Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 13/10/75. The contractual start date was in July 2014. The final report began editorial review in August 2016 and was accepted for publication in May 2017. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Alison Faulkner received consultancy fees for her role in the project.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2017. This work was produced by Simpson et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction, background and aims
Improving the treatment and care of people with mental illness is among the key priorities for health and social care in both England and Wales. 1 However, despite the shift towards community-based models of care, considerable resources are still spent on acute inpatient beds: as much as £585M in 2009–10. 2
In 2014–15, in England, 103,840 people in contact with mental health and learning disability services spent time in hospital. For every 100 female inpatients, 41.9 were detained using the Mental Health Act (MHA) 1983;3 for every 100 male inpatients, 38.5 were detained. 4 In Wales, 9466 admissions to hospital for mental illness took place in 2014–15,5 with 1662 of these taking place using sections of the MHA 1983. 3 Such high numbers of admissions mean that considerable planning and co-ordination is required to ensure that effective care is delivered consistently.
The context and delivery of mental health care is diverging between the countries of England and Wales while retaining points of common interest, thereby providing a rich geographical comparison for research. Across England, the key vehicle for the provision of recovery-focused, personalised, collaborative mental health care is the Care Programme Approach (CPA). The CPA is a form of case management that was introduced in England in 1991 and then revised and refocused. 6 In Wales, the CPA was introduced in 2003,7 but it has been superseded by The Mental Health (Care Co-ordination and Care and Treatment Planning) (CTP) Regulations (Mental Health Measure), a new statutory framework. 8 Data for England show that 403,615 people were on the CPA in 2011–12. 9 Centrally held CPA numbers supplied by the corporate analysis team at the Welsh Government indicate that there were 22,776 people in receipt of services as of December 2011, just 6 months before the introduction of CTP under the Mental Health Measure (James Verrinder, Welsh Government, 2012, personal communication).
In both countries, the CPA or CTP obliges providers to comprehensively assess health/social care needs and risks; develop a written care plan (which may incorporate risk assessments, crisis and contingency plans, advanced directives, relapse prevention plans, etc.) in collaboration with the service user and carer(s); allocate a care co-ordinator; and regularly review care (Table 1). In Wales, as evidence of further divergence, statutory advocacy has been extended to all inpatients. CPA/CTP processes are now also expected to reflect a philosophy of recovery and to promote personalised care. 6,10
| CPA | CTP |
|---|---|
| Was first introduced in England in 1990 via a joint health service/local authority circular | Was introduced on a legislative basis in Wales as part of the Mental Health (Wales) Measure 2010 |
| Identifies the role of the care co-ordinator (initially referred to as key worker) | Confirms the role of the care co-ordinator, who must be a member of one of the specified health or social care professions |
| Requires the development of an individual written care plan | Requires the development of a CTP, to be produced using an all-Wales template |
| Identifies the role of the care co-ordinator in managing plans of care and in ensuring timely review | Identifies the role of the care co-ordinator in managing plans of care and ensuring timely review |
The concept of recovery in mental health was initially developed by service users. It refers to ‘a way of living a satisfying, hopeful, and contributing life even with limitations caused by illness’11 while developing new purpose or meaning. The importance of addressing service users’ personal recovery, alongside more conventional ideas of clinical recovery,12 is now supported in guidance for all key professions. 13–16 To this has been added the more recent idea of personalisation. Underpinned by recovery concepts, the aim of personalisation is for people and their families to take much more control over their own support and treatment options, alongside new levels of partnership and collaboration between service users (or citizens) and professionals. 17 Recovery and personalisation in combination mean practitioners tailoring support and services to fit the specific needs of the individual and enabling social integration through the increased involvement of local communities. 18
The CPA and CTP are central to modern mental health care, and yet there are few studies that explicitly explore the practices of care planning and co-ordination in community services and even fewer that focus on inpatient care planning. A relatively rare example of the former is the recently completed COCAPP (Collaborative Care Planning Project) study,19,20 with this current sister project extending the field of research to the hospital setting. National quality statements include the requirement that service users in adult mental health services jointly develop a care plan with mental health professionals, are given a copy with an agreed review date, and are routinely involved in shared decision-making. 21 National policies1,10 outline the expectations that people will recover from mental ill health and be involved in decisions about their treatment. This holds true for both informal and detained inpatients, with reasonable adjustments made when necessary to ensure that people are supported to live lives that are as full and socially participative as possible. 22 In the light of this, the Care Quality Commission (CQC) recommended that:
Care planning should have clear statements about how a person is to be helped to recover, and follow guidance set out in the national Care Programme Approach. Care plans should focus on individual needs and aspirations, involving patients at all stages so as to reflect their views and individual circumstances.
Reproduced with permission from the CQC © CQC, Monitoring the Mental Health Act in 2011/12, p. 622
However, in care plans checked by the CQC, 37% showed no evidence of patients’ views being included; 21% showed that patients were not informed of their legal right to an independent mental health advocate; and almost half (45%) showed no evidence that patients consented to treatment discussions before medication was administered. The CQC was also concerned that cultures may persist in which control and containment are prioritised over the treatment and support of individuals, and in 20% of visits the CQC expressed concerns about the de facto detention of patients who were voluntary rather than compulsory patients. However, in other settings, excellent practice was found to lead to care and treatment that were in line with policy expectations.
Earlier national reviews across both nations found that service users remained largely mystified by the care planning and review process itself, with significant proportions not understanding their care plans, not receiving written copies of their plan and, often, not feeling involved in writing plans and setting goals. 23,24 Clearly, there are significant problems with inpatient care planning, with the CQC noting a:
significant gap between the realities observed in practice and the ambitions of the national mental health policy.
Reproduced with permission from the CQC © CQC, Monitoring the Mental Health Act in 2011/12, p. 622
The House of Commons Health Committee25 subsequently reported widespread concerns about delays and imbalance in care planning, with a focus on risk rather than recovery. In Wales, the National Assembly’s Health and Social Care Committee reported a low uptake of advocacy services by people admitted to hospital care. 26
Further evidence is clearly needed to develop care planning interventions that embed dignity, recovery and participation for all of those who use inpatient mental health care.
In 2008, the Healthcare Commission27 measured performance on 554 wards across 69 NHS trusts that provided mental health acute inpatient services. The commission found that almost two-fifths of trusts (39%) scored weakly on involving service users and carers; 50% of care plans sampled did not include a record of the service user’s views; and nearly one-third of care records (30%) did not include a record of whether or not the service user had a carer. One-third of all care records sampled (33%) showed that community care co-ordinators provided input into the service user’s care review meetings only ‘some or none of the time’. The commission27 called for more to be done to address the divisions between hospital and community services and to:
ensure that acute inpatient services are more personalised as a basis for promoting recovery.
Reproduced with permission from the Commission for Healthcare Audit and Inspection © Commission for Healthcare Audit and Inspection 2008, The Pathway to Recovery, p. 327
An even earlier study of inpatient stays in England reported that large numbers of patients are admitted for a week or less, which had implications for inpatient and community services, and the authors suggested that the CPA was ‘cumbersome’, ‘rigid’ and ‘impractical’ in relation to short admissions. 28
Although the evidence base for community care planning and co-ordination is sparse,20 research studies exploring care planning and co-ordination in acute inpatient mental health settings are almost non-existent, as will be shown in Chapter 3. This may reflect the reported historical neglect of inpatient care by policy-makers and researchers,29 or some of the ethical and practical challenges faced when conducting research in settings in which a significant proportion of patients are detained under legislation or may lack the capacity to consent. These challenges are addressed directly in this study.
To summarise: the CQC22 identified serious concerns in relation to care planning, patient involvement and consent to treatment for patients detained under the MHA3 and the de facto detention of patients who were voluntary rather than compulsory patients. Earlier reports by the Healthcare Commission27 had identified serious concerns about care planning and called for measures to ensure that acute inpatient services are more personalised as a basis for promoting recovery. To date, there has been almost no research exploring the realities and challenges of planning and providing care and treatment in inpatient settings that includes people detained under the MHA. 3
The design of our initial COCAPP study of care planning and co-ordination in community mental health care settings (Health Services and Delivery Research programme project 11/2004/12), published in Health Services and Delivery Research in February 2016,20,30 has informed the design and procedures of this COCAPP-A (Collaborative Care Planning Project-Acute) inpatient study. Owing to the similarities in the study design and methods, some material in this report has been adapted from that publication, but all data and analysis are new and the results from both studies are compared in Chapter 6 of this report.
Aims
The aim of this study is to identify factors that facilitate or hinder recovery-focused personalised care planning and co-ordination in acute inpatient mental health settings.
We intend the results of this study to complement and build on our study of care planning and co-ordination in community settings20 (Health Services and Delivery Research project 11/2004/12) to provide a whole-systems response to the challenges faced in providing collaborative, recovery-focused care planning. We also aim to respond to the CQC’s22 question of how to embed dignity, recovery and participation in inpatient practice when people are subject to compulsory care and treatment.
As an exploratory study guided by the Medical Research Council31 Complex Interventions Framework, the study will generate empirical data, new theoretical knowledge and greater understanding of the complex relationships between collaborative care planning, recovery and personalisation. It will help identify the key components required and provide an informed rationale for a future evidence-based intervention and evaluation aimed at improving care planning and patient outcomes within and across care settings, likely to be acceptable to service users, families/carers, practitioners and service managers. It will also provide lessons for similar, equally problematic, care planning processes in a range of other health/social care settings. 32
Research question
The main research question for this study is ‘what facilitates or hinders recovery-focused personalised care planning and co-ordination in acute inpatient mental health settings?’. To answer this, the following questions are explored:
-
What impact do national and local policies and procedures have on care planning and co-ordination?
-
What are the key drivers that have an impact on care planning and co-ordination?
-
What are the views of staff, service users and carers on care planning, therapeutic relationships, recovery-orientation and empowerment in acute care settings?
-
How is care planning and co-ordination currently organised and delivered in local services?
-
How, and in what ways, is care planning and co-ordination undertaken in collaboration with service users and, when appropriate, carers?
-
To what extent is care planning and co-ordination focused on recovery?
-
To what extent is care planning and co-ordination personalised?
-
What specific features of care planning and co-ordination are associated with the legal status of service users?
-
Is care planning and co-ordination affected by the different stages of stay on a ward (i.e. at admission, during stay, pre discharge)?
-
What suggestions are there for improving care planning and co-ordination in line with recovery and personalisation principles?
Objectives
This study investigated care planning and co-ordination for inpatients in acute mental health settings. The objectives were to:
-
conduct a literature review on inpatient mental health care planning and co-ordination and review English and Welsh policies on care planning in inpatient settings
-
conduct a series of case studies to examine how the care of people with severe mental illness using inpatient services is planned and co-ordinated
-
investigate service users’, carers’ and practitioners’ views of these processes and how to improve them in line with a personalised, recovery-oriented focus
-
measure service users’, carers’ and staff’s perceptions of recovery-oriented practices
-
measure service users’ perceptions of inpatient care, and their views on the quality of therapeutic relationships and empowerment
-
measure staff’s views on the quality of therapeutic relationships
-
review written care plan documentation and care review meetings
-
conduct a multiple comparisons analysis within and between sites to examine the relationships and differences in relation to perceptions of inpatient care, recovery, therapeutic relationships and empowerment.
Structure of report
This report presents the key findings of our empirical research building on a metanarrative policy and literature review within the context of continuing developments in the organisation, structure and delivery of inpatient mental health care in England and Wales.
In Chapter 2 we outline the methodology and design of the study, including public and patient involvement and ethics issues. In Chapter 3 we outline the methods and findings of the comparative policy analysis and metanarrative literature review. In Chapter 4 we present the results from the within-case analysis, with findings from quantitative and qualitative analyses for both meso- and micro-level data presented for each case study site. Then, in Chapter 5 we draw out comparisons and contrasts across sites set within the cross-national policy contexts and provide summary charts of the factors identified from this cross-case analysis that appear to act as facilitators of and barriers to the provision of recovery-focused, personalised care planning and delivery. Finally, in Chapter 6, we compare the results from this study with those from our earlier community study, consider the limitations of the study and explore the findings in relation to our aims and objectives and recent and ongoing research in relevant and overlapping areas. We end by outlining some tentative implications for mental health care commissioning; service organisation and delivery; clinical practice and health-care professional education and training; and recommendations for future research.
Chapter 2 Methods
Design
We conducted a cross-national comparative study of recovery-focused care planning and co-ordination in inpatient mental health-care settings, employing a concurrent transformative mixed-methods approach with embedded case studies. 33 Concurrent procedures required that we collect quantitative and qualitative data at the same time during the study and then integrate those data to provide a comprehensive analysis of the research problem. One form of data is nested within another larger data collection procedure to allow the analysis of different questions or levels of units in an organisation.
In this study, we nest in-depth micro-level case studies of everyday ‘frontline’ practice and experience with detailed qualitative data from interviews and reviews of individual care plans within larger meso-level survey data sets and policy reviews in order to provide potential explanations and understanding.
At the macro level is the national context. Cross-national comparative research involves ‘comparisons of political and economic systems . . . and social structures’ (p. 93)34 where ‘one or more units in two or more societies, cultures or countries are compared in respect of the same concepts and concerning the systematic analysis of phenomena, usually with the intention of explaining them and generalising from them’ (pp. 1–2). 35 In this study, devolved government and the emergence of similar but distinct health policy, legislation and service development in England and Wales provided the backdrop for the investigation of inpatient mental health care.
Such an approach fits well with a case study method36 that allows the exploration of a particular phenomenon within dynamic contexts whereby multiple influencing variables are difficult to isolate. 37 It allows the consideration of historical and social contexts38 and is especially useful in explaining real-life causal links that are maybe too complex for survey or experimental approaches. 39 So, in this study, we conducted a detailed comparative analysis of ostensibly similar approaches to recovery-focused care planning and co-ordination within different historical, governmental, legislative, policy and provider contexts in England and Wales.
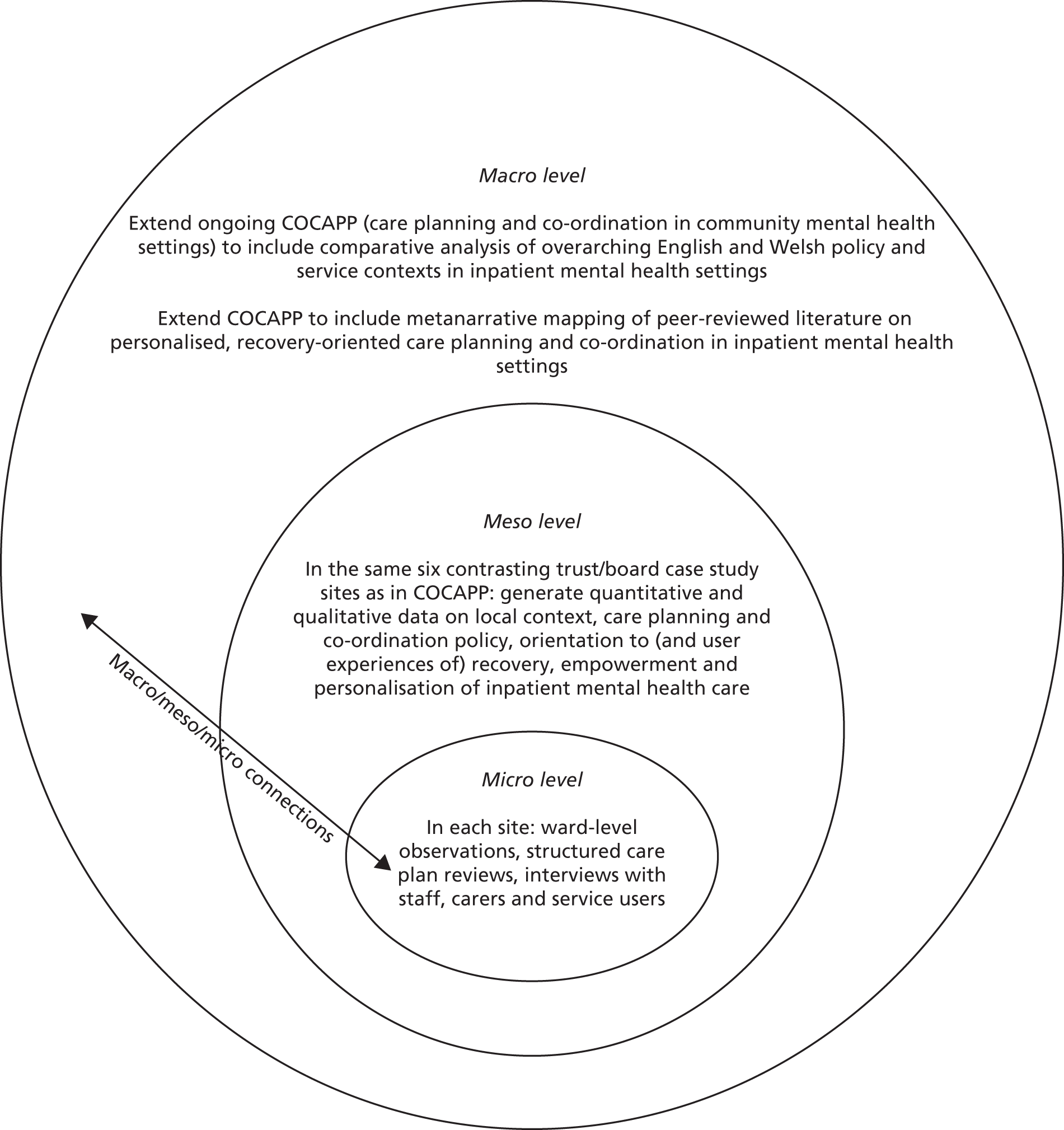
The definitions of the case studies were predetermined40 and focused on six selected NHS trust/health boards. Data collection at this level involved identifying local policy and service developments alongside empirical investigations of care planning and inpatient care, recovery, personalisation, therapeutic relationships and empowerment, employing mixed quantitative and qualitative methods. This design is represented in Figure 1.
FIGURE 1.
Diagram illustrating embedded case study design and integration with (and extension of) initial COCAPP study of care planning and co-ordination in community mental health settings. Adapted with permission from Simpson et al. 20
Theoretical/conceptual framework
Transformative research seeks to include an explicit ‘intent to advocate for an improvement in human interests and society through addressing issues of power and social relationships’. 41 In line with this, transformative procedures require the researcher to employ a transformative theoretical lens as an overarching perspective. 42 This lens provides a framework for topics of interest, methods of collecting data, and outcomes or changes anticipated by the study.
This study is guided by a theoretical framework emphasising the connections between different ‘levels’ of organisation43 (macro/meso/micro) and concepts of recovery and personalisation that foreground the service user perspective and, arguably, may challenge more traditional service/professional perspectives. Furthermore, our research team and processes involve mental health service users throughout. We employed mixed methods across two phases.
Methodology
Phase 1: literature and policy review and synthesis
Literature review on inpatient mental health care planning and co-ordination
We extended our previous review of international peer-reviewed literature, and English and Welsh policies,20 to include recovery-oriented care planning in inpatient settings (macro level). We employed Greenhalgh et al. ’s44 metanarrative mapping method, which focuses on providing a review of evidence that is most useful, rigorous and relevant for service providers and decision-makers and that integrates a wide range of evidence. 45 Our metanarrative mapping method review provides a preliminary map of current mental health care planning and co-ordination by addressing four points: (1) how the topic is conceptualised in different research traditions, (2) what the key theories are, (3) what the preferred study designs and approaches are and (4) what the main empirical findings are. We describe the methods employed in Chapter 3, where we also bring together our broad narrative synthesis.
Comparative analysis of policy and service frameworks
By searching English and Welsh government websites we also identified all key, current, national-level policy and guidance documents directly relating to inpatient mental health care planning and co-ordination across the two countries, along with those which relate directly to the promotion of recovery and the delivery of personalised care. Drawing on these, we produced a narrative synthesis identifying the major themes and areas of policy convergence and divergence (see Chapter 3), and used these materials to lay out the large-scale (or ‘macro-level’) national policy contexts to inform our case study research interviews (see Chapter 4).
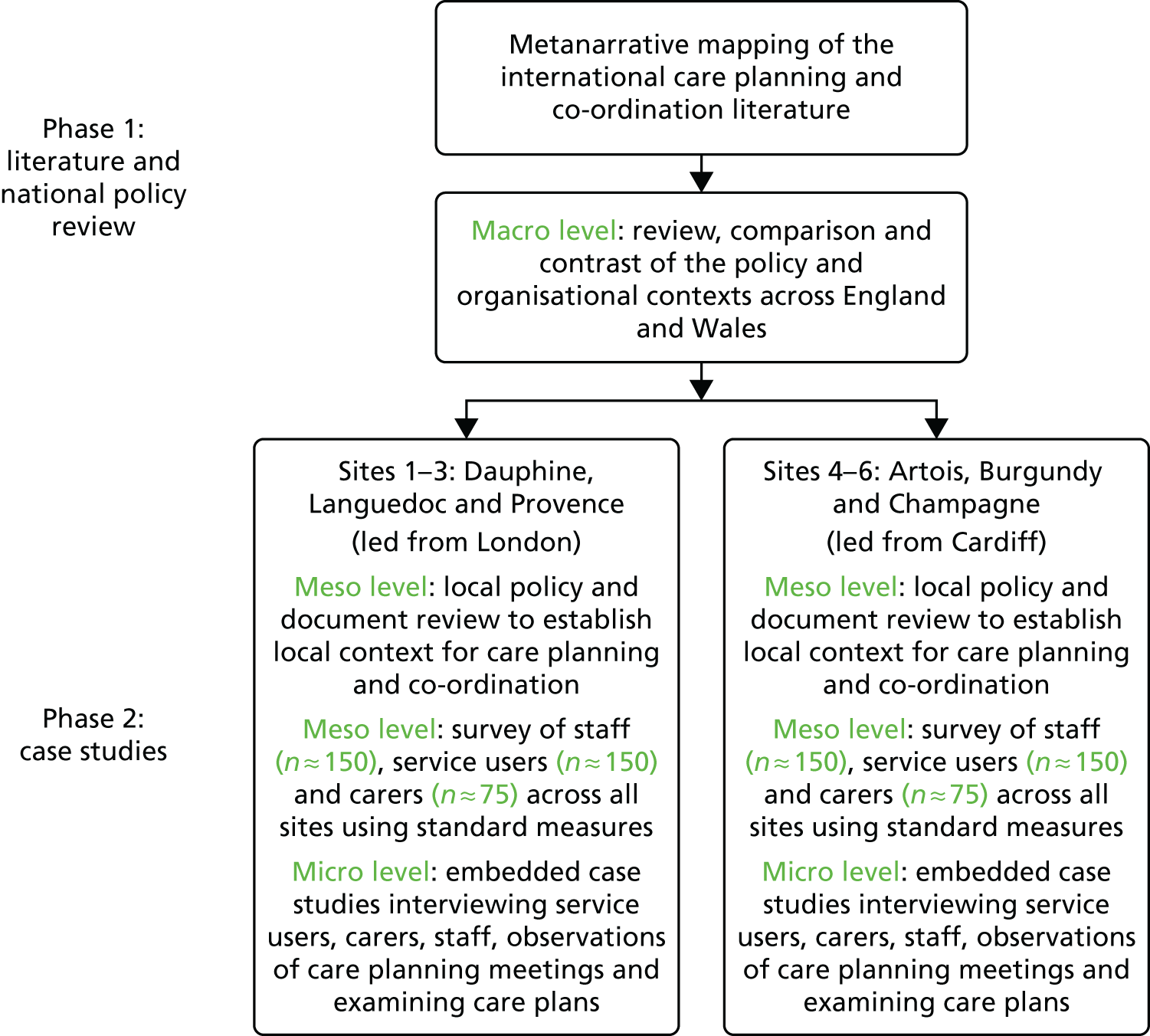
Phase 2: case studies
In phase 2, we conducted six in-depth case study investigations36 in six contrasting NHS trust/health board case study sites in England (n = 4) and Wales (n = 2) (meso level), employing mixed quantitative and qualitative methods. Then, in each site, we secured access to a single acute inpatient ward from which up to six service users, six multidisciplinary staff and four informal carers were sampled as embedded micro-level case studies. 33 Qualitative data were generated related to care planning and co-ordination processes in each inpatient ward (Figure 2).
FIGURE 2.
Sample size and data collection targets for COCAPP-A. Adapted with permission from Simpson et al. 20
Inclusion criteria
Ward inclusion criteria
-
The ward provided an acute mental health care admissions facility to the local adult population.
-
The ward had an established ward manager/team leader in post.
-
The ward was not subject to any plans for closure or merger during the study.
-
The ward was not currently experiencing excessive pressures or responding to elevated levels of untoward incidents (so that we did not add to participant burden).
-
There was multidisciplinary team (MDT) support to participate in the study.
Service user/patient inclusion criteria
-
Was admitted to inpatient unit.
-
Had been on the ward for a minimum of 7 days.
-
Was aged ≥ 18 years.
-
Had a history of severe mental illness.
-
Was able to provide informed consent.
-
Had sufficient command of English/Welsh.
These criteria were deliberately broad to allow the inclusion of patients with organic brain disorders, people with substance abuse and people who were not fluent in English or Welsh, which is very often the case in NHS routine care.
Staff inclusion criterion
-
Any qualified or unqualified staff working on inpatient wards who were involved in care planning or review.
Sampling
We selected the same six case study sites that had participated in the initial COCAPP study to enable us to draw comparisons and connections between community and inpatient services. These sites consisted of four NHS trusts in England and two local health boards (LHBs) in Wales that were commissioned to provide inpatient mental health services. These sites were identified to reflect variety in geography and population and to include a mix of rural, urban and inner-city settings in which routine inpatient care is provided to people with complex and enduring mental health problems from across the spectrum of need. The selection of six sites in the original COCAPP study followed advice from reviewers and was decided pragmatically, balancing variety of settings and populations with logistical and data management pressures in the time available.
In each meso-level trust/health board site, we aimed to survey a large sample of service users, carers and ward staff (see Figure 2). Survey questionnaires focused on recovery-oriented practices (all groups), the quality of therapeutic relationships (service users and staff), feelings of empowerment (service users only) and perceptions of acute mental health care, including involvement in care planning and ward round discussions (service users only).
In each trust/health board site, we also selected a single ward that provided routine inpatient mental health care and met our inclusion criteria (outlined in Ward inclusion criteria). Interview data were generated relating to local contexts, policies, practices and experiences from a range of ward staff purposively selected to include ward managers, psychiatrists, senior nurses, psychologists and occupational therapists (OTs) (meso- and micro-level data).
To generate knowledge about how care is planned, co-ordinated and experienced at the ‘micro level’, we then invited a sample of six service users, who were under the care of that ward and approaching discharge, to be interviewed about their experiences of care planning during their admission. They were also invited to jointly review their inpatient care and aftercare plans, as well as their involvement in developing and implementing those plans in line with recovery and personalisation approaches. In addition, we attempted to interview family members/carers about their experiences of inpatient care planning and co-ordination. A structured review of additional care plans and a non-participatory observation of ward activities discussing and reviewing care plans were also conducted.
Sample size calculations
For the questionnaire survey, an a priori sample size calculation was conducted using the software package G*Power (version 3.1; Heinrich-Heine-Universität Düsseldorf, Düsseldorf, Germany). 46 The sample size was based on completing a multivariate analysis (MANCOVA) for comparing the interaction of within (covariates) and between (sites) factors. Assumptions were based on six groups (sites), four outcome measures (questionnaires) and 10 potential predictors (gender, age, ethnicity, time on CPA, etc.). We calculated the sample size using α level of 0.05, power of 0.8047 and a small effect size (Pillai’s Trace V = 0.10). Given the many potential influences on our outcome measures, we expected the magnitude of the observed relationship to be small. A small effect size was therefore chosen to represent the subtleties in relationships of the data. This calculation suggests that a sample size of 276 is required in order to reach power.
Based on this sample size calculation we aimed to obtain complete questionnaire survey responses from 300 service users (n = 50 per trust/health board), 300 inpatient staff (n = 50 per site) and 150 informal carers (n = 25 per trust/health board). By aiming to sample 300 survey responses we were seeking to include more than the sample size suggested for the service users and inpatient staff. We anticipated that with rates of non-response and incompletion of the questionnaires we would need to oversample to meet our sampling targets. In contrast, we anticipated not to achieve this sample size for informal carers. This was because not every service user would have a carer, and therefore analysis for the informal carers was underpowered (estimated power will be 0.44). The data for the informal carers were, therefore, anticipated to be exploratory in preparation for a future, larger-scale study. Further information on our involvement of carers is given in Chapter 4 (see Recruitment and case study sites).
One ward within each trust/health board was selected to participate in micro-level data collection. We planned to undertake semistructured interviews in each ward with staff (target per ward, n = 6; total, n = 36), service users (target per ward, n = 6; total, n = 36; to include joint review of care plan) and carers (target per ward, n = 4; total, n = 24).
Calculations of the sample size for the qualitative interviews were based on previous research with similar populations by the co-investigators and others; an understanding of the practicalities and time commitments involved in recruiting and interviewing participants and analysing in-depth qualitative data; and the numbers required for us to feel confident that the findings would be transferable to other, similar settings.
In addition, we intended to undertake structured case reviews of care plans for service users on each participating ward (target per ward, n = 10; total, n = 60) and non-participant observation of care planning processes on inpatient units (target per ward, n = 3; total, n = 18).
Instrumentation
Table 2 maps data collection methods against the research questions. Permissions were obtained to use all measures.
-
Documentation and officially collected data: local meso-level CPA policy and procedure documents, CQC, national and local audits and reviews were collated when possible.
-
The Recovery Self-Assessment (RSA)48 is a 36-item scale designed to measure the extent to which recovery-oriented practices are evident in services. It was used in the initial COCAPP study. The scale addresses the domains of life goals, involvement, treatment options, choice and individually tailored services. The total RSA score is obtained by summing the individual items and dividing them by the number of items. Individual item scores range from 1 (‘strongly disagree’) to 5 (‘strongly agree’). A higher total score refers to a more recovery-focused service. The RSA has been tested for use with people with enduring and complex mental health problems and across a range of ethnic backgrounds. To date, no data are available on construct and external validity for this scale. In our community COCAPP study, we assessed the internal consistency of the RSA with Cronbach’s alpha and demonstrated that alpha levels for the total score and subscales were acceptable. 19 The measure was completed by service users, carers and ward staff.
-
The Scale To Assess the Therapeutic Relationship (STAR)49 is a brief (12-item) scale that assesses therapeutic relationships. The patient version was used in the initial COCAPP community study. It has good psychometric properties, the internal consistency and test-retest reliability are acceptable, and it is suitable for use in research and routine care. A total STAR score is obtained by summing the individual items. Scores for individual items range from ‘0’ (‘never’) to ‘4’ (‘always’) and the total possible score ranges from 0 to 48. A higher score refers to a more positive rating of therapeutic relationships. The subscales measure positive collaborations (possible score 0–24), positive clinician input (possible score 0–12) and non-supportive clinician input in the patient version and emotional difficulties in the staff version (possible score 0–12). The measure was completed by service users and ward staff.
-
The Empowerment Scale (ES)50 is a 28-item questionnaire with five distinct subscales: self-esteem, power, community activism, optimism and righteous anger. Empowerment is strongly associated with recovery and ES is the most widely used scale. The development paper for the scale reported a high degree of internal consistency. A further paper confirmed moderate construct validity. 51 A total empowerment score for each service user respondent is obtained by summing individual items and dividing them by the number of items. At the item level the scores range from ‘1’ (‘strongly agree’) to ‘4’ (‘strongly disagree’). A higher total score indicates a higher perceived level of empowerment. Subscale values can also be provided for ‘self-esteem–self-efficacy’, ‘power–powerlessness’, community activism and autonomy’, ‘optimism and control over the future’ and righteous anger’. This scale was completed by service users and was also used in the COCAPP study.
-
The Views of Inpatient Care Scale (VOICE)52 is a 19-item patient-reported outcome measure of perceptions of acute mental health care that includes questions on involvement in care planning and ward round discussions. An innovative participatory methodology was used to involve service users throughout the development and testing of this measure. The VOICE encompasses the issues that service users consider most important and, therefore, it has high face validity. The original development paper for the scale52 reported that the scale had demonstrated high criterion validity and high internal consistency and that the test–retest reliability was high. It is easy to understand and complete, making it is suitable for use by service users while in hospital; it has also been shown to be sensitive to service users who have been compulsorily admitted and who tend to report significantly worse perceptions of the inpatient environment. An overall VOICE total score was obtained by individual item scores; possible total scores range from 19 to 114. Individual item scores range from 1 ( ‘strongly agree’) to 6 ( ‘strongly disagree’). The higher the total score for the VOICE, the more negative the perception of the quality of care on the ward. The measure was completed by service users (see Appendix 1 for all questionnaires).
-
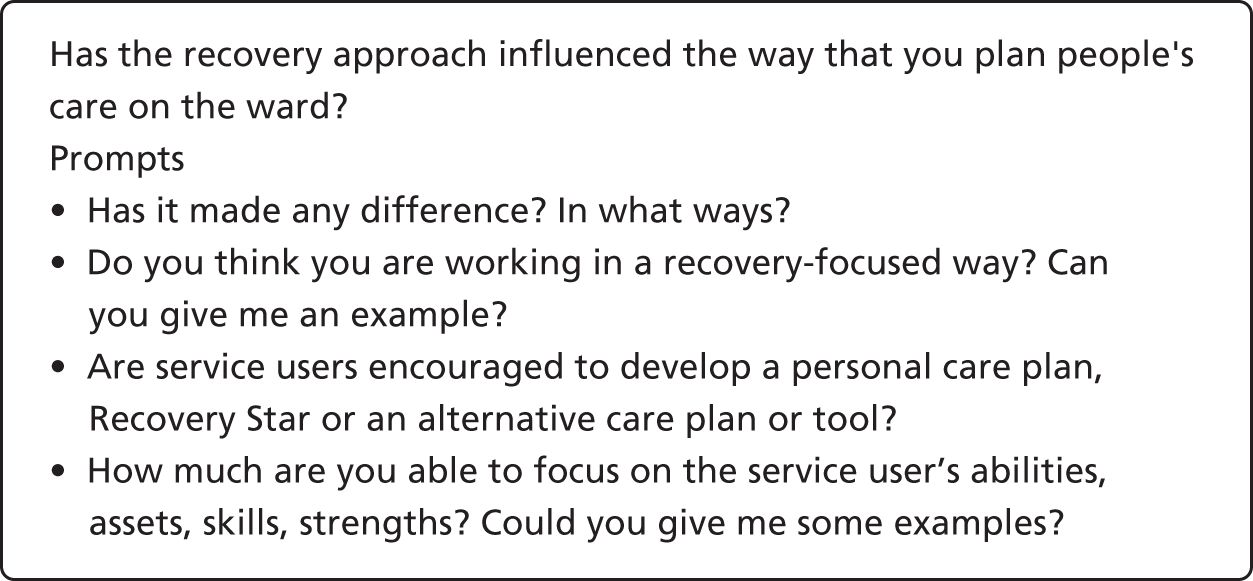
Structured interviews with ward staff, service users and carers: interview schedules were based on those used in the initial COCAPP study and refined by the study team in consultation with our Scientific Steering Committee and Lived Experience Advisory Group (LEAG) and drawing on relevant literature. The aim of all interviews was to explore participants’ views and experiences of care planning and co-ordination, safety and risk, recovery and personalisation, and the context within which these operated. The interview schedules for each group of respondents comprised 19 lead questions, with numerous prompts suggested for the interviewer (Figure 3; the full schedule is in Appendix 2).
-
CPA care plan review: within each ‘embedded case study’, as part of the interview process, the six purposively selected service users were also asked to look at and provide a narrative review of their care plan with the researcher.
-
Structured review of service user care plans: in addition to the narrative care plan reviews above, anonymised information was obtained from the care plans of a series of consecutively discharged patients (including first admissions and readmissions, with replacements for refusals) at each of the six inpatient wards taking part in the study (target at each trust/health board, n = 10; total, n = 60). When consent was provided, anonymous CPA/CTP care plans were systematically reviewed and appraised against a structured template incorporating identified key concepts of good practice in care planning, user and carer involvement, personalisation and recovery (see Appendix 3). The template was specifically developed and informed by CPA good practice checklists developed by service users and staff;53,54 our community care planning study; and the CPA Brief Audit Tool,55 designed and used to assess the quality of CPA care planning for service users who have had more than one compulsory admission in 3 years.
-
Non-participant observation of care planning processes on inpatient units: this included staff–patient assessment/care planning meetings, ward rounds and discharge planning meetings. Observations were informed by a structured guide, developed to identify good practice in involving service users and carers, and a focus on recovery and personalisation. The guide was developed in consultation with an established Service User and carer Group Advising on Research (SUGAR)56 and the LEAG (see Appendix 4).
| Research questions | Data collected to answer the research question |
|---|---|
|
|
|
|
|
|
|
|
|
|
|
|
FIGURE 3.
Example question and prompts.
Research ethics
The study received NHS Research Ethics approval from the National Research Ethics Service Committee London – Fulham (reference number 14/LO/2062) on 29 December 2014.
Considerable attention was given to ensuring the welfare of service users, carers and other participants, as well as that of the researchers. This included providing opportunities for people to pause or withdraw from interviews, assurances of anonymity and confidentiality and responses to concerns for people’s welfare. Careful arrangements were made for the location and conduct of interviews, and all researchers received training, supervision and opportunities for debriefing.
Procedure
We obtained provisional agreement to participate in the study in writing from senior trust/health board managers (e.g. the chief executive) before submitting the research proposal for funding. Following the commissioning of the study, a formal invitation to take part in the study was communicated to a senior manager, such as the chief executive, in each organisation. All accepted, and identified a principal investigator/link person to facilitate research ethics and governance approvals as well as contact with other staff.
We identified suitable local wards meeting the inclusion criteria with the assistance of local NHS trust/health board principal investigators. Ward managers were approached by a researcher who explained the study, responded to any queries and invited them to participate. Nobody declined to take part. We sought consent to participate in the questionnaire survey from two or three wards, one of which was selected for the more in-depth case study of care planning, including interviews.
Questionnaire survey
With help from the clinical teams, researchers, clinical studies officers57 and research nurses distributed information sheets, consent forms and questionnaires to ward staff, service users and carers, and collated the completed questionnaires. We approached additional wards within the host site to enable us to achieve the sample required for the questionnaire survey.
Researchers attended ward staff meetings to explain the study and respond to any questions. All managers and ward staff involved in care planning or care plan review received written and verbal information about the study and were invited to participate in the questionnaire survey (the target was 50 people per trust/health board). We employed the usual procedures for obtaining informed consent with permission to decline or withdraw, and all participants were anonymised.
Staff from participating wards were asked to identify service users who had been on that ward for a minimum of 7 days, and who in their view had the capacity to participate in the study and complete the questionnaire survey (target n = 50 per trust/health board). Staff made the initial approach to the service user, inviting them to meet with the research assistant to find out more about the study. If the service user expressed an interest, the research assistant provided them with written and verbal information about the study, and invited them to ask any questions. During this process the research assistant appraised the capacity of the service user to understand the information and make an informed decision about whether or not to participate. The service user was encouraged to discuss the study with family, friends, advocates or staff if they wanted to. Once informed consent had been obtained, each service user was given the pack of questionnaires to complete, with assistance available from the research assistant if required.
Ward staff were asked to give carer questionnaire packs to carers (family members and friends) who were visiting service users on the ward (target n = 25 per trust/health board). The packs included an information sheet and a freepost return envelope. Researchers working on the ward also approached carers to invite them to complete the questionnaires, with assistance provided if required.
Semistructured interviews
Key personnel, identified using purposive sampling, were invited to participate in interviews for the in-depth case study and to forward local policies and information (target per case study ward, n = 6; total, n = 36). Staff were given written materials that described the purpose of the study and explained what taking part in an interview would entail; this included the option to decline or withdraw from the study at any time. Informed consent procedures were followed. Interviews took place once informed consent had been obtained and at a time convenient to the staff member.
Staff members identified service users approaching discharge who were deemed to have capacity to give informed consent. Subsequently, the research assistant invited these service users to participate in an interview about their experiences of care planning and jointly review their care plan (target per case study ward, n = 6; total, n = 36) (see Care plan review). Once informed consent had been obtained, arrangements were made to conduct the interview at the service user’s earliest convenience. Appraisal of capacity was continuously assessed during the interview. Service users were also asked for their permission for their care plans to be reviewed.
Service users were asked to identify a carer (if applicable) to take part in an interview (target per case study ward, n = 4; total, n = 24). The research assistant either contacted the carer by telephone or approached them on the ward during a visit, in the presence of the service user if possible. If the carer expressed an interest in participating, the research assistant provided them with written information about the study and gave them the opportunity to ask questions. Carers were encouraged to give some time and thought to whether or not they wanted to participate before they signed the consent form, and to discuss it with a family member, friend or member of staff. Once informed consent had been obtained, the carer was invited to participate in an interview at their earliest convenience. The interview took place in the hospital or at their home, depending on their preference. If they requested to be interviewed at home, lone worker policies and procedures were followed.
Care plan reviews
In addition to the service users who consented to interview and a review of copies of their care plans, a total of 10 further service users’ care plans were reviewed by researchers with consent (target per case study site, n = 10; total, n = 60). Potential participants for this part of the study were identified and consented into the study if they had agreed to complete a questionnaire. When care plans were accessed in this way, efforts were made to ensure that the information extracted for research purposes did not include the real names of service user participants or other details that could have identified them. Care plans were systematically reviewed and appraised against a structured template incorporating the identified key concepts of personalisation and recovery. Anonymised demographic, diagnostic and service use data, for example complexity of case/need, were also collated to describe this sample in relation to the wider population of people using acute inpatient mental health services.
Observations of care planning processes
In addition to this, the research team conducted non-participant observations of care planning processes on inpatient units (target per case study site, n = 3; total, n = 18). On each participating acute ward, and with prior agreement, researchers attended and observed at least three meetings during which patient care was routinely discussed and planned. These included individual care planning meetings, discharge planning meetings and ward rounds. Information about the intention of researchers to attend and observe some of these meetings was included on posters displayed in the ward. Researchers took contemporaneous notes of meetings and, with permission, digitally recorded interactions to check for accuracy when the notes were transcribed and analysed. Observations were informed by a structured guide previously developed to identify good practice in involvement of service users and carers and by a focus on recovery and personalisation.
Staff interviews were conducted by academic researchers (SB, NA, RC and MC) and clinical studies officers. Service user and carer interviews were conducted by service user researchers (KB, BE, AM and AF) with one of the academic researchers in attendance, or occasionally by academic researchers (SB, NA and JM). Clinical studies officers undertook care plan reviews using the template provided. Observations were undertaken by academic researchers (SB and RC) and a service user researcher (AF).
Public and patient involvement
The study was developed and designed with full involvement of co-investigator and independent service user researcher AF and in consultation with SUGAR,56 based at City, University of London and facilitated by the chief investigator (AS). In addition, a LEAG was established, consisting of seven service users and one carer with direct experience of inpatient mental health care planning and co-ordination. This separate advisory group of ‘experts through experience’ ensured that more time could be spent exploring the views of service users and carers and ensuring that their perspectives were able to inform the study. Members were recruited via the previous COCAPP LEAG to provide some continuity and ensure geographic spread.
The group was facilitated by AF and it met with members of the research team three times during the course of the study, contributing in the following ways:
-
suggested relevant literature and terms to inform the literature review
-
suggested things to consider when recruiting people for interviews on the ward
-
informed the structured observation guide and advised the research team based on personal lived experiences of ward rounds and discharge meetings
-
advised on the interview schedules, providing suggestions for additional prompts and ensuring consistency
-
provided suggestions on the recruitment of carers
-
discussed with the service user researchers about their experiences of interviewing service users and using the interview schedules
-
provided suggestions on the challenges in gaining access to observe ward rounds
-
provided suggestions for dissemination of the findings from both studies
-
contributed to a co-produced paper for publication on working in partnership.
The 12-member Scientific Steering Committee consisted of representatives with a clinical or research background from each of the participating NHS trusts/health boards and independent academics. One service user and one carer member also represented the LEAG on the Project Advisory Group (PAG), with input from the LEAG timetabled on the agenda of all meetings, which were chaired by Professor John Baker, Professor of Mental Health Nursing at University of Leeds.
Three service user researcher assistants/service user project assistants were employed to work on the study on a temporary contract basis: one based in London and two based in Swansea. All received training and ongoing support during the study.
Analytical framework
We framed our data analysis by drawing on social scientific ideas and the findings of our phase 1 evidence and policy review, an approach used by co-investigators in previous studies58 and in our previous community study. Our concern to explore commonplace practices in inpatient mental health is congruent with interactionist interests in social processes and human action. 59 This perspective also recognises the importance of social structures, so that in any given setting person-to-person negotiations are shaped by the features of organisational context. 60 The immediate context for frontline practitioners and service users in this study is the inpatient ward, each of which we view as a complex open system. Each participating ward also sits within a larger meso-level NHS trust/health board site, which in turn is located within a national-level system of mental health services. This idea of ‘nested systems’ is a feature of complexity thinking,43 and informed our plan to generate, analyse and connect data at different (but interlocking) macro/meso/micro ‘levels’ of organisation. Analysis and interpretation of the case study data were informed by a conceptual framework that emphasised the connections between different (macro/meso/micro) levels of policy and service organisation, and that drew on the findings of the literature and national policy review in relation to care planning, recovery and personalisation.
Quantitative analysis
Preparation of the data
Data from the questionnaires were entered into SPSS version 21 (IBM Corporation, Armonk, NY, USA) and checked and cleaned by a second researcher before statistical analysis. The distribution of the questionnaire data was assessed for normality using descriptive quantitative measures of skewness and kurtosis. Across the sites, normality was assessed for 17 outcomes for service users and 10 outcomes for staff. The outcomes from both groups fell within the range of the normal distribution. There were few deviations from normality (2 out of 27 scale outcomes exceeded the conservative criteria of ± 1) and one was small in the extent of deviation (within ± 2); however, one scale displayed larger deviation of skewness [emotional differences subscale, staff outcome, on the Scale to Assess the Therapeutic Relationship – Clinician Version (STAR-C)]. Parametric tests are robust enough to withstand minor deviations in normality, and therefore the skewness and kurtosis values outlined above do not preclude the use of parametric tests. 61
Comprehensive sensitivity analyses were completed to allow determination of what parameters to use when dealing with missing data. A missing value analysis was completed for the 27 scale outcomes. Moderate to high levels of missing data, not missing at random, were identified on a small number of items (mean level of missing data across the 27 scales/subscales was 20%, range from 6% to 55%). The service user version of the RSA questionnaire in particular had a moderate number of missing data. Mean replacement was used to avoid an unnecessary loss of cases from the analysis. The mean of the available items for the scale and participant was used for replacement of the missing values on the scale. A series of sensitivity analyses were conducted to determine what effect mean replacement would have in the primary analyses at different levels of replacement, ranging from 20% to 50%. A comparison was made between the impact of different levels of mean replacement and a complete case analysis (i.e. participants with no missing values on the scale or subscale). Utilising a 50% mean replacement led to no substantive changes in the key statistical parameters (p-values and associated effect sizes) and the inferences drawn; therefore, it was deemed appropriate to maximise the number of cases included in the analyses.
Exploring the data
Descriptive statistics were calculated for the four questionnaires (VOICE, RSA, STAR and ES). The total scores, subscale means and standard deviations (SDs) were derived to produce a ‘recovery profile’ for each site. When appropriate these scores were compared against reference values (VOICE, STAR and ES) or with the participant groups (RSA). Some further detailed analysis at a descriptive level was completed on the primary outcome scale (RSA) to aid with the triangulation of the qualitative and quantitative data. This was completed at an individual item level on the scale by ranking the mean responses for each question to determine where the most agreement was for the participant groups. The top five items were selected from the questionnaire and presented as a recovery profile for the site. We provide descriptive narratives comparing the results from the community COCAPP study and the COCAPP acute study. We chose to present a comparative analysis descriptively for the within-case analysis and refer the reader to an exploratory inferential analysis in Chapter 5.
Inferential statistics
Several unadjusted one-way analyses of variance (ANOVAs) were conducted to compare differences between the six sites on the RSA, STAR, ES and VOICE measures. Subsequent Tukey’s post hoc tests were conducted to ascertain which measures differed between which locations. A series of one-way analyses of covariance (ANCOVAs) was completed to adjust the analyses for potential confounders. The demographic variables that were chosen for service users were age, gender, ethnicity and living status. Three care-related variables were chosen for service users: previous admissions, time in mental health services and time on the ward. The demographic variables chosen for staff were age, gender, ethnicity, personal experience of mental illness and family experience of mental illness. Two clinical variables were also chosen: time working in mental health services and time working on the ward. The criteria for adjusted analysis between the ANOVA and the ANCOVA were the p-value from the omnibus test, the adjusted means and the p-value from the post hoc test. If the p-value from the omnibus test for the ANCOVAs was not substantively different from the ANOVAs, then no further post hoc analyses were completed. A series of independent t-tests were completed to determine if there were differences between service users and staff on the outcome measures.
To determine if there were any statistical differences in responses between the two COCAPP studies, a series of exploratory two-way ANOVAs were completed. A comparison was made for the main effects of site (trust/health board) and study type (community COCAPP and COCAPP acute) on all of the outcome measures for service users and staff. Analyses for service users were completed for the RSA total score, Scale to Assess the Therapeutic Relationship – Patient Version (STAR-P)] total score and ES total score. A two-way ANOVA for staff was completed for the RSA Total only. When the acquired assumptions were not met, data are not reported.
Correlations
Correlations of the service user data were carried out to identify if there was a relationship between the outcome measures and to determine if there were relationships among patients in terms of views of the inpatient services (VOICE), recovery-oriented focus (RSA), empowerment (ES) and the quality of therapeutic relationship (STAR). Six Pearson’s correlations were carried out to identify if there were relationships between the mean total scores for the measures RSA and VOICE, RSA and STAR-P, RSA and ES, STAR-P and ES, STAR-P and VOICE, and VOICE and ES for all service user participants and by individual site. Cohen’s47 effect sizes were used to describe the data (small, r = 0.10; medium, r = 0.30; and large, r = 0.50). A Pearson correlation was also completed for staff on the mean total scores for the RSA and STAR-C.
For all of the ANOVAs and ANCOVAs, the statistical significance level was set at a level of 0.05. To account for multiple comparisons for the t-tests the significance threshold was raised to 0.005 to accommodate for the number of tests applied (n = 10).
Qualitative analysis
All of the digital interview recordings were professionally transcribed. The transcripts were then checked against the original recordings for accuracy, and any identifying information redacted, before they were imported into QSR International’s NVivo10 qualitative data analysis software (QSR International Warrington, UK) for analysis using the Framework method. 62,63
In this study, members of the research team read numerous transcripts to familiarise themselves with the data. The Framework matrix used was a slight refinement of that used in the COCAPP study, which was developed a priori from the interview schedules, with sections focusing on organisational background and developments, care planning, recovery, personalisation, safety and risk, and recommendations for improvement. Each matrix section also had an ‘other’ column for the inclusion of data-led emergent categories.
Slight amendments to the matrix were made before each transcript was summarised and charted (by RC, SB, AF, AT, BH, MC and FLG) following an agreed format for notation and linking to text. Researchers read and checked samples of each other’s summarising against transcripts to ensure that the approach was accurate and consistent.
Once all charting was completed, second-level summarising was undertaken (by RC, BH, MC, AS and AF) to further précis data and to identify commonalities and differences within trust/health board sites and groups, e.g. senior managers.
Data recorded in the care plan reviews, such as demographic detail, and examples from the template incorporating identified key concepts of good practice in care planning, user and carer involvement, personalisation and recovery were charted (SB). Brief summaries were produced (MC) with particular attention paid to representing the data according to sample characteristics.
Transcripts of the observations and the contemporaneous notes taken by researchers were read (AS and SB) and compared with the structured guide developed to identify good practice in involving service users and carers and a focus on recovery and personalisation. Brief summaries were produced (SB) that included a reference to the context in which the observations were conducted.
Integration and synthesis of data sets
The Framework method was also employed to bring together charted summaries of qualitative data alongside summary statistics of the quantitative measures for each case study site, noting points of comparison and contrast between what we found in our analysis of each type of data.
Armed with our set of six within-case analyses, we then conducted a cross-case analysis to draw out key findings from across all sites. We then considered the relationships between stated orientations to recovery and personalisation in national and local policy and staff interviews, and what we found by studying the accounts of users, carers and ward staff and by reviewing written care plans and undertaking observations. In this way we were able to investigate the data to identify ‘evidence’ at the intersections between macro, meso and micro levels and CPA/CTP care planning, recovery and personalisation, hence the ‘transformative’ nature of the study design. 33 The results of these within-case and across-case analyses are presented in Chapters 4 and 5.
Chapter 3 Policy analysis and literature review
In our earlier investigation into care planning and co-ordination in community mental health settings, we conducted a narrative overview of the policy context in England and Wales in the areas of care planning and co-ordination, combining this with a metanarrative review of research in this area. 20 Here, we extend this to an analysis of policy as it relates to the organisation and delivery of mental health care in hospitals, combined with an extension of our previous metanarrative review into the inpatient area. Again, we pay particular attention to care planning and co-ordination, and to the relationships between these and the aspiration that services be personalised and oriented to recovery. In the context of this project as a whole, this integrated policy and evidence review serves to frame the new empirical findings reported in Chapters 4 and 5. As per the project protocol, the aim was not to generate a pre-fieldwork synthesis leading to propositions to be tested or otherwise investigated.
Metanarrative reviews are a relatively new type of evidence synthesis. 45 They involve the search for traditions within fields of inquiry, paying attention to the ways in which research questions, assumptions and methods coalesce and diverge across different teams, times and places. 46 They also seek to produce outputs that have obvious value to policy-makers, service managers, practitioners and other decision-makers. Metanarrative reviews are open to the inclusion of evidence from studies that have used the full range of research methods, and many (including this one) reflect, to large degree, the standards embodied in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist. 64 When metanarrative reviews break with some other types of evidence, synthesis is in privileging overarching research traditions and the ‘shape’ of fields of study, rather than paying microscopic attention to the detail (including the formally assessed quality) of individual studies.
Search strategy
Step 1: searching
To retrieve literature in this integrated policy analysis and literature review, we initially searched a number of terms and key words (Box 1) individually and then searched these terms combined in clusters (e.g. ‘mental health’, ‘mental illness’, ‘care planning’, ‘care coordination’ hospital, adult followed by ‘patient care planning’, ‘collaborative care’, ‘person-centred care’, ‘personalis*’, hospital, adult) and then combined all. We took care to search in systematic and reproducible ways, reflecting PRISMA guidelines.
Care plan* OR “care and treatment plan*” OR CTP OR “Care Program* Approach” OR CPA OR “wellness recovery action plan” OR WRAP OR “treatment plan*” OR CTO OR “community treatment order*” OR “care coordination” OR (care N2 coordinat*) OR (care N2 collaborati*) OR (discharge N2 plan*) OR “case management” OR (MH “Patient Care Plans”)
Client-cent#red OR patient-cent#red OR person-cent#red OR Customer-cent#red OR recovery-orient* OR recovery focus* OR individuali?ed OR personali?ed OR patient-participation OR client-participation OR customer-participation OR “shared decision making” OR ((client* OR patient*) N3 involv* N3 (decision* OR plan*) OR patient choice
( MH “Recovery” OR (MH “Patient Centered Care“) OR (MH “Mental Disorders+/RH“) OR (MH “Individualized Medicine“) )
detention OR detained OR involuntary OR sectioned
( (MH “Acute Care” AND (MH “Psychiatric Nursing” OR MH “Psychiatric Care” OR MH “Mental Health Services” OR MH “Mental Disorders+”)) OR (MH “Hospitals, Psychiatric“) OR (MH “Psychiatric Patients“) ) OR ( Psychiatric patients OR psychiatric inpatient* OR psychiatric unit* OR acute psychiatric setting* OR (acute OR psychiatric OR mental*) )OR MH “Involuntary Commitment”)
When appropriate, proximity indicators (such as ADJ or N- as appropriate for each database), truncation ($) and wildcard (*) symbols were also used, as were Boolean commands (AND and OR). Key search terms, such as mental health, care planning, care coordination/co-ordination, were also searched by their subject (PubMed medical subject headings) and by keyword.
Inclusion criteria
Research published in English from 1980 onwards focusing on adult mental health inpatient care.
Exclusion criteria
Non-English-language papers and research undertaken in child and adolescent mental health settings.
Verification
The search strategy was verified by a health and social care librarian. In addition, the search terms and strategy were presented for review to, and approved by, the LEAG/PAG.
The databases searched were Applied Social Sciences Index and Abstracts (ASSIA), Cumulative Index to Nursing and Allied Health Literature (CINAHL), Allied and Complementary Medicine Database (AMED), EMBASE, The Cochrane Library, MEDLINE, PsycINFO, Scopus and Web of Science (Table 3).
| Database | Results |
|---|---|
| MEDLINE | 371 |
| CINAHL | 135 |
| ASSIA | 185 |
| EMBASE | 6 |
| AMED | 27 |
| Cochrane database: reviews | 4 |
| Cochrane database: ‘other’ reviews | 1 |
| Cochrane database: trials | 26 |
| PsycINFO | 167 |
| Scopus | 147 |
| Web of Science | 289 |
| Less duplicates | 180 |
| Total | 1178 |
Step 2: sifting and sorting
Using the approach tested in our earlier metanarrative review of research into care planning and co-ordination in community mental health settings,20 the titles of all papers were first reviewed by two members of the project team (BH and MC). Papers for inclusion were labelled ‘yes’ (n = 44) and those not meeting the inclusion criteria were labelled ‘no’ (n = 1001). Papers labelled ‘maybe’, for which inclusion was uncertain (n = 33), were discussed with a third member of the team (AJ) and a decision was made about whether or not to include these. Twenty ‘no’ titles were cross-checked by Aled Jones for accuracy of exclusion and found to be consistent. Aled Jones added a further two papers to the ‘yes’ total following back-chaining, hand-searching and expert group LEAG/PAG discussion. As a result, a total of 46 research papers were included in the metanarrative review.
Step 3: data extraction, analysis and synthesis
Again reflecting PRISMA standards, Aled Jones and Jitka Všetečková extracted relevant information from papers into a template designed by the team for collating information during a previous metanarrative review. 20 The information was then used to generate a focused review of the literature, which is reported in the form of a narrative synthesis under the major headings The context of acute inpatient psychiatric care in England and Wales, Service user and carer involvement incare planning and co-ordination, Outcomes of service user involvement in care planning and co-ordination and Interventions to improve service user involvement in care planning and co-ordination. This synthesis interweaves research evidence with an analysis of prevailing policy contexts. Government and other documents used in our policy analysis were not searched for systematically, but were selected by the team drawing on our collective knowledge of the broad history of the UK’s mental health system (and the changing place of hospitals within it) in the period from the 1950s onwards.
Results
The context of acute inpatient psychiatric care in England and Wales
The research evidence makes reference to difficulties experienced by staff in achieving patient-centred care planning and care co-ordination in acute inpatient mental health settings. The root causes most commonly cited were acuity and rapid turnover of patients; the demand for inpatient beds outstripping supply; and insufficient numbers of nursing staff available to undertake meaningful, patient-centred care planning.
In this first section we contextualise these perceptions through a focused review of policies in England and Wales. Viewed over a period of decades, the story of the mental health system is of an historic shift from care provided in hospitals to care provided predominantly in the community. 65 Organised community care emerged in the 1950s, with early policy initiatives including The Hospital Plan of 1962,66 which foresaw the closure of the Victorian asylums, and Better Services for the Mentally Ill in 1975,67 which introduced locality-based community mental health teams (CMHTs). The number of NHS inpatient psychiatric beds in England and Wales reached a peak of approximately 150,000 beds in 1955 and has steadily declined since this point via a process of deinstitutionalisation. 21 In England, the total number of available mental illness beds (for all ages and for all specialties) dropped from its 1955 peak to roughly 22,300 in 2012; in Wales, the number of adult psychiatric beds fell from 2586 in 1989–90 to 771 in 2013–14. 68 This pattern of psychiatric bed reductions has been mirrored internationally.
The original circular that introduced the CPA into England in 1990 was clear that a formalised process for the planning, co-ordination and review of each individual service user’s care was needed precisely because so many were now living outside institutions. 69 Implicit in the circular was the idea that community care has to be purposively co-ordinated because it draws on the efforts of members of multiple professional groups located in dispersed teams spanning both primary and secondary sectors. Without a formalised system of co-ordination, there remained a risk of fragmented services, unmet needs and lack of clarity in roles and responsibilities. This particular attention to community services has largely continued, with the period from the middle of the 1990s being particularly notable for the intensity with which policy-makers set about their work. 70 In England, new types of community team appeared, offering early intervention to people with psychosis, assertive outreach and (significantly for the hospital components of the system) services providing crisis care and home treatment as an alternative to inpatient admission. 71 In Wales, policy first emphasised the value of the locality CMHT model72 before eventually expanding to the introduction of crisis resolution and home treatment teams to sit in the space between CMHTs and hospitals. 73 It was recently stated that acute psychiatric inpatient services exist in a supportive capacity to community services, providing treatment and care in a safe and therapeutic setting for patients in the most acute and vulnerable stage of mental illness, and whose circumstances or acute care needs are such that they cannot, at that time, be treated and supported appropriately at home or in an alternative, less restrictive setting. 74
However, this dominant narrative of a system moving ever further from its origins in psychiatric institutions risks overlooking the continued position of hospitals within it. Hospitals occupy a significant space, and remain an essential part of local networks of services even though inpatient bed numbers have declined sharply over time and efforts have been made to bolster home treatment to avoid admission whenever possible. Evidence of the part hospitals continue to play is shown in official statistics. As has already been noted in the introduction to this report, in England in 2014–15, 103,840 people in contact with mental health and learning disability services spent time in hospital4 and in Wales 9466 admissions to hospital for mental illness took place in 2014–15. 5
Concerns about a perceived shortage of acute inpatient places in England and Wales are also not a recent phenomenon,75 with some arguing that ‘psychiatric bed numbers (in England) are close to the irreducible minimum if they have not already reached it’. 76 More recently, the coalition government’s care services minister admitted that ‘there is clearly, in some parts of the country, a shortage of beds’. 77 The (then) minister’s reference to ‘some parts of the country’ hints at the variation in the provision of inpatient beds reported by the NHS Benchmarking Network mapping exercise in 2014. Provision across England and Wales ranged from 12 beds per 100,000 (weighted) population to 32 beds per 100,000 (weighted) population, with a median position of 21. 74 (The term ‘weighted population’ refers to the process of adjusting figures to reflect the socioeconomic mix of an area, as this will affect the demands made on the health services. For example, people from areas that are socioeconomically deprived typically have worse health than those living in more affluent areas, and use health services more often as a result.)
A related issue to declining numbers of inpatient beds is the question about the efficiency and effectiveness of bed usage, with evidence emerging that some people are being inappropriately admitted. For example, a sixfold variance across providers in admissions to English adult psychiatric inpatient units has been found, suggesting that 15% of inpatient beds could be decommissioned if the median figure of occupied bed-days was achieved by the worst performers. 78 Similarly, a retrospective review of bed usage in one English NHS service found that approximately one-third of patients admitted over a 32-month period could potentially have been cared for in a community setting. 79
Differences in past and present national mental health policies for England and Wales can clearly be detected (e.g. in the degree to which services should reflect national standards or be flexible to local needs and circumstances, in the use of non-NHS providers, and in the extent to which personal budgets might be used). However, a distinctive feature of current (and recent) macro-level frameworks in both countries is how they seek to direct services to become more recovery-focused and centred on the individual, regardless of the setting in which care is provided. Broad ideals of recovery tailored to the person and of meaningful collaboration run through England’s Five Year Forward View for Mental Health,80 as they did in the coalition government’s Closing the Gap81 and, before that, in No Health Without Mental Health. 1 In Wales, the 10-year strategy Together for Mental Health10 claims similar underpinning values, with references to the promotion of recovery and the delivery of services specified to the person.
References to the part played by hospitals, and to the improvement of care therein, are found in all of these policy documents. The Five Year Forward View for Mental Health80 notes that the severity of the needs of people admitted to hospital have been steadily increasing, with the numbers admitted under sections also rising and black men in particular being over-represented. Closing the Gap81 emphasised the importance of avoiding admission whenever possible while also making sure that local beds were available when needed. No Health Without Mental Health1 addressed acute care pathways and the value of avoiding hospital, and when admissions are necessary making these as effective and as short as possible. In Wales, Together for Mental Health10 acknowledges improvements in the fabric of hospitals and places emphasis on developments such as single-sex facilities, welcoming visiting spaces and a focus on dignity, safety and therapy. Distinctively, the Welsh Government passed primary legislation mandating for care and treatment plans (CTPs) and for care co-ordination by suitably qualified professionals. Independent advocacy is also extended to all inpatients (and therefore not only to those detained under sections of the MHA 19833).
