Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 08/1813/256. The contractual start date was in January 2010. The final report began editorial review in December 2013 and was accepted for publication in May 2015. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
John E Ellershaw reports grants from Marie Curie Cancer Care and the Department of Health End of Life Care Programme outside the submitted work. In addition, Professor Ellershaw has a patent Liverpool Care Pathway logo which is a registered trademark within the UK and European Community issued to Marie Curie Cancer Care and the Royal Liverpool and Broadgreen University Hospitals NHS Trust (joint holders). All Liverpool Care Pathway documentation is copyrighted as Marie Curie Palliative Care Institute Liverpool, a department of the University of Liverpool, Marie Curie Cancer Care and the Royal Liverpool and Broadgreen University Hospitals NHS Trust, using standard Berne Convention. Professor Ellershaw is employed by the Royal Liverpool and Broadgreen University Hospitals NHS Trust and has an honorary contract at the University of Liverpool.
Disclaimer
This report contains quotations from interviews conducted in the course of the research and contains language that may offend some readers.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2016. This work was produced by Perkins et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
Background
The median age of the population is projected to rise across Europe from 75.1 years to an estimated 81.2 years by 2050, with the proportion of the population over the age of 65 years rising to 27.8%. 1 Such projections threaten to place health-care systems across Europe under considerable strain as older age (i.e. ≥ 85 years) brings with it an increased risk of chronic disease. 2 In England and Wales each year around half a million people die, the majority of whom are aged over 65 years. Death occurs mainly after a period of chronic illness such as heart disease, cancer, stroke, chronic respiratory disease, neurological disease or dementia. In those aged ≥ 65 years, the two most likely places of death are hospitals (52%) and nursing homes (22%), with 20% of deaths occurring at home, 5% in hospices and 1% elsewhere. 3
End-of-life care
End-of-life care in the UK has undergone significant development in the last two decades. End-of-life care has been defined by the National Council for Palliative Care as ‘care that helps all those with advanced, progressive, incurable illness to live as well as possible until they die’. 4 The National Council go on to state that end-of-life care ‘enables the supportive and palliative care needs of both the individual and their family to be identified and met throughout the last phase of life and into bereavement. It includes the management of pain and other symptoms and provision of psychological, social, spiritual and practical support’. 4
Historically, underinvestment in both time and financial resource has rendered the quality of end-of-life care as frequently suboptimal, particularly in the acute setting. 5 The Department of Health published its National End-of-Life Care Strategy in July 2008,6 after a 2-year consultation. Its primary aim was to improve the provision of care for all adults approaching the end of their lives, and the support for their families and informal carers. 7 An allied aim was to reduce inappropriate admissions to hospital and enable more people approaching the end of their life to live and die in the place of their choice. It highlighted both the need for ongoing training for all generalist staff who deliver end-of-life care, and the importance of integrated, interprofessional and cross-sector working. 6 The National End of Life Care Programme was established and a number of documents, including the End of Life Care Strategy: Quality Markers and Measures for End of Life Care8 and the Quality Standard for End of Life Care for Adults,9 were published to support the national delivery of high-quality end-of-life care.
The goals of end-of-life care provision are the promotion of the quality of life for ‘dying’ patients (i.e. those with acknowledged life-limiting illness) and a ‘good death’ when the time comes. The evolution of the ‘good death’ concept over time from the prehistoric era to postmodern times10 suggests that general attributes of a good death include effective pain and symptom management, awareness of death, patient’s dignity, family presence, family support and communication among patient, family and health-care providers. Scarre, however, warns against such a narrowly focused definition and questions the very notion of attaining a ‘good death’. 11 He suggests that current definitions reflect its aetiology in the ‘medical model’ with an emphasis merely on providing the right conditions, which he feels omits the importance of the patient’s own self-preparation for death through the development of ‘qualities of character’.
This project sets out to examine the impact of the Liverpool Care Pathway for the Dying Patient (or Liverpool Care Pathway; LCP) on the current practices and experiences of dying in two care settings, nursing homes and intensive care units (ICUs), in England.
Death and dying in the context of nursing homes
Care homes (including nursing homes) are currently second only to hospitals as the most likely place of death for people over the age of 65 years in the UK. In 2011, over 90,000 people aged over 65 years died in care homes. 3 This trend is set to increase owing to the predicted increasing median age of the population1 and the drive to decrease the number of inappropriate admissions to hospital from nursing homes at the very end of life. 6 Age- and sex-adjusted mortality has been shown to be approximately four times higher in nursing homes than in the community12 and, for these reasons, nursing homes are likely to play a significant role in end-of-life care provision now and into the future.
Percival and Johnson explored the factors that influenced good-quality end-of-life care in care homes from the point of view of residents, relatives and staff. 13 While these perspectives are inherently likely to be divergent, the authors identify six key priorities for care:
-
personalised care – maintaining informal relationships; having personal items to hand
-
dignity and respect – attention to cleanliness; explaining while carrying out personal tasks; thoughtfulness on the part of staff; culturally relevant care
-
making time – sitting with residents; listening; touch; patience; reorganising the workload
-
talking about end-of-life issues (and death) – staff personal and professional difficulties; can feel they are protecting residents by not talking about it; most residents wanted to talk about it (especially the practical aspects)
-
relatives’ roles and collaboration – relatives willing to work with staff; their collaboration with staff reassured residents; staying overnight; helping with care; the benefits to staff of having a ‘bond’ with relatives
-
staff support and training – readily admit the need for emotional support for themselves; more likely to be informal; attending funerals; recognition of the importance of ongoing education and training.
However, nursing homes are traditionally staffed by a low-paid workforce with limited access to appropriate sources of expertise and support (e.g. palliative care) and relevant education and training opportunities. Inadequate staffing levels threaten the delivery of complex and emotionally laden care for dying residents14 and staffing levels and training have been the subject of recommendations. 6,15,16 Goddard et al. ’s study17 on the views of a range of care home staff and community nurses illustrated that staff thought that managing the complex needs of residents at the very end of life with a largely unskilled workforce was the greatest threat to the delivery of high-quality end-of-life care in this setting.
Support from external health-care professionals, although vital, is often limited in the care home setting. General practitioners (GPs) usually provide support to individual residents within the nursing homes, but this means that often nursing homes are attempting to co-ordinate a large number of individual practices and doctors. For example, in their survey, Froggatt and Payne18 found that individual care homes in their sample were working with up to 17 practices and 27 GPs, with two-thirds of GPs visiting only when asked. District nurses were generally the most regular visitors to care homes, but, in recognition of the presence of on-site nursing, this was not the case for nursing homes. Links to specialist palliative care, including 24-hour advice, was available for around two-thirds of the sample, but the nature and level of input was not assessed. 18
Death and dying in the context of intensive care units
NHS Choices defines ICUs as ‘specialist hospital wards . . . provid(e)ing intensive care (treatment and monitoring) for people in a critically ill or unstable condition . . . A person in an ICU needs constant medical [and nursing] attention and support to keep their body functioning. They may be unable to breathe on their own and have multiple organ failure. Medical equipment will take the place of these functions while the person recovers’. 19 This definition illustrates the nature of interventions that are generally involved in such care, and the expected and desired outcome of the patient’s recovery. Nevertheless, a significant minority of patients admitted to ICU in England die each year. For example, in 2011–12, 19,567 of the 125,760 total ICU admissions (15.5%) resulted in the death of the patient prior to discharge from the unit. 20 This means that ICU doctors and nurses are exposed to dying and death in their day-to-day work, with the associated potential burdens and opportunities that this may entail.
Death and dying in the ICU, however, can be said to be qualitatively different from death and dying in other settings in that it most often occurs after decisions to withhold and/or withdraw active therapy. 21 Although nurses are not responsible for the decision to withhold/withdraw therapy and, it has been reported, are often not represented in the discussions preceding such decisions,22,23 they are usually most closely involved in providing care at the bedside, interacting with relatives and carers and undertaking the actual withdrawal of those interventions,23,24 requiring considerable ‘emotional labour’. 23,25
Recently, there has been a research focus on understanding the differing perspectives on end-of-life care in the ICU. 24 There is recognition that different professional groups may view the decision about the ‘futility’ of life-sustaining treatment from very different perspectives. 23 For example, it is reported that ICU nurses tend to perceive a direct link between ‘futility’ and dying which ICU doctors often do not. 26 This could lead to friction between professionals about the appropriate timing of end-of-life care. Decisions regarding the transition from active, life-sustaining intervention to care designed to ensure comfort involves complex negotiation within staff groups and between staff, patients and families over a relatively short period of time. 26
The concept of a ‘good death’ is multifaceted and complex in the ICU setting. Thompson et al. 27 illustrate a four-stage process (from the perspective of ICU nurses) to secure a ‘haven for safe passage’:
-
facilitating and maintaining the changing of care goals from curative to palliative
-
getting what is needed: plan of care with focus on comfort care
-
being there: providing support to the patient’s family
-
manipulating the care environment: creating a peaceful environment.
Ryan and Seymour28 reviewed the literature and suggest that a ‘good death’ in this environment has been associated with the some or all of the following:
-
consensual decision regarding the withdrawal of therapy – within staff and between staff and relatives
-
expected (not sudden) and prepared for (by both staff and relatives)
-
under the control of the health-care team – timely – not too fast, not too slow
-
patient comfort maintained (pain and symptom management)
-
natural – free from technological intervention
-
according to the wishes of the patient/family
-
loved ones present at the time of death
-
clear, non-conflicting communication.
End-of-life care tools to support the delivery of high-quality end-of-life care
The end-of-life care strategy6 highlighted and promoted the use of three key end-of-life care tools, which can be used together or separately at different time points in the dying trajectory. The first two of these tools are designed to support appropriate co-ordination and planning of care for people with life-limiting conditions based in the primary care sector. Preferred Priorities for Care promotes timely discussions, documentation and communication about patient’s wishes and choice around their priorities and preferred place of care and death. 29 It is particularly important to offer people with cognitive degenerative illnesses, such as dementia, the opportunity to think, document and share their wishes before they lose the capacity to make complex decisions about their future care as the disease progresses. This document is a patient-held record of such discussions and decisions. The Gold Standards Framework (GSF)30 aims to optimise the quality of care for patients in the last year of life, including enabling choice in place of care and death, through improving the organisation and co-ordination of local services. 31 The GSF began in primary care in the early 2000s (GP surgeries, district nursing services) and has expanded more recently to include nursing and care homes. 32
The LCP33 specifically focuses on the last hours or days of life and can be used to support care wherever people die. The responsibility for use of the LCP document as part of a continuous quality improvement programme sits within the governance of the organisation and the authors stipulate that it must be underpinned by a robust education and training programme. The LCP guides and enables health-care professionals to focus on care in the last hours or days of life, when a death is expected. It is a framework for good practice, and aims to support but not replace clinical judgement. 34 The LCP has been disseminated widely in a variety of settings, including the two settings of interest for this project, ICUs and nursing homes. As the impact of the LCP is a focus of interest in this study, a more comprehensive overview of the LCP is provided below.
An overview of the Liverpool Care Pathway
The care of people who are imminently dying takes place in a number of settings, not all of them specialist in nature, and there is wide variation in understanding of the needs and necessary care required to support patients at the very end of life. 35 The LCP originated in Liverpool and was developed as an end-of-life care tool in the mid-1990s through collaboration between specialist palliative care services at the Royal Liverpool University Hospitals Trust and the Marie Curie Hospice in Liverpool. It aimed to transfer best practice from hospice institutions to the wider context of organisations which provided end-of-life care, for example hospitals, care homes and nursing homes, and was intended to be adapted by organisations to suit their specific organisational contexts. 6 Latterly, its development and dissemination has been overseen by the Marie Curie Palliative Care Institute Liverpool (MCPCIL). 36
The LCP was designed to support clinical decision-making when the multidisciplinary team (MDT) considers that the patient is in the last hours or days of life, and where there is no appropriate reversible treatment available. The challenge in accurately diagnosing the imminently dying phase is identified as a major concern. In this report, the term ‘dying phase’ pertains specifically to the last hours or days of life. Some health-care practitioners and members of the public have articulated concerns that the identification of a person as ‘dying’ could become a self-fulfilling prophecy. A crucial component of the LCP, however, is the continual review of the patient, involving the MDT, which should prompt a reassessment of the patient’s condition. A patient who is no longer thought to be imminently dying should no longer have their care supported by the LCP.
The LCP document is an integrated care pathway with a goal-orientated approach and is organised into three sections: initial assessment, ongoing assessment and care after death (see Appendix 6). One of the most important aims of the LCP is to facilitate the comprehensive documentation of care delivery and outcomes during the last hours or days of a patient’s life in an efficient yet effective manner. Hence the LCP documentation, as with other integrated care pathways, is designed to replace all other documentation in this specific phase of care. 33
The LCP has been reviewed and revised over time. Version 12, published in 2009, was subject to a 2-year international consultation exercise. This version maintained the focus of earlier documents on communication, information and comfort care in the last hours or days of life, and included an algorithm to support staff in reviewing their recognition of the dying phase. It also contained explicit goals to support care with regard to hydration, nutrition and skin integrity. The use of the LCP in hospitals has been the focus of four national audits in England; the latest results are published on the website of the Royal College of Physicians. 37
The LCP has been cited as an example of good practice specifically for care in the last hours or days of life in several national publications38,39 and was disseminated nationally as part of the End of Life Care Initiative to improve care for imminently dying patients in the UK. 6 At the time of writing, in the UK over 2000 organisations were ‘registered’ with the MCPCIL, including hospitals, hospices, care homes and home teams. Additionally, at the time of writing, over 20 countries outside the UK used the LCP to some degree. 34 An International Reference Group, including representation from 12 countries, met annually to oversee the development of the international LCP programme.
A recent independent review of the LCP40 was undertaken in response to growing concerns represented in the media about the use of the LCP to support care for imminently dying people. Reports included stories focused in particular on the challenge of accurately ‘diagnosing dying’, the provision of food and fluids in the last hours or days of life and the use of sedation. The review of the LCP considered written evidence from members of the public and health professionals who had experience of the LCP. They also took evidence from a variety of professional bodies and other relevant organisations and held four public sessions to hear people’s experiences first hand. The review concluded that the LCP represented the right ethical principles for the care of the dying patient and, when the LCP was implemented properly, it could support a peaceful and dignified death. However, the examples of poor care led them to recommend that the LCP be phased out over a 6- to 12-month period to be replaced by individual care plans.
A review of academic literature and hospital complaints was also undertaken as part of the review process. The review focused on the effectiveness of the LCP and other care pathways in end-of-life care. 41 The authors concluded that the evidence base for accurately predicting the imminence of death did not exist. In addition, the authors highlighted a paucity of high-quality, robust empirical studies into how the LCP is used in practice and the impact it has on the care of people who are imminently dying. The authors concluded that independent research focusing on the outcomes and experience of care – as reported by relatives and carers – as well as the quality of dying was urgently required.
Aims of this study
This study sought to develop a comprehensive picture of care in the last hours or days of life in two very different health-care settings, ICUs and nursing homes, in England, half of which used the LCP to support the care of their patients in the last hours or days of life, and half of which did not. It attempted to do so from a variety of perspectives, including undertaking direct observation at the bedside of dying patients, examining the views of bereaved relatives regarding their experience of the last hours or days of their loved one’s life and the views of those directly engaged in the delivery of care. In so doing, it aimed to assess the impact of the LCP in nursing homes and ICUs on the nature and quality of care delivery and outcomes for patients and their relatives and carers. The study was also designed to provide evidence on costs and outcomes. The project aimed to generate evidence to support the commissioning, development, implementation and management of generalist end-of-life care services in the NHS and wider health and social care system.
Section 1
Chapter 2 Methods
Introduction
The LCP is cited as good practice in national health-care documents. 6,38 However, there is limited research evidence on exactly how the LCP is used in practice and the impact it has on the care of people who are dying. This study was designed to produce evidence by examining the impact of the LCP on care in two different settings, ICUs and nursing homes, in England. In so doing, this study met the criteria set out by the National Institute for Health Research Service Delivery and Organisation programme (since renamed Health Services and Delivery Research) in their programme on patient- and carer-centred services. This research also builds on the scoping review of generalist end-of-life care undertaken by Higginson et al. 35 and incorporates an economic component, which aims to compare the costs and outcomes associated with the implementation of the LCP in the two different settings.
Study aim
The aim of this study was to assess the impact of the LCP on care in two different settings: nursing homes and ICUs. The study was designed to examine the impact on patients, carers, bereaved relatives and clinicians including nurses, doctors and other members of the MDT involved in the care of patients in the last hours or days of their lives. The impacts studied include the physical care of the patient; the psychological needs of the patient; the social, spiritual and religious needs of the patient; the information/communication needs of carers; and the economic costs of care.
Piloting and ethics committee review
Given the nature of this study, a detailed pilot study (see Appendix 1) was undertaken to establish the most effective and acceptable ways of approaching patients at the end of their life, their family members and the staff caring for them in nursing homes and ICUs to participate in this study. The main implications of the findings informed the procedure for the main study protocol (see Appendix 2) in terms of the process for patient and relative recruitment and, specifically, for gaining informed process consent. Appendix 3 illustrates a brief summary of this protocol, Appendix 4 includes advisory group membership and Appendix 5 shows the terms of reference for this group.
In line with the recommendations resulting from the pilot phase of this study, a flow diagram was developed to map the consent process for the observational phase of the main study (see Appendix 7).
The pilot study and the subsequent main study received ethics committee approval from the North West Wales Research Ethics Committee (REC) which was authorised to review studies involving patients who might lack capacity. The pilot study was approved in April 2010 (REC reference 10/WNo01/26) and the main study was approved in September 2010 (REC reference 10/WNO01/51).
Research governance
Research and development (R&D) approval was sought and gained in all 12 hospital trusts, and, for the nursing homes, which were under the governance of the then primary care trusts (PCT), letters of access were sought for the data collection in these sites. The researchers collecting data had enhanced Criminal Records Bureau clearance and current Good Clinical Practice training certificates, and were issued with research passports in order to facilitate these processes. Gaining R&D approvals, however, was a complex and often lengthy process, differing logistically and administratively from site to site and which, on occasion, held back the recruitment of patients in research sites for several weeks.
Study design and sampling
The aim of this qualitative, case study-based approach was to collect a range of data from nursing homes and ICUs that used the LCP to support care and matched sites that did not use the LCP. The following types of data form the basis of this study:
-
documentary analysis of Strategic Health Authority (SHA) plans and collection of local end-of-life policy documents
-
a retrospective analysis of 10 deaths in each location using written case notes
-
interviews with staff about local end-of-life care policies and practice (point 1)
-
observation of interactions with dying patients
-
analysis of the case notes pertaining to the observed patient’s death
-
interview with a member of staff who had provided care up to the period of observation (point 2)
-
an interview with a bereaved relative who had been present during the observation
-
economic analysis focused on the 25 observed cases to provide costings to inform future policy/organisation of care delivery.
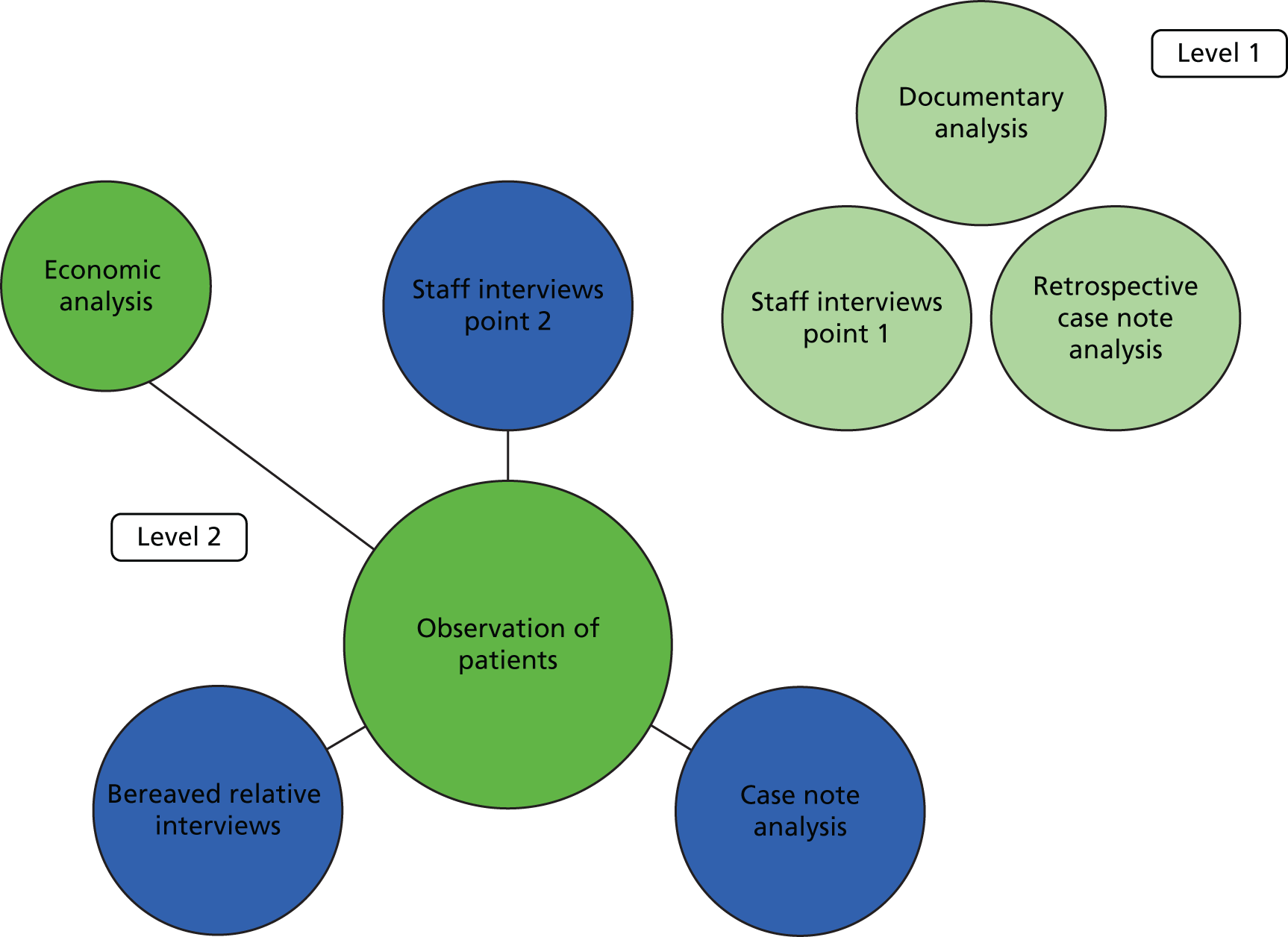
These data work on two levels. Level 1: background, contextual data about views, attitudes and documented practices surrounding end-of-life care in each setting are explored through data types 1–3. This provides a cross-sectional analysis of perspectives in a general sense across all participating sites. Level 2: a case study approach, centred on the observations of patients, allows a detailed contextual analysis of a limited number of events from a variety of relevant perspectives. These are explored through data types 4–8. Figure 1 illustrates how these various elements work together to create an in-depth picture at these two levels.
FIGURE 1.
Overview of data collection methods.
A matched case study design was adopted to collect the data in order to assess the impact of the LCP from different perspectives. The original aim had been to recruit 24 sites, 12 in the north-west and 12 in the south-east, half using the LCP and half not using the LCP.
Identifying potential sites
Appendices 8 and 9 contain flow diagrams that indicate the way in which ICUs and nursing homes were considered, approached and recruited to the study. A ‘master’ list of nursing homes and ICUs in each geographical location was developed. The nursing home list was created using information held on two relevant websites at the time (autumn 2010). These were the Care Quality Commission (CQC) website (www.cqc.org.uk) and the Home Care Choices website (www.homecarechoices.co.uk). The ICU ‘master’ list in the north-west was developed from the acute hospital trusts identified on the then North-West SHA website (www.northwest.nhs.uk). In London and the south-east, it was generated from information held at the time on ‘Dr Foster’ (London, UK; www.drfosterhealth.co.uk/).
Site inclusion criteria
The following criteria were applied to all sites on the two master lists:
-
nursing homes
-
24-hour, ‘on-site’ nursing care
-
within travelling distance of the location of the researcher and each other.
-
-
ICUs
-
level 3 care, i.e. patients who required one-to-one nursing care
-
under the clinical direction of an intensivist
-
> 400 admissions per year (this was amended early in the study to > 6 level 3 beds)
-
> 80% of patients mechanically ventilated
-
general ICU (e.g. not heart and lung, burns or neurological specialty)
-
within travelling distance of the location of the researcher and each other.
-
Definition of a Liverpool Care Pathway-using site (for the purposes of this study)
As part of the national dissemination process of the LCP, organisations interested in using the framework were invited to register their interest with the MCPCIL. While registration was not compulsory, it gave organisations the opportunity to review their practice.
At the time of the commencement of the study, organisational details were held on the MCPCIL national database for 503 care homes and 66 ICUs across the UK.
Any relevant organisation represented on the MCPCIL database within the two geographical locations was potentially eligible for consideration as a ‘LCP-using’ site in this study. Sites were deemed to be eligible for inclusion in the study as a LCP-using site if they had registered with the MCPCIL and/or had used at least one LCP in the previous 6 months to support the care of a dying patient. Potential non-LCP-using sites were matched against those LCP-using sites which agreed to participate in the study.
Matching of sites
The main purpose of matching was to ensure that each of the LCP-using sites within the sample in each setting could be compared with a site that was similar in most important respects apart from LCP implementation and use. In all cases LCP sites were recruited first and then matched with a non-LCP-using site. Matching was based on the following set of key variables in each setting:
-
nursing homes
-
provider type
-
type of care offered
-
size of home
-
CQC rating
-
geographical locality (based on the postcode)
-
deprivation rating.
-
-
ICUs
-
number of beds
-
geographical locality.
-
Recruitment of sites
Overall, 23 sites participated in the study, as shown in Table 1.
| Type of organisation | Location | Total | |
|---|---|---|---|
| North-west | London and south-east | ||
| NH with LCP | 3 | 3 | 6 |
| NH without LCP | 3 | 2 | 5 |
| ICU with LCP | 3 | 3 | 6 |
| ICU without LCP | 3 | 3 | 6 |
| Total | 12 | 11 | 23 |
The recruitment strategy for nursing homes and ICUs was underpinned by three principles:
-
Although the management of an organisation might agree to take part in the study, individual employees had the freedom to decide whether or not they wished to take part.
-
Once an organisation had agreed to participate, meetings were held with staff, individually and in groups, in order to air concerns and clarify procedures. A log of attendance at these meetings was maintained to ensure that, where possible, a minimum of 50% of the staff had received information about the study.
-
Individuals could opt out of the study at any stage without the need for explanation.
Given the nature of the study and the findings of the pilot study, we anticipated reluctance on the part of some staff to consent to participate. Meetings were held to establish the level of organisational interest in taking part. High levels of staff choosing not to participate would have made the observational element of the research difficult to conduct. The purpose of these early meetings was to identify what proportion of staff were unwilling to participate in the study. It was decided that only those organisations in which it was known that a majority of staff were not against participating in the study in principle should be included in the sample.
Nursing homes
A hierarchical ‘top-down’ approach was adopted to the recruitment of nursing homes. Nursing home managers and owners were contacted by telephone to establish LCP-using status, and to ascertain whether or not they would be interested in receiving information about the study. A letter (see Appendix 10) was then sent to all who wished to receive it stating the purpose of the study and the nature of their potential participation. This was followed up by a telephone call to arrange an introductory meeting. If site participation was agreed in principle at this meeting, arrangements were made for the researcher to meet with individuals and groups of staff to give further information about the study.
As previously discussed, the researcher aimed to see at least 50% of the workforce, to give the staff an opportunity to ask questions, express concerns and talk about the proposed research. The researcher would meet the staff in small groups or as individuals, and a record was kept of the names and numbers of staff seen in this way. Visits and meetings were held at different times of the day, including through the night, in order to reach as many staff as possible. Any staff who felt strongly that they did not wish to participate in the study were asked to let the researcher know by e-mail or telephone (to ensure confidentiality), and this information was noted so that these individuals would not be approached for interview or for the observational element of the research.
Intensive care units
A similar recruitment process was adopted in the ICUs. Managers and consultants were approached initially by telephone to check their LCP using status and to gauge initial interest. They were then sent an introductory letter and more information (see Appendix 10). A follow-up telephone call was made, and if there was interest in participation at this stage a face-to-face visit was arranged. If agreement in principle was achieved from ICU managers at this stage, meetings were organised for staff, primarily nurses and doctors, which in the ICU setting were often formal and provided staff with an opportunity to ask questions and/or voice concerns. Again, these meetings were held at various times of the day and night in order to reach as many relevant staff as possible. The researcher kept a record of staff attending these meetings. In some of the larger ICU sites employing over 300 clinical staff, it was only possible to see a small proportion of the workforce. The aim in these large sites was to cascade general written information through the system, using notice boards and by word of mouth. Staff were invited to approach or contact the researcher if they had any questions or concerns about the research.
Challenges in site recruitment and retention
A significant amount of time and resources were used to identify, approach, gain access to and eventually recruit sites to this study. As detailed above, the recruitment process was complex and iterative and, therefore, often protracted. There was a tremendous amount of activity involved in making initial contact with potential sites. Appendix 11 illustrates the level of activity for each site.
Almost all of the issues raised by staff were related to concerns about the observation of their care. In the majority of cases, staff were reassured by the fact that they would not be identified or identifiable and that they had a right to withdraw from the research at any time without giving a reason. Only a small minority of staff (n = 5) in all of the participating sites notified the research team in advance that they would not want to take part in the research study. There were, however, a number of issues, specific to each setting, which impinged on the recruitment and retention of sites to this study.
Nursing homes
Staff turnover in nursing homes was a particular challenge for the recruitment and retention of sites in this study. This was predominantly the case for sites in London and the south-east. Six nursing homes were quite quickly recruited to the study and a significant amount of work had already been undertaken to introduce the research to individual staff in each site. However, three of these subsequently withdrew as a result of a change in the home’s management. Several attempts were made to recruit replacements, but it proved possible to replace only two of the three homes in time for meaningful data collection to take place. An additional problem was experienced with another nursing home in the south-east, where a decision was taken by the management team half-way through the study to opt out of the observational stage of the research. Unfortunately, this happened too late in the course of the study for the site to be replaced.
Similar problems were experienced in the north-west sites. In one, home agreement for the observational phase of the research was withdrawn 5 months after their initial agreement to participate and following a significant amount of data collection (documentary analysis and point 1 interviews had been undertaken). A replacement was found for this nursing home. Another home was taken over by a different management company during the course of the study and, although the home did not formally withdraw, no opportunities for observation were made available to the researcher after this point.
Similar challenges to recruitment and retention have been reported in the literature. For example, Tilden et al. 42 reported a higher rate of turnover of key personnel in ‘non-completer’ sites in their study of the relationship between communication, teamwork and palliative/end-of-life care practices on patient outcomes. They concluded that researchers wishing to undertake large-scale studies in nursing homes should ‘anticipate significant challenges and delays in recruitment and retention of the sample, and should budget accordingly’.
Intensive care units
The speed of recruitment in the ICU setting was slowed by uncertainty about whether or not the LCP was being used. Many of the sites in the north-west had implemented the LCP at some point in some shape or form and it was necessary to recruit from a wider geographical area than originally planned.
In addition, at the time of the recruitment, ICUs were experiencing significant organisational change. Some ICUs were in the process of merging and the allocation of level 3 beds across the sample often changed in response to emergent need; the maximum number of level 3 beds that were available in each site are detailed later (see Table 3). Robust statistics on the proportion of ventilated patients in ICUs at any one time was difficult to locate and the proportion of patients required for inclusion in this study (> 80% mechanically ventilated) was not always reached. Together, these factors made the identification and recruitment of appropriate sites challenging and time-consuming.
Liverpool Care Pathway-using/non-Liverpool Care Pathway-using distinction in nursing homes and intensive care units
Six ‘LCP-using’ sites (coded as NNA sites in the north-west and coded as SNA sites in London and the south-east) and five ‘non-LCP-using’ sites (coded as NNB sites in the north-west and coded as SNB sites in London and the south-east) were recruited to the nursing home sample. However, early on in the data collection it became clear that the distinction between LCP-using and non-LCP-using sites was not clear-cut. A more complex continuum of exposure to the principles and experience in the use of the LCP and of other key end-of-life care initiatives such as the GSF and advance care planning (ACP) existed. Seven of the 11 sites had implemented the GSF and one had recently commenced the North West End of Life Care Six Steps to Success programme for care homes. 43 Both initiatives focus primarily on the last 12 months of life and aim to support the development of a coherent system for planned and co-ordinated care. All 11 managers reported having a process of ACP in place to support the patient choice agenda, and the seven sites using the GSF were also using the LCP to support care in the last hours or days of their patients’ lives. In one site (NNB1) managers reported that although the care provided by nursing home staff was not supported by the LCP, the district nurses who attended the nursing home used the LCP, and another (NNB6), although initially recruited as a non-LCP-using home, began to use it during the course of the study.
In ICUs the situation was more complicated. In those sites recruited as LCP-using, the LCP was not always used. In the main this was because the speed of death was viewed as too quick to allow for the monitoring and assessment of the patient using the LCP documentation. In addition, there was evidence in the case note analysis that three of the sites in the north that had been recruited as non-LCP-using sites (NIB3, NIB4 and NIB5) had used the LCP to support care at the end of life.
The issue of recruiting sites was discussed at the advisory board meetings and with the Department of Health. Given the investment of time in recruiting sites and keeping them on board and the late stage at which some of these issues emerged, a decision was taken, supported by the project advisory board, that these sites should remain in the study. Tables 2 and 3 illustrate the matching characteristics of the samples recruited for nursing homes and ICUs, respectively.
| Geographical location | NH | CQCa rating | Number of beds | Care provided | Provider |
|---|---|---|---|---|---|
| North-west | LCP using | 3 | 32 | Old age | Private |
| Non-LCP using | 2 | 38 | Old age | Private | |
| LCP using | 2 | 62 | Old age | Private | |
| Non-LCP using | 2 | 60 | Old age | Private | |
| LCP using | 3 | 32 | Old age | Private | |
| Non-LCP using | 3 | 32 | Old age | Private | |
| London and south-east | LCP using | 2 | 35 | Old age | Private |
| Non-LCP using | 2 | 30 | Old age | Private | |
| LCP using | 3 | 30 | Old age | Private | |
| Non-LCP using | 3 | 25 | Old age | Private | |
| LCP using | 2 | 37 | Old age | Private | |
| Non-LCP using | – | – | – | – |
| Geographical location | ICU | Maximum number of level 3 bedsa | 1 : 1 intensivist | Type |
|---|---|---|---|---|
| North-west | LCP using | 13 | Yes | General |
| Non-LCP using | 8b | Yes | General | |
| LCP using | 8 | Yes | General | |
| Non-LCP using | 8b | Yes | General | |
| LCP using | 6 | Yes | General | |
| Non-LCP using | 8b | Yes | General | |
| London and south-east | LCP using | 9 | Yes | General |
| Non-LCP using | 11 | Yes | General | |
| LCP using | 11 | Yes | General | |
| Non-LCP using | 11 | Yes | General | |
| LCP using | 6 | Yes | General | |
| Non-LCP using | 6 | Yes | General |
Recruitment of patients, relatives and staff
The process for the recruitment of individuals within participating sites was based on the principles of ‘informed’ and ‘process’ consent. In accordance with best practice,44 the research team sought consent each time data were collected from study participants. The study employed eight types of data collection, some of which were undertaken concurrently and alongside the recruitment of sites and study participants. The specific consent procedure is described within the relevant sections below.
Data collection
Level 1: background, contextual data about views, attitudes, and documented practices surrounding end-of-life care in each setting are explored through data types 1–3
Type 1: documentary analysis of Strategic Health Authority plans and organisational end-of-life care policies
Shortly after the commencement of this study, the SHAs were disbanded and responsibility for end-of-life care was transferred to PCTs and NHS regional offices. Therefore, the documentary analysis of these SHA plans that was originally planned to contextualise this study was refocused to include the collection of information about specific organisational policies and procedures that were expected to more directly underpin the delivery of care.
Key personnel in each site were asked to provide all available current policies, guidelines and frameworks that underpinned the delivery of care to dying patients in each of the sites recruited to the study. Copies were made, wherever possible, of the documentation made available to the researcher. These were then categorised and details entered into a database for ease of comparison of types of documentation available across sites. We had expected that this process would elicit a combination of standard organisational policies as well as locally derived documents. We had planned to analyse these documents in conjunction with the care that we observed and the interviews that were conducted.
As the collection of documents progressed across the sites, we were struck by the huge variation in the number of policies we were given per site, the nature of the policies and the dates of the policies we were handed.
In one site only one policy was provided; in another, 27 policies were provided. In general, ICU sites provided more policies than nursing homes. We are discounting the possibility that what we received was the sum total of their relevant policies in the majority of cases. The variability in what we were given makes interpretation difficult; however, there are a number of possible explanations. We have grouped these under three headings: irrelevance, ignorance and expediency.
-
Irrelevance: policies were not seen as relevant to care at the end of life. Practice was conveyed orally and its relationship to policy was historical.
-
Ignorance: although senior staff had been asked to identify and provide these policies, it is possible that staff were not aware of their existence.
-
Expediency: staff were reluctant to spend time thinking about the policies that might relate to end-of-life care and just gave us what was to hand.
Some or all of the above might have played a role in the variation. Given that protocols and policies pervade the provision of much of NHS care currently, this was perhaps a surprising finding. It raises a number of questions about the relevance of policies and their relationship to the care provided in the last hours or days of life. A more detailed analysis of these documents will be undertaken for journal publication. For this reason, the policy analysis will not be referred to again in this report.
Type 2: retrospective analysis of deaths in each location
The 23 case study sites were asked to provide a consecutive sample of 10 case notes for the most recent ‘expected’ deaths that had occurred in their site, in the 12 months prior to the site being recruited into the current study, wherever possible.
A data capture form was developed [case note analysis form (CNAF)], piloted and refined for use (see Appendices 12 and 13). Researchers also copied the last 24 hours of medication usage from the medication chart. A total of 110 CNAFs were completed for the 11 nursing homes and 120 CNAFs were completed for the 12 ICU sites. Wherever possible, these forms were completed during the early part of data collection in each of the sites. Their completion was time-consuming, but it meant that the researcher had a visible presence in these sites in order to enhance potential recruitment for the observational element.
Type 3: interviews with staff in each site (point 1)
Initially, semistructured interviews were planned with a maximum of six key clinical and (sometimes) administrative staff in each participating site. These are referred to as point 1 interviews throughout this report. Undertaking interviews with a range of staff within each participating site was an important way in which to both publicise and further embed the research study within the site, as well as to gain an important insight to the perspectives of a range of staff regarding the provision of end-of-life care in their site. This was a purposive sample to include, in ICUs, a senior doctor, a junior doctor, a senior nurse, a junior nurse, a health-care assistant and administrators. In nursing homes, the sample included managers, senior nurses, health care assistants and administrators. Members of staff were given written information about the study and a consent form (see Appendix 14) and were given a minimum of 24 hours to consider participation. In total, 138 interviews were undertaken across the 23 sites.
A topic guide (see Appendix 15) was used to draw out experiences of caring in general for patients/residents in the dying phase (last few days or hours of life).
The interviews were designed to ascertain:
-
how care of the dying was organised and managed in each location, including symptom control, ethical issues, spiritual and psychosocial care and relevant policies and documentation (including the use of documents other than the LCP, such as the GSF)
-
the barriers and levers for LCP implementation in those organisations using the LCP
-
how staff felt about care at the end of life, both in general and with respect to the organisation in which they worked
-
how staff defined and assessed the dying phase
-
how patients’ needs and preferences were assessed
-
how relatives were involved in the care of a dying patient
-
the extent and type of training in end-of-life care that was available/had been received.
It is important to note, however, that this was a topic guide rather than a set of questions and interviewees were encouraged to raise and explore any issues that were pertinent to their own experience. All interviews were recorded (with the permission of the participant) and transcribed verbatim before being analysed.
Level 2: case study approach, centred on the observations of patients to allow a detailed contextual analysis of a limited number of events from a variety of relevant perspectives, explored through data types 4–8
The following five ‘types’ of data are all inter-related and driven by the observations of care in the last hours or days of life. The central component of this study was the collection of observational data, alongside the accounts of staff who had delivered care during the observed period, the case notes reporting the care provided and the views of bereaved relatives about the care during the observed period.
Type 4: observations of care in the last hours or days of life
The use of the observational method with ‘vulnerable’ groups, including people who are dying, is not unprecedented. 44–47 Lawton suggests that observational methods enable the researcher to keep the focus on the dying patients, eliciting important data without the need to involve them in long-winded and potentially tiring and distressing interviews. 44 Indeed, many patients who are in the final hours or days of life may be comatose and unable to participate in research that requires their active participation. In this study, ‘overt non-participant observation’ was undertaken of the care provided by staff and relatives to patients in the last hours or days of their lives.
The role of the researcher was designed as the ‘complete observer’ during the observations. 48 Although it was the intention that the research team should have minimal impact on the care being received and provided, there was an agreement that should any suboptimal care be observed the researcher would intervene according to an agreed process (see Appendix 16). This issue is discussed in more detail later in this chapter.
The purpose of the observations was to record the nature and content of interactions between patients, relatives and staff, including the administration of nursing care, drugs, fluid and food as well as their withdrawal. The intention was for the researcher to observe for periods of up to 4 hours at a time, which would enable them to take breaks away from the bedside. Observations took place at all times of the day and night. For this reason, a lone worker policy (Fieldwork Code of Practice) was followed to ensure the safety of researchers (see Appendix 17).
Recording observational notes
A range of observational recording techniques were considered initially for use in this study, including the grid technique (noting down whether or not pre-defined tasks/interventions took place); focused observation (noting down not only whether or not something happens but how it happens and the consequences)49,50 and the contemporaneous narrative method (a non-predetermined approach that involves noting all interventions and interactions relating to care as they occur). The third method was chosen, as it offered the most open, flexible and comprehensive approach to data collection.
The times and duration of events such as nurse, doctor, family and friend visits to the bedside were recorded in the observations alongside the handwritten narrative. Researchers adopted similar approaches to the recording of aspects of the environment, for example whether it was quiet or noisy, lighting and smells, as well as their own thoughts and feelings about the events they were observing. Diagrams of the setting proved to be a useful way of creating a visual representation of the context for ‘thick rich description’ (p. 437). 51
Where possible, following Hammersley and Atkinson,52 the researchers noted their impression of what was actually said by participants in the observations as the events were unfolding. All handwritten observational notes were typed up by a clerical member of the research team for the purposes of analysis.
Recruitment of patients/residents to the observational component
It was expected that the physical health of many patients potentially eligible for inclusion in this study (due to their proximity to death) would prevent them from being able to comprehend information sheets or to provide either verbal or written informed consent. Where this was the case, the consenting procedures were designed to conform to the Mental Capacity Act53 guidance on involving people who lack capacity in research.
The Mental Capacity Act53 recognises the importance of undertaking research to gain knowledge of the care of people who lack capacity, as well as the need to protect their interests and safety, and it contains provisions for the authorisation and regulation of research involving people who lack capacity to consent to taking part in a research study. The Mental Capacity Act53 sets out a clear single test for assessing whether or not a person lacks capacity to take a particular decision at a particular time. It is, therefore, a decision-specific test. An individual cannot be labelled as incapable purely on the basis of a particular medical condition or diagnosis. Section 2 of the Act also warns against making unjustified assumptions about capacity on any grounds but makes particular mention of age, appearance and behaviour.
In those circumstances in which a patient lacks capacity, the Act53 identifies the appointment of a consultee. This is defined as a person who knows the potential particpant and who must be consulted about whether or not it is appropriate to involve the person lacking capacity in the research. In these circumstances, the Act suggests that the researcher must take reasonable steps to identify someone who is engaged in caring for the person who lacks capacity (not in a professional capacity nor for remuneration) or who takes an interest in a person’s welfare and who is willing to be the consultee. It is recognised that the consultee is likely to be a family member or an attorney acting under a lasting power of attorney. For instances where the researcher is unable to find a carer willing to be a consultee, the Secretary of State has issued guidance on nominating an individual. In some cases an Independent Mental Health Capacity Advocate (IMCA) may be the most appropriate person.
The expectation was that the majority of patients would be deemed not to have capacity to provide informed consent to participate in this study; however, at an individual level, a lack of capacity was not presumed to exist. Researchers were required to establish, through consultation with staff and relatives, the patient’s level of consciousness and capacity to make a decision about research participation and to identify the most appropriate person to act as a consultee.
Consent process for observations
Appendix 7 provides a flow diagram to explain the complex process for gaining consent for the observational element of this study. Once a site had agreed to participate in the study, a number of strategies were adopted to ‘publicise’ the research to staff, patients and relatives in advance of asking for any individual’s participation. Information sheets based on generic information about the study (see Appendix 18) and adapted for local use were displayed and made available in accordance with local policy and procedure. These information sheets provided contact details of the researcher should anyone require further information about the study. Background information about the research was provided in this way to give relatives time to think about the research, raise issues and discuss it in less pressurised circumstances.
In the majority of cases, recruitment and consent followed a call from staff to say that a patient in an ICU or a resident in a nursing home was identified by the multidisciplinary health-care team as entering the dying phase. Accurately predicting dying is difficult and this is discussed in more detail in the findings, for example in Chapter 5 (see Physical decline and prognostication), Chapter 9 (see Narratives drawing on clinical data to justify a transition from cure to palliation), Chapter 10 (see The meaning of withdrawal) and Chapter 12 (see The Liverpool Care Pathway and withdrawal). For the purposes of this study, in LCP-using sites, a decision to commence an LCP to support the patient’s care was taken as an identification by the clinical team that a person was thought to be imminently dying. In non-LCP-using sites, the clinical team was able to identify deterioration in the person’s condition which suggested that his or her death was imminent. Once a judgement had been reached that a patient was likely to be in the last hours or days of life, and this understanding had been shared with the patient and/or their relative or consultee, a senior member of staff would ask the patient and/or their relative if they would be willing to talk to a researcher about the end-of-life care study. The decision regarding when and how to recruit the patient and/or relative was made by the staff member most closely involved with the patient’s care. If there was agreement to meet the researcher at this time, the member of staff contacted the researcher, who then travelled to the site.
When the researcher arrived at the site, the first task was to establish whether or not the staff on duty had any reservations about the research and if any member of staff currently involved in the care of the patient did not wish to be involved in the study. The next step was to ascertain the patient’s level of capacity to make a decision regarding participation and the arrangements that had been made for decision-making in the absence of patient capacity. Among the 25 patients enrolled in this study, there were only two instances, both in nursing homes, where the patient was conscious and capable of giving informed consent.
The researcher then approached the patient (where applicable) or designated patient consultee (most often a family member) to discuss the study and give written information and consent forms (see Appendices 19 and 20). Relatives were asked to take as much time as they needed before making their decision known to the researcher.
Where a patient was deemed to lack capacity, the consultee was asked to make two decisions. First, they were asked to decide whether or not the patient would have been likely to agree to take part in the study had they had capacity to make this decision. If the consultee decided that this would have been the case, they were asked to sign a consultee consent form to confirm this (see Appendix 20). Second, they were asked to decide whether or not they themselves were happy to participate in the study and, if this was the case, to sign a second consent form (see Appendix 21). Staff were also given information leaflets and asked to provide informed consent for the observation of their care at the bedside and for being approached to undertake an interview about the observation at a later date, if appropriate (see Appendix 22).
Observation in the vicinity of other patients or residents
In nursing homes there were occasions on which residents had been sharing a room with another resident for a period of time prior to the deterioration in their health. Consequently, care at the end of life was often provided in the presence of another resident. A number of strategies were operated by staff to minimise the distress to the co-resident, including the use of screens and curtains and taking the co-resident to the day room for periods of time during the day. When this situation occurred during an observation, the researcher always introduced herself to the co-resident and any relatives present, explained her role as a researcher and summarised the research. On the four occasions when this scenario occurred, verbal consent was obtained.
It was customary in ICUs for curtains to be drawn around the patient’s bedside at the end of life. Relatives and researchers were contained within this bounded world, which gave little or no access to the care provided to other patients in neighbouring beds.
Absence of relatives
The research team had anticipated that there would be instances in which dying patients were not conscious and did not have relatives or family members who were able to act as consultees and give consent for an observation. In fact, this occurred in two cases in this study. In one case an ICU patient received visits only from a neighbour. The staff reported that the patient had no other contactable family or friends. The consultant discussed the withdrawal of the patient’s treatment with the neighbour. The consultant also asked the neighbour if she would be willing to talk to the researcher about the research. The researcher explained the research to the neighbour; the neighbour was then asked if she thought, knowing all she knew about him, that the patient would have been likely to consent to taking part in the research had he been conscious. The neighbour hesitated and asked the consultant’s opinion. As a result of the consultant’s answer the neighbour reported that the patient could be enrolled in the study. However, on reflection, the neighbour later withdrew her consent to the observation. She reported feeling overwhelmed by all the decisions she was being asked to make and reiterated her status as the patient’s neighbour and not a family member or close friend. She reported feeling that ‘agreeing’ to the withdrawal, and then also to the observation, was too much responsibility for her as a neighbour.
In another example, where the patient had no relatives or friends, the staff contacted an IMCA as they wanted to involve an IMCA in their medical decision-making. Unfortunately, the IMCA representative was unable to visit the ICU for at least 48 hours. The IMCA consulted the patient’s GP by telephone and faxed a report through to the ICU regarding the patient’s attitude to life. The consultants agreed that the patient was dying, that it was not in the ‘best interests’ of the patient to continue treatment and that as far as the IMCA, via the GP, was concerned, he would not want to be kept alive with a poor quality of life. The plan was, therefore, to withdraw treatment.
The researcher discussed the patient’s participation in the study with the IMCA over the telephone. The IMCA was supportive of the research and could not see any reason why the patient might not want to take part. The IMCA agreed over the telephone to the enrolment of the patient into the study, and a member of the clinical staff witnessed this telephone call. However, when the researcher asked the IMCA if she would sign a form confirming the enrolment, the IMCA reported that she would have to check with her manager. After a number of e-mails and telephone calls, the agency providing IMCA support to this ICU reported that they had not been commissioned by the PCT to provide IMCA support for anything other than clinical care. They were, therefore, not willing to provide signed confirmation of what had previously been agreed verbally in relation to this patient. As a consequence, the patient was not enrolled in the study.
Process consent during the observations
Process consent44 or ongoing consent was established to ensure that participants (relatives and staff) were content to continue participating in the research study in the last hours or days of the dying person’s life. This required great sensitivity, with a balance needing to be struck between checking and assuming that continued participation was acceptable. As has been noted in the literature,44,45 deciding when and how often to ask respondents directly if they want to continue participating is a judgement call. The most natural point in the observations for researchers to check consent arose when the researcher took a break, roughly every 3 or 4 hours. In addition, when any ‘new’ people (relatives, friends, staff) entered the bed space, the researcher would, wherever possible, find a suitable time to speak to that person to ensure that they were content with the researcher’s presence. The researcher would also check intermittently that those present were happy for her to continue to be at the bedside, particularly when intimate care was being given to the patient. The experience of being observed was explored with relatives and staff in the interviews following the patient’s death.
Rate of patient/relative recruitment
Based on the likely numbers of ‘expected’ deaths in the ICU and nursing home settings each month, and factoring in the possibility that there would be a low uptake by patients and relatives for the research, a ‘notional target’ was set of up to five observations in each ICU (n = 60) and up to two observations in each nursing home (n = 24) for the proposed data collection period.
A total of 25 observations were undertaken in the period between November 2011 and May 2013. Although it is not possible to identify absolutely all of the reasons that the target number of observations was not reached, several contributory factors are offered in explanation.
First, the project suffered a series of delays. The loss of one researcher for personal reasons and the organisation of her replacement created a 4-month gap during which only very limited contact with sites in London and the south-east was maintained. In addition, a substantial amount of work was required within each site before any data collection could begin. Gaining R&D approval within sites, particularly in the ICU settings, was slow, with different sites requiring different documentation and contact with different members of staff. Although it was essential to contact and provide study information to as close to a majority of staff in each site as possible, this was also time-consuming. Delays in achieving organisational consent to take part in the research meant that the first observation did not take place until December 2011. The data collection period was extended until May 2013 in an attempt to maximise the number of observations. Clearly, this then had an impact on the time that was available to undertake analysis and report on the data.
Second, the recruitment of patients and relatives was complex. Appendix 23 provides a log of referrals that were made to the researchers but, for a variety of reasons, did not result in observations. These reasons included patients dying unexpectedly quickly, staff–relative disputes, patients not meeting the strict inclusion criteria and researcher issues such as a researcher being contacted about a possible observation while he or she was undertaking an observation at another site. In only 25 instances, however, did a patient’s family decline to participate in the study.
Third, over the course of the project there was a marked decline in the willingness of staff to identify patients for inclusion in the study, and also in the willingness of consultees to give consent for participation. Interestingly, 14 of the 25 relatives who declined to enter the study (56%) did so between November 2012 and May 2013. This coincided with a period of intense negative media publicity about the LCP, which gained momentum after November 2012 when an independent review was announced. 40 Sites became unwilling to publicise their use of the LCP. In one site the LCP was renamed as ‘palliative care guidelines’ requiring the research documentation to be amended and resubmitted for ethics approval (see Appendix 24).
Strategies to increase the recruitment of patients and relatives
A number of strategies were implemented to attempt to improve recruitment. Two additional researchers were employed to support the collection of data. These researchers undertook point 1 interviews with staff and collected retrospective case note analysis data. Importantly, they also made frequent telephone calls to each site (sometimes daily and sometimes twice weekly, but at least once a week) to ascertain whether or not there were patients who might be eligible for inclusion in the study. In addition, one of the lead researchers visited the sites to promote the importance of the study and to ascertain whether or not there were any specific barriers to the recruitment of patients and relatives. This ‘supplementary’ activity meant that the primary researchers could concentrate their time on carrying out observations, staff point 2 interviews and bereaved relative interviews. However, despite this increased level of activity, only seven new patients were enrolled into the study between November 2012 and May 2013 (a rate of one per month on average, compared with a rate of 1.6 per month in the preceding 11 months of data collection).
Type 5: interviews with staff following a period of observation
Interviews with staff following the patient’s death formed an important aspect of understanding the care that was observed to have taken place during the observation. These interviews, referred to as point 2 interviews in this report, were conducted with one of the nurses who was most involved in the care of the patient during the observation period. The purpose of these interviews was to explore with staff the care that was delivered (see Appendix 25). Potential staff interviewees received information about the data collection methods at several stages: before, during and after the observation (see Appendices 22 and 26). The aim was to conduct the interview as soon after the patient’s death as was possible. In some cases, interviews took place at the end of the nurse’s shift; in other cases, the interview was conducted the following day. In exceptional circumstances where the staff member had days off after the patient’s death, the interview was arranged at the earliest opportunity. Written consent was recorded for all interviews, which were recorded and transcribed verbatim. Twenty-five staff interviews were undertaken. One interviewee subsequently withdrew consent, because on reflection they felt uncomfortable about the interview being recorded, but another staff member who had also been observed providing care to the same patient agreed to undertake an interview.
Type 6: case note analysis
The third element in the collection of data to support the observations involved the analysis of the patient’s case notes recorded during the observed period. The structured pro forma (see Appendix 7) developed for the retrospective case note analysis was used to extract data in a systematic way. The case notes of the 25 patients whose deaths were observed were examined in this way.
Type 7: interviews with bereaved relatives
The final element in the triangulation of data around the patient’s death was the perspective of relatives present during the observation. The importance of the views of bereaved relatives about care that was provided is reported in the literature. 54 These interviews were designed to elicit information from the relatives about the care that was provided in the last days and hours of life (see Appendix 27). They were not designed to provide proxy data about how the patient might have felt about the quality and timing of care received.
The timing of the interviews with bereaved relatives was important. Ethical concerns about intruding on grieving relatives too soon after the patient’s death needed to be balanced with facilitating recall. The literature suggests that interviews should be conducted 5–6 months following the death of a relative. In this study we allowed relatives to identify the time frame with which they were most comfortable. Relatives received information about the proposed interviews as part of the written information given to them when they initially consented to take part in the study (i.e. prior to the period of observation). At this time they were asked merely to confirm that they would be happy to be approached after the death of the patient to consider participation in an interview (see Appendix 21). They were also asked at this time how soon after the death they were willing to be approached or if they would prefer to contact the researcher themselves when they felt ready to do so. If they did not specify a time for approach at this point, it was agreed that the researcher would contact them no sooner than 1 month after the patient had died to seek their consent for interview. One month was chosen as the time point because this would generally have allowed enough time for patient’s funeral to take place, but was still soon enough after the death to optimise the level of recall. When the researcher telephoned or contacted the relative in accordance with their wishes arrangements were made for the interview. Relatives who gave consent to participate in this interview (n = 22) elected to be interviewed at time points ranging from 38 days to 148 days after the patient’s death. The majority of relatives elected to be interviewed between 2 and 3 months after the death.
Type 8: economic analysis
The economic element to this study was based on a comparative study design examining the benefits and costs associated with care using the LCP as opposed to care without the LCP. This element of the study, including the specific methodology used, is presented in Chapter 13.
Approaches to data analysis
A multistage approach was adopted for the analysis of data.
-
A preliminary analysis of data was conducted as the data were collected.
-
Data from the case notes were analysed in nursing homes thematically, and in ICUs a discourse analytic approach was applied.
-
Data from the point 1 interviews with managerial and senior nurses were analysed to achieve an organisational perspective within sites as well as across sites.
-
Data from the observations of care provided at the end of life were analysed and then cross-checked with data from the case notes and the interviews (staff point 2 and bereaved relative).
-
Economic analysis was applied to the observed deaths using the observation notes and the relative’s responses to the Bereaved Relative Economic Tool.
Analysis of case-note data
Initially, for each of the case notes from each site (n = 230) relevant patient demographic data were extracted, including age; gender; religion; ethnicity; diagnosis; time from admission to death; time from recognition of dying phase to death; preferred place of care; do not attempt cardiopulmonary resuscitation (DNACPR) recorded; and presence or absence of LCP to support care. This enabled a broad, descriptive overview to be constructed and a comparison of the sample on key variables in terms of whether or not the LCP had been used to support care.
A more in-depth analysis of a proportion of nursing home and ICU case-note data was undertaken by HC, EP and MG. It had originally been planned to undertake a discourse analytical approach to these case-note data in each of the settings. Critical discourse analysis55 considers ‘language as social practice’ and acknowledges the importance of the context of language use. 56 The analysis presented centres specifically on the recorded communication between staff and family members regarding the plan of care for patients in the last days of life. However, as a result of major differences in the nature and depth of data recorded, including that pertaining to communication between staff and relatives, this was not possible in the nursing home sites, and a thematic approach to the analysis was adopted in this setting.
Analysis of observations and interviews
The qualitative data derived from the interviews and observations were analysed using the principles of grounded theory. 57 This approach is based on the idea that ‘knowledge’ is constructed and embedded in human perception and social experience. Studies informed by the principles of grounded theory tend to be focused on understanding social processes or actions. They presuppose little knowledge of the topics under investigation and begin with the researcher posing open questions to the research participants. The topic guides used in this study for the interviews allowed respondents the scope to explore in detail their day-to-day roles and experiences of end-of-life care. Similarly, the open, narrative-based approach used to collect the observational data did not impose a framework on the data prior to their analysis.
Data collection was undertaken by SH, TOB, HC and HM. The analysis was undertaken by TOB, MG, SH and EP. The data were coded using the ideas of open coding and constant comparative analysis. Similarities and differences across the data were explored as the data were coded and compared, sometimes word by word or line by line. Concepts and categories were produced and patterns were established that helped to explain the development of a range of core categories within the different data sets. From very early on in the stages of data collection and analysis the researchers SH and TOB met with EP and MG to discuss ideas and concepts. As analysis progressed these meetings became more frequent. A strategic decision was taken to undertake an in-depth analysis of all of the observational data and the accompanying interview and documentary data. A sample of the point 1 interviews was analysed in depth and the findings from this analysis were then cross-checked with other point 1 informants. Only those findings which relate to the in-depth data analysis are presented in this report.
The original aim of the study was to compare care with and care without the use of the LCP. This comparison was based on the assumption that the sites adopting the LCP would have an organisational approach to care at the end of life underpinned by the LCP. In practice, however, the situation was less clear-cut. There were some LCP sites in which only certain groups of staff had received formal training and some non-LCP-using sites in which staff had received some training as part of their previous employment. There were sites that were reported to be using the LCP but did not use it to support all deaths, as well as non-LCP-using sites in which individuals did use it. In addition, some of the non-LCP-using sites adopted the LCP during fieldwork.
The clarity and purity of the original research design was not supported in practice, making the analytical plan difficult to deliver. Therefore, the decision was taken, in conjunction with extensive peer-review comments, to focus on end-of-life care in the environments studied with reference made to deaths that were either supported by the LCP or not supported by the LCP regardless of the site, whenever the data sets allow. However, particular issues relating to the use of the LCP are reported.
Triangulation of data
Once the observations had been analysed, each observation was matched with the patient’s case notes. A timeline framework was then developed for the observation and case-note data, enabling a direct comparison of the observational record with the case-note record. Similarities and differences were recorded and analysed. Comparisons were also made with the staff interview data. Summaries of all of the data sources for the nursing homes and ICUs are provided at the end of Sections 2 and 3.
Structure of the presentation of the findings
Given the collapse of the case match design, the findings are reported in two sections: Section 2 (Findings: dying in nursing homes), and Section 3 (Findings: dying in intensive care units). The data are presented slightly differently in these two sections to reflect the absence of any non-LCP-using deaths in the nursing home observations and the presence of both LCP and non-LCP deaths in the ICUs. Quotes from the participants are illustrative. We have not identified all of the quotes for each point we make and we have, on occasion, used individual situations as cases which are, again, illustrative of the more general points we make.
Although it is acknowledged that nursing homes most frequently refer to their occupants as residents, for the purposes of simplicity in reporting they are referred to as patients in this report.
Section 2 Findings: dying in nursing homes
Chapter 3 Nursing homes: staff interviews (point 1)
Introduction
Section 2 of this report focuses on the data collected from nursing homes. In England and Wales, one-fifth of those aged > 65 years die in care homes. This figure rises to more than one-third in those over the age of 85 years. 58 Planning for and caring for people in the last days and hours of life is, therefore, of considerable importance in this setting. In this chapter of the report we explore how staff talked about end-of-life care in general. In Chapter 4, we examine what the case notes of patients cared for in the last days and hours of life tell us about the care that was provided. In Chapter 5, we report the findings from our observations of patients being cared for up to the point of death and in Chapters 6 and 7 we report the views of the bereaved relatives and the staff who cared for the patient whose death was observed.
We begin in this chapter by presenting the findings from the senior staff interviewed in order to provide an organisational perspective on end-of-life care in these nursing homes. This will form the background for understanding the data derived from the case notes and the specific observations that were undertaken. These point 1 interviews were undertaken to elicit an understanding of generic views of end-of-life care and the way in which it was delivered in nursing homes.
Findings
In total, 11 nursing homes participated in this study, which resulted in a total of 66 point 1 staff interviews. In each home a senior nurse/manager was interviewed and in one home two senior nurses (a manager and a deputy manager) elected to be interviewed together. The demographic details of the 12 participants are outlined in Table 4. More detailed analysis of the extent to which the organisational views of these senior staff were shared by staff, usually health-care assistants, providing day-to-day care will be published in subsequent journal articles. However, the views of more junior staff, primarily nurses, who supported the care of patients observed as part of this study are presented and discussed in Chapter 7 of this report.
| Site | Current post | Gender | Age (years) | Stated nationality (country) | Length of time working in NH setting | Length of time in current post |
|---|---|---|---|---|---|---|
| NNA2S116 | Matron/manager | Female | 55–64 | UK | 14 years | 13 years |
| NNA3S116 | Manager | Female | 45–54 | UK | 22 years | 9 years |
| NNA5S166 | Nurse manager | Female | 45–54 | UK | 22 years | 22 years |
| NNB1S166 | Nurse manager/matron | Female | 45–54 | UK | 25 years | 8 years |
| NNB4S133 | Care services manager/RGN | Female | 45–54 | UK | 10 years | 1 year |
| NNB6S154 | RGN | Female | 55–64 | UK | 1 year 10 months | 1 year 10 months |
| SNA1S166 | Manager | Female | 45–54 | Philippines | 25 years | 12 years 2 months |
| SNA2S136 | Manager | Female | 45–54 | UK | 20 years | 1 year 2 months |
| SNA3S136 | Deputy manager | Male | 55–64 | Mauritius | 12 years | 2 years 7 months |
| SNB1S166 | Manager | Female | 45–54 | UK | 20 years | 4 months |
| SNB2S136 | Managera | Female | 55–64 | UK | 37 years | 6 months |
| SNB2S136 | Deputy managera | Female | 35–44 | India (UK) | 10 years | 4 months |
Six ‘LCP-using’ sites (coded as NNA sites in the north-west and as SNA sites in London and the south-east) and five ‘non-LCP-using’ sites (coded as NNB sites in the north-west and as SNB sites in London and the south-east) were recruited to the nursing home sample. However, early on in the data collection it became evident that the distinction between LCP-using and non-LCP-using sites was not clear-cut. There existed a more complex continuum of exposure to the principles and experience in the use of the LCP and of other key end-of-life care initiatives such as the GSF and ACP. Seven of the 11 sites had implemented the GSF and one had recently commenced the North West End of Life Care Six Steps to Success programme for care homes. 43 Both initiatives focus primarily on the last 12 months of life and aim to support the development of a coherent system for planned and co-ordinated care. All the senior nurses/managers reported having a process of ACP in place to support the patient choice agenda, and the seven sites using the GSF were also using the LCP to support care in the last hours or days of their patients’ lives. In one site (NNB1) managers reported that although the care provided by nursing home staff was not supported by the LCP, the district nurses who attended the nursing home used the LCP; another site (NNB6), although initially recruited as a non-LCP-using home, began to use the LCP during the course of the study. The presence of these end-of-life care initiatives is summarised in Table 5.
| Site | GSFa | ACP | LCP |
|---|---|---|---|
| NNA2 | ✓ | ✓ | ✓ |
| NNA3 | ✓ | ✓ | ✓ |
| NNA5 | ✓ | ✓ | ✓ |
| SNA1 | ✓ | ✓ | ✓ |
| SNA2 | ✓ | ✓ | ✓ |
| SNA3 | ✓ | ✓ | ✓ |
| NNB1 | ✗ | ✓ | ✗ But district nurses do visit dying patients regularly and use the LCP to support their care |
| NNB4 | ✗ But recently completed the training for the Six Steps programme |
✓ Just started as part of Six Steps programmeb |
✗ |
| NNB6 | ✓ | ✓ | ✓ |
| SNB1 | ✗ | ✓ | ✗ |
| SNB2 | ✗ | ✓ | ✗ |
The use or non-use of the LCP to support end-of-life care used to determine participation in this study was not a practical or useful distinction. For this reason, in reporting the findings from these interviews we do not make comparisons between LCP-using and non-LCP-using sites, but we do highlight the end-of-life care tools and processes, including the LCP, that were in place in these sites.
Views on end-of-life care
There was considerable agreement about the best care for patients in the last hours or days of life within the nursing home setting. In all homes, a proportion of elderly patients had been referred from the hospital to the nursing home specifically for end-of-life care. It was generally agreed that dying and death should be planned for and expected, neither sudden nor lingering, comfortable (without pain), peaceful (without agitation, fear or distress) and dignified (keeping patients clean and treating them with respect). Depending on the patient’s wishes, managers reported that patients should be able to die in familiar surroundings with their family members present.
A good death [is] that symptoms are controlled . . . people aren’t in pain, that people are in comfort and they’ve got what they want and the family’s supported . . . we still get sudden deaths you know which are still not very nice but most deaths are . . . good, peaceful.
NNA3S116
She died peacefully in her bed you know with the family aware and visiting . . . and it was what I would call a nice death. In her own bed, not agitated, not distressed, just you know clean and comfortable and surrounded by people who knew her and were fond of her.
NNB4S133
From the perspective of the managers the best place for nursing home patients to receive care at the end of life was in the nursing home. The emergency admission of imminently dying patients to hospital was deemed unlikely to be in the patient’s best interests and represented a failure to plan and organise care appropriately.
This is their home and this is where they have lived and this is where I feel they should die.
NNB1S166
However, there was recognition that there were circumstances in which nursing home patients at the end of their lives were admitted to hospital. To minimise the risk of this outcome and to give the staff the best opportunity to realise a ‘good death’ for a dying patient and their family in the nursing home, respondents highlighted the importance of the following principles, structures and processes:
-
ACP – so that the choices of the patient for his or her end of life can be discussed, documented and shared with all relevant individuals and agencies
-
co-ordinated systems to track and monitor patient status, to recognise imminent death (last hours or days of life) and support the delivery of appropriate care at that time – so that caregiving remains responsive and tailored to emergent need at all stages
-
anticipatory prescribing of medications known to be important in the care of imminently dying patients – so that pain and other symptoms that may be experienced can be controlled in a timely and effective manner without recourse to emergency hospital admission
-
training and links with other health-care professionals.
Each of these key principles, processes and structures will be explored separately.
Advance care planning
Patient choice at the end of life
One important element of a ‘good death’ identified by senior staff was the importance of taking the patient’s stated wishes and choices into account. The promotion of patient choice at the end of life was reported to be a key objective in ACP.
It’s all about . . . anticipating someone’s death and giving them the opportunity to have the death they wanted. Discussing it and not being afraid to broach the subject with someone . . . we’ve got to take away the stigma of death because it’s inevitable. We’re all going to die someday and it should be part of your own choice. I think we’re trying to include it in the patient’s choice.
NNB4S133
All of these senior nurse/managers reported that they had a process in place to facilitate engagement in such discussions and there appeared to be a high degree of correspondence across the sample in the stated purpose, nature and content of these discussions. Offering patients some degree of choice over particular aspects of their own end of life required managers and nurses to have the confidence and skills to open up discussions with patients (where they had capacity) inviting them to contemplate their own death and with relatives to contemplate the death of their loved one. These more experienced respondents broadly felt that they had the skills to meet this challenge.
I think with being experienced and being mature I am well able for that. I think I can do it sympathetically and in a language that they understand and I think I’m approachable enough for them to . . . come to me if they have any questions or anything like that. I think that when you’re running a shift in nursing homes you have to be prepared for that. It’s an unfortunate part of the job. It’s not the nicest part of the job but still in all it’s somebody’s job and that’s ours isn’t it.
NNB4S133
Do not attempt cardiopulmonary resuscitation, hospitalisation and preferred place of death
A major focus of these ACP discussions was to document important decisions about life-saving interventions and the patient’s preferred place of death.
We try and discuss sort of what they want, whether they want to be resuscitated or not, if they want to go to hospital and their preferred place of death really . . . so we discuss that with the resident . . . especially if somebody wants to be resuscitated or not, we try and get that ascertained straight away.
SNA2S136
Although the above example suggests that patients can choose to be resuscitated, this was recognised by others as being a medical decision.
We discuss resuscitation status you know but it’s the GP’s decision at the very end of it.
NNB6S154
One respondent also spoke about the importance of asking patients and relatives to consider other issues that might be part of an advance decision to refuse treatment to ensure that the patient received the ‘best treatment’. While she made it clear that she did not take such decisions on behalf of patients, she illustrated the strong personal beliefs that underpinned her drive to offer these choices:
We would never assist dying but you know we have to look into . . . do we need an advance directive, are they choosing not to have antibiotics for their next chest infection . . . that’s where I would come in. I think people have you know the right to have the best treatment. To prolong someone’s life if they’re not having very good quality of life does that make a lot of sense to keep giving them antibiotics if they have absolutely no quality of life? That’s something they and the family need to decide. I don’t take that decision at all. I just make sure that that it’s legally written properly . . . I would hope . . . in a few months, that we could be sure that everybody who is, wants to be DNR [do not attempt cardiopulmonary resuscitation], it’s signed and it’s written in their chart and it’s on this Coordinate my Care.
SNB1S166
Although the majority of the managers felt that elderly people should be enabled to die in the home, in familiar surroundings, there was recognition that if a patient decided that they did want to go into hospital at the very end of life, their choice should be respected.
We have to respect their wishes. If somebody came to you in the home and said ‘oh I’m not well I want to go to hospital’ we have to record it. We cannot force them, this is their wish.
SNA3S136
At the same time as recognising that patients should be able to make informed decisions about hospitalisation at the very end of life and understand when death is imminent, some respondents were clear that hospitalisation did not offer anything that was not available in the nursing home.
But you have the discussion with them that is there anything in hospital that they can do that we can’t do? Which theoretically there isn’t.
NNA5S166
But then you go and explain to them what would the hospital do that you won’t get in the home? What is the difference? Then you explain to them that ‘you are better cared for here because you have got your own room here. Anything you want we can give it to you here. Your family can be with you here’. So we explain to them afterwards and they will agree. We don’t force them, we don’t pressure them, but we explain clearly to them.
SNA3S136
An additional component of these discussions involved eliciting those elements of care that patients might consider to be important to them in the future.
We find out what they like so even down to . . . there’s patients that would love a hug, there’s patients that would not want a hug, there’s patients who would like to hold their hand, there’s patients that would like their face stroked, there’s patients who wouldn’t. It’s finding out . . . those finer things so it’s there at the end. And also all the spiritual bits, you know, because spirituality is very different, very different to everybody really. So it could be that you want the priest there, you know, every day saying prayers, it could be that you don’t want that, that you want to make friends with somebody that you’ve, you know, fell out with years ago. It could be anything erm it could just be listening to a piece of music, I don’t know. But finding out all that beforehand is really important so that it’s what their wishes are, it’s what we follow out.
NNA2S116
Timing of advance care planning discussions
The GSF promotes early ACP discussions with all residents. It was reported that, for those patients new to the nursing home, these conversations took place soon after admission.
They [manager and other trained staff] make sure that when they come in . . . we don’t do it on the day but within a week we have to have finished the plan. We have to complete an identification form and an advance care plan.
OK so within a week of arrival you have to have completed the advance care form and the DNAR [do not attempt resuscitation] form?
Yes and the care plan as well.
Right OK so with regards to end-of-life decisions, what kind of things are in the advance care plan? What are you asking them at that point?
