Notes
Article history
The research reported in this issue of the journal was funded by the HS&DR programme or one of its preceding programmes as project number 14/19/26. The contractual start date was in October 2015. The final report began editorial review in April 2018 and was accepted for publication in October 2018. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HS&DR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Simon de Lusignan is a Professor of Primary Care and Clinical Informatics and reports that the University of Surrey runs a physician associate course. Jim Parle chairs the UK and Ireland Board for Physician Associate Education and is director of the physician associate programme at the University of Birmingham. Phil Begg is an honorary faculty member at the University of Birmingham and has taught on the physician associate programme since 2008. James Ennis teaches part time on the University of Birmingham physician associate course. Vari M Drennan was a Health Services and Delivery Research Board Member in 2015.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2019. This work was produced by Drennan et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2019 Queen’s Printer and Controller of HMSO
Chapter 1 Background
This study addresses questions about the introduction of a new role, the physician associate (PA), within the hospital medical workforce. It is focused, in the first instance, on providing information that addresses the questions of clinicians, managers and those involved in commissioning services and education programmes in the UK. This chapter provides the background and rationale of the study by presenting contextual information and the evidence at the time the study was commissioned (September 2015). The aims and objectives of the study are presented, followed by brief detail of the advisory process and the public’s role in advising the study team. The chapter concludes with an outline of the rest of the report.
Rationale
Physician associates, previously known in the UK and elsewhere as physician assistants, are a new and rapidly growing occupational group in the UK NHS, with the first significant number of UK-trained PAs graduating in 2009. 1 From 2012, the employment of PAs in medical teams in secondary care was advocated by bodies such as the Royal College of Physicians (RCP),2,3 the College of Emergency Medicine4 and the Department of Health-commissioned Centre for Workforce Intelligence. 5 The increase in the employment of PAs was supported by the doubling of training places to > 200 per annum, as announced by Jeremy Hunt, the Secretary of State for Health, in August 2014, and the increasing number of universities offering PA courses. 6
Although the response from The Patients Association and the British Medical Association to the announcement by Jeremy Hunt was mixed, expressing caution and concern,7 the increase of PAs in the UK was supported by NHS workforce policy and medical royal colleges. Health Education England (HEE), the body responsible for the planning and education of the NHS workforce in England, included PAs in its workforce plans for the first time in 2013 and created a national PA development group. 8 The medical director (MD) of HEE publicly spoke of the need for 5000 PAs in the NHS and the expectation that there will be 500 PAs graduating each year in England by 2018. 9 In Scotland, the inclusion of PAs in NHS workforce planning was agreed in 2012 and PA training was subsequently commissioned from Aberdeen University by the NHS. 10 The Council of the Royal College of Physicians (London) agreed, in March 2014, to establish a Faculty of Physician Associates (FPA) in collaboration with the UK Association of Physician Associates (UKAPA), HEE and other royal colleges to support and develop the role. 11 At least 30 NHS hospital trusts were early adopters of PAs in their medical staffing1,12 and demand was reported to outstrip the supply of UK-trained PAs by 2014. 9 Key drivers of the policy and employer initiatives have been the pressures on the medical workforce, particularly in emergency medicine,4 but more widely linked to the implementation of the EU’s Working Time Directive,13 which currently controls junior doctors’ working hours. 2,3,5,14 PAs were seen as one type of mid-level practitioner (i.e. non-physician clinicians trained to undertake some of the diagnostic and clinical activities of doctors15) that could help address these problems in the immediate and long term without recruiting from another, already-pressured workforce, such as nursing. 5,9,16
Despite this growth of interest and policy support, there was very little published evidence regarding PAs’ contribution to patient care and effectiveness in the secondary care setting. There was, however, published evidence of their contribution in primary care. 17 The National Institute for Health Research (NIHR)-funded study,17 led by the same principal investigator as this report, reported that ‘physician assistants were found to be acceptable, safe, effective and efficient in complementing the work of general practitioners (GPs). Further research is required as to the contribution PAs could make in other services’.
Hospitals are very different from general practice in organisation as well as in type of treatment and care provided to patients. The evidence established in the general practice setting could not automatically be applied to a hospital setting. The primary care study demonstrated that NHS managers, senior clinicians and commissioners were seeking hard evidence to inform their decision-making as to the benefits or otherwise of including PAs in medical teams. 17,18 Patients and representatives from patient organisations also wanted evidence that this professional group was safe and did not result in some patients receiving an inferior service or unnecessary double-handling (i.e. being seen by one professional prior to repeating the consultation with a doctor). 17,19 This study was funded by NIHR as a follow-on study to the primary care research,17 recognising the need for evidence in the hospital setting, where there was increasing employment of PAs in England. 1,8,12
We turn now to provide more detailed information on PAs, PAs in the UK setting and the evidence of their contribution in hospital settings in 2015 (the starting point of this study).
Physician associates
Physician associates are trained at postgraduate level in a medical model to work in all settings and undertake medical history taking, physical examinations, investigations, diagnoses and treatments and to prescribe within their scope of practice as agreed with their supervising doctor. 20,21 PAs have a 50-year history in the USA. 22 By 2014, about 94,000 PAs were employed in US health services;23 of these, an estimated 30% worked in hospitals. 24 A growing number of high-, middle- and low-income countries have developed or are developing PA roles within their health-care workforce to varying degrees, including Ghana, Liberia, South Africa,25 the Netherlands26 and Canada. 27
Reviews of mainly pre-2013 US studies found patients to be very satisfied with PA care and that PAs can provide equivalent and safe care for the case mix of patients they attend. 28–31 The two systematic reviews (one general30 and one specific to primary care31) noted that the quality of most studies was weak to moderate and there was limited evidence on resource utilisation, costs and cost-effectiveness. Three small US studies of PAs in hospital settings published in 2013 and 2014 provided new positive evidence as to the contribution that PAs made to patient outcomes and resource use in a trauma–orthopaedic setting32 and in low- and high-acuity emergency department (ED) settings. 33,34 One study35 had reported that the indirect impact of employing PAs in a general surgical residency programme was to reduce the resident doctor workload, increase the doctors’ ability to attend their training activities and improve results in their American Board of Surgery in Training Examination. In 2014, a study protocol was published for research investigating the substitution of medical doctors with PAs in hospitals in the Netherlands. 36
Physician associates in secondary care in the UK
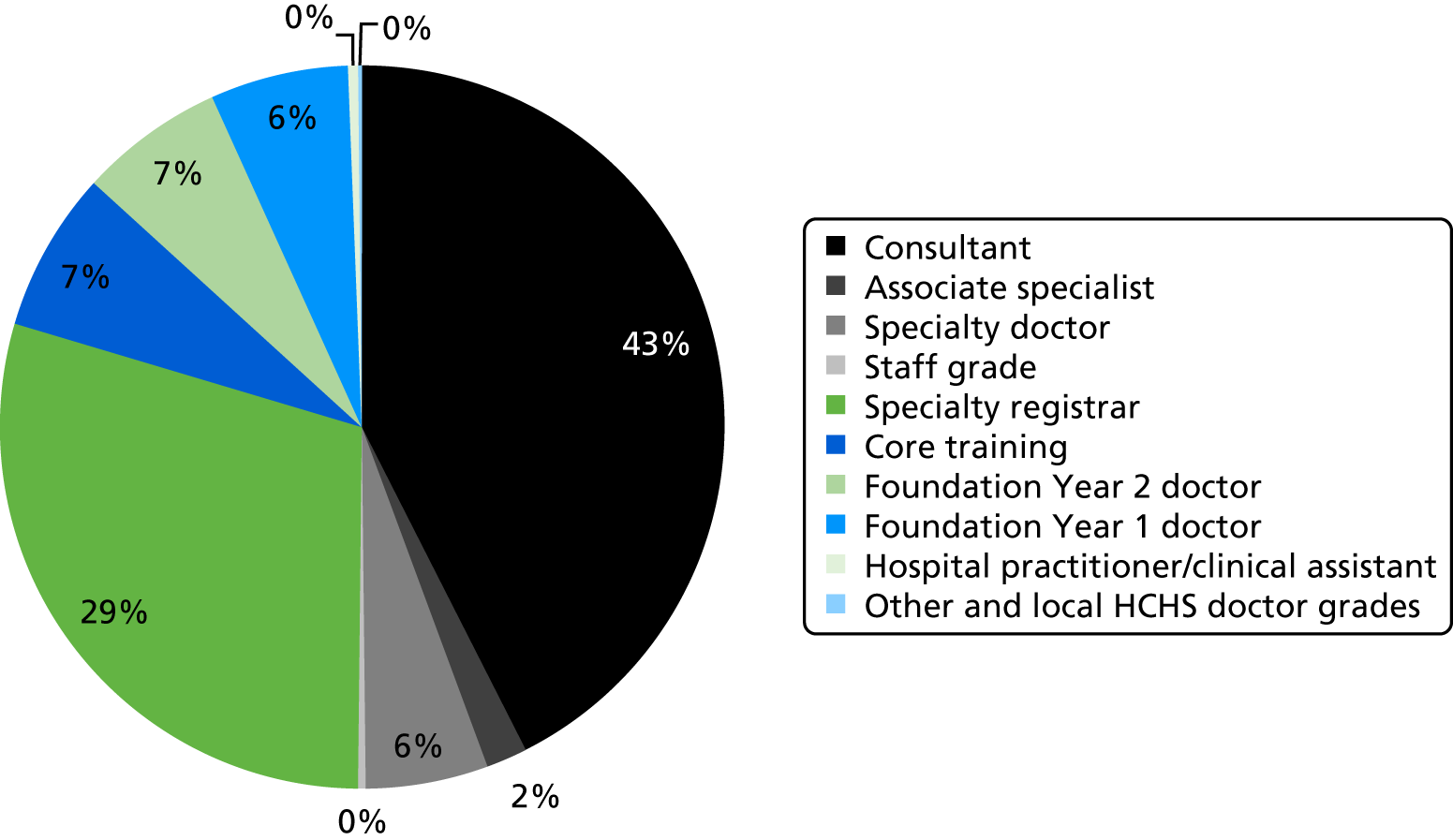
Health policy, NHS funding and concomitant organisational arrangements are devolved to the respective country administrations within the UK. 37 In England, where this study was undertaken, there were 163 NHS trusts (organisations providing NHS services) providing acute secondary care in 2017. 38 The medical workforce in these NHS organisations was formed of doctors of different grades, including training grades. Of the 94,045 full-time equivalents (FTEs) in the medical workforce in these acute secondary care trusts in 2017, 39,993 FTEs (43%) were consultants and 11,871 FTEs (11%) were Foundation Year doctors39 (Figure 1). The NHS workforce descriptor ‘hospital practitioner/clinical assistant’ may include, but is not exclusive to, PA staff; 425 FTEs were recorded in this occupational group. 40
FIGURE 1.
The medical workforce by grade in NHS trusts (excluding psychiatry and community staff). Data were sourced from NHS Digital. 39 HCHS, Hospital and Community Health Service.
In 2015, there was very limited published evidence about the contribution of PAs to hospital care in the UK. A Department of Health-supported pilot project of PAs in England included two PAs in hospitals,41 who worked in EDs. The evaluation concluded that they could make a range of contributions working at the clinical assistant level. 42 A similarly supported pilot project in Scotland included 11 USA-trained PAs working in emergency medicine, intermediate care and orthopaedics. 43 It reported that the PAs were well received by patients, were working safely and at the level of a trainee doctor (in some instances, almost at the level of a specialist trainee). The advantages of their employment were noted to be increased consultant productivity, increased continuity in the consultant team and positive impact on patient throughput. There were, however, issues with PAs’ lack of authority to prescribe medicines and order radiographs (both consequences of a lack of a statutory regulation) and also assuring appropriate medical supervision when there were shortages of medical staff. 43 A commentary in 2013 on the introduction of PAs in one English paediatric intensive care unit described a positive impact on patient care and continuity in the running of the unit and that initial, predictable, implementation problems were soon resolved. 44 A survey,45 conducted in England in 2012, of doctors supervising PAs in primary and secondary care reported that they considered the PA as a flexible member of their team, who was well received by patients and made a positive contribution to patient outcomes and efficiency. The issue of a lack of regulation was seen as the major problem, which also resulted in increased requirement for time from the supervising doctor.
In the UK, there were positive evaluations of US-trained PAs in pilot projects in primary and secondary settings in 2005 (England42) and 2009 (Scotland43). These reports, combined with the first validated PA programme at the University of Wolverhampton in 2004, led to a nationally agreed competency and curriculum statement20 (which was subsequently updated21) and postgraduate programmes in a growing number of universities. PAs were not (and continue to not be) regulated by the state, although application has been made for regulation, supported by HEE and the RCP. 11 The lack of state regulation means that, among other issues, PAs cannot prescribe or order ionising radiation. At present, PAs maintain a voluntary register and undertake revalidation every 6 years. 46 In October 2017, the Department of Health and Social Care announced a public consultation on the inclusion of PAs in UK state regulation processes. 47
There has been an increase in PA employment in UK hospital settings. In 2012, Ross et al. 1 reported that > 200 PAs were employed in 20 hospitals and within 15 medical and surgical specialties. Two years later, in spring 2014, evidence on the UKAPA website (the UKAPA has since disbanded to create the FPA at the RCP and the website has been closed down) showed that PA employment in hospitals had increased by ≥ 50 PAs and in > 30 hospitals. 48 PAs were reported to be in 20 adult and paediatric specialties, including psychiatry, geriatrics, paediatric intensive care, infectious diseases, cardiology, neurosurgery and genitourinary medicine. 48 In 2012, the greatest numbers of PAs were employed in emergency medicine and the medical specialties of respiratory medicine and cardiovascular medicine. 1
Although the rapid spread and growth of PAs in different hospital settings suggested that the role was seen as advantageous by early adopters, there was little evidence available for the public, patients or health service leaders as to the deployment, acceptability, effectiveness and costs of PAs in different types of hospital medical teams. This study aimed to address the evidence gap.
Aims and objectives
The aim of this study was to investigate the contribution of PAs to the delivery of patient care in hospital services in England.
The research questions that have been addressed are:
-
What is the extent of the adoption and deployment of PAs employed in acute hospital medical services?
-
What factors support or inhibit the inclusion of PAs as part of hospital medical teams at the macro, meso and micro levels of the English health-care system?
-
What is the impact of including PAs in hospital medical teams on patients’ experiences and outcomes?
-
What is the impact of including PAs in hospital medical teams on the organisation of services, working practices and training of other professionals, relationships between professionals and service costs?
The full study protocol was published on the NIHR Journals Library website (www.journalslibrary.nihr.ac.uk/programmes/hsdr/141926/#/; accessed 5 February 2019). The study team had the benefit of both an advisory group and patient and public involvement throughout (see Appendix 1). The patient and public voice was important to this study and is detailed in Chapter 2.
The following chapters provide details of the study methods and findings. The report concludes with the discussion and recommendations.
Chapter 2 Methods
This investigation was a follow-on study and used the same theoretical framing and methods as those used by the research team in the original study of PAs in primary care. 17 As an applied health service research study, we used an evaluative framework described by Donabedian49 and applied it to the UK setting by Maxwell. 50 The contribution of PAs, as new types of personnel, was investigated through the dimensions of effectiveness, appropriateness, equity (fairness), efficiency, acceptability and cost in secondary health care. 49,50 The interactions within and between the macro, meso and micro levels of the health-care system in supporting or inhibiting the adoption of PAs as an innovation were also investigated. 51 Furthermore, the study was framed by an awareness of theories concerning substitution and supplementation to task shift from one group of professionals to another30,52 and the potential for contest between professional groups. 53 Overall, the study employed a mixed-methods approach54 in four interlinked workstreams:
-
Investigation of the extent of the adoption, deployment and role of PAs in hospital medical teams through two national electronic surveys: one to MDs of acute trusts and one to PAs (addressed research questions 1 and 2 at the macro and meso levels of the health-care system).
-
Investigation of the evidence of the impact of PAs and factors supporting or inhibiting the adoption of PAs at the macro and meso levels of the system through a review of published evidence for the specialties that most commonly reported employing PAs in the national surveys (workstream 1) and updating the published policy review from the prior study17 (addressed research questions 1, 3 and 4).
-
Investigation, through case study methodology in six hospitals employing PAs, of the impact, contribution and consequences of PAs in the medical teams. This included interviews with patients, managers and team and service members as well as requests for routine management data and observation of PAs at work. It also included a comparison of patient outcomes and service costs in EDs by PAs and Foundation Year 2 (FY2) junior doctors, where these two professional groups are deployed interchangeably (addressed research questions 1–4).
-
A synthesis of evidence from the three workstreams. This was presented and tested at an emerging-findings workshop with invitees from the research participants, the patient and public forum members and other advisors to the study (addressed the overarching study aim).
The following section describes the process of patient and public involvement. The methods of the study itself are then detailed.
Patient and public involvement
The patient and public voice was important to this study. The public and patient representative forum for the previous primary care study17 stressed that the innovation of bringing in a new group of professionals was of concern to the public. Key issues that the forum emphasised in discussion concerned (1) patient choice of the professional to consult or be attended by, (2) whether or not some groups of patients will receive a ‘second-class ‘or inferior service, (3) how patients will judge if this new professional is competent and (4) the ways in which the public and patients are informed of and understand this new role in different settings. Those issues were incorporated in the design of this study.
Within the study itself, the patient and public voice was interwoven in the following ways. First, Sally Brearley, as a public voice representative, was a co-applicant and member of the research team and the study paid for her time. Second, the study advisory group had two public voice members who were reimbursed for their time, following NIHR INVOLVE guidance. 55 Third, two patient and public voice groups were formed: one in London and the other in the West Midlands. Invitations to join were sent to the members of the patient and public group forum involved in the previous primary care study, through the public and patients network of the Centre for Public Engagement (at the Joint Faculty, Kingston University London and St George’s, University of London). Invitations were also circulated through an established patient involvement group of the University Hospitals Birmingham NHS Foundation Trust, Birmingham. Members of these groups who attended research meetings were reimbursed for their time, again following NIHR INVOLVE guidance. 55 The patient and public voice groups met first of all to hear about the study and meet a PA, who was able to describe their work and education and answer questions. The early meetings were used to inform the interview topic guides and interview questions. Later meetings brought members together to help inform the analysis and interpretation of interview transcripts. All patient and public representatives were invited to participate in the final emerging-findings workshop (workstream 4).
We now describe the methods in detail.
Workstream 1: investigating the extent of the adoption, deployment and role of physician associates in hospital medical teams
Two electronic, descriptive, self-report surveys56 using Survey Monkey® (San Mateo, CA, USA) were conducted to map and describe the employment and deployment of PAs in secondary care services in England.
The first survey was of NHS MDs. It was designed by the research team and piloted by a MD. The survey addressed questions of employment and factors supporting or inhibiting that (see Appendix 2). The sample was of MDs in all acute and mental health NHS trusts in England as listed by NHS Choices (the NHS information portal) in December 2015. Contact details were obtained from Binley’s database. 57 The invitation was sent by e-mail in December 2015, and two reminder e-mails were sent.
The second survey was sent to the UK voluntary register and/or UK-trained PAs. It was adapted from the primary care study58 by the research team and piloted by a PA board member of the FPA (see Appendix 3). The questions addressed the PAs’ work settings, activities and supervision. E-mail invitations were sent in February 2016 by the FPA to its members and by university course directors to their alumni. Two reminder emails were sent.
Anonymous responses to both surveys were imported into IBM SPSS Statistics Version 23 (IBM Corporation, Armonk, NY, USA). Data from closed questions were used to produce frequency counts and open responses were analysed for thematic groupings.
This workstream was approved by the Faculty of Health, Social Care and Education Research Ethics Committee at Kingston University London and St George’s, University of London.
All respondents were invited to complete a separate Survey Monkey page (following a link from the completed survey) to provide contact details if they wished to be kept informed of the study progress and outputs.
The findings from this workstream informed workstreams 2 and 3.
Workstream 2: investigating evidence of the impact and factors supporting or inhibiting the adoption of physician associates in the literature and policy
We undertook a systematic review and a policy review.
The systematic review
A systematic review investigated the impact of PAs on patients’ experiences and outcomes, service organisation, working practices, costs and other professional groups for the secondary care specialties of acute medicine, care of the elderly, emergency medicine, trauma and orthopaedics and mental health. These were the specialties that PAs were most frequently reported to work in by the FPA59 and this was confirmed in workstream 1.
The review was conducted as per the international Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. 60 The protocol was published on the International Prospective Register of Systematic Reviews (PROSPERO) as CRD42016032895. 61 In summary, nine electronic databases were systematically searched from 1 January 1995 to the second week of December 2015. The research team undertook periodic update searches, with the last search undertaken on 5 January 2018.
The databases were MEDLINE (via Ovid), EMBASE (via Ovid), Applied Social Sciences Index and Abstracts, Cumulative Index to Nursing and Allied Health Literature Plus (via EBSCOhost), Scopus version 4 (via Elsevier), PsycINFO, Social Policy and Practice (via Ovid), EconLit (via EBSCOhost) and Cochrane Central Register of Controlled Trials. A search strategy is presented in Appendix 4. Lateral searches were also undertaken. 62 Relevant studies were identified first through abstract screening and then through full-text reading by two researchers, with any disagreements resolved by a third researcher. The inclusion criteria were:
-
Articles had to have been peer reviewed.
-
Population – PAs in accordance with the UK definition. 20
-
Intervention – the implementation of PAs in the following secondary health-care specialties: acute medicine, care of the elderly, emergency medicine, mental health and trauma and orthopaedics.
-
Comparison – the comparison group was any health-care professional with whom PAs were compared.
-
Outcome – any measure of impact, informed by recognised dimensions of quality (effectiveness, efficiency, acceptability, access, equity and relevance). 50
-
Study design – any study design that allowed the measurement of the impact of PAs in a primary study.
Articles were excluded if they were not published in English; were from countries not defined by the International Monetary Fund as advanced economies;63 did not provide empirical data; did not provide data for PAs separately from other advanced clinical practitioners, such as nurse practitioners; did not focus on the PAs as the intervention; only provided data before and after a service redesign or educational programme; or only presented literature reviews or commentary.
A data extraction spreadsheet was populated by two researchers independently, with differences resolved by a third researcher. Quality assessment was undertaken with Qualsyst checklists for quantitative and qualitative studies,64 with additional questions from the mixed-methods appraisal tool. 65 No study was excluded on the basis of its quality score, but the limitations of lower-quality evidence were considered in the final synthesis. 66
Owing to the heterogeneity of the included studies, a meta-analysis was not possible, and the results are presented as a narrative synthesis. 67
The policy review
The previous study reported on a review of policy (up to 2013) to identify supporting or hindering factors in the development of the PA profession in the English health-care workforce. 17,18 This policy review68 was therefore updated with a particular focus on secondary care using documentary review methods. 69 Internet searches of relevant English government, NHS and associated agencies’ websites were conducted periodically throughout the study period to identify relevant policy documents and reports on health-care workforce planning, education, regulation and development. The time period was September 2013 to October 2017. These electronic documents were then searched using the ‘find’ function for any references to PAs. A data extraction framework, as used in the previous primary care study, was used to classify the document, note the presence or absence of PAs and record text relevant to the problem analysis that PAs were the policy solution,68 as well implementation concerning the education, employment and deployment of PAs. A narrative synthesis was then undertaken.
Workstream 3: investigating the deployment and contribution of physician associates at the micro level of the health system
A mixed-methods case study design70 addressed all of the research questions at the micro level of the health-care system through investigation in six NHS trusts that employed PAs in their acute care hospitals. Similar methods have been used in other studies investigating new staff groups in NHS hospitals. 71,72 The mixed-methods approach within a multiple case study design70 was designed to both describe and, as far as possible, quantify the impact of PAs in the context of secondary care. The aim was to achieve diversity in the hospitals by geographical location, size and type. At the time of the application for funding, the research team had agreement in principle to participate from trusts in the West Midlands and London that employed PAs. The intention was also to have diversity in the medical and surgical specialties within which PAs were employed. The final decisions regarding the inclusion of hospital trusts in the study was informed by the surveys in workstream 1, as well as the willingness of the trust senior managers and PAs and their consultants to participate. In addition, as PAs are a relatively small staff group and, therefore, potentially identifiable, the design ensured that volunteer PAs came from a specialty in which more than one PA and more than one trust participated. The aim was also to include more than two hospitals employing PAs in emergency medicine (being the acute specialty reported to employ the largest number of PAs). 1 The intention was to report the evidence from the multiple case studies in the manner described by Yin70 as the ‘fourth way’, that is to only present cross-case analysis of the issues of interest rather than from each individual case study site. With this understanding of the reporting intentions, the research team approached hospital executive staff to explain the research and gain formal permission to undertake the study; this was gained from a NHS trust board-level executive (chief executive or MD). Initial meetings were then held with PAs and their consultants to explain the study and ask for volunteers to participate. The sites were recruited sequentially but with data collection being undertaken in two or three sites at a time over a period of between 4 and 6 months. Permission to start data collection was in the control of each hospital research governance team and, in some instances, it took 6 months from the point of overall permission being given to agree. Characteristics of the six hospital trusts are provided in Table 1. At the time of the study, the Care Quality Commission (CQC) rated the overall quality of one of the trusts as ‘outstanding’, one as ‘good’ and the other four as ‘requires improvement’.
| Case study site | Rural/urban locationa | Number of | Annual incomeb | ||
|---|---|---|---|---|---|
| Hospital sites | Inpatient beds | Staffb | |||
| 1 | Urban with major conurbation | 2 | ≥ 1000 | 9001–11,000 | > £500M |
| 2 | Urban with city and town | 1 | 601–800 | 3001–5000 | < £200M |
| 3 | Urban with city and town | 3 | 601–800 | 3001–5000 | £201–500M |
| 4 | Urban with significant rural (rural including hub towns 26–49%) | 2 | ≥ 1000 | 9001–11,000 | > £500M |
| 5 | Urban with major conurbation | 3 | 601–800 | 3001–5000 | £201–500M |
| 6 | Urban with major conurbation | 2 | 201–400 | < 3000 | £201–500M |
The characteristics of some aspects of the medical staffing and training in each of the hospital trusts are given in Table 2.
| Case study site | Number of FTEs | |||
|---|---|---|---|---|
| All doctors | Consultants | FY2 doctors | FY1 doctors | |
| 1 | > 1000 | 401–500 | 41–50 | 41–50 |
| 2 | < 300 | < 100 | 11–20 | 21–30 |
| 3 | 501–700 | 101–200 | 31–40 | 21–30 |
| 4 | > 1000 | 401–500 | 61–70 | 71–80 |
| 5 | 301–500 | 101–200 | 21–30 | 31–40 |
| 6 | 301–500 | 201–300 | < 20 | < 20 |
In overview, data collection in each hospital trust included:
-
interviews with senior managers (including operations directors and human resources), lead consultants, members of the health-care teams (medical, nursing and support staff), PAs and patients
-
requests for relevant routine management information (data and reports) as well as any internal documents, reports or audits on the work or impact of the PAs
-
work activity diaries and observation of the PAs at work
-
for those with PAs working in the EDs, anonymised patient records to allow comparison of patient outcomes and costs for the treatment of patients by PAs and FY2 doctors in the ED, a setting where individual clinicians are allocated to conduct an assessment and propose a plan for the patient.
An overview of the numbers of PAs volunteering to participate and the data collection in each site is provided in Table 3.
| Case study site | Number of | Pragmatic comparative investigation in the ED? | |||
|---|---|---|---|---|---|
| PA participants (number of specialties) | Interviews (all types of participants) | Observation periods (4–9 hours) | Contextual documents (e.g. trust reports and board minutes) | ||
| 1 | 11 (6) | 51 | 24 | 35 | No |
| 2 | 8 (7) | 34 | 15 | 25 | No |
| 3 | 9 (7) | 32 | 25 | 27 | Yes |
| 4 | 2 (1) | 14 | 6 | 19 | Yes |
| 5 | 9 (5) | 24 | 11 | 21 | Yes |
| 6 | 4 (4) | 18 | 7 | 12 | No |
Semistructured interviews
Semistructured interviews were conducted with trust executive-level managers, lead consultants, members of the health-care teams (medical, nursing and support staff), PAs and patients. Topic guides75 appropriate to each group were developed in consultation with the advisory group and the study patient and public forum (see Appendix 5). The topic guides for patients included questions about the patient experience and perceptions of the role as well as acceptability. For managers and senior clinicians, topic guides included questions on factors inhibiting and supporting the employment of PAs as well as the impact on organisation, patient outcomes and costs. The topic guides for professionals included questions on deployment, acceptability and impact on working practices, role boundaries and patient experience. Each group was invited in different ways: senior staff were invited by e-mail and other staff were invited following introductory meetings or introductions by other members of the clinical team. Patients were approached by the clinical team in the first instance. With permission, the interviews were digitally recorded, or notes were taken if preferred. Recordings were transcribed, and the recordings were destroyed at the completion of the study. Transcripts and notes were anonymised. The transcriptions and notes were coded using NVivo version 12 (QSR International Pty Ltd, Melbourne, Australia). Initial coding frameworks were developed by five researchers (CW, MH, LN, JP and VMD). These were developed and agreed with the wider research team as well as the patient and public forum, using a variety of transcripts. Thematic analysis was conducted. 76
Routine data and reports
The managers and clinicians were invited to share any relevant organisational documents or management data for all of the services employing PAs that could assist in answering the research questions concerning deployment, patient outcomes and organisation and cost. Examples were suggested, including patient throughput and outcome data, adverse events/serious untoward incidents, patient feedback, audit reports and expenditure on medical locums. The intention, if data were available, was to compare data before and after PAs were employed in a particular service. These data were to be descriptively analysed and, if appropriate, subjected to tests of significance to explore differences in time periods or between providers. It should be noted that no data of this type were offered from any of the cases study sites, a finding that is discussed in more detail in Chapters 4, 8 and 11.
Work activity diaries and observation of physician associates at work
The PAs were invited to complete work activity diaries, better described as logs. These were adapted from the primary care study17 in discussion with PAs on the research team and also with the advisory group (see Appendix 6). PAs were requested to complete these for 7-day periods up to three times, and for periods likely to demonstrate some differences in their activities (e.g. rotational duties of PAs or rotation times for junior doctors). These work activity diaries were designed to provide detailed information on the deployment, work setting and role of the PA. Data were entered into IBM SPSS Statistics Version 23 and Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA) and were analysed descriptively for summary characteristics and distribution, central tendency, dispersion and measures of the spread of individual variables.
The PAs were invited to volunteer to be observed by a researcher while they were working. This element of the study drew on the ethnographic tradition used in many health service research studies in the UK. 77 For any PA volunteering, permission was also sought from the lead consultant for that service. The PAs sought assent for the researcher’s presence from patients they were attending, in the same way as permission is sought for students to be present during clinical care and treatment (see Appendix 7). Observations of any intimate activities with patients or in which the patient was, or was likely to be, distressed were excluded. PAs were observed for up to three sessions; this was intended to capture diversity in their work or the work environment. These sessions of observations were for all or part of their shift hours, including shifts not in the 09.00–17.00 period and shifts at weekends. Field notes of observations of the PAs’ activities and interactions were made at the time and written up in full later. The analysis method drew on that used in other, similar studies of health professional work in the UK. 78 Rather than trying to impose a coding structure on what were usually fast-moving, dynamic events, the notes were read and particular ethnographic vignettes were identified from each. These were vignettes judged by the observer and one other researcher as being most relevant to the research questions, the theoretical framing of the study or the themes derived from the interview and documentary data. The reading and judgement of the vignettes was conducted with a lens that looked for both confirmatory and also disconfirming evidence of that obtained through sources such as interviews.
Pragmatic retrospective assessment comparing the outcomes and service costs for patients attended by physician associates and Foundation Year 2 doctors in the emergency department
The ED is a setting where PAs are employed and may work in different physical sections [minors, also known as the minor injuries, and majors (i.e. serious illness or trauma79)] alongside, and substituting for, junior doctors. 1,80 Patients, triaged by a clinical professional to these sections of the ED, are assigned and initially assessed by a clinical professional (a PA, a doctor, or, in the case of the minor injuries section, another professional, for example an emergency care practitioner). Consequently, a pragmatic comparison of the patient outcomes and service costs of consultations by PAs and junior doctors (FY2) was undertaken based on the methods and data from two English studies, which compared minor injuries section consultations by nurse practitioners, as the mid-level professional (in the absence of UK data for PAs), with those of doctors. 81,82
Revisions to the protocol
Following the surveys and preliminary recruitment of case study hospitals in 2015 and 2016, it was found that additional ED sites (from the four initially proposed) were required to undertake this element. Although the initial proposal had only included a comparison in the minor injuries section, it became apparent in trying to recruit the hospitals and PAs in January 2017 that PAs were rarely working in the ED at all as they were more frequently assigned to the acute medical assessment units. When they were assigned to the ED, it was usually to the majors section. In addition, practical constraints within trusts made the proposed prospective data collection impractical. Hence, a decision was taken and agreed with NIHR to change to a retrospective analysis of anonymised patient records from hospital databases. This had a concomitant effect in that the proposed linked patient satisfaction surveys could not be conducted. The study protocol was amended twice in pragmatic responses to changing NHS environments.
The pragmatic retrospective record review
In consultation with lead clinicians in EDs, a time period of 16 weeks (covering a national FY2 doctor rotation) in 2016 was designated for data collection. This period was sufficient to ensure that the required sample size of records for patients seen by PAs could be obtained (see Sample size). Each patient case attended by a PA or FY2 doctor in that time period was identified by information management staff and assigned a pseudonymised code number, with the link to the patient-identifiable record kept by the trust. The sample for the primary outcome was identified from the identification (ID) numbers using random sample numbers generated in Stata® version 14.6 (StataCorp LP, College Station, TX, USA) and stratified to ensure equal numbers of cases by type of professional (PA or FY2 doctor) attending the patient and coverage across the period of the rotation. Data items that were requested for the sample included demographics, triage scores, treatment and investigations, prescriptions, diagnoses and outcomes (destinations), time in the ED and reconsultations within seven days. Postcode, to be used to calculate the Index of Multiple Deprivation score as a proxy for socioeconomic status, was requested but information governance review in trusts declined this request as having the potential to make individuals identifiable. Anonymised records were then passed to the research team in a Microsoft Excel spreadsheet and entered onto Stata version 14.6.
For a subsample of 10% of the above sample for the primary outcome, the patient’s full (anonymised) electronic or paper clinical record was supplied by the trust. Each record was assessed by four clinicians in emergency medicine [two emergency medicine registrars (in the final year of their specialty training), one PA (with > 20 years’ experience in emergency medicine) and one emergency medicine medical consultant]. Blinded to each other’s assessments and to the type of professional who was undertaking the patient consultation, they made a judgement as to the clinical adequacy of care. A pro forma (see Appendix 8) was used to guide and record the judgement. The pro forma employed the criteria used in the study by Sakr et al. ,81 which compared consultations between junior doctors and nurse practitioners. When disagreement in judgments was found, the decision of the emergency medicine consultant was used.
Outcome measures
This was a pragmatic study designed to provide information for clinicians, the public, service managers and commissioners on a wide range of measures of quality, satisfaction, impact and cost. The primary outcome was specified in order to assist in calculating a sample size and was a proxy for patient safety and clinical effectiveness, but the goal of this element of the study was to synthesise evidence emerging from all the outcomes, along with the other workstreams, and we therefore used the sample calculation as a guide to avoid futility at either end of the scale.
Primary outcome
The primary outcome was unplanned re-attendance at the same ED within 7 days for the same condition. Unplanned re-attendance by patients, seen in any section, within 7 days for the same condition at the same department is one of the NHS clinical quality indicators for accident and EDs in England. 83
Secondary outcomes
These secondary outcome measures were derived from two studies investigating the substitution of doctors by nurse practitioners in the minors section of the ED. 81,82
-
Measures of consultation processes (taken from the clinical record), including length of consultation (time stamp), use of diagnostic tests, immediate outcomes of the consultation (including prescriptions, treatments, referrals and follow-ups) and associated costs.
-
The clinical adequacy of care. This was an expert clinical judgement. Criteria included record of medical history, examination of patient, requests for diagnostic tests, diagnosis, treatment decisions, referrals and planned follow-up provided by the PA or FY2 doctor at the initial consultation.
Sample size
Anticipated rate of unplanned re-consultation
In the absence of UK data on PAs in the ED setting, we considered three sources of information, including two randomised controlled trials substituting nurse practitioners for doctors in the minors section of the ED. 81,82 First, NHS ED clinical quality indicator data show that unplanned re-attendance at the same ED in England within 7 days for patients seen in any section and by any professional was 7.4%, with individual EDs ranging from 2.4% to 21.7% in December 2014. 84 Second, Sakr et al. 81 reported unplanned reconsultation rates, for the same condition within 28 days, of 8.6% (nurse practitioners) and 13.1% (doctors). Third, Cooper et al. 82 reported rates of 18.3% and 21.5%, respectively. Clearly, the 7-day data at the same ED site will underestimate a 28-day outcome at any ED, urgent care or general practice site. Both studies were conducted in single ED sites and we did not know whether they were high or low on the spectrum seen in the clinical quality indicator data. Taking this into account, we chose Cooper et al. ’s82 18.3% as an anticipated base rate towards the higher end of the observed range.
Minimum clinically important difference
We took the study by Sakr et al. 81 as having the least risk of bias from the comparison and study design. Their sample size calculation was to detect a difference between groups of 2.5% versus 5%. Although this proved to be an underestimate, we were also interested in finding a relative difference of 50%, although in a non-inferiority hypothesis, so we compared 18.3% with 27.4%. It should be noted that as this is a pragmatic study investigating a wide range of measures of impact and cost, we considered that estimating with confidence intervals (CIs)85 and understanding the differences between professions would be more informative for clinicians, service managers and commissioners than a binary hypothesis test on one of the outcomes. We anticipated that 18.3% of patients would reconsult (unplanned) within 28 days for the same problem in any health service. We aimed to test a non-inferiority hypothesis on this primary outcome measure, which stated that PAs do not exceed 27.4% unplanned reconsultations, with 80% power at a 5% significance level. This required 284 patients in each group (calculation from Stata version 11.1 software). We included an extra 20 patients to allow for adjustment for case mix,86 requiring a total of 304 patients in each group (those seen by PAs vs. those seen by FY2 doctors).
Analysis
Data were entered into a patient-level Stata version 14.2 file. Analysis and presentation of these data involved summary measures as cross-tabulation (frequency/proportions) for categorical variables, and location (e.g. means/medians) and dispersion (standard deviations/percentiles) appropriate for continuous variables. The distribution of length of stay in the ED was inspected using a histogram plot. Descriptions of difference at the aggregate level were made between those patients seen by PAs and those seen by FY2 doctors for all patient outcomes. A likelihood ratio (LR) χ2 test was used to assess whether or not the primary and secondary outcomes differed between PAs and FY2 doctors. A logistic regression86 was also carried out for the primary outcome (i.e. the patient making an unplanned reconsultation at the ED within 7 days), while adjusting for confounding factors, such as age, sex and Manchester Triage Score (MTS)87 the latter as a proxy measure of patient acuity. Although the advice of the lead clinicians in EDs and the advisory group was that patient acuity, as recorded through an early warning score,88 was the most appropriate method of classifying differences in patient caseload in the ED, one of the trusts did not supply this variable and missing data, therefore, precluded using that as the main adjustment variable. Because the difference between PAs and FY2 doctors may be different at different sites, an interaction term between profession and site was also tested. The odds ratios (ORs) estimated from the logistic regression were reported and their significance levels were assessed using Wald tests. All p-values are two-sided.
Economic analysis
An analysis of the comparative costs of using PAs and FY2 doctors in the ED was planned from a NHS perspective. The a priori analysis plan was for variables of interest to be extracted from the anonymous patient records, including consultation length (time in and time out in minutes); diagnostic tests ordered (blood, X-rays), treatments (e.g. prescriptions), referrals made and follow-on care recommendations; whether the PA or FY2 doctor sought advice from a senior colleague in the ED during the consultation; and unplanned reconsultations (primary outcome). The protocol stated that if statistically significant differences were observed between the two professional groups in any of these variables, after controlling for case complexity, costs would be attributed. The cost of consultation times would be based pro rata on salaries, with oncosts and overheads, obtained from professional bodies and national sources. 89 The costs of tests and treatments would be obtained from NHS sources90 and local financial managers as needed. It was planned to use a cost–consequences framework91 to indicate differences in costs to the hospital of employing PAs and FY2 doctors in the ED, in relation to appropriateness outcomes, obtained from the record review. However, data limitations restricted the analysis to a comparison of a reduced number of variables and the employment costs of the professionals.
Ethics and governance
The research was undertaken using ethical principles derived from the Medical Research Council92 guidance. Professional and patient participants were volunteers and individual consent to participation was sought. Assurance was given to participating trusts and individuals that they would not be identified in any reports or papers that were published. Data storage and disposal complied with the Data Protection Act 1998. 93
Workstream 3 was reviewed and approved (including amendments) by NHS London – Central Research Ethics Committee (reference 15/LO/1339). For the first case study sites, NHS research governance permission was obtained via the central single process application to the NHS trusts (Integrated Research Application System project ID 181193). The replacement of this system and subsequent delays to all research projects in the transfer are well documented. This study was no exception. Each study site had to then give formal written permission to proceed. The shortest time period from application for local research governance permission was 3 months and the longest was 10 months.