Attention to hospital-based mental health care is also found in guidelines produced by the National Institute for Health and Care Excellence (NICE) that are designed to improve the experiences of people using adult NHS mental health services. 82 Expectations are placed on staff to share decisions with inpatients and to be person-centred, to offer service users daily time with someone they know and to clearly plan and co-ordinate care during admission. Managing transitions out of hospital is also addressed, in recognition of the need to collaboratively co-ordinate discharge with the MDT, service users and their families or other carers.
Despite expectations of excellence, evidence continues to emerge of poor-quality care across the mental health sector. 83 Patients and carers report that many acute wards are not always safe, therapeutic or conducive to recovery, and in some cases they negatively affect the person’s well-being and mental health. 74 However, the availability of robust data and national information on mental health services is limited, which means that quality of services cannot be definitively assessed. 84 Mounting concern about the quality of care has led to the Royal College of Psychiatrists publishing Ten Standards for Adult In-patient Mental Healthcare. 85 This makes the case for maintaining occupancy levels at ≤ 85%; having a maximum of 18 beds on each ward; ensuring that the physical environment is suitable; making sure that the ward serves as a therapeutic space; managing risk and safety in proportionate and respectful ways; sharing information and involving people in care planning; care being oriented to recovery, and being connected to community and other services; psychological interventions being available; care being personalised, with one-to-one contact available every day; and services being socially and culturally sensitive.
Notable variations in the use of inpatient beds, high bed occupancy rates and longer lengths of hospital stays were cited as contributing to a decision to undertake a review of safe staffing for nursing in inpatient mental health settings. 86 Other reasons cited by NICE for undertaking the review of staffing include:
-
increasing numbers of admissions and complexity of issues in service users (which include people who are detained under the MHA 1983, amended 2007)
-
reconfiguration of mental health services
-
loss of experienced inpatient staff to community teams
-
lack of availability of therapeutic interventions
-
lack of ability of staff to establish and maintain therapeutic relationships
-
lack of availability of wider MDT and support services, including crisis resolution and home treatment teams to facilitate early discharge.
The NICE review resulted in the publication of recommendations on the use of two workforce tools and a staffing checklist, and provides advice on how mental health services can review their workforce planning. 87 The framework avoids setting specific staffing levels for mental health inpatient wards and has subsequently been criticised as lacking rigour and independence. 88
It has been highlighted that inpatient nursing numbers fell consistently by 15% between 2009 and 2014 in a context of small increases of the nursing workforce, and since 2010 nursing has experienced ‘debanding’ (a larger fall in the number of staff in senior roles), with the number of band 8 full-time equivalent staff falling by around 18%. 89 Relatedly, requests for temporary (bank and agency) mental health nursing staff increased by two-thirds between 2013 and 2015. Between 2010 and 2015, the number of full-time equivalent psychiatric consultants increased by 6% (the lowest rate of growth across all specialties) and nearly 10 percentage points below growth in the total consultant workforce. The report also suggests that regional workforce variations can be highly significant. For instance, the north-east of England reports the lowest nursing vacancy rates and the highest consultant physician vacancy rates, whereas trusts in London report high vacancy rates for nurses but low rates for consultants.
Inpatient mental health care has also been a regular focus for independent committee investigation, and a picture emerging over time is that of a hospital system under pressure challenging the achievement of policy aspirations and service standards. The most recent report comes from Lord Crisp’s Commission to Review the Provision of Acute Inpatient Psychiatric Care for Adults. 68 This reviewed services in England and, although it found examples of high-quality hospital services, concluded that access is nationally inadequate and, in some instances, potentially dangerous. Recommendations for improvement included reducing waiting times, guaranteeing that admissions take place in hospitals that are local, and reviewing capacity in (and developing) hospital and community-based crisis services in tandem. Similarly concerning findings were produced by the Schizophrenia Commission. 90 Established with support from the charity Rethink, this group’s final report pointed to psychiatric hospitals that were frightening to inpatients, over capacity and staffed by an unstable, low-morale workforce that included large numbers of bank and agency nurses. A few years earlier, the Healthcare Commission had reviewed the quality of inpatient mental health care across England and found wide variations in standards. 27 Looking further back in time, a review of hospital mental health nursing by the Standing Nursing and Midwifery Advisory Committee91 found evidence of poor clinical leadership in a context in which too little attention had been paid to inpatient care.
Common across all these inquiries are concerns over poor or variable standards of care, and calls for investment in (and development of) services. In the current context of demands for parity of esteem, comparisons are also being made with standards prevailing in the physical health-care system. An argument being raised is that the problems endured in the inpatient mental health care system would not be tolerated in other parts of the NHS. The service context in which inpatient care planning and care co-ordination exists has been defined by debates about the correct numbers and usage of both hospital beds and the nursing and medical staff required to deliver efficient and effective services to patients. Resources such as numbers and availability of beds and the ratio of available employees, such as registered nurses, to patients are inevitably important in determining whether or not policy and professional ambitions to provide better mental health services are delivered.
Other initiatives to improve the quality of inpatient care have also emerged. These include work to develop standards and to accredit wards,92 guidance to help service commissioners,93 action by charities to promote good practice94 and research to put hospital-based mental health nursing on a more evidence-based footing. 95 However, there is little direct policy focus on inpatient services despite this being the site of treatment for elevated mental distress and consuming significant resources. Although there has arguably been a renewed interest in mental health policy of late,96 inpatient care has largely been neglected or sidelined in attempts to achieve greater efficiencies elsewhere in the system. Although there is a focus on various types of community teams or alternatives to hospitals, and some focus on new facilities in hospitals, with few notable exceptions little direct research or policy has focused on improving the experience of inpatient mental health care. No sustained efforts have been put into developing and equipping the workforce with the necessary skills to deliver recovery-focused and personalised mental health inpatient care, or to attending to wider structural issues (e.g. housing or discrimination) that hinder positive and timely transitions from hospital.
Service user and carer involvement in care planning and co-ordination within inpatient settings
Service user involvement is a principle of mental health policy in health systems globally and in several supranational strategies to improve mental health. 97,98 Involvement features prominently in English and Welsh health policy documents. The overall intention of policy-makers is that services are provided in accordance with patients’ needs and to enhance service users’ and carers’ control over care delivery. The service user movement has been particularly active in challenging paternalistic assumptions that health-care providers know what is in the best interests of patients when decisions are made by providers on behalf of ‘their’ patients without proper involvement in the process. 99
The definition of the term ‘service user/survivor movement’ used here is derived from Wallcraft and Bryant,100 who refer to people advocating for their individual and collective rights in the face of discrimination. The origins of the movement are in the earliest days of psychiatric hospitals, while a forerunner of modern-day groups was the Alleged Lunatics’ Friend Society, set up in 1845. The mental health welfare and pressure group Mind was formed in 1946, when three mental health welfare groups founded in the early 1900s were merged, and has consistently been a powerful source of advocacy for mental health service users in policy decision-making and service planning. Since the 1980s – and incrementally given more emphasis by each government administration – service user involvement has been a key aspect of mental health policy in the UK. 101 However, although the movement appears to have an influence on the direction of policy-making, there are historical and contemporary concerns regarding the deficient implementation of policies and legislation, especially in relation to inpatient mental health settings. 102
It has been argued that service user involvement has increasingly appeared in government policies not because of concerns about improving service provision, but because certain notions associated with service user movement complement the neoliberal policy aspirations of successive governments. 103,104 For example, it is argued that neoliberal political doctrine appropriates the language of increased individualisation of service user care planning and service delivery as a means of placing unrealistic moral responsibilities and expectations on patients to achieve self-reliance, self-management and self-monitoring, while failing to address the negative impacts of a broad range of government policies and systemic socioeconomic inequities that may undermine the achievement of these objectives. 103,104
The remainder of this section reviews research on inpatient mental health services and its association with service user involvement in care planning and care decisions. Terms and concepts closely linked to involvement, such as patient participation and patient-centred care, are used interchangeably in this literature. Our use of different terminology in this review mirrors the terms and concepts used within publications. Such interchangeability, however, can lead to problems with conceptual clarity across the body of knowledge as a whole.
Care planning inevitably necessitates interactions between different stakeholders (e.g. patients, professionals, carers and relatives) and the context and quality of these interactions may directly affect the way in which the meaning of the event is construed by patients. For example, patient involvement during care planning has long been acknowledged as an essential indicator of high-quality services. 105 Although other professional groups are involved, most of the 24-hour care for patients (and therefore opportunities for patient involvement) is provided by a mix of qualified and unqualified nursing staff. It is unsurprising, therefore, that over the past 20 years there have been a number of research studies about nurse–patient interaction on acute psychiatric wards. 106 Psychiatric nurse Hildegard Peplau, writing in the 1950s, emphasised the need for nurses to construct caring environments in which the shared experiences of nurses and patients formed the bedrock of meaningful partnerships, in contrast to patients passively receiving treatment based on the preferences of professionals. 107
Patient-centeredness, participation and involvement have attracted the attention of researchers. Frequently cited components of best practice are those of mutuality between professionals and patients and truthfulness in decision-making relating to patients’ own treatment and care. 102 These components of best practice are also advocated and integrated in the training of health-care professionals, although there is a relatively underdeveloped understanding of how to measure, research and promote these core components. 108 However, the pursuit of a set of core skills or understanding may be overly ambitious and reductive given that simply being with acutely psychotic patients is shown to be a complex activity that requires a considerable number of adjustments, approaches or interactive techniques. 106
Regardless of arguments for higher levels of patient-/carer-centred and collaborative interaction, it remains questionable whether or not this has been achieved in acute inpatient settings in the UK. 17 For example, recent systematic reviews of service users’ involvement found little evidence of collaboration in community or inpatient mental health services. 102,109,110 Similar shortcomings have been found for this current review. For example:
-
There is a lack of information sharing with patients about the contents of their care plan111,112 and to inform decision-making. 109,113
-
Care plans did not reflect patient involvement in decision-making or patient-identified goals. 114–122
-
There is a lack of carer/family involvement in care planning and a lack of recognition and appreciation of their role from health professionals. 112,115,123
Several issues are identified that affect user involvement and participation in care planning decision-making, including the following.
Staff time
Staff report having insufficient time to involve patients fully in collaborative care planning. 112,124–127 Interestingly, patients report being satisfied with the time made available to talk to staff, despite having little involvement in care planning. 115 There have been several reports over many years of low levels of nurse–patient interaction occurring on acute psychiatric wards. The amount of time spent as a proportion of available nursing time to interact with patients is as low as 4%,128 with a recent review129 concluding that patients spend substantial time apart from staff and that little time is spent delivering therapeutic activities.
Staff attitudes, perceptions and knowledge
A lack of staff commitment to empowering patients125 has been noted, as was the staff perception that patients were not interested in participating in care planning. 121 Staff found engagement and involvement of patients difficult to achieve, and they lacked training, guidance and managerial support. 121,127 Carers’ involvement during care planning was inhibited by a lack of staff understanding when applying theoretical principles of confidentiality to the nuances of practice. 123
Two studies linked staff perceptions and experiences of decision-making to service user involvement. Service user participation in treatment planning is strongly influenced by staff job satisfaction and, interestingly, the extent to which staff themselves are involved in decision-making regarding treatment. 130 Similarly, staff indicated a greater job satisfaction when greater emphasis was placed on collaborative and recovery-focused care planning. 118
Patient perceptions
Patients did not consider their involvement to be linked to meaningful actions or changes, so they refused to participate in care planning125 or lost motivation to be active in treatment planning. 120 In addition, patients described how they were underprepared for care planning meetings and collaborative decision-making, which resulted in attendance becoming stressful and, in turn, led to an avoidance of meetings. 121,131,132
Patients’ capacity for user involvement
It has been argued that the average level of functioning as a result of the acuity of those occupying hospital beds is lower owing to the advent of deinstitutionalisation, thus reducing opportunities for service user involvement. 130 Other studies report similar views, in terms of both increased acuity of inpatients since the advent of deinstitutionalisation that diminish involvement in care planning, and decision-making including deficits in social skills and judgments, attention, concentration, communication difficulties and hypersensitivity towards interpersonal conflict. 133 Similarly, patients’ functioning cognitive capacity and capability to participate in care planning can be lessened by the acuity of their illness. 113,125,130 Patients may, therefore, be unable to participate in care planning at certain points, and instead need safety and the stabilisation of their condition. 102 However, when symptoms improve there is increased participation. 113
Broader contextual issues (1): ‘static’ representations of mental illness and care planning
The realities of non-linear progression of and recovery from mental illness are seldom addressed in the literature. Differing inpatient management approaches may be required according to the severity of symptomatology, although those with more severe symptoms may require more intensive levels of involvement in treatment planning. 134 However, the findings covered in the previous section113,125,130 suggest that the impaired cognitive functioning of those with severe illness symptoms may reduce opportunities for involvement. Taken together, these results indicate the need for prolonged efforts by staff to ensure that opportunities for patient involvement are not limited to those who are less severely ill and have greater cognitive functioning.
Services have reduced care planning to a linear, task-focused event that is defined primarily in terms of outcome (i.e. the completion of a care plan) rather than the process through which this is achieved. 110 A further observation by Bee et al. 110 is that this view of care planning may explain why care quality surveys and audits have historically monitored the extent to which care plans are signed by service users, rather than the degree to which genuine prospective involvement is evident.
Broader contextual issues (2): institution-specific structural and cultural barriers
Hierarchical hospital structures and rules result in tensions when attempts are made to implement service user participation. 135 Tensions were identified when patients’ views challenged staff judgments. Establishing symmetrical therapeutic relationships generally proved difficult. Similarly, themes of hierarchy and power as barriers to involvement appear in other studies of participation in ward rounds and decision planning. 123,132 Power differentials within the interdisciplinary team also lead to a lack of client-centred and collaborative treatment planning. 124
Outcomes of service user involvement in care planning and co-ordination
Patient-centred care and involvement are often presented as overarching idealistic philosophies around which service improvements can be designed. However, there are difficulties in designing studies to capture clear cause–effect relationships between care planning and patient outcomes. Multiple variables may confound any such attempts. These include the contingent complexities of MDT-working across health and social care sectors allied to complex illness and treatment trajectories. This section of the review provides an overview of the outcomes linked to collaborative and individualised care planning.
Patient perceptions of care quality and satisfaction
Increased involvement is positively associated with patients perceiving their care more favourably, especially perceptions that care was delivered with respect and dignity, enhancing patient self-esteem. 112,136 Similarly, the importance of staff–patient relationships based on collaborative care was central to patients’ perceptions of good-quality inpatient mental health. 126,131,137,138
Discharge and readmission
Inappropriate discharge, when a patient is not fully prepared to care for their needs and has inadequate community support, has been associated with early readmission to hospital. 139 This appears to be a longstanding problem in mental health care. For example, the views of patients about to be discharged were studied in relation to involvement in treatment decisions and planning, including discharge information. 111 Over 30% of respondents reported they had not discussed post-discharge follow-up and planning with staff and over 20% reported that they had not been involved in consultation about their discharge. A contemporaneous study exploring readmission noted that people feeling prepared for discharge was strongly influenced by a more individualistic approach. 130 Similarly, inadequate discharge planning (e.g. lack of community referral, unresolved medication non-compliance or financial problems) was found to have a highly significant relationship with readmission within 90 days of discharge. 140
Providing more patient-centred information and individual preparation for discharge is linked with reducing hospital readmission rates. 137,141 A reduction in readmission rates was attributed to providing information about treatment and involving patients in decision-making, and influenced patients; participation in follow-up care after discharge. 137
The hypothesis that length of hospital stay would be shorter the more patients participated in treatment decisions and care planning has been tested. 122,134 Interestingly, no significant relationship between increased involvement and length of stay across a mixed population of inpatients has been found. 122 However, a relationship between increased patient involvement, length of stay and severity of illness has been noted. 134 For example, patients with major affective disorders experienced a reduced length of stay following the introduction of more patient involvement, but those with minor affective disorders showed an increase in length of stay. Caution is needed in interpreting these studies, as both were undertaken in single settings with little effort made to control for multiple potential confounding variables.
In terms of discharge and readmission, the research predominantly focuses on the quality of discharge planning and processes occurring within inpatient wards. However, a notable and significant gap in the literature is in the absence of studies that explore the degree of continuity and co-ordination of care planning with services in other parts of the mental health and social care system. Therefore, we concur with previous reviewers’ conclusions that evidence in support of interventions designed to optimise the transition from inpatient to outpatient is very limited. 139,142
Interventions to improve service user involvement in care planning and co-ordination
Interventions aimed at strengthening service user participation through enhancing employee training, guidelines or legal regulations have had variable results on practices.
Interventions that redesign service delivery
Attempts to improve collaborative care planning and care co-ordination by redesigning some aspects of service delivery have been researched in a variety of countries, including the USA,134,136 Canada,118,124 Sweden,143 Norway,144 Switzerland122 and England. 126
An attempt to encourage more recovery-oriented patient services through the promotion of patient involvement in treatment decision-making has been studied,122 in which opportunities were introduced for patients to participate in regular 3-weekly evaluative treatment planning and treatment conferences. Care plans were jointly agreed, around patient-identified goals, by the patient, nurse and doctor. In addition, recovery-oriented training was delivered to the MDT, which focused on the subjective experiences of patients and case-related supervision. There is no mention of service user involvement or staff consultation during the identification and design of the interventions. Consultation with service users may have revealed patient anxiety linked to involvement in treatment conferences, as identified by others. 131,132 Outcomes (satisfaction, quality of life, hope, therapeutic relationship, perceived coercion and attitude towards and self-evaluation of recovery) were compared pre (n = 34) and post (n = 29) implementation of the changes. The results indicated no significant changes to subjective and functioning variables (e.g. treatment satisfaction, quality of life and perceived autonomy), although some patients’ attitudes towards recovery and their self-assessment of the recovery process improved. The length of hospital stay remained unchanged. The authors concluded that ‘the possibility must be considered that the structural changes and the staff training actually had little observable effect on patient outcomes’. 122
In a separate study, patient outcomes were tested for those receiving increased levels of involvement (n = 35) in treatment planning conferences compared with those receiving usual care (n = 30). 134 The hypothesis that increased patient involvement in planning would result in decreased length of stay was only partially supported. Patients with major affective disorders and ‘schizophrenic disorders’134 showed an 8.2% decrease in hospital stay, whereas patients with minor affective disorders, personality disorders, substance abuse and adjustment disorders showed a 98.8% increase. This indicated to the authors a need for differing inpatient ward management approaches and approaches to engaging with patients according to diagnosis. Those with less severe symptomatology may need less or no involvement in treatment planning as they are expeditiously discharged than those with more severe psychopathology who stay longer in hospital for treatment. There are many limitations to this study, such as a small sample size, the fact that the study was undertaken 30 years ago in a US military hospital with active service personnel and also the fact that length of stay was calculated in an unconventional way, based as it was on military criteria for being fit for active duty.
A study of two models of treatment planning, one with and one without active participation of the patient in formulating a written treatment plan, led to differences in outcomes. 143 The results indicated a positive relationship between active participation and the level of patients’ expectations of improvement, as well as high ratings of the importance of the patients’ own effort in treatment. Expectations of improvement were related to symptom level at discharge and global improvement during treatment, indicating a better outcome for those involved in care planning.
The introduction of an interdisciplinary plan of care incorporating heightened attention to recovery and an interdisciplinary patient-focused approach to care planning was investigated. 118 The interdisciplinary plan of care had a positive impact on both patient and caregiver satisfaction. Patient (n = 46) satisfaction 6 months post implementation was improved in relation to care planning, and patients reported feeling more involved and more respected by staff. Staff (n = 17) reported feeling validated in spending more time with patients, increased job satisfaction and increased involvement in clients’ care.
A quasi-experimental study examined the effectiveness of a self-reported symptom and problem rating scale (BASIS-32) that was completed by patients on admission before being integrated into a treatment plan and reviewed at various time points in collaboration with a clinician. 114 There was significantly more involvement in treatment decisions for patients in the intervention group (n = 23) than for controls, as well as more frequent reports of being treated with respect and dignity by staff. Treatment outcome did not differ between the groups. Major limitations including sample size and single site suggest that caution is required when interpreting these results.
The only study to evaluate an electronic care planning tool reported that nurses believed that the tool was compatible with the way care planning occurred and that it offered advantages over the usual documentation system. 124 Fifty per cent of the nurses interviewed (8/16) commented that the tool could foster improved collaboration and client-centred care, although the existence of a menu from which patient interventions were selected may explain why 50% of respondents were less confident that the tool fostered greater collaboration. There was also uncertainty about improvement to interprofessional practice, with a continued focus on physician-driven discussion on medication and discharge. The acceptability to patients and the effects of the software on patient involvement in care planning were not assessed.
Education and training interventions
A before-and-after evaluation of an 18-day specialist education programme for acute ward-based nurses showed statistically significant improvements in the quality of care planning, initial assessments and the provision of therapeutic care. 117 The quality of care plans was assessed by the degree of individuality versus standardisation of the documentation, evidence in the documents of having verbally consulted with patients about treatment preferences and if risk assessments were undertaken regularly, only once or never. No statistically significant changes were observed in the quality of risk assessments. Improvements in care planning included a > 50% decrease in the use of a standardised/pre-typed care plan, with a parallel increase in the number of individualised care plans. However, this improvement did not appear to extend beyond mere documentation changes, as the involvement of service users in care planning decreased post intervention, with only 20.7% of care plans containing evidence of involvement, compared with 32.9% pre intervention. Qualitative data from patients also confirmed that regular contact with their named nurse was reported by < 30% of patients, and three-quarters of patients reported not being involved in care planning. These mixed results suggest a limited effect of education on workplace cultures.
Patient education and training formed the main components of a quasi-experimental intervention study from Norway. 144 Given the need for educational interventions to be accompanied by broader cultural changes noted in the study above, this project consisted of not only education but also attempts at structural and cultural changes. However, the educational interventions (which included a focus on patient participation in care planning) had no measurable effect on pre- and post-implementation behaviours (knowledge, practice or attitudes towards user participation) of professionals at the intervention hospital (n = 182), compared with at control hospitals (n = 255).
Policy/legal interventions
The introduction in 1992 of the Swedish Compulsory Psychiatric Care Act and the Forensic Psychiatric Care Act has been explored. 116 The main focus of the new legislation was twofold: improved legal safeguards for those detained under compulsory orders and the reduction of violations of patient autonomy. One fundamental aim of the Compulsory Psychiatric Care Act was that a care plan should be drawn up directly after admission that, as far as possible, should be written in conjunction with the patient and their next of kin. The results indicate that few patients reported the existence of care plans. Of those who knew of the existence of the care plan, only a few reported that they or their relatives had participated in its development. There was no change over time in care planning practices, and the aim of the legislation appears not to have been fulfilled.
In contrast, Norway’s introduction of legislation for nursing documentation to be included as ‘an integrated and independent part of the patient medical record’ is more positively evaluated. 119 A seemingly key difference in achieving better outcomes was that staff training was introduced alongside the new legislation. An education day focused on the quality of documentation and instruction on how to improve this. Agreement on areas of improvement was reached during the education day, and 3 months later an analysis of 32 anonymised patient records occurred. These records were compared with professional quality standards enshrined within the legislation and demonstrated that patients appeared, to a much larger extent than before, to be active participants in the development of the nursing plans. However, this conclusion was based on a review of documentation alone, with no data collected about the actual practices of patients and staff during care planning.
Finally, a wide-ranging qualitative study of patient participation in treatment planning found that inpatient facilities that specifically addressed in their local policy the need for client empowerment in treatment planning and how this was to be achieved had greater participation in treatment planning than those that did not. 125 Of all patients participating in the study’s focus groups (n = 72), those on wards with explicit policy statements about patient participation in care planning described how they completed the treatment plan with staff, whereas staff (n = 114) in those areas without specific policies wrote the plans and then invited patients to meetings during which the contents of the plan were explained.
Discussion
As noted in previous reviews,109 most studies of care planning and co-ordination in inpatient mental health services show little involvement of service users and/or carers in the design and implementation of the research process. When carers, relatives or ‘significant others’ do appear in inpatient research, there is a lack of clarity over who these terms refer to. For example, the amalgam term ‘user/carer’ appears in a recent in-depth review of ‘user-led care planning’,110 whereas ‘family/carer’ is a term used elsewhere with no definitions offered of what constituted a carer. 138 The use of undefined amalgam phrases could be misleading, as they conflate social groups with potentially different viewpoints and interests. For example, relatives of patients may not feel comfortable with the ascribed role of carer, preferring instead to preserve their identity as a partner, husband, wife or daughter. The issue here is that relatives may not subjectively care for their patient relative. For example, relatives may be neglectful towards rather than caring of the identified patient. 105 The amalgam phrase ‘users/carers’ or ‘family/carers’ may be useful to services and policy-makers, but the diffuse meanings of these terms suggest that more defined usage is needed in research studies.
Comparable problems with conceptual clarity are also evident in the construction of patient involvement in care planning. There is some evidence in the literature reviewed that policies internationally to promote patient involvement in care planning have resulted in greater inclusivity of patients and some dismantling of power differentials between patients and professionals. However, it is also worth noting that the practical implementation of government policies has been patchy, best summarised as a mixture of local successes and failures. Some have urged a more critical position on the motivations underpinning patient involvement and participation, including care planning and care co-ordination. In short, the argument here is that patient involvement for the most part remains in the gift of provider organisations, in so far as they retain control over decision-making and are accepting of patient involvement as long as it addresses and conforms to organisational agendas and priorities.
A critique of patient involvement as a neoliberal intervention constructs patients as prudent, responsible subjects who plan ahead, maintain control and are constantly engaged in self-surveillance to sustain a healthy lifestyle. 99 Patient involvement constructed in this way works well for those experiencing stability and thus able to focus entirely on self-monitoring and personal improvement. When patients are experiencing economic, relationship or other forms of insecurity, they may prioritise these needs. This notion is summed up in Bourdieu’s concept of ‘distance from necessity’. 99
Our review suggests that professionals take the decision to restrict patient involvement completely when they perceive patients to lack sufficient focus, capacity or capability to engage in care and treatment planning, rather than support patients to undertake more or less involvement depending on the ebb and flow of their mental health status during inpatient stays.
However, there are few studies that explore this further, for example examining how patient involvement in care planning may increase or decrease as a patient’s journey and recovery progress. Most of the research literature therefore positions care planning as static, task focused and linear events, and fails to respond adequately through the design of their studies to the social and organisational context in which care planning exists.
The research literature also indicates that the majority of users and carers feel marginalised during the care planning process. 120,123,127,137 More can be done at the organisational and policy level to enable user involvement. For example, new policy initiatives around patient involvement often do not have sufficient implementation support or show understanding of the historical and contemporary cultures within which mental health care occurs. 127
Our review concurs strongly with these conclusions. Specifically, it is notable how often the literature merely pays lip service to the complex and contingent nature of the work of mental health professionals. Rather than delving into this complexity, researchers will often gloss over issues relating to various inter- and intraprofessional interfaces by reverting to terms such as ‘power differentials’ or ‘hierarchies’. 127 Similarly, little is made of the interaction of professional cultures, patients, relatives, carers and the numerous other social actors that often co-exist within the increasingly populated space of inpatient mental health care.
Conclusion
To summarise, this integrated review of policy and research identifies the continued importance within mental health systems of hospitals, but also the extent to which they are under pressure and have become an increasingly scarce resource. It has been shown that the numbers of inpatient mental health nurses have fallen, and concerns have been raised over poor or variable standards. The evidence suggests – with some notable exceptions – that relatively limited attention has been paid in recent years to the improvement of inpatient mental health services, or to the investigation of personalised processes and interventions promoting recovery and swift, safe returns to the community. This is the case despite the continued large numbers of people admitted each year to inpatient mental health care each year in England and Wales, and the significant resources which continue to be devoted to the hospital parts of the system. In this context there remains a pressing need to establish factors helping and hindering recovery-oriented, individually tailored, inpatient mental health care. The following chapters in this report present findings from this study that set out to do this.
Chapter 4 Results: within-case analysis
Summary of chapter
This results chapter is divided into sections. In Recruitment and case study sites we provide brief summary data of recruitment rates and an explanation of our naming policy for case study sites. Then, in Meso- and micro-level analyses by site, for each site we provide a brief introduction followed by a detailed breakdown of service user and staff participants in the survey study and results of the questionnaire data. When possible, we include reference data that consists of mean scores for participants from other peer-reviewed research studies. The criteria for the selection of reference data was that they were drawn from participants within comparable contexts. When this is not possible, we provide detail of the differing contexts to provide caution to any comparisons made. Finally, we include a brief comparison of the summary scores for the outcome measures from this study with the scores from the community COCAPP study.
This is followed by narrative summaries of meso-level organisational policies, approaches and values in relation to care planning and coordination, recovery and personalisation. This in turn is followed by detailed narrative summaries of micro-level perspectives on care planning and coordination, recovery and personalisation that draw on interview data from service users, carers and staff, with brief illustrative quotations used throughout.
We also include a review of service users’ care plans and observations of ward round meetings. This close examination further enriched and expanded our understanding of the within-case analyses, but cannot be presented in full owing to the limited space available in this report. Each site case study includes a brief summary of the data included.
It should be noted that data extracts (quotations) are labelled with the initial of the site pseudonym (ST, SU and CA for staff, service user and carer, respectively) and the participant’s unique number [e.g. B-ST-001 (Burgundy-Staff-001)].
This chapter thus provides detailed analysis of each site, or each ‘case’, providing deeper contextual information to support the findings and themes identified145 before these are then compared across sites in Chapter 5.
Recruitment and case study sites
Recruitment
Across the six sites, 301 service users completed questionnaires (against a target of 300) and 290 members of staff completed questionnaires (against a target of 300). Unfortunately, and with the support from the Study Steering Committee and the National Institute for Health Research, we had to end the data collection for carers early owing to challenges with data collection. The initial target for recruitment was 150 carers, but we obtained only 28 completed questionnaires before closing this part of the study. This is discussed in the limitations section in Chapter 6.
Across the six research sites we completed 31 interviews with staff (against a target of 36), 36 interviews with service users (against a target of 36) and nine interviews with carers (against a target of 24). A total of 51 care plans were reviewed, against a target of 60, and 12 observations were made, against a target of 18.
More detail is provided in each case study site section.
Case study sites
Each site was given a pseudonym to ensure the anonymity of participants. We used French names to avoid any accidental connection with English or Welsh sites or regions. The site names used were Artois, Dauphine, Languedoc and Provence (sites in England); and Burgundy and Champagne (sites in Wales).
We combine the quantitative and qualitative data analyses and present for each site in alphabetical order.
Meso- and micro-level analyses by site
Artois
History and context
Artois trust provides both primary and secondary mental health services to a population of approximately 1.6 million people. The trust covers a large, predominantly rural geographical area and serves six local authorities. Owing to the large catchment area, ethnicity and deprivation rates vary. According to the 2011 census, in one area 16% of the population were from a non-white background, whereas elsewhere this figure was only 7%. Similarly, deprivation rates vary, from high in the more densely populated urban areas to low in the rural communities of affluence. There are eight adult acute psychiatric wards, with 157 beds available. The main ward used for intensive data collection at this site is mixed gender and has 23 beds: 10 for female patients, 10 for male patients and three that can be used for either male or female patients. There are 43 regular staff working on the ward: one ward manager, one ward consultant, one staff-grade psychiatrist, 14 registered mental health nurses, 22 health-care assistants, one support time recovery worker and three administrative staff.
Adult acute inpatient services: admissions data
There were 1191 admissions to adult acute inpatient care at Artois trust in 2014/15, 61% of which were via the MHA,3 and there were 1296 discharges in total. The mean length of stay for adult acute inpatients at Artois trust in 2014/15 was 42 days, and occupancy rates were 94% for January/February 2016.
Participant characteristics: staff
Sixty-one members of staff from four acute inpatient wards in Artois completed the questionnaires. A large proportion of responses were from nurses (41%) and one-third were from staff who identified as ‘other’ (33%), with a good representation of psychiatrists (11.5%). Just over half of the respondents had been working in mental health for at least 4 years (54%) and one-quarter had been working in mental health for < 1 year (25%). The majority of staff had been working on the ward for < 3 years (72%). Few staff had been working on the ward for > 4 years. Other demographic characteristics of staff in Artois are shown in Table 4.
| Variable | n (%) |
|---|---|
| Gender | |
| Female | 39 (63.9) |
| Male | 20 (32.8) |
| Age (years) | |
| Median (range) | 31 (19–65) |
| Ethnicity | |
| Bangladeshi | 1 (1.6) |
| Asian other | 1 (1.6) |
| Black African | 1 (1.6) |
| Black Caribbean | 2 (3.3) |
| Indo-Caribbean | 2 (3.3) |
| Mixed race | 1 (1.6) |
| White UK/Irish | 50 (82) |
| Profession | |
| Mental health nurse | 25 (41) |
| Psychologist | 1 (1.6) |
| Psychiatrist | 7 (11.5) |
| Employment/recovery worker | 5 (8.2) |
| Other | 20 (32.8) |
| Education | |
| Degree | 20 (32.8) |
| Diploma/similar | 20 (32.8) |
| Postgraduate diploma/certificate | 1 (1.6) |
| Master’s | 3 (4.9) |
| Doctorate | 4 (6.6) |
| Time working in mental health (years) | |
| ≥ 10 | 20 (32.8) |
| 7–9 | 6 (9.8) |
| 4–6 | 7 (11.5) |
| 1–3 | 11 (18) |
| < 1 | 15 (24.6) |
| Time working on the ward (years) | |
| ≥ 10 | 6 (9.8) |
| 7–9 | 5 (8.2) |
| 4–6 | 4 (6.6) |
| 1–3 | 19 (31.1) |
| < 1 | 25 (41) |
| Personal history of mental health problems | |
| Yes | 16 (26.2) |
| No | 43 (70.5) |
| Family history of mental health problems | |
| Yes | 20 (32.8) |
| No | 38 (62.3) |
Participant characteristics: service users
In total, 53 questionnaires were completed by service users on four wards in Artois. The gender distribution of participants was equivalent, and the median age was 42 years. There were responses from diverse ethnicities, with the largest response from those identifying as white UK or Irish. One-third of the respondents had a diagnosis of psychosis/schizophrenia/bipolar-type disorder and one-third identified with two or more diagnostic categories. Just over half of the participants had spent > 10 years in mental health services and just under 50% of participants had been admitted to hospital between two and five times. One-third of participants had been on the ward for 1 week and one-third had been on the ward for > 4 weeks. Almost two-thirds of participants (62%) were in contact with community mental health services. Further details of the demographic characteristics can be found in Table 5.
| Variable | n (%) |
|---|---|
| Gender | |
| Female | 26 (49.1) |
| Male | 27 (50.9) |
| Age (years) | |
| Median (range) | 42 (22–76) |
| Ethnicity | |
| Indian | 2 (3.8) |
| Chinese | 1 (1.9) |
| Asian other | 1 (1.9) |
| Black African | 4 (7.5) |
| Black Caribbean | 1 (1.9) |
| Black other | 2 (3.8) |
| White UK/Irish | 32 (60.4) |
| White other European | 3 (5.7) |
| White other | 6 (7.8) |
| Mental health problem | |
| Psychosis/schizophrenia/bipolar-type disorders | 17 (32.1) |
| Depression/anxiety | 9 (17) |
| Substance user | 2 (3.8) |
| Other | 5 (9.4) |
| Two or more of above | 20 (37.7) |
| Relationship status | |
| Single | 39 (73.6) |
| In an established relationship | 12 (22.6) |
| Length of time with mental health services (years) | |
| ≥ 10 | 27 (50.9) |
| 7–9 | 7 (13.2) |
| 4–6 | 5 (9.4) |
| 1–3 | 5 (9.4) |
| < 1 | 8 (15.1) |
| Number of previous admissions | |
| First admission | 10 (18.9) |
| 2–5 | 26 (49.1) |
| 6–9 | 7 (13.2) |
| ≥ 10 | 9 (17) |
| Contact with community mental health services | |
| Yes | 33 (62.3) |
| No | 17 (32.1) |
| Time on the ward (weeks) | |
| 1 | 17 (32.1) |
| Up to 2 | 9 (17) |
| 2–4 | 10 (18.9) |
| > 4 | 17 (32.1) |
| Frequency contact with family/carer/friends | |
| Daily | 16 (30.2) |
| Weekly | 18 (34) |
| Fortnightly | 3 (5.7) |
| Monthly | 2 (3.8) |
| Other | 14 (26.4) |
| Living status before admission | |
| Independent and single | 22 (41.5) |
| Independent in relationship | 7 (13.2) |
| Living with family | 10 (18.9) |
| Living with friends | 1 (1.9) |
| Living with others | 1 (1.9) |
| Supported housing | 5 (9.4) |
| Homeless | 4 (7.5) |
| Other | 2 (3.8) |
| Previous daytime activity | |
| Full-time employment | 2 (3.8) |
| Part-time employment | 4 (7.5) |
| Sheltered employment | 4 (7.5) |
| Education/training | 20 (37.7) |
| Unemployed | 8 (15.1) |
| Voluntary work | 8 (15.1) |
| Other | 1 (1.9) |
| Two or more of the above | 5 (9.5) |
Summary scores for the questionnaires
Summary scores for four measures, VOICE, ES, STAR-P and RSA, were completed by service users. Staff completed provider versions of the RSA and STAR (STAR-C). When we have the data we also present a comparison of scores from our community COCAPP study.
There was some loss of participants on each of the subscales as a result of missing data. The number of participants is presented alongside the subscales. In particular, the RSA subscale for the service users was subject to quite significant attrition; this will be discussed in Chapter 5. Further participants in this scale were lost in Artois because of a photocopying error whereby a page was missed from the RSA for eight participants and a page was missed from the ES for six participants. Scales with < 50% of missing data were subject to mean replacement; those that had > 50% incomplete could not be included in the data set.
Empowerment Scale
A total ES score for each service user respondent was obtained by summing the scores of individual items. The overall mean score for the sample was above the mid-point for the instrument (Table 6). Out of a possible score of 4, indicating a higher perceived level of empowerment, the mean total score was 2.85 (SD 0.5). This is slightly higher than the reference value, but only marginally. 146 The scores were slightly higher than those of the reference group in all subscales apart from ‘power–powerlessness’, for which the scores were comparable. The Wowra and McCarter146 values relate to data collected in South Carolina, USA; therefore, they are from a different health-care system and also from people in contact with community mental health services.
| Subscale | COCAPP-A acute inpatient, mean (SD) | COCAPP community, mean (SD) | ||||
|---|---|---|---|---|---|---|
| n | Service usera | Referencea | n | Service usera | Referencea | |
| Self-esteem–self-efficacy | 52 | 3.05 (0.71) | – | 67 | 2.57 (0.71) | 2.82b |
| Power–powerlessness | 47 | 2.47 (0.64) | – | 65 | 2.43 (0.50) | 2.51b |
| Community activism and autonomy | 45 | 3.22 (0.62) | – | 66 | 3.13 (0.44) | 3.12b |
| Optimism and control over the future | 53 | 2.89 (0.82) | – | 67 | 2.62 (0.62) | 2.72b |
| Righteous anger | 52 | 2.37 (0.80) | – | 66 | 2.34 (0.70) | 2.34b |
| Total score | 52 | 2.85 (0.50) | – | 67 | 2.62 (0.37) | 2.74 (0.34)b |
A final comparison was made between the scores for empowerment across the two COCAPP studies (acute and community mental health services). The total score and subscales for the ES were marginally higher in the COCAPP-A study from respondents currently in acute mental health wards than the COCAPP study from respondents in contact with community mental health services. See Chapter 5 for some exploratory inferential analyses.
Views on Inpatient Care Scale
A total score on the VOICE for each respondent was obtained by summing the scores of the individual items. The higher the total score (range 19–114), the more negative the perception of the quality of care on the ward. The score for respondents in Artois is shown in Table 7.
| Scale | Service user score, mean SD (n = 53) | Reference value,a mean (SD) |
|---|---|---|
| VOICE totalb | 49.43 (20.16) (range 19.00–106.18) | 55.5 (19.2) male; 52.5 (17.8) female |
The total scores for VOICE were marginally lower than the reference value provided by Evans et al. 52 The mean scores were in the lower half of the scale, suggesting that service users leaned towards a more positive perception of the ward. There is, however, a large range of responses for this measure, demonstrating that some of the participants had a more negative perception of the ward.
Scale to Assess the Therapeutic Relationship
The mean total score for service users on the STAR-P was 29.02 (SD 11.30), 14.99 (SD 6.77) for ‘positive collaboration’, 7.32 (SD 3.41) for ‘positive clinician input’ and 6.77 (SD 3.34) for ‘non-supportive clinician input’. These values align well with the reference values provided by Nolan (Camden and Islington NHS Foundation Trust, 9 March 2016, personal communication) shown in Table 8. Nolan’s study was conducted in acute wards in the UK as part of the protected engagement time study. There were differences in the ‘non-supportive clinician input’ subscale on which the service users scores were on average two points lower than the reference value and only marginally past the mid-point for this subscale.
| Subscale | COCAPP-A (acute inpatient) | COCAPP (community) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| STAR-P (service user) | STAR-C (staff) | STAR-P (service user) | |||||||
| n | Mean (SD) | Reference | n | Mean (SD) | Reference | n | Mean (SD) | Reference | |
| Positive collaborationa | 52 | 14.99 (6.77) | 14.36 (5.99)b | 58 | 17.17 (2.65) | 17.95 (2.98)b | 68 | 17.37 (6.26) | 19.9 (6.7)c |
| Positive clinician inputd | 53 | 7.32 (3.41) | 7.10 (2.91)b | 58 | 10.34 (1.34) | 10.42 (1.23)b | 69 | 8.12 (3.31) | 9.3 (3.0)c |
| Non-supportive clinician inpute (service users)/emotional difficultiese (staff) | 52 | 6.77 (3.34) | 8.78 (2.21)b | 57 | 8.60 (1.53) | 9.61 (1.65)b | 69 | 8.90 (2.35) | 9.3 (3.3)c |
| Total scoref | 53 | 29.02 (11.30) | 30.23 (9.71)b | 58 | 36.08 (4.18) | 37.93 (4.92)b | 68 | 34.51 (10.79) | 38.4 (12.0)c |
The mean total for staff on the STAR-C was 36.08 (SD 4.18), 17.17 (SD 2.65) for ‘positive collaboration’, 10.34 (SD 1.34) for ‘positive clinician input’ and 8.60 (SD 1.53) for ‘emotional difficulties’. All of the subscale values are lower than the reference values, leading to an overall lower average total of approximately 2 points.
When comparing the mean service user and staff scores it is apparent that staff gave higher scores and therefore rated the therapeutic relationship more positively than service users. The total scores are on average 7 points higher for staff than for service users.
Independent samples t-tests were completed to determine if there were significant differences between the perceptions of the therapeutic relationship from service users and staff in the COCAPP-A study. There was a significant difference in the total STAR scores for service users (mean 29.02, SD 11.30) and staff (mean 36.08, SD 4.18) [t(64.9) = –4.28; p < 0.001; 95% confidence interval (CI) –10.35 to –3.77]. Staff perceived therapeutic relationships more favourably than service users. Furthermore, Cohen’s effect size value (d = 0.83) suggests a large practical significance. There was also a significant difference in the responses from service users and staff for two of the subscale scores: non-supportive clinician input and positive clinician input. For the non-supportive clinician input subscale the score for service users (mean 6.77, SD 3.34) was lower than that for staff (mean 8.60, SD 1.53) (t(70.1) = –3.61; p = 0.001; 95% CI –2.84 to –0.82; Cohen’s d = 0.70). For the positive clinician input subscale the score for service users (mean 7.32, SD 3.41) was lower than that for staff (mean 10.34. SD 1.34) (t(66.6) = –6.04; p < 0.001; 95% CI –4.02 to –2.02; Cohen’s d = 1.17). T-test statistics for the remaining subscale are provided in Chapter 5, Table 52.
A final comparison was made between the scores for the therapeutic relationships across the two COCAPP studies (acute and community mental health services). It is clear from the scores in Table 8 that service users in community mental health services score the therapeutic relationship higher than those in acute mental health services.
Recovery Self-Assessment
Mean scores and SDs for the RSA are provided in Table 9. Mean scores for service users and staff on the subscales fell in the moderate to high range (3.06 to 3.45 and 3.15 to 3.53, respectively). The difference in mean total RSA scores was evident, with staff responding with highest ratings [3.36 (SD 0.59)], followed by service users [3.21 (SD 0.96)]. The lowest scoring subscales for service users were ‘choice’ and ‘involvement’, scoring just above three, which within this subscale demonstrates neither a positive nor a negative response. The lowest scoring subscales for staff were ‘involvement’ and ‘diversity of treatment options’. The highest scoring subscale for both service users and staff was ‘life goals’.
| Subscale | COCAPP-A (acute inpatient) | COCAPP (community) | ||||||
|---|---|---|---|---|---|---|---|---|
| Service users | Staff | Service users | Staff | |||||
| n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | |
| Life goals | 49 | 3.45 (1.04) | 54 | 3.53 (0.61) | 65 | 3.48 (1.00) | 38 | 3.68 (0.72) |
| Involvement | 46 | 3.08 (1.14) | 58 | 3.15 (0.68) | 58 | 2.89 (1.11) | 38 | 3.01 (0.81) |
| Diversity of treatment options | 47 | 3.15 (1.04) | 59 | 3.21 (0.77) | 67 | 2.99 (1.20) | 38 | 2.96 (0.87) |
| Choice | 52 | 3.06 (0.99) | 59 | 3.47 (0.67) | 69 | 3.66 (0.90) | 38 | 3.76 (0.64) |
| Individually tailored services | 42 | 3.17 (1.10) | 60 | 3.29 (0.72) | 64 | 3.27 (1.00) | 38 | 3.18 (0.77) |
| Total score | 48 | 3.21 (0.96) | 58 | 3.36 (0.59) | 66 | 3.27 (0.96) | 38 | 3.35 (0.68) |
Independent samples t-tests were conducted to compare the perceptions of recovery-oriented services for staff and service users in acute mental health services. There were no significant differences in the total RSA scores for service users (mean 3.21, SD 0.96) and staff (mean 3.36, SD 0.59) [t(74.5) = –0.963; p = 0.339; 95% CI –0.47 to 0.16; Cohen’s d = 0.19) or the subscale scores (t-test parameters for subscales are provided in Chapter 5, Table 52.
A final comparison was made between the scores for the perceptions of recovery-oriented care across the two COCAPP studies (acute and community mental health services). The RSA total score for service users and staff in community and acute mental health services in Artois was almost equivalent. There are some differences at the subscale level with service users, in acute services score ‘involvement’ and the ‘diversity of treatment options’ marginally higher than those in community mental health services. Service users in acute inpatient services do however score ‘choice’ much lower than those in community mental health services. There are some differences at the subscale level for staff. In our acute study staff score ‘life goals’ marginally lower and ‘involvement’ and ‘individually tailored services’ marginally higher than in our community study. The ‘diversity of treatment options’ scale is higher and the ‘choice’ subscale is lower in the acute study. See Chapter 5 for some exploratory inferential analyses.
A recovery profile from the RSA scale is in Appendix 5.
Narrative summary of interview data: service users, carers and staff
In Artois we conducted interviews with six service users, six staff and five carers.
Care planning and co-ordination
Most staff participants felt that care plans were a necessary and useful part of work done on the ward. They have become an increasingly focal point of care as a consequence of the shift towards a more collaborative approach and shorter inpatient stays. Care plan documents were referred to regularly, especially during handovers and ward rounds. It was also suggested that care plans could be a useful means of encouraging good MDT collaboration and input. Effective communication between all parties (staff and service users) was felt to be crucial to care planning and it was suggested that continual efforts must be made to facilitate this:
With the number of professionals, sometimes it’s difficult to get everyone on board at the same time and get things communicated in a timely manner to make sure that their care [and] . . . treatment is provided as quickly as possible.
A-ST-104
Contrasting responses were received from service users. Only two participants provided positive accounts; others described matters more ambivalently, citing a lack of knowledge and understanding. One participant complained of a lack of continuity in his care throughout the admission process, which had taken considerable time to resolve.
Responses from carers were similarly diverse, with participants having a clear understanding of how care was being planned and co-ordinated, feeling well informed about progress and developments and being kept up to date with any changes as they occur. Two participants described at length the problems that they had experienced as a result of service users refusing to give consent for the disclosure of any information regarding their care:
She wouldn’t tell me whether she was taking medication or not, the nurses obviously couldn’t tell me, so I didn’t know and that was very frustrating, extremely frustrating.
A-CA-102
Staff said that all service users received written copies of their care plans. One participant was, however, keen to note that care plan documents must be regularly updated and (re)considered:
It feels like a very didactic process, this is your care plan, please sign it and then it’s forgotten about and then not really referred to or updated or nurtured.
A-ST-10
As with staff, service users were divided in their responses to the issue of written care plan documents. Only two participants had copies of their care plans, and said that they understood them and found them helpful, with care planned ‘brilliantly’ (A-SU-104) and the range of activities praised. One service user maintained that he did not have a written care plan at all, while another was unsure whether or not he had one. Just one participant mentioned actually referring to her care plan, although she did not do so regularly.
Among carers, there were similarly mixed responses about care plan documentation. Just two participants had seen written care plans, and only one actually had a copy of the document and he had had to request this.
All staff participants interviewed maintained that service user involvement in the care planning process was essential, and that this was actively encouraged on the ward:
Always having the patient’s views . . . on board and working with what . . . they want.
A-ST-101
This was felt to be a fundamental element of the working ethos on the ward: staff noted that matters had improved over time in this respect, and emphasised that service users typically became more involved as their stay progressed.
In contrast to staff views, few of the service users interviewed talked in any detail about being involved in their care planning. One interviewee complained that the focus of his care planning had been almost entirely on medication and that he sometimes felt unable to have a say. Similarly, only one of the carers interviewed reported being satisfied with their level of involvement in care planning; some carers noted that opportunities had been limited because service users refused to grant their permission for this. Interestingly, although documentation was drawn up by staff and then signed by service users, ownership was conceptualised as a shared endeavour between service users and staff: a form of agreement. Only one service user addressed the issue of care plan ownership, and did so in critical terms:
Own it? Oh no, I don’t own it, it just happens.
A-SU-106
Two service user participants raised concerns about the lack of continuity and coherence between inpatient and community services, and felt that this was having a detrimental impact on their care:
Each doctor [from accident and emergency admission onwards] has been good on their own but each one starts again rather than taking the notes from the last doctor and moving forward, they go back to square one again.
A-SU-106
This was also a concern for carers; one participant described having considerable problems with the handover of care from hospital to community services via an intensive support team. Carers were unsure whether or not, and to what extent, any existing care plans had informed service users’ care on the ward.
Staff noted that initial discussions about discharge took place in ward round meetings, at which time arrangements could be made for support (e.g. accommodation) in the community. A separate (formal and specific) discharge meeting was then held 1 or 2 weeks before a service user left. Staff emphasised that all relevant parties were encouraged to attend and felt that such meetings were most successful when they allowed for the communication of up-to-date details about post-discharge practicalities, such as crisis team follow-ups.
However, there was considerable ambiguity regarding post-discharge care planning; most staff seemed unsure whether or not service users were given a copy of their written care plan to take home, or about what happened to the documents after that. One interviewee described being involved in a new development aimed at improving discharge planning on the ward, and explained that service users now received an ‘interim discharge summary’ (A-ST-106) when they left hospital, which set out, for example, medication guidance, visit arrangements and key contact numbers in case of crisis.
In contrast, service users interviewed said that they had not been involved in any formal discussions about their discharge. Only two of the carer participants described being closely involved in discharge preparations and had attended meetings on the ward. One had been supported in visiting care homes that her daughter might be able to live in after leaving the ward, while another praised negotiations related to arrangements for home leave.
Care reviews
Staff participants noted that reviews were carried out during weekly ward round meetings. Care plans were subsequently updated and changes were implemented as required. Staff noted that reviews should reflect careful monitoring of service users’ progress, with all relevant MDT staff working closely together to facilitate this. Most staff maintained that service users were involved as much as possible in care reviews:
We’ll let the doctor know that they’d like to be seen and arrange for that to happen.
A-ST-104
The responses from service user participants were more diverse. One service user maintained that he had not been involved in any reviews and that no one had discussed the process with him. Another understood his care to be reviewed on a regular basis, but without his involvement. Two other participants were satisfied with their involvement, said that they felt listened to and supported, and found review meetings helpful. Most service user interviewees understood that review meetings were fixed (one weekly) and not flexible. Some participants’ families attended, whereas others had decided against this.
Carers talked at greater length about care reviews than did either service users or staff, and most described their experiences in positive terms. Most had attended review meetings regularly, and felt that these were well organised and structured, that they were able to contribute and that their views were listened to:
It’s very nice, it’s not too big . . . I know [the staff], it’s easygoing.
A-CA-101
Most carers viewed review meetings as a good opportunity to be updated on service users’ treatment and progress. Two interviewees complained that they had to take the initiative if they wanted to attend.
Support systems
Most staff had not received any formal training specifically on care planning and reported that they had learned either via job shadowing opportunities or by actually doing care planning. A-ST-101 noted that training opportunities were available to staff, but that it was their responsibility to pursue these.
Staff were unanimous that families, friends and carers were encouraged to be involved in care planning and were invited to contribute to ward round meetings. Staff felt that the trust’s approach was comprehensive and efficient, and described a mutually rewarding communicative relationship, although this was not the case for all carers:
It took me a while to work out what the hell was going on . . . nobody explained to me in [name of ward] what the ward round was and I had the right to be there.
A-CA-102
One staff participant noted that carer involvement had improved since the introduction of a ‘carers lead’ (A-ST-105) on the ward, a system to enable carers to spend time with a staff member. The challenges of involving carers and families were noted by staff, who felt that overinvolvement and unrealistic expectations could be problematic.
Most service users interviewed had family members or friends who supported them and were happy with their level of involvement. One participant complained that his parents sometimes received more information than he was given, which he found frustrating.
Staff noted that the disparity between the 24-hour inpatient care and the working hours of other services created difficulties in arranging meetings and appointments.
On the whole, service users described their relationships with staff in positive terms, and felt able to share their fears and concerns. One participant felt that staff could be inconsistent in their interactions and another complained about the unsatisfactory level of personal engagement between service users and staff. Most service user participants felt that staff attitudes were good, and that they were treated with dignity, respect and compassion. One service user provided a wholly negative account, describing how she was refused a key to her own room when first admitted to the ward, and complained that staff were neglectful of physical needs.
Safety and risk
Staff participants described risk assessment as a key component of care planning on the ward. The importance of careful and continual monitoring and observation was highlighted. Most service user participants reported feeling safe on the ward, and drew comparisons (both positive and negative) with previous experiences on inpatient units elsewhere. Only one service user provided a wholly negative account, maintaining that the reasons for her detention were not justified or explained. All of the carers interviewed felt that service users’ safety had been adequately considered and managed on the ward:
[Staff] did all they could to keep [name] safe.
A-CA-102
Staff participants noted that risk assessments involved the consideration of physiological risks and the close examination of relevant historical factors from service users’ existing notes, and also felt that the safety of the self and of others should be given equal attention. The short- and longer-term significance of risk assessment was emphasised. Although most staff felt that risk assessments were effectively conducted, there was acknowledgement of the potentially detrimental consequences to service users of overestimating risk. Staff maintained that formal and informal admissions to the ward were treated in much the same way, although it was acknowledged that particular attention was given to matters of capacity in formal detentions. Service user participants under detention reported that the process had been satisfactorily explained to them and that their rights had been fully clarified.
Four carers of people detained felt that detention had been necessary and beneficial, and reported that matters had been clearly explained to them. Some had long-term experience of previous detentions and were knowledgeable about the process.
Staff noted that formal discussions about risk took place during weekly ward round meetings, but conceded that service users were not always involved in these discussions. Negotiations around medication were described as especially challenging. None of the service users or carers interviewed mentioned being involved in discussions about risk.
Organisational context
Staff participants were unable to identify any formal policies or specific local developments underpinning the provision of care on the ward, but each recognised different sets of values and principles. These ranged from service user safety to person-centred care, recovery-focused work and good communication between staff, MDT members and service users. Most staff felt that things were done well and with the best of intentions. Challenges faced by staff were acknowledged. These included financial pressures, lack of resources and the requirement for a fast ‘turnaround’ of service users on the ward, which was described as disheartening. Most staff participants emphasised the efforts made to manage these challenges in their everyday work on the ward.
Recovery
Staff participants were familiar with the ‘journey’ metaphor, although none used it themselves, even when they acknowledged its usefulness: most definitions focused on service user choice and empowerment. Some staff were concerned that the notion of recovery could create unrealistic goals for service users and felt that officially sanctioned conceptualisations of recovery were sometimes inconsistent with actual lived experiences.
Only two service users offered a definition of recovery, one describing it in terms of personal wellness and another associating the idea with hospital discharge: they indicated that there had been little sustained or detailed discussion around the subject. Staff and service user participants were aware of divergent conceptualisations of recovery, which was seen as a potential hindrance to effective care planning.
Carer participants gave more detailed definitions of recovery than either staff or service users, and some took great care to acknowledge the process of recovery to be a lengthy and complex one, typically involving ongoing care and medication. They also recognised the non-linear quality of the recovery experience, which was understood to be challenging, noting that the journey metaphor was idealistic and of limited relevance to some.
Staff maintained that they worked in a recovery-oriented way on the ward, although the challenges of doing so were emphasised, with changing organisational objectives and limited resources cited as significant factors. Most carers said that they found it difficult to know whether or not service users’ care had been recovery focused.
Service users seemed more ambivalent about the whole concept of recovery and only two expressed strong feelings as to whether or not their hospital stay had been helpful in this respect. One participant felt that it had, whereas another gave a contrasting view that he felt that he was simply left to occupy himself on the ward.
Most service users seemed to consider hospital a preferable option for them at the current time, but were also aware of the disadvantages of the environment in terms of their well-being:
It’s better than being outside with no help but that maybe the atmosphere in here is a little, it gets into your nerves, they jangle a bit.
A-SU-106
In keeping with staff responses, almost all of the carers interviewed felt that service users’ hospital stays had helped with their recovery, especially in terms of the extent to which they had stabilised and settled the person.
Two carers felt quite strongly that better (and greater) provision of psychological therapies would help with recovery and would have liked to have this in addition to the medication as a means of ‘deeply investigating the causes [of the illness] and trying to right that’ (A-CA-102).
Personalisation
Most of the staff, service users and carers interviewed were unfamiliar with the term ‘personalisation’ but understood it to mean person-centred care. Half of the staff felt that care on the ward was personalised and individually tailored to service users’ needs, although some were more sceptical about the relevance of personalisation to inpatient care:
Personalisation is what we know of them as a patient, not as a person. It’s patientisation . . . [it’s] service userisation.
A-ST-105
Most service user participants felt that their care on the ward had not been personalised and observed that individually tailored care was less possible in hospital than in the community.
Carers’ responses on this subject were mixed. One participant felt that care on the ward had been adequately personalised, and gave examples of staff providing his daughter with crossword puzzles and taking her to have her nails painted and her feet massaged. He also felt that her views and wishes were listened to. Others were less certain, and were reluctant to give a firm opinion. As with staff and service users, carers were aware of the extent to which care could be personalised on the ward.
Two staff interviewees described service user empowerment as a key objective on the ward, but most were more ambivalent about this. Staff emphasised some of the tensions in collaborative decision-making, maintaining that a satisfactory compromise was always sought.
Barriers and facilitators
For most staff, good communication between all parties was seen as a key factor in helping to facilitate recovery-focused and personalised care. It was felt that staff could benefit from listening carefully to families and carers, who often had a good understanding of service users’ needs and wishes. Careful handling of issues pertaining to consent and information sharing were also understood to be important in this respect, with resistance from service users identified as an area of contention:
Most of the patients don’t want any medication or don’t think they’re ill, which is of course part of it, part of being ill a lot of the time, or not wanting their medication, part of why they’ve relapsed, so why they’re here in the first place.
A-ST-103
Service user involvement was seen as another facilitator, as was a comprehensive consideration of service users’ personal histories.
Various suggestions were made about how care planning might be improved. These ranged from extending business hours to maintaining contact with service users after discharge. The potential benefits of involving wider support services more effectively were also discussed, particularly encouraging more professionals to attend ward round meetings.
Several hindrances to the delivery of recovery-focused and personalised care were identified. Inadequate communicative relationships were seen as a major factor, and the lack of one-to-one time available for staff to spend with service users was also a concern. The extensive quantity of paperwork was felt to be a hindrance to staff, as were constant organisational changes.
Care plan reviews
Ten care plans were reviewed on the main ward in Artois for six female and four male service users ranging in age from 23 to 63 years, eight of whom had been formally detained at some point during their admission. For three participants this was their first admission to hospital and for others this ranged from one to nine previous admissions. In five care plans it was clear that the service user had signed the plan, although in only two cases was it clear that a copy had been given to the service user. No care plans were signed by the named nurse. Each of the 10 service users had attended their last ward round, but on only two occasions were carers present, and on four rounds care co-ordinators had attended, suggesting some possible issues with continuity of care. The care plans reviewed had been clearly written by staff to the person; for example, ‘you stated that you felt ready to go home’. In six care plans there was evidence of coproduction, four care plans showed a strengths-based approach and six showed evidence of encouragement to develop self-management approaches. Care plans on the whole lacked a focus on personalisation (4 out of 10), although recovery-oriented care planning was evident (7 out of 10). Four care plans included the person’s views on their safety and risk, and three care plans included the person’s views on their risk management plan. The majority of care plans (9 out of 10) included plans for discharge.
Meeting observations
In Artois one observation of a ward round meeting was completed. Eight people were present, including two members of the research team, two psychiatrists, the service user and his father. The meeting was held in a light, open room with a welcoming layout, plenty of space and chairs arranged in a circle. The meeting began on time and was led by the patient from the start. Formal introductions were not required because there was a well-established relationship; the staff, service user and carer were familiar and comfortable with one another. The interpersonal effectiveness and non-verbal communication of the psychiatrist were impressive throughout, creating a relaxed space for the service user to discuss their care while maintaining a good balance of firmness when required. Many of the questions were framed by using tentative enquiry such as ‘would you mind if . . .?’, ‘would it be OK if . . .?’, which provided scope for negotiation. Plenty of time and patience was provided, which offered the service user adequate opportunity to ask questions. Discussions were handled respectfully, with the use of recapping and summarising to ensure that the information was understood. The service user’s existing knowledge about his condition and medication were used well, and the staff built on this nicely. Physical health was addressed and medical records were consulted openly for the service user to see and discuss. Most of the discussion focused on medication and the request for leave; however, some time was used to explore the service user’s understanding of his illness and his recovery and progress in an open and empowering way, with praise and encouragement given for progress already made. When minor disagreements occurred, these were handled positively and collaboratively, with the service user’s views considered throughout. The patient’s father was able to contribute to the discussion when he wanted to; his main role was to provide moral support, as the service user was able to lead the conversation himself. The end of the meeting was handled efficiently and empathically; the content was summarised and arrangements for future meetings were discussed, as were steps to implement the changes talked about during the meeting.
Burgundy
History and context
Burgundy LHB serves approximately 500,000 people, of whom 1.6% are from black and minority ethnic (BME) groups. It covers a wide geographical area with a mix of urban and rural communities, some of which are densely populated. Twenty-four per cent of the areas measured in the largest urban part of the locale, and almost 30% of a second part, are in the most deprived 20% in Wales. 147 Mental health services are provided in three hospital sites and there are 75 beds in total. The number of available bed-days in 2014/15 was 27,393 and the number of occupied bed-days (excluding leave) was 26,845: a 98% occupancy rate. The number of occupied bed-days (including leave) was 31,710.
Adult acute inpatient services: admissions data
For 2014/15, the number of admissions to inpatient care at Burgundy LHB was 1022. Of these admissions, 362 (35%) involved section under the MHA. 3 The number of discharges from inpatient care, meanwhile, was 929, and the number of emergency readmissions within 30 days (excluding planned readmissions) was 51. The interview data gathered at Burgundy indicate an association between housing and accommodation problems and inpatient admissions, although health board figures for 2014/15 showed that only eight service users were of no fixed abode at the time of their admission.
The health board’s 2014/15 figures for average length of stay emphasise the brevity of admissions. For example, the average length of stay including leave and unadjusted for outliers (i.e. service users staying < 3 or > 60 days) was 34 days (mean) and 9 days (median). Once adjusted for outliers, these figures look slightly different: here, the mean length of stay was 16 days and the median length of stay was 12 days. For service users admitted under MHA section, meanwhile, the mean length of stay was 14 days and the median length of stay was 10 days. The longest stay recorded was 670 days and the shortest was 1 day.
The main ward used for data collection at this site is mixed gender and has 21 beds, with one bed allocated for a child aged between 17 and 18 years (Child and Adolescent Mental Health Services). Staff working on the ward comprise 18 registered mental health nurses, 12 health-care support workers, one activity worker, one OT, one OT assistant, one consultant psychiatrist, one senior house officer and one psychologist (1 day per week).