Actually asking them if they want to be sedated, the first choice . . . of place where they want to . . . be you know when they are passing and if they have any special requests or any person they want to be with them at end of life. Also if they want a vicar or priest to come and give them the last rites.
SNA1S166
Speed in gaining this information was reported to be of particular importance for continuing care patients who had been sent from the hospital setting specifically for end-of-life care. These discussions, which were reported to cover arrangements for cremation or burial, would sometimes happen within 1 or 2 days of the patient’s admission to the nursing home. In the context of a short relationship and from a position of vulnerability, it is not difficult to anticipate that some residents might find this troubling.
I say ‘where would you like to be cared for in the last days of your life, and your end of life care?’ . . . So we have to prepare them for that . . . get all the questions answered before and also whether they are for cremation, for burial, what are your likes and dislikes, who would you like to be with you when you are at end of life care. We have to get all these clear before [they deteriorate] . . . we do that at the start, as soon as they come in . . . I mean . . . at an appropriate time obviously. Maybe after one or two . . . or 48 hours but after that it may not be possible to do that.
SNA3S136
There were examples, however, which illustrated a more sensitive approach, where the timing and pacing of these conversations took into account the perceived disposition of patients and families at the point of admission. Some nurses reported visiting the patient and family prior to admission to try to gauge how appropriate or otherwise it would be to engage in such discussions and when the best time to do this might be.
I usually go out and do the assessments so you get to know the people, OK not that well but you sit and chat with people in the hospital and with families when you meet them and you know whether you can broach the subject of end of life or you shouldn’t broach it just yet. Some people don’t like you to you know, it’s bad enough having to come to a nursing home, they are all distraught, devastated, feel so guilty and they don’t want me sitting there going ‘so end of life what do you think I should do, what would you like to happen to your mum when she dies’. I don’t think it’s appropriate. Once you get to know them a bit better you can sort of broach the subject and I tend to, if you are getting doctor in a few times and they’ve got lots of things going on with them, then you sort of say ‘look what are we doing’.
NNB1S155
In some sites (e.g. NNB6S154 and NNA5S166) the opportunity to involve patients directly in such conversations was reported to be limited as a result of issues of capacity through conditions such as dementia.
The drive to include all patients in the nursing home in such discussions sometimes meant that patients who were not expected to die within, for example, 12 months were participating in ACP discussions. Undertaking such discussions so far ahead, particularly where they included advance decisions to refuse treatment, raised issues about the appropriateness of the timing of these conversations.
Now because we are doing some advance care plans quite well in advance the GPs aren’t as happy to be filling out DNAR forms which I can understand because obviously they need to have a discussion with the relatives and everything but sort of for the DNARs it doesn’t make sense . . . it’s a bit mixed up . . . and I also think with the Harold Shipman thing the doctors aren’t too, not all of them are really happy to be doing a DNAR form for somebody who might die in 3 or 4 years.
NNB6S154
Refusal to participate in advance care planning discussions
Two instances were reported by staff of a patient and their relative refusing to take part in ACP discussions. Both patients were male and in their sixties. In SNA3, although there was recognition that the patient and his brother were finding the discussion difficult, a sense of frustration with this situation was also clearly evident.
So we have a gentleman who is 63 years old . . . he has prostate cancer and we are not able to deliver the [advance] care plan . . . he does not want the care plan, next of kin do not want the care plan also, they think he is too young. He is 63 years old . . . so we are in limbo with that. So these things do happen at times . . . he is not very co-operative at times . . . so we haven’t done the advance care plan we can’t do it.
SNA3S136
In NNA3, the patient and his brother were described as ‘flatly refusing’ to state their wishes. The staff suggested that the reason for this refusal was either that they did not understand or that they were choosing not to think about death.
They won’t do it . . . he’s been with us donkey’s years and he is still refusing and we still every so often say ‘would you like to?’ there’s only him and his brother and they go ‘no, no’ . . . he’s a younger man . . . he’s one of our younger gentlemen that’s in his sixties but . . . erm no they don’t want to be involved in anything like that . . . they’ve not understood or . . . they don’t want to think about it . . . we’re not here to push advance care planning but . . . we do try and do it with the person and the family as soon as possible. But like I say, some families do try and put it off.
NNA3S116
Regular review and sharing of advance care plans
Nursing staff highlighted the importance of the regular review of these plans, as it was acknowledged that patients (and relatives) may well change their minds about particular aspects of their care over time and in response to changing circumstances.
When the time comes that they are poorly . . . they still have that, how they feel and deliberating and they might change their mind . . . so we say to the family we will review the advance care plan every . . . year or if there is any significant change.
SNA1S116
Co-ordinated systems to track and monitor patient status
Gold Standards Framework
As illustrated previously in Table 5, the GSF was reported to have been implemented in seven sites. The GSF aims to promote better quality end-of-life care in nursing homes through proactive planning, enhanced relationships with GPs and other health-care professionals, working with teams to raise staff morale and increasing the practice of ACP, all ultimately with the aim of reducing the number of hospital deaths. 59 The respondents in this study agreed with these aims. Where the GSF and the LCP had been implemented in an organisation, respondents generally believed that they had made a positive contribution to care delivery, particularly in avoiding inappropriate admission to hospital.
I think the Gold Standard and the pathway has made a massive difference that you can go home now [at the end of a shift] and know it’s not going to be left to you, that the next nurses won’t be railroaded and . . . [patients] going into hospital because it’s all organised. Everybody knows what’s going on, the family knows, the GPs know, the out of hours know and we even had a policy . . . with the hospital now . . . so if they go in for something quite acute and they sort it but they’re quite poorly . . . they can fast track them back to us.
NNA2S116
For others, the GSF (and LCP) have also helped to normalise death and dying and allow staff to feel that they have done the best for a patient, even when that patient dies.
Here there’s more of a feeling that there’s care of the dying and you did well while you were caring for the dying and then they died and you reflect on that . . . you know we had someone that came in for a day and died . . . but here it’s more like, well, that’s OK because that’s what he came in for . . . so I think it’s part of, because of the Gold Standards and because of the Liverpool Care Pathway I think it’s just making more people more aware.
SNA2S136
The GSF focuses primarily on patients deemed to be in the last 12 months of their life. The first element it seeks to address is ACP. Staff are encouraged to undertake an advance care plan with a resident ‘soon after admission’30 and there is no doubt that this requirement was successfully achieved in a number of sites; see Advance care planning for further consideration of this element.
The next requirement of the framework is to code the ‘status’ of each patient against a four-stage coding matrix and then to assess and monitor the progress of all patients against this.
We have this coding, this ABCD and A is kind of everybody, B is when people have started to go down but you know nothing drastic but you’re seeing them started to deteriorate a little bit, C is when you think there is only actually a few weeks left which means that they really are going down now and become very poorly so then you look at the whole, the whole of them and see what needs they might have that they won’t be able to do themselves and then . . . at D is like days, so we’re on days, we’re talking about you know getting the GP in and if they’re not eating and drinking, etc., which we just follow protocol, that’s when they go in the pathway [LCP] so we’ve actually got everything in ready.
NNA2S116
Each patient is then to be discussed at a monthly multidisciplinary meeting, which includes professionals external to the home, for example specialist palliative care nurses. In NNA3S116 the nurse reported that health-care assistants also attend these meetings.
But every month, everybody in the home as part of our GSF meetings, gets a full review . . . and that ties in with our care planning as well . . . the carers do come to the meetings as well . . . and it’s just a bit of an education session as well, especially when the Macmillan nurses turn up as well.
NNA3S116
Staff also reported the presence in sites of a process for monitoring, documenting and sharing any changes in the coding of the patient’s status that occurred between meetings. Finally, the GSF encourages critical reflection and discussion between those staff from within the home and those external to it (if appropriate). In NNA5S166 the nurse reported that this kind of debriefing also takes place after a patient’s death in order to highlight any lessons to be learned:
On handover we have GSF meetings so we’re discussing there what went well, what didn’t go well. Because . . . all of our residents that . . . that do pass away, we actually complete a form as to say what went well, what didn’t go well . . . and that’s open for discussion . . . so we highlight problems . . . and if we do have problems we can take it to the end-of-life team.
NNA5S166
The Liverpool Care Pathway for the Dying Patient
As can be seen above, the LCP and the GSF are often seen to be synonymous in settings in which they have been implemented. As with the GSF, there was an overwhelmingly positive view of the LCP and its impact on care.
Before, we used to do our best and we used to think we did a really good job, but I really think since the Gold Standard and since the Pathway . . . I think there’s much more . . . we can do and I think the confidence that we’ve got now, that we can speak to people . . . we didn’t have the confidence about people dying and their wishes and what did they want and how would you cope with it, and how can we help . . . we have now and I think that’s to do with the Gold Standard and with the Pathway.
NNA2S116
Although many respondents spoke of good relationships with their GPs, some described logistical challenges in gaining timely medical input in the care home setting, particularly out of hours. This was a concern for respondents, who regarded this as creating the potential for the inappropriate hospital admission of imminently dying patients. Pragmatic solutions were evident in some sites, for example, to the process for commencement and use of the LCP and the anticipatory prescribing of medication, which are now explored in more detail in the following sections.
Process for commencing the Liverpool Care Pathway to support care
Nursing homes were, by definition, situated within the wider health-care environment and were affected by wider primary care issues in their ability to deliver care at the end of life. Where the LCP was used, some issues were highlighted regarding its use in everyday practice. The main issues related to the timing and purpose of the joint assessment, the GP signature on the LCP and the prescribing of prn [pro re nata (as required)] medication for symptoms that may occur in the last hours or days of life. As with previous versions, commencement of the LCP (version 12) required the signature of the most senior medical professional caring for that patient to confirm the multidisciplinary decision that the patient was imminently dying; that is, they were believed to be in the last hours or days of their life. The use of the LCP to support care is predicated on the requirement that this assessment be undertaken by both a doctor and a nurse. The assessment should involve the consideration of any potentially reversible causes for the patient’s current presenting condition and, where appropriate, should include advice and support from relevant others. 33 After recognition that the patient is imminently dying, the GP should prescribe anticipatory medication for five key symptoms that may occur in the last hours or days of life. In version 12, it is expected that once the LCP has been started, the GP will visit the patient to undertake a further MDT review a minimum of every 3 days, or sooner if either a significant improvement or a decline in the condition of the patient is noted. Three sites (NNB6, NNA3 and NNA5) were using version 12 and four sites (SNA1, SNA2, SNA3 and NNA2) were using an earlier version.
The nurses in sites that had adopted version 12 reported that the level of involvement of the doctor was both important and reassuring.
It gives you more confidence that you’ve got a doctor actually going through it with you.
NNA3S116
This respondent, however, also recognised that gaining this level of involvement was a challenge. Here, and in NNB6, some GPs were reported to ‘struggle’ with the practicalities of a joint assessment of the patient.
Similarly, confirmation of the recognition of imminent death outside normal surgery hours involved ‘out-of hours’ GPs, who were reported to be ‘reluctant’ to make a decision to commence the LCP because they did not know the patient.
I think the only ones we’ve had . . . problems with . . . are the out-of-hours doctors . . . even though we’re a GSF home and we go to GSF meetings at the surgeries, the questions that we’re now raising is the out-of-hours team in that if someone’s condition changes overnight and we’re finding an out of hours and we want to start them on the LCP, they’re actually quite reluctant . . . because they’ve got to make that decision is that person dying? Because they don’t know enough information about that particular resident. It’s not their own GP is it? If it’s something that could be treated. Is it something that’s reversible? So they’re having to make that decision when they don’t really know the patient.
NNA5S166
Four sites that were affiliated with the GSF (SNA3, NNA2, NNA5 and NNB6) used the assessment made as part of the GSF process to recode a patient from code B (months from death) to code C (weeks from death) as a trigger for requesting the prescription of anticipatory medication, rather than on commencement of the LCP, code D, to support care.
. . . the anticipatory meds we usually do before somebody goes on the LCP, but that’s part of GSF programme. [They are prescribed] when somebody’s actually recoded as C, where they’ve got weeks to live. We actually ask for anticipatory meds then.
NNA5S166
There was, however, no evidence in any of these homes that anticipatory medications were used at any time other than when the patient was later recognised to be in the last hours or days of life and the LCP commenced (i.e. recoded on the GSF from C to D).
In three of the sites (NNA2, NNA5 and NNB6), although these medications were requested when the patient was code C, the LCP was commenced at the point of the recoding of that patient from code C to code D. For example:
. . . at C stage, is where we get the anticipated drugs in . . . that’s when we get those in the cupboard at C. And then at D is like days, so we’re on days, we’re talking about you know getting the GP in and if they’re not eating and drinking, etc. . . . that’s when they go on the pathway so we’ve actually got everything in ready.
NNA2S116
The fourth site (SNA3) which reported weekly MDT GSF review meetings and ongoing practical support from the local hospice applied the same procedure as the other three sites to trigger the prescription of anticipatory medication. However, it would appear that a LCP could be signed by a GP but not necessarily implemented immediately. When asked if the LCP could be started at the weekend (when GP cover might be compromised), the respondent explained:
We have someone going on ICP [LCP] as I explained to you we have to have a GP to sign it. Let’s say you are going to start it now, or the next day, maybe next week, maybe 2 weeks’ time. It doesn’t mean you have to start it straight away.
SNA3S136
In SNA1, the recognition of imminent death was reported to be made ‘in house’, at which point the GP could be called to prescribe the prn medication. So, in effect, the LCP could be commenced and the GP would sign the forms later:
No, no, no actually no. We explain to the family that we have started and then we call the GP and they have to sign it. We can decide. Because if in case it happened on a weekend then we don’t wait 2 days before we can start the LCP. They might be dead by then . . . if on the weekday, if the patient is fading and we call them, we are going to say ‘OK doctor can we have the advance medication because it’s Friday’, over the weekend we are going to need it and we have to start the LCP.
SNA1S166
Formal multidisciplinary team review every 3 days
The LCP version 12 promotes a formal MDT reassessment of the patient a minimum of every 3 days, or sooner if either a significant improvement or a decline is noted in the condition of the patient. Again, this was reported to be an important mechanism for the continued medical support of the dying patient.
. . . and the fact it’s got to be reviewed every 3 days by a GP which didn’t happen before . . . so GPs now have to come out to see a patient that’s been on it for 3 days.
NNA5S166
However, the views of staff and GPs were not always aligned in relation to the frequency with which GPs should visit a patient supported by the LCP.
I said ‘now they are on LCP you need to visit every 3 days’. ‘No we don’t it’s once a fortnight’. So I said ‘no, they are on LCP it’s every 3 days’. ‘No you have got it wrong and you have misunderstood it’s every fortnight we visit’. I said ‘but the point of the LCP is that it’s within the last 3 days or the last hours of life, is when we implement, you know we make an assessment to see if they meet that need’. And he said ‘no no you have got it all wrong, she is palliative care’.
NNB6S154
Anticipatory prescribing of ‘as-required’ medications
As we have seen in these respondents’ definitions of a ‘good death’, the ability to control pain and other symptoms was widely deemed to be central to the provision of high-quality care, and important not only for patients but also for their attending family and friends.
I don’t think there’s anything worse for somebody to be called in, a relative, to sit with a resident who’s dying and to see them writhing about in pain or they’re agitated. That’s your lasting memory . . . to think that your mum or your dad or your husband or your wife has died in pain, I don’t think that’s acceptable and I think we’ve failed if that happens.
NNA5S166
The prescription and availability of ‘anticipatory’ medication for five key symptoms – pain, agitation, respiratory tract secretions, nausea and vomiting, and dyspnoea – is promoted in the LCP. The aim of this practice is to ensure that the care of a patient who experiences any of these symptoms in the last hours or days of their life is not compromised. With the focus on avoiding the emergency hospitalisation of dying patients, and the importance of good pain and symptom control in these accounts of a ‘good death’, it was not surprising that many respondents in this study viewed anticipatory prescribing as essential in order to have the drugs available for use ‘as needed’.
Commenting on a time prior to the implementation of the LCP and the GSF in her site, NNA2S116 sums up the concerns that these initiatives were designed to allay.
If they [the patients] need those drugs, it’s going to be a Friday night, middle of the weekend, a bank holiday and I’ve not got them . . . [and the GPs said] that they would come back and give it when it is needed. But obviously that doesn’t work because . . . if you need them in the middle of the night then you’ve got no option but to send them into hospital.
NNA2S116
In the nursing home setting, drugs purchased for a named patient in anticipation of need, but not subsequently used, cannot be used for anyone else. Respondents reported that GPs’ attitudes toward anticipatory prescribing were influenced by the costs associated with throwing away the drugs that were not used.
And some of it was also the money because they were sometimes saying well [if] she doesn’t need them . . . then they’re wasted.
NNA2S116
I mean sometimes we have had anticipatory meds and probably 7 or 8 times out of 10 we don’t actually use any of them and I think that was the problem we had with the GPs when we first started . . . I think it’s been a barrier . . . we’ve had battles I think on the GSF . . . because that’s what we wanted and that’s how we’re being taught . . . but obviously GPs have a budget don’t they so they don’t want to prescribe . . . they don’t want you to get them in stock and then not use them.
NNA5S166
We sort of try and get it a week or two, so when they are a yellow [equivalent to a C on GSF matrix] and we think they are not going to recover. Now we have had a lot where we need to destroy the drugs because they have got better and they have not been used . . . so we have them there I mean so far we have never had to use them. I think the most we have given is two shots of midazolam.
NNB6S154
However, so important was the idea of a comfortable and pain-free death and the significance of the availability of drugs to enable this to be achieved, that respondents were anxious to ensure that, were symptoms requiring their use to emerge in the middle of the night, the drugs would be on hand to administer.
But equally there’s no saying that they’re not going to present [with] something . . . and you’ve not got anything and its 3 o’clock in the morning . . . you need to get a prescription, where do you get one from at 3 o’clock in the morning? So they’re going to wait for the next day. It’s not acceptable.
NNA5S166
In one site, in recognition of the potential waste of resources, steps had been taken to reduce the cost by getting GPs to prescribe smaller quantities of each of the anticipatory drugs in the first instance.
Training
Within all of the end-of-life care initiatives being undertaken in the nursing homes in this study, there was an element of training. Training was mentioned frequently but it was very difficult to get a clear picture of who got trained, how frequently training took place, who provided the training and the exact content of the training.
The examples given of training that had been undertaken did not inspire confidence that it could have prepared staff for the complexities of delivering care at the end of life. The training ranged from a DVD (digital versatile disc) in NNA5 to a National Vocational Qualification Level 3 certificate in SNB1.
I have access to training DVDs, that’s been done through the owners.
NNA5S166
For example, when somebody joins here within a year . . . they will go for an induction day training on palliative care with the hospice, because they have got a team for training there with experts.
SNA3S136
Well the nurses have all been given the choice to go on to it. There’s an end of life what’s it called? Level 3 End of Life Care and I’ve just finished it myself and there’s two nurses signed up for it this time . . . all of the staff just because of the dynamics in this particular building needed to be on the Equality and Diversity course first . . . we don’t have a formal training of any end of life at this moment in the building for staff.
SNB1S166
The picture to emerge was that all respondents thought that training was very important but there was little sense that the organisations within which the nursing home staff were working had a planned programme for training their staff. In some sites, training appeared ad hoc, haphazard and largely informal.
So we tend to be able to free up one or two staff for each training. And a lot of the training goes on throughout the year. I mean I’ve just been . . . up at the hospice . . . ‘opening the spiritual gateway’. That was interesting. That’s a full day’s training.
NNA5S166
We have access to the hospice training. They’ve just run some free training sessions for staff. All grades of staff. I mean it was just a case of turn up. We didn’t have to book it.
NNA3S116
While some of the sites that used the GSF reported training the workforce, those that used the LCP reported that where training existed it was more often targeted at qualified staff.
Everybody’s had training on GSF from the maintenance to the housekeeping. We’ve all had the same training. LCP’s only given to the qualified staff.
NNA5S166
Opinions were divided on whether or not the LCP could be used without training. Some nurses reported that the LCP framework provided its own training.
I like a plan and the LCP for me is a plan. It’s a good guideline too and you can tick off the boxes . . . So what I would try to do myself here is to modify that in a sense that we would roll it out, speak to the GP, do our own training around it as best we can. It wouldn’t be the proper LCP training but enough to say that, this means this, and that means that, and then we would then have a standard at the end and we know and you can actually give yourself some sort of guidance.
SNB1S166
Other nurses reported that implementation without training would have been difficult.
I think if they’d have just given us the LCP and no training and get on with it . . . I don’t think we’d have known what we were doing at all. Because I think when you look at it, it’s quite complicated.
NNA5S166
One nurse, who reported being self-taught with regard to her LCP training, raised a cautionary note. She was discussing a patient she had ‘put on’ the LCP, ‘taken off’ the LCP and ‘put him back on’ the LCP in the space of what appeared to be a couple of weeks.
Maybe I am doing it wrong but I have nobody with me doing it.
NNB6S154
Running alongside the rhetoric of training was a view that experience, although not a substitute for training, was important.
I’m not sure if they have training as such. They do have study days and things and they do erm, most of them are experienced. You know a lot of our staff have been here for many years so we have got experienced care staff.
NNB4S133
However, there was some recognition that perhaps more experienced nurses were the very group of nurses who did require support and training in order to keep up with the changing nursing home population, new ways of providing care and the requirements of regulatory bodies.
Particularly in nursing homes where you are going to be having that poor nurse in the nursing home who might have been in that nursing home 20 odd years and now they are bringing in more complex residents that need more complex nursing needs, they are bringing in the LCP . . . and you know, what proper support and training is she getting?
NNB6S154
Specialist palliative advice and support was reported to be available in all but one of the sites (NNB6). Although it was difficult to gain a clear picture of the breadth and depth of such input, for some sites, collaborations with the local hospice offered the opportunity of specialist support if required.
The local hospice are really actually who we would contact if we have any concerns and they would help and sort of collate an end-of-life care plan.
SNB2S136
Summary
The interviews with senior staff in the nursing homes revealed the complexity of end-of-life care initiatives being introduced into the sector. While there was consensus on what constituted a ‘good death’, there appeared to be a number of ways in which this could be achieved.
There was a strong belief in the importance of ACP and an allied belief that the nursing home was the most appropriate place of care for dying patients. Its importance lay in its relationship with a ‘good death’. The thinking was that gaining an understanding of an individual’s wishes with regard to their own care at the end of life would enable the death, when it came, to be tailored to these needs, and would ensure that inappropriate hospitalisation did not occur. However, the principle of reaching an understanding about what an individual might wish to happen was translated into an imperative which seemed to operate as soon as or shortly after a person was admitted to a nursing home. In only a few cases did nurses report that patients objected to the haste with which these preferences sometimes appeared to be elicited.
The GSF and the LCP were the two most common frameworks used to guide care at the end of life and both were generally well regarded. However, their implementation and use in practice varied enormously, as did the training that accompanied them. Particular problems were identified with the requirement that the GP attend to review the patient for the LCP (version 12) to be commenced and then every 3 days for further MDT review. The nurses in the nursing homes in this study reported a number of strategies to ensure that the anticipatory prn medication had been prescribed and was available in the home should the patient require it. Although the medications were not always used, ensuring that the patient had a comfortable and pain-free death was a major goal of care at the end of life in the nursing homes.
Chapter 4 Nursing homes: retrospective case note analysis
Introduction
In each of the sites in this study case notes of deceased patients were analysed to gain an insight into how care in different settings was documented and described in the very last hours or days of life. The case notes provide a written record of demographic information about each patient as well as information about decisions made, conversations held and care delivered in the last hours or days of life. In 2009 the Nursing and Midwifery Council (NMC) published detailed guidance on record keeping. 60 This document identified a range of clinical, administrative and educational uses of such records. Essentially, the guidance suggests that the purpose of the patient’s notes is to record and communicate patient care, ‘Providing clear, concise documentary evidence of what decisions were made, what care was delivered, what outcomes resulted and how information was communicated to relevant personnel, including patients and those close to them’. Accurate recording keeping is also reported to help to manage risk and improve accountability.
In this chapter we report the analysis of a consecutive sample of case notes from patients who had died within the previous 12-month period in the nursing homes recruited to the study. Data from the case notes of 10 patients per home were extracted using the pro forma previously described (see Appendix 7).
Initially, a sample of 109 pro formas was analysed using descriptive statistics to describe the sample of patients and to provide a summary of some of the main features of care delivered. Sixty patients (55%) had been supported in the last hours or days of life by the LCP. In only one case was the LCP found to have been used to support care in a home that had been recruited as a non-LCP-using care home (NNB6R01) and all of the case notes from homes recruited as LCP-using homes included a completed LCP document.
In terms of the demographic make-up of the two samples, patients in both were generally very elderly (median age LCP = 88 years; non-LCP = 89 years) and were more likely to be female (LCP = 62%; non-LCP = 83%) and to have a diagnosis other than cancer (LCP = 72%; non-LCP = 90%). Religion and ethnicity were not routinely recorded in either sample. Formal documentation of the patient’s preferred place of care (LCP = 82%; non-LCP = 43%) and DNACPR (LCP = 70%; non-LCP = 47%), however, was much more likely to have been recorded for those supported by the LCP.
Although this limited descriptive information was available in the majority of the case notes in this sample, other information recorded tended to be limited. It had originally been anticipated that discourse analysis would be used for both the nursing home and the ICU data analysis. However, the limited information available in the nursing home notes precluded a discourse analytic approach and the decision was made to undertake a thematic analysis focused primarily on what staff chose to record in a patient’s case notes in the period up to that patient’s death.
A total of 39 cases were excluded from the analysis, as an early version of the data extraction tool had been used which gathered data from the patients’ notes in a highly structured format which did not allow for the recording of any narrative data. Seventy case notes formed the sample for the thematic analysis of the patients’ notes. These records came from eight of the sites: five nursing homes in the south-east [three LCP using (n = 30) and two non-LCP using (n = 20)] and three nursing homes in the north-west [one LCP using (n = 9) and two non-LCP using (n = 11)].
Findings
The patients’ case notes included some information on many of the aspects deemed important by the NMC, as outlined above. The information recorded about the patient in the last days and hours of life fell into three broad categories:
-
decisions about future care made with or on behalf of the patient
-
the condition of the patient, actions taken and subsequent outcomes
-
conversations held with and information given to relatives.
Decisions about future care made with or on behalf of the patient
In line with the findings in Chapter 3, ACP and the elements of care deemed appropriate in advance of a patient’s deterioration were features of these records. The most common information recorded was the patients’ preferred place of care and death (72% of cases) and their DNAR status (78% of cases). However, there were interesting differences in the recording of this information between patients who were supported by the LCP and those who were not. In all deaths where the LCP was used to support care, the care home was recorded as being the preferred place of care; where the LCP was not used, this was the case for under half (39%) of cases. Similarly, for the vast majority (97%) of patients supported by the LCP, a DNAR notification or completed form was found in the case notes, whereas this was the case for only just over half (55%) of those patients not supported by the LCP.
These advance notifications were sometimes (although relatively rarely) the result of discussion with the patient; more usually they were a result of discussions with relatives and were often represented as best interest decisions made by GPs and nursing home staff. They could be documented within specific forms (e.g. advance care plans, GSF ‘Thinking Ahead’ or ‘Allow Natural Death’ forms) and/or recorded directly in the notes, for example ‘No hospitalisation’ (SNA2R04) or ‘Not for hospitalisation’ (SNB1R01); ‘for tender loving care in the home’ (SNA1R01); ‘discussed with her sister . . . Not for Resuscitation’ (as part of admission details SNB1R05); or, simply, ‘DNAR’ (NNB6R03).
The main purpose of documenting this information seemed to be to ensure that decisions made in advance of end-of-life care were clearly articulated and accessible to all staff to prevent admission to hospital in the event of further deterioration, or inappropriate life-saving interventions being undertaken in the event of cardiac arrest.
The condition of the patient, actions taken and subsequent outcomes
In the main, regardless of whether the information was documented on the LCP or within the nursing home notes, a major focus of these written records was to record the physical condition of the patient, the care that was delivered in response to this and any subsequent outcomes.
Where the LCP was used to support care, the process required that a series of desired outcomes for patients be regularly assessed (either 4-hourly or 12-hourly) and documented as either ‘achieved’ or ‘variance’. Where outcomes were achieved, it was usual for a staff member to simply insert ‘A’ in the document. The recording of ‘variance’ should have prompted further explanation, although this was relatively rare. The outcomes to be assessed included whether or not the patient had pain, agitation, respiratory tract secretions, nausea and vomiting or dyspnoea. In addition, they included an assessment of whether or not the patient had discomfort resulting from pressure sores, dry mouth, poor micturition or bowel function as well as psychological and emotional distress.
Where the LCP was used to support care, variances were recorded for agitation, respiratory tract secretions or pain. The most common action taken in response to these variances was the use of medication, namely midazolam, glycopyrronium (or hyoscine) and morphine (or oxycodone or diamorphine), respectively. The outcome recorded following the administration of medication was generally that the patient was more comfortable and settled.
SNA3R01 – 23.30: [patient] looks agitated. Action: Injection of midazolam 2.5 mg, s/c given (@23.35). Outcome @ 24.00: Settled well.
SNA2R01 – 06.30: awake and restless. 10 mg midazolam and 10 mg morphine sulphate given. Peaceful and asleep (@ 07.30).
10.30: awake and in pain. 10 mg midazolam and 10 mg morphine sulphate given. Settled and asleep (@ 10.50).
21.00: looks in pain and calling out. 10 mg midazolam and 10 mg morphine sulphate given. Comfortable and slept now (@ 22.30).
Where the LCP was not used to support care, information about the condition of the patient and action taken was recorded as an ongoing narrative within the nursing notes. Although the focus was again on the physical, much more emphasis was placed on summarising the general condition of the patient and any resultant actions and outcomes. Phrases such as ‘All care given’ and ‘TLC’ (tender loving care) were much in evidence within these narratives. Attention was paid particularly to recording staff attempts to administer food and fluids, undertaking regular mouth care, and washing, changing and repositioning the patient.
Day 1 – night: continues to be restless and agitated, pulling everything away. Repositioned, Fluids taken, monitored via fluids chart. TLC given. Medication taken.
Day 2 – 13.05: General condition very poor. Agitated at times. Fluids taken better today using syringe. Dressing to shoulder clean and intact. Cream applied to sore legs and tubi grips. Repositioning regularly. TLC given . . .
Day 2 – night: Continues to be agitated. TLC given. Fluids taken well, please monitor output.
Day 3 – 13.40: Remains very frail. Refused drink and meals. GP visit booked re agitation. Visited by wife. Dressing to left shoulder changed. Skin condition very poor – cream applied and tubi grips to his left. TLC given.
Day 3 – night: All care needs attended to. Very frail. TLC given. Agitated and restless.
Day 4 – 13.40: Poorly, extremely frail. Very thin, writhing in pain. Taking very little fluids or food. Toileted. Repositioned. All care. BP 106/63.
Day 4 – 16.00: General condition very poor. Vomited x3 yellowish secretions – all care given. Washed and changed. Pulse very weak.
Day 4 – 19.15: At 19.15 passed away. Family informed. Doctor contacted – phoned back – is coming shortly.
SNR2R08
In non-LCP notes there were some examples of ‘extended narratives’ which tended to focus on issues or outcomes that either were contrary to those planned or involved important events or some negotiation with outside agencies.
SNB2R10, 09.05 @17.15: [name] from [hospice] visited this afternoon and set up the syringe driver for [patient]. Rang the surgery and asked to speak to [GP] for a prescription for medication to replenish the driver tomorrow. [name] from the surgery said that I could not speak to the doctor as he was running a clinic. I left a message with her for more medications and drug administration charts. I asked her to fax the chart, gave her our fax number but she said that she might not fax the document but keep it in the surgery for [home] to collect in the morning. I explained the importance and she said she will do her best to fax it through.
SNB1R04 – 15.00: At 13.00 he was sitting in an armchair, suddenly heard a big sound and found him lying on the floor. Examined, no injury or bruise noticed. Assisted him to bed, made him in a comfortable position. Informed to IMCA about the fall (left voicemail) because no next of kin. Requested for a GP visit, seen by [GP name] advised to keep him in close observation. NOT For Resuscitation or Not for Hospitalisation. Needs to refer to Palliative Care Team. Made him in a comfortable position.
Reports of communication with relatives
The recording of information relating to what was communicated to relatives and patients in the last days of life was generally limited regardless of the type of documentation used. Patient notes were more likely to capture whether or not communication had occurred rather than the content of that communication or the relatives’ response to it. There were three types of recording in the patient’s notes: (1) a minimalist record asserting that relatives had been informed or were aware of some aspect of the patient’s care; (2) a more fulsome discussion of a more complex situation connected with the patient’s care and its communication to the family; and (3) the reporting of disagreement between staff and relatives and the outcome of that disagreement.
A minimalist record asserting that relatives had been informed or were aware of some aspect of the patient’s care
Although the responses of relatives might have been absent in the case notes, nursing home staff commonly reported assertions about what relatives understood about the patient’s state of health.
Family visited and they are well aware of his deteriorating condition.
SNA3R04
Family know about his condition.
SNA3R07
Spoken to son, aware of condition.
NNA5R10
In the non-LCP documentation, the data in which we were interested were recorded in the ‘daily report’. As with the LCP documentation, there was rarely much detail about the content of conversations. The most common report was that the family had been ‘informed of’ the patient’s deteriorating condition or care. In common with the LCP documentation, the families’ responses were not recorded.
Relative is being brought completely up to date with all the information.
SNB2R01
Patient appears very frail, not responding to call, laboured breathing, informed doctor for a visit, informed her family.
SNB1R01
She is nursed in bed at present to gain strength. Family aware of new plan of care.
SNA1R04
Still agitated and a little bit bubbly. Syringe driver put up. Family informed.
SNA1R01
Relative informed of decision to commence LCP. Will contact if any deterioration.
NNA5RO7
A more fulsome discussion of a more complex situation connected with the patient’s care and its communication to family
On occasions there was a more detailed account of a discussion about a patient’s condition and how certain decisions had been reached.
Repeated to the family how patient’s general condition is and the pressure area which is being monitored as per care plan. Both are aware that due to her deteriorating the area will start to break down and they are aware of this. Had a care plan discussion. N.O.K [next of kin] would like nature to take its course. Relative would like her to just fade away naturally. Also she would like patient not to be resuscitated in case of illness or near death. Both N.O.K. are appreciative of how the staff look after her well. Therefore, she is to be left to be looked after in a place she’s familiar with than the hospital.
SNB1R05
However, the views of relatives on certain aspects of the patient’s care at the end of life were clearly seen as important. The possibility of admitting a patient to hospital at the end of life, and associated issues such as resuscitation, often prompted extensive recording in the notes.
Spoke with relatives regarding the patient. They are concerned that all care should be given to her. We discussed them coming to the meeting on Thursday to give their point of view on the plan for the future for the patient. Should we send her back to hospital if she stops drinking? She is not taking anything except what is being syringed. I explained her quality of life is poor and that she may not recover from this last illness. Relative said no one explained it to him properly – he just wants the best for his mum and for her not to be in pain.
SNB1R03
The reporting of disagreement between staff and relatives and the outcome of that disagreement
Regardless of whether or not the LCP was used to support and document care, where more detailed narrative was found it was often the case that the views of staff differed from those of the relatives. Almost certainly, reports of differences of opinion and how these were resolved were, by their very existence, important. In almost all of the examples identified, the staff member writing the notes emphasised that the views of staff had been over-ridden by a family member’s view. Occasionally, the notes explained why the staff over-rode the views of family members.
Catheter removed at 8:30am. [GP] visited at 12:30 noon. Family were present & discussed with family. [GP] called up & informed that family want re-catheterisation for [pt]. Doctor explained to daughter about the complications, but still they want to do it. Doctor prescribed ‘for catheter’, awaiting catheter from chemist.
SNA2R10
Her son said that she wasn’t like this before. She used to laugh with the nurses when she was in [name] hospital. He suggested to stop her medicines like what he did before, but I said we can’t and won’t do unless advised by the GP.
SNA1R06
In the following examples, the importance of recording something that had been offered but refused becomes clear when the outcomes are serious.
According to NOK [next of kin], patient does not want to go to hospital as she had a bad experience in hospital last December. Ambulance crew wants to take the patient to hospital and spoke to NOK, who strongly disagreed hospital admission. Informed GP over the telephone. DNAR in place. Patient became unconscious at 13:10 and passed away at 13:20. Family advised at 13:30.
SNB1R07
Son was given an option to move his mother to different room (with overhead hoist) but refused. Wants his mum to have comfort of her own room which she knows and feels secure in it.
SNB2R03
On occasion, the views of the relatives were at odds with those of the doctor regarding the decision to hospitalise the patient at the end of life. Again, more extended narratives illustrated and formally documented divergences in opinion, or outcomes of that divergence.
Dr called to confirm to the family re: hospitalization but relative decided – only TLC + stay in the home- came to sign ACP.
SNA1R09
Patient was breathless and wheezing from 7am. Doctor was informed about her condition and also her relative. As per relative, patient doesn’t need any more hospitalization, instead would like to leave her comfortable in Nursing Home. Dr had a chat with daughter and decided to give symptomatic care.
SNA2R04
Deteriorating, family do not want any intervention just TLC. No resuscitation.
NNA5R07
Summary
There were few differences in the demographic make-up of patients whose care was supported by the LCP and those whose care was not. However, it was interesting that people supported by the LCP were much more likely to have their preferred place of care documented and to have a DNACPR in place.
The LCP was designed to support the delivery of care by requiring health-care professionals to regularly assess a series of desired patient outcomes and to take action if any of those outcomes was not ‘achieved’. The structure of the document and the process for documentation within it means that extended narrative is encouraged only in the recording of ‘variance’. Here, staff are expected to highlight where a goal of care was not achieved to illustrate what action was taken and what the subsequent outcome of that action was on the goal of care. In addition, the reporting of variance is encouraged if the patient is found to be in discomfort between the regular assessment times. This is very different from the standard non-LCP approach to recording, which encourages an ongoing narrative approach to the documentation of all relevant information. Thus, although the information recorded in both the LCP and the non-LCP documentation was primarily to do with the physical condition of the patient, the focus of interest was quite different. The LCP narratives were found predominantly for three symptoms (agitation, respiratory tract secretions and pain), the medications used to alleviate them and subsequent outcomes for patients. The non-LCP narratives, in contrast, focused less on symptoms and medications, and more on the delivery of basic elements of care, such as support with eating, drinking, mouth care, repositioning and pressure-area care.
There were few notable differences, however, between the LCP and the non-LCP documentation of communication with families about a patient in the last days and hours of life. In general, the notes were characterised by limited detail and a reliance on unsupported assertions. In situations where more detailed accounts were in evidence, these appeared to reflect the complexity of a patient’s circumstances or a divergence between staff and a patient’s relatives.
Many of the clinical and administrative uses identified by the NMC in their guidance on record keeping were present to a greater or lesser extent in the documentation analysed in this study. Although many professional bodies have issued guidance on how to maintain good records, the evidence suggests that practice is hugely variable. In 1995 the Audit Commission published the results of its study of record keeping in NHS hospitals in England. It reported that records management was given a low priority and that there was a lack of awareness of the importance of good record keeping. It also found that there was a tendency to treat records as personal rather than as corporate assets. 61
Although the Audit Commission study reported in 1995, it would seem from an analysis of the last 72 hours of a patient’s life in nursing homes that not much has changed. The highly selective nature of what was recorded in the notes suggests that the information that was recorded was believed to be significant. There are a number of possible interpretations; for example, it is possible that once a patient has been identified as dying the significance of how much and what gets recorded shifts. The type of issues that were extensively reported might suggest that once a patient is dying the staff focus more on providing justification of events that have happened, are about to happen or might happen in the future. We return to this later in the report after analysing the observational data.
Chapter 5 Nursing homes: observations and case note analysis
Introduction
A major feature of this research project was the undertaking of observations of care provided to patients in the last days and hours of life. This provided the researchers with direct access to care at the end of life as opposed to the self-report present in interviews and the record of care provided in patient records. However, as previously discussed in Chapter 2 of this report, in the context of end-of-life care conducting observations was challenging both for relatives and staff and, potentially, for patients and researchers. Informal observations were undertaken and recorded in field notes, and these field notes form the basis of the analysis presented in this chapter of the report. In addition, in this chapter we examine how the corresponding observational periods were recorded in the patient’s notes.
Findings
A total of eight observations were undertaken in nursing homes: six in the north-west and two in the south-east. In all of these observations, the LCP was used to support the care of the dying patient, regardless of whether or not the home in which the death occurred had been recruited to the study as a LCP-using site or a non-LCP-using site. In addition to the LCP documentation found in the case notes for this sample, there was evidence of GSF documentation in some of the patient files. The absence of any deaths for which the LCP was not used makes it impossible to draw a distinction between care supported by the LCP and care not supported by the LCP. These results do, however, highlight the influence and limitations in practice of the LCP.
It is common to identify the nursing home as the place patients call home. This is often based on a lengthy period of residence during which the patient’s physical space has acquired layers of personalisation and is accompanied by the development of friendships and social relations with staff and other patients. Two patients in the nursing home observations had been discharged directly from hospital to the nursing home in order to receive palliative support. This was the first time that they had been in the home and their rooms did not contain any evidence of the lives they had lived. Table 6 shows how long each of the patients had been in the nursing home prior to their death, along with other relevant demographic information.
| Patient ID | Length of residency to death | Age (years) | Gender | Ethnicity | Religion | PPC | DNACPR | Time from recognition of dying (LCP started) to death |
|---|---|---|---|---|---|---|---|---|
| NNB6P1 | 2 years 6 months 3 days | 95 | F | White British | C/E | Yes | Yes | 45 hours 20 minutes |
| SNA1P1 | 7 days | 86 | F | White British | C/E | No | No | 63 hours |
| SNA1P2 | 13 days | 90 | F | White British | C/E | No | No | 63 hours 45 minutes |
| NNB6P2 | 4 months 26 days | 90 | M | White | R/C | Yes | Yes | 46 hours 30 minutes |
| NNB4P1 | 28 days | 81 | M | Not documented | C/E | No | Yes | 68 hours 15 minutes |
| NNA2P2 | 13 days | 93 | F | White | R/C | Yes | No | 22 hours 30 minutes |
| NNA2P3 | 2 months 30 days | 94 | F | White British | Christian | Yes | Yes | 29 hours 10 minutes |
| NNA2P1 | 1 year 6 months 24 days | 70 | F | White British | R/C | Yes | No | No time of recognition of dying recorded |
Four of the eight patients in the homes were sharing a room with another person with whom, at least in the first instance, they had no previous history or connection. Assessing the impact of death in a shared occupancy room was beyond the scope of this study but it is worthy of further investigation. Patients in these observations were observed over a period of time ranging from 1 day to 8 days. The majority of patients died in the evening or in the early hours of the morning. Two patients died in the late morning.
In the following analysis we combine the data from the observations with the data from all of the relevant available patient notes. It is important to highlight that although all of the case notes analysed included the LCP, the documentation relating to its use was completed in different ways by different personnel in different sites. In some sites the LCP documentation was completed in addition to the usual nursing home charts and recording systems, while in others all documentation had been replaced by the LCP documentation. The analysis focuses on care that starts from the point at which the LCP is introduced and ends with the patient’s death. What happens following a patient’s death in terms of the preparation of the body for viewing and the body’s transfer by undertakers is beyond the scope of this report.
The staff involved in the care of the patient
All of the nursing homes employed a combination of qualified registered general nurses (identified as nurses in the analysis) and health-care assistants (identified as carers in the analysis) to provide care. In the majority of cases health-care assistants, sometimes aided by a qualified nurse, undertook the physical care. Nurses were responsible for monitoring the patient and for administering medication. In all cases but one, a visit by the GP was either observed or mentioned to have taken place during the observational period.
Patient’s level of consciousness
All of the eight patients in the observations were reported by staff to be semiconscious, unconscious or comatose and none of the patients was reported to have capacity to consent to take part in the study. However, while recognising that the patient’s consciousness might fluctuate, and that some of the drugs being administered might interfere with capacity, the researchers observed interactions which suggested that there were was a higher level of consciousness in seven of the eight patients. The issue of consciousness was an interesting and important one.
From a research perspective, it raised issues of informed consent. The researchers had been informed that the patients lacked capacity to understand and discuss their participation in the study and so approval to observe their care had been negotiated with consultees. However, researchers became uncomfortable with this approach where they developed a sense that the patient was neither unconscious nor completely without capacity. In these circumstances the researchers took the opportunity to let the patient know who they were and the purpose of their presence. In all of these cases the patients were asked whether or not they were willing to be involved in the research. The research team discussed this issue of fluctuating or diminishing capacity both as a research challenge and as a research finding.
There were no formal assessments of capacity or consciousness observed. As the patient’s body became weaker as they approached death, different staff appeared to view the patient’s state of consciousness in different ways. Being ‘rouseable’, responding to loud voices and opening eyes were all seen as important indicators of consciousness and were noted as such. However, the existence of these indicators did not appear to fundamentally change how patients were viewed by staff. In the excerpt below signs of consciousness were considered important enough to be reported to the nurse in charge (NIC), although, interestingly, the subtle signs thought to be important by the carer were not recorded in any of the patient’s documentation for that time period.
Day 1;
00:00 Two carers come in to the patient’s room to check whether his pad is dry. After they have turned the patient, one carer says to the other ‘he opened his eyes when we turned him, so I will report this to [name of nurse].’
NNB4P1ON
Consciousness appeared to play a role in decisions about whether or not to undertake some aspects of care. On occasions patients were checked and left on the basis that they were sleeping, while on other occasions patients were checked and provided with care on the basis that they were unconscious. However, patients defined as unconscious were observed to respond to the care being provided with facial gestures, with noises or verbally. This variability associated with defining someone as sleeping or unconscious was reflected in the notes, as will be seen later, where within a short space of time a patient could be reported as deeply asleep, semiconscious or unconscious depending on who was recording it and the circumstances under which this was done.
It seemed that a number of things followed from the presumption that the patient was unconscious or lacked capacity. Rarely were patients accorded any sense of agency. All staff were observed to tell the patient what they were going to do and were doing in terms of the provision of care, but the patient was rarely offered choices or asked questions. This approach was in contrast with that of relatives, who, as will be seen later, despite lacking a clear understanding about the patient’s state of consciousness, were more likely to ask the patient questions and to respond to the answers given.
Defining a patient as semiconscious or unconscious appeared to change the way in which the ‘body’ was viewed. Lacking consciousness appeared to allow some observed behaviours to remain unquestioned and unexplained by both staff and relatives. In the excerpts below, the patient appears very unsettled, but neither the relatives nor the staff respond in any way.
Day 1;
15:09 Patient’s hand comes up and briefly tries to hold the cot side, and then falls back on her bed.
NNA2P2ON
Over the next few minutes these actions are observed a further three times, and then some time later:
16:01 Nurse knocks and comes into the room and looks at patient holding on to the cot side. She moves away from the bed and says ‘Do come down and get me if you need me’ and leaves the room at 16.02
16:23 Patient’s head moves left to right on the pillow briefly.
NNA2P2ON
Although it is clear that the patient’s movements here are observed, neither the staff nor the relatives question the movements or seek to understand them; they are simply witnessed by all around the bedside. While the uncharted nature of dying and death often seemed to leave relatives uncertain of how to interpret what they saw, for staff it was as though the patient’s very status of being unconscious put certain things beyond the need for comprehension.
In another observation the researcher had been informed that the patient was conscious but unable to consent due to dementia. However, on several occasions throughout the observational period this patient appeared to possess capacity.
Day 1;
15:12 Patient has just made us all roar with laughter as he’s just pretended to be dead – patient stopped breathing and stopped blinking with his eyes opened and then when he saw the expressions of alarm, he stopped doing it and grinned. Attending family say that he is always ‘doing mischievous things’.
15:45 He says he doesn’t want to sleep when his relatives ask him
Day 2;
09:12 Suddenly patient opens his eyes and looks over to me [researcher] indicating by lifting his hand to his mouth that he wants a drink. There are no sounds of a nurse or carer so I get up and give him the beaker of juice and watch as he drinks two large swigs.
Day 3;
13:00 The relatives say ‘he can hear us’ they think but is too weak to respond.
NNB6P2ON
Similarly, in SNA1, the patient was described as ‘not conscious’, ‘a bit responsive’, and ‘as though she is in a coma’.
Day 1;
15:20 Relative says ‘There’s nothing going on right now, patient is just lying there. She’s not conscious’.
16:00 Nurse comments that patient ‘is a bit responsive’ when they speak to her
16:45 Relative takes a telephone call. He describes patient’s condition saying ‘She’s not doing anything, her eyes are partially open, it’s as though she is in a coma’.
SNA1P1ON
From the observations it was difficult to assess what staff and relatives meant or understood by someone being unconscious. The relative above continues to talk to the patient and hold her hand, as do the majority of friends and relatives attending the bedside. While it was clear that the patient’s body was failing, there was uncertainty over whether or not the patient could hear or what might be going on in the patient’s mind. Certainly from the activities of the staff the patient’s identity seemed to have been merged into the deteriorating departing body.
Nowhere was this clearer than in the conversations that were had over and within the vicinity of the patient. There were many instances in which, in the presence of the patient, conversations took place involving staff and the patient’s relatives which were about the timing of the patient’s death or the disposal of the patient’s body following the patient’s death:
Day 1;
14:20 (Carer): ‘I don’t think it will be very long, she is very cold to the touch’.
14:40 Nurse to doctor: ‘Her condition has changed twice this morning. I would say she is worse.’
15:00 Relative tells me that that doctor said patient ‘was likely to pass away today, or later on’
15:32 Relative to researcher – Do you know anything about that love?
Researcher – I ask ‘What’s that?’
Relative says ‘Nurse rang yesterday and asked if we wanted her cremated or buried.’
Relative then goes on to discuss his conversation with the undertakers and a non-refundable deposit is mentioned.
16:51 Relative says ‘Doctor says it could be ages, at least she is not dying on her own.’
19:20 Nurse to researcher: She has about another 12 hours.
NA2P2ON
Day 1;
20:50 Carer – ‘She will not pass this night’
21:12 Carer – ‘She is not going to pass away tonight. Normally when patients are close to the end of life, it is 8 or 9 breaths per minute so this is okay’.
SNA1P1ON
In all of the patient notes there were references to the patient’s state of consciousness. The initial assessment recorded on the LCP documentation was always completed, but there was no accompanying evidence to suggest how decisions were made about the states of consciousness that were recorded. Moreover, and notwithstanding that a patient’s condition changed over time, the attribution of different states of consciousness sometimes appeared contradictory.
The documentation completed for SNA1P2ON/CN reported, in different records on the same day, that the patient was semiconscious, conscious, able to communicate and comatose. Similarly, the case-note record for SNA1P1ON/CN records the patient as being comatose and unconscious, and as illustrated in the earlier quote, relatives described the patient as both ‘not conscious’ and ‘as though she is in a coma’. However, a nurse was also heard to report to another carer during the same 90-minute period of the observation that the patient was ‘a bit responsive’. In another site, NNB6P2ON/CN, one set of notes reported a patient as not confused, only for another set of notes at the same time to report the patient as confused.
These reporting differences were interesting in the light of the observations. Although patients’ conditions were observed to fluctuate during the observational period, these were usually minor and on the whole patients declined over time. Clearly any intrusive assessment of consciousness would have been inappropriate for these patients at the end of life. However, it is important to consider whether or not accurately assessing an individual’s consciousness at the end of life is important. This will be discussed further in Chapter 14.
Physical decline and prognostication
Although assessing consciousness did not appear to feature in the nursing home setting, there was an emphasis on monitoring and assessing the physical decline of the patient’s body. This was evident in the monitoring that was conducted by nurses, and to a lesser extent, by health-care assistants. The following extracts reflect the emphasis, particularly by nurses, on recording the pulse rate and the number of breaths the patient took per minute.
Day 6;
20:25 Nurse feels the patient’s right wrist and looks at her watch and her [the patient’s] chest and seems to be counting.
NNB6P1ON
Day 1;
18:00 Nurse: ‘I just want to check your pulse’. She checks patient’s pulse by feeling on the wrist and watching the clock [sic] attached to her top. She comments to the carer ‘It’s 74’
20:50 A new nurse enters the room. She is carrying blood pressure equipment. ‘Hello, I’m (name of nurse). I’m going to take your blood pressure now, OK?’
21:12 Nurse pulls out her mobile phone and stands next to the patient, after a minute she says ‘She is doing thirteen breaths per minute’.
SNA1P1ON
Day 2;
09:50 Another carer comes in and feels patient’s forehead and calls her name very softly. The patient wakes up.
NNA2P1ON
Although the nurses and carers had no influence on the time of death, there was a strong emphasis on monitoring the patient’s deterioration so that the death could more precisely be expected. As can be seen from the previous quotes, staff identified time frames within which the death could be expected. In general, where this was observed to occur the staff were accurate in their predictions. The counting of a patient’s breaths became such a strong feature of nursing visits in the last hours of life that the researcher (with no clinical background at all) also began to record the patient’s breaths.
Although there was a strong emphasis on identifying how close the patient was to death, there remained a focus on care up to the point at which the patient actually died. In some homes the use of hourly charts, which ran alongside the LCP, reflected the intensity with which patients were checked and the importance that was attached to preventing pressure sores. In one case a pressure-relieving mattress had developed a fault which meant that it was not inflating/reinflating as it should have been. The staff decided to swap this mattress with one they knew to be working (SNA1P2ON). This activity involved three staff – two health-care assistants and a registered general nurse – as well as the researcher. The patient died 2 days later.
Provision of physical care
The major focus of all care for the patient was the maintenance of the body’s integrity. Containing leakages, smells and preventing further deterioration of the skin maintained the boundaries of the body. Maintaining the bounded nature of the body was conflated with keeping the patient comfortable, with the provision of care almost always being announced by carers as: ‘We are going to make you comfortable’ (e.g. NNB4P1ON). At night this verbal introduction was also accompanied by the lights being switched on fully:
Day 1;
22:05 There is a knock at the door and two carers come into the room. They switch on the overhead light which startles me [Researcher] but the patient does not react, the resident in the next bed can’t be seen.
NNB6P1ON
This emphasis on ‘keeping the patient comfortable’ and keeping the body bounded translated into three activities:
-
assessing pain, agitation and other symptoms
-
ensuring that the patient was clean, dry and turned
-
maintaining hydration and keeping the mouth moist.
Assessing pain, agitation and other symptoms
Freedom from pain at the end of life was identified by many of the patients in their advance care plan attached to their LCP documents. The assessment of pain and other symptoms took place frequently in the homes, mostly in conjunction with other activities. This assessment involved both observation and questioning, directed to any family member sitting by the bed and on occasions directed to the researcher when the family had gone home.
Given that carers and nurses made frequent visits to the patient’s bedside, ranging from hourly to 3-hourly during the day, there were many opportunities for carers and nurses to observe changes in the patient’s demeanour. In all cases but one, patients also had relatives and or visitors at the bedside for long periods of time during the last days of life. Relatives were often invited to let staff know if the patient’s condition changed or they thought the patient needed something.
Day 1;
18:35 After a period of silence, friend comments that the patient’s breathing is starting to get bubbly. Relative asks if patient has ‘had another shot?’. Friend responds ‘Not since last night.’ Friend reports that staff have told her that they ‘just need to let the staff know if another one is needed and they can give it’ Friend says ‘It’s just starting now’.
SNA1P1ON
The visible symptoms that prompted either questions of others in the patient’s room or the administration of medication by staff were associated with adjectives in the following four domains:
-
bodily discomfort – agitation, twitching, sweating, unsettled, uncomfortable
-
facial expressions – grimacing and frowning
-
noises – moaning and groaning
-
changes in breathing – rattling, bubbly, rasping, wheezy, chesty and rapid.
However, these visible expressions of the body were inconsistently interpreted and responded to. Sometimes they triggered action, while on other occasions they persisted against the backdrop of staff moving in and out of the room and relatives sitting by the bedside.
Perhaps not surprisingly, the acts of turning and washing a patient often elicited a response from the patient, usually in terms of a noise and facial expressions. Whether or not these were deemed to be signs of uncontrolled pain depended on whether or not they persisted after the patient had been turned or washed. Once they had finished providing care, staff were observed to remark that the patient either had settled or remained agitated. Whether or not medication was administered for patients who remained agitated depended on when the last dose had been given and what the NIC felt was appropriate. Carers were heard to remind each other to report the possibility of the patient being in pain to the NIC (e.g. NNB6P2ON, day 2; 10.35).
There were occasions on which patients appeared to be uncomfortable, moving their arms around, shaking their head from side to side or making movements of their legs under the bed covers. As previously mentioned above, it was not always clear why on some occasions these actions were defined as pain related, while on others they went unremarked. Certainly in a number of observed cases, the labelling of the patient as unconscious seemed to have a bearing on this. In one set of circumstances the NIC made the connection of a patient’s agitation with their having a distended stomach. The patient was catheterised and suppositories were given. As the distension was relieved the nurse reported that the patient became more settled (SNA1P2ON).
In the majority of cases where it was established, through either questioning or observation, that there was a symptom that needed relieving, the patient was given medication, with morphine and midazolam being the most common. The route of administration of these drugs was usually via a subcutaneous injection or a continuous subcutaneous infusion via a syringe driver. A small number of patients who were able to swallow were given oral medication. Over the course of the observations the route of administration was tailored to meet the patient’s requirements; tablets were replaced with liquids, subcutaneous injection or continuous subcutaneous infusion via a syringe driver.
However, there were some instances in which a clear request for help was not followed up because, in the eyes of the person who was assessing, the most obvious course of action had already been undertaken.
Day 2;
22:46 Carer and nurse come in. Nurse asks patient how he is and says gently ‘can I check your pad?’ She feels the top of the inside of it with her gloved hand. Patient groans loudly. Carer asks if he has pain. Patient says ‘Yes’ loudly and with feeling . . . Nurse says ‘I can’t give him anything yet’ to carer. She seems at a loss what to do about his pain. We all remain in silence looking at the patient who twitches and scratches his arms and chest. Eventually the carer and nurse leave the room.
NNB6P2ON
Day 1;
18:00 Patient’s mumbling is comprehensible to her son, who responds to her as she mumbles.
Relative told the carer that the patient did not seem settled. Carer said ‘She’s not settled?’ Carer then addresses patient by stating her name as a question ‘[name]?’ I think I heard patient reply ‘Go away’ but I’m not sure. The carer told the relative that ‘my colleague’ had just topped up patient’s morphine, approximately half an hour ago . . . she moved to the side of the patient’s bed and checked the place where the morphine goes into the patient’s arm. She did not appear to find anything wrong. As she was leaving she re-confirmed that the patient had been given morphine quite recently.
SNA1P2ON
All the homes in the study kept drug charts. These provided the formal means by which the administration of medication, dosage, route and timing of delivery could be tracked. In some of the homes staff recorded a narrative which provided the understanding for the administration of prn medication. The routine administration of drugs, for instance, through syringe drivers once in situ was rarely remarked on unless this had to be changed or additional pain relief was required. The variance sheets in the LCP documentation provided support for the administration of pain relief. In NNB6P2ON/CN the nursing notes record on 1 February 2013 that the patient had become very difficult with medicine and personal care, pushing staff away and becoming agitated. In the LCP variance sheet the nurse recorded ‘when personal care was given, was grimacing and became agitated’. The action was recorded as ‘painkillers given 2.5 mls diamorphine’. The outcome was recorded as ‘settled in about 20–30 minutes and went to sleep’.
Ensuring that the patient was clean, dry and turned
All the staff in the homes appeared to balance the benefits of undertaking an activity with the adverse effects of doing so, for example the short-term discomfort from being turned versus the benefit of relieving pressure on the skin. In the last days and hours of life staff were recorded visiting patients hourly to 3-hourly. There were only a small number of observations in which 4 hours had passed between visits. This was more usual at night. Ensuring that the patient was dry seemed to be a priority. If a patient was wet, pads were usually changed. However, if a patient appeared settled and not wet, staff made a decision on the spot as to whether or not they would do anything. If the patient was judged by staff to be asleep then they would most often be left sleeping. However, if the nursing care plan identified 2-hourly turns or repositioning (NNA2P2ON/CN and NNB4P1ON/CN) due to a perceived risk of skin breakdown, this pattern was usually followed. The majority of patients were being nursed on pressure-relieving mattresses and there were three patients (SNA1P2ON, SNA1P1ON and NNA2P3ON) who had pressure sores they had acquired during periods of hospitilisation, and which pre-dated their admission to the home.
In the majority of cases relatives were asked to leave the bed space while the nurses and carers attended to the patient. This sequestration of the patient’s body by nurses and carers for the purposes of care was a major feature of care at the end of life. Relatives were not asked or encouraged to play any part in this and were frequently heard to ask each other, and staff who came into the room subsequently, what care had been given and how they thought the patient was doing. The patient, however, was always given a running commentary on the care that was being provided and what was going to happen next.
Day 1;
16:02 Nurse comes in and asks the relatives to leave and checks patient’s pad by undoing it and looking down. She remarks that it is wet. She asks patient if he has any pain. Patient says ‘No’ Nurse checks his mouth with a torch and tells him he has a touch of thrush. She says ‘The girls are on their way to change you.’
NNB6P2ON
Day 1;
16:00 Nurse tells carer that patient does not appear comfortable on her back as she is making sounds. They should therefore keep her positioned on her side. Nurse tells this to the patient by leaning quite close to her face and speaking loudly ‘I can sense that you are not comfortable on your back. Don’t worry we will put you back’ . . . While carer is putting cream on patient’s heel, Nurse combs the patient’s hair with a brush. She runs the brush through the patient’s hair and then smoothes her hand over her hair.
Day 3;
13:45 Friend tells me that ‘they have been up and turned her’ I say ‘Oh right and what do they think? She says ‘I don’t know because I had to leave the room’. She does not sound particularly happy that she had to leave.
SNA1P1ON
Most patients were washed at the start of the day and additionally if they had been incontinent of urine or faeces. Although it was common for patients to experience some level of discomfort during the process of being washed and turned, this was rarely anticipated by administering pain relief beforehand. In the following example the carers recognised the need to tailor their care to the patient’s needs but were unable to respond to the patient’s pain.
Day 2;
08:23 Two carers come into the room. One of them tells the patient nicely they are going to give him a wash. She asks him if he has pain and he replies ‘I am hurting all over’. She washes his genitals very gently with a flannel and a bowl of water and then applies some sudocrem [Actavis UK Ltd, Devon, UK]. Carer A leads the washing routine and takes her time before turning him saying ‘Let’s give you time to get your breath back’. Patient is saying aargh aargh, but not too loudly. He asks for 5 minutes and says ‘I’m wet’.
08:35 Carer A says ‘We are going to leave you and come back later’. Patient says ‘Yes. Thanks’. She re-does the pad up and says to other carer ‘We will wait until he has some pain relief.’
08:40 Carer A looks at his LCP chart and says I am going to ask the Nurse about the painkillers.’
At 9:45 another carer enters the room to try and feed the patient with porridge which the patient finds too hot. The carer who has gone off to find out whether the patient can be given any analgesia ascertains that the patient was given something at 5am earlier that morning which means that according to the prescribing regime it is too early for the patient to be given any more. The patient finally gets diamorphine at 12 noon according to the notes.
NNB6P2ON
There was a sense that the work of care dominated activity at the end of life in the nursing home setting. Pain created through the provision of care, although brief, was not uncommon, and this raised questions about priorities at the end of life. That said, the adjectives used by the researchers in their observations of care were overwhelmingly positive; they included gentle, sensitive, kind, quiet, caring and soft.
The recording in the notes of the cleaning and turning of patients was largely restricted in the LCP documentation to whether or not it had happened. Where it had not taken place a rationale was supplied, but there was rarely much commentary in the notes regarding this aspect of care.
Maintaining hydration and keeping the mouth moist
All visits by the care staff involved an assessment of the need for mouth care and usually the cleaning of the mouth accompanied by the application of some sort of lubricant to the lips. Attempts at providing fluids varied, as did opinions on whether or not a patient was able to swallow. There were no recorded swallow assessments in the notes, which helps to explain why the method of providing fluids and the consistency of fluids being tried varied according to who was administering the fluids. Staff used specially designed sipping cups, teaspoons and sponges, and were observed using yoghurt, ice cream and thickened fluids such as tea, coffee, juice and Ribena as well as plain water to encourage hydration.
Views differed on whether or not a patient at any point in time could suck or swallow. In one patient’s case carers were heard to offer a patient some sips of water while being uncertain if the patient could actually swallow.
Day 1;
18:45 Two carers have come into the room to change the patient and clean the patient’s mouth. Carer 1 gives the patient mouthcare telling the patient that she is doing so. She asks ‘Would you like some sips of water?’ and I think the patient says ‘Thank you’. Carer 1 tells carer 2 she doesn’t think the patient can swallow, so she will put some water on a sponge so ‘she can suck’. She does this and comments to Carer 2 ‘See she is sucking’.
Day 2;
12:55 The nurse in charge reports that the patient should not be fed ‘otherwise she might choke’. A point that she repeats at 15.15. This particular patient was reported in the LCP progress notes to have taken a few sips of water at 12 noon on the 06.12.12 because she had said she was thirsty. By day 2 (07.12.12) the notes reflect the nurses’ direction that food be omitted, the reason given that the ‘patient appears to be semi-conscious, unable to swallow therefore oral intake omitted’.
SNA1P2ON
Mouth care was the only physical care task that was occasionally undertaken by relatives, often of their own volition.
Day 1;
18:55 Patient opens her eyes a bit. Relative gets a pink mouth sponge and dips it into the pink liquid on the bedside table and gently rubs it around the patient’s lips.
NNA2P3ON
Day 2;
14:50 After a while friend stands up and walks round to the side of the bed. She comments on how the patient’s lips ‘appear to be very dry’. Relative stands up and moves to the dresser where the mouth care sponges are . . . friend runs the sponge over the patient’s lips a couple of times.
SNA1P1ON
Mouth care, although considered to be important by both staff and relatives, was not always welcomed by the patient. In the following examples patients actively attempted to resist this activity.
Day 2;
13:28 Relative tries to clean patient’s mouth with a glycerine mouth sponge saying that she did this yesterday . . . the patient shouts at her and pushes her away. This upsets her and other relative present who both cry a bit.
NNB6P2ON
Day 1;
22:00 The older carer cleans patient’s mouth with a pink sponge and some pink cleaning fluid. The patient is very resistant, but carer is firm and gets the sponge into her mouth.
NNA2P1ON
Day 1;
19:55 The two carers I observed earlier enter the room. One says ‘knock knock’ and explains that they are going to do some mouth care before they finish their shift. They both say ‘Hello (patient’s name). Can I just clean your mouth? Can you open your mouth for me, please?’ The friend still present in the room says ‘She just closed it, didn’t she!’ and laughs. The carer says ‘She knows what we want to do!’ One of the carers spends a long time cleaning the patient’s mouth. She says ‘This is nice and clean now, see’. She comments that there is some ‘dry skin inside her mouth, on her tongue’. The carer uses two sponges and asks the other carer to get her two more because there is still some dead skin on her tongue. When they are finished, the carers say ‘Thank you (name of patient) and then says ‘See you later’. As they are leaving they ask friend if she would like the door open or closed.
SNA1P1ON
The desire to keep the patient’s mouth moist and clean was explained in terms of reducing the discomfort created by the patient breathing through their mouth. Relatives and staff alike also appeared keen wherever possible to enable the patient to eat and drink for as long as possible. Relatives were often more successful than staff in achieving this.
Day 1;
15:51 One of the relatives tries to get patient to drink the beaker of coffee; patient refuses it, grimaces but then drinks it as relative tells him that he needs to drink plenty of fluids.
NNB6P2ON
However, there was little observed discussion between staff and relatives about the strategy with regard to eating and drinking. Providing food and fluid in the absence of a swallow reflex had the potential to cause aspiration with its attendant consequences. Instances were observed where carers and relatives tried to encourage food and fluids but gave up as they could not be certain that the patient could swallow. In the following example there is a clear uncertainty about the plan for this patient with regard to food and fluids and it is the relative who, as the patient’s condition declines, restricts the administration of food and fluids.
Day 2;
22:13 Carer gently cleans patient’s mouth with oral hygiene sticks and removes a fair amount of food (?) yoghurt from her mouth – it seems to have been pocketed inside her cheeks. One carer says to the other – I don’t know how they can say that she is eating and drinking.
Day 3;
13:00 Relative is giving patient a yoghurt drink which she seems to be swallowing most of.
13:30 Relative finishes giving the patient her drink and sits back from the edge of the bed and sits in the chair. She strokes the patient’s hand. She asks patient if she would like some music on ‘or are you not bothered?’ After a while the patient replies in an audible whisper ‘No, I am not bothered.’
Day 7;
09:42 Carer tries patient with a mouthful of porridge, but she is unable to swallow it and so he has to scoop it out of her mouth, he gives her mouth a gentle clean with a swab. He tries her with a sip of tea, no joy, so he wipes her mouth clean.
09:50 Relative arrives
09:55 Carer pops in again with something, food I think but I can’t see. Relative says firmly ‘No, she can’t eat that’.
15:33 Carer comes in with a yoghurt and a beaker of tea and says to relative ‘Shall I give her some of this?’ relative says ‘No thanks. She won’t be able to take it. Just mouth care from now on’. Carer looks disappointed, nods and leaves.
17:10 Same carer knocks at the door. ‘Do you want anything for patient? Some soup or some ice cream?’ ‘No thanks, she can’t eat or drink now’. Carer stands by the screen and looks questioning. Relative adds ‘People don’t want to eat and drink at the end of life’. Carer says ‘okay’ unsurely and leaves.
NNB6P1ON
Interestingly, despite the strong line taken by this relative on eating and drinking there is no direction to care staff in any of the patient’s notes that the frequent assessment of this person’s ability or desire to take food and fluids should be replaced by mouth care or by keeping the tongue and lips moist.
The lack of a consistent line with regard to providing food and fluids was observed in a number of sites. It was not clear what staff were aiming to achieve through the provision of certain foods, for instance porridge and pureed cauliflower, or whether or not a patient’s reluctance to consume these foods had as much to do with taste as ability. Clearly, as the patient approached death the likelihood of their being able to eat reduced. Given that the staff had identified the majority of the patients observed in this study as either semiconscious or unconscious it was surprising to see the focus on feeding patients.
The notes accompanying these observations did not provide any basis for understanding the goal of feeding or providing fluids. There were contradictory references to the patient’s ability to swallow in the same time period and, as previously stated, there were no formal swallow reflex assessments recorded. The detail of foods or fluids, their type, consistency, quantity and frequency to be encouraged were also absent. On the other hand mouth care was usually identified as hourly or 2-hourly. Sips of water were always recorded in the notes. The lack of a shared understanding, between staff and between staff and relatives, about this aspect of care may be a reflection of the lack of a clearly articulated strategy in the patient’s notes.
The provision of physical care, as outlined above, continued in some shape or form up to the point of death. In one case, SNA1P2ON, the patient was washed at 21.25 having had her bowels open. The carers commented to each other that during this they believed her to have smiled. At 22.27 (about 1 hour later) the patient died. In another case, NNB41ON, the patient was turned at 02.00 and mouth care was undertaken and the patient died about 2 hours later at 04.05. One patient (NNA2P3ON) died within 5 minutes of care being provided.
Interaction with relatives
In the nursing homes the patterning of the physical care outlined above provided the framework within which the dying patient was managed. It also appeared to provide the social framework for the experience of dying by the patient’s relatives. Friends and relatives occupied an ambiguous role in the care provided in the homes. They were both at the centre and the periphery of care. Excluded from the hands-on provision of care they were often left as observers at the patient’s bedside. However, their presence was seen as central, providing a context for the patient’s identity, reconnecting the patient to their past and warding off the potential loneliness of dying.
Staff introduced themselves to relatives and always appeared polite and friendly. Staff were also observed to say goodbye to the patient and any remaining family members at the end of their shift. Relatives were provided with chairs, offered drinks and, in many homes, food (sandwiches, biscuits and cakes). Much like the patients, the relatives were well catered for in terms of their physical needs. Relatives appreciated this and were heard to remark on it to each other.
Communication with relatives varied with the members of staff involved. Staff entered the bed space to undertake physical care or offer the relatives refreshments, but were rarely seen to spend time with the patient and or relatives solely for the purposes of communication. ‘Come and get me if you need me’ (NNA2P2ON) was a familiar refrain from staff as they left the bed space.
As previously highlighted, the sequestration of care of the body by staff was reinforced by the exclusion of the relatives from the bed space while this was taking place. Although there are a number of reasons why relatives may be asked to leave, the relatives were never given explanations. Once care had been given, staff made little attempt to report to relatives what had been done or to tell them anything about how they found the patient’s body. In one case where a patient was turned and then turned back because it had become clear that she was struggling to breathe on her back, the lack of communication between the nurse, the carer and the relative led the relative to ask the researcher what had taken place.
Day 1;
16:00 ‘What did they do? Turn her?’ and I say ‘Yes, they turned her, and washed her mouth, and brushed her hair’ relative looks at the patient and touches her shoulder as he sits down.
SNA1P1ON
Interactions with relatives were rarely recorded in any of the LCP documentation. All homes identified that discussions had taken place with relatives about the patient’s deteriorating condition and that an understanding had been reached that the patient was imminently dying. Where the spiritual needs of the patient involved the administration of last rites or the visit of a local vicar, this was observed to be reported to relatives as well as recorded in the nursing notes.
The role of the family
In contrast with the activity of nurses and carers around the bedside, relatives generally sat around the patient’s bed. Being present in this way took many forms and varied over time. There was only one observation in which a relative (a daughter), who was a nurse, took part in providing some aspects of physical care. This particular daughter acted as a co-ordinator as well as a provider of her mother’s care while she was present. She was observed to initiate and provide care, and in relation to food and fluid administration she decided the point at which these activities should cease. The care she provided appeared to draw on her nursing knowledge and skills as well as her knowledge of her mother.
Day 2;
13:05 Relative puts on the patient’s glasses which are in the bedside drawers. She cleans them and puts them on the patient and says ‘Is that better?’ Patient says clearly and audibly ‘No’ Relative says ‘Let’s keep them on and see if you get used to them’.
NNB6P1ON
Although other relatives were less involved in the provision of physical care, helping patients to drink and moistening the mouth and lips were the activities most frequently undertaken. Monitoring the patient’s condition from a lay perspective was actively encouraged by staff, who would frequently ask the relatives how they found the patient that day.