Workstream 4: synthesis of evidence
The evidence from workstreams 1, 2 and 3 was developed into an overall synthesis against the research questions by the research team. This was then discussed in an emerging-findings seminar (see Appendix 9). Participants included those who had advised the research team (patients, members of the public, health professionals and non-clinical health service managers) as well as some of those who had participated. The workshop was organised into presentations followed by round-table discussions in small groups. The presentations were then discussed as a whole group, led by the patient and public representative on the research team. A member of the research team took contemporaneous notes, which were then typed up and circulated to participants. The views, questions and issues raised in the seminar were then incorporated into the final report.
Chapter 3 Findings: evidence from the reviews and surveys
This chapter reports on the evidence identified through workstreams 1 and 2, consisting of a survey across English hospitals, a systematic literature review and a policy review. From macro- and meso-level perspectives of health-care systems, it identifies the factors influencing the extent of the adoption and deployment of PAs in English NHS hospitals as well as research evidence of the impact of employing PAs within the medical and surgical workforce. We report first on the systematic review of evidence, then on the national surveys and finally on the policy review.
The systematic review
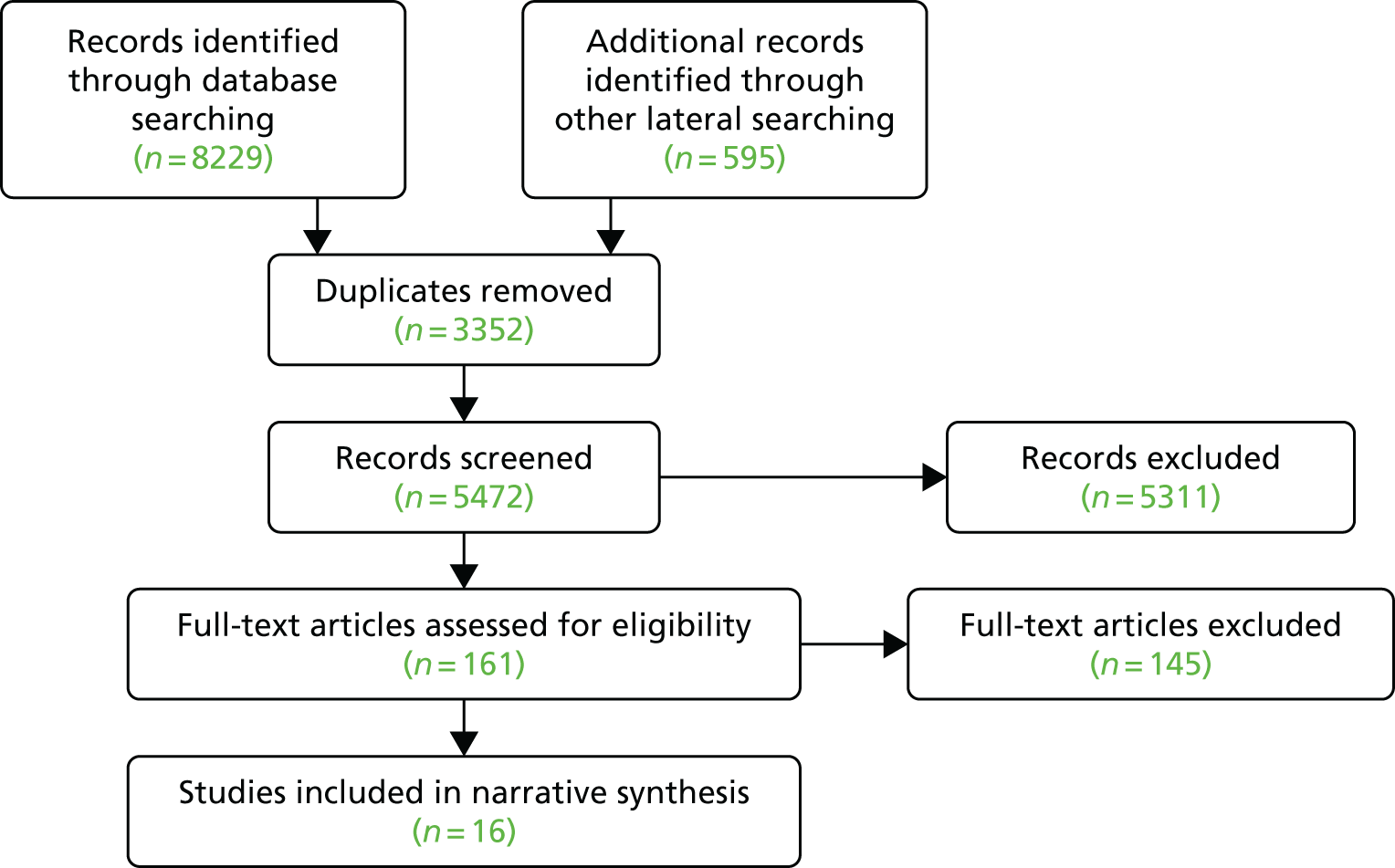
From 5472 references identified through the search strategy, 161 papers were selected for full-text reading, of which 16 papers32,94–108 met the inclusion criteria (Figure 2). Brief characteristics of each of the included studies are presented in Table 4 and in full in Appendix 10. The studies were all from North America (mainly the USA) and addressed different types of questions using a range of methodologies with different outcome measures. Seven studies were in emergency medicine,94–100 six were in trauma and orthopaedics,32,101–105 two were from internal medicine and one was from mental health. 106–108 No studies from acute medicine or care of the elderly were identified.
FIGURE 2.
The PRISMA60 flow diagram of the included papers. Adapted with permission from Halter et al. 109 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/.
| First author, year and study design | Study setting | Intervention |
|---|---|---|
| Emergency medicine | ||
| Arnopolin, 2000,94 comparative retrospective | USA; walk-in urgent care facility | PAs (n = 5) work solo from 08.00–12.00 |
| Ducharme, 2009,95 descriptive retrospective | Canada; EDs in six community hospitals | PAs introduced in EDs under the supervision of a physician |
| Hooker, 2008,96 longitudinal | USA; national sample of ED patient-level data survey | PAs as providers of ED care and prescribers of medication (7.9% of patients were seen by PAs in 2004) |
| Kozlowski, 2002,97 prospective cohort | USA; one suburban ED | PAs were deployed to patients with isolated lower extremity trauma |
| Pavlik, 2017,98 comparative retrospective | USA; one general urban ED | PAs independent of emergency physician |
| Ritsema, 2007,99 retrospective cohort | USA; national sample ED patient-level data survey | PAs attending patients with a long bone fracture |
| Singer, 1995,100 prospective observational | USA; one urban ED | Patients with lacerations assigned to PAs |
| Trauma and orthopaedics | ||
| Althausen, 2013,32 comparative retrospective | USA; trauma care at a level II community hospital | PAs (n = 2) deployed to cover all orthopaedic trauma needs, under the supervision of orthopaedic surgeons |
| Bohm, 2010,101 mixed methods | Canada; one academic hospital arthroplasty programme | Addition of PAs (n = 3) to the operating room team as first assists |
| Hepp, 2017,103 mixed methods | Canada; peripheral hospital | One PA filling provider gaps in preoperative screening, theatre assist, postoperative care and clinic follow-up |
| Mains, 2009,104 prospective cohort | USA; urban, community-based level I trauma centre | Core trauma panel (consisting of full-time, in-house trauma surgeons) plus PAs |
| Oswanski, 2004,105 before and after | USA; level I trauma centre | PAs substituting for doctors in trauma alerts |
| Internal medicine | ||
| Capstack, 2016,106 retrospective comparative | USA; community hospital | Expanded PA group (n = 3) in dyads with physicians (n = 3) for inpatient care |
| Van Rhee, 2002,107 prospective cohort study | USA; two general internal medicine units, teaching hospital | The use of PAs (n = 16) with 64 attending physicians, scheduled to admit to either a PA or a teaching service |
| Mental health | ||
| McCutchen, 2017,108 qualitative | Canada; mental health service | A PA supervised by a psychiatrist |
The studies were of variable methodological quality. The most important methodological flaws in the included studies were the failure to adjust the analysis for confounding variables, the absence of information to evaluate participants’ selection adequacy and the lack of information about baseline and/or demographic information of the investigated patients or PAs. The evidence in the following sections is presented by specialty and framed by the quality dimensions of interest. 50
Emergency medicine
Of the seven studies of emergency medicine,94–100 treatments offered were reported in three studies, a clinical outcome and length of stay were reported in two studies and waiting times were reported in one study. Only two studies reported PAs substituting for doctors. 94,97
Treatments offered
In terms of analgesia prescribing,96,97,99 the studies gave conflicting results. Secondary analysis of national (USA) ED survey data reported a higher proportion of patients receiving prescriptions, and within that for opiate analgesia, when attended by PAs compared to physicians and nurse practitioners. 96,99 This contrasted with a survey study of a similar-quality study, although based on patient self-report, reporting that those attended by an emergency physician had adjusted odds of 3.52 for receiving pain medication compared with those attended by PAs. 97
Clinical outcome of care
A clinical outcome of care was reported in only two studies. 98,100 The older study reported that experienced PAs had no statistically significant difference in wound infection rates compared with other medical staff providers (medical students, residents and attending physicians) in a large sample of patients presenting with lacerations at the ED. 100 The other, newer, large study98 reported a significantly lower 72-hour re-attendance rate to the ED for children aged ≤ 6 years for those patients treated only by a PA (6.8% vs. 8.0% for those treated by an emergency physician; p = 0.03). However, these rates were unadjusted, with PAs seeing the older of the children, who were much less likely to be admitted.
Length of stay
The studies by Arnopolin and Smithline94 and Ducharme et al. 95 showed contradictory results. In the study with PAs as additional staff, patient length of stay was reduced by 30% (mean 80-minute reduction). 94 The study of experienced ED PAs substituting for physicians95 reported a statistically significant longer mean length of visit (8 minutes) for patients of PAs but noted a range of difference (5–32 minutes) by diagnostic group. This study also considered costs through total charge (hospital and physician charge) for the visit and reported a small but statistically significant decrease per patient reported when patients were treated by a PA,95 although, again, this varied by diagnostic group.
Waiting or access outcomes
As an additional staff resource, the PA’s presence significantly reduced the likelihood of a patient leaving without being seen by 44%, and the odds of a patient being seen within their benchmark waiting time was 1.6 times greater; this was further increased to 2.1 if a newly appointed nurse practitioner was present instead. 91
Trauma and orthopaedics
Six papers reported on PAs working in trauma and orthopaedics. 32,101–106 PAs were substituting for doctors (residents105 and GP surgical assistants101,103) in three of these studies.
The impact of PAs on access and service delivery time was ambiguous in three studies. 32,101,105 PAs acting as substitutes for doctors were reported to shorten waiting times in the ED but the authors attributed this in part to other service redesign, such as there being more registered nurses. 32,105 Waiting times for surgical procedures were also reported to be reduced,101 attributed by the authors to the use of two operating theatres by the surgeon, made possible by the PA preparing and finishing the case. However, one study examining in detail the impact of PAs in teams on time to, in and from theatre found no statistically significant difference. 32 In two studies, PAs were found to release the time of doctors for other activities: for supervising physicians for 2 hours a day32,103 and for GPs (not quantified), who had previously acted as surgical assistants. 101
Length of hospital stay was examined in three high-quality studies,32,104,105 with one showing a significant reduction (of 3 to 4 hours) for all patients when PAs were an addition to staffing. 104 The studies in which PAs substituted for doctors found no difference in length of stay. 32,105
Health outcomes were reported as improved in two studies. 32,104 One study reported that the presence of PAs decreased postoperative complications measured by antibiotic and deep-vein thrombosis prophylaxis use. 32 The presence of PAs in the clinical team was found to reduce mortality by 1% for a trauma panel and by 1.5% for general surgery residents’ teams,104 although some of this could be attributed to other contemporaneous service improvements. Two studies found no overall difference between groups in mortality105 and in the likelihood of fracture malunion. 102
Patient satisfaction was surveyed and reported as positive from a small103 and large101 number of respondents, without a comparator, in two studies. 101,103 Responses from staff were more equivocal, with physician team members being positive on the contribution of PAs and nursing staff expressing concern about the overlap of work. 101 A different study found that although staff appreciated the continuity and PA skills in the operating room, they did not consider that the role could offer everything a previous surgical extender did postoperatively, despite being collaborative team members. 103
There was also mixed evidence regarding impact on cost. One study in which PAs were an addition to the team reported specific cost savings in the ED and operating room, although it was noted that only 50% of PA costs were reimbursable. 101 Another study32 suggested that although the costs of employment were similar to those of the GPs assisting in the operating room, there was an opportunity cost for others through released time for supervising physicians.
Internal (acute) medicine
Two studies investigated PAs in internal (acute) medicine and both examined resource use and clinical outcomes. 106,107 Neither study reported any significant differences in length of stay (used as a proxy for severity of illness). Cost in terms of relative value units (based on billing information for physician-ordered items, excluding administrative costs outside the physician’s control) was also mostly similar, although laboratory relative value units were lower for PAs (i.e. they ordered fewer investigations after adjustment for demographics in each diagnostic group). 107 Capstack et al. 106 reported a statistically significantly lower mean patient charge for the expanded PA group with physicians [US$7822 vs. US$7755 for the conventional PA group (3.52% lower, 95% confidence interval (CI) 2.66% to 4.39%; p < 0.001]. Inpatient mortality was stated to be higher for the PA group in pneumonia care only,107 although the authors reported neither the percentage nor the statistical values, and the larger study reported no significant differences in mortality or 30-day all-cause readmission. 106 The authors concluded that PAs used resources as effectively as, or more effectively than, residents107 at the same time as providing similar clinical quality. 106
Mental health
One study was included from mental health services. 108 Participants described improved access to primary care for patients; more timely access to psychiatric appointments and longer appointments; equal team cohesion for the PA or the psychiatrist; decreased waiting times and improved access to tertiary care and screening programmes; and implementation challenges of triage hierarchy and patient understanding of the term ‘physician assistant’.
Summary
Sixteen papers were included; four were published in 2017. 98,102,103,108 Most were from emergency medicine and trauma and orthopaedics specialties, with two from acute medicine and one from mental health. All studies were observational, and quality varied widely. The synthesis was further complicated by the difference between studies in which the PA was a substitute for doctors or was an additional staffing resource, or in which the introduction of PAs was only one of a number of contemporaneous service changes.
Although every paper reported the contribution of PAs as positive overall, it is important to contextualise within these issues of method and methodological quality. Summarising across the specialties, we have reported five studies in which PAs were an addition to the team. 32,95,103,104,108 In these studies, more patients are reported to have been treated; waiting times, time in EDs and time in operating rooms are said to have been shorter and mortality to have been lower; however, assessment of the contribution of PAs as opposed to any increase in team capacity is limited. Eight studies that compared outcomes of care by PAs and physicians when either one or the other was providing care or when PAs were substituting overall for physicians94,97,98,100,101,105–107 presented mixed results: either no or a very small difference in length of stay, reduced resource use but at equal or reduced cost, some time savings to senior physicians, lower analgesia prescribing, no difference in wound infection rate, inpatient mortality or re-attendance or acceptability to staff and patients. In three of the studies carrying out secondary data analysis, we do not know if the PAs were additions or substitutions, but two studies reported higher prescribing by PAs96,99 and one reported no difference in negative outcomes from fracture. 102
The strength of this review was its systematic method. Although it may be considered a weakness that only some specialties were included, this strengthens its applicability to the UK in that these are the specialties most frequently employing PAs in the NHS. We excluded any studies including intensive care data as these overlapped with acute medicine in many abstracts and we could not separately draw these out. Similarly, we excluded studies with medical and surgical specialties combined. We note that this literature appeared to include a greater proportion of studies with stronger study designs, including prospective and randomised designs; in particular, we have excluded the recent matched controlled large study from the Netherlands in which several specialties – some within and some not within our inclusion criteria – were studied. 110,111
A meta-analysis was planned but the heterogeneity of papers precluded this. Although narrative review is more limited in its precision, in following a framework for this, we have aimed to provide a clear rationale for the synthesis and conclusions we draw from it.
All of the included papers were from North America, with the majority from the USA, where health service organisation and the PA role may differ from that in other countries developing the PA role. In the USA, PAs can prescribe and order ionising radiation, and are, as a body, more experienced than those in countries more recently embracing this role.
The studies included in this review can be seen as complex interventions in complex systems and yet this has not been considered in the conclusions drawn by the authors. Well-controlled studies are needed to fill in the gaps in our knowledge about the outcomes of PAs’ contribution to secondary care. The review is published in full elsewhere. 109
We now turn to consider the evidence from the macro level of the policy context in England.
The policy review
At the point when the policy review was finalised in the preceding primary care study17 (in August 2013), it was concluded that ‘there was no reference to PAs in English policy documents’. By the end of the year, that had changed. In response to an acute shortage of doctors in emergency services, HEE (the executive non-departmental body responsible for NHS workforce planning as well as funding of training in England) had identified PAs as one of a number of non-medical roles that it would support to address the shortages. 8 Over the subsequent 4 years, we identified 17 published statements of policy intent at the macro level regarding PAs within the NHS workforce in England. 6,112–127 These are listed by type in Table 5.
| Type of document | Number of statements |
|---|---|
| Secretary for State for Health policy statement6,112–114 | 4 |
| House of Commons Health Select Committee report recommendations115 | 1 |
| Department of Health open consultation116 | 1 |
| NHS England policy statement117–119 | 3 |
| HEE policy statement120–126 | 7 |
| NHS England, HEE, British Medical Association and Royal College of General Practitioners joint policy statement127 | 1 |
| Total | 17 |
In all the policy statements, the problem being addressed was a shortage of doctors. Initially, this was in emergency medicine;6,120 later, GP shortages were the identified problem that a state-supported increased supply of PAs was aimed at addressing. 6,112,115,117–127 In all the policy documents, increased supply of other groups were also specified as in this exemplar from the GP workforce plan. 119
NHS England, HEE and others will work together to identify key workforce initiatives that are known to support general practice – including e.g. physician associates, medical assistants, clinical pharmacists, advanced practitioners (including nursing staff), healthcare assistants and care navigators.
The state support for the training of PAs became marked in 2015, with financial support for numbers of PAs in training increasing by 854% from 24 in 2014/15 to 205 in 2015/16. 121 This was quickly followed by a growth in English universities providing PA courses. 128 The only other group with a large increase in financial support for training over the period was paramedics, with numbers increasing from 853 in 2014/15 to 1231 in 2015/16 (44%). 121
The limitation of the PAs not being within the state regulation framework and, thus, being unable to prescribe or order ionising radiation was noted in the 2014 HEE workforce plans. 120 Two years passed before the intention to consult on the state regulation of PAs was announced113 in November 2016, and a further year passed before this actually commenced (in October 2017). The reasons for this gap between problem identification and action is not apparent in the documents.
At the macro level of the health-care system, sustainability and transformation plans (STPs) were developed in the winter of 2016 across 44 areas of England. 129 These were plans for the NHS and beyond, agreed and informed by health and social care partners across defined geographies. Among other issues, the workforce had to be considered in the plans. We analysed the 41 publicly available plans130 for stated policy intent to develop the PA workforce. We identified that under half were planning to increase the employment of PAs and were specified mainly in support of primary care (Table 6).
| STP reference or otherwise to PAs and ACPs | Number of plans (%) (n = 41) |
|---|---|
| STPs that made no reference in their workforce plans to PAs or advanced clinical practitioners specifically | 19 (46) |
| STPs that specified PAs as new roles being or to be developed | 18 (43) |
| Referred to the primary care sector only | 8 |
| Referred to development both in primary care and in secondary care sectors | 3 |
| Did not specify a sector | 7 |
| STPs that specified developing new or more advanced practitioners (this included terms such as advanced clinical practitioners, and sometimes referred to professions such as nurses, pharmacists, paramedics) | 15 (36) |
| Did not specify the sector | 10 |
| Specified primary care and out-of-hospital care | 5 |
In summary, the policy review identified macro-level support for the development of the PA workforce to address the problem of clinical workload and the immediate and predicted shortages of doctors. The support included not only positive statements but also state funding for training places to increase the supply to employers, particularly general practice. At the meso level, using the STPs as the evidence source, not all plans included the detail of planned growth of advanced clinical practitioners, although this may have been an artefact of the way these were written rather than actual intent. Of those specifying growth in advanced clinical practitioners, four plans did not include PAs and 18 plans did. The majority of plans that specified a sector for support of growth of PAs referred to primary care rather than secondary care.
We now turn to examine the employment of PAs in the secondary care sector through views from the meso and micro levels of the health-care system.
Survey of medical directors
At the time of the survey, there were 214 NHS acute and mental health trusts in England; MDs from 33% of trusts (n = 71) replied. Of these, 68% (n = 48) were acute trusts.
Physician associates were employed in 20 of the responding trusts, only one of which was a mental health trust. Most trusts (n = 16) employed fewer than five PAs but three employed more than 10. MDs reported that PAs were employed in a total of 22 specialties, both medical and surgical (adult and paediatric). The most frequently reported specialties for PA employment were acute medicine (n = 7 trusts), trauma and orthopaedic surgery (n = 6 trusts) and emergency medicine (n = 5 trusts). The majority reported that the supervising doctor was a consultant. Eight MDs reported that their trust was expanding its number of PAs owing to a positive experience to date.
Of the remaining respondents, 61% (n = 44) were considering employing PAs at their trusts and 10% (n = 7) were not considering employing PAs.
Respondents were asked to report supporting and inhibiting factors to the employment of PAs. In general, MDs at trusts employing or considering employing PAs reported multiple supporting factors whereas those at the seven non-employing trusts reported only inhibiting factors.
The most frequently reported supporting factor was to address gaps in medical staffing and to support medical specialty trainees. Other common factors were to improve workflow and continuity in medical/consultant teams, to help address the management of junior doctors’ working hours to be compliant with the EU Working Time Directive,13 and to reduce staff costs.
It was also reported that a number of trusts were piloting or testing out PA roles. Some had specific strategies to increase the numbers of PAs they employed through linking with university PA course providers.
The inhibiting factors that were cited most frequently were the lack of statutory regulation for PAs and the consequent lack of authority to prescribe. The relative lack of PAs to recruit was another commonly reported problem, as was resistance to their employment from (some) consultants. Seven of the 20 respondents reporting PA employment also indicated that PAs had left and not been replaced. Most indicated financial reasons or lack of PAs to recruit. One stated that the consultant considered that a doctor was more effective and efficient than a PA in that particular team. The small number of respondents not considering employing PAs offered a slightly different perspective, suggesting that other professionals – either nurses or doctors – were better placed to meet their trust’s employment needs.
This survey provides evidence of the changing employment context for PAs in England at one point in time and, for this reason, offered insights, not available elsewhere, from those in medical leadership positions within NHS trusts. The survey was conducted at the time of the junior doctors’ strike in England,131 which may help explain the low response rate, although other surveys of NHS MDs report similar rates. 132 The supporting and inhibiting factors reflect those previously reported by us from our survey of the GP employers of PAs. 17 Shortages of doctors have also been the most commonly reported reason for employing PAs in the USA. 133 Although this survey suggested that there was an appetite for employment of PAs in secondary care, it also suggested that there were issues that needed addressing, such as state regulation. Eighteen months later, a consultation on regulation116 was launched; however, this survey suggested that there might be other issues that will need attention, such as senior medical staff resistance to employment.
A full account of this survey has been published elsewhere. 134 We now turn to report findings from the survey of PAs in secondary care.
Survey of physician associates
Out of the 223 PAs on the UK voluntary register and practising in primary and secondary care in the UK at the time of the survey, 63 PAs working in secondary care in England completed the online survey. Of these, 49 provided responses to all 18 questions. Three additional participants started the survey but were filtered out as they were practising in a country other than England.
The majority of respondents had trained in the UK (Table 7) and the mean length of time since qualification was 3.1 years [standard deviation (SD) 2.1 years]. Most worked in large acute hospital trusts. The respondents reported working in 33 medical or surgical specialties; the most frequently reported was acute medicine, followed by elderly care medicine and trauma and orthopaedic surgery (see Table 7).
| Training and work setting characteristics | Number of PAs |
|---|---|
| Country that the PA was trained in (missing data, n = 14) | |
| UK | 48 |
| USA | 1 |
| Hospital type that the PA was employed in (missing data, n = 14) | |
| Acute | 48 |
| Mental health | 1 |
| Number of inpatient beds in employing hospital (missing data, n = 14) | |
| ≤ 250 | 7 |
| ≥ 251 | 31 |
| Unsure | 11 |
| Specialty with more than three respondents (missing data, n = 7) | |
| Acute medicine | 10 |
| Elderly care medicine | 8 |
| Trauma and orthopaedic surgery | 8 |
| Accident and emergency | 7 |
| Neurosurgery | 4 |
The most frequently reported setting that the PAs reported working within was the inpatient ward (n = 38), with 25 describing multiple settings including outpatient clinics and operating theatres. Of the 54 PAs who provided information on their line management arrangements, 44 (82%) were managed solely by consultants. Day-to-day supervision was reported by 48 PAs as being by a consultant or other grade of doctor. Two PAs said that they did not have a day-to-day supervisor. PAs were working within variously configured teams; the most frequently reported team composition (n = 16) was consultant led with other grades of doctors and clinical nurse specialists. PAs were mainly working day shifts (only 1 out of 50 reported working night shifts) from Monday to Friday [although 14 out of 50 (28%) reported working at least one weekend shift during the previous 4 weeks]. Some reported that their work was shaped by the absence of others in the team, for example covering for the clinical nurse specialist or for the registrar when on annual leave or while training.
This cross-sectional survey provided a snapshot of the specialties, teams and working patterns of PAs in secondary care in England and, for this reason, provided new insights, even though the response rate could not be accurately established. The types of specialties reported mirrored those of the annual census by the FPA,59 giving some confidence in the breadth of coverage. The survey provided evidence around questions such as the nature of supervision, to be taken into the next workstream of the overall study, which we report on in Chapter 4. The full report of the PA survey is published elsewhere. 135
Summary
This chapter has presented international evidence as well as evidence from the macro and meso levels of the English health-care system. We now turn to report the findings from the micro level.
Chapter 4 Findings at the micro level: perspectives from hospital senior managers and clinicians
The following six chapters report the findings from workstream 4: the micro level of the study within six hospitals. The research questions (see Chapter 1, Aims and objectives) of deployment and factors supporting and inhibiting PA employment, as well as impact on patient experience and outcomes, organisation of services, working practices and training of other professionals, relationships between professionals and the service costs influenced by deployment were investigated and were reported from different perspectives (see Chapters 4–9). Chapter 10 reports on the pragmatic comparison of patient records for patients attended by PAs and doctors in training in the ED.
This chapter presents the findings from the perspectives of senior managers and senior clinicians in the study hospitals. These were senior members of staff responsible for the strategic direction and management of the hospital and its services, as well as individuals with specific leadership roles in relation to the workforce, professional leadership and medical education and/or PAs. Telephone interviews were undertaken with 21 senior leaders in all of the six hospitals (Table 8). Eight participants were women and 13 were men.
| Type of participant | Number of participants |
|---|---|
| Chief executive | 2 |
| MDa and associate MD | 9 |
| Director of nursing/chief nurse | 2 |
| Director of workforce and organisational development | 3 |
| Director of operations/chief operating officer | 2 |
| Lead consultant for PAs | 3 |
| Total | 21 |
The involvement of senior managers and clinicians in the employment of PAs in their hospitals reflected their respective roles and length of time in their particular trusts. Senior managers and clinicians without a specific lead role had sometimes had prior involvement in the education of PAs or exposure to the use of PAs elsewhere. The consultants with lead roles responsible for PAs each had some previous involvement with PAs, which motivated or inspired them to champion and develop the role. This prior involvement included observations in US hospitals with extensive use of PAs, having PA students on placement and working with PAs while a registrar elsewhere.
Aspects of the participants’ current involvement with PAs included:
-
making decisions at a director level to employ PAs
-
oversight of employment issues
-
promotion of the PA role and the deployment of PAs
-
promoting the training of PAs
-
involvement in governance issues (particularly MDs)
-
setting strategy and developing budgets for the inclusion of PAs.
Irrespective of the hospital, there were similarities in the participants’ views and reported issues, with very few differences. We first present evidence about factors supporting the employment of PAs, issues on governance and then factors inhibiting the employment of PAs. We then turn to report on the perceived impact and contribution of PAs. Finally, themes concerning the development and retention of PAs are described.
Factors supporting the employment of physician associates
In this section, we consider the themes concerning factors supporting the employment of PAs, including issues shaping the decision to employ PAs, decision-making on PA posts and factors for successful adoption and implementation of PAs.
Issues shaping the decision to employ physician associates
Some people spoke explicitly about why PAs had initially been employed in their trusts, whereas others referred to it indirectly in the context of discussing the impact of PAs on the organisation of services. Necessity, in order to address four problems, was the most commonly cited reason for beginning to employ PAs:
-
To address a decrease in the availability of junior doctors and an over-reliance on locums to cover medical shifts.
-
To ensure that junior doctors were able to pursue their training rather than being diverted to cover service rotas – an issue that had been the subject of a deanery review in one trust.
-
To address an increase in workload and challenges in ensuring sufficient medical team presence on inpatient wards.
-
To improve quality of care; this included the necessity to improve the performance of a hospital under scrutiny by the CQC.
Some participants described the problems particularly in relation to shortages of doctors to meet service requirements as ‘a crisis’ or a ‘burning platform’. Many participants discussed redesign of their workforce as an ongoing process. One reason given by some for considering the employment of PAs was to find new sources of staff and not to deplete other groups that had their own shortages:
We’ve looked, over the last 5 years or so, very hard at what work actually needs doing rather than which members of the workforce should be doing it . . . But as time goes on the workforce in every department is limited and so to move pharmacists or nursing staff across to do what have traditional previously been medical roles, means that we’re then robbing another profession of their workforce which they desperately need as well.
ID 46, senior clinician
Decision-making when creating physician associate posts
Most clinicians and senior managers described decisions concerning actual posts for PAs (or others) as being departmentally driven by local assessment of need rather than within an explicit strategic framework:
We have a devolved clinical structure here. It’s up to the clinical business units to decide really on the model of care and the resource that they believe that they need to be able to manage that.
ID 22, senior manager
Only one of the trusts was reported to mention PAs in their workforce development strategy: this is perhaps a reflection of the decentralised approach. At the departmental level, the process was thought to be both considered and opportunistic. Some thought that decisions were often partly principled and partly pragmatic, based on the availability of those with advanced clinical skills and financial considerations. One MD even described the process as ‘completely irrational’, although they thought that it worked well enough.
It was also suggested that people tended to employ staff in roles with which they were already familiar: opting for nurses when colleagues were familiar with the extended nurse role and for PAs when they had encountered PAs before. Other factors, such as the source of the funding for a post, were also reported to be influential. A senior nurse manager explained:
So if we’re using medical money and it’s covering the medical rotas then it has to be a PA rather than . . . a nurse consultant or an advanced nurse practitioner.
ID 26, senior manager
Some interviewees focused on the skills and attributes that were needed and which professional group was likely to have them:
PAs have got those general medical skills, so for example, if on an orthopaedic ward somebody was poorly, a PA could sort that out I think. They could take a history, they could do an assessment, they can do an examination, they can come up with a management plan and I think they could decide what investigations to get. Now, I think it’s pretty unusual that a nurse, an ANP [advanced nurse practitioner] would be able to do that . . . what the nurse practitioners are very good at doing is working to protocol for a specific problem like chest pain or COPD [chronic obstructive pulmonary disease].
ID 27, senior clinician
Given the relative newness of the employment of PAs in secondary care, it was unsurprising that some people noted that the situation was evolving and the use of PAs, alongside other staff, was developing in new specialties.
Successful inclusion of physician associates in the workforce
A wide range of factors were identified as supportive of or conducive to the successful employment of PAs.
Organisational factors
Having the necessity for introducing a change in workforce widely recognised by the senior staff in the organisation was seen as conducive. However, more specifically, the need for support from the top of the organisation was repeatedly stated. This support was from both individuals at the highest level of the organisation (e.g. joint support from medical and nursing directors) and organisational statements and commitment of resources, such as:
-
organisational willingness to embrace cultural change
-
organisational commitment to quality improvement
-
organisation-wide staff engagement programme to encourage acceptance of PAs
-
management support for the business case, particularly if the introduction of PAs needed initial additional finance
-
opportunities for sharing learning from what has worked between different departments
-
identified clinical champions at a senior level.
At the clinical unit or department level, it was considered important to be precise about what was needed and how PAs offered that as well as how they fitted into existing structures. A track record of being innovative was also thought to bode well for the likelihood of welcoming new roles. Clarification about reporting arrangements was also considered to smooth the introduction of PAs. Occasionally, there was a perception that clarity about what was required had not been fully achieved and that PAs had been ‘dumped in’ and then problems had to be sorted out. A number of senior clinicians also cautioned against seeing PAs as ‘a quick fix to medical staffing problems’.
The review of hospital trusts’ public documents (i.e. annual reports, board minutes and operational plans) demonstrated variation between them in the extent of visible senior management and clinician support and resources. In two trusts, there was documented evidence of the chief executive’s and chairperson’s support and celebration of the ‘pioneering’ and ‘innovative’ work within their trust to develop a PA workforce and PA education. Three trusts reported partnership working with other organisations to secure funding and create educational opportunities for PA students and internship posts. By the end of the study period, five trusts had documented descriptions of including and increasing the number of PAs in their workforce planning for their medical establishment.
Understanding of and response to the physician associate role
Understanding the role of PAs by others in the service was reported as important. It was thought to be made easier when people had been exposed to PAs through previous practice or by working with PA students on placements. Many people described the growth of understanding through familiarity as PAs and other health professionals worked together. One person saw advantages of being a relatively small organisation in which people know each other and in which PAs stayed as members of teams for long periods.
In some trusts, considerable efforts had been made to improve the understanding of PA roles. Activities included:
-
information giving at consultants’ meetings
-
coaching for the whole team on working with PAs and what they do
-
explanations of the PA role given to junior doctors during inductions
-
publicly displayed posters introducing PAs
-
promotion of sources of information about PAs.
Clinicians and senior managers either recalled no particularly problematic relationship issues or attitudes, or – more commonly – spoke of initial resistance and concern from groups such as nurses and junior doctors, most of which dissipated as people became familiar with the new roles. Some staff were reported to be positive about having PAs as part of the team, particularly in the context of effective multidisciplinary team working. We return to this in Factors inhibiting the employment of physician associates.
Valued attributes of the physician associate role
Some aspects of the PAs and their roles were described as particularly valuable and valued by doctors and other staff groups, for example:
-
The fact that PAs were trained in the medical model.
-
They supported new junior doctors and freed up their time.
-
PA training promoted caring qualities as well as academic standards.
-
They offered enhanced skills and different skills to doctors and would, therefore, be valuable even if there was not a medical recruitment issue.
-
Their adaptability and flexibility.
One MD said:
So there’s so much they can do in terms of clerking patients, listening to patients and organising things and doing practical things. And it’s not just that they free up doctors to do those things that only doctors do, it’s much more about the positivity of what they bring.
ID 34, MD
A number of the PAs were essentially pioneers in new roles, so some people considered that it was difficult to know how important personal factors might turn out to be in the longer term. It was thought to be good to have a substantial number of PAs in a trust for mutual support and as role models for one another.
Governance issues
It is worth reviewing comments made about governance issues, as these are relevant to both what was considered to work well in employing PAs and what was considered not to work so well in employing PAs. The lack of regulation of the profession was particularly relevant and linked to issues of clinical governance within trusts. The prospect of the regulation of PAs was seen as positive and, indeed, by some, as essential.
In so far as they were discussed, it seemed that trust boards generally were not profoundly involved with the governance arrangements. Typically, detailed work on PAs, including governance arrangements, was taken on by designated PA boards or committees, which had sometimes had changes in leadership. MDs were commonly the link between the PA board and the trust board.
The issues that PA boards or committees considered included:
-
setting up structures (e.g. deciding whether PAs come within medical or nursing administration)
-
the scope of PA roles (i.e. addressing what they could and could not do)
-
clinical supervision arrangements
-
reporting lines to management on non-clinical issues (e.g. leave and rotas)
-
encouraging the organisation with using PAs
-
issues in relation to PAs not being able to prescribe or order ionising radiation
-
the ways in which PAs could work with others [e.g. advanced nurse practitioners (ANPs) and prescribing pharmacists]
-
arrangements for PAs continuing education and study leave.
As mentioned previously, many of these issues linked to factors inhibiting the employment of PAs, which are considered in the following section.
Factors inhibiting the employment of physician associates
Senior managers and clinicians identified the following issues as inhibiting the employment of PAs in secondary care or making it more difficult. These were the lack of regulation with the concomitant lack of authority to prescribe and order ionising radiation, attitudes of others, the lack of PAs to recruit and lack of clarity on governance issues. It should also be noted that one MD thought that too many people focused on the negatives in relation to PAs and one senior manager perceived no negative factors in relation to employing PAs.
Lack of statutory regulation
Senior managers and clinicians saw the absence of regulation as a potential obstacle, particularly as it was associated with a lack of prescribing rights and the right to order ionising radiation. Some senior clinicians felt that it was more important to stress what PAs could do and contribute, rather than dwell on what they could not do. It was viewed by all as a very unsatisfactory situation, described by one senior manager as ‘absolutely bonkers’, explaining that the PAs ‘can put, you know, a chest drain in a patient but they can’t prescribe paracetamol’. This situation was felt by many to detract from the utility of the PAs to the medical team and the service:
I think a number of our consultants kind of stopped at the point where you said ‘Well they [PAs] can’t prescribe and they can’t ask for X-rays’, and metaphorically threw their hands up and said ‘Well what use are they going to be for me then?’.
ID 20, senior clinician
It was thought by many that PAs’ roles were better suited to some contexts and specialties than others, although there was no consensus as to what factors might be positive or negative in this respect.
Attitudes of others and lack of understanding of the role
Almost all of those who were interviewed mentioned the culture of the organisation and the attitudes of other staff as hugely important. Negative attitudes towards new roles were seen to potentially hamper the successful utilisation of PAs. Clinicians and senior managers spoke of initial resistance and initial concerns, most of which dissipated as people become familiar with the new roles. In one trust, it was said that older consultants were starting to welcome PAs, although that was not their initial position, but that they saw the benefits in practice. Some who were resistant or initially unenthusiastic were reported to have become became advocates for the role. In some trusts, there were reported to have been some issues from some junior doctors and nurses concerned or opposed to the deployment of PAs. For the most part, the interviewees reported not so much outright opposition as ‘puzzlement’ and general lack of understanding of what PAs were and what they could do. To some extent, this was also reported to be more of an ongoing issue among doctors in training as they rotated from one hospital to another and had to become familiar with PAs. A number of interviewees considered that there was also some residual suspicion among doctors that PAs might be seen as cheap labour. The advent of PAs as new members of the workforce at an unsettled time for junior doctors when their new contract was being negotiated was considered to have led some to view the PA role with suspicion and concern. This was reported to have largely dissipated as staff came to see the value of PAs.
It was generally argued as unhelpful to view PAs in terms of substitution for junior doctors; however, it was also recognised that this view was not easy to reconcile with reasons given for the introduction of PAs to the workplace (i.e. reasons were often framed in terms of the lack of junior doctors to fill rotas). Interviewees pointed to the types of actions taken to ensure the successful inclusion of PAs in the workforce, described in Successful inclusion of physician associates in the workforce.
The final point that was raised in relation to factors inhibiting employment was the lack of PAs in the UK to recruit.
We turn now to report on the perceived impact of the PAs.
Contribution of the physician associates
The impact of PAs had not been specifically evaluated in any of the hospitals. The general view was that it was hard to separate out PAs from the rest of the team. None of the senior managers could offer routine management data or reports that could quantify impact or costs.
However, all interviewees were able to offer their perceptions of the impact of PAs in contributing to the safe running of the service, greater efficiency, continuity of care for individual patients and continuity across the organisation, and service improvements. In the context of a shortage of junior doctors, the presence of PAs contributed to the safety of the service:
I’ve had times when I’ve been on the wards and for various reasons . . . all the juniors have been away, I’ve had a PA there and actually with a consultant and a PA you can cope . . . so you know, having a PA is absolutely vital and I’ve certainly managed a ward for several days with myself and a PA and felt it’s all been pretty safe.
ID 27, senior clinician
The PAs were reported to contribute to service efficiency through supporting doctors and nurses. Specific examples were given:
-
PAs working shift patterns to complement the junior doctors that enabled an outpatient clinic to extend its hours with greater patient throughput.
-
Increased patient flow through the ED.
-
Improved access for nurses to raise concerns about a patient to a member of the medical team (e.g. when all the doctors were in theatre).
-
In some areas of work, PAs were considered to free up consultants’ time.
-
PAs were also considered to contribute to the hospital meeting national quality targets (e.g. on discharge processes and ensuring policy).
Their presence on the inpatient wards was considered to offer continuity to the medical team that, in turn, supported good patient experience:
I think that they are the glue that pulls the team together, I think they’re a constant source for the nurses for advice and, you know, keeping the patients cared for.
ID 43, senior clinician
There were no quantitative data offered and there was a commonly held view that it was difficult to disaggregate the impact of individual types of staff in team and department provision. Generally, positive answers drew on the PAs’ apparent popularity with patients and the lack of complaints: in some hospitals, PAs were thought to be effective at nipping complaints in the bud. There had also been some positive feedback (e.g. on a hospital website and from surveys of patient satisfaction). In addition, one chief executive noted that the CQC was happy with PAs.
