–87,91,95–102,104,106,108–111,113,114,116–119,128–131 resilience (nine studies),51,83,84,86,87,103,106,108,109,128,137 general well-being (three studies)51,87,107 and self-esteem (10 studies). 51,60–64,106,129–131,134,136 The direct mental health measures were mostly obtained from the CYP (in 56 studies),39,45–64,66–72,74,77,78,81–85,88–94,103–126,129–131,134,136–139 followed by clinicians (36 studies)45,46,48–55,58,59,66,67,69–72,77,78,81,83,84,86,87,91,102,104,106,110,112,118–132,135,138,139 and parents (27 studies). 39,48–50,52,54–56,65,69,73,75,76,79–81,86,87,90–101,104,106,111,127,129–133 Teachers only provided a direct mental health measure in eight studies. 48,65,73,75,76,94–98,101,106 The pattern was similar for the indirect mental health measures, although parents were a more frequent source: there were CYP self-report measures in 29 studies,47,51,56,61–63,66,70–72,78,81–84,86–89,91,95–98,105,107,110,111,113–117,120–126,129–131,136,137 parent report measures in 19 studies,39,52,54–56,58,59,61,66,73,79–81,83,84,86,87,90,95–100,111,129–131,133 clinician report measures in 10 studies54,55,70–72,74,78,87,113,114,118,119,128 and teacher reports in five studies. 73,83,84,87,95–98,111 General functioning data were collected equally by child self-report (11 studies),70,71,74,99,100,104,106,108–110,113,114,116–119,128 parent report (10 studies)65,66,74,87,95–102,111,128 and clinician report (11 studies). 51,53–55,72,78,85,86,91,104,129–131 Teachers only provided data on general functioning in four studies. 65,95–98,101,102 Resilience data were collected from CYP in seven studies,83,84,86,87,103,106,108,109,137 from a parent in one study83,84 and from a clinician in one study. 128 General well-being data were obtained solely from child self-report and in only three studies. 51,87,107 Self-esteem data were collected by child self-report in 10 studies51,57,60–64,106,129–131,134,136 and from a parent in one study. 129–131 Full details of the outcome measures extracted for each study can be found in Appendix 6 ; for a summary of the number of outcome measures of each type, see Table 4 .
As indicated in Table 4 , the majority of outcome measures focused on mental health symptomatology in the CYP, whether directly or indirectly related to the condition of interest. General functioning was measured in a sizeable number (n = 28; 39%) of the papers51,53–55,65,66,70–72,74,78,85–87,91,95–102,104,106,108–111,113,114,116–119,128–131 but few focused on CYP’s resilience, general well-being or self-esteem. Most of the outcome measures were obtained directly from the CYP with clinicians or parents being the most frequent secondary source. Few studies collected outcome data from teachers.
Meta-analysis results
The results of the primary and secondary analyses from the meta-analysis are presented here. Our primary analysis was concerned with the long-term effectiveness of self-care support interventions for CYP’s mental health. Secondary analyses explored a range of comparisons determined a priori through our previous typology, the expertise of the project team and in consultation with the SAG. Analyses were conducted at two follow-up time points: 6 months and 12 months. In interpreting our results, we have adopted standard conventions on effect size179 and study heterogeneity. 144 Regarding effect size, standardised mean differences (SMDs) of 0.2, 0.5 and 0.8 reflect small, medium and large intervention effects, respectively. I 2 measures exceeding 75%, 50% and 25% are taken to reflect high, moderate and low heterogeneity, respectively, across the contributing studies.
Primary analysis
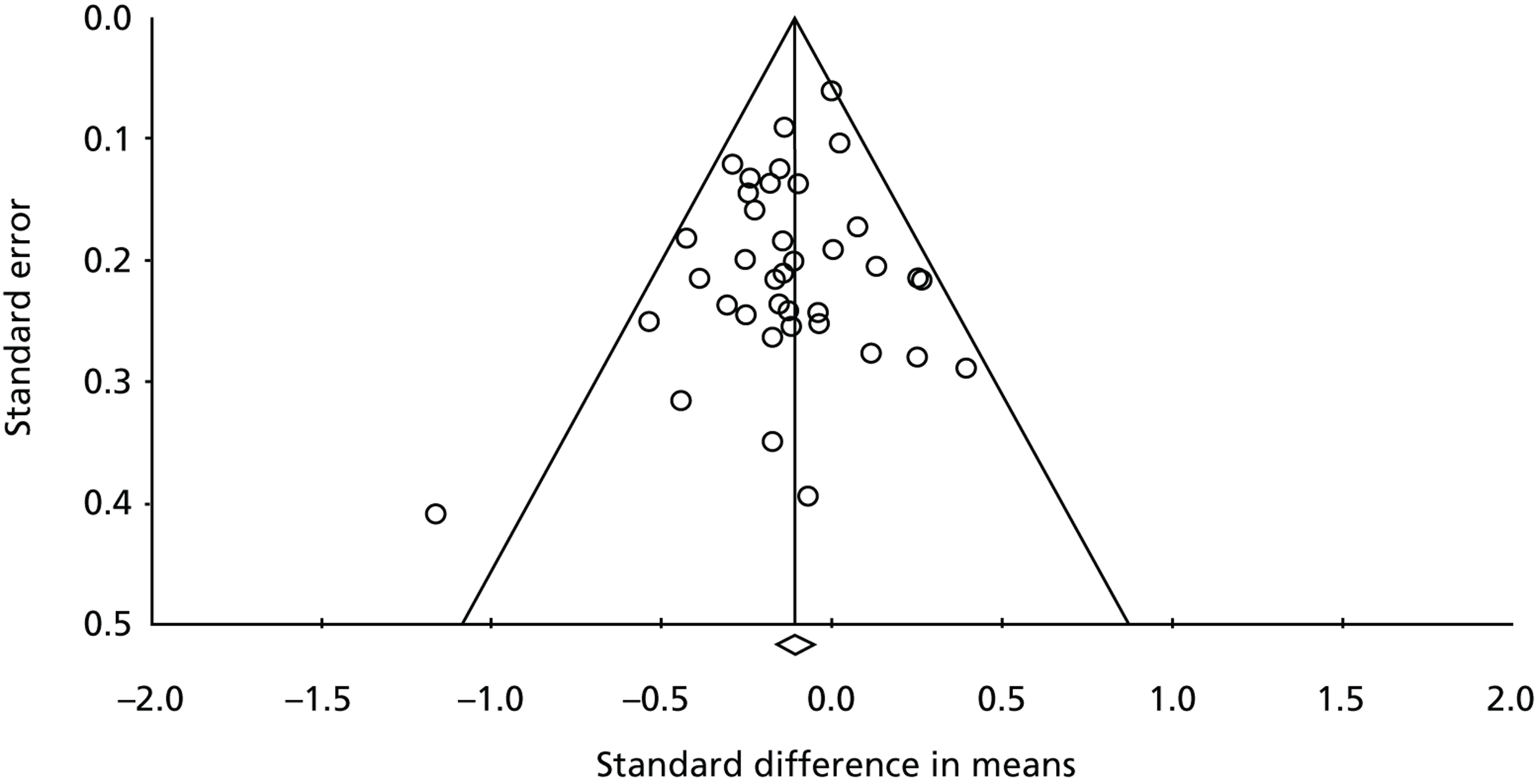
The results of the primary analysis are contained in Table 6 ; forest plots for 6-month (with and without outliers) and 12-month follow-up can be found in Figures 8 , 9 and 10 , respectively.
| Follow-up | Comparisons | Participants | SMD | L 95% | U 95% | I 2 (%) |
|---|---|---|---|---|---|---|
| 6 months, outliers included | 50 | 8362 | −0.34 | −0.46 | −0.21 | 78 |
| 6 months, outliers excluded | 47 | 8210 | −0.20 | −0.28 | −0.11 | 49 |
| 12 months | 48 | 4204 | −0.12 | −0.17 | −0.06 | 13 |
FIGURE 8.
Forest plot for the studies with 6-month follow-up data, outliers included. CI, confidence interval; ES, effect size; IAFS, Intervención en Adolescentes con Fobia Social (Intervention for Adults with Social Phobia); TADS, Treatment for Adolescents with Depression Study.
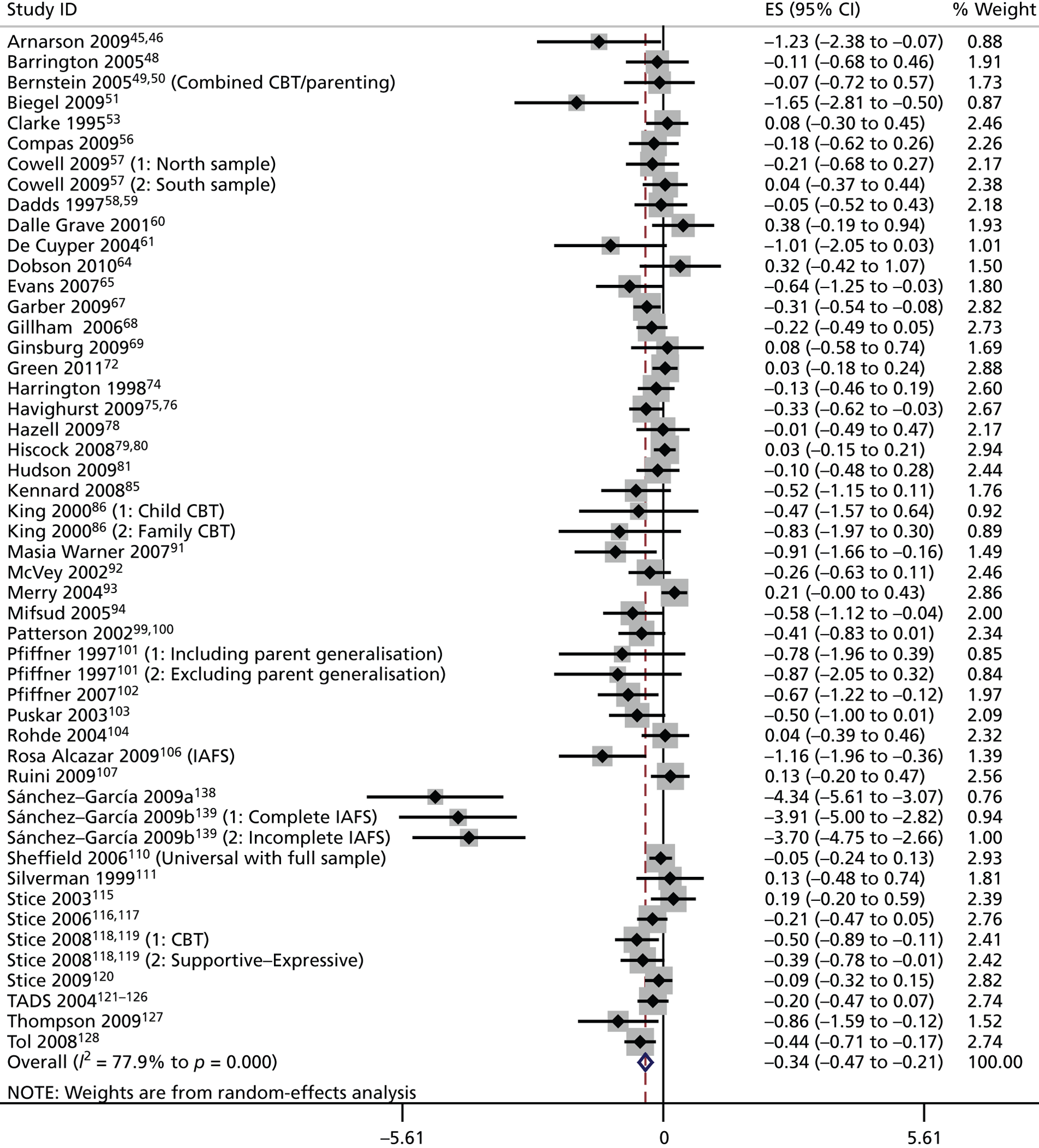
FIGURE 9.
Forest plot for the studies with 6-month follow-up data, outliers excluded. CI, confidence interval; IAFS, Intervención en Adolescentes con Fobia Social (Intervention for Adolescents with Social Phobia); TADS, Treatment for Adolescents with Depression Study.
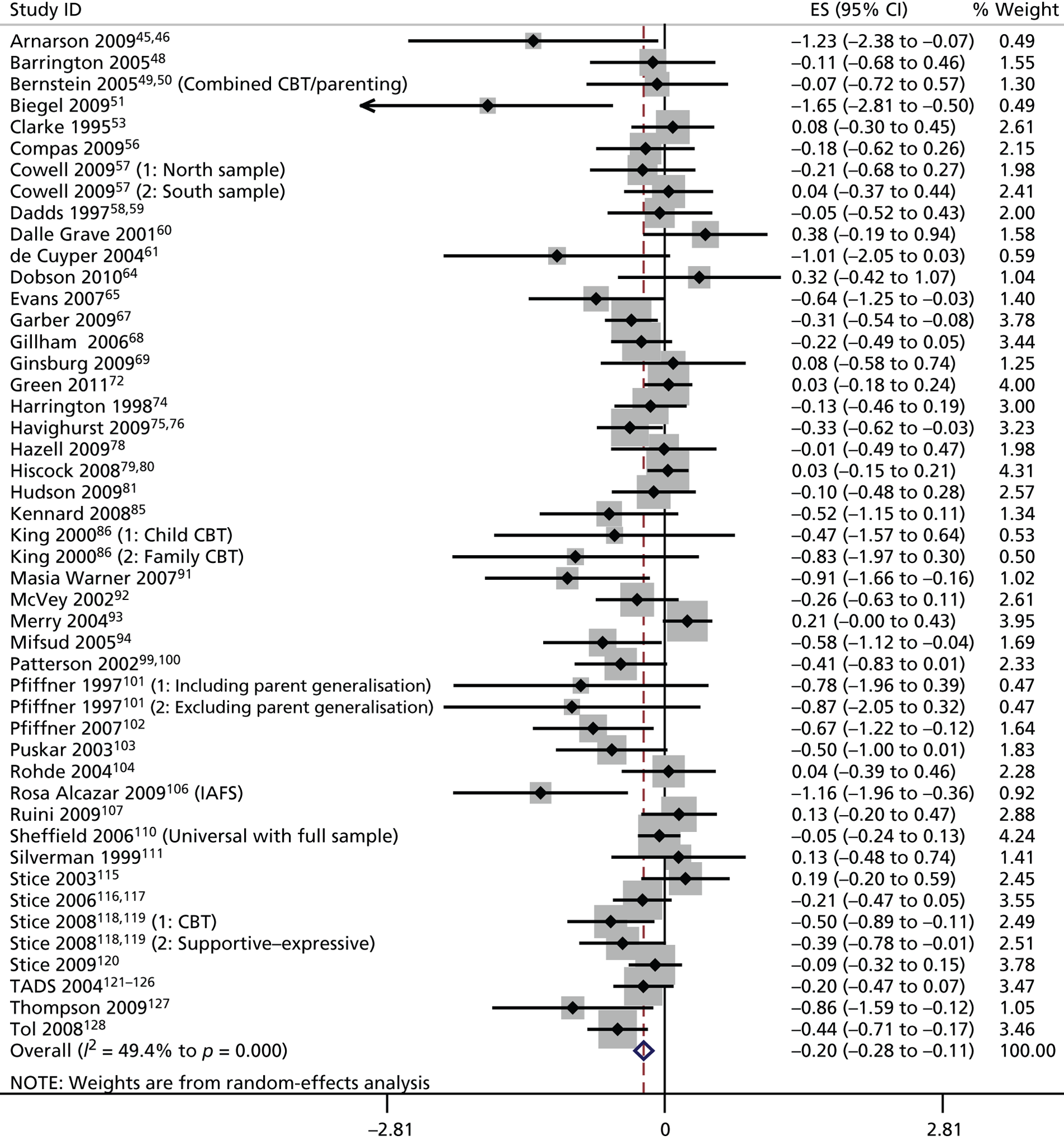
FIGURE 10.
Forest plot for the studies with 12-month follow-up data. CI, confidence interval; IAFS, Intervención en Adolescentes con Fobia Social (Intervention for Adolescents with Social Phobia); TADS, Treatment for Adolescents with Depression Study.
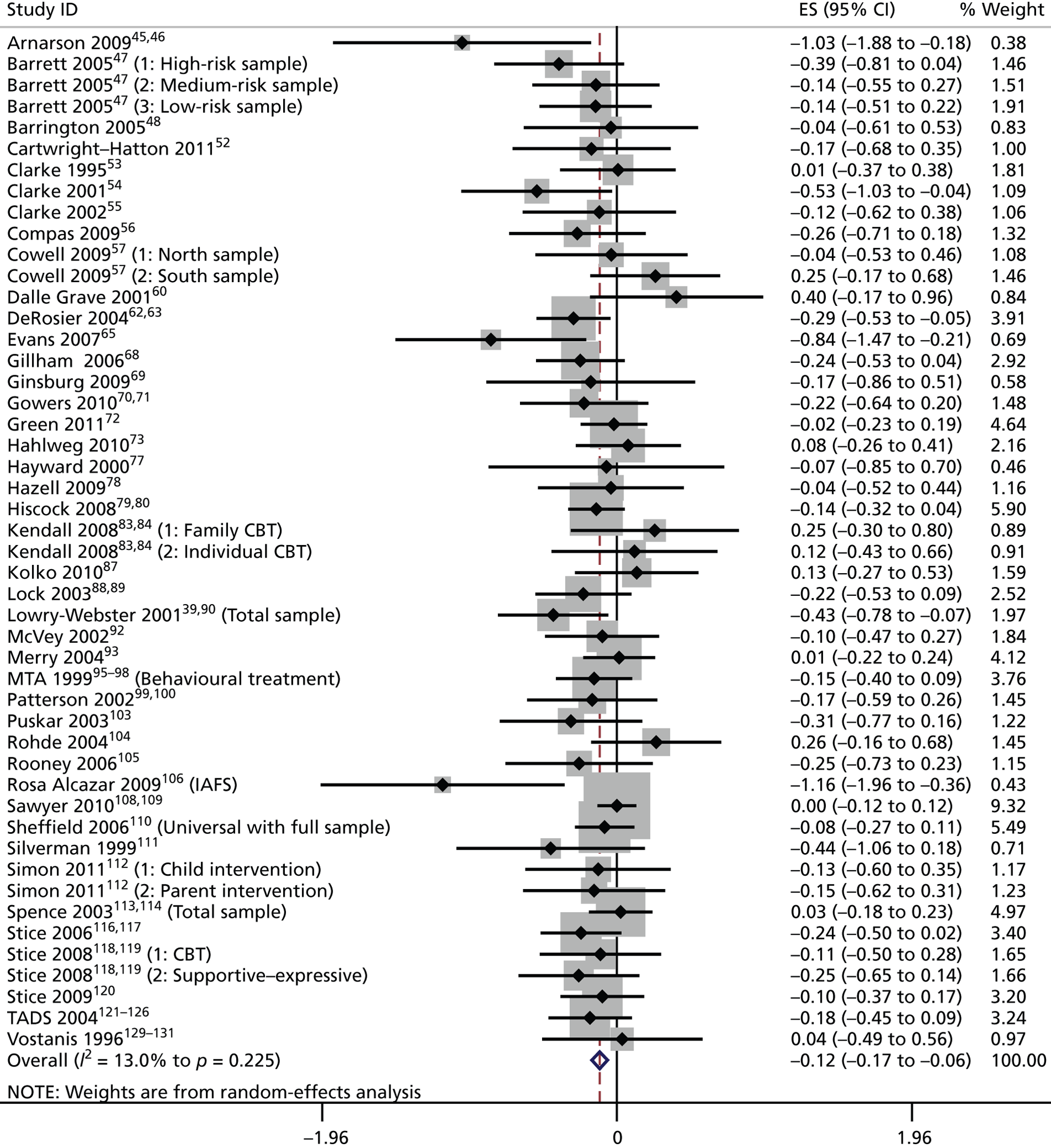
Before discussing the results of the primary analysis, a comment needs to be made about the outliers in the 6-month follow-up data. Three studies from the same research team (Sánchez-García 2009a,138 and the two substudies from Sánchez-García 2009b139) had 6-month data that were included in the primary analysis. However, as is clear from the forest plot in Figure 8 , these studies were outliers. Including these three studies in the meta-analysis meant that inconsistency across the studies, as measured by I 2, increased from moderate to high (see Table 6 ). Accordingly, a decision was made to exclude these outliers, and the analysis with them included is reported here merely for transparency. Furthermore, these outliers were not included in any of our secondary analyses.
The results of our primary analysis imply that self-care support interventions are associated with a ‘medium’ effect on CYP’s mental health in the short to medium term, but the effect declines as time passes (a small intervention effect was sustained at 6-month follow-up, becoming clinically insignificant at 12-month follow-up). I 2 values suggest that there is greater study consistency at the 12-month follow-up than at the 6-month follow-up.
Quality appraisal: sensitivity analysis
As outlined in Chapter 2 , quality appraisal in the meta-analysis was based on a sensitivity analysis using concealment of allocation as a moderator. We deemed ‘high quality’ studies to be those studies where the two assessors agreed that concealment was adequate; ‘low quality’ studies were those where concealment was agreed to be inadequate or reporting was unclear. ‘High quality’ studies were generally in the minority. Table 7 provides details of the sensitivity analysis conducted.
| Follow-up | Quality | Comparisons | SMD | L 95% | U 95% | I 2 (%) |
|---|---|---|---|---|---|---|
| 6 months | High | 7 | −0.04 | −0.21 | 0.13 | 64 |
| Low | 40 | −0.23 | −0.32 | −0.14 | 35 | |
| 12 months | High | 9 | −0.06 | −0.13 | −0.01 | 0 |
| Low | 39 | −0.15 | −0.22 | −0.07 | 19 |
The results of the sensitivity analysis demonstrate a finding similar to the primary analysis when only the ‘low quality’ studies are considered (a ‘medium’ effect that attenuates with time) but a negligible effect across both time points when only the ‘high quality’ studies are considered.
Publication bias
Funnel plots for the two follow-up points are shown in Figures 11 and 12 respectively. The asymmetry in the funnel plots, particularly at 6 months, may reflect some degree of publication bias.
FIGURE 11.
Funnel plot of standard error by standard difference in means for the studies with 6-month follow-up data.
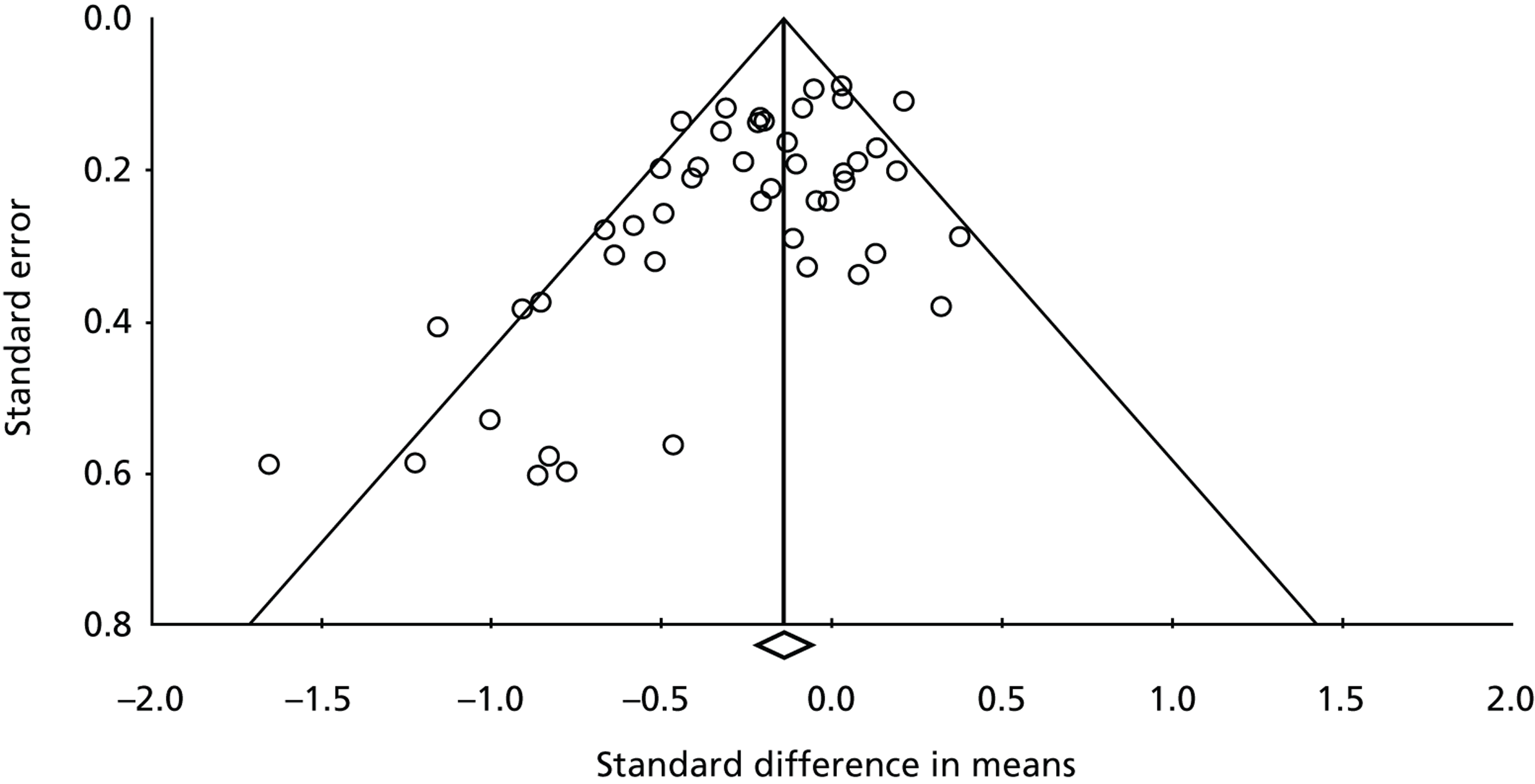
FIGURE 12.
Funnel plot of standard error by standard difference in means for the studies with 12-month follow-up data.
Secondary analyses
The secondary analyses that we carried out related to additional characteristics of the populations and the interventions that might be related to the impact of interventions, namely:
-
intervention level (in terms of whether it was a universal, selective, indicated or treatment intervention)
-
the mental health condition targeted
-
the age of the CYP
-
the theoretical perspective of the intervention
-
the recipient (CYP, parent, family)
-
whether it was school-based or not
-
whether it was group or individual
-
whether the agent was mental health trained or not.
For some dimensions that we had anticipated exploring (e.g. whether the intervention was delivered face to face or via some electronic or telehealth method), we were unable to conduct analyses because there was insufficient variability in the included studies.
Intervention level
This analysis considered whether or not there were differing degrees of effectiveness when the interventions were categorised according to the levels of the intervention hierarchy discussed in Chapter 1 . A summary of the results can be found in Table 8 .
| Follow-up | Level | Comparisons | SMD | L 95% | U 95% | I 2 (%) |
|---|---|---|---|---|---|---|
| 6 months | Prevention | 9 | −0.08 | −0.24 | 0.08 | 64 |
| Selective | 8 | −0.11 | −0.28 | −0.06 | 22 | |
| Indicated | 10 | −0.17 | −0.31 | −0.03 | 41 | |
| Treatment | 20 | −0.38 | −0.55 | 0.22 | 38 | |
| 12 months | Prevention | 16 | −0.07 | −0.14 | 0.00 | 4 |
| Selective | 19 | −0.18 | −0.36 | 0.00 | 26 | |
| Indicated | 6 | −0.14 | −0.26 | −0.01 | 19 | |
| Treatment | 5 | −0.14 | −0.26 | −0.03 | 14 |
An interesting pattern emerges from this analysis in that the effectiveness of the self-care support intervention appears to increase as the interventions become more targeted and specialised. Those classified as treatment interventions are the most effective at 6-month follow-up, with a moderately large effect size, and indicated interventions, the prior intervention level, have a reasonable effect. At 12-month follow-up, selective, indicated and treatment interventions are modestly effective. At both time points, prevention interventions appear to be relatively ineffective. This statement, however, needs to be treated cautiously because (1) this analysis is exploratory and there may well be other factors confounding the results; and (2) the prospective nature and purpose of prevention interventions may be such that it is inappropriate to compare them with interventions designed to treat specific conditions, a point that we will pick up in the discussion.
Mental health condition
Across the two follow-up points, only four conditions had a meaningful number of studies available for analysis: anxiety disorders, depression, serious behaviour problems and eating disorders. The results of the comparisons across these four conditions can be found in Table 9 .
| Follow-up | Condition | Comparisons | SMD | L 95% | U 95% | I 2 (%) |
|---|---|---|---|---|---|---|
| 6 months | Anxiety disorders | 10 | −0.19 | −0.43 | 0.04 | 46 |
| Depression | 18 | −0.19 | −0.32 | −0.06 | 51 | |
| Behaviour problems | 8 | −0.43 | −0.70 | −0.15 | 61 | |
| Eating disorders | 5 | −0.06 | −0.25 | 0.12 | 35 | |
| 12 months | Anxiety disorders | 16 | −0.22 | −0.33 | −0.12 | 0 |
| Depression | 19 | −0.08 | −0.15 | 0.00 | 15 | |
| Behaviour problems | 6 | −0.12 | −0.29 | 0.05 | 38 | |
| Eating disorders | 5 | −0.12 | −0.28 | 0.03 | 6 |
At 6 months, self-care support interventions were most effective for behaviour problems (a moderate effect size), with interventions for anxiety disorders and depression also showing a small effect. The effects appear to be maintained for anxiety disorders at 12-month follow-up. For depression, the effect seems to have attenuated at 12 months. For serious behaviour problems, there was still an effect at 12 months but it was small compared with the effect at 6 months. There were very small effects for eating disorders at the 6-month follow-up point and, interestingly, there is a hint that effects may increase with time.
Age
We divided the studies according to a commonly assumed demarcation between ‘children’ and ‘young people’: the age of 12 years. A summary of the results can be found in Table 10 .
| Follow-up | Age (years) | Comparisons | SMD | L 95% | U 95% | I 2 (%) |
|---|---|---|---|---|---|---|
| 6 months | Under 12 | 24 | −0.24 | −0.37 | −0.12 | 34 |
| 12 and over | 22 | −0.16 | −0.28 | −0.04 | 60 | |
| 12 months | Under 12 | 21 | −0.11 | −0.20 | −0.03 | 3 |
| 12 and over | 21 | −0.09 | −0.17 | −0.01 | 22 |
At 6-month follow-up, self-care support interventions for ‘children’ (aged under 12 years) are slightly more effective than those for ‘young people’ (those aged 12 years and over), with both having small effects. The difference between the SMDs in the two groups (0.06) is, however, negligible. At 12-month follow-up, the effects are attenuated but there is still a modest effect for both age groups.
Theoretical model
As discussed earlier in this chapter, self-care support interventions based on cognitive–behavioural principles and parent training dominated the included studies. This meant that there were few studies considering other models, so this analysis is confined to those interventions using cognitive–behavioural principles, parent training or a mixture of both. This analysis examined whether the principal models identified were effective alone or in combination. A summary of the results can be found in Table 11 .
| Follow-up | Model | Comparisons | SMD | L 95% | U 95% | I 2 (%) |
|---|---|---|---|---|---|---|
| 6 months | CB principles | 26 | −0.15 | −0.27 | −0.03 | 56 |
| Parent training | 10 | −0.23 | −0.40 | −0.05 | 54 | |
| Mixed | 4 | −0.39 | −0.70 | −0.08 | 0 | |
| 12 months | CB principles | 32 | −0.12 | −0.19 | −0.06 | 7 |
| Parent training | 6 | −0.13 | −0.24 | −0.03 | 0 | |
| Mixed | 3 | −0.08 | −0.33 | 0.18 | 0 |
At 6-month follow-up, both models seem reasonably effective, but it is interesting that the effect is much larger in self-care support interventions where the two approaches are combined. This result is not reflected at the 12-month follow-up, however, where all of the approaches, including the combined approach, elicit only modest effects.
Recipient
This analysis examined whether self-care support interventions were more effective when targeted at the CYP alone, the family as a whole or solely at parents. Table 12 contains a summary of the results.
| Follow-up | Recipient | Comparisons | SMD | L 95% | U 95% | I 2 (%) |
|---|---|---|---|---|---|---|
| 6 months | Child/young person only | 27 | −0.20 | −0.32 | −0.08 | 57 |
| Family | 16 | −0.20 | −0.32 | −0.08 | 0 | |
| Parent only | 3 | −0.20 | −0.49 | 0.10 | 69 | |
| 12 months | Child/young person only | 27 | −0.11 | −0.25 | −0.06 | 33 |
| Family | 15 | −0.16 | −0.25 | −0.06 | 0 | |
| Parent only | 5 | −0.11 | −0.25 | 0.03 | 0 |
No clear pattern emerges from these results. At 6 months, self-care support interventions appear to be equally effective (with a small effect size), regardless of whom the recipient of the intervention is. At 12 months, family-targeted self-care support interventions appear to have a slight advantage over the child- or parent-only interventions.
School-based interventions
This analysis examined whether or not school-based self-care support interventions were more effective than interventions conducted in other settings such as hospitals, clinics, other community-based locations and the child or young person’s own home. The results are summarised in Table 13 .
| Follow-up | School based | Comparisons | SMD | L 95% | U 95% | I 2 (%) |
|---|---|---|---|---|---|---|
| 6 months | Yes | 21 | −0.21 | −0.34 | −0.07 | 60 |
| No | 13 | −0.17 | −0.31 | −0.02 | 43 | |
| 12 months | Yes | 24 | −0.13 | −0.22 | −0.05 | 42 |
| No | 12 | −0.12 | −0.22 | −0.03 | 0 |
Whether self-care support interventions are school based or not seems to have no influence on their effectiveness. There is a slight advantage to school-based interventions at 6-month follow-up (both exhibit a small effect) but the difference between the SMDs (0.04) is negligible; at 12 months, they both have a modest effect.
Group versus individual intervention
This analysis examined whether or not group self-care support interventions were more effective than individual interventions. Two sets of analysis were conducted, one looking at those interventions using a group, individual or mixed group/individual format regardless of the recipient (child/young person, parent or family; Table 14 ), and one looking at those interventions targeting only CYP ( Table 15 ).
| Follow-up | Format | Comparisons | SMD | L 95% | U 95% | I 2 (%) |
|---|---|---|---|---|---|---|
| 6 months | Group | 34 | −0.18 | −0.28 | −0.08 | 56 |
| Individual | 10 | −0.24 | −0.40 | −0.08 | 3 | |
| Mixed | 3 | −0.27 | −0.73 | 0.19 | 58 | |
| 12 months | Group | 34 | −0.13 | −0.19 | −0.07 | 14 |
| Individual | 10 | −0.11 | −0.28 | 0.05 | 18 | |
| Mixed | 4 | −0.01 | −0.15 | 0.13 | 13 |
| Follow-up | Format | Comparisons | SMD | L 95% | U 95% | I 2 (%) |
|---|---|---|---|---|---|---|
| 6 months | Group | 29 | −0.19 | −0.30 | −0.07 | 60 |
| Individual | 5 | −0.30 | −0.50 | −0.09 | 0 | |
| Mixed | 3 | −0.27 | −0.73 | 0.19 | 57 | |
| 12 months | Group | 28 | −0.14 | −0.22 | −0.08 | 26 |
| Individual | 5 | −0.16 | −0.43 | 0.11 | 36 | |
| Mixed | 4 | −0.01 | −0.15 | 0.13 | 0 |
For all recipients, individual interventions appeared to be slightly more effective at 6-month follow-up, though both types of intervention could be described as eliciting a small effect. Mixing the two types of intervention elicits the biggest effect but this finding needs to be treated with caution given the number of comparisons (n = 3) available. At 12-month follow-up, there was little to distinguish between group and individual interventions (both having modest effect sizes) and mixing the two appeared to produce no effect.
The findings are similar when only CYP recipients are considered, except that the effect for individual interventions is perhaps more pronounced at 6 months. Again, there is little to distinguish between the two types of intervention at 12 months.
In all, this analysis hints that, despite being in the minority of studies, individual self-care support interventions may be more effective than group interventions.
Mental health or generic agent
This analysis examined whether self-care support interventions delivered by mental health-trained staff (such as clinical psychologists or mental health nurses) were more effective than those where the agent was not mental health trained (general nurses, teachers and educational psychologists, for example). The results are summarised in Table 16 .
| Follow-up | Staff | Comparisons | SMD | L 95% | U 95% | I 2 (%) |
|---|---|---|---|---|---|---|
| 6 months | MH | 20 | −0.21 | −0.33 | −0.09 | 36 |
| Non-MH | 20 | −0.18 | −0.31 | −0.05 | 60 | |
| 12 months | MH | 19 | −0.15 | −0.25 | −0.06 | 9 |
| Non-MH | 22 | −0.10 | −0.18 | −0.03 | 28 |
At 6-month follow-up, there was little to distinguish between the SMDs for mental health and non-mental health-trained staff. At 12-month follow-up, self-care support interventions delivered by mental health-trained staff were only marginally more effective than interventions delivered by non-mental health staff. This suggests that, to be effective, self-care support interventions do not have to be delivered and facilitated by mental health-trained staff, although this is not the same as saying that the agents do not need to have some understanding of mental health in CYP.
Length of intervention
Length of intervention – or perhaps more correctly, contact time with the agent – was examined by making an arbitrary split at 12 hours of contact time so that a ‘short’ intervention was 12 hours or less and a ‘long’ intervention, more than 12 hours. The results of this analysis are presented in Table 17 .
| Follow-up | Length | Comparisons | SMD | L 95% | U 95% | I 2 (%) |
|---|---|---|---|---|---|---|
| 6 months | Short | 19 | −0.14 | −0.26 | −0.01 | 38 |
| Long | 17 | −0.28 | −0.43 | −0.13 | 41 | |
| 12 months | Short | 24 | −0.10 | −0.16 | −0.04 | 0 |
| Long | 14 | −0.13 | −0.28 | −0.01 | 35 |
At 6-month follow-up, the length of the intervention appears to be related to the effectiveness of the intervention, though the effect is attenuated at 12 months. This gives some hints, at least as far as the short-term effectiveness of self-care support interventions is concerned, that length of the intervention or amount of contact time may be important, in that longer interventions appear to be more effective.
Summary of the meta-analysis results
Self-care support interventions appear to be modestly effective in CYP’s mental health, though the generally low quality of the studies considered and the asymmetry in the funnel plots means that this statement has to be made with reservations. Regarding specific dimensions of self-care support that might influence the effectiveness of an intervention, there is some evidence that individual interventions may have an advantage over group interventions, that those delivering and facilitating the interventions need not necessarily be mental health trained, that more contact time with the self-care support agent may be beneficial and that the setting of the intervention (home, school, etc.) is largely irrelevant.
Perceptions review
Description of the qualitative perceptions data
Descriptive details of the qualitative papers included in the perceptions review following quality appraisal are summarised in Appendix 8 . Our initial pool of 33 studies with nominally qualitative data contained 17 studies in which participants’ views on self-care support interventions were obtained from open-ended questions on a satisfaction survey, conducted as part of a controlled or uncontrolled trial; 12 qualitative (focus group or interview) studies; and four service evaluations. Of these, 11 qualitative studies,71,100,147,149,150,152,153–157 one service evaluation148 and one study with data from an open-ended satisfaction survey151 met our quality criteria.
The 13 included papers comprised three British studies (Garraway 2010;153 Gowers 2010;71 Stewart-Brown 2004100), four from the USA,151,152,154,157 two from Australia,149,150 and one each from Jamaica,147 Ireland,148 Hong Kong155 and Denmark in collaboration with Lithuania. 156 A range of mental health conditions were covered: four considered general mental health conditions (where a specific condition was not stipulated),148,152,153,156 three eating disorders71,155,157 and three serious behaviour problems,100,147,150 two mood disorders (anxiety and depression)149,151 and one psychosis. 154 No studies considered self-harm or PTSD. Most of the self-care support interventions were interventions designed to manage the mental health condition rather than prevent it.
There was no particular pattern to the theoretical perspectives that the interventions employed, with social learning theory,100,147 solution-focused therapy,148 behavioural parent training,100,157 family therapy155 and multidimensional, eclectic approaches71,157 all being represented. All but one of the interventions (Garraway 2010153) were professionally led. Interestingly, this exception was unique in that the focus of the intervention – mentoring – was less structured and more informal than the others. There was a mixture of agents delivering and facilitating the intervention, with no real profession dominating. Nine of the interventions were group interventions. All were community-based (clinic, community centre or school) though none were delivered in the home. Only 4 out of the 13 were manualised. Six were targeted at the CYP only, four at parents only and three at the family, including, in one study (Kennedy 2008154), siblings. The interventions in the studies were almost all face to face, with only one (Coyle 2009148) employing computer technology.
Analysis of the qualitative perceptions data
The key message emerging from the included studies is that the acquisition of knowledge and skills is an important feature of interventions – for both parents and CYP – whether as a direct result of the intervention itself or as a result of learning from other participants through the sharing of tips and experiences (see, for example, Eacott 2008149). The skills involved varied from social skills (e.g. Fristad 1998151) to coping skills (e.g. Eacott 2008;149 Garcia 2010;152 Mishara 2006156) to communication skills (e.g. Garraway 2010;153 Kennedy 2008154) and were acquired via a variety of practical methods including homework tasks, workbooks and skills practice, but they might all be loosely termed as behavioural and/or emotional self-management. Peer support also seemed to be an important aspect of the self-care support intervention, being identified in over half of the studies (Eacott 2008;149 Friars 2007;150 Fristad 1998;151 Garcia 2010;152 Garraway 2010;153 Kennedy 2008;154 Zucker 2005157). Peer support provided the opportunity to learn from the experiences of other participants – an experience that could provide normalisation, increased emotional support and decreased isolation, and which attenuated feelings of being ‘different’.
The relationship with the therapist/agent appeared to be important, even to the point of the individual expertise and personal qualities of the agent being more important than the intervention itself (most evident in Garcia 2010,152 Gowers 201071 and Ma 2008155). On the other hand, in one of the studies (Coyle 2009148), the intervention – a facilitated computer game – appeared to be much more appealing than the agent, and the agents, perhaps unsurprisingly, tended to be generally less positive about the intervention than the young people using it.
There were some specific observations from individual studies that are worth mentioning: that the intervention could have an impact on the self-care support agent’s skills as well as those of the child/young person or parent (Baker-Henningham 2009147); that the intervention might not necessarily be suitable for everyone (Friars 2007150) or that specific elements of the intervention might not be liked or suitable (Stewart-Brown 2004100); that families can – indeed, should – be seen as change agents (Ma 2008155), although families do not necessarily have to be supported together (it might be better to support parents and CYP separately); and that a wider view of ‘family’ to include siblings, for example, might be valuable (Fristad 1998151).
However, perhaps the most striking feature of the qualitative studies is a lack of pattern in terms of the intervention, agent, condition or the individual it is targeted at, which could suggest that self-care support approaches are applicable across a range of settings and a range of conditions.
Description of the quantitative perceptions data
As outlined in Chapter 2 , Quality assessment, 36 studies with quantitative perceptions data were selected for the perceptions review. 39,48,51,69–71,73,74,83–85,87,90,91,93,101,102,110,113,118,119,136,158–177 All of these were randomised trials with a true control of some sort, including one (Gowers70,71) which was a mixed-methods study. Eighteen (half) of the studies were also included in the effectiveness review. 39,48,51,69–71,73,74,83–85,87,90,91,93,101,102,110,113,118,119,136 The 36 studies are summarised in Appendix 9 .
In most cases, the quantitative perceptions data were derived from a satisfaction questionnaire (usually study-specific and rarely validated) that had been included as an additional aspect of the trial. Occasionally, related concepts such as ‘usefulness’ (Barrett 2000;158 Merry 2004;93 Webster-Stratton 2001;175 Webster-Stratton 2011177) and ‘helpfulness’ (Ginsburg 200969) were considered instead. Over one-third (13/36) of studies collected data from parents only,48,69,73,87,158,162,164,166,168,169,171,175,177 five from the CYP only,51,83,84,118,119,136,163 10 from both parents and children,70,71,74,85,91,101,159–161,165,167,173,174 four from parents and teachers,102,170,172,176 two from the CYP and teachers,93,113 and two from the CYP, parent and self-care support agent. 39,90,110
Over 80% of the studies were conducted in the USA (16/36)51,69,83–85,87,91,101,102,118,119,163,165,170,172,175–177 and Australia (13/36);39,48,90,110,113,136,158–161,164,167,169,171,173,174 of the remaining studies, only three were conducted in the UK (all in England: Gardner 2006;162 Gowers 2007;70,71 Harrington 199874). A range of mental health conditions were covered, with most studies focusing on serious behaviour problems (16 studies)73,87,101,102,158,162,164,166,168–172,175–177 or mood disorders (11 studies on anxiety disorders;39,48,69,83,84,90,91,159–161,163,165,167,173,174 five on depression85,93,110,113,118,119); there were few studies on eating disorders and no studies on psychosis or PTSD. More than three-quarters (29/36) of the studies concerned management interventions (indicated and treatment-level interventions);39,48,51,70,71,74,83–85,87,90,91,101,102,110,158–168,170,171–177 preventative (selective and universal) interventions were in the minority. Most of the interventions were premised on cognitive–behavioural principles or parent training, and all except one101 were identified as manualised; more than half (20/36) of the interventions were targeted at families,39,48,69–71,74,83,84,87,90,102,158,159–161,165–168,171–174,176,177 one-third (12/36) at the CYP only51,85,91,93,101,110,113,118,119,136,163,170,175 and just four at parents only. 70,162,164,169 Regarding the delivery location, most (14/36) were delivered at a hospital or clinic,48,51,70,71,158–161,166,168,169,171,173–177 with 11 being delivered in a school setting;39,73,90,91,93,102,110,113,136,163,164,170 only three were delivered at home. 74,87,172 One (Gardner 2006162) was delivered in a ‘charity setting’ and two (Khanna 2010;165 March 2009167) were delivered online. The location was unclear in the remaining studies. Psychologists were in the majority as the self-care support agent but they accounted for less than half (14/33) of the interventions;48,69,73,83,84,91,101,102,118,119,163–165,168,171,174 a range of specific (e.g. teachers and counsellors39,90,93,110,113,136,170) and non-specific (e.g. ‘online therapist’,167 ‘certified group leaders’177 and ‘a trained member of the team’70,71) agents provided the support in the other interventions.
