Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 13/114/37. The contractual start date was in May 2015. The final report began editorial review in March 2016 and was accepted for publication in June 2016. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2017. This work was produced by Morrissey et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction and background
People with intellectual and other types of developmental disabilities (IDD), such as autistic spectrum conditions, can face challenges with both adaptive behaviour and general intellectual functioning. As long-stay hospitals for those with IDD were closed from the 1980s onwards, forensic mental health services specifically for those with IDD have increased. These hospital services cater either for people with IDD who have committed criminal acts and are detained under Part III of the Mental Health Act,1 or for those under civil sections whose violent or other challenging behaviour cannot be safely managed in the community. Typically, such patients present with a high level of clinical complexity.
A mapping exercise in 20122 indicated that in the combined NHS and independent sector there were 2393 high, medium and low secure funded beds in 10 strategic health authorities in England, with further access to locked and unlocked forensic rehabilitation beds. In addition, a number of specialised community IDD services provide for those with a forensic history. Inpatient secure beds in particular are high cost, and this is therefore a sector that involves high levels of health expenditure (estimated in 2012 to be £350–430M a year).
Within what we shall henceforth label as the forensic intellectual and developmental disabilities (FIDD) sector, it is notable that there is limited cross-service collation of empirical information on treatment and service outcomes, which in turn limits the ability to measure service effectiveness. 2 This area of service delivery is particularly pertinent in the context of the Department of Health’s Transforming Care programme,3 which aims to move care for people with IDD – including those who have offended – from hospitals to the community with the ultimate aim of closing many hospital beds (indeed, occupied secure beds have already reduced compared with 2012 figures). 3 There is a need to be able to accurately describe the outcomes nationally both for people treated within FIDD services and, in the longer term, those who are discharged from FIDD services, but this is not currently undertaken in a systematic way.
The Clinical Research Group in FIDD funded by the then Mental Health Research Network branch of the National Institute for Health Research (NIHR), which included the authors, considered the research needs in this area in 2013. As a starting point, we know that there are no agreed areas of outcome domains or routine measures employed in this sector. No systematic review has been published in relation to outcomes or outcome measures from such services and, therefore, little is known about the commonality of outcome measures across services. Neither outcome measures developed for mainstream mental health services (explored in a systematic review by Gilbody et al. )4 nor those developed for mainstream forensic services (identified in a systematic review by Fitzpatrick et al. ,5 are necessarily appropriate for FIDD services. The current project therefore aimed to begin to address this existing gap in knowledge by conducting a preliminary study suitable for informing a future primary research project on FIDD service outcomes.
Research group
The research steering group comprised academic and clinical experts in the FIDD field, a systematic review expert, a methodology expert and an ‘expert by experience’ (see Acknowledgements). The group met for two full-day meetings during the project.
Aims of the research
The aims of the research were:
-
To systematically review empirical studies that relate to short- and long-term outcomes from FIDD services including secure, forensic rehabilitation and community forensic services. The review aimed specifically to synthesise the range of outcome domains studied and to identify specific measures that have been employed.
-
To consult a group of FIDD patients/carers regarding the outcome domains of most relevance to these groups of stakeholders.
-
To obtain consensus on appropriate outcome domains and measures for FIDD services based on the expert opinions of professionals and providers.
-
To synthesise the findings and develop a framework of outcomes in order to inform a large-scale primary research project.
Overview of design
The preliminary study needed to examine the evidence from a range of perspectives and, therefore, three stages were planned. The first study was a systematic review and evidence synthesis of outcome domains and measures as found within the FIDD literature. The second was a consultation exercise with FIDD patients and carers and the third was a clinician and expert modified Delphi consensus exercise. The planned timescale of the research was short: May 2015 to February 2016.
This report
This report is divided into four further substantive chapters. Chapter 2 summarises the systematic review and evidence synthesis, which addresses aim 1. Chapter 3 describes the patient and carer consultation, which addresses aim 2. Chapter 4 describes the Delphi study of clinicians, which addresses aim 3. Chapter 5 synthesises the studies and describes the direction for further research and evaluation of services.
Note on terminology
In this report ‘outcome domains’ or ‘subdomains’ refer to specific areas of outcome. These are distinct from outcome ‘measurements/indices’, which refer to how these domains are indexed or measured. Thus, for example, within the patient experience superordinate domain, patient satisfaction would be an outcome subdomain and a patient satisfaction rating scale assessment would be an outcome measure for that domain, whereas the percentage of patients ‘very satisfied’ might be a specific indicator.
Chapter 2 Stage 1: systematic literature review of outcome domains researched in forensic intellectual/developmental disabilities services
Research questions/objectives of the review
The objective of the current review was to identify quantitative studies that examined either short- or long-term outcomes from FIDD service-level treatment. The review sought specifically to identify and categorise the range and type of outcome domains examined in the literature as well as the outcome measures and indicators used to measure these domains. The findings from the studies themselves were therefore not of direct relevance to this review.
Review methods
Search strategy
The search strategy aimed to identify studies from a range of sources. Reports were included regardless of publication status. Searches were conducted on 1 June 2015. The electronic databases searched were MEDLINE, PsycINFO, EMBASE, Allied and Complementary Medicine, Health Management Information Consortium, the British Nursing Index and the Cumulative Index to Nursing and Allied Health Literature from inception to May 2015. A broad search strategy was employed, with intellectual disability terms being combined with forensic terms. For terms specific to intellectual and developmental disabilities, search terms employed were based on those used for a previous Cochrane review. 6 Forensic and offender terms search terms were adapted from a large review for the Department of Health by Duggan et al. 7 The full search terms including ‘explode’ terms, keywords and text words are in Appendix 1.
In addition, the grey literature (opengrey.eu) was searched online on the same date using the same keywords. References of suitable studies were examined to identify additional relevant articles. Finally, expert members of the project steering group were consulted in order to identify any key references not retrieved by the search strategy or in press or unpublished articles and service evaluation reports.
Inclusion and exclusion criteria
Scope
The search related to studies worldwide written in any language. When studies were written in languages other than English, translations were obtained. The search was limited to studies from 1980 onwards, as provision for FIDD patients was either sparse or non-existent prior to this date.
Types of studies
We included any study design, including those at the lower levels of the hierarchy of evidence. Owing to the likely paucity of randomised or controlled studies, the search strategy was designed to capture two primary types of quantitative study:
-
Cohort studies with follow-up. These are studies that report outcomes of intervention at the whole service level from one point in treatment to another (e.g. from admission to present; from admission to discharge) or post discharge, with any length of follow-up.
-
Cross-sectional studies. We also aimed to include cross-sectional studies that reported outcomes either at a single point or for a defined period of time during FIDD service intervention. While the primary goal of such studies is not necessarily to evaluate outcomes from services, studies were included provided they presented data on potential measures or indicators of outcomes. For example, the purpose of the study might be prediction of risk, but outcome data pertaining to ‘incidents of aggression’ in the service may be presented: this was considered to be a potential outcome domain/indicator. This type of study was included within the review for two reasons. First, the aim of the review was to identify outcome domains and outcome indicators appropriate for measuring the effectiveness of FIDD services; the cross-sectional studies provided important information in this regard. Second, FIDD services often provide long-term treatment and, therefore, what happens to patients during treatment and prior to discharge can also be considered an indicator of effectiveness.
Participants and settings
The search strategy sought to capture studies that included data on adults (aged ≥ 18 years) with intellectual and/or developmental disabilities who had current or previous access to specialist FIDD services. Both male and female samples, with a range of offending histories, were included. High-, medium- and low secure inpatient forensic health services, forensic rehabilitation services (service categories 1 and 4 as defined by the Royal College of Psychiatrists, 20132) and community FIDD services were all included. Studies of prison and youth offending services were not considered for this review, as services specifically for people with IDD tend not to exist in these settings. Studies of mixed FIDD and non-FIDD populations were included provided the FIDD data were identifiable.
Intervention
The intervention of interest was at the whole service level, that is, the effect that being treated in the service as a whole has on patients’ outcomes and how that is measured. Studies that evaluated the effects of specific interventions (e.g. sex offender treatment) were excluded. The outcome domains and indicators/measures of such domains were of primary interest, as opposed to the findings of the studies.
Outcomes
There are as yet no agreed outcome measures for use in FIDD services, which was a primary driver for the review. Therefore, inclusive criteria regarding the types of outcomes of interest were adopted. Outcomes were nevertheless broadly conceptualised as falling into the following three overarching domains, reflecting the three key quality areas outlined by the Department of Health in the first NHS Outcomes Framework. 8
Effectiveness
This domain was conceptualised to include any factors that related to the impact of FIDD service-level treatment on the patient, in both the long and short term.
Patient safety
In the current context, the patient safety domain was conceptualised to include outcomes related to avoidable harm such as the extent of restrictive practices in services, and patient injury or death.
Patient experience
This domain was conceptualised to include any factors that related to the patient experience of care, such as patient quality of life, patient satisfaction, etc.
Inclusion and exclusion criteria are summarised in Appendix 2.
Study selection
After removal of duplicates, titles and abstracts of articles were screened against the inclusion criteria. In order to avoid false negatives, all studies that could not be shown to be outside the inclusion criteria were initially included. The full texts of the remaining articles were screened against inclusion and exclusion criteria in order to identify appropriate articles for the review. Two reviewers (CM and NG) independently rated each article using a screening tool developed for the purposes of the study (see Appendix 3). Any disagreements were resolved by a third reviewer (MF).
Data extraction
The articles were subjected to data extraction using a structured form (see Appendix 3). Details regarding the sample, design, service type, methods, outcome domains and related measures were obtained, coded and reported. The information is presented in the form of data summary tables (see Tables 1–6).
Hierarchy of evidence
On the advice of the systematic review consultant on the project, it was decided a priori that no structured quality assessment was to be undertaken. This decision was taken for a number of reasons. First, as noted above, the aim of the current review was to identify the range and type of outcome domains and related measures that have been used in FIDD services research. Its purpose was not to critique the methodology of the studies or to draw robust conclusions about the findings. Furthermore, it was recognised the studies were likely to be heterogeneous and there would be no single quality assessment tool that would be appropriate for included studies. Quality or risk-of-bias ratings would not have influenced the inclusion of studies as, arguably, a poor-quality study could nevertheless have presented outcome domains of interest for the review. We therefore decided simply to code study design using a hierarchy of evidence. The York Centre for Reviews and Dissemination hierarchy of evidence was considered, but it was found that included studies were difficult to classify using that hierarchy. Instead, study designs were coded with reference to the simpler hierarchy of evidence employed by Greenhalgh9 as follows:
-
systematic reviews and meta-analyses
-
randomised controlled trials with definitive results
-
randomised controlled trials with non-definitive results
-
cohort studies (follow participants over time)
-
case–control studies (matched control group)
-
cross-sectional surveys
-
case reports or case series.
Analysis
The broad inclusion criteria applied for the review meant that the included studies represented a wide variety of services, study designs, outcome domains and measures. A method of content analysis10 was used to synthesise the outcome domain types and related measures and indicators. This approach involved an iterative process of identifying categories to capture the outcome measures reported in the studies. Using the aforementioned three core outcome domains (effectiveness, patient safety and patient experience) as an a priori superordinate framework, the outcome measures from all included studies were listed. A process of refining and grouping similar subdomains together was then undertaken. This led to the construction of a ‘framework’ to describe the outcome domains that have been studied in the literature. The number of studies falling into each final outcome domain was also quantified.
Results of the review
Figure 1 shows the flow chart of the study selection process and details number of studies identified at each stage. A list of the 322 excluded studies is available on request from the authors.
FIGURE 1.
Flow chart of study selection process.
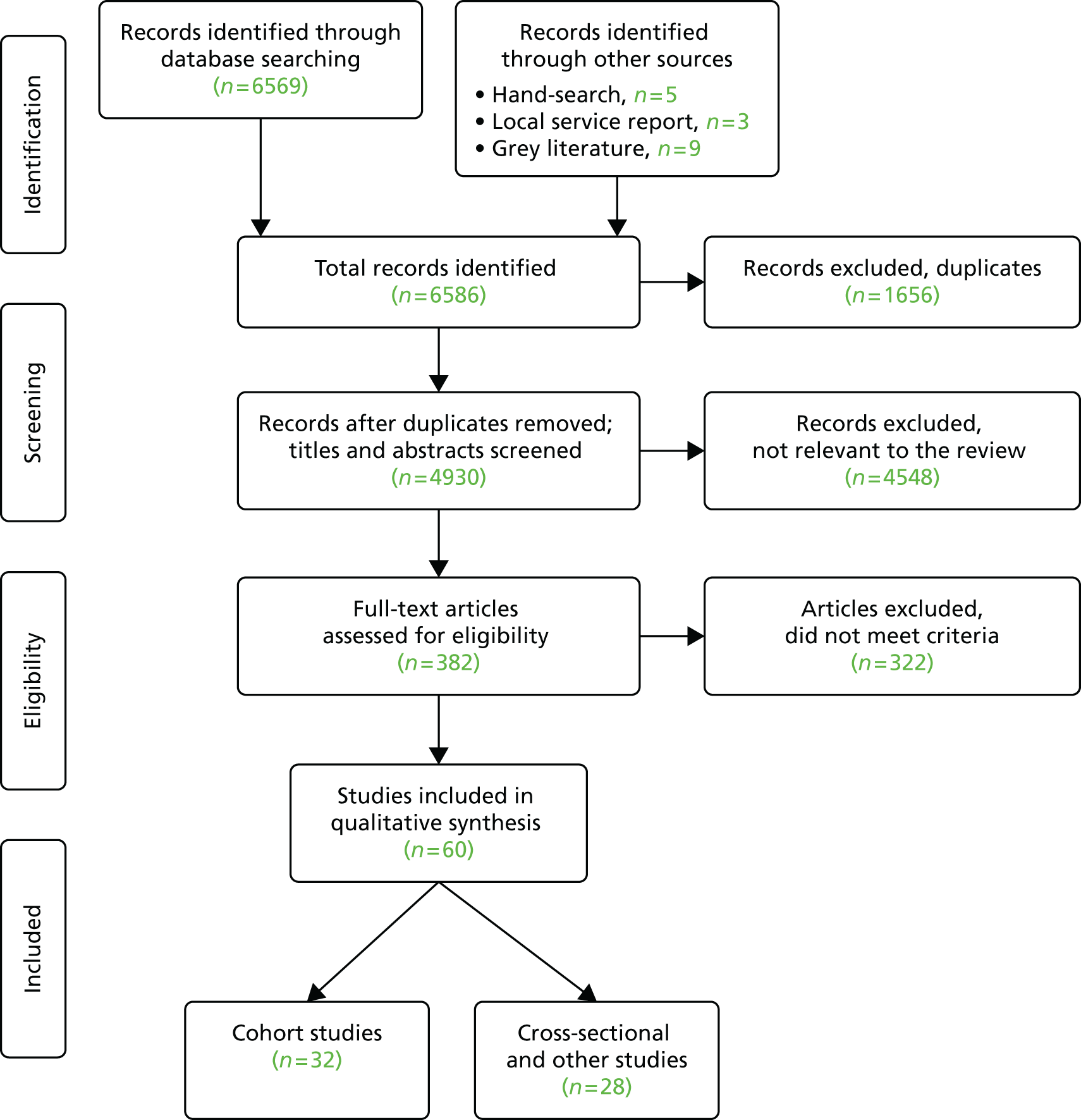
Sixty studies met the inclusion criteria; of these, 28 were cohort outcome studies (type 4) as described (with follow-up from 1 to 20 years) and a further 32 were other study designs. These were primarily cross-sectional studies (type 6) which reported service-level outcome data at one time point, with a small number of case–control and case series designs. Some of these included studies reported overlapping samples. Only two studies were from outside the UK. Most studies were of predominantly male or male-only samples; only two studies reported exclusively on female FIDD samples. Of the 60 included studies, 83% were conducted in a variety of secure inpatient settings, and 17% in community settings. The numbers of participants ranged from 10 to 1891.
Tables 1–6 display the included studies. As the cohort studies are the more ‘prototypical’ studies of outcome, these are tabled separately. Thus, Tables 1–3 show the cohort studies and Tables 4–6 show cross-sectional and other studies in each of the three superordinate domains of effectiveness, safety and patient experience, respectively. Tables 1 and 2 cover the effectiveness studies, Tables 3 and 4 cover safety studies and Tables 5 and 6 cover patient experience studies. Studies can therefore appear in more than one table. The tables present data for each study: study setting; design and the hierarchy of evidence code (1–7; see p. 16); subdomains of outcomes examined in the study, and the indicators or measures used to measure these subdomains.