There was a suggestion that the satisfaction levels of junior doctors in one service area had improved because of the pressure being lifted by the presence of PAs. A few people made particular mention of the impact of PAs on medical education. One MD recalled that he had been initially aware of both positive and negative views on the possible impact on junior doctors’ training and that to some extent views remained mixed. However, generally senior managers and consultants felt that concerns about PAs possibly taking training opportunities away from junior doctors were unfounded, and it was more likely that the role of PAs in service delivery actually freed junior doctors for training. PAs were reported as also contributing positively to the training of junior doctors: in induction, in helping them to understand hospital procedures and sometimes in procedural skills.
Therefore, this group of senior managers and clinicians viewed the PA contribution as positive. However, some also cautioned that to develop the PAs to their greatest utility and also to retain them required investment from the organisation beyond the support for initial introduction. Some of these elements were identified in Governance issues, such as ensuring appropriate clinical supervision. We now discuss the interviewees’ perceptions of the longer-term issues of retaining this staff group.
Developing and retaining physician associates
Senior managers and consultants, with one exception, shared the view that PAs might feel that they lacked career development opportunities. Pay and other factors were considered as relevant, particularly in areas where the cost of living was high. Although recognising a relatively flat career structure, PAs were thought to enter at a relatively high NHS salary level. Some made the point that the assumption that PAs might rapidly leave in order to train as doctors had not been borne out. Some pointed out that the flat career structure of PAs was not unique within the NHS; for example, consultants also tended to have a flat career structure, typically taking a consultant post in their thirties. Although, taking a different view, a chief executive argued that that young people do not think so much in terms of careers for life, so doctors may not stay in medicine and all kinds of changes were needed to maintain a medical workforce. Some considered that it might not be helpful to make comparisons with doctors’ careers; rather, it may be more useful to look at some of the newer roles, such as paramedics and operating department practitioners, who faced similar issues.
Although noting that some PAs wished to continue as they were, with a focus on practical, hands-on care, a variety of observations were made as to how individual hospitals and services provided or were considering providing career development for PAs. These included:
-
opportunities to work across different areas, thereby developing their skills and providing variety to their workload
-
opportunities in quality improvement and patient safety projects
-
senior PA roles for a group of PAs.
Training opportunities were considered essential, and there were examples of shared training with junior doctors and with nurses. One trust gave PAs an annual training bursary. A final observation from some was that career development may become a bigger issue once PAs have been in post for longer periods and more PAs are in posts.
Summary
Senior managers and clinicians described the shortages of doctors together with a need to ensure quality in services as the driving forces in introducing new roles at advanced clinical practitioner level. PAs were only one group that they were considering, but they were mindful of depleting other groups, such as nurses, that were also facing shortages. A variety of change management strategies were described, although not all in place in every hospital, to ensure the successful introduction of this new group. The main inhibitors to employment were thought to be the lack of regulation, with attendant lack of prescribing rights, and the lack of knowledge (with attendant puzzlement rather than hostility) about the role among other staff. Where PAs were employed, they were reported to make significant contributions to efficiency in the organisation and continuity of care for the patients. The lack of PAs for the growing number of jobs meant that PAs could easily move to jobs that offered greater career development. Introducing PAs into a workforce was known to require support structures, ongoing training and provision of appropriate clinical supervision and mentorship. None of the participants were able to quantify impact or costs. They all pointed to the difficulties of separating individual impact/contribution from a team endeavour.
Chapter 5 Findings from the micro level: the deployment of physician associates
This chapter presents a description of the deployment of the PAs recruited into the study by way of an introduction to the participants in the six case study sites. This description comes from three sources of data: work diaries completed by PAs, interview data from the PAs and researcher observations of the PAs in practice. The views of the PAs on their impact, and the challenges associated with their role, are also briefly described.
Description of participants
A total of 43 PAs took part in the case study research. Eighteen PAs returned 23 weekly work diaries, 41 PAs were interviewed and 35 PAs were observed in practice on between one and three occasions each. They worked within 13 adult and paediatric specialties and emergency medicine. The characteristics of participating PAs are not presented individually as these would be likely to identify individual participants; summary characteristics are shown in Table 9.
| Data collection method | Number of PA participants | Total number of data sources |
|---|---|---|
| Weekly work diaries | ||
| Site | ||
| 1 | 4 | 23 diariesa |
| 2 | 3 | |
| 3 | 3 | |
| 4 | 2 | |
| 5 | 3 | |
| 6 | 3 | |
| Total | 18 | |
| Interviews | ||
| Site | ||
| 1 | 11 | 41 interviews |
| 2 | 7 | |
| 3 | 7 | |
| 4 | 2 | |
| 5 | 10 | |
| 6 | 4 | |
| Total | 41 | |
| Observations | ||
| Site | ||
| 1 | 10 | 82 observation sessions |
| 2 | 6 | |
| 3 | 9 | |
| 4 | 2 | |
| 5 | 6 | |
| 6 | 3 | |
| Total | 36 | |
The PA participants worked across a wide range of specialties, similar to what was reported in the annual PA census. 59 The median length of time since qualifying as a PA was 5 years (ranging from the very newly qualified, i.e. in practice for 6 months, to those with more experience, at 9 years) (Figure 3 shows the distribution).
FIGURE 3.
Number of years since qualifying as a PA.
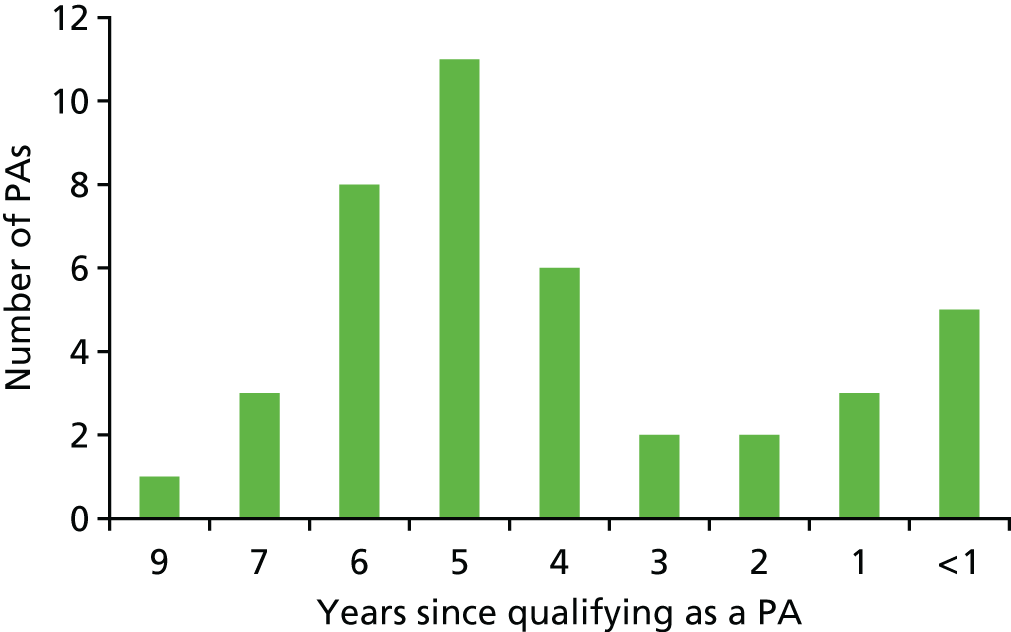
Although a number of PAs had described being in their current post since qualifying, including those with lengthier experience, others described moving between several jobs/specialties in one or more than one trust. In addition, some reported being employed on a rotational basis within their trust (i.e. working in several specialties over the course of 1 to 3 years). The median length of time in their current post was 3 years (range 2 months to 9 years).
Some of the PAs worked in specialties employing clusters of PAs both within and across the trusts, whereas others worked singly or in smaller numbers in medical and surgical subspecialties. However, all the specialties covered by the participating PAs appeared in at least two of our six case study sites.
The physician associates’ working patterns: times and places
Working hours
Work diary entries document 23 working weeks with 107 individual working days. Out of these 107 working days, 100 days were evenly distributed across the normal working week and seven were over weekends (four Saturdays and three Sundays). During these 107 working days, PAs worked a total of 1109 hours and 45 minutes (median 9.5 hours, interquartile range 8.38–12.13 hours). On average, PAs worked 48 hours and 15 minutes per week (median 47.25 hours, interquartile range 40.38–58.75 hours).
The PAs who were interviewed universally described themselves as belonging to the medical team, and their place in work rotas mostly reflected this, with descriptions given of the anticipated medical workforce for particular days or times. As we observed in the diaries, in most specialties, PAs described their main working hours as being daytime, weekday hours. When an extended-hours rota was worked by PAs, this either reflected the nature of the work in the setting (e.g. the ED where PAs worked at any time with consultant-level cover) or had come about over time, usually to address medical workforce gaps, as workload out of hours was described as being higher:
So the minimum we’d have would be one on each side [one 24- and one 28-bed ward] from 8 [a.m.] ‘til 4 [p.m.] but that sort of does vary as well. So, on a bank holiday there might be only one to cover 50 patients, on a weekend there might only be one to cover 50 patients, and on bank holidays and weekends there’s nobody coming at 2 o’clock [p.m.], there’s just that PA.
ID 44, PA
Although the caseload was high, this out-of-hours work was described positively as offering opportunities to expand and develop the PA role:
We realised when we first started working that the weekend and the evenings were the best time for us to get more experience . . . professionally it was really helpful because we could get more, we had more opportunities to practise our procedures because there were less trainees around . . . so, our lead consultant at the time . . . they wanted more cover on the weekends and some more cover out of hours, and then it kind of worked for us in terms of our own learning as well, so it’s kind of what we decided on.
ID 24, PA
For another PA, ‘on-call’ work was seen as desirable but unattainable owing to the limitations on PAs’ independence:
I’ve always wanted to have scope to be able to do more and more, but the limiting factor . . . is experience outside of [medical specialty] . . . Everyone always says how heavy the on-call is, but that’s where you learn your stuff, that’s when you’re exposed to front-door type stuff . . . I think that because we’re so limited in our scope is why we’re not involved in that on-call bit.
Limited in what way specifically?
Certainly the prescribing thing again, it comes back to that, the fact that we’re not independent prescribers.
In line with this pattern, the majority of observations were carried out during the standard working week (between 08.00 and 18.00, Monday to Friday), but four observation sessions took place in the evening, night or daytime weekend shifts.
The work setting
In the interviews, PAs mostly described working in one specialty on hospital assessment units (e.g. the ED or medical assessment units) and specialty-based inpatient ward settings, although a small number described rotational/internship programmes across several specialties, either immediately post qualifying or on a continuing basis. Most described their main work taking place on the ward or unit, with outpatient and theatre duties also forming part of the usual workplace setting for a small percentage of PAs who were interviewed or who completed work diaries. A small number described work that spanned these settings, for example work in an inpatient specialty that included being called to assess patients in the ED or on GP referral units:
Other roles that we do is we also help our SHOs [senior house officers], so they carry our on-call bleep so when they’re busy we carry the on-call bleep or we help them out with it, and that involves seeing patients in [the ED], seeing patients that have [body part] injuries or simple fractures that need to be reduced or manipulated or plastered, we can see them.
ID 160, PA
The breakdown of the working hours by grouped activity setting as reported in the PA work diaries is presented in Figure 4.
FIGURE 4.
Percentage of time spent by type of setting.
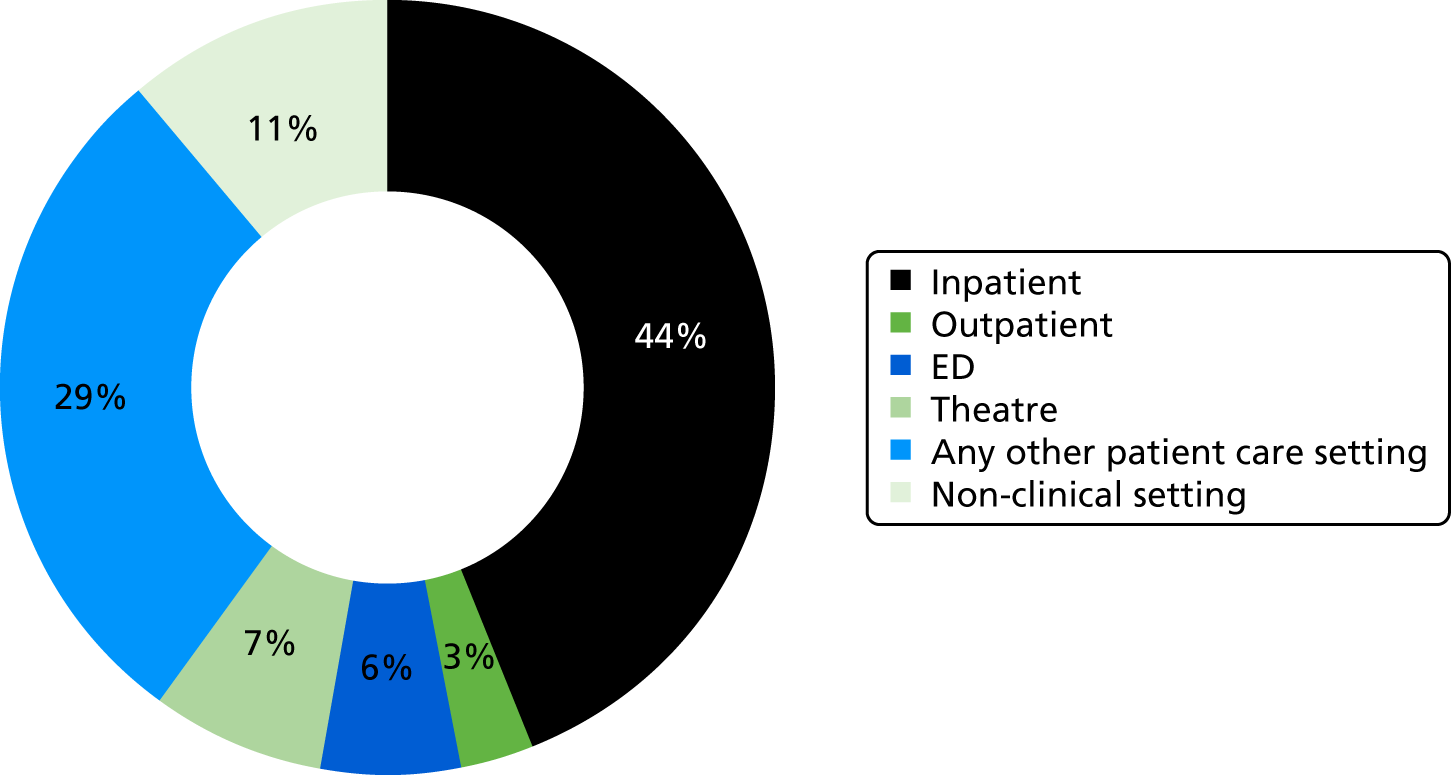
The physician associates’ work activities
An overview of the types of activities that PAs reported carrying out in predefined work diary categories is given in Table 10. Four activities within these categories were commonly described by the PAs during interviews: ward rounds, patient assessment, clinical administration and procedures. Each of these is described here in turn, illustrated by interview quotations and observation note excerpts.
| Activity | Number of daily hours | Percentage of time spent on activitya | Daily frequency | Percentage of total daily frequencya | ||
|---|---|---|---|---|---|---|
| Total | Mean | Total | Mean | |||
| Inpatient ward round (with consultant/registrar) | 160 | 1.50 | 14 | 84 | 0.79 | 10 |
| Inpatient ward round (independent) | 71 | 0.66 | 6 | 42 | 0.39 | 5 |
| Inpatient clerking of new patients | 49.75 | 0.46 | 4 | 40 | 0.37 | 5 |
| Inpatient reviewing patients | 119.25 | 1.11 | 11 | 71 | 0.66 | 8 |
| Inpatient preoperative/postoperative assessment | 15 | 0.14 | 1 | 20 | 0.19 | 2 |
| Inpatient discussion of patient care/case management with clinical colleagues | 68.25 | 0.64 | 6 | 55 | 0.51 | 6 |
| Outpatient clerking new patients | 4.5 | 0.04 | < 1 | 3 | 0.03 | < 1 |
| Outpatient patient consultation | 27 | 0.25 | 2 | 11 | 0.10 | 1 |
| Outpatient preoperative assessment | 0.75 | 0.01 | < 1 | 1 | 0.01 | < 1 |
| Outpatient discussion of patient care/case management with clinical colleagues | 4.75 | 0.04 | < 1 | 3 | 0.03 | < 1 |
| ED clerking new patients | 21.25 | 0.20 | 2 | 13 | 0.12 | 2 |
| ED patient consultation | 41.5 | 0.39 | 4 | 8 | 0.07 | 1 |
| ED discussion of patient care with clinical colleagues | 5.75 | 0.05 | 1 | 3 | 0.03 | < 1 |
| Assisting in theatre/interventional procedures | 78.75 | 0.74 | 7 | 27 | 0.25 | 3 |
| Patient education (any setting) | 25.25 | 0.24 | 2 | 39 | 0.36 | 5 |
| Discussing care with relatives (any setting) | 47.75 | 0.45 | 4 | 64 | 0.60 | 8 |
| Routine procedures (e.g. cannulation) (any setting) | 65.25 | 0.61 | 6 | 82 | 0.77 | 10 |
| TTOs and discharge summaries (any setting) | 103.5 | 0.97 | 9 | 85 | 0.79 | 10 |
| Requesting investigations (any setting) | 62.5 | 0.58 | 6 | 80 | 0.75 | 9 |
| Teaching | 36.75 | 0.34 | 3 | 35 | 0.33 | 4 |
| Own training/study | 17 | 0.16 | 2 | 16 | 0.15 | 2 |
| Networking/attending meetings | 18.75 | 0.18 | 2 | 19 | 0.18 | 2 |
| Strategy/policy/service development | 5.25 | 0.05 | < 1 | 6 | 0.06 | 1 |
| Administration | 27.5 | 0.26 | 2 | 21 | 0.20 | 2 |
| Otherb | 32.75 | 0.31 | 3 | 23 | 0.21 | 3 |
| Total | 1109.75 | 10.37 | N/A | 851 | 7.95 | N/A |
The ward round
In most settings, other than the ED, the ward round appeared to be a central feature of the PAs’ daily work, mostly taking place in the mornings, with PAs describing their work done in preparation for, during and after this daily activity. Ward rounds varied slightly by setting; they were seemingly dependent on whether patients were being reviewed on acute-assessment, high-turnover units where they were not known to the medical team or on a potentially longer stay (even if just for a few days) ward. The composition of the medical team also appeared influential, with rotational on-call consultant, the patient’s own consultant and registrar or junior doctor models all mentioned. In interviews, the tasks associated with ward rounds – for PAs – included preparing notes, offering information, particularly knowing the patient’s test results, answering questions about the patient, scribing into medical notes and getting hold of missing information.
In interview, although the tasks were articulated, it was difficult to accurately judge the level at which the PA was working. During observation, widely varying roles were seen, ranging from participating only in taking instruction and scribing in the notes, to being the main information source for the consultant, as seen in the following excerpt from the researcher’s notes on a 22-bed ward round carried out at the bedside in a surgical specialty, as shown in Box 1.
The PA was on the phone to radiology at the ward staff base as the consultant arrived on the ward. There was a flurry of activity as staff gathered around the consultant and a group of six people started to follow the consultant. The PA finished the phone call and rushed to join the round just as the consultant was moving to bed 2. The ward round moved at pace bed by bed, perhaps spending between one and three minutes at each bedside. When the PA joined at bed 2, the on-call consultant immediately asked the PA what the problem with the patient was and the PA answered ‘complaining of neck pain’. I could not hear the whole conversation as I was at the back of the group, but I could see that the PA and physiotherapist were the only team members the consultant was talking to, and that the PA was also scribing. At bed 3 the ward sister led the conversation, talking directly with the consultant. Here the PA (nor any other member of the team) had any input. At bed 4 the consultant talked first to the patient, then to PA, saying ‘Just remind me . . .’. The PA gave an update about radiology, then the clinical nurse specialist gave another update to the consultant. At bed 5 the consultant went ahead with the PA, talking (I couldn’t hear the content of this). At the bed the consultant asked the ward sister ‘what’s happening here?’, then said to the registrar ‘needs urgent CT’ [computerised tomography], at which the PA says ‘it’s been requested’. As the team left the bedside, the PA said to patient ‘I’ll come back and talk to you after.’ . . . The ward round continued similarly bed by bed with the PA note taking on every patient. At bed 8 I noted that the PA introduced a new patient to the consultant by name and clinical condition and the consultant said to the PA: ‘get him to the CT today’. The ward sister said to the PA ‘CT?’ and the PA said to the ward sister: ‘I’ve discussed with them already, he can go’ (I noted that this was the patient the PA had been on the phone to radiology about immediately prior to the ward round). At bed 10 I noted that the PA presented questions to consultant and the physiotherapist, and the consultant asked the PA if everything else was OK. The PA answers: ‘yes’ but then raised an issue about antibiotics. The patient asked the consultant a question about X-ray results, to which the PA answered.
This observation excerpt supported the description of ward rounds as pivotal points in the PA’s day, for which it was important to be well prepared and from which emerged ‘the jobs’ to be done, described in the following section.
‘The jobs’
Associated with the ward round in many cases, but ongoing throughout the day, were the activities that may be described as enabling patient care decisions – although these are described later in this study report as ‘clinical administration’ by others, no PAs used this term, but variously referred to these activities as ‘ward work’, ‘the jobs’ or ‘clinical jobs’. These activities did not involve direct patient contact, rather they took the form of ordering blood tests and investigational procedures – via a computer system, by telephone or occasionally in person; chasing the date for, or results of, such procedures; reviewing and acting on results; activities related to prescribing; and discharge summaries. In interviews, these ‘jobs’ were mentioned almost in passing by many, even though these were their core role, as if these did not require explanation or attention:
So just doing the preliminary kind of management investigations that needed to be done.
ID 52, PA
These parts of the PAs’ role, however, were clearly on show when observed, as, for many, they took up much of their day and appeared to be closely related to their value in the team in terms of having information ready for the ward round (as previously described), and in enabling medication reviews and readiness for surgery or discharge. There were many examples of these types of work during observation periods, usually interspersed with seeing patients face to face or reporting to seniors – this work took place in PA/doctor offices adjacent to wards or at the staff bases on wards. For example, one observation session included the notes of events in Box 2, which were not continuous.
While the PA was writing on patient history sheet a SHO [senior house officer] asked the PA how to book a CT [computerised tomography] cystogram. The PA said: ‘just do [specialty-specific investigation]’ and the SHO said: ‘they want [specialty-specific investigation], that was the outcome of this morning’. The PA looked on the computer and said: ‘you mean X patient?’. Later in the observation the SHO asked the PA: ‘can you get renal to look at X patient’? The PA replied: ‘CT showed no leak?’. SHO: ‘no’. PA: ‘will do’. The PA went to see a patient at their bed and then returned to the computer. Later again, the PA was looking at the patient list being looked after that day and told me: ‘I can go here, look at the pathology results on screen, need to halve the warfarin.’. The PA went to see another patient at the bed. Back at the staff base the nurse asked about warfarin and the INR [international normalised ratio]. The PA said: ‘hold, no warfarin today’ and then went directly to the patient at the bed and explained this. The PA filled out the warfarin chart and told me [the researcher] not to worry, the PA was not prescribing, but recording the INR. Later the PA went to the outpatient clinic. Here the consultant asked the PA to get bloods done for a patient and the PA directed the patient to as no one was waiting. The PA explained to the patient that they were ‘booked in for Friday’. Back at the computer the PA looked up this patient’s ultrasound results, then the PA’s bleep went off. This was a call from radiology and I heard one half of a discussion about putting in a request for an investigation. After this the PA collected the urgent bloods from phlebotomy and took them directly to the lab. After this the PA bumped into the consultant, who agreed the patient’s booking day of Friday, patted the PA on the arm and thanked them for sorting the bloods. Next, microbiology bleeped the PA. The PA . . . came back with some patient records and said they were going to do two discharge summaries for patients and book [specialty-specific investigation]. Later the PA was on a mobile phone saying: ‘you on call tonight? [first name] clearly handed over, all you need to know is patient has [clinical condition].’. The phone call continued with the PA spelling the patient’s name, and giving the hospital number and patient age, stating that the patient had had surgery, with some problems, had spoken to [other specialty] and looked up the renal function which was ‘fine’.
As noted briefly in the excerpt in Box 2, writing discharge summaries was also observed to be part of the core PA role in all settings. Many PAs listed writing discharge summaries in interviews and, for some, this was described as a fairly independent process following discussion with a senior colleague, but the process was also described as problematic; PAs referred to the process of ‘signing off’ as being hampered by the relationship of discharge summaries to the prescribing of medicines to take home [to take outs (TTOs)]. For example:
Do you find that discharge and TTOs are a challenge for you?
I do, yes, particularly so. It’s been different in every trust I’ve worked at but it has been a common problem throughout and it requires quite a long-winded and often time-consuming process for both myself and the person prescribing the medicines for the patient, as it requires separate log-ins and somebody else to come in and add medicines to an already written discharge letter and then a second sign off by pharmacy . . . in this particular trust, the letter is written by the PA and then somebody has to log in to that same entry and physically, electronically prescribe the medicines, print it and then sign it themselves and the signatures needs to match the person that’s added the medicines to the TTO. It is a long-winded, time-consuming process and quite inefficient, yes.
In observation, the to and fro process was clearly observed as inefficient double-handling of the work, with junior doctors preferring to check the patients’ notes before signing off a summary. Completion of the summaries was also observed as a process that ran parallel to numerous other tasks being carried out, the summary being kept open on a computer while interruptions from staff, patients or relatives occurred or other ‘jobs’ were carried out.
Patient assessment
Patient assessment, as described and observed, took three main forms: with an acutely presenting patient who was not known to the PA (or the medical team), with an outpatient attender and review of an unwell inpatient.
In the ED, medical assessment units and specialty-associated GP referral/assessment beds, PAs were observed doing what they described in interviews as assessing the unwell patient, with a view to presenting their assessment to a senior member of the medical team:
Then as the day goes on, look after the patients that are ward based pre and post op [operative] and take referrals. We do our own clerking on this ward, so they don’t go through the [emergency or acute assessment units], they come straight to us . . . from GP; from other trusts that don’t do a [specialty] service; from our [ED]. We have an on-call registrar and an on-call consultant that accepts referrals each day. Commonly we’ll get a call, or I’ll get a bleep on the ward, saying X is coming up, it’s a 77-year-old man and he’s really unstable, so then I’ll quickly ring the consultant or reg [registrar], just to check they’ve accepted him and they know about this patient. Because there are times when we get [clinical condition] that come over . . . and they often don’t go through our resus [resuscitation section of the ED] unless they’ve been in another hospital resus. They come straight to our assessment bay because on the ward we’ve got an assigned assessment bay. So, they are all quite unstable when they come in. So, this is a ward-based job and also an assessment-service-based job because we don’t admit everyone that comes. So, we could get someone who comes up from a GP and we’ll do an assessment and send them on their way. I’ll be taking an active role in clerking and then referring to a senior.
ID 111, PA
In the excerpt in Box 3, a PA in an ED was observed carrying out face-to-face patient assessment.
The PA was observed at the beginning of their shift, starting work by logging onto a computer, looking at the list of patients waiting and selecting which patient to see. I did not observe this decision being checked by anyone and the PA walked through the ‘majors’ bay, said hello to the nursing staff, picked up the patient’s notes from the nurse’s base desk, read the ambulance and nurse triage notes and blood results and went to a cubicle where the patient was laying on a trolley. The PA spoke directly to the patient and introduced themselves by first name and being a physician associate. The PA asked the patient a large number of medical assessment questions from the general opening: ‘what’s been going on?’ before moving on to the history of the condition and its symptoms, the patient’s past medical history and medications. Throughout this the PA crouched at the trolley, at eye level with the patient, listened to the patient and relative, and made a few notes on a piece of paper. The PA went onto examine the patient and then presented a plan: ‘I suspect we want to involve surgeons for an opinion, you look dehydrated, you’re very warm, I wonder if you need some i.v. [intravenous] antibiotics . . . I’ll chat with the boss, get a chest X-ray and tummy X-ray and fluids and pain relief and go from there’. I noted that the PA did not explain who ‘the boss’ was, nor did the patient ask. The PA went back to the medical office where several doctors were on computers. The PA presented a brief summary of the case to the consultant; the consultant asked further questions and looked at the blood results. I could not hear everything said but it appears that there was agreement to order an X-ray but not yet refer to the surgical team. The PA suggested giving more morphine; the consultant agreed and signed the script the PA had written. The PA then asked a nurse to give morphine and fluids, and to do a screening urine. The PA went back to the office and typed up the patient notes, then asked the consultant ‘Next on the list?’ referring to who should be assessed next. The PA went on to assess the next patient and, after presenting this second case, the consultant pointed out that the X-rays for the first patient were back. The consultant gave the diagnosis, which was less serious than the patient’s earlier presentation had suggested to the PA and consultant and the consultant advised the patient could go home. The PA asked, and the consultant agreed that pain relief was required. The same pattern of initial assessment, discussed with the consultant, continued throughout the shift.
A small number of PAs were observed in the outpatient setting, either seeing routinely booked inpatients, or, as in the excerpt in Box 4, in a clinic assessing acute injuries.
The PA was in clinic with an advanced nurse practitioner and another nurse who was new to the specialty, with the cases being divided between them, selected one at a time from a computer list. They explained to me that there was usually a SHO [senior house officer] or registrar ‘next door’ but not on the day observed. The PA worked in a clinic room assisted by a nurse, for example clerking the patient while the nurse cut off bandage, explaining the type of injury to the patient, examining the injury site and site, showing the patient their X-ray. The PA told me [researcher] that they were following a treatment pro forma for the particular injury site. The PA told the patient: ‘I don’t see anything significant but I’m just going to run past my senior.’. The PA went into theatre [where the senior doctor was], gained an opinion [I did not observe this interaction in theatre] and returned to the patient and explained that the injury would be strapped, but the site would be weak for six months. The PA applied the strapping whilst joking with the patient. After writing the patient notes on a computer, the PA went onto the next patient, following the same pattern of assessing and checking with the senior doctor, whilst also discussing cases and treatments with the nurses the PA was working alongside.
Both of these excerpts (see Boxes 3 and 4) described the PA working without direct supervision at the side of the patient but using the consultant to check each patient plan with after assessment, with patient throughput in the ED or clinic maintained. In another outpatient clinic example, what appeared to be delays were observed with junior medical team members, including the PA, queuing to see the consultant, who was also seeing other patients, to present their initial assessments and questions. The consultant repeated the questions the PA had asked and added more information. Some frustration with waiting time was observed from the patients.
Procedures
Many, but not all, PAs listed specific patient contact procedures they carried out either often or less frequently. Common procedures listed by the majority of PAs, almost in passing, were cannulation and phlebotomy, although many acknowledged the role of the nursing staff in blood taking.
Other practices were described or observed, including urinary catheterisation, arterial blood gases, electrocardiograms, the placement of long intravenous lines, chest drain, extubation, surgical assist roles such as closure, ultrasound for cannulation, lumbar puncture and other specialty-specific procedures. Few of these were observed in practice: only the surgical assist role in holding surgical retractors and testing tissue biopsies using in-theatre equipment and ultrasound-guided cannulation in the ED were observed.
Conducting more procedures appeared to be associated with time since qualification, or personal development over time within a particular specialty. Competence to carry out a procedure was clearly important, with a system and sign-off documents being mentioned by PAs at more than one case study site. Procedures were also, in some cases, a contested area of PA work, with trainee doctors described as ‘competing’ for procedures; views on this varied from a sense that there was plenty work to go round, to a feeling that rotating junior doctors should be allowed the opportunities as they would not be staying in the specialty, to noting the limitations of allowing the junior doctors first refusal on the career development of PAs. All of the views suggested that the PA role was there to fill medical staffing gaps, whichever part of the medical work that entailed.
In one PA’s case, they were also the staff member supervising opportunities for other juniors:
I’m quite good in doing procedure lumbar punctures so my colleagues, doctors came to me and say, could you please supervise me to do this lumbar puncture, I need my clinical placements to be signed off so they were supportive.
ID 184, PA
Limitations on procedures also varied by specialty, with PAs in one specialty reporting that the ward was so short of medical staff that PAs were never released to do what the junior doctors were doing in the first week of their rotations. The reverse was described in another case, in which surgical team shortages were described as being responsible for the PA being pulled off ward work to cover theatre.
Other associated patient-facing activities that were reported or observed included, but were not limited to, giving information to patients and relatives, discussion of DNAR (do not attempt resuscitation) or end-of-life issues and surgical consent.
The degree of PA activity on ward rounds, the ‘jobs’, patient assessment, procedures and the other specific patient-facing tasks varied in PA self-report and observation by setting and by specialty, rather than by PA per se, although there were mentions in interviews of the degree of trust of the senior medical team for the PA to carry out these activities being related to length of experience of the PA in the particular setting and contemporaneous knowledge of the PA’s competence. This is discussed in the following section in terms of the role of the PA in the medical team.
The physician associate as part of the medical team
The work activities and tasks previously described as commonly reported and/or observed give us some indication of the role of the PA in components of care but do not give us a picture of the PA’s overall role, nor of the nuances and variations to that role and place in the team, as observed. We describe this here briefly in terms of membership of the medical team, their place in the medical hierarchy and being a continuous and accessible presence.
A ‘supervised’ but trusted member of the medical team
The PAs told a consistent story about supervision, mentioning consultant- or senior-registrar-level support, which was usually directly available at the point of care or otherwise indirectly by telephone. This supervision was not tied to one particular person, but to whichever senior doctor was on cover for the ward or unit at that point in time.
These descriptions of supervision were supported by the concept of scope of practice being based on trust among the supervising team, as one PA described here:
I think it’s just the fact that we’ve gained a lot of experience. People have got to know us and so there’s trust there with the consultants and some of the middle grades. They’re quite happy as regards what they think we can assess and what we can deal with. They know that we’ll still come and ask for help if we’re stuck or if we’re not happy with something . . .
You mentioned the trust that you’ve built up with the consultants.
Because obviously they have to prescribe drugs and write our X-ray forms, which they’ll quite happily do, and instead of us asking what they think we should give we’re normally telling them what we want our patients to have, and the majority of the time they’re happy to prescribe it for us.
This move within levels of supervision was also articulated by a PA with less experience whose role, nevertheless, was already expanding:
On this ward, I am supervised. However, I’m given what I would consider, for the amount of time that I’ve been here, quite a lot of autonomy. I see my own patients. I don’t need anybody to hover over me to see anything. If I am needing any assistance, I can always ask. There is always somebody about who I can always ask. In terms of supervision, only really when taking consent am I really supervised; just to see that I’m striking home the main points because I’m actually in the process of learning to be able to consent a patient for procedure.
ID 147, PA
This last point related to discussion about PA career structure in the interviews. The interview content here focused on change over time even within one specialty, about moving around specialties and about taking more responsibility. In some settings, this was about new procedures, in others about having one’s ‘own patients’, and in others about opportunities for being part of wider continuing professional development or taking on related roles outside the clinical setting, such as teaching, audit and staff management. These comments were set in the context of – mostly – acceptance of the flat career structure of the PA role, although some concerns about this were also raised:
At the moment, and I think it probably will always be this way, I don’t think we’re ever going to have a set progression like the doctors do is it’s your career will be what you make of it and what you want to do, you will have to push to do that and get it off the ground yourself, essentially, if you like. So, having a consultant who is willing to entertain your silly ideas about what you want to do and enable them is really important and we have that here. I know that if I wanted to do anything, essentially, I know that I’d probably be supported.
ID 8, PA
Supporting and challenging the medical hierarchy
The PAs were clear that they sat in a team, and that was the medical team. Although the setting influenced variations in team members, in general the team was composed of medical strata from consultant to registrars and more junior doctors in training. Most PAs described themselves as being similar in level to Foundation Year doctors (first or second year), with a smaller number considering themselves more akin to registrars. Some of this variation appeared to be related to length of experience in a setting, particularly in having built professional and personal relationships with consultants simply through being a long-term member of the team, and examples of the PA cutting across the medical hierarchy were apparent in interviews and observations, particularly in the PA having direct contact with the consultant:
If it was something sort of out of hours and there were some concerns, I’d phone up the consultants and, you know, we’ve had a really good working relationship, being . . . I’ve worked here for 3 years now so they understand how it will work and I get how they work, so you know, I’d only pester them if it’s necessary.
ID 189, PA
Some PAs could recount instances of being questioned or not being accepted by medical colleagues; most said that these occasions were now much rarer and, in general, they reported acceptance alongside continuing curiosity and requests for role clarification from those who had not previously worked alongside PAs.
Continuity and accessibility
Without exception, PAs mentioned aspects of their role that delivered continuity, on a day-to-day and longer-term basis, on the ward or unit where they were based. In some settings, patient throughput was such that individual continuity of care was not an issue day to day; in other settings, knowledge of the patient was considered to be held only by the PA:
So from Monday to Friday and junior doctors they rotate, they go on nights, go on days, there is also training development and they go on a course and things like so for the patients here was better because this time they know there is more continuous, they know this face and . . . so when the consultant comes he give the consultant handover which is progressive so they don’t repeat every time but they can add on whatever they want to add but there is a bit of continuity of the patient yeah . . .
ID 139, PA
Longer-term team continuity was also described by the PAs, in having a good knowledge of consultants and what they wanted for their patients, and in being a source of knowledge about hospital processes. This was presented by most as a source of knowledge for inducting rotating junior doctors, and direct patient care benefit was also mentioned in a couple of examples of perceived benefit to patients through enacting local clinical care pathways efficiently:
I think generally we probably make things better just because it means that there’s staff in to see patients so they’re not having to wait for a long, long time . . . Also, probably patient safety in some respects because I know in [specialty] there’s, for a lot of the operations you need to do like follow-up like [specialty-specific investigation], things like that and I think previously things were getting missed, you know, so people weren’t getting the follow-ups they might need so . . . And just because we know that kind of how it’s organised just means that things like that aren’t missed.
ID 152, PA
Accessibility for the nursing staff was also mentioned by several PAs in interview and noted widely on observation. For some, this was described as simply being on the ward; for others, it involved more than simply physical accessibility but being approachable and in having long-term relationships with nursing staff, as described by one PA:
But you win hearts and minds very quickly just by being there because ward staff often are frustrated because there isn’t something [in the patient’s medical records] to say ‘What exactly does this say here?’. Or, ‘Can Mr so and so have a drink now?’. And to actually have a PA that even if they’re not physically there they can pick up a phone and bleep and say ‘Mr so and so, can he be drinking no?’. Or, you know, ‘What is, can you come and sort this out for me?’. Once they realise that you are reliable, that you’re going to be there, that you will answer their problems and to be honest you could be a dustbin man and they’d be happy with you.
ID 132, PA
Accessibility to all staff on the ward was also widely observed and, in the vast majority of the interactions observed between PAs and nursing staff, this ‘open access’ appeared unproblematic, friendly and mutually helpful, and implicit to the contribution PAs considered themselves to be making.
Views of the impact of the physician associate contribution
The PAs reported their perceived impact in several ways while commonly being aware that these were anecdotal accounts. PAs described a number of potential areas in which they may have an impact, predominantly in filling gaps in the medical rota, providing direct patient benefit and providing system benefit.
One PA clearly articulated that they were additional, not substitute, members of the team, with benefits:
I think the doctors see that their workload is actually less [OK], that patient care is actually improved in the fact that we’ve got more hands on deck.
ID 88, PA
Some PAs reported junior doctors being able to go off the wards for training as a result of PA presence and in some cases they reported – and were observed – in clinics, assisting in theatre and in medical assessment settings, apparently taking the same role as the junior doctor, for example in settings where patients were allocated – with consultant supervision – to a junior doctor or PA to cover.
When asked directly about the patient’s experience, PAs were clear that this was difficult to judge in team-based settings, but that they had mostly positive experiences with patients who, they considered, were more interested in being well cared for and seen promptly than whether they were seen by a PA or a doctor.
Most PAs said that they did not know about costs but those who were prompted by the interviewer suggested that they must be cheaper than junior doctors, particularly if the PA presence had reduced the locum hours required.
The following quotation highlights that PA deployment has not been without its questions and its doubters, but that PA themselves see it as making an impact:
I think seeing us work is the most important thing. Initially, where would you fit in? Are you a doctor? How would you be able to fit in? But I think by seeing it first hand, it’s worked. A PA on the ward has been able to bring [to] birth a new role, and seeing it work and being effective makes people welcome it more and accept it. I think that because it’s working people are beginning to accept it.
ID 73, PA
Several PAs noted that the researchers would need to ask others on the team to consider their impact, and it is the views of managers, nurses, doctors and patients that we now move onto in Chapters 6–9.
Chapter 6 Findings at the micro level: patient and relative perspectives
This chapter presents the findings from the perspectives of the patients, relatives and carers. Twenty-eight people were interviewed across the six hospitals: 21 patients and 7 relatives. All were adults, with a range of ages, including very elderly people. They were recruited, following introduction by a PA, in the ED, medical and surgical wards. Those patients in the ED had relatively short and contained interactions with a PA. Those participants who were inpatients were variously admitted: as emergencies via the ED, for planned surgery, for medical investigations or with acute medical problems. They had been inpatients for varying amounts of time: described as for ‘3 weeks’ and ‘since last week’. Many patients, including those recruited in the ED, had experiences other recent episodes of acute care, although not necessarily in the same hospital. Many patients had ongoing and chronic conditions. Three of the patients had met more than one PA because either their medical/surgical team included more than one or they had met one in the ED prior to their emergency admission to a team that included a PA/PAs. Relatives were interviewed with their family members. Each interview commenced by checking with the patient (and relative) that they recognised the person the interview was about and that the person had been involved in their care.