Analysis of the quantitative perceptions data
The quantitative perceptions data are limited in that many studies merely report a percentage for satisfaction or the number of respondents satisfied with the intervention. However, a number of salient observations can be drawn from the data, particularly when comparisons have been made within the studies. Firstly, although the overall levels of satisfaction throughout are remarkably high in some instances (e.g. Barrington 2005;48 Ginsburg 2002;163 Harrington 1998;74 Kendall 2008;83 Masia-Warner 200791), there is satisfaction irrespective of whether the participants received the self-care support intervention or the control. Secondly, there were often differences in the CYP’s ratings compared with the parent or teacher ratings, with the child or young person usually being less positive about the intervention than the parent or teacher (e.g. Gowers 2007;70,71 Masia-Warner 2007;91 Molina 2008170). Thirdly, it seems that what adults (parents and teachers) rate highly is not necessarily the same as what CYP rate highly. Elements of the interventions that parents rated highly often related to the specific skills being taught, whereas the CYP seemed more concerned about the activities being fun and enjoyable. A case in point is in Lowry-Webster 2001,39 where both CYP and parents rated specific elements of an intervention for anxiety disorders. Parents rated ‘recognising feelings in others’ as the most useful skill taught whereas the CYP rated ‘relaxation exercises’ as the most useful.
In some studies (e.g. Molina 2008;170 Seeley 2009172), teachers’ satisfaction was generally muted compared with that of parents, and teachers identified some specific issues when they were acting as the self-care support agent. In Merry 2004,93 which examined an intervention for depression, teachers did not like the inflexibility of the manual. Time also seemed to be an issue for teachers; in Molina 2008,170 which examined an intervention for serious behaviour problems, teachers were worried about how much the intervention would impact on their time and on their other duties and responsibilities, and in a study that considered a self-care support intervention for depression (Spence 2003113), they did not have time to complete all the activities specified in the manual.
The two online interventions (Khanna 2010;165 March 2009167) elicit interesting findings regarding satisfaction in that in Khanna 2010,165 the online intervention was rated equally as high as a face-to-face alternative, and in March 2009,167 both children and parents reported only moderate satisfaction levels.
There was evidence that not all children favoured the same intervention, however highly others may have rated it. This was most common in interventions based on cognitive–behavioural principles. For example, in one study (Lowry-Webster 200139), only 66% of CYP said they would use the skills taught, implying that one-third would not; in another (Spence 2003113), almost one-third of CYP said they would not recommend the intervention to others; and in a third study (Shortt 2001173), 17% merely described it as ‘OK’. In an eating disorders intervention (O’Dea 2000136), 10% of CYP did not find the intervention valuable.
Chapter summary: integrating the reviews
In attempting to integrate the effectiveness and perceptions reviews, a number of general observations can be made about the literature as a whole. First, the literature is skewed towards research that attempts to test the effectiveness of self-care support interventions. Research focusing on CYP’s or parents’ views about self-care support interventions is relatively limited; indeed, we found only 12 qualitative studies that met our quality criteria compared with as many as 181 RCTs (although, as outlined in Chapter 2 , we focused only on the 71 RCTs with long-term follow-up data for our effectiveness review). Second, regardless of methodology, most of the literature has emanated from either the USA or Australia, which suggests that these two countries may have different priorities to the UK in terms of self-care support for CYP’s mental health. Third, most of the interventions examined in the various studies concerned mood disorders (anxiety and depression) and behaviour problems, with relatively few considering the more serious mental health problems such as self-harm, psychosis and eating disorders. Fourth, most of the interventions were treatment-level interventions; preventative interventions were in the minority. Lastly, very few of the interventions involved any degree of technology, a particularly salient point given that CYP are often thought to be ‘digitally native’. 180
In terms of integrating the two reviews, a useful starting point is the effectiveness results. We found that self-care support interventions appear to be modestly effective in improving CYP’s mental health symptomatology. The satisfaction data from the perceptions review, however, suggest that CYP and their parents are often satisfied with any intervention, including those, like attention or placebo controls, designed to have no active therapeutic ‘ingredient’. This suggests that whether an intervention is effective or not may not be a principal concern of CYP and their parents – what may be more important is that their needs and concerns receive some form of attention from those providing services. Unfortunately, the satisfaction data do not tell us what specific aspects of the various interventions CYP and their parents are satisfied with, and further work in this area could help unpick this.
Our finding from the effectiveness review that those delivering and facilitating the interventions need not necessarily be mental health trained is complemented by the finding from the qualitative studies that the relationship with the therapist, often known as the ‘therapeutic alliance’, may be more important than the intervention itself. It may be that it is the personal attributes and interpersonal skills of the self-care support agent that matter rather than whether they are mental health trained or not. An additional effectiveness finding – that more contact time with the self-care support agent may be beneficial – is possibly related to this as, clearly, the more time CYP and their families have with staff, the more opportunity there is to develop a therapeutic alliance.
The evidence that individual interventions may be more effective than group interventions is interesting given that peer support – which is necessarily associated with groups and other social networks – was a principal theme emerging from the qualitative studies. It is also a somewhat ironic finding given that, regardless of methodology, the majority of interventions investigated were group interventions. Again, this finding may be related to the therapeutic alliance in that CYP and families undergoing individual interventions are less likely to experience the dilution of individual time and attention that is inevitable in group settings.
Another key theme from the qualitative studies is that the acquisition of knowledge and skills seems to be a crucial aspect of self-care support. Interventions in the qualitative studies appeared to have some flexibility in how knowledge and skills were acquired, in that they were underpinned by a wider range of theoretical models than the interventions in the effectiveness studies, which were largely cognitive–behavioural and parenting interventions. These, and the other manualised interventions in the effectiveness studies, tended to dictate, via specific tasks and activities, exactly how knowledge and skills would be acquired. This did not suit everyone; teachers, in particular, were often dissatisfied with the rigidity of manuals.
Our effectiveness finding that the setting of the intervention (home, school, etc.) is largely irrelevant is reflected across both reviews in that there does not seem to be any sort of overall pattern concerning the location at which the interventions were delivered, other than few took place in the home.
A principal theme emerging from the perceptions studies is that CYP have different views to adults about what is important, or what they like, about interventions. This reinforces the importance of being child-centred when designing interventions for CYP. We have no evidence to suggest that the interventions in the effectiveness studies were anything other than child-centred in their design; the trial designs, however, often fell short in child-centredness in that few outcome measures focused on things that might be important to CYP, such as their strengths (resilience), self-esteem or general well-being. Instead, the focus was largely on mental health symptomatology, perhaps because it was what clinicians and parents (adults) felt was important.
If there is a single message that emerges from our attempt to integrate the effectiveness and perceptions reviews, it is perhaps one of service providers trying to instil homogeneity – in terms of largely manualised, group-based, face-to-face interventions where the only outcome of concern is a reduction in symptoms – in a population of CYP and their families who vary immensely in their needs, their experiences and the resources they have. This opens up issues about choice and flexibility, issues that will be discussed in greater detail in the discussion (see Chapter 6 ).
Chapter 4 Service mapping
This chapter focuses on Stage 1b of the study in that it describes the methods underpinning, and the findings from, the systematic online and offline search conducted to identify mental health self-care support services for CYP across England and Wales. In terms of the study’s research objectives, this addressed objective 1, the provision of a descriptive overview of mental health self-care support services for CYP in England and Wales, and objective 5, an exploration of the interface between the NHS and other service providers in the provision of such services.
This stage of the study, along with the systematic reviews stage (Stage 1a) reported in the previous two chapters, allowed us to examine whether the typology conceived in our previous work on self-care support in CYP’s physical health15 was valid for CYP’s mental health, or whether it required modification. The mapping exercise also provided us with the sampling frame for Stage 2, the case study stage (see Chapter 5 ).
Service mapping: methods
Inclusion criteria
For consistency, we used the same population and intervention definitions that we had used for Stage 1a, the systematic reviews stage (see Chapter 2 , Inclusion criteria). Our population was thus ‘children and young people’, defined as those under the age of 18 years. For interventions, we substituted the term ‘services’ but applied the same defining criteria for self-care support to these services. Thus, we looked for service provision where an agent (e.g. a health, social care or education professional, peer or lay person) facilitated CYP or their parents to take action to promote the CYP’s mental health, prevent mental ill health in the CYP, or maintain or enhance their mental health and well-being following recovery from mental ill health.
Additional inclusion criteria were that the service had to operate in England and Wales and had to be ‘live’ during the 9-month data collection period, October 2011 to June 2012.
Search strategy
The search was conducted ‘online’ and ‘offline’ in that we took advantage of both physical and virtual networks in trying to establish what mental health self-care support services might exist for CYP in England and Wales. In the first instance, an e-mail (see Appendix 10 ) was sent to contacts and networks deemed to have potentially relevant information about current services. This e-mail also included a rider requesting that the e-mail be forwarded to any other networks the recipients thought relevant. We circulated the e-mail directly to the following networks:
-
individual contacts known to the study team and to members of the SAG, for circulation around their networks
-
the National Academic Mailing List Service (JISCMail) lists CAMHS (camhs@jiscmail.ac.uk) and North West Nurses working in CAMHS (nw-camhs-nurses@jiscmail.ac.uk)
-
relevant professional networks such as the Royal College of Nursing Children and Young People’s and Mental Health forums, the Association for Young People’s Health and the CAMHS Nurse Consultants network
-
relevant NIHR clinical research networks, i.e. primary care, mental health and medicines for children networks
-
all primary care trusts, mental health trusts and health boards in England and Wales
-
all directors of children’s services in English and Welsh local authorities
-
relevant voluntary sector organisations, e.g. YoungMinds, 42nd Street and Rethink
-
relevant Contact, Help, Advice and Information Network (CHAIN) groups, e.g. self-management, mentoring and coaching.
An internet search, using the search engine Google, was carried out in order to supplement the information gained via the e-mail requests. In addition, while undertaking the systematic reviews, any English or Welsh services identified in the literature were flagged in the Access database used to manage the systematic reviews as potentially eligible for this stage of the study.
Data extraction and selection of services
Basic details of potential services obtained from any source were logged in an Excel spreadsheet by one member of the study team (Elvey). This spreadsheet contained the fields that we assessed as being important in formally identifying the service as a mental health self-care support service, and for us to be able to provide sufficient information for the service mapping to be meaningful. The fields are listed in Box 3 ; those marked ‘inclusion criterion’ were mandatory for a judgement of inclusion to be made.
Service name.
Service provider including sector (statutory, private, voluntary).
Mental health condition. a
Ages targeted. a
Gender.
Target group (who attends).
Theoretical approach.
Mode of delivery.
Aims of the service tools/techniques used.
Self-care elements. a
Support element.
Facilitator (agent). a
Setting (community, home, etc.).
Geographical location (including whether urban/rural). a
Length of contact.
Timing (frequency of contact).
Service current/dates of service operation. a
a Inclusion criterion.
At the point of identification, we frequently had little information about the service (merely having a website, service name or telephone number, for example) so one member of the team (Elvey) obtained further information by telephoning and e-mailing any relevant contacts. When this team member felt there was enough information to make a judgement, the service was discussed with a second team member (Pryjmachuk) and a decision made on its inclusion in the service map. The principal reasons for exclusion were insufficient information despite repeated attempts at contact; services were no longer operating; services were operating in other parts of the UK besides England and Wales; services were for adults rather than CYP (although a service would be eligible if it also provided support for CYP aged under 18 years); and services with no clear self-care element.
Service mapping: results
The service mapping data were organised using the dimensions in our previous typology as well as a few other dimensions (e.g. urban vs. rural, intervention level) that had relevance to this study. A full summary of the mapping data can be found in Appendix 11 ; a summary of their salient features, tabulated by the typology and other dimensions, is in Table 18 .
| Dimension | Categories (n) | Total |
|---|---|---|
| Location | England (19); Wales (5); online (3) | = 27 providers |
| Urban vs. rural | Urban (14); rural (8); mixed, including online (5) | = 27 providers |
| Provider | NHS/statutory (10); private sector (1); voluntary sector (16) | = 27 providers |
| Condition | Anxiety/depression (7); general mental health (12); self-harm (3); eating disorders (2); behaviour problems (7); psychosis (2) | = 33 services |
| Intervention level | Prevention (9); management (19); unclear or mixed (5) | = 33 services |
| Model | Recovery/empowerment (8); solution-focused (3); cognitive and/or behavioural (11); other (6); unclear (5) | = 33 services |
| Recipient | CYP (28); parents (2); family (3) | = 33 services |
| Agent | A variety of self-care support agents were used across the services | |
| Platform | Manualised? (data not recorded) | |
| Face to face (29); online (4) | = 33 services | |
| Group (16); individual (6); mixed (7); unclear (4) | = 33 services | |
| Delivery location | General community (14); hospital/clinic (4); school (5); online (4); unclear (6) | = 33 services |
Thirty-three individual services were identified across 27 separate service providers, 19 of which operated in England, five in Wales and three were online services operating across the whole of the UK. There was a mixture of urban and rural sites with the urban sites dominating – most of the urban sites were within the major English metropolitan areas (London, Greater Manchester, Merseyside and Yorkshire). Sixty per cent (16/27) of service providers were in the voluntary sector, with the remainder (apart from one private sector provider) being the NHS or the NHS in collaboration with a local authority.
Regarding the age groups covered by the services, six of the voluntary sector sites had an upper age limit above 17 years, offering, for example, services for people aged between 14 and 30 years. This flexibility is at odds with the standard adult/child demarcation at 18 years of age that is usually found in the statutory service providers.
Most of the services were not condition-specific in that almost 40% (12/33) targeted general mental health problems and needs. Seven services targeted mood disorders (anxiety and depression), seven behaviour problems. Only three services targeted self-harm and only two targeted psychosis. There were fewer ‘prevention’ (universal and selective) services than ‘management’ (indicated and treatment-level) services.
There was a mixture of theoretical approaches underpinning the services provided, with no single model dominating, although ‘recovery’ was a guiding principle in around one-quarter (8/33) of services. There was a wide variety of professional and lay people facilitating the services – even within the services themselves – with no particular group dominating; the self-care support agents included social workers, counsellors, nurses, psychologists, youth workers, coaches, school staff, volunteers and CYP themselves. Almost all of the services (28/33) were targeted specifically at the CYP with only a few targeted at parents or the family as a whole. All except the three completely online services and the service with an option for online plus telephone support were face-to-face services; most of the face-to-face services (23/29) involved group sessions or activities, with only six services offering exclusively individual sessions. For those services where the delivery location was known, 19 out of 33 operated in a community setting (which included five services operating within schools), and most of these community services were provided by the voluntary sector. Only four services operated from a hospital or clinic setting; three of these were provided by the NHS and the fourth by the private sector.
Typology modification
As mentioned in the introductory section to Chapter 3 , Stages 1a (the systematic reviews) and 1b (the service mapping) allowed us to assess the relevance of a physical health (long-term conditions) typology from our previous study15 against a mental health data set. During the process of compiling the summary tables for the effectiveness review (see Appendix 7 ), the qualitative and quantitative aspects of the perceptions review (see Appendices 8 and 9 , respectively) and the service mapping discussed above (see Appendix 11 ), it became evident that our previous typology had a reasonable fit but would require some modification to be applicable to a mental health context.
The process of modifying the typology to fit the mental health data set is outlined in Table 19 . Although there are clearly substantial areas of agreement between the two, it is worth commenting on some of the differences. The most salient differences relate to the provider of the intervention/service, the process of self-care and the platform.
| Previous study | This study | Notes |
|---|---|---|
| Theoretical basis | Model | Retained; minor modification to label name |
|
Target
CYP Parents CYP and parents/siblings Peers Professionals Health-care system |
Recipient
CYP (older vs. younger) Parents CYP and parents Family (including siblings) CYP, parents and teachers |
Retained; modification to label name, as ‘target’ was used more specifically to describe the particular client group the intervention/service was designed to help No separate interventions/services identified for siblings though siblings were occasionally included in family sessions No interventions/services identified that were targeted at peers or professionals or the health-care system, though teachers were occasionally targeted as part of an overall package |
|
Location
Home Community (school, camps) Hospital |
Delivery location
Home School Hospital/clinic Community |
Retained; minor modification to label name Slight changes to the categories in that ‘hospital’ was relabelled as ‘hospital/clinic’ and school was separated from community as a separate category |
|
Leadership
Lay led Professional led |
Provider
Statutory sector (health/local authority) Private sector Voluntary sector Agent Lay (e.g. voluntary sector worker, peers, volunteer) Professional (e.g. psychologist, teacher, social worker, nurse) |
Split into two dimensions: ‘provider’ and ‘agent’ Where available, provider proved helpful in understanding the organisation of self-care support The self-care support agent could be categorised into the broad categories of ‘lay’ and ‘professional’ |
|
Focus
Generic Condition-specific |
Condition
General mental health Condition-specific (depression; anxiety disorders; behaviour problems; eating disorders; self-harm; psychosis; PTSD) |
Retained; modification to label name Specific conditions could also be categorised into eight broad areas |
|
Aims/objectives
Increased knowledge Increased self-management skills Improved physical health outcomes Prevention of long-term consequences of condition Improved communication skills (with health-care professionals, parents/young people) Improved family functioning and relationships Improved relationships with health-care professionals Improved psychosocial well-being Increased self-efficacy Enhanced adjustment to the condition Improved social skills Improved problem-solving skills Improved coping skills Increased self-esteem Improved quality of life Increased adherence Increased health locus of control Reduced health-care utilisation |
Process elements
Providing psychoeducation: knowledge of the condition (insufficient on its own to qualify as self-care but a part of many interventions/services) skills for self-management (coping, communication, assertiveness, problem-solving skills) peer support and shared experiences Usually involving skills practice or practical activities of some sort with feedback from the support agent in order to reduce dependence manage symptoms promote ‘recovery’; empower improve family functioning and peer relationships increase social capital; increase social networks improve self-esteem increase resilience |
Dimension replaced with a dimension that identifies the process elements of self-care support for an intervention or service, though there is significant overlap between the ‘core components’ identified by the old and new dimensions |
|
Medium
Face to face Group Dyadic Individual Activities, e.g. role play Discussion Lectures Printed materials Workbooks Diaries Self-care guides, e.g. action plans E-health Websites Chat rooms Mobile phone systems Remote monitoring DVDs Computer and other electronic games |
Platform
Treatment manualised or not (manualised) Face-to-face or remote (i.e. online, telephone) Group or individual (or mixed) sessions |
The old ‘medium’ and ‘individualisation’ dimensions have been integrated into the ‘platform’ dimension Some elements of the subdimensions ‘face to face’ (activities and lectures) and ‘printed materials’ (workbooks, diaries, actions plans) have been integrated into the ‘process elements’ dimension (the ‘usually involving’ subdimension) |
| Individualisation | (see Notes) | Integrated into the ‘platform’ dimension |
Inclusion of the service provider may prove to be important for two inter-related reasons. First, one of our research objectives (objective 5) involved an exploration of the interface between the dominant health-care provider in the UK – the NHS – and other statutory and non-statutory providers. Second, there is a political dimension in that there has been a growing demand from health-care ‘activists’, such as mental health service user groups and the professional health-care community alike, for ‘personalised’ health care regardless of who provides it.
Considering self-care support as a process rather than focusing on its aims/objectives provides a more analytical approach in that self-care support becomes more than a mere set of intentions. There needs to be the acquisition of knowledge and skills, which require input and effort on the child or young person’s (or parent’s) part; opportunities to practise and consolidate these requisite skills with support and facilitation from a self-care support agent; and some positive outcomes for the child or young person and his or her family.
Regarding the platform, the key elements – treatment manualisation, face-to-face or remote contact, and group or individual approaches – may be important when thinking about choice and flexibility, especially when considering with whom that choice or flexibility lies: the child or young person, or some other person or body such as an adult or the provider.
These points, among others, will be considered further in the discussion (see Chapter 6 ). The next chapter – the case study chapter – provides some additional insights into the specific elements of self-care support, allowing us to unpick the dimensions of our ‘new’ typology further.
Chapter 5 The case study
This chapter focuses on Stage 2, the empirical – or ‘primary research’ – aspect of the study, which we conducted using the case study method. We start with an outline of the specific research methods used, after which we provide a descriptive overview of the individual case study sites; we then present our findings, organised according to a number of analytical themes.
This stage of the project was designed to inform research objectives 3 and 4, which were concerned with, respectively, the factors influencing the acceptability of mental health self-care support services for CYP and the barriers affecting the implementation of such services. In addition, as with the mapping exercise (see Chapter 4 ), this stage of the study also helps realise objective 5, which was concerned with the interface between the NHS and other service providers in the provision of mental health self-care support services for CYP.
Methods
Design
Stage 2 was conducted as a collective case study. A case study is an empirical enquiry that focuses on a single phenomenon in its real-life context, especially useful (as in our circumstances) when description or explanation is required. 181 Collective case studies are those in which multiple cases are studied simultaneously or sequentially in an attempt to generate a broad appreciation of a particular issue. 182 Yin181 (p. 6) defines a ‘case’ as a ‘bounded entity’, a broad and flexible definition that allows the case to be as varied as an event, an individual, a service or a policy. In this project we have defined the case as a ‘mental health self-care support service for CYP in England and Wales’.
Sampling and recruitment
A purposive sampling strategy was employed to ensure that the various dimensions of the self-care support typology we derived from the mapping exercise and systematic reviews (see Chapter 4 , Table 19 ) were reflected in our sample. Accordingly, sites were recruited to include a variety of theoretical bases (e.g. cognitive–behavioural, social learning, recovery) and platforms (e.g. face-to-face or remote, group or individual). We also recruited on the basis of organisational characteristics, such as the sector the site operated in (e.g. NHS vs. local authority vs. voluntary sector) and the site leaders (e.g. health professionals vs. other trained workers vs. volunteers). It was also important to include key characteristics of the study population; thus, the sample included sites offering condition-specific and more generic support, CYP from different age groups, and different types of location (urban, rural) across England and Wales. Using the typology and these characteristics, six potential sites were selected from our sampling frame of 33 services (delivered by 27 providers), and these were approached to participate in the study. One site declined to participate so an alternative, similar in terms of typology dimensions and characteristics to the site that declined, was invited to participate and agreed.
The six sites which agreed to participate were:
-
a psychotherapy group for young people aged 14–17 years who self-harm and their families, provided by the NHS in an urban area of England
-
a group intervention (Dina School) for children aged 5–6 years with emotional and behavioural difficulties (EBD), based on The Incredible Years183 programme and provided in rural Wales by the voluntary sector
-
a parenting group for parents of children with EBD, based on The Incredible Years183 programme and operating in rural Wales as a joint NHS/local authority initiative
-
a resilience-focused family support service for families of children aged 5–14 years with emerging EBD, provided by the voluntary sector (but local authority funded) and operating in an urban area of England
-
a national, recovery-focused online support group for young people aged up to 25 years with eating disorders
-
a supported online cognitive–behavioural intervention (Beating the Blues184) provided to young people aged 14–30 years with depression and/or anxiety by the voluntary sector in an urban area of England.
Recruitment of participants at the case study sites was also purposive in that it was driven by the characteristics of the particular self-care model employed. Additionally, to ensure a range of relevant perspectives, the views of younger, as well as older, children, and those of parents and staff with differing roles providing the services were sought.
Regarding the recruitment of service user participants (i.e. CYP and their parents), we received valuable advice from the SAG on engaging these participants in the study. Recruitment documentation (the covering letter, participant information sheets, contact form and consent/assent forms; see Research ethics and governance below) was developed with guidance and feedback from CYP. At five of the sites, staff provided the recruitment documentation to current and ex-service users (or to their parents if they were aged 14 years or below), via the post or by handing the documentation to users when they attended the self-care support service. Participants provided their contact details using the contact form and the researcher (Elvey) telephoned them to arrange the interview. For the eating disorders online support site, the study was publicised, including contact details for the research team, on a web page listing details of current research projects wanting to recruit participants, via an e-mail distribution list of service users who were willing to be contacted about research projects, and via the site’s Twitter feed. CYP participants were eligible to participate only if they were aged between 5 and 17 years. Although two of the sites (sites 5 and 6) did not offer services specifically tailored for CYP, they were eligible for this study because they did offer services to those under the age of 18 years. Non-professional participants (i.e. CYP and parents) were offered £10 in gift vouchers as a token of thanks for their participation.
Recruitment of staff at each site was facilitated via a key contact, usually a service manager, who not only took part in the research, but also identified additional relevant staff to invite as participants. At five of the six sites, staff were provided with the recruitment documentation, either through the post or in person by the researcher; at the eating disorders site, documentation was supplied via e-mail.
Research ethics and governance
Like all empirical research conducted within a university setting, the case study was subject to ethical approval by the host institution, the University of Manchester. Moreover, because the research involved potential access to NHS sites and NHS patients, the ethical aspects of the study required consideration by the NHS National Research Ethics Service (NRES) prior to any consideration by the university. Regulations introduced by NRES in 2011185 allowed an expedited proportionate ethical review in circumstances where a project had no material ethical issues. NRES provides a tool186 to help researchers identify whether there are material ethical issues or not, and use of this tool suggested that our project might be eligible for such an expedited review. This turned out to be the case and a favourable ethical opinion was obtained through proportionate review in March 2012. As is the standard procedure, this favourable opinion was accepted by the University of Manchester Research Ethics Office shortly afterwards. While conducting the case study research, it was necessary, on two occasions (in September 2012 and October 2012), to inform NRES of a ‘substantial amendment’ to the ethics-approved protocol. One amendment was required because one site requested that the wording on the covering letter be modified to remove the term ‘mental health’. The other arose because another site worked predominantly with children aged 5 years, so we asked that our original lower age limit for CYP participants be reduced from 6 to 5 years. Both of these amendments NRES subsequently approved.
Ethical research is underpinned by three inter-related factors: (1) informed consent; (2) the safety of participants and researchers; and (3) the safeguarding of any data obtained during the course of the research.
Regarding informed consent, all identifiable participants received an age-appropriate participant information sheet informing them of the study’s nature and purpose. The participant information sheets and associated consent/assent forms were designed according to NRES guidance. 187 The versions specific to CYP, furthermore, were piloted with colleagues’ children, students at a local secondary school and young people with experience of mental health services, and were subsequently amended as a result of their feedback. Written consent was obtained from all adult participants. In line with NRES guidance,187 all CYP participants aged 15–17 years provided their own written consent; parents provided written consent for children under 15 years old, although, in line with good practice, written assent was also obtained from these children. We needed to take a slightly different approach to consent for the online eating disorders support group (site 5). We were interested in postings on the site’s discussion boards – postings that were both anonymous and publicly available. As the postings were anonymous, it would have been very difficult to obtain individual consent for the use of these postings, so we obtained ‘proxy’ consent to access and use these postings from the eating disorders organisation providing the service.
Regarding the safety of participants and researchers, the principal risks identified for participants were that they might get upset during the interview or disclose information (e.g. in relation to child protection) that would require action by the researcher. Written protocols were prepared for both of these situations. Risks to researcher safety were minimised by adherence to the University of Manchester’s guidance on lone working.
Data safeguarding requires that confidentiality and anonymity issues be addressed, not only in the conduct of the research but also in the reporting and storage of any data associated with the research. To preserve anonymity, the data generated by the research were, wherever possible, stored with identifying features removed. In any case, the data were stored securely, with due regard to confidentiality and in accordance with the University of Manchester’s information governance regulations. When the data were circulated around the study team or SAG, analysed or (as is the case here) reported, we ensured that any identifying features were removed.
At each case study site, we complied with any specific research governance requirements. This included complying with NHS Research and Development requirements at the NHS sites selected.
Data collection and management
Case study research requires data from a variety of sources and, once collected, the data should be managed systematically. 181 Data were obtained through semistructured interviews, documentary review and virtual non-participant observation and, wherever possible, from all three participant categories: CYP, parents and staff.
Semistructured interviews
Semistructured interviews were used as the main data collection technique. They were conducted with staff at all six sites and with CYP and/or parents at all sites except the eating disorders online support site. Pragmatism largely dictated the way in which participants were interviewed in that they were given choices as to which approach they preferred (e.g. telephone vs. face to face; individual vs. group). Forty-two interviews involving 52 participants were conducted; 37 were conducted in person, either at the site’s premises or at the service user’s home, and five were conducted via the telephone. The majority of interviews (35/42) were individual, five were joint interviews with a child or young person plus parent, one was a group interview with a child, parent and sibling and one was a focus group of four young people. The interviews ranged in length from 10 minutes (for some of the youngest children, aged 5 and 6 years) to 1 hour and 20 minutes. Interviews were facilitated by the use of topic guides, copies of which can be found in Appendix 12 . All of the interviews were digitally audio recorded with the permission of participants and the recordings were subsequently transcribed verbatim by a professional company.
Documentary review
Where available, relevant documentary evidence was collected from each site. For sites 5 and 6, documentary evidence was obtained simply from the relevant websites of the services. More comprehensive data were obtained from the other four sites, including a referrer’s leaflet for site 1 as well as a printed self-injury ‘toolkit’ used in providing the self-care support service there; a Microsoft PowerPoint general presentation about the Incredible Years services at sites 2 and 3, and one about the funder’s strategic plan regarding these services; an information leaflet about Dina School training for teachers at site 2; and information leaflets about the site 4 service for referrers, parents and CYP. The documentary evidence largely served to provide a contextual background to, and additional understanding of, the six sites.
Virtual non-participant observation
For the eating disorders online support site (site 5), we collected the data via ‘netnographic’ non-participation observation, adopting the principles of a method designed specifically for health-care research. 188,189 Netnography is a form of ethnography used in the study of online behaviour, and as ethnography concerns everyday routine behaviours in a natural setting,190 netnography was an entirely appropriate method of observing a service that operated entirely online. The service centred around discussion threads that were organised by the providers into nine boards, following themes such as ‘recovery’, ‘caring about someone’, ‘introductions’ and ‘poetry’. Two boards were excluded from the study as the content merely described how to use the boards. All postings over a 4-month period (August to November 2012) were collected from the remaining seven boards. These comprised 114 discussion threads with more than 500 individual messages, each of which was screened for relevance. The postings were copied from the website and pasted into Microsoft Word 2010 documents (Microsoft Corporation, Redmond, WA, USA) prior to analysis.
Regarding management and coding of the data, the three data sets – interview transcripts, background information about the sites (documentary evidence) and the online group postings – were imported into NVivo 10 (QSR International, Warrington, UK), computer software designed to assist in the collection, organisation and analysis of qualitative and mixed-methods data.
Data analysis
The data were analysed using the framework method,191,192 which has five stages: (1) familiarisation; (2) identifying a thematic framework; (3) indexing; (4) charting; and (5) mapping and interpretation. For the interview data, familiarisation was achieved by all of the transcripts being read by the team member who conducted the interviews (Elvey; Kendal also facilitated one group interview), and through other members of the research team (Kirk; Kendal; Pryjmachuk; Catchpole) each reading a sample of transcripts. For the virtual non-participation observation data (site 5’s online postings), Elvey and Kendal undertook an analogous process in that they treated the Word documents into which the postings had been pasted as ‘transcripts’. Following familiarisation, the study’s research questions and the topic guides (see Appendix 12 ) were used to devise an initial thematic framework. Using this initial framework, data from the transcripts (including the online postings) and the background documents obtained from each site were then indexed by Elvey in order to produce an initial chart for each of the six sites. An example of such a chart is provided in Appendix 13 . These six charts were then circulated around team members and a final thematic framework was developed through an iterative process, whereby we met as a team several times to discuss the data and any emerging salient themes. As the final thematic framework emerged, the data from the six initial charts were assimilated into a single chart which was used to guide our analysis and interpretation of the case study findings. The final thematic framework is outlined in Table 22 in the Findings section of this chapter, and Appendix 14 illustrates (using one of the themes, ‘facilitating self-care support’, as an example) how data from each of the initial charts were subsequently assimilated into a single chart.
Characteristics of the case study sites
Details of the six case study sites are summarised in Table 20 and described in detail below.
| Dimension | Site 1: self-harm psychotherapy group | Site 2: Dina School children’s group | Site 3: parenting groups | Site 4: resilience-focused family support | Site 5: eating disorders online discussion board | Site 6: supported online CBT intervention |
|---|---|---|---|---|---|---|
| Mental health condition | Self-harm | Behaviour problems | Behaviour problems | (Emerging) behaviour problems | Eating disorders | Depression; anxiety |
| Target | YP aged 14–17 years who self-harm, plus their families | Children aged 5–6 years with emerging emotional and/or behavioural difficulties | Parents of preschool children aged 2–4 years who wanted support with their child’s behaviour or communication | Families of children aged 5–14 years with emerging emotional and behavioural problems and complex needs but not requiring Tier 3 care | YP up to age 25 years (but including under-18s) | YP aged 14–30 years (case study focused on 14- to 17-year-olds) |
| Model (theoretical or philosophical basis) | Recovery-focused approach; eclectic mix including CBT, DBT, supportive counselling, art and music therapies | Social learning theory; Dina School element of Webster-Stratton’s The Incredible Years183 | Social learning theory; parent training via Webster-Stratton’s The Incredible Years183 | Solution-focused approach; Daniel-Wassell model of resilience194 | Recovery-focused approach | CBT |
| Self-care element | Groups can be chaired by YP; security planning to keep the YP safe; taking ownership, devising alternative strategies to self-harming | Children are introduced to communication and behavioural techniques and encouraged to practise these at home and school; activities involving role play, puppets, video vignettes, etc. | Giving parents skills to manage and facilitate their children in a positive way; practise skills with feedback; peer support | Aims to help children develop resilience via giving children a chance to tell their story and the development of an action plan with goals | Providing peer support | Guided self-help using the Beating the Blues184 programme |
| Self-care agent | Nurse; support worker | Primary school staff (classroom assistants) | Voluntary sector staff with youth and social work backgrounds | Voluntary sector staff with youth and social work backgrounds | Peers; service provider staff (who moderated discussions) | Service manager; volunteer |
| Locale | England | Wales | Wales | England | England and Wales (UK-wide) | England |
| Delivery location | Hospital/clinic | School based | Community (voluntary sector provider premises) | Community (voluntary sector provider premises, home and school) | Online | Community (voluntary sector provider site); online |
| Provider | NHS | NHS/local authority | Voluntary sector | Voluntary sector (but local authority funded) | Voluntary sector | Voluntary sector |
| Platform | Manualised; face-to-face groups | Manualised (number of sessions prescribed); face-to-face groups | Manualised (number of sessions prescribed); face-to-face groups | Manualised (number of sessions prescribed); face-to-face individual support | Moderated online discussion boards; one-to-one online chats with a counsellor | Manualised (number of sessions prescribed); online, supported by face-to-face individual support |
Site 1: self-harm psychotherapy group
This NHS service was designed for young people aged 14–17 years who self-harm; it also offered some support for the families of these young people via family support groups, and families could telephone the service and talk to staff between sessions. The service was run from an outpatient setting at an NHS mental health hospital. The service operated within a recovery-focused philosophy and was eclectic in its approach, in that the group intervention employed elements of group psychotherapy, CBT, Linehan’s dialectical behaviour therapy193 and supportive counselling. Groups ran on a weekly basis (weekday mornings), lasted 2 hours and were led by nurses and support workers. Although the service was manualised – in that there was a specific protocol in place for how the service should be delivered – there was no limit, other than reaching the age of 18 years, to the number of weekly sessions a young person could attend. Young people were referred to the service via community or inpatient services.
Site 2: Dina School
The Incredible Years
The group for children with emotional and behavioural problems (site 2) and the parenting group (site 3) were interconnected, but separate, services. Both operated as part of Webster-Stratton’s The Incredible Years programme183 that had been adopted region-wide (across the local authority area) by the commissioning bodies in the region. The Incredible Years is an evidence-based programme, influenced heavily by social learning theory. It emphasises attachment, relationship building and emotional coaching, with a focus on children learning through play and parents and teachers spending time with children, listening to them and giving them positive feedback. The overall Incredible Years programme comprises universal and targeted (indicated) interventions, both of which were available in the region. At the time of data collection, around half of the region’s schools were Incredible Years schools. In these schools, all staff members were trained in the approach and were thus able to implement the programme universally (in a regular classroom setting, for example) or in a more targeted way.
Dina School
Site 2 was an example of a targeted intervention operating in one of the Incredible Years schools. Known as Dina School, it involved children taking part in 18 weekly, small group sessions, which took place in a room at the children’s school. The groups were facilitated by two classroom assistants, who delivered the programme as set out in the Dina School manual. The programme makes use of a dinosaur puppet called ‘Dina’ (which was also used universally in the main classroom setting) as well as two additional character puppets, ‘Wally’ and ‘Molly’. These puppets were used in role plays, demonstrations of behaviours and communication techniques and in video vignettes. Each session followed a similar format, with a review of the ‘homework’ tasks that were set at the previous session, followed by activities and games and the setting of a further homework task at the end. Parents came to collect their children at the end of the session which coincided with the end of the school day.
Site 3: parenting group
Like site 2, site 3 was a targeted programme. It was one of more than 20 Incredible Years group parenting programmes that operated in the same region as site 2, offering parent training to parents of children aged from 0 years upwards, grouped according to the children’s age. The parenting group participating in this study was for parents of preschool children, aged 2–4 years, who wanted support with their child’s behaviour or communication (e.g. being withdrawn or having tantrums that the parent found difficult to deal with). Parents could self-refer or be referred to the service. The service was provided by a voluntary sector organisation and operated from its premises, although it was commissioned and funded jointly by the NHS and local authority. Parents attended 15 weekly group sessions which were facilitated by two members of staff with backgrounds in family and youth work, and in accordance with the programme manual.
Site 4: resilience-focused family support
Site 4 was a voluntary sector family support service provided to families of children aged 5–12 years with complex emotional and behavioural needs who did not require Tier 3 CAMHS care. Some children were referred to the service because their needs were not seen to warrant CAMHS input; others had attended CAMHS and were subsequently referred to this service for the more generalised support with coping and resilience that it offered. The service is based on the Daniel-Wassell model of resilience,194 a model with six domains – secure base, friendships, talents and interests, education, positive values and social competences – that have some affinity with the principles of recovery. Staff members work through these domains with families to identify the family’s needs and then focus on those domains where the most support is needed. The family support was delivered by a member of staff from the voluntary organisation operating the service. The staff, who had a variety of professional backgrounds including youth work, social work, psychology and nursing, met with the child and his or her parent(s) individually (sometimes together) at home and at school. As with The Incredible Years, this service was manualised with a prescribed number of sessions.
Site 5: online eating disorders discussion board
This site, operated by an eating disorders charity, consisted of online message boards for young people concerned about, or experiencing, eating disorders. The message boards were established around 6 years ago to improve access to support. Although the online eating disorders service was a ‘virtual’ service, operating entirely over the internet, the charity operating the service offered some other services for young people including a telephone helpline and a live online chat service which some message board users had also participated in. Like the self-harm service, this service operated within a recovery-focused philosophy. To post messages, users had to register on the internet site (supplying their name and e-mail address). Although the posts were moderated, they were freely available on the internet for anyone to read. The boards were organised into themes, and users posted messages that mostly described their worries about food or eating, or their experiences of living with eating disorders, as well as messages that sought support from others or offered emotional support and practical tips to others. The boards were moderated by volunteers, many of whom had experienced eating disorders themselves and some of whom had trained in relevant fields such as counselling. Although the service was open to young people up to the age of 25 years, it was eligible as a case study site because those under 18 years of age were represented in the postings. Unlike the other five sites (which were manualised to one degree or another), this service was inherently spontaneous and adaptable.
Site 6: supported online cognitive–behavioural therapy intervention
Site 6 was a charity-operated, supported online CBT service for young people with anxiety or depression aged between 14 and 30 years. Although the service was open to people up to the age of 30 years, it was, like site 5, eligible as a case study site because those under 18 years of age used the service. The service had been established by staff at the site who had had prior experience of anxiety and depression themselves. It was set up in response to a perceived gap in suitable service provision for young people and young adults and aimed to appeal to this group by being accessible and flexible. The site operated as a drop-in centre, whereby people could come without an appointment and access information and advice. Service users came to the charity’s base and worked through a specific online CBT course – Beating the Blues184 – with a volunteer from the charity facilitating the young person through each CBT session. Like most CBT interventions, this service was manualised with a prescribed number of sessions.
Participant characteristics
Table 21 summarises the interviews conducted at each case study site. In total, 52 participants were interviewed between July 2012 and March 2013. The CYP (n = 17) who took part ranged in age from 5 to 17 years. Of these 17 CYP, four were interviewed as a focus group (at the self-harm group psychotherapy site), and six were interviewed along with a parent, five at the family support site and one at the self-harm site. Of the 15 parents who took part, nine were interviewed individually and six along with their child. Two of the individual parent interviews at the parenting site were conducted via the telephone. The service provider staff interviewed (n = 19) included nurses, psychologists, classroom assistants, social workers, youth workers, counsellors and lay volunteers. Three members of staff at the family support, group parenting and eating disorder sites were interviewed over the telephone. The majority of staff and family members were female; two male staff members and three fathers were interviewed. Of the six young people interviewed at the self-harm and anxiety/depression sites, half were male and half female; at the sites where younger children were interviewed, most (8/11) were male.
| Case study site | CYP | Parents | Siblings | Staff | Total |
|---|---|---|---|---|---|
| Site 1: self-harm psychotherapy group | 5a | 1b | – | 4 | 10 |
| Site 2: Dina School children’s group | 6c | 5c | – | 4 | 15 |
| Site 3: parenting group | – | 4c | – | 3 | 7 |
| Site 4: resilience-focused family support | 5d | 5b | 1e | 5 | 16 |
| Site 5: online eating disorders discussion board | – | – | – | 1 | 1 |
| Site 6: supported online CBT intervention | 1c | – | – | 2f | 3 |
| Total all sites | 17 | 15 | 1 | 19 | 52 |
Although the overall quantity of data is sufficient for a case study,195 a few observations need to be made about the relative success of our recruitment strategy across the six sites. Recruitment was relatively successful for all three participant categories across sites 1, 2 and 4, though only having one parental interview at site 1 was disappointing. Site 3’s recruitment was also reasonably successful given that parents were the target of the service and that, as they were under 5 years of age, we did not have ethical permission to interview the children. We did not attempt to recruit parents at sites 5 and 6 because the very nature of the services at these sites meant that it would be difficult to identify parents. The low numbers of staff participants at these two sites was also understandable because these services – both provided by the voluntary sector – had limited resources to employ significant numbers of staff. With site 5, we did not manage to recruit any CYP participants for interview despite advertising on the service provider’s website and through other online networks. Though disappointing, this is not an especially serious recruitment limitation as any interview data obtained would have merely augmented the CYP’s perspectives on self-care support which we obtained via the netnographic non-participation observation data.
Site 6 perhaps created the most significant recruitment issue in that we only managed to recruit one CYP participant at this site. This site was a relatively newly established service which was operated by a small organisation with one full-time member of staff. We recruited via the service manager who asked that we involve only ex-, not current, users of the service. The service manager searched the contact database and telephoned or sent information to all ex-users inviting them to participate in an interview. During the 7 months that we were in contact with the site, only eight people aged 17 years and below accessed the service. Two agreed to be contacted by the research team and subsequently participated in interviews, one of whom has since taken on a role as a volunteer providing the service.
Findings
From the analysis of the case study data, four principal themes emerged, each containing a number of subthemes. These themes and subthemes are summarised in Table 22 and discussed in more detail in the ensuing sections. At this point, however, it can be noted that the first two themes mostly provide contextual detail about, respectively, the users and providers of mental health self-care support services for CYP, whereas the remaining two focus largely on the factors contributing to the acceptability of such services.
| Main theme | Subtheme |
|---|---|
| Having a mental health problem | Understanding the mental health problem Self-care and self-care support |
| Providing self-care support | Service development Training and supervision Integration with other services |
| Accessing self-care support | Referral to services Building and maintaining engagement |
| Facilitating self-care support | Welcoming staff; welcoming organisations Activities to build skills for self-care Sharing experiences and peer support Time and attention |
Having a mental health problem
This theme provides some contextual detail about CYP’s and their families’ understanding of the mental health problems experienced prior to using the services at the case study sites, their understanding of self-care in the context of these problems and their experiences of any self-care support received.
Understanding the mental health problem
The conceptualisation of CYP’s difficulties specifically as mental health problems appeared to be connected to the CYP’s age. The youngest children interviewed, aged 5 and 6 years, did not describe having any mental health problems or difficulties themselves. School staff and parents tended to think that these children mainly lacked confidence or had difficulties expressing or managing their emotions. Some parents described emotional outbursts and tantrums and two described their children as being ‘unhappy’.
I had concerns about his behaviour; he would break down into quite severe tantrums that would last for 20 minutes . . . he would spit all over the seats . . . strip naked and hit and lash and kick; hurt himself, hurt me. And generally I just felt that I had this unhappy child on my hands … I couldn’t go out with him . . . So I was kind of feeling trapped in my own home because of his behaviour.
Parent of younger child
Older, primary school-age children and their parents described various emotional and behavioural problems: being unsettled or disruptive at school; having emotional outbursts at home; having problems with family members or in making friends; lacking confidence; and having communication problems, especially in expressing emotions.
Me and my mum didn’t really use to get along, and not able to cope, like, and with my brother and sister, I didn’t know how to be responsible and stuff.
Child
Young people – that is, older children – who had used the self-harm (site 1), eating disorders online support (site 5) and depression/anxiety (site 6) services had a wide range of experiences, from severe mental health problems and diagnosed conditions, to milder symptoms and difficulties. Some attendees at the self-harm site had been diagnosed with depression and others described feelings of low mood, anxiety and intense feelings. Staff at the self-harm group mentioned a variety of self-harm that users presented with, including cutting and burning. Some CYP attending the self-harm (site 1) and family support (site 4) services had experienced more than one type of difficulty or problem, including being bullied at school, not attending school, displaying signs/symptoms of autism, family relationship problems and misuse of alcohol and/or drugs.