| Study and setting | Design (hierarchy of evidence code, p. 18) | n | Outcome subdomain | Measure/indicator |
|---|---|---|---|---|
| Alexander et al. (2006) 11 | Retrospective cohort study (4) | 64 | Treatment response | Level of CPA support, MHA status and CGIS |
| Medium secure | Follow-up: up to 13 years | Discharge outcome/pathway | Level security/type of placement at discharge | |
| Readmissions | % of patients readmitted to the same unit | |||
| Relapse in MH | % of patients who experienced a relapse in MH symptoms | |||
| Reoffending | Number of patients formally reconvicted, cautioned or who had police contact | |||
| Offender-like behaviour | Behaviour that could be classed as an offence but did not lead to police contact | |||
| Alexander et al. (2010) 12 | Retrospective cohort study (4) | 138 | Length of stay | Mean and median number of days |
| Medium secure | Discharged patients Follow-up: 6 years |
Discharge outcome | % of positive (move to a lower level of security) or negative (move to higher level of security) discharges | |
| Discharge pathway | Level security/type of placement at discharge | |||
| Alexander et al. (2011) 13 | Retrospective cohort study (4) | 138 | Length of stay | Mean and median number of days |
| Medium secure | Follow-up: 6 years | Discharge outcome | % discharged successfully (to a lower level of security) or not (to same/higher level of security) | |
| Alexander et al. (2015) 14 | Retrospective cohort study (4) (arson vs. no arson) |
30 | Length of stay | Discharged patients only; mean and median days |
| Medium secure | Follow-up: 6 years | Discharge pathway | % of discharged patients who moved to either a lower or same/higher level of security | |
| Alexander et al. (2012) 15 | Retrospective cohort study (4) | 145 | Length of stay | Median number of days and age on discharge |
| Medium secure | Discharged patient (personality disorder vs. intellectual disabilities) | Clinical symptoms | PCL-SV pre-treatment scores (clinician rated) | |
| Risk assessment | HCR-20 pre-treatment scores (clinician rated) | |||
| Follow-up: up to 9 years | Reoffending | Reconvictions at 1-, 2- and 5-year follow-up. Categorised as serious/violent offending (as defined by Home Office) | ||
| Time to reoffend | The difference between discharge date and reconviction date for subsequent offence (median) | |||
|
Ayres and Roy (2009)
16
Community |
Case series (7) Follow-up: up to 3 years |
26 | Cost | Average cost saving per patient (based on hourly rate of support) and for the service over 3 years |
| Level of support | Hours per annum providing both direct/indirect support | |||
| Barron et al. (2004) 17 | Cohort study (4) | 61 | Clinical symptoms | ABC and Mini PAS-ADD (clinician rated) |
| Community | Follow-up: 9.5 months average | Treatment response | Categorised treatment use and % with history of service use | |
| Reoffending | Number of patients who reoffended; mean number of offences per patient | |||
| Offender-like behaviour | Telephone call with carers regarding police contact | |||
| Benton and Roy (2008) 18 | Cohort study (4) | 113 | Reoffending | Number of patients arrested and reconvicted and cases dropped |
| Community | Follow-up: up to 3 years | Discharge pathway | Level security/type of placement at discharge | |
| Discharge outcome | % of referrals discharged | |||
| Prevention of inpatient admissions | Number of patients whose inpatient admission was prevented by community treatment | |||
| Butwell et al. (2000) 19 | Cohort study (4) | Up to 278 | Length of stay | Median and mean years, calculated per episode |
| High secure | Follow-up: 10 years | Discharge pathway | Level security/type of placement at discharge | |
| Day (1988) 20 | Cohort study (4) | 20 | Length of stay | Mean number of months |
| Medium secure | Follow-up: 3 years | Treatment response | Categorised as either good (settled and co-operative), fair (continuing lesser problems) or poor (severe problems) | |
| Discharge pathway | % of patients discharged to rehabilitation villa, community or hostel | |||
| Discharge outcome | Level of adjustment at follow-up, based on personal knowledge, hospital notes and liaison with involved agencies | |||
| Readmission | % of patients readmitted to the same unit | |||
| Reoffending | Number who reoffended or returned to prison | |||
| Dickens et al. (2010) 21 | Cohort study (4) | 48 | Length of stay | Mean number of days |
| Medium and low secure | Follow-up: 15 months | Clinical symptoms | HoNOS: change between baseline and final rating. Quartile points used to allow for different lengths of stay (clinician rated) | |
| Fitzgerald et al. (2011) 22 | Retrospective cohort study (4) | 145 | Reoffending | Home Office records; % of patients with general and violent offences |
| Medium secure | Follow-up: 2 years | Risk assessment | OGRS | |
| Gray et al. (2007) 23 | Retrospective cohort study (4) | 145 | Reoffending | Home Office records; % of patients with both general and violent offences |
| Medium secure | Follow-up: 2 years | Risk assessment | HCR-20/VRAG/PCL-SV scores (rated once) | |
| Halstead et al. (2001) 24 | Cohort study (4) | 35 | Length of stay | Mean and median months |
| Medium secure | Discharged patients Follow-up: up to 13 years |
Treatment outcome | Rated as either good (risks reduced, safe for discharge), some (progress made in some areas, risk remains), none (no change) or poor (worse than admission) | |
| Discharge outcome | % of patients discharged | |||
| Discharge pathway | Level security/type of placement at discharge and follow-up | |||
| Relapse in MH | Recurrence of symptoms of illness or challenging behaviour | |||
| Readmissions | % of patients readmitted to hospital | |||
| Offender-like behaviour | Behaviour that could be interpreted as an offence | |||
| Reoffending | Number of patients reconvicted | |||
| Lindsay et al. (2002) 25 | Cohort study (4) | 62 | Offender-like behaviour | % of patients suspected of reoffending |
| Community | Follow-up: 13 years | Reoffending | % of patients with clear evidence of reoffending | |
| Lindsay et al. (2004) 26 | Cohort study (4) | 184 | Reoffending | Number of patients with clear evidence of reoffending |
| Community | Follow-up: 7 years | Harm reduction | Decrease in the number of incidents 2 years before referral vs. incident data at follow-up | |
| Lindsay et al. (2004) 27 | Case series (7) | 18 | Reoffending | Number of patients with clear evidence of reoffending |
| Community | Follow-up: 3 years | |||
| Females only | ||||
| Lindsay et al. (2006) 28 | Cohort study (4) | 247 | Reoffending | Number of patients with clear evidence of reoffending |
| Community | Follow-up: 12 years | Harm reduction | Decrease in the number of incidents 2 years before referral vs. incident data at follow-up | |
| Lindsay et al. (2013) 29 | Cohort study (4) | 309 | Reoffending | Number of patients with clear evidence of reoffending |
| Community | Follow-up: up to 20 years | Harm reduction | Standardised service incident report data; number of offences committed in the 2 years before referral vs. follow-up reoffending data | |
| Lindsay et al. (2010) 30 | Cohort study (4) | 197 | Discharge pathway | Number of patients discharged and level security/type of placement at discharge at the 1-year and 2-year follow-ups |
| Mixed services | Follow-up: 2 years | |||
| Linhorst et al. (2003) 31 | Cohort study (4) | 252 | Reoffending | Local law agency data and arrests frequencies used |
| USA community service | Follow-up: 6 months | Treatment response/engagement | Number of patients who completed treatment | |
| Marks (E Marks, University of Birmingham, 2011, personal communication) | Retrospective cohort study (4) Follow-up: 4 years |
28 | Reoffending | % of patients who reoffended (even if this did not lead to police contact), determined by interview with current care team |
| Length of stay | Mean and median number of years | |||
| Discharge pathway | % of patients in high, medium, low and community services | |||
| Morrissey and Taylor (2014) 32 | Prospective cohort study (4) | 13 | Clinical symptoms | YSQ (patient rated), IPDE Screen and PCL-SV (clinician rated): change in mean scores |
| High secure | Follow-up: 2 years | Discharge outcome | Number of patients remaining in treatment, discharged to a medium secure ward or transferred to another high secure ward | |
| Morrissey et al. (2014) 33 | Cohort study (4) | 70 | Risk assessment | HCR-20: change in mean scores over 5 years |
| High secure | Follow-up: 5 years | |||
|
Morrissey
et al.
(2007)
34
High secure |
Prospective cohort study (4) Follow-up: 2 years |
73 | Discharge outcome | % of patients who made positive (move to a lower level of security) or negative (the same level of security) progress |
| Risk assessment | HCR-20 | |||
| Clinical symptoms | PCL-R (clinician rated) | |||
| Morrissey et al. (2015) 35 | Retrospective cohort study (4) | 68 | Length of stay | Median number of years |
| High secure |
|
24 | Incidents | Frequency per year in the first 4 years of treatment using hospital incident records. Mean number of violent incidents per patient/year |
| Follow-up: up to 6 years | Clinical symptoms | EPS-BRS (clinician rated) and EPS-SRS (patient rated) | ||
| Discharge pathway | Level security/type of placement at discharge | |||
| Discharge outcome | % of patients who moved to a lower level of security | |||
| Readmission | Number of returns from trial leave | |||
| Palucka et al. (2012) 36 | Retrospective cohort study (4) | 20 | Length of stay | Median number of days |
| Canadian inpatient unit | Follow-up: up to 9 years | Discharge outcome | Number of patients discharged | |
| Discharge pathway | Level security/type of placement at discharge | |||
| Reoffending | Any criminal justice involvement (even if charges were not pressed) | |||
| Reed et al. (2004) 37 | Retrospective cohort study (4) | 45 | Length of stay | Mean number of weeks |
| Low secure | Follow-up: up to 14 years | Discharge pathway | Level security/type of placement at discharge | |
| Discharge outcome | Positive (discharged to a level of lower security) or negative (discharged to a level of higher security) outcome | |||
| Incidents | Collected from hospital incident records. The number of incidents at baseline (weeks 6–10 of stay) was compared with the number at the end of stay (last 4 weeks of treatment). Frequency (total number of incidents per month) was adjusted for length of stay. Change in incidents calculated per person per week | |||
| Xenitidis et al. (1999) 38 | Retrospective cohort study (4) | 64 | Length of stay | Mean months of hospital stay |
| Low secure | Follow-up: up to 11 years | Discharge pathway | Level security/type of placement at discharge | |
| Discharge outcome | Good (discharged to community) or bad (not placed in a community setting) outcome | |||
| Incidents | Collected from hospital incident records. The number of incidents at baseline (weeks 6–10 of stay) was compared with the number at the end of stay (last 4 weeks of treatment). Frequency (total number of incidents per month) was adjusted for length of stay |
| Study and setting | Design | n | Outcome subdomain | Measure/indicator |
|---|---|---|---|---|
| Ajmal (2008) 40 | Cross-sectional (6) | 79 | Clinical symptoms | GSI and RSES (patient rated) |
| High secure | ||||
| Beer et al. (2005) 41 | Cross-sectional (6) | 59 | Placement appropriateness | % of patients requiring a less secure placement |
| Low secure | Clinical symptoms | SBS (clinician rated) | ||
| Beer et al. (2005) 42 | Cross-sectional (6) | 68 | Length of stay | Mean number of months |
| Low secure | Placement appropriateness | % of patients requiring less secure care | ||
| Clinical symptoms | Main reason for delayed discharge | |||
| HoNOS-secure (clinician rated) | ||||
| Chaplin et al. (2015) 43 | Cross-sectional (6) | 22 | Risk assessment | HCR-20 median scores |
| Low secure | Incidents | Average per patient at 3-monthly intervals. Coded for severity using the MOAS | ||
| Median number of incidents | ||||
| Length of stay | Median number of days | |||
| Chilvers and Thomas (2011) 44 | Cross-sectional (6) (Males vs. females) |
77 | Clinical symptoms | NAS-PI scores (patient rated) |
| Medium secure | ||||
| Crossland et al. (2005) 45 | Cross-sectional (6) | 60 | Length of stay | Median number of months |
| High, medium and low secure | ||||
| Dickens et al. (2013) 46 | Cross-sectional (6) | 68 | Incidents | Severity rated: near miss, minor, moderate, high or very high |
| Medium and low secure | 16-month period | Incidents/total bed-days × 100. Average number of incidents per 100 occupied bed-days; violent/aggressive incidents and total incidents | ||
|
Esan
et al.
(2015)
39
Medium and low secure |
Cross-sectional (6) (Autism vs. non autism) |
114 | Length of stay | Mean and median months for both discharged and in-treatment patients |
| Discharge outcome | Number of patients with a good (move to a lower level of security) or poor (move to a higher level of security) outcome | |||
| Level of supervision/discharge pathway | Number of patients who were informal, under a MHA Section/guardianship or supervised discharge | |||
| Fitzgerald et al. (2013) 47 | Cross-sectional (6) | 25 | Risk assessment | HCR-20 and VRAG |
| Medium and low secure | Incidents | Number of patients involved in an incident in 6 months | ||
| Hall et al. (2014) 48 | Cross-sectional (6) | 136 | Treatment needs | Clinician ratings |
| Medium and low secure | Security need | Reference group ratings of appropriate security level | ||
| Delayed discharge | Number of patients no longer requiring current security level, main obstacle to progress | |||
| Length of stay | Maximum and average years per level of security | |||
| Incidents | Number of patients with incident in the past 6 months | |||
| Hogue et al. (2007) 49 | Cross-sectional (6) | 228 | Clinical symptoms | EPS-BRS (clinician rated) |
| High, medium, low and community | ||||
| Johnson (2012) 50 | Cross-sectional (6) | 44 | Clinical symptoms | RSES and EBS (patient rated) |
| Medium and low secure | Length of stay | Mean number of months | ||
| Kellet et al. (2003) 51 | Cross-sectional (6) | 45 | Clinical symptoms | BSI (clinical cases) (patient rated) |
| High secure | ||||
| Lindsay et al. (2004) 52 | Cross-sectional (6) | 52 | Offender-like behaviour | % of patients suspected of reoffending |
| Community | Reoffending | % of patients with ‘clear evidence’ of reoffending | ||
| Lindsay et al. (2008) 53 | Cross-sectional (6) | 212 | Risk assessment | HCR-20, VRAG, Static-99, SDRS, RM-2000 |
| High, medium and low secure | Clinical symptoms | EPS-BRS (clinician rated) | ||
| Lindsay et al. (2010) 54 | Cross-sectional (6) | 197 | Risk assessment | VRAG and Static-99 |
| High, medium, low and community | ||||
| Lofthouse et al. (2014) 55 | Cross-sectional (6) | 64 | Length of stay | Mean number of years |
| Rehabilitation, acute admission and residential home | 5 months of data | Risk assessment | CuRV | |
| Incidents | Aggression defined as acts of physical violence, aggression, force to hurt or damage staff, peers or environment. Included verbal abuse. Two researchers rated each incident as aggression present or aggression absent. Number of patients who were aggressive in month 1 vs. month 5 | |||
|
Mansell
et al.
(2010)
56
Medium and low secure |
Cross-sectional (6) NHS vs. private provider units |
1891 | Delayed discharge | % of patients who had completed treatment but did not have any plans to leave the service in the next month |
| Incidents | Average frequency with which another patient was hurt by a patient or staff member (per patient over a 6-month period) | |||
|
McMillan
et al.
(2004)
57
Medium secure |
Cross-sectional (6) 6-month period |
124 | Risk assessment | MDT ratings per patient on risk of physical violence (scale of 0–8) and number of times patient had been violent in 6 months prior to risk assessment |
| Incidents | Author coded each description of incident from computerised record, based on explicit criteria and guidelines | |||
|
Morrissey
et al.
(2007)
58
High secure |
Cross-sectional (6) 12-month period |
60 | Incidents | Coded as either interpersonal physical aggression or verbal aggression/aggression to property. Rated as low, medium or high risk of harm |
| Risk assessment | Number of patients involved in an aggressive incident | |||
| HCR-20 | ||||
| Clinical symptoms | PCL-R and EPS-BRS (clinician rated) | |||
| O’Shea et al. (2015) 59 | Cross-sectional (6) | 109 | Risk assessment | HCR-20 |
| Medium, low and rehabilitation | Incidents | Hospital records in 3-month period following risk assessment for aggression and self-harm. Coded using Overt Aggression Scale. Rated on severity (1–4) | ||
| Number of patients involved in any incident | ||||
| Perera et al. (2009) 60 | Cross-sectional (6) | 388 | Length of stay | Median number of years and % of patients who had stayed longer than 5 years |
| Medium and low secure | Delayed discharge | % of patients assessed as requiring a less secure placement | ||
| Thomas et al. (2004) 61 | Cross-sectional (6) | 102 | Length of stay | Mean and median years |
| High secure | Delayed discharge | Percentage of patients assessed as requiring a less secure placement and main reason for this | ||
| Treatment needs | SDTN scale completed by key worker and RC | |||
| CANFOR-Short and CANDID-Short. Average number of needs and unmet needs | ||||
| Uppal and McMurran (2009) 62 | Cross-sectional (6) | Up to 396 | Incidents | Hospital computerised reporting system. Coded as per the Department of Health:
|
| High secure | 15-month period of incidents (IDD sample included) | |||
| Most frequent location and time of incident. Percentage of incidents which were violent and which were self-harm. Average monthly figure generated |
| Study and setting | Design | n | Outcome subdomain | Measure/indicator |
|---|---|---|---|---|
| Alexander et al. (2015) 14 | Retrospective cohort study (4) | 30 | Seclusion, restraint and intensive observations | Mean number of episodes per patient/month |
| Medium and low secure | Follow-up: 6 years | |||
| Alexander et al. (2010) 12 | Retrospective cohort study (4) | 138 | Seclusion, restraint and intensive observations | Mean number of episodes per patient/month (adjusted for length of stay) |
| Medium secure | Follow-up: 6 years | |||
| Alexander et al. (2011) 13 | Retrospective cohort study (4) | 138 | Seclusion, restraint and intensive observations | Mean and median episodes per patient/month |
| Medium secure | Follow-up: 4 years | |||
| Ayres and Roy (2009) 16 | Case series (7) | 26 | Medication | Case study: reduction in frequency of use of PRN medication |
| Community | Follow-up: up to 3 years | |||
| Butwell et al. (2000) 19 | Cohort study (4) | Up to 278 | Death | Frequency of episodes (number and % of all patients) |
| High secure | Follow-up: 10 years | |||
| (IDD subsample) | ||||
| Morrissey and Taylor (2014) 32 | Cohort study (4) | 13 | Seclusion | Hours per patient for every 6 months of treatment over 2 years |
| High secure | Follow-up: 2 years | |||
| Reed et al. (2004) 37 | Retrospective cohort study (4) | 45 | Seclusion, restraint and relocation | Episodes at baseline (weeks 6–10 of treatment) were compared with end of stay (last 4 weeks of treatment) |
| Low secure | Follow-up: up to 14 years | Mean monthly rates calculated to control for length of stay | ||
| Xenitidis et al. (1999) 38 | Retrospective cohort study (4) | 64 | Seclusion | Episodes at baseline (week 6–10 of treatment) compared with end of stay (last 4 weeks of treatment) |
| Low secure | Follow-up: up to 11 years |
| Study and setting | Design | n | Outcome subdomain | Measure/indicator |
|---|---|---|---|---|
| Esan et al. (2015) 39 | Cross-sectional (6) | 114 | Medication | PRN usage: mean number of episodes (total frequency divided by total number of months of stay to provide an average monthly figure) |
| Medium and low secure | (ASD vs. non-ASD) | Restraint, seclusion and intensive observations | ||
| Mansell et al. (2010) 56 | Cross-sectional (6) | 1891 | Medication | PRN usage: average number of episodes |
| Medium and low secure | 6-month period | Seclusion, restraint, locked areas | Average number of episodes | |
| Access to health care | % of units who reported a delay in patients accessing primary (nurse/dentist) health care | |||
| Mason (1996) 63 | Cross-sectional (6) | 36 | Seclusion | Number of patients secluded; average number of seclusion episodes per patient/year; reason for seclusion and distress-related behaviours after seclusion |
| High secure | 12-month period |
| Study and setting | Design | n | Outcome subdomain | Measure/indicator |
|---|---|---|---|---|
| Fish and Lobley (2001) 64 | Cohort study (4) | 20 | Quality of life | QoLS: change from pre to post move |
| Community | Follow-up: 1 year | |||
| Long et al. (2014) 65 | Cohort study (4) | 10 | Milieu | EssenCes change from pre to post move |
| Low secure | Follow-up: 3 months | Satisfaction | Inpatient satisfaction questionnaire: change from pre to post move | |
| Female only | ||||
| Marks (E Marks personal communication) | Retrospective cohort study (4) | 28 | Quality of life | QoLS scores during treatment |
| Medium secure | Follow-up: 4 years | |||
| Trout (S Trout, National High Secure Learning Disability Service, Rampton Hospital, 2011, personal communication) | Cohort study (4) | 44 | Quality of life | PWI scores: change from pre to post move |
| High secure | Follow-up: up to 2 years | Satisfaction | Service specific evaluation questionnaire using a visual Likert scale via interview |
| Study and setting | Design | n | Outcome subdomain | Measure/indicator |
|---|---|---|---|---|
| Langdon et al. (2006) 66 | Cross-sectional (6) | 18 | Milieu | CIES read aloud to patients, scores during treatment |
| Medium and low secure | ||||
| Mansell et al. (2010) 56 | Cross-sectional (6) | 1189 | Service satisfaction/complaints | Number of patient generated complaints per unit over 6-month period, recorded via standardised survey |
| Medium and low secure | 6-month period | Involvement | Number of patients with an up-to-date and accessible copy of their own care plan and number of visitors for each patient per unit | |
| Steptoe et al. (2006) 67 | Cross-sectional (6) | 28 | Quality of life | SOS and LEC scores during treatment |
| Community | ||||
| Willetts et al. (2014) 68 | Cross-sectional (6) | 45 | Milieu | EssenCES scores during treatment |
| Medium and low secure |
The content analysis of outcomes identified a number of subdomains within each superordinate outcome domain. The final framework of outcome domains is described in Table 7 along with the number of studies that reported outcomes in these domains.
| Effectiveness | Number of studies |
|---|---|
| Discharge outcome/direction of care pathway | 16 |
| Delayed discharge/current placement appropriateness | 6 |
| Length of hospital stay | 22 |
| Readmission (i.e. readmitted to the same setting) | 4 |
| Clinical symptom severity/treatment needs (clinician rated) | 16 |
| Clinical symptom severity/treatment needs (patient rated) | 6 |
| Treatment response | 5 |
| Reoffending (i.e. charges/reconvictions) | 18 |
| ‘Offending-like’ behaviour (which did not result in charges) | 5 |
| Risk assessment measures | 12 |
| Incidents (violence/self-harm) | 14 |
| Security need | 3 |
| Other | 3 |
| Total | 130 |
| Patient safety | |
| Restrictive practices (restraint/relocation//intensive observations) | 12 |
| Restrictive practices (seclusion/segregation) | 9 |
| Medication (i.e. PRN usage/exceeding BNF prescribing limits) | 3 |
| Physical health | 1 |
| Premature death/suicide | 1 |
| Total | 26 |
| Patient experience | |
| Quality of life | 4 |
| Therapeutic milieu | 3 |
| Patient experience: involvement | 1 |
| Patient experience: satisfaction/complaints | 3 |
| Total | 11 |
Discussion: analysis of outcome domains and measures
Domain 1: effectiveness
A total of 53 studies (29 of which were cohort studies) presented data on at least one outcome that measured the effectiveness of FIDD services. Twelve outcome subdomains were identified as a result of content analysis.