The focus of the interview was on their interaction with the PA and their experience and understanding of the PA role. Themes emerging from patients’ and relatives’ interviews were similar and are reported here together. The data are presented under the following themes: experience of the PAs’ involvement in their care, their understanding of the PA role and views about the introduction of the PA role within the NHS.
Experience of the physician associates’ involvement in patient care
Within this theme, we describe the variety of ways that the PA had been involved in patient and relative treatment and care, the overall response to the PA involvement in their care and the contribution they observed the PA(s) making.
Types of involvement
Those patients recruited in the ED described the PA’s clinical assessment, initial diagnosis and management planning within a team that included the triage nurse and a senior doctor:
When I first came in [to ED] I presumably saw a triage nurse who took my blood pressure, took some bloods and then subsequently I saw the lady [PA] who diagnosed me and interviewed me, told me what she planned to do. So, she did an examination, yes, and she scanned me, a urinary scan . . . She then went to consult her superior before she outlined the treatment she was giving.
ID 106, patient
Those patients recruited in the inpatient wards described the PAs involvement (as part of their medical/surgical team) variously, from those reporting that it was quite limited to those reporting frequent involvement that included clinical reassessments and undertaking clinical procedures:
I’ve only seen him once or twice . . . it was just, a very brief chat about, about what they [the surgical team] were going to do.
ID 161, patient
I had a crowd round me, Dr [consultant’s name] and whoever else, doctors, trainees and [PAs name] . . . and he’s [PA] since been round . . . He’s explained things to me in layman’s terms . . . he put a needle in my side and drew a big lot of yellow stuff out of me.
ID 195, patient
Some patients described the PA involvement preoperatively, such as the PA telephoning them at home to confirm details about pre-admission processes or to inform them of postponements and rearrangements. One relative observed a contrast between the work of the PA in the ED, who undertook ‘information gathering, suggesting what was wrong’, with that of the work of the PA in the inpatient team who undertook more organising.
Inpatients frequently described the PA as being the person keeping them informed of their management plan and progress:
Well he’s [the PA] been quite informative . . . keeping me up to date with what’s happening prior to the operation.
ID 181, patient
One patient commented that the PA had also asked their permission and then taught some trainees (although unsure of which discipline) about an aspect of physical assessment because their medical condition made this useful learning for the trainees.
Overall view of the physician associate involvement
All of the patients and relatives were positive about all the treatment and care they had received from their health-care team. Some of those interviewed in the ED had been there for many hours and some inpatients also shared that they were anxiously waiting for results or the next steps in their management plan:
I’ve been here 3 weeks; the care has been excellent. I feel as if I’m going around in circles a bit because the left hand is still chasing the right hand as to what’s wrong.
ID 163, patient
Some patients could not particularly distinguish the PAs’ contribution to their care from the care provided by the rest of the team, which may reflect the level of contact. Those participants who could distinguish the PAs’ contribution to their treatment and care were very positive:
Yeah, he’s [the PA] put me at ease, he’s told me everything he was going to do and why and so forth . . . he’s terrific.
ID 201, patient
Observed contribution of the physician associates
The participants in the ED reported that the contribution the PA made was to conduct a satisfactory assessment, plan and treatment of their presenting problem. One patient and one relative described that they had not waited as long to be seen this time as on other occasions and speculated whether or not having PAs had been instrumental in that.
Inpatients and relatives particularly valued the contribution of the PAs in keeping them informed (previously discussed), in explaining their condition and plan (including self-management information) in a way that they could comprehend, as well as the responsiveness and accessibility of the PAs. An example is given from an observation in Box 5.
The researcher observed a PA checking on a patient in another ward to their main ward. The patient was under their consultant’s care but was on a different ward due to pressure on beds. The PA asked the ward nurse for an update on the patient’s condition. Another nurse overheard the conversation and called to the PA ‘here, doctor’, passing the patient file to the PA to look at. The PA and the nurse discussed how some management plans and requests had not been actioned and what needed to happen.
The PA approached the patient, who was seated on a chair. The patient’s son sat at the end of the bed. The PA knelt down to address the patient, saying ‘good morning. Sir, how are you today?’. The patient appeared confused and his son said that they had not been given up-to-date information on his father’s condition/management plan. The PA clearly outlined the patient’s care to date, the treatment he had received, the reasons for that treatment, which results they were waiting for and what the next steps were. The PA used layman’s terms (e.g. discussing his ‘waterworks’) and recapped the main points at the end of the conversation, to make sure it had been fully understood. Both the patient and the son asked lots of questions, which were all answered by the PA. The PA spent around 15 minutes with the patient and son, ending the conversation with a handshake, followed by a joke about the PA and their ‘cold hands!’. The PA returned to the nurses’ station to type up the notes and fill out forms for further tests.
Some participants described the PA as the ‘liaison’ and ‘a go-between’ the consultant and themselves. Comments were made about the PA helping the patients understand what the management plan was, why it might have changed and what it meant. Several patients commented on the PA’s helpful use of ‘layman’s’ language:
I was waiting all weekend to be set about and sorted out and it wasn’t until the Monday afternoon the gentleman [PA] in question came down and explained to me what was going on and he got it through to me more than anybody else, the consultant and all . . . they [the doctors] were talking before but I didn’t understand what they were saying.
ID 195, patient
Many of these types of comments about the PA’s role as an information giver and communicator also indicated a perception of responsiveness by, and accessibility to, the PA for inpatients. This was contrasted with the doctors by some participants, who were described as ‘coming and going’ and ‘buzz off after the ward round’:
He’s been quite instrumental in helping me understand things because when doctors come they say things that people are writing down and then they walk away. And you find out that they have changed your medication and obviously I need an answer as to why, so I go to him [the PA] and he explains.
ID 143, patient
This patient also commented that the constant presence of the PA on a ward was reassuring as this improved access to someone from the medical/surgical team in an emergency:
He’s [the PA] here all the time so it would be a shame if a role like that didn’t exist in the NHS especially in wards like this where things could be life-threatening and people need to react very fast.
ID 143, patient
Some of the relatives described the PA involvement with them in providing information and reassurance as distinct from the patient:
The initial contact was [PA name] phoned [another relative’s name]. Dad had a bad turn in recovery, he had a respiratory arrest, but I think he choked, but that was the first contact, and then she [the PA] was here as soon as we arrived and she explained everything that was going on.
ID 54, relative
One relative described the PA responding to their concerns about an elderly patient’s wound as having ‘put my mind at rest’, by checking the wound and then asking the nurses to change the dressing. Another relative of an elderly patient also described how the PA was actively following up (and reporting back to them) on referrals and elements of the management plan to make sure the patient was progressing to discharge. This was described a ‘relief’ as on a previous hospital admission it had not felt that way and had been much more burdensome for the relative.
Finally, a few of the inpatients suggested that the PA contributed by helping the senior doctors and consultants work more efficiently. For example, they observed that the PA had items like records, investigation results and scans ready for the senior doctors and consultants to clinically review rather than spend their time gathering or requesting that information.
Although patients and relatives were able to describe the PA involvement and contribution to their care, they did not necessarily understand what a PA was. This is discussed in the following section.
The extent of understanding of the physician associate role
None of the patients or relatives who were interviewed had met a PA prior to this hospital episode. None of them had an accurate understanding of what a PA was. We describe this first before turning to describe their views on the extent to which this concerned or mattered to them.
Understanding of what a physician associate was
None of the participants knew what a PA was, even those who were able to recount that the PA had introduced themselves or been introduced:
She introduced herself as such and also, I saw from her badge, because I sort of saw the title and thought ‘what’s that?’.
ID 54, relative
A few of the participants said they had not realised that they had met a PA until it was pointed out by the interviewer. This was also said in the context of some participants observing that there were large numbers of people involved in their health care and not necessarily knowing exactly who or what many of them were.
Some participants offered accounts of mistaken identity and described thinking that the PA was variously a junior doctor in training, a ‘floating doctor’, ‘like a supply teacher’, a senior nurse or ‘a nice member of staff in the clerking department’.
Some participants took their clues as to the identity of the PA from the clothing or equipment like stethoscopes:
Because of her uniform I gathered she was in nursing, rather than like you with casual clothes on.
ID 159, patient
Some took their clues from the context and the work the PA had been doing:
I thought she was a doctor. But is she?
And what made you think that?
Well ’cos she came to see me, and I was perfectly happy with her expertise and everything else, so I don’t want to give the wrong impression. But I had other things on my mind [than] to ask what her actual title was.
Box 6 illustrates the mistaken identity of PAs as doctors even when they introduced themselves as PAs, as seen in the observations.
The researcher observed a PA completing follow-up jobs from the ward round on a surgical ward. This included completing discharge paperwork, chasing test/scan results and taking bloods. The PA approached a patient on the ward who required a cannula. The patient was lying in bed, with her husband beside and a young child in a pram. The PA approached the bed and introduced themselves, explaining that they were a ‘physician associate, part of the medical team’. The patient commented that they were an ‘experienced’ patient and having seen the cannulation trolley, declared with a wry smile, ‘I know exactly what you are doing here!’. The PA, patient and the family spoke in good humour while the PA prepared the equipment. The patient kept a close eye on the PA, monitoring what they were doing at each stage and inspecting their work carefully. The patient discussed a previous cannulation, which had been very uncomfortable and explained that was the reason she was so cautious. The PA reassured the patient and explained each step of the process as it was being done. The researcher noted that throughout the process, the patient repeatedly addressed the PA as ‘doctor’, despite being introduced to her as a PA. The PA was focused on the task at hand; the cannulation and on reassuring the patient. The PA did not correct her.
The context for most participants was that they saw the PA within the medical team and considered the PA as part of that:
I just knew him as part of that team [the medical team], to be honest, that was with the lady, the consultant. And as I say, they’ve all been terrific, all of them.
ID 201, patient
I thought she [the PA] was one of the junior doctors actually because she was coming around with those . . . and thought no more of it [laughs] you know.
ID 102, patient
Those participants who thought that the PA was a junior doctor added that they were satisfied that the quality of the care the PA provided was very good:
I presumed that he was a fully qualified doctor, his approach and everything was absolutely 100%, that is what, particularly an older person likes, you know what I mean? Yes, to feel that they care and that’s how you felt with him.
ID 120, patient
Most described the PAs within a team context, which was delivering good care, and referring back to senior members of staff, and that was what was important rather than an individual’s title:
[I’m] perfectly happy with her [the PA’s] expertise. She then went to consult her superior before she gave me, outlined the treatment she was giving, very professional, excellent. And to be quite honest with you, these places are very complicated in the number of levels of different jobs, and it’s of little interest to me as a patient unless I’m unhappy with what I’m getting.
ID 106, patient
Some of the participants were curious about PAs and asked the researcher more questions about them to gain a more detailed understanding.
All patients and relatives were content to be attended to by a PA in the future based on their experience in this episode.
Summary
Most participants were not clear about the PA role but were very positive about the involvement of the PA and about the quality of the care they received. Not all patients or relatives knew that they had been treated by a PA, but despite this lack of understanding/awareness about the role, all patients said that they would be happy to be treated by a PA in the future.
Chapter 7 Findings at the micro level: perspectives from the doctors
This chapter presents the findings from the perspectives of the doctors working with the PAs. Forty doctors were interviewed across the six study sites: 23 senior doctors (i.e. consultants), 10 middle-grade doctors (i.e. registrars and senior specialty doctors) and 7 early-career doctors (i.e. Foundation Years/core training doctors). They worked in a wide range of specialties (Table 11).
| Specialty | Numbers of doctors interviewed |
|---|---|
| Geriatrics | 5 |
| Trauma and orthopaedics | 4 |
| Cardiology | 4 |
| Acute medicine | 3 |
| Emergency medicine | 3 |
| Other adult medical and surgical specialties | 12 |
| Paediatric medical and surgical specialties | 9 |
| Total | 40 |
Overall, the analysis was concerned with the way in which PAs work within the teams of doctors, the understanding of their role, the level of work undertaken and views on the perceived impact or contribution to the service as well as to medical training.
We commence with the consultants’ accounts of why PAs have been employed in their services and then turn to descriptions of the work and role the PAs were fulfilling. We describe their views on the contribution made by PAs and of patients’ attitudes to PAs, before turning to factors inhibiting working with or employing PAs. The chapter ends with a discussion of views on the measurement of the impact and costs of PAs.
Factors influencing the employment of physician associates
Most consultants described the main driver for employing PAs initially as a shortage of doctors to cover the medical rotas for their service. They indicated that this shortage had come about through a set of interconnected demand and supply issues: the enforcement of the working time directive on junior doctor hours, the 2016 junior doctors’ employment contract, changes in medical education requirements, reduced numbers of junior doctors in training, difficulties in obtaining visas for overseas doctors as well as the expansion of their service:
We introduced them because of junior workforce doctor issues. So fewer junior doctors being given training numbers and we foresaw that we were going to expand and that we would probably need more junior doctors or more, more people on a junior tier.
ID 89, consultant
Most accounts described the employment of PAs as addressing two main interconnected issues:
-
providing sufficient medical team presence, particularly on inpatient wards during the daytime, to ensure high-quality, efficient and safe patient care
-
ensuring that junior doctors in training were able to meet their training requirements without detriment to the service needs. ID 114, consultantID 68, consultantSeveral of the consultants described that although the initial impetus was to address staffing shortages, it had become evident over time that PAs, particularly experienced PAs, could contribute in a range of ways to service delivery:ID 125, consultantThey also described the way in which this innovation was then taken up by other consultants and services as they observed the contribution the PAs made:ID 119, consultant
One is continuity of care at junior level. People are doing full shifts and so covering wards are quirky . . . You needed somebody who understands the team, who’s a member and part of the team, who knows the ethos of the team, to be able to be there at all times. That was our thought anyway before we employed them [PAs], in that they would be ward based, team based, and they will be there at all time.
You can’t just have them [doctors in training] now doing ward work, that’s not seen as educational or part of their training. They have to be more involved in various other things . . . So that is where PAs come in, for ward work.
[There was] a specific problem to do with excessively long clinic times for complex clinics, which I do one a week, my colleagues each do one a week, [PA name] will come along to these now and she will see these patients and, effectively, she’ll be like another SHO [senior house officer] or another registrar in clinic.
I think consultants started seeing the possibilities as to where else you can use them [PAs] . . . and then everyone goes ’ah, oh they’re quite good, I want one of them, they could do all this and this for me’.
There were consultants who described their ideal team as one staffed with a skill mix of doctors, PAs and other advanced practitioners.
However, at the other end of the spectrum of opinion were a small number of consultants who, having tried PAs as an innovative solution to medical staffing problems, reported not favouring replacing them in their specialty when the current PAs left. Some other consultants reported that they were aware of PAs not being replaced in other departments when they left. These were specialties with high-dependency patients requiring frequent medical procedures and changes in medication. We discuss this in more detail in Factors inhibiting working with and employing physician associates.
Many of the consultants described trying out a variety of new workforce roles. Some consultants reported trying clerical support roles to doctors, such as medical assistants, but ceasing these in favour of PA roles, valued for their clinical knowledge and input. In many of their services, there were also a range of other mid-level posts, such as ANPs, clinical nurse specialists and prescribing pharmacists. In particular, many consultants preferred to use a mid-level profession such as a PA, with their training in the medical model to work in a medical team, because of the work and role they required of them. This was not to say that they did not value the other types of role and described the work as complementary in delivering high-quality and safe patient care. This links to the next theme of the actual work and role of the PAs.
The work and role of the physician associates
The doctors in all of the medical and surgical specialties, apart from emergency medicine, reported that PAs mainly undertook inpatient ward work:
I see our PAs’ role based on the inpatient workload, and delivering the inpatient work, and the quasi-medical management of the patient.
ID 185, consultant
So the main role of the physician associates is the running of the inpatients and the preoperative work-up for the patients coming for surgery that week.
ID 180, mid-grade doctor
The level that they worked at was described as equivalent to a spectrum across Foundation Year doctors and senior house officers (SHOs):
They’re pretty much equal to an FY2. Some of them are almost equal to senior SHOs, after finishing the core training level.
ID 150, consultant
Some of the consultants emphasised that the focus and clinical level to which PAs worked was dependent on the individual’s experience and in-post training. Newly qualified PAs were described as needing support and further in-work development to build their skills and knowledge in that specialty. In one trust, PAs were offered the opportunity to work in different departments to broaden their knowledge and skills.
Building trust in the competency of the individual PAs was a process reported by all three groups of doctors:
When our first PA started, clearly as doctors we weren’t entirely sure, I think a lot of us, what PAs could or could not do. And I think we’ve realised how competent our PAs are and how trustworthy, it’s been, you know, a revelation, we’ve been able to give them more and more jobs to do.
ID 173, consultant
Yeah. The good thing with [name of PA 1] and [name of PA 2] is that I know them, and I trust them and it’s a really good thing because I know they have deep clinical knowledge, so I don’t need to check again the patient if they’re telling me something about the patient.
ID 190, mid-grade doctor
I wouldn’t inherently trust them [PAs in a specialty she had just started working in] because of their job title. If I had asked the PA on the [specialty] ward I would trust him, not because of he’s a PA but because I’ve seen him, I’ve heard him, I know what he’s like and I trust him.
ID 206, early-career doctor
Consultants reported that there had been no patient safety incidents involving PAs. All of the doctors considered the PAs who they worked with to be clinically safe, often citing the PAs as appropriately seeking advice or alerting them to a patient’s deteriorating condition:
Yeah, and they are very careful, they know their limits and they will, you know, just ask for help.
ID 180, mid-grade doctor
All of the consultants and mid-grade doctors described their supervision of the work of the PAs and junior doctors as integral to the work of the team. The type of specialty and the organisation of the medical team were reported to determine the extent of clinical decision-making by PAs and others. For example, in some specialties, all clinical decision-making was undertaken by the consultants and senior registrars:
I think we are quite senior led, as a general rule . . . for example, where our sickest patients are, they would be seen every day by a consultant, and most of the decision-making is taken away from even the senior registrar . . . and then for the other patients, we do operate a system where our department wants the senior registrar to see every patient every day.
ID 51, mid-grade doctor
This senior-led decision-making contrasted with other specialties, such as emergency medicine, in which the PAs were expected to be able to assess, plan and manage certain types of patients, seeking senior advice as necessary:
They’re quite independent, they do a lot of the work themselves; sometimes they come and ask us as registrars like questions just to confirm certain things or like prescriptions. But on the whole, they pretty much do everything, see their own patients and they’re just like a normal member of the team really.
ID 144, mid-grade doctor
A few doctors reported some confusion regarding whether most junior doctors in the team were supervising PAs or working alongside them, a situation compounded by the junior doctors being asked to authorise prescriptions and ionising radiation for patients seen by the PA. We return to this issue in section Lack of authority to prescribe medicines and ionizing radiation. However, it was also linked to the extent to which the PA role was understood:
I think the challenges that we have had is when people haven’t understood what a PA is and what they’re not, and we’ve just had that a couple of times in that some of the doctors haven’t sort of understood what [name of PA] can do and how she sits within the team, and that’s created a little bit of tension that we’ve had to iron out just a couple of times.
ID 199, consultant
Some of the consultants described making it explicit to the new doctors in training about the role of the PA(s) in their team:
So when the junior doctors start, I explain to them what a PA is and how I view them in the team.
ID 119, consultant
Although some of the mid-grade doctors and early-career doctors also reported this type of introduction to the PAs in the team, others described a more ad hoc form of learning about the role, their place in the team and activities that they could (or could not) undertake. This was either from the PAs themselves or through observation of the PAs working in the team:
I think I’m kind of learning through being with them, but I don’t think anyone has ever said what their role is.
ID 207, early-career doctor
Many of the early-career doctors were familiar with the PA role through previous jobs or placements as medical students. They recognised that there was variation in what PAs were allowed to do and that this was something they had to understand early on in that job:
I just had to clarify . . . what they were and weren’t allowed to do, because I think depending on both experience and other bits and pieces, and also what the trust says a PA can and cannot do differs slightly between trusts.
ID 202, early-career doctor
One mid-grade doctor described uncertainty as to what the intended parameters of the role were and queried whether or not the scope of individual PAs had increased over time in an unplanned way. Some of the consultants reported that not all consultants agreed with each other as to the presence of the PAs, the procedures they were allowed to carry out or their position in the team:
I think there still is probably a split among the consultant staff as to what the role of a PA is precisely. I’m not sure that that’s even explicit within the consultant staff what people are happy for them to do and what people aren’t happy for them to do.
ID 89, consultant
We return to this point in section Some specialties with high-dependency patients. First, we consider the consultants’ views on the overall contribution of the PAs to the medical team.
Overall view of the contribution physician associates made
Most consultants provided a positive view of the contribution that PAs made within their specialty. This was echoed by the middle-grade and early-career doctors:
They work alongside our junior doctors, support the junior doctors, and are clinically very valuable. Well, almost invaluable now.
ID 185, consultant
So my experience with PAs has been very good, they are a really important part of the team.
ID 95, mid-grade doctor
The ones [PAs] that we have here are really good, yeah and they’re very useful.
ID 58, early-career doctor
As noted previously, there was a small number of consultants who had a less positive view, which we return to in section The negative views of some doctors and some senior nurses about physician associates.
The contribution of PAs was described by the doctors in terms of (1) supporting good, safe and efficient patient care and (2) supporting the junior doctors in training. The doctors described different ways in which they saw the PAs contributing to the medical team’s work, which we have grouped into five interlinked themes. These were:
-
providing continuity and stability in the medical team
-
undertaking some of the doctors’ workload and filling gaps in rotas
-
enabling doctors to focus on patients who were more acutely ill, were more complex or required assessment or procedures that only doctors could undertake
-
supporting patient flow
-
induction of doctors in short-term training posts and supporting release for training activities.
Providing continuity and stability in the medical team
All of the doctors described the PAs as bringing continuity and stability to the medical team by virtue of their working in one place with one team mainly during weekday daytime hours, in contrast to the junior doctors in training. This meant that the PAs were knowledgeable about the consultants’ usual clinical management, clinical guidelines, trust systems and infrastructure, and this contributed to good and safe patient care:
Our SHO-equivalent doctors rotate all the time . . . so what they [the PAs] really provide is this amazing continuity of how the system works . . . how we care for patients who’ve had [specialty] procedures, how we manage patients with different [specialty] conditions.
ID 51, mid-grade doctor
Junior doctors’ shift patterns meant that they could be absent from the wards for some days, during which period the patients or their condition could have changed. PAs were reported to be an important means for ensuring that the rest of the medical team had up-to-date knowledge about the patients:
It’s that continuity, like I’ve been on call so I’ve not been on the ward for 5 days, I’m like ‘what’s going on?’ and they’re [PAs] like ‘7 and 5 are the sick ones and 10 is the one we’re trying to get out’. And like they know that and that’s very helpful.
ID 207, early-career doctor
Some of the doctors in all groups commented that their continuous presence on the wards meant that the PAs knew the patients and their histories very well, which was an asset to the team, both for patient outcomes and in efficient use of time:
If I have an elderly patient . . . my PA knows what their needs are and everything. So, that makes a big difference for us to make the decisions. So, there’s a good outcome for the patient.
ID 150, consultant
Yes, they’re [the PAs] the continuity, so, and when they go on holiday, it’s a strange experience . . . So, I had one of them on annual leave when I was last covering all the ward patients, and actually it meant that I had to find every single thing about these patients myself, because the SHO had moved into the ward at the same time as me, and the PA normally filled that gap.
ID 30, mid-grade doctor
Nurses on wards were reported to find the continuous presence of the PAs helpful, for example in accessing a member of the medical team:
What nurses want is help if they need some support outside their area of expertise, and they want medical input . . . their assurance comes from knowing they can call someone. The great thing about our PAs is they’re available . . . They’re not stuck in theatre, they’re not in clinic and they’re the conduit to us, and that works very well.
ID 185, consultant
Continuity and stability were also linked to the ways in which PAs contributed to taking some of the medical workload; we now turn to this issue.
Undertaking some of the doctors’ workload and filling gaps in rotas
Many of the doctors across the three groups commented on the PAs’ positive contribution in managing the workload of the junior doctors, and that PAs were missed when they were not on duty:
The experience that I’ve had is that they do make sort of your junior doctor’s day-to-day workload considerably lighter.
ID 12, early-career doctor
I will say that whenever she is not here I miss her and without her it becomes quite difficult at times to manage the ward or do our usual daily work.
ID 91, mid-grade doctor
Although it was not clear in many instances whether the PAs were in addition to the numbers of early-career doctors or substitutes for a doctor’s post, some of the early-career doctors could quantify the impact of the absence of PAs on their workload:
It just takes me longer [without a PA], when I first started here I would often leave reasonably on time, but then as PAs started leaving, that time got later and later, and now commonly I’m leaving an hour and a half or 2 hours or more later.
ID 202, early-career doctor
Several doctors commented on the benefit to patient care of utilising PAs compared with having locum doctors:
Better for patient safety to have the PAs than using people that you don’t know, locums coming in can create chaos.
ID 114, consultant
Although the 2016 junior doctor strike was an unusual event, two of the middle-grade doctors described how the PAs, working with the consultants, had been invaluable in patient care during that time. A more commonly reported experience was that the PA presence enabled doctors to attend the more complex patients.
Enabling doctors to focus on patients who were more acutely ill or more complex
Doctors in all of the groups described the ways in which a PA presence in the team allowed them, and other doctors, to focus on the more acutely ill patients, or those requiring more medical knowledge or requiring procedures that only doctors could undertake:
They’re [PAs] just great at coming in and just taking off those little jobs that will really slow you down unnecessarily and paving the way for the more important sicker patients to get more of your time and attention.
ID 12, early-career doctor
And then for example if you get very complex patients that need us [the doctors] then we can see them and then when you’ve still got a busy department you’ve got trust that actually they can carry on, the PAs, to see the other patients. So you’re not having to then worry, you know that actually you’ve got team members who can see them, so it keeps the flow.
ID 144, mid-grade doctor
The presence of the PAs in the team positively assisted in ensuring that individual patients, and consequently their patients as a population, progressed. This referred to a progression both in their treatment plan and also physically through and out of the hospital. We use the term ‘patient flow’ to describe this concept and discuss this theme next.
Facilitating patient flow
Many of the consultants and middle-grade doctors described the PAs as a positive addition to the medical teams’ ability to efficiently manage the patient flow and deliver a good patient experience:
[The PA] helps the ward round flow and when the ward round flows, jobs get done earlier and when jobs get done earlier, people leave the hospital earlier because everything happens a bit more expediently.
ID 119, consultant
Some of the doctors described this in the context of two types of complexity. The first was the complex system of modern health care with advanced technology and diagnostics. The second was the complexity of the lives of sections of the patient population using the services, including the increasingly aging patient population. This next example describes this interaction and the perceived benefit of the PAs in the team in ‘smoothing’ the processes:
The kind of very advanced care that we can offer to patients in hospitals, it’s such a complex system . . . it brings a multitude of logistical challenges . . . to liaise within teams, to liaise with other departments, to book a test, to get in touch with a GP, to book a bed for a patient which [sic] is frail and elderly, which [sic] need antibiotics a few days before, comes from far away . . . and they [the PAs] can really help for that organisational aspect a lot, and also help in the more clinical aspect . . . I think they [the PAs] smooth things out with many issues that need to be prepared and planned for.
ID 95, mid-grade doctor
Another doctor described the way in which the PAs added to this smoothing of medical care using a mechanical metaphor with the PAs acting like oil:
I don’t think it’s a problem when they’re [the PAs] not there, it’s just better when they are. They’re the lubricant as opposed to, you know, the actual engine.
ID 30, mid-grade doctor
Another way in which the PAs were seen to contribute to patient flow was through the induction of new doctors in training.
Induction of doctors in short term training posts and supporting release for training activities
All doctors described the frequent movement of doctors in training to new teams, departments and hospitals. Many of the consultants and middle-grade doctors described the PAs as important in the induction of doctors new to their service. In some cases, this was a role that was formally assigned; in others, it was viewed as a more informal process in the course of working together:
So, whenever new junior doctors come in, my PA has to become their trainer, to train them how we work in this ward . . . there are a few things we have to do very specifically in this team.
ID 91, mid-grade doctor
The middle-grade and early-career doctors confirmed how helpful they had found the PAs during this period and considered that they had not only helped them personally but also helped patient experience and team efficiency. Some of these doctors described how it was easier, and preferable, to ask a PA about hospital systems and ‘lower-level things’ than to bother a senior doctor.
Some of the consultants and middle-grade doctors noted that the presence of the PAs on the wards allowed the Foundation Year and core trainees to leave the wards to attend other training opportunities, such as in the clinics and theatres. This was said with the proviso that the overall medical staffing level was adequate. Some of the early-career doctors confirmed that this was their experience:
Having the PAs frees me up because as trainees we like to go to clinics.
ID 39, early-career doctor
There was some discussion by a few of the early-career doctors regarding whether or not their learning opportunities to undertake certain procedures were restricted as the experienced PAs were competent in these. There was some speculation regarding whether or not consultants would prefer their experienced PA to carry out these procedures rather than teach each new junior doctor:
If they [PAs] get really good at that [procedures and assisting in theatre] and it’s much easier for the senior doctors, the consultant to say ‘I’d rather have the PA in there, because I don’t have to teach him, he’s done it a thousand times, I want him there’. Rather than get the junior doctor who’s never done it, he has to take time and – if they just fit in the niche, when do we get the opportunity to learn those skills and procedures?
ID 206, early-career doctor
One middle-grade doctor suggested that she had observed such situations. However, other early-career and middle-grade doctors described the ways in which learning opportunities were given to doctors in training by their seniority and there was no ‘competition’ with PAs for opportunities. More than one consultant noted that the workload was such that learning opportunities were plentiful and they remained cognisant of the importance of teaching their doctors in training.
We turn now to the doctors’ views as to patient responses to the presence of a PA in their team.
Patient responses to physician associates in the medical team
Most of the doctors reported that patients and family members were very positive about the PAs’ contribution to their care. They attributed this to factors such as communication style, constant presence on wards, accessibility and reliability:
They’ve got very good feedback from the patients . . . I’ve heard parents complimenting [name of PAs], the way they talk and the way that they’ve been looking after patients. I’ve never heard any of the doctors being complimented by the patients.
ID 186, mid-grade doctor
However, most doctors thought that patients, despite their best efforts in providing introductions, did not understand exactly who or what the PAs were, other than a member of the medical team. They reported that the PAs were always introduced and introduced themselves to patients as such. One doctor described formal introductions by the consultants as part of the ward rounds to separate doctors and PAs:
So normally I’m used to introducing myself as [interviewee first name], I’m a medical doctor, but when the consultants are introducing you to the patients it’s ‘This is Dr [interviewee surname] my medical registrar, this is [PA first name], the PA’, and making it really clear that [PA first name] is not a doctor.
ID 42, mid-grade doctor
Some doctors reported that patients very occasionally asked for explanations of what a PA was but most just accepted them as part of the medical team.
Factors inhibiting working with and employing physician associates
Overall, although the doctors were positive about the contribution of PAs, there were aspects they identified as negative and potentially inhibiting to their employment:
-
lack of authority to prescribe medicines and ionising radiation
-
some specialties with high-dependency patients in which the knowledge and skills of doctors, rather than PAs, were considered more useful to the overall work of the medical team
-
lack of PAs to employ and issues in retention
-
the negative views of some doctors and senior nurses about PAs.
Lack of authority to prescribe medicines and ionising radiation
All of the doctors, when asked if in their view there were factors that inhibited the employment of PAs, cited PA inability to prescribe medicines and order ionising radiation. For some, this was a drawback rather than an absolute reason not to employ or work with them. Most described practices whereby the doctor working with the PA wrote the prescriptions and implied that it was manageable:
I’m more than happy to prescribe for them; more than happy to prescribe all of their radiation . . . It allows me to discuss with them their plans for the patients.
ID 42, mid-grade doctor
However, some described the ways in which this lack of authority added to the workload for the team:
But at the same time if the rules are not changing in, especially in prescription, there will be this misunderstanding because if I’m working with another doctor, my workload is different than working with a physician assistant . . . I can say they [PA] can contribute for 70% [of the work required], but it can be fine when it’s a good day, but if it is a bad day, it’s really bad!
ID 190, mid-grade doctor
All of the doctors considered that PAs, with the appropriate training, should be able to prescribe certain medications and order ionising radiation to improve their utility to the team. There was a degree of puzzlement as to why they could not do so:
This is what I can’t understand. They can see a patient in resus [resuscitation section of ED] but when we come to a prescription of paracetamol, they can’t do it?
ID 150, consultant
One consultant commented that if PAs had the authority to prescribe there would be less that differentiated the PA and the junior doctor role, and that some doctors would see that as problematic.
Some specialties with high-dependency patients
Linked, to some degree, with the inability to prescribe was the reported preference of consultants in some specialties with high-dependency patients to employ doctors, rather than PAs, having worked with PAs:
Actually I think our experience with PAs has, for many of us [consultants], has not been positive . . . but the SHOs are a joy and it’s much easier, and they come in and from day 1 they’re able to do [the required medical work].
ID 53, consultant
Again, this is a very different, difficult environment . . . I’m not sure we would go back to them [PAs] because the doctors just become, within a few months, just become much more useful, I guess . . . the difference between the doctor and them [PAs] is that the doctor has been through, already by the time they get here, multiple other specialties. So, they have a much broader understanding of what else might be going on.
ID 89, consultant
These consultants noted that they only had experience of a small number of PAs and speculated as to the extent to which individual personalities were influential. Although these consultants would not seek to re-employ PAs, others described a lack of PAs to employ, which is now discussed.
Lack of physician associates to employ, retention and career development issues
Many of the consultants described a shortage of PAs to employ as a significant issue. Some described workforce plans that had included multiple PA posts, but they had only managed to recruit one or two PAs. Some consultants then described how without a full complement of PAs, they were unable to create jobs that were attractive to PAs, which meant they then left for more attractive posts. The consultants described the least attractive posts being those that involved only inpatient ward work with high levels of medical clerical work and no clinical development opportunities. A number described rethinking job descriptions in order to attract and retain PAs.
Doctors at all levels discussed the problem as they saw it of the lack of development for PAs and the lack of a clear career progression path:
Something I worry about as an individual is there is no clear progression for them, especially with the young ones. You don’t want to be doing what you’re doing now in 10 years’ time, you want some career progression.
ID 114, consultant
Some consultants described initiatives to support the development of PAs, for example through rotation schemes or training in a specific clinical procedure. However, issues such as confusion over what funding there was was to support PAs’ training and resistance by others to extending their skills were reported to sometimes hamper PA career development. For some consultants, a lack of development opportunities was linked to the problems of retaining PAs. For other consultants, it linked to problems of PAs maintaining up-to-date knowledge. For others, it linked to problems with the position of PAs within the medical team. As they saw it, PAs staying in one specialty would develop deep knowledge of particular types of conditions, diagnostics and treatments – more in depth than junior doctors joining the team. However, they thought that PAs would not have the breadth of knowledge of the junior doctors, but they foresaw this as giving rise to tensions and problems. We turn now to the theme of negative views about PAs.
The negative views of some doctors and some senior nurses about physician associates
Some consultants and other registrars were reported by interviewees to be opposed to the concept of the PA role and, therefore, did not support their employment and avoided working with them. Negative attitudes were demonstrated by the way some registrars worked with the PAs, giving them delegated tasks only and not engaging with them. A consultant noted that some doctors saw PAs as just ‘clerical’ help and treated them that way. Although many consultants said that the junior doctors welcomed the PAs, a few observed that there were sporadic issues of tension between junior doctors and the PAs as to the PA’s position in the team:
Some of the junior doctors are feeling very vulnerable and very defensive about their role and there’s been a fair bit of antagonism with some, again, personalities but it’s a sort of recurring issue. ‘What are they allowed to do, who’s supervising them, is it me?’
ID 89, consultant
One consultant argued that some PAs did not see themselves as assistants to the doctors, particularly those new to the team, but that the doctors did see them that way, and this caused tension. Some of the consultants talked about the frequent change of doctors in their teams and that managing new personalities was always part of their work.
Although most of the doctors reported that nurses, particularly at the ward level, were positive about PAs, some negative views and points of tension were also reported. Some senior nurses were reported to actively block their employment and development, preferring to support ANPs:
She’s [chief nurse] the person who has the worst opinion of our physician associate role . . . her ambition is for more ANPs . . . she wants all development monies to go there.
ID 60, consultant
All of the consultants involved in the introduction of PAs in their trusts talked of having spent considerable efforts in actively engaging with the nurses to allay fears of professional encroachment and do ‘a lot of public relations work about PAs’ (ID 119, consultant).
One part of overcoming some negative views was said to be demonstrating the contribution that PAs could make to services. This links to the next theme of the measurement of impact.
Measurement of the impact and costs
Questions on available evidence about impact and how impact could be measured were particularly directed to the consultants and middle-grade doctors. None of the participants was able to offer any completed internal quantifiable assessment of the impact of the PAs. Most considered that it was a very difficult task to single out one person or type of professional from what was a team activity:
I think it would be extremely difficult to look at patient outcomes because you measure what teams do, you don’t measure what individuals do.
ID 84, consultant
They offered examples from ‘hearsay’ of high levels of patient and family satisfaction – some stating that this had improved since a PA had joined their team, as described in Overall view of the contribution physician associates made. The consultants within the ED setting were able to talk about outcomes for individual patients seen by PAs but pointed out that these were still within a consultant-led and supervised team. Chapter 10 provides this analysis.
Regarding cost, most consultants considered that the employment of PAs rather than doctors, particularly locum doctors, was cost saving. One consultant argued that because of the salary paid to PAs combined with the investment in developing them, particularly those who were newly qualified, the difference in cost between PAs and junior doctors was not as great as some may think. Nearly all of the consultants went on to point out that the major issue for them was not finance (although important) but ensuring that they had the right staffing to provide high-quality, safe and efficient patient care. Some were able to point to aspects of improved patient flow (and consequent reduced costs per patient) in which they thought that the presence of PAs had made a difference:
Overall they have improved our cost, I will say, helping us to reduce the patient stay [in elderly care] . . . but no, I haven’t any analysis for that.
ID 179, consultant
Summary
Forty doctors were interviewed across the six hospital study sites. Initially, the main driver for employing PAs was the shortage of junior doctors and the need to protect their time for their training requirements rather than routine medical inpatient work. Most PAs were employed to undertake the medical inpatient ward work and preoperative preparation as part of the consultant-led medical team. Within the ED, they attended patients independently but as part of the consultant-supervised team. Most doctors of all grades viewed their contribution to the team and patient care positively. However, a few consultants, in high-dependency specialties, considered that doctors were of greater utility in that setting and that they would not replace PAs that left. The continuity and stability the PAs brought to the team were described as an important contribution. This, in turn, ensured a smoother experience for doctors joining the team as well as maintaining or improving quality and safety in patient care. PAs helped junior doctors manage the workload and were missed when they were absent. The presence of PAs on the wards released early-career doctors to undertake training and meant that nurses had easy access to a member of the medical team. PAs were described as contributing to patient flow and patient experience. PAs were considered to increase or significantly contribute to inpatient satisfaction, although most felt that patients did not understand what the PA role was.
The inability of the PAs to prescribe and order ionising radiation was seen as a problem that could be managed, but for some it meant that working with PAs added to their workload, in comparison with a junior doctor who could prescribe. These doctors thought that the PAs should be given the authority to prescribe and order ionising radiation. The lack of supply of PAs to recruit was an inhibiting factor and retention was also reported to be difficult in some areas owing to a lack of development opportunities and no obvious career trajectory. A different problem was identified in the division of views among doctors themselves as to whether or not they supported the concept of the PA role. Tensions were sometimes reported between early-career doctors and PAs. Some differences were noted between doctors of different levels of seniority, with a few (but not all) of the most junior being more likely to perceive PAs as a threat to their training opportunities. A few senior nurses were also thought to view the employment and development of PAs negatively.
The overall consensus was that measurement of the impact on outcomes by individuals and individual roles within hospital teams was very difficult. None of the consultants was able to offer quantifiable evidence, but suggestions were made by some on patient satisfaction levels and shorter lengths of stay in the setting of care of the elderly. No quantifiable evidence was offered on costs, although many consultants argued that using PAs rather than locums to cover gaps would automatically reduce costs. Views were mixed as to the cost of PAs, including their development. The concern of most of the consultants was not about costs but about maintaining the quality and safety of their care to patients. Many of them directed the researchers to the managers for evidence of cost. The next chapter reports their evidence.
Chapter 8 Findings at the micro level: perspectives from the operational managers
This chapter presents the findings from the perspectives of the operational managers. Eleven non-clinical operational managers from five NHS trusts participated. Ten spoke in interviews and one provided written information only. They ranged in their scope of responsibilities and titles, from divisional managers to service business managers and assistant service managers. They worked in medical, surgical and emergency services. All had worked in their posts for ≥ 18 months.
Many had come into their posts when PAs were already employed within the services and described not knowing about this type of professional previously. One had worked in the USA with established physician assistants and was able to contrast between an established model in the USA and one that was a more ‘dynamic’ model of testing and trying out in the UK.