Self-care and self-care support
Just as participants described a wide range of mental health problems and difficulties, their experiences of self-care and support for their problems and difficulties prior to accessing the services were also mixed. Obtaining support was sometimes related to their understanding of the specific mental health problem, as in the case of one young person who had struggled with depression over an extended period:
So had you had any help with your depression before you went to the centre?
No, none, not at all. I had little understanding as well, it wasn’t something that had been spoken about.
Participants generally described undertaking little self-care before coming into contact with the services. Nonetheless, some parents whose children had attended the Dina School groups (site 2) had also previously attended an Incredible Years parenting course and had used some of the approaches at home. A few parents mentioned using techniques from books or television programmes such as Supernanny. Across most of the sites, the situation for many participants was that they came into contact with the services at a point when their problems had emerged, but they had rarely engaged in self-care themselves or received support they were happy with.
With some of the older children (young people), there was some evidence that they could make rational choices regarding self-management, especially when it came to medication:
I usually forget to take it, or I intentionally go out my way not to take it, because I feel as if I don’t need it and it makes me feel different . . . I was on Sertraline, but it kept me awake and then I was on Mirtazapine and then some other things . . . I didn’t like them . . . I don’t feel as if meds help me.
I’m on medication at the moment, because my depression has peaked at the moment . . . so it [the medication] does work.
However, these choices were not always adaptive, as in these examples of young people ‘self-medicating’ with alcohol:
I used to drink and hide in a tree to drink, because my mum wouldn’t allow it, so I used to hide and had to go in a hole and fall out of a tree regularly drinking, that’s how I coped.
Yeah. I used to think alcohol helped me, but it used to just make me worse.
Regarding the support received, there were participants at all of the case study sites with experience of accessing some form of health care or support prior to attending the self-care support service; CAMHS, social services, GPs, psychiatrists, paediatricians, school counselling services and social services were all mentioned. For example, some families had a history of contact with social services due to family situations and some parents had sought help because they were concerned that their child might have an autistic spectrum disorder. There were some reports of positive experiences, such as helpful school counsellors, health visitors and other workers:
My outreach worker who works with me to integrate into the community, because I’m, kind of, agoraphobic, I don’t like people, crowds, so he works with me to try and get me into the community.
Young person
However, many negative experiences were recounted where families had felt dismissed when they raised concerns, for example, about their children’s behaviour or social understanding and had found support hard to access. The mother of one child who had previously been referred to community-based mental health services had found the care provided inadequate:
It didn’t help much, she used to just enjoy going there because I was doing all the talking, they would watch her play, so it wasn’t . . . [helping her with] expressing her feelings . . . and then it just kind of stopped, they were thinking she didn’t need it, but she’d got so much anger at the time, she wanted to leave the house . . . I was worried for her.
Parent
Two settings in particular were singled out for criticism by young people: mainstream schools and inpatient hospital care. Young people had experienced bullying at school, including being bullied about their mental health problems by other students. Some had stopped attending mainstream school and were at school units and felt that staff at mainstream schools often struggled to help students who self-harmed:
They’re not trained in mental health and are only really equipped to do with stuff, like, things to do with education and . . . bullying and peer pressure . . . they’re not equipped . . . they really don’t have a clue when it comes to stuff like mental health and things like self-harm . . . I had a really bad experience with my mentor.
Young person
In terms of hospitals, participants described how support for self-harm in inpatient settings focused mainly on preventing physical harm. For example, two participants reported being restrained and put into seclusion (actions which could both be seen as punitive) when staff found that they were in possession of objects which the staff thought the young people would use to self-harm. Participants had found that they could access either group ‘talking therapies’ or an individual to talk to in the units, but had found this problematic because the therapy was not suitable for them at that stage, or because staff did not spend enough time with them:
There’s people there all the time that you can talk to, [but] I think the therapy puts quite a lot more stress on you at the very beginning . . . you’re taken out of your house . . . kind of throw you in with a bunch of new people, that’s hard to deal with . . . it’s a lot harder to then feel comfortable . . . I think, I had therapy twice, it didn’t work, so they basically just left me.
[My named nurse] was on nights and then when she was on days, she didn’t speak to me anyway, that was so unhelpful. She came to my room at like half past 10 and I’d be talking about stuff and getting upset and minutes later I had to try and sleep.
Yeah I had some nights when mine was . . . on nights and the head of [name of department], so he really didn’t have time [for me].
Running throughout the narratives of the young people was a recurring sense of anxiety around accessing support. Feeling alone, not knowing where to turn for help, discomfort and worry about discussing their problems with family or friends were mentioned repeatedly. The following data extract was taken from one of the site 5 message boards:
When you realise youve got some kind of (eating disorder) what was the first thing you all did? It’s just im stuck and going nowhere, the idea of food and excercise is going round and round in my mind, having crazy thoughts in my head all the time- but i cant tell anyone or even talk about it to anyone because i could shy when it comes to spilling out information about myself . . . any help? Pleasepleaseplease . . . ALSO, if you call the youthline what do they ask you and stuff? because I really wanna call them but im scared of the reponse and over the phone (procedure).
Young person, verbatim message board posting
Providing self-care support
This section explores the findings relating to staff views about providing self-care support services, their reasons for involvement, training and supervision, and the extent to which their service is integrated with other services.
Service development
Staff at the sites became involved in the services for a variety of reasons: a desire to change things or innovate on the basis of personal, often negative, experiences of mental health services; wanting to improve the evidence base for practice; and often just sheer enthusiasm to help CYP. For example, the manager of one site had been motivated to found an independent alternative to traditional ‘clinical’ approaches on the basis of personal negative experiences elsewhere:
I started to experience the onset of depression and anxiety and looked at what sort of support or help was available to me and there was nothing that I felt I would have been likely to access or appealed . . . so I . . . basically came up with a service that I would have liked to see when I was in that situation and applied for funding and got it.
Service lead
At another site, the service lead had been influenced by observations from her own practice, at a time when there was a perceived ‘epidemic’ of self-harm among young people and generally insufficient support available, and when anxiety about the risk of serious harm, including suicide, was high among staff who worked with young people. The rationale behind setting up a group therapy service was that a group approach could be appropriate for young people because of the influence and importance of peer groups to this age group. Moreover, improvements in peers would be clearly visible in a group setting and so serve as a vehicle for hope and optimism in other group members.
The Incredible Years programme, on the other hand, had been adopted at two sites because of its perceived strong evidence base:
I felt really strongly that I knew that the programmes were blueprint [evidence-based] programmes . . . that met the high standards for replicability and for research . . . I really, really like the Incredible Years model.
Staff member
Moreover, service development seemed to be coupled with service leads who were enthusiastic and highly motivated, even to the point of being ‘on a mission’:
So it kind of became my mission and it’s grown into the mission for the Authority to develop all of those programmes.
Service lead
Across all six case study sites, the attributes of the service leads in particular were suggestive of a high level of leadership skills, in that there was evidence of innovation, planning, empathy (for CYP, parents and colleagues), motivation and communication.
Training and supervision
All of the sites except the online eating disorders site (site 5) were manualised, that is there was a specific written manual in place for how the service should be delivered. The Incredible Years sites (sites 2 and 3) and the anxiety/depression site (site 6) were guided by manuals that prescribed the topics to be covered in each session; the self-harm (site 1) and family support (site 4) services had manuals that were less prescriptive.
At the self-harm site (site 1), all staff running the groups were provided with the service manual and, as part of their training, they also observed groups prior to becoming a group leader. Staff running the groups met monthly for group supervision with the service lead. On its initial formation, staff at the family support service (site 4) had been trained in the resilience approach by its architects. New staff members were first introduced to the model and subsequently trained by the service’s current staff, as well as receiving clinical supervision from a psychologist. At the anxiety/depression site (site 6), training was provided by the company supplying the CBT programme and all volunteers had to work through the course before working as a volunteer; there was no formal clinical supervision in place at this site, however.
The two Incredible Years services (sites 2 and 3) were different in that, of all the sites, they had the most structured and formal arrangements for training and supervision. To deliver a programme, staff members were required to undergo formal training. Staff members were regularly supervised by local colleagues and there was ongoing monitoring from the programme base in the USA. The service lead explained why she thought the training and ongoing supervision and support were important:
We’re using an evidence-based programme and actually unless you really are delivering with fidelity we know that you can’t guarantee that you’re going to get the same results as [the] research . . . everybody who delivers the group in [area name] can be sure they’re either going to be able to work with [or get] supervision from someone who’s accredited either as a peer coach or as a mentor . . . I think that is really important in making it effective. These are hard groups to run, so it’s important ensuring that people do get the support.
Service lead
Fidelity was not emphasised as strongly at any of the other sites. This is perhaps because fidelity can be in opposition to flexibility, a characteristic seen by many as a key factor in a service’s accessibility, as will become apparent when the next theme, Accessing self-care support, is discussed.
Integration with other services
As outlined earlier in the site descriptions, the two Incredible Years sites (sites 2 and 3) had been widely adopted by local commissioning bodies. These services were closely integrated with local planning and commissioning structures and with the local education, health and social services sectors. The Incredible Years services were an exception, however. None of the other services had this level of integration with health, education and social care. The family support service (site 4) was integrated in as much as it was run by a voluntary sector organisation but funded by a local authority, with clinical supervision provided by an NHS psychologist. It also had close links with special educational needs co-ordinators (SENCOs) in schools and could form part of an action plan arising from national ‘Common Assessment Framework’196 assessments. Staff at the family support service, however, perceived that there were overlaps between their work and that of the NHS and social services, and that they fitted into a niche between the two.
The self-harm group (site 1) was run from a NHS mental health trust, at a CAMH day service. The service is attached to an inpatient unit with residential and non-residential care and education provision. Self-harm groups using the same principles are run at other NHS locations in the region, and although these groups are integrated with other services to the extent that GPs and consultants can refer CYP to them, they are usually run as ‘standalone’ services with little integration with the NHS CAMHS provider delivering them. The eating disorders (site 5) and depression/anxiety (site 6) services were provided by charities dedicated to helping people with particular difficulties in these areas. The depression/anxiety service was run by a small, relatively new organisation which provided some other activities as well as the supported online CBT, and to some extent could be seen as an alternative, rather than a complement to, statutory services. Regarding the eating disorders charity operating at site 5, integration tended to be limited to ‘signposting’ in that message board posters often offered advice to other board users about how to access statutory services, encouraging users to overcome their anxieties in accessing such services and offering opinions about those services.
Where integration was most evident was in the referral processes at the various sites. This is discussed further in the next section.
Accessing self-care support
This theme, and the next, will present findings on the acceptability of the self-care support services, both in terms of their general accessibility (this theme) and the perceived attributes that services and their staff possess that facilitate CYP and their parents to care for themselves (the next theme). Regarding general accessibility, two key subthemes emerged from the data: one pertaining to referral and one focusing on engagement.
Referral to services
Children, young people and their families had accessed the services via a range of routes, including self-referral, signposting and referral by professionals. The self-harm (site 1), family support (site 4) and parenting group (site 3) services were well integrated into referral pathways and several CYP and parents at these sites had been referred in this way. Several postings on the eating disorders message boards (site 5) mentioned being ‘signposted’ to the board by health professionals, including psychologists and doctors. The parenting group (site 3) and anxiety/depression (site 6) sites encouraged self-referral and publicised their services; some parents had found out about the service through leaflets in their child’s school bag, or through a friend. The anxiety/depression site was advertised through posters and leaflets in shops and bars as well as through presentations at schools and Sure Start centres. At Dina School (site 2), staff at the school had approached the parents of children who they thought would benefit from the service and asked these parents for consent to include their children in the group. Schools were a common source of referrals for the family support service (site 4) and two children who participated in the study had been referred by school staff, one by a SENCO and one by a school nurse. The young person interviewed at the anxiety/depression site (site 6) had self-referred to this service following a presentation at school; in interview, the service manager expressed disappointment that no school nurses had made referrals to the service.
One family who had attended the family support service recalled a long wait (around 2 years) from becoming aware of the programme to the time when they started receiving the support. Waiting times were not cited as a problem, however, by other study participants.
Building and maintaining engagement
In building engagement with health-care services, one of the first barriers to overcome can be the physical access to services. The participants at all of the case study sites seemed to encounter few physical barriers to access, though it should be added that we did not recruit those with probably the best information about barriers to access – ‘dropouts’ from the services – to our sample. For the physically provided services, none of the CYP or parents reported particular problems with travel to the sites. The virtual eating disorders support site could be accessed via the internet at any time, although messages were only uploaded when staff members were available at the service to moderate them (until 20.30 on weekdays and until the afternoon on Saturdays). The Incredible Years services (sites 2 and 3) covered a large rural area and were provided in convenient venues across the region. The young people at the self-harm group site (site 1) were all at school or college and often had to miss school or college to attend the service, though none of the young people interviewed raised this as an issue. These young people were mostly brought by car to the service by their parents. There were several examples of staff working to make services convenient to attend, or taking the service to the families. For example, staff at the family support service (site 4) worked with families in their homes and with children at school. The parenting group (site 3) was generally provided in a group setting but could be run by staff on an individual basis at people’s homes if necessary:
It’s very different to a traditional service where you might send out an invitation and if the parents don’t come then . . . they might say that you might not be able to access the service. With Incredible Years it’s more about going out and getting the parents really. So it’s about awareness raising, training lots of agencies who know about the programme . . . but [also] offering really nice coffee and biscuits. If parents miss a session, [it’s] really important that they have the hand-outs. So, if it’s possible, the leader goes and visits them at home.
Recently we’ve had a case [where] mum . . . is not ever there physically when we turn up for our appointment . . . so our worker . . . she’ll go to the child’s nursery . . . to try and catch mum at a drop-off, just to have that initial face-to-face engagement because we were mindful that this is a mum who is surrounded at the moment by professionals who are all breathing down her neck, and we wanted to make sure that mum had a fair view of where we were in that process, what our role is and that we’re not scary monsters who are trying to trip her up.
Flexibility in service provision seemed to be a key in not only building, but also maintaining, engagement with CYP and their families. As a member of staff at the family support service (site 4) outlines:
It’s looking at each case on an individual basis and thinking about what are the reasons for disengagement, why haven’t they engaged, is this a language issue, did they not understand when the appointment was, is it that the intervention isn’t working for them . . . It’s quite involved; but we don’t just do a kind of, if you don’t pitch up we send you a letter and then if you don’t pitch up again we bin you off to be picked up by some other agency – we will attempt always to get an answer. And then if it’s just that it’s not working, well, then we’ll have a conversation about that and let’s work it out.
Staff member
Another example of the flexible nature of the services was the between-session support that the sites offered. At the self-harm (site 1), family support (site 4) and parenting group (site 3) sites, support in addition to the scheduled sessions was available, including staff being available to parents over the telephone if they wanted to make contact. Staff at these sites emphasised that they worked hard to engage people in the services and to maintain engagement once a supporting relationship had been established. However, a participant who provided clinical supervision at one of the sites provided an alternative perspective on this, suggesting that it was possible to be overly flexible in that, for example, always bringing the service to a family’s home could potentially discourage independence:
I think, the fact that they [the organisation] go out and work with families in their local area, either at home, or in schools . . . that’s really important . . . something that families will like [but] if you’re going to visit somebody at home then . . . how do you evaluate their motivation to change? Because . . . if you’re at home and somebody comes to see you then actually you don’t necessarily need to do anything to engage, other than sit and nod and make the right noises . . . but if you’ve actually got to physically leave the house and go somewhere, then that suggests that your motivation might be greater to engage . . . it’s trying to get the match between that initial buy in to the service [and maintaining engagement].
Staff member (from outside the organisation)
Some staff expressed an awareness of working with parents who were used to being highly monitored by statutory services and said this could sometimes be a challenge when working to engage parents initially. A school-based member of staff, for example, who had referred several children to the service observed:
You do have the odd family who you refer who don’t engage. And it’s very sad really . . . it’s usually . . . parents who have already got to the point of social services . . . [people think] oh, don’t get social services involved, they’ll take my children from me. And once social services are involved . . . they’re breathing down your neck all the time then, aren’t they? I mean, they’re popping in and out of your house all the time, they’re watching your every move, very intrusive.
Staff member
Facilitating self-care support
This theme explores the perceived attributes that services and their staff possess that facilitate CYP and their parents to care for themselves. Key facilitators of mental health self-care support for CYP appear to be organisations and staff that are welcoming; a skills focus whereby CYP and parents are taught relevant self-care skills and then given the chance to practise these skills; opportunities for peer support; and the provision of time and attention.
Welcoming staff; welcoming organisations
Positive staff attitudes appeared to be particularly important. At every site (apart from the online eating disorders service), service users spoke spontaneously and positively about the staff running the service, using adjectives such as ‘nice’, ‘lovely’, ‘good’ and ‘thoughtful’ to describe them. Listening to CYP, allowing them to tell their own story and treating them with empathy and compassion, was also important. This was mentioned particularly by parents at the family support service (site 4) and the young people at the self-harm service (site 1), who liked the manner of the staff and contrasted this with previous, negative experiences at other services. Young people using the self-harm (site 1) and anxiety/depression (site 6) services in particular emphasised the importance of being able to trust staff in order to talk to them openly:
You have to feel comfortable talking to that person, if you don’t like them, then you’re not going to feel comfortable, so you’re not going to engage with them at the level that’s needed to help [you] recover.
Young person
At several sites, CYP and parents perceived staff as wanting to understand and help them and felt that they were treated with care and compassion:
The service worker talked to me as if he’d been there before . . . went out of his way for me.
Young person
It wasn’t just a job to her.
Parent of a younger child
Knowing that the service would accept people for who they were and be open to hearing about their problems was an important attribute of the case study sites operated by voluntary sector organisations. Being non-judgemental or offering non-judgemental support was a particularly positive aspect:
You could be honest and say, ‘This is what my child has done’, and you weren’t judged.
Parent of a younger child
Indeed, contrasts were sometimes drawn with other statutory or conventional health and social care services perceived (unfairly or not) as being judgemental. A worker who referred into the family support service noted:
You’ve got to the point where this has become . . . crisis time: ‘We’ve got a plan here in front of us, you will do this, you will do this, you will do this’ . . . whereas with [site name] it’s not, ‘you will do . . .’ it’s ’these are the suggestions that we can make, that will make things better for you’. So it’s not as judgemental, well, social services aren’t judgemental, I suppose, but it might feel like they are . . . I hear in lots of groups that I go to . . . ‘you’re all judging me, that I’m this, you’re judging me on that’.
Staff member
A similar feeling was expressed in an interview with a young person at another site:
[With the general practitioner (GP) and] even with CAMHS sometimes . . . it seems a bit like I’m being judged, or it doesn’t seem like they’re there for me in the way that I’d like, but it was different with [site name], like, it definitely felt a lot more welcoming.
Okay. Is it the people at the GP and CAMHS? Or is it more general?
I think, it’s more the method, like, I mean, it’s just all about a feeling, it feels like if I’m at the doctors . . . it becomes a thing that I’m ill, or there’s something wrong with me . . . you still sit there and you feel like you’re being judged . . . it definitely affects your confidence when you’re trying to answer, like, the questions, like, confidently and with, like, full honesty . . . I don’t know, like, when I saw my GP I didn’t tell him the whole truth, just because I didn’t feel that comfortable.
Organisational features of the sites were also important in determining how welcoming a service was. In the earlier Service development and Building and maintaining engagement subthemes, we discussed how the service leads appeared to have a high level of leadership skills, and described how staff often worked hard to make services convenient to attend, or took the service directly to the families. There were also some comments about the premises that the services were delivered from. At two of the voluntary sector sites, staff explained that particular efforts had been made to ensure that the physical surroundings were attractive to young people, featuring, for example, bright colours and soft furnishings or having music playing. On the other hand, CYP at one site commented that the rooms in which the groups were held were somewhat small. The physical features of the premises, however, were overshadowed by spontaneous references that CYP and parents made to the welcoming ambience. Indeed, there was often blurring between organisational and individual staff attributes: ‘welcoming’, ‘friendly’ and ‘non-judgemental’ were used by CYP and parents to describe both the staff and the general atmosphere or ambience of the service, often in contrast to other services they had experienced.
Activities to build skills for self-care
The use of skill-building techniques and opportunities to practise such skills in their daily lives was considered an important feature of all six services. Children, young people and parents outlined a variety of practical activities and techniques, including games and exercises, which they had used in formal sessions (in vitro) as well as at home and in school (in vivo). Fittingly, given the nature of this study, most of these activities and techniques were designed to assist the participants in managing (self-managing) the CYP’s condition or problems. For example, in the self-harm group (site 1), young people were supported in devising coping strategies other than self-harming; in site 2, children practised communication skills at home that they had learnt at Dina School; and in the family support group (site 4), families were encouraged to action plan and set goals. For younger children in particular, a large proportion of their narratives consisted of their recollections of the various games and activities in which they had taken part. The youngest children stated that they had gone to Dina School to learn things and that they got ‘prizes’ (plastic chips) for doing well at the activities there:
And what did you get a chip for?
When I’m doing stuff nice.
Many of these activities focused on identifying thoughts and emotions or on learning techniques to relieve anxiety or calm anger. These had been introduced by staff at the sites and also practised by children outside the sessions. The older primary school-aged children seemed to have more insight into the purpose of the activities and techniques:
We used to do these words about temper and then after that to calm me down we used to play a few games.
Child
The parents who were interviewed also seemed to appreciate practical techniques and talked at length about implementing these at home. Reward systems including sticker charts were mentioned frequently, along with techniques designed to help children manage tasks and express their feelings:
I think it is important to have a task and try and complete it and stuff.
Young person
I think she is responding well to positive rewards . . . she loves the reward charts . . . I give her a sticker just on her T-shirt if she’s done something really nice.
Parent of younger child
And from an interview with another parent:
Are there any things in particular that you find helpful?
Well there was the words on the fridge . . . the fridge magnets spelling out, ‘I’m not happy’, ‘I’m . . .’
‘. . . sorry’.
‘Sad’, ‘I’m sorry’ and . . .
‘I love you’.
‘I love you’, yeah. We did that for a while. We lost all the pieces, like, we did it for a while.
Some games and techniques were ‘prescribed’ as part of the manual or workbook for the course. However, most of the activities allowed some personalisation such as tailoring rewards to the individual child. For example, staff at the family support service (site 4) found out what children were interested in or enjoyed and then looked for local activities or clubs they could join, such as football or the Boys’ Brigade. At the self-harm site (site 1), young people put together their own ‘tool boxes’ of distraction techniques, memorabilia and keepsakes that helped them reduce urges to self-harm. The service also provided support for caring for wounds that arose from cutting, and advice on ways to camouflage scars, with an organisation specialising in this visiting the group.
I’ve got this thing called a tool box in my room that I put all my different distraction techniques inside so, like, if I’m having a bad day, even if I’m not having a bad day . . . I could use the different things. And different things work at different times, so one time, like, writing out your feelings might be enough, or drawing might be enough, but sometimes you have to use a range of things to minimise that urge and sometimes nothing works, but . . . at least I’ve tried.
Young person, interviewed with parent
The programmes delivered at sites 2 and 3 (the Incredible Years sites) and site 6 (the anxiety/depression support service) were supplemented by videos for participants to watch that contained vignettes or examples of role plays to augment the situations or techniques that the programmes considered. These were criticised repeatedly by staff and service users for being outdated and participants disliked that they had been filmed in the USA as they would have preferred British accents. One service user found them ‘idealised’ in that the actors looked too ‘perfect’ and suggested that videos featuring real people, not actors, would be more helpful.
Sharing experiences and peer support
Although a key aspect of all of the services at the case study sites was introducing CYP and their families to stock tools and techniques to help them care for themselves, an important aspect of skills building was supporting CYP and parents to discover self-care techniques for themselves. Often, this happened with the support of their peers, especially in the sites operating group-based approaches where other group members could play a key role in generating ideas or giving feedback. For example, children in the Dina School groups (site 2) took part in role plays and other interactions that helped them to think through how they could handle things that children might find difficult, such as sharing:
[Using a puppet to act out] snatching a book, [then discussing], is that kind?, is that unkind? . . . then after a while you’d get them to bring their problems in, you know, if you have a problem on the yard [playground], you know, if someone’s not listening to you, or doesn’t want to play, well, eventually they would come up [and talk about it with the group].
Staff member
Similarly, users of the online support service (site 5) frequently exchanged tips and techniques. Postings on the message boards often included users sharing self-care tips and suggestions with each other, and describing various relaxation or distraction techniques and activities such as reading, knitting, writing, drawing and exercising:
Listening to music is a huge relaxation thing for me, also drawing/writing – either a story, poetry or in a journal. Do you enjoy reading? To begin with i didnt have much concentration for reading, but now I am really enjoying reading again, and i find if i start reading after a meal when i am anxious that I can get lost in the book, and before i know it half an hour has passed. I’ve also tried knitting, but i’m a bit of a perfectionist so that didnt go so well. Hope you are ok, and that some of these tips may help you.
Verbatim message board posting
The following were taken from two other sites:
They discuss coping strategies, like, they’ll say, like, if you get the urge to self-harm, what do you do? And they, sort of, come up with, ‘well, I’ll go and do this, I’ll go and put my favourite music on, my film, go for a walk, walk the dog, talk to my mum’ . . . and I do think it’s very beneficial.
Staff member
I enjoyed the discussion. And what was nice is the feedback we gave each other . . . Because I think, that does you good, to have other people sometimes go, no, you’re good at that or why don’t you try this or why don’t you try that? . . . because you put it into practice with other people, it works better than you just reading books.
Parent
Although the sharing of practical tips and techniques was an important element of peer support, the sharing of the experiences among CYP and parents was perhaps more beneficial. As discussed in the first theme, Having a mental health problem, some participants had not talked about their difficulties with other people prior to coming into the services and had felt alone with their problems. Staff members and attendees at several sites talked about the emotional benefit of being in a group with people who had had similar experiences, in that people who had previously felt isolated with their problems, or uncomfortable about seeking help for them, felt less alone:
It was actually amazing really; firstly because you realise that what your child was doing was normal and that all the other children were doing the same things.
Parent of younger child
I think they listen more to their peers, their peers is pivotal, isn’t it, in adolescence, so I think the peer groups are very important, and that sense of belonging is good. And often . . . I’ve found that every single youngster who attends a group, is excluded from some aspect of their life, either from their family or from a peer group, because they’re bullied or they bully or, you know, they don’t fit somehow . . . So I guess being together with other young people helps you feel, you know, you’re not on your own with this.
Staff member, another site
As well as receiving support from others, satisfaction gained from feeling that they had helped others was also important to some participants:
It was good for [my daughter] to see that she had helped other people, she liked that; that helped her as well.
Parent of older child
As well as perceiving that the sharing of experiences was helpful, staff and parents felt that having a mixture of experiences and people at different stages of illness or recovery within a group provided additional benefits. The self-harm and parenting groups brought together people from different social groups who would normally not socialise together, but who had experienced similar problems, and this seemed to be helpful in terms of giving people a wider perspective on their problems, or perhaps developing empathy:
[They] have a good understanding of each other’s needs . . . it runs well because it’s a mixture . . . they’re all at different stages of their recovery . . . we’ve got young people who have been established for a long time and . . . have almost recovered, others are at the stage of contemplating, sort of, change and in the process of recovery and some that are not ready to change. And that’s, as I say, a very supportive group . . . those that are almost recovered, they do get and understand where [those who are less recovered] are coming from.
Staff member
Very heterogeneous . . . you’d have youngsters in local authority care, and then you’d have very upper middle class young people, who were anxious about exams and stuff like that. And that actually works as well, because kind of sometimes it’s good to see people in other situations . . . you thought your situation was really bad, but actually, there’s people who are worse off, and something about that kind of gratitude about what you have got.
Another staff member, same site
The participant quoted below, who described herself as ‘middle class and educated’ seemed to agree that this could be a benefit:
It sounds awful, but people that you might not necessarily have mixed with before, because you wouldn’t have had the chance, and got to know them . . . different social spheres . . . all of that’s broken down . . . [there can be perceptions that] . . . some backgrounds are better, supposedly, than others. And actually, you know, one of the mums in particular, who hadn’t got any further education . . . was just a fantastic mum. Whenever we’d . . . learn a new principle, when we’d feed back the next week, her and her partner had discussed it, and had both tried it . . . And it was nice to hear about other people, and there is a range of us, you know, people with partners, people without.
Parent of younger child
The ‘sharing experiences’ aspect of peer support was complemented by others including the social aspect and what might be termed an ‘empowerment’ aspect. Regarding the social aspect, service users at the self-harm (site 1) and parenting (site 3) sites enjoyed attending the groups and especially liked the social aspect of getting to know others in the group. The parenting course (site 3) had an arranged ‘buddy system’ where parents were paired up and encouraged to telephone each other between sessions to talk about how they were getting on with their tasks or exercises, and some of these parents also reported forming friendships and continuing to meet socially after the programme had finished. From the focus group:
I prefer group talks, like, talking in groups, instead of taking medication . . . [at first] I was an inpatient so I was really struggling and . . . just having the support off people in the group was what I needed.
We’re good for each other!
We just, like, support people with what’s been going on in their week, and stuff, and it’s nice, because we’re like a little family.
We are like a family aren’t we?
The social benefit of groups was also reported by the staff member at the eating disorders message board service (site 5):
[T]he message board is a really good place to start forging links with other people in a very safe and supported way and it helps to build their confidence . . . when they suggest something to somebody [and they] come back and say, ‘that was really good, I did that and it really worked for me’ [they] make very strong bonds with each other.
Staff member
Some of the group activities also appeared to help empower the CYP. For example, the self-harm groups (site 1) helped participants develop empathy by encouraging the young people to take it in turns to chair the group. Each group began with each member giving an update on how his or her week had been, and a role of the chair was to ensure that each person contributed. Staff observed that some young people in the group seemed unhappy or annoyed when they would have preferred not to contribute but the chairperson still asked them to share their experiences with the group. The staff member who described this thought that this could help young people to appreciate the difficult task that staff sometimes faced in encouraging young people to engage in ‘talking therapies’, and that sometimes encouraging someone to contribute in a group, even if they seemed not to want to, could help develop empathy and leadership skills in the young person.
Although our data demonstrate that peer support is beneficial, the risk of ‘contagion’, or triggering self-harm or problems with eating, was perceived as a key challenge by staff at the self-harm (site 1) and eating disorders (site 5) sites. Staff at both of these services saw risks in group work and worked actively to manage such risks. Unlike the parenting site (site 3), where parents were ‘buddied’ with another parent and encouraged to support each other between sessions, young people at other sites were discouraged from having contact outside of the service. At the self-harm site, young people were actively discouraged from meeting outside the group and, at the online site, interaction was controlled through moderation of the message board postings. This involved screening and editing posts to ensure that they did not contain contact information.
Some people who had attended the self-harm groups (site 1) and parenting courses (site 3) remembered feeling nervous about attending their first session. As it was the first time they had attended anything of that nature, they were unsure what to expect and were nervous about having to talk about their difficulties in front of other people. They felt that groups were only helpful for people who were at a stage of their illness or recovery where they were ready to attend a group. Our interviewees had all settled into the groups and had positive experiences, but they thought that the group setting would not be suitable for everyone; some people simply would not want or choose to discuss their problems in a group setting. Staff at the self-harm group identified managing dominant personalities as a further challenge that they had to be aware of, in order to make sure that all group members had a chance to participate during each session.
Time and attention
Giving CYP time and attention appeared to be a valued characteristic of the services. At four of the six sites, participants valued simply spending time with children, especially when this involved enjoyable activities. A key principle of Dina School (site 2) and the parenting course (site 3) was giving children positive attention. The Dina School groups allowed for each child to receive more attention than would be possible in a regular class. Parents felt that their children enjoyed being in the group and that the environment was more realistic than the regular classroom for them to learn about talking about their feelings. Parents who attended the parenting course found that setting time aside for their children was helpful, including scheduling time to play with them and also having activities together as a reward for good behaviour, and reported that their children were calmer. At the family support service (site 4), a worker described how during school holidays, instead of having appointments with children at their school, she had collected them from home and brought them to the centre, and had been surprised by how much they enjoyed this:
Often I’ll go and pick the children up and bring them here, which they just think is the best thing in the world . . . it’s not that exciting, but it’s just something different . . . that’s what some of them say.
Staff member
Participants of different ages seemed to enjoy positive attention, perhaps away from a school or the clinical or home environment:
Another thing as well that sticks in my mind about the group is when [staff member] actually took us out once into town . . . as a group . . . just to do something nice, instead of being stuck in a small room that’s quite clinical . . . it was good.
Young person
At one site, young people recalled their experiences of being inpatients, when some staff would come to talk to them, but often at inappropriate times or not for long enough. At another, family members of younger children appreciated project workers talking to the children themselves.
I think that young people often really have appreciated the fact that someone has taken the time to listen to them and hear their side of the story.
Staff member
An older sibling of one of the children at the same service singled out the way that the project worker had helped her brother to understand his behaviours and the emotions attached to them, and what might affect these:
When [child’s name] used to get angry we used to talk to him and try and calm him down . . . but we never used to speak to him about why he got angry . . . I think because [project worker’s name] spoke to him and broke it down into steps that he could understand . . . and then she used to ask him stuff about his friends and his family.
Sibling
Although CYP and parents appreciated the time and attention that staff at the sites gave them, staff mentioned that operational constraints sometimes prevented them from providing as much time as they would have liked. The manuals for the Incredible Years services (sites 2 and 3, Dina School and parenting groups) were prescriptive, with themes and associated activities being set out for each session. However, although staff at these sites liked the fact that all the materials for the sessions, and also the letters to send home to parents, were provided (as this made the course easy to deliver), they felt that there was too great a volume of material, and that they had often had to leave out certain aspects in order to complete the sessions on time.
Sometimes it was hard to keep their attention, because we’ve got a programme to deliver and it’s quite a lot to fit into those 2 hours, so sometimes [we] would look at it before and think we’re never going to fit all that in so we’d think, right, we won’t do that activity today, we’ll do that next week and try to fit in an activity where they’d be moving a bit more and try to adapt it a little bit.
Staff member
Both CYP and parent participants at several sites mentioned that they would have preferred more sessions or time with the service – a statement also echoed by staff at some sites – but financial constraints prevented this from occurring. In particular, staff at one of the voluntary sector sites outlined how a scheduled 15-week programme had to be reduced to 12 weeks because of financial and resource restraints.
Now we have this 12-week programme and it used to be a bit more like 15 weeks and we used to be able to be a bit more flexible with what each different family needed . . . I feel I used to do a lot more . . . therapeutic work with the young people and creative work, and some of that has had to be cut because we’re having to be a bit more focused on where we need to get to, which is a bit of a shame . . . I used to do a lot more kind of crafty things . . . than I feel that I’ve got the time to really do now.
Staff member
Summary of the case study findings
This chapter has presented the findings derived from 52 interviews with children, young people, parents and staff, some documentary evidence and over 500 message board postings at six case study sites.
The aim of this stage of the project was to investigate the acceptability of mental health self-care support services for CYP and the interface between mental health self-care support providers, the NHS and other service providers in the statutory, private and voluntary sectors.
A common feature across all the case study sites was the perceived accessibility of the services provided. The self-care support services appeared to offer convenient locations and appointment times, maintained engagement with between-session support, and were staffed by people who were caring and compassionate. Given that self-care support necessarily requires an agent – a professional or lay person to provide that support – it was reassuring to witness passionate, motivated, welcoming, non-judgemental and child-centred staff at all six sites. Where barriers were mentioned, they tended to be discussed in the context of other, sometimes competing, services (including standard NHS and local authority services) rather than with reference to the services at the six sites. These barriers could be seen as criticisms of the other sites and were broadly related to inflexibility: applying (stigmatising) diagnoses and labels, rather than seeing the child or young person as a person needing help and support; being dismissive of, or failing to appreciate, the concerns that CYP and their families might have about having a ‘mental health problem’ or accessing services; adhering rigidly to manualised interventions without questioning the readiness of CYP and their families to self-care or the intervention’s suitability to the CYP; and affording them little choice in their (self-)care.
Taking all of the participants’ perspectives – CYP, parents and staff – into account, we can speculate on some of the key elements of effective mental health self-care support for CYP. From the case study data it seems that, in addition to flexibility, effective mental health self-care support services for CYP seem to be built on straightforward access; positive staff and organisational attributes that are non-judgemental and welcoming; the provision of time and attention; the chance to learn and practise skills relevant to self-care; and systems of peer support which include opportunities to share experiences and practical tips.
If there is an overall constraint, it is regarding the interface with other services. The case study sites cut across the NHS, other statutory providers and the voluntary sector, yet there was no clear pattern of how well these providers worked together, if at all. In the two Incredible Years sites, there was a seamless integration of the health, social care and education sectors; yet in another site (the family support group), even though there was ‘nominal’ integration between health, social care and education, the service preferred to see itself as a ‘niche’ not quite fitting into any of these domains. In the other sites, there was either no visible integration or somewhat erratic integration or, as in the case of one site, an almost defiant refusal to integrate demonstrated by the setting up of an alternative, rather than complementary, service. Where the interface between the sectors worked best was in relation to referral: though only a few services had extremely well-integrated referral pathways, all had some degree of interface, even if it was as simple as merely signposting into, or out of, the self-care support service, or using networks among the sectors to promote self-referral to the service.
Chapter 6 Discussion and conclusion
In the previous three chapters, we presented our findings from the three interconnected stages of the study: the literature reviews, the mapping exercise and the case study. In this chapter, we synthesise the three sets of findings, using an approach similar to that which we used to integrate the effectiveness and perception reviews in Chapter 3 , additionally discussing our findings with reference to current research, policy and practice and with due regard to the aims of the study and our research objectives. Figure 13 outlines this process schematically.
FIGURE 13.
Schematic diagram of the overall study synthesis.
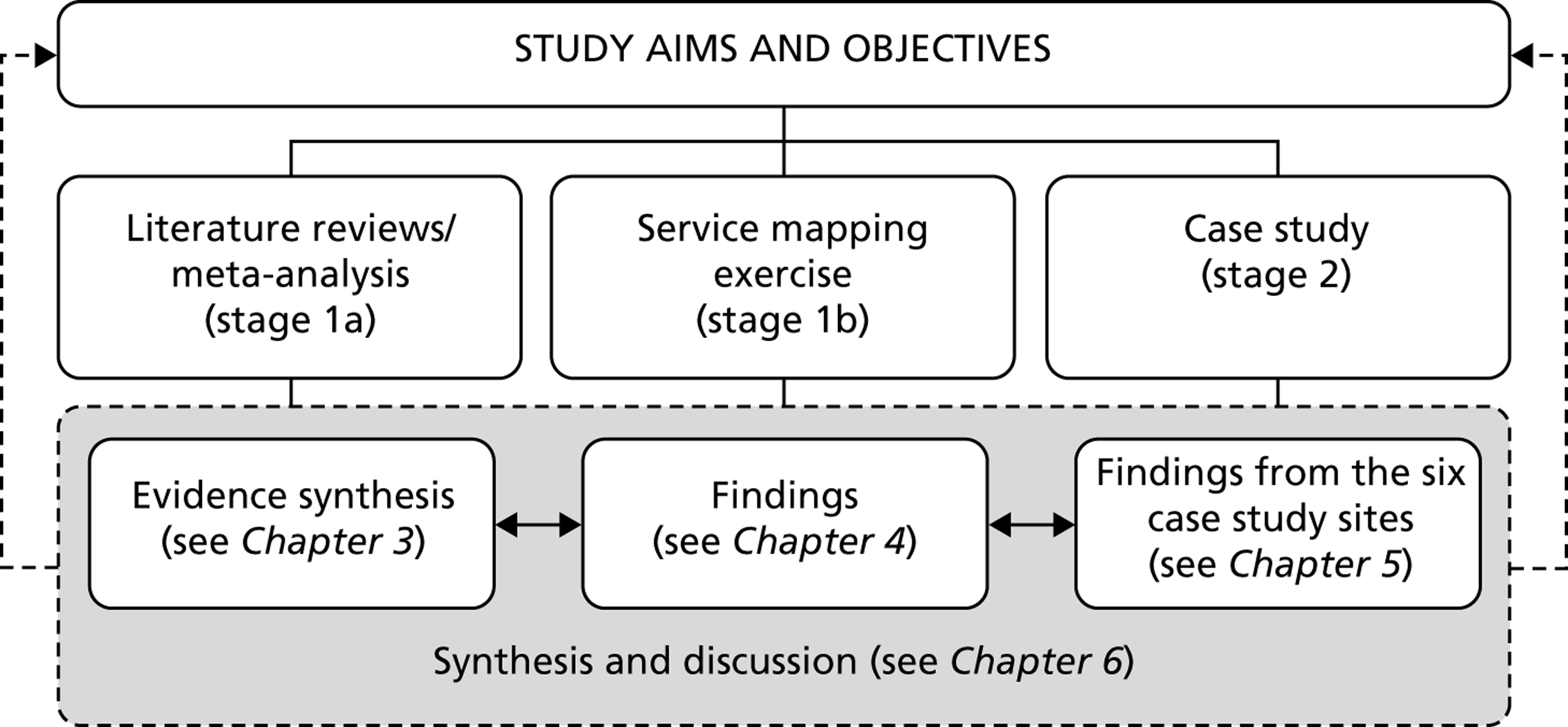
The strengths and limitations of the study and the degree of patient and public involvement (PPI) are then considered. We conclude this chapter, and the report, by discussing the implications for policy and practice that have emerged from our study and by offering some recommendations for further research.
Discussion
We begin the discussion by making some general observations about the evidence that we have obtained. An observation across of all of our data sources is that the interventions and services we examined are largely targeted at CYP with mood disorders or behaviour problems. This is relatively unsurprising given that emotional and behavioural problems are by far the most common problems in CYP’s mental health. 3 However, it is worth noting that there is relatively little about the more serious mental health problems like self-harm, psychosis and eating disorders, given that these are the problems which tend to worry education and health professionals the most. 40,197
Most of the literature we examined originated in the USA and Australia. Again, this is a relatively unsurprising finding given that the most of the manualised treatments seem to emanate from these two countries: The Incredible Years183 parenting and Coping Cat198 CBT programmes in the USA, and the Triple-P164 parenting and FRIENDS199 CBT programmes in Australia, for example. Moreover, the architects of these programmes and their associated research teams are highly active in conducting research and publishing about their respective interventions; indeed, the studies we examined in the systematic reviews were conducted by relatively few research teams. This, of course, does not explain why these approaches originated in the USA and Australia in the first place, but it is notable that they have different health-care systems to that of the UK and no ‘national’ health service. It does, however, raise some questions about their transferability to a UK context, a point made by some of our case study participants when they talked about some of the manualised programmes’ materials.
Most of the interventions and services considered in our study were designed to manage and treat symptoms rather than prevent them. This may reflect the medical dominance in CAMHS provision in most countries – one that tends to have an overemphasis on outcomes relating to symptoms and a focus on deficits rather than strengths. Consequently, the ethical, political and clinical advantages of preventative interventions (normalisation and de-stigmatisation, for instance) may be overshadowed in systems that are concerned with ‘illness’ rather than ‘health’. It may also be that those interested in preventative approaches are those who often sit outside of, or challenge, the traditional medico-scientific culture. A disadvantage of this, however, is that they might not necessarily embrace the ‘hard’ outcomes that are required to further promote an intervention or service as effective in a literature where medico-scientific approaches (such as rigorous RCTs) have the most authority. 200
The remainder of our discussion focuses on four overarching themes that provide a framework for the application of our findings to policy and practice, and in the context of the existing literature. These themes are: what works in supporting self-care in CYP’s mental health?; choice and flexibility; the interface between the NHS and other providers of self-care support; and how self-care support in CYP’s mental health might be conceptualised.
What works in supporting self-care in children and young people’s mental health?
One of the aims of our study was an evaluation of mental health self-care support for CYP. Clearly, in carrying out such an evaluation, we were interested in finding out ‘what works?’ in terms of self-care support, but in asking this question some significant tensions have emerged. These tensions arise because the answer to the question depends on two inter-related factors: how the question is interpreted (whether ‘works’ means effective, enjoyable or satisfying, for example) and who is being asked the question (the researcher, parent, clinician or child/young person).
From the meta-analysis, we found that self-care support interventions appear to be modestly effective in improving CYP’s mental health symptoms, a finding not dissimilar from other reviews and meta-analyses examining psychosocial interventions in CYP’s mental health. For example, meta-analyses on technology-based self-help in CYP,25 parenting for early-onset conduct problems201 and psychological and educational interventions for preventing depression in CYP202 have all identified small to medium intervention effects on relevant mental health symptomatology.
However, two further questions arise here: one concerns the sustainability of these effects, and the other relates to our earlier point about whose perspective – researcher’s, parent’s, clinician’s, or child or young person’s – is the more important when the value of (small to medium) intervention effects on mental health symptomatology is being considered.
Sustainability
An evaluation of CAMHS innovation projects over a decade ago203 identified a number of key elements in services that work, including having a capacity to keep in touch with CYP over the long term and offer additional, short-term intervention or support if needed. This message of sustainability in self-care support interventions has been repeated more recently in both adult mental health12 and CYP’s mental health,204 in mental health promotion in schools200 as well as in a general review of the evidence on self-management. 205 From a service user perspective, it has also been neatly summarised by a SAG member who argued that the principle should be one of ‘give us the skills, remind us of the skills and help us when we get stuck’. Given that our effectiveness review focused on short- to medium-term follow-up (6- and 12-month time points), it can, to some extent, also be seen as a ‘sustainability’ review. Our findings thus suggest that few of the self-care support interventions examined were sustainable, as effectiveness was only moderate at 6-month follow-up and it subsequently declined at 12-month follow-up. Moreover, our effectiveness review found that interventions that were longer also tended to be more effective, an observation that further suggests that a longer-term commitment may be beneficial.