Length of stay
An indirect measure of effectiveness, length of hospital or service stay was one of the most commonly reported outcome domains (22 studies; see Tables 1 and 2). Length of stay was usually reported for discharged patients, although it is well known that this is not a comprehensive measure because of the failure to reflect those patients who have never been discharged. Length of stay can therefore also be described at a fixed point in time for a current hospital population, and this was reported in many of the cross-sectional studies (e.g. Beer et al. ,42 Crossland et al. ,45 Esan et al. ,39 Hall et al. ,48 Johnson et al. ,50 Lofthouse et al. ,55 Perera et al. 60 and Thomas et al. 61). Inevitably, these data are less easy to interpret unless an admission cohort is used (as in Morrissey et al. 35) and the numbers in that cohort who are still in treatment and who have exceeded the mean length of stay of discharged patients are reported. Length of stay was variously reported in days,12,13 weeks, 37 months45 or years. 19,35 This was calculated as either a mean or a median measure. Reported average lengths of hospital stay ranged from 9 years in high secure conditions35 to 55 weeks in low secure conditions. 38
Readmission to the same or another hospital setting was clearly recorded in only four cohort studies11,20,24,35 in which there was follow-up. Only one study11 provided more detail, with the mean number of bed-days for those readmissions being supplied. Studies usually described length of stay in the hospital under study rather than total hospital stay (including in other settings) since first admission.
Discharge outcome/direction of care pathway/delayed discharge
A total of 16 cohort studies (see Tables 1 and 2) examined discharge outcome or direction of care pathway in terms of the level of security of the receiving service or type of community placement (e.g. independent living, supported living, residential accommodation). This was frequently coded as either a ‘successful’ (move to a lower level of security) or ‘unsuccessful’ (move within the same or to a higher level of security) discharge outcome. 12,13,24,34,37,38 Follow-up periods for post-discharge pathway outcome ranged from 2 years23 to 13 years11 for former inpatients and 20 years for a forensic community service. 29
A further six studies reported on current placement appropriateness or delayed discharge. For example, this was reported in terms of the percentage of patients assessed as requiring a less secure placement. 38,42,48,60,61 Similarly, Mansell et al. ,56 in their large cross-sectional study of 1891 patients in medium and low secure units, reported more specifically on the percentage of patients who had ‘completed treatment but did not have any plans to leave the service in the next month’. Reasons for delayed discharge were recorded in around half of these studies.
In summary, discharge outcome was generally reported in relation to a fixed point in time at either discharge from hospital or later follow-up. It is not unusual, however, for some patients to demonstrate initial progress on discharge followed by subsequent regression, placement moves and potential readmission. It was notable that few of the studies described these more complex pathways, which can be common in this population, although there was some attempt by Lindsay et al. ,30 in their study of pathways to secure care, to take this into account.
Clinical symptom or severity ratings/treatment needs
Sixteen studies (see Tables 1 and 2) reported on potential outcome domains relating to clinical symptoms or treatment needs using clinician ratings [often known as clinician-rated outcome measures (CROMs)] and six studies used patient ratings of their symptoms/needs [often reported as patient-rated outcome measures (PROMs)] (see Tables 1 and 2). However, of these, only two cohort studies actually reported change over time in such symptoms during treatment in a service, through repeated measurement on the same patients (i.e. treated clinical symptom ‘change’ as an outcome measure). Thus, Dickens et al. 21 reported on change in 48 patients on the Health of the Nation Outcome Scales (HoNOS-secure) (security scales and clinical scales) during 15 months of treatment in medium- and low secure units, finding significant reduction in severity of symptoms over time. Morrissey et al. 35 reported on change over 2–3 years on the Emotional Problem Scales (EPS)69 as a result of treatment of 68 men in a high secure setting. Both the EPS Behaviour Rating Scale (a CROM) and the EPS Self-Report Inventory, a patient-rated outcome measure (a PROM) designed for an intellectual disabilities population, were employed. It is notable that Morrissey et al. is the only included cohort study that has reported on patient-rated symptom change over time as a result of intervention at the service level.
Relatively few additional included studies reported on patient-rated clinical outcome measures at a fixed time point. Those studies that did so used a range of measures, which included the Young Schema Questionnaire,32 Brief Symptoms Inventory,51 Rosenberg Self-esteem Scale,40 Novaco Anger Scale44 and the Evaluative Beliefs Scale. 50 Of these, only the Novaco Anger Scale was reported to be appropriately adapted for IDD respondents.
Most studies reported CROMs at a fixed point in time. These measures included HoNOS-secure,21,42 EPS,49,53,58 Psychopathy Checklist Revised (PCL-R) and Psychopathy Checklist Screening Version (PCL-SV),23,32,34,53,58 International Personality Disorder Evaluation Screen,32 Clinical Global Impressions Scale,11 Aberrant Behaviour Checklist,17 Mini Psychiatric Assessment Schedules for Adults with Developmental Disabilities17 and the Social Behavioural Schedule. 41 Treatment needs were assessed in one study using the Camberwell Assessment of Needs-Forensic Short Version or the equivalent intellectual disability version, Camberwell Assessment of Needs for Adults with Developmental and Intellectual Disabilities, and a measure called the Security, Dependency and Treatment Needs Scale. 61
Treatment response
Only five studies (see Tables 1 and 2) reported on outcomes that were categorised as global ‘treatment response’. Most of these used qualitative ratings. For example, Day20 coded responses as ‘good’ (settled and co-operative), ‘fair’ (no serious difficulties but continuing lesser problems) or ‘poor’ (severe behaviour problems). Similarly, Halstead et al. 24 coded responses as ‘good’ (risks reduced, safe for discharge), ‘some’ (progress made in some areas, risk remains), ‘none’ (no change) or ‘poor’ (worse than admission). Only one study11 used a psychometric measure to measure this outcome: the Clinical Global Impressions Scale. Finally, Barron et al. 17 recorded whether patients had ‘current’, ‘previous’ or ‘no’ access to particular treatments, such as psychological therapies using standardised definitions, although they did not report the extent to which patients had engaged in these interventions.
Reoffending/‘offending-like’ behaviour/incidents
In total, 18 studies (see Tables 1 and 2) examined formal reoffending (i.e. formal charges and convictions) on follow-up; most commonly these were retrospective discharge cohort studies utilising official records such as police or Ministry of Justice conviction data. The most comprehensive of these reported the percentage of individuals with serious/violent convictions at 1-, 2- and 5-year follow-up and also examined time to reoffend. 15 Barron et al. 17 reported the number of offences committed as opposed to a dichotomy. Gray et al. 23 and Fitzgerald et al. 22 (using the same data set) reported on whether a conviction occurred within 2 years of discharge and was violent or non-violent. A community forensic service study provided more detailed data on the number of participants arrested or reconvicted or cases dropped. 18 One of the few non-UK studies reported ‘any criminal justice involvement’, which included arrest without charge following discharge from an Australian hospital unit, arrest data being likely to be a better reflection of offending behaviour than conviction. 36 Only one linked series of studies attempted to address change in offending behaviour as a result of treatment, comparing the number of formal incidents in the 2 years before referral to a community FIDDs service with those in a follow-up period. 26,28,29
Five studies examined and attempted to measure ‘offending-like’ behaviour in the community that had not been officially recorded. 11,13,24,25,31 This is arguably an important outcome given the frequency with which people with IDD are not progressed through the criminal justice system. 70 These outcome data were generally based on carer report and were described with various definitions, including ‘behaviour which could be interpreted as an offence’ or ‘suspected offending.’ Alexander et al. 11 differentiated between quasi-offending behaviour that led to police contact (but may not have ended with charges) and that which did not. This study also attempted to identify seriousness and persistency of relapse, differentiating between ‘regular, ongoing offending-like behaviour’ and ‘phasic’ or ‘occasional’ relapse. Because of some reliance on carer report in this domain and the retrospective nature of follow-up, the information reported is likely to have poor reliability.
A proxy measure of maintenance of problem behaviour is the occurrence of violent incidents during inpatient treatment, reported in 14 studies. In general, this was recorded from electronic hospital records, and standardised for length of stay (e.g. reported as average incidents per 100 bed-days). Some studies coded severity or used a rating scale such as the Overt Aggression Scale. 43,46 Other reports differentiated between physical violence and verbal aggression/threats. 58 However, measures of change in incident frequency over the course of treatment in FIDD services were reported in only a small number of studies. Xenitidis et al. 38 and Reed et al. 37 calculated change between a 4-week period at baseline and a 4-week period at the end of stay. Morrissey et al. 35 calculated the number of violent incidents in the first year of high secure intervention for each patient and compared that with the number in each subsequent year in treatment. A series of community studies26,28,29 compared the number of incidents 2 years before referral to the service with the number of incidents during intervention and follow-up. No studies reported change in the level of seriousness of incidents over time as an outcome measure.
Although not a type of offending, self-harm is a form of challenging behaviour that can lead to detention and, therefore, may be a target for behaviour change. Self-harm incidents as a service-level outcome indicator were reported in only two studies. 59,62 Neither of these studies reported change over time in self-harm as a result of intervention at the service level.
Risk assessment
A further potential proxy measure of behaviour change as a result of service intervention is the reduction in scores on dynamic structured risk assessment ratings over time. Twelve included studies reported data from such measures gathered in FIDD services. Most commonly, services used the structured clinical judgement tool the Historical, Clinical Risk 20 (HCR-20). 23,33,34,43,53,54,58,59 Other studies reported on static risk assessment measures such as the Violence Risk Appraisal Guide (VRAG),23,53,54 Risk Matrix 2000,53 Offender Group Reconviction Scale22 and Static-99,53 although these would not have utility as outcome measures as they would not be expected to change. The vast majority of these studies reported only cross-sectional data and not within-patient change in such measures over time. Indeed, only one study reported change in scores over 5 years on the clinical risk items of the HCR-20 as an outcome indicator in a FIDD service,33 despite the large number of services that are required to collect routine data on this measure.
In addition to risk assessment tools, patients were assessed for their specific security needs in three studies. This was examined as part of the security items in the HoNOS-secure ratings (e.g. Morrissey et al. 32 and Dickens et al. 21) Thomas et al. 61 used the informant-rated Security, Dependency and Treatment Needs Scale which indicated the type of environment required in terms of level of security.
Domain 2: patient safety
A total of 11 studies (see Tables 3 and 4) reported on some aspect of patient safety, which were classified into five subdomains. Two of these subdomains related to interventions that could be perceived as ‘restrictive practices’71: the first included physical restraint or periods of increased intensive nursing observations, and the second included seclusion/segregation in response to risky or ‘challenging’ behaviour. These were reported either in hours or in terms of the number of episodes. In parallel with recording numbers of violent incidents, mean rates per patient/month or year of treatment were typically reported, in order to control for length of stay. These outcomes could arguably also be construed as an effectiveness indicator if change in rates over time in treatment is measured. Only two studies37,38 reported on such change in seclusion rates in a cohort with follow-up. Only one study reported on the reason for seclusion, and on distress-related behaviours after seclusion, that is, the outcome measured had a specific emphasis on patient safety. 63
Premature death was reported in only one study, which differentiated between natural causes and suicide. 19 Physical health outcomes or access to services was reported by one study only. 56 This is surprising given the higher incidence of premature death and physical health-care problems in forensic psychiatric populations. 72 Use of pro re nata (PRN) medication, which could also be perceived as a restrictive practice, was monitored as an outcome in three studies. The number of episodes of PRN use was recorded in two secure service studies39,56 and via a case study demonstrating a reduction in use in a community patient. 16
Domain 3: patient experience
A total of 11 of the included studies reported on four patient experience-related subdomains (see Tables 5 and 6). Four studies addressed quality of life using a number of rating scales. These included the 10-item Personal Wellbeing Index,73 the only measure specifically designed for people with intellectual disabilities (S Trout, personal communication). Other measures employed were the Quality of Life Questionnaire,74 used among both a medium secure (E Marks, personal communication) and female community sample,64 and the Life Experience Checklist67 in a community sample. When change over time in reported quality of life was examined, this was in relation to a change of environment, that is, a service development. There were no community studies of quality-of-life maintenance over time in discharged FIDD patients.
Three studies addressed satisfaction with services. These related to a specific service development or move, in a community setting,64 a low secure unit65 and a high secure unit (S Trout, personal communication). A range of satisfaction instruments that were service specific and tailored for use with people with IDD were used. Only one study evaluated the number of patient complaints as a service outcome measure. 56
A fourth subdomain of patient experience identified from the literature was the therapeutic environment, reported in three studies using either the Essen Climate Evaluation Scale75 (EssenCES), which was rated by both patients and staff, or the Correctional Institutions Environment Scale. 76 There was no indication that these measures had been specifically adapted for IDD patients in any of the studies. These were typically cross-sectional studies66,68 or evaluated a specific change in environment after 3 months. 65 No identified studies reported long-term change over time in milieu quality, although it is feasible that such measures could be used as a repeated cross-sectional service outcome indicator. Only one community study reported on the level of support that patients received. 16
Finally, patient involvement as an outcome indicator was reported in only one study: Mansell et al. ,56 in their large study, reported the number of patients with an up-to-date and accessible copy of their care plan. This is one of the outcomes addressed by the current Transforming Care programme care and treatment reviews. 3
Conclusions
This systematic review identified 60 studies that either examined substantive outcomes or reported on potential outcome measures from generic treatment in forensic services for people with intellectual and developmental disabilities. Predictably there were no case–control studies that compared FIDD services with some other type of intervention. Around half of the included studies were cohort outcome studies that followed up patients either during or after a period of treatment in such services. The remainder were primarily cross-sectional studies that reported on potential outcome domains at a fixed point in time (although these studies did not necessarily have the explicit aim of evaluating outcomes). Few studies acknowledged the complex outcome pathways common in this clinical population and, interestingly, none mentioned prison as an outcome destination, although this is likely to have been the outcome for some patients.
A broad range of effectiveness outcome domains and measures was identified from the literature, although it is evident that such domains are measured in different ways, with few consistently applied measures other than in the realm of risk assessment. Even apparently categorical data relating to violent incidents or offending were measured differently across studies. Significantly, very few studies examined ‘change’ in patients over their time in treatment using repeated measures of effectiveness, for example change in incident frequency or rated risk, clinical symptoms or progression in achievement of treatment goals. This no doubt reflects the challenges in collecting and analysing longitudinal patient linked data, although it could also relate to the explicit exclusion of studies that evaluated specific treatment interventions as opposed to interventions at the service level. It was notable that that very few of the included service-level outcome studies describe details of the different components of the treatment that patients have received, an issue which needs to be addressed in future research. Finally, there was a relative paucity of reports on patient-rated outcome measures, particularly those relating to treatment progress, recovery and patient experience, and to the quality of community life following discharge from FIDD services.
It is acknowledged that the published research evidence is driven by a range of factors, including the availability of data in services, and does not necessarily reflect the outcomes domains of importance to clinicians, patients and carers. This is addressed in stages 2 and 3 of the project.
Chapter 3 Stage 2: patient and carer consultation groups
Aim
The purpose of consulting patients and carers was to incorporate their views into the framework of outcome domains appropriate for future research on outcomes from FIDD services. It was considered important to obtain perspectives from these different groups, as their views may differ to those of experts in relation to which outcomes are important and relevant.
Consultation methodology
As the consultation related to future research it was construed as patient and carer involvement by the Nottinghamshire Healthcare Foundation Trust Research Governance Group and was therefore deemed not to require a further ethical opinion.
Three patient consultation groups were conducted in May 2015 in the context of routine patient meetings. Patients were provided with information sheets (see Appendix 4), gave written consent to participate and had the opportunity to withdraw at any point. Two groups were conducted in a high-security institution (a NHS service) and one in medium-/low-security institution (an independent sector service). These groups included three female patients, one transgender patient and 11 male patients. Seven were from low- and medium-security institutions and eight were from high-security institutions.
Carer consultation took place in June 2015. Four carers were recruited from one hospital’s carer group and consulted as a group, and two carers were separately recruited and interviewed as a pair. The relatives of those consulted were in three different units at the time of consultation. Of these six carers, one was male and five were female. Carers were provided with an information sheet, and gave written consent to participate, and were provided with travel expenses and costs. Relatives of all carers were in low- or medium secure FIDD care, and one was in a bespoke service within a hospital (these carers expressed a willingness to be identifiable).
All consultation meetings were led by two members of the research team, including in all but one patient group the project lead. An independent advocate was included in the high secure meetings.
A semistructured topic guide was employed to facilitate discussion. This focused on the outcomes that patients and carers would consider important from a period in hospital in the short, medium and longer term (see Appendix 5). The discussion groups ranged in duration from 1 to 1.5 hours, and relative focus on each area depended on the response of the group. Detailed notes or full transcription of consultation meetings was undertaken depending on security restrictions. Interview data were broadly content analysed by the lead researcher according to the three main domains (effectiveness, safety and patient and carer experience), with the initial framework from the stage 1 systematic review used as a starting point (see Table 7). Although a formal qualitative data analysis approach was not undertaken, comments and discussion points were listed under the domain and subdomains already identified. Where appropriate, new subthemes were identified from the consultation data.