Factors supporting the employment of physician associates
The motivating and supporting factors for the employment of the PAs was described predominantly in terms of managing an ongoing shortage of junior medical staff:
So I’ve been doing a juggling act [to cover the medical staffing rota] for the last year and a bit with limited doctors [describes increased recruitment of doctors], which is obviously good, but PAs are still needed . . . For the last 2 years or so, I’ve had two F2s [Foundation Year 2 doctors], this year I’ve been told I’m getting one F2 with no explanation. So, I would not be looking to get rid of PAs anytime soon.
ID 203, manager
Other motivating factors came from the positive value they observed from the PAs’ contribution, which we describe in section Overall positive contribution of physician associates. These factors meant that managers considered that the PAs were in roles complementary to the medical staff and were not substitutes for junior doctors:
We’re not going to put the PAs in to replace the numbers of junior medical staff; we just recognise that there’ll be gaps in junior medical staff rotation and they’re there to support them as well.
ID 100, manager
There were variations in the ways that the PAs were budgeted for, perhaps reflecting the variety of motivating factors. Some of the managers described the costs of the PAs being covered from the medical staff budget through ongoing vacancies. Only one manager suggested that in one specialty the budget for some SHO posts had been permanently changed to support PA employment following changes in allocation from the deanery (part of HEE that allocates doctors in training to hospitals). Two of the managers reported that the PAs were paid from the overall service budget rather than the medical staffing budget. Only one manager was aware of a specific business case having been made within the trust to increase the service budget to include PAs as staff. One reported that business cases were being developed for funding for more PAs in different specialties.
Four managers had been involved in introducing PAs to their service or department. They described working with a lead consultant in managing the process. They reported that although there was initial resistance from other nursing and medical staff, this had dissipated quite quickly. One manager identified the ANPs as the most concerned about the introduction of this new group. Their concerns had been addressed by paying due attention to developing both groups (PAs and ANPs):
But from a starting perspective, it was difficult to manage the expectations of nurses, nurse practitioners, clinicians on what the role was of the PA . . . I think between the advanced practitioners and PAs, that was the biggest stress but the way we designed it, now, because we enhanced both [groups of staff] competencies . . . it has been pretty successful.
ID 205, manager
Aside from these accounts, the managers described good relationships between PAs and other groups of staff.
The three managers who had been involved in the introduction of PAs to a service or department described requiring a period of investment in supporting the PAs to gain the competencies required for that specialty. This was reported as a substantial period for those PAs who were newly qualified but was thought to differ between specialties, with longer training needed for those working with high-dependency or more acutely ill patients.
Overall positive contribution of physician associates
All of the operational managers viewed the PAs and the contribution they made in their services positively:
They’re [the PAs] a really valuable asset in the department now and looking at expanding into seeing how we can have more on the department to help.
ID 205, manager
I value our PAs and I think we need more of them . . .
ID 203, manager
The positive contribution was described within seven interlinking aspects: providing continuity in and accessibility to the medical team, supporting efficient patient flow through the service, supporting doctors in training, reducing the use of locum medical staff, increasing the capacity of senior doctors, contributing to service improvements and offering evidence of successful workforce innovation. The following example indicates the interlinking between these aspects:
They’re [the PAs] providing a good service and looking after our patients on the ward and supporting the doctors, I think those are all positive things, aren’t they?
ID 203, manager
The first and most frequently reported positive contribution the PAs were said to provide was that of continuity in and accessibility to the medical team for patients, nurses and service managers. Most of the managers described the importance of having permanent (as opposed to rotating or short-term) staff within the medical team. This meant that the PAs were familiar with the service and hospital processes, with consultants’ ways of working and with the other clinical and administrative staff:
I think what’s good about them is, they’re static members of staff – unlike your junior doctors that rotate through the department – so I think that’s really, really useful in that they know the department well. They know the processes in the department. They are a reliable firm pair of hands that can work at SHO level, really.
ID 110, manager
This presence on the wards, in particular, was viewed as supporting the patient experience and patient safety:
PAs providing ward cover – this has increased the support to our junior doctors and nurses, increasing the safety of our wards. Patients are seen more regularly, and issues are proactively escalated to senior reg [registrar] or consultant level in a timely fashion.
ID 81, manager
The continual presence of PAs on inpatient wards was contrasted with the doctors, who were described as moving between different areas, such as clinics and operating theatres:
They are ward based, they have fantastic relationships with the nurses and with the patients because they are constantly present, and they don’t tend to sort of float off doing, you know, they don’t get called down to [specialist procedural clinic] and things, which can disrupt continuity of care.
ID 103, manager
Closely linked to this was the contribution to patient flow through the service. Most of the managers described at the service/organisation level the ways in which the PAs helped ensure an efficient patient flow, which also aided patient satisfaction levels. This included not just being a member of the medical team (i.e. a pair of hands) but having a role in ensuring that the processes and medical administration of the team were efficient. Examples were given, such as preparing discharge summaries at the earliest point so that when the clinical decision was taken to discharge there was no delay in the patient leaving the hospital and releasing the inpatient bed for another admission:
PAs provide ward cover so discharge summaries are completed on time, meaning patients leave hospital without delay and bed capacity is released for other patients.
ID 81, manager
This example illustrates this aiding of efficiency in patient flow in a surgical specialty:
[Patient care is organised] . . . much more, much more smoothly, so, so for instance, yeah, patient [name of PA 1] will be highlighting all these patients on the ward up to the consultants [to pre-plan for future surgery], whereas without physician associates that patient on a discharge summary they would be discharged from the ward, they would go home and the discharge summary would slowly make its way across to the admin [administration] team, the patient pathway co-ordinators, and they’d bring the patient back in for a pre-op [preoperative assessment] and then they’d book them, and this whole thing would be delayed by a matter of 2 or 3 weeks . . . [name of PA 1] highlights on there, and then we can pencil them in for their surgery date here and which means that we can, we can line up all of the extra work . . . it’s so much smoother and probably a much quicker pathway for the patient, yeah, well that’s how it benefits me as a manager.
ID 136, manager
The PAs were described as a support to the junior doctors, in induction to the specialty and the hospital, in managing the patient workload, and in helping to cover wards while the doctors went to other areas for their training, hence facilitating junior doctor education:
So we’ve found they’ve been quite well received by the junior doctors . . . especially the ones that come straight out of medical school . . . they’ve [PAs] been quite a helpful support for the junior doctors so they orientate them around the ward, within the hospital as well.
ID 100, manager
Having PAs will stabilise a ward for an afternoon to allow the SHO to go to the clinic that they are required to attend when they’re training.
ID 103, manager
Most of the managers indicated that having PAs as part of the medical team reduced the use of locum episodes. For some, that was through PAs covering work; for others, it was the result of the PAs working additional shifts. All described the advantages in terms of the PA already knowing the service, the processes and the types of patients. From all of the managers’ perspectives, although the reduction in use of locum episodes reduced costs, more importantly it maintained efficiency and quality in the service and patient safety:
The [use of] locums profile has changed [over the period of employing PAs]. I’d have to track back to see if I can find it in the financial data but I know it’s definitely reduced here significantly.
ID 100, manager
For me it’s [having PAs who are permanent members of staff] a safety net and it’s what the department needs and it’s what the patients need . . . [in contrast to locum doctors]. The PAs know this department like the back of their hand and they’ve got the relationships with the consultants, and there’s so many pros to it.
ID 203, manager
A manager whose remit included the ED noted a limitation to rostering, in that, in their trust, the PAs could not be rostered after midnight when there was no consultant physically present.
A few of the managers considered that the employment of the PAs enhanced the capacity of the senior doctors and the medical team more broadly:
PAs have a positive impact on patient experience and outcomes by providing the following services: (1) follow-up clinics – this allows our consultant body to see a higher number of new patients, generating a higher tariff and reducing patient wait times. Follow-up capacity is also increased.
ID 81, manager
Three of the managers noted that PAs in their services were proactive in service improvement activities, undertaking clinical audits and making suggestions for changes in service processes. Two of the managers reported that individual PAs were active in hospital-wide service improvements, for example in relation to patient safety initiatives.
The final positive contribution reported by two managers was that the employment of PAs in one service acted like a pilot and test bed for others to observe and consider innovative ways of addressing workforce issues or longer-term development in staffing their service:
For other services they have that don’t have PAs, they’re saying ‘how can we get a PA into a service and what type of role would we make a PA to do within the service’ and I think it’s helping us to think out of the box.
ID 205, manager
It should be noted in this context that most of the managers described work to support the development of advanced clinical practitioner roles in their services – of which PAs were only one group they were seeking to recruit. The managers variously described this development in terms of a workforce group that was separate but linked to the medical staffing: ‘creating a second-tier rota’ (ID 198, manager) and ‘a brand new rota of PAs and ANPs’ (ID 203, manager). For some managers, this workforce development was specifically linked to the national shortage of doctors in emergency medicine. Others described a number of interlinked factors: providing support to the doctors in training, providing enough medical team staff to cover to all service areas at all times and providing continuity in the medical team staff.
Patient responses to physician associates in the medical team
Many of the managers thought that most patients were not aware that it was a PA attending them, rather than a doctor, despite the PAs introducing themselves as PAs. In some settings, such as the ED, managers thought that patients were more aware of, or accustomed to, being attended to by different types of professionals. They thought that most patients saw PAs as just part of their medical team. Some described positive patient feedback:
Have you had any sense of how patients feel about having physician associates attend them?
I don’t get any complaints from them; I get compliments.
One manager expressed a note of concern about the public confusion about PAs as doctors:
One drawback I’ve observed are patients confusing the PA as a doctor – there is a difficulty to distinguish them as they are wearing the same scrubs, they are part of the ward round, they are always on the ward with doctors and also many of our patients are elderly and confused because of their condition . . . The expectations of patients are that it will be a doctor. The PA even carries a bleep like the doctors.
ID 198, manager
This manager, on reflection, went on to describe the types of action the hospital could put into place to increase patient awareness and knowledge, along the lines observed by the research team in other hospitals, for example different coloured uniforms for PAs and posters around the site explaining PAs.
All of the managers reported that there had never been a complaint regarding the PAs in their service nor had any issues been raised concerning patient safety:
No, never had any – no, we’re quite a big culture of reporting incidents and concerns being raised but there’s nothing been raised with us, no.
ID 100, manager
Measurement of the positive impact and costs
All of the managers were asked about the impact the PAs had made on the service and all were able to state ways in which they observed positive impact, as described in section Overall positive contribution of physician associates. Some were able to be specific, as in these examples:
PAs assisting in theatres – this has seen a reduction in theatre cancellations and increased efficiency due to a lack of junior doctors being available to assist. Resulting in reduced wait times and complaints and income generation.
ID 81, manager
[Following the introduction of PAs] so, we saw more people, we saw them faster, but we didn’t admit more and we were getting them out. So, for us, for that particular case, that was a success and it did what we intended it to do.
ID 205, manager
The managers had mixed views on whether employing PAs reduced costs, were cost neutral, were an expensive staffing option or, as in the example above, increased service income. None, however, was able to share any internal data or reports to support these and similar statements or provide data for the research team to analyse.
Some of the managers identified the difficulty of measuring the impact PAs had within what was essentially a team endeavour and within an ever-changing context:
I know at the moment I don’t have PAs covering a Friday [on inpatient wards] . . . [discusses the value of comparing time of discharge between days the PA is working and Friday, when there are no PAs] . . . but then [that wouldn’t work as] the PAs prepare the discharge summaries for the SHOs for Friday.
ID 103, manager
[Describes implementing a business plan, with key performance measurements, for the employment of PAs] it didn’t quite go as planned because our admissions rose. Over the course of the year, we’re looking at I think we predicted 2 or 3 per cent and they rose by 26 per cent. So, it was hard because our baseline had changed so drastically, it was difficult for that one to say ‘OK, this resource had this impact’, because I was putting in a ton of resource just to deal with the day-to-day activity coming in the department, so it was more difficult to pinpoint exactly what impact the PA had.
ID 205, manager
Views on the reduced use of locum doctors is reported in section Overall positive contribution of physician associates and the cost consequences were described in terms of efficiency and safety rather than just the staffing finances. However, some of the operational managers reported that their PAs cost less than employing locum junior doctors:
The cost question is an easy one, because I’ve costed out quite a bit lately, working out what costs what, and what would equate to whole-time equivalent, I would get more for my money if I went with a physician’s associate as compared with an SHO.
ID 113, manager
It does definitely help with cost because; it’s definitely a lot cheaper to have a band 7 physician associate covering the rota than a locum agency SHO.
ID 98, manager
All indicated that the PAs had a positive impact on the service. They all argued that evidence of this positive assessment of the value of PAs that they and others held was demonstrated through their plans to replace those who left, for recruitment of more PAs and in the planned expansion of PA employment in a different part of their service or specialty.
Inhibiting factors to employing physician associates
When asked about factors that might inhibit the employment of PAs, the managers offered shortage of supply and to some degree the lack of authority to prescribe and order ionising radiation.
A small number of managers described difficulties in recruiting PAs due to the relatively small supply: ‘There’s not many PAs out there . . . so we are struggling with recruitment’ (ID 203, manager). Others described shaping their jobs for PAs in terms of types of work opportunities and career development available in order to be as attractive as possible in what they saw as a very competitive labour market.
A couple of the managers suggested that although PA authority to prescribe and order X-rays did not inhibit them from employing PAs per se, it did limit the overall numbers they would employ for a particular service or department:
The tricky part is the fact they’re not prescribers currently. So, I guess if you have too many, you almost become less efficient . . . I think it becomes difficult to work operationally if you had too many PAs. I think they probably need to keep a balance between how many PAs you have, how many prescribers and medical staff we have.
ID 100, manager
Most of the managers described their services as coping or managing around the PAs’ lack of authority to prescribe medications or order ionising radiation. They all considered it a limitation on using the full potential of the PAs and inevitably created inefficiencies, although they described practices to minimise this:
We always have them [PAs] working in teams [with doctors] so there’s always a way round it [not being able to prescribe], essentially.
ID 100, manager
They can’t do the actual TTO’s, which is the prescribing the actual bit, but you know, they can remind the SHO to do it and get the paperwork done for them to sign off on it.
ID 103, manager
All of the managers considered that having PAs who had the training and authority to prescribe and order ionising radiation would aid efficiency in the medical care of patients:
. . . but if anything was to come out of this [the research], my thing would be prescribing and requesting X-rays would tick many boxes. I’m sure it would help probably, it would definitely help our department 100 per cent and I’m sure it would help other departments as well . . . just being able to request those X-rays. I just don’t see why they can’t.
ID 203, manager
Summary
Overall, the managers who were interviewed were positive about the contribution that PAs made as part of the medical team staffing their services. A key motivating factor for their introduction was the shortage of junior medical staff. However, managers went on to describe the overall value PAs gave to the service in providing continuity and accessibility within inpatient wards for nursing staff, patients and administrators. All of the managers described processes to increase the workforce of advanced clinical practitioners, not just PAs. Although financial efficiency was important to the managers, their views about employing PAs were influenced by factors such as improving the quality and safety of their services. The PAs were not necessarily substitutes or funded from medical staffing budgets; some were in additional service posts that were funded differently. The measurement of impact was described as difficult and although managers could point to ways in which the PAs contributed to more efficient services and increased capacity, they were unable to share hard data on this. The PAs’ inability to prescribe or order ionising radiation was a limitation that was generally ‘worked around’. All of the managers wanted this limitation to be removed. In conclusion, these operational managers considered that the added value the PAs brought to their services outweighed any limitations.
Chapter 9 Findings at the micro level: perspectives from the nurses
Twenty-eight nurses, working in roles including staff nurse, ward manager, clinical nurse specialist and matron, were interviewed about their experiences of working with PAs. They worked in a range of adult and paediatric medical and surgical specialties as well as emergency medicine. The data are presented under the following themes: the work undertaken by the PAs, the contribution made by the PAs and challenges associated with PAs. The identifiers for quotations describe any type of staff nurse as ‘nurse’ and all others as ‘senior nurse’.
The work undertaken by the physician associates
Nurses described the kind of work that PAs were undertaking in their specialties, which included both patient-facing and non-patient-facing work. As part of the medical team, they were described as participating in ward rounds and communicating with patients and relatives. The reviewing of patients was a frequently mentioned task that PAs undertook, and one nurse described how their PA was supervised through this:
I came to understand when they see a patient and assess the patient. After that they come to see the doctor or whoever the consultant is and discuss it. Like junior doctors, student doctors, to discuss the plan.
ID 77, nurse
The PAs were also reported to undertake procedures including taking blood, cannulation and more advanced procedures including central lines and removing drains. In terms of non-patient-facing tasks, PAs were following up and checking blood test results, attending multidisciplinary team meetings, liaising between specialties, and writing the bulk of discharge summaries:
The TTOs [to-take-out medicines], it’s very important and I’m feeling so sorry for them because most of the times the doctors don’t do the TTOs they are the ones who’s doing the TTOs.
ID 82, senior nurse
Although the PAs were seen as undertaking medical roles, many nurses commented on the overlap between the work carried out by PAs and themselves:
We help each other so at times for example if the patient needs blood. So, if the nurse can’t do bloods the PA will go and she will do, but for example if I’m working and if I’m free or if I’m, if, if the PAs are busy I’m more than happy to go and bleed them. So, doesn’t need to be just the nurse or the doctor or the PA, so who’s free will go and do it.
ID 82, senior nurse
Although she works within the medical team, she does take on some of the nursing roles as well as the doctor’s roles. When we fill out the checklists for patients that require further care, nursing home care, residential care, she helps us complete those checklists and also with our audits, our cannula care audits.
ID 66, nurse
We turn now to the nurses’ views on the contribution of the PAs.
The contribution of the physician associates
All of the nurses who were interviewed had positive things to say about their experience of working with PAs. This included general statements, such as:
They are very useful; I am pleased when they’re working.
ID 82, nurse
I think they’re really good, a really good asset to have as a member of the team and as a trust I would say that they’re fantastic to have around.
ID 118, senior nurse
Some examples of the interaction observed between PAs and nurses are provided in Box 7.
This was an observation on a ward in a surgical specialty. Over the course of two different time periods I observed nurses regularly interacting with the PA in different ways. During the ward round a nurse asked the PA whether a patient’s blood had been taken (although in this instance the PA did not know). Nurses frequently came to the PA asking them to do jobs including update a patient’s notes as they were going to be discharged, to do a sick note for a patient, updating a patient’s record who had already been discharged, clarification as to whether a PA needed an outpatient appointment with a specific consultant or just a general one. The PA also received patient information from nurses for the medical team, such as when another department had phoned the ward to let them know that the phosphate levels of a patient who had arrived there were low. The PA also gave instructions to the nursing team; for example, a nurse came to the PA with urine she had collected, and the PA asked her to send it off to check for an infection.
The nurses also gave more detailed comments on the specific ways in which the PAs had made a positive contribution. These are interlinked themes:
-
the provision of stability and continuity in the medical team
-
ease of access for nurses to the medical team for escalation of concerns about deteriorating patients
-
detailed knowledge of patients
-
bridging medicine and nursing
-
relieving the workload
-
enhanced the patient experience.
We now elaborate on these.
The most widely described benefits provided by PAs related to their provision of continuity and stability in the setting in which they were working. This was depicted in a number of ways. First, the majority of PAs were not on a rotational programme, unlike their junior doctor colleagues. This permanency meant that the PAs were recognised as having extensive knowledge of the workings of the particular setting/specialty/team, which made them a useful source of information for all of the health-care professionals with whom they were working.
We are the staff that are consistent, as are the PAs. So, you do get a certain level of knowledge and expertise and that, sometimes you’re like, oh thank goodness, there are other people that, you know, because it’s knowing that it isn’t just knowledge of injuries and patients in that sense. It’s knowledge of processes and the computer systems and the referral.
ID 177, nurse
The nurses reported that the PAs were predominantly working in a ward setting, unlike doctors who had other commitments (e.g. in outpatient clinics and operating theatres). The PAs largely remained on the wards they were attached to. This made them an accessible medical presence for nurses, which was important if they had concerns about patients.
The doctor went away on a cardiac arrest call, or to revive a patient, but there is somebody else on the unit who is more capable, like a doctor level, or they could kind of, if there’s any immediate concerns that we have they can come and take over and do it and nurses feel like there’s somebody around to help them.
ID 178, nurse
Nurses also frequently described using PAs as a means of contacting the doctors (Box 8).
During the observations I saw the nurses use the PAs as a source of knowledge about medical/surgical teams and also as an intermediary. For example, a nurse asked PA what the number was for the [specialty] team bleep. Another nurse wanted to make contact with a certain doctor and asked the PA if they were around the wards. The PA knew that doctor was not on the wards and then tried to contact the doctor using their mobile phone rather than the hospital phone or bleep.
The nurses reported that, in particular, they valued using the PAs as the first step in the escalation process for concerns about deteriorating patients, as illustrated in this quotation and in our observation (Box 9):
If we need any form of escalation, getting in touch with doctors, we can also get in touch with the PAs, the PAs chase the doctors, so their role is quite significant as well . . . to get things going so patients are not left for long hours waiting for a doctor because doctors are doing other things, doctors are in theatres. They’re like the middle person who get things done between both sides, nurses and doctors.
ID 71, senior nurse
During this part of the observation on a unit with very-high-dependency patients the PA was the sole member of the medical team present. During this time a nurse came and asked the PA to check on one of her patients, whom she thought might be having a seizure. The PA proceeded to assess the patient, asking the nurse questions, checking pupil dilation and the patient’s temperature. After letting the nurse know that the PA believed the patient was fine the PA asked the nurse to run an ECG [electrocardiogram] on the patient and to check their electrolytes.
The nurses considered that because PAs were present on a daily basis, usually on weekdays and during daytime hours, they also knew the patients and their histories very well:
Because they’re there on a daily basis, so they will know the day-to-day goings on of the patients. So they’re there Monday to Friday, well, the consultant will be in theatre all the time, but the PAs are supposed to stay on the ward, so if there’s anybody unwell, they should know about it . . . if the patient’s had an X-ray, an ultrasound, they should be able to say ‘This is the X-ray, do you want it?’ and get the consultant to review it and say that they’re happy with it.
ID 121, senior nurse
Some of the nurses described forming close relationships with PAs who remained working in their specialty for a number of years and the trust that built up over time:
I’ve actually found them really good because with the junior doctor rotation, they have rotation every 6 months and with a PA they are, they’ve become like a you know member of the team in regard to that they’re long-standing . . . and you know you can build a more you know good relationship with them kind of thing . . . So, the last PA we had I think she was here for about 3 years before she left.
ID 142, senior nurse
As well as linking the nursing and medical teams, as described previously, PAs were frequently described as an intermediary between the two. The reasons offered for this included PAs being more approachable and less intimidating:
I quite like them in the sense that you always have this like nurse/doctor thing and they’re not really either if that makes sense so, it’s sort of, not a neutral party that’s not quite the right word, but they’re not a nurse or a doctor.
ID 112, senior nurse
And it’s quite nice to have them there to ask, ‘cause you wouldn’t, like, bleep the SHO to be like ‘Can you just give me your opinion?’. But if they’re [the PAs] on the ward it’s quite nice to have them there, like every problem you had kind of went through her so that was, like, quite nice.
ID 167, nurse
As well as bridging between the two professions, the PAs were viewed as a benefit in that they relieved some of the work of the nurses, particularly in relation to the induction of new doctors in training:
Before new doctors come in the nurse in charge would take that responsibility of going through, like inducting them . . . but here the responsibility, if there’s a PA around they will do that job and they will induct so that pressure was taken off us and I think we found it very, professionally very useful and we thought oh gosh, this is good.
ID 178, senior nurse
Many nurses commented that they felt that the PAs they worked with had a positive impact on patient experience. The nurses reported that the constant presence of the PAs on the wards meant that they were a familiar face within the medical team, someone whom patients and their families could easily approach:
[PA 1 first name] and [PA 2 first name] especially are so friendly, like they go over and they’re chatting, and, like, I think the patients feel more like they will discuss things with them more than maybe the consultant . . . Yeah, but I think definitely like they help the patients along.
ID 167, senior nurse
The nurses described the PAs as being very proactive, and appreciated by patients, in communicating the detail of the medical plans and updates of test results. Many nurses spoke positively of PAs’ communication styles, contrasting them with doctors, in explaining medical terminology:
I think PAs tend to have a different approach, a little bit more of a down-to-earth approach, explain things a little bit better and use terminology that people you know understand and things like that.
ID 112, senior nurse
Invaluable with relatives. If you’ve got one team leave and the next team starts, there’s somebody that’s always there constant, really great if we need a relative spoken to, she’s really willing to go and do that.
ID 66, nurse
Most of the nurses did not think that patients understood who and what PAs were:
I wouldn’t particularly say the patients would know that’s a PA. I think they very much I think call them doctors because they see them as part of the ward round and things like that.
ID 112, senior nurse
I think most of the patients, like, love them and I don’t they’re any, I don’t think they consider them any different to doctors either.
ID 167, nurse
Although nurses did not elaborate on the specifics of the cost of employing PAs, many of the senior nurses did speculate that from a trust point of view employing PAs must be cost-effective, as they saw them undertaking the work of the doctors:
And I suppose from a trust point of view it’s cost as well because they’re seeing . . . yeah the cost must be, because they see as much as doctors if not more.
ID 118, senior nurse
We turn now to consider the reported challenges in working with PAs.
Perceived challenges of working with physician associates
Although nurses described the positives that PAs contributed to the service, having PAs as part of the medical team also had some perceived limitations. These were the inability of the PAs to prescribe medicines, lack of clarity over the PA role and impact on nursing roles.
Inability to prescribe
The inability of PAs to prescribe was seen as the biggest drawback to their role by those nurses who were interviewed. This was often mentioned alongside their inability to request ionising radiation, due to the current lack of professional regulation; however, prescribing medication was the issue that was most commonly discussed. The degree to which PAs’ inability to prescribe had an impact varied. The fact that PAs were required to consult a doctor for prescriptions was seen as a step that created a time delay in patient care and flow through the system:
But that’s probably one downside, is that they can’t prescribe, because then things would go even more smoothly and quicker, that they could do the things and prescribe at the same time, and they could assess a patient and prescribe what that patient needed, rather than having to wait for a doctor to be available to prescribe certain medications or fluids, or a blood transfusion or whatever.
ID 121, nurse
On some ward settings with a continuous doctor presence, this delay was viewed as a mild inconvenience with minimal impact, as there was usually a doctor around to ask for a prescription quickly (Box 10).
In this observation there was an instance where both the PA and the junior doctor were present, and the nurse went straight to the doctor to ask for a prescription, and then proceeded to ask the PA to document a patient’s consent for a blood transfusion, suggesting that the nurse knew the limitations of the PA role in relation to prescribing.
The nurses described other elements in their services that mitigated for the PAs’ inability to prescribe. These were elements such as the presence of a ward pharmacist who could prescribe, working in a specialty in which prescription of common types of medication was routinely made for all patients on admission, and the presence of other members of staff, such as nurse practitioners, who could order ionising radiation. We also observed workarounds to these issues in a few settings (Box 11).
This was an observation in which a PA was working in a clinic with specialty-trained nurse practitioners. Several of the patients in the clinic required X-rays and a nurse left their access card in the computer so that the PA could order X-rays using that. The PA was unable to do so using their own access card.
In emergency and urgent care settings, nurses pointed out that PAs were less efficient in a team than nurse practitioners who could prescribe and order ionising radiation:
So I think it’s a really good pathway for a patient to be seen by a PA it’s just a shame that it takes a little bit longer with that review by that doctor again. Whereas with a nurse practitioner, no doctor needs to see them [the patient] unless we want them to or feel that they need to. Whereas PAs they can’t because if they need anything it needs to go through somebody else.
ID 112, senior nurse
In some high-acuity settings, however, there was a feeling that being unable to prescribe had a greater impact. Some nurses questioned the appropriateness of using PAs ‘out of hours’ when there were fewer doctors around, or in settings with fewer doctors when a doctor may be preoccupied with a seriously ill patient:
Because you need a prescription every 5 minutes sometimes, prescribe this, prescribe that, lots of medication, and then it’s not easy, you can’t just write it now, going online, it isn’t easy.
ID 178, nurse
Nursing staff were not opposed to PAs being able to prescribe and many expressed surprise that they were not able to. After working with PAs, many nurses felt that PAs had demonstrated that they were working at a level and in a way that would allow them to prescribe at least the more routine medications. Comparisons were also made with advanced nurses who can prescribe and the implications for the PA role and career owing to PAs being unable to prescribe:
They can’t prescribe, they can’t do X-rays and they have to go through several different people maybe to get what they want. It’s not brilliant for a patient pathway and it’s not brilliant for them either really because it’s not fair when they’re more than capable, they know what they’re sending to X-ray, they know the implication of drugs, they know what drugs to give, but they can’t write it down on a piece of paper, so it just seems, it’s sad really that it hasn’t come about yet.
ID 118, senior nurse
A further challenge of working with PAs related to the lack of clarity about the role, described next.
Lack of clarity on the physician associate role
Some nurses reported a view of a lack of clarity about the PA role, which had been particularly problematic on their introduction into a service. This had also been compounded by issues such as senior levels of grading, which the nurses had resented. The nurses who were interviewed who had experienced this reported that attitudes had changed over time through working with the PAs. However, they noted that there was still a lack of understanding of the role among new nursing staff:
I’m not sure if there’s any negative. I think it’s just, maybe the negative is from staff who maybe don’t understand it. But I think generally people are receptive of their role because unless they tell you that they’re a PA, most times you don’t know, you just figure that they’re a FY1 [Foundation Year 1 doctor].
ID 101, senior nurse
Most of the nurses considered that there had been very little introduction for nurses to the new role. Most of them described working it out for themselves by seeing what the PAs did:
He was introduced ‘oh this is [PA name], this is our physician associate’. OK, what does that actually mean? I didn’t really understand, you know, was he a doctor, was he not? Did he have a clinical background? And really, we’ve never really kind of sat down and chatted about it, I’ve kind of learnt a little bit more on the job about the role.
ID 29, senior nurse
I didn’t know at first and so I was thinking, ‘What are they?’. I thought they were doctors. I even went up to [PA name] and said ‘[PA name], can you prescribe me this?’. But she was saying ‘I cannot do that’. Just not a formal introduction to say that this is a PA and this is what their role is. So, you go along and work with them and that’s the only time you realise their limitations.
ID 77, nurse
In some instances, nurses described introductions not being made and gave reports of nurses working with PAs sometimes for periods of months, mistaking their identity for a doctor if they were not told otherwise:
I think I worked with them for a few months before I actually knew who they were, what they did, or what, like, I didn’t understand the role at all, because it was just something I’d never seen before, and yeah, I just assumed they were all junior doctors.
ID 121, senior nurse
Physician associates themselves were often reported as the key educators on their role:
I came to the ward and they said ‘I’m a physician associate’, I said, ‘OK what do you do?’ and they explained their roles.
ID 82, senior nurse
The lack of clarity and understanding among the nursing staff meant that some of the senior nurses felt that this was an issue that they had a responsibility to help address. Several senior nurses described feeling responsible for junior nursing staff who might not understand the role yet and the implications of the PAs not being regulated. Examples were given of having to explain that the PA could not direct registered nurses to administer medicines in ways not yet prescribed by a doctor. Other examples were given that seemed to be a mixture of legal requirements and hospital regulations:
You have to because if you’ve got a junior nurse they might just allow that person to give that drug and actually we’ve had a few instances where drugs have been removed from like, controlled drugs like morphine removed out of the controlled drug cupboard by a doctor and a PA and actually it has to be two nurses sign out this medicine so then we have to say ‘guys, these are things you have to look out for’ because actually, if that went missing we’d really have to justify what’s happened.
ID 133, senior nurse
In one setting, the senior nurses were requesting the development of written guidance on what the PAs role was and which procedures they were authorised to undertake so that it would be clear to new nursing staff. The role of the PA was also thought by some to have an impact on the nurses; this is discussed next.
Impact on the nurses’ role
Two of the nurses described the way in which the introduction of the PA role affected their role as nurses. The first was in changing the interaction between the ward nurses and the medical team and the second was a more direct impact on a nurse practitioner role. The first nurse suggested that the ward nurses had less interaction with the medical team following the introduction of the PAs. The PAs, being ward based, provided information that nurses might have provided previously, for example on ward rounds, or followed the consultant-led ward round by communicating the decisions to the nurses subsequently. In one nurse’s view, previously a nurse would have been part of the ward round. The second example was from a clinic setting, in which a nurse practitioner reported that her work was changed by the presence of a PA. The following quotation reflects the ambiguity and overlap of roles there can be in patient care:
When the PAs come in, the doctors automatically gravitate towards letting them see the patient over me. And maybe because as a nurse practitioner, and especially because I’m new and my role is new in this clinic, I think too that, you know like, I don’t sort of blame them because I think they would . . . they do have that much more knowledge base. However, they wouldn’t have a nursing input but then the nursing input could be substituted with any other nurse.
ID 101, senior nurse
Summary
This section has provided an analysis of the views of nurses, which were predominantly positive, of the contribution of the PAs to the service and to care of patients. Nurses particularly commented on the stability the PAs brought to medical teams and their continual presence in ward settings. Nurses were able to describe the ways in PAs enhanced the communications between the medical team and the patients and relatives. From the ward nursing team perspective, they identified that the PAs enhanced their access to the medical team in situations when a patient’s condition was deteriorating and of concern. Although PAs were described in mainly positive terms, the limitations to their practice, particularly the inability to prescribe, restricted their utility in some settings – especially those with high-dependency inpatients, those needing frequent prescriptions or in urgent care settings in which many patients could usually be seen by someone working at clinical practitioner level. Many commented on a general lack of clarity as to the PAs’ role and that understanding it seemed to be dependent on working with them. Most of the nurses considered that patients also did not understand who this new addition to the medical team was.
Chapter 10 Findings from the micro level: pragmatic comparison of patient consultations by physician associates and Foundation Year doctors in the emergency department
This chapter reports on the quantitative evidence identified through one strand of the workstream 3 case study, that is, a pragmatic retrospective assessment comparing the outcomes and service costs for patients attended by PAs or FY2 doctors in the ED, using anonymised patient records from hospital databases. These records were analysed to describe and compare PAs’ and FY2 doctors’ consultation records in the ED, including assessment of the study’s primary outcome, that is, re-attendance within 7 days of initial attendance at the ED, as well as of the secondary outcomes of consultation processes, the clinical adequacy of care and economic considerations.
We report first on a description of the consultation records, followed by a comparison of process and clinical outcomes, then the economic analysis.
Description of the consultation records
Study numbers
In the 16-week period studied, 8816 patients attended by PAs or FY2 doctors were identified by the three trusts within the case studies in which PAs worked in the ED. As each trust could provide different data items requested for the study from their routine electronic databases, a data set containing all the data items required to support our analysis has only been collected for the number of patient records required to meet our required sample size of 304 patients in each group, that is, patients whose consultation was attributed to either a PA or a FY2 doctor, to test a non-inferiority hypothesis on the primary outcome measure, which stated that PAs do not exceed a rate of unplanned reconsultations of 27.4%, with 80% power at 5% significance.
With requests for the same number of consultation records for PAs and FY2 doctors in each site, and some replacement consultation records when personnel coding errors were noted, we slightly over-recruited on FY2 doctors’ consultation records and included patient consultation records for 613 ED attendances in total (Table 12).
| Case study site | Number of cases | |||||
|---|---|---|---|---|---|---|
| In the 16-week period | In the sample for analysis | |||||
| PAs | FY2 doctors | Total | PAs | FY2 doctors | Total | |
| 3 | 779 | 3387 | 4166 | 101 | 103 | 204 |
| 4 | 927 | 1864 | 2791 | 102 | 102 | 204 |
| 5 | 1184 | 675 | 1859 | 102 | 103 | 205 |
| Total | 2890 | 5926 | 8816 | 305 | 308 | 613 |
Demography of the patients in the sample
The sample is described in terms of the patients’ age bands and sex only, owing to limitations on the provision of other data items.
The patients consulting both PAs and FY2 doctors show a wide range in ages and a fair spread across the sexes (Table 13). No statistically significant differences were found in patient demographics between groups seen by PAs and those seen by FY2 doctors.
| Patient characteristic | Case type | Unadjusted difference between groups | |||||
|---|---|---|---|---|---|---|---|
| PAs | FY2 doctors | Total | |||||
| Number of patients | Percentage of patients | Number of patients | Percentage of patients | Number of patients | Percentage of patients | ||
| Age band (years) | |||||||
| 0–10 | 17 | 5.6 | 15 | 4.9 | 32 | 5.2 | LR χ2 (10) = 5.4770; p = 0.857 |
| 11–20 | 22 | 7.2 | 27 | 8.8 | 49 | 8.0 | |
| 21–30 | 42 | 13.8 | 44 | 14.3 | 86 | 14.0 | |
| 31–40 | 26 | 8.5 | 26 | 8.4 | 52 | 8.5 | |
| 41–50 | 36 | 11.8 | 28 | 9.1 | 64 | 10.4 | |
| 51–60 | 36 | 11.8 | 28 | 9.1 | 64 | 10.4 | |
| 61–70 | 36 | 11.8 | 40 | 13.0 | 76 | 12.4 | |
| 71–80 | 42 | 13.8 | 42 | 13.6 | 84 | 13.7 | |
| 81–90 | 38 | 12.5 | 42 | 13.6 | 80 | 13.1 | |
| 91–100 | 10 | 3.3 | 15 | 4.9 | 25 | 4.1 | |
| ≥ 101 | 0 | 0.0 | 1 | 0.3 | 1 | 0.2 | |
| Total | 305 | 100.0 | 308 | 100.0 | 613 | 100.0 | |
| Sex | |||||||
| Male | 148 | 48.5 | 134 | 43.5 | 282 | 46.0 | LR χ2 (1) = 1.5541; p = 0.213 |
| Female | 157 | 51.5 | 174 | 56.5 | 331 | 54.0 | |
| Total | 305 | 100.0 | 308 | 100.0 | 613 | 100.0 | |
Characterisation of the clinical condition of the patients in the sample
The clinical condition of the sample of patients on presentation at the ED is characterised through the measures of the acuity of the condition (the early warning score and/or MTS87) as well as the ED stream or area to which the patient is initially allocated. A description of the distribution of acuity of patients seen by PAs or FY2 doctors is given in Table 14.
| Descriptor of patient’s clinical condition | Case type | Unadjusted difference between groups | |||||
|---|---|---|---|---|---|---|---|
| PAs | FY2 doctors | Total | |||||
| Number of patients | Percentage of patients | Number of patients | Percentage of patients | Number of patients | Percentage of patients | ||
| Early warning score at triage (0–20) | |||||||
| Low | LR χ2 (8) = 10.9571; p = 0.204 | ||||||
| 0 | 111 | 36.4 | 85 | 27.6 | 196 | 32.0 | |
| 1 | 40 | 13.1 | 51 | 16.6 | 91 | 14.8 | |
| 2 | 21 | 6.9 | 26 | 8.4 | 47 | 7.7 | |
| 3 | 15 | 4.9 | 24 | 7.8 | 39 | 6.4 | |
| 4 | 6 | 2.0 | 11 | 3.6 | 17 | 2.8 | |
| Medium | |||||||
| 5 | 4 | 1.3 | 2 | 0.6 | 6 | 1.0 | |
| 6 | 2 | 0.7 | 2 | 0.6 | 4 | 0.7 | |
| High | |||||||
| 7 | 2 | 0.7 | 1 | 0.3 | 3 | 0.5 | |
| 8 | 1 | 0.3 | 3 | 1.0 | 4 | 0.7 | |
| Missing | 103 | 33.8 | 103 | 33.4 | 206 | 33.6 | |
| Total | 305 | 100.0 | 308 | 100.0 | 613 | 100.0 | |
| MTS (1–5) | |||||||
| 1 (immediate) | 8 | 2.6 | 1 | 0.3 | 9 | 1.5 | LR χ2 (4) = 18.4277; p = 0.001 |
| 2 (very urgent) | 33 | 10.8 | 33 | 10.7 | 66 | 10.8 | |
| 3 (urgent) | 152 | 49.8 | 194 | 63.0 | 346 | 56.4 | |
| 4 (standard) | 102 | 33.4 | 72 | 23.4 | 174 | 28.4 | |
| 5 (non-urgent) | 4 | 1.3 | 1 | 0.3 | 5 | 0.8 | |
| Missing | 6 | 2.0 | 7 | 2.3 | 13 | 2.1 | |
| Total | 305 | 100.0 | 308 | 100.0 | 613 | 100.0 | |
| ED area patient treated in | |||||||
| Minor | 48 | 15.7 | 18 | 5.8 | 66 | 10.8 | LR χ2 (3) = 23.5973; p < 0.001 |
| Major | 163 | 53.4 | 205 | 66.6 | 368 | 60.0 | |
| Paediatrics | 16 | 5.2 | 8 | 2.6 | 24 | 3.9 | |
| Clinical decision unit or primary care | 4 | 1.3 | 1 | 0.3 | 5 | 0.8 | |
| Missing | 74 | 24.3 | 76 | 24.7 | 150 | 24.5 | |
| Total | 305 | 100.0 | 308 | 100.0 | 613 | 100.0 | |
Descriptively, no differences were seen in the early warning score (although this was only provided by two of the three trusts included in the data set); however, both the MTS87 and the area of the ED in which the patient is seen show statistically significant differences; compared with FY2 doctors, PAs held a higher proportion of consultations in the standard and immediate categories (rather than the urgent category in the majors section of the ED, although in 150 cases the ED area was not available in the data set). In this sample, the number of paediatric patients seen in the sample as a whole was small; PAs saw a greater proportion of these patients.