Different perspectives
One clear finding from our data is that, in evaluating mental health self-care support for CYP, a range of different perspectives surface. Not only is the perceived value of an intervention or service dependent on who is asked, but some biases in the overall literature imply that certain information about interventions and services is valued more than others. Regarding the former, our satisfaction data, for example, noted that adults (parents and teachers) often rated interventions better than CYP, a finding that has been observed elsewhere,206 and in both our satisfaction and qualitative data, there was evidence that CYP did not agree among themselves about the value of a particular intervention or which specific components were the most valuable to them.
Regarding the latter, the dominance of trial studies compared with perceptions studies suggests that an effectiveness perspective is generally more valued. In addition, the observation that most outcome measures in the effectiveness studies were concerned with mental health symptomatology (see Chapter 2 , Table 4 ) also demonstrates a particular (i.e. clinical) perspective regarding the importance of particular outcomes. This contrasts with our previous NIHR study exploring children’s long-term physical health conditions,15 where a much wider range of outcome measures were considered, including health service use, which was notably absent from all of the studies we included. Moreover, the effectiveness of an intervention or service can be measured across many domains, such as a child or young person’s ability to cope or move on from a difficult situation, and not just in improvements in symptoms, and there is evidence that CYP’s problems can be addressed more effectively if their strengths, self-efficacy and resilience are promoted. 204 This is a point that the recent CYP’s IAPT programme seems to have conceded, given that the programme considers a range of outcomes including strengths, general well-being, employment, and education uptake and attendance, as well as mental health symptoms. 31
Choice and flexibility
The most salient finding of our study is, perhaps, the contrast between the effectiveness data and the perceptions data. In comparing the effectiveness and perceptions data, two related tensions arise: the tension between flexibility and fidelity, and the tension between choice and constraint.
Flexibility versus fidelity
Flexibility appears to be a key element of self-care support. Inflexibility of services was a common criticism made about standard CAMHS services by CYP and parents in the case study sites, and flexibility was identified as a valued feature of self-care support in both our previous NIHR report15 and the recent NIHR project on self-care support in adult mental health. 12 However, almost all of the interventions considered in our effectiveness review were manualised, a status that implies that there are ‘rules’ as to how an intervention should be delivered. This raises the issue of fidelity, a concept that it is somewhat at odds with flexibility. Compare, for example, the case study sites that used The Incredible Years, where fidelity to the manual appeared to be paramount (to the service lead, at least), to the perceived inflexibility of some of the manualised interventions that was evident in the perceptions review.
The issue of fidelity in manualised interventions is interesting as there is no consensus on its importance in achieving the best outcomes in psychosocial interventions. The evidence for fidelity in parenting interventions, in particular, is equivocal, with some arguing that it is a necessary component for effectiveness,207 while others argue that there is scant evidence that manuals improve treatment effects. 208 A recent discussion paper from the British Psychological Society209 attempted to reconcile these two positions in the context of the real-life service delivery of parenting programmes, arguing that fidelity is important but not at the expense of acceptability, and that fidelity should be redefined as those principles critical to effectiveness, rather than being seen as the duplication of an original in vitro model.
Choice versus constraint
In attempting to integrate the effectiveness and perceptions reviews at the end of Chapter 3 , we concluded that a key message might be one of service providers constrained by homogeneity, in terms of largely providing manualised, group-based, face-to-face (cognitive–)behavioural interventions. Homogeneity of intervention erroneously assumes homogeneity of recipient, an assumption that has been challenged in many aspects of CYP’s health-care delivery. For example, this has been pointed out in relation to human immunodeficiency virus/acquired immune deficiency syndrome (HIV/AIDS) prevention programmes for CYP210 and the mental health needs of homeless CYP,211 and in a review of CYP’s general perspectives on health and health services. 212 Treating patient groups as homogenous purely on the basis of qualifying for a specific diagnosis has also been critised,208 a fair point given that CYP diagnosed with a specific mental health condition such as anxiety will vary immensely in their needs, their experiences and the resources they have, as will their families. In terms of effectiveness, it might therefore be more appropriate to ask ‘what works for whom and in what circumstances?’ rather than merely asking ‘what works?’.
However, assuming that different things work for different people brings about the question of choice. Choice does not necessarily mean choice only in terms of specific interventions or services. It might also mean choice in terms of specific elements of the service: face to face or telephone, or group or individual. It might mean choice in terms of location: home or school. It might mean choice in the referral process including the opportunity for self-referral, a feature of two of our case study sites and a salient observation in the recent NIHR study on self-care support in adult mental health. 12 Finally, it might mean choice in terms of who makes that choice: the child or young person, a parent or, as is too often the case, the staff providing the service. In other words, choice should mean taking into account the CYP’s and their families’ individual needs. 203
In raising the issue of choice, it is not to say that effectiveness is unimportant, just that some generally effective interventions might not work for some CYP. Standard effectiveness tools such as meta-analysis are not able to assess the issues of accessibility and engagement very well, where choice might be a more significant issue and driver of outcomes. A pragmatic compromise, therefore, is that services should still consider effectiveness when providing interventions but that there should also be a reasonable choice in evidence-based approaches. To some extent, this has been recognised by the CYP’s IAPT programme,31 in that initially only cognitive–behavioural and parent training (the dominant models in terms of effectiveness data) were available but the programme has recently been extended to include other interventions with evidence of effectiveness, such as systemic family therapy and interpersonal therapy. However, even if a range of evidence-based interventions are available, the issue of who makes the choice remains. Moreover, if it is to be CYP and their parents who make that choice, there is a need to ensure that sufficient information about interventions and services, including information about their effectiveness with different CYP, different problems and different circumstances, is available so that CYP and their parents can make informed choices.
A further issue in discussing choice, and a key element of the overall acceptability of a service or intervention, is an appreciation of the CYP’s or their parents’ readiness to self-care. 12,24 Although there was little explicit reference to readiness in our findings, there were definite hints from the case study data that readiness could be an issue in terms of accessing self-care support, and it was a noticeably absent concept in most of the interventions examined in our literature reviews. Our previous NIHR study15 also picked up some hints about readiness in relation to decisions about whether to access services or not. A related concept to readiness is health activation,213 a concept we will discuss further in the Conceptualising self-care support in CYP’s mental health section later in this chapter.
Choice and groups
While discussing choice, it is worth talking about one particular feature of our overall findings. Group interventions and services dominated all of our data sets, although the groups varied from relatively small groups to groups as large as whole primary or secondary school classes. It is not difficult to understand the popularity of groups, given the peer support and shared experience advantages of group approaches in health care identified in this study, our previous study15 and elsewhere,214–216 their relatively low costs compared with individual attention, and the evidence that social support networks are associated with better mental health outcomes, fewer problem behaviours and more health-promoting behaviours in CYP. 217
However, there was some evidence from our meta-analysis that individual interventions may be more effective than group interventions for CYP, though the difference in effect size between the two (a difference in SMD of –0.11 in favour of individual interventions at 6 months) may be insufficient to counter the additional benefits that groups provide and the additional costs involved.
Furthermore, there is evidence that there are some risks to CYP in group interventions. A recent review on the role and impact of social capital on the health and well-being of CYP217 reported that, in certain circumstances, social support networks could increase participation in health-risk behaviours such as alcohol and tobacco misuse, an observation backed up by our case study reports concerning the risk of ‘contagion’ in eating disorders and self-harm groups.
Interface between the NHS and other providers of self-care support
The second aim of our study concerned the interface between the NHS and other providers of self-care support. Compared with our previous study,15 the role of the NHS was less defined in self-care support in CYP’s mental health than it was in CYP’s physical health. In particular, the voluntary sector dominated the services identified in the service mapping. This could, of course, be down to the NHS not publicising any self-care support services it operates in its CAMHS provision; however, it is more likely to be an accurate reflection of current service configuration, given that commissioners of CYP’s mental health services are looking increasingly at alternative providers to NHS organisations to deliver NHS-commissioned and funded services, a situation we found previously in relation to CYP’s physical health. 15 Indeed, the voluntary sector currently has significant involvement – even to the point of subcontracting from the NHS – in two flagship CAMH service innovations in England: the CYP’s IAPT31 and the Better Outcomes New Delivery (BOND) early intervention programmes. 218
The general policy consensus is that the interface between statutory services such as the NHS and the voluntary sector should be one of partnership. 9 In the recent NIHR study on self-care support in adult mental health,12 projects not under the control of the NHS (i.e. voluntary sector projects) were seen as risky by the NHS, which implies a lack of either understanding or communication between one or both parties. This might be down, in part, to tensions between two sets of ‘experts’, each feeling their expertise to be more important than the other’s, and to some extent this parallels the tensions already seen between provider and recipient when we considered the ‘effectiveness’ and ‘acceptability’ of self-care support interventions.
It terms of service provision, it is worth looking at a couple of other salient findings from our study: the location in which the service is provided, and the underuse of technology.
Location of service
The evidence on where services should be located is somewhat equivocal. Our effectiveness review findings suggest that the setting (clinic, home, school, etc.) is a largely irrelevant factor in the effectiveness of an intervention and no argument in favour of any particular location emerged from the perceptions review. This suggests that other factors need to be taken into account when considering the location at which self-care support should be delivered. The case for hospital-based services is generally weak. A recent King’s Fund paper219 argues that health service delivery in general needs fundamental change and that hospital-based care should be reserved for those who cannot be treated more appropriately elsewhere. Our case study data also suggested that inpatient hospital care was not particularly well liked by participants. In terms of mental health provision, current government policy9 is that people with mental health problems – including CYP – should be treated in the least restrictive environment. For CYP, the least restrictive environment usually means school, home or some other community-based location such as a clinic or community centre. All of these locations have advantages and disadvantages. Clinics, community centres and schools often have town centre locations close to transport hubs, a factor seen as important in terms of access214 though our case study data implied that physical access was not necessarily a critical factor for participants. Formal clinics, however, may, at best, reinforce the medicalisation of the CYP’s problems and, at worse, stigmatise the CYP. The family’s own home offers convenience and few access problems but not everyone is comfortable with professionals intervening at home. Perhaps the best candidate for location is schools: schools are part of the CYP’s normal experience, and the fact that most of the studies in the effectiveness review were school based demonstrates that schools are feasible places for delivering such interventions. Moreover, there is evidence that schools are substantially more cost-effective at delivering mental health interventions for CYP than routine CAMHS. 220 On the other hand, there was some evidence in our case study data that schools are not necessarily prepared for the task (as they came in for criticism, along with inpatient hospital care, from some of our participants), and there is some evidence, at least in terms of preventative approaches,200 that schools may need to have the right ethos in place to be centres for mental health support.
Use of technology
Given the commonly held view that CYP are inherently comfortable and confident with new technologies – that they are ‘digitally native’ – there was surprisingly little use of computers and internet technology in the interventions and services we examined. None of the interventions examined in the effectiveness review used computer or internet technology, there were only three such interventions in the perceptions review and only five were identified from the service mapping. This might be because the peer support and shared experience elements of face-to-face, group self-care support are harder to replicate online (though not impossible, as the eating disorders online support case study site has demonstrated); or it might be because NHS services in particular are inherently conservative and have not yet caught up with the technology. 221 On the other hand, it might be that the assumptions about CYP being digitally native are incorrect180,222 – that CYP have no greater a preference for computers and internet technology than adults or that, again, homogeneity is being assumed in CYP when in fact some may embrace technology more than others. This is a salient point because it brings about once more the issues of choice and readiness, in that some CYP may not be ready to use technological interventions and some – as we found in our perceptions review – may not particularly like them. Nevertheless, there is evidence from elsewhere that technology can help in engaging CYP in mental health services: for example, the use of text messaging to reduce ‘did not attend’ rates. 214,223
Conceptualising self-care support in children and young people’s mental health
It is clear from this study that self-care support services in CYP’s mental health do exist, and are being researched, but what is interesting is that very few of these services make explicit reference to ‘self-care’ in their names or service specifications though, occasionally, a related term such as ‘self-help’ or ‘self-management’ may be used. This is in direct contrast to CYP’s physical health where self-care is an established part of the vocabulary. A similar conclusion was drawn in the recent NIHR-funded study on self-care support in adult mental health. 12 One reason for this might be the increasing adoption of ‘recovery’ as a general philosophy of mental health service provision over the last decade or so. In addition, the move towards strengths, rather than deficits, models in CYP’s mental health has brought into focus a related concept: resilience. The key elements of recovery are hope; the establishment of a positive identity; a meaningful life; and taking responsibility for, and control over, one’s own life. 18 All of these elements could describe self-care; indeed, they are implicit, if not explicit, in our definition of self-care (see Chapter 1 ). Moreover, in embracing a philosophy of recovery, the role of mental health practitioners becomes more about doing things with service users than doing things to them, and so, in a recovery framework, mental health practitioners are essentially guides, facilitators and coaches. It is thus not difficult to see how ‘recovery’ might simply be a synonym for self-care in a mental health context, or how it might be encapsulated as part of ‘resilience’ if the self-care support agent helps the CYP identify, and build upon, their strengths; at the very least the concepts are closely related. 12,224
Another interesting dimension in conceptualising self-care support in CYP’s mental health is the observation from the literature review and mapping exercise that most of the interventions and services are targeted at CYP rather than at families. This assumes that CYP are the ‘problem’, and there is perhaps a need within recovery- or resilience-focused approaches to ensure that (a) the emphasis is on strengths rather than problems, and (b) any problems are considered within the context of the family and the CYP’s social networks.
Conceptualising mental health
When considering how self-care support might be conceptualised in CYP’s mental health, it is not surprising to find that conceptualisations of ‘mental health’ can also be somewhat vague. For example, when reporting the case study findings, we noted that conceptualisations of mental health seemed to be connected to the CYP’s age, with mental health being conceptualised in younger children as a lack of confidence or difficulties with emotion and behaviour, and in older children as diagnosed conditions or severe mental health problems. The reasons for this are far from simple; being ‘diagnosed’, for example, may be down to capacity and configuration of local services, the expectations of the child and/or parent, and social constructions of mental illness. There is, nevertheless, a balance to be struck in conceptualising a child or young person’s difficulties as mental health problems or not. A diagnosis is often a criterion that triggers access to a potentially helpful service or it can act as a filter for different interventions and services, as there is evidence in self-care support that different conditions benefit from different approaches. 205 Yet a diagnosis can also have negative connotations (leading to stigmatisation and exclusion, for example), as one of our case study sites made clear when it asked for the removal of any reference to ‘mental health’ from our recruitment materials, even though it was delivering an ostensible mental health service. Maybe choice needs to be considered here too in that CYP should be allowed a choice as to whether they accept a diagnostic label or prefer to focus on, for example, identifying specific needs, feelings and opportunities to develop strengths. This is also reflected in the current debates expressing concerns about the increasing ‘medicalisation’ of emotions and behaviours in CYP. 225,226
It is also worth asking whether CYP’s mental health problems and needs should be considered as long-term conditions because the focus for many families is, as it is for the families of CYP with long-term physical health needs, often more about quality of life and living (well) with a condition than it is about ‘curing’ the condition. Mental health self-care support interventions for CYP need to be considered in a context where the majority of adult mental health problems have their origins in developmental problems in childhood;227 yet, as our study illustrates, what tends to be on offer are relatively short interventions with erratic follow-up periods (often merely for research purposes) for CYP who have problems and mental health needs that are likely to extend into adulthood. Clearly, there is a relationship here with our earlier discussions on sustaining self-care, and a conceptualisation of CYP’s mental health in a longer-term context may help address some of the shortcomings in the sustainability of specific interventions and services.
A conceptual model of mental health self-care support in children and young people
In modifying the typology of self-care support (see Chapter 4 , Table 19 ), we argued that self-care support in CYP’s mental health can be seen as a process. There needs to be the acquisition of knowledge and skills, which require input and motivation on the child or young person’s (or parent’s) part; opportunities to practise and consolidate these requisite skills, with support and facilitation from a self-care support agent; and some positive outcomes for the child or young person and his or her family. Moreover, as we earlier argued, there is some evidence that this process should be long term rather than short term. On the basis of our findings and the discussion herein, a conceptual model of mental health self-care support is proposed in Figure 14 .
FIGURE 14.
A conceptual model of mental health self-care support in CYP.
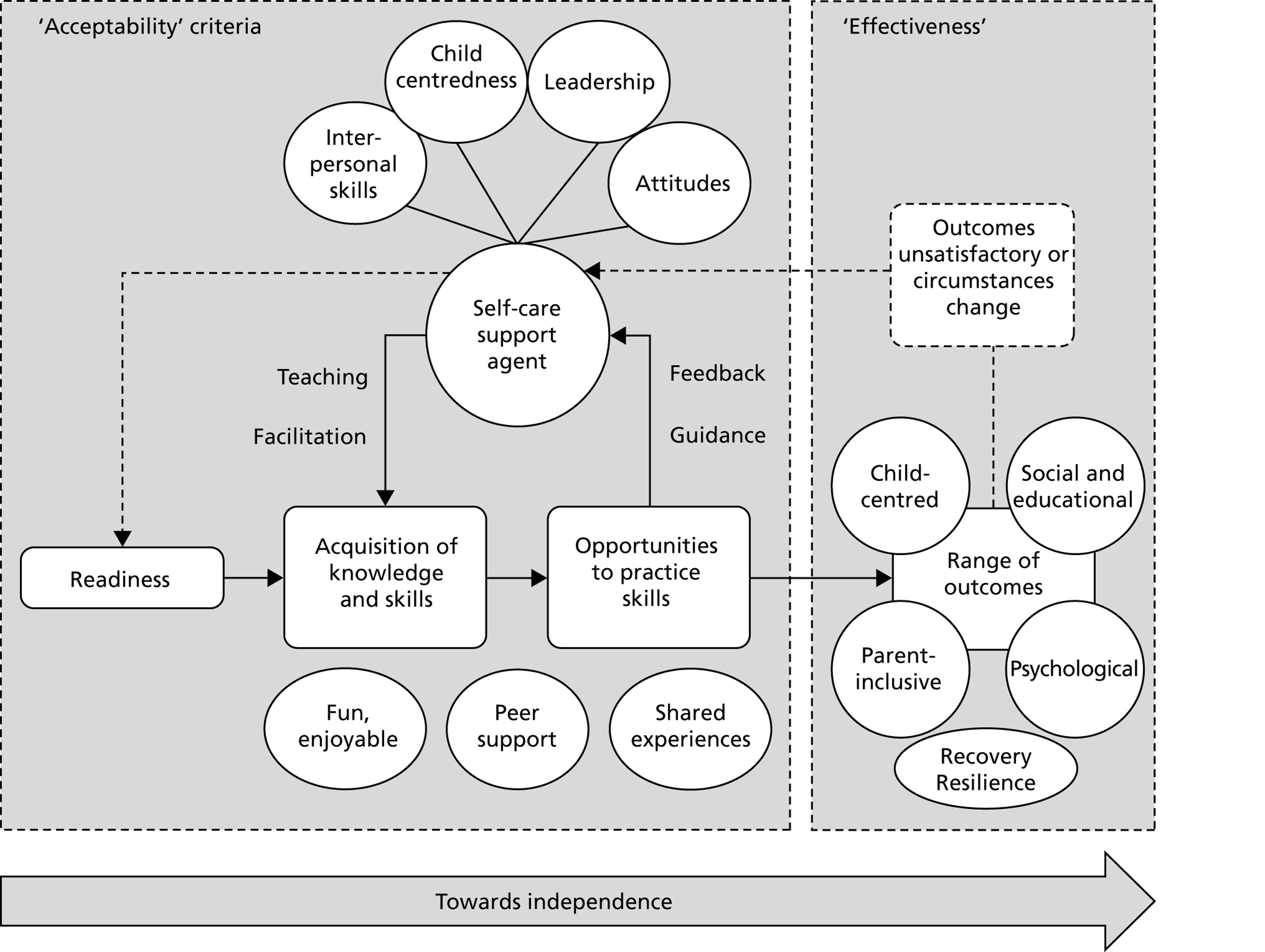
We have discussed a significant number of the elements of this model already, including effectiveness, acceptability, readiness and outcomes. Choice and flexibility, though not explicit in the model, permeate the whole model in that various elements of it, such as the types of skills on offer and the means of acquiring them, the outcomes used and even the self-care support agent, can all be tailored according to the individual needs of the child or young person and his or her family. Two critical elements of the model – skills and the self-care support agent – warrant further discussion, however.
Regarding skills, it seems that skills and the activities that support their development are a central feature of effective self-care support programmes12,15,200,203,205 and of recovery in CYP’s mental health in general. 214,217 However, as mentioned above, choice and flexibility need to be considered when identifying these skills and providing the support CYP and their families need in acquiring them. This raises the issue of the personalisation of health-care services and the associated issue of personal health budgets,219,228 although it seems these two issues raise tensions similar to the ones we identified when discussing effectiveness and acceptability, in that the patient preferences inherent in personalisation have to be reconciled with a co-existing framework of ‘payment by results’ where effectiveness is the key concern. 229
Regarding the self-care support agent, the principal issues that need discussing are the attitudes and attributes of the professional or lay person taking on this role. This involves some discussion of both the attitudes of the agent and their interpersonal skills, as well as some comments about education and training.
Qualities of the self-care support agent
Our case study data suggested that the personal qualities of the staff providing the self-care support were important, with staff generally seen to have positive attitudes such as being non-judgemental, welcoming and an active listener. There were also some hints in the perceptions review that the quality of the relationship with the agent and the expertise of the agent may be as important as, if not more important than, the intervention itself. This is a common theme in the literature: participants in our previous NIHR study15 remarked on the approachability of the self-care support agents and their abilities to listen and be non-judgemental; a recent Health Foundation review on self-management205 found that the attitudes and skills of staff can have a significant effect on perceived levels of engagement and support; and in CYP’s mental health, the ‘therapeutic alliance’ has been identified as a significant but neglected factor in treatment. 230
Leadership in self-care support services may also be an important personal and organisational attribute, and we saw evidence of strong leadership in our case study sites. Effective and consistent leadership was identified as a key element of ‘what works’ in CAMHS provision,203 and the recent NIHR study on self-care support in adult mental health12 noted that charismatic leadership was a feature of many of the projects examined.
Another key personal and organisational attribute is child-centredness. As in our previous NIHR study,15 being child-centred was a feature of most of the case study sites. The general literature indicates that effective patient-centred care requires two specific elements: the straightforward eliciting and discussion of the patient’s perspective and ‘activation’, i.e. a deeper understanding of the individual’s motivation and readiness to become involved in a service, change their behaviour or self-care. 231 This suggests that for the self-care support agent to be truly child-centred, they need to understand not only the CYP’s problems and needs but also recognise the extent to which they are ready. This raises the question of whether or not a readiness measure of some sort, whether standardised and formal like the Patient Activation Measure213 or something more informal like simply asking the question ‘do you feel you are ready?’, should be routinely used in health-care practice.
From an organisational perspective, child-centredness requires – as we saw in the case study sites in this study and in our previous study15 – a friendly, fun, welcoming atmosphere where the CYP’s views are listened to and respected. Above all, child-centredness requires a partnership between the provider and family, one that demands that CYP and their families be seen as part of the care team or, to use a phrase currently gathering momentum in adult mental heath care, as ‘coproducers’ of their care. 232
A consideration of the attributes and skills of the self-care support agent inevitably raises the issue of education and training. None of the attributes and skills required of the support agent necessitate mental health training, and it was interesting to note that our effectiveness data suggested that there is no specific advantage in the agent being mental health trained, although there is some evidence82 in the literature to counter this, and it was notable that around three-quarters of those delivering interventions in the effectiveness studies were specifically trained for the role. What seems to be essential is the ability to understand the CYP’s perspective, and to focus on their needs and the needs of their families, rather than on the needs of the service or the people leading the service. This may require attitude changes among CAMHS staff and those managing services and, certainly, if an eclectic range of interventions is to be made available within CAMHS, then it will require opportunities for staff to retrain and develop new skills. 204 In terms of attitude, in England and Wales at least, our findings suggest that the voluntary sector seems to be ahead of the NHS and other statutory services. However, as our case study data indicate, there is also excellent service provision in the NHS. Thus, it may not matter which sector delivers the service, so long as the staff are child-centred, have opportunities for training and development and are supported by strong leaders. Moreover, there could be considerable benefits for CYP with mental health needs and their families if opportunities are made available for the NHS and the voluntary sector to learn from each other.
Limitations and strengths of the study
All research studies have limitations and in this section the limitations of the various aspects of the study are considered in turn, together with some overall limitations. Some comments are also made throughout about the study’s strengths.
Systematic reviews
As there was a common data pool for the effectiveness and perceptions reviews, the principal issue was the same for both: having to manage an unexpectedly large pool of literature. Although this was clearly related to the issue of how self-care is conceptualised in mental health, the sheer size of the returns we got from our searches and the time available for the systematic reviews meant that we had to make some post hoc, pragmatic decisions, and these decisions, while rational, may have introduced bias into the process. For example, searching electronically in Reference Manager and the Access databases to screen out irrelevant papers on the basis of title or abstract meant that we may have overlooked some relevant papers that manual inspection may have picked up. In hindsight, our search strategy may have been too inclusive although, given that self-care is an unexplored area in CYP’s mental health, we are confident that it needed to be broad.
The reason for the date from which we searched – 1 January 1995 – may have been tenuous, though again the decisions made were rational: it was the date used in our previous self-care support study15 and the year in which major organisational change came about in UK CAMHS provision;38 however, this latter point has less relevance to the international literature.
The effectiveness review and meta-analysis were limited in several ways. Firstly, the post hoc decision to exclude those RCTs with only short-term (postintervention) effectiveness data meant that we had a manageable number of RCTs to describe and meta-analyse, but it also meant that we may have missed some important findings in these studies. Nevertheless, there was an advantage in selecting only those RCTs with longer-term effectiveness data in that sustainable interventions are of more interest to policy-makers and practitioners. A second limitation was the generally poor quality of the included trials. Although we did not include a full Cochrane risk of bias analysis in the effectiveness review, we nonetheless explored the most significant risk – concealment of allocation – finding only seven and nine ‘high-quality’ RCTs at 6- and 12-month follow-ups, respectively. A further limitation is that we did not include cost-effectiveness as a factor in exploring mental health self-care support interventions for CYP.
The perceptions review was limited by the sizeable number of poor-quality studies. For the qualitative aspect, it was also confounded by a relatively small number of studies: just 33 in total, of which only 13 made it through qualitative appraisal. Moreover, of these, only two met all seven of the quality criteria on the quality appraisal tool used. For the quantitative aspect, there were no studies that collected numerical satisfaction data independently of a trial, i.e. all of the satisfaction data were nested within a trial of some sort, controlled or uncontrolled. Furthermore, almost all of these data – including those obtained from high-quality RCTs – were obtained from unvalidated, local satisfaction measures or tentative ‘proxy’ measures, such as attendance at sessions. Standardised statistics such as means and standard deviations were rarely reported; it was unfeasible, therefore, to conduct a second meta-analysis using ‘satisfaction’ as an outcome. It was also difficult to make any sort of quality judgement on the quantitative satisfaction data; indeed, it would have been rational to exclude all of the quantitative satisfaction data, but this would have left us without a ‘majority’ perspective to counterbalance the individual perceptions obtained from the qualitative studies. Again, therefore, a post hoc pragmatic decision was made and only studies initially qualifying for the effectiveness review were included.
Nevertheless, the size of the review is also one of its strengths in that we were able to give a broad overview of recent effectiveness evidence and explore some factors that may or may not be associated with outcome.
Service mapping
The service mapping stage was designed to enable us to provide a descriptive overview of mental health self-care support services for CYP in England and Wales, and was dependent on detective work on our behalf and the information that was volunteered by the networks we had contacted. To a large extent, service mapping is the process of trying to identify the ‘population’ of a particular service, and this brings about an inherent problem: in trying to identify, with little prior information, all members of a population, concepts like ‘sample’ or ‘response rate’ are meaningless. We thus have no way of knowing whether the services that we identified are the total population of mental health self-care support services for CYP in England and Wales, or a sample. If they are a sample, we likewise are unclear whether the sample is large or small, or whether or not it is representative of the total population. We are thus unable to say with any degree of confidence that we have produced a comprehensive overview of self-care support services in England and Wales, and although this is not a fatal aspect of our study, it does nevertheless have some bearing on the case study element in that the service map provided the sampling frame for our case study sites.
We could have been more assertive with the service mapping element by, for example, conducting a postal, telephone or online survey across the major statutory and non-statutory providers. However, we do not know whether or not the considerable additional resources required for this (especially in relation to postal and telephone surveys) would have elicited any more information than that which we gleaned using the methods we employed. Indeed, our experiences of an online survey in our previous study15 suggested that it would not, and this, together with the generally low response rate in postal surveys of health-care professionals,233 explains our approach here. There is nonetheless an argument for carrying out a more comprehensive service mapping exercise, and we make this one of our recommendations for further research.
A further limitation here involved the difficulties we had in tracking down sufficient information about potentially eligible services, when we only had very limited information about a service, such as its name or details of a website or a contact number. Following up these leads required considerable effort on our behalf, and numerous e-mails and telephone calls went unanswered, for a variety of reasons that we can only speculate on (the service having closed without our knowledge or the service having only a single member of staff, for example).
Case study
In selecting the case studies, we were careful to ensure that all of the typology and other relevant dimensions were considered, so that we obtained views on a range of different services. We also tried to ensure that we sought views from all stakeholders – CYP, parents and staff – at each of the sites. Although our case study sites are representative of the self-care support sites we identified in the service mapping, it is unknown how transferable they are to mental health self-care support services for CYP in general, given that we do not know what the true population of such services is. That our case study findings have resonance with other findings on CYP’s mental health services in the literature does, however, suggest some degree of transferability.
Regarding the source of our data for the case studies – CYP, parents and staff – there could be an inherent bias in that we were able only to speak to CYP and parents who had remained with a service. It was not possible for logistical and ethical reasons to recruit CYP or parents who had ‘dropped out’ of the services. In addition, although we managed to obtain ‘virtual’ non-participation observation at our online case study site, we could perhaps have enhanced our data pool by observing sessions at some of the other case study sites. Apart from the fact that it was not part of our original plan to obtain data by such means, there were several other reasons for not carrying out more general non-participation observation, including the ethical complexities of observing, rather than asking for views about, treatment and the practicalities of arranging it.
We outlined in Chapter 5 that the interview format was dictated largely by pragmatism, and that we allowed the sites and individual participants to determine the format most convenient for them. Given the views in the Choice and flexibility theme discussed earlier in this chapter, this was a somewhat fortuitous decision, though it is not without limitations. In the joint CYP–parent interviews, for example, we do not know the extent to which the presence of a parent influenced what the child or young person had to say, nor whether we would have obtained different data had the parent and the child or young person been interviewed separately. On the other hand, the variety of interview formats employed could be seen as a strength of the study in that we still managed to obtain some strong views from CYP regardless of whether parents were present in the interview or not, and the choice and flexibility offered may well have helped recruitment.
That we only managed to interview one young person at site 6 might be seen as inadequate if taken in isolation. However, as part of a collective case study designed to elicit a broad appreciation of a particular issue (see Chapter 5 , Design), we are confident that the limited site 6 data have some value.
Across all stages of the study
Our experiences in conducting this study demonstrate that self-care support in CYP’s mental health is a complex area; there are multiple conditions, a variety of theoretical perspectives (though one or two dominate), widely different content in the services and interventions, and a range of agents and different intervention levels (most notably preventative vs. management interventions). Obviously, self-care support was a common feature of all the services and interventions. However, it may be that the multiple dimensions involved resulted in a somewhat unwieldy study that could have been better co-ordinated had we concentrated on a few specific aspects (e.g. interventions for CYP with mood disorders only) or, given our earlier discussion, avoided confounding management-level and preventative interventions and services by only studying one or the other. Nevertheless, there has been an advantage in exploring so many dimensions in that we are aware of where there are shortfalls in the knowledge, for example in relation to CYP with psychosis or an eating disorder or those who self-harm, and in relation to the use of technology.
Patient and public involvement in the study
One of the study’s strengths was its PPI. We had a significant advantage in this study in that it was planned and conducted with the support and involvement – as co-investigator – of YoungMinds, a specialist mental health charity for CYP and their carers. This was the first time that YoungMinds had been involved in NIHR-commissioned research, and the experience has led to further collaborations, including YoungMinds’ involvement in another NIHR-commissioned research study in which the principal investigator of the present study (Pryjmachuk) is a co-investigator. 7
As with most research projects, there were unexpected issues that prevented us from involving YoungMinds to the extent that we had anticipated. We originally intended to have a separate SAG made up of CYP only. However, when consulting with YoungMinds and other members of the stakeholder group, the consensus was that the CYP known to YoungMinds would be assertive enough to attend a single stakeholder group, and there was thus no need for a separate group. We planned to invite members of YoungMinds’ Very Important Kids (VIKs) – a group of CYP aged 11–24 years who advise YoungMinds on policy and campaign objectives – to this stakeholder group, but we were, unfortunately, unable to recruit any of the VIKs. We did, however, manage to recruit a project worker for the VIKs to the stakeholder group, who spoke on their behalf.
We did manage to involve the VIKs and some other CYP in some aspects of the study; they helped us out with the recruitment documentation for the case study element, giving us feedback about the age appropriateness and readability of the participant information sheets and consent/assent forms. We did plan to put the final results of the study to the VIKs for their views and for their assistance in ensuring that CYP could understand what we had found, but unfortunately, the VIK project ended during this study when its 3-year Big Lottery funding came to an end. Nonetheless, the final results have been put to a SAG that included advocates for CYP and parents, as well as representatives of health, education and social care.
Conclusions
The aims of this study were to identify and evaluate the types of mental health self-care support used by, and available to, CYP and their parents, and to establish how such support interfaces with statutory and non-statutory service provision. Through two inter-related systematic reviews, a mapping exercise and a case study, we are confident that we have achieved these aims. Moreover, in doing so, we have developed a model of self-care support that can help policy-makers and practitioners make decisions about the organisation and delivery of mental health self-care support for CYP and their families, and help researchers identify gaps in the knowledge base that might be resolved with future research in this area.
Contribution of the study
This study makes a contribution to the knowledge base by being the first to formally explore self-care support in the context of CYP’s mental health, an area that is generally under-researched. It is also unique in that it has considered the evidence from a variety of perspectives – including both effectiveness and stakeholder views evidence – and has attempted to integrate those perspectives into a meaningful synthesis.
Implications for health care
In term of implications for policy and practice, we note the following:
-
that self-care support in CYP’s mental health requires a partnership between service providers, the CYP and those who provide care for them
-
that CYP and their families want ongoing support from, and contact with, services
-
that the means by which professionals can support CYP and their families to self-care are not generally considered in the education and training of those working in all four tiers of CAMHS provision
-
that effective services need not necessarily be delivered by mental health-trained staff or by NHS organisations – it is the child-centred skills and attributes of the individuals and organisations that are important
-
that choice and flexibility seem to be important aspects of self-care support in CYP’s mental health, but true choice from a range of interventions is rarely available to CYP (although the continual rollout of the CYP’s IAPT project may resolve this)
-
that practitioners working in CYP’s mental health rarely consider a child or young person’s readiness to engage with a service or commence an intervention
-
that it is important that outcomes other than those relating to mental health symptoms are considered.
Recommendations for research
We make the following recommendations for research into mental health self-care support for CYP, in order of priority:
-
that, because of under-representation in our data, research be undertaken on the potential for self-care support in the more serious mental health problems of psychosis, eating disorders and self-harm
-
that, because of the surprisingly little work on the use and role of technology in self-care support for CYP’s mental health and a lack of consensus on its potential value, research be undertaken exploring the advantages and disadvantages of using computer and internet technology in self-care support
-
that, because there were differences in perceptions of, and satisfaction with, services and interventions, both among CYP and between CYP and adults, more work is conducted on unpicking these differences
-
that, because it is a relatively unexplored, yet important concept in self-care support, the concept of readiness to self-care be explored further
-
that, because it is a relatively unexplored area and there were some potentially valuable findings from our study, research on leadership in CAMHS be commissioned
-
that further research be undertaken on how self-care is conceptualised in CYP’s mental health and, in particular, its links to concepts such as recovery and resilience
-
that, because of the limited service mapping data provided, a more systematic and comprehensive mapping exercise of self-care support services in CYP’s mental health be carried out
-
that work be undertaken on the cost-effectiveness of providing self-care support in CYP’s mental health
-
that there is more testing of interventions and services in real-life environments compared with laboratory or clinical environments (i.e. research on efficacy rather than effectiveness).
Acknowledgements
We express our grateful thanks to all of the participants who took part in this study and to the individual organisations who permitted us to use their service as a case study site. We are also grateful to individuals and organisations that have helped facilitate this study, including Sue Pargeter at the NIHR; the stakeholder group members; Beat; the Open Door Centre; YoungMinds and their Very Important Kids; Claire Hodkinson for her advice on the search strategy; Penny Bee and Judith Gellatly for their advice regarding the effectiveness reviews and the meta-analysis; Shirley Hannan for research governance and finance advice; and the peer reviewers who constructively commented on the original grant application and this report.
Contributions of authors
Steven Pryjmachuk (Professor, Mental Health Nursing) led on the design and conceptualisation of the study; conducted the literature searches for the systematic reviews; contributed to the data extraction and analysis for all aspects of the systematic reviews and meta-analysis, mapping exercise analysis and case study; and led on writing and editing the report.
Rebecca Elvey (Research Associate, Health-care Research) assisted with the literature searches for the systematic reviews; contributed to the data extraction for both systematic reviews and the analysis of the perceptions review; conducted the offline and online search and analysed the data for the mapping exercise; obtained the ethical permissions required; conducted the interviews for the case study; led the analysis of the case study data and the writing of the case study chapter; and reviewed and approved the final report.
Susan Kirk (Reader, Health Service Research) contributed to the design and conceptualisation of the study, data extraction for both systematic reviews, analysis of the perceptions review and case study data analysis; and reviewed and approved the final report.
Sarah Kendal (Lecturer, Mental Health Nursing) contributed to the design and conceptualisation of the study, data extraction for both systematic reviews, analysis of the perceptions review and case study data analysis, and reviewed and approved the final report.
Peter Bower (Professor, Heath Services Research) contributed to the design and conceptualisation of the study; assisted with the data extraction for the meta-analysis; supervised the meta-analysis process; and reviewed and approved the final report.
Roger Catchpole (Education and Training Manager, YoungMinds) contributed to the design and conceptualisation of the study from a PPI perspective, the analysis of the perceptions review and the case study data analysis, and reviewed and approved the final report.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Bright Futures. London: Mental Health Foundation; 1999.
- Meltzer H, Gatward G, Goodman R, Ford T. Mental Health of Children and Adolescents in Great Britain. London: The Stationery Office; 2000.
- Green H, McGinnity A, Meltzer H, Ford T, Goodman R. Mental Health of Children and Adolescents in Great Britain, 2004. Basingstoke: Palgrave MacMillan; 2005.
- Children and Young People in Mind: The Final Report of the National CAMHS Review. London: Department for Children, Schools and Families/Department of Health; 2008.
- Services for Children and Young People with Emotional and Mental Health Needs. Cardiff: Auditor General for Wales; 2009.
- Shepperd S, Doll H, Gowers S, James A, Fazel M, Fitzpatrick R, et al. Alternatives to inpatient mental health care for children and young people. Cochrane Database Syst Rev 2009;2.
- Hannigan B, Edwards D, Evans N, Gillen E, Longo M, Pryjmachuk S, et al. An Evidence Synthesis of Risk Identification, Assessment and Management for Young People Using Tier 4 Inpatient Child and Adolescent Mental Health Services (CAMHS) n.d. www.nets.nihr.ac.uk/projects/hsdr/11102408 (accessed 23 April 2013).
- The NHS Constitution for England: the NHS Belongs to Us All. London: Department of Health; 2013.
- No Health Without Mental Health: A Cross-Government Mental Health Outcomes Strategy for People of All Ages. London: Department of Health; 2011.
- Rogers A, Kennedy A, Nelson E, Robinson A. Uncovering the limits of patient-centeredness: implementing a self-management trial for chronic illness. Qual Health Res 2005;15:224-39. http://dx.doi.org/10.1177/1049732304272048.
- Kennedy A, Rogers A, Bower P. Support for self care for patients with chronic disease. BMJ 2007;335:968-70. http://dx.doi.org/10.1136/bmj.39372.540903.94.
- Gillard S, Edwards C, White S, White R, Adams K, Davies L. The Barriers and Facilitators of Supporting Self Care in Mental Health NHS Trusts. Southampton: National Institute for Health Research Service Delivery and Organisation Programme; 2010.
- Supporting People with Long Term Conditions to Self-Care. London: Department of Health; 2006.
- Your Health, Your Way – A Guide to Long Term Conditions and Self Care. Information for Healthcare Professionals. London: Department of Health; 2009.
- Kirk S, Beatty S, Callery P, Milnes L, Pryjmachuk S. Evaluating Self-Care Support for Children and Young People with Long-Term Conditions. Southampton: National Institute for Health Research Service Delivery and Organisation Programme; 2010.
- Lovell K, Bee P, Richards D, Kendal S. Self-help for common mental health problems: evaluating service provision in an urban primary care setting. Prim Health Care Res Dev 2006;7:211-20.
- IAPT . IAPT: Improving Access to Psychological Therapies – About Us n.d. www.iapt.nhs.uk/about-iapt/ (accessed 20 April 2013).
- Shepherd G, Boardman J, Slade M. Making Recovery a Reality. London: Sainsbury Centre for Mental Health; 2008.
- Every Child Matters. London: The Stationery Office; 2003.
- The Children’s Plan: Building Brighter Futures. London: The Stationery Office; 2007.
- Improving Children and Young People’s Health Outcomes: A System Wide Response. London: Department of Health; 2013.
- Stewart W. A dangerous lesson to forget. TES 2012.
- Research Evidence on the Effectiveness of Self Care Support (Work in Progress 2005–07). London: Department of Health; 2007.
- Elgar F, McGrath P, Watkins P, Clum G. Handbook of Self-Help Therapies. London: Routledge; 2008.
- Ahmead M, Bower P. The effectiveness of self help technologies for emotional problems in adolescents: a systematic review. Child Adolesc Psychiatry Ment Health 2008;2. http://dx.doi.org/10.1186/1753-2000-2-20.
- Stallard P, Simpson N, Anderson S, Hibbert S. The FRIENDS emotional health programme: initial findings from a school based project. Child Adolesc Ment Health 2007;12:32-7. http://dx.doi.org/10.1111/j.1475-3588.2006.00421.x.
- Kendal S. The Use of Guided Self Help to Promote Emotional Wellbeing in High School Students 2009.
- Kendal S, Callery P, Keeley P. The feasibility and acceptability of an approach to emotional wellbeing support for high school students. Child Adolesc Mental Health 2011;29:193-200. http://dx.doi.org/10.1111/j.1475-3588.2011.00602.x.
- Hart A, Blincow D, Thomas H. Resilient Therapy: Working with Children and Families. London: Routledge; 2007.
- Hallam S. An evaluation of the Social and Emotional Aspects of Learning (SEAL) programme: promoting positive behaviour, effective learning and well-being in primary school children. Oxford Rev Educ 2009;35:313-30. http://dx.doi.org/10.1080/03054980902934597.
- IAPT . Children and Young People’s Project n.d. www.iapt.nhs.uk/cyp-iapt/children-and-young-peoples-project/ (accessed 23 April 2013).
- Self-Care – A Real Choice, Self-Care – A Practical Option. London: Department of Health; 2005.
- Francis R. Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry: Executive Summary. London: The Stationery Office; 2013.
- Supporting Self-Care: The Contribution of Nurses and Physicians. Ottawa, ON: Health Canada; 2002.
- Kirk S, Beatty S, Callery P, Milnes L, Pryjmachuk S. Perceptions of effective self-care support for children and young people with long-term conditions. J Clin Nurs 2012;21:1974-87. http://dx.doi.org/10.1111/j.1365-2702.2011.04027.x.
- Kirk S, Beatty S, Callery P, Gellatly J, Milnes L, Pryjmachuk S. The effectiveness of self-care support interventions for children and young people with long-term conditions: a systematic review. Child Care Health Dev 2013;39:305-24. http://dx.doi.org/10.1111/j.1365-2214.2012.01395.x.
- Richardson G, Kennedy A, Reeves D, Bower P, Lee V, Middleton E, et al. Cost effectiveness of the Expert Patients Programme (EPP) for patients with chronic conditions. J Epidemiol Community Health 2008;62:361-7. http://dx.doi.org/10.1136/jech.2006.057430.
- Child and Adolescent Mental Health Services: Together We Stand. London: HMSO; 1995.
- Lowry-Webster HM, Barrett PM, Dadds MR. A universal prevention trial of anxiety and depressive symptomatology in childhood: Preliminary data from an Australian study. Behav Change 2001;18:36-50. http://dx.doi.org/10.1375/bech.18.1.36.
- Pryjmachuk S, Graham T, Haddad M, Tylee A. School nurses’ perspectives on managing mental health problems in children and young people. J Clin Nurs 2012;21:850-9. http://dx.doi.org/10.1111/j.1365-2702.2011.03838.x.
- Systematic Reviews: CRD’s Guidance for Undertaking Reviews in Health Care. York: Centre for Reviews and Dissemination, University of York; 2008.
- Convention on the Rights of the Child. New York, NY: UN General Assembly; 1989.
- Armstrong R, Hall BJ, Doyle J, Waters E. ‘Scoping the scope’ of a Cochrane review. J Public Health 2011;33:147-50. http://dx.doi.org/10.1093/pubmed/fdr015.
- Guideline Development Methods: Information for National Collaborating Centres and Guideline Developers. London: NICE; 2005.
- Arnarson E, Craighead W. Prevention of depression among Icelandic adolescents. Behav Res Ther 2009;47:577-85. http://dx.doi.org/10.1016/j.brat.2009.03.011.
- Arnarson E, Craighead W. Prevention of depression among Icelandic adolescents: A 12-month follow-up. Behav Res Ther 2011;49:170-4. http://dx.doi.org/10.1016/j.brat.2010.12.008.