Day 2;
14:50 Friend comments that the patient’s breathing is starting to sound bubbly again. She moves her head to the patient’s chest and listens.
SNA1P1ON
Some relatives appeared to feel empowered and almost at home in the patient’s room. These relatives also appeared more assertive and familiar with the nursing home staff and routines. Other relatives appeared less certain and more passive. While one set of relatives felt able to adjust the cot sides on the patient’s bed to get physically closer to the patient, another set of relatives worked awkwardly around the physical barrier presented.
Day 1;
18:40 The cot side is down where the relative is sitting which means she can lean over and get closer without being obstructed by the cot sides.
Day 7;
09:51 Relative puts the cot sides down . . . She pulls her armchair up close to patient and holds her hand talking to her, telling her information about people they know.
NNB6P1ON
Day 1;
21:20 Both sisters talk over the patient and each holds her hands. I am struck again by the thought that the cot sides act as a barrier to them getting close to the patient.
NNA2P3ON
In another case, relatives were unable to carry out mouth care for their relative because they were uncertain about how to resolve the lack of oral fluid.
Day 1;
14:55 The family are wondering about his dry mouth. The relative takes the oral hygiene pack and looks at it. There are mouth sponges but no liquid so they don’t know what to do. One of the relatives says ‘I don’t know who to ask’ The other relative says ‘We will ask the nurse when they come.’
NNB6P2ON
The watchful waiting that was observed to characterise the presence of all relatives was interspersed with physical contact and communication. There were no gender differences observed; sons and husbands touched, hugged and kissed the patient in the bed as often as did daughters and wives.
Day 1;
18:15 (Male) relative has been standing at the bedside the whole time, looking at and talking to the patient. Relative held her hand for a while; he commented that this was the warmest she’d been for a while. He repeated ‘Don’t worry, I’m here. I’m here still.’
Day 2;
14:05 Relative says ‘Hello mum, only me, I’m back, you can’t get rid of me that easily’. Relative tells patient about his evening dinner plans and then says ‘Shame you can’t be there!’ Patient shrugs her shoulders and lets out a breath as she relaxes them.
14:20 Her breathing begins to get more irregular and relative says ‘Hello, hello mum.’ Relative continues to stand at the bedside and patient’s breathing becomes regular again. Every now and then relative rubs the top of patient’s right arm with his left hand.
SNA1P2ON
Watching the patient in the bed was punctuated by everyday activities such as reading newspapers and magazines, texting and chatting with other visitors. Occasionally, one of the relatives at the bedside dropped off to sleep. In one instance the breaths of the sleeping relative overlapped with the audible breaths of the patient.
Day 1;
16:45 Relative sits back down and continues to read the magazine. He taps along to the music on the radio. Relative puts down the magazine and looks at his mobile phone . . . Relative texts on his phone, every now and then glancing at the patient.
SNA1P1ON
There were few conversations around the bedside that reconnected the body of the patient with the life that had been lived. Occasionally, visitors appeared. The stories that were told in these circumstances located the visitor’s position in the patient’s life, projecting into the room a character and identity no longer recognisable as the patient in the bed. On these occasions the body in the bed was brought to life.
Day 3;
11:40 The dinner lady walks into the room and says ‘I’ve bought a visitor’. An elderly lady walks in. Conversation continues between the friend who is at the bedside and the new visitor. The new visitor says she’s one of those people who is a good friend of the patient and who could not cope with her deteriorating condition.
They share stories about the patient and the new visitor says ‘I’ve been a terrible friend over the past few years’.
12:00 The new visitor says to patient ‘I must love you and leave you. Thank you for everything you have done over the years.’ She strokes the patient’s hair. She stands up and kisses the patient. When she turns to leave I see she is crying.
SNA1P1ON
Day 2;
16:17 A woman wearing a winter coat enters the room. She tells me that she is the patient’s neighbour. After a moment neighbour stands up and walks to patient’s bedside. She says ‘name of patient’. Patient opens her eyes and appears to look at her. She says ‘It’s (neighbour’s name) . . . she pulls up the comfy chair so it is angled away from me and towards the patient’s face. After several minutes she turns to me and asks me if she has ‘been breathing like this all the time you’ve been here?’ A number of other questions follow about whether the lighting is left on and whether the patient is more comfortable today than yesterday.
16:40 The neighbour continues to sit in the chair watching the patient . . . She told me that she wouldn’t be staying long, she just wanted to sit with patient for a bit. She said ‘There’s no point talking to (name of patient) because she can’t hear, although that’s one of things we don’t know, how much they take in . . . She says ‘But I got a smile . . . so.’
SNA1P2ON
Although it was rare for patients to receive visits from people other than relatives or religious leaders, it was the case that some of the patients had friendships with other residents in the home. However, staff were rarely observed facilitating visits from other residents, with one exception that was notable because the visit was facilitated only once the patient had died.
Day 8;
12:58 Following patient’s death the nurse asks the relative if the patient’s best friend in the home can come in and say her goodbyes. Relative nods.
13:03 I follow Sister to patient’s best friend room. Sister sits best friend down in a chair and explains gently but clearly that patient has just ‘passed away.’ Best friend is really upset and cries and says ‘Can I see her? She’s my best friend’. We go to patient’s room and best friend says her goodbyes tearfully to patient’s body.
SNA1P1ON
The failure to support social relationships where they existed between the dying patient and other residents in the home reflects the common concern of the nursing home staff with the patient’s body rather than with ideas of the patient’s personhood.
The notes were largely silent on the role of the family in care at the end of life. Occasionally the notes referred to the presence of a relative or relatives at the bedside, but more often than not the relatives were absent from the records. They were identified in the notes in terms of next of kin details and whether or not they wanted to be contacted during the night should the patient die, and reappeared in the notes following the patient’s death.
Managing the environment
Although the physical care of the patient received considerable attention from staff throughout the observations, much less attention was paid to the management of the physical environment. In particular, temperature control and noise control were inconsistently managed.
Although carers and relatives were heard to pass comment on the temperature of the patient’s room, most frequently that it was too hot, this rarely resulted in any action. Only once was a window observed to be opened, and once a fan was switched on. However, staff did respond when the environment appeared to have a more direct bearing on the patient. On one occasion, during an observation, the researcher noticed the sun streaming in through a window directly onto the patient. Subsequently, while the researcher was out of the room, action was taken by one of the carers to remedy this.
Day 2;
14:55 When I walk in carer is pouring some water from the jug on the tray stand into a glass. He puts the glass down on the tray. I see the curtain is drawn and he says ‘I’ve just pulled the curtain because the sun was shining’ and he gestures on to his face.
SNA1P2ON
Adjusting the environment to suit the patient at the end of life is difficult because it is not easy to discern what the patient may like. Relatives and staff reported that at the very least they thought that patients were able to hear. As a result, attempts were made to talk to the patient. The use of background music, the radio and the television were in evident in all homes. However, this was not always regulated or tailored to the individual in the bed.
Day 3;
24:11 Carer comes in with a CD player and starts a CD of an Irish male singer, but as he’s singing about dying she switches it off, a bit embarrassed and says ‘I’m not sure it is appropriate’ and leaves.
Day 4; Irish male singer CD playing in the background.
Day 7;
10:55 Relative gets up from chair and puts on music – She shows me the holder it is Handel’s water music. No obvious reaction from patient. Relative sits and strokes patients [sic] hand and forearm.
14.40 Pan pipes are playing in the background.
NNB6P2ON
Day 1;
15:00 Friend reports that the reception is quite poor and that she had had to tune the radio into a number of stations before she found one that would stay on without fading . . . Relative says he will keep radio on. The friend said something like; she liked to dance. The relative now remains on his own sitting with the radio on his lap, changing the station regularly until he finds a song, listens to it and then when it ends switches to another station. After doing this twice he settles on one station.
18:35 When friend arrived, straight after the relative left, friend switched the radio off. Friend reported that it was competing with the TV that was on in another room.
Day 2;
14:50 The radio is on, tuned into a radio station playing what I would describe as light hits from the past. The song currently playing is ‘Ground control to Major Tom’.
SNA1P1ON
Staff often reported, as they switched a radio on, that they liked to have music on in the background to foster a sense for patients that they were not alone. However, as the researchers sat observing, they recognised the incongruence of what was frequently being broadcast; for example, Karen Carpenter singing ‘Top of the World’ might have been difficult for patients to relate to. The unremitting nature of the radio textured the physical space like ever-changing wallpaper, at times soft and inviting and at other times loud and intrusive.
As identified at the beginning of this section, only a few patients were being nursed in a single-occupancy room. Inevitably, the sharing of a room with a person who was dying required some management and this usually took the form of taking the other resident out of the room during the day into some communal space elsewhere. There were times during which the resident sharing the room had visitors who congregated at their bedside.
Day 1; Patient in next bed – relatives of other patient gathered around bed.
16:02 Patient A in next bed clears her throat behind the curtain.
18:05 Patient A is now not in the room and her curtain is drawn back.
19:05 Patient A goes back to bed.
NNA2P2ON
Day 1;
19:10 The other family are talking to patient in next bed in very loud voices drowning out any conversation between patient’s family.
NNA2P3ON
The management of noise elsewhere within the home was hugely variable. The noise of the television emanating from other residents’ rooms, the sounds of patients being escorted from one location to another, and the everyday domestic noises of cleaning and pots and pans, cups and saucers all penetrated the rooms in which people were dying. It is not possible to say what impact, if any, these sounds had on patients; patients rarely appeared to react to them directly. There was only one instance in which the researcher wondered if a patient was affected by noises emanating from outside the room.
Day 2;
13:00 Patient moves left arm out from the blanket. She moves it around for a very short period and then rests it back down. She has begun to make short grunting noises irregularly, or perhaps they are better described as short moans. She seems to react to sound and there are a variety of sounds coming from outside the room. The door is propped open and I can hear a couple of people talking, things being moved about etc. At 13.10 the call bell begins to sound in the Nursing Home. Almost immediately the patient groans and begins to move both of her arms although she does not lift them very high off the bed. This stops after a few moments although the call bell continues to sound and I wonder if the two events . . . are related?
SNA1P2ON
It was interesting that one of the cleaning staff, in acknowledgement of the patient’s imminent death, used a dustpan and brush rather than the vacuum cleaner to clean the patient’s room.
Day 7; The cleaner is using a brush and dustpan on the whole of the floor. She says ‘It’s not fair to use a hoover.’ The relative sits on the edge of the bed so that the cleaner can do under the armchair.
NNB6P2ON
Although the nursing gaze was largely focused on the body, the caring staff passed through the space inhabited by the body, possibly unable to feel the heat and hear the noise that had become the patient’s world.
Impact of the observations on patient care
As observations continued it became clear, from remarks made following a patient’s death by a few relatives, that the presence of the researcher had been reassuring. Relatives suggested that the care their relative had received had been of a higher standard than they might otherwise have received had the researcher not been present.
Day 4;
01:40 As relative is leaving, he says ‘I think she received better care because you were here’. I say ‘Really?’ He says Well, I don’t want to go into it now, but yes.’
SNA1P1ON
Summary of findings
An important feature of care at the end of life in the nursing home was the focus on the patient’s body. The patient’s mind was largely presumed to be absent. This presumption was not always supported by the observations of the researcher and the reporting of consciousness in the notes was contradictory. Patients who were deemed to be unconscious were observed at different times to respond to questions. There was no evidence of the formal assessment of consciousness or capacity in either the observations or the notes. The presumption of a lack of capacity and a belief that the patient was not conscious seemed to determine the care that was given and the way in which it was given.
In the last days and hours of life in the nursing home the maintenance of the patient’s bodily integrity provided the framework within which dying was configured. The activities of containing leakages, relieving pressure and moistening the lips and mouth were undertaken efficiently and with great care. In only one instance did mouth care appear to be given in spite of resistance from the patient. Family members were in the main excluded from the provision of care; in fact, they were almost always asked to leave the bed space. They were rarely informed of what had been done to the patient and often asked staff or the researcher about the care that had been undertaken. There was only one situation in which a relative, who was a trained and practising nurse, undertook a significant amount of her mother’s care.
The issue of the administration of food and fluids was an important one and, along with mouth care, was seen to drive care right up to the point of death. The absence of any formal assessment of a swallowing reflex and the lack of a clear strategy for administering food and fluids led to an inconsistent approach to patient care, occasionally with distressing results for the patient.
Although ‘the body in the bed’ received considerable attention, the management of the patient’s environment, in terms of noise, light and heating, was varied. Providing music ‘for the soul’ became translated into ‘background’ radio or TV, the stations and channels of which were switched as different nurses and relatives appeared and tastes changed.
Once the patient was in the dying phase, little attention was paid to the facilitation and support of friendships that had developed between residents. Indeed, the single example of the facilitation of a visit of another resident came only after the death of the patient.
Chapter 6 Nursing homes: interviews with bereaved relatives
Introduction
There have been many studies of people who have been bereaved to understand their needs for support as well as to understand the health and social care circumstances in which a patient’s death occurred. The views of relatives and carers of people who die have been accessed in research terms in a number of ways, through questionnaires, telephone interviews and face-to-face interviews. A key consideration in all research with people who have been bereaved is the length of time which should be allowed between bereavement and an invitation to participate in a research study. In this study relatives were required to consent to the patient’s participation in the study before any care could be observed. In addition, relatives were asked whether or not they would be willing to take part in an interview to discuss the care observed. Relatives were invited to consider how much time they would prefer to elapse before they were interviewed, and this proved to be a successful way of involving relatives following bereavement. The views of bereaved relatives presented in this chapter provide an important understanding of how the care we observed was interpreted and judged by people close to the patient.
Findings
A total of eight observations were undertaken in nursing homes: six in the north-west and two in London and the south-east. An in-depth interview was undertaken with a relative of seven of the eight observed patients: five in the north-west and two in London and the south-east. We allowed relatives to dictate the point at which the interview was conducted. Although we were keen to interview as soon as possible after the patient’s death, we were also keen to respect the bereaved relatives’ need to grieve. Table 7 provides some of the characteristics of the relatives who were interviewed and the length of time after they were bereaved that they chose to be interviewed.
| Patient identifier | Relationship to patient | Age of relative (years) | Length of time after death relative was interviewed |
|---|---|---|---|
| NNB6P1 | Daughter | 55–64 | 1 month 7 days |
| NNB6P2 | Wife | Over 75 | 2 months 2 days |
| SNA1P1 | Son | 45–54 | 1 month 16 days |
| SNA1P2 | Son | 55–64 | 1 month 17 days |
| NNA2P1 | Son | 45–54 | 3 months 23 days |
| NNA2P2 | Son | 55–64 | 1 month 23 days |
| NNA2P3 | Daughter | 55–64 | 2 months 5 days |
These interviews varied in length from just over 1 hour to just under 2 hours and were, with one exception, conducted in the homes of the relatives. As can be seen from Table 7, four sons, two daughters and one wife were interviewed. All had been present at the patient’s bedside in the hours or days leading up to the death but not necessarily at the point of death.
Relatives’ perception of patient’s deteriorating health prior to admission to the nursing home
The primary purpose of these interviews was to understand relatives’ perspectives of care in the final hours and days of the patient’s life in the nursing home. For the relatives in this study, however, their perspective on care at the end of life was heavily informed by the much bigger story of the patient’s deteriorating health, which began some time prior to admission to the nursing home. These narratives were important to the relatives and considerable effort was expended in the interviews ensuring that the correct chronology was recounted. It became clear, given the universality of the presence of these narratives, that they provided an important context for portraying the circumstances in which the patient was admitted to a nursing home. A central feature of these narratives was the physical and emotional labour expended by relatives to support the patient to live independently. The physical decline of the patient was mapped by doctors’ appointments, emergency admissions and clinical investigations (NNB6P1F1, SNA1P1F1, NNA2P2F1 and NNA2P3F1). Admission to a nursing home heralded a critical point in an individual’s trajectory of decline and failed attempts to keep the patient living independently. However, once the patient had been admitted to the nursing home, the narrative continued to chart repeated infections, failure of wounds to heal effectively, development of pressure sores, renal failure and the progression of dementia. So, in some sense, the admission to a nursing home was simply part of the physical decline associated with old age. What happened after admission was a continuation of the decline that had been in evidence prior to admission. In another sense, admission to the nursing home became the point at which relatives were forced to acknowledge that the strategies that had been put in place in the community were no longer working and that more radical solutions were required to protect the patient.
We sort of looked after her for . . . well as long as you can do in a house . . . we didn’t want her in a home . . . we ended up having to get carers in . . . me still going and the wife . . . four carers a day . . . getting near the end of her being at home . . . she was becoming a danger to herself then.
NNA2P2F1
The physical and emotional demands of caring for these elderly and increasingly infirm patients were present in all of the accounts. The bereaved relatives interviewed in this study were not young (the majority were over 55 years of age) and often held other caring responsibilities. Nevertheless, the admission of a patient to a nursing home was undertaken reluctantly and, in some cases, was associated with a huge sense of guilt and desperation.
I couldn’t cope any more looking after her . . . I couldn’t manage me mum and [daughter’s] baby as well and . . . me sister who probably would have helped, her husband died . . . She [mother] said ‘you must really hate me for putting me in here’ . . . I mean I didn’t want it to happen but I just couldn’t manage any more.
NNA2P3F1
At the point of a patient’s admission to the nursing home, few relatives felt that there were any options other than admission. Medical professionals were reported to be highly persuasive, largely, it would seem, as a result of the way in which they framed the risks that the patient posed both to themselves and to others. ‘A catastrophe waiting to happen’ was how one relative reported a doctor’s view on his mother (NNA2P2F1).
Three patients had lived in the nursing homes between almost 5 months and 2 years prior to their death (see Table 6). Four patients were ‘fast-tracked’ under the continuing care scheme, three from the hospital setting to the nursing home and one from home to the nursing home (NNA2P2F1, NNA2P3F1, SNA1P2F1 and SNA1P1F1). These patients had lived in the home for only a very short period of time before they died.
In the relatives’ accounts of the patient’s death, the age and state of health of the patient were of central importance. All but two of the patients observed in this study (whose relative was interviewed) were over the age of 90 years when they died. The reality of death was a feature of discussions between the patient and their relatives as their lives became underscored by the burden of physical decrepitude. Relatives reported discussions instigated by patients about the manner in which they would like to die and the arrangements for the disposal of their body.
But she told me in the last sort of 3 or 4 months, whatever happens, you must tell people that I’ve had enough now. I’ve had everything in my life, I’ve had a good life, I’ve had extra years as well and I’m not to be resuscitated.
SNA1P2F1
The relatives’ accounts of the progressive deterioration and decline of the patient, while sad and distressing, were tinged with the expectations of a life coming to an end. In short, the death of these patients was expected, sometimes welcomed, often planned for and in the main accepted to be timely. It is this lens through which the care in the nursing homes was viewed and should be understood.
Without exception the nursing homes in the study were described as welcoming and friendly. Staff greeted the relatives, were reported to be courteous and sensitive, offered the relatives unlimited access to the patient and supported visits with refreshments.
. . . the nurse said anything you want . . . they were bringing tea and biscuits all the time and stuff like that they were very good . . . I don’t think nothing [sic] was too much trouble for them.
NNA2P2F1
. . . it was quite a relaxed place, I think we felt no pressure when anything like, it felt like we could just do what we wanted to. I mean we could come in and we could go, we could come and go when we wanted to and nobody was really bothered about that and uh in that sense you’re not being sort of shooed out because of visiting hours or anything like that, you just felt that it was very laid back in that sense yeah, so that was quite nice.
SNA1P1F1
The relatives’ perspectives on care in the final hours and days of the patient’s life in the nursing home fall into four themes:
-
a comfortable and peaceful death
-
interactions between staff, patients and visitors
-
being ‘there’ for the patient
-
the LCP.
A comfortable and peaceful death
Contrary to the view expounded by poet Dylan Thomas, that death in old age should be resisted and fought, the relatives interviewed in this study hoped for a comfortable and peaceful death in which the patient slipped away quietly. The absence of pain and suffering were central components of the deaths they wanted for the patient.
There didn’t seem to be any need for pain relief or anything because she didn’t seem to be in any pain. She was just asleep . . . Basically the important thing was that she died peacefully and comfortably.
SNA1P1F1
Making her comfortable so she wasn’t too agitated which they seemed to do quite well I have to admit. They knew when she hurt and things like that, it was keeping her comfortable . . . I just wanted to say ‘I want you to do anything you can to make mum peaceful and happy and not have to suffer, she’s suffered enough now’.
SNA1P2F1
She wasn’t in any pain at all. So I think, I think they were basically on top of everything. It wasn’t pain. I don’t know what will have caused that agitation. I don’t know what will have caused it. It was err . . . restlessness if you like.
NNA2P2F1
It is important to understand that the deaths in this study were viewed in the context of old age, increasing frailty and hands-on experience of attempts at staving off progressive dependence. Relatives recognised the inevitability of death and focused on the quality of care provided to the patient up to the point of death. The quality of care was measured in terms of the minimisation of physical symptoms (pain, agitation and distress, breathlessness) and the maximisation of comfort care (turning, washing, dressing wounds, providing food and fluids and administering mouth care). These were features of all the relatives’ accounts of care at the end of life for the patient. In the main, relatives felt that this was achieved.
There wasn’t much more they could have done for her, I don’t think . . . it was peaceful, it was in nice surroundings and everybody was nice to her and you couldn’t really ask for more . . . She was given her dignity, they did look after her . . . because some of the awful things I’ve seen previously, because they’re so rushed and stressed they just chuck you in a room and that’s it they forget about you almost, you’re a bit of a nuisance but I never felt mum was like that. I felt they were caring for her, they were actually coming up and checking her and making sure she was all right, trying to talk to her ‘is there anything you want’ . . . which I think was nice.
SNA1P2F1
There was nothing much else they could do, they did everything. They bent over backwards for anything I wanted and all I had to do was phone up and they did the rest.
NNA2P1F1
Everything was just superb.
NNA2P2F1
However, there was one exception to this. One of the relatives, who had spent some time at his mother’s bedside, did not feel that his mother had received enough attention. He reported that from conversations with other family members they felt that the care had been better when the researcher was observing than when she was absent. When asked what in particular had been different, the son reported the regularity and frequency of ‘checks’.
Quite frankly apart from the fact that somebody goes round every now and then, she could have died and nobody been there possibly . . . I mean that might have been fine if she’d died peacefully but she might have been in distress and nobody would have known possibly.
SNA1P1F1
Getting the balance right may be easier to achieve where a dialogue exists between the relatives and the staff. The previous relative’s view is contrasted with that of another relative who felt that, on balance, the staff (in a different site) did too much checking and turning.
I blamed them for wanting to, sort of, go in (to her room), because it’s a very difficult situation. You’ve got somebody that’s really comfortable and you don’t want to be disturbing them too much but the other side to that is you also don’t want to end up with pressure sores if somebody’s going to survive a lot longer.
NNB6P1F1
Interactions between staff, patients and visitors
Relatives viewed staff as intermittent visitors to the patient’s bed space. They interrupted the long vigils adopted by the majority of relatives. Staff were reported to ‘pop’ in, checking the body, offering the relatives refreshments and encouraging relatives to seek them out if they needed anything.
When I was there they kept popping in and out sort of ‘you OK?’ ‘just let us know if you need anything’. They were pretty good like that . . . they just said ‘if you need anything just give us a . . . you know where we are’ and then sometimes they’d pop in anyway just to check her and check her blood or check everything you know check her pulse or something . . . she had pressure relieving mattress and things like that.
SNA1P2F1
From what I could see she was never left on her own. Because do you know I went everyday and (other relative) went at different times. So they didn’t know when I would turn up. But every time I did go . . . there was somebody there.
NNA2P2F1
The relatives all reported being told that if they wanted anything they should find a member of staff or use the room’s buzzer if one was available. One relative reported that they had to go and look for a nurse after they used the buzzer and no one answered.
It was just me and [other relative] at the time . . . what they do they give us a buzzer to buzz ‘em, to sort of see if my mum does go worse, and we buzzed it, but no-one came so [other relative] went looking for the nurse.
NNA2P1F1
Relatives reported that once they had found a nurse, either to seek clarification of an observed behaviour that the patient was exhibiting or to ask the nurse for something, the staff responded quickly. Relatives reported to staff that the patient was in pain and needed medication or needed to be propped up.
I’d have to ask, ‘can you prop her up a bit?’, she seems to sort of, sometimes she slides down the chair and . . . So I’ve had to ask, the nurses did it . . . picked her up and pulled her back again and, you know, but basically they was brilliant, basically you’ve just got to try and catch them ‘cos they’re busy and it was a bit short staffed and they was all looking after everyone else.
NNA2P2F1
In all cases except one the provision of care by staff was undertaken in the relative’s absence. Relatives were reported to be asked to leave the room while care was being delivered. Rarely did relatives know exactly what care was being delivered and rarely did they ask the nurses and carers who were providing it. There seemed to be a tacit acceptance that the body and its physical needs and care was the remit of nurses and carers in the nursing home.
We went out of the room and they did something around her tummy area I think because I saw them pull the sheets back and do something around her tummy area and . . . then when we came back in my mum was peaceful again.
NNA2P2F1
They must have changed the dressing and things like that . . . yeah generally while that kind of stuff was going on we were out of the room . . . and that’s fair enough.
SNA1P1F1
Although relatives accepted that the provision of care was the work of nurses and carers, they reported receiving little information about the care that had been provided in general.
Really there was nobody else there to ask . . . [you] found out by yourself.
NNA2P3F1
Indeed, in their observations the researchers recorded frequently being asked by the relatives about the care that had been provided during the period that the relatives had been out of the room.
While the provision of care was dominated by the nurses and carers, relatives reported their own role as ‘being there’ for the patient and not letting the patient die alone. In one exceptional case a member of staff was reported by relatives to have sat with them, providing comfort and monitoring the patient’s slow decline into death.
[Other relative] went to get the nurse, the nurse came up she . . . stayed until my mum died . . . I don’t like saying it but it took an hour for my mum to die . . . and even the nurse . . . she was crying a bit as well . . . she was just stood at the bed comforting me and [other relative] and just every so often go and taking the pulse . . . she’s not in any pain, don’t worry about the pain, she said it [the breathing] will just go shallower and then all of a sudden it will just stop.
NNA2P1F1
As previously mentioned, one relative, a daughter who was a trained nurse, reported orchestrating the management of the physical and emotional aspects of her mother’s care as well as the hands-on delivery of it. Indeed, her account reflects what the researcher observed. This relative combined the role of daughter and nurse in her narrative.
. . .and it was also good that I was able to do a lot of the care for her and they were helping me almost and I think because again, of my background, I didn’t have to be taught to do it, I was just doing it and it came second nature to me almost . . . at least I felt I could do things and check on her and other things that needed to be done.
NNB6P1F1
This daughter portrayed her role as ‘active’, based on her knowledge, skills and training. For her, using her skill set made her feel useful in an environment in which she could not alter the outcome of certain death. She reported that ‘it took her mind off things, it normalised things’. She contrasted this with other relatives who, lacking this skill set, sat, watched and waited.
I’m sure people that haven’t got the background would feel helpless because you’re almost sitting, waiting and watching . . . Passive relative . . . that’s why I say I just think for anybody else in that situation it would have been maybe a lot harder for them.
NNB6P1F1
Indeed, sitting, watching and waiting was what the majority of other relatives reported doing. But contrary to the daughter’s view that this rendered them helpless, relatives took comfort from the emotional support they believed their presence offered and from their ability to monitor the care that was provided. In general, relatives accepted the environment in which they found themselves and rarely questioned or saw the need to try to change it. They did not expect to be involved in the hands-on care of the patient, but needed to be present for the patient.
‘Being there’ for the patient
Being there for the patient seemed to represent a complex set of thoughts and feelings which related both to the relative and to the patient.
I wanted to be present, I was glad I was, I was glad I was there anyway, ‘cos I missed out on my dad dying, ‘cos I couldn’t get there in time, at least I could hold my mum’s arm, her hand, which I did all the way until she died. Just sort of saying I’m there for her.
NNA2P2F1
The presence of the relative lent a status to the patient as, for example, someone’s mother, father or husband. Bringing the identity to the body was important and in the interviews relatives talked at great length about the person behind the patient. Reconstructing personhood in this way was important because in the last days of life the relatives were often unsure about the patient’s state of consciousness. Most relatives struggled to define or understand the patient’s state of consciousness. One relative (SNA1P1F1) variously described his mother as having been ‘just asleep’, ‘[in] a sleep that went on for a number of days’ and ‘in a black coma’. He also remarked that ‘it didn’t really feel like she was alive in the care home’ and ‘they said she was in a coma [but] I’m curious whether she actually was conscious at all . . . I don’t really know’. Uncertainty over the conscious state of the patient was echoed throughout all the relatives’ accounts. Interestingly, it did not feature as a concern; it existed as a puzzle to which they did not have an answer. This confused and sometimes contradictory sense of a patient’s consciousness was always accompanied by a belief that ‘hearing is the last sense to go’. Relatives reported talking to the patient, playing them their favourite music and reading to them. All of these activities were designed to provide familiarity and comfort to the patient, to recreate a connection with past interests and to reassure.
[T]hrough her dementia she seemed to be more and more into music . . . she would be tapping away . . . we kind of thought . . . if she could hear anything, she’d quite like to hear music . . . if anything was going to make her do something it might be music . . . but . . . there was no feeling of any connection really in the home.
SNA1P1F1
I suppose I was managing to get something through to her. She realised I was there . . . and on Thursday when I came back . . . well, I think she knew I was there, she did sort of say ‘oh hello’. Sort of startled me and said my name but on the Friday when I went through, I thought she’s not mum at all . . . [but] because they say the hearing’s the last thing to go . . . I was talking to her normally, trying to talk to her . . . but she wasn’t really with me.
SNA1P2F1
The provision of food and fluids for patients
The relatives held very mixed views on the appropriateness of providing food and fluids to patients and the timing of this. There was a general agreement, however, that at the very end of life, patients often neither wanted nor were physically able to eat or drink, and to force them to do so was ‘cruel’. For many relatives the acceptance of the patient’s death provided the starting point for understanding this view.
I was asked if I wanted to send her into hospital for subcutaneous fluids by one of the staff nurses. So I sort of said ‘well no, we’ve got an advanced plan in place and I really don’t think that it’s appropriate on two counts: (a) because she’s got C. diff [Clostridium difficile] – I don’t think the hospital’s going to be very impressed at sending somebody in with C. diff and (b) I don’t honestly think it’s going to improve mum’s outcome or ultimately what’s going to happen. I think this is the inevitable and all it would do is to prolong the inevitable for her.
NNB6P1
Another relative reported that as a family (SNA1P1F1) they had already ‘made a conscious decision not to keep feeding, not to keep her alive unnecessarily’.
Three patients were reported by relatives to have been consuming nothing or very little for some considerable period of time. For example, two relatives (SNA1P1F1 and NNA2P1F1) reported that their mothers had not taken any food or drink for the 3 days prior to their deaths, and a wife reported that her husband (NNB6P2F2) had refused food and drink in the last day or so of his life. The relatives in these cases were keen to emphasise that it was not a case of staff ‘saying you’re not going to eat any more’ (SNA1P2F1); it was that the patients had come to a point at which eating and drinking was too much effort or not physically possible.
I think it came to a point where she couldn’t physically do it [feed] herself and she wasn’t accepting stuff and they were giving her the, you know, the supplement drinks and these sorts of things.
SNA1P2F1
Other relatives, however, reported observing staff attempting to get patients to eat and drink up to the point of death. There was one occasion when the participant (who was a qualified nurse) questioned the utility and safety of continuing to try a patient with food and fluids in the face of resistance and a perceived inability to tolerate it, as there seemed to be little or no agreed strategy for feeding.
Bless ‘em they still kept bringing food in and one day they brought something in . . . I wasn’t too sure even what it was . . . was it cauliflower cheese? . . . some of the stuff to be fair they were just winging it . . . there’s no way that’s going down and again I think that was a lack of experience . . . she was struggling to swallow like 6 months ago but she’s certainly not going to swallow that now.
NNB6P1F1
The issue of food and fluids at the end of life is often an emotive one, but in this study relatives adopted a pragmatic approach, principally because they had all decided that the patient’s life was coming to a natural end and they had no desire to prolong the patient’s suffering.
The Liverpool Care Pathway
The inevitability of death and the concomitant desire to promote comfort up to the point of and including the death provides a useful context in which the LCP can be examined. The care of all of the patients whose dying phase was observed in this study was supported, to some extent and in a variety of ways, by the LCP. The relatives’ views on the LCP illustrated a broad spectrum of knowledge, attitudes and beliefs about the LCP in general and, more specifically, its use in the support of their dying relative. Many of the homes in the study used the GSF, although rarely did relatives identify it as such. Where it was used relatives referred to elements of the documentation which are unmistakeably GSF. Most relatives had at least a vague recollection of ACP, including spiritual and religious beliefs and requirements at the end of life, preferred place of death, cardiopulmonary resuscitation and the most important issues for care at the end of life. These conversations also included preferences regarding music and information on key family members, next of kin and important friends.
In a similar vein the majority of relatives had heard of the LCP but could not really describe it. Three relatives were unclear about whether or not the LCP had been used to support the care of their relative.
She mentioned the Liverpool Care Pathway, but to be honest I don’t think we got it.
NNA2P3F1
[T]hey weren’t actually using it as such, were they, on my mum at all? I don’t think they were actually using it on my mum at all.
SNA1P2F1
Knowledge about the pathway was attributed to the media, to discussions with friends and neighbours and to health-care professionals.
I had heard about it in the news and things like that and read about it and it’s been in the paper as well.
SNA1P2F1
Her auntie, she had this pathway thing. And she, well they were very pleased with it.
NNB6P2F1
Relatives also described a range of thoughts and ideas associated with the pathway. These ranged from general care or TLC, to the administration of drugs and stopping someone eating, through to assisted death.
Just formalising what we’ve all known as TLC for so many years . . . when you do feel that somebody’s coming to the end of their life and it’s inevitable . . . that you just make them as comfortable as you can do without causing them any more distress I think.
NNB6P1F1
What’s different about Liverpool Care Pathway to just stopping . . . somebody eating and it would just seem common sense. I can’t really understand what’s odd about it to be honest . . . we wouldn’t have wanted to force feed her . . . we wouldn’t have wanted to have prolonged her life . . . I don’t think she’d have wanted to prolong her life . . . I mean it’s just common sense . . . it seemed normal to me.
SNA1P1F1
I think it’s good myself, other people might not . . . I have heard some people call it assisted death you get all different terms don’t you, but I think it’s good . . . it’s something I’d want if it was for me and I was in the same state as my mother . . . I’m a great believer in things like that anyway . . . whether you want to call it assisted death or pathway or whatever . . . I think if a person is terminal, my mother at that stage was terminal without question or doubt and I know what her feelings would be she didn’t want to die so let her go in her sleep and if that means help her to go to sleep I don’t see a problem with that.
NNA2P2F1
Interestingly, two relatives emphasised that it was just a pathway and not an irreversible route to death. However, one of the relatives, whose mother had had previous experience of the LCP in another home, seemed to suggest that his mother had survived the LCP as though it were a test designed to sort the survivors from those who were going to die.
But they said . . . they can go on it, but . . . they can easily take them off it.
NNA2P3F1
Because when my mum was on the pathway in that [previous care home]. Totally different. She was on like a morphine drip; some medication and morphine drip as well but it was tubes going into her and they explained . . . they said eventually what will happen is basically it will be the morphine that puts her to sleep . . . [but] she kept jumping up and starting hallucinating I thought she’s not going anywhere here making her better if anything . . . I felt this isn’t working . . . anyway she survived that . . . and the doctor took her off it, obviously because she survived it.
NNA2P2F1
These accounts serve to illustrate the complex landscape of knowledge, attitudes and commonly held beliefs that exist and within which end-of-life care resides.
Summary
The importance of the interviews with relatives lies in the understanding that they provide of care in the context of extreme old age and a life that has run its course. For these relatives, the goal was a comfortable death free from pain and suffering. The care that they observed when they sat by the bedside in the main fulfilled this goal, leaving them free to be there for the patient.
Relatives had varying levels of insight regarding the LCP. Some did not know whether or not it had been used to support the care of their relative, and their descriptions of what it involved varied. Interestingly, relatives reported being in support of care that provided comfort and an absence of pain, even if it shortened life. It must be remembered that the relatives in this study had watched the patient’s health decline over a long period up to and including their time in the nursing home, and all but one of the patients were in their eighties or nineties. In this context death was seen as a natural end to life.
Chapter 7 Nursing home: staff interviews (point 2)
Introduction
The death of a patient is an event that most nursing and health-care support workers will encounter as part of their work. Nurses and health-care support staff working in nursing homes will by definition experience a higher proportion of deaths than those in other areas of health care. The focus of this chapter is how these nursing staff approached their role and carried out care in the last days and hours of a patient’s life. In particular, interviews undertaken with nursing staff following observations of a patient’s death explored the care that was provided as well as reflections on that care. It must be remembered, however, that although GPs play an important role in the provision of end-of-life care in this setting, it was beyond the scope of this study to collect their views.
Findings
Eight nursing home staff were interviewed, representing the four sites in which a death was observed, following the death of the patient. The interviews were usually conducted at the end of the nurse’s shift and lasted between half an hour and an hour. All the staff interviewed were qualified nurses, whose characteristics are described in Table 8. They reflected a range of backgrounds, ethnicities and ages. Some of the nurses were unsure of their banding and simply described themselves as ‘staff nurses’. In addition, half of the nurses worked on the night shift. This had clear implications, in their minds, for accessing training and understanding how the patient functioned during the day. This is discussed later. As has been described in detail previously, the LCP/non-LCP distinction between homes was blurred. In this section there are two homes which had been selected for participation in the study on the basis that they did not use the LCP. However, in relation to the patients observed there was evidence of the application of some or all aspects of the LCP which, as reported previously, makes the comparison between LCP-using and non-LCP-using sites impossible.
| Patient identifier | Grade of staff | Age (years) | Sex | Length of time working in NH | Length of interview |
|---|---|---|---|---|---|
| NNB6P1S24 | Staff nurse | 55–64 | F | 2 years 1 month | 52 minutes |
| SNA1P1S23 | Staff nurse | 25–34 | F | 8 months | 46 minutes |
| SNA1P2S23 | Staff nurse | 25–34 | F | 1 year 8 months | 35 minutes |
| NNB6P2S214 | Staff nurse band 5 | 45–54 | F | 4 years 3 months | 25 minutes |
| NNB4P1S24 | Staff nurse band 5 | 35–44 | F | 9 years 6 months | 46 minutes |
| NNA2P2S224 | Staff nurse band 5 | 35–44 | F | 2 years 1 month | 49 minutes |
| NNA2P3S214 | Staff nurse band 5 | 45–54 | F | 7 years 4 months | 40 minutes |
| NNA2P1S214 | Staff nurse | 45–54 | F | 2 years 10 months | 45 minutes |
Nursing home philosophy
All of the nursing staff interviewed had a fundamental belief in the benefits of end-of-life care in the nursing home. They reported that their knowledge of the patient and the fact that it was the patient’s home was an important starting point. They reported being passionate about ACP and keeping patients comfortable in the nursing home environment. The nurses talked about making sure that end-of-life care was pain free and comfortable.
Advanced [sic] care plans are not done just as a paper exercise, but in that we fulfil our promise, when we do that advance care plan because if the decision is to keep them here and for them to die here, then we are saying that we will ensure that they have a peaceful death.
NNB6P1S24
Understanding early on what a patient’s wishes would be were they to become unwell was recognised to be important for staff in achieving the best possible care for that patient.
The majority of the people are on an advanced [sic] care plan; not all of them, because it depends on the circumstances of the resident and the families on the advanced [sic] care plan . . . Occasionally we’ll have an advanced [sic] care plan that says I want my relative to be nursed in hospital; it’s rare but it does happen and people change their minds.
NNA2P1S214
Indeed, the religious and spiritual needs of the patients and their particular preferences for music and foods were all recorded, and observed in most cases to be delivered.
In NNB6 it was recognised that for people with dementia finding out what the patient might want could involve talking to a wider group of people.
Most of ours have dementia, so we need to do what we call a ‘best interest advanced [sic] care plan’ and I always like to include relatives or if there is no relatives, a friend who knows the resident before they came in and would know something about the character and personality to say, what do you think she would like, just to make what they are calling a ‘good death’.
NNB6P1S24
Although the staff were keen on advance care plans, in the case of NNA2P3 one of the relatives raised a note of caution. She was reported to have thought these conversations offensive when taking place too soon after a nursing home admission.
She said it’s something I don’t want to talk about now. Yes, you know, force her mum before her death to discuss how people would treat her . . . they don’t like it.
NNA2P3S214
Clearly such conversations need to be conducted sensitively and it is possible that the enthusiasm of the nurses in the sites might blind them to the individual’s fears about death and dying.
The staff were committed to providing a high level of care and believed that nursing homes were the best environment for elderly and frail people to die.
Training of the nursing home staff
The staff providing care to the patients in this study reported having received end-of-life care training. In some of the nursing homes the GSF was used in conjunction with the LCP.
All qualified actually had a day course on the Liverpool Care Pathway at the Hospice and the senior carers also did the same course the beginning of this year, end of last year. In conjunction with that – because of us doing the Gold Standard Framework – we would have our study days and then every 2 weeks, one of the GSF trainers – would come to the home and have an afternoon of training, so that all members of staff knew about the Gold Standard Framework and end-of-life care because it is important, everybody is included, cleaners, the cooks because they didn’t appreciate what their role was, in caring.
NNB6P1S24
In one site (NNA2) where three members of staff were interviewed, all three nurses reported receiving training. The training was repeated because of the sometimes long gaps between patients dying and the need to keep up to date.
All had training from Sister X several times, because what happens now, maybe one patient becomes poorly and after that there is long gap, but it’s happened about two or three times. They changed the set of papers as well so. So we had about 2–3 sessions from Sister X.
NNA2P3S214
Perhaps not surprisingly, there were issues regarding the way in which night nurses got their training. Four staff were working on nights at the time of the study; not all reported receiving training.
. . . it’s difficult to do on nights, I cannot do the training most of the time because if you’re on night you don’t get the skills and not the training so I won’t get to do it.
NNB4P1S24
The patient’s deterioration
All of the nurses interviewed talked about the patient’s deterioration and this formed an important context for the diagnosis of dying and the steps that needed to be taken by the home to provide end-of-life care. Four of the patients had been admitted with serious health issues and with the expectation that their health would decline. However, the short length of residency in the home set against this decline was reported by staff to make the deterioration difficult to judge. Where patients had been resident for 6 months or more staff reported being better able to chart their deterioration.
I knew that slowly, slowly she was deteriorating. We knew when she’d really stopped eating and drinking.
NNA2P3S214
She was mobile when I came with a frame for short distances and she was quite a feisty lady but suffered a lot of bouts of paranoia where she would think we were poisoning her with any medication or any drinks or anything that we gave her, or any food and on those days she would have nothing. Not a drop of anything because she just mistrusted us. I would say that for a lot of this year you could see she was beginning to deteriorate.
NNB6P1S24
Alongside the general reduction of mobility and the loss of continence and desire to eat and drink, level of consciousness was perceived as another key indicator of dying.
I think her consciousness was starting to go then and she wasn’t fully aware any more then really and that’s when I decided, in my mind, she was probably truly dying at that point then.
NNA2P1S214
I washed and changed her at one point and she never opened her eyes once. So there was varying levels of responsiveness from her.
NNB6P1S24
As observed, consciousness was linked to responsiveness rather than to a detailed neurological assessment. The rule of thumb that seemed to be applied to the definition of a patient’s irreversible decline was their state of consciousness, the nature of their breathing and the colour of their skin.
I started like checking her nails and checking the soles of the feet because these are usually the indications if they’re to die in the next few hours if it’s going to happen.
NNA2P1S214
In reporting the patient’s physical deterioration, nurses made a clear distinction between being old and frail and dying.
There is just a lot of this . . . it’s an attitude – they are elderly, they are frail and it’s immediately they are end of life and she isn’t.
NNB6P1S24
Recognition of dying
The distinction between the recognition of dying and the commencement of the LCP is an important one, as the LCP should be used only when this recognition has occurred. The staff realised that recognising dying was not easy, and in reality a number of things confused the situation.
This is where it’s sometimes difficult with some of our residents. It’s deciding when is the right time.
NNA2P1S214
While the nursing care provided in nursing homes was adjusted to the patient’s bodily decline, the recognition of dying and the commencement of the LCP required nursing homes to involve the GP. Considerations around the involvement of the GP appeared to distort the use of the LCP. The majority of staff reported difficulties getting GPs to visit.
The assessment should be with a doctor but I can’t get the GPs to come out and go through the initial assessment with me and what happened with patient – and it’s happened with all the others – is that I have done the initial assessment on my own, and then I think, yes, I will put her on the Liverpool Care Pathway but then I will get a GP within 24 hours, and when they come I say, please read my assessment and what my comments are and sign if you agree; now they don’t ever read, they just sign it, so I could have written anything to be honest.
NNB6P1S24
As a result, many of the nursing home staff reported bringing forward the GP’s involvement, particularly if the patient’s decline coincided with the weekend.
Before the weekend usually Friday, when the patient is poorly we’ll call the doctor, because if it falls on Saturday we can’t do much. So because Saturday the pharmacy is closed and sometimes, GP won’t be there.
NNA2P3S214
The nurse interviewed in NNB6 reported that she was part of a nursing team involving the local hospice that had been active locally trying to raise the understanding of GPs in relation to end-of-life care in nursing homes. In her view the reluctance of GPs to be involved in the LCP stemmed from the requirement that they reassess the patient at regular short intervals. She reported on several occasions throughout her interview that she thought GPs found the reassessment ‘too much to do’ (NNB6P1S24).
There is no GP will come every 3 days, as they should do when somebody is on the LCP, because they should be doing the reassessment with me but there’s nobody and I am on my own – or whatever nurse is on duty.
NNB6P1S24
Behind the scenes nurses reported talking to people with specialist expertise and taking help and advice where they felt uncertain. In some cases this was from other staff in the nursing home. In other cases it was from hospice experts about drug dosages and maintaining a patient free of pain.
I said that she still complains about pain and she looks uncomfortable when attending her and they said ‘OK you can increase the morphine to 7.5 mg on the syringe driver and keep her with a stat dose of 1.5, 1.25 when needed’.
SNA1P2S23
Commencement of the Liverpool Care Pathway
There seemed to be a variation across sites and patients as to when the LCP was signed and started. Unpicking this variation was complicated because staff often talked about the tools they used, the GSF and LCP in particular, as though they were one and the same thing. In discussing the patient’s deterioration one nurse was able to create a distinction between what she called a ‘palliative period’ and the LCP.
If we feel that we are in what I call a palliative period then we will get the doctor in and say, can we have the four core drugs? We think we are getting within the last few weeks and we will have all that set up and established and from that point on, we will then request a palliative care review every 2 weeks and the doctors are quite happy to come out and do that; it’s just once they’re on the LCP.
NNB6P1S24
However, there was little consistency about the point at which the LCP was started. Views ranged from an informal sense that the patient was dying to the application of an algorithm.
I always go through the algorithm very carefully and the algorithm is a good leader in helping you to make that decision. I found that helpful because I am doing them on my own; it is a bit more support for me and I do find having done the algorithm, that it does tend to be right.
NNB6P1S24
They have a criteria of going on the Pathway, it usually means being nursed in bed; which we would have been doing. Sips and fluids still given but it’s at our discretion; medications are stopped, or acting medications are stopped, although occasionally sometimes antibiotics continue for a few days if it’ll help with their comfort. But most medications are stopped and we no longer actively try and feed them. Food is offered if we think that their swallowing is up to it but we no longer actively try and feed somebody. It gives us permission to say yes this person may be dying.
NNA2P1S214
In the same site in which the nurse reported using the most precise formula for its commencement, another nurse stated ‘Usually you commence, then do the initial assessment, then the doctor comes later’ (NNB6P2S214).
Additional reported difficulties were associated with getting out-of-hours doctors involved who, while attending, were frequently reported not knowing the patient well enough to know whether or not the decline that was observed was as a consequence of the patient being at the end of their life. Again, it is important to remember that it was beyond the scope of this study to collect the views of GPs. As a consequence, nurses reported that while medication changes might be agreed and signed off the LCP documentation was not completed or signed at this stage.
The Care Pathway really commenced around 7–7:30 o’clock. I called the doctors, doctor came, but he has to sign all the forms because he is out of hours and don’t know the patient. So he saw the booklet, so wrote ‘stop giving orally, stop all the oral tablets’ then he signed that.
NNA2P3S214
In this case the LCP documentation was eventually signed off by the patient’s own GP when he was called in as the patient’s condition had deteriorated.
Towards the morning on that shift around 6 o’clock she became a bit breathless and a bit cold in her extremities. Looked very pale, so we called the doctor because the chest was a bit rattlely.
NNA2P3S214
Completion of the Liverpool Care Pathway documentation
Few staff were able to report exactly how the LCP documentation was completed. However, in one site the nurse interviewed reported issues with the completion of the LCP documentation by the carers.
They don’t appreciate that they are not showing what intervention and what care that we are actually giving . . . if they go in and see if she’s wet and they go in and change her then for them that is an A (Achieved), because she is nice and dry. They don’t understand that it was a variance when they went to do the checks and then they have to write down what they did because it just looks like the patient has been laying in bed and not had anything done to her because everything was achieved every time. It is just getting those messages across but they are better than what they were when I first came here.
NNB6P1S24
I would say it is a straightforward thing knowing where to document what and when. Like if there is anything, like if she was restless, I would come and assist or if one of my carers noticed that before me they would tell me and I would go in and assist . . . then I would come back and I would document that she is restless.
NNA2P2S24
All of the staff interviewed thought that the LCP facilitated a comfortable and peaceful death.
Involvement of relatives
The assessments of the patient that brought staff to the understanding that the patient was dying also triggered a review of the knowledge and understanding of the relatives.
So I called her daughters and informed them that there are changes with patient generally because she’s not taking anything orally, also the level of consciousness, very cold, very pale, so far there was no breathing distress or anything, but I told them. So I told them also doctor has signed the medication if needed I’m going to give.
NNA2P3S214
We had informed the daughter of the infection and everything and she could see how down she had gone as well so she started visiting daily and each day she had gone down a little bit, gone down a little bit.
NNB6P1S24
A nurse working on a night shift underlined the importance of the records kept by the home. In observing the decline of the patient, the nurse reported being uncertain about when the patient’s son had last visited and whether or not he was aware of his mother’s deterioration.
If anything happened I had to talk to son; which I knew like last Saturday when I nursed her because I wanted to make sure you know like when you’ve got a very ill patient you’re trying to really familiarise yourself with knowing who’s family, when they die and in case anything happens who you contact and all that . . . Anyway, like, yesterday I was a bit concerned because that’s when she was commenced on the Pathway and there wasn’t nowhere (in the notes) like they said the son came to see his mum, so I was worried thinking that he hasn’t seen his mum.
NNA2P2S224
Anticipatory drugs
One of the most surprising aspects of the interviews with the Nursing Home staff was the importance of the anticipatory drugs and the timing with which they were acquired. In the interviews, getting the GP to prescribe the LCP drugs was seen as important. However, because of the lack of faith expressed by all nursing home staff in the timely arrival of the GP, there was a tendency to acquire the drugs in advance of their need and sometimes in advance of the implementation of the LCP.
Sometimes the medication and Pathway don’t always come together at the same time.
NNA2P1S214
As long as all the medication is in place, you’re not rushing you know. Because if that’s the time, you know that’s the time of death you know, everybody knows that that’s the last few hours or few days, everything’s all in place . . . as long as the syringe driver is in place because we want the death to be peaceful and not in pain . . . If it’s all in place, the medication, it’s fine.
NNB4P1S24
Interestingly, a number of nurses also reported that very few of the deaths in their nursing home had required the administration of the drugs that had been prescribed.
Most of the deaths we have had here, have been symptom free. There has only been two occasions on two different residents where they might have had one dose of morphine and that has been it. But it is very rare that we actually use any of the four core drugs. They are dying from frailty, they are dying from old age; they’re not dying from anything nasty that is causing pain or anything.
NNB6P1S24
Care in the last hours or days of life
Care at this time in a nursing home was a nursing task rather than a medical one. Relatives were only rarely involved in the provision of care and in the interviews, with the exception of one family member a daughter who was also a qualified nurse, it was not felt appropriate that the relatives should undertake nursing tasks. During the observations a number of aspects of care were done frequently. These included mouth care, feeding and encouraging drinking, pressure area care, checking for secretions and pain assessment.
In the interviews, nurses were asked about the relative importance of these tasks and how judgement was applied to the frequency with which they were undertaken. Nurses juggled two different ideas in their answers. The first was the notion that certain things should be assessed, if not carried out, at regular intervals. The second was that discretion and the application of expertise should be allowed to define the frequency with which assessments were made and care was conducted. In relation to the patients whose care was observed, a combination of these two approaches was adopted. However, it seemed that in the fusion of these two ideas some oddities emerged, one of which was explored in the interviews: the relatively common practice of putting the room lights on fully during the checks of a patient at night.
I think the lights should be on because staff are observing as well, you can’t observe breathing and changes or anything in the dark but then always what happened in that room I think the regulator is not perfectly working so the light is quite bright. We can’t reduce it, it was a bright light but as soon as you put off also it was coming on, like then they thought there was a ghost or something because as soon as they put it off it was coming up light.
NNA2P3S224
The frequency with which a task was undertaken and how it was undertaken often reflected the views of the staff rather than the views of the patient or their relatives.
This can also be seen in the pressure area care undertaken for the patients.
Pressure area care
All of the patients observed in the study received regular visits from care assistants to turn the patient. Carers were observed to use their judgement about whether or not to turn a patient but in the interviews there remained an emphasis on 2-hourly turns, reducing to 4-hourly at night.
It’s 2-hourly usually once they go on the Pathway, which is roughly about the same otherwise. Some of the night staff were saying that on their shift . . . if they’re actually on the machine, they go down to 4 hours, they’re not disturbing them too much.
NNA2P1S214
You know the one who is really ill or bed bound we need to do it to prevent the pressure sore . . . most of the residents here we check 2-hourly. We check 2-hourly the residents who move themselves but the one you know, they cannot move they need to be turned 2-hourly to prevent the pressure sore.
NNB4P1S24
In relation to the observed death in NNB4 the nurse reported that she had instructed the staff to reduce the frequency of the turns as it was clear that the patient was dying.
4 o’clock I told them, don’t touch him because I know that’s the last, when I go I told them don’t touch him again because it looks now. So . . . because as long as he’s comfortable not to worry to turn every 4 hours . . . not to turn every 2 hours.
NNB4P1S24
Nevertheless, there was one site in which the nurse seemed to suggest that the prevention of a further deterioration in the patient’s pressure sore demanded frequent turns, despite their painful consequences for the patient.
Always it’s very painful for the patient but we have to do it to prevent pressure sores as we can’t prevent the pressure sore totally. It’s impossible and it’s very painful for patients in the last days . . . and we use a lot of cream to protect the skin but it’s not working, it’s not working and I see the expression on their face when we turn the patient side by side, that expression looks painful.
SNA1P1S23
Food and fluids
The provision of food and fluids was another area in which the goals of care were observed to be inconsistent. In one site care staff were observed to make frequent attempts to get a patient to eat and drink. It appeared that there was no coherent or consistent approach, with different members of staff adopting different strategies. The interview with the member of staff was important because it revealed the various attempts made by the nurse to get the staff to desist from feeding the patient.
The biggest issue is feeding and drinks, and they can’t seem to grasp that the patient wasn’t able to swallow, which she hasn’t been all this week. But they would still go in and because they might get response from her they will try and feed her or give her drinks. So, I have to say, ‘No, you come to me and I will say yes or no whether to give her anything’ and I find that the best way.
NNB6P1S24
The nurse recognised that the actions of the care staff did not match the patient’s ability.
I was doing her mouth care this morning and I was going quite a bit way down her tongue to try and clean it and there was no gag reflex whatsoever, yet one of the girls came to me and said, ‘Patient opened her eyes, shall I give her her breakfast?’ And that was this morning . . . and I just think it’s some guilt.
NNB6P1S24
Despite the nurse’s exhortations, the observations recorded the frequency with which the care staff entered the patient’s room to provide food and fluids. On the patient’s last day of life, her daughter, who was a trained nurse, repeatedly told care staff that her mother was not able to eat or drink.
The nurse’s explanation for the staff’s persistence was interesting.
It does distress them. It is their nature, caring, and they’re thinking she has gone all these days without food and they don’t really grasp that she can’t swallow and it might be a cultural thing because we have quite a few foreign carers and nurses, and I just think they feel they are neglecting if they are not feeding; they don’t see the mouth care and everything like that as part of what the patient needs at that time, if you will.
NNB6P1S24
The nurse went on to report that, for a small group of nursing home staff, there remained a belief that not providing food and fluids right up to the point of death was ‘quickening the death’.
In another site (NNB4P1S24) the nurse reported that, as a member of the night staff, the lack of clear reports in the notes had left her uncertain about whether or not the patient we were observing in the study was able to eat or drink.
Checking for secretions
In all of the sites, nurses reported the importance of managing secretions, as these were uncomfortable for the patient and distressing for the relatives to observe. This was not straightforward, as nurses weighed up the use of the suction machine versus the use of drugs.
If you see them dying so you know, all that suction, it’s not fair to be suctioned regularly. It’s not fair to be suctioned all the time.
NNB4P1S24
In NNA2P1 the nurse reported the difficulty of disentangling the discomfort of secretion from pain and from the agitation associated with dementia.
The main problems I had was excess secretions then, as she moved to the next stage we were unsure whether it was a pain or whether it was an agitation because she’s got dementia it was hard to work out exactly what the signs were so we went down the sedation line first of all with her.
NNA2P1S214
The management of pain
All nurses talked about a pain-free and peaceful death as the goal of care, and the ability to administer pain relief was seen as an important element in achieving this. Staff reported using a range of drugs and routes of administration, and in their accounts staff relied on both the patient’s self-report and the assessment of the patient by the care staff.
On that last day as well to try to keep her comfortable I was the one making decisions, there was definitely more secretions, so she got extra glycopyrronium and there was definitely some sign of pain. I’d decided it was pain because my colleagues, the girls, when they had turned her they said she seemed to be a bit uncomfortable on turning.
NNA2P1S214
She was kept comfortable for quite a while. Then she went on and that’s when we put the syringe driver on . . . because no two people are the same, we have minimum doses we start on and then we . . . obviously decide what this is doing for the patient and if not, we increase it and if then if it’s something we can’t increase, we phone the GP and if it’s something not within our scope . . . but we didn’t need to involve the GP because we managed OK.
NNA2P1S214
The nurse in NNB6P2 talked in detail about the way in which the dosages of pain relief were escalated for the patient in the study. Initially managed on codeine and paracetamol, the patient was believed not to be in any pain. However, it became clear to the care staff that the patient had begun to experience pain and so they began to administer the diamorphine written up in conjunction with the LCP.
He never says he’s got pain . . . but you could see from the face especially facial expressions. That he was in pain . . . They wanted to turn him and he said to them ‘I am in pain’ so they just leave him.
NNB6P2S214
The staff left the patient because the NIC reported that she was unable to increase his diamorphine at that time and it was deemed to be poor nursing to continue while the patient was suffering.
There was a belief that the ability of the nursing home to take care of the patient’s pain had removed some of the incentive to have patients at the end of their life admitted to hospital.
So the patients don’t need to go hospital in a rush, their wishes will be followed, also that they want to stay in their own rooms with their families and everything. Because in the hospital also at an elderly age they don’t want any interference with the resuscitation and everything. It’s like a natural death and with the medication after the doctor has prescribed, after the family agree and the patient has stopped eating and drinking when generally they deteriorate.
NNA2P3S214
However, the administration of drugs often left nurses feeling uncomfortable, particularly if the patient died soon after their administration.
Dying alone
None of the staff thought that their patients should die alone. Two nurses were present at the bedside when the patient died and for one of these nurses this was the first time she had actually seen a patient die. The nurse in NNA2P1 had been summoned by one of the patient’s sons, who had noticed that his mother’s breathing had changed. When the nurse arrived she recognised that the patient was dying and communicated this to the sons.
As soon as I walked in the room I thought she’s dying because I could just tell because of the sort of change because she was blue. She was blue and at that point she wasn’t breathing either, and I thought . . . she was taking her last breath, this was the impression I got because she wasn’t breathing, she went like . . . and her chest was still . . . I said to the boys ‘I think she’s going . . . So the boys both got by her side and then she took a breath.
NNA2P1S214
Having alerted the sons that their mother would die very soon, the nurse stayed in the room and the patient died an hour and a quarter later.
Summary
The interviews with the nursing staff revealed important behind-the-scenes insights into how care at the end of life was organised.
While staff recognised the decline of patients, they reported that this was easier to judge where there was a longstanding relationship with that patient. The recognition of end of life and the commencement of the LCP, although conceptually distinct, were inextricably linked in this study. Unusually, and not observed, the role of the GP was reported to distort the way in which the LCP was commenced. The importance to the nurses of having the anticipatory drugs to hand, were they to be required, was influential in the timing of contacting the GP. All of the nurses reported making sure that medication was in place before the weekend and highlighted issues with the lack of familiarity of out-of-hours doctors with their patients and the implications of this for the signing of the LCP.
There was variation in the way in which the LCP documentation was used. There were reports of it (1) being in place well in advance of the need to use it, attributed to the reported difficulties of getting GPs to visit; (2) being started without the GP’s signature; and (3) being used following discussion with the GP and relatives at the point of need.
The interviews also raised issues of how principles and beliefs, particularly about end-of-life care, are cascaded down to care staff on the ground. The examples provided by staff of a disconnect between the patient’s ability to swallow and the desire for staff to sustain life to its end through feeding and fluids demonstrates the difficulties of implementing end-of-life care even where there is a good understanding of its principles and goals.
All of the staff interviewed thought that the LCP facilitated a comfortable and peaceful death.
Summary of Section 2 findings
Nursing home data
Some interesting convergences and divergences emerged when examining the findings from all the data sources used within this study (interviews, case-note reviews and observations) in relation to care in the final hours and days of life for patients in the nursing home setting.
There was consensus, supported in all interviews and observations, that the nursing home was the patient’s home. Achieving a good death for the patient meant allowing the patient to die in familiar surroundings, free from pain and in contact with people who cared about the patient. Caring for a patient in the place they call home is a desirable goal and there is evidence from many studies that admission to hospital adversely affects the patient. In one study, about one-third of nursing home patients did not survive admission to accident and emergency (A&E), a figure which rises to over half dying within 6 weeks of admission. 62
Establishing the patient’s wishes for their end-of-life care, and in particular agreeing and documenting ‘do not attempt resuscitation’ and ‘not for hospitalisation’ decisions, was reported by staff in the interviews to be important and was evident in the patient’s case notes. Such was the sense of urgency to record these advance preferences that conversations about end-of-life care were reported by staff to take place within days of the patient entering the nursing home, and often months and years before a decision needed to be implemented.
There was considerable emphasis in the interviews, in the observations and, to a lesser extent, in the patient’s notes on the physical care of the patient. This was viewed as taking the form of keeping the patient comfortable and maintaining their dignity up to the point of death. However, there was a sense that the care of the patient’s physical needs formed part of the daily rhythms of the home, while the patient’s emotional and mental needs were rarely addressed.
The extent to which the patient case notes reflected the physical care provided at the end of life was, perhaps as expected, limited. The lack of a clear record of care given and to be given could underpin some of the confusion which arose over the management of the patient at the end of life: in particular, the extent to which patients were or were not conscious and the basis for that judgement, as well as whether or not the patient was able to swallow and the nursing plan associated with the administration of food and fluids.
There were no records of formal assessments of consciousness and yet in the observations there were constant assertions about the state of the patient’s consciousness. It appeared more common for patients to be labelled as not conscious, despite evidence observed by the researcher to the contrary. Explanations given by staff to patients as they went about the physical care of the patient were delivered in a routine ritualistic way which neither invited nor expected an answer. This presumption that patients were not conscious resulted in conversations taking place over the patient; these were felt by the researcher to be insensitive and removing the patient’s agency. It was left to relatives to restore the identity to the body in the bed. This lack of formal assessment of the level of consciousness served to reinforce the focus on the body and a presumption that the patient’s mind was largely absent and, therefore, did not need to be engaged or catered for.
Although staff were well versed in the benefits of the LCP and other end-of-life care pathways this was not matched in the views of the bereaved relatives, who were vague about what it entailed and were often unclear about whether or not it had been used in relation to their relative. The use of the LCP in the nursing home setting was interesting. Given that staff faced difficulties in identifying the point at which a patient’s deterioration had become irreversible, there was considerable uncertainty about when the patient might be in the last days and hours of life. In order to achieve a pain-free death for the patient, staff expressed anxieties about ensuring that the anticipatory drugs were available in case of requirement. This frequently led the nurses to start the LCP some time in advance of its need because of the perceived difficulties of getting a GP to visit who knew the patient. Although considerable effort was expended in getting the anticipatory medications prescribed for the patient, the drugs were not often observed or reported to be used; this was supported by the patient’s clinical records.
In Chapter 8 we turn our attention away from death and dying in the nursing home setting to focus on dying in the ICU setting.
Section 3 Findings: dying in intensive care units
Chapter 8 Intensive care units: interviews with staff (point 1)
Introduction
Technological advances have enabled intensive care facilities to support life during critical illness without modifying the underlying pathology or the process of dying, according to Ravenscroft and Bell. 63 The challenge they identify is not so much the application of those techniques, but the objective defensible decision-making in the initiation, maintenance or withdrawal of support, not only for the patient’s benefit, but to ensure effective and efficient use of resources. Deaths in the ICU setting frequently follow limitation of life-supporting therapies. As a result, ICUs have had to develop expertise in the provision of the care to dying patients and their families. 64 Coombs et al. ’s study26 demonstrated how the transition from curative intervention to end-of-life care was the most challenging and complex part of professionals’ work in this setting.
In this chapter we focus on an analysis of the interviews undertaken with the senior clinical and nursing team to provide an understanding of the organisational context within which end-of-life care was observed. In particular, we focus on the way in which decisions about withdrawal were made and conveyed to relatives, as well as the withdrawal in practice. The interviews include views of staff who used the LCP as well as those who did not. The distinction between these two groups is discussed where relevant.
Findings
In common with the approach adopted in the nursing homes we undertook interviews with a range of staff to provide a general understanding about how end-of-life care was practised within ICUs. A total of 72 interviews were conducted prior to undertaking observations in the ICU: 11 doctors and 61 nurses were interviewed. In all but one of the ICUs, a consultant was interviewed. In one site a junior doctor was interviewed (Table 9).
| Participant | Gender | Age (years) | Ethic group | Years in posta | Years in careera | LCP used in principle | LCP used in practice |
|---|---|---|---|---|---|---|---|
| NIA1S141 | F | 35–44 | White British | 8 | 10 | Yes | Yes |
| NIA2S161 | M | 35–44 | White | 6 | 10 | Yes | Yes |
| NIA6S111 | M | 35–44 | White | 3 | 5 | Yes | Yes |
| NIB3S131 | M | 45–54 | White | 18 | 28 | No | No |
| NIB4S112 | M | 35–44 | White British | 0.5 | 4 | No | No |
| NIB5S161 | M | 45–54 | Asian | 12.5 | 12.5 | No | Yes |
| SIA1S158 | M | 55–64 | White British | 20 | 32 | Yes | Yes |
| SIA2S161 | M | 35–44 | White English | 1.5 | 10 | Yes | No |
| SIA3S141 | M | 35–44 | Mixed Anglo/Asian | 8.5 | 16 | Yes | Yes |
| SIB1S121 | M | 45–54 | White British | 12 | 20 | No | No |
| SIB2S131 | M | 45–54 | White | 10 | 20 | No | No |
In addition, in each ICU, at least one senior grade nurse was interviewed as part of the study. These nurses were either band 6 or band 7 nurses who undertook both clinical and managerial work as part of their role as unit sister, charge nurse or senior staff nurse; unit matrons were excluded from this sample as their role tended to be entirely managerial (Table 10).
| Participant | Gender | Age (years) | Ethnic group | Years in posta | Years in careera |
|---|---|---|---|---|---|
| NIA1S113 | F | 45–54 | White British | 23 | 23 |
| NIA2S113 | F | 55–64 | White | 30 | 30 |
| NIA6S153 | M | 25–34 | Asian | 6 | 12 |
| NIB3S153 | F | 55–64 | White British | 35 | 35 |
| NIB4S133 | F | 35–44 | White | 4 | 13 |
| NIB5S153 | F | 45–54 | White British | 28 | 30 |
| SIA1S143 | F | 35–44 | Asian Indian | 12 | 12 |
| SIA2S113 | F | Declined | Declined | 30 | 30 |
| SIA3S163 | F | 45–54 | White British | 11 | 21 |
| SIB1S143 | M | 45–54 | White British | 10 | 17 |
| SIB2S113 | F | 35–44 | White Australian | 5 | 21 |
| SIB3S153 | F | 35–44 | Asian Filipino | 4.5 | 10.5 |
Dying in intensive care units
In ICUs, death often followed a decision to withdraw or withhold life-sustaining interventions. For this reason, judgements about the point at which interventions were no longer effective received considerable attention in the interviews with doctors and nurses in ICUs.
Doctors viewed the ICU as a specialist resource most appropriately reserved for patients for whom there was an expectation of recovery and survival. Admission to ICU was rationed on the basis of a prospect of recovery; doctors reported that they were effectively labelling those not suitable for ICU admission as ‘dying’.
I would say, particularly when we see referrals . . . from other specialities from medicine or surgery or something like that, and say ‘will you come and see this patient, will you take them to intensive care’ and we go up there and say ‘no that’s not appropriate because this patient is dying’ . . . OK, and dying is a sort of natural physiological process. And sometimes to try and intervene in that isn’t the right thing to do.
SIA2S161
End of life care is really quite difficult in intensive care because generally speaking one has admitted a patient into the intensive care unit because you think they’ve got a chance of survival. And you believe that with the appropriate support, to whatever level, that that patient will then survive . . . If we think someone’s not going to survive, we really shouldn’t admit them.
SIA1S158
The doctors described dying as ‘recognisable’ and ‘obvious’ and generally based their assessment on factors such as the patient’s history, current condition and prognosis, including the patient’s lack of progress, deterioration or reduced prospect of recovery. Nurses were not responsible for the admissions to ICU but, like doctors, reported being able to judge an ICU patient’s failure to respond to treatment. Although nurses reported that the formal acknowledgement of dying was based on repeated medical assessment, they also reported that, as nurses, they were in a prime position to recognise a patient’s deterioration and treatment limitations.
. . . because the nurses are at the bedside 24/7, we are the ones that see the subtle changes in the patient so we are going to pick something up a lot quicker than a doctor will. So I mean, from that point of view they [doctors] do ask for our input during the ward round but at the end of the day the final decision is a medical decision.
SIB2S113
Decision-making about withdrawal
There was agreement between doctors and nurses that decisions regarding withdrawal of treatment were primarily medical but usually drew on the views of the wider team. Although what constituted the ‘team’ varied between sites, and indeed between patients within sites, minimally the consultants reported seeking nurse input. Depending on the unit, such decisions might involve two or three consultants, junior or middle-grade doctors, the senior nurse and the bedside nurse, as well as the patient’s surgical or medical team if applicable.
Doctors were agreed on the importance of collective decision-making, for a number of reasons. There was a view that seeking a range of perspectives from colleagues resulted in more balanced decision-making, ‘balanced’ because the views that contributed to the decision-making were often reflective of different ways of seeing the patient. Medical staff outside the ICU tended to be seen as bringing a more optimistic perspective than their ICU counterparts. Although these views were invited, ICU doctors tended to locate them in ‘unrealistic expectations’ of what could be achieved in ICU. ICU nurses’ views were identified as the ‘most realistic’ in relation to patient outcomes because nurses were at the patient’s bedside every day, observing and recording the patient’s condition. ICU doctors reported having less face-to-face contact with the patient than ICU nurses and, as a result, being more likely to be ‘overly optimistic’ and more willing to keep treating. Where doubts were expressed or opinions were divided, active treatment was more likely to be pursued. However, doctors and nurses agreed that disagreement between staff was rare.
Nurses emphasised a decision to withdraw was often arrived at only when treatment options had been exhausted and that MDT meetings, both formal and informal, ensured that these decisions were thoroughly explored.
Often there’s two consultants nowadays on a ward round, because it’s a like a handover period or whatever, plus senior registrars, nursing staff including senior nursing staff. Physios are nearly always there, dieticians and pharmacists; MDTs every day. So I suspect that’s why that kind of conversation starts to take place because of the volume of expertise . . . and a microbiologist is there.
SIA3S163
While doctors and nurses agreed that decisions to withdraw were usually unanimous, the nature of withdrawal and the speed with which it occurred was reported as hugely variable and often influenced by the senior doctor in charge of the patient’s care. Nurses recognised the individual variability between doctors regarding withdrawal decisions.
People are individuals, consultants are individuals, and they are the ones ultimately making these decisions. Even as a group their name is going to be there so they have think carefully. And I’m never for one minute saying it’s an easy . . . it isn’t easy, but some consultants or intensivists can be much more decisive and others kind of play at the edges a bit. I’m not sure if that’s a kind of defeatist – like ‘I’ll just give them 24 hours, we’ll just give them 24 hours longer’, so it can be . . . I think variability can be unsettling. But then you’ve got to perhaps understand where they’re coming from and talk to them about it. So people think that’s when they’re slow in making that decision when it’s screamingly obvious but then you say to someone ‘well it’s not you making the decision’. You know, you have to talk to them about it.
SIA3S163
I think that sometimes certain consultants go too far and I have actually said to one consultant ‘look you are flogging a dead horse. What exactly do you hope to gain by this? You know this patient is not going to survive. What we are doing is cruel’ [. . .] They just, you know, there comes a point when you know the outcome is not going to be good no matter what you do but some doctors will persist in doing everything, even though you know that outcomes are never going to be positive, and it’s cruel.
SIB2S113
There was a consensus that withdrawal was a doctor-led clinical decision, and that the MDT, family members and relatives, although part of discussions, were not ultimately responsible for the decision.