Process outcomes
The clinical process outcomes within the ED visit have been measured as follows: length of time in the ED, whether or not the patient had an X-ray investigation carried out, whether or not a prescription was issued, whether or not a discharge summary was completed and the destination from the ED (admission rate).
Clinical process outcomes
The proportion of patient visits with each of these process measures reported is shown in Table 14.
Statistical tests have been conducted to see whether or not there are any differences in the clinical process outcomes between PA and FY2 doctors. The difference was tested using LR tests in unadjusted and adjusted analyses. LR χ2 (#) refers to the LR χ2 statistic with # degrees of freedom (df). For adjusted analysis, age, sex, MTS and sites were controlled for and interaction between site and profession is also included if the interaction term is significant.
The results suggest that there are no differences in whether or not prescriptions were given in the ED, whether or not the patient was admitted to hospital or whether or not a discharge summary was completed, but patients seeing a PA differed from those seeing a FY2 doctor regarding whether or not X-ray investigations were conducted. Patients seen by a PA appeared more likely to have an X-ray carried out in the ED than those seen by a FY2 doctor (Table 15). As adjustment for case-mix differences was limited to measures of acuity on presentation, it is not known whether or not any difference in the presenting conditions seen by the PAs or FY2 doctors could have contributed to this finding.
| Processes of care in the ED | Case type | Unadjusted difference between groups | Adjusted difference between groups | |||||
|---|---|---|---|---|---|---|---|---|
| PAs | FY2 doctors | Total | ||||||
| Number of patients | Percentage of patients | Number of patients | Percentage of patients | Number of patients | Percentage of patients | |||
| X-ray investigations conducted? | ||||||||
| No | 162 | 53.1 | 207 | 67.2 | 369 | 60.2 | LR χ2 (1) = 12.7524; p < 0.001 | LR χ2 (3) = 32.63; p < 0.001 |
| Yes | 143 | 46.9 | 101 | 32.8 | 244 | 39.8 | ||
| Total | 305 | 100.0 | 308 | 100.0 | 613 | 100.0 | ||
| Prescriptions given in the ED? | ||||||||
| No | 173 | 56.7 | 158 | 51.3 | 331 | 54.0 | LR χ2 (1) = 2.1104; p = 0.146 | LR χ2 (1) = 1.86; p = 0.172 |
| Yes | 126 | 41.3 | 146 | 47.4 | 272 | 44.4 | ||
| Missing | 6 | 2.0 | 4 | 1.3 | 10 | 1.6 | ||
| Total | 305 | 100.0 | 308 | 100.0 | 613 | 100.0 | ||
| Admitted as an inpatient from the ED? | ||||||||
| No | 191 | 62.6 | 178 | 57.8 | 369 | 60.2 | LR χ2 (1) = 1.5020; p = 0.220 | LR χ2 (1) = 0.78; p = 0.376 |
| Yes | 113 | 37.0 | 129 | 41.9 | 242 | 39.5 | ||
| Missing | 1 | 0.3 | 1 | 0.3 | 2 | 0.3 | ||
| Total | 305 | 100.0 | 308 | 100.0 | 613 | 100.0 | ||
| Discharge summary completed? | ||||||||
| No | 86 | 28.2 | 71 | 23.1 | 157 | 25.6 | LR χ2 (1) = 2.5778; p = 0.108 | LR χ2 (1) = 2.91; p = 0.088 |
| Yes | 117 | 38.4 | 134 | 43.5 | 251 | 40.9 | ||
| Missing | 102 | 33.4 | 103 | 33.4 | 205 | 33.4 | ||
| Total | 305 | 100.0 | 308 | 100.0 | 613 | 100.0 | ||
Emergency department process: length of stay
The length of stay in the ED was available for all cases in the sample. Table 16 shows the distribution of the times.
| Distribution | Length of stay in the ED (hours: minutes) | |
|---|---|---|
| Case type | ||
| PA (n = 305) | FY2 doctor (n = 308) | |
| Mean | 3:03 | 3:48 |
| SD | 1:55 | 2:46 |
| Percentile | ||
| 10 | 1:00 | 1:39 |
| 20 | 1:25 | 2:16 |
| 30 | 1:56 | 2:46 |
| 40 | 2:34 | 3:14 |
| 50 | 3:12 | 3:34 |
| 60 | 3:33 | 3:50 |
| 70 | 3:50 | 3:58 |
| 80 | 3:57 | 4:00 |
| 90 | 4:00 | 5:17 |
| Median | 3:12 | 3:34 |
| Minimum | 0:11 | 0:13 |
| Maximum | 15:29 | 19:31 |
A sharp peak at a length of stay of 3 to 4 hours is noted (Figure 5).
FIGURE 5.
Distribution of length of stay in the ED (all cases).
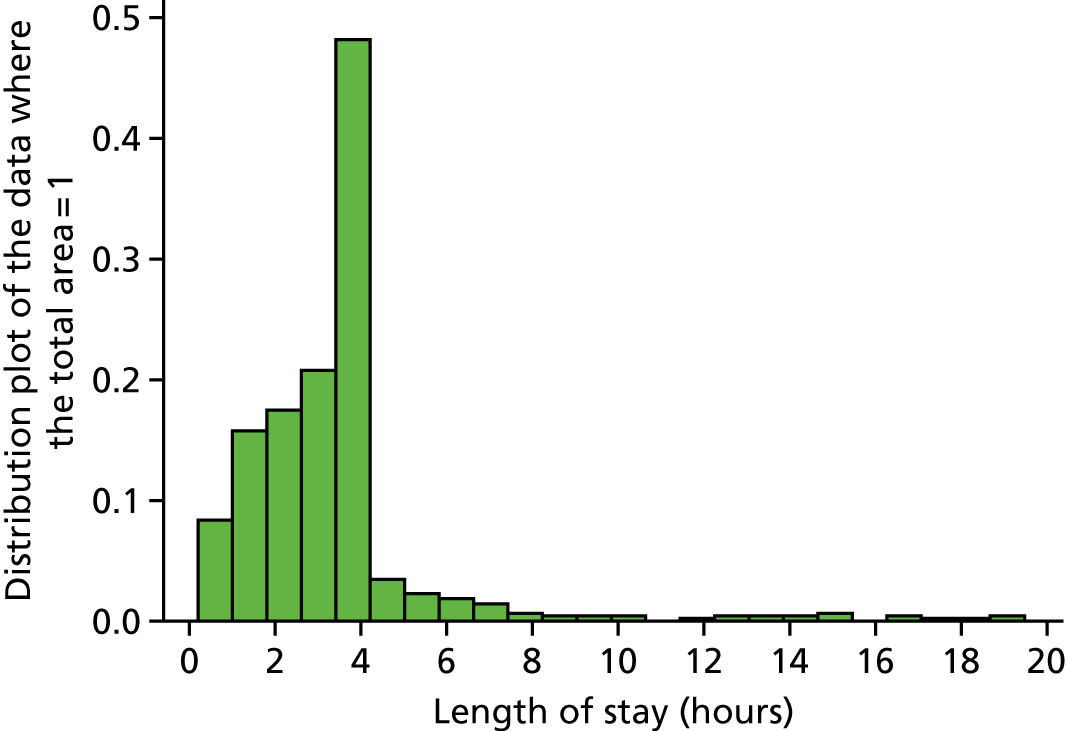
Unadjusted comparisons of the length of stay for patients seen by a PA and those seen by a FY2 doctor suggest that those seen by a PA have a statistically significantly shorter length of stay in the ED, with a mean difference of 45 minutes (t = –3.916, df 611; p = 0.000).
The difference in expected length of stay between PAs and FY2 doctors was also examined after adjustment of other factors using linear regression, including age, sex, MTS (as a measure of acuity), whether or not they were admitted, whether or not an X-ray was taken and whether or not a prescription was given. Overall, across all sites, those seen by a PA, given everything else being equal, can expect a reduction of 0.61 hours (36 minutes) in length of stay in the ED.
Rate of re-attendance at the same emergency department
Re-attendance within 7 days of the index ED visit was found following 8% (n = 48) of the 610 visits for which these data were available (Table 17). Logistic regression was used to model the likelihood of re-attendance. After adjustment for confounding, no statistically significant difference was found in the rate of re-attendance between PAs and FY2 doctors.
| Re-attendance at the same ED within 7 days? | Case type | Unadjusted difference in rate of re-attendance | Adjusted difference in rate of re-attendancea | |||||
|---|---|---|---|---|---|---|---|---|
| PAs | FY2 doctors | Total | ||||||
| Number of patients | Percentage of patients | Number of patients | Percentage of patients | Number of patients | Percentage of patients | |||
| No | 277 | 90.8 | 285 | 92.5 | 562 | 91.7 | OR 1.32, 95% CI 0.73 to 2.4; p = 0.354 | OR 1.33, 95% CI 0.69 to 2.57; p = 0.40 |
| Yes | 27 | 8.9 | 21 | 6.8 | 48 | 7.8 | ||
| Missing | 1 | 0.3 | 2 | 0.6 | 3 | 0.5 | ||
| Total | 305 | 100 | 308 | 100 | 613 | 100 | ||
Clinical review of patient records
In the context of the above finding that the study’s primary outcome – the rate of re-attendance within 7 days – was seen not to differ for patient consultations attributed to PAs and FY2 doctors, a review was carried out of a subsample of 40 of the above ED consultation records (20 PA and 20 FY2). Each record was reviewed by four ED clinicians against pro forma questions. In the following sections, we describe the reviews of the consultation record as well as inter-rater reliability.
Appropriateness of the elements of the consultation records
The reviewers’ assessment – either the agreement of the reviewers or the ED consultant’s judgement – is presented in Table 18. The key consultation components, using the criteria used in the Sakr et al. 81 study (i.e. patient’s medical history, examination of the patient, request for radiography, treatment plan and decision, advice given and follow-up), are each presented separately.
| PA or FY2 consultation record | Judgement of appropriateness | |||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Past medical history | Examination | Request for radiographya | Treatment plan and decision | Advice given | Follow-up | |||||||||||||||||||
| Appropriate | Error or omission | Appropriate | Error or omission | Appropriate | Error or omission | Appropriate | Error or omission | Appropriate | Error or omission | Appropriate | Error or omission | |||||||||||||
| Harm unlikely | Altered treatment | Harm | Harm unlikely | Altered treatment | Harm | Harm unlikely | Altered treatment | Harm | Harm unlikely | Altered treatment | Harm | Harm unlikely | Altered treatment | Harm | Harm unlikely | Altered treatment | Harm | |||||||
| FY2 | ||||||||||||||||||||||||
| Number of records | 14 | 6 | 0 | 0 | 15 | 5 | 0 | 0 | 9 | 0 | 1 | 0 | 14 | 5 | 1 | 0 | 4 | 1 | 1 | 0 | 16 | 3 | 0 | 0 |
| Percentage of records | 70.0 | 37.0 | 0.0 | 0.0 | 75.0 | 25.0 | 0.0 | 0.0 | 45.0 | 0.0 | 5.0 | 0.0 | 70.0 | 25.0 | 5.0 | 0.0 | 20.0 | 5.0 | 5.0 | 0.0 | 80.0 | 15.0 | 0.0 | 0.0 |
| PA | ||||||||||||||||||||||||
| Number of records | 13 | 5 | 1 | 0 | 11 | 7 | 1 | 0 | 9 | 3 | 0 | 0 | 13 | 5 | 1 | 0 | 3 | 1 | 1 | 0 | 13 | 4 | 1 | 0 |
| Percentage of records | 65.0 | 25.0 | 5.0 | 0.0 | 55.0 | 35.0 | 5.0 | 0.0 | 45.0 | 15.0 | 0.0 | 0.0 | 65.0 | 25.0 | 5.0 | 0.0 | 15.0 | 5.0 | 5.0 | 0.0 | 65.0 | 20.0 | 5.0 | 0.0 |
| Not rateda | ||||||||||||||||||||||||
| Number of records | 1 | 1 | 18 | 1 | 29 | 3 | ||||||||||||||||||
| Percentage of records | 2.5 | 2.5 | 45.0 | 2.5 | 73.0 | 7.5 | ||||||||||||||||||
| Total | ||||||||||||||||||||||||
| Number of records | 27 | 11 | 1 | 0 | 26 | 12 | 1 | 0 | 18 | 3 | 1 | 0 | 27 | 10 | 2 | 0 | 0 | 7 | 2 | 2 | 29 | 7 | 1 | 0 |
| Percentage of records | 68.0 | 28.0 | 3.0 | 0.0 | 65.0 | 30.0 | 3.0 | 0.0 | 45.0 | 8.0 | 3.0 | 0.0 | 66.0 | 25.0 | 5.0 | 0.0 | 0.0 | 18.0 | 5.0 | 5.0 | 73.0 | 18.0 | 3.0 | 0.0 |
The results indicate that the reviewers considered the documentation in the consultation record to have been appropriate in the majority of both PA and FY2 doctor cases for each of the key consultation components, and in no component were any errors or omissions seen that resulted in a significant probability that the patient might be harmed.
Nevertheless, in each consultation component a small percentage of consultation records were considered to indicate an error or omission that was unlikely to have resulted in harm or different treatment (defined by Sakr et al. 81 as clinically unimportant), or an error or omission that caused a breach in normal guidelines and procedures that would have altered the patient’s treatment (defined as clinically important). 81
Reviewer judgement of an error or omission seen that caused a breach in normal guidelines and procedures that would have altered the patient’s treatment was seen eight times in three patient records. Two were records of patients attended by FY2 doctors and one was a record of a patient attended by a PA. For one of the FY2 doctors’ patient records, all reviewers agreed that they had been reviewed by a senior doctor. The reviewers disagreed about whether or not a senior doctor had reviewed the two other records.
An error or omission that was unlikely to have resulted in harm or different treatment was seen 45 times in 18 consultation records. These judgments of error or omission were clustered within consultation records, as shown in Table 19. The extent to which these records accurately provide full information on each of the components reviewed is unknown but audits of routine records in EDs have found omissions. 136,137
| Reviewer judgement | Number of components with an error or omission | Number of consultation records | |
|---|---|---|---|
| FY2 doctors | PAs | ||
| All components appropriate | N/A | 12 | 9 |
| An error or omission that was unlikely to have resulted in harm or different treatment | 1 | 2 | 3 |
| 2 | 0 | 1 | |
| 3 | 2 | 2 | |
| 4 | 1 | 1 | |
| 5 | 1 | 2 | |
| Error or omission seen that caused a breach in normal guidelines and procedures that would have altered the patient’s treatment | 1 | 0 | 0 |
| 2 | 0 | 0 | |
| 3 | 0 | 0 | |
| 4 | 0 | 0 | |
| 5 | 0 | 1 | |
| Combination of error or omission | 2 breaches in normal guidelines and 1 unlikely to have resulted in harm | 1 | 0 |
| 1 breach in normal guidelines and 2 unlikely to have resulted in harm | 1 | 0 | |
| Not rated | 0 | 1 | |
| Total | 20 | 19 | |
Review by a senior doctor
The reviewers considered that in just over half of the consultation records, either the treatment plan and decision had not been reviewed by a senior doctor or it was unclear if this was the case (Table 20).
| PA or FY2 doctor consultation record | Treatment plan and decision reviewed by senior doctor? | ||
|---|---|---|---|
| Yes | No | Unclear | |
| FY2 doctor | |||
| Number of records | 7 | 9 | 3 |
| Percentage of records | 35 | 45 | 15 |
| PA | |||
| Number of records | 4 | 12 | 3 |
| Percentage of records | 20 | 60 | 15 |
| Total | |||
| Number of records | 11 | 21 | 6 |
| Percentage of records | 28 | 53 | 15 |
Reviewers’ judgement of who conducted the consultation
The blinding of records to remove any indication of whether the consultation was with a PA or a FY2 doctor was considered to be successful. Reviewers were unable to judge whether the consultation record was that of a PA or FY2 doctor (Table 21).
| PA or FY2 doctor consultation record | Reviewers’ judgement of whether the consultation record was that of a PA or FY2 doctor | |
|---|---|---|
| FY2 doctor | PA | |
| FY2 doctor | ||
| Number of records | 11 | 9 |
| Percentage of records | 55 | 45 |
| PAa | ||
| Number of records | 13 | 6 |
| Percentage of records | 68 | 32 |
| Total | ||
| Number of records | 24 | 15 |
| Percentage of records | 62 | 39 |
Overall, 68% (13/19) of the consultations that were actually with a PA were thought, on the basis of the records, to have been with a FY2 doctor. Sixty per cent (9/15) of the consultations that the reviewers thought were by a PA were actually by a FY2 doctor. The raters were 40% sensitive and 46% specific.
Inter-rater reliability
The assessment of inter-rater reliability using Fleiss’ kappa138 for the review of the key consultation components is presented in Table 22.
| Consultation component | Kappa |
|---|---|
| Medical history | 0.009 |
| Examination | 0.15 |
| Request for radiography | 0.26 |
| Treatment plan and decision | 0.15 |
| Advice given | –0.03 |
| Follow-up | 0.30 |
| Treatment plan reviewed by a senior doctor | 0.32 |
| PA or FY2 doctor | 0.12 |
Taken against the consideration that a kappa score of 0.00–0.20 is ‘poor’, 0.21–0.40 is ‘fair’, 0.41–0.60 is ‘moderate’, 0.61–0.80 is ‘good’ and 0.81–1.00 is ‘very good’139 the inter-rater reliability of the reviewers here was poor when assessing many of the components of the consultation record, improving to fair on request for radiography, the appropriateness of follow-up and whether or not the treatment plan and decision had been reviewed by a senior doctor.
Economic analysis
The economic evaluation set out to compare the costs of using PAs and FY2 doctors in the ED, from the NHS perspective. The main variables of interest, to be extracted from patient records, were also to be analysed as part of the clinical study [these were consultation lengths in minutes, diagnostic tests (blood tests and X-rays) ordered, prescriptions provided, referrals and follow-on care recommended, whether or not the PA or FY2 doctor sought advice from a senior colleague during the consultation, unplanned re-attendance within 7 days (primary outcome) and adequacy/appropriateness of care (obtained through expert review)]. The a priori analysis plan called for calculation of cost differences when statistically significant differences were found in variables, after adjustment for case complexity and consideration of the relative costs to hospitals of employing PAs and junior doctors.
When data collection began, it was found that it was not possible to obtain information on some of the identified indicators. Although time between the first clinical contact and when the patient left the ED was recorded, the patient-facing time of the PA or the FY2 doctor could not be distinguished. Information on blood tests, referrals and follow-on recommendations (other than admissions for inpatient care) and whether or not the PA or FY2 doctor sought advice from a senior colleague during the consultation was not available from all sites.
Of the data that were available, and as reported previously, there were no statistically significant differences between PAs and FY2 doctors with respect to the primary outcome, re-attendance within 7 days, after adjustment for demographic features of patients seen by PAs and FY2 doctors, site and Manchester Triage Score87 (the best available measure of acuity). The patients seen by PAs were observed to receive a significantly higher number of X-rays than those seen by FY2 doctors, after adjustment, but adjustment did not include actual conditions. X-rays could be ordered by any member of the ED team, for example the triage nurse in advance of the patient seeing the PA, and, in any case, PAs are not permitted to independently refer for radiography and have to get requests signed off by authorised colleagues.
Conclusions
Available data for comparing PAs and FY2 doctors were limited. From the information that could be gathered, the evidence suggests that both PAs and FY2 doctors practice equally safely and appropriately in the ED, with no differences in re-attendance rates. Moreover, problems exist in attributing outcomes or processes to individual professional staff because ED care is delivered through consultant-led teams, and both PAs and FY2 doctors routinely take assessments and treatment plans to consultants for checking.
The costs of hiring PAs and FY2 doctors differ. Most PAs are paid at NHS Agenda for Change band 7, although some more-experienced PAs may be at band 8a, and those recently qualified may be hired at band 6. 140 In accordance with validated national unit costs, these hourly rates, inclusive of oncosts and overheads, but excluding qualifications, range from £45 (band 6) to £62 (band 8a). 89 The equivalent hourly rate of FY2 doctors is £30. 89 Note that this figure should be treated with a degree of caution as there is a discrepancy between the mean basic salary for FY2 doctors141 used in the unit cost calculation89 and the national contract basic salary for FY2 doctors. 142 With PAs appearing as a more expensive resource, a strictly financial perspective might suggest that FY2 doctors are better value for money. There are, however, other considerations. Junior doctors have training requirements that mean that they are not always available for direct patient care. There is a shortage of junior doctors, and they are insufficient in number to be the sole source of meso-level care in EDs. Where overall staffing ED shortfalls arise, and hospitals bring in locum FY2 doctors, the real costs are higher. Use of PAs can help to relieve staffing pressures in EDs and improve efficiency in the delivery of care. They are able to safely treat patients with a range of conditions, enabling FY2 doctors, and more-senior colleagues, to cover more complex cases, and for FY2 doctors to thereby gain experience that is consistent with the objectives of the junior doctor training programme. Moreover, the role of individual FY2 doctors in the ED is transient, whereas PAs remain long term and provide continuity.
The final chapter provides a discussion of the findings from across the study.
Chapter 11 Discussion and conclusions
This chapter summarises the findings and presents a synthesis of the study. It draws on the discussions in the emerging-findings seminar that was held with participants in the study, patient and public representatives and advisory group members in December 2017. We first of all address the study questions:
-
What is the extent of the adoption and deployment of PAs employed in hospital medical services?
-
What factors support or inhibit the inclusion of PAs as part of hospital medical teams at the macro, meso and micro levels of the English health-care system?
-
What is the impact of including PAs in hospital medical teams on the patients’ experiences and outcomes?
-
What is the impact of including PAs in hospital medical teams on the organisation of services, working practices and training of other professionals, relationships between professionals and the service costs?
We then present a synthesis against a framework of dimensions to judge the quality of health services. We discuss the strengths and limitations of the study before presenting our conclusions and summary of recommendations.
The extent of the adoption and deployment of physician associates in hospital services
We found that PAs were increasingly being adopted into hospital workforces in England. A small but growing number of hospitals in England were employing PAs to work within a widening range of medical and surgical specialties (see Chapter 3, Survey of medical directors and Survey of physician associates). The growth was evident in comparison with data published for the UK in 20121 and reflects the data captured since in the 2016 UK FPA census. 59 This pattern of small but steady growth in adoption reflects those reported in the USA, the Netherlands and Canada. 22,143,144 We report for the first time that when some PAs have vacated their posts in secondary care they have not been replaced owing to the shortage of PAs to employ. This situation is likely to change with the public-finance-supported growth in training (through HEE) resulting in an estimated 3200 PAs in the UK (mostly England) by 2019. 145
We found that PAs, with the exception of those employed in emergency medicine, were mainly deployed to undertake inpatient ward-based activities of the medical/surgical team during weekdays, mostly in the daytime between 07:00 and 19:00 (see Chapter 3, Survey of physician associates, and Chapter 5, The physician associates’ working patterns: times and places). We found only a small number of PAs spending any time in outpatient clinics and theatres, and when they did it was a minor proportion of their working hours. This finding has also been reported in the USA146 and the Netherlands. 147,148
It was evident that while there was a core role in inpatient care, many of the individual PA roles were ‘bespoke’ or ‘moulded’ in that they were developed/trained to meet the requirements of an individual medical/surgical team, but their activities also reflected the experience, capabilities and competencies of the individual PAs (see Chapter 5 and Chapter 7). The longer a PA stayed in a post, the more skilled and knowledgeable they were reported to become in the work of that specific medical team and specialty. This was contrasted with the greater breadth of knowledge and skills developed by early-career doctors through rotation to different specialties. We found that some PAs had been trained by their consultant(s) to undertake specific clinical procedures in support of faster patient access to these procedures. All grades of doctors described a process of building trust in individual PA’s competencies; this reflects the concept of ‘entrustable professional activities’, which is widely used in medical education literature. 149 Some PAs had additional roles, such as a leadership role for other PAs, mentoring student PAs and hospital-wide involvement in specific initiatives related to quality improvement and patient safety. In addition, some had part-time roles within universities as PA educators.
The factors that support or inhibit the inclusion of physician associates as part of hospital medical teams at the macro, meso and level of the English health-care system
At the macro and meso level of the English health-care system, we found government policy and regional health plans supporting more advanced clinical practice roles, including PAs, in order to address medical workforce shortages (particularly in general practice) and the growing demand for health-care services (see Chapter 3, The policy review). This identifiable policy support was in contrast to the situation at the beginning of 2014, when we noted that PAs were absent from all relevant English policy documents, although they did feature in Scottish policy documents, particularly in relation to rural and remote areas. 17 The policy support identified in this study was more than rhetoric, with public finance assigned to supporting training with a target number of PA graduates, albeit with particular reference to general practice rather than acute hospital service (see Chapter 3, The policy review). By 2017, there were 33 PA studies courses in the UK,150 compared with two in 2013. 17
Our national survey of MDs in England indicated that a growing number were open to more advanced clinical practice roles, including PAs, to address junior doctor workforce shortages and increased patient demand (see Chapter 3, Survey of medical directors). However, the small pool of PAs to recruit from was identified as an inhibiting factor and PAs were not necessarily perceived as the right workforce solution by all MDs or professional leaders. Another important inhibiting factor that was reported was the lack of regulation of the PA role and concomitant lack of authority to prescribe and order ionising radiation. A public consultation was led on this issue by the Department of Health in late 2017 providing further evidence of increased macro-level support in the system. The results of the consultation were finally published in February 2019 with the decision to include physician associates in state regulation. 151
We found that the macro- and meso-level factors enabling and inhibiting the inclusion of PAs in the workforce were amplified and expanded at the micro level of the hospitals (see Chapters 4–9).
At the micro level, it was reported that developing advanced clinical practice roles, such as PAs, was a necessity in the face of the shortages of junior doctors to cover the medical rotas; the need to release junior doctors to undertake their training; the increased workload created by increased patient demand and expansion of services and recognised quality issues in service delivery.
Many different types of stakeholders supported the recruitment of PAs as a new source of advanced clinical practitioners in preference to depleting other staff groups, in particular nursing, which was also experiencing severe shortages. In addition, the PAs’ training in a medical model was reported to be a good fit within the medical/surgical team for undertaking the required medical work. Evidence from North America suggests that similar factors have supported the inclusion of PAs in acute medical/surgical teams. 133,152,153
As part of an innovation and change process,154 many participants within the hospitals identified the benefit of having clinical leadership, ongoing clinical champions for PAs and visible executive-level support (see Chapters 4, 7 and 9). This has previously been described in relation to one acute hospital unit in England. 44 The successful contribution of PAs in one or more consultant teams was identified as leading to other teams creating posts for PAs (i.e. the spread of innovation through diffusion51 rather than a top down managerial-led change). We return to the contribution of PAs in the following section.
Against these supporting factors, inhibiting factors were also identified at the micro level. Foremost among these was the lack of role regulation with attendant lack of authority to prescribe or order ionising radiation. The lack of regulation raised concerns about governance, responsibilities and liabilities (see Chapters 4 and 7), issues that have been raised in other countries where PAs have been developed or piloted and as yet do not have regulation or licensing procedures. 155,156 The extent to which the lack of authority to prescribe or order ionising radiation was viewed as an inhibitory factor varied between specialties.
A few clinical leaders (medical and nursing) were reported to have views that PAs were not the right group to develop or employ, favouring nurses or others. Likewise, some consultants working in some specialties with high-dependency patients, having employed PAs, were not re-appointing when PAs left as they considered doctors to be a better fit to the particular needs of that team and patient group. The extent to which the lack of prescribing or ordering ionising radiation authority, rather than other expressed concerns, was a factor in this experience was not clear.
Overall, the view was that PAs would become much more useful and attractive to the medical/surgical team if they had prescribing authority and there was much puzzlement as to why they did not have these rights. The Netherlands, where the first PA programmes commenced in 2000, agreed the legislation to regulate PAs and give them prescribing authority in late 2017. 157
Finally, the lack of a pool of PAs to recruit from was considered a serious inhibition and this was linked to concerns as to how best to retain PAs in medical/surgical teams. Other evidence from surveying PAs in the UK has suggested that retention might be an issue in some places as some PAs did not consider that they were being effectively used within the clinical team. 158
The impact of including physician associates in hospital medical teams on the patients’ experiences and outcomes
From interviews with inpatients and family members in this study, we found that they perceived the PAs as important in keeping them informed about their medical care and management plan (see Chapter 5). PAs were reported to be caring, approachable and good at communicating. Patients were very pleased with the explanations of important information they received about key aspects of their care. There was an implication that they better understood the explanation from the PA than the more complex language used by some doctors. PAs were trusted within their teams to convey important information to patients. Patients were content, and felt that it was appropriate, to be physically examined and have basic medical procedures carried out by a PA. Overall, inpatients and relatives reported being very happy with the care they received from the PA and the hospital staff.
Patients and relatives did not understand the PA role as a concept, but placed more emphasis on receiving good care, rather than the job role or title of individuals in the team treating them. This contrasted with the patient and public voice representative groups, which considered that it was important that patients understood exactly who and what members of their clinical team were. All participants were happy to have a PA involved in their care in the future. Some additional caveats were added, such as they thought that PAs were a good idea (to assist with staffing pressures) as long as they were properly supervised. In addition, some participants wanted reassurances that this addition to the medical team did not result in fewer doctors. High levels of satisfaction with PA involvement in acute inpatient care for similar reasons has been reported from studies in North America and the Netherlands. 109,110
All types of staff (including in emergency medicine) interviewed across the case study sites reported that patients really appreciated the work of the PAs, as evidenced through positive comments, compliments, gifts and seeking them out to talk to (see Chapters 4 and 6–9). We discuss the patient outcomes in more detail in the following section.
The impact of including physician associates in hospital medical teams on the organisation of services, working practices and training of other professionals, relationships between professionals and the service costs
We consider first the impact on organisation, working practices and costs, before turning to the impact on relationships and on the training of other professionals.
The impact on organisation, working practices and costs
The systematic review found 16 observational studies in the specialties most frequently employing PAs in the UK (see Chapter 3). 109 They were all single-site studies and of variable methodological quality. In four studies of emergency medicine and one study of trauma and orthopaedics in which PAs were an additional resource to the medical team, there were reported reduced waiting and process times, lower charges, reduced re-attendance and admission rates and good acceptability to staff and patients. Analgesia prescribing, operative complications and mortality outcomes were variable. In internal medicine, outcomes of care provided by PAs and doctors were equivalent.
In synthesising the evidence from our study, we draw from our findings reported across Chapters 4–10. We found that, primarily, PAs were deployed to help address gaps in medical rotas. Gaps in medical rotas in hospital teams have been reported as an issue of concern in the NHS. 159,160 There was variability in whether PAs were in addition to or part of the medical rotas. In some services, PAs were part of staffing rotas for what was described as the second-tier staff. This was referring to doctors below registrar level and/or advanced clinical practitioners. In some services, the PAs’ duty times (rotas) were arranged to cover for absences of doctors (e.g. to attend training) and reduce the use of locum doctors. Consultants and operational managers considered locum doctors who were new to their service as less efficient, less safe and more costly than PAs. Reduction in the use of locum doctors, particularly in reaction to costly agency fees, has been a major issue for the NHS, with spending caps imposed in 2016, just before we began the data collection for the case studies, and still in force. 161 However, it was evident that decisions about employing and deploying PAs were not just about finance but also about enhancing the quality of service provision and improving support to junior doctors in training. PAs were substituting for some of the service contribution of the early-career grades of junior doctors but there was variation in the extent to which individual PA posts were substituting for and/or supplementing30,52 the work of junior doctors.
One of the most frequently reported impacts on organisation was that PAs provided continuity of staffing in the medical/surgical team. This, in turn, was seen to provide benefit to other staff and patients through:
-
Continuity in presence on the inpatient wards, thus increased access to the medical/surgical team for patients and nurses.
-
Continuity in knowledge about current inpatient status, management plans and patients’ progress, thus facilitating updating patients and the medical/surgical team, for example on ward rounds.
-
Continuity in knowledge about the policies and practices (clinical and otherwise) of the department, the individual consultants and the trust; this was of particular value for new doctors to that particular workplace.
Similar observations about PAs providing continuity within the medical/surgical team have been made in North America and the Netherlands. 144,146,147
The PAs were reported to work alongside junior doctors in managing the medical/surgical teams’ workloads (although in some specialties the PAs’ full potential was not realised owing to a lack of authority to prescribe and order ionising radiation) and, for doctors in training, PAs were invaluable in induction into policies and working practices. Doctors in training in the UK have described the stress they face in understanding information technology systems, policies and procedures when starting new posts. 162 PAs undertook significant amounts of non-patient-facing clinical work for the medical/surgical team (e.g. preparing discharge summaries). Similar findings have been reported in North America and the Netherlands. 144,146,147 A systematic review of studies of physician time use in hospitals settings found that activities that were indirectly related to a patient’s care used more of hospital physicians’ time than direct interaction with hospitalised patients did. 163 The extent of the patient-facing clinical work delegated to the PAs varied, dependent on the views and attitudes of the senior doctors in the team, as discussed in section The extent of the adoption and deployment of physician associates in hospital services.
The presence of a PA in the team was considered to release the doctors’ time in two ways: first, so that the doctors could attend more complex patients (irrespective of specialty); second, where PAs worked in inpatient settings, it released doctors to attend or remain with patients in outpatient departments and theatre (which was also required training experience). The presence of PAs enabling doctors to undertake required training was also reported and is consistent with reports from the USA. 35
All consultants, registrars and managers reported the PAs to be safe, with no serious incidents or patient complaints recounted. This reflects the evidence found in the systematic review,109 as well as in a Dutch study of PAs in other surgical specialties110 and in a recent single-unit survey in England. 164
Doctors of all grades described a process of establishing an understanding of the PAs’ competency and of building trust in their capabilities through working with them. We have previously referred to the process of entrustable professional activities within medicine149 and we described this process in relation to GPs and PAs in primary care in England. 18
We found that PAs were reported by all stakeholders to contribute to efficiency by smoothing and improving patient flow into, during and out of an episode of treatment/care. PAs were considered to provide ‘oil’ to the system. The extent to which PAs supported the smoothness of patient flow was linked to other attributes of the PA role, discussed previously, such as bringing continuity to the medical team, undertaking non-patient-facing clinical work and providing a communication ‘bridge’ between the medical team, the nursing team and those in roles responsible for patient flow, often nurses. We return to this reported ‘bridging’ role issue in discussing relationships in section The impact on the relationships between professionals and the training of other professionals. We report on the PA support to smoothing patient flow for the first time in the English hospital setting and consider that it needs further investigation in the context of the variety of infrastructure and other support to the medical/surgical team found in NHS. The variability in infrastructure and staffing between NHS hospitals has been well established. 165
All senior managers and clinicians described the difficulty of attributing patient outcomes and cost to an individual professional when clinical provision was team based and affected by multiple other contextual factors. Some thought that the presence of the PAs enabled the senior doctors to be more efficient. Many managers and consultants reported that to some extent PAs reduced the use of expensive locum doctors. Understanding current rates of pay for locum and agency staff in England is not straightforward. Although NHS England imposed caps on agency fees and hourly pay rates in 2016,161 there is considerable evidence that the shortage of doctors has resulted in high demand, which has driven these rates up. 166 From a survey of 68 NHS trusts, the average hourly rate of pay to locum FY2 doctors in 2017 in England was reported to be £50.90 (the maximum reported for the period was an hourly rate of £104.69) plus an average hourly commission rate to the supplying agency of £5.60 (the maximum rate reported was £13.49). 167 Validated national unit costs for staff, such as PAs, on Agenda for Change terms and conditions give hourly rates (inclusive of oncosts and overheads, but excluding qualifications) of £45 (band 6) and £54 (band 7). 89 However, although reducing financial spend on locums was reported as important to the consultants and managers, the primary consideration given for preferring PAs to locum doctors was patient safety and efficiency.
None of the managers or clinicians, in any of the sites, was able to provide any routine data or reports from which the impact of the involvement of PAs could be considered. This absence of data has also been reported from surveyed executives of medical organisations in the USA, who noted the contrast to their primary care services, and similarly could not provide information on patient outcomes or costs that could be attributed to the inclusion or exclusion of PAs in hospital services. 133 Our systematic review did not find robust evidence on cost-effectiveness of the inclusion of PAs in the specialties in which PAs are more frequently found in the UK. 109 A recently reported large, matched, controlled, multicentre study from the Netherlands of several different surgical specialties found no difference in length of stay or quality-adjusted life-years for inpatients of doctor-only teams compared with those treated by mixed doctor and PA teams; the involvement of PAs reduced personnel costs but not overall healthcare costs. 111
The pragmatic retrospective comparison of consultation records for patients seen by FY2 doctors or PAs in the ED found no difference in the primary outcome of rate of re-attendance. A subsample of records of patients seen by FY2 doctors and PAs were reviewed by senior clinicians and judged as equally safe and appropriate. We provide this non-inferiority evidence for the first time in the UK setting.
The impact on the relationships between professionals and the training of other professionals
A number of participants described initial resistance to the introduction of PAs from doctors and nurses. In most services, this was reported to dissipate over time as a result of actually working with PAs (see Chapters 4 and 7–9). Although positive relations were described between PAs, doctors and nurses, there were also occasional reports of doctors and nurses who remained less positive to the introduction of a new professional group. Abbott53 has described the way in which health-care professions are part of an interdependent system in which they jostle over areas of jurisdiction linked to issues of status and control. The dissipation of tension between professional groups through the process of working together has been described both by Abbott53 and in other studies of the introduction of new roles and advanced clinical practitioners,168,169 as well as in our study of PAs in primary care in England. 18
Many stakeholders described the PAs as providing a ‘bridge’ between medicine and nursing in some of the inpatient settings. This was also a finding from our study in general practice. 18 In the inpatient setting, the ‘PA as bridge’ was described as a mechanism for ensuring speedier access for nurses to the medical/surgical team, particularly in relation to patients whose condition was changing or in assisting in planning for their management or discharge (i.e. supporting patient flow). PAs were also described as accessible to others in the nursing team, such as health-care assistants, as well as for non-clinical staff.
Some early-career doctors were reported to be concerned that the presence of PAs would reduce their opportunities for training in certain procedures, as consultants would favour the PAs to do these. Most doctors and PAs described the prioritising of training for doctors and were alert to such problems. To the best of our knowledge, we report this for the first time in the UK setting.
Synthesis
This study is framed by the dimensions proposed by Donabedian49 and Maxwell50 for evaluating health-care services and is applied here to the innovation of PAs in secondary care. The dimensions are acceptability, effectiveness (including safety), equity (fairness) and efficiency (including costs).
Physician associates were an acceptable group of health professionals to contribute to secondary care at the macro, meso and micro levels of the health system. The macro and meso levels of support are in marked contrast to the situation when the primary care study was completed. PA training and employment is now supported at the government level by all countries in the UK.
Physician associates were found to be acceptable and appropriate by most, but not all, doctors, managers and nurses. Patients had little knowledge of the PA role itself but viewed the PAs very positively within the context of the medical/surgical team. Some consultants in specialties with high-dependency patients reported that doctors were more appropriate for the level and/or pace of work, particularly prescribing, required in that setting. Clinicians and managers were supporting the development of many types of mid-level advanced clinical practice roles, of which PAs were one. For many doctors, the training of the PAs in the medical model made the PAs particularly appropriate for the work they required. It should be noted that other hospitals in England have developed medical assistant roles (sometimes called doctors’ assistants or physician assistants) to support doctors. These are trained to the level of health-care assistants to undertake tasks such as phlebotomy and clerical work under the direction of the medical/surgical team. 170 The contribution of different types of roles supporting the medical/surgical team requires further investigation.
For junior doctors and some nurses, there was uncertainty as to the scope of the role, an uncertainty compounded in the eyes of many by their lack of inclusion in the regulatory process for health professionals. Inclusion of PAs in these processes for health professions was viewed as important in terms of their acceptability, their perceived effectiveness (particularly in relation to prescribing and ordering X-ray investigations) and governance.
Physician associates were deployed, within a medical or surgical team, to mainly work in the inpatient ward under the supervision of consultants and their registrars. In the EDs, they worked as part of the team, with early-career doctors and other advanced clinical practitioners, and under senior medical supervision. Their work was described as aiding patient flow and releasing doctor time for more complex, medically unstable patients, for outpatient consultations, for the operating theatre and for training activities. There was no indication that this was inequitable (unfair) to any group of patients.
As part of the medical/surgical team, PAs were reported to be clinically safe in the work they did and to add to patient safety through their knowledge of policy and the practices of the consultants and the organisation. These colleague reports were supported by the finding that the patient outcomes and consultation records of FY2 doctors and PAs in the ED were equally safe and appropriate.
There was difficulty of attributing patient outcomes and cost to an individual professional when the provision was team based and affected by multiple other factors, but, in general, the reported contribution of PAs was highly positive.
Planning and developing a medical and surgical workforce is recognised as internationally challenging. 145,169,171 Medical staffing shortages have continued to rise in England, with a government response during the study period to create an additional 1500 medical student places in England from 2018. 172 The General Medical Council, although welcoming this growth, noted that their presence will not be felt in the workforce as graduates until 2023 and raised questions as to the availability of sufficient capacity within the workplace to train increased numbers. 173 Cyclical shortages of different grades of doctors with attendant reports of increased pressures on the employed doctors has been a recurrent feature of the NHS. 174 Achieving a sustainable medical workforce with the right balance of consultants, GPs, specialty doctors (i.e. not in training posts) and junior doctors has to take account of (1) the service demands, (2) the training requirements for career advancement and (3) the creation of manageable jobs within interesting careers. Having a cadre of flexible, mid-level practitioners, trained in the medical model, who can support doctors, but are not doctors, or intending to replace doctors, may help address inherent tensions between service demands, training requirements and budgetary constraints, as well as mitigate cyclical shortages.