- Barrett PM, Lock S, Farrell LJ. Developmental differences in universal preventive intervention for child anxiety. Clin Child Psychol Psychiatry 2005;10:539-55. http://dx.doi.org/10.1177/1359104505056317.
- Barrington J, Prior M, Richardson M, Allen K. Effectiveness of CBT versus standard treatment for childhood anxiety disorders in a community clinic setting. Behav Change 2005;22:29-43. http://dx.doi.org/10.1375/bech.22.1.29.66786.
- Bernstein GA, Layne AE, Egan EA, Tennison DM. School-based interventions for anxious children. J Am Acad Child Adolesc Psychiatry 2005;44:1118-27. http://dx.doi.org/10.1097/01.chi.0000177323.40005.a1.
- Bernstein GA, Bernat DH, Victor AM, Layne AE. School-based interventions for anxious children: 3-, 6-, and 12-month follow-ups. J Am Acad Child Adolesc Psychiatry 2008;47:1039-47.
- Biegel GM, Brown KW, Shapiro SL, Schubert CM. Mindfulness-based stress reduction for the treatment of adolescent psychiatric outpatients: A randomized clinical trial. J Consult Clin Psychol 2009;77:855-66. http://dx.doi.org/10.1037/a0016241.
- Cartwright-Hatton S, McNally D, Field AP, Rust S, Laskey B, Dixon C, et al. A new parenting-based group intervention for young anxious children: Results of a randomized controlled trial. J Am Acad Child Adolesc Psychiatry 2011;50:242-51. http://dx.doi.org/10.1016/j.jaac.2010.12.015.
- Clarke GN, Hawkins W, Murphy M, Sheeber LB, Lewinsohn PM, Seeley JR. Targeted prevention of unipolar depressive disorder in an at-risk sample of high school adolescents: a randomized trial of a group cognitive intervention. J Am Acad Child Adolesc Psychiatry 1995;34:312-21. http://dx.doi.org/10.1097/00004583-199503000-00016.
- Clarke GN, Hornbrook M, Lynch F, Polen M, Gale J, Beardslee W, et al. A randomized trial of a group cognitive intervention for preventing depression in adolescent offspring of depressed parents. Arch Gen Psychiatry 2001;58:1127-34. http://dx.doi.org/10.1001/archpsyc.58.12.1127.
- Clarke GN, Hornbrook M, Lynch F, Polen M, Gale J, O’Connor E, et al. Group cognitive-behavioral treatment for depressed adolescent offspring of depressed parents in a health maintenance organization. J Am Acad Child Adolesc Psychiatry 2002;41:305-13. http://dx.doi.org/10.1097/00004583-200203000-00010.
- Compas BE, Forehand R, Keller G, Champion JE, Rakow A, Resslund KL, et al. Randomized controlled trial of a family cognitive-behavioral preventive intervention for children of depressed parents. J Consult Clin Psychol 2009;77:1007-20. http://dx.doi.org/10.1037/a0016930.
- Cowell JM, McNaughton D, Ailey S, Gross D, Fogg L. Clinical trial outcomes of the Mexican American Problem Solving program (MAPS). Hispanic Health Care Int 2009;7:179-89. http://dx.doi.org/10.1891/1540-4153.7.4.178.
- Dadds MR, Spence SH, Holland DE, Barrett PM, Laurens KR. Prevention and early intervention for anxiety disorders: a controlled trial. J Consult Clin Psychol 1997;65:627-35. http://dx.doi.org/10.1037/0022-006X.65.4.627.
- Dadds MR, Holland DE, Laurens KR, Mullins M, Barrett PM, Spence SH. Early intervention and prevention of anxiety disorders in children: results at 2-year follow-up. J Consult Clin Psychol 1999;67:145-50. http://dx.doi.org/10.1037/0022-006X.67.1.145.
- Dalle Grave R, De Luca L, Campello G. Middle school primary prevention program for eating disorders: A controlled study with a twelve-month follow-up. Eating Disord 2001;9:327-37. http://dx.doi.org/10.1080/106402601753454895.
- De Cuyper S, Timbremont B, Braet C, Backer VD, Wullaert T. Treating depressive symptoms in schoolchildren. Eur Child Adolesc Psychiatry 2004;13:105-14. http://dx.doi.org/10.1007/s00787-004-0366-2.
- DeRosier ME. Building relationships and combating bullying: Effectiveness of a school-based social skills group intervention. J Clin Child Adolesc Psychol 2004;33:196-201. http://dx.doi.org/10.1207/S15374424JCCP3301_18.
- DeRosier ME, Marcus SR. Building friendships and combating bullying: Effectiveness of SS GRIN at one-year follow-up. J Clin Child Adolesc Psychol 2005;34:140-50. http://dx.doi.org/10.1207/s15374424jccp3401_13.
- Dobson KS, Ahnberg Hopkins J, Fata L, Scherrer M, Allan LC. The prevention of depression and anxiety in a sample of high-risk adolescents: a randomized controlled trial. Can J School Psychol 2010;25:291-310. http://dx.doi.org/10.1177/0829573510386449.
- Evans SW, Serpell ZN, Schultz BK, Pastor DA. Cumulative benefits of secondary school-based treatment of students with attention deficit hyperactivity disorder. School Psychol Rev 2007;36:256-73.
- Gallagher HM, Rabian BA, McCloskey MS. A brief group cognitive-behavioral intervention for social phobia in childhood. Anxiety Disord 2004;18:459-79. http://dx.doi.org/10.1016/S0887-6185(03)00027-6.
- Garber J, Clarke GN, Weersing VR, Beardslee WR, Brent DA, Gladstone TRG, et al. Prevention of depression in at-risk adolescents. JAMA 2009;301:2215-24. http://dx.doi.org/10.1001/jama.2009.788.
- Gillham JE, Hamilton J, Freres DR, Patton K, Gallop R. Preventing depression among early adolescents in the primary care setting: a randomized controlled study of the Penn Resiliency Program. J Abnorm Child Psychol 2006;34:195-211. http://dx.doi.org/10.1007/s10802-005-9014-7.
- Ginsburg GS. The child anxiety prevention study: intervention model and primary outcomes. J Consult Clin Psychol 2009;77:580-7. http://dx.doi.org/10.1037/a0014486.
- Gowers SG, Clark A, Roberts C, Griffiths A, Edwards V, Bryan C, et al. Clinical effectiveness of treatments for anorexia nervosa in adolescents: Randomised controlled trial. Br J Psychiatry 2007;191:427-35. http://dx.doi.org/10.1192/bjp.bp.107.036764.
- Gowers SG, Clark AF, Roberts C, Byford S, Barrett B, Griffiths A, et al. A randomised controlled multicentre trial of treatments for adolescent anorexia nervosa including assessment of cost-effectiveness and patient acceptability – the TOuCAN trial. Health Technol Assess 2010;14.
- Green JM, Wood AJ, Kerfoot MJ, Trainor G, Roberts C, Rothwell J, et al. Group therapy for adolescents with repeated self harm: randomised controlled trial with economic evaluation. BMJ 2011;342. http://dx.doi.org/10.1136/bmj.d682.
- Hahlweg K, Heinrichs N, Kuschel A, Bertram H, Naumann S. Long-term outcome of a randomized controlled universal prevention trial through a positive parenting program: is it worth the effort?. Child Adolesc Psychiatry Ment Health 2010;4. http://dx.doi.org/10.1186/1753-2000-4-14.
- Harrington R, Kerfoot M, Dyer E, McNiven F, Gill J, Harrington V, et al. Randomized trial of a home-based family intervention for children who have deliberately poisoned themselves. J Am Acad Child Adolesc Psychiatry 1998;37:512-18.
- Havighurst SS, Wilson KR, Harley AE, Prior MR. Tuning in to Kids: an emotion-focused parenting program – initial findings from a community trial. J Community Psychol 2009;37:1008-23. http://dx.doi.org/10.1002/jcop.20345.
- Havighurst SS, Wilson KR, Harley AE, Prior MR, Kehoe C. Tuning in to Kids: improving emotion socialization practices in parents of preschool children – findings from a community trial. J Child Psychol Psychiatry 2010;51:1342-50. http://dx.doi.org/10.1111/j.1469-7610.2010.02303.x.
- Hayward C, Varady S, Albano AM, Thienemann M, Henderson L, Schatzberg AF. Cognitive-behavioral group therapy for social phobia in female adolescents: results of a pilot study. J Am Acad Child Adolesc Psychiatry 2000;39:721-6. http://dx.doi.org/10.1097/00004583-200006000-00010.
- Hazell PL, Martin G, McGill K, Kay T, Wood A, Trainor G, et al. Group therapy for repeated deliberate self-harm in adolescents. J Am Acad Child Adolesc Psychiatry 2009;48:662-70.
- Hiscock H, Bayer JK, Price A, Ukoumunne OC, Rogers S, Wake M. Universal parenting programme to prevent early childhood behavioural problems: cluster randomised trial. BMJ 2008;336:318-21. http://dx.doi.org/10.1136/bmj.39451.609676.AE.
- Bayer JK, Hiscock H, Ukoumunne OC, Scalzo K, Wake M. Three-year-old outcomes of a brief universal parenting intervention to prevent behaviour problems: randomised controlled trial. Arch Dis Child 2009;95:187-92. http://dx.doi.org/10.1136/adc.2009.168302.
- Hudson JL, Rapee RM, Deveney C, Schniering CA, Lyneham HJ, Bovopoulos N. Cognitive-behavioral treatment versus an active control for children and adolescents with anxiety disorders: a randomized trial. J Am Acad Child Adolesc Psychiatry 2009;48:533-44. http://dx.doi.org/10.1097/CHI.0b013e31819c2401.
- Hunt C, Andrews G, Sakashita C, Crino R, Erskine A. Randomized controlled trial of an early intervention programme for adolescent anxiety disorders. Aust Psychiatry 2009;43:300-4. http://dx.doi.org/10.1080/00048670902721152.
- Kendall PC, Hudson JL, Gosch E, Flannery-Schroeder E, Suveg C. Cognitive-behavioral therapy for anxiety disordered youth: a randomized clinical trial evaluating child and family modalities. J Consult Clin Psychol 2008;76:282-97. http://dx.doi.org/10.1037/0022-006X.76.2.282.
- Suveg C, Hudson JL, Brewer G, Flannery-Schroeder E, Gosch E, Kendall PC. Cognitive-behavioral therapy for anxiety-disordered youth: Secondary outcomes from a randomized clinical trial evaluating child and family modalities. J Anxiety Disord 2009;23:341-9. http://dx.doi.org/10.1016/j.janxdis.2009.01.003.
- Kennard BD, Emslie GJ, Mayes TL, Nightingale-Teresi J, Nakonezny PA, Hughes JL, et al. Cognitive-behavioral therapy to prevent relapse in pediatric responders to pharmacotherapy for major depressive disorder. J Am Acad Child Adolesc Psychiatry 2008;47:1395-404. http://dx.doi.org/10.1097/CHI.0b013e31818914a1.
- King NJ, Tonge BJ, Mullen P, Myerson N, Heyne D, Rollings S, et al. Treating sexually abused children with posttraumatic stress symptoms: A randomized clinical trial. J Am Acad Child Adolesc Psychiatry 2000;39:1347-55. http://dx.doi.org/10.1097/00004583-200011000-00008.
- Kolko DJ, Campo JV, Kelleher K, Cheng Y. Improving access to care and clinical outcome for pediatric behavioral problems: a randomized trial of a nurse-administered intervention in primary care. J Dev Behav Pediatr 2010;31:393-404. http://dx.doi.org/10.1097/DBP.0b013e3181dff307.
- Lock S, Barrett PM. A longitudinal study of developmental differences in universal preventive intervention for child anxiety. Behav Change 2003;20:183-99. http://dx.doi.org/10.1375/bech.20.4.183.29383.
- Barrett PM, Farrell LJ, Ollendick TH, Dadds M. Long-term outcomes of an Australian universal prevention trial of anxiety and depression symptoms in children and youth: an evaluation of the friends program. J Clin Child Adolesc Psychol 2006;35:403-11. http://dx.doi.org/10.1207/s15374424jccp3503_5.
- Lowry-Webster HM, Barrett PM, Lock S. A universal prevention trial of anxiety symptomology during childhood: results at 1-year follow-up. Behav Change 2003;20:25-43. http://dx.doi.org/10.1375/bech.20.1.25.24843.
- Masia Warner C, Fisher PH, Shrout PE, Rathor S, Klein RG. Treating adolescents with social anxiety disorder in school: an attention control trial. J Child Psychol Psychiatry 2007;48:676-86. http://dx.doi.org/10.1111/j.1469-7610.2007.01737.x.
- McVey GL, Davis R. A program to promote positive body image: a 1-year follow-up evaluation. J Early Adolesc 2002;22:96-108. http://dx.doi.org/10.1177/0272431602022001005.
- Merry S, McDowell H, Wild CJ, Bir J, Cunliffe R. A randomized placebo-controlled trial of a school-based depression prevention program. J Am Acad Child Adolesc Psychiatry 2004;43:538-47. http://dx.doi.org/10.1097/00004583-200405000-00007.
- Mifsud C, Rapee RM. Early intervention for childhood anxiety in a school setting: Outcomes for an economically disadvantaged population. J Am Acad Child Adolesc Psychiatry 2005;44:996-1004. http://dx.doi.org/10.1097/01.chi.0000173294.13441.87.
- MTA Co-operative Group . A 14-month randomized clinical trial of treatment strategies for attention-deficit/hyperactivity disorder. Arch Gen Psychiatry 1999;56:1073-86. http://dx.doi.org/10.1001/archpsyc.56.12.1073.
- Jensen PS, Hinshaw SP, Kraemer HC, Lenora N, Newcorn JH, Abikoff HB, et al. ADHD comorbidity findings from the MTA study: comparing comorbid subgroups. J Am Acad Child Adolesc Psychiatry 2001;40:147-58. http://dx.doi.org/10.1097/00004583-200102000-00009.
- MTA Co-operative Group . National Institute of Mental Health Multimodal Treatment Study of ADHD follow-up: 24-month outcomes of treatment strategies for attention-deficit/hyperactivity disorder. Pediatrics 2004;113:754-61. http://dx.doi.org/10.1542/peds.113.4.754.
- Hoza B, Gerdes AC, Mrug S, Hinshaw SP, Bukowski WM, Gold JA, et al. Peer-assessed outcomes in the multimodal treatment study of children with attention deficit hyperactivity disorder. J Clin Child Adolesc Psychol 2005;34:74-86. http://dx.doi.org/10.1207/s15374424jccp3401_7.
- Patterson J, Barlow J, Mockford C, Klimes I, Pyper C, Stewart-Brown S. Improving mental health through parenting programmes: block randomised controlled trial. Arch Dis Child 2002;87:472-7. http://dx.doi.org/10.1136/adc.87.6.472.
- Stewart-Brown S, Patterson J, Mockford C, Barlow J, Klimes I, Pyper C. Impact of a general practice based group parenting programme: Quantitative and qualitative results from a controlled trial at 12 months. Arch Dis Child 2004;89:519-25. http://dx.doi.org/10.1136/adc.2003.028365.
- Pfiffner LJ, McBurnett K. Social skills training with parent generalization: treatment effects for children with attention deficit disorder. J Consult Clin Psychol 1997;65:749-57. http://dx.doi.org/10.1037/0022-006X.65.5.749.
- Pfiffner LJ, Yee Mikami A, Huang-Pollock C, Easterlin B, Zalecki C, McBurnett K. A randomized, controlled trial of integrated home-school behavioral treatment for ADHD, predominantly inattentive type. J Am Acad Child Adolesc Psychiatry 2007;46:1041-50. http://dx.doi.org/10.1097/chi.0b013e318064675f.
- Puskar K, Sereika S, Tusaie-Mumford K. Effect of the Teaching Kids to Cope (TKC) program on outcomes of depression and coping among rural adolescents. J Child Adolesc Psychiatr Nurs 2003;16:71-80. http://dx.doi.org/10.1111/j.1744-6171.2003.tb00350.x.
- Rohde P, Clarke GN, Mace DE, Jorgensen JS, Seeley JR. An efficacy/effectiveness study of cognitive-behavioral treatment for adolescents with comorbid major depression and conduct disorder. J Am Acad Child Adolesc Psychiatry 2004;43:660-8. http://dx.doi.org/10.1097/01.chi.0000121067.29744.41.
- Rooney R, Roberts C, Kane R, Pike L, Winsor A, White J, et al. The prevention of depression in 8- to 9-year-old children: a pilot study. Aust J Guid Couns 2006;16:76-90. http://dx.doi.org/10.1375/ajgc.16.1.76.
- Rosa Alcázar AI, Olivares-Olivares PJ, Olivares Rodríguez J. The role of non-specific effects in the psychological treatment of adolescents with social phobia. Anuario De Psicología 2009;40:43-61.
- Ruini C, Ottolini F, Tomba E, Belaise C, Albieri E, Visani D, et al. School intervention for promoting psychological well-being in adolescence. J Behav Ther Exper Psychiatry 2009;40:522-32. http://dx.doi.org/10.1016/j.jbtep.2009.07.002.
- Sawyer MG, Pfeiffer S, Spence SH, Bond L, Graetz B, Kay D, et al. School-based prevention of depression: a randomised controlled study of the beyondblue schools research initiative. J Child Psychol Psychiatry 2010;51:199-20. http://dx.doi.org/10.1111/j.1469-7610.2009.02136.x.
- Sawyer MG, Harchak TF, Spence SH, Bond L, Graetz B, Kay D, et al. School-based prevention of depression: A 2-year follow-up of a randomized controlled trial of the beyondblue schools research initiative. J Adolesc Health 2010;47:297-304. http://dx.doi.org/10.1016/j.jadohealth.2010.02.007.
- Sheffield JK, Spence SH, Rapee RM, Kowalenko, Wignall A, Davis A, et al. Evaluation of universal, indicated, and combined cognitive-behavioral approaches to the prevention of depression among adolescents. J Consult Clin Psychol 2006;74:66-79. http://dx.doi.org/10.1037/0022-006X.74.1.66.
- Silverman W, Kurtines WM, Ginsburg GS, Weems CF, Rabian B. Contingency management, self-control, and educational support in the treatment of childhood phobic disorders: a randomized clinical trial. J Consult Clin Psychol 1999;67:675-87. http://dx.doi.org/10.1037/0022-006X.67.5.675.
- Simon E, Bögels SM, Voncken JM. Efficacy of child-focused and parent-focused interventions in a child anxiety prevention study. J Clin Child Adolesc Psychol 2011;40:204-19. http://dx.doi.org/10.1080/15374416.2011.546039.
- Spence SH, Sheffield JK, Donovan CL. Preventing adolescent depression: An evaluation of the Problem Solving For Life program. J Consult Clin Psychol 2003;71:3-13. http://dx.doi.org/10.1037/0022-006X.71.1.3.
- Spence SH, Sheffield JK, Donovan CL. Long-term outcome of a school-based, universal approach to prevention of depression in adolescents. J Consult Clin Psychol 2005;73:160-7. http://dx.doi.org/10.1037/0022-006X.73.1.160.
- Stice E, Trost A, Chase A. Healthy weight control and dissonance-based eating disorder prevention programs: Results from a controlled trial. Int J Eating Disord 2003;33:10-21. http://dx.doi.org/10.1002/eat.10109.
- Stice E, Shaw H, Burton E, Wade E. Dissonance and healthy weight eating disorder prevention programs: a randomized efficacy trial. J Consult Clin Psychol 2006;74:263-75. http://dx.doi.org/10.1037/0022-006X.74.2.263.
- Stice E, Rohde P, Seeley JR, Gau JM. Brief cognitive-behavioral depression prevention program for high-risk adolescents outperforms two alternative interventions: a randomized efficacy trial. J Consult Clin Psychol 2008;76:595-606. http://dx.doi.org/10.1037/a0012645.
- Stice E, Marti N, Spoor S, Presnell K, Shaw H. Dissonance and healthy weight eating disorder prevention programs: long-term effects from a randomized efficacy trial. J Consult Clin Psychol 2008;76:329-40. http://dx.doi.org/10.1037/0022-006X.76.2.329.
- Stice E, Rohde P, Gau JM, Wade E. Efficacy trial of a brief cognitive–behavioral depression prevention program for high-risk adolescents: Effects at 1- and 2-year follow-up. J Consult Clin Psychol 2010;78:856-67. http://dx.doi.org/10.1037/a0020544.
- Stice E, Rohde P, Gau J, Shaw H. An effectiveness trial of a dissonance-based eating disorder prevention program for high-risk adolescent girls. J Consult Clin Psychol 2009;77:825-34. http://dx.doi.org/10.1037/a0016132.
- Treatment for Adolescents with Depression Study (TADS) Team . Fluoxetine, cognitive-behavioral therapy, and their combination for adolescents with depression. J Am Med Acad 2004;292:807-20.
- March J, Silva S, Vitiello B. The Treatment for Adolescents with Depression Study (TADS). J Am Acad Child Adolesc Psychiatry 2006;45:1393-403. http://dx.doi.org/10.1097/01.chi.0000237709.35637.c0.
- Treatment for Adolescents with Depression Study (TADS) Team . The Treatment for Adolescents with Depression Study (TADS): outcomes over 1 year of naturalistic follow-up. Am J Psychiatry 2009;166:1141-9. http://dx.doi.org/10.1176/appi.ajp.2009.08111620.
- Domino ME, Foster EM, Vitiello B, Kratochvil CJ, Burns BJ, Silva SG, et al. Relative cost-effectiveness of treatments for adolescent depression: 36-week results from the TADS randomized trial. J Am Acad Child Adolesc Psychiatry 2009;48:711-20. http://dx.doi.org/10.1097/CHI.0b013e3181a2b319.
- Kennard BD, Silva SG, Tonev S, Rohde P, Hughes JL, Vitiello B, et al. Remission and recovery in the Treatment for Adolescents with Depression Study (TADS): acute and long-term outcomes. J Am Acad Child Adolesc Psychiatry 2009;48:186-95. http://dx.doi.org/10.1097/CHI.0b013e31819176f9.
- Jacobs RH, Becker-Weidman EG, Reinecke MA, Jordan N, Silva SG, Rohde P, et al. Treating depression and oppositional behavior in adolescents. J Clin Child Adolesc Psychol 2010;39:559-67. http://dx.doi.org/10.1080/15374416.2010.486318.
- Thompson MJJ, Laver-Bradbury C, Ayres M, Le Poidevin E, Mead S, Dodds S, et al. A small-scale randomized controlled trial of the revised new forest parenting programme for preschoolers with attention deficit hyperactivity disorder. Eur Child Adolesc Psychiatry 2009;18:605-16. http://dx.doi.org/10.1007/s00787-009-0020-0.
- Tol WA, Komproe IH, Susanty D, Jordans MJD, Macy RD, De Jong JTVM. School-based mental health intervention for children affected by political violence in Indonesia. JAMA 2008;300:655-62. http://dx.doi.org/10.1001/jama.300.6.655.
- Vostanis P, Feehan C, Grattan E, Bickerton WL. Treatment for children and adolescents with depression: lessons from a controlled trial. Clin Child Psychol Psychiatry 1996;1:199-212. http://dx.doi.org/10.1177/1359104596012003.
- Vostanis P, Feehan C, Grattan E, Bickerton WL. A randomised controlled out-patient trial of cognitive-behavioural treatment for children and adolescents with depression: 9-month follow-up. J Affect Disord 1996;40:105-16. http://dx.doi.org/10.1016/0165-0327(96)00054-7.
- Vostanis P, Feehan C, Grattan E. Two-year outcome of children treated for depression. Eur Child Adolesc Psychiatry 1998;7:12-8. http://dx.doi.org/10.1007/s007870050039.
- Conduct Problems Prevention Research Group . Fast track randomized controlled trial to prevent externalizing psychiatric disorders: Findings from grades 3 to 9. J Am Acad Child Adolesc Psychiatry 2007;46:1250-62. http://dx.doi.org/10.1097/chi.0b013e31813e5d39.
- Glisson C, Schoenwald SK, Hemmelgarn A, Green P, Dukes D, Armstrong KS, et al. Randomized trial of MST and ARC in a two-level evidence-based treatment implementation strategy. J Consult Clin Psychol 2010;78:537-50. http://dx.doi.org/10.1037/a0019160.
- McVey GL, Davis R, Tweed S, Shaw BF. Evaluation of a school-based program designed to improve body image satisfaction, global self-esteem, and eating attitudes and behaviors: a replication study. Int J Eating Disord 2004;36:1-11. http://dx.doi.org/10.1002/eat.20006.
- Miklowitz DJ, Axelson DA, Birmaher B, Geore EL, Taylor DO, Schneck CD, et al. Family-focused treatment for adolescents with bipolar disorder: results of a 2-year randomized trial. Arch Gen Psychiatry 2008;65:1053-61. http://dx.doi.org/10.1001/archpsyc.65.9.1053.
- O’Dea JA, Abraham S. Improving the body image, eating attitudes, and behaviors of young male and female adolescents: A new educational approach that focuses on self-esteem. Int J Eating Disord 2000;28:43-57. http://dx.doi.org/10.1002/(SICI)1098-108X(200007)28:1<43::AID-EAT6>3.0.CO;2-D.
- Thompson EA, Eggert LL, Randell BP, Pike KC. Evaluation of indicated suicide risk prevention approaches for potential high school dropouts. Am J Public Health 2001;91:742-52. http://dx.doi.org/10.2105/AJPH.91.5.742.
- Sánchez-García R, Olivares J. Early intervention in children and adolescents with social phobia. Anuario De Psicología 2009;40:75-88.
- Sánchez-García R, Olivares J. Effectiveness of a program for early detection/intervention in children/adolescents with generalized social phobia. Anales De Psicologica 2009;25:241-9.
- Higgins J, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 2011. http://handbook.cochrane.org/ (accessed 23 April 2013).
- Schulz K, Chalmers I, Hayes R, Altman D. Empirical evidence of bias: dimensions of methodological quality associated with estimates of treatment effects in controlled trials. J Am Med Acad 1995;273:408-12.
- Pildal J, Hróbjartsson A, Jørgensen K, Altman D, Gøtzsche P. Impact of allocation concealment on conclusions drawn from meta-analyses of randomized trials. Int J Epidemiol 2007;36:847-57. http://dx.doi.org/10.1093/ije/dym087.
- Wood L, Egger M, Gluud LL, Schulz KF, Jüni P, Altman DG, et al. Empirical evidence of bias in treatment effect estimates in controlled trials with different interventions and outcomes: meta-epidemiological study. BMJ 2012;336:601-5. http://dx.doi.org/10.1136/bmj.39465.451748.AD.
- Higgins J, Thompson S, Deeks J, Altman D. Measuring inconsistency in meta-analysis. BMJ 2003;327:557-60. http://dx.doi.org/10.1136/bmj.327.7414.557.
- Dixon-Woods M, Cavers D, Agarwal S, Annandale E, Arthur A, Harvey J, et al. Conducting a critical interpretive synthesis of the literature on access to healthcare by vulnerable groups. BMC Med Res Methodol 2006;6. http://dx.doi.org/10.1186/1471-2288-6-35.
- Shepherd J. Young people and healthy eating: a systematic review of research on barriers and facilitators. Health Educ Res 2005;21:239-57. http://dx.doi.org/10.1093/her/cyh060.
- Baker-Henningham H, Walker S. A qualitative study of teacher’s perceptions of an intervention to prevent conduct problems in Jamaican pre-schools. Child Care Health Dev 2009;35:632-42. http://dx.doi.org/10.1111/j.1365-2214.2009.00996.x.
- Coyle D, Doherty G, Sharry J. An evaluation of a solution focused computer game in adolescent interventions. Clin Child Psychol Psychiatry 2009;14:345-60. http://dx.doi.org/10.1177/1359104508100884.
- Eacott C, Frydenberg E. At-risk students in a rural context: benefits and gains from a coping skills program. Aust J Guid Couns 2008;18:160-81. http://dx.doi.org/10.1375/ajgc.18.2.160.
- Friars P, Mellor D. Drop out from behavioral management training programs for ADHD: a prospective study. J Child Fam Stud 2007;16:427-41. http://dx.doi.org/10.1007/s10826-006-9096-z.
- Fristad MA, Gavazzi SM, Soldano KW. Multi-family psychoeducation groups for childhood mood disorders: a program description and preliminary efficacy data. Contemp Fam Ther 1998;20:385-402. http://dx.doi.org/10.1023/A:1022477215195.
- Garcia C, Pintor JK, Lindgren S. Feasibility and acceptability of a school-based coping intervention for Latina adolescents. J School Nurs 2010;26:42-5. http://dx.doi.org/10.1177/1059840509351021.
- Garraway H, Pistrang N. ‘Brother from another mother’: mentoring for African-Caribbean adolescent boys. J Adolesc 2010;33:719-29. http://dx.doi.org/10.1016/j.adolescence.2009.10.011.
- Kennedy MG, Schepp KG, Rungruangkonkit S. Experiences of Asian American parents in a group intervention for youth with schizophrenia. J Child Adolesc Psychiatr Nurs 2008;21:220-7. http://dx.doi.org/10.1111/j.1744-6171.2008.00138.x.
- Ma JLC. Patients’ perspective on family therapy for anorexia nervosa: a qualitative inquiry in a Chinese context. Aust N Z J Fam Ther 2008;29:10-6. http://dx.doi.org/10.1375/anft.29.1.10.
- Mishara BL, Ystgaard M. Effectiveness of a mental health promotion program to improve coping skills in young children: Zippy’s Friends. Early Child Res Q 2006;21:110-23. http://dx.doi.org/10.1016/j.ecresq.2006.01.002.
- Zucker NL, Ferriter C, Best S, Brantley A. Group parent training: A novel approach for the treatment of eating disorders. Eating Disord 2005;13:391-405. http://dx.doi.org/10.1080/10640260591005272.
- Barrett P, Turner C, Rombouts S, Duffy A. Reciprocal skills training in the treatment of externalising behaviour disorders in childhood: a preliminary investigation. Behav Change 2000;17:221-34. http://dx.doi.org/10.1375/bech.17.4.221.
- Barrett P, Healy-Farrell L, March JS. Cognitive-behavioral family treatment of childhood obsessive-compulsive disorder: a controlled trial. J Am Acad Child Adolesc Psychiatry 2004;43:46-62. http://dx.doi.org/10.1097/00004583-200401000-00014.
- Barrett P, Farrell L, Dadds M, Boulter N. Cognitive-behavioral family treatment of childhood obsessive-compulsive disorder: long-term follow-up and predictors of outcome. J Am Acad Child Adolesc Psychiatry 2005;44:1005-14. http://dx.doi.org/10.1097/01.chi.0000172555.26349.94.
- O’Leary EMM, Barrett P, Fjermestad KW. Cognitive-behavioral family treatment for childhood obsessive-compulsive disorder: a 7-year follow-up study. J Anxiety Disord 2009;23:973-8. http://dx.doi.org/10.1016/j.janxdis.2009.06.009.
- Gardner F, Burton J, Klimes I. Randomised controlled trial of a parenting intervention in the voluntary sector for reducing child conduct problems: outcomes and mechanisms of change. J Child Psychol Psychiatry 2006;47:1123-32. http://dx.doi.org/10.1111/j.1469-7610.2006.01668.x.
- Ginsburg GS, Drake KL. School-based treatment for anxious African-American adolescents: A controlled pilot study. J Am Acad Child Adolesc Psychiatry 2002;41:768-75. http://dx.doi.org/10.1097/00004583-200207000-00007.
- Hoath F, Sanders M. A feasibility study of enhanced group Triple P-Positive Parenting Program for parents of children with attention-deficit/hyperactivity disorder. Behaviour 2002;19:191-206.
- Khanna MS, Kendall PC. Computer-assisted cognitive behavioral therapy for child anxiety: Results of a randomized clinical trial. J Consult Clin Psychol 2010;78:737-45. http://dx.doi.org/10.1037/a0019739.
- Larsson B, Fossum S, Clifford G, Drugli MB, Handegård BH, Mørch W-T. Treatment of oppositional defiant and conduct problems in young Norwegian children. Eur Child Adolesc Psychiatry 2008;18:42-5. http://dx.doi.org/10.1007/s00787-008-0702-z.
- March S, Spence SH, Donovan CL. The efficacy of an internet-based cognitive-behavioral therapy intervention for child anxiety disorders. J Pediatr Psychol 2009;34:474-87. http://dx.doi.org/10.1093/jpepsy/jsn099.
- Matos M, Bauermeister JJ, Bernal G. Parent-Child Interaction Therapy for Puerto Rican preschool children with ADHD and behavior problems: a pilot efficacy study. Fam Process 2009;48:232-52. http://dx.doi.org/10.1111/j.1545-5300.2009.01279.x.
- Matsumoto Y, Sofronoff K, Sanders M. The efficacy and acceptability of the Triple P-Positive Parenting Program with Japanese parents. Behav Change 2007;24:205-18. http://dx.doi.org/10.1375/bech.24.4.205.
- Molina BSG, Flory K, Bukstein OG, Greiner AR, Baker JL, Krug V, et al. Feasibility and preliminary efficacy of an after-school program for middle schoolers with ADHD: a randomized trial in a large public middle school. J Attention Disord 2008;12:207-17. http://dx.doi.org/10.1177/1087054707311666.
- Nicholson JM, Sanders MR. Randomized controlled trial of behavioral family intervention for the treatment of child behavior problems in stepfamilies. J Divorce Remarriage 1999;30:1-23. http://dx.doi.org/10.1300/J087v30n03_01.
- Seeley JR, Small JW, Walker HM, Feil EG, Severson HH, Golly AM, et al. Efficacy of the First Step to Success intervention for students with attention-deficit/hyperactivity disorder. School Ment Health 2009;1:37-48. http://dx.doi.org/10.1007/s12310-008-9003-4.
- Shortt AL, Barrett PM, Fox TL. Evaluating the FRIENDS program: A cognitive-behavioral group treatment for anxious children and their parents. J Clin Child Psychol 2001;30:525-35. http://dx.doi.org/10.1207/S15374424JCCP3004_09.
- Waters AM, Ford LA, Wharton TA, Cobham VE. Cognitive-behavioural therapy for young children with anxiety disorders: comparison of a Child + Parent condition versus a Parent Only condition. Behav Res Ther 2009;47:654-62. http://dx.doi.org/10.1016/j.brat.2009.04.008.
- Webster-Stratton C, Reid J, Hammond M. Social skills and problem-solving training for children with early-onset conduct problems: who benefits?. J Child Psychol Psychiatry 2001;42:943-52. http://dx.doi.org/10.1111/1469-7610.00790.
- Webster-Stratton C, Reid MJ, Hammond M. Treating children with early-onset conduct problems: Intervention outcomes for parent, child, and teacher training. J Clin Child Adolesc Psychol 2004;33:105-24. http://dx.doi.org/10.1207/S15374424JCCP3301_11.
- Webster-Stratton C, Reid MJ. Combining parent and child training for young children with ADHD. J Child Adolesc Psychol 2011;40:191-203. http://dx.doi.org/10.1080/15374416.2011.546044.
- Sutcliffe K, Brunton G, Twamley K, Hinds K, O’Mara-Eves A, Thomas J. Young People’s Access to Tobacco: A Mixed-Method Systematic Review. London: EPPI-Centre; 2011.
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988.
- Bennett S, Maton K, Kervin L. The ‘digital natives’ debate: a critical review of the evidence. Br J Educ Technol 2008;39:775-86. http://dx.doi.org/10.1111/j.1467-8535.2007.00793.x.
- Yin R. Applications of Case Study Research. London: Sage; 2012.
- Crowe S, Cresswell K, Robertson A, Huby G, Avery A, Sheikh A. The case study approach. BMC Med Res Methodol 2011;11. http://dx.doi.org/10.1186/1471-2288-11-100.
- The Incredible Years Inc . The Incredible Years 2012. www.incredibleyears.com/ (accessed 12 May 2013).
- Ultrasis . Beating the Blues 2013. www.beatingtheblues.co.uk/ (accessed 12 May 2013).
- Department of Health . Governance Arrangements for Research Ethics Committees: A Harmonised Edition 2011. www.gov.uk/government/publications/health-research-ethics-committees-governance-arrangements (accessed 14 May 2012).
- National Research Ethics Service . No Material Ethical Issues Tool 2009. www.nres.nhs.uk/applications/proportionate-review/ (accessed 14 May 2012).
- National Research Ethics Service . Information Sheets & Consent Forms: Guidance for Researchers &Amp; Reviewers 2011. www.nres.nhs.uk (accessed 14 May 2012).
- Salzmann-Erikson M, Eriksson H. LiLEDDA: a six step forum-based netnographic research method for nursing science. Aporia 2012;4:7-18.
- Salzmann-Erikson M, Eriksson H. Fathers sharing about early parental support in health-care – virtual discussions on an Internet forum. Health Soc Care Commununity 2013;21:381-90. http://dx.doi.org/10.1111/hsc.12028.
- Dixon-Woods M. What can ethnography do for quality and safety in health care? [commentary]. Qual Saf Health Care 2003;12:326-7. http://dx.doi.org/10.1136/qhc.12.5.326.
- Ritchie J, Spencer L, Bryman A, Burgess R. Analysing Qualitative Data. London: Routledge; 1994.
- Ritchie J, Lewis J. Qualitative Research Practice: a Guide for Social Science Students and Researchers. London: Sage; 2003.
- Linehan M. Cognitive-Behavioral Treatment of Borderline Personality Disorder. New York, NY: Guildford Press; 1993.
- Daniel B, Wassell S. The School Years: Assessing and Promoting Resilience in Vulnerable Children 2. London: Jessica Kingsley; 2002.
- Baker SE, Edwards R. How Many Qualitative Interviews Is Enough? Expert Voices and Early Career Reflections on Sampling and Cases in Qualitative Research 2012. http://eprints.ncrm.ac.uk/2273 (accessed 31 May 2013).
- The Common Assessment Framework for Children and Young People: a Guide for Practitioners. Leeds: CWDC; 2009.
- Self-Harm: the NICE Guideline on Longer-Term Management. Leicester: British Psychological Society; 2012.
- Kendall PC. The Coping Cat Workbook. Merion Station, PA: Temple University; 1990.
- Barrett PM, Sonderegger R, Sonderegger NL. Evaluation of an anxiety-prevention and positive-coping program (FRIENDS) for children and adolescents of non-English-speaking background. Behav Change 2001;18:78-91. http://dx.doi.org/10.1375/bech.18.2.78.
- Weare K, Nind M. Mental health promotion and problem prevention in schools: what does the evidence say?. Health Promot Int 2011;26:i29-69. http://dx.doi.org/10.1093/heapro/dar075.
- Furlong M, McGilloway S, Bywater T, Hutchings J, Smith SM, Donnelly M. Behavioural and cognitive-behavioural group-based parenting programmes for early-onset conduct problems in children aged 3 to 12 years. Cochrane Database Syst Rev 2012;2.
- Merry SN, Hetrick SE, Cox GR, Brudevold-Iversen T, Bir JJ, McDowell H. Psychological and educational interventions for preventing depression in children and adolescents. Cochrane Database Syst Rev 2011;12.
- Kurtz Z, James C. What’s New: Learning from the CAMHS Innovation Projects. London: Department of Health; 2002.
- Kurtz Z. The Evidence Base to Guide Development of Tier 4 CAMHS. London: Department of Health; 2009.
- De Silva D. Helping People Help Themselves: a Review of the Evidence Considering Whether it is Worthwhile to Support Self-Management. London: Health Foundation; 2011.
- Kramer TL, Phillips SD, Hargis MB, Miller TL, Burns BJ, Robbins JM. Disagreement between parent and adolescent reports of functional impairment. J Child Psychol Psychiatry 2004;45:248-59. http://dx.doi.org/10.1111/j.1469-7610.2004.00217.x.
- Brown ER, Khan L, Parsonage M. A Chance to Change: Delivering Effective Parenting Programmes to Transform Lives. London: Centre for Mental Health; 2012.
- Harwood T, L’Abate L. Self-Help in Mental Health: A Critical Review. New York, NY: Springer; 2010.
- Davis F, McDonald L, Axford N. Technique is not Enough: a Framework for Ensuring that Evidence-Based Parenting Programmes are Socially Inclusive. Leicester: British Psychological Society; 2012.
- National AIDS Programmes: a Guide to Indicators for Monitoring and Evaluating National HIV/AIDS Prevention Programmes for Young People. Geneva: World Health Organization; 2004.
- Stephens J. The Mental Health Needs of Homeless Young People. London: Mental Health Foundation; 2002.
- Children and Young People’s Views on Health and Health Services: a Review of the Evidence. London: National Children’s Bureau; 2005.
- Hibbard JH, Stockard J, Mahoney ER, Tusler M. Development of the Patient Activation Measure (PAM): conceptualizing and measuring activation in patients and consumers. Health Serv Res 2004;39:1005-26. http://dx.doi.org/10.1111/j.1475-6773.2004.00269.x.
- Townley M. An Exploration of how Centres of Excellence Have Implemented Good Practice for Mental Health Services, Aimed at the Transitional Period from Adolescence to Adulthood (Report of a Florence Nightingale Travel Scholarship). London: Florence Nightingale Foundation; 2011.
- Repper J, Carter T. A review of the literature on peer support in mental health services. J Ment Health 2011;20:392-411. http://dx.doi.org/10.3109/09638237.2011.583947.
- Basset T, Faulkner A, Repper J, Stamou E. Lived Experience Leading the Way: Peer Support in Mental Health. London: Together for Mental Wellbeing; 2010.
- McPherson K, Kerr S, McGee E, Cheater F, Morgan A. The Role and Impact of Social Capital on the Health and Wellbeing of Children and Adolescents: a Systematic Review. Glasgow: Glasgow Centre for Population Health; 2013.
- Rees D, Anderson Y. BOND: Better Outcomes New Delivery – Learning from Practice Review. London: YoungMinds; 2012.
- Ham C, Dixon A, Brooke B. Transforming the Delivery of Health and Social Care: the Case for Fundamental Change. London: The King’s Fund; 2012.
- Cost Effective Positive Outcomes for Children and Families: an Economic Analysis of The Place2Be’s Integrated Schoolbased Services for Children. London: The Place2Be; 2010.
- Remote Control: the Patient-Practitioner Relationship in a Digital Age. London: NHS Confederation; 2010.
- Selwyn N. The digital native – myth and reality. Aslib Proc 2009;61:364-79. http://dx.doi.org/10.1108/00012530910973776.
- Hasvold PE, Wootton R. Use of telephone and SMS reminders to improve attendance at hospital appointments: a systematic review. J Telemed Telecare 2011;17:358-64. http://dx.doi.org/10.1258/jtt.2011.110707.
- Take Control: Self-Management in Care and Treatment Planning. Newport: Mental Health Foundation; 2012.
- Davies J. Cracked: Why Psychiatry is Doing More Harm than Good. London: Icon; 2013.
- Classification of Behaviour and Experience in Relation to Functional Psychiatric Diagnoses: Time for a Paradigm Shift (DCP Position Statement). Leicester: British Psychological Society; 2013.
- No Health Without Public Mental Health: the Case for Action. London: Royal College of Psychiatrists; 2010.
- Alakeson V, Perkins R. Recovery, Personalisation and Personal Budgets. London: Centre for Mental Health; 2012.
- Cameron A. Getting it Together for Mental Health Care: Payment by Results, Personalisation and Whole System Working. Bath: National Development Team for Inclusion; 2012.
- Green J. Annotation: The therapeutic alliance – a significant but neglected variable in child mental health treatment studies. J Child Psychol Psychiatry 2006;47:425-35. http://dx.doi.org/10.1111/j.1469-7610.2005.01516.x.
- Michie S, Miles J, Weinman J. Patient-centredness in chronic illness: what is it and does it matter?. Patient Educ Couns 2003;51:197-206. http://dx.doi.org/10.1016/S0738-3991(02)00194-5.
- Gillard S, Turner K, Lovell K, Norton K, Clarke T, Addicott R, et al. ‘Staying native’: coproduction in mental health services research. Int J Public Sector Manag 2010;23:567-77. http://dx.doi.org/10.1108/09513551011069031.
- Cook JV, Dickinson HO, Eccles MP. Response rates in postal surveys of healthcare professionals between 1996 and 2005: An observational study. BMC Health Serv Res 2009;9. http://dx.doi.org/10.1186/1472-6963-9-160.
Appendix 1 Contributing stakeholder advisory group members
| Name | Representing | Role |
|---|---|---|
| Adele Williams | Education | Inclusion Manager, Parrs Wood High School, Manchester, England |
| Nicola Evans | Service users | Parent, Cardiff, Wales |
| Noreen Ryan | Health; health service management | Nurse Consultant in CAMHS, Bolton, England |
| Daryl Nicholas | Service users | Participation Worker, YoungMinds’ VIKs, London, England |
| Kathy Hawley | Self-care expert, Oxford, England | |
| Louise Carpenter | Health | Principal CAMHS Specialist, Wrexham, Wales |
| Sarah Petts | Social care | Home-Start, Tameside, England |
Appendix 2 Screenshot of the Access® database
Screenshot of the Access ® database (PDF download)
Used with permission from Microsoft.
Appendix 3 Copy of the effectiveness review data extraction sheet
HS&DR PROJECT 10/1008/30
EFFECTIVENESS REVIEW DATA EXTRACTION SHEET
General notes
-
If it’s easier, relevant information can simply be copied and pasted from the study PDF.
-
If the information in the paper is not clear or not readily extractable, ‘unclear’ is an appropriate entry for any field.
-
Ignore the greyed out fields. You don’t need to data extract them.
-
If there is more than one intervention, each intervention will be treated as a separate study and alphabetical sequencing added to the Unique ID (22148a, 22148b, etc.). So, for example, an Intervention 1 vs. Intervention 2 vs. Waiting List Control would be extracted as Intervention 1 vs. WL control under 22148a and Intervention 2 vs. WL control under 22148b.
Appendix 4 Example of a combined data extraction sheet for the effectiveness review
Example of a combined data extraction sheet for the effectiveness review (PDF download)
Appendix 5 Copy of the perceptions review data extraction sheet
HS&DR PROJECT 10/1008/30
PERCEPTIONS REVIEW DATA EXTRACTION SHEET
General notes
-
If it’s easier, relevant information can simply be copied and pasted from the study PDF.