Participant characteristics: staff
Forty-three staff from three acute mental health inpatient wards within the locality completed questionnaires. The majority of the responses were from mental health nurses (74%), and a large proportion of the remaining responses identified as ‘other’ for their employment status. Most of the respondents had spent at least 4 years working in mental health (70%); however, over half of the staff had spent < 4 years working on the ward (58%). Only one member of staff disclosed that they had personal history of mental health problems; however, just under one-third disclosed that they had family history of mental health problems. Further details of the demographic characteristics can be found in Table 10.
| Variable | n (%) |
|---|---|
| Gender | |
| Female | 21 (48.8) |
| Male | 20 (48.8) |
| Age (years) | |
| Median (range) | 37 (22–55) |
| Ethnicity | |
| White UK/Irish | 40 (93) |
| White other | 1 (2.3) |
| Black African | 1 (2.3) |
| Profession | |
| Mental health nurse | 32 (74.4) |
| Psychologist | 1 (2.3) |
| Occupational therapist | 1 (2.3) |
| Other | 8 (18.6) |
| Education | |
| Degree | 26 (60.5) |
| Diploma/similar | 8 (18.6) |
| Postgraduate diploma/certificate | 1 (2.3) |
| Master’s | 1 (2.3) |
| Doctorate | 3 (7) |
| Time working in mental health (years) | |
| ≥ 10 | 21 (48.8) |
| 7–9 | 5 (11.6) |
| 4–6 | 4 (9.3) |
| 1–3 | 7 (16.3) |
| < 1 | 5 (11.6) |
| Time working on the ward (years) | |
| ≥ 10 | 7 (16.3) |
| 7–9 | 1 (2.3) |
| 4–6 | 9 (20.9) |
| 1–3 | 13 (30.2) |
| < 1 | 12 (27.9) |
| Personal history of mental health problems | |
| Yes | 1 (2.3) |
| No | 41 (95.3) |
| Family history of mental health problems | |
| Yes | 12 (27.9) |
| No | 29 (67.4) |
Participant characteristics: service users
In total, 48 questionnaires were completed by service users in three wards in Burgundy. The gender distribution of participants was equivalent, and the median age was 46 years. The responses were predominantly from people identifying as white UK, Irish, European or other. One-third of the respondents had a diagnosis of psychosis/schizophrenia/bipolar-type disorder and just over one-third identified with two or more diagnostic categories. Just over half of the participants had spent > 10 years in mental health services and just under 50% of participants had been admitted to hospital between two and five times. A large proportion of participants had been on the ward for 1 week (42%) and just over 20% had been on the ward for > 4 weeks. Just over half of the participants (56%) were in contact with community mental health services. Further details of the demographic characteristics can be found in Table 11.
| Variable | n (%) |
|---|---|
| Gender | |
| Female | 23 (47.9) |
| Male | 25 (52.1) |
| Age (years) | |
| Median (range) | 46.5 (19–75) |
| Ethnicity | |
| Mixed race | 1 (2.1) |
| White UK/Irish | 7 (14.6) |
| White other European | 2 (4.2) |
| White other | 7 (14.6) |
| Mental health problem | |
| Psychosis/schizophrenia/bipolar-type disorders | 16 (33.3) |
| Depression/anxiety | 9 (18.8) |
| Substance user | |
| Other | 4 (8.3) |
| Two or more of above | 18 (38.3) |
| Relationship status | |
| Single | 35 (72.9) |
| In established relationship | 10 (20.8) |
| Length of time with mental health services (years) | |
| ≥ 10 | 25 (52.1) |
| 4–6 | 2 (4.2) |
| 1–3 | 6 (12.5) |
| < 1 | 14 (29.2) |
| Number of previous admissions | |
| First | 10 (20.8) |
| 2–5 | 21 (43.8) |
| 6–9 | 8 (16.7) |
| ≥ 10 | 8 (16.7) |
| Contact with community mental health services | |
| Yes | 27 (56.3) |
| No | 12 (25) |
| Time on the ward (weeks) | |
| 1 | 20 (41.7) |
| Up to 2 | 10 (20.8) |
| 2–4 | 7 (14.6) |
| > 4 | 11 (22.9) |
| Frequency contact with family/carer/friends | |
| Daily | 23 (47.9) |
| Weekly | 11 (22.9) |
| Fortnightly | 2 (4.2) |
| Monthly | 1 (2.1) |
| Other | 10 (20.8) |
| Living status before admission | |
| Independent and single | 22 (45.8) |
| Independent in relationship | 4 (8.3) |
| Living with family | 14 (29.2) |
| Living with others | 1 (2.1) |
| Supported housing | 4 (8.3) |
| Homeless/no fixed abode | 1 (2.1) |
| Previous daytime activity | |
| Full-time employment | 2 (4.2) |
| Education/training | 28 (58.3) |
| Unemployed | 4 (8.3) |
| Voluntary work | 10 (20.8) |
| Two or more of above | 2 (4.2) |
Summary scores for the questionnaires
Views on Inpatient Care Scale
A total VOICE score for each respondent was obtained by summing the scores of the individual items. The higher the total score (range 19–114), the more negative the perception of the quality of care. The scores for respondents in Burgundy are shown in Table 12.
| Scale | Service user score (n = 48)a | Reference valueb |
|---|---|---|
| VOICE total | 45.69 (16.64); range (19.00–84.00) | 55.5 (19.2) male; 52.5 (17.8) female |
The total scores for VOICE were considerably lower than the reference value provided by Evans et al. 52 The mean scores were in the lower half of the scale, suggesting that service users leant towards a more positive perception of the ward. The range of responses for this measure is fairly narrow (19.00–84.00) when taking into account the maximal response score of 114. This demonstrates that the responses from participants were not too extremely weighted towards a negative perception of the ward.
Empowerment Scale
A total empowerment score for each service user respondent was obtained by summing the scores of individual items. The overall mean score for the sample was above the mid-point for the instrument. Out of a possible score of 4, indicating a higher perceived level of empowerment, the mean total score was 2.81 (SD 0.46); this is slightly higher than the reference value. 146 The subscale values were slightly higher than the reference group apart from ‘power–powerlessness’, which was marginally lower (Table 13).
| Subscales | COCAPP-A (acute inpatient) | COCAPP (community) | ||||
|---|---|---|---|---|---|---|
| n | Mean (SD)a | Referencea | n | Mean (SD)a | Referencea | |
| Self-esteem–self-efficacy | 48 | 2.87 (0.89) | – | 74 | 2.60 (0.73) | 2.82b |
| Power–powerlessness | 48 | 2.40 (0.53) | – | 71 | 2.51 (0.54) | 2.51b |
| Community activism and autonomy | 48 | 3.34 (0.55) | – | 70 | 3.07 (0.56) | 3.12b |
| Optimism and control over the future | 48 | 2.95 (0.83) | – | 74 | 2.63 (0.60) | 2.72b |
| Righteous anger | 48 | 2.49 (0.73) | – | 73 | 2.24 (0.69) | 2.34b |
| Total score | 48 | 2.81 (0.46) | – | 73 | 2.62 (0.43) | 2.74 (0.34)b |
A further comparison was made between the scores for empowerment across the two COCAPP studies (acute and community mental health services). Apart from the ‘power–powerlessness’ subscale, the total score and subscale scores for the ES were higher for responses obtained from service users in acute inpatient services than for responses from those in contact with community mental health services. See Chapter 5 for some exploratory inferential analyses.
Scale to Assess the Therapeutic Relationship
For service users the mean total score for the STAR-P was 30.00 (SD 10.15), 15.28 (SD 6.37) for ‘positive collaboration’, 7.47 (SD 3.17) for ‘positive clinician input’ and 7.19 (SD 2.92) for ‘non-supportive clinician input’. These scores closely align with the reference values provided by Nolan (personal communication) shown in Table 14, apart from the ‘non-supportive clinician input’ subscale, for which the service users scores were, on average, 1.5 points lower than the reference value.
| Subscale | COCAPP-A (acute inpatient), mean (SD) | COCAPP (community), mean (SD) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| STAR-P | STAR-C | STAR-P | |||||||
| n | Service user | Reference | n | Staff | Reference | n | Service user | Reference | |
| Positive collaborationa | 47 | 15.28 (6.37) | 14.36 (5.99)b | 43 | 18.86 (2.57) | 17.95 (2.98)b | 73 | 19.81 (4.85) | 19.9 (6.7)c |
| Positive clinician inputd | 48 | 7.47 (3.17) | 7.10 (2.91)b | 43 | 10.95 (1.15) | 10.42 (1.23)b | 74 | 9.46 (2.45) | 9.3 (3.0)c |
| Non-supportive clinician inpute (service users)/emotional difficultiese (staff) | 47 | 7.19 (2.92) | 8.78 (2.21)b | 43 | 9.50 (1.37) | 9.61 (1.65)b | 73 | 9.23 (2.83) | 9.3 (3.3)c |
| Total scoref | 47 | 30.00 (10.15) | 30.23 (9.71)b | 43 | 39.33 (4.31) | 37.93 (4.92)b | 73 | 38.49 (8.55) | 38.4 (12.0)c |
For staff the mean total for the STAR-C was 39.33 (SD 4.31), with scores of 18.86 (SD 2.57) for ‘positive collaboration’, 10.95 (SD 1.15) for ‘positive clinician input’ and 9.50 (SD 1.37) for ‘emotional difficulties’. All the subscale values were marginally higher than the reference values apart from the emotional difficulties subscale, which was marginally lower. Overall, the total score was higher than the reference value.
When comparing the mean total scores for service user and staff, it is apparent that staff give higher scores and therefore rated the therapeutic relationship more positively than service users. It is notable that the total score is at least nine points higher for staff than for service users.
An independent-samples t-test was completed to determine if there were significant differences in the perceptions of the therapeutic relationship between service users and staff. There was a significant difference in the total STAR scores for service users was 30.00 (SD 10.15) and staff was 39.33 (SD 4.31) [t(63.2) = –5.76; p < 0.001; 95% CI –12.57 to –6.10, Cohen’s d = 1.20] and all of the subscale scores (t-test statistics for the remaining subscale are provided in Chapter 5, Table 52).
A final comparison was made of the scores for the therapeutic relationships between the two COCAPP studies (acute and community mental health services). It is clear from the scores in Table 15 that service users in community mental health services scored the therapeutic relationship higher than service users in acute mental health services.
| Subscales | COCAPP-A (acute inpatient) | COCAPP (community) | ||||||
|---|---|---|---|---|---|---|---|---|
| Service usersa | Staffa | Service usersa | Staffa | |||||
| n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | |
| Life goals | 46 | 3.40 (1.01) | 43 | 3.67 (0.70) | 70 | 3.55 (1.06) | 37 | 3.73 (0.70) |
| Involvement | 41 | 3.07 (1.15) | 43 | 3.05 (0.84) | 69 | 2.96 (1.12) | 37 | 2.90 (0.66) |
| Diversity of treatment options | 45 | 3.31 (0.96) | 43 | 3.42 (0.74) | 71 | 3.06 (1.08) | 37 | 3.23 (0.76) |
| Choice | 47 | 3.40 (1.03) | 43 | 3.72 (0.70) | 74 | 3.65 (0.89) | 37 | 3.92 (0.62) |
| Individually tailored services | 41 | 3.28 (0.97) | 43 | 3.34 (0.71) | 66 | 3.27 (1.06) | 37 | 3.10 (0.80) |
| Total score | 46 | 3.32 (0.95) | 43 | 3.45 (0.65) | 71 | 3.33 (0.95) | 37 | 3.41 (0.61) |
Recovery Self-Assessment
Mean scores and SDs for the RSA are provided in Table 15. Mean scores from service users and staff on the subscales fell in the moderate to high range (3.07 and 3.40, and 3.05 and 3.72, respectively). The difference in mean total RSA scores was only marginal; staff had the highest ratings [3.45 (SD 0.65)], followed by service users [3.32 (SD 0.95)]. The lowest scoring subscale was ‘involvement’, with both participant groups showing negligible differences. The highest scoring subscale were ‘choice’ and ‘life goals’ for both groups. Staff rated both of these subscales higher than did service users.
Independent-samples t-tests were conducted to compare the perceptions of recovery-oriented services for staff and service users. There were no significant differences in the total RSA scores for service users (mean 3.32, SD 0.95) and staff (mean 3.45, SD 0.65) [t(79.4) = –0.773; p = 0.442; 95% CI –0.47 to 0.2, Cohen’s d = 0.16] or the subscale scores (t-test statistics for subscales are provided in Chapter 5, Table 52).
A final comparison was made of the scores for the perceptions of recovery-oriented care between the two COCAPP studies (acute and community mental health services). The RSA total scores for service users and staff in community and acute mental health services in Burgundy were almost equivalent. There were some differences at the subscale level, with service users in acute services scoring the ‘life goals’ and ‘choice’ subscales lower than respondents in community services. Conversely, service users scored ‘involvement’ and diversity of treatment options’ subscales higher than did those in community services.
A similar pattern is seen with the responses from staff. An additional difference is that staff working in acute mental health services scored the ‘individually tailored services’ subscale higher than did those in community mental health services. See Chapter 5 for some exploratory inferential analyses.
A recovery profile from the RSA scale is in Appendix 5.
Narrative summary of interview data: service users, carers and staff
In Burgundy, we conducted interviews with six service users on the ward, and six staff. Unfortunately, we were unable to recruit carers for interviews in this site.
Care planning and co-ordination
Staff at Burgundy felt strongly that care and treatment planning needed to be sufficiently flexible and ‘dynamic’ to allow for constant and continual adaptation in order to adequately address the scope and complexity of changes in individual service user progress:
I think usually the nurses on the ward try and review the care plans at least weekly, but some people coming in crisis point can change day to day . . . so it’s about working with that patient and working with their changes, which is always different.
B-ST-101
It was noted that care planning documentation was ‘basic’, making it difficult to incorporate the necessary nuances of care. It was suggested that the documentation did not capture any complete sense of a service user’s identity:
The little things which sometimes are the most important [for an individual] don’t get captured in a dialogue in that care and treatment plan. I think it’s still quite still professionalised . . . rather than the words of the person, that it’s coming out of really.
B-ST-102
Staff were keen to emphasise that the CTP format required by legislation in Wales was not well suited to the typically short-term nature of acute inpatient care. They also felt that the short-term nature of admissions could make the CTP process extremely challenging, because it meant that difficulties with, for example, finances or housing are prioritised over cultural or spiritual needs. When asked to define care and treatment planning, staff primarily associated this with ideas about discharge and recovery.
Interestingly, the legislative requirements of the Mental Health (Wales) Measure 2010 were not emphasised in participants’ narratives: only two raised this at all, and those who did focused on the concerns and anxieties that it had created for practitioners.
Concerns were raised about the lack of continuity of care planning between community and hospital contexts, which were felt to limit the relevance and transferability of CTPs on admission and discharge. As a strategy for addressing this, the ward currently used a separate ‘add-on’ or ‘intervention’/’management’ plan, which mirrored (but did not replace) any existing CTP and was used specifically for the duration of the service user’s stay. Staff reported that, using this system, all service users received a care plan on admission. It was also noted that the intricacy and quantity of paperwork of the existing CTP format could make liaisons with other agencies more complicated, and that this could be better adapted to the ward:
I think I struggle with the principles [of CTP] and how that fits perhaps into the ward – the confusion that still exists is very much present in terms of the fundamentals of it.
B-ST-102
Service user participants reported having contact with mental health services before their admission to inpatient services. Many either had been seen by a crisis team previously or had been transferred from another psychiatric hospital, often following an accident and emergency admission. This suggests that they would have had existing care plans at the time of their admission, although they seemed to have limited knowledge of the implications of this.
Service user responses mirrored concerns raised by staff about the priority necessarily given to housing and accommodation issues in relation to care planning. Accordingly, perhaps, these are the elements of the CTP process in which service users seemed to be most involved. Interview data from the study also suggest that problems in these areas often accompany the worsening mental health conditions that necessitate hospital admissions in the first place:
The main priority [of my care plan] is finding me somewhere to go first basically . . . so that’s the main goal.
B-SU-103
Staff felt that service user involvement and collaboration in care and treatment planning was important. Staff claimed that a lot of the time service users were unwilling or unable to engage with the care planning process and therefore had little awareness of its relevance to them. Most service user participants were unaware that they had a written care plan and those who were reported that they have not seen the document. Only two service user participants were aware that they had a written CTP. After further exploration by our research support nurse, it was confirmed that there were no existing care plans for the remaining four research interview participants. These disparities can perhaps be partly explained by staff presenting idealised versions of their practice during interviews, which may not necessarily reflect the day-to-day reality experienced by service users:
[My care] hasn’t really been planned, they keep giving me different tablets all the time and I’m not quite sure what tablets they’re giving me, I’m just taking them because they’re asking me to.
B-SU-101
No, nobody talks to me about that.
B-SU-104
For the most part, service users believed that staff on the ward provided a good and fair quality of care, but they did not feel that they were actively involved in the care planning. Service user responses substantiated the observations of staff in terms of the apparent willingness of some to actively choose non-involvement. Although service users felt that there was at least the potential for them to be more involved in their care planning, they maintained that this was not necessarily actively encouraged or pursued by staff. Staff felt strongly that service users should have ownership of their care plans, although they were not certain whether or not service users themselves felt that they owned the plans. Responses from service users on this point would seem to indicate that they did not:
They don’t tell me nothing in this ward. They don’t do nothing. They just give you your tablets and feed you food and that’s it like.
B-SU-101
Staff participants emphasised that discharge plans were discussed with service users as soon as possible after their admission, and it was noted that the health board had a 7-day follow-up system with their crisis teams. Weekly discharge planning meetings ere held on the ward so that service user progress could be shared among all staff. Service users themselves, however, were not certain of this. Indeed, in contrast to the staff responses outlined here, discharge had been discussed with only two of the six participants interviewed. For them, the primary focus had been on resolving housing and accommodation problems: moreover, their discharge was contingent on such resolutions:
[Patients are asked] if they feel that everything’s been addressed on [their care plan] and then seeing what we can do prior to their discharge.
B-ST-106
Care reviews
Staff reported that care was reviewed in its most formal sense during weekly ward round meetings, although service user progress was monitored continuously. Staff emphasised that, ultimately, the review process itself had to reflect the individual needs of the service users. Involvement was encouraged as much as possible, as was the involvement of family, friends and carers. It was, however, noted that this could be challenging.
Responses from service users to questions in this category indicated that they had a very limited knowledge or awareness of the review process in relation to care and treatment planning on the ward. Interestingly, service users did not draw any connection between reviews and ward round meetings, and seemed not to understand that this was when reviews of their CTP took place. One participant also suggested that there may be advantages to not being involved in the review process:
Maybe it’s better if I’m not fully aware of the plan, because if I am I could be more guarded in the way I participate . . . Whereas if I’m not fully aware until the end of the plan, maybe there’d be more honesty in the plan, you see.
B-SU-102
Support systems
Staff reported that they had not received any specific training in care planning. They had attended only basic introductory courses at most, or learned about CTP as a part of their wider nursing education, focusing mainly on issues such as the legislative responsibilities of the Measure and the technicalities of the CTP documentation. It was suggested that this lack of training may be detrimental to the overall coherence of the CTP process.
Burgundy has no official policy on family or carer involvement, and some staff participants would have preferred this to be more formalised. According to staff, the involvement of family and carers is encouraged, with invitations issued to attend and participate in ward round meetings. Staff gave little consideration to the extent to which service users could find such meetings stressful or frightening, and that they may, therefore, be deterred from attending them. Nevertheless, the challenges and potential problems of family/carer involvement were widely acknowledged by staff, especially in terms of how this could sometimes create unrealistic expectations for the various parties. Participants also emphasised that service users’ wishes must be respected. Nevertheless, the challenges and potential problems of family/carer involvement were widely acknowledged by staff, especially in terms of how this may sometimes create unrealistic expectations for the various parties. Participants also emphasised that service users’ wishes must be respected, with some staff feeling that there was value and importance in involving advocates and help from other source when possible.
Responses from service users suggested that they had carers, families or friends who supported them and were involved, to some extent, in their care. On the whole, most seemed satisfied with this level of involvement, although one participant would have preferred her family to be more fully involved. Another had been helped by staff on the ward to maintain a good relationship with her daughter by organising special visiting arrangements:
[Having my family more involved] would have been better. Because they could help me to understand [things more fully].
B-SU-101
Service users reported having at least one named nurse and seeing that person regularly. Most described having good relationships with staff with whom they had the most contact. Only one service user described having had a negative experience in terms of her relationship with ward staff, which she attributed to the lack of one-on-one time available for staff–service user interactions. She also commented that the constant presence of students in ward round meetings prevented her from feeling comfortable enough to talk freely to her doctor. All participants agreed that staff attitudes were good, that staff were compassionate and that they treated service users with dignity and respect.
Safety and risk
There was unanimous agreement among staff at Burgundy that risk assessment was a key priority and of primary importance in care planning, although no mention was made of involving service users in discussions about this. All staff participants maintained that formal and informal admissions were handled in the same way. The consequences of detention (e.g. being confined to the ward, administering enforced medication and the importance of reading service users their rights) were also acknowledged. Staff emphasised the need for continual and ongoing risk assessment, and acknowledged the difficulty of adequately capturing this in the CTP document. The value and importance of positive risk taking was mentioned by only two participants.
For service users, meanwhile, there was a feeling that their safety had been considered during their hospital stay. None had had any detailed discussions about their safety, and two participants did not seem familiar with the idea of a risk assessment at all. Most seemed to have limited knowledge and awareness of the subject:
[I don’t think anyone spoke to me about it], no. It was, other patients were on section and I could see what they were going through, say.
B-SU-104
Organisational context
Staff at Burgundy did not, on the whole, feel that the introduction of the Mental Health (Wales) Measure had led to any significant organisational change. In terms of key developments, the shift towards recovery-oriented practices was felt to have had a significant impact for staff. Staff acknowledged that the centralising of services may have made visiting more difficult for carers owing to increased travel distances and poor local transport options. Empowerment and service user choice were seen as the key values or principles that underpinned the provision of services.
Recovery
Staff participants did not offer any standard or dominant definition of recovery. Recovery was not felt to be a new concept in mental health, but most participants (staff and service users) acknowledged its scope and complexity, as well as its potentially disparate interpretations. Service users did not use any single, universal definition of recovery. Interestingly, service user participants did not feel that the ‘journey’ metaphor was especially relevant, and most acknowledged the concept’s complexity and subjective, individual nature:
But how long’s that journey? . . . How long is a piece of string?
B-SU-104
Staff felt that working in a recovery-focused way required flexibility and a consideration of individual differences, which are very difficult to capture in the CTP document. Service users, for the most part, felt that their hospital stay had helped with their recovery, and recognised this as being linked to an ongoing process of continuing to make positive progress.
The Recovery Star is used on the ward, although this is usually done in an informal way, and staff saw this as a useful means of establishing and encouraging service user involvement. Service users are also encouraged to attend regular recovery group meetings. Only one service user cited the Recovery Star approach used on the ward but noted that it was left to her to develop coping mechanisms for her symptoms. Recovery plans were not mentioned by any other service user participants.
Staff felt that involvement, empowerment and drawing on service users’ own existing individual experiences and knowledge were key factors in striving for recovery and working in a recovery-focused way.
Personalisation
Personalisation is not a term used by staff, although they were familiar with the concept and understood the ways in which it related to the notion of person-centred care. Service users were not familiar with the term at all, however, and had not heard it used on the ward. Staff felt that care on the ward was personalised, but recognised that there could be major challenges when it came to delivering this. They identified service user capacity/ability and logistical resources, as well the specific characteristics of inpatient care, as being particular hindrances. It was also noted that medical and psychological therapeutic models of care were in constant tension.
Most service users seemed to feel that their care on the ward was individually tailored and that staff were sensitive to and respectful of their personal needs. One participant, however, maintained categorically that her experience had not been person centred at all. Staff felt that CTP processes facilitated personalised care more now than they did previously, and it was suggested that working in a personalised way could also usefully involve service users and staff getting to know one another better as individuals. The overall sense was that matters had improved in terms of delivering personalised care.
Barriers and facilitators
Staff felt strongly that good relationships and communication were crucial factors in effective care and treatment planning, as was ensuring service user empowerment and involvement. The greatest challenges identified by participants related to a lack of staff collaboration on the ward and to poor continuity of care. Participants noted that unequal power relations in the structural organisation of the ward could be problematic, and that working in a collaborative or democratic way can could difficult as a result. Participants felt that shifting the culture on the ward away from older medical models of care had been challenging for both staff and service users.
Care plan reviews
Ten service users, eight female and two male, were selected for care plan reviews on the main ward in Burgundy. They ranged in age from 18 to 51 years. All service users were informal (i.e. they were voluntarily on the ward) at the time of the reviews and all but one had had previous admissions to hospital. Our review showed no evidence of care plans for four service users and no evidence of service users signing care plans that we could locate. There was no clear evidence that copies had been given to the service user. Only three care plans were signed by the named nurse. There was evidence that only three service users had attended their last ward rounds and that no carers, advocates or care co-ordinators had attended, suggesting potential problems in terms of continuity of care. For the 10 participants reviewed, there was evidence in only one care plan of the person being involved in the drafting of the plan, which had clearly been written by staff: ‘he would prefer to focus on paid roles and work’. This same care plan showed evidence of strengths-based and recovery approaches and, as well as one other, also showed that the service user’s views had been included in safety and risk assessments. There was no evidence that other participants’ views had been included in risk assessment or management. Most care plans showed an orientation to system-based goals only (e.g. medication compliance). Discharge planning was referred to in just one care plan.
Meeting observations
In Burgundy three observations of ward round meetings were completed. Eight people were present in all meetings, including the researcher, the primary nurse, a staff nurse, a note-taker, a student nurse and a student doctor. The meeting was held in a spacious room with four people seated around a long table in the centre of the room, and the atmosphere was relaxed and friendly. There was no prior preparation made (e.g. positioning of the chair) for where the service user would sit, which proved troublesome on one occasion when the service user chose a seat and was then asked to move. The relationships were fairly well established in all three of the observations, so no introductions were offered and the meeting commenced swiftly with questions directed by the psychiatrist. Eye contact and non-verbal communication was good and the atmosphere was quite friendly. In one of the meetings the psychiatrist’s attention appeared divided and he pursued conversation with the primary nurse about arranging a section 117 while trying to maintain cursory conversation with the service user (‘Everything OK?’). Questions were either framed around information that the psychiatrist possessed or based around areas of weakness or difficulties rather than strengths. In two of the meetings the person was referred to in the third person with little regard for their involvement in the conversation. At other times the service user was interrupted while speaking about topics they wanted to explore, which was likely to have left them feeling overlooked or with little understanding or resolution of their query. Disagreements or complaints were actively avoided, responded to with criticism or met defensively: ‘don’t blame me, we want to discharge you, but we’ve got to have the family agreement . . .’ In two meetings there was no mention of the care plan, and in another a service user asked if they could have a care plan on discharge but the topic of conversation was swiftly changed. The focus of the meetings was largely on practical arrangements (becoming more independent or procedures for discharge), with less attention given to the patient’s condition or feelings or to encouraging their progress. The meetings did not have formal endings; one service user marked the end of the meeting themselves, saying ‘is that all?’. An open invitation to ask questions was given in some instances but not others.
Champagne
History and context
Champagne LHB serves approximately 500,000 people living in two demographically divergent areas: one urban and fairly ethnically diverse (20% from BME groups), and the other rural and predominantly white British (96%). Twenty-seven per cent of the small areas measured in the urban part of the locale are among the most deprived 20% in Wales. 147 Adult acute mental health services are provided in two hospital sites, and there are 74 beds in total: this number includes five intensive care beds. The number of available bed-days in Champagne in 2014/15 was 21,545 and the bed occupancy rate was 119.3%, clearly illustrating the high demand for these services in the area.
Adult acute inpatient services: admissions data
The number of admissions to adult acute inpatient care at Champagne LHB in 2014/15 was 502, and there were 492 discharges. Sixty-two per cent of patients were discharged within 1 month and were seen for follow-up within 7 days of their discharge. The average length of stay for adult acute inpatients at Champagne in 2014/15 was 47.46 days. The main ward used for intensive data collection at this site is mixed gender and has 19 beds. Staff working on the ward consist of 11 qualified mental health nurses and 12 health-care support workers. There are typically five staff working in the morning and afternoon and four staff working at night; these would be a mix of registered mental health nurses and health-care support workers.
Participant characteristics: staff
Forty-one staff from three acute mental health inpatient wards within the locality completed the questionnaires. A large proportion of responses were from mental health nurses (76%) and the rest were from a range of professions. The majority of respondents had spent > 4 years working in mental health (63.5%); however, the majority of staff had spent < 4 years working on the ward (80%), with just over one-third working on the ward for < 1 year. A small proportion of staff (17%) disclosed that they had a personal history of mental health problems, whereas nearly half of participants had a family history of mental health problems. Further details of the demographic characteristics can be found in Table 16.
| Variable | n (%) |
|---|---|
| Gender | |
| Female | 26 (63.4) |
| Male | 15 (36.6) |
| Age (years) | |
| Median (range) | 33 (22–60) |
| Ethnicity | |
| White UK/Irish | 34 (82.9) |
| Indian | 3 (7.3) |
| Black African | 1 (2.4) |
| Mixed race | 1 (2.4) |
| Indo-Caribbean | 2 (4.9) |
| Profession | |
| Mental health nurse | 31 (75.6) |
| Occupational therapist | 4 (9.8) |
| Psychologist | 1 (2.4) |
| Psychiatrist | 1 (2.4) |
| Other | 4 (9.8) |
| Education | |
| Degree | 28 (68.3) |
| Diploma/similar | 5 (12.2) |
| Postgraduate diploma/certificate | 2 (4.9) |
| Master’s degree | 3 (7.3) |
| Doctorate | 1 (2.4) |
| Time working in mental health (years) | |
| ≥ 10 | 15 (36.6) |
| 7–9 | 7 (17.1) |
| 4–6 | 4 (9.8) |
| 1–3 | 10 (24.4) |
| < 1 | 5 (12.2) |
| Time working on the ward (years) | |
| ≥ 10 | 2 (4.9) |
| 7–9 | 3 (7.3) |
| 4–6 | 3 (7.3) |
| 1–3 | 19 (46.3) |
| < 1 | 14 (34.1) |
| Personal history of mental health problems | |
| Yes | 7 (17.1) |
| No | 33 (80.5) |
| Family history of mental health problems | |
| Yes | 20 (48.8) |
| No | 21 (51.2) |
Participant characteristics: service users
In total, 48 questionnaires were completed by service users in three wards in Champagne. The gender distribution of participants was almost equivalent, and the median age was 43 years. The responses were fairly diverse in terms of ethnicity, with the largest response from those identifying as white UK or Irish (60%). A large proportion of the respondents had a diagnosis of psychosis/schizophrenia/bipolar-type disorder (42%) and nearly 20% identified themselves with two or more diagnostic categories. Half of the participants had spent > 10 years in mental health services and half of the participants had been admitted to hospital between two and five times. Only 10% of the participants had been on the ward for 1 week and a large proportion of participants had been on the ward for > 4 weeks (60%). Almost two-thirds of participants (62%) were in contact with community mental health services. Further details of the demographic characteristics can be found in Table 17.
| Variable | n (%) |
|---|---|
| Gender | |
| Female | 21 (43.8) |
| Male | 26 (54.2) |
| Age (years) | |
| Median (range) | 43.5 (25–67) |
| Ethnicity | |
| Indian | 2 (4.2) |
| Mixed race | 4 (8.3) |
| Bangladeshi | 1 (2.1) |
| Black African | 1 (2.1) |
| Black Caribbean | 1 (2.1) |
| Black other | 1 (2.1) |
| White UK/Irish | 29 (60.4) |
| White other | 7 (14.6) |
| Mental health problem | |
| Psychosis/schizophrenia/bipolar-type disorders | 20 (41.7) |
| Depression/anxiety | 7 (14.6) |
| Substance user | 3 (6.3) |
| Other | 6 (12.5) |
| Two or more of above | 9 (18.7) |
| Relationship status | |
| Single | 33 (68.8) |
| In an established relationship | 11 (22.9) |
| Length of time with mental health services (years) | |
| ≥ 10 | 24 (50) |
| 7–9 | 2 (4.2) |
| 4–6 | 5 (10.4) |
| 1–3 | 5 (10.4) |
| < 1 | 10 (20.8) |
| Number of previous admissions | |
| First | 7 (14.6) |
| 2–5 | 24 (50) |
| 6–9 | 6 (12.5) |
| ≥ 10 | 10 (97.9) |
| Contact with community mental health services | |
| Yes | 30 (62.5) |
| No | 11 (22.9) |
| Time on the ward (weeks) | |
| 1 | 5 (10.4) |
| Up to 2 | 4 (8.3) |
| 2–4 | 8 (16.7) |
| > 4 | 29 (60.4) |
| Frequency of contact with family/carer/friends | |
| Daily | 16 (33.3) |
| Weekly | 17 (35.4) |
| Fortnightly | 3 (6.3) |
| Monthly | 2 (4.2) |
| Other | 9 (18.8) |
| Living status before admission | |
| Independent and single | 18 (37.5) |
| Independent in relationship | 5 (10.4) |
| Living with family | 10 (20.8) |
| Living with friends | 2 (4.2) |
| Living with others | 2 (4.2) |
| Supported housing | 3 (6.3) |
| Homeless/no fixed abode | 2 (4.2) |
| Other | 3 (6.3) |
| Previous daytime activity | |
| Full-time employment | 7 (14.6) |
| Part-time employment | 2 (4.2) |
| Education/training | 12 (25) |
| Unemployed | 9 (18.8) |
| Voluntary work | 7 (14.6) |
| Other | 9 (18.8) |
Summary scores for the questionnaires
Views on Inpatient Care Scale
A total VOICE score for each respondent was obtained by summing the scores of the individual items. The higher the total score (range 19–114), the more negative the perception of the quality of care on the ward. The score for respondents in Champagne is shown in Table 18.
| Scale | Service user score (n = 47)a | Reference valueb |
|---|---|---|
| VOICE total | 51.56 (16.64), range (20.00–103.00) | 55.5 (19.2) male; 52.5 (17.8) female |
The total scores for VOICE were marginally lower than the reference value provided by Evans et al. 52 The mean scores were in the lower half of the scale, suggesting that service users lean towards a more positive perception of the ward. There is, however, a large range of responses for this measure, demonstrating that some of the participants have a more negative perception of the ward.
Empowerment Scale
A total ES score for each service user respondent was obtained by summing the scores of individual items. The overall mean score for the sample was above the mid-point for the instrument. Out of a possible score of 4, indicating a higher perceived level of empowerment, the mean total score was 2.93 (SD 0.36). This is higher than the reference value. 146 The subscale values for ‘righteous anger’ and ‘power-powerless’ were equivalent. For all other subscales, the scores were higher than the reference group; in particular, the score for ‘self-esteem–self-efficacy’ was considerably higher than the reference value (Table 19).
| Subscales | COCAPP-A (acute inpatient) | COCAPP (community) | ||||
|---|---|---|---|---|---|---|
| n | Mean (SD)a | Referencea | n | Mean (SD)a | Referencea | |
| Self-esteem–self-efficacy | 46 | 3.22 (0.69) | – | 72 | 2.50 (0.73) | 2.82b |
| Power–powerlessness | 47 | 2.54 (0.55) | – | 72 | 2.44 (0.53) | 2.51b |
| Community activism and autonomy | 47 | 3.29 (0.46) | – | 71 | 3.05 (0.58) | 3.12b |
| Optimism and control over the future | 46 | 2.98 (0.66) | – | 72 | 2.51 (0.60) | 2.72b |
| Righteous anger | 46 | 2.31 (0.77) | – | 72 | 2.32 (0.60) | 2.34b |
| Total score | 47 | 2.93 (0.36) | – | 72 | 2.56 (0.38) | 2.74 (0.34)b |
A final comparison was made between the scores for empowerment across the two COCAPP studies (acute and community mental health services). The total score and subscales scores for the ES were higher in the COCAPP-A study than the COCAPP study. Only the ‘righteous anger’ and ‘power-powerless’ subscales were equivalent across services. Scores for ‘self-esteem–self-efficacy’ were considerably higher in acute inpatient care than in community mental health services. See Chapter 5 for some exploratory inferential analyses.
Scale to Assess the Therapeutic Relationship
For service users, the mean total score for the STAR-P was 31.35 (SD 10.15), 15.88 (SD 5.54) for ‘positive collaboration’, 7.85 (SD 3.05) for ‘positive clinician input’ and 7.62 (SD 3.14) for ‘non-supportive relationships’. These scores align well with the reference values provided by Nolan (personal communication) shown in Table 20. There are some marginal differences: service users in the current study scored the ‘positive collaboration’ subscale just over one point higher and the ‘non-supportive clinician input’ subscale just over 1 point lower than the reference value.
| Subscale | COCAPP-A (acute inpatient) | COCAPP (community) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| STAR-P (service user) | STAR-C (staff) | STAR-P (service user) | |||||||
| n | Mean (SD) | Reference | n | Mean (SD) | Reference | n | Mean (SD) | Reference | |
| Positive collaborationa | 46 | 15.88 (5.54) | 14.36 (5.99)b | 41 | 17.63 (2.70) | 17.95 (2.98)b | 69 | 17.13 (5.79) | 19.9 (6.7)c |
| Positive clinician inputd | 46 | 7.85 (3.12) | 7.10 (2.91)b | 41 | 10.34 (1.36) | 10.42 (1.23)b | 70 | 8.01 (3.05) | 9.3 (3.0)c |
| Non-supportive clinician inpute(service users)/emotional difficultiese (staff) | 45 | 7.62 (3.14) | 8.78 (2.21)b | 41 | 8.95 (1.76) | 9.61 (1.65)b | 70 | 9.09 (2.80) | 9.3 (3.3)c |
| Total scoref | 46 | 31.35 (10.15) | 30.23 (9.71)b | 41 | 37.00 (4.84) | 37.93 (4.92)b | 70 | 34.09 (10.13) | 38.4 (12.0)c |
For staff, the mean total for the STAR-C was 37.00 (SD 4.84), with scores of 17.63 (SD 2.70) for ‘positive collaboration’, 10.34 (SD 1.36) for ‘positive clinician input’ and 8.95 (SD 1.76) for ‘emotional difficulties’. All of the subscale values and the total score were marginally lower than the reference values.
When comparing the mean service user and staff scores, it is apparent that staff give higher scores and therefore rate the therapeutic relationship more positively than service users. Total STAR scores were just over 5 points higher for staff than for service users.
An independent samples t-test was completed to determine if there were significant differences between the perceptions of the therapeutic relationship from service users and staff. There was a significant difference in the total STAR scores for service users [31.35 (SD 10.15)] and staff [37.00 (SD 4.84)] [t(68.7) = –3.56, p = 0.001; 95% CI –8.82 to –2.49; Cohen’s d = 0.71]. For the positive clinician input subscale, the scores for service users were lower [7.85 (SD 3.12)] than the scores for staff [10.34 (SD 1.36)] [t (62.9) = –5.06; p < 0.001, 95% CI –3.58 to –1.55; Cohen’s d = 1.03]. T-test parameters for the remaining subscale are provided in Chapter 5, Table 52.
A final comparison was made of the scores for the therapeutic relationships between the two COCAPP studies (acute and community mental health services). It is clear from the scores in Table 20 that service users in community mental health services scored the therapeutic relationship higher than did service users in acute mental health services.
Recovery Self-Assessment
The mean scores and SDs for the RSA are provided in Table 21. The mean scores from service users and staff on the subscales fell in the middle to moderate (3.01 and 3.35, and 2.85 and 3.46, respectively). The difference in mean total RSA scores was almost equivalent. The lowest scoring subscale was diversity of treatment options for both participant groups. Within this subscale the score demonstrates neither a positive nor a negative response. The highest scoring subscale in both groups was life goals.
| Subscales | COCAPP-A (acute inpatient) | COCAPP (community) | ||||||
|---|---|---|---|---|---|---|---|---|
| Service users | Staff | Service users | Staff | |||||
| n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | |
| Life goals | 47 | 3.35 (0.97) | 41 | 3.52 (0.52) | 63 | 3.38 (0.97) | 31 | 3.79 (0.52) |
| Involvement | 44 | 3.11 (1.04) | 38 | 2.85 (0.62) | 56 | 2.70 (1.11) | 31 | 2.92 (0.73) |
| Diversity of treatment options | 46 | 3.01 (0.89) | 41 | 3.06 (0.65) | 65 | 3.05 (1.12) | 31 | 2.94 (0.70) |
| Choice | 48 | 3.25 (0.94) | 40 | 3.46 (0.47) | 70 | 3.66 (0.83) | 31 | 3.70 (0.62) |
| Individually tailored services | 40 | 3.22 (1.10) | 40 | 2.92 (0.49) | 60 | 2.99 (1.06) | 31 | 3.11 (0.75) |
| Total score | 46 | 3.24 (0.84) | 41 | 3.21 (0.46) | 63 | 3.13 (0.87) | 31 | 3.35 (0.56) |
Independent samples t-test were conducted to compare the perceptions of recovery-oriented services for staff and service users. There were no significant differences in the total RSA scores for service users [mean 3.24 (SD 0.84)] and staff [mean 3.21 (SD 0.46)] [t(70.8) = 0.212; p = 0.833; 95% CI –0.26 to 0.32; Cohen’s d = 0.04] or the subscale scores (t-test statistics for subscales are provided in Chapter 5, Table 52).
A final comparison was made of the scores for the perceptions of recovery-oriented care between the two COCAPP studies (acute and community mental health services). The RSA total score for service users in acute mental health services in Champagne is slightly higher than that in community mental health services. Conversely, staff in acute mental health services gave a lower overall RSA total score than did those in community mental health services in Champagne.
There are also some differences at the subscale level. In acute services, service user respondents scored the ‘involvement’ and ‘individually tailored services’ subscale higher than respondents in the community study. Conversely, service users in acute inpatient wards scored the ‘choice’ subscale lower than did those in community mental health services.
There are also some differences at the subscale level for staff. In our acute study, staff scored inpatient services lower on the ‘life goals’, ‘choice’ and individually tailored services’ subscales than did respondents in the community study. To a lesser extent, staff also scored ‘involvement’ lower than in the acute study. Conversely, staff in the acute study scored ‘diversity of treatment options’ higher than did staff in the community study. See Chapter 5 for some exploratory inferential analyses.
A recovery profile from the RSA scale is included in Appendix 5.
Narrative summary of interview data: service users, carers and staff
In Champagne, four staff and six service users on the ward participated in interviews; no carer participants were recruited.
Care planning and co-ordination
Most staff offered detailed definitions of care planning and co-ordination. It was felt that the primary objective of the CTP process is to provide ‘appropriate’ care to service users, from diagnosis and medication to consideration of service users’ lifestyle factors, their personal histories and family circumstances.
Despite the significance attributed to care planning by staff, only one of the service users interviewed was aware of their care being planned: others said that they had received little or no information, or had been obliged to ask for this, and felt that their views had not been listened to in meetings. Only one participant felt that their care was being planned in a helpful way: another talked of being ‘contained’, rather than actually receiving treatment.
There isn’t a treatment plan. There’s no treatment, there’s just containment. Walking to the shop to get a newspaper isn’t treatment. There’s no therapy here.
C-SU-103
The value of longer-term planning was mentioned by one staff participant, especially the need to make early contact with care co-ordinators in the community; individual care plans were considered to be helpful in this respect. Lack of staff resources resulting in insufficient time available to spend with service users was understood to be a hindrance to the CTP process. Concerns about the shift to electronic records featured strongly in staff interview narratives: it was suggested that this has changed the content (as well as the form) of what is written in the care plan documents and has created a barrier in terms of service user involvement:
I think it tends to maybe forget that the patient needs to be involved, whereas when we were writing them you would pick up that patient’s file, get the patient and go somewhere with them, more of a physical thing, chat with them and talk to them.
C-ST-101
One staff participant thought that care planning applications (apps) would be helpful in terms of communicating with service users, for example by providing prompts for forthcoming meetings. Nevertheless, care plans were considered to be helpful because they offered continuity and coherence.
Although staff emphasised that service users should be involved with every aspect of planning their care, concerns were voiced about the impact of unequal power relations on the communicative dynamics of (e.g. ward round meetings), especially when enforced medication is involved. These struggles were also reflected in service users’ responses: only one felt adequately involved in their care, while others talked of not being sufficiently involved or not being involved at all. One service user participant described participating in rushed care planning meetings, while another provided a detailed account of poor communication between staff and outside services, such that visits from professionals not working on the ward were not effectively co-ordinated.
Staff felt that discharge was a primary objective from the time of admission. Discharge planning – carried out during ward rounds – was described as a process that facilitates multidisciplinary participation from ward staff and community support service representatives, involving consideration of service users’ social support needs, including housing.
Service users, however, reported varying degrees of involvement in, and information sharing on, discharge planning. Some described having been party to no discussions at all, and others had a keen awareness of the challenges and complexities inherent in their discharge procedures, accommodation difficulties or homelessness.
The routes of admission of hospital recounted by service user participants indicate degrees of crisis and significant distress followed by, for some, lengthy admissions (11.5 months in one case). One service user talked of attempting suicide, another of being assaulted, two of being sectioned and one of being made homeless.
The ward environment was strongly criticised by one participant, who described the ward as dirty and smelly, and felt that the care she had received was limited to brief interactions with staff centring on medication. Another was critical of the primacy given to medication, and a third refuted the legitimacy of their admission describing their difficulties as physical rather than mental.
One staff participant felt that care planning tended to miss out areas of individual importance in people’s lives, particularly matters of spirituality and sexuality, and another drew a distinction between what was written about care planning in policies and the difficulties of mobilising this in practice. Staff at this site emphasised the usefulness for continuity of having community staff attending discharge meetings.
Care reviews
Staff indicated that weekly review meetings take place with informal reviews on a daily basis during shift handovers. It was noted that review meetings incorporated multiple staff members, and that involvement of service users’ family members and friends was actively encouraged. Concerns were raised about the inadequate time available for reviews and that time-consuming care plan administration detracted from the time spent with service users. It was suggested that service user involvement in reviews could be helped by encouraging staff to make advance arrangements to meet with patients during quieter times on the ward. Staff understood review meetings to serve as an opportunity to evaluate the effectiveness of care planning and to monitor and assess risk.
Service user participants, however, provided negative accounts of their review meetings, describing these as being full of jargon and typically leading to an increase in medication. One service user reported finding it difficult to say everything that they wanted to say during ward round meetings, because of the lack of time available, and emphasised that writing things down in preparation would be useful. Another complained that ward rounds were full of people who ‘don’t really need to be in there, they’re just there to gawk’ (C-SU-103). Service users felt that ward round meetings were repetitive, and one participant was uncertain if she was being listened to.
Support systems
Staff held various ideas about the most important aspects of their roles, including observing and ‘reporting back’ (C-ST-102) about service users’ progress, spending quality time with them, and focusing on their physical as well as mental health needs. Lack of time was once again cited as a hindrance in this respect. Staff provided varied accounts of the training that they had received, ranging from structured, compulsory sessions to informal options and supervision.
One staff participant noted that better collaboration with (and greater support from) other agencies would be helpful, especially in terms of securing housing arrangements for patients after discharge. Staff maintained that family and friend involvement is was as much as possible. One described how, in meetings or discussions, family members or friends are encouraged to express their preferences, and another that this is particularly important in relation to planning leave. It was acknowledged that overinvolvement of family/carers can, however, cause problems, especially in terms of discharge decisions. Effective communication with families/carers was recognised as a means of resolving such difficulties.
Service user participants reported varying experiences of and views about the support they received. Two stated that they did not have a named or primary nurse, and one claimed that ‘you’re pretty much left to your own devices’ (C-SU-105). Another described the relationship with their named nurse as good, but maintained that this was challenged by shift patterns on the ward. One service user noted that their care on the ward had been characterised by poor communication, and that having a solicitor had proved helpful in overcoming this.
Most service users praised the attitude of staff on the ward, believing that staff were compassionate and treated service users with respect and dignity. In contrast, one service user complained that staff continually confused her with a fellow patient, and was very critical of the care that she had received. One reported their discomfort at regularly having to approach and ask staff for their time:
I don’t like to drag people away from their work . . . They don’t mind but you just feel a little bit intrusive, you know what I mean?
C-SU-105
Service users had varying levels and kinds of contact with wider support networks. Two said that they had received occasional help from social workers, and one explained that the relationship with her community psychiatric nurse (CPN) had broken down. Another indicated that although she was aware of the support available from other workers, this process was never discussed with or explained to her.
Safety and risk
Staff emphasised the importance of assessing risk on a continual basis, noting that this was a priority on the ward, to ensure the safety of service users themselves and those around them, during and beyond their hospital stay. Risk assessment was conceptualised as a central part of the care planning process.
Few differences were perceived in care planning between formal and informal admissions, except that the legal aspects were more pertinent when someone had been detained. It was noted that concerns about formal admissions typically arose in relation to requests for leave, child protection and family/home environments. The need for accurate maintenance of medication documentation for audit purposes was also emphasised. One staff member suggested that it might be easier to administer medication to detained service users, while another agreed that enforced treatment necessarily limits service users’ freedom of choice for a time. Another participant felt that greater risks are involved when service users are detained because they are more likely to display aggressive behaviour and less likely to have capacity, noting that this may have a significant impact on how their initial care is planned and coordinated. Only one participant mentioned the value of positive risk-taking.
Most service users believed that their safety had been considered, and said that they felt safe on the ward and that staff handled any disruption or aggressive behaviour competently. One participant, however, described a lack of support for keeping herself safe:
. . . I self-harm and I’ve told them a few times that there’s things that I could use and they’ve said well they have to stay there so the temptation is [still] there.
C-SU-103
Few service users had been involved in any discussions around risk and safety, other than in terms of information about banned items on the ward (e.g. lighters, sharp objects and energy drinks).
Of those service users who had been formally admitted, only one felt that the process had been adequately explained to them. Others described distressing sectioning experiences, devoid of any explanation or helpful information, which they felt to be intrusive and harsh:
. . . nobody talked to me at all about what was going on . . . [it was] terrible . . . Horrible, just horrible because you’ve done nothing wrong.
C-SU-106
Organisational context
Several developments in inpatient care were observed by staff, including an increased focus on involving families and carers, and the implementation of the Measure’s option to allow service users to self-refer. Cutbacks in services and funding were understood to have hindered the effectiveness of care planning and co-ordination, although the Measure was generally felt to have had a positive impact in terms of clarifying expectations and legislative requirements.
Staff provided various accounts that related to the health board’s principles and values. For the most part, these were general conceptualisations, rather than references to specific policies, although it was acknowledged that guidelines do exist.
Recovery
Doubt was cast on the relevance or usefulness of the term ‘recovery’ for some individuals, depending on the nature of their condition. Access to services was acknowledged to be important, and sending people home well was felt to be a primary goal. Another staff participant recognised the ubiquity of the term ‘recovery’, believing that it invoked and represented the shift from asylum-based/medical models of care to newer and more collaborative ones that encourage patient and family involvement. Recovery-oriented practice was seen to have increased the emphasis on leave and discharge, and connections were drawn between recovery and leaving hospital as quickly as possible.
Some staff mentioned the use of recovery tools, although wellness recovery action plans (WRAPs) were not used. Staff noted that although the Recovery Star was used in rehabilitation services at Champagne, it was not used on this ward. Staff maintained that service users’ skills and strengths were recognised and considered. The importance of involving the wider support team (including OTs) was also mentioned.
Service users defined recovery in a variety of ways, and understood this to be a complex and challenging process that necessarily encompassed many different factors. The detrimental impact of mental illness on personal confidence was noted. One participant associated recovery solely with his physical ill health, and another seemed to question the possibility of recovery, given the nature of her illness. Recovery was also associated with improved communicative abilities and self-awareness.
Service users gave mixed views about the ways in which their hospital stay had had an impact on their recovery. Some reported having received practical support, aimed at encouraging service user independence and empowerment. One participant, however, described the ward environment as detrimental to the recovery process: ‘you can’t recover by being locked up in a derelict place . . . filthy everywhere, the patients smell’ (C-SU-102).
None of the participants interviewed indicated that they had been involved in any helpful discussions with staff about their recovery. One service user said that although no one had talked to him about recovery during his time as an inpatient, strategies had been put in place for continuing his medication following discharge, with which he was satisfied. None of the service user participants had recovery plans.
Personalisation
Most staff participants were unfamiliar with the term ‘personalisation’, but all had an awareness of the concept and its association with person-centred care. Only one provided a detailed definition, and did so in positive terms, contrasting current practices with previous ones. Direct connections were also drawn between personalisation and recovery, although it was acknowledged that the term was not used in discussions about care planning.
Most of the service users interviewed were not familiar with the term either, and were unsure about what it might mean, although one participant did associate the term with person-centred/individually tailored care.
Most staff felt that care planning was personalised to a degree; this was linked to the format and structure of written care plan documents, and staff also acknowledged that the successful delivery of a personalised approach depended greatly on the available resources. One member of staff emphasised the extent to which these concerns were related to ethnicity, culture and dignity in terms of behaviours on the ward.
Service users were ambivalent about the personalisation of care planning, although one was very positive about their experiences: ‘without this place it would be the end of me’ (C-SU-105). It was noted that there is, generally, scope for personalisation, although one participant voiced contrasting views and reported that his care had not been personalised or individually tailored in any way at all.
Barriers and facilitators
Factors to help ensure personalised/recovery-focused care included focusing on and regularly reviewing individual needs. Two participants spoke of a lack of resources – especially a lack of nursing staff – and the restrictions that this placed on the time available to spend with service users. Effective communication was seen by staff as important, and an empathic attitude and manner was considered helpful: ‘[to] . . . bear in mind what would you be like in that situation’ (C-ST-102). Integrated care and family involvement were also seen as facilitators.
In terms of barriers, one participant emphasised the problems of delayed discharge caused by the lack of suitable accommodation. The challenge of administering medication for some service users was also seen as a hindrance. It was suggested that delayed discharge is linked to a reduction in the quality of care given to service users. Staff had various suggestions on general improvements to care planning, including investment in service delivery through the provision of more staff. It was noted that, currently, care plans are not comprehensively discussed in ward rounds, and staff felt that this would improve things, especially in relation to risk assessments.
Services users also saw better communication as a means of improving care planning, and some participants felt that an increase in structured ward activities could usefully be made:
. . . have a look around this room, there’s nothing in here, and there’s bits of rubbish everywhere, and it’s like there’s nothing to do.
C-ST-103
Lack of resources was also acknowledged to be having a direct impact on service users; one participant noted that activity/art rooms can only be used as long as there is sufficient staff presence on the ward, which is rarely the case, meaning that activity timetables are rendered redundant.
Care plan reviews
Four participants, three female and one male, were selected for care plans on the main ward in Champagne. They ranged in age from 35 to 49 years. All participants had previous admissions and, although the information provided was unclear, it was determined that one participant had been detained formally. Our review was unable to locate the care plan for one service user. There was no evidence that the remaining care plans had been signed by the service user or that the service user had been given a copy. There was no evidence that the named nurse had signed the care plan. Only one service user had attended the last ward round and no carers attended. The care co-ordinator had attended in only one case and again this suggests potential issues with continuity of care. The care plans had clearly been written by staff and although they demonstrated inclusion of the service users’ views (e.g. ‘patient is happy at present with her current treatment plan although was unsure as to the reason she is prescribed her depot’), there was no clear evidence of coproduction. No care plans demonstrated a strengths-based approach or a focus on personalisation. Two care plans showed some emphasis on person-centred recovery-focused goals, for example supporting a service user to attend church and maintain social activities. Care plans tended to emphasise system-based goals such as medication monitoring and compliance. There was no evidence in the care plans of service user involvement in assessments of safety and risk or in the risk management plans. Discharge planning was evident in care plans, although this seemed somewhat limited (e.g. ‘Integration of the appropriate health and social care services that can support patient to move to [local area] whilst meeting her mental health needs’).
Meeting observations
In Champagne, one observation of a ward round meeting was completed. Eight people were present at the meeting: the researcher, a psychiatrist, the named nurse, two student observers, a note-taker, a doctor and the service user. The meeting was held in an extremely small room. The service user was collected from the ward by the psychiatrist and greeted warmly with a smile and led into the room. Initially, the service user appeared anxious but was reassured by the psychiatrist, with gentle humour, ‘you’re not on trial here, OK?’. The review started with an open enquiry to the service user as to how the week had been. The rest of the meeting focused on exploring the service user’s progress to assess if they were ready for discharge. Focus was placed on self-awareness of relapse indicators and in exploring understanding of potential future problems. There was no evidence of the use of summarising or clarification of what the service user said but sensitive and empathic responses were provided. Emphasis was placed on behavioural patterns and practical strategies rather than feelings and emotions. The service user was knowledgeable about his medication and provided suggestions for changes, which were accepted and adjusted. The psychiatrist and the service user appeared very familiar and comfortable with one another with a well established relationship. This was exemplified by the psychiatrist’s effective use of non-verbal and verbal communication to engage with the service user, who appeared to understand what was being discussed. There was no mention of the care plan in the discussions. Risk and safety were not explicitly mentioned; however, conversations relating to responsibility in decisions around health, in particular the use of substances, were discussed and revisited, with several points reiterated (‘what do you feel is in your control?’). The service user’s relationship with his family was explored, with emphasis placed on concerns about the family’s distress during the last home visit. The service user was asked about updates on his accommodation status, and, interestingly, staff appeared unaware of the progress with this. Discharge was discussed and a date was agreed, and the service user was given the option to invite his parents to the next meeting.
Dauphine
History and context
The trust provides mental health and community services to a population of approximately 750,000 people. It covers an extremely densely populated urban area that is very multicultural. Figures from the 2011 census showed that this site’s catchment area had one of the most ethnically diverse communities in the UK. For example, one area had 45% Asian (Indian, Bangladeshi, Pakistani, Chinese and other Asian), 27% white British/other and 19% black African/Caribbean people, with the remaining 9% split between mixed, Arab and other backgrounds. According to the 2010 English indices of deprivation,148 a high percentage of the areas covered by this site are among the top 10% of the country’s most deprived. Inpatient mental health services are provided from three hospital sites with 251 acute inpatient beds, and community services from 10 CMHTs. There are 17 adult acute mental health wards within the trust. The average occupancy of beds on the wards in 2015 was 84.8%.
Adult acute inpatient services: admissions data
There were 1087 admissions to these wards using the MHA in 2015. The average length of stay for service users discharged from adult acute wards in 2015 was 35 days. The main ward for intensive data collection at this site was mixed and had 19 beds.
Participant characteristics: staff
Fifty-three staff from three acute mental health inpatient wards within the locality completed the questionnaires. Just over one-third of the responses were from mental health nurses; there was a good representation from psychiatrists and employment workers and practitioners who defined themselves as ‘other’. Nearly one-third of staff had spent > 4 years working in mental health; however, the majority had spent < 4 years working on the ward (86.8%). A small proportion of participants disclosed that they had a personal history of mental health problems; however, nearly one-third of participants had a family history of mental health problems. Further details of the demographic characteristics can be found in Table 22.
| Variable | n (%) |
|---|---|
| Gender | |
| Female | 26 (49.1) |
| Male | 24 (45.3) |
| Age (years) | |
| Median (range) | 28 (20–52) |
| Ethnicity | |
| White UK/Irish | 23 (43.4) |
| White other | 1 (1.9) |
| Indian | 3 (5.7) |
| Pakistani | 1 (1.9) |
| Bangladeshi | 6 (11.3) |
| Asian other | 2 (3.8) |
| Chinese | 1 (1.9) |
| Black African | 7 (13.2) |
| Black Caribbean | 4 (7.5) |
| Black other | 1 (1.9) |
| Mixed race | 1 (1.9) |
| Indo-Caribbean | 1 (1.9) |
| Profession | |
| Mental health nurse | 19 (35.8) |
| Social worker | 1 (1.9) |
| Occupational therapist | 1 (1.9) |
| Psychologist | 3 (5.7) |
| Psychiatrist | 9 (17) |
| Employment/recovery worker | 6 (11.3) |
| Other | 13 (24.5) |
| Education | |
| Degree | 17 (32.1) |
| Diploma/similar | 6 (11.3) |
| Postgraduate diploma/certificate | 14 (26.4) |
| Master’s degree | 7 (13.2) |
| Doctorate | 4 (7.5) |
| Time working in mental health (years) | |
| ≥ 10 | 14 (26.4) |
| 7–9 | 4 (7.5) |
| 4–6 | 7 (13.2) |
| 1–3 | 18 (34) |
| < 1 | 10 (18.9) |
| Personal history of mental health problems | |
| Yes | 9 (17) |
| No | 43 (81.1) |
| Family history of mental health problems | |
| Yes | 17 (32.1) |
| No | 35 (66) |
Participant characteristics: service users
In total, 54 questionnaires were completed by service users on three wards in Dauphine. There were slightly more male participants (57%) than female, and the median age was 38 years. There were responses from diverse ethnicities, with a large proportion from Bangladeshi (24%) or white UK/Irish participants (30%). Nearly half of the respondents (46%) had a diagnosis of psychosis/schizophrenia/bipolar-type disorder. Just over one-third of the participants had spent > 10 years in mental health services and just under 50% participants had been admitted to hospital between two and five times. Nearly half of the participants had been on the ward for 1 week and one-quarter had been on the ward for > 4 weeks. Almost half of participants (44%) were in contact with community mental health services. Further details of the demographic characteristics can be found in Table 23.
| Variable | n (%) |
|---|---|
| Gender | |
| Female | 22 (40.7) |
| Male | 31 (57.4) |
| Age (years) | |
| Median (range) | 38 (18–58) |
| Ethnicity | |
| Pakistani | 1 (1.9) |
| Bangladeshi | 13 (24.1) |
| Asian other | 1 (1.9) |
| Black African | 4 (7.4) |
| Black Caribbean | 6 (11.1) |
| Mixed race | 7 (13) |
| White UK/Irish | 16 (29.6) |
| White other European | 3 (5.6) |
| White other | 2 (3.7) |
| Turkish | 1 (1.9) |
| Mental health problem | |
| Psychosis/schizophrenia/bipolar-type disorders | 25 (46.3) |
| Depression/anxiety | 7 (13) |
| Substance user | 1 (1.9) |
| Other | 7 (13) |
| Two or more of above | 8 (14.9) |
| Relationship status | |
| Single | 41 (75.9) |
| In an established relationship | 11 (20.4) |
| Length of time with mental health services (years) | |
| ≥ 10 | 19 (35.2) |
| 7–9 | 4 (7.4) |
| 4–6 | 7 (13) |
| 1–3 | 11 (20.4) |
| < 1 | 12 (22.2) |
| Number of previous admissions | |
| First | 11 (20.4) |
| 2–5 | 28 (51.9) |
| 6–9 | 7 (13) |
| ≥ 10 | 8 (14.8) |
| Contact with community mental health services | |
| Yes | 24 (44.4) |
| No | 16 (29.4) |
| Time on the ward (weeks) | |
| 1 | 26 (48.1) |
| Up to 2 | 5 (9.3) |
| 2–4 | 9 (16.7) |
| > 4 | 13 (24.1) |
| Frequency of contact with family/carer/friends | |
| Daily | 20 (37) |
| Weekly | 15 (27.8) |
| Fortnightly | 7 (13) |
| Monthly | 4 (7.4) |
| Other | 8 (14.8) |
| Living status before admission | |
| Independent and single | 17 (31.5) |
| Independent in relationship | 3 (5.6) |
| Living with family | 14 (25.9) |
| Living with friends | 4 (7.4) |
| Living with others | 2 (3.7) |
| Supported housing | 6 (11.1) |
| Homeless/no fixed abode | 6 (14.8) |
| Other | |
| Previous daytime activity | |
| Full-time employment | 7 (13) |
| Part-time employment | 3 (5.6) |
| Sheltered employment | 4 (7.4) |
| Education/training | 35 (64.8) |
| Unemployed | 2 (3.7) |
| Voluntary work | 2 (3.7) |
| Two or more of above | 1 (1.9) |
Summary scores for the questionnaires
Views on Inpatient Care Scale
A total VOICE score for each respondent was obtained by summing the scores of the individual items. The higher the total score (range 19–114), the more negative the perception of the quality of care on the ward. The score for respondents in Dauphine is shown in Table 24.
| Scale | Service user score (n = 54)a | Reference valueb |
|---|---|---|
| VOICE total | 48.77 (18.60); range (20.00–96.00) | 55.5 (19.2) male; 52.5 (17.8) female |
The total scores for VOICE were marginally lower than the reference value provided by Evans et al. 52 The mean scores were in the lower half of the scale, suggesting that service users lean towards a more positive perception of the ward. There is, however, a moderate range of responses for this measure, demonstrating that some of the participants have a more negative perception of the ward.