Findings
This section of the report summarises the content from the consultation groups, under the three superordinate domain headings. Not all of the original subdomains were commented on in detail in the interviews, and subdomains are therefore combined in the discussion. However, a number of additional outcome subdomains which had not included in the initial framework were identified. Box 1 therefore represents the framework from stage 1 amended to incorporate additional themes generated from patients and carers.
Discharge outcome/direction of care pathway.
Delayed discharge/current placement appropriateness.
Length of hospital stay.
Readmission (i.e. readmitted to the same setting within a specified period).
Clinical symptom severity/treatment needs: patient/carer rated.
Clinical symptom severity/treatment needs: clinician rated.
Treatment response/recovery measures: clinician rated.
Treatment response/recovery measures: patient/care rated.
Reoffending (formal charges/convictions).
‘Offending-like’ behaviour (no formal charges).
Incidents (violence/self-harm) in service.
Risk assessment measures.
Security need (i.e. physical/procedural/escort/leave).
Adaptive functioning.
Engagement in treatment/services.
Patient safetyPremature death/suicide.
Physical health.
Medication (i.e. PRN usage/exceeding BNF limits/side effects/patient experience).
Restrictive practices (restraint).
Restrictive practices (seclusion/segregation).
Victimisation/safeguarding/feeling safe.
Patient and carer experiencePatient experience: involvement.
Patient experience: satisfaction/complaints.
Quality of life: clinician rated.
Quality of life: patient rated.
Therapeutic climate.
Access to work/meaningful activity (when appropriate).
Carer experience: communication.
Carer experience: involvement.
Closeness to ‘home’ area.
Level of support/involvement in community (when appropriate).
BNF, British National Formulary.
Italic = new subdomain following stage 2.
Quotations are included for illustrative purposes. Quotations are referenced only as patient or carer, as linking quotations can lead to potential identification of individuals. In some instances the gender reference in the quotation has been changed in order to preserve anonymity.
Effectiveness domain
Length of hospital stay/readmission/pathways
Length of stay in hospital was identified as an important outcome variable by patients, and a number were frustrated by what they saw as extended time in treatment. However, some of the carers we consulted did not believe a shorter length of stay was necessarily a positive outcome, with fear being expressed by several carer participants regarding premature discharge.
It has to be the right length of stay for that person.
Carer
The fact that the service wasn’t there in the community to start with will make his hospital stay longer. So we can’t just look at the hospital stay – it has to be the overall picture.
Carer
Longer length of stay is not worse – I don’t want him pushed out too soon before he is ready.
Carer
Just because they are out of hospital does not mean they are better.
Carer
Patients in high secure hospital naturally saw a medium secure unit as an appropriate pathway and those in medium and low secure units were looking to community discharge as an indication of progress and positive outcome. Moving up levels of security or readmission to hospital were perceived by patients as negative (albeit sometimes necessary) outcomes. A number of carers noted that frequent changes in hospital or living environment were destabilising and, therefore, constituted a negative outcome.
Placement appropriateness/meeting clinical needs
Placement appropriateness was reported to be very important to carers and patients, with delayed discharge in a progressive direction being a particular concern (e.g. owing to appropriate unit or accommodation availability). Indeed, placement appropriateness in terms of meeting the relative’s specific needs was considered more important to many carers than distance from home:
I would much rather he be further away for 8/9 months [and get the right treatment] than be nearer for 18 months.
Carer
It is very important for people to go to a place where they are happy. Not just because it is closer to family.
Patient
Carers and patients reported that it was important that specific clinical needs were met by appropriate care and treatment in order that progress could be achieved. This included both the model of care (e.g. whether or not it was appropriate for a patient with autism), psychological treatment (e.g. specific treatment programmes) and appropriate levels of meaningful activity being available.
You have to be able to do your offending treatment. I need an arson group and there isn’t one starting.
Patient
[I need] Psychology . . . the Moving On group . . . they make you a pack so you know what to do.
Patient
Other hospitals let patients get real jobs. I want this to happen in this hospital.
Patient
It’s boring here there isn’t enough to do.
Patient
Carers were very clear that their priority for their relatives was an appropriate individualised pathway through hospital care, as opposed to rigid programmes which had to be adhered to regardless of the individual’s needs:
I know from meetings there seemed to be a lot ‘he needed to do this this and this’ – we can’t do this before we do this’ . . . almost setting him up to fail. This is how it works whether you engage or not, whether it’s relevant or not and therefore if it’s not relevant and they’re not going to engage it’s a fail before they’ve started.
Carer
It has got to be individually led.
Carer
He needed an individualised package of support which was right for him.
Carer
Finally, when it came to moving into the community from hospital, carers in particular were concerned that an ‘appropriate’ placement constituted adequate levels of support to keep people safe:
Coming home with me or if he was left in a little flat, he wouldn’t take his medication – he’d go on the drugs and then he would kill somebody or somebody else would kill him.
Carer
I worry about the fact that the service wasn’t there in the community . . . there’s so little support in the community.
Carer
Clinical symptomology/behaviour change
Participants were asked what changes would indicate an improvement in their own or their relatives’ health. Both patients and carers recognised that there would be indicators of clinical improvement which would be reflective of therapeutic change and progress. These included a reduction in the frequency of incidents of violence and self-harm, as well as perhaps less tangible clinical change.
A reduction in incidents. Reduction in restraints, using diversion more frequently, pre-empting incidents.
Carer
[I will know there is change when] he joined in to the real world again because at the moment he is living in . . . his world.
Carer
Clinical progress was typically described by patients as ‘communicating better’ or ‘getting angry less often’:
Before I wouldn’t engage in conversation and now I’ve learnt different strategies so I don’t kick off so often.
Patient
A better attitude towards staff and not taking your bad day out on a staff member.
Patient
Patients also seemed to recognise the difficulty of identifying and measuring progress, often identifying more qualitative changes:
I know what it feels like when I am better . . . I don’t put my head in my hands as much anymore.
Patient
Some people ‘toe the line’ and pretend they’re more agreeable but they aren’t really on the inside.
Patient
There was a feeling expressed by some carers that patients do not really understand what they have to achieve to make progress and that there was too much emphasis on ‘incidents’ in determining progress:
Every time he does something [the goal] gets further ahead. And [name] goes why the hell am I doing this; what’s the point of doing it if I am always going to get failed.
Carer
Furthermore, some carers felt that they were often in a better position than staff to identify nuanced changes in their relative’s functioning, and that this should be included in assessments of change.
[they should get] feedback from families . . . because the families know the person . . . we know our family members best and if the family members flag up a concern or alternatively they say they can see an improvement that should be as critical as the professional.
Carer
A number of patients emphasised that an increase in positive behaviour should be as reflective of change as a decrease in negative behaviour. For example, using low-stimulation areas as opposed to being nursed in seclusion should be seen as positive progress even if incidents were ongoing.
Finally, one carer made the important point that an increase in violent incidents per se need not necessarily be construed as a bad outcome:
It’s important to recognise that even if someone has a bad patch that isn’t a bad outcome – the outcome is how it’s managed. If the staff can see them through the bad patch it’s not necessarily a bad outcome if the service manages it appropriately.
Carer
Similarly, a higher level of observation/staffing was not necessarily seen as negative, if that was necessary for an individual:
I wouldn’t want a reduction [in staffing] because it keeps him happy and safe.
Carer
Finally, a number of participants felt that a concentration on the number of incidents was simplistic and that there should instead be an emphasis on a more nuanced analysis of them:
There is too much focus on incidents and not on understanding them . . . taking it back to the beginning of the process as opposed to just dealing with what the consequences are.
Carer
I get fed up with hearing about the same thing . . . you should just take it off the record and put it somewhere.
Patient
Finally, both patients and carers also spontaneously mentioned engagement with services and therapies as an important positive indicator of clinical progress:
I know when I am doing well. I talk to staff more . . . I’m doing my groups.
Patient
Talking to staff having a good relationship with others. I’m a peer facilitator now.
Patient
. . . at the moment he doesn’t engage in any therapies . . . if it doesn’t meet his criteria he’s not going to bother to engage.
Carer
Reoffending on discharge
Both patients and carers mentioned staying ‘safe’ on discharge as being a positive outcome. Although they talked little about reoffending specifically as an outcome domain which required measurement, a number of the carers considered themselves at potential risk as victims and their own safety was evidently important to them:
If they did say take him home now I’d be too scared.
Carer
Reduction in risk assessment ratings was not mentioned spontaneously, perhaps because patients and carers are less aware of these methodologies than practitioners. Nonetheless, both patients and carers clearly understood the concept of risk reduction and saw it as important.
Adaptive functioning
Patients were very enthusiastic about hospital treatment aimed at improving their life skills such as budgeting and work skills, but some were also fearful that hospital had caused them to lose skills they had previously had:
Since we’ve been locked up here we don’t get a chance to do that sort of thing [budget] so you don’t know what to do when you get it [money].
Patient
I haven’t been given skills like cooking and cleaning . . .
Patient
Other hospitals let patients get real jobs. I want this to happen in this hospital.
Patient
A carer also mentioned loss of adaptive skills as a negative outcome of hospital care:
He used to be able to do those things. He’s lost those skills since he’s been here.
Carer
Patient safety domain
Restrictive practices: seclusion/restraint
The patients we consulted, particularly those in high security, mentioned a reduction in incidents of seclusion as being a relevant outcome indicator. One pair of parents also mentioned reduction in staff assaults and restraint as a pertinent outcome domain for their son.
Once again some interviewees resisted the focus on negative events and considered that positive examples of behaviour, and seclusion avoidance in previously high-risk situations, should be monitored.
Restrictive practices: medication
Although some carers identified medication as having led to improvements, medication reduction was seen to be a relevant goal for some patients and some parents:
A reduction in PRN and other medication [is a goal].
Carer
If he could come off olanzapine, that would be progress.
Carer
It seemed to be important to patients and carers that patients’ experiences of medication were considered, which was an area that had not been considered in the literature. Indeed, a number of patients and carers expressed concerns about perceived overmedication and concurrent side effects and viewed this as a restrictive practice:
He’s never been on this amount of medication . . . he’s so heavily dosed up . . . If he’s been medicated to manage his behaviour he’s not learned how to manage his behaviour.
Carer
Can you be careful about medication and patients being overdosed?
Patient
Victimisation
Patients evidently had a need to feel ‘safe’ in hospital. A number of patients spontaneously mentioned victimisation by other patients as something they had experienced in hospital and, therefore, a reduction in such incidents was considered desirable as a service-level outcome goal.
Patient (and carer) experience domain
Quality of life
Both patients and their carers reported that in hospital and beyond discharge from hospital the quality of life they would achieve was of vital importance to them. In summary, their hopes and priorities were much the same as most people: a home, jobs, relationships and community involvement, but with an emphasis on quality support.
Appropriate accommodation and level of support in the long term
The carers we consulted emphasised that discharge from hospital ‘is not the end of the story’ for them and, therefore, monitoring of long-term outcomes post discharge is important:
[T]here’s a whole long chapter after that . . . and it has to be looked at in the context of that and not well we’ve been discharged from hospital so somebody else – some other authority – can take them over so we’ve got rid of them and that is that file closed.
Carer
In terms of appropriate homes post discharge from hospital, carers expressed a preference for high-quality accommodation that meets their relative’s individual needs in terms of support. They were also clear that inadequate support would lead to increased risk:
He would be in accommodation that was specifically designed for people with autism, but he had sufficient support with people who actually understood his condition and were able to spot the warning signs so I didn’t have to keep flagging them up. And that they would possibly move him into independent living . . . [with] ongoing regular support and checking up which is the low level preventative support [which] stops things happening; you haven’t got a measured outcome of what you stopped because you’ve only got somebody’s idea of what could have happened.
Carer
He needs an individual planned package with sufficient staff with appropriate training. They need to put a tender out for staff who want to work with him.
Carer
[Name] will need 24-hour support for the rest of his life.
For carers in particular, confidence in the long-term nature and consistency of the support received by their relative was vital:
[S]he went from being escorted everywhere to be put in a flat, see you later. That went . . . rapid downhill in less than a year.
Carer
I hope it’s for life.
Carer
We don’t want the care to be changing, we want to know that in future years the care will be the same . . . we need to know he’s going to be cared for the rest of his life.
Carer
I just don’t have much faith in if I wasn’t around I don’t think he’s be very well looked after.
Carer
It was also clear that for some carers back-up of an inpatient service in times of crisis was also important:
[In crisis] for him to go back in a secure unit because he’s a danger when he does deteriorate.
Carer
The patients we consulted typically mentioned wanting ‘supported living’-type arrangements, although some also wanted to live independently, with professional help they could call on should they have the need:
[S]omewhere with staff to help you if you need it.
Patient
I would like to see a doctor when I need to – I don’t want a long wait as things could escalate.
Patient
Meaningful activity
For patients, having paid employment was identified very strongly as an important ‘quality-of-life’ factor in the community. Similarly, hospital patients described wanting more meaningful activity and to experience less boredom:
Best thing was my kitchen cleaner job in my other hospital.
Patient
Having a job keeps you out of trouble.
Patient
I want to do paid work not voluntary.
Patient
A job to keep you busy . . . I had a job in Waitrose before in the shop helping people get their shopping.
Patient
I want to work as a tree surgeon.
Patient
I used to work outside in a charity shop. That was very good.
Patient
Carers naturally also wanted their relatives to be able to achieve goals within their abilities:
We want him achieving something we are proud of like any parent.
Carer
Relationships and community involvement
Relationships with others, including family, friends and pets, and the development of intimate relationships were considered important, particularly by the patients themselves:
I’d like a girlfriend. I need to do more confidence work in psychology.
Patient
I want to have a pet for a companion, to look after it. When you come home from work and the dog is at the door waiting for you.
Patient
Community involvement and the development of social networks on discharge were spontaneously mentioned as important outcomes by both patient and carer groups. Examples given in addition to paid work were church groups, educational programmes and using community facilities.
Carer satisfaction: communication and involvement
The carers we consulted generally had clear views on whether or not they were satisfied with the service their relative was in, and this level of satisfaction evidently was an important outcome for them. Satisfaction clearly led to carers experiencing less worry and concern in relation to their relatives’ well-being:
The hospital are fantastic, the staff are fantastic and at long last somebody is realising the amount of problems he has got and that is one of the problems I had before.
Carer
It is a dream come true. The place where he is now, it’s lovely . . . it’s a dream for places like that to be about.
Carer
They have got the service he needs right now. It’s as good as it gets for me right now.
Carer
The ultimate goal for carers was to feel secure in the knowledge that their relative would be cared for appropriately:
Not having to be worried about him, if we died tomorrow services would be there for him and do what was best for him without thinking of the cost.
Carer
Although some carers were happy with their involvement in the care, others felt that they had had to fight for the right services in the past, and others felt less involved than they should have been in their relative’s current care:
There was nothing much we could say which would be taken on board . . . it was very much ‘no, this is what we think’.
Carer
I was asking for help in the community for years before my son was admitted to hospital.
Carer
Communication with carers was raised as an important issue, with some carers feeling that communication from services was excellent and others feeling that it could have been much better:
We can ring up or turn up at any time.
Carer
I am part of the team there, I go to ward rounds and I feel we all have valid points of view and bring different strengths to the team.
Carer
The staff is supposed to phone me every 6 weeks if there’s been an update but they don’t . . . it’s the only thing I can fault.
Carer
[T]he messages I am leaving . . . there’s no return call and then its days and days and I am sort of banging my head against a wall. And then your relationship with the people dealing with the relative are breaking down because there is a lack of trust, there’s a lack of communication, you are not included in decisions or discussions so the whole thing is really not working is it basically.
Carer
Finally, a need for support for carers was identified, which was not always in place:
The situation, the hospital, impacts on families. How they are getting on impacts on how we feel outside.
Carer
I’ve never been in touch with anybody . . . if I’m ever struggling with anything or having questions I feel are unanswered, if there’s any groups within the hospital for getting to get in touch with, I’ve not been given any information [about them].
Carer
Conclusions
Although necessarily limited in its scope, the consultation with parents and carers validated the importance of some of the outcome domains that have been studied in the literature and that were described in Chapter 2. However, it was clear from the consultation that the original overarching domain of ‘patient experience’ needs to be expanded to include the experience of carers, an area that had not been reflected in the FIDD literature. In addition, the consultation identified a number of further subdomains of outcomes from services that had not been identified in the systematic review of research studies.
These additional subdomains (or areas within subdomains) are summarised as follows:
Effectiveness domain:
-
treatment response/recovery (patient or carer ratings as opposed to clinician ratings)
-
acquiring adaptive functioning skills
-
evidence of engagement with therapies and services.
Patient safety domain:
-
safeguarding/victimisation of patients and patients’ experience of safety
-
overuse of medication (specifically in term of patient perceived overmedication/misuse/side effects).
Patient and carer experience domain:
-
carer experience (including satisfaction, involvement and communication with services)
-
closeness to home area
-
access to work/meaningful activity (in hospital/in community)
-
level of support in the community
-
involvement in the community.
These areas are incorporated into the outcome framework developed at stage 1 in Box 1.
Chapter 4 Stage 3: Delphi survey of professionals
Aims
The aims of stage 3 of the project were to:
-
Gain consensus on expert/senior clinician views on the most important outcome domains for use in future evaluation of FIDD services, based on the domains identified from stages 1 and 2. This included both patient-related outcomes and aspects of the quality of care in services.
-
Identify preferred outcome measures/indicators and their important domains and those being used in services at the time of the study.
Method
The Delphi technique is particularly useful for inquiry into opinion regarding priorities and future areas for research. 77,78 Using an iterative, multistage process, this method seeks to gain a group consensus on a significant issue when agreement is required.
An adapted Delphi method comprising two rounds was conducted online in August 2015. The survey was distributed via a mechanised survey tool (Bristol Online Survey). Within the three overarching outcome domains of ‘effectiveness’, ‘patient safety’ and ‘patient experience’, a list of 31 subdomains/indicators was created from those that had been identified at stages 1 and 2. The Delphi asked participants for their views on the most important/highest priority outcome subdomains using quantitative rating methods. The survey is in Appendix 6.
Participants
Members of the Clinical Research Group in FIDD services were invited to participate in the Delphi exercise. In addition, senior clinicians and commissioners in the field (identified by the Project Steering Group) were contacted. An intended sample size of 15–20 experts was sought in line with Delphi recommendations. 79 Participants were eligible to participate if they had clinical, academic, managerial or commissioning experience of working in FIDD services. No specific exclusion criteria were applied given the purposive sampling method. Individuals were asked to highlight their professional background, current area of work (i.e. clinical/academic/commissioning/managerial), type of FIDD service(s) by level of security in which they were currently working and number of years of experience working within such services.
Procedure
Participants were contacted by e-mail to explain the study and to seek participation. For round 1, 76 individuals were invited to take part. The invitation e-mail provided the rationale and intended aims of the Delphi exercise. The web link, closing date and a contact for further questions were also provided. On opening the link, participants were provided with the information sheet (see Appendix 6) and instructions for completing the survey.