Strengths and limitations
This was a mixed-methodology study that had multiple elements. The major strengths are as follows:
-
the use of multiple methods over a number of workstreams, allowing a macro-, meso- and micro-level view of the research questions
-
undertaking micro-level investigation that included hospitals from a wide range of different sites (both major conurbations and smaller cities/towns, large tertiary referral and small ‘District General Hospital-type’ sites), from a wide range of specialties and with a considerable proportion of the known PA workforce in secondary care in England
-
collection of extensive qualitative data from a wide range of stakeholders utilising individual interviews, allowing analysis of perspectives gathered from senior managers (MDs and trust board members); members of the medical team (senior and junior doctors) and other clinicians, such as nurses; patients; and relatives
-
gathering of quantitative and qualitative data on PAs ‘in action’ in hospitals, using both observation and self-completed diaries
-
carrying out a well-powered quantitative comparative analysis of the documented processes and outcomes of patient care by PAs and FY2 doctors in three EDs in different parts of the country.
The main limitations of the case study elements were largely a result of the difficult circumstances and constraints on research within a highly complex and dynamic system, which was simultaneously under great pressures. 175–179 The protocol was changed twice to try to accommodate real-world changes and priorities. For example, we had intended to compare activity of PAs and FY2 doctors while managing minor cases in EDs but found changes (between the time period we negotiated the research funding and when we commenced recruitment) in how many PAs worked in EDs and in what area of the ED PAs worked in, with most currently working in ‘majors’. This required a change to comparison of ‘majors’ cases instead. This change to ‘majors’ patients also introduced the potential for selection bias in the sample, in that patients in the minors section are attended by the next-available professional whereas patients in the majors section are attended by professionals based on a range of factors, such as severity/immediacy of the injury/illness, number of patients arriving at that time point and the availability of staff, as overseen by a senior doctor in charge. Although there might be the potential for selection bias by a senior doctor in charge in the majors section, three factors in the design mitigated this: (1) the use of three different ED departments rather than a single ED, (2) the overall sample was obtained from a 16-week period at all times of day and night in which there will have been the greatest variation in both the factors referred to above and also individual senior doctors in charge and (3) statistical adjustment for MTS,87 alongside other potential confounding factors, in modelling. The changes also resulted in a very limited economic analysis, unlike the analysis that was planned. There are still relatively few PAs working in secondary care and there is a smaller number within that group who are willing to volunteer to participate in this type of research. However, we successfully recruited six hospitals with PAs (and three with PAs in the EDs) and, within those, 41 PAs willing to participate.
We were unable to access quantitatively measurable data on the effect of the introduction of PA on patient outcomes (other than in the ED) or costs as the hospitals were unable to supply these type of data. In addition, the attribution of changes in quality of patient care, patient safety events or cost savings to the introduction of PAs is problematic when such an introduction commonly went alongside other changes or responses to other significant events, such as unprecedented surges in demand and workforce shortages. However, we were able to describe and scope the range of potential impacts, which could inform the design of future studies either through matched comparisons of medical/surgical teams with and without PAs, such as those used in the Dutch study,110 or in a ‘stepped-wedge’ design (in which the change is introduced sequentially in all sites so that all participants get the intervention, but not simultaneously). 180
Conclusions
Physician associates are a new group of health-care professionals being adopted in a minority but growing number of secondary care hospitals across the UK. The well-documented workforce shortages in the NHS meant that PAs were one of many solutions being followed to address, in particular, the shortage of doctors. PAs were deployed to undertake some of the work of junior doctors, releasing their time to focus on complex and new patients as well as training requirements. The work that PAs undertook was mainly the ward-based activities of the medical/surgical teams and included significant amounts of medical administration. This work was considered to significantly aid patient flow and patient experience. The stability of PAs in the work setting, in contrast to doctors in training, was reported to be valued in inducting new doctors and also contributing to patient and junior doctor experience, patient safety and throughput and the development of trust between PAs and the medical and multidisciplinary teams. Patients were very satisfied with PA care as part of their medical/surgical team but had little understanding of the role. The pragmatic comparative review of ED records of patients attended by PAs and Foundation Year doctors found that they provided equivalent, safe care, suggesting that PAs are another source of advanced clinical practitioners that can be employed in that setting. The main cost benefit identified, but not quantified, by managers and clinicians was thought to be the reduction in employing locum junior doctors. Even when this was discussed, patient safety and experience were the main considerations. Although some specialties with high-dependency patients reported that PAs were less appropriate than junior doctors, most specialties reported inefficiencies and problems in the workflow created by the lack of PA authority to prescribe and order ionising radiation. It is clear from our study that PAs could provide a flexible addition to the secondary care workforce without drawing from existing professions or reducing opportunities for doctors in training. However, their utility in this setting is unlikely to be fully realised without the appropriate level of regulation with attendant authority to prescribe medicines and order ionising radiation within their scope of practice.
Implications
Physician associates have the potential to be a competent and flexible addition to current and future medical and surgical teams. Patients, the public and secondary care professionals need more information to understand both the role and also its potential contribution to acute care medical and surgical teams. Individual employing NHS organisations need to consider their role in this alongside that of national NHS and professional bodies.
Physician associates are a workforce innovation that is not necessarily welcomed by all other professional groups. As an innovation, successful introduction and growth is likely to depend on a planned process with attendant senior levels of support, local champions and embedded governance and review processes. This requires employer organisations to both plan and identify appropriate people and resources. With the expected exponential increase in PAs in England in the next 2 years, this requires prompt consideration.
Findings from this study suggest that the efficiency and contribution that PAs could make to medical and surgical teams in secondary care will be increased by the legal authority to prescribe, which can be achieved only by including PAs in the regulatory framework for health-care professionals. This has implications for policy with regard to regulatory frameworks for health professionals in the UK.
In order for there to be a supply of PAs for secondary care, there needs to be cognisance of this group in health profession education commissioning at a local level. Education commissioners at local levels should consider the contribution PAs could make to a future flexible secondary care, and not just primary care, workforce.
Further investigation
This study has highlighted a number of questions that require further investigation in the context of increasing numbers of PAs and other mid-level practitioners available in the UK to join the NHS workforce. These include:
-
What are the patient outcomes, experiences and service costs for same-specialty medical/surgical teams before and after the introduction of PAs using stepped-wedge quantitative research designs?
-
How does the work of the medical and surgical teams in the same specialties vary between hospitals with different types of infrastructure, technology and patient flow systems and what workforce is required to meet the variation?
-
What is the extent of the use and role of medical assistant roles in different medical and surgical specialties and how does that compare and contrast with the use of advanced clinical practitioners, including but not limited to PAs?
-
What is the influence of sociodemographic and geographic factors, and types of hospitals, such district general or tertiary hospitals, on the demand for PAs and other advanced clinical practitioners, in a secondary care workforce?
-
What factors influence clinician and manager decision-making as to staffing and skill mix in secondary care teams, with particular reference to beliefs, preference, evidence and use of financial data?
-
Can workforce modelling of different permutations of skill-mix support to medical and surgical teams, in which supplementation and/or substitution are explicit, assist managers and clinicians in workforce decision-making?
-
What opportunities are available to retain PAs (and other advanced clinical practitioners) longer term in an essentially flat career structure?
-
What impact will the rapid growth in PA numbers in England over the next 3 years have on perceptions and development of the role?
Acknowledgements
We thank all those who helped with this study – as participants, as advisors, as public voice representatives, as champions for the study within individual NHS trusts and in providing data from hospital information systems. The study was undertaken at a time of increasing workforce pressures in the NHS. So, although timely in providing evidence, this meant that those who helped the study did so in the face of fierce competition for their time and attention. We are therefore very grateful.
Robert Grant (Senior Research Fellow in Quantitative Methods, Joint Faculty of Kingston University and St George’s, University of London) was a member of the research team that obtained the funding until he left his university post in 2017. While a member of the research team, he provided expert statistical advice. Dr Chao Wang (Senior Lecturer in Statistics, Joint Faculty of Kingston University and St George’s, University of London) undertook the statistical analysis and provided statistical advice in preparation of the final report 2018. Morro Touray (Research Fellow in Health Economics, University of Surrey) provided health economics advice and insights to the research team. Dr Cheryl Whiting supported the final preparation of the manuscript.
Contributions of authors
Vari M Drennan (Professor of Health Care and Policy Research) conceived, obtained funding for and led the study. She contributed to all elements of the study, led the emerging-findings seminar and overall synthesis of findings, and drafted the final report.
Mary Halter (Associate Professor of Emergency Cardiovascular and Critical Care Research) conceived and obtained funding for the study. She was project manager and contributed to all elements of the study. She convened the London patient voice groups and led on the surveys, systematic review, data collection and analysis within the EDs. She wrote the initial draft chapters on the PA deployment (see Chapter 5) and the ED element (see Chapter 10). She also contributed important intellectual content to the revisions of the final report.
Carly Wheeler (Research Associate) undertook surveys, the systematic review, data collection and analysis in the case study sites. She helped convene the London patient voice group. She prepared the initial draft of the nurses’ view chapter (see Chapter 9). She also contributed important intellectual content to the revisions of the final report.
Laura Nice (Research Associate) undertook data collection and analysis in the case study sites. She contributed to the West Midlands patient voice group. She wrote the initial draft of the patient and family views chapter (see Chapter 6). She also contributed important intellectual content to the revisions of the final report.
Sally Brearley (Patient and Public Involvement) conceived and obtained funding for the study. She contributed to all elements of the study and chaired all research team meetings. She led on the patient and public involvement, including chairing of the emerging-findings seminar. She contributed important intellectual content to the revisions of the final report.
James Ennis (PA and Lecturer) was awarded the funding and contributed to all elements of the study. He provided PA expertise and knowledge. He contributed to the West Midlands patient voice group and undertook qualitative interviewing and analysis in the study sites. He also contributed important intellectual content to the revisions of the final report.
Jon Gabe (Professor of Sociology) conceived and obtained funding for the study. He contributed to all elements of the study, provided expert knowledge in sociology applied to health care and qualitative methods and undertook analysis of qualitative data. He contributed important intellectual content to the revisions of the final report.
Heather Gage (Professor of Health Economics) conceived and obtained funding for the study. She contributed to all elements of the study, provided expert knowledge in health economics, led on the economic analysis and prepared results for publication. She contributed important intellectual content to the revisions of the final report.
Ros Levenson (Independent Researcher) undertook the senior manager and clinician interviews, leading on the analysis and initial draft of that chapter. She contributed to all elements of the study, including contributing important intellectual content to the revisions of the final report.
Simon de Lusignan (GP and Professor of Primary Care and Clinical Informatics) conceived and obtained funding for the study. He provided expert clinical knowledge and expertise in the organisation of medicine and clinical informatics. He contributed to all elements of the study and contributed important intellectual content to the revisions of the final report.
Phil Begg (Executive Director of Strategy and Delivery in a NHS Trust and Professor) helped conceive the study and was awarded the funding. He provided expert NHS management knowledge of the acute sector organisation and workforce issues. He convened the West Midlands patient voice group. He contributed to all elements of the study and contributed important intellectual content to the revisions of the final report.
Jim Parle (GP and Professor of Primary Care) helped conceive the study and was awarded the funding. He provided expert clinical knowledge, expertise in the organisation of medicine and medical education as well as PA education. He contributed to all elements of the study and led the study elements in the West Midlands. He contributed important intellectual content to the revisions of the final report.
Publications
Halter M, Wheeler C, Drennan VM, de Lusignan S, Grant R, Gabe J, et al. Physician associates in England’s hospitals: a survey of medical directors exploring current usage and factors affecting recruitment. Clin Med (Lond) 2017;17:126–131.
Wheeler C, Halter M, Drennan VM, de Lusignan S, Grant R, Gabe J, et al. Physician associates working in secondary care teams in England: interprofessional implications from a national survey. J Interprof Care 2017;6:1–3.
Wheeler C, Halter M, Drennan MV, de Lusignan S, Grant R, Gabe J, et al. Physician associates working in secondary care teams in England: interprofessional implications from a national survey. J Interprof Care 2017;31:774–6.
Halter M, Wheeler C, Drennan VM, de Lusignan S, Grant R, Gabe J, et al. The contribution of physician assistants/associates to secondary care: a systematic review. BMJ Open 2018;8:e019573.
Drennan VM, Halter M, Wheeler C, Nice L, Brearley S, Ennis J, et al. What is the contribution of physician associates in hospital care in England? A mixed methods, multiple case study. BMJ Open 2019;9:e027012.
Data-sharing statement
All qualitative data generated that can be shared are contained within the report. All data queries and requests should be submitted to the corresponding author for consideration. Please note that exclusive use will be retained until the publication of major outputs. Access to anonymised data may be granted following review.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HS&DR programme or the Department of Health and Social Care.
References
- Ross N, Parle J, Begg P, Kuhns D. The case for the physician assistant. Clin Med 2012;12:200-6. https://doi.org/10.7861/clinmedicine.12-3-200.
- Hospitals on the Edge? The Time for Action. London: RCP; 2012.
- Future Hospital: Caring for Medical Patients. A Report from the Future Hospital Commission to the Royal College of Physicians. London: RCP; 2013.
- Royal College of Emergency Medicine . Emergency Medicine Taskforce Interim Report 2012. CEM6723-EM-Taskforce---Interim-Report-2012-(Final)%20(1).pdf (accessed 31 August 2017).
- Centre for Workforce Intelligence . Big Picture Challenges: The Context 2013. www.gov.uk/government/uploads/system/uploads/attachment_data/file/507359/CfWI_Big_picture_challenges_context.pdf (accessed 31 August 2017).
- BBC News . NHS Plans Rapid Expansion of ‘Doctor’s Assistant’ Jobs 2014. www.bbc.co.uk/news/health-28902132 (accessed 31 August 2017).
- Rawlinson K. NHS Patient Groups Warn More Doctor Assistants may be ‘Healthcare On Cheap’. The Guardian 2014. www.theguardian.com/society/2014/aug/22/fears-nhs-doctors-assistant-recruitment-healthcare-cheap (accessed 31 August 2017).
- Emergency Medicine: Background to HEE Proposals to Address Workforce Shortages. Leeds: Health Education England; 2013.
- Reid W. Plenary Paper Presented at Conference on Physician Associates in the NHS Workforce. Birmingham: University of Birmingham; 2014.
- Nicoll P, MacVicar R. NHS Education for Scotland: Supporting Scottish Remote and Rural Healthcare 2013. www.rrheal.scot.nhs.uk/media/185252/remote%20and%20rural%20healthcare%20updated.pdf (accessed 31 August 2017).
- Royal College of Physicians, Faculty of Physician Associates . Why Did the Royal College of Physicians Agree to Establish the FPA? n.d. www.rcplondon.ac.uk/news/faculty-physician-associates (accessed 31 August 2017).
- UK Association of Physician Associates . Physician Associates Locations 2014. www.ukapa.co.uk/general-public/pa-locations/index.html (accessed 30 October 2014).
- The Working Time Regulations Statutory Instrument 1998, No 1833. London: The Stationery Office; 1998.
- Liberating the NHS: Developing the Healthcare Workforce. London: Department of Health; 2012.
- Task Shifting: Rational Redistribution Of Tasks Among Health Workforce Teams – Global Recommendations and Guidelines. Geneva: World Health Organization; 2008.
- A Strategic Review of the Future Healthcare Workforce: Informing the Nursing Workforce. London: Centre for Workforce Intelligence; 2013.
- Drennan VM, Halter M, Brearley S, Carneiro W, Gabe J, Gage H, et al. Investigating the contribution of physician assistants to primary care in England: a mixed methods study. Health Serv Deliv Res 2014;2.
- Drennan VM, Gabe J, Halter M, de Lusignan S, Levenson R. Physician associates in primary health care in England: a challenge to professional boundaries?. Soc Sci Med 2017;181:9-16. https://doi.org/10.1016/j.socscimed.2017.03.045.
- Halter M, Drennan VM, Joly LM, Gabe J, Gage H, de Lusignan S. Patients’ experiences of consultations with physician associates in primary care in England: a qualitative study. Health Expect 2017;20:1011-19. https://doi.org/10.1111/hex.12542.
- The Competence and Curriculum Framework for the Physician Assistant. London: Department of Health; 2006.
- Physician Associate Managed Voluntary Register . The Revised Competence and Curriculum Framework for the Physician Assistant 2012. www.fparcp.co.uk/about-fpa/Who-are-physician-associates (accessed 31 August 2017).
- Cawley JF, Hooker RS. Physician assistants in American medicine: the half-century mark. Am J Manag Care 2013;19:e333-41.
- US Department of Labor . Occupational Outlook Handbook, 2016–17 Edition, Physician Assistants n.d. www.bls.gov/ooh/healthcare/physician-assistants.htm (accessed 31 August 2017).
- American Academy of Physician Assistants . PAs Practice Medicine Infographic n.d. www.aapa.org/what-is-a-pa/#tabs-2-get-information-on-pas (accessed 31 August 2017).
- Mullan F, Frehywot S. Non-physician clinicians in 47 Sub-Saharan African countries. Lancet 2007;370:2158-63. https://doi.org/10.1016/S0140-6736(07)60785-5.
- van den Driesschen Q, de Roo F. Physician assistants in the Netherlands. JAAPA 2014;27:10-1. https://doi.org/10.1097/01.JAA.0000453240.00098.83.
- Jones IW, Hooker RS. Physician assistants in Canada. Can Fam Physician 2011;57:e83-8.
- Frossard LA, Liebich G, Hooker RS, Brooks PM, Robinson L. Introducing physician assistants into new roles: international experiences. Med J Aust 2008;188:199-201.
- Buchan J, O’May F, Ball J. New role, new country: introducing US physician assistants to Scotland. Hum Resour Health 2007;5. https://doi.org/10.1186/1478-4491-5-13.
- Laurant M, Harmsen M, Wollersheim H, Grol R, Faber M, Sibbald B. The impact of nonphysician clinicians: do they improve the quality and cost-effectiveness of health care services?. Med Care Res Rev 2009;66:36-89. https://doi.org/10.1177/1077558709346277.
- Halter M, Drennan V, Chattopadhyay K, Carneiro W, Yiallouros J, de Lusignan S, et al. The contribution of physician assistants in primary care: a systematic review. BMC Health Serv Res 2013;13. https://doi.org/10.1186/1472-6963-13-223.
- Althausen PL, Shannon S, Owens B, Coll D, Cvitash M, Lu M, et al. Impact of hospital-employed physician assistants on a level II community-based orthopaedic trauma system. J Orthop Trauma 2013;27:e87-91. https://doi.org/10.1097/BOT.0b013e3182647f29.
- Jeanmonod R, Delcollo J, Jeanmonod D, Dombchewsky O, Reiter M. Comparison of resident and mid-level provider productivity and patient satisfaction in an emergency department fast track. Emerg Med J 2013;30. https://doi.org/10.1136/emermed-2011-200572.
- Hamden K, Jeanmonod D, Gualtieri D, Jeanmonod R. Comparison of resident and mid-level provider productivity in a high-acuity emergency department setting. Emerg Med J 2014;31:216-19. https://doi.org/10.1136/emermed-2012-201904.
- Stahlfeld KR, Robinson JM, Burton EC. What do physician extenders in a general surgery residency really do?. J Surg Educ 2008;65:354-8. https://doi.org/10.1016/j.jsurg.2008.06.002.
- Timmermans MJ, van Vught AJ, Wensing M, Laurant MG. The effectiveness of substitution of hospital ward care from medical doctors to physician assistants: a study protocol. BMC Health Serv Res 2014;14. https://doi.org/10.1186/1472-6963-14-43.
- Scotland Office and Office of the Secretary of State for Wales . Devolution of Powers to Scotland, Wales and Northern Ireland 2013. www.gov.uk/guidance/devolution-of-powers-to-scotland-wales-and-northern-ireland (accessed 31 August 2017).
- NHS Choices . NHS Trusts 2017. www.nhs.uk/servicedirectories/pages/nhstrustlisting.aspx#TrS (accessed 31 August 2017).
- NHS Hospital & Community Health Service (HCHS) Monthly Workforce Statistics – Provisional Statistics: HCHS Doctors by Grade and Specialty in Trusts and CCGs – Full Time Equivalent May 2017. Leeds: NHS Digital; 2017.
- National Health Service Occupation Code Manual. Version 14.0. Leeds: NHS Digital; 2016.
- Parle JV, Ross NM, Doe WF. The medical care practitioner: developing a physician assistant equivalent for the United Kingdom. Med J Aust 2006;185:13-7.
- Woodin J, McLeod H, McManus R, Jelphs K. The Introduction of US-trained Physician Assistants to Primary Care and Accident and Emergency Departments in Sandwell and Birmingham. Final Report. Birmingham: University of Birmingham; 2005.
- Farmer J, Currie M, Hyman J, West C, Arnott N. Evaluation of physician assistants in National Health Service Scotland. Scott Med J 2011;56:130-4. https://doi.org/10.1258/smj.2011.011109.
- White H, Round JE. Introducing physician assistants into an intensive care unit: process, problems, impact and recommendations. Clin Med 2013;13:15-8. https://doi.org/10.7861/clinmedicine.13-1-15.
- Williams LE, Ritsema TS. Satisfaction of doctors with the role of physician associates. Clin Med 2014;14:113-16. https://doi.org/10.7861/clinmedicine.14-2-113.
- Royal College of Physicians, Faculty of Physician Associates . Where Are We With Regulation? n.d. www.rcplondon.ac.uk/news/faculty-physician-associates (accessed 31 August 2017).
- Open Consultation. The Regulation of Medical Associate Professions in the UK. London: Department of Health; 2017.
- Ritsema TS, Paterson KE. Results of the Second Annual UK Physician Assistant Census. London; 2012.
- Donabedian A. The quality of care. How can it be assessed?. JAMA 1988;260:1743-8. https://doi.org/10.1001/jama.1988.03410120089033.
- Maxwell RJ. Dimensions of quality revisited: from thought to action. Qual Health Care 1992;1:171-7. https://doi.org/10.1136/qshc.1.3.171.
- Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q 2004;82:581-629. https://doi.org/10.1111/j.0887-378X.2004.00325.x.
- Nancarrow SA, Borthwick AM. Dynamic professional boundaries in the healthcare workforce. Sociol Health Illn 2005;27:897-919. https://doi.org/10.1111/j.1467-9566.2005.00463.x.
- Abbott A. The System of Professions – a Study of the Division of Expert Labour. London: University of Chicago Press; 1988.
- Creswell JW, Clark VL. Designing and Conducting Mixed Methods Research. Thousand Oaks, CA: Sage Publications Ltd; 2007.
- NIHR INVOLVE . Payment and Recognition for Public Involvement n.d. www.invo.org.uk/resource-centre/payment-and-recognition-for-public-involvement/ (accessed October 2017).
- Bowling A. Research Methods in Health. Maidenhead: Open University Press; 2009.
- Binley’s . Database of Hospital Doctors n.d. www.binleys.com/Product/Hospital_Doctors/ (accessed 17 October 2017).
- Drennan VM, Chattopadhyay K, Halter M, Brearley S, de Lusignan S, Gabe J, et al. Physician assistants in English primary care teams: a survey. J Interprof Care 2012;26:416-18. https://doi.org/10.3109/13561820.2012.686538.
- Ritsema TS. Faculty of Physician Associates Census Results 2016. www.fparcp.co.uk/about-fpa/fpa-census (accessed 10 September 2017).
- Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group . Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 2009;62:1006-12. https://doi.org/10.1016/j.jclinepi.2009.06.005.
- Halter M, Wheeler C, Drennan V, Pelone F. Evidence of Impact of Physician Associates in Secondary Care: A Systematic Mixed Studies Review. CRD42016032895 2016. www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42016032895 (accessed September 2017).
- Greenhalgh T, Peacock R. Effectiveness and efficiency of search methods in systematic reviews of complex evidence: audit of primary sources. BMJ 2005;331:1064-5. https://doi.org/10.1136/bmj.38636.593461.68.
- International Monetary Fund . Table B1. Advanced Economies: Unemployment, Employment, and Real GDP Per Capita n.d. www.imf.org/external/pubs/ft/weo/2015/01/pdf/tblpartb.pdf (accessed December 2015).
- Kmet LM, Lee RC, Cook LS. Standard quality assessment criteria for evaluating primary research papers from a variety of fields. Alberta Herit Found Med Res 2004;13:1-11. www.files.deslibris.ca/cppc/200/200548.pdf (accessed November 2015).
- Pluye P, Hong QN. Combining the power of stories and the power of numbers: mixed methods research and mixed studies reviews. Annu Rev Public Health 2014;35:29-45. https://doi.org/10.1146/annurev-publhealth-032013-182440.
- Systematic Reviews. CRD’s Guidance for Undertaking Reviews in Healthcare. York: Centre for Reviews and Dissemination, University of York; 2009.
- Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M, et al. Guidance on the Conduct of Narrative Synthesis in Systematic Reviews. Lancaster: Lancaster University; 2006.
- Walt G, Shiffman J, Schneider H, Murray SF, Brugha R, Gilson L. ‘Doing’ health policy analysis: methodological and conceptual reflections and challenges. Health Policy Plan 2008;23:308-17. https://doi.org/10.1093/heapol/czn024.
- Silverman D. Interpreting Qualitative Data. Methods for Analysing Talk, Text and Interaction. London: Sage Publications; 2014.
- Yin RK. Case Study Research: Design and Methods. Thousand Oaks, CA: Sage Publications; 2018.
- Kessler I, Heron P, Dopson S, Magee H, Swain D. Nature and Consequences of Support Workers in a Hospital Setting. Final Report 2010. www.netscc.ac.uk/hsdr/files/project/SDO_FR_08-1619-155_V01.pdf (accessed October 2017).
- Spilsbury K, Adamson J, Atkin K, Bartlett C, Bloor K, Borglin G, et al. Evaluation of the Development and Impact of Assistant Practitioners Supporting the Work of Ward-Based Registered Nurses in Acute NHS (Hospital) Trusts in England 2010. www.nets.nihr.ac.uk/projects/hsdr/081619159 (accessed October 2017).
- Department for Environment, Food & Rural Affairs . Official Statistics 2011. Rural–Urban Classification of Local Authorities and Other Geographies 2014. www.gov.uk/government/statistics/2011-rural-urban-classification-of-local-authority-and-other-higher-level-geographies-for-statistical-purposes (accessed October 2017).
- NHS Digital . NHS Hospital &Amp; Community Health Service (HCHS): HCHS Doctors, by Grade and Organisation, in NHS Trusts and CCGs in England, As at 31 January to 31 December 2016, Average Full Time Equivalent n.d. https://digital.nhs.uk/catalogue/PUB23470 (accessed October 2017).
- Kvale S. Doing Interviews. London: Sage Publications; 2007.
- Boyatzis RE. Transforming Qualitative Information: Thematic Analysis and Code Development. Thousand Oaks, CA: Sage; 1998.
- Pope C, Mays N, Pope C, Mays N. Qualitative Research in Health Care. Chichester: John Wiley & Sons; 2008.
- McCann, L, Granter E, Hyde P, Hassard, J. Still blue-collar after all these years? An ethnography of the professionalization of emergency ambulance work. Journal of Management Studies 2013;50:750-76. https://doi.org/10.1111/joms.12009.
- Department of Health and Social Care Urgent and Emergency Care Review Team . Safer, Faster, Better: Good Practice in Delivering Urgent and Emergency Care n.d. https://improvement.nhs.uk/resources/safer-faster-better-transforming-urgent-and-emergency/ (accessed 7 March 2019).
- Gipsen K. Presentation at the Physician Assistant in the Workforce Conference. Birmingham: University of Birmingham; 2014.
- Sakr M, Angus J, Perrin J, Nixon C, Nicholl J, Wardrope J. Care of minor injuries by emergency nurse practitioners or junior doctors: a randomised controlled trial. Lancet 1999;354:1321-6. https://doi.org/10.1016/S0140-6736(99)02447-2.
- Cooper MA, Lindsay GM, Kinn S, Swann IJ. Evaluating emergency nurse practitioner services: a randomized controlled trial. J Adv Nurs 2002;40:721-30. https://doi.org/10.1046/j.1365-2648.2002.02431.x.
- A&E Clinical Quality Indicators Data Definition and Implementation Guidance. London: Department of Health; 2010.
- Provisional Accident and Emergency Quality Indicators – England, by Provider for December 2014. Leeds: NHS Digital; 2015.
- Gardner MJ, Altman DG. Confidence intervals rather than P values: estimation rather than hypothesis testing. Br Med J 1986;292:746-50. https://doi.org/10.1136/bmj.292.6522.746.
- Vittinghoff E, McCulloch CE. Relaxing the rule of ten events per variable in logistic and Cox regression. Am J Epidemiol 2007;165:710-18. https://doi.org/10.1093/aje/kwk052.
- Mackway-Jones K, Marsden J, Windle J. Emergency Triage: Manchester Triage Group. London: John Wiley & Sons; 2013.
- National Early Warning Score (NEWS): Standardising the Assessment of Acute Illness Severity in the NHS. London: RCP; 2012.
- Curtis L, Burns A. Unit Costs of Health and Social Care 2017. Canterbury: Personal Social Services Research Unit, University of Kent; 2017.
- NHS Reference Costs 2016. London: Department of Health; 2016.
- Mauskopf JA, Paul JE, Grant DM, Stergachis A. The role of cost-consequence analysis in healthcare decision-making. PharmacoEconomics 1998;13:277-88. https://doi.org/10.2165/00019053-199813030-00002.
- Medical Research Council . Good Research Practice: Principles and Guidelines 2012. www.mrc.ac.uk/research/policies-and-guidance-for-researchers/good-research-practice/ (accessed October 2017).
- Data Protection Act 1998. London: The Stationery Office; 1998.
- Arnopolin SL, Smithline HA. Patient care by physician assistants and by physicians in an emergency department. JAAPA 2000;13:39-40.
- Ducharme J, Alder RJ, Pelletier C, Murray D, Tepper J. The impact on patient flow after the integration of nurse practitioners and physician assistants in 6 Ontario emergency departments. CJEM 2009;11:455-61. https://doi.org/10.1017/S1481803500011659.
- Hooker RS, Cipher DJ, Cawley JF, Herrmann D, Melson J. Emergency medicine services: interprofessional care trends. J Interprof Care 2008;22:167-78. https://doi.org/10.1080/13561820701751468.
- Kozlowski MJ, Wiater JG, Pasqual RG, Compton S, Swor RA, Jackson RE. Painful discrimination: the differential use of analgesia in isolated lower limb injuries. Am J Emerg Med 2002;20:502-5. https://doi.org/10.1053/ajem.2002.34965.
- Pavlik D, Sacchetti A, Seymour A, Blass B. Physician assistant management of pediatric patients in a general community emergency department: a real-world analysis. Pediatr Emerg Care 2017;33:26-30. https://doi.org/10.1097/PEC.0000000000000949.
- Ritsema TS, Kelen GD, Pronovost PJ, Pham JC. The national trend in quality of emergency department pain management for long bone fractures. Acad Emerg Med 2007;14:163-9. https://doi.org/10.1197/j.aem.2006.08.015.
- Singer AJ, Hollander JE, Cassara G, Valentine SM, Thode HC, Henry MC. Level of training, wound care practices, and infection rates. Am J Emerg Med 1995;13:265-8. https://doi.org/10.1016/0735-6757(95)90197-3.
- Bohm ER, Dunbar M, Pitman D, Rhule C, Araneta J. Experience with physician assistants in a Canadian arthroplasty program. Can J Surg 2010;53:103-8.
- Garrison S, Eismann EA, Cornwall R. Does using PAs in the closed treatment of pediatric forearm fractures increase malunion risk?. JAAPA 2017;30:41-5. https://doi.org/10.1097/01.JAA.0000526777.00101.b9.
- Hepp SL, Suter E, Nagy D, Knorren T, Bergman JW. Utilizing the physician assistant role: case study in an upper-extremity orthopedic surgical program. Can J Surg 2017;60:115-21. https://doi.org/10.1503/cjs.002716.
- Mains C, Scarborough K, Bar-Or R, Hawkes A, Huber J, Bourg P, et al. Staff commitment to trauma care improves mortality and length of stay at a level I trauma center. J Trauma 2009;66:1315-20. https://doi.org/10.1097/TA.0b013e31819d96d8.
- Oswanski MF, Sharma OP, Raj SS. Comparative review of use of physician assistants in a level I trauma center. Am Surg 2004;70:272-9.
- Capstack TM, Seguija C, Vollono LM, Moser JD, Meisenberg BR, Michtalik HJ. A comparison of conventional and expanded physician assistant hospitalist staffing models at a community hospital. J Clin Outcomes 2016;23:455-61.
- Van Rhee J, Ritchie J, Eward AM. Resource use by physician assistant services versus teaching services. JAAPA 2002;15:33-8.
- McCutchen B, Patel S, Copeland D. Expanding the role of PAs in the treatment of severe and persistent mental illness. JAAPA 2017;30:36-7. https://doi.org/10.1097/01.JAA.0000521138.61409.04.
- Halter M, Wheeler C, Pelone F, Gage H, de Lusignan S, Parle J, et al. Contribution of physician assistants/associates to secondary care: a systematic review. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2017-019573.
- Timmermans MJC, van Vught AJAH, Peters YAS, Meermans G, Peute JGM, Postma CT, et al. The impact of the implementation of physician assistants in inpatient care: a multicenter matched-controlled study. PLOS ONE 2017;12. https://doi.org/10.1371/journal.pone.0178212.
- Timmermans MJC, van den Brink GT, van Vught AJAH, Adang E, van Berlo CLH, Boxtel KV, et al. The involvement of physician assistants in inpatient care in hospitals in the Netherlands: a cost-effectiveness analysis. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2017-016405.
- Hunt J. Department of Health . New Deal for General Practice 2015. www.gov.uk/government/speeches/new-deal-for-general-practice (accessed November 2017).
- Hunt J. Department of Health . NHS Providers Annual Conference Keynote Speech 30-11-2016 2016. www.gov.uk/government/speeches/nhs-providers-annual-conference-keynote-speech (accessed November 2017).
- Hunt J. Department of Health . Jeremy Hunt Speech to the Royal College of General Practitioners 12-10-2017 2017. www.gov.uk/government/news/jeremy-hunt-announces-salary-supplement-for-trainee-gps (accessed November 2017).
- House of Commons . Health Select Committee Report on Primary Care. HC408 2016. https://publications.parliament.uk/pa/cm201516/cmselect/cmhealth/408/40802.htm (accessed November 2017).
- Department of Health . The Regulation of Medical Associate Professions in the UK: Open Consultation 2017. www.gov.uk/government/consultations/regulating-medical-associate-professions-in-the-uk (accessed November 2017).
- NHS England . General Practice Forward View 2016. www.england.nhs.uk/gp/gpfv/ (accessed November 2017).
- NHS England . The Forward View into Action: Planning for 2015 16 2014. www.england.nhs.uk/publication/the-forward-view-into-action-planning-for-201516/ (accessed March 2018).
- NHS England . Next Steps in the Five Year Plan 2017. www.england.nhs.uk/five-year-forward-view/next-steps-on-the-nhs-five-year-forward-view/ (accessed November 2017).
- Health Education England . Workforce Plan 2014–2015 2014. https://hee.nhs.uk/our-work/planning-commissioning/workforce-planning (accessed November 2017).
- Health Education England . Workforce Plan 2015–2016 2015. https://hee.nhs.uk/our-work/planning-commissioning/workforce-planning (accessed November 2017).
- Health Education England . Workforce Plan 2016–2017 2016. https://hee.nhs.uk/our-work/planning-commissioning/workforce-planning (accessed November 2017).
- Health Education England . Business Plan 2015 n.d. https://hee.nhs.uk/our-work/planning-commissioning/our-business-plan (accessed November 2017).
- Health Education England . Response to the Primary Care Workforce Commission Report 2016. https://hee.nhs.uk/our-work/hospitals-primary-community-care/primary-community-care/primary-care-workforce-commission (accessed November 2017).
- Health Education England . General Practice Nursing Workforce Development Plan 2017. https://hee.nhs.uk/our-work/hospitals-primary-community-care/primary-community-care/general-practice-nursing (accessed November 2017).
- Health Education England . Regulation Consultation Risk Profiles for the Medical Associate Professions 2017. www.gov.uk/government/consultations/regulating-medical-associate-professions-in-the-uk (accessed November 2017).
- NHS England, Health Education England, British Medical Association, Royal College of General Practitioners . Building the Workforce: The New Deal for General Practice 2015. www.england.nhs.uk/commissioning/wp-content/uploads/sites/12/2015/01/building-the-workforce-new-deal-gp.pdf (accessed November 2017).
- Aiello M, Roberts KA. Development of the United Kingdom physician associate profession. JAAPA 2017;30:1-8. https://doi.org/10.1097/01.JAA.0000513357.68395.12.
- NHS England . Delivering the Forward View: NHS Planning Guidance 2016 17–2020 21 2019. www.england.nhs.uk/wp-content/uploads/2015/12/planning-guid-16-17-20-21.pdf (accessed November 2017).
- NHS England . Local Sustainability and Transformation Partnerships n.d. www.england.nhs.uk/stps/view-stps/ (accessed 5 February 2019).
- Hunt J. NHS 7 Day Services and the Junior Doctors’ Strike. London: Department of Health; 2016.
- Monitor, NHS Trust Development Authority . Supporting the Role of the Medical Director 2014. www.gov.uk/government/publications/supporting-the-role-of-the-medical-director (accessed November 2017).
- Moote M, Krsek C, Kleinpell R, Todd B. Physician assistant and nurse practitioner utilization in academic medical centers. Am J Med Qual 2011;26:452-60. https://doi.org/10.1177/1062860611402984.
- Halter M, Wheeler C, Drennan VM, de Lusignan S, Grant R, Gabe J, et al. Physician associates in England’s hospitals: a survey of medical directors exploring current usage and factors affecting recruitment. Clin Med 2017;17:126-31. https://doi.org/10.7861/clinmedicine.17-2-126.
- Wheeler C, Halter M, Drennan VM, de Lusignan S, Grant R, Gabe J, et al. Physician associates working in secondary care teams in England: interprofessional implications from a national survey. J Interprof Care 2017;31:774-6. https://doi.org/10.1080/13561820.2017.1341390.
- Nagurney JT, Brown DF, Sane S, Weiner JB, Wang AC, Chang Y. The accuracy and completeness of data collected by prospective and retrospective methods. Acad Emerg Med 2005;12:884-95. https://doi.org/10.1197/j.aem.2005.04.021.
- Ratnapalan S, Brown K, Cieslak P, Cohen-Silver J, Jarvis A, Mounstephen W. Charting errors in a teaching hospital. Pediatr Emerg Care 2012;28:268-71. https://doi.org/10.1097/PEC.0b013e3182494fb8.
- Fleiss JL. Measuring nominal scale agreement among many raters. Psychol Bull 1971;5:378-82. https://doi.org/10.1037/h0031619.
- Altman D. Practical Statistics for Medical Research. London: Chapman & Hall; 1991.
- NHS Health Careers . Physician Associates: Pay and Conditions 2018. www.healthcareers.nhs.uk/explore-roles/medical-associate-professions/roles-medical-associate-professions/physician-associate (accessed January 2018).
- NHS Digital . NHS Staff Earnings Estimates, December 2017, Provisional Statistics 2009–2017 2018. https://digital.nhs.uk/data-and-information/publications/statistical/nhs-staff-earnings-estimates/nhs-staff-earnings-estimates-december-2017-provisional-statistics (accessed 15 April 2019).
- NHS Employers . Pay and Conditions Circular (Medical &Amp; Dental Staff) 1 2017 2018. www.nhsemployers.org/case-studies-and-resources/2018/03/pay-and-conditions-circular-md-1-2017 (accessed 2 August 2018).
- van Vught AJ, van den Brink GT, Wobbes T. Implementation of the physician assistant in Dutch health care organizations: primary motives and outcomes. Health Care Manag 2014;33:149-53. https://doi.org/10.1097/01.HCM.0000440621.39514.9f.
- Fréchette D, Shrichand A. Insights into the physician assistant profession in Canada. JAAPA 2016;29:35-9. https://doi.org/10.1097/01.JAA.0000484302.35696.cd.
- Health Education England . Facing the Facts, Shaping the Future. A Draft Health and Care Workforce Strategy for England to 2027 2017. https://hee.nhs.uk/our-work/workforce-strategy (accessed 15 April 2019).
- Kartha A, Restuccia JD, Burgess JF, Benzer J, Glasgow J, Hockenberry J, et al. Nurse practitioner and physician assistant scope of practice in 118 acute care hospitals. J Hosp Med 2014;9:615-20. https://doi.org/10.1002/jhm.2231.
- Timmermans MJ, van Vught AJ, Van den Berg M, Ponfoort ED, Riemens F, van Unen J, et al. Physician assistants in medical ward care: a descriptive study of the situation in the Netherlands. J Eval Clin Pract 2016;22:395-402. https://doi.org/10.1111/jep.12499.
- Timmermans MJ, van Vught AJ, Maassen IT, Draaijer L, Hoofwijk AG, Spanier M, et al. Determinants of the sustained employment of physician assistants in hospitals: a qualitative study. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2016-011949.
- Ten Cate O. Nuts and bolts of entrustable professional activities. J Grad Med Educ 2013;5:157-8. https://doi.org/10.4300/JGME-D-12-00380.1.