Empowerment Scale
A total ES score for each service user respondent was obtained by summing the scores of individual items. The overall mean score for the sample was above the mid-point for the instrument. Out of a possible score of 4, indicating a higher perceived level of empowerment, the mean total score was 2.80 (SD 0.38), which is slightly higher than the reference value. 146 The subscale values were also slightly higher than the reference group, apart from righteous anger, which was comparable, and power–powerlessness, which was lower (Table 25).
| Subscales | COCAPP-A (acute inpatient) | COCAPP (community) | ||||
|---|---|---|---|---|---|---|
| n | Mean (SD)a | Referencea | n | Mean (SD)a | Referencea | |
| Self-esteem–self-efficacy | 53 | 2.99 (0.75) | – | 55 | 2.63 (0.72) | 2.82b |
| Power–powerlessness | 53 | 2.32 (0.61) | – | 54 | 2.43 (0.56) | 2.51b |
| Community activism and autonomy | 53 | 3.25 (0.48) | – | 55 | 3.12 (0.58) | 3.12b |
| Optimism and control over the future | 53 | 2.98 (0.67) | – | 57 | 2.70 (0.70) | 2.72b |
| Righteous anger | 53 | 2.34 (0.61) | – | 56 | 2.31 (0.71) | 2.34b |
| Total score | 53 | 2.80 (0.38) | – | 56 | 2.64 (0.40) | 2.74 (0.34)b |
A further comparison was made of the scores for empowerment between the two COCAPP studies (acute and community mental health services). The total score and subscales for the ES were higher for the responses obtained from service users in acute inpatient services than for the responses from those in contact with community mental health services, apart from power–powerlessness, which was lower. See Chapter 5 for some exploratory inferential analyses.
Scale to Assess the Therapeutic Relationship
For service users the mean total score for the STAR-P was 29.17 (SD 10.00), with scores of 14.98 (SD 6.99) for ‘positive collaboration’, 7.16 (SD 3.15) for ‘positive clinician input’, and 7.04 (SD 3.29) for ‘non-supportive relationships’. These scores align well with the reference values provided by Nolan (personal communication) shown below in Table 26, apart from the non-supportive clinician input subscale, for which the service user scores were just over 1.5 points lower than the reference value.
| Subscale | COCAPP-A (acute inpatient) | COCAPP (community) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| STAR-P (service user) | STAR-C (staff) | STAR-P (service user) | |||||||
| n | Mean (SD) | Reference | n | Mean (SD) | Reference | n | Mean (SD) | Reference | |
| Positive collaborationa | 52 | 14.98 (6.99) | 14.36 (5.99)b | 51 | 18.20 (2.35) | 17.95 (2.98)b | 58 | 17.29 (6.03) | 19.9 (6.7)c |
| Positive clinician inputd | 52 | 7.16 (3.15) | 7.10 (2.91)b | 49 | 10.38 (1.07) | 10.42 (1.23)b | 58 | 8.22 (2.79) | 9.3 (3.0)c |
| Non-supportive clinician inpute (service users)/emotional difficultiese (staff) | 52 | 7.04 (3.29) | 8.78 (2.21)b | 50 | 8.86 (1.65) | 9.61 (1.65)b | 58 | 8.02 (3.45) | 9.3 (3.3)c |
| Total scoref | 52 | 29.17 (10.00) | 30.23 (9.71)b | 51 | 37.45 (3.73) | 37.93 (4.92)b | 58 | 33.53 (9.23) | 38.4 (12.0)c |
For staff the mean total for the STAR-C was 37.45 (SD 3.73), with scores of 18.20 (SD 2.35) for ‘positive collaboration’, 10.38 (SD 1.07) for ‘positive clinician input’ and 8.86 (SD 1.65) for ‘emotional difficulties’. The subscale values and total scores were aligned well with the reference values, with negligible differences.
When comparing the mean service user and staff scores, it is apparent that staff give higher scores and therefore rated the therapeutic relationship more positively than service users. The total STAR scores are on average eight points higher for staff than for service users.
An independent samples t-test was completed to determine if there were significant differences in the perceptions of the therapeutic relationship between service users and staff. There was a significant difference in the total STAR scores for service users [29.17 (SD 10.00)] and staff [37.45 (SD 3.73)] [t(65.1) = –5.58; p < 0.001; 95% CI –11.23 to –5.32; Cohen’s d = 1.10] and the subscales. T-test statistics for the subscales are provided in Chapter 5, Table 52.
A final comparison was made of the scores for the therapeutic relationships between the two COCAPP studies (acute and community mental health services). It is clear from the scores in Table 26 that service users score this approximately four points higher in the total STAR-P score for community mental health services than for acute mental health services.
Recovery Self-Assessment
The mean scores and SDs for the RSA are provided in Table 27. The mean scores from service users and staff on the subscales fell in the moderate to high range (3.11–3.49 and 3.47–3.93). The mean total RSA scores for staff were higher [3.74 (SD 0.53)] than those for service users [3.30 (SD 0.89)]. The lowest scoring subscale for both participant groups was involvement. The life goals subscale was the highest scoring subscale for both groups.
| Subscale | COCAPP-A (acute inpatient), mean (SD) | COCAPP (community), mean (SD) | ||||||
|---|---|---|---|---|---|---|---|---|
| Service users | Staff | Service users | Staff | |||||
| n | Mean (SD)a | n | Mean (SD)a | n | Mean (SD)a | n | Mean (SD)a | |
| Life goals | 53 | 3.49 (1.01) | 50 | 3.93 (0.53) | 53 | 3.46 (1.00) | 33 | 3.54 (0.83) |
| Involvement | 53 | 3.11 (1.00) | 51 | 3.47 (0.68) | 46 | 2.93 (1.09) | 33 | 2.99 (0.84) |
| Diversity of treatment options | 51 | 3.29 (0.89) | 51 | 3.72 (0.69) | 53 | 3.21 (1.12) | 33 | 2.98 (0.91) |
| Choice | 52 | 3.23 (0.99) | 51 | 3.73 (0.63) | 55 | 3.69 (0.98) | 33 | 3.46 (0.68) |
| Individually tailored services | 49 | 3.19 (1.14) | 52 | 3.81 (0.66) | 52 | 3.21 (1.07) | 33 | 3.49 (0.86) |
| Total score | 53 | 3.30 (0.89) | 51 | 3.74 (0.53) | 52 | 3.31 (0.96) | 33 | 3.31 (0.75) |
Independent samples t-tests were conducted to compare the perceptions of recovery-oriented services for staff and service users. There were significant differences in the total RSA scores for service users [3.30 (SD 0.89)] and staff [3.74 (SD 0.53)] [t(85.5) = –3.05; p = 0.003; 95% CI –0.72 to –0.15; Cohen’s d = 0.60]. There were also significant differences in two of the subscale scores, ‘choice’ and ‘individually tailored treatment’ [the rest of the t-test statistics for subscales are provided in Chapter 5 (see Table 52)].
A final comparison was made of the scores for the perceptions of recovery-oriented care between the two COCAPP studies (acute and community mental health services). The RSA total score given by service users in acute mental health services in Dauphine is equivalent to that given by service users in our community study. Conversely, staff in the acute study score the overall RSA total higher than respondents in the community study.
There are also some differences at the subscale level, with service users in acute services scoring the ‘involvement’ and ‘individually tailored services’ higher than did service user respondents in the community study. Conversely, service users in the acute study scored the ‘choice’ subscale lower than those in the community study but scored the ‘life goals’ and ‘diversity of treatment options’ subscale comparably.
There are also some differences at the subscale level for staff. In our acute study, the staff members scored all of the subscales higher than did respondents in the community study. See Chapter 5 for some exploratory inferential analyses.
A recovery profile from the RSA Scale is included in Appendix 5.
Narrative summary of interview data: service users, carers and staff
In Dauphine we conducted interviews with six service users, two carers and six staff. The staff interviewed were from varied disciplines and comprised a modern matron, an OT, a psychiatrist, a mental health nurse, a psychologist and a social therapist.
Care planning and co-ordination
Staff spoke of the CPA being a ‘framework’ in which people’s care and needs can be planned, as well as of care plans needing to be holistic and focused on service users’ individual needs and to be informed by knowledge of the person’s background and history. It also required good collaboration within the MDT.
I guess it’s about . . . co-ordinating all the different aspects of their care . . . I’m not saying it always does, but I think it should include things like housing and financial support and family support and psychology support and support from psychiatry and medication if that’s what’s useful.
D-ST-102
Some recognised the care plan as part of a wider dynamic and active approach, and that the written document was only one small aspect, designed to ‘make sure all those things happen’ (D-ST-102). It was important to acknowledge that service user and staff perspectives and interpretations may be very different, and to document these. The care plan must be meaningful to the person and must be regularly updated.
Several staff mentioned that they felt under pressure to reach targets (e.g. owing to cuts), and this did not always allow time for individualised care:
The [NHS] culture is becoming target driven . . . and I think sometimes the CPA just becomes one of the targets.
D-ST-106
Three service users were not aware of their care being planned. One said that they would like the care plan to include physical care. Another said that it was important to have a plan that incorporated continuity of care after discharge:
I have no one out there . . . if there is no network then I’ll fall straight away, which is exactly what happened . . . I think it’s really important to have a care plan.
D-SU-105
One service user who was aware of his care plan said that, based on 15 years of experience using services, it was largely a matter of ‘common sense’ (D-SU-104).
Two carers interviewed were both aware that the care of service users was being planned and co-ordinated. Both also felt that their relatives were well supported and that they had received clear information about their care.
The trust had made attempts to simplify and reduce the complexity of care plans, but many staff still struggled with the logistics of completing various forms and uploading them onto the electronic system. The trust had also introduced the ‘This Is Me’ care plan, which was more personal to the service user; it was described as a ‘golden opportunity . . . to find out what the person is about’ (D-ST-104). Staff described care planning as useful to a degree but that they needed to get the service user to ‘talk about themselves and what they hope for the future’ (D-ST-102) and to obtain a holistic view; the care plan became useless if it was just seen as a ‘tick-box’ exercise. Although care plans were not essential, they did have benefits:
. . . without it stuff would get lost and [then] people won’t get support from the relevant agencies that are needed.
D-ST-102
Several staff mentioned that the care plan was a useful aide memoire, although one staff member said that the plans were not done very well on wards. Care plans were used by the MDT and consultants during ward rounds, and many staff referred to the documents on a regular basis, as they provided structure. One staff member mentioned that the plan was used for controlling and monitoring the team. Several staff thought that an app would be a good idea, but data confidentiality issues remained.
Several service users reported having a care plan in the hospital, but not in the community. A couple had found their care plans useful; others did not have one, could not remember it or said that it had been provided weeks after their admission. Several found the plan unhelpful and not important to their health: ‘it doesn’t really help me because it doesn’t influence . . . me’ (D-SU-104). One felt that she had ownership of her care plan, but she could not find it. Another had refused to sign the care plan as the planned one-to-one meetings had not taken place. One carer was very knowledgeable about the care plan, the other less so. Both said that they would welcome a digital care plan or app, as their relatives were computer literate, used their mobile phones constantly and were responsive to messages received by mobile phone.
All staff spoke about a commitment to involving service users in the writing of care plans, but some also acknowledged that this was not always done and that some staff did not see the care plan as a two-way process. Others barriers to involvement included the structure of and jargon in care plans, a lack of spoken English, severity of illness in the early stages of admission, sensitivity around some issues and a refusal by some service users to become involved. There was also some recognition of the involvement of relational power issues and inequalities:
. . . the power thing, how much do people feel able to say no that shouldn’t be in my care plan or to challenge, you know if someone says oh I need you to sign this care plan.
D-ST-102
Overall, service users spoke of having little or no involvement in the writing of their care plan. Some saw the plan as something produced primarily by the ‘the doctors and his team of professionals’ (D-SU-103) and being much the same for everyone. Although some did not seem concerned about their lack of involvement, others would have liked more:
I would know what was going on. I can give my opinions, I get my rights, I get my choices and preferences.
D-SU-101
Both carers said that they had been satisfactorily involved in discussing and planning care, although one complained that they had been given very short notice about ward rounds. The benefits of carer involvement were clearly articulated:
I’ve felt that my voice has been acknowledged, my presence has been acknowledged, and I’ve been able to share with them what [name] would normally hide. And because of sharing that they’ve, they have a better understanding of how to provide that support for [name], whereas if it was [name] on her own she would minimise a lot of things, which a lot of individuals do because of shame.
D-CA-101
Staff spoke of discharge planning being a phased process over time and taking place in ward rounds, care plan reviews and ad hoc meetings with the involvement of MDT, community teams, the service user and, often, carers. There was some recognition that things did not always go to plan, with pressure on beds and community staff creating tensions.
Services users had generally been involved in discussions about plans for their discharge but the details they gave were often sketchy. Some expressed anxieties about their pending discharge:
I’d like to feel like there’s actually someone there fighting my corner for me. And I’m not feeling any of that, I feel like a statistic, I don’t feel like my consultant has, and I’m being really blunt now, I don’t feel like my consultant has any care about me, I don’t feel secure with my discharge. It’s something I worry about, really regular, and it brings me down quite a lot.
D-SU-105
Both carers said that discharge plans had been discussed with them and with service users from an early stage, but this was not necessarily documented in the care plans.
Care reviews
Staff were consistently clear: care plans were reviewed weekly in psychiatrist-led ward rounds with strong MDT involvement. There was recognition that they tried to involve service users in the meetings but these meetings were often too busy or too long, and people felt that they had too little time or felt too intimidated to contribute. Preparing people for reviews helped but this happened too seldom.
Occasionally, staff were held to account by service users requesting the implementation of care plans.
Half of the service users found the meetings quite useful to determine what was required to be discharged and to be able to plan. Others described them as ‘horrid’ and ‘tedious’. One spoke of being overwhelmed, having no control and feeling scared to say what she felt: ‘I don’t feel welcomed, maybe that’s the word, into my own ward round’ (D-SU-105). Carers said that it was difficult to attend because of the fixed time and short notice, and they had mixed experiences of being heard.
Support systems
Staff members articulated their roles with the MDT, with the consultant clearly seeing the role as providing clear clinical leadership and decision-making and the ward manager trying to provide structure and calm, following and guiding staff to address the service users’ needs. Other staff focused more on their direct clinical and social work with service users. Training was a mix of standard mandatory and discipline specific, with little or no focus on care planning and co-ordination.
Service users and carers spoke very positively about their interactions with most staff and often praised named individuals. Some were aware of having a named nurse but even if they did not they found staff responsive and easy to talk to. Staff were described as ‘fantastic’, ‘cool’, ‘caring’ and ‘respectful’:
They’ll always say please and thank you, and call you by your name, and they’re polite and got manners. So, yeah, but they don’t talk down to you.
D-SU-105
There was some suggestion that dealing with conflict was a challenge for some staff.
The ward team was supported by a mix of external agencies and people, all helping to improve services, with MIND, advocates and even researchers mentioned, and housing advisors being especially praised. One staff member emphasised that efforts were always made to ensure good collaboration and communication between the various parties and organisations involved:
. . . people are proactive at getting them involved, and they’re proactive in coming . . . there’s loads of different things . . . loads of support is available.
D-ST-102
Additional support was also recognised by most service users who described helpful input from social workers, psychologists and family workers. This was echoed by both of the carers, who described widespread collaborative support from professional workers involved in the service users’ care that had been effective and valuable, and that it had had a hugely positive impact on the service users’ progress:
I think they think of everything . . . What do I need to do . . . Do I need to settle her in? Do I need to phone her? Do I need to check in on her? And I think that is something that [name of service user] needs all the time, she needs constant reassurance and I think she gets that.
D-CA-101
Staff also spoke of efforts to involve families/carers on the ward and to a great extent this was reflected in the comments of the carers and most of the service users.
Safety and risk
Staff described various processes and structures to ensure that the safety of patients was paramount, while some also spoke of trying to achieve a balance and said that positive risk-taking was important and valuable:
I think that’s important to not let risk impede care or things that can make a difference.
D-ST-102
Although risk was central to care planning and seen as an important feature of working with service users and families, there was also a recognition that documenting risk issues could be stigmatising and had to be balanced by strengths, positivity and the service user taking responsibility. One staff member emphasised that ‘managing risk should be collaborative’ and that having open and sustained conversations with service users could be helpful in terms of risk assessment and management:
. . . sharing the risk plan and saying, well, what do we need to do to keep you safe? . . . Giving people ownership over, over what they would like to happen.
D-ST-102
Service users had little say on this subject, although most were aware of measures taken to manage risk, such as removing certain items on admission. One service user spoke of staff actively keeping her safe when she had been threatened by another patient and two said that their safety was addressed in their care plans. Two also said that more could be done to address issues of physical health and the environment (e.g. dirty patients, lack of clean air) in relation to safety. When mentioned, service users thought that detained patients were treated similarly to informal patients. Carers thought that the safety of patients was addressed.
Organisational context
Staff said that the trust’s focus on quality improvement had led to significant improvements, including reductions in the levels of violence on wards, improved physical health care and the increased involvement of carers. The introduction of a befriending service, peer support workers and a strong service user organisation within the trust were all important.
There was a strong and consistent view that strong trust values and support from senior staff, which included some people with lived experience of mental illness, was creating a much more positive culture with a focus on dignity, privacy, confidentiality, and feedback from service users to improve services:
I guess stuff to do with respect and that people should be respected . . . people’s needs and people’s culture . . . should be respected, and people should be offered things that are relevant to them.
D-ST-102
The aim, described by D-ST-106, was to provide collaborative, recovery-focused, patient-centred care, and a clear relationship between these values and care delivery on the ward was articulated:
. . . [service users’] wishes and their hopes, and dreams and their beliefs about what is really helpful is for them and what is important to them, it should be valued and encouraged, and acknowledged, and actively included in the care plan.
D-ST-102
Recovery
All staff embraced the idea of recovery, although some were not keen on the name. All described recovery as being very personal and also about helping people come to terms with, make sense of and incorporate their experience of mental illness/distress:
. . . it will never be as such recovery, it’s them living with what is part of them and managing it to the best of their ability and what we’re doing is providing them with the skills and the understanding in order to live with what is part of who they are.
D-ST-101
Some spoke of healing, understanding, resilience, well-being and taking control. One described recovery as perhaps a measured response to a trauma or an episode, whereby the individual is able to understand it and be better equipped to deal with a recurrence. Holistic care needed to be tailored to the person. Another said that some of the recovery journey takes place in mental health services, while some takes place at home and in the community at large:
It’s being able to think with the patient about that, I think, and trying to provide good-quality care where it’s necessary but also being able to withdraw and give ownership back to patients and allowing them to continue that.
D-ST-106
All staff said that a recovery-focused approach informed their practice and care planning that was centred on being person-centred, instilling hope and supporting the person to go back into the community and society. Service users described different levels of recovery, from being able to be discharged to a life free of medication and not needing support, or being able to successfully manage or cope with their mental distress. Another service user described recovery as being more balanced and about being able to think clearer.
All felt that hospital admission had helped in their recovery; they found it difficult to explain how, although for some this was about medication. One said that a greater focus on her strengths would have been more helpful. One carer said:
Recovery is about an individual being given the correct support so that they’re able to deal with situations and deal with them appropriately.
D-CA-101
The carer agreed to an extent with the journey metaphor, but emphasised that service users’ recovery is very much a gradual and non-linear process, and that this dynamic needs to be properly understood and respected:
I think [name of service user]’s at that dip where she’s testing her own control of things, so we allow her to have that dip, because if we don’t . . . she will not be able to reinforce, well you know what? I achieved that, I’ve had a dip, I can go back and try it again.
D-CA-101
The other carer saw recovery as more about the service user returning to a previous state of better mental health. Both carers felt that the care was recovery focused but that this was also shaped by the perspective at different points of the service user. One said that the service user’s care planning had been helping with her recovery by recognising trigger points and particularly stressful issues, and also by providing her with a secure base:
[T]hat is something that has been missing in [her] past. She’s fought battles and nobody’s actually stood behind her, and I think this is the first time that she’s actually experienced it, and she is holding on to that, somebody’s there for me.
D-CA-101
Most staff spoke of the ‘This is Me’ care plans and about encouraging service users to develop them as soon as possible following their admission. These were found to be helpful and were reviewed regularly: ‘I think people really value it because . . . it really helps understand what is going on for that individual’ (D-ST-102). A few staff mentioned the recovery star but did not use it, and some spoke of time pressures limiting just how much they could embrace such tools on the ward. Some service users had used the ‘This is Me’ plans; others had not or were not aware of them. None had been aware of other recovery tools. Carers were unsure. Both of the carers and some service users thought that strengths and achievements were recognised, although the traditional care plan did not reflect this.
Personalisation
Staff thought that personalisation was largely about ensuring that care was personalised and focused on the individual. A couple were aware of personal budgets but all had little involvement in these working on the ward. Staff felt that great efforts were taken to be person-centred but that this was sometimes more challenging when someone had been detained and there was disagreement about why they were there.
Few service users understood or recognised the term personalisation; some thought that it was about their care being personal to them or helping in their recovery or about writing their care plan. One detained service user said that their care was not personalised at all. Another gave an example of how, after another service user had stolen her brand-new pyjamas from her room, staff made sure that her room was locked and that her personal space was protected.
The carers were a little unsure about the term but thought that personalisation meant personal care, or ‘not processed’ (D-CA-101). Both thought that care had been personalised and gave examples of this, including arranging visits from and access to the service user’s children.
Barriers and facilitators
Staff spoke of needing more time to spend with service users, to develop therapeutic relationships, to find out more about them and to develop more collaborative approaches. Some wanted more training and staff who had the right approach. One also wanted education for patients and families ‘to help people become the masters of their own illness and their families to identify and support patients with their specific symptoms’ (D-ST-106).
Limited resources in terms of staff, time and facilities impaired attempts to work on recovery, as did responding to emergencies and people being subject to compulsory detention and safeguarding issues. Service reorganisations and loss of key staff had not helped. Some families did not help recovery-focused work. More time for nurses and other staff to spend with service users was seen as the most important factor that would improve care and care planning.
Care plan reviews
Nine care plans were reviewed on the main ward in Dauphine site for four female and five male service users who ranged in age from 18 to 58 years and of whom two were formally detained. For four participants this was their first admission to hospital and for others the number of previous admissions ranged from one to six. No service users had signed their care plans and only two named nurses had done so. It was not clear whether or not copies of care plans had been given to service users. In only two cases was it clear that the service user had attended the last ward round and there was no evidence that carers or care co-ordinators (seven out of nine service users had allocated care co-ordinators) had attended the previous ward round, indicating possible issues with continuity of care. Care plans were written by staff about patient care, although in most cases (seven out of nine) these did reflect the person’s views to certain extent (e.g. ‘he describes his mood as pleasant’, ‘he denies any hallucinations’). There were limited attempts at co-produced care planning (two out of nine) and strengths-based approaches (three out of nine), although the latter were mostly descriptive. There was limited focus on personalisation (four out of nine), use of personal budgets (two out of nine) and recovery-focused work (two out of nine). There was evidence in one case only of the person’s views of safety and risk planning, and in three care plans there was evidence of the person being aware of their risk indicators as a means to manage risk. Most care plans showed orientation to system-based medical goals such as medication compliance, with rare attention paid to social goals (two out of nine). There was no evidence of encouragement towards self-management in care plans. Discharge planning was addressed in six out of nine care plans.
Meeting observations
Two observations of ward round meetings were conducted in Dauphine. Six people were present in both meetings, including a researcher, the nurse in charge, a junior doctor, a student nurse, a psychiatrist and the service user. Two members of staff from a rehabilitation team attended one of the meetings. The room was spacious, with furniture arranged in a circle helping to create what felt to be a relaxed atmosphere. Both meetings were short, one lasting 7 minutes and the other lasting approximately 12 minutes. The psychiatrist led both meetings and gave no opportunity for other staff to speak, apart from the members of the rehabilitation team. Introductions were not provided because both service users had spent a long period of time on the ward and their relationship with the staff present was well established. For one meeting the service user was asked an open question to start: ‘how are you feeling in your mood, how have things been?’ The psychiatrist gave the service user time to speak but was quite firm at times (‘I’ve already told you we’re going to sort it out’) and interrupted (sometimes quite abruptly) to steer the conversation back on track.
The main focus of the meeting was medication and leave in preparation for discharge. Particular care was taken when considering the person’s safety and mobility issues and explaining the importance of taking medication at certain times in the day to reduce the risk of a fall. Enquiries were also made about practicalities of home life (accessibility and general state of the home) in preparation for discharge. Interestingly, the doctor emphasised the importance of the person’s behaviour on the ward in the next few days, warning them that they ‘need to be good in terms of behaviour’ and not to jeopardise the discharge. The meeting ended informally when the service user requested a cigarette break. For the second observation the psychiatrist initially directed the questions to members of the rehabilitation team and they spoke about the person’s ‘inappropriate behaviour tapering down’ alongside plans for the person’s discharge. The doctor addressed the service user sensitively, asking questions which were met with monosyllabic responses. These questions started quite open and then became more specifically about computer games (‘are you a soldier in the game, do you shoot people?’); it was unclear if the questions were directed out of interest or because they related to risk. The doctor demonstrated what appeared to be genuine interest in the well-being of the service user post discharge, enquiring about friendships and the support that could be put in place for their move to the rehabilitation unit. Praise and encouragement was given in reference to the person abstaining from using drugs. This was reinforced by emphasising the importance of this in relation to the person’s clinical history. A reward, of another computer game, was suggested to mark positive progress. Medication was not discussed in this meeting. During the meeting the doctor reviewed a behaviour contract that had been drawn up by the workers at the rehabilitation unit, but did not seem to engage fully with this and did not ask questions. The service user was given the opportunity to ask questions, reassured when needed and given information about future arrangements.
Languedoc
History and context
The trust provides mental health, learning disabilities, and drug and alcohol services to a population of around 735,000 people. It covers an area that is largely rural with very few urban pockets. According to the 2010 English indices of deprivation,148 this site includes 19 areas that are within the country’s top 10% most deprived. These deprived areas are typically densely populated, urban and with a younger population, although two are officially classified as rural. Around 93% of the population are from white British backgrounds, while the remaining 7% are from BME groups. The trust provides both community and inpatient services and operates from two hospital sites. There are 62 beds available within acute mental health services across the two hospital sites. One of the hospital sites houses a mixed-gender ward for 20 people, while the other hospital has two wards split by gender, with 20 beds available to female service users and 22 beds available to male service users. The demand for beds in 2014/15 is clearly illustrated in the yearly figures for bed occupancy and bed availability. The number of available bed-days from April 2014 to March 2015 was 22,630, and the number of occupied beds (excluding leave) was 20,790: a 92% occupancy rate. The number of occupied bed-days (including leave) was 22,760: a 101% occupancy rate. The number of available beds from April 2015 to December 2015 was 17,050, and the number of occupied bed-days (excluding leave) was 15,805: a 93% occupancy rate. The number of occupied bed-days (including leave) was 17,828: a 105% occupancy rate.
Adult acute inpatient services: admissions data
From April 2014 to March 2015, the number of admissions was 427 across the three wards. Of these admissions, 110 (26%) involved section under the MHA. 3 Three people were detained under Section 136. For the 9-month period in 2015, one ward had twice as many admissions as it did over a 12-month period the previous year. From April to December 2015, the number of admissions to acute inpatient care in the three wards in Languedoc was 669. Of these admissions, 144 (22%) involved sectioning under the MHA. 3 Nine people were admitted on Section 136.
The average mean length of stay from April 2014 to March 2015 was 33 days. Two of the wards had longer average length of stay: on the male ward this was 35 days and on the female ward this was 38 days. The mixed ward had a much shorter length of stay of, on average, 25 days. For April 2015 to December 2015 the average length of stay was 38 days. Again, two of the wards had a longer average length of stay, the male ward at 42 days and the female ward at 44 days. The mixed ward at a different hospital site again had a much shorter length of stay of, on average, 30 days.
The main ward for intensive data collection at this site was a male ward with 22 beds. There was a Section 136 room available within the hospital which could be used for assessment for admission to two acute adult mental health wards.
Participant characteristics: staff
Fifty staff from three acute mental health inpatient wards within the locality completed the questionnaires. Just over half of the responses were from mental health nurses and just over one-third were from staff defining their profession as ‘other’. Just over half of the respondents had spent longer than 4 years working in mental health (56%); however, the majority had spent < 4 years working on the ward (74%). A small proportion of staff disclosed that they had a personal history of mental health problems (12%); however, nearly one-third of staff had a family history of mental health problems. Further details of the demographic characteristics can be found in Table 28.
| Variable | n (%) |
|---|---|
| Gender | |
| Female | 37 (74) |
| Male | 11 (22) |
| Age (years) | |
| Median (range) | 30.5 (19–64) |
| Ethnicity | |
| White UK/Irish | 39 (78) |
| White other | 1 (2) |
| Indian | 2 (4) |
| Asian other | 2 (4) |
| Mixed race | 1 (2) |
| Indo-Caribbean | 3 (6) |
| Profession | |
| Mental health nurse | 26 (52) |
| Occupational therapist | 2 (4) |
| Employment/recovery worker | 1 (2) |
| Psychiatrist | 3 (6) |
| Other | 17 (34) |
| Education | |
| Degree | 18 (36) |
| Diploma/similar | 17 (34) |
| Postgraduate diploma/certificate | 4 (8) |
| Master’s degree | 2 (4) |
| Doctorate | 1 (2) |
| Time working in mental health (years) | |
| ≥ 10 | 18 (36) |
| 7–9 | 3 (6) |
| 4–6 | 7 (14) |
| 1–3 | 17 (34) |
| < 1 | 3 (6) |
| Time working on the ward (years) | |
| ≥ 10 | 3 (6) |
| 7–9 | 2 (4) |
| 4–6 | 6 (12) |
| 1–3 | 19 (38) |
| < 1 | 18 (36) |
| Personal history of mental health problems | |
| Yes | 6 (12) |
| No | 41 (82) |
| Family history of mental health problems | |
| Yes | 16 (32) |
| No | 31 (62) |
Participant characteristics: service users
In total, 47 questionnaires were completed by service users on three wards in Languedoc. There were more male respondents than female (68%), with a median age of 36 years. The responses were from predominantly white UK, Irish European or other service users. One-third of the respondents had a diagnosis of psychosis/schizophrenia/bipolar-type disorder, just over one-third had depression/anxiety and one-quarter identified with two or more diagnostic categories. Just over one-third of the participants had spent > 10 years and just under one-third had spent < 1 year in mental health services. Nearly two-thirds of participants had been admitted to hospital between two and five times (64%). Nearly half of the participants had been on the ward for > 4 weeks and just over half (60%) were in contact with community mental health services. Further details of the demographic characteristics can be found in Table 29.
| Variable | n (%) |
|---|---|
| Gender | |
| Female | 15 (31.9) |
| Male | 32 (68.1) |
| Age (years) | |
| Median (range) | 36 (19–66) |
| Ethnicity | |
| Mixed race | 2 (4.3) |
| White UK/Irish | 35 (74.5) |
| White other European | 4 (8.5) |
| White other | 2 (4.3) |
| Latino | 1 (2.1) |
| Mental health problem | |
| Psychosis/schizophrenia/bipolar-type disorders | 14 (29.8) |
| Depression/anxiety | 17 (36.2) |
| Substance use | |
| Other | 3 (6.4) |
| Two or more of above | 12 (25.6) |
| Relationship status | |
| Single | 30 (63.8) |
| In an established relationship | 16 (34.0) |
| Length of time with mental health services (years) | |
| ≥ 10 | 17 (36.2) |
| 7–9 | 1 (2.1) |
| 4–6 | 8 (17.0) |
| 1–3 | 6 (12.8) |
| < 1 | 14 (29.8) |
| Number of previous admissions | |
| First | 11 (23.4) |
| 2–5 | 30 (63.8) |
| 6–9 | 5 (10.6) |
| ≥ 10 | 1 (2.1) |
| Contact with community mental health services | |
| Yes | 28 (59.6) |
| No | 16 (34.0) |
| Time on the ward | |
| 1 week | 7 (14.9) |
| Up to 2 weeks | 9 (19.1) |
| 2–4 weeks | 8 (17.0) |
| > 4 weeks | 22 (46.8) |
| Frequency of contact with family/carer/friends | |
| Daily | 21 (44.7) |
| Weekly | 11 (23.4) |
| Fortnightly | 3 (6.4) |
| Monthly | 2 (4.3) |
| Other | 9 (19.1) |
| Living status before admission | |
| Independent and single | 15 (31.9) |
| Independent in relationship | 8 (17.0) |
| Living with family | 18 (38.3) |
| Supported housing | 2 (4.3) |
| Hostel | 1 (2.1) |
| Homeless/no fixed abode | 2 (4.3) |
| Previous daytime activity | |
| Full-time employment | 11 (23.4) |
| Part-time employment | 5 (10.6) |
| Sheltered employment | 2 (4.3) |
| Education/training | 17 (36.2) |
| Unemployed | 2 (4.3) |
| Voluntary work | 10 (21.3) |
Summary scores for the questionnaires
Views on Inpatient Care scale
A total VOICE score for each respondent was obtained by summing the scores of the individual items. The higher the total score (range 19–114), the more negative the perception of the quality of care on the ward. The score for respondents in Languedoc is shown in Table 30.
| Scale | Service user score (n = 47)a | Reference valueb |
|---|---|---|
| VOICE total | 49.04 (20.02); range (19.00–109.00) | 55.5 (19.2) male; 52.5 (17.8) female |
The total scores for VOICE were marginally lower than the reference value provided by Evans et al. 52 The mean scores were in the lower half of the scale, suggesting that service users leant towards a more positive perception of the ward. There is, however, a large range of responses for this measure, demonstrating that some of the participants had a more negative perception of the ward.
Empowerment Scale
A total ES score for each service user respondent was obtained by summing the scores of individual items. The overall mean score for the sample was above the mid-point for the instrument. Out of a possible score of 4, indicating a higher perceived level of empowerment, the mean total score was 2.92 (SD 0.34), which is slightly higher than the reference value. 146 The subscale values were all higher than the reference group, apart from righteous anger, which was comparable (Table 31).
| Subscale | COCAPP-A (acute inpatient) | COCAPP (community) | ||||
|---|---|---|---|---|---|---|
| n | Mean (SD)a | Referencea | n | Mean (SD)a | Referencea | |
| Self-esteem–self-efficacy | 43 | 3.07 (0.68) | – | 90 | 2.60 (0.78) | 2.82b |
| Power–powerlessness | 44 | 2.52 (0.45) | – | 90 | 2.45 (0.55) | 2.51b |
| Community activism and autonomy | 44 | 3.41 (0.52) | – | 90 | 3.09 (0.47) | 3.12b |
| Optimism and control over the future | 44 | 3.12 (0.67) | – | 91 | 2.61 (0.65) | 2.72b |
| Righteous anger | 43 | 2.26 (0.73) | – | 91 | 2.21 (0.72) | 2.34b |
| Total score | 44 | 2.92 (0.34) | – | 91 | 2.62 (0.44) | 2.74 (0.34)b |
A further comparison was made of the scores for empowerment between the COCAPP studies (acute and community mental health services). The total score and subscales for the ES were higher in responses obtained from service users in acute inpatient services that in responses from those in contact with community mental health services. See Chapter 5 for some exploratory inferential analyses.
Scale to Assess the Therapeutic Relationship
For service users, the total score for the STAR-P was 27.93 (SD 12.57), 13.85 (SD 7.77) for ‘positive collaboration’, 6.38 (SD 3.85) for ‘positive clinician input’ and 7.71 (SD 3.50) for ‘non-supportive relationships’. These scores align well with the reference values provided by Nolan (personal communication) shown in Table 32. All the values for this study are, however, marginally lower than the reference values for this site.
| Subscale | COCAPP-A (acute inpatient) | COCAPP (community) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| STAR-P (service user) | STAR-C (staff) | STAR-P (service user) | |||||||
| n | Mean (SD) | Reference | n | Mean (SD) | Reference | n | Mean (SD) | Reference | |
| Positive collaborationa | 47 | 13.85 (7.77) | 14.36 (5.99)b | 48 | 18.20 (2.35) | 17.95 (2.98)b | 90 | 18.62 (4.92) | 19.9 (6.7)c |
| Positive clinician inputd | 47 | 6.38 (3.85) | 7.10 (2.91)b | 48 | 10.55 (1.38) | 10.42 (1.23)b | 91 | 8.46 (2.75) | 9.3 (3.0)c |
| Non-supportive clinician inpute (service users)/emotional difficultiese (staff) | 47 | 7.71 (3.50) | 8.78 (2.21)b | 47 | 9.15 (1.46) | 9.61 (1.65)b | 91 | 9.14 (2.87) | 9.3 (3.3)c |
| Total scoref | 47 | 27.93 (12.57) | 30.23 (9.71)b | 47 | 37.98 (4.24) | 37.93 (4.92)b | 91 | 36.07 (9.03) | 38.4 (12.0)c |
For staff, the mean total for the STAR-C was 37.98 (SD 4.24), with scores of 18.20 (SD 2.35) for ‘positive collaboration’, 10.55 (SD 1.38) for ‘positive clinician input’ and 9.15 (SD 1.46) for ‘emotional difficulties’. All of the subscale values and the total score were approximately equivalent for the staff in this study and those in the reference study.
When comparing the mean service user and staff scores it is apparent that staff give higher scores therefore rating the therapeutic relationship more positively than service users. Total scores are on average seven points higher for staff than service users.
An independent samples t-test was completed to determine if there were significant differences in the perceptions of the therapeutic relationship between service users and staff. There was a significant difference in the total STAR scores for service users (mean 27.93, SD 12.57) and staff (mean 37.98, SD 4.24) [t(56.3) = –5.19; p < 0.001; 95% CI –13.9 to –6.17; Cohen’s d = 1.07] and two of the subscales (positive collaboration and positive clinician input). T-test statistics for the subscales are provided in Chapter 5, Table 52.
A final comparison was made between the scores for the therapeutic relationships across the two COCAPP studies (acute and community mental health services). It is clear from the scores in Table 32 that service users scored approximately eight points higher in the total STAR-P score for community mental health services than in the total for acute mental health services.
Recovery Self-Assessment Scale
The mean scores and SDs for the RSA scale are provided in Table 33. Mean scores from service users and staff on the subscales fell in the moderate range (3.12–3.38 and 3.25–3.84, respectively). For the mean RSA total score, the staff scores were marginally higher (mean 3.52, SD 0.63) than those of the service users (mean 3.23, SD 1.10). There is some variability between responses for the service users and the staff. For the service users the lowest scoring subscales were individually tailored services, diversity of treatment options and involvement. For staff the lowest scoring subscale was involvement followed closely by individually tailored services. The highest-rated subscale for service users was life goals and for staff it was choice subscale. The staff scored highly on this subscale, indicating that clinician see this as an area of priority.
| Subscale | COCAPP-A (acute inpatient) | COCAPP (community) | ||||||
|---|---|---|---|---|---|---|---|---|
| n | Mean (SD)a | n | Staffa | n | Mean (SD)a | n | Staffa | |
| Life goals | 46 | 3.38 (1.15) | 50 | 3.68 (0.72) | 81 | 3.31 (1.00) | 28 | 3.82 (0.60) |
| Involvement | 42 | 3.16 (1.25) | 50 | 3.25 (0.70) | 81 | 2.66 (1.12) | 28 | 3.23 (0.63) |
| Diversity of treatment options | 46 | 3.12 (1.12) | 50 | 3.39 (0.73) | 83 | 2.70 (1.04) | 28 | 3.24 (0.64) |
| Choice | 46 | 3.20 (1.23) | 50 | 3.84 (0.66) | 87 | 3.72 (0.86) | 28 | 4.04 (0.50) |
| Individually tailored services | 43 | 3.12 (1.22) | 50 | 3.32 (0.74) | 84 | 3.05 (1.12) | 28 | 3.42 (0.69) |
| Total score | 44 | 3.23 (1.10) | 50 | 3.52 (0.63) | 86 | 3.12 (0.94) | 28 | 3.57 (0.56) |
Independent samples t-test was conducted to compare the perceptions of recovery-oriented services for staff and service users. There were no significant differences in the total RSA scores for service users (mean 3.23, SD 1.10) and staff (mean 3.52, SD 0.63) [t(72.6) = –1.61; p = 0.113; 95% CI –0.73 to 0.08; Cohen’s d = 0.32] or many of the subscale scores (t-test statistics for subscales are provided in Chapter 5, Table 52), apart from the ‘choice’ subscale, where staff (mean 3.84, SD 0.66) scored significantly higher than service users (mean 3.20, SD 1.23) [t(67.8) = –3.15; p = 0.002; 95% CI –1.05 to –0.23; Cohen’s d = 0.65].
A final comparison was made of the scores for the perceptions of recovery-oriented care between the COCAPP studies (acute and community mental health services). The RSA total score for service users in acute mental health services in Languedoc was slightly higher than for those in community mental health services. Conversely, staff gave a marginally lower total RSA score in the acute study than respondents in the community study.
There are some differences at the subscale level, with service users in acute services scoring marginally higher on the ‘life goals’ and ‘individually tailored services’ subscales and considerably higher on the ‘involvement’ and ‘diversity of treatment options’ subscales. Conversely, service users in the acute study scored the ‘choice’ subscale considerably lower than did respondents in the community study.
There are some differences at the subscale level for staff. In our acute study staff scored ‘life goals’, ‘choice’ and individually tailored services’ lower than did respondents in the community study. In contrast, staff scored ‘diversity of treatment options higher’ in the acute study, and scores for ‘involvement’ are comparable across studies. See Chapter 5 for some exploratory inferential analyses.
A recovery profile from the RSA scale is included in Appendix 5.
Narrative summary of interview data: service users, carers and staff
In Languedoc we interviewed six service users, one carer and three members of ward staff. The staff interviewed were a ward manager, an OT and a psychiatrist.
Care planning and co-ordination
Staff expressed contradictory views on care planning processes. Both the ward manager and the OT saw care planning as central to ensuring that all aspects of care were brought together and centred on the patient:
[B]ringing a person’s care all together really, so it’s like a standard to work around, that it’s all centred around the patient’s care, so everything works for them in the best way, I think.
L-ST-103
Care planning supported multidisciplinary working within the ward team but failed to ensure the involvement of the community teams whose members rarely attended planning meetings or CPA reviews. In contrast, the psychiatrist felt that care planning and reviews were no longer significant or helpful and had simply become another tool for measuring achievement of targets against restricted resources.
All but one of the six service users had no idea if their care was planned or co-ordinated, or, if it was, who might be involved in that. Some spoke of ‘trusting’ staff to do what was best to ‘get them better’ (L-SU-101):
I don’t know if there’s anybody, we’re meant to have a named nurse and associate or something, I only found out my named nurse last week and I couldn’t even tell you who the associate is, so I just assume it’s the doctor.
L-SU-105
The one carer interviewed had attended meetings led by the doctor who directed questions at the patient in what seemed a ‘brusque, unhelpful manner’ (L-CA-101), although the parents were asked for their views. The carer would have appreciated if staff had explained what their son was going through, and given them better understanding of how to respond.
Views on documentation differed. The ward manager and the OT spoke of the care plan as an electronic ‘well-being plan’, which was service user focused, built up over time and involved all team members. This was described as a ‘whole document all in one, so it’s a lot better’ (L-ST-103) and was referred to regularly to guide care. All new inpatients have an ‘admission care plan’ for up to 72 hours, addressing safety, medication, observation levels and leave arrangements before the well-being plan is developed. The psychiatrist distinguished between ‘a management plan’ for psychiatrists and a nursing ‘care plan’ for nurses and saw these as separate, but thought that patients liked to see who is doing what with them. The OT wanted to see a mobile phone app introduced and the psychiatrist would welcome being able to e-mail care plans to service users.
All but one of the six service users had not seen or were very uncertain about their care plans, what was in them, what they meant or whether or not they had one. Two had copies of plans that appeared out of date. Some were more aware of care being planned and co-ordinated in the community but did not feel that these plans had influenced their inpatient care. When service users did have sight of care plans, the difficulty appeared to be in how these were worded, as they did not make much sense to the individual:
It’s mad. All these abbreviations, I ain’t got a clue.
L-SU-105
The carer interviewed said their son did have a care plan, and he had given them a copy. It detailed his medication and that he would be assigned a CPN care co-ordinator. However, the carer felt that it would have been more helpful to have something that ‘describes how he’s going to feel’, with personalised targets and things that were going to help.
Routes of admission to hospital recounted by service users indicated degrees of crisis and significant distress. Most had contact with crisis services, police and accident and emergency. Only half were under existing community care, and they reported minimal support. One spoke of a CPN giving him a depot injection every 2 weeks in the community, but ‘she didn’t used to come and talk.’ (L-SU-104).
All staff said that there was a high level of service user involvement in developing care plans, although less so among those admitted compulsorily or in disagreement about treatment. Current use of technology removes staff from the service user as they have to use computers in offices. Service users reported various experiences of care plans. Some seemed aware of them but felt that they were poorly explained and poorly worded. Care plans seemed to be a source of antagonism for some who did not recognise themselves in the descriptions. One suggested the need for an external independent person or advocate to ensure that the care plan reflected the individual’s understanding and that care plans would more directly refer to therapy rather than prioritising medication.
. . . that would have helped me because it would give us somebody to talk to that wasn’t connected to the hospital or ward.
L-SU-106
Workers indicated that discharge planning was something to be considered immediately and reviewed throughout a stay. Giving a provisional discharge date to aim for an early stage worked to motivate some but created anxiety in others. Inpatients tended to be offered periods of graduated leave and sometimes needed to be referred to other services (e.g. drug/alcohol). Multidisciplinary discharge planning included care co-ordinators if possible, with summaries faxed to general practitioners, 48-hour reviews with the crisis team, and 7-day follow-up with community teams if they have one.
Service users described a mix of very detailed planning for discharge, from plans with good multiagency involvement and discussions with service users, to more limited plans for CPN support on discharge, to little discussion at the time of interview. One person spoke of his anxiety about leaving with day leave lined up and little or no preparation for dealing with anxieties and fears. He reported that he was due for discharge but did not feel ready just yet, and advice to contact a crisis team and enrol at recovery college was challenged as he lived one and a half hours away and feared prohibitive travel costs. None of the service users reported actually completing advanced directives, and one carer spoke of their relative having graduated leave days at home but no discussion or planning with the family.
Care reviews
A general view among staff was that review meetings were quite sensitive to service users’ needs, with sufficient time (30–60 minutes) given for discussion per patient. Prompt sheets had been introduced by the consultant to help service users prepare what they wanted to say but they were rarely used ‘partially because they don’t find me too difficult to talk to’ (L-ST-103). Service users’ views were definitely listened to, although there were ‘red lines’, such as refusing all medication when they were clearly very unwell (L-ST-103). A range of staff attended the meetings, which were usually chaired by the consultant, although she occasionally handed over that role to other staff or even the service user.
Service users described ward rounds with doctors, nurses, students and psychologists present and some mentioned that they had the opportunity to invite a carer/family member with some flexibility given to allow attendance. They were given a chance to speak at meetings but did not mention being prepared for these. Most found ward rounds helpful – ‘very, incredibly helpful, yes’ (L-SU-103) – although these were described as largely a chance to ‘catch up’ with the psychiatrist about medication, etc. ‘Sometimes you feel it’s all been decided before you go in, you get that impression . . .’ (L-SU-106).
Some service users spoke of difficulty in addressing things with doctors or raising things in review meetings, and some variation in style of doctors was mentioned. The one carer interviewed spoke of minimal involvement and described one meeting with a psychiatrist as ‘confrontational’ as the service user was ‘accused’ (L-CA-101) in front of family members of frightening staff.
Support systems
Staff reported being a strong supportive MDT but struggled with external agencies at times. Some staff claimed to bring specific skills to care planning. The OT, for example, suggested that they were one of the few people who brought a social dimension to the process, while the psychiatrist brought leadership. All staff said that they had received the basic trust training in the CPA but that they had developed their skills and approaches through practice and by learning from others.
Named nurses were expected to have twice-weekly meetings with service users and all service users were to meet daily with another staff member. Service users either did not know their primary nurse or reported mixed views of the relationship with them. Few service users appeared to have planned times to meet but some spoke of nurses being caring and helpful when approached. One carer described how, when their relationship with the doctor had broken down, they sought out a nurse to speak with who seemed nice.
Service users gave mixed views on staff attitudes; some were sure that staff listened and were respectful and compassionate, and others were less so. Some of this appeared to relate to the use of bank staff and unqualified people who service users worried did not have the training to understand what was going on with them. There was, however, little support for the idea that the caring and compassionate responses actually translated into care plans, and there was a reported mismatch between positive experiences with staff and care plans that were seen as overly negative, which may have led to service users re-evaluating their experiences of staff in a less favourable light.
The family of one service user was concerned that medical staff had been confrontational with their son from the outset after a very serious incident. However, they highlighted that some nursing staff had stood out and ‘went the extra mile’ so that a close bond between them and their son was formed. The family of one service user was concerned that medical staff had been confrontational from the beginning with their son, after a very serious incident. They highlighted, however, that some nursing staff stood out and went the extra mile so that a close bond between them and their son was formed. There was a concern that for some staff it may only be a job, with insufficient time being taken to listen to parents experiencing distress as their relatives were admitted to hospital for the first time.
For the most part, support from staff external to the ward seemed problematic for service users; it appeared that the ward had not been able to build sustainable connections with external agencies or even with CMHT workers. Workers claimed that family involvement was widely encouraged, and about one-third of service users had a relative present at their reviews, although it was recognised that the timing of ward rounds was not always conducive to this. Issues of family difficulties and overinvolvement were raised, which were seen as reasons not to involve the family rather than being recognised as a potential opportunity to engage the person and their family members in some family work. Service users readily identified support from (often several) family members but all either appeared aware that the involvement of family or carers may not be helpful for them or were concerned that this may be a burden to their family members who often had their own difficulties.
Safety and risk
Risk assessments are conducted, which inform the care plan and are regularly updated by nursing staff and reviewed in review meetings. There was no mention of service user involvement. The OT gave examples of concerns about lone working, carrying out cooking assessments with people who might hide knives and helping people with poor personal hygiene to go out in public.
A number of service users said that they did not feel safe on the ward and would have liked more staff to be available. Some said that their concerns about safety from other patients had not been addressed. The carer spoke of the safety of their son being paramount for staff, except when he had left the ward and drank alcohol with staff unaware of his whereabouts.
The psychiatrist viewed care planning as directed by risk concerns and always weighing up the risk against the benefits, such as benefits of medication against possible side effects, or potential benefits and risks of taking leave. The ward manager clearly saw risk as the dominating issue. The OT suggested that psychiatrists tended to be risk adverse but that balancing risks with responsibilities and taking positive risks were necessary to make progress:
. . . if you let the risk rule over the actual care plan then you’re never going to get anywhere.
L-ST-102
Service users had mixed views on whether or not risk was discussed; some service users knew that this was in their care plan but others were uncertain. Some acknowledged that discussions about safety had occurred and staff were open to discussing this, with one person recognising the role of individual agency in the process:
At the end of the day it’s only what I’m willing to tell them isn’t it, so that, yeah, yeah, that was discussed enough.
L-SU-105
Some staff suggested that service users under a section of the MHA3 were less likely to engage in care plan discussions. At least three of the service users had been compulsorily detained; one thought that this meant staff gave more thought to their care, while another thought that he was being ridiculed through the process. They remained uncertain about their rights.
Organisational context
Staff spoke of various initiatives [e.g. productive ward, 6Cs, Accreditation of Inpatient Mental Health Services (AIMS), CQC inspections] and hoped that they helped to raise standards and remind staff of the importance of care planning. However, too often wards had the ‘worst patients, highest intensity of workload caseloads and were fire-fighting’ (L-ST-101). Personal values of caring, respect, honesty and compassion led people into mental health work: a belief that they were essentially good people trying to do good things for others. Some of this was reflected in the ‘vision statement’ of the trust, giving a sense that it was recognised across the organisation.
Recovery
The psychiatrist declared some scepticism about recovery and suggested that policy-makers ‘just come up with different terminology to try and make it sound like we’re doing a better job’ (L-ST-101). She thought that recovery was not appropriate for everyone: that for some it was about symptom management or lifestyle management. She suggested that it was applied differentially – ‘I’ve got hope for you but I’ve not got hope for you’ – and constructed this as ‘elite versus gutter’, suggesting a serious misunderstanding of recovery philosophy. The other staff were more aligned in their thinking and saw recovery as a process:
To me the term recovery is about that person getting back to maybe what they were or to some sort of level where they can have a life and get by and do things that they want to do.
L-ST-102
The contrast between colleagues here is striking and suggests that the ward does not have a unified and agreed approach to promoting recovery-focused care.
Notions of recovery among services users were mixed but most saw it as getting better and regaining a form of their previous life or coming to terms with the impact of their difficulties. Some did not believe that this was possible, while others saw it as a process concurrent with their condition and that they needed to take an active role in making it happen.
Getting better . . . Just like to get yourself back to your daily routines and being normal again I suppose . . . recovery is not always possible but if you think like that you just, I don’t know, you’re just not going to get better are you if you just keep thinking that.
L-SU-101
The carer saw recovery as referring to the service user getting back to their old self, but they also expressed fears that mental illness would have an irreversible impact on the person’s personality and abilities.
Staff felt that service users could be helped to take initial steps towards recovery and that care planning, including the use of Recovery College, could contribute to setting people on a recovery pathway. Most service users felt that hospital had contributed to their recovery, although one person did not feel that anything had helped.
Staff mentioned WRAPs and the Recovery Star but these tools were seen as more suitable for community support and support in the Recovery College. No service users thought that they had been asked to develop a recovery plan or use any recovery-focused tools. Some said that their achievements and strengths were recognised, although specific examples were not provided. Carers felt that some recovery-focused work had occurred but that more specific goal-related support might have been beneficial.
Personalisation
In general, staff spoke fairly vaguely about putting the patient at the centre of their care, and service users often had no idea what ‘personalisation’ referred to:
It doesn’t mean anything, it just sounds like a made-up word.
L-SU-102
Others thought that it was about tailoring the care plan to their individual needs as each person is different, with one likening it to the personal settings on their mobile phone. All staff felt that they worked with service users in a personalised way and gave examples of this.
Overall, service users felt that there were some attempts to provide personalised care and to respond to individual needs, although it was often difficult to elicit examples of these. The carer felt that good attempts had been made and that their son’s individual character had been recognised after some time. Staff highlighted system and structural issues that could work against personalisation (e.g. MHA status and risk behaviours) but also gave examples of when they had been able to provide more personalised care.
Barriers and facilitators
Staff identified factors that would help recovery and personalised care. These included having more medical and nursing staff on the ward, more input from community teams and more time to develop therapeutic relationships:
How much more would I get from them . . . if they didn’t see me as the medic that you just go and see once a week and get your meds signed off.
L-ST-101
The physical environment of the wards was often not conducive to undertaking the work required, and limited ability to work in the community was also a barrier. Poor Wi-Fi access, inflexible information technology and inadequate documentation were all mentioned, as was the amount of time required to complete documentation to the required standard, as major barriers to spending more time on face-to-face work with service users. A lack of stability in accommodation and the failure of community teams to contain concerns about risk were also seen to put added pressures on ward staff.
Some service users asked for more personalised care and more (better paid) nurses, as well as a focus on autonomy and less concern with rules seen as unimportant. More information was also requested, as was more access to care plans so that people could make some sense of what was going on with their care. The carer would have liked to have been introduced to the CPN while their child was still in hospital and had their information needs addressed, such as being told who was in charge at weekends when they needed advice on medications.
Care plan reviews
Ten participants were selected for care plan reviews on the main ward in Languedoc. All of the service users were male and they ranged in age from 26 to 61 years. Seven service users were formally detained during their admission and 3 of 10 had been admitted to hospital previously. In only two cases was it possible to verify that the service user had signed their care plan, whereas five care plans had been signed by the named nurse. All 10 service users had been given copies of their care plans. All service users had attended their last ward round and in four cases carers had also attended; no advocates attended for any of these participants. Care co-ordinators were present for six of the service user participants who had one allocated, suggesting potential issues with continuity of care. One care plan could not be located for the review. In all of the remaining care plans there was evidence that the service user’s views had been included. The ways in which care plans were written varied from those written to the person (e.g. ‘you have voiced an interest in joining the gym’) to those written as if by the person but in formal language (e.g. ‘I will try and build up a therapeutic relationship with my named nurse’). Although there was evidence of attempts at coproduction and a focus on strengths and recovery ideas, for the most part the care plans simply reported discussions and did not show evidence of, for example, using strengths to orient care. There was some evidence of involvement in discussions about safety, risk and risk management. Some reference to discharge planning, usually involving onward referral rather than specific plans for the individual, was evident in all care plans reviewed.
Meeting observations
In Languedoc, two observations of ward round meetings were conducted. Five people were present in both meetings: a researcher, the nurse in charge, a junior doctor, a psychiatrist and the service user. In one of the meetings a crisis team manager attended. The room was quite small, with sofas and a table dominating the room. Some of the staff sat behind the table; the chair that the service user was directed to was close to the psychiatrist with no barrier between the two. One of the meetings focused on discharge and was quite short (5–7 minutes), while another meeting was substantially longer (20–25 minutes) owing to the discussion of complex needs. For both meetings the charge nurse collected the service user from the ward and led them into the room, where they were warmly welcomed. There was little need for introduction in one of the meetings, as the relationship was well established. In the other meeting the doctor was familiar with the service user and used some small talk to remind the person of their previous contact. The meetings were led by the psychiatrist, the atmosphere was relaxed and the other staff were able to ask questions freely. The doctor led the first part of the meeting and then handed over the chairing role to a nurse. Staff showed interest in what the service user had to say, enquired about future plans and worked collaboratively to arrange follow-up meetings. One service user mentioned struggling with some thoughts, which was not really acknowledged and attended to, and it was unclear if this had been spoken about before. It did appear that this service user expected some further support; it was acknowledged that he was trying and that he had support around him, but the doctor voiced ‘I think now, there’s nothing more the ward can offer you’. In one meeting it was mentioned that a discharge care plan would be given to the person but it was unclear if the person had any involvement in the development of this. Staff spoke for a considerable amount of time before one of the meetings, as they were particularly concerned about risk (‘risk is not obvious but subtle until it boils over and he kills someone’). During the meeting, risk was explored openly and quite sensitively (‘How do you feel about certain risks around you? Sometimes you can be impulsive’). Staff clarified what the person thought, details of medication, triggers and what the person’s understanding was of their admission and how the ward could be supporting them at this time. Enquiries were made about the person’s previous episodes of illness and positive encouragement was provided. Medication was discussed and the option of changes to this was given. Activities were also discussed and suggestions were made for coping with triggers. After the meetings, time was given for brief discussions about what to include in the notes.
Provence
History and context
The trust provides both community and inpatient mental health services to a population of approximately 1.5 million. The catchment area is predominantly rural with some urban localities, within which are provided specialist services. According to the 2011 census, > 90% of the population are from white British backgrounds. The English indices of deprivation148 reported that some of the areas within the catchment are affluent and among the least deprived 10% in the country. Adult inpatient services are provided from six hospital sites, with approximately 30 CMHTs and 290 adult psychiatric beds, of which 17 beds are allocated to the ward that was our principal data collection site. The average occupancy rate of beds on the ward was 92%.
Adult acute inpatient services: admissions data
In 2015 the number of admissions excluding transfers was 3195. The number of transfers was 1335 and therefore the overall number of admissions was 4530. Unfortunately, we do not have the number of admissions under the MHA. 3 The average length of stay for service users discharged from the adult acute wards in 2015 was 25 days (excluding leave) and 26 days (including leave).
The main ward for intensive data collection at this site is a mixed ward with 17 beds. There is a Section 136 room available within the hospital that could be used for assessment for admission to two acute adult mental health wards. There were seven qualified members of staff and 11 nursing assistants working on the ward. Typically, two qualified members of staff worked on the morning and evening shift and one worked on the night shift. Four nursing assistants worked on the morning and night shift and three worked on the evening shift.
Participant characteristics: staff
Forty-two staff from three acute mental health inpatient wards within the locality completed the questionnaires. Just over half of the responses were from mental health nurses and just over one-third were from professionals identifying with the ‘other’ category. The majority of respondents had spent at least 4 years working in mental health (62%) and two-thirds had spent < 4 years working on the ward (64%). A small proportion of staff disclosed that they had a personal history of mental health problems and just over one-quarter had a family history of mental health problems. Further details of the demographic characteristics of staff can be found in Table 34.
| Variable | n (%) |
|---|---|
| Gender | |
| Female | 25 (59.5) |
| Male | 16 (38.1) |
| Age (years) | |
| Median (range) | 37 (21–67) |
| Ethnicity | |
| Asian other | 2 (4.8) |
| Black African | 4 (9.5) |
| Indian | 3 (7.1) |
| Indo-Caribbean | 2 (4.8) |
| White other | 2 (4.8) |
| White UK/Irish | 27 (64.3) |
| Profession | |
| Mental health nurse | 23 (54.8) |
| Social worker | 1 (2.4) |
| Psychiatrist | 1 (2.4) |
| Occupational therapist | 1 (2.4) |
| Employment/recovery worker | 2 (4.8) |
| Other | 14 (33.3) |
| Education | |
| Degree | 18 (42.9) |
| Diploma/similar | 12 (28.6) |
| Postgraduate diploma/certificate | 4 (9.5) |
| Master’s | 2 (4.8) |
| Other | 1 (2.4) |
| Time working in mental health (years) | |
| ≥ 10 | 13 (31) |
| 7–9 | 2 (4.8) |
| 4–6 | 11 (26.2) |
| 1–3 | 10 (23.8) |
| < 1 | 5 (11.9) |
| Time working on the ward (years) | |
| ≥ 10 | 5 (11.9) |
| 7–9 | 2 (4.8) |
| 4–6 | 7 (16.7) |
| 1–3 | 15 (35.7) |
| < 1 | 12 (28.6) |
| Personal history of mental health problems | |
| Yes | 6 (14.3) |
| No | 36 (85.7) |
| Family history of mental health problems | |
| Yes | 11 (26.2) |
| No | 31 (73.8) |
Participant characteristics: service users
In total, 42 questionnaires were completed by service users in three wards in Provence. The gender distribution of participants was fairly equivalent and the median age was 40 years. There was some diversity in terms of ethnicity, but the majority of responses, over three-quarters, were from white UK or Irish service users (77%). Nearly one-third of the respondents had a diagnosis of psychosis/schizophrenia/bipolar-type disorder and nearly one-third identified with two or more diagnostic categories. Close to half of the participants had spent > 10 years in mental health services and just under 50% participants had been admitted to hospital between two and five times. A large proportion of participants had been on the ward for 1 week (40%). Just over half of participants (59%) were in contact with community mental health services. Further details of the demographic characteristics can be found in Table 35.
| Variable | n (%) |
|---|---|
| Gender | |
| Female | 23 (45) |
| Male | 27 (53) |
| Age (years) | |
| Median (range) | 40.5 (20–63) |
| Ethnicity | |
| Indian | 1 (2) |
| Bangladeshi | 1 (2) |
| Asian other | 1 (2) |
| Black Caribbean | 2 (4) |
| Mixed race | 1 (2) |
| White UK/Irish | 39 (77) |
| White other European | 1 (2) |
| White other | 4 (8) |
| Mental health problem | |
| Psychosis/schizophrenia/bipolar-type disorders | 16 (31) |
| Depression/anxiety | 10 (20) |
| Substance user | 2 (4) |
| Other | 8 (16) |
| Two or more of above | 15 (30) |
| Relationship status | |
| Single | 33 (64.7) |
| In established relationship | 17 (33.3) |
| Length of time with mental health services (years) | |
| ≥ 10 | 24 (47) |
| 7–9 | 1 (2) |
| 4–6 | 4 (8) |
| 1–3 | 9 (18) |
| < 1 | 12 (24) |
| Number of previous admissions | |
| First | 12 (24) |
| 2–5 | 22 (43) |
| 6–9 | 8 (16) |
| ≥ 10 | 8 (16) |
| Contact with community mental health services | |
| Yes | 30 (58.8) |
| No | 12 (23.5) |
| Time on the ward (weeks) | |
| 1 | 20 (40) |
| Up to 2 | 15 (30) |
| 2–4 | 8 (16) |
| > 4 | 8 (16) |
| Frequency of contact with family/carer/friends | |
| Daily | 31 (61) |
| Weekly | 8 (16) |
| Fortnightly | 2 (4) |
| Monthly | 4 (8) |
| Other | 6 (12) |
| Living status before admission | |
| Independent and single | 17 (33) |
| Independent in relationship | 9 (18) |
| Living with family | 15 (29) |
| Living with friends | 1 (2) |
| Supported accommodation | 2 (4) |
| Hostel | 1 (2) |
| Homeless/no fixed abode | 3 (6) |
| Other | 2 (4) |
| Previous daytime activity | |
| Full-time employment | 11 (21.6) |
| Part-time employment | 3 (5.9) |
| Sheltered employment | 1 (2) |
| Education/training | 17 (36.2) |
| Unemployed | 2 (4.3) |
| Voluntary work | 10 (21.3) |
Summary scores for the questionnaires
Views on Inpatient Care Scale
A total VOICE score for each respondent was obtained by summing the scores of the individual items. The higher the total score (range 19–114), the more negative the perception of the quality of care on the ward. The score for respondents in Provence is shown in Table 36.
| Scale | Service user score (n = 51)a | Reference valueb |
|---|---|---|
| VOICE total | 48.55 (20.07) (range 19.00–101.00) | 55.5 (19.2) male; 52.5 (17.8) female |
The total scores for VOICE were marginally lower than the reference value provided by Evans et al. 52 The mean scores were in the lower half of the scale, suggesting that service users leant towards a more positive perception of the ward. There is, however, a large range of responses for this measure, demonstrating that some of the participants had a more negative perception of the ward.