Ascertaining the views of the patient and their relatives
Involving patients and family members in discussions about withdrawal was considered to be of paramount importance. Within the ICU setting, it was unlikely that patients could be questioned directly, as they were generally either unconscious or heavily sedated and unable to take part in discussions. Doctors reported starting from the premise that where the medical evidence indicated that treatment was not effective there was a default option of withdrawal.
We kind of have a default opinion really where most patients wouldn’t want to be entirely dependent on full time nursing care and be severely mentally impaired and we would generally withdraw treatment, unless we were hearing something very different about what that particular patient would have wanted, but if they had expressed I want that at all costs no matter what the disability, we would change our position in their best interests.
NIA6S111
This default option was reviewed in the light of evidence about what the patient’s wishes might have been in these circumstances. While doctors talked about the patient’s best interests, the determination of best interests was a complex fusion of general and proxy ideas. It did not conform to the definition or test laid out in the Mental Capacity Act (2007). 65 Best interests was constituted in terms of a generalised negative default option: what patients in general would not want as opposed to the considerations each individual might have liked applied to their situation. In determining the patient’s best interests, doctors were reliant on people who had known the patient well and who had some idea about the patient’s views. These people were usually deemed to be the patient’s relatives. Doctors described strategies that they had used with relatives in identifying what a patient’s wishes might have been.
I usually say ‘the decision is made in their best interests but I didn’t know [the patient] and could [you] speak to me, and offer me an opinion, I just wonder what [the patient] would say if he/she was watching us now and knew what we knew now, whether he would offer an opinion to carry on with whatever’. So I try and make it specific that I’m using them as a conduit for the patient’s opinion, whether they’ve either specifically expressed it or what they would think he/she would say in the circumstances and so that is so I am very explicit with it, that ‘it’s our decision but you can help us reach that decision’.
NIA6S111
I try and make it very clear that I’m asking their views on what the patient would want, not because I want them to make a decision about what we want to do long term, but because my decision, our decision on the unit of how we manage that patient must be based on what we think that patient would want us to do. An informed decision of what they’d want us to do.
SIA3S141
Nurses recognised that, in consulting relatives in this way, there was a risk that relatives might begin to feel that they were getting involved in making a decision.
We listen to their [relatives] . . . but we do make it clear that it isn’t their decision at the end of the day. That it is ultimately a medical decision because it’s the doctors that have the knowledge . . . it’s knowing how to kind of say to them ‘I’m sorry but it isn’t your decision’. I think if you can get that over to your relatives it kind of puts the ball back in our court then, therefore we are in control of the decision-making and some of them are grateful for that, it takes the pressure off them.
NIA1S113
Only one nurse reported experience of doctors who routinely involved relatives in decisions about withdrawal.
Pre-withdrawal communication
Medical and nursing staff reported that, prior to the ‘withdrawal conversation’, they worked as a team to establish what information the patient’s relatives understood about the situation and to ensure that the relatives knew that the patient’s condition was deteriorating. Consultants reported that having conversations ‘early on’ with relatives was particularly important in cases when the patient was not improving despite receiving treatment. Much like the nurses, doctors believed that preparatory conversations provided an important context to lessen the shock should the delivery of bad news be required. Erring on the side of pessimism and being proved wrong was seen to be better than giving relatives ‘false hope’. Early conversations were believed to facilitate relatives’ understanding, providing a basis for wider discussions with other family members as well as preparation for discussions about withdrawal. Only one of the doctors interviewed adopted an optimistic approach right up until the time that deterioration was seen as irreversible. He argued that a 20% mortality rate equates to an 80% survival rate (SIA1S158). Most of the doctors, however, felt that it was important to be ‘realistic’ about a patient’s poor prognosis.
I’ll always give them a heads-up early on that things aren’t great.
SIA3S141
As discussed above, the point at which withdrawal was decided was often preceded by a period of deterioration on the part of the patient, during which staff would prepare the relatives for the ‘bad news’ of withdrawal via teamwork and a series of ‘realistic’ conversations. Nurses placed considerable emphasis on communication with relatives that was continuous, honest and consistent.
If they are hearing from each successive person that the condition is deteriorating that the patient is not getting better, eventually it sinks in [. . .] if they are getting people telling them the same thing, on successive days and they are seeing the monitor and the numbers are going down and the support is going up and machines are being added, they know. I mean they might not want to know but they know.
SIB2S113
In the context of ongoing discussions about a patient’s deterioration, doctors and nurses recognised that some relatives might have already come around to the idea of withdrawing treatment before it was actually raised as a possibility. Several of the doctors reported that on occasions relatives ‘jumped at’ the decision to withdraw because they believed that it was in the patient’s interests and that the situation was irreversible.
Sometimes it’s the relatives who want you to stop and it’s us that’s saying ‘well we’re not quite at the hopeless stage yet, it’s very likely that I will be talking to you tomorrow and telling you that we are now, but he might still get better, so we’re still trying’.
NIB3S131
On the other hand, some doctors identified instances in which relatives did not accept that the point of withdrawal had been reached. In line with the strategies reported by the nurses, doctors tended to draw in a second opinion from a colleague in order to confirm both diagnosis and prognosis.
Our job then is kind of to present the information as clearly as possible and from different angles really so they don’t feel they’re just getting one opinion, they’re getting a clear consensus from several doctors ideally of what’s occurring.
NIA6S111
Following the decision to withdraw treatment from a patient, it was the senior doctor’s responsibility to communicate this to the patient’s relatives, and this generally occurred within the context of a formal meeting. Nurses reported that it was important that they attend this meeting in order to provide support and advice following the meeting. If the bedside nurse was inexperienced or the relatives were ‘difficult’, a more senior nurse might replace the bedside nurse.
Mostly the nurse will go, the bedside nurse, will go into the meeting with the consultant. To see the family and also if they expect any problems from the family then the nurse in charge – you know, if it’s a junior bedside nurse – nurse in charge will also go in.
SIA1S143
Depending on the nurse at the bedside, or if it’s a family that we’ve had issues with, then a senior member of the team would often go in with the consultant to be there, rather than maybe a brand new Band 5.
SIB1S143
Nurses were keen to emphasise that the senior doctors were in charge of discussing withdrawal with the relatives and all had different approaches. Doctors reported that these conversations should be clear and free of the use of jargon.
And you say, ‘look, they are dying. We have the ability . . .’, and one of the phrases I commonly use is ‘we have the ability to prolong people’s death as well as their lives’.
NIA1S141
So my technique would be that I would say that the patient, if they were dying, that we need to move towards making him comfortable rather than trying to make quality of life rather than quantity of life. It doesn’t mean we are going to withdraw care it just means we are stopping for example antibiotics, fluids, and explain why.
NIB4S112
Then we would get the family in and then we would explain to the family what the situation is and say that we would not – ‘it is not in the patients best interest to carry on’ [. . .] The majority of the cases they agree because they can see what is going on. And if they don’t agree it’s our job to convince them really to be honest with you. It’s not a decision that they have to make. The GMC [General Medical Council] is very clear as to that you don’t have to offer treatment which you think is inappropriate.
SIA2S161
Although doctors reported the importance of being honest, clear and careful not to provide ‘false hope’ in their communications with patients, nurses reported observing communication which fell short of what doctors themselves recognised as important. Nurses reported that their role in the aftermath of the consultant’s discussion with the relatives was to make sure the relatives had understood what they were being told, answer any questions that might arise and provide comfort.
We have got a particular doctor who really talks way over their [relatives’] heads. And you can see it on their face that they are so confused by what is going on, that they come out of it and they go . . . I have actually had a relative say to me ‘so what exactly did he just say to me?’ And that’s when I say to them, ‘OK look, this is what was just said. We have done everything we humanly can; there is nothing more we can do. And they are like ‘is that what he just said?’ and I am ‘yeah, that’s what he just said’.
SIB2S113
The families always tend to ask questions from the nurse afterwards rather than the doctor. That often happens.
NIA2S113
Then the nurse can back that up again after the meeting. We go over it again. Because sometimes when they’re in the meeting, and they’re upset, they don’t always take everything in.
NIB4S133
Although nurses reported the importance of clear direct communication with relatives, they themselves shied away from using the term ‘dying’ when talking to relatives.
Well, we think of a different word that we can still convey this message you know, ‘because the treatment is not making any better’, and ‘we are going to stop the treatment and make him comfortable’. These kinds of words will give: ‘at the end of the day he is going to die’. And many times, we may probably also tell them ‘we don’t know how long he is going to last’.
NIA6S153
Delays in withdrawal
A number of the consultants interviewed described circumstances in which they would agree to delay the commencement of withdrawing treatment. Agreement to delay treatment withdrawal was contingent on the patient’s condition, as long as the patient remained comfortable, it was not to the patient’s detriment and their best interests were not compromised. Staff framed delays in withdrawal as a means of ‘looking after’ the relatives and of ensuring their well-being. A common reason to agree a delay of withdrawal of treatment from the patient was to allow important relatives to get to the bedside ‘to say goodbye’. Another reason for delaying withdrawal was to give relatives time to hear a second opinion on the patient’s condition; this might be from another ICU consultant, a surgical specialist or other outside specialist. More generally, consultants reported that sometimes relatives needed more time to ‘come to terms’ with the decision.
Some of the doctors reported in the interviews that, although they understood the need to delay withdrawal for the benefit of relatives who needed more time, they would implement a treatment plan of non-escalation rather than maintaining active treatment. Thus, although they would not withdraw active treatment straight away, they would not escalate existing therapies, and should the patient’s condition deteriorate further, staff would not move to redress the deterioration through treatment:
So the main situation when I would go for a non-escalation is when the family just need more time. To get their head around it. It can’t be open-ended because otherwise you are then potentially acting against the patient’s best interests. You may be prolonging their death, rather than prolonging life, but I do think there are periods where you just need a pause for thought and so, ‘OK we’re going to meet again in 12 hours’ time, in the morning, after the ward round and we can discuss this again. You talk amongst yourselves, and if there are signs of improvement by then, we’ll keep moving forward. But if there’s a deterioration overnight, we won’t increase, we’ll let them know, and if we‘re in exactly the same place in the morning then we’ll need to consider.
SIA3S141
I would allow the family who weren’t happy with a withdrawal decision to delay the withdrawal process but I would be very explicit with them that, ‘OK fine we’ll wait and see but we’re not going to increase support if the patient shows signs of deterioration’ and, whilst I wouldn’t say it to the family, I would hope that they would read that as a sign that you know, our reading of the fact that this was futile would be supported by the fact that the patient deteriorated despite ongoing support.
SIB1S121
Relatives’ responses
Nurses, perhaps rather simplistically, identified relatives as either accepting of the patient’s condition or in denial of it. For example, some nurses interpreted relatives’ questions about the length of time it would take for the patient to die as an acceptance of the patient’s irreversible condition and inevitable death:
Sometimes they approach us and say things like: how long’s this going to go on for? Well, quite often it is when they’re not close relatives. You know, when they’re nieces and nephews and they say: ‘how long’s this going to go on for’? Erm, so they’re, quite often they are quite accepting.
NIB3S153
We are talking to the relatives every day, every minute, every hour of the day, over the phone, straight to their face. We’re continuously telling them how their relatives are doing. Yeah? So we have no problem. We can understand. They might tell us first: ‘we don’t [want] them to be treated any more’.
SIA2S113
On the other hand, staff also had to negotiate situations in which relatives were defined as being in denial. Either the relatives were not ready for, not understanding or not in agreement that the patient was deteriorating and/or with the decision to withdraw active treatment. In the nurse interviews, the most common approach to managing relatives who did not agree with the withdrawal of active treatment was to ‘give them time’. This allowed nurses time to talk to the relatives, and the relatives time to process the information.
We will just discuss it with them, find out what their worries and concerns would be and see if we could just address it and just get them to understand the process that we are going through and why we’ve reached that decision.
NIB5S153
They just don’t grasp it, even though you know I have explained to them many times. And that could be difficult really. All you can do is just sit down and then just basically, just try to explain that they’ve come to the point that, you know, they will be able to, you know, understand it, try to understand it better.
SIB3S153
Very occasionally over the years, you’ve had a family that’s said ‘no’. And if they say no [then] there’s no point proceeding with it really, we might as well just back off a bit. Because they will go home and think about it and they will come back ready, either the evening or the next day, they’ll come back and we’ll have the discussion again and they’ll say yes.
NIB3S153
Although the goal of discussions between the medical and nursing team and the relatives was to come to a consensus on the withdrawal of active treatment, there were occasions on which relatives disagreed with the decision. In these very rare cases the nurses reported that the consultant might simply state that the decision was a non-negotiable medical one or that a ‘ceiling of treatment’ had been reached, beyond which there was nothing left.
Withdrawal of active treatment in practice
Moving patients from the category of ‘active treatment’ to ‘withdrawal of treatment’ implied a number of changes in care. However, the degree to which active treatment was actually withdrawn varied between sites and between patients. In very few cases did consultants report the implementation of complete withdrawal of active treatment. In practice, withdrawal ranged from non-escalation, to limitation, to consultants imposing a ‘ceiling’ of treatment for the deteriorating patient. In general, variation in the nature of withdrawal appeared to be based on the individualised nature of care within ICU. For patients on a high level of support – for example, maximum inotropic and ventilator support – it was reported to be unnecessary to withdraw all treatment; simply reducing the inotropes on a patient might bring about the patient’s death before anything else was withdrawn. For patients on lower levels of support, active treatment might be withdrawn in a progressive or step-wise manner. Withdrawal of active therapies included limiting or stopping inotropes, filters, antibiotics, intravenous (i.v.) fluids, nasogastric (NG) or other feed and/or ventilation. If the patient was ventilated, their ventilatory support might be reduced, changed or stopped altogether, with or without subsequent extubation.
I think for us on ITU [intensive therapy unit] it’s easy because you say well, you can do things to bring the end to its end, you know, not continuing infusion or making adjustments to ventilation. You know what you do would in terms of withdrawal of care.
NIA2S161
Decisions about what to discontinue were not straightforward; the ‘grey’ area of (dis)continuing food and fluids was particularly mentioned by doctors. The decision to withdraw food and fluids from patients who did not die quickly was viewed as ‘tricky’.
I don’t feel that maintaining fluids is going to delay death necessarily. There are similar situations we find in ITU and there are patients who do have some sort of consciousness and awareness that sensation of thirst isn’t a very pleasant symptom. I’ve got less of a problem with withdrawing feed because . . . and again, this is in an ITU environment, with sedated patients I’m not sure that . . . I don’t know, can you perceive hunger through sedation? I’m not sure. I suppose just from a personal point of view I’ve got more of a problem with withdrawing fluids than I have with withdrawing feed.
SIB1S121
The withdrawal of active treatment did not mean removing everything; drugs to ensure the patient’s comfort could be commenced, altered or continued if these were already in place. For the doctors, changing from active treatment to the withdrawal of treatment signified a fundamental shift in the care of the patient, namely from medical to nursing care. Typically, good post-withdrawal care was described by consultants as being about patient comfort, dignity, sympathy and peace. The use of such concepts reflected the consultant’s view that withdrawal was also about a shift from intervention to ‘softer’ nursing care. For example, several of the doctors stated that, following the decision to withdraw treatment, patients left the sphere of medical treatment and became ‘nurse level’, with little consultant input unless there were subsequent problems.
But it basically becomes a talk with the nurse looking after the patient ‘Is everything OK? Is the LCP running okay?’ and that will be the ward round for that patient. There wouldn’t be anything active, it’s more ‘is there a problem? Do you need the data changed or anything?’ So it all becomes . . . so it no longer becomes medical it’s all nurse led and then only gets fed up to a doctor if there is a problem with it. So that patient sort of drifts into the background for us and it takes a specific effort almost to remember and at least check in. I remember to check in but I haven’t . . . not everyone checks in on that patient.
NIA6S111
Yes I feel I would be tending to step back [. . .] once that conversation has been had with the family, I would talk with the nursing staff, particularly talking to them or sort of senior experienced sisters who’ve got a lot of experience with this sort of situation, and we would agree a plan, a course of action. Then, if there were any specific complications, talk through them at that particular time . . . and I would expect really then not to have very much input other than say there were problems during the course of that.
SIB1S121
It was clear from the doctor interviews that the ‘withdrawal of treatment’ was a complex directive which took its precise meaning and shape from the individual context in which it was being used.
The nurses supported the idea that once withdrawal of treatment was planned it was their responsibility to manage that withdrawal. The ‘process of withdrawal’ depended on the severity of the patient’s illness and the current level of drug support, and the consultant’s views on the needs of the patient and family. In general, depending on the patient’s condition, the ‘steps’ of withdrawal might include:
-
stopping inotropes (e.g. noradrenaline)
-
reducing oxygen (e.g. from 100% to 21% room air)
-
extubation (if possible)
-
stopping all other active treatment (e.g. NG feed, i.v. fluids)
-
introduction, or continued provision, of i.v. drugs to control pain and ensure comfort.
The order and degree of withdrawal of active treatment was a main focus of discussion for the nurses because they were the staff responsible for providing patient care once the decision to withdraw active treatment was made. In particular, the nurses differentiated between ‘quick deaths’ and ‘slow deaths’, and described how controlling different elements of the withdrawal facilitated a degree of control over the patient’s death and the relatives’ experience of that death.
Not too quick and not too slow
Controlling the speed of death was a feature of the nurse’s narratives. The aim was to reduce or withdraw support so that death came neither too quickly nor too slowly for the relatives. Depending on what was being withdrawn, dying might take from 5 minutes, to a few hours, to several days. Some of the nurses interviewed identified the control of inotropes such as noradrenaline as a significant element relating to the speed of death in ICU. When a patient was on a high or maximum level of inotropic support, its reduction or removal was linked to patients having a ‘quick’ death, which was variously identified by the nurse interviewees as desirable or not desirable, depending on the circumstances.
Inotropes are at such a level that if you turn them off they would die within minutes and sometimes you have to give that family that time. You know it, you can see it in them, they’re not ready for someone to die within 3 minutes of everything being turned off. But you have to make that clear beforehand because if you’re seen fiddling, turning things off in front of them, that can be quite distressing. So you have to make that decision to keep them on because their systolic is so low their heart is going to stop.
SIA3S163
Nurses reported that doctors might request that a syringe pump was allowed to run out rather than be turned off and removed, particularly where the patient was on a high dose of noradrenaline delivered through a syringe driver. However, nurses reported that this had the effect that relatives sat watching the syringe run out in the belief that death would ensue at the last drop.
If that’s [noradrenaline] on a high dose, we usually let the syringe run out. Which I don’t always agree with because the family sit there and watch the syringe till it gets to the last . . . I think it should be done, you know, when everyone’s ready. Rather than ‘the syringe is ticking away’, you know, the family can see. I see them all getting really anxious watching the syringe.
NIB4S133
I can never see much point in having relatives sitting here hour after hour after hour, whilst the syringe pump’s run out. I don’t think that’s fair on relatives. It’s all very well them sitting here by the bed while there’s hope, but once there’s no hope I can’t see the point in dragging it out. ‘We’re going to wait’: I can’t see the point of saying well when that syringe pump runs out in 14 hours. We won’t replace it. I don’t think that’s fair on anybody. Once that decision’s been made, I think it should be done.
NIB3S153
In some sites the reduction of inotropes was accompanied by a reduction in oxygen support.
So we reduce oxygen from 100% to 21% oxygen and stop inotropes. So within 45 minutes there was no blood pressure. And I think death was confirmed within 2 hours.
NIA6S153
If they’re on high ventilation, lots of pressure and that, we leave them on it. But towards the end you might chip the oxygen down. Just to help – I won’t say ‘help’ – but it just sort of stops the dragging on of the death because you’re oxygenating the heart and stuff. So sometimes that is knocked down. Sort of, it’s a feeling, you know, a point where you’re going 3 or 4 hours and there’s still, things are still happening. Then we can put the oxygen down 21% to stop prolonging the inevitable really.
NIB5S153
Nurses reported a delicate balancing act with regard to controlling the speed and nature of the death. They tried to balance the needs of the relatives with the needs of the patient.
Sometimes when patients are dying, they’re gasping. They [relatives] don’t want the ventilator to pump into them. And they get distressed. Then if the doctors agree, we take it off, and put them on oxygen through a [tube], so that they [patients] don’t get distressed or deprived of oxygen.
SIA2S113
The topic of extubation was of central concern to nurses in controlling the speed of death and its presentation.
If I have to decide, I would take the tube out. You know, just leave the patient in peace, and with dignity. And if I’m in charge, and we get a patient that’s still ventilated, and we have withdrawn treatment, I usually suggest to the doctor: ‘I think it’s more dignified if we . . .’ and we’re just like prolonging the inevitable really, which is not fair for the patient and for the relatives.
SIB3S153
While for some nurses extubation allowed the patient to appear more natural and comfortable at the point of death, other nurses felt that extubation could be distressing for the patient.
For the multiorgan failure patient, because it would be uncomfortable sometimes, you know, even if they are sedated if you take them off the breathing tube, they could shock and it would be uncomfortable and cause other difficulties.
SIA1S143
So often we leave the tube in to make it look comfortable for the family. Because you keep them sedated. Which makes the patient more comfortable.
NIB4S113
As with many aspects of end-of-life care in the ICU, there was an acceptance that each case needed to be considered individually. Regardless of the speed of death, nurses were keen to emphasise that nursing care continued.
You’re still giving basic care, you know they still will need mouth, eye care, hygiene needs. If it’s a short thing, you’ve turned the norad [noradrenaline] off and . . . you ain’t going to have a lot of time to do any interventions. All you’re going to do is be there and be supporting the family. I suppose that’s where it does change: if you know it’s going to be quick, you go to more supporting family members, OK? Also ensuring that they are comfortable . . . some people you withdraw treatment on, you know that they’re not going to die straight away, they’re still going to need all their basic care as well.
SIB1S143
However, as identified above, there was a slight shift in focus to incorporate the family and relatives as the patient’s death became more imminent. Relatives were allowed open-access visiting and in some cases were provided with a key to a relative’s room if they needed to stay overnight. In a few cases nurses reported encouraging family members to take part in the provision of care to the patient.
During the care if they [relatives] want to do mouth care or help . . . we don’t let them obviously help much with turns because obviously there’s moving and handling implications. But you know, they can certainly stay in the area. They don’t have to go out, and I think that’s quite important if you are taking the tube out because very often your parameters of your patient changes, sometime the blood pressure drops, or obviously the way they breathe changes, so I think it’s important, possibly if they’re happy to stay, to let them see that you haven’t done anything else other than what you’ve said you were doing. I think if they stand away and then come back and things have changed quite a little bit . . . well, they may well wonder.
NIA1S113
Other nurses reported being selective about the care that relatives were allowed to see.
[W]hat we do now in our intensive care unit is whenever we’re doing patient care or turning patients or mouth care and things like that, we just ask the relatives to sort of leave and we would continue to do that.
SIB3S143
Nurses also had mixed views about privacy and dying, and not all of the ICUs had the facility to create a private space for the patient and relatives.
The rooms are very small. We have no ventilation and no windows. So as you can imagine, if you get five or six people in there it becomes quite claustrophobic. So, as horrible as it sounds, if you have a dying patient you either want them to be in [rooms] 1 or 5 because you can have the relatives around. And it doesn’t matter if five or six or seven relatives come in, there is still room. But some of the smaller rooms, it gets a little bit tricky when there is a huge family and they all want to come in all at once. Then, you have to be horrible to them and say no: ‘look, sorry there is too many people, you have to break it up into groups’. But it does afford some privacy, so there is good and bad about how our unit is set up.
SIB2S113
Where side rooms were not available in some units, patients were separated from other patients in the last days of life by the curtains around the bed space. While there were different views about how effective these were at creating private space, nurses sensed that the patient’s predicament drew the family in to a private world that needed no physical barriers.
Pull the curtains round, if the relatives want. Sometimes they feel claustrophobic, so we’ll keep it open for them. It’s up to them how they want. They want privacy, that’s the only way we can provide privacy. And there will be a nurse there anyway, allocated to that patient, so that they can look after the relatives and the patient’s condition.
SIA2S113
Given that patients were typically heavily sedated or unconscious by the time treatment withdrawal had been discussed and actioned, their religious requirements were often discussed with the patient’s relatives. Although the nurses identified that it was sometimes difficult to assess whose religious needs were being met, they considered the relatives’ needs to be as important as those of the patients.
Well I would ask to see if maybe you know are they Catholic, have they got a particular faith or something like that. Is there anything you want us to do? Would they like a minister or something like that and just see what the relatives say. Sometimes it’s ‘oh I know he would want it’, ‘I’m not particularly bothered’ as a relative, but I know my dad/wife/husband whoever, would want say the priest or whoever. So in that case, or else it could be ‘well he’s not particularly religious but I’d feel comfortable if we had some prayers’. So whatever they want really.
NIA1S113
We would always speak to the family and find out if they [patient] were a religious person, if they would want anybody from the church or a priest or anything to come. We would be guided very much by their family because we don’t know what their religious needs are outside. They might be a very religious patient and we’re not aware of that.
NIB5S153
Although staff aspired to accommodate whatever the patient and their relatives needed, they reported that the ICU design did not readily accommodate religious rituals involving large numbers of people, wailing, crying, religious music chanting and praying.
Doctor and nurse views on the Liverpool Care Pathway
Six sites, three in the north-west and three in London and the south-east, were recruited to the study as LCP-using sites. However, as we have already reported, sites recruited as LCP-using sites did not always use the LCP to support care, while some LCP documentation was evident in some of those sites recruited as non-LCP-using sites. Regardless of whether or not their sites had been recruited as LCP-using sites, the majority of the doctors and nurses interviewed knew about the LCP and were supportive of it both as a document and as a pathway of care. The views of the doctors and nurses about the LCP demonstrated that there was no single or clear-cut understanding of the LCP as either a document or as a plan of care, except perhaps that it was ‘too long’.
On the one hand there were examples of doctors who were signed up to the principles on which the LCP was based.
I firmly believe what we’re doing is a significant advance on managing dying patients and in their best interests and making the dying process a comfortable and dignified process rather than uncomfortable and undignified.
SIA3S141
On the other hand there were doctors who reported that the LCP was ‘just a piece of paper’.
What makes the difference at the end of life is people and not paper and the people aspect of it, they give that personal touch.
NIA1S141
The relationship between withdrawal and the Liverpool Care Pathway
Doctors who had some knowledge or experience of using the LCP reported a conceptual separation between commencement of ‘withdrawal of treatment’ and commencement of the LCP. It was common for doctors to state that one activity took precedence over the other. One doctor described a stepwise process involving the decision to withdraw, and implementation of the LCP prior to the commencement of withdrawal or treatment limitation.
The consultant will have seen the patient and made the decision, will then fill the LCP in at that point having spoken to the family, obviously first.
NIA2S161
The LCP pathway doesn’t teach you to withdraw treatment. LCP pathway tells you and prompts you once you have made that decision.
NIB5S161
For some doctors it seemed that use of the LCP prompted withdrawal of treatment, while for others withdrawal of treatment preceded commencement of the LCP, if indeed the LCP was commenced at all. It was suggested that if the use of the LCP was not separate from and conditional on a decision to withdraw, there was a danger that, almost by default, the patient would be deemed to be dying.
If somebody is sort of being sort of lined up for the LCP 2 days in advance of the decision to withdraw treatment in people’s minds, they may be viewing it as an inevitable end product. It is inevitable that this patient is going to be on the Liverpool Care Pathway; they are already in their minds a dying patient and may stop treating them or having the same degree of vigilance that they would for another patient and I worry about that a little bit.
NIA6S111
For one doctor, the use of the LCP was further qualified by time. This doctor reported that the LCP was not usually commenced unless the patient was still alive half an hour following withdrawal of treatment. This was because it was ‘administratively cumbersome’ to undertake half an hour of paperwork for a patient who would die in 5–10 minutes.
Not a lot of our dying patients go on it. Well, putting them on the Pathway administratively is cumbersome. Signing the Pathway and signing all the drugs and so on takes about half an hour and . . . this is purely a practical consideration but there are a group of patients that would probably die within 5 or 10 minutes of stopping life-sustaining treatment and they will require no medication or anything from the Pathway, so very often they don’t formally get instituted on the Pathway, those patients that appear that they’re going to die within 5 or 10 minutes, because they’re in such a degree of life sustaining treatment, that they are overwhelming likely to die almost instantaneously. Though occasionally they do get formally put on it, but they don’t actually receive any interventions from it. They don’t get their lines removed and so on because they just die within 5 or 10 minutes really, and so pragmatically, what quite often happens is that life sustaining treatment has stopped and then about half an hour or an hour they get put on the LCP . . . then if they’re still alive at half an hour they’re then generally get put on the LCP, simply because of the administrative burden of filling it all in.
NIA6S111
Nurses were more likely than doctors to have been involved in dealing with the completion of the LCP paperwork. For those nurses who had used it, the LCP was regarded as a useful tool for encouraging staff to think about the processes of withdrawal.
I find it useful because it kind of makes you think about, think more about, what levels of care are needed. And it’s kind of indication to think about organ donation, you think about all the comfort of the patient, you think about the relatives, you think about the spiritual care and sometimes you could forget, you know, when you are busy we could, but that paperwork is actually good reminder on all the other areas.
SIA1S143
Another nurse emphasised the way in which the LCP allowed individual level care within a standard of care. Some doctors in this study also reported the LCP as a way of standardising care. It was common for the ICU staff to report the use of the LCP as a checklist and as a reminder to explore a number of domains with the individual patient in mind.
I like it. I think it’s a good tool for people, it has consistency, it’s almost like a checklist to make sure that you do things that’s in the best interests of the patient and the relatives. But maybe that comes from getting experience.
SIA3S163
It allows any variances to be documented so it’s quite nice in the fact that a lot of it is tick box. So you can tick to say ‘yes, I have done that’, ‘yes, I have spoken to relatives’, ‘yes, I have done this, I have considered that’, and then, if I’ve said there’s a variance, then you document at the side why it is different from the actual LCP.
NIA1S113
Some nurses, however, thought that there was a trade-off between tick boxes, which facilitated speedy use of the documentation, and accountability.
Some of it’s good because it’s tick boxes, but it’s got the disadvantage of tick boxes that some of the tick boxes are not signed. If you’re just ticking it, you don’t know who’s ticked it. Really it should be signed because then you know who’s signed it off and who’s done what. Whereas if you’re just ticking it and then sign the bottom and then you come on the next shift, and some of it’s not ticked, the next nurse wants to make sure it’s filled in. But it’s half been done through a shift. There’s no accountability for the ticks except for the line at the bottom of the page.
NIB4S133
This nurse also took issue with the ‘communication’ sections of the document, stating that the information recorded in these sections varied because staff understanding of what constituted ‘communication’ in itself varied. There were broader concerns expressed about the relevance of some of the domains to a setting in which many people died very quickly and as a result of withdrawal of treatment.
In my experience, the patients die so quickly once you stop treatment, then it doesn’t really matter: you’re never going to get through all those aspects of care.
NIB3S153
If the patient is likely to not maintain their own airway and you take the ventilator away, they’re just going to die. And so all the protocols involved in the Liverpool Care Pathway, there would not be time to implement any of those. If the patient is likely to maintain their own airway, then they’re going to be able to be sort of cared for, for a little bit longer. But the idea would be that you wouldn’t then be doing intensive monitoring, and that they may have what was considered to be treatment drugs and the necessary medications discontinued, and just need to have medications for palliation. And that’s where that framework seems to be appropriate, to me.
NIA2S113
We try to use it [LCP] but obviously . . . I think if they die very, very quickly, so that we haven’t really had a chance to fill it all in and you’d be doing it retrospectively [then no point] really no, because some of them, as soon as you withdraw they can die within minutes. Depends on how much support you see we’re taking from them.
NIA1S113
The amount of time required to complete the LCP documentation was discussed in all the doctor and nurse interviews. The documentation was perceived to be too long and an ‘unnecessary distraction’ for which consultants did not have time. There were some doctors who considered that the benefits of using the LCP outweighed the length of time it took to complete the documentation, but these doctors were unusual.
We have to fill out a whole bunch of paperwork when we do any form of intervention in intensive care. It’s a shame if there’s a reluctance. I mean, one must try and advocate practice that limits paperwork wherever possible, but if this is paperwork that occurs around discussions of withdrawal of therapy that will end up in someone dying, and the incrementation [sic] of drugs and therapies that could, in the wrong hands, contribute to the speed of their dying, then it’s appropriate that it’s done, there’s time taken and it’s carefully documented.
SIA3S141
As discussed previously, there was a general view that patients who were expected to die quickly were not considered to receive any benefit from the use of the LCP to support care. In the context of ICU care, the LCP was not considered by most doctors to be a useful tool, being too long and cumbersome. Perhaps ironically, one doctor reported that when the LCP was first introduced into the unit there was ‘initial resistance from the medics’ until they realised that it was mainly to be completed by the nursing staff, and then it got better’ (NIA1S141).
Few of the consultants felt it important, or indeed practical, when talking to relatives to identify the LCP by name as the plan of care to be used to support withdrawal of treatment. In fact, it was common for doctors to report that they referred to the LCP as a ‘protocol of palliative care’ or an ‘end-of-life care plan’. The clinicians reported avoiding use of the term ‘Liverpool Care Pathway’ because of the negative associations with the name reported in the press.
Up and until the press got onto the Liverpool Care Pathway, very few relatives, in my experience, really wanted to go into the details of what is meant by ‘palliative care pathway’. They were happy, they had trust in us to say ‘OK you’ve been looking after my relative to the best of your abilities, we’ve failed to get them, or we’ve not been successful in going through this illness, we don’t have the technology to do it, so we trust you to palliate them as necessary’, but I think that trust has been lost. So the way we’re going to move forward because we’ve identified that it is a problem, we’ve had families proving it’s a problem, we think the problem is with the name. We think the pathway itself is appropriate, but what we must highlight every single time is the communication.
SIA3S41
In ICU the management of pain, secretions and hydration is a central clinical concern for all patients. This is therefore an area in which doctors considered themselves to have developed considerable expertise. Although the majority of clinicians reported that, in general, the LCP as a tool was too cumbersome and lengthy, for some it came into its own in relation to the drug algorithms, which were reported to provide an important structure for drug provision.
We don’t use it from a philosophical point of view, we use it as a purely practical tool to establish what is acceptable and what’s not acceptable. It feels like it gives you, in terms of using drugs, purely to treat, stressing symptoms rather than giving drugs to shorten life. It makes you feel that you are doing the right ethical thing, treating symptoms rather than giving drugs to shorten life. It makes me feel more confident in a way – dare I say, medically, legally – more protected that I am operating within an established framework and, retrospectively, somebody might . . . would not be able to say ‘Why did you give that diamorphine? Was it to shorten their life?’ I said ‘No, it was to treat their symptoms of breathlessness’, so it makes me feel confident that I am acting within medical norms, and to be honest, that’s why I’m using it really.
NIA6S111
In addition, one senior consultant reported that the LCP framework communicates the clinician’s intentions regarding drug administration, which may enable a nurse to react in a timely and responsive manner to the needs of the patient:
It’s been sanctioned as a best practice pathway guideline because we’re not restricted to it in any way; we can deviate from it at any point if we feel the need to. But it means there are clear parameters as to what the nursing staff can do in terms of providing comfort care, which is what they want and what they need in order to make sure it happened. The problem otherwise, without set guidance, is you can have a patient who’s distressed but because a drug isn’t written up or the nurse isn’t sure whether she can give it, the patient doesn’t get the drug and therefore they continue in a state of discomfort.
SIA3S141
Summary
The interviews with staff support the findings of other studies of ICU care which highlight the importance of establishing a prior consensus that the patient’s status is terminal before a decision to withdraw or withhold active treatment can be implemented. 26,66 There was strong agreement between nurses and doctors in relation to care at the end of life on an ICU. In terms of diagnosing dying, both groups drew on factors specifically related to the patient’s medical condition and prognosis. In particular, the patient’s lack of progress and deterioration in spite of ongoing treatment were seen as significant. Both groups also identified that the decision about whether or not a patient was dying was a medical one, although the processes described usually involved collective or team decision-making. Relatives were usually involved in these discussions in some way as doctors reported attempting to discover what the patient might have wanted. Doctors described a rigorous and unhurried process of information gathering at the point when such decisions were made. Nurses also described the consultants’ decision-making process as unhurried, insofar as multiple views were sought and further tests might be tried. The nurses highlighted variability among the consultants with regard to their willingness to make end-of-life decisions, and expressed the difficulty this caused in terms of the well-being of the patient.
Both professional groups identified the pre-withdrawal period as a significant period of communication with relatives. Overall, staff emphasised the importance of providing relatives with ‘realistic’ messages of the patient’s poor prognosis so that relatives were not given ‘false hope’ and were prepared for the eventual bad news of dying, which should then not come as a ‘shock’. This information was disseminated to relatives repeatedly and by different members of staff, with an emphasis on consistency and the presentation of a ‘team front’. Staff felt that this facilitated both relatives’ understanding and their acceptance of the proposed course of action. It was generally agreed that it was the doctor’s responsibility to discuss the withdrawal of life-sustaining interventions with relatives, while it was the nurse’s responsibility to clarify and answer questions once the conversation with the doctor ended.
Both doctors and the nurses were emphatic that, although it was important to provide relatives with open and honest communication, and to invite their opinions, the decision to withdraw treatment was categorically a medical one. Throughout both sets of professionals’ interviews, the justification for this was identified as being for the benefit of the relatives: the onus of making such decisions might weigh heavily on relatives and this was not something the staff felt relatives should have to live with. The discourse of ‘onus’ was a consistent theme from all of the staff interviewed.
However, the doctors described willingness on their part to delay the commencement of withdrawal in order to accommodate relatives; to receive a second opinion; to allow relatives to ‘come to terms’ with the decision; or to await non-present relatives who were travelling from elsewhere – as long as the ‘best interests’ of the patient were not compromised. Like the decision to withdraw, the decision to delay withdrawal was a medical one and might include a change in treatment provision from ‘active’ to ‘non-escalation’ or ‘limitation’.
Doctors identified post-withdrawal care as the domain of the nurses, with little or no further medical input unless there were complications. They described a fundamental shift in care provision from ‘aggressive’ medical interventions to ‘softer’ nursing care that was about the provision of comfort. Doctors talked little about other aspects of end-of-life care in ICU once withdrawal had begun. The nursing staff, on the other hand, had a lot to say about it. Although a patient’s ‘basic’ nursing care (identified predominantly as hygiene and comfort care) was considered relatively standard regardless of the speed of dying, if the patient’s death was slower or more protracted nurses extended their care beyond the patient specifically to include the management of the relatives’ experience. This might include moving the patient to a side room for privacy, facilitating religious rituals, extending visiting hours or providing relatives with overnight accommodation. This might also include allowing relatives to observe elements of care that might otherwise be shielded from them. With regard to the LCP documentation, both professional groups identified it as a good protocol for end-of-life care, although its use was reported very differently. Both doctors and nurses expressed concerns about the LCP as a practical tool, with a focus on its length and its relevance for patients who died very quickly.
Chapter 9 Intensive care units: retrospective case note analysis
Introduction
Following on from the analysis of the interviews of ICU staff, in this chapter of the report we turn to end-of-life care in the ICU through analysis of a patient’s case-note data. The patient case notes highlight how doctors and nurses carefully constructed a narrative to support their decisions to withdraw or withhold active treatment in order that relatives could support a transition from cure to palliation.
There are many types of patient records for a patient being cared for in an ICU. They all have a different purpose and although there is often some overlap they contain a very detailed and complex account of the clinical care observations, medication and treatment provided right up to the patient’s death.
Findings
In a similar set of procedures to the data extraction in the nursing homes, data were extracted from 120 patient case notes using a CNAF (see Appendices 12 and 13). This included a sample of 10 recent deaths from each of the participating ICU sites, half of which had been recruited as LCP-using sites and half of which had been recruited as non-LCP-using sites. However, as for the nursing home sample, these distinctions did not always hold up in practice. For example, three sites in the north that had been recruited as non-LCP-using sites (NIB3, NIB4 and NIB5) provided a total of eight cases for this element of the study that had been supported by the LCP. Similarly, a total of 32 cases were received from six sites recruited as LCP-using sites (NIA1, NIA2, NIA6, SIA1, SIA2 and SIA3) that had not been supported by the LCP. For this reason, Table 11 illustrates the demographic make-up of the sample according to whether or not the LCP was used to support the care of the patient in the last hours or days of their life rather than whether the site was recruited as a LCP-using or non-LCP-using site. Descriptive statistics were initially used to describe the sample and some of the main features of care delivered. Thirty-seven deaths (31%) had been supported in the last hours or days of life by the LCP.
| LCP | Median age (years) (IQR) | Gender = female | Religion = other than Christian | Ethnicity = other than white | Diagnosis = cancer | Preferred place of care documented | DNACPR documented |
|---|---|---|---|---|---|---|---|
| Yes (n = 37) | 65 (56–73) (n = 36) | 41% (n = 37) | 20% (n = 30) | 11% (n = 18) | 5% (n = 37) | 22% (n = 37) | 92% (n = 37) |
| No (n = 83) | 67 (55–80) (n = 83) | 51% (n = 83) | 34% (n = 47) | 40% (n = 25) | 10% (n = 83) | 1% (n = 83) | 86% (n = 83) |
Table 11 illustrates that, on several demographic indices, the sample whose care was supported by the LCP was similar to the sample for whom this was not the case, in terms of the age of patients and the proportion of patients for whom a DNACPR statement had been documented. However, several interesting differences were highlighted, although caution must be exercised owing to the small sample of those supported by the LCP and the high proportion of missing data for these variables. For example, a greater proportion of patients who were other than white and non-Christian formed part of the non-LCP supported sample. The preferred place of care, although documented in only one-fifth of patients in the sample supported by the LCP, was much more likely to be documented here than in those deaths for which the LCP was not used to support care in the last hours or days of life.
For the purposes of this report we focus mainly on the documented communication between ICU staff and family members regarding care at the end of the patient’s life. Of the total of 120 CNAFs, only 104 provided sufficient data for the analysis of communication. There was a focus on the communication between medical staff and family members regarding the care provided to patients who were either unconscious owing to the severity of their condition or heavily sedated. The data were analysed using a discourse analysis approach. What was reported and how it was reported were of interest.
The ICU data draw on a number of different professional records including:
-
critical care unit information given to relatives/communication with relatives document/family communication sheet
-
medical notes/clinical notes/clinical history book
-
critical care daily record/daily assessment sheet/continuing progress/daily observation sheet
-
nursing notes/nursing evaluation/sometimes split into day evaluation and night nursing notes
-
patient care plan
-
multidisciplinary record/multidisciplinary communication sheet
-
LCP documentation
-
drug sheets.
The LCP documentation is not designed to capture large amounts of narrative; rather, it invites consideration of goals which are then marked as achieved or variance. Any recorded variance is then explained briefly on additional variance sheets within the documentation. 36
Three aspects of communication were identified from analysis of case notes regarding care at the end of life:
-
a detailed narrative drawing on clinical data to justify a transition from cure to palliation
-
reports of what relatives were told and relatives’ responses to that information
-
the plan of care.
Narratives drawing on clinical data to justify a transition from cure to palliation
The narratives that underpin the transition from cure to palliation provide the backdrop for communication to relatives regarding care of the patient at the end of life. The discursive components shown in Table 12 draw on a number of linguistic repertoires.
| Main categories | Linguistic repertories | Examples |
|---|---|---|
| A. Patient’s overall state of health |
critical condition/situation
(very, gravely, critically) unwell (very, gravely) ill gravity of situation (very, extremely, desperately) sick (very) poorly |
I explained that [patient] was extremely unwell . . .SIB3R03 |
| B. Patient’s disease progression |
(catastrophic, significant, sudden, worsening) deterioration
(continue to) deteriorate (further, profoundly, rapidly, quickly, progressively) deteriorating condition/situation |
Patient’s condition has progressively deteriorated over the course of the daySIA1R02 |
| C. Physiological markers of patient’s diseases | Although this is individualised and specific to a particular patient, the most often recorded physiological markers include multiple organ failure (at least 3 organ failures) and irreversible neurological damage (brain injury/damage) | Explained that he has severe sepsis with multiorgan failure and is on maximum multiorgan supportSIB3R08 |
| D. Futility of given/ongoing/potential/active treatment |
futile
ineffective not possible inappropriate not working not helping (more often indirectly proven as discussed in the following section) |
Currently treatment is looking ineffective and futile with patient being peri arrest as we speak . . .NIB5R01 |
| E. Patient’s prognosis |
(poor, bleak, extremely poor, extremely bleak) prognosis/outlook/outcome
(no likelihood of, no prospect for, no meaningful chance of) recovery (80%, high, extremely high) mortality (rate/risk), (unlikely to, will not, cannot, low potential to) survive (5%, unlikely chance of, no likelihood of) survival (at risk of) dying (could suddenly) die |
I explained that [patient] is very sick, and may well not survive this hospital admissionSIA1R09 |
| F. Withdrawal and withholding of active treatment |
(not be for, not to attempt) resuscitation/CPR
DNAR Withdraw/withdrawal of (therapy, treatment, care, active management, aggressive therapies) not escalate (care, treatment) extubate/not intubate ventilate/ventilation |
He [patient’s brother] is aware that we will not escalate care on grounds of ethics, and that if there is any deterioration we will embark on sole comfort careSIA1R02 |
| G. Palliative care |
comfort care/(keep) comfortable
palliative care pain free die peacefully/naturally (maintain) dignity End-of-life care (no, avoid) distress (maintain) privacy TLC (allow, let) nature (to) take its course |
Plan to withdraw from active treatment & measures to be put in place to ensure optimum patient comfort is achievedSIB3R07 |
| H. Medical and legal grounds for decision-making | best interests | It is not in [patient’s] best interests to continue treatment . . .NIB4R09 |
Some or all of the Table 12 categories of information formed the narrative argument that justified the transition from cure to palliation in the ICU notes. While there was variation between sites, there was also variation within sites, and this may relate to individual doctor/nurse styles of record keeping and to the fact that a range of documentation was evident (LCP and non-LCP) regardless of the category in which these sites were recruited to the study. For this reason, distinctions between LCP and non-LCP documentation are not drawn. There also appeared to be an overarching logic behind the ways in which the categories were employed in the descriptions of the conversations held with the patient’s relatives. Usually the record of these conversations started with A, the patient’s overall state of health, and/or followed by B, the patient’s disease progression. These two categories of information were used separately or together to orientate family members towards the ‘bad news’: C, physiological markers of the patient’s disease, and/or D, the futility of active treatment. These last two categories, C and D, were used, again either separately or together, to back up or reinforce A and/or B, and to introduce E, the patient’s prognosis. All of the notes contained category E information, perhaps not surprisingly as the patient’s prognosis was a fundamental pre-requisite for F, the withdrawal or withholding of active treatment. Of the last two categories of information conveyed to the relatives, G, the notion of palliative care, was most often discussed in terms of freedom from pain and suffering as well as the promotion of peace and comfort. The types of information subsumed under category H related to the need to place the patient’s medical and legal considerations at the heart of decision-making.
Extracts from NIB3R09 case notes demonstrated the logic outlined above in the medical note record of the conversation with relatives:
Medical note: ‘30/10/2012 09:25 . . . speak to relatives – I think we’ve come to the end.
[consultant]
30/10/2012 11:40 Spoke to mum + others. Staff nurse [name] present.
Told that [patient] is very unwell and getting worse all night and all organs are failing. I told them she is on the maximum O2 and the O2 is not getting through. Pressure on the ventilator is high any more will cause more harm such as a pneumothorax. Her inotropes are back again and gone into very high amount and we cannot give her more since her leg (Lt) is going more purple. So we have to leave it like this.
She has got infection which is getting worse despite changing the antibiotic and I have added another one today.
I also told them her kidneys are not working and overall she is much worse + in these circumstances it is better not to resuscitate if she has a cardiac arrest. This is not in her best interest. I also informed them that I have changed some treatment and going to restart the filter. If she is not responding to the treatment, we should call it a day and keep her comfortable.
They seem to understand this + asked how long she will last. I said ‘I do not know’. We will give her a few hours if she deteriorates, we will discuss again with the view to keep her comfortable.
DNAR form completed. Signed [consultant].
31/10/2012 11:00 42 F bifida/severe CAP + sepsis
(Day 10 in ITU)
Condition worsened yesterday + continued to decline overnight.
DNAR completed yesterday + ceiling of care initiated . . .
31/10/2012 – 11:25 Discussion with family (mum) consultant + SN [staff nurse].
Explained [patient] has deteriorated further + hasn’t responded to maximum treatment overnight. I discussed withdrawal of inotropes and family agreed that we will not renew the adrenaline infusion when it runs out in a few hours- Family will contact other relatives.
These discursive categories were used strategically to prepare the ground for the difficult news that a patient was dying and that medical intervention had reached the limit of its powers. It was clear from the data that doctors’ discussions with a patient’s relatives about the patient’s imminent death reflected a shift from cure to care. This was not just a linguistic device but a very real change in the nature of the patient’s care. The requirement for relatives to make a cognitive shift away from the survival and recovery of the patient to symptom control and death has been discussed elsewhere. 26,67 The speed with which these conversations progressed varied in line with the patient’s condition. This is demonstrated in the cases of SIB3R08 and SIA2R04, below:
D/W partner/son [name]/children. They themselves can see that [patient] is dying. And are in full agreement that we have come to [the end]. Curative Rx [radiotherapy] is not possible. New focus of care will change to palliation.
SIB3R08
I explained to the wife + 2 daughters that the LCP is a comprehensive pathway whereby a medical team identify that a patient is dying and their care switches from active management to palliation. The LCP is designed to ensure the patient is kept calm, pain free and comfortable during the dying process, and that unnecessary/potentially distressing treatment is avoided. The reason for starting the LCP is that [the patient] has a systematic bacterial infection (sepsis) which has affected all his organ systems. The infection + its systemic effects have failed to respond to 72 hours or more of aggressive ITU care and his condition has deteriorated to the point where we do not feel he can ever get better . . .
SIA2R04
Despite the careful construction of a narrative which was designed to lead to the conclusion that the patient was dying, notes often also revealed a glimmer of caution, a small degree of uncertainty which could hold out to a patient’s relative the slim hope of recovery. In some of the notes the use of terms such as realistic, significant recovery, meaningful recovery and significant possibility left some linguistic room for recovery against all odds:
No realistic chance of improving and his deterioration is worsening.
SIA2R09
Dr explained likelihood of significant recovery is poor.
NIA2R10
Without prospect for a meaningful recovery.
SIA3R04
There is a significant possibility he might not survive.
NIA6R04
Will more than likely not recover from this and is most likely at the end of her life.
SIA3R06
While this lack of absolute certainty in the language used to communicate information about prognosis may reflect a wider problem with evidence and its interpretation,68 it is generally considered to be very difficult to predict accurately that a patient is dying. 22,26,45,69 It is clear that despite medical evidence to the contrary there are cases which defy medical expectations; these are often framed as the ‘miracle’.
In this study, the most commonly identified physiological markers used to support the decision that active treatment was no longer of benefit included multiple organ failure (involving at least three organs) and irreversible brain injury/damage. Ravenscroft and Bell’s survey in ICUs also reported multiple organ failure as one of the most common reasons for withdrawal of therapy. 63 In the cases of SIA1R01 and NIB4R03, the role of organ failure supported the notion of a poor prognosis:
Overall, very poor prognosis given 5 organ failures. Family aware of this; DNAR form completed today.
SIA1R01
Discussed end-of-life decisions: – if signs of multi organ failure – esp renal failure this will be indicative of terminal prognosis -will likely withdraw at any time.
NIB4R03
In this study, examination of the notes suggested a multipronged approach to defining the limits of treatment in relation to each individual patient. First, it was reported that staff had done their best, with the limits of active treatment reached or there being no possibility of doing more. Expressions such as on maximum treatment, our best efforts, full treatment and most aggressive therapies were commonly contextualised by disease progression or lack of response or improvement from patient. This is exemplified in the following extracts:
She is going to die regardless of what we do because she has deteriorated despite extremely aggressive treatment on ICU, but also on ward X.
NIB5R07
Advised he is receiving maximum support possible + any further deterioration + we may not be able to support him.
NIA6R04
I explained that his condition has deteriorated further today and we are reaching the limits of our supportive therapies.
SIA3R04
Despite maximal multi-organ support his condition was not improving.
SIA2R10
Told that any attempts to improve [patient’s] health did not help – he is deteriorating rapidly . . . explained that despite all the treatment given there has been no improvement in her condition.
NIB5R06
In many cases, the notes revealed how the concept of futility was actively tested by allowing a trial period during which treatment was continued or given to see if patients improved, responded or deteriorated. The Intensive Care Society’s guidance suggests that ‘when outcome is uncertain, it is worth considering a trial of intensive care treatment on the understanding that it will be withdrawn if ineffective’. 70 However, the nature of active treatment and the length of time allowed to assess efficacy were frequently discussed in the notes, as shown in the following extracts.
[Information Given to Relatives Form] 29/7/12 09:30 Present at interview Son, Daughter + Staff Nurse.
I explained the surgical procedure + the serious nature of a hole in the [-].
Her organs are failing + she is not responding to our treatment. We will continue treatment but I think it is likely that in the next few hours we will reach the limit of our treatments + if she is still continuing to deteriorate continuing Rx [radiotherapy] at this point would not be in her best interests.
Family understand. No further questions. [Signed by the consultant]
29/07 12:05 Present at interview Daughter, Staff nurse, Consultant
I explained that BP is continuing to drop.
Continuing Rx is futile.
I discussed withdrawal of Rx.
[Medical notes] Daughter upset but understands. [Signed by the consultant]
NIA6R09
14/6/12 12:14 Spoke to the relatives at 10:15 Notes written later because of other patient unwell. Told the daughter that [patient] is unwell with multi organ failure + ischemic bowel. Surgeons to have a look at it to see whether they can do anything. If they feel all the bowel is dead it will be open + close + we will withdraw treatment and keep her comfortable. In case of cardiac arrest we will not do CPR [cardiopulmonary resuscitation].
I told her that the decision is a medical one and in all probability she will die.
She accepted the fact.
Pt [patient] returned from theatre. Myself + the medical SPR [specialist registrar] spoke to the whole family + told them that we cannot do any surgery since the entire bowel is black. So we are going to withdraw treatment + keep her comfortable. They agreed. For TLC.
NIB3R06
Reports of what relatives were told and relatives’ responses to that information
Interactions between staff and patients were much in evidence in the ICU patients’ notes. There was lengthy consideration of the families’ responses to what had been communicated and in particular, where there were divergent opinions, how these differences were resolved.
A consistent line was articulated with regard to the relatives’ role in decision-making. Families were not expected to make medical decisions, as this was defined as the doctor’s responsibility. This was evident in the notes:
Aunt informed me that there were more relatives travelling from [name of city] & they were not able to make any decisions until then. I reassured them that there was no decisions for them to make – that once the family were here we would put [patient] onto a ‘t-piece’/macrophon + [patient] would be kept comfortable.
SIA1R06
I have mentioned that we (ITU team) along with medical team have made a decision of DNAR in view of maximum therapy and 4/s organ failure. The outcome is going to be very poor and no further questions from husband.
Have explained that we may make the decision to withdraw active management in next 24 hours . . . [Consultant Anaesthetist].
NIB5R07
[Patient’s] friend spoke to the consultant regarding [patient’s] chances in theatre. [Friend] was very upset following consultation stating that he felt that if there was a chance that the operation could work he should have it irrespective of the likely outcome. I apologised to [friend] and told him that he shouldn’t feel like he has to make the decisions re his friend’s health, that the decisions are for the Drs. NIC also spoke to [friend] and said the same. ITU consultant also spoke with [friend]. I wasn’t present at the time.
SIA1R07
However, although families were not expected to take medical decisions, the voice or opinion of the relative was not absent from the notes. There were three ways in which families’ views were represented in the notes: (1) family agreed to care plan made by staff; (2) family provided proxy views on patient’s preferences for care; and (3) family suggested care plan which was accepted by staff.
Family agreed to care plan made by staff
Not surprisingly, doctors constructed the narratives of the patient’s deterioration with a view to eliciting the relative’s agreement for particular courses of action. Terms such as ‘in (full) agreement with’, ‘agree with/to’ and ‘happy with’ were very often used to convey families’ consent to the doctor’s decision to switch care from cure to palliation and the care plan suggested (see also the following quotes):
Mother and sister spoken to. Emphasis made on fact that there is no likelihood of recovery. Withdrawal discussed. They are all in full agreement. Comfort care at all times. Not for CPR.
SIA1R03
ECG [electrocardiogram] showed brain damage and it was clear we could not help him further to recover back to his old self. Family agreed to withdrawal of all treatment.
NIA2R04
Family provided proxy views on patient’s preferences for care
Some notes recorded that families had ‘expressed’ or ‘stated’ what patients would have wanted in the circumstances:
They [mother and sister] expressed their belief that [patient] had ‘had enough’, his time had come. He has been through so much. [consultant] assured them that we would sedate them for comfort + analgesics if needed.
SIA1R03
Approached by daughter [name] who stated that the family have had a discussion and they were saying [patient] wouldn’t want this invasive support. Therefore discussed regarding how we would keep [patient] comfortable as it was the main issue discussed.
SIA3R02
Family suggested care plan which was accepted by staff
In some notes, families were reported as initiating plans to withdraw/withhold active treatment and provide palliative care. The views and actions of the staff were reported in this context as ‘respecting the family’s wishes’ and responding to family’s preferences:
Following the update the family expressed their wish for pt [patient] to be moved to a side room due to the levels of noise and disturbance in the unit, NIC + Dr agreed to move pt to the side room. In addition to this family requested for the ventilator to be removed. Consultant + NIC informed family of the events that could happen once the ventilator is removed. The family accepted this and NIC and myself removed ventilator. Family requested for endotracheal tube to be removed. NIC explained the events that could take place if tube removed. Family understood NIC confirmed this with consultant. We subsequently removed ET [endotracheal] tube.
SIA1R06
Dr [name] discussed with family that treating was now ineffective. Family expressed wishes that ventilator + tube be removed, so they could spend time with [patient].
SIA1R07
Many notes showed a combination of all three examples:
Consultant Notes 14/06 18:05[Name] – ICU Cons Discussion with [wife] and her son.
We have spoken a couple of times over the past few days and they are well aware that despite aggressive therapies his condition is deteriorating.
I explained that his condition has deteriorated further today and that we are reaching the limits of our supportive therapies. The only cause that we have readily identified is that of infection; yet he has not responded to antibiotic therapy. Currently he continues to have extremely high ventilatory and oxygen requirements and he now also needs cardiovascular support and his renal function is deteriorating.
[Wife] and her son stated that [patient] has always said he would not want a protracted death. We discussed renal support, escalating inotropic therapy and chest compressions in the event of cardiac arrest. I stated that [patient] would not benefit from such therapies on the grounds that they would be futile in the face of continued deterioration. His family stated that he would not wish for such attempts to prolong his life to be attempted.
We also discussed what we would do if his condition deteriorated even further and agreed that in such an event we would call [wife] and her son and would withdraw the supportive therapies while they were present; this based on his previously expressed wishes (above).
SIA3R04
The data suggested that one of the major goals of communication with relatives at the point that treatment was no longer considered beneficial was to get support for decisions that were being formulated or made by the medical team. As already highlighted, the notes were explicit in demonstrating that clinicians did not want relatives to feel responsible for making decisions, particularly those that related to withholding or withdrawing active treatment. These findings are strongly supported by the work of Seymour, who also suggests that families’ participation in decision-making may not be a central aim of clinicians in intensive care. 45 She suggests that the communication with relatives is designed to bring families to a point where they will agree with decisions that have already been taken. Seymour also suggests that sharing responsibility between staff and relatives regarding a patient’s preferences for care provide a way of broadening the basis for withholding or withdrawing treatment. Seymour observed in her study that the views of the family became most important when there was a degree of uncertainty over which way to proceed.
In the majority of notes, families were represented as a single unit, with individual representatives singled out where they had been involved in particular conversations. This created the impression in the notes that families were unified in their understanding of and responses to information that had been communicated. Only occasionally were divergences of opinion between family members recorded.
Nursing Notes 19/05/12 – 14:10
I spoke to the family today after the ward round, explaining how sick their mother is and how dialysis is not an option for her. She has 4 system organ failure, which is not going to improve. There seems to be a slight difference of opinion in the family whether to continue treatment, but at the moment this is not resolved. I emphasised to all the family that the problems with their Mum’s liver is not going to resolve. It appears that they have only recently realised that she was suffering from liver failure. I think they need a little more time to come to terms with the situation.
SIA3R06
In the UK, doctors carry the legal responsibility and accountability for decision-making according to the law, the standards imposed by the General Medical Council and published guidelines. However, it is widely acknowledged and emphasised that families are an intrinsic part of end-of-life decision-making26 and help to make the process of decision-making open and accountable. 71
The plan of care
As Billings points out, in intensive care facilities, deeply anxious patients and families are thrown into a hospital setting that is often strange and frightening, and must work with unfamiliar health-care professionals. 72 In order for families to cope with and accept a terminal prognosis, they need effective and empathetic communication. 73,74 Seymour’s study45 and the study by Cosgrove and Bari74 found that both nursing and medical staff in ICUs saw the delivery of information to families as a major aspect of their role. Nursing and medical staff portrayed their role in giving information as a means of enabling families to adjust to the likelihood of death and facilitating the primary grieving process.
While focusing on communicating the patient’s condition to relatives, the notes also portrayed a narrative around the care that was being provided. Keeping families ‘updated’ and ‘informed’ was invariably recorded in the notes. The word ‘reassure’ or ‘reassurance‘ was used frequently in the notes across all sites and there appeared to be a clear and consistent line articulated in the notes as to what the relatives were told. Once the plan of care had been communicated and was being put into practice, the notes highlighted the relatives’ response, usually in terms of their acceptance of it. There was frequent use of terms such as:
-
they (the relatives) are [(well) aware of]
-
they have clear insight of
-
they (appear to) understand
-
they are (very) understanding
-
they have a good understanding of
-
they (appear to, seem to) accept
-
they (seem) accepting of
-
they are happy with
-
they seem at peace with.
Just as clinicians appeared keen to get the relatives’ support for their treatment decisions, so clinicians also appeared keen to reflect conversations they had had with relatives about a proposed plan of care:
Have explained that we may make the decision to withdraw active management in next 24 hours. Husband was initially very upset to which I have reassured that the ITU management is always to maintain organ support to allow the recovery and in view of the both: had very poor nutritional and very poor natural immunity due to alcoholic liver disease and multiple nutritional deficiencies and ICU outcome is likely to very poor. Husband had no further questions, left the interview room to contact his daughter [Consultant Anaesthetist].
NIB5R07
Summary
The analysis of case notes in relation to the communication between staff and relatives supports other research on end-of-life care in ICUs. 26,45 Limited though they are, the notes revealed the importance to clinicians of building the relatives’ understanding of the treatment and care of the patient in the context of an overall narrative of deterioration and death. The separation of the act of medical decision-making from support for medical decision-making was a very real and important one. Medical staff appeared keen to present in the notes the decisions that were taken as objective evidence-based decisions. They recognised, however, that the emotional connection between relatives needed to be harnessed to the patient’s best interests, even though from the relatives’ point of view this did not necessarily serve their own best interests. It seemed from the notes that as the technology that saved lives became redundant, the efforts of the clinicians became focused on convincing relatives that cure needed to be replaced with care. As the practice shifted, so did the nature of the discourse. Staff of all professions and grades writing in the notes adopted the new discourse of care which was both consistent and persistent. In the next chapter we report the findings from observations undertaken in ICUs.
Chapter 10 Intensive care units: observation and case note analysis
Introduction
In this chapter of the report we focus on the observations of end-of-life care undertaken in the ICUs participating in this study. Although the detailed conversations between clinical staff and relatives about the patient’s condition were not observed prior to a decision that the patient was in the last days or hours of life, subsequent discussions about these conversations were observed between staff, between relatives and between staff and relatives. They were also reported in the case notes which also form part of the data set being analysed here. In all cases the researchers observed the withdrawal of treatment and/or interventions from the patient but not necessarily the patient’s death.
Findings
The sample of ICUs for the study was designed to reflect care in both LCP sites as well as sites that did not use the LCP. However, the opportunity to observe care in each of the 12 sites participating in the study did not occur. In the north-west the observations were undertaken in three LCP-using sites and one non-LCP-using site, and in London and the south-east observations were undertaken in two LCP-using sites and two non-LCP-using sites, making a total of five LCP sites and three non-LCP-using sites. Thus, the 17 observations reported here are based on eight different participating ICUs (Table 13); 10 were undertaken in London and the south-east and 7 in the north-west.
| LCP sites | Deaths observed | Non-LCP-using sites | Deaths observed | Total observations |
|---|---|---|---|---|
| North site 1 | 1 | North site 1 | 1 | 2 |
| North site 2 | 2 | 2 | ||
| North site 3 | 3 | 3 | ||
| South site1 | 4 | South site 1 | 3 | 7 |
| South site 2 | 1 | South site 2 | 2 | 3 |
| Total | 11 | 6 | 17 |
Of the 17 observations, 6 were undertaken in organisations which did not use the LCP, with the remaining 11 taking place in LCP-using organisations. The patients observed had been in an ICU bed from a range of 1–59 days. However, the majority (76%) had been in the ICU for ≤ 5 days (Table 14).
| Patient identifier | Age (years) of patient at death | LCP used (✓) not used (✗) | Length of time in ICU bed | Length of time observed to death | Diagnosis |
|---|---|---|---|---|---|
| NIA2P1 | 83 | LCP documentation not fully completed | 3 days | 12 hours 4 minutes | Bowel obstruction |
| NIA1P1 | 69 | ✓ | 3 days | 35 minutes | Cerebral infarct, MI |
| NIB3P1 | 67 | ✗ | 1 day | 55 minutes | Rheumatoid arthritis, liver disease, sepsis |
| NIA6P3 | 47 | ✓ | 17 days | a26 days after transferb | Hepatitis C, drug and alcohol poisoning |
| NIA6P2 | 71 | ✓ | 2 days | a4 days after transferc | Brain stem infarct |
| NIA6P1 | 45 | Started after 2-hour wait | 4 days | 3 hours 10 minutes | Alcoholic liver failure |
| NIA2P2 | 72 | ✓ | 4 days | 2 hours 30 minutes | Seizure, perforated colon, brain tumour, multiple organ failure |
| SIA1P4 | 50 | ✓ | 9 days | 1 day 1 hour 43 minutes | Variceal bleed, alcoholic liver disease |
| SIA1P3 | 77 | ✓ | 2 days | 39 minutes | Respiratory failure, sepsis |
| SIA1P2 | 58 | ✓ | 1 day | 15 minutes | Sepsis, cardiac arrest, pneumonia |
| SIA1P1 | 77 | ✓ | 5 days | 6 hours 39 minutes | Bradycardia and cardiac arrest |
| SIB2P2 | 74 | ✗ | 59 days | 3 days | Multiorgan failure |
| SIB2P1 | 84 | ✗ | 4 days | 5 minutes | Acute renal failure |
| SIB1P3 | 55 | ✗ | 21 days | 2 hours 36 minutesd | Sepsis, metastatic leiomyosarcoma |
| SIB1P2 | 67 | ✗ | 5 days | 91 minutes | Type II respiratory failure, multiorgan failure |
| SIB1P1 | 81 | ✗ | 2 days | 12 hours | MI, end-state COPD |
| SIA3P1 | 76 | ✓ | 1 day | 55 minutes | COPD |
In two cases, patients did not die on the ICU during the observational period. One of the patients whose care was observed ceased to be supported by the LCP and was transferred to another unit as her condition improved (NIA6P3ON). This patient eventually died in a hospice 26 days later. Another patient was transferred off the ICU to a ward but continued to be supported by the LCP. This patient died 4 days after being transferred. The researcher did not observe the deaths of these two patients. The discussions reported during the observation in which the LCP was withdrawn (NIA6P3ON) provide an important insight into the way in which bodily responses are interpreted differently within lay and medical knowledge and the implications of this (see Divergent views between staff and relatives, later in this chapter).
Apart from the two observations which did not result in the patient dying on the ICU, from the time at which an observation was begun to the point at which a patient died ranged from 5 minutes (SIB2P1ON) to 3 days (SIB2P2ON). All of the observed patients were defined as unconscious, attributed to the severity of the underlying disease processes or the effects of sedation and analgesia.
The use of the Liverpool Care Pathway in Liverpool Care Pathway-using sites
For non-LCP-using sites, there was no evidence to suggest the presence or influence of an end-of-life care pathway. However, for LCP-using sites, the use of the LCP varied enormously between sites and on occasion between patients in the same ICU. The data reported here relate to the 11 observed deaths in five sites which were recruited because they reported using the LCP. Despite the finding in the retrospective case note analysis (see Chapter 9) that some LCP-using sites did not always use the LCP to support care, and that a minority of non-LCP-using sites had supported deaths using the LCP, all 11 observed deaths in LCP-using sites were supported by the LCP.
This section begins by examining the use of the LCP, and in particular the relationship between decisions about care and the use of the LCP. All of the sites used the LCP in different ways.
The major differences in the use of the LCP were:
-
timing of the use of the LCP
-
perceived purpose of use of the LCP
-
the use of documentation
-
communication of LCP use to relatives.
Timing of the use of the Liverpool Care Pathway
The LCP is structured to support care once a person has been recognised to be in the last hours or days of life. In ICUs this is a complicated decision arising from a detailed review of the clinical evidence.
All of the sites using the LCP had access to the ICU LCP documents. Through the retrospective case note analysis (see Chapter 9) it was clear that the LCP was available and used frequently in these sites. However, it was not always used with every dying patient, and, when it was used, it was not always used in the same way. From the notes it was possible to see that a decision to stop active treatment was swiftly followed by the recommendation, ‘for LCP’. However, different ICUs and their staff adopted different approaches to the point at which the LCP forms started to be filled in and consideration was given to achieving the goals outlined in the LCP documentation.
In NIA6P1ON (27 July 2012; 20.15) a nurse reported that it was the ICU’s policy to wait 2 hours after a decision had been made that the patient was not for active treatment before implementing the LCP. In the case of NIA6P1ON, the patient was extubated at 17.45, the LCP documentation was signed by a doctor at 20.15, and a nurse began to complete the LCP assessment elements shortly afterwards. Two months later in the same site, the LCP paperwork was started for another patient as soon as the findings of a magnetic resonance imaging scan and a lumbar puncture revealed a large and irreversible infarct in the patient’s brain stem (NIA6P2CN 18 September 2012; 17.30). The ICU MDT discussion sheet recorded ‘Relatives not present when LCP commenced, but they were aware of patient being extubated and that patient is for TLC. Family finding everything too distressing so have gone home and will return in the morning’.
In NIA2P2ON (7 March 2012) a decision was made at 10.30 for a patient to ‘be put on the LCP’ with the caveat that the LCP would not be ‘started’ until the family arrived, which they did at 13.00.
In SIA1 there was a consistent time lapse between the decision to put a patient on the LCP and its implementation (SIA1P3 and SIA1P1). In the case of SIA1P2 (14 September 2012; 19.30) the nurse was heard to report that it would be unlikely that that they would even get the LCP paperwork started, as the patient was on such a ‘high level of support’ that it was likely that as soon as they started withdrawing the ‘patient would go quickly’.
In the instances outlined above, the variation in the timing of the LCP was associated with the timing of the cessation of active treatment, the likely speed of death once the patient had had active treatment withdrawn and the desire to allow the patient’s relatives and visitors to be present before the patient died. This last point was of considerable importance as clinicians preferred to discuss withdrawal and what would happen after withdrawal with the patient’s family. Clearly, this could not happen unless the family was physically present.
In one site (SIA3P1ON) the consultant had started to complete sections of the LCP documentation prior to the arrival of the patient’s relatives. The consultant sought out the researcher (25 July 2012; 12.55), to tell her that ‘although the family had not yet arrived’ he had decided to start the LCP because the ‘patient was deteriorating’. This decision was based on a clinical judgement but was not associated with any immediate change in the management or treatment of the patient. In fact, the consultant gave explicit instructions that the relatives ‘might need some time at the bedside first, before starting withdrawal’.
Across the ICU sites the intention to use the LCP did not translate automatically and immediately into its implementation. Timing of the use of the LCP reflected its position in the order of priorities. It was considered only once the clinical team had discussed and decided that ‘active’ treatment was no longer of benefit to the patient. Once this decision had been reached the LCP was seen as a flexible response which could be implemented as and when the clinical team felt the circumstances were appropriate. There was a common perception (see staff point 1 and point 2 interviews) that the LCP was seen as a nursing tool. It was a pathway that came into play once the medical and clinical team had decided that active treatment was no longer of benefit to the patient. Some of the delays experienced in LCP implementation were attributed to the difficulties associated with getting doctors to sign the forms.
In the next section we explore what clinicians appeared to think the LCP offered, based on what was observed and what was written in patient case notes.
Perceived purpose of use of the Liverpool Care Pathway
Given the variation in timing of LCP implementation it was not surprising to find that, across the sites, the LCP meant different things to different people. It was common across all sites for the LCP to be associated with ‘withdrawal’. This is not surprising as the decisions that had to take place before the LCP was implemented involved an assessment of the patient’s response to treatment. By definition, the LCP was used only where the clinical team believed that the patient was not deriving any benefit from active treatment. Withdrawal, what is meant by withdrawal, and what happens in practice is hugely complex and is discussed later on. Its importance here, however, is its association with the LCP in the minds of the clinical staff and in their conversations with relatives. Clearly, the decision to cease active treatment is a precursor to withdrawal as well as to the implementation of the LCP. Both stem from a recognition that the patient is entering the last days and hours of life.
In SIA3P1ON (25 July 2012) the nurse was heard telling the relatives as the observation monitors are switched off at 13.20 that ‘they have begun the LCP’. This is curious. The consultant notes, and the conversation held with the researcher by the consultant, indicated that the LCP was started at 12.55. One interpretation of the nurse’s statement could simply be that the use of the LCP had begun earlier. However, the juxtaposition of telling the relatives that the LCP had begun and turning the monitors off seemed to convey the idea that treatment had changed and things were being stopped. In fact, the only thing that had changed at that point was the privacy setting on the monitor, which had been activated to prevent the patient’s relatives from seeing the patient’s vital signs. Intentionally or otherwise, the nurse seemed to be signalling that the LCP was associated with ‘equipment being turned off’.