- NHS Health Careers . Course Finder Physician Associates Studies n.d. www.healthcareers.nhs.uk/career-planning/course-finder (accessed January 2018).
- Department of Health and Social Care . The Regulation of Medical Associate Professionals in the UK 2019. www.gov.uk/government/consultations/regulating-medical-associate-professions-in-the-uk#history (accessed 4 April 2019).
- Gershengorn HB, Johnson MP, Factor P. The use of nonphysician providers in adult intensive care units. Am J Respir Crit Care Med 2012;185:600-5. https://doi.org/10.1164/rccm.201107-1261CP.
- Johal J, Dodd A. Physician extenders on surgical services: a systematic review. Can J Surg 2017;60:172-8. https://doi.org/10.1503/cjs.001516.
- Iles V, Sutherland K. Organisational Change. A Review for Health Care Managers, Professionals and Researchers 2001. www.netscc.ac.uk/hsdr/files/adhoc/change-management-review.pdf (accessed January 2018).
- Jones IW, Hooker RS. Physician assistants in Canada: update on health policy initiatives. Can Fam Physician 2011;57:e83-8.
- Ballweg R, Metzler K. Physician Assistant Staffing in a Rural New Zealand Hospital n.d. www.ruralhealth.org.au/14nrhc/sites/default/files/Ballweg%2C%20Ruth_E2.pdf (accessed January 2018).
- Netherlands Association of Physician Assistants . Independency of Physician Assistants (PA) and Nurse Practitioners (NP) Regulated in the Netherlands 2017. www.napa.nl/english/ (accessed December 2017).
- Ritsema TS, Roberts KA. Job satisfaction among British physician associates. Clin Med 2016;16:511-13. https://doi.org/10.7861/clinmedicine.16-6-511.
- Royal College of Physicians . Census of Consultant Physicians and Higher Specialty Trainees in the UK 2014–15 Executive Summary 2016. www.rcplondon.ac.uk/news/one-fifth-consultants-state-rota-gaps-are-causing-significant-problems-patient-safety (accessed January 2018).
- General Medical Council . GMC Urges Doctors in Training to Share Their Experiences of Rota Gaps 2017. www.gmc-uk.org/news/29301.asp (accessed January 2018).
- NHS Improvement . Reducing Expenditure on NHS Agency Staff: Rules and Price Caps n.d. https://improvement.nhs.uk/resources/reducing-expenditure-on-nhs-agency-staff-rules-and-price-caps/ (accessed January 2018).
- Royal College of Physicians . Being a Junior Doctor: Experiences from the Front Line of the NHS 2016. www.rcplondon.ac.uk/guidelines-policy/being-junior-doctor (accessed January 2018).
- Tipping MD, Forth VE, Magill DB, Englert K, Williams MV. Systematic review of time studies evaluating physicians in the hospital setting. J Hosp Med 2010;5:353-9. https://doi.org/10.1002/jhm.647.
- Newton R, Panchal M, Ahmed N, Yuen S, Thalava R, Puttha R. Safety and health care professionals: satisfaction of the task based role of physician associates, supplementing doctors, in a paediatric unit. Arch Dis Child 2017;102:A1-A218.
- Department of Health . Operational Productivity and Performance in English NHS Acute Hospitals: Unwarranted Variations 2015. www.gov.uk/government/publications/productivity-in-nhs-hospitals (accessed January 2018).
- BBC News . NHS Agency Pay Caps Breached More Than 50,000 Times a Week 2016. www.bbc.co.uk/news/uk-england-36341285 (accessed January 2018).
- Liaison . Taking the Temperature: Review of NHS Agency Spending 2017 2018-Q3 2018. http://liaison.co.uk/taking-the-temperature-update-2017-18-q3/ (accessed March 2018).
- Schadewaldt V, McInnes E, Hiller JE, Gardner A. Views and experiences of nurse practitioners and medical practitioners with collaborative practice in primary health care – an integrative review. BMC Fam Pract 2013;14. https://doi.org/10.1186/1471-2296-14-132.
- Organisation for Economic Co-operation and Development (OECD) . Health Workforce Policies in OECD Countries: Right Jobs, Right Skills, Right Places 2016. www.oecd.org/health/health-systems/health-workforce-policies-in-oecd-countries-9789264239517-en.htm (accessed January 2018).
- McNally S, Huber J. Award-winning new doctors’ assistants freeing time in acute NHS hospitals; pilot reduces doctor overtime and improves efficiency. Health Management 2018;1:56-9. https://healthmanagement.org/c/healthmanagement/issuearticle/award-winning-new-doctors-assistants-freeing-time-in-acute-nhs-hospitals (accessed January 2018).
- Grover A, Orlowski JM, Erikson CE. The nation’s physician workforce and future challenges. Am J Med Sci 2016;351:11-9. https://doi.org/10.1016/j.amjms.2015.10.009.
- Department of Health . Up to 1,500 Extra Medical Training Places Announced 2016. www.gov.uk/government/news/up-to-1500-extra-medical-training-places-announced (accessed January 2018).
- General Medical Council . The State of Medical Education and Practice in the UK 2017. www.gmc-uk.org/publications/somep.asp (accessed January 2018).
- Rivett G. From Cradle to Grave: Fifty Years of the NHS. London: The King’s Fund; 1998.
- Department of Health, Monitor . NHS Providers Urged to Take More Action to Counter Pressures 2016. www.gov.uk/government/news/nhs-providers-urged-to-take-more-action-to-counter-pressures (accessed January 2018).
- BBC News . Junior Doctors’ Strike: All-Out Stoppage ‘A Bleak Day’ 2016. www.bbc.co.uk/news/health-36134103 (accessed January 2018).
- House of Commons . NHS Winter Pressures: 2016 17 Summary Commons Briefing Papers SN07057 2017. https://researchbriefings.parliament.uk/ResearchBriefing/Summary/SN07057 (accessed January 2018).
- House of Commons . NHS Winter Pressures: 2017 18 Summary Commons Briefing Papers. Commons Briefing Papers CBP-8210 2018. https://researchbriefings.parliament.uk/ResearchBriefing/Summary/CBP-8210 (accessed January 2018).
- BBC News . Thousands of NHS Nursing and Doctor Posts Lie Vacant 2016. www.bbc.co.uk/news/health-35667939 (accessed January 2018).
- Hemming K, Haines TP, Chilton PJ, Girling AJ, Lilford RJ. The stepped wedge cluster randomised trial: rationale, design, analysis, and reporting. BMJ 2015;350. https://doi.org/10.1136/bmj.h391.
Appendix 1 Terms of reference for the advisory group and the public and patient involvement group
Advisory group terms of reference
The role
The advisory group will provide critical (but friendly) oversight and advice to the researchers across the breadth of the study. The group will:
-
offer comment and advice on the overall conduct and progress of the research
-
offer comment and advice on the research questions, methods, findings and outputs
-
exchanging ideas and information while ensuring the confidentiality of the research and any other information shared within the meetings
-
offer comment and advice on the dissemination of the research.
The membership
This will include:
-
members of public and patient organisations with particular interests in secondary care provision
-
members of professional organisations with particular interests in secondary care provision
-
members or staff of NHS bodies with a particular remit for workforce development
-
academics both with educational interests and research interests in the PA role.
Frequency and duration of meetings
The group will meet three times over the course of the study (winter 2015 – autumn 2017) for 1 and a half hours per meeting.
Expenses
Expenses will be met.
Funding acknowledgement and disclaimer. The study is called Health Services and Delivery Research programme project: 14/19/26 – Investigating the contribution of physician associates (PAs) to secondary care in England: a mixed methods study. This is independent research funded by the National Institute for Health Research (NIHR) (URL: www.nets.nihr.ac.uk/projectshsdr/141926/; accessed 1 October 2015).
Public and patient involvement group information and terms of reference
Background to the research study
This research study is investigating the contribution of PAs within hospital medical teams in England. PAs are a relatively new, and yet rapidly growing, health profession within the NHS.
Attached to this e-mail is a two-page description of why we are doing the study, how we will be doing it and who the research team and funders are.
Your involvement
We are asking approximately 12 individuals who have expressed an interest in research within the faculty to contribute to this study through the form of a service user group. We are having two of these groups: one in London and one in the West Midlands.
We would ask you to attend four meetings throughout the duration of the study (concluding September 2017). Meetings will take place at [insert] and last no longer than 3 hours. At these meetings we will provide progress updates on the study and would ask you to share your views. There may also be a small amount of reading of study documents required in preparation for each meeting. All discussions within meetings will remain confidential to the group.
The first meeting will take place in the afternoon of [date].
Expenses
In recognition of your time and experience, you would be paid £20 for each meeting that you attend. In addition, your travel expenses to and from each meeting would also be covered.
Next steps and further information
Also attached to this e-mail is a guide for public involvement for you to read for your information.
If you are interested in participating in this service user group, please reply to this e-mail and we will arrange a convenient time to contact you by telephone to discuss the role further.
In addition, if you have any further questions or require more information about the research study or your involvement as part of the service user group, you can also contact the project manager, Dr Mary Halter, using the following details.
Thank you for taking the time to read this and we look forward to hearing from you.
Kind regards,
Professor Vari Drennan, Principal Investigator and Professor of Health Care and Policy Research.
Funding acknowledgement and disclaimer. The study is called Health Services and Delivery Research programme project: 14/19/26 – Investigating the contribution of physician associates (PAs) to secondary care in England: a mixed methods study. This is independent research funded by the National Institute for Health Research (NIHR) (URL: www.journalslibrary.nihr.ac.uk/programmes/hsdr/141926/#/; accessed 7 March 2019).
Appendix 2 Electronic survey of medical directors
Appendix 3 The physician associate survey
Thank you for your interest in completing our survey. You are being invited to take part in this study exploring the contribution that PAs make to clinical teams in secondary care. We are inviting all PAs who are currently working in secondary care in England to participate. This survey is designed to complement the annual census conducted by the Faculty of Physician Associates at the Royal College of Physicians, by gathering additional information about your role for the research study outlined in the e-mail and information sheet. We are looking to explore the specialties that PAs are working in within secondary care, as well as the wider context of deployment.
This survey is anonymous. However, at the end of the survey you will be invited to e-mail the research team in order to be entered into a prize draw to win a £40 book voucher, receive continuing information regarding the project and/or to participate further. If you have any queries or concerns, please do not hesitate to contact me:
Vari Drennan, Principal Investigator and Professor of Health Care & Policy Research, Kingston University and St George’s, University of London [contact details].
Physician associates in secondary care research: physician associate survey
1. Which country are you currently practising in as a PA?
-
England
-
other.
If other – thank you for your interest in our research into PAs in secondary care; however, at the present time we are only able to survey PAs working in England. If you are interested in keeping up to date with the study’s progress, please contact [contact details].
2. As a PA, do you practise in a single job or multiple jobs?
-
single
-
multiple (please specify how many).
3. Which specialty are you working in for each job? Full list of specialties given as drop-down list (e.g. Accident & Emergency, General Acute, Paediatric Accident & Emergency, Acute Medicine, Acute Internal Medicine, Allergy, Cardiology Diabetes, Dermatology, Elderly Care Medicine, etc.)
4. Please select which setting(s) you currently work in (please answer for each job if you work in more than one):
-
emergency department
-
inpatient ward
-
intensive care unit
-
medical assessment unit
-
operating theatre
-
outpatients
-
rehabilitation
-
walk in/out of hours
-
other (please specify).
5. Is the specialty you are currently working in part of a rotation?
-
yes
-
no.
6. If you are on a rotation programme, how long is the programme (in months)?
-
less than 12
-
12–23
-
24–35
-
36 or more.
7. In addition to your current specialty, what other specialties does your rotation programme include? Free-text response
8. Which other health-care professionals make up the specialty consultant-led team in which you work?
-
clinical nurse specialist(s)
-
Foundation Year 1 doctor(s)
-
Foundation Year 2 doctor(s)
-
medical consultant(s)
-
non-career grade doctor(s)
-
physician associate(s)
-
specialty training doctor(s)
-
other(s) – please specify
-
please provide further information if you selected ‘other’.
9. Which type of health-care professional is your line manager?
-
a medical consultant
-
another grade of doctor
-
another type of clinical manager
-
other (please specify).
10. Please can you describe your clinical supervision arrangements day to day/on each shift.
-
e.g. I am supervised by the consultant in charge of the team on each shift.
-
e.g. I am supervised by the registrar on the team when working on the ward and by the consultant when in clinic or theatre.
11. Please can you describe your ongoing clinical/educational supervision.
-
e.g. None, I am only supervised day to day.
-
e.g. I have a clinical supervisor who I go to for XYZ and an educational supervisor who I discuss XYZ with.
-
e.g. I have a lead consultant who I meet with weekly/monthly.
12. Thinking back over the last 4 weeks, please indicate the number of day and night shifts you worked for weekdays and weekends (with week 4 being the most recent week). Drop-down menu.
13. Please describe in broad terms a typical work shift for you.
-
e.g. all shift – working in A&E minors seeing next-in-turn patients
-
e.g. morning – part of consultant ward round; follow-up items from the round such as ordering tests
-
e.g. afternoon – outpatients clinic; meeting with consultant.
14. Are there any factors that change the type of work that you do? – e.g. sickness within the clinical team.
-
yes (if yes please add details)
-
no.
Please could you provide some information regarding the hospital that you work in.
15. Is your hospital acute or mental health?
-
acute
-
mental health.
16. Approximately how many beds does your hospital contain? Drop-down list of numbers.
17. What is the length of your experience post qualification (in years)?
18. In which country did you undertake your PA training?
-
United Kingdom
-
United States of America
-
other (please specify).
19. If you have any additional comments relating to your work role or deployment as a PA, please leave them below.
END OF SURVEY
Thank you for your time and help.
We have a number of reasons why you might wish for us to have your contact details, as follows:
-
You would like to be entered into the prize draw for a £40 book voucher.
-
You may be interested in hearing more about case study work we are aiming to undertake with hospitals that employ PAs.
-
You would like to be kept informed of the study’s progress via newsletters.
-
You would like to see the report of this survey.
As this survey is anonymous please click the following link to provide us with your contact [click here].
Alternatively, you can e-mail us at any time: [contact details].
Appendix 4 Systematic review: example of full search strategy
MEDLINE
Date searched: 24 November 2015.
Date range searched: 1 January 1995 to 1 January 2018.
Preliminary search strategy
| Number and concept | Search terms | Results |
|---|---|---|
| Physician associates | ||
| 1 | exp Physician Assistants/ | 2410 |
| 2 | exp Pediatric Assistants/ | 26 |
| 3 | Physician Assistant$.tw. | 1498 |
| 4 | Feldsher$.tw. | 17 |
| 5 | Clinical Officer$.tw. | 135 |
| 6 | Paramedical Practitioner&.tw. | 0 |
| 7 | Medical Assistant$.tw. | 324 |
| 8 | Allied Health Personnel.tw. | 48 |
| 9 | physician associate$.tw. | 37 |
| 10 | (mid level adj3 provider$).tw. | 124 |
| 11 | ((assistant* or technician* or officer* or associate$) adj2 (physician$ or surgical or clinical$ or practit0069oner$ or medical$ or provider$)).tw. | 24,985 |
| Secondary care | ||
| Emergency medicine | ||
| 12 | exp Emergency Medicine/ and (speciali?ed or specialty or hospital$ or secondary or care or medicine).tw. | 4983 |
| 13 | ((accident and emergency) or A&E department or emergency department or casualty or emergency Medicine).tw. | 47,842 |
| 14 | (emergency adj3 (medic* or servic* or ward* or department)).tw. | 54,262 |
| 15 | (exp critical care/ or exp intensive care/) and (speciali?ed or specialty or hospital$ or secondary or care or medicine).tw. | 23,791 |
| 16 | ((intensive adj3 care) and (speciali?ed or specialty or hospital$ or secondary or care or medicine)).tw. | 71,552 |
| Acute medicine | ||
| 17 | exp Internal Medicine/ and (speciali?ed or specialty or hospital$ or secondary or care or medicine).tw. | 16,968 |
| 18 | (internal medicine and (speciali?ed or specialty or hospital$ or secondary or care or medicine)).tw. | 10,752 |
| 19 | (Acute Medicine or acute internal medicine or acute medical unit$or medical assessment unit$ or acute ward$).tw. | 690 |
| Trauma or orthopaedics | ||
| 20 | (exp Orthopedics/or exp Traumatology/) and (speciali?ed or specialty or hospital$ or secondary or care or medicine).tw. | 3015 |
| 21 | ((Trauma or Orthop?dic$) adj3 (speciali?ed or specialty or hospital$or secondary or care or medicine)).tw. | 7280 |
| 22 | (Orthop?dic surgery or trauma surgery).tw. | 4466 |
| 23 | ((bone$ or joint$ or ligament$ or tendon$ or muscle$ or nerve$) adj3 (operation$or surgery or replacement$)).tw. | 13,668 |
| Care of the elderly | ||
| 24 | (exp geriatrics/ or Ageing/ or exp Aged/or older people.mp. or exp Frail Elderly/) and (speciali?ed or specialty or hospital$ or secondary or care).tw. | 361,294 |
| 25 | ((Older adult or Aged or elderly or geriatric* or older people* or ag?ng) adj3 (speciali?ed or specialty or hospital$ or secondary or care or medicine)).tw. | 15,561 |
| 26 | or/12-25 | 508,965 |
| Primary care | ||
| 27 | exp Primary Health Care/ or exp preventive medicine/ or exp physicians, Primary Care/ | 75,166 |
| 28 | (primary care or primary healthcare or primary health care or primary health service$).tw. | 68,593 |
| 29 | 27 or 28 | 111,510 |
| 30 | exp Family Practice/ or exp Physicians, Family/or exp General Practitioners/or exp General Practice/ | 47,498 |
| 31 | (family practice$ or family practitioner$ or family physician$ family medicine$ or General practice$ or General practitioner$ or GPs).tw. | 47,129 |
| 32 | 30 or 31 | 72,038 |
| 33 | 29 not 32 | 91,680 |
| Outpatient and inpatient care | ||
| 34 | (exp Outpatients/ or Outpatient Clinics, Hospital/ or ambulatory care/) and (speciali?ed or specialty or hospital$ or secondary or care or medicine).tw. | 18,427 |
| 35 | (exp Inpatients/ or Hospitalization /) and (speciali?ed or specialty or hospital$ or secondary or care or medicine).tw. | 49,797 |
| 36 | (ambulatory care or ambulatory emergency care).tw. | 3948 |
| Impact | ||
| 37 | ((outpatient$ or out-patient$) adj3 (speciali?ed or specialty or hospital$ or secondary or care or medicine)).tw. | 11,455 |
| 38 | ((inpatient$ or in-patient$) adj3 (speciali?ed or specialty or hospital$or secondary or care or medicine)).tw. | 24,157 |
| 39 | Treatment Outcome/ or “Outcome and Process Assessment (Health Care)”/ or “Outcome Assessment (Health Care)”/ or Medical Audit/ or Program Evaluation/ | 769,470 |
| 40 | exp Patient Readmission/ or exp Length of Stay/ or exp Clinical Audit/or exp Medical Audit/ | 68,267 |
| 41 | Health Planning/and (organi?ation* or system* or hospital* or Physician* or workforce or staff or professional*).tw. | 2686 |
| 42 | Efficiency, Organizational/ and (organi?ation* or system* or hospital* or Physician* or workforce or staff or professional*).tw. | 8952 |
| 43 | Resource Allocation/ and (organi?ation* or system* or hospital* or Physician* or workforce or staff or professional*).tw. | 1377 |
| 44 | Health Personnel/ and (organi?ation* or system* or hospital* or Physician* or workforce or staff or professional*).tw. | 11,958 |
| 45 | Health Manpower/ and (organi?ation* or system* or hospital* or Physician* or workforce or staff or professional*).tw. | 2123 |
| 46 | Medical Staff/ and (organi?ation* or system* or hospital* or Physician* or workforce or staff or professional*).tw. | 899 |
| 47 | Delivery of Health Care/and (productivity or efficiency or performance or guideline* or quality).tw. | 8411 |
| 48 | ((equity or difference$ disparit$ or inequalit$ or inequit$) adj5 (experience$ or perception$ or view$ or rates or rating or review or audit or impact or influence or effect or outcome or performance or quality)).tw. | 2048 |
| 49 | ((Acceptability or compassion or dignity or satisfaction or dissatisfaction) adj5 (experience$ or perception$ or view$ or rates or rating or review or audit or impact or influence or effect or outcome or performance or quality)).tw. | 16,604 |
| 50 | ((Efficiency or productivity or economic$ or benefit) adj5 (experience$or perception$ or view$ or rates or rating or review or audit or impact or influence or effect or outcome or performance or quality)).tw. | 34,565 |
| 51 | ((Effectiveness or efficacy or effectivity or capability) adj5 (experience$ or perception$ or view$ or rates or rating or review or audit or impact or influence or effect or outcome or performance or quality)).tw. | 35,758 |
| 52 | ((Effectiveness or efficacy or effectivity or capability) adj5 (experience$or perception$ or view$ or rates or rating or review or audit or impact or influence or effect or outcome or performance or quality)).tw. | 35,758 |
| 53 | ((Access$ or responsiveness or timely or timeliness) adj5 (experience$or perception$ or view$ or rates or rating or review or audit or impact or influence or effect or outcome or performance or quality)).tw. | 16,251 |
| 54 | ((Appropriate$ or relevance or relevant) adj5 (experience$ or perception$ or view$ or rates or rating or review or audit or impact or influence or effect or outcome or performance or quality)).tw. | 32,405 |
| 55 | ((Cost$ or afford$ value for money or financ$) adj5 (experience$ or perception$ or view$ or rates or rating or review or audit or impact or influence or effect or outcome or performance or quality)).tw. | 33,373 |
| Impact in secondary care of PAs | ||
| 56 | or/1-11 | 26,515 |
| 57 | 26 or 33 or 34 or 35 or 36 or 37 or 38 | 621,770 |
| 58 | or/39-55 | 959,419 |
| 59 | 56 and 57 and 58 | 1575 |
| 60 | limit 59 to (english language and last 20 years) | 1513 |
Appendix 5 Topic guides for semistructured interviews
Patient interviews
Instructions for the researcher
Confirm that the interviewee understands:
-
the purpose of the research
-
what the interview entails
-
how confidentiality and anonymity will be assured
-
that they can stop at any time without explanation.
And that:
-
they have had the chance to ask questions
-
they are content to be recorded digitally (or not)
-
confirm that the consent form is signed.
Topic areas:
-
Confirm that the person is/has been a patient.
-
Ask them to outline the type of care they have been in receipt of without giving personal medical details (e.g. inpatient for X days).
-
Confirm that the patient has met the PA.
-
Explore what sort of involvement the PA has had with them.
-
Ask them how they understand the role of the PA in the medical/surgical team.
-
Ask them how they found receiving care from a PA.
-
If they were to need similar medical or surgical care, would they be content to receive similar care from a PA in the future as they had this time (and can they explain why) or would they prefer someone different? And if yes, can they explain why?
-
Anything else they would like to say?
Interviewer to probe on all answers to ensure that the meaning is clear (e.g. that is an interesting point, can you explain a bit more about it) and check for understanding (e.g. so can I check I have understood you correctly).
Thank them and ask if they would like to receive updates on the study and a final summary of the findings. If so, could they please give contact details, which will be kept separate from the interview data?
Physician associate interviews
Instructions for the researcher
Confirm that the interviewee understands:
-
the purpose of the research
-
what the interview entails
-
how confidentiality and anonymity will be assured
-
that they can stop at any time without explanation.
And that:
-
they have had the chance to ask questions
-
they are content to be recorded digitally (or not)
-
confirm that the consent form is signed.
Topic areas:
-
Ask them to describe how long they have been a PA, how many posts, type and length as a PA.
-
Ask them to describe the work they undertake, with what type of medical/surgical team.
-
Ask about their supervising doctor and arrangements when they are not there.
-
Ask questions on their views of the factors supporting the adoption of the employment of PAs.
-
Ask questions on the factors inhibiting the employment of PAs.
-
Ask how they have been received in the hospital as a new type of health professional?
-
Ask how they explain to patients, family and staff who they are and what a physician associate is.
-
Questions on their views of their or other PAs’ impact on (ask for examples):
-
Organisation of services.
-
Patient experience and outcomes.
-
Other staff.
-
Costs.
-
-
Anything else they would like to say?
Interviewer to probe on all answers to ensure that the meaning is clear (e.g. that is an interesting point, can you explain a bit more about it) and check for understanding (e.g. so can I check I have understood you correctly . . .).
Interviewer to check for any routine management reports or data or evaluations that the hospital team would be willing to share with the researchers.
Thank them and ask if they would like to receive updates on the study and a final summary of the findings. If so, could they please give contact details, which will be kept separate from the interview data?
Staff interviews
Instructions for the researcher
Confirm that the interviewee understands:
-
the purpose of the research
-
what the interview entails
-
how confidentiality and anonymity will be assured
-
that they can stop at any time without explanation.
And that:
-
they have had the chance to ask questions
-
they are content to be recorded digitally (or not)
-
confirm that the consent form is signed.
Topic areas:
-
Confirm the person’s job role.
-
Ask them to describe their involvement with PA employment in the hospital to date.
-
Ask questions on the factors supporting the adoption of the employment of PAs.
-
Ask questions on the factors inhibiting the employment of PAs.
-
Questions on their views of PAs’ impact on (ask for examples):
-
Organisation of services.
-
Boundaries between the job roles of different types of professionals (e.g. with nurses).
-
Patient experience and outcomes.
-
Other staff.
-
Costs.
-
-
Anything else they would like to say?
Interviewer to probe on all answers to ensure that the meaning is clear (e.g. that is an interesting point, can you explain a bit more about it) and check for understanding (e.g. so can I check I have understood you correctly . . .).
Interviewer to check for any routine management reports or data or evaluations that the hospital team would be willing to share with the researchers.
Thank them and ask if they would like to receive updates on the study and a final summary of the findings. If so, could they please give contact details, which will be kept separate from the interview data.
Senior manager and clinician interviews
Instructions for the researcher
Confirm that the interviewee understands:
-
the purpose of the research
-
what the interview entails
-
how confidentiality and anonymity will be assured
-
that they can stop at any time without explanation.
And that:
-
they have had the chance to ask questions
-
they are content to be recorded digitally (or not)
-
confirm that the consent form is signed.
Topic areas:
-
Confirm the person’s job role.
-
Ask them to describe their involvement with PA employment in the hospital to date.
-
Ask questions on the factors supporting the adoption of the employment of PAs.
-
Ask questions on the factors inhibiting the employment of PAs.
-
Questions on their views of PAs’ impact on (ask for examples):
-
Organisation of services.
-
Patient experience and outcomes.
-
Other staff.
-
Costs.
-
-
Anything else they would like to say?
Interviewer to probe on all answers to ensure that the meaning is clear (e.g. that is an interesting point, can you explain a bit more about it) and check for understanding (e.g. so can I check I have understood you correctly . . .).
Interviewer to check for any routine management reports or data or evaluations that the hospital team would be willing to share with the researchers.
Thank them and ask if they would like to receive updates on the study and a final summary of the findings. If so, could they please give contact details, which will be kept separate from the interview data.
Appendix 6 Work diary
Appendix 7 Observation guide
Instructions to researchers for observations/shadowing
Before commencing
-
Check that the PA understands the following and consents to your presence as a volunteer:
-
That you are looking to understand the types of work they do, with whom and in what ways.
-
That all data are confidential and that you are making notes of types of activities, not personal identifying or clinical information about patients.
-
That you are not clinically trained and can make no judgements of their clinical activities.
-
That should you see acts that are of harm or abuse to a vulnerable adult that you have a responsibility to break confidentiality and report this to the appropriate authority as per hospital policy.
-
-
Agree with the PA at the start for how long and how they would like you to shadow them.
-
Check that they know the patient exclusions to observation (no capacity to consent, no sensitive information will be discussed and no intrusive or intimate procedures will be performed).
-
Check that they have the study script to gain verbal consent of patients and staff.
-
Confirm that they have the patient information leaflets to give to patients and relatives.
Answer any questions they have and confirm that they can ask you to stop at any time without having to give a reason.
On commencement
-
Take written notes as able without intruding or soon after of the types for work they do, with whom and in what ways.
-
Do not document any personal information.
-
Note that patient gives verbal consent.
Thank patient and staff and, most of all, the PA at the end.
Script for physician associate to say to patient/family member/staff member to ask for consent to observation
Note: use the term ‘physician associate’ in full when talking to patients/family members rather than abbreviating to ‘PA’.
Physician associate approaches patient and family member first without the researcher and does their usual introduction. Then asks:
I have a researcher shadowing me today as part of a research study investigating the work of physician associates in hospitals. They are looking at the types of work I do and who I interact with. They are taking notes of this but not of any patient’s details. Is it OK if they observe me while I spend time (or more appropriate word) with you? It’s OK for you to say no without giving a reason and it won’t affect your care or my work (or more appropriate word) with you.
Confirm decision – yes – invite the researcher to shadow.
No – do not invite the researcher to shadow and they remain where they are.
Physician associate notes verbal consent in record.
Appendix 8 Clinical review of emergency department records
Microsoft Excel spreadsheet sent to each reviewer to complete for all records. One column for each record – reviewer to fill in ID number.
| Questionsa |
Insert study ID number from top of record Drop down response options followed by a cell for free text if appropriate |
|
| 1 | Record of the patient’s medical history |
Appropriate Or Error or omission – but unlikely to have resulted in harm or different treatment Or An error or omission seen that caused a breach in normal guidelines and procedures that would have altered the patient’s treatment Or An error or omission seen that resulted in significant probability that the patient might be harmed |
| Free text on rationale or comment on response to item 1 | ||
| 2 | Examination of the patient |
Appropriate Or Error or omission – but unlikely to have resulted in harm or different treatment Or An error or omission seen that caused a breach in normal guidelines and procedures that would have altered the patient’s treatment Or An error or omission seen that resulted in significant probability that the patient might be harmed |
| Free text on rationale or comment on response to item 2 | ||
| 3 | Request for radiography |
Appropriate Or Error or omission – but unlikely to have resulted in harm or different treatment Or An error or omission seen that caused a breach in normal guidelines and procedures that would have altered the patient’s treatment Or An error or omission seen that resulted in significant probability that the patient might be harmed |
| Free text on rationale or comment on response to item 3 | ||
| 4 | Treatment plan and decision |
Appropriate Or Error or omission – but unlikely to have resulted in harm or different treatment Or An error or omission seen that caused a breach in normal guidelines and procedures that would have altered the patient’s treatment Or An error or omission seen that resulted in significant probability that the patient might be harmed |
| Free text on rationale or comment on response to item 4 | ||
| 5 | Treatment plan and decision reviewed by senior doctor |
YES Or NO |
| 6 | Advice given |
Appropriate Or Error or omission – but unlikely to have resulted in harm or different treatment Or An error or omission seen that caused a breach in normal guidelines and procedures that would have altered the patient’s treatment Or An error or omission seen that resulted in significant probability that the patient might be harmed |
| Free text on rationale or comment on response to item 6 | ||
| 7 | Follow-up |
Appropriate Or Error or omission – but unlikely to have resulted in harm or different treatment Or An error or omission seen that caused a breach in normal guidelines and procedures that would have altered the patient’s treatment Or An error or omission seen that resulted in significant probability that the patient might be harmed |
| Free text on rationale or comment on response to item 7 | ||
| 8 | In your view what type of clinician attended this patient? |
Doctor Or Physician associate Or Unable to decide |
| Free text on rationale or comment on response to item 8 |
Appendix 9 Emerging-findings seminar
Appendix 10 Characteristics of the included studies in the systematic review
Adapted with permission from Halter et al. 109 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/.
| Study (first author, year and design), by specialty | Study setting | Intervention | Comparison | Participants | Outcome measures |
|---|---|---|---|---|---|
| Emergency medicine | |||||
| Arnopolin 200094 (comparative retrospective) | USA; walk-in urgent care facility | PAs (n = 5) rotate through the ED. PAs work solo from 08.00–12.00 | 25 physicians rotate through the ED. Physicians work solo from 17.00–21.00 | n = 5345 PA patients, n = 4256 physician patients, June 1995 to June 1996 | Length of visit, total charge |
| Ducharme 200995 (descriptive retrospective) | Canada; EDs in six community hospitals | PAs introduced in EDs under the supervision of a physician | Baseline, 2 weeks and 6 months post implementation | Baseline n = 9585, post implementation. n = 10,007, of which PAs involved in care n = 376 | Leaving without being seen, waiting time, length of stay in ED |
| Hooker 200896 (longitudinal) | USA; national sample of EDs, patient-level data survey | PAs as providers of ED care and prescribers of medication (7.9% of patients seen by PAs in 2004) | Physicians and nurse practitioners | Random sample of patient visits to hospital EDs (n = 1,034,758,313), 1995–2004 | Patient contact growth by provider, medication prescriptions and analgesics (non-narcotic, narcotic, NSAID) by provider |
| Kozlowski 200297 (prospective cohort) | USA; one suburban ED | PAs deployed to patients with isolated lower-extremity trauma | Emergency physicians | n = 384 patients survey (n = 227 PA patients, n = 153 physician patients) in a 9-week period | Analgesia prescribing |
| Pavlik 201798 (comparative retrospective) | USA; one general urban ED | PAs under supervision of emergency physician | Attending emergency physician only | n = 2798 PA-only cases; n = 984 PA with emergency physician; n = 6587 emergency physician only | 72-hour revisits to the ED |
| Ritsema 200799 (retrospective cohort) | USA; national sample EDs, patient-level data survey | PAs attending patients with a long bone fracture | Patients presenting to the ED with a long bone fracture not seen by PAs (medical residents, internists) | n = 2064 patients in two time periods: 1998–2000, n = 834, of whom 3% were seen by a PA, 9% by a resident/intern; 2001–3, 8% PA, 10% resident/intern | Patients with long bone fracture receiving analgesia |
| Singer 1995100 (prospective observational) | USA; one urban ED | Patients with lacerations evaluated by an attending physician and assigned to juniors (i.e. PAs, students, interns and residents) | ED patients whose wounds were managed by students, interns and residents | All patients with lacerations attending the ED, n = 1163. n = 901 seen by a PA, n = 262 by other providers October 1992 to November 1993 | Patient wound infection rate |
| Trauma and orthopaedics | |||||
| Althausen 201332 (comparative retrospective) | USA; trauma care at a level II community hospital | Hospital-employed PAs (n = 2) deployed to cover all orthopaedic trauma needs, under the supervision of 1 of 18 orthopaedic surgeons | Attending surgeon | n = 1104, of whom n = 310 were seen by a PA and n = 687 were not seen by a PA | Time to theatre, time in theatre, complication rates, prophylaxis use, length of stay, cost savings |
| Bohm 2010101 (mixed methods) | Canada; one academic hospital arthroplasty programme | Addition of PAs (n = 3) to the operating room team as first assistants |
Costs: GP first assistants in the operating room Waiting time on list |
Patient satisfaction, n = 1070; interviews of health-care providers and patients, n = 44. Costs, n = 402 surgical procedures conducted in 2006. Time savings, n = 1409 procedures carried out 2006. Waiting list in 2006 | Patient satisfaction, perceptions of PAs among health-care providers and patients, costs, time savings, waiting times, throughput |
| Garrison 2017102 (comparative retrospective) | USA; children’s hospital medical centre | PAs carrying out non-operative management of forearm fractures at clinic visits | Attending physician | Patient charts of those aged 3 to 17 years from February 2012 to January 2013 | Fracture malunion |
| Hepp 2017103 (mixed methods) | Canada; subspecialised upper-extremity surgical programme at a peripheral hospital | One PA filling provider gaps in preoperative screening, theatre assist, postoperative care and clinic follow-up | Usual providers without PA | n = 38 interviews; n = 75 surveys (n = 28 from health-care providers and 47 from patients | Perceptions and experiences with the PA, patient rating of quality of care, expected and actual operating room times, total number of new patients seen |
| Mains 2009104 (prospective cohort) | USA; urban, community-based level I trauma centre | Core trauma panel (consisting of full-time, in-house trauma surgeons) plus PAs | Core trauma panel without PAs or residents | n = 15,297 trauma patients | Overall mortality, mortality with injury severity score of > 15, length of stay |
| Oswanski 2004105 (before–after) | USA; level I trauma centre | PAs substituting for doctors in trauma alerts | General and orthopaedic residents who attend in trauma alerts | n = 293 patients before and n = 476 after | Collaborative relationship, transfer time out of ED, length of stay, mortality rates |
| Capstack 2016106 (retrospective comparative) | Expanded PA group (n = 3) in dyads with physicians (n = 3) for inpatient care | Conventional group: nine physicians and two PAs | Patients (discharged January 2012 and June 2013): n = 6612 in expanded PA group and n = 10,352 in conventional group | 30-day all-cause readmission, inpatient mortality, cost of care and consultant/attending use, length of stay | |
| Internal medicine | |||||
| Van Rhee 2002107 (prospective cohort study) | USA; community hospital | The use of PAs (n = 16) in internal medicine department with 64 attending physicians on rotation, scheduled to admit to either a PA or a teaching service | The teaching service (32 intern/residents with an average experience of 1 year post medical school) | Adult patients discharged with diagnosis of: cerebrovascular accident, pneumonia, acute myocardial infarction discharged alive, congestive heart failure, gastrointestinal haemorrhage: n = 923, of whom n = 409 PA and n = 514 teaching service | Relative value units (costs), length of stay |
| Mental health | |||||
| McCutchen 2017108 (qualitative) | Canada; mental health service | A PA supervised by a by a psychiatrist | None | Multidisciplinary team members of assertive community treatment team | Perceived effect and challenges of delivering psychiatric care with the PA model |
Glossary
- Advanced clinical practitioner
- An experienced, registered health and care practitioner educated to master’s level or equivalent whose work is characterised by complex decision-making in an area of specific clinical competence and a high degree of autonomy.
- Advanced nurse practitioner
- An advanced clinical practitioner who is a registered nurse.
- Agenda for Change
- The NHS Terms and Conditions of Service for all staff apart from doctors and dentists.
- Doctor in training
- See Junior doctors.
- European Union Working Time Directive
- A directive that prevents employees from working for excessively long hours. The UK regulations applied to junior doctors from 1 August 2004; by 2009, the majority were working 48-hour weeks.
- Foundation Year doctor
- A newly qualified (junior) doctor who is undergoing a 2-year postgraduate training programme known as Foundation Year 1 and Foundation Year 2. Foundation Year doctors remain under supervision while they gain experience in a variety of medical/surgical specialties and clinical settings.
- Health Education England
- An executive non-departmental public body and an arm’s-length body of the Department of Health and Social Care, providing system-wide leadership and oversight of workforce planning, education and training across England. It is responsible for allocating £4.8B a year to undergraduate and postgraduate education and training of health professionals.
- Junior doctors
- The term used in the UK to refer to all doctors registered with the General Medical Council but not entered on the specialist register (a register of doctors who are eligible for appointment as substantive, fixed-term or honorary consultants in the NHS).
- Locum doctor
- A doctor who is paid to temporarily stand in for an absent doctor or fill a vacant position.
- Mid-level practitioner
- See Non-physician clinician.
- Non-physician clinician
- A professional health worker who is not trained as a doctor but who is trained to undertake many of the diagnostic and clinical activities of a doctor. They are now variously known as health officers, clinical officers, medical assistants, physician assistants, nurse practitioners and nurse clinicians.
- Nurse practitioner
- See Advanced nurse practitioner.
- Physician associate
- Previously known as physician assistants, a health-care professionals with a generalist medical education at a postgraduate level who works alongside doctors to provide medical care. They are dependent practitioners working with a dedicated supervisor but are able to work autonomously with appropriate support.
- Physician Associate Voluntary Managed Register
- A register of physician associates who have passed the national qualifying examination. It is held by the Faculty of Physician Associates within the Royal College of Physicians. The Department of Health and Social Care has recently had a public consultation regarding whether or not this register should come within the health professions’ regulatory processes and be held by a body such as the General Medical Council or the Health Professions Council.
- Registrar
- A doctor who has completed their Foundation Years training and is undergoing higher-level study and is training in a medical or surgical specialty or general practice.
- Resident
- A US term for a newly qualified doctor, which represents the UK equivalent of a Foundation Year doctor.
- Scrubs
- The blue or green cotton garments that are worn by hospital staff on the wards and in the operating theatre.
- Senior house officer
- Used prior to 2007 to describe junior doctors in their second year after graduating.
- Tariff
- NHS England sets a national tariff for the prices of treatment such as operations to be paid by NHS commissioning organisations to NHS provider organisations such as hospitals.
- To take out
- The prescription medications that a patient is given to take home on discharge from hospital.
- Trust
- The name used to describe a local NHS organisation.
List of abbreviations
- ANP
- advanced nurse practitioner
- CI
- confidence interval
- CQC
- Care Quality Commission
- df
- degrees of freedom
- ED
- emergency department
- FPA
- Faculty of Physician Associates
- FTE
- full-time equivalent
- FY2
- Foundation Year 2
- GP
- general practitioner
- HEE
- Health Education England
- ID
- identification
- LR
- likelihood ratio
- MD
- medical director
- MTS
- Manchester Triage Score
- NIHR
- National Institute for Health Research
- OR
- odds ratio
- PA
- physician associate
- RCP
- Royal College of Physicians
- SD
- standard deviation
- SHO
- senior house officer
- STP
- sustainability and transformation plan
- TTO
- to take out
- UKAPA
- UK Association of Physician Associates