Empowerment Scale
A total ES score for each service user respondent was obtained by summing the scores of individual items. The overall mean score for the sample was above the mid-point for the instrument. Out of a possible score of 4, indicating a higher perceived level of empowerment, the mean ± SD score was 2.85 ± 0.40 this is slightly higher than the reference value. 146 The subscale values were all higher than the reference values, apart from the righteous anger and power–powerlessness subscales, which were comparable (Table 37).
| Subscale | COCAPP-A (acute inpatient) | COCAPP (community) | ||||
|---|---|---|---|---|---|---|
| n | Mean (SD)a | Referencea | n | Mean (SD)a | Referencea | |
| Self-esteem–self-efficacy | 51 | 2.98 (0.77) | – | 76 | 2.73 (0.73) | 2.82b |
| Power–powerlessness | 51 | 2.56 (0.56) | – | 76 | 2.57 (0.48) | 2.51b |
| Community activism and autonomy | 51 | 3.25 (0.48) | – | 76 | 3.14 (0.52) | 3.12b |
| Optimism and control over the future | 51 | 3.00 (0.73) | – | 76 | 2.77 (0.65) | 2.72b |
| Righteous anger | 51 | 2.29 (0.72) | – | 76 | 2.35 (0.56) | 2.34b |
| Total score | 51 | 2.85 (0.40) | – | 77 | 2.73 (0.39) | 2.74 (0.34)b |
A further comparison was made of the scores for empowerment between the two COCAPP studies (acute and community mental health services). The total score and subscales for the ES were higher for responses obtained from service users in acute inpatient services that for those in contact with community mental health services, apart from power–powerlessness and righteous anger, which were comparable. See Chapter 5 for some exploratory inferential analyses.
Scale to Assess the Therapeutic Relationship
For service users, the mean total score for the STAR-P was 29.58 (12.20), with scores of 14.72 (7.22) for positive collaboration, 7.41 (3.38) for positive clinician input, and 7.75 (3.42) for non-supportive relationships. These scores align well with the reference values provided by Nolan (personal communication) shown in Table 38. The score for non-supportive clinician input is, however, marginally lower than the reference score.
| Subscale | COCAPP-A (acute inpatient) | COCAPP (community) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| STAR-P (service user) | STAR-C (staff) | STAR-P (service user) | |||||||
| n | Mean (SD) | Reference | n | Mean (SD) | Reference | n | Mean (SD) | Reference | |
| Positive collaborationa | 50 | 14.72 (7.22) | 14.36 (5.99)b | 39 | 18.21 (3.01) | 17.95 (2.98)b | 74 | 16.15 (6.57) | 19.9 (6.7)c |
| Positive clinician inputd | 50 | 7.41 (3.38) | 7.10 (2.91)b | 39 | 10.67 (1.20) | 10.42 (1.23)b | 75 | 7.83 (3.49) | 9.3 (3.0)c |
| Non-supportive clinician inpute (service users)/emotional difficultiese (staff) | 51 | 7.75 (3.42) | 8.78 (2.21)b | 38 | 8.59 (2.33) | 9.61 (1.65)b | 75 | 8.53 (3.11) | 9.3 (3.3)c |
| Total scoref | 50 | 29.58 (12.20) | 30.23 (9.71)b | 39 | 37.56 (4.82) | 37.93 (4.92)b | 75 | 32.33 (11.91) | 38.4 (12.0)c |
For staff the mean total for the STAR-C was 37.56 (4.82), with scores of 18.21 (3.01) for positive collaboration, 10.67 (1.20) for positive clinician input and 8.59 (2.33) for emotional difficulties. The subscale scores and total score for this study and the reference values are equivalent, apart from the emotional difficulties subscale, which is approximately 1 point higher in the reference value.
When comparing the service user and staff data, it is apparent that staff give higher scores and therefore rate the therapeutic relationship more positively than service users. Total scores are, on average, 8 points higher for staff than for service users. This reflects the pattern seen in the reference values.
An independent samples t-test was completed to determine if there were significant differences in the perceptions of the therapeutic relationship between service users and staff. There was a significant difference in the total STAR scores for service users (mean 29.58, SD 12.20) and staff (mean 37.56, SD 4.82) [t(67.1) = –4.22; p < 0.001, 95% CI –11.4 to –4.20; Cohen’s d = 0.86]. For the positive clinician input subscale, the scores for service users were lower (mean 7.41, SD 3.38) than those for staff (mean 10.67, SD 1.20) [t(63.9) = –6.32; p < 0.001; 95% CI –4.29 to –2.23; Cohen’s d = 1.28]. T-test statistics for the remaining subscales are provided in Chapter 5, Table 52.
A final comparison was made of the scores for the therapeutic relationships between the two COCAPP studies (acute and community mental health services). It is clear from the scores in Table 38 that service users in community mental health services score the therapeutic relationship marginally higher than those in acute mental health services.
Recovery Self-Assessment
Mean scores and SDs for the RSA are provided in Table 39. The mean scores from service users and staff on the subscales fell in the medium to moderate range (2.99–3.36 and 3.46–3.97, respectively). The difference in mean total RSA scores was higher for staff (mean 3.76, SD 0.56) than for service users (mean 3.20, SD 1.00). The lowest scoring subscales were individually tailored services and involvement for service users and involvement for staff. Both participant groups scored highly on the life goals and choice subscales.
| Subscale | COCAPP-A (acute inpatient) | COCAPP (community) | ||||||
|---|---|---|---|---|---|---|---|---|
| Service users | Staff | Service users | Staff | |||||
| n | Mean (SD)a | n | Mean (SD)a | n | Mean (SD)a | n | Mean (SD)a | |
| Life goals | 49 | 3.36 (1.13) | 41 | 3.97 (.60) | 68 | 3.30 (1.10) | 34 | 3.70 (.55) |
| Involvement | 44 | 3.06 (1.20) | 41 | 3.46 (.70) | 69 | 2.86 (1.23) | 34 | 2.86 (.56) |
| Diversity of treatment options | 48 | 3.15 (1.07) | 41 | 3.81 (.66) | 73 | 2.91 (1.16) | 34 | 2.74 (.51) |
| Choice | 51 | 3.26 (1.04) | 41 | 3.79 (.63) | 74 | 3.39 (.98) | 34 | 3.58 (.74) |
| Individually tailored services | 46 | 2.99 (1.08) | 42 | 3.75 (.58) | 71 | 2.89 (1.24) | 34 | 3.08 (.64) |
| Total score | 49 | 3.20 (1.00) | 42 | 3.76 (.56) | 73 | 3.10 (1.03) | 34 | 3.25 (.46) |
Independent-samples t-tests were conducted to compare the perceptions of recovery-oriented services for staff and service users. There was a significant difference in the total RSA scores between service users (mean 3.20, SD1.00) and staff (mean 3.76, SD 0.56) [t(77.6) = –3.33; p = 0.001; 95% CI –0.89 to –0.22; Cohen’s d = 0.70], highlighting that staff rate recovery higher than do service users. A similar trend was found with most of the subscale scores (t-test statistics for subscales are provided in Chapter 5, Table 52), apart from the involvement subscale, on which there is no difference between the scores that staff (mean 3.46, SD 0.70) and service users (mean 3.06, SD 1.20) provided [t(69.8) = –1.89; p = 0.062; 95% CI –0.82 to 0.02; Cohen’s d = 0.41].
A final comparison was made of the scores for the perceptions of recovery-oriented care between the COCAPP studies (acute and community mental health services). The RSA total scores for service users in community and acute mental health services in Provence were almost equivalent. Conversely, staff respondents from acute wards gave an overall higher RSA total score than those from community teams.
There are also some differences at the subscale level, with service users in acute wards scoring the involvement, diversity of treatment options subscales and, to a lesser extent, the life goals and individually tailored services subscales higher than respondents in community services. Similar to the other research sites, service user respondents in acute wards scored lower on the choice subscale than those in the community study.
There were also differences at the subscale level for staff. In our acute study, staff scored all of the subscales considerably higher than respondents in the community study. Interestingly, staff working in the acute wards scored the diversity of treatment options over 1 point higher than respondents in the community study. See Chapter 5 for some exploratory inferential analyses.
A recovery profile from the RSA scale is in Appendix 5.
Narrative summary of interview data: service users, carers and staff
Six staff were interviewed (three nurses, an OT, a therapeutic activity worker and a psychiatrist). Six service users participated, four women and two men, who had a range of contact with services from 1 year to > 10 years. For one service user this was their first admission, whereas two service users had been > 10 times. We conducted interviews with two carers.
Care planning and co-ordination
While some staff described actively involving service users in producing plans, most talked of too little time, few resources and the lack of individualised care plans. One said the CPA was about crisis and risk management with care plans serving only to protect staff against litigation. Communication with and involvement of CMHTs and care co-ordinators was problematic, often delaying discharge. Planning care was the same for detained and informal inpatients but staff thought the status of sectioned service users could be a barrier to engagement.
One service user was not aware of their care being planned and said that planning care meant giving medication and seeing what happened. A second said that staff were trying to get her a social worker and were giving her one-to-one time, but ‘apart from that I don’t really know what they’re up to’ (P-SU-103). Another service user felt relieved that they did not have to co-ordinate their own care, while another spoke of the challenge of moving to another location and not having a care plan with the new care co-ordinator. One carer was aware of co-ordination happening through the community team, while the other was not aware of care being planned.
Staff expressed contradictory views about care plan documentation: some said that digital storage had allowed for wider sharing of information, whereas others spoke of paper plans, failing to complete all of the documentation and community staff not seeing everything. Community care plans did not inform inpatient care. The CQC had criticised a lack of personalised care planning, so more individualised recovery-focused plans were now used, but there were two types of forms, some duplication and insufficient time to complete both.
All service users spoke of their experiences of care planning, with three confirming that they had a care plan. Two were not aware of what was written in the plan and did ‘not feel ownership’; for one this was in part because they did not want to share information about their past illness. One spoke of understanding the care plan’s content. A second service user talked of being well cared-for in hospital and said that their care plan was focused on meeting longer-term accommodation and support needs. A third service user described a regularly updated care plan focusing on safety and risk, and contrasted hospital care experiences with more rapport-based care received in the community. Three service users perceived that staff did little in the way of planning care.
One carer spoke approvingly of distraction techniques being included in the care plan, which the carer saw via the service user. A second carer had never seen a care plan, but thought that it would be helpful for informing them of any progress.
All service users spoke about admissions taking place in the context of self-referral or of family, friend or staff having concerns about their safety. Connections were made between community care and care in the ward, with one service user explaining how hospital staff had been given information about them and others reporting visits by their care co-ordinator. One of the two service users who spoke about their legal status felt that this was not communicated to them clearly.
Staff reported a mix of experiences regarding involvement and collaboration in the production of care plans. Two talked of service users owning their care plans and being involved in reviews and ward rounds. Service users sometimes withheld information or refused copies of their care plans. Care plans could cause upset if the language used was too ‘professional’ and it was important to record information when opinions differed. One described using verbatim quotes in care plans and ensuring that service users were aware when a conversation with a nurse was focused on their care rather than a general chat.
One service user was aware that the care plan had been drawn up and who their named nurse was. Two were troubled by the format of care planning; one wanted the plan to consider her future, her faith and her goals, and she wanted to be more directly involved:
I don’t know if there’s some sort of way if they could sort of write it out on paper while you’re there rather than, because at the moment they type it out and say if you want to make any changes just let me know. And usually you don’t want to just sit there highlighting everything, saying change this. But if they actually sort of created it with you [. . .].
P-SU-106
One service user felt that she had ownership of her care plan, yet she had not written it with staff and did not refer to it much. One carer talked of receiving a care plan that they were not involved in writing, despite being ‘in it together’ (P-CA-101).
Staff said that they placed great emphasis on planning and communicating with community-based colleagues and carers when speaking about discharge planning. The expectation was that they would talk about plans for discharge within 72 hours of a person’s admission, but this was not always possible.
Three service users spoke of being discharged with very little planning or notice, and of being invited into unscheduled meetings with staff to be informed of their imminent departures. One said that discussions about discharge and support with her carer took place only on the day she went home. The eleventh-hour arrangements for discharge were echoed by another service user, who recalled being ‘pulled in out of the blue’ to be told ‘right, you can go’ (P-SU-102). Four service users reported being involved in longer-term discharge planning. One said that discharge was discussed with his wife and with community staff. Carers did not feel informed about discharge arrangements and felt that these were hastily brought forward at short notice. When asked about preparations, one said ‘there wasn’t any’ (P-CA-101).
Care reviews
Weekly reviews for each service user involved members of the MDT, including care co-ordinators where possible, and carers. In the meetings, a clinical review took place for each service user followed by a record of actions to be taken. Care plans could be reviewed following ward rounds and in handovers. One nurse commented that the use of different sets of records by different professional groups was not helpful. Ward rounds could be rushed, with as many as 9–10 people being reviewed within 2.5 hours.
Staff talked of how they involved and listened to service users in reviews, but also of the challenges. Advocacy was mentioned but also that this could antagonise doctors. It was observed how ward rounds could be scary for service users, who might feel judged by the assembled staff.
Service users and carers talked of their experiences of care plan reviews that took place during ward rounds. None had any choice over timing, venue or who was invited other than carers. Their experiences of review meetings in wards rounds were mixed. One service user talked about her care co-ordinator sometimes helping her to prepare, and that ward rounds were sometimes helpful despite the number of people present:
Sometimes you’ve got a load of people in there and you sort of feel a bit like you’re on stage, you know like the spotlight’s on you, sort of thing. But yeah. I’ve had problems with ward rounds but more recently things have been OK, I’ve been able to sort of express myself more.
P-SU-104
Another spoke of being ‘totally involved’, finding ward rounds very helpful and that their ‘wishes and preferences are taken on board’ (P-SU-105) and decisions immediately acted on. A couple of service users, however, described ward rounds as sometimes being organised hastily and ‘quite rushed’, and not helpful: ‘I voice my opinion but they don’t listen’ (P-SU-103). Most talked of not feeling prepared for ward rounds. Two spoke of the ‘power’ in ward rounds and the anxiety they felt at having to ‘sit and wait anxiously’.
[You] shouldn’t really dread ward rounds in a way, but there’s some elements of they don’t really know you, like they just see you once a week and they dictate your life.
P-SU-106
One carer talked of having attended a hastily convened review meeting leading to a discharge that, in the carer’s view, had occurred too early.
Support systems
Staff talked about training for planning care, highlighting both their disciplinary backgrounds and in-service training including classroom sessions, e-learning and mandatory updates. Some also mentioned regular supervision and appraisals and becoming a mentor for student nurses.
Six service users talked of their relationships with named nurses. Five were aware that they had a primary nurse. Most described seeing their primary nurses regularly and having good relationships, and of them being available and good listeners. Most described ward staff as being helpful and said that they trusted them. One-to-one meetings happened, although these were not always pre-arranged. One carer spoke of the person they cared for having good relationships with staff and of being supported, and was aware of the key people on the ward:
They knew how to talk to her and how to get stuff out of her. I mean I found out stuff while she was in there that I didn’t know, because she’d spoken to someone so.
P-CA-101
All service users said that staff treated service users with dignity and respect, although one said that some members of staff were nicer and more compassionate than others. Two spoke of how staff had acted with compassion, care and concern for dignity when helping a distressed woman who had been walking naked through the ward.
Service users also described support from professional and other workers both in hospital and the community. One mentioned he would like to see the community staff visit when the service user is in hospital to build relationships.
Staff talked of working with colleagues to plan care and said that they welcomed links with peer support workers, advocates and others. Helping service users maintain their connections to the community, such as working with families and friends, and welcoming involvement, also brought challenges and frustrations. One spoke of a family member becoming ‘too involved’:
. . . to the point we were asking her not to come in because she wasn’t actually helping in any way and just making things worse.
P-ST-101
Service users spoke of support from family members and other informal carers such as friends and neighbours, but the extent of the help varied. Three described the support they had received from other service users.
The carers felt supported and listened to by staff and knew that community staff were also involved. Carers spoke positively about staff, who they said treated service users with respect, care and compassion. One said, ‘I think they need a medal to be honest with you’ (P-CA-101).
Safety and risk
Ensuring patient safety and managing risk were described by staff as central to their work, with risk assessments ‘coming out of your eyeballs’ (P-ST-101) alongside routine work including observations, ligature audits and clinical reviews. One nurse mentioned reviews at daily handovers and risk assessments shaping what service users could and could not do. One staff member spoke about how difficult it could be to directly address risk during a ward round when the service user was present.
Service users gave examples of when care plans took issues of risk into account, such as recording the use of observations, noting when people have been accompanied off the ward and checking regularly on those who self-harm. One service user talked of safety being considered, saying how ‘they’re there to look after you’ (P-SU-102), but also said that they had not had conversations with staff about safety or risk. Another service user felt that her safety had ‘absolutely’ been considered in her care planning, and gave the examples of her previous risk history being shared with the hospital staff and her observation level being changed when needed. Carers talked about staff taking action to keep people safe, such as removing dangerous objects and conducting frequent observations.
Organisational context
Staff talked about positive developments, including working with only one consultant, the introduction of a housing worker and peer support workers, and greater service user involvement and recovery focus in care planning. A recent duty of candour policy and the introduction of advanced directives were also mentioned. However, changes in shift patterns meant that morning shifts that included ward rounds left little time for anything else. The introduction of a Section 136 room had placed additional demands on staff, as had the introduction of Modified Early Warning Scores, a process for the assessment of physical health.
Recovery
One staff member defined recovery as returning to a ‘normal’ state of functioning. Others spoke of people on a journey to become what they wanted to be, and gave a holistic view of their potential:
[. . .] being able to make improvements in all aspects of their life really. Ensuring stability of their mental health but helping them recover in all aspects of their life as well.
P-ST-104
It was also acknowledged that recovery was an individual process, drawing on personal values and aims, that involved both progress and setbacks. Staff noted the differences in orientation to recovery between hospital and community, including the short-term, sometimes crisis-oriented, nature of the hospital experience.
One service linked recovery to symptoms: ‘getting rid of the voices and what I see. That’s my recovery’ (P-SU-101). Three spoke of returning to a previous state; for example:
[G]etting back to your even normal state that you were a year ago or a few months ago or however long it was, and just feeling healthy and happy and joyful or whatever you want to, and something like that.
[P-SU-102]
Another identified recovery being able:
To do what you want to in your life, as in I want to go to college, I want to finish my degree, I’ve got 2 more years and while I might not be dancing round and everything is wonderful, it’s a slow process but just getting my normal life back really.
P-SU-104
One carer used ‘recovery’ in its clinical sense to indicate that they thought the person would never fully recover, while a second carer embraced a more holistic view of recovery as a process of moving on and learning.
All service users said that hospital had helped their recovery in various ways: by stopping them from hurting themselves; by helping them to feel strong and positive on discharge; by assisting with stabilising mood and feeling safe; and by providing medication and stabilisation. One mentioned that having greater involvement in the planning of her care would have helped with her recovery.
Staff gave divergent responses to questions on the relationships between care, care planning and recovery. One said that recovery had no influence over the way care was planned, but another described how recovery ideas had exerted an impact on his approach to care planning.
Personal recovery plans did not feature strongly in service users’ talk. One said that her care plan focused on helpful distraction techniques, but not on strengths. Another service user talked about achievements being recognised.
Staff gave divergent views on the implementation of recovery-focused care in hospital. For example, a ward manager talked of care plans being very medically driven with almost no focus on strengths and abilities. WRAPs were not used.
Personalisation
Staff were unsure what personalisation meant but offered suggestions, including tailoring care, ensuring that people felt like individuals and care being patient-centred. Only one linked it to personal payments. Service users were also unsure of what was meant by personalisation, although again several felt that it was about tailoring care to the individual. One said:
I don’t know, maybe helping yourself or making your own personal goals maybe? I don’t really know to be honest.
P-SU-103
One carer suggested the idea of personal goals and achievements, while another said:
I guess personalisation means the way her treatment was personalised for her and I guess it was, because everyone is different and everyone needs different help, but I don’t really know what you mean.
P-CA-101
One ward manager said that care was not personalised, as turnover was rapid and the emphasis was on medical treatment. One psychiatrist said that care was not tailored. Others spoke of building rapport and taking account of individual needs. Most service users and carers felt that their care had been personalised to a degree.
Barriers and facilitators
All staff explicitly spoke of the importance of having time to spend with service users, and of talking and listening. This was linked to therapeutic relationships:
I would say that it’s probably being able to build a rapport with a patient, and a therapeutic relationship, that would, I think is the most important thing or tool that I could use as a nurse to, yeah.
P-ST-104
Having more of a recovery-focused approach in the ward was mentioned, as was the importance of instilling hope. Practical help with housing and benefits was seen as important by one staff member, and staff training was seen as important by another.
One carer said that a key challenge was to get more staff. For staff, lack of time and resources featured prominently, encompassing the challenge of staff being deflected by administrative tasks, a reliance on paper (rather than electronic) records, incompatible computer systems, poor communication, and unhelpful separations between hospital and community care.
Closer collaboration between staff and service users in care plan construction was discussed, along with the suggestion that technology might support this (e.g. using tablet computers).
A service user and a carer both spoke of the need for more involvement in care planning and the limited activities available on the ward causing problems for sectioned inpatients who were unable to leave. Carers spoke of the importance of discharge planning, the problem of sudden discharge and lack of accessibility of care plans for visitors in terms of the language used.
Care plan reviews
Eight participants were selected for care plan reviews on the main ward in Provence. These were three female and five male service users who ranged in age from 26 to 43 years; five were formally detained. For three service users this was their first admission to hospital. Three service users had signed their care plans and all care plans had named-nurse signatures. It was clear that only one service user had been given a copy of the care plan and one other had declined the offer. In one case was it clear that a carer had attended a ward round. It was not possible to determine if any service users, advocates or care co-ordinators had attended previous ward rounds, indicating a potential issue of continuity of care. Only four care plans showed evidence of the person’s views being included. The language used varied between describing the service user’s problems in the third person (e.g. ‘describes feeling in his head as ‘chaotic’) and, occasionally, in the first person using quotations in the service user views sections of the plan (e.g. ‘I’m fed up of this’). Most care plans (four out of eight at best for the following categories) did not show evidence of strengths-based approaches, coproduction, personalisation or recovery-focused approaches. When this was evident, the attempt was only partial, suggesting a need for a more sustained focus to achieve these requirements. Seven out of eight care plans showed an orientation towards system-based or medical goals, usually focusing on medication compliance and managing risk, with only one care plan showing person-centred goals and two showing encouragement towards self-management (although these attempts were only partial). Seven out of eight care plans addressed discharge plans. The plans usually showed evidence of a concern about accommodation issues and, in one case, continuity in the form of a request that the care co-ordinator be invited to attend a ward round.
Meeting observations
In Provence, three observations of ward round meetings were conducted. Five people attended all three meetings: two researchers, a senior nurse, a psychiatrist and the service user. In some meetings other clinicians (an OT, a psychologist, a link pathway nurse and a pharmacist) were also in attendance. A carer was present at one of the meetings. For all meetings the nurse collected the service user from the ward, greeting them with warmth and apologising for the delays (20–50 minutes). The meeting was held in a light, spacious room in which chairs were arranged in a circle. The nurse took notes behind a computer, while the doctor, who led the meeting, sat in a large wing-backed chair opposite a seat reserved for the service user. In all meetings, it appeared that the relationship between the doctor, nurse and service user was well established. Introductions were provided for those who had not met. In two of the meetings the service users began speaking without being prompted. One did, however, walk in the room and state ‘I’m terrified’, to which no response was given. Time was provided for the person to speak. The doctor displayed varying levels of interest in what colleagues, the service user and carer had to say. He made good use of clarifying questions when exploring behavioural patterns, but little empathy was displayed. One service user explained that he found it hard to articulate his views; the nurse reassured him that he was coming across fine but the doctor did not respond to this and continued to ask more questions. There were periods of silence during which feelings were not addressed; however, some staff members did interject to empathise but often the conversation was swiftly moved on. At times the doctor appeared disinterested, sitting with his arms crossed, refraining from using eye contact and showing minimal facial expressions throughout. When the doctor mentioned medication he spoke very assertively, stating ‘I will change . . .’ rather than working in collaboration with the person.
The carer was given time to speak and was reassured by the nurse, OT and psychologist about concerns, and it was acknowledged that the process was daunting. The care plan was not discussed during any of the meetings; physical health was, however, explored in one meeting. One meeting was terminated early by the service user because of conflict. In this meeting the doctor began by stating definitively that ‘I spoke to you on Friday; since Friday you have been quite hostile’. The service user agreed that he was angry; however, the ensuing stunted dialogue was matched by the participants’ defensive body language and failed to develop. The conversation was swiftly moved on to medication. Disagreement ensued, which led to the service user storming out of the room (after only a few minutes) saying ‘I want interaction with you; I don’t get one’. The doctor was quite defensive but did try to reassure the service user about the safety of medication; however, his personal questions were not given direct responses. After this meeting the doctor decided that the person did not have capacity and spoke about this in quite a derogatory way. The main focus of the meetings was for medication review, although social outcomes were attended to in one instance. After all of the meetings, the nurse and doctor briefly discussed and agreed what to include in the notes using predefined sections (e.g. Modified Early Warning Score, risk and activities).
Chapter 5 Results: cross-case analysis
Summary of chapter
In this chapter, we conduct a comparison across the six sites. The chapter is in two sections. The first contains a cross-case analysis of scores on the quantitative measures. In the second, we draw on the within-case analysis of the qualitative data presented in the previous chapter and focus on six key areas: care planning and co-ordination, support systems, safety and risk, organisational context, recovery and personalisation. These are then discussed in more detail in the final chapter.
Cross-case analysis of the quantitative data
Unadjusted analyses
Inferential statistics were used to determine if there were any differences across sites for the four questionnaires. Cross-site analyses will be presented for the four service user questionnaires (VOICE, RSA, STAR-P and ES) followed by a cross-site analysis of the two staff questionnaires (RSA and STAR-C). Within-site analyses were completed to determine if there were differences between the perspectives of service users and staff on the questionnaires (RSA and STAR). In addition, several correlations were conducted to determine associations between the questionnaire subscales and totals globally and on a site-specific basis.
Service users
One-way ANOVAs of all subscales were conducted and revealed that there were no global differences across the sites for any of the four questionnaires. Table 40 shows the mean item scores, alongside the parameters of significance.
| VOICE | One-way ANOVA statistics | Site, mean (SEM) | |||||
|---|---|---|---|---|---|---|---|
| Artois | Burgundy | Champagne | Dauphine | Languedoc | Provence | ||
| Mean total score | F(5,294) = 0.49; p = 0.787 | 49.43 (2.77) | 45.69 (2.40) | 51.56 (2.33) | 48.77 (2.53) | 49.04 (2.92) | 48.55 (2.81) |
| RSA | |||||||
| Life goals | F(5,284) = 0.14; p = 0.984 | 3.45 (0.15) | 3.40 (0.15) | 3.35 (0.14) | 3.49 (0.14) | 3.38 (0.17) | 3.36 (0.16) |
| Involvement | F(5,264) = 0.05; p = 0.999 | 3.08 (0.17) | 3.07 (0.18) | 3.11 (0.16) | 3.11 (0.14) | 3.16 (0.19) | 3.06 (0.18) |
| Diversity of treatment options | F(5,277) = 0.56; p = 0.734 | 3.16 (0.15) | 3.31 (0.14) | 3.01 (0.13) | 3.29 (0.12) | 3.12 (0.18) | 3.15 (0.15) |
| Choice | F(5,290) = 0.54; p = 0.748 | 3.06 (0.14) | 3.40 (0.15) | 3.25 (0.14) | 3.23 (0.14) | 3.19 (0.18) | 3.26 (0.15) |
| Individually tailored services | F(5,255) = 0.34; p = 0.891 | 3.17 (0.17) | 3.28 (0.15) | 3.22 (0.17) | 3.19 (0.16) | 3.12 (0.19) | 2.99 (0.16) |
| Mean total score | F(5,280) = 0.13; p = 0.989 | 3.21 (0.06) | 3.32 (0.14) | 3.24 (0.12) | 3.30 (0.12) | 3.23 (0.17) | 3.20 (0.14) |
| STAR-P | |||||||
| Positive collaboration | F(5,288) = 0.45; p = 0.814 | 14.99 (0.94) | 15.28 (0.93) | 15.88 (0.82) | 14.98 (0.97) | 13.85 (1.13) | 14.72 (1.02) |
| Positive clinician input | F(5,290) = 0.99; p = 0.422 | 7.32 (0.47) | 7.47 (0.46) | 7.85 (0.46) | 7.16 (0.44) | 6.38 (0.56) | 7.41 (0.48) |
| Non-supportive clinician input | F(5,288) = 0.77; p = 0.569 | 6.77 (0.46) | 7.19 (0.43) | 7.62 (0.47) | 7.04 (0.46) | 7.71 (0.51) | 7.75 (0.48) |
| Mean total score | F(5,289) = 0.50; p = 0.778 | 29.02 (1.55) | 30.00 (1.48) | 31.35 (1.39) | 29.17 (1.39) | 27.93 (1.83) | 29.58 (1.73) |
| ES | |||||||
| Self-esteem–self-efficacy | F(5,287) = 1.16; p = 0.330 | 3.05 (0.10) | 2.87 (0.13) | 3.22 (0.10) | 2.99 (0.10) | 3.07 (0.10) | 2.98 (0.11) |
| Power–powerlessness | F(5,284) = 1.32; p = 0.257 | 2.47 (0.09) | 2.40 (0.08) | 2.54 (0.08) | 2.32 (0.08) | 2.52 (0.07) | 2.56 (0.08) |
| Community activism and autonomy | F(5,282) = 0.85; p = 0.515 | 3.22 (0.09) | 3.34 (0.08) | 3.29 (0.07) | 3.25 (0.07) | 3.41 (0.08) | 3.25 (0.07) |
| Optimism and control over the future | F(5,289) = 0.48; p = 0.788 | 2.89 (0.11) | 2.95 (0.12) | 2.98 (0.10) | 2.98 (0.09) | 3.12 (0.10) | 3.00 (0.10) |
| Righteous anger | F(5,287) = 0.59; p = 0.707 | 2.37 (0.11) | 2.49 (0.11) | 2.31 (0.11) | 2.34 (0.08) | 2.26 (0.11) | 2.29 (0.10) |
| Total score | F(5,289) = 0.82; p = 0.539 | 2.85 (0.07) | 2.81 (0.07) | 2.93 (0.05) | 2.80 (0.05) | 2.92 (0.05) | 2.85 (0.06) |
Comparison of recovery profiles: Recovery Self-Assessment
In Table 41 we present a comparison summary of the five highest-rated items for service users on the RSA across the sites. The domain that occurs most frequently in the highest-rated items across our six research sites is life goals. Common items within this domain were that staff used a language of recovery, believed that service users could recover and make their own treatment and life choices, and were diverse in terms of culture, ethnicity, lifestyle and interests. Service users in Artois and Languedoc scored the knowledge staff had about special interest groups and activities in the community highly. Other items within the top five rated items were within the individually tailored and choice subscales. For the individually tailored subscale, service users in Artois and Champagne responded highly on the item referring to effort made by the service provider to involve significant others in support and planning. The items that service users scored highly within the choice subscale were related either to staff helping to monitor progress towards personal goals (Artois, Champagne and Burgundy) or to staff not using threats and bribes to influence choice and behaviour (Provence, Languedoc and Dauphine).
| Rank | Artois (mean of 3.52–3.83 on Likert scale) | Burgundy (mean of 3.70–3.81 on Likert scale) | Champagne (mean of 3.63–3.73 on Likert scale) | Dauphine (mean of 3.56–3.98 on Likert scale) | Languedoc (mean of 3.49–3.67 on Likert scale) | Provence (mean of 3.56–4.10 on Likert scale) |
|---|---|---|---|---|---|---|
| 1 | Staff are diverse in terms of culture, ethnicity, lifestyle and interests Life goals |
Staff believe that I can recover and make my own treatment and life choices Life goals |
My service provider makes every effort to involve my significant others and other sources of natural support in the planning of my services, if this is my preference Individually tailored services |
Staff are diverse in terms of culture, ethnicity, lifestyle and interests Life goals |
The role of staff is to assist me, and other people in recovery with fulfilling my individually defined goals and aspirations Life goals |
Staff do not use threats, bribes or other forms of coercion to influence my behaviour or choices Choice |
| 2 | Staff are knowledgeable about special interest groups and activities in the community Life goals |
Staff are diverse in terms of culture, ethnicity, lifestyle and interests Life goals |
Staff believe that I can recover and make my own treatment and life choices Life goals |
Staff use a language of recovery (i.e. hope, high expectations, respect) in everyday conversations Life goals |
Staff do not use threats, bribes or other forms of coercion to influence my behaviour or choices Choice |
Staff are diverse in terms of culture, ethnicity, lifestyle and interests Life goals |
| 3 | My service provider makes every effort to involve my significant others and other sources of natural support in the planning of my services, if this is my preference Individually tailored services |
Staff help to monitor the progress I am making towards my personal goals on a regular basis Choice |
Staff help to monitor the progress I am making towards my personal goals on a regular basis Choice |
Staff believe that I can recover and make my own treatment and life choices Life goals |
Staff believe that I can recover and make my own treatment and life choices Life goals |
Staff use a language of recovery (i.e. hope, high expectations, respect) in everyday conversations Life goals |
| 4 | Staff use a language of recovery (i.e. hope, high expectations, respect) in everyday conversations Life goals |
Staff regularly attend trainings on cultural competency Individually tailored services |
Staff are diverse in terms of culture, ethnicity, lifestyle and interests Life goals |
Staff do not use threats, bribes, or other forms of coercion to influence my behaviour or choices Choice |
Staff are knowledgeable about special interest groups and activities in the community Life goals |
Staff believe that I can recover and make my own treatment and life choices Life goals |
| 5 | Staff help to monitor the progress I am making towards my personal goals on a regular basis Choice |
Staff use a language of recovery (i.e. hope, high expectations, respect) in everyday conversations Life goals |
Staff use a language of recovery (i.e. hope, high expectations, respect) in everyday conversations Life goals |
The role of staff is to assist me, and other people in recovery with fulfilling my individually defined goals and aspirations Life goals |
The achievement of my goals is formally acknowledged and celebrated by the agency Life goals |
The role of staff is to assist me, and other people in recovery with fulfilling my individually defined goals and aspirations Life goals |
In Table 42 we present a comparison summary of the five lowest-rated items for service users on the RSA across sites. The domains that occur frequently within the lowest-rated items across the six sites are diverse, falling within choice, involvement, diversity of treatment options, individually tailored services and life goals. Some items came up frequently across four/five sites. These related to choice, such as access to treatment records and choosing to change the therapist, psychiatrist or other service provider. Other low-rated items were around involvement in staff training and education programs and being regular members of advisory boards and management meetings. A further area related to the diversity of treatment options and opportunities to discuss sexual and spiritual needs and interests.
| Rank | Site | |||||
|---|---|---|---|---|---|---|
| Artois (mean of 2.24–2.89 on Likert scale) | Burgundy (mean of 2.62–3.02 on Likert scale) | Champagne (mean of 2.52–2.88 on Likert scale) | Dauphine (mean of 2.81–2.96 on Likert scale) | Languedoc (mean of 2.68–2.82 on Likert scale) | Provence (mean of 2.75–2.85 on Likert scale) | |
| 1 | I have access to all my treatment records Choice |
I have access to all my treatment records Choice |
I am able to choose from a variety of treatment options at this agency (i.e. individual, group, peer support, holistic healing, alternative treatments, medical) Diversity of treatment options |
I am/can be involved with facilitating staff trainings and education programs at this agency Involvement |
I have access to all my treatment records Choice |
I am given the opportunity to discuss my sexual and spiritual needs and interests Diversity of treatment options |
| 2 | I can choose and change, if desired, the therapist, psychiatrist or other service provider with whom I work Choice |
I am/can be a regular member of agency advisory boards and management meetings Involvement |
I am/can be a regular member of agency advisory boards and management meetings Involvement |
I can choose and change, if desired, the therapist, psychiatrist or other service provider with whom I work Choice |
I am/can be a regular member of agency advisory boards and management meetings Involvement |
I have access to all my treatment records Choice |
| 3 | I am/can be involved with facilitating staff trainings and education programs at this agency Involvement |
This agency actively attempts to link me with other persons in recovery who can serve as role models or mentors by making referrals to self-help, peer support or consumer advocacy groups or programs Diversity of treatment options |
Most of my services are provided in my natural environment (i.e. home, community, workplace) Choice |
This agency provides education to community employers about employing people with mental illness and/or addictions Individually tailored services |
I am/can be involved with facilitating staff trainings and education programmes at this agency Involvement |
I can choose and change, if desired, the therapist, psychiatrist or other service provider with whom I work Choice |
| 4 | I am given the opportunity to discuss my sexual and spiritual needs and interests Diversity of treatment options |
I am/can be involved with facilitating staff trainings and education programs at this agency Involvement |
Staff actively assist me with the development of career and life goals that go beyond symptom management and stabilisation Life goals |
I am given the opportunity to discuss my sexual and spiritual needs and interests Diversity of treatment options |
I can choose and change, if desired, the therapist, psychiatrist or other service provider with whom I work Choice |
Staff focus on helping me to build connections in my neighbourhood and community Individually tailored services |
| 5 | This agency provides education to community employers about employing people with mental illness and/or addictions Individually tailored services |
Staff play a primary role in helping me to become involved in non-mental health/addiction related activities, such as church groups, special interest groups and adult education Life goals |
Staff routinely assist me in the pursuit of my educational and/or employment goals Life goals |
I am/can be a regular member of agency advisory boards and management meetings Involvement |
I am given the opportunity to discuss my sexual and spiritual needs and interests Diversity of treatment options |
I am/can be a regular member of agency advisory boards and management meetings Involvement |
Staff
One-way ANOVAs were conducted for the mean RSA and STAR-C total scores and the subscales for staff (Table 43). There was a significant difference between the research sites in the mean RSA total score [F(5, 279) = 6.35; p < 0.001; η2 = 0.32] and the mean total score for the STAR-C [F(5, 273) = 3.02; p = 0.011; η2 = 0.23]. There were also significant differences found in all of the mean item subscale scores of the RSA and the positive collaboration subscale for the STAR-C (see Table 43).
| Measure | One-way ANOVA statistics | Site, mean (SEM) | |||||
|---|---|---|---|---|---|---|---|
| Artois | Burgundy | Champagne | Dauphine | Languedoc | Provence | ||
| RSA | |||||||
| Life goals | F(5,273) = 4.44; p = 0.001** | 3.53 (0.08) | 3.67 (0.11) | 3.52 (0.08) | 3.93 (0.07) | 3.68 (0.10) | 3.97 (0.09) |
| Involvement | F(5,275) = 4.94; p < 0.001** | 3.15 (0.09) | 3.05 (0.13) | 2.85 (0.10) | 3.47 (0.10) | 3.25 (0.10) | 3.46 (0.11) |
| Diversity of treatment options | F(5,279) = 7.45; p < 0.001** | 3.21 (0.10) | 3.42 (0.11) | 3.06 (0.10) | 3.72 (0.10) | 3.39 (0.10) | 3.81 (0.10) |
| Choice | F(5,278) = 3.14; p = 0.009** | 3.47 (0.09) | 3.72 (0.11) | 3.46 (0.07) | 3.73 (0.09) | 3.84 (0.09) | 3.79 (0.10) |
| Individually tailored services | F(5,239) = 10.95; p < 0.001** | 3.29 (0.09) | 3.34 (0.11) | 2.92 (0.08) | 3.81 (0.09) | 3.32 (0.10) | 3.75 (0.09) |
| Mean total score | F(5,279) = 6.35; p < 0.001** | 3.36 (0.08) | 3.45 (0.10) | 3.21 (0.07) | 3.74 (0.07) | 3.52 (0.09) | 3.76 (0.09) |
| STAR-C | |||||||
| Positive collaboration | F(5,274) = 2.42; p = 0.036* | 17.17 (0.35) | 18.86 (0.39) | 17.63 (0.42) | 18.20 (0.33) | 18.22 (0.36) | 18.21 (0.48) |
| Positive clinician input | F(5,272) = 1.53; p = 0.182 | 10.34 (0.18) | 10.95 (0.18) | 10.41 (0.21) | 10.38 (0.15) | 10.55 (0.20) | 10.57 (0.19) |
| Emotional difficulties | F(5,270) = 1.91; p = 0.092 | 8.60 (0.20) | 9.50 (0.21) | 8.95 (0.27) | 8.86 (0.23) | 9.15 (0.21) | 8.59 (0.38) |
| Mean total score | F(5,273) = 3.02; p = 0.011** | 36.08 (0.55) | 39.33 (0.66) | 37.00 (0.76) | 37.45 (0.52) | 37.98 (0.62) | 37.56 (0.77) |
Recovery Self-Assessment questionnaire
When using Artois and Champagne as reference sites (the sites with the lowest scores), it is apparent that Provence and Dauphine are scored significantly higher for the mean RSA total score (Figure 4). This scale measures some important perceptions that may have a significant effect on patient outcomes and concordance to care and collaboration with service users. Subsequent Tukey’s post hoc tests revealed that staff in Artois (3.36, SD 0.59) scored significantly lower on the subscale than staff in Provence (3.76, SD 0.56; p = 0.009; 95% CI –0.73 to –0.07; Cohen’s d = 0.69) and Dauphine (3.74, SD 0.53; p = 0.009; 95% CI –0.70 to –0.06; Cohen’s d = 0.68). Staff in Champagne (3.21, SD 0.46) scored significantly lower on the subscale than staff in Provence (p < 0.001; 95% CI –0.92 to –0.19; Cohen’s d = 1.07) and Dauphine (p < 0.001; 95% CI –0.88 to –0.19; Cohen’s d = 1.07). There were no significant differences between Artois and Champagne and the other sites on this subscale.
FIGURE 4.
Mean total RSA score for staff (95% CI). Scoring range for the mean is from 0 to 5. *p = 0.05; **p = 0.01. Note that * identifies a significant difference compared with Artois and # identifies a significant difference compared with Champagne. The response range for the items is from 1 to 5.
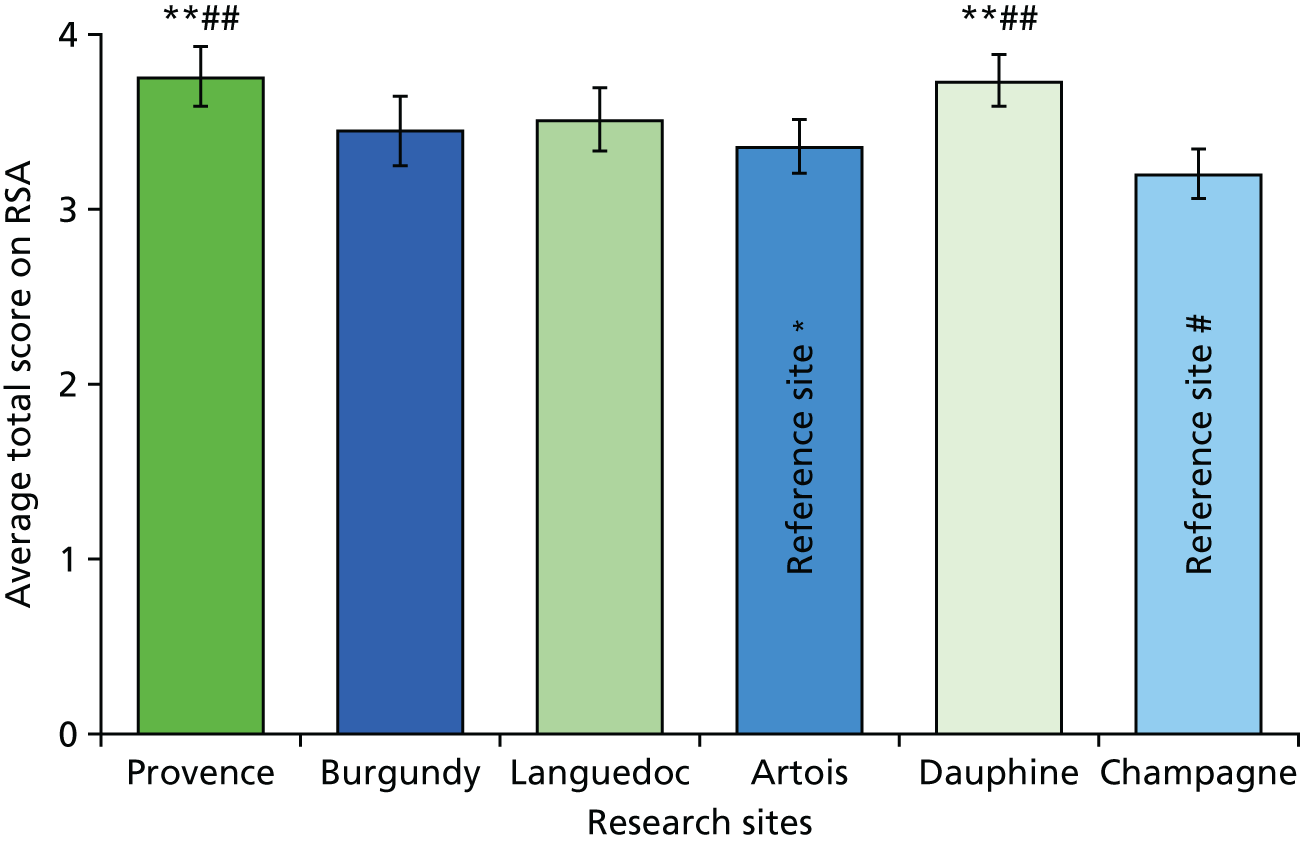
When using Artois and Champagne as reference sites (the sites with the lowest scores), it is apparent that Provence and Dauphine sites are scored significantly higher by staff for the mean life goals subscale score (Figure 5). This scale measures some important perceptions encompassing the extent that staff support the development and pursuit of individually defined life goals such as employment and education. 48 Subsequent Tukey’s post hoc tests revealed that staff in Artois (3.53, SD 0.61) scored significantly lower on the subscale than staff in Provence (3.97, SD 0.56; p = 0.009; 95% CI –0.81 to –0.07; Cohen’s d = 0.75) and Dauphine (3.93, SD 0.53; p = 0.013; 95% CI –0.75 to –0.05; Cohen’s d = 0.70). Staff in Champagne (3.52, SD 0.52) scored significantly lower on the subscale than staff in Provence (p = 0.016; 95% CI –0.84 to –0.05; Cohen’s d = 0.80) and Dauphine (p = 0.023; 95% CI –0.78 to –0.03; Cohen’s d = 0.78). There were no significant differences between Artois and Champagne and the other sites on this subscale.
FIGURE 5.
Mean life goals subscale score for staff (95% CI). Scoring range for the mean is from 0 to 5. *p = 0.05; **p = 0.01. Note that * identifies a significant difference compared with Artois and # identifies a significant difference compared with Champagne. The response range for the items is from 1 to 5.
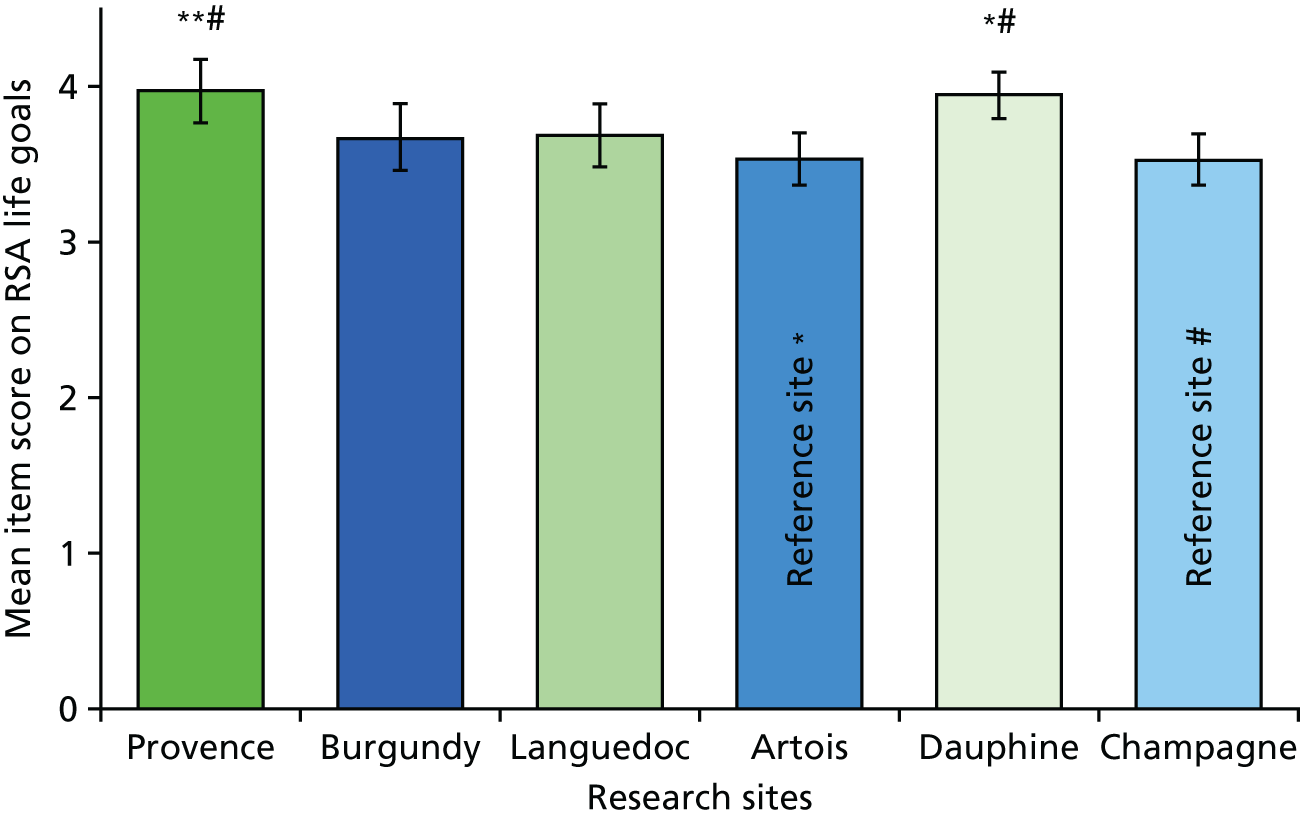
When using Champagne as a reference site (the site with the lowest score), it is apparent that Provence and Dauphine perform significantly better on the RSA involvement subscale (Figure 6). This scale measures some important perceptions encompassing service user involvement, such as the extent to which service users are involved in the development and provision of services, staff training and advisory board meetings. 48 Subsequent Tukey’s post hoc tests revealed that staff in Champagne (2.85, SD 0.62) scored significantly lower on the subscale than staff in Provence (3.46, SD 0.70; p = 0.002; 95% CI –1.07 to –0.16; Cohen’s d = 0.92) and Dauphine (3.47, SD 0.68; p = 0.001; 95% CI –1.05 to –0.18; Cohen’s d = 0.95). There were no significant differences between Champagne and the other sites on this subscale.
FIGURE 6.
Mean involvement subscale score for staff (95% CI). Scoring range for the mean is from 0 to 5. *p = 0.05. Note that * identifies a significant difference compared with Champagne. The response range for the items is from 1 to 5.
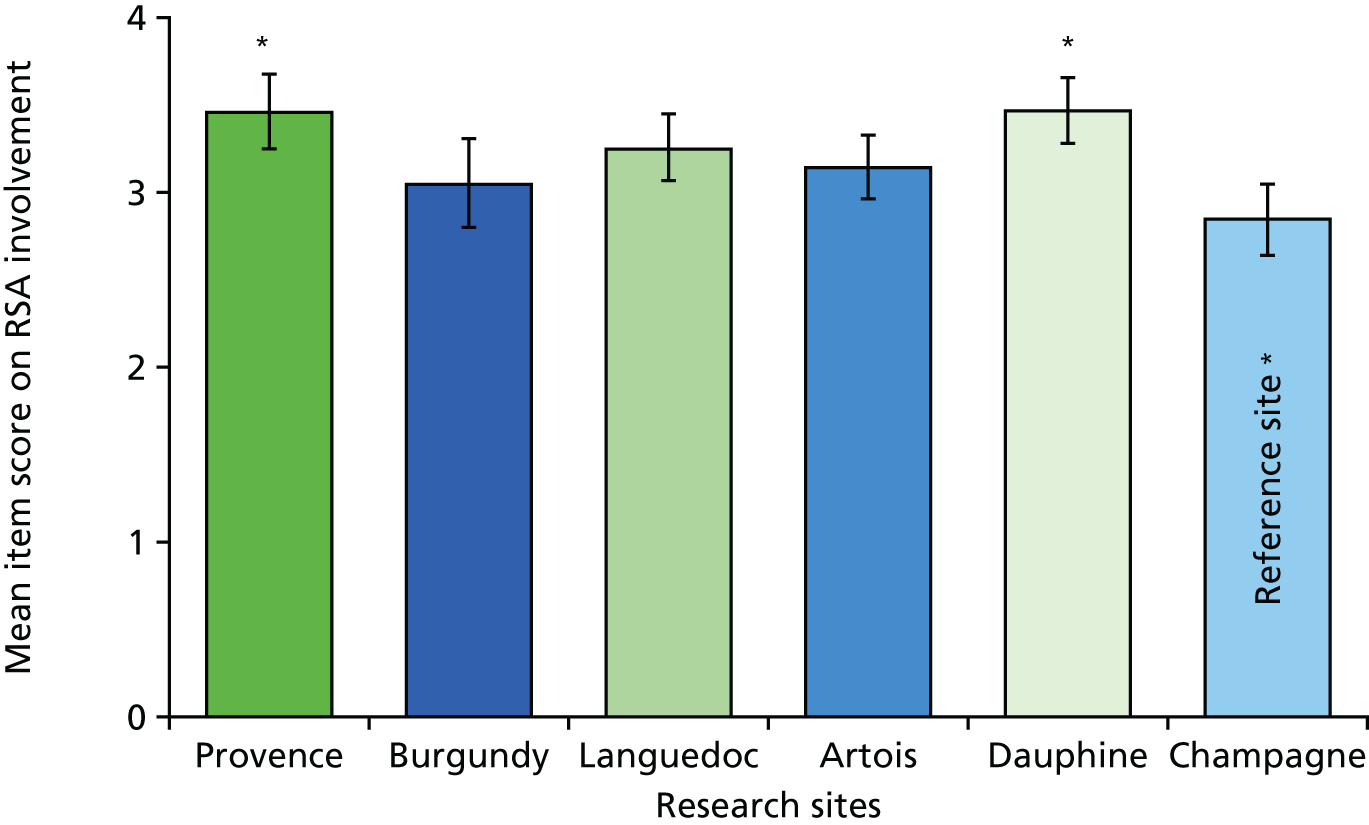
When using Artois and Champagne as reference sites (the sites with the lowest scores), it is apparent that Provence and Dauphine sites were performing significantly better for the mean diversity of treatment options subscale score (Figure 7). This scale measures some important perceptions relating to the extent to which the trust/board provides links to peer mentors and support, variety of treatment options and assistance with becoming involved in non-mental health related activities. 48
FIGURE 7.
Mean diversity subscale score for staff (95% CI). Scoring range for the mean is from 0 to 5. **p = 0.01. Note that * identifies a significant difference compared with Artois and # identifies a significant difference compared with Champagne. The response range for the items is from 1 to 5.
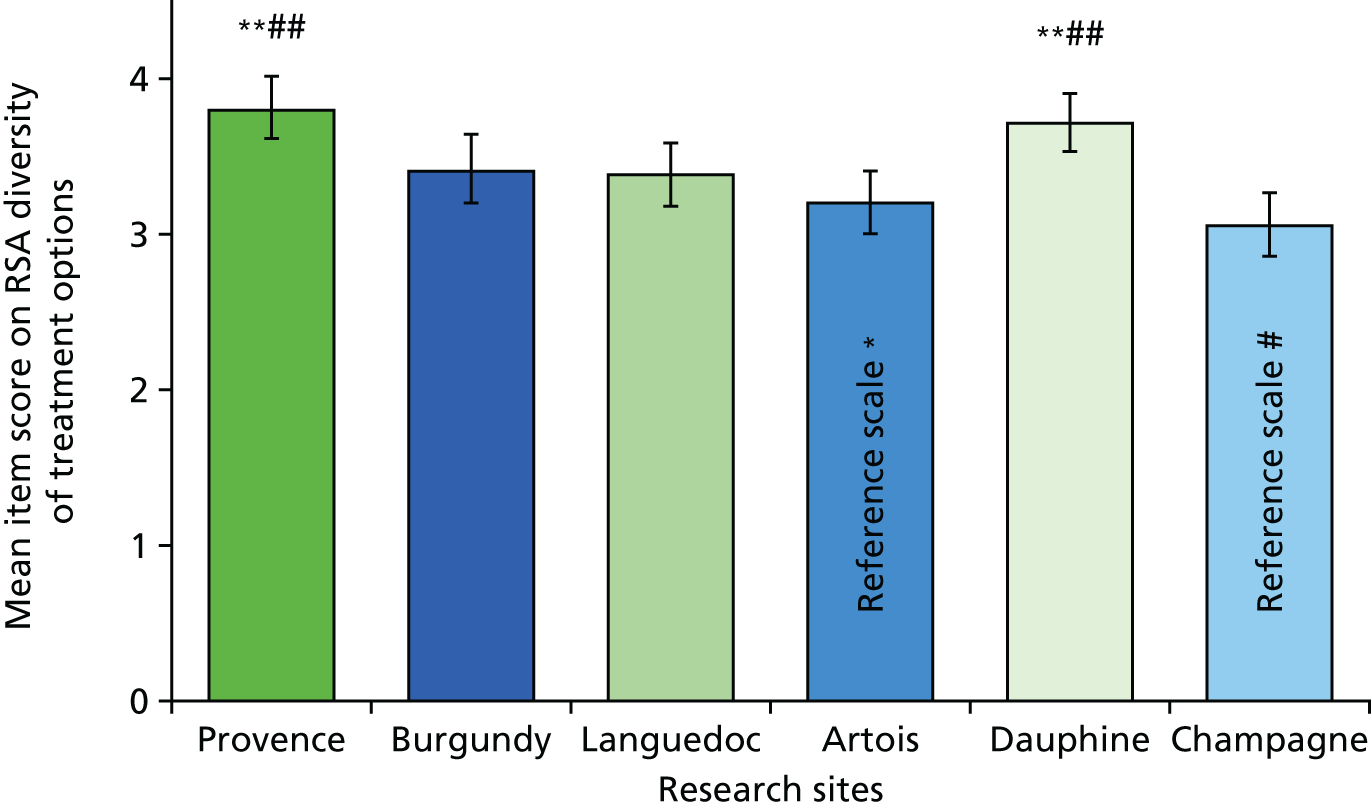
Subsequent Tukey’s post hoc tests revealed that staff in Artois (3.21, SD 0.77) scored significantly lower on the subscale than staff in Provence (3.81, SD 0.66; p = 0.001; 95% CI –1.02 to –0.19; Cohen’s d = 0.84) and Dauphine (3.72, SD 0.69; p = 0.003; 95% CI –1.02 to –0.19; Cohen’s d = 0.70). Staff in Champagne (3.06, SD 0.65) also score significantly lower on the subscale than staff in Provence (p < 0.001; 95% CI –1.20 to –0.30; Cohen’s d = 1.15) and Dauphine (p < 0.001; 95% CI –1.09 to –0.23; Cohen’s d = 0.98). There were no significant differences between Artois and Champagne and the other sites on this subscale.
It is apparent that Languedoc performed significantly better for the mean Choice subscale score than Artois (Figure 8). This scale measures some important perceptions of the extent to which service users have access to their medical records, that the choices of service users are respected and that measures which are considered coercive in nature are not employed. Subsequent Tukey’s post hoc tests revealed that staff in Artois (3.47, SD 0.67) scored significantly lower on the subscale than staff in Languedoc (3.84, SD 0.66; p = 0.033; 95% CI –0.72 to –0.18; Cohen’s d = 0.56). There were no significant differences between Artois and the other sites on this subscale.
FIGURE 8.
Mean choice subscale score for staff (95% CI). Scoring range for the mean is from 0 to 5. *p = 0.05. The response range for the items is from 1 to 5.
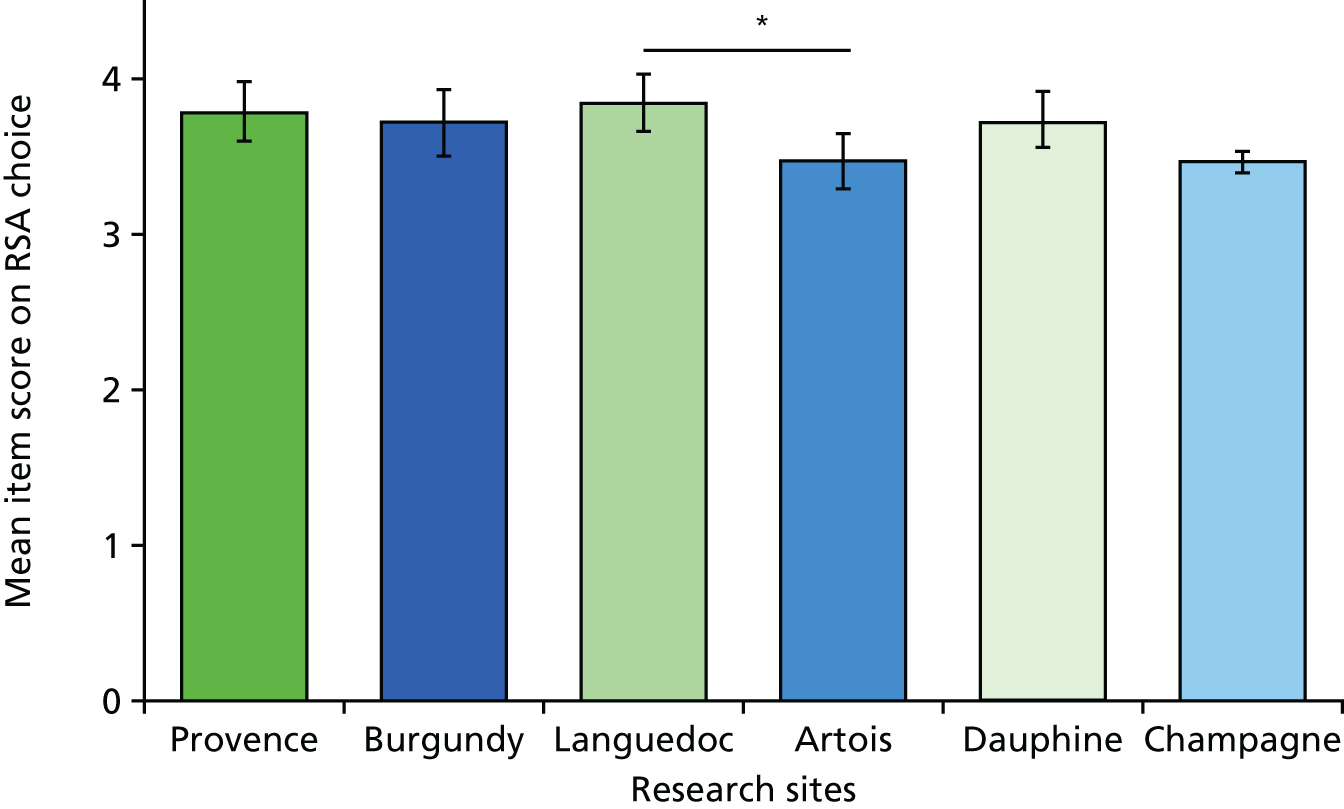
When using Provence and Dauphine as reference sites (the sites with the highest scores), it is apparent that these sites perform significantly better than the other four sites for the mean individually tailored subscale score (Figure 9). This scale measures some important perceptions about the extent to which services are tailored to the individual needs of the service user, their culture and interests and focuses on building community connections. Subsequent Tukey’s post hoc tests revealed that staff in Provence (3.75, SD 0.58) scored significantly higher on the subscale than staff in Languedoc (3.32, SD 0.74; p = 0.028; 95% CI 0.03 to 0.83; Cohen’s d = 0.65), Artois (3.29, SD 0.72; p = 0.009; 95% CI 0.08 to 0.84; Cohen’s d = 0.70) and Champagne (2.92, SD 0.49; p < 0.001; 95% CI 0.41 to 1.25; Cohen’s d = 1.55). Scores between staff in Provence and staff in Burgundy were also approaching significance (p = 0.059; 95% CI –0.01 to 0.82; Cohen’s d = 0.63). Staff in Dauphine (3.81, SD 0.66) also scored significantly higher than staff in Languedoc (p = 0.003; 95% CI 0.11 to 0.87; Cohen’s d = 0.70), Artois (p = 0.001; 95% CI 0.16 to 0.88; Cohen’s d = 0.75), Burgundy (p = 0.009; 95% CI 0.07 to 0.86; Cohen’s d = 0.69) and Champagne (p < 0.001; 95% CI 0.49 to 1.29; Cohen’s d = 0.98). There were no significant differences between Artois, Burgundy, Champagne and Languedoc on this subscale. Scores between staff in Languedoc and Champagne were, however, approaching significance (p = 0.055; 95% CI –0.01 to 0.80; Cohen’s d = 0.64).