If respondents consented to continue, they were asked to provide brief professional background information as described above. Next, participants rated how important each of the 31 outcome subdomains was for the evaluation of (FIDD) services, within the three superordinate domains of effectiveness (15 subdomains presented), patient safety (six subdomains) and patient experience (10 subdomains). A Likert scale anchored 1 (not at all important) to 5 (extremely important) was used to rate each item, with each score having operationalised definitions. For each subdomain participants were able to supply their preferred measures or indicators in a free-text box. Participants were then asked to specify any additional outcome subdomains or indicators which they considered as important from their expert knowledge. Following this, participants were asked to select up to five subdomains which they considered to be the most important/highest priority. This included subdomains already identified as well as any additional items. Finally, in order to fulfil the study’s second aim, all participants indicated the outcome measures used routinely to collect data on all patients in their own service(s). Respondents had 2 weeks to complete the first round. A reminder e-mail was sent 5 days before the closing date to those who had not responded.
Those who completed the first round were invited to take part in the second round (see Appendix 7). The e-mail was sent on an individual basis with the web link, closing date and the participant’s individual round 1 ratings in a portable document format (PDF) attachment. On continuing to the survey web page, further instructions were provided. It was outlined that the second round was an opportunity to reappraise ratings in the light of the average group response, which was provided adjacent to each subdomain. First, participants were asked to rate the importance of each subdomain using the same Likert scale. Second, participants were asked to select up to five subdomains that they perceived to be the most important/highest priority. Participants were reminded that they did not have to change their answer from their original response if they did not wish to do so. Round 2 was available to complete over a 2-week period, with a reminder e-mail sent at the halfway point.
Analysis
Descriptive methods were used to report findings. Frequency data were generated to describe the professional backgrounds of participants. Percentages and average figures were calculated to describe the ratings made in rounds 1 and 2. The consensus level for items rated using the Likert scale was set at an average rating of 4.0 or above (i.e. items rate as either ‘moderately’ or ‘extremely’ important). The percentage of participants who ranked each subdomain in their top five was calculated. Free-text answers were analysed using content analysis.
Ethical and governance considerations
The Delphi study was reviewed by the Nottinghamshire Healthcare NHS Foundation Trust Research and Development Department. As only professionals took part, ethics approval was not deemed to be required and consent was implied by participation. The results were downloaded in an anonymous format onto an encrypted computer. A participant identifying number generated by the Bristol Online Survey was known only to the research assistant. Responses were kept strictly confidential. Direct quotations from free-text answers were anonymised so as not to be traceable back to individuals. Data were stored for the duration of the research project only and then deleted.
Results
Characteristics of participants
A total of 17 respondents completed round 1 (22% response rate). The majority of participants were psychologists and psychiatrists who worked in a clinical role at the time of participation (Figures 2 and 3). Respondents had on average 12.5 years’ experience of working in FIDD services (range 1–25 years). Fifteen of these respondents participated in the second round (88% response rate).
FIGURE 2.
Area of work.

FIGURE 3.
Type of role.

Although all security levels of FIDD services were represented by respondents, the majority were working in medium and low secure care as shown in Figure 4. Seven respondents were working across either two or three different levels of security. Both the NHS and independent sectors were represented.
FIGURE 4.
Type of service currently working in. ASD, autism spectrum disorder; ID, intellectual disability; LD, learning disability.
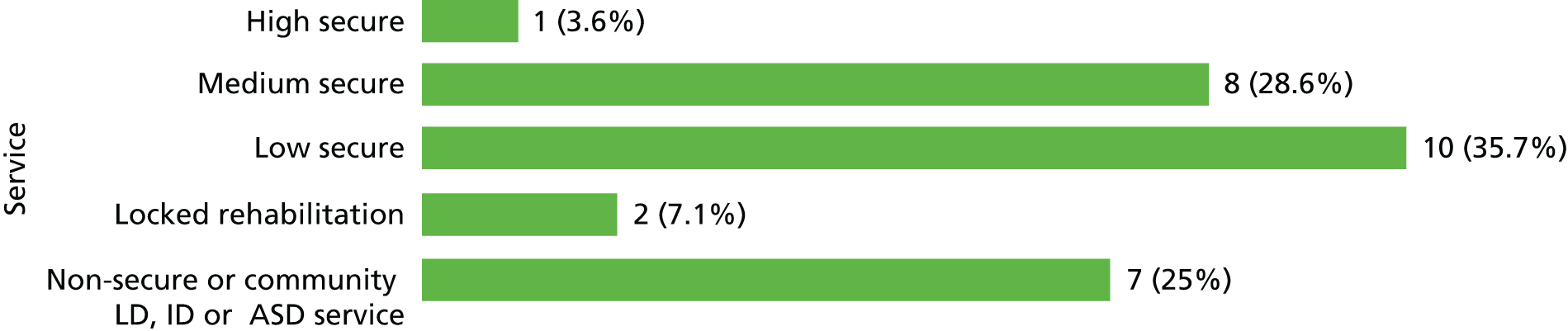
Ratings
In round 1 respondents were asked to rate how important they thought each outcome subdomain was for the evaluation of FIDD services. The subdomains with an average group score from round 1 of 4.0 and above (the consensus threshold level) were presented in round 2. Participants rerated each item. The mean scores were then calculated for each subdomain and are presented in Table 8.
| Effectiveness | R1 | R2 | Change |
|---|---|---|---|
| Discharge outcome/direction of care pathway | 4.53 | 4.80 | +0.27 |
| Treatment response/engagement | 4.65 | 4.73 | +0.08 |
| Reoffending (charges/reconvictions) | 4.59 | 4.60 | +0.01 |
| ‘Offending-like’ behaviour (i.e. behaviour that did not result in charges) | 4.47 | 4.53 | +0.06 |
| Recovery measures/progress on treatment goals (clinician rated) | 4.47 | 4.47 | 0.00 |
| Risk assessment measures | 4.35 | 4.47 | +0.12 |
| Recovery measures/progress on treatment goals (patient rated) | 4.53 | 4.40 | –0.13 |
| Clinical symptom severity/treatment needs (clinician rated) | 4.41 | 4.40 | –0.01 |
| Clinical symptom severity/treatment needs (patient rated) | 4.24 | 4.40 | +0.16 |
| Readmission (i.e. the patient is readmitted within a specified time period) | 4.00 | 4.27 | +0.27 |
| Incidents (violence/self-harm) | 4.29 | 4.20 | –0.09 |
| Delayed discharge/current placement appropriateness | 4.24 | 4.07 | –0.17 |
| Length of hospital stay | 3.65 | 3.40 | –0.25 |
| Security need (i.e. physical/procedural/escort/leave) | 3.94 | N/A | N/A |
| Adaptive functioning | 3.82 | N/A | N/A |
| Patient safety | |||
| Premature death and suicide | 4.59 | 4.73 | +0.14 |
| Victimisation/safeguarding | 4.53 | 4.47 | –0.06 |
| Restrictive practices (i.e. seclusion/segregation) | 4.29 | 4.40 | +0.11 |
| Restrictive practices (i.e. restraint) | 4.29 | 4.33 | +0.04 |
| Medication (i.e. PRN/exceeding BNF prescribing limits) | 4.24 | 4.07 | –0.17 |
| Physical health | 4.12 | 3.87 | –0.25 |
| Patient/carer experience | |||
| Access to work/meaningful activity | 4.65 | 4.60 | –0.05 |
| Therapeutic milieu | 4.41 | 4.60 | +0.19 |
| Support/involvement in community | 4.35 | 4.47 | +0.12 |
| Quality of life (patient rated) | 4.59 | 4.40 | –0.19 |
| Patient experience: involvement | 4.41 | 4.33 | –0.08 |
| Carer experience: communication | 4.18 | 4.20 | +0.02 |
| Patient experience: satisfaction/complaints | 4.29 | 4.07 | –0.22 |
| Carer experience: involvement | 4.06 | 4.07 | +0.01 |
| Quality of life (clinician rated) | 3.94 | N/A | N/A |
| Closeness to ‘home’ area | 3.59 | N/A | N/A |
None of the items was rated as ‘not at all important’ or ‘slightly important.’ There were five items which did not reach the consensus level at round 1 (length of stay, security needs, adaptive functioning, clinician-rated quality of life and closeness to home area). A decision was made to retain one item (length of stay) as, paradoxically, this item was highly ranked in the ‘top five’ domains section. At round 2, two items (length of stay and physical health) did not reach consensus level.
The subdomains that gained the highest ratings at the end of round 2 were discharge outcome, treatment response/engagement, reoffending (effectiveness domain), premature death (patient safety domain), therapeutic milieu and access to meaningful activity (patient experience domain).
Top five outcomes
Participants selected up to five subdomains that they believed were the most important/highest priority for the evaluation of FIDD services. The percentages of respondents who endorsed each subdomain as one of their most important outcomes were calculated for both rounds and are presented in Table 9.
| Effectiveness | R1 | R2 |
|---|---|---|
| Clinical symptom severity/treatment needs | 70 | 80 |
| Reoffending/offending-like behaviour | 59 | 80 |
| Treatment response/engagement/insight | 47 | 73 |
| Risk assessment measures | 41 | 67 |
| Recovery measures/progress on treatment goals | 41 | 67 |
| Discharge outcome/direction of care pathway | 41 | 53 |
| Length of hospital stay | 24 | 13 |
| Adaptive functioning | 24 | 13 |
| Delayed discharge/current placement appropriateness | 18 | 13 |
| Readmission | 18 | 13 |
| Incidents (violence/self-harm) | 18 | 0 |
| Security need (i.e. physical/procedural/escort/leave) | 12 | 0 |
| Patient safety | ||
| Restrictive practices (i.e. seclusion/segregation/restraint) | 12 | 7 |
| Premature death and suicide | 12 | 0 |
| Medication (i.e. PRN/exceeding BNF prescribing limits) | 12 | 0 |
| Physical health | 6 | 0 |
| Patient safety in general | 6 | 0 |
| Victimisation/safeguarding | 3 | 0 |
| Patient/carer experience | ||
| Access to work/meaningful activity (when/where appropriate) | 24 | 13 |
| Patient experience | 24 | 0 |
| Quality of life | 12 | 0 |
| Therapeutic milieu | 6 | 0 |
| Carer experience | 0 | 0 |
| Closeness to home area | 0 | 0 |
| Support/involvement in community (when/where appropriate) | 0 | 0 |
Suggested measures/indicators
Professionals were asked to suggest an ideal or preferred measure/indicator for each subdomain using a free-text response.
Discussion
A total of 15 experts completed both rounds of the survey; they had an average of 12.5 years of experience and represented a wide range of FIDD services. Although the total number of respondents was relatively small, this is common in Delphi studies. As the primary aim is to identify the level of consensus among experts, rather than generalising to a larger population, obtaining a sufficient degree of expertise and a representative panel can be considered more important than obtaining a large sample.
What are the most important/highest priority outcomes?
There were six subdomains which were clearly rated as greatest importance by respondents (shaded in Table 9). Clinical symptom severity, treatment response and reoffending were most frequently endorsed as being within the top five most important subdomains. In addition, recovery/progress on treatment goals and risk assessment measures and discharge outcome were also most commonly ranked as being the most important outcome domains. This broadly concurred with the Likert scale ratings. By the end of the second round, respondents favoured items under the superordinate domain of effectiveness only, with only a few respondents including items from patient safety or patient experience in their top five.
Although in round 1 there appeared to be little difference between the ratings of most domains, if the Likert rating and the top five are combined, the second round identified clear consensus for the nine most highly rated outcome subdomains, as shown in Box 2.
Discharge outcome/direction of care pathway.
Recovery measures/progress on treatment goals.
Global treatment response/engagement/insight.
Clinical symptom severity.
Reoffending (charges/reconvictions) and offender-like behaviour.
Risk assessment.
Patient safetyPremature death and suicide.
Patient experienceTherapeutic milieu.
Access to work/meaningful activity.
It is worth noting that in round 1, reoffending (formal reconvictions) and offender-like behaviour (activity that could be construed as an offence but for which no formal convictions or criminal justice system involvement followed) were similarly rated. One participant emphasised that the latter was ‘as important as formal reconvictions’ to measure. Another respondent highlighted ‘offender-like’ behaviour was of particular importance ‘to capture in an LD [learning disability] population’. In round 2, these two outcomes were therefore presented as one subdomain to reflect this.
Additional subdomains
Only one participant suggested an additional subdomain, degree of patient insight, which did not appear in the original list of items presented in round 1. This was combined with the ‘engagement’ item at round 2, as it was considered to be similar in theme.
Current use of outcome measures
In round 1, participants were asked to indicate any outcome measures used to collect routine data on all patients in the service(s) in which they worked. Table 10 provides a summary of responses. Services routinely measured levels of risk using structured clinical judgement methods (most commonly with the HCR-20). Change on risk measures (such as the HCR 20 and Short-Term Assessment of Risk and Treatability) was clearly considered important, despite the fact that the literature review indicated that there are very few studies that examine change over time in risk measures as a result of treatment. Those that do exist suggest that the measures are quite insensitive to change. It should also be noted that the authors of the HCR-20 caution against ‘totalling up’ of scores, which is the only way of measuring change in rated risk, unless only the summary risk rating (high, medium, low) is used. Totalling of scores is also complicated by the new ‘relevance’ ratings in the HCR-20 latest Version 3, which is now in use. The rated importance of risk measures as an outcome variable by professionals fails to acknowledge such problems and may be driven more by their availability owing to mandated use as part of Commissioning for Quality and Innovation targets.
| Effectiveness | % |
|---|---|
| Risk assessment measures including | |
| HCR-20 | 47.1 |
| Short-term Assessment of Risk and Treatability | 23.5 |
| Dynamic Risk Assessment and Management System | 5.9 |
| Short Dynamic Risk Scale | 5.9 |
| St Andrew’s Sexual Behaviour Assessment Scale | 5.9 |
| Sexual Violence Risk-20 | 5.9 |
| HoNOS-secure | 23.5 |
| HoNOS-LD | 5.9 |
| HoNOS (unspecified) | 11.8 |
| Incident data | 41.2 |
| Length of stay | 41.2 |
| Delayed discharge | 17.6 |
| Discharge outcome/direction of care pathway | 17.6 |
| Recovery star (and versions) | 17.6 |
| Clinical symptom severity measures including | |
| Clinical Outcomes Routine Evaluation – LD | 17.6 |
| Brief Psychiatric Rating Scale | 5.9 |
| EPSs | 5.9 |
| Schedules for Clinical Assessment in Neuropsychiatry | 5.9 |
| Attitudinal, motivational and skills assessments (used pre, during and post psychological interventions) | 5.9 |
| Modified Overt Aggression Scale | 5.9 |
| Number of patients in psychological treatment | 5.9 |
| Brooklands Outcome Scale Secure | 5.9 |
| Security need (e.g. physical/procedural/escort/leave) | 11.8 |
| Patient safety | |
| Restrictive practices | 47.1 |
| Medication | 17.6 |
| Death/suicide | 17.6 |
| Physical health | 11.8 |
| Victimisation/safeguarding | 17.6 |
| Patient/carer experience | |
| Unspecified patient-experience measures | 17.6 |
| Carer Satisfaction Survey | 11.8 |
| EssenCES | 11.8 |
| Patient Satisfaction Survey | 11.8 |
| 25 hours of meaningful activity | 5.9 |
| Friends and Family Test | 5.9 |
| Involvement in community and access to work/meaningful activity | 5.9 |
| Main Identified Problem Scale | 5.9 |
| My Shared Pathway | 5.9 |
There was not a clearly preferred measure of clinical change or treatment progress. Clinical symptoms were most commonly rated using HoNOS-secure or other versions of HoNOS. Patients’ views on their own progress were not routinely collected, despite their rated importance, although a small number of participants mentioned trust-led patient satisfaction surveys or patient self-risk ratings.
Incident data and associated restrictive practices were routinely monitored, but there was no evidence of a standardised coding system across services, which would be necessary for benchmarking purposes. This may reflect the multiplicity of service providers in this sector.
Additional issues raised
Respondents were given the opportunity to provide additional free-text responses in both rounds. The key themes are as follows:
-
Barriers to measuring outcomes: participants reflected on the difficulties of measuring outcomes in FIDD services in general. One participant summarised the issue as ‘a lack of clear objective measures and outcomes for forensic intellectual disabilities services’ suggesting an absence of current guidance and paucity of appropriate outcome measures for the population. Another respondent indicated that ‘there is a huge reliance on clinical judgement and this can be flawed and biased’. As the literature review found, it is notable that the majority of collected data reflect professional opinion and there is a relative dearth of outcomes from the patient perspective.
-
Additional subdomains: participants were given the opportunity to suggest any subdomains which were not presented in round 1. The limited number of extra subdomains suggested that the original list of subdomains was comprehensive. It therefore appeared that the relevant and important items were captured by the framework developed from stages 1 and 2.
-
Discord around direction of ‘positive’ outcomes: with regard to length of stay, the comments of some participants highlighted ambivalence as to the desired direction of this outcome indicator. For example, although having a shorter length of stay may initially appear to be a positive outcome, it was noted that it is ‘important to pick up inappropriate early discharges due to bed pressures’ among inpatient services. It was also noted that, for some forensic patients, an extended length of stay may be clinically appropriate and, therefore, not a ‘negative’ outcome, a theme echoed in the carer interviews. This ambivalence about length of stay as an outcome indicator may be reflected in its relatively low importance rating (indeed, it fell below the consensus threshold in both rounds).
-
Ambivalence regarding closeness to home area: although it is emphasised as being desirable in a range of policy papers, interestingly, closeness to home area was not considered a priority by professionals. One respondent commented that ‘our regional and supra regional Gatekeeper role sometimes experiences the benefit of some “geographical distance”’. This implies that for some patients living near to their family or local authority area may not necessarily be a constructive outcome.
-
Patient-rated outcomes: several respondents recommended using patients’ self-reported data to capture outcomes including patients’ assessment of how safe they perceive they are – often relates to ability to engage in therapeutic change and achieve treatment goals/reduce risk. Professionals also outlined ways that this could be achieved, for example ‘co-production of such [patient satisfaction] measures from within our patient advisors’. It is notable that ‘My Shared Pathway’80 was intended by the Department of Health to be an outcomes monitoring system; it was mandated for use as a CQUINN (Commissioning for Quality and Innovation) target for secure services in 2013 and includes patient ratings of progress on treatment goals. The almost total lack of mention of this tool by clinicians (one respondent) suggests that it is not being used consistently as an outcome measure or indicator by IDD services.
Finally, it is noteworthy that all subdomains were generally rated towards the upper end of the scale, indicating that respondents believed that all items had a degree of importance. Nevertheless, clear consensus around key priorities emerged.
Conclusions
The aim of the Delphi exercise was to obtain an expert group consensus on the most important/highest priority outcomes to be measured in the evaluation of FIDD services in the future. We were therefore interested in service-level outcomes, as opposed to outcomes that clinicians might assess at individual patient level in the consideration of progress and discharge, although these may overlap. A total of 15 experts completed both rounds of the survey. The participants had an average of 12.5 years of experience and represented a wide range of FIDD services.