Discussions between the clinical team revealed that while the LCP was associated with the decision to withdraw active treatment, the implementation of the LCP was not necessarily a trigger for withdrawal (see SIA3P1ON, above). A nurse reported (SIA1P2ON 14 September 2012;19.00) ‘We have done all the (LCP) paperwork but have not withdrawn anything yet’.
Occasionally, in the observations and, less often, in the notes, staff explicitly associated the LCP with ‘palliative care’. This was observed in SIA1 in relation to two of the observed patient deaths. A consultant reported in the notes (SIA1P3CN) that ‘Our plan is to use the LCP in order that comfort needs are met’. While there was a clear association of the LCP with care, and in particular care provided by nurses, the strongest message to emerge from the observations was the association of the LCP with withdrawal. This will be explored in more detail later in this chapter.
The use of documentation
All of the LCP-using sites ran the ICU documentation alongside the LCP documentation, so for each patient an account of the care provided was recorded in a number of places. The names of the documents varied from site to site, but the content was broadly similar and can be grouped into the following types:
-
critical care unit information given to relatives/communication with relatives document/family communication sheet
-
medical notes/clinical notes
-
critical care daily record/daily assessment sheet/continuing progress/daily observations
-
nursing notes/nursing evaluation/sometimes split into day evaluation and night nursing
-
multidisciplinary record/multidisciplinary communication sheet
-
drug sheet.
In order to assess how the LCP was used in practice, we compared the completion of the LCP documentation with what was observed, and what was observed with what was recorded in the various case notes.
Where deaths occurred very soon after the start of the LCP, the LCP documentation was often incomplete. The ICU notes provided a much more detailed account of the patient’s deterioration and what was done by the staff. Although variances were marked on the LCP form, often they were not explained, actions were not described and outcomes were not identified (SIA1P2). Given the short timescales involved, perhaps these discrepancies are not surprising. However, there was one case in which the discrepancies between the LCP documentation, what was observed and what was recorded elsewhere in the notes were quite extensive. Conversations were observed between the clinical team about moving the patient to a ward, and the suggestion that the patient might not die very quickly. In NIA6P2, in section 2 of the form – LCP ICU day 1 – all of the goals were marked hourly as achieved (except Goal f: respiratory support; Goal i: the patient does not have other symptoms; and Goal q: the well-being of the relative or carer). When a patient continues to be supported by the LCP for a second day, the time intervals for recording change from hourly to 4-hourly (for goals a–j) and 8-hourly (for goals k–q). These were completed for the time period 12.00–00.00 (midnight) for goals a–j and for 12.00/16.00 and 00.00 (midnight) for goals k–q.
The major discrepancies in the completion of the documentation related to:
-
the timing of care
-
the assessment of pain and the administration of drugs
-
communication with the relatives.
The nature of these discrepancies are outlined in the case study in Box 1.
When matched with the observational data, none of the times at which turning/rolling, mouth care and assessment of pain were undertaken matched the data recorded on the LCP. The importance of this is simply that as a result of undertaking these activities, observations and decisions were made which were not recorded anywhere. A NG tube that was observed to be removed was also omitted from the record.
19 September 2012; 21.29 Nurse says to Dr ‘Shall I take this out’ (touching the N/G tube) ‘he’s on the LCP, we don’t usually continue feeds when they go to ward’ (NIA6P2ON).
(b) The assessment of symptoms and the administration of drugsAn assessment of a patient’s symptoms (in this case agitation, pain and secretions) would usually be recorded on the variance sheet if the patient was found to be symptomatic and action was required/undertaken. In this case, despite three assessments of pain and the subsequent administration of paracetamol and diamorphine, and three attempts to remove thick sputum using suction, the variance sheets were all left blank.
(c) Communication with the relativesA considerable amount of communication with relatives was observed. This ranged from discussion about arrangements for feeding the patient ‘because the family thought it would be better’ (19 September 2012; 14:35); the name that the patient responds to ‘They keep calling him J’ and that the relatives have told the staff many times that that was not what he was known by (19 September 2012; 14:02); and moving the patient to a ward. None of this communication was recorded on the LCP documentation.
In this patient’s case the LCP records appeared incomplete and, as a result, misleading. It seemed important that a decision was made to move the patient to a ward. Interestingly, the LCP documentation that was completed after the patient’s move off the ICU and on to the ward was more complete, with variances detailed and records made of the communication between staff and family members.
Communication of Liverpool Care Pathway use to relatives
As the study progressed, the environment changed significantly. Negative media coverage of the LCP created huge reluctance on the part of staff to talk to relatives about the use of the LCP. This was openly discussed between staff, observed and reported in the notes. Sites adopted different strategies to discussing the use of the LCP in the care of the patient with the family. At one site (SIA3P1ON 25 July 2012; 11.55) the consultant told the researcher just prior to talking to the family that he discusses the LCP with the family ‘so they know that the patient isn’t just being shoved in a corner’ but is ‘still being actively looked after’. In other sites discussion about the LCP was more restrained, varying from a nurse who reported in SIA1P1ON (15.10) that the patient’s family had not been told that the LCP is being used because of the bad press, to a consultant in NIA2P1ON (19 January 2012; 14.30) who reported ‘it’s another pathway we don’t need to bother relatives with’.
Withdrawal
As has been highlighted, in addition to the initiation of the LCP, the concept of withdrawal was central to the care of these patients in ICU. The following section focuses on the issue of withdrawal in all observed cases regardless of whether or not the LCP was used to support care. It focuses on four specific elements in the process of withdrawal:
-
the decision to withdraw
-
the management of withdrawal
-
the meaning of withdrawal
-
the observed process of withdrawal.
The decision to withdraw
Before discussing in detail what is meant by withdrawal we explore how the decision to withdraw active treatment was communicated and implemented. From the observations of discussions with relatives and the case notes, clinicians presented decisions about the withdrawal of active treatment in terms of the ‘best interests’ of the patient. Death was constructed as preferable to life, and staff did not see prolonging death through active treatment as being in the patient’s best interests.
Patients were explicitly informed, usually by the ICU consultant, that the ‘decision-making’ about withdrawal was clinical and not a decision to be made by relatives.
18.05.12;
10:20 Consultant responds ‘we’re not asking you to make a decision. It’s not a decision the family makes. It’s a decision for consultants to make. The question is: would he be able to sustain life in the long term and the answer is no.
SIB2P2ON
The emphasis on medical decision-making was always explained to the relatives in terms of their benefit, so that they would not have to live with the burden of feeling ‘as though they’d had to choose to end (name of patient’s) life’ (SIB2P2ON). It was also the case that the decision to withdraw had already been made prior to conversations with the family, often during a ward round or MDT meeting. The basis for this decision will be explored in detail in subsequent publications in peer-reviewed journals.
Usually, but not always (see SIB2P1ON), the decision to withdraw was conveyed to the relatives prior to any withdrawal taking place.
25.07.12;
10:18 The nurse told me they had not yet spoken to the relatives, but they were going to. She also told me that they had already had a preliminary conversation about the patient’s deteriorating condition, but they hadn’t yet discussed withdrawal with them, but that withdrawal was likely to be the next step.
SIA3P1ON
The presentation of the decision was carefully constructed. It was almost always preceded by a detailed narrative of the patient’s deterioration, including treatments that might have been tried and complications that had developed.
10.05.12;
13:35 The consultant started the meeting by asking the two relatives what they understood about the patient’s condition. The consultant listened to what the two male relatives reported and at one point checked the patient’s notes, which he had with him. He then explained that, although it had previously appeared that the patient was suffering from a chest infection, for which they had unsuccessfully tried to treat her, they had done an ECHO [echocardiogram] earlier in the day and discovered that, in fact, the patient had cardiac failure. Consultant explained that the symptoms of cardiac failure can sometimes present as respiratory failure for various reasons (which he discussed), but that having done the ECHO they could see that her heart was very damaged and was not pumping properly. He explained that, given the severity of her problems, which he identified as ‘multiple organ failure’ that the treatment they were currently providing was ‘prolonging death, not saving life’ and that the humane thing to do was to ‘let her die’. Consultant said that what they would now do is withdraw the treatment that was ‘prolonging death, rather than saving life’ and that that was the best thing they could do for her.
SIB1P2ON
In only one site (SIB2P1ON 23 April 2012; 12.10), a non-LCP-using site, did the clinical team begin to reduce the patient’s medication without any prior discussion with the patient’s relatives.
In general the issue of withdrawal was always presented in the context of the patient’s decline and the futility of further treatment. The nature of the decline portrayed, in the clinicians’ minds at least, left very little room for doubt that the patient was at the end of their life. For example:
27.7.12;
15:25 Consultant explained that she has continued to deteriorate and in his opinion is not going to survive.
NIA6P1CN
18.9.12;
17:30 Consultant informed family that this is an irreversible process and his clinical condition is unlikely to improve.
NIA6P2CN
15.05.12;
19:15 Consultant explained patient is in decline. Despite all the intensive efforts the patient has failed to improve and nothing we do is likely to change his survival.
SIB2P2CN
Clinicians then focused the discussion with the relatives on the management of withdrawal.
The management of withdrawal
A decision to withdraw active treatment did not mean that everything was just stopped. Different sites adopted different strategies in relation to each patient. Withdrawal was contingent on a number of factors and was deployed to accommodate these factors.
The factors included:
-
the presence of key relatives
-
waiting for the specialist nurse for organ donation
-
allowing the relatives time.
The presence of key relatives
Many instances were observed and reported in the notes of withdrawal being on hold until relatives arrived at the bedside. For example:
17.12.11;
14:20 Staff were waiting for sister-in-law to travel from [name of city].
NIA1P1ON
10.05.12;
15:45 Staff were waiting for relatives to return from putting money in the parking meter.
SIB1P2ON
17.02.12;
12:50 Staff were waiting for the whole family to arrive.
SIB1P1ON
Staff recognised the importance of giving relatives the opportunity to ‘say their goodbyes’ before the patient died and in so doing reflected the delicate balance between the needs of the relatives and the interests of the patient.
Waiting for the specialist nurse for organ donation
There were a few examples in the data where a withdrawal decision was not immediately executed because the staff were waiting for a decision on whether or not the family would be approached regarding organ donation. The policy adopted in most sites where approval for organ donation was considered involved the specialist nurse for organ donation (SNOD) reading the patient’s notes and then calling other sites to see if there was a demand for any of the patient’s organs. This often resulted in quite considerable periods of seeming inactivity.
14.9.12;
20:00 I was introduced to the SNOD at the Pt’s bedside. There was no family present. Curtains are still open as withdrawal hasn’t begun yet. The SNOD told me this Pt [patient] is unlikely to be suitable for organ donation but that it’s her duty to ring round her colleagues just in case ‘there is someone in a worse condition than this Pt is’.
20:20 Am now waiting while the SNOD wanders around the unit trying to get mobile reception. She told me she will need approx. 1–1½hrs. She also told me that she hasn’t yet spoken to the family about donation. She will only do so if there is a potential recipient identified. She said she doesn’t think it would be right to approach them about donation if there’s a chance there won’t be a suitable recipient because sometimes families see donation as a ‘condolence’ in future months, and it wouldn’t be right to offer them that if she couldn’t then follow through.
21:15 Still waiting [for SNOD].
SIA1P2ON
In the end, the SNOD took the decision not to pursue donation because she felt that the family was getting distressed and a picture was emerging that centres were not interested in this patient’s organs. She reported that she would ‘get flack from her manager’ for arriving at this decision but she nevertheless was prepared to stand by her decision in recognition of the needs of the patient’s family.
A similar scenario occurred in the case of SIA1P3ON (14 October 2012; 17.45). The SNOD reported discussing the benefits of donation and the timescales with the neighbour, who had lasting power of attorney in this case, and the patient’s vicar. They felt that they could wait no longer for the SNOD to make enquiries and at 19.30 at their request ‘withdrawal was started’.
Tensions between the interests of the patient and their family and the potential donor recipient were discussed in the interviews by staff (see Chapter 12) who often reported that end-of-life care should mean end-of-life care, not supporting and maintaining life in order to keep the organs functioning for donation (SIA1P4ON, 11 February 2013; 11.50). The detailed analysis of organ donation will be explored in subsequent publications in peer-reviewed journals.
Allowing the relatives time
In the majority of cases staff created the impression that even though a decision had been made to withdraw active treatment, there was no rush to actually make it happen. There were many instances in which staff were observed to check with relatives if they had had enough time with the patient before withdrawal was begun to ‘say their goodbyes and said what they need to’ (SIA1P1ON 19 March 2012; 16.00). In SIB1P2ON (13.35) the nurse asked if there were any other ‘family that they wanted to ask to come in’ before withdrawal began. The relatives were also asked if they would like more time before withdrawal is commenced.
10.05.12;
16:05 The two male relatives return. They walk around the desk at patient’s right-hand side. The son walks up to his mum and kisses her somewhere on the face, though I don’t see where. I also see the husband stroking her chin, between the tube and the strap holding it in. Nurse asks the two relatives if they would like ‘a few more minutes.’
SIB1P2ON
The length of time between a decision to withdraw and the actual beginning of withdrawal varied, but at its maximum it was 6 hours.
The meaning of withdrawal
Withdrawal was described to relatives in different ways. The description of withdrawal prior to its taking place was designed to give relatives a general view of what was involved and what might happen. Phrases such as ‘limiting treatment to keep the patient comfortable’ (NIA6P3ON); ‘not escalating treatment so we won’t replace meds as they run out’ (SIA1P1ON 19.03.12); and ‘not filling syringes when they go through’ (NIB3P1 29 August 2012; 12.10) were all descriptions given to relatives about withdrawal before it took place.
17.02.12;
Noon Consultant continued to explain about what would occur following switching off the ventilator. He said that it was hard to say: sometimes patients ‘slipped away’ within the hour, sometimes it took hours and sometimes it took days or weeks. He said ‘hopefully, in this case, it won’t take long and will be quick’. He said he realised how tired the patient’s wife must be.
SIB1P1ON
Consultants and nurses were observed informing relatives of the difficulty in predicting whether patients would ‘die quickly or over hours’.
17.02.12;
22:15 One of the daughters asked ‘how long will it be now?’ The nurse responds that she doesn’t know, it could be hours or days. The daughter says ‘so it could be days?’ and the nurse responds ‘yes’.
SIB1P1ON
Once withdrawal had started and the patient’s decline was closely monitored, predictions in general became more detailed and more accurate.
The observed process of withdrawal
Withdrawal was a highly complicated and individualised matter. Although some principles emerged about what was withdrawn and when, there were rarely two cases that were identical. In all cases withdrawal was a process in which different treatments and support were reduced or turned off and the patient’s body was monitored to assess its response to the changes. Underlying this process appeared to be a desire to control the speed of the final period of dying so that it was not too quick but also not too slow, and to ‘create a death’ that appeared natural.
Items were withdrawn sequentially but the sequence varied according to the patient’s level of support and condition. The evidence from this study suggested that the tailored approach adopted by all ICUs was designed to withdraw the support on which the patient was most reliant last of all. If the nurse deemed that ‘once the norad is stopped, he’ll go’, other things would be stopped before the noradrenaline so that the patient’s decline was gradual, rather than appearing to be immediate. In line with this was the early removal of support or equipment, which was defined by nurses as ‘not doing anything’.
14.09.12;
21:45 Nurse 1 told the family that she will be reducing the medicine supporting the patient’s heart because it’s not doing anything. She will also reduce the level of oxygen and change the ventilator so that it is only supporting her natural breath.
SIA1P2ON
19.03.12;
17:00 Nurse puts on a green apron and gloves. She then goes to the side of the bed where the ventilator is. The first thing that she does is disconnect one of the bags. She removes the tube and takes it off the hook. I think it’s the bag of feed. She tells the relatives ‘this isn’t actually doing anything’ and says she’s just taking it away to ‘tidy’ the area.
SIA1P1ON
Where possible, it seemed important for staff to construct the withdrawal in a way that meant the patient’s death was not directly attributed to something that had been removed. The next best thing was to create as natural a death as possible while removing the technology that had supported the patient’s life.
The creation of a natural death
The failure of intensive support to save the patient’s life changed the way it was discussed in the case notes. Rather than continuing the narrative of treatment aimed at cure, the interventions were framed as artificially sustaining the physiological functioning of life. In this context the removal of technology was articulated in terms of ‘letting nature take its course’ (SIA1P3ON 14 October 2012; 14.40).
Echoes of this new discourse were seen in the observations as nurses tried to create or manufacture a ‘natural death’ using the slow retraction of support. Nurses appeared to be trying to create a situation in which the removal of technology and certain medications allowed the body to function on its own as a body, even for a short while, until it expired ‘naturally’. The idea of a natural death seemed also to embrace a smooth, calm and peaceful exit.
11.02.13;
15:55 Nurse 1 said that the patient has now taken some breaths on his own, and she’s hoping he will get to the point when all of his breaths are spontaneous; then, she will be able to switch the ventilator setting so that if he naturally stops breathing, it will be natural rather than as a result of her turning the ventilator off. She told me that Relative 1 understands this, and doesn’t want to ‘prolong the agony’, which Nurse 1 thinks is a ‘very brave’ position to take.
SIA1P4ON
The notion of a natural death was appealing to relatives. The family in SIA1P1 decided that an airway tube should remain in situ in the belief that a more natural death would ensue.
19.03.12;
22:30 They decided no, to leave him so that he could go naturally. They were told that if they did take the tube out, he would stop breathing straight away.
SIA1P1ON
Where it was thought that the removal of support might be accompanied by a distressing noise relatives were offered the option of leaving the bedside.
19.03.12;
17:20 Nurse 1 comes back in carrying a large green tube that has a white circular disc at one end. She tells the relatives that [the patient] is now taking very weak breaths and that the machine is finishing the breaths off. She says that at this point, this is no longer natural, so what she is going to do is unhook the ventilation and cap the end of the tube off with the white disc, explaining that this does not block the tube. She explains that the machine will make ‘a noise’ when she does this. ‘Not a terrible noise, but a noise’ and tells them that they do not have to stay while she is doing it.
SIA1P1ON
Nurses often gave relatives an indication of the time frame within which they expected the patient to die once adjustments were made to the supporting technologies.
17.12.11;
15:01 The nurse comes in and puts her arm/hand on the back of the son on the right, says ‘I don’t think it will be long now.’
NIA1P1ON
10.05.12;
15:45 Nurse says when they start to withdraw, she will turn the filter off first, then she will turn the various infusions off. Nurse says that when they turn the noradrenaline off, she will ‘go’ straight away.
SIB1P2ON
The death, however, was not always controlled in the way that the clinical team wanted. Dying too fast or too slow disrupted the expectations and plans of the clinical team. Where it appeared that the death was taking longer than expected, nursing staff progressed their withdrawal to elements which were more critical in the hope that this would ‘move things along’.
11.02.13;
13:30 Nurse 1 enters the bedspace and says ‘Right. I’ve just spoken to the doctor, and we’re going to extubate him.’ She says that at this point, ‘the kindest thing is to take the tube out’. She tells the family: ‘I can’t guarantee that it’ll hurry things along, and I can’t guarantee that it’ll slow things down’ but ‘at this point, it’s cruel to keep him like this.’ She also says ‘I want to be clear that we’re not doing this to hurry things along. We’ve got all the time in the world.’ Relative 1 says: ‘You do what you think is best.’ Nurse 1 asks: ‘Is everyone alright with that?’ She looks around the group, and they all appear to concur. Relative 1 also asks the various members if they are okay with this decision. Nurse 1 turns and asks Relative 2 if he is okay with this, and he nods his head. Various members of the group begin to cry.
SIA1P4ON
There were a number of observed instances in which relatives felt that the death was not proceeding quickly enough. While sticking to the plan of withdrawal, staff often felt the need to justify their actions both to the relatives and to the researcher who was sitting observing.
16.01.13;
19:16 Relative 1 wonders if staff might give the patient an injection to finish her off. Nurse 1 explains that’s not what is going to happen . . . Looking at other Relative 2, Relative 1 asks ‘how long is she going to be like that?’ and ‘You wouldn’t let a dog go on like this’. Relative 2 says ‘Well she’s not a dog is she?’ Nurse 1 explains they are just seeking to keep her comfortable and not much intervention is needed, and as she is young, she could go on like this for some time.
NIA6P3ON
11.02.13;
23:30 Nurse 3 reports they have switched the ventilation to ‘pressure support’, meaning that he is now breathing spontaneously. She tells me that he was ‘dribbling’ a bit and this upset Relative 1. Also, she tells me that Relative 1 has been asking when they can make it happen.
SIA1P4ON
Just as some patients seemed to take an unexpectedly long time to die once withdrawal began, some patients died very quickly. This was also observed when patients were being recruited to the study. In SIA1, a patient who had been identified as ‘for the LCP’ ‘took matters into his own hands’ according to the nurse and declined very quickly: ‘too quickly to even start the LCP paperwork’. The researcher had not reached the site by the time this death occurred. In an observed case a nurse reports to the researcher that she did not even have time to turn the noradrenaline down before the patient died.
14.09.12;
22:08 The nurse tells me that all she did was turn the ventilator down, she deliberately didn’t do the noradrenaline as ‘That’s usually the quick one’.
SIA1P2ON
Divergent views between staff and relatives
It was surprising that the researchers observed few cases in which staff and relatives were observed to hold divergent views. There were, however, two very different cases in which the relationships between staff and patient’s relatives became difficult. At the root of these difficulties was a fundamental difference in views about the management of care and the interpretation of the patient’s response to treatment.
In the case of NIA6P3ON (16.05.12) the family reported understanding the severity of the diagnosis and were heard to say that they understood that the patient’s care was supported by the LCP and that this indicated that she was nearing the end of her life. Despite this, the patient’s mother made a number of comments to staff that suggested that she retained the hope that her daughter would recover. To the clinical staff these views seemed incompatible.
16.05.12;
18:28 I am sitting here day after day willing (name of patient) to open her eyes.
16.05.12;
19:06 I want her to wake up and prove you all wrong.
NIA6P3ON
Over a period of 2–3 hours, shortly after these comments were made the patient sneezed and blinked and gradually opened her eyes for longer and longer periods. When the relatives asked the staff about the meaning of these signs the nurse responded that she ‘does not know’. The researcher subsequently heard the nurse confiding in another nurse that she ‘hates it when relatives ask you about why the patient’s eyes are blinking’. The other nurse said that if she was asked she should say ‘it’s usually just a base function and the body’s way of shutting down’ (NIA6P3ON, 17 May 2012; 13:00).
Although the clinical team continued to incorporate these behavioural signs into the clinical history of decline, the relatives began to feel optimistic. When they expressed their hopes for recovery, the staff relabelled them as false hopes, emphasising that the patient’s vital signs suggested permanent damage to her vital organs. In the absence of a rational clinical explanation the family started talking about miracles and their previous experience of things that had happened against all medical odds.
As the clinical staff’s explanation began to fail to match up to what was being observed, the team drew back from the certainty of decline. They called in neurological experts and began to undertake their own tests of neurological functioning. They moved into an intensive ‘monitoring’ phase. Eventually they recognised that that the patient was recovering some function. She was transferred to a ward and ceased to be supported by LCP.
The clinical staff in the case of SIB2P2ON also found it difficult to deal with the apparent incompatibility of beliefs articulated by the family. Like the relatives in NIA6P3ON above, the family reported understanding the clinician’s view that the prognosis was poor and that the patient was dying. They also appeared to understand the notion of withdrawal. However, the family endlessly frustrated the clinical team with their requests for active treatment, which to the clinical team made no sense at all.
17.05.12;
15:17 Daughter told researcher ‘we understand he is likely going to die, and we accept that. However, we don’t understand why he is not being actively treated.’
SIB2P2ON
The family wanted the patient to be fed, they wanted Holy Water to be put into his i.v. drip, they wanted to make sure he had his insulin as per usual and they did not want him to be given gabapentin as they believed that it made him drowsy and uncommunicative. All of these requests, they felt, would contribute to enabling the patient to remain as communicative and engaged as possible to the point of death. Within the medical paradigm the family’s views made no sense to the staff and little attempt was made to explore them further. In fact, the case notes seemed to suggest that the clinical line regarding withdrawal needed to be held.
17.05.12;
11:00 The daughters seem to think that the pain killer is making him drowsy which is why they don’t want him to have it, but the doctor has explained to them that this pain killer has no effects of drowsiness. Nurse says ‘he’s drowsy because his blood is circulating less strongly and getting less oxygen to his brain’.
SIB2P2ON
At the change of shifts the day nurse in her handover reported:
17.05.12;
19:55 The family have been requesting treatments every hour or half hour and it’s important to be clear that this patient is only for TLC’. The nurse explained that the doctor had spoken to the family and explained why he is not well enough for any kind of active treatment. The nurse said that ‘they understand this, but still ask’. The nurse said that she had been told by a senior nurse to emphasise to the night staff that the family will ask, but treatment will not change.
SIB2P2ON
A number of clashes were observed between the staff and this family, the worst of which resulted in the daughter reporting to the researcher that the consultant was ‘truly the rudest person she had ever met’. The precursor to this clash resulted from the doctor asking the daughter whether or not her father was responding to her. She reported that, ‘at this time he was not’. The consultant said to her ‘then he is no longer with us’ which triggered the following response:
18.05.12;
09:00 In India, doctors keep treating right up until the end. They let the patients die naturally. They do not withdraw, like you’re doing here. They would never do that. Trust me, they never would. My brother, who has come from India cannot believe what you are doing.’ While she is talking, the consultant’s phone rings. He pulls it out of his pocket, turns and starts to leave the room as she is talking. He says ‘How do they die then?’ and she responds ‘Naturally!’ He leaves the room
SIB2P2ON
This family placed great emphasis on the manufacture of a natural death, which made little sense to the clinical staff. They suggested as an explanation that the daughter felt angry and possibly guilty. Conversations that the family held with the researcher revealed that the family were not being deliberately disruptive; they just wanted what they saw as the best for their father.
18.05.12;
09:00 The daughter tells me they want their father to die ‘naturally’, and withdrawing the ventilation is not natural. I asked if she considers the ventilator support to be natural, and daughter says that he’s still got a heart rate, and while there’s a heart rate, there’s hope.
SIB2P2ON
In the main, relatives accepted the clinical accounts of the patient’s decline and the plan of care. However, the two cases cited above demonstrated the gulf between the clinical team’s view of the patient’s body and the relatives’ view of the patient as a person.
Summary
The observations in the ICU were designed to provide an understanding of care once the patient was considered to be in the last days or hours of life. The concept of withdrawal was central to the care of all patients in ICU as well as to the initiation of the LCP.
In general the issue of withdrawal was always presented in the context of the patient’s decline and the futility of further treatment. A decision to withdraw active treatment did not mean that everything was just stopped. Different sites adopted different strategies in relation to each patient. Withdrawal was contingent on a number of factors and was deployed to accommodate these factors.
The factors included:
-
the presence of key relatives
-
waiting for organ donation
-
allowing the relatives time.
Withdrawal was described to relatives in different ways. The description of withdrawal prior to its taking place was designed to give relatives a general view of what was involved and what might happen.
All of the sites used the LCP in different ways and, as previously mentioned, it was observed to be used differently within the same site. The major differences in the use of the LCP involved the timing of its use; differences in perceptions about its purpose; different approaches to completion of the documentation; and variation in the extent to which the use of the LCP was communicated to relatives.
Even though the LCP and withdrawal of active treatment were two separate considerations in practice, they were often conflated and used interchangeably. This is interesting in the context of the interviews in which consultants were keen to maintain a conceptual separation between them. It was not clear whether the LCP was used to reflect what had been done in practice or whether it was used to guide care. Both the implementation of withdrawal and the use of the LCP were portrayed as flexible responses to the patient’s current circumstances. Staff were keen to control the speed of the final period of dying so that it was neither too fast nor too slow and to ‘create a death’ that appeared natural. Only rarely were divergences between staff and relatives views observed. In the two cases reported here the views of the clinical staff seemed to be more important than understanding the basis for this divergence.
Chapter 11 Intensive care units: interviews with bereaved relatives
Introduction
Intensive care units are quite unlike hospital wards; relatives are frequently unprepared for the impact on them of the environment in addition to the psychological stress of the patient’s condition. This chapter focuses on a number of aspects of the care provided to the patient from the bereaved relatives’ point of view.
In this chapter on the interviews with bereaved relatives, we begin by exploring the way in which relatives viewed the patient’s deterioration before going on to examine the impact of the decision to withdraw and the withdrawal process on family members. An important element of these findings relates to their recall of events and their interpretation of what they were told and saw.
Findings
In conjunction with our gaining consent to observe the care of the patient, relatives were invited to be interviewed after the patient had died to explore their perceptions of the care delivered to the patient and to them as the patient’s relative. With the exception of two patients, for each of the observations undertaken in ICUs one relative was identified and agreed to be interviewed: 15 interviews took place. Interviews varied in length between 50 minutes and 2 hours and 15 minutes. In four of the interviews there were a number of relatives present who wanted to comment and contribute to the study. For the purposes of simplicity the primary carer is identified as the main interviewee (see Table 18).
The interviewed relative’s relationship to the patient varied: relatives comprised a husband (n = 1); wives (n = 3); sons (n = 2); daughters (n = 6); a niece (n = 1); a friend (n = 1); and a female cousin (n = 1). Table 15 shows all of the participants present in each of the interviews and the length of time that had elapsed between the patient’s death and the interview. Four of the interviews involved patients who had died in non-LCP-using sites: three in the south and one in the north.
| Patient identifier | Relationship of interviewee to patient | Age (years) of relative interviewed | Time from death of patient to interview |
|---|---|---|---|
| NIA2P1F1 | Husband Daughter |
> 75 | 2 months 28 days |
| NIA1P1 F1 | Wife | 55–64 | 4 months 24 days |
| NIA6P3 F1 | Mother Sister Son |
65–74 | 1 month 11 days |
| NIA6P2 F1 | Wife | 65–74 | 2 months 14 days |
| NIA6P1 F1 | Daughter | 35–44 | 2 months 23 days |
| NIA2P2 F1 | Son Son Son |
25–34 | 2 months 18 days |
| SIA1P4 F1 | Female cousin Partner |
55–64 | 1 month 18 days |
| SIA1P3 F1 | Friend | 35–44 | 1 month 13 days |
| SIA1P2 F1 | Daughter | 25–34 | 1 month 11 days |
| SIA1P1 F1 | Wife | ≥ 75 | 1 month 15 days |
| SIA3P1 F1 | Niece | 35–44 | 1 month 9 days |
| SIB1P2 F1 | Son | 45–54 | 4 months 25 days |
| SIB1P1 F1 | Daughter | 45–54 | 4 months 3 days |
| SIB2P1 F1 | Daughter | 45–54 | 1 month 18 days |
| NIB3P1 F1 | Daughter | 35–44 | 3 months 14 days |
Although the majority of the relatives were interviewed within 3 months of the bereavement, they experienced difficulty reporting the detail of events. While stating that they had understood things at the time they were told, many struggled to reconstruct that understanding, and this is explored in detail throughout this chapter. Related to this is the importance of understanding the variances between what relatives recalled and what was observed and reported by clinical staff.
The bereaved relatives talked at length about the history of the patient’s illness, about how they learned and understood that the patient would not recover and the discussions they had with clinical staff about the withdrawal of active treatment. Despite 11 of the deaths taking place in ICUs which used the LCP, the bereaved relatives’ knowledge about the LCP and its use in relation to the care of their relative was almost non-existent. Only four of the patients whose relative was interviewed died in ICUs which did not use the LCP.
Deterioration of the patient
All of the bereaved relatives were keen to reconstruct the patient’s history of deterioration. Two types of deterioration were described. The first was a slow decline in the patient’s health; the second was a fast and sudden episode resulting in a speedy admission to ICU. The nature of the patient’s deterioration created different expectations and held very different implications for the relatives.
Slow deterioration over time
For over half of the bereaved relatives, the patient’s admission to ICU represented another episode in a history of declining health and increasing dependency. Many of these relatives reported that, on the patient’s admission to the ICU, they felt that recovery was unlikely.
So we kept on having to say ‘look do you realise how poorly dad is mum?’ You know ‘he’s got another chest infection and . . .’ So he was very poorly. We knew he was very poorly. And we knew the chances he would never come out.
SIB1P1F1
Over the years she’s been told she was going to die many times, and she kind of survived . . . but this time, as soon as I saw her I knew, you know, that was probably the end.
SIB1P2F1
What I was worried about even more was had she recovered. She clearly wasn’t looking after herself and she was very determined to stay at home and I just could not see how she was going to return home.
SIB2P1F1
For these relatives, the realisation that death was imminent was not a shock and their accounts bypassed discussions of recovery and moved into a discourse of keeping the patient comfortable and avoidance of suffering.
Rapid onset
At the other extreme were accounts that involved a rapid decline, or the onset of symptoms which may have been present in the past but had been concealed from relatives. These relatives were shocked by the patient’s admission to ICU. Some also reported feeling guilty that they had not known that the patient was so seriously ill and their accounts reflected their hopes of recovery and the difficulties of coming to terms with the patient’s death.
It’s like the day before he was taken in hospital, he was walking around like, joking, and then the next day that happened and we didn’t talk to him no more. You know sort of very quick and I think that’s where it’s sad for some people because you didn’t have time to say goodbye to him, you know, like properly.
SIA1P4F1
Nurse said, she’s got alcoholic liver disease. I was like, no. I thought she doesn’t drink. I’ve never known her to drink. Never seen any evidence of her drinking . . . if she’d of told us she had a drink problem, we might have been able to have done something. But because nobody ever said what it was, we weren’t able to speak to her about this.
NIA6P1F1
We weren’t expecting to lose him. We didn’t have an inkling that we’d lose him and it happened overnight. In a blink of an eye he died.
NIA2P2F1
What I wasn’t happy with was the incredibly rapid change from her being on the ward and just on a drip and suddenly she was in Intensive care.
NIB3P1F1
In this group of bereaved relatives, for whom the patient’s deterioration was fast, the speed of death was reported to have had a lasting impact on some family members, some of whom reported spiralling into depression and requiring counselling as a result.
One relative felt, with hindsight, that her husband’s health had been deteriorating over a long period. It was only once her husband had been admitted to the ICU that she began to piece this deterioration together. Over the previous year her husband had stopped going out and had begun to experience problems with his bowels and breathing, but she had not linked any of the incidents. So for this wife, despite the probably long-standing nature of her husband’s deterioration, she experienced his admission as a big shock and his very poor health status as sudden and unexpected.
I’m trying to remember now exactly what happened because . . . you see he never said anything. He wouldn’t complain about this or say ‘I’m not feeling well today’ . . . all I can remember is that he slept all the time.
SIA1P1F1
This last example is important. It highlights the possibility that medical staff and relatives might not share the same understanding of the patient’s health, even where the patient had been living with a partner for many years and had previously experienced episodes of ill health.
Preceding events
Just as the nature of the patient’s deterioration affected the relative’s perceptions of admission to ICU, so did significant preceding events. In this study, significant preceding events included resuscitation (three patients) and transfer to ICU from a medical ward (one patient).
Three patients were resuscitated: two in hospital (SIB1P1F1 and SIA1P1F1) and one initially in an ambulance and then again in A&E (SIA3P1F1). In one case the patient had had an agreement with relatives that they did not want to be resuscitated and the relatives reported that these wishes had been recorded in the notes as a DNAR directive (SIB1P1F1).
The use of resuscitation in the context of a DNAR is serious. The DNAR acts as an advance directive and supports a patient’s autonomy in circumstances in which the patient is not able to express a view. In this case the relative, a daughter, being interviewed about her father’s death was extremely angry about his resuscitation. She reported that her father had had two previous admissions to hospital and that on his most recent admission to hospital the previous year she, along with her father and mother, had had a discussion with the consultant about not resuscitating and that this had been recorded on his notes. This was confirmed in the patient’s case notes and was reiterated by a consultant on ICU.
The daughter reported that:
My dad was fine with that. He was and that’s why I think he’d got it all in order, in his mind, he knew what was happening. So, like most things, a lot of people do things when they know what you’re dealing with.
SIB1P1F1
Her father was being looked after at home with a significant amount of support from chronic obstructive pulmonary disease (COPD) nurses. Unfortunately, his condition worsened significantly and the nurses had him admitted to a medical ward. It was on a medical ward that he had a heart attack early one morning, was revived and admitted to ICU.
But obviously then they resuscitated, that was hell . . . You know I think if we had got a phone call on that Saturday, to say ‘he’d had a heart attack, he’s passed away’ I think we would have all dealt with it a lot better . . . apart from my mum in some ways not wanting to own up to it, I think we had it all clear in our mind.
SIB1P1F1
The daughter reported that the family felt ‘beaten up with guilt’ about the father’s resuscitation even though it had been beyond their control. She then described a series of events which she reported deepened the family’s guilt. The father had been transferred to ICU at 05.00 (17 February 2012). The patient’s family began to arrive at the hospital, with a total of about 15 relatives present at the patient’s bedside by late morning. The daughter reported that despite being told that the doctor needed to talk to them, they were all kept waiting for the doctor, who, according to the daughter, was dealing with emergencies. The daughter reported that the doctor finally had a meeting with them all at about 14.30/15.00 to discuss withdrawal of intervention. In addition, over the course of the morning the family struggled to keep their car parking tickets valid and to get refreshments, which added to stresses they were already experiencing.
We were saying ‘we should be worrying about dad’ But we were going ‘Oh I’ll go and see what time your car expires. Well if I go and see dad will you put some money in my car in 20 minutes . . . I felt disloyal to my dad that we were worrying about other things.
SIB1P1F1
The daughter blamed the protracted wait on the medical staff, describing them as too busy, off-hand and lacking in care. However, the daughter’s description of this long wait does not tally with what was observed. According to the observational notes and the record of meetings with the consultant and the nurse, the family had wanted to wait until all of the members of the family had arrived before the conversation with the doctor took place. Indeed, in the interview the daughter confirmed this.
Whatever choices we make, it’s got to be unanimous . . . so we felt we all needed to be there.
SIB1P1F1
Some of the family members had had to travel a considerable distance to the site and it was these relatives who were awaited before the consultant could address the relatives. Although this was a site which did not use the LCP, the delay in the withdrawal discussion was, according to the medical and nursing staff and from the observational data, attributable to the wait for all the relatives to arrive followed by a short wait to locate a room big enough to accommodate all the relatives. The daughter went on to praise the communication from the doctor, describing it as excellent. It is difficult to be confident about why there was such a mismatch in the accounts relating to the wait. It is possible that the distress caused by the inadvertent over-riding of the DNAR played a role in this. Its importance here lies less in the divergence of accounts and more in the way in which accounts are constructed and then interpreted by others. The methods adopted in this study enable these differences in accounts to be recognised, even if they cannot always be fully explained.
The second resuscitation example involved an elderly lady who lived alone, sustained by her niece, friends and paid carers. This woman was resuscitated twice, once by the ambulance crew and once in A&E, despite having a long history of COPD.
But in hindsight the doctor said ‘at the time of the ambulance coming out to this call, if they would have had all of her diagnosis in front of them, they would not have resuscitated her at all’ . . . But of course they revived her, they went to the hospital then the casualty department revived her and then when she was sent up to intensive care, they got more of the picture of what was wrong with her and they contacted her GP.
SIA3P1F1
Despite being surprised at the lack of information accessed by the ambulance crew, the niece who was interviewed about this patient’s care did not experience this as either positive or negative. It simply ‘was as it was’; it happened.
In the case of the third resuscitation, the relative (a wife) was grateful for the resuscitation. She had been surprised at the severity of her husband’s condition even though there was some evidence in her account of its longstanding nature. The resuscitation gave the wife a little more time to accommodate the severity of her husband’s condition and to say ‘goodbye’.
By the time I came in and washed all the cups and swilled them, the phone rang, and they said ‘Come at once because his heart has failed – his heart has stopped’. And when I got back there I thought I would have found him dead . . . but he wasn’t he was still awake.
SIA1P1F1
Her husband’s heart failed again the following day.
The doctor said to me ‘his heart has stopped twice and we have resuscitated him twice. If it stops a third time we won’t be able to do any more’ because the resuscitation damages the heart so I knew that after they’d said that, they were not expecting him to pull through.
SIA1P1F1
When the ICU nurse telephoned her at home to tell her that her husband was in his last hours, the relative decided not to await his death at his bedside, choosing instead to see him again when he had died.
So I said to them ‘I’m not coming, it’s too late and I’m very tired so I will come in the morning and see him in the chapel of rest’.
SIA1P1F1
Resuscitation, therefore, was viewed differently in different circumstances. For some relatives, it was entirely negative and created the circumstances in which decisions about withdrawal had to be made. For others, the experience offered the relatives the opportunity for more planned closure.
Admission to the intensive care unit
All of the relatives reported high expectations of the patient’s admission to ICU. The nature of the one-to-one care and the observable complexity of equipment inspired confidence. Relatives reported ICU as providing the best possible chance of recovery.
At that stage I was reasonably hopeful that . . . taking him to intensive care would probably prolong his life . . . I am just grateful that they gave him a chance because it was touch and go whether he did actually go onto ICU . . . But I was just so grateful that they gave him that chance that ultimately wasn’t there.
NIA6P2F1
We were grateful that he got a bed. He’d been treated and we were there with him.
NIA2P2F1
They done all they could do basically for her and, you know, obviously they said it takes time, it doesn’t happen straight away, you know, it has to take time, we have to see if these would work . . . I suppose it was them doing their job, it’s what they are trained for innit to try to save people’s lives so obviously they don’t want to end people’s lives.
SIA1P2 25
For the majority of relatives the clinical picture of the patient’s health emerged quickly. In a few cases diagnosis took some time and relatives reported being unable to form such a clear picture of the patient’s progress.
It kind of meandered. He [the doctor] was very worried initially, and I thought, it doesn’t look good. And, then he . . . there was kind of a bit of hope building up and a bit of momentum, that she was getting a bit better . . . she was deteriorating. They weren’t really specifying anything. They weren’t sort of saying, she’s going to get better. They weren’t saying she isn’t going to get better.
SIB1P2F1
Although the relatives reported that the consultants usually provided very clear messages about the patient’s health, one reported that her mother could not process the information about her husband’s health. She described it as ‘hitting a brick wall’ (SIB1P1F1), with her mother ‘talking about what they’d be doing in a month’s time’ when her husband got out of hospital. Although the family had heard all of the same information, there was a clear divide within the family in terms of how this information was received and understood.
Withdrawal of active treatment
In the observations the withdrawal of treatment was a critical point. Withdrawal represented, for staff and relatives, the failure of treatment, the irreversible decline of the body and the imminence of death. The dependency of the patient on medical technology for life meant that its removal was highly symbolic in the eyes of the relatives.
. . . but in their eyes your mum’s no longer doing anything by herself . . . It’s all the machinery doing it, you know.
SIA1P2F1
However, the fine detail around withdrawal was absent from the relatives’ accounts of the patient’s care in ICU. This was curious. The act of withdrawal was presented almost as less significant than what had gone before and what came afterwards. Clearly the relative’s accounts regarding the withdrawal of active treatment were filtered through the patient’s death. This is important to understand because the accounts provided were highly selective when compared with the observations. Some aspects of care that were observed to be discussed or argued over in the period up to the patient’s death, and in relation to withdrawal in particular, were absent from the relatives’ accounts. Further, without exception, the relatives interviewed were unable to remember some aspects of the care provided and there were some very clear examples of what was remembered being inaccurate.
At first it seemed that the time between death and the point at which the relatives were interviewed had allowed elements of the accounts to become simplified. However, it also became apparent that in reconstructing the death with hindsight, the aspects of withdrawal that may have seemed important at the time had been replaced by other elements.
The narratives of withdrawal were structured around three key stages: the decision to withdraw, the process of withdrawal and the outcome – waiting for death.
The decision to withdraw
Irrespective of whether relatives reported a rapid onset or a slow deterioration, all reported that the clinical staff had been unequivocal about the patient’s condition. Relatives could not always remember the precise details of the patient’s condition but they were clear about its implications. The clinical basis for the discussion with relatives was reported to be the patient’s deterioration or the result of a surgical procedure, radiographs or other tests and investigations.
The surgeon came to see us and explained how bad it was when he had actually opened her up . . . I can’t tell you what his exact words were . . . but he made it very clear to us, no doubt about it.
NIA2P1F1
She just said that they’d done the MRI [magnetic resonance imaging] scan, it had revealed this and basically there was nothing they could do . . . I think deep down I knew, he wasn’t going to get better, he was going to be a vegetable, as a family we said we didn’t want that, but I don’t think I realised the implications of how quickly it was likely to happen.
NIA6P2F1
So then the doctor explained to me, the consultant, explained to me that it was really not looking good . . . so they explained that he’s got organ failure, they were watching, monitoring that . . . But what I clearly know is that they told me that they didn’t think he’d survive the weekend.
SIA1P3F1
In many cases the clinical account of the patient presented by doctors and nurses, according to the relatives, matched the visual image presented by the patient in the bed.
His legs and his feet were enormous . . . all the toxins just built up. His feet they looked like hands they were so fat and his hands were like, you know stress balls as you held his hand it was just water wasn‘t it. Every time you touched him it was like touching fluid. It was like his kidneys were gone . . . and his lungs were filling up as well.
SIA1P4F1
He couldn’t talk, he couldn’t walk, he couldn’t sleep, he could not speak, he couldn’t see. He was just a heart beat on a bed.
NIA2P2F1
It was like something off one of these hospital programs on television . . . she was obviously in a bad way. She was coughing up lots and lots of blood . . . her eyes were getting round, sort of popping out a bit and yellowing.
NIB3P1F1
In the context of irreversible bodily deterioration, ‘suffering’ was viewed as unnecessary. The concept of suffering used by relatives encompassed more than pain. Indeed, relatives recognised that for the most part pain was very well controlled. Suffering related to the altered state the patient was now in, the absence of faculties that had been important to the patient and the loss of dignity.
So it was really hard to see him sort of suffering like that so much. He wasn’t constantly like that, whenever I would come he would always recognise me and talk a bit but he really wasn’t himself . . . So then he was just kind of long silences peppered with him pleading that he was like floating on the ceiling.
SIA1P3F1
I used to say Lord, if you can help him, don’t leave him to be punished. You know because I thought that was just suffering with all those tubes . . . so when he died it was a sort of relief, and I thought well now his troubles are over . . . that was enough for me to say that, that’s what I said ‘if you can’t make him well don’t leave him to suffer.
SIA1P1F1
I knew, she didn’t have no brain activity when they first done it then why prolong something. Why keep on going? That is not the way my mum would have wanted it. My mum likes her pride and dignity, you know what I mean but my mum wouldn’t want to be, no disrespect to you, but my mum wouldn’t want to be laying there alive, but no brain function looking like a fish in a goldfish bowl, she wouldn’t want that. My mum was a very proud woman, so you know she liked her dignity . . . I think my mum had enough suffering throughout the whole years, why let her suffer any more.
SIA1P2F1
In highly complex cognitive manoeuvres, relatives in the interviews reported being clear that the patient was dying while at the same time watching for any sign that might indicate recovery. This sense of hopefulness seemed to sit in some compartment in the human imagination separate from the knowledge of the patient’s physical condition. Not surprisingly, perhaps, so strong was the desire for the patient to live that hope for recovery could be unleashed from sometimes small events that might otherwise appear to be insignificant. Although relatives talked about the clinical ‘team’ and generally reported all members of staff as ‘talking with one voice’ there was an occasion on which the comments from a liver specialist inadvertently raised hopes of recovery and questions about the terminal nature of the patient’s condition.
The liver specialist was like well her liver’s the best it’s been while she’s been in hospital . . . So, we then thought hold on a minute. Is he saying something different from what the other doctor’s said? It made you think, God! They’ve got it wrong. She’s going to be all right.
NIA6P1F1
The example above shows the importance of clear communication and an understanding of the way in which information in this highly emotional environment may be received. In another case a father and daughter were approached by two consultants following a discussion of their relative’s care. Although highly risky, the proposal was to amputate the patient’s leg.
‘It is up to you but I am willing to try if that’s what you want us to do’ he said and the option is to first of all amputate her leg below the knee to try and just get rid of any infection that is coming from there and secondly to put her on dialysis to see if we can just help the kidneys. ‘It is a glimmer’ he said . . . I think if you are given a glimmer of hope you’re just going to go for it because you would never forgive yourself if you didn’t.
NIB3P1F1
Although the operation was reported to have ‘gone as well as could be expected’, the dialysis did not work, and the patient ‘never came round’ from the operation. In the interview the daughter reported that they did not regret the decision they took.
In another case, the relative, a niece, reported that despite knowing about her aunt’s very poor state of health she retained the hope of recovery.
Where there’s life there’s hope . . . I’m not going to say don’t resuscitate, because it seems like you really don’t care about them getting better, you’re really telling us like there’s no quality of life there . . . She did have a really nasty disease, it was killing her and the only comfort you could get was that she did pass away peacefully, that she wasn’t struggling to breathe. And so I had to take comfort from that. Selfishly you just want the person. You just want them whatever. But when you speak to anybody that loved her, the first things they say is ‘she has suffered a lot’.
SIA3P1F1
Although stating that they were clear about the patient’s state of health, and anxious not to let the patient suffer, relatives varied in how they presented their involvement in the decision to withdraw active treatment. Some relatives reported signalling that they did not want to be asked to make a decision, while others reported that their agreement was sought by clinical staff. A very small group of relatives reported that the decision to withdraw was theirs.
The largest group of relatives agreed that the decision to withdraw active treatment had been taken by the clinical staff on the basis of the clinical evidence. This matched what was observed and recorded in the patient’s clinical notes.
You know they don’t leave it up to you. They know when it’s time to turn off or whatever, so you’re not making that decision.
SIA1P1F1
The decision wasn’t there for us to make . . . they just started telling us . . . she isn’t going to improve she isn’t going to get better.
NIA6P1F1
She wasn’t really offering any alternative like well if we did this you might have a chance, it was like he’s really, really unwell. He’s not going to make it.
SIA1P3F1
Again, it is important to emphasise that although relatives reported agreeing with a decision, this did not remove doubts about whether or not this was the best course of action.
I know it wasn’t our decision to make but you just sort of agree to it. And you think, you start to doubt yourself. Did you do the right thing? Because part of you is thinking No! Inside you are thinking do whatever it takes to make her better. But another side’s thinking, you know she’s not going to get better.
NIA6P1F1
Although withdrawal was observed to be a clinical decision, in the interviews three relatives clearly saw themselves as both instrumental in the decision and responsible for the act.
This was before I turned the machine off . . . even when I turned the machine off. I couldn’t stay. I turned the machine off but I couldn’t stay. They never left his side.
NIA1P1F1
They didn’t actually make a decision about anything. They left it up to us as far as I can remember . . . they asked us to; we actually made the decision based on their advice.
NIA2P1F1
Because I was my mum’s carer it was my call if I wanted the machines turned off or not . . . And because it is such a big family, you know, it takes time, and I was like a couple of hours just to think about it.
SIA1P2F1
There was a slight difference between the views of family members and friends when it came to these decisions. Close family were more likely to adopt a shared decision-making approach, with some family members being allocated more weight; for example, in SIB1P1F1 the patient’s wife was given the final say ahead of his children. The way in which these decisions were portrayed by the relatives located the decision in the wishes of the family member as opposed to what the patient might have wanted.
It’s not about a majority decision, it’s got to be unanimous, but the ultimate decision is my mum’s.
SIB1P1F1
However, the friend who was interviewed (SIA1P3F1) located the decision in what they thought the patient would have wanted and aimed to respect their wishes.
We’re making the decisions that we think are in his best interests as his medical team. Which is what I understood to be the legal position as well . . . we have to make the decisions we think are best for him but I did feel very consulted and I actually felt they were the best decisions as well.
SIA1P3F1
Only one friend of a patient was interviewed in this study, so further research would be required to explore subtle differences in the way in which friends and family approach these decisions.
Divergent views of family members
There were many instances in the observations where family members articulated different views about the purpose of care and the lengths or limits to sustaining life. These differences resurfaced in the interviews with the bereaved relatives.
My younger sister wasn’t ready to say goodbye um me and my older sister was ready to say goodbye because we didn’t want my mum suffering no more. I said ‘you don’t want to see an animal suffer’, she said ‘no,’ so I said ‘why let mum suffer?’ I said ‘don’t you think she has been through enough.’ She said ‘yeah, but I’m not ready to say goodbye.’ I said ‘no one ever is ready to say goodbye’ I said to her ‘it’s no disrespect to you, but,’ I said, ‘I can’t go through this no more.’ I said ‘I was mum’s carer, I had to see her suffer’, I says, ‘My mum wants to be at ease now’. I said ‘let her go with her dignity, let her go by herself now’.
SIA1P2F1
There was one very clear case in which a patient’s mother and sister (interviewed together) discussed their different views on withdrawal. As the interview progressed their views merged and diverged, demonstrating the complexity of care at the end of life. For example, on the subject of food and fluids they were agreed.
We said ‘She needs fluid, she needs fluid, you’ve got to give her fluids’. And we all said the same thing, so they put fluids back on.
NIA6P3F1
The sister reported that the response of the staff to this request was that ‘we were prolonging life by doing this’. Although the sister thought that this ‘were a bit shit for them to say’ because the sister was ‘quite happy to prolong her life’, the mother did not want to prolong her daughter’s life.
I was quite happy to prolong her life. I didn’t want her to die.
I didn’t want her to die but I didn’t want to prolong her life how it was, because she wouldn’t have liked it . . . As a mother I just wanted her life to end, quietly and quickly.
NIA6P3F1
The incompatibility of these views meant that agreement was not realistic, but, as it turned out, it was not necessary either. As withdrawal progressed the patient began to show signs of recovery and the expected death did not occur.
Organ donation
Organ donation is usually considered by clinicians prior to withdrawal and discussions were observed between SNODs, clinicians and relatives. All of the patients dying in the ICU were considered to some degree for organ donation, but not all relatives reported being approached by a SNOD.
Again, the recall of relatives was not always accurate, with one relative suggesting that the question over organ donation had been raised once the patient had died.
There was a conversation with, that was after he passed away, there was a conversation about donation, organ donation.
SIA1P3F1
The researcher suggested that the relative might have been mistaken over the timing of this conversation, leading the relative to comment:
It’s weird isn’t it, I can’t really remember the course of events, but there was this feeling of no we don’t want to prolong something, so we said no to organ donation, if it was us we would have donated our own organs but we didn’t know what he wanted so we felt like we couldn’t somehow do it.
SIA1P3F1
Organ donation will be discussed in more detail in subsequent papers. However, one of the few relatives who reported being approached for organ donation refused permission on the grounds that his organs were probably not worth using.
I mean he’s old already and the rest of his organs aren’t any good. What’s the point in getting him cut up just to take tissues. So that was that and he was very nice, he apologised. He said ‘I’m sorry’ you know?
SIA1P1F1
The process of withdrawal
Relatives all reported the willingness of clinical staff to delay the process of withdrawal until relatives were gathered around the bedside. This was appreciated by the relatives and considered to be important.
They said ‘What we’ll do is let all your family know and then we’ll, once you are all together, then we’ll take it off’.
NIA2P2F1
They wanted us to be happy with who was there and have time to sit with him and say goodbye and you know pray and all the things that he wanted and that we could do it at our own pace because they were able to sort of gradually withdraw. So that was all really explained. Again I can’t remember the medical aspects of it, it’s weird isn’t it?
SIA1P3F1
The nuanced and subtle process of withdrawing different aspects of support from a patient on ICU, however, was largely absent from the relatives’ accounts. Invariably these accounts defaulted to switching off ‘the machine’, without any clarification of which machine was being switched off, or to just switching everything off.
I think we just took it that they were going to switch everything off and not give her any medication.
NIA6P1F1
He’d come off everything and obviously if you are not getting anything you are going to pass on at some point aren’t you?
NIA6P2F1
Such was the dependency of the patient on the medical technology that one relative referred to switching the patient off.
That they were switching her off. That they were switching everything, everything were coming off.
NIA6P3F1
Occasionally, relatives reported a more complex withdrawal of different interventions, but a level of confusion and misunderstanding frequently accompanied these accounts.
So that gradually they started taking off the different things . . . the nurse says ‘we’re taking all the things slowly one by one and see how he does’ and then his heart kept going down and then up again. Down and up again. And she told me what she is doing. Then she’d take a few of the things that they had plugged in and I remember her saying that erm she’s going to take, switch off the machine but she’s going to leave him with oxygen. And he had a thing like a pipe for his oxygen.
SIA1P1F1
There were mixed views about the tubes and lines linking the patient’s body to sources of support. Relatives made a distinction between tubes and lines that were in place while the patient was dying and those that remained once the patient had died.
Some relatives were able to see past the tubes and, while sitting at the bedside waiting for the patient to die, did not report any issue with how the patient looked with tubes in situ. Other relatives reported that withdrawal should involve the removal of all the tubes, restoring the patient to the body and divesting its presence from medical mechanics.
We said to the nurses well could we take the tubes out because he’s going now and they were saying well it could be really uncomfortable um, you know, just that process of getting the tube out, so then I was thinking I don’t want it out then because you know I don’t want to cause him, if there’s even a chance that it would cause him more discomfort then . . . you know, we should leave it.
SIA1P3F1
I didn’t like seeing him with the tubes.
NIA1P1F1
Right up until the end was that silly tube that was down his nose . . . you know it just didn’t look comfortable. I know if he could he would have gone and sort of took it off or been saying this is really irritating.
SIB1P1F1
Relatives, taking their lead from the clinical staff, all reported leaving the room while patients were extubated to avoid witnessing the patient’s possible distress.
A number of relatives were confused about the role of the equipment attached to the patient. They were often unclear about the distinction between equipment that monitored the body and equipment that supported the body. Relatives in the LCP sites commonly reported monitors at the patient’s bedside being turned off or turned down. On the whole relatives understood the reason for this and were supportive of it. In the interviews they reported how they had become distracted by or ‘fixated on’ (SIB1P1F1) the flickering monitors, blindly watching numbers and lines moving up and down without really understanding what they meant.
It stopped us focusing on it, then you’d watch him rather than the monitor . . . you missed it, first of all, you kept looking up there and then you thought . . . Oh but you don’t understand it all anyway. Sometimes like it might shoot up but . . . there was nothing to panic about . . . so they didn’t really mean an awful lot to us. You just found yourself looking at them but afterwards you could concentrate more on the patient.
SIA1P4F1
So they definitely turned the monitor around because they wanted to monitor him but I don’t think they wanted us to see. They sort of explained that sort of we’re going to turn this around so you could be with him, but we could obviously hear the noises.
SIA1P3F1
You’re looking at the machines, the machines tell you a lot of what’s going on don’t they. Even though they’d turned all the machines off there was one left on.
NIA6P1F1
Relatives acknowledged that although equipment had been withdrawn the nurses continued to monitor the patient from a distance, enabling the nurse to alert the family to a decline in the patient’s functioning.
The outcome: waiting for death
Relatives reported being well informed about what would happen once active treatment was stopped. While some relatives were told that the patient would die very quickly, others were provided with less clear and certain information.
They told us that they’d switch her off and then . . . she’d die within 2 hours, I’m sure it were 2 hours.
Yes, they said it could be 2 hours, it could be 2 days.
NIA6P3F1
Although machines might have been disconnected and active treatment ceased, relatives reported that care continued. The care reported by relatives during this period in the ICU was without criticism: ‘faultless’ (SIA1P2F1). Relatives commented on a number of aspects of this care.
In the majority of cases the nurses undertook all physical care of the patient. Relatives reported being asked if they wanted to leave while some aspects of care were carried out, but they also felt that if they had wanted to stay in the room this would not have been a problem. One relative reported having been asked if they wished to be involved in washing the patient and combing the patient’s hair. They felt that this had been both appropriate and really important for them. In the observations, this was seen to have taken place. Two relatives, a wife and a niece, reported watching a nurse clean the patient after he had his bowels open. Both were impressed by the nurses’ attitude and the way in which the patient’s dignity was preserved.
I remember going in there and his bowels had opened. And then she went in and she cleaned him . . . she did treat him with dignity nothing less . . . Because the way she used to handle him and stuff like that she would be talking to him and . . . she was very, very good.
SIA1P1F1
I think the treatment was particularly good because you know, he was helpless, he couldn’t do anything for himself and one particular time . . . I mean he had his bowels open and I don’t know how she could stand it but she cleaned him and turned him over and all that sort of thing with no fuss you know. I think that was very good because you see so many other things like on television how people get treated and there was nothing like that, it was all really good. I think he was treated with lots of dignity.
SIA1P3F1
Relatives reported recognising the evidence of good care which had taken place when they were not there, for instance the fact that patient was not lying in the same position on each visit. Relatives reported that nurses were supportive and communicative and explained what they were doing and, in some cases, why they were not going to do things.
Every time you went in there he was in a different position . . . they was always turning him . . . then the last day they said ‘We won’t pull him about any more’ . . . they did wash him.
SIA1P4F1
The relatives were impressed by the way in which the nurses talked to the patient while they were undertaking care and they noticed the small things that were done to personalise and individualise the care that they were giving. The administration to one patient of a chocolate mouthwash took place following a conversation with a relative and was held out as an example of the lengths to which nurses went in tailoring the care to the person.
I thought that was a nice gesture actually. That was treating her like a person and not just someone lay there . . . she went to a lot of trouble to find out what she likes and then went to get it.
NIA2P1F1
In one case, although the nurses were not able to provide a CD player requested by the patient’s friend, the friend did feel that their request had been taken seriously:
They did go and try and find a CD player but then they said ‘Look we just don’t have any and we can’t find one’ and ‘really sorry’ but I mean they didn’t, they weren’t like ‘oh look sorry guys’. I got this sense it was like, ‘we’re really sorry’, but I felt a bit bad for them that we’d asked them to sort of find a CD player when they obviously you know, it’s not what they normally do.
SIA1P3F1
Relatives reported that there was little to do with their time at the bedside other than watch the patient, pray, if it was appropriate, and reminisce. The loosening of restrictions on the number of people at the bedside enabled families to be together both at the bedside and off the ICU.
We had more time to talk and when we went to get coffee while they were giving personal care and stuff we were sharing stories and like laughing and crying and that felt like a good time actually to be away from the patient. Have a bit of a breather but still be really focused on it and kind of preparing ourselves.
SIA1P3F1
The nursing staff were variously reported to have accommodated the needs of relatives by allowing unlimited visiting, providing drinks, sandwiches and overnight accommodation, pleading with security staff over relatives’ over-running parking tickets and securing parking permits.
For those relatives who wanted to be present at the patient’s death there was huge anxiety about leaving the bed space and possibly missing the death.
We so didn’t want to move, you had to be desperate for the toilet before we would leave because your mind is telling you, she is going to go when you go down the corridor and that would have been just awful.
NIA2P1F1
You wanted to be there with him and it’s like you was waiting for him to die, but you was hoping that wasn’t going to happen and the longer it went on, the more time you has to think it’s not going to happen.
SIA1P4F1
Relatives reported the importance of the nurse communicating an observed decline in the patient’s functioning and a broad prediction about the timing of death because it enabled them to organise themselves. Relatives reported attempts by nurses to establish whether or not they wanted to be present when the patient was actually dying. As already identified, not all relatives wanted to be there for the patient’s death.
The gentleman who was looking after her did say ‘You can stay, you’re welcome to stay, or you can go and I’ll call you’ . . . They were pretty sure it would be in the next sort of 12 hours, she’d die and neither of us – and everyone’s different though – and we didn’t want to be there.
NIB3P1F1
Moving the patient
For three patients, withdrawal coincided with a move off ICU, in one case to a side room and in the other two cases onto another ward. Relatives reported understanding the reasons for the move but found it difficult coming to terms with the quality of care that accompanied the move.
Well he was taking up a bed wasn’t he? If I’m bluntly honest, other people would need that bed . . . you’re freeing up that bed and the equipment that somebody else that could use with more chance of staying alive.
NIA6P2F1
The only seriously negative criticisms of care arose in relation to these patients, who, once moved, experienced a dramatic reduction in attention and care compared with that provided in the ICU.
It is worth examining in some detail the case of the patient who was moved into a side ward to accommodate the large number of relatives who visited (up to 22 at one point). The patient had been resuscitated despite having a DNAR recorded in his notes, and was admitted to a non-LCP-using ICU and then provided with a side room just off the main ICU area. The relatives had voiced early criticisms about the length of time they had had to wait to speak to a consultant but the daughter’s account differed sharply from the circumstances that had been observed. Once the consultant had discussed the patient’s case with the relatives, care proceeded with very few complaints. However, the patient was moved into a side room, which the relatives, at first, thought was a good idea. It provided sufficient space for all the family to congregate and initially they ‘thought it was fantastic, but it turned out the worst mistake that was ever made’ (SIB1P1F1). The daughter reported that staff did not come in and check on the patient, and when they needed a member of staff, as when a cannula became disconnected, ‘spurting blood everywhere’, they struggled to find anyone. The bedclothes were not changed despite being covered in the patient’s blood from this episode, and there appeared to be no plan of care and no named nurse as perceived by the daughter in the following quote: ‘no-one had my dad as his nurse’ (SIB1P1F1). As time went on without a nurse attending to ‘an increasingly agitated patient’, the family became more stressed and unhappy. A cup of tea for their frail elderly mother had to be requested several times before a cold, stewed cup of tea arrived.
The nurses when he was on the larger ITU ward . . . used to come in and say ‘I’m just going to check that monitor’ or ‘I’m just going to check’ . . . but in the room I just felt there was no conversation at all. They never spoke to my dad at all . . . whereas in the main ward we felt there was a happy mix of staff leaving us alone to say what we needed to say, and being around if we wanted to ask questions, we felt we were just left.
SIB1P1F1
The criticisms voiced by this daughter were extensive and forced her to consider the consequences of the failure to correctly apply the patient’s DNAR.
If he hadn’t been resuscitated that morning we would have been happy . . . I’m sorry he just didn’t slip away and that was all down to being resuscitated.
SIB1P1F1
This relative was the only one in the study to report that the patient died without dignity.
But those last 6 hours lost it for me for dignity. You know my dad was very much for the NHS, and my mum was exactly the same. But we felt the little touches weren’t there.
SIB1P1F1
The daughter’s account of the care in the side room was supported by the observation undertaken by the researcher.
The patient’s death
Perhaps surprisingly, relatives did identify some confusion about the point of death (this will be explored in detail in a paper focusing on the point of death and the patient’s last offices).
When really they sort of turned the last thing off and we were just waiting. I do remember this tension of has he died or not? You know, I don’t know if he’s actually gone, is he still breathing? And it was a bit like um obviously all those emotions are running really high.
SIA1P3F1
He wasn’t breathing but she needed someone to tell her. Someone in the medical profession to turn around and say ‘he’s died’. ‘He’s gone.’
SIB1P1F1
All of the relatives except one (see SIB1P1F1, above) reported that the patient’s death had been dignified.
I think the staff were amazing and that he did have a dignified and a good death because we were able to do that for him and we were all able to gather there. It was very good, very supportive, very calm, very giving, very compassionate. They gave me as the person that was there, because I was the executive [sic] of his will so gave me a leaflet on next of kin about what to do and explained it so I had a really clear explanation of what to do and they said it’s all in the leaflet. I remember asking at the time it’s all in here isn’t it so my head was a bit like all over the place obviously. So I felt like I knew what to do.
SIA1P3F1
I’m just so glad, my overwhelming thing is I’m so glad he wasn’t on his own. I’m so glad we had that time to say goodbye to him, I’m so glad the staff were so good and that we knew what was happening and that we could be there. So, so glad but it’s so emotionally demanding isn’t it, and then you are kind of grieving, and then you’ve got all this stuff just to do.
SIA1P3F1
Use of the Liverpool Care Pathway
The majority of bereaved relatives (n = 11) had been present in sites which used the LCP. The standard of care described by the relatives was very high and it was difficult for researchers to elicit from relatives ways in which the care could have been improved. However, very few of the bereaved relatives had heard of the LCP. The most common response was that relatives could simply not remember whether or not they had been told anything.
I think two of the doctors went into more lengthy discussion but I really can’t tell you now because I just can’t remember.
SIA1P1F1
I’d never heard of it. It was sort of said that he’s going to be on this Liverpool Path Care, but, now whether the lads knew I don’t know.
NIA6P2F1
I just couldn’t take it in. They were trying to . . . I just didn’t take it in.
NIA1P1F1
When I picked up the belongings, I took a card and some chocolates to the ITU staff because I was so kind of grateful for how they’d looked after him. Um yeah, yeah, it was I think . . . it was called the Liverpool Care Pathways.
SIA1P3F1
Two sets of relatives reported hearing something about the LCP. In the case of NIA6P3F1, the patient’s mother and the sister reported that they thought it had been mentioned but it had not been explained to them at all. The two relatives discussed it between themselves in the following excerpt:
But they didn’t actually explain it to us . . . the only thing they kept saying was that she was being starved to death . . .
Somebody, and I forgot who it were now, he wasn’t in the hospital, it was somebody that said to me. They said the Liverpool Care thing, if you’re old and nobody goes, they give you an injection and you die. That’s what they were told.
NIA6P3F1
Another relative reported that the LCP had been mentioned but she could remember very little about it.
He also mentioned ‘Have you heard of the Liverpool Pathway?’ He was talking and it was, it was all over my head a bit and I’m thinking ‘Is this to do with euthanasia? Oh my God what is this? . . . I thought it was a new way of dying. You know that it was similar to letting somebody go.
SIA3P1F1
This relative went on to explain:
And of course I was crying as well because I was upset and I was trying to be brave. Because I didn’t want to go back and upset everybody else. So I was trying to stop. And he was, he did talk about it but I don’t know what he was saying.
SIA3P1F1
Although all the relatives in the LCP sites reported a high standard of care and attention, they knew little about the LCP and its relationship to the care provided.
Summary
In the complex world of end-of-life care in an ICU, very different views emerged from the interviews with bereaved relatives. With one major exception, care was thought to have been very good, with bereaved relatives reporting that the goals of dying free from suffering and pain and with dignity were achieved.
The nature of the patient’s deterioration and preceding events affected how relatives viewed the admission to ICU and their hopes and expectations of the care that would be provided. When interviewed a comparatively short time after the patient’s death, the relatives appeared to offer a distilled version of the patient’s stay on ICU. Some events which were observed and seemed significant were not mentioned, the chronology of events was occasionally awry and new accounts appeared to be constructed. In many ways these findings are not new but serve to underline the importance of trying to understand these highly emotional stressful events from as many perspectives as possible.
The interviews with relatives highlighted the way in which views within families diverged and converged, and underlined the importance of consistent, clear communication. This was particularly important, as relatives described their ever-present but often muted hopes for the patient’s survival which ran alongside the medical information and clinical appearance of the patient.
Finally, few relatives had heard of or understood the LCP, but all identified the elements of care that made them feel slightly better about the patient’s death.
Chapter 12 Intensive care units: staff interviews (point 2)
Introduction
Caring for the families of patients who are critically ill is an essential component of the nurse’s role on ICU. 60,75 However, little is known about how nurses view this role or about what effects it has on their ‘person’. The aim of the interviews was to provide an opportunity for nurses to talk about the care that had been provided to the patient whose death had been observed and to discuss some of the components of that care. Inevitably, these interviews covered the broader area of end-of-life care and staff views on care in an ICU environment. The sample of deaths observed in the ICU included both those supported by the LCP and some not supported by the LCP. The similarities and differences between these deaths are explored where possible. It is important to note, however, that almost twice as many nurses working on LCP ICUs are represented in the sample and these are drawn from five of the total sites recruited.
Findings
Interviews were undertaken with staff who had provided care to the patients whose death had been observed. As can be seen from Table 16, the majority of the staff interviewed were female and were staff nurses. The majority of the senior staff were working on the ICUs which did not use the LCP. The interviews were conducted as soon after the patient’s death as possible. In the majority of cases the interviews took place at the end of the shift during which the patient died. This in some cases accounts for the short length of the interview. On occasions the interview took place during the nurse’s next shift.
| Patient identifier | Grade of staff | Age (years) | Sex | Length of time working in ICU | Length of interview |
|---|---|---|---|---|---|
| NIA2P1S24 | Staff nurse band 5 | 25–34 | Female | 3 years | 23 minutes |
| NIA1P1S24 | Staff nurse band 5 | 25–34 | Female | 4 years | 18 minutes |
| NIA6P3S224a | Staff nurse band 5 | 35–44 | Female | 3 months | 1 hour 5 minutes |
| NIA6P2S2Da | Staff nurse band 5 | 25–34 | Female | 4 years | 1 hour 2 minutes |
| NIA6P1S214 | Staff nurse band 5 | 25–34 | Female | 3 years 9 months | 58 minutes |
| NIA2P2S24 | Staff nurse band 5 | 25–34 | Female | 1 year 2 months | 47 minutes |
| SIA1P4S23 | Senior staff nurse band 6 | 45–54 | Female | 10 years | 1 hour 14 minutes |
| SIA1P3S24 | Staff nurse band 5 | 25–34 | Female | 9 months | 1 hour 24 minutes |
| SIA1P2S23 | Sister band 7 | 35–44 | Female | 18 years | 55 minutes |
| SIA1P1S21 | Sister band 7 | 45–54 | Female | 1 year 6 months | 38 minutes |
| SIA3P1S24 | Staff nurse band 5 | 18–24 | Female | 3 months | 1 hour 9 minutes |
| SIB2P2S21 | Staff nurse band 5 | 35–44 | Female | 2 years | 59 minutes |
| SIB1P3S24 | Staff nurse band 5 | 25–34 | Female | 1 year 3 months | 1 hour 14 minutes |
| SIB1P2S21 | Junior sister band 6 | 25–34 | Female | 6 years | 40 minutes |
| SIB1P1S21 | Senior sister band 7 | 35–44 | Female | 1 year 6 months | 10 minutes |
| SIB2P1S21 | Senior sister band 6 | 35–44 | Female | 5 years 2 months | 31 minutes |
| SIB2P1S22 | Student nurse | 35–44 | Female | 1 month | 43 minutes |
| NIB3P1S2D | Charge nurse band 6 | 45–54 | Male | 12 years | 52 minutes |
Deterioration of the patient: the clinical context
When discussing the care of the patient who had died on ICU, all of the nurses framed their accounts in terms of the patient’s deterioration. This seemed to be important as all the patients had been admitted to ICU on the basis that there was some hope of recovery.
While you’re still treating them there’s still that sort of glimmer of hope. And when you’re actually withdrawing treatment, you sort of feel like . . . Not that you’ve failed but . . . I don’t know. Like I say just a bit helpless really.