FIGURE 9.
Mean individually tailored services subscale score for staff (95% CI). Scoring range for the mean is from 0 to 5. *p = 0.05; **p = 0.01. Note that * identifies a significant difference compared with Provence, # identifies a significant difference compared with Dauphine and ^ identifies a significant difference between Burgundy and Champagne. The response range for the items is from 1 to 5.
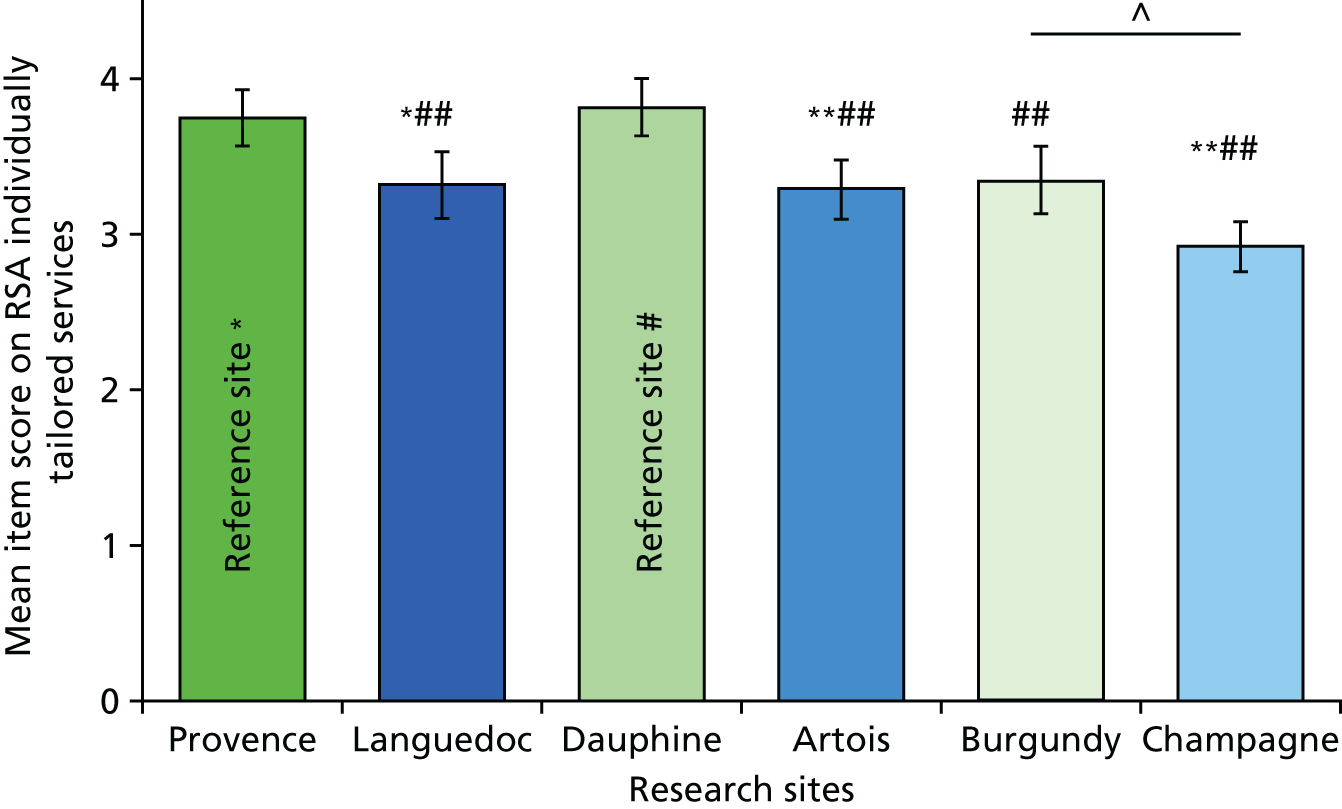
A more detailed analysis was completed for the RSA to look at the individual item level.
Table 44 shows the five highest-rated items for staff in the RSA across the sites. The most frequent responses were in the life goals, individually tailored services and choice subscales.
| Rank | Site | |||||
|---|---|---|---|---|---|---|
| Artois (mean of 3.79– 4.06 on Likert scale) | Burgundy (mean of 4.10–4.44 on Likert scale) | Champagne (mean of 3.80–4.00 on Likert scale) | Dauphine (mean of 4.24 –4.51 on Likert scale) | Languedoc (mean of 4.08–4.18 on Likert scale) | Provence (mean of 4.21–4.59 on Likert scale) | |
| 1 | Staff are diverse in terms of culture, ethnicity, lifestyle and interests Life goals |
Staff do not use threats, bribes or other forms of coercion to influence the behaviour or choices Choice |
Staff do not use threats, bribes or other forms of coercion to influence the behaviour or choices Choice |
Staff are diverse in terms of culture, ethnicity, lifestyle and interests Life goals |
Staff do not use threats, bribes or other forms of coercion to influence the behaviour or choices Choice |
Staff are diverse in terms of culture, ethnicity, lifestyle and interests Life goals |
| 2 | Every effort is made to involve significant others and other natural supports in the planning of a person’s services, if so desired Individually tailored services |
Every effort is made to involve significant others and other natural supports in the planning of a person’s services, if so desired Individually tailored services |
The role of staff is to assist a person with fulfilling their individually defined goals and aspirations Life goals |
Every effort is made to involve significant others and other natural supports in the planning of a person’s services, if so desired Individually tailored services |
Every effort is made to involve significant others and other natural supports in the planning of a person’s services, if so desired Individually tailored services |
The role of staff is to assist a person with fulfilling their individually defined goals and aspirations Life goals |
| 3 | Staff do not use threats, bribes or other forms of coercion to influence the behaviour or choices Choice |
Progress made towards goals (as defined by the person in recovery) is monitored on a regular basis Choice |
Every effort is made to involve significant others and other natural supports in the planning of a person’s services, if so desired Individually tailored services |
Staff do not use threats, bribes, or other forms of coercion to influence the behaviour or choices Choice |
Staff believe that people can recover and make their own treatment and life choices Life goals |
Every effort is made to involve significant others and other natural supports in the planning of a person’s services, if so desired Individually tailored services |
| 4 | Staff listen to and follow the choices and preferences of participants Choice |
The role of staff is to assist a person with fulfilling their individually defined goals and aspirations Life goals |
Staff are diverse in terms of culture, ethnicity, lifestyle and interests Life goals |
Staff use a language of recovery (i.e. hope, high expectations, respect) in everyday conversations Life goals |
Progress made towards goals (as defined by the person in recovery) is monitored on a regular basis Choice |
Staff use a language of recovery (i.e. hope, high expectations, respect) in everyday conversations Life goals |
| 5 | Staff believe that people can recover and make their own treatment and life choices Life goals |
Staff believe that people can recover and make their own treatment and life choice Life goals |
Staff believe that people can recover and make their own treatment and life choices Life goals |
Staff believe that people can recover and make their own treatment and life choices Life goals |
Staff listen to and follow the choices and preferences of participants Choice |
Staff do not use threats, bribes, or other forms of coercion to influence the behaviour or choices Choice |
In the life goals subscale staff in five out of the six sites gave high scores to the item relating to the belief that people can recover and make their own treatment choices. In four of the six sites staff reported that they were diverse in terms of culture ethnicity, lifestyle and interests. In Provence and Dauphine, the use of language of recovery was highly rated by staff.
In the individually tailored subscale, staff in all research sites scored the item referring to making every effort to involve significant others in the planning of a person’s services highly.
In the choice subscale staff in all research sites gave high scores the item referring to not using threats or bribes or other forms of coercion to influence behaviour or choices. In Provence and Champagne staff scored their role in assisting people in fulfilling their goals highly. In Burgundy and Languedoc monitoring of progress towards goals was highly rated by staff. In Artois and Languedoc staff scored listening to and following the choices and preferences of participants highly.
In Table 45 we provide a summary of the lowest-rated items on the RSA for staff members in each of the six study sites. The most frequent responses were from the individually tailored services and involvement subscales.
| Rank | Site | |||||
|---|---|---|---|---|---|---|
| Artois (mean of 3.13–3.24 on Likert scale) | Burgundy (mean of 2.68–2.95 on Likert scale) | Champagne (mean of 2.36–2.65 on Likert scale) | Dauphine (mean of 3.18–3.29 on Likert scale) | Languedoc (mean of 2.59–3.10 on Likert scale) | Provence (mean of 3.13–3.24 on Likert scale) | |
| 1 | Most services are provided in a person’s natural environment (i.e. home, community, workplace) Choice |
This agency provides education to community employers about employing people with mental illness and/or addictions Individually tailored services |
This agency provides education to community employers about employing people with mental illness and/or addictions Individually tailored services |
People in recovery can choose and change, if desired, the therapist, psychiatrist or other service provider with whom they work Choice |
This agency provides education to community employers about employing people with mental illness and/or addictions Individually tailored services |
Most services are provided in a person’s natural environment (i.e. home, community, workplace) Choice |
| 2 | People in recovery are regular members of agency advisory boards and management meetings Involvement |
People in recovery are regular members of agency advisory boards and management meetings Involvement |
All staff regularly attend trainings on cultural competency Individually tailored services |
This agency provides structured educational activities to the community about mental illness and addictions Involvement |
Persons in recovery are involved with facilitating staff trainings and education programs at this agency Involvement |
People in recovery are regular members of agency advisory boards and management meetings Involvement |
| 3 | Persons in recovery are involved with facilitating staff trainings and education programs at this agency Involvement |
Persons in recovery are involved with facilitating staff trainings and education programs at this agency Involvement |
This agency provides structured educational activities to the community about mental illness and addictions Involvement |
This agency provides education to community employers about employing people with mental illness and/or addictions Individually tailored services |
People in recovery are regular members of agency advisory boards and management meetings Involvement |
Persons in recovery are involved with facilitating staff trainings and education programs at this agency Involvement |
| 4 | This agency provides education to community employers about employing people with mental illness and/or addictions Individually tailored services |
This agency provides structured educational activities to the community about mental illness and addictions Involvement |
The development of a person’s leisure interests and hobbies is a primary focus of services Involvement |
Staff actively help people become involved with activities that give back to their communities (i.e. volunteering, community services, neighbourhood watch) Involvement |
Helping people build connections in their neighbourhoods and communities is one of the primary activities in which staff at this agency are involved Individually tailored services |
This agency provides education to community employers about employing people with mental illness and/or addictions Individually tailored services |
| 5 | The development of a person’s leisure interests and hobbies is a primary focus of services Involvement |
All staff regularly attend trainings on cultural competency Involvement |
This agency provides a variety of treatment options (i.e. individual, group, peer support, holistic healing, alternative treatments, medical) from which agency participants may choose Diversity of treatment options |
People in recovery are regular members of agency advisory boards and management meetings Involvement |
This agency actively attempts to link people in recovery with other persons in recovery who can serve as role models or mentors by making referrals to self-help, peer support or consumer advocacy groups or programs Diversity of treatment options |
The development of a person’s leisure interests and hobbies is a primary focus of services Involvement |
In the individually tailored subscale staff in all research sites staff expressed low ratings for the agency providing education to community employers about employing people with mental illness and/addictions. Staff in Champagne and Burgundy scored the regular attendance to trainings on cultural competency low.
In the involvement subscale, staff from five out of the six sites gave low scores to the item referring to people in recovery are regular members of agency advisory boards and management meetings. Along similar lines, staff from four sites gave low scores to the involvement of people in recovery in facilitating staff trainings and education programmes. Staff in Artois, Champagne and Provence scored the item low, referring to the fact that the primary focus of the services is the development of a person’s leisure interests and hobbies. Staff in Dauphine, Champagne and Burgundy gave low scores to providing structured educational activities to the community about mental illness and addictions.
There were no significant differences in the staff responses across sites for the positive clinician input subscale [F(5,272) = 1.53; p = 0.182; η2 = 0.16] and the emotional difficulties subscale [F(5,270) = 1.91; p = 0.092; η2 = 0.16]. There were, however, significant differences found between sites for the positive collaboration subscale [F(5, 274) = 2.42; p = 0.036; η2 = 0.20] and the STAR-C total score [F(5, 273) = 3.02; p = 0.011; η2 = 0.23].
It is apparent that Burgundy performs significantly better than Artois for the mean positive collaboration subscale score (Figure 10). This scale measures some important perceptions about rapport and shared understanding of goals focused on mutual openness and trust. Subsequent Tukey’s post hoc tests revealed that staff in Artois (17.17, SD 2.65) score significantly lower on the subscale than staff in Burgundy (18.86, SD 2.57; p = 0.019; 95% CI –3.20 to –0.18; Cohen’s d = 0.65). There were no significant differences between any of the other sites on this subscale.
FIGURE 10.
Mean STAR-C positive collaboration subscale score for staff (95% CI). Scoring range for the scale is from 0 to 24. *p = 0.05. The response range is from 0 to 48.
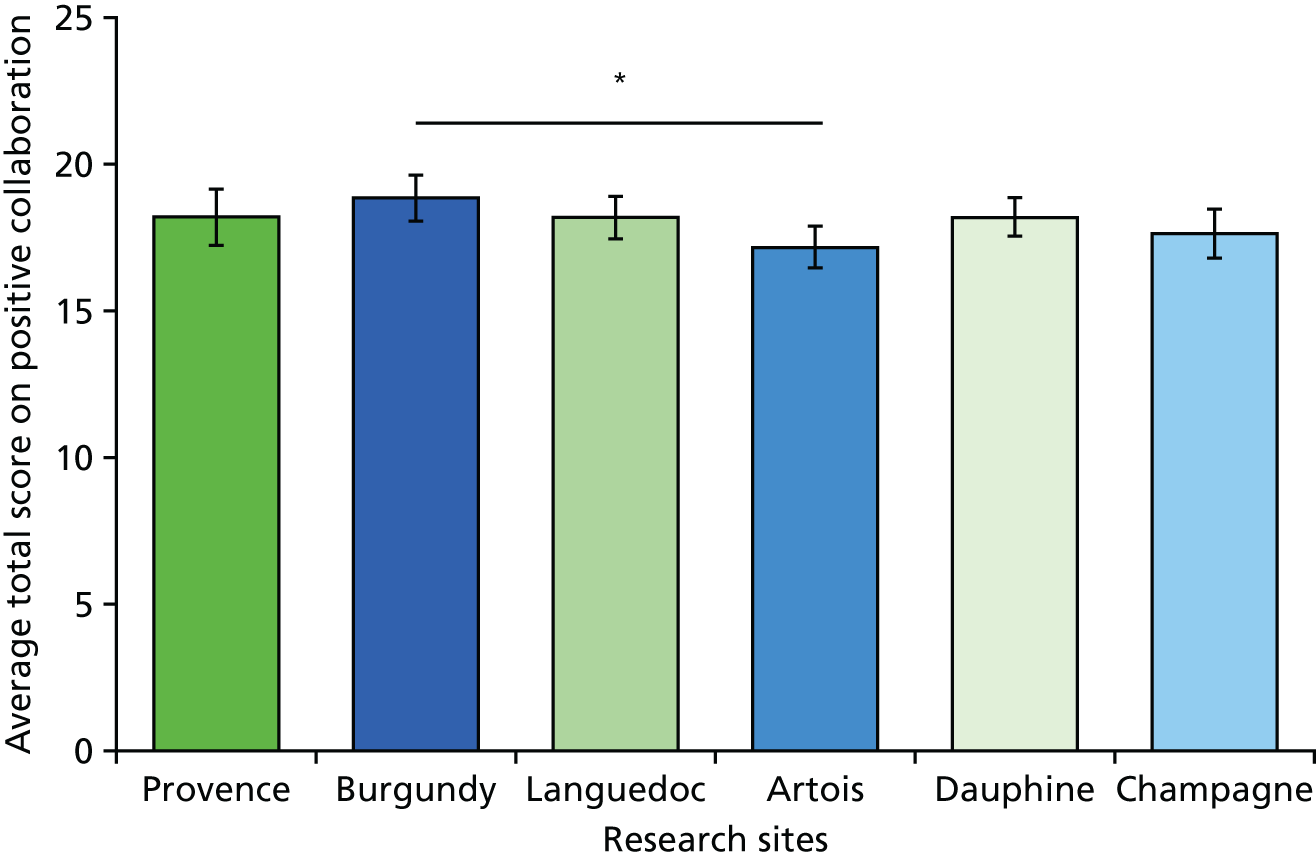
It is apparent that Burgundy performs significantly better than Artois for the mean positive collaboration subscale score (Figure 11). This scale measures some important perceptions that may have a significant effect on patient outcomes and concordance to care and collaboration with service users. Subsequent Tukey’s post hoc tests revealed that staff in Artois (36.08, SD 4.18) scored significantly lower on the subscale than staff in Burgundy (39.33, SD 4.31; p = 0.011; 95% CI –5.76 to –0.75; Cohen’s d = 0.77). There were no significant differences between any of the other sites on this subscale.
FIGURE 11.
Mean STAR-C total score for staff (95% CI). Scoring range for the scale is from 0 to 48. **p < 0.01. The response range is from 0 to 48.
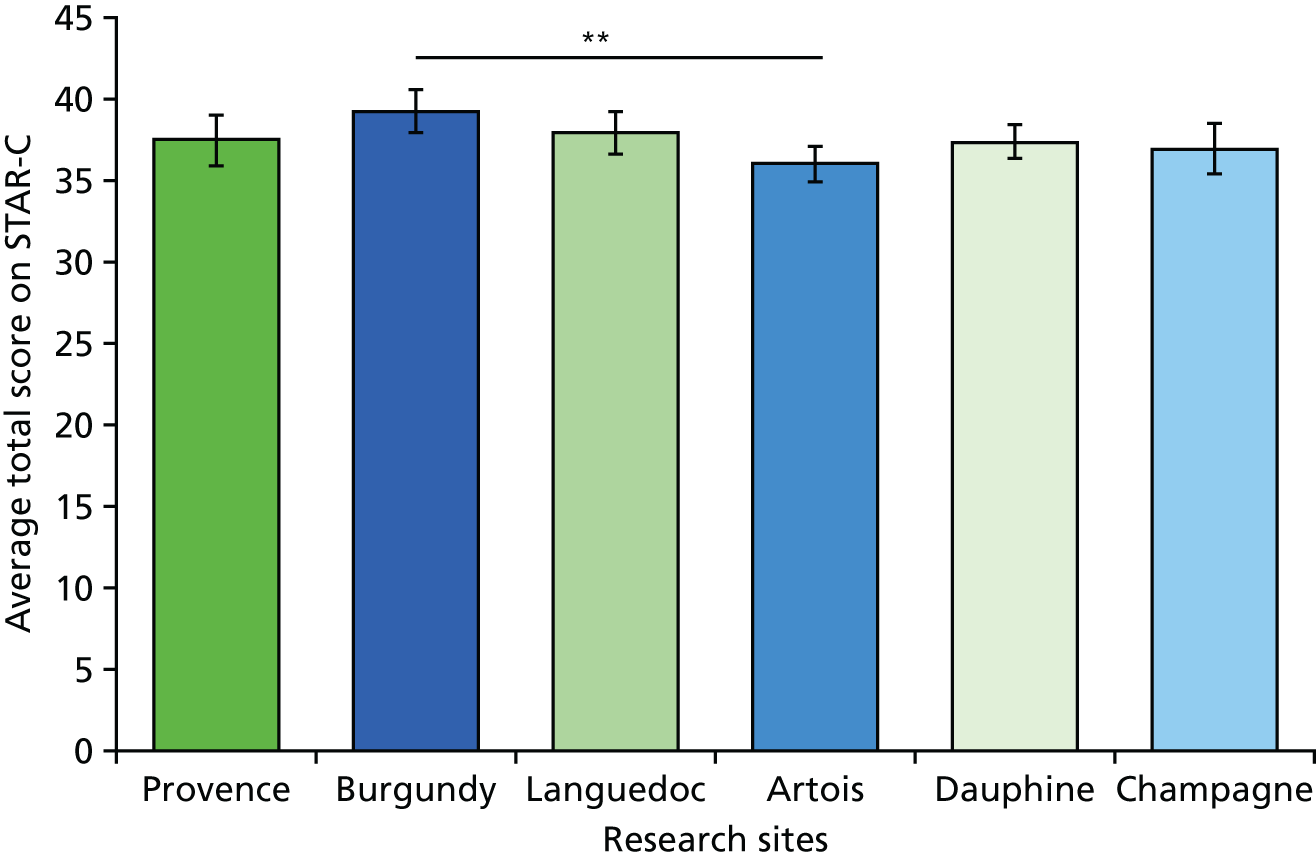
Adjusted analysis
The advantage of using unadjusted ANOVAs to examine the data is that this retains the maximum number of participants in the analysis; the disadvantage is that case-mix differences between the sites could bias the findings. In contrast, the strength of using ANCOVAs is that they adjust for the potential confounders, but this is achieved at the cost of losing participants in the analysis owing to missing data on the covariates. This reduces the statistical power of the analysis and changes the composite of the sample, which poses a problem for the interpretation. Analysing the data using unadjusted and adjusted analyses offers a check on the robustness of the original (unadjusted) findings.
The ANOVAs reported above are not adjusted for potential confounders (i.e. variables that are potentially associated with the outcome variables and which may be differentially distributed across sites). For service users, four demographic variables (age, gender, ethnicity and living status) and three care-related variables (previous admissions, time in mental health services and time on the ward) were identified as potential confounders. These variables were used as covariates in a series of ANCOVAs to determine whether or not they substantively changed the findings from the unadjusted analyses. For staff, five demographic variables (age, gender, ethnicity, personal experience of mental illness and family experience of mental illness) and two measures of clinical experience (time working in mental health services and time working on the ward) were identified as potential confounders for a further series of ANCOVAs. Covariates were all entered at the same time. Potential confounders (for service users and staff) were selected based on factors that would reflect the variation in the population characteristics across the six sites and, therefore, potentially have an impact on the outcome measure. To determine whether or not the adjusted findings were different from the original findings, we compared the p-values for the omnibus ANOVA/ANCOVA, the p-values for the post hoc comparisons, and the unadjusted and adjusted means for each scale and subscale for each site.
Service users
For the service users there were no substantive differences in the adjusted analysis for any of the subscales or the total scores of the VOICE, RSA, STAR-P and the ES (Table 46).
| Measure | One-way ANCOVA statistics | Site, mean (SEM) | |||||
|---|---|---|---|---|---|---|---|
| Artois | Burgundy | Champagne | Dauphine | Languedoc | Provence | ||
| VOICE | |||||||
| Mean total score | F(5, 252) = 0.30; p = 0.913 | 46.85 (2.85) | 46.59 (2.92) | 50.67 (3.13) | 47.60 (2.81) | 49.92 (2.96) | 48.85 (2.85) |
| RSA | |||||||
| Life goals | F(5, 244) = 0.34; p = 0.886 | 3.52 (0.16) | 3.38 (0.16) | 3.46 (0.17) | 3.53 (0.15) | 3.35 (0.16) | 3.30 (0.16) |
| Involvement | F(5, 226) = 0.33; p = 0.897 | 3.03 (0.18) | 3.03 (0.18) | 3.26 (0.20) | 3.11 (0.17) | 3.11 (0.19) | 2.94 (0.18) |
| Diversity of treatment options | F(5, 238) = 0.64; p = 0.670 | 3.19 (0.16) | 3.30 (0.16) | 3.11 (0.17) | 3.34 (0.15) | 3.01 (0.16) | 3.07 (0.16) |
| Choice | F(5, 249) = 0.28; p = 0.926 | 3.13 (0.16) | 3.34 (0.16) | 3.23 (0.17) | 3.30 (0.16) | 3.14 (0.17) | 3.19 (0.16) |
| Individually tailored services | F(5, 217) = 0.59; p = 0.711 | 3.20 (0.19) | 3.28 (0.18) | 3.06 (0.21) | 3.28 (0.17) | 3.05 (0.18) | 2.94 (0.18) |
| Mean total score | F(5, 239) = 0.32; p = 0.899 | 3.24 (0.15) | 3.30 (0.15) | 3.30 (0.16) | 3.34 (0.14) | 3.17 (0.16) | 3.12 (0.15) |
| STAR-P | |||||||
| Positive collaboration | F(5, 248) = 0.20; p = 0.963 | 15.11 (1.04) | 15.13 (1.08) | 15.64 (1.17) | 14.64 (1.02) | 14.22 (1.08) | 14.66 (1.05) |
| Positive clinician input | F(5, 251) = 0.36; p = 0.876 | 7.30 (0.51) | 7.33 (0.52) | 7.52 (0.56) | 7.18 (0.50) | 6.60 (0.53) | 7.34 (0.51) |
| Non-supportive clinician input | F(5, 248) = 0.67; p = 0.648 | 6.83 (0.50) | 7.33 (0.51) | 7.83 (0.55) | 7.04 (0.49) | 7.78 (0.51) | 7.71 (0.49) |
| Mean total score | F(5, 248) = 0.25; p = 0.942 | 29.28 (1.69) | 29.89 (1.75) | 31.11 (1.90) | 28.87 (1.67) | 28.56 (1.76) | 29.50 (1.71) |
| ES | |||||||
| Self-esteem–self-efficacy | F(5, 249) = 1.44; p = 0.209 | 3.00 (0.12) | 2.80 (0.12) | 3.26 (0.13) | 2.96 (0.11) | 3.08 (0.12) | 3.00 (0.12) |
| Power–powerlessness | F(5, 246) = 1.23; p = 0.296 | 2.42 (0.09) | 2.44 (0.09) | 2.56 (0.09) | 2.34 (0.08) | 2.53 (0.09) | 2.58 (0.08) |
| Community activism and autonomy | F(5, 244) = 0.87; p = 0.505 | 3.16 (0.09) | 3.31 (0.08) | 3.28 (0.09) | 3.27 (0.08) | 3.41 (0.08) | 3.24 (0.08) |
| Optimism and control over the future | F(5, 250) = 0.82; p = 0.535 | 2.83 (0.11) | 2.89 (0.12) | 3.02 (0.12) | 2.94 (0.11) | 3.13 (0.12) | 2.99 (0.11) |
| Righteous anger | F(5, 248) = 0.55; p = 0.738 | 2.42 (0.11) | 2.48 (0.11) | 2.39 (0.12) | 2.32 (0.11) | 2.26 (0.12) | 2.29 (0.11) |
| Total score | F(5, 250) = 1.22; p = 0.299 | 2.81 (0.06) | 2.78 (0.06) | 2.96 (0.07) | 2.78 (0.06) | 2.92 (0.07) | 2.86 (0.06) |
Overall, the ANCOVAs for service users show that while there were marginal changes in the adjusted means these changes were not substantive and did not affect the overall pattern of findings. Consistency between the adjusted and unadjusted analyses suggests that the findings are robust.
Staff
In the adjusted analysis there were no global differences in the significance levels for any of the measures for staff (Table 47).
| One-way ANCOVA statistics | Site, mean (SEM) | ||||||
|---|---|---|---|---|---|---|---|
| Artois | Burgundy | Champagne | Dauphine | Languedoc | Provence | ||
| RSA | |||||||
| Life goals | F(5, 230) = 3.99; p = 0.002** | 3.54 (0.09) | 3.68 (0.10) | 3.52 (0.10) | 3.91 (0.10) | 3.70 (0.10) | 4.02 (0.11) |
| Involvement | F(5, 231) = 4.36; p = 0.001* | 3.11 (0.10) | 3.03 (0.12) | 2.87 (0.12) | 3.44 (0.11) | 3.26 (0.11) | 3.51 (0.12) |
| Diversity of treatment options | F(5, 235) = 6.04; p < 0.001** | 3.16 (0.10) | 3.41 (0.12) | 3.07 (0.12) | 3.69 (0.11) | 3.43 (0.11) | 3.80 (0.13) |
| Choice | F(5, 234) = 3.12; p = 0.010** | 3.47 (0.09) | 3.54 (0.10) | 3.44 (0.10) | 3.73 (0.10) | 3.85 (0.10) | 3.83 (0.11) |
| Individually tailored services | F(5, 236) = 9.79; p < 0.001** | 3.28 (0.09) | 3.27 (0.11) | 2.96 (0.11) | 3.83 (0.10) | 3.40 (0.10) | 3.78 (0.11) |
| Mean total score | F(5, 234) = 6.01; p < 0.001** | 3.34 (0.08) | 3.43 (0.09) | 3.21 (0.09) | 3.72 (0.09) | 3.55 (0.09) | 3.81 (0.10) |
| STAR-C | |||||||
| Positive collaboration | F(5, 232) = 2.55; p = 0.029* | 17.08 (0.36) | 18.70 (0.43) | 17.63 (0.43) | 18.39 (0.41) | 18.11 (0.43) | 18.66 (0.47) |
| Positive clinician input | F(5, 230) = 1.47; p = 0.201 | 10.34 (0.17) | 10.92 (0.20) | 10.41 (0.20) | 10.34 (0.20) | 10.57 (0.20) | 10.78 (0.22) |
| Emotional difficulties | F(5, 228) = 2.09; p = 0.068 | 8.45 (0.24) | 9.51 (0.28) | 9.06 (0.28) | 8.81 (0.27) | 9.00 (0.28) | 8.50 (0.31) |
| Mean total score | F(5, 231) = 2.76; p = 0.019* | 35.83 (0.60) | 39.12 (0.71) | 37.08 (0.71) | 37.55 (0.68) | 37.77 (0.72) | 38.07 (0.78) |
Recovery Self-Assessment
For the RSA, Tukey’s post hoc analyses elucidate that two of the five subscales of the RSA and the RSA total score suggested no substantive differences in the adjusted analysis; in the other subscales there were some alterations in the pattern (Figure 12).
FIGURE 12.
Adjusted mean scores for staff (95% CI) on the RSA. (a) RSA life goals subscale; (b) RSA choice subscale; and (c) RSA individually tailored services subscale. *p = 0.05; **p = 0.01. Note that * identifies a significant difference compared with Provence and # identifies a significant difference compared with Dauphine.
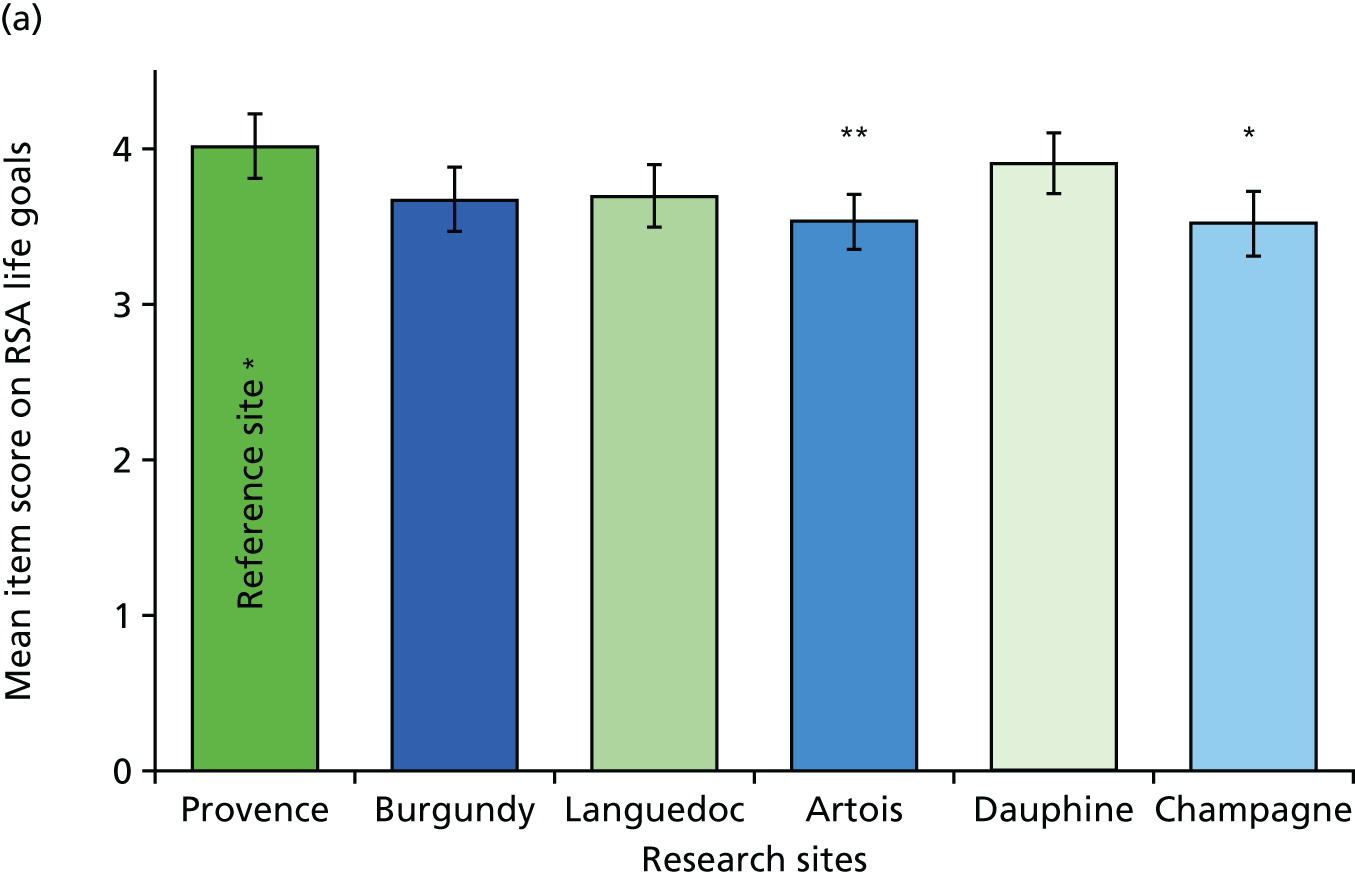
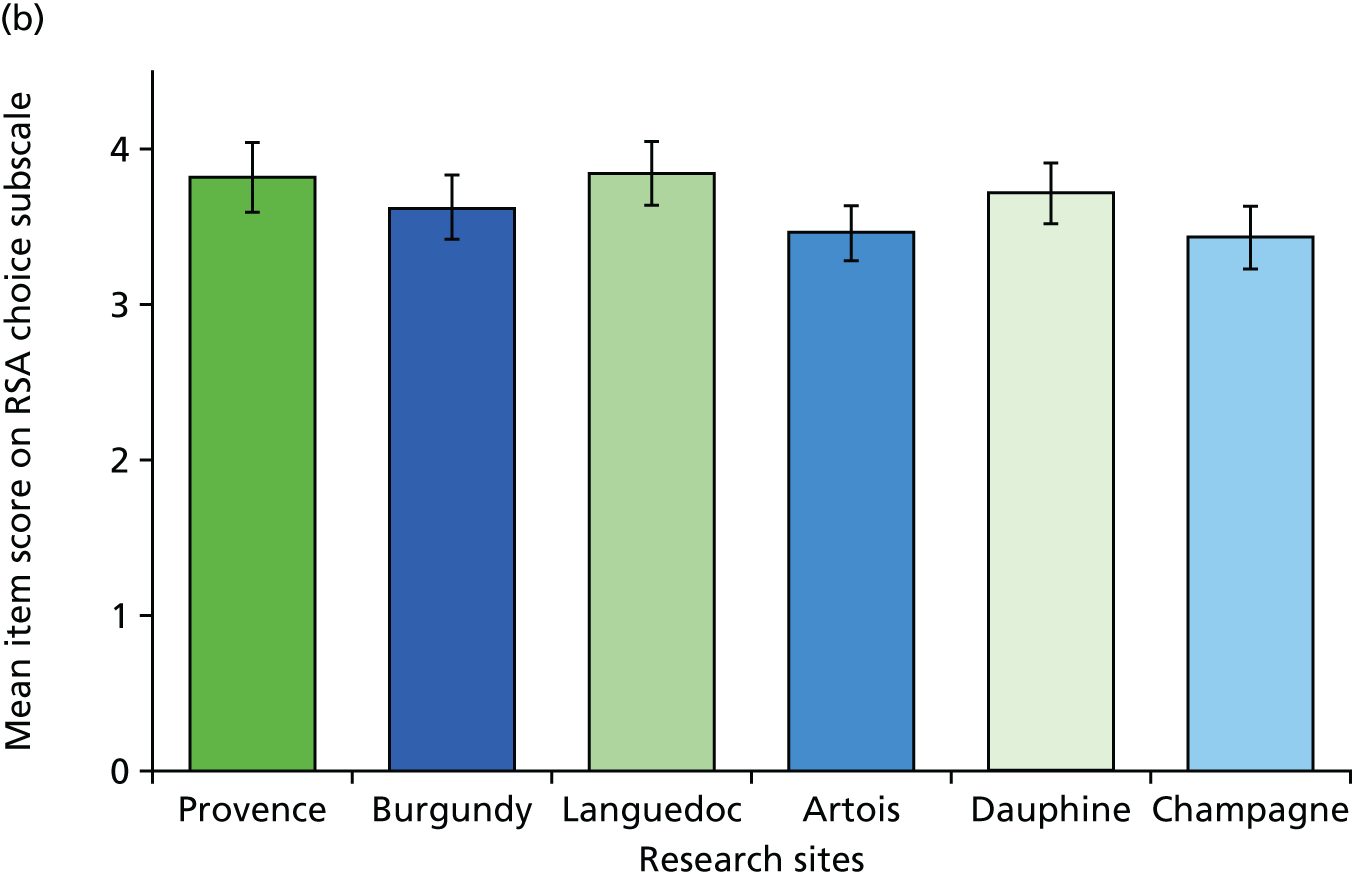
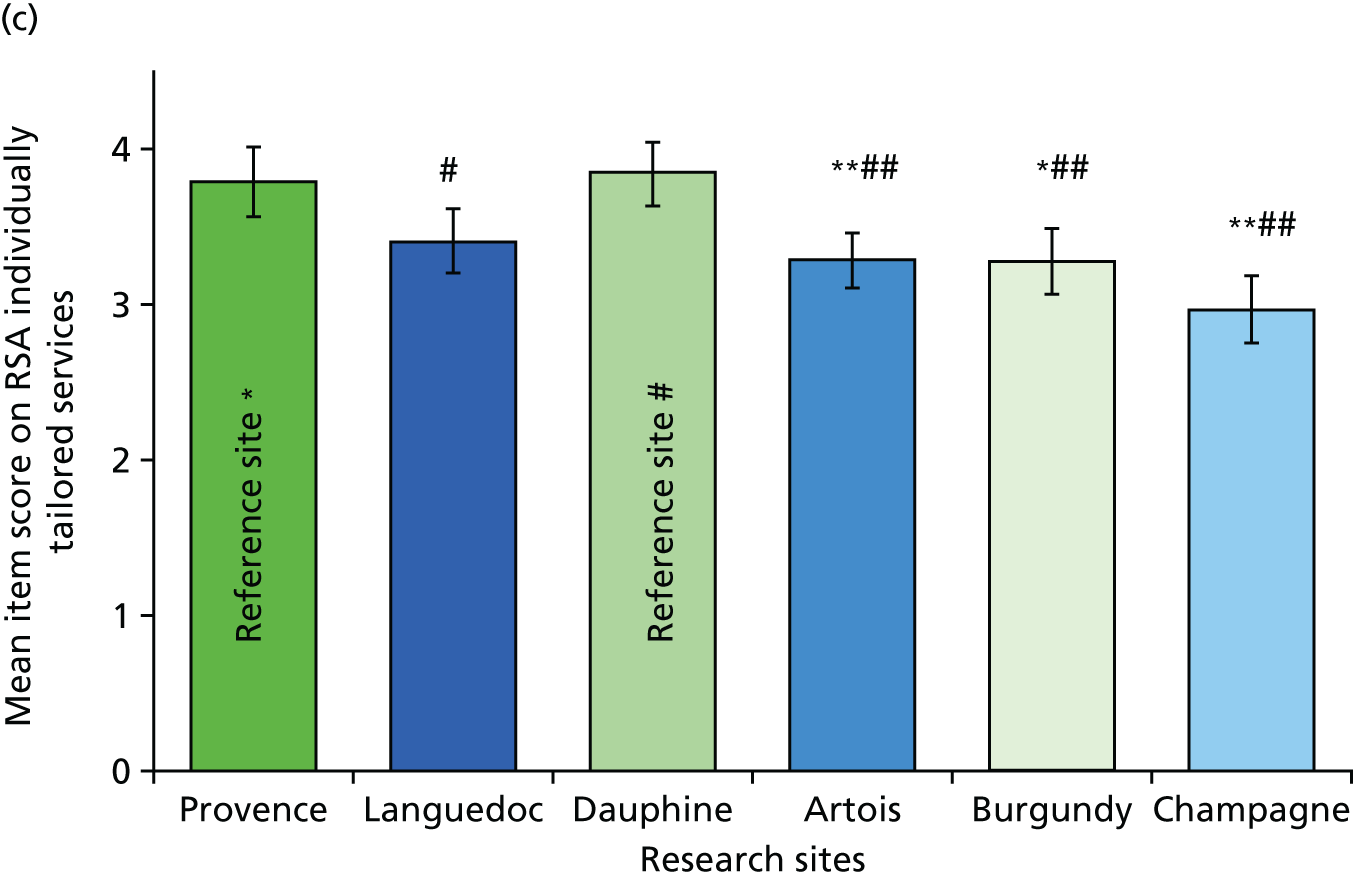
For the RSA, score changes in the adjusted means resulted in a loss of significant difference in the ‘life goals’ subscale between Dauphine (3.91, SD 0.62) and Artois (3.54, SD 0.64; p = 0.075; 95% CI –0.017 to 0.752; Cohen’s d = 0.59) and Champagne (3.52, SD 0.61; p = 0.082; 95% CI –0.022 to 0.800, Cohen’s d = 0.63) (see Figure 12a).The differences between Burgundy and Artois and Champagne remain the same. There was also a loss of significant difference in the ‘choice’ subscale between Languedoc (3.85, SD 0.64) and Artois (3.47, SD 0.64; p = 0.064; 95% CI 0.011 to –0.777; Cohen’s d = 0.59 (see Figure 12b). For the ‘individually tailored services’ subscale, the differences between Provence (3.78, SD 0.66) and Languedoc (3.40, SD 0.66; p = 0.216; 95% CI –0.0077 to –0.835; Cohen’s d = 0.58) (see Figure 12c) were lost. There was also a loss of significant difference between Champagne (2.96, SD 0.66) and Burgundy (3.27, SD 0.67; p = 0.610; 95% CI –0.757 to 0.137; Cohen’s d = 0.47) on this subscale. Changes in the adjusted means in this subscale has resulted in an emergent significant difference between Provence and Burgundy (p = 0.020; 95% CI 0.045 to –0.971; Cohen’s d = 0.58) for this subscale. It should be noted that the change in the means are marginal and the overall pattern of findings remain essentially the same.
Scale to Assess the Therapeutic Relationship – clinician version
The total STAR-C score changes in the adjusted means resulted in a loss of significant difference between Artois (17.08, SD 0.36) and Burgundy (18.70, SD 0.43; p = 0.072) (Table 47). Overall, the total STAR-C score is higher for Burgundy (39.12, SD 0.71) than for Artois (35.83, SD 0.60; p = 0.008) (Table 47); however, this is slightly less significant.
Further STAR-C Tukey’s post hoc analyses elucidate that one of the three subscales of the STAR-C has an alteration in the pattern. The other two remaining subscales remain the same and the total STAR-C score remains significant, with staff in Burgundy scoring the total STAR-C higher (39.12, SD 4.45) than those in Artois (35.83, SD 4.39; p = 0.008; 95% CI –6.08 to –0.504; Cohen’s d = 0.74).
The subscale that shows an alteration in pattern is the ‘positive collaboration’ subscale. The post hoc analyses show that Burgundy (18.70, SD 2.71) is no longer scored statistically higher than Artois (17.08, SD 2.67; p = 0.072; 95% CI –3.323 to 0.066; Cohen’s d = 0.60).
In terms of statistically significant differences between sites, the findings for staff changed more than the findings for the service users in the adjusted analyses. Proportionally, the observed number of changes in significance was small compared with the number of post hoc comparisons conducted, and changes in significance were predicated on relatively small absolute changes in the adjusted means across the various sites and outcome measures. The vast majority of the post hoc comparisons did not change in terms of statistical significance in the adjusted analyses. The findings from the ANCOVAs, therefore, are suggestive of potential site differences on particular measures between particular sites but these findings should be interpreted cautiously as there were no specific a priori hypotheses about site differences and the loss of participants due to missing data on the covariates changes the sample composition.
Correlations between the outcome measures
Service users
Pearson’s correlations were completed at the global level with all participants to determine if there were associations between the responses on the four questionnaire scales. Table 48 shows that there is a strong negative correlation between the RSA and the VOICE (r = –0.70; p < 0.001). This shows that there is an inverse association between the recovery-orientated focus and the negative perception of quality of care among service users. In other words, when recovery-orientated focus was high the quality of care was viewed highly. There is also a positive correlation between the RSA and the STAR-P (r = 0.61; p < 0.001), indicating an association between the recovery-orientated focus and ratings of the quality of therapeutic relationships among service users. There is also a strong negative correlation between the STAR-P and the VOICE (r = –0.64; p < 0.001). There is also an inverse association between the quality of therapeutic relationships and the negative perception of quality of care. In other words, when therapeutic relationships are scored highly, the perception of quality of care is also scored highly. There are negligible relationships between the RSA and the ES, between the STAR-P and the ES and between the VOICE and the ES.
| Measure | n | r | Significance |
|---|---|---|---|
| RSA and VOICE | 285 | –0.690 | < 0.001** |
| RSA and STAR-P | 282 | 0.611 | < 0.001** |
| RSA and ES | 282 | 0.085 | 0.153 |
| STAR-P and ES | 290 | 0.063 | 0.285 |
| STAR-P and VOICE | 294 | –0.641 | < 0.001** |
| VOICE and ES | 295 | 0.055 | 0.349 |
To explore the patterns of the correlation between the RSA and the STAR-P, subsequent correlations were completed at the subscale level. Further analysis could not be completed for the other correlations between the RSA and the VOICE and between the STAR-P and the VOICE because the VOICE scale does not have a subscale breakdown.
Correlation between the Recovery Self-Assessment and the Scale to Assess the Therapeutic Relationship – patient version
There were positive associations found between the positive collaboration subscale, the positive clinician input subscale and the five RSA subscales (Table 49). There were either small or medium correlations between the non-supportive clinician input and the five subscales of the RSA. This is expected, as this subscale is a negatively framed subscale and, therefore, less likely to correlate with the RSA.
| STAR-P subscale | RSA subscale | ||||
|---|---|---|---|---|---|
| Life goals | Involvement | Diversity of treatment options | Choice | Individually tailored services | |
| Positive collaboration | |||||
| r | 0.568 | 0.526 | 0.517 | 0.538 | 0.534 |
| Significance | < 0.001** | < 0.001** | < 0.001** | < 0.001** | < 0.001** |
| n | 284 | 265 | 278 | 290 | 258 |
| Positive clinician input | |||||
| r | 0.555 | 0.512 | 0.474 | 0.520 | 0.492 |
| Significance | < 0.001** | < 0.001** | < 0.001** | < 0.001** | < 0.001** |
| n | 286 | 267 | 279 | 292 | 257 |
| Non-supportive clinician input | |||||
| r | 0.225 | 0.176 | 0.174 | 0.284 | 0.176 |
| Significance | < 0.001 | 0.004 | 0.004 | < 0.001 | < 0.001 |
| n | 284 | 265 | 278 | 291 | 257 |
Although it appears that these questionnaire scales have a strong positive correlation, the results should be taken with caution. There is the possibility that a ceiling effect in the data negatively skewed them. When assessing the correlations by trust/health board, it is apparent that there is some variability (Table 50).
| Measures | Site | |||||
|---|---|---|---|---|---|---|
| Artois | Burgundy | Champagne | Dauphine | Languedoc | Provence | |
| RSA and VOICE | ||||||
| r | –0.585 | –0.608 | –0.649 | –0.805 | –0.773 | –0.704 |
| Significance | < 0.001** | < 0.001** | < 0.001** | < 0.001** | < 0.001** | < 0.001** |
| n | 48 | 46 | 45 | 53 | 44 | 49 |
| RSA and STAR-P | ||||||
| r | 0.516 | 0.548 | 0.618 | 0.707 | 0.651 | 0.635 |
| Significance | < 0.001** | < 0.001** | < 0.001** | < 0.001** | < 0.001** | < 0.001** |
| n | 48 | 45 | 44 | 52 | 44 | 49 |
| RSA and ES | ||||||
| r | 0.204 | –0.087 | –0.072 | 0.089 | 0.129 | 0.224 |
| Significance | 0.169 | 0.566 | 0.639 | 0.528 | 0.416 | 0.121 |
| n | 47 | 46 | 45 | 53 | 42 | 49 |
| STAR-P and ES | ||||||
| r | 0.198 | –0.269 | 0.114 | 0.049 | 0.019 | 0.200 |
| Significance | 0.160 | 0.068 | 0.457 | 0.729 | 0.905 | 0.163 |
| n | 52 | 47 | 45 | 52 | 44 | 50 |
| STAR-P and VOICE | ||||||
| r | –0.625 | –0.763 | –0.659 | –0.740 | –0.653 | –0.534 |
| Significance | < 0.001** | < 0.001** | < 0.001** | < 0.001** | < 0.001** | < 0.001** |
| n | 53 | 47 | 45 | 52 | 47 | 50 |
| VOICE and ES | ||||||
| r | 0.014 | 0.194 | 0.020 | –0.030 | 0.014 | 0.077 |
| Significance | 0.923 | 0.187 | 0.895 | 0.830 | 0.929 | 0.591 |
| n | 52 | 48 | 47 | 53 | 44 | 51 |
The correlation coefficients between RSA and VOICE; RSA and STAR-P and STAR-P and VOICE indicate large correlations across all sites. There is some variability but they all are classed as large effect sizes. The correlation in Dauphine is consistently the highest and Artois is the lowest.
The STAR-P and ES, the RSA and ES, and the VOICE and ES show little variability, with all sites showing a small to moderate association.
Staff
A Pearson’s correlation was completed at the global level with all participants to determine if there were associations between the responses on the two questionnaire scales. This correlation were completed using pairwise deletion. There is a small to moderate correlation between the RSA and STAR-C (r = –0.28; p < 0.001).
When comparing the correlation between the RSA and STAR-C (Table 51), it is clear that there is a considerable degree of variability across sites. There is a large correlation in Burgundy (r = 0.50; p = 0.001). There are moderate or small to moderate correlations in Artois (r = 0.28; p = 0.034), Languedoc (r = 0.35; p = 0.015) and Provence (r = 0.28; p = 0.034). Only small correlations were found in Champagne (r = 0.16; p = 0.331) and Dauphine (r = 0.35; p = 0.015).
| Measures | Site | |||||
|---|---|---|---|---|---|---|
| Artois | Burgundy | Champagne | Dauphine | Languedoc | Provence | |
| RSA and STAR-C | ||||||
| r | 0.284 | 0.503 | 0.156 | 0.108 | 0.351 | 0.284 |
| Significance | 0.034* | 0.001** | 0.331 | 0.457 | 0.015* | 0.034* |
| n | 56 | 43 | 41 | 50 | 47 | 56 |
Comparison of outcome measures between participant groups
We provide a comparison of measures from service users and staff in Chapter 5, Table 52. In order to be cautious with this analysis we raised the threshold for significance to p < 0.005 to correct for the number of comparisons (n = 10).
| Measure | Participant | Site | |||||
|---|---|---|---|---|---|---|---|
| Artois | Burgundy | Champagne | Dauphine | Languedoc | Provence | ||
| RSA | |||||||
| Life goals | Service users | 3.45 (0.15) | 3.40 (0.15) | 3.35 (0.14) | 3.49 (0.14) | 3.38 (0.17) | 3.36 (0.16) |
| Staff | 3.53 (0.08) | 3.67 (0.11) | 3.52 (0.08) | 3.93 (0.07) | 3.68 (0.10) | 3.97 (0.09) | |
| T-test statistics | t(101) = –0.50; p = 0.618 | t(87) = –1.46; p = 0.148 | t(86) = –1.05; p = 0.296 | t(101) = –2.77; p = 0.007 | t(94) = –1.533; p = 0.129 | t(88) = –3.09; p = 0.003 | |
| Involvement | Service users | 3.08 (0.17) | 3.07 (0.18) | 3.11 (0.16) | 3.11 (0.14) | 3.16 (0.19) | 3.06 (0.18) |
| Staff | 3.15 (0.09) | 3.05 (0.13) | 2.85 (0.10) | 3.47 (0.10) | 3.25 (0.10) | 3.46 (0.11) | |
| T-test statistics | t(102) = –0.37; p = 0.714 | t(82) = 0.067; p = 0.947 | t(80) = 1.37; p = 0.176. | t(102) = –2.09; p = 0.039 | t(90) = –0.441; p = 0.660 | t(83) = –1.86; p = 0.066 | |
| Diversity of treatment options | Service users | 3.16 (0.15) | 3.31 (0.14) | 3.01 (0.13) | 3.29 (0.12) | 3.12 (0.18) | 3.15 (0.15) |
| Staff | 3.21 (0.10) | 3.42 (0.11) | 3.06 (0.10) | 3.72 (0.10) | 3.39 (0.10) | 3.81 (0.10) | |
| T-test statistics | t(104) = –0.25; p = 0.803 | t(86) = –0.63; p = 0.533 | t(85) = –0.28; p = 0.778 | t(93.81) = –2.71; p = 0.008 | t(94) = –1.335; p = 0.185 | t(87) = –3.45; p = 0.001 | |
| Choice | Service users | 3.06 (0.14) | 3.40 (0.15) | 3.25 (0.14) | 3.23 (0.14) | 3.20 (0.18) | 3.26 (0.15) |
| Staff | 3.47 (0.09) | 3.72 (0.11) | 3.46 (0.07) | 3.73 (0.09) | 3.84 (0.09) | 3.79 (0.10) | |
| T-test statistics | t(109) = –2.59; p = 0.011 | t(88) = –1.72; p = 0.088 | t(86) = –1.28; p = 0.203 | t(101) = –3.04; p = 0.003 | t(94) = –3.22; p = 0.002 | t(90) = –2.89; p = 0.005 | |
| Individually tailored services | Service users | 3.17 (0.17) | 3.28 (0.15) | 3.22 (0.17) | 3.19 (0.16) | 3.12 (0.19) | 2.99 (0.16) |
| Staff | 3.29 (0.09) | 3.34 (0.11) | 2.92 (0.08) | 3.81 (0.09) | 3.32 (0.10) | 3.75 (0.09) | |
| T-test statistics | t(100) = –0.63; p = 0.531 | t(82) = –0.34; p = 0.731 | t(78) = 1.56; p = 0.122 | t(99) = –3.37; p = 0.001 | t(91) = –0.951; p = 0.344 | t(90) = –4.01; p < 0.001 | |
| Mean total score | Service users | 3.21 (0.14) | 3.32 (0.14) | 3.24 (0.12) | 3.30 (0.12) | 3.23 (0.17) | 3.20 (0.14) |
| Staff | 3.36 (0.08) | 3.45 (0.10) | 3.21 (0.07) | 3.74 (0.07) | 3.56 (0.12) | 3.76 (0.09) | |
| T-test statistics | t(104) = –1.01; p = 0.317 | t(87) = –0.763; p = 0.448 | t(85) = 0.20; p = 0.838 | t(102) = –3.02; p = 0.003 | t(75) = –1.50; p = 0.137 | t(89) = –3.20; p = 0.002 | |
| STAR | |||||||
| Positive collaboration | Service users | 14.99 (0.94) | 15.28 (0.93) | 15.88 (0.82) | 14.98 (0.97) | 13.85 (1.13) | 14.72 (1.02) |
| Staff | 17.17 (0.35) | 18.86 (0.39) | 17.63 (0.42) | 18.20 (0.33) | 18.22 (0.36) | 18.21 (0.48) | |
| T-test statistics | t(108) = –2.27; p = 0.025 | t(88) = –3.44; p = 0.001 | t(85) = –1.84; p = 0.070 | t(101) = –3.11; p = 0.002 | t(93) = –3.71; p < 0.001 | t(87) = –2.83; p = 0.006 | |
| Positive clinician input | Service users | 7.32 (0.47) | 7.47 (0.46) | 7.85 (0.46) | 7.16 (0.44) | 6.38 (0.56) | 7.41 (0.48) |
| Staff | 10.34 (0.18) | 10.95 (0.18) | 10.41 (0.21) | 10.38 (0.15) | 10.55 (0.20) | 10.67 (0.19) | |
| T-test statistics | t(109) = –6.24; p < 0.001 | t(89) = –6.81; p < 0.001 | t(85) = –4.86; p < 0.001 | t(99) = –6.78; p < 0.001 | t(93) = –7.05; p < 0.001 | t(87) = –5.73; p < 0.001 | |
| Emotional difficulties/non-supportive relationships | Service users | 6.77 (0.46) | 7.19 (0.43) | 7.62 (0.47) | 7.04 (0.46) | 7.71 (0.51) | 7.75 (0.48) |
| Staff | 8.60 (0.20) | 9.50 (0.21) | 8.95 (0.27) | 8.86 (0.33) | 9.15 (0.21) | 8.59 (0.38) | |
| T-test statistics | t(107) = –3.72; p < 0.001 | t(88) = –4.73; p < 0.001 | t(84) = –2.39; p = 0.019 | t(100) = –3.51; p < 0.001 | t(92) = –2.60; p = 0.011 | t(87) = –1.30; p = 0.197 | |
| Mean total score | Service users | 29.02 (1.55) | 30.00 (1.48) | 31.35 (1.39) | 29.17 (1.39) | 27.93 (1.83) | 29.58 (1.73) |
| Staff | 36.08 (0.55) | 39.33 (0.66) | 37.00 (0.76) | 37.45 (0.52) | 39.98 (0.62) | 37.56 (0.77) | |
| T-test statistics | t(109) = –4.43; p < 0.001 | t(88) = –5.58; p < 0.001 | t(85) = –3.44; p < 0.001 | t(101) = –5.54; p < 0.001 | t(92) = –5.19; p < 0.001 | t(87) = –3.85; p < 0.001 | |
There are differences in the RSA score in Dauphine and Provence, with the staff in these sites scoring higher overall than service users. Examining this in more detail, it is apparent that in Provence staff score higher in most of the subscales of the RSA. In Dauphine, the differences reside in the choice and individually tailored services subscales. In addition to this, in Languedoc staff score higher in the choice subscale than do service users.
Across all of the six research sites, staff score significantly higher than service users on the scale to assess therapeutic relationships. In Burgundy and Dauphine the same pattern is present across all of the subscales. Positive clinician input was scored higher by staff than service users across the six sites.