In summary, the majority of the most highly rated items came under the superordinate domain relating to effectiveness, with items from patient safety and patient experience domains rated less frequently as a priority. Indeed, consensus was clearer as defined by the top five rating: the domains rated in the ‘top five’ were all in the effectiveness domain with none in the other two domains. Perhaps unsurprisingly, clinician respondents therefore particularly prioritised items that relate to how successful services are in helping patients to reduce their clinical symptoms and progress their treatment goals while they are receiving care, as opposed to items reflecting service quality. These clinical effectiveness outcome domains were found not to be well represented in the literature in stage 1, but were found to be important to the patients and carers, particularly in terms of their own rating, in stage 2. It appears that a variety of measures and indicators could be used to index these outcomes meaningfully (including those developed in the Department of Health-led ‘My Shared Pathway’80), but it seems there are no consistently used outcome measures across the services represented in the survey. It may be concluded that further work needs to be conducted to develop clinical symptom and treatment progress indicators which are both acceptable to clinicians and patients with intellectual disabilities and are valid and reliable.
The majority of the measures that professionals reported were collected routinely in their services were risk assessment measures (such as the HCR-20), and data on incidents and restrictive practices such as seclusion and restraint, which are required by the Department of Health. Length of stay was also routinely collected. Many services collected data on the same outcome subdomain, although the exact measure/indicator will differ (e.g. one way that incidents are coded in each setting differs widely).
The findings suggest that implementing a minimum data set among FIDD services is feasible, at least for some core measures. However, it was apparent that services, while they may collect some similar information, do not necessarily record it systematically on databases and are even less likely to analyse group data on a longitudinal basis, in order to identify change over time in their patients. This was also evident from the paucity of longitudinal studies in the systematic review. This finding may well be because services do not generally have resources to collect and analyse data systematically unless they have research departments (which only applies to some of the larger service providers). It would therefore require a specific research study or direction to services from commissioners to address the issue of developing a core common data set.
Chapter 5 Synthesis of findings and conclusions for future research
Overview
This development project comprised three stages: a systematic review of outcome domains, measures and indicators used in the literature; a series of consultation groups with patients and carers; and a Delphi survey of clinicians and experts. Although they are studies with findings of independent interest, together these allow some conclusions to be drawn about the most important domains and associated measures/indicators for examination in outcome evaluation and research in the forensic intellectual disability field. A key finding is that there appears to be a paucity of widely used, reliable and valid measures and indicators in some of the important domains.
As intended, the project also allowed a group of researchers and an expert by experience in the field to reflect together, through two day-long meetings, on what the future research needs are in relation to outcomes from intellectual disability services.
Final framework of outcome domains
The first output is the final outcome framework which synthesises the evolving framework of outcome domains developed alongside the three studies. For the purposes of this final framework, no domain which had been added at any of the three stages was removed, although a small number were collapsed. For example, ‘closeness to home area’ was subsumed under ‘patient satisfaction’, and ‘treatment response/engagement/insight’ was subsumed under ‘recovery/engagement/progress on treatment goals’, as these were similarly rated by clinicians and were considered to overlap. Table 11 describes this framework and the source of the inclusion of the subdomain. It should be noted that only new domains generated from stage 2 were added to those generated at stage 1 (systematic review). In the event, no new subdomains were added from stage 3.
| Effectiveness | Source |
|---|---|
| Discharge outcome/direction of care pathway | 1 |
| Delayed discharge/current placement appropriateness | 1 |
| Readmission (i.e. readmitted to hospital or prison) | 1 |
| Length of hospital stay | 1 |
| Adaptive functioning | 2 |
| Clinical symptom severity/treatment needs (patient rated) | 1 |
| Clinical symptom severity/treatment needs (clinician rated) | 1 |
| Recovery/engagement/progress on treatment goals (clinician rated) | 1 |
| Recovery/engagement/progress on treatment goals (patient/carer rated) | 2 |
| Reoffending (i.e. charges/convictions) on discharge | 1 |
| Offending-like behaviour (no CJS involvement) on discharge | 1 |
| Incidents (violence/self-harm) (in care setting) | 1 |
| Risk assessment measures | 1 |
| Security need (i.e. physical/procedural/escort/leave) | 1 |
| Patient safety | |
| Premature death/suicide | 1 |
| Physical health | 1 |
| Medication (i.e. PRN usage/exceeding BNF limits/side effects patient rating) | 1/2 |
| Restrictive practices (restraint) | 1 |
| Restrictive practices (seclusion/segregation) | 1 |
| Victimisation/safeguarding | 2 |
| Patient/carer experience | |
| Patient experience: involvement in care | 2 |
| Patient experience: satisfaction/complaints | 1 |
| Quality of life (patient rated) | 1 |
| Therapeutic climate | 1 |
| Access to work/meaningful activity (when appropriate) | 2 |
| Level of support/involvement in community/social network (post discharge) | 2 |
| Carer experience: communication with services/involvement in care | 2 |
These domains are therefore those that we recommend be considered for the purposes of developing benchmarking measurement of outcomes from all FIDD services, and for comprehensive outcome research into such services.
Long list of indicators
The second output is a ‘long list’ of domains alongside suggested measures or indicators of the domains identified in the framework. The stage 1 systematic review identified a range of indicators and measures (see Tables 1–6), which have been used to index the outcome subdomains in the FIDD literature. Similarly, the stage 3 Delphi study gave a consensus on the domains of most importance, and also allowed identification of those measures preferred by clinicians and those that are collected routinely in services. Stage 2 naturally did not include consideration of specific measures, as patients and carers would not necessarily be familiar with these.
Accordingly, information gained from the study as a whole was synthesised to produce a provisional outcome measure or set of indicators for each subdomain. This ‘long list’ was based on a combination of robustness of research findings, clinician preference according to the Delphi exercise and ease of collection and accessibility in services.
The long list is presented in Appendix 8 and will serve as a draft set of important variables for a future minimum data set and longitudinal research study (see below). Importantly, it identifies both the measures to be collected during hospital care and those to be collected post discharge on follow-up in the community. Those areas identified as less important by clinicians but flagged by patients and carers as important have currently been left in the long list. In some areas we recognise that consistency with the relevant NHS Outcomes Framework indicators and Adult Social Care Outcomes Framework should be achieved.
Clearly, further work needs to be undertaken on the precise source of the outcome data in many subdomains and on the exact measurement to be employed. Given the evidence of lack of comparable outcome measures across FIDD services currently, this is a priority task which is all the more important given the current policy context.
Current policy context
During the course of this project NHS England published Building the Right Support,80 along with a National Service Model for people with intellectual and developmental disabilities. 81 These publications are in further response to the abuse that occurred at Winterbourne View3 and focus on transforming services in order to increase community-based services and reduce the use of inpatient beds for people with developmental disabilities, including those with forensic needs. The National Service Model is based around nine clear principles with the person and their family at the centre. Specialist mental health care services, including forensic services, should be offered within community-based settings in order to circumvent admission. However, principle 9 recognises that hospital admission may be required for some individuals, but that change and improvement within services is needed. For example, all hospital-based services need to be integrated into community-based teams, while admissions need to be more clearly justified and associated with active, clear and robust discharge planning to prevent unnecessary hospital stays. Admissions also have to be within the context of a clear care-pathway and subject to a pre-admission Care and Treatment Review.
The findings from our current project outline some of the key indicators that are likely to index treatment outcome as a result of stay in a secure hospital. These effectiveness indicators could be used to routinely measure outcome during and following a hospital stay, and have implications for refining the care pathway for individual service users. In the patient experience domain we also have identified some important indicators for monitoring long-term outcomes for community care for these patients post discharge, which are strikingly consistent with several of the nine principles in the new National Service Model. Accurate collection of such data could support implementation of the model and the vision outlined within Building the Right Support,80 as this framework will allow service providers, NHS England, Clinical Commissioning Groups and those undertaking care and treatment reviews to objectively measure change and progress (or otherwise) in people with IDD who have been in forensic care.
Recommendations for future research
Moving forward from the current preliminary study, our final objective was to inform and underpin a large-scale longitudinal research project on outcomes from FIDD services. We are therefore in the process of developing an outline protocol for further research. As an output of the preliminary studies we have produced a list of key outcome domains (along with preliminary suggestions for measures/indicators with which to index these domains) and we propose to investigate their reliability and validity across a further series of studies. Our overarching goal is to create a standardised index of outcome for application across all IDD secure hospitals in England and to develop a national minimum data set of patients with IDD within secure hospitals which tracks them through their hospital treatment and discharge. Although key effectiveness variables would be the focus, this data set would ideally also include the patient safety and patient experience domain variables which cover some of the overarching principles in the new service framework. This information could potentially be used by NHS England both to monitor patient outcomes objectively and to provide benchmarking across services. It would also enable prediction of those patients who make most progress and the reasons for this, including effective treatments. It should also help to support appropriate care pathways within secure hospitals, and could highlight difficulties that need to be addressed, such as any lack of appropriate treatment provision, which could in turn lead to a reduction in length of stay.
It is proposed that the first workstream would involve an initial refinement of the domains, and the specific indicators of the domains and how they are to be measured. Our current long list, while comprehensive, may have disadvantages with respect to the time and cost of large-scale regular data collection on all variables, some of which may not prove valid or reliable indicators of change. We have already obtained consensus on a smaller subset of priority areas for clinicians, but would propose to undertake a further 1-day face-to-face consensus rating exercise with experts and other stakeholders (e.g. NHS England, patients and carers) with an aim of finalising a shortlist of core outcome measures/indicators for piloting.
Our second workstream would involve piloting our key indicators in several regions within England. We expect that this would be done collaboratively with NHS England and other key stakeholders (e.g. the Care Quality Commission and the Health and Social Care Information Centre). This workstream would allow us to investigate the feasibility of data collection by services and to establish the reliability and validity of our indictors over time. A secondary aim of this workstream would be to reduce the number of indictors further using item response theory methodology.
Within our third workstream, having refined our effectiveness indicators, and developed a reliable, valid and robust set, we would envisage continuing to work collaboratively with NHS England and other partners to create a longitudinal data set of all patients with IDD in secure hospitals. We would collect and refine these data, using a variety of methods, over a minimum period of 5 years. In summary, we therefore envisage the creation of a national FIDD minimum data set, which follows patients longitudinally through secure care to discharge and subsequent long-term follow-up. Patient safety and patient experience would also be monitored at a service level. Although a number of data sources exist (e.g. NHS England’s Transforming Care tracker; NHS Outcomes Framework; Mental Health Minimum Dataset) these do not easily allow identification of FIDD patients, measure treatment outcome (particularly in terms of patients’ progress over time), or adequately track care pathways from secure hospital into the community or to other outcome destinations such as prison. These areas of measurement are necessary if the Department of Health is to achieve its vision as outlined within Building the Right Support80 for forensic patients. It is believed that a robust future research programme will help to support genuine and lasting change within secure IDD services consistent with that vision. The programme should be associated with an improvement in the key indicators for all people with IDD and forensic needs by helping to ensure that they are not admitted to hospital unnecessarily, and, for those who are admitted, that they remain in hospital for no longer than is absolutely necessary.
To summarise, the research priorities are therefore:
-
refining the priority domains and the measures and indicators with which to represent the domains
-
creating a longitudinal minimum data set on all patients in secure services, including follow-up at discharge for a predetermined period.
Limitations
The preliminary research reported in this report was intended only to inform development of future substantive research and there are therefore some limitations. The systematic review was intentionally broadly focused and comprehensive for its primary purpose of identifying how outcomes have been studied in FIDD services, but a synthesis of the findings of the 60 included studies themselves was beyond the scope of the study. Such a synthesis may nevertheless have been of interest, in which case the addition of quality ratings may have identified the studies on which to put most weight, but the reasons for not conducting quality ratings have been clearly outlined. The Delphi survey tapped into the views of only a small pool of 15 experts, and a more comprehensive survey with a larger sample from a more diverse range of professional groups, including more nurses, might have identified more detail and accuracy about data available from services. Furthermore, although carers were represented from three settings, a more structured and representative survey of carer ‘experts by experience’ may have added to the overall picture, but would have been more methodologically complex and time-consuming.
The consultation with patients was limited in a number of ways, particularly in relation to the generalisability of the views of the small number of patients consulted. First, the patients we consulted were detained in two secure settings; we recognise that it was difficult for people with intellectual disabilities in such settings to reflect on a subject (i.e. discharge) of which they have limited choices or control. Furthermore, those willing and able to be consulted were by definition those most able and engaged in services; the voices of those who were the least able or in seclusion or segregation were not heard. In addition, those who had been discharged from services were not consulted in the study, although those former service patients would have had an important perspective on outcomes.
Final remarks
This project comprised preliminary scoping work. While FIDD services serve a unique group of patients, we recognise that the framework we have produced may need to be considered in the context of other frameworks, including the recently proposed Intellectual Disability Outcomes Framework for improving the quality of community services for people with intellectual disability was published while the current work was ongoing. 82 The five domains outlined in that framework (which directly reflect those in the NHS Outcomes Framework83) are nevertheless covered by our three overarching domains of effectiveness, patient safety and patient experience, but it will be important that specific indicators used are common across frameworks when this is meaningful. Finally, we recognise that this preliminary research has not yet identified a ‘definitive’ list of outcome measures/indicators for use in services or future research; this is in large part a result of our finding of a lack of consensus for the use of, or even existence of, measures in some of the domains and reinforces the need for more refinement of measures as a first phase of any future project.
Dissemination strategy
The findings of this report will primarily feed into the design of future substantive research. Findings will be accessible to professional groups and policy-makers through published papers in peer-reviewed journals, and presentation at professional conferences. Patients and carer groups received feedback in the form of the summary in Appendix 9.
Acknowledgements
Dr Mike Ferriter (research consultant) provided expert consultation and advice for the systematic review.
Ms Sam Roberts (librarian, Nottinghamshire Healthcare NHS Trust Library Services) designed and conducted the searches.
Ms Sue Stewart was the carer expert by experience.
We acknowledge the patients and carers from secure intellectual disabilities care who contributed their time to the consultation exercise.
Contributions of authors
The systematic review study selection, data extraction, synthesis and initial write-up of the report were carried out by Catrin Morrissey (Senior Research Fellow, Forensic Intellectual Disability) and Nicole Geach (Research Assistant).
The consultation groups and the Delphi survey were conducted and synthesised by Catrin Morrissey, Nicole Geach and Verity Chester (Research Associate).
Regi Alexander (Consultant Psychiatrist, Intellectual Disability), John Devapriam (Consultant Psychiatrist, Intellectual Disability), Conor Duggan (Head of Research and Development & Emeritus Professor, Research in Forensic Mental Health), Peter E Langdon (Senior Lecturer and Consultant Clinical Psychologist, Intellectual Disability), Bill Lindsay (Clinical Lead and Professor, Intellectual Disability), Jane McCarthy (Consultant Psychiatrist, Intellectual Disability) and Dawn-Marie Walker (Associate Professor, Research Methodology) provided specialist expertise and advice through all stages, contributed to the development of the protocol and commented on and contributed to drafts of the report.
Publication
Morrissey C, Langdon PE, Geach N, Chester V, Ferriter M, Lindsay WL, et al. Systematic review and synthesis of outcome domains for use within forensic services for people with intellectual disabilities. Br J Psych Open 2017; in press.
Data sharing statement
All available data can be obtained from the corresponding author. All data will be shared in a way that safeguards the confidentiality and anonymity of respondents.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- Mental Health Act. London: The Stationery Office; 2007.
- People with Learning Disability and Mental Health, Behavioural or Forensic Problems: The Role of In-Patient Services. London: Royal College of Psychiatrists; 2013.
- Transforming Care: A National Response to Winterbourne View Hospital. Department of Health Review. Final Report. London: Department of Health; 2012.
- Gilbody SM, House AO, Sheldon TA. Outcomes Measurement in Psychiatry. A Critical Review of Outcomes Measurement in Psychiatric Research and Practice. York: NHS Centre for Reviews and Dissemination, University of York; 2003.
- Fitzpatrick R, Chambers J, Burns T, Doll H, Fazel S, Jenkinson C, et al. A systematic review of outcome measures used in forensic mental health research with consensus panel opinion. Health Technol Assess 2010;14. http://dx.doi.org/10.3310/hta14180.
- Hassiotis AA, Hall I. Behavioural and cognitive-behavioural interventions for outwardly-directed aggressive behaviour in people with learning disabilities. Cochrane Database Syst Rev 2008;3. http://dx.doi.org/10.1002/14651858.cd003406.pub3.
- Duggan C, Yang M, Wong S, Kane E, Ferriter M, Beeley C, et al. Building the Evidence Base in Secure Forensic In-Patient Services in England (Including High, Medium and Low Secure Forensic Services). Department of Health Policy Research Programme; 2013.
- The NHS Outcomes Framework 2011/12. London: Department of Health; 2010.
- Greenhalgh T. How to read a paper. Getting your bearings (deciding what the paper is about). BMJ 1997;315:243-6. http://dx.doi.org/10.1136/bmj.315.7102.243.
- Ritchie J, Lewis J, Nicholls CM, Ormston R. Qualitative Research Practice: A Guide for Social Science Students and Researchers. London: Sage Publications; 2013.
- Alexander RT, Crouch K, Halstead S, Piachaud J. Long-term outcome from a medium secure service for people with intellectual disability. J Intellect Disabil Res 2006;50:305-15. http://dx.doi.org/10.1111/j.1365-2788.2006.00806.x.
- Alexander RT, Green FN, O‘Mahony B, Gunaratna IJ, Gangadharan SK, Hoare S. Personality disorders in offenders with intellectual disability: a comparison of clinical, forensic and outcome variables and implications for service provision. J Intellect Disabil Res 2010;54:650-8. http://dx.doi.org/10.1111/j.1365-2788.2010.01248.x.
- Alexander R, Hiremath A, Chester V, Green F, Gunaratna I, Hoare S. Evaluation of treatment outcomes from a medium secure unit for people with intellectual disability. Adv Ment Health Intellect Disabil 2011;5:22-3. http://dx.doi.org/10.5042/amhid.2011.0013.
- Alexander RT, Chester V, Green FN, Gunaratna I, Hoare S. Arson or fire setting in offenders with intellectual disability: clinical characteristics, forensic histories, and treatment outcomes. J Intellect Dev Disabil 2015;40:189-97. http://dx.doi.org/10.3109/13668250.2014.998182.
- Alexander RT, Chester V, Gray NS, Snowden J. Patients with personality disorder and intellectual disability – closer to personality disorders or intellectual disability? A three-way comparison. J Forens Psychiatry Psychol 2012;4:435-51. http://dx.doi.org/10.1080/14789949.2012.694462.
- Ayres M, Roy A. Supporting people with complex mental health needs to get a life! The role of the supported living outreach team. Tizard Learn Disabil Rev 2009;14:29-3. http://dx.doi.org/10.1108/13595474200900006.
- Barron P, Hassiotis A, Banes J. Offenders with intellectual disability: a prospective comparative study. J Intellect Disabil Res 2004;48:69-76. http://dx.doi.org/10.1111/j.1365-2788.2004.00581.x.