NIA6P1S214
The interviews were undertaken after the patient’s death and this may have influenced the structure of these accounts which described the interplay between the patient’s clinical decline, the clinical interventions instituted to address the patient’s decline and the outcome of these interventions.
His heart was restarted in Casualty and he came up to intensive care at 7 o’clock in the evening for monitoring and to see what we could do about this slow heart rate. We needed to give him an infusion of something that’s quite caustic, so it’s only done here, not in general wards . . . And I was taking handover . . . his heart stopped again. And we had to restart it another two times in that episode. By 11 o’clock that night he was then intubated, ventilated, sedated. So, we could get a good look at what was going on with his heart and kidneys. He was on as much noradrenalin as he could be on. Which was maintaining his blood pressure and his blood pressure was still falling. And ventilation-wise he wasn’t really able to get enough oxygen into his blood in spite of his ventilation so it became very apparent that his, his lungs were failing, his heart had failed, his kidneys had failed, he had too many organs failed for us to be able to make him better. But we carried on and on and on, still for full care though if his heart stopped we had said we wouldn’t resuscitate.
SIA1P1S21
She was very severely sick on admission and got intubated because she wasn't able to breathe by herself, she was on a ventilator. And then she became very, very unwell over the last few days where she had maximum treatment of care, ventilation wise and also on medication to support her blood pressure, kidney function, yesterday she had a CT [computerised tomography] scan. She ended up having a multi-organ failure, all her organs failed and . . . she ended up in heart failure, she had a left right sided heart failure and so the heart wasn’t pumping enough and the treatment we were giving was just supporting her blood pressure and the cardio output but she wouldn’t be able to live to survive.
SIB1P2S21
These accounts existed across all sites and formed the basis for discussing detailed aspects of the observed care. In these discussions there were similarities between nurses working in LCP ICU sites and nurses in the non-LCP-using sites, but there were small but subtle differences between the LCP-using and non-LCP-using sites. The differences lay in the role of the nurse following withdrawal. The nature of this distinction will be discussed in the context of the LCP-using and non-LCP-using ICUs.
Liverpool Care Pathway-using sites
Training on end-of-life care and views on the Liverpool Care Pathway
Staff were vague about the training in end-of-life care they had received. None of the staff interviewed in the LCP ICU sites reported receiving formal training in the use of the LCP and it was rare for nurses to report receiving more general end-of-life training.
I have never been trained on it personally but I think there is training available . . . I think I have had general teaching on the main Liverpool Care Pathway. The in-house one is kind of done with a team of in-house so to speak, so it’s not official training. There are some link nurses for bereavement. But we haven’t had any official training actually off them.
NIA1P1S24
I didn’t really do any, you know, training exactly. I didn’t get any teaching on it.
NIA2P2S24
Before I came to this trust I had end-of-life care training and in the rest of the hospital they use a different pathway, it’s a lot more lengthy.
NIA2P1S24
Despite this, the nurses reported that the LCP documentation offered them a framework that they could apply on their own in clinical practice.
I think it gives you a good framework. It gives you a good guide to make sure you’re doing what you should be doing. To make sure that it’s obviously appropriate.
NIA6P1S214
It gives you a prompt really and for peace of mind really even though you know what care to give; it gives you peace of mind.
NIA1P1S24
Whereas we might think about one or two things in the subsection. There might be another two that you might not necessarily automatically think of. So I think it’s good to bring them to your attention, to all the things that are in the subsection. Because you cannot remember 100 things.
SIA1P4S23
In the observations it had been unclear exactly how the LCP documentation had been used. Nurses were observed with the documents in their hands as they moved between the nurses’ station and the bedside, writing on the forms at the end of the bed, and we analysed completed LCPs. But it was unclear whether the forms were being used in real time or were being completed retrospectively at 4-hourly, or longer, intervals. The interviews highlighted that the completion of the forms was secondary to the provision of care; sometimes they were completed contemporaneously just after care had been provided and sometimes this was done retrospectively when nurses were less busy. The act of completing the forms created the prompts for future care. Where nurses reported barely having time to complete the initial assessment page of the LCP documentation, a scanning technique was adopted which took the form of a quick check of the LCP domains.
General views on the Liverpool Care Pathway
Perhaps not surprisingly, given the lack of training received, the interpretation of the LCP documentation and its application varied as nurses applied their judgement to its use. There was a consensus that the LCP was nurse-led, allowing nurses to use their experience and judgement within certain parameters to provide care to the patient at the end of life. We return to this again later.
The LCP for nurses is quite nurse-led and although they have the part where the doctors come in and write we then take over and we use it to our ability and use it for our benefit as well, ultimately for the patient’s benefit but it helps guide us and I think we use it probably a lot more than the doctors use it. I don’t know whether they don’t see it as maybe as important as the nurses do because they have got their medical notes.
NIA2P1S24
Some of the consultants prefer not to, because they don’t really know that much about it probably, it’s not that they have got anything against the LCP, because they have always been intensive care doctors they haven’t used it that often . . . It’s definitely more nurse-led.
NIA1P1S24
The nurses reported a number of (mis)conceptions about the LCP, all of which were grounded in the idea that the LCP required certain actions to be undertaken in a certain way at a specific time. The removal of ‘supportive treatments’ was the most commonly mentioned.
The LCP states that you should remove all supportive treatments. With some patients we could remove the tracheostomy tube but there is a chance that they will occlude their airwave and it’s not a very nice death for the families to witness.
NIA1P1S24
On the Liverpool Care Pathway it specifically says to take the person off monitoring.
NIA2P1S24
Despite its use to some extent in all the deaths observed in LCP-using ICU sites in this study, nurses questioned whether the LCP was always useful in the ICU context, as some patients died very quickly once a decision to withdraw treatment had taken place. This provided staff with less time to go through the documentation and make their assessments.
There have been some cases where I have seen them not go on the LCP but in those cases it would be where the process of them dying was quite rapid.
SIA1P4S23
You start implementing it and often well often you might not even get to the first hour to record anything because they’ve passed away that quickly but I think I can’t recall any time when it’s not been used.
NIA6P1S214
I have got limited experience with the LCP. Some people are put on it promptly, but I do find that in general it probably does take a little bit longer to get it started. Maybe not as long as in this case, but I do find sometimes the nursing staff are maybe wanting to maybe start it possibly quicker than the doctors.
NIA2P1S24
Interestingly, one nurse reported that although they used the LCP in their site, they had adapted it precisely for the cases identified above, namely where a patient was going to die quickly.
A lot of it wasn’t really appropriate so we have adapted it. We tend to use it when patients sort of die very quickly.
NIA1P1S24
The use of the Liverpool Care Pathway
All of the staff acknowledged the controversial nature of the LCP and, while not agreeing with the adverse publicity, the majority of staff chose to talk to the patient’s relatives about the care to be provided without making reference to the LCP.
I made it very clear what was going to happen, what my practices would be, but I didn’t use the word LCP or Liverpool Care Pathway because of the recent poor press. And that wouldn’t have crossed my mind usually except for two or three of my friends have said to me ‘Here do you know anything about this Liverpool business where they starve people to death’ and I was ‘no that’s not what they do . . .’ but of course they have read this bad press.
SIA1P1S21
There was one site, however, where a nurse reported a very frank conversation between the consultant and the patient’s family about the proposal to use the LCP. Interestingly, the nurse’s account of this conversation reflects the impact of the negative media publicity, as the use of the LCP is framed in terms of what it does not mean for the care of the patient rather than what the care entails.
He explained that in this trust we implement the Liverpool Care Pathway. He said that it’s a tool to ensure, not his exact words but . . . to ensure basically that patient’s aren’t left . . . that just because somebody’s passing away or dying, that . . . it doesn’t mean we stop care. It doesn’t mean that we don’t go to them. It doesn’t mean we don’t assist their pain needs. It doesn’t mean that we don’t actively treat certain areas for them, such as pain, agitation, nausea and such, making people comfortable.
SIA3P1S24
Nurses dismissed the LCP’s association with death by starvation, dehydration and oversedation as media hype. In their minds, it simply helped them to give good care.
In relation to the observed deaths, nurses reported that the use of the LCP had been appropriate and, in most cases, timely, with only one nurse suggesting that it might have been better for the patient if the LCP had started sooner (NIA2P1S24).
The Liverpool Care Pathway and withdrawal
The nurses reported that the decision to withdraw treatment was a team decision which preceded the implementation of the LCP. There was recognition that any limitation of treatment, or decisions of not for resuscitation or no active treatment, had become associated with the LCP and that, in practice, they were linked.
He didn’t improve, the consultant came in and he reviewed him and what he said was ‘he’s not improving, we can’t seem to do anything else and we should have that conversation on LCP with the family’.
SIA1P4S23
Once a decision to withdraw had been made and the LCP was started, the nurses felt able to manage the care associated with withdrawal. However, they reported that while they were responsible for this care they were supported in a number of ways by (1) taking advice from consultants and other experts where they felt it was needed, (2) keeping the relatives informed about what they were doing and gaining their views on how certain things were handled, and (3) assessing the impact of the withdrawal process on the patient and making adjustments in their care accordingly. These three elements were present to some degree in all the nurses’ accounts, but constructed differently by nurses in the LCP-using and non-LCP-using sites.
Taking advice from consultants and other experts
Although the nurses viewed care after withdrawal as their domain, they reported involving, and were seen in the observations to involve, consultants and other experts. Consultants were also brought in if the nurse felt that the relatives would benefit from the medical view, with nurses setting up meetings between relatives and the consultant to discuss a change in the patient’s condition.
I said ‘I am afraid he is not going very well today, he has not been very well, I think you should come in and talk to the doctor about how he is’.
SIA1P1S21
Keeping the relatives informed
All of the nurses reported the importance of their conversations with family members regarding the proposal to withdraw active treatment. It provided nurses with an opportunity to impart information as well as to receive information. This dialogue was important because it enabled nurses to identify how the relatives were responding and their understanding of the patient’s condition.
They knew his prognosis was very poor and they knew that to start his heart again would be futile and possibly cruel. And in fact his wife was already saying you know ‘don’t let him suffer. Don’t let this go on forever’. I spoke to her and said ‘he is taking very, very small steps forward at the moment but I don’t know if they will be, if those steps will get him home or if they will just be the only little steps’. And she seemed very comfortable with being able to talk about that.
SIA1P1S21
In the majority of cases the patient being observed in this study had a number of visitors at the bedside. While it was common for patients to have two or three visitors, there were occasions when very large families, for example of more than 10 people, were present at the bedside, which made communication complicated. Selecting a way of communicating with family members at the bedside was an art which sometimes needed refining. The ever-changing bedside population often meant that nurses had to identify key family members and repeat information a number of times in order to ensure that the information reached parties equally.
Because the patient lived with the cousin . . . So, it kind of felt like I should be communicating with her first. But I didn’t. I actually communicated with mum and dad because . . . that just seemed the right thing to do . . . But whatever I told mum and dad, I then told her as well.
SIA1P4S23
Nurses reported that the way in which family members remembered and interpreted what they had been told varied enormously, was not solely a function of family size and was difficult to control. In one case the frequent attempts by the nurse to correct a relative’s misunderstanding left the nurse wondering whether or not she was understanding the point the relative was making.
So I tried to explain to her that he wasn’t breathing enough to take off the mask, he had to be breathing enough to do that. And then he would be weaned onto pressure support, down to pressure support, down to . . . We had to say it a few times for her to realise ‘we’re not taking it away . . .’ She kept on saying ‘so when he’s breathing, you take it away’. To keep bringing her back to saying ‘no when he’s breathing we will wean it down’. ‘Not take it away’. And we kept on seeming to be getting stuck on that point and then after a while I wasn’t sure if she was, if I was understanding what she was asking me. But her understanding was . . . that we would take the ventilator away.
SIA1P4S23
In another case a nurse, overhearing the patient’s granddaughter talking on the telephone, realised that a discussion she had had with the granddaughter had been misinterpreted and/or misreported.
The granddaughter then got on the phone to ring her uncle who had said he wasn’t going to come back, and interestingly she said to him ‘they are going to start turning all the machines off do you want to be here for that’. So that was her perception that we were going to turn off all the machines. And I had already explained to them the day before that there is no such thing as a life support machine to be turned on or off.
SIA1P1S21
These differences between relatives were referred to in other accounts: ‘some family members want to hear; others don’t want to hear’ (NIA6P3S224). In part this was attributed to a relative’s reluctance to accept the patient’s imminent death.
Some relatives can be quite angry with you and sort of blame you in effect . . . You have to try and put yourself in their shoes really and imagine how you might feel if this person was telling you that your relative was dying. And your first emotion might be anger and unfortunately it is directed at the first person you come into contact with which is the nursing staff.
NIA1P1S24
Although nurses in the LCP sites usually managed to resolve these differences, there was one case, in a non-LCP-using site, that became the basis for very strong disagreements between staff and family members.
An additional complication for nurses in their communications with relatives about withdrawal was the unpredictability of the timing of death. Nurses were unable to give a time scale with any degree of certainty. Perhaps because of the clinical picture provided to the family by the clinical team, nurses felt that families expected the patient to die very quickly after withdrawal, which they usually did. However, there were instances in which this did not happen, and a few cases in which the nurses reported the patient ‘rallied’.
His numbers looked better for a while completely off everything, better than they had when he was being treated. And I discussed this with the family because he was making a fool of me and I said to them ‘well in spite of everything I told you he seems to be carrying on a bit longer’.
SIA1P1S21
In these instances, some nurses reported that there was a suggestion from the relatives that they were prolonging the patient’s life in a way that was perceived to be cruel. The relatives’ desire for a natural and quick death, on occasions resulted in subtle requests to the nurse to hasten the patient’s death. Nurses reported their response to this as one of shock and a reiteration that the ‘patient makes the decision in the end’ (SIA1P1S21).
Assessing the impact of withdrawal on the patient
All of the nurses in the LCP sites described withdrawal as a process tailored to the patient’s clinical state. While this process was primarily adjusted to meet the patient’s needs, it also took into account the needs of the relatives.
You can’t get someone to extubation . . . in a flick of a switch. So he was fully ventilated so he needs to be able to breathe himself, for himself without the machine, before you can pull that tube.
SIA1P4S23
This nurse provided extensive detail about the process of withdrawal in the patient whose death was observed in this study. It provides an important example of the way in which assessment informed the care that was given. The initial step required of the nurse was to get the patient on continuous positive airway pressure (CPAP). CPAP is a treatment that uses mild air pressure to keep the airways open.
One of the senior bands was looking after him and she handed over to me that they wanted him to be on CPAP, CPAP is like the lowest amount of ventilation you can have. You have to be able to breathe to do that. So he wasn’t at that point triggering his own breath. So she couldn’t do that. So what she did was she reduced his sedation to a bit, so that he could breathe a bit for himself . . . So that’s what was happening when I came on. So, probably by about sort of 11 or 12 o’clock he was triggering enough breaths for me to then take the mandatory ventilation off . . . I took him to pressure support and to see what he did and then I just brought it down gradually . . . And by 1:30 I [sic] was on CPAP.
SIA1P4S23
At the same time as monitoring the patient’s breathing, the nurse described her visual assessment of the patient’s comfort.
I wanted to see if he was sweaty, was he uncomfortable? Was he moving around? Was his breathing fast? Was he tachycardic? Did his blood pressure shoot up in the air? So . . . all those things would make me think ‘if I started say on 3 mg and he was doing all this what I’ve just said. I would think he needed a bit more’ . . . That’s what I would look for.
SIA1P4S23
In the course of her assessment of the patient she reported that there were some unusual readings on the monitor to which he was attached.
So he was fine for a while and then he was doing that funny little line again. So I thought ‘maybe there’s secretions there again’. Had a little, a little feel and he’d obviously collected it again. And so I suctioned him and obviously when I’m doing this I’m telling him what I’m going to do despite that he’s unconscious . . . I suctioned him again and he did exactly the same so I cleared his chest, that funny line had gone, I couldn’t hear a vibration down the tube, but his respiratory rate kind of went up but didn’t come back down to what is was . . . So I waited a bit because it kind of didn’t go back to lower than normal so . . . I went up with the morphine again.
SIA1P4S23
This account by the nurse provides a useful insight into the considerations that underpinned the adjustments to the care that was observed.
In the process of ‘withdrawing’ the nurses talked at considerable length about the impact of tubes on relatives and on the care being provided. They reported understanding the impact of the environment on the patient’s relatives but, by their own admission, they were sometimes slow to adapt.
There was some equipment that wasn’t even being used which I could have taken away. Sometimes when you walk on intensive care all you see is all the machines and it is quite frightening. If I could have just moved some of those away it might not have been as frightening for her. If she had told me beforehand that these things were frightening her I could have done something about it but she didn’t tell me until afterwards.
NIA1P1S24
The tubes connecting the patients to equipment of varying descriptions were seen by nurses as hugely significant. Although nurses found capping or spigotting tubes and lines relatively straightforward, the removal of these presented some issues. Actually removing tubes that had been discontinued involved weighing up the consequences of doing so. Nurses across all sites reported a requirement for tubes to be left in for a minority of patients for whom a coroner and a post mortem might be involved. There was a tendency, however, to act conservatively, with the majority of all patients in this study dying with some tubes and lines left in.
If the patient needs a post mortem the tubes have to stay in situ and then they will be removed I presume if they are not needed when they leave here. But we do leave every line and every tube in situ including drains and catheters and just make sure they are bunged or spigotted off . . . I think you have to explain why to some extent they do stay in. Because if they don’t know why they have to stay in then they won’t be able to rationalise the reason why we are keeping them in and it is a bit disfiguring when you have got a tube poking out of your mouth.
NIA2P1S24
There was a perception that the visual impact of the tubes disrupted the essence of the patient and created a barrier for relatives. At the same time, withdrawing tubes and lines was not considered to be a quick task, and there was a fear expressed by a number of nurses that the patient might die during the time it took to send the relatives out of the bed space and disconnect the lines.
The family were present when she was extubated, nurse 1 sort of took the tube out and then came out to let the family have some time. Not, not knowing how quickly obviously she would pass away. Erm . . . so hence she still had the lines in. You’ve sort of got the dilemma, do you say to the family after a little while ‘can you leave’, take some of the lines out for the patient’s comfort. And because it’s more pleasant for the family . . . They often retch quite a bit and . . . it’s not particularly pleasant. So in that situation what I’d normally do is just quickly take the tube out and then you just quickly remove some of the monitoring and . . . any lines that I can do quickly. And then let the family come in and see . . . In case they do pass away quickly.
NIA6P1S214
Monitoring
All of the nurses interviewed in the LCP settings reported turning the monitors off or down at the bedside while keeping the monitor at the nurse’s station functioning. The monitors were reported by the nurses to be useful for two reasons. The first reason was that the monitor enabled nurses to be absent from and present at the bedside at the same time. Remote access to the monitor enabled the nurse to track the patient’s physiological functioning. This was considered by nurses to be important so that they could intercede to calm agitation or remove secretions should the monitor alert them to the need. They were enabled to do this at the same time as giving the relatives space and privacy of sorts to be with the patient in their dying hours.
I mean they couldn’t see me and you couldn’t see me but I was watching him through the curtain some of the time to see how they were and what was going on, which is how come I managed to come in just after he did the gurgling noises . . . that wasn’t luck that was because I was keeping an eye, and also I had his vital signs on my monitor outside.
SIA1P1S21
Surprisingly, and despite some views to the contrary, the point of death was not always easily discernible. Nurses saw themselves as interpreting the monitor to get relatives back to the bedside if they wanted to be present at the death and also to confirm or not that the patient had died.
When I looked at the monitor she was actually . . . she still had a heart rate. It was very, very slow.
NIA6P1S214
Nurses in the LCP sites identified a strong nursing role for themselves in this period of withdrawal which involved being there for the relatives and keeping the patient comfortable.
Non-Liverpool Care Pathway-using sites
Six staff were interviewed who were working on ICUs where the LCP had not been used to support a patient in the last days and hours of life. In addition, a student nurse, present during the observations and being mentored by a senior sister, was also interviewed. All of the staff interviewed, with the exception of the student nurse, were aware of the LCP and some had even used the LCP in the past. The more senior members of nursing staff were more likely to have reported using the LCP before.
As previously mentioned, all of the nurses described the clinical context of the patient’s decline and this seemed to be as important for understanding the care in the non-LCP-using sites as in the LCP-using sites.
Training on end of life care and views on the Liverpool Care Pathway
Few members of staff on the non-LCP-using ICU sites reported receiving any training on end-of-life care. One staff nurse, when asked about the provision of end-of-life care training in her ICU, said:
To be honest I really couldn’t tell you. My gut instinct is no.
SIB2S113
Sometimes during the course of other training sessions, for instance on organ donation, the ‘care of the bereaved’ or care of the dying might have been mentioned, but formal, in-depth training on care of the dying was not reported to have been received. Nurses in the non-LCP-using sites had heard of the LCP and some had actually used it in previous jobs, again without being trained to use it. One charge nurse with considerable experience had used the LCP on occasions in the distant past.
My experience of the Liverpool Care Pathway is that it works best in people whose death is not imminent. In intensive care, when you’ve got somebody sedated, ventilated, they are invariably already receiving some dose of opiate . . . the Liverpool Care Pathway does seem to concentrate on the delivery of medication using syringe drivers subcutaneously, and there seems little point to discontinue intravenous opiate, only to start again with subcutaneous opiate.
NIB3P1S213
Clearly, this is a particular interpretation of the LCP and not one which was recognised or implemented in any of the LCP-using sites in this study. Paradoxically, the charge nurse also identified that the length of time it would take to complete the paperwork was a disincentive for using the LCP, while identifying one of the advantages of its use as having the patient’s documentation contained in one place.
I have used Liverpool Care Pathway before and one of the advantages from a purely nursing point of view, in terms of time and so on and so forth, is once you’ve done the work, once you’ve set it up, once somebody is on that pathway, that’s all the documentation that you need. You can tidy everything away and just use that.
NIB3P1S213
In his view, patients who were identified as not likely to recover died very quickly in ICU. Indeed, the patient he was looking after died within 1 hour of withdrawal and the majority of deaths that we observed within the ICU took place on the day of withdrawal, most often within a few hours.
When people are on intensive care and when people are dying on intensive care, they don’t tend to hang about really, they tend to be at the point where as soon as you stop doing something, or even if you continue doing the things that you’re doing, people die anyway . . . I think it’s less useful in intensive care.
NIB3P1S213
This charge nurse reported that it was useful as an aide memoire: ‘It means that you don’t have to sit there thinking: “Oh, have I done this?” ’ (NIB3P1S213). He reported that the downside of using the LCP in this way was that it could also stop people thinking. Interestingly, this was one of the few sites in which the religious and spiritual needs of the patient whose death was observed were not considered. In response to the question from the researcher about the patient’s spiritual needs, the charge nurse demonstrated the reason why some sort of aide memoire might be useful.
I always forget the religious bit . . . because I’m not religious at all. So I always forget that bit . . . It is a timely reminder to me to say oh yeah, do you want to get a priest or a such-a-body . . . But otherwise I would tend to forget all about that, just because it doesn’t really apply to me, which is perhaps a failing on my part.
NIB3P1S213
As the discussion progressed his reply became more confused, moving from his failure to remember (above) to a reluctance to raise it (below).
I didn’t feel comfortable bringing it up, in that they were already aware that she wasn’t going to survive and I kind of thought well I don’t really want to bring the subject up now . . . possibly it was an omission. And again, that would be my fault. It’s not something that occurs to me very often. Had we been using the LCP there would be a box to tick and that would have reminded me to do it.
NIB3P1S213
There were many contradictions about the LCP in the account provided by this charge nurse, but, perhaps more importantly, in his discussion of the LCP he raised questions about his own practice.
Withdrawal
Communication of patient’s decline to relatives
It was in relation to withdrawal that some subtle differences between LCP-using and non-LCP-using sites emerged in the nurses’ interviews. In common with the LCP sites, considerable discussion was reported on how the patient’s decline was communicated to the patient’s relatives and the way in which the nurses interpreted the relatives’ response.
I rang the husband and told him that she hasn’t improved, that she had actually deteriorated overnight and I told him that we have a diagnosis of why she is so unwell and the consultant would like to speak to him. I said ‘When would you be able to come into the hospital’ and he said ‘well about 2 o’clock’ and I said ‘could you make it any earlier?’ and he said ‘no I need to have a shower first, I need to clean the house first’. Right so trying to prolong it a bit. He knew she wasn’t well because he had been spoken to by the doctor yesterday twice.
SIB1P2S21
In this respect the nurses across all sites were very similar. However, it was in the nurse’s role after withdrawal that small differences emerged between the LCP-using and non-LCP-using sites. Nurses in the non-LCP sites reported that the time after withdrawal was ‘a very grey area’ in terms of their role.
Taking advice from consultants and other experts
According to the nurses in the non-LCP-using sites, the consultants were responsible for the decision to withdraw, and on occasions they would take the nurses’ views on board. But the nurses reported that, thereafter, their role was influenced by the consultant; the nurses described the care after withdrawal as consultant led rather than nurse led. In large part what happened depended on the consultant on duty at the time. Nurses took their lead from the consultant, and this might vary depending on who the consultant was. The charge nurse in the following example highlights the prescribed nature of consultant-led care and its consequences for withdrawal and for the nursing care that accompanied it.
Some consultants will say ‘OK, stop that, stop this, take that off’ in that kind of prescriptive way of withdrawing treatment. So, I was told to deal with it in a certain way and that was the way that I dealt with it . . . on occasion it is left to me, it depends on the relationship that you have with the relatives, it depends how much interest your consultant or the doctor may take.
NIB3P1S213
That was the consultant’s decision to keep the ventilator on . . . he wanted her just to feel the same, so we just turned the oxygen down from 28 to normal room air of 21% and that was it. What I would have done differently next time is that, she was on a monitor where she was given the manual press . . . in hindsight I should have just put it on spontaneous mode straight away. She wasn’t lying there for very long but she would have gone quicker, she would have died perhaps earlier . . . the consultant came back and put it on the spontaneous mode and within 10 minutes she passed away.
SIB1P2S21
As can be seen, the nurses’ accounts of the care referenced the consultant’s decisions more frequently than did the accounts provided by nurses in the LCP sites, where care was reported to be more nurse-directed, with experts brought in where the nurse thought it was appropriate. In this context it might not be so surprising that a junior sister of 6 years’ experience expressed a high level of discomfort regarding treatment withdrawal.
I never liked this, withdrawing treatment . . . I always feel uncomfortable by doing it, ‘cos I never know what is the right thing. What would be the right procedure? I think it is necessary to do so but the actual action I am a bit apprehensive about it.
SIB1P2S21
The role of the consultant appeared to dominate the decision to withdraw, the way in which treatment was withdrawn and, to some extent, the care that followed. Nurses in the non-LCP-using ICUs did not identify themselves as leading end-of-life care for the patients whose care was observed in the course of this study. One charge nurse described their role as that of stage management.
I think the longer you’ve worked in critical care, certainly people I know who’ve worked here for a long time, would tend to have quite a business-like approach to it, in that once that decision has been made, then effectively all you’re doing is stage managing it.
NIB3P1S213
Keeping the relatives informed
Communicating with relatives and keeping them informed was as much a feature of non-LCP-using sites as of LCP sites. In common with reports from the nurses on the LCP-using ICUs, there was a view that relatives wanted patients to go naturally and quickly. However, as the interviews with bereaved relatives demonstrated, there were circumstances in which relatives wanted to prolong a patient’s life in the hope of recovery. While a quick death was generally regarded as a good death, where a patient was not deemed to be suffering, there was less emphasis on a speedy death.
Personally for me, if it was me or if it was one of my relatives, I would get it done and dusted as quickly as possible. Not in an unseemly haste, but erm, I would carry on and get everything done . . . probably sounds a bit, erm, uncaring or a bit brutal maybe, but I think once you’ve decided that this person is not benefiting from the treatment and the end result would be death, then, you carry on.
NIB3P1S213
I pulled the curtain and I did ask them if they want to wait a bit longer or if it was OK to stop it now. And he said ‘he didn’t want to wait any longer’ so he was fine for me to stop all the machines.
SIB1P2S21
The managed slow withdrawal of equipment, which was a feature of LCP ICU care, was not much in evidence in the accounts of nurses in the non-LCP-using sites. A slow death was seen as an uncomfortable experience for patients and relatives and to be avoided if possible.
She died in a relatively short time. That’s not always a positive thing, but I think it is when you’re expecting somebody’s death. One of the uncomfortable things about occasionally withdrawing treatment, or being in an end of life situation in intensive care, is that it drags on for 24 or 48 hours, until everybody, even the relatives of the dying person, are sat at the end of the bed thinking: well how much longer is this going to go on for?
NIB3P1S213
Similar problems were reported across all sites in enabling relatives to come to terms with the patient’s imminent death.
What I find happens most of the time, is not so much the family don’t want the treatment to be withdrawn, it’s almost that they feel that they’re the one making that decision, that’s where the problem comes, sort of thing. So, often times, like for example, we call a family, and if I’m the bedside nurse, myself, the doctor, and the consultant, after telling them, or showing them what’s wrong with the patient in terms of letting them know this is failing, that’s failing, I think the next thing is, they feel like they’ve got that switch in their hands, kind of thing, and so nobody wants to turn that switch off.
SIB1P3S24
However, in two cases in the non-LCP-using sites, relationships with relatives became antagonistic, with formal complaints against the staff being threatened.
The first case related to a very large family of Indian origin. The nurse reported in the interview that in India care is purchased. You can have as much or as little treatment as you can afford to pay for. Active treatment to the point of death was more common where families had the resources to fund it. Against this backdrop, staff were struggling to explain to the family that active treatment was not going to be continued.
After half an hour they asked the same questions. It was difficult to deal with that family . . . I think they didn’t understand what you were saying to them. The doctor three or four times explained to them the same thing, the matron spoke to them, the senior doctor spoke to them, but still another family member came and asked the same questions. The doctor did explain to them we can’t restart him . . . the next day they wanted the same, to restart treatment, the patient might even recover. They did understand, but they didn’t.
SIB2P2S21
All nurses were able to identify families in which understanding was impaired by the desire to keep someone alive; in this case a prolonged and bitter argument broke out between staff and relatives with no real resolution.
When the other daughter had a fight with the senior doctor here, I spoke to them and they said ‘We do understand what is happening. He is going to die, he is not going to make it, but she (the daughter) is the one . . . she is not understanding’. They were saying ‘she gets upset because of his dying’ and ‘she’s not understanding as well’. She’s not like accepting it you know fully, so she is just getting frustrated.
SIB2P2S21
In analysing the problems that had arisen with this family the nurse felt that communication had been difficult as a result of the number of family members and their ever-changing presence at the bedside.
In the second case, the relatives were extremely unhappy about the patient’s resuscitation prior to his admission to ICU. The profound impact of this resuscitation on the family was explored in the bereaved relative’s interview. In her interview, the nurse who had provided care to the patient on the ICU provided a very different account of the relative’s response to this event. She seemed unaware of any negative effects it had had on the family.
The family were happy that in a way, even though they didn’t want him resuscitated, they felt like . . . the fact that he’s got lots of children, um, you know if he had died suddenly, they wouldn’t have had the opportunity to come back, you know, and be with him when, he’s, you know . . . So they felt like they were . . . not angry because we resuscitated him, um, and they felt that it gave them opportunity to tell all the family members to come in and see him before he actually passes away.
SIB1P1S21
This was not the view that the bereaved relative reported to the researcher. There are a number of possible explanations for this discrepancy which will be explored in a subsequent paper examining the use of multiple perspectives on events. Further, the nurse’s account of the patient’s transfer to a side room did not reflect the anger and frustration felt by the family, whose interview account and observational record suggested that they felt that the patient had been abandoned.
I think it went well in a lot of sense. I think the only thing I, I could say was the fact that we got to move him to a side room, and the fact that it was little bit of confusion as to who’s looking after him in terms of relatives. When I obviously handed over to them that [name] was gonna be looking after him, but [name] wasn’t within . . . reach for the relatives to, to sort of ask him questions or, get stuff from him. And, um, obviously the nurses at the desk there are coronary care nurses, so they don’t usually look after our patients, so they don’t know anything about him. I felt like, um, at times when the relatives needed stuff, or they wanted to ask a question or something, no one was available. And I think that’s partly the fact that we were quite busy with three admissions in one go and everyone was quite busy.
SIB1P1S23
Assessing the impact of the withdrawal process on the patient
While withdrawal presented many opportunities for nurses in the LCP sites to demonstrate their range of skills and expertise, withdrawal in non-LCP-using sites was presented as a quiet time.
Because all we were doing, all I was doing, essentially while that was going on, was sitting and waiting for things to run out. So essentially, just twiddling my thumbs and waiting for things to run out that were going to run out. It went fairly smoothly I suppose. I would be content that she didn’t suffer any unnecessary interventions, she was sedated, she was on a large dose of morphine, so I think, hopefully, from her point of view, it was a reasonably pleasant way to die.
NIB3P1S213
It was only natural for me to step back at that point, rather than standing and watching over her. Because I wasn’t doing anything physical for her, just making sure, glancing at her, making sure she’s comfortable.
SIB1P3S24
I usually leave the family as much as possible to themselves because this is their last moment, the last time they are with their loved ones so I tend to not to disturb them, I find it’s not appropriate so I do the bare minimum. I am accessible to them, I say ‘I am behind the curtain’ if they need me but I leave them to themselves.
SIB1P2S21
While the nurses in the LCP-using ICUs reported trying to achieve a balance between being present at and being absent from the bedside, the nurses in the non-LCP-using sites reported a more hands-off approach. This was also in evidence in relation to the use of the monitor. In all sites nurses reported that the monitors were a distraction for the relatives and in the majority of cases the monitor was turned off, down or onto a privacy setting. In the LCP-using sites the nurses reported using the monitor to continue their clinical assessment of the patient remotely. In the non-LCP-using sites the nurses reported that the monitor was not needed, although it might be left on.
I think everything sort of went, in terms of him, it was quite peaceful. The other thing that doesn’t normally always happen is monitoring someone that’s dying. We don’t always do that . . . I think that just carried on and no one else just thought, ‘oh we need to take the monitor off’. Since the monitor wasn’t . . . in any way, I don’t think it was . . . a big problem. But normally we would take the monitoring off because we don’t now need it, to, you know, to know that the patient’s died.
SIB1P1S23
Goals of care: Liverpool Care Pathway-using and non-Liverpool Care Pathway-using sites
The goals of nursing care in the LCP-using and non-LCP-using sites were identical: keeping a patient comfortable and pain free and ensuring their dignity. In all but one of the non-LCP cases, the religious and spiritual needs of the patient were reported to have been considered by the nurse.
I make sure that the patient is comfortable and is pain free and I am sure there is no distress, so once that is sorted and I see that then I, then I can focus on the family and make sure they are happy how their loved one died.
SIB1P2S21
From active treatment to withdrawing treatment, the main thing is to just ensure that she’s comfortable really, at that point . . . She had the priest came in.
SIB1P3S24
Achieving privacy for dying patients and their families on ICU was recognised to be a challenge, which all nurses reported managing in the same way, by using the curtains around the bedside.
Men don’t like to be emotional in public. So I drew the curtains just to give him some privacy and also some time alone with his father . . . And then they can let their emotions out and not feel that everybody else is watching them.
NIA1P1S24
She was in an open bay, so I tried to pull the curtains round to get that bit of privacy, even though it wasn’t probably ideal as such, but I feel that it was probably good enough though.
SIB1P3S24
We don’t like anybody to think that anybody dies, we pull all the curtains round all the beds and, everybody kind of looks the other way and pretends that nothing’s happening. Then magically as the curtains are drawn back, there is an empty bed space there . . . it’s a bit like a pantomime really.
NIB3P1S213
Summary
The interviews with the nurses identified some small and subtle differences between nurses working on LCP-using ICUs and those working on non-LCP-using ICUs. It must be remembered, however, that there were many more interviews with nurses in LCP-using sites and the consistency between their views may derive in part from their employment in a small number of ICUs. Nevertheless, the differences in the role of the nurse following a decision to withdraw were interesting and the distinction between nurses leading care and stage-managing care is worthy of further research.
Summary of Section 3 findings
Intensive care unit data
There was incredible consistency across all data sources regarding care at the end of life in ICUs. In the main, the interviews prior to observations reflected the general approach to end-of-life care which was reflected in the care actually seen to be provided in the observations and reported in the case notes. The relatives’ views on the care that was provided did not differ in substance from what was observed but it was selective in certain important respects. We return to this in Chapter 14.
There was agreement that the withdrawal of life-sustaining interventions was ultimately a medical decision. This was what doctors and nurses reported and recorded and what was observed to happen. Relatives confirmed that this was also their experience. However, there were a small group of relatives who, while making reference to the medical decision to withdraw treatment, also reported that they had made the decision to or had been in control of switching off certain machines. Drawing on the interview data it is possible to forward an argument that relatives had been so well informed of the patient’s deterioration or lack of response to interventions and that doctors and nurses were so keen to get relatives on board with the decision to withdraw that relatives felt in control of the withdrawal even though they had not been.
Reaching agreement on a decision to withdraw life-supporting interventions did not automatically lead to withdrawal. Delays in actually implementing the decision were recorded in the patient case notes and in the interviews and were observed. Relatives welcomed the opportunity this presented to make arrangements for other family members to be present and to prepare themselves for the patient’s death.
Laying down a narrative of a patient’s deterioration was seen as an essential precursor to any decision to withdraw or withhold treatment or life-supporting interventions. This appeared to be as important to doctors in the interviews and the records of their contact with the patient as well as in their communication with relatives. The ultimate goal was to ensure that the patient’s physical health was widely understood between the clinical team and the relatives so that there was a shared view of the best course of action. Relatives reported the importance of understanding this deterioration as a basis of their agreement for withdrawal. The physical reflection of a patient’s deterioration, laboured breathing and changes in skin tone, were taken by relatives as signs of suffering, which reinforced the appropriateness of the chosen course of action to withdraw treatment.
There was agreement between doctors and nurses that once a decision to withdraw had been made the physical care of the patient was very much left to the nurses. Relatives communicated principally with nurses once the withdrawal was under way. The nuanced and sensitive steps taken by nurses to achieve a natural death were largely lost on the relatives but there was recognition that the experience for the patient was dignified and respectful.
The role of the LCP in care at the end of life in an ICU was extremely difficult to ascertain. Doctors and nurses were sensitive to the negative media reports about the LCP and did not want to raise unnecessary concerns about the management of these patients in the last hours of life. For this reason, not all relatives were aware of whether or not the patient was being cared for on the LCP. Some relatives expressed some negative views of the LCP, but they did not appear to relate these views to the care of the patient at whose bedside they had sat. Although the principles underpinning the LCP were generally viewed positively by all staff, the documentation was reported and observed to be difficult to operate in practice. This was particularly so in instances where the patient died very quickly after life-supporting interventions were reduced or removed.
Chapter 13 Integrated care pathways: economic evaluation of end-of-life care
Introduction
The purpose of the economic component within this study was to assess the costs and benefits of standard care versus the care supported by the LCP. The study was designed so that, all things being equal, any differentiation between ‘using’ and standard ‘non-using’ sites should be attributable to the care pathway adopted.
Aim
The aim of the economic evaluation was to evaluate the effectiveness with which inputs, processes and outcomes are combined to provide care for patients entering the last days or hours of life. Undertaking such an evaluation presents significant problems for health economic evaluation, as standardised approaches and existing methodological ‘tools’ that can be engaged to produce meaningful outcomes are largely not fit for purpose in this context.
Considerations of the health economic evaluation in this study
In order to assess the cost-effectiveness of the LCP in the ICU and nursing home environments, it was necessary to measure both the difference in costs between the sites using the LCP and the non-using sites, and any variation in a quantifiable outcome. As a general rule, the outcome in an economic analysis is based on the quality-adjusted life-year (QALY). 76 QALYs are a function of the quality of life of a patient and survival. However, as a patient nears the very end of life, survival and quality of life may be of less importance and quality of dying and death may take priority. In particular, the use of the QALY framework requires a detailed analysis of the comparative quantity and quality of life experienced by patients. Such a framework is of limited value in evaluating care provision in the last days of life given that survival is strictly limited and comparative quality of life is largely driven by control of symptoms and distress alongside support for the family.
Many of the adverse consequences resulting from deficits in service provision in the last hours of life are likely to be hidden from view and hence do not directly have a ‘cost’ or ‘price’ associated with them. For example, what is the cost associated with a patient being placed in an isolated room by staff who are unable to correctly deal with the needs of a dying patient? A principal aim of the LCP is to ensure the delivery of a ‘seamless’ service in which care is delivered in a co-ordinated manner to optimise the quality of patients’ remaining life.
The economic analysis attempted to assess, using the data collected around the 25 observations of patient care, the costs of end-of-life care in nursing homes and ICUs with and without the use of the LCP. Bereaved relatives provided their views about the care of patients while in nursing homes or ICUs specifically for this economic evaluation and these data were built into the analysis.
Methodology
There have been a number of studies authored by the National Audit Office7 and Marie Curie Cancer Care77 that have attempted to account for the costs accrued during end-of-life care. However, it is rare that the different care environments and the approaches used have been taken into consideration while also looking at costs. Accordingly, in this study identification of comparative quality of life and resource use was undertaken in close collaboration with health professionals involved in the provision of end-of-life care. Staff and family members were observed giving treatment and care to the patients recruited to the study by the researchers. Notes were recorded about the care delivered, which included timings. Later, the costs associated with each task were calculated and applied. The economic evaluation was based on three data sources:
-
patient observations
-
review of drug charts and interventions
-
bereaved relative economic tool.
Patient observations
For the purposes of the economic analysis the patient observations were used to understand the quality of care provision and the resources used for each patient. Only in this manner could sufficient detail be generated of the broad range of public and private resources utilised by patients in their final hours or days of life. It is well recognised that effective communication between staff and patient/relatives is fundamental to the provision of optimal end-of-life care. In addition a range of subjective elements, for example ‘did the nurse smile and interact positively with the patient and the relatives?’, are likely to be as important in determining ‘quality’ as objective elements such as drug regimens. Equally, accurate allocation of the most important resource (staff) between individual patients requires a detailed knowledge of interactions between staff and patients. All of these aspects featured in the patient observations.
All staff costs were taken from a combination of NHS salary data and allocated in relation to the level of care provided, as measured by the interaction between each staff member and each patient in relation to hospital stay, and Unit Costs of Health and Social Care [Personal Social Services Research Unit (PSSRU)]78 costs.
-
For nursing time in ICU we assigned two different costs: one for contact with the patient, which is £1.62 per minute, and the other for nursing duties for the patient or family without direct contact at £0.67 per minute. These costs are £97 and £40 per hour, respectively. Registered general nurse costs were based on the PSSRU costing document; see Appendix 29 for full costing details.
-
Nursing home nursing staff costs were accounted for at the same level as the ICU nursing staff (£1.62 per minute) for the purpose of the study, in order to keep both sets of costs equal; therefore, if there was a true difference in care it would be due to the amount of care rather than cost differences. In addition, this method was adopted because nursing home providers around the country have varied pay structures and rates, making comparisons difficult. Similarly, costs relating to auxiliary nurses/health-care assistants and carers were calculated at the same rate throughout both sites, assigning a wage of £9.77 per hour, as per NHS Agenda for Change79 band 2 salary structure.
-
Costs assigned to porters within the ICU observations were based on band 2 point 1 in the NHS Business Services Authority, at a cost of £9.77 per hour. 80
-
The school-aged assistance in the south nursing home was paid help; therefore, for the purpose of this study costs have been applied at the National Minimum Wage for 16- to 17-year-olds, which in 2013 was £3.68 per hour. 81
-
In one of the sites the nursing home manager was involved in giving care. For the purpose of the study, the cost applied is at PSSRU rate for a nurse team manager with patient contact at £2.37 per minute. However, we acknowledge that this would vary depending on the nursing home and location.
-
One of the nursing home sites had a sister in the unit. This has been costed at PSSRU rates for a nurse team leader, with patient contact at £2.03 per minute.
-
An important part of end-of-life care is care of the family; during the observations it was noted at times that their family members were brought drinks (tea and coffee). It was not always known which member of staff carried out these hospitality duties, although in some cases it was known, for instance, that volunteers were responsible for this role. For the purposes of consistency it was assumed that individuals who provided tea and coffee in the ICU were hospital volunteers and hence costs have not been assigned.
-
For a number of the resource use items, it has been assumed that they can be separated easily; for example, mouth swabs come in packs of 25, with three swabs in each pack (75 swabs in a box). Therefore, for the purpose of the study it has been assumed that one item can be individually costed. This process has also been carried out for items such as gloves and incontinence pads that come in bundled packs.
The primary analysis was derived from the observational notes captured by the researchers during the last few hours or days of life. Once all observations had been completed, an eligible sample was selected (i.e. had complete data for all of the sources of data being assessed) from each LCP-using/non-LCP-using ICU/nursing home. The information relating to resource use was entered into a Microsoft Excel® table (Microsoft Corporation, Redmond, WA, USA). From this, and using the times noted down by the researchers, a time period was assigned to each action that required resource use.
The final aim was to micro-cost all of the actions observed, using the data sources available. The costs chosen to allocate to the resource use are current NHS figures and recently published costs, although some assumptions still had to be made throughout, and these are outlined later in this chapter (see Limitations and assumptions).
Drug charts and interventions
A detailed analysis was undertaken of drug charts to identify comparative use of medications. In addition, all other diagnostic or therapeutic interventions were identified for each patient. Drug prices were taken from the British National Formulary. 82 Using the drugs charts gathered from the hospitals and nursing homes, any medication that the patients were administered was recorded and costed to the nearest amounts assigned.
When costing drug usage we have costed the whole value of the nearest dosage, therefore not accounting for waste or vial sharing, as it is assumed that the remainder of drug would have been disposed of. All of the drug costs used were sourced from the British National Formulary online 2013 list. For a detailed list of resources, see Appendix 29.
Bereaved relative economic tool
The aim was to review existing measures and identify a suitable quality of dying and death tool for use in this study. If no suitable tool was identified, the next objective was to develop a tool suitable for use in the study.
Suitability of previous outcome measurement tools
Three tools were identified as potentially relevant and were evaluated for use in the study.
Quality of Dying and Death
The Quality of Dying and Death (QODD) questionnaire is a 31-item questionnaire and was developed in order to assess the quality of the dying process. It is completed by family members or clinicians after the patient has died. 83 The QODD questionnaire comprises a number of quantitative questions. The responses from the questions are totalled to a value between 0 and 100, with a higher score denoting a better quality of dying and death. Although there were some elements of the tool that were relevant to this study, such as how the family members’ needs were assessed and their views were taken into consideration in the care of the patient, in this study we were concerned only with care in the last days and hours of life.
Views of Informal Carers – Evaluation of Services
The Views of Informal Carers – Evaluation of Services questionnaire contains 158 questions in eight sections. 84 Section F asks questions specifically about the last 3 days of life and the care given over that time period. The majority of the questions have the options to respond ‘yes’, ‘no’ or ‘don’t know’ and there are spaces to add comments to some questions. Degrees of preference are not measured, which limits the use of this questionnaire for an economic assessment of the quality of care at the end of life.
Evaluating Care and Health Outcomes – for the Dying
Evaluating Care and Health Outcomes – for the Dying has 94 questions divided into nine sections. 85 The time frame of focus is the last days of life and the period immediately after the death of the patient. As the tool was developed based on the LCP domains of care, there was some concern that the use of this tool in the study would be biased towards the LCP-using sites.
Overview of available tools
None of the tools was deemed suitable for use in this study. There were elements within each instrument that would have been inappropriate to the two clinical settings and any attempt to use a subset of questions would have compromised the validity of the tool. As a tool that was sensitive enough to adequately capture the effects of the presence or absence of LCP in supporting care could not be sourced, it was decided that a de novo outcome tool would need to be developed and piloted within the study.
Elements of a good death
Before developing a tool it was important to consider the conceptual and practical elements of a good death that are important to patients, their families and carers at the end of their life. Two key studies have been undertaken to this end.
Steinhauser conducted focus groups and interviews with patients, relatives and individuals providing care to patients at the end of life to establish a list of the components contributing to a good death. 86 Six key factors were identified, which included the management of symptoms and pain; clear communication between health professionals, patients and their families which enabled collective decision-making; being prepared for death; enabling the patient to participate in any spiritual rituals or being able to settle conflicts and say goodbye (termed ‘completeness’); the ability of patients to play a role for the benefit of others (this may be in the form of gifts or spending time with other people); and treating the patient as an individual no matter their level of illness or consciousness.
Low and Payne87 developed a questionnaire to obtain the perceptions on death of health-care professionals working in palliative care. They were concerned specifically with the factors that were perceived to contribute to a good and a bad death. The authors produced a factor analysis of the survey results and found a patient dying without distress to be of fundamental importance to a ‘good death’. This factor encompassed aspects such as a lack of pain and anxiety, as well as family members accepting the prognosis and being at peace. The factors that contributed to the perception of a bad death included elements such as the patient dying without people whom they are close to being around them. In general, the health-care professionals perceived a good death to address any physical or psychological distress of the patient while preparing both them and their family members for what was to come. Aspects of spiritual and cultural rituals were deemed an important contribution to the holistic care of the dying patient.
Development of a de novo outcome measurement tool
Given that most patients at the very end of their life will not be able to complete an outcome measurement tool, it was decided that the views of the patient’s family would be sought. For this reason, the tool’s design needed to take into account the sensitivities of patients and close family members.
The tool in its piloted format contained seven factors which family members were asked to rate on a scale from 1 to 10. This scale was chosen to provide the ability to vary the answers to different elements of the questionnaire by a number of points; in addition, a 1–10 scale is commonly used, which provides familiarity to the assessor and prevents introduction of unnecessary complexity. The poles of the scale represented extremely bad care (1) and care as good as it could be (10).
In line with the layout of the QODD questionnaire, there was an additional box within each question which enabled the responder to discount the domain as an issue, that is, that the patient did not experience the problems identified in the domain.
The relative weight of each of the factors that play a role in enabling a ‘good death’ is thought to differ. 88 In order to apply variable weights in this quality of dying and death outcome tool, the precise magnitude of each of the weights, and their contribution to the estimation of the quality of dying and death as a whole, first needed to be developed. Members of the research team and a convenience sample of relatives were asked to allocate weights to each of the elements in an initial attempt to quantify the preference weights. In this way, it was hoped that the preferences and experiences of the bereaved relatives would contribute to the development of a more sophisticated weighting of the contributing factors.
The information generated from these exercises does not enable precise quantitative weights to be determined. It does, however, allow a form of sensitivity analysis to be conducted, which overcomes the issue of all the factors being weighted with equal importance.
The bereaved relative completed the revised tool at the end of the interview. Respondents were also asked to talk through their response to each item as they made it, and their answers were recorded to provide additional feedback on how the relatives understood and completed the tool.
The final component was then to use the tool to evaluate the quality of dying and death of the patients as perceived by the relatives/carers. A simplifying assumption of linearity was made by which each increment (1–2, 2–3, etc.) was held to have equal value. In this manner the individual values assigned for each patient could be summed and averaged.
Once a detailed cost table for each of the patients sampled had been developed (see Appendix 30 for an example of the detailed cost table for case study 4), a summary of the resource use was derived to show the individual amounts of each resource consumed during the period observed.
It is important to note that the costs accounted for in each of these case studies are not directly comparable, as the length of observed periods differed between cases. Resource use can be calculated only for the time periods that were actually observed, and, similarly, the costs accounted for are not the whole costs of care in the final hours or days of life. The purpose was to focus on the time periods observed to assess any extra care undertaken, including staff care, and time that may have been driven by use of the LCP to support care.
Results
Bereaved relative economic tool results
Data from a total of 22 complete observations and the bereaved relative economic tool formed the focus of this analysis. The challenges to recruitment have been detailed elsewhere in this report, but it is important to highlight that the limited resultant sample has also had a negative effect on the economic analysis. Table 17 shows a breakdown of each of the questionnaires filled in by location and site type. It is important to highlight that the observations in the north non-LCP-using care homes were from the same site, and, although at recruitment this site did not use the LCP to support care, by the time the observations were undertaken the LCP was being used.
| Location | Site type | LCP using or non-using | Number |
|---|---|---|---|
| North | Nursing home | LCP using | 3 |
| North | Nursing home | LCP non-using | 2 |
| North | ICU | LCP using | 6 |
| North | ICU | LCP non-using | 1 |
| South | Nursing home | LCP using | 2 |
| South | Nursing home | LCP non-using | 0 |
| South | ICU | LCP using | 5 |
| South | ICU | LCP non-using | 3 |
In order to analyse the results by institution type and whether or not it was a LCP user, a series of tables were created. This allowed for assessment of overall trends to establish what (if any) were the most important factors to the patient’s family.
The first set of results shows the north nursing home LCP-using sites. As identified in Table 18, the pain management scores are quite varied between patients even though all three observations were undertaken at the same site. The relative of patient NNA2P3 scored pain management at 3 because they believed that the patient had trapped wind and the nurses did not attend to this, although they thought that the pain management through the use of drugs was controlled well. It is interesting to see that the relative of patient NNA2P2 scored 10 across all areas except for breathlessness, which they believed was not an issue. They also believed that the spiritual issues were most important and were pleased with how this was managed. The relatives of patients NNA2P1 and NNA2P2 allocated a score of 10 to personal care and dignity/respect as well as the staff keeping them informed, demonstrating that they felt that both they and the patients were treated well, which was particularly important to the relative of patient NNA2P1. The lowest-rated score from the three observations was for the pain management of patient 3. However, the narrative data collected during the relatives’ allocation of this score reflects uncertainty about the time period to which the pain management question was relevant. In this particular case the patient had been treated on a ward as well as in ICU. Pain management was also the most important factor to this relative, which may account for such a low score. Of the 17 numbered results, nine were scored at 10, two at 9, three at 8, two at 6 and one at 3.
| Site | Patient ID | Pain (question 1) | Breathlessness (question 2) | Agitation (question 3) | Personal care (question 4) | Dignity/respect (question 5) | Spiritual (question 6) | Staff kept family informed (question 7) | Most important | Comments |
|---|---|---|---|---|---|---|---|---|---|---|
| NNA2 | P1 | 8 | 6 | 6 | 10 | 10 | 9 | 10 | Having staff support patient and her needs | Relative felt that making sure her mother was not in pain and being looked after by staff for both her and her mother were constantly the most important factors. Her answers were justified as ‘what felt right’ |
| NNA2 | P2 | 10 | NI | 10 | 10 | 10 | 10 | 10 | Response of staff to patient’s religious beliefs | Relative answered NI to breathlessness as patient did not have any breathing symptoms. All other questions talked through no issues |
| NNA2 | P3 | 3 | NI | NI | 8 | 9 | NI | 8 | Having satisfactory pain and agitation control for the patient | For pain question relative was asking to which period this meant in the dying process. Other NIs not an issue. In addition, score of 3 was given for pain management because patient had wind and relative thought that doctors/nurses did not do anything good to help |
Looking at these results in line with the LCP-using nursing home in the south of England, shown in Table 19, we can see that in these two observations there were no scores of 10, although the results were still at the higher end of the scale. All of the results given (except for the three ‘not an issue’ responses and one declined to answer) were between 7 and 9. It was interesting to see that the relative of patient 2 thought that the management of the patient’s dignity and respect had been very good, although the item was only allocated a score of 8.
| Site | Patient ID | Pain (question 1) | Breathlessness (question 2) | Agitation (question 3) | Personal care (question 4) | Dignity/respect (question 5) | Spiritual (question 6) | Staff kept family informed (question 7) | Most important | Comments |
|---|---|---|---|---|---|---|---|---|---|---|
| SNA1 | P1 | NI | 8 | NI | 6 | 7 | 9 | 8 | That the patient died peacefully and comfortably | Relative did not think patient was in any pain so it was just not an issue. Also agitation not an issue because patient did not appear restless |
| SNA1 | P2 | 8 | NI | 7 | 8 | 8 | No answer | 8 | Keeping her comfortable/not too agitated | Relative commented that patient was not breathless until she was trying to do things and she did not try and do much, so it is difficult to answer – NI. Family member does not really know about spiritual needs, but would not like to say no. For dignity they say this was very good and are a little more positive than for some of the other questions but give an 8 also |
Ideally, the results for the LCP-using nursing homes should be contrasted with the results for those not using the LCP. However, as we have seen, this home began to use the LCP during the course of the study. For the purposes of analysis this site had to be referred to as a LCP-using site in order to avoid introducing bias. Additionally, there are no data at all for the south non-using LCP site.
Table 20 shows the results from the north non-using LCP site (evaluated as a LCP site). There were some interesting reasons given for the scores that were allocated. In the case of the management of pain, breathlessness and agitation, the relative of patient 2 chose not to score 10 because she was not rating for herself and did not really ‘know for sure the way her relative was feeling’. No two of the aspects were scored the same by the relatives, although the scores were always relatively close by 1 or 2 points. The relative for patient 2 believed that all of the care aspects were equally as important, while the relative of patient 1 believed that dignity and personal care were the most important.
| Site | Patient ID | Pain (question 1) | Breathlessness (question 2) | Agitation (question 3) | Personal care (question 4) | Dignity/respect (question 5) | Spiritual (question 6) | Staff kept family informed (question 7) | Most important | Comments |
|---|---|---|---|---|---|---|---|---|---|---|
| NNB6 | P1 | NI | NI | NI | 9 | 10 | 10 | 8 | Maintaining dignity, individuality and personal care | Daughter interviewed: she thought questions 1–3 were not an issue as relative was looked after well, so instead of putting 10, she chose NI |
| NNB6 | P2 | 9 | 9 | 9 | 10 | 9 | 8 | 9 | The seven elements of care were all of equal importance to the relative | The relative believed that particularly for the management of pain, breathlessness and agitation she could not put 10 because although she saw what care was taking place she did not really know and did not believe that she could put 10 |
The results from the family tool for the ICU LCP-using sites are shown below in Table 21. There were six observations of this kind from three sites. As can be seen, the lowest score on any of the care characteristics was 7, which occurred twice: once for keeping the family informed at site NIA6P2 and the other for the management of agitation at site NIA1P1. Observations NIA6P1, NIA6P3 and NIA2P1 all received scores of 10 where rated. The relative of patient NIA6P1 reported being certain that pain management had not been an issue because she had consulted the patient about pain at the time. This relative also reported that the quality of personal care was important to her. The results for patient NIA6P3 were rated as 10 across all care aspects with no ‘not an issue’ given; the results here for this patient were interesting as both the mother and the sister were present during the interview to answer the family tool. As the mother was the primary and intended respondent, her results are shown in Table 21. The sister mostly agreed with her mother’s scores; however, she would have answered 7.5 for ‘staff keeping the family informed’ because she felt that she had not known what the LCP was or how it worked. The relative of patient NIA2P1 believed that breathlessness and agitation was not an important aspect, although all of the other aspects were scored a 10. The relative of patient NIA1P1 believed that all of the aspects being scored were of equal importance, and scored the care 7, 8, 9 and 10, with personal care the best and agitation the worst. Likewise, the relative of patient NIA2P2 scored 8, 9 and 10 as the results for care, with a 10 score for pain management, agitation, dignity and keeping the family informed as the highest results, and for this patient keeping the patient pain free and comfortable were the most important aspects.
| Site | Patient ID | Pain (question 1) | Breathlessness (question 2) | Agitation (question 3) | Personal care (question 4) | Dignity/respect (question 5) | Spiritual (question 6) | Staff kept family informed (question 7) | Most important | Comments |
|---|---|---|---|---|---|---|---|---|---|---|
| NIA6 | P1 | NI | 10 | 10 | 10 | 10 | 10 | 10 | Maintaining patients dignity up until death and that staff treated patient like a person, not just a patient | Daughter interviewed and said pain was not an issue as she asked patient who was able to say they felt none. Also that the personal care was excellent and was the first time she had seen her mother being washed (i.e. she never saw this in the normal ward) |
| NIA6 | P2 | 8 | 8 | 8 | 9 | 9 | No religious needs | 7 | That patient was kept comfortable and in no obvious pain | Relative put 8 for pain as they did not think patient was in pain but saw morphine and so said maybe 8. Also question 7 was answered in two parts for ward 8/9 (‘I would say 9′) and in ICU (‘I’d say 7–8, or 7′) |
| NIA6 | P3 | 10 | 10 | 10 | 10 | 10 | 10 | 10 | The patient’s mother and sister both answered as the sister was there when the interview was being undertaken: both believed that personal care was the most important factor | Although the mother was the primary interviewee, the patient’s sister would have liked to know more from the staff, particularly in the ICU, about the LCP and what it was about. Both the mother and sister agreed on all of the care points, with the exception of question 7 about staff keeping the relatives informed; the mother thought 10 while the sister thought 7.5 |
| NIA2 | P1 | 10 | NI | NI | 10 | 10 | 10 | 10 | Treating the patient as someone who is going to survive and not just a body that is going to die soon. NB Spirituality was the least important aspect | Information unknown |
| NIA2 | P2 | 10 | 9 | 10 | 9 | 10 | 8 | 10 | Keeping patient comfortable and pain free | Information unknown |
| NIA1 | P1 | NI | 8 | 7 | 10 | 9 | No religious needs | 9 | Relative thinks all of equal importance | Information unknown |
The data from the south LCP-using ICU are shown below in Table 22. More observations were undertaken in the south sites than in the north. Results here are more varied; for example, the lowest score was 0 for spiritual care for SIA3P1, in which the family member would have liked some spiritual care for the patient, but had not been asked about this. The relative scored breathlessness, agitation and dignity as 10; however, for breathlessness the relative contemplated answering 8, as they did not know exactly how to respond because the patient was on a ventilator and it was hard to assess breathlessness. The next overall lowest scores were from the relative of observation SIA1P1, who graded pain as 5 and breathlessness as 6. The relative, however, commented that as they did not know the level of pain (if any) that their relative was in they did not want to score it any higher. The remaining aspects – personal care, dignity/respect, spiritual and staff keeping the family informed – were rated 10. This relative believed that keeping the patient out of pain and clean and comfortable were the most important aspects. Observation SIA1P2 also scored 10 for all aspects except for agitation, which was not an issue; the relative believed that all of the aspects were equally important, but so was patient self-respect. For observation SIA1P3 the relative said it was difficult to tell if the patient was in pain, but that they were satisfied when the nurses told them their relative was not in any pain. Overall, they responded with scores of 9 and 10.
| Site | Patient ID | Pain (question 1) | Breathlessness (question 2) | Agitation (question 3) | Personal care (question 4) | Dignity/respect (question 5) | Spiritual (question 6) | Staff kept family informed (question 7) | Most important | Comments |
|---|---|---|---|---|---|---|---|---|---|---|
| SIA1 | P1 | 5 | 6 | NI | 10 | 10 | 10 | 10 | That suffering was not prolonged | Relative did not know if patient was in any pain; therefore, they answered 5 although they did not think he was in any pain. Oxygen did the patient good in terms of his breathing. Agitation and restlessness were not a problem so relative put NI. Personal care is a 10 because nurses brushed his teeth |
| SIA1 | P2 | 10 | 10 | NI | 10 | 10 | 10 | 10 | All of them. Then they go on to say self-respect and talking to the dying patient and telling them what is going on | NI for restlessness although the family say it was an issue they were not pressed to choose a numbered response. 10 for staff keeping them informed although family members feel that a liaison officer may be best placed to talk with the family leaving the nursing staff to care for the patient |
| SIA1 | P3 | 9 | 9 | 10 | 9 | 10 | 10 | 9 | Pain management, dignity and communication | Relative said it was difficult to know if the patient was in pain, but the nursing staff told them he was not. Breathlessness answered as 9 because patient was intubated |
| SIA1 | P4 | 10 | 10 | 10 | 10 | 10 | Not religious | 10 | Keeping the patient out of pain, clean and comfortable | Relative thought that making sure patient was attended to quickly was important and liked how staff responded quickly when family said patient needed checking |
| SIA3 | P1 | NI | 10 | 10 | 8 | 10 | 0 | 9 | Information and care | Patient was not in any pain so NI. Breathlessness was a 10, but that was because the patient was on a ventilator and the family member also considered answering with an 8. Spiritual is 0 because staff did not ask at all |
Only one observation was undertaken in the north non-LCP-using ICU (Table 23). The results were varied and no scores of 10 were awarded, although the relative commented that they were unsure how best to score pain management as their relative had been heavily sedated. The patient did not have breathlessness issues and they were not religious. The relative scored personal care as 6, pain, agitation and dignity as 9 and keeping them informed as 8.
| Site | Patient ID | Pain (question 1) | Breathlessness (question 2) | Agitation (question 3) | Personal care (question 4) | Dignity/respect (question 5) | Spiritual (question 6) | Staff kept family informed (question 7) | Most important | Comments |
|---|---|---|---|---|---|---|---|---|---|---|
| NIB3 | P1 | 9 | NI | 9 | 6 | 9 | No religious needs | 8 | Pain management and that the family was kept informed | Owing to the patient’s sedated state, relative was unsure how to best score pain management |
Three observations were undertaken in the south non-LCP-using ICU sites (Table 24). The lowest score assigned was from SIB2P1 for agitation, to reflect that fact that the relative felt that patient had been uncomfortable. On the other hand, the relative believed that dignity, respect and staff keeping the family informed were all good enough to be scored 10, while the management of pain and breathlessness scored 9 and personal care scored 8. The relatives of SIB1P1 rated 8 for all of the aspects of care overall, with ‘not important’ for spiritual aspects. However, they explained that if they had been asked to rate only the last 6 hours of the patient’s life, the scores would have been much lower: breathlessness, pain and agitation would have been scored as 3, and personal care, dignity and being kept informed as 1. For site SIB1P2, the relatives scored all of the management aspects as 10, except for spiritual, which they did not feel comfortable answering, and staff keeping the family members informed, which they gave an 8, as they believed there were some inconsistencies in what the family had been told by the staff. Overall, the family believed that pain management was most important to the patient, but communication was most important to the family.
| Site | Patient ID | Pain (question 1) | Breathlessness (question 2) | Agitation (question 3) | Personal care (question 4) | Dignity/respect (question 5) | Spiritual (question 6) | Staff kept family informed (question 7) | Most important | Comments |
|---|---|---|---|---|---|---|---|---|---|---|
| SIB1 | P1 | 8 | 8 | 8 | 8 | 8 | NI | 8 | Communication and care | The results shown are for the whole stay. However, the relative said for the last 6 hours, when the patient became more distressed, the scoring should be separate: question 1 = 3; question 2 = 3; question 3 = 3; question 4 = 1; question 5 = 1; question 6 = NI; and question 7 = 1. The answer of NI for religious and spiritual needs is because the patient did not have any. The relative also felt there should have been more compassion shown towards the patient as she thought he might have heard what was happening around him |
| SIB1 | P2 | 10 | 10 | 10 | 10 | 10 | No answer | 8 | Pain is most important to the patient and communication is the most important to the family members | No spiritual needs to be addressed. A score of 8 for communication as there was some inconsistency in what family were being told by the clinical staff |
| SIB2 | P1 | 9 | 9 | 6 | 8 | 10 | 10 | 10 | All of equal importance. There may be a desire to rank highest the thing in which you felt was managed least well but it is the whole package of care that is important | A score of 6 for agitation to reflect that the patient was uncomfortable. Staff let the priest come to address all of the patient’s spiritual needs so this was very good |
Case studies
The data collected for this study are both exploratory and unique and, as can be seen from the preceding findings, hugely complex. A sample of patient observation cases was analysed in more detail to assess the additional costs of care using the family proxy tool results.
The initial costs and outcomes for the non-LCP-using sites were to be compared with those for their LCP-using counterparts given the site type (nursing home or ICU). However, owing to the nature of the research and the skewed nature of the sample, it was not possible to directly contrast the sites as exact opposites; instead, they were examined as individual case studies.
In order to assess the costing aspects of the analysis we will look at seven case studies in depth, one representing each geographical location, setting and condition (LCP using or not), with the exception of the south non-LCP-using nursing home.
Case study 1: north Liverpool Care Pathway-using nursing home
The cost table for the LCP-using nursing home identifies an overall observation period of just under 9 hours. This time period covers 1 day and the observer’s breaks have been removed. The results from this site highlight the different levels/types of staff that were employed and the structure of the nursing home itself. Here, most of the care was undertaken by the carers; there were also sisters employed in this nursing home who had more contact with the patient than the nurses over the period of the observation. The death occurred in the nursing home and a doctor was called in relatively early, but at the point of death the observer did not see a doctor. The total additional cost of care over the 8 hours 55 minutes was £157.03. However, had the nurses or sister provided as much care for the patient as the carers had, this would have been much higher, owing to the wage rate. If we look at the cost table in relation to the family questionnaire results, the scores were all 10, indicating that the family was happy with the care and attention given to the patient (Table 25).
| Site | Overall observation period | Number of days observed | Observed nurse time | Cost | Observed doctor time | Cost | Observed sister time | Cost | Observed carer time | Cost | Porter time | Cost | Resource use list | Cost | Drug use list | Cost | Total cost |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| NNA2P2 | 08:55 | 1 | 2 minutes | £3.24 | 20 minutes | £54.00 | 32 minutes | £64.96 | 208 minutes | £33.69 | 0 minutes | £0.00 | Mouth swabs (× 2) Conti-pad |
£0.54 | Midazolam | £0.60 | £157.03 |
| Site | Patient ID | Pain (question 1) | Breathlessness (question 2) | Agitation (question 3) | Personal care (question 4) | Dignity/respect (question 5) | Spiritual (question 6) | Staff kept family informed (question 7) | Most important | Comments | |||||||
| NNA2 | P2 | 10 | NI | 10 | 10 | 10 | 10 | 10 | Response of staff to patients religious beliefs | Relative answered NI to breathlessness as patient did not have any breathing symptoms. All other questions talked through – no issues | |||||||
Case study 2: south Liverpool Care Pathway-using nursing home
The observation for the south nursing home LCP-using site took place over 2 days, with much shorter observational periods. In total this amounted to around the same number of hours as the north LCP-using nursing home. The cost of care here was much lower than in the north site, although this could have been due to the two short periods as opposed to one full observational period. During the first day, the observer had just missed the administration of morphine to the patient, which cannot be included as, although we knew about it, it was outside the observational period. Similarly, on day 2 of the observations, midazolam, morphine sulphate and haloperidol had been administered 30 minutes before the observer arrived, and so could not be included in the observations. The staffing of this nursing home differs from that of the north as there are more registered general nurses working with auxiliary nurses/carers. There were also no doctors or sisters seen during this time, although the nursing home manager herself took care of patients.
The total cost of care for this case was £70.42, although as the patient died overnight the cost of post-death care could not be included as it was not observed. The cost of care for day 1 was greater than for day 2, although the observation time for day 2 was longer; this was due to the level of staff time spent with the patient. In this site a school-aged helper was employed to bring drinks to the family and patients.
Assessing the cost of care against the family tool we can see that the results are primarily 8, except for agitation of the patient, which scored 7, although it is known that the patient was prescribed medication to ease this. It is also noted in the costing table that the nurses performed mouth care and so maintained personal care (Table 26).
| Site | Overall observation period | Number of days observed | Observed nurse time | Cost | Observed doctor time | Cost | Observed sister time | Cost | Observed health-care assistant time | Cost | Observed auxiliary nurse time | Cost | Observed nursing home manager time | Cost | Observed school helper time | Cost | Resource use list | Cost | Drug use list | Cost | Total cost |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SNA1P2 | 03.10 | 1 of 2 | 17 minutes | £27.54 | 0 minutes | £0.00 | 0 minutes | £0.00 | 26 minutes | £4.21 | 67 minutes | £10.85 | 7 minutes | £16.59 | 0 minutes | £0.00 | Mouth swabs (× 2) | £0.32 | 0 | £0.00 | £59.51 |
| SNA1P2 | 06:10 | 2 of 2 | 6 minutes | £9.72 | 0 minutes | £0.00 | 0 minutes | £0.00 | 7 minutes | £1.13 | 0 minutes | £0.00 | 0 minutes | £0.00 | 1 minute | £0.06 | 0 | £0.00 | 0 | £0.00 | £10.91 |
| SNA1P2 | 09:20:00 | All 2 days total | 23 minutes | £37.26 | 0 minutes | £0.00 | 0 minutes | £0.00 | 33 minutes | £5.34 | 67 minutes | £10.85 | 7 minutes | £16.59 | 1 minute | £0.06 | Mouth swabs (× 2) | £0.32 | 0 | £0.00 | £70.42 |
| Site | Patient ID | Pain (question 1) | Breathlessness (question 2) | Agitation (question 3) | Personal care (question 4) | Dignity/respect (question 5) | Spiritual (question 6) | Staff kept family informed (question 7) | Most important | Comments | |||||||||||
| SNA1 | P2 | 8 | NI | 7 | 8 | 8 | No answer | 8 | Keeping her comfortable/not too agitated | Relative commented that patient was not breathless until she was trying to do things and she did not try and do much, so it is difficult to answer – NI. Family member does not really know about spiritual needs, but would not like to say no. For dignity they say this was very good and are a little more positive than for some of the other questions but give an 8 also | |||||||||||
Case study 3: north non-Liverpool Care Pathway-using nursing home
The north non-LCP-using nursing home was actually a LCP-using site by the time the observation was commenced. The observation was undertaken over 4 days and the combined observation time was 17 hours and 20 minutes, after the break periods were removed, and the total additional cost was £137.67. The greatest costs were incurred on the second observation day as a result of more nurse time and drugs being administered. Once again, the lower than expected cost for the time period could have been because of the short observations over a few days and the time of visits undertaken. A point to note in this site was that it was observed on day 2 that prednisolone and cyclizine were administered, but that they could not be found on the drugs charts and were not therefore included in the costing. In addition, on the first day the observer was told that the patient had received diamorphine hydrochloride, but we also could not include this in the cost, as it was not observed. Nurses and carers predominantly undertook the care in this site, but no sisters were employed and no doctors were observed to provide care. The nursing home environment meant that there were no porters, but undertakers were observed to attend to the patient following death.