Comparison of measures across community and acute mental health services
We now provide an overall comparison of the measures from the study conducted in the community and this study conducted in acute inpatient services. To complement the descriptive analysis in Chapter 4, we provide some exploratory inferential analyses to compare outcomes between the studies. The authors choose to highlight these as analyses as exploratory for two main reasons: (1) a statistical analysis between the two studies was not incorporated into the design of the two independent studies and these are, therefore, not powered for these kind of comparisons; and (2) there were core methodological differences in the way in which data were collected in the two studies, as well as contextual differences between the studies. Table 53 provides a summary table of the measures for service users and Table 54 provides a summary table for staff.
| Measure | One-way ANOVA statistics | Site | |||||
|---|---|---|---|---|---|---|---|
| Artois* | Burgundy* | Champagne* | Dauphine* | Languedoc* | Provence* | ||
| VOICE | |||||||
| COCAPP (acute) | |||||||
| Mean total score | F(5, 294) = 0.49; p = 0.787 | 49.43 (2.40) | 45.69 (2.40) | 51.56 (2.33) | 48.77 (2.53) | 49.04 (2.92) | 48.55 (2.81) |
| COCAPP (community) | |||||||
| Mean total score | This scale was not used in COCAPP (community) | ||||||
| RSA | |||||||
| COCAPP (acute) | |||||||
| Life goals | F(5, 284) = 0.14; p = 0.984 | 3.45 (0.15) | 3.40 (0.15) | 3.35 (0.14) | 3.49 (0.14) | 3.38 (0.17) | 3.36 (0.16) |
| Involvement | F(5, 264) = 0.05; p = 0.999 | 3.08 (0.17) | 3.07 (0.18) | 3.11 (0.16) | 3.11 (0.14) | 3.16 (0.19) | 3.06 (0.18) |
| Diversity of treatment options | F(5, 277) = 0.56; p = 0.734 | 3.16 (0.15) | 3.31 (0.14) | 3.01 (0.13) | 3.29 (0.12) | 3.12 (0.18) | 3.15 (0.15) |
| Choice | F(5, 290) = 0.54; p = 0.748 | 3.13 (0.16) | 3.34 (0.17) | 3.23 (0.17) | 3.30 (0.16) | 3.14 (0.17) | 3.19 (0.16) |
| Individually tailored services | F(5, 255) = 0.34; p = 0.891 | 3.17 (0.17) | 3.28 (0.15) | 3.22 (0.17) | 3.19 (0.16) | 3.12 (0.19) | 2.99 (0.16) |
| Mean total score | F(5, 280) = 0.13; p = 0.989 | 3.21 (0.14) | 3.32 (0.14) | 3.24 (0.12) | 3.30 (0.12) | 3.23 (0.17) | 3.20 (0.14) |
| COCAPP (community) | |||||||
| Life goals | F(5, 394) = 0.65; p = 0.659 | 3.48 (0.12) | 3.55 (0.13) | 3.38 (0.97) | 3.43 (0.14) | 3.31 (0.11) | 3.30 (0.13) |
| Involvement | F(5, 373) = 0.81; p = 0.543 | 2.89 (0.15) | 2.96 (0.13) | 2.70 (0.15) | 2.93 (0.16) | 2.66 (0.13) | 2.86 (0.15) |
| Diversity of treatment options | F(5, 406) = 1.67; p = 0.139 | 2.99 (0.15) | 3.06 (0.13) | 3.05 (0.14) | 3.21 (0.15) | 2.70 (0.11) | 2.91 (0.14) |
| Choice | F(5, 423) = 1.27; p = 0.277 | 3.66 (0.11) | 3.65 (0.10) | 3.66 (0.10) | 3.69 (0.13) | 3.72 (0.09) | 3.39 (0.11) |
| Individually tailored services | F(5, 418) = 1.72; p = 0.129 | 3.27 (0.13) | 3.34 (0.13) | 2.95 (0.13) | 3.23 (0.14) | 3.04 (0.12) | 2.89 (0.14) |
| Mean total score | F(5, 405) = 0.86; p = 0.509 | 3.27 (0.12) | 3.33 (0.11) | 3.13 (0.11) | 3.31 (0.13) | 3.12 (0.10) | 3.10 (0.12) |
| STAR-P | |||||||
| COCAPP (acute) | |||||||
| Positive collaboration | F(5, 288) = 0.45; p = 0.814 | 14.99 (0.94) | 15.28 (0.93) | 15.88 (0.82) | 14.98 (0.97) | 13.85 (1.13) | 17.72 (1.02) |
| Positive clinician input | F(5, 290) = 0.99; p = 0.422 | 7.32 (0.47) | 7.47 (0.46) | 7.85 (0.46) | 7.16 (0.44) | 6.38 (0.56) | 7.41 (0.48) |
| Non-supportive clinician input | F(5, 288) = 0.77; p = 0.569 | 6.77 (0.46) | 7.19 (0.43) | 7.62 (0.47) | 7.04 (0.46) | 7.71 (0.51) | 7.75 (0.48) |
| Mean total score | F(5, 289) = 0.50; p = 0.778 | 29.02 (1.55) | 30.00 (1.48) | 31.35 (1.39) | 29.17 (1.39) | 27.93 (1.83) | 29.58 (1.73) |
| COCAPP (community) | |||||||
| Positive collaboration | F(5, 426) = 3.75; p = 0.002** | 17.37 (0.76) | 19.81 (0.57) | 17.13 (0.70) | 17.29 (0.79) | 18.62 (0.52) | 16.15 (0.76) |
| Positive clinician input | F(5, 431) = 2.80; p = 0.017* | 8.12 (0.40) | 9.46 (0.28) | 8.01 (0.36) | 8.22 (0.37) | 8.46 (0.29) | 7.83 (0.40) |
| Non-supportive clinician input | F(5, 430) = 1.66; p = 0.142 | 8.90 (0.28) | 9.23 (0.33) | 9.09 (0.33) | 8.02 (0.45) | 9.14 (0.30) | 8.53 (0.36) |
| Mean total score | F(5, 429) = 3.45; p = 0.005** | 34.51 (1.31) | 38.49 (1.00) | 34.09 (1.21) | 33.53 (1.21) | 36.07 (0.95) | 32.33 (1.37) |
| ES | |||||||
| COCAPP (acute) | |||||||
| Self-esteem–self-efficacy | F(5, 287) = 1.16; p = 0.330 | 3.05 (0.10) | 2.87 (0.13) | 3.22 (0.10) | 2.99 (0.10) | 3.07 (0.10) | 2.98 (0.11) |
| Power–powerlessness | F(5, 284) = 1.32; p = 0.257 | 2.47 (0.08) | 2.40 (0.08) | 2.54 (0.08) | 2.32 (0.08) | 2.52 (0.07) | 2.56 (0.08) |
| Community activism and autonomy | F(5, 282) = 0.85; p = 0.515 | 3.22 (0.09) | 3.34 (0.08) | 3.29 (0.07) | 3.25 (0.07) | 3.41 (0.08) | 3.25 (0.07) |
| Optimism and control over the future | F(5, 289) = 0.48; p = 0.788 | 2.89 (0.11) | 2.95 (0.12) | 2.98 (0.10) | 2.98 (0.09) | 3.12 (0.10) | 3.00 (0.10) |
| Righteous anger | F(5, 287) = 0.59; p = 0.707 | 2.37 (0.11) | 2.49 (0.11) | 2.31 (0.11) | 2.34 (0.08) | 2.26 (0.11) | 2.29 (0.10) |
| Total score | F(5, 289) = 0.82; p = 0.539 | 2.85 (0.07) | 2.81 (0.07) | 2.93 (0.05) | 2.80 (0.05) | 2.92 (0.05) | 2.85 (0.06) |
| COCAPP (community) | |||||||
| Self-esteem–self-efficacy | F(5, 428) = 0.78; p = 0.563 | 2.57 (0.09) | 2.60 (0.09 | 2.50 (0.09) | 2.63 (0.10) | 2.60 (0.08) | 2.73 (0.09) |
| Power–powerlessness | F(5, 422) = 0.81; p = 0.542 | 2.43 (0.06) | 2.51 (0.06) | 2.44 (0.06) | 2.42 (0.08) | 2.45 (0.06) | 2.57 (0.05) |
| Community activism and autonomy | F(5, 422) = 0.32; p = 0.901 | 3.13 (0.05) | 3.07 (0.07) | 3.05 (0.07) | 3.12 (0.08) | 3.09 (0.05) | 3.14 (0.06) |
| Optimism and control over the future | F(5, 431) = 1.36; p = 0.238 | 2.62 (0.08) | 2.63 (0.07) | 2.51 (0.07) | 2.70 (0.09) | 2.61 (0.07) | 2.77 (0.08) |
| Righteous anger | F(5, 428) = 0.58; p = 0.718 | 2.34 (0.09) | 2.24 (0.08) | 2.32 (0.07) | 2.31 (0.10) | 2.21 (0.08) | 2.35 (0.06) |
| Total score | F(5, 429) = 1.41; p = 0.221 | 2.62 (0.05) | 2.62 (0.05) | 2.56 (0.04) | 2.64 (0.05) | 2.62 (0.05) | 2.73 (0.04) |
| RSA | One-way ANOVA statistics | Site | |||||
|---|---|---|---|---|---|---|---|
| Artois | Burgundy | Champagne | Dauphine | Languedoc | Provence | ||
| COCAPP (acute) | |||||||
| Life goals | F(5, 230) = 3.99; p = 0.002** | 3.54 (0.09) | 3.68 (0.10) | 3.52 (0.10) | 3.91 (0.10) | 3.70 (0.10) | 4.02 (0.11) |
| Involvement | F(5, 231) = 4.36; p = 0.001** | 3.11 (0.10) | 3.03 (0.12) | 2.87 (0.12) | 3.44 (0.11) | 3.26 (0.11) | 3.51 (0.12) |
| Diversity of treatment options | F(5, 235) = 6.04; p < 0.001** | 3.16 (0.10) | 3.41 (0.12) | 3.07 (0.12) | 3.69 (0.11) | 3.43 (0.11) | 3.80 (0.13) |
| Choice | F(5, 234) = 3.12; p = 0.010** | 3.47 (0.09) | 3.54 (0.10) | 3.44 (0.10) | 3.73 (0.10) | 3.85 (0.10) | 3.83 (0.11) |
| Individually tailored services | F(5, 236) = 9.79; p < 0.001** | 3.28 (0.09) | 3.27 (0.11) | 2.96 (0.11) | 3.83 (0.10) | 3.40 (0.10) | 3.78 (0.11) |
| Mean total score | F(5, 234) = 6.01; p < 0.001** | 3.34 (0.08) | 3.43 (0.09) | 3.21 (0.09) | 3.72 (0.09) | 3.55 (0.09) | 3.81 (0.10) |
| COCAPP (community) | |||||||
| Life goals | F(5, 195) = 0.71; p = 0.617 | 3.68 (0.12) | 3.73 (0.11) | 3.79 (0.09) | 3.54 (0.15) | 3.82 (0.11) | 3.70 (0.09) |
| Involvement | F(5, 195) = 0.98; p = 0.429 | 3.01 (0.13) | 2.91 (0.11) | 2.92 (0.13) | 2.99 (0.15) | 3.23 (0.12) | 2.87 (0.10) |
| Diversity of treatment options | F(5, 195) = 2.10; p = 0.068 | 2.96 (0.14) | 3.23 (0.13) | 2.94 (0.13) | 2.98 (0.16) | 3.24 (0.12) | 2.74 (0.09) |
| Choice | F(5, 195) = 3.40; p = 0.006** | 3.76 (0.10) | 3.92 (0.11) | 3.70 (0.11) | 3.46 (0.10) | 4.04 (0.10) | 3.58 (0.13) |
| Individually tailored services | F(5, 195) = 1.74; p = 0.126 | 3.18 (0.13) | 3.10 (0.13) | 3.11 (0.13) | 3.49 (0.15) | 3.42 (0.15) | 3.42 (0.13) |
| Mean total score | F(5, 195) = 0.997; p = 0.421 | 3.35 (0.11) | 3.41 (0.10) | 3.35 (0.11) | 3.31 (0.13) | 3.57 (0.11) | 3.25 (0.08) |
For service users, there are three measures where comparisons can be made between the COCAPP-A inpatient and COCAPP community studies: RSA, STAR-P and ES. For ratings on the recovery focus of services, there were only small differences between the total RSA scores, and can be considered equivalent. At the subscale level service users score the ‘involvement’ subscale higher in COCAPP-A than in COCAPP; for some of the sites there is a marginal difference, while for Champagne and Languedoc this is moderate. The ‘choice’ subscale was scored consistently lower across all sites for COCAPP-A.
A two-way ANOVA demonstrates that there was no significant main effect of site on the RSA total score given by service users [F(5,685) = 0.664; p = 0.651; η2 = 0.005]. There was also no significant main effect of study type (COCAPP vs. COCAPP-A) on the RSA total score [F(1,685) = 0.295; p = 0.587; η2 = 0.000]. There was no significant interaction between the site and study type [F(5,685) = 0.182; p = 0.969; partial η2 = 0.001]. This indicates that there was no main effect of site or study type in the responses provided in the RSA total score.
For the STAR-P scale measuring therapeutic relationships, service users consistently scored the total and subscales lower in COCAPP-A than in COCAPP, suggesting relationships are rated more positively in community services. There was one exception, that service users in Provence scored the ‘positive collaborative’ subscale higher for inpatient services than for community services. It is important to note that Provence scored much lower than the other five sites for this subscale in the community study. The overall difference in total score varied across sites from 2.74 to 8.49 points lower.
A two-way ANOVA could not be completed for the STAR-P total score because the required assumptions for this type of analysis were violated. Levene’s test indicated unequal variances (F = 2.27; p = 0.010).
For the measure of empowerment (ES), service users in the acute study (COCAPP-A) scored higher overall on the total empowerment score than those in the community study (COCAPP). When assessing if there are any patterns within the subscales it appears that the main differences lie with the ‘self-esteem–self-efficacy’ and ‘optimism and control over the future’ subscale being scored higher in COCAPP-A than in COCAPP.
A two-way ANOVA demonstrates that there was no significant main effect of site on the empowerment total score [F(5,719) = 0.681; p = 0.638, η2 = 0.005]. There was, however, a significant main effect of study type (community COCAPP vs. acute COCAPP) on the RSA total score [F(1,719) = 53.89; p < 0.001, 95% CI 0.166 to 0.287; η2 = 0.070], indicating that there was a significant difference in the way empowerment was scored in community mental health services and acute mental health services. There was, however, no significant interaction between the site and study type [F(5,719) = 1.63; p = 0.149; η2 = 0.011]. Subsequent post hoc tests based on the estimated marginal means were completed. Least significant difference post hoc analyses revealed that in Dauphine the total empowerment scores within the community study were lower than those in the acute ward study (mean difference = –0.016, 95% CI –0.310 to –0.003; p = 0.045; η2 = 0.006). In Burgundy, there was a similar trend (mean difference = –0.190, 95% CI –0.339 to –0.041; p = 0.012; η2 = 0.009). In Artois, there was a more pronounced effect in the trend (mean difference = –0.211, 95% CI –0.360 to –0.062; p = 0.005; η2 = 0.011). In Languedoc and Champagne, the most significant difference in response is demonstrated (Languedoc, mean difference = –0.298, 95% CI –0.445 to –0.151, p < 0.001; η2 = 0.022; and Champagne, mean difference = –3.82, 95% CI –0.531 to –0.233; p < 0.001; η2 = 0.034). In Provence, however, there was only a minimal difference, which was not significant (mean difference = –0.123, 98% CI –0.267 to 0.22; p = 0.095; η2 = 0.004). The post hoc analyses outlined above remain uncorrected without adjustments, so they should be taken with caution.
For staff there was only one measure, the RSA, that was used across the two COCAPP studies. In all sites staff rated the ‘diversity of treatment options’ higher in COCAPP-A than in COCAPP. In some sites there was a marginal difference but in other sites this was more noticeable at 0.7–1.0 higher (Dauphine and Provence). Staff in Dauphine and Provence scored all of the subscales and the total RSA score higher in COCAPP-A than did those in COCAPP.
A two-way ANOVA demonstrates that there was a significant main effect of site on the RSA total score given by staff [F(5,474) = 2.377; p = 0.038; η2 = 0.024]. There was also a significant main effect of study type (COCAPP vs. COCAPP-A) on the RSA total score [F(1,474) = 5.929; p = 0.015; η2 = 0.012]. There was also a significant interaction between the site and study type [F(5,474) = 3.998; p = 0.001; partial η2 = 0.040]. This indicates that there was a main effect of site and study type in the responses provided in the RSA total score. Subsequent post hoc tests based on the estimated marginal means were completed. Least significant difference post hoc analyses revealed that in Dauphine the RSA total scores within the community study were lower than those in the acute ward (mean difference = –0.435, 95% CI –0.695 to –0.176; p = 0.001; η2 = 0.022). In Provence there was also a more pronounced trend, with acute wards viewed more recovery-focused than community services (mean difference = –0.511, 95% CI –0.779 to –0.243; p < 0.001; η2 = 0.029). There were no other statistical differences within the effect of study type. The post hoc analyses outlined above remain uncorrected without adjustments so should be taken with caution.
Cross-case analysis of the qualitative data
The following is a narrative summary of the cross-case analysis of the interview data focusing on care planning and co-ordination, support systems, safety and risk, organisational context, recovery and personalisation.
Care planning and co-ordination
Many members of staff across sites talked of the importance of collaborative care planning. Many also spoke of the value of plans being kept up to date with service users actively involved, and of plans being used as a way of pulling together multidisciplinary contributions and of helping manage transitions between hospital and community. However, staff, service user and carer interviews all revealed gaps between shared aspirations and realities, even when service users drew attention to receiving good-quality care. Staff accounts of routine collaboration with service users in care planning contrasted with service user accounts that pointed to lack of involvement. In all sites service users were interviewed who said that they were not involved in the planning of their care, or were unaware of the content of their care plans or had not received copies, or did not feel a sense of care plan ownership. Staff sometimes spoke of service users’ unwillingness or inability to collaborate in care planning, or of the barriers to collaborating brought about by the introduction of electronic records. Lack of a shared language was cited as a barrier in one inner-city site (Dauphine). Staff in Burgundy said how the all-Wales CTP template was not well suited to the short-term nature of acute hospital care, with some domains (e.g. housing) emerging as higher priority than others. As a solution, staff here described having created add-on ‘intervention’ or ‘management’ plans for exclusive use in the inpatient environment. Coherence and continuity in care across hospital and community interfaces were identified as important by many of those taking part, and examples of detailed and collaborative discharge planning involving staff and service users were given. Innovations were also described, such as ‘interim discharge summaries’. However, rapidly arranged discharges were also talked of along with protracted admissions. Across sites carers, too, reported generally low levels of formal involvement in care planning processes, although carers also spoke of high-quality care being provided.
Across sites two types of care plan review were described: formal, typically weekly, multidisciplinary meetings chaired invariably by consultant psychiatrists and daily handovers in which care on a more immediate basis was reviewed by staff. Formal ward rounds were described as key events by staff and as places where progress and plans could be reviewed in a multidisciplinary context also involving service users and carers wherever possible. Service user views and experiences of these differed, within and across sites. For some they were helpful, serving as opportunities for catching up with psychiatrists and the whole MDT. Some service users also described having been supported ahead of time to plan and prepare for formal ward round participation. Others spoke of limited time to fully consider service user needs and issues, of excessive jargon being used and of inflexibility over ward round scheduling.
Support systems
Training and support for staff in care planning varied, from reports of structured sessions to reports of no training whatsoever. In Provence, for example, staff spoke of classroom teaching, e-learning and updates. Irrespective of reported levels of ongoing training, staff across sites talked of their commitments to involving service users and carers and to offering support even if participants were unable to identify specific organisational policies on (for example) carer involvement. Expectations of staff spending dedicated, therapeutic, time with service users were described (e.g. in Languedoc). The majority of service users talked of their positive relations with ward (and community) staff, and of being treated with respect and dignity. One-to-one time was described, and of staff able and willing to listen. For some service users, though, differences in staff approach were described even on the same ward so that some workers were more likely to model particular attentiveness and care than others. Many service users also spoke of having had valuable support from workers not directly attached to the ward (e.g. from social workers). Not all service users had named nurses, however, with shifts creating discontinuities of care also being described. The use of bank staff and staff without qualifications was cited as problems for some. Carers’ experiences were also positive in many instances.
Safety and risk
Assessing and managing risk were invariably seen by staff as central parts of the work of planning and providing care, with formal ward round-based review meetings also being named as a place for risks to be discussed although not necessarily in the presence of service users. Particularly challenging discussions with service users were described in the context of talking through medication. Some staff also talked of the particular issues surrounding risk and decision-making in the care of service users who were detained. Risks mentioned by staff included those to self and others, with some also noting the dangers of overestimating risks and the importance of attending to strengths and of positive risk-taking. A staff view in Burgundy was that the CTP template was not suited to the regular updating of risk assessments. Most service users talked of their safety having been considered and attended to, sometimes giving specific examples of this in action (e.g. through removal of objects and the use of observations), even though risk assessments and management plans were often not actively discussed with them. Others did, however, talk of feeling unsafe in hospital and of asking for more staff.
Organisational context
Staff across sites talked of their awareness of overarching principles underpinning care (e.g. recovery) and of demands for quality, and of specific new initiatives (e.g. the introduction of peer support workers in Dauphine, the use of audit through AIMS in Languedoc, and the introduction of the Measure in the Welsh sites). Staff also spoke of pressures in the system. These included expectations to secure speedy transitions from hospital into the community, high levels of need and limited resources. Centralisation of hospital services was mentioned in one site (Burgundy) as having made it harder for carers to maintain contact.
Recovery
Definitions and understandings of recovery varied among staff, service users and carers, as did views of the role of hospital care in promoting this. Participants, in many cases, were also aware of the disparate meanings of ‘recovery’. Some staff (e.g. in Artois) viewed recovery as problematic in the inpatient context, saying that that this raised expectations or was too poorly understood to help effective care planning. In Languedoc, some antipathy to the idea of recovery was reported by some staff who challenged both its meaning and utility. When some service users said that hospital had helped (e.g. to stabilise medication), others complained of having been largely left to their own devices or subjected to containment. The use of tools to aid recovery (e.g. Recovery Star) were occasionally mentioned (e.g. in Burgundy), but in most cases these were either not deployed or were described as being more suitable out of the acute hospital care context. Service users and carers revealed a range of views around recovery, from the cure of symptoms and to the prospects of life without medication to the idea of coming to terms with difficulties.
Personalisation
The term ‘personalisation’ was not a familiar one, with few revealing knowledge of personal budgets, although across sites there was certainly recognition of the idea that care and services should be oriented to the individual. Although some staff talked of inpatient care as being person centred, there was also widespread recognition of the challenges to this [e.g. tensions between different approaches to providing care, the fact that staff only get to know people as patients and the relative (un)availability of resources]. Within and across sites, there were differences in service user views and experiences of individually tailored care. Some were clear that hospital had been pivotal in their care, and that their personal needs and wishes were attended to. Others were equally clear that their care had not been personalised, or talked of their care at home being more personalised. Carers gave positive accounts of care provided, citing this when asked as having been tailored.
Summary of key barriers and facilitators
Good communication and positive relationships were seen as important by staff, along with regular reviews of service user needs. Time to spend with service users to develop therapeutic relationships was also cited as key, along with good integration and communication with community teams and workers. Less administrative work was asked for, along with more staff, closer collaboration between workers and service users and better management of discharges in timely fashion.
These findings are discussed in more detail in the Chapter 6.
Chapter 6 Discussion
Introduction
In this chapter, we draw on the key findings from both the within-case and cross-case analyses and discuss some of the key issues that have emerged in relation to recovery-focused, personalised care planning. We make connections between the interconnected macro/meso/micro levels and focus on comparisons between this study of inpatient services and our previous study of community services. 19,20 We summarise the impact of public and patient involvement in the study and identify the strengths and limitations of the work. We conclude with recommendations for research and implications of our findings for practice.
Making connections in inpatient mental health care planning and co-ordination
Since the 1990s the focus of policy-makers in mental health has been on community mental health care and alternatives to inpatient services, leaving hospital services neglected. 29 Our policy review shows some encouragement, with recent national mental health policies in England and Wales referring to recovery and personalisation within all mental health services regardless of setting. Three key policies in England34–36 and one key policy in Wales37 remain influential alongside national guidelines produced by NICE for adult NHS mental health services. 38 Despite all of this, there is little contained within these policies that directly focuses on inpatient care. Considering that recent independent reports and inquiries39,40,90 into inpatient psychiatric care highlight that care remains inadequate, this is concerning.
Alongside this has been the Francis Report,149,150 published following an extensive inquiry into failings at Mid-Staffordshire NHS Foundation Trust. The report highlighted the importance of establishing a shared positive safety culture that permeates all levels of the health-care system, which aspires to prevent harm to patients and provide where possible, excellent care and a common culture of caring, commitment and compassion. Although not specifically targeted at mental health hospitals, it might be expected that the level of attention this inquiry and report drew might have wider influence.
Comparison and consideration of our survey results and interview data across sites provides some reason for optimism concerning the overall quality of mental health inpatient care but also indicators of areas to which greater attention may be required.
Interestingly, across the six sites there were no global differences identified across the service user measures. The VOICE measure52 was used to examine service users’ perceptions of inpatient care. Perceptions were generally marginally lower than the reference value provided by Evans et al. 52 However, the mean scores in all six research sites in this study were lower (so more positive) than those reported in a more recently published study which examined different inpatient service models over a period from 2008 to 2010. 151 The mean VOICE score in the COCAPP-A study ranged from 46 to 52 across sites, while the baseline score in the Csipke et al. study151 in a routine care system was at the top end of this (a mean score of 52) and worsened over time to 59. In this scale a higher score denotes a more negative perception of the ward, with possible scores ranging from 19 and 114; it is, therefore, interesting that the Csipke study151 describes a score of 52 on the scale as high and representing a poor view of the ward. It is unclear at what threshold/cut-off points the authors determine a poor view of the ward or, for service users, what a 10- or 15-point difference might ‘feel’ like. It could be argued that a score of 52 falls within the low/mid-range of potential total scores and does not necessarily portray a particularly negative view of the ward. In general, service users in this COCAPP-A study leaned towards a slightly more positive perception of the wards, but there was wide variation in the scores within sites, suggesting a mix of views. To a great extent this was reflected in our interviews in which services users were largely positive about their care, acknowledging being treated with dignity, respect and compassion, with some exceptions. Those carers interviewed also largely spoke very positively about care provided and attitudes of staff.
One of the aims of the study was to explore the CQC’s22 concerns that detained patients are treated with dignity and respect and that they can participate in care planning. Service users across all our research sites reported that staff were kind, compassionate and respected the dignity of them and other patients. This was irrespective of legal status. Carers were also very positive. Staff spoke of the challenges of collaborating on care planning with service users in severe mental distress or lacking insight and this is likely to include those detained under the MHA. 3 However, despite specific questions related to the legal status of services users, this was not explicitly identified as an issue. Further research might investigate in greater depth how staff currently work with such service users and identify any potential changes required that would better enable staff in these situations.
On ratings of the quality of therapeutic relationships, across all six sites staff consistently rated these relationships significantly more positively than did the service users, and are very similar to those reported in the study of protected engagement time undertaken in acute inpatient wards during 2010–13 (Nolan, personal communication). Perhaps tellingly, service users in the COCAPP community study rated therapeutic relationships significantly higher than did their counterparts in this inpatient study. The STAR-P measure used was initially designed for rating the one-to-one relationships that service users have with care co-ordinators in community teams18 so it may be that, despite having a ‘named nurse’, the necessarily more dispersed nature of relationships across a number of ward staff over days and weeks, across shifts and 24-hour care weaken any rating. Inpatient care also, of course, includes the greater likelihood of restrictions, limitations, rules and regulations necessary to provide a safe environment populated by people in the depths of distress and despair. 29 First- or second-hand experience of coercion and containment are also likely to be more prevalent in an inpatient setting. 152 Nevertheless, the data suggest that staff perceive their attempts at developing therapeutic relationships more positively than do those on the other side of the relationship, suggesting the need for further investigation to identify how positive relationships can best be achieved.
In contrast, service users in this study rated their perceptions of empowerment higher than did service users in our community study. In particular, ratings of self-esteem, self-efficacy and optimism and control over the future were higher among inpatients than among service users in the community. This finding initially appears counterintuitive, given that the doors of inpatient units are often locked, reportedly creating feelings of depression and low self-esteem,153 and that service users are more likely to face a range of restrictions. 154 However, on reflection and in the light of some of the qualitative data in which service users outline how the period in hospital had been a necessary and important stage in their recovery, perhaps this is more understandable. In consideration of the more urgent and immediate focus on managing a severe crisis and being supported to take the next steps forward towards discharge and recovery, people do feel empowered and optimistic about the future. Perhaps also, and again reflected in the interview data, despite all the limitations of inpatient care, ward staff do strive to provide a personalised, responsive focus to the individual needs of service users that is reflected in these scores.
This was reflected in the staff interviews where there was a strong perception across sites that staff were very aware of policy drives to provide a greater focus on recovery, to provide respectful, compassionate, dignified care and to improve quality. Most staff articulated clear values and understandings of what they and their colleagues were attempting to achieve and often gave examples to support this. This appeared to reflect core components of the focus on recovery and also the post-Francis culture. It may also be a reflection of some of the other initiatives that have been promoted in an attempt to improve inpatient services, such as the Royal College of Psychiatrists’ AIMS,92 Bright charity’s Star Wards94 and most recently, the mental health nurse-led evidence-based intervention, SafeWards. 155
However, as in the community study, staff also spoke of the socioeconomic context within which they were operating and some of the tensions and pressures that this created when they were unable to fully deliver the levels of personalised, quality care that they wanted to. Although, arguably, this was not articulated as strongly as among community staff who appeared to be under enormous pressures, nevertheless concerns about insufficient funding, and in particular insufficient staff numbers, were highlighted. Increased pressures on beds and demands to maximise throughput and discharge people as soon as possible was evident and made more difficult by those very same pressures on community teams. In some places this appeared to limit the close working and co-ordinated care that is necessary and important in providing safe, effective care across all parts of the interconnected mental health system. Such concerns accurately reflect the data contained in national data sets and reports produced by NHS Benchmarking Network (for data sets and reports, see NHS Benchmarking Network156).
Care planning and review: facilitators and barriers
In terms of planning and reviewing care, we found that the provision of inpatient mental health care planning is centred on two primary processes: the care plan itself and the ward round during which care is regularly reviewed. Both of these processes can be immensely helpful if they are handled well or enormously frustrating if they are not. Barriers and facilitators, as identified in our research interviews with service users and staff across all sites, are summarised in Table 55 and include examples of where these were located in our data set.
| Barriers | Facilitators | |
|---|---|---|
| Planning and review processes | Care plan process
|
Care plan process
|
| Communication |
|
|
| Resources | Time
|
Time
|
Participants reported that the care planning process itself has numerous limitations. A significant limitation is the issue of involvement. In all sites some (although not all), service users reported that either they had not seen a care plan or if a care plan was available it was not one with which they had had much input. The lack of involvement of the person central to the care plan has an obvious immediate limitation in that service users may be unaware of treatment goals, may find those goals incongruent with their own goals and may not be minded to achieve the outcomes desired by the treatment team. To facilitate involvement and collaboration in care planning, staff need to take the initiative to engage with people, titrate this engagement to better fit the individual’s needs and abilities at the time and make efforts to explain and communicate what the care plan is aiming to do.
Staff participants, in suggesting a number of barriers to care planning, provide some explanations for the lack of involvement of service users. They suggest that severity of illness and/or lack of insight sometimes mean that collaborative care planning is difficult to achieve, that there is often insufficient time to devote to this task, that some service users are unwilling or unable to collaborate on care planning, that staff themselves worry about and find it difficult to discuss care with service users, especially when there is likely to be a mismatch in goals and expectations, and that there is limited advice on what a good care plan looks like or on how to identify achievable goals. Some of these barriers, such as staff views on severity of illness, have been found in other studies and highlighted in systematic reviews of barriers to involvement,102 and the consistency of this finding across our study sites can be read in a number of ways. First, it is undoubtedly the case that some people admitted to inpatient services are in severe distress and the process of discussing and negotiating a care plan in those first few days is unlikely to be a priority for them. This is likely to be particularly so in light of increasing rates of compulsory detentions,157 although this was not explicitly articulated by respondents in our study. Experienced inpatient nurses recognise that some service users may be too unwell to be pressed into discussing and agreeing a plan of care. This may explain why in some cases service users reported that their care plan was only presented or discussed a week or more after their admission.
A second reading is that mental health professionals, despite their claimed interest and support of involvement, actually struggle to put this idea into practice and may need some guidance to achieve the aspiration of true collaboration. A possible contributor here was highlighted by both service users and staff, which relates to inflexible documentation and information technology on inpatient wards. In tandem these two elements prevent service users and staff from writing care plans together, as staff have to leave to type up a care plan once it has been discussed, and service users feel removed from the process and unable to alter the document, which can often be presented to them without adequate explanation. The documentation in some settings is set and unalterable and may not fit with the particular needs of the individual involved. For example, in Wales, legislation mandates both the structure and focus of care plans in secondary mental health services.
Another reading based on our research data in which many participants raise the issue of time is that services and staff within them are under significant pressures to meet organisational demands and simply do not prioritise collaboration with service users in their care. Service users reported that time with staff was highly valued but, for the most part, was a limited resource. Time is an important and taken-for-granted feature of social life; it is used by individuals to impose order, understand and handle discontinuities. 158,159 A universal expectation between staff and service users in this current study was that individual one-to-one time would provide the means for problem resolution, help to establish rapport and trust and, ultimately, engender a sense of collaboration towards preferred goals. Time, it seems, was a scarce resource, however, and organisational schedules quickly over-rode those of the service user and their primary nurse. One-to-one time was frequently mentioned by participants but for some this was seen as an unattainable goal: ‘the ideal situation, you’d be having one on one and all the rest of it, but that’s fantasy . . . land that is’ (C-SU-105).
It is not unusual for reports of mental health care to raise the issue of communication as something in need of attention. It is perhaps peculiar that professions that pride themselves on their communicative abilities should continually be seen to have deficits in this area. However, it is because of the importance and focus on communication in these settings that issues are regularly raised and the consistent review of how communication is handled is brought centre stage. We address some communicative issues on ward rounds below. In this section we raise some issues related to the care planning process itself. Care planning of complex issues in partnership with the person can be difficult to achieve and requires skilled negotiation and discussion so that the care plan clearly articulates the focus of care and the expected goals. Some staff were told to avoid these difficult conversations and in some cases care plans were simply shoved under the bedroom door of the service user without the opportunity for discussion. Additionally, care plans can be overly technical, contain many medical terms and generally, it seems, are not written with the service user as reader in mind. In some cases, service users told us that they worried that their status as a mental health patient would lead staff to dismiss or fail to listen to their concerns. However, our survey results also show that service users highly rate staff’s belief in their recovery. It seems that even in difficult situations service users want staff to engage with them, communicate in straightforward terms about what is happening and what the plans are for their care, and show some therapeutic optimism. Service users across all our research sites reported that staff were kind and compassionate and respected their dignity and that of other patients. It seems, then, that, despite pressures on inpatient service delivery, many service users see staff as helpful in their recoveries. This raises the question of whether or not better health outcomes might be forthcoming from more consistent engagement with service users in planning their care.
Ward rounds were of critical importance to service users and staff alike as the site of multidisciplinary discussion, planning and review of care. Ward rounds were, for the most part, consultant led and involved a plethora of medical, nursing and other health and social care professionals. The rounds usually happened weekly at a set time and occupied a whole morning or afternoon for staff involved. Ward rounds were, then, a type of regularity in the weekly timetable for staff and service users alike. However, service users and staff may experience these timetables differently; for example, there may be diverse perceptions of scheduling delays or contradictory understandings of what happened. 160 For service users participating in our study, ward rounds involved anxious hours waiting to be called to attend the meeting followed by sometimes short but overwhelming, intimidating experiences in the meeting itself, as reported previously. 161 Our experience of observing ward rounds revealed to our researchers the high levels of anxiety often experienced by service users at these points, which in other studies has been linked with absconding and conflict. 162 Given the importance of these meetings for both staff and service users, it was noted that few service users were adequately prepared about what to expect in the ward round. Some told us that they had expected to meet only the doctor but found themselves shown into a room full of unfamiliar faces; others felt that their contributions were not valued or that they had been treated in a condescending and rude fashion. For people who are already distressed and anxious about their treatment or future outcomes, it seems that ward rounds handled poorly or are overly rushed can worsen their sense of efficacy and discourage attempts to achieve involvement. Participants found it unhelpful that ward rounds did not discuss or review the care plan but instead focused on medication and an unspecified treatment plan. It seems that parallel processes for care planning were in operation: the care plan created by or with nursing staff and another medical treatment plan that focused on medication.
By contrast, service users report that in some cases ward rounds were of huge importance and very helpful; for example, ‘they’re really good because they put you in a place where you know what’s going to happen next’ (D-SU-102). We heard from both staff and service users that reviewing the care plan in the ward round would be helpful as a way of marking progress towards agreed goals. This finding from our research interviews correlates with the finding in our quantitative survey showing that participants rated highly the recovery language used by staff and the regular monitoring of progress towards recovery goals. Service users who had experience of involving advocates or external independent others found this particularly helpful in ensuring that their needs were attended to in ward round meetings. Continuity of care was raised by staff and service users alike who saw the ward round process as a helpful means to engage with wider professions and external agencies. Additionally, the information needs of service users could be better met with attention to preparation for ward rounds. This should cover the purpose, structure and process of the ward round in addition to preparing a list of what the service user wants to achieve from the meeting. In addition, it was suggested to us that service users be given a summary of outcomes from the ward round as, for many, the experience is rushed and they remain unsure of what has been agreed.
Recovery, therapeutic relationships and care planning
As in the community study, definitions and understandings of recovery varied among staff, service users and carers, as did in this study views on the role of hospital care in promoting recovery. The focus of recovery for many service users was around medication and symptom suppression (perhaps reflecting the primary focus of inpatient care) and therefore a more ‘clinical’ view of recovery than a ‘personal’ view. 12 In some sites, there was greater ambivalence around the idea of suitability or relevance of ‘recovery’ in inpatient care, particularly when people were very unwell. This needs to be challenged, as a message of hope and recovery is important at all stages and especially when the person is least likely to have hope. It is, of course, important to acknowledge that there may be tensions with working in recovery-focused ways when people have had their liberty taken and are detained under the MHA,3 but again this is the very time when a recovery-focused approach would be most powerful and when the use of recovery-focused concepts and language is instrumental.
Our data on recovery show convergence between results from standardised measures and findings from qualitative research interviews. Across five of the six sites service user participants rated highly the use of recovery language from workers and services alongside their perspective that workers believe that people can recover and participate in their own life choices. Service users also rated highly that there is regular monitoring of progress towards their recovery goals. Workers rated these items highly too, suggesting that notions of recovery and therapeutic optimism are supported by those participating in this study. These results from standardised measures are supported by qualitative data that indicate that staff recognise the complex and individual nature of recovery. For example, some staff saw a more recent orientation towards recovery-focused care as representing the shift from previous authoritarian and prescriptive asylum-based care to more collaborative models that encourage patient and family involvement. In contrast to literature on recovery,163 participants across sites did not support the use of a journey metaphor, perhaps highlighting that interruption in the recovery experience signified by hospital admission make these notions difficult to reconcile with current distress. Nevertheless, service users highly rated staff’s belief in their recovery, indicating the value they placed on the contribution of hope and optimism, which is positioned as a critical factor for recovery in much of the literature. 163
As outlined earlier, there was a strong association among service users between their perceptions of recovery-oriented care and their perception of the quality of care on the ward. Likewise, there were close correlations between the therapeutic relationships and the perception of quality of care. These findings were robust and consistent across all research sites, and the correlation between scores for therapeutic relationships and the recovery nature of those services was also found in the community study. Although it is not possible to determine which factor might be influencing which, it does suggest an important interrelationship between service users’ subjective valuing of their relationships with staff, the quality of inpatient care and the recovery-focus of the service. This, and the findings from the interviews in both studies, suggests yet again the importance of ensuring that staff have the time, motivation and skills to work therapeutically and with a focus on recovery.
There was not such a close correlation between scores for therapeutic relationships and perceptions of recovery of services for staff. We cannot be sure why this is the case but we suggest that some core elements of recovery-focused care may be perceived as things that are not possible to modify at the individual level. For example, some people will probably continue to experience recurring mental health crises, challenging some understandings for staff of what ‘recovery’ might be. 164 This reinforces the need for staff to recognise the importance of personal recovery and the ability to grow and maintain relationships even when living with severe mental distress or illness.
It is widely believed that therapeutic relationships are fundamental to good mental health care, and particularly in mental health nursing. 165 In a recent narrative review of the perspectives of mental health nurses and service users on the therapeutic relationship in inpatient psychiatric care,166 it was reported that this was perceived similarly by both nurses and patients. Both felt that the therapeutic relationship consisted of ‘interpersonal interaction between the two, with one party wishing to help and the other wishing to be helped. The relationship rests on trust and respect, establishing a framework in which nurses can care for patients in any number of ways based on various theoretical models, and using a variety of interventions’. 166 Service users described the ideal nurse for the therapeutic relationship as one who is ‘respectful, empathetic, honest, friendly, and available’. 166 They wanted to be treated as equals and hoped to be empowered to manage their illness and their care. At the heart of this is the need for mutual respect but service users reported often feeling that they were treated as ‘problems to be solved, and they also feel that their opinions are not taken into account’ and that nurses could be ‘paternalistic and protectionist’. The paper goes on to report that the lack of time is seen as the major obstacle to achieving therapeutic relationships, both by nurses and by service users. Nurses attributed this shortage of time to the workload of interventions, administrative tasks and poor nurse-to-patient ratios. In contrast, for service users it seemed that nurses were not readily available or accessible and could seem distant and unapproachable.
Our study again underscores the importance of the therapeutic relationship and also echoes concerns identified in reviews of the wider literature that limited staffing and time may militate against the best efforts of staff to develop positive therapeutic relationships and, in particular, make it difficult to find the space and time to ensure that service users are listened to and involved in the planning and delivery of their care.
A consistent finding across all sites in our study is that staff consistently score recovery items more positively than service users. This mismatch is supported by variances in responses in our research interviews in all sites. Here we found ambivalence and different perspectives about the notion of recovery among both staff and service user participants, in line with previous research. 167 The ambivalence seems to relate, in part, to the pace of recovery for some individuals and a concern that there are limited options for those with more long-term enduring, and perhaps complex, mental health problems. The concern that recovery creates ‘unrealistic’ expectations can perhaps be read as anxiety about what services have to offer to achieve this desired outcome. It may be that participants are simply acknowledging that recovery opportunities are hindered in settings where insufficient space is afforded to wider structural and social issues that give rise to and maintain mental distress. All participants appear to recognise the non-linear complex nature of recovery but place the emphasis differently. Workers claim a focus on choice and empowerment while indicating that recovery is not for everyone. Service users appeared to either not recognise or value the term or focus on treatment and discharge. Family members appeared to have more complex understandings and positioned the journey metaphor as idealistic and unlikely to apply to most people.
For some, the idea of recovery has led to greater emphasis on system throughputs in the form of shorter stays and more prompt discharge. The potential benefit of this focus is that individuals maintain contact with their social networks, maintain skills and confidence to participate in community life, and are not harmed by overly long inpatient stays. However, for service user participants and some staff, this appears to raise anxieties that they are being moved through the system much quicker than they would otherwise choose. Such anxieties may be well founded given the rates of suicide among those under the care of crisis resolution home treatment teams. 168
Key elements of care in the form of choice of professional or therapist to work with, diversity of treatment options and access to information about one’s own care were rated lower by service user participants than by staff in most sites. Involvement and collaboration are increasingly watch-words for workers but quantitative results in this study indicate that choice is focused on personal goals and not on wider system issues such as training or involvement in management meetings. This is perhaps not a surprising result as most service users were in hospital for acute exacerbations of their mental health conditions and may not have been keen or appropriate for this type of involvement at this time. We note, however, that service users told us that they felt left to map out their own recoveries on inpatient acute wards and were often left to occupy themselves, a not uncommon complaint. 74 Although in research interviews workers highlighted formal recovery approaches such as the Recovery Star and wellness recovery action plans, we encountered no examples of these being actively used to formally direct or lay out recovery routes for individuals.
In our survey across all sites workers rated education opportunities as low so that knowledge and experience of recovery approaches may be dependent largely on the personal commitment of individual workers. Nevertheless, we found that when recovery-orientation of care was rated highly, so too was the perception of quality of care. We also found a relation between high ratings for therapeutic relationships and recovery orientation. So, despite limited education opportunities, staff are making good contributions to the experience of inpatient mental health care. It would seem that further improvements in recovery-focused services could be achieved with relatively modest but regular opportunities for educational updates. New developments in service user-led design and delivery of staff training in recovery-focused care planning is currently being investigated and may offer a way forward. 169
There was variation in staff perceptions of recovery across sites, with staff in some scoring recovery higher than those in others. It is unclear if those scoring recovery higher were seeing a more positive change in the care, that it was more recovery focused, or that those scoring less positively were more open about some of the pragmatic challenges of working in a recovery-focused way. One site that scored recovery highly, Dauphine, had made local attempts to introduce innovations, such as service user-focused ‘This is Me’ care plans and short summary ‘management plans’, but these were in addition to standard documents and care plans, adding to workload. Other sites that scored lower on recovery were concerned that limited resources and recovery-oriented practice increased the emphasis on early discharge.
Interestingly, in Wales the service users recognised that their goals were being monitored on a regular basis. This was appreciated to a lesser extent in England, with just one site scoring this highly, which may be a positive indication of the use of the structured Mental Health Measure in Wales.
Personalisation
Drawing on the evidence presented here, personalisation is not widely recognised as a concept and not actively used in inpatient services by staff or service users, although there was wide discussion among staff of aiming to provide personal care or a personalised approach to care. Few staff spoke about personal budgets; in some sites staff did have an awareness of these (Dauphine and Provence) but generally they did not appear particularly relevant in inpatient settings.
Staff spoke about some of the constraints and challenges in trying to work in a personalised way and these included a lack of resources, short ward stays, service users being formally detained, disagreements, risk behaviours, limited capacity, and a primary focus on medical treatment. It was recognised that, to enable personalised care, it was necessary to have the time to get to know people as individuals and to provide some element of continuous care. Too often this was difficult to achieve in inpatient settings. Staff in the Welsh sites thought that the format of the CTP process and care plan was supportive of working in a personalised way and helped service users and staff get to know each other better.
Some service users were clear that their care was very personalised and that staff had considered their unique needs, with several good examples provided. Some thought that it was personalised to a degree, and others felt that inpatient care was more routine and standard for all and that individually tailored care was less possible in hospital, especially when people are detained. However, it was clearly possible for some wards and staff to provide care in a more personalised way and support should continue to be given to achieve this everywhere. Personalisation is an integral component of a recovery-focused approach to mental health care and needs to be promoted and supported as such. 170
Safety and risk
Risk and safety remain key concerns for mental health workers171 and, as in our community study, issues around safety and risk are reported to be central to inpatient work for staff. In the mental health system more widely, risk is constructed as an unwanted outcome arising from the actions or behaviours of individuals with mental health problems. In this sense, risk is seen to emanate from the person who is seen as the chief agent of unwanted harmful behaviours. Harm does, of course, occur and mental health services appear to be chiefly concerned with harms from the person to themselves or to others. For example, there are approximately 5500 suicides each year in the UK, 30% of which are known to mental health services. 172–174 The risk of suicide in the transition from inpatient care is now firmly established175 and there is some suggestion that this risk has been transferred from inpatient to crisis resolution and home treatment services. 168,176 Harm to others is a much rarer event but, nevertheless, is likely to have significant negative consequences for the victim, the individual with mental health problems and the wider system, including individual workers, such that risk-averse practice is common. 177 The pressure to ensure safety and avoid blame appears to be omnipresent in mental health services.
Coherence and continuity in care across hospital and community interfaces is known to be important in delivering safe, supportive mental health care and were identified as important by many of those taking part in this study, with examples given of detailed and collaborative discharge planning involving staff and service users. Innovations were also described, such as ‘interim discharge summaries’. However, participants also reported rapidly arranged discharges with little time for discussion or planning. Decisions on movement through phases of inpatient treatment will, in part, depend on the presenting symptomatology of the person, an assessment of their risk status, their needs for treatment and an assessment of their post-discharge needs such as accommodation. 178
Wright et al. 179 note that at key transition points between inpatient and community services there is a tendency to lose the service user voice, which often goes unheard. They note, too, that transitions are, in effect, speeding up owing to the pressure on limited resources and increasingly shorter length of stays on inpatient mental health wards. Transition points in this context have become a point of conflict between different parts of the service and disrupt the continuity of care as disagreements can play out in different constructions of the service users’ problem.
Workers in all sites were at pains to highlight the centrality of risk assessment and management to their practice. People detained under the MHA 19833 (as amended 2007) will have experienced some form of risk assessment in judgements made by workers to make an application for their detention for assessment and/or treatment. Regular review of this risk is essential in judgements made by workers for the purposes of determining the need for ongoing (or indeed termination of) detention. Continued detention in hospital brings with it consequences for the individual and not just in the denial of liberty. For example, the person may be forced to take treatments they would otherwise not choose, they may feel compelled to agree to levels of supervision and intrusion unlike those experienced by any other citizen, and their stay in hospital may be longer than expected.
Staff acknowledged some tensions around sensitive discussions and especially with people detained. Some workers openly acknowledged that this was to avoid difficult conversations but others seemed less aware that in denying service users access to knowledge about their risk they were effectively excluding people from participation in decisions about their care. 180 Previously we have noted that workers position risk assessment as legitimate work despite limitations in the predictive power of these judgements as one way of gaining normative certainty. 181
Here, unlike in the community study, service users seemed to be more aware of their safety being considered and managed in that they understood why certain items were removed or restrictions were imposed, although, sadly, some service users spoke of not feeling safe on wards, as reported in previous studies,182,183 and this needs to be considered in ongoing discussions and policy developments on safe staffing. 184 However, as in the community services, it remained a curious finding that although workers saw risk assessment as central to their efforts, they appeared to largely exclude the service user from meaningful discussions about these.
Reflecting on the accreditation for inpatient mental health services
It is worth reflecting on these findings with reference to the standards for adult inpatient mental healthcare (AIMS) recommended by the Royal College of Psychiatrists85 (see Chapter 3, Results). In the sites in our study, there was an average of 20 beds per ward (ranging from 17 to 23 beds per wards) with only Provence meeting the AIMS target of ≤ 18. Bed occupancy rates in the units in this study were at a mean of 98.8% (ranging from 85% to 105%), compared with a recommended level of ≤ 85% or less, with only Dauphine meeting the target. Overall, service users across all sites largely reported concerted attempts at personalised care and culturally sensitive care, but this stopped short of consistent widespread information sharing and genuine involvement in care planning, as recommended in AIMS. It is not surprising that such bed pressures have an impact on the availability of staff to spend time and work in a more collaborative way with service users. A recovery-based approach was also not consistently reported even though service users saw their hospital admission as a component of their recovery, with some staff across sites expressing ambivalence and uncertainty concerning the relevance of recovery concepts in an inpatient setting. The AIMS standards also recommend good links with and involvement of community agencies and organisations on the ward but these were explicitly identified in only one site (Dauphine). Particularly poor links with the community were mentioned in Champagne and Languedoc. Most service users and carers spoke of being aware of and appreciating patients’ safety being managed, which suggests a proportionate and respectful approach to risk management and safety outlined in AIMS. However, there appeared to be only limited explicit discussion of or involvement in risk assessment or management. We did not consider the ward environment in this study; nor did we explicitly explore access to psychological therapies.
In future, the development and use of a service development tool that helps services to review and improve how they support mental health recovery, such as the Scottish Recovery Indicator 2,185 might prove beneficial, alongside the greater employment of peer workers in supporting service users in identifying and addressing recovery-focused goals. 186
Public and patient involvement
This study was developed and conducted with a high level of service user and carer involvement from the start, including an independent service user researcher as co-investigator. Regular consultations throughout the study with SUGAR, the in-house service user and carer advisory group on research,56 and the project’s specially convened LEAG ensured that the study was conducted with a clear focus on the views and experiences of service users and carers, and that the methods used reflected this.
Additionally, three service user researchers were employed to work alongside the research team, helping with recruitment and interviewing service users and carers and contributing to the interpretation of results. Unfortunately, initial plans to involve two other service user researchers were derailed by the ill health of one person and insurmountable administrative difficulties in the employment of another. Training and support was provided and structured reflection methods were employed to help both the service users and academic researchers to learn from the joint-experience and improve their ways of working. Work is under way to coproduce a paper for publication exploring the benefits and some of the challenges of patient and public involvement in this and the earlier community-focused study in the near future.
Strengths and limitations
The study built on the design and results of an earlier study of care planning and co-ordination in community settings. This provided an opportunity to compare and contrast the results from both studies and to consider the implications for a whole systems approach to improving service delivery. Data were collected from a wide range of participants using a mix of methods from across a reasonable spread of inpatient units and service providers in geographically varied locations in two countries. The use of several quantitative measures with both service users and staff has produced some interesting and significant results, as has the comparison with some measures used in the earlier study. Target numbers were achieved for service users and fell just short for staff, largely when all staff on the wards involved had been approached. Unfortunately, despite considerable efforts by the research team and those supporting the study through the clinical research networks, we were unable to recruit sufficient numbers of carers. Following discussions with the LEAG and the Scientific Steering Committee and, with the agreement of the funders, we closed that aspect of the study. Researchers in the field reported how few carers visit wards, often preferring to meet service users in hospital canteens or off the site entirely. Many service users are not visited or supported by carers. The difficulties of involving carers in studies of inpatient mental health services have been reported elsewhere187 and pose a particular challenge for researchers keen to include the views of family members and friends.
Owing to the nature of the survey, it is not possible to make comparisons between responders and non-responders, as we had no access to data for non-participants. As in the previous study, there was a moderate number of missing data for the RSA completed by service users, possibly owing to some of the difficult language used and the community focus of the measure. As a consequence, a more detailed analysis of covariations within the data was restricted by lack of power. The RSA was selected for use in the first study after consideration of several organisational-focused measures of recovery, and we chose to use it in this study so that a comparison could be made. Nonetheless, this was not a satisfactory measure, as too many participants found some of the language and North American terminology unfamiliar and unclear. The adaptation and revalidation of this measure to a British population or the identification of a more suitable measure would be recommended for future studies.
An oversight during the preparation of the materials resulted in the omission of a key piece of service user demographic information in relation to the admission status of participants, meaning that comparisons between survey respondents could not be made in relation to their informal or detained status. However, aside from the VOICE, the other measures do not have reference data for these categories of service user.
The interview data are rich and the framework method provided a time-consuming but structured and visible method of organising, analysing and comparing those data within and across sites. We believe that the framework method and detailed presentation of results supports the transferability of these findings to other similar services. However, we acknowledge that an alternative method of analysis might more strongly identify themes and the relative strength of those themes. We may attempt to undertake this in a secondary analysis subsequent to this report, as we did on the data on risk in the earlier study. 181 The inclusion of structured care plan reviews and non-participant observations of review meetings allowed triangulation with the data obtained through other methods and provided additional insights and understandings. Obtaining agreement from staff to observe care planning meetings sometimes proved more difficult than obtaining agreement from service users, who were often keen for researchers to be present. It may be understandable that staff are slightly cautious about having their practice observed and appraised by others who they perhaps fear will fail to see the wider picture, but open discussion of practice is an important component in providing quality services and should be encouraged.
The involvement of service users and carers throughout the study as researchers and advisors provided added value to the study by giving additional viewpoints and interpretations.
However, again, the employment of service user researchers on limited time contracts makes the planning and organisation of work logistically challenging and limits involvement at later stages of the study when staff time is at a premium. Employing service user researchers on full contracts may address that problem but this adds to the total costs of studies and is not an attractive or feasible option for all who may be interested in taking up such roles. Structural solutions to these problems need urgent attention.
Table 56 provides an overview of the key findings mapped against the research questions identified at the outset of the study.
| What impact do national and local policies and procedures have on care planning and co-ordination? | |
|---|---|
| Source | Policy narrative review and interviews with ward staff |
| Findings | Policy review highlights
|
| What are the key drivers that have an impact on care planning and co-ordination? | |
| Source | Policy narrative review, local polices/documentation review and interviews with ward staff |
| Findings |
|
| What are the views of staff, service users and carers on care planning, therapeutic relationships, recovery-orientation and empowerment in acute care settings? | |
| Source | Questionnaire survey of ward staff, service users and carers and Interviews with ward staff, service users and carers |
| Findings | Care planning and views of inpatient care
|
| How is care planning and co-ordination currently organised and delivered in local services? | |
| Source | Interviews with service users, carers and ward staff, structured review of care plans and observations of care planning and co-ordination meetings |
| Findings | Care planning and co-ordination
|
| How and in what ways is care planning and co-ordination undertaken in collaboration with service users and, where appropriate, carers? | |
| Source | Questionnaire survey of ward staff, service users and carers; interviews with service users, carers and ward staff; structured review of care plans and observations of care planning and co-ordination meetings |
| Findings | Collaboration with service users and carers
|
| What specific features of care planning and co-ordination are associated with the legal status of service users? | |
| Source | Questionnaire survey of ward staff, service users and carers; Interviews with service users, carers and ward staff; Structured review of care plans and observations of care planning and co-ordination meetings |
| Findings |
|
| Is care planning and co-ordination affected by the different stages of stay on a ward (i.e. at admission, during stay, pre discharge)? | |
| Source | Questionnaire survey of ward staff, service users and carers; interviews with service users, carers and ward staff; structured review of care plans and observations of care planning and co-ordination meetings |
| Findings |
|
| To what extent is care planning and co-ordination personalised? | |
| Source | Questionnaire survey of ward staff, service users and carers; interviews with service users, carers and ward staff; structured review of care plans and observations of care planning and co-ordination meetings |
| Findings |
|
| To what extent is care planning and co-ordination focused on recovery? | |
| Source | Questionnaire survey of ward staff, service users and carers; interviews with service users, carers and ward staff; structured review of care plans and observations of care planning and co-ordination meetings |
| Findings |
|
| What suggestions are there for improving care planning and co-ordination in line with recovery and personalisation principles? | |
| Source | Interviews with service users, carers and ward staff |
| Findings |
|
Conclusions
The findings of this cross-national, multisite mixed-methods study suggest that a lot of positive practice is taking place within acute inpatient wards, with evidence of a widespread commitment among staff to provide safe, respectful, compassionate care with strong values underpinning practice. While ideas of recovery were evident among staff, there was some uncertainty and discrepancy among some about the relevance of recovery ideals and concepts to inpatient care or the ability of people experiencing high levels of distress to engage in recovery-focused approaches. However, service users saw inpatient admissions as an important and often necessary stage in stabilising their mental state and perhaps their lives, with medication an important component, and often appreciated the efforts that were made to keep them safe and to help them take the next tentative steps of their recovery. They also rated highly staff using recovery-focused language and values, and ratings of empowerment among service users were higher than in our community study. Many spoke of care being personalised, with examples given of staff being very responsive and considerate in response to particular needs or concerns. Carers often similarly described positive views of patient care. Perhaps surprisingly, service users experienced this total process as more empowering than many do when receiving community care. However, although they valued the relationships they had with staff on the wards, they did not rate this quite as highly as did the staff. As discussed earlier, this is perhaps not surprising given all of the tensions and anxieties associated with an inpatient stay, but this perhaps can best be summarised as ‘doing well, but could do better’. The big challenge identified by staff is having the time and sufficient numbers to deliver the care and support they want to in the way that they know is required. At a time of continuing and probably growing financial pressures on mental health services, maintaining the well-being of staff is crucial, as personal accomplishment and job satisfaction are important components in maintaining morale and reducing stress and burnout,190,191 and key factors in providing high-quality care.
Where care planning fits in with all this is less clear. Staff were clearly able to articulate the care planning processes and documentation required of them and, as in the community study, described some of their frustrations with lengthy, unwieldy forms and at times distancing computerised systems that required more time in front of monitors than in conversation with service users. Most staff also spoke of their understanding and efforts to involve service users, and carers and families when possible, in the care planning process. However, most service users did not really appreciate the written care plan as an integral or important part of their experience and many did not have a copy or could not find it. A few care plans did not exist. As in the community study, the majority of service users did not feel that they had been genuinely involved in the process. Unfortunately, in relation to service users receiving sufficient time with nursing staff and being involved in planning their care, very little progress appears to have made since the report of the Healthcare Commission of nearly a decade ago. 27
Discussing, co-ordinating and reviewing care in inpatient settings is mainly undertaken in large multidisciplinary meetings that are reportedly beneficial for staff and occasionally helpful for service users and carers, but too often these are intimidating, anxiety-provoking experiences. It may be useful to investigate alternative ways of reviewing care, and perhaps adapting some of the recovery tools may provide a partial solution, but one suspects that pressure of time is at least one factor that inhibits innovative practice. This is an area in which the testing of innovations should be welcomed.
Linked to this is the issue of nurturing and developing relationships with community care co-ordinators, community teams and wider community groups and organisations. We heard of examples in which service users welcomed the approach of having vibrant wards with people inputting from a range of agencies. Such an approach adds to the support provided to service users and also helps break down the barriers and stigma still associated with mental hospitals. Although organising such input no doubt created logistical demands on already busy inpatient staff, the benefits were apparent and should be encouraged.
Issues of risk and safety are ever-present in mental health services and it was clear that this was central to the work of staff, while they displayed an awareness of the sensitivities and challenges involved. Service users, and carers, were often aware of efforts being made by staff to keep them safe and this was frequently appreciated. However, as in the community study, the involvement of service users in discussions about personal risk factors and safety is challenging and requires greater training and support to encourage staff to develop the skills and confidence to undertake such sensitive and important work with confidence. This is particularly so when working with service users who are detained against their will and may strongly resent or deny the explanations for their detention. Such factors should also be considered in decisions around safe, therapeutic staffing levels.
We believe that the findings from across the two studies of care planning and co-ordination in both community and inpatient mental health settings provide strong indicators of the key areas that require attention in developing and improving the quality of recovery-focused services or a suite of interventions or processes that could be tested in future studies across the whole mental health system.
Recommendations for research and implications for practice
Research recommendations
Commission high-quality research to investigate:
-
the effectiveness and cost-effectiveness of innovative organisational approaches to increase direct contact time with service users, carers and social networks with the aim of providing explicit recovery-focused interventions (macro level)
-
how mental health staff can best work collaboratively and in a recovery-focused way with service users detained under the MHA3 and/or in severe distress and/or lacking insight in acute inpatient mental health settings (meso and micro levels)
-
how mental health staff in all settings can implement collaborative working and shared decision-making with mental health service users and carers in risk assessment and management (meso and micro levels)
-
innovative interventions to improve service user experiences of care planning and care reviews in inpatient settings, to provide personalised, recovery-focused care planning and co-ordination (meso level)
-
the use of more explicitly personalised, recovery-focused care planning tools and methods, such as wellness recovery action plans, instead of existing CPA/CTP documentation (macro and meso levels).
Implications for practice
This research suggests that:
-
staff time and therapeutic relationships lie at the heart of safe, effective, compassionate care, care planning, co-ordination and recovery-focused work – acute inpatient ward staff levels need to take account of this so that ‘time to care’, ‘productivity’ and quality improvement initiatives can be operationalised (macro level)
-
care and treatment plans are best developed with the service user and written using everyday language and include goals that are recovery-focused and meaningful to the service user (micro level)
-
inpatient care and treatment planning and review processes need to be designed to enable staff to better promote and support recovery in service users (macro level)
-
staff need to be enabled and encouraged to prepare service users for ward rounds and how best to review their care and treatment in line with identified recovery goals (meso and micro levels)
-
using Commissioning for Quality & Innovation schemes or other initiatives to support service providers in implementing facilitative standards such as AIMS or the Scottish Recovery Indicator 2 may be considered useful by commissioners (macro level)
-
providing education and training that enables all staff to hold difficult, sensitive conversations and negotiate complex issues such as risk and safety with service users and families/carers is important (meso level).
Acknowledgements
Many thanks also to the following people.
Dr Martin Cartwright, Lecturer in Health Services Research: provided independent advice on statistics and contributed to statistical analysis, interpretation and write-up.
Ms Bethan Mair Edwards, Service User Project Assistant in Mental Health: conducted data collection and was a member of the LEAG.
Mr Alan Meudell, Service User Project Assistant in Mental Health: conducted data collection and was a member of the LEAG.
Ms Katherine Barrett, Service User Researcher in Mental Health: conducted data collection.
Ms Nafiso Ahmed, Research Assistant and PhD Candidate in Mental Health: conducted data collection.
Ms Frederique Lamontagne-Godwin, Research Fellow: conducted qualitative data analysis.
Professor John Baker, Chair in Mental Health Nursing: chairperson of the Scientific Steering Committee.
Dr Helen Gilburt, Fellow in Health Policy: member of the Scientific Steering Committee.
Dr Mauro Laudicella, Senior Lecturer in Health Economics: member of the Scientific Steering Committee.
Ms June Hanshaw, Carer and Lived Experience Representative: member of the Scientific Steering Committee and the LEAG.
Mr Isaac Samuels, Service User and Carer: member of the Scientific Steering Committee and the LEAG.
Ms Dorothy Gould, Service User Researcher: member of the Scientific Steering Committee.
Ms Karen Alloway, Senior Research Nurse: member of the Scientific Steering Committee.
Ms Barbara Keogh, Research Nurse and Approved Mental Health Professional: member of the Scientific Steering Committee and support with recruitment and data collection.
Mr Norman Young, Consultant Nurse: member of the Scientific Steering Committee.
Mr Ian Stevenson, Senior Nurse: member of the Scientific Steering Committee and principal investigator.
Mr Adam Baxter, Clinical Research Co-ordinator: member of the Scientific Steering Committee and support with recruitment and data collection.
Mr Habibur Choudhury, Service User Representative: member of the LEAG.
Ms Nelly Adongakulu, Service User Representative: member of the LEAG.
Mr John Tear, Service User Representative: member of the LEAG.
Mr David Hindle, Service User Representative: member of the LEAG.
Ms Neelam Laxhman, Research Assistant: support with recruitment and data collection.
Ms Rebecca Holland, Clinical Studies Officer: support with recruitment and data collection.
Ms Sandra Jumbe, Clinical Studies Officer: support with recruitment and data collection.
Ms Sue Thomson, Research Nurse: support with recruitment and data collection.
Ms Philippa Case, Senior Clinical Research Co-ordinator: support with recruitment and data collection.
Ms Serena Gregory, Senior Clinical Research Co-ordinator: support with recruitment and data collection.
Ms Lauren Wilcock, Clinical Research Co-ordinator: support with recruitment and data collection.
Ms Jo Morris, Clinical Studies Officer: support with recruitment and data collection.
Ms Catherine Sheppard, Clinical Studies Officer: support with recruitment and data collection.
Ms Alexandra Hodges, Clinical Studies Officer: support with recruitment and data collection.
Many thanks to all local principal investigators, research and development managers, service managers, staff, service users and carers who took part in or helped with the study.
Contributions of authors
Professor Alan Simpson, Professor of Collaborative Mental Health Nursing: led on the design and overall management of the study; conducted data analysis and contributed to, and edited, the final report.
Dr Michael Coffey, Associate Professor in Mental Health Nursing: contributed to the design of the study and managed the study in Wales, contributed to the literature and policy review, contributed to training and support of service user researchers, conducted data collection and analysis and contributed to the final report.
Dr Ben Hannigan, Reader in Mental Health Nursing: contributed to the design of the study; contributed to the literature and policy review, contributed to training and support of service user researchers, conducted data collection and analysis and contributed to the final report.
Dr Sally Barlow, Research Fellow in Mental Health: project manager for the study, conducted data collection, contributed to training and support of service user researchers, led on quantitative analysis and write-up, conducted qualitative data analysis and contributed to the final report.
Dr Rachel Cohen, Research Fellow in Health Research: contributed to training and support of service user researchers, conducted data collection and qualitative analysis and contributed to the final report.
Dr Aled Jones, Senior Lecturer in Nursing: led on the literature and policy review and contributed to the final report.
Ms Alison Faulkner, Independent Service User Researcher Consultant; contributed to the design of the study, data collection and qualitative analysis; contributed to training and support of service user researchers; facilitated the LEAG and contributed to the final report.
Ms Alexandra Thornton, Research Assistant: supported the administration of the project, conducted data collection and helped with qualitative analysis and collating the final report.
Dr Jitka Všetečková, Lecturer in Nursing: contributed to the design of the study, data collection and the Scientific Steering Committee.
Dr Mark Haddad, Senior Lecturer in Mental Health: contributed to the design of the study and the Scientific Steering Committee.
Dr Karl Marlowe, Clinical Director and Consultant Psychiatrist, contributed to the design of the study and the Scientific Steering Committee.
Data sharing statement
Data can be obtained from the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health.
References
- No Health Without Mental Health: A Cross-government Mental Health Outcomes Strategy for People of All Ages. London: HM Government; 2011.
- Naylor C, Bell A. Mental Health and the Productivity Challenge. Improving Quality and Value for Money. London: The King’s Fund; 2010.
- Mental Health Act 1983. London: The Stationery Office; 1983.
- Mental Health Bulletin, Annual Statistics 2014–15. Leeds: Health and Social Care Information Centre; 2015.
- NHS Hospital Statistics for People with a Mental Illness 2014–15. Cardiff: Welsh Government; 2016.
- Refocusing the Care Programme Approach: Policy and Positive Practice Guidance. London: DH; 2008.
- Mental Health Policy Guidance: The Care Plan Approach for Mental Health Service Users. Cardiff: Welsh Assembly Government; 2003.
- Mental Health (Wales) Measure 2010: Guidance for Local Health Boards and Local Authorities. Cardiff: Welsh Assembly Government; 2010.
- Mental Health Bulletin: Annual Report from MHMDS Returns – England 2012/13. Leeds: Health and Social Care Information Centre; 2013.