- Benton C, Roy A. The first three years of a community forensic service for people with a learning disability. Br J Forens Pract 2008;10:4-12. http://dx.doi.org/10.1108/14636646200800008.
- Butwell M, Jamieson E, Leese M, Taylor P. Trends in special (high-security) hospitals. 2: Residency and discharge episodes. Br J Psychiatry 2000;176:260-5. http://dx.doi.org/10.1192/bjp.176.3.260.
- Day K. A hospital-based treatment programme for male mentally handicapped offenders. Br J Psychiatry 1988;153:635-44. http://dx.doi.org/10.1192/bjp.153.5.635.
- Dickens G, Sugarman P, Picchioni M, Long C. HoNOS-Secure: tracking risk and recovery for men in secure care. Br J Forens Pract 2010;12:36-4. http://dx.doi.org/10.5042/bjfp.2010.0613.
- Fitzgerald S, Gray NS, Taylor J, Snowden RJ. Risk factors for recidivism in offenders with intellectual disabilities. Psychol Crime Law 2011;17:43-58. http://dx.doi.org/10.1080/10683160903392293.
- Gray NS, Fitzgerald S, Taylor J, Macculloch MJ, Snowden RJ. Predicting future reconviction in offenders with intellectual disabilities: the predictive efficacy of VRAG, PCL-SV, and the HCR-20. Psychol Assess 2007;19:474-9. http://dx.doi.org/10.1037/1040-3590.19.4.474.
- Halstead S, Cahill A, Fernando L, Isweran M. Discharges from a learning-disability medium secure unit: what happens to them?. Br J Forens Pract 2001;3:11-2. http://dx.doi.org/10.1108/14636646200100004.
- Lindsay WR, Smith AH, Law J, Quinn K, Anderson A, Smith A, et al. A treatment service for sex offenders and abusers with intellectual disability: characteristics of referrals and evaluation. J Appl Res Intellect Disabil 2002;15:166-74. http://dx.doi.org/10.1046/j.1468-3148.2002.00111.x.
- Lindsay WR, Smith AH, Law J, Quinn K, Anderson A, Smith A, et al. Sexual and nonsexual offenders with intellectual and learning disabilities: a comparison of characteristics, referral patterns, and outcome. J Interpers Violence 2004;19:875-90. http://dx.doi.org/10.1177/0886260504266884.
- Lindsay WR, Smith AH, Quinn K, Anderson A, Smith A, Allan R, et al. Women with intellectual disability who have offended: characteristics and outcome. J Intellect Disabil Res 2004;48:580-90. http://dx.doi.org/10.1111/j.1365-2788.2004.00627.x.
- Lindsay WR, Steele L, Smith AH, Quinn K, Allan R. A community forensic intellectual disability service: Twelve year follow up of referrals, analysis of referral patterns and assessment of harm reduction. Leg Crim Psychol 2006;11:113-30. http://dx.doi.org/10.1348/135532505X55669.
- Lindsay WR, Steptoe L, Wallace L, Haut F, Brewster E. An evaluation and 20-year follow-up of a community forensic intellectual disability service. Crim Behav Ment Health 2013;23:138-49. http://dx.doi.org/10.1002/cbm.1859.
- Lindsay WR, Holland T, Wheeler JR, Carson D, O’Brien G, Taylor JL, et al. Pathways through services for offenders with intellectual disability: a one- and two-year follow-up study. Am J Intellect Dev Disabil 2010;115:250-62. http://dx.doi.org/10.1352/1944-7558-115.3.250.
- Linhorst DM, McCutchen TA, Bennett L. Recidivism among offenders with developmental disabilities participating in a case management program. Res Dev Disabil 2003;24:210-30. http://dx.doi.org/10.1016/S0891-4222(03)00029-5.
- Morrissey C, Taylor J. Changes in personality disorder traits following 2 years of treatment in a secure therapeutic community milieu. J Ment Health Res Intellect Disabil 2014;7:323-36. http://dx.doi.org/10.1080/19315864.2014.930548.
- Morrissey C, Beeley C, Milton J. Longitudinal HCR-20 scores in a high-secure psychiatric hospital. Crim Behav Ment Health 2014;24:169-80. http://dx.doi.org/10.1002/cbm.1893.
- Morrissey C, Mooney P, Hogue TE, Lindsay WR, Taylor JL. Predictive validity of the PCL-R for offenders with intellectual disability in a high security hospital: treatment progress. J Intellect Dev Disabil 2007;32:125-33. http://dx.doi.org/10.1080/13668250701383116.
- Morrissey C, Hobson B, Faulkner E, James T. Outcomes from the National High Secure Learning Disability Service: findings and challenges. Adv Ment Health Intellect Disabil 2015;9:116-23. http://dx.doi.org/10.1108/AMHID-06-2014-0023.
- Palucka AM, Raina P, Liu SK, Lunsky Y. The clinical profiles of forensic inpatients with intellectual disabilities in a specialized unit. J Intellect Disabil Offending Behav 2012;3:219-27. http://dx.doi.org/10.1108/20420921211327365.
- Reed S, Russell A, Xenitidis K, Murphy DG. People with learning disabilities in a low secure in-patient unit: comparison of offenders and non-offenders. Br J Psychiatry 2004;185:499-504. http://dx.doi.org/10.1192/bjp.185.6.499.
- Xenitidis KI, Henry J, Russell AJ, Ward A, Murphy DG. An inpatient treatment model for adults with mild intellectual disability and challenging behaviour. J Intellect Disabil Res 1999;43:128-34. http://dx.doi.org/10.1046/j.1365-2788.1999.00184.x.
- Esan F, Chester V, Gunaratna IJ, Hoare S, Alexander RT. The clinical, forensic and treatment outcome factors of patients with autism spectrum disorder treated in a forensic intellectual disability service. J Appl Res Intellect Disabil 2015;28:193-200. http://dx.doi.org/10.1111/jar.12121.
- Ajmal MA. Self-esteem and mental health in a forensic learning disabilities setting. Pak J Soc Clin Psychol 2008;6:47-58.
- Beer D, Turk V, McGovern P, Gravestock SM, Brooks D, Barnett L, et al. Characteristics of patients exhibiting severe challenging behaviour in low secure mental health and mild learning disabilities units. J Psychiatr Intensive Care 2005;1:29-35. http://dx.doi.org/10.1017/S1742646405000063.
- Beer D, Spiller MJ, Pickard M, Gravestock S, McGovern P, Leese M, et al. Low secure units: factors predicting delayed discharge. J Forens Psychiatry Psychol 2005;16:621-37. http://dx.doi.org/10.1080/14789940500159475.
- Chaplin E, Eyeoyibo M, Wright S, Xenitidis K, McCarthy J. Historical and clinical items of the HCR-20 as predictors of risk within an intellectual disability population. Adv Ment Health Intellect Disabil 2015;9:62-9. http://dx.doi.org/10.1108/AMHID-01-2015-0002.
- Chilvers J, Thomas C. Do male and female forensic patients with learning disabilities differ on subscales of the Novaco Anger Scale and Provocation Inventory (NAS-PI)?. J Intellect Disabil Offending Behav 2011;2:84-97. http://dx.doi.org/10.1108/20420921111152469.
- Crossland S, Burns M, Leach C, Quinn P. Needs assessment in forensic learning disability. Med Sci Law 2005;45:147-53. http://dx.doi.org/10.1258/rsmmsl.45.2.147.
- Dickens G, Picchioni M, Long C. Aggression in specialist secure and forensic inpatient mental health care: incidence across care pathways. J Forens Pract 2013;15:206-17. http://dx.doi.org/10.1108/JFP-09-2012-0017.
- Fitzgerald S, Gray NS, Alexander RT, Bagshaw R, Chesterman P, Huckle P, et al. Predicting institutional violence in offenders with intellectual disabilities: the predictive efficacy of the VRAG and the HCR-20. J Appl Res Intellect Disabil 2013;26:384-93. http://dx.doi.org/10.1111/jar.12032.
- Hall I, Yacoub E, Boast N, Bates R, Stamps R, Holder S, et al. Secure inpatient services: a needs assessment. J Intellect Disabil Offending Behav 2014;5:38-53. http://dx.doi.org/10.1108/JIDOB-09-2013-0023.
- Hogue TE, Mooney P, Morrissey C, Steptoe L, Johnston S, Lindsay WR, et al. Emotional and behavioural problems in offenders with intellectual disability: comparative data from three forensic services. J Intellect Disabil Res 2007;51:778-85. http://dx.doi.org/10.1111/j.1365-2788.2006.00938.x.
- Johnson P. The prevalence of low self-esteem in an intellectually disabled forensic population. J Intellect Disabil Res 2012;56:317-25. http://dx.doi.org/10.1111/j.1365-2788.2011.01447.x.
- Kellett S, Beail N, Newman DW, Frankish P. Utility of the Brief Symptom Inventory in the assessment of psychological distress. J Appl Res Inellect Disabil 2003;16:127-34. http://dx.doi.org/10.1046/j.1468-3148.2003.00152.x.
- Lindsay WR, Elliot SF, Astell A. Predictors of sexual offence recidivism in offenders with intellectual disabilities. J Appl Res Intellect Disabil 2004;17:299-305. http://dx.doi.org/10.1111/j.1468-3148.2004.00217.x.
- Lindsay WR, Hogue TE, Taylor JL, Steptoe L, Mooney P, O’Brien G, et al. Risk assessment in offenders with intellectual disability: a comparison across three levels of security. Int J Offender Ther Comp Criminol 2008;52:90-111. http://dx.doi.org/10.1177/0306624X07308111.
- Lindsay W, Carson D, O’Brien G, Holland AJ, Johnston S, Taylor JL, et al. The relationship between assessed risk and service security level for offenders with intellectual disability. J Forens Psychiatry Psychol 2010;21:537-48. http://dx.doi.org/10.1080/14789941003653212.
- Lofthouse RE, Lindsay WR, Totsika V, Hastings RP, Roberts D. Dynamic risk and violence in individuals with an intellectual disability: tool development and initial validation. J Forens Psychiatry Psychol 2014;25:288-306. http://dx.doi.org/10.1080/14789949.2014.911946.
- Mansell J, Ritchie F, Dyer R. Health service inpatient units for people with intellectual disabilities and challenging behaviour or mental health problems. J Appl Res Intellect Disabil 2010;23:552-9. http://dx.doi.org/10.1111/j.1468-3148.2010.00568.x.
- McMillan D, Hastings RP, Coldwell J. Clinical and actuarial prediction of physical violence in a forensic intellectual disability hospital: a longitudinal study. J Appl Res Intellect Disabil 2004;17:255-65. http://dx.doi.org/10.1111/j.1468-3148.2004.00213.x.
- Morrissey C, Hogue T, Mooney P, Allen C, Johnston S, Hollin C, et al. Predictive validity of the PCL-R in offenders with intellectual disability in a high secure hospital setting: Institutional aggression. J Forens Psychiatry Psychol 2007;18:1-15. http://dx.doi.org/10.1080/08990220601116345.
- O’Shea LE, Picchioni MM, McCarthy J, Mason FL, Dickens GL. Predictive validity of the HCR-20 for inpatient aggression: the effect of intellectual disability on accuracy. J Intellect Disabil Res 2015;59:1042-54. http://dx.doi.org/10.1111/jir.12184.
- Perera C, Simpson N, Douds F, Campbell M. A survey of learning disability inpatient services in Scotland in 2007. J Intellect Disabil 2009;13:161-71. http://dx.doi.org/10.1177/1744629509339091.
- Thomas SD, Dolan M, Johnston S, Middleton H, Harty MA, Carlisle J, et al. Defining the needs of patients with intellectual disabilities in the high security psychiatric hospitals in England. J Intellect Disabil Res 2004;48:603-10. http://dx.doi.org/10.1111/j.1365-2788.2004.00629.x.
- Uppal G, McMurran M. Recorded incidents in a high-secure hospital: a descriptive analysis. Crim Behav Ment Health 2009;19:265-76. http://dx.doi.org/10.1002/cbm.741.
- Mason T. Seclusion and learning disabilities: research and deduction. Br J Dev Disabil 1996;42:149-59. http://dx.doi.org/10.1179/bjdd.1996.013.
- Fish R, Lobley J. Evaluating a forensic service for people with learning disabilities-comparing approaches. J Intellect Disabil 2001;5:97-109. http://dx.doi.org/10.1177/146900470100500201.
- Long CG, Bell N, Carr A, Cairns L, Webb A, Collins L. The benefits of environmental change in a secure service for people with intellectual disabilities. Adv Ment Health Intellect Disabil 2014;8:309-20. http://dx.doi.org/10.1108/AMHID-11-2013-0063.
- Langdon PE, Swift A, Budd R. Social climate within secure inpatient services for people with intellectual disabilities. J Intellect Disabil Res 2006;50:828-36. http://dx.doi.org/10.1111/j.1365-2788.2006.00847.x.
- Steptoe L, Lindsay WR, Forrest D, Power M. Quality of life and relationships in sex offenders with intellectual disability. J Intellect Dev Disabil 2006;31:13-9. http://dx.doi.org/10.1080/13668250500488652.
- Willets L, Mooney P, Blagden N. Social climate in learning disability services. J Intellect Disabil Offending Behav 2014;5:24-37. http://dx.doi.org/10.1108/JIDOB-10-2013-0025.
- Prout H, Strohmer D. Emotional Problems Scales. Odessa, FL: Psychology Assessment Resources; 1991.
- Lyall I, Holland AJ, Collins S. Offending by adults with learning disabilities and the attitudes of staff to offending behaviour: implications for service development. J Intellect Disabil Res 1995;39:501-8. http://dx.doi.org/10.1111/j.1365-2788.1995.tb00570.x.
- Positive and Proactive Care: Reducing the Need for Restrictive Interventions. London: Department of Health; 2014.
- Davies S, Clarke M, Hollin C, Duggan C. Long-term outcomes after discharge from medium secure care: a cause for concern. Br J Psychiatry 2007;191:70-4. http://dx.doi.org/10.1192/bjp.bp.106.029215.
- Cummins R. Personal Wellbeing Index – Intellectual Disability. Melbourne, VIC: Deakin University; 2004.
- Shalock R, Keith K. Quality of Life Questionnaire. Worthington, OH: IDS Publishing; 1993.
- Schalast N, Redies M, Collins M, Stacey J, Howells K. EssenCES, a short questionnaire for assessing the social climate of forensic psychiatric wards. Crim Behav Ment Health 2008;18:49-58. http://dx.doi.org/10.1002/cbm.677.
- Moos RH. Evaluating Correctional and Community Settings. Oxford: Wiley InterScience; 1975.
- Keeney S, Hasson F, McKenna HP. A critical review of the Delphi technique as a research methodology for nursing. Int J Nurs Stud 2001;38:195-200. http://dx.doi.org/10.1016/S0020-7489(00)00044-4.
- Murphy MK, Black NA, Lamping DL, McKee CM, Sanderson CF, Askham J, et al. Consensus development methods and their use in clinical guideline development. Health Technol Assess 1998;2.
- Ludwig B. Predicting the future: have you considered using the Delphi methodology?. J Extension 1997;35:1-4.
- Building the Right Support. London: NHS England; 2015.
- Supporting People with a Learning Disability and/or Autism Who Display Behaviour That Challenges, Including Those with a Mental Health Condition. Service Model for Commissioners of Health and Social Care Services:. London: NHS England; 2015.
- An Intellectual Disability Outcomes Framework for Improving the Quality of Services for People with Intellectual Disability. London: Royal College of Psychiatrists; 2015.
- The NHS Outcomes Framework 2015/16. London: Department of Health; 2014.
Appendix 1 Search strategy
PsycINFO
Date range searched: 1806 to May week 4 2015.
Date searched: 1 June 2015.
Search strategy
-
exp intellectual development disorder/ (39,999)
-
Learning disorders/ (2170)
-
Developmental Disabilities/ (10,651)
-
((intellectual$ or learning$ or development$) adj3 (impair$ or disab$ or disorder$ or difficult$ or subnormal$ or sub-normal$)).tw. (66,491)
-
((mental$ or development$) adj3 (retard$ or disab$ or defici$ or handicap$ or impairment$ or subnormal$ or sub-normal$)).tw. (58,870)
-
(feeble-minded$ or moron$ or imbecil$ or cretin$).tw. (2851)
-
de lange$.tw. (112)
-
Cri-du-chat.tw. (87)
-
(Wagr adj3 syndrome).tw. (2)
-
(down$ adj3 syndrome$).tw. (6387)
-
(Rubinstein adj3 Taybi).tw. (39)
-
(prader adj3 willi).tw. (637)
-
(williams adj3 syndrome).tw. (1038)
-
fragile X.tw. (1897)
-
((Martin Bell or FRAXE or FRAXA) adj3 syndrome$).tw. (19)
-
(les?h adj3 nyhan$).tw. (184)
-
Adrenoleukodystrophy.tw. (151)
-
(Coffin adj Lowry).tw. (32)
-
Menkes.tw. (60)
-
Glycogen Storage Disease.tw. (43)
-
Mucopolysaccharidosis.tw. (90)
-
Rett$.tw. (1073)
-
Pyruvate Dehydrogenase.tw. (80)
-
or/1-23 (118,478)
-
forensic.tw. (14,524)
-
(secure adj (unit$ or hospital$ or service$)).tw. (676)
-
Criminals/ (11,153)
-
offen$.tw. (36,629)
-
or/25-28 (51,835)
-
24 and 29 (2011)
MEDLINE(R) (via Ovid)
Date range searched: 1946 to May week 4 2015.
Date searched: 1 June 2015.
Search strategy
-
exp Intellectual Disability/ (82,875)
-
Mentally Disabled Persons/ (2227)
-
Learning disorders/ (12,856)
-
Developmental Disabilities/ (15,682)
-
((intellectual$ or learning$ or development$) adj3 (impair$ or disab$ or disorder$ or difficult$ or subnormal$ or sub-normal$)).tw. (48,293)
-
((mental$ or development$) adj3 (retard$ or disab$ or defici$ or handicap$ or impairment$ or subnormal$ or sub-normal$)).tw. (51,852)
-
(feeble-minded$ or moron$ or imbecil$ or cretin$).tw. (1645)
-
de lange$.tw. (793)
-
Cri-du-chat.tw. (368)
-
(Wagr adj3 syndrome).tw. (133)
-
(down$ adj3 syndrome$).tw. (17,498)
-
(Rubinstein adj3 Taybi).tw. (519)
-
(prader adj3 willi).tw. (2673)
-
(williams adj3 syndrome).tw. (1673)
-
fragile X.tw. (4927)
-
((Martin Bell or FRAXE or FRAXA) adj3 syndrome$).tw. (202)
-
(les?h adj3 nyhan$).tw. (969)
-
Adrenoleukodystrophy.tw. (1653)
-
(Coffin adj Lowry).tw. (187)
-
Menkes.tw. (1086)
-
Glycogen Storage Disease.tw. (2005)
-
Mucopolysaccharidosis.tw. (2613)
-
Rett$.tw. (3054)
-
Pyruvate Dehydrogenase.tw. (5100)
-
or/1-24 (17,7158)
-
forensic.tw. (25,673)
-
(secure adj (unit$ or hospital$ or service$)).tw. (315)
-
Criminals/ (1347)
-
offen$.tw. (15,415)
-
or/26-29 (40,461)
-
25 and 30 (718)
EMBASE
Date range searched: 1974 to 2015 week 22.