-
If the information in the paper is not clear or not readily extractable, ‘unclear’ is an appropriate entry for any field.
-
Ignore the greyed out fields. You don’t need to data extract them.
Appendix 6 Details of the outcome measures extracted from the 71 effectiveness randomised controlled trials
| Study ID, condition | Direct CYP mental health measure outcome | Indirect CYP mental health measure | General functioning | Resilience | General well-being | Self-esteem |
|---|---|---|---|---|---|---|
| Arnarson 200945,46
Depression |
Depression diagnosis: clinician-completed diagnostic interview using inconsistent tools (including CAS, A-LIFE and K-SADS) Depression symptoms: child-completed CDI (CDI data reported but not readily extractable) |
|||||
| Barrett 200547
Anxiety disorders |
Anxiety symptoms: child-completed SCAS | Depression symptoms: child-completed CDI | ||||
| Barrington 200548
Anxiety disorders |
Anxiety diagnosis: clinician-completed ADIS Anxiety symptoms: child- and parent-completed SCAS and RCMAS, parent- and teacher-reported BASC |
|||||
| Bernstein 200549,50
Anxiety disorders |
Anxiety diagnosis: clinician-completed ADIS Anxiety symptoms: child- and parent-completed MASC, parent-completed SCARED |
|||||
| Biegel 200951
Generic mental health |
Diagnostic change: based on individual clinician diagnosis Anxiety symptoms: child-completed STAI (State), SCL-90 (Anxiety subscale) Depression symptoms: child-completed SCL-90 (Depression subscale) OCD symptoms: child-completed SCL-90 (OCD subscale) |
Other mental health measures: child-completed STAI (Trait), SCL-90 (Somatisation and Interpersonal Sensitivity subscales) | Global functioning: clinician-completed GAF | Sleep quality: child-completed study-specific measure | Self-esteem: child-completed RSES | |
| Cartwright-Hatton 201152
Anxiety disorders |
Anxiety diagnosis: clinician-completed ADIS Anxiety symptoms: parent-completed CBCL (Anxiety subscale), SCARED, child-completed MASC |
Internalising behaviours: parent-completed CBCL (Internalising subscale) | ||||
| Clarke 199553
Depression |
Depression symptoms: clinician-completed HAM-D, child-completed CES-D | Global functioning: clinician-completed GAF | ||||
| Clarke 200154
Depression |
Depression symptoms: clinician-completed HAM-D, parent-completed CBCL (Depression subscale), child-completed CES-D |
Internalising behaviours: parent-completed CBCL (Internalising subscale) Externalising behaviours: parent-completed CBCL (Externalising subscale) Suicidal ideation: clinician-completed K-SADS (Depression subscale) |
Global functioning: clinician-completed GAF | |||
| Clarke 200255
Depression |
Depression symptoms: clinician-completed HAM-D, parent-completed CBCL (Depression subscale), child-completed CES-D |
Internalising behaviours: parent-completed CBCL (Internalising subscale) Externalising behaviours: parent-completed CBCL (Externalising subscale) Suicidal ideation: clinician-completed K-SADS (Depression subscale) |
Global functioning: clinician-completed GAF | |||
| Compas 200956
Depression |
Depression symptoms: child-completed CES-D, CBCL (Anxiety/Depression subscale), parent-completed CBCL (Anxiety/Depression subscale) |
Internalising behaviours: child- and parent-completed CBCL (Internalising subscale) Externalising behaviours: child- and parent-completed CBCL (Externalising subscale) |
||||
| Cowell 200957
Depression |
Depression symptoms: child-completed CDI |
Global self-worth: child-completed SPP-A/C (Global Self-Worth subscale) Self-conception of health: child-completed CHSCS |
||||
| CPPRG 2007132
Serious behaviour problems |
ADHD, ODD or CD diagnosis: derived from clinician-completed NIMH-DISC parent version | |||||
| Dadds 199758,59
Anxiety disorders |
Anxiety diagnosis: clinician-completed ADIS Anxiety symptoms: child-completed RCMAS |
Internalising behaviours: parent-completed CBCL (Internalising subscale) Externalising behaviours: parent-completed CBCL (Externalising subscale) |
||||
| Dalle Grave 200160
Eating disorders |
Eating disorder symptoms: child-completed EDE-Q (Global scale), ChEAT | Self-esteem: child-completed RSES | ||||
| de Cuyper 200461
Depression |
Depression symptoms: child-completed CDI |
Anxiety symptoms: child-completed STAI (Trait) Internalising behaviours: parent-completed CBCL (Internalising subscale) Externalising behaviours: parent-completed CBCL (Externalising subscale) |
Self-worth: child-completed SPP-A/C | |||
| DeRosier 200462,63
Anxiety disorders |
Anxiety symptoms: child-completed SASC-R | Depression symptoms: child-completed MFQ | Self-worth: child-completed SPP-A/C | |||
| Dobson 201064
Anxiety disorders; depression |
Anxiety symptoms: child-completed BAI, CBCL (Anxiety/Depression subscale), MASQ (Anxiety subscale) Depression symptoms: child-completed CES-D, CDI, CBCL (Anxiety/Depression subscale), MASQ (Depression subscale) |
Self-esteem: child-completed RSES | ||||
| Evans 200765
Serious behaviour problems |
ADHD symptoms: parent-completed BASC (Inattention and Hyperactivity subscales), parent- and teacher-completed DBD (Inattention and Hyperactivity subscales) |
General impairment: parent- and teacher-completed IRS Social skills: teacher-completed SSRS |
||||
| Gallagher 200466
Anxiety disorders |
Clinical severity of anxiety: clinician-completed ADIS Anxiety symptoms: child-completed SPAI-C, SASC-R, RCMAS |
Depression symptoms: child-completed CDI, parent-completed CBCL (Anxiety/Depression subscale) Anxiety symptoms: parent-completed CBCL (Anxiety/Depression subscale) |
Social competence: parent-completed CBCL (Social Competence, Activities and School subscales) | |||
| Garber 200967
Depression |
Depression diagnosis: clinician-completed K-SADS Depression symptoms: clinician-completed CDRS-R, child-completed CES-D |
|||||
| Gillham 200668
Depression |
Depression symptoms: child-completed CDI | |||||
| Ginsburg 200969
Anxiety disorders |
Anxiety diagnosis: clinician-completed ADIS Anxiety symptoms: parent- and child-completed SCARED |
|||||
| Glisson 2010133 Generic mental health | Externalising behaviours: caregiver-completed CBCL (Externalising subscale) | Internalising behaviours: caregiver-completed CBCL (Internalising subscale) | ||||
| Gowers 200770,71
Eating disorders |
Eating disorder symptoms: clinician-completed MRAOS, child-completed EDI |
Aggregate psychiatric symptoms: clinician-completed HoNOSCA, child-completed HoNOSCA-SR Depression symptoms: child-completed MFQ |
Family functioning: child-completed FAD | |||
| Green 201172
Self-harm |
Repetition of self-harm: clinician-completed count (data not readily extractable) Suicidal ideation: child-completed SIQ |
Aggregate psychiatric symptoms: clinician-completed HoNOSCA Depression symptoms: child-completed MFQ |
Global functioning: clinician-completed HoNOSCA | |||
| Hahlweg 201073
Serious behaviour problems |
Externalising behaviours: parent- and teacher-completed CBCL (Externalising subscale) (CBCL teacher data not reported) | Internalising behaviours: parent- and teacher-completed CBCL (Internalising subscale) (CBCL teacher data not reported) | ||||
| Harrington 199874
Self-harm |
Suicidal ideation: child-completed SIQ Hopelessness: child-completed KHQ |
Diagnosis of major depression, conduct disorder and substance abuse: clinician-completed K-SADS |
Family functioning: child- and parent-completed MFAD Social problem-solving: child-completed SPSI (Generation of Alternative Solutions subscale) |
|||
| Havighurst 200975,76
Serious behaviour problems |
Intensity of conduct problems: parent- and teacher-completed ECBI (Intensity subscale) (ECBI teacher data incompletely reported) | |||||
| Hayward 200077
Anxiety disorders |
Social phobia diagnosis: clinician-completed ADIS Social phobia symptoms: child-completed SPAI-C |
|||||
| Hazell 200978
Self-harm |
Repetition of self-harm: clinician-completed count Suicidal ideation: child-completed SIQ |
Aggregate psychiatric symptoms: clinician-completed HoNOSCA, child-completed SDQ Depression diagnosis: clinician-completed K-SADS (Depression scale) Depression symptoms: child-completed MFQ Behaviour disorder diagnosis: clinician-completed K-SADS (Disruptive Behaviour scale) |
Global functioning: clinician-completed CGAS, HoNOSCA | |||
| Hiscock 200879,80
Serious behaviour problems |
Externalising behaviours: parent-completed CBCL (Externalising subscale) | Internalising behaviours: parent-completed CBCL (Internalising subscale) | ||||
| Hudson 200981
Anxiety disorders |
Anxiety diagnosis: clinician-completed ADIS Anxiety symptoms: child- and parent-completed SCAS |
Emotional difficulties: child- and parent-completed SDQ (Emotional subscale) | ||||
| Hunt 200982
Anxiety disorders |
Anxiety symptoms: child-completed RCMAS, SCAS | Depression symptoms: child-completed CDI | ||||
| Kendall 200883,84
Anxiety disorders |
Anxiety diagnosis: clinician-completed ADIS Anxiety symptoms: child-completed MASC |
Depression symptoms: child-completed CDI Internalising and externalising behaviours: parent- and teacher-completed CBCL |
Coping: child- and parent-completed CQ-C | |||
| Kennard 200885
Depression |
Depression relapse: child-completed CDRS-R (Severity subscale) | Global functioning: clinician-completed GAF | ||||
| King 200086
PTSD |
PTSD symptoms: clinician-completed ADIS, parent-completed CBCL (PTSD subscale) |
Anxiety symptoms: child-completed ‘fear thermometer’, RCMAS, parent-completed CBCL (Internalising subscale) Depression symptoms: child-completed CDI Internalising behaviours: parent-completed CBCL (Internalising subscale) Externalising behaviours: parent-completed CBCL (Externalising subscale) |
Global functioning: clinician-completed GAF | Coping: child-completed study-specific coping measure | ||
| Kolko 201087
Serious behaviour problems |
ADHD, ODD or CD diagnosis: clinician-completed K-SADS Externalising behaviours: parent-completed PSC-17 (Externalising subscale) Attention problems: PSC-17 (Attention subscale) (PSC-17 Attention data not reported at follow-up) |
Other mental health disorders: clinician-completed K-SADS Aggregate psychiatric symptoms: parent- and teacher-completed SDQ Anxiety symptoms: child-completed SCARED, parent-completed PSC-17 (Internalising subscale) Depression symptoms: child-completed MFQ |
Impairment: parent-completed CIS | Resilience: child-completed CHIP (Resilience subscale) | General health and well-being: child-completed CHIP (Satisfaction, Comfort, Risks and Achievement subscales) | |
| Lock 200388,89
Anxiety disorders |
Anxiety symptoms: child-completed SCAS, RCMAS | Depression symptoms: child-completed CDI | ||||
| Lowry-Webster 200139,90
Anxiety disorders; depression |
Anxiety symptoms: child-completed SCAS, RCMAS, parent-completed CBCL (Internalising subscale) Depression symptoms: child-completed CDI, parent-completed CBCL (Internalising subscale) |
Externalising behaviours: parent-completed CBCL (Externalising subscale) | ||||
| Masia Warner 200791
Anxiety disorders |
Social anxiety diagnosis (presence and severity): clinician-completed ADIS Anxiety symptoms: child-completed SPAI-C, child- and parent-completed SASA (Fear of Negative Evaluation, Social Avoidance of Distress in New Situations and Social Avoidance of Distress in General Situations subscales) |
Depression symptoms: child-completed BDI-II | Global functioning: clinician-completed CGAS | |||
| McVey 200292
Eating disorders |
Eating disorder symptoms: child-completed ChEAT, SIQYA (Body Image subscale) | |||||
| McVey 2004134
Eating disorders |
Eating disorder symptoms: child-completed ChEAT, SIQYA (Body Image subscale) | Self-esteem: child-completed RSES | ||||
| Merry 200493
Depression |
Depression symptoms: child-completed BDI-II, RADS | |||||
| Mifsud 200594
Anxiety disorders |
Anxiety symptoms: child- and parent-completed SCAS, CATS (Anxiety subscale), teacher-completed CBCL (Internalising subscale) (parent SCAS data only partially reported) | |||||
| Miklowitz 2008135
Bipolar disorder |
Recovery from initial depressive symptoms and recovery from initial manic symptoms: derived from clinician-completed LIFE data | |||||
| MTA 199995–98
Serious behaviour problems |
ADHD/ODD symptoms: parent-and teacher-completed SNAP (ADHD and ODD subscales) |
Anxiety symptoms: child-completed MASC Internalising behaviours: parent- and teacher-completed SSRS (Internalising subscale) |
Social skills: parent- and teacher-completed SSRS (Social Skills subscale) | |||
| O’Dea 2000136 Eating disorders | Eating disorder symptoms: child-completed EDI (Drive for Thinness, Body Dissatisfaction and Bulimia subscales) (EDI-Bulimia data not reported) | Depression symptoms: child-completed BDI Anxiety symptoms: child-completed STAI | Self-worth: child-completed SPP-A/C | |||
| Patterson 200299,100
Serious behaviour problems |
Behaviour problems: parent-completed ECBI (Intensity and Problem subscales), SDQ (Conduct and Hyperactivity subscales) |
Aggregate psychiatric symptoms: parent-completed SDQ (Total) Emotional issues: parent-completed SDQ (Emotional subscale) |
Dysfunctional parent–child systems: parent-completed PSI Peer relationships: parent-completed SDQ (Peer Problems subscale) Prosocial behaviour: parent-completed SDQ (Prosocial Behaviour subscale) |
|||
| Pfiffner 1997101
Serious behaviour problems |
Composite problem behaviour score: derived from parent- and teacher-completed CLAM, SNAP-R and CBCL | Social skills: teacher-completed SSRS and a parent- and teacher-completed study-specific social skills measure | ||||
| Pfiffner 2007102
Serious behaviour problems |
ADHD symptoms: clinician-completed DSM-IV inattention – frequency and severity of inattention (derived from the CSI) |
Social impairment: parent- and teacher-completed SSRS Organisational skills: parent- and teacher-completed COSS |
||||
| Puskar 2003103
Depression |
Depression symptoms: child-completed RADS | Coping: child-completed CRI | ||||
| Rohde 2004104
Comorbid depression/serious behaviour problems |
Depression and conduct disorder diagnoses: clinician-completed K-SADS Depression symptoms: clinician-completed HAM-D, child-completed BDI-II Externalising behaviours: parent-completed CBCL (Externalising subscale) |
Global functioning: clinician-completed CGAS Social adjustment: child-completed SAS-SR |
||||
| Rooney 2006105
Depression |
Depression symptoms: child-completed CDI | Anxiety symptoms: child-completed RCMAS | ||||
| Rosa Alcázar 2009106
Anxiety disorders |
Anxiety diagnosis: clinician-completed ADIS (ADIS data not reported) Anxiety (social phobia) symptoms: child-completed SPAI-C (Social Phobia subscale), SASA, SPS, FNES, parent-and teacher-completed SASA |
Maladjustment: child-completed IE | Assertiveness: child-completed RAS | Self-esteem: child-completed RSES | ||
| Ruini 2009107
Generic mental health (primarily anxiety disorders) |
Anxiety symptoms: child-completed RCMAS, KSQ (Anxiety subscale) | Generic mental health symptoms: child-completed KSQ (Depression, Somatisation and Hostility subscales) | General well-being: child-completed PWB, KSQ (Relaxation, Contentment, Physical well-being and Friendliness subscales) | |||
| Sánchez-García 2009a138
Anxiety disorders |
Anxiety diagnosis: clinician-completed ADIS Anxiety symptoms: child-completed SPAI-C and SASC-R (SPAI-C data not reported) |
|||||
| Sánchez-García 2009b139
Anxiety disorders |
Anxiety diagnosis: clinician-completed ADIS (ADIS data not reported) Anxiety symptoms: child-completed SPAI-C, SASC-R |
|||||
| Sawyer 2010108,109
Depression |
Depression symptoms: child-completed CES-D | Interpersonal competence: child-completed AICQ | Coping: child-completed study-specific coping measure | |||
| Sheffield 2006110
Depression |
Depression diagnosis: clinician-completed ADIS (data reported but not readily extractable) Depression symptoms: child-completed CDI, CES-D |
Hopelessness: child-completed BHS Anxiety symptoms: child-completed SCAS Externalising behaviours: child-completed CBCL (Externalising subscale) Automatic thoughts: child-completed CATS |
Social functioning: child-completed SPSI-R and CASAFS | |||
| Silverman 1999111
Anxiety disorders |
Anxiety symptoms: child-completed ’fear thermometer’, child- and parent-completed RCMAS, FSSC-R |
Depression symptoms: child-completed CDI Internalising and externalising behaviours: parent- and teacher-completed CBCL |
Severity rating: parent-completed study-specific global rating of severity | |||
| Simon 2011112
Anxiety disorders |
Anxiety diagnosis: clinician-completed ADIS Anxiety symptoms: child-completed SCARED |
|||||
| Spence 2003113,114
Depression |
Depression symptoms: child-completed modified BDI, study-specific dysthymia measure (dysthymia measure not reported post intervention) |
Anxiety symptoms: clinician-completed ADIS Internalising behaviours: child-completed CBCL (Internalising subscale) Externalising behaviours: child-completed CBCL (Externalising subscale) |
Social functioning: child-completed CASAFS | |||
| Stice 2003115
Eating disorders |
Bulimic symptoms: child-completed EDE-Q Thin ideal: child-completed I-BSS-R Body dissatisfaction: child-completed SDBPS |
Negative mood: child-completed PANAS-X | ||||
| Stice 2006116,117
Eating disorders |
Bulimic symptoms: child-completed EDE-Q Thin ideal: child-completed I-BSS-R Body dissatisfaction: child-completed SDBPS |
Negative mood: child-completed PANAS-X | Social adjustment: child-completed SAS | |||
| Stice 2008118,119
Depression |
Depression symptoms: clinician-completed adapted K-SADS, child-completed BDI | Bulimic symptoms: clinician-completed EDDI (EDDI data reported in 2008 paper but not reported in 2010 follow-up) | Social adjustment: child-completed SAS | |||
| Stice 2009120
Eating disorders |
Eating disorder symptoms: clinician-completed EDDI, child-completed I-BSS-R (Thin Ideal), SDBPS (Body Dissatisfaction) | Depression symptoms: child-completed CES-D | ||||
| TADS 2004121–126
Depression |
Depression symptoms: clinician-completed CDRS-R, child-completed RADS | Suicidal ideation: child-completed SIQ (Junior Version) | ||||
| Thompson 2001137
Self-harm |
Suicide risk: child-completed HSQ (Suicide Risk items) | Other risks: child-completed HSQ (Related Risk items) | Protective factors: child-completed HSQ (Protective Factors subscale) | |||
| Thompson 2009127
Serious behaviour problems |
ADHD/ODD diagnosis: clinician-completed PACS, study-specific direct ADHD observation measure, parent-completed WWP | |||||
| Tol 2008128
PTSD |
PTSD symptoms: clinician-completed CPSS |
Depression symptoms: clinician-completed DSRSC Anxiety symptoms: clinician-completed SCARED |
General functioning: child- and parent-completed study-specific measure | Hope: clinician-completed CHS | ||
| Vostanis 1996129–131
Depression |
Depression diagnosis: clinician-completed K-SADS Depression symptoms: child- and parent-completed MFQ |
Anxiety symptoms: child- and parent-completed RCMAS | Functioning: clinician-completed SAICA (Adjustment and School Functioning subscales) | Self-esteem: child- and parent-completed SEI |
Appendix 7 Summary table for the 71 included effectiveness studies
| Study ID, locale and quality a | Condition, intervention level and target | Intervention name, model and self-care element | Recipients (with demographics of CYP), platform and delivery location | Agent, agent role and whether or not trained/supervised | Type of RCT, outcome measures and key messages |
|---|---|---|---|---|---|
| Arnarson 200945,46
Iceland Unclear |
Depression Selective YP at risk of depression |
Not explicit (‘prevention programme’) Eclectic model employing developmental theories, psychopathology research, resilience research relating to depression Developing adaptive coping skills to enhance self-esteem and well-being via classroom sessions and a manual and homework book for participants |
CYP (52% female, age range 14–15 years, ethnicity unreported) Manualised; face-to-face CYP groups School |
Psychologists Delivering/facilitating the intervention (running the sessions) Agent trained and supervised |
Two-arm RCT with usual care control Direct MH Compared with usual care, the programme was effective in preventing the first episode of depression and/or dysthymia at 6 months following programme completion; the preventive effects were sustained at 12-month follow-up |
| Barrett 200547
Australia Unclear |
Anxiety disorders Universal General population of primary and secondary school children |
FRIENDS (for children or for youth versions) CB principles CYP are facilitated to work through a workbook; parents have a booklet detailing the strategies discussed in each parent session; flexible implementation to allow for family individuality and the needs of any specific group |
Family (sex unreported, age range 9–16 years, ethnicity unreported) Manualised; face-to-face CYP groups and parent workshops School |
Psychologists Delivering/facilitating the intervention Agent trained and supervised |
Clustered two-arm RCT with usual care control Direct MH, indirect MH Poststudy results indicated significant reductions in anxiety and depression across the high- and moderate-risk groups in both the intervention and control conditions; this trend was evident at 12-month follow-up though reductions in anxiety were greater in the intervention condition |
| Barrington 200548
Australia Unclear |
Anxiety disorders Treatment Children with anxiety disorders and their families |
Not explicit (‘CBT’) CB principles Self-management of anxiety via exposure and self-monitoring sheets; encouraging the child to develop more helpful ways of thinking |
Child, parent or family (65% female, mean age 9.9 years, ethnicity unreported) Manualised; face-to-face individual sessions Hospital/clinic |
Psychologists (CBT trained) Delivering/facilitating the intervention Agent trained (in CBT) and supervised |
Two-arm RCT with usual care control Direct MH Significant improvements were found on all of the anxiety measures over time, but no significant differences were found between the intervention and control groups |
| Bernstein 200549,50
USA Unclear |
Anxiety disorders Treatment Children with mild to moderate anxiety |
FRIENDS (arm 1 = group CBT + parent training; arm 2 = group CBT only) CB principles CYP are facilitated to work through a workbook; parent education and training, including in-session activities and exercises, to help parents understand and support their children |
Arm 1: CYP and parents separately; arm 2: CYP only (66% female, mean age 9.0 years, 97% white) Both arms manualised; face-to-face groups School |
CB therapist, with graduate students and interns as cotherapists Delivering/facilitating the intervention Agent trained and supervised |
Clustered three-arm RCT with no treatment control; both intervention arms were self-care support Direct MH Significant benefits of the two CBT treatments over the control on clinician-, child- and parent-reported measures of child anxiety; however, at follow-up there were no differences between the three groups on remission of baseline anxiety disorders or incidence of new anxiety disorders |
| Biegel 200951
USA Adequate |
Generic MH Treatment Psychologically symptomatic population of YP |
MBSR Mindfulness Group sharing of practice-related and other experiences; instruction in at-home mindfulness practice assignments |
CYP (74% female, mean age 15.4 years, 45% Caucasian) Manualised; face-to-face CYP groups Clinic (implied) |
Master’s-level ‘instructors’ Training the YP in mindfulness; delivering/facilitating the intervention Agent trained; supervision unclear |
Two-arm RCT with usual care control Direct MH, indirect MH, general functioning, resilience, general well-being, self-esteem Relative to the control group, the MBSR group self-reported reduced symptoms of anxiety, depression and somatic distress, increased self-esteem and sleep quality; the MBSR group also showed a higher percentage of diagnostic improvement and significant increases in functioning scores |
| Cartwright-Hatton 201152
UK, England Adequate |
Anxiety disorders Treatment Caregivers of children (9 years and under) with anxiety |
Timid to Tiger CB principles; behavioural parent training Parents are taught techniques that they can use to help their children manage their anxiety |
Parents (children 57% female, mean age 6.6 years, 74% white) Manualised; face-to-face parent groups Clinic |
Psychologists Delivering/facilitating the intervention (running the groups) Unclear whether or not agent trained or supervised |
Two-arm RCT with waiting list control Direct MH, indirect MH Children whose parent(s) received the intervention were significantly less anxious at the end of the study than control group children; relative to controls, treatment gains were maintained at 12-month follow-up |
| Clarke 199553
USA Unclear |
Depression Indicated YP at risk of depression |
Coping with Stress course (modified from Adolescent Coping with Depression course, Clarke 200154) Cognitive (behavioural) principles Teaching new coping mechanisms and strengthening the YP’s repertoire of current coping techniques and strategies |
CYP (70% female, mean age 15.3 years, 92% white) Manualised; face-to-face CYP groups School |
Psychologists; counsellors Delivering/facilitating the intervention (running the groups) Agent trained and supervised |
Two-arm RCT with usual care control Direct MH, general functioning Survival analyses indicated a significant 12-month advantage for the intervention on affective disorder incidence rates but only short-term effects for depressive symptomatology and general functioning |
| Clarke 200154
USA Inadequate |
Depression Selective YP with subsyndromal depression who have depressed parents |
Adolescent Coping with Depression course CB principles; relaxation techniques; conflict reduction techniques Teaching of CB skills using homework activities to practise these skills |
CYP (64% female, mean age 14.5 years, 88% white) Manualised; face-to-face CYP groups Clinic |
‘Therapists’ Delivering/facilitating the intervention; additionally some information-only parent groups Agent trained; supervision unclear |
Two-arm RCT with usual care control Direct MH, indirect MH, general functioning Significant programme effects for depression scores were detected; survival analysis of major depressive episodes during a median 15-month follow-up found a significant advantage for the intervention group |
| Clarke 200255
USA Unclear |
Depression Treatment Depressed YP who have depressed parents |
Adolescent Coping with Depression course CB principles; relaxation techniques; conflict reduction techniques Teaching of CB skills using homework activities to practise these skills |
CYP (sex data erroneous, mean age 15.3 years, 91% ‘non-minority’) Manualised; face-to-face CYP groups Clinic |
‘Therapists’ Delivering/facilitating the intervention; additionally some information-only parent groups Agent trained; supervision unclear |
Two-arm RCT with usual care control Direct MH, indirect MH, general functioning The authors were unable to detect any significant advantage of the programme over usual care for the depression diagnoses, continuous depression measures or functioning outcomes |
| Compas 200956
USA Inadequate |
Depression Selective CYP with a depressed parent |
Family CB intervention CB techniques; parent training Educate families about depression; increase family awareness of the impact of stress and depression on functioning; help families recognise and monitor stress and develop adaptive coping responses; improve parenting skills |
Families (CYP 45% female, mean age 11.3 years, 80% Euro-American) Manualised; face-to-face family groups Location unclear |
Social workers or psychologists Delivering/facilitating the intervention (running the groups) Agent trained and supervised |
Two-arm RCT with attention control Direct MH, indirect MH For the depression scores, the main effect was significant at 12 months but not at 2 and 6 months; for anxiety/depression symptoms, the main effect was significant for the child-reported data at 2, 6 and 12 months but there were no significant effects at any time point on the parent-reported scores |
| Cowell 200957
USA Unclear |
Depression Selective Mexican immigrant women and their children |
MAPS Problem-solving approach embedded into home nursing Group and individual problem-solving activities as well as provision of basic health promotion activities |
CYP and parents separately (CYP sex unreported, mean age 10.4 years, 100% Mexican American) Manualised; face-to-face CYP groups; individual parent sessions Home (mothers); school (CYP) |
Nurses (bilingual) Delivering/facilitating the intervention (running the home-based parent sessions and the children’s groups) Agent trained and supervised |
Clustered two-arm RCT with no treatment control Direct MH There were statistically significant improvements in children’s health conceptions and family problem-solving communication, factors predictive of mental health; however, improvements in children’s depression symptoms in the intervention group were not significant |
| CPPRG 2007132
USA Unclear (but not meta-analysable) |
Serious behaviour problems Selective Children with behaviour problems in ‘high-risk’ neighbourhoods |
Fast Track Program (includes a universal intervention: Promoting Alternative Thinking Strategies curriculum) Parent training; social skills training Training parents in behaviour management and children in social cognitive skills; tutoring in reading, home visiting, mentoring and a universal classroom curriculum |
CYP and parents (mainly CYP) (CYP 31% female, mean age 6.5 years, 47% Euro-American) Manualised; face-to-face CYP groups and individual sessions School |
Educational co-ordinators (CYP); family co-ordinators (parents); also teachers and teaching assistants Delivering/facilitating the intervention (running groups and providing individual support) Agent trained and supervised |
Clustered two-arm RCT with usual care control Direct MH Assignment to the intervention had a significant positive effect in lowering criterion count scores and diagnoses for CD, ADHD and any externalising disorder, and lowering antisocial behaviour scores, but only among those initially at highest risk |
| Dadds 199758,59
Australia Unclear |
Anxiety disorders Indicated General population of schoolchildren aged 7–14 years |
(Based on) Coping Koala CB principles Child develops and implements their own plan for graded exposure; group processes are used to help children learn positive strategies from each other; parents learn how to self-manage own anxiety in order to help their children |
CYP and parents (mainly CYP) (sex inconsistently reported, mean age 9.4 years, ‘majority white’) Manualised; face-to-face CYP groups School |
Psychologists Delivering/facilitating the intervention (running the groups) Agent trained and supervised |
Clustered two-arm RCT with ‘monitoring’ control Direct MH, indirect MH Both intervention and control groups improved at postintervention but at first follow-up, the improvement was maintained only in the intervention group; at 12 months, the two groups converged, but the superiority of the intervention group was evident again at 2-year follow-up |
| Dalle Grave 200160
Italy Unclear |
Eating disorders Universal General population of 11- to 12-year-old school students |
Unclear (‘a school-based eating disorder prevention programme’) CB principles Students apply the prevention programme’s principles through homework and role play |
CYP (58% female, mean age 11.6 years, ethnicity unreported) Manualised; face-to-face CYP groups School |
Psychologists (with experience in eating disorders) Delivering/facilitating the intervention (running the groups) Unclear whether or not agent trained or supervised |
Clustered two-arm RCT with usual care control Direct MH, self-esteem The intervention group eating attitude scores decreased significantly post intervention but at follow-up they partially recovered, restoring the gap between the intervention and control groups; for global eating disorder scores, both groups improved over time; the intervention had no effect on self-esteem |
| de Cuyper 200461
Belgium (implied) Unclear |
Depression Indicated Children with subthreshold depressive symptoms |
Taking Action CB principles Teaching of problem-solving skills, self-monitoring and self-evaluation skills |
CYP (75% female, mean age 10.0 years, 100% white) Manualised; face-to-face CYP groups (parents invited to one session with therapist) Clinic |
Unclear (‘therapist’ and ‘co therapist’) Delivering/facilitating the intervention (running the groups) Unclear whether or not agent trained but supervised |
Two-arm RCT with waiting list control Direct MH, indirect MH, self-esteem At 4-month follow-up there were significant improvements in depression symptoms and self-worth scores in the treatment group; at 12-month follow-up there were further improvements in self-worth, depression and anxiety symptoms and internalising and externalising behaviours |
| DeRosier 200462,63
USA Unclear |
Anxiety disorders Indicated Schoolchildren with social anxiety, bullied by peers or highly disliked |
S.S.GRIN Combination of social learning and CB techniques Didactic instruction combined with active practice (e.g. role playing, modelling, hands-on activities) to enhance social skills and coping skills |
CYP (49% female, mean age 8.6 years, 83% white) Manualised; face-to-face CYP groups School |
School counsellors and interns Delivering/facilitating the intervention (running the groups) Agent trained and supervised |
Two-arm RCT with no treatment control Direct MH, indirect MH, self-esteem S.S.GRIN increased peer liking, enhanced self-esteem and self-efficacy, and decreased social anxiety compared with the control; at 1-year follow-up, further treatment effects were found, including higher social acceptance and self-esteem and lower depression and anxiety |
| Dobson 201064
Canada Unclear |
Depression; anxiety disorders Indicated YP with a high risk of developing anxiety and depression |
Adolescent Coping with Stress course CB principles Teaching YP cognitive restructuring and how to identify and self-manage negative thoughts |
CYP (70% female, mean age 15.3 years, ethnicity unreported) Manualised; face-to-face CYP groups Location unclear |
Psychologists Delivering/facilitating the intervention (running the groups) Agent trained; supervision unclear |
Two-arm RCT with attention control Direct MH, self-esteem Both control and intervention groups exhibited significant improvements in mood symptomatology and self-esteem outcomes post intervention and at the two follow-up points |
| Evans 200765
USA Unclear |
Serious behaviour problems Treatment Secondary school students with ADHD |
CHP-C Psychosocial model centred on academic skills development but also including social skills training; mentoring Learning social skills, e.g. social problem solving; learning to manage ADHD |
CYP (23% female, mean age 11.9 years, 94% Caucasian) Manualised; face-to-face individual CYP sessions School |
‘Mentors’ (mainly teachers) ’Mentoring’; working individually with students Agent trained and supervised |
Clustered two-arm RCT with usual care control Direct MH, general functioning Findings revealed cumulative long-term benefits for the intervention group as measured by parent ratings of ADHD symptoms and social functioning |
| Gallagher 200466
USA Unclear |
Anxiety disorders Treatment Children with social anxiety |
Unclear (no formal name) CB principles (Self-)management of anxiety via education about social anxiety coupled with homework and workbook exercises, which parents help facilitate |
CYP (52% female, age range 8–11 years, 56% white) Manualised; face-to-face CYP groups Location unclear |
Doctoral-level graduate students Delivering/facilitating the intervention (running the groups) Agent trained; supervision unclear |
Two-arm RCT with waiting list control Direct MH, indirect MH, general functioning At 3-week follow-up, children receiving the treatment demonstrated significant improvements on the majority of child, parent and clinician reports of social anxiety and related symptoms; the child’s social competence (general functioning) did not appear to be affected by the treatment |
| Garber 200967
USA Unclear |
Depression Indicated YP at risk of depression |
Unclear (‘Cognitive Behaviour Prevention Program’) CB principles A prevention skills focus; YP are taught cognitive restructuring techniques, problem-solving skills, behavioural activation, relaxation and assertiveness |
CYP (49% female, mean age 8.6 years, 25% self-identified as a minority) Manualised; face-to-face CYP groups (caregivers also receive information sessions) Location unclear |
‘Therapists’ with at least a Master’s in MH Delivering/facilitating the intervention (running the groups) Agent trained and supervised |
Two-arm RCT with usual care control Direct MH The CB prevention programme had a significant prevention effect through the 9-month follow-up period based on both clinical diagnoses and self-reported depressive symptoms |
| Gillham 200668
USA Unclear |
Depression Indicated Children with elevated depressive symptoms |
PRP Depression-prevention curriculum largely based on CB principles Prevention of depression through skills training (e.g. assertiveness, social skills, problem solving); skills practice via skits, group activities, worksheets and homework assignments |
CYP (53% female, age range 11–12 years, 73% Caucasian) Manualised; face-to-face CYP groups Clinic (implied) |
‘Child MH clinicians’ Delivering/facilitating the intervention (running the groups) Agent trained and supervised |
Two-arm RCT with usual care control Direct MH Over the 2-year follow-up, PRP did not significantly prevent depressive disorders overall but significantly prevented depression, anxiety and adjustment disorders among ‘high-symptom’ participants |
| Ginsburg 200969
USA Unclear |
Anxiety disorders Selective Children of anxious parents |
CAPS programme Combination of CB approach and Beardslee’s family intervention for the offspring of depressed parents Prevention of anxiety via psychoeducation and the teaching of specific skills (e.g. problem solving, communication) |
Parents (first two sessions), then any family members (children 45% female, mean age 8.9 years, 90% Caucasian) Manualised; face-to-face individual family sessions Location unclear |
Psychologists Delivering/facilitating the intervention (facilitating the family group meetings) Unclear whether or not agent trained; agent supervised |
Two-arm RCT with waiting list control Direct MH 30% of children in the control group developed an anxiety disorder by the 1-year follow-up compared with none in the CAPS group; parent-reported (but not child-reported) anxiety levels showed significant decreases from pre-intervention to 1-year follow-up in the CAPS but not in the control group |
| Glisson 2010133
USA Adequate (but not meta-analysable) |
Generic mental health Treatment ’Delinquent’ YP and their families |
MST Ecological model; CB therapy and family therapy influenced Reducing family conflict, improving affective relations; decreasing youth association with deviant peers, increasing association with prosocial peers; developing a support network of family, neighbours and friends |
Families (YP 31% female, mean age 14.9 years, 91% Caucasian) Manualised; face-to-face individual family sessions Home |
MST therapists (mostly with Master’s degrees) Delivering/facilitating the intervention Agent trained and supervised |
Two-arm RCT with usual care control Direct MH, indirect MH At 6 months, youth total problem behaviour in the MST was at a non-clinical level and significantly lower than in the control; however, problem behaviour was equivalent and at non-clinical levels in all conditions by the 18-month follow-up, but youth in the MST entered out-of-home placements at a significantly lower rate than control youth |
| Gowers 200770,71
UK, England Adequate |
Eating disorders Treatment YP with anorexia |
Specialised outpatient treatment Multilevel: CB principles; motivational interviewing; education; parental counselling Unclear (implied that the programme is about the child/parent learning to manage behaviour, beliefs and feelings) |
Families (YP 92% female, mean age 14.9 years, ethnicity unreported) Manualised; face-to-face individual family sessions Location unclear (‘outpatients’) |
‘Trained member of the eating disorder team’ Delivering/facilitating the intervention (running the CBT programme and parental counselling) Unclear whether or not agent trained; agent not supervised |
Three-arm RCT with usual care control; only one of two intervention arms was self-care support Direct MH, indirect MH, general functioning There was no difference in treatment effectiveness of specialist outpatient treatment over the community care control at any time point |
| Green 201172
UK, England Adequate |
Self-harm Indicated YP with previous episodes of self-harm |
DGP Eclectic model combining elements of CBT, DBT, social skills training and group psychotherapy YP learn strategies to deal with difficulties using group-based techniques such as role play |
CYP (89% female, age range 12–17 years, 94% white) Manualised; face-to-face CYP groups Clinic |
‘Therapists’ with at least 3 years’ postqualifying experience Delivering/facilitating the intervention (running the groups) Agent trained and supervised |
Two-arm RCT with usual care (but excluding group therapies) control Direct MH, indirect MH, general functioning There was an overall improvement in functioning across the whole cohort (i.e. both intervention and control groups) and the addition of DGP did not result in significant improvements on any of the measured primary or secondary outcomes |
| Hahlweg 201073
Germany Unclear |
Serious behaviour problems Universal General population of parents |
Triple P Parent training Teaching parents skills to manage their children; using a workbook, parents learn to set and monitor their own goals for behaviour change and enhance their skills in observing their child’s and their own behaviour |
Parents (children 49% female, mean age 4.5 years, ethnicity unreported) Manualised; face-to-face parent groups School |
Psychologists Delivering/facilitating the intervention (running the groups) Agent trained and supervised |
Two-arm RCT with no treatment control Direct MH, indirect MH At the 2-year follow-up, Triple P mothers and fathers reported significant reductions in dysfunctional parenting, and mothers also an increase in positive parenting; mothers also reported significant reductions in child internalising and externalising behaviour |
| Harrington 199874
UK, England Inadequate |
Self-harm Treatment YP who have self-poisoned |
Home-based family intervention Family therapy; behavioural therapy; problem solving Improvements in family functioning via goal negotiation and family problem solving |
Families (YP 90% female, mean age 14.5 years, ethnicity unreported) Manualised; face-to-face individual family sessions Home |
Master’s-level child psychiatric social workers Delivering/facilitating the intervention Agent trained and supervised |
Two-arm RCT with usual care control Direct MH, indirect MH, general functioning There were no significant differences in the primary outcomes (suicidal ideation and hopelessness) between the intervention and control groups at either postintervention or 4-month follow-up |
| Havighurst 200975,76
Australia Adequate |
Serious behaviour problems Universal Parents of a targeted preschool child |
Tuning Into Kids Parent training; Gottman’s emotional coaching; some elements of mindfulness Parents were trained to encourage and facilitate emotional competence/emotional intelligence in the child |
Parents (sex and age data inconsistently reported, ethnicity unclear) Manualised; face-to-face parent groups Preschool (implied) |
Unclear (‘the authors of the paper’) Delivering/facilitating the intervention (running the groups) Unclear whether or not agent trained or supervised |
Clustered two-arm RCT with waiting list control Direct MH There was a significant interaction between condition and time for parent-reported behaviour problems, with a reduction for children in the intervention group |
| Hayward 200077
USA (implied) Inadequate |
Anxiety disorders Treatment Adolescent females with social phobia |
CBGT-A CB principles; social problem-solving and assertiveness skills training (Self-)managing anxiety through in vivo and simulated exposure to feared social situations and homework assignments |
CYP (100% female, mean age 15.6 years, ethnicity unreported) Manualised; face-to-face CYP groups Location unclear |
‘Clinician’ plus research assistant Delivering/facilitating the intervention (running the groups) Agent trained; unclear whether or not supervised |
Two-arm RCT with no treatment control Direct MH There was a significant reduction in the number of participants meeting DSM-IV criteria for social phobia in the treated group; however, at 1-year follow-up there were no significant differences by treatment condition |
| Hazell 200978
Australia Adequate |
Self-harm Treatment YP who self-harm |
DGP Eclectic model combining elements of CBT, DBT, social skills training and group psychotherapy YP learn strategies to deal with difficulties using group-based techniques such as role play |
CYP (90% female, mean age 14.4 years, ethnicity unreported) Manualised; face-to-face CYP groups Clinic |
‘Community CAMHS clinicians’ Delivering/facilitating the intervention (running the groups) Agent trained and supervised |
Two-arm RCT with usual care control Direct MH, indirect MH, general functioning More YP in DGP than in routine care had self-harmed by 6 months; there were few differences between the two groups on the secondary outcome measures, other than a trend for greater improvement over time on global symptom ratings in the DGP group |
| Hiscock 200879,80
Australia Adequate |
Serious behaviour problems Universal Mothers of infants |
Toddlers without Tears Parent training (underpinned by attachment and social learning theories) Psychoeducation and training in managing unwanted behaviour in children |
Parents (mothers) (children 49% female, age range 6–8 months, 78% Anglo-Australian) Manualised; face-to-face parent groups Community |
Nurses (maternal and child health nurses) Delivering/facilitating the intervention (running the groups) Agent trained; unclear whether or not supervised |
Clustered two-arm RCT with usual care control Direct MH, indirect MH At both 18- and 24-month follow-ups, child behaviour scores were similar in both the intervention and control groups |
| Hudson 200981
Australia Unclear |
Anxiety disorders Treatment Children with severe broad-based anxiety disorders |
Cool Kids (based on Coping Cat) CB principles; social skills and assertiveness training Training parents to support their children while undertaking graded exposure activities |
Families (children 43% female, mean age 10.2 years, ethnicity data erroneous) Manualised; face-to-face family groups Clinic |
Psychologists Delivering/facilitating the intervention (running the groups) Unclear whether or not agent trained; agent supervised |
Two-arm RCT with attention control Direct MH, indirect MH CBT was significantly more efficacious than the control; compared with the control, significantly more children in the CBT condition did not meet diagnostic criteria for their principal anxiety diagnosis at follow-up |
| Hunt 200982
Australia Unclear |
Anxiety disorders Selective High school first-year students at risk of developing an anxiety disorder |
FRIENDS CB principles; problem solving Teaching problem-solving skills; practising tasks in addition to group sessions |
Families (CYP 43% female, mean age 12.1 years, ethnicity unreported) Manualised; face-to-face CYP groups with some parent sessions School |
School counsellor assisted by teacher Delivering/facilitating the intervention (running the groups) Agent trained; not supervised |
Clustered two-arm RCT with no treatment control Direct MH, indirect MH There was little difference between conditions on self-reported symptoms at 2- and 4-year follow-ups, and no difference on diagnosis or health-care use; when led by school staff, outcomes for FRIENDS may not be as strong as when led by specialist MH staff |
| Kendall 200883,84
USA Unclear |
Anxiety disorders Treatment Children with anxiety |
Arm 1: individual CBT; Arm 2: family CBT (both arms based on Coping Cat) CB principles; relaxation Arm 1: teaching YP skills to manage anxiety via CB techniques and homework tasks; Arm 2: additionally, modifying parental beliefs and expectations, teaching parents constructive responses to their child’s anxious distress and encouraging parents to support the child’s mastery; teaching parents and children effective communication skills |
Arm 1: CYP; Arm 2: families (CYP 44% female, mean age 10.3 years, 85% Caucasian) Arm 1: manualised; face-to-face individual CYP sessions; Arm 2: manualised; face-to-face individual family sessions (CYP and parents separate for two sessions) Location unclear |
Master’s-level therapists and psychologists Delivering/facilitating the intervention (running the sessions) Agent trained and supervised |
Three-arm RCT with attention control; both intervention arms were self-care support Direct MH, indirect MH, resilience The child participants evidenced treatment gains in all conditions, although family CBT and individual CBT were superior to the control in reducing the presence and principality of the principal anxiety disorder, and individual CBT outperformed family CBT and the control on teacher reports of child anxiety; treatment gains, when found, were maintained at 1-year follow-up |
| Kennard 200885
USA Unclear |
Depression Treatment YP recovering from depression (responders to acute phase pharmacotherapy) |
RP-CBT CB principles (especially relapse prevention); little other information Self-care element unclear but implicit in CBT; focus on residual depressive symptoms and promoting wellness |
CYP (48% female, mean age 14.3 years, 74% white) Manualised; face-to-face individual CYP sessions (some family sessions) Location unclear |
CB therapists Delivering/facilitating the intervention (running the individual and family sessions) Agent trained and supervised |
Two-arm RCT with usual care control Direct MH, general functioning Participants in the MM control group had a significantly greater risk of relapse than those in the RP-CBT (+ MM) treatment group |
| King 200086
Australia Unclear |
PTSD Treatment Sexually abused CYP with PTSD symptoms |
Arm 1: individual CBT; Arm 2: family CBT CB principles focusing on PTSD management Arm 1: training in coping skills, psychoeducation, relapse prevention; Arm 2: additionally, parent training in child behaviour management skills and parent–child communication skills; parents self-monitoring own anxiety |
Arm 1: CYP; Arm 2: families (CYP 64% female, mean age 11.5 years, ethnicity unreported) Arm 1: manualised; face-to-face individual CYP sessions; Arm 2: manualised; face-to-face individual family sessions Clinic |
Psychologists Delivering/facilitating the intervention (child and family sessions) Agent trained and supervised |
Three-arm RCT with waiting list control; both intervention arms were self-care support Direct MH, indirect MH, general functioning, resilience Compared with controls, CYP who received CBT exhibited significant improvements in PTSD symptoms and self-reports of anxiety as well as in parent-completed measures and clinician ratings of global functioning; however, parental involvement did not improve CBT’s efficacy; the improvement was maintained at 12-week follow-up |
| Kolko 201087
USA Unclear |
Serious behaviour problems Indicated Children with severe behaviour problems |
PONI Combination of CB principles and parent training Children trained in CB skills to promote self-management; parents trained in positive management and facilitation of children; training in problem-solving skills |
Families (children 35% female, mean age 8.1 years, 80% Caucasian) Manualised; face-to-face (implied) individual family sessions Home |
Nurses (general nurses) Delivering/facilitating the intervention (running the home-based sessions) Agent trained and supervised |
Two-arm RCT with attention control Direct MH, indirect MH, general functioning, resilience, general well-being Both PONI and control cases showed improvements over time on all of the outcomes; the proportion of PONI and control cases diagnosed with ADHD, ODD, CD or other disorders were comparable pre and post treatment, and at 1-year follow-up |
| Lock 200388,89
Australia Unclear |
Anxiety disorders Universal General population of primary and secondary school children |
FRIENDS CB principles Helping children learn skills and techniques that help them cope with, and manage, anxiety and emotional distress through the application of learned coping and problem-solving skills |
CYP (50% female, age ranges 9–10 and 14–16 years, ethnicity unreported) Manualised; face-to-face CYP group (also some parent group sessions) Location unclear |
Teachers Delivering/facilitating the intervention (running the child and parent groups) Agent trained; unclear whether or not supervised |
Clustered two-arm RCT with usual care control Direct MH, indirect MH FRIENDS reduced symptoms of anxiety (but not depression); primary school children reported the greatest changes in anxiety symptoms, suggesting earlier preventive intervention was more advantageous than later intervention; results were maintained only for primary school children |
| Lowry-Webster 200139,90
Australia Unclear |
Anxiety disorders; depression (mainly anxiety) Universal General population of 10- to 13-year-olds (‘universal’), with a ‘high anxiety’ subgroup’ |
FRIENDS for Children; FRIENDS for Parents CB principles (based on Coping Koala) Children taught strategies for coping with anxiety; parents taught management skills to support children |
Families (children 53% female, age range 10–13 years, ethnicity unreported) Manualised; separate face-to-face CYP and parent groups School |
Teachers Delivering/facilitating the intervention (running the child and parent groups) Agent trained and supervised |
Clustered two-arm RCT with waiting list control Direct MH, indirect MH Regardless of their risk status, children in the FRIENDS group reported fewer anxiety symptoms than controls at post-test; in terms of levels of depression, only the high anxiety group who completed FRIENDS evidenced improvements at post-test; at 12-month follow-up, treatment gains were maintained |
| Masia Warner 200791
USA Unclear |
Anxiety disorders Treatment YP with social anxiety |
SASS CB principles; social skills training Unclear (self-care implicit in CB approach); peer support |
CYP (83% female, mean age 15.1 years, 72% Caucasian) Manualised; face-to-face CYP groups (some individual sessions) School |