- Together for Mental Health: A Strategy for Mental Health and Wellbeing in Wales. Cardiff: Welsh Government; 2012.
- Anthony WA. Recovery from mental illness: the guiding vision of the mental health service system in the 1990s. Psychosocial Rehabilitation Journal 1993;16:11-23. https://doi.org/10.1037/h0095655.
- Slade M. Personal Recovery from Mental Illness: A Guide for Mental Health Professionals. Cambridge: Cambridge University Press; 2009.
- Understanding Mental Illness: Recent Advances in Understanding Mental Illness and Psychotic Experiences. Leicester: British Psychological Society; 2000.
- Recovering Ordinary Lives. London: College of Occupational Therapists; 2006.
- From Values to Action: The Chief Nursing Officer’s Review of Mental Health Nursing. London: DH; 2007.
- Fair Deal for Mental Health. London: Royal College of Psychiatrists; 2008.
- Duffy S. Personalisation in Mental Health. Sheffield: Centre for Welfare Reform; 2010.
- Shepherd G, Boardman J, Rinaldi M, Roberts G. Supporting Recovery in Mental Health Services: Quality and Outcomes. London: Centre for Mental Health; 2014.
- Simpson A, Hannigan B, Coffey M, Barlow S, Cohen R, Jones A, et al. Recovery-focused care planning and coordination in England and Wales: a cross-national mixed methods comparative case study. BMC Psychiatry 2016;16. https://doi.org/10.1186/s12888-016-0858-x.
- Simpson A, Hannigan B, Coffey M, . Cross-national comparative mixed-methods case study of recovery-focused mental health care planning and co-ordination: Collaborative Care Planning Project (COCAPP). Health Serv Deliv Res 2016;4.
- NICE Guidance on Improving the Experience of Care for People Using Adult NHS Mental Health Services. NICE; 2011.
- Monitoring the Mental Health Act in 2011/12. Newcastle upon Tyne: CQC; 2013.
- Community Mental Health Services Survey 2011. Newcastle upon Tyne: CQC; 2011.
- Adult Mental Health Services: Follow Up Report. Cardiff: Wales Audit Office; 2011.
- Post-legislative Scrutiny of the Mental Health Act 2007: HC584, First Report of Session 2013–14. London: The Stationery Office; 2013.
- Post-legislative Scrutiny of the Mental Health (Wales) Measure 2010. Cardiff: National Assembly for Wales; 2015.
- The Pathway to Recovery. A Review of NHS Acute Inpatient Mental Health Services. London: Healthcare Commission; 2008.
- Malone D, Fineberg NA, Gale TM. What is the usual length of stay in a psychiatric ward?. Int J Psychiatry Clin Pract 2004;8:53-6. https://doi.org/10.1080/13651500310004498.
- Bowers L, Simpson A, Alexander J, Hackney D, Nijman H, Grange A, et al. The nature and purpose of acute psychiatric wards: The Tompkins acute ward study. J Ment Health 2005;14:625-35. https://doi.org/10.1080/09638230500389105.
- Simpson A, Hannigan B, Coffey M, Jones A, Barlow S, Cohen R, et al. Study protocol: cross-national comparative case study of recovery-focused mental health care planning and coordination (COCAPP). BMC Psychiatry 2015;15. https://doi.org/10.1186/s12888-015-0538-2.
- Developing and Evaluating Complex Interventions. London: Medical Research Council; 2008.
- Challis D, Hughes J, Clarkson P, Abendstern M, Sutcliffe C. A Systematic Evaluation of the Development and Impact of the Single Assessment Process in England. Presentation to the Showcasing Social Care Research Event. London: Department of Health; 2007.
- Creswell J. Research Design: Qualitative, Quantitative and Mixed Methods Approaches. London: Sage; 2009.
- Kohn M. Cross-national Research in Sociology. Newbury Park, CA: Sage; 1993.
- Hantrais L, Mangen S. Cross-national Research Methods in the Social Sciences. London: Pinter; 1996.
- Stake RE. The Art of Case Study Research. London: Sage; 1995.
- Fitzgerald L. Case studies as a research tool. Qual Health Care 1999;8. https://doi.org/10.1136/qshc.8.2.75.
- Platt J. ‘Case study’ in American methodological thought. Curr Sociol 1992;40:17-48. https://doi.org/10.1177/001139292040001004.
- Yin RK. Case Study: Design and Methods. Newbury Park, CA: Sage Publications; 1994.
- Robson C. Real World Research: A Resource for Social Scientists and Practitioners-researchers. Oxford: Blackwell; 1993.
- Sweetman D, Badiee M, Creswell JW. Use of the transformative framework in mixed methods studies. Qual Inquiry 2010;16:441-54. https://doi.org/10.1177/1077800410364610.
- Mertens DM. Transformative Research and Evaluation. New York, NY: Guilford Press; 2009.
- Byrne DS. Complexity Theory and the Social Sciences: An Introduction. London: Routledge; 1998.
- Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q 2004;82:581-629. https://doi.org/10.1111/j.0887-378X.2004.00325.x.
- Wong G, Greenhalgh T, Westhorp G, Buckingham J, Pawson R. RAMESES publication standards: meta-narrative reviews. BMC Med 2013;11. https://doi.org/10.1186/1741-7015-11-20.
- Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods 2007;39:175-91. https://doi.org/10.3758/BF03193146.
- Cohen J. A power primer. Psychol Bull 1992;112:155-9. https://doi.org/10.1037/0033-2909.112.1.155.
- O’Connell M, Tondora J, Croog G, Evans A, Davidson L. From rhetoric to routine: assessing perceptions of recovery-oriented practices in a state mental health and addiction system. Psychiatr Rehabil J 2005;28:378-86. https://doi.org/10.2975/28.2005.378.386.
- McGuire-Snieckus R, McCabe R, Catty J, Hansson L, Priebe S. A new scale to assess the therapeutic relationship in community mental health care: STAR. Psychol Med 2007;37:85-9. https://doi.org/10.1017/S0033291706009299.
- Rogers ES, Chamberlin J, Ellison ML, Crean T. A consumer-constructed scale to measure empowerment among users of mental health services. Psychiatr Serv 1997;48:1042-7. https://doi.org/10.1176/ps.48.8.1042.
- Rogers ES, Ralph RO, Salzer MS. Validating the empowerment scale with a multisite sample of consumers of mental health services. Psychiatr Serv 2010;61:933-6. https://doi.org/10.1176/ps.2010.61.9.933.
- Evans J, Rose D, Flach C, Csipke E, Glossop H, McCrone P, et al. VOICE: developing a new measure of service users’ perceptions of inpatient care, using a participatory methodology. J Ment Health 2012;21:57-71. https://doi.org/10.3109/09638237.2011.629240.
- Gould D. Service Users’ Experiences of Recovery Under the 2008 Care Programme Approach. National Survivors User Network/Mental Health Foundation; 2012.
- Jones A, Bowles N. Best practice from admission to discharge in acute inpatient care: considerations and standards from a whole system perspective. J Psychiatr Ment Health Nurs 2005;12:642-7. https://doi.org/10.1111/j.1365-2850.2005.00886.x.
- CPA Brief Audit Tool (CPA-BAT). London: Centre for Mental Health/Mental Health Act Commission; 2005.
- Simpson A, Jones J, Barlow S, Cox L. SUGAR . Adding SUGAR: service user and carer collaboration in mental health nursing research. J Psychosoc Nurs Ment Health Serv 2014;52:22-30.
- Price J. The role of the clinical studies officer in project recruitment. Ment Health Prac 2010;13:29-33. https://doi.org/10.7748/mhp2010.05.13.8.29.c7731.
- Hannigan B. Connections and consequences in complex systems: insights from a case study of the emergence and local impact of crisis resolution and home treatment services. Soc Sci Med 2013;93:212-19. https://doi.org/10.1016/j.socscimed.2011.12.044.
- Atkinson P, Housley W. Interactionism. London: Sage; 2003.
- Strauss AL. Negotiations: Varieties, Contexts, Processes, and Social Order. San Francisco, CA: Jossey-Bass; 1978.
- Breakwell GM. Research Methods in Psychology. London: Sage; 2012.
- Ritchie J, Lewis J, Nicholls CM, Ormston R. Qualitative Research Practice: A Guide for Social Science Students and Researchers. London: Sage; 2013.
- Ritchie J, Spencer L, Bryman A, Burgess RG. Analyzing Qualitative Data. London: Routledge; 1993.
- Moher D, Liberati A, Tetzlaff J, Altman DG. The PRISMA Group . Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLOS Med 2009;6. https://doi.org/10.1371/journal.pmed.1000097.
- Hannigan B, Allen D. Complexity and change in the United Kingdom’s system of mental health care. Social Theory &Amp; Health 2006;4:244-63. https://doi.org/10.1057/palgrave.sth.8700073.
- A Hospital Plan for England and Wales. London: Ministry of Health; 1962.
- Better Services for the Mentally Ill. London: Department of Health and Social Security; 1975.
- Crisp N, Smith G, Nicholson K. Old Problems, New Solutions: Improving Acute Psychiatric Care for Adults in England. London: The Commission to Review the Provision of Acute Inpatient Psychiatric Care for Adults; 2016.
- The Care Programme Approach for People With a Mental Illness Referred to the Specialist Psychiatric Services. London: DH; 1990.
- Hannigan B, Coffey M. Where the wicked problems are: the case of mental health. Health Policy 2011;101:220-7. https://doi.org/10.1016/j.healthpol.2010.11.002.
- The Mental Health Policy Implementation Guide. London: DH; 2001.
- Adult Mental health Services for Wales: Equity, Empowerment, Effectiveness, Efficiency. Cardiff: National Assembly for Wales; 2001.
- Policy Implementation Guidance on the Development of Crisis Resolution/Home Treatment (CR/HT) Services in Wales. Cardiff: Welsh Assembly Government; 2005.
- Background Briefing Paper. Commission on Acute Adult Psychiatric Care; 2016.
- Shepperd G, Beadsmoore A, Moore C, Hardy P, Muijen M. Relation between bed use, social deprivation and overall bed availability in acute adult psychiatric units and alternative residential options: a cross-sectional survey, one day census data, and staff interviews. BMJ 1997;314:262-6. https://doi.org/10.1136/bmj.314.7076.262.
- Lelliott P. Acute inpatient psychiatry in England: an old problem and a new priority. Epidemiol Psichiatr Soc 2006;15:91-4. https://doi.org/10.1017/S1121189X00004267.
- Mental health sector hit by beds shortage . Health Service Journal 2013. www.hsj.co.uk/news/exclusive-mental-health-sector-hit-by-beds-shortage/5064061.article (accessed 9 August 2016).
- Maximising Resources in Adult Mental Health. London: Audit Commission; 2010.
- It’s intensive, but is it for the best?. Health Service Journal 2012. www.hsj.co.uk/topics/service-design/its-intensive-but-is-it-for-the-best/5048343.fullarticle (accessed 9 August 2016).
- The Five Year Forward View for Mental Health: a Report from the Independent Mental Health Taskforce to the NHS in England. London: NHS England; 2016.
- Closing the Gap: Priorities for Essential Change in Mental Health. London: DH; 2014.
- Service User Experience in Adult Mental Health: Improving the Experience of Care for People Using Adult NHS Mental Health Services. London: NICE; 2011.
- Mental Health Under Pressure. London: The King’s Fund; 2015.
- Is Mental Health Care Improving?. The Health Foundation; 2015.
- Do the Right Thing. How to Judge a Good Ward. Ten Standards for Adult In-patient Mental Healthcare. Royal College of Psychiatrists; 2011.
- Safe Staffing for Nursing in Inpatient Mental Health Settings. London: NICE; 2014.
- Mental Health Staffing Framework. NHS England; 2015.
- Lintern S. Experts Criticise New Mental Health Staffing Framework. Nursing Times; 2015.
- Workforce Planning in the NHS. London: The King’s Fund; 2015.
- The Abandoned Illness: A Report from the Schizophrenia Commission. London: Rethink Mental Illness; 2012.
- Mental Health Nursing: Addressing Acute Concerns. London: Standing Nursing and Midwifery Advisory Committee; 1999.
- Cresswell J, Beavon M. Accreditation for Inpatient Mental Health Services (AIMS). Standards for Inpatient wards: Working-Age Adults. London: Royal College of Psychiatrists; 2010.
- Guidance for Commissioners of Acute Care: Inpatient and Crisis Home Treatment. London: Joint Commissioning Panel for Mental Health; 2013.
- Star Wards . Star Wards n.d. www.starwards.org.uk/ (accessed 12 July 2016).
- Bowers L. Safewards: a new model of conflict and containment on psychiatric wards. J Psychiatr Ment Health Nurs 2014;21:499-508. https://doi.org/10.1111/jpm.12129.
- New Investment in Mental Health Services. Prime Minister’s Office; 2016.
- Improving the Mental Health of the Population. Towards a Strategy on Mental Health for the European Union. (COM (2005) 484); 2005. Brussels: Commission of the European Communities; 2005.
- Improving Health Systems and Services for Mental Health. Geneva: WHO; 2009.
- Bourdieu P, Nice R. Distinctions. A Social Critique of the Judgment of Taste. Cambridge, MA: Harvard University Press; 1984.
- Wallcraft J, Bryant M. The Mental Health Service User Movement in England. London: The Sainsbury Centre for Mental Health; 2003.
- Rose D, Fleischmann P, Schofield P. Perceptions of user involvement: a user-led study. Int J Soc Psychiatry 2010;56:389-401. https://doi.org/10.1177/0020764009106618.
- Storm M, Edwards A. Models of user involvement in the mental health context: intentions and implementation challenges. Psychiatr Q 2013;84:313-27. https://doi.org/10.1007/s11126-012-9247-x.
- Ramon S. Neoliberalism and its implications for mental health in the UK. Int J Law Psychiatry 2008;31:116-25. https://doi.org/10.1016/j.ijlp.2008.02.006.
- Teghtsoonian K. Depression and mental health in neoliberal times: a critical analysis of policy and discourse. Soc Sci Med 2009;69:28-35. https://doi.org/10.1016/j.socscimed.2009.03.037.
- Rogers A, Pilgrim D. A Sociology of Mental Health and Illness. Berkshire: McGraw Hill/Open University Press; 2010.
- Bowers L, Brennan G, Winship G, Theodoridou C. Talking With Acutely Psychotic Patients. Communication Skills for Nurses and Others Spending Time With People who are Very Mentally Ill. London: City University; 2009.
- Peplau H. Interpersonal Relations in Nursing: A Conceptual Frame of Reference for Psychodynamic Nursing. Houndmills: MacMillan Education; 1988.
- Dwamena F, Holmes-Rovner M, Gaulden CM, Jorgenson S, Sadigh G, Sikorskii A, et al. Interventions for providers to promote a patient-centred approach in clinical consultations. Cochrane Database Syst Rev 2012;12. https://doi.org/10.1002/14651858.CD003267.pub2.
- Bee P, Playle J, Lovell K, Barnes P, Gray R, Keeley P. Service user views and expectations of UK-registered mental health nurses: a systematic review of empirical research. Int J Nurs Stud 2008;45:442-57. https://doi.org/10.1016/j.ijnurstu.2007.02.008.
- Bee P, Price O, Baker J, Lovell K. Systematic synthesis of barriers and facilitators to service user-led care planning. Br J Psychiatry 2015;207:104-14. https://doi.org/10.1192/bjp.bp.114.152447.
- Fritz WB. Inpatients’ views of staff-patient discussions about major treatment decisions. Hosp Community Psychiatry 1981;32:791-5. https://doi.org/10.1176/ps.32.11.791.
- Walsh J, Boyle J. Improving acute psychiatric hospital services according to inpatient experiences. A user-led piece of research as a means to empowerment. Issues Ment Health Nurs 2009;30:31-8. https://doi.org/10.1080/01612840802500733.
- Simon D, Loh A, Wills CE, Härter M. Depressed patients’ perceptions of depression treatment decision-making. Health Expect 2007;10:62-74. https://doi.org/10.1111/j.1369-7625.2006.00424.x.
- Eisen S, Dickey B, Sederer L, Dickey B, Sederer L. Improving Mental Health Care: Commitment to Quality. Arlington, VA: American Psychiatric Publishing, Inc.; 2001.
- Howard PB, El-Mallakh P, Kay Rayens M, Clark JJ. Consumer perspectives on quality of inpatient mental health services. Arch Psychiatr Nurs 2003;17:205-17. https://doi.org/10.1016/S0883-9417(03)00096-7.
- Wallsten T, Kjellin L. Involuntarily and voluntarily admitted patients’ experiences of psychiatric admission and treatment – a comparison before and after changed legislation in Sweden. Eur Psychiatry 2004;19:464-8. https://doi.org/10.1016/j.eurpsy.2004.06.029.
- Richards D, Bee P, Loftus S, Baker J, Bailey L, Lovell K. Specialist educational intervention for acute inpatient mental health nursing staff: service user views and effects on nursing quality. J Adv Nurs 2005;51:634-44. https://doi.org/10.1111/j.1365-2648.2005.03550.x.
- Berger JL. Incorporation of the tidal model into the interdisciplinary plan of care – a program quality improvement project. J Psychiat Ment Health Nurs 2006;13:464-7. https://doi.org/10.1111/j.1365-2850.2006.01007.x.
- Karlsen R. Improving the nursing documentation: professional consciousness-raising in a Northern-Norwegian psychiatric hospital. J Psychiat Ment Health Nurs 2007;14:573-7. https://doi.org/10.1111/j.1365-2850.2007.01144.x.
- Daremo A, Haglund L. Activity and participation in psychiatric institutional care. Scand J Occup Ther 2008;15:131-42. https://doi.org/10.1080/11038120801900050.
- Storm M, Davidson L. Inpatients’ and providers’ experiences with user involvement in inpatient care. Psychiatr Q 2010;81:111-25. https://doi.org/10.1007/s11126-009-9122-6.
- Jaeger M, Konrad A, Rueegg S, Rabenschlag F. Patients’ subjective perspective on recovery orientation on an acute psychiatric unit. Nord J Psychiatry 2015;69:188-95. https://doi.org/10.3109/08039488.2014.959561.
- Cree L, Brooks HL, Berzins K, Fraser C, Lovell K, Bee P. Carers’ experiences of involvement in care planning: a qualitative exploration of the facilitators and barriers to engagement with mental health services. BMC Psychiatry 2015;15. https://doi.org/10.1186/s12888-015-0590-y.
- Doran D, Paterson J, Clark C, Srivastava R, Goering PN, Kushniruk AW, et al. A pilot study of an electronic interprofessional evidence-based care planning tool for clients with mental health problems and addictions. Worldviews Evid Based Nurs 2010;7:174-84. https://doi.org/10.1111/j.1741-6787.2010.00191.x.
- Linhorst DM, Hamilton G, Young E, Eckert A. Opportunities and barriers to empowering people with severe mental illness through participation in treatment planning. Soc Work 2002;47:425-34. https://doi.org/10.1093/sw/47.4.425.
- Lloyd-Evans B, Johnson S, Morant N, Gilburt H, Osborn DP, Jagielska D, et al. Alternatives to standard acute in-patient care in England: differences in content of care and staff-patient contact. Br J Psychiatry Suppl 2010;53:s46-51. https://doi.org/10.1192/bjp.bp.110.081117.
- Bee P, Brooks H, Fraser C, Lovell K. Professional perspectives on service user and carer involvement in mental health care planning: a qualitative study. Int J Nurs Stud 2015;52:1834-45. https://doi.org/10.1016/j.ijnurstu.2015.07.008.
- Hurst K, Wistow G, Higgins R. Mental health nursing in acute settings. Mental Health Practice 2004;2:8-11.
- Sharac J, McCrone P, Sabes-Figuera R, Csipke E, Wood A, Wykes T. Nurse and patient activities and interaction on psychiatric inpatients wards: a literature review. Int J Nursing Studies 2010;47:909-17. https://doi.org/10.1016/j.ijnurstu.2010.03.012.
- Holland TP, Konick A, Buffum W, Smith MK, Petchers M. Institutional structure and resident outcomes. J Health Soc Behav 1981;22:433-44. https://doi.org/10.2307/2136683.
- Skelly N, Schnittger RI, Butterly L, Frorath C, Morgan C, McLoughlin DM, et al. Quality of care in psychosis and bipolar disorder from the service user perspective. Qual Health Res 2013;23:1672-85. https://doi.org/10.1177/1049732313509896.
- Cappleman R, Bamford Z, Dixon C, Thomas H. Experiences of ward rounds among in-patients on an acute mental health ward: a qualitative exploration. BJPsych Bull 2015;39:233-6. https://doi.org/10.1192/pb.bp.113.046409.
- Davidson L, Haglund KE, Stayner DA, Rakfeldt J, Chinman MJ, Tebes JK. ‘It was just realizing . . . that life isn’t one big horror’: a qualitative study of supported socialization. Psychiat Rehabil J 2001;24:275-92. https://doi.org/10.1037/h0095084.
- Harden J, Hales RE, Amen D, Lewis G, Miliken C, Orman D. Inpatient participation in treatment planning: a preliminary report. Gen Hosp Psychiatry 1986;8:287-90. https://doi.org/10.1016/0163-8343(86)90011-3.
- Oeye C, Bjelland AK, Skorpen A, Anderssen N. User participation when using milieu therapy in a psychiatric hospital in Norway: a mission impossible?. Nurs Inq 2009;16:287-96. https://doi.org/10.1111/j.1440-1800.2009.00463.x.
- Eisen SV, Dickey B, Sederer LI. A self-report symptom and problem rating scale to increase inpatients’ involvement in treatment. Psychiat Serv 2000;51:349-53. https://doi.org/10.1176/appi.ps.51.3.349.
- Bowersox NW, Bohnert AS, Ganoczy D, Pfeiffer PN. Inpatient psychiatric care experience and its relationship to posthospitalization treatment participation. Psychiat Serv 2013;64:554-62. https://doi.org/10.1176/appi.ps.002342012.
- Hester L, O’Doherty LJ, Schnittger R, Skelly N, O’Donnell M, Butterly L, et al. SEQUenCE: a service user-centred quality of care instrument for mental health services. Int J Qual Health Care 2015;27:284-90. https://doi.org/10.1093/intqhc/mzv043.
- Vigod SN, Kurdyak PA, Dennis CL, Leszcz T, Taylor VH, Blumberger DM, et al. Transitional interventions to reduce early psychiatric readmissions in adults: systematic review. Br J Psychiatry 2013;202:187-94. https://doi.org/10.1192/bjp.bp.112.115030.
- Craig TJ, Bracken J. A case-control study of rapid readmission in a state hospital population. Ann Clin Psychiatry 1995;7:79-85. https://doi.org/10.3109/10401239509149031.
- Ballard FA. Benefits of psychosocial rehabilitation programming in a treatment mall. J Psychosoc Nurs Ment Health Serv 2008;46:26-32. https://doi.org/10.3928/02793695-20080201-01.
- Transition Between Inpatient Mental Health Settings and Community or Care Home Settings. London: NICE; 2015.
- Hansson L, Berglund M. Factors influencing treatment outcome and patient satisfaction in a short-term psychiatric ward. A path analysis study of the importance of patient involvement in treatment planning. Eur Arch Psychiatry Neurol Sci 1987;236:269-75. https://doi.org/10.1007/BF00380951.
- Rise MB, Grimstad H, Solbjør M, Steinsbekk A. Effect of an institutional development plan for user participation on professionals’ knowledge, practice, and attitudes. A controlled study. BMC Health Serv Res 2011;11. https://doi.org/10.1186/1472-6963-11-296.
- Ayres L, Kavanaugh K, Knafl KA. Within-case and across-case approaches to qualitative data analysis. Qual Health Res 2003;13:871-83. https://doi.org/10.1177/1049732303013006008.
- Wowra SA, McCarter R. Validation of the empowerment scale with an outpatient mental health population. Psychiatr Serv 1999;50:959-61. https://doi.org/10.1176/ps.50.7.959.
- Welsh Index of Multiple Deprivation (WIMD). Cardiff: Welsh Government; 2014.
- English Indices of Depriviation 2010. n.d.
- The National Archives . The Mid Staffordshire NHS Foundation Trust Public Inquiry 2013. http://webarchive.nationalarchives.gov.uk/20150407084003/http://www.midstaffspublicinquiry.com/report (accessed 14th July 2016).
- Francis R. Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry. London: The Stationery Office; 2013.
- Csipke E, Williams P, Rose D, Koeser L, McCrone P, Wykes T, et al. Following the Francis report: investigating patient experience of mental health in-patient care. Br J Psychiatry 2016;209:35-9. https://doi.org/10.1192/bjp.bp.115.171124.
- Whittington R, Bowers L, Nolan P, Simpson A, Neil L. Approval ratings of inpatient coercive interventions in a national sample of mental health service users and staff in England. Psychiatr Serv 2009;60:792-8. https://doi.org/10.1176/ps.2009.60.6.792.
- Muir-Cochrane E, van der Merwe M, Nijman H, Haglund K, Simpson A, Bowers L. Investigation into the acceptability of door locking to staff, patients, and visitors on acute psychiatric wards. Int J Mental Health Nurs 2012;21:41-9. https://doi.org/10.1111/j.1447-0349.2011.00758.x.
- Bowers L, Whittington R, Nolan P, Parkin D, Curtis S, Bhui K, et al. Relationship between service ecology, special observation and self-harm during acute in-patient care: City-128 study. Br J Psychiatry 2008;193:395-401. https://doi.org/10.1192/bjp.bp.107.037721.
- Bowers L, James K, Quirk A, Simpson A, Stewart D, Hodsoll J. SUGAR . Reducing conflict and containment rates on acute psychiatric wards: the Safewards cluster randomised controlled trial. Int J Nurs Stud 2015;52:1412-22. https://doi.org/10.1016/j.ijnurstu.2015.05.001.
- Benchmarking Network. NHS; 2016.
- Inpatients Formally Detained in Hospitals Under the Mental Health Act 1983, and Patients Subject to Supervised Community Treatment, England 2014/15. London: Health and Social Care Information Centre; 2015.
- Roth JA. Timetables: Structuring the Passage of Time in Hospital Treatment and Other Careers. Indianapolis, IN: The Bobbs Merrill Company; 1963.
- Coffey M. Time and its uses in accounts of conditional discharge in forensic psychiatry. Sociol Health Illn 2013;35:1181-95. https://doi.org/10.1111/1467-9566.12036.
- Klitzman R. ‘Patient-time’, ‘doctor-time’, and ‘institution-time’: perceptions and definitions of time among doctors who become patients. Patient Educ Couns 2007;66:147-55. https://doi.org/10.1016/j.pec.2006.10.005.
- White R, Karim B. Patients’ views of the ward round: a survey. Psychiatr Bull 2005;29:207-9. https://doi.org/10.1192/pb.29.6.207.
- Bowers L, Simpson A, Alexander J. Real world application of an intervention to reduce absconding. J Psychiatr Ment Health Nurs 2005;12:598-602. https://doi.org/10.1111/j.1365-2850.2005.00879.x.
- Leamy M, Bird V, Le Boutillier C, Williams J, Slade M. Conceptual framework for personal recovery in mental health: systematic review and narrative synthesis. Br J Psychiatry 2011;199:445-52. https://doi.org/10.1192/bjp.bp.110.083733.
- Le Boutillier C, Leamy M, Bird VJ, Davidson L, Williams J, Slade M. What does recovery mean in practice? A qualitative analysis of international recovery-oriented practice guidance. Psychiat Serv 2011;62:1470-6. https://doi.org/10.1176/appi.ps.001312011.
- Scanlon A. Psychiatric nurses perceptions of the constituents of the therapeutic relationship: a grounded theory study. J Psychiatr Ment Health Nurs 2006;13:319-29. https://doi.org/10.1111/j.1365-2850.2006.00958.x.
- Moreno-Poyato AR, Montesó-Curto P, Delgado-Hito P, Suárez-Pérez R, Aceña-Domínguez R, Carreras-Salvador R, et al. The therapeutic relationship in inpatient psychiatric care: a narrative review of the perspective of nurses and patients. Arch Psychiatr Nurs 2016;30:782-7. https://doi.org/10.1016/j.apnu.2016.03.001.
- Aston V, Coffey M. Recovery: what mental health nurses and service users say about the concept of recovery. J Psychiatr Ment Health Nurs 2012;19:257-63. https://doi.org/10.1111/j.1365-2850.2011.01776.x.
- Hunt IM, Rahman MS, While D, Windfuhr K, Shaw J, Appleby L, et al. Safety of patients under the care of crisis resolution home treatment services in England: a retrospective analysis of suicide trends from 2003 to 2011. Lancet Psychiatry 2014;1:135-41. https://doi.org/10.1016/S2215-0366(14)70250-0.
- Fraser C, Grundy A, Meade O, Callaghan P, Lovell K. EQUIP training the trainers: an evaluation of a training programme for service users and carers involved in training mental health professionals in user-involved care planning [published online ahead of print 20 January 2017]. J Psychiat Ment Health Nurs 2017.
- Alakeson V, Perkins R. Recovery, Personalisation and Personal Budgets. London: Centre for Mental Health; 2012.
- Dixon J, Chamberlain M. Medicine, Power, and Discourse. London: Taylor & Francis; 2015.
- Cavanagh B, Ibrahim S, Roscoe A, Bickley H, While D, Windfuhr K, et al. The timing of general population and patient suicide in England, 1997–2012. J Affect Disord 2016;197:175-81. https://doi.org/10.1016/j.jad.2016.02.055.
- Coope C, Gunnell D, Hollingworth W, Hawton K, Kapur N, Fearn V, et al. Suicide and the 2008 economic recession: who is most at risk? Trends in suicide rates in England and Wales 2001–2011. Soc Sci Med 2014;117:76-85. https://doi.org/10.1016/j.socscimed.2014.07.024.
- National Confidential Inquiry into Homicide and Suicide by People with Mental Illness. Annual Report: England, Northern Ireland, Scotland and Wales July 2015. Manchester: University of Manchester; 2015.
- Meehan J, Kapur N, Hunt IM, Turnbull P, Robinson J, Bickley H, et al. Suicide in mental health in-patients and within 3 months of discharge. National clinical survey. Br J Psychiatry 2006;188:129-34. https://doi.org/10.1192/bjp.188.2.129.
- Johnson S. Crisis resolution and home treatment teams: an evolving model. Advanc Psychiat Treat 2013;19:115-23. https://doi.org/10.1192/apt.bp.107.004192.
- Coffey M. ‘A risk worth taking? Value differences and alternative risk constructions in accounts given by patients and their community workers following conditional discharge from forensic mental health services. Health Risk Soc 2012;14:465-82. https://doi.org/10.1080/13698575.2012.682976.
- Bowers L, Chaplin R, Quirk A, Lelliott P. A conceptual model of the aims and functions of acute inpatient psychiatry. J Ment Health 2009;18:316-25. https://doi.org/10.1080/09638230802053359.
- Wright N, Rowley E, Chopra A, Gregoriou K, Waring J. From admission to discharge in mental health services: a qualitative analysis of service user involvement. Health Expect 2016;19:367-76. https://doi.org/10.1111/hex.12361.
- Fricker M. Epistemic Injustice: Power and the Ethics of Knowing. Oxford: Oxford University Press; 2007.
- Coffey M, Cohen R, Faulkner A, Hannigan B, Simpson A, Barlow S. Ordinary risks and accepted fictions: how contrasting and competing priorities work in risk assessment and mental health care planning. Health Expect 2017;20:471-83. https://doi.org/10.1111/hex.12474.
- Jones J, Nolan P, Bowers L, Simpson A, Whittington R, Hackney D, et al. Psychiatric wards: places of safety?. J Psychiatr Ment Health Nurs 2010;17:124-30. https://doi.org/10.1111/j.1365-2850.2009.01482.x.
- Quirk A, Lelliott P, Seale C. Service users’ strategies for managing risk in the volatile environment of an acute psychiatric ward. Soc Sci Med 2004;59:2573-83. https://doi.org/10.1016/j.socscimed.2004.04.005.
- Health Service Journal . NHS Improvement Accused of ‘Dismantling’ NICE Safe Staffing Work 2016. www.hsj.co.uk/topics/workforce/exclusive-nhs-improvement-accused-of-dismantling-nice-safe-staffing-work/7005462.fullarticle (accessed 17 July 2016).
- Scottish Recovery Network . Scottish Recovery Indicator 2: How Recovery Focused Are We? Learning from Four Years of the Scottish Recovery Indicator 2015. https://scottishrecovery.net/wp-content/uploads/2016/04/SRI2_Report_Final_Web.pdf (accessed 6 September 2017).
- Repper J, Aldridge B, Gilfoyle S, Gillard S, Perkins R, Rennison J. Peer Support Workers: Theory and Practice. London: Centre for Mental Health; 2013.
- Nolan F. An Evaluation of Protected Engagement Time on Staff and Patient Outcomes in Acute Mental Health Inpatient Wards: Implications for Mental Health Nursing and Research 2013.
- White M. How effective is productive ward?. Nursing Times 2015;111:22-5.
- Taylor-Watt J, Cruickshank A, Innes J, Brome B, Shah A. Reducing physical violence and developing a safety culture across wards in East London. Br J Ment Health Nurs 2017;6:35-43. https://doi.org/10.12968/bjmh.2017.6.1.35.
- Bowers L, Allan T, Simpson A, Jones J, Whittington R. Morale is high in acute inpatient psychiatry. Soc Psychiatry Psychiatr Epidemiol 2009;44:39-46. https://doi.org/10.1007/s00127-008-0396-z.
- Hannigan B, Edwards D, Coyle D, Fothergill A, Burnard P. Burnout in community mental health nurses: findings from the all-Wales stress study. J Psychiat Ment Health Nurs 2000;7:127-34. https://doi.org/10.1046/j.1365-2850.2000.00279.x.
Appendix 1 Questionnaires: Views on Inpatient Care; Recovery Self-Assessment Person in Recovery; Scale to Assess the Therapeutic Relationship; Empowerment Scale
Appendix 2 Interview schedule example (service user)
Appendix 3 Care plan review structured template
Appendix 4 Non-participant observation guide
Appendix 5 Recovery profiles from the Recovery Self-Assessment
In the following sections, we include a recovery profile for each of the six sites based on individual item analysis of the five highest and five lowest-rated recovery-orientated practices. This is based on the mean scores of all of the respondents and is presented from the perspective of the service user and service provider (staff).
Artois Recovery Profile from the Recovery Self-Assessment
Highest-rated items
Service users
From a possible Likert score of 1 to 5, the mean range of item responses for service users were between 2.24 and 3.83, with the five highest scoring items falling in the range between 3.52 and 3.83. The five highest-rated items for the service users were within the ‘choice’, ‘life goals’ and ‘individually tailored services’ subscales (Table 57). Another highly rated item (not within the top five) fell within the ‘life goals’ domain, referring to staff beliefs in a person’s ability to recover and make treatment and life choices. A further highly rated item was within the ‘choice’ subscale with the item referring to ‘staff not using threats, bribes or other forms of coercion to influence behaviour and choices’.
| Rank | Service users (mean of 3.52–3.83 on Likert scale)a | Staff (mean of 3.79–4.06 on Likert scale)a |
|---|---|---|
| 1 | Staff are diverse in terms of culture, ethnicity, lifestyle and interests Life goals |
Staff are diverse in terms of culture, ethnicity, lifestyle and interests Life goals |
| 2 | Staff are knowledgeable about special interest groups and activities in the community Life goals |
Every effort is made to involve significant others and other natural supports in the planning of a person’s services, if so desired Individually tailored services |
| 3 | My service provider makes every effort to involve my significant others and other sources of natural support in the planning of my services, if this is my preference Individually tailored services |
Staff do not use threats, bribes or other forms of coercion to influence the behaviour or choices Choice |
| 4 | Staff use a language of recovery (i.e. hope, high expectations, respect) in everyday conversations Life goals |
Staff listen to and follow the choices and preferences of participants Choice |
| 5 | Staff help to monitor the progress I am making towards my personal goals on a regular basis Choice |
Staff believe that people can recover and make their own treatment and life choices Life goals |
Staff
From a possible Likert score of 1 to 5, the mean range of item responses for staff were between 2.73 and 4.06, with the five highest scoring items falling in the range between 3.79 and 4.06. The five highest-rated items for the staff were within the ‘choice’, ‘life goals’ and ‘individually tailored services’ subscales (see Table 57). Other highly rated items (not in the top five) were within the ‘life goal’ domain, such as ‘staff play a role in helping people in recovery to become involved in non-mental health/addiction related activities, use a language of recovery in everyday conversations, staff role is to assist a person with fulfilling their individually defined goals and aspirations and facilitate referral to other programmes and services if the trust cannot meet a person’s needs’. In addition to this, an item in the ‘diversity of treatment options’ subscale was scored highly, supporting the notion that ‘people in recovery are given the opportunity to discuss their sexual and spiritual needs and interests’. Another highly rated item was within the ‘choice’ subscale around monitoring progress made towards personal recovery goals.
Lowest-rated items
Service users
From a possible Likert score of 1 to 5, the five lowest scoring items fall in the range between 2.24 and 2.89. The five lowest-rated items for the service users were within the ‘choice’, ‘involvement’, ’diversity of treatment options’ and ‘individually tailored services’ subscales (Table 58).
| Rank | Service users (mean of 2.24–2.89 on Likert scale)a | Staff (mean of 3.13–3.24 on Likert scale)a |
|---|---|---|
| 1 | I have access to all my treatment records Choice |
Most services are provided in a person’s natural environment (i.e. home, community, workplace) Choice |
| 2 | I can choose and change, if desired, the therapist, psychiatrist, or other service provider with whom I work Choice |
People in recovery are regular members of agency advisory boards and management meetings Involvement |
| 3 | I am/can be involved with facilitating staff trainings and education programs at this agency Involvement |
Persons in recovery are involved with facilitating staff trainings and education programs at this agency Involvement |
| 4 | I am given the opportunity to discuss my sexual and spiritual needs and interests Diversity of treatment options |
This agency provides education to community employers about employing people with mental illness and/or addictions Individually tailored services |
| 5 | This agency provides education to community employers about employing people with mental illness and/or addictions Individually tailored services |
The development of a person’s leisure interests and hobbies is a primary focus of services Involvement |
Staff
From a possible Likert score of 1 to 5, the five lowest scoring items fall in the range between 3.13 and 3.24. The five lowest-rated items for the service users were within the ‘choice’, ‘involvement’, and ‘individually tailored services’ subscales (see Table 58).
Burgundy recovery profile from the Recovery Self-Assessment
Highest-rated items
Service users
From a possible Likert score from 1 to 5, the mean range of item responses for service users was between 2.62 and 3.81, with the five highest scoring items falling in the range of 3.70 and 3.81. The five highest-rated items for the service users were within the life goals choice and individually tailored services subscales (Table 59). Other highly rated items related to ‘choice’, such as ‘staff do not use threats, bribes or other forms of coercion to influence my behaviour or choices’. In addition to this, respondents reported that ‘service users that are doing well get as much attention as those with difficulties and that staff are knowledgeable about special interest groups and activities in the community’.
| Rank | Service users (mean of 3.70–3.81 on Likert scale)a | Staff (mean of 4.10–4.44 on Likert scale)a |
|---|---|---|
| 1 | Agency staff believe that I can recover and make my own treatment and life choices Life goals |
Staff do not use threats, bribes or other forms of coercion to influence the behaviour or choices Choice |
| 2 | Agency staff are diverse in terms of culture, ethnicity, lifestyle and interests Life goals |
Every effort is made to involve significant others and other natural supports in the planning of a person’s services, if so desired Individually tailored services |
| 3 | Staff at this agency help to monitor the progress I am making towards my personal goals on a regular basis Choice |
Progress made towards goals (as defined by the person in recovery) is monitored on a regular basis Choice |
| 4 | Staff of this agency regularly attend trainings on cultural competency Individually tailored services |
The role of staff is to assist a person with fulfilling their individually defined goals and aspirations Life goals |
| 5 | Staff use a language of recovery (i.e. hope, high expectations, respect) in everyday conversations Life goals |
Staff believe that people can recover and make their own treatment and life choice Life goals |
Staff
From a possible Likert score from 1 to 5, the mean range of item response for staff was between 2.68 and 4.44, with the five highest items falling in the range between 4.10 and 4.44. The highly rated items for the staff were in the area of ‘life goals’, ‘choice’ and ‘individually tailored services’ (see Table 59). Other highly rated items (not in the top five) related to ‘diversity of treatment options’, such as ‘clearly defined criteria for discharge from hospital and the opportunity for service users to discuss sexual and spiritual needs and interests’. Other strengths were in the area of ‘life goals’, such as ‘staff using a language of recovery, assist individuals in the pursuit of their educational and or employment goals’. In addition to this, respondents agreed that ‘staff were diverse in culture, ethnicity, lifestyle and interests’ and that there were procedures in place for referrals if needed. Participants also strongly agreed that ‘staff listen to and follow the choices and preferences of participants and complementary to this that the trust/board offers services and programs for individuals with different cultures, life experiences, interests and needs’.
Lowest-rated items
Service users
From a possible Likert score from 1 to 5, the five lowest scoring items fall in the range between 2.62 and 3.02. The five lowest-rated items for the service users were within the ‘choice’, ‘life goals’, ‘involvement’ and ‘diversity of treatment options’ subscales (Table 60).
| Rank | Service users (mean of 2.62–3.02 on Likert scale)a | Staff (mean of 2.68–2.95 on Likert scale)a |
|---|---|---|
| 1 | I have access to all my treatment records Choice |
This agency provides education to community employers about employing people with mental illness and/or addictions Individually tailored services |
| 2 | I am/can be a regular member of agency advisory boards and management meetings Involvement |
People in recovery are regular members of agency advisory boards and management meetings Involvement |
| 3 | This agency actively attempts to link me with other persons in recovery who can serve as role models or mentors by making referrals to self-help, peer support, or consumer advocacy groups or programs Diversity of treatment options |
Persons in recovery are involved with facilitating staff trainings and education programs at this agency Involvement |
| 4 | I am/can be involved with facilitating staff trainings and education programs at this agency Involvement |
This agency provides structured educational activities to the community about mental illness and addictions Involvement |
| 5 | Staff play a primary role in helping me to become involved in non-mental health/addiction related activities, such as church groups, special interest groups, and adult education Life goals |
All staff at this agency regularly attend trainings on cultural competency Involvement |
Staff
From a possible Likert score from 1 to 5, the five lowest scoring items fall in the range between 2.36 and 2.65. The five lowest-rated items for the service users were within the ‘involvement’ and ‘individually tailored services’ subscales (see Table 60).
Champagne recovery profile from the Recovery Self-Assessment
Highest-rated items
Service users
From a possible Likert score from 1 to 5, the mean range of item responses for service users was between 2.52 and 3.73, with the five highest scoring items falling in the range between 3.63 and 3.73. The five highest-rated items for the service users were within the ‘life goals’, ‘choice’ and ‘individually tailored services’ subscales (Table 61). Other high-rated items (not within the top five) related to ‘choice’ such as ‘staff do not use threats, bribes or other forms of coercion to influence my behaviour or choices’. Another was in the area of ‘life goals’: ‘the role of staff is to assist me and other people in recovery with fulfilling my individually defined goals and aspirations’. Other highly rated items for staff were in the area of ‘choice’, such as ‘staff do not use threats, bribes or other forms of coercion to influence behaviour or choices’. In addition to this, another strength identified was in the area of ‘life goals’, such as ‘the role of staff is to assist me, and other people in recovery with fulfilling my individually defined goals and aspirations’.
| Rank | Service users (mean of 3.63–3.73 on Likert scale)a | Staff (mean of 3.80–4.00 on Likert scale)a |
|---|---|---|
| 1 | My service provider makes every effort to involve my significant others and other sources of natural support in the planning of my services, if this is my preference Individually tailored services |
Staff do not use threats, bribes or other forms of coercion to influence the behaviour or choices Choice |
| 2 | Agency staff believe that I can recover and make my own treatment and life choices Life goals |
The role of staff is to assist a person with fulfilling their individually defined goals and aspirations Life goals |
| 3 | Staff at this agency help to monitor the progress I am making towards my personal goals on a regular basis Choice |
Every effort is made to involve significant others and other natural supports in the planning of a person’s services, if so desired Individually tailored services |
| 4 | Agency staff are diverse in terms of culture, ethnicity, lifestyle and interests Life goals |
Staff are diverse in terms of culture, ethnicity, lifestyle and interests Life goals |
| 5 | Staff use a language of recovery (i.e. hope, high expectations, respect) in everyday conversations Life goals |
Staff believe that people can recover and make their own treatment and life choices Life goals |
Staff
From a possible Likert score from 1 to 5, the mean range of items for staff was between 2.36 and 4.00, with the five highest scoring items falling in the range between 3.80 and 4.00. The five highest items for the staff were within the ‘life goals’, ‘choice’ and ‘individually tailored services’ subscales (see Table 61). Other highly rated items (not in the top five) were within the ‘choice’ subscale, such as ‘staff listen to and follow the choices and preferences of service users and progress towards goals is monitored on a regular basis’. Another area of strength was within ‘life goals’, such as ‘staff using a language of recovery (i.e. hope, high expectations, respect) in everyday conversations’ and that ‘there are procedures in place to facilitate referrals to other programs/services if needed’.
Lowest-rated items
Service users
From a possible Likert score from 1 to 5, the five lowest scoring items fall in the range between 2.52 and 2.88. The five lowest-rated items for the service users were within the ‘choice’, ‘life goals’, ‘involvement’ and ‘diversity of treatment options’ subscales (Table 62).
| Rank | Service users (mean of 2.52–2.88 on Likert scale)a | Staff (mean of 2.36–2.65 on Likert scale)a |
|---|---|---|
| 1 | I am able to choose from a variety of treatment options at this agency (i.e. individual, group, peer support, holistic healing, alternative treatments, medical) Diversity of treatment options |
This agency provides education to community employers about employing people with mental illness and/or addictions Individually tailored services |
| 2 | I am/can be a regular member of advisory boards and management meetings Involvement |
All staff regularly attend trainings on cultural competency Individually tailored services |
| 3 | Most of my services are provided in my natural environment (i.e. home, community, workplace) Choice |
This agency provides structured educational activities to the community about mental illness and addictions Involvement |
| 4 | Staff actively assist me with the development of career and life goals that go beyond symptom management and stabilisation Life goals |
The development of a person’s leisure interests and hobbies is a primary focus of services Involvement |
| 5 | Staff routinely assist me in the pursuit of my educational and/or employment goals Life goals |
This agency provides a variety of treatment options (i.e. individual, group, peer support, holistic healing, alternative treatments, medical) from which participants may choose Diversity of treatment options |
Staff
From a possible Likert score from 1 to 5, the five lowest scoring items fall in the range between 2.36 and 2.65. The five lowest-rated items for the service users were within the ‘involvement’, ‘individually tailored services’ and ‘diversity of treatment options’ subscales (see Table 62).
Dauphine recovery profile from the Recovery Self-Assessment
Highest-rated items
Service users
From a possible Likert score from 1 to 5, the mean range of item responses for service users was between 2.81 and 3.98, with the five highest scoring items falling in the range between 3.56 and 3.98. The five highest-rated items for the service users were within the ‘life goals’ and ‘choice’ subscales (Table 63). Other highly rated items by the service users were that ‘staff members were knowledgeable about special interest groups and activities in the community’ and that ‘service users who are doing well get as much attention as those who are having difficulties’.
| Rank | Service users (mean of 3.56–3.98 on Likert scale)a | Staff (mean of 4.24–4.51 on Likert scale)a |
|---|---|---|
| 1 | Agency staff are diverse in terms of culture, ethnicity, lifestyle and interests Life goals |
Staff are diverse in terms of culture, ethnicity, lifestyle and interests Life goals |
| 2 | Staff use a language of recovery (i.e. hope, high expectations, respect) in everyday conversations Life goals |
Every effort is made to involve significant others and other natural supports in the planning of a person’s services, if so desired Individually tailored services |
| 3 | Agency staff believe that I can recover and make my own treatment and life choices Life goals |
Staff do not use threats, bribes, or other forms of coercion to influence the behaviour or choices Choice |
| 4 | Agency staff do not use threats, bribes or other forms of coercion to influence my behaviour or choices Choice |
Staff use a language of recovery (i.e., hope, high expectations, respect) in everyday conversations Life goals |
| 5 | The role of agency staff is to assist me, and other people in recovery with fulfilling my individually defined goals and aspirations Life goals |
Staff believe that people can recover and make their own treatment and life choices Life goals |
Staff
From a possible Likert score from 1 to 5, the mean range of item responses for staff was between 3.18 and 4.51, with the five highest scoring items falling in the range between 4.24 and 4.51. The five highest-rated items for the staff were within the ‘life goals’, ‘choice’ and ‘individually tailored services’ subscales (see Table 63). Staff also rated 20 other items highly (a score of > 3.5) on this scale from all subscales but with higher proportions relating to the ‘life goals’ and ‘diversity of treatment options’ subscales.
Lowest-rated items
Service users
From a possible Likert score from 1 to 5, the five lowest scoring items fall in the range between 2.81 and 2.96. The five lowest-rated items for the service users were within the ‘choice’, ‘involvement’, ‘individually tailored services’ and ‘diversity of treatment options’ subscales (Table 64).
| Rank | Service users (mean of 2.81–2.96 on Likert scale)a | Staff (mean of 3.18–3.29 on Likert scale)a |
|---|---|---|
| 1 | I am/can be involved with facilitating staff trainings and education programs at this agency Involvement |
People in recovery can choose and change, if desired, the therapist, psychiatrist or other service provider with whom they work Choice |
| 2 | I can choose and change, if desired, the therapist, psychiatrist or other service provider with whom I work Choice |
This agency provides structured educational activities to the community about mental illness and addictions Involvement |
| 3 | This agency provides education to community employers about employing people with mental illness and/or addictions Individually tailored services |
This agency provides education to community employers about employing people with mental illness and/or addictions Individually tailored services |
| 4 | I am given the opportunity to discuss my sexual and spiritual needs and interests Diversity of treatment options |
Agency staff actively help people become involved with activities that give back to their communities (e.g. volunteering, community services, neighbourhood watch) Involvement |
| 5 | I am/can be a regular member of agency advisory boards and management meetings Involvement |
People in recovery are regular members of agency advisory boards and management meetings Involvement |
Staff
From a possible Likert score from 1 to 5, the five lowest scoring items fall in the range between 3.18 and 3.29. The five lowest-rated items for the service users were within the ‘choice’, ‘involvement’ and ‘individually tailored services’ subscales (see Table 64).
Languedoc recovery profile from the Recovery Self-Assessment
Highest-rated items
Service users
From a possible Likert score from 1 to 5, the mean range of item responses for service users was between 2.68 and 3.67, with the five highest scoring items falling in the range between 3.49 and 3.67. The five highest-rated items for service users were within the ‘life goals’ and ‘choice’ subscales (Table 65). Service users did not identify any other items strongly for them to be considered a strong agreement across the mean responses (a score of > 3.5 on the scale). However, other reasonably highly rated items were in the ‘life goals’ subscale, such as ‘staff are diverse in terms of culture, ethnicity, lifestyle and interests’ and ‘they play a primary role in helping service users to become involved in non-mental health related activities to support recovery’.
| Rank | Service users (mean of 3.49–3.67 on Likert scale)a | Staff (mean of 4.08–4.18 on Likert scale)a |
|---|---|---|
| 1 | The role of agency staff is to assist me, and other people in recovery with fulfilling my individually defined goals and aspirations Life goals |
Staff do not use threats, bribes or other forms of coercion to influence the behaviour or choices Choice |
| 2 | Agency staff do not use threats, bribes or other forms of coercion to influence my behaviour or choices Choice |
Every effort is made to involve significant others and other natural supports in the planning of a person’s services, if so desired Individually tailored services |
| 3 | Agency staff believe that I can recover and make my own treatment and life choices Life goals |
Staff believe that people can recover and make their own treatment and life choices Life goals |
| 4 | Staff are knowledgeable about special interest groups and activities in the community Life goals |
Progress made towards goals (as defined by the person in recovery) is monitored on a regular basis Choice |
| 5 | The achievement of my goals is formally acknowledged and celebrated by the agency Life goals |
Staff listen to and follow the choices and preferences of participants Choice |
Staff
From a possible Likert score from 1 to 5, the mean range of item responses for staff was between 2.59 and 4.18, with the five highest scoring items falling in the range between 4.08 and 4.18. The five highest-rated items for staff were within the ‘choice’, ‘life goals’ and ‘individually tailored services’ subscale (see Table 65). Other highly rated items were within the ‘life goals’ subscale such as ‘diversity of staff in terms of culture, ethnicity, lifestyle and interests and staff using a language of recovery’. Other strengths were ‘procedures in place to facilitate referrals to other services if needed’ and ‘the active role of staff in assisting service users in developing and fulfilling their goals beyond symptom management and in helping people in recovery to become involved in non-mental health related activities’. Other highly-rated items were that ‘people could choose or change their therapist/psychiatrist if they wanted’, ‘that they had the opportunity to discuss their sexual and spiritual needs and interests’ and ‘people in recovery are routinely involved in the evaluation of the agency’s programmes and services and that groups and activities are scheduled in the evening or on weekends so not to conflict with other recovery-oriented activities’.
Lowest-rated items
Service users
From a possible Likert score from 1 to 5 the five lowest scoring items fall in the range between 2.68 and 2.82. The five lowest-rated items for the service users were within the ‘involvement’ and ‘diversity of treatment options’ subscales (Table 66).
| Rank | Service users (mean of 2.68–2.82 on Likert scale)a | Staff (mean of 2.59–3.10 on Likert scale)a |
|---|---|---|
| 1 | I have access to all my treatment records Choice |
This agency provides education to community employers about employing people with mental illness and/or addictions Individually tailored services |
| 2 | I am/can be a regular member of agency advisory boards and management meetings Involvement |
Persons in recovery are involved with facilitating staff trainings and education programs at this agency Involvement |
| 3 | I am/can be involved with facilitating staff trainings and education programs at this agency Involvement |
People in recovery are regular members of agency advisory boards and management meetings Involvement |
| 4 | I can choose and change, if desired, the therapist, psychiatrist or other service provider with whom I work Choice |
Helping people build connections in their neighbourhoods and communities is one of the primary activities in which staff at this agency are involved Individually tailored services |
| 5 | I am given the opportunity to discuss my sexual and spiritual needs and interests Diversity of treatment options |
This agency actively attempts to link people in recovery with other persons in recovery who can serve as role models or mentors by making referrals to self-help, peer support or consumer advocacy groups or programs Diversity of treatment options |
Staff
From a possible Likert score from 1 to 5 the five lowest scoring items fall in the range between 2.59 and 3.10. The five lowest-rated items for the service users were within the ‘involvement’, ‘individually tailored services’ and ‘diversity of treatment options’ subscales (see Table 66).
Provence recovery profile from the Recovery Self-Assessment
Highest-rated items
Service users
From a possible Likert score from 1 to 5 the mean range of item responses for service users was between 2.75 and 4.10, with the five highest scoring items falling in the range between 3.56 and 4.10. The five highest-rated items for the service users were within the ‘choice’ and ‘life goals’ subscales (Table 67). Service users did not identify any other items strongly for them to be considered a strong agreement across the mean responses (a score of > 3.5 on the scale). However, other reasonably highly rated items were in the ‘diversity of treatment options’ subscale, such as ‘service users who are doing well get as much attention as those who are having difficulties’ and ‘the trust attempts to link service users with other people in recovery who act as role models (peer-support)’.
| Rank | Service users (mean of 3.56–4.10 on Likert scale)a | Staff (mean of 4.21–4.59 on Likert scale)a |
|---|---|---|
| 1 | Staff do not use threats, bribes or other forms of coercion to influence my behaviour or choices Choice |
Staff are diverse in terms of culture, ethnicity, lifestyle and interests Life goals |
| 2 | Staff are diverse in terms of culture, ethnicity, lifestyle and interests Life goals |
The role of staff is to assist a person with fulfilling their individually defined goals and aspirations Life goals |
| 3 | Staff use a language of recovery (i.e. hope, high expectations, respect) in everyday conversations Life goals |
Every effort is made to involve significant others and other natural supports in the planning of a person’s services, if so desired Individually tailored |
| 4 | Staff believe that I can recover and make my own treatment and life choices Life goals |
Staff use a language of recovery (i.e. hope, high expectations, respect) in everyday conversations Life goals |
| 5 | The role of staff is to assist me, and other people in recovery with fulfilling my individually defined goals and aspirations Life goals |
Staff do not use threats, bribes or other forms of coercion to influence the behaviour or choices Choice |
Staff
From a possible Likert score from 1 to 5, the mean range of item responses for staff was between 3.13 and 4.59, with the five highest scoring items falling in the range between 4.21 and 4.59. Staff also rated 21 other items highly on this scale (a score of > 3.5) from all subscales, but with higher proportions in the ‘life goals’ and diversity of treatment options’ subscales (see Table 67).
Lowest-rated items
Service users
From a possible Likert score from 1 to 5, the five lowest scoring items fall in the range between 2.75 and 2.85. The five lowest-rated items for the service users were within the ‘choice’, ‘involvement’ and ‘diversity of treatment options’ subscales (Table 68).
| Rank | Service users (mean of 2.75–2.85 on Likert scale)a | Staff (mean of 3.13–3.24 on Likert scale)a |
|---|---|---|
| 1 | I am given the opportunity to discuss my sexual and spiritual needs and interests Diversity of treatment options |
Most services are provided in a person’s natural environment (i.e., home, community, workplace) Choice |
| 2 | I have access to all my treatment records Choice |
People in recovery are regular members of agency advisory boards and management meetings Involvement |
| 3 | I can choose and change, if desired, the therapist, psychiatrist, or other service provider with whom I work Choice |
Persons in recovery are involved with facilitating staff trainings and education programs at this agency Involvement |
| 4 | Staff focus on helping me to build connections in my neighbourhood and community Individually tailored services |
This agency provides education to community employers about employing people with mental illness and/or addictions Individually tailored services |
| 5 | I am/can be a regular member of agency advisory boards and management meetings Involvement |
The development of a person’s leisure interests and hobbies is a primary focus of services Involvement |
Staff
From a possible Likert score from 1 to 5, the five lowest scoring items fall in the range between 3.13 and 3.24. The five lowest-rated items for the service users were within the ‘choice’, ‘involvement’ and ‘individually tailored services’ subscales (see Table 68).
Glossary
- Acute inpatient ward (or unit)
- A mental health hospital ward or unit providing assessment, care and treatment for people who are experiencing a severe episode of mental illness or serious mental distress that cannot be dealt with by a community service. The multidisciplinary team usually includes mental health nurses, health-care assistants, psychiatrists, psychologists and occupational therapists, and sometimes social activities staff, peer workers and administrative workers.
- Care and Treatment Plan
- In Wales, with the passing of the Mental Health (Wales) Measure (2010), this is the document that supersedes the Care and Treatment Plan for all people using secondary mental health services. Care and Treatment Plans must address at least one of eight areas (accommodation; education and training; finance and money; medical and other forms of treatment, including psychological interventions; parenting or caring relationships; personal care and physical well-being; social, cultural or spiritual; and work and occupation).
- Care co-ordination
- The responsibility of a named mental health professional, whose work (under both the Care Programme Approach and the Care and Treatment Plan systems) includes co-ordinating the assessment and planning processes for named individuals using mental health services.
- Care co-ordinator
- Most often a mental health nurse, social worker or occupational therapist who takes responsibility for planning care with the person’s close involvement and ensures that this care is reviewed regularly.
- Care plan and care planning
- The written care plan lies at the heart of the care planning process, and should be collaboratively developed by professionals working in partnership with individual service users and their significant carers. It should include details of goals or intended outcomes, of services to be provided, of plans to be followed in the event of a crisis and of the maintenance of safety.
- Care Programme Approach
- In England, the framework that underpins how services are assessed, planned, co-ordinated and reviewed for someone with severe mental health problems or a range of related complex needs. The approach requires that health and social services assess need, provide a written care plan and allocate a care co-ordinator, and then regularly review the plan with key stakeholders.
- Carer
- Anyone who cares, unpaid, for a friend or family member who, because of illness, disability, a mental health problem or an addiction, cannot cope without their support.
- Clinical studies officer
- A member of research staff employed to support the identification and recruitment of participants in studies supported by Clinical Research Networks.
- Clusters and clustering
- Clusters are the currencies for most mental health services for working age adults and older people in England. Service users have to be assessed and allocated to a cluster by their mental health provider, and this assessment must be regularly reviewed in line with the timing and protocols set out in the mental health clustering booklet. Clusters form the basis of the contracting arrangements between commissioners and providers under Payment by Results (see Payment by Results).
- Community mental health team
- Provides assessment, care and treatment for people who have one or more types of severe mental illness. The team is multidisciplinary and consists of community psychiatric nurses, social workers, support workers, psychiatrists, psychologists, occupational therapists and support and administration staff.
- Community Treatment Order
- The power given to a responsible clinician (usually a psychiatrist) under the Mental Health Act to place certain conditions on the service user that they must follow when they have left hospital. Failure to follow the conditions may lead to the service user being compulsorily recalled to hospital.
- Inpatient/patient
- A person who uses health and social care services, or who is a potential user of health and social care services. The term is used interchangeably with service user in this report (see Service user).
- Local authority
- A broad term used to describe elected councils in England and Wales that have responsibility for the provision of all local government services, including social work, in a specified area.
- Local health board
- In Wales, there are seven local health boards that plan, secure and deliver health-care services in their areas.
- Mental Health Recovery Star
- A tool for supporting and measuring change in people with mental illness and in recovery. It covers 10 key areas, such as managing mental health and social networks, and is underpinned by a five-stage model of change.
- Mental Health Research Network and Mental Health Research Network-Cymru
- Networks in England and Wales (Cymru) (in England, now part of the Clinical Research Network, and in Wales superseded by a new system for supporting research organised and funded through Health and Care Research Wales) that are made up of research-interested clinicians and practitioners working at both national and local levels to enable studies that are included in the national portfolio of research to receive the right support to ensure that they are delivered successfully in the NHS.
- NHS trust
- A public sector corporation within the English NHS generally serving either a geographical area or a specialised function (such as an ambulance service). In any particular location there may be several trusts involved in the different aspects of health care for a resident. Mental health services are usually provided by one NHS trust in an area.
- Payment by Results
- A rules-based payment system recently introduced in England under which commissioners pay health-care providers for each patient seen or treated, taking into account the complexity of the patient’s health-care needs.
- Personalisation
- The enhancement of individual choice and control for eligible adults using health and social care services through person-centred planning and self-directed support. Personalisation underpins the idea that health and social care services should be tailored to the particular needs of individuals, and should enable people to live as independently as possible, exercising choice and control. The use of personal budgets to purchase social care support can be a feature of personalisation.
- Recovery
- The contemporary idea of personal (rather than necessarily clinical) recovery in mental health originated in the service user movement, and is now claimed as the philosophical underpinning for many mental health policies and services, including care planning. A definition often used is a way of living a satisfying, hopeful and contributing life even within the limitations caused by illness.
- Service user
- A person who uses health and social care services, or who is a potential user of health and social care services. The term is used interchangeably with patient or inpatient in this report (see Inpatient/patient).
- Support time recovery worker
- A worker employed to offer day-to-day support of people with mental health problems to support recovery and work with communities to promote better understanding and acceptance of people with these problems.
- Wellness recovery action plan
- A ‘self-management’ tool used in many countries around the world to help individuals take more control of their own well-being and recovery. The plan is underpinned by a number of core principles of recovery, and people work within these principles to create their own plan, which includes a number of components, including the identification of triggers and early warning signs, and associated action plans.
List of abbreviations
- AIMS
- Accreditation of Inpatient Mental Health Services
- AMED
- Allied and Complementary Medicine Database
- ANCOVA
- analysis of covariance
- ANOVA
- analysis of variance
- app
- application
- ASSIA
- Applied Social Sciences Index and Abstracts
- BME
- black and minority ethnic
- CI
- confidence interval
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- CMHT
- community mental health team
- COCAPP
- Collaborative Care Planning Project
- COCAPP-A
- Collaborative Care Planning Project-Acute
- CPA
- Care Programme Approach
- CPN
- community psychiatric nurse
- CQC
- Care Quality Commission
- CTP
- Care Co-ordination and Care and Treatment Planning
- ES
- Empowerment Scale
- LEAG
- Lived Experience Advisory Group
- LHB
- local health board
- MDT
- multidisciplinary team
- MHA
- Mental Health Act
- NICE
- National Institute for Health and Care Excellence
- OT
- occupational therapist
- PAG
- Project Advisory Group
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- RSA
- Recovery Self-Assessment
- SD
- standard deviation
- STAR
- Scale to Assess the Therapeutic Relationship
- STAR-C
- Scale to Assess the Therapeutic Relationship – clinician version
- STAR-P
- Scale to Assess the Therapeutic Relationship – patient version
- SUGAR
- Service User and carer Group Advising on Research
- VOICE
- Views of Inpatient Care Scale
- WRAP
- wellness recovery action plan