The costs in relation to the family questionnaire table show that the family rated personal care as the highest and we can see that the nurses/carers attended to mouth care and making sure that the patient was clean and dry (Table 27).
| Site | Overall observation period | Number of days observed | Observed nurse time | Cost | Observed doctor time | Cost | Observed sister time | Cost | Observed carer time | Cost | Porter time | Cost | Resource use lista | Cost | Drug use list | Cost | Total cost |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| NNB6P2 | 02.22 | 1 of 4 | 11 minutes 30 seconds | £18.36 | 0 minutes | £0.00 | 0 minutes | £0.00 | 83 minutes 30 seconds | £13.53 | 0 minutes | £0.00 | Gloves (× 3); Conti-Pad | £1.09 | 0 | £0.00 | £33.25 |
| NNB6P2 | 04.25 | 2 of 4 | 22 minutes | £35.64 | 0 minutes | £0.00 | 0 minutes | £0.00 | 85 minutes | £13.77 | 0 minutes | £0.00 | Gloves (× 2) | £0.58 | Furosemide 20 mg tablet, ranitidine 150 mg tablet, salbutamol 100 ml, spironolactone 50 mg tablets, Sudocrem | £3.01 | £53.00 |
| NNB6P2 | 07:30 | 3 of 4 | 7 minutes | £11.34 | 0 minutes | £0.00 | 0 minutes | £0.00 | 9 minutes | £1.46 | 0 minutes | £0.00 | Mouth swabs (× 2) | £0.32 | 0 | £0.00 | £13.12 |
| NNB6P2 | 03:03 | 4 of 4 | 21 minutes 30 seconds | £34.83 | 0 minutes | £0.00 | 0 minutes | £0.00 | 21 minutes 30 seconds | £3.48 | Funeral directors (external cost) | £0.00 | 0 | £0.00 | 0 | £0.00 | £38.31 |
| NNB6P2 | 17:20 | All 4 days total | 62 minutes | £100.44 | 0 minutes | £0.00 | 0 minutes | £0.00 | 199 minutes | £32.33 | 0 minutes | £0.00 | Mouth swabs (× 2); gloves (× 5); Conti-Pad | £1.99 | 0 | £3.01 | £137.67 |
| Site | Patient ID | Pain (question 1) | Breathlessness (question 2) | Agitation (question 3) | Personal care (question 4) | Dignity/respect (question 5) | Spiritual (question 6) | Staff kept family informed (question 7) | Most important | Comments | |||||||
| NNB6 | P2 | 9 | 9 | 9 | 10 | 9 | 8 | 9 | The seven elements of care were all of equal importance to the relative | The relative believed that particularly for the management of pain, breathlessness and agitation she could not put 10 because although she saw what care was taking place she did not really know and did not believe that she could put 10 | |||||||
Case study 4: north Liverpool Care Pathway-using intensive care unit
The north ICU LCP-using site was observed over 1 day. This was a relatively short observation, although, perhaps not surprisingly, the costs were greater than those for the nursing home. The difference between the two settings makes comparisons futile. The principal costs were nursing staff and doctors, rather than the lower-band nurses or carers employed in nursing homes. Two different cost levels were attributed to the ICU nurses depending on whether or not they had direct contact with the patient.
The costs depicted in Table 28 shows that the largest component of the total £221.93 cost came from the time that the nursing staff spent with the patient directly, at £152.28, and also the doctor’s time spent with the patient at £48.60. The time spent with the patient by staff appears to coincide with the family member questionnaire results given by the relative, as all of the answers were 10, except for pain, which was not an issue.
| Site | Overall observation period | Number of days observed | Observed nurse time with contact | Cost | Observed nurse time without contact | Cost | Observed doctor time | Cost | Porter time | Cost | Resource use lista | Cost | Drug use list | Cost | Total cost |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| NIA6P1 | 04.57 | 1 | 94 minutes | £152.28 | 20 minutes | £13.40 | 18 minutes | £48.60 | 14 minutes | £2.27 | Mouth Swab pack (× 2), gloves | £0.61 | Hyocine Hydrobromide, Midazolam | £4.77 | £221.93 |
| Site | Patient ID | Pain (question 1) | Breathlessness (question 2) | Agitation (question 3) | Personal care (question 4) | Dignity/respect (question 5) | Spiritual (question 6) | Staff kept family informed (question 7) | Most important | Comments | |||||
| NIA6 | P1 | NI | 10 | 10 | 10 | 10 | 10 | 10 | Maintaining patients dignity up until death and that staff treated patient like a person, not just a patient | Daughter interviewed and said pain was not an issue as she asked patient who was able to say they felt none. Also that the personal care was excellent and was the first time she had seen her mother being washed (i.e. she never saw this in the normal ward) | |||||
Case study 5: south Liverpool Care Pathway-using intensive care unit
The south LCP-using ICU site observation was undertaken over 1 day (as was the case in the north site); this observation was 4 hours and 20 minutes longer, at a total time (after breaks) of 9 hours and 30 minutes. The total additional cost for this site was £306.64. Similar to the north site, the biggest cost driver came from the nursing time spent with the patient, which accounted for £288.36 of the total cost. In this case there was no observed time spent from the nurses without direct contact, or from a doctor. There were porter costs, which were for two porters taking 10 minutes each. In this case, in addition to the drugs prescribed, the patient was given cream for dry skin, mouth swabs, mouth wash and eye drops, which is reflected in the results for personal care and dignity. The responses for pain management and breathlessness were scored lower, but the relative justified this because they did not know what the patient’s level of pain was and so they gave a score of 5. The family member also responded with scores of 10 for spiritual and being kept informed by staff (Table 29).
| Site | Overall observation period | Number of days observed | Observed nurse time with contact | Cost | Observed nurse time without contact | Cost | Observed doctor time | Cost | Porter time | Cost | Resource use lista | Cost | Drug use list | Cost | Total cost |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SIA1P1 | 09:30 | 1 | 178 minutes | £288.36 | 0 minutes | £0.00 | 0 minutes | £0.00 | 20 minutes | £3.24 | Mouth swab pack (× 2), gloves (× 2), mouthwash, E45 cream | £3.60 | Saline 2-ml ampoule, hypromellose eye drops, hyoscine hydrobromide 400 mg, morphine 1 mg/ml, morphine 1 ml | £11.44 | £306.64 |
| Site | Patient ID | Pain (question 1) | Breathlessness (question 2) | Agitation (question 3) | Personal care (question 4) | Dignity/respect (question 5) | Spiritual (question 6) | Staff kept family informed (question 7) | Most important | Comments | |||||
| SIA1 | P1 | 5 | 6 | NI | 10 | 10 | 10 | 10 | That suffering was not prolonged | Does not know whether he was in any pain therefore answers 5 although they do not think he was in any pain. Oxygen did him good in terms of his breathing. Agitation and restlessness was not a problem so put NI. Personal care is a 10 because nurses brushed his teeth | |||||
Case study 6: north non-Liverpool Care Pathway-using intensive care unit
The non-LCP-using ICU site for the north in Table 30 is the shortest observation of all the case studies (3 hours 15 minutes), but despite this the costs are quite substantial. The majority of these costs were derived from two nurses spending 23 minutes each to clean and care for the patient for post-death care. There was only 6 minutes less nursing time spent with the patient that was not direct. In this short period of observed care, the patient was given morphine for pain control. The results from the family tool show that the family thought pain management was high, but were unsure as how best to answer. The relative did not rate personal care during the patient’s end-of-life stage as high, scoring only 6, although we do not know why this is. The remaining results were varied, and owing to the short observation period we cannot be certain of the results in line with the costing. It is important to note that in the absence of attending relatives the nurse remained present at the patient’s bedside until the patient died.
| Site | Overall observation period | Number of days observed | Observed nurse time with contact | Cost | Observed nurse time without contact | Cost | Observed doctor time | Cost | Porter time | Cost | Resource use lista | Cost | Drug use list | Cost | Total cost |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| NIB3P1 | 03:15 | 1 | 88 minutes | £142.56 | 82 minutes | £54.94 | 6 minutes | £16.20 | 18 minutes | £2.92 | Gloves (× 4) | £0.58 | Morphine sulphate | £5.00 | £222.20 |
| Site | Patient ID | Pain (question 1) | Breathlessness (question 2) | Agitation (question 3) | Personal care (question 4) | Dignity/respect (question 5) | Spiritual (question 6) | Staff kept family informed (question 7) | Most important | Comments | |||||
| NIB3 | P1 | 9 | NI | 9 | 6 | 9 | No religious needs | 8 | Pain management and that the family was kept informed | Owing to the patient’s sedated state, relative was unsure how to best score pain management | |||||
Case study 7: south non-Liverpool Care Pathway-using intensive care unit
The final non-LCP-using ICU case study, in contrast to the north non-LCP-using site, was relatively long. Conducted over 1 day, the observation period is 10 hours and 40 minutes after breaks were removed. This also had the highest costs of £415.87, attributable to the length of the observational period and the involvement of nursing care. The most interesting point to note, however, that is both the doctor and the nurse spent 47 minutes each with family members to explain the patient’s care. Surprisingly, it is questionable if this is reflected in the family’s scoring of being kept informed by staff, as they rated this aspect of care as only 8, the same as the results given to the other aspects of care that were rated. The relatives were not pleased with care in the last few hours during the period close to the patient’s death (Table 31).
| Site | Overall observation period | Number of days observed | Observed nurse time with contact | Cost | Observed nurse time without contact | Cost | Observed doctor time | Cost | Porter time | Cost | Resource use lista | Cost | Drug use list | Cost | Total cost |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SIB1P1 | 10:40 | 1 | 136.5 minutes | £221.13 | 47 minutes | £31.49 | 56 minutes | £151.20 | 10 minutes | £1.62 | Gloves (× 8) | £1.16 | Morphine 2.5 mg, 50 ml saline IV | £9.27 | £415.87 |
| Site | Patient ID | Pain (question 1) | Breathlessness (question 2) | Agitation (question 3) | Personal care (question 4) | Dignity/respect (question 5) | Spiritual (question 6) | Staff kept family informed (question 7) | Most important | Comments | |||||
| SIB1 | P1 | 8 | 8 | 8 | 8 | 8 | NI | 8 | Communication and care | The results shown are for the whole stay. However, the relative said for the last 6 hours, when the patient became more distressed, the scoring should be separate: question 1 = 3; question 2 = 3; question 3 = 3; question 4 = 1; question 5 = 1; question 6 = NI; and question 7 = 1. The answer of NI for religious and spiritual needs is because the patient did not have any. The relative also felt there should have been more compassion shown towards the patient as she thought he might have heard what was happening around him | |||||
Case study comparison
Unfortunately, the impact of the LCP in nursing homes could not be assessed owing to the absence of a comparator. The most costly ICU sites, not surprisingly, were those with the longest observations; the south non-LCP-using produced a cost of care of £415.87, while the south LCP-using site produced a cost of care of £306.64. It is hard to interpret the differences in cost across sites, as there were so many variables which could account for them.
Limitations and assumptions
One of the primary limitations of the economic analysis relates to the observational data. Researchers could attend a site only once an institution alerted them to attend. Taking into account travelling time, important medical decisions relating to the patients had often already been made and hence were missed from the observational data. Similarly, because the researchers needed personal time to rest and eat, the observational period was punctuated by gaps in recording. Only activities that were observed and recorded have been costed.
-
Although the observers were able to capture the times each action was carried out accurately, in some situations they were asked to leave and so did not always capture the exact end time of the observation. Therefore, in these circumstances we worked closely with the observers and, using their notes and similar tasks undertaken, calculated an accurate estimate so as not to lose the observation completely.
-
It was assumed throughout the study that all of the patients, in both settings, were assigned a bed. Therefore, the cost of the bed itself was not included in the cost of care. In addition to this, the type of bed a patient had was assumed to be condition related and therefore part of standard care. The full details of each patient’s bed type was not always documented and so to avoid bias this was not costed.
-
The costs attributed throughout the study are based purely on the ‘seen’ costs as opposed to the ‘unseen’ costs.
-
The outcome measurement tool has not been validated. Mayland et al. 89 conducted a review of tools in palliative care and illustrated a lack of appropriate measures for use in the UK population.
-
The use of family members’ valuations may not represent the perspective of the patient or all of the aspects that make up a ‘good death’. The perceptions of health-care providers and family members of what represents a good death can differ substantially. 83 However, the need to be able to measure the impact of palliative care on the family members of the dying patient is essential in an economic evaluation. 90
-
Witnessing a ‘bad death’ can have long-term implications for staff as well as for the patient’s family members. It was not possible in this study to capture the impact on staff of providing care with or without an end-of-life care pathway.
-
The costs included in the case studies for drugs administered to the patients represented the cost of the drugs themselves and the solution/i.v. required for their administration. Although the nursing time to prepare these drugs was recognised as an additional cost, these costs could not be included as these actions were not directly observed by the researchers.
-
It is widely documented that resource costs, especially staff wages, in the south of the country are higher than those in the north. To reduce bias, the standardised prices were adopted for both, as the aim was to evaluate any true differences rather than differences in location.
-
The costs that have been included in the study have not been adjusted for time of day (e.g. any increased staffing costs for night working).
-
Where possible, the costs and resource use were included for the total observation period, to accommodate care given immediately after the death of the patient.
Discussion
The aim of this economic analysis was to quantify the impact of the LCP on care at the end of life and in particular to attribute costs to care provided using the LCP versus standard care. This was not possible because of the methodological challenges discussed earlier in this report, including sampling and site matching issues, particularly in the nursing home setting.
However, notwithstanding the limitations of the data, an approach to costing has been developed. As Smith points out,91 we know precise details on cause and place of death in the population but seldom take note of the experience of death itself. In designing this economic analysis we aimed to capture some of the important aspects to do with the experience of death itself. In the absence of an established and validated outcome tool, a tool was developed and used separately and in conjunction with other data. The economic questionnaire tool was developed to provide a link between the level of care given to patients and how this was received. As patients so close to death could not respond, family members provided proxy data about the possible experience of the care that was provided.
Evaluation of the effectiveness of service provision requires the clinical and economic objectives within the service to be clearly established. If we have not clearly defined such objectives, how can we delineate the extent to which they have been achieved? Measures of ‘success’ are therefore an essential first step in structuring any comparative evaluation. In this evaluation ‘success’ was evaluated in two dimensions:
-
enhancing the quality of life experienced by patients in the last hours of life, and that of their families
-
optimising the efficiency of resource utilisation.
This economic evaluation was designed to ‘piggyback’ onto a detailed qualitative study of care at the end of life. The interviews provided the basis for collecting the data using the economic tool. Its location in the context of a face-to-face interview provided the research team with unique access to the way in which bereaved relatives interpreted and responded to each item in the tool. In addition, the tool in conjunction with the observational and resource data provided a strategy for calculating comparative costs and benefits experienced by patients supported in LCP-using and non-LCP-using units in the last hours of life.
It is important to recognise that the comparisons presented here between LCP-using and non-LCP-using units do not meet the rigorous standards of a randomised controlled trial. Despite attempts to ‘match’ service providers, it was inevitable that the comparison contained a wide range of confounding factors, and hence the results obtained should be interpreted as being indicative rather than definitive. Many non-LCP-using units were found to utilise many aspects of the LCP process, and the LCP-using ICUs varied in their application of the LCP process. Although the ambitious aims of this economic analysis were not achieved, a possible approach to collecting and analysing data for economic analysis at the end of life has been achieved. This now needs to be tested in future studies.
Chapter 14 Discussion and concluding remarks
Overview
This study was designed to examine the impact of the LCP on care at the end of life in ICUs and in nursing homes. Strict inclusion criteria were applied to the selection of nursing homes and ICUs in order that sites could be matched on whether or not they used the LCP. Although the recruitment of matched sites was achieved, the variable participation of sites in this study resulted in the sample becoming skewed. For recruitment reasons, it was not therefore possible to meet the stated aims of the study. Twenty-three sites were recruited to the study, 12 ICUs and 11 nursing homes, and observations were conducted in 12 of these sites (seven of which were LCP sites). Although not able to address the original research question, this study provides a unique insight into care at the end of life in two different settings.
A total of 138 interviews with a range of staff were conducted in the sites to gain an understanding of how care of the dying was organised and managed, including symptom control, ethical issues, and spiritual and psychosocial care. Seventy-two of these interviews took place with ICU staff and 66 took place with nursing home staff. In addition, 10 recent deaths per site (totalling 230) were examined using the patients’ case notes. Relevant policies and documentation pertaining to end-of-life care were also collected. In each site, mechanisms were established to conduct observations of patients receiving care at the end of life. A total of 25 observations were undertaken: 17 in ICUs and eight in nursing homes. For each observation undertaken an interview was carried out (n = 25) with a member of staff who had provided care to the patient in last hours of life. This interview was conducted either at the end of the shift or on the following shift. The case notes recorded during the dying phase were also accessed and analysed. An in-depth interview was also carried out with a relative, who had usually been present in the days and hours prior to the patient’s death (n = 23). This interview was carried out after the patient’s death at a time interval chosen by the relative, most often between 2 and 4 months after the patient’s death.
In this discussion, we explore what the findings tell us about care of people who are dying in these two different settings. The impact of the LCP on care can only be examined in a limited way in relation to the care observed in the ICU. We focus first on the nursing homes and then on the ICUs. We then look at the similarities which emerged across these apparently very different clinical settings before focusing on the economic evaluation in both settings. Finally, we critically review the methods that were used and examine the impact of national events on the study. These limitations of the study are discussed prior to the concluding remarks.
End-of-life care in the nursing homes
The original research design had attempted to match LCP-using and non-LCP-using nursing homes on the basis of a range of criteria in order to assess the impact of the LCP on care. Although, in the main, we were successful in recruiting the sites we had selected on the basis of the predetermined characteristics, as the study progressed it became clear that the distinction between LCP-using and non-LCP-using sites in this setting was blurred. Homes that were reported not to be using the LCP at the time of recruitment were, by the time of data collection, using some or all of its elements. Moreover, as the research progressed only a sample of homes identified deaths for us to observe. Thus, the sample became even more skewed.
The recent drive to reduce the number of hospital deaths6 has reinforced the need to focus attention on improving end-of-life care delivery in the care home setting92 which is currently the second most likely place for people over the age of 65 years to die in the UK. 3 The majority of homes in this study were involved in end-of-life care initiatives (other than the LCP) including the GSF, regional ACP initiatives and the North West End of Life Care Six Steps to Success programme for care homes. 43 Therefore, the environment in which the observations took place was, on paper at least, equipped to undertake end-of-life care using established frameworks either singularly or together.
The patients whose deaths were observed in the nursing homes in this study were extremely elderly. All patients but one were in their eighties or nineties, and there was an expectation by staff and relatives that, in the context of these patients’ declining health, death was a certainty.
Recognising dying and commencing the Liverpool Care Pathway in support of care
The ability to recognise the imminence of death was reported to be improved in this setting where staff had experienced caring for the patient for some time, particularly where the patient had been resident in the home for at least 1 year. However, in two cases, patients had been admitted specifically for end-of-life care and so were defined as dying, although not necessarily imminently, from the point of admission.
In line with the LCP ethos and educational materials to support its use,93 there was evidence that staff in the nursing homes recognised the need to ensure that all reversible causes for any deterioration had been considered and acted on prior to the commencement of the LCP to support care. They also highlighted a number of signs and symptoms that supported their recognition of imminent dying, including level of consciousness and changes in the nature of the breathing and the colour of the skin. These have resonance with recent findings from a study to explore how specialist palliative care staff recognise dying. 94
Implementation of the LCP (version 12) requires a MDT assessment (a minimum of a doctor and a nurse) which, in nursing homes, necessitates the involvement of a GP. Nurses reported difficulties achieving a timely visit from the GP and challenges with out-of-hours GPs who, lacking familiarity with the patient, were reluctant to be involved in the diagnosis of dying. Seymour et al. 95 have also reported variable and inconsistent GP support and poor out-of-hours cover as barriers to end-of-life care in the nursing home setting. As a result, nurses either circumvented the imperative of the MDT assessment by completing the initial assessment themselves and getting the GP to call within 24 hours to confirm the situation; or called GPs out in advance of the need to start the LCP, particularly where the patient’s decline had escalated close to the weekend.
Nurses in this study reported that the main purpose of getting a timely GP visit was to ensure the prescription of prn drugs in anticipation of the five key symptoms that can occur in the last hours or days of life. 93 Nurses stressed the importance of having these in readiness, as they were seen as an important component of a pain-free and peaceful death. Indeed, staff derived considerable satisfaction from having the drugs available in case of the possibility that they be required. In some homes, these drugs designed for use in the last hours or days of life were requested weeks ahead of the patient’s expected death (at GSF Code C/Yellow) and were kept aside for use should they be required when patients were deemed to be in the last hours or days of life (GSF Code D/Red).
Despite this, nurses also reported and were observed to make only minimal use of these drugs at the end of a patient’s life. In the few cases in which the drugs were used, additional expertise was sought, for example from the local hospice, to ensure appropriate use and dosage. In a recent study, Wilson et al. 96 reported similar caution in the use of anticipatory prescriptions in this setting. These authors found that nurses providing end-of-life care for nursing home patients were concerned about avoiding the under- or overuse of medication and the potential for hastening death in their use of anticipatory prescriptions.
Care at the end of life
Research undertaken in UK care homes in the past decade has reported that the quality of care delivery can be inadequate and that dying residents have unmet needs. 97–99 In particular, the management of pain has been reported to be suboptimal. 99–101 The lack of provision of basic care at the end of life has featured in many of the more negative stories that have been presented in the media and were reflected in submissions to the independent review of the LCP. 40
The observations undertaken in the nursing homes revealed consistent monitoring and observation of dying patients with a focus on the provision of physical care. The nursing staff visited patients regularly and sometimes very frequently in the last hours and days of life. In general visits ranged from hourly to 2-hourly to 4-hourly at night. While relatives generally welcomed these frequent visits, the content of the visits was sometimes surprising. In line with the findings of Goddard et al. ,17 pressure area care and the provision of food and fluids were elements of care to which nurses paid particular attention. Interestingly, these were also the main areas of concern raised by relatives in the post-bereavement interviews. The NHS has a zero tolerance policy of pressure sores102 because of their association with poor care. In April 2014, the National Institute for Health and Care Excellence (NICE) issued its latest guidance on the treatment of pressure ulcers,103 and, although it cites the Quality Standard for end of life care among the evidence taken into account, no guidance specifically relating to patients in the last hours or days of life is included. It is possible that the prevention of pressure sores is so firmly embedded in nursing home care that staff find it hard not to turn patients, even at the very end of their life, for fear of being accused of poor care. Staff were also keen to point out to the relatives and the researcher as well as in the notes those pressure areas receiving treatment that had been acquired elsewhere.
Although the LCP framework promotes regular (4-hourly) assessments of the patient’s comfort and suggests that positioning is an area that requires ongoing assessment and monitoring in the last hours or days of life, it does not, for example, stipulate 2-hourly or 4-hourly ‘turns’. 34 Yet staff were extremely reluctant to abandon the repositioning of the patient until very close to the patient’s death.
Nursing home staff were also observed to provide food and fluids to patients up to the point of death. In one case, this continued despite the patient’s lack of a swallow reflex and despite the NIC reporting frequent attempts to stop her care staff from doing so. This case was interesting because on numerous occasions the patient’s daughter, who was a qualified nurse and was present at the bedside, turned away carers bearing food for the patient. This nursing home appeared to have a number of training initiatives in place and operated the GSF and the LCP, and yet the NIC attributed the problem to her staff feeling that the patient was being neglected and possibly starved to death.
Another area of care that caused variation in practice was dealing with the patient’s level of consciousness. There was no evidence in the notes or in the observations of staff undertaking formal assessments of a patient’s mental capacity. However, there appeared to be a presumption of a lack of capacity largely on the basis of the patient appearing unresponsive or sleeping a lot. References to the patient’s state of consciousness as ‘unconscious’ or ‘semi-conscious’ appeared to be devoid of clinical content and based more on a lay understanding of what it was to be conscious. This had implications for the way in which care was subsequently focused and delivered. The presumption of a lack of consciousness or mental capacity effectively rendered the patient subjectively absent (devoid of agency) while remaining the core ‘object’ of care.
The provision of care to patients defined by staff as comatose was observed to be undertaken with care and compassion. Care staff frequently talked to the patient about what they were doing, even in the absence of any ability of the patient to respond, and this is recognised to be an important element of good care at the end of life. 13 However, in these interactions staff were sometimes observed to ignore a patient’s attempt to exert agency, for example in one case where the patient was resistant to attempts to provide mouth care. Instances were also observed in which staff engaged in discussions with relatives regarding the likely timing of the patient’s death at the bedside of the patient, even though it was generally accepted and often remarked that ‘hearing was the last thing to go’. Schou et al. 104 illustrate a similar anonymisation and objectification of patients present in the accounts of general nurses working in hospitals and care homes. In this respect, paradoxically, patients who were deemed unable to respond were treated both as a sentient human being, included in conversation and kept informed, and as an insentient person, exposed to frank discussions about their welfare to which they could not respond. In his classic 1967 sociological study,105 Sudnow identifies in the context of decisions about resuscitation the social death of the patient; a situation in which ‘a patient is treated essentially as a corpse, although perhaps still “clinically” and “biologically” alive’ (p. 74). The patients in Sudnow’s study were labelled according to their social worth, which determined the extent to which resuscitative attempts were made. In this study, the behaviour of staff towards the patient fluctuated, so that the patient was treated in some circumstances as ‘socially dead’ and in others as a sentient human being. The need for seeing a patient through a single lens of a label might be paramount where the label adopted is a summation of key characteristics which staff use almost as a rule of thumb to determine the outcome. In Sudnow’s study, social death became a predictor for biological death. The inconsistent behaviour observed in our study may reflect a more general uncertainty about communicating with patients who do not appear to be conscious.
In this busy environment where staffing levels were often compromised, there was little evidence in the observations of care of staff ‘making time’ to be with dying patients over and above the delivery of physical care described above. Staff were also observed to spend little time at the bedside providing emotional support to attending relatives, although they did ensure that relatives were offered more practical assistance such as food and drink. Involving relatives in the care of patients has also been posited as important in helping to achieve a ‘good death’ in this environment. 13 In this study relatives were frequent visitors to the nursing home and to the patient’s bedside, but they were almost always asked to leave the room while care was given and, when they returned, were rarely informed of the detail of the care the nurses or carers had actually delivered. In only one instance was a relative (who was a qualified nurse) involved in the delivery of personal care to the patient. Most relatives were, however, invited to provide oral care or sips of fluid whenever they felt it appropriate.
The need for ongoing education and training in care in the last hours or days of life has been advocated for staff in the nursing and care home setting. 106 Although training was reported to have taken place in the nursing homes in our study, largely in conjunction with the various frameworks that were being used, the nature and extent of that training was variable. Some homes reported that only qualified staff received training, while others reported that training had been provided for everyone from the cleaning and laundry staff all the way through to the senior nurse managers and even owners. Cavendish106 concluded that training available for health-care assistants and support workers was of variable quality and not sufficiently consistent. Furthermore, although a plethora of courses and different providers existed, it was difficult for organisations to make meaningful choices. The review called for a ‘Certificate of Fundamental Care’ which was launched as the ‘Care Certificate’ in April 2015.
We return to the issue of training later, but this study raises questions about the efficacy of training and the way in which organisations can be enabled to develop a coherent approach to something as complex as the care of people who are dying.
Advance wishes
The concept of ACP was widely supported by nursing homes represented within this sample and all reported having a formal process for engaging in it. Based firmly in the discourse of patient choice at the end of life, these discussions were designed to focus on the views of patients (and often of relatives as proxies) on resuscitation, hospitalisation and preferred place of care and death. In this study it was clear that advance wishes also included religious, spiritual and personal preferences. Staff reported establishing these patient preferences as soon as possible, on occasions very soon after admission. Staff also reported the concerns that such early discussions raised among the patients and their relatives whose views were being sought. However, the pursuit of recording preferences in advance took precedence over the potential for distress among some individuals. Seymour et al. 107 highlighted similar concerns arising from the emphasis placed on the ACP process by ‘top down’ national policy initiatives. They warn against a culture of managerialism whereby the ‘bureaucratisation’ of ACP could lead to a ‘potentially blunt, harmful, one size fits all approach’. They called for such guidance and protocols to be used in support of rather than in place of professional judgement, where conversations emerged from within an established relationship and in light of the risks and benefits for each individual patient. There was also some evidence in our study that some nurses felt more comfortable undertaking these conversations after a relationship had been built between families and staff.
In all observed cases, the nursing home staff in this study had recorded the advance wishes of the patient regarding their religious and spiritual needs, as well as their personal preferences for things such as music at the end of their life. From our observations, and review of the case notes, the patient’s religious needs were always met in line with the recorded wishes. However, the management of the environment received slightly less careful attention. For example, there is a difference between identifying a favourite singer and having that singer played continuously in the background, a distinction that was often not applied in those nursing homes where a patient had provided a musical preference. The use of background radio and TV were routinely observed in the rooms of people who were dying and little additional thought seems to have been applied to its judicious use in the patient’s last days and hours of life.
End-of-life care in intensive care units
In order to understand the complexity of care at the end of life in the ICU it is important to draw on all the data relating to the observations of care. This is a complex world, in which people are admitted on the basis of some chance of recovery, care is provided on a one-to-one basis and the environment is textured by the latest lifesaving technology and machinery. The patient can be stripped of their personhood, through either the use of sedatives or the severity of their condition, and their body is transformed by the lines and tubes that attach it to the ICU life-support equipment. Relatives entering this world are often highly stressed and anxious108–110 and their thoughts and understandings can be disordered. 111 Even where the admission has resulted from a long-standing deterioration in health, and death is recognised as a possibility, many relatives retain hopes of recovery.
In this study, the patients whose deaths were observed were being cared for by staff in five LCP-using sites and three non-LCP-using sites and, where possible, the following discussion will take account of similarities and differences in the care delivered.
Researchers27,28 have described a ‘good death’ in ICU as one where a consensual decision (between staff and between staff and patients and relatives) has been achieved regarding the futility of ongoing treatment; where death is expected and prepared for; where death is neither prolonged nor rushed; where symptoms are managed effectively; where death is natural (free from technology) and conforms to the wishes of the relatives and any previously expressed wishes of patients; and where death is in the presence of family and is characterised by clear and non-conflicting communication. In the main the deaths observed in this study met the criteria outlined above for a ‘good death’, regardless of whether or not the dying was supported by the LCP. Indeed, in line with a study conducted by Fridh et al. ,112 the relatives of 15 patients who had interventions removed and died on the ICU in our study reported that the patient had been treated as a person with their dignity and care maintained right up to and including their death. In two cases in which the patient was transferred out of the ICU once interventions had been withdrawn, the relatives were extremely unhappy about the care that was subsequently provided.
Recognition of dying and withdrawal of treatment
Regardless of whether or not the LCP was used, decisions were made in ICU regarding the extent to which current interventions remained of benefit to the patient. Decisions about withdrawal only followed analysis of the patient’s response to the treatment that had already been provided and usually after a period of intervention, assessment, monitoring and review. General Medical Council Guidance,113 while stressing the importance of multidisciplinary decision-making, and the need to discuss such decisions with patients (where possible) and those close to them, clearly identifies the responsibility for making withdrawal decisions as medical. In all the sites participating in this study, the decision to withdraw active treatment was a medical decision that took account of the views of other relevant clinical experts, usually the nurse but occasionally chest, lung and neurological experts, and relatives.
Relatives were always informed about the decision to withdraw and all of the data sources clearly portrayed this decision as a medical one. The discourse analysis of the ICU notes highlighted the separation of the act of medical decision-making from the gathering of support for the medical decision. In line with the findings of Coombs et al. ,26 communication by staff of this decision was placed in the context of an overall narrative of the patient’s deterioration and irreversible decline. Such an approach has been shown to be instrumental in helping relatives to understand and to be prepared for the inevitability of death. 112 This narrative was carefully crafted in the notes in order to reinforce the decision to withdraw treatment and to illustrate the support of relatives for the change of focus from cure to care.
Thus, although not explicitly seeking the relatives’ consent, the staff, both medical and nursing, aimed to ensure that the relatives were in agreement with the proposed course of action. However, the complexity of such conversations undertaken with highly stressed and vulnerable individuals should not be underestimated. There was evidence that the way in which relatives experienced and constructed their world differed markedly from the way in which health-care professionals constructed that same world. Staff in this study recognised the importance of clear and effective communication. However, while consultants reported that they talked about withdrawal in plain terms without the use of jargon, nurses reported relatives requiring clarification of what the consultant had told them. Against this backdrop, there were also relatives who reported in the bereaved relative interviews that the withdrawal of treatment had been their decision and in one unusual case a relative reported ‘switching off the machine’ themselves, which they clearly did not do. In relation to this last point it is possible to attribute the relatives’ perceptions to poor communication, as indeed Halcomb et al. 114 illustrate in their study of the lived experiences of nurses in ICU. In this study, nurses also reported that relatives felt that they had made the decision to withdraw treatment and put this down to poor handling of discussions with relatives by medics. Although this may be true, it is also possible that these accounts reflect the way in which strong agreement with a decision to withdraw treatment becomes internalised and transformed into ownership of the decision, a process which may be beyond the reaches of even an effective communicator in a clinical setting.
To talk about effective communication in this context does not really do justice to the way in which the worlds of professionals and families collide in these extremely stressful circumstances. High-level communication skills are vital in undertaking such complex conversations, particularly those that seek to involve and include the thoughts and feelings of families, while not appearing to devolve responsibility for the decision to withdraw treatment.
There is an extensive literature on the importance of communication in medical encounters per se and in particular in ICU settings (e.g. see Lautrette et al. ;115 Scheunemann et al. 116 and Siegal117). In his review of the literature, Siegal highlights the enormous scope for communication difficulties in the ICU setting. Using the literature he compiles a list of practices reported to prevent conflict and foster consensus decision-making. While each of the practices seems eminently sensible they are underpinned by a complex set of interpersonal dynamics which are not discussed. It is, perhaps, not surprising that a North American study reported high levels of conflict (63% of cases in ICU) between physicians and family members of critically ill patients in ICU. The study conducted by Schuster et al. 118 involved 100 physicians and 232 surrogate decision-makers (for 175 critically ill patients). Schuster et al. 118 also reported poor concordance between physician and family reports of conflict. They concluded ‘in fact, agreement between physicians and family on whether there was conflict approached the accuracy of flipping a coin’.
Contrary to this North American finding, conflict between a patient’s relatives and clinical staff did not feature prominently in this study. There are many possible explanations for this, including widely varying thresholds at which something may be deemed to be conflict, cultural differences and the status of the patients when the surrogate decision-makers were recruited to the study.
In all sites, once the decision to withdraw had been taken and communicated to the relatives present at the bedside, time was allowed for the decision to be communicated more widely to family members who might wish to be present and ‘say their goodbyes’ to the patient. Relatives attached great importance to this, reinforcing its presence in the notion of a ‘good death’. 28
Relatives’ accounts of withdrawal of treatment
In their accounts of withdrawal of treatment, relatives confirmed that, although they could not often remember the precise details, the message that the patient was not going to survive had been clearly received. Once withdrawal became a reality for relatives, their focus shifted from hope for recovery to the alleviation of suffering and the delivery of a quick, pain-free and peaceful death. However, the interviews revealed instances in which relatives quite strongly disagreed among themselves over whether or not hope for recovery should be abandoned. In this study there was also an instance in which the difference of opinion between relatives angrily spilled out into discussion and disagreement with the consultant.
In common with the findings of Fridh et al. ,112 for some relatives, the medical tubes and lines emanating from the patient were not perceived as problematic while they were active. However, once a decision to withdraw had been taken, some relatives were keen for these to be removed, although they were reluctant to observe their actual removal. There was an emphasis in the accounts of staff and relatives on achieving a natural death, and it is likely that the visual disruption to the patient’s personhood created by the lines and tubes ran counter to this.
Use of the Liverpool Care Pathway in intensive care units
Although the LCP was generally viewed positively, staff held mixed views on the use of the LCP on the ICU. The common assertion was that it was too long and not very useful in cases where the patient died quickly. Doctors’ signatures were hard to obtain and there was reluctance on the part of nursing staff to record all of their observations on the LCP documentation, with the result that information was duplicated across a number of clinical records. It was unclear whether the LCP supported practice (i.e. shaped what was done) or was used mainly to account for what had been done, or a mixture of both. As previously stated, it was regarded mainly as a nursing tool and doctors were less likely to see it as of direct value to their practice. Research has illustrated that once the decision to withdraw treatment has been communicated to the patients and relatives in this setting, the bulk of the technical work of withdrawal and the provision of physical and emotional care for patients and families primarily rests with the nursing staff. 114 The LCP as a framework for the provision of care in the ICU was rarely discussed with or understood by relatives. This was not necessarily surprising as the LCP was just one of many protocols for care that are used in the clinical environment. However, the apparent lack of awareness of the use of the LCP by relatives has been recently portrayed in the media as a failure to communicate the patient’s imminent death to relatives. This was not the case in this study, where all relatives reported being clear about the patient’s deterioration and the ‘futility’ of treatment.
Despite education and training being a cornerstone in the implementation of the LCP, few nurses reported receiving any formal training on its use. It was suggested that the clarity and structure of the framework were self-explanatory.
Differences between Liverpool Care Pathway-using and non-Liverpool Care Pathway-using intensive care units
In all sites withdrawal did not involve simply switching off one machine; sometimes it involved a change in treatment provision from ‘active’ to ‘non-escalation’ or ‘limitation’ as well as reducing particular items of life support. Despite this, when discussing the death afterwards, the relatives often collapsed the withdrawal process into a single event, at a single point in time, even though the reality had been quite different.
Only three very subtle differences were found between LCP-using and non-LCP-using ICU sites. These centred on the period during which interventions were actually withdrawn. The first was a consistent finding in LCP-using ICU sites. Nurses reported and were observed to direct a patient’s care once a decision had been taken to withdraw treatment. As the LCP was viewed by doctors and nurses alike in this study as a nursing tool and was deemed to provide a checklist for most of a patient’s needs in the last hours or days of life, this might not be surprising. Nurses reported involving doctors when they were unsure or wanted their views on the patient’s clinical condition. In non-LCP-using sites the role of the nurse exhibited greater variation, with different consultants directing end-of-life care in different ways. Previous studies support this study’s finding that the LCP is largely regarded as a nursing tool,119 and a number of small-scale qualitative studies in a range of settings, including ICU119–121 also suggest that nurses perceive themselves to be empowered by use of the LCP to support the delivery of care at the very end of life.
The second subtle difference related to the consistency with which nurses in the LCP-using sites aimed to achieve a ‘natural death’ through the phased withdrawal of treatments. Nurses reported and were observed to try to foster the circumstances in which the patient’s ‘last breaths’ were their own. This involved reducing the patient’s reliance on equipment, which was done gradually: neither too quickly nor too slowly. Regular and consistent assessment and monitoring were both observed and reported by nurses to be an important component of this approach to withdrawal. Although some elements of this gradual withdrawal were evident in the observations of non-LCP patient deaths, there were also instances in which ‘everything was just stopped’. The nurses reported different consultant approaches to withdrawal, with some consultants being prescriptive about the order and speed with which interventions were withdrawn.
Finally, the nurses in the LCP-using ICUs reported trying to achieve a balance between being present at and being absent from the bedside in order to give relatives time to be with their loved ones during this period of withdrawal. By contrast, the nurses in the non-LCP-using sites reported a more hands-off approach. This may be an important distinction, as Rusinova et al. 110 found that ‘extended contact between staff and family members was the only related factor associated with anxiety reduction’. Interestingly, in one non-LCP-using site, where the patient was transferred to a side room to allow privacy for the family, a source of conflict arose when the family reported feeling ‘abandoned’ by staff. However, it is important to remember that it is the quality of staff interactions with patients and families rather than the quantity that is likely to influence the perception of support. 111
Care of people dying in the generalist settings of nursing homes and intensive care units
On the surface, it is hard to imagine two more diverse health-care settings in which death could routinely be expected to occur. At one end of the spectrum, the nursing homes recruited to this study attempted to provide a ‘home from home’ for their residents, and those who died in these settings were among the ‘oldest old’. Here, death was an expected outcome following a lengthy period of increasing frailty and decline. Much of the ‘hands-on’ care in this setting was delivered by non-qualified staff. Staffing levels were often challenging and medical input was basic and relatively infrequent. At the other end was intensive care, where the focus was on cure and rehabilitation, and the latest life-saving equipment and interventions were available and utilised. These sites were characterised by high levels of medical and nursing expertise and input and the patients dying in this setting were likely to be considerably younger than those dying in nursing homes. While some deaths occurred after a long-standing disease, others were the result of trauma or injury.
There were a small number of issues common to both settings. Some of these issues were often solved in slightly different ways.
Care at the very end of life
In all settings there was a sense that the care of people very close to death was a nursing responsibility. In the LCP-using sites, regardless of setting, the involvement of doctors was minimal. In non-LCP-using ICU sites the role of the consultant varied according to how the withdrawal of interventions was planned. Nevertheless, providing care was the nurses’ responsibility.
While in ICUs consultants were always on hand if required, difficulties were reported in nursing homes in accessing GPs. In particular, use of the LCP required medical input to the assessment of dying. However, difficulties were reported getting GPs to visit the patient and undertake a joint assessment to recognise the imminence of dying, and subsequently to review care once the assessment had been made.
Withdrawal and withholding interventions
The concepts of withdrawal and withholding interventions at the end of life have received considerable negative media attention recently. The sustained attack on these concepts draws its power from the looseness with which the terms are often used. In ICUs in this study, the withdrawal of technological support resulted from a consultant decision but often with input from nurses and other experts involved in care, including the relatives. It was a decision that was supported and referenced by a host of physiological, neurological and biochemical investigations and results. What was withdrawn and when was entirely dependent on the technological support a patient was receiving and the nature of the patient’s condition. Withdrawal of active therapies included limiting or stopping inotropes, filters, antibiotics, i.v. fluids, NG or other feeds and/or ventilation. If the patient was ventilated, their ventilatory support might be reduced, changed or stopped altogether, with or without subsequent extubation. The slow withdrawal of technological support, which was a feature of care in LCP ICUs, has been discussed in other studies. 45,122 Harvey suggests that this slow withdrawal of technological support mimics the more gradual decline of a natural death. 123 In so doing it allows for the relative’s emotional adaptation but also for a less dramatic disjuncture between life and death, providing the impression of a peaceful death.
In the nursing home setting the concept of withdrawal was not much discussed. The patients in the nursing home were frail and elderly. Their lives had not been supported by technological intervention and so the act of withdrawal seemed irrelevant. However, care at the end of life in nursing homes was often associated in the media124 with the withholding of food and fluids. Whether in response to this negative publicity, the presence of the relatives and/or the researcher, or the beliefs of the care staff, the staff in nursing homes in this study continued to provide food and fluids to patients up to the point of death. However, the issue of withholding was not entirely absent from the nursing home setting. Consideration of resuscitation and hospitalisation at the end of life by staff, patients and their relatives was an important feature of ACP in this setting.
Thus, while in ICUs there was a sense of creating the circumstances in which a natural death could occur, either slowly or quickly, in the nursing homes there was a sense of allowing nature to take its course.
Relatives’ involvement in the provision of personal care
Relatives featured very strongly in the care of patients in both settings. However the extent to which they were engaged in the care being provided varied. In the nursing homes, apart from one unusual case in which the relative was a nurse, relatives were usually asked to leave when personal care was being delivered to the patient, and were rarely involved in anything other than giving the patient sips of fluid or mouth care. In stark contrast, in the ICU relatives were usually given a choice about remaining or leaving when personal care was given, and though some chose to leave while various tubes and machinery were removed, some were actually observed to participate in the delivery of other aspects of personal care.
The accounts of relatives
Relatives and their views are rightly considered to be very important in understanding the care provided to family members. The role of the relative in the patient’s care at the end of life was touched on by staff and by relatives themselves. In the main, the relatives sat by the bedside, talking to and touching the patient. When the interviews with bereaved relatives were compared with the observational, nurse (point 2) interview and case note data, there were some very interesting similarities and differences. There were occasions on which relatives and staff used exactly the same words to describe events and conversations. There were also occasions on which a relative’s account departed substantially from what had been observed, from the accounts provided by staff and from the case notes.
While these differences will be explored in more detail in subsequent papers, it is important to recognise that similar findings have been reported extensively elsewhere. 41 Addington-Hall and McPherson, in an excellent article on issues of validity regarding after-death interviews with bereaved surrogates/family members, highlight the difficulties of research in this area. 54 Approaching relatives too soon after the death of a family member is considered to be both unethical and insensitive. However, although it may be easier to recall information retrospectively if the intervening period is short, the type of information that is retained and reported versus that which is forgotten or omitted may be more than a matter of just recall. In this study, we allowed relatives to identify when they would be willing to be interviewed. Contrary to views often expressed in the literature,125 relatives volunteered to be interviewed sooner after the patient’s death than has previously been considered ethical.
Training
Training is often promoted as a panacea for many of the poor practices that emerge in the workplace, as well as for implementing new initiatives and improving performance. There is extensive management literature assessing the impact of training on performance. Most organisations invest in training because they believe that higher performance will result. 126
The staff in the ICU reported receiving little training on end-of-life care and there were reports that using the LCP document to support care represented a form of self-directed learning. In the nursing homes, there was a strong emphasis on training, and many nurses were reported to have attended end-of-life training courses, but there was no sense of an organisational strategy, or a need for one, with regard to training its workforce. There was no reference to the ‘10 Step Programme’,93 for example, in the interviews in nursing homes using the LCP. This programme accompanies the LCP framework to underpin its systematic implementation and involves changing practice at the strategic, organisational and individual levels to ensure a workforce approach to the education and training of staff.
Interestingly, end-of-life care is rarely represented within the mandatory training provision in either the ICU127 or the nursing home setting,106 further reinforcing this lack of strategic focus.
The two settings used in this research could not have been more different. The ICUs were staffed by highly qualified individuals working in a MDT, in open ‘public’ spaces, with high staff-to-patient ratios and a low turnover of staff. Nursing homes were mainly staffed by health-care assistants, with fewer registered nurses, working in environments that were rarely purpose built and containing a number of confined semiprivate spaces with limited access to doctors. The nursing homes in this study were also characterised by staff whose first language was not English.
Achieving a skilled competent workforce in these two settings with respect to end-of-life care could be expected to require different approaches and different leadership skills. It could be hypothesised that any framework implemented in an organisation with the characteristics of the ICU might achieve a greater standardisation of practice than in an organisation with the characteristics of the nursing home.
Economic evaluation
The economic evaluation was based on the observations of care, analysis of the drug charts and completion of the economic tool by bereaved relatives at the end of the interview conducted by the researchers. This tool, in conjunction with the observational and resource data, provided a strategy for calculating comparative costs and benefits experienced by patients supported in LCP-using and non-LCP-using units in the last hours of life.
The results obtained should be interpreted as being indicative rather than definitive as despite attempts to ‘match’ service providers the comparison inevitably contained a wide range of confounding factors. Many ‘non-LCP-using’ units were found to utilise aspects of the LCP process, and ICUs using the LCP to support care varied in their application of it.
In both settings, relatives were able to discriminate between the different aspects of care provided; so, for instance, different scores were allocated to pain and agitation by a relative. Relatives found completing the tool to be a useful exercise and welcomed the opportunity to justify outlying scores, whether they were high or low. The seven case study analyses demonstrated that it was possible to attribute costs to end-of-life care, but in the context of this study the costings could not be used to compare the costs of care provided using the LCP versus standard care.
The methods
This study was designed to use a number of data sources to examine care at the end of life in the two different settings. Data were collected on care at the end of life in general as well as in relation to the individual patient. In each site, interviews with a range of staff were undertaken (identified in this report as point 1 interviews) about end-of-life care in general, and the case notes from 10 recent patient deaths were analysed to gain an understanding of end-of-life care in these sites. At the patient level, observations of 25 patients in the period up to death were undertaken and combined with the views of staff (referred to as point 2 interviews in this report) and relatives to provide a more nuanced understanding care at the end of life. This also included analysis of the written case notes relating to the patient’s care.
Three distinct methods were therefore used at different times and in different ways to bring together an understanding of the landscape of end-of-life care in these two settings. None of the individual methods used was unproblematic and all had their inherent limitations, as discussed below.
Interviews
A semistructured interview approach was used for all interviews (point 1, point 2, bereaved relatives). The initial focus and some topics of interest were determined by the researcher as a result of the reading of the literature and pilot work, but respondents were encouraged and allowed the time and scope to talk about the topic in question by the use of open-ended and supplementary questioning. In this way, the interviews were more conversational in style, where a rapport could develop between the researcher and the respondent and specific issues arising during the course of the interview could be spontaneously explored as necessary.
Point 1 interviews
These interviews were used to explore the beliefs and practices that underpinned the delivery of care in both settings in order to provide a context for the specific information that was being collected around an observed case. For the purposes of this report an interview with a consultant and a nurse from each site in ICU and the most senior nurse (most often also the manager) in each of the nursing homes were analysed and reported.
These interviews required respondents to focus and comment on what they believed generally to be the case in their organisation regarding the various topic areas under discussion. This included exploring their views on how care was organised and actually delivered to dying patients and their families, which end-of-life care tools had been adopted and were being used, and what education and training opportunities and sources of support were available and being taken up.
All accounts are necessarily partial, and meanings and realities are constructed and reconstructed within the ‘social space’ of the interview. These accounts may, therefore, privilege a more publicly acceptable account in that respondents may wish to show themselves or the staff and services they represent in a favourable light. Arguably, this may be more likely when the subject matter under scrutiny is one as emotionally laden and politically sensitive as caring for dying patients. The responsibility of senior staff to deliver high-quality care is particularly relevant in understanding the accounts given. However, although elements of the public account were undoubtedly evident in these interviews, running through them was a less coherent dialogue that contained a more questioning and less certain view of the practice at the end of life.
We plan to incorporate the views of others from each site representing a more heterogeneous sample in peer-reviewed papers subsequent to this report.
Point 2 interviews
Interviews were also undertaken with the specific purpose of exploring the perspectives of staff involved in the delivery of care to an ‘observed’ patient. One member of staff who had been most closely involved in the delivery of care was interviewed for each observed case. These interviews took place either immediately at the end of the shift or on the following shift and, therefore, offer a perspective that is very close to the point of delivery of care. These interviews, which focused on the way in which care was delivered with reference to a particular patient, allowed an exploration of the thought process and motivations that lay behind aspects of observed care. In this way, these interviews gave a unique insight into issues that were running alongside the delivery of care – a ‘behind the scenes view’ that could neither be observed nor reported elsewhere in this study. These accounts were subject to the same limitations as those described above.
Bereaved relative interviews
An interview was undertaken with 23 bereaved relatives 2–4 months after the death of the patient. Sixteen interviews were undertaken with relatives of patients who had died in ICUs and seven with relatives of patients who had died in nursing homes. These interviews provided a valuable insight into their perspectives on the delivery of care and the dying and death of their relative or friend. However, interviews that take place months after the event may be subject to recall issues, where respondents either unable to remember very much at all, or have since, in the telling and retelling of the story over time, reconstructed an account that differs in some detail from the experience. These issues have already been explored above.
Observations
A total of 25 observations were undertaken within this study: 17 in ICU and 8 in the nursing home setting. The observational method has many advantages over interviewing people to gain an understanding of what they do. It allows care to be observed directly as it unfolds and provides an insight into aspects of that care that for many reasons may not be reported in interviews. However, as with many research methods in the social sciences, observations have some well-reported limitations.
Influence on the environment
There are several potential influences on the environment that is being observed. The potential for those being ‘observed’ to radically change their behaviour in response to the presence of the researcher has been widely discussed in the literature, for example by Denzin and Lincoln128 (see Monahan and Fisher for an interesting discussion on the benefits of observer effects129). Indeed, in this study a family member suggested to the researcher that better care had been provided to his relative as a result of the researcher’s presence. An allied issue is that those being observed may use the researcher as a source of support or information and not see them as separate from the caring team. Again, there were several examples in this study where this occurred, with relatives seeking information from the researcher about what care had been delivered while they had been out of the room.
Recording
Observing at the bedside of a person who is dying and being in the company of their family, friends and staff is potentially fraught with emotional significance and, therefore, likely to be challenging and tiring. Observation involves watching and recording in detail what happens over a given period of time and, in this study, the researchers aimed to remain at the bedside for a maximum of 3 hours, although there were occasions when they chose to remain for longer. They undertook these observations at various times of the day including the evening and overnight. Systematically recording in detail and by hand, sometimes in rooms in which the lighting was dimmed for the comfort of the patient, and over a period of ≥ 3 hours is challenging. It is impossible to record everything that occurs and therefore what does get recorded is necessarily partial and selective, the researcher effectively being the research instrument through which information is filtered.
When the researchers left after a period of observation they sometimes did not return for several hours. If the researcher had been observing during the night and left the patient’s bedside in the morning, they would return home to sleep and then return at a later time if the patient remained alive. There were periods of care that were simply not observed. When comparing observation data with data recorded in case notes, the attribution of timings in the records allowed for closer comparisons to be made.
Response rate
While many of the aspects of observational research outlined above have been well recorded, there is a very much smaller literature on the impact of undertaking observations on the response rate. There can be no doubt that this study experienced a number of setbacks and was ambitious in its conception. However, attempting to observe people as they died in the highly charged negative media spotlight resulted in some of the sites not referring patients to the study for recruitment. Although an incredible amount of work had been invested in recruiting sites and the sites had signed up to have the care they provided observed, this did not translate into observations in half of the sites. This was due not to the absence of deaths but to the gatekeeping role of staff. In line with our views on the protection of the patient and the assurances provided to the ethics committee, we had from the outset accepted this limitation. We did not, however, foresee how this would combine with the adverse publicity to affect our study design so dramatically.
Retrospective case note analysis
A total of 230 case notes were scrutinised to gain information on key elements of end-of-life care as documented in the participating sites. These 230 records were deaths that had taken place in the previous 12-month period, the majority coming in 2011. This method proved to be very time-consuming, both in gaining access to the files and in terms of the wealth of information that it was necessary to review. Poor handwriting and sometimes inconsistent filing added to the challenge. However, it was felt to have the added advantage of making the study visible within sites during the data collection period. The availability of researchers engaged in the task of locating files and undertaking case note reviews meant that they were on hand to discuss the study with staff, or to take referrals.
The case notes from the nursing home sample were relatively impoverished in terms of detail, particularly around the nature and content of the communication that took place. In general there was a more detailed reporting of communication in the ICUs. It was clear that case notes provide a particular account of events, written to serve a specific purpose. 130 Although they did not on their own provide a comprehensive picture of the care delivered, in conjunction with other data they proved to be very useful.
Economic evaluation
In designing this economic analysis we aimed to capture some of the important aspects regarding the experience of death itself. The ‘normal’ tools used in health economics (in particular the estimation of QALYs and incremental cost-effectiveness ratios) are of limited applicability in the evaluation of the care of imminently dying people. The remaining survival (the quantity dimension) is measured in hours rather than months or years, while the ability to enhance the patient experience (the quality dimension) may be entirely dominated by patient symptoms irrespective of the quality and sensitivity with which care is provided.
In the absence of an established and validated outcome tool, a tool was developed and used separately and in conjunction with other data. The economic questionnaire tool was developed to provide a link between the level of care given to patients and how this was received. As patients so close to death could not respond, family members provided proxy data about the possible experience of the care that was provided.
These questionnaires were completed by bereaved relatives in conjunction with the researcher as part of the in-depth interview after the death of the patient. Its location within the context of this interview allowed some exploration of the interpretations and responses of relatives to each of the items on the tool as they completed it. In addition, the tool, in conjunction with the observational and resource data, provided a strategy for calculating comparative costs and benefits of care delivered in LCP-using and non-LCP-using units in the last hours of life.
It is important to recognise, however, that any comparisons made between LCP-using and non-LCP-using units should be interpreted as being indicative rather than definitive. Despite ‘matching’ service providers, the impoverished and arguably skewed sample, particularly of nursing homes, means that a range of confounding factors need to be considered. Many non-LCP-using units were found to utilise many aspects of the LCP process and the LCP-using ICUs varied in their application of the LCP process. Although the ambitious aims of this economic analysis were not achieved, a potential approach to collecting and analysing data for economic analysis at the end of life has been achieved. This now needs to be tested in future studies.
The impact of Liverpool Care Pathway adverse publicity on the project
The research project was undertaken in the context of a heightened public debate regarding the care of dying people, which focused on the LCP. The controversy surrounding the LCP was especially acute between 2012 and 2014 but it can be traced back to articles that first appeared in the mainstream media in 2009. 131
There are undoubtedly many stories of poor care for dying patients. These have come to be routinely associated with the LCP, whether or not the care of the patient was supported by the LCP or if the complaint was related to the LCP. It has commonly and inaccurately been reported, for example, that the LCP is routinely used to ‘finish off’ patients and involves patients being ‘usually denied nutrition and fluids’. 132
Continued media and societal attention led to the national review of the Liverpool Care Pathway. 40 The review found that the LCP is based on sound ethical principles and provides good care when implemented properly. The review drew on a number of different types of evidence, including complaints, a literature review41 and public meetings with over 300 families and professionals. Published in July 2013, it made over 40 useful recommendations, including covering key issues relevant to the ability of the NHS to provide the best quality care for dying patients – such as education, training, research funding, access to specialist palliative care services and the need for care and compassion from all involved in caring for dying patients.
It also identified some key challenges in relation to the LCP and its profile and misrepresentation in the media. The terminology ‘Liverpool Care Pathway’ and in particular the word ‘pathway’ were found to be problematic and it was recommended that these terms be discontinued. The review also recommended that the LCP be replaced in the clinical environment within 6–12 months.
It has been a very challenging time for all professionals involved in caring for dying patients, whether doctors, nurses or other health-care practitioners. It has also been a difficult and uncertain time for patients and their families receiving care in this environment. Since the publication of the review, although media coverage has reduced, there has been concern about a vacuum emerging while national guidance is developed, potentially causing continuing challenges. 133–135 At the end of 2013, interim guiding principles were made available for consultation by the Leadership Alliance for the Care of Dying People, the membership of which included a range of relevant statutory and voluntary sector organisations. The Leadership Alliance published One Chance to Get it Right: Improving People’s Experience of Care in the Last Few Days of Life in June 2014. 136 In it, they confirmed that no new national ‘tool’ would be developed to replace the LCP and highlighted five priority areas that would be used to inform future CQC inspections and clinical guidance on the care of dying adults. Subsequently, NICE published guidelines in December 2015. 137
The controversy has had a much broader impact on work associated with caring for dying patients, including this National Institute for Health Research research project. The negative media publicity had a direct impact on the recruitment of patients to this study and made it difficult to retain the involvement of those sites that had signed up to participate. In nursing homes and in ICUs staff were fearful of associating the care they provided with the LCP and even more fearful of recruiting to a study that had LCP in its title. It is a credit to those organisations that took part that observations, interviews, and case note analyses were undertaken in such a changing and challenging environment.
The media interest in the LCP reflects the wider societal challenges in establishing a helpful debate about death and dying. With strong views on all sides – regarding euthanasia at one extreme and preserving life at any cost at the other – the LCP became the focus of the debate. Its absence from the debate will not remove the need for the debate and the need to improve care for dying patients.
Concluding remarks
This study makes a unique contribution to understanding the complexity of care at the end of life in two very different settings. It highlights the similarities and differences in the perspectives of doctors, nurses, carers and patients’ relatives both within and between settings and between sites where the LCP was used to support care and where it was not. It was not possible to assess the impact of the LCP on practice for methodological reasons (particularly in the nursing home setting). However, the 25 in-depth observations of the care of dying patients that were carried out, and the interviews with the 23 relatives who attended and witnessed the last hours and days of their loved ones’ lives, provide a unique insight to care at the very end of life. This study found no basis for the negative characteristics associated in the media with the use of the LCP. Although there were undoubtedly areas for improvement in the delivery of patient-centred care, in both settings and in all sites (regardless of the use of the LCP to support care), the goals of care at the end of life as described in this study by staff matched the wishes of the relatives for a peaceful and dignified death.
Implications for practice
This study raises a number of implications for practice. These are discussed within the context of the two different settings. However, across all sites staff were inconsistent in their communication with and about the unconscious patient. While they kept the patient informed about the care they were providing on the basis that the patient might be able to hear what was being said, they also talked about the patient with other staff and the patient’s relatives. These conversations often touched on the patient’s physical state, their approaching death and, in some cases, arrangements for their funeral. It is impossible to know what patients heard or the impact of these conversations on them had they been able to hear, but it is important that a consistent approach is adopted which errs on the side of the patient’s best interests.
Nursing homes
-
Documentation of key elements of communication: the retrospective case note analysis of deaths revealed that very little, if indeed anything, had been recorded in the patient’s notes regarding the communication that staff had had with the patient’s relatives. Maintaining good records of these conversations is important to ensure that all staff are aware of what relatives have been told and to assist in the delivery of information in a consistent and accurate way.
-
Consistency and availability of policies to guide care: when staff were asked to produce policies relevant to the care they provided they found it difficult, more so in nursing homes than in ICUs. Policies that were produced varied enormously both in content and in date. It was hard to assess how staff viewed the policies in relation to the care they provided. Clearly, in the provision of end-of-life care there needs to be an up-to-date and coherent approach, which should be identifiable in appropriate policy documents.
-
Lack of distinction between appropriate levels of care and routinised care: although patients in the nursing home setting received frequent visits from staff, these visits were mostly for the purposes of monitoring the patient or to provide physical care. The imperative to relieve pressure areas or provide food very close to death did not appear to be critically assessed by staff. Very few discussions were observed where staff decided not to do something on the basis that it was not appropriate. Given the uncertainty over the timing of death it is possible that staff undertook activities because they simply did not know how long the patient was going to live. Achieving a balance between providing routine care and appropriate care is difficult but the judgements underpinning this distinction may be influenced by training.
-
The focus on the delivery of physical care: while physical care received a lot of attention by nursing home staff, less attention was paid to the patient’s physical environment. The patient’s experiences of noise, light and temperature were frequently not considered, and often seemed to reflect the needs of the staff. This was particularly the case in relation to the playing of background music.
-
Lack of attention to the assessment of consciousness and swallowing: in the nursing home setting there were occasions on which a more formal set of assessment procedures would have improved care. These related to the assessment of the swallowing reflex and the patient’s state of consciousness.
-
The pacing of ACP discussions: the trend towards establishing a patient’s advance wishes regarding their care at the end of life is well established. However, in this study the speed at which staff appeared to want to establish these wishes was in some cases reported to be unseemly. While recognising the importance of establishing the patient’s wishes, it should also be recognised that the pace of these conversations should be individually determined.
-
Reported lack of consistency of GP cover: the reported involvement of the GP in end-of-life care in this study is of concern. A number of consequences flowed from the uncertainty reported by nursing staff of whether or not and when a GP might attend the patient. New meaning was given to the notion of anticipatory prescribing, as nursing staff sought to ensure that a range of drugs designed to make a patient more comfortable at the end of life were available for use. In many cases these were reported to have been prescribed well in advance of need and were often not used. This is clearly a cost which with improved medical cover might be avoided.
-
Systematic delivery of end-of-life care training: finally, it was apparent in all the interviews in the nursing home that although training for end-of-life care was recognised as important, it was rarely delivered in a systematic, rigorous way for all staff across each of the organisations involved in the study. Unless all staff receive high-quality ongoing training, none of the above will change.
Intensive care units
-
Lack of practical information for relatives and carers: the one-to-one care in ICU was perceived by relatives to be of an extremely high quality. Nurses carried out the majority of care once a decision to withdraw treatment had been made. Although the communication between staff and the patient’s relatives about the patient was consistent, on a few occasions relatives reported lacking vital information about purchasing food and hot drinks. Relatives also talked about their car parking concerns and keeping the parking meter topped up. A general reluctance to leave the bedside compounded these issues. More often than not this information was provided, but, where it was not, the relatives identified the stress it produced, over and above that they were already experiencing.
-
Distraction for relatives of the monitor at the bedside after the withdrawal of life-saving interventions: The presence of the monitor at the patient’s bedside was for some relatives a distraction. Relatives found it compelling watching although it took their focus off the patient. In many sites, but not all, the monitor at the bedside was either turned off or rotated out of the relatives’ sight.
-
The impact of staff–relative divergent views on care and treatment: while there were few cases of staff–relative divergent views over a patient’s care and treatment, when these did occur the consequences were far reaching. The divergences in this study occurred as a result of the staff’s inability to understand the relatives’ perspective and the relatives’ inability to understand the goals of care being provided. Despite acknowledging this difference, no attempt was made by staff to resolve it. There were also many cases where family members disagreed with each other. This was not always reflected in discussions between the clinical team or in the notes where the tendency was to refer to the family as a single entity.
Recommendations for future research
In line with the findings of Neuberger,40 which called for more research into how care is delivered to dying patients and their families, this study has generated a wealth of data that would benefit from further analysis.
In making recommendations for further research, we are taking into account the learning derived from undertaking this study with regard to the application of research methods.
-
One of the most important areas for future research is the way in which an organisational culture, regardless of setting, can be created and sustained to promote the practice of good end-of-life care. In this context, the role of leadership, of training and of policy would be fertile areas for further research. Common to all of these areas is the need to develop measurable outcomes to assess their impact on the organisational culture and the delivery of care at the end of life. Studies in these areas will require longitudinal research which should take account of the time-consuming nature of recruiting and retaining organisations in studies of end-of-life care. This has very important implications for the commissioning and funding of future research.
-
Given the growing number of people who receive care in residential and nursing care settings, more research is urgently needed in the following areas:
-
how the relationships between residents can be supported during end-of-life care
-
innovative approaches to building ACP conversations into the day-to-day work of care, to take account of the individuality of each patient and family and to avoid a ‘one size fits all’ approach
-
the role of out-of-hours medical support and how primary care services can be configured to support nursing home staff in achieving a comfortable pain-free death for their residents
-
how consciousness is constructed within the nursing home setting in the last days and hours of life and its importance should be investigated in relation to the delivery of care
-
the way in which nurses and health-care assistants view record keeping and its purpose.
Research in residential and nursing homes needs to take account of the organisational setting in terms of their size, ownership and funding model, and the impact these have on their recruitment and retention in research projects.
-
-
End of life is a feature of intensive care settings. While accepting that withdrawal is a medical decision, it would be useful for research to be undertaken on the relatives’ sense of ownership of the decision and the impact of this on their bereavement. There may also be merit in exploring how the speed of death following withdrawal affects relatives.
At a more theoretical level it would be useful to explore how the private language of nursing and medical staff about a patient’s deterioration reflects what they say and do in practice.
The study demonstrates that it is possible to cost care at the end of life. The approach adopted in this study, however, requires further research to refine and test the tools and processes in larger patient populations.
Acknowledgements
We would like to express our sincere gratitude to the patients and relatives who participated in this study and who allowed the research team into their lives at an emotional and challenging time. We also wish to thank the managers and staff working in the ICUs and in the nursing homes in which this research took place, not only for being open to the observation of their care, but also for sharing their perspectives and experiences of end-of-life care more generally.
Contributions of authors
Elizabeth Perkins (William Rathbone VI Chair of Community Nursing Research Director, Qualitative Research Methods) was a co-applicant on the study. She developed the funding bid and protocol, contributed to the development of the pilot study, supervised data collection, led and contributed to the analysis of data, led and participated in the drafting of the report and reviewed and commented on drafts.
Maureen Gambles (Senior Researcher, End-of-Life Research) was a senior researcher on the study. She undertook the pilot study and contributed to protocol development, data collection, analysis and reporting, contributed to the analysis of data, contributed to the drafting of the report and reviewed and commented on drafts.
Rachel Houten (Researcher, Health Economics) was an economist on the study. For the economic element of the study she contributed to tool development, and also contributed to data analysis and to the drafting of Chapter 13.
Sheila Harper (Postdoctoral Researcher, End-of-Life Researcher) was a researcher on the study. She undertook data collection in London and the south-east ICU and nursing home sites, contributed to the analysis of data, contributed to the drafting of the report and reviewed and commented on drafts.
Alan Haycox (Reader, Health Economics) was an economist on the study. For the economic element of the study he contributed to tool development, and also contributed to data analysis and to the drafting of Chapter 13.
Terri O’Brien (Postdoctoral Researcher, End-of-Life Researcher) was a researcher on the study. She undertook data collection in the north-west ICU and nursing home sites, and contributed to the analysis of data.
Sarah Richards (Researcher, Health Economics) was an economist on the study. For the economic element of the study she contributed to tool development, and also contributed to data analysis and to the drafting of Chapter 13.
Hong Chen (Research Assistant, End-of-Life Researcher) was a researcher on the study. She contributed to data collection in London and the south-east, to the critical discourse analysis of case notes from the ICUs, and to drafting Chapter 9 of the report.
Kate Nolan (Research Associate, Research Nurse) was a researcher on the study. She supported the development of matching criteria and contributed to the identification and recruitment of sites.
John E Ellershaw (Professor of Palliative Medicine, Palliative Medicine) was a co-applicant and is the corresponding author for this study. He developed the funding bid and protocol, contributed to the drafting of the report and reviewed and commented on drafts.
Data sharing statement
This is primarily a qualitative study. The participants in this study were assured that their data would only be shared within the research team. Further information can be obtained from the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Gomes B, Higginson IJ. Where people die (1974–2030): past trends, future projections and implications for care. Palliat Med 2008;22:33-41. http://dx.doi.org/10.1177/0269216307084606.
- Davies E, Higginson IJ. The Solid Facts: Palliative Care. Copenhagen: World Health Organization; 2004.
- Office for National Statistics . Deaths Registered in England and Wales, 2011 n.d. www.ons.gov.uk/ons/rel/vsob1/mortality-statistics--deaths-registered-in-england-and-wales--series-dr-/2011/dr-table5-2011.xls (accessed 15 June 2014).
- Building on Firm Foundations Improving on Care in Care Homes: Examples of Innovative Practice. London: Department of Health; 2007.
- Spotlight on Complaints: A Report on Second-Stage Complaints about the NHS in England 2008. http://webarchive.nationalarchives.gov.uk/20090104012205/http:/healthcarecommission.org.uk/_db/_documents/5632_HC_V18a.pdf (accessed 15 June 2014).
- End of Life Care Strategy: Promoting High Quality Care for All Adults at the End of Life. London: Department of Health; 2008.
- National Audit Office . End of Life Care n.d. www.nao.org.uk/wp-content/uploads/2008/11/07081043.pdf (accessed 15 June 2014).
- Department of Health . End of Life Care Strategy: Quality Markers and Measures for End of Life Care n.d. www.endoflifecare.nhs.uk/search-resources/resources-search/publications/imported-publications/end-of-life-care-strategy-quality-markers-and-measures-for-end-of-life-care.aspx#sthash.Fl0I3dcN.dpuf (accessed 28 November 2013).
- National Institute for Health and Care Excellence . Quality Standard for End of Life Care for Adults n.d. http://publications.nice.org.uk/quality-standard-for-end-of-life-care-for-adults-qs13 (accessed 15 June 2014).
- Grande-Cameron C, Hauldin A. Concept analysis of good death in terminally ill patients. Am J Hospice Palliat Care 2012;29:632-9. http://dx.doi.org/10.1177/1049909111434976.
- Scarre G. Can there be a good death?. J Eval Clin Prac 2012;18:1082-6. http://dx.doi.org/10.1111/j.1365-2753.2012.01922.x.
- Shah SM, Carey IM, Harris T, DeWilde S, Cook DG. Mortality in older care home residents in England and Wales. Age Ageing 2013;42:209-15. http://dx.doi.org/10.1093/ageing/afs174.
- Percival and Johnson . End-of-life care in nursing and care homes. Nursing Times 2013;109:20-2.
- Sims-Gould J, Wiersma E, Arseneau L, Kelley ML, Kozak J, Habjan S, et al. Care provider perspectives on end of life care in long term care homes: implications for whole person and palliative care. J Palliat Care 2010;26:122-9.
- Shield R, Wetle T, Teno J, Miller S, Welch L. Physicians ‘missing in action’: family perspectives on physician and staffing problems in end-of-life care in the nursing home. J Am Geriatr Soc 2005;53:1651-7. http://dx.doi.org/10.1111/j.1532-5415.2005.53505.x.
- Carlson AL. Death in the nursing home: resident, family, and staff perspectives. J Gerontol Nurs 2007;33:32-41.
- Goddard C, Stewart F, Thompson G, Hall S. Providing end-of-life care in care homes for older people: a qualitative study of the views of care home staff and community nurses. J Appl Gerontol 2013;32:76-95. http://dx.doi.org/10.1177/0733464811405047.
- Froggatt K, Payne S. A survey of end-of-life care in care homes: issues of definition and practice. Health Soc Care Community 2006;14:341-8. http://dx.doi.org/10.1111/j.1365-2524.2006.00628.x.
- NHS Choices . Intensive Care n.d. www.nhs.uk/Conditions/Intensive-care/Pages/Introduction.aspx (accessed 15 June 2014).
- Intensive Care National Audit and Research Centre . Key Statistics from the Case Mix Programme Database n.d. www.icnarc.org/documents/Summary%20statistics%20-%202011-12.pdf (accessed 15 June 2014).
- Prendergast TJ, Luce JM. Increasing incidence of withholding and withdrawal of life support from the critically ill. Am J Respirat Crit Care Med 2005;155:15-20. http://dx.doi.org/10.1164/ajrccm.155.1.9001282.
- Coombs MA, Long T. Managing a good death in critical care: can health policy help?. Nurs Crit Care 2008;14:208-14. http://dx.doi.org/10.1111/j.1478-5153.2008.00280.x.
- Pattison N, Carr SM, Turnock C, Dolan S. ‘Viewing in slow motion’: patients’, families’, nurses’ and doctors’ perspectives on end-of-life care in critical care. J Clin Nurs 2013;22:1442-54. http://dx.doi.org/10.1111/jocn.12095.
- Festic E, Wilson ME, Gajic O, Divertie GD, Rabatin JT. Perspectives of physicians and nurses regarding EoLC in the intensive care unit. J Intensive Care Med 2012;27:45-54. http://dx.doi.org/10.1177/0885066610393465.
- McMillen RE. End of life decisions: nurses perceptions, feelings and experiences. Intensive Crit Care Nurs 2008;24:251-9. http://dx.doi.org/10.1016/j.iccn.2007.11.002.
- Coombs MA, Addington-Hall J, Long-Sutehall T. Challenges in transition from intervention to end of life care in intensive care: a qualitative study. Int J Nurs Stud 2012;49:519-27. http://dx.doi.org/10.1016/j.ijnurstu.2011.10.019.
- Thompson G, McClement S, Daeninck P. Nurses’ perceptions of quality end of life care on an acute medical ward. J Adv Nurs 2006;53:169-77. http://dx.doi.org/10.1111/j.1365-2648.2006.03712.x.