Psychologist; ‘peer assistants’ for the weekend activities Delivering/facilitating the intervention (running the group sessions) Unclear whether or not agent trained or supervised |
Two-arm RCT with attention control Direct MH, indirect MH, general functioning There was a significant reduction in social anxiety and better functioning for the SASS group compared with the controls, though parent reports of children’s social anxiety did not discriminate between the two groups; superiority of the intervention was maintained at 6-month follow-up |
| McVey 200292
Canada Unclear |
Eating disorders Universal General population of girls aged around 11 years |
Every Body is a Somebody Unclear (‘life skills promotion approach’) Health promotion (including healthy eating); developing self-esteem and positive body image; social problem-solving skills |
CYP (100% female, mean age 10.9 years, 49% Caucasian) Manualised; face-to-face CYP groups School |
‘The author’ Delivering/facilitating the intervention (running the classroom sessions) Unclear whether or not agent trained or supervised |
Clustered two-arm RCT with usual care control Direct MH There was no programme effect; instead, the findings revealed significant increases in body image satisfaction and decreases in eating problem scores over time for participants in both groups |
| McVey 2004134
Canada Unclear (but not meta-analysable) |
Eating disorders Universal General population of girls aged around 11 years |
Every Body is a Somebody Unclear (‘life skills promotion approach’) Health promotion (including healthy eating); developing self-esteem and positive body image; social problem-solving skills |
CYP (100% female, mean age 11.2 years, 44% Caucasian) Manualised; face-to-face CYP groups School |
‘The author’ Delivering/facilitating the intervention (running the classroom sessions) Unclear whether or not agent trained or supervised |
Clustered two-arm trial with usual care control Direct MH, self-esteem The intervention was successful in improving body image satisfaction and global self-esteem, and in reducing dieting attitude scores post intervention only; the gains were not maintained at 12-month follow-up |
| Merry 200493
New Zealand Adequate |
Depression Universal General population of schoolchildren aged 13–15 years |
RAP-Kiwi CB and interpersonal therapy principles Teaching problem-solving skills via role-play activities |
CYP (52% female, mean age 14.2 years, 59% European) Manualised; face-to-face CYP groups School |
Teachers Delivering/facilitating the intervention (running the classroom sessions) Agent trained; unclear whether or not supervised |
Two-arm RCT with attention control Direct MH Post intervention, depression scores were reduced significantly more by RAP-Kiwi than by the control; group differences, however, averaged across time to 18 months, were significant on one depression measure (RADS) but not the other (BDI-II) |
| Mifsud 200594
Australia Unclear |
Anxiety disorders Treatment Children with high anxiety levels from sociodemographically disadvantaged areas |
Adaptation of Cool Kids CB principles with social skills and assertiveness training; parent training Learning to manage own anxiety; social skills and assertiveness training; structured workbooks supported the training |
Families (children 59% female, mean age 9.5 years, 81% Australian) Unclear whether or not manualised; face-to-face CYP groups (parents attended two sessions) School |
School counsellors with a community-based MH worker Delivering/facilitating the intervention (running the groups) Agent trained; unclear whether or not supervised |
Clustered two-arm RCT with waiting list control Direct MH Children assigned to the intervention group demonstrated a significant reduction in anxiety symptoms relative to controls; differences were maintained 4 months after treatment according to both self-report and teacher-report data |
| Miklowitz 2008135
USA Unclear (but not meta-analysable) |
Bipolar disorder Treatment YP with bipolar disorder and their families |
FFT-A Problem solving Teaching YP problem-solving skills to deal with problems of daily life through role playing and between-session rehearsal |
Families (YP 57% female, mean age 14.5 years, 84% white) Manualised; face-to-face individual family sessions Clinic |
‘Clinicians’ Delivering/facilitating the intervention Agent trained; unclear whether or not supervised |
Two-arm RCT with attention control Direct MH Although there were no group differences in rates of recovery from the index episode, participants in FFT-A recovered from their baseline depressive symptoms faster than controls; the groups did not differ in time to recurrence of depression or mania, but FFT-A participants had a more favourable trajectory of depression symptoms for 2 years |
| MTA 199995–98
USA; Canada Adequate |
Serious behaviour problems Treatment Children with ADHD |
Intensive behavioural therapy Intensive, multimodal behavioural treatment with parent, school and child component, parent training, a summer camp based on behavioural approaches and a school-based intervention integrated into the school year Learning how to self-manage behaviour via a multimodal approach |
Families (children 20% female, mean age 8.4 years, 60% white) Manualised; face-to-face individual CYP sessions and face-to-face parent groups School |
‘Therapist consultants’; behaviourally trained aides Consultants provided: parent training, teacher consultation, supervision for aides; aides provided: intensive behavioural treatments at the summer camp Unclear whether or not consultants trained; agents supervised |
Four-arm RCT with usual care control; only one of three intervention arms was self-care support Direct MH, indirect MH, general functioning For most ADHD symptoms, there were no significant additional benefits of intensive behaviour therapy over the control (community care); a managed medication regime (which was a key element of the two arms not considered and which had no self-care support element) had the best outcomes |
| O’Dea 2000136
Australia Unclear (but not meta-analysable) |
Eating disorders Universal General population of secondary school students |
Everybody’s Different Educational theories of co-operative, interactive and student-centred learning Building self-esteem; home-based activities such as family discussion and positive parental input |
CYP (63% female, mean age 13.0 years, ethnicity unreported) Manualised; face-to-face CYP groups School |
Teachers Delivering/facilitating the intervention (delivering the lessons) Unclear whether or not agent trained or supervised |
Clustered two-arm RCT with attention control Direct MH, indirect MH, self-esteem The eating disorder measures Drive for Thinness and Body Satisfaction were significantly better for the whole intervention group post intervention; however, only Body Satisfaction improvements in a ‘high-risk’ subset were maintained at follow-up |
| Patterson 200299,100
UK, England Unclear |
Serious behaviour problems Selective Families with children aged 2–8 years with a behaviour disorder |
The Incredible Years Primarily behavioural (modelling and experiential learning); Webster-Stratton; parent training Parents set themselves goals, undertake homework each week and report back on progress |
Parents (children ‘just under half girls’, mean age 4.6 years, 91% white) Manualised; face-to-face parent groups Community centre/clinic |
Nurses (health visitors; nursery nurses) Delivering/facilitating the intervention (running the groups) Agent trained and supervised |
Two-arm RCT with usual care control Direct MH, indirect MH, general functioning The intervention significantly reduced child behaviour problems and improved mental health at immediate and 6-month follow-ups but not at 12-month follow-up |
| Pfiffner 1997101
USA Unclear |
Serious behaviour problems Treatment Children with ADHD and their families |
Arm 1: SST; Arm 2: SST-PG Arm 1: SST; behavioural approach (token economy); Arm 2: additionally, parent training in order to generalise from home to school settings Social and problem-solving skills taught via modelling, role play with homework activities; children evaluated each other’s performance |
Arm 1: CYP only Arm 2: families (CYP 30% female, age range 8–10 years, 96% Caucasian) Unclear whether or not manualised; Arm 1: face-to-face CYP groups; Arm 2: additionally, face-to-face parent groups Location unclear |
‘SST expert’ and psychologist Delivering/facilitating the intervention (running the groups) Unclear whether or not agent trained or supervised |
Three-arm RCT with waiting list control; both intervention arms were self-care support Direct MH, general functioning Significant improvement in children’s skill and knowledge, and in parent reports of social skills and disruptive behaviour, occurred for both treatment groups relative to the control group and was maintained at a 4-month follow-up |
| Pfiffner 2007102
USA Unclear |
Serious behaviour problems Treatment Children with inattentive type ADHD |
CLAS programme Social learning principles; token economy; social skills training; parent training; some CB principles Teaching the child self-care (e.g. getting ready for school) and time management skills; teaching parents behavioural strategies for managing ADHD, and how to interact effectively with teachers |
Families (29% female, mean age 8.7 years, 51% white) Manualised (but flexible); face-to-face CYP and parent groups (separately and combined) School (implied) |
Psychologists Delivering/facilitating the intervention (running child and parent sessions; facilitating the child in the home-school environment) Unclear whether or not agent trained or supervised |
Two-arm RCT with mixed waiting list and usual care control Direct MH, general functioning Children randomised to the CLAS programme had significantly fewer inattention symptoms, and significantly improved social and organisational skills, relative to the control group; gains were maintained at follow-up |
| Puskar 2003103
USA Unclear |
Depression Treatment Rural adolescents |
TKC CB principles Teaching coping skills via assertiveness training and social skills training; use of homework assignments and role play |
CYP (82% female, mean age 16.0 years, 99% white) Manualised; face-to-face CYP groups School |
Nurses (Master’s-level with MH experience) Delivering/facilitating the intervention (running the groups) Agent trained and supervised |
Two-arm RCT with usual care control Direct MH, resilience Compared with controls, those receiving TKC significantly improved in depressive symptomatology and Seeking Guidance and Support (coping) scores post intervention and at 6-month follow-up |
| Rohde 2004104
USA Unclear |
Comorbid depression and serious behaviour problems Treatment Depressed YP with comorbid conduct disorder |
CWD-A CB principles; social skills training Learning self-management skills such as mood monitoring and anxiety management; learning social and conflict resolution skills; practice of skills, homework assignments and a relatively small number of therapy sessions |
CYP (48% female, age range 13–17 years, 81% white) Manualised; face-to-face CYP groups (two optional parent sessions) Location unclear |
CDW-A ‘leaders’ assisted by ‘student helpers’ Delivering/facilitating the intervention (running the groups) Agent trained; unclear whether or not supervised |
Two-arm RCT with attention control Direct MH, general functioning CWD-A participants reported greater reductions in depression rating scale scores and improved social functioning post treatment but these were not maintained at 6- and 12-month follow-ups |
| Rooney 2006105
Australia Unclear |
Depression Selective Children aged 8–9 years |
PTP, based on the Aussie Optimism Programme CB principles Learning interpersonal and self-management skills; games and activities used to teach CB skills; worksheets |
CYP (43% female, mean age 9.1 years, ethnicity unreported) Manualised; face-to-face CYP groups School |
Psychologists Delivering/facilitating the intervention (running the groups) Agent trained and supervised |
Clustered two-arm RCT with usual care control Direct MH, indirect MH Compared with the control group, there was a lower prevalence of depressive disorders at postintervention in the intervention group; however, these effects were not maintained over time |
| Rosa Alcázar 2009106
Spain Unclear |
Anxiety disorders Treatment YP with social phobia |
IAFS CB principles; social skills training Self-management of anxiety via CB techniques, homework and exercises |
CYP (68% female, mean age 14.8 years, ethnicity unreported) Manualised; face-to-face CYP groups School |
Psychologists (experienced in treating social phobia) Delivering/facilitating the intervention (running the groups) Agent trained; unclear whether or not supervised |
Four-arm RCT with waiting list control; only one of three intervention arms was self-care support Direct MH, general functioning, resilience, self-esteem IAFS has short- and medium-term effectiveness according to measures of social anxiety and avoidance as well as measures such as assertiveness and adjustment |
| Ruini 2009107
Italy Unclear |
Generic mental health (primarily anxiety disorders) Universal General population of high school students |
WBT Mixed CB principles and Ryff model of well-being Teaching YP to understand and managing own feelings via diary keeping, role playing and group discussions |
CYP (61% female, mean age 14.4 years, ethnicity unreported) Manualised; face-to-face CYP groups School |
Psychologists Delivering/facilitating the intervention (running the sessions) Unclear whether or not agent trained or supervised |
Clustered two-arm RCT with attention control Direct MH, indirect MH, general well-being There were no significant differences for anxiety scores; nevertheless there was a significant effect of WBT on a physiological subscale score which decreased in the WBT group and increased in the control group at post-test but with no effect at follow-up |
| Sánchez-García 2009a138
Spain Unclear |
Anxiety disorders Selective Children with social phobia |
IAFS CB principles; social skills training Getting the child to help themselves with social phobia through the use of exposure, feedback from peers (via an ‘observational test’ exercise) and homework activities |
CYP (76% female, mean age 12.0 years, ethnicity unreported) Manualised; face-to-face CYP groups Location unclear |
Peers, overseen by a psychologist Assisting with the observational test; running the groups Agent trained; unclear whether or not supervised |
Two-arm RCT with waiting list control Direct MH Compared with the control group, there were significant changes in all of the dependent variables assessed in the IAFS condition |
| Sánchez-García 2009b139
Spain Unclear |
Anxiety disorders Treatment Children with social phobia |
IAFS; Arm 1: IAFS without cognitive restructuring; Arm 2: complete IAFS CB principles; social skills training Getting the child to help themselves with social phobia via education, individual behavioural objectives, social skills training and homework tasks |
CYP (73% female, mean age 11.9 years, ‘100% Spanish’) Both arms: manualised; face-to-face (implied) CYP groups Location unclear |
Peers, overseen by a psychologist Unclear (collaborators ‘role-played conversations with participants’) Agent trained; unclear whether or not supervised |
Three-arm RCT with waiting list control; both intervention arms were self-care support Direct MH Compared with the control group, there were significant improvements in all dependent variables in the two treatment conditions (IAFS and IAFS without cognitive structuring) |
| Sawyer 2010108,109
Australia Adequate |
Depression Universal General population of school children |
beyondblue Conceptual model of adolescent depression which emphasised resilience Training in problem-solving, social and coping skills |
CYP (53% female, mean age 13.1 years, ethnicity unreported) Manualised; face-to-face CYP groups School |
Primarily teachers Delivering/facilitating the intervention (running the classroom sessions) Agent trained; unclear whether or not supervised |
Clustered two-arm RCT with attention control Direct MH, general functioning, resilience Changes in depressive symptoms and in the levels of risk and protective factors (interpersonal competence and coping) experienced by children in the two groups did not differ significantly over the study period |
| Sheffield 2006110
Australia Adequate |
Depression Selective/universal High-risk (selective) and general sample (universal) of Australian Year 9 students |
Arm 1: universal intervention; arm 2: indicated intervention Both interventions: CB principles Arm 1: teaching cognitive techniques to challenge irrational thoughts via a variety of approaches that included individual and small-group work, interactive exercises and home tasks and diary keeping; arm 2: teaching interpersonal skills (e.g. assertion and negotiating) and self-reward skills via small-group work and a workbook |
CYP (between 54% and 69% female depending on whether high- or low-risk sample employed; mean age 14.3 years; 88% born in Australia) Both levels: manualised; face-to-face CYP groups School |
Arm 1: teacher; arm 2: trained school counsellors or MH professionals Delivering/facilitating the intervention (running the groups or classroom sessions) Agent trained; supervision optional for arm 1 |
Complex, clustered four-arm RCT with no treatment control; although all three intervention arms were self-care support, for simplicity, only the universal intervention with the total sample and indicated intervention with high-risk sample were included Direct MH, indirect MH, general functioning None of the intervention approaches differed significantly from the no-intervention control condition or from each other on changes in depressive symptoms, anxiety, externalising problems, coping skills or social adjustment |
| Silverman 1999111
USA Unclear |
Anxiety disorders Treatment Children with phobic disorders and their parents |
Unclear (‘self-control’) CB principles Teaching self-observation, ‘self-talk’, self-evaluation and self-reward; teaching parents to support their children through homework and feedback |
Families (children 45% female, mean age 9.5 years, 54% white) Manualised; face-to-face individual family sessions Location unclear |
Psychologists Delivering/facilitating the intervention (running the sessions) Agent trained and supervised |
Three-arm RCT with attention control; only one of two intervention arms was self-care support Direct MH, indirect MH, general functioning Children in the self-control condition showed substantial improvement on all outcome measures; these gains were maintained at 3-, 6- and 12-month follow-up; however, control group children also showed considerable improvement at post-treatment and follow-up |
| Simon 2011112
Netherlands Unclear |
Anxiety disorders Treatment Highly anxious schoolchildren |
Arm 1: child-focused CBT; Arm 2: parent-focused CBT Both arms: CB principles; social learning theory; relaxation training Arm 1: children learn to manage their own anxiety via group work and lay coaching; Arm 2: parents trained as lay therapists to help their child overcome his or her anxieties; parents also worked on their own anxiety and on their coparenting relationship |
Arm 1: CYP; Arm 2: parents (CYP 55% female, mean age 9.9 years, ethnicity unreported) Both arms manualised; Arm 1: face-to-face CYP groups; Arm 2: face-to-face parent groups with some telephone contact Location unclear |
Psychologists; child participants as ‘lay therapists’ Delivering/facilitating the intervention (running the groups and an ill-defined telephone role) Agent trained and supervised |
Three-arm RCT with ‘no treatment’ control; both intervention arms were self-care support Direct MH Both child- and parent-focused CBT showed favourable outcomes compared with the control on the number of symptom-improved children |
| Spence 2003113,114
Australia Unclear |
Depression Universal General population of Australian Grade 8 students |
Problem Solving for Life Broadly CB principles; problem-solving skills training Learning problem-solving skills to manage relationships, situations and feelings; learning cognitive techniques to prevent negative feelings; use of didactic sessions, and individual, small-group and whole-class exercises and activities |
CYP (51% female, mean age 12.9 years, ethnicity unreported) Manualised; face-to-face individual and group CYP sessions School |
Teachers Delivering/facilitating the intervention (running the group and individual sessions) Agent trained; supervision optional |
Clustered two-arm RCT with usual care control Direct MH, indirect MH, general functioning Both high- and low-symptom students demonstrated positive short-term benefits after participating in the intervention condition; however, these benefits were no longer evident by 1-year follow-up nor were they evident at 4-year follow-up |
| Stice 2003115
(implied USA) Unclear |
Eating disorders Selective Adolescent females with body image concerns |
‘Dissonance intervention’ Cognitive dissonance (attempting to avoid internalising the ‘thin ideal’); some CB principles Counter-attitudinal role play getting YP to challenge their ‘thin ideal’ via group work, in-session exercises and homework |
CYP (100% female, mean age 17.4 years, 63% white) Manualised; face-to-face CYP groups Location unclear |
Psychologists (with undergraduate cofacilitator) Delivering/facilitating the intervention (running the groups) Unclear whether or not agent trained or supervised |
Three-arm RCT with attention control; only one of two intervention arms was self-care support Direct MH, indirect MH Participants in both the dissonance group and the healthy weight control group reported decreased thin ideal internalisation, negative affect and bulimic symptoms at end of treatment and at follow-up |
| Stice 2006116,117
USA Unclear |
Eating disorders Indicated YP with body dissatisfaction |
‘Dissonance intervention’ Cognitive dissonance (attempting to avoid internalising the ‘thin ideal’); some CB principles Counter-attitudinal role play getting YP to challenge their ‘thin ideal’ via group work, in-session exercises and homework |
CYP (100% female, mean age 17.0 years, 58% Caucasian) Manualised; face-to-face CYP groups School (implied) |
Graduate student with undergraduate cofacilitator Delivering/facilitating the intervention (cofacilitators assisted with administrative tasks) Agent trained and supervised |
Four-arm RCT with usual care control; only one of three intervention arms was self-care support Direct MH, indirect MH, general functioning At post-test, dissonance participants showed significantly greater reductions in eating disorder risk factors and bulimic symptoms than the assessment-only participants from pre- to post-test; these effects were maintained at short- and long-term follow-up |
| Stice 2008118,119
USA Unclear |
Depression Selective High school students at risk of depression |
Arm 1: brief group CBT; arm 2: group supportive–expressive intervention Arm 1: CB principle, motivational theory; arm 2: non-directive supportive psychotherapy Arm 1: skills training and social support; in-session exercises requiring application of the CB skills taught in the intervention; group activities; motivational enhancement exercises; arm 2: learning strategies to support emotional self-management |
CYP (56% female, mean age 15.6 years, 46% Caucasian) Both arms: manualised; face-to-face CYP groups Location unclear |
Psychologists Delivering/facilitating the intervention (running the groups) Agent trained and supervised |
Clustered four-arm RCT with usual care control; two of three intervention arms were self-care support (CB bibliotherapy was excluded because it was not self-care support) Direct MH, indirect MH, general functioning The group CBT intervention reduced initial symptoms and risk of future depression, although both supportive–expressive therapy and CB bibliotherapy also produced long-term intervention effects; indeed, CB bibliotherapy emerged as the least expensive method of reducing risk of depression |
| Stice 2009120
USA Unclear |
Eating disorders Selective Adolescent females with body image concerns |
‘Dissonance intervention’ Cognitive dissonance (attempting to avoid internalising the ‘thin ideal’); some CB principles Counter-attitudinal role play getting YP to challenge their ‘thin ideal’ via group work, in-session exercises and homework |
CYP (100% female, mean age 15.7 years, 81% white) Manualised; face-to-face CYP groups School |
School nurses and school counsellors (occasionally teachers) Delivering/facilitating the intervention (running the groups) Agent trained and supervised |
Two-arm RCT with attention control Direct MH, indirect MH Compared with the control condition, the dissonance intervention showed significantly greater decreases in ‘thin ideal’ internalisation, body dissatisfaction, dieting attempts and eating disorder symptoms from pre-test to post-test; the effects for body dissatisfaction, dieting and eating disorder symptoms persisted through 1-year follow-up |
| TADS 2004121–126
USA Unclear |
Depression Treatment YP with depression |
Unclear (‘CBT’) CB principles; social problem solving Skills building, flexible tailoring of the treatment to the YP’s needs in a developmentally sensitive fashion; goal-setting with the YP, mood monitoring, teaching social skills such as social engagement, communication, negotiation, compromise and assertion |
CYP (and parents to a small extent) (CYP 54% female, mean age 14.6 years; 74% white) Manualised; face-to-face individual CYP and family sessions Clinic |
CB therapist Delivering the CB intervention Unclear whether or not agent trained or supervised |
Four-arm RCT with usual care control; only one of three intervention arms was self-care support Direct MH, indirect MH Adding CBT to usual care (fluoxetine in this case) meaningfully accelerates recovery from depression relative to fluoxetine alone; adding CBT minimises persistent suicidal ideation and treatment-emergent suicidal events associated with medication |
| Thompson 2001137
USA Unclear (but not meta-analysable) |
Self-harm Selective YP at risk of suicide |
CAST Skills training and social support Providing skills training and social support |
CYP (52% female, age range 14–19 years, 49% Euro-American) Manualised; face-to-face CYP groups School |
Master’s-level teachers, counsellors or nurses Delivering/facilitating the intervention (running the groups) Agent trained and supervised |
Clustered three-arm RCT with usual care control; only one of two intervention arms was self-care support Direct MH, indirect MH, resilience Compared with usual care, the intervention showed significant rates of decline in attitude towards suicide and suicidal ideation and was also effective in reducing depression and hopelessness; reductions in anxiety and anger were greater among females |
| Thompson 2009127
Guernsey Unclear |
Serious behaviour problems Treatment Children with ADHD/ODD and their parents |
Revised NFPP Parent training (underpinned by self-regulation, social learning theory and social/cognitive developmental theory) Training parents so they can provide the support, motivation and ‘developmental scaffolding’ needed to allow their child to reach set goals |
Parents and, for half the sessions, CYP (CYP 24% female, mean age 4.3 years, ethnicity unreported) Manualised; face-to-face individual family sessions Home |
Nurses Delivering/facilitating the intervention Agent trained and supervised |
Two-arm RCT with usual care control Direct MH Effects of the Revised NFPP on ADHD symptoms were large and significant and effects persisted for 9 weeks post intervention; effects on ODD symptoms were less marked |
| Tol 2008128
Indonesia Unclear |
PTSD Indicated Children affected by armed conflicts or political violence |
Unclear CB principles with co-operative play and creative–expressive exercises (drama, dance and music) Sharing of trauma stories; interactive activities; reconnecting the child and group to his/her social context using resiliency-based themes and activities |
CYP (49% female, mean age 9.9 years, 49% ethnicity unreported) Manualised; face-to-face CYP groups School |
‘Interventionists’ (selected from local communities and educated to at least high school level) Delivering/facilitating the intervention (running the sessions) Agent trained; unclear whether or not agent supervised |
Clustered two-arm RCT with waiting list control Direct MH, indirect MH, general functioning, resilience Compared with controls, there was a significant improvement in PTSD symptoms and hope in the treatment group; changes in general remained at 6-month follow-up although the size of differences was smaller; changes in stress-related physical symptoms, depressive symptoms, anxiety and functioning did not differ between groups at follow-up |
| Vostanis 1996129–131
UK, England (implied) Unclear |
Depression Treatment CYP with depression |
Unclear (‘CBT’) CB principles; problem solving Teaching social problem solving, reinforced through practising tasks, homework and self-reinforcement |
CYP (56% female, mean age 12.7 years, 88% white) Manualised; face-to-face individual sessions with CYP School |
Child psychiatrist Delivering/facilitating the intervention (running the sessions) Unclear whether or not agent trained; agent supervised |
Two-arm RCT with attention control Direct MH, indirect MH, general functioning, self-esteem There were postintervention improvements in both the intervention and control groups on all psychosocial measures which were maintained at follow-up |
Appendix 8 Summary of the included qualitative perceptions studies
| Paper, locale and quality score | Condition, intervention type and target | Intervention name, model and self-care element | Recipients, platform and delivery location | Agent and agent role | Data source, methods and key messages |
|---|---|---|---|---|---|
| Baker-Henningham 2009147
Jamaica 6 |
Serious behaviour problems Prevention Preschool children |
The Incredible Years (elements of the teacher programme and Dina Dinosaur classroom curriculum) Webster-Stratton’s social learning approach (involving modelling and experiential learning) Children are encouraged to learn from each other, to solve their own problems with group support and to apply the new skills learnt to their own situations |
Child/young person Face-to-face groups School (classroom based) |
Teacher Delivering and facilitating the intervention (running the classroom sessions) |
Teachers Individual interviews with the teachers The teachers valued the intervention, reporting benefits to their own teaching skills and professional development, their relationships with children, and the behaviour, social–emotional competence and school readiness skills of their students; they also reported benefits to teacher–parent relationships and to the children’s behaviour at home; teachers felt they were able to successfully integrate the programme into their regular practice |
| Coyle 2009148
Ireland 5 |
General mental health problems Management Young people with mental health problems |
Personal Investigator Solution-focused therapy Tasks within the computer game help young people identify problems and develop ways of addressing them |
Child/young person Use of a computer game (with the young person controlling it) in an individual face-to-face session Clinic |
Psychologist, psychotherapist or social worker Supporting the young person playing the game and facilitating conversation |
Therapists; some young people Service evaluation; young person and therapist views obtained from open-ended survey questions Young people found the computer game easy to use and helpful; therapists were generally positive about its impact, but there was a mixed response about using it again; the therapists generally agreed it was a helpful icebreaker that could help engage young people in sessions but there were concerns about young people not engaging sufficiently with the therapist or using the game to exclude the therapist |
| Eacott 2008149
Australia 4 |
Depression Prevention All children in Australian Year 9 (there was an additional focus on those at risk of depression) |
Best of Coping Lazarus and Folkman’s coping theory; CB principles Teaching coping skills and strategies via structured sessions with a student workbook |
Child/young person Manualised; face-to-face groups (classes) School (classroom based) |
Teacher Delivering and facilitating the intervention (running the classroom sessions) |
Young people Individual face-to-face interviews with the young people Unhelpful (non-productive) coping strategies were less likely to be used after completing the programme; the most common benefit was the incidental learning from others in the class group – stories disclosed in terms of obstacles they faced in the past and how they dealt with problems led to a sense of solidarity and shared understanding; relationships concerns rated highly |
| Friars 2007150
Australia 4 |
Serious behaviour problems Management Parents of young people, aged 12–17 years, with ‘disruptive’ behaviour (i.e. ADHD) |
Behaviour management training A behavioural model of parenting Parents are trained in behaviour management techniques to help manage their child’s disruptive behaviour |
Parents Manualised; face-to-face groups Location unclear |
Psychologist Delivering and facilitating the intervention (running the parent groups) |
Parents (including dropouts from the training) Semistructured interviews with parents (unclear whether interviews were individual or group) The programme was helpful in terms of a shared experience; completers found the strategies the programme taught helpful; non-completers tended to be parents of children with more disturbed behaviour, who perceived their children to be more difficult than others, and who experienced more parenting stress; non-completers also felt that the programme was not particularly useful for their child |
| Fristad 1998151
USA 4 |
Depression; anxiety disorders Management Families of children/young people with a mood disorder |
Multifamily psychoeducation group therapy Psychoeducation Parents: support in helping manage their child’s symptoms via a workbook and peer support; children/young people: flexible sessions but generally including peer support, self-management (of symptoms and medication) and, for younger children, social skills training |
Family (child/young person and their parents) Manualised; multifamily face-to-face groups (mixture of parent, child and whole family groups) Outpatient clinic |
Unclear (‘therapist’) Delivering and facilitating the intervention (running the groups) |
Children/young people and their parents Uncontrolled trial with pre/post outcome measures and parent and child views obtained through open-ended survey questions The participants were broadly positive about the intervention; the most helpful aspects were having separate groups for parents and children/young people and creating opportunities for peer support; participants suggested siblings should be included in future groups |
| Garcia 2010152
USA 6 |
General mental health problems Prevention School-aged Latino girls |
Project Wings Model of ‘healthy youth development’, grounded in competence-focused, strengths-based and relationship-centred approaches Training in stress management and coping techniques via a variety of hands-on activities; peer support (‘sharing circles’) |
Child/young person Face-to-face groups School |
University-hired facilitator plus a school-based staff cofacilitator Delivering and facilitating the intervention (running the groups) |
Latino girls Focus groups with the young women and the weekly completion of anonymous ‘note card’ feedback The girls enjoyed the programme and the sharing element and learned new skills; there were some logistical issues (e.g. walking between buildings in winter); acceptability of the programme was largely a factor of the girls connecting with experienced and trained cofacilitators |
| Garraway 2010153
UK, England 7 |
General mental health problems Management African Caribbean teenage boys with ‘psychological and behavioural difficulties’ (e.g. ADHD, depression or schizophrenia) |
Unclear (‘mentoring’) Unclear Providing support to the family when difficulties arise, usually centred on improving communication within the family or providing support in relating to other agencies (e.g. schools or CAMHS) |
Child/young person Face-to-face individual activities (but with the potential for group activities run by some mentors) Community |
Mentor (an unrelated, adult African Caribbean male volunteer) | Young people and the lay mentors Focus groups and interviews with the young people and mentors Mentoring provides a family-like relationship; strong emotional bonds were formed between boys and mentors, facilitated by the perception of shared life experiences; mentoring can assist at-risk African Caribbean youth in coping with life challenges and may help promote positive developmental trajectories |
| Gowers 201071
UK, England 6 |
Eating disorders Management Young people with anorexia |
Unclear (‘specialised outpatient treatment’) Multidimensional approach involving CB principles, motivational interviewing, education and parent counselling Unclear (implied that the programme is about the family learning to manage behaviour, beliefs and feelings) |
Family (child/young person and his or her parents) Manualised; individualised face-to-face sessions Unclear (implied it is an outpatient clinic) |
A trained member of the team Delivering and facilitating the intervention (delivering the CB and parent counselling interventions) |
Parents and young people RCT with child/young person and parent views obtained from focus groups and open-ended survey questions Both parents and young people were more satisfied with specialist than general treatment, with parents in particular much more likely to be satisfied than the young people; satisfaction was largely based on their confidence in ‘expertise’ and on forging good relationships with individual therapists |
| Kennedy 2008154
USA 7 |
Psychoses Management Families of Asian American youth with schizophrenia |
Family-centred programme Self-management, especially in relation to stress, coping and anger A psychosocial approach involving peer support, psychoeducation, medication management and the enhancement of family communication skills |
Family (child/young person, his or her parents and siblings) Face-to-face groups (both separately and combined for the young people, their parents and siblings) Location unclear |
Unclear Delivering and facilitating the intervention (running the groups) |
Parents Semistructured individual interviews with parents Asian American parents value participation in the groups (especially the sharing and peer support aspects) and emphasised their similarities with non-Asian American families who have a mentally ill youth (there are some comments about parents’ views on the use of interpreters but the paper is contradictory in how it reports these) |
| Ma 2008155
Hong Kong 6 |
Eating disorders Management Young women with anorexia nervosa and their families |
Family treatment approach Modified Micucci, no-blame family therapy approach Designed to motivate the self-starving young person to take charge of her recovery and to help parents collaborate as a team in combating anorexia by improving conflict resolution and family relationships |
Family (child/young person and her parents) Unclear (implied that there are face-to-face meetings with the family and therapist) Location unclear |
Family therapist Supporting and facilitating the family |
Young women and their families Focus groups with the families The intervention is seen as a family intervention, with families identifying that they are their own change agents; the relationship with the therapist is linked to positive change |
| Mishara 2006156
Denmark; Lithuania 5 |
General mental health problems Prevention Preschool and first grade children (aged around 6 years) |
Zippy’s Friends Coping skills training based on behavioural approaches such as Webster-Stratton and the PATHS curriculum Coping skills training which encourages children to explore and think for themselves in order to manage their own behaviour |
Child/young person Face-to-face groups School (classroom based) |
Teacher Delivering and facilitating the intervention (running the classroom sessions) |
Teachers Non-randomised, controlled trial with teacher views obtained from session reports, individual interviews and rating scales Teachers reported that children’s enjoyment and participation were high; teachers were generally positive about the usefulness of the sessions though a few minor problems with some activities were identified (no details of these problems are provided, however) |
| Stewart-Brown 2004100
UK, England 5 |
Serious behaviour problems Management Families with children aged 2–8 years with a serious behaviour disorder |
The Incredible Years Webster-Stratton’s social learning approach (involving modelling and experiential learning) Parent training in which parents set themselves goals, undertake homework each week and report back on their progress |
Parents Face-to-face groups Community centre or clinic |
Health visitor or nursery nurse Delivering and facilitating the intervention (running the parent groups) |
Parents RCT with parent views obtained from semistructured interviews and open-ended survey questions Parents generally found the intervention helpful, becoming more skilled in dealing with their children’s problem behaviour and gaining increased confidence that they and their child were ‘normal’; parents had doubts about ‘time out’ as a technique and had difficulty implementing and sustaining any changes because of lack of support from spouses/partners |
| Zucker 2005157
USA 4 |
Eating disorders Management Parents of children aged 7 years or above with an eating disorder |
Group parent training Eclectic parenting approach with elements of emotion-focused therapy, behaviour therapy, social cognitive theory, resilience and mindfulness Teaching parents strategies to manage their child’s eating disorder and supporting parents to implement those strategies; peer support |
Parents Face-to-face groups Outpatient clinic |
Unclear (‘therapist’) Delivering and facilitating the intervention (running the parent groups) |
Parents Focus groups with parents Two key themes emerged from the data: the mutual benefit of combining psychoeducational and skill-based approaches (especially regarding nutrition education, bodily changes associated with weight gain and medication management), and the need to further develop support networks such as a ‘buddy’ system |
Appendix 9 Summary of the quantitative perceptions studies
| Paper and locale | Condition, intervention level and target | Intervention name, model and self-care element | Recipients, platform and delivery location | Agent and agent role | Data source and key messages |
|---|---|---|---|---|---|
| Barrett 2000158
Australia |
Serious behaviour problems Indicated Children, aged 7–9 years with externalising disorders |
RST CB and family therapy principles Teaching the parent child-management techniques and the principles of positive parenting, and teaching the family anger management and communication skills; small-group activities, usually with someone else in the group’s children |
Family Manualised; face-to-face groups Hospital/clinic |
‘Doctoral students’ Delivering/facilitating the intervention (running the groups) |
Parents completed a local ‘social validity’ measure that included questions regarding the usefulness of the treatment Parents reported a high level of consumer satisfaction with RST; although parents found all of the skills useful, the child-focused strategies (i.e. teaching responsibility, identifying feelings in themselves and others, and praise both for their child and from their child) were more strongly preferred |
| Barrett 2004159–161
Australia |
Anxiety disorders Treatment Children with OCD |
FOCUS CB principles Child sessions focused on cognitive training, anxiety management training, building buffer zones with support networks and relapse prevention; parent sessions focused on problem-solving skills and strategies to encourage family support of the child’s progress |
Family (including siblings) Manualised; mixture of face-to-face individual and group sessions Unclear (implied clinic) |
Unclear (‘therapist’) Delivering/facilitating the intervention (running the groups and individual sessions) |
Satisfaction data were obtained from children and parents at the completion of each session Generally, sessions were rated to be fairly helpful/good to quite helpful/good |
|
aBarrington 200548
Australia |
Anxiety disorders Treatment Children with anxiety disorders and their families |
CB therapy CB principles Self-management of anxiety via exposure and self-monitoring sheets; encouraging child to develop more helpful ways of thinking |
Child, parent or family at discretion of therapist Manualised; face-to-face individualised Hospital/community hospital satellite |
Psychologists (Master’s or doctoral level and trained in CBT) Delivering/facilitating the intervention |
Parent ratings of satisfaction using a local four-point scale Parents were very satisfied regardless of whether they were in the intervention or the control group |
|
aBiegel 200951
USA |
Generic mental health Treatment Psychologically symptomatic population of YP |
MBSR Mindfulness Group sharing of practice-related and other experiences; instruction in at-home mindfulness practice |
Child/young person Manualised; face-to-face groups Location unclear (implied clinic) |
Master’s-level ‘instructors’ Training the YP in mindfulness and delivering/facilitating the intervention |
Child ratings of the intervention’s value on a local dichotomous (yes/no) scale and child ratings of its personal importance on a local seven-point scale All who completed the MBSR programme rated the personal importance of the programme moderately high and all indicated that they had obtained something of lasting value |
| Gardner 2006162
UK, England |
Serious behaviour problems Treatment Clinically referred children aged 2–9 years with conduct problems |
The Incredible Years Webster-Stratton’s social learning approach (involving modelling and experiential learning) Parent training in which parents set themselves goals, undertake homework each week and report back on their progress |
Parents Manualised; face-to-face groups (some telephone contact) Charity setting |
Trained group leaders (but not MH trained) Delivering/facilitating the intervention (running the groups; telephone calls are made to encourage progress) |
Parent rating on the 10-item Therapy Attitude Inventory, which included items on parental satisfaction 91% of intervention parents liked the intervention, 75% felt behaviour problems had improved, 97% felt they had learned useful skills, 88% felt the group helped with other family problems |
| Ginsburg 2002163
USA |
Anxiety disorders Treatment Anxious African American youth |
Unclear (‘CBT’) CB principles Learning to self-manage anxiety through using activities and homework assignments |
Child/young person Manualised; face-to-face groups School |
Psychologists Delivering/facilitating the intervention (running the groups) |
YP ratings on a local seven-item satisfaction questionnaire YP’s satisfaction ratings were extremely positive for both the intervention and control groups |
|
aGinsburg 200969
USA |
Anxiety disorders Selective Children of anxious parents |
CAPS Combination of CB approach and Beardslee’s family intervention for the offspring of depressed parents Prevention of anxiety via the teaching of specific skills (e.g. problem solving, communication) and psychoeducation |
Family Manualised; face-to-face individual sessions Location unclear |
Psychologists Delivering/facilitating the intervention (facilitating the family group meetings) |
Parent ratings of the intervention’s helpfulness (13 items on a local five-point scale), and satisfaction with the intervention (three items on a local seven-point scale) Parent satisfaction levels with CAPS were high and most families completed all sessions offered; this suggests that families were engaged in the programme and perceived it to be beneficial |
|
aGowers 200770,71
UK, England |
Eating disorders Treatment YP with anorexia |
Not explicit (‘specialised outpatient treatment’) Multidimensional, involving CB principles, education, motivational interviewing and parent counselling Unclear (implied that the programme is about the family learning to manage behaviour, beliefs and feelings) |
Family Manualised; individualised face-to-face sessions Unclear (implied it is an outpatient clinic) |
‘a trained member of the team ’Delivering/facilitating the intervention (delivering the CB and parent counselling interventions) | Child and parent ratings, on a local seven-point Likert scale, of prior expectations and subsequent satisfaction of any treatment they had received Parents reported being generally satisfied with all treatments but were significantly more satisfied with specialist outpatient treatment (the intervention) than with general CAMHS (the control); the YP had more mixed experiences of treatment, with significantly lower overall satisfaction levels than parents |
|
aHahlweg 201073
Germany |
Serious behaviour problems Universal General population of parents |
Triple P Parent training Teaching parents skills to manage their children; parents learn to set and monitor their own goals for behaviour change in their children |
Parents Manualised face-to-face groups (with optional telephone contact) School based |
Psychologists Delivering/facilitating the intervention (running the groups and making the telephone calls) |
Mothers’ ratings of satisfaction on the 13-item Client Satisfaction Questionnaire 91% of mothers were satisfied with the training, 86% liked the atmosphere during the group sessions and 94% rated the programme as helpful |
|
aHarrington 199874
UK, England |
Self-harm Treatment YP who have self-poisoned |
Home-based family intervention Family therapy; behavioural therapy Improvements in family functioning via goal negotiation and family problem solving |
All family members (YP plus at least one parent) Manualised; face-to-face individual family sessions Home based |
Master’s-level child psychiatric social workers Delivering/facilitating the intervention |
Child and parent ratings of satisfaction on a local eight-point Likert scale Intervention group parents were significantly more satisfied than control group parents; there was no difference between the groups as far as the YP were concerned |
| Hoath 2002164
Australia |
Serious behaviour problems Treatment Parents of children aged 5–9 years with ADHD |
Enhanced Group Triple P Parent training; behavioural, social learning theory and child developmental approaches Teaching parents strategies to encourage their child’s social and language skills, emotional self-regulation, independence and problem-solving abilities |
Parents Manualised face-to-face groups (with weekly telephone contact from the fifth session) School |
Psychologists Delivering/facilitating the intervention (running the groups and providing weekly telephone support) |
Parent ratings of satisfaction on the 13-item Client Satisfaction Questionnaire There was a high level of parent satisfaction with the intervention |
|
aKendall 200883,84
USA |
Anxiety disorders Treatment Children with anxiety |
Family CBT (based on Coping Cat) CB principles; relaxation Teaching children skills to manage anxiety; modifying parental beliefs and expectations, teaching parents constructive responses to their child’s anxiety; teaching parents and children effective communication skills |
Family Manualised; face-to-face groups Location unclear |
Master’s-level therapists and doctoral-level psychologists Delivering/facilitating the intervention (running the sessions) |
Child ratings of the therapeutic relationship on a local seven-item, five-point scale There were no significant differences in the children’s perceptions of the therapeutic relationship between the intervention and control conditions |
|
aKennard 200885
USA |
Depression Treatment YP recovering from depression |
RP-CBT CB principles (especially relapse prevention) Self-care element unclear but implicit in CBT; a focus on residual depressive symptoms and promoting wellness |
Child/young person Manualised; face-to-face individual (YP mainly; some family) sessions Location unclear |
CBT therapists Delivering/facilitating the intervention (running the individual and family sessions) |
Child and parent ratings of satisfaction using the eight-item Client Satisfaction Questionnaire Child-reported satisfaction levels were significantly higher in participants who received RP-CBT in addition to medication management; parent-reported satisfaction levels were similar but not statistically significant |
| Khanna 2010165
USA |
Anxiety disorders Treatment Children aged 7–13 years diagnosed with anxiety |
CCAL and ICBT CB principles; both interventions were based on Coping Cat Teaching children skills to manage anxiety; teaching children effective communication skills |
Child/young person (some parent sessions) Manualised; face-to-face (ICBT) and computerised (CCAL) individual sessions CCAL, online; ICBT, location unclear |
Psychologists Coaching the CYP with completion of the intervention; conducting two parent sessions |
Child and parent ratings of satisfaction on the eight-item Client Satisfaction Questionnaire There was no difference in child-reported satisfaction between the two CBT interventions (ICBT and CCAL), but the child-reported ratings were higher than those of the control; there was no difference across all three conditions (CCAL, ICBT and the control) on parent ratings of satisfaction |
|
aKolko 201087
USA |
Serious behaviour problems Indicated Children with severe behaviour problems |
PONI Combination of CB principles and parent training Children trained in CB skills to promote self-management; parents trained in problem-solving skills and positive management of children |
Family Manualised; face-to-face individualised Home based |
General nurses Delivering/facilitating the intervention (running the home-based sessions) |
Parent ratings on the eight-item Client Satisfaction Questionnaire and Barriers to Treatment Participation scales Parents in the PONI group reported greater satisfaction and fewer obstacles to treatment on three of the four Barriers to Treatment Participation factors; PONI was associated with higher rates of treatment initiation and completion than the control |