Date searched: 1 June 2015.
Search strategy
-
exp mental deficiency/ (124,913)
-
intellectual impairment/ (12,230)
-
developmental disorder/ (27,419)
-
Learning disorders/ (21,725)
-
Developmental Disabilities/ (24,896)
-
((intellectual$ or learning$ or development$) adj3 (impair$ or disab$ or disorder$ or difficult$ or subnormal$ or sub-normal$)).tw. (69,880)
-
((mental$ or development$) adj3 (retard$ or disab$ or defici$ or handicap$ or impairment$ or subnormal$ or sub-normal$)).tw. (69,505)
-
(feeble-minded$ or moron$ or imbecil$ or cretin$).tw. (2271)
-
de lange$.tw. (1017)
-
Cri-du-chat.tw. (483)
-
(Wagr adj3 syndrome).tw. (157)
-
(down$ adj3 syndrome$).tw. (22,586)
-
(Rubinstein adj3 Taybi).tw. (652)
-
(prader adj3 willi).tw. (3535)
-
(williams adj3 syndrome).tw. (2497)
-
fragile X.tw. (6134)
-
((Martin Bell or FRAXE or FRAXA) adj3 syndrome$).tw. (226)
-
(les?h adj3 nyhan$).tw. (1152)
-
Adrenoleukodystrophy.tw. (2064)
-
(Coffin adj Lowry).tw. (219)
-
Menkes.tw. (1331)
-
Glycogen Storage Disease.tw. (2559)
-
Mucopolysaccharidosis.tw. (3866)
-
Rett$.tw. (4102)
-
Pyruvate Dehydrogenase.tw. (6090)
-
or/1-25 (257,407)
-
forensic.tw. (40,822)
-
(secure adj (unit$ or hospital$ or service$)).tw. (577)
-
exp offender/ (8941)
-
offen$.tw. (23,256)
-
or/27-30 (65,604)
-
26 and 31 (1413)
Allied and Complementary Medicine
Date range searched: 1985 to May 2015.
Date searched: 1 June 2015.
Search strategy
-
exp learning disability/ (3019)
-
exp mental retardation/ (2432)
-
exp Developmental disabilities/ (849)
-
((intellectual$ or learning$ or development$) adj3 (impair$ or disab$ or disorder$ or difficult$ or subnormal$ or sub-normal$)).tw. (7938)
-
((mental$ or development$) adj3 (retard$ or disab$ or defici$ or handicap$ or impairment$ or subnormal$ or sub-normal$)).tw. (4951)
-
(feeble-minded$ or moron$ or imbecil$ or cretin$).tw. (9)
-
de lange$.tw. (15)
-
Cri-du-chat.tw. (8)
-
(Wagr adj3 syndrome).tw. (0)
-
(down$ adj3 syndrome$).tw. (825)
-
(Rubinstein adj3 Taybi).tw. (5)
-
(prader adj3 willi).tw. (78)
-
(williams adj3 syndrome).tw. (74)
-
fragile X.tw. (81)
-
((Martin Bell or FRAXE or FRAXA) adj3 syndrome$).tw. (1)
-
(les?h adj3 nyhan$).tw. (4)
-
Adrenoleukodystrophy.tw. (4)
-
(Coffin adj Lowry).tw. (0)
-
Menkes.tw. (0)
-
Glycogen Storage Disease.tw. (8)
-
Mucopolysaccharidosis.tw. (4)
-
Rett$.tw. (71)
-
Pyruvate Dehydrogenase.tw. (7)
-
or/1-23 (11,351)
-
forensic.tw. (226)
-
(secure adj (unit$ or hospital$ or service$)).tw. (22)
-
exp crime/ (312)
-
offen$.tw. (339)
-
or/25-28 (698)
-
24 and 29 (193)
Health Management Information Consortium
Date range searched: 1979 to March 2015.
Date searched: 1 June 2015.
Search strategy
-
exp learning disabilities/ (6239)
-
((intellectual$ or learning$ or development$) adj3 (impair$ or disab$ or disorder$ or difficult$ or subnormal$ or sub-normal$)).tw. (4440)
-
((mental$ or development$) adj3 (retard$ or disab$ or defici$ or handicap$ or impairment$ or subnormal$ or sub-normal$)).tw. (3030)
-
(feeble-minded$ or moron$ or imbecil$ or cretin$).tw. (7)
-
de lange$.tw. (0)
-
Cri-du-chat.tw. (0)
-
(Wagr adj3 syndrome).tw. (0)
-
(down$ adj3 syndrome$).tw. (254)
-
(Rubinstein adj3 Taybi).tw. (0)
-
(prader adj3 willi).tw. (3)
-
(williams adj3 syndrome).tw. (0)
-
fragile X.tw. (12)
-
((Martin Bell or FRAXE or FRAXA) adj3 syndrome$).tw. (0)
-
(les?h adj3 nyhan$).tw. (0)
-
Adrenoleukodystrophy.tw. (0)
-
(Coffin adj Lowry).tw. (2)
-
Menkes.tw. (0)
-
Glycogen Storage Disease.tw. (0)
-
Mucopolysaccharidosis.tw. (3)
-
Rett$.tw. (6)
-
Pyruvate Dehydrogenase.tw. (0)
-
or/1-21 (8443)
-
forensic.tw. (427)
-
exp secure mental health services/ (195)
-
exp psychiatric secure units/ (133)
-
(secure adj (unit$ or hospital$ or service$)).tw. (553)
-
offenders/ (1921)
-
offen$.tw. (1971)
-
or/23-28 (3691)
-
22 and 29 (189)
British Nursing Index Healthcare Databases Advanced Search platform
Date range searched: 1994 to May 2015.
Date searched: 1 June 2015.
Search strategy
-
BNI; (exp AND MENTAL AND RETARDATION).ti,ab (0)
-
BNI; ((mental* OR development*) adj3 (retard* OR disab* OR defici* OR handicap* OR impairment* OR subnormal* OR sub-normal*)).af (1904)
-
BNI; ((intellectual* OR learning* OR development*) adj3 (impair* OR disab* OR disorder* OR difficult* OR subnormal* OR sub-normal*)).af (7333)
-
BNI; (feeble-minded* OR moron* OR imbecil* OR cretin*).af (8)
-
BNI; Cri-du-chat.af (5)
-
BNI; (Wagr adj3 syndrome).af (0)
-
BNI; (down* adj3 syndrome*).af (453)
-
BNI; (Rubinstein adj3 Taybi).af (1)
-
BNI; (prader adj3 willi).af (27)
-
BNI; (williams adj3 syndrome).af (16)
-
BNI; “fragile X”.af (49)
-
BNI; ((Martin Bell OR FRAXE OR FRAXA)).af (2)
-
BNI; ((les?h adj3 nyhan*)).af (1)
-
BNI; Adrenoleukodystrophy.af (0)
-
BNI; (Coffin ADJ Lowry).af (0)
-
BNI; Menkes.af (3)
-
BNI; “Glycogen Storage Disease”.af (3)
-
BNI; Mucopolysaccharidosis.af (2)
-
BNI; Rett*.af (26)
-
BNI; “Pyruvate Dehydrogenase”.af (0)
-
BNI; “de lange*”.af (20)
-
BNI; 1 OR 2 OR 3 OR 4 OR 5 OR 6 OR 7 OR 8 OR 9 OR 10 OR 11 OR 12 OR 13 OR 14 OR 15 OR 16 OR 17 OR 18 OR 19 OR 20 OR 21 (7790)
-
BNI; forensic.af (904) results.
-
BNI; exp SECURE PSYCHIATRIC HOSPITALS/ OR exp MENTALLY DISORDERED OFFENDERS/ (770)
-
BNI; (secure ADJ (unit* OR hospital* OR service*)).af (527)
-
BNI; offen*.af (1270)
-
BNI; 27 OR 28 OR 29 OR 30 (2057)
-
BNI; 26 AND 31 (364)
Cumulative Index to Nursing and Allied Health Literature (via EBSCOhost)
Date range searched: 1806 to May week 4 2015.
Date searched: 1 June 2015.
Search strategy
-
S1. (MH “Intellectual Disability+”) (14,423)
-
S2. (MH “Mentally Disabled Persons”) (2211)
-
S3. (MH “Developmental Disabilities”) (4374)
-
S4. TX ((mental* OR development*) N3 (retard* OR disab* OR defici* OR handicap* OR impairment* OR subnormal* OR sub-normal*)) (40,779)
-
S5. TX ((intellectual* OR learning* OR development*) N3 (impair* OR disab* OR disorder* OR difficult* OR subnormal* OR sub-normal*)) (61,814)
-
S6. TX (feeble-minded* OR moron* OR imbecil* OR cretin*) (1735)
-
S7. TX Cri-du-chat (159)
-
S8. TX (Wagr N3 syndrome) (23)
-
S9. TX (down* N3 syndrome*) (8682)
-
S10. TX (Rubinstein N3 Taybi) (58)
-
S11. TX (prader N3 willi) (806)
-
S12. TX (williams N3 syndrome) (796)
-
S13. TX “fragile X” (1781)
-
S14. TX ((Martin Bell OR FRAXE OR FRAXA) N3 syndrome*) (25)
-
S15. TX (les?h N3 nyhan*) (150)
-
S16. TX Adrenoleukodystrophy (161)
-
S17. TX (Coffin N1 Lowry) (25)
-
S18. TX Menkes (277)
-
S19. TX “Glycogen Storage Disease” (220)
-
S20. TX Mucopolysaccharidosis (186)
-
S21. TX Rett* (3568)
-
S22. TX “Pyruvate Dehydrogenase” (196)
-
S23. TX “de lange*” (805)
-
S24. S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 (83,897)
-
S25. TI forensic or AB forensic (2740)
-
S26. TX (secure N1 (unit* OR hospital* OR service*)) (1797)
-
S27. (MH “Mentally Ill Offenders”) (1376)
-
S28. TI offen* or AB offen* (3951)
-
S29. S25 OR S26 OR S27 OR S28 (8721)
-
S30. S24 AND S29 (1195)
Appendix 2 Inclusion and exclusion criteria
Type of study
-
Any study design
AND
-
Presents quantitative data post 1980
AND is one of the following:
-
in press, in preparation or published in a book or scientific, peer-reviewed journal
-
unpublished service evaluation report
-
grey literature.
Exclude: qualitative data only.
Type of service/participant
All of the following apply:
Study includes data relating to:
-
service includes forensic mental health service(s)
-
IDD- or LD-specific service(s)
-
adult services (≥ 18 years).
If service is mixed the IDD data are identifiable as a separate group.
Exclude: child or adolescent services.
One or more of the following apply:
-
high, medium or low secure service
-
locked rehabilitation service
-
community forensic service.
Non-UK equivalent of any of the above.
Exclude: prison studies; probation.
Intervention
-
Study evaluates/considers outcomes arising from the service as a whole.
-
Study presents data on measures of effectiveness, quality or patient experience.
Exclude: studies that evaluate a specific/singular intervention (e.g. anger management).
Appendix 3 Screening tool and data extraction form
Screening tool
Data extraction tool for included studies
Appendix 4 Patient and carer information for consultation groups
Appendix 5 Topic guides for consultation groups
Appendix 6 Delphi information sheet and round 1 questionnaire
Appendix 7 Delphi round 2 questionnaire
Appendix 8 Provisional ‘long list’ of measures/indicators
| Effectiveness domain | Measure/indicator (individual-/patient-level data) |
|---|---|
| Direction of care pathway (compared with 12 months ago) | % of patients who (compared with 12 months ago) are
|
For those discharged, community status:
|
|
| Readmitted (community) | For those discharged to community:
|
| Length of hospital stay | Date of hospital admission – current date. If discharged, length of stay on discharge date |
| Clinical symptoms (patient rated) | Clinical Outcomes Routine Evaluation – LD (total score) (12-item outcome measure validated on intellectual disabilities) |
| Clinical symptoms (clinician rated) | HoNOS-secure clinical scale items (total score); Clinical Global Impression Scale |
| Recovery/engagement/progress on treatment goals (clinician rated) | Team rating, for example:
|
| Or | |
|
|
| Recovery/engagement/progress on treatment goals: (patient/carer rated) | Parallel ratings to be developed |
| Adaptive functioning | HoNOS-secure rating (item 10) |
| Risk assessment | HCR-20-V3 summary rating:
|
| HCR-20-V3 clinical items total | |
| HoNOS-secure rating A (risk of harm) | |
| Incidents | Mean number contact violent/sexual incidents per month of inpatient stay (past 12 months) (agreed definition required) |
| Mean severity of incidents (past 12 months) Each incident coded, for example:
|
|
| Mean self-harm incidents per month (past 12 months) (agreed definition required) | |
| Mean severity of incidents (past 12 months) | |
Each incident coded:
|
|
| Level of security appropriate to current needs | HoNOS-secure item C (compared with actual level) OR Security, Dependency and Treatment Needs scale |
| Reoffending (community) | In past 12 months:
|
| Offence-like behaviour (community) | In past 12 months: Number of incidents using same definition of ‘incident’ as for inpatient (service or carer records using structured format) |
| Patient safety domain | Measure/indicator (service-level data) |
| Premature death/suicide | Number of premature/unexpected deaths (past 12 months) (as NHS Outcomes Framework) |
| Reason code | |
| Physical health | HoNOS-secure item B (mean for service) |
| HoNOS-LD (if community) | |
| Self-harm | Self-harm incidents (12 months) |
| Medication | Number of patients exceeding BNF limit (past 12 months) |
| Number of PRN episodes (past 12 months) | |
| Medication (patient rating) | Patient survey rating with pictorial rating, for example:
|
| Seclusion | Mean number of seclusion episodes per inpatient month (past 12 months) Or Number of episodes per month per 10 inpatient beds (see NHS benchmarking) |
| Effectiveness domain | Measure/indicator (service-level data) |
| Restraint | Mean number of restraints per inpatient month (past 12 months) Or Number of restraints per month per 10 inpatient beds (see NHS benchmarking) |
| Victimisation/SG | Number of patient on patient assaults recorded (past 12 months) |
| HoNOS-secure scales item F | |
| Patient survey rating, for example: | |
| % of patients who endorse ‘I feel safe and secure in this service’ | |
| Patient/carer experience domain | Measure/indicator (all rated once in a 12-month period) (service-level data) |
| Patient complaints | Mean number of patient generated complaints per inpatient month |
| Patient involvement | Patient survey rating with pictorial rating, for example:
|
| (Or CTR rating achieved?) | |
| Quality of life | MANS–LD or European Quality of Life-5 Dimensions |
| Stability: number of home moves in past 12 months (community) | Number of home moves |
| Access to work and meaningful engagement | Mean number of hours meaningful activity per patient per week |
| % in paid work (community) (see NHS Outcomes Framework83) | |
| Carer experience | |
| Involvement | Carer survey rating, for example (% rating ‘enough’ involvement):
|
| Communication | Carer survey rating, for example (% carers rating good communication):
|
| Therapeutic climate | Friends and Family Test (% who would recommend service) At least 50% sample staff EssenCES within 12-month period At least 50% sample patient EssenCES (intellectual disabilities adapted) within 12-month period Mean total score on three EssenCES subscales |
| Level of support (patient-rating) | Patient/service user survey rating, for example (% rating good support):
|
| Level of support (carer-rating) | (% rating good support)
|
| Social network (community) | Social Network Guide (Tizard Centre 2006, personal communication) |
Appendix 9 Summary of research for public and patient involvement dissemination
Health Services and Delivery Research Programme research project 13/114/37
What happens to people who are in secure services for people with intellectual and developmental disabilities?
Looking at the previous research and consulting with patients in hospital, their carers and their clinicians.
What we wanted to do
-
We are a group of researchers who work in different secure services.
-
This is a report on some work we did in 2015.
-
We want to know what happens when patients with IDD are in secure hospital and after hospital. We call this ‘outcomes’.
-
We want to know things like: how do they change, where do they end up and what support do they get later on?
-
This small piece of work was part of planning our next big research project, which will take 5 years.
-
Because it will be a big project we want to do it properly.
-
So we want to know what questions to ask, what things are important to measure and how to measure them.
-
To help to decide this we looked at work by other researchers, and we talked to secure patients and carers, and their doctors, nurses and psychologists.
-
We wanted to find out to find out what these people thought we should look at when we are doing our big research project.
-
The work was paid for by the NIHR.
What we did
-
We looked carefully at 60 studies from around the world.
-
We talked to 11 patients and six carers and 15 clinicians.
-
We put all this information together.
What we decided
The main three areas we decided we should look at in future research were:
-
Does secure hospital treatment make people better?
-
How safe are patients in hospital?
-
What is hospital like for patients and their carers? And what is their experience on discharge from hospital?
We will talk about each of these.
-
Does secure hospital treatment make people better?
The conclusions were that in our next research the most important things to measure are:
-
How peoples’ mental health symptoms change and how patients see that change.
-
Whether people are reaching their goals for treatment and how patients see their progress.
-
How peoples’ behaviour changes (e.g. do they harm others or themselves any less often?).
-
Whether people do actually commit offences or harm others when they come out of hospital.
-
How people move through the hospital system and how fast do they do that?
-
-
How safe are patients in hospital?
The conclusions were that in our next piece of research we should look at:
-
How often people are secluded or restrained?
-
How many people feel they are on too much medication?
-
How many people died or took their own life?
-
How often other patients are harmed by other patients?
-
-
What is hospital like for patients and their carers and what happens on discharge?
The conclusions were that in our next research project we should look at:
-
How satisfied patients are with their care?
-
How satisfied carers are with their care?
-
How involved patients and carers feel in the care – do they have a say?
When they leave hospital:
-
Where do people go?
-
How much support do people get when they leave hospital?
-
How involved they are in the community?
-
Whether patients have enough to do in hospital and after hospital.
-
Do they go back to hospital or prison?
-
We have suggested ways to measure all these things.
We plan to apply for funding from NIHR to collect information on ALL people with LDs and autism who go through secure hospitals. We want to describe their characteristics in detail and to see what happens to them over 5 years. We want to know what happens both while they are in hospital and after hospital.
List of abbreviations
- ASD
- autistic spectrum disorder
- CROM
- clinician-rated outcome measure
- EPS
- Emotional Problem Scales
- EssenCES
- Essen Climate Evaluation Scale
- FIDD
- forensic intellectual and developmental disabilities
- HCR-20
- Historical, Clinical Risk 20
- HoNOS
- Health of the Nation Outcome Scales
- IDD
- intellectual and other types of developmental disabilities
- LD
- learning disability
- NIHR
- National Institute for Health Research
- PCL-R
- Psychopathy Checklist Revised
- PCL-SV
- Psychopathy Checklist Screening Version
- portable document format
- PRN
- pro re nata
- PROM
- patient-reported outcome measure
- VRAG
- Violence Risk Appraisal Guide