- Ryan L, Seymour J. Death and dying in intensive care: emotional labour of nurses. End Life J 2013;3:1-9. http://dx.doi.org/10.1136/eoljnl-03-02.1.
- NHS Improving Quality . Preferred Priorities for Care n.d. www.nhsiq.nhs.uk/resource-search/publications/eolc-ppc.aspx (accessed 3 June 2016).
- Gold Standards Framework . The Gold Standards Framework n.d. www.goldstandardsframework.org.uk (accessed 3 June 2016).
- Thomas K. Care For the Dying at Home. Oxford: Radcliffe Medical Press; 2003.
- Badger F, Plumridge G, Hewison A, Shaw SL, Thomas K, Clifford C. An evaluation of the impact of the Gold Standards Framework on collaboration in end-of-life care in nursing homes. A qualitative and quantitative evaluation. Int J Nurs Stud 2012;49:586-95. http://dx.doi.org/10.1016/j.ijnurstu.2011.10.021.
- Ellershaw J, Murphy D, Ellershaw J, Wilkinson S. Care of the Dying: A Pathway to Excellence. Oxford: Oxford University Press; 2011.
- Marie Curie Palliative Care Instititute Liverpool n.d. www.mcpcil.org.uk (accessed 3 June 2016).
- Higginson IJ, Shipman C, Gysels M, White P, Barclay S, Forrest, et al. Scoping Exercise on Generalist Services for Adults at the End of Life: Research, Knowledge, Policy and Future Research Needs. Report 1: Overview and Recommendations for Future Research in Generalist End of Life Care. London: NCCSDO; 2007.
- Ellershaw J, Ellershaw J, Wilkinson S. Care of the Dying: A Pathway to Excellence. Oxford: Oxford University Press; 2011.
- Royal College of Physicians and Marie Curie Cancer Care . The National Care of the Dying Audit of Hospitals 2014 n.d. www.rcplondon.ac.uk/projects/outputs/national-care-dying-audit-hospitals (accessed 14 March 2016).
- Improving Supportive and Palliative Care for Adults with Cancer. London: NICE; 2004.
- Our Health, Our Care, Our Say: A New Direction for Community Services. London: Department of Health; 2006.
- Neuberger J. More Care Less Pathway: A Review of the Liverpool Care Pathway n.d. www.gov.uk/government/uploads/system/uploads/attachment_data/file/212450/Liverpool_Care_Pathway.pdf (accessed 15 June 2014).
- Parry R, Seymour J, Whittaker B, Bird L, Cox K. Rapid Evidence Review: Pathways Focused on the Dying Phase in End of Life Care and Their Key Components n.d. www.gov.uk/government/uploads/system/uploads/attachment_data/file/212451/review_academic_literature_on_end_of_life.pdf (accessed 15 June 2014).
- Tilden VP, Thompson SA, Gajewski BJ, Buescher CM, Bott MJ. Sampling challenges in nursing home research. J Am Med Dir Assoc 2013;14:25-8. http://dx.doi.org/10.1016/j.jamda.2012.08.015.
- Cheshire and Merseyside Strategic Clinical Networks . Programme Overview n.d. www.cmscnsenate.nhs.uk/strategic-clinical-network/our-networks/palliative-and-end-life-care/six-steps-sucess-end-life-care/care-homes/programme-overview/ (accessed 3 June 2016).
- Lawton J. Pearls, pith, and provocation, gaining and maintaining consent: ethical concerns raised in a study of dying patients. Qual Health Res 2001;11:693-705. http://dx.doi.org/10.1177/104973201129119389.
- Seymour J. Critical Moments – Death and Dying in Intensive Care. Buckingham: Oxford University Press; 2001.
- Mills M, Davies HTO, Macrae WA. Care of dying patients in hospital. BMJ 1994;309:583-6. http://dx.doi.org/10.1136/bmj.309.6954.583.
- Buckingham RW, Lack SA, Mount BM, MacLean LD, Collins JT. Living with the dying: use of the technique of participant observation. Can Med Assoc J 1976;115:1211-15.
- Gold R. Roles in sociological field observation. Social Forces 1958;36:217-33. http://dx.doi.org/10.2307/2573808.
- Adler P, Adler P, Denzin K, Lincoln Y. Collecting and Interpreting Qualitative Materials. Thousand Oaks, CA: Sage; 2004.
- Fasschnach G. Theory and Practice of Observing Behaviour. London: Academic Press; 1982.
- Patton MQ. Qualitative Research and Evaluation Methods. Thousand Oaks, CA: Sage; 2007.
- Hammersley M, Atkinson P. Ethnography: Principles in Practice. London: Routledge; 1995.
- Mental Capacity Act. London: HMSO; 2005.
- Addington-Hall J, McPherson C. After-death interviews with surrogates/bereaved family members: some issues of validity. J Pain Symptom Manage 2001;22:784-90. http://dx.doi.org/10.1016/S0885-3924(01)00330-X.
- Fairclough N, Wodak R, Van Dijk T. Discourse Studies: A Multidisciplinary Introduction. London: Sage; 1997.
- Wodak R, Wodak R, Meyer M. Methods of Critical Discourse Analysis. London: Sage; 2001.
- Charmaz K. Constructing Grounded Theory: A Practical Guide through Qualitative Analysis. London: Sage; 2006.
- Seymour J, Witherspoon R, Gott M, Ross H, Payne S, Owen T. Dying in Older Age: Reflections and Experiences from an Older Person’s Perspective. London: Help the Aged; 2005.
- Gold Standards Framework . Care Homes Training n.d. www.goldstandardsframework.org.uk/care-homes-training-programme (accessed 3 June 2016).
- The Code: Professional Standards of Practice and Behaviour for Nurses and Midwives. London: NMC; 2015.
- Setting the Record Straight: A Study of Hospital Medical Records. London: Audit Commission; 1995.
- Ahearn D, Jackson T, McIlmoyle J, Weatherburn AJ. Improving end of life care for nursing home residents: an analysis of hospital mortality and readmission rates. Postgrad Med J 2010;86:131-5. http://dx.doi.org/10.1136/pgmj.2008.076430.
- Ravenscroft AJ, Bell MD. ‘End-of-life’ decision making within intensive care – objective, consistent, defensible?. J Med Ethics 2000;26:435-40. http://dx.doi.org/10.1136/jme.26.6.435.
- Carlet J, Thijs LG, Antonelli M, Cassell J, Cox P, Hill N, et al. Challenges in end-of-life care in the ICU: Statement of the 5th International Consensus Conference in Critical Care: Brussels, Belgium, April 2003. Intensive Care Med 2004;30:770-84. http://dx.doi.org/10.1007/s00134-004-2241-5.
- Mental Capacity Act Code of Practice. Norwich: The Stationery Office; 2007.
- Barton E, Aldridge M, Trimble T, Vidovic J. Structure and variation in end-of-life discussions in the surgical intensive care unit. Commun Med 2005;2:3-20. http://dx.doi.org/10.1515/come.2005.2.1.3.
- Morgan J. End-of-life care in UK critical care units – a literature review. Nurs Crit Care 2008;13:152-61. http://dx.doi.org/10.1111/j.1478-5153.2008.00274.x.
- Trevena LJ, Davey HM, Barratt A, Butow P, Caldwell P. A systematic review on communicating with patients about evidence. J Eval Clin Prac 2006;12:13-2. http://dx.doi.org/10.1111/j.1365-2753.2005.00596.x.
- Gott M, Barnes S, Parker C, Payne S, Seamark D, Gariballa S, et al. Dying trajectories in heart failure. Palliat Med 2007;21:95-9. http://dx.doi.org/10.1177/0269216307076348.
- Cohen SL, Bewley JS, Ridley S, Goldhill D. Guidelines for Limitations of Treatment for Adults Requiring Intensive Care. London: The Intensive Care Society; 2003.
- Jecker NS, Pearlman RA. Medical futility: who decides?. Arch Internal Med 1992;152:1140-4. http://dx.doi.org/10.1001/archinte.1992.00400180012002.
- Billings JA. The end-of-life family meeting in intensive care part I: indications, outcomes, and family needs. J Palliat Med 2011;14:1042-50. http://dx.doi.org/10.1089/jpm.2011.0038.
- Adolph MD, Frier KA, Stawicki SPA, Gerlach AT, Papadimos TJ. Palliative critical care in the intensive care unit: a 2011 perspective. Int J Crit Illn Inj Sci 2011;1:147-53. http://dx.doi.org/10.4103/2229-5151.84803.
- Cosgrove JF, Bari F. End-of-life care on the Intensive Care Unit in England and Wales: an overview for hospital medical practitioners. Surgery 2012;30:563-6. http://dx.doi.org/10.1016/j.mpsur.2012.07.002.
- Hardicre J. Nurses’ experiences of caring for the relatives of patients in ICU. Nursing Times 2003;99.
- Prieto L, Sacristán JA. Problems and solutions in calculating quality-adjusted life years (QALYs). Health Qual Life Outcomes 2003;1. http://dx.doi.org/10.1186/1477-7525-1-80.
- Marie Curie Cancer Care . Understanding the Cost of End of Life Care in Different Settings n.d. www.mariecurie.org.uk/documents/healthcare-professionals/commissioning-services/understanding-cost-end-life-care-different-settings.pdf (accessed 15 June 2014).
- Curtis L. Unit Costs of Health and Social Care 2011 n.d. www.pssru.ac.uk/project-pages/unit-costs/2011/index.php (accessed 15 June 2014).
- NHS Emplyers . Agenda for Change Pay and Conditions Circulars n.d. www.nhsemployers.org/your-workforce/pay-and-reward/pay/pay-and-conditions-circulars/agenda-for-change-pay-and-conditions-circulars (accessed 3 June 2016).
- NHS Business Authority n.d. www.nhsbsa.nhs.uk/ (accessed 15 June 2014).
- HM Government . National Minimum Wage Rates n.d. www.gov.uk/national-minimum-wage-rates (accessed 15 June 2014).
- Joint Formulary Committee . British National Formulary n.d. www.bnf.org/bnf/index.htm (accessed 15 June 2014).
- Levy CE. Quality of dying and death in two medical ICUs: perceptions of family and clinicians. Chest 2005;127:1775-83. http://dx.doi.org/10.1378/chest.127.5.1775.
- Department of Health . First National VOICES Survey of Bereaved People: Key Findings Report. Appendix B: Survey Questionnaire n.d. www.gov.uk/government/uploads/system/uploads/attachment_data/file/216896/VOICES-Survey-Appendix-B.pdf (accessed 15 June 2014).
- Mayland C, Williams E, Ellershaw J. Assessing quality of care of the dying: the development and initial validation of a postal self-completion questionnaire for bereaved relatives. Palliat Med 2011;26:897-90. http://dx.doi.org/10.1177/0269216311424953.
- Steinhauser KC. In search of a good death: observations of patients, families, and providers. Ann Intern Med 2000;132:825-32. http://dx.doi.org/10.7326/0003-4819-132-10-200005160-00011.
- Low J, Payne S. The good and bad death perceptions of health professionals working in palliative care. Eur J Cancer Care 1996;5:237-41. http://dx.doi.org/10.1111/j.1365-2354.1996.tb00241.x.
- Hales SZ. Review: the quality of dying and death: a systematic review of measures. Palliat Med 2010;24:127-44. http://dx.doi.org/10.1177/0269216309351783.
- Mayland CR, Williams EMI, Ellershaw JE. How well do current instruments using bereaved relatives views evaluate care for dying patients?. Palliat Med 2008;22:133-44. http://dx.doi.org/10.1177/0269216307085742.
- Gomes BH. Optimal approaches to the health economics of palliative care: report of an international think tank. J Pain Symptom Manage 2009;38:4-10. http://dx.doi.org/10.1016/j.jpainsymman.2009.04.008.
- Smith R. A good death: an important aim for health services and for us all. BMJ 2000;320:129-30. http://dx.doi.org/10.1136/bmj.320.7228.129.
- National Council for Palliative Care/End of Life Care Programme . Building on Firm Foundations. Improving End of Life Care in Care Homes: Examples of Innovative Practice 2007. www.ncpc.org.uk/sites/default/files/BuildingOnFirmFoundations.pdf (accessed 14 March 2014).
- Ellershaw JE, Wilkinson SM. Care of the Dying: A Pathway to Excellence. Oxford: Oxford University Press; 2011.
- Latten R. Diagnosing Dying: Exploring the Process by Which Hospice Staff Recognise the Last Days of Life 2015.
- Seymour JE, Kumar A, Froggatt K. Do nursing homes for older people have the support they need to provide end-of-life care? A mixed methods enquiry in England. Palliat Med 2011;25:125-38. http://dx.doi.org/10.1177/0269216310387964.
- Wilson E, Marbey H, Brown J, Payne S, Seale C, Seymour J. How do community nurses decide when to use anticipatory prescriptions in end of life care and what do they worry about? Findings from a qualitative study. BMJ Support Palliat Care 2014;4. http://dx.doi.org/10.1136/bmjspcare-2014-000653.3.
- Addington-Hall J, Higginson I. Palliative Care for Non Cancer Patients. Oxford: Oxford University Press; 2001.
- Reynolds K, Henderson M, Schulman A, Hanson LC. Needs of the dying in nursing homes. J Palliat Med 2002;5:895-901. http://dx.doi.org/10.1089/10966210260499087.
- Gallagher R, Krawczyk M. Family members’ perceptions of end-of-life care across diverse locations of care. BMC Palliative Care 2013;12. http://dx.doi.org/10.1186/1472-684X-12-25.
- Barber ND, Alldred DP, Raynor DK, Dickinson R, Garfield S, Jesson B, et al. Care homes’ use of medicines study: prevalence, causes and potential harm of medication errors in care homes for older people. Qual Saf Health Care 2009;18:341-6. http://dx.doi.org/10.1136/qshc.2009.034231.
- Kinley J, Hockley J. A baseline review of medication provided to older people in nursing care homes in the last month of life. Int J Palliat Nurs 2010;16:216-23. http://dx.doi.org/10.12968/ijpn.2010.16.5.48142.
- National Patient Safety Agency . 10 for 2010: Pressure Ulcers n.d. www.nrls.npsa.nhs.uk/resources/collections/10-for-2010/pressure-ulcers (accessed 15 June 2014).
- Pressure Ulcers: Prevention and Management of Pressure Ulcers. London: NICE; 2014.
- Schou K, Alvsvåg H, Blåka G, Gjengedal E. The (dis)appearance of the dying patient in generalist hospital and care home nurses’ talk about the patient. Nurs Philos 2008;9:233-47. http://dx.doi.org/10.1111/j.1466-769X.2008.00374.x.
- Sudnow D. Passing On: The Social Organisation of Dying. Upper Saddle River, NJ: Prentice Hall; 1967.
- Cavendish C. The Cavendish Review: An Independent Review into Healthcare Assistants and Support Workers in the NHS and Social Care Settings 2013. www.gov.uk/government/uploads/system/uploads/attachment_data/file/236212/Cavendish_Review.pdf (accessed 14 March 2016).
- Seymour J, Almack K, Kennedy S. Implementing advance care planning: a qualitative study of nurses’ views and experiences. BMC Palliat Care 2010;9. http://dx.doi.org/10.1186/1472-684X-9-4.
- Gries CJ, Engleberg RA, Kross EK, Zatzick D, Nielsen EL, Downey L, et al. Predictors of symptoms of posttraumatic stress and depression in family members after patient death in the ICU. Chest 2010;137:280-7. http://dx.doi.org/10.1378/chest.09-1291.
- McAdam JL, Dracup KA, White DB, Fontaine DK, Puntillo KA. Symptom experiences of family members of intensive care unit patients at high risk for dying. Crit Care Med 2010;38:1078-85. http://dx.doi.org/10.1097/CCM.0b013e3181cf6d94.
- Rusinova K, Kukal J, Simek JR, Cerny V. Limited family members/staff communication in the intensive care units in Czech and Slovak Republic considerably increases anxiety in patients’ relatives – the DEPRESS Study. BMC Psychiatry 2014;14. http://dx.doi.org/10.1186/1471-244X-14-21.
- Crunden E. A reflection from the other side of the bed: an account of what it is like to be a patient and a relative in an intensive care unit. Intensive Crit Care Nurs 2010;26:18-23. http://dx.doi.org/10.1016/j.iccn.2009.09.001.
- Fridh I, Forsberg A, Bergbom I. Close relatives’ experiences of caring and of the physical environment when a loved one dies in an ICU. Intensive Crit Care Nurs 2009;25:111-19. http://dx.doi.org/10.1016/j.iccn.2008.11.002.
- General Medical Council . Treatment and Care towards the End of Life: Good Practice in Decision Making 2010. www.gmc-uk.org/Treatment_and_care_towards_the_end_of_life___English_1015.pdf_48902105.pdf (accessed 15 June 2014).
- Halcomb E, Daly J, Jackson D, Davidson P. An insight into Australian nurses’ experience of withdrawal/withholding of treatment in the ICU. Intensive Crit Care Nurs 2004;20:214-22. http://dx.doi.org/10.1016/j.iccn.2004.05.010.
- Lautrette A, Darmon M, Megarbane B, Joly LM, Chevret S, Adrie C, et al. A communication strategy and brochure for relatives of patients dying in the ICU. N Engl J Med 2007;356:469-78. http://dx.doi.org/10.1056/NEJMoa063446.
- Scheunemann LP, McDevitt M, Carson S, Hanson LC. Systematic review: controlled trials of interventions to improve communication in intensive care. Chest 2011;139:543-54. http://dx.doi.org/10.1378/chest.10-0595.
- Siegal M. End-of-life decision making in the ICU. Clin Chest Med 2009;30:181-94. http://dx.doi.org/10.1016/j.ccm.2008.11.002.
- Schuster RA, Hong SY, Arnold RM. Investigating conflict in ICUs – is the clinician’s perspective enough?. Crit Care Med 2014;42:328-35. http://dx.doi.org/10.1097/CCM.0b013e3182a27598.
- Walker R, Read S. The Liverpool Care Pathway in intensive care: an exploratory study of doctor and nurse perceptions. Int J Palliat Nurs 2010;16:267-73. http://dx.doi.org/10.12968/ijpn.2010.16.6.48825.
- Jack B, Gambles M, Murphy D, Ellershaw JE. Nurses’ perceptions of the Liverpool Care Pathway for the dying patient in the acute hospital setting. Int J Palliat Nurs 2003;9:375-81. http://dx.doi.org/10.12968/ijpn.2003.9.9.11764.
- Clark J, Marshall B, Sheward K, Allan S. Staff perceptions of the impact of the Liverpool Care Pathway in aged residential care in New Zealand. Int J Palliat Nurs 2012;18:171-8. http://dx.doi.org/10.12968/ijpn.2012.18.4.171.
- Cook DJ, Giacomini M, Johnson N, Willms D. Life support in the intensive care unit: a qualitative investigation of technological purposes. CMAJ 1999;161:1109-13.
- Harvey J. The technological regulation of death: with reference to the technological regulation of birth. Sociology 1997;31:719-35. http://dx.doi.org/10.1177/0038038597031004005.
- Riley-Smith B. More than a thousand care home residents die thirsty. The Telegraph 2013. www.telegraph.co.uk/news/health/10421787/Liverpool-Care-Pathway-Back-to-the-old-days-of-patients-dying-in-agony.html (accessed 14 March 2016).
- Stroebe N, Stroebe W, Schut H. Bereavement research: methodological issues and ethical concerns. Palliat Med 2003;17:235-40. http://dx.doi.org/10.1191/0269216303pm768rr.
- Alliger GM, Tannenbaum SI, Bennett W, Traver H, Shortland A. A meta-analysis on the relations among training criteria. Personnel Psychol 1997;50:341-58. http://dx.doi.org/10.1111/j.1744-6570.1997.tb00911.x.
- Royal College of Physicians . National Care of the Dying Audit for Hospitals – England, 2014 n.d. www.rcplondon.ac.uk/resources/national-care-dying-audit-hospitals (accessed 13 June 2014).
- Denzin NK, Lincoln YS. Handbook of Qualitative Research. Thousand Oaks, CA: Sage; 2000.
- Monahan T, Fisher JA. Benefits of ‘observer effects’: lessons from the field. Qual Res 2010;10:357-76. http://dx.doi.org/10.1177/1468794110362874.
- Berkenkotter C, Ravotas D. Genre as tool in the transmission of practice over time and across professional boundaries. Mind Culture Activity 1997;4:256-74. http://dx.doi.org/10.1207/s15327884mca0404_4.
- Devlin K. Sentenced to death on the NHS. The Telegraph 2009.
- Groves J, Martin D, Doughty S. 60,000 patients put on death pathway without being told but minister still says controversial end-of-life plan is ‘fantastic’. Mail Online 2013. www.dailymail.co.uk/news/article-2255054/60-000-patients-death-pathway-told-minister-says-controversial-end-life-plan-fantastic.html (accessed 15 June 2014).
- Bingham J. More dying in agony after scrapping of care pathway, leading nurse claims. The Telegraph 2013. www.telegraph.co.uk/health/healthnews/10413287/More-dying-in-agony-after-scrapping-of-care-pathway-leading-nurse-claims.html (accessed 15 June 2014).
- Pemberton M. Liverpool Care Pathway: back to the old days of patients dying in agony. The Telegraph 2013. www.telegraph.co.uk/health/10421787/Liverpool-Care-Pathway-Back-to-the-old-days-of-patients-dying-in-agony.html (accessed 18 November 2013).
- Editorial . Dignity in death: the triumph of politics over evidence. Lancet Oncol 2013;14. http://dx.doi.org/10.1016/S1470-2045(13)70559-X.
- One Chance to Get it Right: Improving People’s Experience of Care in the Last Few Days and Hours of Life. London: Department of Health; 2014.
- Care of Dying Adults in the Last Days of Life. London: NICE; 2015.
- National Institute for Health and Care Excellence . British National Formulary (BNF) Controlled Drugs and Drug Dependence n.d. www.evidence.nhs.uk/formulary/bnf/current/guidance-on-prescribing/controlled-drugs-and-drug-dependence (accessed 3 June 2016).
Appendix 1 Pilot study report
Appendix 2 Final study protocol
Appendix 3 Brief summary of the research
Appendix 4 Original advisory board membership
| Name | Title | Role |
|---|---|---|
| Julia Addington-Hall | Professor, End of Life Care, School of Health Sciences, University of Southampton, Southampton, UK | Advisory Group Member |
| Rebecca Bancroft | Dr, Consultant Geriatrician, Royal Liverpool and Broadgreen University Hospitals NHS Trust, Liverpool, Liverpool, UK | Advisory Group Member |
| Jayne Brown | Dr, Senior Research Fellow, University of Nottingham, Nottingham, UK | Advisory Group Member |
| Barbara Burkey | Mrs, lay representative | Advisory Group Member |
| Maureen Coombs | Dr, Consultant Nurse, Intensive Care Unit, Southampton University NHS Hospitals Trust, Southampton, UK | Advisory Group Member |
| Massimo Costantini | Dr, Head Regional Palliative Care Network, National Cancer Research Institute, Genova, Italy | Advisory Group Member |
| Steve Dewar | Mr, Research and Innovation Director, Marie Curie Cancer Care, London, UK | Advisory Group Member |
| Joy Duxbury | Dr, Reader in Mental Health Nursing, Divisional Leader for Mental Health, University of Central Lancashire, Preston, UK | Advisory Group Member |
| John Ellershaw | Professor of Palliative Medicine, Director Marie Curie Palliative Care Institute, chief investigator | (Initially CHAIR); Advisory Group Member |
| Katharine Froggatt | Dr, Senior Lecturer, Observatory of End of Life Care, University of Lancaster, Lancaster, UK | Advisory Group Member |
| Jane Harper | Dr, Consultant, Intensive Care Unit, Royal Liverpool and Broadgreen University Hospitals NHS Trust, Liverpool, UK | Advisory Group Member |
| Chris Haywood | Mrs, Head of Hospice Services, Willowbrook Hospice, Liverpool, UK | Advisory Group Member |
| Irene Higginson | Professor of Palliative Care and Policy, Division of Health and Social Care Research, King’s College London, London, UK | Advisory Group Member |
| Louise Jones | Dr, Head of Unit, Marie Curie Palliative Care Research Unit, University College London, London, UK | Advisory Group Member |
| John Joshua | Mr, Assistant Network Director (Communications and Involvement), Greater Manchester and Cheshire Cancer Network, Manchester, UK | Advisory Group Member |
| Barbara Monroe | Dame, Chief Executive, St Christopher’s Hospice, London, UK | Advisory Group Member |
| Sheila Payne | Professor, Help the Hospices Professor of Hospice Studies, Observatory of End of Life Care, University of Lancaster, Lancaster, UK | Vice Chair (and later Chair) |
| Kathy Rowan | Professor, Director, Intensive Care National Audit and Research Centre, London, UK | Advisory Group Member |
| Jane Seymour | Professor, Sue Ryder Care Professor of Palliative and End of Life Studies, University of Nottingham, Nottingham, UK | Advisory Group Member |
| Eleanor Sherwin | Ms, End of Life Care Programme, Department of Health, London, UK | Advisory Group Member |
| PMG | All members of the Project Management Group | Advisory Board Members |
Appendix 5 Advisory group terms of reference
The Impact of the Liverpool Care Pathway on care at the end of life Advisory Group
Terms of Reference
Background to the Project
The research builds on the scoping review of generalist end-of-life care undertaken by Higginson et al. 34 (2007) and focuses on providing evidence on the impact of the Liverpool Care Pathway on care at the end of life in two generalist settings: Nursing Homes and Intensive Care Units in the north-west of England and London and the south-east. In essence this study is a matched case study design where half of the sample will have registered to use the Liverpool Care Pathway and half will not. It involves the collection of data using: interviews, observations, case note analysis and documentary analysis of the SHA's plans for end-of-life care and end-of-life care policies in place within individual sites.
The study will provide evidence on costs and outcomes to enable the comparative cost-effectiveness underlying the implementation of LCP in different sub-groups of patients and in different contexts to be evaluated. The project will generate evidence relevant for the commissioning, development, implementation and management of generalist end-of-life care services in the NHS and wider health and social care system. Importantly, this study involves the views of bereaved relatives as well as those of staff and other key stakeholders and the ethical issues involved in the conduct of this study are complex.
Purpose of the Advisory Group
To provide relevant specialist advice and support (clinical and research) at all stages of the project including: setting up (design and implementation), conduct, findings and dissemination. The majority of the communication between Advisory Group members will take place electronically but the group will have the opportunity to meet formally once per year (a total of 3 times during the life of the project).
Specific Terms of Reference
-
To receive regular (6 monthly) updates re project progress (electronically).
-
To provide feedback/support (electronically) on the 6 monthly updates (as and when required/requested).
-
To offer advice/support (electronically) in response to ‘ad hoc’ requests regarding specific issues/challenges throughout the project.
-
To agree that information about the study, including emergent findings, that is shared within meetings, or via electronic means, remains confidential until publicly available.
-
To have the opportunity to attend the bi-annual meeting of the Advisory Group.
This bi-annual meeting shall be considered in quorum if:
-
at least 50% of the members are present, and
-
the Chair or the Deputy Chair is present.
Appendix 6 Liverpool Care Pathway for the Dying Patient: model document
Appendix 7 Research process flow chart
FIGURE 2.
Research process flow chart. a, Written consent for ‘significant other’ here includes permission to approach for interview after the death of the patient.
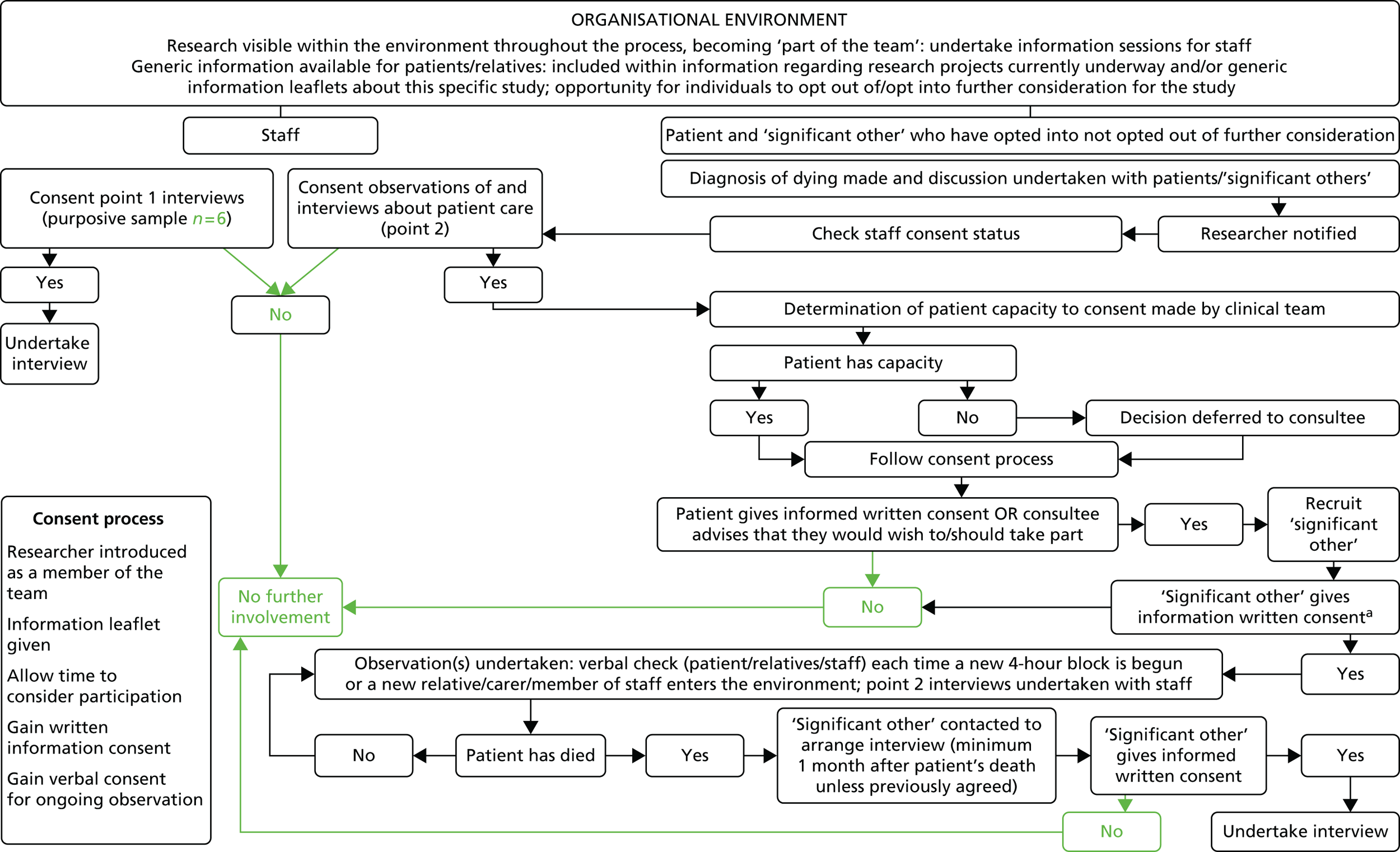
Appendix 8 Intensive care unit recruitment flow diagram
FIGURE 3.
Intensive care unit recruitment flow diagram. L&SE, London and the south-east.
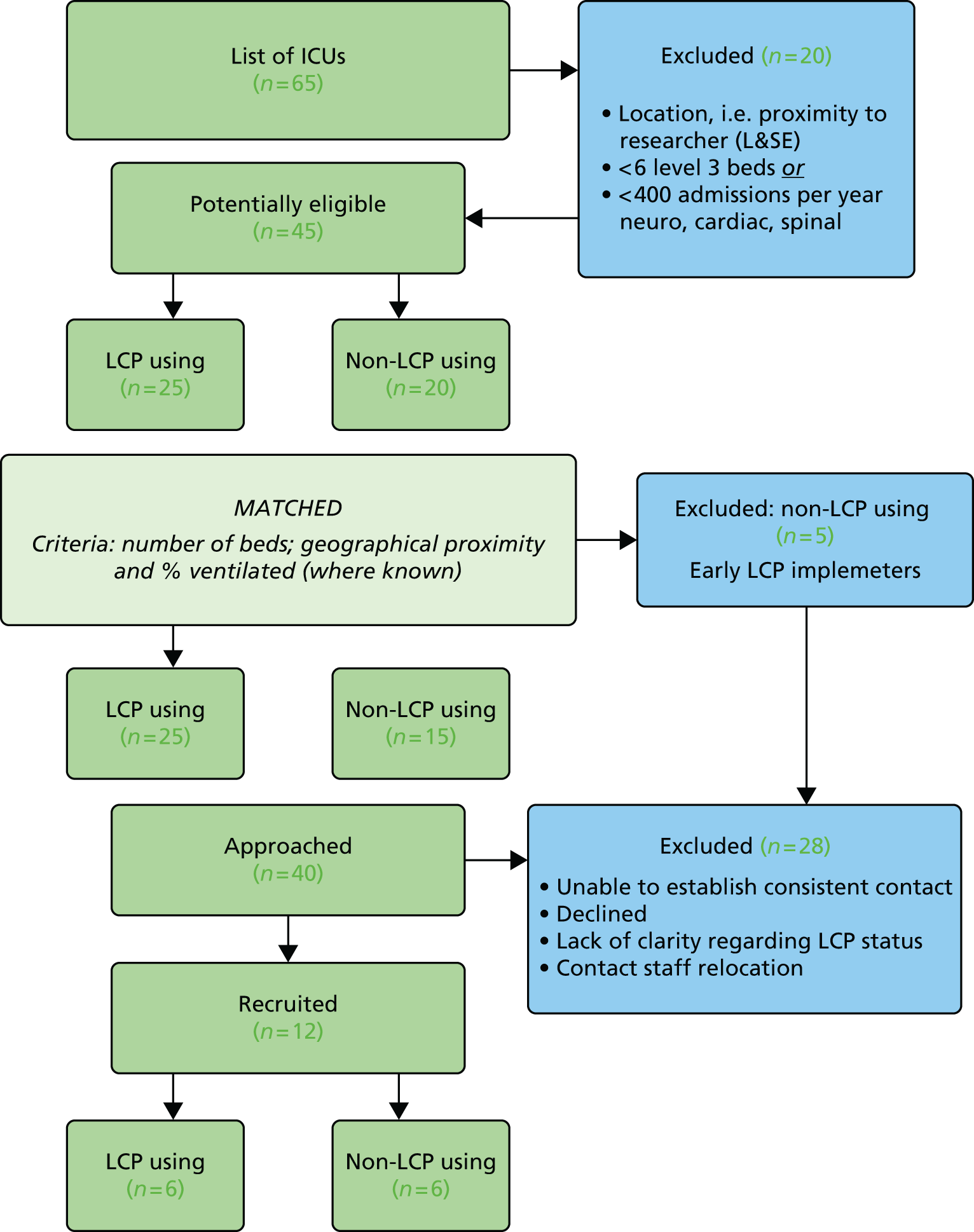
Appendix 9 Nursing home recruitment flow diagram
FIGURE 4.
Nursing home recruitment flow diagram. L&SE, London and the south-east.
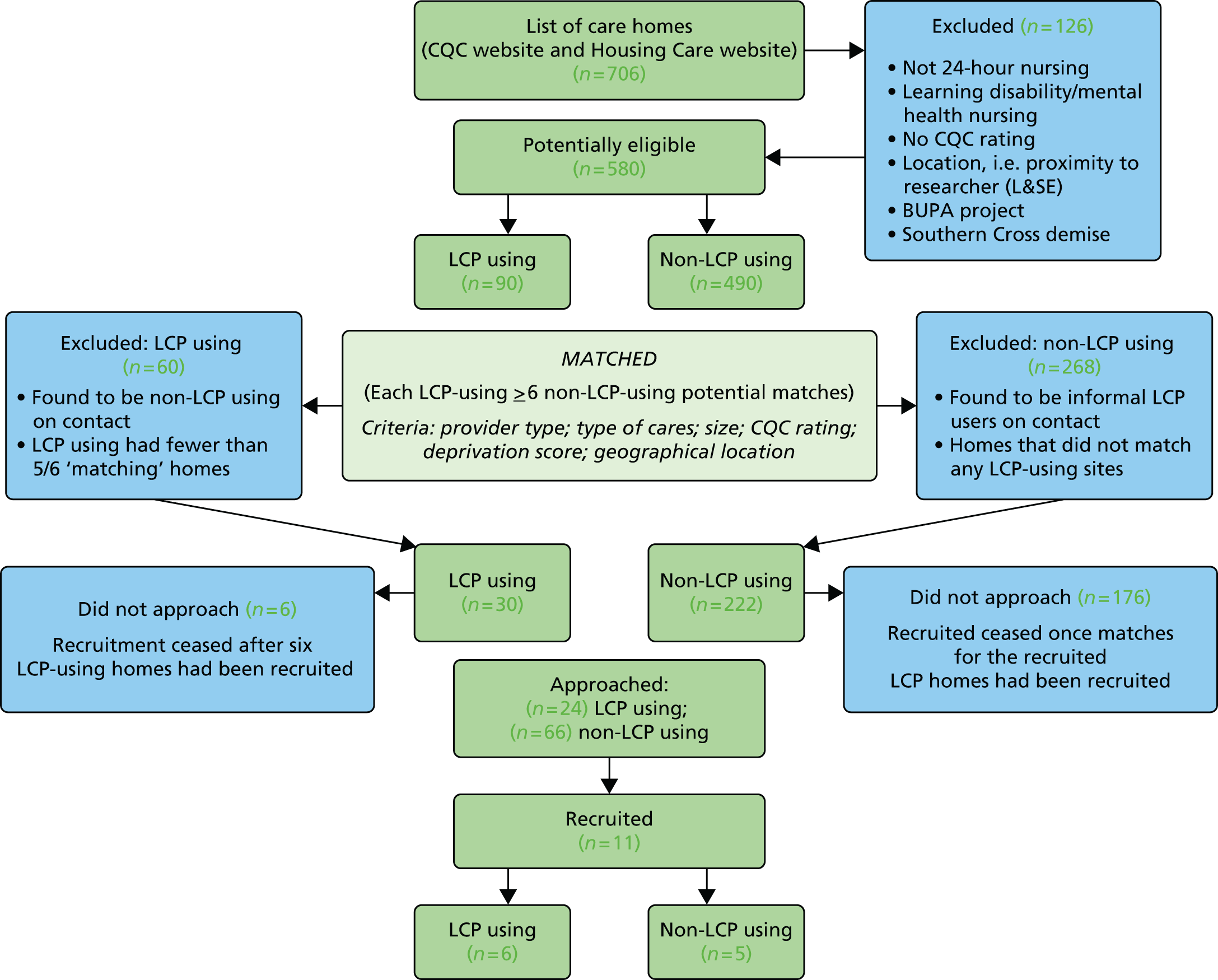
Appendix 10 Introductory letter regarding research: nursing homes and intensive care units
Appendix 11 Level of activity to recruit sites
| Site | Date of first contact | Number of telephone calls | Date of recruitment | Number of visits to site | Comments |
|---|---|---|---|---|---|
| Nursing home (1) | 17 December 2010 | 6 | N/A | 1 | |
| Nursing home (2) | 20 December 2010 | 6 | N/A | – | |
| Nursing home (3) | 20 December 2010 | 4 | N/A | – | |
| Nursing home (4) | 20 December 2010 | 19 | 13 January 2011 | 1 | Site withdrew from the study 27 May 2011 |
| Nursing home (5) | 14 January 2011 | 18 | 27 January 2011 | 1 | No observations offered |
| Nursing home (6) | 14 January 2011 | 10 | N/A | – | |
| Nursing home (7) | 12 April 2011 | 7 | N/A | – | |
| Nursing home (8) | 12 April 2011 | 6 | N/A | 1 | |
| Nursing home (9) | 19 April 2011 | 3 | N/A | – | |
| Nursing home (10) | 19 April 2011 | 10 | N/A | – | |
| Nursing home (11) | 20 April 2011 | 5 | N/A | 1 | |
| Nursing home (12) | 24 May 2011 | 22 | 30 June 2011 | 1 | |
| Nursing home (13) | 24 May 2011 | 16 | N/A | 1 | |
| Nursing home (14) | 24 May 2011 | 20 | 30 June 2011 | 1 | |
| Nursing home (15) | 10 June 2011 | 17 | 26 August 2011 | 1 | |
| Nursing home (16) | 30 June 2011 | 7 | N/A | – | |
| Nursing home (17) | 30 June 2011 | 9 | N/A | – | |
| Nursing home (18) | 7 July 2011 | 8 | N/A | 1 | |
| Nursing home (19) | 8 July 2011 | 4 | N/A | – | |
| Nursing home (20) | 8 July 2011 | 8 | N/A | – | |
| Nursing home (21) | 12 July 2011 | 8 | N/A | 1 | |
| Nursing home (22) | 12 July 2011 | 6 | N/A | 1 | |
| Nursing home (23) | 22 July 2011 | 5 | N/A | – | |
| Nursing home (24) | 30 August 2011 | 10 | N/A | 1 | |
| Nursing home (25) | 1 September 2011 | 9 | 13 October 2011 | 1 | |
| Nursing home (26) | 14 September 2011 | 3 | N/A | – | |
| Nursing home (27) | 14 September 2011 | 3 | 11 October 2011 | 1 | |
| Nursing home (28) | 14 September 2011 | 3 | N/A | 1 | |
| Nursing home (29) | 2 November 2011 | 1 | N/A | – | |
| Nursing home (30) | 2 November 2011 | 1 | N/A | – | |
| Nursing home (31) | 2 November 2011 | 1 | N/A | – | |
| Nursing home (32) | 2 November 2011 | 1 | N/A | – | |
| Nursing home (33) | 30 August 2011 | 10 | 4 October 11 | 1 | |
| Nursing home (34) | 30 August 2011 | 6 | 9 November 2011 | 1 | |
| Nursing home (35) | 12 September 2011 | 9 | N/A | – | |
| Nursing home (36) | 12 September 2011 | 1 | N/A | – | |
| Nursing home (37) | 12 September 2011 | 7 | N/A | 1 | Change of manager |
| Nursing home (38) | 12 September 2011 | 9 | N/A | – | |
| Nursing home (39) | 12 September 2011 | 5 | N/A | – | |
| Nursing home (40) | 12 September 2011 | 5 | N/A | – | |
| Nursing home (41) | 3 October 2011 | 3 | 10 November 2011 | 1 | |
| Nursing home (42) | 3 October 2011 | 5 | N/A | – | |
| Nursing home (43) | 3 October 2011 | 2 | N/A | – | |
| Nursing home (44) | 13 October 2011 | 7 | N/A | 1 | |
| Nursing home (45) | 13 October 2011 | 4 | N/A | 1 | |
| Nursing home (46) | 13 October 2011 | 4 | N/A | – | |
| Nursing home (47) | 13 October 2011 | 4 | N/A | – | |
| Nursing home (48) | 13 October 2011 | 2 | N/A | – | |
| Nursing home (49) | 13 October 2011 | 2 | N/A | – | |
| Nursing home (50) | 13 October 2011 | 1 | N/A | – | |
| Nursing home (51) | 13 October 2011 | 1 | N/A | – | |
| Nursing home (52) | 19 October 2011 | 5 | 6 December 2011 | 1 | |
| Nursing home (53) | 19 October 2011 | 5 | N/A | – | |
| Nursing home (54) | 14 November 2011 | 2 | 21 November 2011 | 1 | |
| Nursing home (55) | 14 November 2011 | 1 | N/A | – | |
| Nursing home (56) | 14 November 2011 | 7 | N/A | 1 | |
| Nursing home (57) | 21 November 2011 | 5 | N/A | – | |
| Nursing home (58) | 25 November 2011 | 1 | N/A | – | |
| Nursing home (59) | 25 November 2011 | 3 | N/A | – | |
| Nursing home (60) | 25 November 2011 | 1 | N/A | – | |
| Nursing home (61) | 25 November 2011 | 1 | N/A | – | |
| Nursing home (62) | 25 November 2011 | 2 | N/A | – | |
| Nursing home (63) | 25 November 2011 | 1 | N/A | – | |
| Nursing home (64) | 2 November 2011 | 1 | N/A | – | |
| Nursing home (65) | 2 November 2011 | 1 | N/A | – | |
| Nursing home (66) | 2 November 2011 | 5 | N/A | – | |
| Nursing home (67) | 2 November 2011 | 5 | N/A | – | |
| Nursing home (68) | 2 November 2011 | 4 | N/A | – | |
| Nursing home (69) | 2 November 2011 | 5 | N/A | – | |
| Nursing home (70) | 2 November 2011 | 1 | N/A | – | |
| Nursing home (71) | 9 November 2012 | 1 | N/A | – | |
| Nursing home (72) | 20 November 2012 | 1 | N/A | – | |
| Nursing home (73) | 20 November 2012 | 1 | N/A | – | |
| Nursing home (74) | 20 November 2012 | 1 | N/A | – | |
| Nursing home (75) | 4 December 2012 | 11 | N/A | – | |
| Nursing home (76) | 4 December 2012 | 6 | N/A | – | |
| Nursing home (77) | 4 December 2012 | 7 | N/A | – | |
| Nursing home (78) | 4 December 2012 | 4 | N/A | – | |
| Nursing home (79) | 4 December 2012 | 2 | N/A | – | |
| Nursing home (80) | 4 December 2012 | 6 | N/A | – | |
| Nursing home (81) | 4 December 2012 | 3 | N/A | – | |
| Nursing home (82) | 4 December 2012 | 4 | N/A | – | |
| Nursing home (83) | 4 December 2012 | 6 | N/A | – | |
| Nursing home (84) | 4 December 2012 | 4 | N/A | – | |
| Nursing home (85) | 4 December 2012 | 1 | N/A | – | |
| Nursing home (86) | 11 December 2012 | 1 | N/A | – | |
| Nursing home (87) | 11 December 2012 | 1 | N/A | – | |
| Nursing home (88) | 11 December 2012 | 1 | N/A | – | |
| Nursing home (89) | 11 December 2012 | 1 | N/A | – | |
| Nursing home (90) | 11 December 2012 | 1 | N/A | – | |
| ICU (1) | 1 February 2011 | 7 | 17 August 2011 | 2 | |
| ICU (2) | 2 March 2011 | 3 | 28 June 2011 | 2 | |
| ICU (3) | 18 March 2011 | 5 | N/A | – | |
| ICU (4) | 11 April 2011 | 4 | 31 August 2011 | – | |
| ICU (5) | 10 March 2011 | 5 | N/A | 1 | |
| ICU (6) | 10 March 2011 | 12 | 22 August 2011 | 2 | |
| ICU (7) | 14 March 2011 | 3 | N/A | – | |
| ICU (8) | 14 March 2011 | 9 | 14 September 2011 | 2 | |
| ICU (9) | 20 April 2011 | 2 | N/A | – | |
| ICU (10) | 20 April 2011 | 2 | N/A | – | |
| ICU (11) | 3 May 2011 | 3 | N/A | 1 | |
| ICU (12) | 14 March 2011 | 1 | N/A | – | |
| ICU (13) | 17 March 2011 | 2 | N/A | 1 | |
| ICU (14) | 17 March 2011 | 1 | N/A | – | |
| ICU (15) | 18 March 2011 | 1 | N/A | – | |
| ICU (16) | 4 April 2011 | 6 | N/A | – | |
| ICU (17) | 18 August 2011 | 9 | 2 November 2011 | 1 | |
| ICU (18) | 23 September 2013 | 4 | N/A | – | |
| ICU (19) | 19 October 2011 | 5 | 21 November 2011 | 1 | |
| ICU (20) | 6 April 2011 | 13 | N/A | – | |
| ICU (21) | 23 September 2011 | 9 | N/A | – | |
| ICU (22) | 2 November 2011 | 3 | N/A | – | |
| ICU (23) | 2 November 2011 | 1 | N/A | – | |
| ICU (24) | 4 April 2011 | 3 | N/A | – | |
| ICU (25) | 24 June 2011 | 8 | 13 September 2011 | 1 | |
| ICU (26) | 4 April 2011 | 1 | N/A | – | |
| ICU (27) | 29 March 2011 | 9 | N/A | 2 | |
| ICU (28) | 29 March 2011 | 2 | N/A | – | |
| ICU (29) | 20 July 2011 | 5 | N/A | 1 | |
| ICU (30) | 18 August 2011 | 1 | N/A | – | |
| ICU (31) | 29 March 2011 | 18 | 9 June 2011 | 2 | |
| ICU (32) | 29 March 2011 | 9 | 6 December 2011 | 1 | |
| ICU (33) | 4 April 2011 | 8 | 24 August 2011 | 2 | |
| ICU (34) | 4 April 2011 | 1 | N/A | – | |
| ICU (35) | 29 March 2011 | 2 | N/A | – | |
| ICU (36) | 31 August 2011 | 2 | N/A | – | |
| ICU (37) | 29 March 2011 | 2 | N/A | – | |
| ICU (38) | 6 April 2011 | 1 | N/A | – | |
| ICU (39) | 6 April 2011 | 1 | N/A | – | |
| ICU (40) | 6 April 2011 | 3 | N/A | – |
Appendix 12 Retrospective case note analysis form (first version)
Appendix 13 Retrospective case note analysis form (final version)
Appendix 14 Staff point 1 interviews: information and consent
Appendix 15 Topic guide point 1 interviews with staff
Appendix 16 Suboptimal care process
Appendix 17 Lone worker policy: fieldwork code of practice
Health and Community Care Research Unit (HaCCRU)
Community Visiting/Fieldwork Divisional Safety Code
Health and safety are an integral part of the duties of all members of staff, for which they are held accountable at all levels. Staff should be encouraged to regard good safety practice as the norm, and to help in establishing and observing high standards of health and safety.
For the purpose of this document, Community Visiting or fieldwork are defined as any field or survey work carried out by staff of the Health and Community Care research Unit for the purpose of teaching and/or research in places which are not under University control, but where the University is responsible for the safety of its staff and/or students and others exposed to their activities. These procedures are concerned with protecting the personal safety of staff in relation to the unlikely event of an attack on them during fieldwork. The safety of all researchers is paramount. If at any stage during fieldwork the researcher feels threatened, they should act on their instincts, and if necessary abandon an interview or meeting in the most appropriate way.
This departmental safety code for community visiting/fieldwork constitutes a generic risk assessment of the main risks whilst carrying out community visiting/fieldwork. Provided the precautions specified in this code are followed, risks will be adequately controlled to a low, or very low level. However, neglecting them may result in significant risk of injury or ill health.
All fieldwork requires risk assessment. There must be a separate risk assessment for each Research Project. Those preparing proposals for research projects should prepare a risk assessment together with the proposal, so that it can be established at the planning stage that all research projects have been risk assessed.
Individuals doing such work need to ensure that risks are assessed and appropriate precautions taken. These should always include the precaution that people doing such work should inform either a colleague or the departmental office of the areas/addresses being visited. In addition, following risk assessment, appropriate precautions from among those listed on the form should be selected. Either working in pairs or regularly reporting back should be the norm. A risk assessment proforma for community visiting is attached.
There must always be at least two fieldwork supervisors, of which at least one must be a member of staff, with adequate, clear deputising arrangements. Fieldwork guidance can be found in the UCEA Code (www.liv.ac.uk/intranet/safety/codes_of_practice).
Field workers should be aware that the University does not carry any special insurance cover specifically for field/community work. Individuals can choose to take out additional personal insurance if they wish.
Appendix 18 Generic information about the study
The impact of the Liverpool Care Pathway on end-of-life care
The last days or hours of a person’s life can be an emotional and sometimes anxious time for the person themselves and their relatives and friends. The quality of care provided at this time can impact on patient comfort and have important and lasting effects on the emotional well-being of those left behind.
The Liverpool Care Pathway (LCP) was developed to provide health-care professionals with a guide for ‘good practice’ at this time, to enhance the physical, emotional and spiritual well-being of patients and their relatives/friends. Although the LCP is now used widely in organisations such as this, we still do not know exactly how it is used and what impact it has on the quality of care provided.
A research study that is aiming to find out how the LCP is used and what impact it has on the quality of care delivered in the final days or hours of a person’s life is currently being undertaken in this [unit/home]. The research will involve asking patients (where appropriate and possible) and their relatives for permission to observe care as it is delivered and to talk to relatives after the death of the patient about their views on the way their loved one was cared for.
We understand that asking people if they would be happy for a researcher to observe care at a time when they may be trying to come to terms with the news that the end of life is near may be very distressing. We are bringing this research to the attention of everyone who is admitted to this [Intensive Care Unit/Nursing Home] in the hope that people can have time to think about whether they would wish to be involved in the research if it becomes appropriate for them and to give them the opportunity to make their wishes known to those caring for them.
Please let us know if you would like further information or you would like to talk to someone about this study. Please also let us know if you would prefer not to be approached at any time in the future to be part of this research.
Appendix 19 Patient information and consent
Appendix 20 Consultee information and consent
Appendix 21 Relative information and consent
Appendix 22 Staff point 2 interviews: information and consent
Appendix 23 Log of referrals that were made to the researchers but that did not result in observations
| Category | Number | |
|---|---|---|
| Researcher unavailable | 29 | |
| Undertaking data collection at another site | 16 | |
| On annual leave | 6 | |
| On other study business | 7 | |
| Patient died unexpectedly quickly | 18 | |
| Relative declined either to speak to the researcher or to enter the study | 25 | |
| No relatives/IMCA present (and patient lacked capacity) | 5 | |
| Patient did not meet inclusion criteria | 24 | |
| ICU: not level 3 care | 8 | |
| Being transferred out/condition improved | 6 | |
| Burns unit | 1 | |
| Organ donation | 3 | |
| Withdrawal of treatment not commenced | 1 | |
| Nursing home: transferred to hospital | 5 | |
| Staff decision | 8 | |
| Relatives likely to be too upset/too difficult | 5 | |
| Junior staff member not confident to contact researcher | 1 | |
| Other | 2 | |
| Researcher declined | 24 | |
| Preparatory work in site not complete | 2 | |
| Late referral/not enough time to get to patient | 18 | |
| Lack of clarity regarding gaining consent | 3 | |
| Other | 1 | |
| Total | 133 |
Appendix 24 Relative information and consent (amended for one site)
Appendix 25 Staff point 2 interview topic guide
Draft topic guide
The interview will be based on the observations made by the researcher and will focus specifically on the following themes:
-
Can you describe the care that you personally provided for the patient and their relatives/friends?
-
What, in your opinion, worked well and why?
-
What, in your opinion, could have been done better and why?
-
How typical is this death of the way in which patients die in this setting?
-
Do you have anything further you would wish to add?
Appendix 26 Staff point 2 interviews: information and consent
Appendix 27 Bereaved relative interview topic guide
Draft topic guide
1. Can you describe the last hours or days of life of your relative/friend as you experienced it at the bedside?
-
General description – environment, sounds, smells, general perceptions.
-
What went well?
-
What could have gone better?
2. Can you tell me anything about the following:
-
your relative/friend‘s comfort – physical/emotional
-
your relative/friend’s dignity
-
the way in which staff delivered care
-
your relative/friend’s and/or you own understanding of what was going on
-
the way that staff spoke to you and your relative/friend
-
the way that staff involved you and your relative/friend in decisions about the care
-
what happened immediately after your relative/friend died?
3. Is there anything else you would like to add about the care delivered to your relative/friend in the last hours or days of their life and the care provided to you and others at the bedside?
4. How did you feel about the researcher being present in the room during the last hours or days of your friend/relative’s life?
Appendix 28 Bereaved relative 2: information and consent
Appendix 29 Economic costing workings
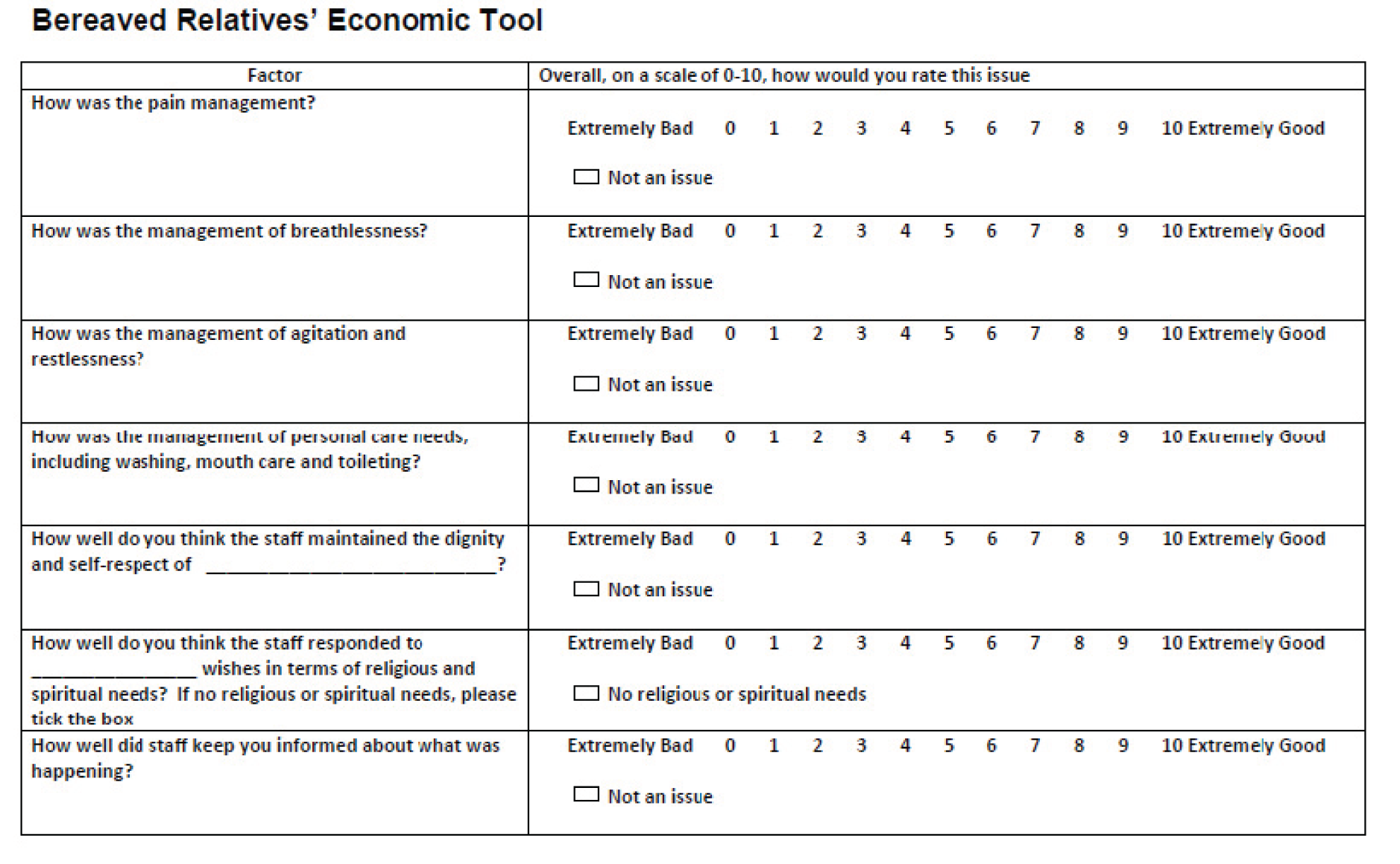
Drug costs
Hyoscine (non-proprietary): prescription-only medicines138
Injection, hyoscine hydrobromide 400 mg/ml, net price 1-ml ampoule = £4.12; 600 mg/ml, 1-ml ampoule = £2.53 (www.medicinescomplete.com/mc/bnf/current/PHP8558-hyoscine-non-proprietary.htm).
Midazolam (non-proprietary): controlled drugs schedule 3138
Injection, midazolam (as hydrochloride) 1 mg/ml, net price 2-ml ampoule = £0.50, 5-ml ampoule = £0.60, 50-ml vial = £7.87; 2 mg/ml, 5-ml ampoule = £0.65; 5 mg/ml, 2-ml ampoule = £0.58, 10-ml ampoule = £2.50.
Morphine sulfate (non-proprietary): controlled drugs schedule 2138
Injection, morphine sulfate 10, 15, 20, and 30 mg/ml, net price 1- and 2-ml ampoule (all) = £0.72–1.40.
Intravenous infusion, morphine sulfate 1 mg/ml, net price 50-ml vial = £5.00; 2 mg/ml, 50-ml vial = £5.89.
Sodium chloride intravenous infusion (non-proprietary): prescription-only medicines138
Intravenous infusion, usual strength sodium chloride 0.9% (9 g, 150 mmol/l each of Na+ and Cl-), this strength being supplied when normal saline for injection is requested. Net price 2-ml ampoule = £0.21; 5-ml ampoule = £0.29; 10-ml ampoule = £0.34p; 20-ml ampoule = £1.04; 50-ml ampoule = £4.27.
Hypromellose (non-proprietary)
Eye drops, hypromellose 0.3%, net price 10 ml = £1.39.
Hyoscine (non-proprietary): prescription-only medicines138
Injection, hyoscine hydrobromide 400 mg/ml, net price 1-ml ampoule = £4.12; 600 mg/ml, 1-ml ampoule = £2.53.
E45® Itch Relief Cream (Reckitt Benckiser)
Cream, urea 5%, macrogol lauryl ether 3%, net price 50 g = £2.55, 100 g = £3.47, 500-g pump pack = £14.99.
Mouthwash solution tablets
Consist of tablets which may contain antimicrobial, colouring and flavouring agents in a suitable soluble effervescent base to make a mouthwash suitable for dental purposes. Net price 100-tablet pack = £15.09.
Furosemide (non-proprietary): prescription-only medicines138
Tablets, furosemide 20 mg, net price 28 = £0.80; 40 mg, 28 = £0.73; 500 mg, 28 = £4.22.
£0.80/28 tablets = £0.029 per tablet.
Ranitidine (non-proprietary): prescription-only medicines138
Tablets, ranitidine (as hydrochloride) 150 mg, net price 60-tablet pack = £1.48; 300 mg, 30-tablet pack = £1.57.
1.48/60 tablets = £0.025 per tablet.
Spironolactone (non-proprietary): prescription-only medicines138
Tablets, spironolactone 25 mg, net price 28 = £1.43; 50 mg, 28 = £2.15; 100 mg, 28 = £2.32. Label: 21.
£2.15/28 tablets = £0.077.
Salbutamol (non-proprietary): prescription-only medicines138
Aerosol inhalation, salbutamol (as sulfate) 100 mg/metered inhalation, net price 200-dose unit = £1.50. Counselling, administration.
Brands include AirSalb® and Salamol®.
Nebuliser solution, salbutamol (as sulfate) 1 mg/ml, net price 20 × 2.5 ml (2.5 mg) = £1.91; 2 mg/ml, 20 × 2.5 ml (5 mg) = £3.82. May be diluted with sterile sodium chloride 0.9%.
Sudocrem® (Forest)
Cream, benzyl alcohol 0.39%, benzyl benzoate 1.01%, benzyl cinnamate 0.15%, hydrous wool fat (hypoallergenic lanolin) 4%, zinc oxide 15.25%, net price 60 g = £1.38, 125 g = £2.00, 250 g = £3.35, 400 g = £4.71.
Staff costs
Porter salary
NHS band 2 – point 1 – £14,294 (www.nhscareers.nhs.uk/working-in-the-nhs/pay-and-benefits/agenda-for-change-pay-rates/).
Based on NHS Business Services Authority: www.nhsbsa.nhs.uk/Documents/NHSBSACorporatePoliciesandProcedures/Annual_Leave_Policy.pdf
Based on a working week of 37.5 hours for 39 weeks per year so 7.5 hours per day.
£366.51 per week → £73.30 per day → £9.77 per hour → £0.162 per minute.
Auxiliary nurse/health-care assistant/carer
Nursing health-care assistants usually work a 37.5-hour week on a shift or rota system, typically including nights and weekends. Part-time and flexible working is often available.
Under NHS Agenda for Change, health-care assistants are on the band 2 salary scale. From April 2012 this ranged from £14,153 to £17,253 per year. For the purpose of this study we have put health-care assistants on the start of band 2 – given a working week of 37.5 hours for 39 weeks per year so 7.5 hours per day.
£366.51 per week → £73.30 per day → £9.77 per hour → 0.162 per minute.
www.hospitaldr.co.uk/guidance/nurses-and-nhs-managers-pay-scales-for-20122013
www.sammons.co.uk/uploads/File/Healthcare/2011/Jan/Sammons%20Healthcare%20Salary%20Survey%202010.pdf
Healthcare Salary Survey: March 2010
NHS band 6 – point 21 – £25,783 – given a working week of 37.5 hours for 39 weeks per year so 7.5 hours per day then £88.15 per day so £11.75 per hour and £0.196 per minute.
Nursing home sister
Cost at PSSRU78 rates for a nurse team leader with patient contact at £2.03 per hour.
| Nurse cost table | Per hour general | Per minute general | Per hour with patient contact | Per minute with patient contact |
|---|---|---|---|---|
| Nurse day ward/24 hours | 40 | 0.67 | 97 | 1.62 |
| Nurse team manager | 58 | 0.97 | 142 | 2.37 |
| Nurse team leader | 50 | 0.83 | 122 | 2.03 |
| Consultant doctor | 162 | 2.70 |
‘After-School’ helper
Corporate report. National minimum wage: government response to the Low Pay Commission’s 2013 report.
Minimum wage 16- and 17-year-olds – £3.68 per hour.
Per minute £0.061.
Nursing home manager
Cost at the PSSRU78 rate for a nurse team manager with patient contact at £2.37 per hour.
Resource use
Swabsticks
Lemon/blackcurrant glycerin swabsticks: price £3.89 (www.psuk.co.uk/polo/products/lemon_blackcurrant_glycerin_swabsticks/).
Lemon glycerin or blackcurrant glycerin swabstick for quantity: 25 × 3.
Hence £0.16 per 1 × 3 pack.
Gloves
Prestige (Performer) Sterile Soft Vinyl Powder-Free Exam Gloves × 50 pairs (www.midmeds.co.uk).
£11.99 (excluding VAT); £14.39 (including VAT); so one pair (including VAT) = £0.29.
Incontinence underpads
75 cm × 57 cm 5-ply × 100.
£17.99 (excluding VAT); £21.59 (including VAT); so £0.22 for one pad.
Appendix 30 Observations: example of timings for economic costings in case study sites
North
NIA6: north intensive care unit Liverpool Care Pathway-using site
| Time | Action (observation notes) | Action (summary) | Action (drug charts) | Dose | Elements to cost | Costs (£) | Total cost for actions (£) |
|---|---|---|---|---|---|---|---|
| 18.40 | Observation start time | ||||||
| 18.45 | M, Pt is conscious with [what looks like] a Ryles tube in her left nostril | Ryles tube inserted | Nurse time (9 minutes) | 1.62 × 9 = 14.58 | 14.58 | ||
| 18.50 | AW comes in and says ‘I’m just going to give you something to help your breathing’. S/N says ‘I’ll just get her a drink’, to the relatives | Injection given | Hyoscine hydrobromide | 400 mg/i.v. | Injection, drug Nurse time (3 minutes) |
4.12 – Hyoscine hydrobromide 1.62 × 3 = 4.86 nursing time |
8.98 |
| 19.00 | S/N brings a plastic cup of water and a straw in and gives it to the Brother . . . She then comes round the bed to see father (man in front of me) and crouches down by him and says to him and the rest of the relatives, that she is going to get them a room and a key so they have a place to rest if need be. Husband says ‘Thanks A’, and she leaves the curtains at 19.05hrs | Nurse gives family a room to sleep in | Nurse time (5 minutes) | 0.67 × 5 = 3.35 | 3.35 | ||
| 19.40 | AW comes in with the new nurse and introduces her to the family | New nurse is introduced to the family | Nurse time (3 minutes) | 0.67 × 3 = 2.01 | 2.01 | ||
| 20.00 | S/N AW comes in . . . says her BP has dropped now so it may not be long | Nurse observes BP | Nurse time (4 minutes) | 0.67 × 4 = 2.68 | 2.68 | ||
| 20.15 | Pt is about to start on the LCP now, since Policy is to wait 2hrs after withdrawal, and Dr has signed it now. S/N F will start the nursing bits off now | Patient started on LCP now – tubes, etc., removed | Nurse time (4 minutes), doctor signed LCP (3 minutes) | 1.62 × 4 = 6.48 3 × 2.70 = 8.10 |
14.58 | ||
| 20.20 | S/N F comes in with an injection and says ‘I’m just going to give her something for her breathing’ . . . S/N F gives the injection slowly into a central line in Pt’s neck, on the right side and gives her a bit of suctioning. She is gentle and explains what she is doing to the Pt. She repositions Pt’s head on the pillow and leaves. [takes her about 20 mins] | Given injection for breathing | Midazolam | 2.5mg/i.v. | Nurse time (20 minutes), injection | 1.62 × 20 = 32.40 nurse time 0.65 for 5-ml ampoule of midazolam |
33.05 |
| 20.30 | F comes in and explains she’s already had something for secretions. I think she says she’ll check if she can have anything else, but I can’t hear very clearly as F speaks very low – she leaves | Nurse says pt given something for secretions | Nurse time (2 minutes) | 0.67 × 2 = 1.34 | 1.34 | ||
| 20.35 | D picks up an oral sponge and wipes Pt’s mouth | D (relative) wipes patient’s mouth with oral sponge | Mouth swab cost | 0.16 per 1 × 3 pack | 0.16 | ||
| 20.35 | There is a monitor above my head and slightly to my right but I can’t see if it’s on from my angle | Monitor mentioned in family room | Nurse observation (1 minute) | 0.67 | 0.67 | ||
| 21.50 | S/N F mops Pt’s mouth with a tissue. . . . still in purple latex gloves | S/N F mops Pt’s mouth with a tissue | Nurse time (4 minutes), gloves | 1.62 × 4 = 6.48 0.29 gloves |
6.77 | ||
| 21.56 | S/N F comes in with fresh mouth sponges and gives oral care saying to Pt ‘Just washing your mouth so it tastes a bit better’ | S/N F comes in with fresh mouth sponges and gives oral care | Nurse time (2 minutes) Mouth sponge |
1.62 × 2 = 3.24 0.16 |
3.40 | ||
| 22.00 | Brother comes out from the curtains and S/N F speaks to him . . . she comes back to the station where I am, and gives him a bereavement leaflet and he heads off to the relatives room | Nurse spends time with relatives | Nurse time (5 minutes) | 0.67 × 5 = 3.35 | 3.35 | ||
| 22.31 | The Dr comes to verify the death. I watch him through a chink in the curtains, listen to her chest with his stethoscope, checks pupil reactions with the light from a ophthalmoscope and feel for a pulse at the wrist. He signs the verification form [now he has come from the bedside to the staff station] | Dr certifying patient death | Doctor time (15 minutes) | 2.70 × 15 = 40.50 | 40.50 | ||
| 22.50 | I follow Night Sr D to the bedside and there is a male S/N there. Night Sr lays Pt’s bed straight and tries to close the body’s eyes with her fingers. They drift back half open . . . I watch Night Sr and Night S/N lay the body out . . . Night Sr removes the catheter and tells body what she is doing – she says ‘we are just going to give you a bit of a freshen up, alright’. Male S/N starts to wash the body, quick and efficient with a light touch. Night Sr puts bungs in the remaining lines and clamps them off. They each wash one side of the body and cover up bits that they have done with the top sheet. They put a paper shroud on her. F comes to help and they roll the body on her side and F washes her back and bottom, Night Sr combs her hair . . . F puts on a large incontinence sheet next to the body whilst the other two hold the body on her side and then they work the plastic/paper white body bag underneath. Two dressings on the front shins of the patient are left in place | Three staff members clean and dress the patient ready to be taken | Night sister time (21 minutes), S/N time (18 minutes), S/N F Time (9 minutes) | 1.62 × 48 = 77.76 | 77.76 | ||
| 23.20 | Shroud is on and she is in the body bag . . . They put another ID band on her right leg with name and her hospital number on it | Prepare patient ready to be taken by porters | Nurse time (4 minutes) | 1.62 × 4 = 6.48 | 6.48 | ||
| 23.30 | Porters come for the body | Porters arrive to take body | Porter × 2 (7 minutes) | 0.162 × 14 = 2.27 | 2.27 | ||
| 21.50 | Time of death |
Glossary
- Continuing care scheme
- NHS continuing health care is free care outside hospital that is arranged and funded by the NHS. It is available only for people who need ongoing health care and meet the eligibility criteria (definition from NHS Choices: www.nhs.uk/CarersDirect/guide/practicalsupport/Pages/NHSContinuingCare.aspx, accessed 15 June 2014).
- Level 3 care
- Patients requiring advanced respiratory support alone or basic respiratory support together with support of at least two organ systems. This level includes all complex patients requiring support for multiorgan failure (reproduced under the terms of the Open Government Licence from Department of Health. Comprehensive Critical Care: A Review of Adult Critical Care Services. London: Department of Health; 2000).
- Not for active treatment
- Phrase used here for simplicity. In the section on withdrawal it becomes clear that a decision that a patient should not receive active treatment does not rule out the provision of a number of activities that elsewhere might be interpreted as active treatment, for example feeding, antibiotic administration and some tests and investigations.
List of abbreviations
- A&E
- accident and emergency
- ACP
- advance care planning
- CNAF
- case note analysis form
- COPD
- chronic obstructive pulmonary disease
- CPAP
- continuous positive air pressure
- CQC
- Care Quality Commission
- DNACPR
- do not attempt cardiopulmonary resuscitation
- DNAR
- do not attempt resuscitation
- GP
- general practitioner
- GSF
- Gold Standards Framework
- ICU
- intensive care unit
- IMCA
- Independent Mental Capacity Advocate
- ITU
- intensive therapy unit – used interchangeably with ICU
- i.v.
- intravenous
- LCP
- Liverpool Care Pathway for the Dying Patient
- MCPCIL
- Marie Curie Palliative Care Institute Liverpool
- MDT
- multidisciplinary team
- NG
- nasogastric
- NIC
- nurse in charge
- NMC
- Nursing and Midwifery Council
- PCT
- primary care trust
- prn
- pro re nata
- PSSRU
- Personal Social Services Research Unit
- QALY
- quality-adjusted life-year
- QODD
- Quality of Dying and Death
- R&D
- research and development
- SHA
- Strategic Health Authority
- SNOD
- specialist nurse for organ donation
- TLC
- tender loving care