| Larsson 2008166
Norway |
Serious behaviour problems Treatment Children aged 4–8 years, diagnosed with ODD or CD |
The Incredible Years, parent and child elements Webster-Stratton’s social learning approach (involving modelling and experiential learning) Parent training in which parents set themselves goals, undertake homework each week and report back on their progress |
Child/young person and parents (separately) Manualised; face-to-face groups Clinic |
MH-trained staff Delivering/facilitating the intervention (running the groups) |
Parent ratings on a local seven-point consumer satisfaction scale Slightly more mothers than fathers rated the programme good or very good (93.8% compared with 83.7%); over 90% of both mothers and fathers would recommend or strongly recommend it |
|
aLowry-Webster 200139,90
Australia |
Principally anxiety disorders Indicated ‘Universal’ population of 10- to 13-year-olds, with a subgroup identified as ‘high anxiety’ |
FRIENDS for Children; FRIENDS for Parents CB principles (based on Coping Koala) Children taught strategies for coping with anxiety; parents taught management skills to support children |
Family Manualised; face-to-face groups (separately for the children and parents) School based |
Teachers Delivering/facilitating the intervention (running the child and parent groups) |
Children, parents and teachers completed local acceptability measures 66% of children said they would use the skills that they learnt in the FRIENDS programme and 85% of children rated the programme as somewhat enjoyable or higher; 71% of parents rated the programme as somewhat useful or higher in terms of enhancing their child’s coping skills; parents rated all of the skills taught in the programme as useful but ‘recognising feelings in others’ was rated as the most useful; this was slightly different from the ratings evidenced by children who rated ‘relaxation exercises’ as the most useful; the programme was rated as acceptable by teachers on all aspects measured |
| March 2009167
Australia |
Anxiety disorders Treatment Children aged 7–12 years with anxiety disorders |
BRAVE for Children – ONLINE CB principles Cognitive strategies of coping, problem solving and self-reinforcement of ‘brave’ behaviour are taught; parents are empowered to help their children acquire and use the skills presented in the programme |
Child/young person and parents Manualised; computerised individual sessions Delivered online |
Unclear (‘online therapist’) E-mailing families during the intervention with weekly feedback plus telephone calls at the beginning and midway during the intervention |
Parent and child ratings on a local eight-item satisfaction scale Children and parents reported moderate levels of satisfaction following treatment |
|
aMasia-Warner 200791
USA |
Anxiety disorders Treatment YP with social anxiety |
SASS CB principles; social skills training Unclear (self-care implicit in CB approach); peer support |
Child/young person Manualised; face-to-face groups School based |
Psychologists; ‘peer assistants’ for the weekend activities Delivering/facilitating the intervention (running the group sessions) |
Child and parent ratings on four questions on a local treatment satisfaction scale For YP, satisfaction did not differ by treatment group but intervention group parents were more satisfied than control group parents |
| Matos 2009168
Puerto Rico |
Serious behaviour problems Treatment Parents of children aged 4–6 years with a diagnosis of ADHD |
Parent–child interaction therapy Behavioural management; coaching Helping parents manage their child’s behaviour more effectively; parents are taught and given time to practise specific communication and behaviour management skills |
Family Manualised; face-to-face groups Clinic |
Psychologists Delivering/facilitating the intervention (running the groups) |
Mothers’ ratings on the TAI and a local TES (TAI data presented were of limited value); mothers’ reports on the TES indicated they felt comfortable and understood by their therapists as well as confident and supported |
| Matsumoto 2007169
Australia |
Serious behaviour problems Universal Japanese parents with children aged 2–10 years |
Triple P Parent training; behavioural, social learning theory and child developmental approaches To learn and practise positive parenting skills in a self-regulatory framework; peer support, friendship and feedback from other parents and opportunities for parents to normalise their parenting experience through group interaction |
Parents Manualised face-to-face groups (with additional telephone contact) Unclear (implied clinic) |
Accredited Triple P trainers Delivering/facilitating the intervention (running the groups and providing telephone support) |
Parent ratings of satisfaction on the 13-item Client Satisfaction Questionnaire Parents’ ratings of satisfaction with the programme ranged from 4.9 to 6.2; parents rated the items ‘quality of service received’, ‘type of help expected’ and ‘overall satisfaction’ highest, and the item ‘improvement in partnership’ lowest |
|
aMerry 200493
New Zealand |
Depression Universal General population of school children aged 13–15 years |
RAP-Kiwi CB and interpersonal therapy principles Problem solving; role-play activities |
Child/young person Manualised; face-to-face groups School based |
Teachers Delivering/facilitating the intervention (running the classroom sessions) |
Child ratings of enjoyment and usefulness on a local scale; teachers provided verbal feedback on the intervention Students rated both RAP-Kiwi and the control as reasonably enjoyable and useful; teachers were less positive about RAP-Kiwi than the students in that they felt being tied down to delivery as prescribed in the manual was inflexible |
| Molina 2008170
USA |
Serious behaviour problems Treatment US ‘Middle-Schoolers’ with ADHD |
Challenging Horizons Program Behavioural approach; social skills training After-school programme targeting educational, social and recreational skills, homework completion and school and home behaviour |
Child/young person Manualised; face-to-face groups School |
‘Counsellor’ Delivering/facilitating the intervention (running the groups; liaising with parents) |
Parent and teacher ratings on, respectively, 10- and 13-item local satisfaction scales Satisfaction with the programme was promising; more than 70% of the parental ratings indicated a positive reaction, including benefits gained from the programme and desire for continued participation; teacher ratings of satisfaction were generally positive as well but somewhat muted compared with those of parents |
| Nicholson 1999171
Australia |
Serious behaviour problems Treatment Children with ODD and conduct problems in stepfamilies |
BFI Behavioural principles Standard behavioural family intervention approaches were supplemented by components that focused on co-operative parenting and conflict resolution skills; involves review of homework assignments, discussion and identification of skills deficits, and active skills training |
Family Manualised; face-to-face groups Clinic |
Psychologists Delivering/facilitating the intervention (one arm of the trial – self-directed BFI – had the same intervention with no therapist involvement) |
Parent/step-parent ratings on a local 13-item satisfaction questionnaire Both programmes were evaluated positively; significantly higher ratings of satisfaction were obtained for the therapist-directed intervention than the self-directed intervention |
|
aO’Dea 2000136
Australia |
Eating disorders Universal General population of secondary school students |
Everybody’s Different Educational theories of co-operative, interactive and student-centred learning Building self-esteem; home-based activities such as family discussion and positive parental input |
Child/young person Manualised; face-to-face groups School based |
Teachers Delivering/facilitating the intervention (delivering the lessons) |
Children anonymously completed a local evaluation questionnaire exploring the value of the intervention Most students found the programme valuable though a small percentage rated the programme as not valuable; a majority would participate in another similar programme |
|
aPfiffner 1997101
USA |
Serious behaviour problems Treatment Children with ADHD and their families |
SST Social skills training; behavioural approach; parent training Social and problem-solving skills taught via modelling and role play with homework activities; children evaluated each other’s performance |
Child/young person Face-to-face groups Location unclear |
‘SST expert’ plus a psychologist Delivering/facilitating the intervention (running the groups) |
Child and parent ratings on a local consumer evaluation questionnaire A majority of the children reported that the group helped them get along better with other children, and most reported liking the group ‘pretty much’ or ‘a lot’; all parents in the parent group found the group useful |
|
aPfiffner 2007102
USA |
Serious behaviour problems Treatment Children with inattentive type ADHD |
CLAS programme Behavioural approach; parent training; social skills training; some CB principles Teaching the children self-care skills (e.g. getting ready for school) and time management (skills that were shared with teachers so that they were able to reinforce in the classroom); teaching parents strategies for managing ADHD using behavioural techniques; teaching parents how to effectively interact with teachers |
Family Manualised; face-to-face groups Implied school based |
Psychologists Delivering/facilitating the intervention (running the child and parent sessions; facilitating the child in the home-school environment) |
Parents and teachers completed a consumer satisfaction survey (little methodological detail was reported) The intervention was well received by parents, teachers and children; all of the parents were very satisfied with the intervention and the majority rated the strategies and skills taught as being useful or very useful; the majority of teachers thought the intervention was appropriate for treating children’s attentional, academic and social skills problems and would recommend it to others, with most agreeing that minimal effort was required to participate in the intervention; most children reported liking the group either ‘pretty much’ or ‘a lot’, and most believed that it helped them do better at home and at school |
| Seeley 2009172
USA |
Serious behaviour problems Indicated Students meeting criteria for ADHD |
First Step to Success Coaching Through instruction, role playing, cueing, prompting and feedback, parents learn how to teach and encourage relevant skills in their child and how to communicate and co-operate with the child’s teacher in prompting and reinforcing these skills at school |
Child and parents (and, indirectly, teachers) Manualised; face-to-face individual sessions Home |
Behavioural coach (normally school professional) Delivering/facilitating the intervention (running the sessions; liaising between teachers and parents) |
Parent and teacher ratings on, respectively, 12- and 13-item local satisfaction scales Satisfaction ratings were quite favourable based on parent report, whereas teachers reported more moderate satisfaction ratings, especially on ‘the program did not take much of my time’, ‘the program did not interfere with my other teaching activities/responsibilities’ and ‘the program was effective’ items |
|
aSheffield 2006110
Australia |
Depression Indicated High-risk Australian Year 9 students |
Not explicit (‘universal’ and ‘indicated’) CB principles Universal: teaching CB techniques via individual and small-group work, interactive exercises and homework tasks; indicated: teaching interpersonal skills (e.g. assertion and negotiating) and self-reward skills via small-group work and a workbook |
Child/young person Manualised face-to-face groups (universal: whole class; indicated: small groups) School based |
Trained school counsellors or MH professionals Delivering/facilitating the intervention (running the groups) |
Child, teacher and counsellor ratings on a local 10-point Likert scale The mean evaluation rating was significantly higher for the indicated than for the universal intervention; teacher/counsellor evaluations indicated that satisfaction was higher among group leaders from the indicated intervention compared with the universal intervention; student attendance for the universal intervention was extremely high; for the indicated intervention, attendance was less good but still around 75% |
| Shortt 2001173
Australia |
Anxiety disorders Treatment Children aged 6–10 years with separation anxiety, generalised anxiety disorder or social phobia |
FRIENDS for Children; FRIENDS for Parents CB principles (based on Coping Koala) Children taught strategies for coping with anxiety; parents taught management skills to support children |
Family Manualised; face-to-face groups Clinic |
‘Clinical masters trained doctoral candidates’ Delivering/facilitating the intervention (running the groups) |
Children and parents completed a local satisfaction questionnaire The programme received positive evaluations from parents and children alike; 44% of children would ‘often’ and 56% would ‘sometimes’ use the FRIENDS strategies; 83% of children rated the programme as ‘fun’ and 17% rated it as ‘OK’ |
|
aSpence 2003113
Australia |
Depression Universal General population of Australian Grade 8 students |
Problem Solving for Life programme Broadly CB principles Learning problem-solving skills to manage relationships, situations and feelings; learning cognitive techniques to prevent negative feelings; individual, small-group and whole-class interactive exercises and activities |
Child/young person Manualised face-to-face groups School based |
Teachers Delivering/facilitating the intervention (running the group and individual sessions) |
Children and teachers completed a rating scale evaluation form 42% of the children would, 31% might and 27% would not recommend the course to others; 34% would, 49% might and 17% would not use the skills taught in everyday life; 90% of teachers thought the course was effective and 88% said they would teach the course again; teachers did not have time to complete all of the tasks required in some sessions |
|
aStice 2008118,119
USA |
Depression Selective High school students at risk of depression |
Brief group CBT and group supportive–expressive therapy (both are self-care support interventions) CBT: CB principles; motivational theory; supportive–expressive therapy: non-directive supportive psychotherapy CBT: skills training; social support; skills practice, group activities and motivational enhancement exercises; supportive–expressive therapy: learning strategies to support emotional self-management |
Child/young person Manualised; face-to-face groups Location unclear |
Psychologists Delivering/facilitating the intervention (running the groups) |
Child ratings of satisfaction and the degree to which they felt prepared to avoid future depression on a local five-point Likert scale 76% of the group CBT condition and 71% of the supportive–expressive condition indicated they were pleased or extremely pleased with the intervention; 84% of the group CBT participants and 63% of the supportive–expressive participants felt they were prepared to avoid future depression |
| Waters 2009174
Australia |
Anxiety disorders Treatment Children aged 4–18 years with anxiety disorders |
Take ACTION CB principles Teaching coping, problem-solving and social skills via activities and homework |
Children and parents (separately) Manualised; face-to-face groups Clinic |
Psychologist Delivering/facilitating the intervention (running the groups) |
Child and parent ratings using two local five-point satisfaction scales Parents reported high levels of satisfaction with the treatment |
| Webster-Stratton 2001175
USA |
Serious behaviour problems Indicated Children aged 4–8 years diagnosed with early-onset CD |
The Incredible Years (Dina School element) Webster-Stratton’s social learning approach (involving modelling and experiential learning) Parent training in which parents set themselves goals, undertake homework each week and report back on their progress |
Children/young people Manualised; face-to-face groups Clinic |
MH-trained clinicians Delivering/facilitating the intervention (running the groups) |
Parents completed a local ‘social validity’ measure that included questions regarding the usefulness of the treatment 88% of parents found the programme useful |
| Webster-Stratton 2004176
USA |
Serious behaviour problems Treatment Children aged 4–8 years diagnosed with ODD |
The Incredible Years Webster-Stratton’s social learning approach (involving modelling and experiential learning) Parent training in which parents set themselves goals, undertake homework each week and report back on their progress |
Children/young people, parents and teachers Manualised; face-to-face groups Clinic |
MH-trained clinicians Delivering/facilitating the intervention (running the groups) |
Parents and teachers completed local seven-point consumer satisfaction scale Consumer satisfaction with the parent, child and teacher elements was high; parents and teachers are more satisfied when teachers are also involved in the training |
| Webster-Stratton 2011177
USA |
Serious behaviour problems Treatment Young children with ADHD |
The Incredible Years, parent and child elements Webster-Stratton’s social learning approach (involving modelling and experiential learning) Parent training in which parents set themselves goals, undertake homework each week and report back on their progress |
Child/young person and parents (separately) Manualised; face-to-face groups Clinic |
‘Certified group leaders’ Coaching; delivering/facilitating the intervention (running the parent and child groups) |
Parents completed a local 59-item questionnaire concerned with satisfaction and usefulness of the programme Mothers generally rated the intervention higher than fathers but both were satisfied |
Appendix 10 E-mail circulated to identify service provision in England and Wales
Mental health self-care support for children and young people
Do you know of any projects or initiatives that focus on mental health self-care support for children and young people and/or their families and carers?
The School of Nursing, Midwifery and Social Work at the University of Manchester is conducting a study into mental health self-care support for children and young people. The study is in collaboration with the charity YoungMinds, and is funded by the NHS National Institute for Health Research.
Part of the study involves carrying out some case studies on mental health self-care support initiatives or projects that are directed at children and young people and/or their families and carers. Although we are picking up some initiatives and projects through a literature review and an Internet search (which are also part of the study) and through our networks, we are also aware that many initiatives/projects will be local and won’t necessarily be widely publicised. Some examples of the types of projects we’re interested in include:
-
Interactive, online support for children and/or their families and carers
-
Peer support programmes
-
Guided self-help initiatives (regardless of theoretical model or media used)
-
Whole school approaches to mental health where self-management is a key element
-
Parenting programmes where changes in children’s mental health is a clear outcome
-
Summer schools/activity holidays where self-management is a key element
If you’re aware of any such initiatives and projects operating in England and Wales (we are limited to these areas because of our research funding stream) regardless of whether the NHS is involved or not, we’d be delighted to hear about them. You can contact either the project Researcher, Dr Bec Elvey (rebecca.elvey@manchester.ac.uk, 0161 306 7784) or the Principal Investigator, Dr Steven Pryjmachuk (steven.pryjmachuk@manchester.ac.uk, 0161 306 7859). Further information about the project can be found on the funder’s website: http://www.sdo.nihr.ac.uk/projdetails.php?ref=10-1008-30
* Please feel free to circulate this email round your networks *
Appendix 11 Mapping of mental health self-care support services for children and young people across England and Wales
| Service | Location, urban/rural and provider | Condition, intervention level and target | Model, self-care element and agent | Recipients, platform and delivery location | Notes |
|---|---|---|---|---|---|
| 1a | England Urban Voluntary sector |
Anxiety disorders Indicated CYP aged 7–19 years experiencing worry, fear or panic attacks |
Self-empowerment; solution-focused approach Helping CYP to help themselves through psychoeducation and the use of exercises and activities Counsellor; youth worker; occupational therapist; nursery nurse |
Child/young person Face to face; mainly groups Community |
Three services delivered by the same voluntary sector provider, all 5–6 weeks long |
| 1b | General mental health Selective CYP aged 7–19 years experiencing low self-esteem/confidence |
Unclear CYP supported, through a range of activities, to explore feelings and develop coping strategies to increase confidence and self-esteem Voluntary sector staff |
Child/young person Face to face; mainly groups; gender specific Community |
||
| 1c | General mental health Selective CYP aged 7–19 years at risk of becoming a victim |
Self-empowerment Giving CYP the necessary skills to prevent them becoming a victim; teaches self-empowerment and rights, strategies for self-protection; encouragement to speak out/ask for hep Voluntary sector staff |
Child/young person Face to face; mainly groups Community |
||
| 2a | England Urban NHS |
Self-harm Treatment YP aged 14–17 years who self-harm, plus their families |
Recovery-focused approach; eclectic mix including CBT, DBT, supportive counselling, art and music therapies Groups can be chaired by YP; security planning to keep the YP safe; taking ownership, devising alternative strategies to self-harming Nurse; support worker |
Child/young person Face-to-face groups Hospital/clinic |
Case study site
Groups are flexible and ongoing, with YP usually attending for 4–5 months; provided at several other sites |
| 2b | Eating disorders Treatment YP aged 12–18 years with eating disorders |
Recovery-focused approach Little information supplied (but self-care implicit in recovery-focused approach) Nurse; support worker |
Child/young person Face-to-face groups Hospital/clinic |
Same provider as service 2a above | |
| 3 | England Urban Voluntary sector (but local authority funded) |
(Emerging) behaviour problems Indicated Families of children aged 5–14 years with emerging emotional and behavioural problems and complex needs but not requiring Tier 3 care |
Solution-focused approach; Daniel-Wassell model of resilience Aims to help children develop resilience via giving them a chance to tell their story and the development of an action plan with goals Voluntary sector staff with youth and social work backgrounds |
Child/young person Face-to-face individual support Community (voluntary sector provider premises, home and school) |
Case study site
12-session programme that follows an evidence-informed model using a framework with six domains |
| 4 | England Urban Voluntary sector |
(Psychosis) Indicated Group and peer support YP aged 12–18 years who hear or see things that others do not |
Romme and Escher’s Hearing Voices approach; recovery Provides support in coping with, or recovering from, voice-hearing experiences; various unstructured or semistructured activities to increase empowerment, coping strategies and skills Service provider staff plus any volunteers (including YP themselves) |
Child/young person Face-to-face groups Community |
Weekly groups; no limit on how long YP can attend for |
| 5 | England (multisite) Urban Voluntary sector |
General mental health Selective YP aged 14–18 years at risk of, or who have, mental health problems |
Recovery An emotional health and well-being programme with a follow-on leadership programme; both aim to build confidence, help the YP learn new skills, and reflect on and understand own mental health through various activities including art, drama, dance and music Service provider staff (two facilitators, typically experienced in youth work but not mental health trained) |
Child/young person Face-to-face groups Community |
Delivered at three sites; programme consists of four half-day sessions |
| 6 | England Urban NHS |
General mental health Indicated CYP aged 5–12 years with complex mental health and emotional needs and their families |
Uses Webster-Stratton’s The Incredible Years (social learning theory) Helping children and parents manage the child’s behaviour Unclear (’various’) |
Child/young person Face-to-face individual, group and family therapies Unclear (but including schools) |
Service is a day treatment programme |
| 7 | England Rural Voluntary sector |
(Emerging) behaviour problems Indicated School-aged CYP with emerging behavioural and emotional difficulties |
Solution-focused approach Aims to help children recognise, express and manage their feelings and improve school attendance; various activities including workshops with stories, puppets and creative activities Teachers, teaching assistants, pastoral support staff, SENCOs |
Child/young person Face to face; mainly groups, some individual sessions School |
Up to 10 sessions |
| 8 | England Rural NHS |
(Emerging) behaviour problems Indicated CYP aged up to 19 years with emerging behavioural and emotional difficulties for whom Tier 1 services have not worked but specialist CAMHS referral is inappropriate |
Solution-focused approach; early intervention Focuses on getting the CYP to use their own resources; affirmations and self-management of specific issues, e.g. sleep problems, anger CAMHS staff, school nurses, pupil support workers |
Child/young person Unclear (’various’ but implied face to face) Unclear (implied school) |
|
| 9 | England Urban; rural Voluntary sector |
Anxiety disorders; depression Indicated; treatment CYP aged 16–17 years with low-level anxiety or depression |
IAPT framework; CB principles Guided self-help approaches in anxiety and depression; uses standard packages such as Fear Fighter, MoodCalmer, Beating the Blues ’Psychological wellbeing practitioners’ |
Child/young person Face-to-face or computerised individual sessions with telephone support Community or online |
Predominantly adult service that also works with 16- to 17-year-olds |
| 10 | Wales Urban; rural NHS |
Behaviour problems (ADHD, ODD, CD) Indicated Parents of children aged 6–12 years referred to Tier 3 CAMHS for ADHD or CD, or any other parents who might benefit |
Social learning theory; parent training via Webster-Stratton’s The Incredible Years Giving parents skills to manage and facilitate their children in a positive way; practise skills with feedback; peer support Educational psychologist plus a cofacilitator |
Parents Face-to-face groups Community |
Separate service to service 11 below |
| 11 | Wales Rural Voluntary sector |
Behaviour problems (ADHD, ODD, CD) Indicated Parents of children with behavioural and/or emotional difficulties |
Social learning theory; parent training via Webster-Stratton’s The Incredible Years Giving parents skills to manage and facilitate their children in a positive way; practise skills with feedback; peer support Voluntary sector staff with youth and social work backgrounds |
Parents Face-to-face groups Community (voluntary sector provider premises) |
Case study site |
| 12 | Wales Rural NHS; local authority |
Behaviour problems (ADHD, ODD, CD) Indicated Children aged 5–6 years with emerging emotional and/or behavioural difficulties |
Social learning theory; Dina School element of Webster-Stratton’s The Incredible Years Children are introduced to communication and behavioural techniques and encouraged to practise these at home and school; activities involving role play, puppets, video vignettes, etc. Primary school staff (teaching assistants) |
Child/young person Face-to-face groups School |
Case study site
Groups of six children with two facilitators |
| 13a | England Urban NHS; local authority |
General mental health Indicated CYP, aged 14–18 years, referred to Tier 2 and 3 CAMHS |
Mindfulness To help YP with their ’experience’, not tell them what to do; practise mindfulness techniques between sessions with feedback from facilitator MH staff (e.g. primary MH worker, clinical psychologist; MH nurse; psychotherapist) |
Child/young person Face-to-face groups Location unclear |
Two services delivered by the same provider |
| 13b | Anxiety disorders Treatment Families of CYP aged 8–12 years with generalised anxiety having a medium impact on family life |
CB principles Programme based on a CB workbook devised by a team member; parent learns strategies to help their child with skills practice at home Unclear (’various’) |
Family Face-to-face groups of six to seven families Location unclear |
||
| 14 | England Urban Voluntary sector |
Depression; anxiety Indicated YP aged 14–30 years |
CB principles Guided self-help using the Beating the Blues programme Service manager; volunteers |
Child/young person Online, supported by face-to-face individual support Community (voluntary sector provider site); online |
Case study site
Young adult service which 14- to 17-year-olds can access |
| 15 | Wales Rural Voluntary sector |
General mental health Selective; indicated YP, aged 16–25 years, at risk of mental health problems or already suffering mental distress, e.g. depression or anxiety or who are self-harming |
Recovery; early intervention To stop the process of desocialisation and to end isolation via practical action such as encouraging and enabling service users to pass their driving test or encouraging them into volunteering roles; to increase self-esteem and interaction with others Project worker |
Child/young person Face-to-face individual support and group activities Location unclear |
Young adult service which 16- to 17-year-olds can access |
| 16a | England Urban Voluntary sector |
General mental health Selective YP aged 13–25 years |
Model unclear Focus on promoting skills and self-esteem; offers peer support, a drop-in service, one to one in schools and an 8-week counselling programme Service provider staff |
Child/young person Face-to-face individual support and group activities Community (provider premises) |
Three young adult services delivered by the same service provider which 13- to 17-year-olds can access |
| 16b | Self-harm Unclear YP aged 13–25 years |
Psychoeducational approach Unclear (focus on safeguarding) Service provider staff |
Child/young person Face-to-face individual sessions Community (provider premises) |
||
| 16c | Anxiety disorders Unclear Females aged 17+ years |
Model unclear Unclear Service provider staff |
Child/young person Face-to-face groups Community (provider premises) |
||
| 17 | England Rural NHS |
General mental health Selective; indicated CYP up to age 19 years with any MH or emotional well-being concern that is not immediate high risk |
CAPA Aims to promote emotional/holistic well-being through various activities designed to encourage responsibility and provide opportunities to develop and practise independence and life skills; activities such as homework, thought diaries, relaxation techniques, physical exercise and setting a routine/structure Primary MH worker |
Family Face-to-face individual support Location unclear |
Assessment plus six follow-up appointments offered |
| 18 | England (multisite) Urban Voluntary sector |
General mental health Universal YP aged 16–25 years whether MH service user or not |
Mixed model, designed to avoid the ’recovery rhetoric’ A participatory project giving YP the opportunity to design and deliver services; self-care activities for peers around building emotional resilience; activities such as chill-out sessions, climbing, anger management, boxing, ’walk and talk’ MH-trained youth workers |
Child/young person Various face-to-face group and individual activities Community |
Young adult service, delivered across three sites, which 16- to 17-year-olds can access |
| 19 | England Urban Voluntary sector |
Self-harm Indicated; treatment Young females who self-harm |
No specific model used Aims to raise awareness and emotional literacy to reduce self-harm through unstructured shared activities, e.g. creative writing activities; encouraged to develop and implement own coping strategies ’Counsellor’ |
Child/young person Face-to-face groups Community |
10-week programme |
| 20 | Online Urban; rural Voluntary sector |
General mental health Universal YP aged 16–25 years |
Unclear Provides emotional and peer support on general health and well-being including mental health Peers; the site workers who are from mental health voluntary organisations |
Child/young person Moderated discussion boards and live chat room Online |
Service for people up to the age of 25 years which 16- to 17-year-olds can access; live chat sessions held twice a week |
| 21 | Online Urban; rural Voluntary sector |
General health and well-being including mental health Universal YP aged up to 18 years |
Unclear Provides peer and professional support for depression, mental health, phobias, self-esteem, eating disorders and self-harm Peers; service provider staff |
Child/young person Moderated discussion boards; one-to-one online chats with a counsellor Online |
|
| 22 | Online Urban; rural Voluntary sector |
Eating disorders Universal; selective YP aged up to 25 years |
Recovery-focused approach Providing peer support Peers; service provider staff (moderated discussions) |
Child/young person Moderated discussion boards; one-to-one online chats with a counsellor Online |
Case study site
Service for people up to the age of 25 years which 16- to 17-year-olds can access |
| 23 | England Rural Private sector |
Mainly psychosis Treatment Males aged 14–19 years |
Recovery; psychosocial and rehabilitation approaches An approach that facilitates education, vocational skills, social integration and daily living skills for the service users Multidisciplinary facilitators |
Child/young person Various face-to-face individual and group sessions Hospital |
Residential unit providing Tier 4-type services |
| 24 | England Rural Voluntary sector |
General mental health Selective YP aged 14–17 years with emotional and behavioural problems who are at risk of developing mental health problems |
Coaching Coaching (little other information) Professional coach |
Child/young person Face-to-face groups with some individual sessions Location unclear |
Six 2.5-hour groups plus one-to-one sessions |
| 25 | England Urban NHS |
Anxiety disorders Indicated YP aged 16–18 years with anxiety, low self-esteem or low mood who do not attend mainstream CAMHS |
CB principles Workshops use a well-being, non-stigmatising approach and are aimed at increasing access to CB-based intervention for YP who do not attend mainstream CAMHS Clinical and assistant psychologists |
Children/young people Face-to-face group workshop, with individual pre- and postworkshop sessions Schools; youth centres |
Workshops are held in partnership with schools who arrange day release from classes and assist with recruitment |
| 26 | Wales Urban NHS |
Depression Indicated CYP up to age 18 years with depression/low mood |
CB principles Enhanced guided self-help; the use of workbooks and support sessions focusing on five areas: thoughts, feelings, body sensations, behaviours and situations CAMHS practitioner |
Child/young person Face-to-face individual sessions Location unclear |
10 sessions |
| 27 | England Urban NHS |
Serious behaviour problems Treatment CYP from the age of 9 years with CD |
CB principles Unclear (self-care implied by having a facilitated CB approach) CAMHS practitioner |
Child/young person and parents (separately) Face-to-face parent and child groups Clinic |
14 weekly sessions |
Appendix 12 The case study topic guides
Topic guide for children and young people
Context/history
-
Length of time of condition
-
Self-care before the project – what did they do and who helped them?
-
Difficulties experienced around self-care
The self-care service
-
Who told them about the service?
-
Why were they interested in going/taking part?
-
Pattern/frequency of use of the service
-
What do they like about it?
-
What don’t they like about it?
-
Do they feel it has helped them? If so, how?
-
Could the project be improved? If so, how?
Self-care
-
Who can best support them?
-
How would they like to receive the support?
-
Barriers and enablers
-
Have they used other similar services? If so, how does this one compare?
Topic guide for parents and carers
Context/history
-
Length of time child has had condition
-
Self-care before the project
-
Who helped/supported them
-
Difficulties experienced around self-care and/or encouraging child’s involvement
The self-care project
-
Who told them about the project?
-
Why were they interested in going/taking part?
-
What do they like about it?
-
What don’t they like about it?
-
Do they feel it has helped them? If so, how?
-
Do they feel it has helped their child? If so, how?
-
Could the project be improved? If so, how?
Self-care
-
Who can best support them?
-
Who can best support their child?
-
How would they like to receive the support?
-
How do they think their child should receive the support?
-
Have they used other similar services? If so, how does this one compare?
Topic guide for service providers
Role in the self-care project
-
Current role
-
Previous role (development of project)
-
Preparation for role in self-care project
-
Specific training/education
-
Additional needs for training/education in the area of self-care
View of the project
-
What works well and why? (enablers)
-
What does not work well and why? (barriers)
-
Perception of its impact on children/parents (long and short term)
-
Perception of the impact of the model on use of primary care, hospital and other support services
Integration with other self-care support
-
How does the project fit/link with ‘mainstream’ health service support?
-
How does the project fit/link with lay forms of self-care support?
-
How does the project fit/link with self-care support from social care/educational sectors?
Appendix 13 Initial framework chart for site 4
| Initial thematic framework | Data source | |||
|---|---|---|---|---|
| CYP | Families | Staff | Documents | |
|
Context
Experiences of illness/problems |
Not getting on with parent and siblings; having a bad temper; behavioural problems | Difficulty understanding instructions, not speaking up in class, not settling into school; not dealing with unfamiliar people; unable to differentiate friend from non-friend; unsettled by change; angry; soiling; behaviour in class, not listening, stamping | Families with complex needs that do not meet CAMHS thresholds (which are quite high); unsettled in classroom; not listening in class; struggling with peer relationships; not sticking to task; not working within social boundaries | |
|
Context
Experiences of self-care/support (what they’ve done to self-care and been helped with) |
At school, saw one of the teachers to express their feelings, but school gives limited support; ongoing support from school counsellor | There are proactive parents who read up on things; many parents are aware of Supernanny and similar approaches but doing this without support is often unrealistic | ||
|
Context
Experience of other services (self-care and otherwise) |
Went to CAMHS but staff only talked to parent while child did colouring, child didn’t mind but no help; CAMHS for a few weeks (for soiling) but appointments stopped before problem resolved | |||
|
The service
How project fits in with other services/forms of support |
Bridges a gap between primary care and mental health services; CAMHS access criteria have become more tightly applied (perhaps not higher); there are few – and increasingly fewer – services that provide intensive individual work of this type; reinforces parts of work done in some schools by learning mentors, and work done at CAMHS (solution-focused therapy), but the service is better equipped for intensive individual work, also schools are less able to access a child’s home life; service staff find organisations for children to attend, suited to their interests, e.g. Boys’ Brigade, football, a local mentoring/buddy system; some cases have been referred to CAMHS initially but after discussion agreed the service will work with the family instead; often work in situations with child protection concerns or ‘care situations’; many skills in this service are the same as found in CAMHS: social skills, engagement skills; we use solution-focused skills, we use some systemic-practice skills: ‘we don’t have workers who have qualifications in those things but they are skills that they have developed through experience and through going on some training courses’ (staff C3); learning mentor sometimes attends session with child, to learn about strategies | Information booklets for referrers, CYP and parents | ||
|
The service
Reason for involvement |
Come from Tier 3–4 settings, where often there has been little early intervention; wanted to work at this level | |||
|
The service
Referral routes |
Via social worker, school | Agreement with CYP | IFS (integrated family support) service has school-facing workers; SENCO at local primary school refers children having difficulties; CAMHS refer children who don’t meet their criteria (recent-onset EBD/coping problems), and those coming to the end of CAMHS work (to maintain progress, meet a newly arisen need or give more generalised support with coping and resilience); general practitioners (GP); self-referral | Information booklet for referrers |
|
The service
Approach (including theoretical basis) and aim |
Based on Assessing and promoting emotional resilience in vulnerable children (Wassell and Daniel) model which has six domains of resilience (education, talents and interests, social competencies, positive values, secure values, and friendships); aim to build resilience in the domains where it’s needed most for the child; early intervention for behavioural and emotional difficulties, focusing on what’s behind the behaviour, building emotional resilience and well-being; a common-sense approach, uses everyday language, not ‘mental health’ language; work with child plus their support network, a participative approach; solution focused, goal driven, structured; holistic – try and see what’s going on underneath a situation; try to empower families to make changes they would like to; flexible approach | Service provider document on resilience; information booklets for referrers, CYP and parents | ||
|
The service
Likes (works well) |
Like playing games with staff; generally enjoyed spending time with staff (attention?) | Staff spoke to child about reasons behind angry behaviours as well as behaviours themselves; situations were broken down into steps child could understand; staff look at the situation from different angles – work with child at school and also see home situation, so feel they see things through her eyes; staff bonded well with children, who often were not comfortable around unfamiliar people; staff showed care and commitment (not just a job); regular contact between appointments | Families appreciate someone taking the time to listen to them and their ‘story’; talking to children about things they can engage with easily – friends – not ‘mental health’; referrer/supervisor thinks staff at site are highly skilled; flexibility – mixture of individual and family sessions, travel to schools and homes, if someone misses a session, try and re-engage them (not throw them out) – helps to make families feel they can work with them, a voluntary service, not statutory which can be threatening – with this one, there is not the fear of having children taken away, more relaxed, less judgemental | |
|
The service
What has helped (impact) |
Identify which tools and techniques they liked to use | Child able to manage anger better – outbursts are shorter and employs techniques, e.g. going to sit quietly on trampoline; identified various tools used at home to improve behaviours; teachers see improvement in child’s behaviour in class | Parents and schools report improved behaviours – interacting better with peers, family relationship with school can improve; can successfully put in more structure and consistency at home | |
|
The service
Challenges |
Child was upset when service ended; concern that other children noticed they were receiving a ‘treatment’ | It does not work for everyone; difficult to keep track of people for more than about 6 months; suggestion that staff being so highly skilled can lead them to work ‘above and beyond’ the model (‘too holistic?’), also questions the benefit of working ‘with’ some younger children – maybe should work with their parents alone as ‘cotherapists’ | ||
|
The service
Not like (did not work well) |
Struggled to engage with some of the games, etc., as he felt too old | |||
|
The service
What has not helped (impact) |
Child still does not understand some of the concepts (about recognising who is a friend) | |||
|
The service
Improvements suggested |
Would have liked support for longer; could show carer tools they could use with child that carer can engage with more | |||
Appendix 14 The theme ‘facilitating self-care support’ in the final framework chart
| Theme: facilitating self-care support | |||||
|---|---|---|---|---|---|
| Site | Source | Subthemes | |||
| Welcoming staff; welcoming organisations | Activities to build skills for self-care | Sharing experiences and peer support | Time and attention | ||
| Site 1 | CYP | Relaxed atmosphere, where it is easy to open up; staff are approachable, this is very important; it’s very important to feel comfortable with (or ‘like’) the therapist; negative experiences regarding this in other services | ‘Tool boxes’ of distraction techniques, memorabilia and keepsakes that helped them reduce urges to self-harm | Best people to provide support are other people, friends who understand your experience including self-harm; support from others in the group, talking to them is more important than the tasks (describe close ties – they have become friends and also like a family unit; also risks here in sharing (contagion) | Talking to them is more important than the tasks |
| Parents | Staff are approachable to parents – important | Staff work to include families, talk to them when come to collect YP from group | |||
| Staff | YP enjoy the groups; relaxed atmosphere helps | Working with the group dynamic – may help YP see others’ perspectives, so what it might be like for their families; some strategies from DBT – self-regulation, alternative strategies; aim is harm reduction; YP give each other good ideas for distraction techniques | Sharing, thinking of things for others can take you away from yourself; peer support – because YP will sometimes listen to peers better than anyone else; sense of belonging a group can give; benefit of seeing others with similar experiences, including from different social background | ||
| Documents | Some details in the self-injury ‘toolkit’ | ||||
| Site 2 | CYP | Getting rewards (prizes) for activities | Pinpointed activities they enjoyed – colouring, tidying up, watching video vignettes, watching the puppets; liked getting stickers and prizes; having a snack | ||
| Parents | Giving praise increased confidence; working towards goals reduced tantrums; concentration improved | Child enjoyed attending; pleased that child was getting attention in a nice small group, this made child feel special | |||
| Staff | Want children to enjoy the group | Based on child-directed play, coaching in social skills, giving effective praise; children taught techniques to others in their class; child increased in confidence, making eye contact, talking; helps children to cope and improves classroom performance | Children get the benefit of positive adult attention; operational constraints on time and attention | ||
| Documents | Giving positive attention is part of philosophy of Incredible Years | ||||
| Site 3 | Parents | Like the group mediator and thought she had good group management skills; enjoyed being in the group, having fun | Liked having a toolkit they could use, generally like the approach, including focus on play and praise; normalising aspect; parent learnt how to calmly explain a situation to him and give consequences, e.g. a reward for good behaviour; child playing more | ||
| Staff | If someone misses a session, try and re-engage them (not throw them out) | Based on child-directed play, coaching in social and academic skills, giving effective praise; play is important | Parents enjoy meeting others with shared experiences; buddy system | Parents report immediate positive effects from having a ‘play time’ with children each day – children are calmer; operational constraints on time and attention | |
| Documents | Giving positive attention central to philosophy of Incredible Years | ||||
| Site 4 | CYP | Like playing games with staff; generally enjoyed spending time with staff (attention?) | Like playing games with staff; generally enjoyed spending time with staff (attention?) | ||
| Parents/sibling | Staff showed care and commitment (not just a job); regular contact between appointments; staff bonded well with children, who often were not comfortable around unfamiliar people | Staff spoke to child about reasons behind angry behaviours as well as behaviours themselves; situations were broken down into steps child could understand; staff look at the situation from different angles – work with child at school and also see home situation, so feel they see things through her eyes | Staff showed care and commitment (not just a job); regular contact between appointments; would have liked support for longer; sibling talked about project worker taking time to break things down when explaining to brother | ||
| Staff | Can successfully put in more structure and consistency at home; reinforces parts of work done in some schools by learning mentors and work done at CAMHS (solution-focused therapy), but the service is better equipped for intensive individual work, also schools are less able to access a child’s home life; service staff find organisations for children to attend, suited to their interests, e.g. Boys’ Brigade, football, a local mentoring/buddy system | Families appreciate someone taking the time to listen to them and their ‘story’; talking to children about things they can engage with easily – friends – not ‘mental health’; service being a different experience for CYP | |||
| Documents | CYP leaflet written in child-friendly way | Skills relating to resilience described in the information leaflets for parents, CYP and referrers | |||
| Site 5 | CYP (online postings) | Various relaxing or distracting activities including reading, knitting, writing, drawing, exercising; can be difficult to concentrate, especially on reading; setting goals for self (go out and meet friend) | Wants to hear from people experiencing similar problems; find ideas from other service users helpful; like talking to others with similar experiences; find writing about their experiences helpful; glad to find others have similar feelings; feel they can be open on the site, not hide who they are; enjoyment from reassuring other people | ||
| Staff | Had personal experience of ED and recovered and had an interest in working in the field; also risks here in sharing (cf. contagion in self-harm group) | ||||
| Documents | Website is attractive and welcoming | ||||
| Site 6 | CYP | Being able to trust staff | |||
| Staff | CBT based, with human interaction to make it less cold; not clinical, friendly and laid back | Experienced onset of depression and anxiety, had previously studied counselling and came up with ideas for the type of service he would like to use | |||
| Documents | Website is attractive and welcoming | ||||
Appendix 15 Dissemination plans
| Audience | Platform | Progress |
|---|---|---|
| Children, young people and parents | Lay summary in print form | Late 2014; awaiting approval of the final report |
| Lay summary on YoungMinds’ website | Late 2014; awaiting approval of the final report | |
| End-of-project workshop | Late 2014; will be mainly for providers, practitioners and service users (CYP and families) | |
| The academic community | Papers from the study presented at conferences and seminars | Papers have already been presented at national and international mental health nursing (USA, UK) and family nursing conferences (USA) Poster on the case study has been presented at a methodological conference (Canada) Seminar held at the EPPI-Centre, Institute of Education, London (Any other opportunities as they arise) |
| Publications in the peer-reviewed press | In addition to the NIHR monograph, papers on the following aspects of the project will be worked on during 2014–15:
|
|
| E-dissemination | Reference to the NIHR monograph, once published, to be circulated around relevant Twitter feeds | |
| The professional community | Accessible summary in print form for practitioners, commissioners and managers | Late 2014; awaiting approval of the final report |
| E-dissemination | The accessible summary to be freely downloadable (from YoungMinds’ and the University’s websites) Reference to the report once published to be circulated around relevant Twitter feeds and e-mail lists |
|
| End-of-project workshop | See above |
List of abbreviations
- ADHD
- attention deficit hyperactivity disorder
- CAMH
- child and adolescent mental health
- CAMHS
- child and adolescent mental health services
- CBT
- cognitive–behavioural therapy
- CD
- conduct disorder
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- CMA
- Comprehensive Meta-Analysis
- CPPRG
- Conduct Problems Prevention Research Group
- CYP
- children and young people
- EBD
- emotional and behavioural difficulties
- EBM
- evidence-based medicine
- EPPI-Centre
- Evidence for Policy and Practice Information and Co-ordinating Centre
- IAPT
- Improving Access to Psychological Therapies
- MTA
- Multimodal Study of Children with ADHD
- NIHR
- National Institute for Health Research
- NRES
- National Research Ethics Service
- ODD
- oppositional defiant disorder
- portable document format
- PICOS
- Population, Interventions, Comparators, Outcomes and Study designs
- PPI
- patient and public involvement
- PTSD
- post-traumatic stress disorder
- RCT
- randomised controlled trial
- SAG
- stakeholder advisory group
- SENCO
- special educational needs co-ordinator
- SMD
- standardised mean difference
- VIK
- Very Important Kid